Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 08/1808/239. The contractual start date was in June 2009. The final report began editorial review in January 2013 and was accepted for publication in August 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Harvey et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction and background
In this introduction we present the policy context within which the research was set, and outline its aims and objectives. The literature which informed the analytical framework for the study is presented in Chapter 2 .
In 2008 when the National Institute for Health Research (NIHR) Service Delivery and Organisation (SDO) Programme Management Practice call was announced, the Griffiths report into management in the NHS1 was over 25 years old. Although Griffiths (p. 1)1 focused on general managers who ultimately would be accountable for the performance of NHS organisations,2 middle managers in health care have subsequently been identified as key strategic actors. Hence, predictably, in many organisations the number and variety of their roles steadily increased. 3,4 The NIHR SDO Programme call seemed to reflect the need for organisation and management researchers to more directly address the concerns and challenges facing management5 and to realise the potential of research evidence to improve managerial practice and decision-making. 6 It also mirrored the more general emphasis on evidence-based practice that now predominates in health care.
During the development phase of the present research, the role and responsibilities of the NHS manager were being expressed in various ways. For example, they have been described as enablers within the framework of ‘system management, regulation and decision-making that guarantees safety, quality, equity and value for money’ (p. 71). 7 The NHS was deemed to be ‘rapidly becoming a rules-based system’ (p. 5)8 where managers are expected to ‘build capacity, to manage choice and competition’, and hold the organisation to account ‘through assurance mechanisms’ (p. 71)7 and transparent performance metrics. 9,10 In 2010 when the fieldwork commenced, the then new coalition government had announced a 45% reduction in management costs (to be implemented over the next 4 years). This was classed as the ‘largest reduction in administrative costs in NHS history’ (p. 43). 11 Thus, NHS managers and their work is a subject of enduring concern. In recent years in particular this has been set alongside the increasing involvement of clinical staff in management.
NHS management came increasingly into the media spotlight and to the fore of government concern during the period of data collection for this study (which took place during 2010–12; see Chapter 3 , Introduction). Thus, the King’s Fund report on leadership and management in the NHS, published in 2011 (p. 8),12 highlighted the ‘spectacular management failures of NHS management and leadership’ revealed by enquiries into the Maidstone and Tunbridge Wells NHS Trust and the Mid Staffordshire NHS Foundation Trust. The juncture between the drafting of this report and the preparation of the present final version, saw the publication of the Mid Staffordshire NHS Foundation Trust Public Enquiry (Francis Report). 13 The report identifies catastrophic failures of care associated with the trust’s ‘ingrained culture of tolerance of poor standards’ (p. 43). 13 The trust board and senior leaders are held accountable for undue attention to financial issues and for paying ‘insufficient attention to the risks in relation to the quality of service this entailed’ (p. 45). 13 The subsequent government response, Patients First and Foremost: The Initial Government Response to the Mid Staffordshire NHS Foundation Trust Public Inquiry 14 signals measures to reduce ‘paperwork, box ticking and duplicating regulation and information burdens by at least one third’ and to set up a barring list for unfit managers, based on the barring scheme for teachers. The NHS Leadership Academy’s programmes are identified as a key arena for the harnessing of leadership skills to the provision of high-quality care. One part of this has been renewed attention to the challenges of the clinical manager role, i.e. those staff whose work combines the management/leadership of others with clinical work. For example, Patients First and Foremost14 identifies ward managers (termed nursing supervisory ward managers) as key to the delivery of safe, high-quality care to patients.
These recent calls are part of a longstanding agenda to reform clinical work and to improve efficiency and quality by forging more effective working relationships between clinicians and management in the NHS. 15,16 The most recent Labour government10 and the current Coalition government11 alike have emphasised the need to empower clinicians and promote clinical leadership. The White Paper Equality and Excellence: Liberating the NHS,11 which presaged the Health and Social Care Act of 2012,17 puts a strong emphasis on empowering front-line health care professionals and the incorporation of managerial and leaderships skills at all levels of clinical engagement (concerning not only doctors, but also other clinical staff). This seems to echo Griffiths’1 decades-earlier belief that clinicians are natural managers whose talents need to be encouraged and enabled. This expectation sits alongside the intent to reduce management costs by at least 45% between 2010 and 2014 and to remove layers of management in the NHS with the introduction of Clinical Commissioning Groups.
The NHS Modernisation Agenda and measures in its wake are premised on well-functioning relationships between doctors and managers18 and other clinical staff. Yet from the perspective of clinicians [by which we mean the spectrum of practitioners to include doctors, nurses, midwives and allied health professionals (AHPs)], the role of general middle managers has shifted over the last 20 or so years from that of administrators, who ‘provided an environment for clinical work to be done’ to controllers and implementers of top-down government policy. 19,20 Clinicians themselves have been increasingly recruited into roles which involve management as well as clinical duties. Hospital clinical directors were the vanguard of this phenomenon. It was noted early on21,22 that being a clinical director or the equivalent is a potential threat to the professional identity of the individual concerned as well as to collegiality and the autonomy of the professional group. Whether or not the long-standing tension between clinical professionals and general managers, and the particular challenges of the ‘hybrid’ clinical–manager role, are diminishing16,22 remains open to empirical investigation, especially as it is likely to be quite variable according to specialism and span of responsibility and control within an organisation.
When this research was at planning stage, the NHS Employers deputy director had stressed that ‘managers must look at what they can do to create a sense of identity among staff’ within their organisations, particularly in the midst of merger and restructuring activity in the NHS. 23 Yet relatively little consideration had then, or has since, been given to the identity of managers themselves within the health sector generally or in hospitals specifically, and even less to how this may influence how they go about their work. This especially has been the case at ranks below the top management or executive team level and particularly at the level of junior, or ‘front-line’, clinical and non-clinical managers.
An extensive and longstanding literature exists on the ethnography of management. 24,25 However, much of it focuses on private rather than on public sector organisations, such as the NHS. Hence the aim of this research was to undertake ethnographic research within the hospital sector to explore the identities of clinical and non-clinical middle and junior health-care managers and to chart the kind of work they do, including the mobilisation of their identities within the distinctive organisational context of the NHS. As part of this we wanted to investigate whether or not managers with different clinical and non-clinical backgrounds, and at middle and junior levels, have different sources of identification, leading to different identities, which, in turn, might shape their interpretations of their roles and the ways in which they carry them out.
Definitions
Middle and junior managers
Chapter 2 describes how the academic literature has sought to define junior and middle managers. It is somewhat vague and inconsistent. In general, definitions of middle managers are broad in conception and typically see them as below executive level, and above managers who oversee ‘front-line’ operations. Junior managers, by contrast, are generally defined as ‘front-line’ or ‘first-line’ managers, concerned with operational rather than strategic management and with a supervisory component; in fact, they are referred to as ‘supervisors’ in some contexts. The NIHR SDO Programme call did not define junior or middle managers. For the purposes of this research, we define middle managers as those in a management role below executive board level but above the level of ‘front-line’ operational management, whom we take to be junior managers. Within the pay grade structure this equates to those on Agenda for Change (AfC) bands 4–7 being classed as junior managers and those on band 8 and above (but not full members of the executive board) as middle managers. Even so, as discussed in Chapter 3 , actually distinguishing middle and junior managers (especially from job titles) and, to a lesser extent, clinical and non-clinical managers was problematic.
Identity
Once the research commenced we elected to adapt the model of social identity proposed by Ashforth et al. (pp. 328–31). 26 Here social identity is placed on a continuum from (i) the ‘core’ of identity (such as ‘I am’ a nurse, a manager), (ii) the ‘content of identity’ (e.g. values, motivations, beliefs, stereotypical personal traits), to (iii) the ‘behaviour of identity’ (i.e. the work that they do). As a composite we refer to elements of an identity, such as self-definition, values and work, as ‘facets of identity’.
Identities may conflict, converge and combine,26,27 thus we considered middle and junior managers as carriers of multiple identities. 13,27 This approach has an affinity with the recently published (after the completion of our research) Foresight report28 on future identities in the UK, which emphasises that contemporary identities are ‘multiple, culturally contingent and contextual’ (p. 1). 13 Managers’ identities may be seen as inherently in flux, as an organisation comprises ‘a series of influential discourses, often competing against each other, which create the possibilities of conflicting identities’ (pp. 212–13). 29 In this context, managers have been identified as ‘boundary spanners’,30 ‘translators’ and ‘integrators’,31,32 with a key role in mediating and facilitating between ‘tribes’, while not really coalescing into a ‘tribe’ themselves.
Wider research on the mobilising potential of identity has tended to focus on how shared identities, such as those associated, for example, with ethnicity, age or gender, or on how identification with a particular issue, such as racism, ageism or sexism, are collectively organised to effect change (e.g. social movements research). We are aware of no existing research which looks, as we do here, at how individual managers mobilise their identities in organisational contexts. We focus on the ‘mobilising capacity’ of those facets of their identities that strengthen and weaken their ability to influence others and the enactment of this capacity in the context of their work with others, which we call their ‘mobilising strategies’ (these concepts were derived inductively from the data).
Effectiveness
It has been argued that ‘the way that professionals view their role identity is central in how they interpret and act in work situations’ (p. 1515)33 and hence, comprehending managers’ identities seems essential to understanding their work performance and the performance of their team, unit or organisation. However, as has long been recognised34 linking facets of identity to managerial performance is particularly problematic. Our focus is on managers’ own self-reported effectiveness and what influences this in their assessments. We adopted a general definition of effectiveness as a multidimensional concept concerned with the attainment of desired outcomes. 24,35
Research aims and objectives
As advised by Mintzberg24 more than 40 years ago now, we sought to locate managerial work in the context of organisational structures and processes. Through this we hoped to discover whether or not managers with clinical and non-clinical responsibilities and at middle and junior levels have different sources of identification, leading to different identities, which might shape their interpretations of their roles and the ways in which they carried them out.
The primary typology of managers was based on the two dimensions of management level (middle or junior managers) and clinical engagement (whether the manager is counted as clinical or non-clinical staff). This generated four primary groups: junior clinical (JC), junior non-clinical (JNC), middle clinical (MC) and middle non-clinical (MNC). We also employ a more fine-grained categorisation according of ‘work groups’ (which maps back onto the four ‘primary groups’) for some aspects of the analysis which follows.
In summary, the aims and objectives of the research were:
-
to chart the work of middle and junior health-care managers, including identity work, and to produce an ethnography of the lived experience of middle and junior management within the specific context of the NHS
-
to explore the identities of managers (goals, values, motivations, beliefs and interaction styles) and how these are constructed, and further, how the performance of managers’ roles is shaped by these identities
-
to capture how middle and junior health-care managers leverage their identities to create success, establish trust and broker alliances to exert influence in different and various spheres and to determine how they interpret and take forward their ‘project’ to achieve organisational, group and personal goals within the framework of the NHS
-
to determine the influence of managerial identities on organisational processes and outcomes.
Structure of the report
Chapter 2 provides an outline of the key bodies of research relevant to the research and outlines the analytical framework that guided the conduct of the study and data analysis. Chapter 3 details the research methodology and Chapter 4 provides an overview of the two research sites (two acute hospital trusts). Chapters 5–8 set out the research findings. Specifically, Chapter 5 explores the ‘facets of identity’ of the four main categories of manager. Chapter 6 analyses what managers do in their work, based on the more fine-grained work groups. In Chapter 7 we consider the managers’ self-reported accounts of how effective they are as managers and what facilitates and what inhibits their effectiveness. Finally, in Chapter 8 , we report on how managers seek to mobilise their identities to exert influence in the various and different spheres in which they operate. Chapter 9 summarises the main findings and outlines the recommendations for practice and for future research. Although of necessity the chapters build on and relate to each other, the report has been written in such a way that readers interested in particular findings can also read each chapter as a stand alone.
Chapter 2 Analytical framework
This chapter presents the analytical framework for our study. The first part (see Identity, Professions, and Junior and middle managers) offers a brief overview of research in three topic areas relevant to our investigation. The aim of the overview is not to provide a comprehensive survey of the literature, but rather to establish the key reference points germane to our conceptualisation of identity and its mobilisation in the context of managerial work in the NHS. The second part of the chapter (see Analytical framework) lays out our analytical framework.
Identity
Identity is defined as ‘a self-referential description that provides contextually appropriate answers to the question “Who am I?”’ (p. 327). 26 Identity as a concept helps to ‘capture the essence of who people are’ and ‘to explain why people think about their environments the way they do and why people do what they do in these environments’ (p. 334). 26
Identification is ‘the process by which people come to define themselves, communicate that definition to others and use that definition to navigate their lives’ (p. 334). 26
An individual’s self-concept consists of (a) personal identity, or ‘a person’s unique sense of self’ (p. 260)36 and encompasses their idiosyncratic characteristics, such as bodily attributes, psychological traits and interests, and (b) social identity, or ‘a person’s sense of belonging to some human aggregate’ (from a small group to a nation) (p. 21). 37 The focus of our project is on social identities.
Research on identity is prominent in anthropology, organisation science, philosophy, psychology and sociology. Of these, the research in sociology and organisation science is most relevant to the project topic.
In sociology, research on identity consists of two distinct strands (1) a (sociological) social psychology strand, which focuses on individual agency, and (2) a collective identity strand, which focuses on group agency.
The social psychology strand focuses on the identities of individuals and encompasses two inter-related research traditions. The first (e.g. identity theory38) emphasises ‘internalized role-identity meanings’ and examines ‘how the social positions that people occupy become stable, internalized aspects of their self-concepts’. The second (e.g. social identity theory39) emphasises ‘culture and situational context’ and investigates how ‘cultural meanings associated with identities are imported by actors into local interactions and how situational environments shape the localized meanings of the situationally relevant identities’ (pp. 480–4). 40
The collective identity strand focuses on the identities of groups, or collective identities, and examines how collective identities are constructed and influence mobilising joint action. The collective identities examined in this strand are primarily associated with the ‘holy trinity’ of social categories: gender/sexuality, race/ethnicity and class (p. 1). 41 A notable example of research in this strand is the studies of social movements. 40,42
In organisation science, research on identity traces its roots to the works of Simon43 and March and Simon,44 but has gained strength from the late 1980s following the publications by Albert and Whetten45 and Ashforth and Mael. 37 Recently, research on identity has been deemed ‘one of the fastest growing, most fertile, and . . . most contested’ research areas in organisation science46 impacting nearly all research domains in the field. 26 Identity and identification are considered as ‘root constructs in organizational phenomena’ because ‘they speak to the very definition of an entity – an organization, a group, a person’ and because they ‘situate the organization, group, person’, which is essential for interaction between the entities (p. 13). 47,48
Research shows that identity and identification are essential for the well-being of both individuals and collectives (groups and organisations).
For individuals, the two basic motives for – and the outcomes of – social identification are (1) self-enhancement and (2) uncertainty reduction. Self-enhancement (or self-esteem) underpins the striving for positive intergroup distinctiveness: ‘a belief that “we” are better than “them”‘. Uncertainty reduction is associated with social categorisation: ‘People . . . like to know who they are and how to behave and who others are and how they might behave’ (p. 120). 48 An additional motive/outcome, specific to work context, is employee strengthening, or a process of increasing individual capacity to endure stress and take on new challenges. Employee strengthening is associated with a particular type of social identity, dubbed ‘positive identity’, variously interpreted as ‘infused with virtuous qualities’, entailing ‘subjective feelings of self-regard’, or keeping ‘the multiple facets of the identity . . . in a balanced . . . relationship’. Positive identity leads to employee strengthening, because it helps to build social resources, i.e. ‘the number, breadth, diversity, and quality of relationships employees have at work’ (pp. 268–73). 46
With regard to collective outcomes, research has mainly focused on organisational identification, showing that such identification job satisfaction, intrinsic motivation, task performance, employee turnover, co-operation, teamwork, information sharing, organisational citizenship, creative and helping behaviours, customer orientation, improved organisational control, and positive evaluation of the organisation (though this list may be misleading) (pp. 336–7). 26
Despite the wealth of research on identity, considerable gaps remain in our understanding of this phenomenon, especially with regard to work-related identities.
Thus, the research on work-related identities has focused largely on the identification with the organisation as a whole (‘organisational identity’), whereas other loci of identification, namely work groups, organisational units and occupations, have received little attention (p. 348). 26 In particular, research on occupational and professional identification has been ‘sporadic’, though more frequent recently33,49,50 and the topic of managerial identity has been particularly neglected (for notable exceptions). 50,51 Hence, researchers have primarily concentrated on how managers manage the identities of other groups (e.g. medical professionals; see Covaleski et al. 52) and of the organisation as a whole, but largely disregarded the identities of the managers themselves. Within the research on the identities of managers, the identity of junior and middle managers has received much less attention than the identity of senior management; and the identities of those working in public service contexts have received far less attention than those working in the private sector (p. 5). 53
Our project addresses these gaps, contributing both to better understanding of management in the NHS and to the broader research on identity.
We also note that research on mobilising identities has been mainly confined to identity mobilisation in the context of social movements, with particular reference to social category identities, such as gender, race and class. We were unable to find any research on identity mobilisation in the organisational context and with reference to occupational/professional work.
Professions
The changing role of the professional worker in the 21st century has been identified as of critical sociological importance. 54
Early accounts of professions were based primarily on studies of the liberal professions (especially medicine) and focused on their distinctiveness from other occupations, cataloguing their traits and documenting their (successful) quest for power and autonomy. 55–57 These accounts clearly differentiated between professionals and managers. 58 The latter were described as depending for their power on their position within, and knowledge, of a particular organisation, whereas that of the former stemmed from abstract knowledge and was independent from organisations.
More recently, however, the emphasis has shifted to reflect new realities as the privileged position of traditional professions has been threatened by globalisation, technological change, neo-liberal ideologies,59 the encroachment of managerialism60 and the spread of ‘new professions’ (such as ‘knowledge workers’). 61,62 The boundary between managers and professionals has also been blurred by the increasing professionalisation of management and the co-optation of professionals into managerial jobs. Yet, although some have argued that the rise of new forms of professionalism advances co-operation and reduces barriers between occupational groups, others have observed the persistence of the classic patterns of professionalism, based on status hierarchy and exclusion. 63
Particularly germane to this research is the literature on the relationships between managers and (other) professionals in health care. For expediency, in what follows we present a stylised composite picture of this literature.
Most has focused on clinicians – as managers and vis-à-vis managers. Clinical and managerial logic are usually portrayed as incompatible and hence conflicting. Yet, with the advent of New Public Management (NPM), clinicians have been drawn into management processes, both indirectly, by having to contend with the increasing organisational constraints (e.g. leaner budgets, closer control of performance), and directly, by assuming managerial roles64,65 and moving into ‘hybrid’ (clinical and managerial) organisational positions. 66 As Kirkpatrick et al. (p. 121)67 relate with reference to physicians, extending clinical leadership in the hospital sector has become an ‘international fashion’ though how it is enacted and the level of engagement varies considerably and depends very much on local conditions. Research frequently has found that clinicians are reluctant to engage in managerial work,68 but are also uncomfortable with the idea of non-medics taking decisions that affect patient care69 and may be motivated to enter management by the desire to influence the direction of change. 66 Nurses see management as a step up the nursing career ladder, whereas medics see it as a step away from what really matters. 70 Most clinicians, on entering management, strive to maintain their clinical responsibilities and are keen to disassociate themselves from the term ‘management’. 71 This has led some to conclude that the boundaries between medicine and management are no longer sustainable. 72 As Kuhlmann et al. relate, organisations, such as hospitals, are ‘“switchboards” of clinical practice, where “medicine meets management” and control is made and remade’ (p. 723). 72
In post, many clinical managers see themselves as performing a critical boundary role, translating between different groups,33 and nurses in particular come to espouse managerial definitions of professional work. 73 At the same time, many feel isolated from other clinicians (the feeling exacerbated by hostility from their former colleagues)66 and ‘caught in the middle’ between the expectations of subordinates (to represent clinical interests) and the demands of senior management (to run efficient and effective services). 74 Qualitative research by Spehar et al. 75 in Norway on nurses’ and physicians’ journeys into management found that most had not anticipated a career in management but were persuaded into it. Most were thrown into the position unprepared for the challenges, which they had to learn to deal with ‘on the fly’ (i.e. with insufficient training).
Getting into management does not necessarily mean subjugating a clinical agenda to a managerial one. Indeed, as a detailed analysis of one US manager reveals, it can mean finding oneself on the boundaries of several discourses, such as the profession-specific discourse of medicine; the resource-efficiency and systematisation discourse of management; and the ‘inter-personalising discourse devoted to hedging and mitigating contradictions’ (p. 15). 76 In the UK, clinical directors have been shown to subvert market discourse by making rhetorical appeals to ‘service quality’ and to ‘market demand’ in order to bargain for extra resources, defend the status quo,77 and to counter managerialism by asserting their capacity to be ‘close to the customer’ in a way that management cannot. 78
Nor do the differences between clinical and managerial logics necessarily lead to a conflict. As Reay and Hinings79 demonstrated, based on their research on health care in Canada, a rivalry between these logics may be managed by a collaboration that allows the collaborators to maintain their independence (e.g. differentiating medical decisions from managerial decisions, seeking informal input from medics as part of decision-making processes, and working together against the Government). Similarly, drawing on ethnographic case studies of Dutch health-care organisations, Stoopendaal80 suggests that rather than provoking conflict between different interest groups, the position of non-clinical managers as ‘outsiders’, can allow managers to serve as a tie connecting these groups.
Clinicians may also become ‘managerialised’ without entering the ranks of management. As Waring and Currie81 argue, medics may draw managerial expertise into their professional practice in order to stave off managerial encroachment by taking responsibility away from managers (‘co-optation’), adapting existing professional systems to better reflect the aspirations of policy (‘adaptation’) or circumventing management systems (‘circumvention’) by emphasising the superiority of their own systems.
Yet, however blurred, boundaries between clinicians and managers persist, even when clinicians become managers. Thus, Hoque et al. 82 showed a clear divide between consultant managers and non-consultant managers in how they perceived each other and their own roles: whereas non-clinical managers spoke of being an interface between management and medical staff, promoting a quality service, fulfilling the daily needs of clinicians and patients, and improving the environment in terms of training, recruitment and personnel; clinicians alternatively talked about having a blueprint for the NHS and delivering it. Consultant managers, who retained a ‘strong identification with their profession’ were also left feeling unduly constrained, whereas non-consultant managers saw themselves as agents of government and their role as delivering targets and centrally derived objectives.
Junior and middle managers
The literature on managers mirrors management hierarchy, with senior managers attracting the most attention and junior managers the least. Furthermore, whereas the research on middle managers generally and in the NHS in particular, has burgeoned in the past two decades, the research on junior managers peaked between the 1940s and 1970s, and then petered out recently, with a paucity of studies in the health-care context.
Junior managers
The delineation of junior management has been a contentious issue. Some authors have used terms such as ‘junior manager’, ‘front-line manager’, ‘shop-floor manager’, ‘team leader’ and ‘supervisor’ interchangeably,83,84 whereas others have distinguished between supervisors, who engage with workers directly and only implement decisions at an operational level, and front-line managers, who deal with workers through the supervisor and possess delegated authority. 85 We follow Hales86 in treating supervisors and ‘first-’ or ‘front-line’ managers as parts of one entity, in which various functions of ‘management’ and ‘supervision’ are distributed in different ways among different positions, and refer to them jointly as junior managers.
Traditionally, the role of junior managers (as depicted, for example, in the research on industrial supervisors and foremen that proliferated from the 1940s to the 1980s87,88) was fairly clearly and consistently defined as encompassing planning, scheduling and allocating work, monitoring output and conduct of work, checking equipment, ensuring safety and cleanliness, dealing with unforeseen staffing, equipment and production problems, maintaining discipline, handling disputes, training, counselling and record keeping. 89,90
More recently, in his review and survey of 135 organisations in the south of England, Hales86 relates that organisational changes, such as the spread of team-working, flattening of organisational hierarchies and devolution of budgetary responsibilities from middle to junior management, have engendered a shift in the junior manager’s role. Though some have suggested that these changes entail the decline of supervisory responsibilities, Hales86 asserts that they have strengthened the supervisory core of junior manager’s responsibility (especially in the light of increasing external regulations), while adding a panoply of managerial responsibilities, relating to stewardship, translating strategy into operations and business management.
Given this intensification of core supervisory duties with additional devolved managerial responsibilities, Hales (p. 174)91 suggests that junior managers construct a ‘precarious coping identity’, which may have potentially negative consequences for their work performance.
The literature highlights the importance of junior managers, who ‘direct as much as two-thirds of the workforce and are responsible for the part of the organisation that typically defines the customer experience’ (p. 2). 92 Yet, it also acknowledges that junior managers are primarily seen as ‘cogs in the system’ and have limited flexibility in decision-making. They have considerable power over operational matters, some power over the people management, little or no power over resources, and a limited capacity to influence upwards in the organisation. 93
Overall, however, our review indicates that, in the past two decades, there has been insufficient research on junior management, particularly in professional organisations and the health-care sector. Our project, therefore, fills a gap in the literature.
Middle managers
Similar to junior management, the delineation of middle management has been a thorny issue: the boundaries of the ‘middle’ are contingent on organisational structure and so the ‘middle’ may extend across several levels of management. 51 Generally, however, ‘middle management’ refers to the managers situated ‘below the top managers and above first-level supervision’ (p. 1192). 94
Also similar to junior management, there have been considerable debates about the impact of organisational changes on the role and responsibilities of middle managers (for an overview, see Thomas and Linstead51). Some believe that changes such as developments in information technology (IT) have significantly limited the role and undermined the position of middle managers,95 whereas others hold a more optimistic view, suggesting that ‘a slimmer middle management in a time of rapid change has a more important role to play than in the past’ (p. 43). 3 In the context of NPM, the position of middle managers has been equally equivocal: strengthened by the emphasis on management96 but threatened by the focus on cost-improvements.
There is a burgeoning literature that argues that organisational performance is heavily influenced by what happens in the middle of the organisation, rather than at the top (for overviews, see Dopson and Fitzgerald3 and Wooldridge et al. 94), and that middle managers are key strategic actors. Middle managers are a linking-pin between the strategic apex of the organisation and the operating core (p. 70). 97 They ‘mediate, negotiate and interpret connections between organisations’ institutional (strategic) and technical (operational) levels’ (p. 6). 98 Nurse managers appear to be particularly well suited for linking operational and strategic management71 and managing relationships between various categories of staff (particularly doctors and nurses). 3 Middle managers are seen to perform the critical roles of interpreting and framing strategic objectives for front-line staff, ‘selling’ strategic ideas to executive management and elaborating on the detailed content of strategic change99,100 and boundary-spanning. 101 Their work also frequently goes beyond their job description (which generally concerns standard general management roles, such as staff management, representation, monitoring performance standards) to embrace the management of major organisational changes (e.g. the relocation or expansion of a service to a new site, the adoption of new technology; the reconfiguration of staff skills to provide more effective use of resources). (See Fitzgerald66 for clinical directors.)
Yet, similar to clinical managers, middle managers also feel ‘caught in the middle’, being required to be both team players and executioners. 101,102 Further, at least in the NHS, middle managers’ potential strategic contribution is constrained by ‘a powerful professional cadre of core employees’ (i.e. medics) and by ‘the changing priorities of government policy’ (p. 1326). 103 Although frequently portrayed as instruments of Government in the public sector in respect of cost control and targets,104 middle managers tend to resist changes that they see as politically imposed and unnecessary or inimical to public services. ‘Hybrid’ managers, drawn from the clinical ranks, have an additional challenge of experiencing the conflict between their professional and managerial roles. 4,64,70
A new twist on junior and middle management has been introduced by a recent shift of emphasis by policy-makers from management to leadership. 99,100,105 Leadership has been advocated as means of reinvigorating public services (p. 770)106 and viewed as an ‘identity’ that should be utilised across organisations, not just by those at the top. In particular, in the NHS, various grades of staff (from matrons to operating assistants) have been given the designation ‘leader’. 107 This move might have been particularly welcomed by clinical managers that have been traditionally reluctant to identify themselves as managers. However, although there is much talk about the shift to leadership, there is little detail about how it is exercised in practice. Thus, Martin and Waring107 note that the effectiveness of newly designated leaders is limited, they can be effective only as long as what they do is consistent with the existing organisational arrangements and power structures.
Analytical framework
We use the term ‘analytical framework’ to signal that we consider our work as exploratory rather than aimed at testing or refining particular theories.
This analytical framework consists of a set of ‘sensitising’ concepts108 and ideas that guided our empirical investigation.
Identity
In order to examine the process and outcomes of mobilising identities, we needed first to map the social identities of the junior and middle managers in the NHS and establish what was characteristic of their identities. Although we acknowledge that social category identities (such as gender) and non-work-related identities (e.g. parent) might be important, our project focused on occupational/professional identities.
To describe the managers’ identities we adapted the model of social identity proposed by Ashforth et al. (pp. 328–31). 26 Their original model portrays social identity as a continuum that encompasses (moving from the narrow to the broad formulation): (1) core of identity, including self-definition (‘I am “A”’), importance (‘I value “A”’), and affect (‘I feel about “A”’); (2) content of identity (i.e. values, goals and beliefs, stereotypic traits, knowledge, skills and abilities); and (3) behaviour of identity. Our adapted version of their model is presented in Figure 1 .
FIGURE 1.
A model of identity.
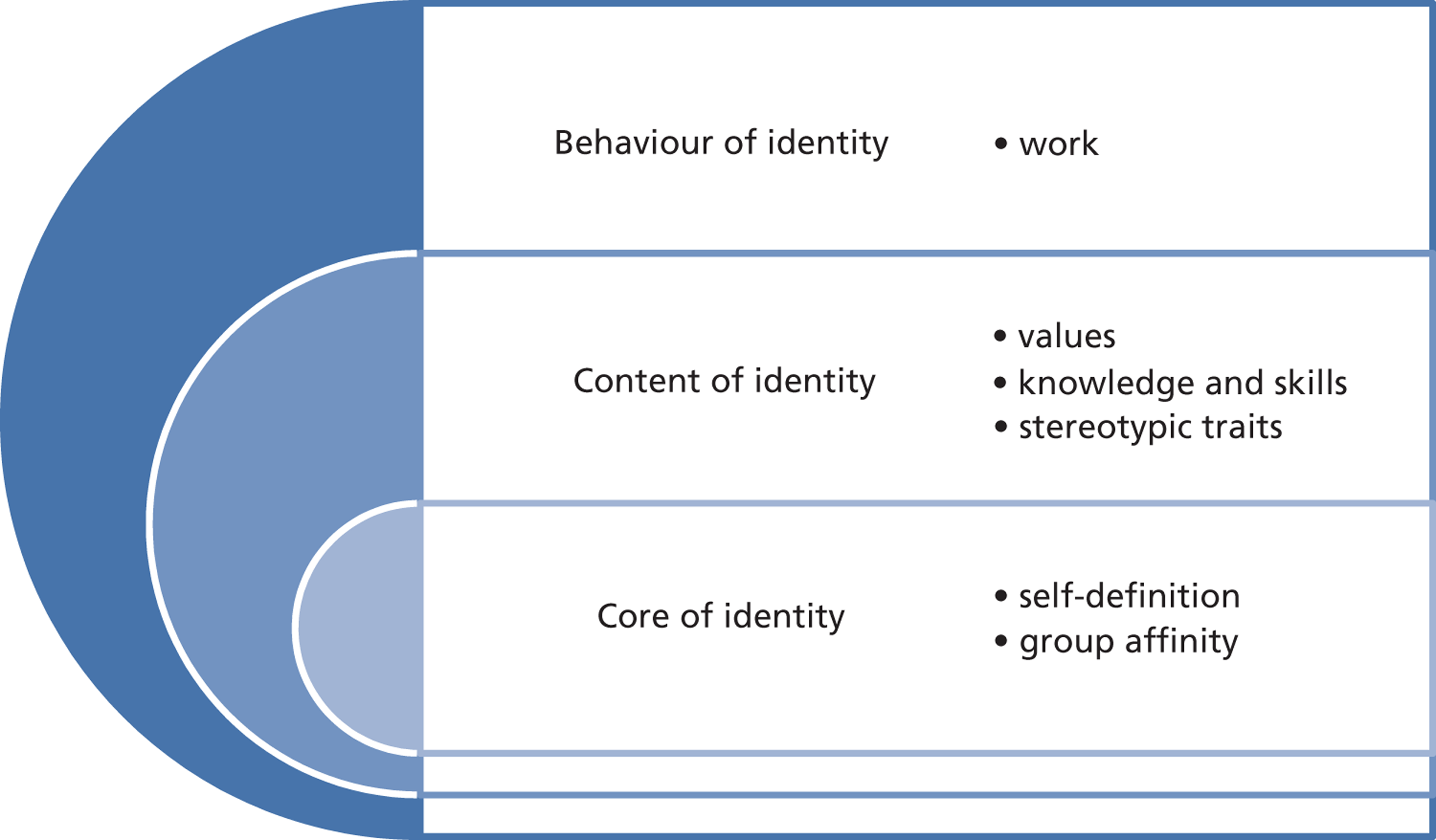
We refer to particular elements of an identity, such as self-definition, values and work, as the facets of identity.
An individual’s identities may:
-
conflict – when there is ‘an inconsistency between the contents of two or more identities, such as a clash of values, goals, or norms’
-
converge – so that different identities become aligned and reinforce each other, and/or
-
combine – so that different identities are compartmentalised (pp. 354–9). 26
Social identities are ‘relational and comparative’ (p. 16)39 because individuals develop the self-definition and the evaluative component of identity by contrasting the group with which they identify with a salient other group.
An individual’s identity is further ‘verified or falsified by experiences provided by interactions with similar others’ and by the ways one is described by others (p. 208). 109
Identities evolve, fluctuate and change. Individuals learn identities through the processes of identity enactment and sense-making (reflecting on the reactions to the identity enactment). ‘Much if not all activity involves active identity work: people are continuously engaged in forming, repairing, maintaining, and strengthening or revising’ (p. 626). 110
Effectiveness
Within the framework of NPM it is usual to connect effectiveness with quality, safety and financial targets. 111,112 This ties effectiveness to objective ‘performance indicators’ which in turn are associated with the attitudes, actions and achievements of individuals. Accordingly, we expected that these ‘hard’, evidential forms of effectiveness would be vital for most managers.
However, we also anticipated that managers would imbue the notion of effectiveness with a wider meaning, because in the health-care environment the achievement of effectiveness occurs in the ongoing interaction between people. Thus effectiveness is also ‘softer’, diffuse, processual and difficult to tie to hard outcome measures.
Mobilising identity
As noted above, the extant literature provides little, if any, guidance on identity mobilisation in organisational context and on the mobilisation of occupational/professional identities. Perhaps, even more importantly, it only discusses identity mobilisation as a group phenomenon that contributes to collective action. In contrast, this research does not deal with group or collective action (indeed, one would be hard pressed to conceive of the grounds for and the forms of such action in our empirical context). Hence, we had to navigate the uncharted waters and develop our own conceptual structure to explore how junior and middle managers mobilised their identities.
The dearth of existing research on the mobilisation of individual identities means that we need to anticipate some of our results not yet presented in order to explicate our analytical framework. As discussed in Chapter 8 , we found that identity mobilisation was an individual rather than a group project, even though the individuals mobilised their social identities as members of particular professional groups. This identity mobilisation mainly took the form of individual action and was directed at the members of other groups within the organisation: the junior and middle managers’ subordinates, superiors and peers (colleagues at the same ‘lateral’ level of organisational hierarchy). The goal of this mobilisation was to influence these others to act in the way that would enable them to achieve their own effectiveness (variously defined, as above). To influence others, the managers drew on the specific facets of their identities that strengthened their ability to influence others. We termed these facets mobilisation capacity. The enactment of the mobilisation capacity in the context of a relationship between the manager and others we termed mobilisation strategy.
Chapter 3 Methods
Introduction
We ascertained that the best way to capture the lived experience of middle and junior, clinical and non-clinical, managers was to situate their work within its organisational context. This follows from our theoretical approach. Identities are recognised to be highly contextual. In other words, they are formed in interaction with others and can alter in their emphasis according to the interaction context in which the individual is engaged. 13 Thus workplace organisational contexts – which in the case of hospital trusts are likely to be wide in scope for some managers (see Chapter 6 , General parameters of managers’ work) – are important to capture empirically because they facilitate the formation and enactment of identities.
Two large hospital trusts in the same region with similar organisational structures (at the start of the fieldwork) were selected for study (see Chapter 4 ). To recap, we endeavoured to collect rich, ethnographic data to enable us to provide an account of the every-day work of these categories of manager, and to capture any associations between their sense of identity, how they mobilised their identities in the course of their work, and how this contributed or detracted from their self-reported effectiveness.
The main data collection method was one-to-one, in-depth, semistructured interviews, including a reflection on respondent-generated schematic work diaries. This was supplemented by shadowing of a number of respondents and the observation of meetings. The fieldwork took place consecutively in the two hospital trusts over approximately 24 months between 2010 and 2012. The research was approved by the Regional Research Ethics Committee in December 2009 (i.e. before the harmonised edition of the Governance Arrangements for Research Ethics Committees,113 which excludes research on NHS staff by virtue of their professional role from the National Research Ethics Committee, came into effect).
The two research sites
Case studies are an appropriate method to use when posing ‘how’ and ‘why’ questions, when the researcher has little control over events, and when the ‘focus is on a contemporary phenomenon in a real-life context’ (p. 2). 114 Case studies are generalisable to theoretical propositions, not to populations or universes. 114
The case study hospital trusts were both multisite organisations which had not yet achieved foundation trust status: we refer to them as Metropolitan Hospital Trust (Metropolitan; case study 1) and Cityscape Hospital Trust (Cityscape; case study 2). As discussed further in Chapter 4 , at the design, inception and negotiation of access for the study (via senior board-level individuals in each trust), the two trusts were virtually identical in size and structure. Our initial expectation was that using very similar organisations would enable us to identify whether or not the association between identity and work activity was common for managers in both trusts following Yin’s114 concept of multiple-case design using literal replication with embedded units of analysis [i.e. the four groups generated from the primary typology based on the two dimensions of management level (middle or junior managers) and clinical engagement (clinical or non-clinical staff)].
However, this was impeded by organisational restructuring at Cityscape following changes in key members of their executive team. Even though Metropolitan was not undergoing the same degree of organisational change, it was not static either. In fact, the dynamics that the two trusts faced such as multisite working, year-on-year efficiency savings and cost improvement programmes, and mergers of services are mirrored by trusts across the country.
Once the full phase of data analysis began (see Data analysis), it became apparent that the organisational factors affecting the work of the middle and junior managers were of a similar order across the two trusts. A further factor inhibiting comparison was the distribution of respondents (see Sampling method). For example, all scientist managers were located at Metropolitan and the majority of nurse middle managers at Cityscape.
We, therefore, did not seek to compare the two trusts but rather combined the two sets of data for analysis to generate cross-case theoretical generalisations, drawing out specific references to any organisational differences where they mattered for aspects of the managers’ work where appropriate.
Sampling method
The intention was to recruit 24 middle managers (12 clinical and 12 non-clinical) and 24 junior managers (12 clinical and 12 non-clinical) at each site, constituting a total sample of 96. We chose these numbers as they were deemed large enough to capture internal variation within each of the four categories for what we anticipated to be a diversity of jobs and sufficient for any differences across categories – such as between middle and junior managers, and between clinical and non-clinical managers – to emerge.
Respondents were purposively sampled and drawn in consultation with human resources (HR) staff in the two trusts with the aim of maximising variance across the organisation (i.e. managers were chosen from a wide range of directorates/divisions and specialities/departments occupying a variety of comparable roles across the two trusts). Prospective participants were contacted by HR staff by letter and those opting into the research then contacted the research team directly (see Appendices 1–3 ).
As shown in Table 1 , slightly more respondents were recruited from Metropolitan (52%) than from Cityscape (48%), and there is slightly more clinical (53%) than non-clinical staff (47%) in the overall sample.
| Category | Metropolitan | Cityscape | Total | ||||
|---|---|---|---|---|---|---|---|
| Junior | Clinical | 11 | 12% | 10 | 11% | 21 | 23% |
| Non-clinical | 9 | 10% | 6 | 7% | 15 | 16% | |
| Middle | Clinical | 12 | 13% | 15 | 16% | 27 | 30% |
| Non-clinical | 15 | 16% | 13 | 14% | 28 | 31% | |
| Total | 47 | 52% | 44 | 48% | 91 | 100% | |
The achieved sample reflects difficulties in recruiting certain types of staff, predominantly non-clinical staff, notably JNC managers at Cityscape. Also, within the MC category, we experienced particular difficulties recruiting doctors (nurses, midwives and scientists are the major work category for MC managers, Table 2 ). This may reflect the more general observation within the two trusts of generating the involvement, participation and presence of medical doctors. For example, our observations showed that both trusts (but Cityscape in particular) experienced difficulties in getting medical doctors to attend meetings in sufficient numbers. It may also be the case that doctors were less likely to opt into the study, as they are less likely to think of themselves as ‘managers’.
| Work group | Metropolitan | Cityscape | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| MC | MNC | JC | JNC | MC | MNC | JC | JNC | ||
| 1. Consultant managers | 3 | 3 | 6 | ||||||
| 2. Nurse and midwife managers | |||||||||
| (a) Middle | 4 | 10 | 14 | ||||||
| (b) Junior | 5 | 8 | 13 | ||||||
| 3. Scientist managers | |||||||||
| (a) Middle | 5 | 5 | |||||||
| (b) Junior | 4 | 4 | |||||||
| 4. AHPs | 2 | 2 | 4 | ||||||
| 5. Managers of clinical units | |||||||||
| (a) Middle | 10 | 2 | 9 | 21 | |||||
| (b) Junior | 5 | 3 | 8 | ||||||
| 6. Managers of corporate units | |||||||||
| (a) Middle | 5 | 4 | 9 | ||||||
| (b) Junior | 4 | 3 | 7 | ||||||
| Total | 12 | 15 | 11 | 9 | 15 | 13 | 10 | 6 | 91 |
The slight shortfall in the overall number of interviews (n = 91) against the target (n = 96) is not significant as it was still possible to reach analytical saturation when analysing the data for the four primary categories.
The sample is predominantly (75%) female. The only subcategory in which males exceed females is the MC managers at Metropolitan.
Table 2 illustrates the job titles of managers in each of the four overarching categories of managers. The NHS grading and pay system AfC115 allocates posts to one of nine pay bands based on the knowledge, responsibilities, skill and effort needed for the job. Band was not available for the whole sample. However, for those providing this information, all of the middle managers (both clinical and non-clinical) were within bands 8a–d, with one respondent in band 9. The JC managers were mainly band 7, with some band 6. JNC managers ranged mostly from band 5 to band 7, though one was band 4. Generally speaking, those classed as middle managers had larger ‘spans of responsibility’ than junior managers. ‘Span of control’ (defined as the number of the manager’s direct reports) often was larger for junior managers than for middle managers, though, again, there was variation within this (see Chapter 6 ).
Blurred boundaries
As already discussed, the terms middle and junior manager are contested terms. Grouping respondents into the four primary categories was not always straightforward. This is well illustrated by the following scientist manager:
Well, whether I’m classed as a middle or junior manager, or am I healthcare professional? Actually, I’m probably all of them.
MC 21
The boundaries of the middle extend across various levels of management and depend on specific organisational structures. 51 Unsurprisingly, therefore, some of those we classified as ‘middle’, self-identified as ‘senior’. The term ‘junior manager’ was particularly unfamiliar to most respondents. For example, when asked if the terms junior manager and middle manager were familiar, one respondent commented:
Not really, no, which is why I signed up in the first place, because I thought well, as far as I know, I was a middle manager because I manage some things in quite a lot of detail and I don’t manage others and there are people above me and there are people below, so I am probably in the middle then so . . .
MC 14
The line between clinical and non-clinical staff was not straightforward either. Some managers whose roles were non-clinical, and are classified as such here, were clinically qualified (e.g. in nursing or the allied health professions). The following radiography services manager was on AfC band 8a as a result of her clinical qualifications, but the scope of her activity was more similar to JNC managers on band 7. Highlighting the complexity, but also connectedness, she mused,
You know, you can’t think of yourself as . . . it’s hard to know whether you’re a middle manager, senior manager, or clinical person because you can one minute find yourself doing something which you regard as fairly low level, and the next minute you can be doing something that you think is very strategic and you feel it’s a higher level. But the whole thing goes together and so it’s hard to know, you know, you work as a team and the whole team working at all these different levels is about what you want to do.
MNC 45
Work categories
In some of the analysis – mainly Chapter 6 , which provides a textured account of ‘what managers do’ – we further subdivided the sample into what we call ‘work groups’ as follows:
-
group 1: consultant managers
-
group 2: nurse and midwife managers
-
– middle (e.g. matron),
-
– junior (e.g. ward sister)
-
-
group 3: scientist managers
-
– middle (e.g. consultant scientist)
-
– junior (e.g. team leader)
-
-
group 4: AHPs
-
group 5: managers of clinical units
-
– middle (e.g. division general manager, service manager)
-
– junior (e.g. administrative manager)
-
-
group 6: managers of corporate units
-
– middle (e.g. chief accountant, head of contracts and commissioning)
-
– junior (e.g. booking centre manager, business change manager).
-
Data collection
Interview questions
The flexible schedule of questions for the semistructured interviews was devised based on issues raised in the literature review (see Chapter 2 ) and the related concerns of the research proposal. Questions were grouped under six headings: current role; professional background; day-to-day work; management work; effectiveness/accountability; and mobilising identities. The content of the questions varied slightly to reflect what was anticipated to be the different work of clinical and non-clinical managers and of middle and junior managers (see Appendices 4 and 5 ).
Pilot interviews
The questionnaires were piloted with four managers at Metropolitan (two JNC managers, one MC manager and one MNC manager). As we judged the questions to appropriately capture the issues of interest, these interviews were included in the final sample of 91 respondents.
Diaries
Part of the interview involved using the diary-interview method. 116 The intention was that managers would keep a simple, brief, schematic diary for up to 3 working days prior to the interview (see Appendix 6 ). This was intended to generate the outline of a ‘concrete’ description of how they had spent the proceeding days (rather than a potentially idealised appraisal of their work) to be explored and fleshed-out during the interview (thus the diaries were a tool to generate interview data rather than data for analysis in their own right). This was modified during the course of data collection as it was found that some respondents routinely kept their own electronic diaries that could be used to the same end, and this was viewed by the team as preferable to duplicating effort by asking the respondent to replicate this process. Where a respondent had neither a paper nor an electronic version of the diary they were asked to choose a recent day to talk through.
The interview process
All of the interviews took place at the manager’s workplace, usually in their office or, if this was shared and a colleague was present, elsewhere in the work area. The length of interviews was on average 1 hour, although when the interviewee chose to extend them they were longer. The large majority of the managers spoke expansively about their work, generating a rich and detailed corpus of data for analysis (see Data analysis).
All consented for their interview to be audio-recorded. These were then professionally transcribed in full. Equipment failure meant that three interviews were not transcribed or transcribed only in part. In these instances the interviewer wrote up as much as they could capture immediately on its conclusion.
Shadowing
The weight of the analysis in this report rests on the interview data. However, we also wished to consider practices and discourses as they occurred in vivo and in situ117 [i.e. not only to explore what managers say they do (in interview) but what they actually do in ‘real-time’]. Shadowing involves observation and also asking questions which prompt a running commentary which helps to clarify and reveal purpose from the person shadowed. 118
In total, 16 managers were shadowed: four middle managers (two clinical and two non-clinical) and four junior managers (two clinical and two non-clinical) from each trust. Those shadowed were selected, post-interview, from the interview sample to represent a range of professional background characteristics, operating at a range of levels within the organisations.
The original intention was for shadowing to take place over 2 days, but, in practice, we had to negotiate what the managers felt to be ‘realistic’ and this was generally 1 day only. In view of restrictions of the Ethical Approval, we were required to withdraw during shadowing from situations which directly involved patient contact (on grounds of confidentiality). Hence, if shadowing took place in a ward or clinic, for example, we retired to a position some distance from the patient–staff interactions, such as the nursing station. Field notes were written immediately after the shadowing sessions.
Observations
Observation of meetings took place at both case study sites (12 observations per case study, n = 24) where middle and junior managers (including those who had been interviewed and, in some cases, shadowed) were present. These were varied. At Metropolitan, meetings observed included six operations group meetings, three directors group meetings and three directorate-level meetings. At Cityscape, a much wider range were observed, such as a review of services meeting, waiting-list meetings, divisional meetings, a project group meeting, a reconfiguration group meeting, a quality and performance meeting and an executive board meeting. The more dispersed spread of meetings at Cityscape to some extent reflects the more diffuse and project management working that characterises this trust.
We had hoped direct observation of interaction between different categories of managers at different levels of the hierarchy would enable us to see how, for example, those attending emphasised or de-emphasised certain aspects of their identities when interacting with colleagues (e.g. as clinician, as manager, as long-standing member of staff, etc.), thereby providing contextual information for the analysis of the interview data. However, many of the meetings observed – and, significantly, this seems to be a feature of key hospital acute trust meetings – had large numbers of people present (often between 15 and 25, or sometimes more) which made it very difficult to know the background of all present. In addition, some, such as operations group meetings at Metropolitan, appeared to be largely briefing meetings and, consequently, dialogues between those present was limited. That said, field notes from meetings furnished us with some useful background information about contextual factors and the ‘burning’ issues within the trusts which aided in the interpretation of the interview data.
Data analysis
The project generated a large volume of qualitative data in the form of interviews and field notes. As is common in qualitative research, the analysis ran alongside data collection. Thus the work to generate an initial coding frame began while the fieldwork was taking place at Metropolitan, the first research site. This was fleshed out and finalised while it proceeded there and began at Cityscape. The process of developing a coding frame is itself part of the analytical process, providing the researcher with an initial template against which to assess the data still being collected.
Data coding (interviews)
To promote reliability and validity we put in place a coding agreement process, which involved double-coding subsets of early interview transcripts and field notes from Metropolitan (site 1). Research team meetings were held to:
-
develop initial codes, check and re-check them against the interview data and to generate an agreed on coding frame
-
all of the interviews were then coded by two of the team members using NVivo [initially NVivo7 (QSR International, Southport, UK), then imported into NVivo9]
-
tree nodes were organised under six main categories: how work is experienced; identity; mobilising identity; the organisation; what work they do; and who (the latter covering such matters as educational and work background, prior experience and training). This was supplemented by the use of free nodes as the analysis progressed.
(See coding frame in Appendix 7. )
Rather than generating a coding frame for the shadowing data we drew on field notes to illustrate some of the issues which arose in interviews in relation to the mobilising of identities (reported in Chapter 8 ).
The analytical process
The data were analysed using qualitative and quantitative methods.
The qualitative analysis was based on the constant comparative method. 119,120 First, transcripts were read to ensure familiarisation with the data. The second step consisted of developing the coding frame, as already described. The third step involved the coding process, and the fourth step was the analysis of the NVivo nodes to explore associations and any possible patterns between key matters of interest such as identity, the work managers do, their self-reported effectiveness, and how they might mobilise their identities to achieve their goals. Themes of interest were highly interwoven with each other and embedded in the narrative accounts of personal experience making the analytical process particularly challenging.
The quantitative analysis methods were chosen depending on the objectives of the analysis and the type of data. As noted under The two research sites, case study research is concerned mainly with ‘how’ and ‘why’ questions rather than enumerating ‘who does what’. 114 However, quantitative analysis can be instrumental both for summarising ‘who does what’ and for examining the ‘how and why’.
Thus in Chapter 6 , in line with the objective to chart the work of MC and JC and MNC and JNC managers, we have summarised the more quantifiable aspects of the content of work (what managers do) and the form of work (how they do it) by providing numerical comparisons between the four primary manager groups and also between the nine work groups. Some of the data for these comparisons were quantitative in nature, such as the number of staff managers are responsible for and the average number of work hours per week. These were captured in descriptive statistics per group. Other data, such as cross-site working and responsibilities outside the trust, were partly translated into binaries (e.g. whether a manager worked across two sites or more) and presented as the numbers of respondents in each group who did cross-site work and had external responsibilities.
In Chapter 5 , in line with the objective to explore the identities of MC and JC and MNC and JNC managers, we undertook more extensive quantitative analysis. Following the theoretical model presented in Chapter 2 , which depicts identity as a continuum of facets, from the core of identity (self-definition and group affinity) to the content of identity (values, stereotypical traits, knowledge and skills) to the behaviour of identity, we sought to uncover the potential patterns of association (a) between the core and content facets of identity and the managerial groups, and (b) between the self-definition and other core and content facets of identity. Our initial intuition, which was derived from both the theory and the qualitative analysis of the data, was that the functional differences between clinical and non-clinical managers and the positional differences between junior and middle managers may relate to the differences in the facets of identity. Our other intuition was that the self-definition may be congruent with other facets of identity. To facilitate pattern recognition, we used the method of ‘quantitising’ or ‘the numerical translation, transformation, or conversion of qualitative data’ (p. 208). 121 Quantitative treatment of qualitative data is commonly undertaken ‘to form qualitative data in ways that will allow analysts to discern and to show regularities or peculiarities in qualitative data they might not otherwise see or be able to communicate, or to determine that a pattern or idiosyncrasy they thought was there is not’ (p. 210). 121
Thus, we extracted from the interview transcripts the responses pertaining to specific facets of identity, namely, self-definition as a manager, group affinity, values, and knowledge and skills (covering general educational qualifications, management qualifications, training, job tenure and work experience outside of the NHS) and grouped them into categories. Some data, such as the information on a person’s general educational qualifications, yielded themselves more easily to categorisation. (For example, for general educational qualifications, we mapped the highest reported level of education onto the Framework for Higher Education Qualifications (FHEQ)104 and then coded it into Level 5 or below, Level 6, Level 7, or Level 8.) For other data, we had to devise the categories based on our reading of the data and the extant theoretical constructs. (For example, for values, we distinguished between the responses reflective of a public service ethos and responses indicative of a performance ethos.) Then we coded the individual responses into these categories and constructed the contingency tables, cross-tabulating (a) a particular facet of identity with managerial groups and (b) self-definition with another facet of identity.
Here it should be noted that where data are listed as ‘missing’, this should not be interpreted as missing in the conventional sense employed in, for example, survey research. Rather it reflects the flexibility of qualitative interviews where not all questions are asked of all respondents.
We constructed contingency tables for all core and content facets of identity, with the exception of job tenure. (As job tenure was reported in years or months, we have provided descriptive statistics by managerial group and self-definition category and conducted Kruskal–Wallis and Mann–Whitney tests to establish whether or not the differences between groups or categories are significant). We then analysed these data using the Fisher’s exact probability test or chi-squared test, as appropriate, to establish whether or not there was a significant association between particular facets of identity and managerial groups or between self-definition and other facets of identity. Where the tests showed a significant association, we followed these with analysis of the strength of association, using Cramer’s V, and the analysis of the reduction in the error of predicting (a) a particular facet of identity from the managerial group (or vice versa) and (b) self-definition from another facet of identity (or vice versa), using Goodman–Kruskal’s λ. The results of these analyses are presented in the text and tables. In both chapters we also provide the qualitative analysis that supplemented the quantitative analysis.
Anonymity and confidentiality
We assured anonymity and confidentiality to our respondents. To preserve this, where respondents held quite distinctive roles, these have been made deliberately vague. Equally, where respondents talk about particular work areas or kinds of patient-related work these have been made as non-specific as possible to avoid identification. We have also avoided giving too much specific detail on the organisational structures of the two trusts in Chapter 4 . In Chapters 5 – 8 we use abbreviations (JC, MC, JNC and MNC) to describe manager level. The accompanying numbers are those allocated to the interviewee from 1 to 91. Where the number is preceded by P (e.g. P4) this indicates that this was a pilot interview.
Chapter 4 Research setting: case study sites
This chapter presents the background information on the two case study sites and provides the context for our analysis. It describes the activities, structure and performance of the two trusts and the recent organisational changes and management development initiatives within them.
As noted in Chapter 3 , the two sites were chosen because of their geographical proximity and organisational similarities (e.g. both being large acute trusts). The description in this chapter highlights further similarities and differences between the sites.
The data for the chapter were obtained from various sources, including:
-
publicly available documents produced by the trusts themselves (e.g. annual reports, websites)
-
independent publications/websites [e.g. Healthcare Commission; Care Quality Commission (CQC); internal documents, such as organisational charts and quality accounts, field notes from observations of meetings (see Chapter 3 ); and policy documents].
We have not referenced any of these sources either in this chapter or in the References section of the report in order to preserve the anonymity of the participating organisations.
Much of the information reported in this chapter comes from the financial year 2010–11, which provided a near complete overlap with the timing of the fieldwork undertaken.
The two hospital trusts
It should be noted that the research took place before the implementation of the Health and Social Care Act of 201217 which has established different commissioning arrangements to those described below and elsewhere in the report.
Both trusts are based in medium-sized cities in England and, at the time of the research, belonged to the same strategic health authority regions.
Metropolitan, which was formed in the late 2000s, comprises two hospital sites and liaised with two primary care trusts (PCTs) in its area. Formed in the early 2000s, Cityscape consists of three hospital sites and liaised with three PCTs.
Each trust employs over 10,000 staff and provides services for 2–3 million people in their city, surrounding areas, and nationally for specialist services. Metropolitan has approximately 1700 beds and Cityscape 1900 beds. Both trusts claim in their annual reports that they are among the largest teaching trusts in England and have among the country’s busiest emergency departments (each with over 160,000 accident and emergency patients treated annually). They also have high aspirations. Thus, at the time of the fieldwork Metropolitan was aiming to be the country’s best acute teaching hospital, whereas Cityscape wished to be the number one provider of emergency and specialist services in England.
When the research began (June 2009), based on the Healthcare Commission Annual Health Check for the 2008–9 financial year, both trusts were rated ‘good’ for use of resources (the effectiveness of resource utilisation). For quality of services (covering a range of areas such as patient safety, cleanliness and waiting times), Metropolitan was rated as ‘fair’ and Cityscape was rated as ‘good’.
At the start of the research period, both trusts were in the process of applying for foundation trust status and were seeking to achieve it by the end of our 3-year project, but neither did.
Both trusts were engaged in organisational change programmes (see Organisational change and management development initiatives within the trusts).
Financial performance
In 2010/11 Metropolitan achieved a surplus of £5M despite making cost savings of over £24M. Given changes to funding formulas, commissioners’ budgets, etc., the trust was aiming to achieve a surplus of £3M in 2011/12 despite having to make cost savings of over £30M. The XYZ Change programme (see below) was considered the key mechanism for achieving cost savings.
Cityscape achieved a surplus of £1M with cost savings of £31M in 2010/11, and was seeking to make further savings of nearly £40M in 2011/12.
Clinical performance indicators
Metropolitan achieved the 18-week referral target with a figure of 95%, Cityscape also achieved the target. Metropolitan’s emergency department dealt with 97% of patients within 4 hours, whereas Cityscape’s dealt with 94%. At Metropolitan 87% of cancer patients were cared for within 62 days of urgent referral against the national target of 85%, and 97% of cancer patients were cared for within 31 days of diagnosis against the national target of 96%. Cityscape also achieved both national cancer targets.
The larger of the two hospitals within Metropolitan was inspected by the CQC mid-way through 2010/11 and was assessed as meeting all essential standards of quality and safety. All three hospitals at Cityscape were assessed during the same period and were found to be compliant with all 16 outcome requirements.
Organisational structures
At the time when research access to the trusts was initially negotiated, they had similar organisational structures.
Metropolitan consisted of several clinical and corporate directorates each led by a clinical director, a general manager and a clinical lead, and was supported by heads of service and matrons that led each of the 50 or more service areas within the directorates. Each corporate directorate was led by an executive and a deputy.
Cityscape comprised a series of clinical and corporate directorates. Each clinical directorate was headed by a clinical director and a general manager and each corporate directorate by an executive or associate director. However, in 2010 a new structure was introduced, and the trust was organised into clinical divisions, with each division containing a number of clinical business units (CBUs) containing a number of services (a structure adopted by several other hospital trusts in England in recent years).
Therefore, the overall structure of both trusts consists of two blocks: (1) corporate and (2) clinical.
Corporate block
The corporate block consists of corporate directorates and is similar across the two trusts.
Thus, both trusts have eight corporate directorates, each led by a director who is a member of the board. In both trusts, four of these directors are executive directors and the other four are associate directors/advisors to the board.
The four executive directors’ directorates are nearly identical in name/function in both trusts and include (1) nursing, (2) medical, (3) finance and procurement and (4) HR.
The other four directorates somewhat differ in name and function and include:
-
in Metropolitan: (1) ‘trust secretary’ (e.g. governance, policies and procedures), (2) estates and facilities, (3) information and communication technology (ICT), and (4) operations
-
in Cityscape: (1) strategy, (2) research and development (R&D), (3) corporate and legal affairs, and (4) communications and external relations.
Clinical block
The clinical blocks are also similar across the two trusts, but there is a difference in the degree of aggregation and number of levels, owing to the corporate restructuring in Cityscape.
Metropolitan is divided into several clinical directorates, each encompassing a range of specialist services (about 10 on average), with some services further subdivided into smaller service areas, units or departments.
Cityscape is divided into clinical divisions (a smaller number than the clinical directorates at Metropolitan), each comprised two to four CBUs, with each unit encompassing a range of specialist services.
Figure 2 depicts the levels of hierarchy in each trust.
FIGURE 2.
Clinical block: hierarchical structure. CBU, clinical business unit.
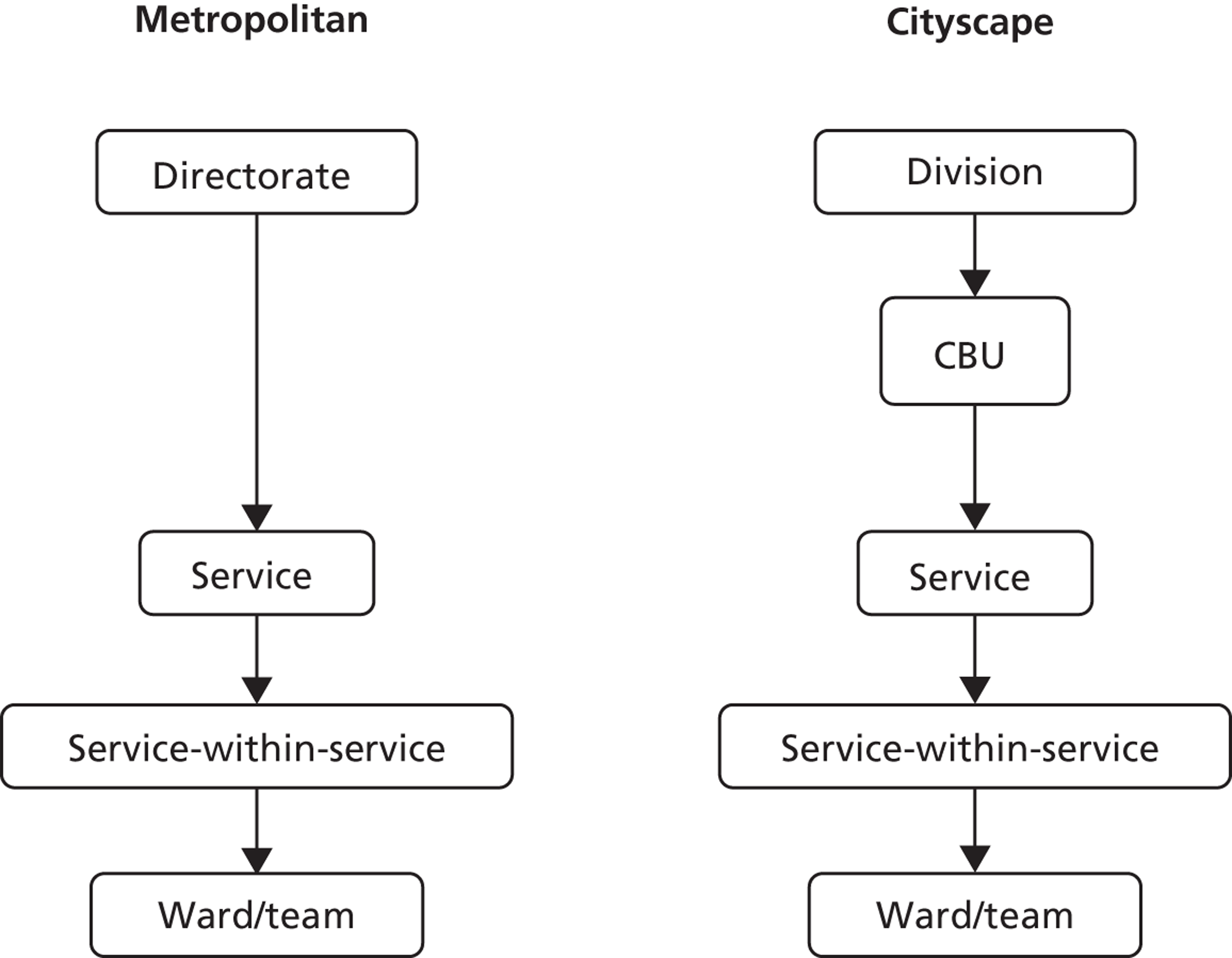
Thus, a Cityscape division is broader in scale and scope than a Metropolitan directorate, and a Cityscape clinical business unit (CBU) provides an intermediate hierarchical level, absent in Metropolitan.
Organisational change and management development initiatives within the trusts
In this section we describe the organisational change programmes and management development initiatives that were under way in the two trusts during the period of the research. This provides an important contextual background to the interview data reported in the subsequent chapters, as these changes and initiatives had impacted on the work of the managers in the study. A more detailed breakdown of different types of management training and education activity appears in Chapter 5 .
Metropolitan Hospital Trust
When the research commenced, the key organisational change activity at Metropolitan was the XYZ Change programme. The broad aims of the programme were to improve the quality of patient care and patient safety and to ensure improvements for other key stakeholders (e.g. visitors and staff), as part of the trust’s overall objective to be the best acute teaching organisation in the country, noted earlier. According to the chief executive, this programme was about sharing what the trust does well and making improvements in less successful areas. A key component of the programme was staff involvement and engagement. It was reported that over 800 ideas had been provided by staff regarding possible improvements either individually or through focus groups and workshops. The programme was concerned with enhancing services but this had to be done while ensuring financial savings.
The programme was inaugurated by a series of launch events, which involved most of the workforce and identified three areas for action: (1) improvements in communications; (2) development of management standards; and (3) improvements in staffing. In response to these, it was proposed to introduce monthly briefings led by the executive team, to which all staff would be invited, to develop some organisation-specific management standards, and to provide workforce reporting tools, which would allow managers to share key staffing information with their teams.
With regard to management development, Metropolitan felt it necessary to create managers’ standards that were specific to the organisation. Although recognising that a number of established frameworks were already in existence [e.g. the Leadership Framework (of the NHS Leadership Academy) and the Medical Leadership Competency Framework], the trust felt that there was the need for a common framework for managers. It stressed the importance of developing the standards in consultation with managers themselves. A website was created to provide information and support for managers so that they could access the knowledge and skills to help them develop themselves and their teams. The standards were split into three main areas, leading, managing and communicating.
A leadership skills programme for AfC band 7 staff had been introduced with over 100 staff having completed it. In addition, a leadership programme specifically for first-line managers/supervisors at bands 5 and 6 was scheduled for introduction.
The trust recognised the importance of appraisals and had agreed a new policy that all staff on AfC conditions of service should have a personal development and performance review which would result in a personal performance rating. By mid-2011, over 1000 managers had undertaken training to conduct these reviews.
The Improving Working Lives 122 Steering Group was tasked with responding to issues identified in the national staff survey (which was circulated to all staff for completion, not just a sample). Key issues related to supporting staff well-being, involving staff, appraisals and development of managerial skills. Reports specific to each directorate were produced so that locally specific issues could be addressed.
Cityscape Hospital Trust
As mentioned earlier, during the research period Cityscape replaced its directorate structure with a divisional structure. This was driven by the appointment of several new key senior staff to the executive board. The reorganisation was intended to improve governance, enable matrix-based management (instead of silo working) and allow managers to focus on strategic issues rather than operational concerns. It was also intended to increase clinical engagement and enhance quicker, more local decision-making.
The old structure had comprised quite a large number of clinical and corporate directorates. The new structure consisted of a much smaller number of clinical divisions, each containing a number of CBUs (see Figure 2 ). The divisions were charged with the strategic ‘visioning’, whereas the day-to-day operational matters were delegated to the CBUs. The number of corporate divisions was also reduced vis-à-vis the old directorates.
Each clinical division was headed up by a triumvirate of a doctor (divisional director, with membership in the executive team), a nurse/midwife and a manager, and supported by a finance manager and an HR business partner. It was envisaged that the divisional posts would be held by senior doctors and would increase medical engagement and contribution to the leadership and management of the trust. Each CBU was led by a doctor and a lead manager, and most also had a lead nurse. One of the consequences of the new structure was that the posts of clinical director, general manager and head of nursing no longer existed.
The structural change occurred as part of a broader review of operational and strategic issues in response to a report provided to the trust board. The report stated that the organisation was not operating efficiently or effectively as it could do in terms of operational matters and was deficient in terms of strategic vision. It noted that, although the trust had shown good ratings over a number of years on some performance measures (e.g. Healthcare Commission Annual Health Check), other evidence (e.g. from national patient surveys and staff survey results) suggested that the performance did not measure up to the trust’s expectations. The structural change also affected the delivery of patient services. For example, one of the divisions rationalised provision of services from three of the hospitals in the trust, down to two.
Cityscape felt that there were seven key areas requiring improvement: (1) governance, (2) performance management, (3) performance basics, (4) infrastructure, (5) organisational capability, (6) business and partnerships, and (7) irritants. In addition to these, the trust put emphasis on the identification and adoption of ‘key values’. As a result, the following five ‘key values’ were developed with the involvement of staff:
-
treating patients and staff with dignity and respecting their views
-
listening effectively and delivering on promises
-
focusing on essentials
-
the importance of teamwork
-
encouraging creativity and innovation to solve problems.
Regarding the management performance, the trust felt that there was an excess of data without a focus on essentials. The report proposed to use the Balanced Scorecard method to provide a common basis for reporting performance at all levels (‘from ward to board’). It also recommended regular performance management meetings both with divisions and within divisions so that performance could be clearly understood, discussed and improved. The review which generated the report also recognised that the existing practice of ‘soft cost savings’ would be unable to achieve future larger-scale savings and that a transformation would be required. This transformation, in turn, would require leadership. The trust, however, recognised that it had neither effective mechanisms for spotting and nurturing talent nor systems in place to support the people struggling with their roles.
With regard to management development, Cityscape provided short courses in-house on various aspects of management and occasionally supported staff to take relevant external courses and qualifications. (Further information is provided in Chapter 5 .)
Cityscape had embarked on a process of identifying leadership competences and behaviours deemed necessary to support the trust’s key values. At the time of our fieldwork, over 300 senior leaders had undertaken a leadership excellence programme that included 360 degree feedback and executive coaching. A clinical leadership development programme had also recently been launched.
For non-managerial staff, Cityscape had an internal vocational qualification programme designed to synchronise with the FHEQ and Credit Framework (see Chapter 5, General education qualifications). The trust had also become the first NHS-approved provider of apprenticeships in health and social care, and customer services.
Cityscape circulated the National Staff Survey to a random sample of 1500 of its 10,000 staff, unlike Metropolitan which circulated it to all staff. Key issues that the trust recognised needed attention related to: communication (particularly between senior managers and staff); quality of appraisals; recognition and reward; work–life balance and employee well-being; and training/development opportunities. Cityscape intended to introduce quarterly staff polls designed to facilitate feedback with a view to enhancing engagement.
Summary
As can be seen from the description of the two case study sites in this chapter, they are similar in many ways. Arguably, Cityscape considered structural reforms to be more important than cultural/training activities in seeking to deal with financial pressures and enhance services. Metropolitan’s XYZ Change programme was intended to facilitate engagement from all staff in seeking to make financial savings and develop services. The description of these activities reported in this chapter has deliberately reflected a corporate perspective. The subsequent results chapters report the perceptions of the middle and junior managers with respect to these corporate activities.
Chapter 5 Identifying identities
This chapter provides the starting point and foundation for our investigation, as it examines the identities of junior and middle managers. Our analysis follows the model of identity outlined in Chapter 2 and covers the core of identity, namely, self-definition and group affinity, and identity content (i.e. values, stereotypical traits and knowledge and skills). It also considers potential connections between self-definition and other facets of identity. The behaviour of identity is analysed in Chapter 6 .
Self-definition
The focus of our inquiry was on work-related identities and, in particular, on the professional identity of the respondents as managers.
Self-definition as a manager
In establishing the respondent’s self-definition, we relied primarily on the interview responses directly referring to self-definition (e.g. how the respondent would describe themselves in a social situation), supplementing this with the common pattern of reference to oneself (e.g. ‘as a manager, I always . . .’).
The preliminary analysis led us to categorise the responses into three types:
-
‘I am a manager’ – respondent clearly defined themselves as a manager.
-
‘I am a manager, but . . .’ – respondent defined themselves as a manager but qualified this definition [e.g. by making a reference to their ‘primary’ occupation, such as ‘I am a scientist manager’ (MNC, MI 22)].
-
‘I am not a manager’ – respondent was adamant not to define themselves as a manager.
The data are reported in Table 3 .
| Self-definition | Management category | Total | |||
|---|---|---|---|---|---|
| JC | JNC | MC | MNC | ||
| ‘I am a manager’ | 4 | 7 | 3 | 16 | 30 |
| % within self-definition | 13 | 23 | 10 | 53 | |
| Expected count | 7.2 | 4.8 | 8.9 | 9.2 | |
| Observed count as % of expected count | 56 | 146 | 34 | 174 | |
| ‘I am a manager, but . . .’ | 8 | 2 | 3 | 6 | 19 |
| % within self-definition | 42 | 11 | 16 | 32 | |
| Expected count | 4.5 | 3 | 5.6 | 5.8 | |
| Observed count as % of expected count | 178 | 67 | 54 | 103 | |
| ‘I am not a manager’ | 9 | 5 | 20 | 5 | 39 |
| % within self-definition | 23 | 13 | 51 | 13 | |
| Expected count | 9.3 | 6.2 | 11.5 | 12 | |
| Observed count as % of expected count | 97 | 81 | 174 | 42 | |
| Subtotal (without missing) | 21 | 14 | 26 | 27 | 88 |
| % within subtotal | 24 | 16 | 30 | 31 | |
| Missing | 0 | 1 | 1 | 1 | 3 |
| Total | 21 | 15 | 27 | 28 | 91 |
Overall, 33% (30 of 91) of the respondents defined themselves as managers, 21% (19 of 91) did so with reservations and 43% (39 of 91) declined to identify themselves as managers.
There was a significant (Fisher’s exact p = 0.00018) and moderate (Cramer’s V = 0.38) association between management category and self-definition.
[Here and elsewhere the measures of association were calculated excluding the missing values. To describe the magnitude of association we used the following convention: the values of Cramer’s V between 0.10 and under 0.20 were interpreted as ‘weak association’, between 0.20 and under 0.40 as ‘moderate’, between 0.40 and under 0.60 as ‘relatively strong’, and between 0.60 and under 0.80 as ‘strong’ (p. 203). 123]
Comparison of the observed and expected cell frequencies showed that self-definition as:
-
manager was more common for non-clinical managers and less common for clinical managers
-
manager with reservations was more common for JC managers and less common for JNC and MC managers
-
not a manager was more common for MC managers and less common for MNC managers.
To explore whether the differences in self-definition could be attributable to management level or to clinical engagement, we aggregated the data, first, into junior and middle management categories, and second, into clinical and non-clinical categories. (We have omitted the data tables because of space constraints.)
We found no significant association of self-definition with management level and self-definition [χ2 (2, N = 88) = 1.68, p = 0.432], but significant [χ2 (2, N = 88) = 17.94, p = 0.0001] and relatively strong (Cramer’s V = 0.45) association with clinical engagement. Knowing the manager’s clinical engagement reduced the error in predicting self-definition by 27% (Goodman–Kruskal’s λ = 0.27, 95% CI 0.0 to 0.5), and knowing self-definition reduced the error in predicting clinical engagement by 39% (λ = 0.39, 95% CI 0.1 to 0.7). In other words, it would be more likely, for instance, for a clinical manager to define themselves as not a manager, but even more likely for someone who defined themselves as not a manager to be a clinical manager.
Incidentally, 16% of all non-clinical managers (7 of 43; all middle managers) had clinical backgrounds, including nursing, allied health professional (AHP) and ambulance services. Of these, three identified themselves as managers, three as managers with reservations, and one as not a manager.
Expanded self-definitions
A definite ‘yes’: ‘I am a manager’
Three-quarters (23 of 30) of those who defined themselves as managers were non-clinical managers.
Many defined themselves as just ‘a manager’, but quite a few felt the need to specify it further as an ‘NHS manager’ (MNC 17, MNC 42, MNC 103) or ‘hospital manager’ (MC 107, MNC 4) and some went into yet further detail [e.g. ‘a quality and safety manager’ (MC 95)].
The need for an expanded self-definition seemed to arise both from the desire to clarify one’s position within the variety of managerial jobs:
What I find being a manager here, and what I find being a manager in the posts I had before . . . it’s very, very different in different places and in different roles.
JC 29
and from the perceived need to explain and even justify themselves:
I sometimes say I work in a hospital as a kind of like easier way of . . . getting around the question of . . . ’What does an NHS manager do?’
MNC 17
A qualified ‘yes’: ‘I am a manager, but . . . ’
Of 19 respondents who provided this answer, four (one from each management category) saw themselves as a ‘specialist’ first and a manager second:
I think of myself primarily as an accountant . . . in terms of . . . the technical side . . . and then secondarily . . . as a manager.
JNC 3
Four (all nurse managers) described themselves as being ‘half and half’ (MC 18) (i.e. equally a nurse and a manager):
[It] depends what you’re dealing with at the time, what sort of projects and what focus you’ve got at the time. I suppose if people ask what I do, I say I’m a nurse more often than I would say I’m a ward manager . . .
JC 51
Four qualified their self-definition as manager by adding a reference to their original occupation, such as: ‘I am an occupational therapist’ (MNC 104), ‘I am a scientist manager’ (MNC 22); and the remaining seven provided other caveats, for example:
I heard recently that the NHS now has more managers than it does have beds, but in that criteria I’m not classed as a manager because . . . I do still do clinical work.
JC 12
Those who espoused a dual identity spoke of the challenges such identity presented:
It’s almost having an internal battle with yourself, from the body of the managerial head and the lead nurse head . . . It varies from day to day which one takes priority . . . It depends on the demands and the needs of the Service at the time, so it’s not something that you would say the one is above the other, they’re equal in my head in a way . . .
MNC 73
A definite ‘no’: ‘I am not a manager. . . ’
Of the 39 respondents who declared that they were not managers:
-
over two-thirds (27 of 39, including 23 clinical managers) identified with their original occupation; of the sample overall, two-thirds of consultant managers defined themselves as doctors, a half of scientist managers as scientists, and more than one-third of nurse managers as nurses
-
four (all non-clinical) reported that they would just say that they work for the NHS
-
the remaining eight provided no alternative self-definition, but instead mainly explained why they did not define themselves as managers.
Some respondents preferred to be identified as a leader (five MC managers and one JC manager):
It’s about am I a leader or am I a manager? I’d like to think that I’m a leader [ . . . ] Because . . . I’ve always associated being a manager as office type documentation . . . and I think managing people is more leading . . . So that’s why I find it difficult when people say: ‘Oh, you’re a manager’. I’m, actually . . . a leader, I don’t think I’m a manager.
JC 77
‘Leader’ seemed to be a more palatable term than ‘manager’, possibly reflecting the recent emphasis on leadership in the NHS. 124
Some responses reflected an instrumental approach to self-definition, suggesting that they would choose which hat to wear depending on the situation:
It depends in what context really. I think if it was outside work I would say I’m a doctor. In context of [Cityscape] I would probably say I’m a divisional director for Primary Care . . . And then caveat that by saying ‘I’m also a . . . practising orthopaedic surgeon’ . . . Because, I think, people understand what you mean when you say you’re a doctor . . . And I guess at the heart of it I am a doctor . . . Although I do management, at the heart of what I do I am still doctor.
MC 70
‘Reluctant managers’: reluctant to manage or be labelled?
The above results indicate that the managerial identity of our respondents was problematic in its very core (self-definition).
The interview responses recall the term ‘reluctant manager’, coined independently by Scase and Goffee,125 in reference to middle managers in the private sector, who had become reluctant to manage in response to changes in the structure of large corporations, and by Pollitt et al. ,126 in reference to attempts to turn doctors into resource managers in the NHS. The term has been later employed by Currie98 to describe the plight of nurses as middle managers in the NHS.
Our results suggest that ‘reluctant manager’ is a more widely spread phenomenon, restricted neither to middle management nor to managers with clinical backgrounds.
Our findings also paint a more nuanced portrait of a ‘reluctant manager’.
Thus, some respondents were, indeed, reluctant to be a manager. They resented the fact that progressing through the ranks in the NHS meant taking on managerial responsibilities:
. . . You haven’t got an option, have you, in the NHS? . . . As you go up the bands, you naturally gain managerial responsibilities . . . I think it’s wrong . . . You’re either a clinician or you’re not, and I’m not sure why we’re expected to be two things.
JC 39
Yet, more frequently, the respondents were accepting of managerial work, but nevertheless reluctant to define themselves as a manager:
I still always see myself as a scientist doing a managerial job . . . Some weeks, if I spend a lot of time doing purely managerial work . . . you do see yourself slightly differently . . . but I rarely see myself as a manager.
MC 15
Among those reluctant to be called a manager, some showed a passive hesitancy to define themselves as managers because they felt they did not ‘qualify’ to be classed as such:
I see myself as this uneducated woman who’s masqueraded . . . You talk to some of these people [managers], and they’ve got degrees and diplomas. I’ve never done anything.
MC 55
More often, however, respondents demonstrated an active rejection of the label ‘manager’:
I am a professional providing leadership and service and having to manage to keep it working. I would never describe myself as a manager.
MC 21
Many of those were at pains to differentiate between ‘managing’ and ‘being a manager’ and would admit to the former but not to the latter:
I am an accountant, not a manager, but I do manage people on a day-to-day basis and manage budgets.
JNC P1
For these respondents, the behaviour of identity (‘managing’), which resides on the periphery of identity formulation, did not penetrate into the identity core (i.e. their self-definition). In their eyes, ‘doing a managerial job’ did not make them managers.
In contrast, some respondents who did define themselves as managers noted that their work effectively dictated their identity:
Yes, you have to [identify oneself as a manager] because it’s always the management work will have to take the priority.
JC 5
Both the passive hesitancy and the active rejection indicate the existence of a stereotype of a manager that lays some distance away from the self-image of these respondents. The difference is that, for those who showed a passive hesitancy to define themselves as managers, to be called a manager meant ‘measuring up’, whereas for those who showed an active rejection it implied ‘stooping down’.
We proffer three (not mutually exclusive) explanations for the respondents’ attempts to dissociate themselves from the label ‘manager’.
First, these attempts may be motivated by the desire to maintain credibility. Prior research suggests that practitioners moving into management face a threat to their credibility as practitioners without gaining credibility as managers (e.g. see Willmot127 for charge nurses). Some of the responses reflected this motivation:
[There is a view that] NHS managers [are] all failed clinicians, and the only reason they go into management is because they can’t do their job.
JC 39
Second, these attempts may stem from the perceived insecurity of a manager’s position, as ‘from the mid-1990s onwards the government’s efficiency drive . . . continued to target middle managers’. 98,103 This insecurity appeared to intensify following the White Paper, Equity and Excellence: Liberating the NHS, in which the Government promised to ‘reduce the NHS’s management costs by more than 45%’ over 4 years (p. 43). 11 Several respondents [in particular four JNC managers, two from each trust (JNC 53, JNC 54, JNC 88 and JNC 105)] described the recent experiences of having their jobs ‘restructured’ or downgraded from a higher to a lower band, for example:
We were all called to a meeting, came in here, and my job had gone . . . without being warned or any suggestion that that was going to happen.
JNC 53
Third, these attempts may indicate that the job of NHS manager is considered to be a morally tainted occupation. ‘Moral taint occurs where an occupation is generally regarded as somewhat sinful or of dubious virtue (e.g. exotic dancer, pawnbroker, tattoo artist, psychic, casino manager)’ (p. 415). 37 In the case of health-care managers, the moral taint is associated with the claims that managers do not add value but instead somehow ‘take money away from the frontline staff’:
If you asked me what I did for my job . . . I’d never say I’m a manager in the NHS. [ . . . ] It’s like saying you’re a tax inspector.
MNC 61
I am a PPP, that is, a pen-pushing parasite . . . I am part of the fat . . . The people who really do the work in the NHS are the frontline nurses and doctors and healthcare assistants and theatre practitioners.
MNC 25
One of the bad things about being an NHS manager is it’s not one of those things you brag about because people look down on NHS managers . . . Because doctors are good, nurses are good and managers are bad.
MNC 42
Incidentally, respondents who defined themselves as managers talked about the ‘stigma’ of being an NHS manager more frequently than those who did not.
Group affinity
In terms of group affinity, we distinguished three types of responses, depending on whether or not the respondent identified with:
-
particular individual(s), rather than any group
-
work team
-
peer group [‘colleagues the same level as me’ (JC 12)].
The data are presented in Table 4 (and Table 22 in Appendix 8 ).
| Group affinity | Management category | Total | |||
|---|---|---|---|---|---|
| JC | JNC | MC | MNC | ||
| Individual(s) | 0 | 1 | 4 | 3 | 8 |
| Work team | 1 | 1 | 3 | 5 | 10 |
| Peer group | 4 | 1 | 5 | 3 | 13 |
| Missing | 16 | 12 | 15 | 17 | 60 |
| Total | 21 | 15 | 27 | 28 | 91 |
Over a quarter of the respondents who discussed the issue (8 of 31) perceived affinity only with a particular individual or individuals. We suggest that the lack of identification with any group narrows the person’s support base and makes this base vulnerable to any changes. To illustrate, one respondent related that he had developed a strong relationship with a colleague, only to find himself isolated when the colleague moved to a new post (MC 47).
One-third of the respondents (10 of 31) identified with their work team and the remainder (13 of 31) with their peers. The affinity with work team provides more social resources than the affinity with an individual, but these resources are less rich and varied than those that a peer group can provide:
The management group within the Directorate [i.e. the peer group] . . . understand some of the trust issues, whereas . . . people in radiotherapy [i.e. the work team] haven’t come out of the silo of radiotherapy because that is what they do all day long. So if you go into a room of . . . managers external from radiotherapy, you start to . . . understand the trust’s financial position, the trust’s strategies . . . Whereas people here don’t want to know about the trust’s financial situation even if you tried to tell them.
MNC 26
Both the internal (within the trust) and the external peer groups were quoted as important:
When you get to a senior level . . . you have your peer support within the organisation, but it’s quite useful to have that peer networking support outside the organisation. So I have got colleagues in dermatology around the country that I class as . . . peer support, so we bounce ideas off each other, and if we’re having a difficult time we can share those experiences.
MC 8
There were some examples of formal arrangements for building peer support within the trusts [e.g. the trust-level ‘sisters’ timeout days’ at Metropolitan (JC 40)]. Yet, it appeared that across the trusts some previously established peer networks were withering away:
The problem is, nowadays in physiology we don’t have the same sort of regional associations that we used to, [when] I would call on my peer in [another hospital] . . . to get some ideas from her. . . . It is lack of time and co-ordinating that sort of meeting, and I think it is a great shame because . . . it served a purpose. Now we just cope within our own trust . . . Something big has been lost there.
MNC 22
Although it appeared as if clinical managers were more likely to identify with peer group and non-clinical with work team, no significant association between group affinity and four management categories (Fisher’s exact p = 0.623), management level (Fisher’s exact p = 0.458) or clinical engagement (Fisher’s exact p = 0.394) was found.
Values
In terms of values, we distinguished two types of responses:
-
those reflective of public service ethos, and
-
those indicative of performance ethos.
Public service ethos is a well-established construct that encompasses public service belief (i.e. motivation to work for the public services, e.g. ‘altruism, compassion’), practice (i.e. organisational values supporting this motivation, e.g. accountability, fairness) and public interest (i.e. acting ‘in the interests of the common good’) (p. 34). 128 In our study, public service ethos was manifested in the work motivation to ‘make a difference to the patient’:
My values are that the patient should always be at the centre of everything that we do . . . It’s not about me, or the team, it’s about the patient.
MC 76
Performance ethos is a novel concept, introduced (but not defined) by Casey and Allan. 129 We define it as the work motivation to ‘get things done’, as manifested in the following quote:
Motivation is leading things forward, getting things done, . . . finding the inefficient areas and actually making them efficient, finishing things off, . . . getting it ticked off and getting the business, whatever it is, done and up and running.
MNC 75
The data are presented in Table 5 (and in Table 23 in Appendix 8 ).
| Values | Management category | Total | |||
|---|---|---|---|---|---|
| JC | JNC | MC | MNC | ||
| Performance ethos | 1 | 3 | 2 | 7 | 13 |
| Public service ethos | 5 | 8 | 9 | 9 | 31 |
| Missing | 15 | 4 | 16 | 12 | 47 |
| Total | 21 | 15 | 27 | 28 | 91 |
Two-thirds of respondents (31 of 47) subscribed to the public service ethos. No significant association was found between values and management category (Fisher’s exact p = 0.482), management level (Fisher’s exact p = 0.215) or clinical engagement (Fisher’s exact p = 0.111).
Self-selection mechanisms were certainly at play. Most of the managers with private sector experience noted that they had become disenchanted with the ethos of profit maximisation and were attracted to the NHS by the desire to do good:
I was fed up of working in the private sector and all that mattered was the bottom line . . . In the public sector for me it was more about . . . what can I do to make a difference to the patient.
MNC 87
Yet, the dividing line between the public service ethos and the performance ethos was not very sharp. Many pointed out that ‘making a difference to someone’s life’ should not be narrowly interpreted in terms of the direct contact with patients but involves a bigger picture:
Part of being a physician is about determining best patient care, practice, pathways, and those sorts of things, and . . . you cannot do that in a void, so it needs to be done with directing . . . so one has a management role in terms of the team.
MC 59
The results were in agreement with the prior research, which has indicated that the public sector managers are less motivated by economic incentives and have a stronger desire to serve the public interest than the private sector managers. 130
Stereotypical traits
The responses clearly pointed to the existence of a stereotype of a manager. The respondents associated ‘being a manager’ with:
(a) a certain level in organisational hierarchy:
I’m a therapy radiographer who is in a manager’s position. [ . . . ] I’m a radiographer, because the manager is hierarchy, whereas my job is I’m a radiographer although I’m not on a machine day to day.
JC 26
I suppose my idea of an NHS manager would be somebody like one of the directors.
MC 23
(b) line management:
I don’t really think of myself in that light [as a manager] because to me you manage if you manage people and I don’t manage people. [ . . . ] . . . I do project management, I do training, I do support, admin . . .
JNC 54
(c) a particular job title and remuneration level:
When you read my job description, it says manage this, manage that, manage the other . . . but the word ‘manager’ isn’t actually in the job title or in the pay packet.
JNC 38
(d) decision-making power:
Yes, I do see myself as a manager; I probably don’t see myself as a manager . . . in the same sense as other managers within the hospital, who . . . have quite a high profile . . . I don’t have the same profile . . . as . . . the general managers . . . I think if you spoke to any diagnostics manager they would probably feel the same. They’re not part of the bigger management scheme they sit on the periphery feeding in. Complying; meeting targets and so on, but not necessarily a voice within the trust.
MNC 22
Knowledge and skills
To assess the respondents’ knowledge and skills we examined their self-reported general education qualifications, management education, vocational qualifications and other training, tenure in the current job, and work experience outside the NHS.
General education qualifications
To delineate the levels of general education qualifications we adapted the FHEQ:131
-
Level 5 or below: secondary education qualifications [including General Certificate of Secondary Education (GCSEs), A levels, and Ordinary National Certificate (ONC)].
-
Level 6: undergraduate degree qualifications, such as Bachelor’s degrees and graduate diplomas (including nursing, optician, occupational therapy and accounting qualifications).
-
Level 7: postgraduate degree qualifications, such as Master’s degrees and postgraduate diplomas [including advanced midwifery and advanced the Chartered Institute of Personnel and Development (CIPD) qualifications].
-
Level 8: doctoral degrees (including PhD, MD and professional degrees in medicine).
The data are presented in Table 6 .
| General education qualifications | Management category | Total | |||
|---|---|---|---|---|---|
| JC | JNC | MC | MNC | ||
| Level 5 or below | 0 | 5 | 0 | 2 | 7 |
| % within level | 0 | 71 | 0 | 29 | |
| Expected count | 1.5 | 1 | 2.3 | 2.2 | |
| Observed count as % of expected count | 0 | 500 | 0 | 91 | |
| Level 6 | 10 | 4 | 10 | 15 | 39 |
| % within level | 26 | 10 | 26 | 38 | |
| Expected count | 8.1 | 5.7 | 12.8 | 12.4 | |
| Observed count as % of expected count | 123 | 70 | 78 | 121 | |
| Level 7 | 7 | 2 | 8 | 8 | 25 |
| % within level | 28 | 8 | 32 | 32 | |
| Expected count | 5.2 | 3.7 | 8.2 | 7.9 | |
| Observed count as % of expected count | 135 | 54 | 98 | 101 | |
| Level 8 | 0 | 1 | 9 | 1 | 11 |
| % within level | 0 | 9 | 82 | 9 | |
| Expected count | 2.3 | 1.6 | 3.6 | 3.5 | |
| Observed count as % of expected count | 0 | 63 | 250 | 29 | |
| Subtotal (without missing) | 17 | 12 | 27 | 26 | 82 |
| % within subtotal | 21 | 15 | 33 | 32 | |
| Missing | 4 | 3 | 0 | 2 | 9 |
| Total | 21 | 15 | 27 | 28 | 91 |
The associations between general education qualifications and management category, management level and clinical were significant and moderate (Fisher’s exact p-values of 0.00065, 0.065, and 0.005, and Cramer’s V of 0.38, 0.30 and 0.38, respectively).
Comparison of the observed and expected cell frequencies suggested that:
-
on Level 5 and below, JNC managers clearly predominated
-
on Level 6, JC and MNC managers were somewhat over-represented, whereas the remaining two categories were under-represented
-
on Level 7, JC managers were over-represented and JNC managers were under-represented
-
on Level 8, MC managers were over-represented and other categories unrepresented.
The Kruskal–Wallis test also showed a significant difference in general education level by management category [H (3) = 11.94, p = 0.0076]. The general education level of MC managers was one level higher (mean = 7.0) than that of MNC (6.3), JC (6.4) and JNC managers (5.9).
The findings were broadly in line with our initial intuition. Thus, a middle management position would likely require higher educational credentials than a junior management position; and, indeed, the observed frequencies for middle managers were in line with the expected frequencies for Level 7. Clinical qualifications would entail formal education at least to Level 6 (with higher levels required for doctors); and, indeed, on Levels 6 and 7, JC managers were over-represented. The combination of clinical engagement and middle rank would likely result in over-representation of MC category at the top end of education qualifications. (Of 27 MC managers in the sample, six were medical consultants and another five were consultant clinical scientists.)
However, the finding that the general education level of non-clinical managers was significantly lower than that of clinical managers with the same management rank was troubling. As educational credentials affect one’s status in a professional bureaucracy, these disparities may have a significant impact on managers’ identities.
Knowing the management category, management level or clinical engagement did not materially reduce the error of predicting the level of education, but knowing the education level reduced the error of predicting management category by 18% (λ = 0.18, 95% CI 0.0 to 0.4), management level by 10% (λ = 0.10, 95% CI 0.0 to 0.7) and clinical engagement by 18% (λ = 0.18, 95% CI 0.0 to 0.5). In other words, if an individual occupied a certain management position, it did not necessarily follow that they had the educational credentials common to this position; however, having the educational credentials common to the position made it more likely that an individual would be occupying this position. This one-way tendency suggested that, although the educational attainment was likely to be ‘rewarded’ by a particular position in the management hierarchy, the hierarchy itself did not clearly correspond to the hierarchy of educational credentials.
Management qualifications and training
We classified the management qualifications and training undertaken by the respondents into three categories:
-
Higher education qualifications [i.e. those within the FHEQ (e.g. a Bachelor degree in Management)].
-
Vocational qualifications [i.e. those within the Qualifications and Credits Framework (QCF)/National Qualifications Framework (NQF) for England and Northern Ireland regulated by the Office of Qualifications and Examinations Regulation (Ofqual) (e.g. a Level 4 certificate in Management); these included qualifications awarded by the National Examining Board for Supervision and Management (NEBS), the Chartered Management Institute (CMI) and the Institute of Leadership and Management (ILM) (the correspondence between the levels of higher education qualifications and vocational qualifications is detailed in Appendix 9 )]. [NEBS merged in 2001 with the Institute of Supervision and Management to form ILM; its qualifications were mapped onto the QCF using the information provided by ILM (no date).]
-
Learning and development programmes that do not lead to the award of higher education or vocational qualifications, namely:
-
– National level programmes provided by professional bodies, including Association of Clinical Biochemists (ACB), Healthcare Financial Management Association (HFMA), Institute of Healthcare Management (IHM), Royal College of Nursing (RCN), and The King’s Fund, and ranging from a week-long course by ACB to a five-module 12-month programme delivered by an RCN-trained local facilitator. 132–135
-
– Regional level programmes, namely an NHS-wide programme for people from black and minority ethnic backgrounds delivered by the Strategic Health Authority and the two leadership programmes offered by a regional ‘leadership academy’; these programmes were delivered via a series of events and activities (e.g. forums, action-learning sets, coaching/mentoring) over a period from 3 months to 1 year.
-
– Organisation level programmes provided by the trusts, namely (i) HR training events (1 day or less) and (ii) leadership programmes, ranging from a 3-day workshop on ‘empowerment’ to a 12-month coaching programme (Metropolitan offered three different leadership programmes, Cityscape offered one) (information from the organisational documents).
-
These learning and development programmes do not map onto the frameworks for higher education and vocational qualifications and are not directly comparable to formal qualifications. Although some of these programmes provided fairly extensive training and development opportunities, they arguably did not provide these to the same level as the courses leading to the award of recognised higher education and vocational qualifications.
The data on the respondents’ management qualifications and training are presented in Table 7 . (For respondents with several types of management education and training, we report the highest level and give priority to the recognised qualifications.) For the analysis of association, owing to computational constraints, we had to aggregate the data for learning and development programmes. The disaggregated data on these are presented at the bottom of the table.
| Management qualifications and training | Management category | Total | |||
|---|---|---|---|---|---|
| JC | JNC | MC | MNC | ||
| Higher education qualifications Level 6 | 0 | 0 | 0 | 2 | 2 |
| % within level | 0 | 0 | 0 | 100 | |
| Expected count | 0.5 | 0.4 | 0.6 | 0.6 | |
| Observed count as % of expected count | 0 | 0 | 0 | 333 | |
| Higher education qualifications Level 7a | 0 | 1 | 4 | 10 | 15 |
| % within level | 0 | 7 | 27 | 67 | |
| Expected count | 3.7 | 2.5 | 4.5 | 4.3 | |
| Observed count as % of expected count | 0 | 40 | 89 | 233 | |
| Vocational qualifications Level 5 | 2 | 5 | 3 | 1 | 11 |
| % within level | 18 | 45 | 27 | 9 | |
| Expected count | 2.7 | 1.9 | 3.3 | 3.1 | |
| Observed count as % of expected count | 74 | 263 | 91 | 32 | |
| Learning and development programmes | 12 | 5 | 15 | 8 | 40 |
| % within level | 30 | 13 | 38 | 20 | |
| Expected count | 9.9 | 6.8 | 11.9 | 11.4 | |
| Observed count as % of expected count | 121 | 74 | 126 | 70 | |
| None | 5 | 2 | 1 | 1 | 9 |
| % within level | 56 | 22 | 11 | 11 | |
| Expected count | 2.2 | 1.5 | 2.7 | 2.6 | |
| Observed count as % of expected count | 227 | 133 | 37 | 38 | |
| Subtotal (without missing) | 19 | 13 | 23 | 22 | 77 |
| % within subtotal | 25 | 17 | 30 | 29 | |
| Missing | 2 | 2 | 4 | 6 | 14 |
| Total | 21 | 15 | 27 | 28 | 91 |
| Addendum: disaggregated data on learning and development programmes | |||||
| National programmes | 1 | 1 | 5 | 1 | 8 |
| Regional programmes | 0 | 1 | 0 | 1 | 2 |
| Trust programmes | 11 | 3 | 9 | 5 | 28 |
| Unspecified | 0 | 0 | 1 | 1 | 2 |
Less than one-third (28 of 91) of respondents had recognised management qualifications, and only 16% (15 of 91) had those at the advanced level. Just two respondents had an MBA (both MNC managers). About one-third (28 of 91) had only ‘in-house’ training, and 10% (9 of 91) had no management training.
The associations of management qualifications and training with management category and clinical engagement were significant and moderately strong (Fisher’s exact p-values of 0.00089 and 0.025 and Cramer’s V of 0.38 and 0.37, respectively) and with management level – significant and relatively strong (Fisher’s exact p = 0.001, Cramer’s V = 0.46).
Comparison of the observed and expected cell frequencies showed that:
-
among the respondents with the higher education qualifications in management, MNC managers were over-represented, whereas other management categories were under-represented
-
among the respondents with vocational management qualifications, JNC managers were over-represented, whereas other categories were under-represented
-
among the respondents who had undertaken learning and development programmes, clinical managers were over-represented, whereas non-clinical managers were under-represented
-
among the respondents with no management education, junior managers were over-represented, whereas middle managers were under-represented.
These findings indicate that there were considerable disparities in terms of management qualifications and training between management categories, levels of management and clinical engagement.
The error in predicting the management qualifications and training was unaffected by the knowledge of management category, management level or clinical engagement (λ of 0.05, 0 and 0, respectively), but knowing the management qualifications and training reduced the error in predicting management category by 26% (λ = 0.26, 95% CI 0.0 to 0.5), management level by 25% (λ = 0.25, 95% CI 0.0 to 0.7) and clinical engagement by 29% (λ = 0.29, 95% CI 0.0 to 0.7). These findings echo the results on general education qualifications. Thus, if an individual occupied a certain management position it did not necessarily mean that they had the management qualifications and training common to this position; although having the management qualifications and training common to the position made it more likely that an individual would occupy this position.
Of additional note is the variety of management qualifications and training programmes reported by respondents. This variety suggests the multitude of opportunities for professional training and development, but also gives a cause for concern, as it indicates the lack of standardisation in educational and training prerequisites for management posts. Prior research suggests that management has a more ‘craft-like’ knowledge base than the liberal professions and thus has to constitute its expertise ‘through educational and bureaucratic credentials’ (p. 584–5). 136 Hence, if this is typical, the lack of a clear credentialing system for managers in UK health care might weaken the expert power base of NHS managers.
Tenure in the current job
We used respondents’ tenure in the current job as a proxy for the development of job-specific skills. The data are presented in Table 8 .
| Job tenure (years) | Management category | Total | |||
|---|---|---|---|---|---|
| JC | JNC | MC | MNC | ||
| Mean | 4.50 | 2.65 | 3.70 | 2.51 | |
| Median | 5.00 | 2.25 | 3.25 | 1.50 | |
| Minimum | 1.00 | 1.00 | 1.00 | 0.02 | |
| Maximum | 12.00 | 6.50 | 9.00 | 16.00 | |
| Count | 19 | 12 | 24 | 26 | 81 |
| Missing | 2 | 3 | 3 | 2 | 10 |
| Total | 21 | 15 | 27 | 28 | 91 |
The results of the Kruskal–Wallis test [H (3) = 10.14, p = 0.018] indicate that the job tenures were significantly different between the four categories of respondents. JC managers were in their current post the longest (4.5 years on average), whereas MNC managers were in post the shortest (2.5 years on average).
Work experience outside the NHS
Over a half of the respondents (54 of 91) had never worked outside the NHS, whereas one-third (30 of 91) had. The aggregate data are presented in Table 9 . More detailed information on the prior employment is presented in Table 10 .
| Work experience outside the NHS | Management category | Total | |||
|---|---|---|---|---|---|
| JC | JNC | MC | MNC | ||
| Yes | 4 | 11 | 0 | 15 | 30 |
| % within positive answer | 13 | 37 | 0 | 50 | |
| Expected count | 7.1 | 5 | 8.2 | 9.6 | |
| Observed count as % of expected count | 56 | 220 | 0 | 156 | 54 |
| No | 16 | 3 | 23 | 12 | |
| % within negative answer | 30 | 6 | 43 | 22 | |
| Expected count | 12.9 | 9 | 14.8 | 17.4 | |
| Observed count as % of expected count | 124 | 33 | 155 | 69 | |
| Subtotal (without missing) | 20 | 14 | 23 | 27 | 84 |
| % within subtotal | 24 | 17 | 27 | 32 | |
| Missing | 1 | 1 | 4 | 1 | 7 |
| Total | 21 | 15 | 27 | 28 | 91 |
| Sector | Industry | Management category | Total | |||
|---|---|---|---|---|---|---|
| JC | JNC | MC | MNC | |||
| Private sector | Health care (e.g. nursing home) | 3 | 0 | 0 | 2a | 5 |
| Health-care related (e.g. pharmaceutical industry) | 0 | 1 | 0 | 2 | 3 | |
| Not health care | 0 | 9 | 0 | 9 | 18 | |
| Public sector | Health care (e.g. army) | 1 | 0 | 0 | 0 | 1 |
| Not health care (e.g. education) | 0 | 1 | 0 | 4 | 5 | |
| Subtotal | 4 | 11 | 0 | 17 | 32 | |
| No prior experience outside the NHS | 16 | 3 | 23 | 12 | 54 | |
| Missing | 1 | 1 | 4 | 1 | 7 | |
| Total | 21 | 15 | 27 | 28 | 91 | |
The associations of work experience outside the NHS with management category and clinical engagement were significant [χ2 (3, N = 84) = 30.76, p < .0001 and Yates’ χ2 corrected for continuity (1, N = 84) = 1.2, p = 0.2733, respectively] and relatively strong (Cramer’s V of 0.61 and 0.56, respectively), but not significant with management level [Yates’ χ2 corrected for continuity (1, N = 84) = 1.2, p = 0.2733].
The error in predicting work experience outside the NHS was reduced by knowing the management category by 37% (λ = 0.37, 95% CI 0.0 to 0.9) and clinical engagement by the same amount (λ = 0.37, 95% CI 0.0 to 0.7), and knowing whether or not the respondent had previously worked outside the NHS reduced the error in predicting management category by 19% (λ = 0.19, 95% CI 0.0 to 0.4) and clinical engagement by 54% (λ = 0.54, 95% CI 0.4 to 0.7).
Facets of identity: an interim summary
Table 11 brings together the findings on the associations between the facets of identity and management category, management level, and clinical engagement.
| Facet of identity | Management category | Management level | Clinical engagement |
|---|---|---|---|
| Self-definition | Significant and moderate association
|
No significant association | Significant and relatively strong association
|
| Group affinity | No significant association | No significant association | No significant association |
| Values | No significant association | No significant association | No significant association |
| Knowledge and skills | |||
| General education qualifications | Significant and moderate association
|
Significant and moderate association
|
Significant and moderate association
|
| Management qualifications and training | Significant and moderate association
|
Significant and relatively strong association
|
Significant and moderate association
|
| Tenure in the current job | Significant difference between the groups | ||
| Work experience outside the NHS | Significant and strong association
|
No significant association | Significant and relatively strong association
|
Connections across the facets of identity
We also examined potential associations between self-definition and other facets of identity: group affinity, values, and knowledge and skills.
We employed two types of grouping of self-definition:
-
the original grouping into three categories: (a) ‘I am a manager’, (b) ‘I am a manager, but. . .’, and (c) ‘I am not a manager’
-
an alternative grouping into two categories: (a) ‘definite’ managerial identity (‘I am a manager’) and (b) ‘reluctant’ managerial identity (all other responses).
Depending on whether or not the analysis with the original or the alternative grouping showed significant association, we reported the data using one or the other grouping. Where the analysis showed no significant association, we reported the data using the original grouping. To conserve space, the data tables are presented in Appendix 8 ( Tables 22 – 27 ), but the results of analyses are summarised in Table 12 .
| Facet of identity | Self-definition | |
|---|---|---|
| Original grouping | Alternative grouping | |
| Group affinity | ||
| No significant association (Fisher’s exact p = 0.10) | Significant and relatively strong association (Fisher’s exact p = 0.057, Cramer’s V = 0.43) | |
| % reduction in error in predicting: | ||
| Self-definition from group affinity | 22% (λ = 0.22, 95% CI 0.0 to 0.7) | |
| Group affinity from self-definition | 0% (λ = 0) | |
| Values | ||
| No significant association | No significant association | |
| (Fisher’s exact p = 0.309) | (Fisher’s exact p = 0.242) | |
| Knowledge and skills | ||
| General education qualifications | No significant association | No significant association |
| (Fisher’s exact p = 0.379) | (Fisher’s exact p = 0.309) | |
| Management qualifications and training | No significant association (Fisher’s exact p = 0.095) | Significant and moderate association (Fisher’s exact p = 0.034, Cramer’s V = 0.34) |
| % reduction in error in predicting: | ||
| Self-definition from management qualification | 19% (λ = 0.19, 95% CI 0.0 to 0.6) | |
| Management qualifications from self-definition | 0% (λ = 0) | |
| Tenure in the current job | No significant difference between the groups | No significant association between the groups |
| (Kruskal–Wallis H = 0.29, 2 df, p = 0.865) | (Mann–Whitney U = 685.5, z = 0.54, two-sided p = 0.5892) | |
| Work experience outside the NHS | Significant and moderate association [χ2 (2, N = 82) = 7.74, p = 0.02; Cramer’s V = 0.31] | Significant and moderate association |
| % reduction in error in predicting: | ||
| Self-definition from management qualification | 17% (λ = 0.17, 95% CI 0.0 to 0.4). | 10% |
| Management qualifications from self-definition | 10% | 10% |
The results showed:
-
A significant and relatively strong association between group affinity and self-definition which ran contrary to our initial intuition that identification with the management profession would be linked to a stronger peer group affinity. In fact, those who defined themselves as a manager more often expressed affinity with individuals and work teams, than with a peer group.
-
No significant association between values and self-definition, indicating that the public service ethos predominated and neither affected nor was affected by identification with managerial profession (or lack of thereof).
-
No significant association between general education qualifications and self-definition, suggesting that the identification with the managerial profession was unrelated to general educational credentials.
-
A significant and moderate association between management qualifications and training and self-definition, which suggests that higher education qualifications in management strengthen managerial identity, but other forms of management education and training do not.
-
No significant relation between tenure in the current job and self-definition, suggesting that, contrary to our initial intuition, the practical experience of managing did not affect identification with management profession.
-
A significant relation between work experience outside the NHS and self-definition which indicates that work experience outside the NHS strengthens the identification with management profession.
Summary
Our main findings are as follows.
The junior and middle managers were not a homogeneous group on most examined facets of identity. The cleavages ran between all four categories of managers (JC, JNC, MC and MNC), though the differences by clinical engagement were more common than those by management level.
The professional identity of the respondents as managers was not particularly strong: 43% of respondents did not define themselves as managers and another 21% defined themselves as managers with some reservations. The main dividing line was between non-clinical managers, who were more likely to define themselves as managers, and clinical managers, who tended to espouse their ‘primary’ clinical identity.
The respondents who had higher education qualifications in management were more likely to define themselves as managers, as were those who had previously worked outside the NHS.
Only 42% of respondents reported peer group affinity. Those who defined themselves as managers were more likely to identify with individual(s) or a work team than with a peer group. Hence, the collective identity of the respondents as managers was not particularly strong.
The main unifying facet of the respondents’ identities was values, as the majority espoused a public service ethos, and there were no significant difference in values between either junior and middle or clinical and non-clinical managers.
There were considerable differences within the sample on all assessed aspects of knowledge and skills.
The disparities between general education and management qualifications and training were broadly in line with the anticipated differences owing to job requirements (between junior and middle managers and clinical and non-clinical staff), but were more extensive than expected. Although general education qualifications and, even more so, management qualifications and training were instrumental in predicting the management category, management level and clinical engagement (thus giving more credence to the anticipated differences), there was no similar tendency in the opposite direction, as management category, management level and clinical engagement did not affect the prediction of either general education qualifications or management qualifications and training. Hence, the managerial hierarchy did not appear to be congruent with the hierarchy of educational credentials.
The tenures in the current post were on average rather short (< 5 years), and the differences between management categories, though small, were significant: JC managers were in post on average about 4.5 years, 2 years longer than JNC managers, and MC managers were in post for about 3.7 years, or over 1 year longer than MNC managers. Yet, the experience of a managerial job did not significantly influence the respondents’ identification with the management profession.
Work experience outside the NHS also considerably differed between the management categories and this difference ran along the clinical engagement dimension rather than the management level, as non-clinical managers were more likely to have worked outside the NHS.
Implications
Our findings indicate that the managerial identity of junior and middle NHS managers was not sufficiently strong, as many respondents were reluctant to define themselves as managers. As noted in Chapter 2 , social identity leads to uncertainty reduction. Regardless of whether or not the individual managers accept it, the managerial identity is foisted on them by their position, and hence they cannot fully disclaim it. Those who prefer to distance themselves from a managerial identity face a challenging task of constructing an alternative identity that has to be congruent with their position and be recognisable to, and validated by others. It may complicate their relationships, as other people would find it difficult to place them. As one respondent observed:
If I didn’t [think of myself as a manager] it would confuse the staff, because we’ve had a supervisor in the past who was very, very friendly with the staff and it had confusing and conflicting friendships and things.
JNC 101
Furthermore, a positive social identity helps to build social resources and increases the individual’s ability to endure stress and take on new challenges. In this light, our finding that a managerial identity was problematic for many respondents gives a cause for concern, because an insufficiently delineated or partially adopted identity may negatively affect both individual outcomes (e.g. self-esteem) and organisational outcomes.
In contrast to the previous accounts of ‘reluctant managers’, we found, however, that the respondents were not so much reluctant to manage as reluctant to associate themselves with the label ‘manager’.
The interview responses suggested to us two potential explanations of such reluctance. First, the reluctance to call oneself ‘manager’ may stem from the difficulties of defining what it means to be a manager. Considerable diversity of the pathways into management, of the prerequisites for occupying a managerial position (see Knowledge and skills), and of the authority, responsibilities and activities associated with management (as noted above and described in greater detail in the following Chapter 6 ) make ‘manager’ a very broad and diverse category. This diversity is further compounded by the dualism of many management positions, which combine clinical and managerial duties. The language markers also do not provide clear guidance, as the term ‘manager’ does not always appear in the job titles of managerial positions. As a result, defining oneself as a manager increases rather than decreases the ambiguity of self-definition.
Second, the reluctance to identify oneself as ‘manager’ may stem from the negative image of NHS managers, propagated by politicians and the media, which in turn influence the public opinion. Our findings echoed those of the earlier research, which had shown that the managers were aware of this negative image, held by ‘their staff the media, the public and even their immediate families’ (p. 110). 137,138 Although our research did not pertain to the analysis of the reasons why politicians and the media tend to vilify the NHS management, the extant literature suggests that such vilification is a long-standing phenomenon. Thus, Learmonth139 found that NHS managers were held in very low esteem by the ‘general population’ and were ‘overwhelmingly . . . gratuitously insulted’ by the press. More recently, a report by The King’s Fund Commission on leadership and management in the NHS (p. 1)12 noted that ‘in the public sector – and in the NHS in particular – whenever politicians talk about management it is almost invariably a pejorative term. It is often equated sneeringly with bureaucracy. Whole political careers have been built on attacking it’ and deriding managers as ‘men in grey suits’ and ‘pen pushers.’ The report also noted that the public appears to take ‘its cue from the political attacks on bureaucracy’; it quoted the results of a recent poll by Ipsos MORI showing that ‘85 per cent of the public supported proposals to reduce the number of managers in the NHS by one-third’ (p. 2). 12 One possible explanation for these tendencies, with regard to middle management in NHS, has been proffered by Hyde et al. 140 Hyde et al. 140 trace their roots to the more general stereotype of middle management, dominant in both academic and popular management literature, and quote Mills,141 Whyte,142 Handy,143 Peters144 and Kanter145 as the prominent examples of portraying a middle manager as ‘someone stuck in their role with limited hopes of progression, with few managerial skills and little managerial ability’, ‘a person who slavishly dotes on paperwork and petty rule enforcement’, ‘obstructive and afraid of change’ (p. 13). 140 They note that ‘on the whole, this view has gone largely unchallenged, with only a small number of commentators identifying positive features of middle managerial work’ (e.g. Hassard et al. 146 and Huy147).
Hyde et al. 140 further argue that, as a consequence of such stereotyping, middle managers have become ‘a mythical or fantasy group of others’, with whom barely anyone identifies (p. 14). 140 This mythical group, however, serves ‘a useful scapegoat function in that policy failures can be blamed on poor middle management’ (p. 18). 140
We concur with this interpretation. We believe that it is, indeed, expedient for politicians to shift the blame for the public sector problems from the policy-makers onto the policy ‘implementers’ (i.e. managers). It is certainly easier to attribute the problems to the shortcomings of a particular group of individuals and to devise solutions by targeting such groups rather than to examine the underlying systemic issues and develop more comprehensive remedies. It is particularly convenient that the scapegoat group already has a poor reputation, lacks voice/representation, and is a group with which barely anyone wants to identify (even if they formally belong to the group).
Putting these findings into our theoretical framework of identity, we observe incongruence between the respondents’ role identities and group identities. Role identity refers to the shared expectations regarding behaviour that are attached to a ‘position’ in a social network (p. 559). 38 Group identity refers to ‘that part of the individuals’ self-concept, which derives from their knowledge of their membership of a social group . . . together with the value and emotional significance of that membership’ (p. 255). 148 By and large, the respondents are more likely to identify with management as a role and are less likely to identify with managers as a group.
Social identity theory offers two basic motives of group identification: uncertainty reduction and self-enhancement. Uncertainty reduction is associated with social categorisation: ‘people strive to reduce uncertainty about their social world and their place in it – they like to know who they are and how to behave and who others are and how they might behave’ (p. 120). 149 Self-enhancement is associated with the positive intergroup distinctiveness [i.e. ‘a belief that ‘we’ are better than “them”’ (p. 120)149]. In our context, identification with ‘managers’ as a group does not appear to provide either uncertainty reduction or self-enhancement, thus undermining the motives for group identification.
Our findings that the respondents were more likely to report an affinity with individuals or their work group rather than with their peer group, and that those respondents who did identify themselves as managers were less likely to identify with their peer group than other respondents, further amplify this point. They suggest that the respondents were not only reluctant to identify with managers as an abstract category, but also did not strongly identify with other managers in their own organisation.
The consequences of low identification of the ‘de facto’ managers with managers as a social group and with managers as a peer group in their own organisation are far-reaching. Thus, the low identification creates a self-perpetuating cycle: as fewer individuals opt to identify with a group, the group distinctiveness and attractiveness decrease, weakening its pull on prospective members. A smaller and weaker group becomes yet more vulnerable to vilification and scapegoating. This in turn contributes to low morale and high turnover in the management ranks (p. 18). 140 Scapegoating also obscures the group’s vital role in and contribution to the organisation and misguides the problem identification and the search for solutions. It undermines the group’s status and reduces its power to influence other groups. The low identification also presents a barrier to peer support and knowledge transfer.
Potential practical solutions to the problem of low identification with other managers as a social and a peer group may entail:
-
promoting a better understanding of the role of managers, to which both research on management and management education should contribute ( Chapters 6–8 below offer our research input and Chapter 9 highlights the implications for management education)
-
promoting intra- and inter-organisational peer networks (Group affinity above highlights both the importance of peer networks and the apparent withering away of the previously established networks, as reported by our respondents)
-
promoting the status of management as an occupational group by its further professionalisation via (i) establishing an NHS-wide system of accreditation and qualification prerequisites for managers and (ii) creating a professional association of NHS managers (these suggestions are further developed in Chapter 9 , Management education and training)
-
promoting a better-informed and more positive image of NHS management in political circles and in the media (in this, a professional association of NHS managers may be particularly instrumental).
Finally, we suggest reinstating the term ‘manager’. The waves of change in both the private and public sectors, in the UK and internationally, have already seen the replacement of the term ‘administrator’ (still enduring, however, in degree title, i.e. ‘Master of Business Administration’) by the term ‘manager’ and, more recently, ‘leader’. The reasons for these changes have been amply documented elsewhere (e.g. Learmonth,150 Parker151 and O’Reilly and Reed152), and we will not rehearse them here. We would, however, argue that the frequent name changes contribute to the lack of distinctiveness and attractiveness of managers as a group, noted earlier. We would further caution, following Martin and Learmonth (p. 10–11)124 that, as leadership discourse becomes ubiquitous (and management goes out of use), leadership is likely to lose ‘the positive cultural valences currently ascribed’ to it, which hinge on a contrast between management and leadership. This may then prompt a search for a new ‘Holy Grail’, with detrimental consequences for the group image. We also note the dangers of leadership discourse per se. As suggested by Martin and Learmonth,124 leadership discourse is often used to ‘seduce’ and co-opt the dissent, align individual aims with the policy aims and mask the contradictions ‘between claimed decentralization and actual retention of power by the centre’. We add that the discourse of leadership focuses attention on an individual, rather than organisational context. The ‘individualisation’ of issues, or the interpretation of organisational problems as stemming from the qualities of an individual (e.g. personality traits, leadership style), diverts the attention from the examination of organisational-level causes, such as strategy, structure and culture, and places the responsibility with the individual rather than the system.
We therefore advocate a ‘return to management’ (i.e. the use of terms ‘manager’ and ‘management’) in order both to strengthen management and managers as a group and to focus the attention on the organisational roots of problems and the organisational solutions to those.
Chapter 6 What do junior and middle managers do?
This chapter addresses the aim of the project to ‘chart the work of middle and junior healthcare managers . . . and to produce an ethnography of their lived- experience’. It provides the empirical evidence to illuminate the perennial question ‘What do managers do?’ in the NHS context.
We begin by developing a fine-grained typology of junior and middle managers’ ‘work groups’, proceed to present the general parameters of managers’ work and, finally, offer a series of work profiles of the groups.
We note that, as the work of most managers includes a combination of managerial and technical components, we use the term ‘managers’ work’, rather than ‘managerial work’, to denote the whole complex activities of a manager.
A typology of managers’ work groups
Our study used a primary typology based on two dimensions: (1) management level (junior or middle) and (2) clinical engagement (whether the manager is counted as clinical or non-clinical staff).
Our examination of the managers’ work, however, revealed a greater complexity of roles which led us to develop a more fine-grained typology, which disaggregated the clinical and non-clinical categories based on the nature of their work:
-
Within clinical managers, taking into account the differences between clinical professionals, we distinguished between: (1) medical consultants, (2) nurses, (3) health-care science scientists, and (4) AHPs.
-
Within non-clinical managers, taking into account the differences between clinical and corporate units, we distinguished between managers working in (a) clinical units and (b) corporate units.
Table 13 presents the typology with illustrative examples from the sample.
| Clinical engagement | Management level | ||
|---|---|---|---|
| Middle | Junior | ||
| Clinical managers | Medical consultants |
Group 1: consultant managers Examples: clinical director, CBU medical lead, consultant – head of service |
(Theoretically empty cell) |
| Nurses |
Group 2a: middle nurse managers Examples: matron, nurse consultant, divisional head of nursing |
Group 2b: junior nurse managers Examples: ward sister, ward manager, deputy sister |
|
| Scientist managers |
Group 3a: middle scientist managers Examples: consultant scientist – head of service |
Group 3b: junior scientist managers Examples: team leader, laboratory manager |
|
| AHPs | (Empirically empty cell) |
Group 4: AHP managers Examples: clinical specialist – team leader |
|
| Non-clinical managers | Clinical units |
Group 5a: middle managers of clinical units Examples: directorate general manager, service manager |
Group 5b: junior managers of clinical units Examples: administrative manager |
| Corporate units |
Group 6a: middle managers of corporate units Examples: chief accountant, head of corporate contracts and commissioning |
Group 6b: junior managers of corporate units Examples: manager (booking centre), assistant manager (medical records) |
|
General parameters of managers’ work
‘General parameters’ here refer to the more quantifiable aspects of the content of work (what managers do) and the form of work (how they do it). A richer qualitative picture of the managers’ working lives is presented in Work profiles of managers’ work groups.
To assess the content of work, we considered the scale and the scope of their activities.
The scale of activities reflects:
-
the span of responsibility, defined as the size of organisational unit over which the manager has responsibility
-
whether or not the manager has staff or functional responsibility over the unit
-
the span of control, defined as the number of the manager’s direct reports
-
any cross-site work; and
-
any responsibilities outside the trust.
The scope of activities is characterised by relative weights of ‘the strictly managerial component’ of a manager’s job, which reflects the ‘responsibility for getting others to do things’, and the technical component, which reflects the manager’s specialist contribution to a work process through what they do themselves’ (p. 20). 153
To assess the form of work, we considered the length of their average work day and the proportion of work time devoted to scheduled meetings.
The scale of activities
The span of responsibility
The span of responsibility is, to a considerable extent, determined by the manager’s position within the organisational hierarchy and reflects the organisational structure.
As described in Chapter 4 , the two trusts had similar structures, although Cityscape had introduced an additional level of hierarchy by creating CBUs. Figure 3 presents the hierarchy of organisational units.
FIGURE 3.
Hierarchy of organisational units.
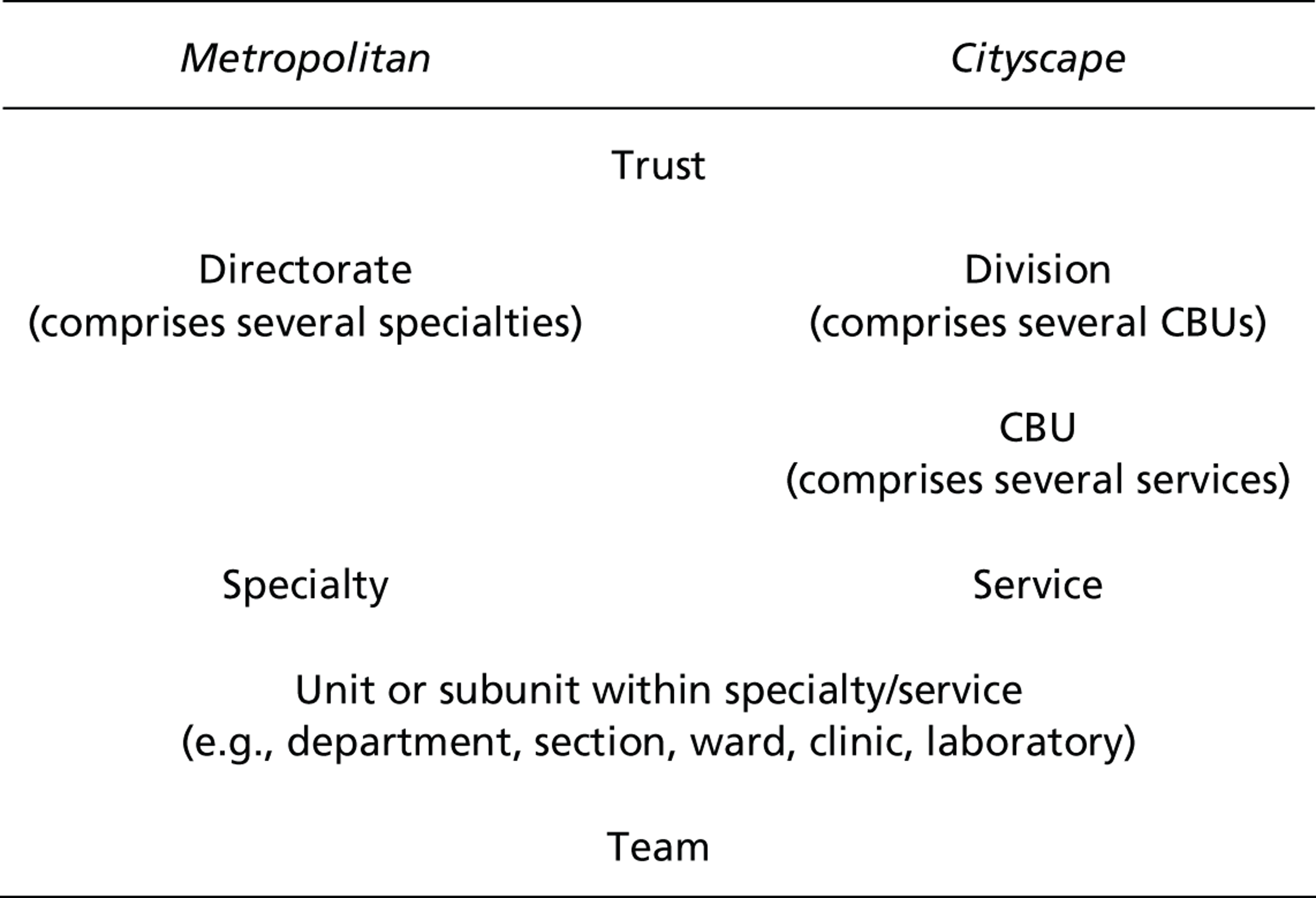
The span of responsibility of the respondents encompassed the entire range of organisational structural units: from team to trust ( Table 14 ).
| Category | Team | Unit, subunit, ward, clinic, laboratory | Specialty or service | Group of services or specialties | CBU | Division or directorate | Trust | Total |
|---|---|---|---|---|---|---|---|---|
| JC | 10 | 10 | 1 | 21 | ||||
| 2b Junior nurse managers | 4 | 9 | 13 | |||||
| 3b Junior scientist managers | 2 | 1 | 1 | 4 | ||||
| 4 AHP managers | 4 | 4 | ||||||
| JNC | 3 | 3 | 3 | 4 | 2 | 15 | ||
| 5b Junior managers of clinical units | 1 | 1 | 2 | 4 | 8 | |||
| 6b Junior managers of corporate units | 2 | 2 | 1 | 2 | 7 | |||
| MC | 4 | 7 | 1 | 7 | 8 | 27 | ||
| 1 Consultant managers | 2 | 1 | 3 | 6 | ||||
| 2a Middle nurse managers | 4 | 1 | 6 | 3 | 14 | |||
| 3a Middle scientist managers | 4 | 1 | 5 | |||||
| 5a Middle managers of clinical units | 2 | 2 | ||||||
| MNC | 2 | 6 | 3 | 2 | 6 | 9 | 28 | |
| 5a Middle managers of clinical units | 2 | 6 | 3 | 2 | 6 | 19 | ||
| 6a Middle managers of corporate units | 9 | 9 | ||||||
| Total | 9 | 19 | 17 | 8 | 9 | 14 | 1 | 91 |
Junior clinical mangers had the smallest span of responsibility. Thus, junior nurse managers were responsible for a ward (ward sister), a clinic (charge nurse) or a team within ward (deputy sister). Junior scientist managers had a wider range: from team to specialty/service. AHP managers were all team leaders or clinical specialist lead.
Junior non-clinical managers were more broadly spread, between team and group of services/specialties, with the two ‘outliers’ in the group of junior managers of corporate units (these were the managers within the R&D department who had trust-wide responsibility for narrow areas of activity, e.g. research governance).
Middle clinical managers mostly had a wide span of responsibility [almost one-third of them (8 of 27) were responsible for a clinical directorate/division], but there was some variation by work group. Consultant managers and middle nurse managers were responsible for wider entities (from specialty/service up to and including directorate/division) than middle scientist managers (units or subunits).
The span of responsibility of MNC managers covered nearly the whole range of organisational unit levels, but there was a significant split within the category by work group. Although middle managers of clinical units were responsible for anything between unit and division, all middle managers of corporate units had trust-wide responsibilities.
Two further considerations impacted the span of responsibility:
Temporal differences in the span of responsibility Some clinical managers regularly assumed an expanded span of responsibility when they were assigned (as many ward sisters were) a bed or a staff ‘bleep’.
Additional trust-wide roles Some managers had additional trust-wide roles, such as being a lead on a specific project.
Staff versus functional responsibilities
The assessment of the scale of activities also took into account whether the manager primarily had staff responsibility (i.e. was accountable for the entire staff, operations and performance of an organisational unit) or functional responsibility (i.e. was only responsible for a particular aspect of the unit’s operation).
-
Primarily staff responsibility All JC managers, most JNC managers and some MC (namely, all consultant managers and middle scientist managers and some middle nurse managers) and MNC managers (namely, some middle managers of clinical units) had the full responsibility for their unit and its staff.
-
Primarily functional responsibility The remainder of respondents had responsibility only for a specific functional area. In particular, all middle managers of corporate units had trust-wide responsibility for a specific function (e.g. corporate communications, contracts and commissioning, occupational health).
The contrast between staff and functional responsibilities is reflected in Table 15 , which presents the data on the total number of staff for whom the respondents reported responsibility.
| Category | Mean | Minimum | Maximum | Missing | Total count |
|---|---|---|---|---|---|
| JC | 18 | 2 | 46 | 3 | 21 |
| 2b Junior nurse managers | 24 | 2 | 46 | 2 | 13 |
| 3b Junior scientist managers | 8 | 4 | 10 | 1 | 4 |
| 4 AHP | 8 | 3 | 10 | 0 | 4 |
| JNC | 22 | 0 | 90 | 2 | 15 |
| 5b Junior managers of clinical units | 21 | 0 | 55 | 1 | 8 |
| 6b Junior managers of corporate units | 24 | 0 | 90 | 1 | 7 |
| MC | 314 | 0 | 2000 | 9 | 27 |
| 1 Consultant managers | 855 | 130 | 2000 | 3 | 6 |
| 2a Middle nurse managers | 201 | 0 | 800 | 3 | 14 |
| 3a Middle scientist managers | 11 | 9 | 13 | 2 | 5 |
| 5a Middle managers of clinical units | 3 | 3 | 3 | 1 | 2 |
| MNC | 139 | 2 | 2000 | 8 | 28 |
| 5a Middle managers of clinical units | 207 | 3 | 2000 | 5 | 19 |
| 6a Middle managers of corporate units | 12 | 2 | 34 | 2 | 9 |
| Total | 131 | 0 | 2000 | 22 | 91 |
The notable discrepancy between the number of staff in a manager’s responsibility (presented in Table 15 ) and the span of responsibility (see Table 14 ) is attributable to the fact that most clinical managers had staff responsibility for their unit and thus reported being responsible for the entire staff of their unit, whereas most non-clinical managers had functional responsibility and thus reported only the number of their direct reports.
Span of control
For junior managers the span of responsibility was normally equivalent to the span of control, whereas for middle managers the span of responsibility considerably exceeded their span of control, as they had few direct reports (who in turn supervise the rank-and-file employees or other managers).
The span of responsibility of middle managers (numbering in hundreds of members of staff) was on average much broader than the span of responsibility of junior managers (numbering in dozens), but their span of control (below 10) was much narrower than that of junior managers.
Cross-site work
Some managers were responsible for the units that operated on several sites ( Table 16 ).
| Category | Frequency | Percentage | Total |
|---|---|---|---|
| JC | 2 | 10 | 21 |
| 2b Junior nurse managers | 0 | 0 | 13 |
| 3b Junior scientist managers | 0 | 0 | 4 |
| 4 AHP | 2 | 50 | 4 |
| JNC | 7 | 47 | 15 |
| 5b Junior managers of clinical units | 5 | 63 | 8 |
| 6b Junior managers of corporate units | 2 | 29 | 7 |
| MC | 9 | 33 | 27 |
| 1 Consultant managers | 1 | 17 | 6 |
| 2a Middle nurse managers | 4 | 29 | 14 |
| 3a Middle scientist managers | 2 | 40 | 5 |
| 5a Middle managers of clinical units | 2 | 100 | 2 |
| MNC | 8 | 29 | 28 |
| 5a Middle managers of clinical units | 6 | 32 | 19 |
| 6a Middle managers of corporate units | 2 | 22 | 9 |
| Total | 26 | 29 | 91 |
Very few JC managers (only AHPs) worked across sites, which is understandable given that they had to directly supervise staff providing patient care. The proportion of MC and MNC managers working across sites was near the average for the sample overall. Interestingly, JNC managers were the ones most frequently stretched across the sites (nearly a half of the category reported working across sites), with almost two-thirds of junior managers of clinical units working across two or more sites.
Responsibilities outside the trust
Some managers had responsibilities that spanned outside their trust, as shown in Table 17 .
| Category | Frequency | Percentage | Total |
|---|---|---|---|
| JC | 3 | 14 | 21 |
| 2b Junior nurse managers | 1 | 8 | 13 |
| 3b Junior scientist managers | 2 | 50 | 4 |
| 4 AHP | 0 | 0 | 4 |
| JNC | 7 | 47 | 15 |
| 5b Junior managers of clinical units | 4 | 50 | 8 |
| 6b Junior managers of corporate units | 3 | 43 | 7 |
| MC | 7 | 26 | 27 |
| 1 Consultant managers | 1 | 17 | 6 |
| 2a Middle nurse managers | 3 | 21 | 14 |
| 3a Middle scientist managers | 3 | 60 | 5 |
| 5a Middle managers of clinical units | 0 | 0 | 2 |
| MNC | 9 | 32 | 28 |
| 5a Middle managers of clinical units | 6 | 32 | 19 |
| 6a Middle managers of corporate units | 3 | 33 | 9 |
| Total | 26 | 29 | 91 |
The different responsibilities outside the trust between management categories and work groups were similar to those for cross-site work. Again, JC managers were the least frequently involved, whereas the JNC managers were those most frequently involved (especially junior managers of clinical units) and MC and MNC managers were around the sample average.
The most commonly cited responsibilities outside the trust were (with the number of respondents in brackets) working with an independent sector treatment centre (ISTC) (n = 7), dealing with external contractors (n = 4), providing services for public and private sector organisations (n = 4), managing commercial and non-commercial trials (n = 2), and commissioning with NHS and non-NHS organisations (n = 2).
The scope of activities
The scope of activities refers to the relative balance between the strictly managerial and the technical components of managers’ work.
In the circumstances, it was difficult to ascertain this balance for non-clinical managers, but in the case of clinical managers the distinction between managerial and technical (i.e. clinical) work was fairly straightforward. Table 18 presents descriptive statistics on the relative proportion of clinical work in the total work time for clinical managers.
| Category | Mean | Minimum | Maximum | Missing | Total count |
|---|---|---|---|---|---|
| JC, including | 48 | 20 | 60 | 5 | 21 |
| 2b Junior nurse managers | 47 | 20 | 60 | 3 | 13 |
| 3b Junior scientist managers | 53 | 40 | 60 | 0 | 4 |
| 4 AHPs | 50 | 50 | 50 | 2 | 4 |
| MC, including | 18 | 0 | 80 | 8 | 27 |
| 1 Consultant managers | 60 | 50 | 80 | 3 | 6 |
| 2a Middle nurse managers | 10 | 0 | 50 | 3 | 14 |
| 3a Middle scientist managers | 17 | 10 | 20 | 2 | 5 |
| 5a Middle managers of clinical units | 0 | 0 | 0 | 0 | 2 |
| Total | 32 | 0 | 80 | 56 | 91 |
Junior clinical managers devoted, on average, nearly 50% of their work time to clinical duties, and the differences between work groups within the category were relatively minor. In contrast, MC managers, on average, devoted just under 20% of their work time to clinical work, but there was a substantial variation within the category between work groups. Consultants spent on average 60% of their work time doing clinical work; middle nurse managers only 10%; and middle scientist managers 17%. (The two middle managers of clinical units, classified as ‘clinical’ but not engaged in any hands-on clinical practice, were divisional quality, safety and risk managers.)
The form of work
To give some idea of the demands that the work placed on the respondents, we asked them to estimate the average number of hours they worked per week ( Table 19 ).
| Category | Mean | Minimum | Maximum | Missing | Total count |
|---|---|---|---|---|---|
| JC | 49 | 40 | 60 | 7 | 21 |
| 2b Junior nurse managers | 50 | 40 | 60 | 3 | 13 |
| 3b Junior scientist managers | 46 | 40 | 52.5 | 1 | 4 |
| 4 AHP | 45 | 45 | 45 | 3 | 4 |
| JNC | 45 | 40 | 50 | 4 | 15 |
| 5b Junior managers of clinical units | 48 | 45 | 50 | 4 | 8 |
| 6b Junior managers of corporate units | 44 | 40 | 50 | 0 | 7 |
| MC | 57 | 40 | 80 | 11 | 27 |
| 1 Consultant managers | 65 | 50 | 80 | 0 | 6 |
| 2a Middle nurse managers | 55 | 43.5 | 65 | 8 | 14 |
| 3a Middle scientist managers | 45 | 40 | 50 | 3 | 5 |
| 5a Middle managers of clinical units | 52 | 40 | 63.5 | 0 | 2 |
| MNC | 49 | 37.5 | 60 | 16 | 28 |
| 5a Middle managers of clinical units | 47 | 37.5 | 60 | 11 | 19 |
| 6a Middle managers of corporate units | 53 | 45 | 60 | 5 | 9 |
| Total | 51 | 37.5 | 80 | 38 | 91 |
For the sample as a whole, the average work week (51 hours) was nearly 2 days longer than the official work week (37.5 hours). The majority of respondents worked more than the official hours. Many commented that theirs was not a ‘9 to 5’ job and that they normally did not take time for lunch:
We don’t get lunch, no lunch, no, no. Not in the NHS.
MNC 17, directorate assistant general manager
Those who reported the time they started work (38% of the sample) began their work day, on average, at 07.45 in the morning and noted that they preferred to arrive before their subordinates did in order to have some ‘quiet’ time to catch up on e-mails and paperwork.
Middle clinical managers worked the longest hours, with consultant managers having especially heavy workloads. (Some of them had full-time consulting work and did their management duties on top of that.)
Time in meetings
Time in meetings refers to the time spent in formal pre-arranged meetings, as opposed to the casual ‘drop ins’.
I spend a lot of my time in meetings because people come in here all the time to ask me things, but I guess we’re not talking about that.
MC 41
Time in meetings as a proportion of total work time was recorded as directly reported by the respondents or as calculated based on the number and duration of meetings the respondents attended (e.g. per day or week) and on the assumption of a ‘normal’ 40-hour work week (rather than the actual hours at work reported).
As detailed in Table 20 , on the whole, the managers spent just over a quarter of their work time in formal meetings, but there was considerable variation by category and work group. JC managers were the least taxed by meetings, spending on average 11% of their work time in the meetings, whereas middle managers (both clinical and non-clinical) spent about one-third of their time in meetings.
| Category | Mean | Minimum | Maximum | Missing data | Total n |
|---|---|---|---|---|---|
| JC | 11 | 0 | 20 | 7 | 21 |
| 2b Junior nurse managers | 12 | 0 | 20 | 3 | 13 |
| 3b Junior scientist managers | 14 | 8 | 20 | 2 | 4 |
| 4 AHP | 4 | 4 | 4 | 2 | 4 |
| JNC | 27 | 5 | 50 | 5 | 15 |
| 5b Junior managers of clinical units | 25 | 12 | 50 | 3 | 8 |
| 6b Junior managers of corporate units | 29 | 5 | 50 | 2 | 7 |
| MC | 33 | 5 | 75 | 6 | 27 |
| 1 Consultant managers | 27 | 10 | 38 | 2 | 6 |
| 2a Middle nurse managers | 37 | 5 | 75 | 2 | 14 |
| 3a Middle scientist managers | 34 | 30 | 40 | 2 | 5 |
| 5a Middle managers of clinical units | 21 | 8 | 33 | 0 | 2 |
| MNC | 35 | 0 | 90 | 4 | 28 |
| 5a Middle managers of clinical units | 35 | 10 | 90 | 3 | 19 |
| 6a Middle managers of corporate units | 33 | 0 | 80 | 1 | 9 |
| Total | 28 | 0 | 90 | 22 | 91 |
The information collected from the observations at meetings and the shadowing of respondents showed that the meetings were frequently conducted in an atmosphere of high stress, pressure and urgency. This atmosphere reflected both the nature of the topics under discussion and the behaviour of the meeting participants. Some participants arrived late, some left early (after the discussion of a particular item of interest). While waiting for other participants to arrive, those present engaged in a discussion of work-related matters, rather than a general social chat. The impression given was that no time could be wasted. During the meeting most participants were multitasking, sending text messages on their mobile phones or using laptops to answer e-mails. The mobile phones were ringing frequently, and the participants often went outside, into the corridor, to answer these calls. Many of these calls were of an urgent nature, requiring immediate attention. Thus, one of the participants commented after the meeting that he took a call to give advice on a patient who was in operating theatre undergoing surgery and ‘whose chest was open’. (These observations were taken at a quality and performance meeting, an executive board meeting and a divisional management team meeting, all at Cityscape.)
Work profiles of managers’ work groups
Group 1: consultant managers
All consultant managers were involved clinically (see Table 18 ) and some continued to work full clinical sessions. Consequently, many perceived their managerial work as ‘an addition’ to their clinical responsibilities.
All defined themselves as ‘doctors’ first, but also talked about being leaders rather than managers (reserving the latter label for day-to-day running of operations), and were deeply engaged in their ‘leadership’ roles, describing them as intrinsic to their interpretation of their role as physicians:
Part of being a physician is about determining best patient care, practice, pathways, and those sorts of things, and I suppose one could argue that you can’t do that in a void. So it needs to be done with directing . . . and then I suppose that one of the responsibilities of being a senior clinician is to facilitate change, benefit, positivity and those sort of things.
MC 59
All stressed their focus on strategy, with regard to both their specialty and trust-wide issues. Most offered the examples of large-scale organisational changes they initiated and/or led, such as redesigning services, merging sites and bringing different teams together.
All emphasised that they were accountable for the quality, performance and finances of their organisational units, but not all were equally empowered to make decisions. The higher-level consultant managers (i.e. clinical directors of directorates/divisions) appeared to have considerable influence with their trust boards and more discretion to make decisions. In contrast, heads of service and CBU leads felt ‘stuck in the middle’, channelling directions from ‘above’ to those ‘below’ them and channelling the voices of their units to those ‘above’, and constrained by the slowness of decision-making processes.
All worked very long hours, with 12-hour days and taking work home being the norm, and described their positions as intense and unsustainable in the long term. On their managerial days, many had to attend ‘back-to-back meetings’ and some were critical of the number and the content of the meetings they were expected to attend. They described their roles as ‘wicked’ (see Effective management as a ‘wicked problem’ in Chapter 7 ) and impossible for one person, especially in the context of cost-cutting while delivering quality services.
The tensions between managerial and clinical responsibilities, well documented in the extant literature on professions (see discussion in Chapter 2 , Professions), were clearly evident in the interview responses, which frequently referred to ‘conflict’, ‘juggling’ and ‘balancing’.
Yet, despite the demanding roles, consultant managers also reported great satisfaction from their work and their efforts to benefit the patients and improve the quality of care:
The reasons I do it [the job] is you want to be involved in the decision-making and making the lot of patients and your colleagues within the environment you have influence better . . . and you know it is rewarding and challenging to be involved in.
MC 70
Group 2: nurse managers
Middle nurse managers
Divisional heads of nursing were responsible clinically and operationally for nursing and clinical staff in their respective divisions (with responsibility for advising on professional standards and a particular focus on quality, behaviour and discipline, auditing, performance and nurse education).
All adopted a trust-wide perspective and were heavily involved in networking and building strong relationships to facilitate ‘influence’. They emphasised having strong support both from above (e.g. the chief executive officer and chief nurse) and from below (lead nurses). They focused on being ‘doers’ and achieving change in order to provide better and more efficient services for patients and were able to give concrete examples of their achievements, such as procuring funding for a theatres project board (MC 57), developing strategy for infection prevention (MC 60), and devising an electronic handover system (MC 83). It transpired, however, that, although their focus was supposed to be on strategy, recently operational issues tended to take priority.
Similarly to consultant managers, heads of nursing felt under pressure to juggle competing priorities. As noted by one head of nursing:
While capacity and capability is being concentrated on, sickness absence is getting worse. Focus on sickness and sickness improves. Focus on appraisal, appraisal improves. Focus on incidents and they improve, meanwhile other things get worse.
Observation at quality and performance meeting, Cityscape
All reported long working hours and intense working days. They attended back-to-back meetings but also engaged in many other face-to-face interactions (e.g. walkabouts, supervisions, mentoring). As one respondent remarked:
I don’t believe the job can be run in an office, a lot of it is face-to-face contact.
MC 60
All commented on getting work satisfaction from seeing change that benefits patients and staff and described ‘paperwork’ (reports, documentation) as the least satisfying part of the job, often interrupted and delayed by having to deal with staff issues.
Lead nurses had direct line managerial responsibilities for nurse practitioners. Work was divided between 3 days clinical, 1.5 days managerial and 0.5 days training. Clinical days involved carrying out procedures for clinics while also being responsible for addressing staff queries and compiling referral lists. Clinical days were described as tiring, owing to staff shortages and a heavy workload, with frequent extra clinics scheduled. Management days were devoted to incident reports, appraisals and staff competency assessments and were described as ‘calmer’, although back-to-back meetings were often attended and there were numerous interruptions throughout the day.
The matron role involved line managerial responsibilities for ward sisters and also, for some respondents, for specialist nurses. They had little, if any, ‘hands on’ clinical input, although the clinical side was deemed a priority, realised through the interaction with patients and the clinical input into decision-making. As one respondent remarked:
It’s all about the clinical . . . although I’m not as expert as I used to be because that’s all about the care of the nurses.
MC 85
Days usually started with ward walkabouts and matron’s rounds to pick up problems on the wards and with staffing issues. All the matrons were involved in bed management and, at Cityscape, were rostered for this role. They attended a lot of meetings and were involved in cost improvements, final approval for investigations about complaints, staff budgeting, payment of invoices, and HR issues such as appraisals and disciplinary and sickness reviews. Some matrons commented that their time was wasted doing clerical work such as filing and typing, when they could have been on the wards. All complained about the amount of e-mails they received. Work was described as unpredictable and with frequent interruptions. Some matrons discussed their role in the management of change and wider trust issues such as the patient experience, but, on the whole, they were little involved in strategy.
Nurse/midwife consultants’ responsibilities were split between clinical practice (50%) and research, education and leadership (50%). Nurse/midwife consultants were passionate about their specialist areas and were involved in both strategy development (identifying the short- and long-term strategic objectives for their area) and strategy implementation (setting up and running clinics and training programmes). Their involvement in strategy-making was, however, curtailed by lack of time, as their other work was very demanding and described as ‘back-to-back nearly every day’ (MC 23) and ‘one thing on the back of another on the back of another’ (MC 9). There was a contrast between their profile within and outside the trust: they had a fairly high standing nationally (in terms of their research activities, attending conferences and writing journal articles) but complained of the trusts’ lack of understanding of their roles.
Junior nurse managers
This group included ward sisters, ward managers (nurse managers in charge of wards; the titles ‘ward sister’ and ‘ward manager’ appeared to be interchangeable), deputy sisters and a charge nurse (nurse manager in charge of an outpatient clinic). All were JC and on AfC band 7 (except for deputy sisters who were band 6).
Ward sisters, ward managers and charge nurses
Ward sisters/managers and charge nurses had a dual job role, normally defined as 50% clinical and 50% non-clinical (i.e. managerial).
In their managerial capacity, ward sisters/managers (but not charge nurses) had ‘24 hour overall care responsibility for the patients’, being ‘overall responsible for everything that happens with the patients’ (JC 6). In this capacity, they worked both directly and through deputy sisters (who were in charge of the teams within ward).
In their clinical capacity, they were also directly involved in and responsible for the care of some of the patients on their ward. In this capacity, they worked on the same level as their direct reports.
Their span of responsibility covered a single ward or clinic and was nearly equal to their span of control. A representative example would be a ward manager, who had 30 direct reports, including three deputy sisters (band 6), 18 qualified nurses (band 5), eight auxiliaries (band 2) and one receptionist (band 2). Their span of responsibility, however, regularly exceeded their span of control, as they had staffing or bed occupancy responsibility for several wards on a rota basis (for a day or a week at a time).
The 50/50 split in their job role manifested itself in the split of the work week into 3 clinical days and 2 management days (JC 65, ward sister) or some variation thereof, depending on the length of a shift on the ward. In practice, however, this split rarely materialised, with the clinical work always taking the priority and pushing the managerial work to the margins. These nurse managers frequently had to step in and substitute for the missing members of their staff, working clinically during the times formally allotted for their managerial responsibilities. Most of the wards did not have the full complement of staff, and this staff shortage was exacerbated by sickness absences.
Their managerial work was both very extensive in terms of the variety of activities and intensive in terms of the time and effort they required. It encompassed:
-
general management, including managing the work flow (e.g. organising admissions, planning discharges), communicating with patients (e.g. telling them their ‘plan of action’, dealing with patient complaints), monitoring the work of subordinates on various aspects of the standards and quality of care (e.g. auditing patient observation charts), and supplies management
-
staff management, including nearly the full suite of HR functions: recruitment and selection (e.g. interviewing job candidates), performance management (e.g. appraisals), training (e.g. mentoring nursing students), attendance and sickness absence management [e.g. meeting with staff ‘who have triggered the sickness policy and reviewing them at various stages’ (JC 51)], and ‘management of change and redeployment’ (JC 56)
-
information management (e.g. weekly sickness and absence returns)
-
financial management, i.e. having responsibility for the pay and non-pay budget of their ward (without, however, having any control over the monies, e.g. being unable to reallocate the money saved in one area for other needs).
These managers did primarily operational work and had little, if any, opportunities for feeding into strategy formulation, with minor exceptions (e.g. one ward sister was the directorate’s representative for the trust’s strategy group for a particular problem area). Yet, on the local level, many showed considerable initiative in introducing changes into their work areas that went beyond the mere maintenance of status quo, but were aimed at developing the service. These ‘entrepreneurs’, however, admitted difficulties in finding the time to devote to such projects and in getting their proposals through the decision-making channels.
The pace of work was relentless and highly intense. All reported constant interruptions and being called out to perform managerial duties while doing clinical work, and doing clinical work on non-clinical days. Most came to work half an hour earlier than required and left an hour later than the formal end of their day, in order to catch up with managerial duties. Many also did extra clinical shifts on top of their normal workload because of staff shortages.
These managers described their work as ‘fire fighting’ (JC 12) and ‘juggling’ (JC 56, JC 62, JC 51). It was highly stressful, with the ‘normal’ stress of coping with the demands of patients and staff exacerbated by increasing demands of internal reporting and financial constraints leading to the closure of vacant posts or the inability to fill vacancies and stringent controls over the use of temporary staff.
Their plight was neatly summed up by a ward manager, who described their position as
The jam in the middle of the sandwich, because you get battered from above [their superiors] . . . and then from below [their subordinates].
JC 6
The working environment of these managers was also highly stressful. The notes from shadowing of JC 40, for instance, showed that the respondent worked in a small, poorly ventilated office, with no windows, crowded with furniture. The respondent tended to keep the office door open because the office was too hot and stuffy and also because the staff members kept going in and out of the office. Thus, the staff members came into the office to collect their duty rosters, use the fax and the photocopier that were housed in the office, and to discuss the matters with the respondent. There were incessant interruptions and a considerable background noise from the phones ringing, buzzers and alarms going off, and the staff talking.
Deputy sister
The role and work of a deputy sister were similar to those of a ward sister, scaled down to the level of a team within a ward, but, unlike ward sisters, deputy sisters had no formally defined job role split into clinical and non-clinical duties, and their job was defined primarily as clinical (despite having a considerable managerial component). Thus, they had only one non-clinical day a month, and even that was frequently lost owing to staffing problems. Their span of responsibility varied, being normally the same as their span of control (the team), but frequently changing to a different group of staff when they were in charge of a shift (as the shift members were not necessarily in their team) or expanding to the whole ward when they were on duty (in the absence of ward sister). Therefore, in terms of managerial duties, deputy sisters did the same general work management as ward sisters during their shifts and the same staff management and information management as ward sisters (but just for the team). The pace of work was similarly relentless and the level of stress was equally high (so much so that one of the respondents had previously taken a long leave with stress and depression). However, deputy sisters still managed to be as ‘entrepreneurial’ as ward sisters, succeeding in introducing significant changes in their work arrangements (e.g. creating a day room for patients, eliminating unnecessary paperwork or reorganising the shifts).
Group 3: scientist managers
Scientist managers had a range of responsibilities for the delivery of their service specialities, including clinical responsibilities (e.g. carrying out tests, responding to requests from medics), managerial responsibilities (e.g. line management, cost improvement, adhering to waiting list targets), and R&D. Quality and safety was an important requirement in their line of work and all were heavily involved in auditing and inspections.
All stressed the importance of their clinical work and of staying involved in the direct patient/laboratory practice for their sense of identity and as feeding into their managerial role. They reported getting a ‘buzz’ from clinical practice and still being enthused by what their respective scientific subjects had to offer. The managerial work, however, tended to dominate and push their ‘hands-on’ scientific work to the margins. Most found people management to be both challenging and satisfying, but all were critical about being subject to micro-management and having to provide frequent reports and statistics (which they perceived as ‘wasted time’).
Most were engaged in the work that spanned or went beyond the trust boundaries. In particular, they were involved in research and teaching, and in professional associations at national and international levels. Some were also involved in income generation and working under contract with private providers. Their ‘external profile’ was therefore quite high. Yet, within the trust they perceived their specialist areas to lack visibility and themselves to lack influence (despite being advisors for their speciality across the trust), which was a source of frustration to them. They talked about being constrained by the slow decision-making processes within the trust and the NHS more generally.
Most scientist managers led fairly small teams, but these were not always ‘compact’, as, frequently, parts of the team were located on different sites and hence challenging to manage.
Most described their daily work as unpredictable and intense – too much to do, with the added pressure of being short-staffed and under resourced – and some admitted to being unable to meet their patient waiting-time targets.
Group 4: Allied Health Professional managers
All AHP managers were involved clinically and their workloads were geared towards clinical rather than managerial responsibilities. They talked about the patient care being their priority, although they were also responsible for staff and the daily operational running of a team. Their staff responsibilities entailed dealing with sickness absence, organising cover, and advising, teaching and mentoring junior members of their teams. All worked in interdisciplinary teams, which included nurses, other AHPs and consultants, and hence they often attended multidisciplinary team meetings.
They described their work as unpredictable:
Every day is different because sometimes you don’t have enough staff. Sometimes you do have enough staff but you are under pressure from clinicians – there is more that needs to be done, but your resources just can’t cope.
JC 94
and intense:
I like a bit of a buzz in the office and it gets the adrenaline going. But it can get too much quite easily and it does quite frequently. And then you realise it’s the end of the working day and I’ve not written my notes up and of course legally that’s unacceptable. So they might roll over to the next day which I know is not ideal, but I might stay late to finish them.
JC 90
All had heavy workloads and were under pressure to see more patients and reduce waiting lists.
Work satisfaction was primarily derived from their clinical work, but also from fostering a happy team and from teaching. Dissatisfaction stemmed from feeling ‘stuck in the middle’ and ‘not listened to’.
Group 5: managers of clinical units
This group was very diverse in terms of the hierarchical levels and functional spheres of their responsibilities. What united them was that, unlike other groups of managers in the clinical block, these managers, as a rule, did not have any clinical duties.
[Note that several managers in this group did have clinical duties, but these appeared to be the exceptions driven by idiosyncratic circumstances. Specifically, one CBU manager did, on average, about 1 clinical day a week to keep up their professional registration; and some service managers had about 20% of their workload as ‘hands-on clinical’, but reported that this share was gradually reducing (MNC M1).]
We further divided this group into two subgroups:
-
middle managers, who operated on the level of directorate/division, CBU or service and were all within AfC band 8
-
junior managers who operated within a service and were predominantly AfC band 5.
Middle managers
General managers
The remit of these managers was neatly summed up by a directorate assistant general manager as ‘split in half’: ‘one is to deliver performance’ (in accordance with performance targets) and ‘the other is to deliver the budget’ (including cost reduction) (MNC 17).
The precise meaning of this remit varied, however, by hierarchical level.
Thus, a directorate general manager was responsible for the whole clinical directorate, with 2000 staff and a budget of over £100M. In addition to delivering ‘the services. . . within a particular financial envelope’ and ‘all of the required performance targets’, this manager was also accountable for developing the directorate strategy and agreeing it with the trust, and it was this strategic work that occupied most of their time. The strategic work was largely ‘technical’ in that it concerned annual planning, business analysis and financial forecasting and was conducted in tandem with technical specialists (e.g. discussing the assumptions for the financial forecast with the directorate finance manager; amending the draft annual plan with a deputy general manager; agreeing job descriptions for the senior roles in a new ‘particularly large project’ within the directorate – with the trust’s director of strategy). In contrast to the span of responsibility, the span of control was fairly narrow (about a dozen staff, all of whom were ‘fairly senior’, i.e. heads of service and directorate assistant general managers), and the staff management work was also strategic, as the manager devoted a considerable amount of time and reflection to the performance appraisal of the direct reports. Meetings accounted for about half of work time, but the boundary between meeting time and other work time was blurred as much time was devoted to preparation for meetings, and the meetings themselves were ‘working’ meetings, rather than ‘information dissemination’ ones. The pace was fairly sedate; the meetings were all scheduled; there were no interruptions; and the manager was one of a very few in the whole sample who kept ‘normal’ working hours (08.30 to 17.30) (MNC 30).
One level down were directorate assistant general managers (in Metropolitan) and CBU managers (in Cityscape), who were responsible for a set of clinical services within the directorate/division, with a staff of several hundred and a budget in the region of £15–30M. Their work combined strategy development and implementation, with the emphasis on the latter. In terms of strategy development, they provided input from their services into directorate/divisional planning, led on specific service projects within the trust (e.g. ‘developing the acute oncology service’) and, in some cases, on the regional level (e.g. sitting on the regional ‘cancer commissioning board’) (MNC 4), and initiated their own projects, which had strategic ramifications for the division and the trust [e.g. medical workforce change, using physician’s assistants instead of junior doctors (MNC 73)]. In terms of strategy implementation, the scope of their activities was extensive, encompassing finance [‘either generating income or reducing costs’ (MNC 7)], HR and operations [‘monitoring of day-to-day activity, making sure that systems are in place, meeting with the staff, walking the patch’ (MNC 4)]. Yet, they had considerable assistance from the management teams below them and worked through them:
Whilst I might be the one that sets up the action plans, I might be the one who sends people off to do certain tasks . . . actually it’s not me that does it, it’s we who do it, there’s a raft of us who do.
MNC 73
Their work was a mixture of planned and unplanned activities. The emphasis was on ‘putting processes in place . . . to make things smoother’, and hence work was geared towards the scheduled, but they also had to be reactive and ‘drop everything. . . [to] get something sorted there and then’ and were not averse to stepping up to the coalface to ‘keep things going’:
If my admin manager is off . . . I . . . go in there and fill and get it working.
MNC P2
They spent over one-third of their work time in meetings (with one ‘outlier’ spending as much as 90% of their time). The majority of these, however, were not ‘just . . . “sit in” meetings . . . listening what they’ve got to say’, but ‘meetings with people to make sure that things are done or . . . planned systems are changed and so . . . quite important’ (MNC 4).
Many considered themselves both managers (those who ‘get the process done’) and leaders (those who ‘help people to do it’, by ‘role modelling and making sure people understand which direction we are going and why we are headed in this direction’) (MNC 7).
Their work days were long (mostly 07.30 till 18.00) and hectic; but the majority appeared to relish being busy:
A not so good day would be when I’m tied to my desk and things are going so well I don’t need to go and do anything, because I hate not being busy!
MNC 7
and enjoy the challenge:
Having that and 15 other things on your plate at the same time, it does give you a buzz.
MNC 17
Finally, further down, were service managers responsible for a specific service or department. The core of their work was operational but they also had a strategic role, both leading on a particular aspect of the service delivery at a higher level of hierarchy (e.g. directorate) (MNC 45) and doing ‘service level strategy’ (i.e. ‘interpreting’ the trust strategy and ‘applying’ it to their ‘individual speciality’). As one of them noted:
[The trust] strategy is just a strap-line . . . it can be very generic and every speciality is going to interpret that strategy in a different way . . . [so] there is a lot of devising your own goals.
MNC 1
These middle managers were the closest to the coalface and, although, in principle, they had junior managers to line manage the ‘rank and file’, in practice, because of staff shortages and pressure to deliver on performance targets (such as waiting times), the line managers were too preoccupied with their clinical duties to offer sufficient managerial support. Thus, a service manager lamented that the line management system was:
Working poorly . . . because all of the line managers are in clinical roles . . . My deputies are 70 per cent clinical and 30 per cent managerial in theory, [but] in practice it’s more 90 per cent to 10 per cent.
MNC 22
Consequently, instead of delegating routine staff management duties to their deputies, service managers had to directly look after the entire staff of their service and devoted over one-third of their time to these matters (e.g. performance appraisals, ‘return to work’ procedures). Staff management was the main source of unpredictability in their job:
No two days are ever really the same, and there are all sorts of things that are thrown into that pot . . . and it’s mainly staff and their issues.
MNC 22
Similar amounts of time were devoted to the general work management, ‘mak[ing] sure everybody is . . . in the right place and we can cover what we need to cover’ (MNC 45). This entailed scheduling work, checking supplies, doing the invoices, liaising with other services, and other operational matters. Although general managers at all levels were accountable for the service delivery, it was the responsibility of service managers to deliver the service on the day-to-day basis.
The dual challenge of staff management and general management work was reflected in the long hours these managers worked. On being asked what it is like to be a manager in the NHS one replied:
You have to be of a strong constitution physically because a lot of managers in my position do hours beyond what they’re paid for.
MNC 45
Functional specialist managers
In contrast to general managers, the specialist managers on this level were responsible for a more narrow scope of activities within their function. Yet, similarly to general managers, specialist managers had a dual focus on both strategic and operational matters. Thus, a divisional finance and performance manager was in charge of producing the business cases for developing specific services within the division and taking them for approval to a commercial executive board, but also had operational responsibility for monthly reporting on the financial position of the division to the trust executive directors (MNC 75). A divisional HR lead was responsible for planning ‘what is it we need from staff moving forward to the next 5 years to become a hospital of choice for Planned Care’, but also for ‘hand-hold[ing] managers operationally . . . on sickness management or disciplinary or investigations . . . ’ (MNC 98).
Junior managers
In comparison with middle managers of clinical units, junior managers of clinical units were a more homogeneous group, comprising mainly administrative managers on band 5. These managers were in charge of administrative and clerical staff [e.g. ‘medical secretaries, medical support secretaries, admin officers, analysts, filing clerks, receptionists’ (JNC 24)] within one or, more commonly, several clinical specialty areas.
Their span of responsibility was between 5 and 55 staff, with the added challenge that some managed employees located on two or three different sites (JNC 24 and JNC 97). Their span of control was either the same or smaller than their span of responsibility, as some administrative managers had managers below them who directly managed staff.
The work focus of this group was overwhelmingly operational, though some reported being involved in the annual business planning for their units.
The main foci of work were general work management (e.g. dividing the incoming work between staff, scheduling the clinics) and staff management (e.g. organising training, monitoring performance and sickness absences). Administrative managers were also responsible for reporting on and achieving mandatory targets in their areas (e.g. waiting lists). Some also did a share of ‘hands-on’ administrative or clerical work alongside their subordinates either on a regular basis or stepping-in as required because of staff shortages.
Staff management was the main source of variability and unpredictability in their job and also made their work spill over into their non-work time:
Every day is different . . . Although . . . we have meetings booked in, calendars and things, but I don’t know what I’m coming in to every day . . . I have phone calls Friday night, Saturdays and Sundays from staff regarding personal issues and things.
JNC 24
They worked long hours:
It’s not a 9 to 5 job.
JNC 105
at a high pace, with constant interruptions; and the majority found their workload excessive:
Ideally, this particular role should be a more operational role . . . and then . . . a people role, it should be split . . . I could split, there could be two of me and still not enough time really.
JNC 24
It’s like your washing basket, there’s no end to it.
JNC 106
Group 6: managers of corporate units
Middle managers
These managers had specific functional areas of responsibility that encompassed the trust as a whole. For example, a head of corporate contracts and commissioning managed the provision or the purchase of clinical services for the trust; an assistant director of finance for financial management managed the preparation of the trust’s financial plan for the year and the reporting on the actual position vis-à-vis the plan throughout the year (MNC 11); an assistant director of learning and organisational development looked after ‘the learning, training and education of all medical, clinical and non-clinical staff’, including mandatory training, management training, continuous professional development, succession planning and ‘any of the policies that link in with learning’ [e.g. induction, performance management, study leave, secondment (MNC 20)].
Most in this group were heavily involved in the development of trust strategy. For some, strategy formulation was literally part of their job description. Thus, a deputy director of strategy was ‘responsible for advising the trust on strategy and . . . the development of the five year business plan of the trust’ and also led on strategy development for individual strategies in the trust (e.g. the cancer strategy) (MNC 42). Others provided the crucial inputs. So, a chief accountant was responsible for developing ‘a medium term planning scenario: . . . what is our activity in the current financial year, what will it be next year and what will it be for the next three years after that . . . ’ (MNC 25). Yet others were in charge of specific strategic projects such as an occupational health manager who was responsible for the trust’s health and well-being strategy (MNC 10).
Thus, their span of responsibility was trust-wide in scale, but narrow (functionally focused) in scope. Unlike other managers, they were not accountable for the performance of front-line staff or actual service delivery. The exception to this was an occupational health manager, who was effectively service manager of a service that provided services to the employees of the trust, but also to other NHS organisations and some businesses and non-profits in the region. This manager managed three teams: nursing, counselling and administrative (34 members in total).
The span of control for this group was quite modest (fewer than 10 members of staff), and staff management occupied very little of their time and attention. General work management was also of very minor concern. The main focus of their work was technical (e.g. accounting, designing corporate communications) and focused on processes (e.g. commissioning) rather than people. At the same time, the work on processes and systems often entailed extensive interactions with both internal and external constituencies and was accomplished through formal and informal meetings, with formal meetings occupying, on average, more than one-third of the time for this subgroup (but ranging from ‘nearly none’ for a chief accountant to 80% for an assistant director of learning and organisational development). For instance, the work of a head of performance improvement primarily involved working with the divisions and specialities to identify any problem areas and devise the solutions for improvement.
Their work, in contrast with the other groups, appeared to be more sedate and predictable (e.g. following the annual planning cycle) and to have fewer interruptions:
This isn’t a role that needs to react today, or very rarely needs to react today . . . [It is] complete opposite to being in the ambulance service which is you need to react in the next minute. So . . . there are occasions when something needs to happen quickly, but even quickly for a contractor means in the next few days.
MNC 86
Yet, unplanned activities and interruptions were still a feature of their working life it was just that they were of a different magnitude from those confronting the managers in clinical units:
Let me give you an example of the interruptions that I will get. They will be because somebody suddenly wants a presentation, so the interruption isn’t a 10-minute interruption . . . I’ve suddenly got to find half a day to get something scoped out and worked up and get data for it and I’ve got to ask the team to go and find things . . . that will support it. So I will be working on the council strategy at one point, then all of a sudden . . . my manager . . . will say: ‘I need a tender . . . for demand and capacity across the [region] . . . Can we get that tender put together with the proposal document and it needs to be done by Friday?’ So you’ve suddenly got to find a day . . . It is not like when I was an operational manager where suddenly someone would come to you and they needed a decision on it and it might take you half an hour to work it out, but once you’d done that you could move on . . . Because it is strategy, everything about strategy tends to take bigger chunks of your time.
MNC 42
Although these managers did not, as a rule, complain about stress and pressure, they did tend to work long hours (e.g. MNC 11 reported working 60 hours a week).
One of the respondents provided a metaphor that could sum up the role of managers in this group:
A catalyst . . . to achieving what needs to be achieved’ within the trust.
MNC 86
Junior managers
Junior managers of corporate units were a diverse group with three responsible for ‘patient services’ (appointment bookings and medical records), two managing IT services, and two managers from the R&D department. There was a marked difference between managers of patient services and the rest of the group in terms of the span of responsibility and the nature and pace of work they did.
Managers of patient services supervised between 14 and 90 staff and staff management duties, which were predominant in their workload, were also the main source of unpredictability and stress in their work (in particular owing to the staff sickness absence). They were also under significant pressure to deliver targets, such as for answering a telephone call in a specified amount of time in the booking centre, though in some areas (medical records) targets (e.g. percentage of medical records being at the correct place for the correct time) were less numerous and challenging. Yet, performance management appeared to be a less onerous task than for junior managers of clinical units, thanks to the computerised surveillance in some areas (such as a booking centre, where the manager was able to monitor the performance of every staff member ‘on screen’, e.g. the speed of response, the call duration, etc.).
Research and development and IT managers had few staff (the largest number was 10, supervised by a head of software development) and devoted little time to staff management. The main component of their work was ‘technical’ (i.e. hands-on specialist work), but this involved a considerable amount of interaction within and, even more extensively, outside their work unit. In particular, one IT manager, though having no direct reports, had worked with 15 different teams across the trust. Similarly, a R&D manager responsible for commercial trials worked with many stakeholders both within and outside the trust and consequently spent about half of their time in meetings.
Summary
Below we sum up the main findings on ‘what do managers do?’ (a schematic summary can be found in Appendix 10 ).
Junior clinical managers had a span of responsibility from team to specialty, with all AHP managers having the smallest span (team) within this category, junior nurse managers ranging between team and unit (ward), and junior scientist managers between team and specialty. Junior nurse managers had a heavy staff management load, whereas the other two groups had a medium load. Although none of the AHP managers and only one junior nurse manager (specialist nurse) had work that spanned outside the trust, half of junior scientist managers did. Junior scientist managers were also the only group that worked across sites. All work groups within this category had an approximately 50/50 split between management and clinical responsibilities, worked about 50 (or just under) hours a week, and spent only a small fraction (about one-tenth) of their time in meetings. They had little involvement in strategy; though junior nurse managers were notable for their local entrepreneurial initiatives.
Junior non-clinical managers had a span of responsibility from a team responsibility to trust-wide responsibility. Junior managers of clinical units worked primarily across a group of specialties or services, often across sites, and half had work spanning trust boundaries. Junior managers of corporate units, with a couple of exceptions, managed smaller entities (teams or units), though nearly half worked across sites, and one-third was engaged in work spanning trust boundaries. They had no clinical involvement, worked about 45 hours a week, and spent a quarter of their time in meetings. They had little, if any, involvement in strategy.
Middle clinical managers had a span of responsibility from specialty to directorate/division. Consultant managers and middle nurse managers managed larger entities, from specialty to directorate/division, with the number of staff ranging from about 150 to 2000, respectively, whereas middle scientist managers mostly managed units within specialties, with about a dozen staff. Staff management responsibilities of consultant managers and middle scientist managers were considered fairly light, responsibilities of middle nurse managers were considered medium. Consultant managers had the heaviest clinical load (clinical/managerial split of 50/50), middle scientist managers a medium load (20/80), and middle nurse managers the least heavy (10/90; with some internal variation: nurse consultants, 50/50; matrons, 0/100). Just about one-fifth of consultant managers and middle nurse managers were involved in work outside the trust, as were most of the middle scientists. Consultant managers worked the longest hours (65 hours a week on average), middle nurse managers less so (55 hours a week on average), and middle scientist managers less still (45 hours a week on average). All spent about one-third of their time in meetings. Consultant managers had significant input into the trust strategy, whereas the two other groups had a minor input (though nurse consultants and middle scientist managers had a considerable impact on strategy outside the trust, via their role in professional associations).
Within the category of MNC managers, middle managers of clinical units had general responsibility for managing wide entities (a group of services or a directorate/division). Their staff management load was heavy and half of them worked across sites. Their strategic role consisted of strategy translation and elaboration. In contrast, middle managers of corporate units worked on the trust level but had only functional responsibility for their specialist area and their staff management load was low; only a few were engaged in work across sites. They had a strong input into strategy development in their specific functional areas. In both groups, about one-third of managers had responsibilities that spanned the trust boundaries, the managers worked on average about 50 hours a week and spent one-third of their time in meetings.
Implications
The portrayal of ‘what managers do’ helps to illuminate the construction of identities and has implications for research and practice in itself.
Managers’ work represents the behavioural aspect of identity. In our theoretical model, behaviour lies on the periphery of identity, farthest removed from the identity core (i.e. self-definition and group affiliation). Such positioning implies a possibility of only a tenuous link between the identity core and behaviour. Indeed, our analysis in Chapter 5 (see ‘Reluctant managers’: reluctant to manage or be labelled?) showed that some respondents admitted to ‘managing’ but not to ‘being a manager’. Our analytical description of managers’ work allows us to examine the extent of congruence between what the respondents did and how they defined themselves.
Our findings reflect the breadth and depth of the activities associated with management performed by the respondents. These findings support our conclusion in Chapter 5 that the low identification of the respondents with managers as a group stemmed primarily from the insufficient distinctiveness and attractiveness of the group, rather than from their behaviour (their work activities).
The implications for research stem from our fine-grained description of work groups within the broader categories of JC, MC, JNC and MNC managers. Although we do not claim to have ‘discovered’ such groups as scientist managers, managers of clinical units and managers of corporate units, we do note that to date the research on managers in health care has been predominantly based on nurse managers (including ward sisters and matrons) and doctor managers. Such selectivity may lead to a bias in the representation and assessment of the characteristics and role of NHS managers.
With regard to practice, a more inclusive picture of the NHS managers’ activities may serve to inform policy-making and media coverage. As we discussed in Chapter 5, Implications, politicians and the media seem to employ a negative stereotype of the NHS manager to scapegoat NHS management for the problems of health-care systems. Our portrayal of junior and middle NHS managers runs contrary to this stereotype. Although the vagaries of reporting did occupy a not insignificant portion of their time, none of the respondents could be fairly described as a ‘pen-pusher’. The scale, scope and sheer intensity of their work were striking, as were the challenges they coped with. The extent and importance of the functions performed by the respondents attested to the significance of their input into organisational operations. Although we obviously do not expect our findings to immediately and directly redress the situation, we hope that our research would contribute to building a more positive assessment of the managers and their work and altering political, media and public opinions.
Chapter 7 Effectiveness
Conceptualising effectiveness
A series of questions were asked in interview to explore managers’ self-reported effectiveness and what influences this. As befits the flexible format of semistructured interviews, not every question was asked of every respondent, but they included:
-
What does being an effective manager mean to you?
-
How is success as a manager measured in the trust?
-
Can you identify any specific incidents that have really required you to exercise all your managerial and personal skills in managing them effectively?
Effectiveness is a multidimensional concept to do with the attainment of a range of desired outcomes. 34,35 Within the framework of NPM, it usually is associated with ‘hard’, evidential measures of clinical activity and the achievement of financial targets. 111,112 Accordingly, we anticipated that these would be vital indicators of effectiveness or the inverse for the managers, but we also expected managers to characterise effectiveness in wider and perhaps alternative terms, for the following reasons. First, in much of health care, effectiveness is accomplished through ongoing interactions between many people. In other words, it is takes place in the complex, messy, lived-reality of managerial work. Second, as discussed in Chapter 5 , many respondents construe management as what they do (managing), not that they are (a manager). Hence, they may seek to establish ‘softer’ assessments of effectiveness which have a closer fit with their sense of identity as ‘reluctant managers’. This may not always connect directly with specific transactions captured in conventional ‘hard’ outcome measures.
Two overarching sensitising concepts,108 ‘transactional effectiveness’ and ‘processual effectiveness’ were derived inductively from analysis.
-
Transactional effectiveness: ‘hard’, demonstrable and visible performance measures, such as meeting an array of organisational targets, personal and team awards, and other achievements.
-
Processual effectiveness: ‘softer’ and more nebulous. Evident, for example, in ‘smooth-running’ and in work ‘getting done’. Achieved by communicating and enabling others.
As we will discuss, transactional and processual effectiveness can be mutually reinforcing, but they also may be in tension.
It should also be noted that for clinical managers our focus is on effectiveness in relation to their managerial work, not their clinical activity.
Processual effectiveness
Effectiveness as embodied knowledge
In response to questions such as ‘what makes an effective manager?’ or ‘how do you know when you are effective?’, some managers demurred from hard measures in favour of the more diffuse indicator of being able to make ‘things work’ or ‘run smoothly’:
I don’t know, the job gets done I suppose is the only answer I’ve got.
MNC 26
You kind of aim for everybody feeling satisfied at work and having completed what they want to complete, and going home happy. But that isn’t something that’s necessarily measurable. Do you know what I mean? It wouldn’t be a twenty per cent, ten per cent, it would be hard to measure.
JC 58
Thus awareness of personal effectiveness is embodied:
I know in myself whether things are going well or not. I think everybody does deep down, don’t they.
JC 5
And it is naturally acquired from knowing people well (and related to tenure in the organisation):
You learn to know when people are having a bad day, a good day. Same with my team, you know when they’re stressed, or they’re anxious, or things haven’t gone right. You can tell by their body language, how they behave.
MC 8
This way of thinking was most common among, but not limited to, managers whose span of responsibility was relatively small. It was not, for example, ordinarily expressed by those with large spans of responsibility such as MNC managers of corporate units.
Effectiveness as communicative competence
Some time ago Luthans154 identified that the most effective managers spend most time on communication and HR management activities. Seemingly mundane activities such as listening, chatting and creating a good atmosphere are so highly valued that managers in general often endow them with extraordinary value. 155 For example, the objective of a simple ‘walk around’ a clinical area by a directorate general manager was intended to encourage her staff to feel comfortable with her. Then, as she put it, ‘maybe they’ll think I’m human’ (MNC 30) and understand her decisions, such as turning down a staffing request.
Being a practical problem-solving ‘sort of person’ with ‘common-sense’, or, as a matron put it, someone who needs to ‘see, touch, smell, feel’ (MC 55) what is going on, was voiced by those especially attuned to the processual side of effectiveness. This supports Fournier’s62 findings from outside health care that being an effective manager is a personal quality associated with the ‘the sort of person’ one is and cannot easily be learnt through, for example, leadership courses.
Many clinical and a number of non-clinical managers associated facets of identity such as the power of ‘personal qualities’ or a ‘positive personality’ with the capacity to ‘lead by example’, ‘role model’, ‘create an ethos’, exude ‘positivity’, unlock ‘energy’ and thereby to motivate and challenge others to achieve their objectives. They adduced that this equipped them for being effective with a ‘light touch’ (thus avoiding the negatively valued personal micro-managing often associated with the traditional ‘manager’), but at the same time enabling them to deliver on targets keenly monitored by their own line managers.
Thus as a result of its potential to enable and empower others, communicative competence is a key dynamic for achieving effectiveness, as exemplified by the following divisional director:
At the start, when I first started doing it, it was about solving the problem. For me now, in the role I’m in, it’s about getting others to understand the problem, to feel engaged about it and feel empowered to do something about it. So my role very much now is more about being a leader than being a doer and, you know, that is something that I have grown into with time because that wasn’t . . . and some of the softer skills I have picked up along the way you know, the difficult conversations, getting people to feel enthused and empowered to do things.
MC 70
Clinical managers, particularly, drew associations between empowerment, personal effectiveness and quality of care, as expressed by the following ward manager speaking about her staff:
By empowering them, it kind of makes my job easier in the long run because I can rely on them in my absence, or even when I’m here to just get on with the job in hand and they don’t have to keep coming to me and saying is it alright, shall I do this? [ . . . ] There’s a big emphasis on team work and we’re all here to benefit patients, working as a team, we pull together as a team, whether that’s involving the reception staff a little bit more in something else, you know, delegating on a daily basis. And, you know, I want to make sure that my patients are cared for in a very safe environment.
JC 51
This thinking corresponds with recent policy recommendations for NHS management, captured, for example, by the No More Heroes subtitle of the King’s Fund’s’ The Future of Leadership and Management in the NHS. 12 It has been argued that effective leadership is shared and distributed99 and that ‘effective leaders need to work through others to achieve their objectives, motivating and engaging followers’ (p. iv). 105
Links between processual and transactional effectiveness
As noted earlier, ideally, processual and transactional effectiveness mutually reinforce each other. The managers recognised this. For example, many JC and MC managers, in particular, doubted ‘hard’ targets could be met without due attention to the ‘softer’ processual aspects of ‘being a manager’.
Effective, I think it’s . . . being able to meet all of your targets, but also aware of staff and how they feel, and obviously the input that they have towards those targets. You need to enable to your staff as well, if they have got some good ideas, listen to them, involve them. I think if you involve your staff in decision-making . . . you are more likely to get buy-in from them.
JNC 97
This explicates how processual effectiveness should feed and nurture transactional effectiveness. However, this was not always the case. By way of illustration, a midwife consultant spoke of how the push to meet targets negatively affects crucial team building:
The culture at the minute is about hitting targets, doing things, and so it is not about team working, and setting strategies for the future, it’s almost meeting the targets already a month behind.
MC 9
As discussed in Effective management as a ‘wicked problem’, this indicates that effectiveness in one sphere may detract from effectiveness in another.
Transactional effectiveness
Box 1 lists service improvement targets and other outcomes managers contend with.
National reporting (e.g. QCQ/ KPIs, Quality and Safety Standards, QRPs, 18-week referral-to-treatment times, external accreditation, auditing of clinical support services).
Internal reporting such as, patient quality and safety (e.g. infection control, nutritional assessment), length of stay, incident reporting.
Financial and corporateCIP, business planning.
Project workSetting up or development of specific services or quality improvement initiatives.
Human resourceFor example, appraisals, mandatory training, sickness monitoring.
CIP, cost improvement planning; KPI, key performance indicators; QRP, quality and risk profile.
As might be expected, meeting targets is a crucial indicator of effectiveness for most managers and, conversely, not meeting them usually signals need for improvement. We recognise that these various forms of transactional effectiveness are real, ‘objective’ pressures on managers, but (as outlined in Conceptualising effectiveness) our focus is on their self-reported experience of dealing with them.
Clinical managers
Ensuring that their clinical team/unit delivers on service improvement, HR, and financial targets is a routine feature of many MC and JC managers’ work and they worried about the ever-expanding, ever-changing list. A consultant midwife remarked:
There have been so many quick changes from the government that we’re just jumping from one thing to the next, to the next, to the next, and nothing is sustained, and it’s all blown in the water afterwards. But as long as you’ve met it on that date and done it on that date, that is how managers are driving us . . . Where is it going to end?
MC 9
A divisional head of nursing explained that a main component of her working day involved:
A lot of chasing up of my teams to ensure that we’re on track to meet the CIP targets and ensure that . . . what we’re trying to do is, when I talk about the targets is always ask them about the safety and quality aspects first to ask how that is going, because I don’t think nurses or medics are driven by finance at all, and so we try very hard, at all of our meetings, that we put quality and risk and safety at the top of the agenda before we talk about the bottom-line finance bit.
MC 83
Junior clinical managers, particularly ward managers, spoke of the quantity of benchmark information they have to produce. By way of illustration:
My Mondays are basically built around looking at the audits, so that’s what I spend the majority of, between 8 and 12 o’clock on a Monday doing, it’s the first job I do, start the audit. I do an audit of the observations, I’ll pick ten random observations charts and I’ll look to see has everything been done properly . . . is all the data there, is it filled in correctly and, if it’s not, then we’ll fail the audit. I am responsible, and I get the staff involved in these as well because they’re looking after the patients clinically, but I need to know how many patients have got indwelling catheters, how many have got central lines in, how many people have got vents in and has the correct protocol been adhered to, have they been inserted correctly, if they haven’t who inserted them, so I’ve somebody tracking it back to find out to report to their manager that they’re not doing their job properly.
JC 6
Managing this process was highly demanding. Thus, the above ward manager explained that, although her team is highly successful in meeting targets and she derived much satisfaction from this, managers at her level are the ‘jam in the sandwich, . . . getting it in the ear’ from superiors who demand targets be met, irrespective of challenges such as the pressure for cost improvement and staff shortages, and from their own staff whom they have to subject to extra work.
Non-clinical managers
As reviewed in Chapter 6 , the MNC and JNC managers are internally diverse groups in terms of hierarchical level and functional sphere of responsibility. However, most were tasked with meeting service improvement and financial targets, which were fundamental gauges of their effectiveness.
As might be expected, targets, per se, elicited less adverse commentary from non-clinical managers than from clinical managers. The probable reason is that this work is an intrinsic ‘given’ to most. However, they were tasked with making sure staff delivered on targets and ‘targets within targets’ and this invariably brought challenges. Hence, as a deputy general manager explained in relation to clinical staff:
When they say to me, I just want to see patients, I’m like, ‘Good, just tell me how many you saw, and what you did with them, and what you need to be able to do that better and we’ll run the rest. We’ll sort the other bits out’. So, if we were in a sink-making business and they said I just want to make pink sinks all day, and they were happy doing that, I’d say fine, just tell me how many you made, and I’ll do the counting.
MNC 7
Relatedly, many recognised the ‘target fatigue’ expressed by staff they manage:
What people have got into is fatigue; ‘Oh yes, well, they’re asking for it this week, but by next week there’ll be something else, I’m not bothering about that’. And I think, that’s a fair criticism, if I’m honest.
MNC 3
Some JNC managers spoke of relentless pressure to meet targets under difficult conditions such as low- or under-staffing (see also Chapter 8 ). For example, after recounting that she is asked ‘everyday’ for a new set of reports, an administrative manager covering three clinical areas explained that it was highly unrealistic and, hence, not surprising that waiting-list targets were not met:
In neurology virtually everybody goes for tests, well you’ve got to have those tests and everything else and then they go on the waiting-list and they’ve got to be done in 18 weeks and the tests have got targets for six weeks and some go for one test and then go for another. So you’ve already exceeded your 18 weeks before you’ve even got your diagnosis.
JNC 106
Although meeting targets like these meant considerable work for clinical and non-clinical managers alike, it does have positive potential as ‘hard evidence’ of effectiveness that can be presented to one’s team or to individuals to demonstrate their hard work is worthwhile. At the time of our research there was discussion within Government of removing some waiting-time targets. However, those mentioning this felt it was important that some (if not all) targets were retained. Thus a service manager explained that although it would be good to have some leeway on breaches, it would be demoralising for her staff if diagnostic targets were eliminated as they would feel that they were doing a disservice to their patients (MNC 22).
A number of MNC managers in corporate services explained that their work is mostly ‘developmental’ or ‘problem-related’ which often involves facilitating others to meet performance objectives. It is difficult to measure and hence for them to know if they have been effective or not. As a performance improvement manager related, his work is lacking in ‘bite-size chunks that can be measured’ (MNC 100). Likewise, an assistant director of finance explained, in the absence of delineated targets, she and her colleagues needed to find their own ways of ‘demonstrating we are good’ (MNC 11).
Project work
Project work concerns specific activities, such as:
-
Initiatives arising from the NHS Institute for Innovation and Improvement, such as the Productive Ward, High Impact Actions for Nursing and Midwifery, Back to Basics, Root Cause Analysis (mainly concerning JC staff such as ward managers and team leaders).
-
Strategic projects that are clinical and clinical-related (e.g. infection prevention, pathway developments, educational programmes, skill-mix changes, maximisation of theatre use). Non-clinical developments around, for example, communication and brand development (mainly middle managers).
-
Service reconfiguration, for example, bringing services together across sites, and/or service developments such as care pathway work (mainly, but not exclusively, concerning MC managers).
The diversity of project work, coupled with space limitations within the report, precludes us from including data extracts to illustrate the wide range of project work; but, in brief, managers generally spoke positively about project work. Although it’s long-term and protracted nature could be frustrating, especially when it involved engaging interdisciplinary teams across services, satisfaction was derived from delivering effectively.
Human resource functions
Most managers were responsible for meeting annual staff appraisal completion targets, sickness absence targets of ≤ 5% and releasing staff for training. They reported that it was nigh on impossible for them to be fully effective in these domains because they would need staff resources that invariably were in short and diminishing supply (this was especially marked at Cityscape, where the financial state at the time of the study meant that managers were unable to replace staff and some reported severe shortages and had heard of potential down-grading/rebanding; see Chapter 8 ).
Effectiveness as collectively achieved
Most managers felt they brought something unique to their roles which they associated with certain qualities or blends of skill that enable them to mobilise others effectively. However, only a minority spoke of their personal, individual successes, such as annual internal trust awards, work within a professional association, research or publication. In fact, it was more common for them to attribute their effectiveness to the team/others they manage. This links back to the point that many felt you can only be really effective, especially in initiating change, when you ‘bring the team with you’.
Never expecting the team to do something you would not do oneself was voiced particularly, but not exclusively, by clinical managers. Thus a matron explained:
I have responsibility for ensuring quality is maintained, improved, that the operational side of things runs for wards within my area of responsibility, and also standards in a more general sense . . . Now there’s ways that you can do that isn’t there; one way to do it is to go and do it yourself, you know you go and you peer at everything and every difficult meeting you sit in on it to make sure it goes as it should. But to me you don’t . . . the thing for me, my philosophy has always been if I look after my staff they will look after the patients and in that way will look after me and will make my job work, or make it productive.
MC 68
An example relating to efficiency in project work is the Productive Ward initiative (taken up in several clinical areas in both trusts), which aims to improve ward processes and environments to release nurses for patient care (with the objective of thereby improving quality and safety). For example:
So, on the admissions ward I’m just trying to say, look when we get an acute admission in we will identify nurses with nurse 1, nurse 2, nurse 3, a bit like they would in trauma. Nurse 1 does this, nurse 2 does this, nurse 3 does this, and we all help get the patient in the bed, settled, get them on the monitor, get them monitored, get some vital signs written down. Hopefully it does lend itself then to us working a little bit more efficiently, fostering more teamwork as well.
JC 51
Conversely, personal effectiveness could be compromised by others. However, when managers – across all four primary categories – spoke about this, typically it was not in reference to their team as a collective, but to particular individuals, such as people who were obstructive or failed to provide the input or quality of input that a manager needed in order to deliver in a timely and effective manner on work of various kinds.
The contribution of feedback to effectiveness
The managers spoke of a range of constraints and enablers to the achievement of effectiveness. Most drew a strong association between communicative competence and effectiveness. The actual ways they ‘communicated for effectiveness’ and the identity constraints on this are discussed in Chapter 8 . Here we address how the ways others communicated with them, specifically in relation to feedback (sometimes also framed as support), contributed to self-reported effectiveness.
Effective communication is a recursive process: if a manager communicates effectively with others, usually this enhances their own competence. But this can be undermined if others do not communicate effectively with them. The importance of feedback is apparent in that it commonly was the first thing raised by managers in response to our questions about effectiveness.
Feedback can come from a variety of sources within the organisation, including line managers, their own staff, peers and previous line managers in the organisation, patients and relatives/visitors. It can be more formal, such as in appraisals and patient satisfaction surveys, and more informal, such as in one-to-one conversations, various meetings and e-mails.
As one might expect, positive feedback was highly valued:
If we do well on our [nursing, care quality] metrics we’ll get an e-mail to say, ‘you’ve done really well this month, that’s excellent, keep up the good work’ sort-of-thing, which I pass onto my staff, obviously.
JC 77
There is the formal [trust name] honours, so there is a staff recognition programme, but individuals within the executive team, particularly [the chief executive], will personally come and tell you when you’ve done something good. And clinical directors, I have had, you know, positive comments from clinical directors on stuff that I have done. So people are very good at giving that one-to-one feedback on how you’ve done.
MNC 42
However, many reported that line managers and others above them in the hierarchy give feedback only very infrequently or only when they have done something wrong or not right. Many managers, middle and junior, clinical and non-clinical alike, shared the frustrations evident in the following remarks:
December to May was horrendous, the worst working months of my career. And that was because of lack of support actually. So I’m quick, but often I will need to say, ‘Okay, I’m just doing this, am I on the right track?’ And all you need to do is say ‘yes’ or ‘no’. And I wasn’t getting that. So what I was doing was doing something because I wasn’t getting that and then being publicly pulled apart for having got it wrong.
MNC 11
This is regrettable; lack of feedback and poor-quality feedback have the potential to contribute to ineffectiveness by breeding uncertainty and, in some cases, the undermining of managerial and other facets of self-identities. 48 The personal uncertainties that can accumulate over time are communicated by the following middle scientist manager working in a support service:
I am managing the show now, but am I doing it right? And, you know, we don’t get patted on the head a lot, so you know my boss said to me recently, yeah he thought I was doing okay, there was nothing really he had a problem with; some things could be better, some things had gone very well. But that doesn’t really say should I in general learn something to do something else better. So I sort of feel there’s this bit of an unanswered question hanging over me, which is am I properly equipped to deliver what people expect me to deliver, do I understand what I’m expected to deliver? Because part of me feels my job is to sort of give the rugby hand-off to management as much as possible, so I can keep everything else going. But I don’t think that’s necessarily the right attitude, because I actually need not to be handing these people up, I need to be engaging with them. That’s how I feel. But then I don’t have vehicles to do that, so there’s a slight sort of worry, there’s a bit of a vacuum there in engagement, and even if I did engage what would it look like?
MC 21
However, it was also possible for managers to read something positive into lack of feedback. Perhaps on the premise that ‘no news must be good news’, some interpreted silence as indicating that they must be doing well, otherwise surely someone would have told them. However, as thoughts of this kind often were accompanied in interviews by the citing of ‘hard’ evidence of effectiveness (such as audit results), this suggests an awareness that it is risky to rely too much on this assumption.
It is also worth noting that lack of feedback, or only negative feedback, from above could be offset by positive feedback and support from below and laterally from peers in the organisation (as well as from outside). Some managers interpreted this as what ‘really matters’. For example, when asked how success was measured, a quality, safety and risk manager commented:
Lots of ways really, there’s all the targets stuff, but not just that way. There’s feedback from colleagues, formal and informal and feedback from patients and relatives. I am often in very close contact with patients and relatives. I always give relatives my number when I am dealing with them and say, ‘look if you are anxious about anything, don’t sit at home and worry, ring’, and people do and you think, well, people must have confidence then that you will do something about it.
MC 107
Thus, so far in the chapter we have considered the various ways in which the managers construe effectiveness and some of the contributors to achieving or not achieving it. We now turn to how the organisational contexts within which they work can enable and constrain the achievement of effectiveness. This also serves as a basis for the discussion of identity constraints on effectiveness in Chapter 8 .
Effective management as a ‘wicked problem’
The sheer complexity of health-care management has led to its characterisation as a ‘wicked problem’. A wicked problem is not ethically deplorable; rather it is a problem which defies easy solution because it is embedded in a complex open system (p. 160). 156 It has no quick fixes or simple solutions. 157 It is worth recalling that Cityscape and Metropolitan are among the largest in England, which one would expect to contribute to the ‘wickedness’ of managing in these organisations.
Many managers were alert to this:
I think what’s frustrating is the size of the beast. It’s that bit that you can’t just go and change anything, because there are so many different facets that are affected by any decision that you make. So we’ve been trying to improve our theatre utilisation, we can’t just say right I’ve got a surgeon, let’s go. It’s a surgeon, an anaesthetist, theatre staff, recovery staff, beds. You could do all this and then on the day we’ve had that many emergencies there are no beds, so patients get cancelled. We always say it’s a bit like treading mud really, because you know you really feel tired of getting somewhere, and then you know something else blocks it, there’s lots of blockers unfortunately that are out of your control. In effect really, nothing is directly in your control.
MNC 87
Wicked problems arose from the need to work across organisational and professional boundaries of various kinds and to varying extents, such as:
-
spatial (e.g. across hospital sites)
-
clinical and managerial specialisms
-
professional (e.g. clinical, non-clinical)
-
cultural (e.g. different working practices and emotional attachments to them).
(See also The scale of activities in Chapter 6. )
Wicked problems could be exacerbated poor communication and failures of communication (and felt lack of trust), especially from ‘above’ in the hierarchy, and by resource deficits (e.g. staff, equipment).
‘Knock-on’ and ‘ripple-effects’
As discussed in Chapter 6 , the span of responsibility of many middle managers (scientist managers excluded) and, notably, also some juniors, within the organisations was quite large and, in some cases, extended beyond (e.g. dealing with social services, private sector, commissioners). Some spoke of ripple effects. For example:
What we change here will directly affect the X [anonymised] division because we are the service provider to X division because we provide theatre provision. So if we change this and say, actually, this is not going to operate every afternoon any more, we’re going to send the staff home, X division drivers, their targets, their patients, will be immediately affected. So you have to think about everybody else . . . And you can’t work in isolation, patient care isn’t delivered in isolation, it affects imaging, it affects pharmacy, it affects the discharge team, you can’t just say we’re going to do this bit without having everybody else’s influence.
MC 57
A charge nurse related how they had been trying for 2.5 years to set up a nurse-led clinic for a particular aspect of patient care [detail not provided to preserve anonymity], but momentum had faded as ‘stumbling block after stumbling block’ was met, such as the need for pharmacy back-up not available owing to staff shortages (JC 12).
An additional challenge, especially for those whose work spanned different parts of the organisation, was that being effective in one area has the potential for negative ‘knock-on’ effects elsewhere, as exemplified by the following assistant manager (medical records), who talks sympathetically about clinic co-ordinators:
A lot of departments have found themselves very short staffed now [ . . . ] I suppose, for a clinic co-ordinator, if you are dealing with booking patients appointments, referrals, making sure that they hit all the government targets for the waiting-list times, preparing notes for clinics, hitting the clinics, booking the notes elsewhere afterwards is going to be one of your less priorities. But then that causes us the problems. So I can understand why things are happening . . . It really does take minutes to do the whole task, but departments are struggling and it’s having a knock-on effect on us.
JNC 84
Hence knock-on effects can arise from a lack of personal control over the constellation of factors contributing to a managerial problem. For example, a MNC manager recounted:
As a manager of elective services you have to balance your budget, you have to make sure that you don’t have too many patients that are cancelled, you have to meet an 18-week target, you have to meet a cancer target, etcetera and deliver savings schemes. In winter a lot of emergencies, those emergencies sitting in surgical beds make cancellation rates go up, spend more money in beds, because it actually costs more to treat a medical patient on a ward than it does a surgical patient. So your cancellation rates go up . . . You struggle to get your cancer patients and your 18-week elective patients in on time, your theatre utilisation drops through the floor because you can’t get your patients in, you’ve got to do initiatives out of hours to get that work in. So as a manager you’ve no influence on those medical patients being in your beds.
MNC 61
The span of responsibility of JC managers (e.g. junior nurse managers, AHP managers) generally was more circumscribed than their MC managers. However, the scope and volume of some JNC managers’ work was surprisingly large and growing (see Chapter 6 ). Some spoke with unease of trying to reduce waiting lists under ever-increasing pressure of targets that could not be met owing to barriers such as staffing shortages (this was especially marked at Cityscape).
Organisational cultures and silos
The mangers often perceived organisational cultures, or ways of working within the NHS generally and within the two trusts specifically, as inhibiting their ability to be effective. In particular, many MNC and JNC managers who had previously worked in private sector organisations were frustrated by what they saw as the slow pace of decision-making and change in their trusts. They recognised, however, that this was often an inevitable consequence of the sheer complexity of NHS organisational processes.
Many of the middle managers spoke of the ongoing challenges associated with mergers of hospital sites (see Chapter 4 ). At the basic level, they experienced practical difficulties, such as precious time taken up travelling between distant sites (often on the bus) when they could have been ‘getting things done’. There were also practical challenges of working on service mergers. Thus:
[Several years after the merger] as I sit here today, we have two pharmacy systems that operate independently on each campus, we still have two patient activity database systems, so we’re recording all the patients we see and what treatments they’ve had, on two campuses. That kind of infrastructure is not yet merged . . . and we’ve got people on different campuses, different cultures, different gradings of people doing the same kind of job.
MNC 25
Emotive elements came into play. As a middle manager in a corporate unit related:
I still think of myself as an X hospital person because that’s where I started out you know. And I think probably even if people have been recruited in later times, if they’re mainly based at the X hospital] they probably still see themselves as an X person.
MNC 104
Hence middle managers faced major challenges as they sought to deal effectively with two sets of working practices and with bringing together and harmonising operating procedures and working practices. As a directorate general manager explained:
We are very silo’ed the accountability style works very, very well, in terms of I know what I’ve got to answer to in my box, and I do answer to that, it’s quite a robust process, but where there’s stuff which I do that might have implications for somebody else, or even benefits for [ . . . ] personally I would have a situation where the acknowledgement of performance was probably for clinical directors and general managers like myself was you know 60 per cent credit you get for what you deliver down your own lines. But actually the remaining 40 per cent is about achieving whole-organisational aims. And, you know, there’s no point if one part of the organisation is going off track big style on its finances, and you either have to performance manage it because you believe they could be on track, so you performance manage it hard to get them on track, or you have to say well maybe we need to do something different as an organisation, maybe there’s a collective responsibility in this somewhere, and let’s take a collective approach to sorting it.
MNC 30
This contributed to a ‘systems-wide’ view of what it means to be effective as an individual manager. The tendency for many middle managers’ responsibility to span across groups of services, CBUs, divisions and directorates – and for those who manage corporate units, the trust as a whole – encourages them to think about their effectiveness in systems terms. As a composite, ‘systems thinkers’ tend to eschew ‘silo-working’ and seek to encourage those who work within units and specialties/services to think beyond the local. They tend to be frustrated by the slow and protracted process of decision-making and speak of challenging the unthinking replication of traditional ways of working that characterises NHS hospitals.
Effectiveness as a ‘catch 22’
Many clinical and a minority of non-clinical managers believed that an undue focus on performance management, with numerous hard reporting targets, risks compromising patient care and drains resources (e.g. treating patients in the private sector in order to meet targets). This was illustrated by a divisional head of nursing who referred to a requirement to report any grade 3 or 4 pressure ulcers. Given that the trust should have the minimum of pressure ulcers (some are unavoidable), she felt this was appropriate. However, the time put into ‘massive reports’ could be counterproductive since:
What we need to do is cut through that and do the education and training with staff on the ground and clinical leadership about how to prevent them, but we spend our time doing the reports.
MC 60
Along similar lines, a deputy sister remarked:
It was called Back to Basics, but it’s not back to basics whatsoever because we are not actually doing the care that we should be doing with patients. We’re actually, you know, patients get a quick wash and then it’s back to paperwork [ . . . ] All the targets, that is how we’re judged, not on how many thanks we get, not on how many successful discharges we get etcetera, etcetera. They just look at the statistics and that is it.
JC 67
Moreover, meeting trust-level targets intended to protect patient care at the collective level (e.g. not jeopardising contracts) has the potential to be detrimental to individuals:
If I have a patient who is going to breach the six week target by one day my managers would have me cancel somebody out of a slot that they are in if moving them would not cause them to breach but would allow me to slot this other patient in two or three days earlier, which has absolutely no clinical consequences for that person whatsoever, quite probably. But because it moved them to the other side of a reporting threshold there is all sorts of grief [which] will [then] not happen all the way up the system. But the person who we have kicked-out of a slot might be the one who, you know, will have difficulty getting time off work to get in that slot in the first place.
MC 32
Hence vicious circles can develop whereby breeches generate paperwork which consumes precious time, and risks yet more breeches in environments where staff and time are both finite resources. In other words effectiveness can be compromised.
Somewhat ironically, ‘target culture’ could lead to a manager and their team being negatively evaluated for being effective. For example, a consultant midwife, who viewed herself as a ‘change agent’, related that she and her team had successfully instituted a programme of training for the treatment of two clinical procedures [detail excluded to preserve anonymity] which they felt could be improved on. In the case of the first, the very success of their work meant that not much more could be achieved. Yet, to the dismay of the team, a raised target was imposed. In the case of the second procedure, initiating a successful improvement programme for an aspect of care – involving substantial staff training and improved recording – had thrust the aspect of care into the light (which would not have been the case for other units) and led to the unit being deemed an ‘outlier’. As the manager concerned related:
Even though we have written saying this is why, and actually we’re very proud of our now increased rate of [named procedure] . . . it’s like, ‘no, you’ve got to reduce it’. So what do you do with that? Do you bury it all and fudge the figures, or do you not do any more training and knowing that actually ultimately its women [patients] that will do worse out of it?
MC 9
Effectively combining managerial and clinical work
The objective of combining clinical work and management is that by positively reinforcing each other they will increase overall effectiveness (see discussion in Chapter 2 ). Many clinical managers supported this objective. As discussed further in Chapter 8 , they spoke of mobilising their clinical expertise to get people to listen to them. A divisional head of nursing related:
People have this view that you’ve got management over here and clinical work over here, and that the two don’t meet. Actually, if you manage them well together, you’ll improve the quality and reduce cost before you have to do anything else. You don’t have to take dramatic action and change, if the two are working closely aligned you’ll improve patient care dramatically, and along the way you’ll make efficiency savings.
MC 57
Others spoke more in terms of the potential for this to happen and used specific examples (which were not the everyday norm) by way of illustration. For example, a matron (MC 72) attributed her ability to assess that a proposed skill mix on a clinical unit undergoing change would not be effective at the level of care needed to her capacity to engage in clinical work alongside her staff. The following divisional director spoke of how his clinical identity could be mobilised to convince on matters of finance and how a steely managerial stance could be employed to make clinical colleagues aware that cost savings were needed:
Even when we were having conversations about cost improvement savings, efficiency savings, as you’re still bringing a clinical aspect to that you still think ‘okay and what would that mean on the ward and stuff like that’. But, equally, there is a steel core if you like that realises that we do have to do those things. It’s like, I had a meeting with all the heads of service last week and said, look we have to close a ward, okay this is the outcome from this meeting, but we have to close a ward in a safe way, okay so we have to come up with a way of doing this, okay, that is safe. But the bottom line is that we have got to find £800,000.
MC 70
Although counterbalancing the clinical and managerial aspects of one’s role usually was challenging, the managers seemed to feel that equipoise (however shaky) could be striven for. In the eyes of many, this enabled clinical managers to work quite effectively. Even so, doing ‘two jobs’ could result in having, as a ward manager put it, ‘not have enough time to do everything, so you end up having to cut corners and doing half a job’ (JC 39). The following junior manager describes the tensions in some detail:
I’ve been working more clinically lately, I would say just over a quarter of what I’m doing in a month now is clinical, and the other three quarters is more ward manager role. But actually that’s making it quite difficult for me to feel on top of my management role, so there is always conflict. There’s been times when I’ve needed to be much more managerial, for instance, when we decamped to here and the reduction of the ward, we were increasing our beds, there was an awful lot of treatment going on, so I was constantly interviewing and shortlisting, so I wasn’t working very much clinically then. I think I might have actually got stuck in a little bit of a . . . well I don’t say stuck but so I was working then perhaps one long day a month, which was okay, but maybe not enough. It’s kind of finding that middle ground isn’t it, but I’m very conscious that when I’m working clinically out there, yes it’s great for the team, you know, I’m hopefully working as a good role model, it’s good for the patients because I’m an experienced nurse, but I’m also aware that actually, you know, I haven’t been in my emails for a week, what’s in there? [ . . . ], you do start to think about well I’m out here doing clinical shifts I’m not picking up that other work that needs to be done.
JC 51
Summary
This chapter has explored managers’ self-reported effectiveness and what contributes to and detracts from it. Through this we have contributed to our aim of determining the influence of managerial identities on organisational processes and outcomes. We have seen that ‘transactional effectiveness’; that is, ‘harder’, demonstrable measures of performance, such as organisational targets, work output, awards and other personal or collective achievements, are the visible front of a more diffuse dimension of effectiveness which we have called ‘processual’. As would be expected, we found that this enables transactional effectiveness, but we also found that some construe it as a form of effectiveness in its own right that can actually be compromised by undue attention to transactional effectiveness.
The analysis shows that communicative competence, encompassing feedback, is a key contributor to effectiveness/ineffectiveness. However, achieving effectiveness is a ‘wicked’ problem that defies easy solution because the managerial work that produces or fails to produce it is embedded in the complex open system of the hospital as an organisation. Although the managers’ span of responsibility and scope of activity (see Chapter 6 ) varied considerably according to their clinical or non-clinical status and position in the hierarchy (middle or junior and variations within this), this was something with which they all wrestled.
As outlined in Chapter 2 , identities are ‘relational and comparative‘. 39 They are learnt through identity enactment and sense-making. 110 This chapter has explored this process in relation to self-reported effectiveness. Through this we have contributed specifically to our research aim 2, of exploring how the performance of roles are shaped by identities, and aim 3, of determining the influence of managerial identities on organisational processes and outcomes (see Chapter 2 , Research aims and objectives).
We have seen that ‘transactional effectiveness’, that is, ‘harder’, demonstrable measures of performance, such as organisational targets, work output, awards and other personal or collective achievements, are the visible front of a more diffuse dimension of effectiveness which we have called ‘processual’. This brings us back to the observation first made in Chapter 5 and reiterated at the start of this chapter, that many respondents construe management as what they do (managing) not what they are (a manager). This suggests, at least for some, that knowledge of effectiveness becomes embodied through the activity of managing which has at its core engagement with others. Various values, knowledge and skills, and self-perceived ‘personal qualities’ or traits – the ‘content’ of identity – were frequently drawn together under what we have termed ‘communicative competence’. This is a highly valued as a resource for effectiveness which was often attributed by respondents to ‘leadership’ or being a good leader, a quality which was seen to have the inherent capacity to motivate or empower others to positively achieve in their work.
In Chapter 6 we reflected critically on contemporary leadership discourse, remarking, along with others,124 that it carries the risk of vesting responsibility for (in)effectiveness in individuals and individual qualities (that is, the ‘content of identity’) while deflecting it away from organisational-level causes. Yet we have seen here that respondents drew a strong connection between ‘leadership’ qualities and processual effectiveness, that is, their capacity to ‘manage’. As noted above, this can be distinguished from ‘being a manager’ (which is, perhaps, more closely associated with transactional effectiveness measures). Yet, at the same time, respondents were more or less aware (according to their work group) that the capacity of their leadership skills, communicative competence and so on, to work for them in the achievement of effectiveness was both enabled and constrained by the organisational contexts in which they worked. This has been evident in various ways in the chapter, such as in the value placed on feedback from various tiers of the organisation. Moreover, the analysis suggests an awareness, which again, varies by work group, that achieving effectiveness is a ‘wicked’ problem that defies easy solution because the managerial work that produces or fails to produce it is embedded in the complex open system of the hospital as an organisation. Although the managers’ span of responsibility and scope of activity (see Chapter 6 ) varied considerably according to their clinical or non-clinical status and position in the hierarchy (middle or junior and variations within this), this was something with which they all wrestled. We now go on to look at this in more detail in Chapter 8 which explores the behaviour of identity in relation of the managers’ capacity to ‘mobilise’ others.
Chapter 8 Mobilising identities
Introduction
This chapter aims to capture how health-care managers mobilise their identities to exert influence in the different and various spheres in which they operate. We explore the different strategies our respondents utilise to mobilise their identities.
We define ‘mobilising identity’ as using facets of identity, such as values, knowledge and blend of skill to achieve a range of managerial objectives (as appropriate to a manager’s role, see Chapter 6 ).
The following aspects of identity mobilisation are important to bear in mind:
-
Identity mobilisation is not always immediately recognisable and is not necessarily a deliberate, pro-active process. In some instances, an identity is sufficiently strong and accepted by others for its bearer not to have to assert it as it may be embodied. Identity mobilisation also may not be conscious. Thus, a manager may interpret their managerial skill as their personal trait, such as the capacity to motivate or engage others.
-
Individual identities are socially situated and relational (see Chapters 2 and 5 ). A sense of self is developed by enacting identities and interpreting the responses to those enactments. 26 Individuals utilise different mobilising strategies depending on the context, that is, who they engage with, what they are trying to achieve, and how others perceive their identity and respond to their identity enactments.
-
The ability to mobilise identity effectively is influenced by the organisational context in which managers work most notably its power structures and the place of the individual within it in terms of position and tenure/experience (see also Chapter 7 ).
With the above points in mind, to conduct our analysis we looked at both who the respondents tried to influence (above, below, laterally) and how they mobilised or attempted to mobilise their identities. We draw on the primary typology based on two dimensions: (1) management level (junior or middle) and (2) clinical engagement (whether the manager is a member of clinical or non-clinical staff) and give consideration to key work group subcategories within them (see Table 2 ).
Junior managers of clinical units (group 5b)
Within this group we focus specifically on administrative managers who manage the work of clerical staff within a specialty in a clinical directorate or a group of services within a CBU. To recall their key features (see Chapter 6 ), most have a relatively high span of responsibility from a team, to a specialty/service, or to a group of services. The majority have cross-site responsibilities and some work with external agencies.
The content of their work, which mainly involves service delivery targets, such as managing waiting lists, requires many to mobilise ‘upward’, to influence medical consultants, and ‘downward’, to influence their line reports. Influencing upward is, however, a challenge, as their mobilisation capacity is low vis-à-vis medical consultants. Their identity is purely managerial and not very strong at that. Half do self-define as managers, but some prefer to hide behind the phrase ‘I work for the NHS/in a hospital’. Many went into work straight after school, and their education credentials (both general and managerial) are not particularly high. Their position in the organisational hierarchy, as reflected in their AfC banding is not very high, either (all band 5, except for one band 4). They are labelled ‘administrators’ rather than managers, and their work lacks visibility and is not accorded much respect:
[People] see the title of admin manager and they think you just deal with invoices or something. They have no understanding at all of what we have to deal with, very wide, broad, diverse.
JNC 24
Many spoke forcefully, and in some cases with despair, of their inability to mobilise an identity positively valued by others ‘above’. The following are fairly typical:
The consultants . . . they just swan in, swan out! Everything’s . . . happening for them . . . they just turn up and the patient is there . . . If you approach them and say, you know, you’ve got X amount of patients that you need to get in, they just say, ‘It’s not my problem, it’s management’ . . . take no responsibility.
JNC 97
Could one stand up to them? [consultants]
You wouldn’t, you wouldn’t be able to . . . you just couldn’t, no . . . ‘Consultantists’ we call it!
JNC 106
The main, if not the only, facet of their identity they seem to be able to draw on, when trying to influence ‘upward’, is knowledge and skills derived from their work experience:
I’ve got huge amounts of experience in very wide, diverse roles . . . it’s a very board skill-set you need to do these jobs, and I can do it successfully because of the broad skills I’ve got.
JNC 24
Yet, despite its advantages, skills honed from work experience outside the NHS, appears difficult to mobilise in the context of their current job. They spoke of the contrast between the NHS and the ‘real world’, where their identities were more highly valued and could be more effectively mobilised. Thus, one related that in the ‘real world’ she was used to change happening more quickly and that when she had asked someone to do something, they did it right away (JNC 24). The following incident observed during a shadowing session further illustrates the problem:
A secretary has ‘refused’ to do some allocated work and ‘walked out with stress’. The manager related that she would have liked to have told this person to ‘get your arse back here and do your job’, but she knows that HR will require her to ‘pussyfoot around’, ‘mollycoddle’ and ‘support’ the person. Also she relates that consultants develop a close relationship with ‘their’ Secretaries and ‘protect’ them. Things escalate later in the day when her line-manager (an AGM) calls to say that another member of the team has sent a text message to a consultant in the middle of a meeting to tell her about the walkout. The rest of the meeting is then hijacked by this issue, leaving the AGM with a plethora of unaddressed agenda items.
Tenure within the organisation (though not necessarily in the same job) transpires to be more valuable than ‘real world’ skills, as it allows administrative managers to build rapport with powerful individuals:
I’ve got a fantastic relationship with all of them [consultants] . . . Yes, they can come and shout at me as well, but, you know, that’s what you expect from clinicians . . . and I get on quite well with the general surgeons because the two are sort of linked together anyway, so I already knew the surgeons and now obviously I’m managing their admin service, so they already know me, I already know them. But the other areas, I know some of them, but not as well as I would like to be honest.
JNC 105
A manager of several surgical areas spoke of how, in a prior role, she had made a consultant aware of the difficulty getting patients onto lists,
[Doctors] just think you pick up the ‘phone and the patient will say yes straight away. We had a consultant in [named area] once and I said, ‘I can’t get anybody on your list’. He said, ‘Oh, I’ll try’, and he came and sat at the desk, and he goes ‘I can’t believe it’. Anyway he gave up in the end. He said, ‘you’re right, they don’t want to come in’.
Interviewee 106
Mobilising ‘downward’ is not always easy owing to pressured work environments and, sometimes, the reluctance of subordinates (e.g. to speed up or take on more work). However, administrative managers draw on a combination of management experience, their status vis-à-vis their subordinates, and their technical expertise/skills to attain their goals. Their technical skills (the ability to do the same work as their subordinates) and their affinity with their work unit allow them to identify themselves and be identified as ‘part of the team’. In turn, their interpersonal skills, refined through experience, enable them to choose the right management style when dealing with their staff:
You’ve got to keep trying to motivate your staff, we’re forever asking them to do more, and . . . as long as you’ve built up a good relationship with your staff they will help you . . . you know, they’ll moan about it and they’ll say they’re not going to do it, but then actually they do then come forward and help in the end. But I think that’s about building the kind of . . . the right relationship with your staff. I tend to be firm but fair, I’m quite friendly with everybody, I’m approachable, but they know when I’m in a bad mood also.
JNC 105
They are also skilled at employing a range of tactics – from persuasion to assertion. Explaining, cajoling and negotiating often come first, but, when it does not work, there is a need to be firm:
It’s like today, I have had to talk to somebody about time-keeping and I have actually asked them to reduce their hours because they can’t get in on time . . . and it’s not as if it’s a one off, it’s regular, three, maybe four times a week . . . and it is the third time I’ve discussed it with her and it’s everybody else’s fault but that person’s . . . You know I’m not prepared to pay you for that time that we’re losing and she has agreed you know . . . I’ve said to her . . . ‘It’s not fair to the other staff who see you coming in late on a regular basis and you’re not making the time up, how do you think they feel, you know, they think she’s getting away with it.
JNC 97
Junior nurse managers (group 2b)
Within this group we focus on the most representative case of ward managers and ward sisters. Half of them self-identified as nurses and another one-quarter as ‘50/50’ (nurse/manager), but all stressed the importance of their clinical work, which amounted to at least half (and usually more) of their time. Their dual identity as nurses and managers was their strongest asset.
Their job required ward managers and sisters to mobilise both downward (ward staff) and upward (matrons, lead nurses and medics).
In their relationship with middle nurse managers, there was a noteworthy disparity in perceptions and expectations. Middle nurse managers emphasised the continuing significance of their clinical identities and the importance of the ‘back to basics’ care [see Middle nurse managers (group 2b)], but junior nurse managers saw the clinical identity of their superiors as compromised by their lack of actual engagement in clinical practice and criticised the nursing expertise of middle nurse managers as outdated. Middle nurse managers emphasised empowering their staff, but junior nurse managers experienced this as being left to their own devices (JC 51) and described their role as ‘isolating’ and ‘lonely’ (JC 62). Junior nurse managers also saw themselves as taking a clinical perspective, whereas middle nurse managers adopted a managerial perspective (with a narrow focus on budgets and targets). Thus, junior nurse managers’ mobilising capacity vis-à-vis middle nurse managers rested on their clinical values and expertise. Yet, they also occasionally used their knowledge of and relationships with the higher ranks of the nursing hierarchy to influence their line managers. Thus, one ward sister reported that, although she would normally turn first to her matron as her line manager, she would also always liaise with the lead nurse (the matron’s line manager), with whom she had built up a strong relationship over the years of working in the trust (JC 62).
In their attempts to influence medics, junior nurse managers utilised both their clinical identity, in its facets of clinical expertise and hands-on clinical work, and their managerial identity, in its facets of job (and organisational) tenure. This particularly came out in the shadowing data. Although junior nurse managers showed deference to medics as manifested, for instance, in addressing them by their formal title (JC 56 and JC 39), they did not shy away from pressing their point, when necessary. One respondent reported complaining to a consultant about the behaviour of junior doctors on her ward who were not doing their job and creating extra work for the nursing staff (JC 6). Another used her long working relationship with a medic to speed up the confirmation of a diagnosis for a patient who had to be transferred to another ward (shadowing, JC 56). They also employed their connections with medics to influence their immediate superiors. Thus, a ward sister related that, when a series of patient operations had to be cancelled, she knew she could draw on her relationship with the clinical lead to ensure that the matron was actively involved in the situation (JC 62).
Finally, in other attempts to exert upward influence, when this influence was not directed at a particular category of staff, but at several levels of organisational structure (i.e. when trying to obtain additional resources, equipment and staff), junior nurse managers drew on their tacit organisational knowledge. They understood that, to get what they wanted, in an organisational context where decision-making processes are slow and protracted, they had to demonstrate persistence – building a case, following up requests and reinforcing messages:
A lot of . . . ward sisters have said, how do you get all the stuff you’ve got. I say . . . I just nag until they shut me up . . . I don’t give up. I’m like a terrier . . . It takes months . . . it took me two years to get a bath. Two years of nagging, chasing, . . . going through different departments . . . you’re passed from pillar to post, they’ve all got to agree . . . and it took two years.
JC 6
The downward influence was a combination of mobilising their clinical and their managerial capacities. The junior nurse managers’ involvement in patient care allowed them to influence subordinates by leading by example and modelling desired behaviours. As Bolton158 asserts, nurses are firmly attached to their professional image (however over-idealised), socialised not only to put on a uniform but also to embody whole sets of attitudes to their work and role. Indeed, mobilising their clinical identity and their commitment to a public service ethos was an important strategy to get the ward staff to do what they wanted them to do and was perceived to engender respect. Many said they could ring staff to cover at short notice and that they co-operated because the staff knew their manager would also do it as part of the team.
The managerial experience of junior nurse managers, in turn, allowed them to engage a variety of management styles relevant to the individual and the situation. They described facets of their identity as, on the one hand, being supportive, empathetic and team players and, on the other, ‘bossy’, ‘scary’ and resorting to ‘nagging’ (JC 6, JC 40, JC 51, JC 77).
Allied Health Professional managers (group 5)
The AHP managers (all AfC band 7), of whom there was only four, managed clinical teams of occupational therapists, physiotherapists or radiographers. With one exception they did not self-define as a manager and instead strongly identified with their clinical specialty. Yet, all did manage and hence possessed a dual clinical and managerial identity.
All engaged ‘upward’ with doctors and non-clinical managers and managed ‘downward’ to their teams. One (JC 90, an occupational therapist) referred to ‘lateral’ engagement with physiotherapists which she depicted as ‘strained’.
Like other clinical managers, AHP managers mobilised facets of both their clinical and managerial identity. This was especially evident in their descriptions of influencing upward, when they utilised one or the other identity depending on who they dealt with, and emphasised their clinical expertise when dealing with medics:
I’m sure certainly when it comes to any dealings I might have with our doctors because they know who I am, they don’t know who our managers are, that’s more helpful if I’m looking at altering a clinic time or if I’m saying to them, that treatment takes this length of time, you can’t refer six people in 1 day, etc. They take it from me; they wouldn’t from a non-clinical manager.
JC 13
As well as their managerial savvy when dealing with non-clinical managers:
Big brother is watching us in our clinical work. They can see how many times we saw a patient, how long we spent with them . . . I’m able to kind of defend what we’re doing through the fact that we have got outcome measures that show that things are going well.
JC 90
Allied Health Professional managers also relied on the facets of both their clinical identity when mobilising downwards, such as their continuing professional practice, which enabled them to lead by example, and their managerial identity, such as interpersonal skills:
Before I went into management . . . I always thought of . . . the power and authority to ask people to do things and them to do it for you and all that. But I’ve found the greatest challenge of management is people skills, and I think generally I’m very good with people skills. I easily . . . make a rapport with people, because I was always able to motivate others, I find it very easy to convince people to . . . I’m quite unfazed by pressure . . . I’ve got a calm personality and I found it very easy when I started this because a lot of people expected it to be a challenge for me to get people to recognise my authority, but for some reason . . . I just manage to reason with people better.
JC 94
We might advance that even though they cast these skills as a part of their personality, they actually are mobilising managerial skills honed over the years. Another important skill was to be able to translate demands from non-clinical managers ‘above’ into comprehensible and palatable messages to clinical staff ‘below’. As an occupational therapist commented, they were stuck in the middle being a ‘filter’ or ‘stop-gap’ (JC 13).
At times, it was difficult to differentiate which identity was mobilised as the managerial and clinical aspects of the work intermingled and they tried to juggle both loads. This was particularly evident in data from the shadowing of a physiotherapy manager. Over the course of the day she carried a management ‘to do’ list literally on the back of an envelope. When, at various points, the researcher asked her what she counted as management, she responded that it was difficult to define, as, for example, clinical work involved managing people and management meetings concerned service development. During the afternoon, she was working at her computer sorting out staffing cover for the outpatient clinic alongside patient numbers, but was frequently interrupted by her staff coming into the (shared) room with queries about patients, car parking and other matters. The researcher asked how often the staff came to ask for advice like this. She responded that it happened ‘all the time, it’s sort of part of the job’. To underscore the challenges of fitting in management time, when she was leaving the department, she stopped by the reception to query whether she would be able to see a patient with a junior colleague on a certain day – she could do this only if she had a management slot that she could use for it.
Middle non-clinical managers of clinical units (group 5a)
Middle non-clinical managers comprised general managers, assistant general managers and operation and service managers. For the sake of brevity we refer to them jointly as ‘general managers’.
Their responsibilities included delivering services within their respective areas within a particular financial envelope, managing performance targets and being involved in strategy planning. They also had to ensure that their staff:
Are doing what they need to do at the right time, in the right place, in the right way.
MNC 30
In contrast to the groups examined above, the main focus of identity mobilisation of general managers was neither upward nor downward but was, instead, directed laterally, as the avowed challenge of their jobs was dealing with medical consultants.
In contrast to other non-clinical managers, general managers also appeared to feel little or no disadvantage as a result of to their lack of clinical identity:
It’s not stopped me from doing anything . . . you know being non-clinical enables me to ask daft questions, and those daft questions are often useful, . . . whereas if I was clinical I’m not sure it would wash so much . . . so you know it can be an advantage.
MNC 87
Indeed, they seemed to be a perfect example of health managers as ‘outsiders’, who could serve as a link between different interest groups by virtue of such a position. 80
What did weaken their position, however, was the occupational taint associated with middle management in the NHS and the lower status of their occupation vis-à-vis that of the medical consultant. Nevertheless, general managers were highly committed to their work, stressing that they enabled the clinicians to concentrate on patients while they dealt with ‘the background issues’ (MNC 79). They also noted their responsibility for the ‘bigger picture’ and the trust as a whole (whether or not they agreed with what was been asked of them) (MNC 103). (This reflects the system-level thinking associated with effectiveness by non-clinical managers generally, discussed in Chapter 7. ) This appeared to accord with how they were perceived by their main constituents, consultants. As was evident from the interviews with consultant managers, although consultants did view management per se with suspicion, they showed respect for and appreciation of the specific general managers they worked with, recognising their expertise and acknowledging their role in sheltering themselves from the demands of senior management.
Aware of the so-called ‘them and us’ attitude that purportedly exists between doctors and managers,65 general managers understood the need to engage in long-term relationship building:
I keep my door open because my core business is the consultant staff . . . everything kind of hinges on them.
MNC 17
They believed they possessed considerable interpersonal skills, often developed through the experience of work in the private sector and through ‘learning on the job’. These skills were particularly important in dealing with medics, because general managers typically lacked both the authority to demand compliance and the status to impose their will. They therefore had to use ‘softer’ tactics of persuading, negotiating, ‘putting ideas into people’s heads’, ‘selling’ ideas98 and ‘translating’ (i.e. interpreting the ‘demands from above’ as relevant, meaningful and of value to their audience).
It would be really nice if I didn’t have to do all of this running around trying to . . . cover clinics because you have to use all of your skills of persuasion to get doctors to do something that they don’t want to do, and when . . . you’ve got patients arriving, you’ve got to get something like that covered. Sometimes you just feel like putting your hands up and saying . . . ‘I can’t be bothered . . . just do it’ . . . [but] you can’t do that.
MNC 79
Tailoring the message to a particular audience was of particular importance. Several spoke of using an evidence-based approach (facts and statistics) with medics (MNC 17, MNC 87, MNC 104); some talked about using a more ‘emotive’ language and lines of argument with the nurses.
They also spoke of utilising informal, one-to-one interactions, networking, and engaging the support of the senior clinical staff as important strategies of influencing clinicians. Thus, one general manager had circulated a paper covering the points she wanted one of her clinical leads to take on board. Alongside this, she spoke to her clinical superior (whom she knew well) and used this to tell him what to ‘feedback’ to the clinical lead (MNC P2).
Tenure in the organisation afforded general managers tacit knowledge of organisational processes and the opportunity to develop relationships. One interviewee explained that because she had worked with medics for many years, she had a strong understanding of doctor–manager relations and the power dynamics involved. She commented that she was not afraid to ‘get cross’ and mobilise her status as a general manager, when necessary (MNC 30). This mobilisation was implied rather than explicitly evoked, but it was an unspoken presence and appeared related to the general managers’ position within the upper echelons of AfC banding and their links to senior management.
Yet, the clinical respect for general managers was perceived as fragile. Some described an unspoken acceptance of poor behaviour by medics. Having been on the receiving end of such behaviour, one of the respondents intended to leave the NHS (MNC P2); and several admitted that one had to have a strong enough personality to be able to cope with medical staff.
Overall, the general middle managers appeared to draw on their tacit organisational knowledge and a set of skills and strategies that were continually utilised and developed in the enactment of ‘doing’ management. Although such skills and strategy utilisation were often taken for granted, it was clear they were presented as part of an accepted discourse of good management.
Middle nurse managers (group 2a)
Middle nurse managers were a diverse group comprising divisional heads of nursing, CBU lead nurses, nurse/midwife consultants and matrons. For this analysis, we elected to concentrate on matrons (all AfC band 8) because they sit in the middle of this group and have a key role engaging clinical staff ‘below’ (such as ward managers/sisters) and ‘above’ (consultants and more senior nurses).
Matrons were reintroduced to the NHS in the NHS Plan of 2000 and ‘intended to provide a clear focus for clinical leadership across a group of wards and a highly visible, accessible and authoritative figure on whom patients can rely to ensure that the fundamentals of care are right’ (p. 6). 159 When bolstered by experience, and their managerial position, their credibility as a ‘true’, or ‘shop floor’ nurse who embodies nursing values and practice, was a potent combination for influencing others. Their effectiveness in their role, however, very much depended on whether or not they were able to build relationships and support this credibility by interpersonal trust.
Matrons’ identity was deeply rooted in their core nursing skills, general nursing mind-set and their ‘feel’ for the ward environment. They emphasised their no-nonsense, ‘back to basics’ approach; some contrasted that with their image of other ‘new’ nurses, who were ‘too posh to wash’ and did not ‘believe that they should be in the sluice and emptying commodes, doing bed baths and washing’ (MC 55). Yet, as discussed in Junior nurse managers (group 2b), junior nurse managers often were sceptical of the matrons’ expertise because they no longer directly practiced nursing.
One of the key words describing the matron’s role was visibility. They were expected to be ‘visible’ to patients and their relatives and to provide a point of contact and a sense of reassurance. Visibility was also essential for influencing their subordinates. Their time-consuming managerial work, however, made it difficult to achieve this visibility:
We’ve had one or two operational things pulled away from us, so that we don’t spend as much time managing beds, which we’d got heavily involved in, and actually it was loathe, hate and abhor. So now we’re trying to get back to our roots, the visible, being able to help people. So you go round, you meet people, you try to answer their questions, just see how things are going.
MC 68
As their managerial work made it impossible for them to be directly ‘watching over’ their subordinates, they strived to:
Put time into people at the front end . . . showing people that I trust them to do things and to develop.
MC 68
They also placed a high value on being approachable and communicating with staff they line managed.
In mobilising upward, building relationships was also important:
One of the things I dreaded when I had to move was to form those new relationships with the consultants in particular. The junior doctors are fine, but I do . . . it’s a confidence thing . . . But having said that, the ophthalmologists love me, and they all talk to me and they’re fine, and I’m with them. But I haven’t made great strides to meet the others, to meet ENT or plastics or maxfax, if I’m totally honest . . . I know that I need to make that effort to get in there, because if I want to influence anything they’ve got to know who I am and what I’m capable of, and you know that I’ve got some credibility, but I do find it difficult.
MC 55
Their identity, in a sense, was not strong enough to carry them and they had to ‘prove’ that they were capable of performing their role.
One matron who had a track record as someone willing to take risks and prepared to deal with contingencies related how she was asked by senior management to open an additional unstaffed ward during a winter bed crisis and had to ‘rattle some very senior cages’ in order to obtain the necessary staff and equipment. Her reputation as ‘reasonable’ lent credence to her demands, but she opined that one could not be seen to cry wolf too often (MC 68).
Thus, matrons’ identities as ‘shop floor nurses’ allowed them to connect with their subordinates and to influence upwards, but these identities had to be bolstered by actions that supported this claim.
Middle scientist managers (group 3a)
The middle scientist managers interviewed were heads of services and defined themselves as ‘scientists’ rather than managers:
I am a clinical scientist in the health service. The fact that I don’t get to do much science anymore is unfortunate, but where I come from is being a scientist.
MC 32
Alongside the daily responsibilities in their particular service areas, scientist managers were involved in national committees and national auditing.
Describing themselves as ‘the link between the laboratory and the clinicians and the outside world’ (MC 14), scientist managers may be seen as organisational ‘boundary spanners’. 30 They were primarily involved in mobilising ‘down’ (their team of scientists, which often included laboratory workers, administrators and/or nurses) and ‘laterally’ (with consultants throughout the trust and the general manager for their service area).
In attempting to influence downward, all emphasised the importance of their ongoing clinical involvement, which also informed the managerial side of their work:
If I don’t do [science] then . . . I have lost what I came in for and I have lost some of the information or . . . feedback which is . . . important to my managerial work. I wouldn’t be working on the shop floor anymore and I would have lost some of that contact . . . it is useful to know, not just what you’re telling people to do, but to experience some of the consequences of what you are telling them and asking people to do.
MC 32
All appeared less confident in enacting their managerial identity and, unlike most other work groups, directly spoke of their lack of management training and experience as hampering their work:
I don’t know whether this is where my lack of management training shows. I perhaps could manage these things better if I had more training or experience simply in management.
MC 32
Those who had received some management training highlighted the need to support managerial knowledge with skills, which had to be honed through experience:
Well . . . when you get out . . . actually doing it and being ground down by too much to do, a lot of that stuff goes out of my head and it’s not embedded well enough to be part of [my] normal working.
MC 21
Although the managers in other work groups emphasised their strong interpersonal skills, scientist managers appeared to be in the process of developing those, but lamented the time and organisational constraints that prevented them from doing so:
Increasingly what would be nice is to have the time to engage people . . . to gradually build a case, but of course I don’t have the time to go and meet with everyone. I would like to bump into people more often and that’s an issue about site location. Some of the people I need to influence as opposed to bludgeon, are over at [the other site] and I don’t see them . . . It’s about just getting out there and talking to people, in some ways I’m getting better at it, in others because the trust has become bigger I’m less good . . .
MC 21
In attempting to influence upward, scientist managers appeared to be on a more secure ground. Their interactions with medical consultants were on equal terms, because of the parity in clinical status and expertise. Thus, a consultant scientist spoke of being sufficiently medically trained:
To know what a clinician is going to be doing with their patients, what they are worried about, what they won’t understand, what they won’t or what they will be able to do with the results . . .
MC 14
Indeed, he reported needing to ‘translate’ science for medics and commented that, although he understood their job, they did not have the scientific training to understand his.
They also had considerable experience of dealing with medics, were unfazed by ‘tantrums and shouting’, and knew how to utilise their established relationships with consultants:
If I need support or help in moving things forward I tend to talk to the clinicians that are in charge of the services, that use our service. So for example we’ve got one of the lead consultants who sends us patients . . . so he’s a useful contact . . . if you need support in a particular area . . . And there’s a few other clinicians like that . . .
MC 15
Their interactions with general managers were less amicable. They derided them as ‘NHS managers, not real managers’ (MC 15), criticised ‘needless management’ (MC 32), and commented that they had a tendency to ‘say one thing and do another’ (MC 21). They were also frustrated by the general managers’ lack of clinical knowledge and perceived that this hampered their ability to ‘sell’ scientific ideas to senior managers. Yet, similar to consultant managers, scientist managers were grateful to their immediate general managers for sheltering them from the pressures of senior management.
Consultant managers (group 1)
Consultant managers had a wide span of responsibility and typically managed large numbers of staff. Like most other clinical managers, they defined themselves primarily as clinicians:
At the heart of it I am a doctor. Although I do management, at the heart of what I do I am still a doctor . . . in terms of everything I do, it comes from the context of being a doctor.
MC 70
Often they had taken on the management role because they were ‘passionate’ about developing their service and/or felt the time was ‘ripe for change’ more generally. The managerial role was portrayed as a demanding and time consuming ‘add-on’ to their core identities as clinicians and clinical leaders. Yet they saw no fundamental opposition between their clinical and their managerial role:
So, the core identity is being a physician . . . but part of being a physician is about determining best patient care, practice, pathways, and those sorts of things, and I suppose one could argue that you cannot do that in a void . . . So, one manages the team so the rest of the doctors in the team, associated with the nurses, the admin people, has a responsibility . . . I suppose that one of the responsibilities of being a clinician, a senior clinician, is to facilitate change, benefit, positivity, and all those sort of things.
MC 59
Unlike most other work groups who primarily had to exercise influence downward and upward, consultant managers were mainly engaged in managing their former peers (other consultants), i.e. laterally. Another distinctive characteristic was that those former peers were likely to become actual peers again, as most consultant managers took on the managerial job only temporarily. (In contrast, other clinical managers, both junior and middle, had worked their way up to a management role and were likely either to stay in it or move up to a higher post.) The upshot of this was that the identity of consultant managers was ‘suspended’, hovering precariously over the ‘pool’ of their peers, into which they would eventually ‘drop back’. This created a challenge to mobilising their identity for lateral influence:
Taking the team with you is very difficult because . . . you’re basically up there to be shot at . . . [It’s] extremely tricky, because at some point I’ll give this role up, and then you just pop down to being one of the team again.
MC P4
If you continue in this role too long, you almost get to the point where you can’t move forward, can’t move anything forward, and everyone is hating you. Then you drop back in and then you feel despised and hated and not part of a team and someone else has to take it over.
MC 47
Although it seems an oxymoron to suggest that the consultant manager’s identity is vulnerable, this is, in fact, an apt way to describe it. On the clinical side, they feared loss of credibility among their peers, the very people whom they looked to for confirmation of a valued identity and who now thought that they had:
. . . Gone over to dark side . . .
[A consultant once] stood at the door at my office and said, ‘I’m not coming in because that is management carpet and I’m on workers’ lino.’ And he was a friend, but at that moment I had my clinical director hat on in his mind and therefore I was management on the carpet.
MC 49
On the managerial side, they lacked the authority to sanction, because their consultant peers were powerful enough to refuse both to listen and to act:
I can’t tell my consultant colleagues to do anything because they just go: ‘Make me!’
MC P4
To counteract these vulnerabilities, consultant managers had to press the valued aspects of their identity to the fore by continuing to carry the clinical load to show that they stood:
‘Shoulder-to-shoulder’ and saying ‘Why would I want to shaft us because actually I’m shafting myself as well as you’.
MC 47
Another way of countering these vulnerabilities was to espouse a system- or trust-level view, which placed them more effectively as outsiders to their peer group:
You are in a role which people understand that you’re not part of the team. So I’m coming in as clinical director, but actually I’m going to provide a service for you as well . . . I am now going to come to you and explain the costs of that service that you are missing, because I am providing the costs and it gives me a very different lever than if I had been a cardiologist.
MC 49
However, this view was not easily digested by their peers, who, as several respondents recounted, were heavily inclined to see the individual picture rather than the wider perspective.
Finally, consultant managers tried to draw on their management team (e.g. general managers and matrons) to counterbalance the force of peer consultants. Also, one consultant manager recalled using nursing staff as a lever to achieve the successful merger of services across two sites:
The rotation of nursing staff [between sites] has been the catalyst . . . It doesn’t matter how much resistance my consultant colleagues put up, if the nurses are doing it, it’s going to happen . . . I talk to them, I talk to them, I spend hours doing walk around management, because it is incredibly time consuming, but it is also just so important . . . I try to give them my vision, if you like, and try to encourage them and show them the advantages. But most of them are really receptive . . . and take it on and you don’t really need to push . . . The give was much more obvious.
Interviewee 47
In conclusion, consultant managers struggled to mobilise their dual or hybrid identity as clinicians and as managers to influence their peers, because, for their peers, this undermined their credibility. Yet, consultant managers developed strategies to bolster their influence, by strengthening both their clinical identity (through continuing engagement in clinical practice) and their managerial identity (such as by espousing a systems view and trying to communicate their vision to the subordinates).
Summary
In this chapter we have been concerned with the ‘behaviour of identity’ (see Figure 1 , Chapter 1 ), that is, the ways in which various work group subcategories mobilise facets of their identity to achieve their managerial objectives. We have focused on the ‘who’ and the ‘how’ of identity mobilisation, bearing in mind our overarching approach to identity which emphasises its contextual and relational features.
The analysis shows that, in terms of ‘who’ respondents tried to influence, there was evidence of mobilising their identities to influence downward (their subordinates), upward (their superiors) and laterally (colleagues operating at the same or similar level of the organisational hierarchy).
In terms of the ‘how’ of identity mobilisation, the analysis shows a combination of:
-
mobilisation capacity, i.e. the facets of identity that a manager could draw on in trying to influence others (e.g. continuing engagement in clinical practice, tacit organisational knowledge derived from the tenure in the job or the organisation), and
-
mobilisation strategy, i.e. the enactment of this capacity in interaction with others (e.g. leading by example, building trust).
Respondents mobilised both their managerial identities and their ‘other’ ‘core’ professional self-identities [clinical (e.g. nurse) or non-clinical (e.g. accountant)]. In comparison with the mobilisation capacities of other identities, which were fairly explicit, a key finding is that the mobilisation capacity of managerial identity was more veiled and often appeared ‘in disguise’, referenced by the respondents as their personal characteristics (i.e. ‘content of identity’). Thus, they frequently referred to their experience, or tenure, within the organisation as a resource they used to influence others. Yet we wish to emphasise that their notion of experience actually implied skilled knowledge of organisational context (e.g. decision-making structures) that had been honed over time. Indeed, the problem that managers faced when they did not have these kinds of skill was evident in the not uncommon reference to the challenges of being new to a role and not yet having built up the valuable personal connections and insider knowledge that come with experience in the specific work environment. Similarly, as also seen in Chapter 7 , managers often cited their ability to communicate with others as their personality trait. Yet, on closer examination, this encompassed a plethora of specific skills associated with the management profession, such as the skill of translating specific demands placed on their subordinates by the organisation (e.g. adherence to targets) in terms that were clear and meaningful to their audience.
In Chapter 6 we considered the variation in the span of responsibility and scope of activity of managers according to their clinical or non-clinical status and position in the hierarchy (middle or junior and variations within this). In Chapter 7 we saw how the achievement of self-defined effectiveness is enabled and constrained by the organisational context within which the managers work. These two points have been drawn together in the present chapter in our analysis of the constraints that hierarchies of various kinds (both within and between work subgroups) place on the capacity of managers to mobilise others in pursuit of their objectives, thereby further contributing to our research aim of determining the influence of managerial identities on organisational process and outcomes (see Chapter 2, Identity). As highlighted throughout this report, there were significant differences in identity (its core, content and behaviour) both between and within the four primary categories of managers. As the analysis shows, the ‘who’ and the ‘how’ of mobilising identities also varied. Table 21 summarises the overall findings of the chapter.
| Work group | Challenges: where do the identities need to be mobilised? | Mobilisation capacity | Mobilisation strategy |
|---|---|---|---|
| JNC managers | |||
| Administrative managers | Upward: for general work management – medical consultants (in order to achieve the service delivery targets, e.g. scheduling clinics) | Limited Lack of clinical identity is a disadvantage when dealing with medics. Managerial identity affords insufficient mobilisation capacity vis-à-vis (senior) clinicians (low status in organisational hierarchy, insufficient education credentials) The main mobilisation capacity is the organisational tenure (experience) |
Building relationships with individual medics |
| Downward: for staff management – subordinates (administrative and clerical) (in order to overcome the problems of insufficient staffing and heavy workload) | Considerable Managerial identity vis-à-vis subordinates is sufficient to ensure compliance The main mobilisation capacities are work experience outside the NHS and the tenure in the job and in the organisation, as these allow them to hone the array of interpersonal skills and management styles |
Using a variety of influence tactics, ranging from persuasion to assertion/pressure; deploying specific tactics depending on situation and individual(s) | |
| JC managers | |||
| Junior nurse managers (group 2b – ward managers and ward sisters) | Upward: (1) Middle nurse managers (2) Medics (3) ‘Anonymous’ decision-makers (several levels of organisational structure, e.g. to obtain new equipment) |
Considerable Dual identity: clinical is primary, managerial is secondary The main capacities of clinical identity are clinical knowledge and current clinical work. The main capacity of managerial identity are tenure and associated knowledge of organisational processes |
Based on the tenure and resulting organisational knowledge: knowing ‘how’, tenacity when dealing with decision-making authorities Based on the tenure and resulting long-term relationships with medics and middle nurse managers: knowing ‘who’ Based on current clinical work: combating the ‘managerialist’ rationale |
| (1) Middle nurse managers | Stronger clinical identity than the one perceived to be possessed by middle nurse managers | ||
| (2) Medics | Clinical expertise and work and organisational tenure (relationship building) | ||
| (3) ‘Anonymous’ decision-makers | Tacit organisational knowledge | ||
| Downward: subordinates (primarily other nurses) | Considerable The main capacities of clinical identity are clinical skills and current clinical work The main capacities of managerial identity are tenure and knowledge and interpersonal skills derived from experience |
Based on clinical capacity: working alongside, stepping in, leading by example Based on managerial capacity: employing a variety of influence tactics depending on the situation (‘firm but fair’, empowering vs. ‘bossy’) |
|
| AHPs | Upward: to medics and non-clinical managers | Considerable Dual identity: clinical and managerial Skilled at presenting a different ‘face’ depending on the situation, i.e. to medics – mobilising their clinical identity; to non-clinical managers – demonstrating their management savvy |
No defined strategies |
| Downward: team members (staff) | Considerable Mobilising capacity is the behaviour of identity, i.e. work (continuing engagement in clinical practice) |
Leading by example Interpersonal skills |
|
| MNC managers | |||
| Middle general managers (group 5a) | Lateral: medical consultants | Considerable Identity solely managerial Mobilisation capacity is reflective of strong managerial identity, supported by education, training and experience (both within and outside the NHS), and the resultant skills |
Skilful use of ‘softer’ tactics of persuading, negotiating, ‘putting ideas into people’s heads’, ‘selling’ the ideas and ‘translating’ the demands from above |
| MC managers | |||
| MC nurse managers – matrons | Upward: medical consultants | Dual identity: clinical and managerial Considerable mobilisation capacity rooted in clinical identity, but the clinical credibility had to be proven by enacting appropriate behaviours |
Building relationships to create trust |
| Downward: nursing staff | Dual identity: clinical and managerial Limited mobilisation capacity of the clinical identity due to the scepticism of the nursing staff stemming from the matron’s lack of engagement in clinical practice Limited mobilisation capacity of the managerial identity |
Empowering the front-line staff | |
| Scientist managers – heads of service (group 3a) | Downward: subordinates (teams consisting of technical specialists, but also administrators and nurses) | Dual identity: clinical and managerial Mobilisation capacity of clinical identity is considerable and supported by ongoing engagement in clinical practice, but that of managerial capacity is limited, owing to the lack of training and experience |
Leading by example Influencing through clinical expertise Attempting to develop and deploy interpersonal skills |
| Lateral: medical consultants and general managers | Mobilisation capacity of clinical identity is strong. Clinical identity is solely relied on in these relationships | Using clinical and specialist scientific expertise | |
| Consultant managers | Lateral: medical consultants | Dual identity: clinical and managerial Mobilising capacities of both are limited owing to the vulnerability of their position vis-à-vis their peers |
Ongoing clinical engagement (embodying the identity) Espousing a systems view Communicating the vision to subordinates and the management team to counter the resistance of medical consultants |
Chapter 9 Conclusion
Introduction
Little research attention has been given to the identities of managers within the health sector generally or in hospitals specifically, and even less to how their identities may influence their work and their effectiveness.
The category ‘NHS manager’ is internally broad and diverse. Managers are situated at different organisational levels in a variety of clinical and non-clinical roles. Their work calls for them to engage with an array of other organisational members. In an attempt to capture this diversity in a way that could reasonably be operationalised for empirical research, we employed a primary typology of managers based on the two dimensions: management level (middle or junior managers) and clinical engagement (whether the manager is counted as clinical or non-clinical staff). This generated four primary categories of managers: MC, JC, MNC and JNC. During the data analysis it became apparent that a finer-grained categorisation according to ‘work groups’ (which maps back onto the four primary groups) would be useful to elucidate some components of their work. We hoped to discover whether managers from different clinical and non-clinical backgrounds and at middle and junior levels have different sources of identification, leading to different identities, which might shape their interpretations of their roles and the ways in which they performed them.
On the premise that the work managers do is facilitated and constrained by organisational contexts and processes, we elected to take a case study approach focusing on two acute hospital trusts. The original intention was to interview 12 managers in each of the four primary categories in each trust, making an overall total of 96. (In actuality 91 respondents were recruited; see Chapter 3. ) The interviews were supplemented by the shadowing of a number of respondents and the observation of meetings.
In this final chapter we return to the original questions of the research and summarise the main findings from Chapters 5–8 . We also reflect on the strengths and limitations of the research and the challenges we experienced in conducting the research and analysing the data. Finally we draw out some implications for practice and make recommendations for future research.
Research questions and analytical approach
Research questions
To reiterate, our objectives were to:
-
to chart the work of middle and junior, clinical and non-clinical managers; including identity work and to produce an ethnography of the lived experience of middle and junior management within the specific context of the NHS
-
to explore the identities of managers (goals, values, motivations, beliefs and interaction styles) and how these are constructed, and further, how the performance of managers’ roles is shaped by these identities
-
to capture how managers leverage their identities to create success, establish trust and broker alliances to exert influence in different and various spheres, and to determine how they interpret and take forward their ‘project’ to achieve organisational, group and personal goals within the framework of the NHS
-
to determine the influence of managerial identities on organisational processes and outcomes.
Analytical approach
The research was exploratory rather than aimed at testing or refining particular theories. Thus the interviews were conceived to capture the following broad themes: current role; professional background; day-to-day work; management work; effectiveness/accountability; and mobilising identity. A set of ‘sensitising’ concepts108 broadly guided the data analysis (as depicted in Chapter 2, see Figure 1 ). To describe identities we adapted Ashforth et al. ’s26 model of identity which portrays social identity as a continuum encompassing (moving from the narrow to the broad formulation): (1) core of identity, including self-definition (e.g. ‘I am “A”’, ‘I value “A”’, ‘I feel about “A”’); (2) content of identity (i.e. values, goals and beliefs, stereotypic traits, knowledge, skills and abilities), and (3) behaviour of identity (pp. 328–31). 26 We have referred to the elements of an identity, such as self-definition, values and work, as ‘facets of identity’.
Facets of identity are relational and comparative. They are situationally produced and hence evolve, fluctuate and change over time. Individuals may hold several identities (the most obvious example, for some, being that of ‘manager’ and ‘clinician’) that may conflict, converge and combine in different ways in different work contexts at different points in time. Our approach to the study of the behaviour of identity or identity mobilisation was to explore associations between the self-reported facets of identity, how the managers reported going about their work, and their self-assessments of their effectiveness.
Main findings
The research generated a rich, complex and wide-ranging body of data. The extent to which the findings can be extrapolated beyond the two case study trusts is difficult to assess. On the one hand, as emphasised in Chapter 2 and elsewhere, it is important to appreciate that identities are formed in interaction with others and can alter in their emphasis according to the interaction context in which individuals are engaged. Thus the specific organisational contexts of these two trusts are likely to be important. On the other hand, as noted in Chapter 3, The two research sites, we found that the organisational factors affecting the work of the managers in the study were of a broadly similar order across the two sites, even though the trusts’ organisational structures were somewhat different (see Chapter 4, Organisational structures), this suggests that many of the findings are theoretically generalisable to other sites. That said, a cautionary note is called for as these two trusts are among the largest in England, and each has more than one physical site, which may make them more complex than other trusts.
The four preceding chapters presented the research findings. We recap on these in what follows.
Facets of identity
In relation to facets of identity, Chapter 5 showed that cleavages ran between all four primary categories (JC, JNC, MC and MNC). It was found that:
-
The professional identity of respondents as managers was not particularly strong (almost half did not self-define as managers). The main dividing line was between non-clinical managers, who were more likely to define themselves as managers, and clinical managers, who tended to espouse their ‘primary’ clinical identity and distance themselves from the managerial identity.
-
Those respondents who had higher education qualifications in management were more likely to define themselves as managers, as were those who had previously worked outside the NHS.
-
Those who defined themselves as managers were more likely to identify with individuals or a work team than with a peer group (i.e. people at the same level as themselves).
-
Our results paint a more nuanced portrait of a ‘reluctant manager’ than conveyed to date and indicate that this is a more widely spread phenomenon than hitherto reported, restricted neither to middle management nor to managers with clinical backgrounds.
The scale, scope and form of work: what managers do
Chapter 6 addressed the question ‘What do managers do?’ We explored the general parameters of their work covering its ‘content’ (e.g. the ‘scale’ and ‘scope’ of their activities) and its ‘form’ (how they do it). We have reported differences between the ‘content’ and ‘form’ of clinical and non-clinical managers’ work and between that of junior and middle managers. However, we also found that the boundaries between them are blurred (i.e. there are variations within and similarities across the types of manager). The picture that emerged was complex and therefore not easily summarised; however, we did find the following:
-
The majority of the respondents across the sample worked more than their official hours.
-
Many reflected on the unpredictability of their working days. They reported frequent interruptions and having to juggle their responsibilities in the context of staff shortages and heavy workloads.
-
There were some marked differences between middle and junior managers along expected lines, such as middle managers were far more likely to be involved in strategy formation than junior managers and tended to spend more time in meetings. There was also the obvious difference that clinical managers split their time between management and clinical work and non-clinical managers did not.
-
However, on some dimensions, such as ‘span of responsibility’, ‘span of control’ and cross-site working, internal variations by ‘work group’ meant that comparisons between the four primary groups were not particularly meaningful.
-
This variety was added to by internal diversity even within a ‘work group’. For example, within the ‘work group’ of consultant managers, clinical directors perceived themselves as having some scope for decision-making, whereas heads of services felt ‘stuck in the middle’ with little power to make decisions.
Hence the overall finding on ‘what managers do’ is that variation exists not only across the four primary categories but also within them (as shown by the finer-grained analysis of the ‘work groups’).
Effectiveness
Our analysis of self-reported effectiveness revealed that ‘hard’, demonstrable measures of performance, which we call ‘transactional effectiveness’, were important to all four primary groups of managers and hence to organisational processes and outcomes. However, many were also concerned with ‘softer’ indicators of their personal effectiveness, which we call ‘processual effectiveness’, involving activities such as enabling others, supporting and developing a team. The analysis showed that:
-
managers felt that ‘processual effectiveness’ contributed to ‘transactional effectiveness’; however, for some, it was a form of effectiveness in its own right that could be compromised by undue attention to ‘transactional effectiveness’
-
‘processual effectiveness’ was especially relevant to managers with smaller spans of responsibility (it was not, for example, so significant to middle managers of corporate units)
-
being a skilled or competent communicator was viewed as a key contributor to effectiveness generally
-
personal feedback was a gauge of effectiveness for most categories of manager; however, many reported that feedback from their own managers was lacking and/or that the only feedback that they got was of a negative kind
-
personal effectiveness could be challenged by the sheer size and complicity of the hospital as an organisation, effectiveness in one area could be compromised by ‘knock-on’ or ‘ripple-effects’ from another
-
the objective of combining clinical work and management is that they positively reinforce each other and thereby increase overall effectiveness; however, lack of time and volume of work often made this a potential more than a reality.
Mobilising identities
Chapter 8 showed that managers mobilise their identities to influence downward (their subordinates), upward (their superiors) and laterally (colleagues operating at the same or similar level). We explored the ‘mobilising capacities’ of the four primary groups (focusing on selected work groups), that is, the facets of identity that a manager could draw on in trying to influence others, and the ‘mobilising strategies’ (i.e. the enactment of these capacities) that they employed. We found that:
-
Respondents mobilised both their managerial identities and their other professional identities (e.g. nurse, doctor, accountant or scientist).
-
In comparison with the mobilisation capacities of other identities, which were fairly explicit, the mobilisation capacity of managerial identity often appeared ‘in disguise’. Thus, many managers made reference to their experience, or tenure, within the organisation as a resource to influence others and often cited their ability to communicate with others as their personality trait. Yet experience actually implies an in-depth knowledge of organisational context. Similarly, the ability to communicate with others encompasses a raft of management skills, such as the skill of translating specific demands placed on their subordinates by the organisation (e.g. adherence to targets) in terms that were clear and meaningful to other audiences.
-
The research revealed that the ‘mobilising capacities’ of the various groups of managers were subject to various identity constraints arising from those they sought to mobilise for effectiveness, ‘above’, ‘below’ and ‘laterally’, as well as from the wider organisation (such as its culture or available resources) and their workload. For instance, for clinical managers, it was constricted by the juggling of clinical and non-clinical work within time constraints.
Strengths and limitations
To our knowledge, this is the first study to explore the associations between managers’ self-identity and how it is mobilised to achieve their goals (i.e. for effectiveness in the course of their daily work in interaction with other staff).
To some extent the strengths of this research are also its limitations. The interview data were rich and nuanced. They provided a textured and complex picture of each manager’s work and their experience of it. However, the sheer variety and complexity of issues raised meant they were a challenge to analyse comparatively by primary category. As discussed in Chapter 3 , we used the method of ‘quantitising’, or the ‘numerical translation, transformation, or conversion of qualitative data’121 to explore patterns which otherwise might not have been so readily apparent in qualitative data. However, given the flexibility of qualitative interviews not all questions were asked of all respondents and this meant that data were not available for all tabulations, particularly in respect of the content of work and scale of activities.
Quite early on in the research it became apparent that the sheer scope of the sample would raise a question mark over the validity of the four primary categories for some aspects of the analysis. Although breaking the sample down into the ‘work groups’ helped to deal with this during the data analysis, it was not a complete solution as some work groups had quite small numbers and there was internal variation even within those. On the one hand, as outlined in Main findings, this points to what appears to be a valuable finding – and, hence, a strength of the research – that there are more differences within and commonalities across the four primary categories than we had anticipated. Yet on the other hand, we cannot be sure that this is not an artefact of small numbers.
As outlined in Chapter 3 , it had been our original intention to study two similar organisations to enable us to identify whether or not the association between identity and work activity was common for managers in two hospital trusts, thus enhancing the potential reliability of the findings. This was impeded by organisational restructuring at one site (Cityscape). However, we found that the two trusts faced similar dynamics such as multisite working, year-on-year efficiency savings, cost improvement programmes and mergers of services, which seems to be mirrored by hospital trusts across the country. Moreover, challenges of recruiting respondents such as ours who have pressured and busy jobs meant that we could not balance categories of respondents across the trusts. For example, all of the matrons were from one trust and all of the scientist managers were from the other. Hence we did not seek to compare the two trusts but rather combined the two sets of data for analysis to generate cross-case theoretical generalisations.
A related analytical challenge came from the variability of the issues raised in the interviews. Although the topic guides (see Appendices 4 and 5 ) were lengthy in the number of questions, the interview transcripts show that we soon settled on a common core. Yet, even so, as befits semistructured interviews, respondents varied in what they focused on most; in other words, on what mattered to them, and hence what was most important for us to capture. However, this did make it hard to compare them on some facets of their identity and on the ‘content’ and ‘form’ of their work.
The key research concepts, namely, identity, mobilising identity and effectiveness, are ‘slippery concepts’ that are difficult to operationalise in research terms. In fact, respondents largely seemed to find it relatively easy to talk about their identities as managers, clinicians, colleagues and so on. However, it was far more difficult to capture how they mobilised facets of their identities in their work and especially how this might contribute to effectiveness. Many found it hard to give concrete examples of being ‘effective’ and even more difficult to account for how they had achieved this, although we have, of course, been able to draw inferences ourselves on this from issues raised across each interview. The shadowing data were useful in helping us to tease out some elements of how those concerned mobilised their identities in the course of their everyday work. Within the limitations of word length we have employed some of these in Chapter 8 . We had anticipated that observations of meetings would be similarly useful in seeing identities ‘in action’, but as remarked on in Chapter 3 , they proved less useful than we had hoped because (in large meetings in particular) many participants were not actively engaged (e.g. in briefing meetings). Even so, the meetings were useful in providing us with a rich insight into the organisational structures and processes of the two study sites and the issues they faced at the time of the research. This assisted us in the interpretation of the issues raised in the interviews.
Implications for practice
As remarked on in Chapter 1 , the period during which this research was conceived and accomplished has been one of quite rapid change for NHS management, particularly in the wake of the White Paper Equity and Excellence: Liberating the NHS 11 and subsequent changes following the Health and Social Care Act of 2012. 17 Although the bedding in of the reforms and the recommendations of the Francis Report11,13,14 post-date the conduct of the research presented in this report (and hence did not directly inform the analysis) our findings do have implications for some of the issues that they raise. We incorporate some of these into the discussions of implications for practice that now follow.
Identity mobilisation and effectiveness
Across the primary categories, and for those with clinical roles particularly, managers distanced themselves from an identity as ‘a manager’. This is potentially problematic because a strong identity is associated with uncertainty reduction and employee strengthening (i.e. helping to deal with stress and facing new challenges).
‘Mobilising capacities’ derive from various facts of their identities including, the ‘content of identity’ (i.e. values, goals and beliefs, stereotypic traits, knowledge, skills and abilities). 26 Although these are appropriately interpreted as managerial skills built up from tenure and from experience in managing and acquiring specific tacit organisational knowledge, the managers tended to present them as personal qualities that were ‘given’ to them. Thus, they underestimate their work-related skills and the capacity to develop them further to enable effectiveness. This suggests that much more could be done within organisations not only to foster individual awareness of the knowledge and skill that accrues from experience qua skill, but also to enable the wider cultivation of such skills among coworkers.
Managers often felt that their mobilising capacity was inhibited by other ‘work groups’ (upwards, downwards and laterally in the organisation). Although the hierarchical power structures that commonly exist in complex organisations, such as the NHS (which is divided along professional lines as well as those of status), inhibit the capacity of the work groups studied (including those at the apex, i.e. medical consultants) to mobilise their managerial identities, it was evident that various strategies were to hand or could be devised to achieve their objectives.
Many managers adopted wide definitions of effectiveness which encompass but also go beyond ‘hard’ performance measures. Although they generally identify themselves as able communicators and as supportive of those they manage, their own capacity to be effective appears to be compromised by poor quality feedback from ‘above’.
The capacity to be effective is also affected by the complex organisational environments which they work in, which are hard to navigate. The recent NHS reforms11 place considerable emphasis on the incorporation of values of performance and quality into front-line care. The implication is that ‘toxic cultures’ – as identified by the Francis report into the Mid Staffordshire NHS Foundation Trust13 and discussed in the government report, Patients First and Foremost14 – which place targets and related financial concerns before quality of care, can be circumvented if managers are enabled to focus on care rather than the financial bottom line. Our respondents recognised that reducing unnecessary bureaucracy is not the same as reducing targets that measure quality assurance. However, many managers demurred from the overly simple equating of effectiveness with the meeting of various targets, some of which they saw as inimical to their capacity to deliver the best quality care. Thus our research broadly supports the policy of Patients First and Foremost to ‘ensure that paperwork, box ticking and duplicatory regulation and information burdens are reduced’ (p. 16). 14
Management education and training
Although the research did not directly focus on management education and training, these issues were considered within the analysis of identity, specifically in relation to the ‘knowledge and skills’ facet of identity (within the identity content). As noted in Chapter 1 , in the wake of the Bristol, Maidstone and Tunbridge Wells, and Mid Staffordshire inquiries and prior failures of leadership and management in the NHS, concern has been raised as to whether or not a system of professional accreditation and a professional association of NHS managers should be put in place, similar to those of the General Medical Council, the Health Professions Council and the Nursing and Midwifery Council. 12 Our findings, relevant to both the issue of professional qualifications and the issue of professional association, now follow.
Professional qualifications
With regard to professional qualifications, although the analysis of selection criteria for managerial positions in the NHS was not in the direct remit of our study, our investigation did show that only less than one-third of our respondents had recognised management qualifications. Our analysis also indicated that if an individual occupied a certain management position it did not necessarily follow that they had the management qualifications and training commensurate with this position (see Chapter 5, Management qualifications and training). These findings give rise to significant concerns. Obviously, the possession of management qualification is neither the sole indicator of requisite knowledge, skills and abilities nor the sole predictor of the subsequent performance in the post. Yet, obtaining formal higher education or vocational qualifications in management does lead to the development of relevant knowledge, skills and abilities; and using the management qualifications as a selection criterion does improve the quality of selection decision. The lack of attention to management qualifications in the selection process hinders the aim of ‘hiring the best talent’ by making the process of identifying such talent less robust. It also sends a wrong message to aspiring managers, downplaying the role of education in developing knowledge and skills and reducing the clarity in career paths into management.
From the focal point of our project – that of identity – the issue of professional qualifications also assumes a wider significance. Our findings show that ‘higher education qualifications in management strengthen managerial identity, but other forms of management education and training do not’ (see Chapter 5, Connections across the facets of identity). If we believe that a strong – and positive – identity is important, then the emphasis on management qualifications, particularly the higher education ones, is one of the instruments to achieve the greater identification of managers with management.
Furthermore, the disparity in the strength of identification with management as opposed to other professions in the health-care setting is partly related to the disparity in the bases of expert power of management vis-à-vis other professions. As we noted in this report, prior research suggests that because management has a more ‘craft-like’ knowledge base than the liberal professions, it has to constitute its expertise through educational credentials136 (see Chapter 5, Management qualifications and training). If one effectively removes the educational credentials as a criterion for being a manager, one further weakens the position of management in a professional organisation setting (such as NHS).
We, therefore, advocate strengthening the role of management qualifications as a prerequisite for NHS management.
We also maintain that, contrary to the conclusion of the King’s Fund report, ‘establishing a system of accreditation and . . . making the acquisition of a qualification a prerequisite for certain jobs’ does not necessarily lead to the creation of ‘a new form of professional accreditation for NHS management . . . [and] an entire new industry of NHS qualifications’ (p. 30). 12 Arguing against a system of accreditation and qualification prerequisites on the grounds of the potential costs of creating an NHS-specific accreditation and qualifications system is akin to throwing out the baby with the bathwater.
The King’s Fund report states that ‘the skills needed [for NHS management] are diverse and in many cases generic’ (p. 30). 12 We agree and therefore see no reason why the existing management qualifications could not be utilised for the purposes of selection in the NHS. This obviates the need for an NHS-specific system, but retains the emphasis on qualifications.
We also note that the King’s Fund report’s apparent assumption that a system of accreditation and qualification prerequisites does not exist in the NHS is not entirely accurate. Our findings indicate that what is missing is a formalised and standardised NHS-wide system. What is available is an array of local arrangements. In particular, as described earlier (see Chapter 5, Management qualifications and training), the interview responses revealed a wide variety of management qualifications (higher education and vocational) and a yet wider variety of learning and development programmes in circulation. Our analysis also indicated that having the management qualifications and training commensurate with the management position made it more likely that an individual would occupy this position. Since we did not distinguish in the analysis between the ‘prerequisites’ and the ‘postrequisites’ (i.e. qualifications and learning and development programmes undertaken before and after assuming the management position), the picture is somewhat blurred, but it does suggest that there are arrangements whereby those individuals with management qualifications and/or training are selected for management positions and any individuals selected for management positions without prior management qualifications and/or training then acquire these. This means that, in the absence of an NHS-wide solution to the challenge of matching the individual’s knowledge and skills to the requirements of a management position, some organisations are developing their own local solutions. Although we have no means of ascertaining whether local solutions would be more or less effective than an NHS-wide solution, we are certain that devising local solutions is less efficient. In particular, whereas the management qualifications are comparable by level within higher education qualifications and vocational qualifications frameworks (as presented in Appendix 9 ), the knowledge and skills developed via numerous learning and development programmes not leading to the award of qualifications are not. Given the variety of national, regional and organisational level programmes indicated in our description in Chapter 5, Management qualifications and training, an informed assessment and comparison of the quantity and quality of training received through these programmes would appear to be beyond the means of an individual organisation.
The King’s Fund Commission’s proposed alternative to the development of an NHS-wide accreditation and qualifications prerequisites system is for organisations themselves and ‘their boards (especially their non-executives) to ensure that they have competent, effective and sustainable management arrangements’ (p. 30). 12 Although we agree that organisations and their board should have the ultimate responsibility, our argument above suggests that in the absence of an NHS-wide system such responsibility would be too difficult and, indeed, costly to discharge.
The alternative also raises the perennial question of who would be watching the watchers. The King’s Fund suggestion – that ‘a national NHS leadership centre should consider whether the effectiveness of senior management and leadership should be considered by the CQC as an important determinant of organisational performance and be taken into account in processes for registering and licensing health care providers’ (pp. 30–1)12 – brings in an NHS-wide body by stealth, undermining its position against such body. It proposes to monitor the ‘outputs’ (the effectiveness of management) and to regulate on the basis of such monitoring, but without allowing an NHS-wide institution to control the ‘inputs’ (the quality of management resource). However, prior research and our own analysis in Chapter 7 of this report indicate that measuring effectiveness of management, albeit important, is difficult. It is certainly more difficult – and post hoc – than assessing management knowledge, skills and abilities ex ante. In addition, limiting the remit of any oversight over management to ‘senior management and leadership’ only is risky as the ‘failures of management and leadership’ are rarely limited to the top management team and the development of management cadre should begin from the bottom.
Finally, from the point of view of strengthening the managerial identity and improving its attractiveness, any local arrangements for prerequisites for management jobs are counterproductive. Managers, whether within an organisation or in society generally, are already an extremely disparate group, divided by boundaries of level, function, organisation and industry. Anything that further raises these boundaries, such as local prerequisites, lowers the potential for unity within the group and increases the uncertainty associated with what ‘manager’ is. Simply put, if different organisations within the NHS have different criteria for selecting the candidates for management positions, being an NHS manager becomes a less attractive proposition.
Taking a broader perspective, the ongoing debate about the status of management as a profession highlights that, in contrast with the established professions, management as an occupational group lacks barriers to entry, such as ‘a formal educational requirement and a system of certification and mandatory continuing education’ (pp. 4–8). 12 In a professional organisation, such as the NHS, the status disparity between the groups with and without barriers to entry would be felt particularly acutely. Introducing barriers to entry would improve the quality of management not only directly but also indirectly, by enhancing its status and hence attractiveness.
There may then be merit in establishing an NHS-wide system of accreditation and qualification prerequisites as (a) a more efficient (and possibly more effective) solution to the problem of matching individuals and jobs than the current array of local arrangements and (b) a way to strengthen management identity and make it more attractive/positive.
With regard to management education, the King’s Fund Commission champions ‘leadership development’ programmes, with a national NHS leadership centre at the helm and with links to ‘private sector and business schools’ (p. 29). 12 Although we support the principle of continuing professional development, we caution that ‘leadership development’ is too often taken to mean a substitute for professional education – a ‘top-up’ to whatever prior education the person possesses. We maintain that professional development, as a further ongoing education and training, should be taken in tandem with the core management qualifications requirement.
Further, we express concern with potential proliferation of such programmes from the point of view of quality assurance. In our study, the programmes quoted by the respondents under this banner widely varied in terms of content, duration and modes of delivery, and the forms of assessment were rarely specified. Evaluating the learning outcomes and comparing these across the programmes and vis-à-vis some standards would be difficult if not impossible.
Although the research team may be suspected of a bias on this matter, as its members are university academics, we see no reason why either the ‘primary’ professional education or further professional development in management cannot be delivered by the existing accredited institutions of higher education and vocational training. This would assure the quality of provision and a more efficient use of resources. Furthermore, it may be advisable to develop, within the existing higher education and vocational programmes, the stronger emphasis on management in the public sector, possibly with specialist routes. It would, however, be unwise to limit the remit of a programme solely to management/leadership in the NHS, as it may lead to the ‘parochial’ treatment of issues and prevent knowledge transfer from other segments of public sector and the private sector.
Thus, concentrating the professional management education (including further professional development) within the existing accredited institutions of higher education and vocational training may be merited.
Professional association
Having a professional association has always been and remains one of the hallmarks of a profession. The lack of comprehensive associations of managers is one of the weaknesses of management as a (would be) profession generally, not just in the context of health care. There are, of course, manager associations within particular sectors and sector segments, but these associations tend not to cover the whole segment, let alone sector or nation, and to have an advisory rather than regulatory remit.
In UK health care, to our knowledge, there is only one professional association of managers – HFMA. Its membership is limited to finance staff in health care. Another association, British Association of Medical Managers, created in 1990, closed in 2010. It only covered doctors in management positions. This state of affairs is lamentable.
The King’s Fund report advises against creating an association for the managerial profession on the grounds that vesting it with powers to regulate entry into the profession would increase bureaucratisation and preclude ‘hiring the best talent’ and that the costs of such association would outweigh the benefits.
Our counterarguments regarding ‘barriers to entry’ were presented above. To recap, we maintain that establishing such barriers would be instrumental to strengthening the quality and identity of management in the NHS. Whether or not the regulatory powers should be delegated to a professional association is a separate matter. We believe it is a feasible option, but the matter needs a comprehensive investigation, using the analysis of the experience of professional associations with regulatory powers in the UK and elsewhere.
The benefits of a professional association, however, are wider than those deriving from regulating the entry into a profession. Through the lens of identity, a professional association of managers in the NHS could serve a set of both practical and symbolic purposes. On the level of identity core, it would provide a clearly defined group one can identify with. If the distinctiveness of a group is relatively low, the psychological benefit of uncertainty reduction associated with affiliating with such group would also be low. Professional association would represent the managers in governmental policy-making and in the media, and work on correcting the misapprehensions and improving the public image of NHS management.
Management education and training
Finally, we suggest that the results of our study may inform management education and training in the NHS and in the public sector more generally. In line with our findings, we believe that management education and training need to stress the importance of management and managers in organisations and to instil a greater pride in the profession of management. We also believe that management education and training should devote more attention to developing the skills of communicating organisational objectives to other stakeholders, such as translating these objectives into the different occupational and professional languages employed by the stakeholders and aligning the objectives of the stakeholders with those of the organisation.
Recommendations for further research
Our primary recommendation follows from the exploratory nature of this study. Given the variation not only across but also within primary categories and work groups, it would be valuable to extend the research with larger numbers of respondents. There is also scope to explore each of the work groups in greater detail in their own right than has been possible here. This particularly applies to hitherto under-researched ‘work groups’, such as scientist managers and AHP managers.
Given the exploratory nature of the research most of our implications for practice (see Implications for practice) are suggestive rather than definitive. Hence our recommendations for further research are a call for additional investigation into these areas. Briefly, they are as follows.
An over-riding finding from which most others follow is that many respondents were struggling with their identities as managers. To recap, most were not reluctant to manage but to self-identify as ‘a manager’. Given that a strong identity is associated with uncertainty reduction and employee strengthening, we advocate for more research on how positive managerial identities can be enabled within specific organisational contexts and at different levels within the organisation. This applies not only to managers’ self-identities but also to identities conferred on them by others, such as other NHS staff groups and the general public. In particular, since our study focused on managers themselves and their own perception of their identities, it would be valuable to complement the study by examining how different groups of managers are perceived by other organisational members.
Following on from this, we propose that more research knowledge is needed on how ‘veiled’ skills, such as those that derive from tenure and experience and are often framed as personal traits (the ‘content of identity’), in the workplace seem to function as skills that enable effective managing (the ‘behaviour of identity’), even though they are not recognised as such. To the extent that they are effective enablers, further research should be able to discover how they may be re-envisaged as skill and facilitated in management education, training and development.
As recapped in Implications for practice, we have found that less than one-third of the respondents had recognised management qualifications and that the qualifications that they did have were not necessarily commensurate with their current positions. We have suggested that management qualifications might foster stronger identification of NHS managers with management. However, our study did not set out to directly research this issue. Hence we would recommend further study of managers’ own perceptions of this issue and how it might be tackled, something which may vary across work categories and finer-grained work groups. The same point applies to the issue of professional association.
Finally, we have found that the managers generally felt that the mobilising capacity of work group identity was inhibited by other work groups (upwards, downwards and laterally in the organisation). There is, therefore, considerable need to explore the perceptions that staff groups have of the work that other staff groups do (including non-managers) and, if inaccuracies exist, to identify how they might be overcome to enable more effective working between groups. It is also of note that although feedback from above was valued, many managers reported that it was infrequent and tended to occur only when there was a problem. More detailed research on both vertical and horizontal feedback channels might profitably identify how feedback can be improved and whether this in turn can enhance managerial effectiveness.
Acknowledgements
We are grateful to NIHR SDO for funding this project and would like to acknowledge the managers who generously gave of their time. We would also like to thank our colleagues who worked with us in various capacities during the project: Dr Jackie Goode, Professor Ellen Kuhlmann, Ms Nicola Selby and Ms Sophie Wilson.
Contributions of authors
Dr Janet Harvey (Senior Research Fellow, Health Services Research, University of Leicester, and for majority of the project, Assistant Director at the Centre for Research in Social Policy, Loughborough University). Principal investigator for the first 3 years of the project, leading on project design and contributing to the literature review, data collection and ongoing data analysis. Dr Harvey also contributed to the early stages of writing this report and latterly acted as an advisor to the team, giving critical advice covering content both factual and intellectual, and contributed to the revision of draft report and preparation of final report.
Professor Ellen Annandale (Professor of Sociology, University of York). Principal investigator from July 2012 to completion of final report in June 2013. Contributed to development of the proposal, literature review, fieldwork, development of coding frame, NVivo data coding, NVivo data analysis (see Chapters 6–8 ), writing of Chapters 3 and 7–9 , commented on all chapter drafts, edited complete report, and contributed to the revision of draft report and preparation of final report.
John Loan-Clarke (Senior Lecturer in Organisational Development, Loughborough University). Contributed to development of the proposal, literature review, fieldwork, development of coding frame, NVivo data analysis (see Chapter 4 ), writing of Chapters 1, 2 and 4 , commented on some aspects of draft chapters.
Dr Olga Suhomlinova (Lecturer in Management, University of Leicester). Contributed to, development of the proposal, literature review, fieldwork, development of coding frame, NVivo data analysis (see Chapters 5 and 6 ), writing of Chapters 2, 4–6 and 8 , commented on all chapter drafts, and contributed to the revision of draft report and preparation of final report.
Dr Nina Teasdale (Research Fellow, University of Leicester). Contributed to fieldwork, literature review, development of coding frame, NVivo data coding, NVivo data analysis (see Chapters 6 and 8 ), writing of Chapters 2, 4, 6 and 8 , commented on all chapter drafts, and contributed to the revision of draft report and preparation of final report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- NHS Management Enquiry Report. London: The Stationery Office; 1983.
- Strong P, Robinson J. The NHS Under New Management. Buckingham: Open University Press; 1990.
- Dopson S, Fitzgerald L. The role of the middle manager in the implementation of evidence-based health care. J Nurs Manag 2006;14:43-51. http://dx.doi.org/10.1111/j.1365-2934.2005.00612.x.
- Hewison A. Editorial. Middle management and nursing. J Nurs Manag 2006;14:1-4. http://dx.doi.org/10.1111/j.1365-2934.2005.00621.x.
- Starkey K, Madan P. Bridging the relevance gap: aligning stakeholders in the future of management research. Br J Manage 2001;12:3-26. http://dx.doi.org/10.1111/1467-8551.12.s1.2.
- Shortell SM, Rundall TG, Hsu J. Improving patient care by linking evidence-based medicine and evidence-based management. JAMA 2007;298:673-6. http://dx.doi.org/10.1001/jama.298.6.673.
- Our NHS, Our Future: Interim Report. London: DH; 2007.
- Framework for Managing Choice, Cooperation and Competition. London: DH; 2008.
- Developing the NHS Performance Regime. London: DH; 2008.
- High Quality Care for All. NHS Next Steps Review. London: DH; 2008.
- Equity and Excellence: Liberating the NHS. London: DH; 2010.
- The King’s Fund . The Future of Leadership and Management in the NHS: No More Heroes. Report from The King’s Fund Commission on Leadership and Management in the NHS 2011. www.kingsfund.org.uk/sites/files/kf/future-of-leadership-and-management-nhs-may-2011-kings-fund.pdf (accessed 8 February 2014).
- Report of the Mid Staffordshire Foundation Trust Public Inquiry. Executive Summary. London: The Stationary Office; 2013.
- Patients First and Foremost: The Initial Government Response to the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Degeling P, Maxwell S, Kennedy J, Coyle B. Medicine, management, and modernisation: a ‘danse macabre’?. BMJ 2003;326:649-52.
- Hunter DJ, Gabe J, Kelleher D, Williams G. Challenging Medicine. London: Routledge; 2006.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Davies HTO, Hodges CL, Rundall TG. Views of doctors and managers on the doctor–manager relationship in the NHS. BMJ 2003;326:626-8. http://dx.doi.org/10.1136/bmj.326.7390.626.
- Wall A. Being a Health Service Manager–Expectations and Experience: A Study of Four Generations of Managers in the NHS. London: Nuffield Trust; 2001.
- Davies HTO, Harrison S. Trends in doctor–manager relationships. BMJ 2003;326:646-9. http://dx.doi.org/10.1136/bmj.326.7390.646.
- Thorne ML. Being a clinical director: first among equals or just a go-between?. Health Serv Manage Res 1997;10:205-15.
- Witman Y, Gerhard AC, Smid PL, Meurs PL, Willems DL. Doctor in the lead: balancing between two worlds. Organization 2011;18:477-95.
- Santry C. Trusts contest figures for yearly management costs. Health Serv J 2008;24.
- Mintzberg H. The Nature of Managerial Work. New York, NY: Harper & Row; 1973.
- Parker M. Organizational Culture and Identity. London: Sage; 2000.
- Ashforth BE, Harrison SH, Corley KG. Identification in organizations: an examination of four fundamental questions. J Manage 2008;34:325-74. http://dx.doi.org/10.1177/0149206308316059.
- Delmestri G. Streams of inconsistent institutional influences: middle managers as carriers of multiple identities. Hum Relat 2006;59:1515-41. http://dx.doi.org/10.1177/0018726706072848.
- Final Project Report. London: The Government Office for Science; 2013.
- Mischenko J. Exhausting management work: conflicting identities. J Health Organ Manag 2005;19:204-18. http://dx.doi.org/10.1108/14777260510608943.
- Adams JS, Dunnette MD. Handbook of Industrial and Organizational Psychology. Chicago, IL: Rand McNally; 1976.
- Eyres J. Clinicians and Managers: Viva La Difference n.d. www.hsj.co.uk/resource-centre/clinicians-and-managers-vive-la-difference/1807972.article#.UvfT3klFDIU (accessed 9 February 2014).
- Kitchener M. The bureaucratization of professional roles: the case of clinical directors in UK hospitals. Organization 2000;7:129-54. http://dx.doi.org/10.1177/135050840071007.
- Chreim S, Williams BEB, Hinings CRB. Internal influences on the reconstruction of professional role identity. Acad Manage J 2007;50:1515-39.
- Hales CP. What do managers do? A critical review of the evidence. J Manage Stud 1986;23:88-115. http://dx.doi.org/10.1111/j.1467-6486.1986.tb00936.x.
- Van Peursem K, Prat M, Lawrence S. Health management performance: a review of measures and indicators. Accounti Audit Accountabil J 1995;8:34-70. http://dx.doi.org/10.1108/09513579510103254.
- Postmes T, Jetten J, Postmes T, Jetton J. Individuality and the Group: Advances in Social Identity. London: Sage; 2006.
- Ashforth BE, Mael F. Social identity theory and the organization. Acad Manage Rev 1989;14:20-39. http://dx.doi.org/10.2307/258189.
- Stryker S. Identity salience and role performance: the relevance of symbolic interaction theory for family research. J Marriage Fam 1968;30:558-64. http://dx.doi.org/10.2307/349494.
- Tajfel H, Turner JC, Worchel S, Austin WG. Psychology of Intergroup Relations. Chicago, IL: Nelson-Hall; 1986.
- Owens TJ, Robinson DT, Smith-Lovin L. Three faces of identity. Annu Rev Sociol 2010;36:477-99. http://dx.doi.org/10.1146/annurev.soc.34.040507.134725.
- Appiah KA, Gates HL, Appiah KA, Gates HL. Identities. Chicago, IL: University of Chicago Press; 1995.
- Cerulo KA. Identity construction: new issues, new directions. Annu Rev Sociol 1997;23:385-409. http://dx.doi.org/10.1146/annurev.soc.23.1.385.
- Simon HA. Administrative Behavior: A Study of Decision-making Processes in Administrative Organization. New York, NY: Macmillan; 1947.
- March J, Simon H. Organisations. New York, NY: Wiley; 1958.
- Albert S, Whetten DA. Organisational identity. Res Organ Behav 1985;7:263-95.
- Dutton JE, Roberts LM, Bednar J. Pathways for positive identity construction at work: four types of positive identity and the building of social resources. Acad Manage Rev 2010;35:265-93. http://dx.doi.org/10.5465/AMR.2010.48463334.
- Albert SB, Ashforth B, Dutton J. Organizational identity and identification: charting new waters and building new bridges. Acad Manage Rev 2000;25:13-8. http://dx.doi.org/10.5465/AMR.2000.2791600.
- Hogg MA, Burke PJ. Contemporary Social Psychology Theories. Santa Clara, CA: Stanford Social Sciences; 2006.
- Pratt MG, Rockmann KW, Kaufmann JB. Constructing professional identity: the role of work and identity learning cycles in the customization of identity among medical residents. Acad Manage J 2006;49:235-62. http://dx.doi.org/10.5465/AMJ.2006.20786060.
- Thomas R, Davies A. Theorising the micro-politics of resistance: new public management and managerial identities in the UK public services. Organ Stud 2005;26:683-706. http://dx.doi.org/10.1177/0170840605051821.
- Thomas R, Linstead A. Losing the plot? Middle managers and identity. Organization 2002;9:71-93. http://dx.doi.org/10.1177/1350508402009001356.
- Covaleski MA, Dirsmith MW, Heian JB, Bucknell SS. The calculated and the avowed: techniques of discipline and struggles over identity in big six public accounting firms. Admin Sci Quart 1998;43:298-327. http://dx.doi.org/10.2307/2393854.
- Ainsworth S, Grant D, Iedema R. ‘Keeping things moving’: space and the construction of middle management identity in a post-NPM organisation. Discourse Commun 2009;3:5-25.
- Bourgeault IL, Benoit C, Hirschkorn K. Introduction: comparative perspectives on professional groups current issues and critical debates. Curr Sociol 2009;57:475-85. http://dx.doi.org/10.1177/0011392109104350.
- Freidson E. Profession of Medicine. New York, NY: Harper & Row; 1970.
- Larson MS. The Rise of Professionalism: A Sociological Analysis. Berkeley, CA: University of California Press; 1977.
- Abbott A. The System of Professions: An Essay on the Division of Expert Labor. Chicago, IL: University of Chicago Press; 1988.
- Exworthy M, Halford S. Professionals and the New Managerialism in the Public Sector. Buckingham: Open University Press; 1999.
- Faulconbridge J, Muzio D. Organizational professionalism in globalizing law firms. Work Employ Soc 2008;22:7-25. http://dx.doi.org/10.1177/0950017007087413.
- Evetts J. The construction of professionalism in new and existing occupational contexts: promoting and facilitating occupational change. Int J Sociol Social Pol 2003;23:22-35. http://dx.doi.org/10.1108/01443330310790499.
- Dent M, Whitehead S. Managing Professional Identities: Knowledge, Performativity and the ’New’ Professional. London: Routledge; 2002.
- Fournier V. The appeal to ‘professionalism’ as a disciplinary mechanism. Sociol Rev 1999;47:280-307.
- Kuhlmann E. Postmodern times for professions – the fall of the ‘ideal professional’ and its challenges to theory. Knowl Work Soc 2004;2:69-85.
- Ferlie E, Pettigrew A, Ashburner L, Fitzgerald L. The New Public Management in Action. Oxford: Oxford University Press; 1996.
- Forbes T, Hallier J. Social identity and self-enactment strategies: adapting to change in professional–manager relationships in the NHS. J Nurs Manag 2006;14:34-42. http://dx.doi.org/10.1111/j.1365-2934.2005.00614.x.
- Fitzgerald L. Moving clinicians into management: a professional challenge or threat?. J Manag Med 1994;8:32-44. http://dx.doi.org/10.1108/02689239410073420.
- Kirkpatrick I, Bullinger B, Dent M, Lega F. The development of medical–manager roles in European hospital systems; a framework for comparison. Int J Clin Prac 2012;66:121-4.
- Dopson S, Stewart R. Information technology, organizational restructuring and the future of middle management. New Tech Work Employ 1993;8:10-2. http://dx.doi.org/10.1111/j.1468-005X.1993.tb00030.x.
- Buchanan D, Jordan S, Preston D, Smith A. Doctor in the process: the engagement of clinical directors in hospital management. J Manag Med 1997;11:132-56. http://dx.doi.org/10.1108/02689239710177774.
- Opdahl Mo T. Doctors as managers: moving towards general management? The case of unitary management reform in Norwegian hospitals. J Health Organ Manage 2008;22:400-15.
- Bolton SC. Multiple roles? Nurses as managers in the NHS. Int J Public Sector Manage 2003;16:122-30. http://dx.doi.org/10.1108/09513550310467975.
- Kuhlmann E, Burau V, Larsen C, Lewandowski R, Lionis C, Repullo J. Medicine and management in European healthcare systems: how do they matter in the control of clinical practice?. Int J Clin Prac 2011;65:722-4. http://dx.doi.org/10.1111/j.1742-1241.2011.02665.x.
- Causer G, Exworthy M, Exworthy M, Halford S. Professionals and Managers in the Public Sector. Maidenhead: Open University Press; 1998.
- Braithwaite J. An empirically based model for clinician-managers’ behavioural routines. J Health Organ Manage 2004;18:240-61.
- Spehar I, Frich J, Kjekshus LE. ‘Clinicians’ experiences of becoming a clinical manager: a qualitative study. BMC Health Serv Res 2012;12:1-11.
- Iedema R, Degeling P, Braithwaite J, White I. It’s an interesting conversation I’m hearing: the doctor as manager. Organ Stud 2012;25:15-33. http://dx.doi.org/10.1177/0170840604038174.
- Whittington R, McNulty T. Market-driven change in professional services: problems and processes. J Manage Stud 1994;31:829-45. http://dx.doi.org/10.1111/j.1467-6486.1994.tb00641.x.
- Clarke J, Newman J. The Managerial State: Power, Politics and Ideology in the Remaking of Social Welfare. London: Sage Publications Limited; 1997.
- Reay T, Hinings CR. Managing the rivalry of competing institutional logics. Organ Stud 2009;30:629-52. http://dx.doi.org/10.1177/0170840609104803.
- Stoopendaal A. Healthcare executives as binding outsiders in fragmented and politicised organisations. J Manage Market Healthcare 2009;2:184-94. http://dx.doi.org/10.1179/175330309791011145.
- Waring J, Currie G. Managing expert knowledge: organizational challenges and managerial futures for the UK medical profession. Organ Stud 2009;30:755-78. http://dx.doi.org/10.1177/0170840609104819.
- Hoque K, Davis S, Humphreys M. Freedom to do what you are told: senior management team autonomy in an NHS acute trust. Public Admin 2004;82:355-75. http://dx.doi.org/10.1111/j.0033-3298.2004.00398.x.
- Allan P. Research notes. Managers at work: a large-scale study of the managerial job in New York City government. Acad Mange J 1981;24:613-19. http://dx.doi.org/10.2307/255579.
- Pavett CM, Lau AW. Managerial work: the influence of hierarchical level and functional specialty. Acad Manage J 1983;26:170-7. http://dx.doi.org/10.2307/256144.
- Lowe J, Blythe P, Turnbull P. Reassessing Human Resource Management. London: Sage; 1992.
- Hales C. Rooted in supervision, branching into management: continuity and change in the role of first-line manager. J Manage Stud 2005;42:471-506. http://dx.doi.org/10.1111/j.1467-6486.2005.00506.x.
- Guest RH. Of time and the foreman. Personnel 1956;32:478-86.
- Child J, Partridge B. Lost Managers: Supervisors in Industry and Society. Cambridge: Cambridge University Press; 1982.
- Dunkerley D. The Foreman: Aspects of Task and Structure. London: Routledge and Kegan Paul; 1975.
- Kerr S, Hill KD, Broedling L. The first-line supervisor: phasing out or here to stay?. Acad Manage Rev 1986:103-17. http://dx.doi.org/10.2307/258334.
- Hales C. Structural contradiction and sense-making in the first-line manager role. Ir J Manage 2007;28.
- De Smet A, McGurk M, Vinson M. Unlocking the Potential of Front-Line Managers 2009. www.mckinsey.com/insights/organization/unlocking_the_potential_of_frontline_managers (accessed 14 April 2014).
- Isosaari U. Power in health care organizations: contemplations from the first-line management perspective. J Health Organ Manage 2011;25:385-99.
- Wooldridge B, Schmid T, Floyd SW. The middle management perspective on strategy process: contributions, synthesis, and future research. J Manage 2008;34:1190-221. http://dx.doi.org/10.1177/0149206308324326.
- Gratton L. The end of the middle manager. Harvard Bus Rev 2011;89.
- Currie G, Brown AD. A narratological approach to understanding processes of organizing in a UK hospital. Hum Relat 2003;56:563-86. http://dx.doi.org/10.1177/0018726703056005003.
- Balogun J. From blaming the middle to harnessing its potential: creating change intermediaries. Br J Manage 2003;14:69-83. http://dx.doi.org/10.1111/1467-8551.00266.
- Currie G. Reluctant but resourceful middle managers: the case of nurses in the NHS. J Nurs Manag 2006;14:5-12. http://dx.doi.org/10.1111/j.1365-2934.2005.00613.x.
- Currie G, Lockett A, Suhomlinova O. The institutionalization of distributed leadership: a ‘Catch-22’in English public services. Hum Relat 2009;62:1735-61. http://dx.doi.org/10.1177/0018726709346378.
- Ford J. Discourses of leadership: gender, identity and contradiction in a UK public sector organization. Leadership 2006;2:77-99. http://dx.doi.org/10.1177/1742715006060654.
- Carlström ED. Middle managers on the slide. Leadership Health Serv 2012;25:90-105. http://dx.doi.org/10.1108/17511871211221028.
- Thomas R, Dunkerley D. Janus and the bureaucrats: middle management in the public sector. Public Policy Admin 1999;14:28-41. http://dx.doi.org/10.1177/095207679901400103.
- Currie G, Procter SJ. The antecedents of middle managers’ strategic contribution: the case of a professional bureaucracy. J Manage Stud 2005;42:1325-56. http://dx.doi.org/10.1111/j.1467-6486.2005.00546.x.
- Currie G. The influence of middle managers in the business planning process: a case study in the UK NHS. Br J Manage 1999;10:141-55. http://dx.doi.org/10.1111/1467-8551.00116.
- Leadership and Engagement for Improvement in the NHS. London: The King’s Fund; 2012.
- Martin GP, Currie G, Finn R. Leadership, service reform, and public-service networks: the case of cancer-genetics pilots in the English NHS. J Public Admin Res Theory 2009;19:769-94. http://dx.doi.org/10.1093/jopart/mun016.
- Martin GP, Waring J. Leading from the middle: constrained realities of clinical leadership in healthcare organizations. Health 2013;17:358-74. http://dx.doi.org/10.1177/1363459312460704.
- Blumer H. What is wrong with social theory?. Am Sociol Rev 1954;19:3-10. http://dx.doi.org/10.2307/2088165.
- Rowley TJ, Modoveanu M. When will stakeholder groups act? An interest-and identity-based model of stakeholder group mobilization. Acad Manage Rev 2003;28:204-19. http://dx.doi.org/10.2307/30040709.
- Alvesson M, Willmott H. Identity regulation as organizational control: producing the appropriate individual. J Manage Stud 2002;39:619-44. http://dx.doi.org/10.1111/1467-6486.00305.
- Hunter DJ. The Health Debate. Bristol: The Policy Press; 2008.
- Klein R. The New Politics of the NHS: From Creation to Reinvention. Oxford: Radcliffe Publishing; 2010.
- Governance Arrangements for Research Ethics Committees: A Harmonized Edition. London: Department of Health; 2011.
- Yin RK. Case Study Research: Design and Methods. London: Sage Publications; 2009.
- Agenda for Change: The Final Agreement. London: DH; 2004.
- Zimmerman DH, Wieder DL. The diary interview method. Urban Life 1977;5:479-98. http://dx.doi.org/10.1177/089124167700500406.
- Zilber TM. Institutionalization as an interplay between actions, meanings, and actors: the case of a rape crisis center in Israel. Acad Manage J 2002;45:234-54. http://dx.doi.org/10.2307/3069294.
- McDonald S. Studying actions in context: a qualitative shadowing method for organizational research. Qualitative Res 2005;5:455-73. http://dx.doi.org/10.1177/1468794105056923.
- Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. London: Sage Publications; 2006.
- Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ 2000;320:114-16. http://dx.doi.org/10.1136/bmj.320.7227.114.
- Sandelowski M, Voilis CI, Knelf G. On quantitizing. J Mixed Meth Res 2009;3:208-22. http://dx.doi.org/10.1177/1558689809334210.
- Improving Working Lives. London: NHS Employers; 2009.
- Reay LM, Parker RA. Designing and Conducting Survey Research: A Comprehensive Guide. San Francisco, CA: Jossey-Bass; 1992.
- Martin G, Learmonth M. A critical account of the rise and spread of ’leadership’: the case of UK healthcare. Soc Sci Med 2012;74:281-8. http://dx.doi.org/10.1016/j.socscimed.2010.12.002.
- Scase R, Goffee R. Reluctant Managers: Their Work and Lifestyles. London: Unwin Hyman Limited; 1989.
- Pollitt C, Harrison S, Hunter D, Marnoch G. The reluctant managers: clinicians and budgets in the NHS. Financ Account Manage 1988;4:213-33. http://dx.doi.org/10.1111/j.1468-0408.1988.tb00069.x.
- Willmot M. The new ward manager: an evaluation of the changing role of the charge nurse. J Adv Nurs 1998;28:419-27. http://dx.doi.org/10.1046/j.1365-2648.1998.00635.x.
- Rayner J, Lawton A, Williams HM. Organizational citizenship behavior and the public service ethos: whither the organization?. J Bus Ethics 2012;106:117-30. http://dx.doi.org/10.1007/s10551-011-0991-x.
- Casey R, Allen C. Social housing managers and the performance ethos towards a ‘professional project of the self’. Work Employ Soc 2004;18:395-412. http://dx.doi.org/10.1177/09500172004042775.
- Boyne GA. Public and private management: what’s the difference?. J Manage Stud 2001;39:97-122.
- The Quality Assurance Agency for Higher Education, Office of Qualifications and Examinations Regulation, Scottish Credit and Qualifications Framework, CCEA, Credit and Qualifications Framework for Wales, and The National Qualifications Authority of Ireland . Qualifications Can Cross Boundaries – a Rough Guide to Comparing Qualifications in the UK and Ireland 2011. www.qaa.ac.uk/Publications/InformationAndGuidance/Documents/Quals_cross_boundaries.pdf (accessed 26 July 2012).
- Healthcare Financial Management Association . E-learning n.d. www.hfma.org.uk/e-learning (accessed 26 July 2012).
- Royal College of Nursing . RCN Clinical Leadership Programme 2012. www.rcn.org.uk/development/practice/clinical_governance/leadership (accessed 9 February 2014).
- Institute of Healthcare Management . Education n.d. www.ihm.org.uk/education_portfolio (accessed 5 October 2012).
- NHS . Breaking Through Programme 2009. www.nhsbreakingthrough.co.uk/About-the-NHS/Institute-for-innovation-and-improvement.aspx (accessed 9 February 2014).
- Reed MI. Expert power and control in late modernity: an empirical review and theoretical synthesis. Organ Stud 1996;17:573-97. http://dx.doi.org/10.1177/017084069601700402.
- Preston D, Loan-Clarke J. The NHS manager: a view from the bridge. J Manage Med 2000;14:100-8. http://dx.doi.org/10.1108/02689230010346411.
- Merali F. NHS managers’ views of their culture and their public image: the implications for NHS reforms. J Manage Med 2003;16:549-63. http://dx.doi.org/10.1108/09513550310500409.
- Learmonth M. Managerialism and public attitudes towards UK NHS managers. J Manage Med 1997;11:214-21. http://dx.doi.org/10.1108/02689239710177314.
- Hyde P, Granter E, McCann L, Hassard J, Dickinson H, Mannion R. The Reform of Health Care: Shaping and Resisting Policy Developments. London: Palgrave Macmillan; 2012.
- Mills CW. White Collar: The American Middle Classes. Oxford: Oxford University Press; 1953.
- Whyte WH. The Organization Man. London: Penguin; 1960.
- Handy C. The Empty Raincoat: Making Sense of the Future. London: Hutchinson; 1995.
- Peters T. Liberation Management. New York, NY: Macmillan; 1992.
- Kanter RM. The Change Masters: Corporate Entrepreneurs at Work. London: Routledge; 1989.
- Hassard J, McCann L, Morris J. Managing in the Modern Corporation: The Intensification of Managerial Work in USA, UK and Japan. Cambridge: Cambridge University Press; 2009.
- Huy N. In praise of middle managers. Harvard Bus Rev 2001;79:72-9.
- Tajfel H. Human Groups and Social Categories: Studies in Social Psychology. Cambridge: Cambridge University Press; 1981.
- Hogg MA, Burke PJ. Contemporary Social Psychological Theories. Stanford, CA: Stanford University Press; 2006.
- Learmonth M. Doing things with words: the case of ‘management’ and ‘administration’. Public Admin 2005;83:617-37. http://dx.doi.org/10.1111/j.0033-3298.2005.00465.x.
- Parker M, Learmonth M, Hardin N. Unmasking Health Management 2004.
- O’Reilly D, Reed M. The grit in the oyster: professionalism, managerialism and leaderism as discourses of UK public service modernization. Organ Stud 2011;32:1079-101. http://dx.doi.org/10.1177/0170840611416742.
- Hales C, Mustapha N. Commonalities and variations in managerial work: a study of middle managers in Malaysia. Asia Pac J Hum Resou 2000;38:1-25. http://dx.doi.org/10.1177/103841110003800102.
- Luthans F. Successful vs. effective real managers. Acad Manage Exec 1988;2:127-32. http://dx.doi.org/10.5465/AME.1988.4275524.
- Alvesson M, Sveningsson S. Managers doing leadership: the extra-ordinarization of the mundane. Hum Relat 2003;56:1435-59. http://dx.doi.org/10.1177/00187267035612001.
- Rittel HWJ, Webber MM. Dilemmas in a general theory of planning. Policy Sci 1973;4:155-69. http://dx.doi.org/10.1007/BF01405730.
- Governance for Health in the 21st Century. Copenhagen: WHO Regional Office for Europe; 2011.
- Bolton SC. ‘Making up’ managers: the case of NHS nurses. Work Employ Soc 2005;19:5-23. http://dx.doi.org/10.1177/0950017005051278.
- Implementing the NHS Plan – Modern Matrons. Health Service Circular Series. London: DH; 2001.
Appendix 1 Letter to prospective staff interviewees
This was printed on the letterhead of the particular Trust and sent out by their HR Department.
Dear. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
‘Mobilising Identities: The Shape and Reality of Middle and Junior Managers’ Working Lives’
Please find herewith information concerning the above research project, the purpose of which is to investigate the working lives of NHS managers operating in areas other than the most senior tier. We wish to interview those engaged in management who are medically/clinically trained and also those who are from a general management background.
We are now writing to ask whether you would be prepared to be interviewed, to gain your views and experiences concerning your day-to-day work as someone who manages in the NHS and also to explore how elements concerned with your professional background and identity feed into this process. Relatively little is known about the professional orientation and experiences of NHS managers at this level of the organisation and the Department of Health is keen to investigate and take into account such knowledge.
The project is funded by the NHS SDO ‘Service Organisation and Delivery’ programme and is part of their Management Practices Programme of research. The research team is a joint collaboration by an experienced team of researchers from the universities of Loughborough, Leicester and Bath.
If you are willing to be interviewed, please complete the attached form and return it in the enclosed prepaid envelope. You will subsequently be contacted by a member of the research team, who will agree an interview time and venue with you (interviews will last for approximately one hour).
We would like to take this opportunity to assure you of complete anonymity in terms of information you contribute to the study. Reporting of the results of the study will be organised in such a way that those participating in the project will not be individually identified in any way.
Appendix 2 Participant information sheet
PROJECT INFORMATION SHEET
Project title
Mobilising identities: the shape and reality of middle and junior manager’ working lives
Sponsor NHS Service Delivery and Organisation (SDO)
Project based at Loughborough University, The University of Leicester and The University of Bath
Project description
It is now well-recognised that managers play a central role in leadership, organisation and service delivery in the public sector. Middle managers, in particular, have been identified as ‘key strategic actors’ in terms of how effectively organisations operate and, in many organisations, the number and variety of the roles they play has steadily increased. Currently, little consideration has been given to the accounts of managers themselves, particularly at the middle and junior levels, concerning how and why they operate in particular ways and what affects their professional backgrounds and identities play in this process.
The purpose of the research, therefore, is to investigate the working lives of middle and junior managers in the NHS. It will look at managers who are medically/clinically trained, and those who are not but who come from a general management or other backgrounds; in order to identify the similarities and differences in the way that they operate. The research will also explore the identities held by middle and junior managers and the effect these identities have on the way they conduct their work and how they relate to others with whom they come into contact in the workplace. It will then look at how this feeds into the performance of their roles and influences leadership effectiveness.
This will build on existing research that has described the working lives of managers more generally and will help to increase our specific knowledge about middle and junior managers, about whom relatively little is known. It will also tell us about these groups in the health-care setting. This will provide valuable learning to the NHS and groups, such as patients, who use its services, about what goals, values and beliefs motivate middle and junior managers and how this may relate to the performance of their roles.
How the research will be conducted?
To conduct the research we are using a range of methods that include:
-
One-to-one Interviews We will interview both middle and junior managers to gather accounts of managers’ daily working lives and their own sense of personal and professional identity and how this is may influence the ways in which they work to achieve personal and organisational goals. Interviews will last approximately 1 hour and with the participants’ consent, these will be recorded and fully transcribed. Prior to the interviews, we will ask interviewees to keep a brief, simple schematic diary of their meetings, tasks, activities and contacts for the previous 3 working days.
-
Observation and Shadowing We will observe managers’ work in action; that is, carrying out the work that they regularly undertake. This will involve shadowing a small number of middle and junior managers over a 2-day period and the observation of some directorate, departmental and unit meetings.
Whom we would like to participate
We intend to interview both women and men, middle and junior managers, from both clinical and non-clinical backgrounds and from a variety of different departments, specialisms and directorates. Individuals have been randomly selected for interview according to these criteria’ from the Human Resource directorate.
Anonymity, confidentiality and right to withdraw
All participants who agree to take part will be asked to sign a consent form. They will be guaranteed both anonymity and confidentiality, and will have the right withdraw their participation at any stage of the research. All data will be treated as personal data under the 1998 Data Protection Act and stored securely for a period of 5 years.
Research outcomes
Both preliminary and overall findings will be presented to participating hospitals and the findings will also be presented at conferences and published in scientific journals.
Project team
Dr J Harvey, (Principal Investigator) Assistant Director, Centre for Research in Social Policy, Loughborough University
Dr E. Annandale, Reader in Sociology, Department of Sociology, University of Leicester
Mr J Loan-Clarke, Senior Lecturer in Organisational Development, Business School, Loughborough University
Dr O Suhomlinova, Lecturer in Management, School of Management, University of Leicester
Dr E. Kuhlmann, Senior Lecturer in Sociology, University of Bath
Dr J Goode, Senior Research Associate, Centre for Research in Social Policy, Loughborough University; and
Dr N Teasdale, Research Associate, Department of Sociology, University of Leicester.
If you require more information or to discuss the research further please contact:
Dr J Harvey
Centre for Research in Social Policy; Loughborough University (contact details provided)
Appendix 3 Consent form
PARTICIPANT CONSENT FORM
Mobilising identities: the shape and reality of middle and junior managers’ working lives
Purpose of the study The purpose of the research is to investigate the working lives of middle and junior managers in the NHS. It is funded by the NHS R&D SDO.
It will look at managers who are medically/clinically trained and those who are not but who come from a general management background; in order to identify the similarities and differences in the way that they operate. The research will also explore the identities held by middle and junior managers and the effect these identities might have on the way they conduct their work and how they relate to other groups with whom they come into contact in the workplace. It will then look at how this feeds into the performance of their roles and influences the achievement of personal and organisational goals as a result of their work.
| Declarations for the participant to sign project title: Mobilising Identities: The Shape and Reality of Middle and Junior Managers’ Working Lives | (Tick as appropriate) |
|---|---|
| I confirm that I have read and that I understand the information sheet dated. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . .for the above study | □ |
| I confirm that I have had the opportunity to consider the information, ask questions about the research and have had these answered satisfactorily | □ |
| I confirm that I understand that the research has been reviewed and received ethical clearance through the appropriate NHS and University channels | □ |
| I confirm that I understand that data will be collected via a brief diary, an interview and some shadowing and observation, at times convenient to participants | □ |
| I confirm that I understand that data collected during the study will be viewed and analysed by members of the research team | □ |
| I confirm that I understand that all data will be treated as personal under the 1998 Data Protection Act and will be stored securely | □ |
| I confirm that I understand that all data will be treated confidentially and will be anonymised so that my participation in the research will not be identifiable | □ |
| I confirm that I understand that my words may be quoted in publications, reports and other research outputs, but my name will not be used and any details identifying me will be removed | □ |
| I confirm that I understand that my participation is voluntary and that I am free to terminate the interview or my active involvement in the research process at any time, without giving any reason, by advising the researchers of this decision | □ |
| I agree to take part in the research study | □ |
Participant consent form
Name of research participant . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Date. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Signature of research participant. . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . .
Research team
Dr J Harvey, (Principal Investigator) Assistant Director, Centre for Research in Social Policy, Loughborough University
Dr E Annandale, Reader, Sociology Department, University of Leicester
Mr J Loan-Clarke, Senior Lecturer in Organisational Development, Business School, Loughborough University
Dr O Suhomlinova, Lecturer in Management, School of Management, University of Leicester
Dr E Kuhlmann, Senior Lecturer in Sociology, University of Bath
Dr J Goode, Senior Research Associate, Centre for Research in Social Policy, Loughborough University; and
Dr N Teasdale, Research Associate, Sociology Department, University of Leicester.
If you require more information or to discuss the research further, please contact:
Dr J Harvey
Centre for Research in Social Policy (CRSP)
Loughborough University
Telephone: (removed for report), e-mail: (removed for report)
Appendix 4 Interview schedule for middle managers
1. Current role
1.1 What is your current job title(s)?
1.2 How long have you occupied your current post?
1.3 Can tell me about your main duties, responsibilities and areas of jurisdiction; including (roughly) the number and categories of staff you manage?
2. Professional background
2.1 Can you tell me briefly about your professional background and qualifications?
2.2 Have you ever worked outside of the NHS? (If ‘yes’: Do you think this has influenced your management practice?)
2.2 What management training have you undertaken (if any)?
2.3 Are you a member of any professional association or network? (It maybe that there are ‘expected’ as managers to belong to certain networks, for example.)
3. Day-to-day work
3.1 What are your main activities during a working day?
3.2 Can we talk about the diary you completed? Can you talk me through 1 day of it in more detail (researcher to choose the day – ask how the respondent felt about various issues/events)?
3.3 Are these documented diary-days typical days for you in terms of the components of work involved? (Why? Why not?)
3.4 Roughly how much time do you spend in meetings? What meetings do you regularly attend?
3.6 What’s a good day like? What’s a bad day like?
4. Management work
4.1 Why did you choose to get involved in a management role in the NHS?
4.2 What are the main challenges of being in a management role in the NHS? Greatest satisfactions? Greatest downsides?
4.3 Are you directly involved in strategy within the trust – that is in terms of implementing strategy and/or the formulation of strategy? (If ‘yes’: At what level?)
4.4 What are your goals/targets as a manager? (Prompt: Are these set by you/by others? How much discretion do you have?)
4.5 How do you go about achieving these goals/targets? (Prompt: Are there particular skills, tactics or strategies you deploy to further these goals? How far do these goals coincide or diverge from your own professionally derived goals?)
4.6 How do the current organisational structures affect the way you work?
4.7 Is there a body of knowledge you can call upon to inform your role as a manager? (Prompt: Are there identifiable skills involved?)
5. Effectiveness/accountability
5.1 What does being an effective manager mean to you? (Prompt: How do you create and judge success in your role?)
5.2 How is success as a manager measured in the trust? Criteria of effective performance (e.g. performance targets, annual ‘quality’ account and other metrics, financial targets of various kinds, organisational and national priorities)?
5.3 Is success incentivised? Are there any sanctions imposed for not achieving targets/success?
5.4 If there were two things you could change to help you more effectively achieve your management goals, what would they be?
5.5 From what sources do you derive support in doing your job effectively?
5.6 Who are the people you get on with the best in your work? (Prompt: Why is this?)
5.6 Can you identify any specific incidents that have really required you to exercise all your managerial and personal skills in managing them effectively? (Can you talk me through such an incident?).
5.7 Are there some areas of your work where you find it easier to exercise influence than others? (Prompt: What does this depend on?)
5.8 How do you get people to act in the ways you want them to? Get them to do what you want them to?
6. Mobilising identity (using particular identity-derived elements of professional and individual background to create influence and leverage advantage in an occupational situation)
6.1 Can you tell me about something you have achieved in the organisation of which you are particularly proud, why you felt this was important and how you achieved the result you wanted?
6.2 Conversely, can you tell me about something in which you were involved in the trust that you felt turned out badly and caused you some concern? (Prompt: Why did this particularly concern you? What did you try to do about it?)
6.3 What things do you fall back on when the going gets tough?
6.4 Multidisciplinary teams seem to be an increasing feature of the NHS – how well do people from different professional backgrounds work together? (Prompt: Do you find some groups easier to work with than others?)
6.5 In your view, are there differences in the way managers from clinical (medicine, nursing, etc.) and non-clinical (general management) backgrounds operate? What about managers at different levels of the organisation, do they operate differently? How well do the different levels of management relate to each other? (Prompt: Is communication good between them?)
6.6 How far do you see yourself operating within the wider hospital trust or do you operate more locally at the level of the ward or department? (Prompt: What are your operating boundaries here?)
7. Identity
7.1 How much does your work define you as a person?
7.2 Do you think of yourself primarily as a ‘manager’? (If ‘yes’: Get them to expand on this. If ‘no’: Why not?).
7.3 (For clinical managers only.) Which are you first – a clinician or a manager? (Are the lines between ‘clinician’ and manager blurring?)
7.4 (For clinical managers only.) Have there been occasions when being a clinician as well as a manager has helped you to resolve management issues?
7.5 (For non-clinicians only.) Given that this is predominantly a clinical environment, has it ever felt difficult that you don’t have a clinical background?
7.6 (For non-clinicians only.) Are there times in your management role where not being a clinician has helped you?
7.7 What motivates you in your role as manager? (Prompt: What values do you bring to your role as a manager?)
7.8 How would you describe your management style?
7.9 What ethical issues do you face in a management role in the NHS (Prompt: Where do you derive your ethical compass from?)
7.10 (Dis-identification.) What alienates and frustrates you within this organization? (Incentives.) What energies and excites you about this organization? (Prompt: Which part of your work do you most enjoy/least enjoy?)
7.11 Are there particular aspects of your work that you particularly hold dear/that are particularly important to you (to a greater degree than other aspects)? (Prompt: What? Why?)
7.12 If you have to leave/jettison certain aspects of the job, what goes first and why?
7.13 Who do you most closely identify with in the trust, as having the most in common with you? (Prompt: Whose goals do you see as most aligned with your own?)
7.14 Would you say you have a strong sense of self-identity? How does this express/manifest itself? (Prompt: Does this express itself in your work?)
7.15 How do you envisage your long-term career? Do you see yourself continuing in a managerial role in the NHS?
7.16 Is there anything else you would like to say about the issues we have discussed?
Appendix 5 Interview schedule for junior managers
1. Current role
1.1 What is your current job title(s)?
1.2 How long have you occupied your current post?
1.3 Can tell me about your main duties, responsibilities and areas of jurisdiction; including (roughly) the number and categories of staff you manage?
2. Occupational background
2.1 Can you tell me briefly about your job history and qualifications?
2.2 Have you ever worked outside of the NHS? (If ‘yes’: Do you think this has influenced the way you work in this job?)
2.3 Have you had any management training for this job?
2.4 Are you a member of any professional association or network? (It maybe that there are ‘expected’ as managers to belong to certain networks, for example.)
3. Day-to-day work
3.1 What are your main activities during a working day?
3.2 Can we talk about the diary you completed? Can you talk me through 1 day of it in more detail (researcher to choose the day – ask how the respondent felt about various issues/events)?
3.3 Are these documented diary-days typical days for you in terms of the components of work involved? (Why? Why not?)
3.4 Is attending meetings part of your job? (If ‘yes’: What meetings do you attend regularly?)
3.5 What’s a good day like? What’s a bad day like?
4. Management work
4.1 How and why did you become involved in a management role in the NHS?
4.2 What are the main challenges of your job? Greatest satisfactions? Greatest down-sides?
4.3 What are your goals in your job? (How far are these set by you and how far by others? If others: Who?) How do these goals impact on your job? How much discretion do you have?
4.4 How do you go about achieving these goals? (Prompt: Are there particular skills, tactics or strategies you deploy to further these goals? How do you feel about the goals you have to meet?)
4.5 What proportion of your work is routine and how much of it involves responding to events as they unfold?
4.6 What sort of skills do you need to do your job? How do you gain these?
5. Effectiveness/accountability
5.1 What are the targets/performance indicators for the group/unit you manage/people you supervise? Who sets them and how often are they monitored? How far do they coincide or diverge from your own views of what is important?
5.2 What does being an effective manager/supervisor mean to you? (Prompt: How do you create and judge success in your role?)
5.3 Are you specifically rewarded for success? Are there any sanctions imposed on you for not achieving targets/success?
5.4 If there were two things you could change to help you more effectively achieve your work goals, what would they be?
5.5 Where do you go for support if you need it to get your job done?
5.6 Can you identify any specific incidents that have really required you to exercise all your skills in managing them effectively?
5.7 Who are the people you get on with the best in your work? (Prompt: Why is this?)
5.8 Are there some areas of your work where you find it easier to exercise influence than others? (Prompt: What does this depend on?)
5.9 How do you get people to act in the ways you want them to?/get them to do what you want them to?
6. Mobilising identity (using particular identity-derived elements of professional and individual background to create influence and leverage advantage in an occupational situation)
6.1 In your view, are there differences in the way clinical and non-clinical (general management) managers at your level operate?
6.2 How well do people with different professional backgrounds work together? (Prompt: Do you identify more with some groups than others/find some groups easier to work with than others?)
6.3 Can you tell me about something you have achieved in the organisation that you are particularly proud of, why you felt this was important and how you achieved the result you wanted?
6.4 Conversely, can you tell me about something you were involved with in the trust that you felt turned out badly and caused you some concern? (Prompt: Why did this particularly concern you? What did you try to do about it?)
6.5 What do you fall back on when the going gets tough?
6.6 In your view, are there differences in the way managers from clinical (medicine, nursing, etc.) and non-clinical (general management) backgrounds operate? What about managers at different levels of the organisation, do they operate differently? How well do the different levels of management relate to each other? (Prompt: Is communication good between them?)
6.7 How far do you see yourself as a part of the wider hospital trust or do you operate more locally at the level of the ward or the department? (Prompt: What are your operating boundaries here?)
7. Identity
7.1 How much does your job define you as a person?
7.2 Do you think of yourself primarily as a ‘manager’? Why/Why not? (Probe if this is a term they would use to describe themselves.)
7.3 (For clinical managers only.) Which are you first – a clinician or a manager? (Are the lines between ‘clinician’ and manager blurring?)
7.4 (For clinical managers only.) Have there been occasions when being a clinician has helped you resolve management issues? (Prompt: Does this ever hinder you?)
7.5 (For non-clinicians only.) Given that this is predominantly a clinical environment, has it ever felt difficult that you don’t have a clinical background, when trying to get across your point of view?
7.6 (For non-clinicians only.) Are there times when not being a clinician has helped you as a manager?
7.7 What motivates you in this job?
7.8 How would you describe your management style?
7.9 What ethical issues do you face in your role? (Where do you derive your ethical ‘compass’ from?)
7.10 (Dis-identification.) What alienates and frustrates you within this organisation? (Incentives.) What energies and excites you about this organisation? Which part of your work do you most enjoy/least enjoy?
7.11 Are there particular aspects of your work that you particularly hold dear/that are particularly important to you (to a greater degree than other aspects)? (Prompt: What? Why?)
7.12 If you have to leave/jettison certain aspects of the job, what goes first and why?
7.13 Who do you most closely identify with in the trust as having most in common with you? (Prompt: Whose goals do you see as most aligned with your own?)
7.14 Would you say you have a strong sense of self-identity? How does this express/manifest itself? (Prompt: Does this express itself in your work?)
7.15 Do you see yourself continuing in a managerial role in the NHS in the future?
7.16 Is there anything else you would like to say about the issues we have discussed?
Appendix 6 Participant diary template
| Job title | ||
|---|---|---|
| Date | Activities, tasks and meetings | Groups and/or job titles of those interacted with |
| 8.30 a.m. – 10.30 a.m. | ||
| 10.30 a.m. – 12.30 p.m. | ||
| 12.30 p.m. – 2.30 p.m. | ||
| 2.30 p.m. – 4.30 p.m. | ||
| 4.30 p.m. – 6.30 p.m. | ||
Appendix 7 The coding frame in NVivo
The following appendix describes the main tree nodes developed within the coding frame in NVivo.
Who
|
||
|
||
|
|
|
|
||
|
||
|
||
|
||
|
||
|
||
|
||
|
|
|
|
||
|
What
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
||
|
|
|
|
|
|
|
||
|
|
How work is experienced
|
|
|
|
||
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Identity
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Mobilising identity
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Organisation
|
||
|
|
|
|
|
|
|
|
|
|
||
|
||
|
|
|
|
|
Appendix 8 Self-definition and other facets of identity
The following tables supplement the presentation in Chapter 5 .
| Group affinity | Self-definition | Total | |
|---|---|---|---|
| ‘I am a manager’ | ‘I am a manager, but’ and ‘I am not a manager’ | ||
| Individual | 4 | 4 | 8 |
| % within ‘Individual’ | 50 | 50 | |
| Expected count | 2.7 | 5.3 | |
| Observed count as % of expected count | 150 | 75 | |
| Work team | 5 | 5 | 10 |
| % within ‘Work team’ | 50 | 50 | |
| Expected count | 3.3 | 6.7 | |
| Observed count as % of expected count | 150 | 75 | |
| Peer group | 1 | 11 | 12 |
| % within ‘Peer group’ | 8 | 92 | |
| Expected count | 4.0 | 8.0 | |
| Observed count as % of expected count | 25 | 138 | |
| Subtotal (without missing) | 10 | 20 | 30 |
| % within subtotal | 33 | 67 | |
| Missing | 20 | 38 | 58 |
| Totala | 30 | 59 | 88 |
| Values | Self-definition | Total | ||
|---|---|---|---|---|
| ‘I am a manager’ | ‘I am a manager, but’ | ‘I am not a manager’ | ||
| Performance ethos | 5 | 5 | 3 | 13 |
| Public service ethos | 14 | 5 | 12 | 31 |
| Subtotal | 19 | 10 | 15 | 44 |
| Missing | 11 | 9 | 24 | 47 |
| Totala | 30 | 19 | 39 | 88 |
| General education qualifications | Self-definition | Total | ||
|---|---|---|---|---|
| ‘I am a manager’ | ‘I am a manager, but’ | ‘I am not a manager’ | ||
| Level 5 | 3 | 1 | 3 | 7 |
| Level 6 | 11 | 10 | 16 | 39 |
| Level 7 | 9 | 5 | 10 | 25 |
| Level 8 | 1 | 1 | 9 | 11 |
| Subtotal | 24 | 17 | 38 | 82 |
| Missing | 6 | 2 | 1 | 9 |
| Totala | 30 | 19 | 39 | 88 |
| Meanb | 6.3 | 6.4 | 6.7 | |
| Median | 6 | 6 | 7 | |
| Count | 24 | 17 | 38 | |
| Management qualifications and training | Self-definition | Total | |
|---|---|---|---|
| ‘I am a manager’ | ‘I am a manager, but’ and ‘I am not a manager’ | ||
| Higher education qualifications | 11 | 6 | 17 |
| % within level | 65 | 35 | |
| Expected count | 6 | 11 | |
| Observed count as % of expected count | 183 | 55 | |
| Vocational qualifications | 4 | 7 | 11 |
| % within level | 36 | 64 | |
| Expected count | 3.9 | 7.1 | |
| Observed count as % of expected count | 103 | 99 | |
| Learning and development | 10 | 30 | 40 |
| % within level | 25 | 75 | |
| Expected count | 14 | 26 | |
| Observed count as % of expected count | 71 | 115 | |
| None | 2 | 7 | 9 |
| % within level | 22 | 78 | |
| Expected count | 3.1 | 5.8 | |
| Observed count as % of expected count | 65 | 121 | |
| Subtotal without missing | 27 | 50 | 77 |
| % within subtotal | 35 | 65 | |
| Missing | 3 | 8 | 11 |
| Totala | 30 | 58 | 88 |
| Tenure in the current job (years) | Self-definition | ||
|---|---|---|---|
| ‘I am a manager’ | ‘I am a manager, but’ | ‘I am not a manager’ | |
| Mean | 2.98 | 3.80 | 3.44 |
| Median | 2 | 2.25 | 2.5 |
| Minimum | 0.02 | 0.83 | 0.08 |
| Maximum | 12 | 16 | 10 |
| Count | 29 | 18 | 33 |
| Work experience outside the NHS | Self-definition | Total | ||
|---|---|---|---|---|
| ‘I am a manager’ | ‘I am a manager, but’ | ‘I am not a manager’ | ||
| Yes | 16 | 5 | 8 | 29 |
| % within positive answer | 55 | 17 | 28 | |
| Expected count | 10.3 | 6.72 | 12 | |
| Observed count as % of expected count | 155 | 74 | 67 | |
| No | 13 | 14 | 26 | 53 |
| % within negative answer | 30 | 33 | 60 | |
| Expected count | 18.7 | 12.3 | 22 | |
| Observed count as % of expected count | 30 | 114 | 118 | |
| Subtotal (without missing) | 29 | 19 | 34 | 82 |
| % within subtotal | 35 | 23 | 41 | |
| Missing | 1 | 0 | 5 | 6 |
| Totala | 30 | 19 | 39 | 88 |
Appendix 9 Education and vocational qualifications
| Main stages of education/employment | FHEQ in England, Wales and Northern Ireland | Vocational qualifications QCF/National Qualifications Framework for England and Northern Ireland | ||
|---|---|---|---|---|
| Level | Level | |||
| Professional or postgraduate education, research or employment | 8 | Doctoral degrees | 8 | Vocational qualifications Level 8 |
| Higher education, advanced skills training | 7 | Master’s degrees, postgraduate diplomas, postgraduate certificates | 7 | Fellowships NVQ Level 5 Vocational qualifications Level 7 |
| Entry to professional graduate employment | 6 | Bachelor’s degrees with honours, bachelor’s degrees, graduate diplomas, graduate certificates | 6 | Vocational qualifications Level 6 |
| Specialised education and training | 5 | Foundation degrees, HND | 5 | NVQ Level 4, HND, vocational qualifications Level 5 |
| Qualified/skilled worker, entry to higher education, completion of secondary education | 4 | HNC, CertHE | 4 | Vocational qualifications Level 4, HNC |
| Progression to skilled employment, continuation of secondary education | 3 | NVQ Level 3, vocational qualifications Level 3, GCE AS, A Level advanced diplomas | ||
| Secondary education Initial entry into employment or further education | 2 | NVQ Level 2, vocational qualifications Level 2, GCSEs at grade A*–C | ||
Appendix 10 What do managers do?
| Category | Scale of responsibility | Clinical vs. managerial responsibilities | Staff management load | Work week (hours) | Time in meetings as % of work time | % within the group with responsibilities outside trust | % within the group involved in cross-site work | Strategic input |
|---|---|---|---|---|---|---|---|---|
| JC | Team to specialty | ∼ 50/50 | 49 | 11 | 14 | 10 | ||
| 2b Junior nurse managers | Team to unit | ∼ 50/50 | Heavy | 50 | 12 | 8 | 0 | Informal, through local entrepreneurship |
| 3b Junior scientist managers | Team to specialty | ∼ 50/50 | Medium | 46 | 14 | 50 | 0 | None |
| 4 AHP managers | Team | ∼ 50/50 | Medium | 45 | 4 | 0 | 50 | None |
| JNC | Team to group of specialties, trust | 45 | 27 | 47 | 47 | |||
| 5b Junior managers of clinical units | Team to group of specialties | 0/100 | Heavy | 48 | 25 | 50 | 63 | None |
| 6b Junior managers of corporate units | Team to specialty, trust | 0/100 | Heavy | 44 | 29 | 43 | 29 | None |
| MC | Specialty to directorate | 20/80 | 57 | 33 | 26 | 33 | ||
| 1 Consultant managers | Specialty to directorate | 50/50 | Low | 65 | 27 | 17 | 17 | Considerable, strategic leadership of clinical services |
| 2a Middle nurse managers | Specialty to directorate | 10/90 | Medium | 55 | 37 | 21 | 29 | Minor (but nurse consultants have considerable regional or national leadership in their area) |
| 3a Middle scientist managers | Unit to specialty | 20/80 | Low | 45 | 34 | 60 | 40 | Minor within the trust, but some impact regionally/nationally through representation in professional bodies |
| 5a Middle managers of clinical units | Directorate | 0/100 | Medium | 52 | 21 | 0 | 100 | None |
| MNC | 49 | 35 | 32 | 29 | ||||
| 5a Middle managers of clinical units | Unit to directorate | 0/100 | Heavy | 47 | 35 | 32 | 32 | Strategy translation and elaboration (‘strategy is just a strapline’) |
| 6a Middle managers of corporate units | Trust | 0/100 | Low | 53 | 33 | 33 | 22 | Considerable, in specific functional areas |
Glossary
- Agenda for Change
- The NHS grading and pay system Agenda for Change allocates posts to one of nine pay bands based on the knowledge, responsibilities, skill and effort needed for the job.
- Cityscape
- Case study site two.
- Junior clinical managers
- Including ward sisters, ward managers, deputy sisters, occupational therapist team leader and chief renal technician (Agenda for Change banding 5–7).
- Junior non-clinical managers
- Including administrative managers, booking centre managers and research managers (Agenda for Change banding 4–7).
- Medics
- Term used to refer to all doctors, including junior doctors as well as consultants.
- Metropolitan
- Case study site one.
- Middle clinical managers
- Including clinical directors, heads of service, consultant scientists, matrons, divisional head of nursing and nurse consultants (Agenda for Change banding 8a–8d).
- Middle non-clinical manager
- Including directorate general manager, directorate assistant general manager and clinical business unit manager (Agenda for Change banding 8a–8d and 9).
List of abbreviations
- ACB
- Association of Clinical Biochemists
- AfC
- Agenda for Change
- AHP
- allied health professional
- CBU
- clinical business unit
- Cityscape
- Cityscape Hospital Trust
- CQC
- Care Quality Commission
- FHEQ
- Framework for Higher Education Qualifications
- HFMA
- Healthcare Financial Management Association
- HR
- human resources
- ILM
- Institute of Leadership and Management
- IT
- information technology
- JC
- junior clinical
- JNC
- junior non-clinical
- MC
- middle clinical
- Metropolitan
- Metropolitan Hospital Trust
- MNC
- middle non-clinical
- NEBS
- National Examining Board for Supervision and Management
- NIHR
- National Institute for Health Research
- NPM
- New Public Management
- PCT
- primary care trust
- QCF
- Qualifications and Credits Framework
- R&D
- research and development
- RCN
- Royal College of Nursing
- SDO
- Service Delivery and Organisation