Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/2002/16. The contractual start date was in February 2012. The final report began editorial review in June 2013 and was accepted for publication in October 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Morris et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction and background
Epidemiology
Estimates of the prevalence of childhood disability in the UK vary from 5% to 18%, depending on the definition or indicator of disability. 1 Most commonly, an estimate of 1 in 20 children is cited. 2 Based on the Family Resource Survey (2004–5), there are an estimated 952,741 ‘disabled’ children in the UK, which is 7.3% of the population of children aged 0–18 years (8.8% boys and 5.8% girls). 3,4 However, the survey used a definition that broadly comprises any long-term health conditions, including neurodisability, but also, for instance, health conditions such as diabetes, arthritis and asthma.
Neurodisability is an umbrella term for conditions associated with impairment of the nervous system and includes conditions such as cerebral palsy, autism and epilepsy; it is not uncommon for neurological impairments to co-occur. Aside from asthma, neurodisability probably represents the largest proportion of significant childhood disability. 5 Individually, many conditions that result in a neurodisability are rare, whereas, grouped together, they are relatively common.
Neurodisability is a UK term; there is a subspecialty of paediatric training within the Royal College of Paediatrics and Child Health devoted to this group of children. However, the term neurodisability is not defined, and there is no universally recognised agreement as to which conditions are included. The term has arisen as a way of describing a group of conditions which give rise to similar problems, health and educational needs, and which are commonly managed by the multidisciplinary teams skilled in multisystem health conditions.
Without a clear and agreed definition, it is not possible to derive consistent and reliable estimates of the prevalence of neurodisability to inform needs assessment and appropriate resource planning. The lack of a definition of neurodisability, and lack of clarity about which conditions are included, also hinders effective communication, especially when considering health outcomes and the planning and evaluating of health services, multiprofessional teams and care pathways.
In other English-speaking countries, the term neurodevelopmental disorders is used to describe similar conditions in children. For instance, we found a definition of neurodevelopmental disorders as ‘disorders where motor, cognitive, behavioural, and/or language functioning are affected by central nervous system impairments, resulting in a variety of challenges associated with ambulation, information processing, self-regulation and communication’. 6 To our knowledge, no definition is widely agreed on.
Health services for neurodisability
Although neurodisability comprises a heterogeneous group of conditions, these conditions have much in common in terms of resulting health-care needs. Children and young people affected by neurodisability have a range of impairments; some of these are relatively minor, but many give rise to complex health-care needs. As a consequence, they are among the most frequent and intensive users of the NHS, requiring care and support from health services across primary and community care, hospital services and specialist centres.
Although largely unable to cure the neurological impairments, health services aim to optimise functioning and to maintain/improve the health and well-being of these children, most of whom can be expected to survive into adulthood. 7 Funding and provision of health services for disabled children are recognised to be highly variable. 8 A report by Sir Ian Kennedy into improving health services for children and young people acknowledged that children ‘do not always get the attention and care from health care services that they need’. 9 He also recommended the need to identify a ‘common vision’ between families and professionals for what services are seeking to achieve (p. 54). 9 A further level of complexity is that NHS care for children is often integrated with education and social care services.
Disabled children are known to face health and social disadvantage. Thus, over recent years, a range of initiatives have sought to improve health and social care provision, for example the National Service Framework for Children, Aiming High for Disabled Children, and the Centre for Excellence and Outcomes in Children and Young People’s Services. The Every Child Matters outcome framework has provided a useful means to develop indicators assessing educational and social care outcomes for children and, with adjustments, is proposed to be appropriate and meaningful for disabled children. 10
Nevertheless, it has been difficult to assess the impact of NHS care on disabled children, as there is no overall measure of their health outcomes. Hence, identifying outcome measures of how the NHS is impacting on the health of children with neurodisability would be extremely useful, particularly if the measurement was grounded in the perspectives and priorities of children, young people and their parents. Identifying an agreed set of health outcomes between families and professionals would also provide a focus for the combined efforts of the NHS. In fact, such outcomes could constitute the ‘shared vision’ of what health services are trying to achieve for disabled children, as recommended by Sir Ian Kennedy.
Health outcomes
Outcomes of a health condition or injury can be considered within the bio-psychosocial framework expressed through the World Health Organization’s (WHOs) International Classification of Functioning, Disability and Health (ICF). 11 The WHO ICF classifies components of health and functioning as ‘body structures and functions’ and ‘activities and participation’. Thus, a disease or injury may lead to impairments of body structure or function, limitation in activities and/or restriction in participation. These impairments, limitations and restrictions are collectively referred to as disability, and the relationships between these components are mediated by environmental and personal factors. Key environmental factors are health-care services, systems and policies, and social interventions.
In the context of neurodisability, it is often difficult for health services to make changes in chronic impairments of ‘body functions and structures’. Consequently, there may be a greater likelihood of health and social interventions maintaining or improving ‘activities’ and/or the ‘participation’. Clearly, the constructs assessed using outcome measures should be those most appropriate to assessing likely impacts of health care, and must be credible to patients, in this instance children and young people affected by neurodisability, and their parents. 12,13
Patient-reported outcome measures
Patient-reported outcome measures (PROMs) assess the quality of care delivered to NHS patients from the patient perspective. PROMs measure a patient’s health at a single point in time, and are collected through short, self-completed questionnaires. PROMs aim to assess components of health, which are largely the components of the ICF under the rubric of health status or health-related quality of life (HRQoL). A wide range of generic and condition-specific PROMs has been developed for children and young people. 14 Identifying PROMs for neurodisability requires, first, identification of the precise constructs to be measured and, then, the gathering of evidence of psychometric performance of available measures. 12
Language and cultural issues can affect how people interpret and/or respond to questions; hence, one cannot simply assume that PROMs perform consistently across languages and cultures. 15 Therefore, for example, the Food and Drug Administration guidance on PROMs recommends that evidence be provided of the process used to test measurement properties across different language and cultures. 15
Structured reviews have identified generic and condition-specific PROMs that can be used with children. 14 Others have discussed conceptual issues pertaining to what such instruments measure for children and young people affected by neurodisability. 16–18 However, no systematic reviews have comprehensively appraised published research about the psychometric performance of generic PROMs when used with children and young people affected by neurodisability.
Children and young people have the right to report on their own health. 12 Although there has been wide recognition that children’s voices should be heard in research and service design, this is often not the case19 and, in particular, the voices of disabled children are frequently overlooked. Chronological age is not a clear criterion for judging when children are capable to self-report their health by completing a questionnaire, although children aged ≥ 8 years are widely believed to be competent. 12 Parent and carer proxy reports are the only way to assess outcomes for children cognitively unable to self-report, but these do represent a different perspective to the child’s own view. However, as it is parents who typically seek health care on their child’s behalf, they need to be offered an opportunity to report their perspective. Ideally, both children’s and parents’ reports should be collected so that both perspectives are represented independently. 12
NHS Outcomes Framework
The NHS Outcomes Framework is part of a strategy that aims to deliver ‘the outcomes that matter most to people’. 20 Domain 2 of this framework will detail indicators of the ‘quality of life of people with long-term conditions’. Much of the detail is still being determined and will evolve over the coming years. 20
Proposed indicators include PROMs. There continues to be a substantive programme of methodological, applied and policy research about PROMs funded by the National Institute for Health Research (NIHR), Medical Research Council and the Department of Health. Much of the work has focused on adults and less on children. There is a clear direction of travel whereby PROMs look set to be one of the key performance indicators in the UK and other health systems. 13
As part of consultations on the initial proposal for the NHS Outcomes Framework , the Royal College of Paediatrics & Child Health proposed, pragmatically, that there should be a single PROM ‘for a basket of conditions’ rather than aiming to have one for every diagnosis. 21
The identification of suitable outcome measures will improve the evaluation of integrated NHS care for the large number of children affected by neurodisability, and has the potential to encourage the provision of more appropriate and effective health care. This research sought to contribute to positively improving children’s health outcomes by providing a high-quality means for measuring them. Identifying a common purpose for NHS services will improve health outcomes for children and young people affected by neurodisability. 9 Establishing appropriate outcome measures will help to ensure that NHS resources are deployed effectively and in an efficient manner.
Chapter 2 Aims and objectives
This research aimed to determine (a) which outcomes of NHS care should be assessed for children and young people affected by neurodisability and (b) the extent to which they can be measured by existing PROMs.
To address this aim, the study had the following objectives:
-
to identify key health-care outcomes, beyond measures of morbidity and mortality, that are regarded as important by children with neurodisability and parents
-
to ascertain what outcomes of services health professionals think are important for this group and to assess the extent to which they agree with families’ views
-
to seek consensus between families and professionals on what health outcomes are important and assess the usefulness of candidate generic PROMs for routine use in the NHS
-
to identify generic PROMs which have been evaluated using English-language questionnaires, and identify which best map onto outcomes identified as most important by families and professionals
-
to appraise evidence of the psychometric performance of these PROMs when evaluated with general population samples and/or children with neurodisability
-
to make recommendations about the use of generic PROMs to measure health-care outcomes for children with neurodisability.
As part of this research, the serendipitous opportunity arose to develop and determine agreement on a definition of ‘neurodisability’, in terms of the types of conditions it includes. Hence, the following objective was in addition to those specified in the protocol:
-
vii. to develop and test agreement with a definition of neurodisability that would be acceptable and meaningful to both families and health professionals.
The research design comprised three main work streams to address these aims and objectives:
-
a systematic review of the psychometric properties of generic PROMs used to measure the health of children and young people
-
qualitative research involving focus groups and interviews with children and young people affected by neurodisability, and separately with parents
-
an online Delphi survey with health professionals working with children and young people affected by neurodisability.
Finally, a consensus meeting with a small group of young people, parents and professionals was convened to seek agreement on a core set of more important aspects of health that could represent key health outcomes for neurodisability.
The report
The approach taken for each work stream, and findings from each approach, are described separately in the report. We begin by describing the public and patient involvement (PPI) in the research (see Chapter 3 ). Then, we describe the systematic review (see Chapter 4 ), the qualitative research (see Chapter 5 ) and online Delphi survey (see Chapter 6 ). In practice, these activities were carried out in parallel. In Chapter 7 we describe the consensus meeting. These sections are followed by a narrative synthesis (see Chapter 8 ), where the findings of each component of the research are brought together, conclusions are drawn, and relevant implications for health policy and research are considered.
Chapter 3 Public and patient involvement
We define PPI using the NIHR INVOLVE terminology as ‘where members of the public are actively involved in research projects and in research organisations’, as distinct from being research participants. 22 In this research, the members of the public involved were parents of children and young people. This chapter describes how parents of children affected by neurodisability were involved as part of the research team, and discusses the impacts that parent involvement had on the research, parents and the researchers. This chapter is intended to describe the PPI activities and provide reflections rather than be a rigorous appraisal of the involvement. The report takes in to account the recommendations for complete and transparent reporting of PPI in health services research. 23
Peninsula Cerebra Research Unit and public and patient involvement
Involving stakeholders and members of the public in research is believed to improve the utility of applied health service research. 22 The Peninsula Cerebra Research Unit (PenCRU) at University of Exeter Medical School is committed to involving families of disabled children in all aspects of the research process. PenCRU achieves this involvement through recruiting and retaining a ‘Family Faculty’. Our rationale for involving families of disabled children in research embraces the philosophical as well as pragmatic advantages and policy-relevant advantages. 24
The PenCRU Family Faculty is currently a cadre of several hundred parents of disabled children, mostly resident in Devon, who have indicated a willingness to be involved in research. We have learned to be flexible in our approaches to PPI in the context of childhood disability research. We understand that being involved in research is not a top priority for these parents and, therefore, provide opportunities for them to be involved in research at a level that suits their situation and the time they have available. Therefore, while our overall approach and ethos is to seek to work in partnership with families, in practice our methods for PPI vary from being wholly collaborative to, in other instances, being relatively consultative.
Methods
The chief investigator (CM) conceived the idea for the research based on policy relevance and personal interests, skills and experience; we do not believe that parents in the Family Faculty would have suggested the topic. However, the proposal was discussed and endorsed by the PenCRU advisory group prior to applying for funding. One parent participated as a co-applicant on the application, although their contribution to the protocol was consultative regarding the salience of the research rather than methodological.
Subsequent to funding being approved by NIHR, the opportunity to be involved in the research was advertised to the Family Faculty by e-mail. Including the parent who was a co-applicant, five parents volunteered to become involved. Four of these parents participated alongside members of the research team in the first co-investigator meeting held in Exeter, UK, in November 2012, and three participated in the co-investigator meeting held towards the end of the project, in April 2013.
Parents participated in several meetings during the research to help develop and review appropriate topic guides for the qualitative research (described in more detail in Chapter 5 ), to hear progress and ask questions about the systematic review, contribute to and refine the definition of neurodisability, and to reflect on the outcomes suggested by professionals in the Delphi survey (see Chapter 6 ). Parents also communicated and contributed by e-mail, particularly in relation to developing the definition. The time that parents contributed to the research was acknowledged financially, and their expenses were reimbursed.
The Research Fellow (AJ) convened involvement activities with support from the PenCRU Family Involvement Co-ordinator (CMc) and chief investigator (CM). Meetings were held generally during the school day (10 a.m. to 1 p.m.) and, although they were structured with an agenda, the meetings were informal and discursive, and followed by a sociable lunch.
Parents were provided opportunities to comment on the final report and conclusions and recommendations, and helped to write the plain English summary. They will help to produce plain language summaries for subsequent academic papers produced from the research, and help in implementing the dissemination strategy for the findings.
Measuring the impact of the PPI was not a formal element in the protocol. Nevertheless, we sought the views of the parents who had been involved using a feedback questionnaire. We asked parents how they had been involved in the research; their general experience of being involved; what were positive or good things about being involved; whether there were any parts of the experience of being involved that were not so good or could have perhaps been better; whether or not they felt that they had an impact on the way the research was done; whether or not being involved had any particular impacts on them; and whether or not they felt part of the research team. Members of the whole research team were offered the opportunity to comment by e-mail on whether they felt parents having been involved had an impact on the research or on them personally.
Parent feedback
Parents who gave feedback generally described their involvement as having been part of a ‘group of parents’ involved with the research team. They recalled the co-investigator meetings, other meetings, being sent documents and commenting on these by e-mail. They described their experience generally as interesting and educational, and appeared to have enjoyed meeting other members of the team and adding their own perspectives to those expressed by others in the team. There were indications that they felt that any impact they might have had on the research was as a group, rather than by them as individual parents. Their impression was that their greatest impact on the research was their contributions to the definition of neurodisability.
While they did feel involved in the research, they did not feel that they were necessarily integral to the research team, and one expressed that they felt in some ways the research could have been carried out without them. One parent indicated that they would have liked greater involvement in the interviews and analysis for the qualitative research but also appreciated that parents are busy and they may not have been able to be more involved, even if the opportunity had been offered. One indicated that they wished that they could have been more help to the team, which was expressed as a slightly negative reflection.
Researcher perceptions
Members of the research team in Exeter felt that parents made significant and valuable contributions both at co-investigator meetings and through their other contributions. In the first co-investigator meeting, parents were noted to have made important contributions in the small group discussion planning the qualitative research. At the second co-investigator meeting, parents were felt to have provided important perspectives to the general discussions interpreting the findings of the three research streams, and in particular the discussion on how to approach and conduct the consensus meeting. Involving parents at these meetings meant that documents and presentations had to be prepared in accessible formats, which may have taken a little more time. The feeling generally among researchers appeared to be that parents’ input positively influenced the dynamics of discussion.
The researchers involved in the Delphi survey that developed the definition of neurodisability felt that the contributions of parents made by e-mail and at meetings were invaluable. The two meetings the Exeter team had with parents to develop the topic guides for the qualitative research were felt to have been crucial to developing an appropriate format for these events. Researchers carrying out the systematic review found it difficult to find ways to involve parents meaningfully and usefully in that aspect of the research due the technicalities of psychometric evaluation, and the tasks associated with systematic reviews generally.
Feedback from members of the research team based elsewhere in the UK was that the approach taken to PPI in this research was laudable, and went beyond the ‘tick-box’ approach that they had observed previously with some other projects. One researcher who was less familiar with childhood disability felt educated to the demands of parenting disabled children by meeting and talking with the parents, and remarked profound admiration for their contributions to the research given the demands of their daily lives.
Discussion
There was a general feeling that this project presented a number of challenges for enabling the full collaborative involvement of parents, especially given the technical nature of the systematic review. There are several opportunities for PPI when conducting systematic reviews: suggestion of the topic and development of specific research questions; in the development of the protocol and determining the appropriate inclusion and exclusion criteria; and in the conduct of the review by helping to draft or review the report. 25 For this project, the opportunity to involve parents in each of these activities was somewhat compromised due to the topic and research questions having been predetermined, and the technical understanding required for appraising the psychometric aspects of PROMs.
There were greater opportunities for involving parents as part of the research team in planning the qualitative research and Delphi survey with professionals. Pragmatically, there were few opportunities to involve parents in the analysis of qualitative data, as members of the research team (AA and AF) who led this aspect of the analysis were based in London. Planning more substantive involvement of parents throughout the qualitative analysis may well have provided enhanced insight and depth of analysis; nevertheless, it would also have taken more time, and would have needed to be factored into the overall project management.
We have learned from this project that full collaborative involvement of families in designing and managing the project would have provided greater scope for impacting on the research from the start, and also may have enabled us to plan greater opportunities for involvement throughout. Developing a more detailed plan for involvement activities as part of the protocol may have been beneficial. In addition, producing a plain language summary of the protocol would have been helpful to assist parents to understand the context and purpose of the study; the plain language summary would have aided advertising of the opportunity for being involved. Time and interest of parents permitting, providing a package of introductory training for parents about PROMs and appraising measurement properties would have been ideal.
In terms of evaluating the impact of involving parents in childhood disability research generally, it may be useful to record the preconceived notions and plans that researchers take into meetings with parents, and recording afterwards what, if anything, has changed by the end of the meeting. Involving disabled children and young people more fully as partners in research requires resources to identify interested young people and to support them throughout their involvement. There remains scope for methodological research to learn more about appropriate approaches to PPI in the childhood disability research context.
Summary
There was a strong commitment to involving parents of children and young people affected by neurodisability in this research. In practice, a number of challenges were identified. In particular, the topic and technical methodology presented opportunities for more innovative involvement activities, such as a plain language summary of the protocol, or providing training. On balance, involvement of parents was perceived positively by those parents involved and by the researchers.
Chapter 4 Systematic review of patient-reported outcomes for children and young people
Aims and objectives
The aims of the review were to identify generic PROMs used to measure the health of children and young people and to appraise psychometric evidence of the performance when evaluated using English-language questionnaires.
The objectives for the systematic review were:
-
to identify eligible candidate generic PROMs for measuring the health of children and young people
-
to identify peer-reviewed publications of studies in which the psychometric performance of candidate PROMs had been evaluated in general populations
-
to identify peer-reviewed publications of studies in which the psychometric properties of candidate PROMs had been evaluated specifically in a population of children and young people affected by neurodisability
-
to appraise the methodological quality of the identified studies that evaluated psychometric properties of candidate PROMs
-
to appraise the evidence for the psychometric properties of candidate PROMs both in general populations and with children and young people affected by neurodisability.
Methods
The systematic review was designed in two stages. In stage 1, we sought to identify all generic PROMs used to measure the health of children and young people < 18 years of age. In stage 2, we identified and critically appraised peer-reviewed publications of studies in which the psychometric performance of identified candidate PROMs had been evaluated with children and young people. In stage 2, studies were categorised depending on whether they evaluated PROMs in (i) a general population of children or (ii) children and young people affected by neurodisability.
The systematic review was conducted following the general principles published by the NHS Centre for Reviews and Dissemination. 26 The systematic review team developed a detailed protocol for the review from the original proposal (www.netscc.ac.uk/hsdr/files/project/HSR_PRO_10–2002–16_V01.pdf). We applied to publish the full protocol with PROSPERO in February 2012; however, we were informed that, as a methodology review, our systematic review did not meet their inclusion criteria at the time. However, the protocol was published on the Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for the South West Peninsula (PenCLAHRC) website (http://clahrc-peninsula.nihr.ac.uk/patient-reported-outcome-measures-in-children-with-neurodisability.php). The protocol was updated to take account of methodological decisions that were required as the review progressed.
Stage 1: identification of patient-reported outcome measures
Search strategy
The search strategy was designed by an information specialist (MR) following consultation with the systematic review team, and with reference to the methodological filters published by the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) group27 and the construct filters developed by the Oxford PROMs group. 28 The strategy used a combination of medical subject headings (MeSH) and free-text terms. Search terms were grouped as follows:
-
group 1: general names for measures (e.g. questionnaires, instruments or tools)
-
group 2: multidimensional health construct terms (e.g. quality of life or health status)
-
group 3: terms to describe children and young people (e.g. children, teenagers or adolescents).
The terms within each group were combined with a Boolean OR command and were searched in combination using a Boolean AND command. Piloting this search strategy produced a total of 38,893 citations. Systematic screening of this number of citations was judged to be too burdensome within the confines of the resources allocated to the project. A fourth set of terms was therefore added to increase the specificity of the search:
-
group 4: terms relevant to psychometric performance (e.g. validity or reliability).
As this project was conceived to inform the NHS Outcomes Framework in the UK, we were interested only in PROM questionnaires that were available and evaluated in English; hence, the search was limited to English language. The search was also limited by date to publications from 1992, as the team agreed that it was unlikely that PROMs had been developed before this date.
The search strategy was designed for MEDLINE (via OvidSP) and modified for EMBASE and PsycINFO (via OvidSP) and Cumulative Index to Nursing and Allied Health Literature (CINAHL) (via EBSCOhost). The searches were run on 20 and 21 March 2012. Separate searches were carried out on the Oxford PROM bibliographic database and Patient-Reported Outcome and Quality of Life Instruments Database. Reference lists of systematic reviews were also checked. 14,29–32 The search strategy (for MEDLINE/OvidSP) is shown in Appendix 1 . All search results were exported to reference manager software (EndNote X6, Thomson Reuters, CA, USA) and deduplicated. EndNote was used to manage the citation database throughout the project.
Inclusion and exclusion criteria
The aim of this stage of the review was to identify potential candidate PROMs. Eligibility criteria were developed to guide selection ( Table 1 ).
| Inclusion criteria | Specification |
|---|---|
| Population | Children and young people < 18 years old |
| Instruments | Generic PROMs used in the English language; child self-report and/or parent (primary carer) reported |
| Evidence | Indication of testing/reporting of psychometric performance, such as aspects of validity or reliability |
| Study design | Any type of study design |
| Date | 1992 to March 2012 |
| Language | English language |
| Exclusion criteria | Specification |
| Instrument not used in a population of children (< 18 years) | |
| Condition-specific PROMs | |
| Instruments administered by an interviewer | |
| Any instrument where the proxy respondent is not a parent or primary carer (e.g. clinicians or teachers) | |
| English-language version not used |
Study selection
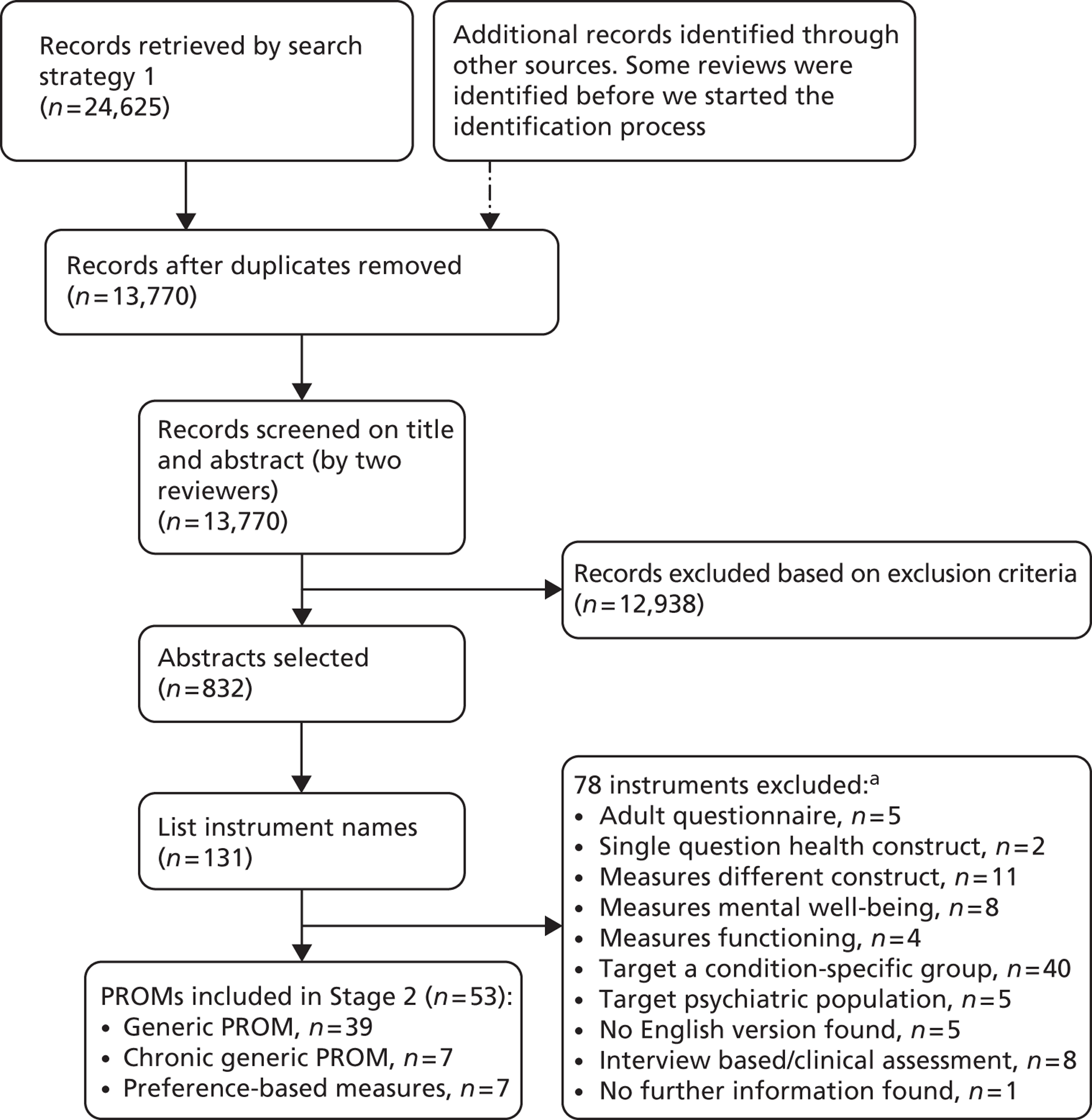
Two groups of reviewers (group 1: AJ, VS, SB; group 2: CM, JTC, MR, DM, RW, RA) independently screened all titles and abstracts to locate papers in which potential candidate PROMs were cited. Discrepancies were discussed and resolved with the arbitration of a third reviewer (either CM or AJ), where necessary. A flow chart describing the process of identifying relevant literature for this stage of the review can be found in Figure 1 .
FIGURE 1.
Flow chart showing identification and selection of potentially eligible candidate PROMs. a, Some instruments were excluded for more than one reason.
Data extraction
The result of this stage of the search was a list of potentially eligible candidate PROMs. Names and acronyms of all PROMs cited were extracted by one reviewer (AJ) who applied the eligibility criteria. Where there was insufficient detail provided in the paper to address all eligibility criteria, additional information was sought by internet searching.
Stage 2: identification of studies evaluating psychometric performance of patient-reported outcome measures
Search strategy
The search for the second stage of the review was designed using the names, alternative names and standard acronyms of the candidate PROMs identified in stage 1. For each candidate PROM, an individual search strategy was created to identify studies where the PROM had been used and evaluated in general populations (search 2.1). Three groups of search terms were used:
-
group 1: name(s) of the PROM
-
group 2: terms to describe children and young people
-
group 3: psychometric terms (e.g. validity or reliability).
The electronic search was designed for MEDLINE (via OvidSP) and modified for EMBASE and PsycINFO (via OvidSP). No language or date limits were applied to the search. The search used in MEDLINE (OvidSP) can be found in Appendix 2 . In total, 51 searches were run on each of the three databases between 18 July and 5 September 2012.
A further search strategy was designed to identify studies where candidate PROMs might have been used specifically with neurodisability (search 2.2). Three groups of search terms were used:
-
group 1: name(s) of the PROM
-
group 2: terms to describe children and young people
-
group 3: neurodisability terms, including key exemplar conditions.
The terms used included MeSH terms, and variations of the three exemplar conditions set out in our original proposal, namely cerebral palsy, autism and epilepsy. The search was designed in MEDLINE (OvidSP) and modified for EMBASE, PsycINFO and the Allied and Complementary Medicine Database (via OvidSP), CINAHL (via EBSCOhost) and NHS Database of Economic Evaluations. Searches were run between 12 and 25 September 2012. The strategy used for MEDLINE/OvidSP can be found in Appendix 3 .
Backwards citation chasing (one generation) was carried out using all reference lists from papers included in this stage of the review. Forward citation chasing was carried out between 28 January and 6 February 2013 using Science Citation Index and Social Science Citation Index (via Web of Knowledge) for included studies. Search results were exported into separate EndNote libraries created for each PROM.
We sought to locate a copy of each questionnaire; if a copy was not readily available, authors and/or developers of the PROMs were contacted to request a copy. We also contacted the authors or developers of all PROMs for which no evidence of the psychometric performance in an English-speaking population was found.
Inclusion and exclusion criteria
The aim of this stage of the review was to identify evidence for the performance of candidate PROMs when evaluated with children and young people. Criteria to guide inclusion and exclusion are shown in Table 2 .
| Inclusion criteria | Specification |
|---|---|
| Population | English speaking children and young people < 18 years old |
| General and/or neurodisability populations | |
| Instruments | Generic PROMs as listed as a result of stage 1; child self-report and parent (primary carer) reported measures are eligible |
| English version of the instrument administered | |
| Evidence | Reporting of any aspects of psychometric performance, including reliability, validity, responsiveness, precision, interpretability, acceptability and feasibility |
| Study design | Studies specifically designed to evaluate psychometric properties. Cross-cultural studies were included if referencing an English-language version of the instrument |
| Date | Inception of databases to September 2012 |
| Forward citation chasing until February 2013 | |
| Language | English version of the PROM administered |
| Paper written in English | |
| Exclusion criteria | Specification |
| Instrument/study design | Adult PROMs |
| PROM was used only as a ‘gold standard’ to test other instrument | |
| Incidental mention of psychometric evidence in studies designed not designed to evaluate those properties, e.g. trials of interventions | |
| Studies addressing ‘preference weighting or scaling’ issues for preference-based measures | |
| Population | Fewer than 10% of the sample were < 18 years |
| Data presentation | Data regarding neurodisability not reported separately in mixed samples of chronic conditions |
Study selection
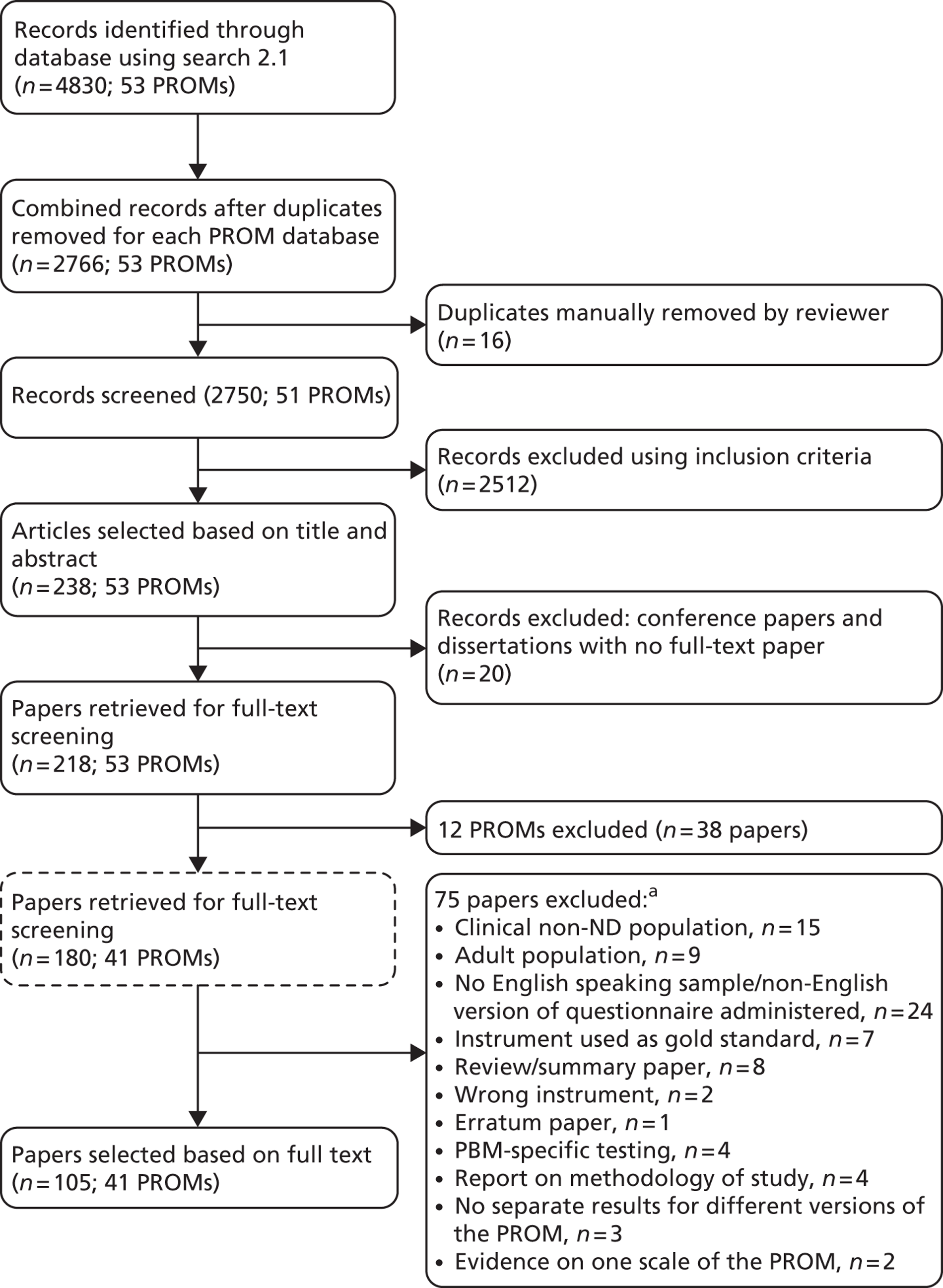
Titles and abstracts of all unique citations were screened against the eligibility criteria by one reviewer (AJ) and a sample of 10% of decisions was checked by a second reviewer, (CM) with disagreements resolved by discussion with a third (CJ) where necessary. The full text of any potentially relevant article was retrieved and screened using the same procedure. A flow chart describing the process of study selection for this stage of the review can be found later in this chapter ( Figure 2 ).
Data extraction
Data were extracted using standardised, piloted data extraction forms. For each included candidate PROM, the following were extracted: name of PROM and acronym, purpose of measurement, number of items, the responder, completion time, age range, recall period, response options, key reference paper, and types of domains/dimensions assessed.
We determined that there were three types of eligible candidate generic PROMs: (i) generic PROMs, designed for use across all people; (ii) chronic-generic PROMs, intended for use across people with chronic conditions; and (iii) preference-based measures (PBMs). Scores from generic and chronic-generic PROMs are typically determined directly from responses to items in the questionnaires. PBMs have two components; the responses to patient questionnaires are transformed using a weighting system, based on valuation of health states by a reference population, to produce a single index score between 1 and 0 (or less), where 1 equates to full health and 0 is dead. 33,34
The domain scales and items of each candidate PROM were inspected with reference to the WHO’s International Classification of Functioning, Disability and Health, Children and Youth Version (ICF-CY)11,35 to provide an indication of the constructs each instrument was measuring. It was not our aim to allocate every item from candidate PROM questionnaires to a precise ICF code using proposed linking rules. 36 Instead, our mapping sought to use the ICF-CY to describe what the scales of each candidate PROM proposed to measure. We coded at the higher levels of the ICF-CY, and also identified separately constructs not represented in the ICF-CY.
For each paper describing a study evaluating the psychometric performance of an eligible candidate PROM, the following descriptive data were extracted: instrument version, first author name, publication year, study aim, study population, number of participants, age range, mean age [standard deviation (SD)], and setting/country where the study was conducted. Data were extracted by one reviewer (KA/AJ) and checked by a second reviewer (AJ/KA), with disagreements resolved by discussion with a third (CM) where necessary.
For each included paper, the methodological quality of the study and the completeness of the report were assessed using the COSMIN checklist. 37 The COSMIN checklist assesses the methods and reporting of internal consistency, reliability, measurement error, content validity, structural validity, hypothesis testing, cross-cultural validity, criterion validity and responsiveness. Cross-cultural validity is not reported as we only included studies using an English version of the eligible PROMs. The checklist was administered by one reviewer (CM) and a 10% sample was rated by a second (AJ). Studies that used Rasch analysis were also assessed by one of the team with expertise in these techniques (AT). The COSMIN checklist uses a ‘worst score counts’ rating for methods used to test psychometric properties, producing a quality assessment of excellent, good, fair or poor. 37 Any discrepancies were resolved by discussion, or with the involvement of a third reviewer (CJ), where necessary.
Then, any data on evidence of the psychometric properties or performance of instruments were extracted including content validity (theoretical framework and/or qualitative research), construct validity (structural validity and hypothesis testing), internal consistency, test–retest reliability, proxy reliability, precision, responsiveness, acceptability and feasibility. Data were extracted by one reviewer (KA/AJ) and checked by a second reviewer (AJ/KA), with disagreements resolved by discussion with a third (CM) where necessary.
Appraisal of evidence for psychometric performance
Our original proposal focused on evidence of psychometric properties when evaluated with children and young people affected by neurodisability. However, we were mindful that some emerging PROMs may have only been tested with general populations, and it would be advantageous to be aware of the state of the evidence of the psychometric performance of such PROMs. Therefore, the evidence of psychometric performance for each instrument was organised by whether the sample in the study was (i) a general population of children and young people, (ii) children and young people with mixed chronic conditions that included neurodisability, or (iii) specifically, children and young people affected by neurodisability.
Evidence for each of these populations was studied separately for the three groups of PROMs: generic PROMs, chronic-generic PROMs, and PBMs.
Appraisal criteria
Standardised criteria and thresholds were used to judge the evidence of psychometric performance of each candidate PROM. 38,39 The criteria used to assess and select patient-completed instruments included their appropriateness for measuring the health of children and young people affected by neurodisability, and an appraisal of their validity, reliability, responsiveness, precision, interpretability, acceptability and feasibility. 38 A summary of the criteria and indices used to judge psychometric properties is provided in Table 3 .
| Psychometric property | Indicative criteria |
|---|---|
| Content validity | Clear conceptual framework consistent with stated purpose of measurement |
| Qualitative research with potential respondents | |
| Construct validity | Structural validity from factor analysis |
| Post-hoc tests of unidimensionality by Rasch analysis | |
| Hypothesis testing, with a priori hypotheses about direction and magnitude of expected effect sizes | |
| Tests for differential item and scale functioning between sex, age groups and different diagnoses | |
| Reproducibility | Test–retest reliability ICC > 0.7 adequate, > 0.9 excellent |
| Child- and parent-reported reliability ICC > 0.7 | |
| Internal consistency | Cronbach’s alpha coefficient: α > 0.7 and < 0.9 |
| Responsiveness | Longitudinal data about change in scores with reference to hypotheses, measurement error, minimal important difference |
| Precision | Assessment of measurement error; floor or ceiling effects < 15%; evidence provided by Rasch analysis and/or interval level scaling |
| Acceptability | Non-participation or non-response to surveys |
| Proportion of missing data | |
| Appropriateness | Content pertinent to children and young people affected by neurodisability |
| Excellent psychometric performance when evaluated with children and young people affected by neurodisability |
To demonstrate content validity, PROM developers should describe a clear conceptual framework underpinning the instrument, and incorporate qualitative research with potential respondents to inform development of the items in the questionnaire. This is also likely to ensure that the questionnaire has face validity to future potential respondents.
Construct validity concerns whether or not a scale is measuring what is stated as the purpose of measurement. Construct validity can be seen as comprising two aspects, internal and external. Internal construct validity is concerned with the valid structure of the scale, and is often examined through factor analysis. 40,41 Item response theory approaches also can apply an initial factor analysis, as they assume unidimensionality,42 but Rasch analysis often implements a post-hoc test of unidimensionality based upon analysis of the residuals. 43 External construct validity can take several forms; for example, hypothesis testing examines evidence of whether scales correlate well with other scales measuring a similar construct (convergent validity) or correlate poorly with instruments that are measured something unrelated (divergent validity). Correlations are considered low if r < 0.3, moderate if r lies between 0.30 and 0.49 and high if r < 0.5. 44 Hypotheses should be stated a priori, including the postulated direction and magnitude of correlation. 37 Discriminative validity describes whether or not an instrument detects ‘known differences’ between respondents.
Internal consistency is the extent to which all items in a scale are measuring the construct of interest and is assessed by Cronbach’s alpha statistic (α). Scales with an α statistic between 0.7 and 0.9 are considered to be composed of items that adequately measure a uniform construct. 45 The statistic assumes unidimensionality. If the assumption of local independence is violated, or there are simply a large number of items, Cronbach’s alpha may be inflated and/or an unreliable indicator. 45
All scores from PROMs include some level of measurement error, which can be estimated using calculations such as standard error of measurement;45 Rasch analysis estimates the measurement error for individual items (and persons) rather than the average of the scale level. 46
The reliability of instruments is determined by repeating administration on different occasions when respondents have not changed with respect to the construct being measured (test–retest). The level of agreement is also reported where child and parent responses are typically compared (inter-rater reliability). 38 Reliability coefficients are directly related to the variability in the population in which they are used;45 however, intraclass correlation coefficients (ICCs) exceeding 0.7 are generally regarded to indicate reliability for population-based research and ICCs exceeding 0.9 are considered to indicate reliability for use clinically with individuals. 45
Responsiveness describes the ability of instruments to detect important change when it has occurred. 47 Methods for evaluating responsiveness are either distribution based [effect size, minimal detectable change (MDC)] or anchor based [minimal important difference (MID)]. The effect size is a standardised measure of the magnitude of change, calculated by dividing the amount of change by the SD of the baseline score. 44 MDC is an indication of the amount of change required to have confidence that it is change beyond measurement error; a common standard is to use a 90% confidence level (MDC90). 48 The MID is the mean change in score reported by the respondents who indicate that they had noticed some small change. 49
Precision is concerned with the number and accuracy of distinctions made by an instrument. 50 Indices include how well the possible responses to each item are distributed over a true range. Use of Rasch analysis in scale development has suggested that scale scores vary in their precision (standard error) across the spectrum of the scale, with greater precision at the centre of the scale. Interval-level scales, such as those derived in the weighting of PBMs, inherently offer greater precision. A further aspect of precision is to examine whether there is any evidence of floor or ceiling effects, typically judged to occur when more than 15% of respondents’ scores aggregate at one end of the scale. 38
Acceptability to respondents is influenced by the design of a questionnaire, the number of items and the time necessary to complete the questionnaire. 51 Cognitive interviewing is a process to investigate how potential respondents understand PROM questions.
Appropriateness in this context is also dependent on evidence of excellent psychometric properties of candidate PROMs when evaluated with children and young people affected by neurodisability. Given that the purpose of the review is to identify and recommend a generic PROM for children < 18 years, and with different diagnoses under the umbrella of neurodisability conditions, we looked particularly for evidence of group invariance across age groups and different conditions. This would indicate that valid comparisons could be made across age and diagnostic groups.
Two practical issues considered were interpretability and feasibility. Interpretability is concerned with how meaningful the scores are produced by an instrument; indicators of interpretability are their face validity to those using the scores from PROMs. 51 Feasibility is also concerned with the researchers’ perspectives, and assesses whether or not the instrument is easy to administer and process, in terms of managing data and the calculation of scores. 52
Summarising evidence of psychometric performance
Several similar systems have evolved for summarising evidence to support psychometric properties of PROMs in systematic reviews. In our original protocol, we proposed using the system of the Oxford PROMs group: 0 for not reported; – for no evidence in favour; + for some evidence in favour; ++ for some good evidence in favour; and +++ for good evidence in favour. 28 The COSMIN group later proposed something similar: + positive rating; ? for an indeterminate rating; – negative rating; and 0 for no information available. 53 On balance, we elected to use a combination of these systems to summarise available evidence ( Table 4 ).
| Rating | Definition |
|---|---|
| 0 | Not reported |
| ? | Not clearly determined (poor study) |
| – | Evidence not in favour |
| +/– | Conflicting evidence |
| + | Some evidence in favour |
| ++ | Some good evidence in favour |
| +++ | Good evidence in favour (multiple studies) |
Summary ratings of evidence of psychometric performance were made using data extracted from included studies, with reference to whether or not standard criteria33,34 were met. When making the ratings, we also took account of the methodological quality of studies, number of studies, and giving further weight to any apparently independent studies that appeared not to have been conducted by the original developers. 54 We made an overall judgement separately for evidence emerging from studies conducted with (a) samples from general populations and (b) samples of young people with neurodisability.
Results
Search results stage 1: identification of patient-reported outcome measures
The first search, to identify potentially eligible PROMs, resulted in 13,770 records after duplicates were removed. Following screening of the records by two independent reviewers, 832 abstracts were reviewed for names and/or acronyms of potentially eligible PROMs. This resulted in a list of 131 PROMs (see Appendix 4 ), of which 78 were excluded based on the exclusion criteria. The flow chart in Figure 1 illustrates the different steps in the selection process.
In total, stage 1 identified the names of 53 potentially eligible candidate PROMs, including 39 generic PROMs, seven chronic-generic PROMs and seven PBMs.
Search results stage 2: identification of studies evaluating psychometric performance of candidate patient-reported outcome measures
Search for eligible studies in general population samples (search 2.1)
The combination of the searches for each of the 53 individual PROMs in general populations resulted in 4830 records. Screening the deduplicated file of 2750 records resulted in 238 records that were selected for full-text screening. In total, we retrieved 218 full-text papers. We excluded 12 further PROMs (and their corresponding 38 papers), as they did not match our inclusion criteria. These were instruments that were developed for adults or were dimension-specific to mental health, assessed health-related behaviours, or were screening tools.
This reduced the number of eligible papers to 180, which described 41 PROMs. Another 75 records were excluded on closer examination of the full text; most papers were excluded because they had not administered an English version of the PROM (n = 24) or because a clinical but non-neurodisability group of children and young people had been studied (n = 15). The flow chart in Figure 2 shows the different steps in the process and details on the different exclusion criteria and number of papers excluded. This search process resulted in the selection of 105 papers reporting on psychometric evidence on one of the 41 eligible candidate PROMs.
FIGURE 2.
Flow chart showing identification and selection of studies evaluating psychometric performance of PROMs in general populations (search 2.1). ND, neurodisability. a, Some papers were excluded for more than one reason.
Search for eligible studies in neurodisability samples (search 2.2)
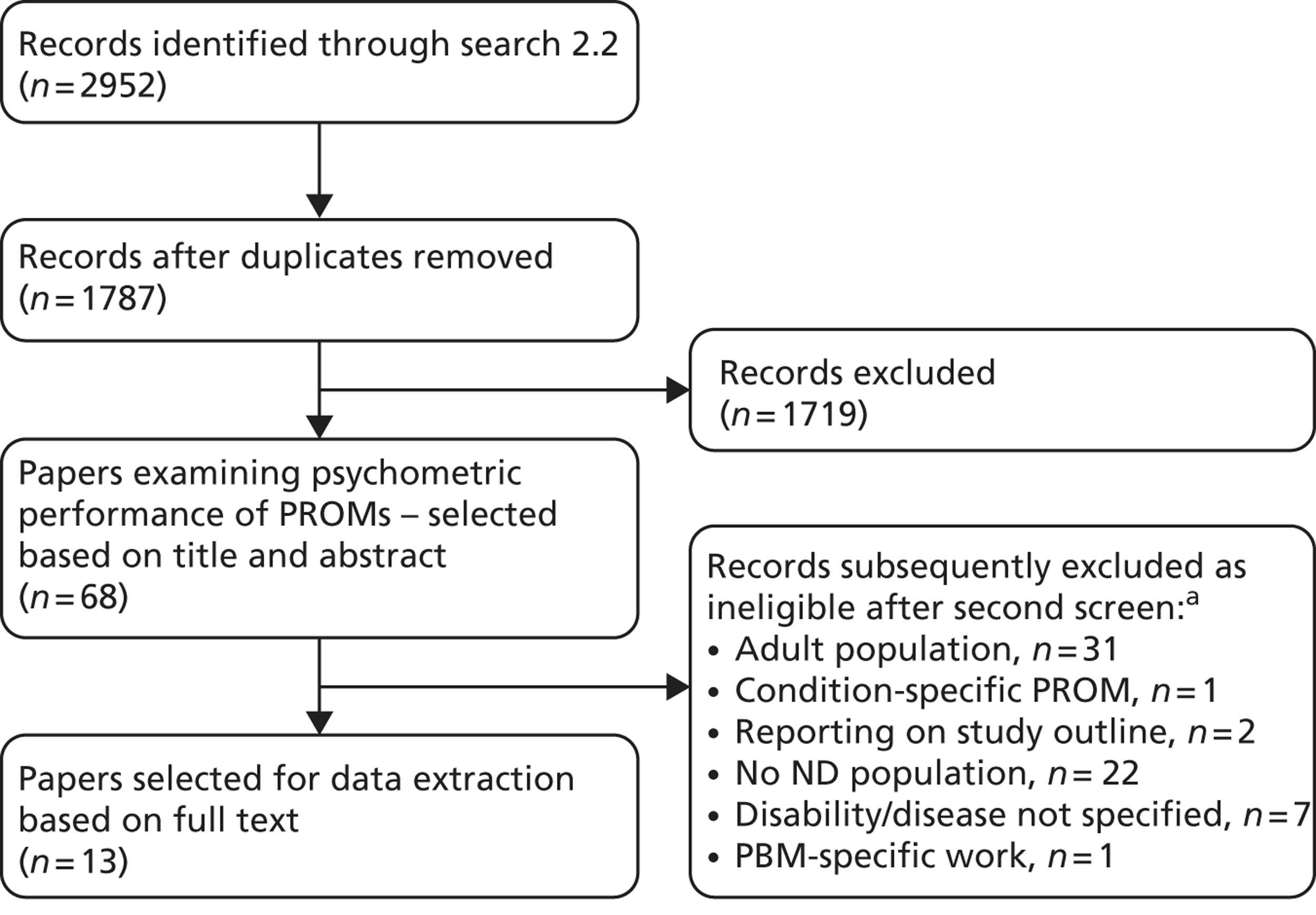
The combination of searches for the 53 individual PROMs used with neurodisability resulted in 2952 records. A total of 68 papers studying psychometric properties were selected based on title and abstract. After full-text screening, 13 papers were identified as eligible: nine were duplicates from search 2.1 and four new papers were selected for data extraction. Figure 3 gives an overview of the selection process.
FIGURE 3.
Flow chart showing identification and selection of studies evaluating psychometric performance of PROMs in neurodisability (search 2.2). ND, neurodisability. a, Some papers were excluded for more than one reason.
Citation chasing
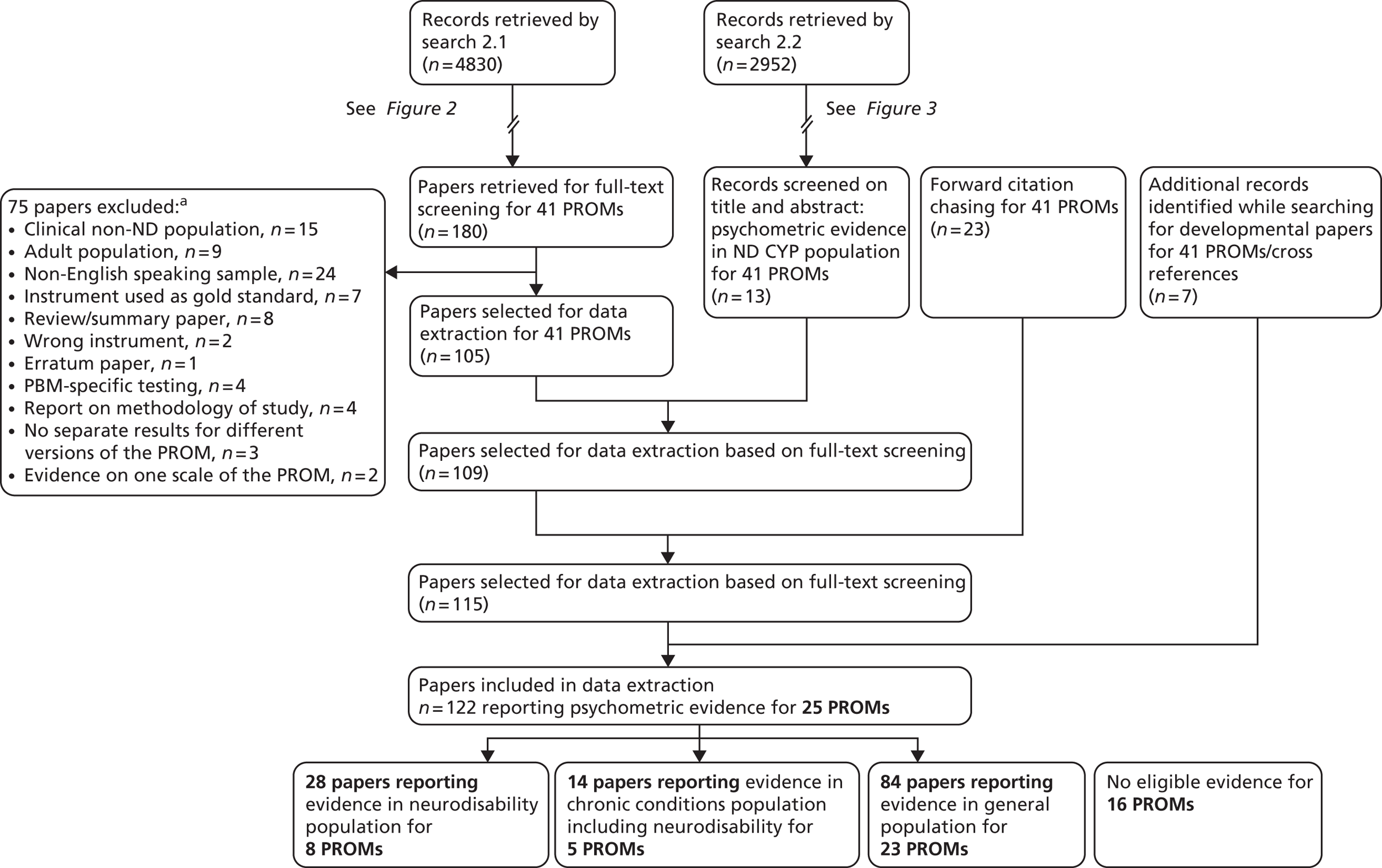
The forward citation chasing used 80 references; this resulted in 7858 records (5654 after deduplication). Filtering the EndNote file to only select records that mentioned validity (and derivatives, e.g. validation) or reliability (and derivatives) reduced the number of records to 235. Screening the titles and abstracts of these 235 records revealed 23 papers reporting on studies examining psychometric properties of a selected PROM in a population of children and young people with neurodisability. This strategy highlighted four papers not otherwise identified, which were included in data extraction. A further 10 papers were identified while searching for the key reference paper and were also included for data extraction.
Search results summary
In total, 126 papers were selected for data extraction. These papers report evidence from evaluations of the psychometric performance of 25 PROMs (notwithstanding that some PROMs have more than one version) evaluated in an English-language questionnaire. No evidence was found for 16 other PROMs.
Eligible evidence was found for:
-
19 generic PROMs
-
two chronic-generic PROMs
-
four PMBs.
The evidence is grouped according to the study population:
-
Eighty-four papers report results collected in a general population.
-
Fourteen papers report evidence for a PROM administered in a group of children with various chronic conditions including neurodisability; the results are not presented separately for each individual chronic condition.
-
Twenty-eight papers present results gathered in a neurodisability population.
The flow chart in Figure 4 illustrates the process of the selection of papers for data extraction.
FIGURE 4.
Summary of selection of papers for data extraction. CYP, children and young people; ND, neurodisability. a, Some papers have been excluded for more than one reason.
Data presentation
The results are presented within each category of PROM:
-
generic measures
-
chronic-generic measures
-
preference-based measures.
The following data are presented for each type of PROM:
-
Descriptive characteristics of all versions of the candidate PROMs.
-
There are substantively different versions of some PROMs, either with different target age groups, varying items, domains or dimensions assessed, or responder, short and long versions, or revised versions. Each variation has been catalogued.
-
-
Content assessed by the PROMs coded using the WHO ICF-CY.
-
The items of the questionnaires were mapped, as far as possible, to the chapter levels and domains of the WHO ICF-CY version.
-
-
Evidence of psychometric performance for candidate PROMs.
The data were further categorised by the sample with which the evaluation was conducted:
-
general population
-
mixed chronic conditions population including neurodisability
-
neurodisability population.
The evidence in each of the study populations is presented as follows:
-
a description of the study reported in the selected paper: instrument version, author, publication year, aim or purpose, study population, number of participants, age range, mean age (SD) and setting/country
-
the methodological quality of the paper rated following the COSMIN checklist
-
a summary of evidence of the psychometric performance of the PROM with reference to whether or not the study population was a sample of the general population or neurodisability.
Generic patient-reported outcome measures
Initially, in stage 1, 30 generic PROMs were identified. For 11 PROMs, no evidence was found from eligible studies meeting our inclusion criteria: Pictured Child’s Quality of Life Self Questionnaire [Autoquestionnaire de Qualité de Vie Enfant Image (AUQUEI): QUALIN,55 AUQUEI Soleil,56 AUQUEI Ours,57 OK.ado Questionnaire58], the Child’s Health Assessed by Self-Ladder (CHASL),59 the Duke Health Profile – Adolescent version (DHP-A),60 Health And Life Functioning Scale (HALFS),61 How Are You? (HAY),62,63 the Illness Perception Questionnaire (IPQ, IPQ Revised, Brief IPQ),64 Infant Toddler Quality of Life (ITQoL long and short versions),65,66 Nordic Quality of Life (QoL) Questionnaire,67,68 Quality of Life Questionnaire for Children (QLQC),69 the Quality of My Life (QoML)70 and the Dutch Organization for Applied Science Research – University Medical Centre Leiden [Toegepast Natuurwetenschappelijk Onderzoek – Academisch Ziekenhuis Leiden (TNO-AZL)] questionnaires [TNO-AZL Questionnaire for Preschool Children’s Health-Related Quality of Life (TAPQOL),71 TNO-AZL Questionnaire for Children’s Health-Related Quality of Life (TACQOL)72 and TNO-AZL Questionnaire for Adult Health-Related Quality of Life (TAAQOL)73].
The authors and or developers of these PROMs were contacted to verify that we had identified all available peer-reviewed papers. We received responses from the authors of the AUQUEI, the CHASL, the HALFS, the Nordic Quality of Life and the QLQC who sent us a full-text version of the PROM; no additional eligible papers were received. The characteristics of these PROMs can be found in Appendix 5 .
Generic PROMs with evidence from studies using an English-language questionnaire that have more than one version include:
-
Child Health and Illness Profile (CHIP) – age groups and short/long (four versions)74
-
Child Health Questionnaire (CHQ) – child/parent and short/long (three versions)75–77
-
Functional Status II Revised (FSIIR) – age group and short/long (six versions)78
-
KINDL – age group (three versions)82
-
Pediatric Quality of Life Inventory (PedsQL) – age group and short/long (10 versions)83–85
-
Personal Wellbeing Index (PWI) – revised and age groups (three versions)86
-
Student Life Satisfaction Scale (SLSS)87/Multidimensional SLSS (MSLSS) – revised and short/long (three versions)88–90
-
Youth Quality of Life instrument (YQoL) – short/long (two versions). 91
Generic patient-reported outcome measures: general characteristics
Table 5 contains descriptive characteristics for all identified versions of the 19 candidate generic PROMs, including the purpose of the instrument, number of items, age range, responder (self or proxy), response options, completion time (as mentioned in the key reference paper or manual), recall period, and the domains or dimensions assessed.
| Acronym | Author | Purpose | n of items | Age range | Responder | Response options | Completion time | Recall period | Domains/dimensions |
|---|---|---|---|---|---|---|---|---|---|
| CHAQ | Singh 199492 | To measure functional status (functional ability in daily living activities) | 30 Four disability related and two VAS |
0–18 years | Proxy | Four-level difficulty scale + VAS for pain and overall well-being | < 10 minutes | Past week | Dressing and grooming, arising, eating, walking, hygiene, reach, grip, and activities + (VAS) pain, overall well-being |
| CHIP-CE CRF | Riley 199874 | To broadly describe the health of children so that infrequent but important differences in health could be identified | 45 | 6–11 years | Self | Five graduated circle responses (frequency) with cartoons at beginning/end | 20 minutes | Past 4 weeks | Satisfaction, comfort, resilience, risk avoidance, achievement |
| CHIP-CE PRF (45) | Riley 199874 | To broadly describe the health of children so that infrequent but important differences in health could be identified | 45 | 6–11 years | Proxy | Five-option frequency scale (never–always) | 15 minutes | Past 4 weeks | Satisfaction, comfort, resilience, risk avoidance, achievement |
| CHIP-CE PRF (76) | Riley 199874 | To broadly describe the health of children so that infrequent but important differences in health could be identified | 76 | 6–11 years | Proxy | Five-option frequency scale (never–always) | 20 minutes | Past 4 weeks | Satisfaction (health, self), comfort (physical and emotional, restricted activity), resilience (family involvement, physical activity, social problem-solving), risk avoidance, achievement (academic performance, peer relations) |
| CHIP-AE | Riley 199874 | To broadly describe the health of adolescents so that infrequent but important differences in health can be identified | 138 | 1–17 years | Self | Mostly five-option frequency scale (no days–15 to 28 days) | 30 minutes | Past 4 weeks | Satisfaction, discomfort, resilience, risks, achievement |
| Healthy Pathways | Bevans 201093 | To broadly describe the health of youth in transition from childhood to adolescence and identify differences in health | 88 | 9–11 years | Self and proxy | Five-point Likert scale | 20 minutes | Past 4 weeks | Comfort, energy, resilience, risk avoidance, subjective well-being, achievement |
| CHQ-PF28 | Kurtin 199475 | To measure the physical and psychosocial well-being of CYP | 28 | 5–18 years | Proxy | Response options vary from four to six levels | 5–10 minutes | Past 4 weeks; global health items: in general; global change items: as compared with 1 year ago | General health, change in health, physical functioning, bodily pain, limitations in school work and activities with friends, behaviour, mental health, self-esteem, time and emotional impact on the parent, limitations in family activities and family cohesion |
| CHQ-PF50 | Landgraf 199876 | To measure the physical and psychosocial well-being of CYP | 50 | 5–18 years | Proxy | Response options vary from four to six levels | 10–15 minutes | Past 4 weeks; global health items: in general; global change items: as compared with 1 year ago | General health, change in health, physical functioning, bodily pain, limitations in school work and activities with friends, behaviour, mental health, self-esteem, time and emotional impact on the parent, limitations in family activities and family cohesion |
| CHQ-87 | Landgraf 199777 | To measure the physical and psychosocial well-being of CYP | 87 | ≥ 10 years | Self | Response options vary from four to six levels | 16–25 minutes | Past 4 weeks; global health items: in general; global change items: as compared with 1 year ago | General health, change in health, physical functioning, bodily pain, limitations in school work and activities with friends, behaviour, mental health, self-esteem, time and emotional impact on the parent, limitations in family activities and family cohesion |
| CHRS-PF | Maylath 199094 | To assess a child’s perception of general health | 17 | 9–12 years | Proxy | Five-point response scale rating agreement | 5 minutes | Today or ‘in general’ | No information |
| CHSCS | Hester 198495 | To measure a child’s perceptions of his or her health and health-related behaviours | 45 | 7–13 years | Self | Four-point Likert scale: more positive health perception, to more negative health perception | 20–30 minutes | No information | Activity exercise, personal grooming, physical, nutrition, behaviour, emotional, dental health, sleep, friends, substance use, general health, and family |
| COOP/WONCA | Nelson 198796 | To assess adolescents’ health and social problems (using a single-item picture-and-words chart) | 6 | Adolescent | Self | Five-point Likert-type scale with descriptors and cartoons | 4–5 minutes | During the past month | Physical fitness, emotional feelings, school work, social support, family communications, health habits |
| CQoL | Graham 199797 | To measure the child’s function, together with their own upset and satisfaction for each of the domains measured | 15 | 9–15 years | Self and proxy | Seven-point Likert scale rating of function, upset and satisfaction | 10–15 minutes | Over the past month | Activities, appearance, communication, continence, depression, discomfort, eating, family, friends, mobility, school, sight, self-care, sleep, worry, overall |
| ExQoL | Eiser 200098 | Computer-based assessment of quality of life as a result of perceived discrepancies between a child’s actual and ideal selves | 12 | 6–12 years | Self | VAS: not like me–exactly like me | 20 minutes | Not used | Symptoms (sleep, aches, food allergies, sickness), social well-being, school achievements, physical activity, worry, and family relationships |
| FSIIR long version, infants | Stein 199078 | Describes children’s functional status in the previous 2 weeks | 22 | Up to 1 year | Proxy | Three-point Likert scales: (1) difficulty; (2) extent this is due to illness | 20 minutes | Last 2 weeks | General health, responsiveness |
| FSIIR long version, toddlers | Stein 199078 | See above | 30 | 1–2 years | Proxy | See above | 5–30 minutes | Last 2 weeks | General health, responsiveness |
| FSIIR long version, preschoolers | Stein 199078 | See above | 40 | 2–4 years | Proxy | See above | 15–30 minutes | Last 2 weeks | General health, activity |
| FSIIR long version, school-age children | Stein 199078 | See above | 40 | 4 years and older | Proxy | See above | 15–30 minutes | Last 2 weeks | General health, interpersonal functioning |
| FSIIR-7 | Stein 199078 | See above | 7 | 0–16 years | Proxy | See above | 10 minutes | Last 2 weeks | General health |
| FSIIR-14 | Stein 199078 | See above | 14 | 0–16 years | Proxy | See above | 10 minutes | Last 2 weeks | General health |
| GCQ | Collier 199799 | To assess discrepancy between a child’s perception of their actual and desired lives | 25 | 6–14 years | Self | Five-point Likert scale: (1) child most like you; (2) child you would like to be | 15 minutes | Today | Perceived and preferred quality of life |
| KIDSCREEN-52 | Ravens-Sieberer 200579 | To assess children’s health and well-being; can be used as a screening, monitoring and evaluation tool | 52 | 8–18 years | Self and proxy | Five-point Likert scale assessing frequency or intensity | 15–20 minutes | Last week | Physical well-being, psychological well-being, moods and emotions, self-perception, autonomy, parent relations and home life, social support and peers, school environment, social acceptance (bullying), financial resources |
| KIDSCREEN-27 | Ravens-Sieberer 200780 | See above | 27 | 8–18 years | Self and proxy | Five-point Likert scale assessing frequency or intensity | 10–15 minutes | Last week | Physical well-being, psychological well-being, autonomy and parents, peers and social support, and school environment |
| KIDSCREEN-10 | Ravens-Sieberer 201081 | See above | 10 | 8–18 years | Self and proxy | Five-point Likert scale assessing frequency or intensity | 5 minutes | Last week | Physical activity, depressive moods and emotions, social and leisure time, relationship with parents and peers, cognitive capacities and school performance |
| KINDL: Kiddy-KINDLR | Bullinger 199482 | To assess the physical, mental and social well-being of children and adolescents using age-appropriate versions | 12 | 4–7 years | Self by interview | Three-point Likert scale assessing frequency | 15 minutes | Last week | Physical health, general health, family functioning, self-esteem, social functioning, school functioning |
| KINDL: Kid-KINDLR | Bullinger 199482 | To assess the physical, mental and social well-being of children and adolescents using age-appropriate versions | 24 | 8–12 years | Self and proxy | Five-point Likert-scale assessing frequency | 5–10 minutes | Last week | Physical health, general health, family functioning, self-esteem, social functioning, school functioning |
| KINDL: Kiddo-KINDLR | Bullinger 199482 | To assess the physical, mental and social well-being of children and adolescents using age-appropriate versions | 24 | 13–16 years | Self and proxy | Five-point Likert-scale assessing frequency | 5–10 minutes | Last week | Physical health, general health, family functioning, self-esteem, social functioning, school functioning |
| PedsQL Infant Scales | Varni 201183 | To assess the core dimensions of health according to the WHO as well as school functioning using age-appropriate versions | 36 45 |
1–12 months 13–24 months |
Proxy | Five-point Likert scale rating frequency | < 4 minutes | Past month | Physical functioning, physical symptoms, emotional functioning, social functioning, cognitive functioning |
| PedsQL Pediatric Quality of Life Inventory Trade Mark 4.0 Generic Core Scales | Varni 199984 | 21 23 |
2–4 years 5–7 years 8–12 years 3–18 years |
Self and proxy (proxy only age 2–4 years) | Physical functioning, emotional functioning, social functioning, school functioning | ||||
| PedsQL Short Form 15 Generic Core Scales | Chan 200585 | 2–4 years 5–7 years 8–12 years 13–18 years |
Self and proxy (proxy only age 2–4 years) | Physical functioning, emotional functioning, social functioning, school functioning | |||||
| ComQOL-S5 | Cummins 1997100 | To describe current health status and perceived importance and satisfaction with selected life domains | 21 | 11–18 years | Self | Mostly five-point Likert scale rating frequency, importance and satisfaction | 15–20 minutes | Stated for each items | Material well-being, health, productivity, intimacy, safety, place in community, emotional well-being |
| PWI-PS | Cummins 200586 | To assess degree of satisfaction with seven life domains | 7 | Up to 5 years | Proxy | Eleven-point happiness scale | 10–20 minutes | Not stated (today) | Standard of living, health, life achievement, personal relationships, personal safety, community connectedness, future security |
| PWI-SC | Cummins 200586 | To assess degree of satisfaction with seven life domains | 7 | 5–18 years | Self | Ten-point scale from very sad to very happy | 10–20 minutes | Not stated (today) | Standard of living, health, life achievement, personal relationships, personal safety, community connectedness, future security |
| QoLP-AV | Raphael 1996101 | To assess quality of life in three broad domains of adolescent functioning: being, belonging and becoming | 54 | 14–20 years | Self | Five-point Likert scale rating importance, satisfaction, control and opportunities | 40 minutes | Not stated (today) | Being: physical, psychological, spiritual Belonging: physical, social, community Becoming: practical, leisure, growth |
| SLSS | Huebner 199187 | To assess satisfaction with life as a whole | 7 | 7–14 years | Self | Six-point Likert scale rating agreement | < 5 minutes | Not stated | Family, friends, school, living environment, self |
| MSLSS | Huebner 199488 | To assess satisfaction with life as a whole and specific life domains | 40 | 8–18 years | Self | Six-point Likert scale rating agreement | 10 minutes | Not stated | Family, friends, school, living environment, self |
| BMSLSS | Seligson 200389 | To assess satisfaction with life as a whole and specific life domains | 6 | 8–18 years | Self | Seven-point Likert scale rating satisfaction | Less than 5 minutes | Past several weeks | Family, friends, school, living environment, self |
| MSLSS-A | Gilligan 200790 | 53 | Six-point Likert scale rating agreement | Past several weeks | Family, same-sex friends, school, opposite-sex friends, living environment, and self | ||||
| WCHMP | Spencer 1996102 | To assess parent-reported health and morbidity in infancy and childhood | 10 | Up to 5 years | Proxy | Four response options and free text | 10 minutes | Not stated | General health status, acute minor illness, behavioural, accident, acute significant illness, hospital admission, immunisation, chronic illness, functional health, HRQoL |
| YQoL-S | Edwards 200291 | To assess adolescents’ perceived quality of life in a broad sense | 13 | 11–18 years | Self | Five-point Likert scales with anchors for each point; 11-point rating scales with anchors each side of the scale | 5–10 minutes | In general or during the past month | Relation parents, future aspirations, loneliness, confidence, joy/happiness, satisfaction, lust for life, overall quality of life |
| YQoL-R | Edwards 200291 | To assess adolescents’ perceived quality of life in a broad sense | 56 | 11–18 years | Self | Five-point Likert scale with anchors for each point; 11-point rating scales with anchors each side of the scale | 15–20 minutes | In general or during the past month | Sense of self, social relationships, culture and community, and general quality of life |
After contacting the authors or developers of the PROMs, we received a free copy of the questionnaires and manuals for the CHIP, and paid for the Quality of Life Profile – Adolescent Version (QoLP-AV)101 and FSIIR. 78 For the Healthy Pathways,93 the Child Health Ratings Scale (CHRS)94 and the Exeter Quality of Life Measure (ExQoL),98 we located a copy of the items but had no instructions. The Comprehensive Health Status Classification System (CHSCS) has 45 items; the development paper provides instructions, details of the first eight items, and broadly describes the topics covered by the other items. 95 The Child Quality of Life Questionnaire (CQoL) has 15 items; instructions, an exemplar item, and domains covered by the remaining items are reported in the developmental paper. 97 Data for the CHQ were obtained from the website www.healthactchq.com; exemplar items and general information are provided.
Three PROMs provide different versions according to age group for self-report:
-
CHIP (two versions; youngest: 6 years old)74
-
KINDL (three versions; youngest: 4 years old)82
-
PedsQL (three versions of short and longer forms; youngest: 5 years old). 83–85
Instruments providing only a self-report version were:
-
Healthy Pathways (9–11 years)93
-
CHSCS (7–13 years)95
-
Dartmouth Primary Care Cooperative Information Project (COOP) (adolescent)96
-
ExQoL (6–12 years)98
-
Generic Children’s Quality of Life Measure (GCQ) (6–14 years)99
-
Comprehensive Quality of Life Scale – school version, fifth edition (ComQoL-S5) (11–18 years)100
-
SLSS (7–14 years)87
-
MSLSS (8–18 years)88
-
Brief MSLSS (BMSLSS) (8–18 years)89
-
YQoL – Surveillance version (YQoL-S) (11–18 years)91
-
YQoL – Research version (YQoL-R) (11–18 years). 91
Instruments providing only a proxy version were:
-
Child Health Assessment Questionnaire (CHAQ)92
-
CHRS – Parent Form94
-
FSIIR78
-
Warwick Child Health and Morbidity Profile (WCHMP). 102
The number of items ranged from 6 (COOP and BMSLSS) to 138 [CHIP – Adolescent Edition (CHIP-AE)]. Other PROMs with < 10 items were FSIIR-7, Personal Wellbeing Index – Pre-School (PWI-PS), Personal Wellbeing Index – School Children (PWI-SC), SLSS, KIDSCREEN-10 and WCHMP. The longer questionnaires require the longest completion times: CHIP-AE (30 minutes) and QoLP-AV (40 minutes).
Most questions used a Likert-scale response option; exceptions included the CHAQ [pain and overall well-being use a visual analogue scale (VAS)] and ExQoL (each statement is rated on a VAS ranging from ‘not like me’ to ‘exactly like me’). The CHIP – Child Edition (CHIP-CE) self-report version uses a scale of circles of increasing sizes to as the response options.
Three PROMs incorporate illustrative elements: CHIP-CE (drawings illustrate the question, and a ‘fun break’ page is provided where a child can make a drawing); COOP (response option is illustrated with a drawing); and ExQoL (each statement is accompanied by a picture).
The shortest recall period is ‘today’, and the longest recall period is ‘1 month’.
A note on the CQoL is that each question/statement is required to be rated for ‘health state’, ‘upset’ and ‘satisfaction’; this may become repetitive and confusing.
Generic patient-reported outcome measures: content mapping
The ICF-CY was used as a framework to report on the content assessed by the different PROMs. We mapped the items on the ICF-CY chapter headings using the 1424 ICF-CY core sets as a guide. This yielded a profile across ICF-CY categories for each of the PROMs.
The items or domains of the questionnaires were mapped onto the chapter headings of the ICF-CY (ICF-CY content mapping for generic PROMs can be seen in Table 6 ). If we could not identify a chapter that described the item or domain we used the additional ICF-CY categories (general health/mental health or physical health not covered by the generic or specific ICF-CY core sets) or categorised them under ‘other’.
| ICF-CY chapter | CHAQ | CHIP | HP | CHQ | CHRS | CHSCS | COOP | CQoL | ExQoL | FSIIR | GCQ | KIDSCREEN | KINDL-Kiddy | KINDL-Kid | KINDL-Kiddo | PedsQL | PWI | ComQol-S5 | QoLP-AV | SLSS | MSLSS | MLSS-A | BMSLSS | WCHMP | YQoL-S | YQoL-R | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 10 | 27 | 52 | ||||||||||||||||||||||||||
| Body functions | ||||||||||||||||||||||||||||
| Mental | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| Sensory and pain | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||||||||
| Voice and speech | ||||||||||||||||||||||||||||
| Cardiovascular, haematological, immunological and respiratory systems | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||||||||||||
| Digestive, metabolic and endocrine | ✗ | ✗ | ||||||||||||||||||||||||||
| Genitourinary and reproductive | ✗ | ✗ | ✗ | |||||||||||||||||||||||||
| Neuromusculoskeletal and movement | ✗ | ✗ | ||||||||||||||||||||||||||
| Skin and related | ||||||||||||||||||||||||||||
| Activities and participation | ||||||||||||||||||||||||||||
| Learning and applying knowledge | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||||||
| General tasks and demands | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||||||||||||
| Communication | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||||||||||
| Mobility | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||||||||||
| Self-care | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||||
| Domestic life | ✗ | ✗ | ✗ | |||||||||||||||||||||||||
| Interpersonal interactions and relationships | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| Major life areas | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||
| Community, social and civic life | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||
| Other | ||||||||||||||||||||||||||||
| General health – not defined | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||
| Mental health – not defined | ✗ | ✗ | ✗ | |||||||||||||||||||||||||
| Physical health – not defined | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||||||
| Environment | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||||
| Accidents/injuries | ✗ | |||||||||||||||||||||||||||
| Achievements in life | ✗ | ✗ | ✗ | |||||||||||||||||||||||||
| Being able to do what you want to do | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||||
| Challenging behaviour | ✗ | |||||||||||||||||||||||||||
| Food | ✗ | ✗ | ||||||||||||||||||||||||||
| Functional status | ✗ | |||||||||||||||||||||||||||
| Functioning of family | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||||
| Future aspirations | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||||||||
| Having fun (enjoyment) | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||||||
| Health condition/treatment | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||||||
| Health habits | ✗ | ✗ | ||||||||||||||||||||||||||
| Making decisions | ✗ | ✗ | ✗ | ✗ | ||||||||||||||||||||||||
| Quality of life | ✗ | ✗ | ||||||||||||||||||||||||||
| Satisfaction with life | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||||||||||||||
We had full-text versions of all questionnaires except for two PROMs. For the CHQ we used the domains and exemplar items available online (www.healthactchq.com). The CQoL was mapped on to the ICF-CY using the variables reported in the developmental paper. 97 We paid to receive a full-text questionnaire (and manual) of the QoLP-AV and the FSIIR.
Overall, the domain ‘activities and participation’ is most covered by the generic PROMs (see Table 6 ). The CHQ, CHIP, CQoL, PedsQL, QoLP-AV and the YQoL-R each cover a minimum five of the nine chapters. None of the items of the CHRS, SLSS and WCHMP cover an ICF-CY Activity and Participation domain.
‘Mental functioning’ and ‘sensory functions and pain’ are the most commonly covered domains in the ICF-CY Body Functions and Structures section.
Many PROMs have at least one item that maps on to the environment domain and ask about health in general. From the topics not covered by the ICF-CY, ‘being able to do what you want to do’, ‘having fun’ and ‘satisfaction with life’ score highest.
The Healthy Pathways, KIDSCREEN-52 and the QoLP-AV broadly seem to cover aspects of both ‘body functions’ and ‘activities and participation’.
Generic patient-reported outcome measures: psychometric performance with general population
We found 73 papers that reported evidence from studies of the evaluation of the psychometric performance of 19 generic PROMs. Some have also been tested in a sample with neurodisability. The PROMs that have most studies reporting evidence are:
-
CHIP (n = 6)
-
CHQ (n = 8)
-
KIDSCREEN (n = 12)
-
PedsQL (n = 16)
-
SLSS/MSLSS (n = 22).
First, we describe the studies, reporting the instrument and version under study, the author and publication year of the paper, the aim of the study and a description of the study population, the number, age range and mean age (SD) of the participants included and the study setting and country ( Table 7 ). The methodological quality of these studies is reported in Table 8 .
| Instrument version | Author | PY | Aim/purpose | Study population | n | Age range | Mean age (SD) | Setting, country |
|---|---|---|---|---|---|---|---|---|
| CHAQ (PR) | Nugent103 | 2001 | Develop (cross-cultural adaptation) and test (validation) British parents’ version of the CHAQ and CHQ | (1) 219 JIA patients; (2) 221 healthy children (siblings or children from local school) | 440 (1) 219; (2) 221 |
6–18 years | Not stated | (1) Different children’s hospitals, UK; (2) local schools, UK |
| CHAQ30 | Lam104 | 2004 | Evaluate relative discriminant validity of three new versions of the CHAQ | (1) Paediatric patients with musculoskeletal disability; (2) non-disabled controls | 149 (1) 48; (2) 101 |
(1) 2.1–17.5 years; (2a) 1.1–16.8 years; (2b) 2.4–11.0 years | (1) 9.60; (2a) 6.15; (2b) 6.12 | (1) Hospital for Sick Children, Canada; (2a) dermatology and ears, nose and throat clinics (HSC, Canada); (2b) summer day camps, Canada |
| CHIP-AE | Starfield105 | 1993 | To develop a reliable, valid and practical instrument to assess health in 11- to 17-year-olds and its initial testing | (1) Adolescents with acute illness, chronic illness (diabetes, cystic fibrosis, sickle cell anaemia), or emotional and or behavioural problems; (2) healthy adolescents | 121 Mentally ill 17, chronic 33, acute 22, healthy 49 |
11–17 years | Not stated | (1) Two large inner-city hospital emergency departments, five specialty clinics and an outpatient clinic; (2) five different community youth groups, USA |
| CHIP-AE | Starfield106 | 1995 | To test the reliability and validity of the CHIP-AE | General paediatric population | 3451 | 11–17 years | Not stated | Eight public middle or junior high schools and public high schools in both urban and rural communities, USA |
| CHIP-CE | Rebok107 | 2001 | To test children’s ability to respond to the CHIP using cognitive interviews | (1) General paediatric population; (2) chronically ill children (kidney/cardiac condition) | 114 (1) 96; (2) 18 |
5–11 years | Not stated | (1) Children in day care or after-school programmes, USA; (2) clinics at one hospital, USA |
| CHIP-CE CRF | Riley108 | 2004 | To evaluate (assess reliability and validity) and revise the CHIP CE/CRF | (1) Clinical paediatric population; (2) general paediatric population | 1708 (1) 446; (2) 1240 |
5–12 years | 8.13–8.69 depending on sample | (1) Hospital clinic in Providence, Rhode Island, and a health-maintenance organisation, USA; (2) public schools two states, USA |
| CHIP-CE PRF | Riley109 | 2004 | The objectives of this study were to describe the development, testing, and final versions of the CHIP-CE/PRF | (1) Parents of clinical paediatric population; (2) parents of general paediatric population | 1049 (1) 466; (2) 583 |
6–11 years | 8.49 (1.60) | (1) Attendees of health maintenance organisation, (California) and a well child check-up (Rhode Island), USA; (2) four schools (east coast) USA |
| CHIP-CE PRF | Riley110 | 2007 | To test the reliability and validity of the CHIP-CE (PRF) global score | General paediatric population | 583 | 6–11 years | Not stated | Recruited through elementary schools in three sites, USA |
| Healthy Pathways | Bevans93 | 2010 | To describe the development of the Healthy Pathways, child-report scales: content validity and first psychometric analyses | General paediatric population | 2095 | Grades 4–6 | Elementary school 10.2 (0.8); middle school 11.6 (0.6) | Children recruited from regular education classrooms in 34 elementary or middle schools, USA |
| Healthy Pathways | Bevans111 | 2012 | To describe the development of the Healthy Pathways, parent-report scales: content validity and first psychometric analyses | General paediatric population | 1527 | 9–14 years | 4th grade 9.6 (0.6); 5th grade 10.6 (0.7; 6th grade 11.6 (0.6) | Children recruited from regular education classrooms in 34 elementary or middle schools, USA |
| CHQ-CF87 | Landgraf77 | 1997 | To examine tests of item scaling assumptions and differences in health scores as reported by children representing three predominant cultural groups in the USA | (1) General population; (2) CYP with ADHD; (3) children undergoing haemodialysis | 354 (1) 278; (2) 56; (3) 20 |
(1) 10–15 years; (2) 9–16 years; (3) 10–19 years | (1) 13.0 (1.1); (2) 11.8 (1.9); (3) 16.0 (2.7) | (1) US middle schoolchildren (predominantly African American), USA; (2) children from an ADHD clinic (predominantly Caucasian), USA; (3) children in a haemodialysis clinic (predominantly Spanish American), USA |
| CHQ-PF50 | Landgraf76 | 1998 | Development and evaluation of Canadian-French, German and UK translations CHQ-PF50 and comparison with US data | (1) UK: CYP with acute respiratory disorders; Canada: childhood cancer survivors; (2) US household survey (62% reported one or more chronic condition) | 818 (1) 145; (2) 398 |
4–19 years | (1) Variety of ages; (2) 12 | (1) UK: questionnaire administered during routing office visits; Canada: as part of a feasibility study; (2) national random sample, USA |
| CHQ-CF87 | Waters112 | 1999 | Examine the psychometric properties of the CHQ-CF-87 and -PF-50 and test whether or not the assumptions underlying the scales and items developed in the USA also hold true in an Australian population | General child and adolescent population | 449 (1) 171; (2) 278 |
(1) 12–18 years; (2) 10–15 years | (1) 13.9; (2) 13.1 (1.1) | (1) Three urban schools, a small inner-city primary government school, a large secondary government school in an outer geographic area and a large combined primary–secondary independent school in a central area, Australia; (2) household data collected for CHQ manual included for comparative purposes, USA |
| CHQ-PF50 | Waters112 | 1999 | Examine the psychometric properties of the CHQ-CF-87 and -PF-50 and test whether or not the assumptions underlying the scales and items developed in the USA also hold true in an Australian population | Parents of general child and adolescent population | 647 (1) 249; (2) 398 |
(1) 5–18 years (2) 4–19 years | (1) 8.8 (primary), 13.0 (secondary); (2) 12.0 | See above |
| CHQ-PF50 | Waters113 | 2000 | To investigate the psychometric properties of the CHQ-PF-50 in an Australian population and compare results with those from a US population | General child and adolescent population | Total 5794; (1) 5414 (AUS); (2) 380 (USA) | 5–18 years | 11.58 (3.52) | (1) Data from a health study conducted in schools, Australia; (2) data from a household survey, USA |
| CHQ-PF50 | Nugent103 | 2001 | To cross-culturally validate a British English version of the CHQ and CHAQ in healthy children and children with JIA | (1) Children with JIA; (2) healthy children | 440 (1) 219; (2) 221 |
(1) Not stated; (2) 6–18 years | (1) 9.6; (2) 10.1 (3.1) | (1) Children involved in a study of JIA, UK; (2) children from local schools and healthy siblings of children with JIA, UK |
| CHQ-CF87 | Waters114 | 2001 | To evaluate the psychometric properties of the CHQ-CF87 and the health and well-being of an adolescent population in school | General child and adolescent population | 2361 | 12–18 years | 15.13 (1.75) | Students from a class or year group across a number of schools completed the questionnaire during class time, Australia |
| CHQ-CF80 | Waters114 | 2001 | To evaluate the psychometric properties of the 80-item self-report version of the CHQ and the health and well-being of an adolescent population in school | General child and adolescent population | 2361 | 12–18 years | 15.13 (1.75) | Students from a class or year group across a number of schools completed the questionnaire during class time, Australia |
| CHQ-PF50 | Hepner115 | 2002 | Replication of previously obtained factor structure in a minority sample (low-income families) | (1) General paediatric population; (2) clinical paediatric population | (1) 43; (2) 108 | 5+ years | Not stated | (1) Participants registered with or attending community health centres. Questionnaire mailed or administered in person; (2) participants approached in paediatrics office in a community health centre (Arizona), USA |
| CHQ-PF50 | Drotar116 | 2006 | To test the factor structure of the CHQ-PF-50 with a sample of children and adolescents with chronic conditions and physically healthy children seen in a paediatric setting | (1) Children with chronic conditions, including epilepsy; (2) general paediatric population | 661 (1) 329 (epilepsy 25); (2) 332 |
5–18 years | (1) 12.3 (3.5); (2) 11.4 (3.5) | (1) Patients identified through clinics at a large tertiary care centre, USA; (2) healthy patients from ambulatory paediatric clinics and normative controls from a community-based sleep study, USA |
| CHRS | Maylath94 | 1990 | To test the reliability and validity of the CHRS in school children | General child and adolescent population | 1141–1159 | 9–12 years | Not mentioned | Fourth to sixth grade students at nine public and private schools in Indiana, including rural, metro, suburban and town districts, USA |
| CHSCS | Hester95 | 1984 | To report the development of the CHSCS along with initial tests of reliability and validity | General child and adolescent population | 940 | 7–13 years | Not stated for overall group | Children from two rural, mountain communities, USA |
| COOP | Wasson117 | 1994 | Report on the development, testing and use of single item picture-and-word charts in an adolescent population | (1) School students; (2) adolescents from private physicians offices | 658 (total) (1) 490; (2) 168 |
12–21 years | Median – 15 | (1) Four schools, USA; (2) 18 private physicians offices, USA |
| CQoL | Graham97 | 1997 | To report the psychometric properties of the CQoL in four groups of children: chronic physical problems, psychiatric disorders, severe learning difficulties and a general sample | (1) Clinical (including neurological disorders) CYP population; (2) general child and adolescent population | 102 (1) 77 (neurodisability 26) (2) 25 |
(1) 9–15 years(2) 13–14 years | (1) 12.51 to 12.97 (1.44 to 1.79) depending on group (2) 14.03 (0.25) |
(1) Children from outpatient department of one hospital, one psychiatric outpatient clinic and parents of children with severe learning difficulties, UK; (2) children attending a regular secondary school, UK |
| ExQoL | Eiser98 | 2000 | To report the development and psychometric properties of the ExQoL | (1) Clinical paediatric population (asthma); (2) general paediatric population | 127 (1) 58; (2) 69 |
(1) 6–12 years (2) 6–11 years | (1) 8.95; (2) 7.49 | (1) One rural GP practice, UK; (2) one local school, UK |
| FSIIR-14 | Stein78 | 1990 | To describe the initial development and psychometric testing of the FSIIR in CYP with and without chronic conditions | (1) CYP with significant chronic illness; (2) general child and adolescent population | 739 (total) (1) 462; (2) 276 |
0–16 years | Not stated | Recruited at a hospital, (USA): (1) chronic ongoing health conditions; (2) well patients receiving routine care |
| GCQ | Collier118 | 2000 | To measure the quality of life of children using the GCQ | General child and adolescent population | 720 | 6–14 years | 10.3 (2.4) | Schools across a county; one primary and one secondary tested in each of the following categories: rural affluent, rural low affluence, urban affluent and urban low affluence, UK |
| KIDSCREEN-52 | Ravens-Sieberner79 | 2005 | To describe the development and psychometric properties of the KIDSCREEN-52 questionnaire in 12 European countries | General child and adolescent population | 22,296 UK 1983 |
8–18 years | Children 9.6, adolescents 14.3 | Questionnaires were completed in class time in a number of representative schools (UK) |
| KIDSCREEN-27 | Erhart119 | 2006 | To test if the KIDSCREEN-27 is able to detect mental health problems, provided a principal component analysis for summative scaling is applied | General child and adolescent population | 22,830 Ireland 1240, UK 1877 |
8–18 years | Children 9.6, adolescents 14.3 | Ireland: questionnaires completed in class time in a number of representative schools; UK: questionnaires either completed in class time or sent by mail to people sampled by telephone |
| KIDSCREEN-52 | Robitail120 | 2006 | To assess the psychometric properties of the KIDSCREEN-52 proxy measure in terms of reliability, construct and external validity | General child and adolescent population | 2526 UK 105 |
8–18 years | 12.4 (2.5) | Questionnaire completed in school class time |
| KIDSCREEN-52 | Berra121 | 2007 | To compare three different sampling and questionnaire administration methods in terms of participation, response rates, and external validity | General child and adolescent population | 22,827 Ireland 1240; UK 1877 |
8–18 years | Children 9.7 (1.1), adolescents 14.4 (1.7) | Ireland: questionnaires completed in class time in a number of representative schools; UK: questionnaires completed in class time or sent by mail to people sampled by telephone |
| KIDSCREEN-27 | Ravens-Sieberer80 | 2007 | To assess the construct and criterion validity of the KIDSCREEN-27, a shorter version of the KIDSCREEN- 52 | General child and adolescent population | 22,827 Ireland 1240, UK 1877 |
8–18 years | Children 9.7 (1.1), adolescents 14.4 (1.7) | Ireland: questionnaires completed in class time in a number of representative schools; UK: questionnaires either completed in class time or sent by mail to people sampled by telephone |
| KIDSCREEN-27 | Robitail122 | 2007 | To assess the structural and cross-cultural validity of the KIDSCREEN-27 questionnaire | General child and adolescent population | 22,827 Ireland 1240, UK 1877 |
8–18 years | Children 9.7 (1.1), adolescents 14.4 (1.7) | Ireland: questionnaires completed in class time in a number of representative schools; UK: conducted computer assisted telephone interviews or administered questionnaire during class time |
| KIDSCREEN-52 | Ravens-Sieberer123 | 2008 | To assess the reliability and validity of the European KIDSCREEN-52 in children and adolescents | General child and adolescent population | 22,827 Ireland 1240, UK 1877 |
8–18 years | Children 9.7 (1.1), adolescents 14.4 (1.7) | Ireland: questionnaires completed in class time in a number of representative schools; UK: conducted computer assisted telephone interviews or administered questionnaire during class time |
| KIDSCREEN-10 | Erhart124 | 2009 | To test the psychometric properties and measurement results of the KIDSCREEN-10 Mental Health Index in schoolchildren from 15 European countries | General adolescent population | 78,000 UK 15,382 |
11, 13 and 15 years | Not stated | Completed in schools by a representative sample of school children; UK |
| KIDSCREEN-52 | Erhart125 | 2009 | To assess if the Rasch-scaled KIDSCREEN-52 generic HRQoL measure was valid in children with and without CP | (1) Children with CP; (2) general child and adolescent population | 4042 (1) UK/Ireland 320 (PR), 315 (SR); (2) UK/Ireland 828 (PR), 1503 (SR) |
8–12 years | 10.5 (1.5) | (1) Selected randomly from population-based registers and researchers administered questionnaires in family home; (2) data collected through either telephone interviews or completion of questionnaire in schools during class time; UK, Ireland |
| KIDSCREEN-10 | Ravens-Sieberer81 | 2010 | To assess the criterion and construct validity of the KIDSCREEN-10 questionnaire | General child and adolescent population | 22,830 Ireland 1240, UK 1877 |
Children 8–11 years, adolescents 12–18 years | Children 9.7 (1.1), adolescents 14.4 (1.7) | Ireland: questionnaires completed in class time; UK: conducted computer assisted telephone interviews or administered questionnaire during class time |
| KIDSCREEN-27 | Lloyd126 | 2011 | To examine the psychometric properties of an internet version of the KIDSCREEN-27 | General child and adolescent population | 3440 | 10 and 11 years | Not stated | Pupils in one year group from 217 schools completed the questionnaire in class time online, Northern Ireland |
| KIDSCREEN-10 | Stevens127 | 2012 | To further examine the practicality and validity of the CHU-9D and KIDSCREEN-10 | General adolescent population | Kidscreen 630; CHU-9D 636 | 11–17 years | 14.5 (2.0) | Completed online, recruited via independent market research company, Australia |
| KINDL-Kid | Wee128 | 2005 | To evaluate the psychometric properties of the KINDL questionnaire in an Asian population | (1) Clinical child and adolescent population (diabetes mellitus); (2) general child and adolescent population | 69 (1) 30; (2) 39 |
8–12 years | (1) 10.7 (1.35); (2) 10.6 (1.23) | (1) Patients seen at a hospital; (2) recruited at community libraries, Singapore |
| KINDL-Kiddo | Wee128 | 2005 | To evaluate the psychometric properties of the KINDL questionnaire in an Asian population | (1) Clinical child and adolescent population (diabetes mellitus); (2) general child and adolescent population | 63 (1) 31; (2) 32 |
13–16 years | (1) 14.5 (1.48); (2) 14.3 (0.87) | (1) Patients seen at a hospital, Singapore; (2) randomly recruited outside three community libraries, Singapore |
| KINDL-Kid | Wee129 | 2007 | To report the psychometric properties, in particular factor structure, of KINDL (Singapore) questionnaires among school-going children | General child and adolescent population | 328 | 8–12 years | 9.6 (1.31) | Students in three primary and five secondary schools completed the questionnaire during class time, Singapore |
| KINDL-Kiddo | Wee129 | 2007 | To report the psychometric properties, in particular factor structure, of KINDL (Singapore) questionnaires among school-going children | General child and adolescent population | 1026 | 13–16 years | 14.0 (1.00) | Students in three primary and five secondary schools completed the questionnaire during class time, Singapore |
| PedsQL 4.0 (SR and PR) | Varni130 | 2001 | To report on the reliability and validity of the PedsQL in a diverse sample of healthy children and paediatric patients with acute or chronic health conditions | Healthy, acutely ill and chronically ill children | 717 (healthy) | 2–18 years | 9.3 (4.37) | Telephone interviews or outpatient clinics, USA |
| PedsQL 4.0 (SR and PR) | Varni131 | 2002 | To report on the sensitivity, responsiveness, and impact on clinical decision-making at the point of service for the PedsQL 4.0 in diverse paediatric samples | (1) Cardiology, orthopaedics and rheumatology sample; (2) general child and adolescent population | 1019 (1) 289; (2) 730 |
2–18 years | (1) 10.15 (4.59); (2) 9.3 (4.37) | (1) Recruited from three types of specialty clinics at one hospital; administered in person or by telephone; (2) administered in clinicians office or by telephone, USA |
| PedsQL 4.0 (SR and PR) | Varni132 | 2003 | To determine the feasibility, reliability, and validity of the PedsQL 4.0 | General child and adolescent population | 10,241 English 4363 (PR), 2520 (SR) |
2–16 years | 7.9 (4.0) | Postal survey, USA |
| PedsQL 4.0 SF15 (SR and PR) | Chan85 | 2005 | To assess the reliability and validity of the PedsQL 4.0 SF15, a shortened version of the 23-item PedsQL | General child and adolescent population | 451 | 2–18 years | 9.3 (3.0) | Telephone interviews or outpatient clinics, USA |
| PedsQL 4.0 (SR and PR) | Upton133 | 2005 | To test the psychometric properties of the UK-English version of the PedsQL | (1) General paediatric population; (2) CYP with chronic conditions (e.g. asthma, diabetes) | 1399 self-report; 970 proxy report (1) 1034; (2) 365 |
2–18 years | SR 12.58 (2.6); PR 11.86 (2.3) | 23 schools (South Wales) and outpatient clinics, UK |
| PedsQL 4.0 (SR and PR) | Varni134 | 2006 | To test reliability and validity of the PedsQL in CYP with ADHD | (1) CYP with ADHD; (2) CYP with CP; (3) healthy children | (1) 72 (72 SR/69 PR); (2) 58 (57 SR/57 PR ; (3) 3260 (3256 self/3251 proxy) | 5–16 years | (1) 10.95 (3.13); (2) 9.79 (3.14); (3) 10.75 (3.1) | Postal survey, USA |
| PedsQL 4.0 (SR and PR) | Varni135 | 2007 | To test how young children can self-report HRQoL using PedsQL | (1) Children with chronic conditions (e.g. ADHD and CP); (2) healthy children | 8591 (SR) 8406 (PR) (1) 2603 SR (2556 PR); (2) 5988 SR (5399 PR) |
5–16 years | Not stated | Outpatient clinics and telephone interviews, USA |
| PedsQL 4.0 (SR and PR) | Varni136 | 2007 | To test the reliability and validity of the PedsQL parent-proxy report | (1) Children and adolescents with a chronic health condition (e.g. ADHD, CP, diabetes); (2) healthy children | 13,878 (1) 3652 (CP 250; ADHD 108); (2) 9467 |
2–16 years | Not stated | Outpatient clinics and telephone interviews, USA |
| PedsQL 4.0 (SR) | Varni137 | 2008 | To investigate the longitudinal factor structure of the self-report PedsQL 4.0 | General child and adolescent population | 2887 English: 1157 |
5–17 years | T1 9.93 (3.14); T2 10.96 (3.15) | Mail survey, USA |
| PedsQL 4.0 (PR) | Huang138 | 2009 | To establish clinically meaningful cut-off scores of the PedsQL in children | General child and adolescent population including those with special health-care needs and chronic conditions | 1745 | 2–18 years | 10.3 (4.6) | Telephone interviews, USA |
| PedsQL 4.0 (SR and PR) | Iannaccone139 | 2009 | To test reliability and validity of the PedsQL with SMA | (1) Children with SMA; (2) general child and adolescent population | (1) 176; (2) 1134 | 2–18 years | (1) 8.53 (4.75); (2) 9.73 (3.28) | (1) Outpatient clinics, USA and Canada; (2) outpatient clinics, telephone interview or postal survey, USA and Canada |
| PedsQL 4.0 (SR) | Varni140 | 2009 | To use factor analysis to test for variance in PedsQL scores across different modes of administration | (1) Children with clinical conditions (including CP); (2) general child and adolescent population | (1) 676 (CP: 70); (2) 1629 | 5–18 years | In person: 12.32 (3.59) Mail: 10.24 (3.19) Telephone: 11.43 (3.28) |
(1) Outpatient clinics and telephone administration, USA; (2) postal survey and telephone administration, USA |
| PedsQL 4.0 (SR and PR) | Davis141 | 2010 | To test reliability and validity of the PedsQL with DMD | (1) Children with DMD; (2) general child and adolescent population | (1) 44; (2) 275 | 8–18 years | (1) 12.85 (3.05) (3) 13.07 (2.02) |
(1) Outpatient clinics, USA; (2) outpatient clinics, telephone or mail administration, USA |
| PedsQL 4.0 (SR and PR) | Limbers142 | 2011 | To test reliability and validity of the PedsQL with ADHD | (1) Children with ADHD; (2) general child and adolescent population | (1) 183; (2) 1453 | 5–18 years | (1) 11.08 (3.7; (2) 9.21 (4.46) | (1) Outpatient clinics, USA; (2) outpatient clinics, telephone or mail administration, USA |
| PedsQL Infant 36-item (PR) | Varni83 | 2011 | To report on feasibility, internal consistency reliability, and validity of the PedsQL Infant Scales in healthy, acutely ill, and chronically ill infants | Parents of infants aged 1–24 months | 420 | 1–12 months | 6.60 months (3.84) | Attendees of general paediatric clinics, coming for chronic illness care, acute illness care or well-child check (USA) |
| PedsQL Infant 45-item (PR) | Varni83 | 2011 | To report on feasibility, internal consistency reliability, and validity of the PedsQL Infant Scales in healthy, acutely ill, and chronically ill infants | Parents of infants aged 1–24 months | 263 | 13–24 months | 18.84 months (3.96) | Attendees of general paediatric clinics, coming for chronic illness care, acute illness care or well-child check (USA) |
| PedsQL 4.0 (SR) | Awasthi143 | 2012 | To test the psychometric properties of the PedsQL in Indian adolescents | General child and adolescent population | 385 English: 264 | 10–19 years | 13.6 (1.6) | Two schools, India |
| ComQol (SR) | Gullone144 | 1999 | To psychometrically evaluate the ComQol with adolescents | General adolescent population | 264 | 12–18 years | 14.92 (1.71) | Seven high schools, Australia |
| PWI-SC (SR) | Tomyn145 | 2011 | To psychometrically evaluate the PWI-SC with adolescents | General adolescent population | 338 | 12–20 years | 15.70 (1.75) | Seven high schools, Australia |
| QoLP-AV (SR) | Raphael101 | 1996 | To validate the QoLP-AV in adolescents | General adolescent population | 160 | 14–20 years | 17.4 (1.7) | One secondary school, Canada |
| SLSS | Huebner87 | 1991 | To report the development and validation of the SLSS | General child and adolescent population | Study (1) 254; study (2) 329 | 7–14 years | (1) 10.54; (2) 9.25 to 13.32 | (1) Two schools, USA; (2) four schools, USA |
| SLSS | Huebner146 | 1991 | To investigate the construct validity of the SLSS | General child and adolescent population | 254 | 7–14 years | 10.54 | Schools from two districts, USA |
| SLSS | Huebner147 | 1993 | To further examine the psychometric properties of the SLSS | General child and adolescent population, including some at risk for academic failure | 56 At risk 28, general 28 |
8–12 years | At risk, 10.2 (1.5); general, not stated | School classrooms, USA |
| SLSS | Huebner148 | 1993 | To investigate further the psychometric characteristics of the SLSS and determine its appropriateness for use with Black children | General child and adolescent population | 221 | 13–18 years | 15.5 (1.5) | School classrooms, USA |
| SLSS | Dew149 | 1994 | To investigate the psychometric properties and correlates of the SLSS with an adolescent sample | General child and adolescent population | 222 | 13 to 18 years | 15.5 (1.5) | School classrooms, USA |
| MSLSS | Huebner88 | 1994 | To develop and validate a multidimensional life satisfaction scale for preadolescent children | General child and adolescent population | 312 | 8–14 years | 10.9 (2.0) | School classrooms, USA |
| MSLSS | Huebner88 | 1994 | To develop and validate a multidimensional life satisfaction scale for preadolescent children | General child and adolescent population | 413 | 8–11 years | 8.97 (0.91) | School classrooms, USA |
| SLSS | Huebner150 | 1994 | To explore the convergent and discriminate validity of the SLSS | General child and adolescent population | 235 | 10–14 years | 11.72 (4.63) | School classrooms, USA |
| SLSS | Gilman151 | 1997 | To explore the convergent and discriminant validity of the SLSS | General child and adolescent population | 99 | 11–14 years | 12.6 (1.1) | School classrooms, USA |
| SLSS | Gilman151 | 1997 | To determine the comparability and stability of children’s SLSS scores | General child and adolescent population | 73 | 11–14 years | 12.7 (1.09) | School classrooms, USA |
| MSLSS | Greenspoon152 | 1997 | To examine the reliability and validity of the MSLSS | General child and adolescent population | 314 | 8–15 years | 11.0 (1.7) | Classrooms in three schools, Canada |
| MSLSS | Greenspoon153 | 1998 | To assess the relative goodness-of-fit of the MSLSS using confirmatory factor analytic procedures | General child and adolescent population | 314 | 8–15 years | 11.0 (1.7) | School classrooms, Canada |
| MSLSS | Huebner154 | 1998 | To compare the psychometric properties of the MSLSS across ethnic groups | General child and adolescent population | 725 | 8–14 years | 9.9 (1.7) | Classrooms in seven schools, USA |
| MSLSS | Huebner155 | 1998 | To evaluate the psychometric properties of the MSLSS with middle school students | General child and adolescent population | 291 | 11–14 years | 12.89 (0.99) | Classrooms in two schools, USA |
| SLSS | Huebner156 | 1999 | To explore the discriminant validity of global self-esteem and global life satisfaction in children | General child and adolescent population | 290 | 11–14 years | 12.9 (0.99) | Classrooms in two schools, USA |
| SLSS | Huebner156 | 1999 | To further explore the discriminant validity of global self-esteem and global life satisfaction in children | General child and adolescent population | 183 | 8–11 years | 9.07 (0.92) | Classroom in one school, USA |
| MSLSS | Gilman157 | 2000 | To investigate the psychometric properties of the MSLSS | General child and adolescent population | 321 | 14–18 years | 16.14 (1.1) | Classrooms in two schools, USA |
| MSLSS | Huebner158 | 2002 | To investigate correspondence between parent and adolescent ratings in typically achieving adolescents and adolescents with mild mental disabilities | (1) Clinical (mild mental disability); (2) general adolescent population | (1) 80; (2) 80 | 1 –18 years | (1) 15.8 (1.07); (2) 16.5 (1.76) |
School classrooms, USA |
| BMSLSS | Seligson89 | 2003 | To investigate the psychometric properties of the BMSLSS | General child and adolescent population | 221 | 11–14 years | 12.33 (0.97) | Classrooms in one school, USA |
| BMSLSS | Seligson89 | 2003 | To investigate the psychometric properties of the BMSLSS with older adolescents | General child and adolescent population | 46 | High school students (not stated) | 15.65 (0.99) | Classrooms in one school, USA |
| MSLSS | Seligson89 | 2003 | To investigate the psychometric properties of the BMSLSS with older adolescents | General child and adolescent population | 46 | High school students (not stated) | 15.65 (0.99) | Classrooms in one school, USA |
| BMSLSS | Seligson159 | 2005 | To investigate the psychometric properties of the BMSLSS and SLSS with younger children | General child and adolescent population | 518 | 8–11 years | 9.34 (0.95) | Classrooms in three schools, USA |
| BMSLSS | Funk160 | 2006 | To investigate the psychometric properties of the BMSLSS with high school students | General child and adolescent population | 146 | 14–18 years | 15.95 (1.29) | Classrooms in three schools, USA |
| MSLSS-A | Gilligan90 | 2007 | To examine the factor structure, reliability and stability of the MSLSS-A | General child and adolescent population | 266 | 14–18 years | 16.20 (1.28) | Classrooms in two schools, USA |
| MSLSS SLSS |
Haranin161 | 2007 | To examine the validity of the MSLSS and SLSS and relationships between life satisfaction and behaviour problems | General child and adolescent population | 1201 | 10–19 years | 14.62 (2.06) | Classrooms in five schools, USA |
| MSLSS | Sawatzky162 | 2009 | To evaluate the measurement validity of the MSLSS | General child and adolescent population | 7305 | 12–18 years | 15.2 (1.5) | Students in 49 schools, Canada |
| BMSLSS | Huebner163 | 2011 | To evaluate the psychometric properties of the BMSLSS with secondary school students | General adolescent population | T1: 421; T2 284 | T1: 12–15 years; T2: 13–16 years | Not stated | Students in class from one school district, USA |
| WCHMP | Spencer102 | 1996 | To validate the WCHMP | General and clinical child population | 228 | 0–5 years | Not stated | Health clinics, developmental units and outpatient departments, UK |
| WCHMP | Spencer164 | 2000 | To further validate the WCHMP | General child population | 2072 | T1: 8 weeks; T2: 8 months | Not stated | Health visitor visits, UK |
| YQoL | Patrick165 | 2002 | To develop a quality of life measure for adolescents | Adolescents including samples of general population, ADHD and mobility disability | 236 ADHD 68, mobility disability 52 |
12–18 years | Not stated | Outpatient clinics, USA |
| Instrument version | Author | PY | Internal consistency | Reliability | Measurement error | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness |
|---|---|---|---|---|---|---|---|---|---|---|
| CHAQ | Nugent103 | 2001 | Good | Good | Fair | |||||
| CHAQ30 | Lam104 | 2004 | Fair | Fair | ||||||
| CHIP-AE | Starfield105 | 1993 | Poor | Excellent | Fair | |||||
| CHIP-AE | Starfield106 | 1995 | Good | Good | Good | |||||
| CHIP-CE | Rebok107 | 2001 | Excellent | |||||||
| CHIP-CE CRF | Riley108 | 2004 | Excellent | Good | Excellent | Good | ||||
| CHIP-CE PRF | Riley109 | 2004 | Excellent | Good | Good | |||||
| CHIP-CE PRF | Riley110 | 2007 | Poor | Good | Excellent | Good | ||||
| Healthy Pathways | Bevans93 | 2010 | Good | Excellent | Excellent | Good | ||||
| Healthy Pathways | Bevans111 | 2012 | Good | Good | Excellent | Good | Good | |||
| CHQ-CF87 | Landgraf77 | 1997 | Good | Good | ||||||
| CHQ-PF50 | Landgraf76 | 1998 | Good | |||||||
| CHQ-CF87 and CHQ-PF50 | Waters112 | 1999 | Good | |||||||
| CHQ-PF50 | Waters113 | 2000 | Excellent | Excellent | Excellent | Good | ||||
| CHQ-PF50 | Nugent103 | 2001 | Good | Good | Fair | |||||
| CHQ-CF80 and CF87 | Waters114 | 2001 | Good | Good | ||||||
| CHQ-PF50 | Hepner115 | 2002 | Poor | |||||||
| CHQ-PF50 | Drotar116 | 2006 | Poor | |||||||
| CHRS | Maylath94 | 1990 | Poor | Fair | Excellent | Good | ||||
| CHSCS | Hester95 | 1984 | Poor | Fair | Excellent | Fair | ||||
| COOP | Wasson117 | 1994 | Poor | Fair | Excellent | Poor | ||||
| CQoL (SR and PR) | Graham97 | 1997 | Poor | Poor | Fair | |||||
| ExQoL | Eiser98 | 2000 | Poor | Poor | Fair | |||||
| FSIIR | Stein78 | 1990 | Good | Poor | Good | Good | ||||
| GCQ | Collier118 | 2000 | Poor | Fair | Good | |||||
| KIDSCREEN-52 | Ravens-Sieberner79 | 2005 | Excellent | Excellent | Excellent | |||||
| KIDSCREEN-27 | Erhart119 | 2006 | Good | |||||||
| KIDSCREEN-52 | Robitail120 | 2006 | Excellent | Good | Excellent | |||||
| KIDSCREEN-52 | Berra121 | 2007 | ||||||||
| KIDSCREEN-27 | Ravens-Sieberer80 | 2007 | Good | Fair | Good | |||||
| KIDSCREEN-27 | Robitail122 | 2007 | Good | |||||||
| KIDSCREEN-52 | Ravens-Sieberer123 | 2008 | Good | Good | Good | Good | ||||
| KIDSCREEN-10 | Erhart124 | 2009 | Good | Good | Good | |||||
| KIDSCREEN-52 | Erhart125 | 2009 | Good | Good | Good | |||||
| KIDSCREEN-10 | Ravens-Sieberer81 | 2010 | Good | Good | Good | Good | ||||
| KIDSCREEN-27 | Lloyd126 | 2011 | Good | Good | Good | |||||
| KIDSCREEN-10 | Stevens127 | 2012 | Good | |||||||
| KINDL-Kid and -KIDDO | Wee128 | 2005 | Poor | Good | ||||||
| KINDL-Kid and -KIDDO | Wee129 | 2007 | Excellent | Excellent | ||||||
| PedsQL 4.0 (SR and PR) | Varni130 | 2001 | Excellent | Excellent | Good | |||||
| PedsQL 4.0 (SR and PR) | Varni131 | 2002 | Fair | Fair | ||||||
| PedsQL 4.0 (SR and PR) | Varni132 | 2003 | Good | Good | Poor | Good | ||||
| PedsQL 4.0 and SF15 (SR and PR) | Chan85 | 2005 | Good | Good | ||||||
| PedsQL 4.0 (SR and PR) | Upton133 | 2005 | Poor | Good | ||||||
| PedsQL 4.0 (SR and PR) | Varni134 | 2006 | Fair | Fair | ||||||
| PedsQL 4.0 (SR and PR) | Varni135 | 2007 | Fair | Fair | Fair | |||||
| PedsQL 4.0 (SR and PR) | Varni136 | 2007 | Fair | Fair | ||||||
| PedsQL 4.0 (SR) | Varni137 | 2008 | Excellent | |||||||
| PedsQL 4.0 (PR) | Huang138 | 2009 | Good | |||||||
| PedsQL 4.0 (SR and PR) | Iannaccone139 | 2009 | Fair | Good | Good | |||||
| PedsQL 4.0 (SR) | Varni140 | 2009 | Poor | |||||||
| PedsQL 4.0 (SR and PR) | Davis141 | 2010 | Poor | Fair | Fair | |||||
| PedsQL 4.0 (SR and PR) | Limbers142 | 2011 | Fair | Fair | Fair | |||||
| PedsQL Infant 36 and 45 (PR) | Varni83 | 2011 | Excellent | Excellent | Excellent | Good | ||||
| PedsQL 4.0 (SR) | Awasthi143 | 2012 | Fair | Poor | Good | |||||
| ComQol (SR) | Gullone144 | 1999 | Fair | Fair | Good | |||||
| PWI-SC (SR) | Tomyn145 | 2011 | Excellent | Excellent | Good | |||||
| QoLP-AV (SR) | Raphael101 | 1996 | Good | Excellent | Fair | Good | ||||
| SLSS | Huebner87 | 1991 | Fair | Fair | Poor | Fair | Fair | |||
| SLSS | Huebner146 | 1991 | Fair | Fair | ||||||
| SLSS | Huebner147 | 1993 | Fair | |||||||
| SLSS | Huebner148 | 1993 | Fair | Poor | ||||||
| SLSS | Dew149 | 1994 | Fair | Fair | Fair | |||||
| MSLSS | Huebner88 | 1994 | Fair | Fair | Fair | Fair | ||||
| SLSS | Huebner150 | 1994 | Fair | |||||||
| SLSS | Gilman151 | 1997 | Fair | Fair | Fair | Fair | ||||
| MSLSS | Greenspoon152 | 1997 | Fair | Fair | Fair | |||||
| MSLSS | Greenspoon153 | 1998 | Fair | Fair | ||||||
| MSLSS | Huebner154 | 1998 | Fair | Fair | Fair | |||||
| MSLSS | Huebner155 | 1998 | Fair | Fair | Fair | Fair | ||||
| SLSS | Huebner156 | 1999 | Fair | Fair | ||||||
| MSLSS | Gilman157 | 2000 | Fair | Fair | Fair | |||||
| MSLSS | Huebner158 | 2002 | Poor | |||||||
| BMSLSS and MSLSS | Seligson89 | 2003 | Fair | Fair | ||||||
| BMSLSS and SLSS | Seligson159 | 2005 | Fair | Fair | Poor | |||||
| BMSLSS | Funk160 | 2006 | Fair | Fair | Fair | Fair | Poor | |||
| MSLSS-A | Gilligan90 | 2007 | Fair | Fair | Fair | Fair | ||||
| SLSS and MSLSS | Haranin161 | 2007 | Fair | Fair | ||||||
| MSLSS | Sawatzky162 | 2009 | Excellent | Excellent | ||||||
| BMSLSS | Huebner163 | 2011 | Fair | Fair | Fair | |||||
| WCHMP | Spencer102 | 1996 | Fair | Fair | Fair | |||||
| WCHMP | Spencer164 | 2000 | Fair | |||||||
| YQoL | Patrick165 | 2002 | Fair | Fair | Excellent | Fair | Fair |
Generic patient-reported outcome measures: summary of evidence in a general population
A summary of the evidence of the psychometric performance of each generic PROM in a general population is shown in Table 9 . We present an overall rating for each psychometric property based on the evidence in the selected papers and also taking into account the quality of the papers.
| Instrument version | Content validity | Structural validity | Construct validity | Internal consistency | Test–retest reliability | Proxy reliability | Precision | Responsiveness | Acceptability |
|---|---|---|---|---|---|---|---|---|---|
| CHAQ | 0 | 0 | 0 | + | + | – | – | 0 | – |
| CHIP-CE | ++ | + | + | ++ | +/– | 0 | + | 0 | + |
| CHIP-AE | ++ | 0 | + | ++ | +/– | 0 | + | 0 | + |
| Healthy Pathways | + | ++ | + | + | 0 | – | ++ | 0 | + |
| CHQ-50 | 0 | +/– | +/– | + | +/– | 0 | – | 0 | + |
| CHQ-80/87 | 0 | 0 | +/– | + | 0 | 0 | – | 0 | + |
| CHRS | + | + | + | +/– | 0 | 0 | 0 | 0 | 0 |
| CHSCS | + | + | + | – | – | 0 | 0 | 0 | 0 |
| COOP | + | 0 | +/– | ? | + | 0 | 0 | 0 | + |
| ExQoL | ? | 0 | ? | + | 0 | 0 | 0 | 0 | 0 |
| FSIIR | ? | + | + | + | 0 | 0 | 0 | 0 | – |
| GCQ | + | 0 | + | + | 0 | 0 | 0 | 0 | 0 |
| KIDSCREEN-52 | ++ | +++ | ++ | + | +/– | – | + | 0 | + |
| KIDSCREEN-27 | 0 | ++ | + | + | +/– | 0 | + | 0 | + |
| KIDSCREEN-10 | 0 | + | ++ | + | + | – | + | 0 | + |
| KINDL Kid | 0 | 0 | +/– | 0 | 0 | 0 | + | 0 | + |
| KINDL Kiddo | 0 | +/– | +/– | +/– | 0 | 0 | + | 0 | + |
| PedsQL | 0 | ++ | +/– | + | +/– | – | +/– | ? | + |
| PedsQL Infant Scales | + | + | + | + | 0 | 0 | +/– | 0 | + |
| ComQoL-S5 | 0 | 0 | + | – | ? | 0 | 0 | 0 | + |
| PWI | 0 | + | + | +/– | 0 | 0 | 0 | 0 | + |
| QoLP-AV | + | + | + | + | 0 | 0 | 0 | 0 | 0 |
| SLSS | + | ++ | ++ | ++ | + | 0 | 0 | 0 | + |
| MSLSS | + | + | ++ | + | + | 0 | 0 | 0 | + |
| BMSLSS | 0 | ++ | ++ | ++ | + | 0 | 0 | 0 | + |
| WCHMP | + | 0 | 0 | + | +/– | 0 | 0 | 0 | 0 |
| YQoL | + | + | + | + | + | 0 | 0 | 0 | 0 |
Strong evidence was found for the content validity of the CHIP and KIDSCREEN-52, with extensive qualitative research having been used to generate the items. The evidence of content validity for the KIDSCREEN versions with 27 and 10 items was rated lower, as fewer of the concepts are covered. No evidence of work to determine the content validity with children and young people was found for CHAQ, CHQ, KINDL (although this was examined in a German study), PedsQL and PWI. The manual of the PWI mentions that the child versions (preschool and schoolchildren) are based on the adult versions. These versions do not appear to have been adapted with input from qualitative research with children and young people.
Good evidence for structural validity was found for the Healthy Pathways, KIDSCREEN-52 and 27, the PedsQL, the SLSS and BMSLSS, and most robust for the Healthy Pathways and KIDSCREEN which have undergone good quality studies using Rasch analysis.
Good evidence was found to support the internal consistency of the domain scales for most PROMs. The internal consistency of some domains of the CHQ, KINDL and PedsQL were below accepted criteria (α < 0.7) and hence received an equivocal rating overall. Evidence from hypothesis testing generally supported construct validity of domain scales.
Test–retest reliability was examined for half of the PROMs; if tested, results were inconclusive. Evidence from different studies of the CHIP, KIDSCREEN and PedsQL either supported stability (ICC > 0.7) or did not (ICC < 0.7). The reliability between self- and proxy report was studied only for a few PROMs and tests generally showed negative results, in that reliability between children and proxy reports was usually below recommended criteria on one or more domains (ICC < 0.7).
Evidence for precision is provided for the Healthy Pathways and KIDSCREEN based on Rasch analysis. Little is known about the responsiveness of these instruments.
Generic patient-reported outcome measures: psychometric performance in neurodisability population
A total of 10 papers report evidence of a generic PROM evaluated with children and young people with chronic conditions including neurodisability ( Table 10 ). The CHQ and the PedsQL are most tested; respectively, three and five papers have been included in the data extraction. With the exception of the paper on the BMSLSS and SLSS, the methodological quality of the reported studies was rated fair to poor ( Table 11 ).
| Instrument version | Author | PY | Aim/purpose | Study population | n | Age range (years) | Mean age or median (SD) | Setting, country |
|---|---|---|---|---|---|---|---|---|
| CHQ-PF28 | Pencharz166 | 2001 | Evaluate and compare the psychometric properties of the CHQ-PF-28 in a paediatric clinical sample | CYP with musculoskeletal disorders, including children with CP and MD | 166 MD 8, CP 8 |
5–16 | 11.0 (2.9) | Hospital and paediatric rehabilitation centre, Canada |
| CHQ-PF50 | Vitale167 | 2001 | Evaluate and compare the psychometric properties in a paediatric orthopaedic sample | Children with a range of musculoskeletal problems, including CP | 242 CP 23 |
5–18 | 12 | Physician’s office, USA |
| CHQ-PF50 | Drotar116 | 2006 | To test facture structure of the CHQ-PF-50 in a sample of children and adolescents with chronic conditions and physically healthy children seen in a paediatric setting | (1) Children with chronic conditions, including epilepsy; (2) general paediatric population | 661 (1) 329 (epilepsy 25); (2) 332 |
5–18 | (1) 12.3 (3.5); (2) 11.4 (3.5) | (1) Outpatient clinics, USA; (2) controls from sleep study, USA |
| CQoL (SR and PR) | Graham97 | 1997 | To develop a QoL measure for 9- to 15-year-old children, and test it in one healthy and three clinical samples | (1) Children with chronic physical disorders, including neurological disorders; children with mental retardation; children with psychiatric disorders; (2) general paediatric population | 102 (1) 77; (2) 25 |
(1) 9–15; (2) 13–14 | (1) 12.51–12.97 (1.44–1.79) depending on group; (2) 14.03 (0.25) | (1) Outpatient departments and support groups, UK; (2) one local school, UK |
| PedsQL 4.0 (PR) | McCarthy168 | 2005 | To test reliability and validity of the PedsQL with traumatic brain injury | Children and adolescents with TBI or an extremity fracture | 391 | 5–15 | 10.6 (3.2) | Telephone interviews, USA |
| PedsQL 4.0 (SR and PR) | Varni135 | 2007 | To test how young children can self-report HRQoL using PedsQL | (1) Children with chronic health conditions, including ADHD and CP; (2) healthy children | 8591 (SR); 8406 (PR) (1) 2603 (2556 PR); (2) 5988 (5399 PR) |
5–16 | Not stated | Outpatient clinics and telephone interviews, USA |
| PedsQL 4.0 (SR and PR) | Varni136 | 2007 | To test the reliability and validity of the PedsQL parent-proxy report | (1) Children with chronic health conditions, including ADHD and CP; (2) healthy children | (1) 3652 (total), CP 250, ADHD 108; (2) 9467 | 2–16 | Not stated | Outpatient clinics and telephone interviews, USA |
| PedsQL 4.0 (SR) | Varni140 | 2009 | To test factorial invariance for the self-reported PedsQL across different modes of administration | (1) CYP with chronic health conditions, including CP; (2) general child and adolescent population | (1) 676 (total), CP 70; (2) 1629 | 5–18 | In person: 12.32 (3.59) Mail: 10.24 (3.19) Telephone: 11.43 (3.28) |
(1) Outpatient clinics and telephone administration, USA; (2) postal survey and telephone administration, USA |
| PedsQL 4.0 (SR) | Young169 | 2009 | To test the reliability and validity of the web-based administration of the PedsQL | Children with complex physical health conditions, including CP | Total 69, CP 19 | 8–13 | 11.00 (1.55) | Clinics in six hospitals/home completion, Canada |
| BMSLSS SLSS |
McDougall170 | 2012 | To assess to psychometric properties of the BMSLSS and SLSS in youth with chronic conditions | Adolescents with chronic conditions (including CP, acquired brain injury and ASD) | Total 439, CP 150 (35%), acquired brain injury 59 (14%), ASD 35 (7%) | 11–17 | Not stated | In a treatment office or adolescent’s home, Canada |
| Instrument version | Author | PY | Internal consistency | Reliability | Measurement error | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness |
|---|---|---|---|---|---|---|---|---|---|---|
| CHQ-PF28 | Pencharz166 | 2001 | Fair | |||||||
| CHQ-PF50 | Vitale167 | 2001 | Fair | |||||||
| CHQ-PF50 | Drotar116 | 2006 | Poor | |||||||
| CQoL (SR and PR) | Graham97 | 1997 | Poor | Poor | Fair | |||||
| PedsQL 4.0 (PR) | McCarthy168 | 2005 | Good | Good | Poor | Good | ||||
| PedsQL 4.0 (SR and PR) | Varni135 | 2007 | Fair | Fair | Fair | |||||
| PedsQL 4.0 (SR and PR) | Varni136 | 2007 | Fair | Fair | ||||||
| PedsQL 4.0 (SR) | Varni140 | 2009 | Poor | |||||||
| PedsQL 4.0 (SR) | Young169 | 2009 | Poor | |||||||
| BMSLSS and SLSS | McDougall170 | 2012 | Excellent | Excellent | Excellent |
Eight generic PROMs have been tested in a neurodisability population: CHIP, CHQ (three versions), CQoL, KIDSCREEN-52, PedsQL and YQoL ( Table 12 ). A total of 25 papers were found reporting evidence on five generic PROMs tested in a solely neurodisability population. The CHQ (seven papers) and PedsQL (13 papers) have been studied more frequently, but the same developer reported most of the studies of the PedsQL.
| Instrument version | Author | PY | Aim/purpose | Study population | n | Age range (years) | Mean age (years) (SD) | Setting, country |
|---|---|---|---|---|---|---|---|---|
| CHIP-CE (PR) | Riley171 | 2006 | To test reliability and validity of the CHIP-CE with children with ADHD | Children with ADHD in a clinical trial | 1476 | 6–18 | Not stated | Outpatient clinics, Europe |
| CHIP-CE (PR) | Schacht172 | 2011 | To test reliability and validity of the CHIP-CE with ADHD | Children with ADHD in five clinical trials | 794 | 6–15 | 9.7 (2.3) | Outpatient clinics, Europe and Canada |
| CHQ-CF87 | Landgraf77 | 1997 | To test reliability and validity of CHQ-CF87 with ADHD | General population and subgroup of children with ADHD | Total 354, ADHD 56 | 9–16 | 11.8 (1.9) | Postal survey, USA |
| CHQ-PF50 | Wake173 | 2003 | To test reliability and validity of the CHQ-PF50 with CP | Children with CP | 80 | 5–18 | 11.25 (3.5) | Outpatient clinics, Australia |
| CHQ-PF50 | Rentz174 | 2005 | To test reliability and validity of the CHQ-PF50 with children with ADHD | Children with ADHD in a clinical trial | 921 | 6–18 | 11 | Outpatient clinics, USA |
| CHQ-PF28 | Vitale175 | 2005 | To determine the efficacy and sensitivity of the CHQ in children with CP | Children with CP | 180 | 5–18 | 10.7 | Completed before treatment for CP at one hospital, USA |
| CHQ-PF50 | Thomas-Stonell176 | 2006 | To test responsiveness of the CHQ-PF50 with TBI | Paediatric patients with TBI | 33 | 4–18 | 12.5 (4.5) | Inpatient clinic, Canada |
| CHQ-PF50 | McCullough177 | 2009 | To test reliability and validity of CHQ with children with CP | Children with CP | 818 | 8–12 | Not stated | Home visits, Europe |
| CHQ-PF28 KIDSCREEN-10 (SR and PR) | Davis178 | 2010 | To compare reliability and validity of the CHQ-PF28 and KIDSCREEN-10 | Children with CP | PR 204, SR (54) | 4–12 | 8.25 (2.51) | Outpatient clinics, Australia |
| KIDSCREEN-52 | Erhart125 | 2009 | To test reliability and validity of KIDSCREEN-52 in children with CP | Children with CP | Total 828, UK 144 | 8–12 | 10.5 (1.5) | Home visits, Europe |
| PedsQL 4.0 (SR and PR) | Eiser179 | 2003 | To test inter-rater reliability (mother or child) and validity | (1) CYP who had survived a CNS tumour; (2) CYP with leukaemia | (1) 23; (2) 45 | > 8 | (1) 13.74 (3.06) (2) 13.51 (3.15) | (1) & (2) Recruited at clinic appointment, completed at home, UK |
| PedsQL 4.0 (SR and PR) | Varni134 | 2006 | To test reliability and validity of the PedsQL with children with ADHD | Children with ADHD | SR 72, PR 69 | 5–16 | 10.95 (3.13) | Postal survey, USA |
| PedsQL 4.0 | Varni180 | 2006 | To test reliability and validity of the PedsQL with children with CP | Children with CP | SR 7, PR 224 | 2–18 | SR 8.1 (4.25) PR 7.8 (4.0) | Outpatient clinics, USA |
| PedsQL 4.0 (SR and PR) | Palmer181 | 2007 | To examine the internal consistency and construct validity of the PedsQL brain tumour module and generic core scales | Children with brain tumours | Total 99 (51 children, 99 parents) | 2–18 | 9.76 (4.52) | Outpatient clinics from one hospital, USA |
| PedsQL 4.0 | Majnemer182 | 2008 | To test inter-rater reliability of PedsQL | Children with CP | 48 | 6–12 | 9.9 (1.9) | Outpatient clinics, Canada |
| PedsQL 4.0 | Oeffinger183 | 2008 | To test longitudinal validity of PedsQL | Children with CP | 381 | 4–18 | 11.0 (4.4) | Outpatient clinics, USA |
| PedsQL 4.0 (PR) | Limbers184 | 2009 | To examine the feasibility, reliability and validity of the PedsQL parent proxy in school-aged children with Asperger’s syndrome | Children with Asperger’s syndrome | 22 | 6 –12 | 9.25 (2.15) | Waiting rooms for group social skills class, USA |
| PedsQL 4.0 | Iannaccone139 | 2009 | To test reliability and validity of the PedsQL with SMA | Children with SMA | 176 | 2–18 | 8.53 (4.75) | Outpatient clinics, USA |
| PedsQL 4.0 | Davis141 | 2010 | To test reliability and validity of the PedsQL with children with DMD | Children with DMD | 44 | 8–18 | 12.85 (3.05) | Outpatient clinics, USA |
| PedsQL 4.0 | Dunaway185 | 2010 | To test reliability of telephone administration | Children with SMA | 20 | 2–18 | 8.4 (not stated) | Outpatient clinics, USA |
| PedsQL 4.0 | Limbers142 | 2011 | To test reliability and validity of the PedsQL with children with ADHD | Children with ADHD | 183 | 5–18 | 11.08 (3.7) | Outpatient clinics, USA |
| PedsQL 4.0 | Shipman186 | 2011 | To test reliability and validity of the PedsQL with children with ASD | Children with ASD | 39 | 12 –8 | 14.8 (not stated | Outpatient clinics, USA |
| PedsQL 4.0 | Green187 | 2012 | To test reliability and validity of the PedsQL children with TBI | Children with TBI | 33 | 15–18 | 16.5 (1.0) | Outpatient clinics, Australia |
| YQoL | Patrick165 | 2002 | To develop a quality of life measure for adolescents | Adolescents including samples of general population, ADHD and MD | Total 236, ADHD 68, MD 52 | 12–18 | Not stated | Outpatient clinics, USA |
The content validity of two instruments (CQoL and YQoL) has been tested in a neurodisability sample and evidence was very favourable for the CQoL. Some good evidence in favour of the structural validity has been found for all PROMs except the CQoL from factor analysis, and for the KIDSCREEN-52 in a study using Rasch analysis with responses from a large sample of children with cerebral palsy ( Table 13 ).
| Instrument version | Author | PY | Internal consistency | Reliability | Measurement error | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness |
|---|---|---|---|---|---|---|---|---|---|---|
| CHIP-CE (PR) | Riley171 | 2006 | Good | Fair | Good | |||||
| CHIP-CE (PR) | Schacht172 | 2011 | Fair | Fair | Fair | |||||
| CHQ-CF87 | Landgraf77 | 1997 | Good | Good | ||||||
| CHQ-PF50 | Wake173 | 2003 | Fair | Good | ||||||
| CHQ-PF28 | Vitale175 | 2005 | Fair | |||||||
| CHQ-PF50 | Rentz174 | 2005 | Good | Fair | Good | Good | ||||
| CHQ-PF50 | Thomas-Stonell176 | 2006 | Fair | |||||||
| CHQ-PF50 | McCullough177 | 2009 | Excellent | Excellent | ||||||
| CHQ-PF28 | Davis178 | 2010 | Fair | Fair | ||||||
| KIDSCREEN-52 | Erhart125 | 2009 | Good | Good | ||||||
| KIDSCREEN-10 (SR and PR) | Davis178 | 2010 | Fair | Good | Fair | |||||
| PedsQL 4.0 | Eiser179 | 2003 | Poor | Poor | ||||||
| PedsQL 4.0 (SR and PR) | Varni134 | 2006 | Fair | Fair | ||||||
| PedsQL 4.0 | Varni180 | 2006 | Fair | Good | Fair | |||||
| PedsQL 4.0 (SR and PR) | Palmer181 | 2007 | Poor | |||||||
| PedsQL 4.0 | Majnemer182 | 2008 | Fair | |||||||
| PedsQL 4.0 | Oeffinger183 | 2008 | Poor | Poor | ||||||
| PedsQL 4.0 (PR) | Limbers184 | 2009 | Poor | Poor | ||||||
| PedsQL 4.0 | Iannaccone139 | 2009 | Fair | Good | Good | |||||
| PedsQL 4.0 | Davis178 | 2010 | Poor | Fair | Fair | |||||
| PedsQL 4.0 | Dunaway185 | 2010 | Poor | |||||||
| PedsQL 4.0 | Limbers142 | 2011 | Fair | Fair | Fair | |||||
| PedsQL 4.0 | Shipman186 | 2011 | Poor | Fair | Fair | |||||
| PedsQL 4.0 | Green187 | 2012 | Poor | |||||||
| YQoL | Patrick165 | 2002 | Fair | Fair | Excellent | Poor | Fair |
Not all domain scales of the CHQ-PF50 and PedsQL reached acceptable criteria for internal consistency. There is stronger evidence from test–retest reliability studies that responses to the PedsQL were stable.
The KIDSCREEN-52, CHIP and YQoL show the most promising results, with a caveat that all evidence for the YQoL is drawn from one paper. Table 14 provides a summary of the performance of generic PROMs in a population of children and young people with a neurodisability.
| Instrument version | Content validity | Structural validity | Construct validity | Internal consistency | Test–retest reliability | Proxy reliability | Precision | Responsiveness | Acceptability |
|---|---|---|---|---|---|---|---|---|---|
| CHIP-CE (PR) | 0 | + | + | + | 0 | 0 | + | 0 | + |
| CHQ-CF87 | 0 | + | 0 | + | 0 | 0 | 0 | 0 | + |
| CHQ-PF28 | 0 | + | 0 | – | 0 | 0 | – | 0 | + |
| CHQ-PF50 | 0 | + | +/– | +/– | 0 | 0 | – | +/– | +/– |
| CQoL | ++ | 0 | 0 | ? | ? | 0 | 0 | 0 | 0 |
| KIDSCREEN-52 | 0 | + | ++ | 0 | 0 | 0 | + | 0 | + |
| KIDSCREEN-10 | 0 | 0 | 0 | + | + | 0 | 0 | 0 | 0 |
| PedsQL | 0 | + | ? | +/– | ++ | – | +/– | 0 | ++ |
| SLSS and BMSLSS | 0 | + | + | + | + | 0 | 0 | 0 | 0 |
| YQoL | + | + | + | + | + | 0 | 0 | 0 | 0 |
Chronic-generic patient-reported outcome measures
In the selection process, five families of chronic-generic PROMs were identified. For three chronic-generic PROMs no evidence was found in an English-speaking population: the Child Health Ratings Inventory (CHRIs),188 the Children’s Life Quality Index (CLQI)189 and the Perceived Illness Experience scale (PIE and PIE-R). 190,191 The authors and or developers of these PROMs were contacted to verify that we had not missed any peer-reviewed papers; no response was received. These PROMs are not included in the report; characteristics of these PROMs can be found in Appendix 6 .
Patient-reported outcome measures with evidence that have more than one version include:
-
DISABKIDS Chronic Generic Module (DCGM or DISABKIDS) – age group and short/long (three versions). 192–194
Chronic-generic patient-reported outcome measures: descriptive characteristics
Instructions and items of the Functional Disability Inventory (FDI)-Child Form are available in the paper of Walker and Greene. 195 We contacted the author of the DISABKIDS and paid to receive all three versions of the instrument and the manual.
Table 15 contains descriptive characteristics for all identified versions of the 19 candidate generic PROMs including the purpose of the instrument, number of items, age range, responder (self or proxy), response options, completion time (as mentioned in the key reference paper or manual), recall period, and the domains or dimensions assessed.
| Acronym/name | Author | Purpose of PROM | n of items | Age (years) | Responder | Response options | Completion time | Recall period | Domains/dimensions |
|---|---|---|---|---|---|---|---|---|---|
| DISABKIDS-Smileys-6 | Chaplin 2008192 | To assess health status and well-being in young children | 6 | 4–7 | Self and proxy | Five-point scale of smiley faces | < 5 minutes | Lately | Single summary score (health and well-being) |
| DCGM-37 | Simeoni 2007193 | Assess quality of life aspects related to being ill | 37 | 8–18 | Self and proxy | Five-point Likert scale rating frequency | 10–15 minutes | Past 4 weeks | Independence, emotion, social inclusion, social exclusion, limitation, treatment |
| DCGM-12 | Bullinger 2002194 | Assess quality of life aspects related to being ill | 12 | 8–18 | Self and proxy | Five-point Likert scale rating frequency | 10 minutes | Past 4 weeks | Independence, emotion, social inclusion, social exclusion, limitation, treatment |
| FDI | Walker 1991195 | To assess a child’s perception of its difficulty completing daily activities due to pain (functional impairment) | 15 | 8–17 | Self and proxy | Five-point Likert scale rating difficulty of completing an activity | 5–10 minutes | Last few days | Physical activities, daily activities |
The DISABKIDS has two age group versions: one for children aged 4–7 years and one for those aged 8–18 years. The number of items ranges from 6 (DISABKIDS-Smileys) to 37 (DISABKIDS-37); these were derived from the original 56-item pilot version. The FDI has one version for 8- to 17-year-olds; the FDI has 15 items. Both the DISABKIDS and the FDI have self-report and proxy report versions. All instruments can be completed in < 10 minutes.
The DISABKIDS-Smileys-6 version employs illustrated response options as ‘smiley faces’.
The recall period for the FDI is the ‘last few days’, while the DISABKIDS-Smileys uses ‘lately’ and the recall period for the DISABKIDS-37 and DISABKIDS-12 is ‘the past 4 weeks’.
Chronic-generic patient-reported outcome measures: content mapping
The FDI is aimed at measuring a child’s ability to complete daily activities and those are the ICF-CY chapters broadly covered by the items. No additional aspects are assessed.
All versions of the DISABKIDS focus strongly on how children ‘feel’. They are not aimed at abilities or functioning; none of the items specifically assesses what the child can or cannot do. The DISABKIDS-Smileys-6 asks children how they ‘feel in general’ as well as about themselves. The DISABKIDS-12 focuses on how children feel about their life and their medical treatment. In addition to those items probing emotional well-being, the DISABKIDS-37 covers more topics: running, sleep, play, school (concentration) and friends.
Table 16 summarises the content mapping for the chronic-generic PROMs.
| ICF-CY | DCGM-37 | DCGM-12 | DISABKIDS-Smileys-6 | FDI |
|---|---|---|---|---|
| Body functions | ||||
| Mental | ✗ | ✗ | ✗ | |
| Sensory and pain | ✗ | |||
| Voice and speech | ||||
| Cardiovascular, haematological, immunological and respiratory systems | ✗ | ✗ | ||
| Digestive, metabolic and endocrine | ||||
| Genitourinary and reproductive | ||||
| Neuromusculoskeletal and movement | ||||
| Skin and related | ||||
| Activities and participation | ||||
| Learning and applying knowledge | ||||
| General tasks and demands | ✗ | |||
| Communication | ||||
| Mobility | ✗ | ✗ | ||
| Self-care | ✗ | ✗ | ||
| Domestic life | ✗ | |||
| Interpersonal interactions and relationships | ✗ | ✗ | ✗ | |
| Major life areas | ✗ | ✗ | ||
| Community, social and civic life | ✗ | ✗ | ✗ | |
| Other | ||||
| General health – not defined | ✗ | |||
| Mental health – not defined | ||||
| Physical health – not defined | ||||
| Environment | ✗ | |||
| Being able to do what you want to do | ✗ | ✗ | ||
| Condition/treatment | ✗ | ✗ | ||
| Functioning of family | ||||
| Having fun (enjoyment) | ✗ | |||
Chronic-generic patient-reported outcome measures: evidence of psychometric performance in a general population
Evidence of the psychometric performance was found for two of the five identified chronic-generic PROMs ( Table 17 ). The FDI has been tested in a general population, and the DISABKIDS-37 and DISABKIDS Smileys-6 have both been tested in a mixed chronic condition sample including neurodisability.
| Instrument version | Author | PY | Aim/purpose | Study population | n | Age range (years) | Mean age (SD) | Setting, country |
|---|---|---|---|---|---|---|---|---|
| FDI | Walker195 | 1991 | To describe the development and validation of the FDI for school-age children and adolescents | (1) Adolescents with acute minor illnesses; (2) CYP with abdominal pain; (3) general CYP population | 157 (1) 47; (2) 69; (3) 41 |
(1) 9–17; (2) 8–16; (3) 8–16 | (1) 14; (2) not stated; (3) not stated | (1) Adolescents attending outpatient clinics, USA; (2) participants in a study of paediatric abdominal pain, USA; (3) well patients attending routine examinations, USA |
Only one paper reports evidence, of varying quality (poor–good), for the FDI in a general population ( Table 18 ). In conclusion, we found some good evidence in favour of content validity, internal consistency and hypothesis testing of the FDI ( Table 19 ).
| Instrument version | Author | PY | Internal consistency | Reliability | Measurement error | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness |
|---|---|---|---|---|---|---|---|---|---|---|
| FDI | Walker195 | 1991 | Poor | Fair | Good | Fair |
| Instrument version | Content validity | Structural validity | Internal consistency | Construct validity | Test–retest reliability | Proxy reliability | Precision | Responsiveness | Acceptability |
|---|---|---|---|---|---|---|---|---|---|
| FDI | + | 0 | + | + | 0 | – | 0 | 0 | 0 |
Chronic-generic patient-reported outcome measures: evidence of psychometric performance in neurodisability population
The DISABKIDS-37 and DISABKIDS-Smileys-6 have both been tested in with children and young people with chronic conditions including neurodisability ( Table 20 ).
| Instrument version | Author | PY | Aim/purpose | Study population | n | Age range (years) | Mean age or median (SD) | Setting, country |
|---|---|---|---|---|---|---|---|---|
| DCGM-37 (SR) | Petersen196 | 2005 | To develop and test a chronic-generic HRQoL measure | CYP with different chronic health conditions | 360 CP 21, epilepsy 37 |
6–19 | 12.48 (2.55) | Outpatient clinics, UK and six other European countries |
| DCGM-37 (SR and PR) | Schmidt197 | 2006 | To test cross-cultural validity of the DISABKIDS in children with different chronic conditions | Seven CYP groups with different chronic conditions, including CP and epilepsy | 122 CP 27, epilepsy 45 |
8–16 | 12.12 (2.57) | Seven hospitals, UK and six other European countries |
| DCGM-37 (SR and PR) | Simeoni193 | 2007 | To shorten and test the shortened version of the DISABKIDS in children which chronic diseases | CYP with chronic health conditions, including CP and epilepsy | 122 CP 27, epilepsy 45 |
8–16 | 12.20 (2.80) | Various clinical settings, UK and six other European countries |
| DISABKIDS-Smileys-6 (SR and PR) | Chaplin192 | 2008 | To test the reliability and validity of the DISABKIDS Smiley in children with a chronic disease | CYP with different chronic medical conditions, including CP and epilepsy | 435 CP 56; epilepsy 40 |
4–7 | 6.04 (1.57) | Hospital clinics, UK and six other European countries |
Four papers report evidence of the psychometric performance of the DISABKIDS-37 and Smileys-6; these were studies mostly of good to excellent methodological quality ( Table 21 ).
| Instrument version | Author | PY | Internal consistency | Reliability | Measurement error | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness |
|---|---|---|---|---|---|---|---|---|---|---|
| DCGM-37 (SR) | Petersen196 | 2005 | Good | Excellent | Good | |||||
| DCGM-37 (SR and PR) | Schmidt197 | 2006 | Good | Good | Good | Good | ||||
| DCGM-37 (SR and PR) | Simeoni193 | 2007 | Good | Good | Good | Good | ||||
| DISABKIDS-Smileys-6 | Chaplin192 | 2008 | Poor | Fair | Excellent | Fair |
There is some good evidence available in favour of content validity, structural validity and test–retest validity of both versions. Some good evidence in favour of hypothesis testing and precision is reported for the DISABKIDS-37. The study evaluating the internal consistency of the Smileys-6 version was not considered equivocal in terms of evidence to support this property. Overall, there appears to be evidence that the DISABKIDS-37, and to a lesser extent the Smileys-6, have performed well in samples of children and young people with chronic conditions that included neurodisability ( Table 22 ).
| Instrument version | Content validity | Structural validity | Construct validity | Internal consistency | Test–retest reliability | Proxy reliability | Precision | Responsiveness | Acceptability |
|---|---|---|---|---|---|---|---|---|---|
| DCGM-37 | +++ | + | ++ | ++ | + | – | + | 0 | +/– |
| DISABKIDS-Smileys-6 | ++ | + | 0 | +/– | + | 0 | 0 | 0 | 0 |
Preference-based measures
We found six eligible PBMs. Two PBMs were not included for further analyses, as no evidence was found in an English-speaking population: 16 Dimensional (16D)198/17 Dimensional (17D),199 and Assessment of Quality of Life Mark 2 – 6D Adolescents (AQoL-6D). 200 Characteristics of these excluded PROMs can be found in Appendix 7 .
Preference-based measures with evidence that have more than one version include:
Preference-based measures: general characteristics
A free sample copy of the English version of the European Quality of Life-5 Dimensions-Youth (EQ-5D-Y),204 the Child Health Utility 9D (CHU-9D)201 and HUI2202 and 3203 is available online or can be requested (respective websites: www.euroqol.org; www.shef.ac.uk/polopoly_fs/1.44111!/file/Health-Questionnaire-final-watermarked.pdf; www.healthutilities.com). The items of the CHSCS – Preschool (CHSCS-PS)205 are included in a paper by Nathan. 206
Table 23 contains descriptive characteristics for all identified versions of the included PBMs including the purpose of the instrument, number of items, age range, responder (self or proxy), response options, completion time (as mentioned in the key reference paper or manual), recall period, and the domains or dimensions assessed.
| Acronym/name | Author | Purpose | n of items | Age | Responder | Response options | Completion time | Recall period | Domains/dimensions assessed |
|---|---|---|---|---|---|---|---|---|---|
| CHU-9D | Stevens 2009201 | A symptoms and function profile, used to create a preference-based score of HRQoL | 9 | 7–11 (used: 7–17, tested: 5–7) years | Self and proxy | Five ordinal levels, by which more or less of the attribute is distinguished | 3–5 minutes | Today/last night | Worried, sad, pain, tired, annoyed, school work, sleep, daily routine, activities |
| EQ-5D-Y | Ravens-Sieberer 2010204 | A function and symptoms profile, used to create a preference-based score of HRQoL | Five- and 100-point VAS | 7–12 years | Self and proxy | Three ordinal levels (no, some, severe problems), and a VAS for overall health | A few minutes | Today | Mobility, self-care, usual activities, pain or discomfort, feeling worried/sad/unhappy General health |
| HUI2 | Torrance 1996202 | A function and symptoms profile, used to create a preference-based score of HRQoL | 7 | 12+ years (SR); 5+ years (PR) | Self and proxy | Three to five ordinal levels, by which more or less of the attribute is distinguished | 8–10 minutes | Different versions: Usually, past 4 weeks, past 2 weeks, past week | Sensation, mobility, emotion, cognitive, self-care, pain, fertility |
| HUI3 | Feeny 1995203 | A function and symptoms profile, used to create a preference-based score of HRQoL | 8 | 12+ years (SR); 5+ years (PR) | Self and proxy | Five to six ordinal levels, by which more or less of the attribute is distinguished | 8–10 minutes | Different versions: Usually, past 4 weeks, past 2 weeks, past week | Vision, hearing, speech, ambulation/mobility, pain, dexterity, emotion, cognition |
| CHSCS-PS | Saigal 2005205 | A function and symptoms profile for infants | 12 | 2–5 years | Proxy | Three to five ordinal levels of functioning | Less than 10 minutes | Past week | Vision, hearing, speech, mobility, dexterity, self-care, emotion, learning and remembering, thinking and problem solving, pain, behaviour and general health |
All the PBMs have a single form for all age groups:
-
CHU-9D (7–11 years originally, now extended to 17 years old)
-
EQ-5D-Y (7–12 years old)
-
HUI (12 years and onwards for self-report, 5 years and onwards for proxy report)
-
CHSCS-PS (2–5 years old).
The CHSCS-PS for infants is a proxy report questionnaire; the other PBMs have both self-report and proxy report versions for all age groups covered. The number of items ranges from 5 for the EQ-5D-Y to 12 for the CHSCS-PS. PBMs use ordinal-level response options by which more or less of the attribute is distinguished. All instruments can be completed in less than 10 minutes. The shortest recall period is ‘today’ (CHU-9D, EQ-5D-Y) and longest recall period ‘the past 4 weeks’ (HUI2 and HUI3).
Preference-based measures: content mapping
The CHU-9D and EQ-5D-Y, and the HUI2, HUI3 and CHSCS-PS, are similar in the content they cover, and the way in which their questions are phrased.
All of the PBMs examined have relatively few items compared with the generic and chronic-generic PROMs. Nevertheless, they seem to cover a variety of ICF-CY chapters in both of the domains ‘body functions’ and ‘activities and participation’ ( Table 24 ). The HUI2, a seven-item questionnaire, covers eight ICF-CY chapters. Mental functioning and sensory functioning and pain are covered by all PBMs.
| ICF-CY | CHU-9D | EQ-5D-Y | HUI2 | HUI3 | CHSCS-PS |
|---|---|---|---|---|---|
| Body functions | |||||
| Mental | ✗ | ✗ | ✗ | ✗ | ✗ |
| Sensory and pain | ✗ | ✗ | ✗ | ✗ | ✗ |
| Voice and speech | ✗ | ✗ | ✗ | ||
| Cardiovascular, haematological, immunological and respiratory systems | |||||
| Digestive, metabolic and endocrine | |||||
| Genitourinary and reproductive | ✗ | ||||
| Neuromusculoskeletal and movement | ✗ | ✗ | ✗ | ||
| Skin and related | |||||
| Activities and participation | |||||
| Learning and applying knowledge | ✗ | ✗ | ✗ | ||
| General tasks and demands | ✗ | ||||
| Communication | ✗ | ||||
| Mobility | ✗ | ✗ | ✗ | ✗ | |
| Self-care | ✗ | ✗ | ✗ | ✗ | |
| Domestic life | |||||
| Interpersonal interactions and relationships | |||||
| Major life areas | ✗ | ||||
| Community, social and civic life | ✗ | ||||
| Other | |||||
| General health – not defined | ✗ | ||||
| Mental health – not defined | |||||
| Physical health – not defined | |||||
| Environment | |||||
Preference-based measures: psychometric performance in a general population
We found evidence of the psychometric performance of five PBMs tested in a general population, including both versions of the HUI from 10 papers ( Table 25 ).
| Instrument version | Author | PY | Aim/Purpose | Study population | n | Age range (years) | Mean age (SD) | Setting, country |
|---|---|---|---|---|---|---|---|---|
| CHU-9D | Stevens201 | 2009 | To develop content for a descriptive system amenable to valuation | General child and adolescent population | 74 | 7–11 | Not stated | Two schools, UK |
| CHU-9D | Stevens207 | 2010 | To identify the dimensions of HRQoL for a generic PBM. Explore a common HRQoL framework across ages | General child and adolescent population | 74 | 7–11 | Not stated | Two schools, UK |
| CHU-9D | Stevens208 | 2011 | To pilot and assess the performance of the CHU-9D, and make refinements to be amendable to health state valuation | (1) General paediatric population; (2) a clinical paediatric sample with a wide range of health problems | (1) 150; (2) 95 | 7–11 | Not stated | (1) Two schools, UK; (2) one children’s hospital, UK |
| CHU-9D HUI2 |
Ratcliffe209 | 2012 | To assess construct validity in adolescent general population sample | General adolescent population | 500 | 11–17 | 14.0 (1.9) | Community sample, recruited via independent market research company, Australia |
| CHU-9D | Stevens127 | 2012 | To further examine the practicality and validity of the CHU-9D | General adolescent population | 636 | 11–17 | 14.5 (2.0) | Completed online, recruited via independent market research company, Australia |
| CHU-9D EQ-5D-Y |
Canaway210 | 2013 | To assess feasibility, acceptability, construct validity and reliability of the EQ-5D-Y and CHU-9D in young children | General child population | 160 | 6–7 | Not stated | Six mainstream schools, West Midlands (UK) |
| EQ-5D-Y | Jelsma211 | 2010 | To investigate the performance of the EQ-5D-Y instrument and compare it with the standard EQ-5D in high school children | General child and adolescent population | 521 | 13–19 | 15.5 (1.3) | Pupils from all classes in one high school completed questionnaire during lesson time, South Africa |
| EQ-5D-Y | Ravens-Sieberer204 | 2010 | To examine the feasibility, reliability, and validity of the newly developed EQ-5D-Y | General child and adolescent population | Total 2809, English 258 | 13–19 | 15.5 (1.3) | Pupils from mainstream schools completed questionnaire during lesson time |
| EQ-5D-Y | Wille212 | 2010 | To develop and pilot the EQ-5D-Y and compare results to the adult version EQ-5D | General child and adolescent population | Total 2976, English 517 | 13–19 | 15.5 (1.3) | Pupils from one school in South Africa and 29 schools in Germany and Spain, South Africa and four European countries |
| EQ-5D-Y HUI2 and HUI3 |
Oluboyede213 | 2013 | To investigate the practicality, validity and reliability of the EQ-5D, EQ-5D-Y and HUI | General adolescent population | 49 | 11–18 | 12 (median) | Pupils from one school and adolescent family members of staff members from one university, UK |
The methodological quality of studies examining the content validity of the CHU-9D was rated as excellent. The hypothesis testing was also rated as good quality. The development process of the EQ-5D-Y included the revision of the content and wording of EQ-5D to ensure relevance and clarity for young respondents. After translation of the resulting modified version, cognitive interviews were conducted in Germany, Italy, Spain and Sweden to test the instrument’s comprehensibility in children and adolescents. 207 No information supporting content validity was found for the HUI2, HUI3 and CHSCS-PS. Table 26 reports the methodological quality of the studies reporting evidence.
| Instrument version | Author | PY | Internal consistency | Reliability | Measurement error | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness |
|---|---|---|---|---|---|---|---|---|---|---|
| CHU-9D | Stevens201 | 2009 | Excellent | |||||||
| CHU-9D | Stevens207 | 2010 | Excellent | |||||||
| CHU-9D | Stevens208 | 2011 | Excellent | Good | ||||||
| CHU-9D and HUI2 | Ratcliffe209 | 2012 | Good | |||||||
| CHU-9D | Stevens127 | 2012 | Good | |||||||
| CHU-9D and EQ-5D-Y | Canaway210 | 2013 | Poor | Good | ||||||
| EQ-5D-Y | Jelsma211 | 2010 | Excellent | |||||||
| EQ-5D-Y | Ravens-Sieberer204 | 2010 | Fair | Excellent | ||||||
| EQ-5D-Y | Wille212 | 2010 | Poor | |||||||
| EQ-5D-Y and HUI2/3a | Oluboyede213 | 2013 |
No good evidence was found for test–retest reliability, internal consistency, structural validity and measurement error. Overall, there appears little evidence to substantiate the performance of PBMs based on standard psychometric criteria. Few conventional psychometric properties of these PBMs appear to have been examined. Of all PBMs, the CHU-9D has been tested more extensively, with some limited evidence in favour for content and construct validity.
Table 27 shows an overall appraisal of the PBMs performance in a general population.
| Instrument version | Content validity | Structural validity | Internal consistency | Construct validity | Test–retest reliability | Proxy reliability | Precision | Responsiveness | Acceptability |
|---|---|---|---|---|---|---|---|---|---|
| CHU-9D | ++ | 0 | 0 | + | 0 | 0 | +/– | 0 | + |
| EQ-5D-Y | 0 | 0 | 0 | + | +/– | 0 | +/– | 0 | + |
| HUI2 | 0 | 0 | 0 | 0 | 0 | 0 | +/– | 0 | 0 |
| HUI3 | 0 | 0 | 0 | 0 | 0 | 0 | +/– | 0 | 0 |
| CHSCS-PS | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Preference-based measures: psychometric performance in a neurodisability population
No papers were found reporting on the psychometric performance of the four PBMs in samples of children and young people with mixed chronic conditions that included neurodisability. The proxy-report version of the EQ-5D (not the Youth version) has been used with children with attention deficit hyperactivity disorder (ADHD), the HUI3 has been used with children and young people with autistic spectrum disorder, and the HUI2 and CHSCS-PS have also been evaluated in a neurodisability population ( Table 28 ). No studies were found evaluating the CHU-9D with children and young people affected by neurodisability.
| Instrument version | Author | PY | Aim/purpose | Study population | n | Age range (years) | Mean age (SD) | Setting, country |
|---|---|---|---|---|---|---|---|---|
| CHSCS-PS | Saigal205 | 2005 | To develop a multidimensional health status classification system for preschool children | (1a) VLBW children and (1b) general population sample; (2) VLBW children; (3) children with CP | (1a) 101; (1b) 50; (2) 150; (3) 222 | 1–6 | (1a) 3.05 (0.09) (1b) 3.04 (0.08) (2) 3.88 (0.62) (3) 3.79 (1.01) | Outpatient clinics, Canada and Australia |
| EQ-5D (PR) | Matza214 | 2005 | To test EQ-5D with children with ADHD, correlations with CHQ-PF50 and CHIP-CE | Children with ADHD receiving treatment | Total 126, UK 83 | 7–18 | 10.2 (USA), 12.6 (UK): SD not stated | Outpatient clinics, USA and UK |
| HUI2 (SR and PR) | Glaser215 | 1999 | To assess inter-rater reliability of the HUI | Children who were CNS tumour survivors | 30 | 6–16 | 10.5: SD not stated | Outpatient clinics, UK |
| HUI3 | Tilford216 | 2012 | To test HUI3 with children with ASD | Children with ASD | 150 | 4–17 | 8.6 (3.3) | Outpatient clinics, USA |
Little evidence of the performance of the four tested PBMs in a neurodisability population could be gleaned ( Table 29 ). Most evidence pertained to construct validity using hypothesis testing; there was one poor-quality reliability study comparing self and proxy reports of the HUI2. An overall appraisal of the PBMs’ performance in a neurodisability population is provided in Table 30 .
| Instrument version | Author | PY | Internal consistency | Reliability | Measurement error | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness |
|---|---|---|---|---|---|---|---|---|---|---|
| CHSCS-PS | Saigal217 | 2005 | Good | |||||||
| EQ-5D (PR) | Matza214 | 2005 | Fair | |||||||
| HUI2 (SR and PR) | Glaser215 | 1999 | Poor | |||||||
| HUI3 | Tilford216 | 2012 | Good |
| Instrument version | Content validity | Structural validity | Construct validity | Internal consistency | Test–retest reliability | Proxy reliability | Precision | Responsiveness | Accessibility |
|---|---|---|---|---|---|---|---|---|---|
| EQ-5D (PR) | 0 | 0 | +/– | 0 | 0 | 0 | 0 | 0 | 0 |
| CHSCS-PS | 0 | 0 | + | 0 | 0 | 0 | 0 | 0 | 0 |
| HUI2 | 0 | 0 | 0 | 0 | 0 | ? | 0 | 0 | 0 |
| HUI3 | 0 | 0 | + | 0 | 0 | 0 | 0 | 0 | 0 |
Discussion
This systematic review focused on the identification of generic, multidimensional PROMs for children and young people, and appraisal of the psychometric performance when using English-language versions with samples of the general population and/or neurodisability.
Key findings
We identified 25 PROMs: 19 generic PROMs, 2 chronic-generic PROMs and 4 PBMs. In total, 126 papers reporting evidence of the psychometric performance of 25 PROMs were selected. The psychometric performance has been tested either in a general population (84 papers, 23 instruments), a chronic-condition population including neurodisability (14 papers, five instruments) or a neurodisability population (28 papers, eight instruments).
Patient-reported outcome measures not selected for further consideration
There were 13 PROMs for which the evidence was so limited or of such poor quality that they could not be considered psychometrically robust compared with other candidate PROMs; all were developed prior to the year 2000. We found only one eligible paper reporting an evaluation of psychometric performance for CHAQ, CHRS, CHSCS, COOP, ExQoL, FSIIR, GCQ, QoLP-AV and FDI, and only two papers for CQoL, PWI/ComQOL-S5, WCHMP and YQoL. The available evidence precludes a full understanding of their psychometric properties as generic PROMs in general populations, and particularly with children and young people affected by neurodisability.
Patient-reported outcome measures selected for further consideration
Twelve PROMs were selected as potentially psychometrically more robust, based upon the quality and quantity of evidence available for appraisal. The candidate generic PROMs included CHIP, CHQ, Healthy Pathways, KIDSCREEN, KINDL, PedsQL and SLSS/MLSS. The DISABKIDS was the only chronic-generic PROM to stand out in the appraisal. The four PBMs all showed some potential: CHU-9D, EQ-5D-Y, HUI and CHSCS-PS. These are discussed in further detail, taking into account the age range of the target population, availability of self- and/or proxy report versions, content assessed, content validity, and their psychometric performance in different populations.
Child Health and Illness Profile
The CHIP has four versions: a self-report and two proxy report versions for 6- to 11-year-olds and a self-report adolescent edition (for 11- to 17-year-olds). The CHIP-AE was developed based on the literature, the involvement of focus groups and expert panels, and pretesting in four groups of teenagers with different health states. 105 Three studies using cognitive interviews were conducted to develop the CHIP-CE. 107 They tested children’s ability to convert their health experiences into scaled responses and examined type of response format and recall period most effectively used by children. At least some good evidence in favour of the CHIP-CE and AE has been reported for precision, hypothesis testing and internal consistency. Structural validity has been tested for the CHIP-CE but not for the CHIP-AE. In addition, the reliability and validity of the CHIP-CE has been tested in an ADHD population, reporting evidence in favour of the instrument.
The use of circles of increasing sizes to clarify the response options and drawings to illustrate the questions makes the CHIP-CE more attractive to children. The developers of the CHIP prefer self-report over proxy-report, offering only a self-report version for adolescents.
All versions of the CHIP contain items that question mental functioning, sensory functioning and pain and nearly all chapter headings of the ICF-CY ‘activities and participation’ domain. The CHIP items ask ‘how often’ something occurs, broadly assessing functioning. The length of the questionnaires is a disadvantage of the instrument. For children 6–11 years old, the self-report questionnaire contains 45 items. The adolescent version takes up to 30 minutes to answer all 138 questions.
Child Health Questionnaire
The CHQ has two proxy versions, of different lengths (50 and 28 items), and one self-report version (87 items). The proxy version covers a broad range from 5 years of age; self-report is recommended from the age of 10 years. The different versions of the CHQ have been studied across general, mixed chronic conditions and neurodisability, and findings have been reported in 19 papers.
The content validity appears not to have been tested. The CHQ covers all ‘activities and participation’ chapters in the ICF-CY, as well as mental functioning and sensory functioning and pain. The CHQ items broadly focus on a child’s abilities, limitations and functioning. Evidence of structural validity, internal consistency, and test–retest reliability is inconsistent.
Healthy Pathways
The Healthy Pathways (child report and proxy report) is a recent instrument, published in 2010, targeted at children between 9 and 12 years old. The conceptual framework for the CHIP was the starting point for the Healthy Pathways. The selection of additional items was influenced by other questionnaires and/or generated by a panel of test developers, child health experts and clinicians. Items were then pilot tested with 200 children. However, no new qualitative work was carried out with children. 93,111 The Healthy Pathways is a rather long instrument, with 88 items, although studies report few missing responses.
Structural validity has been tested using both factor analysis and Rasch analysis, providing persuasive evidence of the unidimensionality of all scales but one (balanced nutrition). At least some good evidence in favour has been reported for precision, hypothesis testing and internal consistency. The Healthy Pathways ICF-CY profile shows a good coverage of both ‘body function’ and ‘activities and participation’. The questionnaire asks how often something occurs, assessing a child’s functioning. We found no studies that have been conducted with children and young people affected by neurodisability.
KIDSCREEN
The KIDSCREEN has three versions, differing in length, all available for self-report and proxy report. The KIDSCREEN questionnaires are available in various languages. The development of the first version, the KIDSCREEN-52, involved literature searches and expert consultation, as well as focus group discussions with children and adolescents. After translation and back-translation, cognitive interviews and pilot tests were performed. 79
Twelve papers have been published examining psychometric properties of the KIDSCREEN family in a general population. There is at least some evidence in favour of all three versions of the KIDSCREEN for all psychometric properties, including factor analysis and Rasch analysis to support the structural validity of the instruments. In addition, psychometric performance of the KIDSCREEN-52 and -10 has been tested with children with cerebral palsy, reporting minimal evidence of structural invariance compared with general population samples. 125
All versions target children and adolescents from 8 to 18 years. The KIDSCREEN asks how a child ‘feels’ (e.g. ‘has your child felt fit and well?’) as well as what a child has been able to do (e.g. ‘has your child been physically active?’). The theoretical model implies seeking to assess aspects of both well-being and functioning.
KINDL
Two papers report on the psychometric evidence of the English-language version of KINDL. The content validity has been examined with a German population. The instrument was derived from a conceptual model, in which the four main components of quality of life were included in interviews with children (several school classes). 218 The items were constructed and pretested in two pilot studies involving 28 children each. 219
There are different age group versions. The KINDL has 24 items and covers a broad range of concepts: mental functioning, sensory functioning and pain, general tasks and demands, relationships and some major life areas, as well as family functioning, having fun and some items on a child’s health condition. The items are targeted to capture how a child is doing and feeling, asking questions such as ‘during the past week, I played with friends’ and ‘during the past week I felt different from other children’.
Pediatric Quality of Life Inventory
The PedsQL has three versions, according to age, for both the self-report and proxy report questionnaires. The PedsQL is one of three extensively studied instruments. In total, 16 papers report on the PedsQL psychometric performance in a general population, five studies tested the PedsQL in a chronic conditions population and 13 papers report on its performance in a neurodisability population. The PedsQL covers all activity and participation domains, except for communication, learning, and tasks and demands. It also contains items on mental functioning and sensory functioning and pain. Asking ‘how much of a problem your child has had with’ physical, emotional, social and school functioning, the PedsQL mainly assesses functioning. The developers suggest that it can be completed in less than 4 minutes.
No evidence was found that qualitative work has been conducted to develop the questionnaire. Good evidence was found for structural validity from factor analysis, but not Rasch analysis, and hypothesis testing. Evidence of internal consistency, test–retest validity and precision was found to be inconsistent.
Student Life Satisfaction Scale/Multidimensional Student Life Satisfaction Scale
The SLSS family contains the self-report SLSS, for 7- to 14-year-olds, the self-report MSLSS/MSLSS-A and the BMSLSS, for 8- to 18-year-olds. Twenty-three papers report psychometric evidence of the performance of the SLSS family, including one recent paper reporting a study in which the BMSLSS and the SLSS have been tested with a chronic conditions sample including children and young people with cerebral palsy and acquired brain injuries.
The development of the SLSS and MSLSS involved consultation with adolescents; no content validity reports were found for the BMSLSS. Good evidence in favour of construct validity, internal consistency, hypothesis testing, and test–retest reliability was found for all versions.
Whether or not the construct assessed by the SLSS, MSLSS and BMSLSS is really HRQoL is debatable. Few items could be mapped onto the ICF-CY; all three versions focus mostly on satisfaction with life and emotional well-being.
DISABKIDS
The DISABKIDS family of PROMs were produced as part of an EU-funded project. The DCGM has a long and a short version (DCGM-37 and DCGM-12). Recently, a version has been developed for 4- to 7-year-olds: the DISABKIDS-Smileys-6. DISABKIDS has been validated for use in seven languages. The DISABKIDS-37 was developed using literature searches, expert consultation and focus groups with 360 children and adolescents with different chronic health conditions and their families. 196 Child and parent focus groups were conducted to develop the DISABKIDS-Smileys-6. 192
Four papers report favourable evidence for the DISABKIDS-37 across psychometric properties, including Rasch analysis to support structural validity, and the Smileys-6 version has been evaluated with a chronic conditions population. The 12-item version has not been tested thus far. All versions of the DISABKIDS are strongly focused on how a child feels; they are not aimed at abilities or functioning. The DISABKIDS-Smileys-6 asks the child how they feel in general as well as about him- or herself and among others (school and doctor), using smileys as response options. The DISABKIDS-12 focuses on how a child feels about their life and their medical treatment. In addition to those items probing emotional well-being, the DISABKIDS-37 covers more topics: running, sleep, play, school (concentration) and friends.
Child Health Utility 9D
The CHU-9D was developed with and for children between 7 and 11 years old. The CHU-9D is the only PBM for which qualitative research was conducted to develop the instrument; interviews were undertaken with over 70 children aged 7–11 years to generate the items and response options. 201 A self-report and a proxy report version are available. It consists of nine domains (worried, sad, pain, tired, annoyed, school work, sleep, daily routine and activities) and uses five levels within each domain. The CHU-9D aims to assess a child’s health status by asking how a child is doing, but also probes for a child’s well-being (e.g. ‘I do not feel worried today’, vs. EQ-5D-Y: ‘I am not worried today’).
The CHU-9D has since been evaluated across older age groups, but without further qualitative research to examine content validity. Some evidence in favour has been reported for hypothesis testing. Precision was rated equivocal; although the scales of PBMs are interval level, there were very large observed ceiling effects. The instrument has not been tested yet in a neurodisability population.
European Quality of Life-5 Dimensions-Youth
European Quality of Life-5 Dimensions consists of five attributes (mobility, self-care, usual activity, pain/discomfort, and anxiety/depression). Only one study was found evaluating a proxy-report version of the original version. The EQ-5D-Y assesses a child’s current health status; it primarily measures functioning, asking only how a child is doing (e.g. ‘I have no pain’, ‘I am not worried’), with three response levels per attribute. The EQ-5D-Y is available in various languages. The development process of the EQ-5D-Y included the revision of the content and wording of the EQ-5D to ensure relevance and clarity for young respondents. After translation, cognitive interviews were conducted in Germany, Italy, Spain and Sweden to test comprehensibility to children and adolescents. 212
Five papers were found which reported psychometric evidence in a general population; some favourable evidence was reported from hypothesis testing and there was conflicting evidence for precision and test–retest reliability. Some hypothesis testing has been done to establish construct validity with children and young people with ADHD.
Health Utilities Index
The HUI2 uses seven domains (sensation, mobility, emotion, cognitive, self-care, pain and fertility) using three to five levels, describing 24,000 unique health states. The HUI3 uses eight domains (vision, hearing, speech, ambulation, dexterity, emotion, cognition and pain) and five or six levels. Both questionnaires have a self-report version for adolescents (≥ 12 years) and one proxy version targeting children ≥ 5 years.
Four papers were found for the HUI2 and HUI3 (two studies in a general population and two in a neurodisability population); few properties were studied and little evidence in favour was reported. Of all PBMs, the HUI covers mostly ‘Body Functioning’ chapters (including the less prevalent chapter genitourinary and reproductive functioning). The HUI2 and HUI3 measure functioning, asking about a child’s abilities and limitations.
Comprehensive Health Status Classification System – Preschool
The CHSCS-PS was developed for children aged 2–5 years. The CHSCS-PS is based conceptually on the HUI. No additional information supporting content validity was found. One study involved hypothesis testing in a sample of young children with cerebral palsy, providing some evidence in favour of the instrument.
Methodological reflections
The methodology for developing and evaluating PROMs has progressed over recent years. Most notably, there has been an increasing use of Rasch analysis to evaluate the structural validity and provide evidence for the precision of scores across the spectrum of measurement scales. Rasch analysis can also be used to test for any evidence of group invariance for items across age groups, sex, and between those with different diagnoses. Evaluation of these aspects of generic PROMs appears to have been relatively unexplored. An exception is that item invariance between general populations and children with cerebral palsy has been evaluated for KIDSCREEN, with only minor differences reported. 125 Therefore, although several generic PROMs have been used with children and young people affected by neurodisability, little can be concluded with respect to whether or not generic PROMs perform consistently across the various conditions within neurodisability.
The International Society for Pharmacoeconomics and Outcomes Research Good Research Practices Task Force for Developing Pediatric Patient-Reported Outcomes sets out five good practices relevant for PROMs for children and young people: (i) attention to age groups and age-based cut-offs, (ii) establishing content validity using concept elicitation to inform item generation, and cognitive interviews to assess and refine all aspects of the draft instrument, (iii) consideration of whether or not proxy report is necessary, (iv) ensuring that the instrument is designed and formatted appropriately for the target age group, and (v) considering cross-cultural validation.
Age groups
Some PROMs seek to cover all age groups with a single instrument, particularly the chronic-generic instruments and PBMs but also some of the generic tools. Other generic instruments have tailored instruments to specific age groups by modifying the content being assessed, the number of items in the questionnaire, or the response style. Whether or not different age group versions are necessary depends on whether or not the constructs assessed are likely to change with the age and context of young people’s lives, and whether or not the items of the questionnaire are appropriate for the cognitive development of potential respondents.
Content validity
Guidance suggests that children and young people can be content experts; however, varying efforts have been made to establish the content validity of the PROMs included in this review with children and young people. A few instruments stand out as having evidence from extensive qualitative research to generate the constructs and items in general populations (KIDSCREEN, DISABKIDS and CHU-9D). However, only two studies97,165 were identified in the review reporting qualitative research examining the content validity of PROMs with young people with neurodisability, respectively, for the CQoL and YQoL. In fact, the content of the KIDSCREEN has been compared with the life priorities identified by young people with cerebral palsy; while some overlap was found with the content assessed by KIDSCREEN, other key domains identified by young people were not represented. 220
Determining the content validity within age group strata has also been relatively neglected. For instance, the development of the CHU-9D included extensive qualitative research with children aged 7–11 years but we did not find evidence that content validity has been examined with adolescents, even though use of the instrument has been generalised to this older age group and other properties have begun to be assessed.
Proxy reports
We found no good evidence of the reliability between reports by children or young people and proxy reports by parents. Our findings are similar to those reported by Eiser and Morse,221 that reliability is often better for physical functioning and poorer for emotional and social domains. The evidence suggests poor reliability (below the recommended criterion of ICC > 0.7) for some domains of all candidate PROMs when this property has been assessed. It would be misleading to recommend a measure for which only some domains are reliable.
This adds weight to the argument that young people and parents generally have different perceptions about the content assessed in questionnaires, and scores from young people and parents should not be considered comparable, or be aggregated in analyses. 221
Proxy reports may still have a use, for instance for very young children and/or those without the cognitive capacity to respond. Five PROMs were identified that were developed, or have separate versions, to specifically target preschool children under 5 years: FSIIR, PedsQL Infant Scales, PWI-PS, and WCHMP, and the CHSCS-PS.
Age-appropriate design and formatting
The candidate PROMs identified varied in design and formatting. Few papers in the review documented evidence that questions were comprehensible and/or checked whether or not response options were appropriate across age groups, or reported whether or not any design features met with approval from potential participants. Cognitive interviews or focus groups appear to have been relatively neglected in the development of all but a few instruments.
Cross-cultural issues
As the focus of this review was English-language PROMs, we did not encounter cross-cultural validity issues for many PROMs. The KIDSCREEN and DISABKIDS instruments were developed as international collaborative projects, and considerable efforts were made to check the consistency of translated versions. The issue of cross-cultural validity was also encountered with the few papers where English-language versions were used in Singapore and India, where language and meaning may vary contextually. Rigorous testing of PROMs should be undertaken when translating versions from other languages.
Strengths and limitations
This was a comprehensive systematic review utilising a two-stage search strategy to maximise the possibility of identifying all candidate PROMs, and any eligible evidence of their psychometric performance in general and neurodisability populations. In addition, we contacted the authors of instruments for whom no evidence was found and conducted a forward citation search using a key reference for each PROM.
Our aim was only to appraise evidence of the psychometric performance of generic PROMs with children and young people affected by neurodisability. However, we decided to include appraisal of evidence from studies with general populations in order not to exclude emerging measures or those instruments with promising possibilities for use with neurodisability. This made the task much larger, but makes the findings more likely to represent the actual state of knowledge about psychometric performance of generic PROMs. We included studies with children and young people with chronic conditions, providing that the samples included neurodisability. Hence, there is a body of research that was not included in this review, which is those studies examining performance of PROMs with children and young people with conditions that would not be considered neurodisability (e.g. arthritis or asthma).
Excluded from the scope of the review were clinical assessments and instruments designed to be administered by clinicians or trained assessors. Hence, there are several outcome measures that may be commonly used in research that would not be consistent with the definition of a PROM. Examples include various forms of adaptive behaviour assessments, and for instance, the interview-administered Assessment of Life Habits (LIFE-H). 222 Also specifically excluded were domain-specific instruments. Thus, instruments that only measure one aspect of health, for example the Strengths and Difficulties Questionnaire, which is often used to assess mental health and behavioural problems, were not considered. 223
There are some limitations to this systematic review; most are a consequence of the strict inclusion criteria. Limiting the search to studies where an English version of the PROM was administered excluded some PROMs from further analyses. In addition, cross-cultural validity was not comprehensively assessed for the selected PROMs. Two PROMs excluded from this review that may warrant further investigation are ITQoL (for infants), which was developed in the Netherlands and for which an English translation is available but no published studies of this version were found, and the TNO-AZL family (TACQOL, TAPQOL and TAAQOL). If studies were included that were conducted using versions of questionnaires in languages other than English, then further evidence would emerge, for instance regarding the KINDL and the plethora of translated versions of the more popular instruments such as PedsQL. Nevertheless, psychometric performance cannot be assumed across languages and cultures;217 therefore, in our view, limiting the review to evaluations of English-language versions is a relative strength of the review.
The WHO ICF-CY was used to create a content profile for each of the questionnaires. In carrying out this analysis, many items could not be mapped readily onto the ICF-CY, and some items could not be mapped at all. This is both a problem with the conceptualisation and design of the ICF-CY, which focuses on function and is less concerned with aspects of well-being, and problematic because the questionnaires conflate these concepts. PROMs are often composed of items that assess various concepts in a single item; the latter is also problematic in view of the cognitive task faced by respondents.
Another problem encountered with using the ICF-CY to describe the content of the questionnaires was how to deal with the way a question is asked. For example, the KIDSCREEN asks ‘have you felt fit and well?’ and the CHIP asks ‘how often did you play hard enough to start sweating and breathing hard?’. Both questions can be mapped on ‘b130 Energy and drive functions’; however, each item assesses something quite different, and may be answered differently. The KIDSCREEN predominantly assesses how children and young people feel about their health; the CHIP focuses mostly on functioning, asking what children and young people can do. Describing the content of PROMs using the ICF-CY is likely to lead to a loss of information, without reference to the context and precise focus of the question.
The COSMIN checklist was used to rate the methodological quality of the studies. The aim and purpose of this exercise should be carefully considered in future systematic reviews, as it is a time-consuming task. There is undoubted benefit from identifying and considering the methodological quality of studies evaluating psychometric properties of PROMs. However, in our quality assurance checks with a second reviewer, we found an issue in the consistency of how those making the ratings interpret of some parts of the COSMIN checklist. The most difficult COSMIN item to code consistently was ‘how missing items are dealt with’, and this item has a strong influence on the overall quality rating for most psychometric properties. The procedures for handling missing data may not have been reported in all papers that were included in the review, but may have been detailed in other papers or be detailed in the manual of the PROM.
We did not examine the methods used to derive the preference weights applied in the scaling of the PBMs appraised in the review; the methods for creating the preference weighted scales were assumed to meet the requirements for creating interval-level measurement. 224 As the fundamental purpose of preference-based measurement is to quantify the value or strength of preference for health change, the means for assuming and eliciting preference values should be critically assessed. 225 Not all of the standard criteria for appraising PROMs are proposed to be appropriate for evaluating PBMs; for instance, the requirement for internal consistency may conflict with the underlying theory. 225 Nevertheless, most criteria for face, content and construct validity and test–retest and proxy reliability remain applicable;225 these properties of PBMs were found to be largely untested with children and young people.
Our inclusion criteria only considered published peer-reviewed studies that specifically set out to evaluate psychometric properties of PROMs. Hence, we will have excluded studies that may present incidental evidence of psychometric performance. For instance, there may be indications of ability to measure change, over time or with interventions, for any candidate PROMs that have been used in longitudinal observational or experimental studies. In addition, we will have omitted any information that may be contained in manuals, if these data have not been published in peer-reviewed journals.
Summary
This systematic review aimed to identify eligible candidate generic PROMs, and to identify and appraise evidence of the psychometric performance of these PROMs in both general and neurodisability paediatric populations.
We identified 41 potentially eligible candidate PROMs; a total of 126 papers were identified that reported evidence of the psychometric performance of 25 PROMs that had been evaluated using English-language versions: 19 generic PROMs, two chronic-generic PROMs and four PBMs. Twelve candidate PROMs were selected as having more favourable evidence regarding their performance. Robust evidence was lacking in one or more respects to support the psychometric performance for all candidate PROMs that were appraised in this review, both in a general population and, more crucially, with children and young people affected by neurodisability. No evidence was found for any of the candidate PROMs to support the responsiveness to detect meaningful change.
The most studied generic PROMs are CHQ (two proxy versions and one self-report version), KIDSCREEN (three versions of different lengths), PedsQL (three versions for different age groups) and SLSS/MSLSS (three versions of different lengths). Of the generic PROMs, only the KINDL and the PedsQL cover all age categories from infancy to adolescence. For self-report questionnaires for children aged 8 years to adolescence, there is stronger evidence of the structural validity and precision of the Healthy Pathways and KIDSCREEN from Rasch analysis in general populations, and for the KIDSCREEN-52 in those with cerebral palsy.
The DISABKIDS was the only chronic-generic PROM in this review for which reasonable eligible evidence was found. As one would expect, it has been evaluated only with children and young people with chronic conditions, and these do include neurodisability. Promising evidence of psychometric performance was found.
Few conventional psychometric properties of the PBMs have been examined with children and young people. The CHU-9D has been tested more extensively, with some limited evidence in favour. However, the CHU-9D has not been tested with children and young people affected by neurodisability.
Whether generic, chronic-generic or PBM, each candidate PROM appraised has a different conceptualisation of what they purport to measure; some PROMs focus more on functioning, other PROMs focus more on well-being, and still others assess aspects of both well-being and functioning in the same instrument. The selection of any instrument should be consistent with the purpose of measurement, and have face validity to potential respondents.
Chapter 5 Qualitative research with children and young people affected by neurodisability, and parents
Aims and objectives
The qualitative research with children and young people affected by neurodisability, and with parents, used a mix of focus groups and individual interviews to identify their perspectives on important health-care outcomes, and the extent to which candidate generic PROMs represent these health outcomes.
The aim from the study protocol addressed by the qualitative research was:
to identify key health-care outcomes, beyond measures of morbidity and mortality, that are regarded as important by children with neurodisability, and parents.
The specific objectives were:
-
to identify, broadly, what outcomes children and parents expect from the NHS
-
to present candidate generic PROMs, with example items, to determine whether or not these instruments measure outcomes that children and parents value
-
to consider pragmatic approaches which might motivate children to want, and be able, to complete PROM questionnaires, such as novel technology.
Methods
Theoretical framework
This was an applied health services research project with specific objectives and required to relate to the other research streams. This qualitative research was not seeking to elicit a deep understanding of the ‘lived experience’ of the young people and parents. Hence, the analytical approach reflected these issues and purposefully addressed focused policy-relevant questions. The WHO ICF-CY was used as a theoretical framework to link the findings to the other research streams.
Topic guide development
The first discussions to develop a topic guide were convened in a meeting of the qualitative research team and four parents, held as part of the co-investigator meeting in autumn 2011. These discussions highlighted two key issues. First, there was a need to distinguish between ‘health outcomes’ as defined for this research study, and people’s experiences of health services; second, the concept of ‘health outcomes’ was not readily understood by parents.
Parents
Members of the team in Exeter convened two meetings with several parents from the PenCRU Family Faculty; these meetings sought to explore ways in which ‘health outcomes’ could be introduced and understood in the context of this research. The method that appeared to work best used the term ‘aspects of health’, with prompts to build discussion around issues arising such as communication and pain; showing parents examples of PROM questionnaires was also helpful to focus discussions on topic.
In addition, an exception question was added to the parent topic guide. Exception questions are used in family therapy and ask participants to focus on times when a problem does not occur or has not occurred; the inclusion of the question helped to move participants’ focus away from problems with the health system to the differences they would expect to see in their child if the health system were perfect. A hypothetical situation was proposed to parents of ‘an ideal world’, where all services were provided satisfactorily. Given the scenario, parents were asked to consider what improvements in their children’s health they would expect, and ways in which they would want the NHS to improve their child’s health generally.
After a break, parents were shown examples of PROM questionnaires, including the HUI, EQ-5D-Y, KIDSCREEN, and PedsQL with self-report and proxy report versions. Parents were asked for their views on the format and wording of the questionnaires but also on whether or not they felt that the questionnaires addressed the outcomes previously identified as important.
Children and young people
For children and young people, an approach was developed using a hypothetical character in order to depersonalise issues and to encourage them to raise issues that they might otherwise be reluctant to reveal. They were presented with a scenario where an imaginary young person was affected by a health condition, and asked to suggest what health problems they had. Participants were then asked about ways in which the character’s health could be improved. After a break, participants were shown examples of PROM questionnaires, and exemplar questions were extracted from PROMs that were ‘blown up’ as posters, on which young people could write directly or make suggestions for the facilitator to annotate.
The approach was piloted with an established disabled young people’s group in Torbay that was convened on behalf of the local authority by The Children’s Society. The pilot focus group was led by AF and observed by CM. Some modifications were made in the light of this experience, particularly that prompts were helpful to encourage young people to consider aspects of physical, emotional and social health and that there should be less focus on the potential health problems of the character.
This led to the development of a poster to introduce the concept of ‘health outcomes’ to the participants ( Figure 5 ). The poster showed a disabled young person, images of various health professionals, and a road leading to a sunny destination. Participants were invited to give the disabled young person a name and then asked to talk about which health outcomes would be important to the character when they arrived in ‘Outcomes Town’. To help structure the conversation in a way that enabled the participants to better understand and engage with the concept of outcomes, the facilitator (AF) introduced broad outcome areas, including physical health, emotional and mental health, and social and community life. This facilitated discussion of more specific topics; issues such as communication, pain and having friends were introduced as appropriate. Prompts were used to explore participants’ views on (i) how the character in the poster might feel about each of the issues, (ii) whether or not an issue was likely to be important to them and (iii) what could be done could help improve the outcome. This structured conversation gave the participants the opportunity to explore and define the outcomes according to the importance they attached to them.
FIGURE 5.
Poster used to conceptualise the journey towards outcomes.

After the outcomes discussion, the children and young people were shown examples of PROM questionnaires in small groups. They were encouraged to write on these forms to express their reactions, and supported by the facilitator (AF) and support staff to explore and evaluate the content of the forms in small groups. The small groups then came back together to discuss the forms as a single group and were asked to make suggestions on how the forms could be improved to be more attractive to other children and young people affected by neurodisability.
Adaptations and modifications to the methodology
After the fourth focus group, three themed posters were developed to help participants to explore key emerging concepts from the research in more detail ( Figure 6 ). The posters encouraged the participants to explore some of the physical health outcomes, mental and emotional health outcomes, and wider life outcomes that were emerging from the research, and to suggest additional outcomes that they felt were missing.
FIGURE 6.
Three health posters used to conceptualise physical health outcomes, mental and emotional health outcomes.


Further significant modifications to the topic guide were required to include young people with profound communication impairments. This group was included by using a ‘Talking Mat framework’ ( Figure 7 shows an example). The facilitator (AF) collaborated with a speech and language therapist to create cards with illustrations that would be mostly familiar to young people using augmented communication to represent all the aspects of health that had been identified in the previous focus groups.
FIGURE 7.
Example of Talking Mat board used to enable young people with communication impairments to express their views.

A total of 157 cards were compiled as a resource to facilitate discussion about 10 outcome topics: moving about, senses and pain, mental functions, activities, communication, participation, education, feelings, body functions, and diet. Participants were invited in turn to choose which of the outcome topics they wished to discuss. Subsets of symbol cards were then presented, relating to the specific outcome selected. For example, when a participant selected the illustrated card for ‘mental functions’, they were then presented sequentially with cards that related to sleep, memory and concentration. Participants were asked if each of these symbols was for them ‘good’, ‘bad’ or ‘sometimes good and sometimes bad’, and asked to indicate which topics were ‘more important’ to them, ‘somewhat important’ or ‘not important’.
Young people’s personal choices of outcome cards were grouped on their Talking Mat boards, and their interactions were captured using audio recording and photographs of completed boards.
Recruitment and sampling
Interviews and focus groups were led by AA and AF of Council for Disabled Children (CDC). CDC is the leading national policy and practice improvement organisation for disabled children in England. CDC has considerable experience of consulting disabled young people and their parents on a broad range of issues. CDC maintains networks of disabled young people’s groups and parent groups. These networks provided expedient sampling frames for contacting children, young people and parents, including various conditions and age groups. CDC is also able to contact large numbers of families of disabled children through news items on their website and using Twitter and Facebook social networking sites.
The Making Ourselves Heard network comprises 271 contacts across England, including the major providers of services to disabled children from within the voluntary sector and local authority leads from within both youth services and disabled children’s teams. CDC also contacted professionals working with individual and groups of disabled children and young people who applied to be on the Department for Education Young People’s Advisory Group. CDC works closely with the National Network of Parent Carer Forums, which is the umbrella body for all 152 local authority forums for parents of disabled children.
An invitation was advertised through these networks and using other media for individuals and groups of young people affected by neurodisability, and similarly but separately for parents, to volunteer to participate in this research. Volunteers registered their interest directly with CDC. Volunteer individuals and group leaders were screened by telephone to ensure that they were eligible, as CDC has a non-categorical approach to disability and some volunteers were not affected by health conditions included within the project definition of neurodisability.
Focus groups and interviews were purposively selected and strategically arranged to capture diagnostic, demographic and geographic variation. For instance, two groups were held in London in order to include black and minority ethnic communities. Interviewees were subsequently selected to address gaps identified in the sampling frame; for instance, interviews were arranged in the north-west, where it had not been possible to arrange a focus group.
Procedure for interviews and focus groups
The focus groups were organised with support from local professionals, working with parents and children and young people, who recruited participants and provided them with information about the study. The focus groups took place in a range of locations that the participants were familiar with: six took place at weekends or in evenings in premises that the groups used for regular meetings, and two took place in rooms in a school during the school day. Individual interviews were held at the participants’ homes.
At the start of the focus group sessions, the convenors of the group introduced facilitators from CDC, who then introduced themselves to the group and explained the purpose of the project and consent forms were obtained for all participants. For children < 16 years, the consent forms were signed by their parents in advance of the meeting. Participants were also asked to complete a form providing demographic details about themselves and/or their child.
The facilitator then explained how the focus groups would be audio recorded and transcribed, and that this information would be treated confidentially. It was made clear that if at any point a participant said something that they wished to retract, either during or after the meeting, this would be removed from the transcript. All participants were happy with this, and none asked for information to be withdrawn at any point.
The facilitators then began with an introductory activity to establish a relaxed atmosphere. For the children and young people, the facilitator introduced him- or herself and told the group about something he or she was looking forward to doing in the coming week, and asked the participants to do the same. Parents were asked to say who they were and three things about themselves, including how they chose to relax.
Data management and analysis
All audio recordings were transcribed verbatim and checked by the interviewers. Documents used in the data collection and notes were also catalogued. Data were entered into NVivo 10 (QSR International, Warrington, UK) for management and analysis.
The framework approach was developed as a systematic and rigorous methodology for applied qualitative research and was used for the analysis. 226 Framework uses a structured and transparent approach to qualitative data collection and analysis. 227 Framework analysis involves five distinct stages: (i) familiarisation with the data immersion in the raw data (listening to recordings and reading transcripts) to gain an overview of the whole; (ii) identifying a thematic framework – identifying both the key concepts and issues a priori and those emerging from the data of individual respondents and recurring concepts; (iii) indexing – applying the framework to the transcripts, annotating the transcripts with identification codes referring to themes and subthemes; (iv) charting – extracting data from its original context, summarising and grouping it in chart form according to the thematic reference; and (v) mapping and interpretation – reviewing the charts and research notes to compare and contrast, search for patterns and connections and provide explanations for the findings.
Two researchers (AA and VS) read the transcripts from four focus groups, including three with parents and one with young people, to develop the thematic framework used in the analysis. More salient issues grounded in the data were allowed to emerge; nevertheless, the interpretation of the findings was heavily influenced by the prestated research objectives and the ICF-CY. The same two researchers (AA and VS) then both coded six transcripts, including two parents’ and two young people’s focus groups and two interviews (one with a parent and one with a young person). Double coding and subsequent comparison enabled us to check for consistency in the application of the index. The reliability of the coding was checked in NVivo. Nodes (themes) were discussed when the disagreement rate between the two researchers was higher than 2% and Cohen’s kappa < 0.40. Differences arising in interpretation between the researchers were resolved through discussion.
One researcher (AA) then coded all materials from focus groups and interviews, working closely with the facilitator of the young people’s groups and interviews (AF). This was particularly important when coding material from the Talking Mat group. Once all of the material had been coded, two researchers (AA and AF) led on analysis. The data were themed into key concepts, with researchers identifying which outcomes appeared to carry the most weight for participants based on frequency and depth of discussion. Researchers then created maps to identify and illustrate the number and nature of relationships between these identified key outcomes. Several team teleconferences and face-to-face meetings were helpful for considering issues that arose as analyses progressed. The identification of the relationships between the key concepts as shown in the maps enabled the researchers to propose an overarching hierarchy, within which the relationships between outcomes could be contained and explained. As the study progressed, the team discussed whether or not any new issues were emerging and judged that data saturation had been achieved.
The emerging findings were presented at a co-investigator meeting that included parents who were involved in the study and researchers not directly involved in the qualitative work stream. This generated particularly useful discussions and feedback, which aided refinement of the analysis.
The sample size was determined pragmatically, initially, to enable a broad range of participants from different parts of England to be involved in focus groups and/or interviews.
Where extracts of representative quotes are presented in the results, the identification code FGP (focus group parents) is used for parents’ focus groups, those from parents’ interviews are coded IP (interview parents), children and young people’s focus groups are coded FGCY (focus group children and young people), and interviews with children and young people are coded ICY (interview children and young people). For all extracts, square brackets containing three dots [. . .] indicate short sections of omitted speech. All names are aliases.
Approvals
The procedures were approved by National Research Ethics Service (NRES) Committee North East – County Durham & Tees Valley (reference 11/NE/0364); two protocol amendments were approved in relation to refining procedures and topic guides. The study was co-sponsored by the University of Exeter and Royal Devon and Exeter Foundation Trust. Indemnity was provided through the University of Exeter.
Results
Sites and participants
In total, 54 children and young people participated in the research: 50 participated in focus groups and 4 in interviews. There were 53 parents who participated in the research: 47 in focus groups and 6 in interviews ( Table 31 ). The children and parents were not related.
| Participant(s) | Type | Location | Familiar environment | Familiar group | Number of participants |
|---|---|---|---|---|---|
| Parents | Focus group | Stoke-on-Trent | Y | Y | 7 |
| Parents | Focus group | Hull | Y | Y | 8 |
| Parents | Focus group | Exeter | N | N | 8 |
| Parents | Focus group | Westminster | Y | Y | 6 |
| Parents | Focus group | Chelsea and Kensington | Y | Y | 7 |
| Parents | Focus group | York | Y | Y | 11 |
| Parent | Interview | Seascale | Y | N/A | 1 |
| Parent | Interview | Croydon | Y | N/A | 1 |
| Parent | Interview | Beaconsfield | Y | N/A | 1 |
| Parent | Interview | Wigan | Y | N/A | 1 |
| Parent | Interview | Preston | N | N/A | 1 |
| Parent | Interview | Luton | Y | N/A | 1 |
| C&YP | Focus group | London | Y | Y | 7 |
| C&YP | Focus group | Dudley | Y | Y | 10 |
| C&YP | Focus group | Northampton | Y | Y | 4 |
| C&YP | Focus group | Leicester | Y | Y | 6 |
| C&YP | Focus group | Peterborough | Y | Y | 7 |
| C&YP | Focus group | Birmingham | Y | Y | 8 |
| C&YP | Focus group | York | Y | Y | 6 |
| C&YP | Talking Mat session | Mirfield | Y | Y | 5 |
| C&YP | Interview | Leicester | Y | N/A | 1 |
| C&YP | Interview | St Leonards-on-Sea | Y | N/A | 1 |
| C&YP | Interview | St Leonards-on-Sea | Y | N/A | 1 |
| C&YP | Interview | Bognor Regis | Y | N/A | 1 |
The characteristics of participants are shown in Table 32 . There was variation by deprivation in the areas where participants lived, as a direct consequence of our purposive sampling. Ethnicity was mixed, although the majority of participants who identified themselves were white British.
| Characteristics | Children and young people | Parents |
|---|---|---|
| Number of children, range (mean) | – | 1–6 (2.4) |
| Sex (male/female) | 34/20 | 33/20 |
| Age of child, range (mean; SD) in years | 8–25 (16.5; 4.1) | 4–23 (11.6; 4.4) |
| IMD quintiles | ||
| 1 (less deprived areas) | 7 | 8 |
| 2 | 13 | 4 |
| 3 | 9 | 2 |
| 4 | 7 | 5 |
| 5 (more deprived areas) | 6 | 16 |
| Missing | 12 | 18 |
| Ethnicity | ||
| African | 0 | 2 |
| African + white British | 1 | 1 |
| Asian UK/other | 1 | 1 |
| Black UK | 0 | 2 |
| Indian | 2 | 0 |
| White British | 41 | 28 |
| White Irish | 0 | 2 |
| White Irish + Brazilian | 0 | 1 |
| White other | 2 | 0 |
| Other (not detailed) | 0 | 2 |
| Missing | 7 | 14 |
| Neurological diagnosis | ||
| Acquired brain injury | 0 | 2 |
| ADHD | 1 | 0 |
| ADHD/ASD | 0 | 1 |
| ASD | 16 | 13 |
| Awaiting diagnosis | 2 | 0 |
| Cerebral palsy | 9 | 18 |
| Developmental delay | 1 | 3 |
| Down syndrome | 1 | 6 |
| Duchene muscular dystrophy | 5 | 0 |
| Learning disability | 3 | 4 |
| Syndrome | 6 | 5 |
| Missing | 10 | 1 |
| DLA CC | ||
| Higher rate | 16 | 36 |
| Middle rate | 10 | 11 |
| Lower rate | 3 | 0 |
| None | 2 | 0 |
| Missing | 23 | 6 |
| DLA MC | ||
| Higher rate | 16 | 29 |
| Lower rate | 9 | 18 |
| None | 2 | 0 |
| Missing | 27 | 10 |
The ‘primary’ neurodisability diagnosis shown in Table 32 was a pragmatic judgement (made by CM); many participants had indicated more than one impairment, or complex disability. In addition to the listed primary diagnoses, the parents of seven children reported that their children had epilepsy/seizures and the parents of four children reported sensory impairments. Some parents reported having more than one child with a neurodisability: eight parents said that they had two children and three parents had three children affected by a neurodisability. Some children and young people also stated they had several impairments, including seven children who additionally recorded epilepsy and four who were recorded with sensory impairments.
Some missing data resulted from parent groups, with parents arriving late and leaving early. In addition, some parents did not turn over the demographic data sheet and provide those data. A number of parents of children taking part gave their child’s name in the box asking for diagnosis. Some stated that they did not want to give information on Disability Living Allowance (DLA).
Health outcomes
Parents and children and young people were asked to identify health outcomes that were important to them. Because of a need to have a common language for outcomes across the different strands of research within this project, it was decided that they would be, as far as was possible, mapped onto the outcomes defined by the WHO ICF-CY. To maximise intercoder reliability, ICF-CY chapter headings were chosen as far as was possible, with subheadings being utilised only when unavoidable. The ICF-CY health outcomes identified were:
-
communication
-
mobility
-
sensory functions
-
sleep
-
pain
-
interpersonal interactions and relationships
-
making decisions and choices
-
neuromusculoskeletal and movement-related functions
-
self-care, which includes having a good diet, exercise, washing, dressing and toileting
-
major life areas, for example education and work
-
functions of cardiovascular and respiratory systems, including endurance and fatigue
-
community and social life, including recreation, sports and leisure
-
other mental functions, which encompasses consciousness, orientation, social skills, intellectual cognitive functioning, energy and drive
-
temperament, which encompasses behaviour, mood, emotion, anxiety, attention and concentration
-
body structures
-
genitourinary and reproductive functions (continence, enuresis)
-
functions of digestive system including constipation, swallowing and drooling.
In addition to these outcomes defined by the ICF-CY, two additional themes emerged from the data that could not be mapped directly onto the ICF-CY: (i) emotional well-being and (ii) gaining independence/future aspirations.
Outcomes identified
Parents and children and young people were encouraged to identify and explore the importance and meaning of a range of health outcomes. Within these discussions, parents and young people did not generate discretely defined health outcomes. Through the process of analysis, it seemed that the most probable explanation for this was that parents and young people do not think about individual health outcomes in isolation. Rather, they view outcomes as strongly interrelated, facilitating or inhibiting each other.
A number of key outcomes emerged from their accounts that seemed to be given more weight than others. Generally, this was because of the extent to which they affected other outcomes. However, some seemed intrinsically to hold more value for participants. Key outcomes included communication, mobility, pain, self-care, temperament, relationships, social life, emotional well-being and developing independence. These key outcomes are discussed below in the context of their relation to other outcomes and life aspirations.
Communication
Communication was regarded as a highly important outcome by both parents and children and young people. They identified some shared elements, particularly the importance of communication in relation to decision-making and social interactions. Both parents and children and young people distinguished between different types of communication – basic and social.
Parents with children with profound communication impairments wanted children to be able to indicate choice. Many parents identified a link between profound communication impairments and challenging behaviour, where children were using behaviour to communicate feelings or desires:
And he can’t tell us if he’s feeling depressed or angry or, he can scream and wave his arms around and that’s how we know something’s not quite right.
FGP2
There was an underlying anxiety from some parents about safeguarding issues for children who could not communicate. A lot of parental effort goes into translating non-verbal communication for substitute carers:
We felt that we had to really constantly talk to the staff because we were conscious that Stan couldn’t tell them, so we were always having to say now if this happens, if this happens.
IP3
Communication is thus seen as a critical gateway to independence; parents seem much more confident about their children managing without them where they are confident that they can communicate their needs and desires, and prioritise teaching them how to communicate choice:
And they can make choices. [ . . . ] Teach them to say yes or no [ . . . ] Just a big thing is yes and no. It’s a huge thing is yes or no. [ . . . ]
Needing help to go to the toilet and needing to be fed they’re all about personal dignity [ . . . ] some of these children will never experience, and that independence of, I’m going to eat that bit but I’m not going to eat that because I don’t like that or I don’t want it.
FGP1
The relationship between communication and taking part in decision-making was recognised by children and young people, who saw communication as a vital element of independence and crucial to taking part in decision-making about their lives, both highly valued outcomes. Not being able to communicate was a source of anxiety for children and young people, associated with being marginalised or excluded from making decisions about their own lives, with other people taking decisions on their behalf without taking their preferences into account ( Box 1 ).
I suppose support for young people, depending on their, how they can communicate, for them to be able to say what they need or any discomfort that they have or, instead of just having an expert saying this is what you need, listen to the individual sometimes.
FGCY2
It’s easy for someone to decide for you, but they don’t really know how you feel about, you know, what you want or need . . . I think if the other person can’t communicate then what they want might not get done.
FGCY2
But the only person that can tell people about it is yourself really, isn’t it?
ICY4
Children and young people believed that children affected by neurodisability should be supported by health services to be able to communicate to the best of their ability, encompassing a wide range of communication techniques and assistive technology to enable them to take part in the decision-making process. Children and young people also recognised the role that their parents played in understanding and transmitting their communication to others, especially other adults. These points were endorsed by a young person who participated using an eye-gaze computer to communicate:
Why are friends and family important to young people?
Because the parents can understand what the people are saying and understand them as well. Yeah, communication for parents.
ICY1
All children and young people with complex communication impairments taking part in the Talking Mat sessions selected communication as one of their key outcomes. They chose symbols for ‘choice’, ‘listen to me’, ‘people don’t listen to me’, ‘independent’ and ‘people ignoring me’ as aspects of communication that were important to them ( Figures 8 and 9 , FGCY7).
FIGURE 8.
Results of Talking Mat session showing the importance of communication.

FIGURE 9.
Talking Mat showing a link between aspects of communication and friends.

One aspect that was articulated repeatedly by children and young people as one of the most importantelements of communication was being able to communicate with health professionals. This was raised in the context of the importance that children and young people placed on being able to express their views and convey information to professionals in order to help determine treatments that could lead to better health outcomes:
People messing you about like when you’re in hospital and stuff, they don’t understand you and stuff. And not necessarily just in hospital as well like in care and stuff because they don’t understand what you, what your needs are and stuff like that.
FGCY3
Parents with children with more moderate communication impairments wanted them to have support that would help them to develop social communication ( Box 2 ). They were frustrated about what they perceived to be a loss of potential speech (or development in speech) because of a lack of therapeutic input, or other interventions such as cochlear implants.
She can talk and they discharged her because they said that she can make every sound of the alphabet but she is difficult to understand. So you need to listen to her in context and we don’t always understand what she’s saying.
FGP5
Because my daughter can’t, non [sic] verbalise at all, but the speech therapy see more of a swallowing issue for further problems as opposed to, they’re not looking at it for, like let’s see if we can develop her to socially communicate, be more independent.
FGP5
Eventually we did get her a communication device. Actually if we’d have had it much earlier [ . . . ] Would have had a much better outcome for Katie [ . . . ] She would have been communicating from a very young age.
FGP3
Both parents and children and young people identified communication as critical to the ability to form friendships and interact socially; not being able to communicate socially would lead to difficulties in forming relationships and be a cause of frustration and distress:
Because they won’t be able to understand one another, basically . . . They would probably get annoyed, frustrated and all that, angry.
ICY1
Mobility
Mobility was another area that was an important outcome for both parents and children and young people. Both groups identified the relationship between mobility and the ability to make choices. For children and young people, mobility was closely associated with making choices about being able to go where they want in order to access a range social and community activities while spending time with friends and family, without always needing somebody with them to support them, and was therefore also strongly related to community and social life:
Being able to move when you want to move and not when other people just want to move you, as well, so you’ve got a choice over where you’re going and what you’re doing.
FGCY2
A disabled person needs some help but sometimes they like to do things themselves . . .
But sometimes they get stuck . . . it [mobility] would help them if they don’t want to go about with someone with them all the time.
FGCY8
Achieving this level of mobility was an aspiration for children and young people and provided them with a sense of freedom and independence that they regarded as a key part of living an ordinary life. For parents, there was the very basic fact that, for children without functional communication, mobility might be the only way in which they were able to indicate a positive, or negative, choice:
The way he communicates to me is, if he wants a drink he will pull my arm until he gets what he wants. That’s basically how he communicates, so anything he wants, and he just pulls me.
IP4
Parents were concerned about the impact of mobility on social interaction, most commonly in relation to play when parents talked about the way in which lack of, or poor, mobility impacted on their child’s ability to join in and keep up with other children, and then on their self-esteem:
It’s not that they’re being mean, but they don’t play with Dan, because he can’t, so they end up getting too busy and zooming off somewhere else, and he feels that a lot, I think. [. . .] he seems to have become quite passive, to me, [. . .] but I think a lot of it is I’m not going to bother now, which worries me.
IP6
Children and young people shared this recognition of the way that their mobility impacted on their ability to participate in social and community activities with friends. There was a particular concern about how their level of mobility affected the extent to which they could attend school, take part in sporting activities and keep up with non-disabled peers:
Because I’m not really fast at the moment, and all my other mates are, so I can’t really catch up.
FGCY1
Elements of children and young people’s physical functioning played a big role in determining their degree of mobility. Neuromuscular functioning in particular was seen as critical for mobility, with a particular emphasis on the importance on muscle and joint functioning in being able to move around to the greatest degree possible:
My problems with my leg, legs I struggle to straighten it . . . it’s just so difficult because you have to really concentrate really hard and you have to like go like, you have to start slow and then go quicker . . . It’s really hard to do things quickly so it’s impact on me.
FGCY4
This was often related to spasticity, but hypermobility and dyspraxia were also mentioned. Physiotherapy input was highly valued by parents, and also by some of the children and young people, as a key route for maximising neuromuscular functioning and, therefore, mobility:
He had a surgery on his hip and if like physio and occupational therapy provided a programme he needed he would have, would have been able to use a standing frame, even a walking frame. He is not able to use any of them.
FGP1
Effective mobility aids were important for the quality of life children and young people, who recognised the importance of achieving a level of neuromuscular functioning that enabled them to use their equipment comfortably and effectively:
I was just going to say like having mobility aids can be, help give you more a sense of freedom and independence to move around and to do more what you please.
FGCY2
I’ve got a dislocated hip on one side and for me I can only spend about half an hour in my [wheel]chair and then I need to get out again. So if the NHS could help me with that then that would be a lot better.
FGCY4
Wheelchair users had a specific concern about maintaining sufficient motor skills to enable them to operate their wheelchairs independently, as losing this ability undermined their ability to get around independently. For children and young people with complex communication impairments, who were all wheelchair users, their mobility equipment was more important to them than their ability to stand or walk ( Figure 10 ).
FIGURE 10.
Talking Mat showing importance of equipment for moving and moving about (FGCY7).

A number of parents voiced concerns about what they perceived to be ‘low expectations’ from professionals. This crossed a number of different outcome areas, including mobility. For example, one mother was frustrated that her child had been discharged from physiotherapy services because she could now walk, when the mother felt that her daughter’s gait was still ‘peculiar’. She wanted more input so that her daughter would be able to walk and present herself more ‘normally’. This possibly indicates a difference between the goals of professionals and parents. For the physiotherapist, mobility is the goal and this has been attained. For this parent, mobility is an end in itself, but she additionally has a higher-level goal, which is about her daughter standing out less from her community and her peers.
Parents talked about the way in which a number of neurodisabling conditions, such as autism, meant that their concerns around mobility were not in relation to any physical difficulties, but rather because their child did not necessarily have the cognitive abilities that would enable them to be safely mobile:
If she sees something she fancies. She ran out of the house and she stopped a taxi in the road, and she lay on its bonnet and was shouting ow, ow. She’d seen something on the telly.
FGP3
Pain
Children and young people were concerned with the direct physical discomfort caused by pain but also by the negative impact of pain on a wide range of physical, mental, emotional and social outcomes and overall quality of life. As a result, children and young people regarded pain as one of the major barriers to their life aspirations, one that affected ‘everything’ (FGCY1 + ICY4), and one of the aspects of their health that they wanted the health service to improve.
This prioritisation of pain was linked to the strong feeling that if pain was not managed adequately then the consequences were serious and widespread and it could become a barrier in relation to a range of health outcomes that children and young people valued. The most prominent outcomes that were raised by children and young people as being negatively impacted on by pain were communication, physical endurance, mobility, the ability and desire to interact socially with others, the ability perform mental tasks and school attendance ( Box 3 ).
I think it’ll [pain] bring them generally down, as well, because [ . . . ] you can’t socialise with anyone or [ . . . ] can’t be independent because the pain isn’t handled well, then I guess you become just, I don't know, bring yourself down, I guess.
FGCY2
If you’re in less pain there’d be a happier impact, if you’re in more pain it would have a bad impact on yourself.
FGCY2
It might mean you can’t talk to anybody because you’re in pain.
FGCY2
Because if it hurts you, you don’t want it to go on and on.
FCCY1
It would get too tiring for them, plus they get too exhausted as well.
ICY4
If they’re so much in pain then it can cause somebody to be emotional and sometimes trying to find the words to tell someone that you are actually really upset or really angry then it can be even quite hard and it doesn’t always come across the way you want it to.
FGCY4
The impact that pain could have on school attendance, and participation at school, was important to children and young people, both in terms of learning new knowledge and skills, which was highly valued for gaining qualifications that would be beneficial after they left school, and as an important site of social interactions with peers. Pain, especially when it affected mobility, was frequently mentioned as a one of the main factors related to neurodisability that disrupted children’s and young people’s school experiences. This disruption was related to the negative effect pain has on the ability to concentrate and perform complex mental tasks, and to the way pain limits mobility and can cause long-term school absence:
If you’re in a lot of pain then, and that’s not being managed properly, then it’s going to affect what you can and can’t do as well, and whether you can enjoy doing those things, concentration and things like that.
ICY3
Children and young people who used mobility aids were concerned that if equipment was poorly fitting this could cause pain, which could then become a major barrier to mobility:
If you have splints or orthotics on your legs it’s just making sure they fit properly otherwise that can cause quite a lot of pain [ . . . ]
And so if they weren’t fitting properly what’s the negative impact of that?
Well, it hurts quite a lot and it affects how I walk because if they hurt then obviously I can’t walk as far and I have to take them off and it means I can’t get round places that I need to go to.
FGCY4
For wheelchair users, being able manage the potential side effects, especially minimising discomfort resulting from long periods of sitting in a fixed position, and reducing the risk of pressure sores, was a major concern. Parents were also concerned about pain caused by poor equipment products, including incontinence products leading to sores and pain. There was frustration from parents about what was felt to be avoidable pain:
The nappies that we’ve got keep him dry. So if he soils or wees at night, we don’t have to change the sheets any more. He obviously still has the soreness issue. So it would be nice to have some that were the, like what you get Pampers and everything where they’ve got the layer that protects the skin. It just seems to be basic, very basic nappies.
IP5
Parents of children with communication difficulties were very anxious about pain being missed or misunderstood and, therefore, not managed appropriately and effectively.
Self-care
Self-care was another pervasive outcome area for parents, but one that was not of equal concern for children and young people. As an outcome in and of itself parents were looking for their children to achieve the maximum amount of self-care possible and wanted health professionals to factor in the impact of interventions or procedures on self-care:
Once the gastrostomy was put in there was absolutely no effort and no plan to keep up the [feeding] skills.
FGP1
Parents identified neuromusculoskeletal functioning as an obstacle to self-care and valued interventions and exercises that were focused on helping their child to be more independent with their self-care:
We want Stan to focus on things that are going to be useful to him and functional to him, so transfers out of his wheelchair to go to the toilet and things like that [ . . . ] as parents we would like to think that in the future when he’s going to the toilet he has got some kind of privacy or dignity. [ . . . ] But in physiotherapy sessions they’ll work on things like side sitting, which, he’s not going to be able to use that in any kind of functional way.
IP3
For children and young people, there was some concern that neuromusculoskeletal functioning restricted their ability to carry out self-care independently, or made carrying out self-care tasks more difficult and time-consuming. At best, this was regarded as an inconvenience that children and young people learned to cope with; at worst, it was described as being highly distressing:
They become tired and it makes it very difficult, like for instance going to the toilet, getting yourself dressed if your legs, if you try to do any little things then it can hurt and become all of a sudden very difficult.
FGCY8
Some parents who wanted their children to have a greater level of independence prioritised toileting as a key outcome. Mothers highlighted concerns about the fact that they still needed to support pubescent children with washing and going to the toilet when more usual age-appropriate behaviour is a child’s increased desire for privacy. Toileting was also a priority for parents because of the logistics of changing children who are not continent; parents saw continence and independent toileting as opening up a greater range of social opportunities. The poor quality of continence products was also raised as an issue in this context, with parents feeling that the products did not support toilet training, for instance if no ‘pull-up’ products were provided.
Anxiety was also identified as an obstacle to self-care. For children and young people with high levels of anxiety, this could paralyse them in many different aspects of functioning, of which self-care and particularly dressing was identified as one. Self-care was also seen as critical to children and young people gaining independence and parents often talked about the two concepts in tandem:
If they understood why they felt stressed [ . . . ] if they had strategies that they were taught that would help to bring all of these down then they would be able to dress, they would be able to be more independent.
IP2
Daniel nowadays he loves his independence when he can shower himself and wash himself, but at the moment I have to supervise him.
FGP3
Children and young people did not make the same explicit link between self-care and independence, but there was recognition of how requiring self-care support from family or friends could influence these relationships. This resulted in some children and young people identifying being able to carry out self-care tasks, or being able to help more with them, in order to minimise the disruption to relationships:
Yes, and so I want to get stronger in my hips, so. My daddy doesn’t, well, at the moment my daddy lifts me and I want to be able to help him so if I had more strength in my legs I could help daddy more with lifting.
FGCY4
Temperament
Temperament was one of the topics that featured more strongly for parents than for children and young people. While children and young people recognised that difficulty in controlling emotions was an obstacle for them, it was a persistent, recurring theme for parents. This may partly be a reflection of the difference between being on the receiving end and the delivery end of severe anxiety or challenging behaviour; it is also likely to reflect a difference in disability represented by the children and young people and children of the parents involved.
Parents frequently mentioned a reduction in their children’s frustration and challenging behaviour as a desired outcome. They also referred to examples of children being able to manage their behaviour better with pleasure and with reference to another desired outcome, such as consequently getting on better at school:
He’s learnt to handle himself better and [ . . . ] he’s no longer on school action.
FGP3
Parents’ accounts indicate a clear relationship between behaviour and communication:
We’ve had problems with him kicking out and being frustrated and knocking teachers to the ground and just being really, really cross and it’s because he’s, somebody can’t understand him.
FGP1
Ellie is quite extreme [ . . . ] In that she punches herself if it’s, if there’s something that she doesn’t like. [ . . . ] And then if that doesn’t work she’ll bite herself, and then if that doesn’t work she’ll bite you. [ . . . ] It’s communication.
FGP3
Parents felt that anxiety caused their children emotional distress. Although anxiety is separate from challenging behaviour, parents were clear that it often led to challenging behaviour when children were unable to communicate clearly what was making them anxious:
Last year when he was doing GCSEs he got very agitated. And he was pulling his hair all the time and getting up in the night and crying and all sorts of bad things.
IP1
I heard Connor screaming and I came running and Evan had, [pauses to control emotions] sorry, he’d wrapped a cord round his neck and he was going blue and he did it because I wasn’t there and he needed me. [ . . . ] And he’s so helpless he just and so emotional and he was really angry with me and he didn’t do it because he wanted to die he did it because he was [ . . . ] really distressed, mentally ill.
IP2
Parents identified a number of areas where they felt that poor outcomes led to increased anxiety and or challenging behaviour. These included sleep and ‘sensory processing’ difficulties. Anxiety was also identified as a barrier to sleep and both anxiety and challenging behaviour were identified as barriers to learning and to interpersonal relationships.
For some children and young people, there was recognition that being unable to control emotions such as anger and frustration can result in verbal or physical outbursts that have a negative impact on their relationships:
At school when people annoy me, I get really frustrated. I get really annoyed, and I shout at them, and there’s no need for me to shout at them, and I just need to calm down . . . because then people would think that I’m a better friend.
FGCY1
Interpersonal relationships and interactions
Interpersonal relationships and interactions, especially relationships with friends and family, emerged as a key overarching outcome for children and young people. Making and building friendships with other children and young people is a hugely important part of most children’s and young people’s lives and is regarded as an absolutely fundamental element of having a happy and ordinary life. Making and maintaining friendships was described as crucial for maintaining good mental health and positive emotional well-being:
If you don’t play with your friends you lose them, but if you see your mates you’re more than happy.
FGCY1
Not being able to spend time with friends or to build friendships was a major cause of anxiety for children and young people, who worried about being isolated and lonely, which was identified as a major contributor towards feeling depressed:
If you don’t have a group of friends at school, then you’re a bit like ‘what’s the point of living?’
FGCY2
Wanting their children to be able to form and maintain friendships and relationships with siblings was a recurrent theme for parents. As was the case for children and young people, this seemed to be about wanting their children to have a happy, ordinary life. The lack of any friends at school was one of the factors that caused one parent to consider that her son might have a neurodisability. It was an area of priority for parents to the extent that one had decided to have more children so that her disabled child would have friends. Parents frequently mentioned concerns about their children not having any friends and described situations where their children were left behind, not included or, in the worst instances, bullied. They wanted them to be able to keep up, and to be included with their peers. One woman described, through an interpreter, her desire for her 11-year-old son to have friends of his own age:
So she wants him to socialise more with normal people, normal kids [ . . . ] She said when he goes to the park he’ll play with the little babies.
FGP4
Parents valued children and young people developing and forming friendships, for instance:
Evan now will admit to having friends at school, which is a huge difference, he never would have before.
IP2
A wide range of health outcomes, such as being in pain, having limited mobility or having problems with communication, were identified by children and young people as having a major negative impact on their ability to build and maintain positive personal relationships with friends and family. For children and young people, managing these aspects of their health in a way that minimises its impact on their personal relationships is a hugely important outcome that the health service should support them to achieve:
I think there needs to be working together with the schools and the doctors . . . socially, if you can’t see your friends and things like that, there’s that risk of not staying in contact, maybe losing those friends . . . I think with there being such a big focus obviously with the NHS on fixing you, that is forgotten and because that’s forgotten it has a bigger impact than it needs to have.
ICY3
Relationships with parents were also very important to children and young people but, in addition to the emotional importance of having strong family relationships, there was an extra element to relationships with parents. Children and young people were aware of the role that parents played in providing extra support for them as a result of their neurodisability. This includes parents’ role in understanding children’s communication, providing care and support with managing a health condition, self-care and providing transport. Children and young people described the importance of balancing these two elements of their relationships with their parents and not allowing their neurodisability to disrupt their family relationships by forcing them to prioritise their health issues rather than other activities. A young person interviewed, who used an eye-gaze computer to communicate (ICY1), said that they did not let their health condition get in the way of their family relationships, but that the NHS did not do enough to support this. Another young person suggested:
I think your family and stuff like that, it can affect being able to see them and having that relationship with them, because you’re restricted . . . your family then starts to become second, whereas for a lot of people. . . it’s their number one priorities, friends and family, but I think definitely for a disabled young person, it’s changed around and it’s almost like the doctors are the number one priority for them.
ICY3
Parents never mentioned this aspect of their relationships with their children and this may reflect a taboo. Once parents have processed the loss of the child they had imagined they were having and have bonded with their disabled child, it may be important not to articulate the additional demands. There may also be a concern for their child’s self-esteem and, therefore, a concern not to locate the problem in the child, or it may simply be that they take it for granted.
Children and young people were also concerned that this increased dependence on parents for support could inhibit their opportunities to interact with other children and young people without supervision, which is something they valued for building friendships and feeling independent and having an ordinary life:
Your friends and family are always there for you and sometimes when your mum and dad takes you out and then it, and then you get embarrassed by your parents being around . . . it could be a big problem for some young children if they need their parents with them . . . it’s not really a social life it’s more like a medical social life.
ICY2
This was also true for parents, with many expressing a desire for their children to be able to form friendships and loving relationships. Conversely, not having friendships was seen as extremely negative and distressing. Parents also recognised that challenging behaviour and anxiety were barriers to their children forming successful relationships.
Social relationships were a major part of children’s and young people’s lives, and were identified by them as being directly related to their emotional well-being. Minimising the disruption to these relationships caused by neurodisability was one of their key overarching outcomes.
Community and social life
Community and social life were spoken of as a key priority by parents and children and young people. As outlined above, this was an area strongly linked to interpersonal interactions and relationships, with a mutually reinforcing feedback mechanism; being able to take part in social and community activities was a major factor in influencing children and young people’s ability to build friendships, and being able to take part in social activities with friends was one of the most valued benefits of having personal relationships.
However, the concept was broader than a social life; it was about being included within one’s community and being able to participate in sports and leisure activities. Parents talked about community and social life being fundamental to having a life and enjoying life. They wanted their children to enjoy life, to be having fun, and identified a relationship between community and social life and emotional well-being:
But the fact she is now living a life that’s having fun and doing things and taking part in theatre productions and all sorts of stuff, but the most important thing, she’s relaxed and you can physically see that with her.
FGP6
This prioritisation seemed to be in part because they could identify the positive benefits for their children’s well-being of their children enjoying life: ‘he loves it and he laughs [ . . . ] must be good for his emotional well-being’ (IP3). However, parents also seemed to have an eye on the future; there was a strong desire for their children to be included, to be a part of the community. This seemed, in part, to be about them being able to live an ordinary life, but it was also about their children being a part of something when they were no longer around to make sure it happened:
He’s becoming part of the community, which is what I really wanted for him [ . . . ] he goes and he gets his Coke and his packet of cheese and onion crisps, and they have it on the bar waiting for him now. Hello [son’s name], how are you? And it’s, it’s what I want for him when he’s older, they’ll know him, and when I’m long gone, he’ll be part of something, he’ll have people that know him and that can chat to him and say hello.
IP6
When parents talked about social opportunities, there was often a palpable sense of loss. This was partly for their child, but also for the family as a whole. Parents often talked about the places that they could not go or the things they could not do as a family:
And it’s difficult because a lot of the things that we don’t do as a family are because of Matthew’s behaviour, not so much because of his health. So we generally don’t go to the cinema together as a family because Matthew is unpredictable as to whether he would sit and watch the film. [ . . . ] We don’t go for bike rides together as a family.
IP5
The importance that children and young people placed on participating in social and community life was closely related to the importance of friendships and relationships with family. The interaction of these two factors had a major influence on children’s and young people’s emotional well-being and mental health, and even on their perception of their wider health:
I think it, having a social life, could impact on your health as well because if you’ve got one and able to go out and see friends and family members or anyone [ . . . ] So you’ll feel happy in yourself and sometimes being happy and being with people you know and going out, it can benefit it on your health. So I think it’s really important that all disabled people should have some sort of social life because it can have a positive effect and sometimes even improve your health.
FGCY4
The importance of participating in social activities with friends and family meant that any outcomes that enabled or prevented them from being able to participate in activities with friends took on great significance:
Well, for instance like I can’t go on day trips and I can’t go to the theme park, right, and it’s ruining my parents’ and my life. So every day I have to stay in bed at a certain time and I get out for half an hour, then I get back in bed, so it’s hard for me.
FGCY1
For a number of children and young people, physical play was an important part of their social life, and having the physical functioning to be able perform physical exercise as part of play and sporting activities was an important outcome.
For other children and young people, getting out in the community was not as difficult as being able to carry out tasks that enabled them to participate in social activities. This was related to fine motor control and physical endurance, two aspects of health that could prevent children and young people from socialising with their peers in the way they wanted. While a young person might have enough mobility to get to a fast food restaurant or a theme park, if they did not have the fine motor skills to manipulate money to pay for things or be able to hold an ice cream, or were unable to meet the requirements to go on a ride, their ability to socialise was still restricted.
Sleep and food issues were also mentioned as barriers. Both could prevent opportunities that are a normal part of most childhoods, such as play dates and sleepovers. For some families, this also meant that they could not have friends to stay, or that going on holiday was problematic.
Emotional well-being
Emotional well-being was a strong theme in discussions with parents and children and young people. Parents would often prioritise well-being over other outcomes:
My main objective is to make sure he’s happy and he’s comfortable.
IP4
I just want him to be happy.
IP6
One parent talked about the fact that she and her partner supported their son in walking, although they had been advised by the physiotherapist that it was bad for his hips, because he got so much pleasure from it and she felt that it had a positive impact on his emotional well-being:
I don’t know what benefits it gives him health, like physical health wise. [ . . . ] But mental health wise it’s so powerful because you can see on his face he just loves it and he laughs, and he just loves it, so it must be doing something good for his emotional well-being.
IP3
Children and young people frequently related other health outcomes to the impact that they would have on their emotional well-being, and this was a consistent way children and young people used to explain why an outcome was important to them ( Box 4 ). Children and young people referenced being happy, feeling sociable and relaxed as positive aspects of their emotional well-being, while anxiety, depression and frustration were mentioned as negative consequences of not being able to meet a range of outcomes.
Make sure the person’s happy. I think that’s really important.
FGCY2
If you can’t go out or you can’t meet with these people and you’re in really deep depression that you can’t do anything, so . . .
FGCY2
Relax and be yourself . . . In a good way.
ICY2
I feel just very happy with the migraine tablet’s helped me out.
FGCY1
I feel angry and afraid sometimes.
FGCY1
They’d get in a lot more pain, more frustrated and all that. And they wouldn’t be happy either.
ICY1
I’d rather my medication not be changed that I’m happy with who I am I’m happy with how it affects my life.
FGCY3
It would make you depressed because you wouldn’t be able to make any friends.
FGCY4
I think it might affect other things as well, how happy you are as a person.
ICY3
It upsets them because they’re sitting at home feeling bored.
FGCY8
A number of parents of children with physical disabilities identified a link between physical ability and positive self-esteem. One mother felt that her son struggled with his physical disability and that when he was able to kick a football after a tendon transfer operation it increased his self-esteem:
His self-esteem, you could see it coming out of his ears.
IP6
Even if children were profoundly physically disabled, parents felt that things such as physiotherapy relaxed their children and boosted their confidence. The importance of self-esteem was also evident for children and young people, who referred to things in their lives that made them feel positive. A number of participants expressed the importance of self-esteem in relation to their neurodisability, and how children and young people should be supported to come to terms with their disability and its impact on their life:
Telling them what will happen, explaining it to them slowly and helping them get over what they can’t have . . . Helping them understand what they’ve got when they’re young and helping them learn to, to deal with it . . . and always teach them to have a positive outlook on life.
FGCY8
And sometimes even knowing things that you could have done years ago that you can’t now that can be quite emotional because I used to do a bit of walking and obviously I can’t so much now. I’m more or less wheelchair bound and sometimes that can be quite frustrating not for just me but for my parents and family around me. So having some, having people who understand that would make it easier.
FGCY4
Often a parent’s desire for improvements or interventions was about wanting their child to be happier in themselves; thus, one parent wanted her son to sleep better because she felt he was happier when he did. Another talked about the benefits of music therapy because it made her son relaxed. Another wanted her son to be out of pain because of the negative impact this had on his well-being and state of mind. One mother felt that her daughter’s mental health and well-being had improved as a result of having a proper communication system in place:
She’s physically relaxed, you’re seeing her as a proper person.
FGP4
Parents identified a number of undesired consequences that came from lack of emotional well-being, such as anxiety and depression, including self-harming. For some children, there were physical manifestations of this poor mental health, such as stomach cramps or migraines.
Parents wanted their children to feel good about themselves and to have a positive self-image, to be able to value their strengths.
Gaining independence, future aspirations
Parents valued interventions and support that increased their children’s independence. This was regardless of cognitive and physical ability:
In an ideal world he probably might, as I say, have been able to look after himself.
FGP5
Washing and toileting independently, being able to communicate and to communicate choice were concepts most frequently referred to in relation to gaining independence. Whether or not this was the case, parents were keen that their children’s dignity was protected and respected. So, ideally, they might want their child to be able to self-toilet, but they definitely wanted continence products which did not leak when their children soiled themselves in public. For children with more profound disabilities, parents wanted them to have the personal dignity of continence or at least to have the independence that came from pull-ups as opposed to nappies.
This may reflect the way in which parents try to ‘future proof’ for their children. A number of the quotes in Box 5 refer to a time when parents will not be around to care for their children, and it is very clear that parents feel more secure about the idea that their children will be looked after well in their absence if their children can communicate need and indicate choice. So, there may be an aspiration to enable greater independence, as well as a strong pragmatic desire to prevent poor care in the future or, in the worst-case scenario, harm.
So she’s living her life independently [ . . . ] because Georgia’s communication doesn’t stop on my door. It doesn’t stop anywhere. It’s everywhere.
FGP6
If they can learn to communicate better then they can tell people what they want when you’re not with them.
FGP4
I would like to know that he, other people could understand him because it makes them afraid of him, people are afraid of him. My own family don’t want to know and would never look after him and I just, I sort of fear for the future really.
FGP6
Let’s see if we can develop her to socially communicate, be more independent.
FGP5
I think it’d be nice for him to be able to go and say, this is where I want to go, mum, I don’t want to go that way, I want to go this way.
IP4
The concept of gaining independence was slightly wider than wanting children to be as independent as possible; parents wanted their children to reach their potential. There was anger from a number of parents about what they perceived to be low expectations from professionals about what their children might achieve:
He hasn’t seen a speech therapist for 18 months. [ . . . ] And the last time we saw her she just turned round and said, ‘Liam’s Liam’. That doesn’t help me. Oh, I hate that. I hate that [ . . . ] what does that mean ‘Liam’s Liam’? Which is annoying. And it’s low expectation.
FGP5
They wanted their children to be the best they could be, whatever that might mean; they felt that, too often, because the best that might be achieved might not be the norm, there was a prevailing attitude that a low level of achievement was good enough. Parents talked about therapies being withdrawn as soon as progress was beginning to be made.
Children and young people made far less direct references to gaining independence and future aspirations, and they did not talk about future developments in the way that parents did. As reported above, they were concerned with being able to make choices and participate in activities independently, but this was in the context of developments in the present or near future, rather than longer-term aspirations. Where children and young people did raise issues of future independence, this tended to be in relation to issues common to all young people, such as education, qualifications and employment, and the additional support that disabled people require to achieve these.
The nature of the relationship between outcomes
As is evident throughout, parents and children and young people do not view health outcomes individually. Outcomes were always spoken of in terms of whether they impacted on, or were impacted by, other outcomes. The research team observed that greater weight was given by participants to those health outcomes with the greater number of inter-relationships.
In looking more closely at the inter-relationships and focusing on the way in which participants spoke about certain outcomes as having an impact on, or being impacted on by other outcomes, outcomes could be conceptualised and, it seemed, were experienced as an interdependent hierarchy ( Figures 11 and 12 ).
FIGURE 11.
Hierarchy of outcomes described by parents.
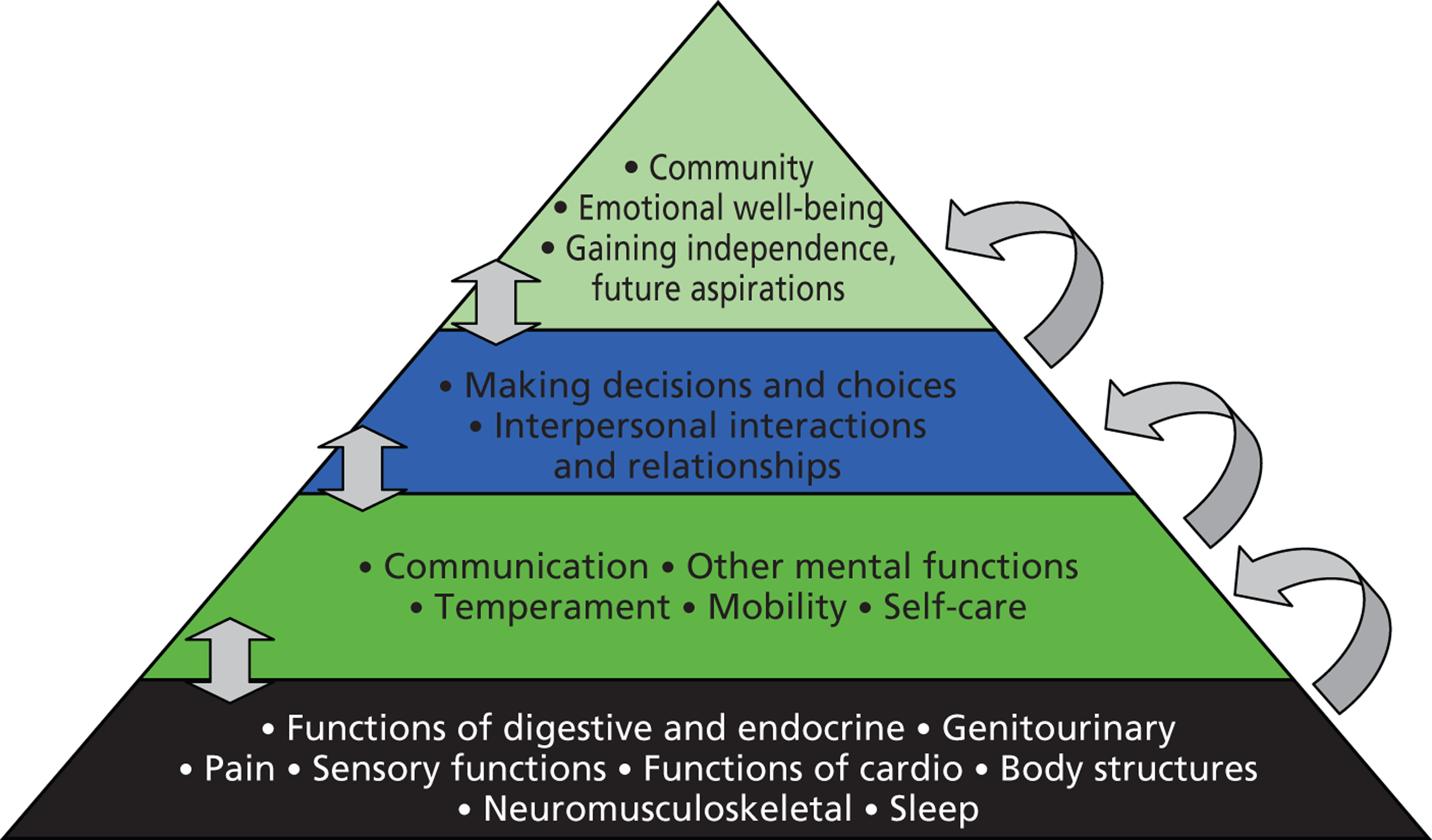
FIGURE 12.
Hierarchy of outcomes described by children and young people.
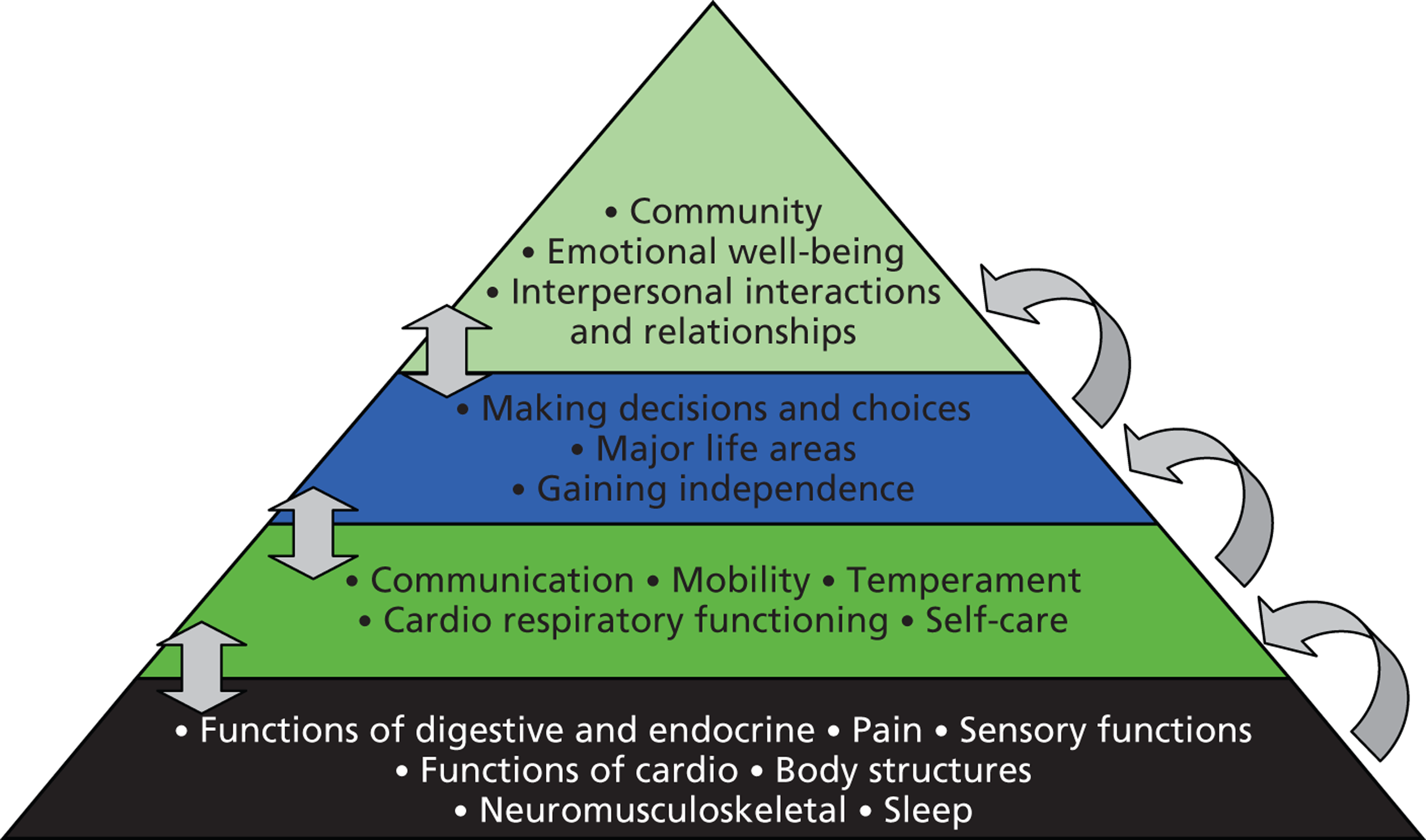
Within the hierarchy, the highest-level overarching outcomes were identified as being of critical importance. These higher-level outcomes were frequently described by participants as the end goal for health services, and the ultimate positive consequence of achieving other, lower-level health outcomes that sit beneath them in the hierarchy:
Huge differences in terms of Daisy being able to make clear choices, having key words to be able to slow herself down without the anxiety building up to her thumping somebody [ . . . ] Huge differences in terms of her whole wellbeing, her mental health and wellbeing. [ . . . ] she is now living a life that’s having fun and doing things [ . . . ] but the most important thing, she’s relaxed and you can physically see that with her.
FGP6
Lower in the hierarchy are fundamental or foundation outcomes related to more basic physical and mental health functioning. These foundation-level outcomes are not necessarily perceived as goals in their own right but take on importance due to their consequences on the achievement of other, higher-level outcomes:
Obviously if you’re in a lot of pain you don’t really concentrate that much on other things and going out with friends and just having a life like everybody else would be is quite restricted because of that.
ICY3
In between higher-level and foundation outcomes are intermediary concepts, more complex than basic outcomes related to physical and mental health functioning. These intermediary outcomes, including communication, mobility, decision-making, learning and applying knowledge, are enabled by a combination of foundation outcomes but are not necessarily regarded as ‘ultimate’ outcomes. The weight given to them is based on their role in facilitating (or blocking) the achievement of higher-order outcomes such as gaining independence.
Two overarching outcomes that were shared by parents and children and young people were emotional well-being and social and community life. Parents also prioritised gaining independence, while children and young people placed a far greater emphasis on the importance of interpersonal interactions and relationships.
Emotional well-being was frequently mentioned by both parents and children and young people as an overarching outcome. As set out in the previous section, and the quote above, parents commented on how interventions or procedures would impact on emotional well-being.
Social and community life was also highly valued by both sets of participants, with other outcomes being valued for their contribution to enabling children and young people to take part in social and community activities. Parents identified the ability to participate in social and community life as being central to ‘living a life’. Other outcomes such as mobility were referenced in terms of the way in which they presented an obstacle or made a contribution to children’s ability to participate socially.
Gaining independence and future aspirations were identified as a key aspiration in all discussions and interviews with parents. Other outcomes such as mobility and communication were identified as being of value in supporting independence and were prioritised for that reason.
There was often a different quality to parental discourse on these three higher-level aspects of health, and they spoke about these areas with clear emotion:
He wheeled himself off round the corner, and I said where are you going? [ . . . ] they said he’s coming to sit with the lads, stop cramping his style, and he went and sat with all these lads, and I just, I nearly cried, I thought it was fantastic.
IP6
Children and young people prioritised social interactions and relationships. Minimising the impact that neurodisability has on their relationships with friends and family was a consistent theme and affected the value that they placed on a wide range of other outcome areas, and was often referred to as the ultimate goal of meeting other health outcomes.
Feedback on exemplar questionnaires
In the second part of the interview or focus group, participants were asked to reflect on a small selection of example PROM questionnaires, in terms of presentation and content. Young people were only asked about the self-reported questionnaires. Parents were asked for their views on questionnaires for children and young people to complete, and those designed for parents to complete about their child.
Purpose and context of patient-reported outcome measure questionnaires
There were immediate concerns from both parents and young people surrounding the purpose of the questionnaire; they wanted the beginning of the form to clearly set out why the questions were being asked and what would be done with the information:
There’s no explanation as to, not only just the purpose of what the forms are for, but what they’re hoping to achieve by us filling in the forms in the first place.
FGP2
It should be borne in mind that for many parents, completing questionnaires, such as those required for DLA, can directly affect their income. There was clearly a concern that filling in this form could have a negative impact on services. Although parents understood that the results would be aggregated, there were still concerns about the inadequacies of the questionnaire in measuring health improvements in disabled children that might then lead to a failure to adequately fund services, or to their child receiving the wrong service:
Will they, in a sense, diagnose your child with something completely different than what happened, based on just this simple test?
FGP2
Confidential or not I would expect severe repercussions if we put the right or wrong thing.
FGCY3
Some participants, both parents and children and young people, struggled not to see the form as an assessment method:
Is there hope that through this form that you will be passed on or fed through to the relevant services available or does that need to be a separate question again?
FGP2
A number of parents argued against the questionnaire being presented within health settings for that reason; their children were often upset by appointments, and filling out the questionnaires at that time would give an unduly negative perspective on how they felt about life.
Face validity issues
There were major concerns about the language used in the questionnaires, in that it may be upsetting for those completing them, especially children and young people. The language was perceived as negative and focused around children and young people’s deficits as opposed to celebrating what they were able to achieve ( Figure 13 ):
And then you’d actually want to go away and commit suicide, wouldn’t you, when you realise [ . . . ] That you have trouble getting along with the world, you have other kids who don’t want to be with you. [ . . . ] I don’t want Daniel to say yes to that. [ . . . ] I don’t want them to be even, have that in their head.
FGP3
I feel afraid and scared, I feel sad or blue, I feel angry, I have trouble sleeping, I worry about what will happen to me, I have trouble getting along with kids, other kids don’t want to be my, my God. [ . . . ]
FGP5
They’re all really negative, aren’t they?
FGP3
Lots of negative questions in, for instance instead of saying, I feel sad or I feel really unhappy, it never really gave you an option of, no, I feel fine or I feel really happy. It was always negative, almost presuming something was always going to be wrong . . . I think they’re too negative.
CYFG4
FIGURE 13.
Feedback from young people about questionnaires (FGCY3).
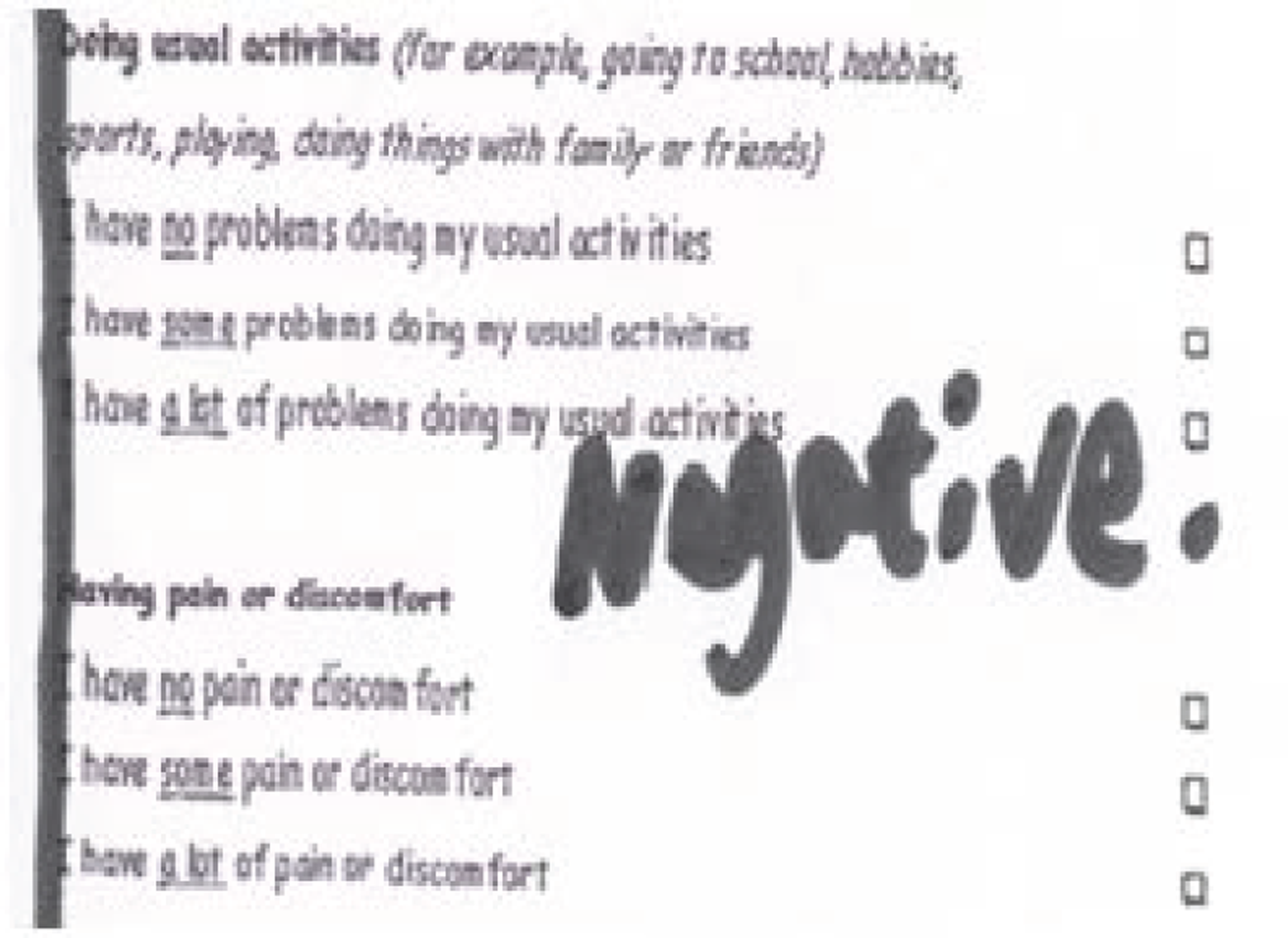
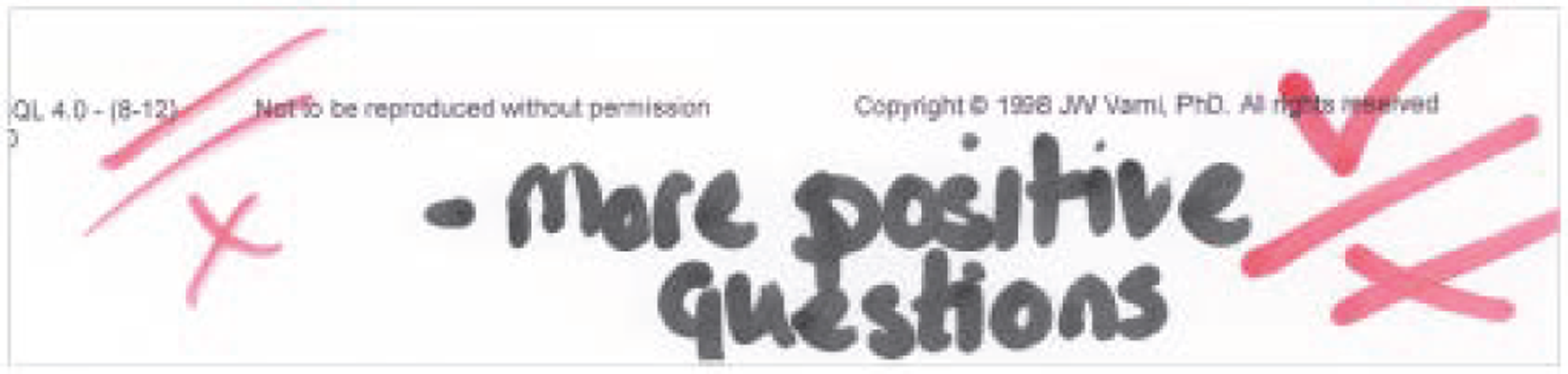
Some parents with profoundly disabled children indicated that they would feel alienated by a questionnaire that did not enable them to capture their child’s level of functioning:
To me, straightaway it’s not relevant because my child can’t do any of these things yet.
FGP2
Parents felt that they wanted to be able to give details of their child’s condition and/or their developmental age so that it gave some context to their answers:
It may be never, but it’s OK for it to be never.
FGP3
They also wanted to be able to measure small improvements or capabilities:
I can say she can dress herself, but washing she could never wash herself.
FGP4
A specific issue for parents of children with cognitive impairment but who were physically able was that a child might, theoretically, physically be able to do something but not be able to do it safely or reliably without supervision. For example, parents wanted to indicate that they had problems with running – not because they could not run but, rather, because they had a tendency to run off.
Children and young people who were wheelchair users felt marginalised by the questions on mobility that related to walking and running rather than giving them the opportunity to answer based on how easily they were able to get around. This marginalisation caused a negative feeling towards the forms and led to wheelchair users not valuing the questionnaires:
Because all of them ones would be four for me because I’m a wheelchair user so most of them . . . it’s not putting into consideration wheelchair users.
FGCY4
I think it’s hard because I suppose young people walking can be a problem but for people who are in wheelchairs . . . you can still go more than one block but you don’t necessarily walk.
FGCY2
That’s not relevant to all to all young people because they can’t walk. So it’s how would you get about better?
CYFG8
Parents also recognised the problem of focusing on walking rather than mobility:
It would be more important for Stan to be able to go in the shop [ . . . ] it doesn’t matter how he gets there.
IP3
Participants’ views on the appropriateness of the questions appeared mixed. Many parents and children and young people agreed that the questionnaires did measure outcomes of concern to them, if indirectly. However, a reasonably common initial response was that they did not:
They’re like, no, they’re like a million miles away from asking any relevant questions.
So what should they be asking, then?
Can your child walk? [ . . . ]
Can your child talk? [ . . . ]
Can your child see?
FGP2
This often seemed to be related to the level or type of a child’s disability, and so parents of profoundly disabled children, or children and young people themselves, often felt alienated by the questionnaires which they felt assumed too high a higher level of functioning in some or all areas, depending on their child’s condition:
For the likes of us isn’t that depressing? [ . . . ] it does make you realise what they can’t do.
FGP1
No one is ever perfect . . .
FGCY5
Sometimes, when aspects of health that might affect a question were explored, parents and children and young people did then feel that the key areas were covered by some of the questions. Children and young people often expressed approval of specific questions as covering an important outcome area, but the way in which the question was asked undermined their approval, and led the participants to dislike the forms generally.
Parents’ initial responses might be that the form did not cover the right areas, but then they might see that ‘anxiety’ or ‘challenging behaviour’ could map onto questions about ‘feeling afraid’ or ‘feeling angry’. However, even when they agreed that there was overlap, they were not always happy with the way in which some topics were addressed. This may have been related to degree of disability and the extent to which parents wanted more finely graded questions and response options which would enable them to track the small improvements that they might be able to expect in their child’s condition.
There were a number of areas that were frequently identified as being inadequately captured, such as continence and food intolerances, and also children’s ‘levels of frustration’.
The proxy-reporting problem
Some parents suggested they would not feel comfortable completing a questionnaire as a proxy for their child. Parents indicated that they would not know how to respond; this was particularly problematic for children with communication difficulties:
For me with this one, my child can’t communicate, so I couldn’t actually answer most of the questions. So I wouldn’t know if he’s fit or well or if he felt full of energy or sad or lonely because he can’t tell me.
FGP2
Many parents indicated that they would not know how their child was getting on at school and that they would need the teacher or teaching support assistant to provide them with that information. For some children, their only social interaction outside of the family was at school, so again parents felt that they did not hold the knowledge necessary to answer those questions. For a few children and young people, there was a concern that the questions relating to social functioning at school may be difficult for children and young people to answer truthfully:
I know it’s a bit anonymous but, it’s anonymous but some people may still not want to put forward their opinion.
And why do you think that might be?
Because people may feel, the parents may think, oh actually they’ve got loads of friends, and they’re probably a bit scared to say whether or not they have loads of friends.
FGCY2
However, it also reflected parents’ acknowledgement that they might hold a different perspective to that of their child. Some parents additionally felt that there might be a difference between their assessment of whether or not their child felt a certain way and their child’s lived experience. The example most commonly cited was around the concept of loneliness for children with autism:
I can definitely say, yes, he seemed lonely to me. But has your child felt lonely? I haven’t the foggiest. He’s usually happiest on his own, so maybe he’s not lonely.
IP2
The same issue arose with questions relating to sleep and bathing, with parents feeling that their assessment may differ to their children’s responses.
Cognitive challenges
Three main cognitive challenges were raised: (i) understanding the question, (ii) the recall period and (iii) feeling able to respond accurately and completely. For children and young people, the language used in the questionnaires was a barrier to understanding, as there were a number of words and phrases that participants did not understand:
Some could be rewritten so it’s a bit easier, because it’s for a little kid to read it should be a bit more simple.
FGCY3
Parents also felt that some of the language used in the questionnaires was not accessible for young people. A number mentioned simple things such as the use of the words ‘male’ and ‘female’, which they felt were less familiar words to their children.
Children and young people felt that some questions asked them to make difficult judgements that they were not sure how to answer, for instance about their relationships with others. They felt that they may not have all the information necessary to fill in the forms ‘accurately’, or were not able to give a response:
Have your parents treated you fairly, what do they mean by that, and what’s that, it doesn’t explain what that’s got to do with your health, that could mean anything?
ICY3
Parents worried that children with cognitive impairments would not understand some of the concepts they were being asked about, particularly that children with autism might have an overliteral interpretation of questions; one parent reflected that, for her son, energy was all about ‘kcals’ (kilocalories), and he would not appreciate that he was being asked if he had felt energetic.
Parents and children and young people repeatedly described questions as too vague or unclear. They were concerned that some questions were not specific enough. Again, this was particularly an issue of concern for parents of children with autism:
So if you are told that it’s hard to pay attention in class, he would say no. If you say, Andrew, are you paying attention to what you’re meant to be paying attention to in class, that’s an entirely different thing.
FGP3
Another concern was that some questions contained more than one possible answer. These were described as vague; for example, the question on getting on well at school could be answered from the perspective of attainment, social interaction or behaving well in class.
Children and young people were concerned with answering the question accurately but were unsure what factors they could include when deciding how to answer the question. They were uncertainties about how they should answer questions that related to activities that they could complete but only with assistance, and how ‘non-health’ factors should influence their answers:
Doesn’t give option of non-health barriers.
CYFG5
Yeah, but that’s not by yourself then, is it, if you’ve got support?
FGCY4
Parents also raised an issue about the difference that environment makes and the fact that a lot of time and energy goes into adapting environments to ensure that they meet the needs of their children both physically and emotionally, but that this does not necessarily happen equally in every environment. This could, therefore, mean that the answer to ‘have you felt sad’ or ‘have you felt lonely’ might reflect something situation-specific as opposed to a pervasive feeling:
They could be happy at home, but they can be miserable in school if they’ve not got the right support.
FGP4
The recall period was also queried. Parents suggested that 1 month was too long a period for young people to reflect on, and that they themselves would find it challenging to be asked to remember back over the last week or month. They felt that children very much lived in the moment and should be asked about that day; however, they were also concerned that because functioning might fluctuate considerably, children might be asked on a particularly good or bad day, which then would not give an accurate reflection. Children and young people’s attitudes to the recall period were mixed, with no clear agreement about an appropriate time frame.
Parents suggested that there were too many response options for young people but not quite enough for themselves. This was partly about a desire to be able to answer accurately and partly about a desire to be able to capture more finely graded improvements:
In his case he’s somewhere between, I don’t know, two or three.
IP1
Both parents and children and young people consistently wanted comment boxes so that they could explain why they were answering in the way that they were and provide greater details and context about their answers. Parents wanted to give a context to the answers relating to the fact that they had no expectation of some areas of functioning improving:
It may be never, but it’s OK for it to be never.
FGP3
For children and young people, they felt that the tick-box format of the response mechanism did not give them adequate opportunity to provide all the information they wanted to about the questions they were being asked, and why they had answered in the way they had:
You haven’t got space to put in a comment and I don’t think that should be a compulsory part of it, but I think you should at least have that chance to comment on things and make yourself clear about what you’re trying to say.
IYP3
Many of the children and young people struggled to comprehend the complexity of the response options, despite the instructions provided in the questionnaire. This included the way the responses were set out, the language used and the format of the scales. The level of complexity meant that some participants were unable to understand how they should use the response mechanism to answer the question:
It’s hard for me to walk more than one block, yes or no, I don’t really get, it’s hard for me to walk more, never, I don’t understand that, they need to be more clearer.
ICY2
The use of pictures, symbols and simple scales was consistently proposed by children and young people and parents as a means of making the forms more interesting and more accessible ( Figure 14 ).
FIGURE 14.
Young people’s comments on PROM questionnaire (FGCY3).
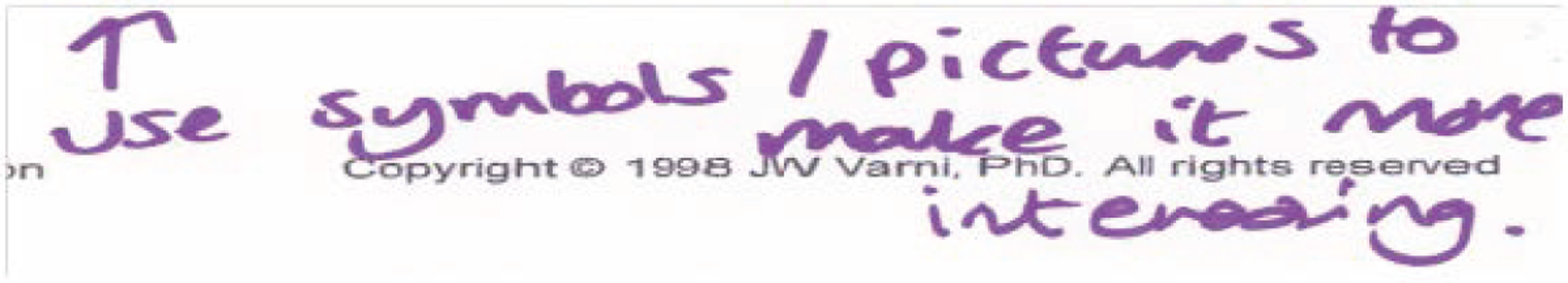
Encouraging completion of questionnaires
The initial response to the appearance of the questionnaires was overwhelmingly negative; they were described as being too dry and formal ( Figures 15 and 16 show some examples). Children and young people repeatedly compared them to exam papers and found this intimidating, and their comments written directly on the questionnaires strongly reflected this. Parents felt that the questionnaires aimed at children and young people needed to be more colourful and engaging but they also thought that more should be done to make them appealing to parents, describing them as looking ‘very official’ (FGP5).
FIGURE 15.
Young people’s comments on a PROM questionnaire (FGCY3).
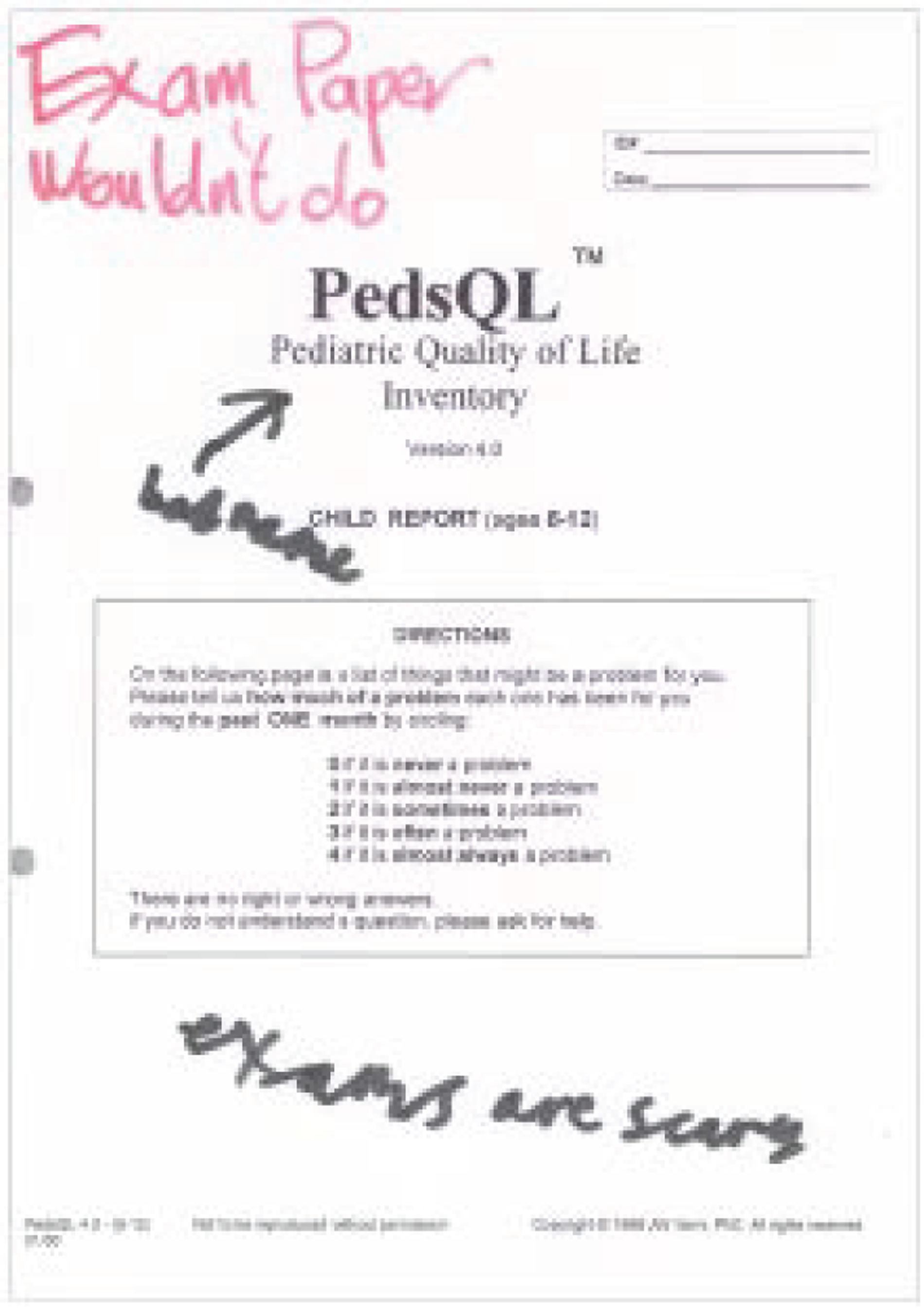
FIGURE 16.
Young people’s feedback on format of PROM questionnaires (FGCY3).
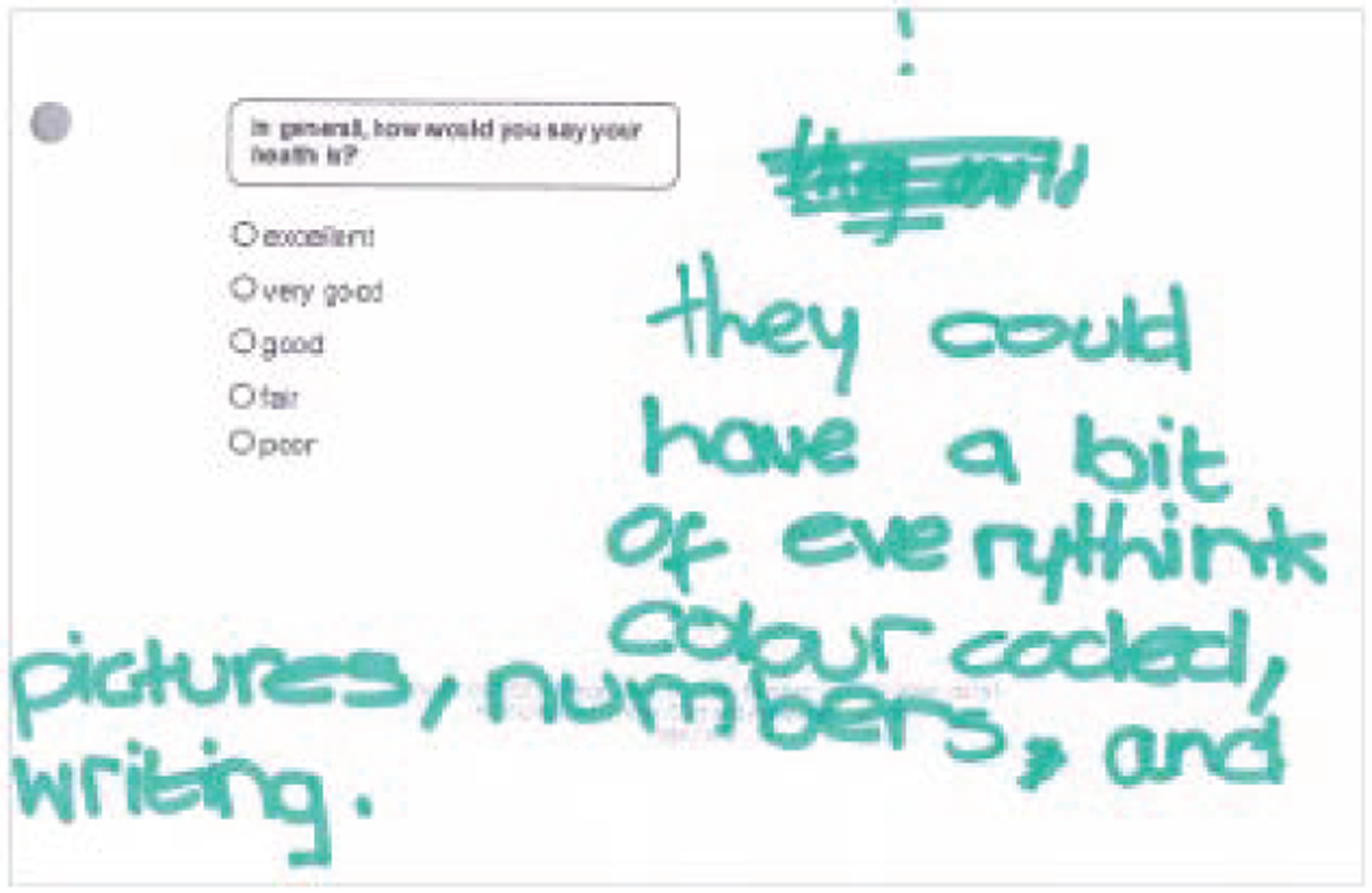
Parents and children and young people suggested use of symbols, emoticons, and traffic lights as more appropriate and familiar response options. They argued that the forms needed to be more accessibly worded and more attractively designed:
Each individual is different, so some people need help, some people just need pictures to let them understand what the question means.
FGCY3
For some children with information-processing issues, parents indicated that the questionnaire would need to be presented in a format which allowed for one question to be shown at a time.
Having an online or touch-pad version of the questionnaire was a popular suggestion for parents and children and young people. For young people, it was felt that this would enable one question to be presented at a time and would overcome some problems for those with fine motor control issues, allowing them to complete the questionnaire independently rather than requiring a scribe. Young people also expressed that they would feel more comfortable with a computerised version of the form as this is a medium that they spend a lot of time interacting with, and it would seem more fun and appealing than a paper version:
They can express themselves into the computer . . . it’s more easy because there’s lots of new products going around, iPads and they can just click, it’d be easier for them.
ICY2
Because [on paper] maybe you’d need someone to do it for you but if you’re on the computer you can just sit down and do it yourself easier.
FGCY2
I spend a lot of mine time on the computer so I’d be better at it really.
FGCY5
Parents felt that, for them, a digitally presented questionnaire would enable them to have the best of both worlds: a short, basic questionnaire which captured more detail where appropriate, but which allowed them to skip past those capacities that were irrelevant to their child.
Discussion
Key findings
Health outcomes
Children and young people and parents viewed health outcomes as inter-related and with reference to a hierarchy. Participants clearly identified the contribution that ‘foundation’ and ‘intermediary’ outcomes made to a smaller set of higher-level outcomes that they felt were most important to achieve in order to have a good quality of life.
The outcomes that were mentioned more frequently in discussions were communication, mobility, pain, self-care, temperament, interpersonal relationships and interactions, community and social life, emotional well-being and gaining independence/future aspiration.
The three that seemed to be consistently identified as higher-level outcomes by children and young people were interpersonal relationships and interactions, community and social life and emotional well-being. For parents, the three were community and social life, gaining independence/future aspiration and emotional well-being.
While these higher-level outcomes might appear to fall outside the sole influence of health services, young people and parents focused on the way in which health services could contribute to them. For instance, the way continence is managed and the efficiency with which wheelchairs and other equipment are provided and maintained impacts on the ability of children and young people to engage in social opportunities.
Where children and young people’s priorities differed from those of parents, this seemed to be due to the impact of lived experience. So, for instance, children described pain as pervasive and impacting on many areas of life. For parents, pain was something that needed to be effectively managed, but they identified far fewer related outcomes. Conversely, the issues of self-care and future independence featured heavily for parents but less so for children and young people. It seemed that this reflected the impact on parents of living with the responsibility of taking care of another person, and their concern about that person’s well-being at those times when they would not be around to do this.
The issue of lived or personal experience had wider implications for the research. Parents approached the outcomes discussion from a position informed by their own experiences, and were clear and open about prioritising those outcomes that were an issue for their child, and which they thought that the health services could and should be impacting on. They were, therefore, less likely to mention improvements in functioning which they felt their child had no prospect of attaining; as a corollary for some parents the desired outcome was maintaining the level of functioning their child already had.
This may explain why sleep did not emerge strongly in the analysis, although it is an area that has commonly been raised as a concern for this group of children. The topic of sleep did arise, but was not discussed extensively in most groups. Where children and young people needed little sleep, they were more likely to see it as a bonus than as an issue, and saw lack of sleep as problematic only if it made them feel tired. For many parents, sleep was not an issue for their child. Parents of children with autism were particularly concerned about sleep. For these parents, it was likely to be identified as problematic only when children were younger or had challenging behaviour and, therefore, in situations where the fact that they were awake meant that they needed to be looked after. This meant that for those parents affected it was a huge issue, but the numbers affected were relatively small.
This personal perspective also meant that the outcomes prioritised by parents might be affected by their experience of services. In the same way that they prioritised those outcomes that they felt were achievable, they prioritised those where they felt that the health service had underperformed and their child had lost out as a result. So, parents who felt let down by the physiotherapy service, in that their child has lost functional ability, or missed out on gaining it, would be more likely to identify musculoskeletal functioning and mobility as high on their list of desired outcomes than another parent whose child had the same condition but who felt that they were getting the interventions or therapies they required.
Feedback on questionnaires
The examples of PROM questionnaires were felt to be dry in appearance, inaccessible and often negative in their use of language. Parents of children with profound difficulties could feel alienated from a set of questions that seemed far removed from their own child’s abilities. The questions were felt not to be appropriate for children with neurodisability without the additional option of comment boxes so that parents could qualify their answers in relation to their child’s diagnosis, functioning and reasonable expectation of improvement.
This was particularly the case for parents of children with autism, who wanted to be able to explain that their children might have a cognitive rather than a physical difficulty with aspects of physical functioning in terms of doing something safely or proportionately.
While the shorter, more generic, questionnaires generally covered the types of areas that parents wanted to be covered, they felt that there were key areas of functioning missing and that the concepts and response mechanisms were too crude to capture useful information about improvements or deteriorations in their child’s functioning. Even with the more detailed questionnaires, parents felt that because they conflated outcomes such as eating, bathing, dressing and toileting they did not allow them to accurately reflect their child’s ability.
A number of parents identified a difficulty in having the right information to complete the questionnaire in instances where they felt that the school rather than they would hold that knowledge. Parents were also uncomfortable in completing the questionnaire as their child’s proxy, feeling that this might lead to a very different assessment than if the child completed it themselves.
Both parents and children and young people wanted the forms to be designed in a more accessible and inviting way and to use tools such as emoticons, with which their children were familiar as communication aids, as response choices.
The idea of presenting the questionnaire digitally was universally popular in that it would enable the form to be presented in a way that might work better for those with information-processing difficulties – presenting one question at a time – but would equally enable parents to have a more personalised questionnaire where areas of functioning relevant to their child might be expanded.
Strengths and limitations
A methodological strength of this research was the gathering of views of a wide range of young people and parents. Young people and parents were drawn from socioeconomically diverse backgrounds, and from areas around England. The participants also included young people with a range of conditions and wide levels of functional ability. We were successful in including children and young people with profound communication impairments using the Talking Mat framework. However, engaging with these children was resource intensive ,and time constraints meant that we were not able to explore their views about the PROM questionnaires. Nevertheless, the sample could not be considered comprehensive of all the conditions under the umbrella of neurodisability. This may impact on the omission of any key outcomes that might be more specific and/or important for certain conditions; there may be different priorities for subgroups of children and young people, for instance those with acquired brain injuries.
In this research, a major challenge was finding ways to focus on ‘health outcomes’, which many participants found to be nebulous. For the majority, ‘health outcomes’ was an abstract concept that required considerable explanation. Hence, we tended towards using posters and prompts that presented them with a series of outcome areas to explore in conversation. This approach may have affected the scope of the ideas that participants generated. Nevertheless, as a result of the introduction of a series of general and then more specific topics to participants, they were able to explore outcomes areas through a structured and depersonalised conversation.
The networks that CDC maintains provide an expedient means to enable a range of disabled young people and their parents to have their say on relevant matters. CDC routinely consults with parents and young people about their experiences of health care, public services and other salient issues. This open consultative approach may have been a distraction in some early parent focus groups. Once this was identified as an issue, strategies and changes to the topic guide were put in place to minimise this problem in later groups. Nevertheless, it was sometimes difficult to steer some parents away from talking about their broad experiences of the health system. In contrast to the parents, children and young people were not preoccupied with experience of services, but they were keen to stress the importance of being able to communicate with health professionals as an important factor on influencing their health.
Data were coded at focus group rather than individual participant level and we did not seek to accurately map whether or not views had links to particular diagnoses in any systematic way. Rather, the approach was non-categorical, aside from the stand-out observations noted in the results.
The views of parents and young people overlapped on some topics but there were also differences. There were almost certainly differences in the characteristics of the children and young people who participated compared with the children of participating parents. For instance, some of the children of the parents who took part had profound cognitive impairments and challenging behavioural problems which are not represented in the young people’s data.
Summary
In terms of the objectives set for the qualitative research for this study, we have been able to clearly identify those outcomes prioritised by children and young people and parents, and the decision-making processes which underlie that prioritisation. This provides valuable information to clinicians and health commissioners in understanding what patients and their families want and expect from the health services.
Presentation of the examples of PROMs determined that these do measure some of the key outcomes identified by children and young people and parents, but:
-
do not capture all of the health concepts that participants see as important to measure
-
are not worded or presented accessibly for all children and young people affected by neurodisability
-
do not enable parents and children and young people to capture more finely graded improvements and, therefore, may not capture improvements made by children with more severe and complex needs
-
do not take into account cognitive difficulties with physical tasks and are therefore seen as unsuitable for many children with autism.
Pragmatic approaches that might motivate children and young people to want to complete PROM questionnaires were identified:
-
the use of emoticons for response options
-
accessible wording and more colourful presentation
-
the use of digital presentation.
Chapter 6 Online Delphi survey with health professionals
Aims and objectives
The aim of the online Delphi survey was to ascertain what outcomes health professionals in England think are important for children and young people affected by neurodisability.
The objectives were:
-
to recruit a multidisciplinary group of health professionals working with children and young people affected by neurodisability in England, and retain their engagement over time
-
to identify the current health outcomes that health professionals routinely prioritise when working with children with neurodisability
-
to focus attention on health outcomes that can be assessed using PROMs as reported by children and young people, and on outcomes other than mortality and morbidities
-
to seek agreement broadly among health professionals on a suite of health outcomes which the NHS could view as important goals for children and young people affected by neurodisability.
It became apparent that, as there was no agreement about what conditions constitute ‘neurodisability’, it would be helpful to clarify and agree a definition. Consequently, a fifth objective was:
-
5. to seek consensus on a definition of neurodisability.
Methods
Recruitment and sampling
We sought a multidisciplinary group of health professionals working with children and young people affected by neurodisability in England. The rationale for focusing on England, rather than UK-wide, was consistency with the qualitative research stream being conducted by the CDC with young people and parents in England, and mindfulness of any cultural differences that might exist in delivering health services in the devolved nations.
The sample of health professionals was recruited initially through an invitation sent to the lead contact person at child development teams (CDTs) in England. The British Academy of Childhood Disability (BACD) maintains a national database of CDTs throughout the UK. On our behalf, following payment of an administrative fee, the BACD administrator e-mailed the lead person with a request to forward an invitation to take part in the survey to a range of their professional colleagues. The administrator sent two reminder e-mails.
In a subsequent phase of purposive sampling, conducted in order to recruit representatives of professions underrepresented after our initial round of invitations, we approached the following professional societies with a request to forward invitations to their members:
-
Association of Paediatric Chartered Physiotherapists
-
Association for Child and Adolescent Mental Health
-
British Paediatric Neurology Association
-
British Society of Children’s Orthopaedic Surgery
-
British Association of Paediatricians in Audiology
-
British Association of Paediatric Surgeons
-
British Association of Prosthetists and Orthotists
-
British Paediatric Neurosurgical Group
-
British Psychological Society – Division of Clinical Psychology
-
College of Occupational Therapy: Children, Young People and Families Specialist Section
-
Royal College of Ophthalmologists
-
Royal College of Speech and Language Therapists
-
Society of British Neurological Surgeons
-
Special interest group in autism for speech & language therapists
-
London Special Interest Group for Autism Spectrum Disorders (Royal College of Speech and Language Therapists)
-
Child and Adolescent Mental Health Services Outcomes Research Consortium.
Professionals volunteered to take part in the Delphi survey by identifying themselves to the research team using an online form. Volunteer professionals were asked to provide details of their profession, region of England where they were employed and their e-mail address.
Survey procedures
Data were collected using several iterative rounds of an online Delphi survey, an established method for seeking consensus. 228 Recommended procedures for conducting Delphi surveys were followed, including beginning with open questions before moving to more specific closed questions, and retaining non-responders in future rounds. 229 In each round, participants were emailed a unique web-link to an online survey system. Participants who connected through the link were presented with a mix of open questions with free-text response boxes, or asked to rate their agreement with statements using four-point Likert response options: ‘strongly disagree’, ‘agree’, ‘disagree’ and ‘strongly agree’. Non-responders were sent reminder e-mails, which included an option to withdraw from the survey.
Question development
Health outcomes
In round 1, participants were invited to state, using free text, what aspects of health they tried to influence and/or improve when working with children and young people affected by neurodisability; examples (‘improve communication’, ‘reduce pain’, etc.) were provided in order to encourage respondents to be precise and to focus on outcomes. Participants were also asked to indicate if they used PROMs and, if so, to state which PROMs they used.
In round 2, survey participants were presented with the list of aspects targeted by respondents in round 1, classified according to the WHO ICF-CY domains. Participants were invited to rate their agreement with the list as broadly covering health outcomes that the NHS should routinely assess for children and young people affected by neurodisability. They were also invited to suggest additional key aspects of health that they felt should be considered, although they were reminded that not all aspects of health could be included.
Many respondents in round 1 stated the very general goals of ‘improve general health’ or ‘improve quality of life’. In order to elicit more specific outcomes in round 2, we asked them what they used as an indicator to find out whether or not things were going well for the child.
In round 3, participants were presented with a revised list and the rationale behind it. We removed two items, ‘activity and participation’ and ‘body functioning’, as both are top-level concepts in the ICF-CY. Other modifications were based on participants’ feedback, and also comments from parents, taking into account the following three criteria:
-
Can the aspect of health be measured validly and reliably using a questionnaire?
-
Is the aspect of health common to many children and across all ages?
-
Can a health service be expected to influence that problem?
Participants were again invited to rate their agreement with the list as presenting appropriate NHS outcomes for children and young people affected by neurodisability.
The candidate PROMs identified in the systematic review measure subtly different tenets of health, some of which distinguish ‘functioning’ and ‘well-being’. Therefore, we also invited participants to comment on whether the NHS should target ‘functioning’, as in what a child can do or does, and/or ‘well-being’, as in how children and young people feel about their health.
In round 4, we focused on gathering professionals’ views on the aspects of health that were assessed by the candidate PROMs emerging in the systematic review. In total, 23 health-related concepts, representing different aspects of health, were selected and presented to participants. Respondents were asked to rate to what extent they thought the NHS should be responsible for these as health outcomes. Participants were also invited to volunteer for the consensus meeting.
Definition of neurodisability
An initial version of the definition was drafted following discussion at the first co-investigator meeting (November 2011), with input from parents. In each of the first three rounds of the survey, participants were asked to rate their agreement with the definition presented from ‘strongly disagree’ to ‘strongly agree’. There was an opportunity to make comments and suggestions using free text.
The level of agreement with the definition in each round, and participants’ specific feedback, was reflected upon by the team, and further iterations of the definition were revised and tested.
Once an acceptable definition was achieved among the survey participants in this work, we sought an international perspective. An invitation and link to a survey was sent by e-mail to (i) the country leads for the European Academy of Childhood Disability, and (ii) International Collaborators of the CanChild Centre for Childhood Disability Research, McMaster University, ON, Canada. We invited a rating of agreement with the definition from international colleagues, from ‘strongly disagree’ to ‘strongly agree’, comments on the definition, and details of any terms synonymous with neurodisability used in their other countries/languages.
The full text of the questions employed in each of the four rounds is included in Appendix 8 ; in summary, questions in each round addressed:
-
aspects of health that clinicians target (rounds 1 + 2)
-
use of PROMs in clinicians’ practices and indicators for ‘well-being’ (rounds 1 + 2)
-
aspects of health that NHS should routinely assess (rounds 2 + 3)
-
appropriateness of constructs of health covered by candidate PROMs (round 4)
-
definition of neurodisability (rounds 1 + 2 + 3).
Analysis
We used an a priori criterion of 67% approval (agree or strongly agree) to appraise whether or not statements were generally acceptable to participants. 229 Free-text responses were categorised and analysed thematically, with reference to the WHO ICF-CY where appropriate (by AJ in discussion with CM). Comments and feedback from participants in each round were categorised, and considered in discussions by the team to inform further rounds of the survey.
Ethics
Formal ethics approval is not required for research with health professionals in the NHS; however, the procedures for the Delphi survey were included in the study approved by NRES Committee North East – County Durham and Tees Valley (reference 11/NE/0364).
Results
Survey response
In total, 309 health professionals registered their interest in participating in the Delphi survey; registrants identified themselves as being from a range of professions. Although we principally targeted English health professionals, there were 14 registrants who identified themselves as working outside England. Their views on the definition of neurodisability were considered eligible and they were retained in the survey. However, participants from outside England were not included in the Delphi process for developing consensus on an appropriate suite of health outcomes, in order to be consistent with the purpose of the research and data collected from families in England.
Responses to all four rounds including only participants from England were, respectively, 233 out of 284 (82.0%), 232 out of 294 (78.9%), 227 out of 293 (77.5%) and 191 out of 292 (65.4%) ( Figure 17 and Table 33 ).
FIGURE 17.
Flow chart showing responses to the Delphi survey regarding health outcomes (rounds 1–4), including only participants from England.
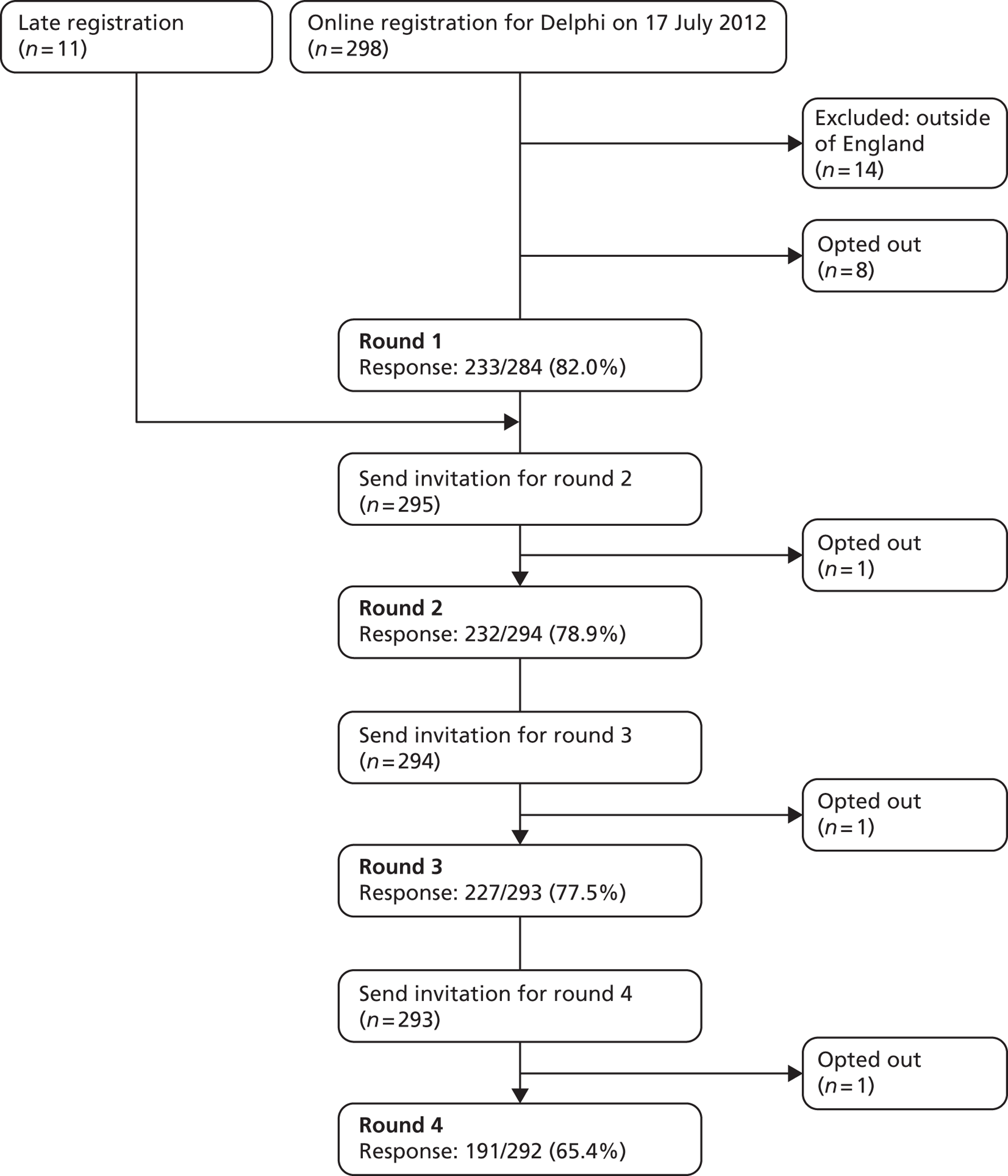
| Professions | Round 1, n (%) | Round 2, n (%) | Round 3, n (%) | Round 4, n (%) |
|---|---|---|---|---|
| Audiologist | 1 (0.4) | 1 (0.4) | 1 (0.4) | 1 (0.5) |
| C&A psychiatrist | 5 (2.1) | 5 (2.2) | 5 (2.2) | 4 (2.1) |
| Child development worker | 1 (0.4) | 1 (0.4) | 1 (0.4) | 1 (0.5) |
| Neurosurgeon | 1 (0.4) | 2 (0.9) | 2 (0.9) | 2 (1.0) |
| Nurse | 9 (3.9) | 9 (3.9) | 5 (2.2) | 4 (2.1) |
| Occupational therapist | 14 (6.0) | 15 (6.5) | 14 (6.2) | 11 (5.8) |
| Ophthalmologist | 0 (0.0) | 1 (0.4) | 1 (0.4) | 1 (0.5) |
| Orthopaedic surgeon | 6 (2.6) | 5 (2.2) | 7 (3.1) | 5 (2.6) |
| Orthotist | 19 (8.2) | 20 (8.6) | 19 (8.4) | 17 (8.9) |
| Paediatric neurologist | 5 (2.1) | 7 (3.0) | 6 (2.6) | 4 (2.1) |
| Paediatric oncologist | 1 (0.4) | 1 (0.4) | 1 (0.4) | 1 (0.5) |
| Paediatric surgeon – other | 2 (0.9) | 2 (0.9) | 2 (0.9) | 2 (1.0) |
| Paediatrician in ND | 4 (1.7) | 3 (1.3) | 4 (1.8) | 3 (1.6) |
| Paediatrician | 76 (32.6) | 73 (31.5) | 73 (32.2) | 63 (33.0) |
| Physiotherapist | 61 (26.2) | 59 (25.4) | 61 (26.9) | 50 (26.2) |
| Prosthetist | 2 (0.9) | 2 (0.9) | 1 (0.4) | 0 (0.0) |
| Psychiatrist | 1 (0.4) | 1 (0.4) | 0 (0.0) | 0 (0.0) |
| Psychologist | 8 (3.4) | 8 (3.4) | 7 (3.1) | 7 (3.7) |
| Rehabilitation medic | 1 (0.4) | 1 (0.4) | 1 (0.4) | 1 (0.5) |
| S&L therapist | 15 (6.4) | 15 (6.5) | 15 (6.6) | 13 (6.8) |
| Teaching assistant | 1 (0.4) | 1 (0.4) | 1 (0.4) | 1 (0.5) |
| Total | 233 | 232 | 227 | 191 |
Responses to the first three rounds that included iterations of the definition, and participants from outside England, were, respectively, 245 out of 290 (84.4%), 242 out of 300 (80.6%) and 237 out of 297 (79.7%) ( Figure 18 and Table 34 ).
FIGURE 18.
Flow chart showing responses to the Delphi survey regarding iterations of the definition (rounds 1–3), including participants from outside England.
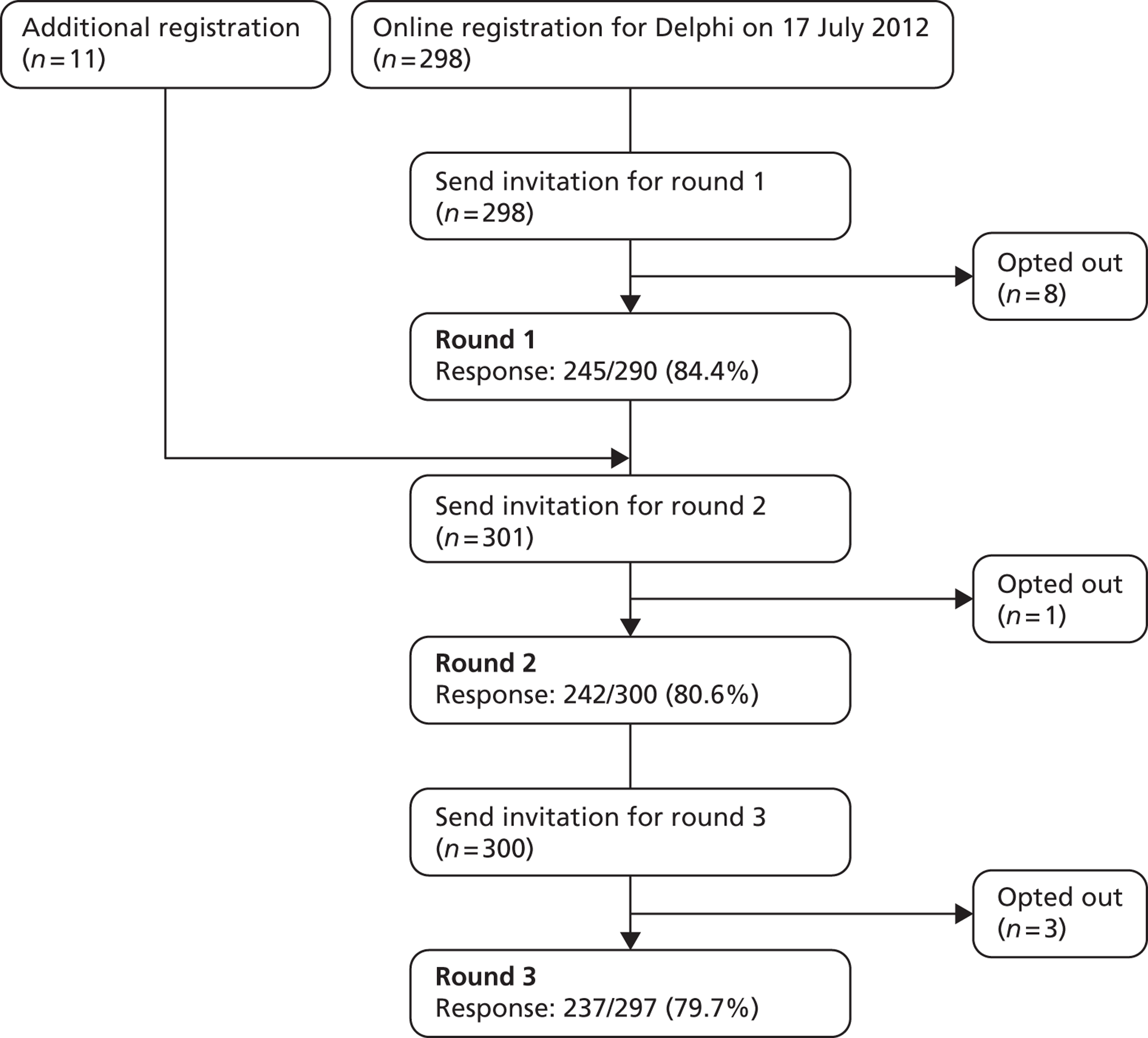
| Professional group | Round 1, n (%) | Round 2, n (%) | Round 3, n (%) |
|---|---|---|---|
| Audiologists | 1 (0.4) | 1 (0.4) | 1 (0.4) |
| C&A psychiatrist | 5 (2.0) | 5 (2.1) | 5 (2.1) |
| Child development worker | 1 (0.4) | 1 (0.4) | 1 (0.4) |
| Neurosurgeons | 1 (0.4) | 2 (0.8) | 2 (0.8) |
| Nurses | 10 (4.1) | 10 (4.1) | 6 (2.5) |
| Occupational therapists | 14 (5.7) | 15 (6.2) | 14 (5.9) |
| Ophthalmologists | 0 (0.0) | 1 (0.4) | 1 (0.4) |
| Orthopaedic surgeon | 6 (2.4) | 5 (2.1) | 7 (3.0) |
| Orthotists | 20 (8.2) | 20 (8.3) | 19 (8.0) |
| Paediatric neurologists | 7 (2.9) | 9 (3.7) | 8 (3.4) |
| Paediatric oncologist | 1 (0.4) | 1 (0.4) | 1 (0.4) |
| Paediatric surgeons – other | 2 (0.8) | 2 (0.8) | 2 (0.8) |
| Paediatrician in ND | 4 (1.6) | 3 (1.2) | 4 (1.7) |
| Paediatricians | 79 (32.2) | 75 (31.0) | 75 (31.6) |
| Physiotherapists | 66 (26.9) | 64 (26.4) | 66 (27.8) |
| Prosthetist | 2 (0.8) | 2 (0.8) | 1 (0.4) |
| Psychiatrists | 1 (0.4) | 1 (0.4) | 0 (0.0) |
| Psychologists | 8 (3.3) | 8 (3.3) | 7 (3.0) |
| Rehabilitation medicine | 1 (0.4) | 1 (0.4) | 1 (0.4) |
| S&L therapists | 15 (6.1) | 15 (6.2) | 15 (6.3) |
| Teaching assistant | 1 (0.4) | 1 (0.4) | 1 (0.4) |
| Total | 245 | 242 | 237 |
Consensus among professionals
Health outcomes
In response to the open-ended question in round 1, about which aspects of health professionals sought to influence and/or improve when working with neurodisability, we received 1524 suggestions from 233 respondents. Some respondents stated aspects of health in general terms, such as ‘improve function’, ‘maintain/improve comfort’, ‘maintain/increase participation’, ‘improve general health’, ‘improve quality of life’ and ‘help the child have fun’. Other respondents were more specific, identifying targets such as ‘improving upper and lower extremity use’, ‘increasing fine motor skills (this includes dexterity, digit strength, manipulations)’, ‘improving motor co-ordination’ and ‘improving gross motor skills: rolling, sitting, moving on the floor, crawling, standing, walking, running, jumping, co-ordination, balance, core stability, etc.’.
All 1524 aspects of health were mapped to the WHO ICF-CY,35 using the most detailed level of ICF coding possible. Together, as a group, respondents targeted aspects of health across all broad domains of the ICF-CY ( Figure 19 ). Some aspects of health were cited more frequently than others; aspects of health that were mentioned 20 times or more are highlighted ( Figure 20 ), although we did not assume that frequency denoted or equated to importance.
FIGURE 19.
Aspects of health reported by professionals as coded using the ICF-CY.
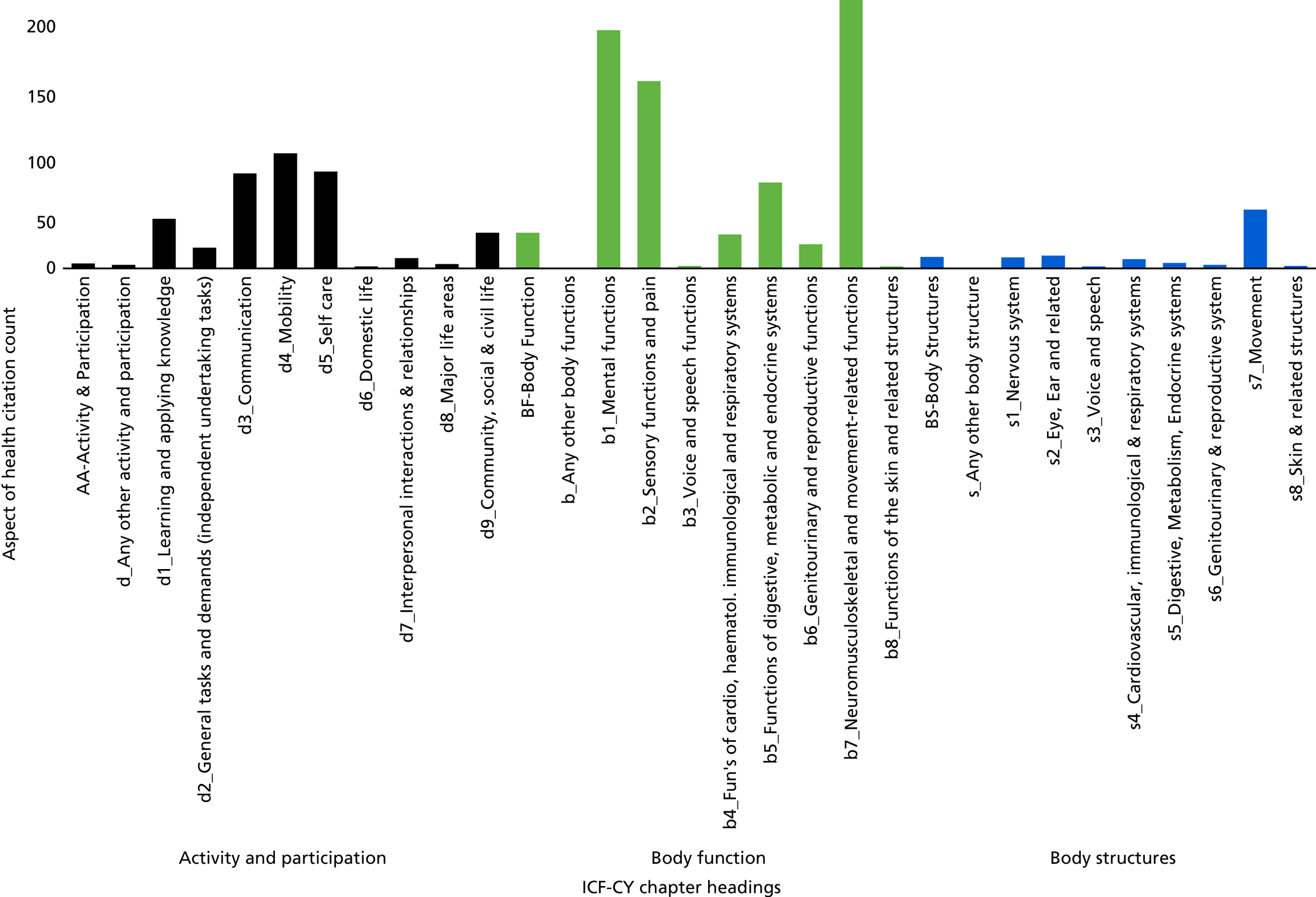
FIGURE 20.
Most frequently mentioned aspects of health in round 1, ordered by WHO ICF-CY domain.
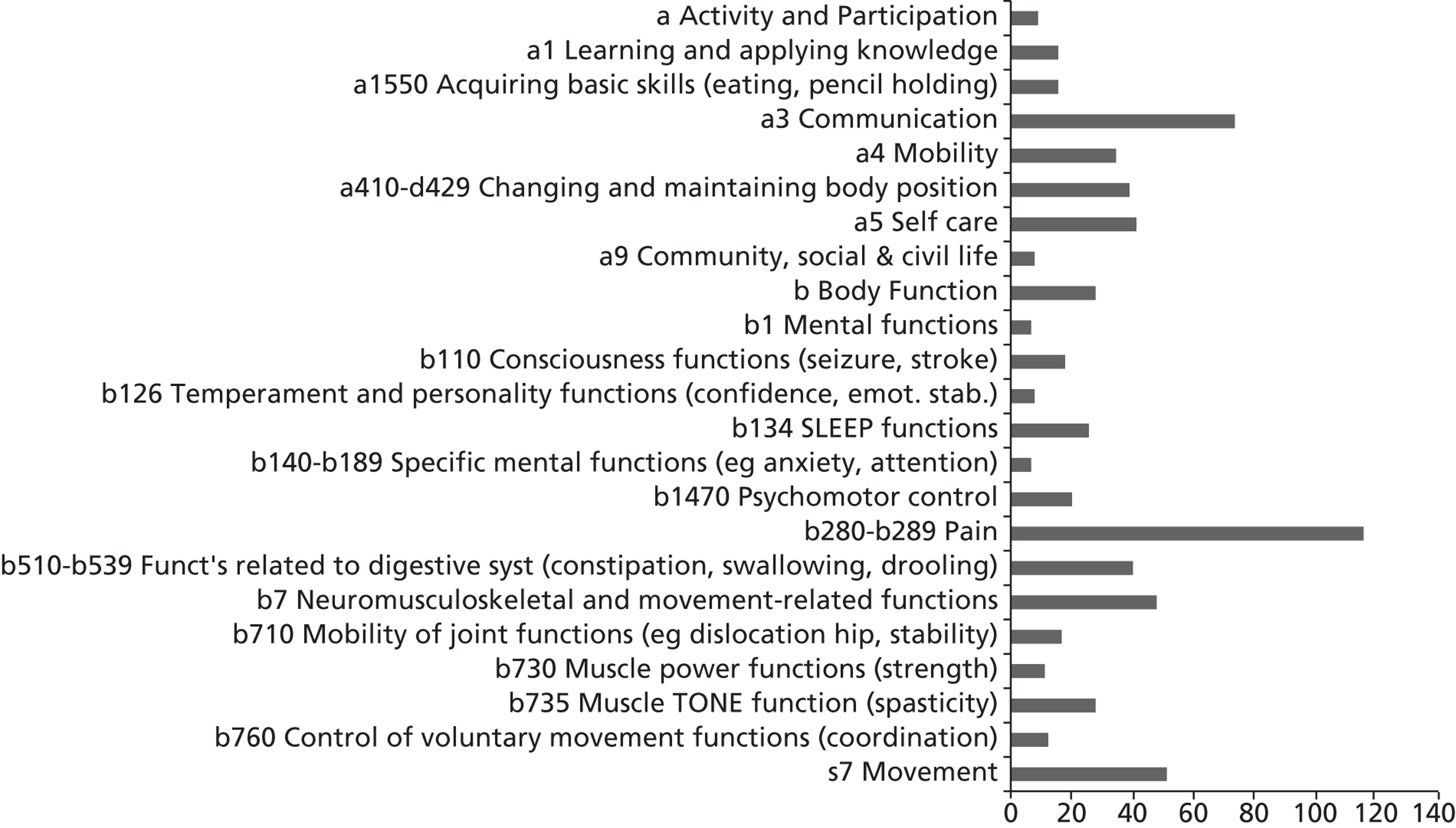
Most (78.2%) respondents indicated that they were not using PROMs; of those who told us they did use PROMs, more frequently mentioned instruments were condition-specific PROMs or mental health questionnaires (e.g. Strengths and Difficulties Questionnaire).
When, in round 2, participants were presented with the list of aspects targeted by respondents in round 1, coded to ICF-CY domains ( Table 35 ), 211 out of 232 (90.9%) of respondents agreed or strongly agreed that that the list broadly included some of the aspects of health that they target, and 207 out of 232 (89.2%) agreed or strongly agreed that these were appropriate health outcomes for the NHS.
| Aspect of health | n |
|---|---|
| Pain | 118 |
| Communication | 80 |
| Movement (in ‘body structures’), e.g. reduce/prevent contractures and deformity; muscle length and joint range of movement | 60 |
| Neuromusculoskeletal and movement-related functions: improve gross and fine motor function; improve quality of movement | 57 |
| Self-care, e.g. improve independence in all activities of daily living (washing, toileting, dressing, eating) | 51 |
| Functions related to digestive system, e.g. constipation, swallowing, drooling | 50 |
| Changing and maintaining body position, e.g. sitting, standing, lying down | 49 |
| Mobility (in ‘activity and participation’), e.g. improve transfer | 45 |
| Body function, e.g. improve function, functional abilities (very general) | 39 |
| Muscle tone function, e.g. spasticity | 39 |
| Sleep functions | 37 |
| Psychomotor control, e.g. manage behavioural problems | 32 |
| Consciousness functions, e.g. seizure, stroke | 30 |
| Mobility of joint functions, e.g. improve mobility and ease of movement of joints | 29 |
| Learning and applying knowledge: acquiring skills; learning to read, write | 28 |
| Acquiring basic skills, e.g. learning to co-ordinate fine motor function to improve eating, pencil holding | 28 |
| Control of voluntary movement functions, e.g. co-ordination of movements, improve head and trunk control | 25 |
| Muscle power functions: muscle strength | 24 |
| Activity and participation | 22 |
| Community, social and civic life, e.g. engage in social clubs; recreation and leisure | 21 |
| Temperament and personality functions: confidence, emotional stability | 21 |
| Mental functions, e.g. improve mental health issues; reduce emotional and behavioural difficulties | 20 |
| Specific mental functions, e.g. anxiety, attention | 20 |
In round 3, 209 (92%) agreed or strongly agreed with a revised list of aspects of health, based on feedback received from round 2 and input from parents ( Table 36 ). Further comments received regarded adding or changing examples, missing items that needed to be added, overlapping redundant items, and aspects of health that were not perceived to be influenced directly by NHS services. We considered that we had dealt with all arising issues by the end of round 3; suggestions had been either integrated into the list, or dismissed as ineligible if:
-
they could not feasibly be measured using a self- or a parent-completed questionnaire
-
they were not common to children with differing neurodisabilities, and across age groups
-
they could not reasonably be expected to be influenced by the NHS.
| Mental functions, e.g. mental health issues |
| Consciousness functions, e.g. seizures, stroke |
| Temperament and personality functions: confidence, emotional stability |
| Sleep |
| Specific mental functions, e.g. anxiety, attention |
| Psychomotor control, e.g. behavioural problems |
| Pain |
| Functions related to digestive system, e.g. constipation, swallowing, drooling |
| Urinary functions (continence, enuresis) |
| Neuromusculoskeletal and movement: gross and fine motor function; quality of movement |
| Mobility of joint functions, e.g. mobility and ease of movement of joints |
| Muscle power functions: muscle strength |
| Muscle tone function, e.g. spasticity |
| Control of voluntary movement functions, e.g. movements, head and trunk control |
| Learning and applying knowledge: acquiring skills; learning to read, write |
| Acquiring basic skills, e.g. fine motor function to improve eating, pencil holding |
| Communication |
| Changing and maintaining body position, e.g. sitting, standing, lying down |
| Mobility (in ‘activity and participation’), e.g. moving, making transfers between posture |
| Self-care, e.g. independence in all activities of daily living (washing, toileting, dressing, eating) |
| Community, social and civic life, e.g. engaging in social clubs; recreation and leisure |
| Movement (‘body structures and functions’), e.g. gait, deformity; muscle length and joint range of movement |
In terms of the precise focus for professionals regarding aspects of health, 212 (93.4%) indicated that they targeted ‘functioning’, and 190 (83.7%) indicated that they targeted ‘well-being’, suggesting considerable overlap in these goals.
In round 4, respondents rated the following as being the greatest responsibility of the NHS: pain, hearing, seeing, vision, mobility, communication, manual ability, sleep and toileting. Those aspects of health that were rated as less the responsibility of the NHS were play, relationships with family, sport and leisure, learning and applying knowledge, and relationships with friends ( Table 37 ). Note that no aspects of health were rated as outside the responsibility of the NHS, taking into account the grouped responses.
| Aspect of health | n | Min. | Max. | Mean | SD |
|---|---|---|---|---|---|
| Pain | 191 | 2 | 7 | 6.22 | 0.90 |
| Hearing | 191 | 1 | 7 | 5.99 | 1.02 |
| Seeing and vision | 191 | 1 | 7 | 5.97 | 1.01 |
| Mobility (e.g. walking, getting around) | 191 | 2 | 7 | 5.57 | 1.11 |
| Communication, speech and language | 191 | 2 | 7 | 5.43 | 1.04 |
| Manual ability | 191 | 1 | 7 | 5.17 | 1.21 |
| Sleep | 191 | 2 | 7 | 5.08 | 1.03 |
| Toileting (e.g. continence) | 191 | 2 | 7 | 5.07 | 1.16 |
| Sexual health | 191 | 2 | 7 | 4.84 | 1.24 |
| Emotional well-being (feeling depressed, happy, nervous, anxious) | 191 | 1 | 7 | 4.60 | 1.22 |
| Self-care – eating (eat well, need help eating, diet, dietary habits) | 191 | 1 | 7 | 4.54 | 1.27 |
| Regulation of emotion (e.g. tantrums, behavioural control) | 191 | 1 | 7 | 4.36 | 1.27 |
| Self-care – hygiene (e.g. washing, brushing teeth) | 191 | 1 | 7 | 4.24 | 1.48 |
| Self-care – dressing | 191 | 1 | 7 | 4.21 | 1.49 |
| Concentration | 191 | 1 | 7 | 4.11 | 1.30 |
| Autonomy, independence | 191 | 1 | 7 | 4.11 | 1.39 |
| Fitness and stamina | 191 | 1 | 7 | 3.97 | 1.34 |
| Self-care – personal safety (avoiding risks, safety issues) | 191 | 1 | 7 | 3.97 | 1.34 |
| (Engagement in) play | 191 | 1 | 7 | 3.91 | 1.38 |
| Relationships with family | 191 | 1 | 7 | 3.57 | 1.30 |
| Sport and leisure | 191 | 1 | 7 | 3.44 | 1.48 |
| Learning and applying knowledge (e.g. learning, problem solving) | 191 | 1 | 7 | 3.41 | 1.48 |
| Relationships with friends | 191 | 1 | 7 | 3.40 | 1.34 |
Inspection of mean scores within professions revealed some minor variations. The varying number of professionals in each group affects the overall mean scores. The small numbers presented by some professions make further statistical analysis or interpretation inappropriate.
Definition of neurodisability
Agreement with the proposed definition was extremely high in every round (89.0%, 90.1%, 93.6%), far exceeding the a priori expressed criteria. However, there were a number of queries, comments and suggestions which informed revisions following each round.
In round 1, participants raised queries about whether or not both congenital and acquired conditions were included, and requested that it be made more explicit that these were long-term conditions with a broad range of severity and complexity, some of which vary over time. Participants were keen for the wording to be consistent with the WHO ICF-CY; hence, we added that the impairments created ‘activity limitations’.
In round 2, participants commented that the revised definition was too long, the inclusion of examples was contested, and some participants were uncertain whether or not neuromuscular and sensory conditions were included. We retained the key concepts from round 2, namely a group of conditions, congenital or acquired, long term, variable, limiting, comorbidity, and including undiagnosed neurological conditions. Nevertheless, we revised the definition to explicitly include neuromuscular conditions, and re-presented two versions of the definition in round 3, one with and one without examples, and invited participants to indicate a preference.
There was broad endorsement of the version presented in round 3, with 93% of participants agreeing or strongly agreeing. However, in response to a direct question about including example conditions, 75% of respondents favoured their omission. Parents working with the team thought that the examples may help some parents but also considered that they could be misleading, especially if a child’s actual diagnosis was not listed and/or was very different from the examples.
Iterations of the definition are provided in Appendix 9 .
From our international survey, we received 22 responses from a variety of professions and one parent ( Table 38 ); 60% of participants had English as their native language. Participants endorsed the definition generally, with 18 out of 22 agreeing or strongly agreeing. Terms being used in other countries include neurodevelopmental disorder or conditions, and neurological disorders or conditions; terms are used in other languages with similar meaning. There were indications that no terms were consistently used or widely agreed upon. The most common feedback from international colleagues was to use terminology consistent with the WHO ICF-CY. 35
| Profession | n (%) |
|---|---|
| Occupational therapist | 4 (18.1) |
| Paediatrician | 4 (18.1) |
| Paediatric neurologist | 3 (13.6) |
| Parent | 1 (4.5) |
| Physiatrist | 2 (9.1) |
| Physiotherapist | 4 (18.1) |
| Psychologist | 1 (4.5) |
| S&L therapist | 1 (4.5) |
| Social science researcher | 1 (4.5) |
| Social work | 1 (4.5) |
| Total | 22 |
| Country | |
| Australia | 3 (13.6) |
| Belgium | 1 (4.5) |
| Canada | 8 (36.4) |
| France | 1 (4.5) |
| Israel | 1 (4.5) |
| Former Yugoslav Republic of Macedonia | 1 (4.5) |
| Switzerland | 1 (4.5) |
| Netherlands | 2 (9.1) |
| Turkey | 1 (4.5) |
| UK | 1 (4.5) |
| USA | 2 (9.1) |
| Total | 22 |
The final recommended definition from this process was:
Neurodisability describes a group of congenital or acquired long-term conditions that are attributed to impairment of the brain and/or neuromuscular system and create functional limitations. A specific diagnosis may not be identified. Conditions may vary over time, occur alone or in combination, and include a broad range of severity and complexity. The impact may include difficulties with movement, cognition, hearing and vision, communication, emotion and behaviour.
Discussion
Key findings
Consensus on key health outcomes
Our iterative approach to seek consensus took account of the frequency with which key health outcomes were mentioned by participants, appropriateness of the concept as a NHS outcome, and the extent to which the NHS might influence the outcome. Those aspects of health that were rated by participants as most commonly targeted, and viewed as the responsibility of the NHS, were predominantly located in the WHO ICF-CY ‘body functions and structures’ – pain, hearing, seeing, sleep and toileting – or were those domains of ‘activities and participation’ most readily influenced by provision of available assistive technologies: mobility and communication. Less frequently endorsed as the responsibility of the NHS, by consensus among participants, were play, relationships with family, sport and leisure, learning and applying knowledge, and relationships with friends. Nevertheless, the WHO ICF-CY chapter titled ‘Community, social and civic life: e.g. engaging in social clubs; recreation and leisure’ did appear in the list of outcomes as broadly endorsed as important.
Arguably, some aspects of health could be deemed morbidities. Aspects of health such as seizures, stroke, constipation, incontinence, respiratory functioning, spasticity, muscle strength and power, and gait may be better measured by quantitative means rather than self-reported using questionnaires. The same could be argued about impairments of aspects of health such as seeing and hearing. We list below a summary selection of outcomes identified in the Delphi survey that would be likely to be amenable to self-reporting using PROMs:
-
mental health
-
confidence, emotional stability
-
anxiety, attention
-
sleep
-
pain
-
toileting
-
movement ability
-
manual ability
-
acquiring skills
-
communication
-
mobility, e.g. moving around environments, making transfers between postures
-
self-care: independence in all activities of daily living (washing, toileting, dressing, eating)
-
social, e.g. engaging in social clubs; recreation and leisure.
Many participants recognised that there were limitations to the extent to which they felt that the NHS could be responsible for aspects of health that are influenced by multiple environmental factors, especially those that take place in settings away from NHS services. Participants noted the need to discuss treatment and therapeutic goals with families and to negotiate priorities. In this way, perhaps, professionals are seeking to have at least some influence on those aspects of health more distal to health services’ sphere of direct influence; that is, in contrast to managing pain, which is clearly perceived as mostly a direct responsibility of health services.
Definition of neurodisability
Contributions from parents and professionals have helped to produce a definition of neurodisability that appears to be clear and generally, if not universally, approved. The definition will help to discriminate between children affected by neurodisability and those with other long-term conditions, such as impairments of the endocrine, respiratory or musculoskeletal systems. Although children with such conditions share some characteristics with those affected by neurodisability, there are sufficient differences to make this an important distinction.
Although there was large agreement with the definition in the Delphi survey, with 93% of participants agreeing or strongly agreeing, there were a small number of people who disagreed. One reason for disagreeing was inconsistency with the ICF terminology. We addressed this to some extent in the final version by using ‘impairment’ in the first sentence, but we preferred ‘functional’ rather than ‘activity’ limitations in the last sentence because of the broader interpretation of ‘functioning’, although some inconsistency with the ICF remains. Nevertheless, we were reluctant to become ‘instructive’ about ICF terminology at the expense of clarity. One could be critical of the lack of details regarding ‘causality’ within the definition, to which we would emphasise that our definition is intended to be descriptive of a phenomenon, rather than an explanatory model. One could also suggest that there should be more explicit, detailed inclusion and exclusion criteria, which we did debate. Ultimately, we prioritised producing a concise definition that would be accessible by any of our intended users, many of whom would not be familiar with the ICF or medical terminology.
It could be argued that finding a definition of neurodisability is an issue parochial to the UK. However, our international survey identified that similar grouping of conditions is made commonly in other countries, but that terminology is applied inconsistently. We believe that there is a need for international consensus, as people with neurodisability represent a group with particular difficulties, who are often vulnerable and require advocacy. Therefore, it is important to be able to identify people with neurodisability in order to then identify their needs, and the needs of their carers and families. Hence, working towards international agreement for a definition is desirable, to improve clarity of communication to enable sharing of knowledge, experiences, and use of findings from research.
Strengths and limitations
A strength of this study is the multidisciplinary and geographically diverse sample of people who participated, comprising paediatricians, paediatric neurologists, paediatric surgeons and a wide range of allied health professionals, all working with children and young people affected by neurodisability. Their views may or may not accurately represent the views of the broader population of health professionals. We recognise that our participants were the ones motivated to volunteer and take part in the study, which may mark them as different to their colleagues.
Our sample was composed of mainly community and hospital-based professionals. Professionals working in CAHMS were represented in smaller proportions to some other professions, and may be under-represented. We did not purposively seek to recruit any GPs; while their caseloads are varied, they and primary care would be expected to co-ordinate some aspects of health care for neurodisability.
Therefore, a major methodological limitation is the unequal proportions of health professions represented. The professions of respondents will have influenced the frequency with which certain aspects of health were mentioned and endorsed in the survey. Hence, there is a risk that professions with large or small proportions of representatives will have biased the overall consensus. We could argue that these proportions broadly represent the numbers of health professions who interact with families in paediatric neurodisability, with more paediatricians and therapists involved, while general audiologists and surgeons with a mixed child/adult caseload may see fewer children. However, such arguments are tenuous; we recognise the methodological limitation of our sample, without discounting the potential validity of their views.
The online Delphi survey was an efficient and economical means of gathering the views of a large number of health professionals. We sought to provide the opportunity to participate in the survey as widely as possible to as many different professions frequently involved in the health care of children and young people affected by neurodisability. However, our ability to contact and invite eligible professionals was always mediated through third-party organisations. Invitations were largely sent by e-mail; as health professionals receive large numbers of e-mails, they make rapid decisions about whether to respond to or delete non-essential communications.
A particular challenge was the unexpected large-scale organisational change to NHS e-mail addresses that was wholly beyond our control. This meant that some of our invitations could not be delivered to participants who had volunteered to participate, and the security system within the proprietary online survey process then considered them as withdrawn. Considerable efforts were made to contact these professionals and register their new e-mail addresses. There does not appear to be any systematic bias with attrition; there were a small number of participants who actively withdrew during the course of the survey, and some non-responders to each round.
We used the WHO ICF-CY terminology and definitions to code the information on aspects of health that professionals provided, and then presented these ICF terms back to them without precise definition. While no participants raised this as an issue, and there is increasing awareness of the ICF and related terminology, it is possible that professionals may have interpreted particular health outcome terms inconsistently. There were subjective judgements made in the process of coding in the Delphi survey, and we sought opportunities to confirm our interpretations in later consensus work.
Summary
We recruited a large multidisciplinary sample of health professionals working with children and young people affected by neurodisability. Over four rounds of an online Delphi survey, professionals identified the aspects of health that they targeted, and agreed broadly on a core set of domains that represent appropriate outcomes for NHS care. Some of the aspects of health that professionals target are neurological symptoms, and outcomes in these domains are less amenable to being assessed by using PROMs. A subset of outcome domains was identified that may be more feasible to assess using PROMs. In addition, participants in the Delphi survey helped to develop a definition of neurodisability, which was generally approved, and also broadly endorsed by a small number of international colleagues.
Chapter 7 Consensus meeting
Aims and objectives
At this stage of the project it was evident that no candidate PROM had emerged that was likely to fulfil the requirements of young people, parents and professionals. Furthermore, preceding research activities had gathered ample feedback on the questionnaire design and format. Therefore, the aim of this part of the research was to seek agreement between families and professionals on which aspects of health should be assessed as outcomes of NHS care.
The objectives were:
-
to bring together a nominal group of various participants who had taken part in previous elements of the study
-
to provide a forum whereby the participants could discuss the health outcomes that were identified by young people, parents, health professionals, and from questionnaires
-
to observe whether or not the group could negotiate and agree on appropriate health outcomes to assess for children and young people affected by neurodisability.
Methods
The methodological rationale for the consensus meeting was to convene a representative group of relevant stakeholders, and to use an interactive exercise to enable participants to explore their various perspectives. The participants were a nominal group in terms of seeking consensus,230 although we did not impose all the elements of conventional nominal groups; for instance, we did not ask participants to prepare statements and we did not impose a structure of ordering which participants could speak and when. The activity selected was a ‘Q-sort’. The chief investigator had experience of this working well for prioritising outcomes in a separate NIHR-funded research study about outcomes for young children with autism. 231 The sorting activity is one stage of Q Methodology,232 originally developed by Stephenson. 233
Q Methodology has its foundations in approaches to using factor analysis as means to identifying types of people based on how they respond to cognitive tasks. 232 We did not set out to apply the statistical methodology. Rather, we used the Q-sort task to observe the processes and discussions that the participants go through when prioritising the concepts of health outcomes we presented to them, in order to gain insight in to their various attitudes and beliefs. The Q-sort task we used seeks to force participants to make a choice about ordering concepts on a grid; the result was a ‘forced choice frequency distribution’ representing their views. We were interested to see whether or not the participants would be able to reach consensus within groups, and also to compare the results between the groups.
Participants
Participants were invited from those who had taken part in earlier components of the research. Young people and parents who had taken part in focus groups or interviews were selected and approached by the CDC. Health professionals were selected from those who had participated in all four rounds of the online Delphi survey, and a further selection was made to include a range of the different professions. Ideally, we sought to balance, broadly, the numbers of family and health professional representatives who participated.
Preparations
A central London venue was considered most accessible for participants from around England. The Royal College of Paediatrics and Child Health was selected as the venue, being both fully accessible and consistent with the ethos of the research. A meeting room was identified that was large enough for the number of participants, and allowed them to move around during the meeting, taking into account that some young people used powered wheelchairs. A separate meeting room was reserved to provide a breakout room for carers not participating in the meeting, and for anyone who wanted to use a quiet space away from the event.
In advance of the meeting, a list of the health outcomes was compiled from those issues identified (i) from the qualitative research with children and young people and parents; (ii) through the online survey with health professionals; and (iii) from the content of eligible PROM questionnaires. Duplicates were identified and removed from the list ( Table 39 ). There was debate about several aspects of health, for example whether or not they were eligible as being ‘morbidities’ (e.g. seizures) or perceived as self-reportable by young people (e.g. safety).
| Cards depicting: | Qualitative work with children and parents | PROMs | Delphi survey with health-care professionals |
|---|---|---|---|
| Play | ✗ | ✗ | ✗ |
| Sport | ✗ | ✗ | |
| Independent | ✗ | ✗ | ✗ |
| Communication | ✗ | ✗ | ✗ |
| Memory | ✗ | ✗ | |
| Concentration | ✗ | ||
| Emotional well-being | ✗ | ✗ | ✗ |
| Fitness and stamina | ✗ | ✗ | |
| Breathing | ✗ | ||
| Learning | ✗ | ✗ | ✗ |
| Let me decide | ✗ | ✗ | ✗ |
| Muscle strength | ✗ | ||
| Moving my body | ✗ | ✗ | ✗ |
| Manipulating objects | ✗ | ✗ | |
| Moving about | ✗ | ✗ | ✗ |
| Pain | ✗ | ✗ | ✗ |
| Worried | ✗ | ✗ | |
| Personality/confidence and self-esteem | ✗ | ✗ | ✗ |
| Family | ✗ | ✗ | ✗ |
| Friends | ✗ | ✗ | ✗ |
| Hearing and seeing | ✗ | ✗ | ✗ |
| Self-care | ✗ | ✗ | ✗ |
| Eating nutrition | ✗ | ✗ | ✗ |
| Self-care hygiene | ✗ | ✗ | ✗ |
| Safety | ✗ | ✗ | ✗ |
| Sexual health | ✗ | ✗ | |
| Sleep | ✗ | ✗ | ✗ |
| Social life/go out | ✗ | ✗ | ✗ |
| Continence | ✗ | ✗ | ✗ |
| Education | ✗ | ✗ | |
| Drool, swallowing, constipation | ✗ | ✗ | |
| Body structures | ✗ | ✗ | |
| Control behaviour | ✗ | ✗ | |
| Change body position | ✗ |
The final list of 33 ‘aspects of health’ or ‘health outcomes’ were then represented on laminated cards, with an illustration inspired by the signs from the Talking Mat system used with young people with communication difficulties in the qualitative research. There were some aspects of health that overlapped conceptually, but a decision was made to present these items individually and allow the participants to decide if they could be collapsed as a group concept.
A Q-sort grid was created depicting a ‘normal distribution’ of boxes matching the size of the cards; the grid encourages participants to rank fewer items at the margins of the grid than at the mid-range of the scale ( Figure 21 ). The scale identified the horizontal boxes as ranging from ‘less important’ to ‘more important’ for the NHS to focus on. Participants were asked to discuss the aspects of health, and then allocate each concept to a different box on the grid based on their perception of the importance of the aspect of health as an outcome of NHS care. We emphasised that, while the scale was ordered by importance, no item was being considered as unimportant.
FIGURE 21.
Q-sort grid shape used to create forced choice distribution.
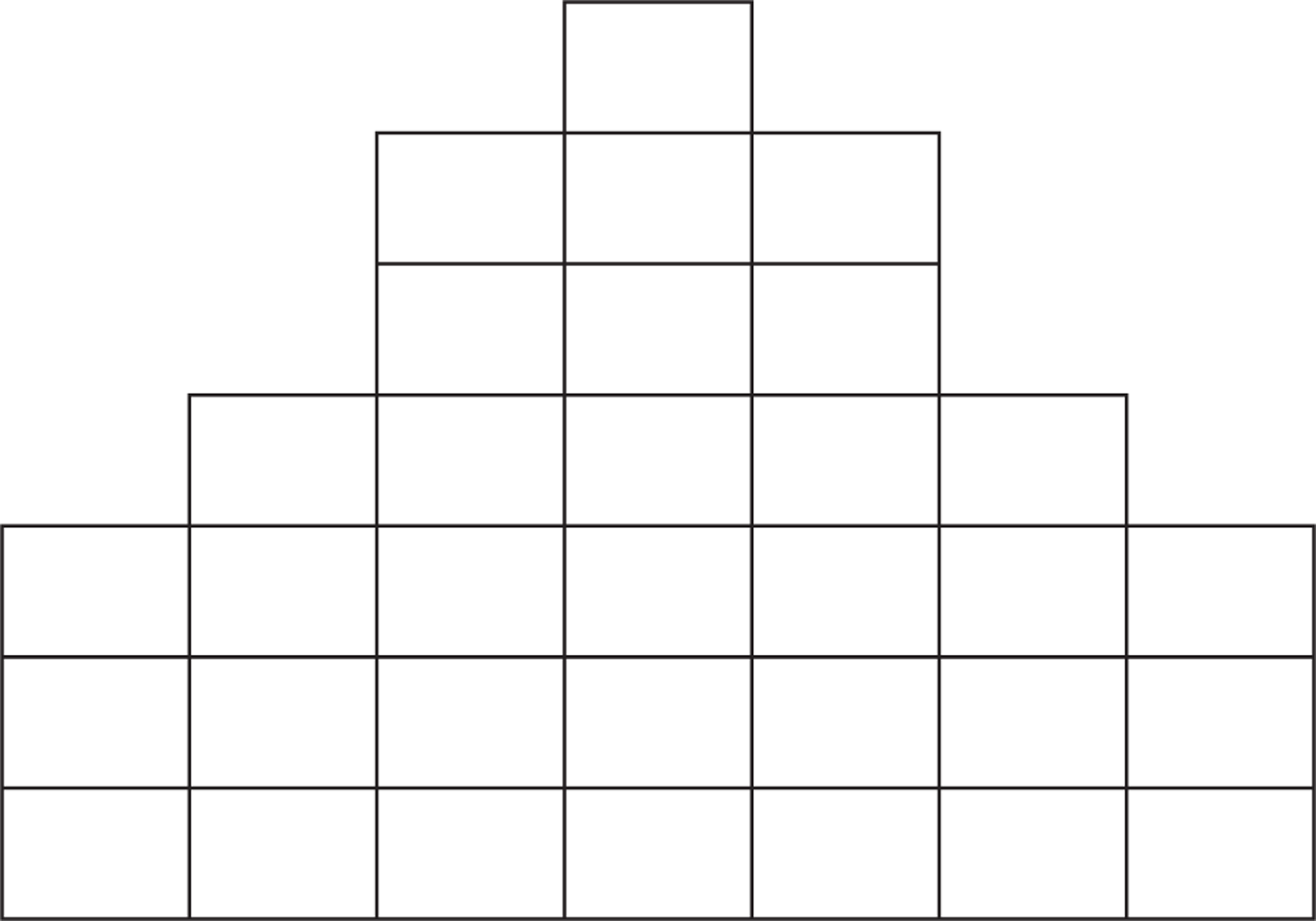
Procedures
The meeting hosts and facilitators were four members of the research team (CM, AJ, AA and AF). Participants were welcomed informally on arrival at the venue. Once everyone had convened, the meeting began with all participants introducing themselves, and then the chief investigator (CM) described the background to the research, the scope of what was meant by health outcomes in this research and the purpose of the meeting. Participants were invited to ask questions and request clarification.
The Q-sort activity was introduced and instructions explained, and again questions were invited. The meeting was then divided into two groups, predefined by the organisers, which sought to mix young people with parents and professionals from different health specialities (see Appendix 10 ). Each group was facilitated by two of the organisers, who were able to provide clarification about the concepts portrayed on the cards and encourage all participants to engage in the activity.
The groups worked through the Q-sort exercise for 90 minutes at separate ends of the same large room, and then broke for lunch. The groups reconvened after lunch for 15 minutes to review their decisions about relative placements of cards on the grids. Finally, the groups came together to compare which aspects of health had been prioritised, and make any final comments.
The small group discussions were audio recorded, but were not transcribed. The facilitators made written field notes of pertinent points made by participants, and also recorded the processes through which the groups negotiated discussions and decisions. Photographs were used to record processes and the positions of cards on the grids.
Analytical approach
The final positions of the cards on the grids were of interest, but we were as interested in the negotiations and decision-making processes that the groups went through in considering the issues. Indeed, we were keenly aware that the task might not be completed, depending on how the groups functioned. We were conscious in advance that various factors might affect the way individuals representing different perspectives would interact in the group discussions.
The facilitators debriefed immediately after the event, and subsequently shared their notes. Participants were e-mailed to thank them for their contribution, and a feedback form was included in order to gather any additional comments about their experience of the meeting. The report of the meeting and findings was drafted by the chief investigator and modified and agreed by the facilitators. A summary version of the report was shared with participants, inviting feedback on both the representativeness of the report and the meeting and activity.
Ethics
The consensus meeting was included in the procedures approved by NRES Committee North East – County Durham and Tees Valley (reference 11/NE/0364). Consent forms were not required for participation in the event; signed consent forms were used to permit use of photographs of the event for dissemination purposes. Participants gave consent to be named in the report but were assured that they would not be identified with any specific comments.
Results
There were 15 participants at the meeting: 3 young people affected by neurodisability, 5 parents and 7 health professionals (physiotherapist, occupational therapist, 2 paediatricians, nurse, paediatric surgeon, child and adolescent psychiatrist); apologies were received from a speech and language therapist and an orthopaedic surgeon.
Interpretation of the concepts
The participants generally shared an understanding of most of the concepts presented, but there were several exceptions that required explanation and generated discussion. For example, ‘family’ was explained as relationships with family members, but participants also raised the importance of family roles and taking part in family activities. ‘Education’ was explained as being involved in school and education, but created debate about the extent to which the NHS could be expected to have influence on school life, and certainly not on academic performance.
Participants thought that some concepts were not easy to distinguish from each other and, therefore, found them difficult to separate for prioritisation. For instance, both groups linked the concepts of ‘emotional well-being’, ‘self-confidence’ and ‘worry’, and ‘self-care’ with ‘independence’. Connections were also made between ‘fitness and stamina’ and ‘muscle strength’, and ‘change body position’ with ‘moving my body’. Queries were raised regarding whether or not it was realistic to assess some of the concepts using questionnaires.
Approaches to prioritisation
Various issues arose in the process of prioritising concepts as an important focus for the NHS. Participants recognised some concepts as being more readily influenced by health services. They distinguished other concepts as broader ‘life outcomes’ that would be influenced by many factors. Physical outcomes were perceived as more amenable for health services to influence, including ‘pain’, ‘communication’, ‘continence’ and ‘moving my body’. Broader life outcomes that might be harder for health services to influence included ‘emotional well-being’, ‘making decisions’, ‘friends’, ‘family’, ‘social life’ and ‘play’.
There was debate about what constitutes ‘the NHS’ and health services for children and young people affected by neurodisability, particularly as integration of health services with education and social care is commonly pursued. There was also debate about how the concepts might be prioritised variously, depending on how the children and young people are conceptualised. For instance, ‘sport’ was suggested as being more important for older children; it was suggested that ‘continence’ might be more of a priority for some people, and ‘worry’ might be more of a focus for people with mental health issues. Participants also asked whether or not comparisons with children and young people without neurodisability might be relevant.
The groups engaged well with the task, but most found the task challenging. More discussion focused on how to arrange the ‘most important’ half of the grid than concerned the ‘least important’ items. Health outcomes placed towards the least important columns generally remained fixed after placement, and did not generate much discussion.
Group dynamics during the task
Participants represented views grounded in their individual social roles, informed by their personal experiences. There were differences between the focuses of different professions. Some participants digressed from the task; professionals were prone to raise service issues such as commissioning targets and the reorganisation of the NHS, and parents raised service user issues about the adequacy and access to services. Nevertheless, discussion was generally cordial and respectful and there was no evident disagreement between parents and health professionals. The group was supportive of the young people taking part; however, one young person chose not to engage with the activity as he found the social nature of the task challenging. One facilitator had a sense that the group was reluctant to challenge decisions proposed by the young people, and that a change may have taken place after the break when the group had forgotten that it was the young person who had originally placed that card.
Prioritised health outcomes
As expected, there was variation between the priorities selected by each group ( Figures 22 and 23 ); however, certain health outcomes were common higher priorities selected by both groups. Among concepts ranked as more important in both groups were:
-
communication
-
emotional well-being.
Also highly ranked in both groups were:
-
pain
-
sleep
-
moving about
-
independence
-
worry.
FIGURE 22.
Health outcomes ranked as more important focus for the NHS by each group.
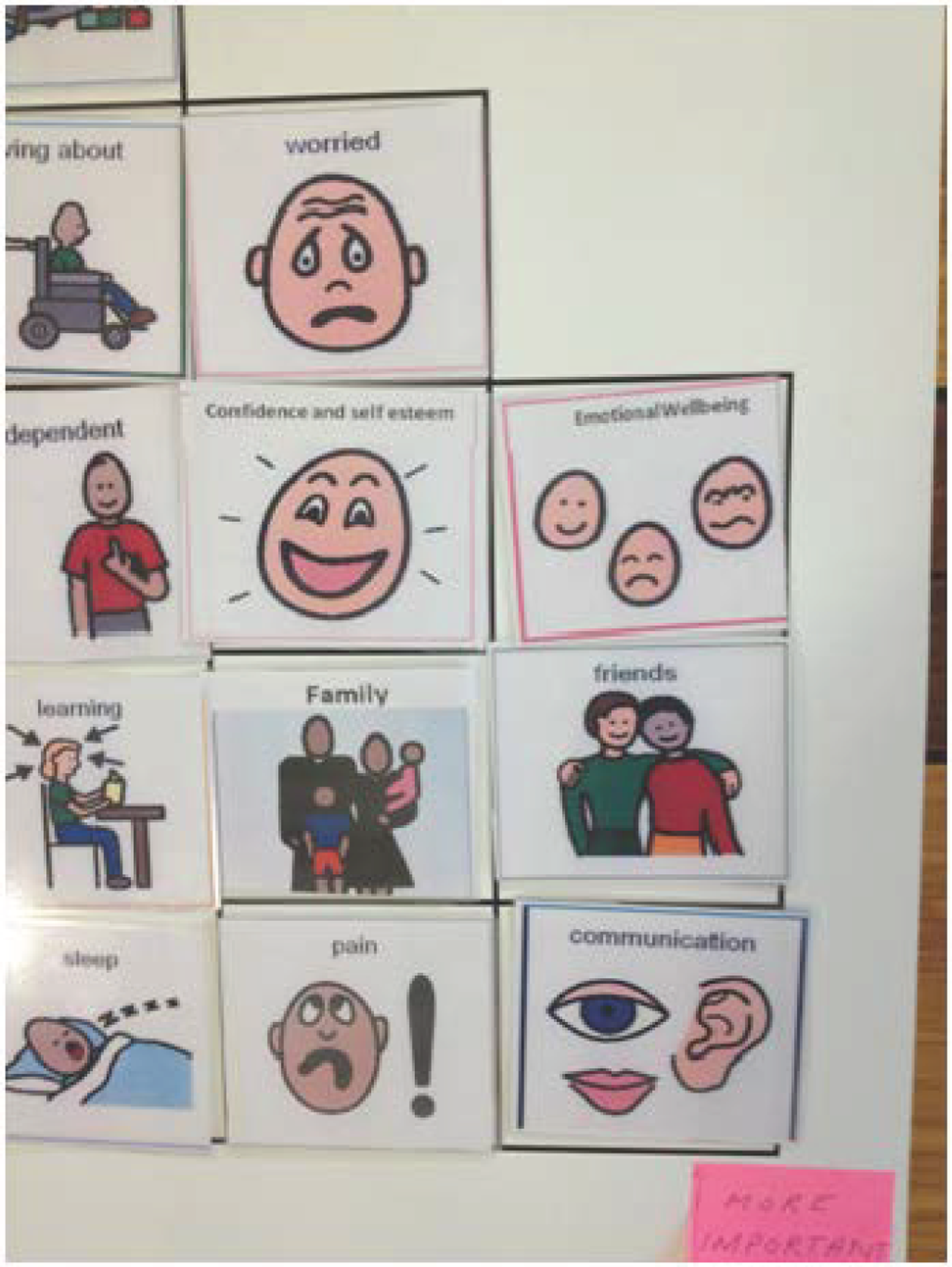
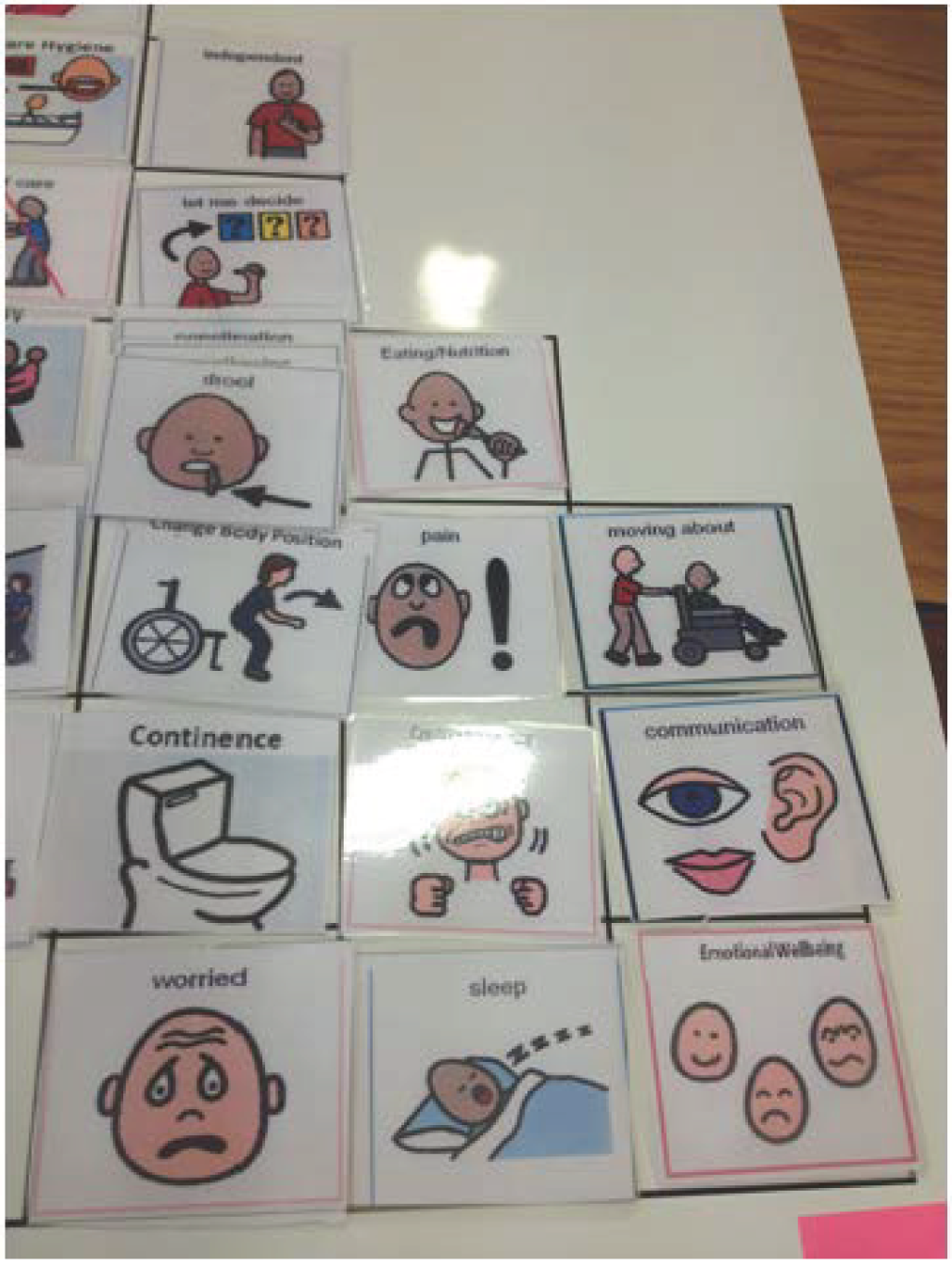
FIGURE 23.
Completed Q-sort grid from one group.
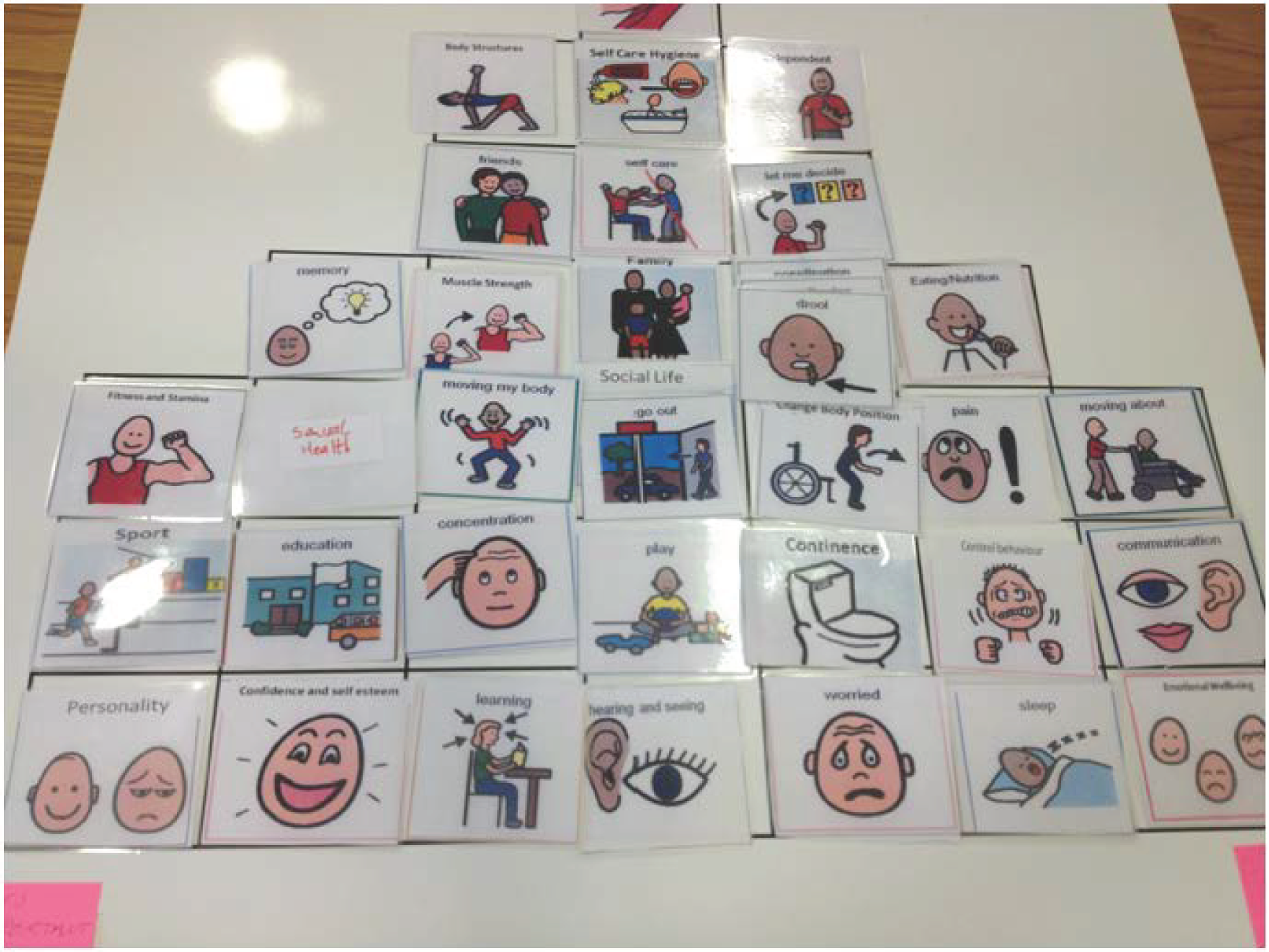
‘Sexual health’ and ‘concentration’ were concepts ranked as of lesser important by both groups. Otherwise, there was little overall consistency between the groups; some concepts, for example ‘control behaviour’, were ranked at opposing ends of the framework. The differences are largely explained by understanding the varying approaches each group took to the ranking, and the stage that discussions had reached when the session ceased.
Feedback from participants
General feedback was that participants enjoyed the event and the opportunity to hear different perspectives and felt able to express their views. Feedback on the activity specifically indicated some difficulties in dealing with and ranking the large number of concepts that were presented. One parent suggested that it was a pity nobody from the Department of Health was present to hear the views expressed.
Discussion
Key findings
The meeting was in many ways successful, and some consensus emerged that there are several stronger candidates for more important outcomes that it might be appropriate to assess for children and young people affected by neurodisability:
-
communication
-
emotional well-being
-
pain
-
sleep
-
moving about (mobility)
-
independence
-
worry.
In defining these concepts, we drew on the WHO ICF terminology; each concept is defined in the ICF except well-being, which can be considered synonymous with the WHO definition of ‘quality of life’. 234
Strengths and limitations
When plans for the consensus meeting were discussed at the second co-investigator meeting, some among the research team questioned the utility of the exercise, particularly whether or not the activity really would produce any new information over what the preceding work had identified. Others argued that the novel aspect of the consensus meeting was that it was the only time in the research when family and professional representatives of the participants would interact together to discuss and debate the issues. The event appeared to be highly valued by the participants as an opportunity to be actively engaged in the project, and their contribution was certainly informative. Bringing young people, parents and professionals together provided insight into factors likely to enable further development from the emergent findings. The meeting was only feasible to arrange as a one-day event, which limited what could be achieved.
The group were, for the most part, able to work together in pursuance of a common purpose, guided by the facilitators. The purpose of the event, composition of participants, motivation of the participants, the location and room environment, and the Q-sort activity all appeared to provide conditions that were conducive to addressing a challenging problem in a collaborative way. All ‘small groups’ have to find their own way to work together, and not all small groups succeed. We were not aware of any overt individual or role power imbalances among participants that might have affected overall group decision-making. Two of the three young people appeared to find it easy to integrate with their small groups. Unfortunately, one of the young people found the experience overwhelming, and withdrew; this was probably in relation to the social aspects of the exercise, and could have been anticipated and accommodated with further preparation.
The cognitive task was made challenging by the large number of concepts that participants had to understand, recall and rank. It has long been recognised that people find it difficult to discern more than a handful of categories in any reliable way. 235 It may have been helpful to carry out a preliminary grouping of the concepts, and/or include a stage to see whether or not some concepts could have been eliminated prior to moving to the ranking Q-sort task. Having gained experience with the Q-sort, and using a smaller number of concepts, it may be useful to structure the sorting exercise as a series of separate activities, each using a specific case study. This could reduce the number of variables that arose in discussions, such as age and problems associated with different diagnoses. In addition, some constructs may have appeared similar, despite being conceptually distinct in terms of ICF terminology and definitions.
Summary
A small group of young people, parents and health professionals who had taken part in previous elements of the study participated in a consensus meeting. An interactive Q-sort activity was used to promote discussion and encourage a prioritisation of the various health outcomes that had emerged from the research. There appeared to be broad agreement on a group of more important outcomes for children and young people affected by neurodisability.
Chapter 8 Synthesis of findings
This research aimed to determine (a) which outcomes of NHS care should be assessed for children and young people affected by neurodisability, and (b) the extent to which they can be measured by generic PROMs. Principally, the research design comprised three studies:
-
a systematic review of the psychometric properties of generic PROMs used to measure the health of children and young people, and particularly those with neurodisability
-
qualitative research with children and young people affected by neurodisability, and parents of children and young people affected by neurodisability
-
an online Delphi survey with health professionals working with children and young people affected by neurodisability.
We also convened a consensus meeting to bring together young people affected by neurodisability, parents and health professionals to seek agreement on key health outcomes.
The WHO ICF was used as a means to code health outcomes and, hence, connect findings emerging from different aspects of the research.
At the outset of the research there was no agreed definition of neurodisability. Hence, we also took the opportunity to address the lack of an agreed definition of neurodisability, using the Delphi survey and involvement of parents working with the research team.
Definition of neurodisability
It is clearly crucial to know which children and young people are being considered in this research, in terms of inclusion in the various studies and the inferences of the findings. An unanticipated element of this research was defining ‘neurodisability’. The term is commonly used to describe a group of children or subspecialty of paediatrics, particularly in the UK; neurodevelopmental disorders or conditions and other terms are used in the same context in other English-speaking countries. Nevertheless, there appeared to be no accepted definition of any of these terms. Therefore, early in the detailed planning of the research, we sought to develop and seek agreement on a definition of neurodisability.
Using contributions from health professionals participating in the first three rounds of the online Delphi survey, and incorporating the views of a small group of parents involved with the research team, we produced a definition of neurodisability. We also sought international perspectives on the resulting definition using networks of colleagues. The following definition was approved generally, if not universally:
Neurodisability describes a group of congenital or acquired long-term conditions that are attributed to impairment of the brain and/or neuromuscular system and create functional limitations. A specific diagnosis may not be identified. Conditions may vary over time, occur alone or in combination, and include a broad range of severity and complexity. The impact may include difficulties with movement, cognition, hearing and vision, communication, emotion and behaviour.
This definition will help to identify children and young people affected by neurodisability, and may be useful in discriminating them from others with different long-term conditions, such as impairments of the endocrine, respiratory or musculoskeletal systems. Although children with such disabling conditions share characteristics with those affected by neurodisability, there are sufficient differences to make this an important and useful distinction, both in this and other research, and also in health services design, audit and evaluation.
Key health outcomes
We sought to identify key health-care outcomes, beyond measures of morbidity and mortality, which children and young people affected by neurodisability and parents regard as important. We carried out focus groups and interviews with both children and young people affected by neurodisability, and separately also with parents.
Children, young people and parents viewed health outcomes as inter-related and with reference to a hierarchy. Participants identified clearly the contribution that foundation and intermediary outcomes made to a smaller set of higher-level outcomes that they felt were most important to achieve in order to have a good quality of life. Health outcomes that were highlighted more frequently by young people and parents were communication, mobility, pain, self-care, temperament, interpersonal relationships and interactions, community and social life, emotional well-being, and gaining independence/future aspirations. Some parents were also particularly concerned with sleep and/or behavioural problems. In terms of hierarchy, children and young people identified interpersonal relationships and interactions, community and social life and emotional well-being; parents identified community and social life, gaining independence/future aspiration and emotional well-being.
We also sought to ascertain what outcomes of NHS care health professionals considered important for children and young people affected by neurodisability, through four rounds of the online Delphi survey. Professionals identified targeting aspects of health across the spectrum of WHO ICF-CY. In the domains of ‘body functions and structures’, goals targeted pain, hearing, seeing, mental health, sleep and toileting; in ‘activities and participation’, goals targeted mobility, communication, manual ability, self-care and social activities. Professionals also identified seeking to improve emotional functioning and well-being. Some aspects of health that professionals indicated they target were specific neurological symptoms: seizures, stroke, spasticity, constipation or incontinence, breathing problems, vision and hearing loss, muscle strength and gait. Some of these health issues could be considered as measures of ‘morbidity and or mortality’, which were excluded from our scope, as these are captured in other ways and less amenable to self-report using generic PROMs.
Young people, parents and professionals all recognised that health services influence each of the outcomes to varying degrees. Although they recognised their importance as outcomes, professionals suggested that health services were less able to influence play, relationships with family and with friends, sport and leisure, learning and applying knowledge. Young people and parents also recognised that health services could play less of a role in influencing some valued higher-level outcomes, but considered that appropriate and adequate core health services provision was crucial to achieving in these outcome domains.
We sought consensus among young people, parents and professionals on what aspects of health might be important to assess as outcomes of NHS care. The aspects of health and outcomes identified by the systematic review, qualitative research and Delphi survey were aggregated and presented to a nominal group of young people, parents and professionals. The consensus meeting appeared to identify several stronger candidates for health outcomes for children and young people affected by neurodisability: communication, emotional well-being, pain, sleep, mobility, independence and worry.
Thus, there does appear to be some consistency among young people, parents and professionals regarding an emerging suite of more important health outcomes:
-
communication
-
emotional well-being
-
pain
-
mobility
-
independence/self-care
-
worry/mental health
-
social activities
-
sleep.
A further subset that parents rated as important, and professionals also identified were:
-
behaviour
-
toileting
-
safety.
One cautionary note concerns how these terms are defined, and operationalised in the context of measurement. We used WHO terminology consistently within each aspect of this research, and also to provide a framework to link findings from different parts of the research. We have recognised earlier in the report that there are elements of subjectivity in the process of coding and prioritising outcomes. However, we point to original quotes from participants in the qualitative chapter, and the iterative process of the Delphi survey and participants at the consensus meeting support the internal validity of our findings.
Candidate patient-reported outcome measures
We sought to identify all generic PROMs for children and young people, and then sought evidence from peer-reviewed publications describing studies conducted to evaluate the psychometric performance of PROMs when using English-language versions of the questionnaires. We separately appraised instruments that were generic (meant to be suitable for all children), chronic-generic (intended for to be suitable for children with health conditions), or PBMs. We also considered evidence separately depending on whether the research had been conducted with general populations or with children and young people affected by neurodisability.
We identified 41 potentially eligible PROMs, and identified 126 papers that reported evidence of the psychometric performance of 25 PROMs using English-language versions. Twelve candidate PROMs were selected as having more favourable evidence regarding their psychometric performance. Robust evidence was lacking in one or more respects to support the psychometric properties for all candidate PROMs appraised in this review, both in general populations and with children and young people affected by neurodisability. No evidence was found to support the responsiveness of any of the candidate PROMs to detect meaningful change in either general population or neurodisability.
We identified those aspects of health assessed by candidate generic PROMs through the systematic review, and coded these pragmatically using the WHO ICF-CY. Each PROM questionnaire assesses a range of constructs, but each does so in a slightly different way. The most notable difference was in how some PROM questions assess functioning as what people do, or can do, and other questions assess well-being as how people feel about their health. A few PROMs focus predominantly on either functioning or well-being, but all of our candidate PROMs conflated these concepts. As with our previous note on defining outcomes above, it is necessary to audit closely how the constructs measured by PROMs are defined, and whether or not these are consistent with the style and context of the questions being asked.
For children aged 8 to 18 years, there is favourable psychometric evidence for the KIDSCREEN, including Rasch analysis in general populations, and for the KIDSCREEN-52 with children with cerebral palsy. The Healthy Pathways is a promising instrument with some good evidence in favour, including from Rasch analysis; however, only two recent papers are published. The DISABKIDS was the only eligible chronic-generic instrument for which favourable evidence was found of psychometric performance in children and young people affected by chronic conditions, including neurodisability. The version of DISABKIDS Smileys-6, aimed at children 4 to 7 years old, was the only competitive candidate PROM to utilise emoticons in the response options. This was something preferred by children, young people and parents in the qualitative research. The PedsQL and KINDL have versions to include younger children, but evidence for their psychometric robustness is weaker. The CHU-9D emerged as the PBM that has been evaluated more extensively, with some limited evidence in favour. However, the CHU-9D has not been tested with children and young people affected by neurodisability.
The fact that some newer PROMs have been subjected to greater methodological scrutiny, and thus more robust psychometric evidence, probably reflects the emerging awareness of higher standards required for scale development and methods for psychometric evaluation. The ability of developers of PROMs to fund research generally drives evaluation of the instruments. Hence, the lack of robust evidence for some older measures may be an artefact of the research process rather than mean that some scales perform poorly per se. Some older PROMs have become more established by frequency of use in research, even though robust psychometric evidence is lacking. Nevertheless, one can only make decisions based on the available evidence. There remains much scope for research to evaluate generic PROMs, particularly testing item invariance across neurodisability conditions, and responsiveness of PROM scores to meaningful change.
The selection of any instrument should be consistent with the purpose of measurement and psychometric properties; nevertheless, the questionnaire must have face validity to potential respondents. There appears only partial overlap between the suite of key outcomes identified by young people, parents and professionals, and the content assessed by more competitive candidate PROMs. Looking broadly at WHO ICF-CY domains, each of these PROMs appears to assess some aspects prioritised; notably, though, communication is not represented in any of these PROMs, and mobility is tainted by a focus on walking/running rather than ‘moving around’, which, if more broadly conceived, would include use of assistive technology.
We presented examples of four commonly used PROM questionnaires as part of the qualitative research. General feedback on the questionnaires suggested poor face validity for using these to measure NHS care. Even though many questions were felt to be relevant, other key outcomes were identified as missing. In addition, participants disliked questions that were perceived as negatively phrased, verifying what colleagues had previously proposed. 17 Response options were not perceived to reflect the health of children and young people affected by neurodisability appropriately, nor were they perceived likely to capture salient improvement or deterioration. The exemplar questionnaires we used were chosen as more commonly used instruments, and feedback may not reflect across all PROMs. Nor did we seek specific feedback on the PROMs individually, as they were simply conversation aids.
Careful cognitive interviewing should be undertaken with children, young people and parents to examine the face validity of any candidate instruments before selecting any PROMs. Key issues to consider are the content assessed, appropriate phrasing of questions, whether or not the proffered response options are likely to capture differences or changes in health that are meaningful and realistic for the population being studied, and length of questionnaire. Our qualitative research identified that some questions present cognitive challenges that young people and parents felt made responding difficult. Scale developers could do more work to ensure that such problems do not present, and those considering using PROMs in research or other contexts may want to pilot specific questionnaires for themselves.
Parents identified discomfort in being able to respond to some questions as their child’s proxy, particularly about emotional domains and about activities that take place away from them, such as at school and with friends. Hence, there may be consideration as to whether or not these questions should be asked of parents, especially as ample evidence identified in this review suggests strongly that proxy reporting is statistically unreliable. Parents may be required to report on behalf of those children who do not have the cognitive capacity to respond, but the questions parents are asked should reflect issues about which they feel able to respond. There were some outcomes that parents felt were more important to assess than did children and young people, including toileting, behaviour and safety, probably reflecting their roles as carers. These may be important outcomes to include in ‘parent’ reported instruments, but less relevant to include in self-reported questionnaires for children and young people.
Implications for health services
The Department of Health continues to pursue a commitment to a focus on outcomes. The NHS Outcomes Framework 2010–11,20 cited in our original proposal, has progressed to the NHS Outcomes Framework 2013–14. 236 Allied work has produced the Public Health Outcomes Framework. 237 There remains a commitment to assess the HRQoL of people with long-term conditions as part of the NHS Framework;236 presumably, this would include children and young people affected by neurodisability.
A recent consultation commissioned by the Department of Health was the Children and Young People’s Health Outcomes Forum; this pertained to all children and young people, not only those affected by neurodisability. The forum recommended ‘specific outcome measures and indicators for the very wide variety of illnesses and conditions of children and young people including where appropriate patient rated outcomes’ (p. 12). 238 The Department of Health’s response does not appear to address this recommendation directly; nevertheless, such a commitment is integral to the NHS Outcomes Framework. 236 Thus, there appears to be a strong case for further research to address both the technical measurement issues and the potential barriers to the implementation of PROMs as routine outcome indicators for disabled children.
Existing PROMs would need to be refined if they were to cover comprehensively the key outcomes that the children and young people with neurodisability, parents, and professionals ranked as appropriate and important. To move from the themes we identified to questionnaire items would be a natural next step in PROM development; this would require agreement on how to define the concepts, and further research with families and professionals. Research would also ensure that the questions and response options have face validity, and that the resulting measurements are robust across the range of standard psychometric properties.
One strategy could be to consider a battery of condition-specific PROMs, as usually these might include items thought to be more relevant to people with particular diagnoses. Such instruments have been developed for several conditions including epilepsy and cerebral palsy; however, this approach would isolate children and young people with rarer forms of neurodisability, and exclude those children without any diagnostic label. Having identified several key domains as part of this research, another approach could be to critically review existing ‘domain-specific’ instruments for each of these as discrete outcomes.
More recent psychometric approaches, using Rasch analysis, allow for the co-calibration of ‘banks of items’ and scales from condition-specific, domain-specific and generic instruments which measure the same construct. Thus, in future, a carefully designed and integrated approach might emerge that offers inclusivity, flexibility and choice to young people. This has been the strategy adopted in the USA by the Patient Reported Outcomes Measurement Information System initiative, funded by the National Institutes of Health. In fact, one potentially eligible instrument under development as part of this project was not identified or appraised in our review. The Quality of Life in Neurological Disorders (Neuro-QOL) measurement system was initially devised for adults but, more recently, a children’s version has been proposed. 239 Notably, there is only partial coverage of the key domains proposed by our research in the content of Neuro-QOL, and examination of included items suggests there may be similar problems with face validity identified with other PROMs.
The response by the Department of Health to the Children and Young People’s Health Outcomes Forum does focus on children and young people’s experiences of care. There is an important distinction between the health outcome constructs assessed by PROMs and those issues assessed by patient-reported experience measures (PREMs), and the two must not be conflated. The development and appraisal of PREMs, to assess how health services are experienced, for example in terms of whether or not professionals were respectful and supportive, waiting times and so forth, is a separate though related line of enquiry, evaluation and research. In fact, there was considerable confusion about what exactly the term ‘outcomes’ meant to participants in this research. Everyone wants to improve outcomes for children and young people but there are many different perceptions of what such outcomes might be, and some participants struggled to understand outcomes in any defined way.
The Children and Young People’s Health Outcomes Forum also recommended that outcomes for children and young people be considered in 5-year age bands, and the Department of Health’s response was broadly affirmative: ‘all data will be presented in 5 year age bands up to 25 to enable effective transition to be monitored’ [with caveat] ‘where technically feasible and statistically robust’ (p. 13). 240 This raises important considerations: whether or not the health outcomes assessed should be different for these age categories, whether or not questionnaires should be formatted differently, or whether or not it is the presentation of the data within each age bands that is most important. The upper age categories of 15–20 years and 20–25 years also introduce a complexity that was not addressed in this research, as our systematic review focused on PROMs for children and young people < 18 years of age.
There is scope for health services policy to address how health outcomes should be measured for disabled young adults between 18 and 25 years, for instance whether or not it is sensible to leap to the constructs assessed by adult PROMs, such as the Short Form Questionnaire-36 items and/or the EQ-5D. There is also an emerging classification of PROMs specifically for young adults. Alternatively, one could consider using the concepts identified in this research, and test the appropriateness of extending the age range of existing candidate PROMs for young people to 20 or 25 years, as part of work to evaluate other psychometric properties. There is widespread recognition of the need for attention to supporting transition between child and adult services, though practice remains inconsistent. Assessing outcomes with a common metric through these age bands would seem to offer advantages in terms of monitoring and evaluation of services.
There is political momentum for integrating educational, health and social care services for disabled young adults. As part of the Children and Families Bill,241 legislation will introduce ‘Education, Health and Care Plans’ for students with special educational needs, which will include many children and young people affected by neurodisability. The government has stated that these plans will be clearly focused on both short and long term outcomes that are important to the child and their family, across education health and social care, and services will be expected to work together to achieve these outcomes. In addition, the emerging roles of paediatric public health services, to be delivered in the community by local authorities rather than the conventional NHS, are an example of where the traditional boundaries of the NHS are becoming blurred.
This creates further complexity to outcome measurement and monitoring: does it make sense to seek to measure NHS outcomes as distinct from integrated cross-sector outcomes? Many health professionals in our research felt that there were limitations to the extent to which the NHS (as they perceived it) could be responsible for more distal aspects of health influenced by multiple environmental factors, including social interventions that they regarded as social care. From the perspectives of families of children and young people with neurodisability, who receive support from a range of public services, partitioning NHS outcomes from those of other services may lack credibility. Increasingly, integrated education, health and social care services are promoted as likely to be more family centred and efficient.
Although this research did not find adequate evidence of psychometric performance for any particular PROM, we did identify a number of issues that might be worth considering as part of any implementation of a PROMs strategy with disabled children and young people. First and foremost, there are important contextual factors to consider; families are all too familiar with completing various questionnaires and forms to apply for entitlements, and may be suspicious that data from the questionnaires will affect service provision and other support. Therefore, it would be advisable to provide transparent information about how information will be used, in order that reliable and complete information can be gathered. We also identified several other factors that might be likely to encourage participation in completing questionnaires to maximise response. Nevertheless, our research also identified that young people and parents often disliked aspects of the exemplar questionnaires. This was especially the case when the wording of the questions and response options did not allow them to express accurately the information they wanted to convey. This is a challenge for the implementation of PROMs in this context and probably also for other long-term conditions.
Children, young people and parents in our qualitative research would prefer questionnaires to be designed in more accessible formats; there were suggestions that standard paper versions looked like ‘exam papers’. Electronic administration using computers appeared to be popular, especially if the administration could be individualised in some ways; personalised PROMs that are reflexive to responses and hence explore the most relevant areas of functioning are likely to be better received. Electronic formats that enable children with communication difficulties to participate seem entirely fair, and feasible. Our qualitative research included children with profound communication difficulties who, given appropriate time and support, were able to express clearly their views on important health outcomes. Therefore, adequate planning should enable these children to participate in self-completing PROMs, and some young people may need personal assistance.
Our review included evaluations only of English-language versions of PROMs; hence, there may potentially be an accessibility issue for people for whom English is not their first language. Current policy using PROMs in the NHS appears to offer telephone support rather than providing alternative language versions. If alternative language versions were to be considered, then recommended guidance for evaluating translations indicates that this would require substantial work. 242,243
One final implication for health services policy concerns the recommendation in the report by Sir Ian Kennedy that a common vision needs to be developed of what health services are trying to achieve for children and young people. This research has identified a suite of key health outcomes that appeared to be shared as important by young people, parents and professionals. Identifying these health outcomes may present an incremental step towards developing a common vision, although further work is required to ensure that these are shared more widely, and agreed by stakeholders who were not represented in the research, particularly those responsible for commissioning health services.
Our consensus meeting showed that young people, parents and professionals could be brought together and work together collaboratively, given that there is appropriate motivation, environment and support. Furthermore, the opportunity to participate in the consensus meeting appeared to be highly valued by the participants. This approach would seem a valuable and important opportunity to be seized, at a national level in the first instance, and then locally. Involving service users in designing services is already widely encouraged in the NHS; nevertheless, this opportunity may still fall within the remit of health services research, as facilitation requires an appreciation of the complexity of the various social roles of the stakeholders, and negotiating the varying priorities of the participants.
Such strategies require broad support from all the health professions, who want to see how individual, as well as combined, therapeutic contributions influence the shared vision and goals. If the shared vision is too distal and removed from the day-to-day activities of health professionals, then the vision will lack credibility and not be wholly shared. This issue will be particularly pertinent for professionals involved in hospital settings, who may be more focused on managing acute or chronic neurological symptoms. There could be a role for widespread consultation with relevant professional bodies regarding a core set of goals.
The findings from this research substantively inform what outcomes health services might seek to achieve for children and young people with neurodisability, and selection of PROMs for the NHS Outcomes Framework. Furthermore, we have identified several factors that could be considered in terms of implementing routine use of PROMs with disabled children, with respect to contextual issues, format and administration.
A summary of the implications for health services emerging from the evidence in this study is shown in Box 6 .
Evidence from this research suggests that:
-
Children and young people with a wide range of neurodisabilities can contribute their views on what they believe are important health issues for them, and these do not always concur with parents’ views.
-
Young people, parents and professionals agreed generally on a suite of more important health outcomes.
-
None of the current PROM questionnaires adequately captures all of the key important constructs.
-
Young people, parents and professionals do not always readily understand or interpret ‘health outcomes’ in the same way.
-
The purpose of measuring health outcomes using PROM questionnaires should be explained clearly and transparently.
-
Appropriate consideration to administration and presentation of PROM questionnaires would enable more young people to self-report their health.
-
Current questionnaires may not have face validity to potential respondents.
-
The appropriate age range and categories for measuring health outcomes is a key consideration.
-
The feasibility and utility of measuring outcomes for the NHS and/or other public health, social care and education services merits consideration.
Implications for research
There are a number of research opportunities arising directly from this work, and also some implications for those using PROMs in research and/or interpreting research incorporating data emanating from PROM questionnaires.
First, there is scope for studies to build further consensus around the suite of key outcomes identified in this research. Such work could replicate the consensus meeting on a larger scale and more nationally, and include a wider range of stakeholders including those responsible for commissioning services and potentially representatives of professional societies. Bringing together young people with neurodisability, health professionals, and those responsible for services might lead us further towards the shared vision of what the NHS should be seeking to achieve for these children and young people.
The content of what is assessed by PROM questionnaires needs to closely match this vision, or at least the component domains. Thus, the constructs, items and response options used in PROM questionnaires should be refined to ensure that they match purpose of measurement, and have face validity to respondents. This might be achieved through cognitive interviewing with a diverse range of potential respondents, using the more promising PROMs as a starting point. It may be necessary to add domains to cover key outcomes such as communication.
Using reports of parents and carers as proxies for outcomes designed to be measured from the perspectives of children and young people appears wholly unsatisfactory. However, there will always be children and young people who do not have the developmental cognitive capacity to self-report, and it is usually parents and carers who seek health care for their children. Therefore, parent-report probably can provide important insights. Nevertheless, we advocate that the appropriate content of a parent questionnaire should differ from the children and young people’s version. Parent questionnaires should assess items and concepts that are important to parents, and in ways that parents feel they can respond accurately. The potential for a proxy-reported PROM, but based on the domains of more importance to parents, would seem a promising line of enquiry for research.
Although some children do not have the cognitive capacity to complete PROM questionnaire themselves, this should not be readily assumed. Many children with moderate intellectual delay and/or communication impairments will be able to self-report their health if provided with appropriate technology, time and support. Research could pilot practical methods for ensuring that all children who could self-report their health are not excluded as a result of design and administration processes and procedures.
Finally, providing that a candidate PROM could be produced that appropriately captures content representing the purpose of measurement, that is to say the ‘right outcomes’, and that the questionnaire has face validity and is acceptable to respondents, it should be tested. Such evaluation might be a short-term longitudinal study with children and young people with a range of diagnoses, with perhaps 6 to 12 months’ follow-up for each subject. This research could assess the extent of any item invariance across different neurodisability conditions and age groups, and also determine the magnitude of meaningful differences in scores, or change in scores.
A summary of the implications for research emerging from the evidence in this study is shown in Box 7 .
Evidence from this research suggests that:
-
Further research to build consensus between families and professionals on a shared vision for health services for neurodisability would be beneficial.
-
There is potential to devise separate PROM questionnaires for young people and parents, capturing their different priorities for health outcomes.
-
Generic and/or chronic-generic PROMs require refinement in order to capture all key important health outcomes for neurodisability.
-
Cognitive interviewing with young people with neurodisability and parents would help to improve the face validity of questions and response options.
-
Formats for administering PROMs with children and young people that are that are inclusive, attractive and expedient should be tested.
-
The extent of any item invariance across different neurodisability conditions and age groups should be assessed in well-designed studies.
-
The size of meaningful change or difference in PROM scores needs to be determined in well-designed studies.
Summary
This research involved a comprehensive systematic review of generic PROMs; qualitative research with a diverse group of children and young people affected by neurodisability, and parents; and an online Delphi survey with a multidisciplinary group of health professionals. The findings would appear to substantively inform the NHS regarding what health services might seek to achieve, and inform selection of PROMs for the NHS Outcomes Framework . Furthermore, we have identified several key factors that might be considered in terms of implementing routine use of PROMs with disabled children and their families.
Acknowledgements
This project benefited significantly through the involvement of several parents of disabled children. We are grateful to Kim Antonio, who collaborated on the application for funding; Kim Antonio, Tricia Stone, Julia Melluish, Antonia East also collaborated in various aspects of the research. We are grateful to Camilla McHugh (PenCRU Family Involvement Coordinator) and Anna Stimson (PenCRU Administrator), at the University of Exeter, for facilitating and supporting the involvement of parents in this research, and providing administrative support. PenCRU receives core funding from the charity Cerebra, which enables the group to maintain a Family Faculty and involve families of disabled children in research. The project benefited from pump-priming funding from NIHR PenCLAHRC; the authors are grateful to Becky Taylor (formerly PenCLAHRC Research Fellow) who carried out valuable development work for the research, including securing ethics approval through NRES for the qualitative research and online Delphi survey. We are also grateful to colleagues at PenCRU (Sarah Bailey) and the PenCLAHRC Evidence Synthesis Team (Darren Moore, Rebecca Whear, Rebecca Abbott), University of Exeter, who assisted with tasks associated with the systematic review. We are also grateful to those people who work ‘behind the scenes’ at various organisations, and whose work facilitates the financial and regulatory processes required to support research. Finally, we appreciated the comments and suggestions on the report from anonymous reviewers and editors. Finally, we appreciated greatly the comments and suggestions on the report from anonymous reviewers and editors, and the work of Katrina Strachan for copy-editing and Norma Sweeney for managing the production of the report.
Contributions of authors
Christopher Morris (Senior Research Fellow, Child Health) conceived the research, gathered the team, drafted the protocol, led the application for funding, managed all aspects of the research, drafting and editing of the final report.
Astrid Janssens (Research Fellow, Child Health) led the systematic review and managed the online Delphi survey, contributed to the qualitative research, and assisted in the drafting and management of the production of the final report.
Amanda Allard (Principal Officer, Council for Disabled Children) contributed to the design of the protocol, application for funding, led the qualitative research with parents and oversaw the research with children and young people, drafted the qualitative chapter, and commented on the final report.
Joanne Thompson Coon (Senior Research Fellow, Evidence Synthesis) contributed to the design of the protocol, application for funding, oversaw the conduct of the systematic review and drafting of that chapter, and commented on the final report.
Valerie Shilling (Research Fellow, Child Health) contributed to the design of the protocol, application for funding, contributed to the qualitative research and drafting of that chapter, and contributed to various sections of the final report.
Richard Tomlinson (Consultant Paediatrician) contributed to the design of the protocol, application for funding, contributed to the online Delphi survey and drafting of that chapter of the final report.
Jane Williams (Consultant Paediatrician) contributed to the design of the protocol, application for funding, contributed to the online Delphi survey and drafting of that chapter of the final report.
Andrew Fellowes (Health and Participation Officer, Council for Disabled Children) led the qualitative research with children and young people, and drafted the qualitative chapter, and commented on the final report.
Morwenna Rogers (Information Specialist) contributed to the design of the search strategies for the systematic review, carried out the searches and managed the reference libraries, and contributed to the systematic review chapter of the final report.
Karen Allen (Associate Research Fellow, Child Health) undertook data extraction for the systematic review, and organisation and presentation of the data in the systematic review chapter of the final report.
Bryony Beresford (Professor, Social Policy) contributed to the design of the protocol, application for funding, contributed to analysis, interpretation and presentation of the qualitative research chapter of the final report.
Colin Green (Professor, Health Economics) contributed to the design of the protocol, application for funding, and commented on the systematic review chapter of the final report.
Crispin Jenkinson (Professor, Health Services Research) contributed to the design of the protocol, application for funding, contributed to the systematic review chapter of the final report.
Alan Tennant (Professor, Rehabilitation Studies) contributed to the design of the protocol, application for funding, contributed to the conduct of the systematic review, and commented on various sections of the final report.
Stuart Logan (Professor, Paediatric Epidemiology) contributed to the design of the protocol, application for funding, contributed to the systematic review and online Delphi survey, and commented on the final report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Read J. Can We Count Them? Disabled Children and their Households: Full Research Report. The Economic and Social Research Council (ESRC) End of Award Report. Swindon: ESRC; 2007.
- Nessa N. The Health of Children and Young People. London: Office for National Statistics; 2004.
- Blackburn CM, Spencer NJ, Read JM. Prevalence of childhood disability and the characteristics and circumstances of disabled children in the UK: secondary analysis of the Family Resources Survey. BMC Pediatr 2010;10.
- Chung R, Donaldson D, Herring I, McColl H, Snow J, Cockerham J, et al. Family Resources Survey, Office for National Statistics. London: National Centre for Social Research; 2004.
- Horridge KA. Assessment and investigation of the child with disordered development. Arch Dis Child Educ Pract Ed 2011;96:9-20. http://dx.doi.org/10.1136/adc.2009.182436.
- Farmer JE, Deidrick KK, Farmer JE, Donders J, Warschausky S. Treating Neurodevelopmental Disabilities: Clinical Research and Practice. New York, NY: The Guildford Press; 2006.
- Johnson S, Fawke J, Hennessy E, Rowell V, Thomas S, Wolke D, et al. Neurodevelopmental disability through 11 years of age in children born before 26 weeks of gestation. Pediatrics 2009;124:e249-57. http://dx.doi.org/10.1542/peds.2008-3743.
- State of Healthcare 2008. Norwich: The Stationery Office; 2008.
- Kennedy I. Getting it Right for Children and Young People: Overcoming Cultural Barriers in the NHS so as to Meet their Needs. London: Department of Health; 2010.
- Sloper P, Beresford B, Rabiee P. Every Child Matters outcomes: what do they mean for disabled children and young people?. Child Soc 2009;23:265-78. http://dx.doi.org/10.1111/j.1099-0860.2008.00185.x.
- International Classification of Functioning, Disability and Health. Geneva: WHO; 2001.
- Morris C, Gibbons E, Fitzpatrick R. Child and Parent Reported Outcome Measures: A Scoping Report Focusing on Feasibility for Routine Use in the NHS. Report to the Department of Health. Oxford: University of Oxford; 2009.
- Fitzpatrick R, Smith PC, Mossialos E, Papanicolas I, . Performance Measurement for Health System Improvement: Experiences, Challenges and Prospects. Cambridge: Cambridge University Press; 2009.
- Solans M, Pane S, Estrada MD, Serra-Sutton V, Berra S, Herdman M, et al. Health-related quality of life measurement in children and adolescents: a systematic review of generic and disease-specific instruments. Value Health 2008;11:742-64. http://dx.doi.org/10.1111/j.1524-4733.2007.00293.x.
- Guidance for Industry: Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labelling Claims. Rockville, MD: Department of Health and Human Services, Food and Drug Administration, Centre for Drug Evaluation and Research; 2009.
- Ronen GM, Fayed N, Rosenbaum PL. Outcomes in pediatric neurology: a review of conceptual issues and recommendations. The 2010 Ronnie Mac Keith Lecture. Dev Med Child Neurol 2011;53:305-12.
- Waters E, Davis E, Ronen GM, Rosenbaum P, Livingston M, Saigal S. Quality of life instruments for children and adolescents with neurodisabilities: how to choose the appropriate instrument. Dev Med Child Neurol 2009;51:660-9. http://dx.doi.org/10.1111/j.1469-8749.2009.03324.x.
- Colver A, Jessen C. Measurement of health status and quality of life in neonatal follow-up studies. Semin Neonat 2000;5:149-57. http://dx.doi.org/10.1053/siny.1999.0002.
- Hallet C, Prout A. Hearing the Voices of Children: Social Policy for a New Century. New York, NY: RoutledgeFalmer; 2003.
- The NHS Outcomes Framework 2011/12. London: Department of Health; 2010.
- Royal College of Paediatrics and Child Health . Response to Transparency in Outcomes 2010. www.rcpch.ac.uk/doc.aspx?id_Resource=7722 (accessed 7 April 2011).
- Staley K. Exploring Impact: Public Involvement in NHS, Public Health and Social Care Research. Eastleigh: INVOLVE; 2009.
- Staniszewska S, Brett J, Mockford C, Barber R. The GRIPP checklist: strengthening the quality of patient and public involvement reporting in research. Int J Technol Assess Health Care 2011;27:391-9. http://dx.doi.org/10.1017/S0266462311000481.
- Morris C, Shilling V, McHugh C, Wyatt K. Why it is crucial to involve families in all stages of childhood disability research. Develop Med Child Neurol 2011;53:769-71. http://dx.doi.org/10.1111/j.1469-8749.2011.03984.x.
- Kreis J, Puhan MA, Schunemann HJ, Dickersin K. Consumer involvement in systematic reviews of comparative effectiveness research. Health Expect 2013;16:323-37. http://dx.doi.org/10.1111/j.1369-7625.2011.00722.x.
- Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. York: Centre for Reviews and Dissemination, University of York; 2008.
- Terwee CB, Jansma EP, Riphagen II, de Vet HCW. Development of a methodological PubMed search filter for finding studies on measurement properties of measurement instruments. Qual Life Res 2009;18:1115-23. http://dx.doi.org/10.1007/s11136-009-9528-5.
- Jenkinson C, Gibbons E, Fitzpatrick R. A Structured Review of Patient-Reported Outcome Measures (PROMs) for Stroke. Oxford: University of Oxford, Patient-reported Outcome Measurement Group and UK Department of Public Health; 2009.
- Schmidt LJ, Garratt AM, Fitzpatrick R. Child/parent-assessed population health outcome measures: a structured review. Child Care Health Dev 2002;28:227-37. http://dx.doi.org/10.1046/j.1365-2214.2002.00266.x.
- Connolly MA, Johnson JA. Measuring quality of life in paediatric patients. Pharmacoeconomics 1999;16:605-25. http://dx.doi.org/10.2165/00019053-199916060-00002.
- Davis E, Waters E, Mackinnon A, Reddihough D, Graham HK, Mehmet-Radji O, et al. Paediatric quality of life instruments: a review of the impact of the conceptual framework on outcomes. Dev Med Child Neurol 2006;48:311-18. http://dx.doi.org/10.1017/S0012162206000673.
- Matza LS, Swensen AR, Flood EM, Secnik K, Leidy NK. Assessment of health-related quality of life in children: a review of conceptual, methodological, and regulatory Issues. Value Health 2004;7:79-92. http://dx.doi.org/10.1111/j.1524-4733.2004.71273.x.
- Brazier J, Deveril M, Green C, Harper R, Booth A. A review of the use of health status measures in economic evaluation. Health Technol Assess 1999;3:i-iv.
- Brazier J, Ratcliffe J, Salomon JA, Tsuchiya A. Measuring and Valuing Health Benefits for Economic Evaluation. Oxford: Oxford University Press; 2007.
- International Classification of Functioning, Disability and Health – Children and Youth Version: ICF-CY. Geneva: WHO; 2007.
- Cieza A, Geyh S, Chatterji S, Kostanjsek N, Ustün B, Stucki G. ICF linking rules: an update based on lessons learned. J Rehabil Med 2005;37:212-18. http://dx.doi.org/10.1080/16501970510040263.
- Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res 2010;19:539-49. http://dx.doi.org/10.1007/s11136-010-9606-8.
- Fitzpatrick R, Davey C, Buxton MJ, Jones DR. Evaluating patient-based outcome measures for use in clinical trials. Health Technol Assess 1998;2:i-iv.
- Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007;60:34-42. http://dx.doi.org/10.1016/j.jclinepi.2006.03.012.
- Kaiser HF. The application of electronic computers to factor analysis. Educ Psychol Measure 1960;20:141-51. http://dx.doi.org/10.1177/001316446002000116.
- Fayers P, Machin D. Quality of life: the Assessment, Analysis and Interpretation of Patient-Reported Outcomes. Chichester: John Wiley & Sons; 2007.
- Hambleton RK, Swaminathan H, Rogers HJ. Fundamentals of Item Response Theory. Newbury Park, CA: Sage Press; 1991.
- Tennant A, Conaghan PG. The Rasch measurement model in rheumatology: what is it and why use it? When should it be applied, and what should one look for in a Rasch paper?. Arthritis Rheum 2007;57:1358-62. http://dx.doi.org/10.1002/art.23108.
- Cohen J. Statistical Power Analysis for the Behavioural Sciences. Mahwah, NJ: Lawrence Earlbaum Associates; 1988.
- Streiner DL, Norman GR. Health Measurement Scales: a Practical Guide to their Development and Use. Oxford: Oxford University Press; 2003.
- Smith EV. Understanding Rasch measurement: detecting and evaluating the impact of multidimensionality using item fit statistics and principal component analysis of residuals. J Appl Measure 2002;3:205-31.
- Kirshner B, Guyatt G. A methodological framework for assessing health indices. J Chron Dis 1985;38:27-36. http://dx.doi.org/10.1016/0021-9681(85)90005-0.
- Haley SM, Fragala-Pinkham MA. Interpreting change scores of tests and measures used in physical therapy. Phys Ther 2006;86:735-43.
- Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials 1989;10:407-15.
- Kessler R, Mroczek D. Measuring the effects of medical interventions. Med Care 1995;33:AS109-19.
- Ware JE, Brook RH, Davies AR, Lohr KN. Choosing measures of health status for individuals in general populations. Am J Public Health 1981;71:620-5. http://dx.doi.org/10.2105/AJPH.71.6.620.
- Aaronson NK. Assessing the quality of life of patients in cancer clinical trials: common problems and common sense solutions. Eur J Cancer 1992;28A:1304-7. http://dx.doi.org/10.1016/0959-8049(92)90504-U.
- Schellingerhout JM, Verhagen AP, Heymans MW, Koes BW, de Vet HC, Terwee CB. Measurement properties of disease-specific questionnaires in patients with neck pain: a systematic review. Qual Life Res 2012;21:659-70. http://dx.doi.org/10.1007/s11136-011-9965-9.
- McDowell I, Newell C. Measuring Health. A Guide to Rating Scales and Questionnaires. New York, NY: Oxford University Press; 1996.
- Manificat S, Dazord A, Langue J, Danjou G, Bauche P, Bovet F, et al. A new instrument to evaluate infant quality of life. Qual Life Newsletter 1999;23:7-8.
- Gayral-Taminh M, Bravi C, Depond M, Pourre F, Maffre T, Raynaud J-P, et al. Auto-évaluation de la qualité de vie d’enfants de 6 à 12 ans: analyse du concept et élaboration d’un outil prototype. Santé Publique 2005;17:35-4. http://dx.doi.org/10.3917/spub.051.0035.
- Manificat S, Dazord A. Children’s quality of life assessment: preliminary results obtained with the AUQUEI questionnaire. Qual Life Newsletter 1998;19:2-3.
- Manificat S, Dazord A. Assessing adolescent’s quality of life: validation of a new questionnaire. Qual Life Newsletter 2002;28:2-3.
- Norton-Broda M. The Relationship of Parental Health-Promoting Lifestyles to School-Age Children’s Self-Esteem, Perceived Health Status, Health Beliefs, and Health Behaviors. Austin, TX: University of Texas-Austin; 1988.
- Parkerson GR, Broadhead WE, Tse CK. Validation of the Duke Social Support and Stress Scale. Fam Med 1991;23:357-60.
- Bastiaens L, Dello Stritto C. Validity and reliability of the Health And Life Functioning Scale n.d.
- Le Coq EM, Boeke AJP, Bezemer PD, Bruil J, van Eijk JT. Clinimetric properties of a parent report on their offspring’s quality of life. J Clin Epidemiol 2000;53:139-46. http://dx.doi.org/10.1016/S0895-4356(99)00158-4.
- Maes S, Bruil J, Rodriguez-Marin J. Assessing quality of life of children with a chronic illness 1995:637-52.
- Weinman J, Petrie KJ, Moss-morris R, Horne R. The illness perception questionnaire: a new method for assessing the cognitive representation of illness. Psychol Health 1996;11:431-45. http://dx.doi.org/10.1080/08870449608400270.
- Landgraf JM. The Infant/Toddler Child Health Questionnaire: Conceptual Framework, Logic, Content and Preliminary Psychometric Results. Boston, MA: HealthAct, Inc.; 1994.
- Klassen AF, Landgraf JM, Lee SK, Barer M, Raina P, Chan HWP, et al. Health related quality of life in 3 and 4 year old children and their parents: preliminary findings about a new questionnaire. Health Qual Life Outcomes 2003;1.
- Lindström B, Köhler L. Youth, disability and quality of life. Pediatrician 1991;18:121-8.
- Lindström B, Eriksson B. Quality of life among children in the Nordic countries. Qual Life Res 1993;2:23-32. http://dx.doi.org/10.1007/BF00642886.
- Bouman NH, Koot HM, Van Gils APM, Verhulst FC. Development of a health-related quality of life instrument for children: the quality of life questionnaire for children. Psychol Health 1999;14:829-46. http://dx.doi.org/10.1080/08870449908407350.
- Feldman BM, Grundland B, McCullough L, Wright V. Distinction of quality of life, health related quality of life, and health status in children referred for rheumatologic care. J Rheumatol 2000;27:226-33.
- Fekkes M, Theunissen NCM, Brugman E, Veen S, Verrips EGH, Koopman HM, et al. Development and psychometric evaluation of the TAPQOL: a health-related quality of life instrument for 1–5-year-old children. Qual Life Res 2000;9:961-72.
- Theunissen NCM, Vogels TGC, Koopman HM, Verrips GH, Zwinderman KA, Verloove-Vanhorick SP, et al. The proxy problem: child report versus parent report in health-related quality of life research. Quality Life Res 1998;7:387-97. http://dx.doi.org/10.1023/A:1008801802877.
- Vogels T, Verrips GHW, Verloove-Vanhorick SP, Fekkes M, Kamphuis RP, Koopman HM, et al. Measuring health-related quality of life in children: the development of the TACQOL parent form. Qual Life Res 1998;7:457-65. http://dx.doi.org/10.1023/A:1008848218806.
- Riley AW, Forrest CB, Starfield B, Green B, Kang M, Ensminger M. Reliability and validity of the adolescent health profile-types. Med Care 1998;36:1237-48. http://dx.doi.org/10.1097/00005650-199808000-00011.
- Kurtin PS, Landgraf JM, Abetz L. Patient-based health status measurements in pediatric dialysis: expanding the assessment of outcome. Am J Kidney Dis 1994;24:376-82.
- Landgraf JM, Maunsell E, Speechley KN, Bullinger M, Campbell S, Abetz L, et al. Canadian-French, German and UK versions of the Child Health Questionnaire: methodology and preliminary item scaling results. Qual Life Res 1998;7:433-45. http://dx.doi.org/10.1023/A:1008810004694.
- Landgraf JM, Abetz LN. Functional status and well-being of children representing three cultural groups: initial self-reports using the CHQ-CF87. Psychol Health 1997;12:839-54.
- Stein RE, Jessop DJ. Functional status II(R). A measure of child health status. Med Care 1990;28:1041-55. http://dx.doi.org/10.1097/00005650-199011000-00006.
- Ravens-Sieberer U, Gosch A, Rajmil L, Erhart M, Bruil J, Duer W, et al. KIDSCREEN-52 quality-of-life measure for children and adolescents. Expert Rev Pharmacoecon Outcomes Res 2005;5:353-64. http://dx.doi.org/10.1586/14737167.5.3.353.
- Ravens-Sieberer U, Auquier P, Erhart M, Gosch A, Rajmil L, Bruil J, et al. The KIDSCREEN-27 quality of life measure for children and adolescents: psychometric results from a cross-cultural survey in 13 European countries. Qual Life Res 2007;16:1347-56. http://dx.doi.org/10.1007/s11136-007-9240-2.
- Ravens-Sieberer U, Erhart M, Rajmil L, Herdman M, Auquier P, Bruil J, et al. Reliability, construct and criterion validity of the KIDSCREEN-10 score: a short measure for children and adolescents’ well-being and health-related quality of life. Qual Life Res 2010;19:1487-500.
- Bullinger M, von Mackensen S, Kirchberger I. KINDL – Ein Fragebogen zur Erfassung der gesundheitsbezogenen Lebensqualität von Kindern. Sonderdruck Zeitschrift für Gesundheitspsychologie 1994;1:64-77.
- Varni JW, Limbers CA, Neighbors K, Schulz K, Lieu JE, Heffer RW, et al. The PedsQL Infant Scales: feasibility, internal consistency reliability, and validity in healthy and ill infants. Qual Life Res 2011;20:45-5. http://dx.doi.org/10.1007/s11136-010-9730-5.
- Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care 1999;37:126-39. http://dx.doi.org/10.1097/00005650-199902000-00003.
- Chan KS, Mangione-Smith R, Burwinkle TM, Rosen M, Varni JW. The PedsQL: reliability and validity of the short-form generic core scales and Asthma Module. Med Care 2005;43:256-65. http://dx.doi.org/10.1097/00005650-200503000-00008.
- Cummins RA, Lau ALD. Personal Wellbeing Index – School Children (PWI-SC). 3rd edn. Melbourne, VIC: Deakin University; 2005.
- Huebner E. Initial development of the Student’s Life Satisfaction Scale. School Psychol Int 1991;12:231-40. http://dx.doi.org/10.1177/0143034391123010.
- Huebner ES. Preliminary development and validation of a multidimensional life satisfaction scale for children. Psychol Assess 1994;6:149-58. http://dx.doi.org/10.1037//1040-3590.6.2.149.
- Seligson JL, Huebner E, Valois RF. Preliminary validation of the Brief Multidimensional Students’ Life Satisfaction Scale (BMSLSS). Soc Indicat Res 2003;61:121-45.
- Gilligan TD, Huebner S. Initial development and validation of the Multidimensional Students’ Life Satisfaction Scale-Adolescent Version. Appl Res Qual Life 2007;2:1-16. http://dx.doi.org/10.1007/s11482-007-9026-2.
- Edwards TC, Huebner CE, Connell FA, Patrick DL. Adolescent quality of life, part I: conceptual and measurement model. J Adolesc 2002;25:275-86. http://dx.doi.org/10.1006/jado.2002.0470.
- Singh G, Athreya BH, Fries JF, Goldsmith DP. Measurement of health status in children with juvenile rheumatoid arthritis. Arthrit Rheum 1994;37:1761-9. http://dx.doi.org/10.1002/art.1780371209.
- Bevans KB, Riley AW, Forrest CB. Development of the healthy pathways child-report scales. Qual Life Res 2010;19:1195-214. http://dx.doi.org/10.1007/s11136-010-9687-4.
- Maylath NS. Development of the Children’s Health Ratings Scale. Health Educ Q 1990;17:89-97. http://dx.doi.org/10.1177/109019819001700109.
- Hester NO. Child’s Health Self-Concept Scale: its development and psychometric properties. Adv Nurs Sci 1984;7:45-5.
- Nelson E, Wasson J, Kirk J, Keller A, Clark D, Dietrich A, et al. Assessment of function in routine clinical practice: description of the COOP chart method and preliminary findings. J Chron Dis 1987;40:558-63. http://dx.doi.org/10.1016/S0021-9681(87)80033-4.
- Graham P, Stevenson J, Flynn D. A new measure of health-related quality of life for children: preliminary findings. Psychol Health 1997;12:655-65. http://dx.doi.org/10.1080/08870449708407412.
- Eiser C, Vance Y, Seamark D. The development of a theoretically driven generic measure of quality of life for children aged 6–12 years: a preliminary report. Child Care Health Develop 2000;26:445-56.
- Collier J. Developing a generic child quality of life questionnaire. Br Psychol Soc 1997;28:12-6.
- Cummins RA. The Comprehensive Quality of Life Scale – Adult. Melbourne, VIC: Deakin University; 1997.
- Raphael D, Rukholm E, Brown I, Hill-Bailey P, Donato E. The Quality of Life Profile – Adolescent Version: background, description, and initial validation. J Adolesc Health 1996;19:366-75. http://dx.doi.org/10.1016/S1054-139X(96)00080-8.
- Spencer NJ, Coe C. The development and validation of a measure of parent-reported child health and morbidity: the Warwick Child Health and Morbidity Profile. Child Care Health Dev 1996;22:367-79. http://dx.doi.org/10.1046/j.1365-2214.1996.811811.x.
- Nugent J, Ruperto N, Grainger J, Machado C, Sawhney S, Balidam E, et al. The British version of the Childhood Health Assessment Questionnaire (CHAQ) and the Child Health Questionnaire (CHQ). Clin Exp Rheumatol 2001;19:S163-7.
- Lam C, Young N, Marwaha J, McLimont M, Feldman BM. Revised versions of the Childhood Health Assessment Questionnaire (CHAQ) are more sensitive and suffer less from a ceiling effect. Arthrit Care Res 2004;51:881-9. http://dx.doi.org/10.1002/art.20820.
- Starfield B, Bergner M, Ensminger M, Riley A, Ryan S, Green B, et al. Adolescent health status measurement: development of the Child Health and Illness Profile. Pediatrics 1993;91:430-5.
- Starfield B, Riley AW, Green BF, Ensminger ME, Ryan SA, Kelleher K, et al. The adolescent child health and illness profile. A population-based measure of health. Med Care 1995;33:553-66. http://dx.doi.org/10.1097/00005650-199505000-00008.
- Rebok GW, Riley A, Forrest C, Starfield B, Green B, Robertson J, et al. Elementary school-aged children’s reports of their health: a cognitive interviewing study. Qual Life Res 2001;10:59-70.
- Riley AW, Forrest CB, Rebok GW, Starfield B, Green BF, Robertson JA, et al. The Child Report Form of the CHIP-Child Edition: reliability and validity. Med Care 2004;42:221-31. http://dx.doi.org/10.1097/01.mlr.0000114910.46921.73.
- Riley AW, Forrest CB, Starfield B, Rebok GW, Robertson JA, Green BF. The Parent Report Form of the CHIP-Child Edition: reliability and validity. Med Care 2004;42:210-20. http://dx.doi.org/10.1097/01.mlr.0000114909.33878.ca.
- Riley AW, Chan KS, Prasad S, Poole L. A global measure of child health-related quality of life: reliability and validity of the Child Health and Illness Profile – Child Edition (CHIP-CE) global score. J Med Econ 2007;10:91-106. http://dx.doi.org/10.3111/200710091106.
- Bevans KB, Riley AW, Forrest CB. Development of the Healthy Pathways Parent-Report Scales. Qual Life Res 2012;21:1755-70. http://dx.doi.org/10.1007/s11136-012-0111-0.
- Waters E, Wright M, Wake M, Landgraf J, Salmon L. Measuring the health and well-being of children and adolescents: a preliminary comparative evaluation of the Child Health Questionnaire in Australia. Ambulat Child Health 1999;5:131-41.
- Waters E, Salmon L, Wake M. The parent-form Child Health Questionnaire in Australia: comparison of reliability, validity, structure, and norms. J Pediatr Psychol 2000;25:381-91. http://dx.doi.org/10.1093/jpepsy/25.6.381.
- Waters EB, Salmon LA, Wake M, Wright M, Hesketh KD. The health and well-being of adolescents: a school-based population study of the self-report Child Health Questionnaire. J Adolesc Health 2001;29:140-9. http://dx.doi.org/10.1016/S1054-139X(01)00211-7.
- Hepner KA, Sechrest L, Bissell K. Confirmatory factor analysis of the Child Health Questionnaire-Parent Form 50 in a predominantly minority sample. Qual Life Res 2002;11:763-73.
- Drotar D, Schwartz L, Palermo TM, Burant C. Factor structure of the Child Health Questionnaire-Parent Form in pediatric populations. J Pediatr Psychol 2006;31:127-38. http://dx.doi.org/10.1093/jpepsy/jsi078.
- Wasson JH, Kairys SW, Nelson EC, Kalishman N, Baribeau P. A short survey for assessing health and social problems of adolescents. Dartmouth Primary Care Cooperative Information Project (The COOP). J Fam Prac 1994;38:489-94.
- Collier J, MacKinlay D, Phillips D. Norm values for the Generic Children’s Quality of Life Measure (GCQ) from a large school-based sample. Qual Life Res 2000;9:617-23.
- Erhart M, Ravens-Sieberer U. Health-related quality of life instruments and individual diagnosis -- a new area of application. GMS Psycho Social Medicine 2006;3:1-13.
- Robitail S, Simeoni M-C, Erhart M, Ravens-Sieberer U, Bruil J, Auquier P, et al. Validation of the European proxy KIDSCREEN-52 pilot test health-related quality of life questionnaire: first results. J Adolesc Health 2006;39:596.e1-10. http://dx.doi.org/10.1016/j.jadohealth.2006.01.009.
- Berra S, Ravens-Sieberer U, Erhart M, Tebé C, Bisegger C, Duer W, et al. Methods and representativeness of a European survey in children and adolescents: the KIDSCREEN study. BMC Public Health 2007;7. http://dx.doi.org/10.1186/1471-2458-7-182.
- Robitail S, Ravens-Sieberer U, Simeoni M-C, Rajmil L, Bruil J, Power M, et al. Testing the structural and cross-cultural validity of the KIDSCREEN-27 quality of life questionnaire. Qual Life Res 2007;16:1335-45. http://dx.doi.org/10.1007/s11136-007-9241-1.
- Ravens-Sieberer U, Gosch A, Rajmil L, Erhart M, Bruil J, Power M, et al. The KIDSCREEN-52 quality of life measure for children and adolescents: psychometric results from a cross-cultural survey in 13 European countries. Value Health 2008;11:645-58. http://dx.doi.org/10.1111/j.1524-4733.2007.00291.x.
- Erhart M, Ottova V, Gaspar T, Jericek H, Schnohr C, Alikasifoglu M, et al. Measuring mental health and well-being of school-children in 15 European countries using the KIDSCREEN-10 Index. Int J Public Health 2009;54:S160-6.
- Erhart M, Ravens-Sieberer U, Dickinson HO, Colver A. European SPARCLE and KIDSCREEN Groups . Rasch measurement properties of the KIDSCREEN quality of life instrument in children with cerebral palsy and differential item functioning between children with and without cerebral palsy. Value Health 2009;12:782-92. http://dx.doi.org/10.1111/j.1524-4733.2009.00508.x.
- Lloyd K. Kids’ Life and Times: using an Internet survey to measure children’s health-related quality of life. Qual Life Res 2011;20:37-44. http://dx.doi.org/10.1007/s11136-010-9728-z.
- Stevens K, Ratcliffe J. Measuring and valuing health benefits for economic evaluation in adolescence: an assessment of the practicality and validity of the Child Health Utility 9D in the Australian adolescent population. Value Health 2012;15:1092-9. http://dx.doi.org/10.1016/j.jval.2012.07.011.
- Wee H-L, Lee WWR, Ravens-Sieberer U, Erhart M, Li S-C. Validation of the English version of the KINDL® generic children’s health-related quality of life instrument for an Asian population — results from a pilot test. Qual Life Res 2005;14:1193-200. http://dx.doi.org/10.1007/s11136-004-2957-2.
- Wee H-L, Ravens-Sieberer U, Erhart M, Li S-C. Factor structure of the Singapore English version of the KINDL children quality of life questionnaire. Health Qual Life Outcomes 2007;5.
- Varni JW, Seid M, Kurtin PS. PedsQLTM 4.0: reliability and validity of the Pediatric Quality of Life Inventory™ Version 4.0 Generic Core Scales in healthy and patient populations. Med Care 2001;39:800-12.
- Varni JW, Seid M, Knight TS, Uzark K, Szer IS. The PedsQL 4.0 Generic Core Scales: sensitivity, responsiveness, and impact on clinical decision-making. J Behav Med 2002;25:175-93.
- Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL* 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambulat Pediatr 2003;3:329-41. http://dx.doi.org/10.1367/1539-4409(2003)003%3C0329:TPAAPP%3E2.0.CO;2.
- Upton P, Maddocks A, Eiser C, Barnes PM, Williams J. Development of a measure of the health-related quality of life of children in public care. Child Care Health Develop 2005;31:409-15. http://dx.doi.org/10.1111/j.1365-2214.2005.00520.x.
- Varni JW, Burwinkle TM. The PedsQL as a patient-reported outcome in children and adolescents with Attention-Deficit/Hyperactivity Disorder: a population-based study. Health Qual Life Outcomes 2006;4.
- Varni JW, Limbers CA, Burwinkle TM. How young can children reliably and validly self-report their health-related quality of life?: an analysis of 8,591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes 2007;5.
- Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children’s health-related quality of life: an analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes 2007;5.
- Varni JW, Limbers CA, Newman DA, Sied M. Longitudinal factorial invariance of the PedsQL 4.0 Generic Core Scales child self-report Version: one year prospective evidence from the California State Children’s Health Insurance Program (SCHIP). Qual Life Research 2008;17:1153-62. http://dx.doi.org/10.1007/s11136-008-9389-3.
- Huang IC, Thompson LA, Chi YY, Knapp CA, Revicki DA, Seid M, et al. The linkage between pediatric quality of life and health conditions: establishing clinically meaningful cutoff scores for the PedsQL. Value Health 2009;12:773-81. http://dx.doi.org/10.1111/j.1524-4733.2008.00487.x.
- Iannaccone ST, Hynan LS, Morton A, Buchanan R, Limbers CA, Varni JW, et al. The PedsQL in pediatric patients with spinal muscular atrophy: feasibility, reliability, and validity of the Pediatric Quality of Life Inventory Generic Core Scales and Neuromuscular Module. Neuromusc Disord 2009;19:805-12. http://dx.doi.org/10.1016/j.nmd.2009.09.009.
- Varni JW, Limbers CA, Newman DA. Using factor analysis to confirm the validity of children’s self-reported health-related quality of life across different modes of administration. Clinical Trials 2009;6:185-95. http://dx.doi.org/10.1177/1740774509102309.
- Davis SE, Hynan LS, Limbers CA, Andersen CM, Greene MC, Varni JW, et al. The PedsQL in pediatric patients with Duchenne muscular dystrophy: feasibility, reliability, and validity of the Pediatric Quality of Life Inventory Neuromuscular Module and Generic Core Scales. J Clin Neuromusc Dis 2010;11:97-109. http://dx.doi.org/10.1097/CND.0b013e3181c5053b.
- Limbers CA, Ripperger-Suhler J, Heffer RW, Varni JW. Patient-reported Pediatric Quality of Life Inventory™ 4.0 Generic Core Scales in pediatric patients with attention-deficit/hyperactivity disorder and comorbid psychiatric disorders: feasibility, reliability, and validity. Value Health 2011;14:521-30. http://dx.doi.org/10.1016/j.jval.2010.10.031.
- Awasthi S, Agnihotri K, Chandra H, Singh U, Thakur S. Assessment of health-related quality of life in school-going adolescents: validation of PedsQL instrument and comparison with WHOQOL-BREF. Natl Med J Ind 2012;25:74-9.
- Gullone E, Cummins RA. The comprehensive quality of life scale: a psychometric evaluation with an adolescent sample. Behav Change 1999;16:127-39. http://dx.doi.org/10.1375/bech.16.2.127.
- Tomyn AJ, Cummins RA. The subjective wellbeing of high-school students: validating the Personal Wellbeing Index–School Children. Soc Indicat Res 2011;101:405-18. http://dx.doi.org/10.1007/s11205-010-9668-6.
- Huebner E. Further validation of the Students’ Life Satisfaction Scale: the independence of satisfaction and affect ratings. J Psychoeduc Assess 1991;9:363-8. http://dx.doi.org/10.1177/073428299100900408.
- Huebner E, Alderman GL. Convergent and discriminant validation of a children’s life satisfaction scale: its relationship to self- and teacher-reported psychological problems and school functioning. Soc Indicat Res 1993;30:71-82. http://dx.doi.org/10.1007/BF01080333.
- Huebner E, Dew T. An evaluation of racial bias in a life satisfaction scale. Psychol Schools 1993;30:305-9. http://dx.doi.org/10.1002/1520-6807(199310)30:4%3C305::AID-PITS2310300404%3E3.0.CO;2-F.
- Dew T, Huebner E. Adolescents’ perceived quality of life: an exploratory investigation. J School Psychol 1994;32:185-99. http://dx.doi.org/10.1016/0022-4405(94)90010-8.
- Huebner E. Conjoint analyses of the Students’ Life Satisfaction Scale and the Piers-Harris Self-Concept Scale. Psychol Schools 1994;31:273-7. http://dx.doi.org/10.1002/1520-6807(199410)31:4%3C273::AID-PITS2310310404%3E3.0.CO;2-A.
- Gilman R, Huebner E. Children’s reports of their life satisfaction: convergence across raters, time and response formats. School Psychol Int 1997;18:229-43. http://dx.doi.org/10.1177/0143034397183004.
- Greenspoon PJ, Saklofske DH. Validity and reliability of the multidimensional students’ life satisfaction scale with Canadian children. J Psychoeduc Assess 1997;15:138-55. http://dx.doi.org/10.1177/073428299701500204.
- Greenspoon PJ, Saklofske DH. Confirmatory factor analysis of the multidimensional Students’ Life Satisfaction Scale. Personality Individ Diff 1998;25:965-71. http://dx.doi.org/10.1016/S0191-8869(98)00115-9.
- Huebner E. Cross-racial application of a children’s Multidimensional Life Satisfaction Scale. School Psychol Int 1998;19:179-88. http://dx.doi.org/10.1177/0143034398192006.
- Huebner ES, Laughlin JE, Ash C, Gilman R. Further validation of the Multidimensional Students’ Life Satisfaction Scale. J Psychol Assess 1998;16:118-34. http://dx.doi.org/10.1177/073428299801600202.
- Huebner E, Gilman R, Laughlin JE. A multimethod investigation of the multidimensionality of children’s well-being reports: discriminant validity of life satisfaction and self-esteem. Soc Indicat Res 1999;46:1-22.
- Gilman R, Huebner E, Laughlin JE. A first study of the Multidimensional Students’ Life Satisfaction Scale with adolescents. Soc Indicat Res 2000;52:135-60.
- Huebner E, Brantley A, Nagle RJ, Valois RF. Correspondence between parent and adolescent ratings of life satisfaction for adolescents with and without mental disabilities. J Psychoeduc Assess 2002;20:20-9. http://dx.doi.org/10.1177/073428290202000102.
- Seligson JL, Huebner E, Valois RF. An investigation of a brief life satisfaction scale with elementary school children. Soc Indicat Res 2005;73:355-74. http://dx.doi.org/10.1007/s11205-004-2011-3.
- Funk BA, Huebner E, Valois RF. Reliability and validity of a brief life satisfaction scale with a high school sample. J Happiness Stud 2006;7:41-54. http://dx.doi.org/10.1007/s10902-005-0869-7.
- Haranin EC, Huebner E, Suldo SM. Predictive and incremental validity of global and domain-based adolescent life satisfaction reports. J Psychoeduc Assess 2007;25:127-38. http://dx.doi.org/10.1177/0734282906295620.
- Sawatzky R, Ratner PA, Johnson JL, Kopec JA, Zumbo BD. Sample heterogeneity and the measurement structure of the Multidimensional Students’ Life Satisfaction Scale. Soc Indicat Res 2009;94:273-96. http://dx.doi.org/10.1007/s11205-008-9423-4.
- Huebner ES, Antaramian SP, Hills KJ, Lewis AD, Saha R. Stability and predictive validity of the Brief Multidimensional Students’ Life Satisfaction Scale. Child Indicat Res 2011;4:161-8.
- Spencer NJ, Coe C. Validation of the Warwick Child Health and Morbidity profile in routine child health surveillance. Child Care Health Dev 2000;26:323-36. http://dx.doi.org/10.1046/j.1365-2214.2000.00148.x.
- Patrick DL, Edwards TC, Topolski TD. Adolescent quality of life, part II: initial validation of a new instrument. J Adolesc 2002;25:287-300. http://dx.doi.org/10.1006/jado.2002.0471.
- Pencharz J, Young NL, Owen JL, Wright JG. Comparison of three outcomes instruments in children. J Pediatr Orthopaed 2001;21:425-32. http://dx.doi.org/10.1097/01241398-200107000-00002.
- Vitale MG, Levy DE, Moskowitz AJ, Gelijns AC, Spellmann M, Verdisco L, et al. Capturing quality of life in pediatric orthopaedics: two recent measures compared. J Pediatr Orthopaed 2001;21:629-35. http://dx.doi.org/10.1097/01241398-200109000-00015.
- McCarthy ML, MacKenzie EJ, Durbin DR, Aitken ME, Jaffe KM, Paidas CN, et al. The Pediatric Quality of Life Inventory: an evaluation of its reliability and validity for children with traumatic brain injury. Arch Phys Med Rehabil 2005;86:1901-9. http://dx.doi.org/10.1016/j.apmr.2005.03.026.
- Young NL, Varni JW, Snider L, McCormick A, Sawatzky B, Scott M, et al. The Internet is valid and reliable for child-report: an example using the Activities Scale for Kids (ASK) and the Pediatric Quality of Life Inventory (PedsQL). J Clin Epidemiol 2009;62:314-20. http://dx.doi.org/10.1016/j.jclinepi.2008.06.011.
- McDougall J, Wright V, Nichols M, Miller L. Assessing the psychometric properties of both a global and a domain-specific perceived quality of life measure when used with youth who have chronic conditions. Soc Indicat Res n.d.:1-15. http://dx.doi.org/10.1007/s11205-012-0200-z.
- Riley AW, Coghill D, Forrest CB, Lorenzo MJ, Ralston SJ, Spiel G, et al. Validity of the health-related quality of life assessment in the ADORE study: Parent Report Form of the CHIP-Child Edition. Eur Child Adolesc Psychiatry 2006;15:I63-71. http://dx.doi.org/10.1007/s00787-006-1009-6.
- Schacht A, Escobar R, Wagner T, Wehmeier PM. Psychometric properties of the quality of life scale Child Health and Illness Profile-Child Edition in a combined analysis of five atomoxetine trials. Atten Defic Hyperact Disord 2011;3:335-49. http://dx.doi.org/10.1007/s12402-011-0066-y.
- Wake M, Salmon L, Reddihough D. Health status of Australia children with mild to severe cerebral palsy: cross-sectional survey using the Child Health Questionnaire. Develop Med Child Neurol 2003;45:194-9. http://dx.doi.org/10.1111/j.1469-8749.2003.tb00930.x.
- Rentz AM, Matza LS, Secnik K, Swensen A, Revicki DA. Psychometric validation of the child health questionnaire (CHQ) in a sample of children and adolescents with attention-deficit/hyperactivity disorder. Qual Life Res 2005;14:719-34. http://dx.doi.org/10.1007/s11136-004-0832-9.
- Vitale MG, Roye EA, Choe JC, Hyman JE, Lee FY, Roye DP. Assessment of health status in patients with cerebral palsy: what is the role of quality-of-life measures?. J Pediatr Orthopaed 2005;25:792-7. http://dx.doi.org/10.1097/01.bpo.0000164870.26632.6b.
- Thomas-Stonell N, Johnson P, Rumney P, Wright V, Oddson B. An evaluation of the responsiveness of a comprehensive set of outcome measures for children and adolescents with traumatic brain injuries. Pediatr Rehabil 2006;9:14-23. http://dx.doi.org/10.1080/13638490500050097.
- McCullough N, Parkes J, White-Koning M, Beckung E, Colver A. Reliability and validity of the Child Health QuestionnairePF-50 for European children with cerebral palsy. J Pediatr Psychol 2009;34:41-50. http://dx.doi.org/10.1093/jpepsy/jsn048.
- Davis E, Shelly A, Waters E, Davern M. Measuring the quality of life of children with cerebral palsy: comparing the conceptual differences and psychometric properties of three instruments. Develop Med Child Neurol 2010;52:174-80. http://dx.doi.org/10.1111/j.1469-8749.2009.03382.x.
- Eiser C, Vance YH, Horne B, Glaser A, Galvin H. The value of the PedsQL™ in assessing quality of life in survivors of childhood cancer. Child Care Health Dev 2003;29:95-102.
- Varni JW, Burwinkle TM, Berrin SJ, Sherman SA, Artavia K, Malcarne VL, et al. The PedsQL in pediatric cerebral palsy: reliability, validity, and sensitivity of the Generic Core Scales and Cerebral Palsy Module. Develop Med Child Neurol 2006;48:442-9. http://dx.doi.org/10.1017/S001216220600096X.
- Palmer SN, Meeske KA, Katz ER, Burwinkle TM, Varni JW. The PedsQL Brain Tumor Module: initial reliability and validity. Pediatr Blood Cancer 2007;49:287-93. http://dx.doi.org/10.1002/pbc.21026.
- Majnemer A, Shevell M, Law M, Poulin C, Rosenbaum P. Reliability in the ratings of quality of life between parents and their children of school age with cerebral palsy. Qual Life Res 2008;17:1163-71. http://dx.doi.org/10.1007/s11136-008-9394-6.
- Oeffinger O, Bagley A, Rogers S, Gorton G, Kryscio R, Abel M, et al. Outcome tools used for ambulatory children with cerebral palsy: responsiveness and minimum clinically important differences. Develop Med Child Neurol 2008;50:918-25. http://dx.doi.org/10.1111/j.1469-8749.2008.03150.x.
- Limbers CA, Heffer RW, Varni JW. Health-related quality of life and cognitive functioning from the perspective of parents of school-aged children with asperger’s syndrome utilizing the PedsQL. J Autism Devel Disord 2009;39:1529-41.
- Dunaway S, Montes J, Montgomery M, Battista V, Koo B, Marra J, et al. Reliability of telephone administration of the PedsQL Generic Quality of Life Inventory and Neuromuscular Module in spinal muscular atrophy (SMA). Neuromusc Disord 2010;20:162-5. http://dx.doi.org/10.1016/j.nmd.2009.12.002.
- Shipman DL, Sheldrick RC, Perrin EC. Quality of life in adolescents with autism spectrum disorders: reliability and validity of self-reports. J Devel Behav Pediatr 2011;32:85-9. http://dx.doi.org/10.1097/DBP.0b013e318203e558.
- Green L, Godfrey C, Soo C, Anderson V, Catroppa C. Agreement between parent-adolescent ratings on psychosocial outcome and quality-of-life following childhood traumatic brain injury. Devel Neurorehabil 2012;15:105-13. http://dx.doi.org/10.3109/17518423.2011.638331.
- Parsons SK, Shih MC, Mayer DK, Barlow SE, Supran SE, Levy SL, et al. Preliminary psychometric evaluation of the Child Health Ratings Inventory (CHRIs) and Disease-Specific Impairment Inventory-Hematopoietic Stem Cell Transplantation (DSII-HSCT) in parents and children. Qual Life Res 2005;14:1613-25. http://dx.doi.org/10.1007/s11136-005-1004-2.
- Beattie PE, Lewis-Jones MS. A comparative study of impairment of quality of life in children with skin disease and children with other chronic childhood diseases. Br J Dermatol 2006;155:145-51. http://dx.doi.org/10.1111/j.1365-2133.2006.07185.x.
- Eiser C, Kopel S, Cool P, Grimer R. The Perceived Illness Experience Scale (PIE): reliability and validity revisited. Child Care Health Devel 1999;25:179-90. http://dx.doi.org/10.1046/j.1365-2214.1999.00116.x.
- Kiernan G, Gormley M, MacLachlan M. The Revised-Perceived Illness Experience Scale (R-PIE): data from the Barretstown studies. Behav Med 2004;30:23-31. http://dx.doi.org/10.3200/BMED.30.1.23-34.
- Chaplin JE, Koopman HM, Schmidt S. DISABKIDS Group . DISABKIDS smiley questionnaire: the TAKE 6 assisted health-related quality of life measure for 4- to 7-year-olds. Clin Psychol Psychother 2008;15:173-80. http://dx.doi.org/10.1002/cpp.570.
- Simeoni M-C, Schmidt S, Muehlan H, Debensason D, Bullinger M. DISABKIDS Group . Field testing of a European quality of life instrument for children and adolescents with chronic conditions: the 37-item DISABKIDS Chronic Generic Module. Qual Life Res 2007;16:881-93. http://dx.doi.org/10.1007/s11136-007-9188-2.
- Bullinger M, Schmidt S, Petersen C. DISABKIDS Group . Assessing quality of life of children with chronic health conditions and disabilities: a European approach. Int J Rehabil Res 2002;3:197-206. http://dx.doi.org/10.1097/00004356-200209000-00005.
- Walker LS, Greene JW. The functional disability inventory: measuring a neglected dimension of child health status. J Pediatr Psychol 1991;16:39-58. http://dx.doi.org/10.1093/jpepsy/16.1.39.
- Petersen C, Schmidt S, Power M, Bullinger M. DISABKIDS Group . Development and pilot-testing of a health-related quality of life chronic generic module for children and adolescents with chronic health conditions: a European perspective. Qual Life Res 2005;14:1065-77. http://dx.doi.org/10.1007/s11136-004-2575-z.
- Schmidt S, Debensason D, Muhlan H, Petersen C, Power M, Simeoni MC, et al. The DISABKIDS generic quality of life instrument showed cross-cultural validity. J Clin Epidemiol 2006;59:587-98. http://dx.doi.org/10.1016/j.jclinepi.2005.09.012.
- Apajasalo M, Sintonen H, Holmberg C, Sinkkonen J, Aalberg V, Pihko H, et al. Quality of life in early adolescence: a sixteen-dimensional health-related measure (16D). Quality Life Res 1996;5:205-11.
- Apajasalo M, Rautonen J, Holmberg C, Sinkkonen J, Aalberg V, Pihko H, et al. Quality of life in pre-adolescence: a 17-dimensional health-related measure (17D). Qual Life Res 1996;5:532-8. http://dx.doi.org/10.1007/BF00439227.
- Moodie M, Richardson J, Rankin B, Iezzi A, Sinha K. Predicting time trade-off health state valuations of adolescents in four Pacific countries using the assessment of quality-of-life (AQoL-6D) instrument. Value Health 2010;13:1014-27. http://dx.doi.org/10.1111/j.1524-4733.2010.00780.x.
- Stevens KJ. Developing a descriptive system for a new preference-based measure of health-related quality of life for children. Qual Life Res 2009;18:1105-13. http://dx.doi.org/10.1007/s11136-009-9524-9.
- Torrance GW, Feeny D, Furlong W, Barr RD, Zhang Y, Wang Q. Multiattribute utility function for a comprehensive health status classification system: Health Utilities Index Mark 2. Med Care 1996;34:702-22. http://dx.doi.org/10.1097/00005650-199607000-00004.
- Feeny D, Furlong W, Boyle M, Torrance GW. Multiattribute health status classification systems: Health Utilities Index. Pharmacoeconomics 1995;7:490-502.
- Ravens-Sieberer U, Wille N, Badia X, Bonsel G, Burström K, Cavrini G, et al. Feasibility, reliability, and validity of the EQ-5D-Y: results from a multinational study. Qual Life Res 2010;19:887-97. http://dx.doi.org/10.1007/s11136-010-9649-x.
- Saigal S, Rosenbaum P, Stoskopf B, Hoult L, Furlong W, Feeny D, et al. Development, reliability and validity of a new measure of overall health for pre-school children. Qual Life Res 2005;14:243-57. http://dx.doi.org/10.1007/s11136-004-4228-7.
- Nathan PC, Furlong W, Horsman J, Van Schaik C, Rolland M, Weitzman S, et al. Inter-observer agreement of a comprehensive health status classification system for pre-school children among patients with Wilms’ tumor or advanced neuroblastoma. Qual Life Res 2004;13:1707-14.
- Stevens KJ. Working with children to develop dimensions for a preference-based, generic, pediatric health-related quality-of-life measure. Qual Health Res 2010;20:340-51. http://dx.doi.org/10.1177/1049732309358328.
- Stevens KJ. Assessing the performance of a new generic measure of health related quality of life for children and refining it for use in health state valuation. Appl Health Econ Health Policy 2011;9:157-69. http://dx.doi.org/10.2165/11587350-000000000-00000.
- Ratcliffe J. An assessment of the construct validity of the CHU9D in the Australian adolescent general population. Qual Life Res 2012;21:717-25. http://dx.doi.org/10.1007/s11136-011-9971-y.
- Canaway A, Frew E. Measuring preference-based quality of life in children aged 6–7 years: a comparison of the performance of the CHU-9D and EQ-5D-Y – the WAVES pilot study. Qual Life Res 2013;22:173-83.
- Jelsma J. A comparison of the performance of the EQ-5D and the EQ-5D-Y health-related quality of life instruments in South African children. Int J Rehabil Res 2010;33:172-7. http://dx.doi.org/10.1097/MRR.0b013e32832bb0f7.
- Wille N, Badia X, Bonsel G, Burström K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010;19:875-86. http://dx.doi.org/10.1007/s11136-010-9648-y.
- Oluboyede Y, Tubeuf S, McCabe C. Measuring health outcomes of adolescents: report from a pilot study. Eur J Health Econ 2013;14:11-9. http://dx.doi.org/10.1007/s10198-011-0340-0.
- Matza LS, Secnik K, Mannix S, Sallee FR. Parent-proxy EQ-5D ratings of children with attention-deficit hyperactivity disorder in the US and the UK. PharmacoEconomics 2005;23:777-90. http://dx.doi.org/10.2165/00019053-200523080-00004.
- Glaser AW, Furlong W, Walker DA, Fielding K, Davies K, Feeny DH, et al. Applicability of the Health Utilities Index to a population of childhood survivors of central nervous system tumours in the U.K. Eur J Cancer 1999;35:256-61. http://dx.doi.org/10.1016/S0959-8049(98)00367-0.
- Tilford JM, Payakachat N, Kovacs E, Pyne JM, Brouwer W, Nick TG, et al. Preference-based health-related quality-of-life qutcomes in children with autism spectrum disorders: a comparison of generic instruments. Pharmacoeconomics 2012;30:661-79.
- Saxena S, Carlson D, Billington R. The WHO quality of life assessment instrument (WHOQOL-Bref): the importance of its items for cross-cultural research. Qual Life Res 2001;10:711-21.
- Bullinger M. KINDL – a questionnaire for health-related quality of life assessment in children. Zeitschrift für Gesundheitspsychologie 1994;1:64-77.
- Ravens-Sieberer U, Bullinger M. Assessing health-related quality of life in chronically ill children with the German KINDL: first psychometric and content analytical results. Qual Life Res 1998;7:399-407. http://dx.doi.org/10.1023/A:1008853819715.
- Young B, Rice H, Dixon-Woods M, Colver AF, Parkinson KN. A qualitative study of the health-related quality of life of disabled children. Dev Med Child Neurol 2007;49:660-5. http://dx.doi.org/10.1111/j.1469-8749.2007.00660.x.
- Eiser C, Morse R. Quality-of-life measures in chronic diseases of childhood. Health Technol Assess 2001;5:1-157.
- Noreau L, Fougeyrollas P, Vincent C. The LIFE-H: assessment of the quality of social participation. Technol Disabil 2002;14:113-18.
- Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry Allied Disciplin 1997;38:581-6. http://dx.doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2006.
- Brazier J, Deverill M. A checklist for judging preference-based measures of health related quality of life: learning from psychometrics. Health Econ 1999;8:41-5. http://dx.doi.org/10.1002/(SICI)1099-1050(199902)8:1%3C41::AID-HEC395%3E3.3.CO;2-R.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analyzing Qualitative Data. New York, NY: Routledge; 1994.
- Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ 2000;320:114-16. http://dx.doi.org/10.1136/bmj.320.7227.114.
- Hsu CC, Sandford BA. The Delphi technique: making sense of consensus practical assessment. Res Eval 2007;12:1-10.
- Sinha IP, Smyth RL, Williamson PR. Using the Delphi technique to determine which outcomes to measure in clinical trials: recommendations for the future based on a systematic review of existing studies. PLoS Med 2011;8. http://dx.doi.org/10.1371/journal.pmed.1000393.
- Fink A, Kosecoff J, Chassin M, Brook RH. Consensus methods: characteristics and guidelines for use. Am J Public Health 1984;74:979-83. http://dx.doi.org/10.2105/AJPH.74.9.979.
- McConachie H, Parr J, Glod M, Hanratty J, Livingstone N, Oono IP, et al. MeASURe: Measurement in autism spectrum disorder under review. Health Technol Assess 2013.
- Watts S, Stenner P. Doing Q Methodological Research: Theory, Method & Interpretation. London: Sage Publications Limited; 2012.
- Stephenson W. The Study of Behavior: Q-Technique and its Methodology. Chicago, IL: University of Chicago Press; 1953.
- WHOQOL Measuring Quality of Life. Geneva: WHO; 1997.
- Miller GA. The magical number seven, plus or minus two: some limits on our capacity for processing information. Psychol Rev 1956;63:81-97. http://dx.doi.org/10.1037/h0043158.
- The NHS Outcomes Framework 2013/14. London: DH; 2012.
- Public Health Outcomes Framework 2013 to 2016 and Technical Updates. London: DH; 2013.
- Children and Young People’s Health Outcomes Forum: Recommendations to Improve Children and Young People’s Health Results. London: DH; 2013.
- Cella D, Lai JS, Nowinski CJ, Victorson D, Peterman A, Miller D, et al. Neuro-QOL: brief measures of health-related quality of life for clinical research in neurology. Neurology 2012;78:1860-7. http://dx.doi.org/10.1212/WNL.0b013e318258f744.
- Improving Children and Young People’s Health Outcomes: a System Wide Response. London: DH; 2013.
- Children and Families Bill. London: Department for Education; 2013.
- Wild D, Eremenco S, Mear I, Martin M, Houchin C, Gawlicki M, et al. Multinational trials-recommendations on the translations required, approaches to using the same language in different countries, and the approaches to support pooling the data: the ISPOR Patient-Reported Outcomes Translation and Linguistic Validation Good Research Practices Task Force report. Value Health 2009;12:430-40. http://dx.doi.org/10.1111/j.1524-4733.2008.00471.x.
- Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2005;8:94-104. http://dx.doi.org/10.1111/j.1524-4733.2005.04054.x.
Appendix 1 Stage 1: MEDLINE (OvidSP) search strategy
-
"outcome assessment (Health Care)"/ (40,965)
-
tool*.ti,ab. (308,915)
-
instrument*.ti,ab. (157,993)
-
questionnaire*.ti,ab. (243,762)
-
index.ti,ab. (373,496)
-
indices.ti,ab. (90,324)
-
scale*.ti,ab. (357,341)
-
survey*.ti,ab. (328,968)
-
feedback.ti,ab. (68,626)
-
interview*.ti,ab. (183,596)
-
(outcome* adj2 measure*).ti,ab. (125,463)
-
(outcome* adj2 assessment*).ti,ab. (4843)
-
PROMS.ti,ab. (73)
-
(measur* adj2 (quality or health or outcomes)).ti,ab. (28,910)
-
(assess* adj2 (quality or health or outcomes)).ti,ab. (42,593)
-
(patient report* adj2 outcome* adj2 (measure* or assessment*)).ti,ab. (648)
-
(self report* adj2 outcome* adj2 (measure* or assessment*)).ti,ab. (649)
-
(parent report* adj2 outcome* adj2 (measure* or assessment*)).ti,ab. (19)
-
(child report* adj2 outcome* adj2 (measure* or assessment*)).ti,ab. (1)
-
(patient assess* adj2 outcome* adj2 (measure* or assessment*)).ti,ab. (34)
-
(self assess* adj2 outcome* adj2 (measure* or assessment*)).ti,ab. (30)
-
(parent assess* adj2 outcome* adj2 (measure* or assessment*)).ti,ab. (0)
-
(child assess* adj2 outcome* adj2 (measure* or assessment*)).ti,ab. (0)
-
(carer assess* adj2 outcome* adj2 (measure* or assessment*)).ti,ab. (0)
-
(caregiver assess* adj2 outcome* adj2 (measure* or assessment*)).ti,ab. (0)
-
or/1-25 (1,874,632)
-
"quality of life"/ (96,741)
-
quality of life.ti,ab. (115,675)
-
QOL.ti,ab. (14,555)
-
HRQOL.ti,ab. (5284)
-
QL.ti,ab. (964)
-
HRQL.ti,ab. (1899)
-
health utilit*.ti,ab. (841)
-
health outcomes.ti,ab. (13,869)
-
patient outcome*.ti,ab. (18,437)
-
(patient reported adj2 outcome*).ti,ab. (2051)
-
(self reported adj2 outcome*).ti,ab. (985)
-
(parent reported adj2 outcome*).ti,ab. (39)
-
(proxy reported adj2 outcome*).ti,ab. (2)
-
(child* adj3 outcome*).ti,ab. (9789)
-
(patient assessed adj2 outcome*).ti,ab. (39)
-
(self assessed adj2 outcome*).ti,ab. (42)
-
(parent assessed adj2 outcome*).ti,ab. (0)
-
((health or functional) adj status).ti,ab. (44,733)
-
(well being or wellbeing).ti,ab. (35,877)
-
functioning.ti,ab. (95,274)
-
activit*.ti,ab. (1,958,867)
-
participation.ti,ab. (78,859)
-
or/27-48 (2,308,026)
-
child*.ti,ab. (868,176)
-
infant*.ti,ab. (272,358)
-
(young adj people).ti,ab. (13,154)
-
(pediatric or paediatric).ti,ab. (158,131)
-
adolescen*.ti,ab. (143,298)
-
teenager*.ti,ab. (9191)
-
or/50-55 (1,215,742)
-
reliab*.ti,ab. (257,841)
-
valid*.ti,ab. (311,171)
-
evaluation.ti,ab. (685,857)
-
repeatability.ti,ab. (11,261)
-
acceptability.ti,ab. (14,434)
-
responsiveness.ti,ab. (72,770)
-
feasibility.ti,ab. (78,334)
-
psychometric.ti,ab. (19,445)
-
57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 (1,303,471)
-
26 and 49 and 56 and 65 (8559)
-
limit 66 to (english language and yr="1992 -Current") (7255)
Appendix 2 Stage 2.1: MEDLINE (OvidSP) search strategy
-
child/ (1,273,968)
-
child*.ti,ab. (891,994)
-
adolescent/ (1,484,571)
-
adolescent*.ti,ab. (133,832)
-
infant/ (596,913)
-
infant*.ti,ab. (279,971)
-
1 or 2 or 3 or 4 or 5 or 6 (2,675,732)
-
reliab*.ti,ab. (266,400)
-
valid*.ti,ab. (326,487)
-
responsive*.ti,ab. (151,564)
-
evaluation.ti,ab. (706,297)
-
repeatab*.ti,ab. (16,575)
-
feasib*.ti,ab. (147,155)
-
acceptab*.ti,ab. (93,849)
-
psychometric.ti,ab. (20,216)
-
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 (1,533,356)
*Names of individual instruments identified in stage 1, plus their abbreviations and synonyms, were added to this search to create a separate and unique search strategy for each instrument.
Appendix 3 Stage 2.2: MEDLINE (OvidSP) search strategy
-
(15D or 16D or 17D or 15 dimensional or 16 dimensional or 17 dimensional).ti,ab. (1766)
-
(AQol or "adolescent quality of life instrument" or "adolescent quality of life mark" or AQol*).ti,ab. (78)
-
(Auquei* or "Autoquestionnaire Qualite de Vie Enfant Image").ti,ab. (17)
-
"Self evaluation of the quality of life of infants".ti,ab. (0)
-
"Pictured Child's Quality of Life Self Questionnaire".ti,ab. (0)
-
Auto Questionnaire Enfant Image.ti,ab. (0)
-
(qualin or "infant's quality of life").ti,ab. (6)
-
(OK*ado or OK ado).ti,ab. (6)
-
"adolescent quality of life questionnaire".ti,ab. (0)
-
(sqlp or "subjective quality of life profile questionnaire for parents").ti,ab. (11)
-
(chaq or Child Health Assessment Questionnaire).ti,ab. (153)
-
chasl.ti,ab. (0)
-
"Child's Health Assessed by Self-Ladder".ti,ab. (0)
-
"Child Health Assessment Ladder".ti,ab. (0)
-
"Health Perception Ladder".ti,ab. (0)
-
(CHIP AE or CHIP CE or "Child Health and Illness Profile").ti,ab. (101)
-
(CHQ or child health questionnaire).ti,ab. (556)
-
(chris or Child Health Ratings Inventories).ti,ab. (335)
-
(CHRS or Children's Health Ratings Scale).ti,ab. (353)
-
(CHSCS PS or "Comprehensive health status classification system for preschool children" or CHSCS*PS).ti,ab. (2)
-
(child health utility or CHU 9D or CHU9D or CHU?9D).ti,ab. (6)
-
CLQI.ti,ab. (1)
-
children* life quality index.ti,ab. (4)
-
(coop or cooperative information project).ti,ab. (311)
-
(CQOL or "child quality of life questionnaire").ti,ab. (21)
-
(disabkids* or dcgm*).ti,ab. (48)
-
(TNO AZL or TNO?AZL or ducatqol or dux* or tapqol or taiqol or taaqol or tacqol).ti,ab. (265)
-
(Euroqol or EQ 5D or EQ 5D* or EQ?5D or (EQ vas or EQ?vas)).ti,ab. (3053)
-
(Exqol or EHRQOL or exeter health related quality).ti,ab. (1)
-
functional disability inventory.ti,ab. (21)
-
(disab* and FDI).ti,ab. (42)
-
(FSIIR or functional status II).ti,ab. (30)
-
generic health questionnaire.ti,ab. (9)
-
(GHQ or general health questionnaire or generic children* quality or GCQ).ti,ab. (3635)
-
(GWBS or general wellbeing scale or general well being scale).ti,ab. (65)
-
"health and life functioning scale".ti,ab. (2)
-
(HALFS and function*).ti,ab. (0)
-
(HAY adj5 (scale* or questionnaire)).ti,ab. (26)
-
("how are you" adj10 (scale* or questionnaire*)).ti,ab. (7)
-
HPCRS.ti,ab. (0)
-
healthy pathways child report scale*.ti,ab. (2)
-
(HSCS PS or HSCSPS or health status classification system).ti,ab. (26)
-
(HSQ or health status questionnaire).ti,ab. (441)
-
(hui or health utilities index).ti,ab. (910)
-
comprehensive health status classification system.ti,ab. (3)
-
chscs.ti,ab. (7)
-
(IPQ or illness perception* questionnaire).ti,ab. (333)
-
(ITQoL or "infant toddler quality of life scale" or (infant toddler and "quality of life")).ti,ab. (19)
-
kidscreen.ti,ab. (102)
-
(KINDL or KINDLR).ti,ab. (113)
-
nottingham health profile.ti,ab. (952)
-
("Nordic quality of life questionnaire" or Nordic QOLQ or Nordic quality of life questionnaire).ti,ab. (0)
-
(pediatric healthquiz or pediatric health quiz or paediatric healthquiz).ti,ab. (1)
-
(pedsql or "pediatric quality of life inventory").ti,ab. (558)
-
(PIE scale* or "perceived illness experience").ti,ab. (8)
-
PWI SC.ti,ab. (0)
-
personal wellbeing index.ti,ab. (16)
-
(comqol or "comprehensive quality of life scale").ti,ab. (11)
-
(QLQC or "quality of life questionnaire for children").ti,ab. (38)
-
(QoLAQ or "quality of life assessment questionnaire").ti,ab. (4)
-
(("quality of life profile" and adolescent) or QOLP AV).ti,ab. (13)
-
("quality of my life questionnaire" or QoML).ti,ab. (2)
-
(quality of well being scale or quality of wellbeing scale or "quality of well being self administered" or "quality of wellbeing self administered" or QWB).ti,ab. (233)
-
(RAND and (health insurance or health survey)).ti,ab. (382)
-
(RAND HIS or RAND HSMC).ti,ab. (0)
-
(CHSQ or child health status questionnaire).ti,ab. (5)
-
(SF and health survey).ti,ab. (3631)
-
(MOS SF* or short form health survey).ti,ab. (2564)
-
(sickness impact profile or SIP questionnaire).ti,ab. (984)
-
(student* life satisfaction scale or slss or mslss).ti,ab. (44)
-
(ducatql or dux 25 or tapqol or taiqol or tacqol or tno azl).ti,ab. (88)
-
(wchmp or (warwick child health and morbidity profile)).ti,ab. (7)
-
(whoqol or "world health organisation quality of life").ti,ab. (1011)
-
(yoq or youth outcome questionnaire).ti,ab. (7)
-
(YQOL or "youth quality of life instrument*").ti,ab. (21)
-
or/1-75 (20,532)
-
child/ (1,286,269)
-
child*.ti,ab. (904,151)
-
adolescent/ (1,501,263)
-
adolescent*.ti,ab. (136,775)
-
infant/ (602,198)
-
infant*.ti,ab. (283,092)
-
77 or 78 or 79 or 80 or 81 or 82 (2,705,447)
-
exp Nervous System Diseases/ (1,920,850)
-
Neurologic Manifestations/ (7306)
-
Autistic Disorder/ (14,797)
-
developmental disabilities/ or learning disorders/ or intellectual disability/ or motor skills disorders/ (69,477)
-
exp cerebral palsy/ (14,642)
-
(cerebral adj palsy).ti,ab. (13,270)
-
epilep*.ti,ab. (87,953)
-
autis*.ti,ab. (19,133)
-
(neuro-motor adj disease*).ti,ab. (2)
-
(neuromotor adj disease*).ti,ab. (18)
-
(neuromotor adj disorder*).ti,ab. (52)
-
(neuro-motor adj disorder*).ti,ab. (1)
-
(neuromotor adj dysfunction*).ti,ab. (59)
-
(neuro-motor adj dysfunction*).ti,ab. (0)
-
neurodisabilit*.ti,ab. (82)
-
(neuropsychiatric adj disease*).ti,ab. (1022)
-
(neuropsychiatric adj dysfunction*).ti,ab. (63)
-
neuro-psychiatric.ti,ab. (406)
-
((Child* or infant* or adolescen*) adj4 disab*).ti,ab. (8648)
-
or/84-102 (1,959,092)
-
76 and 83 and 103 (1258)
Appendix 4 List of identified, non-eligible questionnaires
| Instrument | Adult questionnaire | Dimension specific | Other construct | Functioning | Mental well-being | Condition-specific (non-ND) | Psychiatric setting | No English version | Interview based/clinical instrument | Other |
|---|---|---|---|---|---|---|---|---|---|---|
| AAOS Instrument: American Academy of Orthopaedic Surgeons Instrument | ✗ | |||||||||
| ATOM: Adolescent Treatment Outcomes Module | ✗ | |||||||||
| BASES: the Behavioural, Affective, and Somatic Experiences Scale | ✗ | |||||||||
| BFSC: Benefit Finding Scale for Children | ✗ | |||||||||
| CAFAS: Child and Adolescent Functional Assessment Scale | ✗ | ✗ | ||||||||
| CAVE: Quality Life scale in childhood epilepsy | ✗ | |||||||||
| CCIIS: Children’s Critical Illness Impact Scale | ✗ | |||||||||
| CCQ: Child’s Caregiver Questionnaire | ✗ | |||||||||
| CDLQI: Children’s Dermatology Life Quality Index | ✗ | |||||||||
| CFQ-R: Revised CF Quality of Life Questionnaire (Cystic Fibrosis) | ✗ | |||||||||
| CGAS: Children’s Global Assessment Scale scores | ✗ | ✗ | ||||||||
| Check your health measures | ✗ | |||||||||
| CHS: Children’s Health Scale/Child Health Status/Child Health Scale | ✗ | ✗ | ||||||||
| CHSA: Children’s Health Survey for Asthma | ✗ | |||||||||
| CHSI: Child Health Status Index for Ontario children National Health Interview Survey | ✗ | ✗ | ||||||||
| CIQ: Caregiver Impact Questionnaire | ✗ | |||||||||
| CIS: Columbia Impairment Scale | ✗ | |||||||||
| COSA: the Child Occupational Self Assessment | ✗ | |||||||||
| CPCHILD: Caregiver Priorities and Child Health Index of Life with Disabilities | ✗ | |||||||||
| C-QoL: Child’s Quality of Life | ✗ | ✗ | ||||||||
| DAWBA: Development and Wellbeing Assessment | ✗ | ✗ | ✗ | |||||||
| FAQ: Gillette Functional Assessment Questionnaire | ✗ | |||||||||
| FAQLQ-PF: Food Allergy Quality of Life Questionnaire – Parent Form | ✗ | |||||||||
| GAF: Global Assessment of Functioning | ✗ | ✗ | ✗ | |||||||
| GBB-24: Giessen Subjective Complaints List-24 questionnaire | ✗ | |||||||||
| GBI: Glasgow Benefit Inventory | ✗ | ✗ | ||||||||
| GCBI: Glasgow Children’s Benefit Inventory | ✗ | |||||||||
| GHAC: General Health Assessment for Children | ✗ | |||||||||
| GOS: Glasgow Outcome Scale | ✗ | |||||||||
| Holmes’ Quality of Life Index | ✗ | |||||||||
| I AM I | No information | |||||||||
| IDQOL: Infants’ Dermatitis Quality of Life Index | ✗ | |||||||||
| IMPACT: inflammatory bowel disease HRQoL questionnaire | ✗ | |||||||||
| IMPACT II: inflammatory bowel disease HRQoL questionnaire | ✗ | |||||||||
| Infant Health Quality of Life Risk Scores | ✗ | |||||||||
| ITP-Child Quality-of-Life Questionnaire (immune thrombopenic purpura) | ✗ | |||||||||
| JAQQ: Juvenile Arthritis Quality of Life Questionnaire | ✗ | |||||||||
| JSCA-QOL: Quality of Life Questionnaire for Japanese School-aged Children with Asthma | ✗ | |||||||||
| JWHS-76: Juvenile Wellness and Health Survey | ✗ | |||||||||
| LAQ-G: Generic Lifestyle Assessment Questionnaire | ✗ | |||||||||
| MAHSC: Multi-Attribute Health Status Classification | ✗ | |||||||||
| MMQL: Minneapolis-Manchester Quality of Life Instrument | ✗ | |||||||||
| MPQOLQ: Miami Pediatric Quality of Life Questionnaire | ✗ | |||||||||
| PAQAQ: Paediatric Asthma Quality of Life Questionnaire | ✗ | |||||||||
| PEDI: Paediatric Evaluation and Disability Inventory | ✗ | |||||||||
| PediQUEST: Paediatric Quality-of-Life Evaluation of Symptoms Technology | ✗ | |||||||||
| PedsQL Diabetes Module | ✗ | |||||||||
| PEMQOL: Paediatric Enuresis Module on Quality of Life | ✗ | |||||||||
| PinQ: continence-specific paediatric quality-of-life measurement tool | ✗ | |||||||||
| PODCI: the Paediatric Outcomes Data Collection Instrument | ✗ | |||||||||
| POEM: Patient Oriented Eczema Measure | ✗ | |||||||||
| PQ-LES_Q: Paediatric Quality of Life Enjoyment and Satisfaction Questionnaire | ✗ | ✗ | ||||||||
| PQoL: Perceived Quality of Life | ✗ | |||||||||
| PRISM: Pictorial Representation of Illness and Self Measure | ✗ | |||||||||
| PRQL: Paediatric Rheumatology Quality of Life scale | ✗ | |||||||||
| PSPCSA: Pictorial Scale of Perceived Competence and Social Acceptance for Young Children | ✗ | |||||||||
| QLSI-C: Quality of Life Systemic Inventory – Module for Cancer | ✗ | |||||||||
| QOL: QOL Questionnaire | No information | |||||||||
| QOLAQ: Quality of Life Assessment Questionnaire | ✗ | |||||||||
| QOLCE: Quality of Life in Children with Epilepsy | ✗ | |||||||||
| QOLQA: Quality of Life Questionnaire for Adolescents | ✗ | |||||||||
| QVCE-50: Quality of Life in Epilepsy Inventory for Adolescents (Brazilian version) | ✗ | |||||||||
| SAC: Short form Assessment for Children | ✗ | |||||||||
| Satisfaction with Life Scale | ✗ | |||||||||
| SEIQoL: Schedule for the Evaluation of Individual Quality of Life | ✗ | |||||||||
| Skindex Quality of Life Questionnaire | ✗ | |||||||||
| SPPC: Self-Perception Profile for Children | ✗ | |||||||||
| SRS-22: Scoliosis Research Society | ✗ | |||||||||
| SRS-24: Scoliosis Research Society | ✗ | |||||||||
| SWLS: Satisfaction with Life Scale | ✗ | ✗ | ||||||||
| SWLS-C: Satisfaction with Life Scale | ✗ | |||||||||
| TedQL.4 | ✗ | |||||||||
| The Terrible–Delighted Scale | ✗ | |||||||||
| T-QoL: Teenager’s Quality of Life Questionnaire (dermatology-specific) | ✗ | |||||||||
| VSP-A: Vecu et Sante Percu de l’Adolescent | ✗ | |||||||||
| WeeFIM | ✗ | |||||||||
| WEMWBS: Warwick–Edinburgh Mental Wellbeing Scale | ✗ | |||||||||
| YAQL: Young Adult Quality of Life | ✗ | |||||||||
| Total | 5 | 2 | 11 | 4 | 8 | 40 | 5 | 5 | 8 | 2 |
Appendix 5 Characteristics of excluded generic patient-reported outcome measures
| Acronym/name | Author | Purpose | n of items | Age range | Responder | Response options | Completion time | Recall period | Domains/dimensions |
|---|---|---|---|---|---|---|---|---|---|
| QUALIN: Infant’s Quality of Life | Manificat 199955 | To assess children’s perceived satisfaction with different life domains | 34 | 0 to 1 years 1 to 3 years |
Proxy | Six-point response scale rating agreement | 10 minutes | Not stated | No information |
| AUQUEI Ours: Auto Questionnaire Enfant Image Child Pictured Self Report | Manificat 199857 | To assess children’s perceived satisfaction with several paediatric life domains | 28 | 3 to 6 years | Self (by interview) | Four-level response continuum (happy–sad faces) | 10 to 15 minutes | Not stated | Leisure, family environment, duties and external world/autonomy |
| AUQUEI Soleil: Pictured Child’s Quality of Life Self Questionnaire | Gayral-Taminh 200556 | To assess children’s perceived satisfaction with several paediatric life domains | 33 | 6 to 10 years | Self | Four-level response continuum (happy–sad faces) | 15 minutes | Not stated | Leisure, separation, duties, parents |
| OK.ado questionnaire: Adolescent quality of life questionnaire | Manificat 200258 | To assess children’s perceived satisfaction with several adolescent life domains | 33 | 11 to 18 years | Self | Five-level response continuum (feeling very badly, feeling very well) | 10 minutes | Not stated | Leisure and relationships, school, family, self-esteem and self-image |
| CHASL (HPL): Child’s Health Assessed by Self-Ladder (Health Perception Ladder) | Norton-Broda 198859 | To assess a child’s global impression of their own health | 1 | 9 to 12 years | Self | Five-rung Cantril ladder with graphic representation | 1 minute | Today | Perceived health status |
| DHP-A: Duke Health Profile – Adolescent version | Parkerson 199160 | To assess a child’s health and emotional well-being | 17 | 13 to 18 years | Self | Three-point response scale rating agreement | 5 minutes | Today or past week | Physical health, mental health, social health, general health, perceived health, self-esteem |
| HALFS: Health and Life Functioning Scale | Bastiaens 200461 | To assess a child’s functioning on different life domains | 10 | 6 to 12 years | Proxy | Three-point response scale rating frequency of the statement | 5 minutes | Not used | Functioning in general health, academics, leisure, family relations, social life |
| HAY: How Are You? | Le Coq 2000,62 Maes 199563 | To assess the prevalence of complaints and symptoms and general performance in daily life | 29 | 8 to 12 years | Self and proxy | Four-point response scale rating frequency or performance | 10 minutes | No information | Physical functioning, cognitive functioning, social functioning, physical complaints, happiness |
| IPQ: Illness Perception Questionnaire | Weinman 199664 | To assess the cognitive representation of illness | 68 | Not stated | Self | Five-point Likert scale rating agreement | 15 minutes | Not used | Identity, cause, timeline, consequences, cure/control |
| IPQ Revised | Weinman 199664 | To assess the cognitive representation of illness | 56 | Not stated | Self | Five-point Likert scale | 15 minutes | Not used | Identity, cause, timeline, consequences, cure/control |
| Brief IPQ | Weinman 199664 | To assess the cognitive representation of illness | 8 | Not stated | Self | Eleven-point scale | 3 minutes | Not used | Identity, cause, timeline, consequences, cure/control |
| ITQOL: Infant Toddler Quality of Life Questionnaire (long version) | Landgraf 1994,65 Klassen 200366 | To assess the core dimensions of health according to the WHO for preschool children | 97 | Up to 5 years | Proxy | Response options vary from four to six levels | 20 minutes | Most scales: past 4 weeks; global change items: compared with 1 year ago | Physical functioning, growth & development, bodily pain, temperament & moods, general behaviour, getting along, general health perceptions, parental impact (emotional, time), family activities, family cohesion, change in health |
| ITQOL: Infant Toddler Quality of Life Questionnaire (short version) | Landgraf 1994,65 Klassen 200366 | To assess the core dimensions of health according to the WHO for preschool children | 47 | Up to 5 years | Proxy | Response options vary from four to six levels | 10 minutes | Most scales: past 4 weeks; global change items: compared with 1 year ago | Physical functioning, growth & development, bodily pain, temperament & moods, general behaviour, getting along, general health perceptions, parental impact (emotional, time), family activities, family cohesion, change in health |
| Nordic Quality of Life Questionnaire for children | Lindstrom 1991,67 199368 | To assess health and welfare of children and young people | 60 | 12 to 18 years 2 to 18 years |
Self and proxy | Different for all questions | 20 minutes | Three months | Global sphere, external sphere, interpersonal and personal sphere |
| QLQC: Quality of Life Questionnaire for Children | Bouman 199969 | To assess three broad domains of functioning in children: physical, psychological and social functioning | 118 | 8 to 12 years | Self or proxy | Three-point response scale rating frequency | 15 minutes | The last 12 months | Physical complaints & limitations & handicaps, general wellbeing, cognitive functioning, self-concept, anxious-depressed feelings, relation with parents & peers, school functioning, social conflicts, leisure activities |
| QoML: Quality of My Life | Feldman 200070 | To assess quality of life and health-related quality of life as two separate constructs in CYP | 3 | 8 to 12 years | Self or proxy | Two 100 mm VAS a 5-point scale | < 5 minutes | Today | Quality of life and health-related quality of life |
| TAPQOL: TNO-AZL Questionnaire for Preschool Children’s Health-Related Quality of Life | Fekkes 200071 | To assess CYP’s health status, weighted by the emotional response of the children themselves to their health status problems | 32 43 |
Up to 18 months 18 months, up to 6 years |
Proxy Proxy |
Three-point scale rating frequency of occurrence and four-point scale rating the child’s state | 10 minutes | Recent weeks | Stomach problems, skin problems, lung problems, sleeping problems, appetite, problem behaviour, anxiety, liveliness, social functioning, motor functioning, communication |
| TACQOL: TNO-AZL Questionnaire for Children’s Health-Related Quality of Life | Theunissen 198972 | To assess CYP’s health status, weighted by the emotional response of the children themselves to their health status problems | 63 | 8 to 15 years 6 to 15 years |
Self Proxy |
Three-point scale rating frequency of occurrence and four-point scale rating the child’s state | 10–15 minutes | Recent weeks | Body functioning, motor functioning, cognition, peer interaction, positive and negative emotions |
| TAAQOL: TNO-AZL Questionnaire for Adult Health-Related Quality of Life | Vogels 199873 | To assess a person’s health status, weighted by the emotional response of the person to his/her health status problems | 45 | ≥ 16 years | Parent-report | Three-point scale rating frequency of occurrence and four-point scale rating the impact | 10–20 minutes | Last month | Gross and fine motor functioning, pain, sleeping, cognitive and social functioning, daily activities, sexual activity, vitality, happiness, depressive moods, aggressiveness |
Appendix 6 Characteristics of excluded chronic-generic patient-reported outcome measures
| Acronym/name | Author | Purpose | n of items | Age range | Responder | Response options | Completion time | Recall period | Domains/dimensions |
|---|---|---|---|---|---|---|---|---|---|
| CHRIs: Child Health Ratings Inventory | Parsons 2005188 | To assess the general health status at different times to evaluate treatment | 20 | 5 to 13 years | Self | Five response options, pictorially represented | 10–25 minutes | Last 4 weeks | Physical functioning, role functioning, emotional functioning, energy |
| CHRIs: Child Health Ratings Inventory | Parsons 2005188 | To assess the general health status at different times to evaluate treatment | 20 | 13 to 18 years 5 to 18 years |
Self Proxy |
Five-point Likert scale, rating frequency or intensity | 10–25 minutes | Last 4 weeks | Physical functioning, role functioning, emotional functioning, energy |
| CLQI: Children’s Life Quality Index | Beattie 2006189 | To assess how much a child has been affected by their health problem | 12 | 5 to 12 years | Proxy | Four-point Likert scale rating frequency | 10 minutes | Last 3 months | No dimensions defined |
| PIE: Perceived Illness Experience Scale | Eiser 1999190 | To assess a patient’s overall illness experience | 40 | 8+ years | Self and proxy | Five-point Likert scale rating agreement | 10–15 minutes | Not stated | Interference with activity, disclosure of illness, school/work, peer rejection, parental behaviour, manipulation, preoccupation with illness, treatment, physical appearance |
| PIE-R: Perceived Illness Experience Scale - Revised | Kiernan 2004191 | To assess a patient’s overall illness experience | 36 | 7+ years | Self and proxy | Five-point Likert scale rating agreement | 10–15 minutes | Not stated | Interference with activity, disclosure of illness, school/work, peer rejection, parental behaviour, manipulation, preoccupation with illness, physical appearance, food |
Appendix 7 Characteristics of excluded preference-based measures
| Acronym/name | Author | Purpose | n of items | Age | Responder | Response options | Completion time | Recall period | Domains/dimensions assessed |
|---|---|---|---|---|---|---|---|---|---|
| 16D: 16 Dimensional | Apajasalo 1996198 | A function and symptoms profile, used to create a preference-based score of HRQoL for economic evaluations | 16 | 12 to 15 years | Self | Five ordinal levels on each dimension, by which more or less of the attribute is distinguished | 5–10 minutes | Today | Mobility, vision, hearing, breathing, sleeping, eating, speech, excretion, school and hobbies, mental function, discomfort and symptoms, depression, distress, vitality, appearance, friends |
| 17D: 17 Dimensional | Apajasalo 1996199 | A function and symptoms profile, used to create a preference-based score of HRQoL for economic evaluations | 17 | 8 to 11 years | Self | Five ordinal levels on each dimension, by which more or less of the attribute is distinguished | 5–10 minutes | Today | Mobility, vision, hearing, breathing, sleeping, eating, speech, excretion, school and hobbies, learning and memory, discomfort and symptoms, depression, distress, vitality, appearance, friends, concentration |
| AQoL-6D: Assessment of Quality of Life Mark 2 – 6D adolescents | Moodie 2010200 | A function and symptoms profile, used to create a preference-based score of HRQoL for economic evaluations | 20 | 15+ years | Self | Six ordinal levels, by which more or less of the attribute is distinguished | 5–10 minutes | Past week | Physical ability, social and family relationships, mental health, coping, pain, vision, hearing and communication |
Appendix 8 Questions used in the Delphi survey
Round 1
-
Rating agreement with definition of neurodisability (strongly agree, agree, disagree, strongly disagree, no opinion) + option to comment.
-
Which aspects of health do you try to influence and/or improve when working with children and young people with neurodisability? Please state as many as apply, such as ‘improve communication’, ‘reduce pain’, etc. (free-text box).
-
Do you use PROMs in your clinical work or in research with children affected by neurodisability? (Yes, No) + Which PROM questionnaire do you use? (free-text box).
Round 2
-
Rating agreement with revised definition (strongly agree, agree, disagree, strongly disagree, no opinion) + option to comment.
-
Here we listed the aspects of health that were most frequently mentioned. Young people and parents will also be asked to comment on this list in the qualitative stream.
-
-
Looking at the table, to what extent do you agree that the list broadly includes some of the aspects of health you target in your professional work? Participants were asked to rate their agreement (strongly agree, agree, disagree, strongly disagree, no opinion) + option to comment.
-
And do you agree this list covers broadly the health outcomes that the NHS should assess routinely for these children? Participants were asked to rate their agreement (strongly agree, agree, disagree, strongly disagree, no opinion) + option to comment.
-
Many of you told us that you try to improve children’s quality of life and/or well-being. What do you use as (an) indicator(s) that things are going well for the child? (free-text box).
Round 3
List of aspects of health as presented in Round 3
Mental functions, e.g. improve mental health issues; reduce emotional and behavioural difficulties
Consciousness functions, e.g. seizure, stroke
Temperament and personality functions: confidence, emotional stability
Sleep functions
Specific mental functions, e.g. anxiety, attention
Psychomotor control, e.g. manage behavioural problems
Pain
Functions related to digestive system, e.g. constipation, swallowing, drooling
Urinary functions (continence, enuresis)
Neuromusculoskeletal and movement-related functions: Improve gross and fine motor function; improve quality of movement
Mobility of joint functions, e.g. improve mobility and ease of movement of joints
Muscle power functions: muscle strength
Muscle tone function, e.g. spasticity
Control of voluntary movement functions, e.g. co-ordination of movements, improve head and trunk control
Learning and applying knowledge: acquiring skills; learning to read, write
Acquiring basic skills, e.g. learning to coordinate fine motor function to improve eating, pencil holding
Communication
Changing and maintaining body position, e.g. sitting, standing, lying down
Mobility (in ‘activity and participation’), e.g. improve transfer
Self-care, e.g. improve independence in all activities of daily living (washing, toileting, dressing, eating)
Community, social and civil life, e.g. engage in social clubs; recreation and leisure
Movement (in ‘body structures’), e.g. reduce/prevent contractures and deformity; muscle length and joint range of movement
-
If you look at the list, would you agree that this list now represents appropriate NHS health outcomes for children and young people with neurodisability? If you disagree, please use the free-text box below to add any missing health aspects. It would be helpful to argue your choice using the above mentioned inclusion criteria.
-
We are looking for a patient-reported outcome measure (PROM) for children and young people to assess NHS care. Your feedback on the aspects of health you focus on as a clinician has triggered discussion about whether, in your view, health care should target functioning and/or well-being. Option A, functioning, as in what children and young people can do. Option B, well-being, as in how children and young people feel about their health. (Participants could tick both options.)
-
Participants were presented with two revised versions of the definition: one with and one without exemplar conditions. Please indicate below to what extent you agree with this revised definition? Additionally, they were asked to choose which one they preferred (only one option possible).
-
Round 4
This research considers what outcomes of NHS care should be measured for children affected by neurodisability. We have identified 23 distinct concepts measured by relevant questionnaire-based patient-reported outcome measures (PROMs). These are listed below. Please consider each concept in turn, and rate to what extent you think the NHS should be responsible for the following patient outcomes:
-
fitness and stamina;
-
mobility;
-
manual ability;
-
regulation of emotion;
-
emotional wellbeing (feeling depressed, happy, nervous, anxious, etc.);
-
concentration;
-
learning and applying knowledge;
-
communication, speech and language;
-
hearing;
-
seeing and vision;
-
pain;
-
sleep;
-
toileting;
-
self-care: hygiene;
-
self-care: dressing;
-
self-care: eating;
-
self-care: personal safety;
-
autonomy/independence;
-
relationships with family;
-
relationships with friends;
-
sexual health;
-
sport and leisure;
-
engagement in play.
Appendix 9 Version iterations of the definition of neurodisability at each round
Version 1
Neurodisability is an impairment of functioning relating to any condition that affects the brain and/or nervous system. This may, for example, result in predominantly physical difficulties (such as cerebral palsy), learning and communication difficulties (such as autism), or other medical conditions (such as the problems associated with epilepsy). However, some children with a neurodisability will not have been given a specific diagnosis.
Version 2
Neurodisability includes a group of congenital or acquired long-term conditions with a broad range of severity and complexity, some of which can vary over time. Neurodisability is a consequence of impairment of the brain, central or peripheral nervous system that creates activity limitations. This may result in physical difficulties (such as cerebral palsy), learning difficulties (such as intellectual disorders), and social/communication difficulties (such as in autism), or other medical conditions (such as the problems associated with epilepsy). Sensory, behavioural and emotional difficulties are all included if they are a consequence of neurological impairment. Some children affected by neurodisability are diagnosed with specific syndromes and conditions, whilst for others a specific diagnosis may not be possible.
Version 3
Neurodisability includes a group of congenital or acquired long-term conditions, which can co-occur, with a broad range of severity and complexity, some of which can vary over time. Neurodisability is a consequence of impairment of the brain, central or peripheral nervous system that creates activity limitations. This may result in physical difficulties (such as cerebral palsy), learning difficulties (such as intellectual disorders), and social/communication difficulties (such as in autism), or other medical conditions (such as the problems associated with epilepsy). Sensory, behavioural and emotional difficulties are all included if they are a consequence of neurological impairment. Some children affected by neurodisability are diagnosed with specific syndromes and conditions, whilst for others a specific diagnosis may not be possible.
Version 4
Neurodisability describes a group of congenital or acquired long-term conditions that are attributed to disturbance of the brain and or neuromuscular system and create functional limitations. A specific diagnosis may not be identified. Conditions may vary over time, occur alone or in combination and include a broad range of severity and complexity. The impact may include disturbances of movement, cognition, hearing and vision, communication, emotion and behaviour.
Appendix 10 Consensus meeting participants
Group A
Shaym Chandegra, young person.
Adam Dewhurst, young person.
Diane Kay, parent.
Sue Redmond, parent.
Mahima Rupasinghe, paediatrician.
Dido Green, occupational therapist.
Lynne Watson, nurse.
Group B
Stewart Hatton, young person.
Mary Busk, parent.
Asia Fazal, parent.
Michele Hopwood, parent.
Sarah Beasley, physiotherapist.
Katherine Telford, child and adolescent psychiatrist.
Nigel Hall, surgeon.
Andrew Lloyd Evans, paediatrician.
Apologies received
Speech and language therapist.
Orthopaedic surgeon.
List of abbreviations
- ADHD
- attention deficit hyperactivity disorder
- AUQUEI
- Pictured Child’s Quality of Life Self Questionnaire (Autoquestionnaire de Qualité de Vie Enfant Image)
- BACD
- British Academy of Childhood Disability
- BMSLSS
- Brief Multi-dimensional Student Life Satisfaction Scale
- CDC
- Council for Disabled Children
- CDT
- Child Development Team
- CHAQ
- Child Health Assessment Questionnaire
- CHASL
- Child’s Health Assessed by Self-Ladder
- CHIP
- Child Health and Illness Profile
- CHIP-AE
- Child Health and Illness Profile – Adolescent Edition
- CHIP-CE
- Child Health and Illness Profile – Child Edition
- CHQ
- Child Health Questionnaire
- CHRIs
- Child Health Ratings Inventory
- CHRS
- Children’s Health Ratings Scale
- CHSCS
- Comprehensive Health Status Classification System
- CHSCS-PS
- Comprehensive Health Status Classification System – Preschool
- CHU
- Child Health Utility 9D
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CLQI
- Children’s Life Quality Index
- ComQOL
- Comprehensive Quality of Life Scale
- ComQOL–S5
- Comprehensive Quality of Life Scale – School version, fifth edition
- COOP
- Dartmouth Primary Care Cooperative Information Project questionnaire
- COSMIN
- COnsensus-based Standards for the selection of health Measurement INstruments
- CQoL
- Child Quality of Life Questionnaire
- DCGM
- DISABKIDS Chronic Generic Module
- DHP-A
- Duke Health Profile – Adolescent version
- DLA
- Disability Living Allowance
- EQ-5D
- European Quality of Life-5 Dimensions
- EQ-5D-Y
- European Quality of Life-5 Dimensions-Youth
- ExQoL
- Exeter Quality of Life Measure
- FDI
- Functional Disability Inventory
- FGCY
- focus group children and young people
- FGP
- focus group parents
- FSIIR
- Functional Status II Revised
- GCQ
- Generic Children’s Quality of Life Measure
- HALFS
- Health And Life Functioning Scale
- HAY
- How Are You?
- HRQoL
- health-related quality of life
- HUI
- Health Utilities Index
- HUI2
- Health Utilities Index version 2
- HUI3
- Health Utilities Index version 3
- ICC
- intraclass correlation coefficient
- ICF
- International Classification of Functioning, Disability and Health
- ICF-CY
- International Classification of Functioning, Disability and Health, Children and Youth Version
- ICY
- Interview Children and Young People
- IP
- interview parents
- IPQ
- Illness Perception Questionnaire
- ITQoL
- Infant Toddler Quality of Life
- MDC
- minimal detectable change
- MeSH
- medical subject heading
- MID
- minimal important difference
- MSLSS
- Multidimensional Student Life Satisfaction Scale
- NIHR
- National Institute for Health Research
- NRES
- National Research Ethics Service
- Neuro-QOL
- Quality of Life in Neurological Disorders
- PBM
- preference-based measure
- PedsQL
- Pediatric Quality of Life Inventory
- PenCLAHRC
- Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for the South West Peninsula
- PenCRU
- Peninsula Cerebra Research Unit
- PIE
- Perceived Illness Experience (Scale)
- PIE-R
- Perceived Illness Experience (Scale) – Revised
- PPI
- public and patient involvement
- PROM
- patient-reported outcome measure
- PREM
- patient-reported experience measure
- PWI
- Personal Wellbeing Index
- PWI-PS
- Personal Wellbeing Index – Pre-School
- PWI-SC
- Personal Wellbeing Index – School Children
- QLQC
- Quality of Life Questionnaire for Children
- QoL
- quality of life
- QoLP-AV
- Quality of Life Profile – Adolescent Version
- QoML
- Quality of My Life
- SD
- standard deviation
- SLSS
- Student Life Satisfaction Scale
- TAAQOL
- TNO-AZL Questionnaire for Adult Health-Related Quality of Life
- TACQOL
- TNO-AZL Questionnaire for Children’s Health-Related Quality of Life
- TAPQOL
- TNO-AZL Questionnaire for Preschool Children’s Health-Related Quality of Life
- TNO-AZL
- Dutch Organization for Applied Science Research – University Medical Centre Leiden (Toegepast Natuurwetenschappelijk Onderzoek – Academisch Ziekenhuis Leiden)
- VAS
- visual analogue scale
- WCHMP
- Warwick Child Health and Morbidity Profile
- WHO
- World Health Organization
- YQoL
- Youth Quality of Life instrument
- YQoL-R
- Youth Quality of Life instrument – Research version
- YQoL-S
- Youth Quality of Life instrument – Surveillance version