Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/1007/47. The contractual start date was in September 2011. The final report began editorial review in March 2013 and was accepted for publication in October 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
David Roberts has declared a competing interest. Capsticks LLP acts on behalf of, and so has a financial relationship with, a number of organisations who participated in this research.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Birks et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
. . . there are no easy answers when it comes to making mistakes. That needs to be said outright lest someone, especially someone in training who is less experienced, think that admitting a mistake stops at quality control or sharing responsibility, and that there is then some way around the difficult task of actually taking responsibility for the mistake. Within the culture of medicine and even more broadly in modern society there seems to be a drive for finding the easy way out. In this case there is none, and it needs to be made very clear that this is a defining moment in the life of a physician with regard to integrity and professionalism
Reproduced from Medical Errors and Medical Culture. There is no Easy Way Around Taking Responsibility for Mistakes, Lyckholm L, Vol. 323, p. 570, 20011 with permission from BMJ Publishing Group Ltd.
Estimates suggest that approximately 1 in 10 patients admitted to hospital will experience some sort of unintended harm; approximately half of these cases are thought to be preventable. 2,3 In a recent review of prevalence studies, between 3% and 16% of hospitalised patients were found to have suffered harm from medical care. 4 This represents a significant proportion of patients, and the Department of Health in the UK has identified quality and safety of care as a major concern. 5 The recent publication of the Francis report has brought this into even sharper focus. 6 Internationally, other agencies are dedicated to co-ordinating improvement efforts [e.g. the Agency for Healthcare Research and Quality (AHRQ) and The Joint Commission (TJC) – formerly the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) – in the USA, and the Australian Commission on Safety and Quality in Healthcare (ACSQH)]. A central component of a just patient safety culture is thought to include the disclosure of serious medical incidents to patients who have been affected or their families, often termed open disclosure. 7 The concept of openly disclosing the details of medical incidents has been adopted by several organisations, including ones in Canada,8 New Zealand,9 the UK,10,11 the USA12 and Australia,13 which implemented a national open disclosure policy in 2003. However, it is estimated that as few as 30% of harmful errors may currently be disclosed to patients. 14
Historically, the disclosure of adverse events to patients was neglected. Prior to the 1970s there was a general acceptance of medical expertise; medical notes were rarely seen by patients or families and, if required, often had to be obtained through a legal process. Discussions recognising this as problematic appear to have emerged during the 1970s and early 1980s, when it was identified that patients suffering from ‘medical mishap’ were often unable to find out who was responsible for an error or whether or not anyone had been at fault. 15 The importance of transparency in relation to improving quality and safety in health care became increasingly discussed in the wake of seminal documents such as To Err is Human 16 in the USA and An Organisation With a Memory 17 in the UK. Standards that promote open communication with patients following events where errors have occurred are rapidly emerging in both the UK and a wider international setting. 4,17–19 Advocates of open disclosure propose that failing to communicate effectively with patients following errors could reduce patient trust in health services, perhaps with negative consequences for future care, and may increase the likelihood of litigation. Patient trust may be diminished if they consider that their health service provider has not honoured their commitment to care for patients by apologising. There is some evidence, mainly emerging from the USA, to support such concerns. 20,21
In the UK, the National Patient Safety Agency (NPSA) relaunched its Being Open framework in November 2009. 11 The framework describes Being Open as being about the way in which health-care organisations and their staff communicate with patients and/or their carers following a patient safety incident, and sets out 10 key principles that underpin the successful facilitation of this process. These include providing a genuine and timely apology for what has happened, keeping patients and/or their carers informed about the progress made with the incident investigation, reassuring patients and/or carers that the incident is being taken seriously and ensuring that measures are taken to prevent the incident from happening again.
An apology is described as different from an admission of liability, and though an apology may be referred to in legal proceedings, the NHS Litigation Authority (NHSLA) stresses that this should in no way deter those involved from providing explanations and apologies following adverse events. 22 Being Open suggests that good communication and trust are fundamental to the relationship between health-care professionals and patients, but also that it is the ethical course of action. The Being Open framework was part of a broader NPSA initiative in the UK to create an open and fair culture in the NHS. The NPSA stressed that open disclosure should be explicitly linked to systems of incident reporting and analysis in health-care organisations. 23 Reorganisation within the NHS meant that on 1 June 2012 the key functions and expertise for patient safety developed by the NPSA transferred to the NHS Commissioning Board. It was anticipated that this would ensure that patient safety remains at the heart of the NHS and builds on the learning and expertise developed by the NPSA in driving patient safety improvement. The Board will continue to use the National Reporting and Learning System (NRLS) to identify important patient safety issues at their root cause. Health-care organisations are expected to report patient safety incidents to the NRLS as previously. The approach to monitoring safety within UK NHS trusts is therefore unchanged, and the stance that disclosure should be part of safer patient care remains.
Despite limited empirical work assessing the effectiveness of implementing open disclosure policies (largely undertaken in the USA, Australia and New Zealand), a review of the available literature in 2008 revealed increasing recognition of open disclosure as an important issue for both organisations and patients. 24 The review also highlighted key debates around the ethical principles of ‘being open’ versus the legal liability and economic risk involved. The absence of investigation into non-hypothetical scenarios and individuals’ actual experiences of open disclosure was also noted. With growing acknowledgement of the challenges associated with open disclosure, the literature in this field has rapidly expanded, and there is now a need to update the synthesis undertaken in 2008 to identify a point from which to move forward, particularly in relation to the UK. Further work undertaken by Iedema et al. includes the assessment of open disclosure in terms of the impact on patients and health-care staff in Australia. 25–27 Qualitative analysis of interviews with 131 clinical staff and 23 patients/family members indicated that, despite some uncertainty surrounding the use and consequences of open disclosure, the system was strongly supported. 24 Further work has examined 119 patients’ and family members’ responses to questions about whether or not, and how, they experienced disclosure. 27
Complementary work by Gallagher et al. has conducted an investigation into patients’ and doctors’ attitudes towards the disclosure of medical errors, which highlighted the need for doctors to meet patients’ expectations of an apology following medical errors and also to provide information about the error. 28 Further work by Gallagher et al. ,29 in line with findings from other studies,30,31 has discussed the increasing need and desire for open disclosure of medical errors.
Although the ethical arguments for the open disclosure of adverse events to patients are strong, there are many stakeholders (e.g. patients and clinicians, hospital managers, health policy-makers, unions, equipment companies, insurers, legal advisers and indemnifying organisations) involved in the delivery of such a framework at a variety of levels. (Future reference to stakeholders will include the aforementioned groups, although this is not intended as an exhaustive list.) The complexities of the differing perspectives of all of these stakeholders means that implementation of any initiative is challenging. Embedding incident disclosure into national and local culture within the NHS is a substantial challenge for NHS managers, as well as for the individuals involved in direct patient care. It has been suggested that this is due to a culture that favours risk aversion over patient-centred disclosure, despite the suggestion that the latter produces better financial and relational outcomes. 32 Current barriers to disclosure, such as fear of litigation or damaged reputation, can obstruct clinicians in maintaining good relationships with patients and becoming more open to learning from error or mistakes. If such barriers are not recognised, challenged and addressed appropriately and overtly, they may cause significant problems for the implementation of a more open safety culture.
There appears to be a small but significant literature within the area of patient safety which looks at the open disclosure of adverse events, including the important area of the impact of open disclosure on the health professionals involved in the error and the link between disclosure and systems improvement. 33 However, this research is almost exclusively grounded in contexts outside of the UK, and much of the empirical work is based on training scenarios rather than in situ practice. We know little about how the policy of open disclosure is being, or might be, implemented and applied locally or nationally in the UK and how it is, or will be, aligned with current incident reporting and analysis systems in health-care organisations. As is the case with many patient safety outcomes, there is also a lack of knowledge around how open disclosure might best be evaluated and improved. In addition to examining the current breadth and quality of the literature in the area of open disclosure to date, this research will provide information about the implementation and current stakeholder perceptions of open disclosure within the UK.
Aim
The overall aim of this project was to critically evaluate and extend both the evidence base and practice in relation to the implementation of a policy of open disclosure of adverse events to patients within the UK.
Objectives
-
To extend a previous literature review of open disclosure conducted by one of the applicants in 2008.
-
To identify the strategies which have been considered or used to encourage an open disclosure culture, and to assess the evidence of effectiveness of such strategies.
-
To identify and critique the various ways in which open disclosure has been conceptualised and measured.
-
To determine the understanding of, views on and interpretation of a policy of open disclosure of adverse events among a variety of UK stakeholders.
-
To identify specific situations and ways in which the various stakeholders have been involved in the disclosure of adverse events in the UK, and their experiences of this.
-
To explore how open disclosure can be linked effectively into safety and quality management systems at all levels.
-
To explore the extent to which disclosure activity is actually linked in practice to safety and quality management.
-
To develop a summary of evidence-based guidance for managers to facilitate the implementation of open disclosure in individual trusts.
The objectives were addressed in three main phases, each of which built on the previous work. The first phase comprised a focused literature review, summarising current knowledge on different stakeholder roles, current interventions and proposed interventions, underpinning theory and the ways in which current strategies feed into established reporting systems. The second phase involved individual interviews, with the objective of generating new knowledge about UK-based stakeholders’ views on their roles in and experiences of open disclosure of safety incidents in health-care settings. The third phase involved the development of a set of short pragmatic suggestions aimed at NHS trust executives and managers, to facilitate the implementation and evaluation of open disclosure in UK NHS trusts.
The main product of this research was intended to be new information which can be used to:
-
identify areas where current evidence and knowledge remain sparse
-
supplement the current guidance on implementing open disclosure
-
inform training and support for organisations and individuals in this area
-
identify continuing barriers to the implementation of open disclosure
-
identify well-developed models for open disclosure.
We also aimed to produce a series of short and pragmatic guidelines for NHS trust managers to facilitate the implementation and evaluation of open disclosure initiatives.
Chapter 2 Methods
This study addressed the objectives via three main phases of work. A review phase and a qualitative phase directly contributed to a synthesis of the information, to address specific issues in relation to delivery of the Being Open guidance in the UK in the final phase of the study.
Phase 1: reviews
The reviews were conducted to capture data from a diversity of sources, in a systematic way, to identify how open disclosure (an openness with patients about avoidable potentially harmful incidents) has been conceptualised, the key ethical and legal debates associated with the process, the roles of the different stakeholder groups and the outcomes that have been used to assess its impact.
A more focused review of the effectiveness of open disclosure interventions to date was carried out to sit within this broader conceptual synthesis.
Two previous reviews have been conducted, both of which involved one of the current project team (RI). The authors of these reviews planned to search five electronic databases using terms related to open disclosure, as well as the websites of health and government regulatory bodies in a number of countries. 34,35 Although both of these reviews are seminal pieces of work and comprehensive, the authors adopted a less standard systematic search strategy than the strategy presented in this work. In the previous work, searching was stopped after three databases had been searched as it was considered they had ‘reached saturation’ (the same articles began to appear), whereas all literature identified will be considered in this work. This makes the current work the most comprehensive exploration of previous literature to date.
Objectives
Review 1: scoping review
The aim of this review was to identify and critique the literature around open disclosure, including (i) the ways in which it has been conceptualised and discussed within current systems of quality and safety, (ii) the wider debates around legal and ethical issues in open disclosure, (iii) the outcomes used to explore its impact, (iv) the roles of stakeholder groups, (v) the relationship between open disclosure policy and systems of reporting and monitoring adverse events worldwide and (vi) the extent to which open disclosure policies appear to have been informed by research evidence.
Review 2: effectiveness review
This review was carried out to identify, assess and summarise the effectiveness of open disclosure and strategies/interventions that have been explicitly used with the intention of promoting and supporting open disclosure of patient safety incidents in a health-care context.
Definitions
Patient safety incident
The term patient safety incident refers to any unintended or unexpected incident which could have, or did, lead to harm for one or more patients. 23
Open disclosure
There is no agreed international definition of open disclosure, but its underlying principle involves clinicians informing patients and/or family members when a safety incident has occurred. Many policies describe the use of an honest and consistent approach to communication which should happen as soon as possible following the incident (e.g. Canadian Patient Safety Institute,8 New Zealand Health and Disability Commissioner,9 NPSA,10,11 Joint Commission Resources Inc.,12 ACSQH13). Elements of such policies, including that of the UK, commonly include saying sorry for what has happened; keeping patients and/or their carers informed about the progress of the incident investigation; reassuring patients and/or carers that the incident is being taken seriously; and ensuring measures are taken to prevent the incident from happening again. 11
Search strategy
The aim of the search was to systematically identify literature on the open disclosure of adverse events in health care to inform both systematic reviews. A broad search strategy was initially developed on MEDLINE (Ovid SP) using the two main concepts of open disclosure and adverse events. A range of text words, synonyms and subject headings for each of the two concepts were identified by scanning key papers identified at the beginning of the project, and through discussion with the review team and collaborators, and the use of database thesauri. The terms for open disclosure were combined with those for adverse events using the AND Boolean operator (see Appendix 2 for the full search strategy). The MEDLINE strategy was adapted for use in each database. These searches are considerably more detailed than those adopted in the previous literature reviews. 34,35
Retrieval of studies was restricted to those published after 1980 as little literature appears before this date. The early reports which reinvigorated the drive for higher-quality and safer patient care began to appear from the early 1990s, and a period of 10 years prior to this was felt reasonable to capture the vast majority of the literature. No language restrictions were applied to the search strategy, to ensure that non-English-language papers were retrieved. Study design filters were not applied to the search strategy, so that any literature – including papers about the effectiveness of specific open disclosure interventions, reviews, opinion pieces, policy documents and discussion articles – was identified by the search.
A wide range of electronic resources were searched, including databases, research registers, trials registers and other internet resources, to retrieve both published and unpublished literature, grey literature and ongoing research. The resources searched covered literature from the medical, health, nursing, social science and legal fields. The full list of searched databases can be seen in Appendix 3 .
The above searches were supplemented by searching key patient safety organisation websites and government agency websites to identify reports, policy documents and grey literature not indexed in the electronic databases. Further references were identified by scanning the reference lists of key papers and reports identified during the searching process, from the personal collections of the review team and consultations with key personnel from patient safety organisations, and by hand-searching the reference lists of key seminal papers.
Records were managed within an EndNote library (EndNote version X3; Thomson Reuters, CA, USA). After deduplication, 10,527 records in total were identified.
The literature search was designed and carried out by an information specialist from the Centre for Reviews and Dissemination, University of York, with input from the review team. Peer review of the search strategy was undertaken by a second information specialist at the Centre for Reviews and Dissemination. Searching of the legal databases was carried out by an information specialist from Capsticks (a specialist health and social care law firm), using a search strategy adapted from the initial MEDLINE strategy.
Inclusion criteria
Review 1: scoping review
Types of literature included
-
Available in English.
-
Produced after 1980 following the rise of patient safety/medical error research.
This could be any of the following:
-
policy documents
-
opinion pieces
-
research that has investigated
-
– perceptions or experiences of open disclosure
-
– ethical or legal issues in open disclosure
-
– the process or outcomes of open disclosure
-
– the role of any stakeholder in open disclosure
-
-
accounts of stakeholders’ experiences of open disclosure, including those of patients, patient support groups, health professionals, health-care managers and litigation services
-
literature developed to guide patients, health-care providers or litigation services about open disclosure
-
grey literature reporting activities/initiatives/research that focuses on open disclosure.
Types of participants included
Participants could be stakeholders in open disclosure from any health-care context in any location, including:
-
health service users who may have been affected by safety incidents (patients, relatives, carers)
-
potential health service users
-
representatives or members of support groups for health service users
-
health-care professionals
-
health-care managers
-
representatives or members of medical litigation services
-
professional/regulatory bodies such as the General Medical Council (GMC) or Nursing and Midwifery Council (NMC).
Nature of content
The content of the literature could be any of the following:
-
conceptualisation of open disclosure
-
discussion of the principles or implementation of open disclosure
-
discussion of the ethics of open disclosure
-
discussion of legal issues relating to open disclosure
-
reporting or describing criteria for assessing quality and/or consequences of open disclosure
-
reporting the implications of open disclosure for health services
-
discussion of the roles of any of the stakeholders in the open disclosure process
-
discussion or development of open disclosure policies or experiences of its use
-
professional expectations from bodies/regulatory bodies.
Exclusion criteria
Documents were excluded if they:
-
did not include stakeholders in open disclosure from a health-care context, i.e. none of the types of participants described above
-
described/discussed/reported disclosure relating to deliberate acts of harm
-
were not available in English
-
were produced before 1980.
Additional criteria for the effectiveness review
Population
These could be stakeholders in open disclosure from any health-care context in any location, including health service users, potential health service users, representatives or members of support groups for health service users, health-care professionals, health-care managers and representatives or members of medical litigation services.
Intervention
We included open disclosure as an intervention. Interventions that were explicitly intended to promote, enhance or support open disclosure were also included.
The following comparisons were included:
-
Open disclosure versus against non-disclosure. Any intervention which involved an act of informing a patient and/or family member or representative that a patient safety incident had occurred. Characteristics of open disclosure interventions were likely to differ, however seemed likely to include elements commonly identified in open disclosure policy (see definition above).
-
Interventions to promote or support open disclosure in combination with open disclosure versus against open disclosure alone.
Any intervention that was explicitly intended to promote, enhance or support open disclosure of patient safety incidents in a health-care context was included. It was anticipated that candidate interventions would be, for example, training or education in communication techniques and peer support groups.
Studies of interventions using actual events (real cases) or hypothetical scenarios were included. Studies where the intervention aimed to promote or improve communication of illness (‘bad or sad news’), such as diagnosis of cancer or terminal illness, were excluded. Studies of interventions relating to deliberate acts of harm were also excluded.
Outcomes
Outcomes included (but were not restricted to):
-
patients’ and/or health professionals’ attitudes relating to the intervention
-
rates and patterns of uptake of the intervention (among patients and/or health professionals) and of any behaviours/practices it was designed to promote
-
other behaviours relating to health service delivery or use
-
patients’ assessments/evaluations of health-care quality, including their perceptions of involvement, of the quality of their interactions with health-care professionals, and of their safety
-
patients’ health status and sense of well-being
-
psychological effects on staff.
Study design
The following study designs were included:
-
Randomised controlled trials (including cross-over trials and cluster trials). Investigators allocated participants to groups using randomisation.
-
Quasi-experimental studies (non-randomised controlled studies, before-and-after studies and interrupted time series). Investigators allocated participants to groups using a non-random method.
It was not anticipated that many studies of these designs would be available. Therefore, observational data were included if there was a comparison group, as in the following studies:
-
Cohort studies A defined group of participants is followed over time and a comparison is made between those who did and those who did not receive the intervention.
-
Case–control studies Groups from the same population, with (cases) and without (controls) a specific outcome of interest, are compared to evaluate the association between exposure to an intervention and the outcome.
Case series and case reports were excluded.
Study selection
Four reviewers screened citations of the title and abstract for potential relevance, with all citations being viewed by two reviewers. Full papers were obtained for citations judged potentially relevant. On receipt of the full paper, one reviewer applied the inclusion criteria for all papers to identify material of relevance. A second reviewer screened a random subset (10%) of the sample to ensure that no potentially relevant papers were missed and that the inclusion/exclusion criteria were applied consistently. Where decisions were unresolved, the two reviewers discussed the decision, and a third party was consulted if agreement could not be reached.
Information extraction
Review 1
Given the complexity and variety of literature explored, we specified that data extraction would be based on the study objectives to ensure that the review had a clear and consistent focus and was carried out in a systematic way.
Given the ultimate aim of developing current guidance on open disclosure in the NHS, we extracted data from the reviewed papers that related to any of the 10 principles of open disclosure described in the Being Open framework. These were:
-
acknowledgement
-
apology
-
truthfulness, timeliness and clarity
-
professional support
-
recognise patient and caregiver expectations
-
risk management and systems improvement
-
individual/multidisciplinary team responsibility
-
clinical governance
-
continuity of care
-
confidentiality.
It was anticipated that this would provide an idea of those aspects of the framework for which there was currently supporting literature and those that had been implemented in health care, and the extent to which implementation had been perceived as successful. It would also highlight the areas of the framework for which there was less evidence or support, that were less clearly defined or enacted or that had been less successfully implemented to date. Both intended and unintended outcomes were documented during this process.
On this basis we extracted:
-
author/investigator
-
date
-
location
-
type of literature
-
population
-
study design (if applicable)
-
outcomes/arguments/guidance, which were summarised in relation to
-
– acknowledgement
-
– truthfulness, timeliness and clarity of communication
-
– apology
-
– recognising patient and carer expectations
-
– professional support
-
– risk management and systems improvement
-
– multidisciplinary responsibility
-
– clinical governance
-
– confidentiality
-
– continuity of care.
-
There were two stages of information extraction: in the first stage, a basic extraction that provided an outline of the paper, and in the second, a more detailed extraction in which particular aspects of the work were drawn out, depending on the type of material and its salience to the review objectives and domains outlined in the Being Open guidance.
Review 2
The following data were extracted from included studies (where available):
-
general information (author, article title, type of publication, country of origin, source of funding)
-
study characteristics (aims and objectives, study design, inclusion/exclusion criteria, recruitment procedures, unit of allocation)
-
participant characteristics (of both health-care workers/managers and patients, including age, gender, ethnicity, profession/position of health-care worker, disease or condition/adverse event details of patient)
-
intervention and setting (setting where the intervention was delivered, description of the intervention and comparator)
-
outcome data (for intervention and comparator groups the following were reported: number enrolled, number included in analysis, number lost to follow-up, withdrawals and exclusions. For each reported outcome the following were extracted: definition of outcome, measurement tool used, length of follow-up, results of study analysis).
Data collection and analysis
In the larger primary review (review 1), each included paper was summarised to provide an overview of research, discussion and policy or guidance documents relating to open disclosure of error.
In the smaller systematic review of interventions (review 2), no formal pooling of data was appropriate owing to a lack of studies with a comparator group and uncontrolled before-and-after designs. Findings were grouped into two sections:
-
studies where disclosure was the intervention
-
studies where interventions were intended to promote or support disclosure.
In each of these sections the included studies were described in terms of their setting, participants, methods, intervention, outcomes, outcome measures and reported findings, and linked to tabulated descriptions of studies.
Phase 2: interviews
Ethical approval
Ethical approval for this phase of the project was obtained from the Bradford NHS Research Ethics Committee (ref. 10/1007/47). Research governance approval was obtained from the relevant NHS trusts (see Appendix 4 ).
In-depth individual interviews were used to describe, explore and explain stakeholders’ views and experiences of open disclosure in health care. The rationale for selecting a qualitative approach was threefold. Firstly, little research has been conducted in the UK in this area to date; qualitative methods are ideally suited to reveal the range of views or practices and key issues that might be missed through the use of more structured data collection instruments. Secondly, in-depth interviews are the most effective and valid way of exploring people’s experiences, beliefs and meanings, from the perspective of the respondent, in order to provide a ‘rich’ data set which is grounded in the experiences of the interviewees themselves. Thirdly, one of the strengths of qualitative research is that it can identify the complex ways in which particular beliefs or experiences are likely to influence behaviour.
Perspectives were likely to vary according to stakeholder, health-care setting and participant demographics; therefore, we employed sampling strategies and data collection techniques that allowed for an inductive, hypothesis-generating approach to interpretation of the data.
Populations studied
In order to explore the views of a range of stakeholders who might contribute to open disclosure, with diverse clinical backgrounds and differing degrees of patient contact in a variety of health-care contexts, study participants were strategically selected from four different groups:
-
Policy-makers Individuals with a current or previous position of responsibility for developing health policy, and in particular the Being Open guidance.
-
Professional organisations Individuals from professional organisations that represent or regulate the health professions.
-
NHS managers and health professionals Health-care managers included members of the senior management team, some of whom had dual clinical and management roles. Health professionals were staff who carried out work on the ‘shop floor’, from matron and consultant level to junior doctors and nurses (from band 5 up).
-
Patients and patient organisations Participants were approached through national patient groups. Participants could include patient advocates and those with experiences of disclosure or a lack of disclosure.
Details of the original sampling framework and the planned participant numbers in each group are shown in Appendix 1 .
Recruitment and consent
Recruitment procedures were tailored according to the stakeholder groups. Policy-makers, leaders of professional and patient organisations and senior managers were contacted in the first instance by a targeted letter from the research team. All other participants were contacted, in the first instance, by an appropriate member of the identified organisation. In all cases, potential participants were sent information about the study and asked to return a short slip (or contact the research team by e-mail or telephone if preferred) to discuss participation.
A member of the research team then contacted respondents to explain the nature and purpose of the study. In the case of patient participants, we emphasised that the research would not directly help them to seek a remedy or redress for any problems they may have experienced related to the disclosure of adverse events. Where people expressed willingness to participate, the researcher made arrangements to hold an individual interview at a time and place convenient for the respondent. A small number of interviews were conducted over the telephone if specifically requested by the participant.
Prior to the commencement of interviews, the researcher reminded participants of the purpose of the research; asked respondents if they had any further questions; checked that they were still happy to take part; and reminded them that they could stop the interview or withdraw from the study at any time.
Data collection
The aim of the interviews was to explore:
-
stakeholders’ general awareness and understanding of open disclosure
-
their personal experiences and perceptions of both the principle of openness in relation to disclosure of adverse incidents and the Being Open guidance, in the context of their own position in relation to health care
-
their views on the contribution that they might make to promote and enhance open disclosure
-
their thoughts about the Being Open guidance.
Although all interviews shared these aims, the emphasis in the interviews varied by stakeholder group. Interviews with policy-makers focused on the development of the Being Open guidance and perceptions of its current use. With professional organisations, the translation of national and local guidance into practice was emphasised, along with the perceived contribution that such organisations can make to support health professionals in delivering open disclosure. Interviews with NHS managers and staff explored experiences of open disclosure and of implementing the Being Open guidance specifically. We also explored the challenges of discussing adverse events with patients. Representatives from patient organisations were asked about their perceptions of open disclosure in the policy context and from a broader patient perspective, and patients were asked to share their individual experiences and beliefs.
A core topic guide (see Appendix 5 ) covering these investigative areas was developed and piloted. This was refined before interviews commenced with the target populations. Interviews opened with questions exploring respondents’ broad understanding of the term ‘open disclosure’, the reasons for implementing open disclosure, experiences or beliefs about the Being Open guidance and, finally, where the challenges lie. Modified versions of the topic guide were developed for use with each stakeholder group. After initial interviews, some minor alterations were made to the wording of the guide to be used with NHS managers, to make it more sensitive to exploring the experiences of this group.
Data analysis
Interviews were audiotaped and fully transcribed. Transcripts were analysed using framework analysis. 36 This approach was selected for several reasons. Firstly, it is especially well suited to applied qualitative research, in which the objectives of the investigation are typically set a priori, and shaped by the information requirements of the funding body, rather than wholly emerging from a reflexive research process. Secondly, framework analysis provides a visible method which can be scrutinised, carried out, and discussed and operated by individuals in a team. Lastly, the approach lends itself to reconsidering and reworking ideas because the analysis follows a well-defined procedure, which can be documented and accessed by several members of a research team.
Framework analysis comprised the following steps:
-
Familiarisation with the data, sometimes referred to as ‘immersion’.
-
Thematic analysis, carried out in order to develop a coding scheme.
-
Systematic coding of the data.
-
Charting of data using a Microsoft Excel 2010 spreadsheet (Microsoft Corporation, Redmond, WA, USA). Charts contained summaries of data (supported by references to data points in the original transcripts), so the research team was able to build a matrix to see across cases and the range of data under themes.
-
Mapping and interpretation of the data in order to explore relationships between the codes.
Each of the three researchers (YB, RH, KB) most involved in fieldwork took a sample of interviews, and initial data were open coded. The coding framework emerged from a focus on the questions posed by the research document, but at initial stages was also open to emergent codes. The coding framework was further developed through discussions with members of the wider research team with extensive qualitative (VE) and clinical (IW) experience, to discuss emerging codes and categories, the interpretation of key texts and potential new lines of enquiry. The coding framework is included in Appendix 6 .
Data sampling
Sampling decisions always fluctuate between the aims of covering as wide a field as possible and conducting analyses which are as deep as possible. 37 A strategic decision was made to aim for depth in analysing the qualitative interview data, as we sought to present findings which were ‘rich’ in relevant information. All interviews were coded, and 33 interview transcripts were selected for in-depth analysis, to represent diversity in the total data set of 86 interviews. The interviews were selected strategically from the complete data set using maximum variation sampling;38 that is to say, they included ‘typical’ cases (reflecting the views of the majority of respondents), ‘deviant’ cases (extreme cases of the phenomena under investigation) and ‘critical’ cases (those that appeared to be especially information rich and thus particularly illuminating). These 33 interviews related to 33 participants (four policy-makers, four professional organisations, 10 health-care managers, 12 health professionals and three patients/family members who had experienced error). Although these transcripts formed the basis of the analysis, data from across the whole sample contributed to the analysis. The selected transcripts included interviews with males and females, who had wide-ranging views and experiences of open disclosure (see Appendix 7 for a detailed participant breakdown).
Rigour and transparency in the analytic process
Analytic rigour and accurate interpretation of data were promoted and enhanced in a number of ways. The three team members most closely involved in fieldwork (YB, RH, KB) met frequently to discuss data collection and analysis. At regular intervals, meetings were held with members of the wider research team with extensive qualitative (VE) and clinical (IW) experience, to discuss emerging codes and categories, the interpretation of key texts and potential new lines of enquiry. In this way, the combined insights of those ‘handling’ the data closely and members of the team with a wider perspective of methodological and open disclosure issues could be incorporated into the coding framework to be used for all data analysis (see Appendix 6 ). In addition, a small subsample of transcripts coded using this agreed framework (n = 5) were examined by a member of the wider research team (VE) as an independent check on the assignment of codes to data.
The framework approach to data analysis allowed data to be compared within cases, facilitating the exploration of contextual meaning; comparing cases across the data set facilitated the search for regularities (key themes) and exceptions (negative cases). The use of memos during initial stages of analysis provided a visible ‘audit trail’ as the analysis moved from ‘raw’ data, through interpretation to the production of findings. A reflexive approach has been taken throughout the entire research process, from the initial development of the research questions, through data collection and analysis (for a full statement on reflexivity see Appendix 8 ).
Chapter 3 Results
Phase 1: review 1
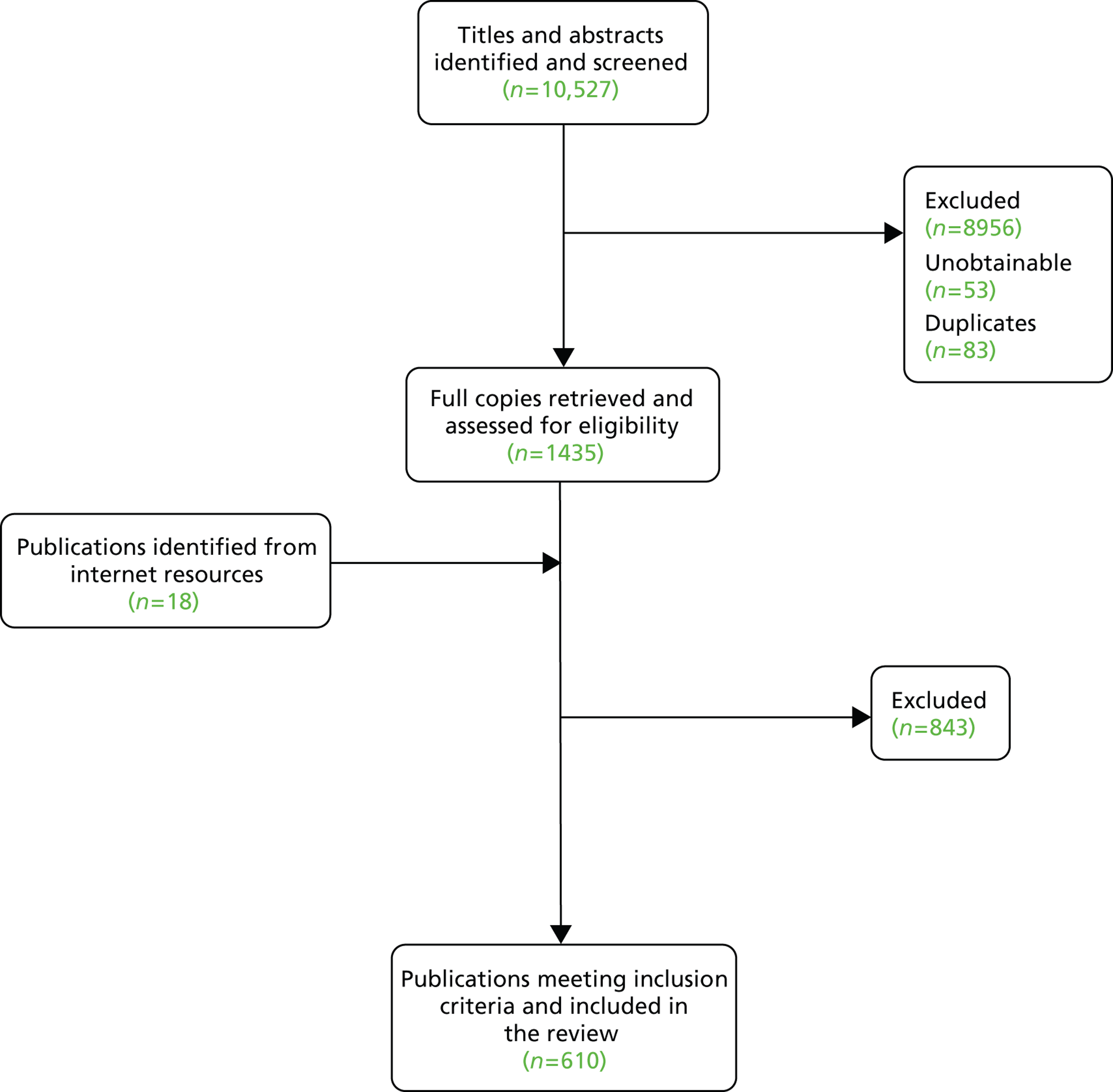
The searches identified over 10,000 pieces of literature. Of these, 1435 full copies were retrieved and 610 pieces of literature were included in the final review. Full details of the literature selection process are illustrated in Figure 1 .
FIGURE 1.
Selection of literature.
A broad description of the literature
Literature published over a 22-year period was examined, with the majority of papers published from 2001 onwards. A broad description of the literature is presented below. We were interested in capturing the volume and type of literature and the pattern of publications over time, which has been little discussed in previous reviews.
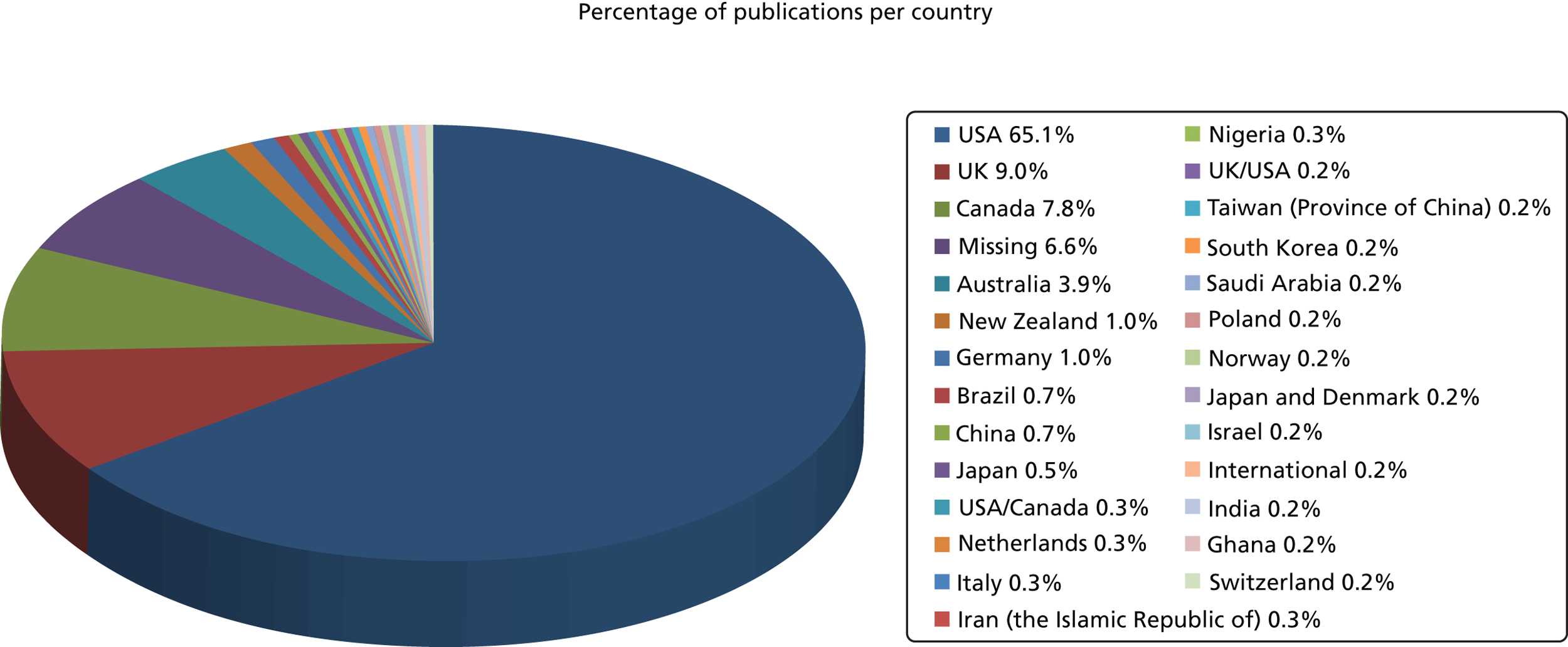
The majority of literature discussing open disclosure is from the USA (65.1%). A further 20% is from Canada, the UK and Australia. The remainder consists primarily of single publications from a range of countries, and in just under 7% of papers the country of origin was not clear. Further details are shown in Figure 2 .
FIGURE 2.
Countries of origin of the literature.
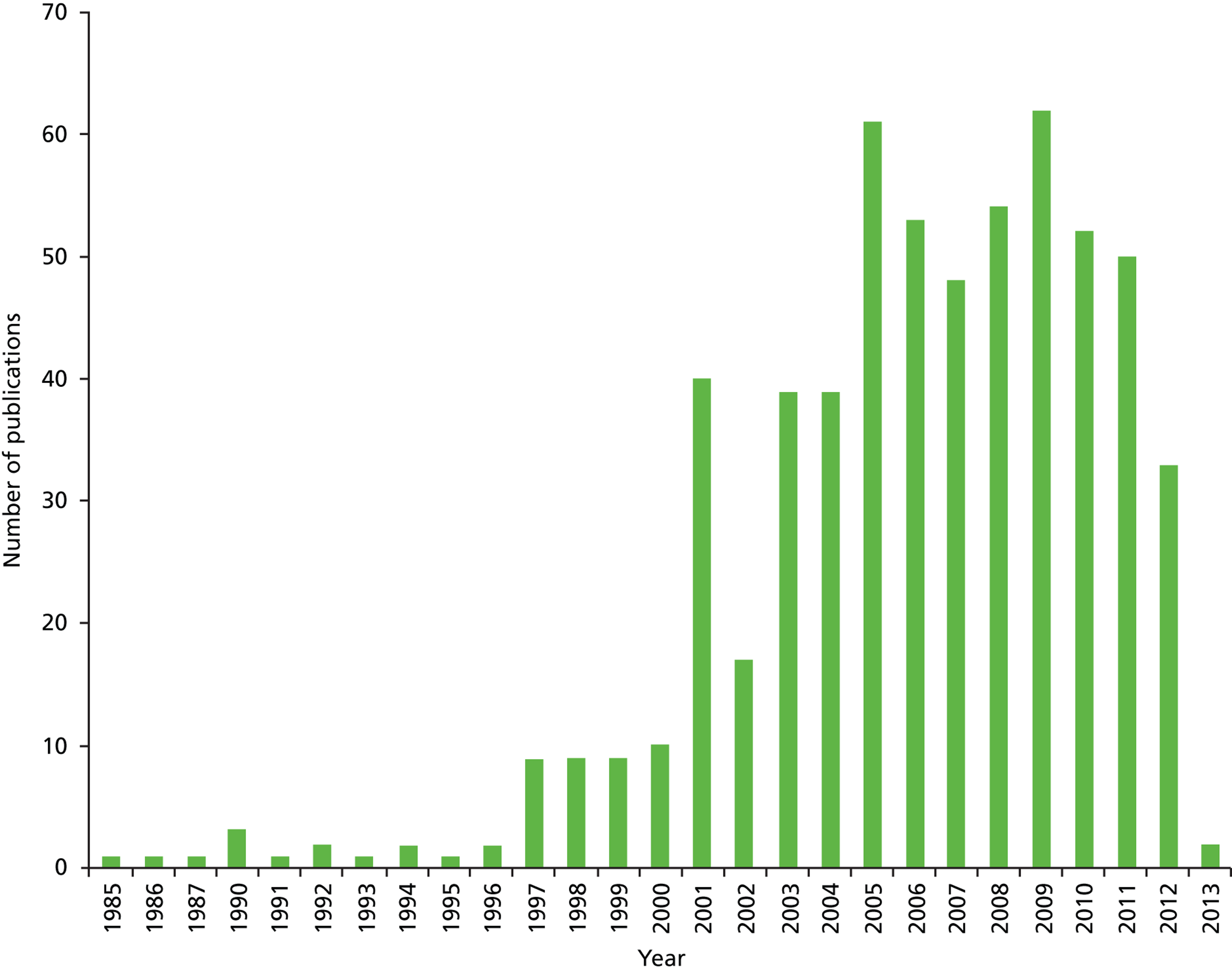
The literature search was restricted to 1980 onwards as previous work had demonstrated a surge in safety literature in the 1990s,39 and this was felt to be an appropriately sensitive time frame in which to capture the main body of literature. Figure 3 demonstrates that until 2000 there were few publications per year relating to open disclosure. From 2001, the number of publications suddenly increased to an approximate average of 50 publications per year. The rise in publications is likely to reflect the increased awareness of patient safety issues and the publication of articles now regarded as seminal pieces in the safety literature, such as To Err is Human in 1999;16 this article drew attention to the consequences and cost of medical error in the US health system and other health systems worldwide.
FIGURE 3.
Number of publications per year.
The majority (just over two-thirds) of the literature comprised opinion or ‘think’ pieces, journalistic-type articles and a variety of articles containing reports of other (previously published) publications and guidelines. Thirty-five per cent consisted of either primary research or papers which were judged to be of seminal importance to the topic, largely based on authorship by well-published or well-cited figures in the open disclosure field. There were small pockets of literature emerging from Europe, Asia and sub-Saharan Africa, as well as the better-known literature from North America and Australia, where discussion of the area of disclosure of adverse events is well established. Largely, this consists of descriptive literature outlining what clinicians feel about disclosing error and harm and what they report that they do in relation to disclosure, as well as descriptions of patient preferences and experiences in the context of open disclosure. There is little primary research and referencing back to early publications is common, with key messages largely unchanged. Clinicians, in principle, and for the most part, agree that patients should be informed of errors in their care that cause harm but are challenged by mixed messages from their institutions about what they perceive to be their legal status in this context. This is further exacerbated by concerns about their skills in disclosing error, due to a lack of specific training or exposure to this kind of communication. Additionally, the literature includes inconsistent terminology and ideas about which events should be disclosed, which adds further confusion.
Patients unequivocally report that they want disclosure of all unanticipated events and errors that occur during care. In some literature, the barriers to disclosure are explored more deeply and there are some in-depth critiques of what ‘telling the truth’ means. Although a good understanding of the concepts that underpin openness is valuable, such theoretical accounts may have limited application in changing the current culture in health care or persuading the NHS to fully implement the policy of open disclosure rigorously and consistently. However, these accounts have been included alongside more practical accounts and primary research to fully illustrate the types of literature available to inform each principle.
Main findings
Given the challenges which open disclosure appears to present for some individuals and health-care organisations, it is surprising how little attention the topic has received in the UK. There is good reason to think that open disclosure may be different in different contexts. 40 In the limited evidence available, UK doctors were more likely than US doctors to agree that significant medical errors should always be disclosed to patients, and more US doctors reported that they had not disclosed an error to a patient because they were afraid of litigation. 40 The context of care may influence both how professional values are expressed and the extent to which behaviours are in line with stated values. Lessons may be learned from the largely US and other literature about the implementation of a policy of open disclosure, but the clinical negligence contexts in each country may have implications for how open disclosure is perceived locally. A large and growing body of literature exists in relation to open disclosure. Much of this is in practice journals and summarises a small number of frequently cited pieces of original research in the area. Thus, although there appears to be a great deal of activity in this field, there is limited underpinning primary research to substantiate conclusions; received truth is perpetuated from past references often based on small before-and-after studies or single cases.
Following detailed data extraction and appraisal of the literature, the results were synthesised under the specific principles of Being Open. Although there are vigorous and ongoing debates within the literature related to open disclosure, the nature of the UK health-care context, and in particular the NHS, means that some of these debates have less relevance than in other countries. This is reflected in the attention afforded to some of the areas presented in this review and we did not seek to capture the very valid but less applicable areas within State and Federal statute in other international contexts. The large volume of literature on this topic has been surprising, but the aim of this project was to examine open disclosure specifically in a UK context. The legal frameworks and statutory requirements differ in various contexts and therefore some of the literature is less applicable to the UK. The review will address the international literature but focus on its applicability to a UK context, concentrating on lessons which can be learned to specifically address the implementation of open disclosure policy and duty of candour in relation to unanticipated outcomes in the UK.
A complete list of included literature sources is included in Appendix 9 .
Acknowledgement
The Being Open guidance10 states that all patient safety incidents should be acknowledged and reported as soon as they are identified. In cases where the patient, or his or her family and carers, inform health-care staff that something untoward has happened, this must be taken seriously from the outset. Any concerns should be treated with compassion and understanding by all health-care professionals. However, the literature suggests that defining the events that warrant disclosure presents a fundamental challenge for organisations, managers and clinicians. Although a number of definitions of what constitutes an error or an adverse event exist, there is much less clarity about what should be disclosed. Often the need to disclose has been associated with whether or not an event is classed as an error or constitutes harm. This is further complicated by an abundance of diverse error definitions in the literature. The terminology used to describe and categorise errors is also complex and includes an array of synonyms such as ‘bad outcome’, ‘sentinel event’, ‘adverse event’, ‘mishap’, ‘mistake’, and ‘untoward incident’. All are used as synonyms or (partial) explanations of the word ‘error’. 41 Additionally, errors can occur through acts of commission or omission; that is, not only as a result of what is done, but also as a result of what is not done. 41 The guidance suggests that ‘error’ refers to ‘any unintended or unexpected incident that could have or did lead to harm for one or more patients receiving NHS-funded healthcare’. 10 ‘Error’ seems to be problematic in its definition, and although harm, certainly in a biomedical context, may be easier to define, it does not address issues of culpability. Although this appears to be a well-defined principle, the discussions in the literature reflect continued ambiguity about the events that individuals feel are covered by any principle of openness.
Definitions of error or harm
Patients and clinicians appear to define error differently. 42 From the patient perspective, the distinctions between the terms ‘error’, ‘adverse event’ and ‘unexpected outcome’ seem relatively unimportant. Such definitions are largely constructed from the systems perspective and may be at odds with the way in which patients interpret harm. In the patient experience, harm is perceived, and regardless of how members of the health-care community and legal profession wish to classify this harm, patients who perceive that they have suffered as a result of their treatment feel that they deserve a timely, supportive and informative conversation about their concerns. In 2003, the College of Physicians and Surgeons of Ontario recognised this with the publication of its policy on disclosure of harm. 43 This describes a definition of harm as a concept which is not always preventable nor necessarily an indicator of substandard care. According to this definition, harm refers to any unintended outcome arising during the course of treatment, which may be reasonably expected to negatively affect a patient’s health and/or quality of life. Such outcomes may occur as a result of individual or systemic acts or omissions, and include adverse events related to the care and/or services provided to the patient rather than to the patient’s underlying medical condition. This is a considerably broader definition than many and has the potential to address the broader nature of patient concerns which are often raised but not addressed.
What should be disclosed?
The definitions of which events should be disclosed have subtle differences but there are common recommended elements of disclosure including ‘an expression of sympathy or regret’,10 as well as the provision of practical and emotional support for the patient. Most guidance is keen to stress that disclosure discussions should ensure that no speculation, opinion or attribution of blame occurs and that an apology to patients by health-care providers is not taken as an admission of liability. The Canadian Patient Safety Institute44 has non-binding disclosure guidelines for adverse events which state that all harm must be communicated to patients, irrespective of the reason for the harm. There does not appear to be any consensus about the obligation to disclose adverse events with minor consequences,16,20,21,28,45–48 despite the fact that most patients express the desire to be informed of these types of errors. It is proposed that the need for disclosure is proportionate and increases as the harm or risk of harm to the patient increases. 49 Others have proposed the ‘view from below’, putting oneself in the patient’s position to determine how he or she would want the situation to be handled. 50 Disclosure should be the norm, with practitioners expected to justify why there should be any exception to this rule. The 2008 Veterans Health Administration (VHA) directive, Disclosure of Adverse Events to Patients,51 is one of the few policies which has been explicit about its stance on serious and minor errors and events, stating that even when a near miss occurs, disclosure of such ‘close calls’ is recommended if the patient may have become aware that something strange had occurred. 52,53 One account describes the useful role lay members can play in informing decisions with regard to disclosure. Even in well-motivated organisations which try to implement openness, it can be useful to have lay members as part of a review board to ensure decisions remain patient centred. 54
Truthfulness, timeliness and clarity of communication
Being Open guidance10 stresses the three principles of truthfulness, timeliness and clarity, mentioning specifically an ‘appropriately nominated person’, a step-by-step explanation which is timely and based on fact and that patients and families should be kept up to date with the progress of any investigation. Additionally, communication should be clear and unambiguous with a single point of contact.
Why is truthfulness important?
There are a number of involved critiques of why disclosure should occur, which refer to philosophical underpinnings. The most powerful argument in favour of disclosure is deontological in nature. This deontological perspective, which is the perspective of duty-based ethics, is largely attributed to German philosopher Immanuel Kant and suggests that, in principle, all errors must be disclosed. 55,56 In this argument, truth-telling is not mandated by the specific detail of the situation. Therefore, factors such as whether or not an error is serious, or does or does not cause harm, or indeed whether or not an institution or practitioner is liable for harm, are not relevant. The duty is simply one of honesty. The same ethical principles insist that any proposed ethical rule must be universally applicable; it must bind everybody in all situations or else individuals are unable to know if they are bound by it or not. An in-depth but accessible critique of this perspective as it applies to disclosure is presented by Scheirton. 41 In this critique, the reader is asked to imagine that we propose a rule that therapists, nurses, pharmacists and physicians should generally tell the truth but that sometimes it may be acceptable to hide the truth or even lie (for example, in the case of an error). The outcome for patients in this scenario, as soon as they learn about this rule for health-care practitioners, is likely to be suspicion. One family member’s account of non-disclosure refers to the fact that they ‘know of no other industry where honesty is optional’. 57 A practitioner may be telling the truth, but the patient knows this may not be the case, as the practitioner is ethically allowed not to tell the truth sometimes. Therefore, in this paradigm the practitioner’s moral duty to tell the truth cannot logically accommodate exceptions for errors.
Scheirton also describes patient rights as the other side of a similar argument, as the flip side of duties. 41 Laws, professional bodies and institutions agree that patients have a right to be informed about their own medical situation and health care. This right is not conditional upon the individual qualities of the patient or their condition. It is argued that any information is the patient’s and it does not matter whether the particular condition or intervention is the result of an error or some other cause. The patient’s right is to be informed, and this should be honoured by the health-care practitioners who have entered into a therapeutic relationship with the patient.
The picture of disclosure and non-disclosure
A recent paper looking at error and disclosure in emergency care in the USA has outlined the scale of non-disclosure,58 at least in one context. A large number of medication errors (13,932) from 496 emergency departments were analysed. Physicians were responsible for 24% of errors, nurses for 54% and most occurred in the administration (36%). Although 3% of the errors resulted in harm, in only 2.7% of these cases were patients or family members notified. Other work59 indicates that willingness to disclose was related to the severity of the error, with the majority of near misses not even reported to the head of department or the hospital error committees. Such studies indicate that health professionals still hesitate in their reports of many errors or adverse events unless serious harm occurs. A small number of papers have looked at the kinds of factors which may affect whether or not a patient or his or her family experiences disclosure. 60–63 These tend to be conducted in survey work directed at either clinicians or patients. One study60 conducted with patients who had experienced error suggests that patients were less likely to report that disclosure had occurred if they were older than 50 years, did not generally report good health, experienced preventable events, or were still affected by the event at the time of the interview. Disclosure seems to have been more likely to occur when events required additional treatment and among patients who reported good health. 60 This suggests that disclosure occurs when individuals and organisations feel compelled to do so because the error is more visible. 61 Although there is little work directly addressing attitudes to and rates of disclosure in Britain, one paper looking at trainee anaesthetists as recently as 2009 reported that, although 57% had made an error which caused harm, only 68% of these had informed the patient. In the 32% of cases where the patient had not been told, a number of reasons, including negligible perception of patient harm, fear of litigation, fear of organisational or professional reprisal, and the patient having moved, died or remained unconscious were cited as reasons for non-disclosure. 62 This highlights the need for further training among this group of clinicians in relation to both current duty of candour and also medico-legal aspects of care. Other work in the UK63 has demonstrated norms of selective disclosure in medical trainees whereby errors were disclosed informally to colleagues, particularly when teams were seen as supportive, but formal reports and disclosures to patients were rare.
The disclosure gap
There is an increasing literature stressing the importance of disclosing health-care errors, but the available, largely USA-based evidence suggests that this enthusiasm for what is seen by many as the moral imperative may not be reflected in practice. 60,64–66 Disclosure still remains an elusive concept for some and the evidence from a number of surveys points to a marked difference between what patients want from their health-care provider, in terms of honest conversations about mistakes and errors, and what clinicians (doctors in particular) say they would provide. 67,68 This term has been referred to as the ‘disclosure gap’. 69 Several sources give a number of well-cited reasons to explain this mismatch between patient expectations and health-care provider practice, which are discussed at length in a wide variety of outputs from academic papers to short journalistic pieces. However, they seem to fall into four main areas. 69
-
Truthfulness requires an admission of a mistake. For clinicians, admitting that they have harmed a patient is psychologically difficult. As well-trained and compassionate individuals they have a professional and often personal commitment to helping patients. The challenge to this identity posed by unanticipated outcomes and errors in particular is uncomfortable. Many physicians are upset by an allegation that they have been negligent, even if this turns out not to be the case. 70 This is further complicated by a culture of self-regulation and one where the belief is that health-care professionals heal rather than harm.
-
Health-care professionals undergo extensive training, both initially and as part of continuing professional development. However, this rarely extends to conducting the challenging conversations that are required by disclosures of errors or mistakes. 71,72 US work by Gallagher revealed that only 9% of physicians reported receiving any training in disclosing medical errors. 71 Where work has used standardised patients to explore skills in error disclosure, current evidence suggests that doctors are relatively lacking in such skills. 73,74 There is no literature to support training input in the UK.
-
It seems likely that health-care organisations and the individuals who work within them may not fully appreciate how important full disclosure is to their patients, and thus make interpretations about what it is important to disclose. In fact, many examples are given where individuals argue that they are protecting patients from difficult information. A number of studies show that physicians are less likely to tell patients about errors if the error is not obvious to the patient. 67,71
-
In the extensive literature from the USA, one of the arguments is that the biggest barrier to full disclosure is fear of litigation. 75 Risks and costs associated with malpractice are high, and physicians and institutions are worried that admitting an error will increase the likelihood that patients will sue them. The emphasis on this has changed with a number of reforms in state law and in the policy adopted by a number of large insurers, but physicians remain sceptical about the power of such ‘apology clauses’ to protect them in practice. Additionally, most clinicians do not understand the law or update themselves, as they are too busy with clinical decision-making and practising medicine. 70
Delaying disclosure or non-disclosure
Common objections to open disclosure policies suggest that disclosures may not always be in the best interest of the patient. Some work suggests that even if many physicians are perceived to prefer to limit disclosure for their own rather than patients’ interests, or that as a society we believe paternalism is no longer acceptable, there may still be good reasons not to inform a patient of an error, or at least not to disclose immediately. 41 The idea that information conveys power to the patient is sometimes questioned in relation to whether or not such information may also harm them. Does the patient’s right to information always trump emotional well-being? It has been suggested that if an error has no consequences for the patient’s well-being and disclosure does not empower the patient, but is more likely to cause distress or reduce the patient’s trust, then non-disclosure for the sake of sustaining the therapeutic relationship may be the ethical course. 76 However, this rule of therapeutic exception means that the burden of proof is on the one who wishes to use the exception. 41 At this point, proving that full disclosure will create an unreasonable risk of serious harm to the patient before the patient has the information is impossible. Unless research could demonstrate that patients would like clinicians to judge whether or not information relating to an error would be more distressing than non-disclosure, this reasoning ultimately fails. Largely, the limited literature suggests that the opposite appears to be the case, as patients have indicated when surveyed that they would prefer to be told about errors. 28 However, a patient can only judge how distressing the conversation might be after the event, and often such surveys are conducted in patients who have not experienced error and, as such, lack ecological validity. Even bearing this in mind, the best argument for non-disclosure of errors may be difficult to navigate with conviction. Aside from the well-intentioned motive of protecting the patient from what might be judged to be additional distress, the decision not to disclose for whatever reason may backfire. Another member of the team may (inadvertently) disclose the error, the patient may request copies of his or her records, or the error may be discovered during another procedure or even at post-mortem.
The literature here highlights the consistent findings in relation to the disclosure gap. This work comes largely from the USA, but some UK evidence also exists which indicates that disclosure policy is at best inconsistently applied. 28,41,76 There remain considerable challenges for and barriers to the principles and enactment of any policy of open disclosure, which range from a well-intentioned but paternalistic view of protecting patients and families from additional distress to a self-preserving strategy based on fear of reprisals from a legal or professional perspective.
Apologies
Being Open guidance10 stresses that patients and families should receive a sincere apology and this may include expressions of regret for the harm. The wording of the apology should be agreed as early as possible and a decision about who should apologise and how would be based on local circumstances. Characteristics of the person to apologise may include judgements of seniority, relationship to the patient, and experience and expertise in the type of patient safety incident that has occurred. The role of both verbal and written apology is stressed and the time frame suggested is ‘as soon as possible’. The purpose of the verbal apology is stated as allowing face-to-face contact between the patient/family and the health-care team. It is stressed that an apology should not be withheld on the basis of setting up a more formal enquiry, organisational apprehension or staff availability. The guidance also relates evidence from focus groups that families are more likely to seek legal advice if apologies are not forthcoming.
The issue of an apology is related to, but distinct from, openness. The decision about whether or not and when to give an apology, and about what an apology is, seems to be complicated in the literature by the open disclosure process. Individuals often feel they are unable to apologise as this may be construed as an admission of fault or negligence, or that a full investigation has to have been completed before an apology can occur; that is, that an apology can only occur once fault has been determined. A key recommendation of the various global policies on medical error disclosure is to apologise to the patient, which is thought to reduce anger and increase trust. 77 Apologies are recommended elements and processes of all disclosure policies, which generally include who, when, where and what to disclose, as well as how disclosure should be conducted. In a number of descriptive accounts from patients, the concept of an appropriate and sincere apology is often raised as a key element of the perception of an adequate or inadequate disclosure. There are often repeated and strong claims for the power of disclosure and apologies in a number of contexts. Allan suggests that apologies are powerful factors in the healing of harmed patients. 78 This may or may not be the case, but there appears to be little evidence to support this belief. Although a lack of openness, accompanied by little information and no apology, often causes a prolonged and distressing period for patients or their families, we know very little about what ‘good’ disclosure conversations might look like from the patient perspective beyond some common-sense recommendations. The fact that an apology is made does not necessarily make a situation better for the patient who has been harmed and there is little to substantiate this claim. It has been articulated that some feel that the ability of current laws to protect against use of apologies in legal proceedings is perceived as inadequate in the US and Australian contexts. 79
What is an apology?
An apology refers to an encounter between two parties in which one party, the offender, acknowledges responsibility for a harm or grievance and expresses regret or remorse to the aggrieved party. 80 Building on this core definition, Lazare, who has published extensively on the concept of apology,80 outlines the vital components of an apology to include:
-
acknowledging offence
-
providing an explanation for committing the offence
-
expressing remorse
-
offering reparation.
However, it is thought that an apology may have a number of functions. For patients an apology can restore self-respect and dignity, facilitate forgiveness and provide the basis for a reconciliation with an individual health-care professional or institution; for the physician, it is thought to moderate feelings of guilt, shame and fear of retaliation. For both parties, it may strengthen a previously satisfactory relationship, or restore one that has been damaged. 80 However, reassuring though these statements are, there is currently little empirical evidence which can support these claims beyond expert opinion.
What do apologies achieve?
Zammit81 suggests that although people often fear giving an apology as it implies an admission of guilt, the reality may be that the courts have a certain respect for apologies; apologies may actually be viewed favourably. However, this work also suggests that there is little evidence that apologies reduce malpractice claims, as the studies cited in support of this claim are often based on scenarios and have little ecological validity. Additionally, the dangers of unskilled apologies, or weak and insincere apologies made by clinicians who are unsure whether an apology may be protected or not, may actually inflame rather than calm an angry patient or family. This point relates specifically to training in open disclosure conversations, which will be followed up in a section addressing training (see Professional support).
Recognising patient and caregiver expectations
Being Open recognises the need to fully inform patients and families and to attempt to ensure that the process of disclosure meets their expectations. Although there are some practical suggestions for an appropriate attitude from the health-care organisation reflecting sympathy and respect, addressing additional support needs and informing the family of any appropriate support networks is less well reported; we know relatively little about the patient experience of disclosure.
What do patients and families say they want?
Since 1996 there has been some evidence that patients report a wish for an acknowledgement of even minor errors, that they may wish to be referred to another doctor if other treatment is required and that they are more likely to litigate if they have not had an error disclosed. 21 Since this paper, there has been a limited amount of work exploring how patients feel after an error and exploring their responses to disclosure. In survey work the majority of patients clearly indicate that they would want full disclosure of medical error and wish to be informed of error immediately upon its detection. 82 Patients also clearly support reporting of errors to government agencies, state medical boards and hospital committees focused on patient safety. Patients also indicate that they support teaching health-care professionals error disclosure techniques, with honesty and compassion endorsed as a priority for educators who teach clinicians about error management. 83 Patients are clear that, as the person who has experienced harm, they are important, and if apologies are perceived to be driven by regulatory standards and institutional policies alone, and are felt to be insincere and purely managing risk to the organisation, then this may well carry its own risks in terms of the subsequent patient or family response to any apology. One study which explored how patients had experienced disclosure and error described patients reporting that the actual error was less concerning than the continued relationship with their health-care provider. 84 These individuals described being treated not as experts in their own experience of care, but as outsiders. The authors described this as patients feeling like a foreigner in a strange land experiencing a different culture and language, and highlight how poor communication suggests a conflict between a model of person-centred care, with the patient–provider relationship at its heart, and the business or corporate model of health care. A number of other studies have suggested that when poor communication occurs, it can be perceived as medical error by the patient. 28,85
Patients are known to value apologies and expressions of remorse, empathy and caring. They indicate that what they want from disclosure is an explanation of any potential harm and an acknowledgement of responsibility, and they need to see efforts to prevent recurrences; however, these are often reported as missing elements in the disclosure process. 82,83 For many patients, actions and evidence of learning were most important. Current reports of patients’ accounts of apology and disclosure suggest that clinicians’ and organisational responses continue to fall short of expectations. 86
These accounts of what patients seek from open disclosure and apologies largely emanate from the US literature, often from surveys where it is unclear whether or not the population has experienced harm or error. However, from the few findings available from other contexts, these desires would seem to be relatively consistent. Okamoto,87 for example, found that individuals in Japan reported that after the immediate disclosure of a medical error by senior medical personnel, medical providers should create an environment where communication is repeated and continuous to accommodate the shifting nature of the perspectives of those who have experienced the error. Although the severity of the outcome remains the most important single factor in a patient’s choice of actions following an error, the professional’s approach to the error is regarded as essential in the overall evaluation of consequences. In errors with a severe outcome, an honest, empathic and accountable approach to the error decreased the probability of participants’ support for strong punitive action against the physician involved by 59%. These judgments in this scenario study were only marginally affected by respondents’ characteristics. 88
These findings are consistent but come from a context which is quite different from the UK and the NHS in particular. Though it seems unlikely that UK participants would expect different standards in relation to open disclosure or apology, we know little about this.
Real accounts of disclosure by patients and families
There is still relatively little work exploring real accounts of disclosure and error, what worked well and what was less successful from either a clinical or a patient perspective. A number of individual accounts of what non-disclosure or poor disclosure feels like from the patients’ perspective are reported, often by the individuals themselves,57,89 but few accounts exist in the academic literature.
One of the few pieces of work exploring this directly is a focus group study with patients who had been subject to iatrogenic harm. 85 This paper describes how trauma as a result of harm developed in two ways, from the incident itself and/or from the manner in which the event was subsequently handled. This has been previously described by Vincent. 90 Those who experienced what they felt had been skilled communication (demonstrable respect, active listening, caring) with their provider reported less emotional trauma. The medical error literature has often ignored financial trauma but the participants in this group all mentioned the devastating impact of financial problems following an incident; this may be from bills for health care but also from loss of income, either temporarily or permanently. This paper also identified a cycle where patients tried to work out what happened, what would happen next and finally whether or not they would ever be the same. Often patients reported working through the process, feeling very alone. Participants pointed out the importance of having information to help them cope, but also reported having great trouble obtaining it. There were reports of frustration resulting from poor information about their situation causing anger and a perceived need for battles or conflict. The provision of adequate information was often accompanied by relief. Patients reported a perceived need to ‘threaten’ to get action. Some of the group reported that apologies did not routinely happen, but an apology remained important to their ability to resolve their situation and was associated with organisations or individuals taking responsibility for the harm that occurred. Where the communication process was seen as satisfactory, the patients were usually able to continue their relationship with the provider. Those patients who experienced a ‘good’ communication process with their provider also perceived a ‘no fault’ event. These patients were more likely to call these events ‘mistakes or complications’. Conversely, those patients who were dissatisfied with their communication with the provider had a tendency to see incompetence or malicious intent. Most patient anger was directed at the way in which they were treated rather than at the event itself. 91
The 100 Patient Stories project27 is the most comprehensive attempt to date to gather the accounts of patients and relatives of patients who have experienced harm in their health care. From this work, so far, the investigators have been able to gather that most individuals appreciated the opportunity to meet staff and have the adverse event explained to them. There were a number of concerns about how disclosure took place, including disclosure not occurring promptly or being conducted too informally; disclosure not being adequately followed up with tangible support or change in practice; staff not offering an apology; and disclosure not providing opportunities for individuals who have experienced error or harm to meet with the staff originally involved in the adverse event. This work suggests that the practice which is likely to best represent how individuals would prefer to experience disclosures is likely to consist of a combination of formal open disclosure, a full apology and an offer of tangible and material support. 25
There is little to suggest that the experiences of patients who have experienced harm and/or disclosure in the UK are likely to be more or less positive than those described so far in other contexts. Although financial issues are often overlooked, as health care is usually free at the point of care in the UK, the subsequent financial burden for some patients is likely to be substantial if their ability to work is affected or ongoing care is required for a member of their family. The majority of accounts raise the challenges associated with obtaining accurate and timely information, and the frustration, anger and sense of having to engage combatively with an organisation. Another strong account directed towards health-care providers summarises messages from three individuals who had experienced error, either as individuals or to a family member. 92 These accounts leave the reader in no doubt as to the profound effects that poorly conducted disclosure or non-disclosure has on patients and their families. They describe a sense of betrayal and abandonment, likening their experience to a ‘hit-and-run health care accident’ where they were abandoned by a clinician who was both personally afraid and worried about the legal implications of the error. The non-disclosure of medical error is described as ‘the most destructive phenomenon in health care’, eroding trust and confidence and reflecting an ‘intolerable lack of integrity’ which was perceived to be the result of poor leadership. One relative described knowing that something had gone wrong, and that the outcome of the given explanation did not fit that explanation, but experiencing being faced with ‘stonewalling, lack of empathy, and lack of information that would have been helpful’. She perceived this as ‘emotionally and viscerally insulting’ to her intelligence, and believed that if disclosure had occurred and the organisation had given an expression of regret and instigated an investigation, this would have made a great deal of difference to the following period in her life – a period she goes on to describe as ‘2 years of solitary confinement in a prison of inconsolable pain’. The silence is not perceived as passive by these individuals; it is perceived as an active and abusive strategy by individuals and organisations. In contrast, one account describes a senior clinician coming to a child’s home, taking responsibility for the error and maintaining a relationship with the child’s family all through the process of investigation. This was interpreted as a courageous act by the family and they reported this as directly influencing their decision not to litigate.
The perception of some commentators is that organisations and the individuals who work within them have a general lack of knowledge of the suffering inflicted on patients and families when they do not disclose. One participant in the work by Sheridan et al. 92 stated: ‘When they harm us, it is typically a passive event. When they consciously withhold information, cover up what happened, or seek to discredit us in courts of law to preserve their precious financial resources, they are actively harming us’. This US article also points out that consumers do not wish to litigate for monetary gain for the sake of it. Rather, they suggest that people may risk their homes because they cannot pay medical bills and that medical error expenses are an additional harm to the patient and his or her family. The accounts conclude that if hospitals disclose errors and adverse events and work with the patient and/or family to improve the system, they may well eliminate many lawsuits and at the same time continuously improve the system so that the same errors do not repeat themselves. The strength of these accounts may reflect a situation where the consequences for individual families of ongoing medical costs can be more catastrophic than is common in the UK, but this should probably not be based on an assumption and requires more examination in the UK context.
Professional support
The relevant literature and guidance for UK clinicians and managers would seem to be clear and originates from a number of sources including the Being Open guidance itself. 10,11,22,23 In the UK, open disclosure and appropriate apologies or expressions of regret are not the same as admitting legal liability or negligence. Openness and honesty towards patients are supported and actively encouraged by many professional bodies, including the Medical Defence Union (MDU), the Medical Protection Society (MPS) and the GMC for doctors, and the NMC for nurses and midwives.
The MDU advises that, if something goes wrong, patients are entitled to a prompt, sympathetic and, above all, truthful account of what has happened, and it encourages its members to apologise where appropriate. 93 This approach has been given legislative support in section 2 of the Compensation Act, which reads: ‘An apology, offer of treatment or other redress, shall not of itself amount to an admission of negligence or breach of statutory duty’. 94 Doctors’ ethical responsibilities are also clearly set out in guidance from the GMC, which states:95
If a patient under your care has suffered harm or distress, you must act immediately to put matters right, if that is possible. You should offer an apology and explain fully and promptly to the patient what has happened, and the likely short-term and long-term effects. Patients who complain about the care or treatment they have received have a right to expect a prompt, open, constructive and honest response including an explanation and, if appropriate, an apology. You must not allow a patient’s complaint to affect adversely the care or treatment you provide or arrange.
However, this statement is framed in the context of harm or complaints rather than being aimed at a more overarching spirit of openness. The GMC has also indicated that saying sorry and providing an explanation to a patient or relative seldom does any harm and can often avoid a complaint. 96
The role of training and support has been identified by a number of sources as fundamental to the success of any open disclosure policy. Leape97 believes that hospitals must expand the training of physicians to ensure that patients are treated with openness, honesty and compassion, and, when indicated, are given an apology and compensation. Most physicians and other health-care professionals have little or no training in the communication skills required for effective disclosure of adverse events or errors but there are increasing efforts to teach these skills. 69 Recent studies have used standardised patients and role play to teach practising doctors, surgeons and medical residents these skills. 73,98 As well as providing a relatively safe environment in which to practise, this approach also allows individuals to receive feedback to improve their communication. This method could be used for any training, from the highest level of management to risk managers and front-line clinicians. Although the majority of training is directed at medical professionals, a number of barriers to nurse involvement in disclosures have been identified, principally in the area of training and knowledge of how to disclose incidents,99 alongside uncertainty around the information that they could and should reveal. 100,101
The evidence for the effectiveness of such interventions has been captured in detail in the second, more specific review addressing effectiveness specifically (see Phase 1: review 2).
It is thought that patients often litigate to get information after failing through their routine contacts with professionals and organisations. Doctors are often more likely to explain than admit errors. 102 There are a small number of accounts in the literature by health-care professionals discussing cases where they (or one of their colleagues) have made an error, often accompanied by their account of disclosure or, in some cases, no disclosure. 103 There are big challenges in terms of addressing difficult concepts such as guilt and shame in the professional education and continuing professional development of health-care professionals. However, one suggestion is that a more candid discussion of such issues from senior members of professions may help junior staff to talk publicly about their own errors and address the associated emotions that arise as a result of error. Ofri104 suggests that, for junior staff, witnessing the fact that these professionals continue to practise successfully despite their errors may be an important lesson, demonstrating that it is possible to survive the distress associated with error and not be defined by it. Making an error has been highlighted as a defining moment in the life of a physician with regard to integrity and professionalism. 1 A number of accounts have reflected on this, and the way in which a senior physician deals with a more junior colleague who has made a mistake may be crucial in the way this situation is modelled for trainees in any profession. 105,106
An overview of the literature suggests that though professional, regulatory and indemnifying bodies support professionals to be open, the norms within practice seem somewhat removed from this. Discussing a change of ‘culture’ seems overly vague but there is a sense that medical societies, certifying boards and accrediting bodies all play a role in integrating this into practice alongside institutions and professionals, and a more consistent and joined-up approach to education needs to be undertaken. Whether or not this requires statutory support is unclear, but it is likely to require to tackle the issue of openness within health care using both bottom-up and top-down approaches which are reinforced throughout career pathways. Information on the educational approaches which are most effective is lacking.
Risk management and systems improvement
The importance of investigation of adverse events is emphasised in the Being Open guidance,10 which stresses the need to embed this within a process which aims to improve systems of care. Local Being Open policies should be integrated into local and national incident reporting and risk management policies. The framework is aimed at boards and health-care staff responsible for clinical governance infrastructure rather than front-line clinicians, with the emphasis on systems rather than individual failures.
No-blame culture
Although the general thrust of patient safety literature is directed towards the promotion of what is often termed a ‘no-blame’ culture as encouragement to promote the reporting of error, the idea of ‘no-blame’ is questioned by some as being misdirected. 107 Robinson107 suggests that this focus will only lead organisations to identify patterns of risk, but stop short of investigating primary causes. This may feel like a safe climate for professionals, but it is unlikely to address the fears around damaged reputation. However, the assumption that removal of penalties will automatically create a climate of honesty is unproven. Occasionally the source of risk is the individual personality, not the system, and those people have to be identified if they falsify documentation or are dishonest. It is important that institutions do not defend their own staff against a patient or family in the name of a ‘no-blame’ culture. 107
Learning from mistakes and error
Part of the rationale for disclosure is to allow learning to occur. This is obvious when disclosure occurs to the system and to colleagues, but is perhaps less recognised in terms of the potential contribution of the patient and family perspective to enhancing learning. Firstly, some valuable lessons may not be learnt if disclosure does not occur for all patients for the majority of events. Secondly, the process of disclosure is often one of information-giving rather than a dialogue around issues. A number of individuals highlight the role that patients and families may have. 84 Patients and their families often have a unique perspective on their experiences and can provide information and insights that health-care providers and systems administrators may not appreciate or know. 108 Allowing patients and families to engage in a dialogue as part of disclosure allows them to describe what may be important insights into factors leading up to and following health-care incidents, and emotional harms that occur when these incidents are inadequately communicated or responded to, and to make a potential contribution to patient safety. 109
Evidence for the effect of disclosure on risk management outcomes
Calvert et al. 110 have explored the strength of evidence around a number of common statements concerning the belief that disclosure of a medical error improves a patient’s confidence in the physician and leads to improved outcomes, and conclude that they are based on expert opinion rather than concrete evidence. The idea that physicians and other staff may experience a resolution of anxiety and guilt that can improve their well-being after an error may be true, but in terms of quality of evidence this is based on survey data. 110 There is limited evidence that disclosure increases assessments of quality by patients. 111 Mazor has conducted a number of manipulated scenario and other studies in an attempt to build what we know about how patients may respond to disclosure. 13,20,47,86 Some of her work suggests non-disclosure increases the likelihood of swapping to a new clinician and leads to reduced satisfaction and trust in clinicians. 112 Her work suggests that non-disclosure increases the likelihood of seeking legal advice and is associated with a more negative emotional response in one experimental condition, although this was not consistent across conditions. 113 Interestingly, neither the existence of a positive relationship nor an offer to waive health-care costs had a significant impact on outcomes. 113
A current study114 to look at the effect of medical liability reforms and patient safety initiatives is under way and may be able to answer the questions surrounding the effect on liability of offer with disclosure. The experience of a number of US providers has pushed the perspective that open disclosure can be a useful risk management strategy. It is suggested and borne out by some patient accounts that litigation is often initiated by an injured patient in order to get the answers that they feel unable to get from their health-care provider. 41 Practitioners and organisations, when they fear litigation, may avoid open and honest discussion with the injured patient. However, the widely described experience of the Veterans Affairs (VA) Medical Center in Lexington, KY, has not resulted in higher liability as might be suspected. 52 The VHA is not generally representative of the US health-care system,41 but many authors have remarked on the low rates of litigation. 115–117
In 2005, the Sorry Works! Coalition was formed to promote an approach to medical and surgical errors that incorporates full disclosure, apology and reparation. 48 However, a number of papers suggest that there is little evidence to support the perspective that disclosure or apology will deter patients from seeking litigation,117,118 even if disclosure meets the patients’ expectations. 20 Early adopters of this approach have reported reduced liability costs, but the extent to which these results stem from effective disclosure and apology practices, versus compensation offers, is unknown. A survey study119 using vignettes examined the effects of different compensation offers on individuals’ responses to disclosures of medical errors compared with explanation and apology alone. Although two-thirds of these individuals wanted compensation offers, increasing the offer amount did not improve key outcomes. Full compensation offers did not decrease the likelihood of seeking legal advice and increased the likelihood that people perceived the disclosure and apology to be motivated by providers’ desire to avoid litigation, which suggests this relationship is complex. Conversations with patients may benefit from separating disclosure conversations and compensation offers and from excluding physicians from compensation discussions. 119 However, Boothman, a well-known advocate of moving compensation discussions away from the courts, has said it is important to move discussions of compensation into the hands of physicians, hospitals and patients in an attempt to defuse the adversarial nature of the process. 120
Systems for compensation
A number of health-care systems have adopted different ways of addressing compensation for error. New Zealand, Sweden and Denmark have replaced litigation with administrative compensation systems in which patients who sustain an avoidable medical injury can apply directly, without any legal representation, for compensation. However, fear of discipline arising from complaints and threats to reputation remain a concern for doctors and are factors that are still thought to be a factor in inhibiting disclosure. 121,122 Suggested advantages of this system are a focus on compensation and learning from system errors rather than attributing blame, as well as allowing injured patients to access compensation for their injuries quickly without the additional stress and cost of the legal system. However, upper limits attached to claims may not adequately compensate over time for care costs. It has been suggested that many of these early compensation mechanisms which occur in the disclosure with offer programmes, particularly in the USA, are capable of causing patients to reach a financial settlement before considering their future medical costs or the need for non-economic damages. 123
Apology laws
An admission of error to a patient is not the same as the admission of liability for the damages the patient has suffered. In the USA this is the basis of a series of ‘apology laws’ that prohibit or limit the use of an apology in the case against a health professional or organisation in litigation. 124–126 At least 36 states have passed, and others are considering passing, immunity for apology laws and five states have passed mandatory disclosure laws. 127 However, there continue to be a number of authors who warn individual clinicians to be wary of making an admission of liability during the open disclosure process. 128–130 Professional journals sometimes carry ‘health warnings’ which highlight the problems associated with saying ‘sorry’. 131 Although litigation is feared by clinicians, most patients do not bring a legal challenge to court and physicians substantially overestimate the risk of being sued. When a clinician has apologised to a patient, the legal case against him or her is likely to viewed differently by a jury, who will be more likely to concern themselves with establishing just compensation rather than negligence in the face of an honest clinician who has apologised. 132
Apology laws emerged in the USA in the 1990s as part of efforts to enhance medical error reporting and patient safety. As outlined earlier, it is thought that more disclosures and apologies, combined with early settlement offers by hospitals, has led to a dramatic decrease in claims of malpractice in the USA. However, the actual impact of apologies and of apology laws on litigation is less clear because both are components of broader regulatory and institutional efforts to overcome the complex problem of resistance to disclosure. Early settlements may well drive down the cost and number of claims with or without an apology. 133 Some consider that apology laws are unnecessary for the open disclosure of adverse events and that they will make it more difficult for individuals to pursue negligence claims. 134 But others suggest that apology laws are unlikely to shield people in the case of gross negligence. 135 The most important distinction among apology laws is whether or not admissions of fault are protected. However, there are many variations in these laws between states. Some protect oral, but not written, statements;46 some mandate that hospitals or their physicians notify patients of medical errors leading to adverse outcomes, moving beyond voluntary disclosure52–54,57 with laws to protect the required disclosure from being used as evidence of fault in any legal action. Some have suggested that apology laws usually do not protect physicians who expressly admit fault or use explanations or statements that can be interpreted as admitting fault, and that in such cases physicians could find themselves in difficulty regarding explanations and disclosure of error. 136 The perception of a lack of explicit legal protection for the admission of faults and the fear that an apology will expose physicians to higher risk of litigation certainly causes concern in the USA. If this is the perception of clinicians in the UK then it is likely to have a similar effect. However, the NHSLA, which indemnifies NHS trusts for claims in England, stresses that apologies and explanations should be provided and to do so will in no way affect the availability of the trust’s indemnity. 22 However, although risk managers in the USA tend to support disclosure, they are much less enthusiastic than physicians about offering an overt apology. 61,137 We have little evidence that would allow us to determine the position of risk managers in the NHS.
Dissenting views on the need for apology laws do exist138 although they seem to exist in a Canadian rather than a US context. Objections seem to rest on the premise that whereas apology laws exist to protect admissions of liability, a better course is to express sympathy, discuss the facts and promise investigation, followed up with further disclosure after a review has determined the most likely causes of the situation. If an error has occurred and physicians or institutions admit an error that caused harm, then they should encourage their liability insurer to negotiate reasonable compensation without requiring their patient to sue them.
Consistency of patient experience
Some take a broader view of the culture in relation to apologies, looking at smaller steps leading to culture change. If the broader approach of health care were to apologise for relatively minor violations like being late or forgetting to do things, then apologising for bigger things should be easier. Woods139 discusses this idea and points out that it seems convenient for organisations to believe that litigation is driven by opportunistic solicitors and patients who see a way to profit from error in a way that seems to be beyond the control of clinicians and organisations. However, she suggests that this may not be so if people feel they have been treated honestly, and that if information has been shared perhaps people will sue less. 139 Nonetheless, she cautions against the use of apology and openness as a risk management strategy in itself, something that is seen as out of keeping with the rest of the patient experience. Patients are perceptive to change. If no trust has been established by offering apologies and courtesy throughout care, then any perception that an organisation is offering one up after a poor outcome to lower liability may well make them angry. 139 These suggestions link to the observations of others who have pointed out that there is a general failure of openness across information-giving to patients, which means they are often unprepared for what the system might consider disappointing, but not unexpected, outcomes. As such, informing and managing expectations before, during and after treatment should always be part of decision-making, ensuring that all possibilities have been discussed. 140 Difficult and possibly adversarial situations can arise when anxieties during care and then afterwards have been ignored, and defensive and/or slow responses will cause problems. Others have observed that apologies might be easier if patients are better prepared for complications or poor outcomes as a possibility. 141
The responsibility/role of the patient and family
A slightly different perspective discusses patients having rights in relation to disclosure, but on the basis that with rights come responsibilities. 142 The emphasis here is that patients cannot expect the right of disclosure without taking an active role in making challenges and information-giving in relation to safety. The examples given in this work sit within a previously described literature in which patients are expected to contribute their knowledge and input for the greater safety good. However, other work has demonstrated how challenging these kinds of roles can be for patients and families who experience this process as outsiders to a system in which they only know what the system chooses to disclose to them, and where the implications and assumptions underlying roles are often not well thought through. 39 There appears to be little work exploring the roles that patients might play in informing disclosure policy and in directly informing improvement after errors.
Liang143 suggests the patient/family should be asked to assist in the error investigation by the error disclosure team during the initial contact, if appropriate, or by the patient care liaison at a later time. It is proposed that this could range from discussion of any factor, problem and/or witnessed error that may or may not have contributed to the negative outcome to a full debriefing on all stages of care, from before admission to the event itself and even the time following the event. This kind of approach is consistent with the systems nature of error and outcomes and is indicative of a more equal partnership approach between health-care providers and patients. Additionally, the patient and/or family have a vested interest in corrective action at the facility, which may allow something constructive to emerge from an otherwise destructive situation. Perspectives gathered in the 100 Patient Stories work support the view that patients and families feel they have a valuable perspective to contribute. 27
Implementing disclosure policy
Sorensen et al. 144 examined the implementation of open disclosure policy and concluded that health service managers must formulate their own local approaches. This would include identifying ‘the circumstances under which open disclosure is conducted, who should be involved, where and when discussions take place and how patients are informed of the process, the plan of remedy and the means for feedback of investigative results’ (p. 231). They too identify a gap where open disclosure policy fails to be applied by those who have to undertake the process, and find that the necessary links between policy-makers, those who have to conduct disclosure conversations and those who hold knowledge that may improve the process remain unconnected. The organisational components required to improve practice include improved competence at both the organisational and individual levels, but also the removal of barriers such as the covering up of errors and a lack of commitment to disclosing error. The identification of this organisational competency, they propose, would link the two currently predominantly discussed areas of policy development and clinician–patient communication. On a practical level, it is proposed that this would consist of networks where good practice can be shared, allowing managers to examine models of care and appraise their possible implementation within their own local context. This would allow more support for managers to move beyond what is referred to as a complacency which talks about principles but fails to support their enactment in practice. 145,146
There is little knowledge of how open disclosure policies are being implemented in the UK, but one recent cross-sectional survey of UK risk mangers147 identified that 98% of the participants reported that they were familiar with the Being Open guidance and 82% stated that they implemented it more than half the time when incidents occur. However, provision of timely information was not reported as routine, with two-thirds of the discussions taking place 3–6 weeks after the investigation. The frequency of taking responsibility for harm was low for incidents of different severity levels but significantly lower for less serious ones. Long-term follow-up of patients and ex-gratia payments to patients occurred less than half the time. The most highly rated barriers to being open were reported by risk managers as clinical staff’s fear of negative reactions from patients or their families and anxiety about litigation. Support practices for staff, such as debriefing and training on being open, were acknowledged as highly important but not always available. The authors concluded that though awareness of the importance of open disclosure appeared to be high in their respondents there was still considerable scope for improvement in the consistent application of the guidance.
Accounts of open disclosure policy perceived as successful
Instances where local policies of open disclosure have been successfully implemented do exist and are frequently cited moving through the chronology of the literature. Such examples of implementation are rarely discussed in the academic literature and are often limited to risk management conferences and professional journals. There are a number of examples of individuals from practice who talk persuasively for the power of disclosure of adverse events in terms of institutional learning and patient- and clinician-centred outcomes, but a substantial evidence base has yet to be established. These individuals are often interviewed as part of more journalistic literature discussing the challenges they experienced in implementing disclosure policy within their organisation. Often these policies emerged from serious errors within their organisation. Such accounts must be taken at face value but have strong messages for the UK in terms of how implementation may be able to succeed in the face of the barriers that are frequently cited in literature from all contexts. It seems to be agreed that a number of key actions and individuals need to be mobilised. Disclosure needs to take place systematically and based on agreed protocols, with tangible support in the case of psychological health-related problems, accompanied by clear and demonstrable efforts to learn from events and make the system for providing health care safer. Much more could be done relatively quickly by hospital management and department leaders, who are identified as key in implementing such comprehensive incident management approaches, educating staff in collaboration with professional organisations and professional curricula and promoting an organisational culture that supports open communication and learning from critical incidents. 148 Although the principles espoused in policies such as Being Open seem simple, operationalising these locally is often the point at which a number of questions arise. 149 All accounts stress that a focus on the patient perspective, not that of the organisation, is key to making implementation credible. Resistance from the system to disclosure should be expected and will need to be overcome.
Julie Morath from the Children’s Hospitals and Clinics of Minnesota describes the commitment required to change and describes a ‘wholesale revamping of philosophy at the hospital, not just the implementation of a new policy handed down by risk management’. 150 She has also highlighted that a focus on limiting organisational liability does not fit well with full disclosure and should not compromise the philosophy. Jo Shapiro from Brigham and Women’s Hospital, Boston, MA, describes the use of Boothman’s principles as the basis for the hospital’s process and describes having to convince her institution that it was the right thing to do. 151,152 The approach at Brigham is grounded within the Center for Professionalism and Peer Support, which is able to offer a support hotline 24 hours a day and uses a ‘train the trainer’ model to engage all staff with the principles of and skills need for disclosure. She credits the success at Brigham to the joined-up approach between risk management, human resources, patient safety, and senior clinicians and managers. There are monthly symposia and staff evaluate the effectiveness of full disclosure with patients and families. Families continue to seek care, and safety is reported to have improved, as have attitudes.
Richard Boothman is another well-known individual within US health care who has disseminated his practice from the University of Michigan Health System (UMHS). Boothman describes what started out as an effort to save money changing into a major patient safety and patient communication agenda, and describes the issue of claims as ‘background noise’. 153 As soon as UMHS learns of an error, risk management staff are assigned to talk to patients. They apologise, letting the patient and/or family know that UMHS will investigate the error and that whatever is learned from the investigation, as well as any new practices to prevent the error in the future, will be shared with them. If UMHS has made an error, compensation will also be offered. They will, however, vigorously defend their organisation if no error is identified. Another initiative involves a team in risk management which supports doctors who find themselves in difficult positions, helping them decide on an honest approach with patients. Sincere apologies are encouraged, with support given to help clinicians make sure their conclusions and evaluations are sound, that the event is discussed in context and that disclosure and follow-up plans are supported. As with the approach described by Shapiro, the emphasis is on the whole team. Additionally, Boothman describes the way in which the publicity of UMHS’s success has led to more reports of near misses and patient injuries. 153
In 2003, Trillium Health Centre in Toronto, ON, identified the need to develop a disclosure protocol as part of its risk management approach. Key to this was training provided through a ‘train the trainer’ model and this account also stresses the need to address and change norms which happened slowly over time. 154 Sisters of Mercy Health System in St. Louis, MO, has described the questions it asked itself in developing a policy for open disclosure. 155 The process was clearly iterative and took a great deal of negotiation in defining the policy; however, the advice from this risk management system was to begin a defined output and to choose a strong facilitator and multidisciplinary team members. Further steps involved looking at the process and policy of other successful organisations and examining how these might apply to this organisation in light of current guidance and statute. A number of other accounts of the application of policies with the support of insurers can be drawn upon to examine concrete suggestions for change, at least from the US literature. 156–160 Common to these accounts is a sense of enthusiasm, but also often a charismatic individual driving the process forward. There seem to be fewer of these accounts outside of the US context and we found only one in the UK, which described Liverpool Women’s NHS Foundation Trust’s approach to embedding quality improvement and patient safety in the organisation. 161
In a recent critique of the Consultation Draft of the Australian Open Disclosure Framework, Parker162 suggests that there appears to be movement towards ethical practice being prioritised over organisational and individual learning from error, rather than an organisational risk-management approach. However, a note of caution is stressed with the emphasis still being one of stating regret rather than accepting responsibility. As has been pointed out previously, expressions of regret are not apologies, as an apology presupposes the fault that health professionals are advised to avoid admitting. A criticism levelled by Parker is that this may represent a continuing insincerity on the part of health professionals and their institutions regarding the kind of apologies that patients look for, and suggests that though open disclosure policies and practices are inconsistent and unclear about complete disclosure, admission of fault and genuine apology, they will continue to lack respect for and empathy towards patients harmed by health care. Finally, it is suggested that the National Open Disclosure Standard should be revised to encourage and support full disclosure and genuine apology, but that if this fails, statutory reform should be considered. This would chime with the recommendations of the Francis report6 in the UK.
Individual/multidisciplinary team responsibility
The Being Open framework10 stresses the role of all staff and suggests that this should be reflected in the way that communication occurs when things go wrong. Multidisciplinary involvement is specifically drawn out. Much of the literature is focused on the role of doctors in the disclosure process; however, there is recognition that a number of other people may be involved in this. A small number of papers discuss a multidisciplinary approach but most argue for the role of an individual profession, usually a physician or a risk case manager.
Some argue that disclosure should be conducted by someone who is one step removed from the error; that contact between the family or patient and those directly involved in an adverse outcome undermines the systems approach. The delivery of health care is conducted in teams and errors typically involve several members of the team, including nurses, physicians, pharmacists and others. When an error occurs, there needs to be communication between the team members to discuss not only what went wrong but who should tell the patient or family. These interprofessional team conversations can be challenging and most team members are not experienced in conducting this type of conversation about a difficult issue such as disclosing an error. Given the complexity of these conversations and the need for consistency, there is a lack of research about how team members should participate in the disclosure process. Who should tell the patient: one individual or several team members?69
Whereas some suggest that disclosure should be undertaken by the clinician with responsibility for the patient’s care, or a delegated representative, others warn that delegation of this responsibility to a member of the team who does not have sufficient knowledge to answer all the patient’s questions may be problematic. Some policies specifically assign this task to the clinician who has overall responsibility for patient care,163 but in certain settings other health-care professionals and/or senior administrators may be better placed to disclose, particularly if they are more knowledgeable about the consequences of the error. The same policy163 also recommended that at least one other member of staff is present during the disclosure process. The VHA suggests that in instances with minor harm, an informal process is indicated involving the clinical team, but in more serious cases of harm the institution should be represented by one or more of its leaders in a more formal approach. 51 The Australian Council for Safety and Quality in Health Care stipulates clear guidance for the qualities and skills of the individuals involved in disclosure,164 stating that the individual making the disclosure should be the most senior health-care professional who is responsible for the care of the patient. In serious incidents that person should have the support of a senior staff member with good communication skills. The Council goes on to describe an individual who should be known to the patient; familiar with the facts of the incident and care of the patient; senior enough to be credible; trained in open disclosure; in possession of good interpersonal skills and the ability to communicate clearly in everyday language; able and willing to offer reassurance and feedback to the patient and family; and willing to maintain a medium- to long-term relationship with the patient where possible.
However, a contrary view142 suggests the practitioner should not initially participate as a member of the disclosure team because the emotional stress generated from the error could result in ineffective communication or conflict. Liang142 argues for an objective approach which is characterised as calm, non-reactive, caring and honest, and composed of senior institutional representatives such as a risk manager. Although concern for distress in clinicians is valuable, others observe that health-care practitioners who make an error may need to personally make amends and, hopefully, be forgiven by the patient. It is their therapeutic relationship with the patient that may need to be maintained to rebuild trust and preserve continuity of care where possible. Thus, others view delegation not as the rule, but as the exception.
A large body of publications comes from a risk management perspective in literature from the USA, and many of the most vocal and proactive proponents of open disclosure, with or without compensation, are from a risk management perspective. The role of risk management in the UK is less discussed and possibly less defined than in the USA. In the UK, who risk managers are and what they do may differ from trust to trust. Risk managers usually work away from front-line care. Their focus is on service quality and safety, and they occupy an important position in the handling of incidents. They assist clinicians and patients in resolving incidents, and they guard the service against undue risk. Their perspective is often couched in terms of operating a policy of disclosure while keeping liability minimised. 165 The role of clinicians involved in error disclosure, and the personal nature of their involvement, is seen as a disadvantage in some accounts, where they are perceived to weaken the approach to dealing with incidents, disclosure and blame. Risk managers may regard themselves as less personally implicated and therefore more able to be proactive about disclosure and incident investigation; however, with this comes a less pressing perception that an apology may be required. In a critique of the role, Iedema suggests that the current stance adopted by risk management dilutes the function of the role in avoiding simplistic assumptions about incident causality, service responsibility for an error and disclosure. 33 He also suggests that clarity of role remains ill-defined for risk managers and health-care professionals over the main components of patient safety related to systems thinking and just culture. 166 Other work suggests that risk managers have more favourable attitudes towards disclosing errors to patients compared with physicians, but are less supportive of providing a full apology. These differences may create conflicts between risk managers and physicians regarding disclosure. If clinicians are to be clear about the nature of disclosure conversations and encouraged to disclose then greater collaboration between risk management and clinicians needs to take place. 137 Certainly, in the USA, where communication after an event can be viewed as evidence, it is likely that risk managers will be keen to promote expressions of empathy but guard against full apologies. 167 There appears to be no exploration of whether or not such a divergence of views exists among risk managers in the UK context.
Although historically the role of discloser has often fallen to the doctor, there appears to be an increasing awareness of the role that nurses may have to play. Nurses are intimately involved in patient care and, inevitably, in the patient safety incidents that occur. This may create additional dilemmas for nurses when faced with the responsibility of disclosure and has been identified as posing challenges when continuing to provide day-to-day care. 100,168,169 Though a small number of papers make comment on the potential role of the nurse,170,171 empirical literature exploring nurse disclosure is limited. The literature suggests that while nurses are confident in reporting safety incidents through organisational mechanisms, feelings about the contribution of nurses to disclosing those incidents are more varied. Nurses expressed a desire for a more senior member of staff, such as the lead physician or nurse manager, to be primarily responsible for the disclosure of more serious events99 but reported discontent with exclusion from the planning and delivery of such disclosures. 100 Uncertainty around what and how to tell patients about issues arising in their care appears to leave nurses feeling that they cannot freely address patients’ queries about their care, which may result in inaccurate, incomplete or ill-timed disclosures. 100
Disparity between the perceived potential contribution that nurses can make to disclosure and their current contribution was evident. For example, in an emergency care setting nurses reported much lower rates of disclosure conversations than physicians. 172,173 Furthermore, in simulated error disclosures nurses expressed a lack of clarity about the nature of their input and expressed fears around overstepping professional boundaries. 174 A secondary, supportive contribution was apparent across the reviewed papers, whereby nurses balanced being the patient’s advocate and supporting doctors; this meant offering additional explanation and comfort to the patient, or contributing detail to the knowledge of the medical team about the circumstances of the incident or the patient involved.
Recent studies described facilitating a more active contribution for nurses in accounts of training for multiprofessional teams. 174,175 Nurses described this as a valuable opportunity to explain their contribution to an incident and be apportioned blame fairly when the patient was in contact with a number of health-care professionals, but the tendency for lead physicians to drive and manage the process of disclosure in practice was identified as a key limitation.
A hierarchical structure within health care has been highlighted in relation to junior and senior doctors and medical students, and in relation to nurses. Ineffective team working, specifically with regard to exclusion of nurses from decision-making processes, has been cited as an obstacle to nurses ensuring that events are disclosed. 100,168,174 Even when empowered to disclose an event, the likelihood of a nurse challenging the decision of a physician or taking the lead for the disclosure was perceived to be rare. 174 Nurses often perceive more than medical staff that they will be punished or treated unfairly by managers or the organisation, supporting the notion that a fair blame environment that encourages consideration of systems factors in patient care may foster a more open and honest culture. 100,169,176,177 Nurses perceive that exclusion from disclosure planning or delivery may expose them to disproportionate blame for an incident, especially where an error was made. 175,178
Although the majority of literature within this review came from or was directed towards doctors, nurses and risk managers, a number of outputs were seen in journals specifically addressing dentists, podiatrists, pharmacists, physiotherapists, laboratory-based health professionals and general practitioners. However, there was notable bias towards secondary care literature and primary care was identified as an area that required further work.
Clinical governance
Being Open stresses the support of quality and improvement processes and the importance of disseminating lessons learned to health professionals, alongside implementation of learning and subsequent monitoring of change.
The application of this approach is articulated in the seminal documents relating to patient safety, To Err is Human 16 and, in the UK, An Organisation with a Memory. 17 The Joint Commission, one of the most influential organisations to develop patient safety-related standards for hospitals, explicitly links disclosure of errors and adverse events to hospital accreditation. They require that a ‘responsible licensed independent practitioner or his or her designee clearly explains the outcomes of any treatments or procedures to the patient and, when appropriate, the family, whenever those outcomes differ significantly from the anticipated outcomes’. 179 However, many hospitals in North America had developed error disclosure protocols addressing the patient’s right to be informed some years before these documents existed, for example the Royal Victoria Hospital in Montreal, QC,180 Minneapolis Children’s Hospital and Clinics, MN,181 and the Dana-Farber Cancer Institute in Boston, MA. 163 More recent model disclosure programmes and policies are those of the University of Illinois Medical Center, UMHS, Kaiser Permanente, Catholic Health Initiatives and COPIC Insurance Company, which covers a number of Colorado providers. 151,152 However, the best-known examples are probably the VA medical centres. 52 In each of these examples, a set of policies and procedures has been developed to address medical errors committed while caring for patients. In the case of the VA it is required that a mistake be disclosed to the patient, usually by the leader of the treatment team. The 2008 policy of the VHA on Disclosure of Adverse Events to Patients starts out by emphasising that:
VHA facilities and individual VHA providers have an ethical and legal obligation to disclose to patients adverse events that have been sustained in the course of their care, including cases where the adverse event may not be obvious or severe, or where the harm may only be evident in the future.
VHA 200851
Litigation
One way of measuring disclosure of medical error might be supposed to be examining litigation activity. The most commonly asserted claim for the advantages of disclosure is the link between disclosure, apology and reduced litigation or malpractice activity. 52 There are number of problems with assuming this link, and indeed there is disagreement in the literature about the strength of this assertion. There is an extensive body of literature which discusses the advantages of disclosure in terms of reduced litigation. It is argued that patients who feel that they have been deprived of full disclosure and, if required, an appropriate apology may be more likely to pursue malpractice litigation. 52 Some evidence (controlled and uncontrolled) suggests that full disclosure, apology and fair compensation may result in lower litigation costs arising from medical error. The University of Michigan has reported that since it adopted a policy of full disclosure of medical error in 2001, a marked reduction in claims and decrease in legal expenses has occurred. 182 A similar experience has been reported by the Lexington VA Medical Center in Lexington, KY. After it adopted a full disclosure and fair settlement approach, the hospital had more settled claims, fewer plaintiffs’ verdicts and reduced payments per claim,183 and subsequently adopted a full disclosure policy across all hospitals in the VA system. 52 The remainder of the literature in this area tends to cite these two papers as evidence of the link between disclosure and reduction in litigation (the publication regarding VA centre experience has been cited by 399 related articles to date). However, in both of these studies disclosure was combined with financial settlement and hence it is impossible to disentangle the effects of the two. We would argue that no clear link has been established between disclosure and reduction in litigation. A review by the Canadian Patient Safety Institute in 2007 also came to similar conclusion. 184
Advocates of a fault-based civil compensation system suggest that the award of damages is not only intended to compensate the patient but to act as a deterrent, reducing medical error and resulting injury to patients. 185 Negligence law is generally treated with suspicion by health-care professionals but is viewed by others as one system to promote the implementation of mechanisms to improve care to patients. 186 This is unlikely to persuade individual practitioners who have committed an error to disclose it to the patient, but there may be good legal reasons for disclosing error even in the face of an increased risk of litigation. 41 Although the error itself can instigate legal action, failing to disclose may deprive the patient of a timely opportunity to receive treatment for the injury, thus potentially increasing the amount of damages awarded. 187
Few cases are resolved through a trial; many are resolved through negotiations following an assessment of risk by both parties. As a result, using reported court cases is unlikely to be useful as a way of examining disclosure effectiveness. However, fear of litigation continues to be cited as a reason preventing disclosure. Lord Woolf,188 with reference to the UK context, has alluded to a role for lawyers with regard to their primary responsibility to facilitate a settlement rather than to encourage litigious exchanges, and has promoted better co-operation and understanding between the courts and the medical profession. Barach189 has suggested that if the fear of litigation continues to undermine the efforts to improve patient safety through disclosure as a mechanism for learning, then transforming the present unsatisfactory situation into a culture promoting safety for patients may never be fully realised. This said, current evidence, albeit further survey work, suggests that full disclosure seems to have little effect on the likelihood that an injured patient will seek legal advice, and although the positive results of individual systems, such as the one in Michigan, are able to describe a decrease in malpractice suits, even the most enthusiastic supporters such as Boothman suggest that it is probably overstating the case to directly link the policy to fewer claims for compensation. 190 The effect of disclosure practice on litigation in terms of numbers and value of claims is by no means clear. Studdert et al. ,191 in a somewhat controversial mathematical modelling study, concluded that the number of malpractice lawsuits is likely to rise if and when full disclosure occurs. However, the literature is vocal on the benefits of disclosure in reducing litigation and the size of settlements. 52,124,153,192,193 Hickson et al. 194 concluded that nearly half of all perinatal injury actions were motivated by parents’ suspicion of a cover-up. Another study suggests that patients are significantly more likely to sue if their physician failed to disclose an error. 21 Patients want to know the facts when an injury has occurred as a result of medical error.
Scheirton41 suggests that law follows ethics, and that as more and more hospitals adopt policies on error disclosure, and professional associations and quality assurance organisations insist on such policies, the courts may start to adopt these standards as normative. The MPS argues for changes whereby health-care managers facilitate and encourage organisations to develop policies and processes to support open disclosure alongside notification of both adverse events and near misses. Crucially, it envisages that this will include strategies which provide ongoing support, training, mentorship and investment in leadership by example. It feels that this will allow staff to be effective in participating in open discussions in health care and will allow them to fulfil their professional obligations. 195
Duty of candour
As early as 1995, a discussion around a duty of disclosure highlighted that doctors suggested they did not have time to disclose, that they had not done so in the past and were unlikely to start without some kind of professional obligation to do so. 196 This was proposed as a measure to increase trust in hospitals and doctors and possibly defuse negligence cases. Some have observed that there may be many incentives to conceal an error when we compare the possible consequences of concealment with those of disclosure. If a clinician or organisation does not disclose an error in particular, this might never be discovered and there may be no legal sanctions or negative effects, including any impact on reputation. If the error is discovered and the patient actually sues, some have argued that the legal consequences seem very similar to those that would occur if disclosure had occurred right from the start. 197 Thus, the current sanctions for non-disclosure would seem to some to be inadequate.
The codes of a number of professional bodies and indemnifying bodies advocate openness as a professional obligation, including the British Medical Association (BMA), the GMC, the NMC and the MPS. However, in response to a persisting lack of consistency in openness with patients over error, there have been calls to introduce a statutory duty of candour in the UK. Others argue that openness should be encouraged through supporting a culture of change rather than a change in the law.
After much lobbying and debate, the UK introduced a contractual duty of candour for health-care institutions which came into effect in April 2013. This duty is imposed by the NHS Commissioning Board on all contracts with NHS providers. The Department of Health suggests this will cost £130M over a 10-year period, the cost being incurred by clinical commissioning groups taking over the contracts in breach of duty and costs associated with the disclosure of events to patients. However, it is also thought that savings will be in the region of £541M over the same period. 198,199 An amendment to the Health and Social Care Bill was rejected, meaning that no law would be enacted to require the NHS to be open with patients about errors that cause harm. A coalition of patients’ charities and health organisations had lobbied for the amendment and a further new report has stressed the importance of transparency. 200 Critics argued that the measure would be woefully inadequate to protect patients’ rights because it would lack statutory force and would not apply to non-hospital care providers such as general practitioners (GPs) and dentists. 201 A compromise was introduced: a ‘contractual’ duty of candour, a standard clause to be included in hospitals’ contracts. Recent events related to the questioning of the quality and safety of care in the NHS, and the Francis report6 and most recent report by Berwick et al. ,200 may lead to this being reviewed with a view to mandating statute; however, it is to date unchanged.
Confidentiality
There was very little literature specifically addressing the area of confidentiality within disclosure of adverse events to patients. As the review concerned itself with disclosure to patients rather than the broader topic of whether or not events are disclosed to systems either local or nationally, this may be one area of the Being Open guidance which requires further examination specifically. Similarly, we did not approach whistleblowing as an area within this review. The area of confidentiality with respect to patients did raise one interesting account, which to some extent addresses how confidentiality may be more difficult to manage once the error has been disclosed to a patient or family. In one disclosure scenario where the parents of a baby had been alerted to an error while their baby was still in the care of the unit, the family alerted other families within the same neonatal unit to be vigilant about the care of their babies following this disclosure. 202 Staff described the dilemma their unit faced as they had to talk to many families as a result of one disclosure discussion, and the time this took. The implication of this did not seem to be that the parents should not talk to other patients but they did seem to be arguing that the disclosure should have been delayed until the parents did not have ‘access’ to other parents. However, that parents should be vigilant about the care of their children, and that they should question it, seems to be exactly the message given in the pamphlets and books produced around the world to encourage patients to contribute to the greater safety agenda. There is a real question about what harmed patients may do with disclosed information, and it seems impossible to control who patients choose to discuss their error with once it has been disclosed. The Being Open guidance10 seems more focused on ensuring confidentiality within the organisation to protect the no-blame systems approach, but how and whether or not it applies to patients and families is less clear.
Continuity of care
It is well established that patients and families wish to have early, and complete, information wherever and whenever possible. However, what is often lacking is an understanding of the ongoing nature of the disclosure process. If patients are alerted to an error or adverse event as soon as it becomes apparent then it is likely that there are a number of facts to be established and that an ongoing discussion will be required. Further information will emerge, and in time the nature of any further treatment or compensation will need to be discussed alongside any system learning. 203 The literature suggests that it is still common for medical organisations to approach open disclosure with less than a high-level commitment and belief in the process. 27 Disclosure should begin shortly after a medical incident is recognised, and not when all the internal fact-finding and analysis are complete. Those affected need specific and timely information and the use of any generic approach is unlikely to be helpful. Clinicians require support to effectively deliver an apology and demonstrate empathy for the patient and family. In some situations this may require coaching and role playing before the first disclosure meeting.
As part of a continuing package of care and skilled disclosure process it is crucial that the care team does not abandon patients or families when something goes wrong. Disclosure needs to be viewed as a process, not a single meeting. 31 It is unlikely that affected people will understand all the components or complexities of an incident in one meeting. Organisations should expect a multivisit process, even if the clinicians are involved only in the initial meeting. A single meeting often cannot deal with more than reviewing the event, expressing an apology or expression of regret and answering questions. Subsequent meetings allow for additional questions, further information disclosure, discussion of steps taken to lessen the chance of a recurrence and possibly financial discussions. Any attempt to define a number of meetings in advance is unlikely to be helpful as different individuals and different errors will require a flexible approach. Those affected need someone who can help them collect information, find answers to questions, provide updates and help complete any financial support arrangements. 85 This person must be seen as someone who is supportive of those who have been affected, not someone who is seeking to play down the incident, obscure the content of information, or protect the medical system or clinicians involved. 156
Amori and Popp203 suggests that the role of a skilled risk manager who is committed to effective disclosure is in determining where the family is in the process of coming to terms with an adverse outcome. This allows both coaching and support for the staff involved, ensuring the proper timing and mechanisms for the various conversations that need to take place. 203 Whoever leads the process must be available when needed by the patient or family, even when the timing is inconvenient.
Summary
A huge body of work exists which discusses open disclosure of adverse events; however, key messages, although useful and positive, are often handed down as received wisdom on the basis of little theoretical underpinning or research. There seems to be broad agreement that open disclosure is the ‘right’ thing to do. However, justifications often sit within a context of reducing costs to organisations in terms of lawsuits. If being open is the right course of action, and in some contexts the legal one, then perhaps it does not require such evidence and the focus of research should lie more within implementation and monitoring and the most effective and acceptable models of training. Gallagher et al. 204 have identified that more work is needed to examine how open disclosure is operationalised in practice, and how staff negotiate the systems within which they operate as well as interactions with patients. Research needs to focus on how we can best capture dimensions of quality in relation to disclosure conversations and whether or not these are measurable.
Phase 1: review 2
Results of the search
After deduplication, 10,527 records were identified. Screening of the titles and abstracts identified 21 references that potentially fulfilled the inclusion criteria for this review and copies of the full papers were sought. A total of 10 studies (11 publications) fulfilled the eligibility criteria and were included in the review. 52,205–214 In two studies the intervention was disclosure (combined with another intervention)52,208 and in eight studies (nine publications) the interventions were intended to promote or support open disclosure. 205–207,209–214 Two studies included a comparator group52,212 and eight were uncontrolled before-and-after design. 205–211,213,214 Two literature reviews were identified117,215 and one of the included studies52 was identified from the reference list of the review by Kachalia et al. 117 Three references to completed research funding grants were identified. 216–218 Authors identified as the award holder were contacted but we were unable to identify any publications for inclusion. One ongoing study was identified. 219 Figure 4 explains the study selection process.
FIGURE 4.
Study selection flow chart.
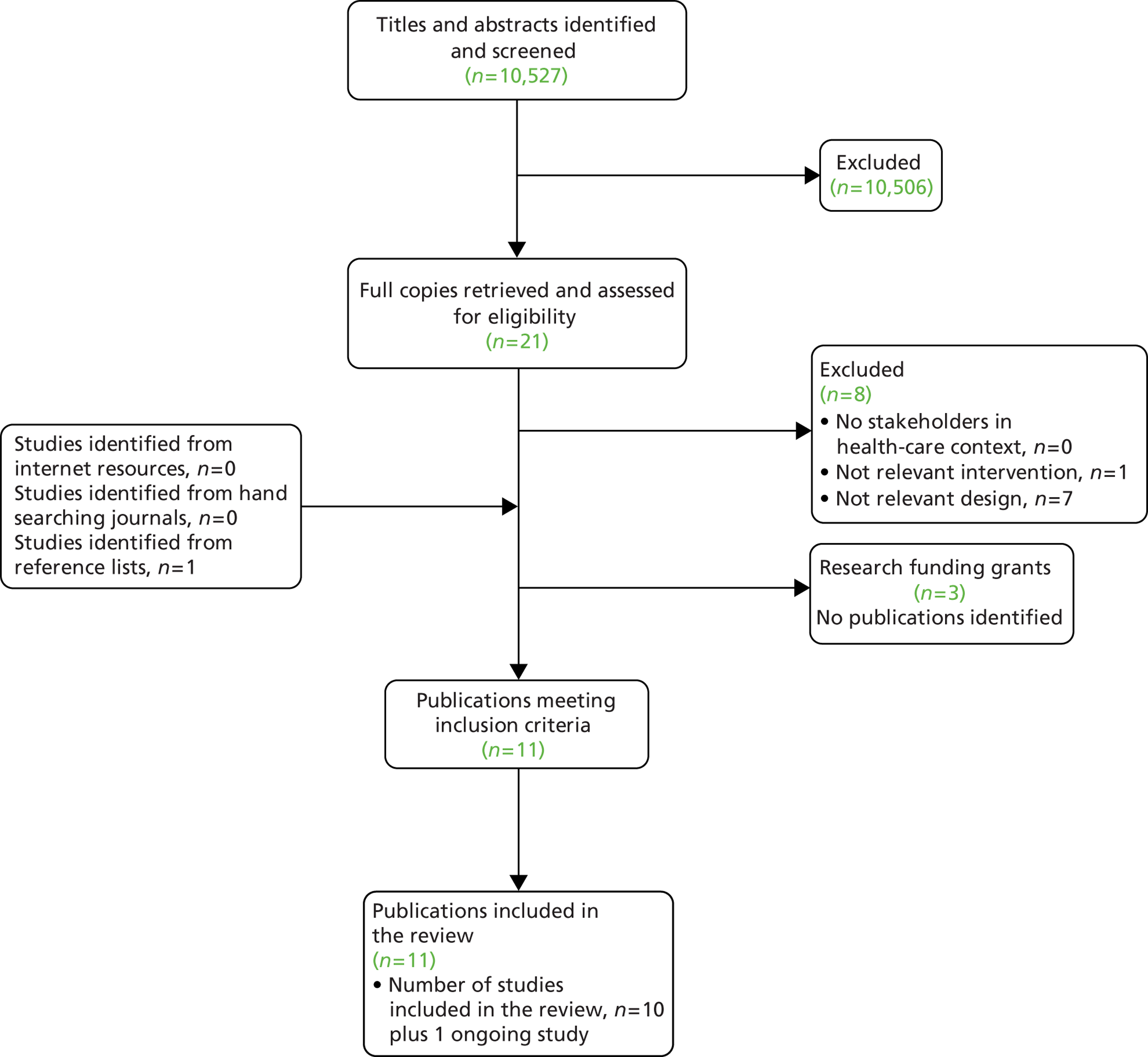
Excluded studies
Eight studies were excluded after reviewing the papers. 98,220–226 Seven studies were excluded on the basis of the study design. One study225 was excluded as the intervention was not open disclosure or an intervention to support open disclosure. A list of the excluded studies detailing the reason(s) for exclusion is available in Appendix 10 .
Ongoing studies
One ongoing study was identified. Researchers in the USA are undertaking a randomised controlled study of training physicians in disclosure. 219 The intervention includes a disclosure training webcast, practice and feedback with standardised patients, and a refresher training webcast. The primary outcome is patient satisfaction with a disclosure that they experience, measured using the Patient Assessment of Disclosure Quality. The project was due to complete in 2012.
Included studies where the intervention was disclosure
Two studies included disclosure as an intervention,52,208 combined with another intervention; in both cases this was an offer of financial compensation ( Table 1 ).
| Author/year/country | Study type | Participants | Interventions | Outcome: outcome measure | Reported findings |
|---|---|---|---|---|---|
| Kachalia 2010208
USA |
Uncontrolled before-and-after | Public academic medical centre and health system (UMHS) | Disclosure-with-offer programme Programme first introduced in July 2001, and by February 2003 disclosure programme fully integrated with patient safety efforts. Identifies patient injuries through various means. Experienced risk managers lead investigations and mediate patient concerns as facts are collected and conclusions are disclosed. Settlements, if made, generally occur in the institution’s name, not those of individual caregivers |
|
|
|
|
||||
|
|
||||
|
|
||||
| Kraman 199952
USA |
Retrospective cohort | Intervention (n = 1): VA medical centre, Lexington, KY Control (n = 38): VA medical centres located east of the Mississippi River between 1990 and 1996 |
Intervention: risk management policy Where patient injury is caused by accidents or negligence the following procedure is followed:
|
Tort claim experience during 7-year period: tort claim data from Department of Veterans Affairs tort claim information system | Liability payments at intervention facility were moderate and comparable with those of similar facilities |
Kachalia 2010
Kachalia et al. 208 compared civil claims and costs at UMHS before and after implementation of a disclosure-with-offer (of compensation) programme (July 1995 to September 2007). Once fully implemented, the disclosure-with-offer programme was fully integrated with other efforts to improve patient safety. Experienced risk managers with clinical backgrounds led the investigations and mediated patient concerns through a process of collation of facts, evaluation of care quality and disclosure of the conclusions. The authors report that UMHS emphasises honesty and transparency with patients and staff, regardless of whether or not events resulted from error. After full implementation of the programme, the average monthly rate of new claims and lawsuits both decreased. Time to resolution decreased and average monthly cost rates also decreased for total liability, patient compensation and non-compensation-related legal costs. The authors acknowledge that the study design cannot establish causality.
Kraman 1999
This was a retrospective cohort study52 of the effects of a new risk management policy intervention which was implemented at one Department of Veterans Affairs facility in Lexington, KY. The policy had two components: disclosure of the incident to the affected patient (or family) and assistance with filing a claim for compensation. The comparator group comprised 38 facilities where there was no organised effort to standardise or track the notification of affected patients. The main outcome was tort claim experience during the 7-year period, measured using data from the Department of Veterans Affairs tort claim information system. It was reported by the authors that liability payments at the intervention facility were moderate and comparable with those of similar facilities (analysis based on 35 facilities in the comparator group). No data were provided; however, a bar chart depicting liability payments ranked the intervention facility eighth out of 36 (first = lowest liability payments, 36th = highest liability payments). The authors draw attention to issues with the comparator facilities and the analysis which should be taken into account in interpreting the findings.
Included studies where the intervention was intended to support or promote disclosure
Eight studies (nine publications) were included in which the interventions aimed to promote disclosure. 205–207,209–214 One included a comparator group212 and seven were uncontrolled before-and-after design. 205,207,209–211,213,214 Study characteristics are provided in Table 2 .
| Author/year/country | Study type | Participants | Interventions | Outcome: outcome measure | Reported findings |
|---|---|---|---|---|---|
| Gunderson 2009205 (plus Gunderson 2008206) USA |
Uncontrolled before-and-after | Students (n = 18) from the six health sciences colleges (medicine, nursing, pharmacy, applied health, public health and dentistry) at the University of Illinois at Chicago | Educational module on full disclosure Conducted as part of a 30-hour 2-week patient safety elective in spring of 2006. The 3-hour module consisted of:
|
|
|
|
|
||||
| Halbach 2005207
USA |
Uncontrolled before-and-after | Third-year medical students (n = 572) attending 4-week family medicine clerkship in years 2000–1, 2001–2 and 2002–3 | 4-hour curriculum to raise awareness about medical errors and patient safety:
|
|
|
|
|
||||
|
|
||||
|
|
||||
| Kiersma 2009209
USA |
Uncontrolled before-and-after | First-year pharmacy students (n = 160) |
|
|
|
|
|
||||
|
|
||||
| Madigosky 2006210
USA |
Uncontrolled before-and-after | Second-year medical students (n = 92) | Patient safety and medical fallibility curriculum (10.5 contact hours). Addressed five main themes: patient safety overview, error reporting systems, vs. human approach, safety tools and ethics/disclosure. Involved mixture of lectures, panel discussion, demonstration and interactive forums. Disclosure techniques involved role play disclosing an error to an attending, supporting a peer who experiences an error and assuming role of an attending to disclose an error to a patient |
|
|
|
|
||||
|
|
||||
| Moskowitz 2007211
USA |
Uncontrolled before-and-after | Third-year medical students (n = 229) | 1-day programme on patient safety. Included two plenary sessions, lunch discussion with dean of medical college and two 1-hour workshops selected from a list of nine topics (one topic was discussing medical errors with patients) |
|
|
| Paxton 2010212
USA |
Controlled before-and-after | Intervention (n = 51): third- and fourth-year medical students and physician assistant students rotating on the general surgery service from January 2007 to June 2008 Control (n = 24): third-year medical students |
Intervention: Medical Errors Educational Intervention 2-hour session comprising small-group discussion with slide presentation. Slides covered six major medical errors subjects including error disclosure. Frequent breaks throughout session allowed students opportunity to describe their own experiences with medical errors Control: no medical error education tool |
|
|
| Posner 2011213
Canada |
Uncontrolled before-and-after | Obstetrics and gynaecology residents (postgraduate years 2 to 5): year 2 (n = 4); year 3 (n = 2); year 4 (n = 2); year 5 (n = 6) Female (n = 8); male (n = 6) |
2-hour workshop on disclosure Facilitated by a physician risk manager. Objectives of the workshop were to review the circumstances when a disclosure discussion is appropriate, who should participate in disclosure discussions, when and where disclosure should take place, what to disclose and how to say it, the role of apology and what should be documented Disclosure in objective structured clinical examination performed by students before and after the intervention |
|
|
| Wayman 2007214
USA |
Uncontrolled before-and-after | Registered nurses on paediatric oncology ward at children’s hospital (n = 16). All female. Fourteen (88%) had fewer than 5 years of experience, two had more than 20 years of experience. Representative of 36% of the nurses working on the ward at the time | Simulation-based medical error disclosure training Three disclosure or adverse event scenarios were developed. Scenarios varied in the level of adverse effects to the patient. Two scenarios involved chemotherapy and the third involved blood transfusion. Instructors from the Centre for Advanced Paediatric Education who were skilled in role playing and debriefing led the training. Trained parents were incorporated as actors in the simulation scenarios |
|
|
|
|
||||
|
|
||||
|
|
Setting
All studies took place in North America, seven in the USA and one in Canada. 213 The majority of studies took place in educational establishments, six in training schools/colleges or universities205,207,209–212 and one in a specialised simulation-based training centre. 214 In one study it was unclear from the published report where the intervention took place. 213
Participants
The majority of participants were students from a variety of health-related disciplines including medicine, nursing, pharmacy and dentistry. 205,207,209–212 Two studies recruited qualified health-care professionals (paediatric oncology nurses, and postgraduate obstetrics and gynaecological residents). 213,214
Interventions
In all eight studies the interventions were delivered as educational or curricular modules and workshops (either solely about disclosure or incorporated into a broader theme of patient safety). They included features such as didactic lecture sessions, pre reading materials, DVD materials, observation, small-group work, and discussions and role play or simulated training to practise open disclosure, often including feedback sessions. Further details of content are described in Table 2 .
Outcomes/outcome measures
A variety of outcomes were evaluated related to knowledge about safety and disclosure, perceived self-efficacy to perform disclosure and confidence in dealing with error and disclosure. These included perceived self-efficacy to understand full disclosure, conduct a full disclosure, admit an error to a supervisor and admit an error to a patient,205 self-awareness about patient communication and safety,207 students’ knowledge of medication safety,209 students’ confidence in medication safety,209 comfort with the skills of disclosure,210 attitudes and beliefs about patient safety,211 knowledge about medical error212 and perceived self-efficacy in communication. 214 Four studies also carried out descriptive evaluations of the curriculum. 207,209,210,214
Outcome measures were nearly always designed for the study itself with no validation reported. These included a true/false questionnaire,209 multiple choice questionnaire212 and a number of rating scales. 207,209,214 Role play in which participants enacted disclosure with patient actors was measured by subjective evaluation,205 a checklist of performed tasks extracted from the guidelines for disclosure of adverse events developed by the Canadian Patient Safety Institute213 and a Likert-type scale self-assessment of comfort with skills of disclosure. 210
Reported findings
All studies evaluating outcomes such as knowledge and confidence reported positive results, comparing pre- with post-test scores. Although one study included a comparator group, results were presented for within-group analyses only and did not compare the outcomes for intervention versus comparator groups. 212
Summary
This review examined evidence for the effectiveness of open disclosure and interventions to support open disclosure. To our knowledge, this is the first time a systematic review of this topic has been undertaken. Findings from this review indicate that there is almost no evidence for the effectiveness of open disclosure, nor of interventions intended to support or enhance open disclosure. This finding is in line with a previous, wide-ranging review of the open disclosure literature. 35
Phase 2: qualitative interviews
We generated an extremely rich data set. From our initial analysis of the sampled interviews we identified six primary themes and produced descriptive summaries of our data relating to these, using subheadings to help organise the material.
The primary themes are briefly described below.
Primary theme: broad understandings of open disclosure
When asked what they understood by the term ‘open disclosure’, stakeholders were all able to give an answer, and most talked about honesty and transparency. Despite some variations in its conceptualisation, from a very broad principle to a discrete set of behaviours, there was agreement across the sample that open disclosure in principle was the right thing to do. Most respondents defined the term open disclosure in terms of being ‘honest’ and ‘transparent’. Typically, open disclosure was reduced to quite a simple set of values to be applied to practice.
Although widely understood, the conceptualisation varied. Some respondents suggested that it is a patient’s right to know what has happened in the course of their care, whatever the outcome. Others articulated a position of openness as a way of providing an opportunity for patients to be involved in their care, recognising that patients may have a unique perspective and know or capture different information to that available to and from health professionals.
Other respondents conceptualised open disclosure in the context of, and with reference to, the Being Open policy framework. These respondents conceptualised open disclosure in terms of specific behaviour and processes. They tended to focus on how and when the process of open disclosure should be initiated and how it should proceed. A number of participants indicated the importance of face-to-face discussion and that a dialogue should follow between patients and/or families and those providing or overseeing care provision. Dialogue was described as critical in enabling patients and their families or carers to engage with health professionals, to ask questions, to be listened to and to promote the understanding of all parties.
The idea that there is ‘no one size fits all’ and that the disclosure process must be flexible and responsive to individuals’ needs was identified.
Respondents identified the importance of health professionals choosing language carefully when communicating with patients and families, specifying the need to avoid using jargon or technical terms which can hinder understanding and be misinterpreted.
Primary theme: motivators
A dominant theme throughout the interviews was the role and conduct of the person or team who was responsible for disclosing information to a patient. Respondents discussed the motivators for health professionals to disclose, placing emphasis on the proposed relationship between open disclosure and the likelihood of litigation. Explicit links were made between openness and health professionals’ self-preservation. Respondents commonly expressed beliefs that being open and honest might minimise complaints and the likelihood of litigation, and that this was a main driver for health professionals and managers. Openness with patients was also described as the essence of behaving professionally and providing a good standard of care.
Primary theme: the Being Open guidance and framework
Although nearly all of those interviewed seemed to have a good understanding of the term ‘open disclosure’, very few were familiar with the Being Open guidance – the exceptions being those patients and families interviewed who had first-hand experience of error and identified a lack of its application, and those involved in developing the guidance or associated policies. Only a minority of health-care managers indicated any degree of familiarity with its 10 guiding principles. Health professionals rarely had any knowledge of these nor of the existence of any national guidance; however, some respondents were aware of a local Being Open policy at their trust, and despite a lack of awareness of the NPSA Framework, most participants talked about open disclosure in terms that reflect the concept as delivered through the 10 principles.
Primary theme: ‘good’ disclosures
Although respondents lacked clarity around the Being Open guidance, it was clear from the numerous accounts of direct and indirect involvement in disclosures that there some common features which marked a better or worse disclosure. From these accounts, it was evident that open disclosure can take many forms and that the several different approaches described by interviewees were perceived to yield positive outcomes. The common features described as important for delivering effective and appropriate disclosures included the degree to which (a) responsibility was accepted on behalf of an individual, team or organisation, (b) language was used that patients understood, (c) an apology was given, (d) the reasons for the event were explained, and (e) the patient perceived the health provider to be genuine, transparent and compassionate.
The opportunity to prepare for a disclosure was described as important by some respondents, including taking time to consider what to say and who should deliver the information, speaking to other members of staff and having opportunities to pre-empt how the information might be received before approaching the patient or carers. Any recommendation of this approach may, however, present a dilemma. The desire to prepare for disclosure, while potentially enhancing the discussion, may also lead to negative feelings and uncertainty for the patient if dialogue with them is delayed as a consequence.
Although some common features of more effective disclosures were evident, scrutiny of accounts of disclosure suggest that the parameters of a ‘good’ disclosure are extremely difficult to delineate. Even in those disclosures perceived as effective, the tendency to attribute blame to team members and to deliver patients a monologue rather than engage them in dialogue was apparent. Moreover, qualities such as the degree to which patients perceive the provider as genuine and compassionate are subjective and complex to evaluate.
Primary theme: uncertainty
Although respondents expressed clarity around some common features of good or poor open disclosure, uncertainty and confusion about how to manage specific situations was apparent. Uncertainty was expressed specifically in relation to identifying an adverse event, handling complex circumstances, defining the circumstances in which disclosure is needed and deciding who should speak with patients and carers. Issues around the timing and nature of an apology were identified as a further source of confusion.
Definitional uncertainties
Considerable uncertainty was expressed by many stakeholders around defining when to be open and what constitutes an incident of the kind that needs to be disclosed. The primary concern appeared to be how to define an incident when little or no harm has been caused.
Circumstances of the event
Respondents recognised the complexity of the system in which disclosure is to be enacted. There was widespread acknowledgement from most respondents that health care is a complex system and unpicking events in any health-care incident is made more arduous by its complexity. The diversity of events that occur within this system creates a lack of clarity around how to proceed with disclosure in any given situation, as each circumstance is unique.
In spite of the complexity that characterises health care, some respondents suggested that the standardisation of process would aid the disclosure practice.
Although each situation is unique, common situations that presented dilemmas were reported, particularly missing information and the delayed discovery of an event. Missing information about what has happened was often mentioned by respondents in the context of decisions around whether or not to disclose and when to begin the disclosure process. Our findings revealed uncertainty and mixed messages around the level of information needed to begin the disclosure process.
Patients and families reinforced the notion that disclosure should begin as soon as it becomes apparent that something has gone wrong, even if not all the facts are clear. They were unequivocal about the need to be included from the outset in the process, the dialogue and the incident investigation.
The late discovery of an event was also a source of uncertainty. A number of respondents discussed the difficulties associated with making a disclosure when the event only became apparent after some time. The challenges associated with a late discovery included patients not being on site, uncertainty about how to make contact and uncertainty about whether or not to tell them at all.
Primary theme: professional and organisational context
Features of the professional and organisational context appeared to be significant drivers of decisions made around whether or not to be open with patients and the circumstances in which to do this.
Patient–professional relationships
The patient–professional dynamic was frequently discussed. Despite espousing openness, stories told by health professionals and managers directly involved in the practice of disclosure (or decision-making about disclosure) suggested that decisions about whether or not to share information with a patient, what information to share and when to do this were made by health-care providers. Dilemmas were generally presented when the patient had come to no harm and would not otherwise find out that something had gone wrong. The perspective presented in such circumstances reinforced the position that information about the patient was perceived as the property of the health-care provider rather than of the patient.
The health-care team’s judgement of the degree of resulting patient harm appeared to be a central driver of practice. Current guidance from the GMC,95 local policy and national Being Open guidance10 suggest that health providers must inform patients of events which caused them harm. Some respondents in management roles referred to these sources of guidance as a reason for not talking to patients about non-harmful events and for health professionals to use their own judgement regarding what information to disclose.
The changing dynamic of power relations between doctor and patient also created a sense of confusion for some professionals about the type of information to provide to patients. With more access to information, particularly from online sources, patients were described as more questioning and active in decisions about their care and as having higher expectations of the care they received. Both health professionals and managers described not always knowing how to respond appropriately, particularly when issuing information about things that have gone wrong.
Overview of main findings
There was inevitable overlap in terms of the issues that featured under the primary theme headings. Further consideration supported the development of a more theorised analysis that may help to explain why implementation of the Being Open framework, and indeed the principles of open disclosure more generally, are not consistently evident in practice. The analysis highlights the complexities of interpreting and acting on widely endorsed moral principles that underpin calls for open disclosure, and the inevitable limitations of attempts to promote good practice by prescribing quite standardised communication procedures.
Support for the values that underpin calls for open disclosure
Our interviews revealed broad-based and strong support for the idea of open disclosure. Strong associations were made with moral concepts of honesty, openness and transparency.
Being honest and open . . . the basics of being a good human being. You should be honest and open whether you’re a builder, or an engineer or a pilot, it doesn’t really matter, that’s just being a good person.
Manager 1
The principles behind it are laudable, understandable; I don’t think there’s anything that you can argue against on sort of moral grounds, on ethical grounds, transferring that into practice is much more difficult than you would expect.
Health professional 6
These broad value statements were associated, by some, with the rights of individuals to know about all aspects of their care and the obligations of health professionals to tell them about all matters that affect them or influence their care. Both health professionals and patients suggested that it is a patient’s right to know what has happened in the course of their care, whatever the outcome; that they have ownership of any information in relation to their health and their body.
Deference to professionals is definitely moving away. There’s a sense in which people have a sense of having rights . . . and patients regard themselves as having rights to this information as I think we would probably say that they do, both legal rights to information that’s relevant and also moral rights to information.
Professional organisation 2
If we don’t adopt sort of an open approach to mistakes and errors we are never going to treat them as human beings because they have a right to know, it’s their bodies, not ours, we only look after it but it belongs to them. And it should be treated with respect and so should their wishes and feelings.
Health professional 2
Anything that happens in the course of health care, including errors and omissions in health care, it should be the absolute, unequivocal right of the patient, or in the case of them being dead or lacking capacity, then their next of kin know about.
Patient organisation 1
The links between learning from safety incidents and improving care for the future were also apparent, and were linked to patient involvement in promoting safer care. Some stakeholders in senior positions (often slightly removed from the clinical front line) identified coming from a general stance of openness as an identified way of engaging with related concepts of patient ownership of health-care decisions and entitlement to a fully informed perspective. This included the view that patients may have a unique perspective and know or capture different information.
If the patient is still on the ward and you know the patients and the relatives become involved in it . . . and they can often help us as well.
Health professional 3
The patient or the family say . . . had you asked me, I could have told you that when I came into A&E [accident and emergency], I did report the symptoms . . . sometimes it’s one person’s word against another, you know. It may be recorded in the notes, patient attended A&E; didn’t report this symptom, that symptom; full record taken. But the patient will say, oh no! I did say exactly I was having a bad headache or, you know, I was reporting these symptoms. So even from a practical reason, it’s bad practice not to involve people from an early stage.
Patient organisation 2
The other thing we need to do is be much better at involving patients in their own safety so giving them permission to challenge us when they think something’s going to go wrong . . . patients might just get a better sense of where the risk areas are but most of the evidence suggests that it improves their safety.
Professional organisation 3
Multiple meanings of open disclosure
Individuals held various ideas about what open disclosure entails in practice. When people talked about open disclosure in terms of communicative actions or processes, there was no consistent, clear, comprehensive definition in evidence. References to a number of features of communication were present in many of the accounts of examples of open disclosure, and were lamentable in their absence from accounts of examples where disclosure was deemed not to have occurred.
The common features described as important for delivering effective and appropriate disclosures included the degree to which (a) responsibility was accepted on behalf of an individual, team or organisation, (b) language was used that patients understood, (c) an apology was given, (d) the reasons for the event were explained, and (e) the patient perceived the health provider to be genuine, transparent and compassionate. The quote below provides a typical description of a ‘good’ disclosure that is representative of many of the examples given; the features commonly emphasised by respondents across the sample are shown in bold text.
If we take where I had to go and do it because I had made a mistake or played a part in the mistake, it was a young lad with his mum and I just said, you know . . . it was about analgesia and because it clearly hadn’t worked so I had then subsequently given him the right intravenous formulation and I said ‘I’m really sorry, as you know I came to review you because your pain relief didn’t seem to be working and I know now why it wasn’t working and I’m sorry to have to tell you that we gave a drug that’s normally taken orally, I gave it into your vein’. That didn’t really mean anything to them so I tried to explain why that was important and why that shouldn’t happen, told them what I’d done about it and really in that particular instance it was about the main reason there’s a problem in this particular drug is that it wasn’t made . . . usually the problem is around sterility, is it made in a sterile environment, if it’s going intravenously. So I had to wait for someone from pharmacy to ring and talk to the manufacturer and in fact this was made in a sterile fashion. So I explained it to him I said ‘You don’t seem to have come to any harm from what has happened but clearly it is something that wouldn’t normally . . . this should not normally happen’ and I told them why it had happened, the nurses giving the drugs for some reason despite it saying ‘IV [intravenous] morphine’ had thought I must have meant Oramorph and given it to him. My part was that I didn’t ask to see the little vial of morphine which you would normally get with an intravenous morphine so I had played a part and I think I just told them what had happened and told them what would happen as a result so that it would be reported formally and we would have a look at it to see if there were any things we could put in place to stop it from happening again and I just apologised and they were fine and I never heard anything else about it.
Manager 10
Instances in which poor disclosures were described reinforced the importance of accepting responsibility, explaining things clearly, and instigating and maintaining contact with the patient and family as early as possible.
He came in for surgery . . . and it didn’t go quite right. It was part of the risks, one of the things that went wrong is part of the risks that they do, they sign the consent and are given the information and I think that was the start of it because I don’t know how much this gentleman actually realised could go wrong with what he sees as quite routine surgery . . . So it started off quite badly in that sense because his family have said well we didn’t realise that was one of the side effects, that was one of the risks. So he was then passed from the orthopaedic department to the vascular department and again the vascular people were saying well actually it is the orthopaedic department, they have made a bit of a blunder and then of course the orthopaedic department are then saying no you can’t say that because it was a risk . . . actually the patient has got quite a bad history, a lot of comorbidities and so it was a disaster waiting to happen. And it’s been going on . . . he’s had recent meetings where nobody has actually been clear. Now in the patient[’s] and the patient’s relative[’s minds] it’s that, we are not being clear to him because we’ve got something to hide. And actually when you come down to it we haven’t got anything to hide at all. But that is how they perceive it, that we are hiding and we are actually not . . . you know you can bring people in but they have this preconceived idea that hospitals don’t make mistakes or if they do we hide it.
Health professional 3
A number of respondents (mainly policy-makers and managers) were keen to ‘pin down’ exactly what should be done to ensure open disclosure and saw the prescription of a standardised process as the key to this.
What I am clear on is that when you are in distress, process is really important. And if it’s one thing that happens in one trust and it’s different to another trust or whatever, I think the public are bemused and upset . . . so I do think we should certainly have some sort of standardisation of process . . . if you walk through the door of Primark, it says Primark, you know what you’re going to get. If you walk through the door of Hugo Boss, you know what you’re going to get, you know, it varies in cost and quality. If you go through the door that says NHS, you don’t think it’s going to vary in terms of cost and quality from another door that says NHS . . . So we should have standardised processes around handling something like this.
Policy stakeholder 5
However, others, specifically clinicians, emphasised the complexities of practice and insisted there could be no ‘one size fits all’ approach for disclosure, with each encounter requiring careful situational interpretation and value judgements which would always be needed to communicate appropriately about safety problems.
I think we should work towards that being a kind of professional value and responsibility rather than something that is enshrined in some sort of legislative framework because I think it is too difficult to put in there. And I think every circumstance needs individual interpretation on what the best thing to do . . . my concern is that kind of legal, making it a legal duty would lead to inappropriate responses sometimes for patients.
Health professional 10
We suggest that the distinction between agreement about the importance of several moral concepts that supported the case for open disclosure and diversity of opinion about how these concepts should be interpreted and reflected in practice is one important key to understanding why the NPSA’s Being Open guidance, or even the concept of openness more generally, is not consistently implemented. When individuals want to act well they appear to be attempting to integrate a number of values into their decision-making and action. Judgements about the particular situation are context dependent and interpretive, and consider how a particular action may be related to other matters, morally or otherwise. As people do not always agree about what is required to reflect moral values, these can be variously interpreted and multiply realised in practice, although some actions are quite closely tied to particular moral concepts.
We draw on this distinction again below when we consider uncertainties and tensions in judgement; however, before doing so we consider the policy itself and its use.
The Being Open Framework and its use
Very few of the stakeholders we interviewed were familiar with the Being Open document. A number suggested this was because they did not have time to read all the policy documents that were issued and relevant to them. Some of the principles of Being Open were reflected in local trust policies on open disclosure, and we stress again that both types of guidance reflect the underlying moral concepts that were widely endorsed by stakeholders.
Being completely open about what’s happened, why it’s happened and informing those involved and affected.
Manager 2
It is common sense . . . it is basically just about not lying to people, being honest, being open, being explicit and sorting out problems when they occur.
Health professional 1
One reason offered for the limited use of Being Open was the fact that it was not designed for timely, practical application at the time of the safety incident.
In common with other policies we have in this organisation . . . it’s just not easy to draw out the information you actually want on the spot. So when an incident happens, you don’t have time to go and spend an hour wading through the policy and picking out the key points and making a plan, what you need is just do this, do that, do that first.
Manager 8
If you start getting into fifty pages for a policy, nobody’s going to read that, they won’t have time to read that and I think it’s about taking what’s in the national stuff but also then translating that to what’s workable locally . . . thinking about anything that can make it more manageable for the staff on the ward, sometimes it might be a checklist, sometimes it might be a flowchart, as I say, something that people can see at a glance and think, ‘that’s what I need to do’ or ‘this is the person that I need to ask’.
Manager 9
Some of the stakeholders who were familiar with the Being Open document raised concerns about the scope of application and particularly the way it made different recommendations for incidents of different severity. Incident severity was consistently identified as a key determinant in deciding whether or not to follow the guidance. Notably, most health professionals and managers reported enacting the principles espoused through the Being Open guidance in circumstances of moderate or severe patient harm. Respondents repeatedly indicated that the Being Open process was not followed for near misses or minor incidents. Furthermore, it was often argued that disclosing events that were minor or did not result in harm may not be in the patient’s or the organisation’s interests.
The Being Open policy does say that there is no obligation to report, to let people know about near misses . . . or I think the low harm ones, again, it’s whether it does more harm than good.
Manager 8
As things stand at the moment, we would expect to disclose to a patient any harm, moderate or severe harm, that has been caused by the treatment that they have received from us . . . I would imagine that (the Being Open process) happens more where there’s a serious incident . . . If there was very limited or no harm we would expect clinicians to use their discretion as to whether it is in the patient’s best interest at that moment, and I think that is based on the national policy.
Manager 6
I do not think that if things are minor or near misses you necessarily want to think about that in terms of patient involvement, but for serious incidents the family is told by the investigating team at CSU [commissioning support unit] level that an investigation is being undertaken and that the results of that investigation will be shared with them.
Manager 4
Uncertainties and tensions in judgements about whether and how to discuss safety issues
Between them, the stakeholders we interviewed identified a range of issues that they deemed salient to considerations of whether or not and how safety issues should be discussed with patients and family members. These included, but were not restricted to, ideas about why health professionals or managers did not behave well. There was widespread recognition of uncertainty and complexity, especially in relation to the multiple values at stake in the complex situations referred to earlier in which decisions about the ‘right thing to do’ are being made. The diversity of events that occur within health care creates a lack of clarity around how to proceed with disclosure in any given situation as each circumstance is unique.
Health care is just not that cut and dried, so when something goes wrong it’s usually a bit of a jigsaw.
Policy stakeholder 2
Respondents also recognised the complexity of the system in which disclosure is to be enacted. There was widespread acknowledgment from most respondents that health care is an intricate system and unpicking adverse events that occur within it is made more arduous by its complexity.
The main issues appear to be interlinked but we have separated them here to allow for examination of each in turn.
The first main consideration seems to involve whether or not the event or issue should be disclosed or discussed. Considerations include the type of incidents which need to be discussed and why, the implications for the patient and his or her family, which health professionals and health services are involved and whether or not there are opportunities to learn from the incident.
Simply identifying what it was necessary to disclose presented a source of confusion for a number of those interviewed across all stakeholder groups, with the exception of patients and families. Although the guidance appears to offer clarity on this in principle and suggests ‘providing a full and frank explanation of the circumstances without regard to any other factor which might have influence in the situation’,10 many of those interviewed identified exceptions to this and circumstances in which it was not always considered necessary to disclose.
I am not saying that we would absolutely always at all costs think well we’ve found this we’d better let the family know, I think you’ve always got to weigh up what the risks and benefits are of talking to the family as well.
Manager 11
Somebody reports an incident because there was a delay in taking somebody to theatre because the theatres were full and then that person deteriorated and died, and you know they might be aged ninety-five and came in seriously ill in the first place with an acute abdomen, and yes it’s a report of an incident because there’s no barrier, people can report anything they like and they report it as an incident involving inappropriate delay . . . what do you go to the relatives and say, do you say well I’m terribly sorry she died, she was very seriously ill and elderly but there was a three-hour delay before theatre which isn’t desirable. Well I suppose that is what you would say being open but then where does that leave the relatives thinking for the rest of their life that their mother or father would have you know lived another two years if it hadn’t been for a three-hour delay in the hospital?
Policy stakeholder 4
I think truth will out and so I support the concept of openness and as an institution we will support it very, very strongly. But you will always get examples where you know it may not be in the interests of the patient to reveal all.
Professional organisation 4
Uncertainties around what types of incidents should be disclosed were often related to particular areas; for example, where there was a near miss or the patient appeared to have suffered no harm.
As things stand at the moment, we would expect to disclose to a patient any harm, moderate or severe harm, that has been caused by the treatment that they have received from us . . . I would imagine that [the Being Open process] happens more where there’s a serious incident . . . If there was very limited or no harm we would expect clinicians to use their discretion as to whether it is in the patient’s best interest at that moment, and I think that is based on the national policy.
Manager 6
I didn’t disclose it actually but we had a patient who . . . was receiving chemotherapy for leukaemia and she was on the ward and . . . the chemotherapy came up for her and one of the nurses had to make it up as pharmacy had sent it up to be reconstituted on the ward, and the nurse did that . . . and she came to me a little bit later and said ‘I’ve just thought about it and actually I’ve given the wrong dose’. And we sat down and worked it out and she’d given too much but not enough that it would make any difference. It wouldn’t put the patient at risk but it was a bit more than she should have had and she was a very anxious girl . . . she’d had a rough time . . . I know she’d been through a lot and . . . she was quite emotionally fragile and we discussed what we should do about it and whether we should tell her or not. And we . . . decided between us really that . . . it would probably be detrimental to tell her that it had happened because she was so emotionally fragile we felt she might lose a bit of confidence, she’d be upset, she’d be worried . . . and we thought it would probably just do more harm than good by telling her about it really.
Health professional 9
Sometimes . . . the risk is that . . . you might undermine the confidence in the system that’s one thing, perhaps you undermine . . . the patient’s confidence in you as a practitioner . . . you make the patient feel anxious and insecure without any real benefit . . . if you undermine that trust what’s the benefit.
Health professional 10
They [health-care team] had a patient who fell off the operating table. Now potentially that is very serious, you can do huge damage if you are unconscious and you fall like a sack of potatoes from a height like that onto a stone floor in an operating theatre. But there wasn’t any damage and it was then questioned whether the patient needed to be told that they had fallen off the operating table because there was . . . no actual consequential damage to the patient . . . and that is a grey area which I think is quite difficult to work out.
Professional organisation 5
Situations where events might be seen as routine or unavoidable imperfections in care were also highlighted.
You know one surgeon said to me when this was first being discussed, he said: ‘well if I was taking out somebody’s gall bladder and I made a tiny nick on the liver which bled for two seconds and then I cauterised it and it stopped would I have to go to the patient afterwards and tell them this is what had happened?’ He said, ‘because that would happen kind of twenty times in an average operation.’ I said well of course not you know that’s just normal dissection in surgery that’s not an error or an avoidable incident. He said: ‘well what if the scrub nurse reported me to the GMC and then I was accused not just of doing it but not disclosing it, what would happen then?’.
Policy stakeholder 4
The arguments that there are more or less severe harms, and that disclosure may cause a particular patient more harm were individual and complex. If the situations were considered as a spectrum, it would be possible to ask questions of a similar situation, replacing variables to try to identify at what point a situation becomes an event that requires disclosure. However, if the relationship between patient and health-care professional or organisation is viewed as one of transparency and is focused on facilitating involvement in care generally, then the ‘step up’ to disclosure of minor events may not be required. The discussions may take place within ongoing conversations rather than being viewed as ‘incidents’ per se.
There will be gains and losses for both patients and health professionals in decisions about whether or not to disclose. For example, we might ask what the patient could gain or lose from the discussion of the error described above by health professional 9 in relation to the chemotherapy dosing error. It is possible to argue that the right to know what has happened to you as a result of your care is a matter of treating patients with dignity, of an individual or organisation respecting the fact that it is the right of an individual to know about events, whether they harm or not. Although this may vary across situations and patients, needing to know that things have occurred in order to be able to move forward responsibly is highlighted by some and there is an increasing expectation that patients and families will be informed.
I see it as being entirely open and honest about things that have happened in health care. Which have caused harm or may have caused harm. It’s as simple as that, that people’s treatment and health care belongs to them. It doesn’t belong to the institution or the health professional who has been treating them, and with that goes the information around what happens. Anything that happens in the course of health care, including errors and omissions in health care, it should be the absolute, unequivocal right of the patient, or in the case of them being dead or lacking capacity, then their next of kin know about.
Professional organisation 1
Deference to professionals is definitely moving away. There’s a sense in which people have a sense of having rights . . . and patients regard themselves as having rights to this information as I think we would probably say that they do, both legal rights to information that’s relevant and also moral rights to information.
Professional organisation 2
Some patients are real experts on their conditions, more than we could ever be. That dynamic has changed and therefore being open is way more relevant than it used to be.
Policy stakeholder 2
Health professionals may perceive a number of negative consequences from the disclosure of safety events. Professionals often identified impacts in terms of their professional identity, even in cases where they were not at fault or where no consequences arose for their employment, or no litigation or investigation ensued. However, professional self-integrity is also maintained by doing what a professional perceives to be the right thing.
There are a number of issues specific to the health-care organisation which principally concern reputation and litigation. There appears to be uncertainty in relation to the impact of disclosure on organisational issues. There are general ideas that being open and honest with patients will lead to less litigation but also a recognition that this cannot be guaranteed. Respondents explicitly discussed the value of openness for minimising the likelihood of becoming involved in complaints or legal proceedings.
The fact that he had discussed it [the error], had been open about it, hadn’t tried to conceal it, meant that the patient wasn’t moved to make a complaint.
Professional organisation 3
I think if we are not being open there are all kinds of consequences and one may be a complaint. But you know could be legal action, whatever. Which is one of the many reasons why being open makes sense.
Manager 6
We are taught that if you’re open and honest and frank with your patient and apologise if appropriate then the subsequent difficulties in terms of litigation and what have you for the doctor will be reduced.
Professional organisation 6
I’ve learned that it’s [being open] also quite a self-preserving thing to do . . . the worst thing . . . is if they [patients] get it into their heads that there’s some sort of cover up going on, then they get the bit between their teeth and solicitors get involved and it’s all very difficult.
Health professional 4
If you are very honest and straightforward and treat the patients right then often they feel that, they take a generous view towards the mistake as opposed to getting very litigious about it, which I think they are more inclined to do if there’s a big cover up and people aren’t honest.
Health professional 1
I think the culture is, you say sorry, you explain what’s happened and you do it promptly and openly and honestly . . . I think the understanding now is that it’s much less likely to go to litigation if you are open and honest and say, ‘I’m sorry’.
Manager 2
Health professionals described situations in which they perceived that an open and honest disclosure had enhanced patient satisfaction with the outcome, the ongoing patient–practitioner relationship and the way that the event was handled. Critically, even in such instances, health professionals described their initial fear that open disclosure might actually invite complaints or litigation.
Part of me was telling me you shouldn’t do this, why ask for trouble, this is going to just lead to litigation or complaints . . . just let it be and hopefully things will quieten down. But you know every time I’ve done this has been a positive and rewarding experience, I’ve not regretted it.
Health professional 5
Through the course of my career, so many times I’ve seen very bad things have happened and patients have in the end not taken any kind of legal action and not taken grievance with the doctors when they’ve immediately said: ‘Look, I’m very sorry, this went wrong and this is why it went wrong and this is what we’re going to do to try and fix it’.
Health professional 4
Despite concerns regarding the likelihood of openness inviting complaints or legal action, many health professionals recognised the patient’s and carer’s right to take legal action and distinguished this from their decision to be open and honest.
I think there are going to be times where I might meet with a family . . . who have got a threshold for complaining . . . who would you know take this opportunity with both arms and take it forward to a full litigation process and what have you but that is their right at the end of the day and it shouldn’t in principle put me off being honest and upfront with my patients.
Health professional 5
If I’d made a mistake I’ve got to go and see that person and say look I am sorry it was my fault, I am not saying it was right, you know it was me that did it and I did it and it was an error and I apologise. And if they then want to take that further well that is their prerogative.
Health professional 2
If errors have been made, and those errors are to lead to long-term health problems, then it seems to me entirely appropriate, or where it’s appropriate, for patients to make claims for compensation, in order that they can, quite directly, be compensated for errors that have been made.
Professional organisation 2
However, links between communication processes in relation to disclosure of error were not uniformly linked to outcomes at the organisational or the patient level. Patients will vary in their propensity to take legal action and what satisfies in one context cannot be guaranteed in another.
A number of respondents indicated a clash between the principles underpinning open disclosure and maintaining their professional identity, reputation and relationships with colleagues. Openness about incidents was perceived by some to have broader implications for breaching professional loyalties and to some degree siding with the patient. This concern may add an additional complexity and sense of confusion about the appropriate course of action to take following an adverse incident.
There is a sense in the medical profession I think, that they look after their own. They look after their own. They look after their own interests. I still think there’s a kind of us and them between doctors and patients . . . at the moment I still think there is a kind of defensive mechanism, defensive instincts that you should cover up, look inside, protect the interests of the profession and the hospital and I still think it can be very difficult for patients to make inroads against that. My sense at the moment is that there’s a lot of, there are big changes taking place, but they haven’t bedded down in certain kinds of areas, and I don’t think there’s an instinctive culture of openness and candour.
Professional organisation 2
Therefore, in each context individuals will consider the attitudes of their colleagues, the stance that they perceive their employer will take or has taken and the likelihood of litigation, although this is not an exhaustive list of variables.
The opportunity to learn from error or improve care is also a factor in decisions about disclosure of patient safety events. Transparency around errors was identified as particularly important at the early stages of the process in facilitating learning.
I think as well, it’s [openness] important because medicine has not always been great at learning from its mistakes. And partly that’s been because there has been a culture of concealing them.
Professional organisation 2
[Not] being open with patients or families is, on the one hand, fairly terrible dereliction of duty to another human being, and a dereliction of ethical and moral duties. But it’s also perpetuating a culture where people go into denial – where people refuse to accept that there’s been error, or when there has been error, fail to investigate the root causes and any lessons that there might be to help prevent reoccurrence.
Patient organisation 1
There was notably less reference to disclosure as a proactive way of engaging with patients to enhance the quality and safety of their care, and that of service delivery more broadly, than to benefits associated with reduction of complaints or litigation.
The first issues may be moderated by how disclosure is or is not conducted. There were uncertainties and value tensions in relation to a number of areas. For example, deciding who should disclose error involved judgements balancing closeness to the patient, seniority, competence, well-being of the patient and available support for health-care professionals involved.
Many felt strongly that information should be delivered by the senior clinician closest to the patient if the incident was serious, and that junior staff should not lead formal disclosures. Others highlighted individual responsibility.
The obligation is on the person who made the mistake . . . I think there’s a problem, documented to the point of absurdity, that dehumanising in medicine and dehumanising particularly in the hospitals, and if a doctor or another health professional makes a mistake, and three months later, someone, an administrator comes round to your house and knocks on the door and says, ‘oh by the way, a mistake was . . .’ it seems to me you further entrench those kinds of . . . if I make a mistake, and I harm somebody, then I’ve got a responsibility to discuss the mistake I’ve made with them.
Professional organisation 2
However, other respondents highlighted that junior staff may often be present or directly involved in an event and therefore make a critical contribution to its disclosure. Moreover, some respondents suggested that decisions around who should be involved in a disclosure should be undertaken on a case-by-case basis to ensure that the most appropriate person or team is involved.
If something’s been designated as a serious incident and there’s been an incident investigation and there’s a formal ‘being open’ meeting set up with the relatives, that’s where I think you can’t leave junior staff unsupported to do it on their own. But, on an everyday basis, they’re the actual first people who would probably see that something’s gone wrong and so, of course, if they do, you can’t, well, we shouldn’t have a system which says they shouldn’t apologise.
Policy stakeholder 3
There isn’t clear guidance but we almost don’t mind that so much because sometimes if you say it has to be the lead consultant that person may not be the best person, they may not have the best communication skills or they may be too emotionally involved to do it so sometimes it’s better to have lots of flexibility in that and sometimes the family has been really close to a certain nurse who’s actually quite gentle and they might, their communication skills might be amazing, they might be the perfect person.
Policy stakeholder 2
The different standpoints presented regarding responsibility for disclosure are likely to give rise to confusion among health-care team members when presented with an adverse event.
Apology appeared to be critical to a good disclosure. Patients expressed an understanding and acceptance that mistakes will be made but were unanimous in their expectation of an authentic and timely apology. In situations where individuals had fought for insights into health-care incidents, the lack of any genuine and sensitive apology was often highlighted as particularly distressing.
‘All these meetings,’ he said [Chief Executive], ‘and you’ve never had an apology’, but he said, ‘if that’s what you want I’ll go over and write you a letter of apology now’. I thought just go you condescending, patronising man.
Patient 2
Never had a proper apology, a genuine apology . . . given a sort of a one-paragraph apology from the legal authorities . . . signed by the chief executive but it was clearly dictated by a solicitor, and it was the minimal possible grouping of words that would technically satisfy the NHS’s requirement that apologies are given for accidents, but it was meaningless.
Patient 3
And the apology came after two and a half years . . . one two-sentenced paragraph and one one-sentence paragraph, and it started off with the chief executive two and a half years down the line said: ‘it has come to my attention that’, as if oh suddenly somebody’s just dropped this on my desk, I didn’t know anything about it and, ‘the standard of care was not everything it should have been’, and that’s life-changing disabilities, and ‘there have been some unfortunate side effects’. I mean that’s how he actually phrased it!
Patient 3
Many other stakeholders suggested that an apology is a necessary and unquestionable aspect of disclosure.
We really need to question how we’ve got to a situation where we’re even questioning whether we should apologise or not. Why are health-care staff having conversations about whether it’s appropriate to offer an apology ’cause it should be a no brainer.
Policy stakeholder 3
The expectation on anyone and everyone in the NHS should be, you apologise and you apologise early on, irrespective of what your role is.
Policy stakeholder 2
If you’ve got someone who is man enough to say, ‘look this is what’s happened and we are very sorry, it shouldn’t have done, we are taking steps to sort it out and so it doesn’t happen to anyone else, we are willing to accept blame’, you will then get people who will say, ‘well all right, they made a mistake and it is not good, it shouldn’t happen but it did. And we can move on, and we feel that our concerns have been addressed properly’ . . . a simple ‘I am sorry’ works wonders . . . just tell them the truth, they are not idiots.
Health professional 2
Despite this recognition, uncertainty over whether or not to apologise, when to apologise, who should offer an apology and what this might include persists. A number of respondents discussed the variation in apology depending on level of harm.
So the way that the ‘being open’ policy is structured is . . . you have a formal ‘being open’ discussion with patients and carers when they suffer from moderate harm, severe harm or when a patient’s died . . . if there’s minor harm, then you just leave it up to the health-care team and if there’s no harm, then they can just make a decision about whether an apology is appropriate on a case-by-case basis. So, in some ways, one of the weaknesses with the policy as it’s written, is that we’ve linked the level of apology to the level of patient harm.
Policy stakeholder 3
We also identified the reluctance of staff to reveal that something has gone wrong in the process of care as inhibiting apology.
I don’t think often that members of staff do apologise, I think things are still covered up to a degree.
Health professional 2
Organisational incident reporting systems were described as a barrier to giving a timely apology, as the reporting process and subsequent investigation (where relevant) was perceived to inhibit open discussion of events with patients and carers. Having to wait until information was gathered and documentation completed before issuing an apology was seen by some respondents as creating unnecessary delay. Incorporating apology into the uncertainty of the situation following an error is supported by some, and the need to apologise on different levels at different times in a process was stressed.
The internal bureaucracy that we’ve created around incidents and incident reporting, and claims and complaints, and time frames to respond to these things, acts as a barrier . . . it just creates a level of bureaucracy that can sometimes get in the way of a prompt apology.
Policy stakeholder 2
What I think needs to be clear is what you’re saying sorry for is the outcome and I don’t think that’s clear, so you’re saying, I’m sorry this has happened, this is awful, I’m really sorry this person’s died, we don’t know what happened but we’re going to find out.
Manager 3
Linked to the earlier issue of more general transparency in health-care consultations, guidance on apologies was seen to miss the point if saved only for moderate and serious harm.
I think what is wrong with the ‘being open’ policy . . . the expectations should be on health-care staff to apologise even for minor things and the policy as it currently is written is that there’s no requirement to offer an apology or it’s left down to fight the local jurisdiction as a team . . . if there was no harm. But, if you can actually instil a culture where, even if someone’s delayed in outpatients, someone offers them an apology and that’s not an incident, that’s just an efficiency issue. And, if people get into that habit of good customer service, then maybe it’ll be more ingrained in NHS staff to apologise irrespective of the severity of outcome. And it’ll make apology exercising more pervasive per say.
Policy stakeholder 3
Organisational, professional and policy support (what can be done to promote open disclosure?)
Policy is able to provide guidance to support the disclosure of adverse events to patients. However, rigid recipes for what to say and do will inevitably be limited and can lead to problems if they are not used in combination with discretion and judgement. Employing guidance for the disclosure of adverse events requires a number of sophisticated moral and value judgements which are contextual, usually unique and may or may not lead to a desired behaviour. Individuals are required to recognise a problem and also the individual components that make a particular issue a problem in that situation. As well as making their own judgements, they may be required to support junior colleagues to make judgements, individuals who may not have the experience or confidence to do so. Guidance conflates moral concepts with behaviours, and thus inevitably runs the risk of not being consistent in its outcomes. Therefore, the problem is not that individuals behave badly, but that the guidance fails to address the conflicting but multiple defensible values at play.
Organisational culture and managerial leadership can act as a facilitator of or a barrier to open disclosure and good disclosure practice. A reluctance to be open and honest about mistakes made in care can be due to fears of the repercussions for the health professional(s) involved. This may even extend to deliberately concealing mistakes in an attempt to protect their job or reputation.
[We] had to dismiss a number of staff who have made medicine errors . . . not . . . as a result of the medicine error, it’s been as a result of them trying to cover up and hide the fact and the potential harm that could have come to the patient because they’ve either hidden it or falsified documentation to try and hide it.
Manager 5
Sometimes there’s a culture of well if I admit I am wrong . . . my employer would sack me because I’ve been open and honest and if I don’t say anything they can’t sack me . . . if you are there in a situation where you know that something is not right and you daren’t say anything because you are frightened of what might happen to you, you won’t say it, it’s your job. And I think that goes with colleagues as well, you may have a colleague who is not performing well but you don’t always say something because you don’t want to upset them.
Health professional 2
There may be numerous reasons for a health professional’s decision to conceal either their error or that of a colleague, but the most feared repercussions were of damaging professional standing or of disciplinary action. Current organisational support systems to support health professionals dealing with the experience of making an error may be inadequate.
There’s a sort of culture of disclosing mistakes in most trusts but where I think things probably fall down if you look at the most extreme cases is in terms of support for doctors and other health-care professionals.
Professional organisation 4
I don’t think we do talk very openly about these things at the moment and the levels of support are poor . . . I think at the moment the feeling is just go to an occupational health service but doctors don’t do that, just don’t do it . . . I think you need better support services for doctors because a lot hangs in our decisions, both in terms of consequences for patients and use of resources . . . I think there’s certainly benefits for the health service in providing better support and certainly a duty of candour without appropriate support would be, I don’t think would be useful or productive.
Professional organisation 6
The big gap is how we support staff. I think we’re really not good at that and I think we think they’re more robust than they are over these things because they don’t show it outwardly, they go away and feel it deeply. I think we don’t know the toll it takes on staff until it is too late.
Policy stakeholder 2
Health professionals commonly described the feeling that they experienced when realising they had made an error and the concerns this raised for them as an individual. Failure to manage these concerns may present a greater likelihood of either non-disclosure or a poor disclosure of the incident to the patient and/or carer. An individual who is struggling to manage his or her own anxiety is unlikely to provide the support required by patients and families in the event of a health-care incident.
Where I think doctors get very worried . . . is about the prospect that is then going to lead to litigation, a referral to the GMC . . . if you then say to a patient I am sorry, I blew it, I should have seen that sign, I should have picked this up earlier. If by apologising and saying . . . that’s a lesson I must learn and if you think then those words are going to be quoted in a GMC hearing . . . then you are much less likely to say I am sorry I blew it, you are much more likely to say I am really sorry about what happened to your husband, it is really tragic what happened but actually I did everything I could and you . . . take a defensive pose.
Professional organisation 7
I think there’s still a fear of the action that might be taken against you, but I think people are much more aware of, and responsible really about the failure to disclose a mistake that they’ve made . . . there’s still a concern I guess for everyone that there will be a whole weight off something coming on them.
Health professional 11
Furthermore, respondents identified links between reluctance to discuss mistakes and the inhibition of an open culture leading to reduced likelihood of learning from events.
I think as well, it’s [openness] important because medicine has not always been great at learning from its mistakes. And partly that’s been because there has been a culture of concealing them.
Professional organisation 2
[Not] being open with patients or families is, on the one hand, fairly terrible dereliction of duty to another human being, and a dereliction of ethical and moral duties. But it’s also perpetuating a culture where people go into denial – where people refuse to accept that there’s been error, or when there has been error, fail to investigate the root causes and any lessons that there might be to help prevent reoccurrence.
Patient organisation 1
I imagine if you’re a unit that works on total honesty, total disclosure you’ll probably find the quality of care in that unit is far better because it is just symptomatic of openness which can only be good.
Professional organisation 4
Staff often seem to be very doubtful about whether they should actually tell people about what has happened. So I would say the more scared staff are about what the consequences might be for them, the more chances are that they’re unlikely to tell the person something has happened.
Patient organisation 2
The need to develop a culture of improvement and transparency with relation to error and unintended harm was clearly articulated by the majority of respondents. The importance of incentivising the desired behaviours is crucial to success. When staff or patients are concerned or suspect error the organisation needs to be receptive and welcome reports. This would be echoed in current patient safety thinking which emphasises feedback and learning, but existing systems, particularly those used to capture patient feedback, need to be improved.
There first of all on the whole needs to be a no-blame culture which is often misunderstood, it doesn’t mean nobody’s ever held to account because there are negligent acts but when there’s a genuine error, that well you know was in good faith as it were, then I think first of all not to take appropriate disciplinary action and then to provide the sort of counselling and support.
Policy stakeholder 4
And it’s about placing responsibility on organisations to ensure that staff aren’t unfairly dealt with if they have unintentionally been involved in mistakes which have led to harm. Or unfairly dealt with if they’ve been open about incidents with patients and families where the organisation is worried about the consequence for itself. A lot of this is about raising awareness, about facilitating a change in culture, about showing understanding and support for people.
Professional organisation 5
It was also noted by some that patients should be given access to information regarding the incident report, and be included in its dissemination and learning.
I think we could be much more transparent not just about reporting the incident but also reporting what subsequently happened and how people have been allowed to learn really.
Policy stakeholder 5
Creating an open environment which facilitates staff to feel confident about being honest with patients and colleagues after making a mistake, and able to handle uncertainties associated with adverse events, was recognised as a key prerequisite to facilitating open disclosure.
There was little evidence of any training for staff in disclosing events, with many admitting that they did not know such training was even available.
I’ve never, me personally, I’ve never received training along those lines.
Health professional 6
I haven’t had any personal training. Certainly, the trust offers a sort of day if you like around breaking bad news, however, I think that tends to be more related to breaking, you know, cancers and diagnoses type thing, rather than adverse events that happened.
Health professional 12
No there isn’t any training, the only training is life experience, nursing experience and, as you go along.
Health professional 3
However, training was highlighted, described as being necessary to improve both the culture and the practice of open disclosure. There was demand for training to be administered locally and internally by trusts, and to be inclusive, involving clinical and managerial staff at all levels.
They’ve got to have training and to understand what the policy means to them at their level, and what they should be dealing with at their level, and what they should be escalating to more senior people to come in and support them . . . handling a patient’s negative impression of something at an early point is so important.
Professional organisation 8
Different people expressed different opinions as to the best way to implement training to support open disclosure. A bottom-up approach, where training takes place on the ‘shop floor’ and juniors learn by example from their seniors, led by clinicians, was contrasted with a more top-down approach. Few made a case for continuous training integrated into basic training and reiterated as part of ongoing development, including individuals from across the organisation to ensure a uniform and coherent message in terms of practice.
To be honest, it’s people who’ve led by example. So, consultants who’ve shown that actually they’re open and honest and they’re still practising, they haven’t been struck off . . . it’s partly leadership by example and I mean I was, I did have particularly good bosses for a lot of the time I was training, so I did pick up some particularly good habits and I try to pass them on to my juniors. And juniors pass through lots of consultants, so if they pick up good things off each consultant, they should pick up a lot of good things and that should help disseminate good practice.
Health professional 7
It all boils down to see one, do one, teach one, which the educationalists say that but actually I think that worked quite well for doctors for a few hundred years. You watch people who are good at things and you think, ‘that went well, I might do that myself’.
Health professional 4
I think the policy needs to be clear, I think it needs to be. I think it’s up to senior people in an organisation to train people within that organisation so that they understand at their level what is expected to comply with that policy of openness.
Health professional 12
What might be useful is in formulating effective training programmes for junior medics, junior nurses, medical students, that sort of thing. I should think a lot of that sort of stuff’s been hijacked by non-clinicians and doesn’t reflect the reality of the situation often and there are some people that are very good at it.
Health professional 4
I think if we are going to talk about training you’d need to talk about it at undergraduate level so it would need, in my personal opinion it needs to be written in at the bottom end of medicine not at the top end.
Professional organisation 5
Doctors should ideally get it just through their training . . . inductions and so on are the ideal place to introduce how to report a problem and just encourage doctors that that’s something that they can do without fear and all the rest of it.
Health professional 7
If you are really going to get into the culture you’ve got to do it at undergraduate level, you’ve got to do it to medical students who then grow up with those ideas and it’s the same as any other education in life, if you take small children you can educate them much more freely than everyday teenagers because they will mop the knowledge up more easily. And I think that is true of undergraduate and postgraduate medicine as well, I think undergraduates will take it on board and accept it as part of the culture . . . so I think that is where it needs to be pitched at.
Professional organisation 5
Conception of formal training appeared isolated, specific to professional groups and stand-alone. We suggest that this is likely to perpetuate the professional tensions between groups already evident in the literature. Methods involving video filming practice in real-time and inviting clinicians to feedback on their own performance, discussion of complex events in multiprofessional groups, and reflection on the knowledge and questions that patients and families have about their care and about unexpected outcomes and clinical incidents, address the considered exploration of the evident tensions in patient safety events. Such methods could be used to underpin specific training in relation to disclosure conversations and encourage reflexive practice.
The wider concept of a statutory duty of candour was multiply described and has been a point of debate throughout the life of the project. This was raised as a broader contextual factor that might influence decisions around disclosure. Most policy-makers, patients and families expressed unremitting support for a statutory duty. In contrast, most health professionals and managers expressed reservations, although there were some exceptions to this. Those in favour of a legal duty of candour argued that it would be the most effective way of initiating culture change around open disclosure.
Passing a law doesn’t change the culture, but the creation of that law has helped create a change in culture, a change in attitudes. It’s a demonstration that society is no longer prepared to accept that behaviour. Similarly, with using seat belts or drink-driving, it wasn’t the passing of the actual legislation that led to people changing their behaviour. It was cultural change underpinned by society making that strong, unequivocal statement this is no longer acceptable in this society.
Professional organisation 1
I would like to see a legal underpinning, I think it’s very, very difficult to have it as a voluntary thing . . . it would be hard to police but all professional practice is hard to police and I just think a lot of it would be dealt with at the procedural level so if you’re receiving an incident report to a risk management system in the hospital which is what happens at the moment then part of the procedure would be, you know, has the conversation taken place with the relatives or the patient if they’ve survived.
Policy stakeholder 4
We see it [substandard care] all the time and I hate it. And you just think, oh, if that’d been my mother, I’d be distraught, so I don’t think you should, it should be legal.
Manager 7
You’re relying on people’s personal integrity, I don’t think that’s enough, I just don’t think it’s enough.
Patient 3
It’s just saying look if you screw up you’ve got to be honest and is it really that harmful to put that into law?
Manager 3
I believe and my organisation believes that all of this also needs to be underpinned with a completely unequivocal understanding that these things are requirements. That at the end of the day they’re not optional . . . I believe there’s a lot of confusion around on the part of health professionals, managers and institutions about whether it’s really absolutely required upon them to be fully open and honest.
Professional organisation 1
The NHS is a public service and we have a duty to be honest. So I think if there are people out there that aren’t honest, it should be made a statutory requirement.
Manager 12
There were acknowledged tensions and limitations highlighted in relation to the ongoing lack of clarity that would remain in terms of defining an incident.
[It] would help to move everything towards disclosure when it should be disclosed, but it isn’t obviously going to be able to deal with some of those areas of uncertainty.
Policy stakeholder 4
The alignment of professional and regulatory drivers requires professional directives and engagement of high-profile physician leaders; professional incentives in the form of revalidation, indemnity and professional development will need to be linked to patient-centred outcomes to align values in the direction of openness.
If I do something when I’m on my own and nobody else is aware of it, how is that going to be legally enforceable? I think that’s the difficulty of it and you know when these things are legally enforceable, if you don’t do it are you going to get a policeman knocking on your office door and saying, ‘you’re under arrest for not telling this person about X, Y and Z’? I think it makes the whole process more likely to go underground, rather than less. I think people would be less inclined to engage with it, if there was a legal status to it, than not.
Health professional 6
It’d be almost impossible to enforce and really challenging because how you do it is as important as doing it. And I think forcing people to be open and everyone doing it really, really badly will actually cause more harm than good.
Manager 2
I think we should work towards that being a kind of professional value and responsibility rather than something that is enshrined in some sort of legislative framework because I think it is too difficult to put in there. And I think every circumstance needs individual interpretation on what the best thing to do . . . my concern is that kind of legal, making it a legal duty would lead to inappropriate responses sometimes for patients.
Health professional 10
The identified need for opportunities for the careful exploration of held and multiple values which may conflict were apparent in our data. For any identified situation there is a need for a forum where individuals can discuss interpretations and reason through situations in a supported way, rather than over-reliance on a prescribed recipe outlined in guidance. This may promote a more reflexive approach which is likely to be critical to underpinning attempts to enhance safety and suggested methods for achieving both a more open culture but also more skilful disclosure.
Chapter 4 Discussion
This project set out to critically evaluate and extend both the evidence base and practice in relation to the implementation of a policy of open disclosure of adverse events to patients within the UK. The findings have been presented and the implications of both reviews and the primary research will be summarised here in relation to our original purpose highlighted below. The project set out to:
-
identify current areas where evidence and knowledge remain sparse
-
supplement the current guidance on implementing open disclosure
-
inform training and support for organisations and individuals in this area
-
identify continuing barriers to the implementation of open disclosure
-
identify well-developed models for open disclosure
and:
-
develop a series of short and pragmatic guidelines for NHS trust managers to facilitate the implementation and evaluation of open disclosure initiatives.
The following discussion will situate the findings from the reviews and the qualitative work within our research aim. We have been able to identify current areas where evidence and knowledge remain sparse and within identified limits we are able to supplement the current guidance on implementing open disclosure. The supplementation of the guidance is reviewed in the context of findings from the work conducted within the context of this report. Similarly, we have been able to identify issues and evidence which can inform training and support for organisations and individuals in open disclosure practice.
The gaps observed in the literature in relation to open disclosure of adverse events to some extent mirror observations which have been made in relation to patient safety research in a broader sense. Although patient safety research has made progress since To Err is Human 16 and evidence of success is apparent, this largely falls in quite specific clinical areas such as decreasing catheter-related infections227 or surgical checklists. 228 Shekelle et al. ,229 in their appraisal of patient safety science, have suggested that a view that patient safety interventions have improved outcomes for patients is not entirely convincing based on a number of other reports (e.g. Landrigan et al. 230). Their view that the science behind patient safety improvement is still developing and maturing holds true for the related area of disclosure of adverse events. Shekelle et al. have made four key recommendations for improving evaluation of safety initiatives: describing the theory, describing the practice in detail, detailing the implementation process and assessing the outcomes including unintended effects. They also stress the importance of attention to context when making conclusions about successful implementation. 229 The literature reviews that we have produced have emphasised the gaps that still exist in relation to these recommendations when considering open disclosure. Although the reviews have highlighted the lack of conventional empirical studies as a means of evaluation, they have located a body of useful opinion which raises a number of issues and provides useful illustrations. However, the area is undertheorised.
The development of theory is perhaps particularly important in relation to the design and evaluation of efforts to improve communication with patients and families about safety incidents that have (or may have) affected their care. The significance of the multiplicity of value considerations at play in these situations needs to be taken seriously, and considerations of context will be both particularly difficult and particularly important for good judgement both in and of practice. In relation to the conceptualisation of open disclosure, both the literature reviews and the interviews have highlighted the challenges in conceptualising acts of disclosure as processes, because these cannot be prescribed in any simple or linearly direct way from a broader principle of openness in health care or the moral concepts that lie behind this.
The act of disclosing (Being Open) and the broader issue of openness or transparency in health-care systems more generally are often discussed interchangeably but conceptually are quite different. There is a definitional problem around the area of Being Open which is highlighted in both the literature reviews and the qualitative data. Open disclosure in relation to so-called ‘never events’ presents a picture of greater agreement in that health services are morally obliged to communicate with patients and families in a way that is somehow ‘open’. However, what exactly is required and why still seems to be open to interpretation. Events that are catastrophic, life-changing for all concerned and considered avoidable are the main focus of the Being Open guidance. However, the language of the Being Open guidance strays into a much wider domain which speaks to a broader perspective on openness. The broader principle of transparency within health care is highlighted in the content of the second Francis report6 and in the very recent report by Berwick et al. ,200 which address a broader concept of openness and duty of candour. However, the lack of distinction between moral constructs and behaviour may cause confusion for those attempting to implement the guidance in that the definitions provided within it allow for interpretation, and it is this that appears to cause tensions within our data.
An alternative approach in addressing the disclosure of adverse events is to focus on the wider problem of candour on a bigger scale and to change the emphasis from candour associated with discrete events to candour associated with health care per se. This emerged as a theme in both the literature and in our primary data. If health-care providers were generally more open with patients then openness in the aftermath of error may be easier to achieve. However, there is a lack of exploration of the impact of such a blanket promotion of general candour, and even if such a culture were promoted and existed, the reliance on interpretation would still require good judgement in the promotion of moral behaviour. Organisations need to be clear about the focus of attempts to change. It is relatively easy to capture whether or not events are disclosed but more challenging to capture a change in broader concepts of openness. This broader focus would increase patients’ confidence that all aspects of their care are being shared with them, extending from everyday decision-making about their care to a more involved consent process. This is not to say that care should be one long disclosure process but more to emphasise a culture shift which sees candour incorporated into everyday conversations in relation to care, which may in itself help with the process when things do go wrong.
There was little literature from the UK which allowed us to determine understanding, views and interpretation of a policy of open disclosure of adverse events among UK stakeholders, but the qualitative data from the wide variety of stakeholders we were able to access has provided a valuable starting point on which to base future efforts to promote both disclosure of discrete events and a wider principle of openness in care provision.
Many of our stakeholders were willing and able, in the context of anonymised individual interviews, to articulate clear examples of situations where they had made errors or had been involved in situations where errors needed to be or were disclosed. However, the reluctance of those who we approached to engage in focus group discussions highlights the considerable challenge of embedding discussion of real error and disclosure events into quality and safety improvement efforts at national and organisational level. The persistent reluctance of individual clinicians and managers to engage in reflective and reflexive processes around particular errors hampers attempts to unpick ways in which this is embedded and linked to quality and safety reporting and management in practice. This is an important finding and reflects the continued lack of confidence of individuals employed in health care that the professional and organisational systems in which they work will be supportive in managing the context in which a particular event has occurred.
The previous sections have presented the findings from the literature reviews and the primary research. The following section will discuss how the synthesis of these findings might further inform an evidence base and practice in relation to the implementation of a policy of open disclosure of adverse events to patients within the UK. Although no formal mixed-methods synthesis was applied, we have summarised the findings from both phases and presented them as a matrix (see Table 3 ) to allow simple comparisons of the evidence in relation to each of the 10 principles of Being Open. The matrix summarises areas of convergence or divergence between the reviewed papers and our primary data, and identifies where gaps in knowledge remain. This synthesis has been used to explore ways in which future research might further inform and extend current practice and implementation of open disclosure and produce a series of short and pragmatic guidelines for NHS trust managers to inform and facilitate the implementation and evaluation of open disclosure initiatives.
During the course of the work reported here there has been a fast-paced change in the landscape of the NHS. Significant challenges to the belief that the NHS presents a safe and high-quality service at point of care have been raised. The recent Francis report6 has highlighted the urgent need to address transparency and openness within the NHS, and the decision to implement a contractual duty of candour within health care from April 2013 has been challenged by Francis, with a recommendation for a statutory duty of candour. Although the debate appears to have moved from a contractual duty of candour to a statutory duty, the implications of this for organisations and individuals remains unclear. The current attention to openness within the NHS means that our examination of the existing evidence and thinking around open disclosure of unanticipated outcomes in health is not only useful but timely.
A synthesis of the literature exploring open disclosure and primary data from stakeholder interviews reveal that although knowledge around some of the concepts presented in the 10 principles of Being Open is well established, little is known about the way in which other principles feature in practice or in the perceptions of stakeholders.
This discussion will examine areas where literature exists and which are aligned with the issues raised by respondents in our primary data collection, and raises novel concepts which are highlighted in the primary data but where little literature exists. We also propose to look at the areas where little evidence was identified from either phase and begin to situate our findings within a broader theoretical perspective of safety and organisational change.
A summary of the evidence and brief synopsis of the synthesised findings is presented in Table 3 .
| Being Open principle | Reviews | Primary data/interviews | Synthesised findings/conclusions |
|---|---|---|---|
| Acknowledgement | Clear events for disclosure are serious errors which lead to harm that is obvious to the patient. Difficulties with definitions of what should be disclosed persist. Terms are inconsistent and patients, professionals, organisations and the legal profession do not view or define patient safety incidents uniformly. Harm is usually conceptualised within a biomedical model, discounting patient reports of incidents which are sometimes dismissed or treated with discourtesy | Concern around defining an incident particularly related to minor/little or no events. Borderline cases present definitional difficulties. Widely held understanding that only events of moderate to severe harm are disclosed. Opinion divided over whether or not to tell the patient as soon as event becomes apparent or wait until information is gained from an investigation. Patients stress disclosure should begin immediately, irrespective of missing information | Differences of opinion remain about which kinds of incidents should be mentioned to patients and families. Further work could investigate conceptual variations between clinicians and patients to establish what is relevant to patients. Beginning the process of disclosure as soon as an event is discovered may help patients to feel more confident and trusting in the process. Being honest about uncertainty and missing information seems preferable to withholding information which patients may perceive as covering up |
| Truthfulness, timeliness and clarity of communication | The disclosure gap persists. The number of errors disclosed to patients does not map to the number of errors that occur. Although the principle of disclosure is largely supported by most people, there are a number of identified barriers including fears around litigation, being unfairly punished, tarnished reputation and loss of trust. Additionally, clinicians report a need to gatekeep information to protect patients, despite evidence suggesting that patients wish for honest disclosure of all incidents | Wide support for ideas of truthfulness, timeliness and clarity of communication being important although evidence suggests challenges associated with translating principles into practice. Uncertainty over how to react when information is missing or discovery of event is delayed. Concern over how to deal with complex circumstances where causes are unclear. Dilemma over who should disclose, where and how. Fear of legal action and desire to self-preserve seemed to be more active drivers for clinicians’ openness than concern for patient. Gatekeeping approach endures with clinicians deciding whether or not it is in patient’s best interest to disclose | There appears to be a need for standardisation of the process associated with disclosure to ensure quality and consistency in how being open is practised. Perhaps patients should be asked who they would like to lead the disclosure process. Organisations and individuals may need to consider the use of language carefully, avoid jargon and technical terminology and check patients’ understanding of the discussions. It would appear that disclosure should begin as soon as it becomes apparent that something has gone wrong and should be considered as a process, ongoing from its inception to final closure and not regarded as a single entity |
| Apology | Apology has a strong presence spanning ethical, legal and medical literature. It appears to be regarded as a fundamental feature of disclosure. Widely documented debates focus on whether or not apology can be used as evidence of fault, and what constitutes an apology. Less practical guidance is available | Evidence of conflicting opinion on apology. Some support waiting until investigations complete before apologising. Others see delay as missing the point that apology must be prompt even if all that can be said initially is ‘sorry for the outcome’. Patients stated apologies must be sincere and timely to be authentic | Some feel that apologising for any untoward event, like being late for an appointment, should be actively encouraged. It is thought that by doing so, saying sorry and empathising with patients becomes commonplace and part of the culture. Clinicians need to be clear and confident about associations between apology and liability |
| Recognising patient and carer expectations | There seemed to be a lack of focus on the need to think about patient expectations. Patients’ actual expectations of disclosure were only studied in a small number of papers | Managers and professional organisations highlighted the need to consider patient and carer expectations within disclosure. Health professionals did not conceptualise disclosure as a dialogue, in direct contrast to expressed patient perspective | By considering disclosure as a dialogue in which the patient is an active participant, health professionals might acknowledge the need to adjust the interaction to respond to patients’ expectations. Policy material could make explicit reference to the role of the patient within disclosure |
| Professional support | Clear and consistent messages from professional bodies, NHSLA and Being Open guidance. Openness should be the norm and expressions of regret and apologies are not the same as admissions of liability. The discussion of apologies in a wider international literature may be confusing for the UK context. Professionals receive little training in disclosure but this is identified as a key to any successful implementation. Patient reports identify unskilled and clumsy disclosures which often add insult to injury. The evidence for the effectiveness of current training is weak | Evidence that openness is considered part of duty of care, adhering to guidance from professional bodies. Support to implement professional guidance from local trusts often reported as lacking. Reluctance to be open attributed to fears of negative repercussions relating to professional identity, reputation and litigation. Sparse evidence of training despite most viewing it as critical to adopting a culture of openness. Suggested that training should be inclusive and delivered to both clinicians and non-clinical stakeholders and at all levels | Professional bodies could facilitate dissemination of guidance on being open to optimise clinician engagement. Most people believe that support is critical to both clinicians and patients/families if a change in culture is to succeed. This needs to take place throughout any disclosure process, inside and outside of office hours. Training may be best delivered locally and internally through trusts, although more evidence for effectiveness of different models is required. Training of all staff who may be involved in disclosure is required but awareness of transparency should exist throughout the organisation |
| Risk management and systems improvement | The majority of literature is focused towards a ‘no-blame’ culture although there is little evidence that this will create a climate of openness. The wider effort to involve patients in ensuring their own safety seems to offer few opportunities within the disclosure context. Little evidence to support statements in support of disclosure in relation to reducing litigation, improving well-being for patients and clinicians, patient satisfaction. Areas of policy development and communication cited as key for embedding a culture of openness | Openness is seen as presenting an opportunity for patients to be involved in their care and offer a unique perspective, capturing different information from health professionals. Discussed by many as minimising likelihood of becoming involved in complaints or legal proceedings. Openness often linked to risk management processes. Such links highlight reactive rather than proactive link between openness and quality and safety via these risk management processes | Expert opinion stresses links between openness about adverse events and reduced organisational risk. Openness may have practical benefits, enabling learning from mistakes, improving systems and finding solutions; however, the mechanisms by which this may occur are under-researched. There is a consistent emphasis on culture change from the negative associations with reporting incidents to a focus on positive outcomes of learning from mistakes, and improving practice and care |
| Multidisciplinary responsibility | The majority of literature focuses on the role of doctors but recognition that a number of key professions may have useful roles within disclosure process. No clear consensus as to who should disclose. Given the complexity of disclosure conversations there is a lack of research about how team members could or should participate. The role of risk managers is more widely discussed in the US literature and the role of risk managers in the UK is less well defined in relation to disclosure conversations. Nurses are identified as often feeling excluded and vulnerable in relation to disclosure | Evidence of constant dilemma over who should disclose. Often seen as responsibility of senior clinician closest to patient, particularly for serious incidents. Lack of consensus over role of junior staff and whether or not to ‘burden’ them with responsibility of disclosing. Question of how to gain experience if responsibility not shared. Nurses reported limited opportunities to be involved. Scarce evidence of multidisciplinary disclosure. The role of risk managers is clearer at some trusts displaying practice consistent with Being Open guidance. Patients ask for those directly involved to disclose events | There remains a lack of evidence to support what might be considered best practice with relation to individual vs. team disclosures and the role of risk management in the UK. Accounts suggest that junior staff are often ‘protected’ from being involved in disclosures rather than using such opportunities for learning and modelling best practice. Patients express a desire to interact with staff involved in error and reports often describe staff who meet patients as courageous and authentic. Lack of evidence to underpin the effect of this on patients or health professionals remains the case |
| Clinical governance | The implementation of learning and subsequent monitoring of change is challenging in relation to fostering a culture of openness with patients. Over-reliance on measurement and reporting open disclosure conversations may miss the point. The focus on moderate to severe harms may miss opportunities for organisational learning. The policy and patient perspectives seem to indicate disclosure within an ethical framework rather than focusing on governance and risk management. Lack of information about what a ‘good’ disclosure looks like, and the reports of unskilled and insincere disclosures, supports the need to ensure a focus on quality as well as quantity is maintained | Statutory duty is supported by policy-makers and patients/families to initiate cultural change. Contrasts with most clinicians/managers who oppose it as difficult to police and promoting a negative image of clinicians. There is a suggestion from practice that professionals may not give the best care when they feel policed rather than valued | The recent debate on duty of candour as a contractual rather than statutory duty was contentious; however, the recent Francis report and new announcements with relation to statutory duty of candour may have implications for the current Being Open guidance. However, the implications of what this statutory duty will mean for organisations and individual clinicians remains unclear. Championing a no-blame culture may be challenging but there is an enduring concern that genuine mistakes should not be punished to ensure that health professionals are confident to be open and feel supported by their organisation Over-reliance on measurement and reporting of open disclosure could reduce the principle of openness to numbers of disclosures, with a focus on documentation of disclosures which may lose information on aspects that represent a good-quality disclosure |
| Confidentiality | There is little focus on issues of confidentiality within the literature. Discussions about confidentiality seem to centre more on internal rather than outward, patient-facing conversations. Some literature discusses the right of an organisation to protect an individual staff member from being exposed to patient or family contact | Confidentiality of any party involved in disclosure was not identified as a concern among most interviewees. Some patient respondents identified difficulty in accessing information in relation to their case. They were often told the information was confidential as a justification for not sharing this | The links between the principles underpinning confidentiality in relation to individuals or information are underexplored. It is unclear how confidentiality sits in relation to disclosure of events to patients. Sometimes patients perceive the principle of confidentiality as a barrier to accessing information in relation to an error or harm. It is not possible to legislate for confidentiality in patient accounts of error once these have been disclosed |
| Continuity of care | It is well established that patients and families express a desire to have early and complete information wherever and whenever possible. There is a small literature emphasising the ongoing nature of disclosure conversations in relation to individual events and the importance of having one individual as a common point for patients and families. Current expert consensus would appear to be that continuity of care seems to be the ability to convey a supportive dialogue for those affected, even when emotions run high. Continuity does not relate well to playing down the incident, obscuring the content of information or being perceived as protecting the medical system or clinicians involved | Ongoing support and dialogue described as critical to enable patients and families/carers to engage with health professionals, ask questions and be listened to, to promote understanding for all parties | It seems unlikely that one approach will provide perceived continuity of care for all affected individuals. It is likely that there will be a need to be flexible. Disclosure processes require judgements to be made responding to individuals’ needs. Current consensus stresses the need to adopt an empathic and transparent process focused on the need of the patient or family rather than focusing on the risk to the organisation |
An abundance of literature was identified in relation to four of the principles of the Being Open guidance: acknowledgement, apology, professional support, and truthfulness, timeliness and clarity of communication. These issues were also some of the most pertinent arising in stakeholder interviews. It was apparent that these issues were perceived as critical to open disclosure by all stakeholders, but also as problematic when not implemented effectively.
The acknowledgement of an adverse event demonstrates one such example of where there was a large amount of literature and was widely discussed by respondents. There was an emphasis in the literature review on the importance of health professionals and organisations acknowledging events (e.g. Mazor et al. ,20 Gallagher et al. ,28 Wojcieszak et al. ,48 Berlinger,50 Anon.,231 Brahams232), and this belief was echoed by patients and many other stakeholders in interviews. Despite this, one of the most commonly reported features of poor or non-disclosure emerging throughout this project was the lack of consistent acknowledgement of adverse events (e.g. Pham et al. ,58 White et al. ,62 Kroll et al. ,63 Martinez and Lo,66 Garbutt et al. ,68 Gallagher et al. ,71 López et al. 111). The primary reason cited for this in our interview data seems to be the difficulty health professionals experience in defining an adverse event and the particular circumstances in which disclosure is required. Most interview respondents raised the difficulty of knowing which events should be disclosed; as the Being Open and GMC guidance both use patient harm as the determinant for whether or not disclosure is needed,11,95 respondents who were familiar with either defined the need for disclosure in these terms. The dissonance between patient or family and health professional definitions of harm shown in the review69,233 may mean that the use of patient harm to define what should be disclosed is problematic. Although one solution may be to define the types of events that warrant disclosure, it was apparent from the range of search terms required to capture all of the relevant literature (see Appendix 2 ) that numerous terms were used to describe adverse events in health care. The use of diverse terminology means that even when issuing guidance in relation to events that warrant disclosure, organisations, health professionals and patients may not always attribute the same type of event to each term.
The literature and the interviews relating to the topic of acknowledgement demonstrate the complexity of developing appropriate strategies to ensure that open disclosure occurs; at a basic level, simply recognising that an event has taken place and that disclosure is needed can be challenging. In the context of patient safety and protecting patients from harm, decisions regarding events that warrant disclosure become additionally complex as they appear to link the potential for patient harm and what may be the subjective judgements of providers. An additionally complicating aspect seems to be that the further from obvious error with apparent harm an event moves, the more opaque the decision seems to become. However, when conceptualised in the context of care quality, the complexity relating to terminology may be lessened. In providing high-quality care, health providers may need to consider whether or not a general principle of adopting an open and ongoing dialogue with patients may contribute to improvements in patients’ perceptions of quality and commitment to it; this includes discussions about everything that occurs in their care, including minor or more serious undesirable events.
Discussion of patient–provider communication featured prominently in the interview data and in the literature around the ethics of disclosure and disclosure training. This evidence relates closely to the principle of truthfulness, timeliness and clarity of communication. Data from both the reviews and interviews consistently demonstrated that most stakeholders strongly support the principle of being truthful with patients (e.g. Kohn et al. ,16 NHSLA,22 Scheirton,41 Shapiro152). This consensus about broad values sits alongside reports from practice in which interviewees describe staff withholding information from patients. The discrepancy might be variously explained by failures to reflect the key value of truthfulness appropriately in practice and/or by appropriate efforts to balance this value with other values that suggest different ways of acting in particular circumstances.
We found it striking that a number of health professionals considered it their prerogative or role to determine the type of information patients and carers needed to know, and that they used the aim of protecting patients from harm as the primary reason for withholding information. They seemed to have few reasons that might strengthen their imperative to act on considerations of truthfulness, but potential to develop these can be found in the reasoning of some of their peers who gave accounts of what seemed to be more open and truthful disclosures. The professionals who seemed to adopt more truthful practices were not neglectful of considerations of harm, but also mentioned considerations of who owned the information, and of patients’ rights to know. The language of rights and concepts of information ownership that they used might not be ideal, but could be further explored and developed for use in efforts to encourage a greater emphasis on truthfulness in relation to the discussion of safety incidents.
Similarly, the literature and patient accounts suggest that timely and clear communication are central to good disclosure, and though this view was reflected in interview data, descriptions of the complexities that prevented this happening were also described. More complex (but possibly common) scenarios in which information was missing or the discovery of an event was delayed led to uncertainty regarding when communication with the patient should take place and what this might include. There is a tension between acknowledging promptly and presenting a delayed, but more complete, picture of the implications and cause of errors. Early disclosure conversations may leave patients with uncertainty in relation to their current condition and vulnerable to delayed and unclear communication from health providers. Communication could be further hampered by dilemmas regarding who should disclose, where and how.
One of the most widely discussed barriers to truthfulness was health professionals’ fears regarding litigation. This was discussed in interviews and apparent in the literature. Concerns about litigation and studies of the impact of disclosure on litigation commonly featured in the reviews, particularly those originating from the USA (e.g. Gallagher et al. ,67,71 Studdert et al. ,79 Wu et al. 193). In relation to these, numerous articles presented disclosure as a strategy for health professionals to protect against litigation, suggesting that openness with patients may prevent legal action (e.g. Boothman et al. ,32,182 Kraman and Hamm,52 Kachalia et al. 208). However, a marked lack of any evidence to support this widely held belief was apparent from the reviews. The stakeholder interviews suggested that though health professionals were aware of the potential for litigation in relation to adverse events, this did not appear to be such a pervasive fear in our UK sample. Health-care managers discussed the possibility of litigation more than front-line staff, suggesting that this may be a more salient barrier for managers attempting to manage organisational risk than for clinicians. However, where health professionals made reference to litigation, it was generally to suggest that their fears had not been realised in their own experience, and that patients had not pursued legal action as a result of disclosure. The literature review suggests that patients often litigate to obtain information that they feel they have failed to access through other discussions and this was reinforced by the patient respondents in our sample. However, litigation may be pursued as a legitimate claim for loss of earnings or care costs even though individual patients and families are happy with explanations of error and apologies.
Professional support is identified as a principle of Being Open which can be conceptualised as support for professionals in a number of ways. Support may be in the form of support from professional organisations, the organisation that employs the health professional and managerial support. Additionally, support may be from peers and may occur within and between professional groups. Support can be enacted in ways that promote learning and inform how to disclose effectively, and as emotional and instrumental interventions for health professionals to cope with the burden of clinical work and emotional responses to adverse outcomes that may impact on their ability to disclose effectively. With regard to the former, although training was developed to accompany the Being Open guidance and support its implementation, both the review and interviews revealed a lack of awareness of its availability. No evaluation of any training specifically associated with the UK Being Open guidance was identified in the reviews. Only interviewees involved in developing or delivering the training, and senior leaders in one trust in which it was used, were aware of its existence. Those who were aware of the training package cited cost as the main barrier to wider uptake. Beyond the training that was explicitly developed in relation to the UK guidance, there was a wider absence of any evaluation of training approaches to support disclosure, although in the accounts of successful implementation of a disclosure policy, training was always featured as key to success. 150–152,154 Interview participants consistently articulated the view that professional training is imperative to support and enhance the disclosure process. Such findings suggest that while professional support and training are widely recognised as valuable, little is known about the most acceptable and effective models on which to base such interventions. Further research may help to clarify the most effective training models, the most appropriate outcomes on which to judge effectiveness and ways to support implementation. Iedema234 suggested that the promotion of reflexivity may be critical to underpinning attempts to enhance safety, and suggested methods for achieving this, such as video filming real-time clinical practice and inviting clinicians to feedback on their own film, and reflection on the knowledge and questions that patients and families have about their care and about unexpected outcomes and clinical incidents. Such methods could be used to underpin specific training in relation to disclosure conversations and encourage reflexive practice, enabling individuals and teams to reflect upon and appraise their actions in light of a range of salient values.
With reference to broader support for health professionals, interviewees recognised the lack of support available to staff to manage their experience of making an error or of being involved in an adverse event; this is reflected in a growing body of literature about the distress experienced by health professionals in these situations. This literature was not included in this review but has a growing evidence base. 235 A small number of papers referred to the belief that disclosure may help professionals involved in error to come to terms with their own associated distress; however, while this may convey empathy in some situations this may not always be the case, and we currently know little about how disclosure affects either health professional or patient well-being. Interview respondents (particularly those representing professional bodies) indicated that without the necessary support for health professionals, they may not be as willing to disclose events or may do so with low levels of commitment or skill. This belief is reflected in the broader literature (e.g. Levinson,69 Stroud et al. 73). There is a well-established literature and understanding (shown through our interview data) that broader professional support is important to enhance open disclosure, but the availability of support appears to be inconsistent and, as with training, based more on the motivation of well-intentioned institutions than evidence-based guidance. US-based accounts of providers who have implemented such support are enthusiastic152 but no evaluation data seem to be available.
Apology was one of the most widely debated issues identified in the review, spanning the medical, ethical and legal literature. Literature reporting patients’ beliefs indicated that a genuine and timely apology was one of the most important aspects of effective disclosure. 86 Policy material from the NHSLA also supported the notion that health professionals should be free to give an apology without fear of the possible impact it may have on a claim. 22 Although the value of apology was widely discussed, health professionals and managers described several dilemmas in deciding when to apologise, who should apologise and what this should include. Additionally, there is a sense that although the message seems to be that apologies are welcomed by patients, and often by professionals and their regulatory organisations, this may sometimes conflict with interpretations of that message from those involved in risk management. This can be understood as reflecting different interpretations of the concept of apology and how it relates to a range of values and consequences. For instance, the legal system in the USA in particular means that the caveats placed on apology translate to nervousness around the timing and content of apology, which may appear to convey insincerity and a lack of empathy if not handled sensitively by the individual or team making the disclosure. The absence of pragmatic guidance around apology to support professionals to translate the principle into practice was evident; however, as we have emphasised throughout this discussion, the presence of guidance that may be interpreted as a recipe for what to say is unlikely to facilitate any progress towards helping individuals in appraising their moral reasoning about apologies. In the UK, an apology is clearly articulated as not being the same as an admission of fault. There seems to be a present need, articulated in patient accounts, to distinguish between an ‘apology’ whereby a health-care provider accepts responsibility for something that happened or did not happen and apologises for this, and the situation where a provider expresses sympathy or regret at an outcome but fails to take responsibility for harm. Confusing these two situations appears to have the potential to cause more harm than good when a patient feels that failing to accept responsibility for an error fails to address the impact it has had.
Continuity of care and multidisciplinary team responsibility were primarily highlighted by our interview respondents but had a less established literature. Continuity of care may relate to the implications of disclosure for the ongoing treatment of the patient but was also conceptualised in relation to the ongoing nature of a disclosure process. Often ‘good disclosures’ or training for disclosure models were represented in the literature in terms of a single conversation between patient and provider. Interview data and a small number of written accounts suggested that conceptualising disclosure as an ongoing dialogue between patient and health-care team was of great importance for ensuring real transparency. 31,85 Only a small number of professional respondents recognised disclosure as a dialogue, suggesting that mismatched expectations of the disclosure process between patient and provider may be an issue. Preparing health professionals for a disclosure conversation may exacerbate the belief that disclosure occurs at a single point in time; therefore, defining disclosure more explicitly as an ongoing process in any guidance, but also in training and education, may be helpful.
A failure to recognise disclosure as a process over time may be part of a broader lack of recognition of patient and carer expectations about disclosure. Patient and carer expectations of communication with health professionals are referenced in broader health-care literature, particularly in relation to patient involvement and shared decision-making. However, the literature that focused on open disclosure revealed that patient and carer expectations of disclosure, and the ability of health professionals to recognise these, received little attention. In contrast, interviewees who were health-care managers and representatives of professional organisations consistently raised the need to consider and respond to patient and carer expectations. More work may be needed to establish the most effective way to support health professionals in determining patient expectations and representing these in disclosure dialogue, in order to promote responses and reactions that meet the needs of patients or carers and allow them to contribute to the disclosure discussion.
Interview data revealed a lack of consistent agreement regarding who is responsible for leading disclosure communications with patients and carers, and this appeared to contribute to inconsistency and some confusion for both clinicians and patients. Although Being Open identified multidisciplinary team responsibility as one of the 10 principles, most respondents identified the most senior doctor in the team as responsible for disclosure. Perceptions of the roles of other team members varied widely, particularly in relation to nurses and junior team members. In keeping with the limited literature that we found,99,100,168–170 nurses were not depicted as central to disclosure conversations by respondents, despite the common belief that nurses are often closer to the patient than other team members. There was divergence between interviewees regarding the degree of responsibility that should be held by junior team members. Some felt that junior staff should be protected from challenging discussions with patients, whereas others suggested that involvement in disclosure is critical to their learning and may also be helpful for the patient if the junior team member was directly involved in the incident. Interestingly, although the literature around disclosure training demonstrates that much of the training has been directed at junior medical staff, studies exploring the role of the wider multidisciplinary team in disclosures beyond the lead doctor were limited. 175 Such findings suggest that although multidisciplinary responsibility is identified as a principle of Being Open, there is a lack of clarity about what role each team member should play and how teams can work together to deliver more effective disclosures.
Reference was made to the majority of the principles in the Being Open guidance to at least some extent in both the literature and interviews, but we noted an absence of evidence from existing literature or our interviews that related explicitly to three of the principles: confidentiality, risk management and systems improvement and clinical governance.
Confidentiality around disclosure was not raised by patients or other stakeholders as a primary concern and this was reflected in the absence of literature that discussed this. Moreover, it was apparent from interviews with patients and health professionals that concerns about breaking confidentiality may be used by health-care providers as a reason for delaying or not revealing certain information to patients. Being unable to discuss an error with those directly involved seemed to be a particular frustration for families for whom this was an important part of the process of coming to terms with what had happened. In the literature, limited work made reference to the level of confidentiality offered to the health professionals involved in an incident, but it was not clear how confidentiality would be conceptualised in the context of open disclosure beyond patient confidentiality that is part of day-to-day practice. Confidentiality regarding serious adverse events was highlighted as challenging, and many respondents identified that in the case of serious errors information was often widely discussed within the organisation beyond the immediate team and risk management. Teams may wish to explore the motives around maintaining confidentiality in relation to health-care staff in their reporting of error and harm to patients, and the value of this approach in relation to both patient expectation and learning. Issues around confidentiality may be particularly challenging in the area of mental health care where patients may not wish discussion about their care to take place with family members or representatives, and this requires further exploration.
Implications of disclosure for risk management and systems improvement were discussed in the context of clinical governance by some health-care managers, but these were not addressed as distinct issues. Literature from the USA reports the role of risk managers in relation to incident disclosure to some extent, but work originating from the UK does not explore the role of this group, which may be very different from the US context. The explicit links between disclosure, risk management and clinical governance remain underinvestigated. Establishing which outcomes might link these areas requires more examination. Interview data linking disclosure with risk management, clinical governance or systems improvement were limited to the reporting of risk incidents and action taken with staff as a result. The contribution of patient perspectives was described by some interviewees as a source of information that might guide systems improvement but is currently not exploited to its full potential. This strategy relates closely to a broader literature on patient involvement,236 but respondents did not explicitly make this link. Risk management, clinical governance and systems improvement may each be critical to open disclosure and informed by open disclosure, but these principles are currently under-represented in the literature.
The recent debate on duty of candour as a contractual rather than statutory duty was contentious; however, the recent Francis report6 may mean that this is reviewed and changed to a statutory requirement. Since 1 April 2013 the new standard NHS contract has been used by all organisations commissioning NHS services, with the exception of services commissioned under primary care contracts. The contract requires all NHS and non-NHS providers of services to NHS patients to comply with the duty of candour. Unlike professional ethical duty (e.g. Good Clinical Practice), the contractual duty of candour only applies to incidents that result in moderate to severe harm or death. This will present considerable challenges for both organisations and professional bodies in terms of clinical governance and monitoring. The impact of contractual or statutory duty of candour is unknown but there seems to be a concern from practitioners that an over-reliance on measurement and reporting of open disclosure could reduce the principle of openness to numbers of disclosures, with a focus on documentation. This may result in the loss of information regarding which criteria represent a good quality disclosure. The interviews suggest that the messages from the various sources and organisations that clinicians look to for support are interpreted inconsistently and differently. In the UK, the requirement to be open about adverse events is currently disseminated as guidance, although a contractual duty of candour may mean that the pace of change is accelerated. Those in favour of statutory duty of candour feel that genuinely essential practice can only be achieved through this route. 201 NHSLA guidance emphasises openness, and the MDU and MPS have publicly advocated candour. However, the evidence in the literature and the interviews in this study demonstrates that despite this practice is often different, and more recently, A Promise to Learn 200 has called for a clearer supervisory and regulatory system, with clearer incentives which do not conflict, to ensure that individuals and organisations feel confident in being transparent.
The challenge of defining appropriate outcomes for individual trusts to allow them to demonstrate both quality and quantity of disclosure needs further clarification. The current emphasis is on championing a no-blame culture, despite a lack of evidence that this improves safety in health care. The concept of just blame is becoming increasingly discussed, but there is an enduring concern that genuine mistakes should not be punished to ensure that health professionals are confident to be open and feel supported by their organisation. This has been reinforced by Berwick et al. 200 in their recent report into the NHS, which has called for recognition that transparency is essential and that organisations, health professionals and patients should expect and insist on it. This recommendation was balanced with a clear message that blaming staff should end and that they should be trusted to do the right thing with adequate support throughout their careers.
Although this report concentrated on open disclosure, we are aware that there are a number of theoretical perspectives which might be brought to bear on any examination of the disclosure of adverse events. The area itself is undertheorised but there appear to be several useful perspectives from related fields which might be employed to progress thinking in this area and inform future research questions. Patient safety more generally draws upon a theoretical body of work around systems and behavioural change in health professionals and organisations. There is also a body of change management, transformational, entrepreneurial and ethical leadership, and organisational change literature equally relevant to this report. Although a detailed analysis of appropriate theoretical models is beyond the scope of this work, we are aware of some approaches which appear to sit well with our current analysis of the available literature but in particular with our interview findings.
In theory, the UK NHS is a collection of organisations that share, to a greater or lesser extent, a common mission and values. It is referred to as a ‘national institution’ and described by both staff and patients in a way that depicts a well-recognised brand. However, Checkland et al. 237 suggest it is more accurate to consider it as a heterogeneous and evolving organisation, which is becoming more diverse as it evolves in response to the considerable changes which have occurred in recent years. This makes it a complex adaptive system, and as such there are a number of theories through which we would be able to view the attempts to introduce greater transparency around adverse events. The purpose of the complex adaptive systems perspective is to draw attention to basic tenets or principles rather than provide hard and fast rules about what works. The recommendation of this approach is that policy should avoid elaborate checklists or specific instructions for change. The idea that health-care systems are complex adaptive systems has been established for a number of years, and several influential papers from a number of authors in mainstream medical journals are emphasising the usefulness of the complex adaptive systems lens in understanding improvement and transformation in health care. 238,239
The majority of literature on transformation in health care describes change on a relatively small scale, often by one organisation or service. 240 Generally it lacks both definition and an evidence base. 241 Best and Holmes240 define large-scale transformation in health-care interventions as change which is aimed at ‘system wide change affecting multiple organizations and care providers with the significant goal of significant improvements in the efficiency of healthcare delivery, the quality of patient care, and population-level patient outcomes’ (p. 422). Embedding a culture of openness in the NHS can, at least to some extent, be considered a large-scale transformation. Therefore, this work may be usefully employed here. Lanham et al. 242 has stressed the need to move away from top-down efforts and focus instead on the natural creativity of health professionals to adapt and develop new ways of achieving quality – a suggestion which was recently endorsed by Berwick et al. 200 in their report on the NHS. However, this can only be achieved when positive conditions allow a supportive work environment. Those working in health care need to be able to make use of relationships and skills within the system, and it may be at this point that complex adaptive systems theory is able to link into the systems theory. The focus of systems theory on just blame may complement organisational theory in terms of supporting the development of a culture where candour is able to become a more ingrained cultural norm in health care.
Work from a realist review of large system transformation (LST) in health care has identified a number of findings which may be applied to the practice of disclosure but are, as yet, largely untested outside of individual accounts. 240 Our review highlights examples where the principles of LST, which makes use of the engagement of individuals at all levels in leading change, have been applied. There are examples in practice-based literature where this need has been recognised, and where there are identified individuals leading on efforts to mobilise delivery of change in terms of disclosure. 150–154 This would suggest that each trust should have an individual lead for openness. However, engagement at the levels of policy, regulation and indemnity bodies through to risk management and patients all need to be considered. The model of more distributed responsibility may be useful and possibly more sustainable, but in the few reported examples where organisations are perceived to have adopted more transparent ways of working, they appear to have significant figureheads usually accompanied by a stakeholder, often from among relatives who have been instrumental in helping to bring about change. Distributed leadership appears to focus on practice and relationships in leadership as well as developing leadership through mentoring. Pedagogical approaches which support and model good practice to promote leadership may be useful models with effective feedback loops to further bolster learning and development. A number of recommendations for LST change have been suggested by Best and Holmes240 and are discussed below in relation to open disclosure.
Ensuring that it is valuable and safe for staff to engage in good disclosure practice is crucial to success. The need to promote the reflection of important values and principles in practice, and to provide cultural and interpretive support for those values, is likely to be important and has been highlighted in our data. When staff or patients are concerned, or suspect error, the organisation needs to be receptive and welcome reports. This would be echoed in current patient safety thinking which emphasises feedback and learning. A Promise to Learn 200 emphasises the need to engage both staff and patients in gathering information about risks and harm and the involvement of both in establishing the important information that needs to be collected. Additionally, it seems important to focus on how this might be achieved, as this will avoid measures that could potentially influence behaviours in negative and unintended ways, and employ metrics which capture things of importance to both clinicians and patients.
Clarification of concepts, and consistency and transparency of definition have also been highlighted as important. There is a pervasive problem around definitions of error and harm which are defined solely by one side (the provider) and are driven by definitions of events which are classed as moderate or severe. We would suggest that the naming of harm, beyond so-called ‘never events’ (or those that the organisation judges to have harmed the patient), appears to be open to interpretation and would benefit from such examination and consistency. This lack of clarity was conspicuous in the accounts of stakeholders in our data. Unless definitions are applied and seen to be used consistently, patients will be frustrated by such inconsistencies and report this in their accounts of instances where they seek an apology. Incentivising acting on feedback should include patient feedback but has to be sustained to avoid gaming.
Open disclosure could connect to the valued commitment to learn from previous safety problems to prevent future errors and harms. Careful analysis of events is an important step but will not predict how things might happen in the future. Analysis of events should be viewed as an opportunity for sensitive discussion and planning of how to avoid the situation or, more realistically, how to handle a situation if it happens again. Although the aspiration of the NHS may be zero harm, in the journey to this aspiration the usefulness of the approach of handling how to disclose error must not be forgotten. Broader literature on quality and safety will need to address how the aspiration of zero harm can be made to sit more comfortably with values and behaviour in relation to open disclosure where the very aspiration of a service has been challenged by the occurrence of error. It is exactly this tension which was raised by our stakeholders, and failure to address this as part of ongoing support and development is unlikely to result in changes in action.
The importance of engaging physicians and their indemnity and professional bodies in LST change has been identified. The issue of who makes decisions about disclosure and how it is done seem largely to fall in the domain of doctors, although our data do support the active participation and in some cases leadership of nursing colleagues. Transformative initiatives are often championed by nurses or non-clinical mangers (who have less power) involved in the system and the literature identified the frustration expressed by nurses in relation to their involvement in disclosure. Although doctors in the UK tend not to operate as independent practitioners (though GPs and those in private practice may be an exception to this), their collegial regulatory framework is geared towards detecting extreme examples of poor practice or unethical behaviour to protect the profession rather than monitoring quality. That gives them a great deal of power in responding to transformative events. Our interviews supported this and it was clear that professional regulatory guidance had most influence on the moral perspective articulated in practice. The influence of professional regulation was apparent during the duty of candour debate, with the medical profession objecting to a legal duty of candour on the grounds that their professional regulatory framework already meant they had a duty to be open with patients. Nurses and patient organisations, on the other hand, were supportive of regulation around openness in care which went beyond a statutory duty. As doctors often have a power of veto when other groups adopt a normative aspirational target, the engagement of the medical profession in making this a normative aspiration seems essential and the current literature and our interview data would suggest that this is currently equivocal.
The role of situated judgement in both the literature review and the interviews with stakeholders has been discussed in all sections, and the importance of attention to context in both practice (for professionals) and in evaluating practice (for those who would judge them) is clear. Context has emerged in the theoretical literature as important and is discussed separately from effectiveness of interventions. 243,244 In a systematic review of interventions, context was highlighted as poorly described and reference to the general lack of understanding that still exists in relation to context in patient safety practice interventions was made. 243
Implications for research suggested by some patient safety researchers are that there needs to be clarity about both theory and concepts in relation to any safety practice244 and this could equally apply to the broader but related value of openness in health care. Defining the events to be disclosed without due care and attention to the multiple values inherent in decisions about disclosure behaviour fails to address contextual issues and thus the effectiveness of guidance such as Being Open.
Providing care for individual patients and organisation of care for populations are related but different endeavours and this may lead to tensions, which has been highlighted by Shale245 in relation to the concept of ethical leadership. Health-care professionals and health-care organisations aspire to provide the best possible care for individuals but the reality of health care, especially in a system such as the NHS, is that this is achieved through providing shared resources at a population level. Thus, there is an inherent challenge in managing a shared resource in an ethical way which often differs from managing a resource for an individual. Therefore, managing the reputation of an organisation to maintain the trust of the larger population may conflict with disclosing information about an individual error.
Such dilemmas are apparent at all levels from the boardroom to the bedside and solutions present a constant challenge. These observations were reflected in every interview and by the differing perspectives represented in the review literature. Such work may also be useful in starting to unpick why moral values do not automatically translate into ethical action.
Shale245 also points out the importance of doing the right thing in the right way and this point is particularly salient in disclosure conversations. Training, where it exists, focuses on raising awareness of the moral and legal imperative, but occasionally also on how to have a challenging conversation. In both the literature review and our interview findings, clinicians highlight their anxiety about having disclosure conversations and patients highlight the damage that can be done by the right thing being done in the wrong way. A doctor who wishes to tell a patient that an error in his or her care has occurred is ethically correct, but blurted out in the wrong circumstances and in the wrong way, it would not be considered an action which was necessarily morally strong. So the skill involved in doing the moral thing in the right way is important. Finding the right place, having all the information and rehearsing this all underpin efforts to train people to do this well, if the ethical course of action is to be carried out in a morally appropriate way. Preferences of the family or patient need to be taken into account; therefore, the person disclosing should have good knowledge of the individual being dealt with, and this has implications for who discloses. Moral communication requires skills and these skills need to be practised and experienced. There are the real skills of expressing the situation clearly, listening and tailoring information to suit the context. However, the degree of emotional intelligence required in such situations is important in relation to managing difficult conversations; being able to express empathy, and managing anger and distress are all important in making the communication with the patient or family sensitive. Equally important are the skills enabling the professional to self-manage his or her own emotional response, as feelings of defensiveness, distress, shame and anger are often cited by professionals in relation to errors. Forgiveness may not be forthcoming from the patient and family and dealing with this response when an individual and an organisation feel they have acted with integrity can be hard to accept.
Interventions to train people in disclosure may well find the work around ethical leadership and emotional intelligence useful as a starting point for their construction. Although emotional intelligence theory would not state that managing emotions either in oneself or in others is easy, or that every individual can become skilled in such conversations, it does support the notion that skills can be developed and that levels of improvement can be measured. The simple ethical question of ‘is it the right thing to do?’ to disclose error is easily answered. An ethical perspective and our data suggest that the answer is yes, but any exploration of its enactment highlights the numerous challenges associated with action. It is both emotionally and legally sensitive and takes considerable skill that is not captured well by current guidance, which is unlikely to be able to address the complexity of decision-making underpinning disclosure of an adverse event, whether serious or associated with less or no apparent harm.
There is an inherent sense of risk for organisations in relation to disclosure and the wider principle of candour. In order to achieve an open culture they must be prepared to give up some control. Patient safety initiatives are, for the most part, aimed at exerting as much control over processes as possible, limiting the points where initiative or opinion come into play in order to prevent error, and checking the process at as many identified points as possible to reduce the likelihood of mistakes. However, disclosure requires a degree of resilience and the ability to manage uncertainty if organisations and individuals are to deal with errors and disclosure effectively. The process linking the monitoring of quality and safety is unlikely to be able to measure or quantify a sea change in openness which may be imperceptible even to those using health-care services, and so cannot be conceptualised in the same way as the majority of safety interventions. Disclosure of adverse events should be focused around informing future practice and improving quality and safety but it has wider implications for the staff and patients involved. For these reasons, sitting disclosure entirely within the current patient safety theoretical models is unlikely to fully address its challenges, and theoretical models which are able to address the complexity of values within health care and emotional intelligence in practice are also likely to be useful.
Strengths and weaknesses of the work
The review was extensive. All identified potential sources published over a 22-year period were searched. This inevitably produced a large volume of literature but should ensure that most relevant literature has been appraised and included. Publications were not excluded on grounds of quality and peer-reviewed publications sit alongside journalistic literature and guidance from professional bodies. This was necessary to gain a wider sense of the movement in the attitudes as well as the evidence base within the field of open disclosure, much of which has involved disparate, common-sense responses adopted by individual organisations or in particular areas.
A large part of this literature originates in the USA and refers to US health systems, and for this reason applicability in other countries may be limited. However, the range of interventions described from different countries with different health-care systems illustrate that similar approaches are being adopted within many systems. The practitioner–patient relationship, which is at the heart of all health organisations and systems, appears to have key similarities worldwide; that is, a knowledge and status imbalance which means that the ability of a patient to access information in relation to their care, and to fully contribute to making an impact on safety-related behaviours within health care, depends upon a number of things. The behaviour of patients is likely to be profoundly affected by the information their health-care professional chooses to share with them and the extent to which the health-care system is prepared to engage in dialogue after an error or adverse event. The review conducted here has illustrated how few empirical findings exist in relation to open disclosure and how few models of good practice have been described or tested, and indeed, how unclear the possible outcome measures that are applicable to such work are. These factors make any recommendations challenging from the perspective of both generalisability and a lack of any firm evidence base on which to base them.
There may be examples which have not been captured by the searches where implementation of disclosure policy is being conducted consistently and linked to safety outcomes within organisations and is being evaluated. Such accounts may not have been written up for dissemination.
The searches were conducted in 2011 and rerun at the end of 2012. Although we have not systematically searched all reports published since this date, we have, through monitoring relevant publications, attending conferences and maintaining contact with experts in the field through the project steering group, closely observed the field for any new themes or ideas. We are not aware of any literature which would change our overall conclusions.
The qualitative component of this project makes an original contribution to the field of patient safety research by providing empirical data relating to stakeholders’ awareness and understanding of open disclosure and their personal experiences and perceptions of both the principle of openness in relation to disclosure of adverse incidents and the Being Open guidance, in the context of their own position in relation to health care. A major strength of the study was the deliberate inclusion of a wide range of participants (drawn from different stakeholder groups) in order to capture a broad range of views and perspectives from people with varying disciplinary and professional characteristics as well as patients and families who had been affected by health-care error.
In-depth interviews proved to be a highly effective way of exploring people’s knowledge, beliefs and experiences in relation to open disclosure of adverse events and policy implementation, allowing the interviewers to probe and clarify responses in order to produce a rich data set that was grounded in the experiences of interviewees themselves. Individual interviews yielded highly detailed information on aspects of process (e.g., on the nature of communication between patients and health-care professionals) which contributed to identification of the ways in which particular beliefs or experiences were likely to influence behaviour.
Although the original protocol had planned to conduct focus groups, a number of challenges meant that we were unable to achieve this. Research governance processes took longer than expected which, given the 18 months available to conduct this study, meant that the time available to achieve these was short. This, coupled with the reluctance of stakeholders to discuss this topic in groups, meant that the qualitative data are based on interview data rather than a combination of methods. However, the breadth of the interviews was extensive and it seems unlikely that focus groups would have resulted in a change in our conclusions.
There are well-recognised limitations to the qualitative approach used in the study. One of the obvious disadvantages is that it does not support the formulation of quantitative estimates of either the frequency or distribution of particular views or experiences within a population. The current study was designed in order to explore how knowledge, beliefs and experiences in relation to open disclosure of adverse events and policy implementation might vary according to job role, professional discipline and distance from direct patient care. It is feasible, therefore, that findings from the current study could be used to usefully inform future survey work to investigate the significance of such contextual variables in a quantitative fashion.
Owing to the large number of data collected, and the complexity of that data, analysis of the study data is currently primarily descriptive in nature, which imposes limitations on the generalisability of the study findings at this point in time. Although the analysis that has been undertaken enables us to meet the study objectives, and to comprehensively answer the research questions (as stated in the protocol), further analyses are possible. These will be carried out prior to the production of papers for publication in order to develop theoretical hypotheses and to refine an explanatory model. This should allow for inferential and theoretical generalisation from the study findings.
The evidence-based guidance for managers to facilitate the implementation of open disclosure had been planned as a consultation event. The lack of evidence currently available to support this activity meant that the work is only able to support a short pragmatic set of suggestions which have emerged from the work covered, and we remain somewhat tentative in suggesting these in light of our work as presented here. What is apparent from this project is the need for a focused programme of work to determine an evidence base for almost every aspect of open disclosure policy. Until this time, such guidance is advice based on expert opinion but little more. There appears to be a fundamental problem with attempts to simplify and standardise an area as complex as disclosure, which has been clearly articulated in work by several authors in the reviews and in our stakeholder interviews, and has been further supported by extended discussions in our synthesis and calls from both the Francis6 and Berwick200 reports which have been published as this research was ongoing.
The majority of work in the literature and in primary research has engaged with secondary care services. However, error occurs in all areas of both health and social care. Although we were able to interview some primary care practitioners, they made up a small number within our sample and we acknowledge that the generalisability of this work to other areas may be limited. This said, the principles of transparency in care may encounter some differences of context but the issues raised by our predominantly secondary care-focused sample of stakeholders have many themes which are likely to translate well to other settings.
Finally, we would highlight a limitation which has been articulated in other work reviewing LST. 240 The time frame in which to conduct this work was short (18 months). Although this was useful in providing focus and discipline and keeping us aligned with the fast-paced change in policy and structure within the NHS, it has posed a challenge in making less time for reflection on the complexity of disclosure values and practice and the wider literature which might apply. Thus, our work and discussion has been limited by what we have been able to achieve within this time frame. We intend to extend this work with further analysis of our findings in the future.
Chapter 5 Conclusion
Health-care reforms are often difficult to enact and the changes that policy-makers envisage and aspire to may not translate into practice, or change may take longer because working practices are institutionalised. This is apparent in a policy of open disclosure and is complicated by the levels at which the policy needs to be delivered. The US VA classifies the strength of patient safety interventions based on the probability that they will reduce risks; checklists are classed as weak interventions. Being Open is, in fact, a clear set of guidance rather than a checklist per se, but short pieces of advice run the risk of being used in such a way. It is intended to act as a simple reminder of what to do, but unless it is coupled with attitude change and efforts to remove barriers to actually disclosing, it will continue to have limited impact. This has been demonstrated by both the reviews of the literature and the interviews with stakeholders.
Both the literature reviews and participants’ accounts identified a range of benefits of a more open culture as well as reasons for the reluctance within health-care institutions to fully implement policies of open disclosure in an international context and, more specifically, in the context of the Being Open guidance. Virtually all stakeholders discussed the need for cultural change when considering ways to make Being Open become more ingrained in health-care practice. Respondents explicitly referred to how a change was needed from persistent negative associations in relation to reporting incidents towards a focus on the positive outcomes of learning from mistakes, and improving practice and care. Although there was a lack of familiarity with the guidance itself beyond general principles, there was a widely held belief that poor implementation may be due to a lack of appreciation of hypothesised benefits. Despite the enthusiasm for a move to a culture of openness, issues around defining the events that should be disclosed persist, and there is a pressing need to establish a robust evidence base in relation to open disclosure practice. Health-care institutions and the individuals who work within them need to be receptive and responsive to patient concerns about unanticipated outcomes in relation to their care, whether these are mistakes, errors or simply a case of unmet expectations. This approach may allow patients to participate in the broader agenda of contributing to improving quality and safety of care. The nature of the patient–professional relationship would seem to be crucial in achieving a disclosure which supports information-giving to patients and families and mitigates risk for the organisation, but this is currently unsupported by established training or professional support.
A number of gaps in the evidence base persist and current practice is based mostly on expert consensus rather than an existing evidence base. This needs to be addressed if culture change is to occur and disclosure is to be performed consistently and with skill. At a fundamental level, there is a tension between the pragmatic guidance issued by a number of professional bodies and organisations and the more in-depth critiques of what being consistent and transparent in health care really means. The tension between a more reflexive sociological approach and a systems failure paradigm has not been fully resolved. There appears to be a protective agenda from the systems approach which focuses on learning and the non-attribution of blame. However, the literature and respondent accounts highlight that emotions are a very real part of disclosure for both patients and their families and the members of the health-care teams involved. Further work needs to focus on how these two paradigms can be used to inform disclosure of events to patients and support for patients and professionals, and to provide learning for health-care systems effectively.
It has been suggested that there are several common contextual factors which contribute to successful implementation of safety practices: commitment from the top, dedicated staff and financial resource, an open process to encourage buy-in and enthusiasm from end users, and sheer persistence. 246 In the small number of reports of institutions where authors report progress in open disclosure, these factors are all apparent, and it would seem that efforts to improve open disclosure practice in the UK will require the same. The impetus for change is currently strong, with influential reports and public opinion very much behind increased openness in health care and more transparency in relation to learning from error, and we would suggest that efforts towards change should ensure that this normative cultural change in the policy and public spheres is captured and facilitated in practice. This will require visible support from influential parties such as professional and indemnifying organisations and senior members of trust boards to facilitate clinicians in having the confidence to negotiate complex decision-making in relation to disclosure practice, and to promote skill-building throughout careers through formal support and insightful mentoring.
Chapter 6 Future research
This work has highlighted that there are a number of areas which require further investigation.
At the level of individual health-care trusts we have little information about how the Being Open guidance is being interpreted and implemented in local policy. Mapping this would allow the identification of any potentially well-developed implementation which could be tested in other settings. More work is required to better understand the facilitating and impeding factors that have the greatest influence on disclosure and how these might vary by context (at the level of profession, trust, patient and clinician characteristics). Exploration of the links between outcomes of interest for risk managers (and those concerned with clinical governance) and open disclosure is needed to determine whether or not outcomes relating to safety can be used as proxy measures for a successful disclosure process.
Very little is currently known about the influence of specific factors such as how the level of training undertaken, speciality or professional environment might affect attitudes towards disclosure, or the effect of particular training models in supporting or discouraging disclosure. Future research will need to determine whether or not educational and institutional interventions actually reduce the influence of impeding factors or enhance the influence of facilitating factors. This requires good-quality effectiveness studies with robust controlled studies and appropriate outcomes that reflect both patient-centred outcomes and clinician and organisational outcomes. Future studies should explore the mechanisms through which open disclosure might address and reduce some of the psychological and health-related consequences of error for patients, their families and the health-care providers involved.
Observational work in any context is challenging but in the context of disclosure conversations this may be even more so. Practitioners often find the observation of practice challenging, and using observational methods in relation to disclosure conversations would pose many difficulties for consent and methods. This said, there seems to be a need for a number of interesting but methodologically challenging studies. Being able to understand in more detail the impact of organisational culture and leadership styles on disclosure practice at the hospital and departmental level, and the ways in which individuals interact during specific disclosure conversations, seems essential for understanding and improving the status quo. These studies are likely to employ complex mixed-methods approaches to capture observational, experiential and quantitative outcomes in relation to disclosure practice. What is also clear is that any evidence base is unlikely to be able to make hard and fast statements about what works. More likely are broad statements about what tends to work, for whom and in what circumstances. Best and Holmes240 also suggest realist evaluation as a tool to generate such statements to understand and explain different outcomes. The realist review is still an emergent field but may be a useful way to take forward a more detailed examination of contexts where openness is perceived to be established. Future research might examine which disclosure styles patients perceive as competent, and assess their causal impacts on objective and relational disclosure outcomes. The involvement of patients and the insights this perspective may bring to the prevention of adverse events and promotion of service improvement should also be considered. The need to observe and explore real-time disclosure as well as in anticipation of and after disclosure interactions is apparent.
Most of the work looking at disclosure takes place in secondary care and the majority of respondents we engaged with were based in secondary care. There is almost no literature addressing other contexts more specifically, either internationally or in the UK. We know little about some health-care contexts, such as private health care, social care providers, general practice, learning disability or mental health settings as five examples, but this is not an exhaustive list. These areas require focused exploration to determine the transferability of findings from other, more general contexts.
Chapter 7 Summary of evidence-based guidance for managers to facilitate the implementation of open disclosure in individual trusts
As part of the commissioning brief for this project we were asked to produce some short evidence-based pragmatic guidance which NHS managers may wish to consider in relation to developing and implementing local policy for open disclosure. The lack of a robust evidence base in relation to the majority of individual Being Open principles, and the arguments presented in this work for the problems associated with the use of such guidance to improve or guide practice, means that the following suggestions are based largely on expert opinion and consensus. In using them organisations should be mindful of their extensive and inherent limitations. As such, they are tentative observations. These would need to be revisited and revised as the evidence base in relation to specific principles develops.
Organisations may wish to consider assembling a multidisciplinary team to establish the working definitions to which the policy will apply. As part of this they may wish to consider the following factors in team composition. All levels of the organisation, from the board down, should be represented, including senior and junior doctors and nurses, and service managers including clinical governance and risk management. Consideration should be given to the inclusion of lay members to keep policy and practice focused on the needs of patients and families who have experienced harm. This is supported by the findings from both reviews and our interviews with stakeholders.
In considering the specific principles of the Being Open guidance, we suggest the following points for consideration by trusts.
Acknowledgement Try to ensure that everyone in the organisation is working to the same definition of an event that requires disclosure and that patients and families are also clear about the events that will be disclosed. Explore and acknowledge the difficulties associated with definitions. Consider a small group who can discuss any contentious events, perhaps with lay representation to enhance transparency.
Truthfulness, timeliness and clarity of communication Try to ensure that patients and families are given information relating to events as soon as possible. Although investigations may be ongoing, convey this uncertainty to families and keep them updated with facts as they emerge.
Apology Apologies are important to families. These should be sincere and issued as soon as any error or mistake is established. Trusts may wish to provide regular updates and support to ensure that clinicians and risk management are clear about both professional and legal obligations in relation to open disclosure.
Recognising patient and carer expectations If the expectations of the patients and carers are established before, during and after treatment, this may help in discussing perceptions of harm and error when outcomes are unexpected. This can be facilitated by ensuring that accurate information is given, that patients and families understand possible outcomes and risks and that information is updated if and when necessary to manage expectations.
Professional support Trusts may wish to consider the availability of professional support for those involved in disclosure. This may take the form of individuals who model good practice within the institution or specific training available in open disclosure. There is little evidence for any particular model of training over another, but given the observed complexity of decision-making in relation to disclosure and disclosure work, opportunities to practise conversations and apply reflexive thinking alongside reflection on real disclosure are likely to provide the most useful approaches. Consider multidisciplinary training and support. Working alongside patient groups and advocates to ensure that such training is also focused on the needs of patients is also likely to be important.
Risk management and systems improvement Patients may have useful insights into systems informed by a unique perspective and as experts in their own care. Viewing the disclosure process as a conversation will allow patients and families to add their views on factors which may have contributed to errors or harms.
Multidisciplinary responsibility Errors are usually systemic in nature, involving a number of team members. There is no evidence to support any particular discipline as being more effective in disclosure. Trusts may consider exploring the use of team disclosure and consulting with patients about the information they require to tailor the best approach and the best team to be involved in the disclosure process.
Clinical governance Try to ensure that the focus of disclosures remains in the realm of quality. Counting and recording disclosures is important but not at the expense of monitoring quality. A more reflective approach to capturing performance of the organisation in relation to disclosure processes is likely to yield more sophisticated insights into quality and help to inform future efforts to improve. Asking individuals how the process met their needs and what could be improved, in the case of both individuals enacting disclosures and families, may be useful.
Confidentiality Try to ensure that issues of confidentiality are not invoked to prevent patients from accessing information or discussions which they need to understand error or harm. Being unable to discuss an error with those directly involved can be a particular frustration for families, for whom this may be part of the process of coming to terms with what has happened to them. Try to support clinicians to be able to talk directly with patients and families.
Continuity of care The focus of open disclosure should be on the care of patients rather than on mitigating organisational risk. Preserving continuity of care by respecting patient choice and consulting with them about what their care preferences are moving forward after an adverse event are likely to contribute to maintaining the patient–provider relationship in the best interests of the patient.
Acknowledgements
The Being Open research team would like to thank all the patients, their family members and representatives, clinicians, policy stakeholders and managers who gave their time and views so generously to inform this project. We would also like to thank all our clinical collaborators, some of whom facilitated our contact with others who took part in the project. Without the support and co-operation of all those involved this project would not have been possible.
We would like to thank the reviewers of this report for their insightful and thoughtful input which has helped us in further shaping our thoughts and presentation of the work undertaken within this project.
We would also like to thank Sally Baker for her valuable contribution in the administrative support for this study and Karen Scott, Head of Information at Capsticks, who supported the searches of the legal literature.
Contributions of authors
Professor Yvonne Birks, Professor of Health and Social Care, was the principal investigator and responsible for conception and design of the study, drafting and revision of the report and supervision.
Dr Reema Harrison, Research Fellow, contributed to data collection, data analysis and drafting of the report.
Ms Kate Bosanquet, Research Fellow, contributed to data collection, data analysis and drafting of the report.
Ms Jill Hall, Research Fellow, contributed to data collection, data analysis and drafting of the report.
Mrs Melissa Harden, Information Specialist, was responsible for the conception and design of search strategies and contributed to revision of the report.
Professor Vikki Entwistle, Professor of Health Services Research and Ethics, contributed to conception and design of the study, interpretation of data and drafting of the report.
Professor Ian Watt, Professor of Primary and Community Care, contributed to conception and design of the study, interpretation of data and revision of the report.
Mr Peter Walsh, Chief Executive of Action Against Medical Accidents, contributed to conception and design of the study and revision of the report.
Mrs Sarah Ronaldson, Research Fellow, contributed to conception and design of the study and revision of the report.
Dr David Roberts, Partner at Capsticks LLP, contributed to conception and design of the study and revision of the report.
Dr Joy Adamson, Senior Lecturer in Epidemiology and Deputy Director of York Trials Unit, contributed to conception and design of the study and revision of the report.
Dr John Wright, Director of the Bradford Institute for Health Research, contributed to conception and design of the study and revision of the report.
Professor Rick Iedema, Professor of Communication, contributed to conception and design of the study, interpretation of data, and drafting and revision of the report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Lyckholm L. Medical errors and medical culture. There is no easy way around taking responsibility for mistakes. BMJ 2001;323. http://dx.doi.org/10.1136/bmj.323.7312.570.
- Baker GR, Norton PG, Flintoft V, Blais R, Brown A, Cox J, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. CMAJ 2004;170:1678-86. http://dx.doi.org/10.1503/cmaj.1040498.
- Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, et al. The nature of adverse events in hospitalized patients. N Engl J Med 1991;324:377-84. http://dx.doi.org/10.1056/NEJM199102073240605.
- Jha AK, Prasopa-Plaizier N, Larizgoitia I, Bates DW. Patient safety research: an overview of the global evidence. Qual Saf Health Care 2010;19:42-4. http://dx.doi.org/10.1136/qshc.2008.029165.
- Equity and Excellence: Liberating the NHS. London: Department of Health; 2010.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Pace WD, Staton EW. Improving the disclosure of medical incidents: A genuine apology is only the first step in the process. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d4340.
- Canadian Patient Safety Institute . Canadian Disclosure Guidelines. Being Open With Patients and Families 2011. www.patientsafetyinstitute.ca/English/toolsResources/disclosure/Documents/CPSI%20Canadian%20Disclosure%20Guidelines.pdf (accessed 2 December 2012).
- New Zealand Health and Disability Commissioner . Guidance on Open Disclosure Policies 2007. www.hdc.org.nz/media/18328/guidance%20on%20open%20disclosure%20policies%20dec%2009.pdf (accessed 2 December 2012).
- Being Open: Communicating Patient Safety Incidents with Patients and their Carers. London: NPSA; 2005.
- Being Open: Communicating Patient Safety Incidents with Patients, their Families and their Carers. London: NPSA; 2009.
- 2011 Comprehensive Accreditation Manual for Hospitals: The Official Handbook. Oakbrook Terrace, IL: Joint Commission Resources Inc.; 2010.
- Open Disclosure Standard: A National Standard for Open Communication in Public and Private Hospitals, Following an Adverse Event in Healthcare. Canberra: Australian Commission on Safety and Quality in Healthcare; 2003.
- Blendon RJ. Common concerns amid diverse systems: health care experiences in five countries. Health Aff 2003;22:106-21. http://dx.doi.org/10.1377/hlthaff.22.3.106.
- Anon . Medicolegal. What should a doctor tell?. Br Med J (Clin Res Ed) 1985;290:780-1. http://dx.doi.org/10.1136/bmj.290.6470.780.
- Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Washington, DC: Institute of Medicine; 1999.
- An Organisation With a Memory. London: Department of Health; 2000.
- Revisions to Joint Commission Standards in Support of Patient Safety and Medical Health Care Error Reduction. Oakbrook, IL: Joint Commission on Accreditation of Health Care Organizations; 2001.
- The National Medical Error Disclosure and Compensation Act. 109th Congress, 1st Session. Washington, DC: Government Printing Office; 2005.
- Mazor KM, Simon SR, Yood RA, Martinson BC, Gunter MJ, Reed GW, et al. Health plan members’ views about disclosure of medical errors. Ann Intern Med 2004;140:409-18. http://dx.doi.org/10.7326/0003-4819-140-6-200403160-00006.
- Witman AB, Park DM, Hardin SB. How do patients want physicians to handle mistakes? A survey of internal medicine patients in an academic setting. Arch Intern Med 1996;156:2565-9. http://dx.doi.org/10.1001/archinte.1996.00440210083008.
- Apologies and Explanations. London: NHSLA; 2009.
- National Patient Safety Agency (NPSA) n.d. www.npsa.nhs.uk (accessed 3 March 2013).
- Iedema RAM, Mallock NA, Sorensen RJ, Manias E, Tuckett AG, Williams AF, et al. The National Open Disclosure Pilot: evaluation of a policy implementation initiative. Med J Aust 2008;188:397-400.
- Iedema R, Sorensen R, Manias E, Tuckett A, Piper D, Mallock N, et al. Patients’ and family members’ experiences of open disclosure following adverse events. Int J Qual Health Care 2008;20:421-32. http://dx.doi.org/10.1093/intqhc/mzn043.
- Iedema R, Jorm C, Wakefield J, Ryan C, Sorensen R. A new structure of attention?: Open disclosure of adverse events to patients and their families. J Lang Soc Psychol 2009;28:139-57. http://dx.doi.org/10.1177/0261927X08330614.
- Iedema R, Allen S, Britton K, Piper D, Baker A, Grbich C, et al. Patients’ and family members’ views on how clinicians enact and how they should enact incident disclosure: the ‘100 patient stories’ qualitative study. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d4423.
- Gallagher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. Patients’ and physicians’ attitudes regarding the disclosure of medical errors. JAMA 2003;289:1001-7. http://dx.doi.org/10.1001/jama.289.8.1001.
- Gallagher TH, Levinson W. Disclosing harmful medical errors to patients: a time for professional action. Arch Intern Med 2005;165:1819-24. http://dx.doi.org/10.1001/archinte.165.16.1819.
- Loren DJ, Klein EJ, Garbutt J, Krauss MJ, Fraser V, Dunagan WC, et al. Medical error disclosure among pediatricians: choosing. Arch Pediatr Adolesc Med 2008;162:922-7. http://dx.doi.org/10.1001/archpedi.162.10.922.
- Manser T, Staender S. Aftermath of an adverse event: supporting health care professionals to meet patient expectations through open disclosure. Acta Anaesthesiol Scand 2005;49:728-34. http://dx.doi.org/10.1111/j.1399-6576.2005.00746.x.
- Boothman RC, Blackwell AC, Campbell DA, Commiskey E, Anderson S. A better approach to medical malpractice claims? The University of Michigan experience. J Health Life Sci Law 2009;2:125-59.
- Iedema R, Jorm C, Wakefield J, Ryan C, Dunn S. Practising open disclosure: clinical incident communication and systems improvement. Sociol Health Illn 2009;31:262-77. http://dx.doi.org/10.1111/j.1467-9566.2008.01131.x.
- Iedema R, Sorensen R, Piper D, Brownhill S. Open Disclosure: A Literature Review. Sydney: Australian Commission on Safety and Quality in Health Care and University of Technology; 2008.
- Piper D, Iedema R. Literature Review: Incident Disclsoure Policy, Legal Reform and Research Since 2008. Sydney: Centre for Health Communication (University of Technology) and Australian Commission on Safety and Quality in Health Care; 2011.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analysing Qualitative Data. London: Routledge; 1994.
- Flick U. An Introduction to Qualitative Research. London: Sage; 2006.
- Kuper A, Lingard L, Levinson W. Critically appraising qualitative research. BMJ 2008;337:687-9. http://dx.doi.org/10.1136/bmj.a1035.
- Watt I, Birks Y, Entwistle V, Gilbody S, Hall J, Mansell P, et al. A Review of Strategies to Promote Patient Involvement, A Study to Explore Patient’s Views and Attitudes and A Pilot Study to Evaluate the Acceptability of Selected Patient Involvement Strategies 2009. www.haps.bham.ac.uk/publichealth/psrp/PS034_Project_Summary.shtml (accessed 30 March 2013).
- Roland M, Rao SR, Sibbald B, Hann M, Harrison S, Walter A, et al. Professional values and reported behaviours of doctors in the USA and UK: quantitative survey. BMJ Qual Saf 2011;20:515-21. http://dx.doi.org/10.1136/bmjqs.2010.048173.
- Scheirton LS. Proportionality and the view from below: analysis of error disclosure. HEC Forum 2008;20:215-41. http://dx.doi.org/10.1007/s10730-008-9073-6.
- Fein SP, Hilborne LH, Spiritus EM, Seymann GB, Keenan CR, Shojania KG, et al. The many faces of error disclosure: a common set of elements and a definition. J Gen Intern Med 2007;22:755-61. http://dx.doi.org/10.1007/s11606-007-0157-9.
- Flemons WW, Davies JM, MacLeod B. Disclosing medical errors. CMAJ 2007;177. http://dx.doi.org/10.1503/cmaj.1070114.
- Canadian Patient Safety Institute . Background Paper for the Development of National Guidelines for the Disclosure of Adverse Events Canada 2006. www.patientsafetyinstitute.ca/English/toolsResources/disclosure/Documents/Background%20Paper%20for%20the%20Canadian%20Disclosure%20Guidelines.pdf (accessed 2 December 2012).
- LeGros N, Pinkall JD. The new JCAHO patient safety standards and the disclosure of unanticipated outcomes. Joint Commission on Accreditation of Healthcare Organizations. J Health Law 2002;35:189-210.
- Lamb RM, Studdert DM, Bohmer RMJ, Berwick DM, Brennan TA. Hospital disclosure practices: results of a national survey. Health Aff 2003;22:73-8. http://dx.doi.org/10.1377/hlthaff.22.2.73.
- Mazor KM, Simon SR, Gurwitz JH. Communicating with patients about medical errors: a review of the literature. Arch Intern Med 2004;164:1690-7. http://dx.doi.org/10.1001/archinte.164.15.1690.
- Wojcieszak D, Banja J, Houk C. The Sorry Works! Coalition: making the case for full disclosure. Jt Comm J Qual Patient Saf 2006;32:344-50.
- Hébert PC, Levin AV, Robertson G. Bioethics for clinicians: 23. Disclosure of medical error. CMAJ 2001;164:509-13.
- Berlinger N. What is meant by telling the truth: Bonhoeffer on the ethics of disclosure. Stud Christ Ethics 2003;16:80-92. http://dx.doi.org/10.1177/095394680301600206.
- Disclosure of Adverse Events to Patients, VHA Directives 2008–002. Washington, DC: Department of Veterans Affairs; 2008.
- Kraman SS, Hamm G. Risk management: extreme honesty may be the best policy. Ann Intern Med 1999;131:963-7. http://dx.doi.org/10.7326/0003-4819-131-12-199912210-00010.
- Matlow A, Stevens P, Harrison C, Laxer R. Achieving closure through disclosure: experience in a pediatric institution. J Pediatr 2004;144:559-60. http://dx.doi.org/10.1016/j.jpeds.2004.01.013.
- Wetzel TG. When errors occur, ‘I’m sorry’ is a big step, but just the first. Hosp Health Netw 2010;84:41-2.
- Bernstein M, Brown B. Doctors’ duty to disclose error: a deontological or Kantian ethical analysis. Can J Neurol Sci 2004;31:169-74.
- Kant I. Practical Philosophy. Cambridge: Cambridge University Press; 1996.
- Mantone J. Clarion call. National forum on patient safety stresses disclosure. Mod Healthc 2005;35.
- Pham JC, Story JL, Hicks RW, Shore AD, Morlock LL, Cheung DS, et al. National study on the frequency, types, causes, and consequences of voluntarily reported emergency department medication errors. J Emerg Med 2011;40:485-92. http://dx.doi.org/10.1016/j.jemermed.2008.02.059.
- Linthorst GE, Kallimanis-King BL, Douwes Dekker I, Hoekstra JBL, de Haes JCJM. What contributes to internists’ willingness to disclose medical errors?. Neth J Med 2012;70:242-8.
- López L, Weissman JS, Schneider EC, Weingart SN, Cohen AP, Epstein AM. Disclosure of hospital adverse events and its association with patients’ ratings of the quality of care. Arch Intern Med 2009;169:1888-94. http://dx.doi.org/10.1001/archinternmed.2009.387.
- Loren DJ, Klein EJ, Garbutt J, Krauss MJ, Fraser V, Dunagan WC, et al. Medical error disclosure among pediatricians: choosing carefully what we might say to parents. Arch Pediatr Adolesc Med 2008;162:922-7. http://dx.doi.org/10.1001/archpedi.162.10.922.
- White SM, Deacy N, Sudan S. Trainee anaesthetists’ attitudes to error, safety and the law. Eur J Anaesthesiol 2009;26:463-8. http://dx.doi.org/10.1097/EJA.0b013e328324b6d1.
- Kroll L, Singleton A, Collier J, Rees Jones I. Learning not to take it seriously: junior doctors’ accounts of error. Med Educ 2008;42:982-90. http://dx.doi.org/10.1111/j.1365-2923.2008.03151.x.
- Gallagher TH, Lucas MH. Should we disclose harmful medical errors to patients? If so, how?. J Clin Outcomes Manag 2005;12:253-9.
- Leape LL, Berwick DM. Five years after To Err Is Human: what have we learned?. JAMA 2005;293:2384-90. http://dx.doi.org/10.1001/jama.293.19.2384.
- Martinez W, Lo B. Medical students’ experiences with medical errors: an analysis of medical student essays. Med Educ 2008;42:733-41. http://dx.doi.org/10.1111/j.1365-2923.2008.03109.x.
- Gallagher TH, Garbutt JM, Waterman AD, Flum DR, Larson EB, Waterman BM, et al. Choosing your words carefully: how physicians would disclose harmful medical errors to patients. Arch Intern Med 2006;166:1585-93. http://dx.doi.org/10.1001/archinte.166.15.1585.
- Garbutt J, Brownstein DR, Klein EJ, Waterman A, Krauss MJ, Marcuse EK, et al. Reporting and disclosing medical errors: pediatricians’ attitudes and behaviors. Arch Pediatr Adolesc Med 2007;161:179-85. http://dx.doi.org/10.1001/archpedi.161.2.179.
- Levinson W. Disclosing medical errors to patients: a challenge for health care professionals and institutions. Patient Educ Couns 2009;76:296-9. http://dx.doi.org/10.1016/j.pec.2009.07.018.
- Wei M. Doctors, apologies, and the law: an analysis and critique of apology laws. J Health Law 2007;40:107-59.
- Gallagher TH, Waterman AD, Garbutt JM, Kapp JM, Chan DK, Dunagan WC, et al. US and Canadian physicians’ attitudes and experiences regarding disclosing errors to patients. Arch Intern Med 2006;166:1605-11. http://dx.doi.org/10.1001/archinte.166.15.1605.
- Kaldjian LC, Jones EW, Wu BJ, Forman-Hoffman VL, Levi BH, Rosenthal GE. Reporting medical errors to improve patient safety: a survey of physicians in teaching hospitals. Arch Intern Med 2008;168:40-6. http://dx.doi.org/10.1001/archinternmed.2007.12.
- Stroud L, McIlroy J, Levinson W. Skills of internal medicine residents in disclosing medical errors: a study using standardized patients. Acad Med 2009;84:1803-8. http://dx.doi.org/10.1097/ACM.0b013e3181bf9fef.
- Chan DK, Gallagher TH, Reznick R, Levinson W. How surgeons disclose medical errors to patients: a study using standardized patients. Surgery 2005;138:851-8. http://dx.doi.org/10.1016/j.surg.2005.04.015.
- Studdert DM, Brennan TA. No-fault compensation for medical injuries: the prospect for error prevention. JAMA 2001;286:217-23. http://dx.doi.org/10.1001/jama.286.2.217.
- Rosner F, Berger JT, Kark P, Potash J, Bennett AJ. Disclosure and prevention of medical errors. Committee on Bioethical Issues of the Medical Society of the State of New York. Arch Intern Med 2000;160:2089-92. http://dx.doi.org/10.1001/archinte.160.14.2089.
- Cohen JR. Future research on disclosure of medical errors. Ann Intern Med 2004;141. http://dx.doi.org/10.7326/0003-4819-141-6-200409210-00017.
- Allan A, McKillop D. The health implications of apologizing after an adverse event. Int J Qual Health Care 2010;22:126-31. http://dx.doi.org/10.1093/intqhc/mzq001.
- Studdert DM, Piper D, Iedema R. Legal aspects of open disclosure II: attitudes of health professionals – findings from a national survey. Med J Aust 2010;193:351-5.
- Lazare A. Apology in medical practice: an emerging clinical skill. JAMA 2006;296:1401-4. http://dx.doi.org/10.1001/jama.296.11.1401.
- Zammit R. How to say you are sorry: a guide to the background and risks of apology legislation. Masters Abstr 2009;48.
- Massó Guijarro P, Aranaz Andrés JM, Mira JJ, Perdiguero E, Aibar C. Adverse events in hospitals: the patient’s point of view. Qual Saf Health Care 2010;19:144-7. http://dx.doi.org/10.1136/qshc.2007.025585.
- Hobgood C, Peck CR, Gilbert B, Chappell K, Zou B. Medical errors – what and when: what do patients want to know?. Acad Emerg Med 2002;9:1156-61.
- Kooienga S, Stewart VT. Putting a face on medical errors: a patient perspective. J Healthc Qual 2011;33:37-41. http://dx.doi.org/10.1111/j.1945-1474.2010.00121.x.
- Duclos CW, Eichler M, Taylor L, Quintela J, Main DS, Pace W, et al. Patient perspectives of patient–provider communication after adverse events. Int J Qual Health Care 2005;17:479-86. http://dx.doi.org/10.1093/intqhc/mzi065.
- Mazor KM, Greene SM, Roblin D, Lemay CA, Firneno CL, Calvi J, et al. More than words: patients’ views on apology and disclosure when things go wrong in cancer care. Patient Educ Couns 2013;90:341-6. http://dx.doi.org/10.1016/j.pec.2011.07.010.
- Okamoto S, Kawahara K, Algren M. Transformative possibilities of communication in medical error cases in Japan. Int J Qual Health Care 2011;23:26-35. http://dx.doi.org/10.1093/intqhc/mzq064.
- Schwappach DLB, Koeck CM. What makes an error unacceptable? A factorial survey on the disclosure of medical errors. Int J Qual Health Care n.d.;16:317-26. http://dx.doi.org/10.1093/intqhc/mzh058.
- Micalizzi DA. The aftermath of a ‘never event’. A child’s unexplained death and a system seemingly designed to thwart justice. Mod Healthc 2008;38:24-5.
- Vincent CA, Pincus T, Scurr JH. Patients’ experience of surgical accidents. Qual Health Care 1993;2:77-82. http://dx.doi.org/10.1136/qshc.2.2.77.
- Lamb R. Open disclosure: the only approach to medical error. Qual Saf Health Care 2004;13:3-5. http://dx.doi.org/10.1136/qshc.2003.008631.
- Sheridan S, Conrad N, King S, Dingman J, Denham CR. Disclosure through our eyes. J Patient Saf 2008;4:18-26. http://dx.doi.org/10.1097/PTS.0b013e31816543cc.
- Medical Defence Union (MDU) n.d. www.themdu.com (accessed 30 April 2013).
- The Compensation Act 2006. London: The Stationery Office; 2006.
- Good Medical Practice. London: General Medical Council; 2001.
- Holden J. Apologies and legal liability. Saying sorry is not the same as admitting legal liability. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b520.
- Leape LL. Apology for errors: whose responsibility?. Front Health Serv Manage 2012;28:3-12.
- Keller DR, Bell CL, Dottl SK. An effective curriculum for teaching third-year medical students about medical errors and disclosure. WMJ 2009;108:27-9.
- Wagner LM, Harkness K, Hébert PC, Gallagher TH. Nurses’ perceptions of error reporting and disclosure in nursing homes. J Nurs Care Qual 2012;27:63-9. http://dx.doi.org/10.1097/NCQ.0b013e318232c0bc.
- Shannon SE, Foglia MB, Hardy M, Gallagher TH. Disclosing errors to patients: perspectives of registered nurses. Jt Comm J Qual Patient Saf 2009;35:5-12.
- Fein S, Hilborne L, Kagawa-Singer M, Spiritus E, Keenan C. Conceptual Model for Disclosure of Medical Errors. Rockville, MD: Agency for Healthcare Research and Quality; 2005.
- Duke MB, Wilson JF. Responding to medical error: factors that influence the likelihood of disclosure by medical residents. J Investig Med 2007;55.
- Dunavan CP. Los Angeles Times – Southern California Edition. 2006.
- Ofri D. Ashamed to admit it: owning up to medical error. Health Aff 2010;29:1549-51. http://dx.doi.org/10.1377/hlthaff.2009.0946.
- Singer PA. Commentary: learning to love mistakes. BMJ 2001;322.
- Wu AW. Commentary: doctors are obliged to be honest with their patients. BMJ 2001;322:1238-9.
- Robinson J. Consumer comments: A duty of candour: will it really make amends?. Br J Midwifery 2003;11.
- Donaldson LJ. Put the patient in the room, always. Qual Saf Health Care 2008;17:82-3. http://dx.doi.org/10.1136/qshc.2007.025262.
- Allen S. Story telling an innovation to improve healthcare incident disclosure. Women Birth 2011;24. http://dx.doi.org/10.1016/j.wombi.2011.07.081.
- Calvert JF, Hollander-Rodriguez J, Atlas M, Johnson KE. Clinical inquiries. What are the repercussions of disclosing a medical error?. J Fam Pract 2008;57:124-5.
- López L, Cohen AP, Schneider EC, Weingart SN, Epstein AM, Weissman J. Predictors of disclosure of hospital adverse events and its impact on patient’s quality ratings. J Gen Intern Med 2008;23:374-5. http://dx.doi.org/10.1001/archinternmed.2009.387.
- Mazor KM. Understanding patients’ perceptions of medical errors. J Commun Healthc 2009;2:34-46. http://dx.doi.org/10.1179/cih.2009.2.1.34.
- Mazor KM, Reed GW, Yood RA, Fischer MA, Baril J, Gurwitz JH. Disclosure of medical errors: what factors influence how patients respond?. J Gen Intern Med 2006;21:704-10. http://dx.doi.org/10.1111/j.1525-1497.2006.00465.x.
- Buckley J. Open Disclosure and Medical Claims Study n.d. www.cf.nlm.nih.gov/hsr_project/view_hsrproj_record.cfm?PROGRAM_CAME=search_fields.cfm&NLMUNIQUE_ID=20104205&SEARCH_FOR=20104205 (accessed 2 December 2012).
- Wu AW. Handling hospital errors: is disclosure the best defense?. Ann Intern Med 1999;131:970-2. http://dx.doi.org/10.7326/0003-4819-131-12-199912210-00012.
- Hall MA. Law, medicine, and trust. J Nurs Law 2003;9:33-84.
- Kachalia A, Shojania KG, Hofer TP, Piotrowski M, Saint S. Does full disclosure of medical errors affect malpractice liability? The jury is still out. Jt Comm J Qual Patient Saf 2003;29:503-11.
- Hobgood C, Tamayo-Sarver JH, Elms A, Weiner B. Parental preferences for error disclosure, reporting, and legal action after medical error in the care of their children. Pediatrics 2005;116:1276-86. http://dx.doi.org/10.1542/peds.2005-0946.
- Murtagh L, Gallagher TH, Andrew P, Mello MM. Disclosure-and-resolution programs that include generous compensation offers may prompt a complex patient response. Health Aff 2012;31:2681-9. http://dx.doi.org/10.1377/hlthaff.2012.0185.
- Mitka M. Disclosing medical errors does not mean greater liability costs, new study finds. JAMA 2010;304:1656-7. http://dx.doi.org/10.1001/jama.2010.1422.
- Malcolm L, Barnett P. Disclosure of treatment injury in New Zealand’s no-fault compensation system. Aust Health Rev 2007;31:116-22. http://dx.doi.org/10.1071/AH070116.
- Cunningham W. The immediate and long-term impact on New Zealand doctors who receive patient complaints. N Z Med J 2004;117.
- Teninbaum GH. Saying ‘sorry’; isn’t enough. Health Aff 2010;29. http://dx.doi.org/10.1377/hlthaff.2010.0992.
- Robbennolt JK. Apologies and legal settlement: an empirical examination. Mich Law Rev 2003;102:460-516. http://dx.doi.org/10.2307/3595367.
- Disclosing Medical Errors: A Guide to an Effective Explanation and Apology. Oak Park, IL: Joint Commission Resources; 2007.
- Wojcieszak D, Saxton JW, Finkelstein MM. Ethics training needs to emphasize disclosure and apology. HEC Forum 2008;20:291-305. http://dx.doi.org/10.1007/s10730-008-9077-2.
- Sorry Works! Coalition . States With Apology Laws 2008. www.sorryworks.net (accessed 13 March 2013).
- Butcher L. Lawyers say ‘sorry’ may sink you in court. Physician Exec 2006;32:20-4.
- Slovenko R. Saying you’re sorry in a litigious society. Med Law 1992;11:669-71.
- Slovenko R. Admission or Apology in Liability Prevention n.d.
- Mlott K. Don’t say you’re sorry: surviving a lawsuit by Jay Weaver in the September issue. EMS Magazine 2007.
- Robbennolt JK. Apologies and medical error. Clin Orthop Relat Res 2009;467:376-82. http://dx.doi.org/10.1007/s11999-008-0580-1.
- Dresser R. The limits of apology laws. Hastings Cent Rep 2008;38:6-7. http://dx.doi.org/10.1353/hcr.0.0015.
- Bailey TM, Robertson EC, Hegedus G. Erecting legal barriers: new apology laws in Canada and the patient safety movement: useful legislation or a misguided approach?. Health Law Can 2007;28:33-8.
- MacDonald N, Attaran A. Medical errors, apologies and apology laws. CMAJ 2009;180. http://dx.doi.org/10.1503/cmaj.081997.
- Miller LA. Apology, disclosure, and unanticipated outcomes. J Perinat Neonatal Nurs n.d.;25:10-1. http://dx.doi.org/10.1097/JPN.0b013e3182076850.
- Loren DJ, Garbutt J, Dunagan WC, Bommarito KM, Ebers AG, Levinson W, et al. Risk managers, physicians, and disclosure of harmful medical errors. Jt Comm J Qual Patient Saf 2010;36:101-8.
- O’Connell D. Apology laws. CMAJ 2009;180. http://dx.doi.org/10.1503/cmaj.1090007.
- Woods MS. Commentary: Let’s start admitting our mistakes. Clin Advis Nurse Pract 2008;11.
- O’Connell D, Reifsteck SW. Disclosing unexpected outcomes and medical error. J Med Pract Manage 2004;19:317-23.
- Renwick KK. Should doctors disclose mistakes?. West J Med 2000;172. http://dx.doi.org/10.1136/ewjm.172.1.10-a.
- Liang BA. A system of medical error disclosure. BMJ Qual Saf 2002;11:64-8. http://dx.doi.org/10.1136/qhc.11.1.64.
- Liang BA, Coulson KM. Legal issues in performing patient safety work. Nurs Econ 2002;20:118-25.
- Sorensen R, Iedema R, Piper D, Manias E, Williams A, Tuckett A. Health care professionals’ views of implementing a policy of open disclosure of errors. J Health Serv Res Policy 2008;13:227-32. http://dx.doi.org/10.1258/jhsrp.2008.008062.
- Walshe K, Shortell SM. When things go wrong: how health care organizations deal with major failures. Health Aff (Millwood) 2004;23:103-11. http://dx.doi.org/10.1377/hlthaff.23.3.103.
- Sorensen R, Iedema R, Piper D, Manias E, Williams A, Tuckett A. Disclosing clinical adverse events to patients: can practice inform policy?. Health Expect 2010;13:148-59. http://dx.doi.org/10.1111/j.1369-7625.2009.00569.x.
- Pinto A, Faiz O, Vincent C. Managing the after effects of serious patient safety incidents in the NHS: an online survey study. BMJ Qual Saf 2012;21:1001-8. http://dx.doi.org/10.1136/bmjqs-2012-000826.
- Manser T. Managing the aftermath of critical incidents: meeting the needs of health-care providers and patients. Best Pract Res Clin Anaesthesiol 2011;25:169-79. http://dx.doi.org/10.1016/j.bpa.2011.02.004.
- Porto GG. Disclosure of medical error: facts and fallacies. J Healthc Risk Manag 2001;21:67-76. http://dx.doi.org/10.1002/jhrm.5600210411.
- Anon . MN hospital creates a culture of full disclosure. Healthc Risk Manag 2005;27:53-5.
- Shapiro E. Disclosing medical errors: best practices from the ‘leading edge’: part I. Care Manage 2008;14:14-8.
- Shapiro E. Disclosing medical errors: best practices from the ‘leading edge’: part II. Care Manage 2008;14:11-7.
- Boothman RC. Apologies and a strong defense at the University of Michigan Health System. Physician Exec 2006;3:7-10.
- Droppo L. Trillium Health Centre’s journey to disclosure. Healthc Q 2005;8:151-6. http://dx.doi.org/10.12927/hcq. 17682.
- Ott M. Key considerations on drafting a policy on disclosure of unanticipated outcomes. J Healthc Risk Manag 2001;21:27-34. http://dx.doi.org/10.1002/jhrm.5600210406.
- Quinn RE, Eichler MC. The 3Rs program: the Colorado experience. Clin Obstet Gynecol 2008;51:709-18. http://dx.doi.org/10.1097/GRF.0b013e3181899cc2.
- Powell SK. When things go wrong: responding to adverse events: a consensus statement of the Harvard hospitals. Lippincotts Case Manag 2006;11:193-4. http://dx.doi.org/10.1097/00129234-200607000-00001.
- Sullivan RP, Waldemayer CR, Bunting RF. Building confidence into communication of bad news: the role of the patient advocate. J Healthc Risk Manag 2010;29:33-7. http://dx.doi.org/10.1002/jhrm.20032.
- Liebman CB, Hyman CS. A mediation skills model to manage disclosure of errors and adverse events to patients. Health Aff 2004;23:22-3. http://dx.doi.org/10.1377/hlthaff.23.4.22.
- McDonald TB, Helmchen LA, Smith KM, Centomani N, Gunderson A, Mayer D, et al. Responding to patient safety incidents: the ‘seven pillars’. BMJ Qual Saf 2010;19. http://dx.doi.org/10.1136/qshc.2008.031633.
- Scholefield H. Embedding quality improvement and patient safety at Liverpool Women’s NHS Foundation Trust. Best Pract Res Clin Obstet Gynaecol 2007;21:593-607. http://dx.doi.org/10.1016/j.bpobgyn.2007.02.005.
- Parker M. A fair dinkum duty of open disclosure following medical error. J Law Med 2012;20:35-43.
- Conway JB, Nathan DG, Benz EJ, Shulman LN, Sallan SE, Ponte PR, et al. Key Learning from the Dana-Farber Cancer Institute’s 10-Year Patient Safety Journey n.d.
- Australian Commission on Safety and Quality . Open Disclosure Resources and Supporting Materials n.d. www.safetyandquality.gov.au/our-work/open-disclosure/open-disclosure-resources-and-supporting-materials (accessed 10 November 2012).
- Berry M. Legally speaking. Saying the right thing when things go wrong. RN 2004;67:59-61.
- Iedema R. Attitudes toward error disclosure need to engage with systems thinking. Jt Comm J Qual Patient Saf 2010;36:99-100.
- Saxton JW, Finkelstein MM. Adverse event management: your evidence to decrease professional liability risk. J Med Pract Manage 2008;24:5-8.
- Katsuhara Y. What moral requirements cause ethical dilemmas among nurse executives?. Jpn J Nurs Sci 2005;2:57-65. http://dx.doi.org/10.1111/j.1742-7924.2005.00028.x.
- Luk LA, Ng WIM, Ko KKS, Ung VH. Nursing management of medication errors. Nurs Ethics 2008;15:28-39. http://dx.doi.org/10.1177/0969733007083932.
- Armstrong D. The power of apology: how saying sorry can leave both patients and nurses feeling better. Nurs Times 2009;105:16-9.
- Steefel L. To tell the truth – or not?. Nursing Spectrum 2002;3:8-9.
- Hobgood C, Weiner B, Tamayo-Sarver JH. Medical error identification, disclosure, and reporting: do emergency medicine provider groups differ?. Acad Emerg Med 2006;13:443-51. http://dx.doi.org/10.1111/j.1553-2712.2006.tb00324.x.
- Hobgood C, Xie J, Weiner B, Hooker J. Error identification, disclosure, and reporting: practice patterns of three emergency medicine provider types. Acad Emerg Med 2004;11:196-9. http://dx.doi.org/10.1197/j.aem.2003.08.020.
- Jeffs L, Espin S, Rorabeck L, Shannon SE, Robins L, Levinson W, et al. Not overstepping professional boundaries: the challenging role of nurses in simulated error disclosures. J Nurs Care Qual 2011;26:320-7.
- Jeffs L, Espin S, Shannon SE, Levinson W, Kohn MK, Lingard L. A new way of relating: perceptions associated with a team-based error disclosure simulation intervention. BMJ Qual Saf 2010;19:i57-60. http://dx.doi.org/10.1136/qshc.2009.036418.
- De Freitas GF, Hoga LAK, Fernandes MDP, González JS, Ruiz MCS, Bonini BB. Brazilian registered nurses’ perceptions and attitudes towards adverse events in nursing care: a phenomenological study. J Nurs Manag 2011;19:331-8. http://dx.doi.org/10.1111/j.1365-2834.2011.01208.x.
- Al-Hashemi J. The role of the advanced scrub practitioner. J Perioper Pract 2007;17:76-80.
- Nicklin W, Mass H, Affonso DD, O’Connor P, Ferguson-Paré M, Jeffs L, et al. Patient safety culture and leadership within Canada’s Academic Health Science Centres: towards the development of a collaborative position paper. Nurs Leadersh 2004;17:22-34. http://dx.doi.org/10.12927/cjnl.2004.16243.
- Patient Safety Standards. Patient Safety and Medical/Health Care Error Reduction Standards. Oakbrook Terrace, IL: Joint Commission for Accreditation of Healthcare Organizations; 2001.
- Peterkin A. Guidelines covering disclosure of errors now in place at Montreal Hospital. CMAJ 1990;142:984-5.
- Morath J, Hart LG. Partnering with families: disclosure and trust. National Patient Safety Foundation/JCAHO Patient Safety Initiative 2000: Spotlighting Strategies, Sharing Solutions. Chicago, IL; 2000.
- Boothman RC, Imhoff SJ, Campbell DA. Nurturing a culture of patient safety and achieving lower malpractice risk through disclosure: lessons learned and future directions. Front Health Serv Manage 2012;28:13-28.
- Kraman SS, Hamm G. Bad modeling?. Health Aff 2007;26. http://dx.doi.org/10.1377/hlthaff.26.3.903.
- Canadian Patient Safety Institute . The Impact of Disclosure of Adverse Events on Litigation and Settlement: A Review for the Canadian Patient Safety Institute 2007. www.patientsafetyinstitute.ca/English/toolsResources/disclosure/Documents/The%20Impact%20of%20Disclosure%20on%20Litigation%20a%20Review%20for%20the%20CPSI.pdf (accessed 2 December 2012).
- Liang BA. The adverse event of unaddressed medical error: identifying and filling the holes in the health-care and legal systems. J Law Med Ethics 2001;29:346-68. http://dx.doi.org/10.1111/j.1748-720X.2001.tb00353.x.
- Ranke BA, Moriarty MP. An overview of professional liability in occupational therapy. Am J Occup Ther 1997;51:671-80. http://dx.doi.org/10.5014/ajot.51.8.671.
- Kapp MB. Legal anxieties and medical mistakes: barriers and pretexts. J Gen Intern Med 1997;12:787-8. http://dx.doi.org/10.1046/j.1525-1497.1997.07167.x.
- Woolf L. Clinical negligence: what is the solution? How can we provide justice for doctors and patients?. Med Law Int 2000;4:133-44. http://dx.doi.org/10.1177/096853320000400204.
- Barach P. The end of the beginning: lessons learned from the patient safety movement. J Leg Med 2003;24:7-27. http://dx.doi.org/10.1080/713832128.
- DerGurahian J. When sorry is enough. Study finds owning up to mistakes better approach. Mod Healthc 2009;39.
- Studdert DM, Mello MM, Gawande AA, Brennan TA, Wang YC. Disclosure of medical injury to patients: an improbable risk management strategy. Health Aff 2007;26:215-26. http://dx.doi.org/10.1377/hlthaff.26.1.215.
- Kraman SS, Cranfill L, Hamm G, Woodard T. John M. Eisenberg Patient Safety Awards. Advocacy: the Lexington Veterans Affairs Medical Center. Jt Comm J Qual Improv 2002;28:646-50.
- Wu AW, Cavanaugh TA, McPhee SJ, Lo B, Micco GP. To tell the truth: ethical and practical issues in disclosing medical mistakes to patients. J Gen Intern Med 1997;12:770-5. http://dx.doi.org/10.1046/j.1525-1497.1997.07163.x.
- Hickson GB, Clayton EW, Githens PB, Sloan FA. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA 1992;287:1359-63. http://dx.doi.org/10.1001/jama.1992.03480100065032.
- Medical Protection Society . A Culture of Openness: The MPS Perspective 2011. www.medicalprotection.org/uk/booklets/a-culture-of-openness (accessed 13 March 2013).
- Ritchie JH, Davies SC. Professional negligence: a duty of candid disclosure?. BMJ 1995;310:888-9. http://dx.doi.org/10.1136/bmj.310.6984.888.
- Woffen T. Patient safety and legal challenges: disclosure of medical error, class actions, and reporting systems. Masters Abstr 2008;47.
- A Consultation on Strengthening the NHS Constitution. London: Department of Health; 2012.
- Lintern S. Duty of candour will cost NHS £130m in 10 years. Health Serv J 2012. http://www.hsj.co.uk/news/duty-of-candour-will-cost-nhs-130m-in-10-years/5052712.article#.U6KKWvidXTo (accessed 19 June 2014).
- A Promise to Learn – A Commitment to Act. London: Department of Health; 2013.
- Limb M. Peers’ rejection of statutory duty of candour is a missed opportunity, say campaigners. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e1116.
- Koh THHG, Alcock G. Open disclosure: appropriate timing is crucial. Int J Qual Health Care 2007;19. http://dx.doi.org/10.1093/intqhc/mzm036.
- Amori G, Popp PL. The timing of early resolution: working at the patient’s pace. J Healthc Risk Manag 2007;27:19-23. http://dx.doi.org/10.1002/jhrm.5600270305.
- Gallagher TH, Wu AW, Iedema R, Levinson W. Disclosing Unanticipated Outcomes to Patients: International Trends and Norms. Seattle, WA: University of Washington; 2009.
- Gunderson AJ, Smith KM, Mayer DB, McDonald T, Centomani N. Teaching medical students the art of medical error full disclosure: evaluation of a new curriculum. Teach Learn Med 2009;21:229-32. http://dx.doi.org/10.1080/10401330903018526.
- Gunderson A, Tekian A, Mayer D. Teaching interprofessional health science students medical error disclosure. Med Educ 2008;42:531-2. http://dx.doi.org/10.1111/j.1365-2923.2008.03050.x.
- Halbach JL, Sullivan LL. Teaching medical students about medical errors and patient safety: evaluation of a required curriculum. Acad Med 2005;80:600-6. http://dx.doi.org/10.1097/00001888-200506000-00016.
- Kachalia A, Kaufman SR, Boothman R, Anderson S, Welch K, Saint S, et al. Liability claims and costs before and after implementation of a medical error disclosure program. Ann Intern Med 2010;153:213-21. http://dx.doi.org/10.7326/0003-4819-153-4-201008170-00002.
- Kiersma ME, Darbishire PL, Plake KS, Oswald C, Walters BM. Laboratory session to improve first-year pharmacy students’ knowledge and confidence concerning the prevention of medication errors. Am J Pharm Educ 2009;73:1-8. http://dx.doi.org/10.5688/aj730699.
- Madigosky WS, Headrick LA, Nelson K, Cox KR, Anderson T. Changing and sustaining medical students’ knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med 2006;81:94-101. http://dx.doi.org/10.1097/00001888-200601000-00022.
- Moskowitz E, Veloski JJ, Fields SK, Nash DB. Development and evaluation of a 1-day interclerkship program for medical students on medical errors and patient safety. Am J Med Qual 2007;22:13-7. http://dx.doi.org/10.1177/1062860606296669.
- Paxton JH, Rubinfeld IS. Medical errors education: a prospective study of a new educational tool. Am J Med Qual 2010;25:135-42. http://dx.doi.org/10.1177/1062860609353345.
- Posner G, Nakajima A. Assessing residents’ communication skills: disclosure of an adverse event to a standardized patient. J Obstet Gynaecol Can 2011;33:262-8.
- Wayman KI, Yaeger KA, Sharek PJ, Trotter S, Wise L, Flora JA, et al. Simulation-based medical error disclosure training for pediatric healthcare professionals. J Healthc Qual 2007;29:12-9. http://dx.doi.org/10.1111/j.1945-1474.2007.tb00200.x.
- Benedetti DJ, Gallagher T. Evaluating disclosure and offer programs to enhance the response to medical injuries. J Investig Med 2009;57:118-19.
- Gallagher TH. Enhancing the Disclosure of Medical Errors to Patients n.d.
- Gallagher TH. Using Team Simulation to Improve Error Disclosure to Patients and Safety Culture n.d.
- Stewart VT. Putting a Face on Hospital Medical Errors n.d.
- Gallagher TH. Training Doctors to Disclose Unanticipated Outcomes to Patients: Randomized Trial n.d.
- Barrios L, Tsuda S, Derevianko A, Barnett S, Moorman D, Cao CL, et al. Framing family conversation after early diagnosis of iatrogenic injury and incidental findings. Surg Endosc 2009;23:2535-42. http://dx.doi.org/10.1007/s00464-009-0450-2.
- Bell SK, Moorman DW, Delbanco T. Improving the patient, family, and clinician experience after harmful events: the ‘when things go wrong’ curriculum. Acad Med 2010;85:1010-17. http://dx.doi.org/10.1097/ACM.0b013e3181dbedd7.
- Daud-Gallotti RM, Morinaga CV, Arlindo-Rodrigues M, Velasco IT, Martins MA, Tiberio IC. A new method for the assessment of patient safety competencies during a medical school clerkship using an objective structured clinical examination. Clinics (Sao Paulo) 2011;66:1209-15. http://dx.doi.org/10.1590/S1807-59322011000700015.
- Gillies RA, Speers SH, Young SE, Fly CA. Teaching medical error apologies: development of a multi-component intervention. Fam Med 2011;43:400-6.
- Hannawa AF. When the Truth Hurts: Toward a Validation of the Physician Mistake Disclosure (PMD) Model 2009;70.
- Kim S, Brock D, Prouty CD, Odegard PS, Shannon SE, Robins L, et al. A web-based team-oriented medical error communication assessment tool: development, preliminary reliability, validity, and user ratings. Teach Learn Med 2011;23:68-77. http://dx.doi.org/10.1080/10401334.2011.536896.
- Wu AW, Huang IC, Stokes S, Pronovost PJ, Wu AW, Huang IC, et al. Disclosing medical errors to patients: it’s not what you say, it’s what they hear. J Gen Intern Med 2009;24:1012-17. http://dx.doi.org/10.1007/s11606-009-1044-3.
- Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 2006;355:2725-32. http://dx.doi.org/10.1056/NEJMoa061115.
- Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat A-HS, Dellinger EP, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009;360:491-9. http://dx.doi.org/10.1056/NEJMsa0810119.
- Shekelle PG, Pronovost PJ, Wachter RM, McDonald KM, Schoelles K, Dy SM, et al. The top patient safety strategies that can be encouraged for adoption now. Ann Intern Med 2013;158:365-8. http://dx.doi.org/10.7326/0003-4819-158-5-201303051-00001.
- Landrigan CP, Parry GJ, Bones CB, Hackbarth AD, Goldmann DA, Sharek PJ. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med 2010;363:2124-34. http://dx.doi.org/10.1056/NEJMsa1004404.
- Anon . MPs: make disclosing errors a duty. Nurs Times 2010;106.
- Brahams D. GMC’s sifting and investigation of complaints must be ‘transparent’. Lancet 2000;356. http://dx.doi.org/10.1016/S0140-6736(05)73164-0.
- Anon . Disclosure gap is apparent with docs. Healthc Risk Manag 2005;27:138-9.
- Iedema R. Creating safety by strengthening clinicians’ capacity for reflexivity. BMJ Qual Saf 2011;20:i83-6. http://dx.doi.org/10.1136/bmjqs.2010.046714.
- Sirriyeh R, Lawton R, Gardner P, Armitage G. Coping with medical error: the case of the health professional. A systematic review of papers to assess the impact of involvement in medical errors on healthcare professionals’ psychological well being. Qual Saf Health Care 2010;19:1-8.
- Entwistle VA, McCaughan D, Watt IS, Birks Y, Hall J, Peat M, et al. Speaking up about safety concerns: multi-setting qualitative study of patients’ views and experiences. Qual Saf Health Care 2010;19. http://dx.doi.org/10.1136/qshc.2009.039743.
- Checkland K, Harrison S, Snow S, Mcdermott I, Coleman A. Commissioning in the English National Health Service: what’s the problem?. J Soc Policy 2012;41:533-50. http://dx.doi.org/10.1017/S0047279412000232.
- Plsek PE, Greenhalgh T. The challenge of complexity in health care. BMJ 2001;323:625-8. http://dx.doi.org/10.1136/bmj.323.7313.625.
- Plsek PE, Wilson T. Complexity, leadership, and management in healthcare organisations. BMJ 2001;323:746-9. http://dx.doi.org/10.1136/bmj.323.7315.746.
- Best A, Greenhalgh T, Lewis S, Saul JE, Carroll S, Bitz J. Large-system transformation in health care: a realist review. Milbank Q 2012;90:421-56. http://dx.doi.org/10.1111/j.1468-0009.2012.00670.x.
- Best A, Holmes B. Systems thinking, knowledge and action: towards better models and methods. Evid Policy 2010;6:145-59. http://dx.doi.org/10.1332/174426410X502284.
- Lanham HJ, McDaniel RR, Crabtree BF, Miller WL, Stange KC, Nutting PA. How improving practice relationships among clinicians and nonclinicians can improve quality in primary care. Jt Comm J Qual Patient Saf 2009;35:457-66.
- Taylor SL, Dy S, Foy R, Hempel S, McDonald KM, Øvretveit J, et al. What context features might be important determinants of the effectiveness of patient safety practice interventions?. BMJ Qual Saf 2011;20:611-17. http://dx.doi.org/10.1136/bmjqs.2010.049379.
- Øvretveit JC, Shekelle PG, Dy SM, McDonald KM, Hempel S, Pronovost P, et al. How does context affect interventions to improve patient safety? An assessment of evidence from studies of five patient safety practices and proposals for research. BMJ Qual Saf 2011;20:604-10. http://dx.doi.org/10.1136/bmjqs.2010.047035.
- Shale S. Moral Leadership in Medicine: Building Ethical Healthcare Organizations. Cambridge: Cambridge University Press; 2011.
- Farley DO, Battles JB. Evaluation of the AHRQ patient safety initiative: framework and approach. Health Serv Res 2009;44:628-45. http://dx.doi.org/10.1111/j.1475-6773.2008.00931.x.
- Dingwall R, Daly J, MacDonald I, Willis E. Researching Health Care: Designs, Dilemmas, Disciplines. London: Tavistock/Routledge; 1992.
- Mauthner NS, Doucet A. ‘Knowledge once divided can be hard to put together again’: an epistemological critique of collaborative and team-based research practices. Sociology 2008;42:971-85. http://dx.doi.org/10.1177/0038038508094574.
Appendix 1 Sampling strategy for qualitative interviews
| Group | Recruitment strategy | Recruitment for individual interviews and/or focus groups | Sampling notes |
|---|---|---|---|
| Senior managers (n = 10) | Participants recruited from local trusts. Targeted written explanations with an invitation to be interviewed | Individual interviews only. Afocus group of these senior figures likely to be impractical | Senior-level managers in secondary and primary care including chief executives, medical directors and directors of nursing and midwifery |
| NHS litigation (n = 5) | Individual interviews only. Afocus group of these senior figures likely to be impractical | Authority and key senior figures in NHS litigation (as identified by DR from the team) | |
| Professional bodies (n = 10 maximum) | Targeted written explanations with an invitation to be interviewed. Start with board members and key contacts identified by the team. Senior colleagues may suggest someone to take part | Participants will be invited for interview. The practicalities of a focus group will be explored and pursued as practical | BMA, GMC, the Royal Colleges, RCN, RCM, NMC, Royal College of Pharmacists |
| Patient groups (maximum three focus groups) | Disseminate invitations via the patient groups and key contacts within the groups. Individuals will be asked to take part in a focus group | A focus group will be explored and pursued as practical with AvMA, WHO and PA | Contacts via AvMA, National Patient Champions, WHO, AIMS, MRSA support groups and other patient support groups. Patients who have been part of a disclosure and those who have not Maximum of three focus groups |
| Health professionals (n = 50 maximum) | Individual participants invited via publicity within trusts across the UK and through key contacts within the trusts approached. Focus groups will take place in trusts across Yorkshire | Participants will be invited for individual interviews. Separate focus groups will be set up in more local trusts as this is a more feasible approach | Ensure representation from health professionals at all levels and in all professions including doctors, nurses, midwives, pharmacists and other allied health professionals Focus groups likely to consist of one group of health professionals. Once analysis starts the team may consider a more mixed group of it is considered appropriate Maximum of five focus groups |
| PALS (one focus group) | Individual participants invited via publicity within trusts across the UK and through keycontacts within the trusts approached | Individual interviews only. Afocus group of these people is likely to be impractical | As broad a representation of trusts as possible. Ensure a mental health trust if at all possible |
| Other (n = 5 maximum) | Individuals who emerge as significant players in the field of open disclosure in the UK who have not been previously considered will be invited by letter or, if appropriate, in an opportunistic strategy. These people may emerge in the course of visits to other participants or in the course of meetings to disseminate the project. They may also become apparent from ongoing monitoring of the project at team meetings | Participants will be invited for interview. If there is a significant group who would provide useful data in a focus group setting, this will be considered | Maximum of one focus group if appropriate |
Appendix 2 Search strategy
Health-related databases
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations
OvidSP, http://ovidsp.ovid.com/
1948 to November week 2, 2011.
Searched on 18 November 2011; 3222 records were retrieved.
-
Disclosure/ (9552)
-
Truth Disclosure/ (10,655)
-
disclos$.ti,ab. (45,475)
-
(nondisclos$ or undisclos$).ti,ab. (641)
-
(candour or candor or candid).ti,ab. (413)
-
duty of care.ti,ab. (489)
-
duty to advise.ti,ab. (8)
-
apolog$.ti,ab. (768)
-
sorry.ti,ab. (321)
-
openness.ti,ab. (2522)
-
being open.ti,ab. (277)
-
((express$ or show$ or communicat$ or convey$) adj2 regret$).ti,ab. (123)
-
((express$ or show$ or communicat$ or convey$) adj2 remorse).ti,ab. (15)
-
((express$ or show$ or communicat$ or convey$) adj2 sympathy).ti,ab. (45)
-
or/1-14 (66,283)
-
Medical Errors/ (10,486)
-
Diagnostic Errors/ (27,982)
-
exp Medication Errors/ (9010)
-
Iatrogenic Disease/ (11,989)
-
Malpractice/ (24,338)
-
(adverse adj2 (event$ or incident or incidents or outcome$)).ti,ab. (82,145)
-
(safety adj2 (incident or incidents)).ti,ab. (178)
-
(serious adj2 (incident or incidents)).ti,ab. (173)
-
(sentinel adj2 event$).ti,ab. (564)
-
((critical or clinical or medical or healthcare) adj2 (incident or incidents)).ti,ab. (1729)
-
((harm or harms or harmful) adj3 (event$ or incident or incidents or outcome$)).ti,ab. (591)
-
(unexpected adj2 (event$ or incident or incidents or outcome$)).ti,ab. (1151)
-
(unintended adj2 (event$ or incident or incidents or outcome$)).ti,ab. (121)
-
(unintentional$ adj2 (event$ or incident or incidents or outcome$)).ti,ab. (67)
-
(unanticipated adj2 (event$ or incident or incidents or outcome$)).ti,ab. (156)
-
((unexpected or unintended or unintentional$ or unanticipated) adj2 injur$).ti,ab. (1281)
-
(medical adj (accident$ or injur$)).ti,ab. (321)
-
(surgical adj (accident$ or injur$)).ti,ab. (703)
-
((patient$ or inpatient$ or outpatient$ or consumer$ or citizen$ or public or user$) adj3 adverse).ti,ab. (10,028)
-
((patient$ or inpatient$ or outpatient$ or consumer$ or citizen$ or public or user$) adj3 (harm or harms or harmful)).ti,ab. (2763)
-
((patient$ or inpatient$ or outpatient$ or consumer$ or citizen$ or public or user$) adj3 (mistake$ or error or errors)).ti,ab. (3712)
-
((professional$ or worker$ or dentist$ or nurs$ or doctor$ or physician$ or surgeon$ or surgical$ or surger$ or pharmac$ or human or practitioner$ or psychiatrist$ or psychologist$ or anaesthe$ or anesthe$ or GP) adj3 (mistake$ or error or errors)).ti,ab. (4085)
-
((medical or diagnos$ or treatment$ or medication$ or healthcare or care or hospital$ or system$) adj3 (mistake$ or error or errors)).ti,ab. (17,663)
-
misdiagnosis.ti,ab. (6617)
-
(iatrogenic or iatrogenesis).ti,ab. (18,465)
-
(negligence or negligent).ti,ab. (3159)
-
malpractice.ti,ab. (7847)
-
litigat$.ti,ab. (4718)
-
(legal adj (action$ or proceeding$)).ti,ab. (857)
-
(lawsuit$ or law suit$).ti,ab. (2425)
-
near miss.ti,ab. (688)
-
near misses.ti,ab. (402)
-
err is human.ti,ab. (249)
-
things go wrong.ti,ab. (63)
-
or/16-49 (213,095)
-
15 and 50 (3156)
-
open disclosure.ti,ab. (42)
-
((communicat$ or discuss$ or convers$ or talk$ or explain$ or explanation$ or tell$ or told or acknowledg$ or consult$ or inform$ or notif$) adj3 (patient$ or family or families or inpatient$ or outpatient$ or consumer$ or citizen$ or public or carer$ or caregiver$ or user$) adj3 (adverse or harm$ or error or errors or mistake$ or incident or incidents)).ti,ab. (301)
-
51 or 52 or 53 (3423)
-
limit 54 to yr="1980 -Current" (3222)
Key
/ = indexing term [medical subject heading (MeSH)]
exp = exploded MeSH
$ = truncation
.ti,ab. = terms in either title or abstract fields
adj2 = terms within two words of each other (any order)
EMBASE
OvidSP, http://ovidsp.ovid.com/
1980 to week 45, 2011.
Searched on 18 November 2011; 3655 records were retrieved.
-
*interpersonal communication/ (29,453)
-
disclos$.ti,ab. (50,225)
-
(nondisclos$ or undisclos$).ti,ab. (683)
-
(candour or candor or candid).ti,ab. (434)
-
duty of care.ti,ab. (573)
-
duty to advise.ti,ab. (8)
-
apolog$.ti,ab. (801)
-
sorry.ti,ab. (367)
-
openness.ti,ab. (2813)
-
being open.ti,ab. (317)
-
((express$ or show$ or communicat$ or convey$) adj2 regret$).ti,ab. (129)
-
((express$ or show$ or communicat$ or convey$) adj2 remorse).ti,ab. (12)
-
((express$ or show$ or communicat$ or convey$) adj2 sympathy).ti,ab. (47)
-
or/1-13 (83,329)
-
exp medical error/ (66,530)
-
exp *iatrogenic disease/ (124,806)
-
sentinel event/ (118)
-
malpractice/ (28,065)
-
negligence/ (2761)
-
lawsuit/ (7778)
-
(adverse adj2 (event$ or incident or incidents or outcome$)).ti,ab. (108,362)
-
(safety adj2 (incident or incidents)).ti,ab. (216)
-
(serious adj2 (incident or incidents)).ti,ab. (245)
-
(sentinel adj2 event$).ti,ab. (653)
-
((critical or clinical or medical or healthcare) adj2 (incident or incidents)).ti,ab. (2047)
-
((harm or harms or harmful) adj3 (event$ or incident or incidents or outcome$)).ti,ab. (714)
-
(unexpected adj2 (event$ or incident or incidents or outcome$)).ti,ab. (1400)
-
(unintended adj2 (event$ or incident or incidents or outcome$)).ti,ab. (132)
-
(unintentional$ adj2 (event$ or incident or incidents or outcome$)).ti,ab. (70)
-
(unanticipated adj2 (event$ or incident or incidents or outcome$)).ti,ab. (198)
-
((unexpected or unintended or unintentional$ or unanticipated) adj2 injur$).ti,ab. (1330)
-
(medical adj (accident$ or injur$)).ti,ab. (342)
-
(surgical adj (accident$ or injur$)).ti,ab. (779)
-
((patient$ or inpatient$ or outpatient$ or consumer$ or citizen$ or public or user$) adj3 adverse).ti,ab. (13,061)
-
((patient$ or inpatient$ or outpatient$ or consumer$ or citizen$ or public or user$) adj3 (harm or harms or harmful)).ti,ab. (3311)
-
((patient$ or inpatient$ or outpatient$ or consumer$ or citizen$ or public or user$) adj3 (mistake$ or error or errors)).ti,ab. (4391)
-
((professional$ or worker$ or dentist$ or nurs$ or doctor$ or physician$ or surgeon$ or surgical$ or surger$ or pharmac$ or human or practitioner$ or psychiatrist$ or psychologist$ or anaesthe$ or anesthe$ or GP) adj3 (mistake$ or error or errors)).ti,ab. (4883)
-
((medical or diagnos$ or treatment$ or medication$ or healthcare or care or hospital$ or system$) adj3 (mistake$ or error or errors)).ti,ab. (19,843)
-
misdiagnosis.ti,ab. (7808)
-
(iatrogenic or iatrogenesis).ti,ab. (21,661)
-
(negligence or negligent).ti,ab. (3538)
-
malpractice.ti,ab. (8078)
-
litigat$.ti,ab. (5423)
-
(legal adj (action$ or proceeding$)).ti,ab. (962)
-
(lawsuit$ or law suit$).ti,ab. (2480)
-
near miss.ti,ab. (808)
-
near misses.ti,ab. (516)
-
err is human.ti,ab. (280)
-
things go wrong.ti,ab. (97)
-
or/15-49 (386,847)
-
14 and 50 (3407)
-
open disclosure.ti,ab. (44)
-
((communicat$ or discuss$ or convers$ or talk$ or explain$ or explanation$ or tell$ or told or acknowledg$ or consult$ or inform$ or notif$) adj3 (patient$ or family or families or inpatient$ or outpatient$ or consumer$ or citizen$ or public or carer$ or caregiver$ or user$) adj3 (adverse or harm$ or error or errors or mistake$ or incident or incidents)).ti,ab. (400)
-
51 or 52 or 53 (3776)
-
limit 54 to yr="1980 -Current" (3655)
Key
/ = indexing term (EMTREE heading)
* = focused EMTREE heading
exp = exploded EMTREE heading
$ = truncation
.ti,ab. = terms in either title or abstract fields
adj2 = terms within two words of each other (any order)
PsycINFO
OvidSP, http://ovidsp.ovid.com/
1806 to November week 3, 2011.
Searched on 18 November 2011; 697 records were retrieved.
-
interpersonal communication/ (12,219)
-
disclos$.ti,ab. (15,916)
-
(nondisclos$ or undisclos$).ti,ab. (388)
-
(candour or candor or candid).ti,ab. (732)
-
duty of care.ti,ab. (176)
-
duty to advise.ti,ab. (4)
-
apolog$.ti,ab. (1521)
-
sorry.ti,ab. (234)
-
openness.ti,ab. (6694)
-
being open.ti,ab. (197)
-
((express$ or show$ or communicat$ or convey$) adj2 regret$).ti,ab. (120)
-
((express$ or show$ or communicat$ or convey$) adj2 remorse).ti,ab. (50)
-
((express$ or show$ or communicat$ or convey$) adj2 sympathy).ti,ab. (125)
-
or/1-13 (37,231)
-
Errors/ (6987)
-
Misdiagnosis/ (333)
-
professional liability/ (1723)
-
litigation/ (919)
-
(adverse adj2 (event$ or incident or incidents or outcome$)).ti,ab. (8032)
-
(safety adj2 (incident or incidents)).ti,ab. (43)
-
(serious adj2 (incident or incidents)).ti,ab. (97)
-
(sentinel adj2 event$).ti,ab. (53)
-
((critical or clinical or medical or healthcare) adj2 (incident or incidents)).ti,ab. (2099)
-
((harm or harms or harmful) adj3 (event$ or incident or incidents or outcome$)).ti,ab. (292)
-
(unexpected adj2 (event$ or incident or incidents or outcome$)).ti,ab. (531)
-
(unintended adj2 (event$ or incident or incidents or outcome$)).ti,ab. (90)
-
(unintentional$ adj2 (event$ or incident or incidents or outcome$)).ti,ab. (12)
-
(unanticipated adj2 (event$ or incident or incidents or outcome$)).ti,ab. (101)
-
((unexpected or unintended or unintentional$ or unanticipated) adj2 injur$).ti,ab. (416)
-
(medical adj (accident$ or injur$)).ti,ab. (34)
-
(surgical adj (accident$ or injur$)).ti,ab. (6)
-
((patient$ or inpatient$ or outpatient$ or consumer$ or citizen$ or public or user$) adj3 adverse).ti,ab. (771)
-
((patient$ or inpatient$ or outpatient$ or consumer$ or citizen$ or public or user$) adj3 (harm or harms or harmful)).ti,ab. (881)
-
((patient$ or inpatient$ or outpatient$ or consumer$ or citizen$ or public or user$) adj3 (mistake$ or error or errors)).ti,ab. (767)
-
((professional$ or worker$ or dentist$ or nurs$ or doctor$ or physician$ or surgeon$ or surgical$ or surger$ or pharmac$ or human or practitioner$ or psychiatrist$ or psychologist$ or anaesthe$ or anesthe$ or GP) adj3 (mistake$ or error or errors)).ti,ab. (1063)
-
((medical or diagnos$ or treatment$ or medication$ or healthcare or care or hospital$ or system$) adj3 (mistake$ or error or errors)).ti,ab. (2637)
-
misdiagnosis.ti,ab. (903)
-
(iatrogenic or iatrogenesis).ti,ab. (1173)
-
(negligence or negligent).ti,ab. (906)
-
malpractice.ti,ab. (1104)
-
litigat$.ti,ab. (2642)
-
(legal adj (action$ or proceeding$)).ti,ab. (649)
-
(lawsuit$ or law suit$).ti,ab. (807)
-
near miss.ti,ab. (147)
-
near misses.ti,ab. (114)
-
err is human.ti,ab. (45)
-
things go wrong.ti,ab. (56)
-
or/15-47 (31,213)
-
14 and 48 (620)
-
open disclosure.ti,ab. (27)
-
((communicat$ or discuss$ or convers$ or talk$ or explain$ or explanation$ or tell$ or told or acknowledg$ or consult$ or inform$ or notif$) adj3 (patient$ or family or families or inpatient$ or outpatient$ or consumer$ or citizen$ or public or carer$ or caregiver$ or user$) adj3 (adverse or harm$ or error or errors or mistake$ or incident or incidents)).ti,ab. (92)
-
49 or 50 or 51 (722)
-
limit 52 to yr="1980 -Current" (697)
Key
/ = subject heading
$ = truncation
.ti,ab. = terms in either title or abstract fields
adj2 = terms within two words of each other (any order)
Health Management Information Consortium (HMIC)
OvidSP, http://ovidsp.ovid.com/
1979 to September 2011.
Searched on 18 November 2011; 236 records were retrieved.
-
"disclosure of information"/ (401)
-
"duty of care"/ (2)
-
openness/ (23)
-
disclos$.ti,ab. (947)
-
(nondisclos$ or undisclos$).ti,ab. (18)
-
(candour or candor or candid).ti,ab. (21)
-
duty of care.ti,ab. (127)
-
duty to advise.ti,ab. (1)
-
apolog$.ti,ab. (48)
-
sorry.ti,ab. (52)
-
openness.ti,ab. (391)
-
being open.ti,ab. (33)
-
((express$ or show$ or communicat$ or convey$) adj2 regret$).ti,ab. (7)
-
((express$ or show$ or communicat$ or convey$) adj2 remorse).ti,ab. (1)
-
((express$ or show$ or communicat$ or convey$) adj2 sympathy).ti,ab. (5)
-
or/1-15 (1803)
-
exp errors/ (910)
-
iatrogenic disease/ (39)
-
exp medical malpractice/ (1085)
-
clinical negligence/ (94)
-
legal proceedings/ (480)
-
litigation/ (351)
-
adverse events/ (420)
-
(adverse adj2 (event$ or incident or incidents or outcome$)).ti,ab. (1413)
-
(safety adj2 (incident or incidents)).ti,ab. (113)
-
(serious adj2 (incident or incidents)).ti,ab. (73)
-
(sentinel adj2 event$).ti,ab. (20)
-
((critical or clinical or medical or healthcare) adj2 (incident or incidents)).ti,ab. (326)
-
((harm or harms or harmful) adj3 (event$ or incident or incidents or outcome$)).ti,ab. (49)
-
(unexpected adj2 (event$ or incident or incidents or outcome$)).ti,ab. (23)
-
(unintended adj2 (event$ or incident or incidents or outcome$)).ti,ab. (16)
-
(unintentional$ adj2 (event$ or incident or incidents or outcome$)).ti,ab. (0)
-
(unanticipated adj2 (event$ or incident or incidents or outcome$)).ti,ab. (8)
-
((critical or clinical) adj2 (incident or incidents)).ti,ab. (297)
-
((unexpected or unintended or unintentional$ or unanticipated) adj2 injur$).ti,ab. (64)
-
(medical adj (accident$ or injur$)).ti,ab. (72)
-
(surgical adj (accident$ or injur$)).ti,ab. (5)
-
((patient$ or inpatient$ or outpatient$ or consumer$ or citizen$ or public or user$) adj3 adverse).ti,ab. (191)
-
((patient$ or inpatient$ or outpatient$ or consumer$ or citizen$ or public or user$) adj3 (harm or harms or harmful)).ti,ab. (276)
-
((patient$ or inpatient$ or outpatient$ or consumer$ or citizen$ or public or user$) adj3 (mistake$ or error or errors)).ti,ab. (165)
-
((professional$ or worker$ or dentist$ or nurs$ or doctor$ or physician$ or surgeon$ or surgical$ or surger$ or pharmac$ or human or practitioner$ or psychiatrist$ or psychologist$ or anaesthe$ or anesthe$ or GP) adj3 (mistake$ or error or errors)).ti,ab. (245)
-
((medical or diagnos$ or treatment$ or medication$ or healthcare or care or hospital$ or system$) adj3 (mistake$ or error or errors)).ti,ab. (681)
-
misdiagnosis.ti,ab. (54)
-
(iatrogenic or iatrogenesis).ti,ab. (101)
-
(negligence or negligent).ti,ab. (587)
-
malpractice.ti,ab. (200)
-
litigat$.ti,ab. (566)
-
(legal adj (action$ or proceeding$)).ti,ab. (134)
-
(lawsuit$ or law suit$).ti,ab. (38)
-
near miss.ti,ab. (32)
-
near misses.ti,ab. (80)
-
err is human.ti,ab. (24)
-
things go wrong.ti,ab. (72)
-
or/17-53 (5580)
-
16 and 54 (207)
-
open disclosure.ti,ab. (12)
-
((communicat$ or discuss$ or convers$ or talk$ or explain$ or explanation$ or tell$ or told or acknowledg$ or consult$ or inform$ or notif$) adj3 (patient$ or family or families or inpatient$ or outpatient$ or consumer$ or citizen$ or public or carer$ or caregiver$ or user$) adj3 (adverse or harm$ or error or errors or mistake$ or incident or incidents)).ti,ab. (38)
-
55 or 56 or 57 (236)
-
limit 58 to yr="1980 -Current" (236)
Key
/ = subject heading
exp = exploded subject heading
$ = truncation
.ti,ab. = terms in either title or abstract fields
adj2 = terms within two words of each other (any order)
The Cochrane Library
Wiley, http://onlinelibrary.wiley.com/
-
Cochrane Database of Systematic Reviews (CDSR), Issue 11, November 2011
-
Database of Abstracts of Reviews of Effects (DARE), Issue 4, October 2011
-
Health Technology Assessment (HTA) Database, Issue 4, October 2011
-
Cochrane Central Register of Controlled Trials (CENTRAL), Issue 4, October 2011.
The above four databases were searched on 22 November 2011, via The Cochrane Library.
Ninety-three records were retrieved in total: 10 from CDSR, 1 from DARE, 0 from HTA, 82 from CENTRAL.
| ID | Search | Hits | |
|---|---|---|---|
| #1 | MeSH descriptor Disclosure, this term only | 80 | |
| #2 | MeSH descriptor Truth Disclosure, this term only | 167 | |
| #3 | disclos*:ti,ab | 1409 | |
| #4 | (nondisclos* or undisclos*):ti,ab | 27 | |
| #5 | (candour or candor or candid):ti,ab | 10 | |
| #6 | "duty of care":ti,ab | 0 | |
| #7 | "duty to advise":ti,ab | 0 | |
| #8 | apolog*:ti,ab | 11 | |
| #9 | sorry:ti,ab | 4 | |
| #10 | openness:ti,ab | 69 | |
| #11 | being NEXT open:ti,ab. | 4 | |
| #12 | ((express* or show* or communicat* or convey*) NEAR/2 regret*):ti,ab | 3 | |
| #13 | ((express* or show* or communicat* or convey*) NEAR/2 remorse):ti,ab | 0 | |
| #14 | ((express* or show* or communicat* or convey*) NEAR/2 sympathy):ti,ab | 2 | |
| #15 | (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14) | 1680 | |
| #16 | MeSH descriptor Medical Errors, this term only | 82 | |
| #17 | MeSH descriptor Diagnostic Errors, this term only | 211 | |
| #18 | MeSH descriptor Medication Errors explode all trees | 147 | |
| #19 | MeSH descriptor Iatrogenic Disease, this term only | 61 | |
| #20 | MeSH descriptor Malpractice, this term only | 10 | |
| #21 | (adverse NEAR/2 (event* or incident or incidents or outcome*)):ti,ab | 24,785 | |
| #22 | (safety NEAR/2 (incident or incidents)):ti,ab | 2 | |
| #23 | (serious NEAR/2 (incident or incidents)):ti,ab | 6 | |
| #24 | (sentinel NEAR/2 event*):ti,ab | 9 | |
| #25 | ((critical or clinical or medical or healthcare) NEAR/2 (incident or incidents)):ti,ab | 55 | |
| #26 | ((harm or harms or harmful) NEAR/3 (event* or incident or incidents or outcome*)):ti,ab | 62 | |
| #27 | (unexpected NEAR/2 (event* or incident or incidents or outcome*)):ti,ab | 200 | |
| #28 | (unintended NEAR/2 (event* or incident or incidents or outcome*)):ti,ab | 7 | |
| #29 | (unintentional* NEAR/2 (event* or incident or incidents or outcome*)):ti,ab | 2 | |
| #30 | (unanticipated NEAR/2 (event* or incident or incidents or outcome*)):ti,ab | 19 | |
| #31 | ((unexpected or unintended or unintentional* or unanticipated) NEAR/2 injur*):ti,ab | 46 | |
| #32 | (medical NEXT (accident* or injur*)):ti,ab | 1 | |
| #33 | (surgical NEXT (accident* or injur*)):ti,ab | 31 | |
| #34 | ((patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) NEAR/3 adverse):ti,ab | 2215 | |
| #35 | ((patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) NEAR/3 (harm or harms or harmful)):ti,ab | 162 | |
| #36 | ((patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) NEAR/3 (mistake* or error or errors)):ti,ab | 149 | |
| #37 | ((professional* or worker* or dentist* or nurs* or doctor* or physician* or surgeon* or surgical* or surger* or pharmac* or human or practitioner* or psychiatrist* or psychologist* or anaesthe* or anesthe* or GP) NEAR/3 (mistake* or error or errors)):ti,ab | 93 | |
| #38 | ((medical or diagnos* or treatment* or medication* or healthcare or care or hospital* or system*) NEAR/3 (mistake* or error or errors)):ti,ab | 401 | |
| #39 | misdiagnosis:ti,ab | 43 | |
| #40 | (iatrogenic or iatrogenesis):ti,ab | 287 | |
| #41 | (negligence or negligent):ti,ab | 18 | |
| #42 | malpractice:ti,ab | 12 | |
| #43 | litigat*:ti,ab | 50 | |
| #44 | (legal NEXT (action* or proceeding*)):ti,ab | 7 | |
| #45 | lawsuit*:ti,ab. | 8671 | |
| #46 | law NEXT suit*:ti,ab | 1 | |
| #47 | "near miss":ti,ab | 11 | |
| #48 | "near misses":ti,ab | 6 | |
| #49 | "err is human":ti,ab | 1 | |
| #50 | "things go wrong":ti,ab | 0 | |
| #51 | (#16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50) | 35,181 | |
| #52 | (#15 AND #51) | 103 | |
| #53 | (open NEXT disclosure):ti,ab | 0 | |
| #54 | ((communicat* or discuss* or convers* or talk* or explain* or explanation* or tell* or told or acknowledg* or consult* or inform* or notif*) NEAR/3 (patient* or family or families or inpatient* or outpatient* or consumer* or citizen* or public or carer* or caregiver* or user*) NEAR/3 (adverse or harm* or error or errors or mistake* or incident or incidents)):ti,ab | 6 | |
| #55 | (#52 OR #53 OR #54) limited to CDSR, DARE, HTA, CENTRAL | 94 | |
| #56 | (#52 OR #53 OR #54), from 1980 to 2011 limited to CDSR, DARE, HTA, CENTRAL | 93 | |
Cumulative Index to Nursing and Allied Health Literature (CINAHL)
Via EBSCOhost.
Inception to 9 December 2011.
Searched on 21 December 2011; 1300 records were retrieved.
| # | Query | Results |
|---|---|---|
| S62 | S59 or S60 or S61 Limiters - Published Date from: 19800101- | 1300 |
| S61 | TI ( (communicat* or discuss* or convers* or talk* or explain* or explanation* or tell* or told or acknowledg* or consult* or inform* or notif*) N3 (patient* or family or families or inpatient* or outpatient* or consumer* or citizen* or public or carer* or caregiver* or user*) N3 (adverse or harm* or error or errors or mistake* or incident or incidents) ) OR AB ( (communicat* or discuss* or convers* or talk* or explain* or explanation* or tell* or told or acknowledg* or consult* or inform* or notif*) N3 (patient* or family or families or inpatient* or outpatient* or consumer* or citizen* or public or carer* or caregiver* or user*) N3 (adverse or harm* or error or errors or mistake* or incident or incidents) ) | 183 |
| S60 | TI "open disclosure" OR AB "open disclosure" | 26 |
| S59 | S53 and S58 | 1165 |
| S58 | S10 or S54 or S55 or S56 or S57 | 11,431 |
| S57 | TI ( (express* or show* or communicat* or convey*) N2 sympathy ) OR AB ( (express* or show* or communicat* or convey*) N2 sympathy ) | 28 |
| S56 | TI ( (express* or show* or communicat* or convey*) N2 remorse ) OR AB ( (express* or show* or communicat* or convey*) N2 remorse ) | 4 |
| S55 | TI ( (express* or show* or communicat* or convey*) N2 regret* ) OR AB ( (express* or show* or communicat* or convey*) N2 regret* ) | 29 |
| S54 | TI "being open" OR AB "being open" | 67 |
| S53 | S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38 or S39 or S40 or S41 or S42 or S43 or S44 or S45 or S46 or S47 or S48 or S49 or S50 or S51 or S52 | 60,878 |
| S52 | TI "things go wrong" OR AB "things go wrong" | 59 |
| S51 | TI "err is human" OR AB "err is human" | 124 |
| S50 | TI "near misses" OR AB "near misses" | 194 |
| S49 | TI "near miss" OR AB "near miss" | 234 |
| S48 | TI ( lawsuit* or "law suit*" ) OR AB ( lawsuit* or "law suit*" ) | 1609 |
| S47 | TI ( "legal action*" or "legal proceeding*" ) OR AB ( "legal action*" or "legal proceeding*" ) | 295 |
| S46 | TI litigat* OR AB litigat* | 1731 |
| S45 | TI malpractice OR AB malpractice | 2361 |
| S44 | TI ( negligence or negligent ) OR AB ( negligence or negligent ) | 1625 |
| S43 | TI ( iatrogenic or iatrogenesis ) OR AB ( iatrogenic or iatrogenesis ) | 1587 |
| S42 | TI misdiagnosis OR AB misdiagnosis | 765 |
| S41 | TI ( (medical or diagnos* or treatment* or medication* or healthcare or care or hospital* or system*) N3 (mistake* or error or errors) ) OR AB ( (medical or diagnos* or treatment* or medication* or healthcare or care or hospital* or system*) N3 (mistake* or error or errors) ) | 5467 |
| S40 | TI ( (professional* or worker* or dentist* or nurs* or doctor* or physician* or surgeon* or surgical* or surger* or pharmac* or human or practitioner* or psychiatrist* or psychologist* or anaesthe* or anesthe* or GP) N3 (mistake* or error or errors) ) OR AB ( (professional* or worker* or dentist* or nurs* or doctor* or physician* or surgeon* or surgical* or surger* or pharmac* or human or practitioner* or psychiatrist* or psychologist* or anaesthe* or anesthe* or GP) N3 (mistake* or error or errors) ) | 1521 |
| S39 | TI ( (patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) N3 (mistake* or error or errors) ) OR AB ( (patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) N3 (mistake* or error or errors) ) | 1332 |
| S38 | TI ( (patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) N3 (harm or harms or harmful) ) OR AB ( (patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) N3 (harm or harms or harmful) ) | 1281 |
| S37 | TI ( (patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) N3 adverse ) OR AB ( (patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) N3 adverse ) | 2580 |
| S36 | TI ( "surgical accident*" or "surgical injur*" ) OR AB ( "surgical accident*" or "surgical injur*" ) | 35 |
| S35 | TI ( "medical accident*" or "medical injur*" ) OR AB ( "medical accident*" or "medical injur*" ) | 79 |
| S34 | TI ( (unexpected or unintended or unintentional* or unanticipated) N2 injur* ) OR AB ( (unexpected or unintended or unintentional* or unanticipated) N2 injur* ) | 611 |
| S33 | TI ( unanticipated N2 (event* or incident or incidents or outcome*) ) OR AB ( unanticipated N2 (event* or incident or incidents or outcome*) ) | 80 |
| S32 | TI ( unintentional* N2 (event* or incident or incidents or outcome*) ) OR AB ( unintentional* N2 (event* or incident or incidents or outcome*) ) | 27 |
| S31 | TI ( unintended N2 (event* or incident or incidents or outcome*) ) OR AB ( unintended N2 (event* or incident or incidents or outcome*) ) | 45 |
| S30 | TI ( unexpected N2 (event* or incident or incidents or outcome*) ) OR AB ( unexpected N2 (event* or incident or incidents or outcome*) ) | 281 |
| S29 | TI ( (harm or harms or harmful) N3 (event* or incident or incidents or outcome*) ) OR AB ( (harm or harms or harmful) N3 (event* or incident or incidents or outcome*) ) | 268 |
| S28 | TI ( (critical or clinical or medical or healthcare) N2 (incident or incidents) ) OR AB ( (critical or clinical or medical or healthcare) N2 (incident or incidents) ) | 1083 |
| S27 | TI sentinel N2 event* OR AB sentinel N2 event* | 399 |
| S26 | TI ( serious N2 (incident or incidents) ) OR AB ( serious N2 (incident or incidents) ) | 68 |
| S25 | TI ( safety N2 (incident or incidents) ) OR AB ( safety N2 (incident or incidents) ) | 145 |
| S24 | TI ( adverse N2 (event* or incident or incidents or outcome*) ) OR AB ( adverse N2 (event* or incident or incidents or outcome*) ) | 16,562 |
| S23 | (MH "Legal Procedure+") | 3916 |
| S22 | (MH "Negligence") | 3985 |
| S21 | (MH "Malpractice") | 6020 |
| S20 | (MH "Iatrogenic Disease") | 1129 |
| S19 | (MH "Sentinel Event") | 631 |
| S18 | (MH "Adverse Drug Event") | 2596 |
| S17 | (MH "Adverse Health Care Event") | 2237 |
| S16 | (MH "Failure to Diagnose") | 1025 |
| S15 | (MH "Human Error") | 454 |
| S14 | (MH "Diagnostic Errors") | 4111 |
| S13 | (MH "Medication Errors") | 7424 |
| S12 | (MH "Treatment Errors") | 4066 |
| S11 | (MH "Health Care Errors") | 1914 |
| S10 | S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 | 11,321 |
| S9 | TI openness OR AB openness | 814 |
| S8 | TI sorry OR AB sorry | 245 |
| S7 | TI apolog* OR AB apolog* | 391 |
| S6 | TI "duty to advise" OR AB "duty to advise" | 8 |
| S5 | TI "duty of care" OR AB "duty of care" | 333 |
| S4 | TI ( candour or candor or candid ) OR AB ( candour or candor or candid ) | 132 |
| S3 | TI ( nondisclos* or undisclos* ) OR AB ( nondisclos* or undisclos* ) | 167 |
| S2 | TI disclos* OR AB disclos* | 5581 |
| S1 | (MH "Truth Disclosure") | 5370 |
Science Citation Index (SCI)
Social Sciences Citation Index (SSCI)
Conference Proceedings Citation Index – Science (CPCI-S)
Conference Proceedings Citation Index – Social Science & Humanities (CPCI-SSH)
Web of Science – ISI Web of Knowledge, www.isinet.com/
SCI, 1899 to present; SSCI, 1956 to present; CPCI-S, 1990 to present; CPCI-SSH, 1990 to present.
The above four databases were searched together with the strategy as set out below on 6 December 2011; 3778 records were retrieved in total.
| Query number | Results | Query |
|---|---|---|
| # 45 | 3778 | #44 Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=1980-2011 |
| # 44 | 3785 | #43 OR #42 OR #41 Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 43 | 2145 | TS=((communicat* or discuss or discussed or convers* or talk* or explain* or explanation* or tell* or told or acknowledg* or consult* or inform or informs or informed or informing or notif*) SAME (patient* or family or families or inpatient* or outpatient* or consumer* or citizen* or public or carer* or caregiver* or user*) SAME (adverse or harm or harms or harmful or error or errors or mistake* or incident or incidents)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 42 | 43 | TS="open disclosure" Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 41 | 1724 | #40 AND #12 Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 40 | > 100,000 | #39 OR #38 OR #37 OR #36 OR #35 OR #34 OR #33 OR #32 OR #31 OR #30 OR #29 OR #28 OR #27 OR #26 OR #25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 39 | 112 | TS="things go wrong" Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 38 | 195 | TS="err is human" Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 37 | 2818 | TS=(lawsuit* or "law suit*") Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 36 | 948 | TS=("legal action*" or "legal proceeding*") Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 35 | 10,948 | TS=litigat* Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 34 | 5625 | TS=malpractice Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 33 | 3358 | TS=(negligence or negligent) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 32 | 13,183 | TS=(iatrogenic or iatrogenesis) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 31 | 5123 | TS=misdiagnosis Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 30 | 82,099 | TS=((medical or diagnos* or treatment* or medication* or healthcare or care or hospital* or system*) SAME (mistake* or error or errors)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 29 | 12,738 | TS=((professional* or worker* or dentist* or nurs* or doctor* or physician* or surgeon* or surgical* or surger* or pharmac* or human or practitioner* or psychiatrist* or psychologist* or anaesthe* or anesthe* or GP) SAME (mistake* or error or errors)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 28 | 17,176 | TS=((patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) SAME (mistake* or error or errors)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 27 | 6815 | TS=((patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) SAME (harm or harms or harmful)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 26 | 42,210 | TS=((patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) SAME adverse) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 25 | 448 | TS=("surgical accident*" or "surgical injur*") Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 24 | 272 | TS=("medical accident*" or "medical injur*") Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 23 | 1680 | TS=((unexpected or unintended or unintentional* or unanticipated) SAME injur*) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 22 | 437 | TS=(unanticipated SAME (event* or incident or incidents or outcome*)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 21 | 237 | TS=(unintentional* SAME (event* or incident or incidents or outcome*)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 20 | 462 | TS=(unintended SAME (event* or incident or incidents or outcome*)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 19 | 2944 | TS=(unexpected SAME (event* or incident or incidents or outcome*)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 18 | 2159 | TS=((harm or harms or harmful) SAME (event* or incident or incidents or outcome*)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 17 | 4755 | TS=((critical or clinical or medical or healthcare) SAME (incident or incidents)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 16 | 407 | TS=(sentinel SAME event*) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 15 | 486 | TS=(serious SAME (incident or incidents)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 14 | 1242 | TS=(safety SAME (incident or incidents)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 13 | 82,616 | TS=(adverse SAME (event* or incident or incidents or outcome*)) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 12 | 59,602 | #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 11 | 188 | TS=((express* or show* or communicat* or convey*) SAME sympathy) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 10 | 42 | TS=((express* or show* or communicat* or convey*) SAME remorse) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 9 | 386 | TS=((express* or show* or communicat* or convey*) SAME regret*) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 8 | 8673 | TS=openness Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 7 | 618 | TS=sorry Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 6 | 2060 | TS=apolog* Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 5 | 6 | TS="duty to advise" Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 4 | 452 | TS="duty of care" Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 3 | 775 | TS=(candour or candor or candid) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 2 | 763 | TS=(nondisclos* or undisclos*) Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
| # 1 | 46,329 | TS=disclos* Databases=SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan=All Years |
Latin American and Caribbean Health Sciences Literature (LILACS)
http://bases.bireme.br/cgi-bin/wxislind.exe/iah/online/?IsisScript=iah/iah.xis&base=LILACS&lang=i
Searched on 20 December 2011; 83 records were retrieved.
disclos$ or nondisclos$ or undisclos$ or candour or candor or candid or apolog$ or sorry or openness [Words field]
934 records
AND
error$ or mistake$ or adverse or harm$ or misdiagnosis or sentinel or safety or iatrogenic or iatrogenesis or negligence or negligent or malpractice or litigat$ or "NEAR-MISS" or "NEAR-MISSES" [Words field]
42,474 records
83 records
Key
$ = truncation
PASCAL
Dialog, www.dialog.com/
1973 to December week 3, 2012.
Searched on 9 January 2012; 921 records were retrieved.
| Set | Items | Description |
|---|---|---|
| 1 | 16,404 | DISCLOS?/TI,AB,DE |
| 2 | 243 | (NONDISCLOS? OR UNDISCLOS?)/TI,AB,DE |
| 3 | 173 | (CANDOUR OR CANDOR OR CANDID)/TI,AB,DE |
| 4 | 0 | DUTY(W)OF(W)CARE/TI,AB,DE |
| 5 | 0 | DUTY(W)TO(W)ADVISE/TI,AB,DE |
| 6 | 286 | APOLOG?/TI,AB,DE |
| 7 | 63 | SORRY/TI,AB,DE |
| 8 | 2026 | OPENNESS/TI,AB,DE |
| 9 | 73 | BEING(W)OPEN/TI,AB,DE |
| 10 | 76 | (EXPRESS? OR SHOW? OR COMMUNICAT? OR CONVEY?)(2N)REGRET?/TI,AB,DE |
| 11 | 9 | (EXPRESS? OR SHOW? OR COMMUNICAT? OR CONVEY?)(2N)REMORSE/TI,AB,DE |
| 12 | 21 | (EXPRESS? OR SHOW? OR COMMUNICAT? OR CONVEY?)(2N)SYMPATHY/TI,AB,DE |
| 13 | 19,178 | S1:S12 |
| 14 | 39,042 | ADVERSE(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 15 | 109 | SAFETY(2N)(INCIDENT OR INCIDENTS)/TI,AB,DE |
| 16 | 97 | SERIOUS(2N)(INCIDENT OR INCIDENTS)/TI,AB,DE |
| 17 | 151 | SENTINEL(2N)EVENT?/TI,AB,DE |
| 18 | 750 | (CRITICAL OR CLINICAL OR MEDICAL OR HEALTHCARE)(2N)(INCIDENT OR INCIDENTS)/TI,AB,DE |
| 19 | 321 | (HARM OR HARMS OR HARMFUL)(3N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 20 | 745 | UNEXPECTED(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 21 | 61 | UNINTENDED(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 22 | 31 | UNINTENTIONAL?(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 23 | 89 | UNANTICIPATED(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 24 | 452 | (UNEXPECTED OR UNINTENDED OR UNINTENTIONAL? OR UNANTICIPATED)(2N)INJUR?/TI,AB,DE |
| 25 | 78 | MEDICAL(W)(ACCIDENT? OR INJUR?)/TI,AB,DE |
| 26 | 216 | SURGICAL(W)(ACCIDENT? OR INJUR?)/TI,AB,DE |
| 27 | 6560 | (PATIENT? OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR USER?)(3N)ADVERSE/TI,AB,DE |
| 28 | 986 | (PATIENT? OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR USER?)(3N)(HARM OR HARMS OR HARMFUL)/TI,AB,DE |
| 29 | 2779 | (PATIENT? OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR USER?)(3N)(MISTAKE? OR ERROR OR ERRORS)/TI,AB,DE |
| 30 | 8055 | (PROFESSIONAL? OR WORKER? OR DENTIST? OR NURS? OR DOCTOR? OR PHYSICIAN? OR SURGEON? OR SURGICAL? OR SURGER? OR PHARMAC? OR HUMAN OR PRACTITIONER? OR PSYCHIATRIST? OR PSYCHOLOGIST? OR ANAESTHE? OR ANESTHE? OR GP)(3N)(MISTAKE? OR ERROR OR ERRORS)/TI,AB,DE |
| 31 | 24,079 | (MEDICAL OR DIAGNOS? OR TREATMENT? OR MEDICATION? OR HEALTHCARE OR CARE OR HOSPITAL? OR SYSTEM?)(3N)(MISTAKE? OR ERROR OR ERRORS)/TI,AB,DE |
| 32 | 2086 | MISDIAGNOSIS/TI,AB,DE |
| 33 | 21,351 | (IATROGENIC OR IATROGENESIS)/TI,AB,DE |
| 34 | 2975 | (NEGLIGENCE OR NEGLIGENT)/TI,AB,DE |
| 35 | 1937 | MALPRACTICE/TI,AB,DE |
| 36 | 1605 | LITIGAT?/TI,AB,DE |
| 37 | 194 | LEGAL(W)(ACTION? OR PROCEEDING?)/TI,AB,DE |
| 38 | 390 | (LAWSUIT? OR LAW(W)SUIT?)/TI,AB,DE |
| 39 | 302 | NEAR(W)MISS/TI,AB,DE |
| 40 | 165 | NEAR(W)MISSES/TI,AB,DE |
| 41 | 48 | ERR(W)IS(W)HUMAN/TI,AB,DE |
| 42 | 23 | THINGS(W)GO(W)WRONG/TI,AB,DE |
| 43 | 105153 | S14:S42 |
| 44 | 431 | S13 AND S43 |
| 45 | 15 | OPEN(W)DISCLOSURE/TI,AB,DE |
| 46 | 514 | (COMMUNICAT? OR DISCUSS? OR CONVERS? OR TALK? OR EXPLAIN? OR EXPLANATION? OR TELL? OR TOLD OR ACKNOWLEDG? OR CONSULT? OR INFORM? OR NOTIF?)(3N)(PATIENT? OR FAMILY OR FAMILIES OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR CARER? OR CAREGIVER? OR USER?)(3N)(ADVERSE OR HARM? OR ERROR OR ERRORS OR MISTAKE? OR INCIDENT OR INCIDENTS)/TI,AB,DE |
| 47 | 924 | S44:S46 |
| 48 | 921 | S47/1980:2012 |
Health Systems Evidence
www.mcmasterhealthforum.org/healthsystemsevidence-en
Searched on 6 January 2012; 13 records were retrieved.
Using the open search box the following terms were entered:
disclos* OR nondisclos* OR undisclos* OR candour OR candor OR apolog* OR sorry OR openness
Key
* = truncation
Social science databases
Applied Social Sciences Index and Abstracts (ASSIA)
CSA Illumina, www.csa.com/csaillumina/
1987 to December 2011.
Searched on 20 December 2011; 199 records were retrieved.
((DE="disclosure") or(DE="truth telling") or(DE="duty of care") or(DE="apologies") or(DE="openness") or(DE="regret") or(DE="remorse") or(DE="sympathy") or(KW=disclos*) or(KW=(nondisclos* or undisclos*)) or(KW=(candour or candor or candid)) or(KW="duty of care") or(KW="duty to advise") or(KW=apolog*) or(KW=sorry) or(KW=openness) or(KW="being open") or(KW=((express* or show* or communicat* or convey*) WITHIN 2 regret*)) or(KW=((express* or show* or communicat* or convey*) WITHIN 2 remorse)) or(KW=((express* or show* or communicat* or convey*) WITHIN 2 sympathy))) and((DE=("errors" or "human error" or "near misses")) or(DE=("misdiagnosed" or "misdiagnosis")) or(DE="iatrogenic effects") or(DE="medical malpractice") or(DE="medical negligence") or(DE="critical incidents") or(DE="harm") or(DE="mistakes") or(DE=("litigation" or "claims" or "class action suits")) or(KW=(adverse WITHIN 2 (event* or incident or incidents or outcome*))) or(KW=(safety WITHIN 2 (incident or incidents))) or(KW=(serious WITHIN 2 (incident or incidents))) or(KW=(sentinel WITHIN 2 event*)) or(KW=((critical or clinical or medical or healthcare) WITHIN 2 (incident or incidents))) or(KW=((harm or harms or harmful) WITHIN 3 (event* or incident or incidents or outcome*))) or(KW=(unexpected WITHIN 2 (event* or incident or incidents or outcome*))) or(KW=(unintended WITHIN 2 (event* or incident or incidents or outcome*))) or(KW=(unintentional* WITHIN 2 (event* or incident or incidents or outcome*))) or(KW=(unanticipated WITHIN 2 (event* or incident or incidents or outcome*))) or(KW=((unexpected or unintended or unintentional* or unanticipated) WITHIN 2 injur*)) or(KW="medical accident*" or "medical injur*") or(KW="surgical accident*" or "surgical injur*") or(KW=((patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) WITHIN 3 adverse)) or(KW=((patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) WITHIN 3 (harm or harms or harmful))) or(KW=((patient* or inpatient* or outpatient* or consumer* or citizen* or public or user*) WITHIN 3 (mistake* or error or errors))) or(KW=((professional* or worker* or dentist* or nurs* or doctor* or physician* or surgeon* or surgical* or surger* or pharmac* or human or practitioner* or psychiatrist* or psychologist* or anaesthe* or anesthe* or GP) WITHIN 3 (mistake* or error or errors))) or(KW=((medical or diagnos* or treatment* or medication* or healthcare or care or hospital* or system*) WITHIN 3 (mistake* or error or errors))) or(KW=misdiagnosis) or(KW=(iatrogenic or iatrogenesis)) or(KW=(negligence or negligent)) or(KW=malpractice) or(KW=litigat*) or(KW=("legal action*" or "legal proceeding*")) or(KW=(lawsuit* or "law suit*")) or(KW=("near miss" or "near misses")) or(KW="err is human") or(KW="things go wrong"))
Key
DE = subject heading
KW = searches the title, abstract, descriptor and identifier fields
WITHIN 2 = terms within two words of each other (any order)
* = truncation
“ “ = phrase search
Law databases
Lawtel
Westlaw
Lexus
Reports/conference proceedings/grey literature
National Technical Information Service (NTIS)
Dialog, www.dialog.com/
1964 to January week 1, 2012.
Searched on 9 January 2012; 217 records were retrieved.
| Set | Items | Description |
|---|---|---|
| 1 | 9931 | DISCLOS?/TI,AB,DE |
| 2 | 58 | (NONDISCLOS? OR UNDISCLOS?)/TI,AB,DE |
| 3 | 168 | (CANDOUR OR CANDOR OR CANDID)/TI,AB,DE |
| 4 | 0 | DUTY(W)OF(W)CARE/TI,AB,DE |
| 5 | 0 | DUTY(W)TO(W)ADVISE/TI,AB,DE |
| 6 | 51 | APOLOG?/TI,AB,DE |
| 7 | 10 | SORRY/TI,AB,DE |
| 8 | 379 | OPENNESS/TI,AB,DE |
| 9 | 25 | BEING(W)OPEN/TI,AB,DE |
| 10 | 2 | (EXPRESS? OR SHOW? OR COMMUNICAT? OR CONVEY?)(2N)REGRET?/TI,AB,DE |
| 11 | 0 | (EXPRESS? OR SHOW? OR COMMUNICAT? OR CONVEY?)(2N)REMORSE/TI,AB,DE |
| 12 | 5 | (EXPRESS? OR SHOW? OR COMMUNICAT? OR CONVEY?)(2N)SYMPATHY/TI,AB,DE |
| 13 | 10,604 | S1:S12 |
| 14 | 516 | ADVERSE(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 15 | 192 | SAFETY(2N)(INCIDENT OR INCIDENTS)/TI,AB,DE |
| 16 | 72 | SERIOUS(2N)(INCIDENT OR INCIDENTS)/TI,AB,DE |
| 17 | 40 | SENTINEL(2N)EVENT?/TI,AB,DE |
| 18 | 246 | (CRITICAL OR CLINICAL OR MEDICAL OR HEALTHCARE)(2N)(INCIDENT OR INCIDENTS)/TI,AB,DE |
| 19 | 36 | (HARM OR HARMS OR HARMFUL)(3N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 20 | 145 | UNEXPECTED(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 21 | 12 | UNINTENDED(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 22 | 10 | UNINTENTIONAL?(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 23 | 57 | UNANTICIPATED(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 24 | 100 | (UNEXPECTED OR UNINTENDED OR UNINTENTIONAL? OR UNANTICIPATED)(2N)INJUR?/TI,AB,DE |
| 25 | 34 | MEDICAL(W)(ACCIDENT? OR INJUR?)/TI,AB,DE |
| 26 | 4 | SURGICAL(W)(ACCIDENT? OR INJUR?)/TI,AB,DE |
| 27 | 242 | (PATIENT? OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR USER?)(3N)ADVERSE/TI,AB,DE |
| 28 | 131 | (PATIENT? OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR USER?)(3N)(HARM OR HARMS OR HARMFUL)/TI,AB,DE |
| 29 | 604 | (PATIENT? OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR USER?)(3N)(MISTAKE? OR ERROR OR ERRORS)/TI,AB,DE |
| 30 | 1536 | (PROFESSIONAL? OR WORKER? OR DENTIST? OR NURS? OR DOCTOR? OR PHYSICIAN? OR SURGEON? OR SURGICAL? OR SURGER? OR PHARMAC? OR HUMAN OR PRACTITIONER? OR PSYCHIATRIST? OR PSYCHOLOGIST? OR ANAESTHE? OR ANESTHE? OR GP)(3N)(MISTAKE? OR ERROR OR ERRORS)/TI,AB,DE |
| 31 | 7343 | (MEDICAL OR DIAGNOS? OR TREATMENT? OR MEDICATION? OR HEALTHCARE OR CARE OR HOSPITAL? OR SYSTEM?)(3N)(MISTAKE? OR ERROR OR ERRORS)/TI,AB,DE |
| 32 | 20 | MISDIAGNOSIS/TI,AB,DE |
| 33 | 61 | (IATROGENIC OR IATROGENESIS)/TI,AB,DE |
| 34 | 220 | (NEGLIGENCE OR NEGLIGENT)/TI,AB,DE |
| 35 | 462 | MALPRACTICE/TI,AB,DE |
| 36 | 1877 | LITIGAT?/TI,AB,DE |
| 37 | 207 | LEGAL(W)(ACTION? OR PROCEEDING?)/TI,AB,DE |
| 38 | 320 | (LAWSUIT? OR LAW(W)SUIT?)/TI,AB,DE |
| 39 | 63 | NEAR(W)MISS/TI,AB,DE |
| 40 | 47 | NEAR(W)MISSES/TI,AB,DE |
| 41 | 11 | ERR(W)IS(W)HUMAN/TI,AB,DE |
| 42 | 4 | THINGS(W)GO(W)WRONG/TI,AB,DE |
| 43 | 13,784 | S14:S42 |
| 44 | 117 | S13 AND S43 |
| 45 | 1 | OPEN(W)DISCLOSURE/TI,AB,DE |
| 46 | 144 | (COMMUNICAT? OR DISCUSS? OR CONVERS? OR TALK? OR EXPLAIN? OR EXPLANATION? OR TELL? OR TOLD OR ACKNOWLEDG? OR CONSULT? OR INFORM? OR NOTIF?)(3N)(PATIENT? OR FAMILY OR FAMILIES OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR CARER? OR CAREGIVER? OR USER?)(3N)(ADVERSE OR HARM? OR ERROR OR ERRORS OR MISTAKE? OR INCIDENT OR INCIDENTS)/TI,AB,DE |
| 47 | 260 | S44:S46 |
| 48 | 217 | S47/1980:2012 |
Dissertation Abstracts
Dialog, www.dialog.com/
1861 to December 2011.
Searched on 9 January 2012; 411 records were retrieved.
| Set | Items | Description |
|---|---|---|
| 1 | 10,298 | DISCLOS?/TI,AB,DE |
| 2 | 169 | (NONDISCLOS? OR UNDISCLOS?)/TI,AB,DE |
| 3 | 332 | (CANDOUR OR CANDOR OR CANDID)/TI,AB,DE |
| 4 | 0 | DUTY(W)OF(W)CARE/TI,AB,DE |
| 5 | 0 | DUTY(W)TO(W)ADVISE/TI,AB,DE |
| 6 | 1799 | APOLOG?/TI,AB,DE |
| 7 | 73 | SORRY/TI,AB,DE |
| 8 | 4576 | OPENNESS/TI,AB,DE |
| 9 | 160 | BEING(W)OPEN/TI,AB,DE |
| 10 | 50 | (EXPRESS? OR SHOW? OR COMMUNICAT? OR CONVEY?)(2N)REGRET?/TI,AB,DE |
| 11 | 12 | (EXPRESS? OR SHOW? OR COMMUNICAT? OR CONVEY?)(2N)REMORSE/TI,AB,DE |
| 12 | 108 | (EXPRESS? OR SHOW? OR COMMUNICAT? OR CONVEY?)(2N)SYMPATHY/TI,AB,DE |
| 13 | 17,191 | S1:S12 |
| 14 | 1189 | ADVERSE(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 15 | 26 | SAFETY(2N)(INCIDENT OR INCIDENTS)/TI,AB,DE |
| 16 | 41 | SERIOUS(2N)(INCIDENT OR INCIDENTS)/TI,AB,DE |
| 17 | 24 | SENTINEL(2N)EVENT?/TI,AB,DE |
| 18 | 1655 | (CRITICAL OR CLINICAL OR MEDICAL OR HEALTHCARE)(2N)(INCIDENT OR INCIDENTS)/TI,AB,DE |
| 19 | 111 | (HARM OR HARMS OR HARMFUL)(3N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 20 | 391 | UNEXPECTED(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 21 | 108 | UNINTENDED(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 22 | 14 | UNINTENTIONAL?(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 23 | 116 | UNANTICIPATED(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 24 | 133 | (UNEXPECTED OR UNINTENDED OR UNINTENTIONAL? OR UNANTICIPATED)(2N)INJUR?/TI,AB,DE |
| 25 | 11 | MEDICAL(W)(ACCIDENT? OR INJUR?)/TI,AB,DE |
| 26 | 11 | SURGICAL(W)(ACCIDENT? OR INJUR?)/TI,AB,DE |
| 27 | 217 | (PATIENT? OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR USER?)(3N)ADVERSE/TI,AB,DE |
| 28 | 225 | (PATIENT? OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR USER?)(3N)(HARM OR HARMS OR HARMFUL)/TI,AB,DE |
| 29 | 572 | (PATIENT? OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR USER?)(3N)(MISTAKE? OR ERROR OR ERRORS)/TI,AB,DE |
| 30 | 669 | (PROFESSIONAL? OR WORKER? OR DENTIST? OR NURS? OR DOCTOR? OR PHYSICIAN? OR SURGEON? OR SURGICAL? OR SURGER? OR PHARMAC? OR HUMAN OR PRACTITIONER? OR PSYCHIATRIST? OR PSYCHOLOGIST? OR ANAESTHE? OR ANESTHE? OR GP)(3N)(MISTAKE? OR ERROR OR ERRORS)/TI,AB,DE |
| 31 | 3906 | (MEDICAL OR DIAGNOS? OR TREATMENT? OR MEDICATION? OR HEALTHCARE OR CARE OR HOSPITAL? OR SYSTEM?)(3N)(MISTAKE? OR ERROR OR ERRORS)/TI,AB,DE |
| 32 | 170 | MISDIAGNOSIS/TI,AB,DE |
| 33 | 150 | (IATROGENIC OR IATROGENESIS)/TI,AB,DE |
| 34 | 573 | (NEGLIGENCE OR NEGLIGENT)/TI,AB,DE |
| 35 | 336 | MALPRACTICE/TI,AB,DE |
| 36 | 2536 | LITIGAT?/TI,AB,DE |
| 37 | 361 | LEGAL(W)(ACTION? OR PROCEEDING?)/TI,AB,DE |
| 38 | 812 | (LAWSUIT? OR LAW(W)SUIT?)/TI,AB,DE |
| 39 | 54 | NEAR(W)MISS/TI,AB,DE |
| 40 | 42 | NEAR(W)MISSES/TI,AB,DE |
| 41 | 22 | ERR(W)IS(W)HUMAN/TI,AB,DE |
| 42 | 16 | THINGS(W)GO(W)WRONG/TI,AB,DE |
| 43 | 13,285 | S14:S42 |
| 44 | 280 | S13 AND S43 |
| 45 | 9 | OPEN(W)DISCLOSURE/TI,AB,DE |
| 46 | 133 | (COMMUNICAT? OR DISCUSS? OR CONVERS? OR TALK? OR EXPLAIN? OR EXPLANATION? OR TELL? OR TOLD OR ACKNOWLEDG? OR CONSULT? OR INFORM? OR NOTIF?)(3N)(PATIENT? OR FAMILY OR FAMILIES OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR CARER? OR CAREGIVER? OR USER?)(3N)(ADVERSE OR HARM? OR ERROR OR ERRORS OR MISTAKE? OR INCIDENT OR INCIDENTS)/TI,AB,DE |
| 47 | 414 | S44:S46 |
| 48 | 11,296 | 47/1980:2012 |
| 49 | 411 | S47/1980:2012 |
Inside Conferences
Dialog, www.dialog.com/
1993 to 6 January 2012.
Searched on 9 January 2012; 29 records were retrieved.
| Set | Items | Description |
|---|---|---|
| 1 | 1049 | DISCLOS?/TI,AB,DE |
| 2 | 11 | (NONDISCLOS? OR UNDISCLOS?)/TI,AB,DE |
| 3 | 30 | (CANDOUR OR CANDOR OR CANDID)/TI,AB,DE |
| 4 | 0 | DUTY(W)OF(W)CARE/TI,AB,DE |
| 5 | 0 | DUTY(W)TO(W)ADVISE/TI,AB,DE |
| 6 | 244 | APOLOG?/TI,AB,DE |
| 7 | 49 | SORRY/TI,AB,DE |
| 8 | 230 | OPENNESS/TI,AB,DE |
| 9 | 2 | BEING(W)OPEN/TI,AB,DE |
| 10 | 1 | (EXPRESS? OR SHOW? OR COMMUNICAT? OR CONVEY?)(2N)REGRET?/TI,AB,DE |
| 11 | 0 | (EXPRESS? OR SHOW? OR COMMUNICAT? OR CONVEY?)(2N)REMORSE/TI,AB,DE |
| 12 | 0 | (EXPRESS? OR SHOW? OR COMMUNICAT? OR CONVEY?)(2N)SYMPATHY/TI,AB,DE |
| 13 | 1608 | S1:S12 |
| 14 | 668 | ADVERSE(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 15 | 91 | SAFETY(2N)(INCIDENT OR INCIDENTS)/TI,AB,DE |
| 16 | 6 | SERIOUS(2N)(INCIDENT OR INCIDENTS)/TI,AB,DE |
| 17 | 2 | SENTINEL(2N)EVENT?/TI,AB,DE |
| 18 | 166 | (CRITICAL OR CLINICAL OR MEDICAL OR HEALTHCARE)(2N)(INCIDENT OR INCIDENTS)/TI,AB,DE |
| 19 | 9 | (HARM OR HARMS OR HARMFUL)(3N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 20 | 28 | UNEXPECTED(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 21 | 6 | UNINTENDED(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 22 | 0 | UNINTENTIONAL?(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 23 | 6 | UNANTICIPATED(2N)(EVENT? OR INCIDENT OR INCIDENTS OR OUTCOME?)/TI,AB,DE |
| 24 | 11 | (UNEXPECTED OR UNINTENDED OR UNINTENTIONAL? OR UNANTICIPATED)(2N)INJUR?/TI,AB,DE |
| 25 | 9 | MEDICAL(W)(ACCIDENT? OR INJUR?)/TI,AB,DE |
| 26 | 5 | SURGICAL(W)(ACCIDENT? OR INJUR?)/TI,AB,DE |
| 27 | 68 | (PATIENT? OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR USER?)(3N)ADVERSE/TI,AB,DE |
| 28 | 27 | (PATIENT? OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR USER?)(3N)(HARM OR HARMS OR HARMFUL)/TI,AB,DE |
| 29 | 149 | (PATIENT? OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR USER?)(3N)(MISTAKE? OR ERROR OR ERRORS)/TI,AB,DE |
| 30 | 673 | (PROFESSIONAL? OR WORKER? OR DENTIST? OR NURS? OR DOCTOR? OR PHYSICIAN? OR SURGEON? OR SURGICAL? OR SURGER? OR PHARMAC? OR HUMAN OR PRACTITIONER? OR PSYCHIATRIST? OR PSYCHOLOGIST? OR ANAESTHE? OR ANESTHE? OR GP)(3N)(MISTAKE? OR ERROR OR ERRORS)/TI,AB,DE |
| 31 | 1542 | (MEDICAL OR DIAGNOS? OR TREATMENT? OR MEDICATION? OR HEALTHCARE OR CARE OR HOSPITAL? OR SYSTEM?)(3N)(MISTAKE? OR ERROR OR ERRORS)/TI,AB,DE |
| 32 | 54 | MISDIAGNOSIS/TI,AB,DE |
| 33 | 219 | (IATROGENIC OR IATROGENESIS)/TI,AB,DE |
| 34 | 181 | (NEGLIGENCE OR NEGLIGENT)/TI,AB,DE |
| 35 | 227 | MALPRACTICE/TI,AB,DE |
| 36 | 1198 | LITIGAT?/TI,AB,DE |
| 37 | 23 | LEGAL(W)(ACTION? OR PROCEEDING?)/TI,AB,DE |
| 38 | 72 | (LAWSUIT? OR LAW(W)SUIT?)/TI,AB,DE |
| 39 | 54 | NEAR(W)MISS/TI,AB,DE |
| 40 | 29 | NEAR(W)MISSES/TI,AB,DE |
| 41 | 8 | ERR(W)IS(W)HUMAN/TI,AB,DE |
| 42 | 19 | THINGS(W)GO(W)WRONG/TI,AB,DE |
| 43 | 5214 | S14:S42 |
| 44 | 16 | S13 AND S43 |
| 45 | 1 | OPEN(W)DISCLOSURE/TI,AB,DE |
| 46 | 12 | (COMMUNICAT? OR DISCUSS? OR CONVERS? OR TALK? OR EXPLAIN? OR EXPLANATION? OR TELL? OR TOLD OR ACKNOWLEDG? OR CONSULT? OR INFORM? OR NOTIF?)(3N)(PATIENT? OR FAMILY OR FAMILIES OR INPATIENT? OR OUTPATIENT? OR CONSUMER? OR CITIZEN? OR PUBLIC OR CARER? OR CAREGIVER? OR USER?)(3N)(ADVERSE OR HARM? OR ERROR OR ERRORS OR MISTAKE? OR INCIDENT OR INCIDENTS)/TI,AB,DE |
| 47 | 29 | S44:S46 |
| 48 | 29 | S47/1980:2012 |
Ongoing research resources
PROSPERO
Searched on 6 January 2012; 0 records retrieved.
disclos* OR nondisclos* OR undisclos* OR candour OR candor OR apolog* OR sorry OR openness
Key
* = truncation
Health Services Research Projects in Progress (HSRProj)
www.cf.nlm.nih.gov/hsr_project/home_proj.cfm
Searched on 9 January 2012; 33 project records retrieved.
Using the advanced search with ‘project status’ set to ‘all’ and ‘states’ set to ‘all’.
(((disclose or discloses or disclosure or disclosures or disclosed or disclosing or nondisclose or nondisclosure or nondisclosures or nondisclosed or undisclose or undisclosed or candour or candor or candid or apology or apologies or apologise or apologize or apologised or apologized or apologising or apologizing or sorry or openness) AND (adverse OR harm OR harms OR harmful OR mistake OR mistakes OR error or errors OR misdiagnosis OR iatrogenic OR iatrogenesis OR negligence OR negligent OR malpractice OR litigate OR litigates OR litigation OR miss OR misses OR err OR incident OR incidents)))
National Research Register Archive
www.nihr.ac.uk/Pages/NRRArchiveSearch.aspx (contains records of projects from 2000 to 2007 only).
Searched on 6 January 2012; 63 records retrieved.
(disclos* or nondisclos* or undisclos* or candour or candor or apolog* or sorry or openness or communicat* or discuss* or convers* or talk* or explain* or explanation* or tell* or told or acknowledge* or consult* or inform* or notif* ) all fields
AND
(adverse or harm or harms or harmful or mistake* or error or errors or misdiagnosis or iatrogen* or negligence or negligent or malpractice or litigat* or miss or misses or err or incident or incidents) in title field
Key
* = truncation
ClinicalTrials.gov
http://clinicaltrials.gov/ct2/search
Searched on 5 January 2012; 125 records retrieved.
disclose OR discloses OR disclosure OR disclosures OR disclosed OR disclosing OR "duty of candour" OR "duty of candor" OR apology OR apologies OR apologise OR apologize OR apologised OR apologized OR apologising OR apologizing OR sorry OR openness | received on or after 01/01/1980 | updated on or after 01/01/1980
Clinical Controlled Trials
www.controlled-trials.com/mrct/searchform
Searched the metaRegister (including all active and archived registers) on 9 January 2012; 245 records retrieved.
(disclos* OR candour OR candor OR candid OR apolog* OR sorry) AND (adverse OR sentinel OR harm* OR mistake* OR error OR errors OR misdiagnosis OR iatrogen* OR negligence OR negligent OR malpractice OR litigat*)
Key
* = truncation
World Health Organization (WHO) International Clinical Trials Registry Platform Search Portal (ICTRP)
http://apps.who.int/trialsearch/Default.aspx
Searched on 6 January 2012; 54 records retrieved.
disclos* OR candour OR candor OR candid OR apolog* OR sorry OR openness
Key
* = truncation
Appendix 3 Databases searched
The following databases were searched.
Health related
-
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations.
-
EMBASE.
-
PsycINFO.
-
HMIC.
-
The Cochrane Library:
-
CDSR.
-
DARE.
-
HTA Database.
-
CENTRAL.
-
-
CINAHL.
-
SCI.
-
LILACS.
-
PASCAL.
-
Health Systems Evidence.
Social science
-
ASSIA.
-
SSCI.
Law
-
Lawtel.
-
Westlaw.
-
Lexus.
Reports/conference proceedings/grey literature
-
NTIS.
-
CPCI-S.
-
CPCI-SSH.
-
Dissertation Abstracts.
-
Inside Conferences.
Ongoing research
-
PROSPERO.
-
HSRProj.
-
National Research Register Archive.
-
ClinicalTrials.gov.
-
Current Controlled Trials.
-
WHO ICTRP.
-
The websites and databases of relevant organisations [e.g. AHRQ, Canadian Patient Safety Institute (CPSI), Institute for Healthcare Improvement (IHI), NPSA, National Patient Safety Foundation (NPSF), Alexandria Patients Safety Alliance (APSA), Action Against Medical Accidents (AvMA), Joint Commission Journal on Quality and Patient Safety (JCJQS), Sorry Works in the USA, Safety Improvement for Patients in Europe (SIMPATIE)].
-
Personal contact with key personnel in organisations that are actively developing work to involve patients in efforts to improve their own safety (e.g. AHRQ, CPSI, IHI, NPSA, NPSF).
Appendix 4 Ethical permission
Appendix 5 Example topic guide
Topic guide
Health professional interviews
Outline of the project. Define adverse event.
General awareness of disclosure and current practice
Can you talk to me about open disclosure in health care – what does this term mean to you?
Personal experiences of disclosure
If an adverse event occurred in your ward/unit what role might you expect to play in its disclosure?
How would you feel about disclosing an adverse event?
How well-prepared do you feel if that situation was to arise now?
What would you want to achieve through the disclosure?
What do you think the patients would want from the disclosure?
What factors do you think might influence your approach to the disclosure or the things you might say?
What would your main concerns be about disclosing an event to patients or their friends or relatives?
Have you had any experience of disclosing an adverse event to a patient or their friends or relatives?
If yes go to Q4.
Can you tell me a bit about your experience?
What role did you play in the disclosure?
How did you feel about disclosing the event?
How well-prepared did you feel for that situation?
What did you want to achieve through the disclosure?
What do you think the patient wanted from the disclosure?
What factors do you feel influenced your approach to the disclosure or the things that you said?
What challenges did you face, if any?
How did you feel after the disclosure – would you have done anything differently?
Knowledge and perceptions of open disclosure policy
You might be aware of the Being Open framework which relates to the policy of open disclosure in the NHS. The framework sets out 10 key principles of open disclosure that NHS staff should use when communicating with patients, their families and carers about a patient safety incident. Are you aware of the being open policy or framework?
If yes go to 6.
If no go to 8.
Can you tell me a bit about the policy and how it works in practice from your own experiences?
What do you consider to be the main challenges in its use?
What kinds of things might you expect to see in the 10 key principles that you might need to consider in the process of disclosing an incident?
SHOW PARTICIPANTS THE FRAMEWORK
What are your initial thoughts about this framework?
Do you see any parts that you think might raise some challenges or are there any things that you would feel concerned about looking at this?
Disclosure, quality and patient safety
Can you tell me a bit about the disclosure policy that operates in your trust?
What are you required to do, when and who is responsible for disclosing what types of incidents?
How does it link into the incident reporting system, if at all?
Do you think there is a link between disclosing adverse events to patients and enhancing the quality or safety of their care?
Appendix 6 Coding framework
Why Being Open is important: for and against (including consequences) – BRIEF ONLY
-
Respect for the patient as a person.
-
Showing trustworthiness of professional, organisation or profession.
-
Implications for ongoing care relationship.
-
What matters to the patient/family (including implications for them going forward).
-
Impact on the professional going forward.
Uncertainties/complexities of what and whether to disclose
-
‘The problem’ – definitions and thresholds.
-
Who might be responsible – error or not.
-
Patient and their likely response.
-
‘Salience’ of the event – is it important to tell.
Whether and where disclosure is done and not done (descriptive/epidemiology)
-
Relationship, history, context.
-
Setting/specialty.
How it’s done (descriptive including examples)
What makes for better and worse disclosure (evaluative comments)
-
Medium – person, letter, phone.
-
Person – involved with incident, seniority, experience, role.
-
Where.
-
When.
-
If in person – sincerity, genuine.
-
Relationship history.
-
Ongoing process of disclosure.
-
Flexibility, subtlety, sensitivity – attitude, sincerity.
-
Formality/formulaic.
-
Resultant feelings – patient – clinician.
Issues influencing whether, how, when and awareness of it (all include what’s missing and what’s needed)
-
National policy on Being Open.
-
Local policy on Being Open.
-
Health professional
-
hearing mixed messages (or consistent messages) about value/appropriateness of being open
-
vulnerability to/trust of patient
-
vulnerability to/trust of employing organisation
-
tension between requirement/pressures of employing organisation and professional body
-
place in hierarchy/seniority/experience
-
perceptions of expectations on you and perceived norms (profession, organisation, team, patient)
-
concerns re difficult conversations and personal ability to conduct and handle them well
-
attitudes to open disclosure (normative beliefs?)
-
past personal experiences of open disclosure
-
awareness of others’ experiences of open disclosure (or not)
-
concern for self (including reputation, job security)
-
education/training on open disclosure.
-
-
Professional organisations
-
principle of being open
-
specific guidance/policy – awareness of and driving force behind.
-
-
NHS organisations
-
processes for disclosure/follow-up post event
-
resources/staff allocated to it
-
reporting for learning
-
(whose) awareness/promotion of principle/policy of being open
-
support for staff involved in adverse outcomes/errors
-
reputation concerns
-
litigation concerns
-
costs/financial issues relating to being open or not and the consequences.
-
-
Policy framework
-
forked tongues (policies that pull in different directions)
-
measurement of effective disclosure and of patient safety problems/success in addressing these
-
reporting for learning.
-
-
Legal framework
-
duty of candour.
-
Suggestions or solutions to improve open disclosure
-
Duty of candour.
-
Training/education.
Appendix 7 Key characteristics and numbers of study participants by stakeholder group
| Group | Salient characteristics | Recruitment | Sampling notes |
|---|---|---|---|
| Policy-makers (n = 7) | Individuals who had been involved in health at political policy level, with an interest in open disclosure of adverse events currently or in the recent past | Targeted letters to those involved in health policy with a role in patient safety or the Being Open guidance | Deliberately identified those involved in the development or implementation of Being Open |
| Representatives from professional organisations (n = 16) | Organisations which regulate or indemnify health professionals in the UK | Targeted letters to leaders of 23 professional organisations in the UK | |
| NHS managers and health professionals (n = 54) | NHS managers working in clinical or non-clinical roles. Included risk managers Some managers have both clinical and non-clinical roles 13 doctors; 22 nurses; two pharmacists 17 NHS managers |
Targeted letters to senior managers in the five recruited trusts, and information disseminated through them to health professionals with our contact details | Efforts were made to recruit from a variety of ranks and professions but junior doctors were difficult to recruit |
| Patients and patient organisations (n = 5) | Individuals either represented patient organisations or had experienced error or harm | Information distributed to patient organisations and sent out to patients via the organisations with contact information Targeted letters to leaders of patient organisations |
Patients with positive experiences of disclosure were sought through health-care trusts but none were identified |
| Other relevant individuals (n = 2) | Targeted letters to those identified as potentially suitable by other respondents |
Appendix 8 Detailed statement for reflexivity
Team data analysis
At significant points during the process of data analysis, the researchers most closely involved in data collection and the early stages of analysis (YB, RH, KB) met with members of the wider research team with extensive qualitative (VE) and clinical (IW) experience, to discuss emerging codes and categories, the interpretation of key texts and potential new lines of enquiry, thereby drawing on the combined insights of those ‘handling’ the data closely and members of the team with a wider perspective of methodological and open disclosure issues.
Reliability of coding
Towards the end of the analysis of the qualitative data, a member of the wider research team (VE) examined five transcripts which had been coded by the members of the team most closely involved in data collection and analysis (YB, RH, KB), as an independent check on the assignment of codes to data.
Comparison of data within and across cases in the data set
This was facilitated by the use of the analytic matrix which forms the basis of the framework approach. Comparing data within cases allowed for the exploration of contextual meaning, while comparing cases across the data set facilitated the search for regularities (key themes) and exceptions (negative cases).
Use of memos
The careful use of memos (by the prime analysts) during initial stages of analysis provided a visible ‘audit trail’ as the analysis moved from ‘raw’ data, through interpretation, to the production of findings.
Attention to ‘negative’ cases
Analysis included a search across the data set for ‘negative’ cases (evidence that contradicts, or appears to contradict, the explanations being developed) and alternative ways of explaining the data were considered. Systematic searching for negative cases or ‘outliers’ can help illuminate the connections that link the other cases together.
Reflexivity
Reflexivity relates to sensitivity to the ways in which the researcher and the research process may shape the data collected, including the role of prior assumptions and experience.
Prior assumptions and experience
Within the context of the current study, the members of the research team involved in face-to-face contact with study participants needed to consider the ways in which their interactions with participants might be influenced by their own professional background, experiences and prior assumptions. The two interviewers (RH and KB) were both academic research fellows from non-clinical backgrounds. An important question we needed to address in drawing conclusions from the data concerned whether or not knowing about our professional background could have impacted on participants’ willingness to talk openly about experiences, or how this knowledge might have shaped what was said.
Awareness of social setting and the social ‘distance’ between the researcher and the researched
The majority of interviews were conducted in participants’ workplaces or homes (for patients), either face to face or over the telephone, as this was usually more convenient for them. Although we were invited in as researchers, we were also mindful that we were guests in the participants’ work or living spaces; respondents were therefore given the lead in ‘setting the pace’ of the interview. By deliberately adopting a ‘back seat’ approach in setting the scene for the interview to take place, the researchers hoped that participants would feel they were exercising a measure of control over the interview process.
Fair dealing
Dingwall247 has suggested that one way of reducing bias in qualitative research is to ensure that the research design explicitly incorporates a wide range of different perspectives, so that the viewpoint of one group is never presented as if representing the sole truth about any situation, an analytic technique he has referred to as ‘fair dealing’.
Our study was designed to elicit contributions from a broad range of stakeholders in open disclosure. During the analytic process no particular group’s views were ‘privileged’ over those of others; that is to say, data analysis included a process of constant comparison between accounts of each group of participants, to uncover similarities and differences, which were subsequently highlighted (for example, health professionals identified a lack of certainty around what should be disclosed to a patient or carer, more so than other participants).
A main goal of data analysis was the identification of common themes that emerged from comparison across cases (individual interviews). However, equal importance was attached to focusing on the minutiae of individuals’ accounts relating to specific incidents of disclosure; in the analysis, we sought to identify the views and experiences of individuals, as well as the majority, where these were divulged.
Awareness of wider social and political context
As a research team, we discussed the fact that participants recruited from a policy level, professional organisation or national ‘consumer’ group might show a strong commitment to a particular personal or political agenda, or wish to raise particular issues during group discussions which may relate only tangentially, or not at all, to the main purpose of the discussion. We discussed how we might handle this situation if it arose and decided to emphasise the purpose of the research prior to interview and through the questions and probes used. This strategy appeared to be successful in keeping participants engaged in the research process.
The role of the research team as collaborators in knowledge production
Collaborative research is highly valued for its ability to bring together multiple researchers with distinctive and specialist perspectives to tackle large or complex research problems, though frequently the ‘putting together’ of multiple perspectives in the construction of knowledge is not described. 248
Within the Being Open research team, there was a strong commitment from the outset to work collaboratively in the collection, analysis, interpretation and reporting of the qualitative data, though individual involvement with the various stages of the research process necessarily varied. The three team members most closely involved in fieldwork (YB, RH, KB) met frequently (on average at least once per week) to discuss the progress of fieldwork and reflect on data collection; meetings intensified during the early stages of analysis, when themes and codes were beginning to be identified. At this crucial stage, input was sought from other members of the research team with extensive experience of qualitative research and a broad knowledge of patient safety research (VE, IW) to assist with ‘firming up’ the coding framework. During the early stages of analysis, an all-day meeting was convened in a location away from the interruptions of the office environment, which served as a kind of ‘interpretative retreat’. Throughout the day, we explored a sample of transcripts to gain a sense of the data that were emerging, the effectiveness of the topic guides and whether or not there may be additional participants who we wanted to invite to take part. A more intense focus on a subset of transcripts (which had been sent to VE in advance) in a further half-day analysis session was used to draw up the coding framework that would serve to underpin the analysis (and interpretation) of all the interview data. This endeavour resulted in an analytic strategy that was informed by insights from team members with a broad understanding of the research field and methodological issues, and those with field-based contextual and experiential understanding.
Potential for psychological harm
Members of the research team involved in fieldwork (RH, KB) were acutely sensitive to the possibility that focusing on the research topic could potentially provoke anxiety in the research participants concerning the disclosure of adverse events. At the end of each interview, researchers took time to ensure that participants were not feeling distressed by their participation; in these interviews, none of the participants expressed such concerns or appeared to be distressed or uneasy.
Appendix 9 Reference list of included literature for reviews
References are arranged chronologically by date for unauthored citations followed by alphabetically for first author.
Anon. Disclosure of documents by doctors. Br Med J 1985;290:1973–4.
Anon. Needle stick: hospital refused to show patient the incidence report, court says patient can sue. Legal Eagle Eye Newsletter for the Nursing Profession 1998;6:8.
Anon. Legal questions. Explaining an error: how to break the news. Nursing 1999;29:30.
Anon. Here’s how to admit you made a mistake. ED Manag 2000;12:124–5.
Anon. Medical mistakes: tell patients, families say risk managers in national survey. QRC Advis 2000;16:12.
Anon. Should patients, families be told of mistakes? Healthc Risk Manag 2000;22:88–90.
Anon. An ethical dilemma: Medical errors and medical culture. BMJ 2001;322:1236–7.
Anon. Policy and procedure manual: guidelines for disclosure and discussion of conditions and events with patients, families and guardians. Kennedy Inst Ethics J 2001;11:165–8.
Anon. Disclosure requires some hard choices. Healthc Risk Manag 2001;23:137–9.
Anon. Legal questions. After an error: should you tell all? Nursing 2001;31:25.
Anon. News & trends. JCAHO wants doctors to admit errors. Bus Health 2001;19:14.
Anon. Patients must be told of errors. OB-GYN Malpractice Prevention 2001;8:64.
Anon. Plan how you’ll disclose unanticipated outcomes. Healthc Risk Manag 2001;23:139–40.
Anon. The insider: hospital mistakes must be disclosed to patients. Ohio Nurses Rev 2001;76:10.
Anon. John M. Eisenberg Patient Safety Awards. Individual lifetime achievement: Julianne M. Morath, RN, MS. Jt Comm J Qual Improv 2002;28:637–45.
Anon. Open disclosure: an Australian project. Nurs Ethics 2002;9:557–8.
Anon. Mandatory patient safety training, from the board room to linen room. Healthc Benchmarks 2002;9:1–5.
Anon. Telling patients about mistakes made in their care is the right thing to do and may reduce lawsuits. AHRQ Research Activities 2002;263:9.
Anon. Sometimes it might just pay to say you’re sorry. Patient Care Manag 2003;19:3–4.
Anon. Disclosure to patients of in-hospital medical errors has increased, but there is room for improvement. AHRQ Research Activities 2003;275:8.
Anon. Experts are uncertain whether full disclosure of medical errors will help avoid lawsuits. AHRQ Research Activities 2003;280:7.
Anon. Fear of lawsuits may make physicians reluctant to disclose medical errors to patients. AHRQ Research Activities 2003;273:12.
Anon. Disclosure of medical errors. Ann Emerg Med 2004;43:432.
Anon. Disclosure of errors preferred by patients. J Fam Pract 2004;53:525–6.
Anon. Summaries for patients. The effects of telling patients about medical errors. Ann Intern Med 2004;140:I17.
Anon. By the numbers does your organization have a board-approved policy for disclosure? Mod Healthc 2004;34:9.
Anon. Doctors’ disclosure of medical errors improves patient satisfaction but may not prevent legal action. AHRQ Research Activities 2004;286:22.
Anon. More hospitals disclosing errors. OR Manager 2004;20:32.
Anon. Nearly half of surveyed hospitals don’t disclose serious errors to patients. Brief Patient Saf 2004;5:4.
Anon. Physicians say they favor disclosure of medical errors to patients and families, but disclosure often does not occur. AHRQ Research Activities 2004;290:14.
Anon. Professional update. Can apologizing actually prevent a malpractice lawsuit? Contemp OB/GYN 2004;49:25.
Anon. ‘I’m sorry’. Lancet 2005;366:1138.
Anon. Medical liability system hinders improvements in patient safety: Joint Commission expert panel offers solutions to crisis. Jt Comm Perspect 2005;25:9–10.
Anon. Bad news bearers: telling patients about infections: straightforward apology can head off lawsuit. Hosp Infect Control 2005;32:110, 115–16.
Anon. Disclosure gap is apparent with docs. Healthc Risk Manag 2005;27:138–9.
Anon. Disclosure process starts with an apology, then info. Healthc Risk Manag 2005;27:55–6.
Anon. How to discuss AEs with patients and families: establish a foundation of trust. Patient Educ Manag 2005;12:67–9.
Anon. ‘I’m sorry’ laws vary, require physicians’ finesse. Healthc Risk Manag 2005;27:129–30.
Anon. Insurer sees good results from disclosure, apologies. Healthc Risk Manag 2005;27:112.
Anon. MN hospital creates a culture of full disclosure. Healthc Risk Manag 2005;27:53–5.
Anon. On its web site, a hospital apologizes for a fatal error. Healthc Risk Manag 2005;27:21.
Anon. Risk managers, doctors disagree on ‘full disclosure’. Healthc Risk Manag 2005;27:137–8.
Anon. Saying ‘I’m sorry’ is starting to pay off with reduced lawsuits and legal costs: some providers seeing dramatic cutbacks in settlement amounts. Healthc Risk Manag 2005;27:109–12.
Anon. Survey: doctors respond differently after error. Healthc Risk Manag 2005;27:139.
Anon. When doctors hide medical errors. New York Times 2006;9.
Anon. Bad news bearers: telling patients about infections straightforward apology can head off lawsuit. Patient Educ Manag 2006;13:33–6.
Anon. Case study. Disclosing errors and examining mistakes: Kaiser Permanente keeps patients informed and involved. Jt Comm Perspect Patient Saf 2006;6:9–10.
Anon. Critical care’s efforts to disclose medical errors and adverse events may not increase lawsuits. Healthcare Purchasing News 2006;30:8.
Anon. Federal bill promotes apologies and negotiations. Contemp OB/GYN 2006;51:26–7.
Anon. How you can encourage doctors to disclose errors. Healthc Risk Manag 2006;28:115.
Anon. Physicians still resist full disclosure of errors. Healthc Risk Manag 2006;28:112–15.
Anon. Professional update. Harvard adopts disclosure and apology policy. Contemp OB/GYN 2006;51:22.
Anon. Professional update. The art of presenting bad news vs the risk of getting sued. Contemp OB/GYN 2006;51:25.
Anon. Professional update. Washington state tort reform law incorporates apology clause. Contemp OB/GYN 2006;51:16.
Anon. Surgeons less likely to disclose errors: study says surgeons provide fewer details. Same-Day Surg 2006;30:124–5.
Anon. Surgeons vary widely in their approaches to disclosing medical errors to their patients. AHRQ Research Activities 2006;311:3.
Anon. What patients want to know about adverse events. Bandolier 2006;13:4.
Anon. Attorney: openness can actually reduce lawsuits. Hosp Infect Control 2007;34:76–8.
Anon. Full disclosure of medical errors to patients is becoming more and more transparent. AHRQ Research Activities 2007;328:6.
Anon. NQF updates list of safe practices, urges disclosure. Healthc Risk Manag 2007;29:5–7.
Anon. Patient safety pulse: your patient safety news. Making the case for apologies. Jt Comm Perspect Patient Saf 2007;7:2.
Anon. Studies reveal that error disclosure is similar among American and Canadian doctors, despite different malpractice environments. AHRQ Research Activities 2007;317:7–8.
Anon. When you have a serious adverse event should you apologize, waive charges? University of Michigan system cuts number of pending cases by 80%. Same-Day Surg 2007;31:29–32.
Anon. Will more hospitals adopt apology-and-disclosure policies? Contemp OB/GYN 2007;52:28.
Anon. Majority of hospitals won’t bill for ‘never events’. Healthc Benchmarks Qual Improv 2008;15:7–9.
Anon. Few medical trainees are trained to disclose errors to patients by the time they assume some patient care. AHRQ Research Activities 2008;340:2–3.
Anon. How an apology may help you avoid litigation. Urol Times 2008;36:30.
Anon. Most patients want doctors to disclose severe medical errors. AHRQ Research Activities 2008;335:3.
Anon. Doctors, admit your mistakes. Consum Rep 2009;74:12.
Anon. Are ED nurses left out if errors are disclosed? ED Nursing 2009;12:69.
Anon. Avoid a bungled apology: first, get all the facts. Second of a two-part series. ED Legal Lett 2009;20:137, 140–1.
Anon. Don’t inform a patient about this type of error. ED Nursing 2009;12:68.
Anon. Facts concealed from family: no negligence, but civil fraud lawsuit can go forward. Legal Eagle Eye Newsletter for the Nursing Profession 2009;17:7.
Anon. Making it easier to apologize. Can Nurse 2009;105:6.
Anon. Nurses feel left out of the medical error disclosure process. AHRQ Research Activities 2009;347:23–4.
Anon. Openness is the best policy with patients, says NPSA. Nurs Stand 2009;24:6.
Anon. Patient safety pulse: your patient safety news. Study spotlights medical error disclosure. Jt Comm Perspect Patient Saf 2009;9:2.
Anon. Professional update. Nurses often excluded from error disclosure. RN 2009;72:15.
Anon. Should you tell patients a drug error was made? ED Nursing 2009;12:68–9.
Anon. Some pediatricians would disclose errors only if harm is evident. AHRQ Research Activities 2009;343:4–5.
Anon. Study finds failure to include nurses in process of admitting errors to patients, families. Healthcare Purchasing News 2009;33:12.
Anon. Survey responses: do you tell patients about errors? Nursing 2009;39:26.
Anon. Summaries for patients. Does admitting mistakes to patients lead to more lawsuits. Ann Intern Med 2010;153:I-28.
Anon. If providers apologize, will there be a lawsuit? ED Manag 2010;22:20–1.
Anon. Clinical rounds. Disclosing errors: physicians and risk managers disagree. Nursing 2010;40:21.
Anon. Disclosure-with-offer program provides more transparent culture. Patient Saf Monit J 2010;11:1–3.
Anon. Study recommends disclosure of medical mistakes that affect multiple patients. AHRQ Research Activities 2010;362:20–1.
Anon. Study recommends disclosure of medical mistakes that affect multiple patients. Healthcare Purchasing News 2010;34:8.
Anon. $3.3M verdict after surgeon says ‘sorry’. Same-Day Surg 2011;35:116–7.
Anon. Court weighs ‘I’m sorry’ vs ‘I’m responsible’. Same-Day Surg 2011;35:118–19.
Anon. Difference between ‘sorry’ and ‘my fault’. Same-Day Surg 2011;35:118.
Anon. Doc tells patient provider not happy. Same-Day Surg 2011;35:120.
Anon. Hasty error disclosure can damage others. Same-Day Surg 2011;35:121.
Anon. Must be 50 ways to say you’re sorry. Same-Day Surg 2011;35:119.
Anon. Study examines barriers to adverse-event disclosure. Jt Comm Perspect Patient Saf 2011;11:2.
Anon. Take a pause after the apology. Same-Day Surg 2011;35:117.
Anon. When, how to disclose a provider’s errors. Same-Day Surg 2011;35:119–20.
Anon. Amy Francis Inquest: Patient Died After Attempt to Remove Wrong Organ. BBC; 2012. URL: www.bbc.co.uk/news/uk-wales-south-east-wales-16533134 (accessed 20 January 2012).
Agency for Healthcare Research and Quality (AHRQ). Links to Documents and Resources Relating to Being Open. URL: www.ahrq.gov (accessed 2 December 2012).
Action Against Medical Accidents (AvMA). Legal Duty of Candour – ‘Robbie’s Law’. URL: www.avma.org.uk/pages/legal_duty_of_candour_-_robbies_law.html (accessed 2 December 2012).
Action Against Medical Accidents (AvMA). Links to Documents Relating to Being Open. URL: www.avma.org.uk/pages/about_us.html (accessed 2 December 2012).
Aasland OG, Forde R. Impact of feeling responsible for adverse events on doctors’ personal and professional lives: the importance of being open to criticism from colleagues. Qual Saf Health Care 2005;14:13–17.
Agapito JC. Scientia et Mores: veracity, ethics and the radiation therapist. Can J Med Radiat Technol 1998;29:18–23.
Aitkenhead AR. Anaesthetic disasters: handling the aftermath. Anaesthesia 1997;52:477–82.
Allan A. Apology in civil law: A psycho-legal perspective. Psychiatr Psychol Law 2007;14:5–16.
Allan A, McKillop D. The health implications of apologizing after an adverse event. Int J Qual Health Care 2010;22:126–31.
Allen G. Evidence for practice: Perceptions of error definition, reporting, and disclosure. AORN J 2006;84:494, 496–7.
Allen S. Story telling an innovation to improve healthcare incident disclosure. Women Birth 2011;24(Suppl. 1):23.
Allman J. Bearing the burden or baring the soul: physicians’ self-disclosure and boundary management regarding medical mistakes. Health Commun 1998;10:175–97.
Almaramhy H, Al-Shobaili H, El-Hadary K, Dandash K. Knowledge and attitude towards patient safety among a group of undergraduate medical students in Saudi Arabia. Int J Health Sci (Qassim) 2011;5:59–67.
Amatuzio J. To tell you the truth. Minn Med 2005;88:60.
American Society for Healthcare Risk Management. Disclosure of Unanticipated Events: Creating an Effective Patient Communication Policy. Chicago, IL: American Society for Healthcare Risk Management of the American Hospital Association; 2003.
American Society for Healthcare Risk Management. Disclosure of Unanticipated Events: The Next Step in Better Communication. Chicago, IL: American Society for Healthcare Risk Management of the American Hospital Association; 2003.
American Society for Healthcare Risk Management. Disclosure: what works now and what can work even better. J Healthc Risk Manag 2004;24:19–26.
Amori G, Popp PL. The timing of early resolution: Working at the patient’s pace. J Healthc Risk Manag 2007;27:19–23.
Appelbaum PS. Law & psychiatry: reforming malpractice: the prospects for change. Psychiatr Serv 2011;62:6–8.
Applegate WB. Physician management of patients with adverse outcomes. Arch Intern Med 1986;146:2249–52.
Armstrong D. The power of apology : how saying sorry can leave both patients and nurses feeling better. Nurs Times 2009;105:16–19.
Asghari F, Fotouhi A, Jafarian A. Doctors’ views of attitudes towards peer medical error. Qual Saf Health Care 2009;18:209–12.
Atterbury C. Apologies go a long way towards making amends adverse incidents. Nurs Stand 2003;17:30.
Atwood D. Impact of medical apology statutes and policies. J Nursing Law 2008;12:43–53.
Aubrey ME. The error of our ways. CMAJ 2001;165:270–2.
Ausman JI. Trust, malpractice, and honesty in medicine: should doctors say they are sorry? Surg Neurol 2006;66:105–6.
Bacon AK, Morris RW, Runciman WB, Currie M. Crisis management during anaesthesia: recovering from a crisis. Qual Saf Health Care 2005;14:e25.
Baggett P. I’m sorry: apologizing for a mistake might prevent a lawsuit. Tex Med 2005;101:56–9.
Bailey TM, Robertson EC, Hegedus G. Erecting legal barriers: new apology laws in Canada and the patient safety movement: useful legislation or a misguided approach? Health Law Can 2007;28:33–8.
Bakalar N. Medical errors? Patients may be the last to know. New York Times 2006;29:F7.
Baker KR. Can I say ‘I’m sorry’? Drug Top 2011;155.
Baker S, Lauro C, Sintim-Damoa A. Malpractice allegations and apology laws: benefits and risks for radiologists. J Am Coll Radiol 2008;5:1186–90.
Bancroft NP. Physician shame: An obstacle to disclosing adverse outcomes. Clin Manag 2007;15:3–10.
Banik DMR, Simon SR. Medical errors: Do physicians want to tell? Do geriatric patients want to know? J Am Geriatr Soc 2005;53:S68.
Banja J. Moral courage in medicine – disclosing medical error. Bioeth Forum 2001;17:7–11.
Banja J. CM ethics Medical errors 101: a primer. Case Manager 2005;16:57–9.
Banja JD. Disclosing medical error: how much to tell? J Healthc Risk Manag 2003;23:11–14.
Banja JD. Ethically speaking: the case manager’s response to harm-causing error. Case Manager 2005;16:60–4.
Banja JD. Problematic medical errors and their implications for disclosure. HEC Forum 2008;20:201–13.
Barach P. The end of the beginning: lessons learned from the patient safety movement. J Leg Med 2003;24:7–27.
Barach P, Cantor MD. Adverse event disclosure: benefits and drawbacks for patients and clinicians. In Clarke S, Oakley J, editors. Informed Consent and Clinician Accountability: The Ethics of Report Cards on Surgeon Performance. Cambridge: Cambridge University Press; 2007. pp. 76–90.
Barron WM, Kuczewski MG. Unanticipated harm to patients: deciding when to disclose outcomes. Jt Comm J Qual Patient Saf 2003;29:551–5.
Barsella RM. It’s hard to say ‘I’m sorry’. NurseWeek 2007;14:30–1.
Bartlett P. Doctors as fiduciaries: equitable regulation of the doctor-patient relationship. Med Law Rev 1997;5:193–224.
Baum M. Making Amends misses the point. BMJ 2004;328:407.
Baumrucker SJ. A medical error leads to tragedy: how do we inform the patient? Am J Hosp Palliat Care 2006;23:417–21.
Bayley C. Turning the Titanic: changing the way we handle mistakes. HEC Forum 2001;13:148–59.
Bayley C. Medical mistakes and institutional culture. In Sharpe VA, editor. Accountability: Patient Safety and Policy Reform. Washington, DC: Georgetown University Press; 2004. pp. 99–119.
Baylis F. Errors in medicine: nurturing truthfulness. J Clin Ethics 1997;8:336–40.
Beer Z, Guttman N, Brezis M. Discordant public and professional perceptions on transparency in healthcare. QJM 2005;98:462–3.
Bell SK, Smulowitz PB, Woodward AC, Mello MM, Duva AM, Boothman RC, et al. Disclosure, apology, and offer programs: stakeholders’ views of barriers to and strategies for broad implementation. Milbank Q 2012;90:682–705.
Berlin L. Reporting the ‘missed’ radiologic diagnosis: medicolegal and ethical considerations. Radiology 1994;192:183–7.
Berlin L. Malpractice issues in radiology. Admitting mistakes. AJR Am J Roentgenol 199;172:879–84.
Berlin L. Will saying ‘I’m sorry’ prevent a malpractice lawsuit? AJR Am J Roentgenol 2006;187:10–15.
Berlin L. The mea culpa conundrum. Radiology 2009;253:284–7.
Berlinger N. What is meant by telling the truth: Bonhoeffer on the ethics of disclosure. Stud Christ Ethics 2003;16:80–92.
Berlinger N. Avoiding cheap grace. Medical harm, patient safety, and the culture(s) of forgiveness. Hastings Cent Rep 2003;33:28–36.
Berlinger N. Fair compensation without litigation: addressing patients’ financial need in disclosure. J Healthc Risk Manag 2004;24:7–11.
Berlinger N, Wu AW. Subtracting insult from injury: addressing cultural expectations in the disclosure of medical error. J Med Ethics 2005;31:106–8.
Bernstein M, Brown B. Doctors’ duty to disclose error: a deontological or Kantian ethical analysis. Can J Neurol Sci 2004;31:169–74.
Bernstein M, Hébert PC, Etchells E. Patient safety in neurosurgery: detection of errors, prevention of errors, and disclosure of errors. Neurosurg Q 2003;13:125–37.
Berry M. Saying the right thing when things go wrong. RN 2004;67:59–61.
Bismark M, Paterson R. ‘Doing the right thing’ after an adverse event. N Z Med J 2005;118:U1593.
Bismark MM. The power of apology. N Z Med J 2009;122:96–106.
Bluebond-Langner R, Rodriguez ED, Wu AW. Discussing adverse outcomes with patients and families. Oral Maxillofac Surg Clin North Am 2010;22:471–9.
Boden TW. It’s hard for me to say I’m sorry. MGMA Connex 2011;11:36–9.
Boivin J. Confidence gained: full medical error disclosure improves quality of care. Nurs Spectr (N Engl Ed) 2005;9:13.
Bonnema RA, Gosman GG, Arnold RM. Teaching error disclosure to residents: a curricular innovation and pilot study. J Grad Med Educ 2009;1:114–18.
Boothman RC. Apologies and a strong defense at the University of Michigan Health System. Physician Exec 2006;32:7–10.
Boston Bar Association. Medical Malpractice: Emerging Issues in Apology Disclosure and Peer Review. Boston, MA: BBA Continuing Legal Education; 2010.
Bovbjerg RR. Medical safety: from stories to policy. Health Aff 2001;20:241–2.
Bovbjerg RR, Tancredi LR. Liability reform should make patients safer: ‘Avoidable classes of events’ are a key improvement. J Law Med Ethics 2005;33:478–500.
Boyle D, O’Connell D, Platt FW, Albert RK. Disclosing errors and adverse events in the intensive care unit. Crit Care Med 2006;34:1532–7.
Boyte WR. Casey’s legacy. Health Aff 2001;20:250–4.
Bradley C, Brasel K. Disclosing medical error #194. J Palliat Care Med 2009;12:555–6.
Bradley CT, Brasel KJ. Core competencies in palliative care for surgeons: interpersonal and communication skills. Am J Hosp Palliat Med 2007;24:499–507.
Brahams D. Should doctors admit their mistakes? Med Leg J 2005;73:41–4.
Brandom BW, Callahan P, Micalizzi DA. What happens when things go wrong? Paediatr Anaesth 2011;21:730–6.
Brazeau C. Disclosing the truth about a medical error. Am Fam Physician 1999;60:1013–14.
Bressler HJ. Safety issues as exemplified by the activities of the Joint Commission on Accreditation of Healthcare Organizations: context for the safety and disclosure standards. J Health Law 2002;35:179–87.
Brooke PS. Legal questions. Revealing medication errors: is honesty the best policy? Nursing 2005;35:29.
Brooke PS. Legal questions. Reporting med errors: who needs to know? Nursing 2008;38:11.
Bruder KL, Gambone JC. Patient safety series: understanding and implementing the regulatory requirements. ACOG Clin Rev 2003;8:1–5.
Buckley J. Open Disclosure and Medical Claims Study. URL: www.cf.nlm.nih.gov/hsr_project/view_hsrproj_record.cfm?PROGRAM_CAME=search_fields.cfm&NLMUNIQUE_ID=20104205&SEARCH_FOR=20104205 (accessed 2 December 2012).
Buerhaus P. Is hospital patient care becoming safer? A conversation with Lucian Leape. Interview by Peter I. Buerhaus. Health Aff 2007;26:w687–96. [Erratum published in Health Aff(Millwood) 2007;26:following w696.]
Burchardi H. Are we honest enough with our patients? Intensive Care Med 1998;24:1237–8.
Butcher L. Lawyers say ‘sorry’ may sink you in court. Physician Exec 2006;32:20–4.
Bute JJ. Review of medical errors and medical narcissism. Health Commun 2006;20:105–7.
Calvert JF Jr, Hollander-Rodriguez J, Atlas M, Johnson KE. Clinical inquiries. What are the repercussions of disclosing a medical error? J Fam Pract 2008;57:124–5.
Camire E, Moyen E, Stelfox HT. Medication errors in critical care: risk factors, prevention and disclosure. CMAJ 2009;180:936–43.
Canadian Patient Safety Institute. Canadian Disclosure Guidelines. Being Open with Patients and Families. URL: www.patientsafetyinstitute.ca/English/toolsResources/disclosure/Documents/CPSI%20Canadian%20Disclosure%20Guidelines.pdf (accessed 2 December 2012).
Canadian Patient Safety Institute. Background Paper for the Development of National Guidelines for the Disclosure of Adverse Events Canada. URL: www.patientsafetyinstitute.ca/English/toolsResources/disclosure/Documents/Background%20Paper%20for%20the%20Canadian%20Disclosure%20Guidelines.pdf (accessed 2 December 2012).
Canadian Patient Safety Institute. Disclosure Training Programs. URL: www.patientsafetyinstitute.ca/English/toolsResources/disclosure/DisclosureTraining/Pages/default.aspx (accessed 2 December 2012).
Canadian Patient Safety Institute. The Impact of Disclosure of Adverse Events on Litigation and Settlement: A Review for the Canadian Patient Safety Institute 2007. URL: www.patientsafetyinstitute.ca/English/toolsResources/disclosure/Documents/The%20Impact%20of%20Disclosure%20on%20Litigation%20a%20Review%20for%20the%20CPSI.pdf (accessed 2 December 2012).
Cantor MD. Telling patients the truth: a systems approach to disclosing adverse events. Qual Saf Health Care 2002;11:7–8.
Cantor MD, Barach P, Derse A, Maklan CW, Wlody GS, Fox E. Disclosing adverse events to patients. Jt Comm J Qual Patient Saf 2005;31:5–12.
Casey JM, Afable RF. Contract or covenant? Health Prog 2004;85:25–7.
Clark C. Medical error second victims get some help finally. Health Leaders Media, 17 January 2013. URL: www.healthleadersmedia.com/content/QUA-288425/Medical-Error-Second-Victims-Get-Some-Help-Finally## (accessed 5 February 2013).
Coustan DR, Mathieu PL, Rakatansky H, Sullivan FW, Hamolsky MW. Commentaries on reporting physicians’ mistakes. R I Med J 1990;73:336–44.
Cramer H, Foraita R, Habermann M. Nursing errors and the consequences. Results of a survey of nurses from inpatient care institutions. Pflege 2012;25:245–59.
Dalton GD, Samaropoulos XF, Dalton AC. Improvements in the safety of patient care can help end the medical malpractice crisis in the United States. Health Policy 2008;86:153–62.
Danesh HN. The Ethics of Disclosure: How an Ethical Decision Making Framework Can Contribute to Determining When Disclosure is Appropriate. Dissertation Abstracts International 2010;72:1406.
Darr K. Communication: the key to reducing malpractice claims. Hosp Top 1997;75:4–6.
Darr K. Uncircling the wagons: informing patients about unanticipated outcomes. Hosp Top 2001;79:33–5.
Daud-Gallotti RM, Morinaga CV, Arlindo-Rodrigues M, Velasco IT, Martins MA, Tiberio IC. A new method for the assessment of patient safety competencies during a medical school clerkship using an objective structured clinical examination. Clinics (Sao Paulo) 2011;66:1209–15.
Daugherty CG. Revealing a medication error. Am Fam Physician 2000;62:315.
Davies JM. Disclosure. Acta Anaesthesiol Scand 2005;49:725–7.
de Cassia Pires Coli R, dos Anjos MF, Pereira LL. The attitudes of nurses from an intensive care unit in the face of errors: an approach in light of bioethics. Rev Lat Am Enfermagem 2010;18:324–30.
De Freitas GF, Hoga LAK, Fernandes MDP, González JS, Ruiz MCS, Bonini BB. Brazilian registered nurses’ perceptions and attitudes towards adverse events in nursing care: a phenomenological study. J Nurs Manag 2011;19:331–8.
Demorest BH. When it’s okay to say you’re sorry. Surv Ophthalmol 2001;46:190–1.
Department of Health. A Consultation on Strengthening the NHS Constitution. London: The Stationery Office; 2012.
DerGurahian J. When sorry is enough. Study finds owning up to mistakes better approach. Mod Healthc 2009;39:17.
DeVita MA. Honestly, do we need a policy on truth? Kennedy Inst Ethics J 2001;11:157–64.
Dewan JA. Adverse events: accountability and disclosure attitudes of student nurse anesthetists (SRNAs). State of the Science Oral and Poster Sessions: part 2. AANA J 2006;74:465.
Dickens B. Disclosing adverse outcomes in medical care: FIGO Committee for the Ethical Aspects of Human Reproduction and Women’s Health. Int J Gynaecol Obstet 2010;111:192.
Dickens BM. Medical errors: legal and ethical responses. Int J Gynaecol Obstet 2003;81:109–14.
Dietz I, Borasio GD, Molnar C, Müller-Busch C, Plog A, Schneider G, et al. Errors in palliative care: kinds, causes, and consequences: a pilot survey of experiences and attitudes of palliative care professionals. J Palliat Med 2013;16:74–81.
Dintzis S, Gallagher TH. Anatomic pathologists’ attitudes and experiences regarding error disclosure. United States and Canadian Academy of Pathology, Annual Meeting, Washington, DC, 20–26 March 2010.
Dintzis SM, Gallagher TH. Disclosing harmful pathology errors to patients. Am J Clin Pathol 2009;131:463–5.
Dintzis SM, Stetsenko GY, Sitlani CM, Gronowski AM, Astion ML, Gallagher TH. Communicating pathology and laboratory errors: anatomic pathologists’ and laboratory medical directors’ attitudes and experiences. Am J Clin Pathol 2011;135:760–5.
Donn SM, McDonnell WM. When bad things happen: adverse event reporting and disclosure as patient safety and risk management tools in the neonatal intensive care unit. Am J Perinatol 2012;29:65–70.
Donohue P, Boss R, Valdez RC, Shepard J. Inherent risks vs. medical errors in the NICU: parent perceptions and physician disclosure. Acta Paediatr 2009;98:9–10.
Doucette E, Fazio S, LaSalle V, Malcius C, Mills J, Archer TR, et al. Full disclosure of adverse events to patients and families in the ICU: wouldn’t you want to know? Dynamics 2010;21:16–19.
Downing L, Potter RL. Heartland Regional Medical Center makes a ‘fitting response’ to medical mistakes. Bioeth Forum 2001;17:12–18.
Dresser R. The limits of apology laws. Hastings Cent Rep 2008;38:6–7.
Droppo L. Trillium Health Centre’s journey to disclosure. Healthc Q 2005;8:151–6.
Duclos CW, Eichler M, Taylor L, Quintela J, Main DS, Pace W, et al. Patient perspectives of patient-provider communication after adverse events. Int J Qual Health Care 2005;17:479–86.
Duke MB, Wilson JF. Responding to medical error: factors that influence the likelihood of disclosure by medical residents. J Investig Med 2007;55:S310.
Dunavan CP. Doctor files. Sometimes, it has to be said: ‘I made a mistake’. Los Angeles Times – Southern California Edition, 27 March 2006.
Dyer C. NHS staff should inform patients of negligent acts. BMJ 2003;327:7.
Eadie A. Medical error reporting: should it be mandatory in Scotland? J Forensic Leg Med 2012;19:437–41.
Edwin A. Non-disclosure of medical errors an egregious violation of ethical principles. Ghana Med J 2009;43:34–9.
Eisenberg D. When doctors say, ‘we’re sorry’. Time 2005;166:50–2.
Elhence P. Ethical issues in transfusion medicine. Indian J Med Ethics 2006;3:87–9.
Elwy AR. Patients’ and Providers’ Perceptions of Communicating an Adverse Event. URL: www.cf.nlm.nih.gov/hsr_project/view_hsrproj_record.cfm?PROGRAM_CAME=search_fields.cfm&NLMUNIQUE_ID=20094071&SEARCH_FOR=20094071 (accessed 2 December 2012).
Erlen JA. Medication errors: ethical implications. Orthop Nurs 2001;20:82–5.
Espin S, Levinson W, Regehr G, Baker GR, Lingard L. Error or ‘act of God’? A study of patients’ and operating room team members’ perceptions of error definition, reporting, and disclosure. Surgery 2006;139:6–14.
Etchegarary JM, Gallagher TH, Bell SK, Dunlap B, Thomas EJ. Error disclosure: a new domain for safety culture assessment. BMJ Qual Saf 2012;21:594–9.
Ethics Committee of the American Society for Reproductive Medicine. Disclosure of medical errors involving gametes and embryos. Fertil Steril 2006;86:513–15.
Evans SB, Decker R. Disclosing medical errors: a practical guide and discussion of radiation oncology-specific controversies. Int J Radiat Oncol Biol Phys 2011;80:1285–8.
Evans SB, Yu JB, Chagpar AB. Medical error disclosure attitudes among radiation oncologists. Int J Radiat Oncol Biol Phys 2011;81:S563.
Everett JP, Walters CA, Stottlemyer DL, Knight CA, Oppenberg AA, Orr RD. To lie or not to lie: resident physician attitudes about the use of deception in clinical practice. J Med Ethics 2011;37:333–8.
Fallowfield L. Communication with patients after errors. J Health Serv Res Policy 2010;15(Suppl. 1):56–9.
Fasler K. Integrating disclosure, patient safety and risk management activities. J Healthc Risk Manag 2008;28:19–25.
Faunce TA, Bolsin SN. Fiduciary disclosure of medical mistakes: the duty to promptly notify patients of adverse health care events. J Law Med 2005;12:478–82.
Federico F. Hospitals disclosing harm. Health Aff 2003;22:248; author reply 249.
Fein S, Hilborne L, Kagawa-Singer M, Spiritus E, Keenan C. Conceptual Model for Disclosure of Medical Errors. Rockville, MD: Agency for Healthcare Research and Quality; 2005.
Fein SP, Hilborne LH, Spiritus EM, Seyman GB, Keenan CR, Shojania KG, et al. Shades of gray: the spectrum of medical error disclosure and its influences. J Gen Intern Med 2004;19:210.
Fein SP, Hilborne LH, Spiritus EM, Seymann GB, Keenan CR, Shojania KG, et al. The many faces of error disclosure: a common set of elements and a definition. J Gen Intern Med 2007;22:755–61.
Feinmann J. You can say sorry. BMJ 2009;339:b3057.
Feinmann J. Why sorry doesn’t need to be the hardest word. BMJ 2011;342:1238–9.
Fentiman I. Litigation and doctor-patient communication. Clin Risk 2003;9:180–1.
Fiesta J. Legal aspects of medication administration. Nurs Manage 1998;29:22–3.
Fischer MA, Mazor KM, Baril J, Alper E, DeMarco D, Pugnaire M. Learning from mistakes. Factors that influence how students and residents learn from medical errors. J Gen Intern Med 2006;21:419–23.
Fisseni G, Pentzek M, Abholz H-H. Responding to serious medical error in general practice – consequences for the GPs involved: analysis of 75 cases from Germany. Fam Pract 2008;25:9–13.
Fleming C. New Health Affairs: Some Physicians Not Always Honest With Patients. Health Affairs Blog; 8 February 2012. URL: http://healthaffairs.org/blog/2012/02/08/new-health-affairs-some-physicians-not-always-honest-with-patients (accessed 2 December 2012).
Flemons WW, Davies JM, MacLeod B. Disclosing medical errors. CMAJ 2007;177:1236.
Flotta D, Rizza P, Bianco A, Pileggi C, Pavia M. Patient safety and medical errors: knowledge, attitudes and behavior among Italian hospital physicians. Int J Qual Health Care 2012;24:258–65.
Fox PK, Patterson S. Practical ethics. To apologize or not, that is the question. Hosp Health Netw 2006;80:24.
Fox R. I am sorry that we lost your leg. J R Soc Med 1996;89:181.
Freckelton I. Apologies, medicine and the law. J Law Med 2008;16:200–8.
Freeman Cook A, Hoas H, Guttmannova K, Joyner JC. An error by any other name. Am J Nurs 2004;104:32–43.
Freitas GF. Daily activities of nursing auxiliaries and technicians in relation to ethical events. Rev Lat Am Enfermagem 2009;17:449–54.
Frenkel DN, Liebman CB. Words that heal. Ann Intern Med 2004;140:482–3.
Friedman AL, Lee KC, Lee GD. Errors in ABO labeling of deceased donor kidneys: case reports and approach to ensuring patient safety. Am J Transplant 2007;7:480–3.
Gallagher TH. A 62-year-old woman with skin cancer who experienced wrong-site surgery: review of medical error. JAMA 2009;302:669–77.
Gallagher TH, Bell SK, Smith KM, Mello MM, McDonald TB. Disclosing harmful medical errors to patients: tackling three tough cases. Chest 2009;136:897–903.
Gallagher TH, Cook AJ, Brenner RJ, Carney PA, Miglioretti DL, Geller BM, et al. Disclosing harmful mammography errors to patients. Radiology 2009;253:443–52.
Gallagher TH, Denham CR, Leape LL, Amori G, Levinson W. Disclosing unanticipated outcomes to patients: the art and practice. J Patient Saf 2007;3:158–65.
Gallagher TH, Garbutt JM, Waterman AD, Flum DR, Larson EB, Waterman BM, et al. Choosing your words carefully: how physicians would disclose harmful medical errors to patients. Arch Intern Med 2006;166:1585–93.
Gallagher TH, Greene S, Roblin D, Calvi J, Horner K, Prouty C, et al. Patients’ views on delayed diagnosis in cancer. JClin Oncol 2010;28(Suppl. 1):6098.
Gallagher TH, Lucas MH. Should we disclose harmful medical errors to patients? If so, how? J Clin Outcomes Manag 2005;12:253–9.
Gallagher TH, Studdert D, Levinson W. Disclosing harmful medical errors to patients. N Engl J Med 2007;356:2713–19.
Gallagher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. Patients’ and physicians’ attitudes regarding the disclosure of medical errors. JAMA 2003;289:1001–7.
Gallagher TH, Waterman AD, Garbutt JM, Kapp JM, Chan DK, Dunagan WC, et al. US and Canadian physicians’ attitudes and experiences regarding disclosing errors to patients. Arch Intern Med 2006;166:1605–11.
Garbutt J, Brownstein DR, Klein EJ, Waterman A, Krauss MJ, Marcuse EK, et al. Reporting and disclosing medical errors: pediatricians’ attitudes and behaviors. Arch Pediatr Adolesc Med 2007;161:179–85.
Ghalandarpoorattar SM, Kaviani A, Asghari F. Medical error disclosure: the gap between attitude and practice. Postgrad Med J 2012;88:130–3.
Gooderham P. Disclosure of medical error. J R Soc Med 2005;98:437; author reply 437.
Grayson M. Human nature. Hosp Health Netw 2004;78:8.
Greene DA. Nursing experiences with disclosure of errors to patients. South Online J Nurs Res 2008;8:2.
Gu X, Itoh K. Patient views and attitudes to physician’s actions after medical errors in China. J Patient Saf 2012;8:153–60.
Gutheil TG. Commentary: Systems, sensitivity, and ‘sorry’. J Am Acad Psychiatry Law 2006;34:101–2.
Hammami MM, Attalah S, Al Qadire M. Which medical error to disclose to patients and by whom? Public preference and perceptions of norm and current practice. BMC Med Ethics 2010;11:17.
Hannawa AF. Negotiating medical virtues: toward the development of a physician mistake disclosure model. Health Commun 2009;24:391–9.
Hannawa AF. Shedding light on the dark side of doctor–patient interactions: verbal and nonverbal messages physicians communicate during error disclosures. Patient Educ Couns 2011;84:344–51.
Hannawa AF. ‘Explicitly implicit’: examining the importance of physician nonverbal involvement during error disclosures. Swiss Med Wkly 2012;142:w13576.
Harrington B. Medical errors and medical culture. Changing the culture of blame requires a revolution. BMJ 2001;323:570–1.
Hatlie MJ, Sheridan SE. The medical liability crisis of 2003: must we squander the chance to put patients first? Health Aff 2003;22:37–40.
Hébert PC. Patients must be told of unintended injuries during treatment. BMJ 1999;318:1762. [Erratum published in BMJ 1999;319:1253.]
Hébert PC, Levin AV, Robertson G. Bioethics for clinicians: 23. Disclosure of medical error. CMAJ 2001;164:509–13.
Hébert PC, Levin AV, Robertson G. Disclosure of medical error. In Singer PA, Viens AM, editors. The Cambridge Textbook of Bioethics. Cambridge: Cambridge University Press; 2008. pp. 257–65.
Henry LL. Disclosure of medical errors: ethical considerations for the development of a facility policy and organizational culture change. Policy Polit Nurs Pract 2005;6:127–34.
Hevia A, Hobgood C. Medical error during residency: to tell or not to tell. Ann Emerg Med 2003;42:565–70.
Hingorani M, Wong T, Vafidis G. Patients’ and doctors’ attitudes to amount of information given after unintended injury during treatment: cross sectional, questionnaire survey. BMJ 1999;318:640–1.
Hobgood C, Hevia A. Disclosing medical error: a professional standard. Hosp Physician 2004;40:41–52.
Hobgood C, Hevia A, Hinchey P. Profiles in patient safety: when an error occurs. Acad Emerg Med 2004;11:766–70.
Hobgood C, Hevia A, Tamayo-Sarver JH, Weiner B, Riviello R. The influence of the causes and contexts of medical errors on emergency medicine residents’ responses to their errors: an exploration. Acad Med 2005;80:758–64.
Hobgood C, Peck CR, Gilbert B, Chappell K, Zou B. Medical errors – what and when: what do patients want to know? Acad Emerg Med 2002;9:1156–61.
Hobgood C, Tamayo-Sarver JH, Elms A, Weiner B. Parental preferences for error disclosure, reporting, and legal action after medical error in the care of their children. Pediatrics 2005;116:1276–86.
Hobgood C, Tamayo-Sarver JH, Weiner B. Patient race/ethnicity, age, gender and education are not related to preference for or response to disclosure. Qual Saf Health Care 2008;17:65–70.
Hobgood C, Weiner B, Tamayo-Sarver JH. Medical error identification, disclosure, and reporting: do emergency medicine provider groups differ? Acad Emerg Med 2006;13:443–51.
Hobgood C, Xie J, Weiner B, Hooker J. Error identification, disclosure, and reporting: practice patterns of three emergency medicine provider types. Acad Emerg Med 2004;11:196–9.
Hofmann PB. Telling patients of mistakes. Hastings Cent Rep 2006;36:7.
Holden J. Saying sorry is not the same as admitting legal liability. BMJ 2009;338:370.
Huntoon MA, Levy RM. How to keep a bad outcome from becoming a lawsuit. Pain Med 2008;9(Suppl. 1):128–32.
Hurst JA. Puzzling out disclosure programs: where do you fit into the picture? Nursing 2011;41:50–4.
Ibrahim A, Garba ES, Asuku ME. Challenges in disclosure of adverse events and errors in surgery; perspectives from sub-Saharan Africa. Pan Afr Med J 2012;12:82.
Iedema R, Allen S. Anatomy of an incident disclosure: the importance of dialogue. Jt Comm J Qual Patient Saf 2012;38:435–42.
Iedema R. Attitudes toward error disclosure need to engage with systems thinking. Jt Comm J Qual Patient Saf 2010;36:99–100.
Iedema R, Allen S, Britton K, Piper D, Baker A, Grbich C, et al. Patients’ and family members’ views on how clinicians enact and how they should enact incident disclosure: the ‘100 patient stories’ qualitative study. BMJ 2011;343:d4423.
Iedema R, Jorm C, Wakefield J, Ryan C, Dunn S. Practising Open Disclosure: clinical incident communication and systems improvement. Sociol Health Illn 2009;31:262–77.
Iedema R, Jorm C, Wakefield J, Ryan C, Sorensen R. A new structure of attention?: Open disclosure of adverse events to patients and their families. J Lang Soc Psychol 2009;28:139–57.
Iedema R, Sorensen R, Manias E, Tuckett A, Piper D, Mallock N, et al. Patients’ and family members’ experiences of open disclosure following adverse events. Int J Qual Health Care 2008;20:421–32.
Iedema RAM, Mallock NA, Sorensen RJ, Manias E, Tuckett AG, Williams AF, et al. The National Open Disclosure Pilot: evaluation of a policy implementation initiative. Med J Aust 2008;188:397–400.
Itoh K, Andersen HB. Patient reactions to staff apology after adverse event and changes of their views in four year interval. In Palanque PVJWM, editor. Human Error, Safety and Systems Development. Lecture Notes in Computer Science. Berlin: Springer-Verlag Berlin; 2010. pp. 28–43.
Itoh K, Andersen HB, Madsen MD, Ostergaard D, Ikeno M. Patient views of adverse events: comparisons of self-reported healthcare staff attitudes with disclosure of accident information. Appl Ergon 2006;37:513–23.
Jeffs L, Espin S, Rorabeck L, Shannon SE, Robins L, Levinson W, et al. Not overstepping professional boundaries: the challenging role of nurses in simulated error disclosures. J Nurs Care Qual 2011;26:320–7.
Jeffs L, Espin S, Shannon SE, Levinson W, Kohn MK, Lingard L. A new way of relating: perceptions associated with a team-based error disclosure simulation intervention. BMJ Qual Saf 2010;19(Suppl. 3):i57–60.
Jerrold L. Litigation, legislation, and ethics: hiding the truth. Am J Orthod Dentofacial Orthop 1997;111:455–6.
Johnson C. We made a mistake. Nurs Manage 2000;31:22–4.
Johnson C, Horton S. Owning up to errors: put an end to the blame game. Nursing 2001;31:54.
Johnstone M. Clinical risk management and the ethics of open disclosure when things go wrong: implications for the nursing profession. Australas Emerg Nurs J 2007;10:215–6.
Johnstone M. Clinical risk management and the ethics of open disclosure: part I. Benefits and risks to patient safety. Australas Emerg Nurs J 2008;11:88–94.
Johnstone M. Clinical risk management and the ethics of open disclosure: part 2. Implications for the nursing profession. Australas Emerg Nurs J 2008;11:123–9.
Jones JW, McCullough LB, Richman BW. What to tell patients harmed by other physicians. J Vasc Surg 2003;38:866–7.
Josefson D. Hospitals must inform patients of errors. BMJ 2001;323:9.
Kachalia A, Kaufman SR, Boothman R, Anderson S, Welch K, Saint S, et al. Liability claims and costs before and after implementation of a medical error disclosure program. Ann Intern Med 2010;153:213–21.
Kachalia A, Shojania KG, Hofer TP, Piotrowski M, Saint S. Does full disclosure of medical errors affect malpractice liability? The jury is still out. Jt Comm J Qual Saf 2003;29:503–11.
Kachalia A, Shojania KG, Hofer TP, Saint SK. How does full disclosure of medical mistakes impact malpractice liability? J Gen Intern Med 2003;18:133.
Kaldjian LC, Jones EW, Rosenthal GE. Physician disclosure of medical errors: a literature-based framework of relevant beliefs, values, fears, and barriers. J Gen Intern Med 2003;18:233.
Kaldjian LC, Jones EW, Rosenthal GE. Facilitating and impeding factors for physicians’ error disclosure: a structured literature review. Jt Comm J Qual Saf 2006;32:188–98.
Kaldjian LC, Jones EW, Rosenthal GE, Tripp-Reimer T, Hillis SL. An empirically derived taxonomy of factors affecting physicians’ willingness to disclose medical errors. J Gen Intern Med 2006;21:942–8.
Kaldjian LC, Jones EW, Wu BJ, Forman-Hoffman VL, Levi BH, Rosenthal GE. Disclosing medical errors to patients: attitudes and practices of physicians and trainees. J Gen Intern Med 2007;22:988–96.
Kalra J. Disclosure of medical error – Response. J R Soc Med 2005;98:437.
Kapp MB. Medical mistakes and older patients: admitting errors and improving care. J Am Geriatr Soc 2001;49:1361–5.
Kapp MB. Resident safety and medical errors in nursing homes: reporting and disclosure in a culture of mutual distrust. J Leg Med 2003;24:51–76.
Katsuhara Y. What moral requirements cause ethical dilemmas among nurse executives? J Jpn Acad Nurs Sci 2003;23:1–10.
Kaul TK. Catastrophic situation & communication. J Anaesthesiol Clin Pharmacol 2008;24:381–2.
Kiersma ME, Darbishire PL, Plake KS, Oswald C, Walters BM. Laboratory session to improve first-year pharmacy students’ knowledge and confidence concerning the prevention of medication errors. Am J Pharm Educ 2009;73:99.
Kilpatrick K. Apology marks new era in response to medical error, hospital says. CMAJ 2003;168:757.
Kim KS, Kwon S-H, Kim J-A, Cho S. Nurses’ perceptions of medication errors and their contributing factors in South Korea. J Nurs Manag 2011;19:346–53.
Kim S, Brock D, Prouty CD, Odegard PS, Shannon SE, Robins L, et al. A web-based team-oriented medical error communication assessment tool: development, preliminary reliability, validity, and user ratings. Teach Learn Med 2011;23:68–77.
Kirshtein J. Hospital errors. ‘Doctors, admit your mistakes’. Consum Rep Health 2010;75:5.
Kmietowicz Z. NHS Constitution is ‘patchy, low key, and inconsistent,’ says review. BMJ 2012;345:e7494.
Knifed E, Goyal A, Bernstein M. Moral angst for surgical residents: a qualitative study. Am J Surg 2010;199:571–6.
Koh THHG, Alcock G. Open disclosure: appropriate timing is crucial. Int J Qual Health Care 2007;19:326.
Kondro W. Adverse events disclosure. CMAJ 2008;178:1128.
Kraman SS, Hamm G. Risk management: extreme honesty may be the best policy. Ann Intern Med 1999;131:963–7.
Krizek TJ. Surgical error: ethical issues of adverse events. Arch Surg 2000;135:1359–66.
Kroll L, Singleton A, Collier J, Rees Jones I. Learning not to take it seriously: junior doctors’ accounts of error. Med Educ 2008;42:982–90.
Kronman AC, Paasche-Orlow M, Orlander JD. Factors associated with disclosure of medical errors by housestaff. BMJ Qual Saf 2012;21:271–8.
Ladouceur R. Owning up to medical errors. Can Fam Physician 2007;53:201.
Lamb R. Open disclosure: the only approach to medical error. Qual Saf Health Care 2004;13:3–5.
Lamb RM, Studdert DM, Bohmer RMJ, Berwick DM, Brennan TA. Hospital disclosure practices: results of a national survey. Health Aff 2003;22:73–83.
Lape CP. Disclosing medical mistakes. J Gen Intern Med 1998;13:283–4.
Lazare A. Apology in medical practice: an emerging clinical skill. JAMA 2006;296:1401–4.
Leape L. Doctors and patients. Disclose, apologize, explain. Newsweek 2006;148:50.
Leape L, Berwick D, Clancy C, Conway J, Gluck P, Guest J, et al. Transforming healthcare: a safety imperative. Qual Saf Health Care 2009;18:424–8.
Leape LL, Berwick DM. Five years after To Err Is Human: what have we learned? JAMA 2005;293:2384–90.
Leape LL. Apology for errors: whose responsibility? Front Health Serv Manage 2012;28:3–12.
Lesnewski R. A piece of my mind. Mistakes. JAMA 2006;296:1327–8.
Leung GKK, Patil NG. Patient safety in the undergraduate curriculum: medical students’ perception. Hong Kong Med J 2010;16:101–5.
Levinson W. Disclosing medical errors: we’re halfway there. Arch Pediatr Adolesc Med 2008;162:991–2.
Levinson W. Disclosing medical errors to patients: a challenge for health care professionals and institutions. Patient Educ Couns 2009;76:296–9.
Levinson W, Gallagher TH. Disclosing medical errors to patients: a status report in 2007. CMAJ 2007;177:265–7.
Liang BA. A system of medical error disclosure. Qual Saf Health Care 2002;11:64–8.
Liang NL, Herring ME, Bush RL. Dealing honestly with an honest mistake. J Vasc Surg 2010;51:494–5.
Liebman CB, Hyman CS. A mediation skills model to manage disclosure of errors and adverse events to patients. Health Aff 2004;23:22–32.
Limb M. Peers’ rejection of statutory duty of candour is a missed opportunity, say campaigners. BMJ 2012;344:e1116.
Lintern S. Duty of candour will cost NHS £130 million in 10 years. Health Serv J 2012.
Linthorst GE, Kallimanis-King BL, Douwes Dekker I, Hoekstra JB, de Haes JC. What contributes to internists’ willingness to disclose medical errors? Neth J Med 2012;70:242–8.
Localio AR. Patient compensation without litigation: a promising development. Ann Intern Med 2010;153:266–7.
López L, Weissman JS, Schneider EC, Weingart SN, Cohen AP, Epstein AM. Disclosure of hospital adverse events and its association with patients’ ratings of the quality of care. Arch Intern Med 2009;169:1888–94.
Loren DJ, Garbutt J, Dunagan WC, Bommarito KM, Ebers AG, Levinson W, et al. Risk managers, physicians, and disclosure of harmful medical errors. Jt Comm J Qual Patient Saf 2010;36:101–8.
Loren DJ, Klein EJ, Garbutt J, Krauss MJ, Fraser V, Dunagan WC, et al. Medical error disclosure among pediatricians: choosing carefully what we might say to parents. Arch Pediatr Adolesc Med 2008;162:922–7.
Love D. Advancing Communication of Medical Error: Bridging the Gap Between Transgression and Transparency. Masters Abstracts 2011;49:3526.
Luk LA, Ng WIM, Ko KKS, Ung VH. Nursing management of medication errors. Nurs Ethics 2008;15:28–39.
Lyckholm L. Medical errors and medical culture. There is no easy way around taking responsibility for mistakes. BMJ 2001;323:570.
Lynch TG. Editorial comment: regarding ‘Moral angst for surgical residents: a qualitative study’. Am J Surg 2010;199:577–9.
MacDonald N, Attaran A. Medical errors, apologies and apology laws. CMAJ 2009;180:11.
Madden B, Cockburn T. Bundaberg and beyond: duty to disclose adverse events to patients. J Law Med 2007;14:501–27.
Magnavita N, Magnavita G, Fileni A, Bergamaschi A. Ethical problems in radiology: medical error and disclosure. Radiol Med 2009;114:1345–55.
Malaty W, Crane S. How might acknowledging a medical error promote patient safety? J Fam Pract 2006;55:775–80.
Malcolm L, Barnett P. Disclosure of treatment injury in New Zealand’s no-fault compensation system. Aust Health Rev 2007;31:116–22.
Manser T. Managing the aftermath of critical incidents: meeting the needs of health-care providers and patients. Best Pract Res Clin Anaesthesiol 2011;25:169–79.
Manser T, Staender S. Aftermath of an adverse event: supporting health care professionals to meet patient expectations through open disclosure. Acta Anaesthesiol Scand 2005;49:728–34.
Mantone J. Clarion call. National forum on patient safety stresses disclosure. Mod Healthc 2005;35:10.
Martinez W, Lo B. Medical students’ experiences with medical errors: an analysis of medical student essays. Med Educ 2008;42:733–41.
Mason DJ. To forgive, divine: it’s time to drop the veil of secrecy about disclosing errors. Am J Nurs 2005;105:11.
Massó Guijarro P, Aranaz Andrés JM, Mira JJ, Perdiguero E, Aibar C. Adverse events in hospitals: the patient’s point of view. Qual Saf Health Care 2010;19:144–7.
Mastroianni AC, Mello MM, Sommer S, Hardy M, Gallagher TH. The flaws in state ‘apology’ and ‘disclosure’ laws dilute their intended impact on malpractice suits. Health Aff 2010;29:1611–19.
Matheson GO. Who said medicine means never having to say you’re sorry? Phys Sportsmed 2005;33:2
Matlow A, Stevens P, Harrison C, Laxer R. Achieving closure through disclosure: experience in a pediatric institution. J Pediatr 2004;144:559–60.
Matlow A, Stevens P, Harrison C, Laxer RM. Disclosure of medical errors. Pediatr Clin North Am 2006;53:1091–104.
Matlow AG, Moody L, Laxer R, Stevens P, Goia C, Friedman JN. Disclosure of medical error to parents and paediatric patients: assessment of parents’ attitudes and influencing factors. Arch Dis Child 2010;95:286–90.
Maurer MJ. Nurses’ Perceptions Of and Experiences With Medication Errors. PhD thesis. Toledo, OH: University of Toledo; 2010.
Mavroudis C, Mavroudis CD, Naunheim KS, Sade RM. Should surgical errors always be disclosed to the patient? Ann Thorac Surg 2005;80:399–408.
Maxston BE, Fenna N. Disclosing your mistakes to patients: a legal perspective. Dent Pract Manage Spring 1992:9–11.
Mazor KM. Understanding patients’ perceptions of medical errors. J Commun Healthc 2009;2:34–46.
Mazor KM, Greene SM, Roblin D, Lemay CA, Firneno CL, Calvi J, et al. More than words: patients’ views on apology and disclosure when things go wrong in cancer care. Patient Educ Couns 2013;90:341–6.
Mazor KM, Reed GW, Yood RA, Fischer MA, Baril J, Gurwitz JH. Disclosure of medical errors: what factors influence how patients respond? J Gen Intern Med 2006;21:704–10.
Mazor KM, Simon SR, Gurwitz JH. Communicating with patients about medical errors: a review of the literature. Arch Intern Med 2004;164:1690–7.
Mazor KM, Simon SR, Yood RA, Martinson BC, Gunter MJ, Reed GW, et al. Health plan members’ views about disclosure of medical errors. Ann Intern Med 2004;140:409–18.
Mazor KM, Simon SR, Yood RA, Martinson BC, Gunter MJ, Reed GW, et al. Health plan members’ views on forgiving medical errors. Am J Manag Care 2005;11:49–52.
McAuliffe DM. The requirement to disclose unanticipated outcomes. Fla Nurse 2001;49:13–14.
McBride JL. Five ways to respond to a medical mistake. Fam Pract Manag 2009;16:40.
McCaffrey J. Honest talk. Disclosure is not about asset protection – it is about doing the right thing. Hosp Health Netw 2003;77:94.
McCarthy M. Medicare to shift stance on medical errors disclosure. Lancet 2001;357:128.
McDonald TB, Helmchen LA, Smith KM, Centomani N, Gunderson A, Mayer D, et al. Responding to patient safety incidents: the ‘seven pillars’. Qual Saf Health Care 2010;19:e11.
McDonnell WM, Guenther E. Narrative review: do state laws make it easier to say ‘I’m sorry?’. Ann Intern Med 2008;149:811–16.
McKinney EMH. Medical Error: Overcoming Barriers to Truthful Disclosure. Dissertation Abstracts International Section B: The Sciences and Engineering 2009;70:2801.
McKinney M. Going beyond saying you’re sorry. More hospitals using quick remediation strategies following medical errors. Mod Healthc 2011;41:32–3.
McLennan S, Beitat K, Lauterberg J, Vollmann J. Regulating open disclosure: a German perspective. Int J Qual Health Care 2012;24:23–7.
McNeill PM, Walton M. Medical harm and the consequences of error for doctors. Med J Aust 2002;176:222–5.
Medical Protection Society (MPS). Briefing Paper: Culture of Candour. London: MPS; 2010.
Medical Protection Society (MPS). A Culture of Openness in NHS Scotland. London: MPS; 2011.
Micalizzi DA. The aftermath of a ‘never event’. A child’s unexplained death and a system seemingly designed to thwart justice. Mod Healthc 2008;38:24–5.
Miller LA. Apology, disclosure, and unanticipated outcomes. J Perinat Neonatal Nurs 2011;25:10–11.
Mitka M. Disclosing medical errors does not mean greater liability costs, new study finds. JAMA 2010;304:1656–7.
Mlott K. Don’t say you’re sorry: surviving a lawsuit by Jay Weaver in the September issue. EMS Magazine, December 2007, p. 14.
Monson MS. Legal checkpoints. Disclosing adverse events: you said it, now write it. Nurs Manage 2006;37:16–17.
Moskop JC, Geiderman JM, Hobgood CD, Larkin GL. Emergency physicians and disclosure of medical errors. Ann Emerg Med 2006;48:523–31.
Moskowitz A. Survey: physicians more likely to disclose obvious medical errors. Ocular Surgery News 2006;24:163.
Moskowitz E, Veloski JJ, Fields SK, Nash DB. Development and evaluation of a 1-day interclerkship program for medical students on medical errors and patient safety. Am J Med Qual 2007;22:13–17.
Murtagh L, Gallagher TH, Andrew P, Mello MM. Disclosure-and-resolution programs that include generous compensation offers may prompt a complex patient response. Health Aff (Millwood) 2012;31:2681–9.
Myers V. When something goes wrong: how to disclose an error. Am Nurse Today 2001;6. URL: www.americannursetoday.com/article.aspx?id=8302&fid=8276# (accessed 27 February 2013).
Nassrally MS. Difficulty in admitting error. An equally hard thing: supporting the admission of error. BMJ 2012;344:e3563.
National Patient Safety Agency. Being Open E-learning Module. URL: https://report.npsa.nhs.uk/boatoolelearning/course/courselaunch.htm (accessed December 2011).
National Patient Safety Agency. Being Open: Communicating Patient Safety Incidents With Patients and Their Carers. London: National Patient Safety Agency; 2005.
National Patient Safety Agency. Being Open: Communicating Patient Safety Incidents With Patients, Their Families and Their Carers. London: National Patient Safety Agency; 2009.
Newell A. Bulletin board. Apologies can heal: new book helps providers say ‘I’m sorry’. Nurs Womens Health 2007;11:205–6.
Newfield JS. The evolution of the apology. Home Health Care Manag Pract 2007;19:137–9.
Nicklin W, Mass H, Affonso DD, O’Connor P, Ferguson-Pare M, Jeffs L, et al. Patient safety culture and leadership within Canada’s Academic Health Science Centres: towards the development of a collaborative position paper. Nurs Leadersh 2004;17:22–34.
Gara N, on behalf of Government Affairs and Reimbursement Committee of the American Association of Physicians Assistants.. Apologizing for adverse outcomes. JAAPA 2007;20:47–8.
Nie Y, Li L, Duan Y, Chen P, Barraclough BH, Zhang M, et al. Patient safety education for undergraduate medical students: a systematic review. BMC Med Educ 2011;11:33.
Noland CM, Rickles NM. Reflection and analysis of how pharmacy students learn to communicate about medication errors. Health Commun 2009;24:351–60.
Northcott H, Vanderheyden L, Northcott J, Adair C, McBrien-Morrison C, Norton P, et al. Perceptions of preventable medical errors in Alberta, Canada. Int J Qual Health Care 2008;20:115–22.
Nowicki M, Chaku M. Do healthcare managers have an ethical duty to admit mistakes? Healthc Financ Manage 1998;52:62–4.
Nwomeh BC, Caniano DA. Emerging ethical issues in pediatric surgery. Pediatr Surg Int 2011;27:555–62.
O’Connell D. Apology laws. CMAJ 2009;180:644.
O’Connell D, Reifsteck SW. Disclosing unexpected outcomes and medical error. J Med Pract Manage 2004;19:317–23.
O’Connell D, White MK, Platt FW. Disclosing unanticipated outcomes and medical errors. J Clin Outcomes Manag 2003;10:25–9.
O’Connor E, Coates HM, Yardley IE, Wu AW. Disclosure of patient safety incidents: a comprehensive review. Int J Qual Health Care 2010;22:371–9.
Ofri D. Ashamed to admit it: owning up to medical error. Health Aff 2010;29:1549–51.
Ogundiran TO, Adebamowo CA. Surgeon–patient information disclosure practices in southwestern Nigeria. Med Princ Pract 2012;21:238–43.
Okamoto S, Kawahara K, Algren M. Transformative possibilities of communication in medical error cases in Japan. Int J Qual Health Care 2011;23:26–35.
O’Neill AT. Patients deserve full disclosure. BMJ 2012;344:29.
Oppenheim EB. New JCAHO standards create affirmative duty to disclose hospital error. Trauma 2004;46:79–99.
O’Reilly KB. Fear of Punitive Response to Hospital Error Lingers. American Medical News, 20 February 2012. URL: www.amednews.com/article/20120220/profession/302209938/2/ (accessed 12 March 2013).
Ornstein H, Baum N. The power of saying ‘I’m sorry’: a well-planned apology can go a long way towards patient satisfaction. Podiatry Manag 2008;27:49–50.
Ott M. Key considerations on drafting a policy on disclosure of unanticipated outcomes. J Healthc Risk Manag 2001;21:27–34.
Overly FL, Sudikoff SN, Duffy S, Anderson A, Kobayashi L. Three scenarios to teach difficult discussions in pediatric emergency medicine: sudden infant death, child abuse with domestic violence, and medication error. Simul Healthc 2009;4:114–30.
Pace WD, Staton EW. Improving the disclosure of medical incidents: a genuine apology is only the first step in the process. BMJ 2011;343:d4340.
Panting G. How to avoid being sued in clinical practice. Postgrad Med J 2004;80:165–8.
Parker M. A fair dinkum duty of open disclosure following medical error. J Law Med 2012;20:35–43.
Pedley L. Medication errors and ethical nursing practice. Perspectives 2002;26:10–13.
Pelletier LR. On truth telling. J Healthc Qual 2001;23:2.
Pelletier E, Robson R. Giving back the pen: disclosure, apology and early compensation discussions after harm in the healthcare setting. Health Q 2008;11:85–90.
Pelt JL, Faldmo LP. Physician error and disclosure. Clin Obstet Gynecol 2008;51:700–8.
Pendrak R. Anger management in disclosure of adverse events: how to deal with anger and other emotions in adverse events and error disclosure. J Healthc Risk Manag 2005;25:8.
Penson RT, Svendsen SS, Chabner BA, Lynch TJ Jr, Levinson W. Medical mistakes: a workshop on personal perspectives. Oncologist 2001;6:92–9.
Perez B, Didona T. Assessing legislative potential to institute error transparency: a state comparison of malpractice claims rates. J Healthc Qual 2010;32:36–41.
Peterkin A. Guidelines covering disclosure of errors now in place at Montreal Hospital. CMAJ 1990;142:984–5.
Peterson LM, Brennan T. Medical ethics and medical injuries: taking our duties seriously. J Clin Ethics 1990;1:207–11.
Pfrimmer DM. Nursing’s role in disclosure and apology. J Contin Educ Nurs 2010;41:342–3.
Pham JC, Story JL, Hicks RW, Shore AD, Morlock LL, Cheung DS, et al. National study on the frequency, types, causes, and consequences of voluntarily reported emergency department medication errors. J Emerg Med 2011;40:485–92.
Philpott S. The truth, the whole truth and nothing but the truth? Nurs N Z 2005;11:16–18.
Pinker S. Quebec moves toward full disclosure of medical errors. CMAJ 2002;166:800.
Pinto A, Faiz O, Vincent C. Managing the after effects of serious patient safety incidents in the NHS: an online survey study. BMJ Qual Saf 2012;21:1001–8.
Pollack C, Bayley C, Mendiola M, McPhee S. Helping clinicians find resolution after a medical error. Camb Q Healthc Ethics 2003;12:203–7.
Pollock G, Pesto MM, Sirridge M, Van Way CW III. Disclosing medical errors in Missouri: how to say ‘I’m sorry’. Mo Med 2010;107:338–44.
Popp PL. How to – and not to – disclose medical errors to patients. Manag Care 2002;11:52–3.
Popp PL. How will disclosure affect future litigation? J Healthc Risk Manag 2003;23:5–9.
Porto GG. Disclosure of medical error: facts and fallacies. J Healthc Risk Manag 2001;21:67–76.
Posner G, Naik V, Bidlake E, Nakajima A, Sohmer B, Arab A, et al. Assessing residents’ disclosure of adverse events: traditional objective structured clinical examinations versus mixed reality. J Obstet Gynaecol Can 2012;34:367–73.
Powell SK. When things go wrong: responding to adverse events: a consensus statement of the Harvard hospitals. Lippincotts Case Manag 2006;11:193–4.
Purtilo RB. Beyond disclosure: seeking forgiveness. Phys Ther 2005;85:1124–6.
Quinley K. ‘Sorry works’ – or does it? Insurance coverage implications of patient apology programs. Med Mal Law Strat 2007;25:3–4.
Quinn RE, Eichler MC. The 3Rs program: the Colorado experience. Clin Obstet Gynecol 2008;51:709–18.
Quirk M, Mazor K, Haley H-L, Philbin M, Fischer M, Sullivan K, et al. How patients perceive a doctor’s caring attitude. Patient Educ Couns 2008;72:359–66.
Rait JL, Van Ekert EH. Legal aspects of open disclosure II: attitudes of health professionals – findings from a national survey. Med J Aust 2011;194:48.
Rajendran PR. Ethical issues involved in disclosing medical errors. JAMA 2001;286:1078.
Raju TNK, Suresh G, Higgins RD. Patient safety in the context of neonatal intensive care: research and educational opportunities. Pediatr Res 2011;70:109–15.
Rathert C, Phillips W. Medical error disclosure training: evidence for values-based ethical environments. J Bus Ethics 2010;97:491–503.
Reitman V. Healing Sound of a Word – Sorry. Los Angeles Times, 24 March 2003. URL: http://articles.latimes.com/print/2003/mar/24/health/he-risk24 (accessed 16 April 2012).
Remakus BL. Talking about our mistakes. Maybe we should, in spite of what our lawyers and insurance companies say. Med Econ 2005;82:64–5.
Renwick KK Jr. Should doctors disclose mistakes? West J Med 2000;172:10.
Rickles NM, Noland CM, Tramontozzi A, Vinci MA. Pharmacy student knowledge and communication of medication errors. Am J Pharm Educ 2010;74:60.
Ritchie JH, Davies SC. Professional negligence: a duty of candid disclosure? BMJ 1995;310:888–9.
Robbennolt JK. Apologies and medical error. Clin Orthop Relat Res 2009;467:376–82.
Roberts RG. The art of apology: when and how to seek forgiveness. Fam Pract Manag 2007;14:44–9.
Robertson G. Fraudulent concealment and the duty to disclose medical mistakes. Alta Law Rev 1987;25:215–23.
Robertson GB. When things go wrong: the duty to disclose medical error. Queens Law J 2002;28:353–62.
Robinson AR, Vanni AJ, Anderson RJ. Medical students’ attitudes on disclosure of medical errors. J Gen Intern Med 2003;18:252.
Robinson J. Consumer comments. A duty of candour: will it really make amends? Br J Midwifery 2003;11:542.
Rohrich RJ. It’s okay to say ‘I’m sorry’. Plast Reconstr Surg 2007;120:1425–7.
Roland M, Rao SR, Sibbald B, Hann M, Harrison S, Walter A, et al. Professional values and reported behaviours of doctors in the USA and UK: quantitative survey. BMJ Qual Saf 2011;20:515–21.
Roman L. Finding the words: how to handle difficult conversations. RN 2007;70:34–8.
Rowe M. Doctors’ responses to medical errors. Crit Rev Oncol Hematol 2004;52:147–63.
Salladay SA. Ethical problems. Medication error: shrouded in secrecy. Nursing 1998;28:72–3.
Sanford DE, Fleming DA. We meant no harm, yet we made a mistake; why not apologize for it? A student’s view. HEC Forum 2010;22:159–69.
Saxton JW, Finkelstein MM. Adverse event management: your evidence to decrease professional liability risk. J Med Pract Manage 2008;24:5–8.
Scheirton LS. Proportionality and the view from below: analysis of error disclosure. HEC Forum 2008;20:215–41.
Schneck LH. Oops . . . disclosing medical errors and adverse outcomes, establishing dialogue with patients. MGMA Connex 2003;3:28–30.
Scholefield H. Embedding quality improvement and patient safety at Liverpool Women’s NHS Foundation Trust. Best Pract Res Clin Obstet Gynaecol 2007;21:593–607.
Schoonover-Shoffner K. Editorial. A confession. J Christ Nurs 2008;25:183.
Schuer KM, Quality Care Committee of the AAPA. Disclosure of medical errors: the right thing to do. JAAPA 2010;23:27–9.
Schuling J, Conradi MH. Errors in general practice: what should the doctor do next? Int J Risk Saf Med 1998;11:165–70.
Schulte D. What you should know about Michigan’s new ‘I’m sorry’ law. J Mich Dent Assoc 2011;93:16.
Schulte DJ. New ‘I’m sorry’ law does not immunize physicians from admitted malpractice. Mich Med 2011;110:6.
Schwappach DLB, Koeck CM. What makes an error unacceptable? A factorial survey on the disclosure of medical errors. Int J Qual Health Care 2004;16:317–26.
Schwartz B. Errors in dentistry: a call for apology. J Am Coll Dent 2005;72:26–32.
Schwartz B. Apology legislation: the time has come. J Can Dent Assoc 2009;75:621.
Scott H. Health professionals must learn to say sorry. Br J Nurs 1999;8:792.
Selbst SM. The difficult duty of disclosing medical errors. Contemp Pediatr 2003;20:51–2.
Shannon SE, Foglia MB, Hardy M, Gallagher TH. Disclosing errors to patients: perspectives of registered nurses. Jt Comm J Qual Patient Saf 2009;35:5–12.
Shapiro E. Disclosing medical errors: best practices from the ‘leading edge’: part I. Care Manag 2008;14:14–18.
Shapiro E. Disclosing medical errors: best practices from the ‘leading edge’: part II. Care Manag 2008;14:11–17.
Sheridan S, Conrad N, King S, Dingman J, Denham CR. Disclosure through our eyes. J Patient Saf 2008;4:18–26.
Sheu S-J, Wei I-L, Chen C-H, Yu S, Tang F-I. Using snowball sampling method with nurses to understand medication administration errors. J Clin Nurs 2009;18:559–69.
Shift TJ. Sample disclosure note to put in patient record. Healthc Risk Manag 2006;28:41.
Silversides A. Apologies abound: advances in adverse-event disclosure. CMAJ 2009;180:382.
Simone JV. Simone’s OncOpinion. Telling patients the truth. Oncology Times 2007;29:3–5.
Simons SL. Full disclosure when bad things happen. Neonatal Netw 2007;26:131–2.
Singer PA. Commentary: learning to love mistakes. BMJ 2001;322:1238.
Singh V, Panda M, Cunningham CJ, Hetzler DC. Disclosure and documentation of unintended medical events: what do healthcare providers believe? American Federation for Medical Research, Southern Regional Meeting, New Orleans, LA, 17–19 February 2011.
Skarsgard ED. Managing the adverse event occurring during elective, ambulatory pediatric surgery. Semin Pediatr Surg 2009;18:122–4.
Slovenko R. Saying you’re sorry in a litigious society. Med Law 1992;11:669–71.
Slovenko R. Admission or apology in liability prevention. American College of Forensic Psychiatry, 28th Annual Symposium, San Francisco, CA, 15–18 April 2010.
Slovenko R. Expression of sorrow or apology. Am J Forensic Psychiatry 2010;31:17–34.
Smith ML, Forster HP. Morally managing medical mistakes. Camb Q Healthc Ethics 2000;9:38–53.
Sokol DK. The hardest thing: admitting error. BMJ 2012;344:e3085.
Sokol DK. ‘The patient would have died anyway’. BMJ 2013;346:f285.
Somerville M. Litigation: a saying-sorry way to heal the wounds. Directions for Canadian Healthcare: a Framework for Sound Decisions: Do we care? conference proceedings, 1998:150–1.
Sorensen R, Iedema R, Piper D, Manias E, Williams A, Tuckett A. Health care professionals’ views of implementing a policy of open disclosure of errors. J Health Serv Res Policy 2008;13:227–32.
Sorensen R, Iedema R, Piper D, Manias E, Williams A, Tuckett A. Disclosing clinical adverse events to patients: can practice inform policy? Health Expect 2010;13:148–59.
Sorokin R, Riggio JM, Hwang C. Attitudes about patient safety: a survey of physicians-in-training. Am J Med Qual 2005;20:70–7.
Sorokin R, Riggio JM, Moleski S, Sullivan J. Physicians-in-training attitudes on patient safety: 2003 to 2008. J Patient Saf 2011;7:133–8.
Sparkman CA. Legislating apology in the context of medical mistakes. AORN J 2005;82:263–6.
Springer R. Taking the OR to the office: Disclosing unanticipated events. Plast Surg Nurs 2005;25:199–201.
Spurgeon D. Quebec doctors must tell patients about medical ‘accidents’. BMJ 2002;325:1192.
Stetsenko GY, Gallagher T, Sitlani C, Gronowski AM, Astion M. Medical error disclosure: attitudes and experiences of laboratory medical directors. Am J Clin Pathol 2009;132:41.
Stoffan PM, O’Toole P. Admitting mistakes is not enough. Health Aff 2001;20:258–60.
Stokes SL, Wu AW, Pronovost PJ. Ethical and practical aspects of disclosing adverse events in the emergency department. Emerg Med Clin North Am 2006;24:703–14.
Stow J. Using medical-error reporting to drive patient safety efforts. AORN J 2006;84:417–20.
Straumanis JP. Disclosure of medical error: is it worth the risk? Pediatr Crit Care Med 2007;8:S38–43.
Stroud L, McIlroy J, Levinson W. Skills of internal medicine residents in disclosing medical errors: a study using standardized patients. Acad Med 2009;84:1803–8.
Studdert D, Mello M, Gawande A, Brennan T. Open disclosure: details matter – response. Health Aff 2007;26:904–5.
Studdert DM, Mello MM, Gawande AA, Brennan TA, Wang YC. Disclosure of medical injury to patients: an improbable risk management strategy. Health Aff 2007;26:215–26.
Studdert DM, Piper D, Iedema R. Legal aspects of open disclosure II: attitudes of health professionals – findings from a national survey. Med J Aust 2010;193:351–5.
Studdert DM, Richardson MW. Legal aspects of open disclosure: a review of Australian law. Med J Aust 2010;193:273–6.
Sullivan RP, Waldemayer CR, Bunting RF Jr. Building confidence into communication of bad news: the role of the patient advocate. J Healthc Risk Manag 2010;29:33–7.
Sulmasy DP. Dignity, vulnerability, and medical error. Health Prog 2006;87:12–14.
Surbone A, Rowe M, Gallagher TH. Confronting medical errors in oncology and disclosing them to cancer patients. J Clin Oncol 2007;25:1463–7.
Suziedelis AK. Physicians and the burden of medical error. Health Care Ethics USA 2003;11:E3.
Swanson DS. Physician gag clauses – the hypocrisy of the Hippocratic Oath. South Ill Univ Law J 1997;21:313–34.
Sweet MP, Bernat JL. A study of the ethical duty of physicians to disclose errors. J Clin Ethics 1997;8:341–8.
Symon A. Improving communication: apologies and explanations. Br J Midwifery 1997;5:594–6.
Tanasiewicz M, Bednarski J, Galazka A. The truth, misunderstanding or lie? Different forms of doctor–patient relations. Bull Med Ethics 2005;209:13–17.
Tapper R, Malcolm L, Frizelle F. Surgeons’ experiences of complaints to the Health and Disability Commissioner. N Z Med J 2004;117:U975.
Taylor D, Hassan MA, Luterman A, Rodning CB. Unexpected intraoperative patient death – the imperatives of family- and surgeon-centered care. Arch Surg 2008;143:87–92.
Taylor J. Compensation culture. Do patients justice. Health Serv J 2008;20:20–2.
Teninbaum GH. Saying ‘sorry’ isn’t enough. Health Aff 2010;29:2127.
Thompson DA, Cowan J, Holzmueller C, Wu AW, Bass E, Pronovost P. Planning and implementing a systems-based patient safety curriculum in medical education. Am J Med Qual 2008;23:271–8.
Thomson L. Patient safety corner: critical incidents and disclosure following critical patient incidents. Manitoba RN J 2011;36:21.
Thurman AE. Institutional responses to medical mistakes: ethical and legal perspectives. Kennedy Inst Ethics J 2001;11:147–56.
Tieman J. Enforcing a new openness. JCAHO to hospitals: let patients know when their care hasn’t met standards. Mod Healthc 2001;31:4–5.
Tammelleo AD. Failure to disclose colon nicked during hysterectomy. Medical Law’s Regan Report 2006;39:4.
Tammelleo AD. Failure of Dr. to notify Pt. of botched surgery. Medical Law’s Regan Report 2007;40:1.
Traynor K. Patient safety standards focus on medical-error reduction, patient notification. Am J Health Syst Pharm 2001;58:1389.
Truog RD, Browning DM, Johnson JA, Gallagher TH. Talking With Patients and Families About Medical Error. Baltimore, MD: Johns Hopkins University Press; 2010.
Wachter RM. Entering the second decade of the patient safety movement: the field matures: comment on ‘disclosure of hospital adverse events and its association with patients’ ratings of the quality of care’. Arch Intern Med 2009;169:1894–6.
Waite M. To tell the truth: the ethical and legal implications of disclosure of medical error. Health Law J 2005;13:1–33.
Waite MA. Patient Safety and Disclosure of Medical Error: The Legal and Ethical Implications of Human Error in Medicine. Masters Abstracts 2006;44:2152.
Wakefield J, Jorm C, Ryan C. Open disclosure: details matter. Health Aff 2007;26:903–4.
Walsh P. How real is the NHS commitment to ‘Being open’? Health Care Risk Report 2009;15:12–13.
Walsh P. Don’t be daunted by duty of candour. Health Serv J, 2012. URL: www.hsj.co.uk/resource-centre/best-practice/patient-safety-resources/dont-be-daunted-by-the-duty-of-candour/5043539.article#.U2ojfPldWVM (accessed 20 May 2012).
Warriner DR. Apologies and legal liability. Three little words. BMJ 2009;338:b521.
Watling CJ, Brown JB. Education research: communication skills for neurology residents: structured teaching and reflective practice. Neurology 2007;69:E20–6.
Wears RL, Wu AW. Dealing with failure: the aftermath of errors and adverse events. Ann Emerg Med 2002;39:344–6.
Weber LJ. The ethics of withholding information about mistakes. Health Prog 1994;75:65.
Wei M. Doctors, apologies, and the law: an analysis and critique of apology laws. J Health Law 2007;40:107–59.
Weinstein L. A multifacited approach to improve patient safety, prevent medical errors and resolve the professional liability crisis. Am J Obstet Gynecol 2006;194:1160–5.
Weiss GG. Medical errors. Should you apologize? Med Econ 2006;83:50–4.
Weiss PM. To err is human – to air is humane: disclosing adverse events to patients. Obstet Gynecol Surv 2007;62:217–18.
Weiss PM, Miranda F. Transparency, apology and disclosure of adverse outcomes. Obstet Gynecol Clin North Am 2008;35:53–62.
Weissman JS, Annas CL, Epstein AM, Schneider EC, Clarridge B, Kirle L, et al. Error reporting and disclosure systems: views from hospital leaders. JAMA 2005;293:1359–66.
Weng L, Joynt GM, Lee A, Du B, Leung P, Peng J, et al. Attitudes towards ethical problems in critical care medicine: the Chinese perspective. Intensive Care Med 2011;37:655–64.
Weselake T, French J. The ethics of disclosure – perspectives of radiation therapists and patients regarding disclosure of radiation therapy errors. Can J Med Radiat Technol 2004;35:10–14.
Wetzel TG. When errors occur, ‘I’m sorry’ is a big step, but just the first. Hosp Health Netw 2010;84:41–2.
White AA, Bell SK, Krauss MJ, Garbutt J, Dunagan WC, Fraser VJ, et al. How trainees would disclose medical errors: educational implications for training programmes. Med Educ 2011;45:372–80.
White AA, Gallagher TH, Krauss MJ, Garbutt J, Waterman AD, Dunagan WC, et al. The attitudes and experiences of trainees regarding disclosing medical errors to patients. Acad Med 2008;83:250–6.
White SM, Deacy N, Sudan S. Trainee anaesthetists’ attitudes to error, safety and the law. Eur J Anaesthesiol 2009;26:463–8.
Wilson J, McCaffrey R. Disclosure of medical errors to patients. Medsurg Nurs 2005;14:319–23.
Winer IK. What physicians can do to reduce the risks of malpractice and litigation. J Med Pract Manage 1993;8:213–18.
Witman AB, Park DM, Hardin SB. How do patients want physicians to handle mistakes? A survey of internal medicine patients in an academic setting. Arch Intern Med 1996;156:2565–9.
Woffen T. Patient Safety and Legal Challenges: Disclosure of Medical Error, Class Actions, and Reporting Systems. Masters Abstracts 2008;47:2018.
Wojcieszak D, Banja J, Houk C. The Sorry Works! Coalition: making the case for full disclosure. Jt Comm J Qual Patient Saf 2006;32:344–50.
Wojcieszak D, Saxton JW, Finkelstein MM. Ethics training needs to emphasize disclosure and apology. HEC Forum 2008;20:291–305.
Woods MS. Commentary: Let’s start admitting our mistakes. Clin Advis Nurse Pract 2008;11:142.
Woodward HI, Mytton OT, Lemer C, Yardley IE, Ellis BM, Rutter PD, et al. What have we learned about interventions to reduce medical errors? Annu Rev Public Health 2010;31:479–97.
Woolf L. Clinical negligence: what is the solution? How can we provide justice for doctors and patients? Med Law Int 2000;4:133–44.
Sorry Works! Sorry Works! Making Disclosure a Reality for Healthcare Organizations. URL: www.sorryworks.net (accessed 30 March 2013).
Wright J, Opperman G. The disclosure of medical errors: a catalyst for litigation or the way forward for better patient management? Clin Risk 2008;14:193–6.
Wu A, Pronovost P. Telling patients the truth. Health Aff 2003;22:249.
Wu AW. Handling hospital errors: is disclosure the best defense? Ann Intern Med 1999;131:970–2.
Wu AW. Commentary: doctors are obliged to be honest with their patients. BMJ 2001;322:1238–9.
Wu AW. Is there an obligation to disclose near-misses in medical care? In Sharpe VA, editor. Accountability: Patient Safety and Policy Reform. Washington, DC: Georgetown University Press; 2004. pp. 135–42.
Wu AW, Cavanaugh TA, McPhee SJ, Lo B, Micco GP. To tell the truth: ethical and practical issues in disclosing medical mistakes to patients. J Gen Intern Med 1997;12:770–5.
Wu AW, Folkman S, McPhee SJ, Lo B. Do house officers learn from their mistakes? JAMA 1991;265:2089–94.
Wu AW, Folkman S, McPhee SJ, Lo B. Do house officers learn from their mistakes? Qual Saf Health Care 2003;12:221–6.
Wu AW, Huang IC, Stokes S, Pronovost PJ. Disclosing medical errors to patients: it’s not what you say, it’s what they hear. J Gen Intern Med 2009;24:1012–17.
Wusthoff CJ. Medical mistakes and disclosure: the role of the medical student. JAMA 2001;286:1080–1.
Yardley IE, Yardley SJ, Wu AW. How to discuss errors and adverse events with cancer patients. Curr Oncol Rep 2010;12:253–60.
Zammit R. How to Say You Are Sorry A Guide to the Background and Risks of Apology Legislation. Masters Abstracts 2009;48:2012.
Zimmerman R. Doctors’ new tool to fight lawsuits: saying ‘I’m sorry.’ Malpractice insurers find owning up to errors soothes patient anger. ‘The risks are extraordinary’. J Okla State Med Assoc 2004;97:245–7.
Zimmerman TM, Amori G. Including patients in root cause and system failure analysis: legal and psychological implications. J Healthc Risk Manag 2007;27:27–34.
Zimmermann PG, Kobs A, Heilicser B. Managers forum. Telling patients about a mistake. J Emerg Nurs 2002;28:456–7.
Appendix 10 Studies excluded at second stage
| Author and year | Title | Reason for exclusion |
|---|---|---|
| Barrios 2009220 | Framing family conversation after early diagnosis of iatrogenic injury and incidental findings | Study not a controlled design or uncontrolled before and after |
| Bell 2010221 | Improving the patient, family, and clinician experience after harmful events: the ‘when things go wrong’ curriculum | Study not a controlled design or uncontrolled before and after |
| Daud-Gallotti 2011222 | A new method for the assessment of patient safety competencies during a medical school clerkship using an objective structured clinical examination | Study not a controlled design or uncontrolled before and after |
| Gillies 2011223 | Teaching medical error apologies: development of a multi-component intervention | Study not a controlled design or uncontrolled before and after |
| Hannawa 2009224 | When the truth hurts: toward a validation of the physician mistake disclosure (PMD) model | Study not a controlled design or uncontrolled before and after |
| Keller 200998 | An effective curriculum for teaching third year medical students about medical error and disclosure | Study not a controlled design or uncontrolled before and after |
| Kim 2011225 | A web-based team-oriented medical error communication assessment tool: development, preliminary reliability, validity, and user ratings | Intervention not open disclosure or intervention to support open disclosure |
| Wu 2009226 | Disclosing medical errors to patients: it’s not what you say, it’s what they hear | Study not a controlled design or uncontrolled before and after |
Appendix 11 Patient and public involvement
The majority of this work was directed at exploring implementation of policy and stakeholders were varied. We had the expertise of Peter Walsh as a leading national patient representative who was able to ensure representation for patients and the public as part of this work. Peter advised on patient and public involvement at a national level.
Peter Walsh is the chief executive of AvMA and brings a wealth of experience from both the voluntary sector and the patient perspective to this project. He is also a WHO-appointed patient safety champion, a member of the National Patient Safety Forum and an executive member of the Clinical Disputes Forum. He has been involved in several research projects looking at patient perspectives on patient involvement in safety in health care and is well networked with the NPSA and WHO.
Peter was involved in this work from its inception. He helped to write the grant proposal and was an applicant for the funding. Peter has been involved in managing the delivery of the research, assisting with recruitment of stakeholders, designing recruitment materials and writing the final report, and will be involved in future dissemination of the findings of this report to both lay and professional organisations.
List of abbreviations
- ACSQH
- Australian Commission on Safety and Quality in Healthcare
- AHRQ
- Agency for Healthcare Research and Quality
- ASSIA
- Applied Social Sciences Index and Abstracts
- AvMA
- Action Against Medical Accidents
- BMA
- British Medical Association
- CDSR
- Cochrane Database of Systematic Reviews
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CPCI-S
- Conference Proceedings Citation Index – Science
- CPCI-SSH
- Conference Proceedings Citation Index – Social Science & Humanities
- DARE
- Database of Abstracts of Reviews of Effects
- GMC
- General Medical Council
- GP
- general practitioner
- HMIC
- Health Management Information Consortium
- HSRProj
- Health Services Research Projects in Progress
- HTA
- Health Technology Assessment
- JCAHO
- Joint Commission on Accreditation of Healthcare Organizations
- LILACS
- Latin American and Caribbean Health Sciences Literature
- LST
- large system transformation
- MDU
- Medical Defence Union
- MeSH
- medical subject heading
- MPS
- Medical Protection Society
- NHSLA
- NHS Litigation Authority
- NMC
- Nursing and Midwifery Council
- NPSA
- National Patient Safety Agency
- NPSF
- National Patient Safety Foundation
- NRLS
- National Reporting and Learning System
- NTIS
- National Technical Information Service
- SCI
- Science Citation Index
- SSCI
- Social Sciences Citation Index
- TJC
- The Joint Commission
- UMHS
- University of Michigan Health System
- VA
- Veterans Affairs
- VHA
- Veterans Health Administration
- WHO
- World Health Organization
- WHO ICTRP
- WHO International Clinical Trials Registry Platform Search Portal