Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 08/1809/232. The contractual start date was in December 2008. The final report began editorial review in October 2012 and was accepted for publication in July 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors:
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Hanratty et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background, context and scope
Introduction
As life expectancy increases, older adults are living and dying with multiple conditions. Their health-care needs are complex, and may involve a range of professionals working in different settings. Ensuring that the patients experience co-ordinated and coherent care, and that moves occur because of individual needs rather than system imperatives, is crucial to patients’ well-being. Such patient-focused care has attracted much attention in recent years in an effort to improve individual outcomes1 and promote cost-containment and efficient use of resources.
At the end of life, a move into or out of hospital, a care home or a hospice is potentially one of the most disruptive events for older adults and their carers, with consequences for their mental, physical and emotional well-being. Older adults are particularly sensitive to the consequences of inadvertent alterations to their care, for example existing medication regimes failing to be maintained or follow-up blood tests not being performed. Patients’ experiences of moving between places of care offer an opportunity to explore the extent of integration at the interfaces between different professional roles, services and approaches to care. Understanding the challenges of providing high-quality care at transitions between care settings for older adults is a crucial step towards improving patients’ and families’ experiences of care in the final months, weeks and days of life.
Background
More people are living into old age across the world. There are currently 650 million people aged over 60 years, and expected to reach 2 billion by 2050. 2 In England, almost two-thirds of the half a million people who die each year are aged over 75 years. 3 While some deaths may be unexpected, most deaths follow a period of chronic illness requiring ongoing management, often in different care settings.
Definition and importance of transitions
A transition occurs between two locations or settings of care, for example moving from hospital to a care home. It may also represent a shift in the nature of care, such as the decision not to continue with curative treatments. For some older adults with chronic progressive conditions, the realisation or acknowledgement that the aim of treatment is to control symptoms, and no longer to prolong life, may come late in the illness. In a number of common conditions, such as heart failure, the course of an illness may be unpredictable. In such cases, clinical considerations and the wishes of patients and family have to be weighed and discussed to judge the appropriate time to move towards palliative care. Therapies that improve symptoms may also lengthen survival and the possibility of a change of gear from curative to palliative care may never arise. The nature and location of care are interdependent and changing one may naturally influence the other; a move to a hospice or a return to primary care, for example, may offer an opportunity to broach sensitive subjects that are overlooked in the faster-paced world of acute medicine. Hence, although this study has focused on transition as a change in setting, it will have relevance to the relationship between active and palliative care.
For many older adults, the majority of transitions will take place in the 12 months before death. The proportion of people admitted to hospital in their last year of life rises with age. People over the age of 85 years are less likely to be admitted to hospital in their last year, but, when they are, they remain in hospital for longer periods than younger adults. 4 Although improved detection and treatment of disease means that some older adults are surviving with multiple comorbidities and complex health-care needs, recent decades have seen reductions in morbidity and functional decline among older adults. 5–7 Increasing survival has not invariably led to more years of sickness and disability, and the total time spent in hospital at older ages has not increased, though the last year of life remains a time of high health service utilisation. 8–10 Patterns of hospital and other service utilisation suggest that rapid increases in the costs of end-of-life care are unlikely to be realised. Nevertheless, the large number of older decedents will mean that costs are still considerable. Findings from time-to-death cost analyses are not entirely consistent across different health systems and study methodologies. Approaching death is associated with increased health service expenditures, and costs of care for decedents in the year before death are greater than for comparable survivors. 11–16 In some countries, this effect is diminished in extreme old age because of substitution of care in other settings (such as care homes) for hospital admission. 17,18 The overall effect of increased survival appears to be to delay the years of high spending to the end of life, with some shift away from acute care costs. Transitions, therefore, are likely to be a major contributor to overall health-care costs. Ensuring that they are necessary and that they enhance health outcomes and experiences should, therefore, be a priority.
Terminology
There are many different, overlapping, concepts, processes and labels applied to the organisation of care that is provided by multiple players. Many of them originate from work in the US health-care market, and have meanings specific to their original context. Transitional care, for example, is focused on processes and defined as a set of actions to ensure co-ordination and continuity of health care as patients transfer between different locations or levels of care within the same location. 19 This is similar to the more broadly defined ‘integrated care’ – a process of reducing fragmentation, improving connections between the different components of health and social services and delivering continuity of care. 20,21 Case management is a tool that is well established within the US-managed care system,22 which aims to integrate services around the needs of people with complex long-term conditions. 23 Case management encompasses case-finding, assessment, care planning, and care co-ordination.
Amid some definitional and conceptual confusion, it is possible to observe common components of initiatives to improve care across settings. Multidisciplinary teams have been identified as a means of providing integrated care, though moves to achieve this have not focused specifically on transitions between settings. Many initiatives to integrate care rely on having a dedicated worker, often a nurse, who co-ordinates, and may also provide care. The evidence for such approaches to management preventing readmissions to hospital or improving quality of care at the end of life is limited, as studies have focused on highly selected patient groups, often excluding people who are known to be terminally ill, or living in the community. 24,25 In some circumstances, case management has been able to improve the experience of patients and carers and reduce use of hospital services,23 and there is some evidence to support the adoption of disease-specific strategies to improve transitions between care settings for older adults. Cameron and Gignac26 recommended that recognising the changing needs of relatives caring for stroke survivors who moved from hospital to home would assist professionals in providing more timely and appropriate support. For heart failure patients, a nurse-directed, multidisciplinary intervention was found to improve the quality of life and reduce hospital use for elderly patients. 27 Continuity of care is a common thread across almost all of this work, either as a core component or as an outcome of any intervention.
Care across transitions and continuity of care
In the last decade, Service Delivery and Organisation (SDO) has funded a range of work on the concept, measurement and promotion of continuity of care. 28 Freeman et al. 29 originally defined continuity as the experience of a co-ordinated and smooth progression of care from the patient’s point of view. He went on to propose a six-dimension model of continuity, that was later refined to three: (1) informational continuity relates to the use of past information to ensure that current care is appropriate; (2) relationship continuity refers to a therapeutic relationship with a health professional; (3) management continuity is concerned with a consistent and coherent approach to the management of a health condition across boundaries, which is responsive to changing needs. 30 Continuity is thus framed as an individual, relational concept, experienced by patients and carers and dependent on their preferences, priorities and perceptions. The SDO-funded projects that followed took a broad and sometimes divergent approach to defining continuity. As a group, they developed a more complex, fragmented concept that emphasised the quality and strength of partnerships. Continuity of care was understood to be a process, an outcome, or some combination of the two by different research teams.
The individual research projects concerned specific disease or patient groups, and the work with cancer patients is most relevant to the subject of our study. Nevertheless, there are three findings from the overall body of work on continuity that are relevant to this study of transitions. First, certain groups were identified as disadvantaged by an inability or reluctance to negotiate continuity: for example, patients who were too ill, or facing socioeconomic or cultural barriers. Such people were under-represented in the empirical work, and were highlighted, along with people with multiple comorbidities, as a group requiring future research. Older adults in the last year of life could be expected to fall into this category. Second, in most projects, transitions between care settings was an issue that emerged as important to service users. This was synthesised by researchers into their understanding of continuity, but it was not the focus of study for any of the projects. Finally, the synthesis and conceptual analysis of the overall SDO programme on continuity identified a number of implications for research that are likely to be pertinent to any study of transitions. The gaps in our understanding included carers’ views and experiences of continuity for themselves and those they support; if and how health professionals see themselves, patients and carers in partnership and what would facilitate this; how patients and carers see themselves as being in partnership; and how leadership and culture can encourage continuity of care.
Areas of enquiry that are relevant to the study of transitions between care settings
There are multiple ways of looking at health-care utilisation, and there are separate bodies of literature, beyond end-of-life care, that may provide important context for any enquiry into transitions between settings. The next section briefly considers readmissions to hospital, delayed discharges and care-home transfers.
Readmissions to hospital
Readmissions to hospital shortly after discharge are among the most common and potentially distressing transitions for individuals. They are monitored as a marker of quality of care, and a potentially avoidable cost. 31 Although analyses of hospital admissions and discharges are rarely specific to the last year of life, they are relevant to end-of-life care because of high utilisation rates in the period before death. Data from different countries across the world provide a common picture of frequent transfers for older people following an acute hospital admission.
In England, in 2007–8, over 1 million (1,130,271) people aged 75 years or older were discharged from hospital and almost 160,000 (159,134) older adults were readmitted within 28 days. This equates to 14.2% of older adults being readmitted to hospital within 28 days of discharge. 32 Readmission rates within 28 days have risen considerably in recent years, from 10% in 1998 to 13.9% in 2008 for older adults aged 75 years or older. 33 Overall in England, between 1998–99 and 2007–8, the number of emergency readmissions in England rose by 52%, from 359,719 to 546,354. Financial penalties for hospitals in England and Wales were introduced in 2011 as part of the Payment by Results initiative. 34 Local commissioners are no longer paying for emergency readmissions within 30 days of discharge following a planned stay. The Department of Health also expected commissioners to deliver a 25% reduction in readmissions following a non-elective admission.
The picture is similar in the USA. Medicare provides health coverage for all people who are aged over 65 years and some people under that age who live with a disability. Analysis of claims data showed that around one in five of the approximately 12 million Medicare recipients who were discharged from hospital in 2003–4 were readmitted within 30 days, and more than one in three were readmitted within 90 days of discharge. Over the age of 70 years, readmission became more likely with increasing age, up to the age of 89. 35 In the month after leaving hospital, a significant proportion of Medicare recipients aged over 65 years are transferred multiple times between different places of care. Analysis of data from 1997–8 showed that 18% of older adults moved twice, while up to 25% had complex patterns of care in a range of different settings. Overall, 46 distinct patterns of care were described, but the majority (61.2%) of people underwent only one transfer; 18% had two transfers and 4% more than four transitions in the 30 days after discharge from hospital. Eight per cent of this older patient population died within 1 month of leaving hospital. 1 Information on how the method of payment for care influences movements after hospital discharge is limited, but appears to suggest that patients whose health care is provided on a fee-for-service (FFS) basis rather than as managed care will experience more frequent transfers. In a study of 1055 older adults who passed through acute-care units, two-thirds of managed-care patients and three-quarters of those receiving FFS health care had two or three transitions, and a slightly higher proportion of FFS were transferred four to six times, all in the 3 months after discharge (14.6% vs. 13.8%).
A wide range of interventions to reduce emergency or unplanned readmissions have been tried, most with limited success. 33,36 However, discharge planning,37 self-management and multidisciplinary interventions with heart failure patients38–40 have had some success.
Transitions for care-home residents
Patterns of hospital utilisation by care-home residents have been studied extensively in the USA, through analysis of large, nationally representative survey data. 41 Data from the national Long Term Care Survey in 1992–94 showed that 18% of over-65-year-olds in long-term care (around 5 million people) were admitted to hospital in a 2-year period and almost one-quarter (22.4%) of these people moved again. 42 Commentators have questioned the appropriateness of transitions of nursing home residents to hospital, particularly at the end of life. 43,44 Estimates of the proportion of emergency department attendances or admissions that were not in the patients’ best interests are as high as 36–40%. In the UK, there is a perception that residents of nursing homes are still sent into acute hospitals to die,45 and the probability of readmission to hospital within a short period of discharge is considerably higher for nursing home residents. 46–48 Analysis of data from the Cambridge City Over-75s Cohort Study49 found that 15% of deaths in acute hospitals were from (predominantly residential) care homes. The more recent introduction of initiatives to improve end-of-life care in the care-home sector may lead to future changes. 45 For residents in care homes who are not close to death, specialist in-reach nursing teams in the UK have been employed to try to avert hospital admissions. 50 An evaluation of the impact of the nursing team in four residential homes included the convening of an expert panel, who judged that 197 admissions were avoided for 131 residents. However, the cost savings from the intervention were only modest, which may limit its wider adoption.
Delayed discharges
Frequent transitions are generally held to be undesirable for individuals and care systems, but delayed transfers may also be a source of great distress to older adults and their families. Older people are more likely than those in other age groups to remain in hospital when their care might be more appropriately provided elsewhere. People with multiple comorbidities and a need for high levels of support are most often affected and there is a range of service-related factors, such as the availability of community support, or internal hospital processes, that may contribute to delays. Research into the reasons why the discharge of patients from hospital may be delayed is suggestive of a complex set of influences, which means that simple solutions are unlikely to be successful. However, recent reviews have found the literature to be of poor quality, with a tendency to neglect patient and family perspectives. 51,52 The provision of rehabilitation services and residential care places, internal hospital processes, and co-ordination and communication with social care service processes and staff are all common causes of delay. This can be exacerbated by discharge planning being delayed until the patient is ready for hospital discharge. Aside from the additional costs of delayed hospital discharge, qualitative interviews indicate that uncertainty in having their hospital discharge delayed and guilt about being identified as a ‘bed blocker’ can cause considerable anxiety and stress to patients at the end of life. 53,54 When provision for support outside hospital is in place, arranging timely and appropriate transport can cause further delays. 55
Care pathways
Care pathways have been developed for a range of conditions, often involving professionals working together with a focus on continuity of care. 56 In end-of-life care, the Liverpool Care Pathway (LCP) extends good practice, based on hospice care, to other settings. 57 However, while the LCP takes a patient-focused approach that maximises quality of life and involves and supports carers, it is concerned with the last days before death. Greater attention to communication and work across settings is found in the Gold Standards Framework (GSF) for patients in the last months of life. 58 This aims to support generalist professionals to work together to provide high-quality care regardless of the setting. The GSF proposes a three-stage approach to care: identify, assess and plan. Anticipating needs through advance planning and enabling death in the place of choice are at the heart of the GSF, but it does not specifically address transitions or their management. All of these structured approaches to care could be incorporated into the planning and management of transitions, but this would be contingent on close communication and joint working across settings. In the UK, at least, there is anecdotal evidence to suggest that both continue to be a problem.
Researching end-of-life transitions
Three contrasting approaches to the study of transitions between care settings at the end of life can be identified in the research literature. All are likely to produce complementary yet different perspectives on experiences of transitions.
The first involves quantitatively analysing patterns of service utilisation. For example, a population-based study in the Netherlands identified an increase in service utilisation of formal care in the last 3 months of life, with half of community-dwelling older people experiencing transitions to institutional care, in most cases to hospitals. 59 Two separate studies based on surveys of GPs in Belgium and the Netherlands found that, among non-sudden deaths, the majority of patients were transferred between settings. 60,61 In the Belgian study, 37% of patients were transferred once in their final 3 months, 16% were transferred twice and 10% were transferred three times or more. Figures reported in the Dutch study were similar: 38%, 21% and 8%, respectively. In both studies, more than 70% of those living at home had at least one transfer; care home residents in the Netherlands were, however, much more likely than their Belgian equivalents to have moved at least once (92% and 36%, respectively).
A second method used to study end-of-life transitions is sequential analysis of changes in health and symptom control for individual patients across different settings. Trask et al. ’s62 mortality follow-back study is typical of this approach, using telephone-administered questionnaires to collect nationally representative data from bereaved relatives in the USA. They studied relatives’ perceptions of distressing pain in cancer patients in their last care settings and found that transitions were not necessarily associated with improvement in symptom control. Similarly, in a comparison of hospice and hospital care for cancer patients in the last 3 months of life in the UK, the transition from one setting to the other appeared to make little difference in the experience of pain and breathlessness, although participants rated pain control by the hospice as more effective. 63
The third approach to the study of transitions at the end of life has been to explore people’s perceptions using qualitative methods. Many studies of this type have collected bereaved family carers’ retrospective accounts or professionals’ perspectives, rather than those of older adults themselves. For example, Harrison and Verhoef64 interviewed 33 carers to explore their perceptions of co-ordination of care. Levine65 conducted six focus groups with 56 carers in New York, in a well-recognised study of carers’ journeys through the health-care system. Many more studies, including some of those funded under the SDO continuity stream, will have collected data on experiences of transitions when exploring other issues.
Summary
The preceding background has emphasised the importance of transitions to patients, families and health systems. Older adults with complex health-care needs are likely to be more vulnerable than other sections of the population to the effects of moving from one place of care to another. To minimise the impact on patients’ and carers’ well-being, care should be co-ordinated and consistent across settings. To achieve this, we need to draw on and combine the strengths of the different settings and approaches in health and social care provision.
Quality improvement initiatives in health services have been criticised for missing the obvious in patient care – the need for caring – and focusing on technical aspects of health services. 66 Many of the recent initiatives in integrated or guided care and care pathways are aimed at quality improvement, but share similarities with the hospice approach. The hospice movement has traditionally been interested in holistic care, with continuity across time and settings, rather than efficiency and cost-effectiveness. A focus on bridging the gap between these approaches may be a particularly effective way of addressing any shortcomings in current experiences of care. The following study aims to combine perspectives from health services research and end-of-life care, to this end.
To improve patients’ and carers’ experiences of end-of-life transitions, we need to appreciate the complexity of their journey. Current knowledge of transition experiences in health systems outside the USA is limited, as is the application of components of managed or integrated care in other health systems. Financial incentives are in their infancy in the UK and elsewhere, and their consequences for transitions are as yet unknown. For older adults’ transitions between care settings to be better understood, we need to gauge the frequency and nature of transitions in the last year of life; deepen our understanding of the consequences of transitions for carers; and understand how decisions are made and what the constraints are for professionals who commission and provide care.
The major part of the following study adopts the third approach to the study of transitions described above, and uses qualitative methods to explore patient, carer and professional experiences. However, we also analyse quantitative data on service utilisation and a structured questionnaire to capture carers’ proxy views of patient experiences in different settings.
Theoretical framework
We sought an appropriate theoretical framework within which to site our study from the previously funded SDO work on continuity. Freeman et al. ’s29 three-dimensional construct of continuity (informational, relationship and management) was used to inform our work. Continuity was considered as both a part of the process of transitions and an outcome of good care across transitions. Throughout this project, Donabedian’s approach to quality, examining structure, process and outcome, provided an underlying framework for our thinking. 67,68
To understand end-of-life transitions, we wished to explore patient, family and staff experiences and explore how these were influenced by wider factors in both their surrounding social networks and the wider health and social care system. Our choice of methodology allowed us to gain insight into how ‘end-of-life care’ was constructed through the relations between the different categories of participants. It also enabled us to begin to understand the diverse and dispersed nature of ‘palliative care’ within systems of health and social care, and wider policy frameworks.
We took a mixed-methods approach in this study. Mixed-methods research involves the collection and analysis of data, and integration of findings, using both qualitative and quantitative approaches. Such approaches are especially suitable for understanding complexity and for enabling understanding of both the experiential and ‘systems’ factors surrounding any given phenomena. 69,70 In this report, we present findings that have been combined at the analysis stage, based on the ‘following a thread’ technique. 69,71
The majority of our work in this project was qualitative, and we approached the analysis of our qualitative data with a broadly social interactionist lens. We were interested in how patients, families and staff interact and attribute meaning to others’ behaviours, in order to understand how transitions were experienced. This approach allowed us to consider carers’ and patients’ negotiation of their roles, the social construction of patient and professional behaviours, and how all of these link to service structures. We aimed to gain an in-depth understanding of transitions, set within social and organisational contexts.
Chapter 2 Objectives
The aim of this study was to understand the patterns, potential causes and consequences of transitions between settings and their association with older people’s experiences at the end of life. The three conditions under study, heart failure, stroke and lung cancer, will provide information on care provided across contrasting disease trajectories. Whereas cancer patients commonly undergo a steady progression with a clear terminal phase, gradual decline in people with heart failure is characterised by episodes of acute deterioration and some recovery, with a more sudden and seemingly unexpected death. 72 Older stroke patients, meanwhile, have a trajectory marked by episodes of sharp decline.
Objectives
-
To explore the effect of transitions towards the end of life on health status, quality of life, symptom control and satisfaction with care.
-
To understand the factors that influence decisions about transitions in the nature and location of care.
-
To elicit patient and provider views on the appropriateness of different transition patterns and the factors that constrain or shape decisions.
-
To describe transitions in and out of hospital at the end of life for older people with selected conditions in England.
-
To identify individual- and service-level factors associated with frequency of transitions.
The major part of this project used qualitative interviews to address objectives 1 to 5. A structured questionnaire was administered to bereaved carers to inform objective 1, while quantitative data were analysed to complete objective 4.
Rationale: interviews with patients
The aim of this section of the study was to explore older adults’ own experiences of moving between care settings in their last year of life. Previous research into end-of-life care has rarely sought out care recipients’ perspectives, relying instead upon carers as a proxy voice for people who have died73 or are too unwell to be interviewed. Our aim, in interviewing patients themselves, was to understand how relationships with carers and professionals affect older adults’ experience of transitions at the end of life. We anticipated that patients’ accounts of how their care was delivered and experienced, and how they interpreted their interactions with professionals and carers, would provide new and valuable insights into older people’s experiences of end-of-life care. In order to provide representation of the settings and services involved in transitions at the end of life, we interviewed people identified by secondary care and specialist nurse teams.
Rationale: interviews with bereaved family carers
Bereaved family carers were interviewed to provide a proxy view of patients’ experiences and explore their own perspectives on the transitions experienced by the decedent. The interviews explored the reasons underlying any moves, the experiences and consequences for decedent and family, and perceptions of care across settings. Carers were able to provide a different and often complementary perspective to the patients’ reports of experiences in their last months. In addition, the carers had insights into the time around the death and beyond, which is often the subject of great scrutiny.
Rationale: interviews with professionals
Professionals were interviewed with the aim of understanding their perspectives on decision-making concerning transitions, and the organisation and management of transitions between care settings for older adults at the end of life. Participants were made aware that the study team was particularly interested in care for older adults who die with lung cancer, heart failure or stroke. However, many of the professionals had a broader remit focused on older people, palliative or end-of-life care. This is reflected in their interview data, which are not solely concerned with these conditions.
Senior professionals responsible for providing or commissioning health or social care services for older people, and with some insights into transitions between care settings, were the target participants. Senior staff were considered more likely to have an overview of the way services are provided, interfaces with other settings and services, and views and insights about the reasons why services are organised as they are, including alternative models of care, and piloting and developing new services. Insights from both providers and commissioners were sought as a means of gaining insights into different stages and levels of the structure, organisation, planning and delivery of care.
The sampling frame covered medical and nursing staff in different settings, with representation of ambulance, paramedic and out-of-hours services, as well as a range of commissioners. Most senior social care interviewees were commissioners rather than providers of services, although some had direct contact with patients and their relatives in making assessments and commissioning care for individuals.
Chapter 3 Methods
Issues, problems and responses
Research ethics and research governance approvals
To conduct this study, which included interviews with 191 individuals, approval from research ethics committees (RECs) and NHS and social care research governance approvals were obtained. Standard application procedures to NHS RECs were followed for all components of the project, except for the research with professionals, where a fast-track process for low-risk studies was followed (proportionate ethical review) and permission granted within 2 weeks. Ensuring that appropriate research governance approvals were in place was a far more time-consuming process, as procedures were locally derived and frequently opaque. Changes to the information technology (IT) supporting the central application process for research governance approvals (Integrated Research Application System or IRAS) produced a 4-month delay in the processing of our application for professional interviews, and we were obliged to send all the application paperwork to each trust in addition to making a centralised online application.
Two primary care trusts (PCTs) refused permission to interview carers in their area. One gave no reasons; the other was critical of the study design, stating that GPs would be unlikely to be able to identify carers. A resubmission of the application to this PCT was also unsuccessful. Seeking permission for professional interviews was complicated by variation between organisations in interpretation of the national guidance. We sought permission to conduct telephone interviews with staff members, unless they preferred to meet the researcher. Some organisations considered themselves to be participant identification centres, while others argued that they were research sites. This was not resolved with intervention from the lead PCT and, consequently, the time taken to approve the study ranged from a few days to more than 3 months. Both researchers were in possession of NHS research passports, but almost all trusts also insisted on additional local approval procedures for individual researchers. In total, across the project we applied for NHS research governance approval 86 times.
Staffing
Recruitment and retention of staff, along with contractual difficulties, were responsible for delays to the start of the project in the south. An extension to the end of the project within original resources was granted to enable the work to be completed.
Qualitative interviews
Recruitment and data collection from patients
We sought a purposive sample of older adults aged over 75 years who had moved at least once between care settings in the 3 months leading up to the interview, and for whom specialist health professionals answered ‘no’ to the question ‘would you be surprised if this patient was to die in the next 12 months?’. This ‘surprise’ question is commonly used to identify individuals nearing the end of life,74,75 in particular where prognosis is complex, as is the case with heart or renal failure, for example. 76 Along with the criteria listed above, participants had to be aware of their heart failure, stroke or lung cancer diagnosis. Our initial aim was to interview 10 patients for each of these three conditions.
Potential participants were identified and invited by their specialist health professionals to contact the research team. On receipt of an expression of interest, a researcher telephoned the patient to explain the study and, if appropriate, send further information by post. All of the interviews were arranged and conducted by one member of the research team between June 2009 and July 2010. They took place at the participants’ place of residence and lasted an average of 1 hour.
Interviews followed a flexible person-centred topic guide that covered interviewees’ social background, family circumstances and their experiences as a patient. Participants were asked about their illness, the health and social care they received, their experiences of the transitions that they had experienced, and how they felt about these moves between care settings. People were encouraged to talk about issues which were important to them, and to share their perspectives on the quality of the care received in different settings as well as on the impact of transfers between places of care. A comprehensive list of prompts for the interviewer ensured consistency across interviews. All interviews were audiotaped with permission, transcribed verbatim by a professional transcriber and anonymised by the research team.
Recruitment and data collection from bereaved caregivers
Family carer interviewees were identified in a two-stage process. Primary care research networks (PCRNs) in three NHS regions of England first advertised the study to GP practices enrolled with their Primary Care Incentive Scheme for research participation. Comprehensive local research networks facilitated the involvement of general practices by funding service support costs.
Support from primary care research networks
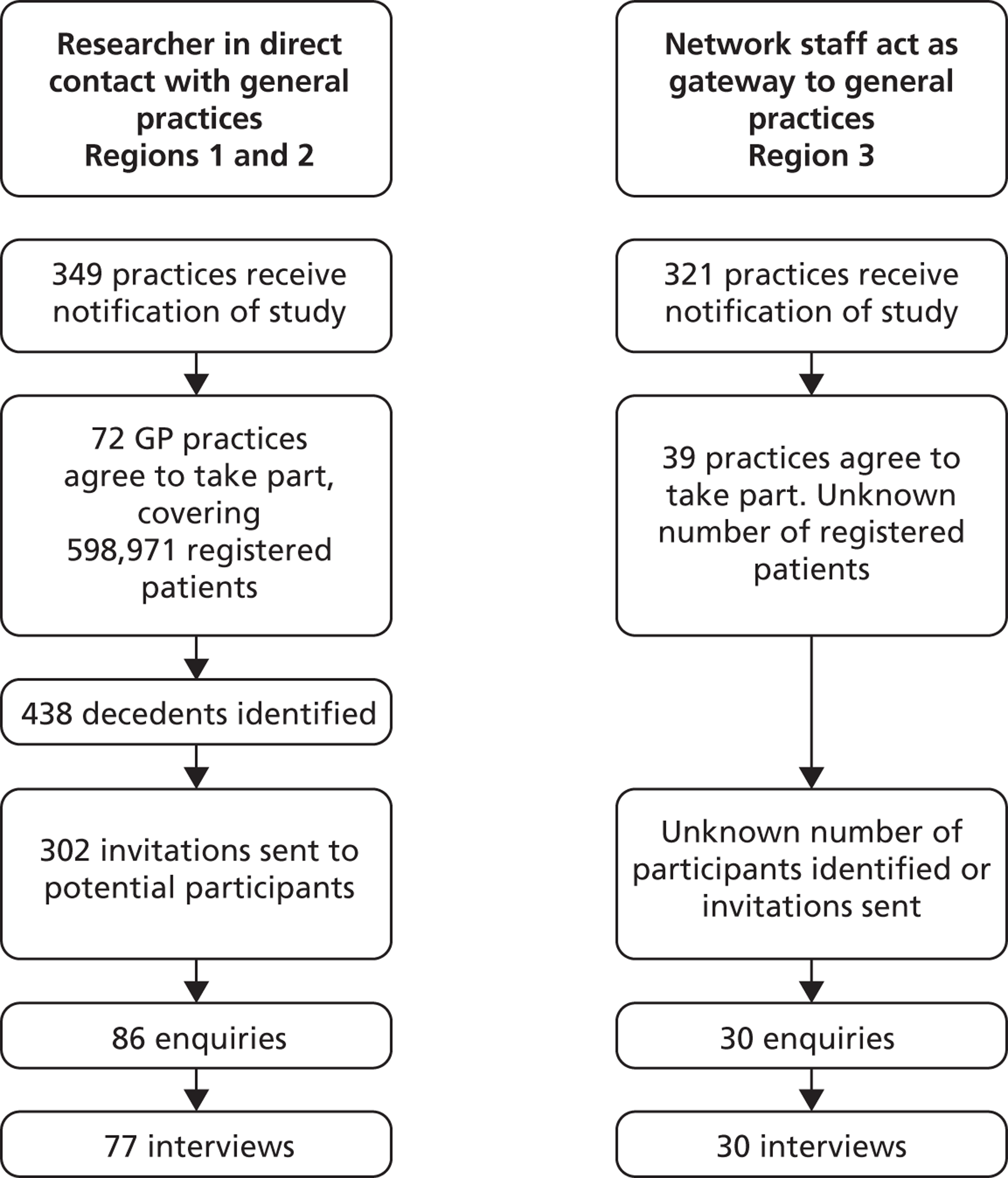
Two approaches to recruitment were adopted once GP practices were recruited to the study (Figure 1). 77 In the north-west region, the Merseyside and Cheshire PCRN and the North Lancashire PCRN worked directly with GP practices. PCRN staff visited each practice assisted with database searches and distribution of recruitment materials to eligible individuals and collected some data about practice involvement in the study. In other areas [South Central Strategic Health Authority (SHA) (Portsmouth, Southampton, Hampshire, Isle of Wight PCTs), parts of the South West SHA that were encompassed by the same primary care research network (Devon, Plymouth, Torbay, Somerset, Bath and North Somerset, Bristol, Swindon, Wiltshire, Dorset, Bournemouth and Poole, Greater Manchester)], PCRN staff dealt with initial enquiries from practices and passed on formal expressions of interest as they arose to the research team, who then supported practices through their involvement. In all regions, participating practices were provided with the recruitment materials: invitation letters, participant information sheets, reply slips and stamped envelopes.
FIGURE 1.
Recruitment of family carers by general practices.
General practices were asked to identify people who had died within the last 3–9 months aged 75 years or older with lung cancer or heart failure or following a stroke. Most were able to scrutinise a list of patients who had died, though appropriate read codes were made available for searching electronic databases if required. The list of eligible decedents was restricted to individuals who had experienced more than one transition between care settings in the last 3 months of their lives.
Identification of carers
The primary care team identified carers for each decedent in cases where the team knew the carer as a result of providing care to the patient. The GP took responsibility for inviting carers into the study. Most were family members or friends. A small number of care-home professionals who had known the decedent well and were able to talk about transitions and end-of-life experiences were also included.
Interviews were conducted between 3 and 9 months following the death. Within end-of-life care research, 3 months after bereavement is acknowledged as an appropriate minimum threshold for inviting bereaved people to participate in research. This is because, by 3 months, memories are sufficiently fresh for a person to provide details about the experience, but enough time will have passed for most individuals to feel able to speak with a research interviewer about their experiences without feeling too upset to do so. Care was taken to avoid holding any interviews around the first anniversary of the death.
Interviews were conducted at a time and a place chosen by each participant. For the majority, this was a face-to-face interview in their own home. Written informed consent was obtained from all participants and interviews were conducted by a research team member experienced in working with vulnerable adults and older people. One family carer living in Scotland and one care-home professional were interviewed by telephone, while two participants chose to be interviewed in the researcher’s office and one at their own place of work. Another care-home owner chose to be interviewed face to face at the care home where she lived.
Some carer participants chose to be interviewed with a relative or friend present. In some cases, this was prearranged, but, in others, the person was present when the interviewer arrived. Informed consent was received from and documented with all individuals. Additional participants were almost always female: one widow and two widowers were accompanied by their daughters; another widow had a female friend with her; five sons and one daughter had their spouses present.
Most interviews opened with a question to prompt an overview about the transitions experienced in the last year of life. This approach was used in order to tailor the subsequent questions. Where it was difficult to obtain this overview, interviewees provided detailed accounts of each setting and transition. The interviewers then probed for details about the final transition, and asked a series of structured questions. If interviewees were reticent after probing, structured questions were introduced sooner. If interviewees had an account they wanted to provide about later transitions, this was explored before the introduction of structured questions.
Administration of questionnaire
The previously validated VOICES survey78 was used in this study with minor modifications. We added a small number of open questions after separate blocks of questions to invite the participants to give examples to clarify their answers (e.g. if a participant’s answer indicated that the nurses had treated the patient with dignity and respect, we asked the participant to offer an example of such behaviour). Responses to open questions were coded if appropriate and reported with the VOICES data. In addition, we inserted two questions that have been used elsewhere, to ask about co-ordination of care. VOICES is available elsewhere;78 additional questions are available from the author on request. The questionnaire was administered face to face as part of the interview, and responses were entered into a touchscreen computer by choosing responses from drop-down menus of options. The interviewers were also able to type short open answers using the onscreen keyboard. The structured questions were followed in sections appropriate to the interviewee’s circumstances, and not all were applicable to every interviewee. The questions on places of care were completed first, followed by medications, GP care, out-of-hours services, and the circumstances of the death, finishing with questions that required the respondent to take an overview of the care transitions. A small number of participants expressed discomfort about the specificity of the structured VOICES questions and, to avoid distress in these cases, open questions were substituted for the same themes.
All of the interviews were audio recorded with permission and transcribed in full. With the exception of one telephone interview (two separate conversations 2 weeks apart), each interview was conducted on a single day, sometimes with short breaks. The recorded interview duration was 90 minutes on average, but varied between 45 and 180 minutes.
Recruitment and data collection from professionals
After research governance approval had been granted, some organisations provided assistance with recruitment and in other organisations the researcher sent invitations directly to individuals. Five individuals already known to the study team (three of whom had expressed interest in earlier phases of the study) participated after direct invitation. Four organisations granted permission to recruit on the grounds that they would nominate potential participants to be sent invitations. One of these organisations (social care) sent the invitations to potential participants and the researcher was asked to wait for a direct response before making any contact with the potential participants. Six organisations circulated information to a large number of potential participants, but there were no restrictions on the research team to also make contact. Other invitations were sent on the basis of organisation structures and contacts, recommendations from other professionals, and the results of telephone calls to establish the most appropriate people to invite. All of the social care organisations provided assistance with recruitment.
Telephone interviews
The majority (37) of interviews were conducted on the telephone, but six were face to face in a private room at the participant’s place of work. Four of the professionals interviewed by telephone were at home for the interview, and the other 33 were at work. The interviews were 36–90 minutes in length.
Interviews followed a topic guide. Professionals were asked to talk about what their role involved and how this fitted within their service or organisation. They were then asked to discuss challenges associated with transitions at the end of life for older people, and to provide information about good practice and any pilot initiatives. Some had identified key issues in advance which they wanted to mention. Each individual was asked if they would like to explore commissioning or provision (the opposite of their own role); how care was organised for individuals without readily accessible family carers; which pieces of strategy or guidance they work within; and what impact they saw the (at that stage planned) changes within NHS structures having on the care of older adults at transitions between care settings. Short summaries of particular experiences of care derived from the interviews with bereaved carers were sent to participants in advance. These scenarios were identified from an initial analysis of the first 60 interviews with carers. They were chosen to reflect themes and issues that were frequently occurring, or that reflected particularly challenging circumstances for the service providers. Each scenario was a composite of data from a number of different interviews, with important demographic data modified to ensure that the individuals involved remained anonymous. The scenarios were carefully selected to ensure that individuals were not able to recognise or asked to respond to patient care in which they were directly involved. The interviewees were invited to share their perceptions of the events, with prompts about whether or not such things could occur in their area and what provision was or could be implemented to minimise the chances of poor care.
Interviews were audio recorded with permission. Assurances were given about the study team’s commitment to confidentiality for the participants, including not publishing job titles that would identify an individual and restricting information available data on any participant’s location. Written informed consent was obtained for all participants. For participants interviewed by telephone, the consent form was sent in advance by e-mail or post. Verbal consent was obtained at the time of the interview and forms were signed by the participant and interviewer and exchanged after the interview. Audio recordings were transcribed in full by a professional transcriber.
Qualitative data analysis
A common approach was taken to data analysis across all three sets of interviews. For the patient and carer interviews, three researchers familiarised themselves with the data by reading and rereading the transcripts and identified key issues, concepts and themes. These served as a basis for developing a coding framework of initial categories and themes, which was tested on a 10% sample of transcripts before being used to code all transcripts line by line. Two researchers coded the same 20 transcripts, and a third researcher coded a further 10. Any discrepancies were discussed and, if agreed, the minor modifications were made to the coding framework.
Each major theme was allocated to a chart in Microsoft Excel (Microsoft Corporation, Redmond, WA, USA), with a row for every case and a column for each category. Data were entered into the relevant cells and summaries were prepared at the base of every column. The data were compared within and across cases, searching for commonalities and differences. This enabled the research team to identify patterns and main issues arising from the interviews. The original transcripts and field notes were referred to in order to ensure that analysis took the context of interviews into account.
In the case of the professional interviews, the thematic framework brought together key themes emerging from those transcripts with a priori issues and questions derived from the aims and objectives of the study and concepts raised by respondents in the first two phases. One researcher, in discussion with two others, tested and adapted the framework on the basis of a 25% sample of interviews transcribed. All transcripts were subsequently coded line by line by one researcher, using NVivo software (version 9.2, QSR International, Warrington, UK) to manage the data. A second researcher double coded five transcripts to check the validity of the framework. The NVivo programme’s framework matrix function was used to allocate each theme to a chart, with a row for every source and a column for each category. Data were mapped and interpreted by searching for associations between themes and identifying the commonalities and differences in interviewees’ attitudes.
The researchers involved discussed and refined their analysis throughout the process, drawing on their different backgrounds (medicine and public health, nursing, psychology, sociology and social policy) and their different relationships with the data (study design, interviewers or data analysts) to reach agreement. Findings were discussed with an external group of research partners, comprising people who had themselves provided care for older adults and were keen to ensure relevance to patients’ needs.
Chapter 4 Analysis of linked Hospital Episode Statistics and mortality data
The aim of this section of the project was to analyse data on care received by older adult patients with specific causes of death, in the year before death. Hospital Episode Statistics (HES) records details of each episode of inpatient care provided by a consultant. Total length of each admission (made up of all consultant episodes), dates of admission and discharge, destinations, procedures undertaken and specialty of treatment are recorded.
Linked HES and mortality data were obtained for patients aged ≥ 75 years who had been admitted to hospital with a diagnosis of heart failure or lung cancer in the 12 months before their death. At the time of the study, it was not possible to select a group of individuals using mortality data and then extract HES data relating to their hospital use. The study data set was, therefore, defined by diagnoses recorded by HES and not by cause of death. Hence, patients who had received hospital treatment for specified conditions but did not have any of these recorded as a cause of death would still be included in the study. As the starting point for the study data set was hospital admissions, the data provide a reflection of resource use, but are liable to inaccuracies within HES. Deficiencies in the quality of HES data are well recognised, including many mistakes of coding and omission. 79,80 People who died without any inpatient episodes in the 12 months before death would not be included in this study. However, we know that 78% of all deaths recorded by the Office for National Statistics (ONS) are associated with one admission in the last year of life; the same is true for 88% of all age cancer deaths and 66% of deaths from cardiovascular disease. 81
Pseudonymised HES containing records of admitted patient care in England, linked to ONS mortality data, were selected for years 2000–1 to 2010–11. The data were restricted to people aged > 74 years with diagnoses of either lung cancer or heart failure [International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes I50–I50.9, I11.0. I42.0, I25.5, I42.9, C33.0–34.9]. HES data variables were selected relating to diagnosis, length of stay and discharge destination. No variables that would identify geographical locations for patients or institutions or dates of birth were used in this analysis. The Index of Multiple Deprivation (IMD) was provided with the data, calculated from the postcode of residence provided on hospital admission. Mortality data were obtained only for patients who had been in hospital in the year before their death and, therefore, had a record in the HES. Cause of death and whether this took place at home or in a communal establishment were extracted. Data were reported to be cleaned prior to being released for analysis.
Data management
The data were provided in a .ZIP file, copied from the encrypted hard disk onto a non-networked computer, and then expanded. PASW Statistics version 18 (SPSS Inc., Chicago, IL, USA) was used to import the delimited files into a statistical and data management environment. Loading syntax kept the variable names from the HES data set.
Plan for analysis
There are 20 diagnosis fields within the HES data set. The study data set was then defined by searching for the diagnostic codes. Heart failure admissions were restricted to the primary diagnosis, in line with the approach taken in the national audit of heart failure care. 82 A broader definition was used for lung cancer admissions, using positions 1–10. The data set was ordered according to patient ID and increasing date of discharge. Using the date of admission, spells were identified if they had occurred in the 12 months preceding the date of death. The total number of bed-days within the 12 months before death was calculated from the sum of the spell durations. The ONS file was expanded and imported into PASW. The ‘merge files add variable’ command was used to join the ONS fields to the HES records using the common ID. Deaths were allocated to the final spell for each case in the data set.
The rank of the IMD was recoded into quintiles (with the recode into different variable command), using publicly available data from the Communities and Local Government website83 to provide cut off ranks for each quintile. Patients who died in hospital on their last admission were identified using the discharge method and discharge destination variables. For all other cases, the time in days between last admission and death was calculated using the ‘date wizard’ function. For deaths within each patient group, the number of admissions, bed-days in year before death and the time between the last admission and death were calculated.
Chapter 5 Findings
Participant characteristics
Patients: participant characteristics
Thirty people were interviewed (Table 1). Thirteen of the 20 people with heart failure who were sent information about the study agreed to be interviewed (four female and nine male). Thirty-five older adults with lung cancer expressed interest, but only 14 were interviewed (three male and 11 female). One of the patients died before the interview date and 20 others were too unwell to participate at the time. We interviewed three stroke patients. Other planned interviews were cancelled because of deterioration in the patient’s condition, or death. Lung cancer patients were aged 73–89 years, heart failure patients were aged 69–88 years and stroke patients were aged 81–93 years. Four of the interviewees (three heart failure patients and one person with lung cancer) were interviewed despite being younger than the inclusion criteria minimum age of 75 years, as they had been invited by their responsible clinicians to take part in the study. We monitored the sociodemographic composition of the sample, based on IMD, derived from the participants’ postcodes, and used the last reported occupation to allocate the participant to one of the five categories in the National Statistics Socioeconomic Classification. 84 Our aim was to make sure that people from disadvantaged areas were represented, and this was the case, without intervention.
| Characteristics | Heart failure | Lung cancer | Stroke | All |
|---|---|---|---|---|
| Age, years (median, range) | 77 (69–88) | 80 (73–89) | 85 (81–93) | |
| Male | 9 | 3 | 2 | |
| Female | 4 | 11 | 1 | |
| Social classificationa | ||||
| 1 and 2 | 6 | 4 | 3 | |
| 3 | 1 | 0 | 0 | |
| 4 and 5 | 6 | 10 | 0 | |
| IMD | ||||
| Quintile 1 | 16 (53%) | |||
| Quintile 2 | 3 (10%) | |||
| Quintile 3 | 8 (27%) | |||
| Quintile 4 | 1 (3%) | |||
| Quintile 5 | 0 (0%) | |||
| Living circumstances | ||||
| Home, alone | 3 | 5 | 1 | |
| Home, with others | 9 | 7 | 1 | |
| Institution | 1 | 2 | 1 | |
| Totals | 13 | 14 | 3 | |
Carers: participant characteristics
One hundred and eighteen carers were interviewed (77 from 302 invitations from GPs in the south, 30 from an unknown number of GP invitations in the north-west and 11 recruited via other means) (Table 2). They ranged in age from 38 to 87 years (median 66 years). The majority (75%) were female; around half (47%) had been the spouse or partner of the patient. More carers were recruited from the southern regions (73%) and a disproportionate number were from less disadvantaged areas. The participants’ postcodes were used to allocate an IMD score to the carer, which was then placed into quintiles based on the scores for England. This provided a measure of relative disadvantage across our sample.
| Characteristics | n (%)a |
|---|---|
| Age, years (median, range) | 65.5 (38–87) |
| Sex | |
| Male | 30 (25.4) |
| Female | 88 (74.6) |
| Marital status | |
| Married or cohabiting | 42 (35.6) |
| Widowed | 59 (50) |
| Single | 12 (10.2) |
| Divorced or separated | 1 (< 1) |
| N/A | 4 (3.4) |
| Relationship to the decedent | |
| Spouse or partner | 56 (47.5) |
| Child | 53 (44.9) |
| Other relative | 6 (5.1) |
| Friend | 1 (< 1) |
| Professional | 2 (1.2) |
| Decedent resident in | |
| North-west | 32 (27) |
| South-central or south-west | 86 (73) |
The patients whose care was the subject of the interviews had a median age of 84 years (range 66–97 years) and half of them were female (Table 3). Treatment had been received for at least one of the three main study conditions (heart failure, lung cancer or stroke) by 82 (77%) of the decedents. The sample was supplemented by carers of people who had had chronic obstructive pulmonary disease (COPD) (18.6%), colorectal cancer (7.6%) and breast cancer (2.5%). The vast majority of decedents had lived at home (84%) or in a care home (9%), and hospital was the most usual place of death (58%). Thirty-two per cent of patients had died in their own or a relative’s home (n = 17) or in a care home (n = 19). Reported levels of comorbidities were low.
| Characteristics | n (%)a |
|---|---|
| Age, years (median, range) | 84 (66–97) |
| Sex | |
| Male | 62 (52.5) |
| Female | 56 (47.5) |
| Main condition | |
| Heart failure | 40 (33.9) |
| Stroke | 27 (22.9) |
| Lung cancer | 16 (13.6) |
| COPD | 22 (18.6) |
| Colorectal cancer | 9 (7.6) |
| Breast cancer | 3 (2.5) |
| Cancer unknown primary | 1 (< 1) |
| Reported comorbiditiesb | |
| COPD | 4 (3.4) |
| Colorectal cancer | 3 (2.5) |
| Breast cancer | 2 (1.7) |
| Heart failure | 1 (0.8) |
| Stroke | 1 (0.8) |
| Place of residence 3 months before death | |
| Own home | 99 (83.9) |
| Relative’s home | 4 (3.4) |
| Care home | 11 (9.3) |
| Hospital | 3 (2.5) |
| Other | 1 (< 1) |
| Place of death | |
| Hospital | 68 (57.6) |
| Care home | 19 (16.1) |
| Own home | 17 (14.4) |
| Relative’s home | 2 (1.7) |
| Hospice | 11 (9.3) |
| Ambulance/A&E | 1 (< 1) |
| Transitions in the last year of life | |
| One or more in last 12 months | 118 (100) |
| One or more in last 6 months | 114 (96.6) |
| One or more in last 3 months | 110 (93.2) |
The carer and patient interviewees had different socioeconomic profiles, with a disproportionate number of patients drawn from the most disadvantaged areas (Table 4). Carers from the south were predominantly resident in more advantaged areas. However, it is important to note that not all of the carers were co-resident with the person receiving care. When the IMD is examined by decedent diagnosis, there is a significant gradient only for COPD, where fewer carers were found in the least disadvantaged quintiles (Table 5).
| IMD quintiles | Number (%) of interviewees, north-west | Number (%) of interviewees, southern regions | Totals, N (%) |
|---|---|---|---|
| Quintile 1 (most deprived) | 4 (12.5) | 1 (1.2) | 5 (4.3) |
| Quintile 2 | 9 (28.1) | 3 (3.5) | 12 (10.3) |
| Quintile 3 | 8 (25.0) | 17 (20.0) | 25 (21.4) |
| Quintile 4 | 6 (18.8) | 29 (34.1) | 35 (29.9) |
| Quintile 5 (least deprived) | 5 (15.6) | 35 (41.2) | 40 (34.2) |
| Totals | 32 (100) | 85 (100) | 117a (100) |
| IMD quintiles | All cancers, n (%) | Heart failure, n (%) | Stroke, n (%) | COPD, n (%) | Totals, N (%) |
|---|---|---|---|---|---|
| Quintiles 1, 2 and 3 | 10 (35.7) | 14 (35) | 8 (28.6) | 11 (50) | 43 (36.4) |
| Quintile 4 | 8 (28.6) | 11 (27.5) | 9 (32.1) | 7 (31.8) | 35 (29.7) |
| Quintile 5 | 10 (35.7) | 15 (37.5) | 11 (39.3) | 4 (18.2) | 40 (33.9) |
| Totals | 28 (100) | 40 (100) | 28 (100) | 22 (100) | 118 (100) |
Professionals: participant characteristics
Forty-three professionals were interviewed from 10 PCTs, four PCT provider arms, four acute hospital trusts, two ambulance trusts, five social care organisations and five hospices. Interviewees were drawn from the north-west (n = 20) and south-central and south-west NHS regions (n = 23), but no staff participated from any of the 11 care trusts in England. The roles of the interviewed staff are shown below (Table 6).
| Roles | North-west, n | South-central and south-west, n | Totals, N |
|---|---|---|---|
| Social care commissioner | 6 | 1 | 7 |
| Social care operational | 1 | 1 | 2 |
| Health commissioner | 1 | 6 | 7 |
| Community matron | 3 | 1 | 4 |
| GP | 4 | 1 | 5 |
| Hospital doctor | 0 | 4 | 4 |
| Hospice senior staff | 3 | 2 | 5 |
| Senior/specialist acute nursing staff | 0 | 5 | 5 |
| Urgent/out-of-hours service | 1 | 0 | 1 |
| Ambulance service | 1 | 2 | 3 |
| Totals | 20 | 23 | 43 |
Questionnaire findings: carers’ views of end-of-life care transitions
Overview of care
A minority of respondents reported that care from health and social services had been well co-ordinated (42%) or flexible to the needs of the patient (47%) (Table 7). Half of the participants were aware of a main contact person for the decedent at their general practice, hospital or elsewhere in their last 3 months. Most often, that contact person had been the GP, either alone or in combination with nurse, consultant or care-home colleagues. Only 26 (22%) of all respondents judged that any of the transitions in the final 3 months of life could have been avoided. Ratings of both the amount and the nature of help and support were not high; 42% received as much help and support as needed (Table 8).
| Care from health and social services | Responses, n (%) | |||
|---|---|---|---|---|
| Yes | No | Don’t know | N/A or no response | |
| Well co-ordinated | 50 (42.4) | 36 (30.5) | 12 (10.2) | 20 (16.9) |
| Consistent | 60 (50.8) | 31 (26.3) | 7 (5.9) | 20 (16.9) |
| Flexible to decedent’s needs | 55 (46.6) | 30 (25.4) | – | 33 (28) |
| Everyone involved had enough information about decedent’s needs | 61 (51.7) | 26 (22) | 11 (9.3) | 20 (16.9) |
| Decedent had a main contact person at hospital, general practice or elsewhere over last 3 months | 59 (50) | 27 (22.9) | 7 (5.9) | 25 (21.2) |
| Could any of the transitions in last 3 months have been avoided? | 26 (22) | 54 (45.8) | 5 (4.2) | 33 (28) |
| Questions | Responses, n (%) |
|---|---|
| Who was main contact person in last 3 months? | |
| GP, alone or in combination with nurse, consultant, care home | 33 (28.0) |
| District or specialist nurse | 3 (2.5) |
| Social worker | 4 (3.4) |
| Care home | 5 (4.2) |
| Hospital consultant or ward staff | 7 (5.9) |
| Not applicable or no recorded response | 66 (55.9) |
| Do you feel your family got as much help and support as you needed when caring for the decedent? | |
| Yes, as much as needed | 50 (42.4) |
| Yes, some support but not as much as needed | 10 (8.5) |
| No, although we tried to get more help | 10 (8.5) |
| No, but we did not ask for more help | 15 (12.7) |
| We did not need any help | 6 (5.1) |
| No recorded response | 27 (22.9) |
Care from general practitioners and out-of-hours care
Almost all of the decedents had seen their GP in the last 3 months of life, and the respondents gave high ratings to all aspects of the care provided. A minority received no home visits and a number were seen at home at a frequency equivalent to more than twice each week. Out-of-hours care was sought by around 30% of people in their final months. Only one used NHS Direct and most telephoned the out-of-hours service or their own GP, which resulted in a home visit. Advice to go straight to hospital was uncommon (4%). Table 9 presents carers’ views of GP care and Table 10 presents carers’ views of out-of-hours care.
| Questions | Responses, n (%) |
|---|---|
| Did the decedent have any contact with his or her GP in last 3 months of life? | |
| Yes | 103 (87.3) |
| No | 9 (7.6) |
| Don’t know | 1 (< 1) |
| No response | 5 (4.2) |
| In your opinion, did the GP know enough about their condition or treatment? | |
| Yes | 85 (72) |
| No | 10 (8.5) |
| Don’t know | 9 (7.6) |
| Not applicable or no recorded response | 14 (11.9) |
| Did you have confidence and trust in the GPs who were caring for them? | |
| Yes, in all of them | 84 (71.2) |
| Yes, in some of them | 10 (8.5) |
| No, not in any of them | 9 (7.6) |
| Don’t know | 0 |
| Not applicable or no recorded response | 15 (12.7) |
| Do you feel that the GPs had time to listen and discuss things? | |
| Yes, definitely | 81 (68.6) |
| Yes, to some extent | 11 (9.3) |
| No | 4 (3.4) |
| Don’t know | 2 (1.7) |
| Not applicable or no recorded response | 20 (16.9) |
| Were you able to discuss with the GP any worries or fears that you may have had about his or her condition, treatment or tests? | |
| Yes, I discussed them as much as I wanted | 71 (60.2) |
| Yes, I discussed them, but not as much as I wanted | 4 (3.4) |
| No, although I tried to discuss them | 5 (4.2) |
| No, but I did not try to discuss them | 6 (5.1) |
| Don’t know | 0 |
| I had no worries or fears to discuss | 9 (7.6) |
| Not applicable or no recorded response | 23 (19.5) |
| How much of the time were you treated with respect and dignity by the GP? | |
| Always | 91 (77.1) |
| Most of the time | 8 (6.8) |
| Some of the time | 1 (< 1) |
| Never | 2 (1.7) |
| Don’t know | 0 |
| Not applicable or no recorded response | 16 (13.6) |
| How often did the GP visit at home during the last 3 months of life? | |
| Once | 11 (9.3) |
| Two to five times | 50 (42.4) |
| Six to 10 times | 10 (8.5) |
| Eleven to 15 times | 5 (4.2) |
| Sixteen to 20 times | 1 (< 1) |
| More than 21 times | 3 (2.5) |
| Did not visit, no visits were needed | 15 (12.7) |
| Did not visit, but wanted the GP to visit | 1 (< 1) |
| Not applicable or no recorded response | 22 (18.6) |
| Questions | Responses, n (%) |
|---|---|
| In the last 3 months, did the decedent ever need to contact a doctor for something urgent in the evening or at a weekend? | |
| Not at all | 47 (39.8) |
| Once or twice | 26 (22) |
| Three to four times | 6 (5.1) |
| Five or more times | 3 (2.5) |
| Don’t know | 7 (5.9) |
| No recorded response | 29 (24.6) |
| For the 35 decedents who reported using OOH services, who did the decedent contact (last time this happened)? | |
| Own GP or OOH number | 25 (71.4) |
| NHS Direct | 1 (2.8) |
| District nurses | 3 (8.6) |
| No recorded response | 6 (17.1) |
| What happened as a result of making contact in the evening or weekend | |
| Advised to call 999 | 3 (8.6) |
| Advised to go to A&E | 1 (2.8) |
| The OOH service called an ambulance | 1 (2.8) |
| They were visited by their own GP at home | 2 (5.7) |
| They were visited by another GP at home | 13 (37.1) |
| Advice was given over the phone, no visit | 1 (2.8) |
| No recorded response | 14 (40.0) |
| Was this the right thing for them to do or not? | |
| Yes | 26 (74.3) |
| No | 3 (8.6) |
| Don’t know | 3 (8.6) |
| No recorded response | 3 (8.6) |
Medication
Deficiencies in the information relating to medication, or choice of medication, were reported by few respondents, with misunderstandings or errors recalled by 14 carers (12%) (Table 11).
| Questions | Responses, n (%) | |||
|---|---|---|---|---|
| Yes | No | Don’t know | N/A or non-response | |
| Was the decendent or carer given enough information about the medications that the decendent was taking? | 42 (35.6) | 19 (16.1) | 2 (1.7) | 55 (46.6) |
| Was the decedent or carer given enough choice about the medications that the decendent was taking? | 21 (17.8) | 14 (11.9) | 8 (6.8) | 75 (63.6) |
| Were there any incidents when there was a misunderstanding or error regarding mediations? | 14 (11.9) | 61 (51.7) | 4 (3.4) | 39 (33.3) |
| Throughout the last 3 months, did all the professionals know enough about the decedent’s medication? | 53 (44.9) | 7 (5.9) | 9 (7.6) | 49 (41.5) |
Death and bereavement
Carers of two-thirds of decedents believed that their relative or friend was aware that they were about to die, though a substantial proportion of decedents (40%) had not been told by a health professional or family member. Fewer than one-third had expressed a preference for place of death but, for almost all of these, the preferred place was home. Most respondents felt that the choice over place of death was sufficient, and around one-quarter said that it was important to have choices. In retrospect, 85 (72%) participants felt that the decedent died in the right place (Table 12).
| Questions | Responses, n (%) |
|---|---|
| Did the decedent know they were likely to die? | |
| Yes | 78 (66.1) |
| No | 20 (16.9) |
| Not sure | 3 (11) |
| Not applicable or no recorded response | 9 (7.6) |
| Who had told them they were likely to die? | |
| Hospital doctor | 19 (16.1) |
| GP | 2 (1.7) |
| Family member | 3 (2.5) |
| No one | 47 (39.8) |
| Don’t know | 7 (5.9) |
| Not applicable or no recorded response | 40 (33.9) |
| Did the decedent ever say where they would like to die? | |
| Yes | 34 (28.8) |
| No | 64 (54.2) |
| Not sure | 2 (1.7) |
| Not applicable or no recorded response | 18 (15.3) |
| Where did they say they would like to die? | |
| Home | 32 (27.1) |
| Hospice | 2 (1.7) |
| Hospital | 1 (< 1) |
| Care home | 1 (< 1) |
| Somewhere else | 1 (< 1) |
| Not applicable or no recorded response | 81 (68.6) |
| Did you have enough choice about where the decedent died? | |
| Yes | 25 (21.2) |
| No | 13 (11) |
| Don’t know | 10 (8.5) |
| Not applicable or no recorded response | 70 (59.3) |
| How important to the carer/decedent was it to have choices? | |
| Very important | 23 (19.5) |
| Fairly important | 10 (8.5) |
| Not important | 3 (2.5) |
| Not applicable or no recorded response | 82 (69.5) |
| On balance, did the decedent die in the right place? | |
| Yes | 85 (72) |
| No | 9 (7.6) |
| Not sure | 7 (5.9) |
| Don’t know | 6 (5.1) |
| No recorded response | 11 (9.3) |
Care homes
Ten decedents were living in a care home for most of the last 3 months of life, but 19 died in a care home. Seven people moved into a home within 1 month of their death. Care needs that could not be met at home were the most frequently cited reason for admission (Table 13).
| Questions | Responses, n (%) |
|---|---|
| During the last 3 months, was the decedent admitted to a care home at all? | |
| Yes | 19 (16.1) |
| All other responses | 99 (83.9) |
| During the last 3 months, did the decedent live for most of the time in a care home? | |
| Yes | 10 (8.5) |
| All other responses | 108 (91.5) |
| Where was the decedent living when they were admitted to a care home? | |
| Own home | 8 (6.8) |
| With friends or relatives | 1 (< 1) |
| Other care home | 2 (1.7) |
| Hospice | 1 (< 1) |
| Other | 12 (10.2) |
| Not applicable or no response | 94 (79.7) |
| How long did they spend in a care home on the last admission? | |
| One week or less | 2 (1.6) |
| One to 4 weeks | 5 (4.2) |
| More than 4 weeks | 2 (1.6) |
| Not applicable or no response | 109 (92.4) |
| Why was the decedent admitted to a care home? | |
| Care needs | 11 (9.3) |
| Respite | 4 (3.4) |
| Rehabilitation | 2 (1.7) |
| Not applicable or no response | 101 (85.6) |
Care at home
Most decedents had spent time at home in the last 3 months of life. Relatively small proportions of carers recalled care from specialist nurses, but social carers were a commonly reported component of end-of-life care. Informal carers were the most frequently cited additional sources of care. Twenty-seven patients (23%) were known to have had their care needs assessed on at least one occasion. This led to observed changes in the care received for 15 patients. All of the health and social services involved in the care worked well together (definitely or to some extent) for 20 (17%) respondents. Six carers reported that the services did not work well together. Help to meet personal care needs was reported as sufficient for 42 decedents (45%).
In the last 3 months of life, 45 (38%) of carers reported that the decedent had experienced pain. Forty of these had treatment for the pain; 21 had their pain relieved some or all of the time. Thirty-three carers (32%) felt that all or most of the community staff knew enough about the decedent’s condition or treatment.
Care in hospital
Forty-five (38%) of the decedents experienced pain during their hospital stay, the majority of whom received treatment for the pain (Table 14). The question of whether or not the treatment relieved their pain was answered by a low proportion of respondents. More than half of carers felt that the hospital staff treated their relative with respect and dignity most or all of the time, and a similar proportion had sufficient opportunities to talk privately with their relative or friend while they were an inpatient.
| Questions | Responses, n (%) |
|---|---|
| During this hospital stay, did they experience any pain? | |
| Yes | 45 (38) |
| No | 36 (30.5) |
| Don’t know | 9 (7.6) |
| Not applicable or no recorded response | 28 (23.7) |
| Did they have any treatment of their pain? | |
| Yes | 40 (33.9) |
| No | 6 (5) |
| Don’t know | 3 (2.5) |
| Not applicable or no recorded response | 69 (58.5) |
| Did the treatment relieve their pain? | |
| Completely, all of the time | 12 (10.2) |
| Some of the time | 11 (9.3) |
| Partially | 2 (1.7) |
| Not at all | 2 (1.7) |
| Don’t know | 8 (6.8) |
| Not applicable or no recorded response | 83 (70.3) |
| Did you have confidence and trust in the staff who were caring for them? | |
| Yes, in all of them | 48 (40.7) |
| Yes, in some of them | 26 (22) |
| No, not in any of them | 10 (8.5) |
| Don’t know | 1 (0.8) |
| Not applicable or no recorded response | 33 (28) |
| Do you feel that the staff had time to listen and discuss things? | |
| Yes, definitely | 31 (26.3) |
| Yes, to some extent | 31 (26.3) |
| No | 16 (13.6) |
| Don’t know | 1 (0.8) |
| Not applicable or no recorded response | 39 (33.1) |
| Were you able to discuss with the any worries or fears that you may have had about his/her condition, treatment or tests? | |
| Yes, I discussed them as much as I wanted | 25 (21.2) |
| Yes, I discussed them, but not as much as I wanted | 11 (9.3) |
| No, although I tried to discuss them | 12 (10.2) |
| No, but I did not try to discuss them | 6 (5.1) |
| Don’t know | 4 (3.4) |
| I had no worries or fears to discuss | 6 (5.1) |
| Not applicable or no recorded response | 54 (45.8) |
| How much of the time were you treated with respect and dignity by the doctors, nurses and other hospital staff? | |
| Always | 43 (36.4) |
| Most of the time | 21 (17.8) |
| Some of the time | 9 (7.6) |
| Never | 6 (5.1) |
| Don’t know | 4 (3.4) |
| Not applicable or no recorded response | 35 (29.7) |
Twenty-eight (24%) carers reported that they were involved a little or not at all in decisions about care. However, levels of confidence and trust in staff were high; 74 (63%) had confidence and trust in some or all of the staff and 62 (52%) reported that the staff had time to listen and discuss things, although 29 (25%) did not discuss worries or fears as much as they would have liked. Forty-nine (42%) reported that most or all of the staff knew enough about the decedent’s condition or treatment. Overall ratings of the care were excellent or good for just over half of doctors (51%) and nurses (56%). Around one-quarter of carers perceived a change in the decedent’s quality of life (23%) or health (24%) as a result of the hospital admission. Reported practical problems during hospital stays were few. Sixteen people had problems with car parking, and 15 with extra expenses incurred as a result of the hospital admission.
Care experiences of decedents with different conditions
A higher proportion of patients with cancer died at home compared with people with other diagnoses [12 (41%) where home includes relatives’ homes and care homes]. Eleven (38%) cancer patients died in hospital compared with 27 (69%) heart failure patients, 17 (61%) people with stroke and 13 (59%) with COPD. Carers of people with heart failure and stroke were less likely than others to report that the care received was flexible to the patients’ needs or that they had enough information and help. However, the ratings of GP care were similar across the diagnostic groups.
Reported differences by socioeconomic status of carer
There was a general tendency observed throughout the data set for more advantaged carers to be critical, particularly in relation to information giving and participating in decision-making processes. However, it is important to note that carers from advantaged areas were over-represented. Carers in more advantaged IMD quintiles appeared to be less likely to report that care was flexible, that they had enough information, or that care was excellent or good. They were more likely to report that some of the transitions in the last 3 months could have been avoided. However, with increasing advantage, carers were more likely to report that they were able to discuss their concerns with the staff and that professionals had time to listen. Selected findings are presented in Table 15 but interpretation of these data should be cautious because numbers in each IMD quintile are small.
| Questions | Quintiles 1 and 2 (most disadvantaged), n (%) | Quintile 3, n (%) | Quintile 4, n (%) | Quintile 5 (least disadvantaged), n (%) | Total responses to this question, N |
|---|---|---|---|---|---|
| Yes, care flexible to decedent’s needs | 9 (75) | 12 (63) | 18 (72) | 16 (55) | 55 |
| Yes, everyone involved had enough information about decedent’s needs | 13 (76) | 14 (67) | 17 (61) | 17 (53) | 61 |
| Overall help and support was excellent or good | 12 (86) | 8 (60) | 10 (100) | 9 (64) | 37 |
| Transitions could have been avoided | 3 (20) | 5 (31) | 8 (31) | 9 (33) | 85 |
| Given enough choice about place of death | 8 (53) | 4 (33) | 4 (50) | 9 (69) | 48 |
| Having choice in place of death very important | 6 (60) | 6 (67) | 3 (50) | 8 (73) | 36 |
| Given enough information about medications | 10 (77) | 7 (58) | 12 (71) | 13 (65) | 62 |
| Given enough choice of medications | 9 (75) | 6 (68) | 4 (40) | 2 (18) | 43 |
In multivariate analyses (not presented), neither age of patient or carer, IMD nor diagnosis were significant influences on place of death or responses to questions on the overall co-ordination of care.
-
Most decedents spent time at home in the last year of life and were admitted to hospital. Up to one in five decedents in this study spent some time in a care home.
-
The GP was the main contact person for most families and the care they provided was rated more highly than hospital care.
-
Practical problems associated with transitions were seldom reported.
-
Most admissions to hospital were precipitated by deterioration in health status.
-
Many respondents considered that care received was not well co-ordinated, and many reported that they needed more help and support and more time to discuss their concerns.
-
There was a tendency for carers of people with heart failure and stroke and those from more disadvantaged areas to report poorer experiences.
-
Few respondents felt that any of the transitions could have been avoided.
Qualitative data findings
The following section synthesises data from the 191 qualitative interviews in this study: 30 interviews with patients, 118 with bereaved caregivers and 43 with health and social care professionals. As the volume of data is large, it is possible to present only an overview of the work here. More detailed and reflective interpretations of the data will be presented elsewhere. The few direct quotations that are included have been chosen to represent the larger body of data.
Satisfaction
We did not ask patients and carers directly about whether or not they were satisfied with services, but most raised issues in their interviews that are relevant to the domains of satisfaction. The literature on satisfaction is extensive, yet data from our participants was encompassed by the domains proposed by Donabedian67 more than three decades ago: accessibility, continuity, efficacy, availability, finances, the physical environment, the technical aspects and art of care. The patient interviewees raised many issues relating to continuity, availability and the art of care. The great majority of the bereaved family carers spoke openly and in detail about the decedent’s illness, end-of-life care transitions, their own roles as family carers, and their experiences when the decedent was dying and care after the decedent’s death. Many of the carer participants also wanted to share their perspectives on how they were coping in their bereavement.
Overall, the carer participants fell into three groups: approximately one-third of participants were very satisfied with the care provided; approximately one-third were generally happy but felt that attention to one or more specific issues could help improve end-of-life care for others; and approximately one-third had some serious concerns about the care received. None of the carers was universally critical.
Synthesised findings from patients, carers and professionals
Six separate themes are reported, based on analysis across the three data sets, from patients, carers and professionals:
-
an imperfect system with beacons of excellence
-
perspectives on the carer’s role
-
general practitioner and out-of-hours care
-
communication and expectations about death and dying
-
choice and the influence of personal finances
-
interprofessional relationships.
An imperfect system with beacons of excellence
Patients’ experiences of transitions between care settings at the end of life were characterised by disjointed care provision, with essential components of care, such as organising medication or getting input from social services, apparently dependent upon system imperatives and processes instead of being tailored to individual needs. Older adults reported feeling unsupported and unheard as they changed care setting, with many participants devoid of an ongoing relationship with a family doctor. 85 The carers’ narratives supported the patients’ impressions of a system that presented an uncoordinated front to families and was not focused on the patients’ experiences. Such discontinuity was observed between services, when, for example, an absence of in-hospital physiotherapy delayed hospital discharge, disrupting social care arrangements. It also emerged in descriptions of transitions into hospital, when the constraints of the ambulance service result in patients being discharged and admitted to different hospitals within hours for the same problem.
Beacons of excellence
For patients, even where the overall experience of transitions was not wholly good, individual health professionals were singled out for praise and not held accountable for broader deficiencies within the system. Similarly, almost all of the carers’ criticism of services related to the ways in which systems were organised and resources allocated. Bereaved family members were very appreciative of the care provided for the decedent and for them by health and social care professionals. Some individuals were identified as providing particularly high-quality care; often, this was where the bereaved family carer considered that the member of staff had provided care which demonstrated personal concern, a personal sense of vocation or what they considered to be beyond usual procedural expectations. Examples included doctors and nurses providing follow-up visits or telephone calls, staff attending patients’ funerals (in their own time) and taking time to communicate clearly and to ensure that care was fully co-ordinated. Some participants discussed strategies that they had developed to overcome poor care provision by particular individuals. This included direct challenges, explanations and demonstrations of appropriate care for inexperienced staff such as junior doctors and domiciliary or care home staff.
Family carers expressed awareness of the pressures faced by staff with large numbers of patients to care for and limited time available. In hospital settings and for domiciliary carers, these pressures were described as acutely observable. For GPs and community nurses, this awareness was often presumed rather than observed, and was used as a context for the carers’ gratitude for professionals’ attentions.
Perspectives on the carer’s role
Patients’ views of carers
Patients’ accounts highlighted the roles adopted by carers across transitions. While at home, the carer is often the main co-ordinator of care, taking responsibility for liaising with a range of professional carers. During and after a transition into hospital or other institution, the carer is required to take on a supporting role as professionals take over the responsibility for the patients’ well-being. Carers described how they became advocates, filled perceived gaps in the care and maintained continuity and support. The carers’ influence on decision-making in hospital was perceived by all to be limited, despite their unique insight into the individualised care required. Patients observed great flexibility in the way that carers switched between these two contrasting roles of supporter and co-ordinator, particularly when admissions and readmissions were frequent. 86
Carers’ views
Family carers considered themselves to be the people primarily responsible for co-ordinating care and ensuring that the care recipient’s needs were met. They typically went to enormous efforts to maintain a focus on ensuring their provision of high-quality care. The extent of the efforts undertaken is evident from their retrospective accounts in bereavement, where family carers pondered how they were able to sustain such emotionally and physically demanding caring tasks, and often recognised that they negated their own needs.
Yes, I mean at the time you just grit your teeth and get on with it, and you do what you do, and do it all the time. You know people said to me, oh fancy doing all that nursing. I said, well it didn’t seem like nursing to me at the time. It was just what we needed to do to get through every day, so we did it.
59-year-old widow of 72-year-old man who died with heart failure, S103
Many carers identified a tipping point in the care recipient’s physical condition, beyond which they would request professional assistance. They expected professionals to be responsive when the care recipient’s condition reached the limits of their competence and they did not seek a partnership relationship with professionals. Transitions were often associated with such points in the caring trajectory when care needs exceeded family carers’ ability to provide care, and guilt was a common response from family carers. This applied even where help with caring was considered essential by health professionals. In these circumstances, if a move to an institution followed, family carers would continue to provide emotional support with regular visits as appropriate, often working alongside or supplementing professional carers’ input in all settings except hospice.
Professional’ views of carers
Interviewed professionals held conflicting views of family carers as both a resource for professionals providing care and a group who require care and support themselves. For many professionals, their ability to empathise with the difficulties and demands of family caring at the end of life was supported by examples from their own personal experiences, and reflections on how family caring may be experienced by people who have not worked in health and social care services.
Carers as a resource for professionals
Professionals identified two main ways in which family carers can be a resource for their own work. Firstly, the simple presence or absence of a carer can affect transitions between care settings, enabling older adults to stay at home for longer, reducing the chances of admission to a hospital, hospice or care home, and enabling transitions to occur in a timely manner. Carers provide a point of liaison between professionals and their patients or clients, and supply key information about the patient’s condition, needs, preferences and treatment. For individuals without readily available family carers, professionals can sometimes provide enhanced support. Some of this support is provided through established procedures, and some is freely given by staff who see the particular needs and have a personal and professional wish to increase support. However, this generally did not substitute completely for the involvement of family carers, so that professionals felt that these individuals were far more likely to receive care in an institutional setting than those with carers.
If there is nobody in the home with the person, it’s not practical for them to stay at home unfortunately.
So what tends to happen if there isn’t anybody available?
They tend to go into residential care or nursing care depending on the needs at that time.
Community matron, north (15)
Historically that has been a big problem because they are the ones that end up going into hospital because they haven’t got anybody else to care for them. Erm . . . or into a care home.
Health commissioner for end-of-life care, north (20)
The more the family is able to take on then quite often the quicker we are able to get them home.
Specialist stroke nurse in an acute trust, south (31)
Carers as a challenge to professionals
Family carers’ presence and their relationships with the care recipient and professionals can also mean that they are well placed to defend a patient’s case, seek clarification from or challenge professionals. While some professionals viewed this involvement positively in ensuring patients received the best possible care, others resented the style of and expectations behind some interventions from family carers. Working with carers is recognised as sometimes quite challenging for professionals, particularly in situations of rapid change, where conflict or limited understanding exist, and where professionals do not have an existing relationship with patients and their family carers. Most accounts recognised the importance of engaging appropriately with family carers and with patients in these circumstances to resolve misunderstandings and to enable the best possible care for patients.
Co-patients
Professionals also recognised the demands placed on family carers and the limits of carers’ abilities to positively influence decision-making about transitions between care settings when a care recipient is at the end of life. This awareness extends to the emotional and physical burdens of family caring and the vulnerability of accompanying the care recipient through their end-of-life journey, as well as carers’ own needs, which may include existing medical conditions, and anxiety, fear and panic arising from the responsibilities of their family caring role.
You have two people who are going through this illness, you have, well you have the patient and their significant other, and then if you have got other family members, they are all going through that experience too and everybody is going through it at a different point.
Palliative care nurse specialist in an acute hospital, south (16)
The emotions that are aroused when family carers feel unsupported are perceived by professionals to lead to some admissions that might have been avoided otherwise. Participating professionals felt more generally that family carers’ lack of support may impede their ability to provide high-quality end-of-life care in appropriate settings. Professionals felt that support for family carers should be enhanced while exercising their family carer role and also in bereavement, but they acknowledged that family carers are often unaware of existing support opportunities and services. Family carers’ lack of expertise in end-of-life care may be associated with unrealistic expectations and poor understanding of the ways in which complex systems function. Family carers may also hold ideas about appropriate nature and settings for end-of-life care which conflict with views held by professionals.
We may come out with a different conclusion than the family, we might be actually saying to the service user, yes, we can manage and support you at home, with a package of care and of course daughter has already made her mind up mom is best placed in care.
Senior social care manager, north-west (38)
They [family carers] may not always be informed, they may not always be aware and I think sometimes their expectation of what can be delivered is not realistic.
Matron for older people’s services in an acute hospital, south (18)
General practitioner and out-of-hours care
A high proportion of the patients in this study did not have a relationship with a single GP who provided continuity of care and ongoing support. Patients with lung cancer were more likely to see the hospital as the focus of their care while they were receiving active treatment. In common with others with chronic illness, many patients with heart failure were reluctant to consult services, feeling that they had exhausted everything that the professionals had to offer. Relationships with health professionals had often lasted many years, and this aspect of the participants’ biography clearly influenced their perceptions of how much choice and control they had over their own care. Two broad sets of experiences were evident. A majority had maintained a traditional doctor–patient relationship, with the doctor influential at significant moments in the interviewees’ lives; the decision to retire early from work, or caring for a spouse in their terminal illness, for example. A reluctance to disobey the doctor was typical of this group; they adopted the attitude that the doctor knows best.
A smaller group of interviewees had lost trust in their health professionals over many years, as their doctors failed to meet their expectations. Patients with heart failure often tolerated a high burden of symptoms; this was particularly the case for the most disadvantaged interviewees. Some of these were reluctant to request input from GPs until they were too unwell to be cared for at home and had no option but to accept the need for urgent hospital admission.
Among all patients, when communication within consultations was discussed, it was to report less satisfactory experiences. A significant minority reported that they could not talk to their family doctors. Too much attention given to the computer within consultations gave an impression that the doctor was not listening. One female participant described her doctor as ‘playing the piano’ on his computer. Use of language that the participants did not understand further distanced the patient from explanations and perhaps understanding of their care.
Dr A, when I go to see her, she always got a blinking, clicking away at the television in front of her, listening to you, and I always think, oh she is taking no darn notice of me, here.
And, he [a hospital doctor] looked after me, but they didn’t explain. Well he might have explained but I couldn’t understand what it was. Well I think it’s these words, you know, a bit too high up for me.
Female with heart failure, age 84 years
People who saw little of their family doctors also relied more than other respondents on the community nurse as a source of advice and support.
He [the GP] doesn’t listen to you and he won’t come out and visit you. I have always relied on [. . .] the specialist community nurse. I mean my trust is in her.
Female with heart failure, age 69 years
The GP has a role as gatekeeper to other community services and specialist care, so that a poor relationship or limited contact may influence access to other aspects of health and social care. The implications of this for the patients were neither acknowledged nor discussed, but examples were presented of how it increased the stress and burden on the carers.
Carers and general practitioners
Many carers rated the care from their GPs highly; they trusted the GP as someone known to them and to the patient, and who knew them. In GPs, they looked for responsive, empathetic and expert partners in care who are flexible and honest. Taking time for their patient was particularly appreciated. GPs were described as looking out for them, working in tandem with the carer. Some GPs provided continuity, and although this was valued, it was not an essential criterion for satisfaction with care. Family carers did not see GPs as providing a co-ordinating role, but were surprised and pleased when GPs liaised with other services on their behalf. How GPs perform their role seems to be more important than the actions themselves in how family carers understand the role of the GP. For example, a trusted GP was regarded very positively by a family for telephoning through a prescription for steroids, while a GP prescribing by telephone for a woman living in a care home was regarded very negatively by her son living 100 miles away, who had difficulty making contact with the GP.
Carers were less satisfied when the GP did not take time to come and see the patient at home or in a care home, or spent very little time with patients when they did. Failure to meet carers’ expectations, such as taking necessary steps for admission into hospital when carers felt that this was needed, was a source of dissatisfaction. Carers also regretted that when the GP was unavailable continuity was lost, though they were keen not to blame individual doctors for this.
Professionals and general practitioners
The professional interviews examined both GPs’ experiences and perceptions of their own roles in relation to end-of-life transitions, and other health and social care providers’ and commissioners’ experiences of working with GPs and their views about the roles that GPs play.
The GPs interviewed in this study shared an involved, committed approach to transitions at the end of life. They understood it to be an area of care which fell under the responsibility of general practice and was not distinct from their general work. All of the doctors were aware of the challenges inherent in this area; in particular, how difficult it may be to identify when an individual is nearing the end of life. GPs described how they are involved in co-ordinating care, including involvement in decision-making before transitions happen and avoiding admissions to hospital, and in following up after transitions have occurred.
General practitioners perceived decision-making around transitions at the end as an area in which they exercised their professional judgment and discretion. GPs value being able to work autonomously, making decisions which they consider to be in patients’ best interests rather than working within what they might see as rigid policy guidance or according to colleagues’ guidance. They were less likely to identify policy as a guide, with only one GP singling out the GSF as having an impact on practice. However, they also acknowledged that exercising professional judgement might not produce a body of GPs who all work in the same way.
When discussing their involvement in transitions at the end of life, the GPs highlighted the importance of having a good relationship with patients and carers. This was perceived to be essential to providing appropriate care. Knowledge of a patient’s medical history and social context limited the need for information from other professionals, enabling doctors to provide timely care.
If you were asking me for example about how to get the best care for an elderly relative of yours at the end of their life then I would say do your best to get to establish a relationship with one GP from the practice, and erm . . . and try and do that and try and erm . . . work on that basis, really, because that, as I keep saying, is key.
General practitioner, north (24)
Establishing trust between the patient and the GP was felt to be important for the success of doctors’ interventions in transitions at the end of life. Having an honest conversation with patients was upheld as a goal, although achieving this level of communication in practice was often difficult. One professional admitted to not discussing transitions about which it was felt he could do nothing. Another interviewee referred to a more generalised reluctance among professionals to discuss end-of-life issues.
There is quite a reluctance amongst doctors to talk about this [planning for end of life], probably more of a reluctance amongst doctors than patients, although some patients don’t want to.
General practitioner, north (41)
They valued establishing trust and having honest discussions with patients and family carers. This might, as described by one of the interviewees, involve shouldering the responsibility for a decision that another professional might otherwise be reluctant to support.
Ultimately I have made, you know it’s my head on the block if I have made the wrong decision but you know I have said I will take responsibility for that capacity decision, therefore, I am taking responsibility for saying yes, she can go home, so if something goes wrong it’s me, that is going to be held to account not you [social worker], don’t worry.
General practitioner, north (23)
Other professionals on general practitioners’ role in transitions at the end of life
Other professionals identified a number of specific expectations of GPs in end-of-life care. They expected GPs to play a leading role in transitions at the end of life. In contrast with their own roles, other professionals usually expected the GP to have continuity in their professional relationships with patients and their families in ways that should enable co-ordination of care. GPs were expected to identify end of life, talk with patients about planning for death, document these conversations and their outcomes, and to make referrals to appropriate services. GPs were also expected to verify and certify deaths, to reduce further distress for bereaved relatives of a post mortem and coroner’s involvement. For some respondents, alongside these expectations of GPs, lay a hope that GPs were a potential solution to many difficulties in transitions between care settings and interfaces between services.
While other professionals expected GPs to be pivotal in transitions at the end of life in the ways described above, they were critical of how well doctors fulfilled this role. They regretted that the conversations between doctors and patients, which they saw as an essential foundation for care provision, did not systematically take place. This was perceived as distressing for patients and relatives as well as putting other professionals in delicate situations.
A lot of these patients don’t know that they have a terminal illness. They are never told and it’s not our place to tell them really. We feel that needs to come from the GP . . . the GP or the consultant.
Community matron, north-west (28)
It’s really back to that old chestnut about how, at what point somebody has a conversation with somebody [. . .] and that includes primary care, and I still think we have got a bit of a long way to go with that, you know. We are still finding that it’s sometimes quite late in the day, that a conversation about somebody’s prognosis takes place, and obviously until you have had that, it is quite difficult to put all the planning in place
Director of nursing in a primary care cluster, south (22)
The tension stemming from professionals’ expectations of GPs in transitions at the end of life, on the one hand, and their criticism of GP limitations, on the other, was echoed in their attitudes to the system’s shift towards greater provision of care in the community. Several professionals and clinical commissioning groups, saw this as an opportunity to strengthen GP involvement in end-of-life care provision. Many others, staff working in the acute setting in particular, were concerned that primary care was not equipped to manage those patients most likely to undergo transitions at the end of life.
The expectation of expertise was a major challenge to the GPs’ central role. They were open about the difficulties that they may have in identifying which of the many people encountered in routine general practice are most likely to be at the end of life, in order to know with whom to initiate discussions about preferences and to implement appropriate care. Already-stretched resources and pressures associated with mismatches between acute and community provision were cited by GPs as barriers to good end-of-life care provision.
Many of the other professionals work within strict guidelines and protocols, and have few opportunities to exercise their own professional judgement. This contrasts with what they regard as the more wide-ranging role of GPs. When GPs choose not to undertake their role in ways that dovetail with other professionals’ procedures, this can create difficulties for the other professionals and, they feel, the wider delivery of end-of-life care. Tensions also arise between other professionals and GPs when doctors fail to engage with procedures.
A common complaint was that GPs did not communicate their decisions and care planning in ways that are meaningful for, and fit with, the procedures of other professionals and services. In these situations, both GPs and other professionals are dissatisfied because they have not fulfilled expectations of each other.
GPs are difficult people to pin down (laughs) and get them to write things in patients’ notes. I have often said I wouldn’t let him or her out through the door, until she has documented it. There is no point saying over your shoulder ‘no heroics for Mrs Smith’ you know, that needs documenting properly. I would be chasing after them saying, what do you mean, no heroics?
Urgent care services manager in a primary care trust, north-west (37)
. . . Not having GPs on board: as a team we felt that that was quite a big, erm . . . a very significant erm . . . area, because we can all name GP practices within this area that, that is oh no that one will have to go here or there, you know they just will not deal with the Liverpool Care Pathway, they won’t put them on it, or they feel that there is something wrong here, or, and they just, decline to engage with the nurses.
Health needs assessor in a primary care trust, south (40)
They don’t like doing them [Ambulance Anticipatory Care Plans] because it’s another form to fill out, so we have got a lot of resistance from GPs.
Clinical assurance quality lead for ambulance services, south (12)
Different and non-compatible IT systems for GP surgeries, acute settings, ambulance and out-of-hours services are also acknowledged as impeding communication between professionals. A number of other professionals also suggested that prognostication is difficult and that GPs probably do not see sufficient numbers of people at the end of life to develop expertise in end-of-life care.
While a small number of family carers spoke about NHS Direct or contacting known district or specialist nursing services for advice, most family carers relied on their GPs and paramedic responses when they judged that the care recipient’s needs had reached a critical point. Out-of-hours GP services were also accessed with mixed results. Some family carers valued the full evaluation that this allowed, while others were concerned about waiting times and a high probability of a hospital admission being recommended by a GP who did not know the care recipient or their needs. In general, there seemed to be limited awareness among family carers of any services other than the GP or ambulance service.
GP out-of-hours service provision was highlighted as an obstacle to continuity of care, and staff from the acute setting, in particular, felt that the service’s involvement often led to inappropriate transfers and unnecessary admissions into hospital.
I think the out of hours doctors system I am afraid has a lot to answer for, there seems to be a lot of disquiet amongst the patients and amongst my colleagues, about the support from that particular service.
. . . It’s somebody that doesn’t know who they are, and if they don’t know who they are, they perhaps are more likely to suggest that they come in to hospital rather than . . . I have to say there are still elements where it sounds like they don’t go out and visit at all but are doing a telephone consultation and then making a decision.
Palliative care nurse specialist in an acute hospital, south (16)
. . . There is a big difference between taking calls in-hours from people’s GPs versus out-of-hours from a deputising service. And, I think the feeling of all of us is that we are not infrequently, not all the time, but not infrequently, admitting people who really, it’s not appropriate. They are end stage dementia in a care home, and been deteriorating for quite some time and now they have got really unwell. If it was in-hours maybe their own GP would go out and see them and maybe have a have a conversation about what they thought the best thing was. But if that happens at 9 o’clock at night the nursing home are either going to phone an ambulance or they are going to phone the out of hours service, who will turn up and go – this person looks horrible and phone an ambulance.
Consultant in the acute medical unit of a hospital, south (36)
Many of the data reinforced the influence of past experiences on use of services. Family carers relied on their understanding of health services gained over a lifetime, rather than acting on new information or being signposted to specialist services. Where carers had professional experience of health and social care services, or had access to such expertise through social networks, this was drawn upon as a source of confidence when liaising with professionals. Experience in qualified and senior roles was mentioned much more frequently than domiciliary or care-home caring roles. However, several family carers on low incomes and with no experience in health or social care also expressed confidence about interactions with professionals. These family carers, who were predominantly located in north-west England, used a strong sense of justice and fairness as their motivation and source of confidence. Several older family carers with professional experience in nursing, social care and allied health professional roles were very aware of its currency and seemed to disregard this experience because they had retired more than 10 years ago.
Communication and expectations about dying and death
Breaking bad news sensitively about terminal diagnoses and prognoses is very important to older adults. Its relevance to subsequent use of services, and transitions between services, is well known but often overlooked. In this study, patients recalled the way in which their diagnosis and its implications had been discussed with them. The pace and clarity of the communication and the presence of supporters were important factors to patients. Patients with heart failure were different from the others, as none had been given information on the likely prognosis associated with their diagnosis. 87
Sensitively conducted initial discussion can also greatly help carers in understanding the nature of the condition and the likely pattern of events and services required. Even when faced with the news that the individual may die soon, family carers were aware of and appreciated the efforts of clinicians in taking the time to provide explanations in a supportive manner. This experience colours attitudes to services and individuals. It may also influence the way in which carers choose to bring services in, with all the implications that this has for the number and timing of transitions.
. . . that was clever of the consultant wasn’t it, because [specialist nurse] was already in that room . . . it was nicely done . . . He was a charming man, perfectly charming, very handsome man, I might tell you and he conducted his consultation beautifully really. You felt you could ask him any questions, which is what it’s all about. In fact he did say ‘have you any questions’, well, I couldn’t think of a thing to ask . . . he said ‘well we will find a little room and you can . . .’ and this is when she [specialist nurse] went through all the bits and pieces and she was the one that said, that we could have carers in and the palliative nurse in and all this you see and I am thinking oh, oh do I need it, because [husband] at that time you see, he hadn’t had the fall then . . . he was really, I was going to say as fit as a fiddle but no he wasn’t as fit as a fiddle but he was fairly active. And it was later on, but you see she had already, if you think about it now, she had already put the paving stones down right at the beginning, which is how it should be . . .
76-year-old widow of 85-year-old man who died with lung cancer, S160
Bereaved family carers’ accounts presented several examples of anticipated and well-managed deaths within the prevalent cancer-derived model. There was a strong sense of expectation about being able to anticipate, acknowledge and plan for dying. Many carers and patients expected and asked for prognoses in terms of months or weeks. Where estimates were given, accuracy was expected. Even small discrepancies between the prognosis and actual date of death for a patient with heart failure were considered worthy of comment. Deaths that met the carers’ expectations were considered to be appropriately managed.
Choice and the influence of personal finances
The patient interviewees expressed strong views on welfare services and paying for care that are outwith the research questions addressed in this report, and are described in detail elsewhere. 88
Choice for carers
In general, the concept of choice had little meaning for the bereaved carers participating in our study. Younger carers (including both spousal and intergenerational carers in their early 70s or younger) were more likely to be constructively critical of services and care provision than older carers. Yet even for younger carers, there appeared to be limited orientation to the idea of being presented with choices about possible ways forward. Many seemed to understand care provision decisions as a ladder in which the next step should be taken if the previous one was no longer adequate. There was a general acceptance of professionals’ expertise. When faced with questions about choices or the extent of their involvement in decision-making, several carers appeared confused. The extent of this confusion was such that after several similar questions, the interviewers felt that they should limit or reword further questions about a concept which clearly had limited or no resonance for family carers. Despite explanations about choices, decision-making and their involvement, many family carers went on to provide an answer which was broadly evaluative of the care provided, rather than answering the specific question raised.
Some family carers recalled a discussion about wishes for the location and nature of end-of-life care. There was no mention of documenting wishes except with regards to resuscitation. In many instances, discussion about initiating or changing treatment or transitions between care settings did not include patients’ wishes.
The only thing the doctor said, and I do believe that this was contributed to the way he was, on the Thursday night when he went in, he saw a young doctor a registrar and he said to him, ‘Do you want to be resuscitated?’, the usual questions, so he said, ‘Cor too right I do, I have got plenty to do’, he was writing a book at the time. When we saw the specialist the next morning, [partner] was fine, specialist spoke to him, my daughter and I were in there with him, and he said to him, ‘Because you do know that we won’t resuscitate if anything goes wrong . . . he was so forthright it took us by surprise, erm he just said of course you know if things go wrong, he said to him I am going to keep you in for 10 days, to erm, change your medication make sure we have got it right, so that there is not too much pressure on your heart and your kidneys function properly and get rid of this water off your body. No indication that there was anything life threatening at all and within an hour of him saying that to him, he started to go down hill. As though he had lost right, that’s it, he had lost the will.
70-year-old bereaved partner of 89-year-old man who died with COPD, S110
Some health professionals displayed insight into the importance of discussing wishes with patients. Others made firm recommendations, which may have given the impression that they were disregarding patients’ expressed wishes. Family carers were generally overwhelmed by any strongly stated suggestions that contradicted their relatives’ wishes, and were ill equipped to challenge senior clinicians. When this followed a discussion about future preferences for care, it was clearly perplexing and uncomfortable for patients and their family carers. However, the tendency to selectively implement different elements of end-of-life guidelines was a theme running through the family carers’ accounts.
. . . [community matron] took all her tests and oxygen, she said we need to see the respiratory nurse, that is not always a good sign . . . she is in the hospital and she comes out when you are quite poorly but that doesn’t mean it’s just not going to be another chest infection . . . She says, ‘I want you into hospital immediately’. So mom said, ‘I am not going into hospital’. So, [respiratory nurse] phones up her boss, and says, ‘I have spoken to the family they don’t, [mother] wants to stay at home, I am suggesting she gets into hospital’, so, she then starts to talk to me about dying while mom is still in the bed. And then she turned round and said to me, ‘Get downstairs, I need to talk to you’. She said, ‘[mother] I am going to take [participant] downstairs and I am going to talk to her’. So I looked at her and I said to her, ‘You are not like Herr Flip with the Mafia are you?’, I said something along those lines, she said, ‘We need to talk about this urgently’. So we sat there and she did have a face on and she said, ‘Right your mom is very, very ill, her oxygen levels are terrible and I need to get her into hospital’. I said, ‘Well she doesn’t want to go’. And all the way through this, [community matron] has been saying, mom doesn’t need to go into hospital mom can be here. And she will get us help, she will get us nurses, although I didn’t know what that entailed, at all.
60-year-old daughter of 87-year-old woman who died with COPD, S163
Family carers with higher incomes or whose deceased family member had a higher income also had the ability to exercise choice through purchasing care themselves. A very small number spoke about paying for private health care or using occupational health insurance schemes to access tests and specialist consultations more quickly than through health service provision. More commonly, families were paying for domiciliary carers and care-home places. Several carers also reflected on the significance of accumulated self-funded costs of medical supplies such as incontinence pads and incidental expenses such as transport for visiting and paying for television and telephone in hospital.
Paying for care was only rarely described using the language of choice. The majority of self-funded care was domiciliary and care-home care where the care recipient was means-tested and required to pay because of their income or savings. In most of these situations, family carers described how the care was no different than if it had been funded care. Some family carers with higher incomes in the south and south-west felt that their being self-funding for care-home places enabled them to exercise greater influence about the timing of transitions. Carers were able to make decisions about an appropriate care home, and did not have to wait for funding decisions to be agreed and for social workers to navigate the system and set up the place for their relative.
Families often made a choice to fund supplementary care which could enable someone to be involved in activities and care at a day centre, for example. Their accounts implied that statutory provision would otherwise fall short of what they considered to be acceptable care for an older adult living at home at the end of their life.
For some families, paying for and employing a carer allowed a decedent to have continuity of care provided by a trusted person at a convenient time. This was contrasted with district nursing and also domiciliary carer provision where continuity in timing and personnel was less usual.
One of the times that she came out of hospital it was a case of well can we have any day activities for her, or anything else like that, no there is nothing you can do, so mom is just going to sit there, just rotting away so we found a private place as a day care centre, for her to be stimulated, but one of the problems was that all the time the social workers would deem her as just too old, to do anything and that was the problem.
61-year-old son of 89-year-old woman who died following a stroke, NW007
I had employed you know at my own expense this retired nurse, and near the end she came in, no she wouldn’t work weekends because her husband didn’t like it, so five days a week she would come in, and that’s right she would do the washing and all the personal stuff and aided by me because left over from my wife’s treatment I had a seat over the bath . . .
So the alternative would have been . . .
Erm . . . more work for the district nurses, I suppose. This way she got a regular, because the district nurses are not time whereas D called at the same time every morning, just every morning that’s right, because she did all the toiletry work, yes.
81-year-old husband of 84-year-old who died with lung cancer, S144
Many older adults were on low incomes and did not have savings available to pay for care. Family carers from socioeconomically disadvantaged groups were under-represented in our sample, and we do not have any examples of people on lower incomes reflecting on their inability to exercise choice through purchasing care.
Money to pay for care opens up choices about the nature, quality and type of care which are not available to those on lower incomes. This was a theme running through the interviews. Even where the actual care provision may be similar, whether means-state or self-funded, paying for care provides opportunities to influence the care setting and the timing of transitions. Where care was funded by family carers rather than care recipients, taking on this agency role appeared to be a positive thing for the carers, contributing to how fulfilled they felt in their role.
Professionals and choices
Professionals acknowledged that taking patient choice and preferences into account was an integral part of their work relating to transitions at the end of life. Interviewees provided examples of patient choice being adhered to in the hospice, hospital, care home and community settings.
Proximity to home or relatives and familiarity were singled out by professionals as guiding patient choice. Personal preferences and fear of their privacy being invaded were also mentioned as patient reasons for accepting or declining care. While they referred to several different reasons guiding patient choice, professionals mainly equated patient choice with one preference: wanting to be cared for and to die at home. Conversely, patients reported that they rarely opted for a care home as their preferred place of care and nor did they wish to be admitted into hospital. Although professionals viewed taking patient choice as part of decision-making around transitions at the end of life, they discussed what they felt were limits to the patient choice agenda.
Interviewees underlined their belief that older adults may not wish to choose where they are to be cared for. It was, therefore, not simply a matter of professionals listening to a patient’s choice and working towards complying with it. Determining what the patient wanted was a potentially delicate task for professionals, given the unappealing nature of the choices with which patients were sometimes presented. A paradox was further highlighted whereby elderly patients, used to being told what to do by professionals, were now expected to have a say in their care plans.
Professionals were wary of situations where patient choice did not agree with what they thought was best for them. This could be a source of tension, and allowing an uninformed decision to supersede professional judgement was felt by some to be problematic. Following a patient’s wishes might involve providing care in a manner which professionals did not perceive to be optimal for the patient, with the potential for favouring what they felt were unnecessary transitions. One professional admitted that, rather than offering a choice in particular circumstances where it was felt to be futile, he might not seek out patients’ involvement.
The extent to which patients had an effective choice with regards to transitions at the end of life was felt to be strongly limited by the availability of resources. The availability of carers was identified by professionals as a key determinant of whether or not a patient could be cared for at home. The choice open to isolated patients was, therefore, acknowledged to be particularly restricted. For those patients whose family disagreed with their relative, interviewees deemed the impact of patient choice to be similarly limited.
Patient choice was also felt to be constrained by the availability of services and information. Professionals regretted that the lack of flexibility and responsiveness of services, particularly in the community, hindered compliance with patient choice and preferences. Interviewees also noted that patients had a choice only if they were informed of the different options available to them. Mixed messages from professionals working disjointedly were thought to be common but particularly unhelpful.
Interprofessional relationships
The impact of deficiencies in interprofessional working on carers
Carers’ perceptions of uncoordinated care, gaps in service provision and fragmentation of services have been described in earlier sections of this report. Relationships between aspects of the NHS, particularly primary and secondary health care, were most prominent in carers’ accounts, perhaps because they were most visible to them. Carers regretted that communication and handovers between professionals did not always take place where they felt them to be necessary, and perceived frequent, repeated (and by implication unnecessary) assessments and interventions to be the consequence. Families felt compelled to take responsibility themselves and fill gaps left by deficiencies in interprofessional communication and working.
When I actually took her up to the ward, I felt a real pressure to tell them as much as I possibly could then, because I was handing over to night time staff, without English as a first language. And it was a case of trying to explain to them that she can’t do anything for her self, and really, not feeling that that was documented sufficiently. I mean it may have been, but I didn’t feel that it was documented sufficiently. And I was aware of the fact I was entrusting my mother to their care and not knowing whether they knew that she is paralysed, and she can’t talk. I said to them, she has got a really high pain threshold and if she is in pain, she really is in pain, please take it seriously. Erm . . . you know it was just the pressure I felt to get that information across to them [final hospital admission].
45-year-old carer for female patient age 78 who died with stroke, S143
I wouldn’t have minded if they, if the Macmillan had been the co-ordinator in the last 3 weeks or if her GP had been the co-ordinator in the last 3 months, but somebody, even then I am looking as though, I view it as though I was the co-ordinator, and I don’t mind.
53-year-old carer for a male patient aged 90, who died with colorectal cancer, NW019
It [hospital to care home] wasn’t very well planned as I say because I don’t think there was a handover with the information for the staff at the home. I think they just arrived in wheelchairs and they were just left there [laughs].
69-year-old carer of 71-year-old woman who died following colorectal cancer, S181
It’s the communication within the hospital, I know they are a bit pushed, erm . . . and they were putting up signs, I forget what happened but they restricted her fluid intake to get her sort of salt levels right, you know that was, you know, what was needed for her, and one I think they didn’t actually tell the carers at first and of course they overlooked the fact that it’s not just nursing staff there, carers come in, would you like a drink of water or whatever, so unless it’s actually spelt out very clearly to the carers they are going to give her a drink of water aren’t they and then they wonder why the salt balance isn’t coming back, you know.
64-year-old carer of 91-year-old man who died following a stroke, S180
Carers expressed a belief that lack of co-ordination had an adverse effect on care provision for the patient, as well as on the carers themselves. It was a source of frustration, and the resulting mixed and inconsistent messages that they received from staff caused them confusion and worry. A small number of carers identified the division of funding between health and social care as an issue that left them feeling stranded between the two services.
All her notes are there, and she was under so many clinics, what with macular degeneration, pace maker, cancer, dementia, but actually no one ever ties it together when they are in A&E, my dad was the same they didn’t know he had cancer when he was taken in poorly, see until you tell them what is wrong with them, there doesn’t seem to be a tie up.
Daughter of 78-year-old woman who died with breast cancer, S142
Professionals on interdisciplinary working
One of the main themes to emerge from professionals’ interviews was the concept of a divide between those who worked in health care, on the one side, and social care staff, on the other. There were relatively fewer accounts of successful collaboration between the two workforces, and professionals described working relationships characterised by friction and discord.
In my limited experience of working with social workers locally it’s about some sort of antagonism that I don’t understand, so professional experience is an experience that makes them not trust GPs.
GP (23)
Silos with bridges
In their descriptions of the interface between health and social care services, professionals’ accounts pointed to functional relationships when colleagues worked in the same setting, such as a hospice or acute hospital. However, when liaison across settings was required, social care and health were felt to be resistant to influence from the other side.
Relatives still feel that as a consultant, you can somehow influence it [laughs]. So often they will come to us and say, what are you going to do. And we will say, actually, we are fairly limited in what we can do, we can’t influence whether social services will take you home, we can’t influence whether rehab will take you. We can only scream and shout and stamp our feet which actually doesn’t achieve very much anyway.
Consultant geriatrician, south (34)
The absence of a common understanding or shared goal and the different languages of health and social care were themes running through health and social care accounts.
There is still a lot of myth around what social services do and what health do. And that’s amongst staff, professionals. The nursing, health staff think that we can just take people off into residential care and they almost prescribe services. They prescribe us [laughs]. ‘They need residential care’ – I mean the number of times we hear that is just frightening. This is where I believe social work is so vital, because we are about ensuring people’s rights. It’s about rights versus risks, means versus wants.
Social care commissioner (29)
We say that people are medically fit but they are not fit. You know I think the public would have a vision of these older people sitting next to their bed with their coat on and their case packed, but in fact a lot of these people are very, very frail, and what we are saying is there is nothing more medically that the hospital can do, but no one would say that these people are fit. And yet that is the language that is used. Their physical and mental health could be deteriorating rapidly, but what we do, because of this great pressure to empty hospital beds, we move people in the last two or three days of their life. And you could say that is actually quite cruel.
Social care commissioner, older people’s services (32)
Explaining the tension between health and social care
Professionals acknowledged that health and social services did not work well together. They proposed a range of reasons for deficiencies in joint working but most related either to funding or to the differing approaches to providing care.
Health and social care funding
Disagreements over funding were reported to arise most often because health and social care budgets were separate. However, the funding source was not the only cause of frustration identified by interviewees. Social care professionals expressed dissatisfaction with the Continuing Healthcare89 funding procedure, criticising its complexity for delaying care provision.
Emphasis on the contrasting approaches to care provision
The second group of explanations put forward by professionals to account for the disjointed working relationship between health and social care was a difference in their approaches to providing care. The different pace of work, contrasting emphases on legislative and regulatory frameworks were prominent in accounts from all disciplines.
Another thing for me, too, is the rate of work of social services – because they are dealing far more with chronic long term issues – is inordinately slow. Because in health . . . time is of the essence in palliative care and so . . . trying to encourage someone to see that actually no, next week is not good enough for this particular patient, it may well be good enough for someone else, but not for this person, its quite hard. But I also recognise that for social services their mode of operation is, on the whole, about long term issues, not about short term ones.
Hospice medical director (26)
It’s just such a lengthy process trying to tap into respite. You are ringing the social worker up, is there a bed available. Well I can’t sanction it, it’s got to go the . . . and then that takes a couple of days or its next week, and it’s just so convoluted trying to get the services that you need.
Community matron (15)
We have found, especially latterly with the pressure on social workers, that care for people when they are going home, tends to take even longer. Even pinning a social worker down is a lot harder than it used to be to get things started. And their condition can sometimes be quite different by the time they are ready to go home, than when they were actually assessed.
Community matron (42)
We have got the NHS and Community Care Act that gives us the framework to carry out our assessments, we have got the National Assistance Act to use. Health can use these as well, but I don’t think they think about things in relation to legislation. We have got the Mental Capacity Act that is fundamental to everything we do when people are coming to the end of their lives and they have lost the capacity to make their own decisions. Say a person is coming to the end of their life, and they may be at home and they don’t want to move from home into a nursing environment. But because of their mental health capacity we have to be the decision makers if it’s regarding social care. If it’s health care then obviously it’s a health care professional that has to be the decision maker. Then there is the court of protection that we can get involved in there . . . It happens time and time again, particularly with hospital discharges where they just expect us to rush in and put the person into care, without proper planning, without multi-professional assessments.
Social care commissioner (29)
The medical model of end-of-life care
End-of-life care was understood by all our professional interviewees to be an area where health care takes the lead, despite criticisms from social care of the appropriateness of a medical model. Examples of successful joint commissioning were given but the perception of leadership from health care left some social care staff uncertain of their contributions.
Older people in hospital are generally not looked after in the way that you and I would want them to be looked after. I think that the health service is too busy. I think there is a lack of information. I don’t believe older people get a fair deal, which is why we need to keep them at home
Social care manager (19)
Now someone specialises in your heart, or your lungs, I mean it’s getting to the stage now where somebody specialises in a part of your heart, and older people tend to have several conditions and we can’t cope with that. The health service is constantly talking about pathways. Well most older people would be on more than one pathway and these pathways don’t necessarily fit together neatly. And we can’t cope and God help them if they are then put on the end of life pathway. But they are already on the dementia pathway. And they are quite often pulling in different directions. The old style doctors [geriatricians] have retired, or died. It is very specialist, very clinical.
Social care commissioner, older people’s services (32)
Care homes
Across health, social care and ambulance services, interviewees perceived care homes to be a cause of some unnecessary transitions. Staff skills, experience, continuity and confidence were identified as influential factors, along with a reluctance to take responsibility for dying residents and a rigid adherence to protocols. Many calls to the ambulance service were felt to be unnecessary. Understanding of the impact of a low-wage economy and feeling of isolation from the NHS among care home staff was appreciated by the specialist nursing staff who worked closely with this sector.
District nurses
District nurses were perceived as the glue between many services in the community. Referred to as ‘admission avoidance teams’ by ambulance professionals, and heavily relied upon by GPs, it was clear that all participants appreciated their central role in end-of-life transitions. Other nursing staff pointed to a lack of leadership among district nurses, which limited the extent of the influence that they might have.
Impact of the health and social care divide on transitions at the end of life
Some of the professionals interviewed did acknowledge that the tensions between health and social care staff could hinder timely provision of care for end-of-life patients, especially in relation to disagreements about funding. The majority of interviews, however, reflected professionals’ propensity to attribute what they deemed inappropriate care to their social or health-care counterparts. Referring to resources in the community, for example, health-care professionals regretted that social care services were not responsive enough to provide timely care for patients. Health professionals perceived social care services to be difficult to access and regretted what they saw as a lack of commitment. Professionals provided examples of mistrust between health and social care which reinforced their description of a tense working relationship. Examples were given of social care staff asking to verify the data provided by specialist nurses, doctors who felt that social workers’ questioning of their medical decisions were ‘stalling tactics’, and one GP described a social workers’ lack of trust in his generalist expertise. Conversely, social care voiced concern about the levels of health support available in the community. Social care professionals were particularly critical of a health-care service which they perceived to be too fragmented to provide adequate care for older adults.
Professionals from both social and health care did recognise that their colleagues faced pressures and not all of their concerns took the form of blame. What professionals were less inclined to voice was the impact which the tensions between health and social care – as opposed to failings from social care or health care, depending on which side of the boundary professionals stood – had on care provision. Interviewees hinted at the impact of distrust on professionals’ decision-making around transitions at the end of life. Two of the interviews mentioned that the health and social care divide was perplexing for relatives who were not familiar with it. However, the link between interprofessional tensions on the one hand, and the consequences for care provision on the other, appears to be relatively absent from professionals’ interviews. What does clearly emerge from them is that the absence of a good working relationship causes professional frustration, is time-consuming, and has the potential to have a negative impact on care provision for older adults at the end of life.
How relationships might improve
Professionals’ awareness of the boundary between health and social care prompted them to suggest ways in which it could be softened. Greater integration, better co-ordination and improved communication links were considered key areas for fostering co-operation. Both health and social care professionals advocated joint funding where it was not already in place. In so far as it might promote common budgets and joint commissioning, the 2012 Health and Social Care Act90 was seen by a few professionals as a potential means of improving the working relationship between health and social care. Positive views were, however, outnumbered by those of professionals who perceived the reforms to be destabilising, rather than an opportunity for beneficial change.
Carers’ views on how end-of-life care should change
From their perspectives in bereavement, many family carers offered suggestions about how to improve end-of-life care. Many suggestions related to improved communication and transfer of key information between professionals. In particular, this concerned integration of IT systems to enable transfer of information between primary and secondary care and care homes, and also verbal handover of key information between professionals at interfaces between settings and at shift handover. Family carers often found themselves providing information at these interfaces, and expressed concern about potentially poor-quality care for people without readily available primary carers.
Family carers also made suggestions about improving their own contributions through better understanding of medical conditions and what to expect. Specific suggestions included having a particular person to co-ordinate all care and support the family in instances where people die at home. Moving to care homes was another area of concern, and many family carers suggested that advice and experience about what to look for when choosing a care home, how to identify high-quality nursing homes, and information and support on how to negotiate problems and delays in funding care were missing.
-
Patients’ and carers’ experiences of transitions were of a disjointed system, where organisational processes were prioritised over individual needs. Carers felt unheard and unsupported, with little control or opportunities for effective advocacy.
-
Factors that made transitions more likely or more problematic were:
-
Patient factors
-
non-cancer diagnoses
-
older age
-
unanticipated deterioration in health status
-
absence of a carer.
-
-
Health service factors
-
no ongoing relationship with a GP
-
out-of-hours doctors
-
limitations to professional prognostication and communication.
-
-
Interface factors
-
structural factors, e.g. separate health and social care budgets
-
differing approaches to protocols and guidelines
-
a lack of shared responsibility for patients across settings
-
provision of information and support to aid family decisions.
-
-
-
Carers are pivotal to care across transitions, but there is no shared understanding of their role and their expectations. Many of them lack the knowledge and support to fulfil their role as they would like. There was a particular need for more support in arranging transfers to care homes. Staff view carers either as patients in their own right who require help or as resources who smooth the professional’s path.
-
Choice is not a concept recognised by patients or carers. Greater material advantage did confer the ability to purchase services that could influence the timing and nature of transitions.
-
A mismatch was observed between the rhetoric of choice and the selective application of end-of-life policies. Choice was offered to patients and carers by some staff only if they made the ‘right’ selection.
-
Out-of-hours GP services and care homes were identified by many as the weakest links in transitions at the end of life. Staff confidence and training and closer working relationships with the health service were identified as potential solutions.
-
Older people without carers or those living alone were restricted in their care choices, and it was acknowledged that their care might be disadvantaged by their circumstances.
-
GPs saw themselves as central figures in end-of-life transitions. Other disciplines and carers concurred with this, but were critical of their abilities and expertise. Clinical skills, communication and ability to co-ordinate and organise care were brought into question.
-
Stereotypical divisions between health and social care were described, with differences in culture, language and approaches to patients or clients. Relationships were good when professionals were co-located. Structural changes in budgets and organisations were perceived to be a possible answer. The dominance of the medical model in end-of-life care was perceived to be unhelpful in creating close working relationships between health and social care.
-
The impact of interprofessional tensions on patients and families was unacknowledged by staff.
Analysis of linked hospital and mortality data
The following analysis is based on records of 187,225 people aged ≥ 75 years who died between 2000 and 2010, following admissions to hospital with heart failure in the previous 12 months, and 113,079 people who died following an admission with lung cancer. It is important to note that these cases do not represent a complete picture of deaths from lung cancer or heart failure; rather, they are deaths of people who had been admitted to hospital and their records coded with these conditions. For each individual, data on hospital utilisation relate to the 12 months prior to their date of death, and not to HES data years.
Demographic characteristics
The demographic characteristics of both patient groups are shown in Table 16. People admitted with lung cancer were younger, more of them were men and more were living in disadvantaged areas compared with the heart failure patients. A similar proportion of both groups died in hospital.
| Characteristics | Heart failure cases | Lung cancer cases |
|---|---|---|
| Sex, n (%) | ||
| Male | 84,205 (45) | 65,130 (57.6) |
| Female | 103,020 (55) | 47,949 (42.4) |
| Age (years), n (%) | ||
| 75–84 | 91,473 (48.9) | 87,119 (77) |
| 85–94 | 85,090 (45.4) | 24,972 (22.1) |
| 95+ | 10,674 (5.7) | 997 (< 1) |
| IMD quintiles, n (%) | ||
| 1 (most disadvantaged) | 36,793 (19.6) | 28,099 (24.8) |
| 2 | 39,095 (20.9) | 24,440 (21.6) |
| 3 | 40,439 (21.6) | 22,619 (20) |
| 4 | 38,103 (20.3) | 20,465 (18.1) |
| 5 (least disadvantaged) | 31,590 (16.9) | 16,715 (14.8) |
| Year of death, n | ||
| 2001 | 20,381 | 9999 |
| 2002 | 20,179 | 10,169 |
| 2003 | 20,227 | 10,694 |
| 2004 | 19,036 | 10,680 |
| 2005 | 19,149 | 11,194 |
| 2006 | 17,673 | 11,498 |
| 2007 | 17,609 | 11,878 |
| 2008 | 17,731 | 12,221 |
| 2009 | 17,327 | 12,376 |
| 2010 | 17,930 | 12,381 |
| Died in hospital, n (%) | 99,298 (53) | 60,646 (53.6) |
Deaths in hospital
Just over half of all deaths occurred in hospital (53%) in both groups, with a downward trend over time. People with lung cancer from the least disadvantaged areas were less likely to die in hospital, but the same was not true for people with heart failure (Figures 2 and 3). A higher proportion of females than males with heart failure died in hospital, and among lung cancer cases, a higher proportion of males compared with females with lung cancer (not shown).
FIGURE 2.
Proportion of deaths in hospital for lung cancer cases by IMD, 2001–10.
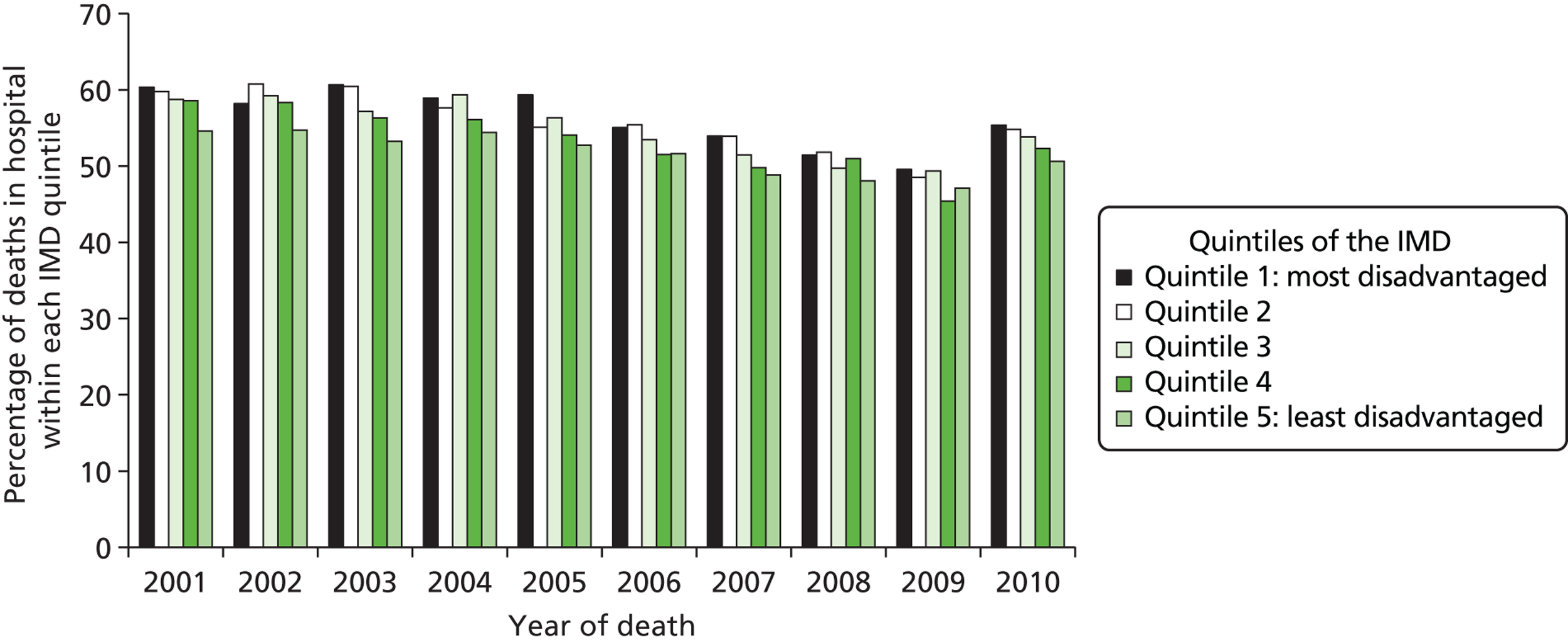
FIGURE 3.
Proportion of deaths in hospital for heart failure cases by IMD, 2001–10.
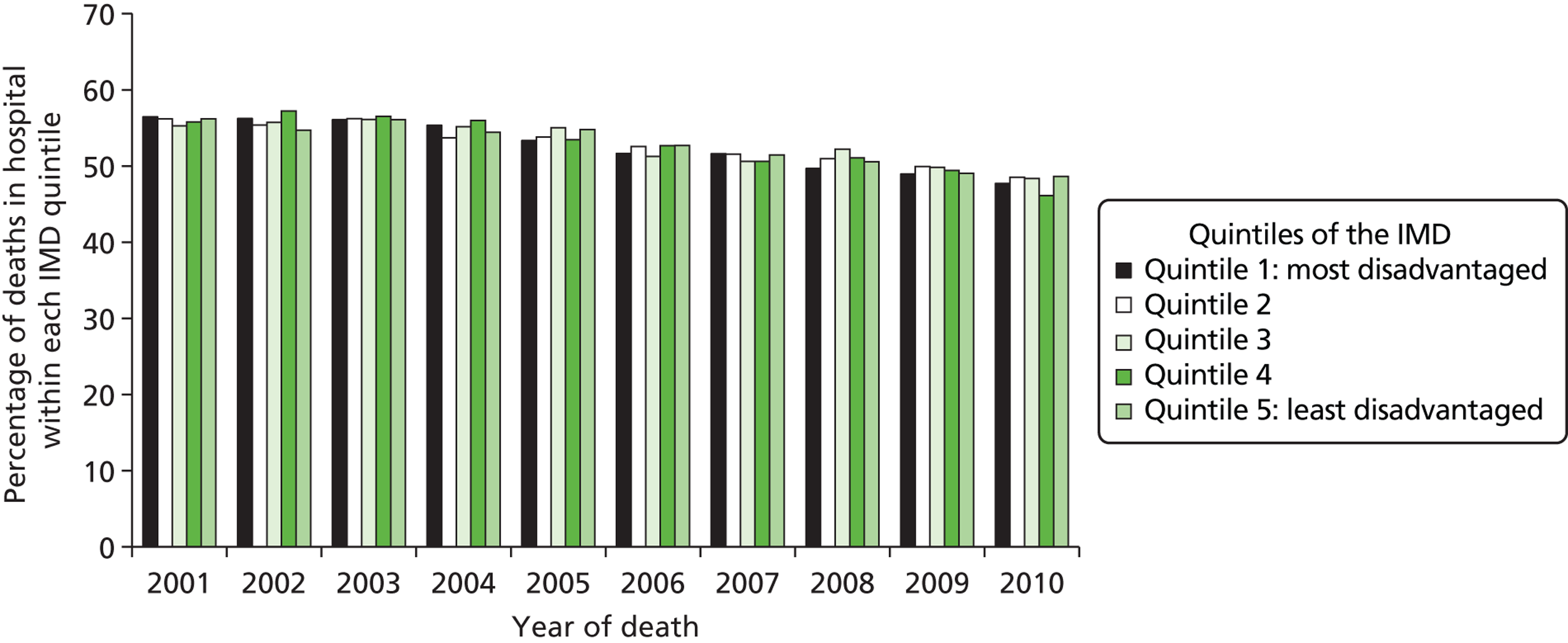
Time between last hospital admission and death
The time between the last hospital admission and date of death gives the best available indication in this data set of the proximity of the final transition to death.
A majority of lung cancer patients had been admitted to hospital in the 3 months before death. A higher proportion of heart failure patients had a longer gap between admission and death. Table 17 presents time between admission and death for all patients. Within 1 month of death, almost 60% of lung cancer patients and 50% of heart failure patients had undergone a transition into hospital. Within 3 months, 85.5% of lung cancer patients and 72% of heart failure patients had been admitted to hospital.
| Weeks before death | Lung cancer cases, n (cumulative %) | Heart failure cases, n (cumulative %) |
|---|---|---|
| 1 | 26,886 (23.8) | 44,611 (23.8) |
| 2 | 16,240 (38.1) | 21,279 (35.2) |
| 3 | 13,096 (49.7) | 15,345 (43.4) |
| 4 | 10,086 (58.6) | 11,278 (49.4) |
| 5 | 7674 (65.4) | 8991 (54.2) |
| 6 | 5765 (70.5) | 7020 (58.0) |
| 7 | 4583 (74.6) | 5912 (61.1) |
| 8 | 3525 (77.7) | 4963 (63.8) |
| 9 | 2824 (80.2) | 4357 (66.1) |
| 10 | 2333 (82.2) | 3817 (68.1) |
| 11 | 2026 (84) | 3371 (69.9) |
| 12 | 1620 (85.5) | 3074 (71.6) |
| > 12 | 16,432 (100) | 53,224 (100) |
| Total | 113,090 | 187,242 |
Source of admission
The majority (92.6%) of the admissions in this data set were transitions from the patient’s usual place of residence. Fewer than 1% were from residential or care homes, and a similar number (< 1%, n = 148) from a non-NHS hospice.
Ninety-four per cent were emergency admissions. Overall, 33.5% of admissions resulted in death, 56% in discharges back to the person’s usual residence, and fewer than 3% in discharges to a residential or care home.
Factors associated with high numbers of admissions in the last year of life
Heart failure cases with three or more admissions in the last year of life and lung cancer cases with four or more admissions were above the 90th centile for admissions. Table 18 compares the characteristics of cases who experienced frequent admissions. The source of admission was the usual place of residence for the majority of cases. The cases who were admitted frequently differed from the study population in age and gender. Proportionately more men with heart failure were admitted often, and proportionately more women with lung cancer.
| Characteristics | Lung cancer cases, n (%) | Heart failure cases, n (%) |
|---|---|---|
| Sex | ||
| Male | 8766 (63.9) | 5208 (50.5) |
| Female | 4959 (36.1) | 5114 (49.5) |
| IMD quintile | ||
| 1 | 3309 (24.1) | 2209 (21.4) |
| 2 | 2951 (21.5) | 2212 (21.4) |
| 3 | 2838 (20.7) | 2279 (22.1) |
| 4 | 2521 (18.4) | 1965 (19) |
| 5 | 2071 (15.1) | 1604 (15.5) |
| Age (years) | ||
| 75–84 | 12,271 (89.4) | 5915 (57.3) |
| 85–94 | 1437 (10.5) | 4035 (39.1) |
| 95+ | 15 (0.1) | 367 (3.6) |
| Source of admission | ||
| Usual residence | 12,340 (89.9) | 8662 (83.9) |
| A&E, other hospital | 1202 (8.8) | 1459 (14.1) |
| Care home | 52 (< 1) | 86 (< 1) |
| Other | 131 (1) | 115 (< 1) |
| Totals | 13,725 | 10,322 |
Descriptive analysis of these data has identified the importance of age, sex and socioeconomic status as influences on frequency of admission to hospital in the last year of life (Table 19). In multivariate analysis, younger age and male sex were associated with numbers of hospital admissions above the 90th centile for both lung cancer and heart failure patients. People in the most disadvantaged areas were less likely to be admitted frequently, adjusting for age and sex.
| Characteristics | Heart failure cases, adjusted odds ratio (95% confidence interval) | p-value | Lung cancer cases, adjusted odds ratio (95% confidence interval) | p-value |
|---|---|---|---|---|
| Sex | ||||
| Males | 1.196 (1.149 to 1.245) | < 0.001 | 1.309 (1.261 to 1.359) | < 0.001 |
| Females (ref. category) | ||||
| Age (years) | ||||
| 75–84 | 1.826 (1.638 to 2.035) | < 0.001 | 10.361 (6.219 to 17.261) | < 0.001 |
| 85–94 | 1.356 (1.216 to 1.512) | < 0.001 | 3.878 (2.322 to 6.477) | < 0.001 |
| 95+ (ref. category) | ||||
| IMD quintiles | ||||
| 1 | 1.162 (1.088 to 1.242) | < 0.001 | 0.906 (0.854 to 0.961) | 0.001 |
| 2 | 1.112 (1.04 to 1.188) | 0.002 | 0.957 (0.901 to 1.017) | 0.151 |
| 3 | 1.112 (1.041 to 1.187) | 0.002 | 1.008 (0.948 to 1.071) | 0.806 |
| 4 | 1.015 (0.948 to 1.086) | 0.672 | 0.988 (0.928 to 1.051) | 0.684 |
| 5 (ref. category) | ||||
| Source of admission care home | ||||
| Yes | 0.957 (0.769 to 1.190) | 0.691 | 0.881 (0.660 to 1.176) | 0.389 |
| No (ref. category) | ||||
The sociodemographic profiles and patterns of service utilisation for the two patient groups are in keeping with established knowledge of the epidemiology of both conditions. Lung cancer patients are generally younger than patients with heart failure, with a higher proportion drawn from lower socioeconomic groups. The time from diagnosis to death is shorter than for many other cancers. Admissions for lung cancer have risen over time, while total time in hospital has fallen. Within HES, an admitted patient is one who occupies a hospital bed, including those who are subsequently sent home without treatment, or undergo a day-case procedure and are discharged without an overnight stay. In such cases, their data would contribute to admissions data but not to the duration of the spell. This would account for lung cancer attendances for assessment or treatment as a day case. The proportion of lung cancer admissions who are day cases has been shown elsewhere to be around 60%, but this falls rapidly in the last 8 months of life. 91
Approximately two-thirds of deaths in England occur in people aged 75 years and over, with slightly more deaths in females than males. The cases in this study represent approximately 9% of average annual deaths in this age group. 92 Both lung cancer and heart failure patients are important groups in any study of hospital use. Heart failure is one of the top 10 diagnoses underlying admission to hospital, and almost 70% of admissions are among people aged 75 years and over, most of these as emergencies. 82 Halting the rise in emergency inpatient admissions for cancer patients was a particular focus of the Cancer Reform Strategy. 93 Cancer patients accounted for around 12% of inpatient bed-days in England. Of all the cancer sites, lung cancer accounted for the second highest number of emergency bed-days, with the cost of lung cancer admissions the third highest overall. 94
In the last year of life of people aged ≥ 75 years, with diagnoses of lung cancer or heart failure:
-
The majority (94%) of hospital admissions were emergencies, from the usual place of residence.
-
Eighty-five per cent of lung cancer cases and 72% of heart failure cases underwent a transition into hospital in the last 3 months of life.
-
Heart failure cases spent a median of 13 days in hospital in their last year of life, and lung cancer cases a median of 15 days.
Frequent admissions (> 90th centile) were associated with younger age and male sex but not admission from a care home. Living in more disadvantaged areas was associated with an increased likelihood of frequent admissions for heart failure cases. Lung cancer cases in the most disadvantaged areas were less likely to be admitted frequently to hospital.
Chapter 6 Answering our research questions
In our original proposal, we identified a gap in the research knowledge relating to older adults’ experiences of transitions at the end of life. Despite anecdotal evidence of distressing, unnecessary and costly hospital admissions near to death, there has been little published academic work in this area. We set out to gain a deep understanding of the patients’ perceptions through interviews, and planned to follow that with a more structured approach to data collection with bereaved carers. After a small number of interviews with carers, it became clear that this would not do justice to the richness of the data the carers wished to share, and we sought permission to conduct in-depth interviews with the relatively large group of bereaved carers.
Our original objectives were to:
-
explore the effect of transitions towards the end of life on health status, quality of life, symptom control and satisfaction with care
-
understand the factors that influence decisions about transitions in the nature and location of care
-
elicit patient and provider views on the appropriateness of different transition patterns and the factors that constrain or shape decisions
-
map (describe) transitions in and out of hospital at the end of life for older people in England
-
identify individual- and service-level factors associated with frequency of transitions.
The structured data collected from carers have provided some common information on satisfaction with different aspects of care in a range of settings, but primarily home and hospital. The mix of patient diagnoses has meant that there was no shared concept of symptom control. Questions on pain control were asked of all carers but were relevant to only a proportion. Carers’ feelings about how well the condition was managed did emerge from the interviews, but not in a format that leant itself to ready comparison across the whole sample. All three sets of interviews have contributed to the data to inform our understanding of perceived quality of life, satisfaction with care and the influences on decisions and consequences of transitions for patients and families. The interview data have also identified some individual- and service-level factors that are important to note. However, early in the data collection with professionals, it became apparent the notion of an appropriate move was too simplistic and did not reflect the multiple, interacting influences on decisions that were apparent to professionals and families. In answer to this question, we have presented an overview of the factors that emerged as most influential, and most often raised by participants.
Reasons for diversions from original protocol
Our work differs from the original protocol in the following ways.
1. Addition of patient interviews
This was suggested by reviewers of the original application.
2. Addition of qualitative interviews with bereaved carers to questionnaire administration
We sought permission from the funder to do this, after reviewing data from the first few interviews. The interviewees were sharing rich and useful qualitative data with the researchers that were not being adequately captured in the quantitative responses. This added to the workload of the project, as the time taken to analyse 118 lengthy in-depth interviews was considerable. No additional resources were required.
3. Design of linked data analysis
Data analysis was limited to patients with heart failure and lung cancer, in line with the patient interviews. Constraints of data availability meant that we were able to analyse data relating to people who were admitted to hospital and died, rather than data on people who died from specific causes.
Chapter 7 Implications
In this section, we consider what our findings may mean for care transitions in England, and identify priorities for future research. Comparisons are made with the work on transitional care from the USA to draw out the implications of our findings for developing interventions appropriate to the UK context.
Key implications
Older adults are important consumers of health and social care services. As we are living longer, a greater proportion of deaths occur in older age, and needs for care and support have become more complex. Frailty, multiple comorbidities and reduced family size are some of the challenges that current systems will need to anticipate and accommodate. As the population of older adults continues to grow in number, it will become increasingly important that services meet the needs of older adults in an effective and efficient manner. Data from this study will help to inform a response to the changing end-of-life care needs for older adults.
The key implications from our work are:
-
The role of the carer in transitions should be scrutinised, putting aside past assumptions and practices. Enabling family carers to have a stronger voice, particularly in hospital settings, has the potential to improve older patients’ experiences of care transitions.
-
Patients and carers are already engaged in self-management. Identifying ways to enhance their skills would be welcomed and may reduce unnecessary end-of-life transitions.
-
Ensuring that people who live alone, or have no family carers, are given the same choices and care as others is a challenge for existing services.
-
A critical examination of the traditional model of GP care at the end of life is required, and their role in care transitions in particular.
-
The impact of interprofessional disagreement and discord on patients’ experiences must be acknowledged and addressed. The question of how professionals should co-ordinate care for older adults across settings and sectors is an important underlying issue.
Caregivers
A key finding from our interviews is that different understandings of the carers’ role among professionals, carers and patients may be a barrier to carers’ effective involvement in care. To the patients, carers were an essential part of the team. The carers’ own accounts suggested that they wished to have their insights into the patients’ needs listened to and incorporated into plans of care, but this seldom happens in current practice. Although professionals articulated support for the principle of including the carer, this masked an underlying ambivalence. Carers were either regarded as a useful resource or as potential patients, depending on whether the personal or professional lens was dominant. The concept of the carer as a co-worker, articulated in the End of Life Strategy,95 was an aspiration for some carers, but fell between the two portrayals of carers in the professional accounts.
It is clear that professional detachment that leads to the objectification of carers as a useful resource is undesirable. However, professionals are also required not to empathise so closely with carers’ situations that they become reluctant to engage with them as co-workers. Finding the point of equipoise between conflicting professional constructs of caregivers is essential to good care, but it is not a new challenge. Most of the professionals’ views fitted within two of the carer–service provider models developed by Twigg and Atkin almost 20 years ago. 14 Twigg and Atkin’s typology presented carers as a resource and as co-clients. Data from our study formed similar patterns, despite differences in client group and professional roles. Our respondents’ perception of carers extended further, to encompass being a resource for patients, with carers also seen as a source of information for professionals. However, our interviewees did not articulate Twigg and Atkin’s fourth model of the superseded carer, where the aim is to dispense with the need for informal care by maximising the patients’ independence.
Alongside problems that appear to arise from the way in which the carers’ roles are constructed, our findings revealed some very practical challenges to those providing end-of-life support at home. Carers described not knowing how and where to find the information and help that they need, and this lack of knowledge was often associated with a reliance on their own biographical experiences of services. Carers who were better off displayed a more sophisticated understanding and confident interaction with service providers, which raises the possibility that the current approach to carers may be reinforcing entrenched social divisions in access to care. Assessment of carers’ needs is enshrined in policy within the End of Life Strategy, and in practice with the local authorities’ statutory duty to assess needs. National Institute of Health and Care Excellence (NICE) guidance suggests regular assessment of the needs of end-of-life carers, yet few of our interviewees recalled any assessment of either patient or carer needs.
One of the most striking findings of our analysis of the carers’ role is how little has changed over recent decades. Researchers commented on how policy for carers had come in from the cold in the 1990s. 96 Since then, a carers’ strategy has been introduced and particular attention paid to their situation at the end of life. 3,97 Yet despite all of these developments, carers’ experiences have changed little over time. Our data question the value of the current framework for carer assessments, and suggest that it is either poorly implemented or ineffective. Practitioners need to be reflective, aware and cautious in how they bring their own experiences to bear on caring for carers. Why this may not be achieved with training and continuing professional development is unclear. Most importantly, our data raise the question of why, despite wide recognition of their importance, carers’ experiences have remained immune to new initiatives and policies. Our data would support active intervention with carers, including development of methods to assess their needs for support and care, and identifying ways in which they may find their voice and exert greater influence on care across settings.
Professional co-ordination of care
Our findings from all three groups of participants identified the need for an identified individual professional or team to support patients and carers and to co-ordinate care. The GP has a view across settings and an awareness of the contribution of different services, all of which may not be as readily available in specialist practice. The position of lynchpin in a system of multiple components is one that the GPs assume is their own, a stance supported by the majority of carers, who identified the GP as the main contact person in the last few months of life. Respondents to the questionnaire were positive about GPs’ personal care for the decedents, suggesting that they had time to listen to family concerns and visited the home when needed. However, in the interviews, patients and carers revealed limited expectations of the GP as co-ordinator or someone who would take overall responsibility for their care. They were more likely to expect a family member to assume this task.
Other professionals were in accord with the GPs’ views of what their role should be, but critical of how well they performed it. Much of this discord had its roots in differing attitudes to pathways and other forms of guidance for clinicians. Disciplines such as nursing and the ambulance service, where performance management may be based upon adherence to regulations and implementation of guidelines, were frustrated by GPs’ use of clinical freedom to justify disregarding standard protocols. GPs were also perceived by some professional interviewees to see too few dying patients in any one year for them to develop expertise. A GP may have relatively limited exposure to palliative care patients with complex needs, but the GP will have been the responsible doctor for the majority of older adults who die while resident in the community. Their training should equip them with the skills to know when they need to draw in expertise from other professionals, and to share responsibility for a patient’s care.
Specialist nurses were the other group of professionals to emerge from our data as natural candidates to be care co-ordinators. They play a particularly important role with patients who do not have a trusted relationship with a GP. Specialist nurses frequently take on a co-ordination role in the UK, usually for particular patient groups, and often by default. For many years, Macmillan nurses have been providing support to cancer patients that has encompassed aspects of case management. In recent years, community matrons have been appointed with an explicit responsibility to act as case managers, usually for patients with complex long-term conditions, though none of our carer or patient interviewees had any experience of their services.
The appointment of a key professional to manage the range of services and relationships between them is central to many service developments in the USA, within managed or integrated care. In the NHS, the Evercare pilots were the first widespread implementation of case management for frail elderly people. They introduced specialist nurses to organise and co-ordinate care, but although some qualitative benefits were apparent on evaluation, they had little impact on the number of hospital admissions. 98 In Evercare and other defined programmes, the need for training in care co-ordination is accepted, whereas in the NHS, professional competency in co-ordinating care has often been assumed, and the question to be answered is which discipline or professional group should take responsibility. Our data suggest that definition of the skills required, and identification of any gaps in expertise would be helpful, irrespective of the disciplinary background of the professional involved.
There was a widely held perception among our professional interviewees that ownership of end-of-life care lies with health services, which may make it difficult for social care staff to see themselves as legitimate candidates to be leaders in this area. GPs were perceived to be the natural co-ordinators, but other professionals felt that they lacked the expertise to bring a package of care together. In practice, the time doctors are able to devote to organising care will be limited, and appointment of additional staff to take on this role would be costly. If greater co-ordination of care at the end of life is to be delivered within existing resources, it may require more widespread acknowledgement of the importance of this task, with clarification and agreement of responsibilities for doctors, specialist nurses and staff in social care. Possession of the knowledge and skills to be an effective co-ordinator cannot be assumed. Challenging the dominance of health care in end-of-life care may allow a broader range of professionals to contribute to improving the overall continuity and co-ordination of care.
Performance measurement and incentives
To date, payment structures for health professionals do not appear to have provided incentives to promote improved care across transitions. In our study, the Quality and Outcomes Framework (QOF) and Quality, Innovation, Productivity and Prevention programme (QIPP) were rarely mentioned by the professional interviewees. The QOF provides payments for regular multidisciplinary meetings to discuss patients who are approaching the end of life. If ownership of end-of-life care by health services is challenging to other care providers, it is possible that existing financial incentives are also too closely aligned to the behaviour of health professionals. The QOF has provided financial incentives for primary care across a range of clinical processes, but it has stopped short of defining ways of working across primary and secondary care that could influence the experiences of people moving between settings.
Quality incentives focused on individual settings that fail to take into account care across locations are unlikely to influence transitions. 19 Aligning financial and structural incentives to improve patient flow across settings has been identified as a factor that should contribute to improving transitional care within case management in the USA. 99 However, this is unproven and it is important to note that improved patient flow may not be synonymous with improved patient experiences. In the UK, the formation of Health and Wellbeing Boards should offer an opportunity for some of the longstanding deficiencies in cross-sectoral working to be overcome. It may be timely to consider how financial incentives could better contribute to promoting closer working between health and social care for older adults at the end of life.
Self-management
Many patients and carers within this study felt that they were managing their own care, with carers playing a major role liaising with services. The promotion of self-care to reduce demands on the NHS has grown in parallel with the ageing population and financial constraints, but it has never played any more than a minor role in end-of-life care. As more and more deaths occur in older age, the challenge of distinguishing between frail old age and imminent death becomes increasingly difficult. Self-management of transitions has had much attention within US transitional care research relating to chronic illness. Programmes have been developed for patients with complex needs and their caregivers to learn self-management skills to help them ensure that needs are met in transition from home to hospital in particular. A typical programme includes a focus on medication self-management, use of a dynamic patient-centred record, timely specialist or GP follow-up and awareness of red flags to identify deteriorating health.
Neither our questionnaire nor the qualitative interviews with carers identified concerns with medication or errors in prescribing. Deficiencies in transfer of information across settings did feature in patient, carer and professional accounts, and appeared to be particularly problematic in relation to care homes. Timeliness of follow-up and patient recognition of deteriorating health may be closely related issues. Sudden or severe deterioration in condition prompted hospital admission for many of the decedents discussed in our carer interviews. It was unclear whether or not an understanding of the warning signs and action required would have changed the course of events. Training for patients and carers in ‘red flag’ recognition may offer the potential to reduce admissions and maintain constant health status, but it would require evaluation among older people, and at the end of life. The question of whether or not training in self-management would be acceptable and valuable to carers and patients in end of life care should be considered. It would have the support of many carers and may enhance patients’ experiences and reduce resource use.
Interventions to enhance the experience of transitions
Studies from the USA have identified a range of strategies to reduce readmissions and enhance transitional care for adults with chronic illness. A recent review identified nine interventions that had a positive effect on measures related to hospital readmissions. 100 Having a nurse as a leader or clinical manager was a common feature of these nine successful interventions. Encouraging patients and families to play a more active part in their care, guidance from a ‘transition coach’ and interventions to improve communication across settings have been shown to reduce the rate of readmission to hospital for adults over 65 years in the USA. 101 Although these were concerned with a wider population of older adults, our findings support some of the areas identified in that work and identify other issues specific to end-of-life care, and the English context. Other possible components of an intervention suggested by our analysis (listed below) include developing a shared understanding of the carers’ role, clarifying professional responsibilities and enhancing their ability to co-ordinate care, ensuring that carers’ needs for information are identified and met. 68
Development of future interventions
Concepts and theory
-
Harmonising understanding of the carers’ role.
-
Questioning or affirming the centrality of GP care.
-
Consideration of the consequences for patients and families of interprofessional tensions in order to understand how to overcome them.
-
Understanding the constraints on the work of other disciplines.
-
Developing models for shared responsibility for patients across settings.
Skills
-
Communication between professionals that is timely and crosses settings.
-
Carers’ and patients’ ability to recognise deteriorating health condition and pre-empt an urgent need for a transition.
Strengths and limitations
We believe that this is the first study in the UK to focus on transitions between settings for older adults at the end of life. Other studies have considered transitions from life prolonging to palliative care. 102,103 Our use of qualitative and quantitative methods and inclusion of different constituencies involved in care transitions have provided both a broad overview and rich insights into the influences on patients’ experiences. Participants were drawn from three NHS regions of England, and should be representative of a range of health economies and social contexts. Our patient and carer interviewees were recruited via health professional gatekeepers, using an ‘opt-in’ approach. This strategy for recruiting potentially vulnerable interviewees is favoured by research ethics and governance committees. It aims to reduce the possibility of causing distress by approaching people who were not suitable for interview; allows selection by patient or carer characteristics, such as diagnosis, prognosis or time after death; and complies with data protection regulations. However, both the use of gatekeepers and an opt-in approach to recruitment may adversely influence sample selection and be criticised for limiting transferability of our findings. The patient interviewees were disproportionately drawn from disadvantaged areas of the north-west, while people from poorer areas were under-represented among the carers. Our inclusion of the voices of a hard-to-reach group is a strength of the study, but the paucity of more disadvantaged carers is a limitation. However, the number of interviews with carers was large for a qualitative study, and offers the potential for selective analysis of data from a more socially balanced sample as well as robust subgroup analyses by diagnoses or transition type to be conducted. In recruiting the professional interviewees, we sought broad representation of disciplines, and a bias to senior staff. This approach meant that analysis of data from our participants provides a valuable strategic view of care across transitions, but the number of people in some specific, patient-facing roles was limited.
Our qualitative data collection with carers has resulted in an extensive and unusually rich resource, which will form the basis of future analyses. It may be used to answer many different questions beyond those posed in this project. This study was not designed to produce a large quantitative data set from bereaved carers, though we did complete a questionnaire with bereaved carers. The collection of qualitative data, combined with the researchers’ sensitivity to the well-being of the interviewees, resulted in incomplete responses being recorded for a number of survey questions. As the VOICES survey is being used widely by the Department of Health in England to provide a nationally representative body of data, the value of smaller-scale data collection using VOICES may be limited in the future.
The general limitations of routine HES and mortality data have been widely discussed and will not be rehearsed again here. The requirement to construct a data set starting from HES data rather than deaths was a specific limitation for this study. Recent changes in the way that data are made available should now allow application of the approach used here with data defined from mortality statistics.
Recommendations on priorities for future research
Our findings suggest that the following should be priorities for future research:
-
Investigation of why the experiences of end-of-life carers appear to have been immune to policy interventions in recent years.
-
Exploration of the acceptability, potential scope and ways of facilitating self-management with patients and carers, to reduce unnecessary end-of-life transitions. Our data suggest that patients and carers wish to take control of their care, even at the end of life, but they may lack some of the knowledge and confidence to do so effectively. Whether or not intervention to promote self-management of some aspects of care at the end of life would be widely acceptable to patients, families or professionals requires investigation.
-
Exploration of the consequences for patients and families of interprofessional tensions and identifying ways to reduce them. This should include questioning or affirming the centrality of GP care.
-
Exploring ways to ensure that people who live alone, or without carers, exercise choices and receive equitable end-of-life care.
-
Identification of any unmet needs for training for professionals involved in co-ordinating end-of-life care across settings. Work with GPs and specialist nurses is needed, in particular, to identify gaps in their knowledge and skills relating to co-ordination of services.
-
A systematic review of the international literature on interventions to improve patient experiences of transitions. This was beyond the resources of this project. As comparison of our findings with work from the USA points to a common core of component activities, a systematic evaluation of the literature would be helpful to inform design and refinement of interventions relevant to the NHS context.
-
Development and testing of an intervention to enhance patients’ experiences across transitions. Our data provide a broad basis for such work in the future,68 and suggest that interventions in the following areas may offer the greatest potential benefits:
-
harmonising understanding of the carers’ role and enhancing their ability to influence patients’ experiences of care in hospital settings
-
improving carers’ and patients’ ability to recognise deteriorating health and pre-empt an urgent need for a transition.
-
Summary
This study has described deficiencies and challenges in current care that are shared by people with different conditions and in different regions of England when they undergo transitions between settings. There is a growing body of opinion that argues that current models of care are not best suited to our changing population. A patient in extreme old age, with comorbidities, frailty and no clear diagnosis may require different care from that of the individual with a condition that leads to a steady, progressive and easily identifiable decline. The deficiencies in care identified by our work support a call for change, but this study has also highlighted the extent to which patients with different conditions share common experiences at the end of life. The need for greater attention to basic components of care is well recognised, and clearly observed in our data. This will benefit all patients, not just those in transition. Dignity and good communication are essential, for example. Improvement of care across transitions requires critical re-examination of well-established thinking, particularly around the involvement of patients and carers in health care, the role of the GP at the centre of care, and the ways in which professionals and services work together. A focus on these three broad areas offers the potential to reduce the number and enhance the experience of transitions for older adults at the end of their lives.
Acknowledgements
This work would not have been possible without the generosity of patients, carers and professionals who gave their time to be interviewed and share their experiences with us. We are also grateful for the invaluable support provided by the primary care research networks and local research governance staff.
Contributions of authors
Barbara Hanratty had the original idea for the study, put together the first draft of the report and contributed to aspects of the design and analysis.
Elizabeth Lowson put together the first draft of the report and contributed to aspects of the design and analysis.
Gunn Grande contributed to aspects of the design and analysis.
Sheila Payne contributed to aspects of the design and analysis.
Julia Addington-Hall contributed to aspects of the design and analysis.
Nicole Valtorta put together the first draft of the report and contributed to aspects of the design and analysis.
Jane Seymour contributed to aspects of the design and analysis.
All authors have seen and approved a final version.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med 2004;141:533-5. http://dx.doi.org/10.7326/0003-4819-141-7-200410050-00009.
- 10 Facts on Ageing and the Lifecourse. Geneva: World Health Organization; 2011.
- End of Life Care Strategy. London: The Stationery Office; 2008.
- Henderson J, Goldacre MJ, Griffith M. Hospital care for the elderly in the final year of life: a population based study. BMJ 1990;301:17-9. http://dx.doi.org/10.1136/bmj.301.6742.17.
- Fries JF. Frailty, heart disease, and stroke: the Compression of Morbidity paradigm. Am J Prev Med 2005;29:164-8.
- Fries JF. The compression of morbidity (1983). Milbank Q 2005;83:801-23.
- Mor V. The compression of morbidity hypothesis: a review of research and prospects for the future. J Am Geriatri Soc 2005;53:S308-9. http://dx.doi.org/10.1111/j.1532-5415.2005.53496.x.
- Busse R, Krauth C, Schwartz FW. Use of acute hospital beds does not increase as the population ages: results from a seven year cohort study in Germany. J Epidemiol Commun H 2002;56:289-93. http://dx.doi.org/10.1136/jech.56.4.289.
- Himsworth RL, Goldacre MJ. Does time spent in hospital in the final 15 years of life increase with age at death? A population based study. BMJ 1999;319:1338-9. http://dx.doi.org/10.1136/bmj.319.7221.1338.
- Dixon T, Shaw M, Frankel S, Ebrahim S. Hospital admissions, age, and death: retrospective cohort study. BMJ 2004;328. http://dx.doi.org/10.1136/bmj.38072.481933.EE.
- Breyer F, Felder S. Life expectancy and health care expenditures: a new calculation for Germany using the costs of dying. Health Policy 2006;75:178-86. http://dx.doi.org/10.1016/j.healthpol.2005.03.011.
- Roos NP, Montgomery P, Roos LL. Health care utilization in the years prior to death. Milbank Q 1987;65:231-54. http://dx.doi.org/10.2307/3350021.
- Seshamani M, Gray AM. A longitudinal study of the effects of age and time to death on hospital costs. J Health Econ 2004;23:217-35. http://dx.doi.org/10.1016/j.jhealeco.2003.08.004.
- Twigg J, Atkin K. Carers Perceived: Policy and Practice in Informal Care. Buckingham: Open University Press; 1994.
- Werblow A, Felder S, Zweifel P. Population ageing and health care expenditure: a school of ‘red herrings’?. Health Econ 2007;16:1109-26. http://dx.doi.org/10.1002/hec.1213.
- Zweifel P, Felder S, Meiers M. Ageing of population and health care expenditure: a red herring?. Health Econ 1999;8:485-96. http://dx.doi.org/10.1002/(SICI)1099-1050(199909)8:6%3C485::AID-HEC461%3E3.0.CO;2-4.
- Hogan C, Lynn J, Gabel J, Lunney J, O’Mara A, Wilkinson A. Medicare Beneficiaries’ Costs and Use of Care in the Last Year of Life. Washington, DC: Medicare Payment Advisory Commission; 2000.
- Seshamani M, Gray A. Ageing and health-care expenditure: the red herring argument revisited. Health Econ 2004;13:303-14. http://dx.doi.org/10.1002/hec.826.
- Coleman EA, Boult C. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc 2003;51:556-7. http://dx.doi.org/10.1046/j.1532-5415.2003.51186.x.
- Mur-Veeman I, Hardy B, Steenbergen M, Wistow G. Development of integrated care in England and the Netherlands: managing across public–private boundaries. Health Policy 2003;65:227-41.
- Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc 2003;51:549-55. http://dx.doi.org/10.1046/j.1532-5415.2003.51185.x.
- Kane R, Kaye N, Mollica R, Riley T, Paul Saucier T, , et al. Managed Care: Handbook for the Aging Network. Minneapolis, MN: University of Minnesota National LTC Resource Center; 1996.
- Ross S, Curry N, Goodwin N. Case Management: What It Is and How It Can Best be Implemented. London: The King’s Fund; 2011.
- Golden AG, Tewary S, Dang S, Roos BA. Care management’s challenges and opportunities to reduce the rapid rehospitalization of frail community-dwelling older adults. Gerontologist 2010;50:451-8. http://dx.doi.org/10.1093/geront/gnq015.
- Boling PA. Clin Geriatr Med 2009;25:135-48. http://dx.doi.org/10.1016/j.cger.2008.11.005.
- Cameron JI, Gignac MA. ‘Timing It Right’: a conceptual framework for addressing the support needs of family caregivers to stroke survivors from the hospital to the home. Patient Educ Couns 2008;70:305-14. http://dx.doi.org/10.1016/j.pec.2007.10.020.
- Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med 1995;333:1190-5. http://dx.doi.org/10.1056/NEJM199511023331806.
- Parker G, Corden A, Heaton J. Continuity of Care: Synthesis and Conceptual Analysis of the NIHR, Service and Delivery Organisation Programme’s Research. London: NIHR Service and Delivery Organisation programme; 2009.
- Freeman G, Shepperd S, Robinson, I, Ehrich, K, Richards S. Continuity of Care: Report of a scoping exercise for the National Coordinating Centre for Service Delivery and Organisation. London: NIHR Service and Delivery Organisation programme; 2001.
- Freeman G, Woloshynowych M, Baker R, Boulton M, Guthrie B, Car J, et al. Continuity of Care: What Have we Learned Since 2000 and What are Policy Imperatives now?. London: National Coordinating Centre for Service Delivery and Organisation; 2007.
- Ashton CM, Kuykendall DH, Johnson ML, Wray NP, Wu L. The association between the quality of inpatient care and early readmission. Ann Intern Med 1995;122:415-21. http://dx.doi.org/10.7326/0003-4819-122-6-199503150-00003.
- Compendium Indicators: Emergency Readmission Rate within 28 Days of Discharge from Hospital. London: National Clinical and Health Outcomes Knowledge Base; 2009.
- Hudson B. Emergency readmission rates: everybody’s business. Community Care 2008;1750. www.communitycare.co.uk/2008/12/01/emergency-readmission-rates-everybodys-business/#.U2JqN9ySgpE (accessed 20 April 2013).
- Payment by Results Guidance for 2011–12. Leeds: Department of Health; 2011.
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. New Engl J Med 2009;360:1418-28. http://dx.doi.org/10.1056/NEJMsa0803563.
- Linertova R, Garcia-Perez L, Vazquez-Diaz JR, Lorenzo-Riera A, Sarria-Santamera A. Interventions to reduce hospital readmissions in the elderly: in-hospital or home care. A systematic review. J Eval Clin Pract 2011;17:1167-75. http://dx.doi.org/10.1111/j.1365-2753.2010.01493.x.
- Shepperd S, McClaran J, Phillips CO, Lannin NA, Clemson LM, McCluskey A, et al. Discharge planning from hospital to home. Cochrane Database Syst Rev 2010;1. http://dx.doi.org/10.1002/14651858.CD000313.pub2.
- Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disorders 2006;6.
- Rich MW. Heart failure in the elderly: strategies to optimize outpatient control and reduce hospitalizations. Am J Geriatr Cardiol 2003;12:19-24. http://dx.doi.org/10.1111/j.1076-7460.2003.01752.x.
- Gwadry-Sridhar FH, Flintoft V, Lee DS, Lee H, Guyatt GH. A systematic review and meta-analysis of studies comparing readmission rates and mortality rates in patients with heart failure. Arch Intern Med 2004;164:2315-20. http://dx.doi.org/10.1001/archinte.164.21.2315.
- Barker WH, Zimmer JG, Hall WJ, Ruff BC, Freundlich CB, Eggert GM. Rates, patterns, causes, and costs of hospitalization of nursing-home residents – a population-based study. Am J Public Health 1994;84:1615-20. http://dx.doi.org/10.2105/AJPH.84.10.1615.
- Murtaugh CM, Litke A. Transitions through postacute and long-term care settings: patterns of use and outcomes for a national cohort of elders. Med Care 2002;40:227-36.
- Terrell KM, Hustey FM, Hwang U, Gerson LW, Wenger NS, Miller DK. Quality indicators for geriatric emergency care. Acad Emerg Med 2009;16:441-9. http://dx.doi.org/10.1111/j.1553-2712.2009.00382.x.
- Saliba D, Kington R, Buchanan J, Bell R, Wang MM, Lee M, et al. Appropriateness of the decision to transfer nursing facility residents to the hospital. J Am Geriatr Soc 2000;48:154-63.
- Partridge J. Why are nursing home residents sent in to hospital to die?. Postgrad Med J 2008;84. http://dx.doi.org/10.1136/pgmj.2008.070656.
- Ahearn DJ, Jackson TB, McIlmoyle J, Weatherburn AJ. Improving end of life care for nursing home residents: an analysis of hospital mortality and readmission rates. Postgrad Med J 2010;86:131-5. http://dx.doi.org/10.1136/pgmj.2008.076430.
- Dobrzanska L, Newell R. Readmissions: a primary care examination of reasons for readmission of older people and possible readmission risk factors. J Clin Nurs 2006;15:599-606. http://dx.doi.org/10.1111/j.1365-2702.2006.01333.x.
- Quinn K, Courts C. Sound Practices in Medicaid Payment for Hospital Care. Hamilton, NJ: Center for Health Care Strategies, Inc.; 2010.
- Fleming J, Zhao J, Farquhar M, Brayne C, Barclay S. Cambridge City Over-75s Cohort Study C. Place of death for the ‘oldest old’: > or =85-year-olds in the CC75C population-based cohort. Br J Gen Pract 2010;60:171-9. http://dx.doi.org/10.3399/bjgp10X483959.
- Szczepura A, Nelson S, Wild D. In-reach specialist nursing teams for residential care homes: uptake of services, impact on care provision and cost-effectiveness. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-269.
- Glasby J, Littlechild R, Pryce K. All dressed up but nowhere to go? Delayed hospital discharges and older people. J Health Serv Res Policy 2006;11:52-8. http://dx.doi.org/10.1258/135581906775094208.
- Hubbard G. A Research Review on Tackling Delayed Discharge. Edinburgh: Scottish Executive Social Research; 2004.
- Kydd A. The patient experience of being a delayed discharge. J Nurs Manag 2008;16:121-6. http://dx.doi.org/10.1111/j.1365-2834.2008.00848.x.
- Swinkels A, Mitchell T. Delayed transfer from hospital to community settings: the older person’s perspective. Health Soc Care Comm 2009;17:45-53. http://dx.doi.org/10.1111/j.1365-2524.2008.00796.x.
- Ingleton C, Payne S, Sargeant A, Seymour J. Barriers to achieving care at home at the end of life: transferring patients between care settings using patient transport services. Palliat Med 2009;23:723-30. http://dx.doi.org/10.1177/0269216309106893.
- Luhrs CA, Penrod JD. End-of-life care pathways. Curr Opin Suppor Palliat Care 2007;1:198-201. http://dx.doi.org/10.1097/SPC.0b013e3282f1aae6.
- Ellershaw JE, Murphy D. The Liverpool Care Pathway (LCP) influencing the UK national agenda on care of the dying. Int J Palliat Nurs 2005;11:132-4.
- Shaw KL, Clifford C, Thomas K, Meehan H. Review: improving end-of-life care: a critical review of the gold standards framework in primary care. Palliat Med 2010;24:317-29. http://dx.doi.org/10.1177/0269216310362005.
- Klinkenberg M, Visser G, van Groenou MI, van der Wal G, Deeg DJ, Willems DL. The last 3 months of life: care, transitions and the place of death of older people. Health Soc Care Comm 2005;13:420-30. http://dx.doi.org/10.1111/j.1365-2524.2005.00567.x.
- Van den Block L, Deschepper R, Bilsen J, Van Casteren V, Deliens L. Transitions between care settings at the end of life in belgium. JAMA 2007;298:1638-9.
- Abarshi E, Echteld M, Van den Block L, Donker G, Deliens L, Onwuteaka-Philipsen B. Transitions between care settings at the end of life in the Netherlands: results from a nationwide study. Palliat Med 2010;24:166-74. http://dx.doi.org/10.1177/0269216309351381.
- Trask PC, Teno JM, Nash J. Transitions of care and changes in distressing pain. J Pain Symptom Manage 2006;32:104-9. http://dx.doi.org/10.1016/j.jpainsymman.2006.03.007.
- Addington-Hall JM, O’Callaghan AC. A comparison of the quality of care provided to cancer patients in the UK in the last three months of life in in-patient hospices compared with hospitals, from the perspective of bereaved relatives: results from a survey using the VOICES questionnaire. Palliative Med 2009;23:190-7. http://dx.doi.org/10.1177/0269216309102525.
- Harrison A, Verhoef M. Understanding coordination of care from the consumer’s perspective in a regional health system. Health Serv Res 2002;37:1031-54. http://dx.doi.org/10.1034/j.1600-0560.2002.64.x.
- Levine C. Rough Crossings: Family Caregivers’ Odysseys Through the Healthcare System. United Hospital Fund of New York; 1998.
- Feinstein AR. Is ‘quality of care’ being mislabeled or mismeasured?. Am J Med 2002;112:472-8. http://dx.doi.org/10.1016/S0002-9343(02)01043-4.
- Donabedian A. A founder of quality assessment encounters a troubled system firsthand. Health Aff (Millwood) 2001;20:137-41.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1655.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c4587.
- Seymour J. Combined qualitative and quantitative research designs. Curr Opin Support Palliat Care 2012;6:514-24. http://dx.doi.org/10.1097/SPC.0b013e328358214e.
- Moran-Ellis J, Alexander V, Cronin A, Dickinson M, Fielding J, Sleney J, et al. Triangulation and integration: processes,claims and implications. Qual Res 2006;6:45-59. http://dx.doi.org/10.1177/1468794106058870.
- Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. BMJ 2005;330:1007-11. http://dx.doi.org/10.1136/bmj.330.7498.1007.
- McPherson CJ, Addington-Hall JM. Judging the quality of care at the end of life: can proxies provide reliable information?. Soc Sci Med 2003;56:95-109. http://dx.doi.org/10.1016/S0277-9536(02)00011-4.
- Moss AH, Lunney JR, Culp S, Auber M, Kurian S, Rogers J, et al. Prognostic significance of the ‘surprise’ question in cancer patients. J Palliat Med 2010;13:837-40. http://dx.doi.org/10.1089/jpm.2010.0018.
- Murray S, Boyd K. Using the ‘surprise question’ can identify people with advanced heart failure and COPD who would benefit from a palliative care approach. Palliat Med 2011;25. http://dx.doi.org/10.1177/0269216311401949.
- Moss AH, Ganjoo J, Sharma S, Gansor J, Senft S, Weaner B, et al. Utility of the ‘surprise’ question to identify dialysis patients with high mortality. Clin J Am Soc Nephrol: CJASN 2008;3:1379-84. http://dx.doi.org/10.2215/CJN.00940208.
- Hanratty B, Lowson E, Holmes L, Addington-Hall J, Arthur T, Grande G, et al. A comparison of strategies to recruit older patients and carers to end-of-life research in primary care. BMC Health Serv Res 2012;12. http://dx.doi.org/10.1186/1472-6963-12-342.
- Addington-Hall J. Sample VOICES Questionnaires University of Southampton 2012 n.d. www.southampton.ac.uk/voices/sample_voices_questionnaires/ (accessed 1 July 2012).
- Spencer S. Hospital Episode Statistics (HES): Improving the Quality and Value of Hospital Data. Leeds: The Health and Social Care Information Centre; 2011.
- Goldacre M, Croft GP. HES For Physicians: A Guide to the Use of Information Derived from Hospital Episode Statistics. London: Royal College of Physicians; 2006.
- Verne J, Lyons P. Pattern of Hospital Admission in the Final Year of Life n.d.
- National Heart Failure Audit 2010–2011. London: University College London; 2012.
- Department for Communities and Local Government . English Indices of Deprivation 2010 2011. www.gov.uk/government/publications/english-indices-of-deprivation-2010 (accessed 20 April 2014).
- Hanratty B, Holmes L, Lowson E, Grande G, Addington-Hall J, Payne S, et al. Older adults’ experiences of transitions between care settings at the end of life in England: a qualitative interview study. J Pain Symptom Manage 2012;44:74-83. http://dx.doi.org/10.1016/j.jpainsymman.2011.08.006.
- Office for National Statistics . The National Statistics Socioeconomic Classification 2010. www.ons.gov.uk/ons/guide-method/classifications/current-standard-classifications/soc2010/soc2010-volume-3-ns-sec--rebased-on-soc2010--user-manual/index.html#skiptotop (accessed 20 April 2014).
- Lowson E, Hanratty B, Holmes L, Addington-Hall J, Grande G, Payne S, et al. From ‘conductor’ to ‘second fiddle’: older adult care recipients’ perspectives on transitions in family caring at hospital admission. Int J Nurs Stud 2013;50:1197-205. http://dx.doi.org/10.1016/j.ijnurstu.2012.02.005.
- Hanratty B, Lowson E, Holmes L, Grande G, Jacoby A, Payne S, et al. Breaking bad news sensitively: what is important to patients in their last year of life?. BMJ Support Palliat Care 2012;2:24-8. http://dx.doi.org/10.1136/bmjspcare-2011-000084.
- Hanratty B, Lowson E, Holmes L, Grande G, Addington-Hall J, Payne S, et al. Funding health and social services for older people – a qualitative study of care recipients in the last year of life. J R Soc Med 2012;105:201-7. http://dx.doi.org/10.1258/jrsm.2012.110189.
- Department of Health . National Framework for NHS Continuing Healthcare and NHS-Funded Nursing Care 2012. www.gov.uk/government/uploads/system/uploads/attachment_data/file/213137/National-Framework-for-NHS-CHC-NHS-FNC-Nov-2012.pdf (accessed 20 April 2014).
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Pring A, Verne J. End of Life Care for Cancer Patients in the South West: Trends in Hospital Care, Place and Cause of Death Summary. Bristol: South West Public Health Observatory; 2009.
- Ruth K, Verne J. Deaths in Older Adults in England. Bristol: South West Public Health Observatory, National End of Life Care Intelligence Network; 2010.
- The Cancer Reform Strategy. London: The Stationery Office; 2007.
- White J. The Impact of the Lung Cancer Specialist Nurse on Inpatient Stays for Patients With Lung Cancer 2010. www.rcplondon.ac.uk/sites/default/the-impact-of-the-lung-cancer-nurse-specialist-on-inpatient-stays-for-lung-cancer.pdf (accessed 20 April 2014).
- End of Life Care Strategy. London: Department of Health; 2008.
- Twigg J, Atkin K. Carers Perceived: Policy and Practice in Informal Care. Buckingham: Open University Press; 1994.
- Recognised, Valued and Supported: Next Steps for the Carers Strategy. London: The Stationery Office; 2010.
- Gravelle H, Dusheiko M, Sheaff R, Sargent P, Boaden R, Pickard S, et al. Impact of case management (Evercare) on frail elderly patients: controlled before and after analysis of quantitative outcome data. BMJ 2007;334. http://dx.doi.org/10.1136/bmj.39020.413310.55.
- Tahan HA. One patient, numerous healthcare providers, and multiple care settings: addressing the concerns of care transitions through case management. Prof Case Manag 2007;12:37-46. http://dx.doi.org/10.1097/01269241-200701000-00008.
- Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The importance of transitional care in achieving health reform. Health Aff 2011;30:746-54. http://dx.doi.org/10.1377/hlthaff.2011.0041.
- Coleman EA, Parry C, Chalmers S, Mahoney E. The influence of system change on improving quality of care transitions. J Am Geriatr Soc 2006;54.
- Gott M, Ingleton C, Bennett MI, Gardiner C. Transitions to palliative care in acute hospitals in England: qualitative study. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d1773.
- Murray SA, Kendall M, Boyd K, Grant L, Highet G, Sheikh A. Archetypal trajectories of social, psychological, and spiritual wellbeing and distress in family care givers of patients with lung cancer: secondary analysis of serial qualitative interviews. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c2581.
Appendix 1 Publications and conference presentations
Papers published using data from patient interviews:
Hanratty B, Holmes L, Lowson E. et al. A comparison of strategies to recruit older patients and carers to end of life research in primary care. BMC Health Serv Res 2012;12:342.
Hanratty B, Lowson E, Holmes L, Grande G, Addington-Hall J, Payne S, Seymour J. Funding health and social services for older people – a qualitative study of the views of care recipients in the last year of life. J Royal Soc Med 2012;105:201–7.
Hanratty B, Lowson E, Holmes L, Grande G et al. Breaking bad news sensitively: what is important to patients in their last year of life? BMJ Palliat Support Care 2012;2:24–8.
Lowson E, Hanratty B, Holmes L, Addington-Hall J, Grande G, Payne S, Seymour J. From conductor to second fiddle: transitions in family caring at older people’s hospital admission. Int J Nurs Stud 2012;50:1197–205.
Hanratty B, Holmes L, Lowson E, Grande G et al. Older adults’ experiences of transitions between care settings at the end of life in England – a qualitative interview study. J Pain Symptom Manag 2012;44:74–83.
Other papers from patient, carer and professional data, quantitative analyses are in production.
Conference proceedings
Hanratty B, Addington-Hall J, Grande G, Payne S, Seymour J. A study of socioeconomic disadvantage and end-of-life hospital admissions for older people with heart failure and lung cancer in England. BMJ Palliat Support Care 2013;3:132.
Valtorta N, Lowson E, Hanratty B, Addington-Hall J, Grande G, Payne S, et al. Recognising the influence of interprofessional working on end-of-life care transitions for older adults: the views of patients, bereaved carers and professionals. BMJ Palliat Support Care 2013;3:132–3.
Thompson E, Holmes L, Addington-Hall J, Grande G, Payne S, Seymour J, et al. From conductor to second fiddle: transitions in family caring when community-dwelling older people are admitted to hospital. Aging Clin Exp Res 2011;23:135.
Holmes L, Thompson E, Addington-Hall J, Grande G, Payne S, Seymour J, et al. Transitions between care settings for older adults at the end of life. Aging Clin Exp Res 2011:23:111.
Hanratty B, Thompson E, Holmes L, Addington-Hall J, Grande G, Payne S, et al. Who should pay for our care? A qualitative study of the views of older adults at the end of life. Aging Clin Exp Res 2011;23:111.
Holmes L, Addington-Hall J, Grande G, Payne S, Seymour, J, Hanratty, B. Transitions between care setting in the last year of life for people living with heart failure, stroke and lung cancer: a qualitative study. Palliat Med 2010;4:S190.
Holmes L, Addington-Hall J, Grande G, Payne S, Seymour J, Hanratty B. Out of Control? Experiences of transitions between care settings at the end of life for older adults with heart failure: a qualitative study. J Epidemiol Comm Health 2010;64:S129.
Conference presentations
Thompson E, Hanratty B, Holmes L, Addington-Hall J, Grange G, Payne S, et al. From Conductor to Second Fiddle: Informal Caring Transitions at the End of Life at Older People’s Hospital Admission. Marie Curie Cancer Care Palliative Care Annual Research Conference – Improving end of life care: generating the evidence to understand new services for a changing society, London, 25 March 2011.
Holmes L, Hanratty B, Thompson E, Addington-Hall J, Grande G, Payne S, et al. Who stays? Who Goes? Who Decides? Bereaved Carers’ Perspectives on Older People’s Transitions Between Places of Care at the End of Life. Marie Curie Cancer Care Palliative Care Research Conference – Improving end of life care: generating the evidence to understand new services for a changing society, London, 25 March 2011 (winner of a poster prize).
Hanratty B, Thompson E, Holmes L, Addington-Hall J, Grande G, Payne S, et al. Who Should Pay for Our Care? A Qualitative Study of the Views of Older Adults at the End of Life. VII European Congress – Health and Active Ageing for all Europeans ‘II’, Bologna, Italy, 14–17 April 2011.
Thompson E, Holmes L, Addington-Hall J, Grande G, Payne S, Seymour J, Hanratty B. From Conductor to Second Fiddle: Transitions in Family Caring when Community-Dwelling Older People are Admitted to Hospital. VII European Congress – Health and Active Ageing for all Europeans ‘II’, Bologna, Italy, 14–17 April 2011.
Holmes, L, Thompson E, Addington-Hall J, Grande G, Payne S, Seymour J, et al. Transitions Between Care Settings for Older Adults at the End of Life. VII European Congress – Health and Active Ageing for all Europeans ‘II’, Bologna, Italy, 14–17 April 2011.
Hanratty B, Lowson E, Holmes L, Grande G, Addington-Hall J, Payne S, et al. Who Should Pay for Our Care? Views of Older Adults at the End of Life. HSRN/SDO Network annual conference: Delivering better health services, Liverpool, 7–8 June 2011.
Holmes L, Lowson E, Addington-Hall J, Grande G, Payne S, Seymour J, et al. Transitions Between Care Settings for Older Adults at the End of Life. HSRN/SDO Network annual conference: Delivering better health services, Liverpool, 7–8 June 2011.
Hanratty B. Transitions Between Care Settings at the End of Life. North American Primary Care Research Group Annual Meeting, New Orleans, LA, December 2012.
Hanratty B, Addington-Hall J, Grande G, Payne S, Seymour J. A Study of Socioeconomic Disadvantage and End-of-Life Hospital Admissions for Older People with Heart Failure and Lung Cancer in England. Marie Curie Cancer Care Palliative Care Annual Research Conference, London, March 2013.
Valtorta N, Lowson E, Hanratty B, Addington-Hall J, Grande G, Payne S, et al. Recognising the Influence of Interprofessional Working on End-of-Life Care Transitions for Older Adults: The Views of Patients, Bereaved Carers and Professionals. Marie Curie Cancer Care Palliative Care Annual Research Conference, London, March 2013.
Appendix 2 Study materials
The invitation letters, participant information sheets and consent forms were similar for all three groups. Materials for carer and professional interviews are included in this appendix.
Invitation letter to carer participant

SURGERY LETTER HEADED PAPER
Dear [Name of potential participant],
[GP Surgery name here] is involved in a study with the University of [Liverpool or Southampton], which aims to understand more about older people’s experience of health and social care at the end of life. We are writing to you because your own doctor or nurse has suggested that you may be eligible to take part.
The researchers are interested in talking to local people who cared for a relative or friend aged over 75 years who died recently with heart failure, stroke or lung cancer. People who take part will be asked to spend up to an hour and a half talking about their experiences and any services that their relative or friend received.
We have enclosed an information sheet about the study with this letter. If, after reading it, you think that you may wish to be interviewed, please contact the researchers. You can either send them your name and telephone number in the stamped-addressed envelope, or contact them by telephone [researcher telephone number]. If you don’t want to take part, then you do not need to do anything. No one will contact you.
If you have any questions please contact [Researcher name] on [Researcher number] or email [Researcher name] at [email address].
Thank you very much for taking the time to read this letter. We realise that it may be upsetting to talk and think about your experiences at this time, and hope that this letter has not brought back too many painful memories. We hope you will share our interest in improving care for people at the end of their lives, and understand why we have contacted you at this sensitive time.
Yours sincerely,
[GP Surgery name here]
Participant information sheet: caregiver interviews
Participant information sheet
Research into services for people at the end of life
You are being invited to take part in a study, which aims to help to improve care for older people with serious illnesses. We are interested in the experience of the people caring for their relatives or friends who died of either lung cancer, heart failure or stroke.
We would like to find out more about why older adults move from one place of care to another to receive care; what their experiences were, and how they and their family felt about the care. It does not matter if they moved from their own home or a relative’s house, to a hospital, care home or hospice. We are interested in all of these experiences.
We are interested in speaking to carers of people who died with stroke, lung cancer or heart failure. This is because carers are the people most likely to know about the care the older person received in the months before their death. They are also most likely to be able to tell us about the things that could improve the care given, and also the things that affected the family the most.
Part 1 of this leaflet tells you why the research is being done and what would be involved if you choose to take part.
Part 2 is further information you should read if you choose to take part. Feel free to discuss this research with anyone that might help you to make a decision on whether to take part in it including friends and family.
Part 1
What is the purpose of this study?
Older people are sometimes moved between different health care settings such as hospital, hospices and their home at the end of life. We are studying the statistics about people moving in and out of hospital and other places. But we need your help, to tell us the real story behind the numbers.
We would like to know about your experiences of caring for someone who was moved between different places in the last 3 months before they died. We would like to ask you about where they received care, such as home, hospital, care home or hospice; why they moved, or did not move from one place to another, and how they and you felt at the time about any moves. We are also interested in how the care that your relative/loved one/friend received affected you and your family. This may have been emotionally, socially, physically, or financially. We are also particularly interested in the care that they received just before they died (from about 3 months before they died).
Why have I been chosen?
We would like to talk to people who have looked after, and cared for people over 75 years old who died with stroke, lung cancer or heart failure. This is because we are interested in talking to people who know about the care the person over 75 years old was receiving before they died. You do not have to have lived with them, or be a member of their family. You just need to have played a close part in looking after them. You might have been their friend or neighbour or a paid carer for example. We would still like to talk to you.
This information sheet has been sent to you from the GP practice you are registered with. They identified you as someone who may wish to take part.
If you think that there is someone else who may be able to help us and who would be interested in talking to us, then please pass this information on to them.
Do I have to take part?
Taking part or not is entirely up to you. We will not contact you again, unless you send the reply slip back to the research team. If you would like to take part, you will need to return the reply slip at the end of this information sheet. I will then phone you and arrange a time to interview you at a place and time of your choosing (most people choose their home).
The research will not affect your health or medical care in any way. Whether you take part or not, any care you receive from your doctor will not change. If you decide to take part and then change your mind, your doctor or nurse will not know.
What will happen to me if I take part?
If you send the reply slip back to the research team, a researcher, [Name], will phone you within a week or so and tell you more about the study and answer any questions you may have. You can also phone [Name] directly (her number is below) if you want to take part or find out more information. If you decide not to take part at this point, she will not contact you again.
If you do decide to take part, we would arrange to meet you wherever may be convenient for you, at a convenient time. We will answer all your questions about the study and ask you to sign a form saying you are happy to talk to us. If you agree, we will record the interview so that the interviewer can remember more accurately what you said.
The interview will not last longer than 90 minutes, and we will stop at any time if you wish. Whatever you tell us will be confidential. No one will be able to identify you from any of the reports we produce and no-one will know that it is you that made any particular comments. Only if the researcher uncovers information that suggests that you, or others, are at risk of coming to any harm, will they break this promise of confidentiality.
What are the possible disadvantages and risk in taking part?
A possible risk is that we might upset you by asking questions about the few months before your loved one died. If this happens, we can move on to another question, return another day, or just finish the interview there and then.
What are the possible benefits?
We cannot change the experience that you or your loved one have had, but we might be able to use the information that you give us, to make the experience better in the future for other people.
Sometimes, people find it helpful to talk to someone about what happened, the good things and the bad things. Some people find it comforting to know that by giving their opinion, they might help to improve care services in the future.
What happens when the research study stops?
After your interview, we will telephone you the following week to check that you were happy with the way in which the interview was conducted. After that we will not contact you again. If you would like to receive a newsletter summary of the outcome of the study (which could take up to two years, as it is a big study) then we will be happy to send one to you.
What if there is a problem?
If there are any problems with the research that we can sort out, we will try and do this. If you are unhappy about the questions, or anything to do with the researcher, we will tell you who to contact. The details of this are in part 2.
Will my taking part be kept confidential?
YES. All details about your participation will be kept confidential.
However, if we think that there may be a risk of you or someone else being harmed in any way, we will break confidentiality and report what you have told us to the relevant authorities.
Contact Details:
Any questions, queries or problems please contact [Name] on [Number]. Or if you or your relatives would like to send us an email, the address is; [Email]. If you would like to call Louise instead of sending the reply slip, to confirm your interest in taking part, you can also do this.
Please note that the researcher is not a medical doctor, and she is not able to act as your advocate. She will not be able to help you to complain about your care in any way. Details of the NHS Complaints Procedure can be obtained from your hospital doctor or GP. The researcher can answer questions relating to this research and the person you speak to on the telephone will be the same person who visits you, if you decide to take part.
Part 2- Please read this if you are interested in taking part in the study.
What will happen if I decide not to carry on in the study?
Nothing at all will happen. If you decide not to carry on, after you have replied to us, please phone us and let us know.
Can I complain?
If you are unhappy with the research in any way please tell us. We will try to put things right. If you would prefer to talk to someone outside the research team or if you are not happy with the way we deal with your problem you can formally complain through the NHS Complaints Procedure. Details can be obtained from your hospital doctor or GP.
Am I likely to be harmed?
In the very unlikely event that something does go wrong and you are harmed whilst taking part in this research there are no special compensation arrangements. If the harm is due to someone’s negligence then you may have grounds for a legal action for compensation against the University of Liverpool, who employs the researcher, but you may have to pay your legal costs. The normal NHS complaints mechanisms will still be available to you, if appropriate.
Will all my thoughts and answers be kept confidential?
Yes. Any information about you will have your name and address removed. The only person that knows what you said is the researcher who interviewed you. Any tapes will be kept secure and then destroyed and any written information will be kept strictly confidential. The procedures for handling, processing, storage and destruction of data from the study are complaint with the Data Protection Act 1998. After five years, recordings will be destroyed.
Involvement of the GP
Your general practitioner (GP) or nurse has suggested that you might be interested in taking part in the study. We will not ask for any personal or medical information about you from them. We will not tell your GP that you are taking part in the study, unless you ask us to do so.
What are you going to do with the results of the study?
The results of this study will be published in academic journals, and presented at conferences, and reports will be prepared for the NHS and the participants. You will not be identified in any publication even if we use your words. We are happy to send you a newsletter with a summary of the findings if you wish.
Who is organising and funding the research?
Researchers from the University of Liverpool are organising this research. Other Universities are also part of the team, although they will not see any identifiable information. The main research is funded by the NHS and it is being conducted in two regions of England.
Who has reviewed the study?
This study has been given favourable ethical opinion for conduct in the NHS by the Liverpool Central Ethics Committee.
Please keep this information sheet. If you would like to ask any other questions regarding the research, or what is expected from you, please ring [Name] on [Number] (Monday to Friday 9am–5pm). Or, [Name] email address is [Email].
[Name] will contact you to arrange an interview time within a week or so of her receiving your reply slip. Or, you can call [Name] and let her know that you are interested in taking part.
Thank you for taking the time to read this information.
Poster to advertise study
Publicity: participant information leaflet
Publicity: press release
HELP IMPROVE END OF LIFE CARE TO OLDER PEOPLE THROUGH UNIVERSITY OF LIVERPOOL STUDY
Researchers at the University of Liverpool are conducting an interview study with family members and friends of people aged 75 or older who have died in the last year with lung cancer, heart failure or after a stroke. The Liverpool study, in collaboration with the Universities of Oxford, Southampton, Manchester, Lancaster and Nottingham, will provide data on the experiences of UK patients in order to build a national picture of the difficulties patients face when moving through the health and social care system towards the end of life.
The team has been funded by the National Institute of Health Research for three years to study how well the health system looks after elderly patients as they move between home and hospital, care home or hospice. In the last months of their lives, older people often transfer many times between different places of care. This might mean going into hospital or hospice, returning home after treatment, or moving into a care home or the home of a friend or relative. Previous studies in the United States have found that many transfers do not improve the control of pain or quality of life, even though that is the intention. This study will help us to understand what is happening in the UK, and whether health and social services are organised in the best possible way to care for older adults.
Dr Barbara Hanratty, from the University’s Institute of Psychology, Health and Society, said: “Our studies have so far highlighted the ways that patients find it difficult trying to negotiate their way through health and social care services when they are unwell. Patients have told us about many problems ranging from communication with health professionals to practical issues such as transportation to hospitals, and inappropriate equipment being delivered to their homes. We are keen to talk to families and carers of who have been bereaved, so that we can understand how well care was organised for them in the crucial weeks and months before their relative died. “People have a great deal of contact with health and social services in their final year of life and can experience frequent transfers between places of care, so it is essential that we have data that shows us whether the movement of patients across many services has a positive or negative outcome on their quality of life.”
Family members and friends aged 18 years or older and who can give an account of the older person’s care can take part. No one will be interviewed in the first three months after someone has died.
To find out more about the study please contact the researcher [Name], on [Email] or telephone: [Number].
Letter of invitation to professional interviewees
11/NW/0466 Transitions for older adults: Professional perspectives
Letter of invitation to potential participants Version 1.0 27 June 2011

Dear [Name of potential participant],
Researchers at the University of Liverpool would like to invite you to take part in a telephone interview.
We are conducting research into the causes and consequences of transitions between different places of care for older people in the last few months of their life. We are looking at transfers between all care settings, including hospitals, care homes, hospices and older adults’ own homes.
We are seeking your help to understand the perspectives of health and social care providers and commissioners whose work has relevance to the care that older people receive in the last months of their lives. Interviews with patients and bereaved family caregivers have already provided insights into older adults’ experiences of transfers between places of care. We also wish to understand the different constraints and pressures faced by people who work with older adults’ services, and how these may influence the care provided as older adults move from one place to another.
Interviews will be conducted by telephone (or face-to-face if you prefer) at a convenient time for you. People who take part will be asked to spend no more than an hour talking about their perspectives on transfers between care settings. We will provide short descriptions of typical patterns of care received by older people, to help interviewees to reflect on what happens in their area of work.
A leaflet and information sheet about this study is enclosed with this letter. If you have any questions, please contact [Name] by telephone [Number] or by email: [Email].
We will contact you by telephone in the next two weeks, to ask if you would like to take part. If you have already decided, please feel free to get in touch before then, by telephone or email, or alternatively by returning the reply slip by post.
Thank you for taking the time to read this letter. We hope that you will share our interest in improving care for people at the end of their lives. If you feel that a colleague may also be interested in being interviewed as part of this study, please pass on this information to them, or provide us with their contact details so that we can send information to them.
Yours sincerely,
Ms [Name], Research Assistant and
Dr Barbara Hanratty, Clinical Senior Lecturer
Study website: www.transitionsattheendoflife.org
Participant information sheet: professional interviewees
Participant information sheet
Research into transfers between care settings for older adults at the end of life
You are being invited to take part in a study, which aims to understand the circumstances in which older adults with serious illnesses transfer between care settings in the last few months of their lives, and how services can better meet the needs of older adults and their families. The care settings involved homes, including sheltered accommodation and homes shared with relatives.
We are interested in the perspectives of people working in health and social care, including service managers and commissioners with insights into these services. We are particularly interested in the services available for older adults who die with lung cancer or heart failure, or following a stroke, as well as chronic obstructive pulmonary disease (COPD), breast and colorectal cancers. We would like to know what health and social care providers and commissioners see as the key challenges to providing good end of life care across settings, and the changes they would like to see implemented.
Part 1 of this leaflet tells you why the research is being done and what would be involved if you choose to take part.
Part 2 is further information you should read if you choose to take part. Feel free to discuss this research with anyone that might help you to make a decision on whether to take part in it.
Part 1
What is the purpose of this study?
At the end of life, older people are sometimes moved many times between different health care settings such as hospital, hospices, care or nursing homes, and their home. We are studying the statistics about people moving in and out of hospital and other places, and we have spoken with patients, and bereaved family caregivers about their experiences. But we need your help, to understand health and social care professionals’, service managers’ and care commissioners’ perspectives.
We would like to know about your job role and your involvement with care for older adults at the end of life, including transfers between care settings. We would like to ask you about what you see as the key barriers and facilitators of good end of life care in the context of transfers between care settings, and any suggestions to improve provision. We would also like to ask you to discuss some scenarios involving older adults and their families, drawing on your professional experience and insights into the structure of services and how they work in practice. We would be particularly interested in any insights you can give into care available to older adults who die with lung cancer, heart failure or following a stroke, as well as chronic obstructive pulmonary disease (COPD), breast and colorectal cancers.
Why have I been chosen?
We wish to talk to a wide range of health and social care professionals, service managers and commissioners with insights into the care older adults receive in their last few months of life. This is because we are interested in developing a breadth of understanding about how transfers between care settings are understood in each type of care setting, within primary care, and by those who have an overview of all service provision within a local area.
If you think that there is someone else who may be able to help us and who would be interested in talking to us, then please pass this information on to them.
Do I have to take part?
Taking part or not is entirely up to you. If you would like to take part, you will need to contact the researchers by telephone, email or by returning the reply slip at the end of this information sheet. We will then phone you and arrange a time to interview you at a time of your choosing. Most people will be interviewed by telephone.
If we do not hear from you, we will try to contact you by telephone in the next two weeks, to ask if you would like to take part.
Taking part is confidential, and your colleagues and employer will not be informed whether or not you were interviewed.
What will happen to me if I take part?
If you contact the research team, a researcher, [Name], will ‘phone you within a week or so and tell you more about the study and answer any questions you may have. You can also ‘phone [Name] directly (her number is below) if you want to ask questions or volunteer to participate.
If you do decide to take part, we would arrange to interview you at a convenient time. Most people will be interviewed by telephone, but if you would prefer to meet the researcher, we will try to organise a face-to-face interview. We will answer all your questions about the study and ask you to sign a form saying you are happy to talk to us, and send it back to us. If you agree, we will record the interview so that the interviewer can remember more accurately what you said.
The interview will not last longer than 60 minutes, and we will stop at any time if you wish.
Whatever you tell us will be confidential. The research is taking place over a wide geographical area in north west, south central and south west England, so individuals will not be identifiable from their job titles. No one will be able to identify you from any of the reports we produce and no-one will know that it is you that made any particular comments.
Only if the researcher uncovers information that suggests that you, or others, are at risk of coming to any harm, will they break this promise of confidentiality
What are the possible disadvantages and risk in taking part?
The disadvantages and risk in taking part are very low. We are asking for an hour of your time to talk about your professional perspectives. We will ensure that you are not identified by your employer, colleagues or clients.
What are the possible benefits?
While we cannot directly change services or your job circumstances, we might be able to use the information that you give us, to make recommendations about how services could be improved in the future.
What happens when the research study stops?
After your interview, we will telephone you the following week to check that you were happy with the way in which the interview was conducted. After that we will not contact you again. If you would like to receive a newsletter summary of the outcome of the study (which could take about a year, as it is a big study) then we will be happy to send one to you.
What if there is a problem?
If there are any problems with the research that we can sort out, we will try and do this. If you are unhappy about the questions, or anything to do with the researcher, we will tell you who to contact. The details of this are in part 2.
Will my taking part be kept confidential?
YES. All details about your participation will be kept confidential.
However, if we think that there may be a risk of you or someone else being harmed in any way, we will break confidentiality and report what you have told us to the relevant authorities.
Contact Details:
Any questions, queries or problems please contact [Name] on [Number] or [Email].
Please note that the researcher is not a medical doctor. The researcher can answer questions relating to this research and the person you speak to on the telephone will be the same person who interviews you, if you decide to take part.
Part 2 – Please read this if you are interested in taking part in the study.
What will happen if I decide not to carry on in the study?
Nothing at all will happen. If you decide not to carry on, after you have replied to us, please phone us and let us know.
Can I complain?
If you are unhappy with the research in any way please tell us. We will try to put things right. If you would prefer to talk to someone outside the research team or if you are not happy with the way we deal with your problem you can formally complain through the NHS Complaints Procedure.
Am I likely to be harmed?
In the very unlikely event that something does go wrong and you are harmed whilst taking part in this research there are no special compensation arrangements. If the harm is due to someone’s negligence then you may have grounds for a legal action for compensation against the University of Liverpool, who employs the researcher, but you may have to pay your legal costs. The normal NHS complaints mechanisms will still be available to you, if appropriate.
Will all my thoughts and answers be kept confidential?
Yes. Any information about you will have your name and address removed. The only person that knows what you said is the researcher who interviewed you. Any tapes will be kept secure and then destroyed and any written information will be kept strictly confidential. The procedures for handling, processing, storage and destruction of data from the study are complaint with the Data Protection Act 1998. After five years, recordings will be destroyed.
What are you going to do with the results of the study?
The results of this study will be published in academic journals, and presented at conferences, and reports will be prepared for the NHS and the participants. You will not be identified in any publication even if we use your words. We are happy to send you a newsletter with a summary of the findings if you wish.
Who is organising and funding the research?
Researchers from the University of Liverpool are organising this research. Other Universities are also part of the team, although they will not see any identifiable information. The main research is funded by the NHS and it is being conducted in three regions of England.
Who has reviewed the study?
This study has been given favourable ethical opinion for conduct in the NHS by the North West Ethics Committee.
Please keep this information sheet. If you would like to ask any other questions regarding the research, or what is expected from you, please ring [Name] on [Number] (Monday to Friday 9am-5pm). Or, [Name]’s email address is [Email].
[Name] will contact you to arrange an interview time within a week or so of her receiving your reply slip. Or, you can call [Name] and let her know that you are interested in taking part.
Thank you for taking the time to read this information.
Consent form for professional interviewees
11/NW/0466 Transitions for older adults: Professional perspectives
Consent Form Version 2.0: 07 July 2011
Consent form: participant copy
Transitions between services for older adults
Please initial each box.
| 1 | I confirm that I have read and understand the information sheet dated . . .. . .. . .. . .. . .. . .. . .. . ...(version . . .. . .. . .. . .) for the above study. I have had the opportunity to consider the information, ask questions and have had these answered satisfactorily. | □ |
| 2 | I understand that my participation is voluntary and that I am free to withdraw at any time, without giving any reason, without my legal rights being affected. | □ |
| 3 | I agree to take part in the above study and that the interview can be audio taped. I understand that direct quotes will be used but in a way where I will not be identified. | □ |
| 4 | I understand that data collected during the study, may be looked at by individuals from regulatory authorities. I give permission for these individuals to have access to my data. | □ |
Name of participant. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .
Signed. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .Date. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .
Name of person taking consent. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .
Signed. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . .. . ..Date. . .. . .. . .. . .. . .. . .. . .. . .. . ...
Contact: [Name] [Number], [Address].
Topic guide: patient interviews
Transitions between services: patients’ perspectives
1. Introduction.
2. Life history.
3. Understanding of illness.
4. Nature of transitions.
5. Understanding of transitions.
6. Effects of transitions.
7. Ending.
8. Questions.
1. Introduction
Name and position of researcher within University of Liverpool.
Outline and purpose of study.
2. Brief life history
Childhood and family background.
School life/education.
Working history.
Living arrangements before illness/after illness.
Family life now and before illness (include marital status and number of children/grandchildren, if any).
Changes throughout life for significant items above.
3. Illness understanding
Duration and course of illness.
First diagnosed, how long, other illnesses.
Who diagnosed and explained illness?
Key professionals/family members involved in care.
Family knowledge.
Family expertise.
Family support.
Family issues that have increased/reduced support.
Own knowledge of illness.
Changes since diagnosis.
Perceived gaps in knowledge.
Perceptions of type/amount of information.
Expectations for the future.
Knowledge of expected course.
Emotions (e.g. hope/denial/frustration/upset/control).
4. Nature of transitions
How many in last 12 months?
Where to/where from?
Why?
Who made the decision (patient/carer/family/services, etc.)?
Feelings about decision.
How many in last 3 months?
Where to/from?
Why?
Who made the decision (patient/carer/family/services, etc.)?
Feelings about decision.
Feeling about nature of care.
For patient/family/care staff.
Knowledge of team/familiarity with main health professionals.
How do they feel about the number/nature?
Perceptions of information.
Choice.
Practicalities.
Care services.
Perceptions of need for improvements.
5. Understanding of transitions
Transitions explained? How? By whom?
How did you feel?
How did family feel?
Understanding of place of care now.
Feelings about staying (if would like to move on, prompt for reasons).
6. Effects of transitions
Physical/mental/emotional/social.
Impact on physical health problems (changes in pain, discomfort, medication).
Impact on psychological well-being (increase or decrease in subjective well-being/anxieties and fears).
Emotional: do you feel more or less comfortable/happier/peaceful?
Social: more/fewer visitors/change in surroundings?
Effect on close family/distant family/primary caregiver.
Has transition influenced relationship between family members (e.g. strained/closer/stronger relationships)?
Practical issues: bus routes, areas, distances, childcare, visiting times.
Financial.
Have there been any financial changes due to the transitions?
Resulting in transitions.
Cost of old setting/new setting.
Other –?
Any other issues that the interviewee would like to raise?
7. Ending
Confidentiality.
Anonymous data.
No health-care-related impact.
Ability to withdraw at any time.
Use of results without names.
Use of results.
Published journals, articles, conferences.
DoH who funded research want to know experiences.
Option of newsletter on summarising results.
Topic guide: caregiver interviews
This topic guide follows the structure of the VOICES questionnaire that it replaced or supplemented. Order of topics guided by participant.
Introduction
Name and position of researcher.
Outline and purpose of study.
Confidentiality.
Hospital admissions
Reasons for admissions.
Decision makers.
Involvement in decisions.
Understanding of reasons and choices.
Practical concerns.
Time in hospital
Experience of symptoms.
Perceptions of treatment.
Perceptions of staff (humanity, caring, professionalism, technical ability, willingness to listen).
Involvement in decision-making.
Understanding of choices, treatment options.
Perceptions of outcome of time in hospital (changes in symptom control, quality of life, benefits for carers).
Perceptions of information provided.
Repeat for hospice, as appropriate
Care at home
Questions following structure above, considering:
-
assessment of needs
-
contact with out-of-hours services
-
GP and district nurses, specialist nurses, social care
-
medication – access and understanding.
Death and bereavement
Preferences for place of care and death.
Preferences for transitions and how they influenced actions.
Overview of continuity and consistency of care
Perceptions of joint working, communication, continuity (relational, informational).
Factors leading up to transitions.
Control of transitions, carer involvement.
Overview of care received.
Other aspects of transitions identified by participant
Closing
Thanks.
Confidentiality.
Use of data, reports, feedback to participants.
Questions, concerns.
Topic guide: interviews with health and social care providers and commissioners
Introduction
Study aims, confidentiality, audio recording, informed consent.
Socio-demographic data
Interviewee’s job title, responsibilities, role in end-of-life care and transitions between settings, key national guidance relevant to role.
Introductory questions
-
What are the key circumstances/factors in which older adults may transition between settings?
-
Description of typical patterns of care in their area for people at the end of life with, for example, heart failure, stroke, lung cancer, etc. – key sources of support and care, typical use of institutional and community care.
-
Perceptions of key problems, challenges or threats with transitions between care settings for older people at the end of life.
Perceptions/views prompted by scenarios
Scenario 1: Inappropriate transition(s), as perceived by family caregivers.
Scenario 2: Transition(s) avoided and care perceived as positive by family caregivers.
Scenario 3: The important role of caregivers – contrasting experiences of two patients, one with a network of supportive family and the other with no family caregivers.
Where possible, scenarios constructed from interviews with family caregivers will be sent to provider and commissioner interviewees in advance of their interviews. Scenarios will be used to provoke discussion (within the interviewees’ area of expertise) on the following topics:
-
perceptions of transitions including appropriateness or inappropriateness, patients’ best interests and benefits
-
barriers and facilitators of positive experiences of transitions
-
barriers and facilitators to avoid unnecessary transitions
-
family caregivers and statutory services, including interfaces and provision for older people without family caregivers
-
community/hospital interfaces, including co-ordination, communication and medication safety
-
relationships between transitions to palliative and terminal care, and transitions between settings
-
age – including effects on experiences of transitions, and adaptations of services to accommodate differences.
Conclusion
Clarifications, any additional points.
Thanks and information about availability of study findings.
Scenarios for phase 3 interviews
A. Inappropriate transitions, as perceived by caregivers:
-
multiple admissions to hospital or other institution
-
late admission to hospice or late implementation of specialist palliative care
-
death in hospital shortly after admission from home or care home
-
delayed transitions between institutions.
B. Transitions avoided and care perceived as positive by caregivers.
C. Transitions avoided because of the role of the caregivers.
A 1. Multiple admissions to hospital or other institution
Case 1. Mrs S, an 82-year-old lady with cancer, lived alone in a rural area. In the last 4 months of her life, she was admitted to hospital, went home and was readmitted less than 24 hours later. She moved into one care home, was transferred to a second care home, and then readmitted to hospital when she fell out of bed and cut her head.
Case 2. Mr W, an 89-year-old gentleman with heart failure and diabetes, lived with his disabled wife in a small town. He was admitted to hospital six times in the last 5 months of his life.
Case 3. Late admission to hospice or implementation of specialist palliative care.
Mrs C, aged 88, had cancer and a stroke. She was cared for at home by her children. (She required help with mobility, continence and eating.) She had one short stay in a nursing home for respite. In the nursing home, she fell out of her bed multiple times, breaking some ribs, and spent one entire night on the floor. Two weeks before she died, Mrs C was admitted to hospital, and on the day of her death, she was transferred from hospital to a hospice.
Case 4: Death in hospital shortly after admission from care home.
Mrs S, aged 92 with heart failure, lived with her son and his wife. She was admitted to hospital with a chest infection and discharged to a care home for recovery. From the care home, she was readmitted to hospital and died 1 hour later.
Case 5: Death in hospital shortly after admission from home.
Mr M, 86 years old with colorectal cancer, lived at home. He was admitted to hospital and discharged to a relative’s home. He went back to his own home and collapsed. The ambulance staff resuscitated him and took him to hospital where he died 18 hours later.
Case 6: Delayed transitions between institutions.
Mrs H, aged 90 with heart failure, lived alone. In the last 6 months of her life she was admitted to hospital, and then transferred to a local community hospital for rehabilitation. She then moved backwards and forwards between the two hospitals four times whilst she was waiting to move into a care home. When the funding was organised, she did move into the care home but died shortly afterwards.
B. Transitions avoided and care perceived as positive by caregivers
Mrs J, aged 83, a retired academic, was admitted to hospital with a suspected brain tumour. While she was an inpatient, she had a stroke, which affected her sight, speech and physical functioning. Her family decided that she should return home from hospital. Community services provided carers and district nurses around the clock until Mrs J died, at home with her family around her.
C. Transitions avoided because of the role of the caregivers
Mr S, aged 78, had lung cancer and lived with his wife in a rural area. He spent 2 weeks in hospital, then went home for 5 weeks before his death. They had no regular input from community or palliative care services. Mr S fell a couple of times, and his wife telephoned paramedics to help to get him off the floor. Each time, the paramedics wanted to take him to hospital, and the GP had to be contacted to intervene. On the day that he died, Mr S fell, but they decided to leave him on the floor to avoid another argument about admission to hospital. The district nurse was expected later, but Mr S died on the floor before she arrived.
Glossary
- Carer
- Carer, caregiver and bereaved caregiver are terms used in this document to describe someone who provides unpaid support to family or friends.
- Care trust
- Care trusts are organisations that work in both health and social care. They carry out a range of services, including social care, mental health services and primary care services.
- Episode
- Term used in Hospital Episode Statistics: an episode is a single period of care under one consultant.
- Spell
- Term used in Hospital Episode Statistics: a patient’s entire stay in hospital is a spell. A spell can contain one episode, or several episodes. If the patient is transferred to another hospital, dies or is discharged, the episode and the spell end. The vast majority of spells contain only one episode.
List of abbreviations
- COPD
- chronic obstructive pulmonary disease
- FFS
- fee-for-service
- GP
- general practitioner
- GSF
- Gold Standards Framework
- HES
- Hospital Episode Statistics
- IMD
- Index of Multiple Deprivation
- IT
- information technology
- LCP
- Liverpool Care Pathway
- ONS
- Office for National Statistics
- PCRN
- primary care research network
- PCT
- primary care trust
- QOF
- Quality and Outcomes Framework
- REC
- research ethics committee
- SDO
- Service Delivery and Organisation
- SHA
- Strategic Health Authority