Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/1008/17. The contractual start date was in April 2011. The final report began editorial review in July 2013 and was accepted for publication in November 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Kessler et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background and overview
Support workers: policy agendas and building upon previous research
Over recent years, health-care support workers – employees working alongside and typically assisting the registered nurse (RN) – have become an increasingly important part of the nursing workforce in the acute care sector. This is reflected not only in the growing number of such workers, but also in their development as the main bedside presence and principal provider of the fundamentals of care. 1 Thus, the number of full-time equivalent workers ‘supporting doctors and nurses’ in the English NHS rose from 93,000 in 1995 to some 117,000 in 2010, a rise of around 26%. 2 This importance has, however, generated dilemmas and tensions for policy-makers and practitioners at different levels of the NHS. Comprising unregistered employees, positioned in Agenda for Change (AfC) pay bands 2 to 4, the health-care support workforce has often been presented as a ‘flexible’, low-cost source of labour, yet in the absence of regulation this same workforce has also been viewed as generating potential risks and uncertainties. For example, the absence of minimum entry and training requirements has prompted concerns about this workforce’s capability and capacity to deliver safe care. 3
Against such a backdrop, this report presents the findings from a 2-year study examining and contributing to organisational initiatives designed to help develop a high-performance nurse support workforce in acute health-care settings. Such support workers have variously been labelled as health-care assistants (HCAs), nursing assistants, nursing auxiliaries, assistant practitioners (APs) and clinical or health-care support workers. These various job titles are not without significance. In part, they point to the long-standing contribution made by support workers to the provision of health care in England; a support role has been a feature of the country’s modern nursing workforce since its inception in the mid-nineteenth century, and the various titles often equate to their use in different historical periods. 4
Moreover, these differing job titles sometimes denote contrasting signals sent by trusts to various stakeholders on the character and contribution of the nurse support role; for example, the terms ‘auxiliary’ and ‘assistant’ have somewhat different connotations in terms of how the support role is to be viewed, not least in relation to the RN. In the main, however, the different titles are no longer indicative of meaningful substantive difference. Indeed, in general, trusts refer to support workers at pay bands 2 and 3 as ‘HCAs’ and those at pay band 4 as ‘APs’. Where the report refers to support workers at these different levels, it uses these terms. Where these workers are referred to more generically, across the different pay bands, the term ‘nurse support worker’ is used.
In exploring the nurse support worker’s role in acute health care, this study is designed to develop and strengthen the evidence base on the deployment and management of such workers. In so doing, it seeks to draw lessons and provide guidance to policy-makers, and more especially practitioners, in addressing the dilemmas and tensions faced, as well as the opportunities presented, in the increasing use of this group of employees. In pursuing these objectives, the study builds upon research into the nurse support workforce previously undertaken by the investigators. Between 2008 and 2010, in parallel projects funded by the National Institute of Health Research (NIHR), Kessler et al. 1 at the University of Oxford explored the nature and consequences of the HCA role at AfC pay bands 2 and 3, while Spilsbury et al. 5 at the University of York concentrated on the development of AP roles, typically positioned at AfC pay band 4. The current study, undertaken between 2011 and 2013, brought together these researchers to focus on the nurse support workforce across AfC pay bands 2 to 4.
The 2008–10 Oxford and York studies1,5 were prompted by the patchy evidence base on the nurse support workforce – its shape, management and consequences for various stakeholders. This patchiness arguably reflected a limited research interest in a low-status role, traditionally performing ‘mundane’, auxiliary tasks. 6 Indeed, while the role is a long-standing feature of the modern nursing workforce,4 there was a general reluctance on the part of policy-makers and practitioners at different levels of the NHS to develop and perhaps fully acknowledge the nurse support workers’ contribution to the delivery of care. Thus, Thornley7 referred to the HCA as an ‘invisible worker’, while the general orientation of the nursing establishment to the role was captured by the regulatory body for nursing at the time, the UK Central Council for Nursing, Midwifery and Health Visiting,8 when it noted its preference for registered professionals to deliver all care.
In important respects, this picture has significantly changed, with the nurse support worker assuming increased importance in the delivery of bedside care. In the late 1980s, Project 2000 not only removed an intermediate level of nursing, the state enrolled nurse (SEN), but, perhaps more significantly, placed nurse education within higher education establishments and led to the award of a nursing diploma. The government’s acceptance of Project 2000 reforms depended on the introduction of a new category of support worker, the HCA, to support RNs and make up for the loss of student numbers from the ward due to the supernumerary status awarded to student nurses. The introduction of the HCA grade was also accompanied by the government’s plans for formal training of this group of workers through vocational qualifications,9 but this was not fully realised in practice. 10 The recent move of nurse education to an all-graduate profession by 201311 further substantiates the future role of the HCA in supporting a smaller, highly skilled, registered nursing workforce. Simultaneously, the roles of RNs have been developed to take on a wider range of tasks. Indeed, the need for nurses to address and service new NHS performance regimes, based on the achievement of targets and the application of more robust systems of audit, has impacted upon their engagement in the fundamentals of care.
As nurses were withdrawn from the bedside, the HCA appeared to step in to fill this space. Indeed, national policy-makers explicitly presented HCAs as a key resource in these terms. Taking on more ‘routine’ bedside tasks, HCAs were viewed as relieving RNs of ‘burdens’, allowing them to deepen their specialist and advanced skills. As the Department of Health noted:12
As existing staff develop into new roles . . . so the time of more highly skilled staff can be used more effectively. For instance suitably skilled support workers could carry out some of the current tasks of registered nurses, freeing up these nurses to contribute more fully with their skills.
p. 1312 © Crown Copyright. Contains public sector information licensed under the Open Government Licence v1.0. URL: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.nationalarchives.gov.uk/doc/open-government-licence/open-government-licence.htm
The enhanced use of HCAs was also presented by policy-makers as an end in its own right, making a distinctive and positive contribution to care quality. In the late 1990s, the then health minister, John Denham, stressed that:13
Health care assistants are an invaluable and important part of the NHS . . . they make an important contribution to the direct care of patients as well as supporting a range of health professionals in a wide variety of ways [emphasis added].
Moreover, the HCA was seen as a way of addressing supply-side difficulties in the recruitment of RNs through a ‘grow your own approach’. 14 Indeed, providing career opportunities for HCAs connected to the government’s broader agenda on widening participation and improving access to the professions. 15 The NHS Skills Escalator and a new career framework sought to establish the organisational infrastructure for new and clearer career pathways for nurse support workers (and other work groups in the NHS). 16 As the Department of Health noted:17
We want to open up opportunities for people who join NHS organisations at relatively low skill levels to progress their skills through investment in their training and development to professional levels and beyond.
p. 1717 © Crown Copyright. Contains public sector information licensed under the Open Government Licence v1.0. URL: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.nationalarchives.gov.uk/doc/open-government-licence/open-government-licence.htm
In the context of these developments, the evidence base on the nature of the nurse support workforce and its consequences for various stakeholders remained limited and uneven. Indeed, there were relatively few attempts to draw upon established analytical and theoretical frameworks to enhance understanding of the health-care support role: its development, form and impact. In the case of the AP role, an unregistered band 4 role analogous to the old SEN, this was perhaps unsurprising. It was relatively new, being introduced under the AfC agreement, signed by the government and NHS unions in late 2004. 18 More surprising was the underdeveloped nature of the research literature on the standard and long-standing nurse auxiliary role. Certainly, research was emerging which provided greater insight into various features of the broader nurse support workforce. Surveys were building up a picture of the personal characteristics of the HCAs, revealed as principally made up of middle-aged and experienced women. 19 However, with some notable exceptions,7,10,20 these data were not framed by, and failed to feed into, debates on the gendered nature of the care workforce and the consequences of this gendering for various associated processes and outcomes.
Studies were also highlighting nurse and nurse manager perspectives on the HCA contribution to service delivery,21 albeit against the backdrop of ongoing uncertainty about variability in its use. 22–26 Yet again, however, these data were seldom connected to well-developed debates on interoccupational relations, and the contested nature of the division of labour. This was despite the attention drawn to the fluidity of occupational boundaries in health and other sectors,27,28 and to the nature of power-driven professionalisation projects seeking occupational closure. 29 Nurse professionalisation figured prominently in this literature, but with a focus mainly on the nursing–doctor rather than the nurse–support worker relationship. 30
The most developed research stream on the use and management of nurse support workers had developed in relation to skill mix: the ratio of registered to non-registered nursing staff on any given shift. In part, this stream was framed by a narrow, largely technical prescriptive debate on the appropriate algorithms for such a ratio: whether it should be, for example, linked to ward size and or patient acuity. 31 More generally, however, this stream was associated with a research literature on skill-mix dilution, the depletion of RN numbers relative to HCAs. For some commentators, HCAs as a ‘cheap’ resource had opportunistically been used by health-care managers to substitute for nurses as a means of controlling or reducing costs in periods of financial strain, a process predicated on the devaluation and under-rewarding of the HCAs’ skills. 10,31,32
Notwithstanding these debates and material, the research literature on health-care support workers remained partial in substantive terms, methodologically eclectic and significantly undertheorised, encouraging a more structured and systematic approach to the study of the nurse support workforce. The 2008–10 Oxford and York projects1,5 sought to develop such an approach. While designed as separate studies, with somewhat different methodologies, they shared an interest in mapping the incidence, use, management and impact of the component parts of the nurse support workforce, respectively at pay bands 2 and 3 and pay band 4. Indicative of shifting occupational jurisdictions, the studies confirmed the growing but uneven deployment and contribution made by nurse support workers to the delivery of bedside care, while at the same time highlighting ongoing ambiguities among stakeholders about such roles. The HCA post-holders themselves were revealed as typically satisfied with their working lives but retained concerns about being (over) used by nurses to undertake ‘dirty work’. In the main, RNs emerged as welcoming and valuing the support provided by HCAs, but with residual doubts about their own accountability for the performance of these workers and some uncertainty about how the HCA role impacted on their professionalisation project. Patients appeared to form closer emotional relationships with HCAs than nurses, while often being unable to distinguish between registered and unregistered staff and displaying some confusion about the relative contribution of the respective work groups to their care.
Yet the most striking findings from these earlier Oxford and York studies1,5 related to organisational or trust approaches to the management of the nurse support workforce: such approaches emerged as fragmented, ad hoc and possibly disordered. In general, this might be traced to the relatively weak institutionalisation of the nurse support role, as reflected in its unregistered status. Thus, in contrast to the RN and other strongly institutionalised NHS professions and allied professions, there were no standard regulations to guide trusts on the recruitment, training and development of HCAs. The result was a patchwork of different practices between trusts and underdeveloped systems to manage HCAs. The lack of order was particularly reflected in the degraded relationship between pay banding, training and the nature of the role performed; most HCAs were to be found at pay band 2, but performing very different sets of tasks with different levels of qualification.
A new public policy context
In providing baseline data on the nature and consequences of nurse support roles in acute health-care settings, the Oxford and York studies1,5 were able to formulate a research agenda for follow-up work on this part of the nursing workforce. Such an agenda provided the foundation for the current study. It was an agenda given added weight by the continued and indeed deepening public policy interest in nurse support workers. This deepening of interest in HCAs reflected an important shift of emphasis in debate among NHS policy-makers and practitioners on the role, closely associated with high-profile cases of failure in the delivery of health and social care. Such failures ranged from broad concern about the absence of dignity and compassion in the provision of care to older people to more specific instances of institutional failure, most obviously apparent at Mid Staffordshire NHS Foundation Trust and Winterbourne View. The causes of these failures have been presented as complex and varied. 32 However, the increasing use of the unregulated HCA in the provision of frontline care inevitably encouraged a focus on and consideration of the role’s contribution to such failures. If the Oxford and York 2008–10 studies1,5 were rooted in policy assumptions about the value of HCAs in improving care quality, the current study was framed by concerns about the risks associated with the use of such workers.
These concerns were not new. A decade ago, McKenna et al. warned that ‘the increasing reliance on HCAs raises serious quality and safety questions’ (p. 457),33 while a survey of chief executives in health and social organisations found that over half (52%) felt there was ‘considerable’ or ‘moderate’ risk from the use of support workers. 34 More recently, however, such concerns have come to the fore, reflected not least in terms of a sharper debate on whether or not support workers should be registered. The General Secretary of the Royal College of Nursing (RCN)35 has criticised the level of quality of training received by health-care assistants. In a considered review of the evidence on the use of HCAs, Griffiths and Robinson36 concluded that the use of health-care support workers might well constitute a risk to public safety.
The present study
Focus and debates
This new public policy backdrop added particular significance and urgency to the present study. It encouraged a continuation of attempts to strengthen the evidence base on the nature and consequences of nurse support roles, and more particularly to focus on key issues highlighted in the earlier Oxford and York studies. 1,5 More specifically, this follow-up project centred on three related but distinct themes associated with the use and management of HCAs, each theme, in turn, concentrating on the pursuit of a particular objective:
-
innovation: to identify and facilitate the development of innovative and sustainable management and working practice as it relates to support worker roles in an acute health-care setting
-
evaluation: to evaluate various acute trust policies and practices designed to improve the efficiency and effectiveness of stakeholder interaction with support worker roles
-
engagement: to secure the engagement of various stakeholders in sharing knowledge, practice and learning on support worker roles.
Clearly, these themes cover a defuse range of issues, precluding the development of a strong central narrative and reducing our capacity to draw upon a single, unifying theoretical or analytical framework. This diffusion of interest might be related to the ‘follow-on’ status of the project. Building on previous, more tightly focused research, the current study was, in a sense, ‘mopping up’ and digging deeper into often loosely connected aspects of health-care support worker roles and their consequences. The central themes – innovation, evaluation and engagement – were an important organising device, but they were typically dealing with different sorts of issues: respectively, the incidence and development of new practices, the outcome of initiatives and the sharing of ideas and approaches. The current study, therefore, remains somewhat fragmented and might, by analogy, in part be viewed as a collection of self-contained ‘short stories’ rather than an integrated ‘novel’.
This is not, however, to detract from important cross-cutting issues and shared lessons emerging from the project or from our capacity to link the study to broader theoretical debates. The project’s predominant theme related to workforce change in the NHS, and in particular the challenges and difficulties faced in bringing about and sustaining such change. This was self-evidently the case in considering innovation, with its focus on the introduction of new ways of using and managing nurse support workers. Indeed, while centring on outcomes, the evaluation theme was still exploring initiatives which changed approaches to health-care delivery, particularly in terms of the new contribution made by the support worker. Moreover, although our engagement theme sought to encourage the sharing of views, and practices, this sharing principally related to changes in approaches to the use and management of nurse support workers.
A focus on workforce change, concentrating on the use and management of nurse support workers, encouraged a connection between the current study and a number of closely related theoretical debates. The first such debate related to organisational architecture, and, more specifically, to those organisational features that might facilitate or inhibit workforce change. An extensive literature provides a variety of organisational change models,37,38 rooted in differing assumptions about the drivers, nature and outcome of change. In crude terms, a distinction is often made between rational, often top-down, strategic change and normative, typically bottom-up, incremental or organic change, with very different prescriptive implications. Taking an inductive approach, the current study did not adopt a particular model of change. It was, however, sensitive to these different models and sought to explore which more usefully characterised and explained change in the management and use of nurse support workers.
The second debate linked to the literature on interoccupational relations,27,28 and, more particularly, role boundaries and jurisdictions, which, as noted, had previously devoted only limited attention to the positioning of the nurse support role. An acknowledgement that job territories are often contested, especially by occupations seeking to professionalise, encouraged an interest in how the development of the nurse support role was viewed by adjacent groups, most obviously RNs: whether changes to the nature of the nurse support role and its contribution to health care were welcomed or resisted.
The third and closely related debate touched on by the project was associated with the institutionalisation of new ways of using and managing nurse support workers. For (neo) institutional theorists, change had traditionally been problematic and not easily accommodated; after all, institutions are viewed by such theorists as enduring and constraining. 39 More recently, however, there has been a growing emphasis within this literature on agency, reflected in the figure of the institutional entrepreneur (IE),40 well placed and motivated to pursue institutional change, and the notion of institutional work, routine activity designed to ‘create, maintain and disrupt’ institutions. 41 This interest in institutional change at the workplace has increasingly been used by institutional theorists to examine the emergence of new work roles and practices, not least in health care,42–44 but again with little inclination to embrace the development of the nurse support role. The current project provided an opportunity to explore whether or not and how new ways of using and managing nurse support workers had become legitimised and taken for granted: in other words, institutionalised.
Approach
The research on the three themes – innovation, evaluation and engagement – was overseen by an advisory group comprising national and regional employer and employee representatives, plus academics with an expertise and interest in the nursing workforce (see Appendix 1 for list of members) and key actors from the project’s case study trusts (see Chapter 3, Focus and methods and Chapter 4, Introduction). Patient representatives were also members of the advisory group (see Appendix 2 for a more detailed statement on patient/public involvement in the project). The advisory group was a virtual network for the duration of the study. It was kept informed of project developments as well as being asked to comment on draft research instruments and papers. It was also sent research findings as they emerged. The group met once, on 19 April 2012, halfway through the project, with 20 members and senior case study representatives attending. This meeting reviewed and discussed available findings from the project and commented on the plans for future work.
The project also maintained a dedicated and openly available website for the posting of project documents and findings. 45 The material on this site complemented that produced by the previous Oxford and York studies,1,5 coming to constitute a significant and accessible repository for research data on nurse support workers. Indeed, indicative of the value of this site, there have been almost 3000 visits (according to Google Analytics website data) since the project began in 2011, with recent monthly averages of almost 50 hits per month from search engines, implying that the traffic is not simply generated from our own project mailings.
The NIHR-approved research protocol was granted full NHS ethical approval (11/LO/0770). Trust research and development approval was successfully sought prior to carrying out the fieldwork in all innovation case (IC) studies and evaluation case (EC) studies. The project fulfilled all university requirements for the ethical conduct of research.
The main body of the report is structured around the three main themes: Chapters 2 and 3 focus on the innovation theme, the former considering the scoping and survey work on this theme and the latter on the related case study work; Chapter 4 concentrates on the evaluation theme; and Chapter 5 examines the engagement theme. In each of these chapters, we present the context for the work undertaken, the methods used and the findings. A final chapter provides an overview and discussion.
Chapter 2 Innovation: scoping and survey
Innovation in the public services, and particularly in the NHS, has attracted increasing attention among policy-makers and practitioners over recent years as a means of both meeting pressures on, and improving the quality of, service provisions. 46 The NHS Modernisation Agency, established in 2001, was focused on innovation as the development and testing of new ideas, a role taken on by the National Institute for Innovation and Improvement in 2005. Indeed, the current NHS chief executive has stressed that:47
We need to do things differently. We need to radically transform the way we deliver services. Innovation is the way – the only way – we can meet [new] challenges. Innovation must become core business for the NHS.
Innovation Health and Wealth: Accelerating Adoption and Diffusion in the NHS. 47 © Crown Copyright. Contains public sector information licensed under the Open Government Licence v1.0. URL: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.nationalarchives.gov.uk/doc/open-government-licence/open-government-licence.htm
This interest connects to an extensive and well-developed research literature, which has debated the nature of innovation: its definition, incidence and diffusion. In general, innovation has been seen to relate to ‘change’ and ‘difference’, with a particular emphasis on the ‘new’ as applied to ‘products’ as well as to ‘processes’. 48 This ‘newness’ might, in turn, be seen to refer to the completely original, or as Van de Ven49 has suggested, to something novel to those involved. As these authors note:49
As long as the idea is perceived as new to the people involved, it is ‘innovation’ even though it may appear to others to be an imitation of something that exist elsewhere.
p. 491
As a ‘process innovation’, new approaches to the use and management of the workforce have been a key feature in the NHS change agenda over recent years; for example, the Modernisation Agency had a changing workforce programme and, indeed, new ways of working have consistently informed contemporary developments in policy and practice in the NHS. The Oxford and York studies1,5 revealed examples of innovative practice in the use and management of HCAs. These examples were, however, unevenly distributed within and between trusts, raising three primary questions considered in the current study:
-
What form does innovation in the management and use of nurse support workers take?
-
As a means of characterising and categorising innovation in relation to nurse support roles, the current study distinguished various dimensions of innovative practice:
-
A new way of working within an established role, centred on the range and nature of the tasks performed. The extension of a nurse support role to take on new tasks might be seen as indicative of this form of innovation.
-
A new role, bundling tasks and responsibilities in a distinctive way. The development of a distinctive, specialist nurse support role by a trust might be viewed as illustrative of this type of innovation.
-
A new way of managing, associated with the systems used by trusts to manage HCAs in terms of their recruitment, retention, development and performance.
-
-
-
How is innovation distributed?
-
The different dimensions provided the basis for exploring patterns in the distribution of innovation both between and within trusts. This was essentially a mapping exercise, indicating the incidence of innovation and its location.
-
-
What explains patterns of innovation?
-
The uneven distribution of innovative practice encourages consideration of why some organisations or clinical areas are able to innovate, while others, delivering broadly similar services, are not. It suggests that there might be drivers, systems and styles which stimulate, support and sustain innovative practice.
-
The three questions were examined in a number of related but distinct phases:
-
scoping: a series of scoping interviews with senior trust managers as a means of both highlighting examples of innovation and providing context for the design of a survey
-
surveying: a national survey of directors of nursing and senior human resource managers at all English acute trusts
-
case study work: six case studies selected to reflect different forms of innovation:
-
management: values-based recruitment at York Hospitals NHS Foundation Trust
-
management: a HCA development nurse role at University College London Hospitals (UCLH) NHS Foundation Trust
-
new role: a colorectal support worker (C-SW) at Hillingdon Hospitals NHS Foundation Trust
-
new role: a dermatology support worker at Oxford University Hospitals (OUH) NHS Trust
-
new role: a band 4 educator role with responsibility for training clinical support workers (CSWs) at OUH
-
new way of working: AP specialists at South Devon Healthcare NHS Foundation Trust.
-
This chapter concentrates on the scoping and surveying phases of the innovation theme and the next chapter focuses on the case study phase.
Scoping
Focus and methods
The scoping phase, conducted during the summer and autumn of 2011, aimed at developing an appreciation of the range and nature of innovative practices emerging within trusts across England. The findings from this phase were valuable in their own right, identifying practices, examples and debates on the management and use of nurse support workers. However, they were also used to inform the design of the national survey (see National survey, below). It was crucial to build a picture of the types of innovative practices being considered and implemented by trusts as a means of exploring their take-up and use in a more structured and systematic way through a survey. Moreover, without prejudging the outcome of the survey, these scoping meetings were used to explore the possibility of case study and evaluation work with trusts.
Conducted during 2011, the scoping phase comprised face-to-face interviews and meetings with key actors at different levels of the NHS – national, regional and local. A total of 116 actors were covered during this phase including:
-
national employee (RCN and UNISON) and employer representatives (NHS Employers)
-
regional workforce leads (in the east of England, the south-west, the north-west, Yorkshire and Humberside, London, Scotland and Wales)
-
directors and assistant directors of nursing, HR directors, education leads and practice development nurses (PDNs) from trusts
-
representatives from a miscellaneous range of organisations including higher education institutions (HEIs) and the Nursing and Midwifery Council (NMC).
This total included 12 one-to-one interviews; eight meetings involving two to three participants; four meetings covering five to six participants; and two more significant events involving trust support worker education leads in different regions of the country, one covering 15 and the other covering 35 participants. As a scoping or exploratory phase, these interviews and meetings were conducted in a flexible way, using open questions encouraging participants to highlight examples of innovative practice in the use and management of nurse support workers, why and how such practices were introduced and with what perceived impact on various outcomes. In the main, full notes were taken of the interviews and meetings. These examples were then classified and coded according to the three dimensions of innovation highlighted earlier to reveal the incidence and patterns of such innovation. Participants were also asked to raise more general issues: prevailing practice, emerging developments, and areas of debate or contention. The responses to these issues were processed to establish patterns and trends. For example, the prevailing practices and emergent trends raised by the respondents were again coded against our three forms of innovation. Similarly, areas of debate or contention were coded according to the substantive issue at stake to distinguish a spectrum of concerns.
Findings
Figure 1 sets out innovative practice as it relates to the use and management of support workers along the three dimensions distinguished: new ways of working, new roles and new management practices. It is clear that most of the innovation has taken place along the new management dimension. Thus, there have been instances of trusts drafting their own codes of conduct for HCAs, establishing clearer career pathways for their HCAs, and creating champions for the role and dedicated corporate educators. Most striking, however, is the concentration of new management practice associated with the recruitment of HCAs and preparation for performing the role. In the absence of minimum entry requirements and with trusts recruiting from low-paid, low-status jobs from across the labour market,1 these new practices suggested that trusts have been seeking to develop and ensure the capabilities of starter HCAs.
FIGURE 1.
Innovative practice.
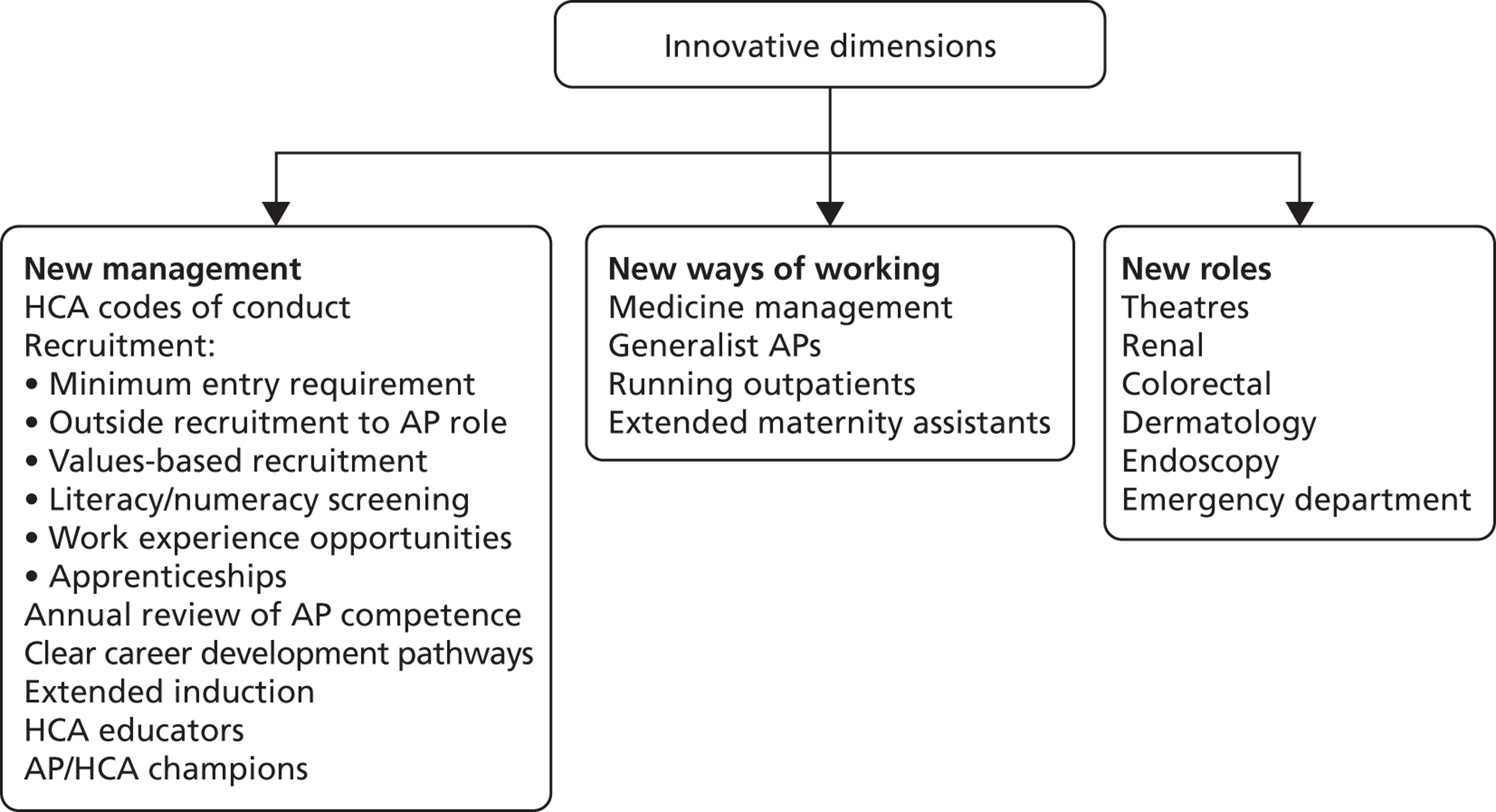
New recruitment practices have included the strengthening of entry requirements. In some cases this has been by stipulating a requisite qualification, typically National Vocational Qualification (NVQ) level 2, and in others it has been by recruiting straight on to an apprenticeship scheme. The new practices have also been apparent in numeracy and literacy tests, designed to filter out applicants deficient in these basic capabilities. Perhaps the most novel development relates to the use of values-based recruitment, which moves selection beyond capability to focus on the attitudes and beliefs of applicants: whether or not these are appropriate for care work and aligned with those of the trust. Finally, the introduction of extended induction programmes arguably reflects attempts to better prepare individuals for the HCA role, particularly before they join the ward team and begin delivering direct patient care.
The scoping phase revealed far fewer examples of new roles or ways of working, perhaps a reflection of the clinical governance issues generated by such change. New ways of working were highlighted, in particular the extension of AP roles to take on drugs administration and the greater use of maternity care support workers to perform more direct care duties. New specialist roles were being developed in clinical areas – theatres, emergency departments, endoscopy and dermatology – typically graded at pay band 4. However, changes involving the performance of new tasks, whether within an existing or in a new role, often had important implications for clinical practice, requiring revisions to trust policy and mechanisms to ensure patient safety and minimise risk. Dealing with such issues could be time-consuming, procedurally complex and sometimes contentious.
These difficulties informed broader debates among NHS policy-makers and practitioners on the management and use of nurse support roles in acute care settings. These debates were indicative of differences in approach to these roles and signalled continuing uncertainty as to how to deploy and deal with them. The debates often revolved around dilemmas or competing views along five dimensions, set out and discussed below:
-
Careers ←→ Costs
-
Developing career pathways for nurse support workers provided new opportunities, seen as a way of retaining this valued part of the workforce. However, career progression also incurred pay bill costs as employees were upgraded, not easily met in times of financial pressure.
-
-
Sweating ←→ Elevating
-
New roles and ways of working could be developed at pay band 4, but an alternative, perhaps cheaper and less difficult option was to ‘sweat’ those in band 2, in other words find ways of generating more work and effort from those in the lower band. This dilemma was deepened by the fact that trusts were sometimes uncertain about the tasks performed by their band 2s, particularly relative to those undertaken by band 3 HCAs. Such uncertainty was encouraging particular trusts to clarify and ‘sort out’ the tasks respectively undertaken by band 2 and 3 HCAs before considering the development of new roles at band 4.
-
-
Trained ←→ Registered
-
Traditionally, skill-mix ratios are based upon a distinction between unregistered and registered nursing staff. However, as AP training has developed and intensified, this distinction has become increasingly problematic, especially where trusts have been seeking to replace a band 5 RN with an AP. If APs continue to be counted as unregistered, their increased use inevitably dilutes skill mix and in so doing raises trust concerns about how such dilution might be perceived.
-
-
Assistant practitioners ←→ Registered nurses
-
Partly related, there is a debate on the relative worth of using band 4 APs or band 5 RNs. Some trusts question the value for the money of the former: the cost difference between the two is not great, and nurses as registered professionals are seen as a more cost-effective option.
-
-
‘Growing your own’ ←→ In-role development
-
The development of career pathways allows trusts to ‘grow their own’ nurses, but this might well be in tension with a trust’s interest in retaining those experienced staff in nurse support roles who might otherwise seek to move into RN roles. Nurse training takes support workers away from the trust, depleting workforce experience and stability.
-
National survey
Focus and methods
Findings from the scoping phase provided the basis for a more structured and systematic mapping of innovative practice in the management and use of nurse support workers by surveying directors of nursing and human resources (HR) in English acute trusts. A draft of the survey was developed and refined in response both to comments from the study’s advisory panel and to a pilot conducted among a national network for support worker co-ordinators.
The mapping of innovative practice comprised a number of elements, reflected in the final survey design. The first provided an overview of employment trends, with the aim of highlighting changes in the structure of the nursing workforce over the last 2 years. To this end, respondents were asked whether they had ‘increased’ or ‘decreased’ (or ‘not changed’) nursing staff at each of the pay bands from 2 to 6 inclusive. The second element centred on those factors driving trusts to innovate in the use and management of nurse support workers. The survey included a range of possible drivers such as efficiency gains and service delivery pressures, asking whether or not these had been influential, as well as directing respondents to specify ‘the most’ influential driver. The third element focused on organisational infrastructure. It had become clear during scoping that workforce innovation depended on the development of a supportive infrastructure: systems to facilitate, nurture and sustain innovation. Respondents were asked whether or not systems that constituted such an infrastructure were in place (‘yes’ or ‘no’); for example, a HCA champion at trust level or a HCA working group.
The centrepiece of the survey was three dimensions of innovation: management, new roles and new ways of working. Selectively drawing upon some of the innovations highlighted during the scoping phase, respondents were asked whether or not they had introduced a given number of such practices along each of these dimensions (‘yes’ or ‘no’), and, indeed, whether they had been introduced in ‘most’ or only ‘part of the trust’. Respondents were provided with an opportunity at the end of the questionnaire to provide additional comments on any of the issues covered in the survey (see Appendix 4 for questionnaire).
The survey was conducted online and invitations to participate were sent to the directors of nursing and of HR at all acute trusts in England during November 2011. To ensure that as many trusts as possible were covered, the final reminder sent in December asked those who had yet to complete the survey to forward it to the most appropriate person in their organisation. The survey was closed in January 2012 and the response details are available in Table 1. In total, 94 trusts took part in the survey, representing a response rate of 57%. The respondent in 90% of the trusts was the most senior nursing or HR director. This represents a very good response rate for a voluntary and independent survey among senior managers in the NHS. The original decision to cover both directors from any given trust was driven by an appreciation that the respective directorates were likely to be involved in innovations related to the nursing workforce. It was also informed by an interest in whether or not the views of the respective functional professionals on nurse support roles were aligned. It was disappointing that the response rate among HR directors was considerably lower than that among nursing directors, despite the promotion of the survey by the Healthcare People Management Association (HPMA). This limited the intended comparison of views between the two groups, although there were glimpses of how perspectives on the nurse support role might vary by function (see Miscellaneous, below).
| Position | Opted out | Returned | Multiple returns | Respondents |
|---|---|---|---|---|
| Head of nursing | 13 | 69 | 3 | 66 |
| Head of HR | 5 | 28 | 9 | 19 |
| Other nursing/HR manager | 4 | 16 | 7 | 9 |
| Total | 22 | 113 | 19 | 94 |
| Response rate | 56.97%a | |||
Using data from the Department of Health, Monitor and the Audit Commission non-response analysis was carried out to ascertain if there was any bias in the type of trust that chose to respond to the survey. The analysis revealed that there was no significant difference between those trusts that responded and those that did not on background variables such as foundation trust status, regional location, trust type, nursing workforce size or financial well-being. We can, therefore, be confident that the results of the survey are likely to be representative of the wider population of English NHS acute trusts.
The survey findings are presented under the following headings:
-
the workforce trends for pay bands 2 to 6 during the last 2 years
-
common drivers of nurse support worker development
-
managerial infrastructure for nurse support workers
-
innovative practices to manage nurse support workers
-
innovative nurse support worker roles or ways of working
-
miscellaneous.
Where respondents provided comments on particular questions, they are referred to in the appropriate section.
Findings
The workforce trends for pay bands 2 to 6 during the last 2 years
The workforce trends highlighted in Table 2 need to be treated with some care, being based on the impressions of respondents rather than on hard data. As a means of ensuring a high response rate, the survey was deliberately designed to ask for views rather than hard data on changes in employment level between bands. We felt that if respondents had to seek out harder, more precise data on staff numbers, usually from other staff and departments in the trust, they would have been less likely to complete the survey. However, these trends do suggest considerable dynamism and change in the nature of the workforce over the last 2 years. Interpreting the picture presented is far from straightforward. In a period of financial pressure and broader resource constraint, it is clear that trusts are not simply decreasing numbers in the nursing workforce. Rather, it appears that they are increasing and decreasing numbers of nursing staff, with important differences in the net flow between pay bands. In part, these patterns might reflect broader organisational changes; for example, one respondent noted that the trust had mainly increased the size of its nursing workforce on taking over community care services from the primary care trust. Staff flows also appeared sensitive to regional or local labour market factors. As another respondent suggested:
We find band 6 nurses extremely difficult to recruit and so have converted some posts to band 5 to enable us to fill vacancies and grow our own. There is some evidence that this is a London phenomenon due to the cost of living at a time when people are embarking on life commitments such as starting a family.
Trust_42
| Pay band | Increased | Decreased | No change | Count (n) |
|---|---|---|---|---|
| Nurse support workers at pay band 2 | 59.5 | 8.3 | 32.1 | 84 |
| Nurse support workers at pay band 3 | 44.6 | 21.7 | 33.7 | 83 |
| Nurse support workers at pay band 4 | 54.7 | 8.0 | 37.3 | 75a |
| RNs at pay band 5 | 56.8 | 21.0 | 22.2 | 81 |
| RNs at pay band 6 | 35.0 | 23.8 | 41.3 | 80 |
More generally, these data suggest three trends in employment centred on different pay bands:
-
Stability: the first is concentrated on RNs at band 6, with employment relatively stable: almost half of the respondents (41%) indicate no change in the employment of nurse in this pay band.
-
Churn: the second covers band 5 nurses and band 3 HCAs and displays considerable churn. A significant proportion of trusts, around half, are increasing the numbers employed in these bands, while at the same time, close to one-quarter are decreasing numbers employed at these levels. The band 3 HCA role is not used extensively by trusts, limiting the weight that can be placed on volatility of employment at this level. As the entry grade for RNs, the churn at pay band 5 is noteworthy and might well be related to trust variation in approaches to the band 4 AP role. Thus, the increased use of band 4 APs is often traded off against band 5 posts, perhaps accounting for the noteworthy minority of trusts decreasing employment at this level. Yet it is equally apparent that many trusts, well over a half (57%), are increasing their number of band 5 nurses, perhaps reflecting grade dilution with the employment of fewer band 6 nurses.
-
Expansion: the third pattern is characterised by increasing employment, with little sign of any decrease in numbers. This would seem to relate to those parts of the nursing workforce which trusts appear to be most keen on using and developing. More specifically, this pattern embraces band 2 HCAs and band 4 APs. In the case of both groups, well over half of trusts have increased levels of employment at these levels, with only 8% decreasing employment. The increase in band 2 HCAs lends some credence to the suggestion that trusts are seeking to ‘sweat’ the role in financially difficult times, employing more staff at the ‘low-cost’ end of the nursing workforce. Where APs replace band 5 nurses, it might similarly reflect a dilution of skill mix. As one of the respondents commented, ‘As we develop band 4’s they will replace some band 5’s’.
It also suggests a shift from the tardiness displayed by trusts in developing and using the AP role,5 along with a greater appreciation and understanding of the contribution to be made by such a role in the restructuring of their nursing workforce. Certainly, the AP role continues to be a source of some contention and debate with trusts. As one respondent stressed:
I have considered introducing the band 4 AP, but the lack of registration and ability to administer drugs does not appear to offer any efficiency savings.
Trust_91
Moreover, in an echo of the concerns raised in the scoping phase about the value for money of a band 4 AP, another argued that:
There needs to be a full cost–benefit analysis of band 4 roles on general wards to show whether there is an added value to the role. I personally believe that bands 2 and 3 already provide competent basic care and competency based clinical skills to patients and so am unclear what the added value of a band 4 is. There needs to be a clear steer on the administration of medications by any group of clinical support workers at 2, 3 or 4 and if there is a national push for unregistered staff to provide medications then there should be some form of registration or regulation with an appropriate body.
Trust_23
However, the balance of comments suggested that more trusts were seeking to develop AP roles for the first time. Nine respondents commented that this was the case, including those noting:
We are currently developing band 4 roles and a strategy for associate/assistant practitioners.
Trust_89
We are working to develop the band 4 AP workforce.
Trust_57
Common drivers of nurse support worker development
Table 3 indicates that trusts have been driven to address their nurse support workforce by a combination of factors. However, the primary drivers are service redesign (79%) and attempts to improve patient experience (73%). Other notable drivers are efficiency gains (65%) and service delivery pressures (49%).
| Driver | % (n) |
|---|---|
| Service redesign | 78.7 (70) |
| Improving patient experience | 73.0 (65) |
| Efficiency gains | 65.2 (58) |
| Service delivery pressures | 49.4 (44) |
| Financial pressures | 38.2 (34) |
| National and/or regional policy initiatives | 31.5 (28) |
| Trust restructuring | 29.2 (26) |
| Difficulties in recruiting and/or retaining RNs | 21.3 (19) |
| Other (e.g. patient safety, patient complexity, turnover of support workers, providing a career framework) | 7.9 (7) |
| No significant nurse support worker developments | 4.5 (4) |
When respondents were asked to choose between the drivers and specify the single most important one (Table 4), patient experience emerged as the principal driver, highlighted by well over one-third of respondents (39%), compared with service redesign (19%). At the same time, the table suggests that some trusts are being driven by more immediate pressures. A crude distinction can be made between drivers that suggest a proactive or strategic approach to the nurse support workforce, such as service redesign and improvements in the patient experience, and a more ad hoc and reactive approach reflected in the importance of efficiency gains, financial pressures, service pressures and recruitment and retention difficulties among nurses. In total, these more ad hoc and opportunistic pressures are driving nurse support workforce developments in well over one-third of trusts (39%).
| Most important driver | % (n) |
|---|---|
| Improving patient experience | 38.6 (32) |
| Service redesign | 19.3 (16) |
| Efficiency gains | 18.1 (15) |
| Financial pressures | 8.4 (7) |
| Service delivery pressures | 7.2 (6) |
| Difficulties in recruiting and/or retaining RNs | 4.8 (4) |
| Trust restructuring | 2.4 (2) |
| National and/or regional policy initiatives | 1.2 (1) |
Managerial infrastructure for nurse support workers
The three questions on managerial infrastructure were indicative of the kind of system which might stimulate and support innovation in the management and use of nurse support workers. The findings presented in Table 5 cast some doubts on whether or not such systems are in place. Certainly, around half of trusts had a designated nurse support worker champion at senior levels (48%), but given that many trusts have a senior (nurse) manager responsible for the development of the nursing workforce, it is perhaps surprising that more were unable to respond positively to this question. Indeed, suggestions that the lack of a champion reflects the absence of a supportive infrastructure for innovation finds some confirmation in the fact that only a minority of trusts have a strategy group (30%) and a written strategy covering this group (29%). A number of respondents in their open comments indicated that support workers were covered by more broadly based nursing strategies and associated working groups. Indeed, seven nursing directors volunteered this comment in the survey. However, in combination, responses to these questions still cast some doubt on the strength of the infrastructure to develop nurse support workers in innovative ways.
| Infrastructure | Yes | No | n |
|---|---|---|---|
| Designated nurse support worker champion at divisional or trust management level | 48.3 | 51.7 | 89 |
| Established support worker strategy group | 30.2 | 69.8 | 86 |
| A written nurse support workforce strategy | 28.9 | 71.1 | 83 |
Innovative practices to manage nurse support workers
A significant proportion of trusts have adopted new management practices designed to more tightly regulate entry into HCA roles within the trusts. Thus, Table 6 indicates that over two-thirds of trusts are using numeracy and literacy tests to screen band 2 candidates across most of their organisations, while a similar proportion have extended induction programmes for this group of workers (69%).
| Practice | Most of the trust | Some of the trust | No | n |
|---|---|---|---|---|
| Candidates at pay band 2 are screened for numeracy and literacy | 68.2 | 12.5 | 19.3 | 88 |
| All new pay band 2 staff recruited to an apprenticeship programme | 7.8 | 23.3 | 68.9 | 90 |
| An off-ward induction programme for new pay band 2 staff lasting 3 or more days | 69.2 | 12.1 | 18.7 | 91 |
| New pay band 2 recruits must achieve training targets to be confirmed in post | 39.3 | 16.9 | 43.8 | 89 |
| Guaranteed pay band 4 role to APs on completion of training | 27.1 | 17.1 | 55.7 | 70 |
| Forum/support group at division or trust level attended by nurse support workers | 20.5 | 25.3 | 54.2 | 83 |
However, other practices which might be seen to strengthen and regulate nurse support work preparation and engagement have been unevenly taken up. Only a small proportion of trusts recruit all band 2s onto an apprenticeship programme across most of the trust (8%), and barely more than one-third require band 2s to achieve training targets before they are confirmed in post (39%).
Guarantees for APs to receive a band 4 role on completion of training is not a comprehensive practice, with over half of trusts suggesting that the AP post is not confirmed in these circumstances (56%). Similarly, the direct nurse support worker voice remains fairly weak, with over half of trusts indicating that they have no dedicated forum anywhere in the trust above ward level for them (54%). Certainly, some trusts had explicitly engaged nurse support workers in more broadly based forums, thereby ensuring a fuller integration within the nursing workforce. As one respondent noted:
We have made a conscious effort to include support workers in other forums e.g. as infection control champions; tissue viability links; in addition to staff nurses completing these roles. Hence we involve HCAs in trust forums but not always in groups of only HCAs.
Trust_77
However, the absence of a dedicated HCA space raises issues about the effectiveness of the nurse support worker voice, with previous research suggesting that their view can be lost when combined with others. 1
Innovative nurse support worker roles or ways of working
Table 7 indicates that trusts are beginning to develop new nurse support roles. This is particularly marked in the case of maternity support workers, where the overwhelming majority of trusts have a support role delivering direct care; only 1 in 10 trusts reported this not to be the case (9%). A support role that works across professional boundaries is also a common feature in trusts (72%), although it is less established, with 50% of trusts reporting the role as occurring in only some parts of the organisation. Likewise, a critical care support role features in over half of the trusts (55%), but the majority of that occurrence is only in some parts of the organisation (30%).
| New role | Most of the trust | Some of the trust | No | n |
|---|---|---|---|---|
| Critical care support worker role with patient care duties | 25.6 | 29.5 | 44.9 | 78 |
| Health-care support worker role that works across different professional boundaries | 22.0 | 50.0 | 28.0 | 82 |
| Maternity support worker role with direct care duties | 43.8 | 47.5 | 8.8 | 80 |
In terms of new ways of working, some trusts are seeking to clarify and sharpen responsibility for the performance of tasks. Table 8 points to a clear majority of trusts revising job descriptions for bands 2 and 3 (74%) in most or some parts of the trust. The issuing of guidelines for the delegation of tasks to nurse support workers also appears to be fairly prevalent (63%), although it is perhaps noteworthy that over one-third of trusts (37%) have no such guidelines anywhere in the trust. While the only substantive change in ways of working included in this section of survey, the administration of medicine, has not been widely taken up, it is still striking that nurse support workers undertake this activity in at least some parts of the organisation in almost one-fifth of trusts (18%).
| New way of working | Most of the trust | Some of the trust | No | n |
|---|---|---|---|---|
| Revised job descriptions for pay bands 2 or 3 in the last 2 years | 32.2 | 41.4 | 26.4 | 87 |
| Code of conduct for nurse support workers | 31.8 | 6.8 | 61.4 | 88 |
| Nurse support worker role that includes the administration of medicine | 4.9 | 13.4 | 81.7 | 82 |
| Guidelines for the delegation of tasks to nurse support workers | 40.5 | 22.8 | 36.7 | 79 |
In concentrating on the development and use of AP roles as a new of way working, Table 9 reveals the relatively high incidence of a preceptorship programme for newly qualified workers in these roles in at least some part of their organisation: well over half of trusts have such programmes (59%). In contrast, formal evaluation of the role and revalidation of AP competence are considerably less common.
| Most of the trust | Some of the trust | No | n | |
|---|---|---|---|---|
| Annual revalidation of AP competence | 10.0 | 15.0 | 75.0 | 60 |
| Formal evaluation of AP roles | 28.1 | 23.4 | 48.4 | 64 |
| A preceptorship programme for newly qualified APs | 46.0 | 12.7 | 41.3 | 63 |
Miscellaneous
A number of additional findings emerged from the survey, based on further statistical analysis and on the open comments made by respondents. First, as a means of seeking to categorise trusts by innovative approach in the use and management of nurse support workers, cluster analysis was undertaken. This drew upon data from the survey which related to new management practices, new roles and ways of working, including new approaches to the AP role, and trust infrastructure. The findings suggest five different types of trust summarised in Table 31, which can be found in Appendix 5.
The surveyed trusts are fairly evenly distributed across these five types, suggesting a variability of approach and perhaps an uncertainty as to how to approach and deal with the nurse support role. These five types can be labelled and briefly summarised as follows.
-
The non-innovator: a low take-up of any form of any innovation, alongside poorly developed infrastructure to support such developments. It is noteworthy that this type comprises the smallest number of trusts, just eight, suggesting that a significant majority of trusts are seeking to innovate in certain ways.
-
The regulatory innovator: mainly innovating in terms of the management of nurse support roles, in particular regulating entry into the role. These trusts have introduced numerical/literacy screening, extended induction programmes and revised job descriptions. However, they show few signs of more ambitiously innovating in relation to roles and or ways of working.
-
The grounded innovator: grounded in terms of both establishing infrastructure for the development of nurse support roles and concentrating their innovation mainly on AP rather than on band 2 HCA roles. This is the most common type of trust, covering 13 organisations, providing some support for the suggestion that trusts are now moving forward with the development of band 4 roles.
-
The focused innovator: centred on developing new roles rather than any other form of innovation and in the absence of developed infrastructure.
-
The full innovator: innovating along all three dimensions – roles, management and ways of working – and underpinned by a strong infrastructure. Clearly, these are the most innovative trusts, but just as there are few non-innovators trusts, there are relatively few (nine) full innovator trusts.
A second miscellaneous finding emerges as a glimpse of the divergence of perspective between nurse and HR directors on innovation associated with the nurse support workforce. While most innovative developments affecting nurse support workers are driven by the nursing directorate, the HR function plays a part, with a general interest in workforce planning and a more direct role in certain initiatives, especially those linked to the recruitment and selection of nurse support workers. A divergence of view is brought into sharp focus by survey comments from a HR director and nurse director at the same trust, the former suggesting that there is considerable scope to further extend the support worker role and the latter arguing quite the reverse:
This is an area in which I am particularly interested. We are not doing enough, in my view, to develop the nurse support workforce particularly at assistant practitioner band 4 level. There is a divergence of views within the organisation, those that are very keen and those that are not.
Trust_29_director of human resources
We have looked at the workload of the nursing staff in the clinical area, and I personally believe that use of non-clinical support workers for tasks like admin, housekeeping support, and decontamination, to allow trained nurses more time to care for patients, is a better use of untrained clinical support workers to provide direct patient care.
Trust_29_director of nursing
This was one of the few trusts which provided a response from both the nursing and the HR directors, although in hinting at a divergence of view between the two functional professionals, this finding encourages more focused work on this issue.
Third, a number of respondents highlighted the significance of a competency framework or model as the basis for innovating around nurse support roles. The survey did ask a few questions about competencies, but the open comments suggest that they are being used to confirm HCA appointments, develop AP roles, review capabilities and distinguish roles, and establish career pathways and performance manage, as follows.
-
Confirm HCA appointments:
-
‘We have a centralised recruitment for trainee HCAs with a nine day skills training programme then completion of portfolio and clinical competencies over six months before they become qualified HCAs.’ [Trust_114 (emphasis added)]
-
-
Develop AP roles:
-
‘As we develop band 4s we will utilise competencies and training in administration of medicines in a controlled way to benefit patient care.’ [Trust_18 (emphasis added)]
-
-
Review capabilities and distinguish roles:
-
‘We have introduced a full week’s refresher training for nursing assistants to ensure competence and clarity of roles.’ [Trust_40 (emphasis added)]
-
-
Establish carer pathways and performance manage:
-
‘Our support worker programme is undergoing many changes and developments to ensure that quality patient care is delivered at all levels, and to provide a robust career pathway linked to education and competency attainment. We are just beginning the implementation of this work, with a CSW framework from recruitment, cadets and apprentices, through to AP levels.’ [Trust_119 (emphasis added)]
-
Finally, comments suggested that many trust were on the cusp of developing new approaches to the management and use of nurse support workers. The survey was, arguably, conducted in a period of uncertainty with the trusts awaiting a more detailed report on Mid Staffordshire by Robert Francis, and the government’s response, before addressing the issue of unregistered nursing staff. Some trusts were more explicit about their forthcoming intention to develop this part of the nursing workforce:
We are working towards implementing our 3-year workforce strategy that aims to improve productivity by maximising benefits of new roles i.e. APs and reduce reliance upon temp staff along with many other goals.
Trust_1
Overview: discussion and lessons
Process and product innovation has assumed increasing importance to NHS policy-makers and practitioners as a means of delivering cost-efficient and effective care services. As a process innovation, new developments in the structure of the nursing workforce – in particular the distribution of tasks and responsibilities – have figured prominently on this agenda. There have, however, been few attempts to map innovative practice in the management and use of nurse support workers: in other words to explore what form innovation has taken, how it has been distributed by trust and clinical area and what has driven it. Distinguishing between innovations associated with the management of nurse support workers, their ways of working and their roles, the scoping phase of the research, based on consultation with over 100 policy-makers and practitioners at different levels of the NHS, has presented a picture of patchy, uneven and uncertain developments. Innovation had been most evident in the management of nurse support workers, particularly during recruitment and preparation for the role; this form of innovation might be more straightforward than in relation to new roles or ways of working where issues of clinical governance add a layer of complexity to the process. Indeed, these complexities seemed to generate a number of dilemmas and competing views within trusts on the use and management of the nurse support workforce.
Of value in their own right, the findings from the scoping phase also fed into the design of a national survey, which provided a more detailed, structured and systematic picture of innovation. In important respects, the survey findings reinforced those presented in the scoping phase. The increasing employment of band 2 and 4 nurse support workers suggested that trusts were concentrating their efforts at these levels. Driven by an interest in improving patient experience and service redesign, the infrastructure to support innovation remained fragile, although some innovative practice had become relatively widespread. Again, these practices relate mainly to the management of nurse support workers: numeracy and literacy tests and extended induction. The adoption of codes of practice and guidelines for the delegation of tasks suggests that systems were being put in place to develop new ways of working, and new roles were being developed, particularly in maternity care. However, the cluster analysis revealed the tentativeness of trust approaches to innovation. Certainly, this analysis suggested that there were few non-innovative trusts; in other words, most trusts were innovating in some way. However, there were also few fully innovating trusts, and the fairly even distribution of the trusts across the five types pointed to the diversity of approaches being adopted.
Such diversity encourages consideration of why and how certain trusts were able to innovate, and in the next chapter, attention turns to the case study phase of the innovation theme, which sought to address these questions.
A number of lessons can be drawn from the scoping and survey phases of the innovation stream:
-
Given the relatively high incidence of new ways of managing, this approach to innovation appears to be more viable and lower risk than one based upon new roles or ways of working. New ways of managing generate far fewer clinical governance issues than other forms of innovation, and are less likely to be contested by various stakeholders from within trusts.
-
While dilemmas remain about how to use and manage support workers, if trusts are to make progress on the innovative deployment of this group of workers, these dilemmas need to be systematically worked through, with any uncertainties and tensions directly addressed.
-
Certainly, the dilemmas or trade-offs highlighted are not easily reconciled. However, any resolution might usefully be related to local trust circumstances and needs: the state of the local labour market for the nurse support workers; the capacity to recruit and retain RNs; and or the financial well-being of the trust. Thus, the decision to employ APs, or to develop nurse support workers as a means of ‘growing your own nurses’, might be linked to a trust’s ability to attract nurses. Difficulties in this respect are likely to encourage the search for alternative sources of nursing labour. Similarly, the development of career pathways for support workers might be associated with the ‘tightness’ of the local labour market for ‘low-paid, low-skilled’ jobs. Career pathways are a useful way of retaining nurse support workers, who might otherwise seek alternative job opportunities, providing the trust with value for money.
-
Despite the limited incidence of new roles and ways of working, there were examples of such practices in these areas, suggesting scope for the sharing of ideas and approaches. It was not, however, immediately apparent what institutional spaces or network at national, regional or indeed trust level might provide the opportunity to share such ideas and approaches. There were laudable examples of attempts to engage, for example a national network of trust AP education leads, but greater consideration should be given to the development and resourcing of such spaces and networks.
-
Many trusts need a more robust infrastructure for developing the support worker role, for example in the form of a support worker champion at senior management levels and or nursing strategies sensitive to the contribution of such workers.
-
If support workers are to be used and managed more innovatively, there needs to be a closer alignment between functional views and approaches, particularly in the case of the nursing and HR management teams.
Chapter 3 Innovation: case studies
Focus and methods
The primary aim of the IC studies was to develop an understanding of the development of a new role or practice in a given trust, examining the details of how and why it emerged and evolved within a specific organisational context. If the scoping and survey phases were designed to map the form taken by, and the distribution of, innovation, the case study phase sought to explain innovative management and the use of nurse support workers in particular trusts. More specifically, why were some trusts able to innovate in these respects, while others, providing similar health-care services, were not?
Table 10 sets out the six IC studies. The cases were purposefully selected to fall within three dimensions of innovation. Two cases focused on new approaches to management: values-based recruitment and the introduction of a HCA development nurse. Three cases examined new roles: a C-SW; a surgical assistant practitioner; and a band 4 educator role with responsibility for training CSWs. Finally, one case study looked at new ways of working: APs in specialist clinical areas. In all cases, the role or practice was new to the trust, although not necessarily unique to the NHS. The six trusts explicitly agreed to attach their names to the presentation of the material in this report. The cases were, after all, examples of ‘good practice’, and in general the trusts were proud of their achievement in ‘successfully’ introducing them.
| Trust | Innovation | Fieldwork dates | Level of staff interviewed | Total | ||
|---|---|---|---|---|---|---|
| Trust managers | Service managers | Ward staff | ||||
| York | Values-based recruitment | December 2011–March 2012 | 6 | 7 | 5 | 18 |
| South Devon | APs as flexible resource | August 2012 | 7 | 2 | 8 | 17 |
| Hillingdon | Stoma care support worker | June–November 2012 | 4 | 3 | 4 | 11 |
| UCLH | HCA development nurse | July 2012 | 4 | 0 | 14 | 18 |
| OUH | Surgical assistant practitioner | January 2013 | 1 | 0 | 3 | 4 |
| OUH | CSW trainer at band 4 | December 2012–May 2013 | 8 | 0 | 3 | 11 |
| 30 | 12 | 37 | 79 | |||
Carried out between the winter of 2011 and the early summer of 2013, the cases were mainly based upon interviews with a vertical slice of trust actors who had a stake in the innovation under consideration. Table 10 sets out those interviewed in the respective cases. In total, there were 79 interviews carried out. These interviews were typically supplemented by relevant documentary material, for example trust policies, job descriptions and training programmes.
In general, the interviewees were asked fairly open questions about:
-
the context for the innovation, including trust structure, culture and history
-
the nature and aims of the innovation
-
the design and implementation of the innovation
-
the impact of the innovation on various stakeholders and outcomes
-
the broader lessons.
All interviews were recorded and transcribed. The transcriptions were read through on a number of occasions with a view to establishing whether or not there was an agreed narrative from the stakeholders on the development of the innovation, its aims, design features and consequences, and, if not, where differences of view lay. A draft case report was fed back to the respective trusts, providing the opportunity for inaccuracies and misinterpretation to be picked up.
This section presents an overview of the findings from the respective cases. A final section provides a summary and discussion. To protect the identity of those we interviewed, and to provide consistency between the case study reports, the quotes within the text use the identifier IC plus attributions related to three broad job areas: trust manager, which may include senior and executive managers, personnel within HR, the education and learning teams and external managers; service manager, which can include matrons, divisional managers and senior nurses not working on wards; and ward staff, which can include ward or clinic managers, medical staff, nurses, HCAs and APs. Where an interviewee could be easily identified owing to their specific role, they were contacted to give their approval prior to the case study report being made public. Approval was given in all instances.
Values-based recruitment
Context
This case study deals with a new values-based approach to the recruitment and retention of HCAs introduced by York Teaching Hospital NHS Foundation Trust in 2010. The innovative character of this initiative was reflected in the fact that it had won the 2011 HPMA award for innovation in HR and a similar Health Service Journal (HSJ) award in 2012. The trust’s interest in such an approach was underpinned by two broad considerations. The first related to a high turnover among its 500-or-so HCAs, particularly in the first 6 months of employment, which the trust found to be associated with recruits not being fully aware of the nature of the HCA job:
So many people just came and didn’t have a clue really what they were going to be doing . . . They come and think, ‘oh I thought I was only making tea’. And you think, ‘gosh no, there’s a whole host of things, and tea isn’t one of them’.
IC1_ward staff_1
The second consideration was values based, and reflected York’s interest in aligning its values, revolving around ‘caring and ‘compassion’, with those of new HCAs:
We wanted to be able create the opportunity for the individual to demonstrate their caring disposition.
IC1_trust manager_1
The new recruitment model
York’s new approach to HCA recruitment comprised a number of elements:
-
A new band 2 HCA job description placed emphasis on personal disposition rather than formal qualification. The person specification was modified to reduce the need for ‘relevant work experience’ and the need for a NVQ level 2 qualification. There was a sharper focus on an understanding of the HCA role and an ability to demonstrate a caring orientation.
-
A new application process sought to address the high turnover of HCAs, stemming from the failure of candidates to fully appreciate the HCA role. The centrepiece of the change was a mandatory open day: ‘On the open day, they come and talk to other healthcare assistants, and they get a view of what the job actually entails. They can look around at the stands, and it’s a really good push into what the role is’ (IC1_trust manager_2). Only those attending were provided with a unique identification number which allowed them access to the application form. As a means of providing more detailed information about the role, the trust also produced a 10-minute film made available on DVD and online, involving HCAs talking about their role.
-
A new selection process sought to ensure a better fit between applicant and clinical area, with shortlisted candidates having the opportunity to list their order of preferred wards. Moreover, the old standard list of interview questions was replaced by an open, scenarios approach, better able to assess whether or not candidates had a caring disposition.
-
A new 2-week HCA induction programme was introduced, with new recruits only taking up their post on the ward on its completion. Replacing an often deferred corporate induction of a couple of days, the new programme ensured that HCAs were better prepared for their role, and so more able to deliver compassionate care and become more appreciative of what the role involved before ‘hitting the ward’.
Key processes and actors
The emergence of York’s new recruitment model rested on a number of processes and actors.
Identifying health-care assistant recruitment as a legitimate issue of concern
Informally, HCA turnover had been a concern for some time, particularly among the trust’s matrons:
We were a very sort of tight knit group of matrons and the problem with retention in terms of health-care assistants was not something strange that had escaped our attention.
IC1_service manager_1
However, defining high HCA turnover as an issue worthy of further action had to be sanctioned by senior trust managers:
The assistant chief nurse and [recruitment manager] along with their line managers, the chief nurse and HR director had initial meetings to say we’re getting feedback from matrons and ward sisters that the health-care assistants . . . don’t understand what the role’s about.
IC1_trust manager_2
Devising the means to address concerns about health-care assistant recruitment
The trust’s attempts to deal with the recruitment of HCAs rested on close working relationships between different trust functions, particularly the nursing directorate and the HR directorate. The latter was crucial in presenting substantive ideas; thus, the notion of values-based recruitment came from HR. However, the former was essential in carrying these forward and ensuring ‘buy-in’ from nurses and ward sisters to any changes in recruitment procedures.
A third partner in the design process was the trust’s applied learning and research directorate. This was a standalone directorate at York, rather than more typically a part of the HR function, and it acted as a useful resource in designing and delivering a new, credible induction programme.
In the initial stages, there was some informal working between these partners, especially the assistant chief nurse and the recruitment manager, testing ideas and establishing a ‘direction of travel’. These relations were, however, formalised and extended by the establishment of a small working group comprising matrons and ward sisters, which allowed ideas to be sharpened.
Implementation
The implementation of the new recruitment model was an iterative process, with trust managers regularly seeking the views of nursing staff, and ‘tweaking’ in response to staff views:
We had focus groups, we went to matron meetings to get their feedback. We tried to pull from a whole kind of range of nursing staff, so we didn’t just talk to the health-care assistants, we spoke to some of the staff nurses that dealt with them, we spoke to ward sisters, we spoke to matrons . . . And the feedback we got was really beneficial in terms of how we shaped the process.
IC1_trust manager_3
Equally crucial was formal sanctioning and buy-in from the trust’s senior management, which lent legitimacy and credibility to the initiative, and, more prosaically, helped to address certain obstacles:
We needed that board level sign up because there was an issue when we needed the freedom to really change things, not just tweak things . . . I think it was helpful because you know that you did have the ability to change things and actually just to have, if you’re wanting to do it quickly you need that kind of senior sign up.
IC1_trust manager_3
There was strong ongoing support from the chief nurse for the initiative:
It is important that you’ve got the support of your chief nurse and your director of HR who can help overcome some of those obstacles . . . because there are resource implications.
IC1_trust manager_3
Impact
There were some organisational concerns raised about the introduction of values-based recruitment at York. For example, it was suggested that setting up the model was time consuming:
. . . probably just the time to set it up. Because there was a lot of work in, you know, producing the DVD, getting people to come and feel confident enough as a HCA to stand up and talk to a room of what can be a 100 people.
IC1_trust manager_4
More generally, however, responses to the new model were positive, with a number of benefits being highlighted.
Quality
In providing applicants with a fuller appreciation of the HCA role, the new process walked a fine line between realism and deterrence: more information about the HCA role might as easily have discouraged as encouraged applicants. However, the trust produced data that revealed the effectiveness of open days in attracting those interested in the HCA role: between May 2010 and April 2011, the average attendance was around 100. The average number submitting a formal application had fallen from some 100 to 67, suggesting some ‘deselection’ among those attending the open days. The enthusiasm of those who did apply was reflected in the fact that the numbers of those not attending interviews when called fell by over two-thirds.
Preparation
The new induction was seen to better prepare HCAs for their role, particularly in terms of competence. As well as contributing to high-quality care, better preparation was viewed as lowering HCA turnover by reducing initial difficulties and stress. The value of the new induction programme was certainly not uncontested. There was, for example, a 2-week lag between the appointment of a HCA and their taking-up of the role on the ward, which caused some ward manager concern. In general, however, HCAs were seen as more equipped for their role following the new extended induction:
They seem to fit in the team quickly, they pick things up much faster, they have an understanding of what is expected of them, their documentation is pretty quick really, they know what they should be doing and what they shouldn’t be doing.
IC1_ward staff_2
Symbolism
The new recruitment process, with its open day and extended induction, also signalled the greater support or value placed by the trust on the HCA:
It’s nice that they’re actually thinking about us [HCAs] now; that they’re thinking, ‘oh yes well they’re doing this role so we need to put some training in’.
IC1_ward staff_1
Retention
There was circumstantial evidence to suggest that HCA retention had improved under values-based recruitment. The trust’s need for fewer rounds of HCA recruitment suggested that HCAs were more inclined to stay. Figures backed this up: turnover reduced from 17% to 12% in the immediate aftermath of the changes and this lower figure has been sustained for 3 years. Indeed, given the costs invested in HCAs who had previously left, this high HCA retention rate was seen to render the initiative highly cost-efficient.
Values
There was similarly anecdotal evidence to suggest that the new interview process was effectively seeking to probe the dispositions of prospective HCAs. As a HCA who had been through the process noted:
They were definitely trying to find out sort of about your personality as well rather than what you are on paper . . . There was quite a lot of that and there was lots of kind of smiling and laughing and it did feel quite relaxed and I did feel that I could bring my personality across and I wasn’t just kind of reciting the notes in my head and answering sort of regimented questions.
IC1_ward staff_3
Overview
Figure 2 provides an overview of York’s new approach to HCA recruitment. It can be seen that the initiative was embedded in two closely related but analytically distinct streams of development based on retention and on values, which fed into the design of the new recruitment model in various ways.
FIGURE 2.
Tracking the initiative.
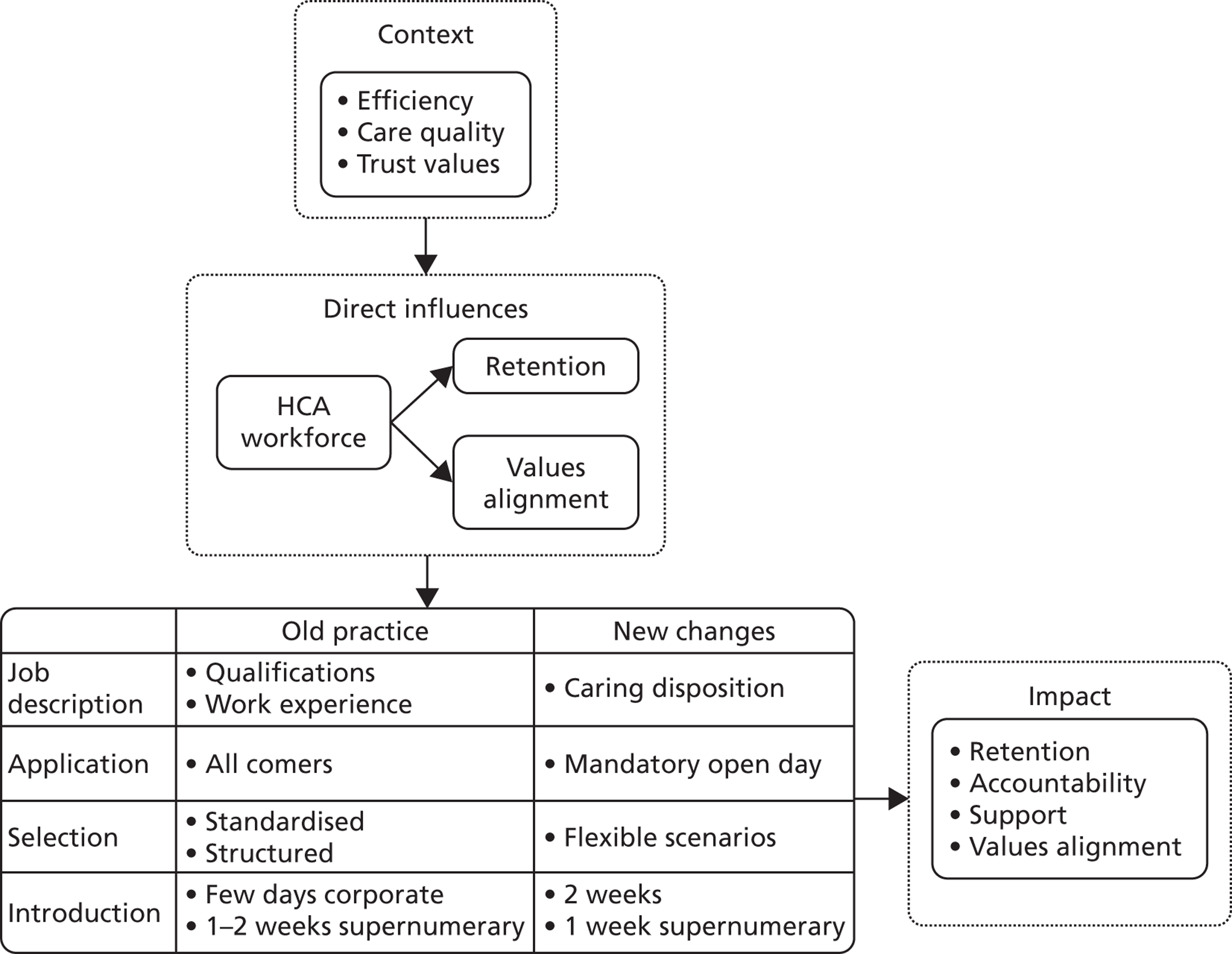
Developing assistant practitioners as a flexible resource
Context
This case study explored the development of the AP role at South Devon Healthcare NHS Foundation Trust (henceforth referred to as Torbay). The AP role was first introduced at Torbay in 2006 and, with the foundation degree (FD) taking 2 years to complete, the first cohort of APs qualified in 2008. Two further cohorts have since completed their training. With three cohorts active, in the summer of 2012 there were around 30 APs in the trust, with another 14 trainees in either the first or the second year of their FD. The emergence of the AP role at Torbay some 7 or 8 years ago placed the trust at the vanguard of developments in the south-west.
This leading position was indicative of an organisational culture, which, in a more general sense, displayed a capacity to innovate. Torbay had won the HSJ Acute Healthcare Organisation of the Year Award in November 2011, with the judges commenting that ‘the trust works as a team in an integrated way to deliver best outcomes and innovations in care with high levels of clinical engagement’.
Inevitably, questions arise as to how Torbay was able to develop such an innovative culture, with suggestions that the trust’s structure played a part. As a medium-sized district general hospital, with its acute services located on a single site, Torbay was a relatively compact organisation. The workforce was relatively stable, with low turnover. These characteristics fostered an open and friendly organisational culture, encouraging the kind of direct personal interaction needed to raise, share and develop new ideas.
The culture and working environment provided the backdrop to, and fostered, Torbay’s lead role in developing APs. Initially, this lead role assumed a somewhat opportunistic form. There was money available from the Strategic Health Authority (SHA) for a pilot to develop an educational programme to support band 4 APs. In 2006, Torbay worked with a trust in Cornwall on such a programme, with an initial intake of around 20 trainee APs covering community and mental health as well as acute health care. The opportunistic nature of this involvement was further reflected in the absence of clearly articulated objectives underpinning Torbay’s development of the AP role:
It was a gamble. But we made it work and that was the impetus to do more. There were pound signs and, ‘oh we’ve got some money coming in, let’s take it, let’s see if we can do something that would actually benefit the patients’, without really understanding what the [AP] role would be.
IC2_trust manager_1
However, this initial opportunism was quickly transformed into a more strategic approach to the AP role, characterised by a number of features, each discussed below.
Clarifying the assistant practitioner role
The trust felt that the AP role needed to be sensitive to the particular needs of the clinical areas:
The trust didn’t use a one model fits all. So like if every ward needs a band 4, I don’t think they’ve ever seen it that way, but they also recognised that there are some things that band 4s will never do and you need a registration for.
IC2_trust manager_2
Narrow and deep
The trust acknowledged that the AP role was most likely to become established where a ‘critical mass’ of post-holders could develop within a given clinical area. This would allow APs to support one another and to become a ‘fixture’ within the ward team:
We needed to go deep rather than wide . . . and it really did work, because it was sort of safety in numbers because there was at least two in, or two wards, they would work closely together, would have one on each ward, so there was a presence being seen.
IC2_trust manager_1
An emergent approach
Torbay’s approach was based on learning through practice. By taking the lead in the region, the trust was often the first to confront the difficult issues, such as clarifying the contribution to be made by APs and the design and management of a viable FD programme, and, in so doing, learned from the experience and sharpened their approach going forward:
Torbay has done this with their band 4s over the past five years and they’ve had really a lot of quite I suppose difficult discussions and challenging problems in order for them to do that.
IC2_trust manager_2
Objectives
A variety of aims came to inform Torbay’s interests in the AP role, some formally stated by senior management and others more informally articulated in the organisation.
Career opportunities
Senior managers at Torbay viewed the AP role as a means of developing career opportunities for HCAs at bands 2 and 3, particularly as pathways into registered nursing became limited and problematic. Nurse training represented a significant leap for HCAs, with progression to a band 4 AP role seen as more manageable. The use of the AP role to develop such career opportunities for bands 2 and 3 HCAs was not, however, an end in itself. It was viewed as a means of retaining and making the most of the unregistered part of the workforce, which had considerable skill, experience and potential:
What we said is it’s not a stepping-stone to become a nurse; it’s a different type of role and it’s valued and it’s better paid, and it gives you opportunities to think about a different future career if you want to, but at the same time you know you could stay there as well.
IC2_trust manager_3
Flexibility: crossing boundaries
The AP role was seen as much more flexible than the RN role, with scope to develop ‘bolt-on’ competencies to undertake particular tasks. One manager described this flexibility as ‘The ability to have a modular content backed up by the academic theory, [with] assessment in clinical practice to do “strange jobs” that really nobody thought of doing before’ (IC2_trust manager_1).
Specialisation
Torbay saw the potential for the AP role to fill service gaps, and, in so doing, establishing a new area of expertise within the nursing workforce:
If you’re just going to use them like a member of the workforce, that for me is well why bother to even train people at band 4; band 2s and 3s are doing that. If you’ve got somewhere, for example, the stroke clinic where you’ve got a band 4 that does some occupational therapy, physiotherapy and some nursing care as well, that person is valuable in terms of care plans, patient journey, discharge planning liaison, a whole slew of things that are very specific around stroke care.
IC2_trust manager_2
Nurse shortages
The AP role was seen to address future shortages of RNs:
We know that we’re going to see less RNs coming through and I think we have to proactively try and work with the [AP] role to make it a role that we want and it works for us.
IC2_service manager_1
Cost reductions
Among staff within clinical areas, cost control was seen as informing the trust’s use and development of the AP role, particularly at ward level:
I feel it’s [the use of APs] a cheaper option. We run on four trained at the moment, and then they’re saying we can have three trained plus an AP and I think that’s the way it is. I think they’re saving money, truthfully.
IC2_ward staff_1
Nurse relief
The AP was viewed as a means of taking away certain tasks from a nurse, and so allowing them to concentrate on ‘more pressing’ activities:
[The development of the AP] was taking out some of the more basic standard levels of perhaps dressings and chaperoning to allow us to use our specialist, clinical nurse skills.
IC2_ward staff_2
Design
Torbay’s AP initiative had the following design features:
-
trainee assistant practitioners (TAPs) recruited from HCAs within the trust
-
a 2-year FD delivered by South Devon College (SDC), but with significant input from Torbay’s education department (ED) and other staff members
-
TAPs mainly employed as band 3s
-
two study days, although one of these was taken from their own time
-
band 4 on qualification
-
a preceptorship programme, also involving RNs.
The design of this initiative was based on a ‘virtuous triangle’, set out in Figure 3.
FIGURE 3.
A virtuous triangle at Torbay.
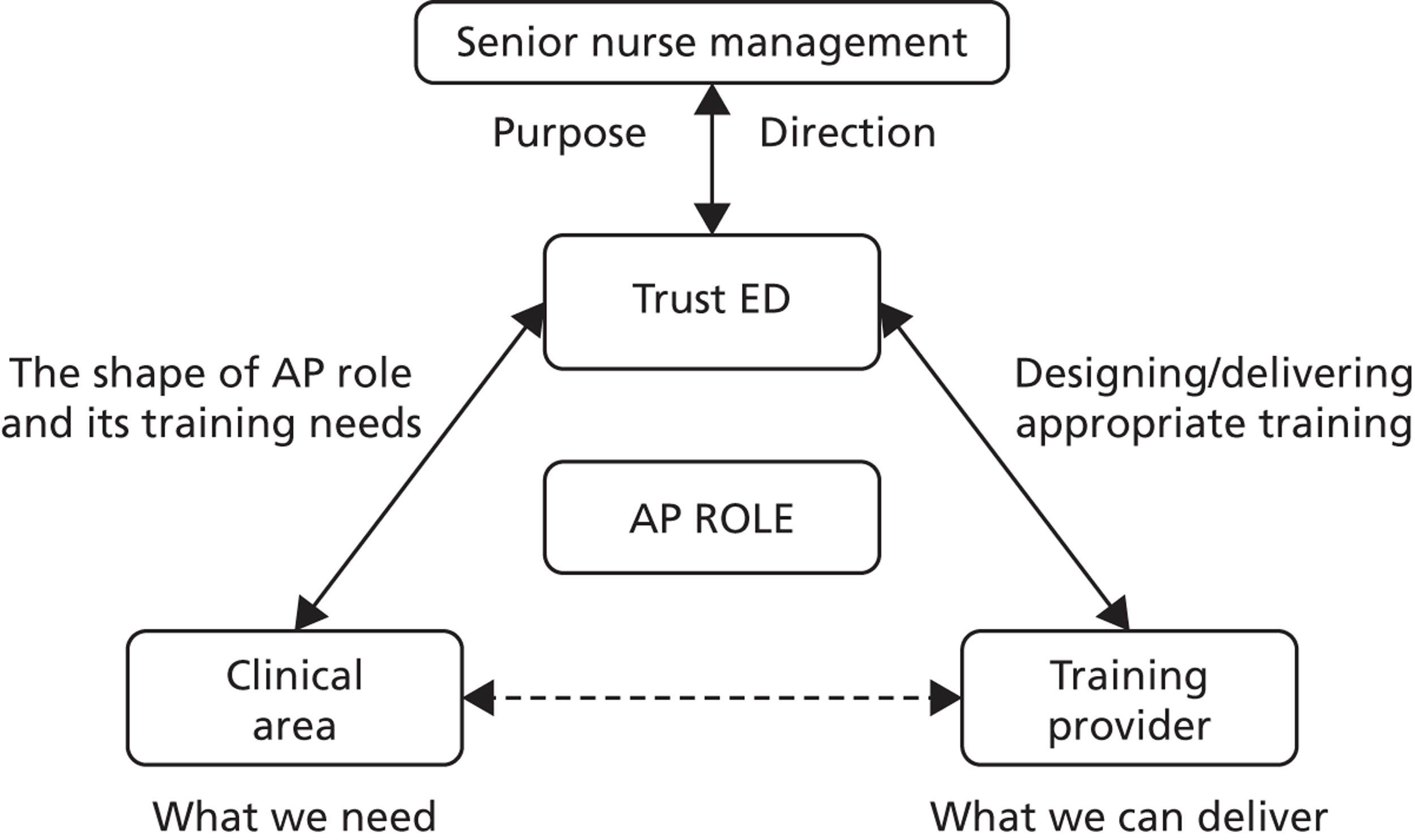
This ‘triangle’ rests on two key relationships. The first was between the trust’s ED and SDC as the provider of the FD taken by the TAPs. This relationship was strengthened by idiosyncratic features, particularly the fact that the key point of contact at SDC had formerly worked at Torbay, and indeed had been involved in the initial AP pilot.
The quality of the Torbay–SDC relationship ensured that the delivered FD was sensitive to the needs of discrete clinical areas:
Working with SDC was a revelation really because they were hungry for doing something that actually would link them in to us, but also it was actually sort of saying we’ve got enough people locally, we’ve got a local workforce, we need to tap in to it.
IC2_trust manager_5
This relationship also allowed Torbay to develop a cross-subsidising funding model. SDC had agreed to expand its AP programme to include self-funders, alongside those on the programme employed by and supported by the trust. These funders needed placements and, in providing them, Torbay generated an income stream which supported its internal candidates.
The second key relationship was between the trust’s ED and clinical areas interested in introducing an AP role. The most important aspect of this relationship was establishing a clear role for the AP. This was ‘hammered out’ in intense discussions between ward managers and the ED. The clinical areas brought to these discussions a full appreciation of clinical requirements, work routines and what a distinctive AP role might be able to bring to care delivery. The ED brought a capacity to clarify issues and sort out any ‘blockages’. For example, with a need to amend trust policy and develop protocols, allowing APs to undertake certain clinical procedures, the ED engaged the pharmacist in the development the AP role:
Over the years pharmacy started to teach on the AP programme, so they’re setting learning standards with me as to what they’re teaching. So they’re knowing the education they’ve given and feeling more comfortable because they know the standard of teaching.
IC2_trust manager_1
Impact
The impact of the AP role at Torbay can be considered from the perspective of different stakeholders, each discussed below.
Assistant practitioner post-holders
While some APs saw the role as a stepping-stone into nursing, many regarded it as an end in its own right, allowing considerable scope for personal development:
I really enjoyed my job as a HCA but I wanted to progress a little bit further, I wanted some promotion, I also kind of felt I deserved some promotion; that I’d been in the trust a long time and had given a long service to the trust. But having children at home and a husband that worked away, I didn’t want to go and do my training, I didn’t want the responsibility of having to take three years out unpaid, as it would have been if I’d gone on to do my nurse training.
IC2_ward staff_3
A few concerns were raised about the impact of the AP role on post-holders. For example, it was suggested that, having taken up an extended role, APs might be somewhat frustrated at not being able to push the boundaries further:
They’re [APs] getting frustrated with their job descriptions and they want to do more, and I’m having to say to them ‘look, I’m really sorry but you aren’t registered and you can’t do more’.
IC2_trust manager_4
Nurses
For some nurses, the AP represented a general challenge to the nurse status and role:
Some trained nurses do feel threatened because they’ve got this cheaper nurse coming up who they definitely are replacing trained nurses.
IC2_ward staff_1
More specifically, APs with more specialist or practiced skills were sometimes seen to erode nurse capability:
They’re [APs] actually better cannulators than a lot of the RNs. So they’ll end up putting canullas in here, there and everywhere around the ward for patients, for their treatment . . . because they’re handing it over to the APs to do, they’re losing that skill.
IC2_ward staff_4
At the same time, nurses often viewed APs as relieving them of certain tasks, allowing them to concentrate on core activities, with positive consequences for patient care:
That shows very well in breast care, that they [APs] will do stuff that’s seen as mundane but they’ll love it because they’ll give more time to the patient in clinics with sort of smaller breast operations, which relieves the RNs to do psychosexual counselling, the more advanced dressings.
IC2_trust manager_1
Patients
Interviewees suggested that the APs contributed to patient care by taking on technical tasks and not, therefore, having to seek the RNs to carry out certain clinical procedures. This often improved the capacity of a service or clinic, speeding up the flow of patients, reducing service pressures and allowing patients to be dealt with in a more timely manner.
The colorectal support worker
Background
This case study focuses on the development of a role designed to provide support for the delivery of stoma care at Hillingdon NHS Foundation Trust (henceforth referred to as Hillingdon). Developed under the job title ‘colorectal support worker’, the role was based within a team of specialist coloproctology nurses. This specialist nursing team had four members: a colorectal nurse and a senior colorectal nurse, working alongside the one C-SW, and headed by a nurse consultant. Most of the patients undergoing colorectal surgery at Hillingdon were located on a single ward, although the team were responsible for patients needing stoma care help throughout the hospital.
The specialist nursing team was involved in three broad areas of activity:
-
consultant- and nurse-led clinics
-
on-ward work, immediately prior to and following the surgery
-
community, typically post-operative, outreach work, involving home visits.
Within this set-up, the C-SW was seen as an innovative role, not only within the trust but also across the NHS:
We think it is the only one in the UK, because I haven’t come across any more.
IC3_service manager_1
The C-SW role was designed principally to engage in on-ward work dealing with those patients in need of stoma care. The number of stoma patients in the trust at any given time varied. During the research fieldwork, there were 13 patients in need of stoma care at Hillingdon. Over the year, it was estimated the trust would deal with between 80 and 100 stomas, with the C-SW likely to be involved in most of these cases.
The role had emerged 3 years ago but then developed organically, rather than in response to any clear-cut strategic initiative. More specifically, the role was a response to the confluence of two broad sets of factors: institutional and personal.
Institutional
At an institutional level, various developments had impacted on ways of working within the specialist nursing team, creating the space for a new support role:
-
General pressure. Partly in response to public health campaigns, awareness of cancer and the number of cases picked up had increased.
-
More acute patients. The increasing scale of care needs had been accompanied by the growing acuity of patients treated in a hospital setting. The requirement for more intense care from RNs had, in turn, generated a need for more support, whether in providing such care or in undertaking more routine tasks.
-
New models of care. The trust’s enhanced recovery programme (ERP) had placed new demands on specialist nurses, for example in running enhanced recovery clinics. It also generated a specific need for patients more quickly to become comfortable with, and capable of, dealing with their stomas.
-
Staffing. These developments placed pressure on the specialist team’s staffing capacity: ‘It’s very easy for the stoma care nurses to get pulled in to other areas with their consultants and things like that at MDT [multidisciplinary team] meetings and all of the sort of upper echelons of patient care’ (IC3_trust manager_1).
Personal
The institutional factors combined with the availability of a worker already present within colorectal surgery particularly well suited to take up a specialist support role. As a consequence, the development of the role became inextricably linked to the personal circumstances of this individual. A number of characteristics of the post-holder are worth noting:
-
Experience in care work prior to joining the trust, combined with a personal disposition displaying enthusiasm for taking on an expanded and specialist technical role: ‘Initially she [the post-holder] was quite despondent about what healthcare assistants could do. She is quite an assertive person and kind of felt that she wanted more, she wanted to be a bit more autonomous, whereas on the wards it was kind of quite limited’ (IC3_trust manager 2).
-
Experience of working in the trust. The post-holder had worked at Hillingdon for 8 years in a HCA post, before taking on the new specialist support role.
-
Experience as a HCA working with colorectal patients on the ward before moving into the specialist nursing team. This was reinforced by a 6-month period working on a temporary basis with the specialist colorectal nursing team, which then became a permanent post.
Design and implementation
This confluence of institutional need, and the availability of a person with the background and skills to meet it, was appreciated by the nurse consultant leading the team of specialist colorectal nurses, and taken forward by her, with the support of others, through various processes.
Shaping the role
The C-SW role was initially formalised with the development of a job description by the HR department. Initially, the role was graded at band 2, although at the time of the fieldwork, the C-SW had moved onto pay band 3 and it was envisaged that she would move onto band 4 on completing the FD. The job description listed no fewer than 26 main duties. Exactly half of these were patient-centred, including teaching patients to look after their stomas and ensuring that patients were given appropriate food and nutritional information.
Funding
The C-SW role, along with the two specialist colorectal specialist nurses, was funded by a firm producing stoma care products. Given the scale of stoma care at Hillingdon, it was unlikely that the trust would attract sponsorship for a third specialist nurse. However, a C-SW role (particularly one working 25 hours per week) represented a viable, lower-cost sponsorship option.
Training
The post-holder had already achieved a NVQ level 3 in her capacity as a HCA. As a C-SW, this was supplemented by a 1-week dedicated training course on stoma care. Less formally, the post-holder had, over the years, acquired relevant tacit skills and knowledge:
Working on the colorectal ward, you had to have a certain amount of knowledge and training anyway.
IC3_ward staff_1
The acquisition of experience, knowledge and skills allowed the post-holder gradually to push the role’s boundaries, affecting how others viewed and engaged with it. As nursing and clinical staff became more aware of and confident in the post-holder, increasingly they drew upon her:
Over the last year or so things have evolved and the job itself has matured in a way that she’s taken on more and more responsibility as she’s got on . . . Overall she has been fairly well supervised and trained to fulfil this role and she’s not just been let go on her own, but she’s sort of coming to a stage where she could do it independently or with advice.
IC3_ward staff_2
In terms of general functioning, the C-SW role largely involved on-ward pre- and post-operative patient-centred work. The nature of the C-SW engagement with patients was intense and sustained, reflected in the following description of her role by the post-holder:
I always see them first day post-op. I like to see them before they have their surgery, just to introduce myself so that they know a familiar face when I see them on the first day post-op and basically review the stoma and everything because at that time they don’t want to do anything. Then they gradually get a little bit better and a little bit more mobile, and I start educating them about it; start teaching them about their diet and giving tips. Then I discharge them as well back into the community.
IC3_ward staff_3
More specifically, the C-SW’s impact assumed a number of forms, each discussed below.
Patient teacher
The core of the C-SW role revolved around preparing and providing support for patients in the future management of their stoma:
The nurses are always busy; there is always something to do, but when the girls are in clinic or doing ERP clinics she will be on the ward; if there’s teaching for the stomas to be done, she will do the teaching of the stomas.
IC3_service manager_2
Emotion manager
This sustained and close contact with the patient allowed the C-SW to manage patient emotions in invariably difficult circumstances:
[Patients] come in confused and worried and depressed, and the stoma care nurse can only give them five or 10 minutes a day and they might see them twice and that’s it. The [C-SW] will see them nearly every day on the ward; she becomes a constant to them and so is much more supportive to their actual needs. She is the most important psychological support for that patient and their subsequent recovery, because the aim is to get them back and living a normal life and doing everything they ever did before.
IC3_trust manager_1
Another ‘pair of eyes’
The C-SW came to represent another ‘pair of eyes’ with the capacity to feed insights on the patient into broader clinical deliberation and decision-making. For example, discharge decisions were often informed by the C-SW’s perception of the patient’s readiness to leave hospital based on whether or not they could manage their stoma care.
In acting as another ‘pair of eyes’, the C-SW was often able to connect to, and articulate, the patient’s perspective, a capacity drawn upon by other carers. As a consultant noted:
If I’ve got a patient with a stoma, I usually take [the C-SW] along with me on the ward round, and I find it very useful to get her side of the story. She always has a different angle on how the patient should be managed. She’s been trained over the years as a HCA on the ward, so she has a more holistic view rather than the stoma nurses who will be looking at stomas and the technical problems with it.
IC3_ward staff_2
Relief
The C-SW role was designed to relieve specialist colorectal and ward nurses of the main responsibilities for stoma care, allowing them to concentrate on other tasks. The C-SW appeared to be fulfilling this relief role:
So it takes the workload off them as well for them to do other things like clinics and work in the community and all that. So in that sense it does help.
IC3_ward staff_2
Expert and mentor
Dedicated to specialist tasks, the C-SW had clearly become an expert in stoma care:
[The C-SW role] is a useful resource because the stoma nurses obviously have got other things on their plate. They’re working at the clinic, which [the C-SW] doesn’t, and so she’s purely dedicated to the ward as such. And, you know, the first port of call would be her if there was any problem on the ward in terms of primary management of stomas.
IC3_ward staff_2
This expertise allowed the C-SW to act as a mentor to others, including registered ward nurses, specialist colorectal nurses, HCAs and student nurses. Each is illustrated by a quote below.
When we have newly qualified nurses joining the team, [the C-SW] is there to teach them, to help them.
IC3_service manager_3
[The C-SW] is able to tell [name of colorectal nurse] quite a lot of things. [The latter] has not got a lot of back knowledge, whereas [the C-SW] has built up her knowledge over time from first of all being on the ward, enjoying looking at stoma patients, which not many people do, and then doing the temporary post and then moving into it as a full-time job.
IC3_service manager_1
As the time’s gone on she’s [the C-SW] very much more been a link to the other health-care assistants on the ward in terms of getting them more involved in learning stoma care and engaging them in teaching patients as well.
IC3_ward staff_4
Most of the students that we have on placement will work with [the C-SW] who will show them about the stoma care.
IC3_service manager_1
Impact
The C-SW role had a largely positive impact on a range of stakeholders. However, a few qualifications are worth noting. First, the C-SW’s capacity to impact in these ways was closely tied to the personal characteristics of the post-holder, someone known and trusted by these various actors. It was, therefore, not a contribution easily replicated by another taking on this role.
Second, there was some resistance to the C-SW role. As an expert, the C-SW might challenge the registered and higher-graded professional:
Registered practitioners maybe feel a bit intimidated because she’s [the C-SW] doing teaching on the ward and obviously teaching patients and seeing patients on her own without that direct supervision and that has caused a bit of a problem.
IC3_trust manager_2
Third, the specialist nature of the C-SW role might encourage ward staff to ‘dump on’ her all those tasks associated with the stoma care, with detrimental consequences for the quality of the C-SW’s working life and perhaps for patient care more widely:
Most ward staff, because there’s a stoma care nurse, it’s not their job to change bags, so some would be happy to leave a patient with a leaking bag until they found a stoma care nurse to come and do it.
IC3_service manager_1
Figure 4 summarises the C-SW’s various contributions.
FIGURE 4.
The C-SW’s contribution to stoma care.
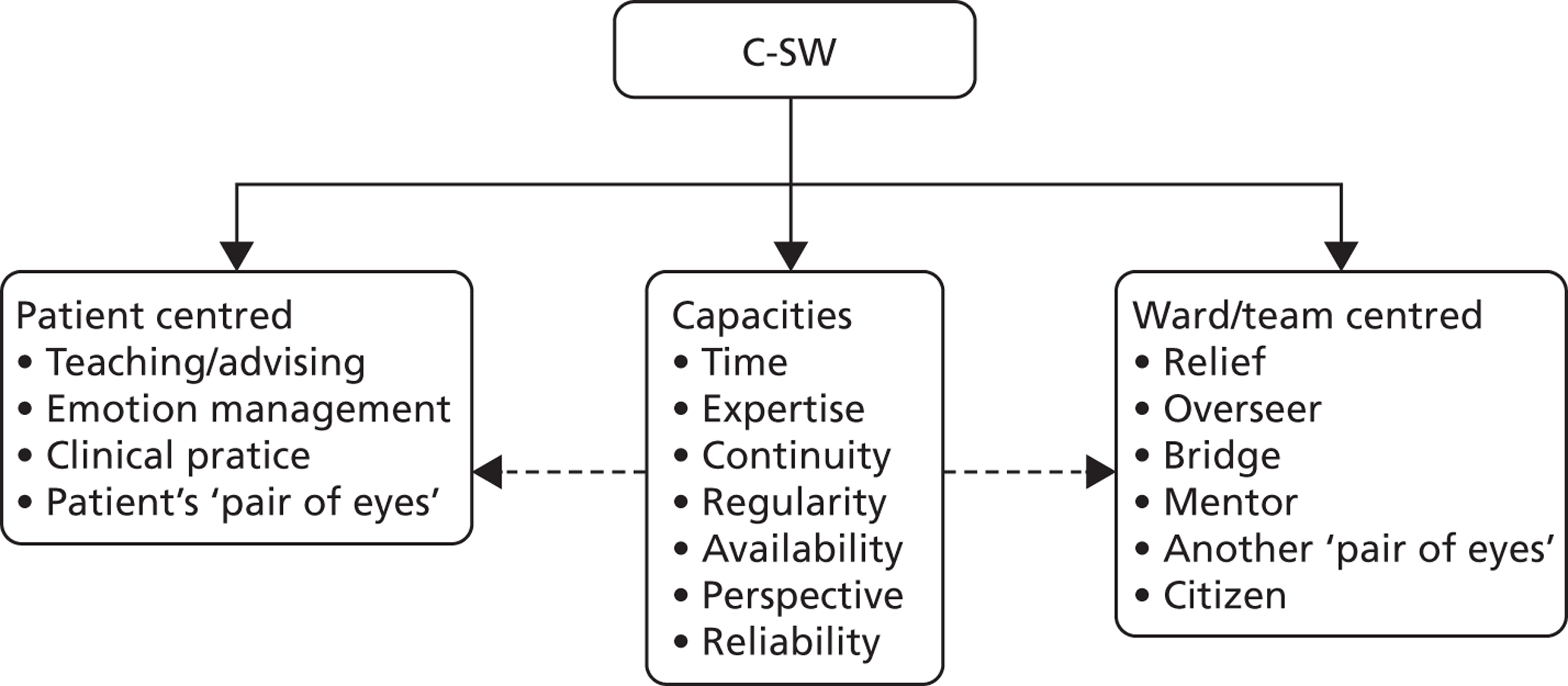
The health-care assistant development nurse
Context
This case study explores the introduction of a dedicated corporate role, the HCA development nurse (HCA-DN), to support the management of HCAs at UCLH. One of the first trusts to acquire foundation status in 2004, UCLH is a large organisation comprising seven hospitals, some specialist and some general, located on different sites in central London and employing around 7000 staff in total.
The emergence of the HCA-DN role reflected an increasing focus on the unregistered component of the trust’s nursing workforce in the delivery of patient care:
The heads of nursing, corporate nursing and the trust itself has a commitment to training and development and to healthcare assistants and to that support. Otherwise we wouldn’t have I suppose the [HCA-DN] post we have.
IC4_trust manager_1
Driven by financial pressures, this focus was integral to an attempt to review the trust’s traditionally rich skill mix. Indeed, there was a growing interest not only in the balance between unregistered and registered staff, but in the distribution between HCAs at band 2 and band 3 in the trust. UCLH had a relatively high proportion of its HCA workforce at band 3: the trust’s 428 HCAs were spilt roughly half and half between band 2s and band 3s.
From a financial perspective they [HCAs] save the trust money and if we can bolster them as much as possible, then it’s fantastic not just for their self-esteem and their educational purposes but also from the trust’s financial perspective, and I think you’re foolish if you don’t utilise them to their fullest potential.
IC4_ward staff_1
The trust’s greater interest in the nurse support workforce was also influenced by perceived challenges to the future supply of RNs with implications for the nature of the nurse role:
We looked at the demographics of the nursing workforce . . . and thought that first of all we might be limited in the numbers of registered nurses and it was thought that the assistant practitioner would be assistants to some of the day to day delivery of care, the sort of routine stuff that didn’t need a more advanced assessment of the patient’s needs.
IC4_trust manager_2
The health-care assistant development nurse role
The HCA-DN post was initially supported by SHA funding. It was filled on secondment by a clinical practice facilitator (CPF) from within the trust (initially for 3 months), who had since remained in the role. In a large and complex organisation, these background characteristics were not without significance: the post-holder understood the trust’s systems and routines and had credibility in the role.
In terms of purpose and focus, the HCA-DN role was principally seen by senior nurse managers as a way of developing training standards on entry to the trust, and supporting the establishment of clearer career pathways for HCAs:
What was very frightening to us when we were first expanding the numbers was that for band 2s these are people who could be working in Woolies one day and here tomorrow. There’s not a lot of training in between and what we wanted to try and do is make sure that at least there were very clear induction standards, very clear development programmes associated with these roles, and hence the development of [the HCA-DN] role.
IC4_trust manager_2
In practice, the role’s remit was broader, covering nurse support workers at bands 2 to 4, and concentrating on a number of aspects of HCA training and development:
-
assessing the capabilities (numeracy and literacy) of candidates for HCA posts
-
developing and delivering corporate HCA induction
-
developing and delivering in-house HCA training
-
managing accredited training/education programmes, including the apprenticeships and the FD
-
supporting HCA career development
-
liaising with and supporting wards in the development of their more bespoke training.
Working with wards to address their particular HCA training and development needs involved the HCA-DN connecting to another key role within the trust, the CPF. Graded at band 6, typically performed by a RN and found in many of the trust’s wards, the CPF’s main purpose, according to the job description, was ‘. . . to support and develop band 5 and band 6 nursing staff and healthcare assistants through facilitation in clinical practice and promotion/implementation of relevant education and development pathways’ [emphasis added]. 50
The training and development of health-care assistants
The HCA-DN role had been responsible for developing a number of initiatives related to HCA training and development. These are set out in Figure 5.
FIGURE 5.
Training and development initiatives.
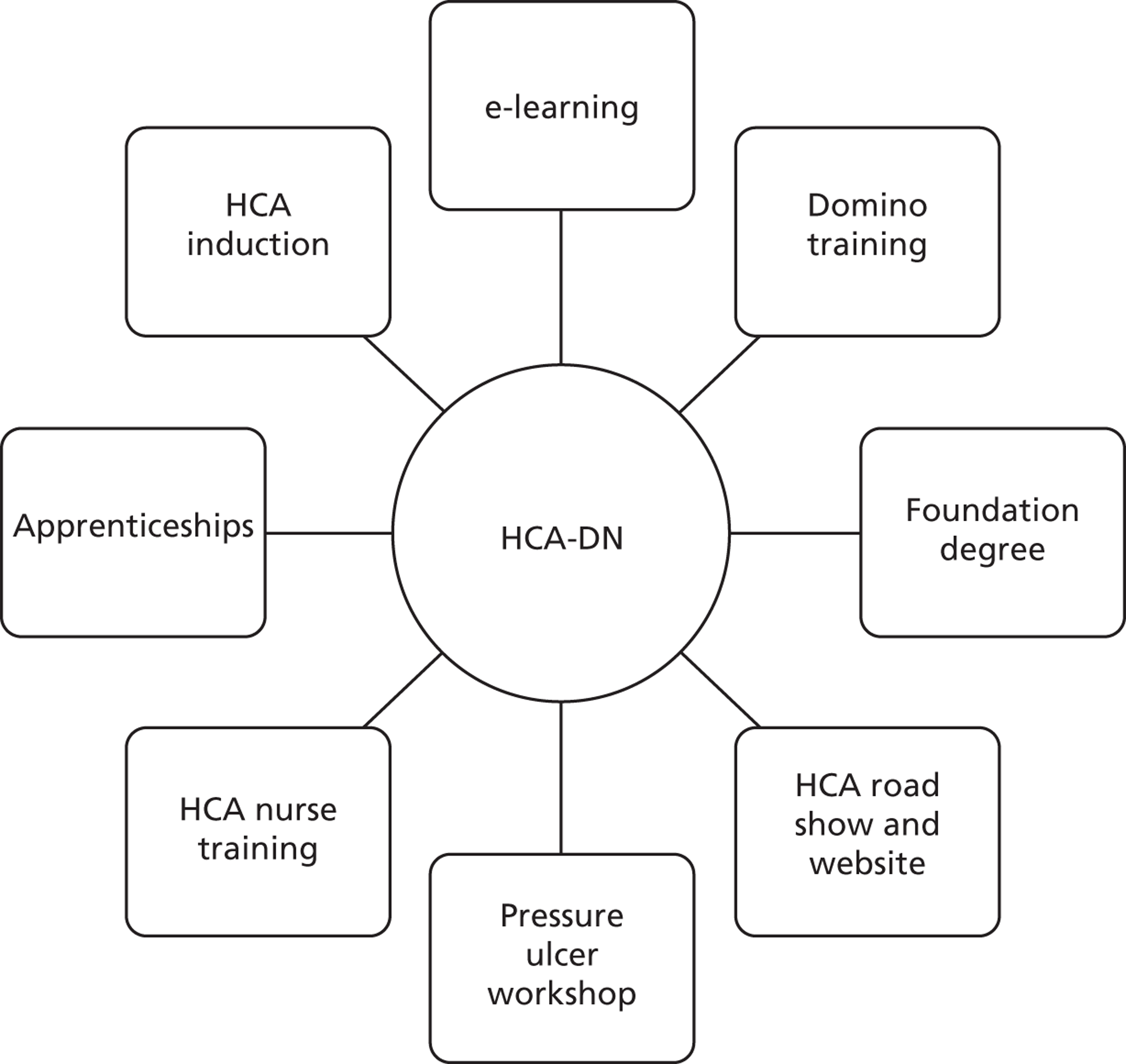
Health-care assistant induction
The HCA-DN was heavily involved with HCAs as they entered the trust. This involvement was reflected in some work around recruitment practices, such as establishing whether or not applicants had basic numeracy and literacy skills. It was also aimed at establishing whether or not HCA applicants had appropriate values and capabilities:
One of the things that the [HCA-DN’s] been trying is scenario-based assessment so that we understand the values around individuals that we appoint, but we’ve got much more clarity around, you know, basic life skills like numeracy, literacy and communication.
IC4_trust manager_2
At the outset, the HCA-DN role was seen to be particularly concerned with establishing an acceptable level of basic competence in newly recruited HCAs:
The priority was getting the induction programme right, getting the right competencies.
IC4_trust manager_3
Consulting with a range of staff, the HCA-DN developed, piloted and implemented a new induction programme. The corporate element of the new induction (including infection control, moving and handling) was held before HCAs began on the ward. The HCA training element was usually held within 5 to 6 weeks of their being in post. This part of the induction covered 4 days of HCA skills, including communication and washing. Each recruit was given a competency pack for their first 6 months that formed their probationary period and had to be achieved to attain a permanent contract.
e-learning
A more recent initiative, designed to underpin the induction process, was the development by the HCA-DN of an e-learning package to support competencies and development online. This e-learning focused on mandatory training and the development of certain basics, such as vital signs, and, given the scattered nature of the trust across central London, provided an efficient means of dealing with such training.
Still a work in progress, this e-resource, in a more general sense, enabled the HCA-DN to track that HCAs were getting the support they needed:
I’ll be able to monitor who logs on, when they log on, if they complete a whole module or whether they do the whole package in one go, and if they haven’t passed, do they go back and log on again, how many times they’ve actually completed a module, how many tries they’ve had and not completed.
IC4_trust manager_3
Domino training
A more specific initiative centred on a half-day study day preparing HCAs to recognise the signs of deteriorating patients. This programme, run monthly under the title ‘Domino’, extended the delivery of a programme from medical and registered nursing staff to HCAs. Domino was based on the critical care Patient Emergency Response Team training given to nurses and junior doctors. Domino was piloted for HCAs in 2009 and ‘went live’ in 2010.
Pressure ulcer workshop
The HCA-DN instituted additional study days on other topics of relevance to HCAs. In identifying such topics, the HCA-DN was again sensitive to the views of others, with pressure ulcers emerging as an issue worthy of a study day:
We’re sort of having very preliminary discussions about having a mandatory study day to cover some of the things that maybe are required . . . so around pressure ulcers, for example, maybe patient falls.
IC4_trust manager_3
Accredited programmes
The HCA-DN was responsible for various aspects of accredited programmes available to nurse support workers: their design, publicising and recruiting to them and dealing with the HEIs. In the case of band 2 and 3 HCAs at UCLH, the main available programme was the apprenticeship. The trust’s apprenticeship programme began in 2010 and focused on existing staff. At the time of the research fieldwork, a proposal was pending on a new approach to recruitment, with all future recruitment to the HCA role via a 1-year apprenticeship contract at band 2 level, supported by all new job descriptions, and promotion to the band 3 level restricted to internal candidates only.
In the case of APs, the main programme was the FD. In 2010, UCLH had its first large cohort of APs passing through the London South Bank University FD. Originally, the cohort was for 10 trainee clinical APs at band 3 level but this was extended to 20. The original 10 were guaranteed a band 4 role on completion. There was a forum for APs held quarterly by the HCA-DN to facilitate networking and support. Each session had an external speaker. A band 4 booklet of competencies and expectations was being piloted at the time.
Road show and website
The HCA-DN communicated with HCAs on various types of issues, with two main systems developed to support this activity. Established by the HCA-DN in 2009, the HCA road show was a monthly event open to nurse support workers from across the trust and held on a rotating basis between the different UCLH sites. The road show had evolved to serve a number of purposes: connecting with HCAs and other staff groups from across the trust for the HCA-DN to find out about their concerns and issues; an opportunity for HCAs to raise queries, not least in relation to their current training; and an information and learning space for HCAs, with speakers coming along to make formal presentations.
The second communication initiative was the establishment of a dedicated HCA website. This website played an important role in informing HCAs about the availability of different study days and programmes, along with details about how courses might be accessed:
[The HCA-DN] has written loads of stuff online which are all around processes of applying, when they have workshops, you know, what’s entailed.
IC4_trust manager_1
The role in practice
As a single post-holder working in a large and multi-site organisation, the HCA-DN needed considerable skill in taking these initiatives forward and in establishing wider commitment to them across the trust. A consideration of process issues suggests the importance of three organisational characteristics (Figure 6): institutions, actors and systems.
FIGURE 6.
Elements of process in developing HCA initiatives. N&M, Nursing and Midwifery.
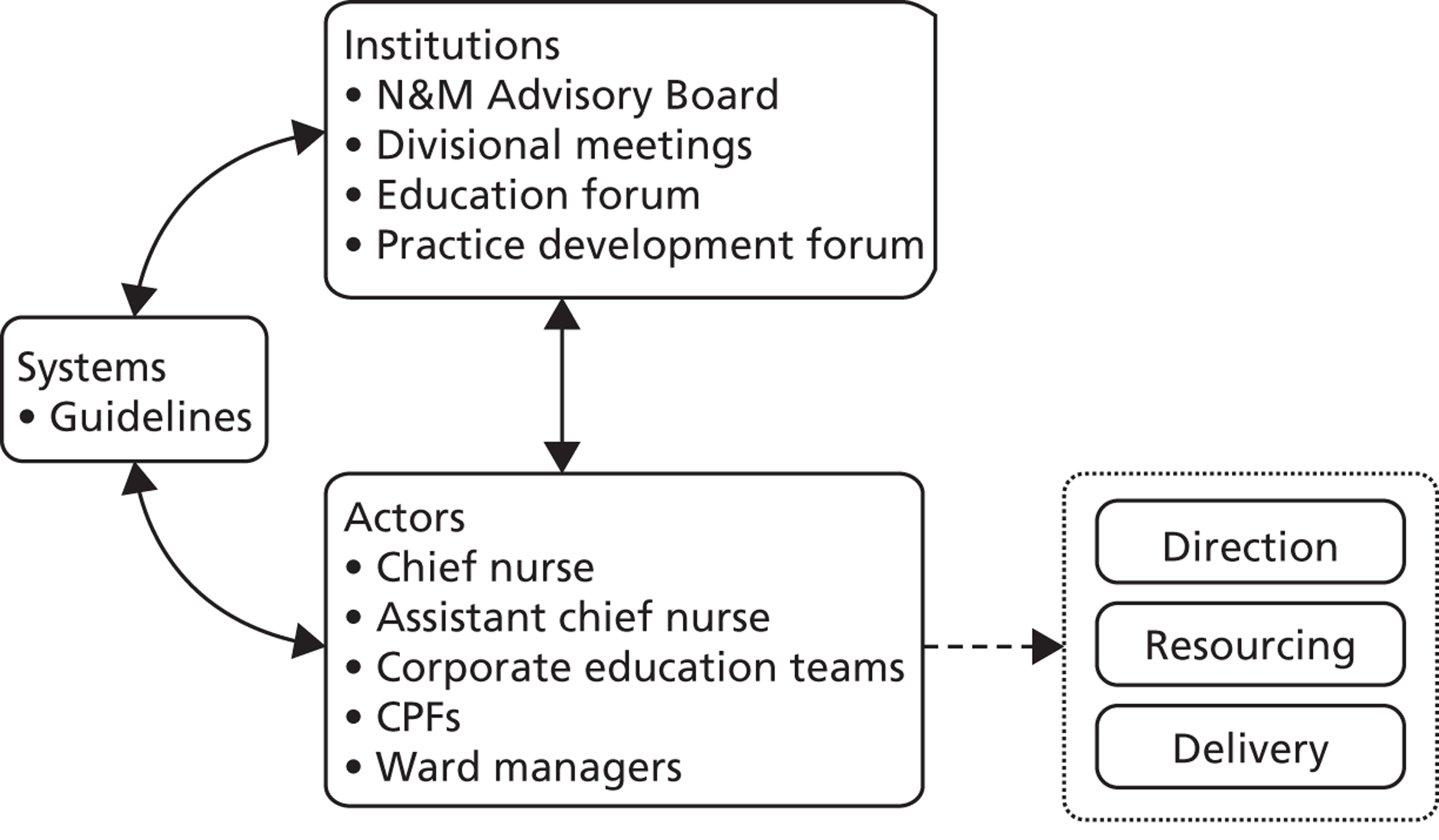
Institutions
There were a number of formal institutions or bodies within UCLH that played an important part in both discussing and formally signing off a HCA-DN initiative. At the peak of the trust was the Nursing and Midwifery Advisory Board, comprising the chief and assistant chief nurses and the heads of nursing. This board introduced trust-wide initiatives with significant implications for the nursing workforce. The HCA-DN had sought sign-off from this board on the development of HCA competencies and on the design of a new approach to HCA recruitment based on the use of numeracy and literacy tests.
At the next level, divisional meetings involving the relevant head of nursing and her matrons were used as a means of developing or fine-tuning a proposal. For example, the HCA-DN used these meetings to develop specialist modules on certain HCA programmes, particularly the FD.
There were also a couple of bodies, specifically concerned with training and education, which played a role in the development of HCA initiatives. The education forum, convened by the assistant chief nurse, brought HEI providers to the trust for discussions on an accredited training programme. More important in this context was the CPF forum, a monthly meeting for CPFs across the trust. The extension of the Domino programme to HCAs, for example, was signed off at this forum.
Actors
At UCLH, a number of actors were crucial to the functioning of the HCA-DN role. The support of the chief nurse was important in setting the broad direction for the development of the trust’s unregistered workforce:
[The HCA-DN] needs the chief nurse’s support as well. It would be true to say that the chief nurse is essential; they’re going to drive the direction that this goes in.
IC4_trust manager_2
If the chief nurse set the direction, the assistant chief nurse leading on education and research was needed to ‘make things happen’: pushing decisions to action and ensuring that the necessary resourcing was in place. The assistant chief was particularly accessible to the HCA-DN.
The HCA-DN’s line manager and, in particular, the corporate team of nurse educators and facilitators played an important part in actually delivering aspects of the HCA-DN’s programme. For example, the teaching on the study days would often come from this team.
Systems
Two systems were particularly important in allowing the HCA-DN to take forward initiatives in such a large and complex organisation. The first was the emphasis placed by the trust on guidance to divisions and clinical areas. Guidance was less prescriptive and more flexible than rules, and, in a large, complex and diverse organisation such as UCLH, played a role in giving effect to some of the HCA developments. The second was the HCA-DN’s use of networking to test, consult and build alliances in support of various initiatives:
[The HCA-DN] has done a lot of work around sort of networking with the ward sisters and trying to understand what it is that we want in terms of development. So therefore she’s got quite a lot of our buy-in for that.
IC4_ward staff_2
Impact
The HCA-DN’s impact on the training and development of nurse support workers was seen as significant and beneficial. Views on the positive contribution made by the HCA-DN were often provided in an unprompted way, and suggested that the HCA-DN had made a tangible difference to improving these aspects of the HCAs’ working lives and changing the trust’s capacity in these respects:
The trust has put a lot of funds and effort into it recently, certainly the recruitment of [name of HCA-DN] . . . Giving someone of [name of HCA-DN’s] level and experience a whole-time equivalent job to spend putting together training for them, and to be fair pretty much every course that we run for qualified staff, [the HCA-DN] has adapted. So the work [HCA-DN’s name] done has been fantastic. So asking me the question now, I do think we have great learning and development opportunities for unqualified staff.
IC4_ward staff_2
For some, the HCA-DN role had provided trust focus and direction on HCA training and development:
What [HCA-DN’s name] has done is given it a bit more focus. Everybody knows [HCA-DN’s name], she’s done a lot of good work for lots of other projects within the trust and I think that now she’s sort of taken this on-board, it’s got a bit more direction.
IC4_ward staff_1
In the HCA focus group, the name of the HCA-DN was mentioned on no fewer than 18 separate occasions, providing some insight into how HCAs viewed and used the role. Thus, HCAs perceived the role and engaged with it as a channel for raising concerns, accessing opportunities and sorting out problems. Each of these areas is illustrated with a quote below.
[HCA-DN’s name] was one of the persons I said, ‘sorry, I’m not here just to do domestics, I’m here because I want to become a nurse; I give up my degree in biomedical because I want to be a nurse, I don’t want to be a domestic’.
IC4_HCA_focus group
So you have, so you have regular e-mails from [HCA-DN’s name] letting you know about things. There’s the website to check things on. And so there’s the availability of study days, courses that you can do.
IC4_HCA_focus group
I didn’t know what to do because I finished my nursing from [name of country], came here, was not able to work as a nurse because of the English exam. So then I approached [HCA-DN’s name] what to do, then she told me if you’re going to go back to nursing, do this course and then go.
IC4_HCA_focus group
Data on the scale and coverage of many of the in-house initiatives developed by the HCA-DN are presented in Table 11. Some noteworthy achievements stand out from these figures. Most striking, perhaps, is the significant number of HCAs completing the Domino and pressure care programmes. The number of HCAs who had been through the new induction programme, close to 100 over the last 2 years, was also striking.
| Course | Year | |
|---|---|---|
| 2011 | 2012 | |
| Induction | 57 | 25 |
| Domino | 101 | 75 |
| Pressure area care | 105 | 23 |
| Band 2 | 21 | 15 |
| Band 3 | 34 | 7 |
| Band 4 | 5 | 10 |
Consultant-driven innovation: the surgical assistant practitioner role
This case study focuses on a band 4 AP role developed in the dermatology department of OUH NHS Trust. Introduced in 2011 and to date held by one post-holder, the role was labelled surgical assistant practitioner (SAP). In examining the nature and consequences of this role, four actors were interviewed in March 2013: the post-holder herself, a consultant dermatologist, a specialist nurse and the trust’s AP lead. During the fieldwork, the SAP was observed working alongside a consultant during a procedure.
The SAP role generates interest within the context of this project as an innovative development both within the trust and more generally across the NHS. Pushing role or practice boundaries perhaps further than any other innovative development considered in the project, this unregistered support role was designed to perform relatively complex clinical tasks, including minor surgical procedures.
Background
The development of the SAP role took various turns, emerging in an iterative rather than in a fully formed way. Asked if the nature of the AP role was clear from the outset, the post-holder noted:
No, it’s just evolved really.
IC5_SAP_1
Indeed, despite clinical consultant interest in it, the role initially emerged through discussion between the AP lead in the ED and a specialist nurse in the dermatology department, within the broader context of the trust’s second cohort of APs around 2008–9. These discussions, which also involved the potential AP post-holder, considered service gaps in dermatology that might be filled by an AP role. This encouraged an initial focus on how such a role might contribute to service flows in the outpatient clinic, with the aim of relieving nurses of aspects of work in this area and allowing them to concentrate more on their specialist tasks. All patients were seen in the dermatology department on an outpatient basis, with any surgery being performed as day surgery.
Against the backdrop of these discussions, a person had been selected for the AP support role in dermatology and had begun the FD. However, around 1 year into the degree, the specialist nurse who had originally sponsored the role as a support for the department’s clinics left the trust. At around the same time, the value of a role supporting the department’s day surgery work became apparent, particularly to one of the department’s consultant dermatologists, resulting in a shift in the role’s focus from the general clinics to the operating theatres.
The emergence of a support role centred on the dermatology department’s surgical activities was related to the confluence of two sets of factors: institutional need and personal circumstance. Institutionally, the need for such a role to contribute to surgical work was linked to the nature of the service provided by the dermatology department, and by the performance management regime underpinning it. Physically, and indeed clinically, the department was divided into two main parts. The upstairs section, comprising consultant-led general clinics, dealt with the full range of conditions: ‘. . . leg ulcers, anything to do with your skin, so eczema, psoriasis’ (IC5_specialist nurse_1).
A tumour clinic was also run upstairs, a ‘one-stop’ service which provided those in need of skin surgery with a same-day service. This same-day surgery was provided downstairs in the department’s operating theatres, along with elective surgery. These operating theatres were staffed by a number of clinical consultants – the department had a team of four consultants working on tumours along with two band 6 specialist nurses and the band 4 SAP.
Within the context of this set-up, a SAP role, able to undertake a wide range of tasks, many overlapping with those performed by the specialist nurses, was seen as a means of addressing service capacity and workload pressure. Such a role could undertake and finish off work, freeing up consultants and specialist nurses to see more patients:
With the one-stop service we try and do as much as we can on the same day, and we have so many referrals it’s really hard to keep on top of all the skin cancers that we need to perform surgery on. So having that supportive role, somebody to stitch up a hole while you’re doing the paperwork, it means that we can get through everything so much faster.
IC5_specialist nurse_1
More specifically, such a role provided a greater a range of options in terms of staff deployment, particularly important given variation in and uncertainty about the availability of staff on any given shift:
The way we’ve done that is that we have clinics which are designed to see, screen and recommend treatment for patients at the same time as the theatre is open downstairs, so that they can be seen and treated at a one-stop. The difficulty with that is staffing it really, and so the way we’ve staffed it is by having a consultant downstairs and a consultant upstairs and if one of the consultants is away on holiday, the other consultant comes up and then covers the clinic, and then supervises the nurses and junior doctors downstairs; which is why it’s essential that we have the flexibility we’ve got from the girls [the nursing staff in the operating theatres].
IC5_consultant_1
The personal circumstances contributing to the development of the SAP role were apparent in a potential post-holder with a profile particularly well suited to the role. In part, this profile was characterised by a work history which provided the post-holder with a firm platform to develop in an extended unregistered role. Prior to joining the trust, the post-holder had been involved in nursing work in the military. More significantly, the post-holder had some experience of the trust and the department prior to taking up the SAP role:
I worked with them beforehand anyway and they know that if I was never happy I’d always come and find them, and there is a massive amount of trust involved in this and I think that’s one thing that needs to be stressed, you know, that they have to trust me.
IC5_SAP_1
In fact, the post-holder had taken up a band 2 HCA post around 7 years before commencing the FD. This allowed her to develop an appreciation of the department’s systems, team members and ways of working. Equally significantly, it provided an opportunity for the department’s clinical and nursing staff to get to know her and to build trust in her personality and skills.
The disposition to take on more complex tasks was the final feature of the personal profile underpinning the emergence of the SAP role:
I’ve known [post-holder’s name] for I don’t know, seven or eight years now, it was very obvious early on that she had the competence to do this.
IC5_consultant_1
This approach to identifying development potential in an individual and then building upon it encouraged the view that an evolutionary, ‘grow-your-own’ process was the ‘best’ way to develop an extended support role within the department:
The problem is identifying those HCAs that will have the competence and confidence to be able to do those, it’s much more of a sort of an evolutionary ad hoc thing, it’s very difficult to find the individual right for the job, you know, we have to grow our own almost.
IC5_consultant_1
The development of the role
If institutional need and personal circumstance provided the basis for the role, these drivers still needed to be converted into a process that provided for the development and emergence of the SAP role. As played out in the dermatology department of OUH, a number of features of this process are worth highlighting. The first was the emphasis placed on competence as a means of cutting through formalities and any apparent barriers to change. It was a view summed up by the consultant in noting the range of complex tasks undertaken by the unregistered band 4 SAP:
As long as the competencies are in place to demonstrate ability and safety, then to be honest that’s far more important than a name or a label.
IC5_consultant_1
The second feature of the process was a willingness to push boundaries. Without in any way compromising patient safety, the role was developed to undertake the complex clinical tasks associated with skin surgery, and systems were found to facilitate this extension.
The third feature was the importance of the consultant’s authority and support in giving effect to the changes needed to establish the SAP role:
So long as they know that they’ve got the support of the consultant, then it gives them the confidence to proceed.
IC5_consultant_1
The importance of the consultant’s support was particularly apparent in his engagement with the post-holder; indeed, this consultant–post-holder relationship was pivotal to the development of the role. The relationship provided the basis for a shaping of the role, and more tangibly drawing out the requisite competencies. It was also a supportive relationship, with the consultant acting not only as a mentor but more actively as a trainer, facilitating on-the-job learning for the post-holder:
I do like the surgical side, and because I’ve worked down here with him very closely, he said I’d like to develop you into doing anaesthetics. And because I’d given injections and done a little bit of minor surgery in the RAF [Royal Air Force], he said let’s have a go and see where you develop. So I started off doing a little bit of suturing, then some minor procedures, and then it’s just developed and snowballed from there really.
IC5_SAP_1
The significance of the consultant–post-holder relationship should not, however, detract from the importance of other relationships to the development of the role, in particular that between the trust’s AP lead and the post-holder. The AP lead was another key support for the post-holder, particularly during the FD. More specifically, the AP lead was able to give effect to the consultant’s aspirations for the role by developing appropriate specialist competencies to be built into the second year of the FD. The development of the role also required an education provider able and willing to provide bespoke programmes sensitive to the needs of the trust and the role it was seeking to develop.
Issues of clinical governance needed to be addressed. They were dealt with by putting in place thorough systems, demonstrably ensuring that the post-holder had acquired the requisite competencies without any risk to patient safety. Certainly, staff trust in the post-holder’s sensitivity to these safety issues underpinned this approach. There was a confidence in the SAP’s awareness of her limits and boundaries.
However, formal and comprehensive guarantees of competence were in place, for example reflected in the number of times a procedure had to be practiced and witnessed before the competence was signed off:
We ensured that her competencies were such that they were kind of unassailable, they were better than had been done for the junior doctors, better than I’d had as a trainee.
IC5_consultant_1
There were specific clinical governance issues to be addressed, in particular related to prescribing and the administration of local anaesthetic. These took time to sort out. Indeed, it was suggested that ‘. . . we worked around it rather than work through it. And then did it properly afterwards’ (IC5_consultant_1).
The final aspect of the process relates to the involvement of the nursing directorate or nurse management in the development of the role. This involvement was limited. As a consultant-driven initiative, the role had a particular credibility and legitimacy, with responsibility at the end of the day presented as lying with the consultant:
As long as they know that they’ve got the support of the consultant, then it gives them the confidence to proceed. I would always ultimately be responsible for what goes on surgically and if there are issues with the nurses.
IC5_consultant_1
The post-holder formally took up the SAP role on the completion of the 2-year FD. During the period of the FD, the post-holder was working at band 3, with 2 days per week off for study (one of these in her own time). On completion, she moved on to pay band 4. The role developed during the period of the FD, with the support of the AP lead, the consultant and other colleagues. On completion of the FD, the SAP role was striking in terms both of the range and complexity of the tasks performed.
Unable to secure patient consent for a surgical procedure, the SAP was not in a position to run lists, and therefore concentrated on providing assistance to the specialist nurses and the consultants with their lists. However, with the exception of the issue of acquiring patient consent, there was very little to distinguish the SAP role from that of the specialist nurse. Thus, the SAP tasks included administering local anaesthetic; conducting shave and puncture biopsies; removing moles; undertaking suturing; applying dressing; and dealing with after-care.
Impact
The consequences of the SAP role can mainly be seen in terms of positive service outcomes. At the outset, it was suggested that, given staffing and workload pressures, particularly associated with a same-day surgical service, an extended support role contributed to departmental capacity and flexibility:
From an efficiency perspective, it just means that we can ride the peaks and troughs of a busy clinical service, you know, more or less able to deal with whatever comes at us. So it means that we’re pretty rock solid.
IC5_consultant_1
A more detailed consideration of the role highlights how it contributed to these ends and, arguably, also to improvements in service quality. Thus, the impact of the role can be seen to lie in a number of areas, each discussed below.
Sequential working
The SAP worked sequentially with the consultant in two senses. First, she prepared patients, allowing the consultant to come in and begin his work with speed and confidence. As indicated, this preparation involved not only clinical tasks, such as the administration of the local anaesthetic, but the ‘softer’ tasks of relaxing and putting the patient at ease:
He [the consultant] knows that my local [anaesthetic] will have been done properly, that the patient’s completely nice and numb, comfortable, warm, reassured. I’ve been with that patient all the time, whereas he’ll have to go in and out to see other rooms, so I’ve very often escorted the patient all the way down and I’m there right until the very end, which he won’t be.
IC5_SAP_1
Second, the SAP worked in sequence with the consultant by finishing off a surgical procedure and associated activities, allowing the consultant to move on to deal with another patient.
Partnership working
As well as working alone and in sequence, the SAP acted alongside the consultant and the specialist nurse, again allowing a patient to be dealt with in a timely and speedier fashion. A specialist nurse provided an example:
So we work together most days, so if I have a surgical list I might go in and consent the patient, while I’m doing that, she’s drawing up the local anaesthetic. And then she’ll numb the patient. I might remove the lesion and leave her to stitch up while I do the paperwork. So potentially that patient’s time on the bed is halved, the paperwork takes up, you know, as long as the surgery, so while I’m doing the paperwork she can be finishing off and stitching up.
IC5_specialist nurse_1
Time
As implied, the SAP appeared to have more time to engage with patients, relaxing them, dealing with anxieties and putting them at ease:
So once you’ve reduced somebody’s blood pressure by being relaxed with the anaesthetic, then usually the operation is a doddle.
IC5_SAP_1
Accessibility
Accessibility to the SAP also contributed to a positive patient experience. To the patient, the SAP was far less intimidating than the consultant or indeed the nurse:
I’ve been able to chat to them and explain to them what’s going to happen in more detail, in layman’s terms. I’m not as intimidating as a doctor, who’s quite loud and I can relax them and say, ‘well this is what’s going to happen’.
IC5_SAP_1
Expertise
In focusing on the performance of particular support tasks, the SAP became expert in their performance: a degree of specialisation bred increased proficiency. This was seen to be the case in relation to the administration of local anaesthetic:
I’ve done so many [local anaesthetics] now, so on the sites that are very painful or if people have a needle phobia, I get given those patients because it doesn’t bother me.
IC5_SAP_1
In a slightly less positive vein, the consequences of the SAP might also be seen in terms of certain tensions. These were apparent in how others in the department viewed the role. Pushing the boundaries of the nurse support role meant that there had been some resistance from RNs in the department:
There are some other nurses in the department who haven’t been so accepting and have made comments, but they’re in the minority, and actually there’s only one that I can really think of who’s really made a fuss of it.
IC5_specialist nurse_1
Summary
A summary of the features and issues associated with the development of the SAP role is presented in Figure 7.
FIGURE 7.
The development of the SAP role.
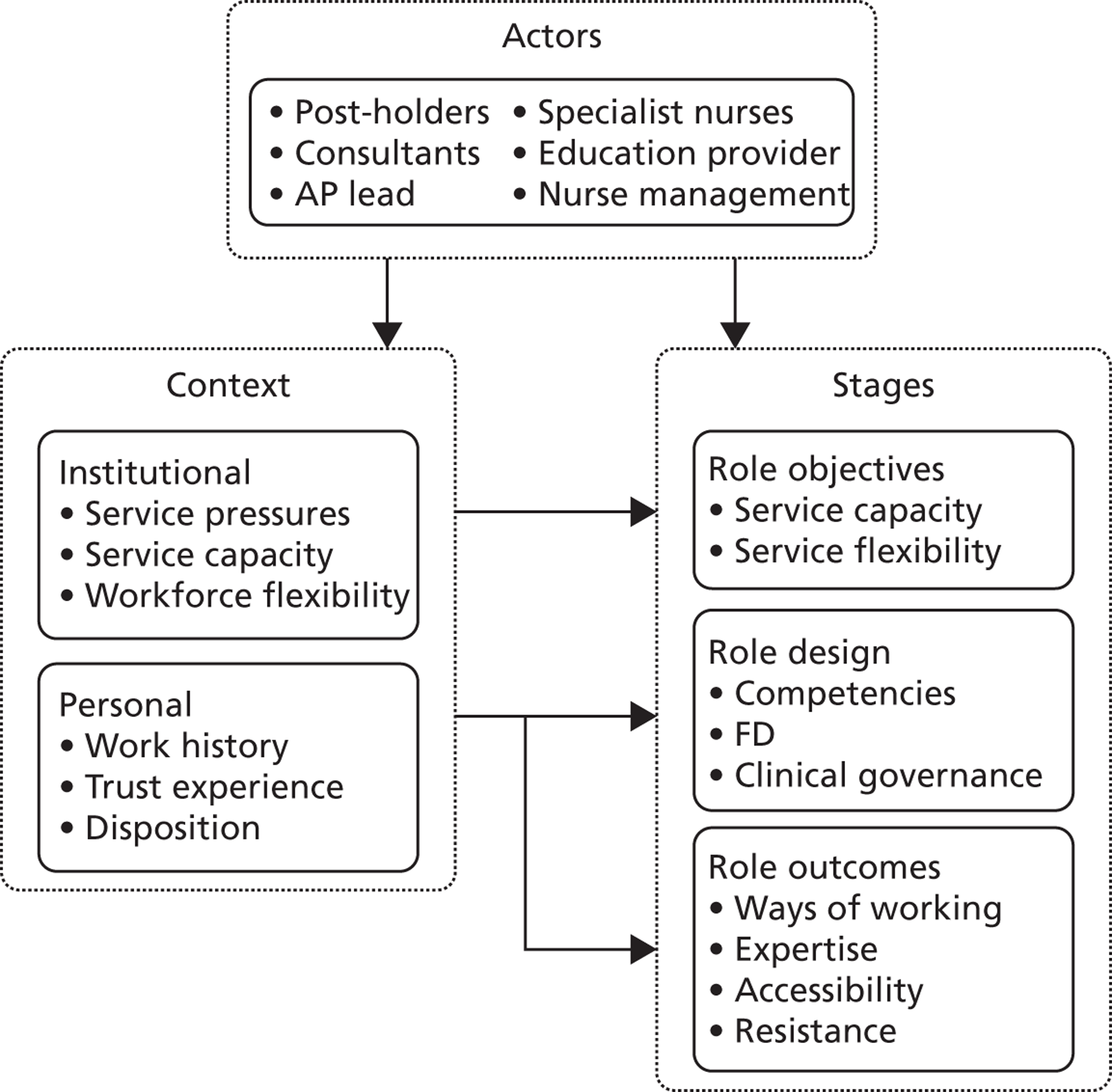
The role of the clinical support worker trainer at band 4
This case study explores the development of a new educator role at OUH, specifically designed to help CSWs at pay bands 2 and 3 undertake training, particularly those on the Qualification and Credit Framework (QCF) diplomas and apprenticeships. The trust viewed the role as a means of strengthening its capacity to train CSWs, increasing both the scale of such training and the speed of completion. The fieldwork was undertaken in two phases. The first comprised interviews with key members of the trust’s CSW training team and with the CSW trainer herself, conducted at the end of 2012, soon after role had been introduced. The second phase involved repeat interviews with these actors, plus interviews with three CSWs engaging with the CSW trainer. These interviews were carried out in May 2013, some 6 months after the role had been introduced and been given time to ‘bed down’. The second-phase CSW interviewees were employed in different clinical areas: maternity, neuroscience and orthopaedics. In total, 11 interviews were completed.
Context and objectives
The CSW trainer was designed as a corporate role, working in a small team positioned in the nursing directorate and responsible for the training and development of the trust’s CSWs at bands 1 to 4. The emergence of the CSW trainer role was related to two sets of factors. The first was strategically driven, being tied to a broader initiative on the management and development of CSWs at the trust. OUH had decided to set up what it labelled as a CSW academy, with the CSW trainer role long envisaged as an integral part of it.
The rationale for the CSW trainer role within the CSW academy was associated with a perceived need to improve the trust’s approach to the training of CSWs, particularly at bands 2 and 3. Much of this training had been centred on the acquisition of NVQs (levels 2 and 3), although at the time the CSW trainer post took effect, the national training regime was underpinned by the QCF providing level 1 and 2 diplomas, and, when linked to functional skills, an apprenticeship. The trust was seen as ‘lagging’ in the number of CSWs seeking such accredited qualifications and in the pace and scale of completion.
The problem was seen to lie in the limited support available to CSWs undertaking this programme. In large part, this limited support derived from a lack of assessors in the trust. Indeed, it was the need for a dedicated corporate assessor for trainee CSWs across the trust that underpinned the introduction of the CSW role. The job description for the post noted one of the overall objectives: ‘[t]o effectively assess NVQ/QCF learners’ performance, knowledge and understanding against the national occupational standards’. 51
In more general terms, the CSW trainer role was a means of providing support to trainees during diploma and apprenticeship programmes. Formal training for CSWs was a far from straightforward process: not only had many trainees been away from formal learning for some time, but typically the requisite training involved juggling ongoing work and domestic responsibilities. In this context, support from a dedicated CSW trainer role was seen as assuming different forms. In part, it was related to ongoing advice, particularly on time management. Indeed, the CSW trainer’s contribution in this respect was reflected in another job description objective: ‘[t]o support a cohort of learners to achieve key performance targets relating to achievement and timely success rates’. 51
In addition, such support had a more personal dimension, with the CSW trainer available to deal with the stresses and strains likely to emerge during the training period. As the job description notes, the trainer role seeks ‘to provide pastoral support’ for trainees.
A significant dimension of this support was accessibility: the CSW trainer needed to be someone CSWs could relate to and readily approach in seeking support. The job description explicitly presented the CSW trainer’s post as a ‘role model’, and suggested the need to appoint an individual with a personal and professional background compatible with such a requirement. 51
The second set of factors driving the introduction of the trainer role was more opportunistic, reflecting immediate needs and pressures. Other initiatives associated with the CSW academy, particularly a new recruitment system and induction programme, were generating unexpected demands on other team members. The academy team was small, comprising only three other staff members, with the intensity of work exacerbated by the lack of replacement cover while the academy lead took 1 year’s sabbatical leave. In such circumstances, the CSW trainer role was perceived as crucial in relieving other team members of certain duties in relation to supporting CSW trainees, freeing the team up to concentrate on these other initiatives and activities:
[We] weren’t doing a good enough job really in supporting, there was just too much to do in terms of launching the academy, trying to support that initiative and also trying to run apprenticeships and trying to make them effective, trying to meet targets from [college name] who have the overall managerial responsibility for the apprenticeships. So really we felt that we needed someone dedicated to [QCF] assessment and to support apprenticeships.
IC6_trust manager_1
Implementation and operation
The CSW trainer took up her post in September 2012. Graded at pay band 4, the post was internally funded and due to last until May 2013. This period of employment was subsequently extended until the end of 2013. The appointee came from outside the trust but had experience as a qualified nurse. As a new role to the trust, issues arose as to how it would establish itself and operate in practice. These processes unfolded iteratively: ‘I don’t think any of us really knew what was going to happen’ (IC6_CSW trainer_1).
In the event, the role developed along three activity tracks: assessor, champion and team. Each of these is discussed below.
An assessor track
The assessor track revolved around the range of tasks associated with managing a group of CSW trainees. At the outset, the post-holder took on six trainees but this rapidly increased to a steady-state number of 19, broken down into seven taking the apprenticeship and 12 taking the standalone QCF diploma. This aspect of the role centred on a one-to-one CSW trainer–trainee relationship. The trainer quickly established a routine of face-to-face meetings with each trainee every 2 weeks.
Such meetings were supplemented by the CSW trainer’s engagement with relevant actors at ward level. This included witnessing and assessing the performance of competencies, as well as dealing with ward managers in facilitating the CSW’s training and development: ‘I always liaise with the managers and try and get them onside’ (IC6_CSW trainer_1).
Closely related, the assessor role involved various activities related to the local accrediting college. For example, the post-holder was involved with the college in carrying through a diagnostic process, which evaluated the capabilities of potential trainees. This determined the appropriate level of training and, where necessary, connected the trainee to a bridging programme allowing them to build up capabilities.
Clinical support worker champion track
Working across a large and dispersed trust, as well as ‘starting from scratch’, championing the CSW role was a challenging aspect of the job. It was initially taken forward by the post-holder developing regular ‘drop-in sessions’ on the various trust sites. At the outset, these sessions introduced interested parties to and informed them about the presence of the new CSW trainer role. As an appreciation of the role developed, these sessions provided advice and information to CSWs on available training and dealt directly with CSW queries and problems associated with ongoing training.
This champion track had other dimensions. For instance, the CSW trainer made an effort to make the trust’s libraries more accessible to CSWs, not least by ensuring that the libraries acquired publications and other sources of use and relevance to CSW trainees. Moreover, the CSW role was increasingly contacted by ward managers seeking to develop competencies for their CSWs, as a means of explaining and encouraging the process: ‘She’s now sort of helping go round, as I was saying we’re doing competency workshops’ (IC6_trust manager_1).
Team track
The final track involved the CSW trainer in tasks somewhat beyond the training needs of established CSWs and more supportive of the broader activities of the CSW academy. Most striking in this respect was the work undertaken by the post-holder in helping the team to deliver the trust’s CSW induction. In part, this support was organisational and administrative: ensuring that speakers were available, rooms were booked and the appropriate paperwork was available. More substantively, the CSW was also contributing some of the teaching on the induction, for instance on the communication sessions.
Impact
Responses to the CSW trainer role from various stakeholders were extremely positive. In general, the role was seen as having taken on more than envisaged:
She’s taken on a lot more than we’d first anticipated, she’s sort of taken on organising key skill sessions and booking rooms for that and liaising with the key skills tutor and liaising with the students, even [when] they’re not her students.
IC6_trust manager_1
At corporate level and in terms of impact on the trust’s CSW academy, the consequences of the role included:
-
Freeing up other teams members to concentrate on other tasks:
-
‘[It’s] freed them up to do other things. I’m always willing to put my hand to whatever’s happening if I can help’ (IC6_CSW trainer_1).
-
-
Increasing the CSW academy’s capacity, with a tangible impact on the number of CSW trainees it could manage:
-
‘With our capacity we couldn’t have considered taking on another cohort of apprentices or people just wanting to do standalone QCF awards, but her [the CSW trainer] coming in that September time for when they started, she helped with their recruitment and the interviewing and taking them on, with their induction taking them through their programme’ (IC6_trust manager_1).
-
-
Providing a contact point, not least through the drop-in sessions for CSWs, allowing them find out more and seek advice on training opportunities:
-
‘There was certainly a gap in the market: they all knew about NVQs, and they all wanted to do them, but up till now there’d never been any way of them accessing it, they didn’t know who to go to or where to go’ (IC6_CSW trainer_1).
-
At an interpersonal level, the role impacted by providing various forms of support to trainees, again with meaningful corporate consequences such as improved and quicker completion rates. The CSW trainer noted that 18 of her 19 trainees were on schedule with their training. Asked to reflect on the various ways in which the CSW trainer had impacted on their learning and helped to keep them on schedule, CSWs noted:
I see her as a mentor that helps me with . . . [as] a lot of stuff is written in such a way that you don’t understand it. She helps you break it down.
IC6_CSW_1
If I’ve got some question I can always phone to her or e-mail to her that I’ve got problem, ‘can we just meet?’ And it’s not a problem at all.
IC6_CSW_2
More generally, the CSW interviewees highlighted the trainer’s role in:
-
reassuring
-
problem solving
-
mentoring
-
planning
-
witnessing
-
clarifying.
The capacity of the CSW trainer to contribute in these different ways can be related to the structure of the role and to three associated factors: personality, background and skills. In terms of role structure, the post was designed as a dedicated trainer role with a core focus on the direct relationship with the CSWs, and as a consequence the post-holder had more time to devote to the CSWs:
I can give all my time to it now really, whereas they’re [other members of the CSW academy] constantly having to deal with the AP course, that takes a lot of time up.
IC6_CSW trainer_1
It will also be recalled that, as a band 4 role, the post was designed to be more accessible to CSWs than the other, higher-graded members of the CSW academy. There were signs of such accessibility:
I suppose they just feel a bit more comfortable; sometimes I think they’re aware [that other members of the CSW academy] are quite high up nurses and, you know, a little bit wary of them. Whereas with me they’re, especially after they’ve known me for a few weeks, because we do have a little bit of a laugh and coffee together and so it’s quite informal.
IC6_CSW trainer_1
Most of the CSWs were unaware of the CSW trainer’s work background, and placed greater weight on her personality and style:
She’s [the CSW trainer] just got really positive body language; she’s not in your face; she’s quite calm; she never raises her voice and if I was struggling to get words out like on a piece of paper, she’s like, ‘I can see like you’re struggling, let’s just look at it a different way’. Like she’s just more relaxed about it and I never walk out thinking that made no entire sense.
IC6_CSW_1
In terms of skills, it was clear that the post-holder was extremely well organised: she was juggling a range of tasks, including meeting all 19 trainees at least every other week. For one CSW, the regular meetings provided a structure and regularity of contact which had been absent in her previous assessor relationship. Indeed, this CSW asserted that without the CSW trainer she would have given up her training:
[Without the CSW trainer] I’d probably be looking at stopping it, to be honest; because [before] I wasn’t doing much with it at all . . . The structure wasn’t there and I know she’s very busy, I wasn’t seeing her that often, to be honest, I’d have probably looked at giving up if, if I’m honest.
IC6_CSW_1
Summary
Figure 8 summarises the form assumed, and objectives achieved, by the CSW trainer role.
FIGURE 8.
Summarising the CSW trainer role.
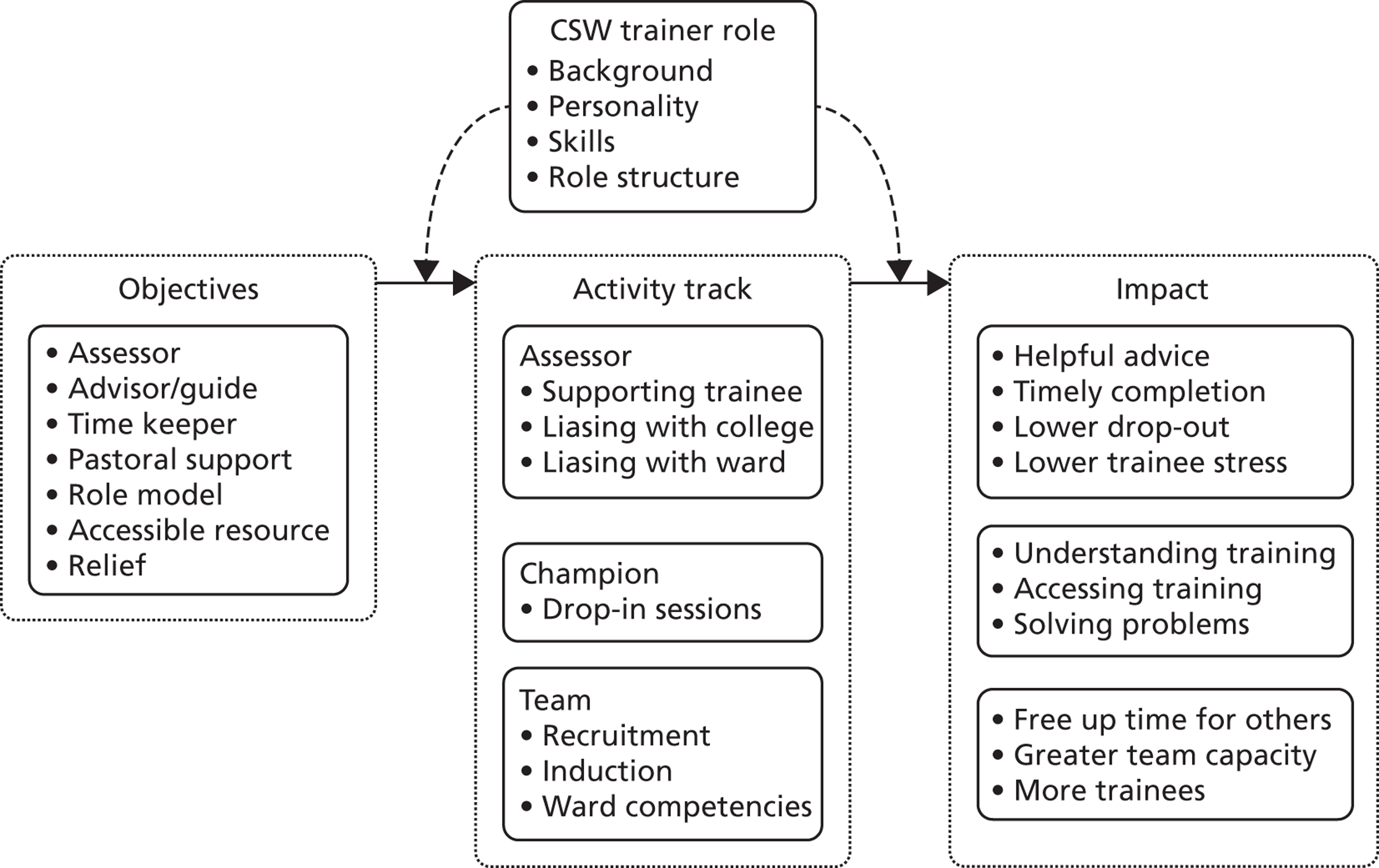
Overview: discussion and lessons
The purpose of the innovation studies was to examine how and why trusts were able to introduce new nurse support roles and new management or working practices. These innovative interventions were defined as being new to the trust rather than unique to the NHS. There was an interest in why some trusts were able to take such steps while others were not, and what circumstances and organisational architectures permitted and supported them. In exploring various types of innovation, the cases have highlighted important differences in the conditions, processes and outcomes underpinning the introduction of new management practices, new support roles and new ways of working. These differences have included the following:
-
New management practices are likely to be less threatening to other groups of staff than new work roles and ways of working, which might well challenge job boundaries and status.
-
New work roles and ways of working represent more of a challenge to ward routines than new management practices, and therefore are more difficult to establish and sustain.
-
New management practices are less likely to generate clinical governance issues which draw in a distinctive range of actors and often involve more complex and extended procedures.
-
There is often a stronger training dimension associated with a new support role or way of working than with a new management practice.
Equally striking, however, are the similar lessons to be drawn from innovating in these various ways. These lessons relate to context, systems and actors:
-
Context:
-
Trusts seeking to innovate in the management and use of nurse support workers are often innovative in other aspects of care delivery.
-
Such innovative trust cultures are found within compact rather than large, sprawling trusts, with the personal interaction and networks needed to generate, share and develop ideas more likely in the former than in the latter.
-
Innovation associated with nurse support workers is often initially opportunistic, rather than planned or strategic. The rationale and objectives underpinning such innovation might well emerge and be sharpened once the initiative has been implemented and ‘bedded down’.
-
New nurse support roles and practices develop iteratively, as confidence, trust and understanding grow. Indeed, in doing so, innovation sometimes evolves in unexpected ways: for example, a new role might take on more than originally envisaged.
-
-
Systems and processes:
-
Innovations need to be resourced; various sources are available and can be used to ‘pump-prime’ an initiative.
-
Innovation in the use and management of nurse support roles needs to be seen as legitimate by key trust stakeholders: it has to address a ‘real’ issue or concern and be seen as an effective way of dealing with it.
-
Innovation rests upon effective communication with those involved in, and affected by, the innovation. Such communication serves various purposes: testing ideas, getting feedback and informing.
-
While formal structures might facilitate such communication, more informal contact and interaction often facilitates effective communication.
-
The bottom-up rather than top-down introduction of an innovation, sensitive to ward-based needs and circumstance, is often more likely to be accepted, particularly by those at ward level.
-
-
Actors:
-
Actors from a range of functional areas within a trust – nursing, HR, education – often need to work in partnership in taking forward an innovation; they bring complementary capacities and insights to the process.
-
Access to, and the support of, senior management, particularly senior nurse management, is often crucial to those taking forward an innovation. Senior management commitment legitimises innovation, while also helping to identify and remove barriers to it.
-
Key individuals within the trust, ‘institutional entrepreneurs’, are often important in driving through and sustaining an innovation, becoming a hub for processing issues and maintaining essential relationships.
-
A powerful internal sponsor, for example a clinical consultant, is likely to add weight to calls for the introduction of an innovation related to nurse support workers.
-
Trust insiders – those with some knowledge and experience of a trust – are more likely to achieve traction in performing a new role and developing a new practice. They will be better known and trusted by others, and have a deeper understanding of trust routines and systems.
-
Actors external to the trust can be crucial players in innovation, suggesting the need to develop constructive relationships with them. This is particularly the case where accredited training is involved, requiring outside education providers.
-
Chapter 4 Evaluation
Introduction
This chapter presents the findings from cases designed to evaluate trust initiatives taken to develop the use and management of nurse support workers. The purpose of these cases was to assess the impact of various types of initiatives on a range of stakeholder outcomes. Six cases were selected, covering four different trusts. These initiatives assumed different forms and focused on nurse support workers in different pay bands. Four of the evaluations centred on new ways of working:
-
recalibrating the distribution of tasks between support workers and nurses (see Developing the support workforce using the Calderdale Framework)
-
developing the new band 3 maternity care assistant (MCA) role (see The developing of maternity care assistants)
-
extending the band 4 AP role to administer medication (see The administering of medicine by assistant practitioners)
-
rolling out a band 4 cohort for the first time in this trust (see Rolling out the assistant practitioner role).
The other evaluations explored new ways of managing nurse support workers:
-
introducing a set of band 2 beginner or probationary competencies (see Beginner competencies for band 2 health-care assistants)
-
introducing a new induction programme (see A new health-care assistant induction programme).
In general, our evaluation model was based on tracking the initiative, carrying out fieldwork at two points in time: gathering benchmark data before an initiative had been introduced or at the early stages of its implementation; and then, some time after the initiative had bedded down or been fully implemented, to explore its impact. However, the consistent application of this model was dependent on the support that the case trusts were able and willing to provide. Moreover, it was difficult to control for factors influencing outcomes between the two points in time.
In the main, the cases evaluated an initiative by elucidating its stated and perceived objectives, where possible, and the extent to which they had been achieved. Evaluation was also based on assessment of how the initiative impacted on various actors with a stake in it: typically, the support workers themselves, coworkers and, to a lesser extent, patients. The intention was to involve trust stakeholders in the evaluation. All evaluated initiatives were selected by the trust, reflecting their interests and priorities. Feedback was given to the trusts at various stages of the evaluation, allowing findings to input into how the initiative unfolded. Beyond these forms of involvement, engagement with the trusts was uneven. At one trust (initiatives 1 and 2), a working group of stakeholders, including a patient representative, met on two occasions: at the outset of the evaluation and to discuss early findings. At another trust (initiative 3), a feedback and discussion session involving stakeholders from across the trust was convened. The researchers maintained ongoing contact with the other trusts (initiatives 4–6), albeit mainly with senior nurse managers, providing regular briefing on the research.
The findings from each of the case study evaluations are presented in turn. They are structured according to a similar template setting out:
-
the context, including details on the evaluated initiative
-
the research methods and
-
the findings.
In contrast to the ICs, the ECs are presented anonymously. Our EC trusts displayed considerable bravery in allowing us to report in a ‘warts-and-all’ way on initiatives with unknown consequences. In the event, they faced many difficulties; indeed, in some instances, they might be deemed to have failed. In these circumstances, it was felt appropriate to protect their identity.
Developing the support workforce using the Calderdale Framework
Context
This evaluation focuses on the use of the Calderdale Framework (CF)52 in one NHS hospital trust in the north of England. This organisation had expressed concern about the nursing and support worker skill mix and was keen to find ways to support its services in developing the support worker roles in ways which would promote quality of care to patients and better support the registered nursing workforce. This was recognised as a priority given the changing context of health-care delivery, forecasts of a future reduction in the numbers of RNs and financial pressures.
At the outset, senior managers indicated that the nursing support workforce in the organisation comprised predominantly band 2 AfC workers who supported the registered nursing workforce (at band 5 and above). 18 However, despite this uniform banding for support workers, there was recognition and concern about the wide variation in roles and responsibilities of these staff at band 2 and the education and training that they had received, particularly when taking on extra responsibilities. The organisation was looking to ‘take stock’ of the nursing support workforce and consider its potential for the future through new ways of working and, potentially, new roles at bands 3 and 4 of the AfC. 18 It was anticipated that this would help the organisation develop a workforce ‘fit for purpose’.
The CF was perceived by the organisation as supporting it to gain a better understanding of their current and future nursing support workforce, as well as providing a possible infrastructure to underpin role developments for the non-registered nursing workforce. Originating in Calderdale and Huddersfield NHS Foundation Trust, the CF was first utilised to facilitate change to service delivery by the community rehabilitation teams. It had since been used by a range of other organisations and services (including housing adaptations and social care). The CF focused on engaging clinical staff through a ‘bottom-up’ approach to service and workforce change. The emphasis was on encouraging the development of competency-based training for staff taking on new roles and standardising the processes within an organisation. This had had particular value for considering the roles of support workers.
The CF comprised seven stages: (1) awareness raising; (2) service analysis; (3) task analysis; (4) competency identification; (5) supporting systems; (6) training; and (7) sustaining. Each stage encourages ownership of the process by clinical staff.
Methods
The CF was introduced to the organisation in November 2011. Following some introductory sessions with the CF facilitators, a decision was taken to implement it in one clinical area (which will be referred to as the pilot site). Concurrently, the CF facilitators trained three staff from the organisation in how to use the framework in other clinical areas. A substantial component of this training involved staff from the organisation shadowing the CF facilitators working with the pilot site. This pilot site was a ward, and this forms the focus for data collection. Organisation staff trained in using the framework went on to administer the framework in two additional clinical areas (referred to as sites A and B). The views of senior staff on how these have progressed with implementation have also been gathered.
Over the evaluation period (November 2011 to June 2013), the organisation progressed to stage 4 of the CF – competency identification. The progress of the organisation through these different stages, as well as the challenges this raised for the organisation, constitute this EC study. The case site evaluation has not been compromised by the organisation being only part way through the process: this is an evaluation of workforce change in real-world contexts. However, it has not been possible to gather before-and-after outcome data.
Data collected for the study (and up to the point of reporting in June 2013) comprised the following (summarised in Figure 9):
-
observations (non-participant) of meetings associated with implementation of the CF and involving a range of staff from the organisation, including introductory meetings (n = 2, December 2011), awareness-raising meetings in the pilot site (n = 3, May/June 2012), service analysis meeting for the pilot site (n = 1, June 2012), task analysis meetings for the pilot site (n = 2, July 2012) and competency identification meeting for the two pilot sites (n = 1, April 2013)
-
survey of all ward-based registered and non-registered nursing staff in the pilot site to explore their perceptions about their role and working environment at point of implementation of the CF (89% response rate; n = 23)
-
interviews with ward-based registered and non-registered nursing staff in the pilot site at point of implementation of the CF (n = 10) and at 1 year (n = 6)
-
interviews with senior nurses (including ward managers, matrons, workforce development lead, deputy director of nursing (workforce), director for staff development at point of implementation of the CF (n = 3) and at 1 year (n = 6)
-
interviews with external partners for the implementation of the CF at point of implementation of the CF (n = 3) and at 1 year (n = 3).
FIGURE 9.
Summary of data collection points to evaluate implementation of CF.
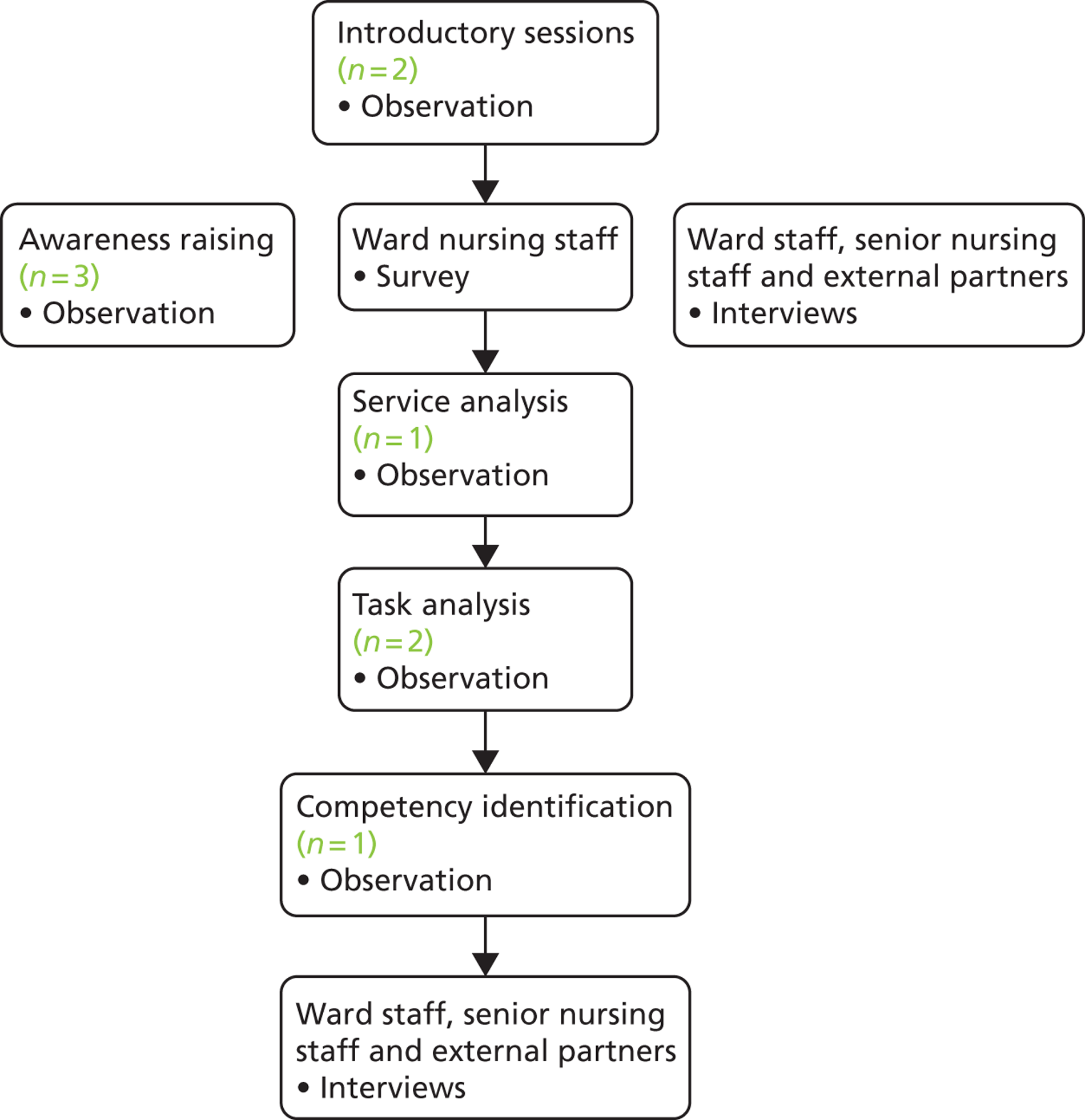
Sampling of participants for the interviews was purposive with the aim of representing the range of staff in the organisation involved in implementing the CF, including ward-based staff, senior nurses and external partners. The survey used a census approach and was administered to all registered and non-registered nursing staff (n = 26) in the pilot site. Observation of meetings was purposive but included staff who attended the different meetings. Accounts from different participants have been compared and contrasted. Descriptive summary statistics were used to analyse quantitative survey data.
Findings
The evaluation findings presented are the processes of implementing the CF within the organisation. The findings reflect the drivers for change nationally and locally, the opportunities and challenges of implementing the approach for developing support worker roles, and consideration of the future potential for support worker roles in the organisation.
Meeting an ambitious NHS agenda
Senior nurses in the organisation summarised a range of national drivers that were influencing their focus on the roles of nurse support workers. These included:
-
a recognition of changes in service delivery and the health-care roles required to deliver services
-
a projected forecast of fewer RNs in the workforce over a 10-year period
-
changes in nurse education to an all-graduate profession and
-
financial pressures which required the organisation to ensure effective use of their resources, including their human resource, to promote quality of care while controlling costs: ‘Rather than recruiting straight in to band fives, it may be having gone through the framework that we look at different levels and we can get more for our money. I think that’s the way it’s going and I don’t think any of us are naïve enough to believe that’s not the case. I guess it’s a prime opportunity for us to make it work for us in a way that we feel it’s going to work for us if it does’ (EC1_senior nurse_1a).
Support workers were considered a ‘stable’ human resource (often recruited from the local population) that, with investment, would support organisations to deliver its health-care agenda of the future. The CF was viewed as an approach that had the potential to support the organisation in considering how they would meet demands for services through the best use of staff, a significant number of whom were support workers.
In addition, the CF was presented as able to help organisations reconsider the traditional deployment of the workforce to meet these changing demands:
A lot of trusts will say we haven’t got the time to do that . . . but if you’ve got a clean page, a bottom-up situation to do it in, to go through that type of exercise, you’ll probably finish up with a staffing structure in an environment that’s totally different to what it is at the moment.
EC1_external partner_3
Managing professional lethargy and resistance and changing organisational cultures were recognised as key influences on whether or not roles for support workers were going to be able to develop to their full potential within the organisation. The CF was seen as the model to address these issues, with its ‘bottom-up’ approach engaging clinical staff throughout the process.
Senior staff in the organisation viewed the CF as useful in reviewing and developing support workers’ roles and, in particular, for considering the appropriate delegation of tasks from the registered to non-registered workforce. The CF recognised that services were changing in response to patient need, suggesting the need for a health-care workforce ‘fit for purpose’ in delivering quality of care for patients. Where non-registered support workers took on the work of registered professionals, risks had to be managed in delegation of work and staff had to be confident about role boundaries and about sources of help when care demands fell outside their level of skill. The CF was perceived to provide the opportunity for this careful planning and preparation.
However, use of the CF at this organisation was considered opportunistic rather than planned, as the organisation was offered financial support from the (former) SHA to work with the Calderdale team:
It came along at a time when we were saying we felt as an organisation we were behind the times in terms of introducing support worker roles . . . So the opportunistic funding and [name] secondment and having been exposed to the introductory session delivered by the Calderdale team, this model resonated with [the organisation].
EC1_senior nurse_4a
Getting the ‘band 2 house in order’
The profile of nursing support workers in the organisation was predominantly band 2. At the outset, the organisation considered addressing this skills gap by creating new roles and ways of working, available to nursing support workers at higher band levels. However, as the Calderdale process commenced, the focus of change became less clear. Discussions about band 2 nursing support worker roles highlighted wide-ranging discrepancies in tasks and responsibilities, as well as in preparation for practice. It was going to be difficult to develop new roles when the organisation had not sorted these fundamental issues related to the band 2 workforce:
We haven’t got our band 2 house in order . . . so the various competencies of our band 2 workforce, what we use isn’t sorted and how can you start to introduce new roles at potentially a higher band if you don’t sort that bit first?
EC1_senior nurse_4b
Indeed, this concern about discrepancies informed the use of the CF, with sensitivity to the privileged status of clinical areas involved in the process:
Individuals that have gone through a more structured process should be able to be more confident in how they demonstrate their abilities and how they apply that caring to the setting that they are working in. And that’s good. That’s positive. But if it fails to create a sustainable model we will continue creating haves and have nots.
EC1_senior nurse_6b
Opportunities and challenges
As the organisation considered the utility of the CF, developments focused on one ward area: this forms much of the focus for our evaluation. The survey of staff (see Appendix 6) at the outset of the Calderdale process revealed a workforce largely satisfied with their roles and place of work, regardless of banding (see Appendix 7, Table 33). The workforce was predominantly female, aged over 30 years, and nurse support workers comprised one-third of the workforce (see Appendix 7, Tables 34–39).
The manager of the ward put the team forward after the introductory sessions as a way of trying to support the careers of support workers:
With Calderdale there’s a potential for their [support worker] development, academic – well not necessarily, not even thinking about academically, but with financial remuneration to move up a different grade and to be, in their eyes, recognised for what they’re already doing.
EC1_senior nurse_2a
The clinical area progressed the Calderdale initiative through awareness-raising sessions to brief the entire ward nursing team and facilitate their engagement with the process. There remained a level of confusion at this stage about what Calderdale could offer the clinical area; many RNs felt that the roles of the nursing support workers were already more developed in their ward than in other clinical areas in the trust. This created challenges in considering whether or not and how the support worker roles might further develop. Nurses expressed concern about continuing to develop the roles of support workers without mechanisms for the support workers to be held accountable for their practice:
If we’re technically always going to be responsible for them, no matter how much their role develops, there’s always going to be an element of ’well the nurse was in there as well’ or ‘they knew I was doing it’ or ‘so and so showed me how to do it this way so it’s their fault, not mine’ . . . I think that’s what’s good, which came out of the Calderdale Framework, is that everything we’re doing technically should be documented to say yes, ‘they’ve had this training’, which I do think is a really good step forward.
EC1_nurse_6a
It also emerged that support workers were concerned that they were not being provided with recognition through banding or receiving any financial reward for taking on extra duties:
I don’t mind taking on jobs but there’s so many jobs you can do without getting paid and then sometimes, you know, it tips you over the edge because you’re just getting the same wage as someone that isn’t even doing half of them jobs.
EC1_HCA_3a
At the awareness-raising sessions, senior nurses clearly stated that the Calderdale process would be organic, but many support workers hoped that the process would lead to rebanding:
I’m holding out for the Calderdale Framework . . . So my understanding is that they’re going to be pulling out segments of what our job is going to be . . . and we’re going to be band 3 and possibly one or two band 4.
EC1_HCA_2a
The Calderdale process progressed through the service and task analysis stages. These stages facilitated the enthusiastic engagement of staff in considering service change and the risks associated with delegating across role boundaries. The process identified various tasks to delegate to support workers, including taking blood from a Hickman line, cannulation and the second checking of blood products and controlled medications with a RN. The possibility of introducing a band 4 AP was also discussed, such a role supporting the RNs with telephone triage (using a protocol), patient admission assessments and wound management and care. However, this suggestion was ‘parked’, given reports that the Calderdale work might not progress on the ward until ‘bigger’ organisational issues were addressed related to banding and training.
As the evaluation concluded, the organisation was seeking to address some of these ‘bigger’ organisational issues, prompted by the competency identification stage. The pilot site was described as having reached a ‘hiatus’ or a ‘lull’ while the organisation sought to address a range of issues, not least related to a recent merger with another large trust, with some concern that the process would lose momentum within the clinical area:
Although it’s kind of frustrating because you want to carry on and you don’t want to lose the momentum and we’ve still got the enthusiasm on [name ward] and it’s about how do you keep that engagement and that buy-in with this kind of lull really.
EC1_senior nurse_1b
At ward level, staff commented that they understood the process might have ‘fallen flat on its face’ (HCA_2b). For some support workers and senior nurses, this had created disappointment:
It’s been put on the back burner so it’s something that’s going to happen at some point but it’s not as imminent as we all thought it was going to be . . . then you just kind of feel like is this going to happen in my lifetime, let alone being enthusiastic.
EC1_HCA_2b
Some felt that the organisation had moved the focus away from CF to the higher education certificate for support workers and this reinforced perceptions of ward staff that the organisation kept changing their focus in relation to the development of the support workforce.
Looking back over the previous year, senior nurses and external partners highlighted key issues as creating challenges for the Calderdale process:
-
The steering group for the implementation of Calderdale. Key senior organisational staff from HR and the training department had been largely excluded from the process:
-
‘They should have had human resources involved from the outset and they should have had education providers involved from the outset so, either within their own training department, or people who did have relationships with in terms of higher education or further education for the vocational link’ (EC1_external partner_2b).
-
-
There were concerns about the expectations placed on staff who had taken on the Calderdale facilitator training programme to ensure that the framework was sustainable in the longer term in the organisation. For facilitators, the concern was whether or not they would have time to implement the framework while trying to fulfil clinical responsibilities:
-
‘The downside of it is how time-consuming it was. You could almost, I almost feel like it could be a full time job in developing them in terms of working through the process and keeping that momentum going and maybe pushing things through with a tighter timeframe’ (EC1_senior nurse_1b).
-
It is important to recognise that two clinical areas (sites A and B) were simultaneously progressing their teams through the Calderdale process, facilitated by the organisation’s trained facilitators. Areas for development of support worker roles were identified, but these areas were placed on hold while wider organisational issues were resolved. In addition, some of these developments had come up against professional resistance and so these teams were reconsidering their proposed changes for support worker roles.
Looking to the future for support worker roles
Despite slow progress and the organisation reconsidering how best to progress the Calderdale work, many ward-based staff and senior nurses indicated that progressing the work had been a useful exercise. It had forced some difficult conversations related to role boundaries and helped the organisation to consider delegation and the associated management of risk:
Calderdale absolutely has its place and what I really like is that it’s a robust process that you work through and you’ve got the evidence behind it and that’s not to say that you don’t do that in any of the changes that you make, but because it is a set process and steps that you go through, and the tools that it provides you with are easy to use . . . I like the fact that it engages everybody at all levels . . . and for our integrated services certainly I can still see real potential around that, really pushing some boundaries that perhaps we haven’t done.
EC1_senior nurse_1b
However, the opportunities for furthering the work were reliant on a number of inter-related factors:
-
There are wider organisational discussions following the merger of the organisation with another large NHS trust to determine whether or not the CF provides a useful way forward for service and role developments. Despite positive reports on the impact of the process on localised teams, some staff members had raised concerns about the process, in particular whether or not it would create even greater inconsistencies in support worker roles across the organisation.
-
Without the backing of key ‘enablers’ for the work, such as the HR department and the organisation’s learning and development department, it was questionable whether or not CF would be taken forward.
-
There were key decisions to be made around training packages and, more importantly, how such packages could be funded to ensure sustainability of the initiatives.
-
Despite continuing trust commitment to creating career opportunities for support workers, there was a concern that staff, particularly support workers, would feel disheartened if time invested in the CF did not change their roles or banding: ‘It’ll be really great to have some career development for the healthcare assistants because I’m absolutely passionate about that . . . They shouldn’t be abused at all, and if we are not careful, they will be’ (EC1_senior nurse_3b).
Summary
This EC study has focused on the implementation of the CF in one NHS hospital trust in the north of England. This framework provided a bottom-up, step-by-step approach for considering service delivery and workforce development.
The evaluation has highlighted the enthusiasm at both service and corporate levels for the development of support worker roles and career opportunities. However, there were a number of key lessons to be learnt, albeit within the context of an organisation still part way through the change process:
-
There were risks and benefits associated with ‘opportunistic’ change. The chance of financial support for the Calderdale process was attractive to the organisation, coinciding with commitment to address nurse support roles and skill mix in pursuit of improved care quality. However, in early discussions it became apparent that the organisation needed to concentrate on getting some ‘order’ in the band 2 nursing support workforce, prior to developing new roles (at bands 3 and 4) or new ways of working which would require extra skills and training. This was noted once the process had got under way and a number of service-level staff had started to engage with the process.
-
There were significant challenges facing the project teams. The merger with another NHS trust further complicated the landscape, and begged questions about the suitability of the CF in the merged trust; nurse support workers at the different organisations had been trained in different ways and there was variation in the banding of support workers across the organisation.
-
Focusing on a defined clinical area, the CF was reliant on an enthusiastic ward manager, supportive of their support workers. It was, therefore, questionable whether or not the CF would be taken up in all areas. Indeed, there were concerns about how to use the framework within areas resistant to change in support worker roles.
-
A significant question also related to the training packages required to support any new roles for support workers emerging from the CF. At an organisational level, there was uncertainty about how this would be funded and how the initiative might become sustainable.
In conclusion, the CF had prompted discussion within the organisation about the nursing support workforce. It provided an opportunity for considering step-by-step change revolving around complex issues associated with the redistribution of tasks between registered and non-registered staff. In looking to the future, the trust was hopeful that any obstacles would be overcome, with support workers in different clinical areas seeing their roles, banding and career opportunities develop. However, as the evaluation concluded, it remained uncertain whether or not the CF would be the vehicle for such change.
Beginner competencies for band 2 health-care assistants
Context
This case evaluates an attempt to introduce beginner competencies for band 2 HCAs across a trust. This initiative was taken alongside the development of the new 2-week induction programme, also evaluated as part of this project (see A new health-care assistant induction programme). Indeed, these beginner competencies were embedded in the induction and integral to the trust’s broader pursuit of a more robust approach to the recruitment and development of its HCAs. The principle of a new competency framework for the trust’s band 2 to 4 HCAs was signed off by its nursing board in December 2011, and by mid-2012, beginner competencies had been formulated and disseminated to the wards. There were 19 such competencies. These included soft skills, such as communication and ensuring patient privacy, dignity and respect, and hard skills, for example monitoring fluid balance and meeting nutritional and hydration needs. To acquire these competencies, HCAs were to be assessed and signed off by an on-ward mentor and in the process were required to collect a portfolio of evidence indicative of requisite skill and knowledge.
The beginner competencies were seen by the trust to serve a number of related purposes:
-
Preparation for new starters. The competencies were rooted in and represented an extension of the induction process. A booklet of competencies was handed out in the first week of the induction programme, and the teaching was aligned with these competencies. However, the induction programme was not designed to deliver ‘competent’ HCAs to the wards, with the beginner competencies being taken back to the ward for development and sign-off.
-
Probation. The acquisition of these competencies was explicitly tied to successfully completing a probationary period: starter HCAs were given 6 months to acquire the competencies as a condition of confirmation in the post.
-
Developing within band. As originally envisaged, there were different levels of competence in band 2 associated with the beginner, the proficient and the expert. This was designed to provide a structured within-band as well as a between-band route to individual development. At the time of the research, only the beginner competencies had been developed and rolled out. Indeed, on completion of the research the competencies at the proficient and expert levels had yet to be formulated.
-
Standardising competencies. The beginner competencies were to be rolled out to all band 2 HCAs in the trust. Those HCAs already in post were also scheduled to achieve sign-off of the competencies in 6 months, a means of providing the trust with some assurance on the baseline capacity of its band 2 HCA workforce.
-
Development route. In the medium and longer term, the roll-out of competencies to band 3 HCAs was seeking to provide clear achievable career development routes for the trust’s staff.
Our evaluation centred on the beginner competencies introduced on to the 2-week induction and rolled out to band 2s across the trust, with a view to assessing how they had been received and used at ward level.
Methods
The methodological approach was influenced by progress made by the trust on introducing the beginner competencies across the organisation. On the assumption that the beginner competencies would be taken up and administered both to HCA inductees and existing band 2 HCAs on the ward, the evaluation was to be conducted in two phases: collecting data just before and approximately 6 months after the beginner competencies had been introduced. The first phase was undertaken as envisaged and comprised:
-
Interviews with three members of the trust’s learning and development team, plus the deputy chief nurse responsible for developing the beginner competencies and managing their roll-out.
-
Interviews with nurses in three clinical areas on different trust sites undertaken in May 2012, examining whether or not the take-up of the beginner competencies might be sensitive to area needs and circumstances. Six staff members in each clinical area were interviewed, covering ward managers, nurses, HCAs and practice nurses in trauma, oncology and a general medical ward.
As planned, the beginner competencies were introduced by the trust on to the new induction programme for new starters and for existing band 2 HCAs on the wards. However, it remained uncertain whether or not the wards had taken up these competencies for their existing band 2 HCAs. The second phase, therefore, involved the following:
-
Checking progress, by repeating interviews with the three members of the trust’s learning and development team.
-
Tracking the take-up of the beginner competencies on the wards for new starters, by including a question on this issue in the follow-up induction survey (see A new health-care assistant induction programme). Respondents were given the options of stating that they had not received the new beginner competencies booklet; had none of their competencies signed-off; had some of their competencies signed off; or had all of their competencies signed off.
-
Examining the impact of beginner competencies for existing band 2 HCAs by repeating interviews in two of the original clinical areas: trauma and the general medical ward. In the former, the ward manager and PDN were interviewed, and in the latter the matron was interviewed. However, it became clear that the beginner competencies had not been effectively implemented. In such circumstances there was seen to be little value in repeating the full phase 1 interview programme, and this aspect of the evaluation focused on how and why beginner competencies for existing band 2 HCAs had not been taken forward at ward level.
Findings
The findings are presented in three parts: the first draws upon the phase 1 data to explore views about how the beginner competencies might be received at ward level; the second examines the survey data on the sign-off of new starter competencies; and the third uses phase 2 data to consider if beginner competencies were taken up, and, if not, what barriers inhibited roll-out.
Views on the planned initiative
The trust-wide beginner competencies were not being introduced onto a ‘blank canvas’. Some wards had already taken steps to develop their own competencies, sensitive to specific clinical needs, but the picture was uneven: one of the three wards covered, trauma, had its own PDN, and HCA starter competencies were already well developed; another, oncology, also had its own PDN and there were plans to introduce ward-based competencies; while the third, the general medical ward, had neither a PDN nor local beginner competencies. Against such a backdrop, a trust-wide initiative was likely to prompt different ward-based responses: in trauma, it was seen as an uncontentious overlay onto its existing system; in the other two it was viewed as more likely to encourage a change in practice.
Indeed, generally, views on the prospect of beginner competencies were mixed. In substantive terms, some welcomed the initiative, and particularly the associated evidence captured by the portfolio, as likely to bring some structure to the development of band 2 HCAs:
It’s something to be welcomed. It will highlight those people that are doing the job to the right level, it will identify training needs for those people that haven’t had the training to do the job, and it will make sure that all of us, whatever level, work to the right job that we're being paid to do.
EC2_ward manager_1
There was caution, suggesting that this approach represented a likely threat, particularly to long-serving HCAs, whose capabilities would have to be (re)assessed and who might perceive themselves as ‘too old’ for further development:
Many of them have been on their job for a very long time and have been doing the same things and treated in the same way for a long time, and it will be terrifying to have to prove what they do.
EC2_ward manager_1
There were also some concerns about process. On the cusp of the trust introducing the initiative, a ward manager expressed considerable uncertainty about how to implement it, while one of the PDNs interviewed claimed to know nothing about it:
I understand the rationale for its introduction, but what I’m not clear about is the implementation, if that’s clear. So I’ve kind of thought, where are we with this now?
EC2_PDN_1
Table 12 draws upon the new induction cohort surveys to highlight progress made on the sign-off of beginner competencies. Clearly, implementation had been problematic. With the follow-up survey administered in May 2013, even those on the last of the inductions (October 2012) should have had the 6 months needed to complete the competencies booklet. It can be seen that only 12%, or 2 of the 17 respondents, had done so, with well over half of the respondents either not having received the booklet or yet to have a single competence signed off.
| Competency status | Follow-up inductees (n = 17) |
|---|---|
| Not received booklet | 29 |
| No competencies signed off | 29 |
| Some competencies signed off | 29 |
| Achieved final sign-off | 12 |
The barriers to rolling out
If rolling out the beginner competencies to inductees had proved difficult, there were grounds for arguing that take-up among existing band 2 HCAs was even slower. This was despite the fact that matrons had been keen to ensure that existing band 2 HCAs were covered by the beginner competencies:
When we spoke to the matrons, they felt that all of their band 2s should be doing those competencies because they’d come at a higher level, they’d not demonstrated competence at the beginner level.
EC2_trust manager_1
There was some uncertainty as to how extensively the beginner competencies had been rolled out to existing HCAs: an attempt by the trust’s learning and development team to check progress, as part of our evaluation, elicited little response from the wards. On the basis of the follow-up interviews, it appeared unlikely that this silence implied compliance: a host of difficulties in implementing the initiative were raised. These difficulties, some of which were foreshadowed in the phase 1 research, were assumed to relate to principle, process and practice:
-
Principle
-
For some, a reliance on competencies for developing, particularly starter, HCAs was flawed, provoking some ‘push back’ at ward level. In part, this stemmed from the task-centred nature of competencies, seen as understating the importance of HCA values and attitudes to care delivery:
-
The difficulty with managing some of these processes is that in many ways what you value most about individuals delivering the kind of job that actually we’re all delivering, it’s adaptability, flexibility, care, compassion, it’s all stuff that is very difficult to measure’ (EC2_matron_2).
-
-
More prosaically, some felt that requiring new starters to acquire a broad range of competencies within 6 months and before probation was completed was ‘quite a tall order’:
-
‘I’m not saying people shouldn’t have the competencies but now there’s competencies for every bit of kit including possibly, you know, a dustpan and brush on the ward nowadays. It’s just overwhelming and people are just becoming stressed-out with what they are expected to achieve and have signed-off’ (EC2_ward manager_3).
-
-
-
Process
-
A variety of process concerns with the beginner competencies were raised. In a large trust, this initiative was one of a number being taken forward at the time, and was seen as ‘lost’ among the others. Indeed, in chasing-up on progress, the learning and development team found that many wards had misunderstood the initiative:
-
‘People thought the competencies were just for new staff’ (EC2_trust manager_4).
-
-
Partly related, given the build-up of initiatives in the trust, some were ‘overwhelmed’ by yet another. More specifically, there were concerns about the paperwork associated with the beginner competencies; as noted, there were 19 such competencies, set out in considerable detail for wards:
-
‘As for the competencies, there’s pages of them; you’ve got to be realistic in terms of what you can expect of them [HCAs] and what you can expect of staff on the ward who are supervising them . . . It’s a sort of monstrous growth industry that is almost becoming unmanageable in terms of volume and complexity’ (EC2_ward manager_3).
-
-
-
Practice
-
Finally, there were perceived practical difficulties in implementing the initiative. The most acute related to finding a supervisor with the time to mentor and sign-off competencies:
-
‘I spoke to somebody who probably attended induction. She was saying that she’s been given somebody as a supervisor but she never works with them; she feels quite upset and wants to leave the ward’ (EC2_trust manager_5).
-
-
In more general terms, concerns were raised about the development of a portfolio of evidence and this was seen as far from straightforward, requiring time and resource from various parties, not least the HCA post-holders themselves:
-
‘It’s a struggle enough to get band 5 nurses to be able to put a portfolio of evidence together’ (EC2_PDN_1).
-
-
Summary
The introduction of band 2 HCA beginner competencies at this trust was designed to pursue a number of objectives. Embedded in a new induction programme and tied to the successful completion of the probationary period, the trust was seeking to strengthen HCA preparation for the performance of their role and provide a clear basis for confirmation in post. As applied to band 2 HCAs already in post, the initiative was aimed at establishing a clear baseline of capability among this part of the workforce, and a platform for its future development. This evaluation has cast considerable doubt on the effective fulfilment of these objectives. The phase 1 data suggested that there was some ward-level support for the initiative, seen as contributing to the more structured development of HCAs. However, concerns were raised, a number of which were borne out when the initiative was rolled-out across the trust.
The survey data cast doubt on the take up of the competencies for inductees even after at least 6 months in the post. The roll-out of the competencies to existing band 2s had also failed to materialise. In terms of our methods, this undermined the value of the planned extended phase 2 interview programme. As a consequence, the evaluation concentrated on evaluating the difficulties faced by the trust in introducing the beginner competencies.
There were general concerns of principle about the use of competencies, inevitably task centred, in developing HCAs. However, many of the difficulties were more prosaically related to process and practice. In process terms, there appeared to have been problems in clearly communicating the coverage of the initiative and its implementation. Alongside a wealth of other trust initiatives, beginner competencies also became ‘lost’, not least because of the paperwork associated with them. In practical terms, concerns about depleted supervisory capacity emerged, inhibiting sign-off of HCA competencies.
A new health-care assistant induction programme
Context
This case evaluated the introduction of a new induction programme for HCAs at a large multisite trust. The new programme was part of a suite of measures adopted by the trust, which included a new approach to recruitment using numeracy and literacy tests along with an assessment centre, and apprenticeship and competency frameworks (see Beginner competencies for band 2 health-care assistants). In the words of the deputy director of nursing, presenting them to the nursing board in November 2011, these measures sought:
To develop a rigorous and comprehensive recruitment and development pathway for [HCAs] that will support our delivery of excellent patient care and uphold trust values.
The previous induction comprised a corporate day plus 3 clinically focused days specifically for HCAs. However, according to the trust’s induction handbook, this programme:
. . . no longer met the needs of the HCAs or the clinical areas and that a more robust and effective programme was required that would benefit patients, individuals and the trust.
As the handbook continued, the previous programme was:
. . . not giving HCAs the opportunity to learn practically those skills needed to fulfil their role.
In seeking to address these concerns, the new induction programme, designed principally by the trust’s support worker training and development team, had four stated aims, to:
-
produce a competency-based induction which provides a platform from which HCAs can grow into highly skilled and knowledgeable practitioners
-
provide an induction which meets the needs of the clinical areas
-
demonstrate that HCAs are valued and to improve staff retention
-
raise care standards which reflect the core values of the trust.
To be held once every 2 months, the new induction was extended to 2 weeks (10 working days including 1 day for the trust induction). It operated on the assumption that entry HCAs would complete the 2 weeks before moving on to their wards, so ensuring that they were ‘safe’ when they did so. The substance of the induction did not change greatly, but clearly participants were to spend longer on topics, with more scope to practice skills, as well as being exposed to a wider range of contributors. The new induction provided for 2 days on different forms of communication; and days respectively on maintaining patients’ hygiene needs, tissue viability, moving and handling, and safeguarding to practice.
In evaluating the new induction programme, the fieldwork mainly focused on aims 2–4, whether or not, and in what sense, they were met.
Methods
The following methods were used to evaluate the new induction programme:
-
Interviews were carried out (December 2012) with three trust training and development leads responsible for design and delivery of the new programme before it started and then after it had been operating for approximately 1 year (May 2013).
-
Interviews were also conducted 6 months later (May 2013) with two ward managers and PDNs on different trust sites and in different clinical areas, inter alia to gather their views on the new induction.
-
A focus group was held for HCAs (n = 17) on attending the final 5-day induction in January 2012, prior to the introduction of the new 2-week programme.
-
A survey was administered to four cohorts of HCA inductees. The first of these cohorts (cohort 1) comprised those participating in the final 5-day induction in January 2012. The succeeding three cohorts (cohorts 2–4) covered those HCAs involved in the new, 2-week programmes run during May, July and October 2012. Each of these four cohorts was surveyed twice: initially to generate baseline data (on the final day when they had completed their induction) and then following up at the end of 2012 (see Appendix 8 for baseline questionnaire). It was hoped that the impact of the new induction might be revealed by attitudinal and behavioural differences between the old and the new induction cohorts.
The surveys sought data on personal characteristics of the HCA inductees and on their work histories and qualifications. A number of survey measures were connected to the trust aims of the new induction (see Appendix 9 for scale mean scores). These included:
-
an intention-to-leave scale (aim 3)
-
an explicit evaluation of the induction programme (baseline) and its value once in post (follow-up survey) (aims 2 and 4)
-
a clinical confidence scale, dealing with the confidence of the respondent to perform various clinical tasks (aims 2 and 4)
-
a psychological contract scale asking respondents what they felt the trust ‘owed’ them (baseline) and whether or not the trust had delivered (follow-up) (aim 3)
-
a job satisfaction scale (aim 3)
-
a motivation scale (aim 3)
-
a caring behaviour scale (aims 2 and 4).
Table 13 presents the survey responses by cohort and baseline/follow-up. The numbers attending induction were between 14 and 27, and, with some turnover among HCAs, the numbers responding to the follow-up survey were particularly small. For analytical purposes, the three new induction cohorts (2–4) were combined, but with only four of the old induction (cohort 1) responding to the follow-up survey, the value of comparing the new and old induction cohorts was substantially weakened.
| Cohort | Baseline (2012) | Follow-up (2013) | ||||
|---|---|---|---|---|---|---|
| Sample (n) | Respondents (n) | Response (%) | Sample (n) | Respondents (n) | Response (%) | |
| 1 | 27 | 17 | 63 | 8 | 4 | 50 |
| 2 | 14 | 12 | 86 | 9 | 3 | 33 |
| 3 | 19 | 17 | 89 | 16 | 7 | 47 |
| 4 | 25 | 17 | 53 | 16 | 7 | 44 |
Table 14 provides a profile of the old induction cohort (1) and the combined new induction cohorts (2–4). It is clear that the old and the new induction cohorts differ in important respects: the old induction cohort tends towards being more ethnically diverse, younger and with fewer domestic responsibilities than the new induction cohorts. Perhaps most striking is the fact that the old induction cohort comprised HCAs with a higher level of formal education than the new induction cohorts: almost three-quarters of cohort 1 were graduates or postgraduates compared with one-third of cohorts 2–4. There are grounds for arguing that cohort 1 was less typical of the HCA intake at the trust than the cohorts 3–4. Indeed, survey data on the background of HCAs from this trust, generated during an earlier research project,1 indicated that the cohort 2–4 profile was much more typical than that of cohort 1. Certainly, the distinctive character of cohort 1 suggests that the survey data should be treated with care (see Table 14).
| Background | Baseline (2012) | |
|---|---|---|
| Cohort 1 (n = 17) | Cohorts 2–4 (n = 46) | |
| Age: < 30 years | 81 | 49a |
| Female | 71 | 87 |
| Ethnicity: BME | 44 | 28 |
| Married or with long-term partner | 50 | 67 |
| Children | 25 | 47 |
| Sole or main income earner | 40 | 33 |
| Attended local primary school | 29 | 40 |
| Graduate/postgraduate qualification | 73 | 33b |
Findings
The findings are presented in two main parts. The first concentrates on the survey results and the second draws upon the focus group and interview material to interpret and add insight to the survey data.
In general terms, the survey data suggest that the new induction had essentially failed to meet its stated aims, not least reflected in the pattern of attitudinal and behavioural responses from the old induction cohort and the new induction cohorts.
Table 15 presents the survey results on how HCAs directly viewed the induction (baseline survey) and how useful the induction proved to be once they had settled down on their wards (follow-up survey). If anything, the old induction cohort are more positive about their induction programme than the new induction cohorts are about theirs. For example, the baseline surveys indicate that despite the new induction programme being a week longer than the old, under half (41%) of the latter ‘strongly agree’ that they were given enough time to ask questions, compared with one-third of the former (65%). The follow-up surveys reveal no differences between the old and new induction in providing HCAs with requisite skills and knowledge; indeed, in both groups only around one-quarter suggested that induction is effective in these terms.
| Features of induction | Baseline (2012) | Follow-up (2013) | ||
|---|---|---|---|---|
| Cohort 1 (n = 17) | Cohorts 2–4 (n = 46) | Cohort 1 (n = 4) | Cohorts 2–4 (n = 17) | |
| The induction programme covered the topics I needed to learn about | 29 | 24 | – | – |
| The language used in the induction sessions was easy to understand | 53 | 35 | – | – |
| The general atmosphere during the induction programme helped me to learn | 18 | 35 | – | – |
| Information was clearly presented during each of the sessions | 47 | 26 | – | – |
| Enough time was given to each topic | 35 | 26 | – | – |
| I was given enough time to ask any questions I had | 65 | 41 | – | – |
| Following induction, I clearly understand the role of the CSW at this trust | 47 | 35 | – | – |
| The induction programme provided me with the skills I needed | – | – | 25 | 18 |
| The induction programme provided me with the confidence I needed | – | – | 0 | 18 |
| The induction programme provided me with the knowledge I needed | – | – | 25 | 25 |
| The induction programme helped me to do my job better | – | – | 25 | 24 |
Table 16 sets out HCA confidence in performing a range of clinical tasks, immediately on completion of the induction (baseline) and after being on the ward for some time (follow-up). On some tasks the new induction cohorts (2–4) were more confident than the old cohort (1) at the conclusion of the induction programme (baseline): most of the former (89%) agree that they were confident in recording a patient’s fluid intake, while fewer than three-quarters of the latter were similarly confident. However, on other tasks, such as assessing a patient’s nutritional status, the old induction cohort was more confident than the new, and in general there were few noteworthy differences between the cohorts. Indeed, on settling into their wards (follow-up), confidence was very similar between the cohorts (with the exception of vital signs where, against expectation, the old induction cohort was more confident than the new).
| Task | Baseline (2012) | Follow-up (2013) | ||
|---|---|---|---|---|
| Cohort 1 (n = 17) | Cohorts 2–4 (n = 46) | Cohort 1 (n = 4) | Cohorts 2–4 (n = 17) | |
| Assessing skin integrity of a patient | 82 | 78 | 75 | 100 |
| Recording a patient’s vital signs | 71 | 67 | 100 | 56 |
| Recording a patient’s fluid intake | 71 | 89 | 75 | 94 |
| Assessing a patient’s nutritional status | 82 | 76 | 75 | 81 |
| Effectively communicating with a patient | 94 | 98 | 100 | 100 |
| Assisting a patient to meet hygiene needs | 88 | 94 | 100 | 100 |
| Identifying if a patient is in poorly controlled pain | 65 | 65 | 100 | 94 |
| Assisting a patient to mobilise | 94 | 91 | 100 | 100 |
Finally, the survey data cast doubt on the capacity of the new induction to improve staff retention and signal the value placed by the trust on HCAs. Turnover was much higher among the old induction cohort (1) than the new (2–4). Exactly half of cohort 1 had left the trust by the time of the follow-up survey, while most of the new induction cohorts were still in place (75% or more). However, as Table 17 indicates (follow-up survey), cohort 1 were much more likely than cohorts 2–4 to feel that the trust had delivered on what they ‘owed’ employees. Both new and old induction cohorts had similar expectations about what the trust ‘owed’ them at the outset (baseline survey) but it can be seen, for example, that while exactly half (50%) of the old induction cohort felt that the trust had delivered on ‘training to my job’ to a ‘very great extent’, the equivalent figure for the new induction cohort was under one-third (31%).
| Feature of the psychological contract | Baseline (2012)a | Follow-up (2013)b | ||
|---|---|---|---|---|
| Cohort 1 (n = 17) | Cohorts 2–4 (n = 46) | Cohort 1 (n = 4) | Cohorts 2–4 (n = 17) | |
| Career advancement | 25 (41) | 30 (33) | 0 | 13 |
| Long-term job security | 24 (47) | 39 (44) | 25 | 38 |
| Good career prospects | 29 (53) | 37 (38) | 50 | 25 |
| Support with any personal problems | 29 (24) | 17 (15) | 0 | 13 |
| Up-to-date training and development | 71 (82) | 61 (60) | 50 | 38 |
| Policies/procedures that help me do my job | 65 (71) | 63 (58) | 50 | 19 |
| Training to do my job | 71 (82) | 70 (63) | 50 | 31 |
| Support when I want to learn new skills | 53 (77) | 57 (48) | 50 | 13 |
| Fair pay for the responsibilities in my job | 65 (82) | 57 (57) | 25 | 38 |
| Constructive feedback on my performance | 44 (88) | 50 (57c) | 25 | 13 |
In suggesting that the new induction had not had the expected impact, the survey findings need to be treated with care. As implied, the striking differences in the background profiles between the old and new induction cohorts might have confounded the impact of any change in the design in the programme. There were, however, other indications, drawn from the qualitative data, that the new induction was not meeting trust objectives:
-
Timing. The trust’s intention to ensure that HCAs attended induction before moving on to the wards was not met. Certainly, a higher proportion of those on the new induction than on the old induction had not yet been on the wards, but in two of the former cohorts half of the participants had already been working on their wards. This was seen as partly related to the timing of the inductions, held every other month; if newly appointed HCAs had just missed an induction, it was a long wait until the next one. There were also suggestions that the HR function had not always been timely in providing new HCAs with their joining instructions.
-
Length. A 2-week induction took HCAs away from the ward for what was perceived, particularly by ward managers, as too long a time: this not only had staffing implications but was costly for wards already paying those HCAs attending the induction.
-
Coverage. There were concerns, again expressed by ward managers, about the content of the programme and the failure to cover what they viewed as some essential aspects of care, such as life-support training. Moreover, some ward managers felt that the coverage of the programme was not sensitive enough to their specific needs:
-
‘Trauma [manager] felt that their [HCAs] don’t do observations so they shouldn’t have to attend, but I did clarify that they didn’t have to attend that session . . . Neuro [manager] felt that they wanted information about setting up a bed space’ (EC3_trust manager_4).
-
These concerns were raised despite an extensive trust consultation on the design of the new induction programme. However, this consultation mainly involved matrons rather than ward managers, the workplace needs of the latter perhaps not directly informing the process. There were also some genuine dilemmas faced by the trust in developing a 2-week induction. There might well be calls for a more regular induction, but a longer induction is inevitably resource intensive and requires considerable organisational effort, not easily managed in a busy trust. Moreover, wards might well want their HCAs on the wards as soon as possible, but they also want them on the wards ‘safe’, arguably requiring a thorough induction.
Summary
A more robust induction for HCAs, better preparing them for their role before they ‘hit the ward’, has increasingly been seen by trusts as a means of ensuring and improving care quality standards, not least given considerable unevenness in the skills and experience of those taking up the post. This evaluation of a 2-week HCA induction, introduced by a trust to replace a 1-week induction, suggests the need for some sensitivity to the challenges faced in adopting such an approach. The evaluation casts some doubt on whether or not the trust aims for the new induction were met: many HCAs had started working on the wards before completing the induction; some clinical areas felt that the new induction was not meeting their needs; and, while the survey data must be treated with care, attitudinal and behavioural responses from HCAs attending the old and the new induction were not compatible with the increased efficacy of the latter. It is not being suggested that a 2-week induction is invariably problematic. However, in setting one up, organisational issues have to be managed: for example, the contributors/presenters must show ongoing commitment; HR must provide timely joining instructions; and the ‘right’ people need to be consulted on the design of the programme. Some ‘hard’ choices need to made about the purpose of the induction; if wards want ‘safe’ HCAs at the outset, a long induction might well be needed, which takes time and resources to organise and, therefore, might not be as frequent as desired and might also take HCAs away from the wards for longer than is ideal.
The development of maternity care assistants
Context
The primary focus of this evaluation was a 9-month accelerated development programme (ADP) for MCAs at a two-site trust in the south of England. This programme, however, was embedded in a broader organisational change initiative centred on the trust’s maternity services, with implications for how the evaluation was conducted and the issues captured by it. Responsible for over 6000 births, the trust provided a hospital-based maternity service – comprising a 16-bedded central delivery suite (CDS), two postnatal wards with a total of 55 beds, an antenatal ward and a 24-hour antenatal assessment unit – and a community-wide service. The change initiative was essentially directed at the hospital’s CDS and its community service. In both service areas, the change rested on a radical shift in skill mix, MCA numbers increasing as the number of band 7 registered midwives fell. In the CDS, the number of whole-time equivalent (WTE) MCAs increased from 12 to 19, as WTE midwives dropped by three. In the community, the number of WTE band 7 midwives went down from 35 to 10, with WTE MCAs rising from 6 to 18.
In the community, this shift in skill mix was part of a major restructuring of the service. Formerly attached to GP surgeries, the trust’s community midwives had traditionally worked as lone, semiautonomous practitioners with their own caseload of between 80 and 100 pregnant women. The reorganisation created 10 area teams, with each managed by a band 7 registered midwife and staffed by four WTE band 6 midwives and two MCAs. The respective teams were designed to work in a more corporate fashion, responsible for around 400 pregnant women, dealt with and managed jointly by team members. The former band 7 community midwives were eligible to apply for one of the new band 7 team leader posts. The unsuccessful candidates and those choosing not to apply were downgraded to a band 6 post, albeit with protected pay and conditions for a period of 5 years. The reorganisation in the CDS and the community service were predicated not only on the use of a higher number of MCAs, but also on an extension of the MCA role to take on more tasks from the midwives, those so doing becoming band 3 MCAs. The accelerated MCA development programme was introduced to bring the band 2 MCAs up to a band 3 level.
The ADP was delivered on the basis of a partnership between the trust’s maternity services and HR directorate’s learning and research function. From the former, the deputy director of midwifery in post when the programme started played the lead role in the development of the programme, while from the latter a vocational team leader was centrally involved.
The ADP began in October 2011 and was characterised by the following features:
-
It was an apprenticeship accredited by City and Guilds, London.
-
In line with the standard apprenticeship programme, it comprised:
-
functional skills
-
generic modules (delivered by the learning and research department)
-
specialist modules (delivered by the maternity department)
-
the acquisition of relevant competencies (developed and signed off at ward and team levels).
-
-
It was designed to be completed in 9 months, compared with the 18 months usually taken by participants.
-
The intake was 15 MCAs, made up mainly of band 2s from within the trust but also of new external candidates.
-
An upgrading for band 2 to 3 MCAs on completion of the programme.
-
Study time of 2 or 3 days per month.
-
Candidates were expected to complete in the summer of 2012.
The close relationship between the ADP and the reorganisation of maternity services impacted on our evaluation in various ways. First, it was difficult to disentangle engagement with, and perceptions of, the ADP from the changes associated with the broader reorganisation of the CDS and community service. Second, this close relationship influenced the nature of the evaluation. Ostensibly, interest remained centred on the ADP: how its delivery was viewed and experienced, and how participants fared. However, closely related was a concern with the development the MCA role – whether or not, as envisaged, it had extended to allow MCAs to take on tasks from registered midwives.
Methods
The evaluation was conducted in two phases, which involved the following:
-
Phase 1: Spring 2012 (around half way through the ADP)
-
Interviews with 14 managers, midwives and MCAs plus a focus group involving eight MCAs.
-
A department-wide survey of midwives and MCAs with an overall response rate of 55% (midwives 54%, n = 117; and MCAs 58%, n = 41; see Appendix 10 for the phase 1 questionnaire). This survey was designed to collect baseline data in relation to a number of variables, for example job satisfaction, work pressure and perceived control, with a view to assessing whether or not these had changed following the assumed completion of the ADP and the emergence of the band 3 role.
-
-
Phase 2: May 2013 (after the ADP was due for completion)
-
Eighteen follow-up interviews with managers, midwives and MCAs (six of the MCAs were involved in both phases of the research).
-
A follow-up survey of midwives and MCAs with an overall response rate of 56% (midwives 52%, n = 114; and MCAs 63%, n = 53). Data tracking of the progress made by the ADP cohort of MCAs.
-
As part of the second phase follow-up research, interviewees were asked about developments subsequent to the first phase fieldwork, which might form a backdrop to views on the ADP programme and the role of the MCAs. Two such developments were worth noting. First, the deputy of midwifery services leading the reorganisation had left the trust. Second, concerns and misunderstandings had arisen about the pay protection arrangements as part of the reorganisation. Given the stress generated by the reorganisation (see Phase 1: the reorganisation, below). The departure of the deputy chief midwife might well be seen to have diffused certain tensions. The concerns associated with pay protection might well have created new ones.
Findings
Phase 1: the reorganisation
The ADP was embedded in a change of skill mix, as numbers of band 7 midwives were reduced and band 3 MCAs increased within the context of a broader reorganisation of community maternity services. These changes generated considerable concerns among midwives, a number of whom had been downgraded. Despite the pay protection, this downgrading was seen to impact on the midwives’ identity and status:
The identity thing’s really important. I remember walking into this building for a quiz night that they were running, and one of the band 7s who had been demoted to a band 6, those were her words. It is like bereavement: when someone’s died and you’ve had to tell a new person for the first time again. They had to go through that cycle of telling everybody again for the first time what their new role was.
EC4_trust manager_6
Such concerns were deepened by a feeling that the changes were designed to save costs, with the development of the MCA within the context of the ADP presented in these terms. More profoundly, there was unease at the development of an extended MCA role. The MCA role at the trust had traditionally been fairly evenly split between a focus on patient care and clerical work. For the midwife, an extended MCA role was often presented by department management as a means of relieving midwives of certain burdens, perhaps related to paperwork. This would ‘free’ them up to concentrate on their direct relationship with ‘mums’, although, for the MCA, such a shift was not necessarily as well received. As an MCA responding to the survey noted:
Sadly my role as an MCA has changed vastly . . . The majority of my time is spent being at the desk inputting patients, which the midwives do not have time to do. This leaves little for patient care.
EC4_MCA_survey
However, for the midwives, the concerns were in the other direction, revolving around the capacity of MCAs to take on more complex clinical tasks:
I am very concerned about the MCA role in the community – taking over important midwives [sic] roles with insufficient training to be fully competent.
EC4_Midwife_survey
Phase 1: the accelerated development programme
Around halfway through the ADP, views on the delivery of the programme were mixed. Delivery of the different components of the programme had fared unevenly. The mandatory training modules delivered through the learning and research department were perceived by MCAs to have been accessible, timely and effective. However, the specialist modules proved problematic, with the maternity department being unable to resource them.
Views on progress at this stage of the programme were also varied. While management remained fairly confident of timely completion, the MCAs themselves expressed greater concern:
I think everyone’s behind.
EC4_MCA_focus group
The problems were partly related to juggling the intensive study needed with work and domestic responsibilities:
If you’ve got families and you work full time and you’re so busy at work, I don’t know where you’re going to fit it all in.
EC4_MCA_focus group
There were more specific concerns about the level of support at workplace level, particularly revolving around the MCAs’ relationship with their mentor, crucial in assessment and sign-off of competencies. For a number of the MCAs, finding time to spend with mentors, whether due to workplace pressures or simply due to differences in rostering, proved difficult.
Phase 2: the accelerated development programme
Table 18 presents MCA progress by phase 2, and reveals that only 4 of the 15 MCA starters on the ADP had completed in a timely fashion. Another five MCAs (one of whom had since left the trust) who had completed 75% or more of their modules were thought likely to complete, albeit at ‘best’ 18 months after the start of the 9-month programme, while five of the participants had been classified as ‘drifters’ (< 75% complete), were not up to date with their modules and were thought to have little prospect of completing in the foreseeable future. It is striking that the completing MCAs were markedly older than the drifters and likely completers. The four oldest MCAs on the ADP, who were in their forties and late thirties, were the timely completers; it is possible that they had grown-up children and, therefore, fewer domestic responsibilities to manage alongside the training.
| MCA | Course completion (%) | Length of service as MCA (months) | Maternity workplace | Age (years) |
|---|---|---|---|---|
| 1 | 100 | 18 | Community | 40 |
| 2 | < 75 | 3 | Community | 27 |
| 3 | < 75 | 40 | Community | 32 |
| 4 | < 75 | 40 | Community | 32 |
| 5 | 90 | 4 | Hospital | 21 |
| 6 | 100 | 1 | Hospital | 49 |
| 7 | < 75 | 1 | Hospital | 36 |
| 8 | 85 | 3 | Hospital | 23 |
| 9 | Resigned | 2 | Community | 20 |
| 10 | 75 | 7 | Community | 20 |
| 11 | 100 | 24 | Community | 48 |
| 12 | 100 | 12 | Community | 37 |
| 13 | 75 | 1 | Hospital | 22 |
| 14 | 90 | 3 | Community | 22 |
| 15 | < 75 | 12 | Hospital | 22 |
With a timely ADP completion rate of less than one-quarter, concerns raised by MCAs during phase 1 about its tardy progress appeared to be well founded. In the wake of this outcome, there was some debate between trust stakeholders from the learning and development department and the maternity services about the time frame for the programme. For example, learning and research suggested a commitment, which they met, to deliver the mandatory modules in 9 months, rather than the complete apprenticeship programme. Certainly, the difficulties associated with workplace learning, assessment and competence sign-off were reiterated, particularly by the MCAs. More specifically, a number of points were raised by MCA participants on the nature of the programme:
-
The relationship between the MCA and their assessor or mentor, usually a registered midwife within their team, was crucial to progress made on the ADP: assessors supported workplace learning and signed off competencies. In some cases this relationship was effective, but more typically, MCAs found it difficult to maintain contact and work with their assessor:
-
‘My first mentor was a band 7 midwife and she just didn’t have time at all and I don’t think we both understood how much work had to go into it from my side and hers’ (EC4_MCA_5).
-
-
MCAs faced intense pressures while participating in the programme, particularly given the limited study time:
-
‘It was very unrealistic in the first place. They were panicking to get us qualified within a certain amount of time which personally I don’t think worked because it just put a lot of people under a lot of pressure’ (EC4_MCA_9).
-
-
There were questions raised by MCAs about the relevance of certain modules:
-
‘I don’t think they adapted or even actually set up the delivery of the education and of the units from a maternity point of view’ (EC4_MCA_9).
-
-
MCAs were also concerned about the delays caused by the need for some MCAs to acquire functional skills:
-
‘If we would have done the diploma bit straight off and carried it on while we were doing the key [functional] skills, it would have been much easier’ (EC4_MCA_17).
-
Phase 2: reorganisation and the extended maternity care assistant role
It has been stressed that the ADP was not an end in its own right but a means to extending the MCA role in the context of skill-mix dilution. Given the low completion rate on the ADP, questions were inevitably raised about whether or not this affected the efficacy of the change in skill mix and the broader reorganisation of maternity services at the trust. There were strong grounds for arguing that ADP completion was not the sole determinant of MCA role extension. Informally, there appeared to have been some MCA ‘task creep’ as MCAs progressed through the ADP and had competencies signed off, allowing them to extend their role:
Not a huge amount has changed in my clinical skills other than I was doing it before but then obviously I’ve got more competencies: baby screening, neonatal screening, that’s the heel prick test. I’ve been doing those really since I started, but that was part of the course as well as.
EC4_MCA_9
I felt like I was doing what I already was doing because when I agreed to do the course, my assessor got me going straightaway. So as soon as I started I was doing blood pressures and taking blood, so my role hasn’t really changed that much I don’t think.
EC4_MCA_17
However, phase 1 and 2 survey data throw some light on whether or not the MCA band 3 role had been accepted and settled down, and, more generally, whether or not MCAs and midwives were recovering from the reorganisation. Table 19 presents the survey findings broken down by results for midwives and MCAs.
| Scale | Midwife | MCA | Contrastsa | ||
|---|---|---|---|---|---|
| 2012: A | 2013: B | 2012: C | 2013: D | ||
| MCA evaluation | – | 3.14 | – | 3.43 | D > B |
| MCA role extension | 2.89 | 3.04 | 3.50 | 3.61 | C > A; D > B |
| Quality of patient care | 2.75 | 3.01 | 3.32 | 3.74 | C > A; D > B; D > C |
| Motivation at work | 3.75 | 3.70 | 3.95 | 3.91 | – |
| Perceived control | 3.46 | 3.52 | 3.44 | 3.46 | – |
| Work pressure | 3.74 | 3.51 | 3.19 | 2.92 | A > C; B > D; A > B |
| Managerial support | 3.42 | 3.75 | 3.83 | 3.87 | C > A; A > B |
| Team member tensions | 2.94 | 2.76 | 2.76 | 2.74 | – |
| Job satisfaction | 2.81 | 3.04 | 3.49 | 3.53 | C > A; D > B |
| Intention to leave | 2.42 | 2.43 | 2.00 | 2.09 | A > C |
A number of features stand out from this table:
-
Two scales explored how well the MCA band 3 had settled down: an MCA evaluation scale used in the follow-up survey examined whether or not over the last 12 months MCAs had taken on more tasks and become more confident in doing so; and an MCA role extension role scale, used in both surveys to explore the scope for the MCAs to take on more tasks. Table 19 suggests that, on both scales, MCAs were significantly more positive than midwives about how effectively their role had developed.
-
At phase 2, midwives were more neutral and less negative than previously about the new MCA role, although this was not a statistically significant improvement (3.04 compared with 2.89 at phase 1).
-
On general attitudes to work and employment, MCAs were more positive than midwives at both phases. For example, in both surveys MCAs had higher levels of job satisfaction and perceived less work pressure than midwives.
-
However, midwife attitudes to work and employment had improved between the two phases: for instance, the mean score for work pressure had decreased from 3.74 to 3.51, while the mean score for managerial support had significantly increased. Indeed, while in the first survey midwives were more likely to leave the trust than MCAs, in the second there was no statistically significant difference between the two groups.
-
Again, MCAs were significantly more positive about patient care quality than midwives in both surveys. However, there had also been notable changes in perceptions between the surveys. In particular, the mean score for MCAs on quality of patient care was significantly higher in 2013 (3.74) than in 2012 (3.32). The score for midwives had also increased, but this was not statistically significant and therefore must be treated with caution.
A more positive view about the MCA role, particularly among midwives, should not, however, detract from the ongoing debate and uncertainty around the MCA role extension. In part, this was reflected in tensions about whether or not MCAs should perform certain tasks, such as the resuscitation of babies. It was also apparent in the inappropriate delegation of tasks by midwives to MCAs:
There have been times where I’ve needed to remind the midwives about their professional boundaries and their rules and regulations and, you know, that is a midwife’s responsibility, not a maternity care assistant’s.
EC4_trust manager_2
Summary
This evaluation has been complex, comprising a number of threads. Principally, the focus was on a trust’s ADP for band 2 MCAs, fast-tracking them to band 3. The programme was, however, seen as intimately related to a broader reorganisation of the trust’s maternity services, in part predicated on a shift in skill mix as band 3 MCAs increased and replaced a diminishing number of band 7 midwives, and also to a significant change in work organisation, especially on the community side. The evaluation of the ADP has, as a consequence, inevitably involved some assessment of an extended MCA role within the context of organisational change.
In seeking to deliver apprenticeship training to band 2 MCAs in a 9-month period, the ADP met with only limited success: only 4 participants out of 15 completed the programme in a timely way. The stresses faced by MCAs in undertaking the programme were flagged up during phase 1 fieldwork and, given phase 2 outcomes, these concerns were clearly well founded. MCAs faced major difficulties in completing the programme in 9 months given the need to juggle work, domestic and learning pressures. Crucially, many MCAs also had difficulties in developing a relationship with their mentor, an aspect important to the workplace learning and competency sign-off underpinning the programme.
Against the backdrop of these findings, it is intriguing to note that between phases 1 and 2 the MCA role de facto appeared to have extended and increasingly been accepted, especially by midwives. This found some support in the survey data, indicated by higher means scores on the MCA evaluation scale among both midwives and MCAs between the two surveys. Indeed, MCA perceptions of patient care quality were significantly higher between the two surveys. It might also be argued that, even if they did not complete the ADP on time, many MCA trainees were iteratively acquiring competencies and developing capabilities through workplace learning, allowing them to push role boundaries. In short, cumulative workplace learning and skills acquisition might have played a more important part in MCA role extension than formal completion of the ADP programme.
The administration of medicine by assistant practitioners
Context
This case focuses on the evaluation of a trust’s proposal to extend the administration of medicines to APs at pay band 4. The development of the AP role in this way has attracted increasing attention across the NHS. 53 There have, however, been few detailed cases exploring such an initiative: how it has been viewed by various stakeholders and taken forward within a particular organisational context. Indeed, the nature of this evaluation shifted over the period of the project in response to changing contextual circumstances. At the outset, with much of the trust preparation for implementation apparently complete, the intention was to conduct a before-and-after evaluation of a 6-month pilot involving the sign-off of relevant competencies and the administration of a specified list of drugs by APs. However, clinical governance issues arose which delayed the pilot by almost 1 year, encouraging a more detailed consideration of the design and implementation of the initiative and how various stakeholders viewed it.
The medicines management (MM) initiative can be related to the broader development of the AP role at the trust. The role had first emerged in 2005 somewhat opportunistically as the trust drew upon SHA financial support for AP training. The role was then taken up widely across the trust – with 100 APs in post and a further 70 in training by 2013 – and on the basis of a more strategic approach. Thus, the trust envisaged the AP role gradually extending over the years to take on more tasks, with the MM by post-holders being part of this planned process.
A new build on the trust’s main site gave added impetus to the development of the AP role. With 75% single-room occupancy and an absence of central ward stations, this new building had major implications for the delivery of nursing care and skill mix. RNs would be less able to take responsibility for a bay of patients, instead becoming central co-ordinators of care directly delivered by non-registered staff. The AP MM pilot was, therefore, important to the trust in preparing for the transfer of many of its services to a new building.
The MM pilot comprised the following six elements:
-
selection of a given range of drugs (n = 8):
-
oral paracetamol
-
oral codeine
-
oral ibruprofen
-
intravenous paracetamol
-
subcutaneous enoxaparin
-
intravenous venfor
-
intravenous tinzaparin
-
intraperitoneal heparin
-
-
administered by APs in specified clinical areas:
-
medicine: accident and emergency and acute assessment unit (AAU)
-
surgery: day surgery, recovery and urology
-
renal: dialysis unit and home team
-
-
identification of 12 APs from these clinical areas to take part
-
a period of training for the APs, made up of 3 days’ dedicated ‘classroom’ training on aspects of MM, completion of the online package dealing with the theoretical aspects of MM and a test of the APs’ calculative skills
-
post training, the formulation of an individual action plan for the acquisition of the relevant competencies and their sign-off at ward level
-
development of standard operating procedures (SOPs) for the administration of the relevant drugs.
As the evaluation fieldwork began, the first four elements had been completed with an expectation that the SOPs would shortly be in place. In the event, agreeing and signing off the SOPs proved difficult, delaying the start of the pilot.
Methods
The fieldwork was designed to take place in two phases. The first phase, conducted during March–May 2012, with the MM pilot still on schedule, involved:
-
An AP focus group including eight of those involved in the pilot.
-
Interviews with 19 staff, covering those with a stake in the initiative, including six APs, five ward managers, three RNs and five senior managers.
-
A survey of band 4 to 7 nursing staff in four clinical areas (with a response rate of 43%; n = 65; see Appendix 11 for the questionnaire): renal, the AAU and a control ward not part of the pilot. The survey asked three sets of questions related to preparation for the initiative, its perceived impact on nurses and its impact on care quality.
The second phase, conducted during March–April 2013, was more limited. The pilot had not started as planned and it was therefore decided to evaluate the design and implementation of the initiative and how different stakeholders viewed it. Twelve interviews were completed: two APs, four ward managers, and six senior managers including those from nursing, HR and pharmacy (eight of these interviewees had been involved in the phase 1 fieldwork).
The findings are presented in three parts: the first (drawing mainly upon phase 1 interview data) evaluates stakeholder views about the drivers and rationale for the MM initiative; the second (based on phase 1 and 2 interview data and the phase 1 survey) evaluates the design and implementation of the pilot; and the third (mainly based on phase 1 survey and interview data) evaluates views on the nature of the initiative, and particularly its perceived impact on various stakeholders and outcomes.
Findings
Drivers and rationale
As was the case in many trusts, the effective use of APs was seen by matrons and ward managers as resting on their capacity to administer medicines. This was especially the case where APs were replacing RNs:
The biggest thing that will help wards to develop the band 4 role and identify where they can release some band 5 roles, is band 4s being able do some drugs. That ‘these people are no good to me if they can’t do drugs’, is what I’m often being quoted by ward managers.
EC5_trust manager_6
However, MM at the trust assumed a distinctive form within the context of the new build, where it was associated with a major future restructuring of the nursing workforce. While this restructuring was associated with a change in the mode of care delivery, it also involved a dilution in skill mix as APs replaced nurses, encouraging many at ward level to equate the MM initiative with cost-saving:
They’re trying to save money, if I’m being truthful, they’re trying to get us to almost be what the band 5s are doing and it’ll be cheaper in the long run because they’re paying us less.
EC5_AP_6
At the same time, it was hoped that the administration of medicine by APs would positively impact on care quality. As APs administered medicines, nurses would be ‘freed up’ to concentrate on other essential (patient-centred) tasks. More directly, it was felt that, in administering medicine, APs might be in a position to ensure greater continuity of care, able to deliver certain drugs without the need to call on nurses.
Design and implementation
While closely associated with top-down, strategic developments at the trust, the MM pilot was informed by ‘bottom-up’ input. Clinical areas were asked to volunteer for participation in the pilot and identify a limited number of drugs that might usefully and viably be administered by APs in those areas. The design and implementation of the initiative then comprised three main elements. The first design feature was the formal training of the APs to administer drugs. This was positively viewed by both nurse managers and APs:
The training they did was extremely good and I think it was probably more thorough than a lot of the registered nurses get. So I think from that perspective, they came out feeling confident.
EC5_ward manager_2
These positive views should not, however, detract from residual concerns, particularly among nurses, about the level of AP preparation. Drawing on the survey data, Table 20 indicates that under one-quarter (22%) of nurses were confident about AP preparation to administer drugs, with only just over one-quarter (28%) agreeing that APs were clear about their responsibilities in this respect.
| Statement | APs | Nurses | ||||
|---|---|---|---|---|---|---|
| Disagree | Neutral | Agree | Disagree | Neutral | Agree | |
| I am confident that APs have been well prepared to administer medication | 14 | 29 | 57 | 41 | 37 | 22 |
| APs on my ward/unit are clear about their responsibilities for administering medication | 0 | 43 | 57 | 39 | 33 | 28 |
The second design feature related to the management of the clinical governance issues associated with the administration of medicine by APs. While this initiative was nursing led, its approval lay within the trust’s medicine governance process and heavily rested on the involvement of the pharmacy directorate:
The real challenge has not been with guidelines or the law or anything, it’s been convincing our pharmacy colleagues and our medicines governance process, that this is OK.
EC5_trust manager_11
The trust’s medicine governance committee (MGC), chaired by the trust’s principal pharmacist (service development), was central to ratifying the principle and detail of the MM initiative. This committee had called for the pilot as a prelude to rolling out MM by APs across the trust, and had called for the use of SOPs to underpin this process. It was difficulty in formulating and signing off the SOPs that delayed the pilot. While views varied on the source and nature of these difficulties, in substantive terms they mainly centred on the form assumed by the SOPs. Nursing and HR were seeking generic SOPs, based on the three main routes of administration – oral, subcutaneous and intramuscular – while pharmacy remained committed to more detailed SOPs, sensitive to each particular drug and the clinical area in which it would be administered.
The third design element more generally related to preparation for the initiative within the selected clinical areas. Certainly, there were some concerns among APs about the level of the support they would receive in preparing for MM from their colleagues, especially in terms of the requisite workplace supervision and sign-off of competencies:
This ward is so busy we just don’t get the time and the backup which we need quite often to do the medicine management and the additional roles.
EC5_AP_7
In more general terms, there was uncertainty about how clearly the MM initiative had been communicated. As the survey indicated (Table 21), only just over one-quarter (29%) of APs agreed that the initiative had been clearly explained to them and were clear about how it would work on their wards. This perceived lack of clarity was even more striking among nurses, with very few (13%) agreeing that it had been clearly explained to them.
| Statement | APs | Nurses | ||||
|---|---|---|---|---|---|---|
| Disagree | Neutral | Agree | Disagree | Neutral | Agree | |
| The role of an AP administering medication has been clearly explained to me | 43 | 29 | 29 | 70 | 17 | 13 |
| I am clear about how the role of an AP administering medication will work on my ward/unit | 43 | 29 | 29 | 63 | 22 | 15 |
Perceived impact
Perceived impact was evaluated by reference to different stakeholders: APs, nurses and patients. While in general APs welcomed the opportunity to administer medicine in broadening their work remit, there were a number of residual concerns:
-
Unwanted responsibilities. Some APs felt that administering medicine would fundamentally alter their role, undermining their preference to deliver close and sustained direct care. One AP stressed that she had not undertaken nurse training for fear that the drugs administration would undermine her scope to give direct care, and yet now as an AP she was being drawn into this very activity.
-
Ambiguity. APs felt that, in administering medicines, they would be placed in a somewhat ambiguous position, vulnerable to being ‘dragged’ in different directions. Continuing to count as unregistered members of the staff team, but with responsibilities significantly overlapping with those of the nurse, they could readily and unpredictably be required to act in different capacity – as a carer or a nurse – with little control over their working lives.
-
Unused skills. APs were worried about the possibility of infrequent or irregular use of their MM skills. Infrequent use of such skills raised the possibility that they would be lost.
-
Cheap labour. Some APs cast doubt on whether or not MM was an appropriate task for unregistered staff, suggesting that this was drifting into a ‘cheap’ form of labour, albeit with limited power to resist for fear of being left behind:
-
‘I don't really think it is a band 4 role to do drugs when band 5s get paid. I will do it because I don’t want everybody else to have that extra skill that I haven’t got’ (EC5_AP_6).
-
Residual uncertainties about how the MM initiative would impact on nurses were also apparent. The survey data presented in Table 22 suggest some differences of view between nurses and APs in this respect. Thus, APs slightly overstated nurse concerns about the extension of their role to administer drugs. While close to half (43%) of the APs agreed than nurses were ‘unhappy’ about APs administering medicine, only one-third (33%) of nurses actually agreed that they were ‘unhappy’. Indeed, the absence of nurse ‘unhappiness’ might well be accounted for by the fact that a significant proportion of nurses, close to half (44%), agreed that the MM initiative would ‘allow them to spend more time on other essential work’. APs also overstated concerns about nurse accountability, with all APs agreeing that nurses had such concerns and a lower proportion of nurses agreeing they did so. At the same time, with close to three-quarters of nurses (72%) having such concerns about their accountability, this was clearly an issue which worried nurses:
I don’t want somebody else making drug errors that could come back on my PIN [personal identification number] and therefore I could lose my PIN because she’s made a drug error.
EC5_nurse_2
| Statement | APs | Nurses | ||||
|---|---|---|---|---|---|---|
| Disagree | Neutral | Agree | Disagree | Neutral | Agree | |
| Most nurses I know are unhappy about APs being trained to administer medication | 29 | 29 | 43 | 43 | 24 | 33 |
| The administration of medication is an appropriate task for APs to perform on my ward/unit | 14 | 43 | 43 | 49 | 19 | 32 |
| Nurses on my ward/unit are concerned about their accountability when APs administer medication | 0 | 0 | 100 | 15 | 13 | 72 |
| APs administering medication will allow me to spend more time on other essential work | – | – | – | 35 | 20 | 44 |
The likely impact of the MM initiative on patients, in terms of care quality, was slightly contested (Table 23). In general, the benefits derived from continuity of care were challenged by those suggesting that the ward team’s capacity to deliver the fundamentals of care might be reduced if APs administered medicines, particularly if they continued to be counted in the unregistered numbers. Moreover, the perceived risks associated with the initiative were highlighted in the survey, with a not-inconsiderable minority of nurses, over one-quarter (28%), agreeing that patient safety would be put at risk by the initiative. Clearly, APs were much more sanguine, all of them discounting the possibility of any risk associated with the initiative. Indeed, the survey data again revealed a sharp contrast between nurse and AP views on the impact of the initiative on patients: significant majorities of APs agreed that the patient experience ‘would be improved’, allowing them to ‘respond more immediately to patient need’. Nurses were markedly less likely to agree that the initiative would lead to such outcomes.
| Statement | APs | Nurses | ||||
|---|---|---|---|---|---|---|
| Disagree | Neutral | Agree | Disagree | Neutral | Agree | |
| APs administering medication will improve patients’ experiences on my ward/unit | 0 | 29 | 71 | 30 | 33 | 37 |
| On my ward/unit patient safety is likely to be put at risk by APs administering medication | 57 | 43 | 0 | 43 | 30 | 28 |
| APs trained in administering medication will be able to respond more immediately to patient needs | 0 | 14 | 86 | 28 | 24 | 48 |
Summary
In evaluating the design and implementation of a trust’s AP MM pilot, this case has highlighted the importance of contextual factors. In part, the trust was driven down this route by a new build that would radically alter care delivery systems, with implications for the structure of the nursing workforce and the richness of the skill mix. Context was also a significant influence on the way the pilot was taken forward, with the tensions between nursing and pharmacy over the form assumed by the SOPs slowing down and influencing the character of the pilot. Much of the preparation for the pilot, particularly a well-received training programme for APs, was put at risk by the failure to develop an agreed approach to the development of the essential protocols.
There are broader lessons to be drawn from these particular difficulties in terms of the potentially contested nature of an extended AP role and the consequent need to develop a partnership between functions, as well as agreed systems, at the outset of such a process.
In evaluating stakeholder perceptions of the MM initiative, it became clear that AP and nurse views differed markedly. In general, APs were much more positive than nurses about the process in terms of preparation and impact on care quality. This finding should not, however, detract from the more nuanced picture of how these actors regarded the pilot. APs retained various doubts about their future role, the levels of support provided at ward level, and how they would be used by their colleagues if they acquired responsibility for MM. Nurses expressed considerable concern about their accountability for APs administering drugs, although a significant proportion of nurses felt that they would be ‘freed up’ to focus on ‘more essential tasks’. Perhaps most telling was the ongoing uncertainty about the impact the initiative would have on patient care: some suggested risks, while others saw the initiative as improving the patient experience, allowing APs to ‘respond more immediately to patient needs’.
Rolling out the assistant practitioner role
Context
This evaluation focuses on the introduction of an AP role across a trust. The trust in question was a single site, ‘medium-sized district general hospital’ in the east of England with 450 beds and a nursing workforce of 2000 full-time equivalent employees (including registered and unregistered workers). Initially driven by a SHA workforce group, funding a project co-ordinator’s post, the trust was at the forefront of developing the AP role in the region. Launched in June 2010, the trust’s initiative was distinctive in seeking to introduce the AP role throughout the trust, in general as well as in more specialist clinical areas. The initiative comprised the following elements:
-
the appointment of a cohort of 25 TAPs embedded in nine clinical areas: emergency assessment unit (EAU); trauma and orthopaedics; respiratory medicine; gastroenterology; general medicine; general surgery; rehabilitation; endoscopy; and the stroke unit
-
at least two TAPs in each of these clinical areas
-
internal and external recruitment on to the TAP programme
-
funding the AP through the loss of a band 5 nurse post
-
TAP recruitment on to pay band 3, moving to band 4 on qualifying as an AP
-
a training programme made up of:
-
a 2-year FD, with TAPs given 2 study days per week
-
a set of competencies
-
five practical assessments covering, for example, total patient care, wound care, and care of the deteriorating patient
-
-
a 4-day preceptorship programme.
The evaluation centred on four aspects of the initiative:
-
reasons for its introduction
-
design and implementation
-
learning and training components (FD, competencies and assessments)
-
development of the (T)AP role within clinical areas.
Methods
Covering this first trust cohort of 25 TAPs, the research was carried out at two points in time:
-
phase 1: March 2010, 18 months into the TAP programme – 19 interviews with various stakeholders, and a focus group covering 10 TAPs
-
phase 2: December 2012, after the programme had been completed – 24 interviews with a similar range of staff.
Those covered by the fieldwork included:
-
19 (T)APs (seven at both phases)
-
seven ward managers and a matron (one at both phases)
-
six nurses (one at both phases)
-
10 senior managers (four at both phases).
Rapid feedback on the findings was given to the trust after each phase. In March 2013, a presentation was made at the trust, engaging stakeholders in a discussion of the full findings.
Findings
Reasons
The decision to introduce the AP initiative was a top-down decision taken by trust senior management:
We had to make it work; had we gone from the bottom-up it would never have happened.
EC6_trust manager_4
It was a decision informed by a number of objectives:
-
The trust had faced difficulties in recruiting band 5 nurses, with such recruitment problems seen as likely to deepen in the future. Rather than providing a stepping-stone to nursing, the AP role was viewed as a means of reconfiguring the distribution of nursing tasks by developing an extended senior support role.
-
The central objective underpinning the initiative was to use the AP role as a leader for the delivery of the fundamentals of care. This was reflected in the AP job description, which summarised the role as ‘acting as a team leader for the delivery of daily personal care activity with patients’.
-
To address nurse shortages and to create new leaders at the bedside, band 4 was seen as a career grade for the trust’s band 2 and 3 HCAs.
-
The use of the AP role to address cost pressures was fully acknowledged by senior nurse management at the trust, reflected in the fact that its introduction was predicated on the loss of a band 5 nurse within the respective clinical areas to fund it.
Design and implementation
The design and implementation of the AP initiative involved a range of actors and processes, presented in Figure 10.
FIGURE 10.
Design and implementation of AP initiative.
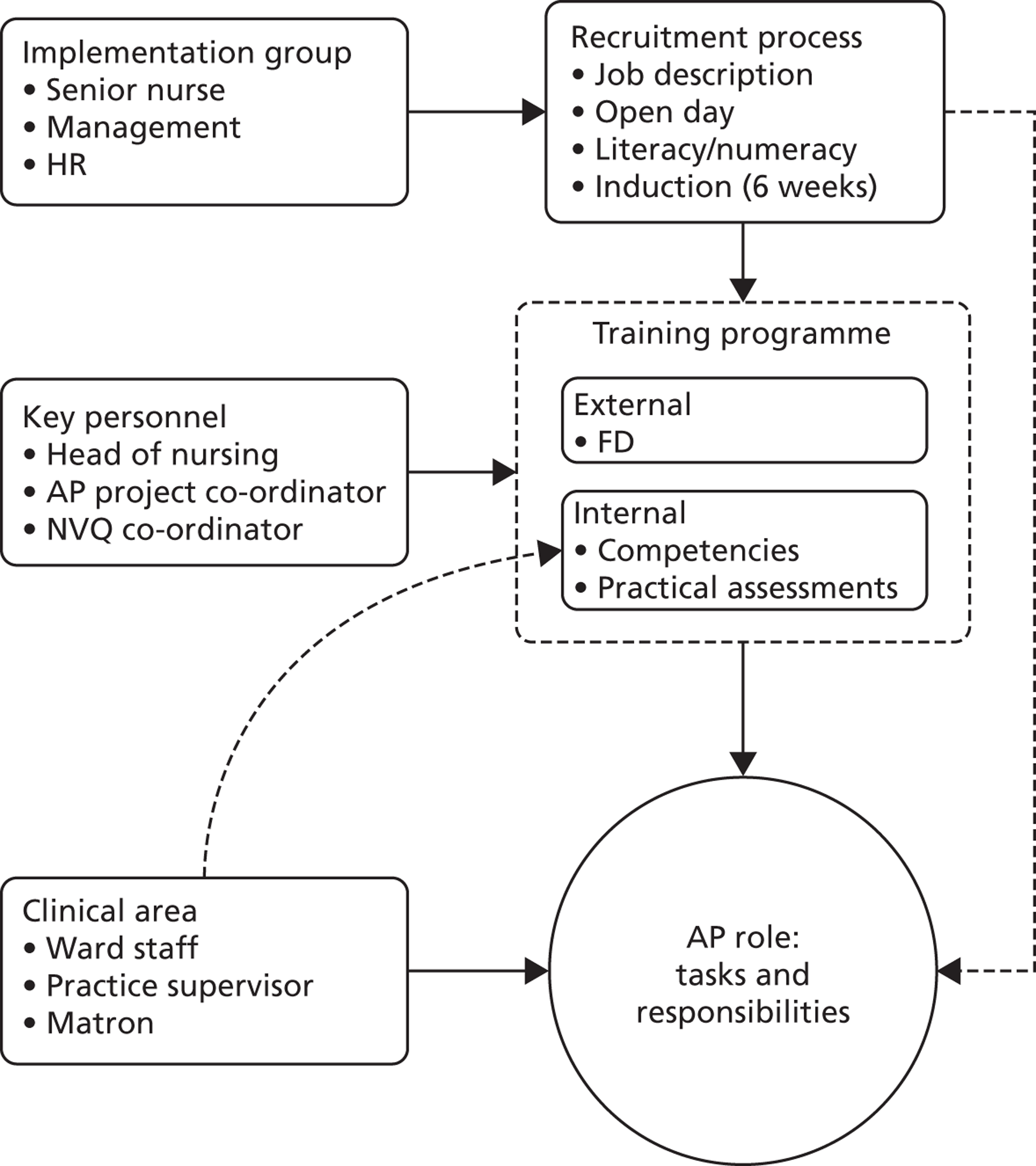
It can be seen that the initiative was managed by a trust implementation group from different directorates including nursing and HR. This group developed the TAP and AP job descriptions, which provided the basis for recruitment to the programme. The initiative was led by the head of nursing. However, the key figure, working full time on the initiative, was the project co-ordinator who:
-
provided ongoing support and advice to TAPs
-
worked with the FD provider
-
liaised with ward managers, not least to ensure that TAPs fitted in and developed a clear role
-
acted as an assessor, particularly on the practical assessments.
At the heart of the process was the development of an AP role with a given set of tasks and responsibilities designed to meet service and trust needs. In general, this process comprised two main elements:
-
Covered by the upper part of the figure, the first related to the formalities of the role, particularly the training programme designed to ensure that those recruited could perform the role.
-
Represented by the bottom half of the figure, the second was a less formal element, taking place within clinical areas, to shape the AP role to meet specific clinical needs and circumstances.
The findings as they relate to these two elements are presented for each phase in turn.
Phase 1: the training programme
Trainee assistant practitioner engagement with the FD was relatively unproblematic. This should not detract from the challenges faced by TAPs during their studies. Many of the TAPs were driven by a three-way set of pressures: they had returned to formal learning after many years away from an institutional educational environment; they were working on their wards in a new capacity, having to balance work and study pressures; and they had ongoing domestic obligations to meet. In such circumstances, it was unsurprising that many TAPs found their studies difficult, time-consuming and often stressful. Indeed, one of the more frequent calls from the TAP interviews was for more study time:
It was a little bit stressful to begin with because we’re expected to work on the wards as well as do all our assignments and all our study, so it was a lot to try and juggle. You had to definitely learn how to organise your time, but as it progressed, got slightly more relaxed and it was quite nice to realise that I could actually write an assignment.
EC6_TAP_10
The practical assessment and in particular the acquisition of the competencies were more problematic. The main cause of concern lay in supervision, sign-off and support at ward level:
My last mentor, I had to force and force and force to actually get time with her.
EC6_TAP_9
We never really got time with our practice supervisors, our mentors, we got given two lots of competency packs to sign-off and no one to practice with. We were supposed to have one specific individual who was supposed to help us do that, as well as our work-based learning, and we weren’t even being put on the same shifts as them.
EC6_TAP_10
Phase 1: the trainee assistant practitioner role at ward level
There was some variation between wards in how TAPs were being used, with three main approaches apparent. In the first approach, the TAP was already performing an extended role, having acquired and been signed off on many of the requisite competencies (endoscopy and stroke):
If I’m totally honest with you I do absolutely everything that the, I’m working as a band 4 now as if I was qualified and I have been for the last 10 months, a year probably. And there’s really no difference in my role than there is of the registered nurse, there is nothing that they do that I don’t apart obviously give medication.
EC6_TAP_8
In the second approach, the TAP was still being used essentially as a HCA. This was by far the most common situation across the wards and led to frustration among TAPs:
We do get treated like nursing assistants the majority of the time, especially if you’re on an early shift, which means you then don’t learn any new skills.
EC6_TAP _9
The third approach involved the TAP drifting between roles. On some shifts the TAP acted as a carer, on others as a learner TAP and on yet others as a practising TAP:
But that’s the main thing, when I come on to a shift I have to establish at what level I’m going to be practising, whether I’m going to be practising [as a HCA] or just learning new skills or I’m going to be practising as a TAP in training, or I’m going to be practising as a TAP as I am going to be.
EC6_TAP_14
This uncertainty might have reflected that the TAPs were only part way through the programme. A number of ward managers remained uncertain as to how they would use the qualified AP. Indeed, there was still a lack of understanding about the (T)AP role among team members. However, in some areas this uncertainty took the form of a more forthright hostility. This was most apparent among nurses, who sometimes felt threatened by the role, but such hostility was also apparent among HCAs and ward managers:
A lot of people are threatened by us.
EC6_TAP_3
There was a lot of hostility when I first started on that ward, not only from nurses, from [HCAs] as well.
EC6_TAP_14
It hasn’t been all bad but it has been quite difficult. I don’t think it was really explained as to what our role was going to be and we just kind of appeared on the wards one day and everyone was like, ‘who are you and what can you do and why do you do it?’
EC6_TAP_10
These negative responses were particularly directed at externally recruited TAPs:
[There was resistance] from, people who didn’t think it was right that I got a band 3 post having never worked for the trust before.
EC6_TAP_7
Phase 2: the training programme
On the return visit to the trust, the first cohort should have completed the training programme and been settled into their AP roles. Certainly in terms of formal outcomes, the training had been successful. From an original cohort of 25, four had pulled out of the FD early on, leaving a cohort of 21, of whom 19 passed the FD. Despite the ward-based supervision difficulties, the (T)APs had also managed to acquire the relevant competencies and completed the practical assessments.
Phase 2: the assistant practitioner role at ward level
Even on APs’ successful completion of the training, embedding the role at ward level proved to be much more problematic. Before considering the deployment of, and engagement with, the AP on the wards, a couple of contextual points are worth noting. Between the first and second phases of fieldwork, the trust had recruited a group of around 40 nurses from Portugal at band 5. Given that one of the rationales for the AP programme was to address recruitment difficulties at this level, this overseas recruitment strategy was seen by some as negatively affecting perception of the value and utility of the APs.
There should have been a change of uniform for APs on completion of their training and becoming an AP, but as a cost-saving measure this had not occurred. For the APs, this reneging on a change of uniform was symbolically significant.
At phase 2 there was again variation between clinical areas in how the AP role had been used and viewed post training, with a number of patterns emerging. The first was a ‘smooth transition’ pattern where APs had up-skilled and moved into a clear and distinctive band 4 role (endoscopy and stroke):
Throughout my training, particularly in my second year of training I was working to a band 4 role.
EC6_AP_8
The second was a ‘sudden change’ pattern where the TAP role had taken on a more extended role post training with a sharp shift of responsibility (EAU):
I’ve got too much responsibility, and it sounds terrible moaning, but sometimes it is a bit too much and I’m thinking it can be a bit scary.
EC6_AP_12
The third, a ‘carer pattern’ where the AP role remained, centred on caring, with little if any extension (some general medical and surgical wards):
I don’t do anything differently to the other band 2s on the ward. I’m in the carer numbers on the ward off duty . . . I’m actually de-skilling.
EC6_AP_15
Finally, a fourth to emerge was an ‘unstable pattern’, where the use of the AP was still uncertain, varying often by shift (some general medical and surgical wards):
Some days we’ll go in and we’ll be under the trained [side of the skill mix], some days we’ll go in, it’s the, it’s the not knowing. You can’t grow into a role if one day you’re being a [HCA], the next day you’re being trained and then the next day you’re expected to do management.
EC6_AP_4
The prevailing pattern was largely influenced by whether the AP counted in the registered or unregistered numbers. In a few clinical areas – those with a ‘smooth transition pattern’ – the APs were counted in the registered numbers. In the ‘unstable pattern’, APs were counted in the nurse numbers, but could slip back into the unregistered numbers. In the ‘carer pattern’, APs were still counted in the unregistered numbers.
For those APs covered by the ‘carer pattern’, there was a considerable disillusionment. They perceived themselves as ‘glorified HCAs’, with few opportunities to use their newly acquired knowledge and skills:
I feel sometimes I get de-skilled, you don’t do the skills that I’m trained to do, and then you might go a couple of months without not doing anything like that and then another time you’re expected to do everything.
EC6_AP_4
Those falling within the ‘unstable’ and the ‘carer’ patterns perceived themselves as being used opportunistically by nurses, engaged to undertake tasks when needed but more routinely used as carers. The APs viewed this uneven use as detrimental in a number of ways: they were often being pulled in different direction; where they did combine extended and carer activities it led to work pressure and intensity; and uncertainty developed among others – doctors and patients – about how they should be viewed and used.
There were indications post training that APs were taking on certain leadership tasks in relation to new TAPs and HCAs, although in this respect there was, again, some unevenness between clinical areas:
When we went for the job we were told that, both my colleague and I that work on the same ward, we were told that we would be like the role model for the [HCAs] and it would be up to us to do the fundamental care, and that would be where we would be focused and it would be very much teaching. Which hasn’t necessarily happened.
EC6_AP_4
I’m mentor to the new TAP who’s a band 2 and I do manage all the band 2s.
EC6_AP_8
Summary
This initiative was seen as worthy of evaluation given its attempt to embed the AP role across a trust, in general surgical and medical wards as well as specialist clinical areas. The trust had made a strategic decision to use the AP role to restructure its nursing workforce in pursuit of a number of objectives: addressing recruitment difficulties among nurses; developing a new leader in the delivery of the fundamentals of care; making medium-term financial savings; and creating new career pathways for band 2 and band 3 HCAs.
In general terms, any evaluation needed to focus on whether or not and in what ways these objectives had been met. However, it has been argued that in examining such questions it was important to assess two aspects of the initiative: the formal training and learning aspects, and the less tangible, but equally significant, use of the AP role at ward level. In this case, the relative success of the formal learning and training component, in terms of completion rates and general perceptions of the process, has been accompanied by difficulties in ensuring the adoption and use of the AP role on wards as envisaged.
This finding derives from the views and experiences of various actors from across the trust with a stake in the initiative. The phase 1 material suggested that, in general, the TAPs were finding it difficult to move beyond caring activities, and sometimes faced resistance from team members to an extension of their role. During this period, however, they were focused on their training, which, while often stressful and intense, was generally progressing well. With only 3 days per week on the ward, their roles were always likely to be slightly uncertain and distorted. More telling was the phase 2 material which indicated that, in many clinical areas, ward use and engagement with the role remained uncertain. Indeed, if the general tenor of the phase 1 TAP interviews was upbeat and optimistic, the prevailing ‘mood’ at phase 2 was one of AP disillusionment with their role and prospects.
Certainly, the initiative had fared unevenly between clinical areas. The general roll-out across the trust provided an opportunity to compare how the role would ‘take’ in different clinical areas, and it was clear that problems were most apparent on the general wards than in the specialist areas such as endoscopy. However, the broader picture to emerge raised questions about the achievement of the trust’s objectives. There were some signs that the AP was emerging as a team leader for HCA carers, but that APs were not yet fully developed leaders of fundamental care. Most striking was the difficulties APs faced in extending their roles in an ordered and sustainable way: many claimed to be ‘glorified carers’, at ‘best’ used opportunistically by nurses to undertake more complex tasks. It was a finding that casts some doubt on the capacity of APs to address band 5 recruitment difficulties and to provide a worthwhile or meaningful career route (in terms other than a rise in pay banding).
A number of reasons emerged as possibly explaining the problems faced by the APs in gaining acceptance at ward level:
-
The value and contribution of the AP was distorted by the view that they were a cost-saving measure.
-
The initiative was driven by the trust senior management, and perhaps therefore seen as an imposition before an understanding and consensus on the value of the AP role had been established.
-
APs expressed concern at the lack of understanding about their role, particularly among team members.
-
There was a residual degree of ‘resistance in principle’ to the AP role within the trust, which proved difficult to break down. Some staff were opposed to the AP role in principle as a threat to the nursing profession and its status.
-
Practical issues were raised rendering the use of APs problematic in the trust, leading to a ‘resistance in practice’. The role assumed by the AP was often crucially related to whether they were included in the trained or untrained numbers: counted in the untrained numbers, they were typically carers; counted in the trained number, they had greater scope to play an extended role. The AP’s inability to administer drugs was also seen by some as a constraint on their use.
Despite, or perhaps because of, the difficulties faced with the first cohort of APs, the trust had moved ahead with a second cohort. There had been some organisational learning from the first AP cohort, resulting in important changes to the design of the programme as summarised in Table 24. The trust’s second AP cohort, much smaller than the first, at 10, was recruited solely from internal candidates rather than also drawing upon external candidates; promotion to band 4 was to be dependent on the availability of a role at that level upon the completion of the programme, rather than being guaranteed; and the number of study days was cut by half, from 2 to 1.
| Features of programme | Cohort 1 | Cohort 2 |
|---|---|---|
| Numbers | 21 | 10 |
| Clinical areas/funding | Top-down | Bottom-up: wards to volunteer |
| Recruitment | Internal and external | Internal only |
| Training/learning | FD | FD |
| Competencies | Competencies | |
| Practical assessments | Practical assessments | |
| Pay banding/progressions | Guaranteed band 4 | Band 4 only if role available |
| Study days | 2 | 1 |
| Supervision | One practice supervisor | Two practice supervisors |
| AP co-ordinator | 30 hours per week | 15 hours per week |
Overview: discussion and lessons
This chapter has explored attempts to evaluate a diverse range of initiatives related to the use and management of nurse support worker roles, a diversity reflecting our interest in encouraging trusts to select initiatives which they felt might usefully be assessed. It was clear that the case study trusts faced difficulties in introducing and embedding new support worker policies and practices, in turn weakening our capacity to evaluate some of them. In certain instances, it proved difficult to apply our ‘before’ and ‘after’ evaluation model, with the proposed initiative delayed and contested within the trusts. This is not to detract from the evidence base established by the six evaluations presented in this chapter. In a number of cases, the evaluation cast some doubt on the efficacy of the initiative, suggesting a guarded approach to its adoption by other trusts. For example, few MCAs completed the ADP. In another trust, the 2-week induction programme for support workers did not appear to better engage or prepare the HCA recruits for their new role than the old, shorter programme. Moreover, the CF made only limited progress on recalibrating the distribution of tasks, while the take-up of beginner competencies was extremely uneven. It was evident from these ECs that, once introduced, those factors delaying the introduction of an initiative could also, on occasion, subvert it.
At the same time, there were instances where the evaluation provided some support for the initiative, strengthening the evidence base for its use: for example, despite the difficulties with the ADP, the new and extended MCA role had gained some acceptance within the maternity services workforce; in another trust, the roll-out of the first cohort of APs was founded upon the successful completion of an intense training programme by most of the TAPs.
A number of lessons can be drawn from the six ECs, categorised in the same fashion as those presented at the end of Chapter 3:
-
Context
-
New initiatives are sometimes tied to broader organisational changes, which can influence the implementation and consequences of the initiative. Trusts need to consider this interaction effect in planning the development of an initiative, displaying sensitivity to any detrimental linkages between the initiative and broader organisational changes. For example, the disruption to registered midwives’ status and responsibilities caused by general restructuring of community maternity services, generated a negative perception of the MCA role and the associated ADP, and, more tangibly, weakened the midwives’ capacity to support it.
-
Careful consideration needs to be given to the unintended consequences of an initiative. The difficulties faced in implementing the CF were in part related to a failure to foresee the resource implications of the training required to recalibrate the distribution of tasks. Similarly, the problems with the 2-week induction programme were associated with an unforeseen need to release the newly recruited support workers for an extended period of time, with the ward bearing the cost of the worker being away from the bedside.
-
Given the range of initiatives typically being pursued by a trust at any one time, there is a danger that any one such initiative might become ‘lost’ or overlooked at the ‘busy’ ward level. To avoid this fate, trusts need to prioritise initiatives for ward managers, and continue to monitor progress on those deemed high priority.
-
-
Systems and processes
-
Even in those cases where the evaluation was not particularly positive, some care is needed in ‘writing off’ the initiative. Where problems arose, they often lay in the implementation, with the substantive value of the initiative remaining an open question. In others words, a ‘better approach’ to the implementation of some of these initiatives might well have enhanced their take-up and positive impact. It follows that careful consideration needs to be given by trusts to how an initiative is to be introduced.
-
More specifically, any new initiative needs to be properly resourced. For example, the appointment of a dedicated and fully funded AP project co-ordinator to provide support for APs in the ‘roll-out’ case ensured that most TAPs successfully completed their training.
-
Where initiatives relate to new ways of working and new roles, clinical governance issues assume particular importance and need to be dealt with before the initiative is scheduled for implementation or publicised. This can be a difficult and protracted process, as illustrated in the case of the MM initiative. Clinical governance issues bring in new actors, such as trust pharmacists; new procedures, for instance the drafting of protocols; and new approval mechanisms, for example sanctioning and monitoring by the trust’s MGC.
-
-
Actors
-
The implementation of an initiative is often contentious and might well generate resistance from actors threatened by it. Steps need to be taken to minimise resistance, not least through addressing any perceived concerns. This might be achieved by ensuring that stakeholders are fully informed about an initiative and extensively involved in the associated change processes.
-
Closely related, the longer-term sustainability of an initiative can be subverted by the resistance from key actors. In the AP roll-out case, it was noteworthy that while most TAPs successfully completed their training, the acceptance of the AP role remained contested, particularly by RNs.
-
Accountability for the support worker, particularly as the role becomes more extended, is a recurring source of concern among registered health-care professionals. This was raised as a ‘worry’ among registered midwives as the MCA role developed and among RNs as the AP took on the management of medicines. There might well be national, and indeed local, guidance on the issue of accountability, but risk-averse registered professionals still remain unclear about their responsibility and, as a consequence, are often unwilling to delegate. Steps need to be taken to ensure that health-care professionals are fully aware of, and understand the nature of, their accountability for support workers.
-
The expectations of staff involved in a new initiative need to be carefully managed. The slow roll-out of the CF in the selected ward and indeed across the trust, for example, frustrated staff expectations of work reorganisation and associated training opportunities. Similarly, APs were all trained up to manage medicines, only for the pilot to be delayed to allow the SOPs to be agreed and signed off. Staff expectations generated by an initiative need to be realistic and trusts must try to meet those expectations. This might be achieved by ensuring that staff are well informed about the initiative; that the initiative is not ‘oversold’ in terms of its benefit for staff; that the resourcing is adequate and firmly in place; and that systems needed to implement the initiative have been agreed.
-
Chapter 5 Engagement
Context and focus
The engagement theme was designed to follow up on a number of findings from the original Oxford and York studies. 1,5 First, these studies revealed the highly fragmented and uneven nature of approaches to the management and use of nurse support roles across and, indeed, even within trusts. It was a finding explained by the long, path-dependent development of the HCA role, in the absence of a regulatory framework which might otherwise have ensured some control or standardisation of approach. This is not to detract from important uniformities across the NHS. In examining the nature and consequences of HCAs in different NHS trusts, these original studies did reveal shared patterns, for example in the background of those performing the role and in how HCAs related to various stakeholders. However, equally striking was the variation in approach to deploying and dealing with the nurse support role.
There is nothing intrinsically problematic about variation: it might well reflect a legitimate sensitivity to local trust circumstances and needs in relation to the use and management of the nurse support role. It was clear, however, that such variation was more a response to ad hoc, uncertain and idiosyncratic trust engagement with the role, displaying little, if any, strategic intent. This was particularly manifest in uneven practice within the same trust, often by clinical area or ward, generating opaqueness about the form and contribution of nurse support workers to the delivery of care, and in turn severely constraining the scope for workforce planning and an appreciation of workforce capacity at the corporate level.
Such unevenness and fragmentation was problematic in various senses. They implied the absence of opportunities and spaces within which trusts might share ideas, approaches and practices associated with the nurse support role. This absence was reflected in a duplication of time and effort as trusts ‘reinvented’ existing HCA policies and practices. There were attempts to develop networks, typically of trust education leads, in particular regions. However, engaged sporadically, the general picture was characterised by an absence of shared learning around the nurse support role.
Second, the Oxford and York studies1,5 highlighted the importance of a stakeholder approach, in other words an approach which involved actors with an interest in the nurse support role: senior and ward-based nurse managers, RNs, practice and development nurses, HR managers, HCAs themselves along with their RCN and UNISON representatives, and patients and their representatives as well as education providers. These stakeholders were revealed as bringing distinctive perspectives to consideration of the nurse support role and how it might be used and managed.
As a means of providing an opportunity and space for stakeholders to explore the management and use of the nurse support role, four regional workshops were convened by the current study during 2012. An end-of-project stakeholder conference was also organised to present and discuss the project findings (a full list of delegate organisations can be found in Appendix 12). It can be seen from Table 25 that, in total, over 100 participants attended the regional workshops. Reflecting the stakeholder approach, these attendees had a variety of backgrounds, being drawn from SHAs, employee representative bodies such as the RCN, and education providers. The majority came from trusts in the respective regions, with over 50 trusts in total taking part in the workshops. These trust participants were from a range of positions, including directors and assistant directors of nursing, HR managers, ward managers, education leads, PDNs, RNs and nurse support workers.
| Location | Date | Attendees (n) |
|---|---|---|
| Leeds | 17 May 2012 | 33 |
| London | 28 June 2012 | 21 |
| Birmingham | 17 October 2012 | 35 |
| Taunton | 14 November 2012 | 20 |
The aims of the regional workshops were to:
-
share views, knowledge, information and practice on the development, management and use of support workers
-
codesign support worker roles and ways of working sensitive to the needs of the respective groups
-
establish clearer, stronger and more productive relationships among the stakeholders in the context of developing support worker roles
-
develop a toolkit for the better management of support workers.
In pursuing these objectives, the workshops were organised as facilitated discussions revolving around a number of questions related to the current and future use of nurse support workers. The questions are set out in Table 26. In the main, the same questions were considered at the respective workshops, although it can be seen they were modified in some respects. More specifically, the discussion questions were fine-tuned in the light of experience. For example, at the Leeds workshop certain questions did not encourage the expected form of discussion and so were tweaked for the subsequent workshops. In addition, the London workshop was organised on a slightly different basis from the other three. In contrast to the other, day-long, stand-alone workshops, the London workshop took place as the morning session of a broader NHS London event. As a consequence, we did not have as long with the participants and the questions were framed slightly differently to cover the relevant issues. At all four workshops, participants discussed the questions in small, rotating groups, which provided them with an opportunity to engage and share practices and views with as many attendees as possible. Notes were taken at each workshop and each group feedback session was recorded and transcribed. In addition, the written material from the group discussions, such as the ‘post-it notes’ and flip chart presentations, was collected. Given that the material was tied to specific questions, it was possible to develop and identify patterns from the articulated views, ideas and practices. These outputs were used to produce a report on each workshop, subsequently posted on the project website. The workshops also supported the development of a nurse support worker management toolkit. The respective workshops sought views and ideas were presented to participants for comment.
| Question number | Question text | Workshop |
|---|---|---|
| 1 | What do HCAs currently do? | Leeds, Birmingham |
| 2 | How do you view the HCA role? | London |
| 3 | What distinguishes band 2, 3 and 4 HCAs? | Taunton |
| 4 | What good practices are there in relation to the roles and management of the HCA? | All |
| 5 | What could be improved about the role and management of the HCA? | All |
| 6 | How do you see the HCA role of the future? | All |
| 7 | How do we move towards the vision? | Leeds, London |
| 8 | What do managers need to do to fulfil the ideal role? | Birmingham, Taunton |
| 9 | What do HCAs need to do? | Birmingham, Taunton |
| 10 | What support do others need to help HCAs fulfil the ideal role? | Birmingham, Taunton |
| 11 | What are the challenges and barriers? | All |
In covering four different regions we were seeking to ensure comprehensive coverage: gathering views, ideas, examples and practices from across much of England. There might have been scope to explore regional differences in the issues raised and discussed. However, this approach was not, in the main, adopted – the workshop discussions and feedback not being controlled in a tight enough way to allow this sort of analysis. It is important to stress that these workshops were ends in their own right, allowing participants to share views, ideas and practices, rather than principally a means of collecting research data.
This chapter presents the themes and findings emerging from the workshops. It is divided into four main parts: the first deals with shared views on the current state of the HCA role (questions 1–3); the second covers ‘good practice’ and opportunities for improvement (questions 4–5); the third considers the future of the nurse support role (questions 6–12); and the final section discusses the management toolkit.
Current state of the nurse support role
The starting point for the workshop discussions was a sharing of views on the current role of the nurse support worker; this provided baseline material for a series of questions on the future development of such a role, considered later in proceedings. In exploring the current role, there was also a particular interest in drilling down to distinguish between the shape and nature of band 2, 3 and 4 nurse support roles. It was the attempt to probe these issues which led to modifications in the opening question. The question was framed in the most open terms at the London workshop: participants were asked how they ‘viewed the HCA role’.
As set out in Table 27, the points raised were grouped under three conceptually distinct headings. The first heading was ‘work emphasis’: comments dealing with the weight placed by workshop participants on different aspects of the HCA role. In turn, this emphasis was revealed as having different dimensions related to:
-
the stakeholder – the HCA being patient focused
-
the activity – the HCA being viewed as providing hands-on care at the frontline and
-
the locus of support – the HCA being seen to provide direct assistance mainly to the nurse, albeit with some mention of direct support to the patient.
| Areas | Comments |
|---|---|
| Work emphasis | Patient focused |
| Supporting service users on their road to recovery | |
| Frontline – delivering large proportion of direct care | |
| Supporting role to implement good patient care | |
| Supporting the professional workforce | |
| Supporting the ward community | |
| Supporting the delivery of essential nursing care/duties | |
| Contribution | Important to maintaining patient care |
| Vital to the modernisation of the NHS | |
| An essential workforce undertaking extended invasive clinical tasks | |
| Crucial to the care team | |
| Crucial to service delivery | |
| Pivotal to good patient care | |
| Back bone of patient care/services | |
| Have many hidden talents | |
| Better communication skills and add value to patient care | |
| More knowledgeable than are given credit for | |
| Treatment | Undervalued and not used to full potential |
| Not valued as part of the team | |
| Valued by immediate manager but not by senior managers | |
| Underutilised | |
| An underrated role |
The second heading was the perceived ‘contribution’ of HCAs, and included comments based on normative and value-based judgements. It can be seen that these judgements were invariably positive, the HCA being viewed as ‘important’, ‘essential’ and ‘vital’. More noteworthy, perhaps, were comments that suggested that the HCA had something distinctive to contribute to care quality: better patient communication skills and ‘more knowledge’ (although about what remained unclear). The third heading touched on the treatment of HCAs, generating fewer comments but with a consensus on the ‘undervaluation’ of this work group.
The Leeds workshop elicited views distinguishing the tasks performed by different bands of nurse support workers according to three categories: personal, technical and ‘other’. These activities can be found in Tables 40–42 in Appendix 13 and incorporate the views from the Leeds, Birmingham and Taunton workshops. This is a dense presentation of the material, reflecting the fact that participants articulated the tasks performed by the respective bands in different ways: as a generic bundle, for example ‘support patients and carers’, although more typically they are listed as specific tasks. Moreover, certain tasks are repeated both within a given band and between them, providing an indication of the weight placed on that task and of where the same tasks might be performed by different bands.
A number of points from the tables are worth highlighting:
-
It is clear that band 2 HCAs concentrate on the personal care of patients, while bands 3 and 4 perform a much wider range of technical tasks.
-
This is not to detract from instances where band 2 HCAs appear to be involved in quite complex technical activities. Thus, mention is made of band 2s undertaking cannula care, performing the removal of urethral catheters, and supervising patients taking medication.
-
There is also a significant overlap between the tasks performed by band 2 and band 3 HCAs. This is reflected not only in the list of activities under the band 2 and 3 heading but also in the repetition of tasks under the respective headings. These shared tasks include, for instance, observation and venepuncture.
-
At the same time, these tables reveal some important differences in the tasks undertaken by the different bands; as expected, tasks become more complex on moving up the band levels.
‘Good practice’ and opportunities for improvement
The ‘good practice’ highlighted at the workshops was coded according to key aspects of the nurse support worker role and its management: more specifically, whether such practices related to recruitment, induction, development, training, supervision and support; the role and ways of working; and miscellaneous elements such as rewards and communication. Table 44 in Appendix 14 presents all such practices raised under these headings broken down by regional workshop.
In general terms, the good practice raised by participants assumed three forms. First, it emerged as a broad approach rather than as specific practices, mainly relating to established, often nationally driven, ways of using and managing nurse support workers. For example, in the training domain, reference was consistently made to the increasing use of apprenticeships as the basis for entry to, and training within, the HCA roles. Second, there was a bundle of newer practices, somewhat akin to the policies and practices dealt with in our innovation theme, becoming increasingly popular across trusts. Indeed, the increasing uptake of such practices suggested a new model for managing nurse support workers. This range of practices is presented in Figure 11. It includes a ‘tightening’ of recruitment with the use of numeracy and literacy tests; a shift in selection methods with the use of a values-based approach; and more clearly distinguishing bands 2 and 3 roles on the basis of discrete and clearly defined competence, and establishing associated portfolios and booklets to regulate the acquisition of such competencies.
FIGURE 11.
Emerging standard practice.
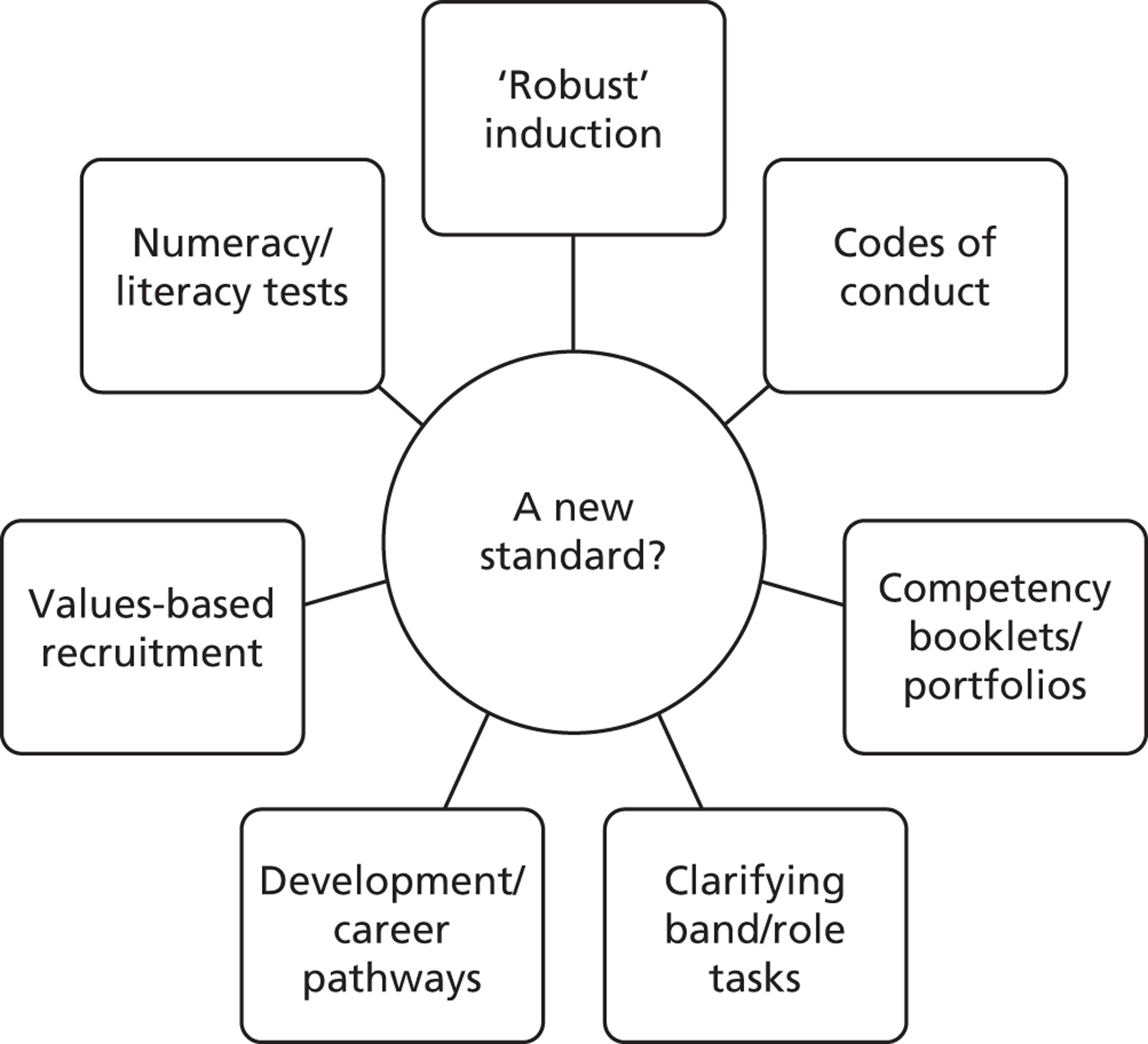
Third, there was more distinctive or unusual ‘good practice’. A selection of these practices is presented in Figure 12. These more novel practices are being adopted on a more uneven and selective basis by trusts. For example, one trust had developed ‘buddy shifts’ to provide time and space for HCAs to complete their competencies, while another allowed individuals to shadow an AP before deciding to apply for the role.
FIGURE 12.
Good practice as distinctive practice.
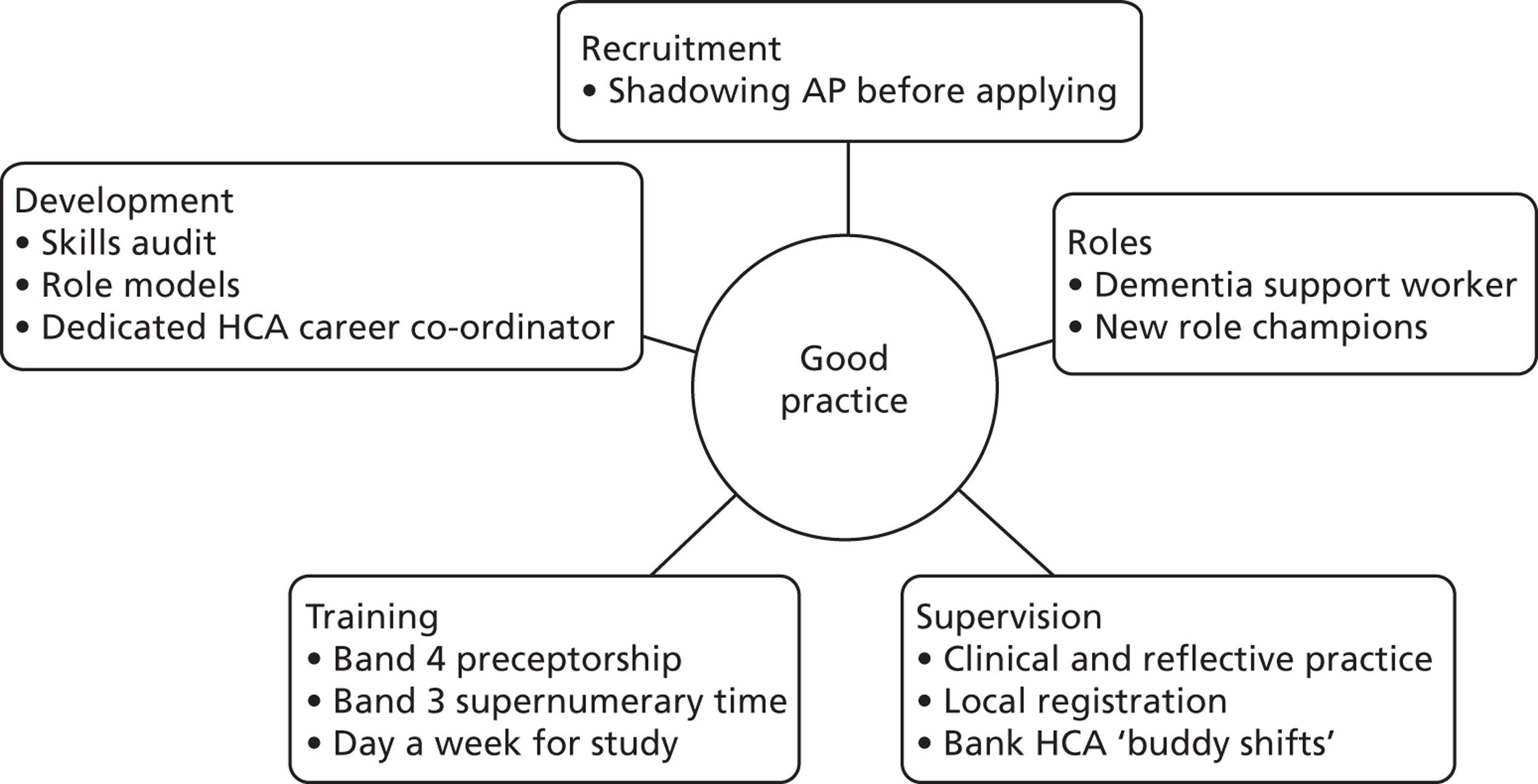
It is perhaps a testament to the variable and uneven development of trust approaches to the use and management of nurse support workers that many of the activities raised as ‘good practice’ also emerged as areas of potential improvement. Recoding the points made in accordance with the headings used above, there was a striking frequency with which similar areas for improvements were raised across the regions. A summary of these suggested improvements can be found in Table 28.
| Domain | Suggested improvement |
|---|---|
| Recognition and engagement | Recognition of roles’ contribution to safe effective care |
| Patients know and recognise role of HCA/registered staff | |
| More uniformity of role with appropriate recognition | |
| Alter wording used for HCAs, i.e. do not refer to as ‘unqualified’ – alter perceptions of registered staff | |
| Need to lift profile of role in trust | |
| Improve voice with a monthly chaired forum by HCA, i.e. forum similar to nursing and midwifery quality forum | |
| Improve team awareness and responsibility awareness | |
| Knowing limitations | |
| Greater consideration of support workforce when devising policies | |
| Education of the registered workforce about what HCAs can and cannot do | |
| Organisational commitment to develop non-registered roles | |
| No longer use negative wording in relation to the role, e.g. non-registered | |
| Not to be seen as the ward’s ‘go-to’ person for all the undesirable jobs | |
| Integration – take out snobbery | |
| Stop the stigma of being ‘just’ a HCA | |
| Encourage HCA ambassadors | |
| Organisational champion for the support worker staff group | |
| Recruitment | Better recruitment processes (nursing not HR) |
| Recruitment on attitudes, values and beliefs | |
| Numeracy and literacy assessment | |
| Roles and ways of working | Continuity of care, follow patients out of hospital into community |
| Nationally standardised role of AP and clear parameters of role training, education and governance | |
| Cross-sector working, i.e. AHP and nursing | |
| Supervision | Regulation of the non-registered workforce or some similar system |
| Governance boundaries | |
| Organisation codes of conduct (developed regionally) | |
| Clarity, i.e. accountability, role boundaries | |
| Consistency from registered workforce in the appropriate delegation of tasks | |
| Improved mentoring by higher-band registered staff | |
| RN role supporting development of HCA, listening to HCAs | |
| Consistency – clinical supervision and reflective practice for all HCAs | |
| Training | Clarify/standardise education requirements in relation to bands 2 to 4 – involve HCAs in mentoring and educating other HCAs |
| Agree national training and development programmes that allow transferability and partiality rather than trust guidelines and frameworks | |
| A passport-type approach for the region | |
| Quality assurance of HCA training and development programmes | |
| HCAs given more time for learning | |
| HCAs should be given ‘study time’ when doing FD | |
| Career development | Define the difference between bands 2 to 4 in role expectations |
| Role differentiation, e.g. what differences and does everybody understand? | |
| Better information on career development | |
| Defined career progression not cheap labour | |
| Clear national career framework with progression mapped out | |
| Support and development of HCAs could be improved, lots of on-the-job learning, so experience only as good as your mentor |
Many of the improvements are driven by the need for consistency, clarity and understanding. More specifically, the need for consistency emerges in terms of the delegation of tasks by RNs to HCAs and in the level of supervision and support received by nurse support workers, particularly during training and development. The need for greater clarity assumes a number of forms related to nurse accountability, an issue which feeds into the registration of support workers; and the distribution of tasks and responsibilities, especially by band, with implications for career development and work organisation. Similarly, the need for understanding is presented in a variety of ways. In part this is associated with a fuller appreciation of the nature of nurse support roles by members of the ward team and by patients, but it is also derived from a sensitivity to nurse support workers as a discrete occupational group, reflected in calls for more effective forms of voice for these employees.
Vision: the future of the nurse support worker
The final element of the workshop activity, a visioning exercise, sought to generate views and ideas on the future role of the nurse support worker, in a structured way. The questions posed examined what form the role might take, the challenges and barriers faced in moving towards it, and the conditions or requirements for achieving it. There were significant overlaps in the points made in response to these questions and, indeed, some restatement of the themes raised in relation to ‘improving’ on the current nurse support role. As a consequence, the aggregated responses from the four workshops were recoded and rationalised. Figure 13 presents the findings on the views expressed. The future of the role is presented in the figure as ‘the aspiration’ and the features of that role draw upon the domains used on the preceding sections. Clearly, the ‘achievement’ of this aspiration involves addressing certain challenges and overcoming barriers. These are expressed in the figure under headings: attitudes, behaviours, systems and resources.
FIGURE 13.
The future of the nurse support role. FE, further education.
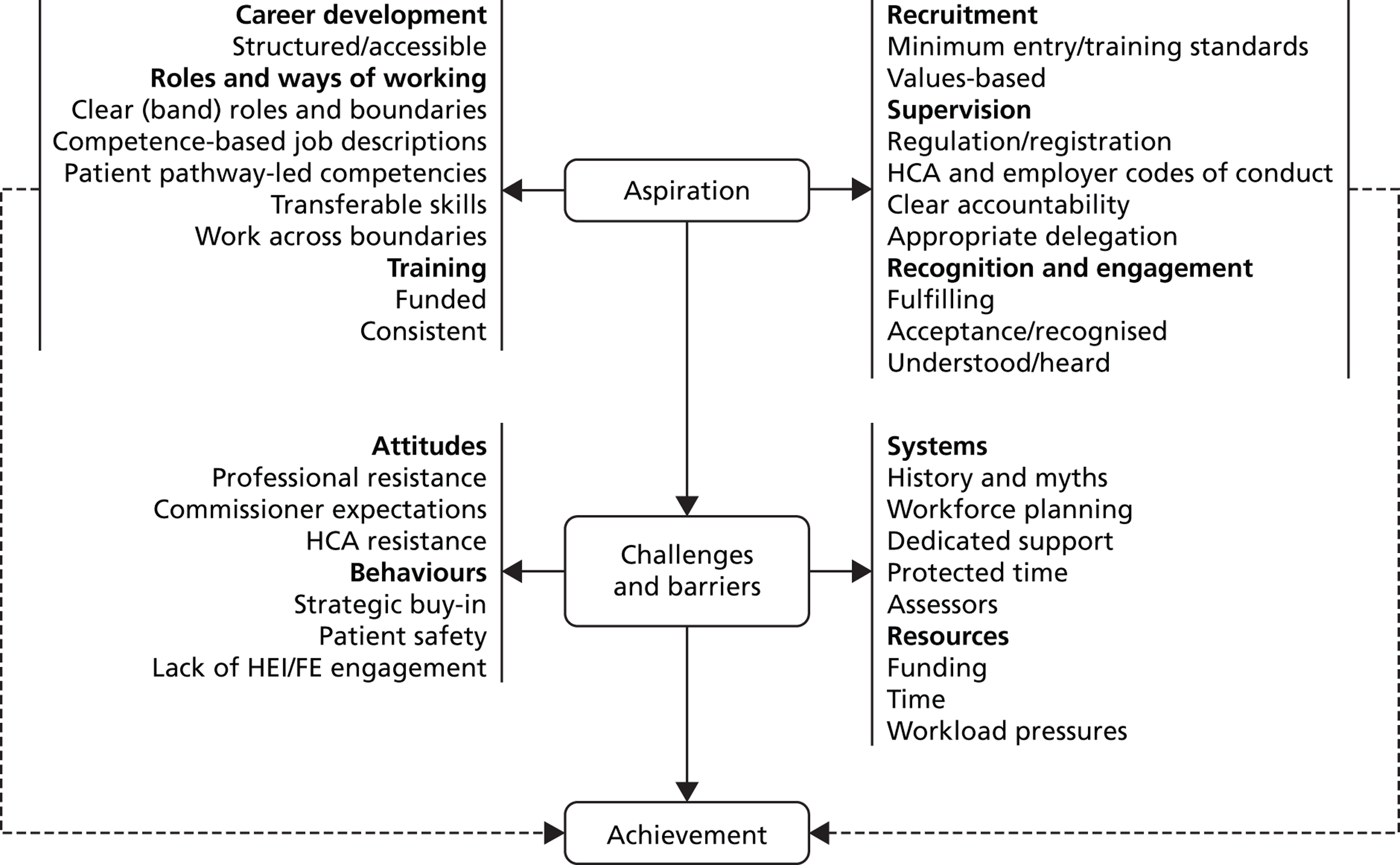
A number of features of the figure are worth highlighting. In terms of aspirations for the role, a series of points centre on the nature of the role and its ways of working. In particular, competencies assume prominence with an emphasis on competence-based job description and competencies more closely aligned with, and rooted in, patient care pathways. ‘Boundaries’ also emerge as significant, albeit in various ways. In part, there is a theme which touches on flexible occupational boundaries, especially in allowing support workers to span or cross disciplines, for example nursing and various forms of therapy. However, there is also an emphasis on clearer and sharper boundaries, not least in distinguishing between roles at different levels of banding.
The Leeds workshop, in particular, dealt with the issue of boundaries in some detail, producing different models to distinguish between the pay bands. One of these is presented in Table 29 (a further two can be found in Appendix 15), and suggests that while drawing upon shared values of care, the bands might be differentiated along three axes: supervision versus autonomy; reporting versus treating; and awareness versus skill/knowledge.
| Band 2 | Band 3 | Band 4 |
|---|---|---|
| Core values | Core values | Core values |
| Greater supervision | More autonomy | Even more autonomy |
| Recognise issues and report | Recognise issues and react | Recognise issues and treat within protocol |
| Technically aware | Technically skilled | Technically skilled with knowledge |
While emphasis is placed on ‘clear accountability’ and ‘appropriate delegation’, it is striking that considerable attention is given to the issue of recognition and engagement: ensuring that nurse support workers are heard, accepted and appropriately valued. Indeed, shifting attitudes are presented as a key challenge to the development of the future nurse support role. A residual degree of nurse professional resistance, particularly to the AP role, was highlighted, as well as a reluctance, perhaps on the part of older, more experienced support workers, to shift habits and established ways of working. In broader terms, systems and ways of working also remained deeply embedded in the trust and ward, rendering change problematic.
The phrase ‘history and myths’, raised at one workshop, captured the ‘stickiness’ of practice around the support role. More prosaically, prevailing systems were also seen to work against the capacity of support workers to develop within the role and, in particular, acquire requisite competencies. The pressures faced at ward level, the general absence of protected time for workplace learning and the shortage of assessors and effective mentors were seen by workshop participants as barriers to be overcome in any moves towards the aspirational nurse support role.
Exploring the potential for the development of a ‘toolkit’ to support the development and management of support worker roles
Introduction
The concept of a ‘toolkit’ to support stakeholders in the development and management of support worker roles in acute care was based on a previous toolkit produced by the Working in Partnership Programme to support the development of HCAs within general practice. 54 Our vision was that a toolkit for acute care might be useful to a range of stakeholders including:
-
support staff – including staff newly appointed to an assistant role as well as supporting career progression of assistant staff through the levels of the NHS Career Framework
-
employers of support staff in acute care – who currently employ support workers or may be considering introducing new support workers roles (such as AP roles)
-
acute trusts – who want to maximise the potential support staff resource within the organisation
-
education providers – providing education and training for the development of the support workforce and
-
patients – who come into contact with, and experience care delivery by, support workers.
During the research study, we have explored the potential for the development of the toolkit. In particular, we have sought opinion from a range of stakeholders on whether or not a ‘toolkit’ would be useful and to whom and, if considered useful, what form it should take and what content would be useful.
Our approach
At the respective regional workshops, an introductory presentation outlined our vision for the toolkit and broad areas for inclusion in the toolkit, including (i) role description for support workers, (ii) support worker role integration, (iii) support worker training development and progression, (iv) management of support workers, (v) recruitment and induction of support workers and (vi) support worker role impact (see Appendix 16). To explore stakeholder perspectives on the potential value of developing a toolkit, we posed the following four questions:
-
Where do you go for guidance to inform management and development of support worker roles?
-
Would a ‘toolkit’ be useful (and for who)?
-
If you would find a toolkit useful, what form would it take and what would it include?
-
Have we got the right six items (see Appendix 16, slide 4) and are they all important or are some more important than others?
This consultation has guided our considerations about the potential utility of developing a toolkit. The main findings of the consultation and our plans for taking the toolkit forward are outlined below.
Findings
Sources of guidance to inform management and development of support worker roles
Participants identified a range of sources that they used when considering the management and development of support worker roles (Table 30).
| Type | Source |
|---|---|
| Internal | Colleagues (ward manager, other professionals) |
| HR | |
| Trust board | |
| Clinical Risk Department | |
| Vocational Education Department | |
| Learning and Development Department | |
| External | Professional bodies (RCN) |
| (Former) SHA | |
| Unions (UNISON) | |
| Sector skills councils (Skills for Health, Skills for Care) | |
| Awarding bodies (City and Guilds, Skills Funding Agency) | |
| Benchmarking – local, nationally, globally | |
| Networks (practice, education) | |
| Other NHS trusts | |
| Higher/further education institutions | |
| Department of Health | |
| NHS Scotland | |
| NLIAH Wales | |
| Skills for Life | |
| NHS Employers | |
| Social Care Institute for Excellence | |
| Health-care cluster groups | |
| National Apprenticeship Service |
Sources included both internal and external support to their organisation, electronic searches for relevant support (using Google and other library databases) and nursing journals. The source of support would largely depend on the type of support worker role.
Participants identified a recent proliferation of sources of guidance to support them in practice when considering the development and management of support worker roles. In addition, participants identified other toolkits for AP roles, including the East Midlands Assistant Practitioner Project Toolkit55 and the NHS Education for Scotland Healthcare Support Workers Toolkit. 56 Other toolkits we identified include the West Yorkshire Lifelong Learning Network Assistant Practitioner Toolkit57 and NHS Scotland’s Assistant Practitioner Project. 58
The utility of a toolkit, the content and target audience
The stakeholders gave mixed responses to whether or not a toolkit would be useful and there were a range of views about who this should be targeted at if taken forward. Many of the participants indicated that they did not like the term ‘toolkit’ and at later workshops the toolkit started to be referred to as an information repository on the guidance of participants.
Participants highlighted that the main challenge for the information repository, if taken forward, would be in maintaining its currency. There were concerns that a proliferation of information from a range of organisations would mean that it would quickly become out of date. This raised questions about where the information resource would be ‘housed’ and whose responsibility it would be to maintain the information, especially given that the research is funded for a defined time period. The overwhelming consensus was that any toolkit/repository should be an electronic resource, underpinned by a good search engine for ease of use so that interested parties could locate information they required in an accessible and simple way.
Despite these reservations, participants indicated the sorts of information that would be useful in such a repository. The main feedback was to create an area that had the following features:
-
signposts to existing national and regional resources about support worker role development and management
-
shares ‘best’ practice and case studies (related to recruitment, induction, training, role integration and transition, supervision, mentoring, competencies, job descriptions)
-
profiles the evidence base for support worker roles (particularly related to ‘benefit realisation’) and how to access evaluation and/or research reports and
-
includes a discussion forum for sharing information about courses and study days related to support worker roles.
These reflected, and added to, the areas that we had identified based on our earlier Oxford and York studies1,5 and as outlined in the presentation. One area where there was less enthusiasm was for information to be held in the repository about the management of the support workforce. This was because participants felt that the area was too broad and something that would be embedded in local HR procedures.
Participants expressed that this information repository could most usefully be housed on a national employer or organisation website because these are sites that many stakeholders already access. In addition, this would ‘endorse’ the information repository and may promote the use of the resource by a range of stakeholders. A search of existing national websites (as described by participants) revealed sites that may be part fulfilling the suggestions of participants. For example, NHS Employers hosts a Support Workforce website59 that includes a ‘tools and resources’ section. The RCN hosts a ‘HCA & AP’ website60 that includes a range of resources aimed at support workers (e.g. ‘first steps’) and their colleagues (e.g. ‘accountability, delegation and professional issues’).
Summary
The consultation with participants at the workshops, representing a range of stakeholders, was useful for exploring the potential for the development of a toolkit as part of the current research study. A key requirement of any toolkit or information repository, from the perspective of these stakeholders, was to ensure that it had ‘currency’. This raises a number of challenges in producing a toolkit or information repository that is ‘fit for purpose’ as requested through the consultation. We will, therefore, utilise the existing project website45 to provide access to information requested by participants, including signposts to useful resources, case studies and examples of ‘best’ practice and the evidence-base for support worker roles. We will not be able to manage a discussion forum and we will have to state the date of publication. However, while considering the development of the toolkit or repository, we have commenced discussions with national organisations to determine options for keeping the information up to date and adding new materials as published. This would be the most suitable option for ensuring maintenance of the resource.
Details of the web pages will be disseminated through a variety of strategies, including publications, conferences and signposting from other national and regional web sites. This is the most pragmatic way forward with this work and to ensure the longer-term engagement of stakeholders.
Overview: discussion and lessons
As an end in their own right, the regional workshops provided an opportunity for stakeholders to share ideas and ‘good’ practice on the management and use of the nurse support worker role. Indeed, the perceived value of these workshops to participants was indicative of the absence of available institutional spaces to discuss such issues and a signal to policymakers of the need to establish them. The workshops confirmed the diversity of trust policy and practice on approaches to the deployment and treatment of support workers even within the same region. There was, however, a strong consensus on the challenges facing trusts as they dealt with and developed the support worker role and on how those challenges might be addressed. These shared views emerged from the design of the four regional workshops, in particular the facilitated discussion, which allowed participants to address issues in a structured and systematic way. Thus, participants initially examined the current approaches to the use and management of nurse support workers in their trusts; how they might better use and manage such workers in the future; and the steps needed to make the move from current, typically problematic practice, to the future desired and improved practice. These workshop deliberations provide the platform for a number of substantive lessons:
-
Nurse support workers are highly valued members of the ward, primarily engaged in patient-centred bedside work. At the same time, they are often undervalued and under-rewarded, and indeed subject to ‘weakly’ developed management practices, not least reflected in a lack of clarity around the distinction between band 2 and 3 roles.
-
Against the backdrop of these concerns, there is scope to develop distinctive good practice, highlighted by examples of leading edge roles and approaches to recruitment, development, training and supervision. If some trusts are able to pursue such approaches, there is further scope to examine why some others have not been able to do so and how they might be encouraged in this respect.
-
More telling is the emergence of a shared perceived approach to the future management of nurse support workers. This is based on a set of agreed practices, including values-based recruitment; more robust induction programmes, in terms of length and issues covered; clear sets of competencies associated with different bands; and providing the basis for more developed career pathways.
-
Trusts face significant challenges in developing such an approach. There are embedded and underdeveloped extant systems likely to undermine or inhibit progress. There is pressure on the resources needed to develop it. Moreover, attitudes and behaviours among certain stakeholders are likely to question it. Given these challenges, and on the assumption that this model is seen as worth pursuing, policy-makers and practitioners at different levels of the NHS – national, regional and local – need to consider in a structured and systematic way how these challenges might be addressed and overcome.
Chapter 6 Summary and conclusions
Reviewing the study
As concerns among policy-makers, practitioners and service users about the quality of frontline health care have come to the fore in recent years, so attention has increasingly focused on the structure and capability of the nursing workforce, and particularly on the role of the nurse support worker within it. This interest in the nurse support worker is hardly surprising. While a long-standing component of the nursing workforce, the support worker has over the last few decades emerged as the main bedside presence, making a crucial contribution to providing the fundamentals of care. 1 Despite, or perhaps because of, their unregulated status, the use of support workers in this way has often been encouraged by policy-makers and practitioners, who view them as ‘freeing up nurses’ and providing a ready source of flexible and cost-efficient labour. As support workers are unregistered workers, positioned at AfC pay bands 2–4, there has, however, been an undercurrent of caution regarding their use, particularly as the role has extended. Most recently, this caution has deepened just at the point when the cost and productivity pressures facing the NHS have prompted trust managers to reconsider how they organise their nursing workforce and, as part of this process, how the nurse support role might be used and managed. In short, a deepening caution about the deployment of support workers has emerged at the very time when mounting pressure is encouraging their greater use.
Against this backdrop, our study on the development of a high-performance support workforce in acute care is particularly timely. This timeliness is reflected in a series of public policy developments related to support workers, arising during the period of our research. In part stimulated by the second Francis Report on Mid Staffordshire3,61 but also by compelling evidence pointing to the lack of dignity and compassion in the delivery of care, especially to older people,62,63 these developments have included the publication of a Skills for Health Code of Conduct and minimum training standards for support workers64 and a series of recommendations on the recruitment, training and development of support workers made by the government-commissioned Cavendish Review. 65
The value of our current project is also enhanced by its positioning. It is a follow-up study, building on previous research carried out at the University of Oxford1 on support workers at AfC pay bands 2 and 3 and at the University of York5 on APs at band 4. While independently conceived, both studies sought to strengthen the evidence base on nurse support workers by a structured and systematic examination of who support workers were, in terms of their background and motivation, what they did and how they were viewed and used by different stakeholders. Moreover, these initial studies were in large part diagnostic, highlighting the problems faced by trust managers in their use and management of nurse support workers. The York and Oxford studies revealed significant challenges and some disordered policies and practices related to this group of workers. In contrast, the current study has been concerned with how trusts have sought to change their approaches to nurse support workers, not least in response to some of the problems highlighted in the previous studies. Analysing these changes in trust approaches to support workers has revealed new sets of challenges, but also allowed this study to contribute to and help to formulate a much more constructive, applied and forward-looking agenda on the utilisation of such workers.
The three themes constituting the current project followed on from specific aspects of the previous Oxford and York studies1,5 and each considered discrete sets of questions.
-
The innovation theme drew upon the uneven incidence of new practice in the use and management of support workers, as revealed by the previous studies. 1,5 Questions remained about the incidence of different forms of innovation – new roles, ways of working and management – as well as about how and why some trusts were able to innovate in these respects, while others were not. Different phases of research were undertaken as part of the theme – scoping discussions, a national survey and case studies of different types of innovation – designed to address these questions.
-
The evaluation theme explored the consequences of different initiatives taken by trusts in relation to the management and the use of their nurse support workforce. More specifically, this part of the project evaluated whether or not and how such initiatives impacted on various outcomes and stakeholders, thereby strengthening the evidence based on the use of certain policies and practices. In pursuing this theme, we engaged with trusts on the evaluation of the initiative in question. This engagement was not as structured or organised as hoped, but the trusts involved did select the evaluated initiatives and were informed about the research process and its findings on an ongoing basis.
-
The engagement theme was driven by findings from the initial Oxford and York studies,1,5 which suggested the fragmented, arguably disordered nature of trust policy and practice on the use and management of support workers. In the absence of a national regulatory model ensuring standardisation in the recruitment, training and management of support workers, trust approaches had developed in incremental, diverse and disconnected ways. The engagement phase of the research brought together the actors with a stake in the support worker role, as a means of sharing ‘good practice’, identifying and addressing common problems and issues, and exploring ways forward. In pursuing these ends, four regional workshops were organised, complemented by an end-of-project conference convened in July 2013 to present and discuss the findings from all three project themes.
The current study, therefore, had a diffuse focus, but this should not detract from the possibility of examining cross-cutting issues and findings, drawn from the application of a common set of research methods. Indeed, methodologically, while a variety of research techniques were used, the core of our project revolved around 12 case studies: six ICs and six ECs. While these cases, particularly the former, derived from purposeful sampling, their broader value lay in the scope they provided for naturalistic generalisation. 66 This form of generalisation is rooted in the view that, where a case is detailed and in-depth enough, the reader might be able to relate the findings to their own circumstances and needs. As Melrose67 notes, ‘Naturalistic generalisation invites readers to apply ideas from natural and in-depth depictions presented in case studies to personal contexts’ (p. 341).
It was this search for naturalistic generalisation that encouraged us to name the case study trusts wherever possible: we felt that identifying a trust allowed the reader to relate to it and, indeed, if useful, to follow up and contact it. This naming of the organisations involved proved viable in the case of the six innovation trusts, perhaps unsurprisingly given that the trusts involved typically viewed their innovation as a ‘success story’. Such an approach was much more problematic in relation to our ECs. These trusts were embarking on an initiative with uncertain outcomes, and subsequently found themselves facing major difficulties and, in some instances, short-term failure. The identities of the ECs were, therefore, protected. However, it was these very difficulties and failures that arguably provided an alternative basis for naturalistic generalisation. Few trusts would claim not to have experienced problems in implementing an initiative, allowing readers from other trusts to empathise with developments in our ECs and meaningfully draw upon the case findings to examine issues in their own trusts.
In substantive terms, the range of issues considered in this study should also not obscure a unifying interest in workforce change in acute health care. More specifically, all three research themes centred on how trusts sought to change the ways in which they used and managed nurse support workers. This common concern with workforce change was much greater than originally envisaged. While the innovation and engagement themes were always designed to explore change in relation to support workers, the evaluation theme was originally presented as focusing much more on outcomes: whether or not various support worker initiatives met their stated objectives. Certainly, the ECs examined such outcomes, but the difficulties trusts faced in implementing the initiatives ensured that, in addition, they provided considerable insight into the nature of the change process.
A shared interest in workforce change centring on the nurse support role in acute health care provided an opportunity to draw upon different research literatures as a means of understanding such change. The literatures, to some extent overlapping, related to:
-
different models of organisational change
-
interoccupational relationships and role boundaries or jurisdictions
-
institutional approaches to change, in particular focusing on embedding and legitimising new work practices.
In this concluding chapter, our research findings are related to the general features of the analytical and theoretical frameworks associated with the three literatures. Detailed lessons for policy-makers and practitioners at different levels of the NHS were presented in a section at the end of each of our four substantive chapters (see Chapters 2–5).
Models of change: bottom-up or top-down?
Over the years, a range of change models have been presented in the organisational studies literature, based on very different assumptions about and observations on the nature of ‘effective’ change. 37,38 Such models have variously been rooted in notions of organisational learning; in the underlying importance of power and processes of conflict resolution; and in a view of change as essentially an interactive process, based on a negotiated order. However, perhaps the sharpest divide has been between two models of change. One is a mechanistic model based on the top-down introduction of change, underpinned by a strategic, structured and systematic approach, setting out clear goals and the means of achieving them. The other is an organic model driven by the bottom-up pursuit of change, advanced in an ad hoc and opportunistic manner, with goals and means emerging in an incremental, albeit still ordered, way. 68,69 Our study suggests that in seeking to change the use and management of nurse support workers, these models are far from mutually exclusive.
Indeed, what is striking from our study is the need for a local balance between top-down planned strategic and bottom-up opportunistic incremental approaches, sensitive to various contingencies, in particular the nature of the change and its stage of development. In terms of stage of development, most striking in our study was how many of the innovative cases originated in the seizing of an opportunity, often by those at lower levels of the trust and in discrete clinical areas, without much initial clarity or planning on the development of the new practice: at Torbay, for example, the chance of external funding used to train APs in a select range of wards; at Hillingdon, external sponsorship for a C-SW role in a specialist team of nurses; and at OUH, the availability of an individual particularly well suited to help out in the operating theatres of the dermatology department. This contrasts with ‘less successful’ changes, particularly from within our evaluation theme, which were top-down, broadly based and developed by trusts in quite a detailed and meticulous way: for instance, the roll-out of the APs across all clinical areas in a trust; the development of a new induction programme explicitly linked to beginner competencies; and the introduction of an ADP related to the extended use of MCAs as part of a broader reorganisation of maternity services.
While successful change was often stimulated in a bottom-up and less ordered way, taking forward and consolidating a change often relied on top-down backing, typically from senior nurse and HR managers. In the absence of such backing, there was a danger that a change would remain a disconnected experiment, liable to ‘fizzle out’. Indeed, our bottom-up examples of change did not remain opportunistic and ad hoc for long, with focused objectives quickly emerging: for example, at Torbay, the AP training initiative quickly developed into a more strategic ‘narrow and deep’ approach to the use of APs in the trust.
More specifically, senior management backing for emergent change took various forms in our cases. In some instances, senior management visibly endorsed the change, sending a strong validating signal to matrons, ward managers and other stakeholders. More tangibly, senior managers provided necessary resources and were able to address relevant governance issues: presenting and arguing for the formalisation of the initiative in relevant decision-making committees. This sort of backing was particularly apparent in the introduction of values-based recruitment at York and the introduction of the CSW trainer role at OUH and the HCA development nurse role at UCLH. Moreover, the absence of such senior management backing might be seen as contributing to the delayed MM pilot. At this trust, the chief nurse who was committed to, and focused on, the pilot was succeeded by an individual with other competing priorities.
The need for senior management backing for change in the use and management of nurse support workers was also reflected in the partnership working by senior managers in developing initiatives. This was again seen in the case of values-based recruitment at York, where senior managers in three functions – nursing, HR and organisational development – made complementary contributions to the initiative. In fact, the absence of this functional co-operation in the introduction of the new 2-week induction at one of our ECs contributed to some of the problems it faced. HR had failed to provide timely joining instruction for new HCAs, with the result that they missed their scheduled induction programme, undermining the objective of ensuring that all starter HCAs completed the programme before ‘hitting the ward’.
Given the value of top-down support, particularly in driving forward an initiative, it is perhaps a cause of some concern that our study found that the conditions for such support often appeared to be lacking. This was reflected in two sets of findings. First, the national innovation survey suggested that the organisational infrastructure to underpin the development of nurse support roles was typically quite weak; for example, the proportion of trusts with senior management champions for support workers was surprisingly low. In the wake of our findings, there is a clear need for such trust champions to develop, indicative of broader senior management commitment to and enthusiasm for the nurse support role. Moreover, while the survey response rate from HR directors was weak, where we were able to match nurse and HR director responses in the same trust, striking differences were revealed in views on whether or not and how the nurse support roles might be developed. Given the importance of partnership working, steps are required to ensure that functional views are aligned and a consensus is built within trusts on the management and use of support workers.
Second, the scoping exercise suggested that there was a considerable degree of residual uncertainty, yet to be worked through, about how to address issues around the future use and management of the nurse support role. This organisational hesitancy, in some cases paralysis, in dealing with the dilemmas associated with the role might have reflected the timing of the scoping phase: the second Francis report61 on Mid Staffordshire had yet to be published, with some trusts clearly awaiting its recommendations and the government’s response to them, before tackling uncertainties associated with the support role. However, even in the wake of the Francis report,3 key dilemmas remained: whether or not to create career pathways for support workers which might be costly; whether or not to employ unregistered APs rather than band 5 RNs; and whether or not to ‘sweat’ band 2 HCAs before developing more extended band 3 and band 4 roles.
The lessons drawn at the end of Chapter 2 sought to provide some guidance on how such uncertainties might be addressed, with a particular emphasis on the need for trusts to display some sensitivity to their local circumstances. Thus, for example, the tightness of local labour markets might influence responses to the uncertainties. Where it is difficult to recruit and retain nurse support workers, the development of a career pathway to attract and keep them might assume considerable importance. Similarly, difficulties in recruiting and retaining RNs might encourage ‘grow your own’ strategies, predicated on pathways for support workers through to pre-registration training.
A key finding from our study, therefore, suggested the value of a balance between top-down and bottom-up models of change, albeit with our results also casting some doubt on whether or not the systems and structures were in place in trusts to achieve this balance. It has been argued that such a balance needs to be sensitive to the stage of development: the initiation of a change might well come from below, but taking it forward and consolidating it often requires support from above. This emphasis on the bottom-up initiation of change should not, however, detract from at least a few examples of ‘effective’ change stimulated from the top down: for example, at York, the introduction of values-based recruitment, rooted in a recognition of the high and rapid turnover among HCAs; at OUH, the appointment of a CSW trainer to deal with low HCA completion rates on accredited programmes; and at UCLH, the creation of the HCA nurse development post to address the perceived paucity of training opportunities for HCAs. What appeared to distinguish these cases from the ‘less successful’ examples of top-down change were their sharper focus and the fact that they were much less ambitious in terms of scale. They were also dealing with a problem or need widely recognised and acknowledged within the trust.
Interoccupational relations: boundaries and jurisdiction
As the nurse support role has extended its activities and assumed increasing importance at the bedside, so the challenge to occupational jurisdictions and job boundaries has come to the fore as an issue of debate among policy-makers, practitioners and other commentators. This challenge is most intense at the RN–support worker interface. However, this should not detract from concerns about job boundaries at pay bands 2, 3 and 4, and in particular, how these bands might be substantively differentiated.
The nurse–support worker interface
There has been a long-standing overlap between the tasks performed by RNs and support workers, a legacy of nursing’s quasiprofessional status and its failure to achieve occupational closure on the creation of a nurse registrar at the beginning of the twentieth century. 70 Nursing has remained an activity open to ‘unqualified’ workers, with few, if any, nurse activities, beyond the dispensing of controlled drugs, protected in statute. This has created an uneasy relationship between the ‘nurse establishment’ – the RCN, the chief nurses and the nurses’ regulatory body – and support workers, particularly as RNs have sought to pursue and bolster their professional status.
The uneasiness of this relationship with support workers might be seen to partly lie in nurse uncertainty about how to take forward their professionalisation project. 29 Over the years, the nurse establishment has oscillated between two possible approaches to this project, with very different implications for the positioning of the support worker:
-
Specialism–discard: the first is based on occupational closure around a discrete set of specialist tasks, with nurses discarding more ‘routine’ tasks as they move on to develop this deepening expertise. Abbott27 refers to professions passing on ‘dangerously routine tasks’, which might otherwise undermine claims to specialist expertise, to subordinate occupations, a process also stressed by Hughes71 who more specifically refers to nurses delegating such tasks to nurse aides as they move up the occupational hierarchy. It is an approach to professionalisation that views the support worker as a convenient depository of routine tasks for nurses as they acquire more expertise and take on specialist roles.
-
Holism–hoard: the second approach to professionalisation is rooted in claims to professional status on the basis of the holistic provision of care. These holistic claims, often found among quasiprofessionals72 – teachers and social workers as well as nurses – are clearly at odds with the former approach to professionalisation. Rather than professional status resting upon specialist expertise, it is seen to lie in an occupation’s capacity to recognise and meet the users’ needs in the round, from the most basic to the more complex. A holistic narrative suggests that, rather than discarding or delegating tasks to the nurse support worker, the nurse needs to retain or hoard tasks. Indeed, in this context, the nurse support worker becomes less a ‘convenient depository’ and more a potential threat to nurse claims to provide all-round care.
This is not the place for a detailed discussion of the debates within nursing over the relative merits between these competing approaches, or which should be or indeed has been privileged. Briefly, there has been a secular trend towards a specialism–discard approach over recent decades as nurses have departed from the bedside to take on other, often more specialist roles and tasks. 73 In part, this has been driven by the profession itself, but it has also been steered by government policy, with its deepening emphasis on the nurses’ role in the performance management of the ward. More recently, however, such a trend has elicited a rebuke from the nursing establishment – the chief nurse and the RCN – stressing the value of a holism–hoard approach and reflected in warnings that nurses should never be too posh to wash. 74 This uncertainty, perhaps ambiguity, in the preferred approach to professionalisation was also manifest in our previous studies: the earlier Oxford1 project, in particular, revealed that while in interview nurses stressed the positive impact made by support workers on their working lives, in the questionnaire they were somewhat more qualified in their views, suggesting a more grudging acknowledgement of the HCA contribution.
The findings from the current study suggested that profession–support worker jurisdictional issues were at their most pressing and intense in relation to the band 4 AP role. Moreover, given the findings from our national innovation survey that trusts were increasing rather than decreasing their use of APs, these jurisdictional issues are likely to be increasingly to the fore. Four of our cases explored the development of APs: the roll-out of APs across a trust (the roll-out case), the MM (the MM case) by APs, the specialist use of APs at Torbay and the development of a band 4 surgical AP role in dermatology at OUH. A further two cases explored a band 3 role, which had also advanced quite deeply into professional territory: the raft of MCAs at one of our evaluation trusts (the MCA case) and the single C-SW at Hillingdon.
The results from these six cases suggest that some care is needed in generalising about the impact of extended support roles on occupational jurisdictions at the nurse interface. The one generic issue to emerge at this interface was nurse accountability for the tasks performed by nurse support workers with extended roles. Nurses often felt vulnerable, with their registration perceived as being ‘on the line’ if any mistakes were made by the unregistered workers under their supervision. These concerns were apparent despite clear NMC guidance on ‘appropriate delegation’, stressing that nurses are accountable for the decision to delegate to the nurse support workers but not for the performance of the tasks. In others words, if the nurse makes an informed and responsible decision to delegate, they cannot be held accountable if the nurse support worker then goes on to make a mistake. However, perceptions matter, with nurse uncertainty about accountability still generating concerns and influencing the propensity to delegate. It is a finding which suggests that trusts need to ensure that their nurses fully understand their accountability for nurse support workers, with assurance given that as long as they adhere to NMC guidance their registration will be safe.
Despite this generic nurse concern about accountability, the nature and consequences of the impact of extended roles are more usefully seen as related to certain contingencies, in particular why and how the support role was being extended. Thus, AP roles and the extended band 3 roles were introduced in our cases for a number of reasons, with different outcomes for nurse–support worker relations:
-
meeting service needs: the specialist Torbay APs, Hillingdon C-SW and OUH SAP cases
-
addressing recruitment difficulties among band 5 nurses: the roll-out case
-
substituting (typically associated with the search for cost savings): the MCA, MM, roll-out cases
-
creating a new leadership role at ward level: the roll-out case.
The development of AP/band 3 roles appeared less of a challenge to RN jurisdictions where they were clearly designed to meet specific service needs. Typically, this was a bespoke process, with clinical areas working through whether or not and why they needed such a role, and, if they did, how precisely it would fit into care delivery and its associated routines. Where the need for an extended AP/band 3 support role was clear and those within the clinical area were involved in its design and introduction, it was typically not seen as a threat to nurses or challenged by them. Such roles were seen as complementary to those of the RNs and with a clear added value. The Torbay case, in particular, highlights this non-threatening approach: the selective introduction of APs only into ward areas which had seen the need for such a role – cancer services and breast care – and following detailed working through of what form the role would take and its training requirements. At Torbay, the AP role was seen to provide a means of developing expertise in certain clinical procedures, which might otherwise not exist. This benefit also derived from the C-SW role at Hillingdon, with the C-SW able to work very closely with patients in managing their stomas prior to discharge. It was an approach predicated on the view that APs and extended band 3s might be needed and could fit in well in certain clinical areas, but not necessarily all.
Nurse jurisdictions appeared much more directly challenged where the AP/band 3 roles were seen as part of a broader attempt at substitution, whether as a means of saving costs and/or dealing with shortages in registered nurses. By definition, substitution dilutes skill mix and involves support workers taking on tasks previously performed by RNs. As noted, depending on how the nurses’ professionalisation project is perceived, this process is not necessarily problematic for nurses. For nurses, the real concern with APs/band 3s lies in the perception that they might be taking on core rather than marginal, routine tasks. This concern was clearly illustrated by the MM case, where the planned MM prompted nurses to question whether or not there were any tasks, other than the handling of controlled drugs, protected for them. According to the survey in this case, APs themselves appeared to be somewhat more sanguine about taking on this role, although in interview even APs voiced some concern about taking on MM. Many such APs had been keen to remain as support workers as a means of retaining direct contact with patients. The same responsibility for drugs which had contributed to nurses being driven away from the bedside was seen as likely to affect support workers at this level in the same way. Similarly, registered midwives, particularly in the community services, displayed concern at the increasing role played by band 3 MCAs in conducting home visits.
Perhaps the most striking example of nurse resistance to the AP role was in our roll-out case. The attempt to introduce the AP role across the whole of this trust provided a particularly stark contrast with Torbay’s more selective approach. Indeed, the roll-out case lends some support to the view that the AP role might be better suited to some clinical areas than to others. In certain, specialist clinical areas in the roll-out case, such as endoscopy and stroke, the AP role was broadly accepted by RNs. However, in the general medical and surgical wards, the APs’ contribution to health-care delivery was less obvious, with the post-holders finding it much harder to gain acceptance.
Interestingly, resistance at the roll-out case was not only from nurses but also from band 2 and 3 HCAs. This was a consequence of design features of the roll-out trust’s AP programme, which allowed outside applicants into TAP posts. ‘Parachuted in’ over the heads of existing HCAs who were not selected for the programme, these external TAP recruits caused resentment among HCAs. However, it was the resistance of the nurses which proved particularly significant in the roll-out case, reflected in trained APs often being restricted to the performance of basic care tasks, with little use being made of their extended skills. Indeed, the roll-out case illustrated the fact that, even where an AP training programme appears to be successful in terms of completion rates, unless the role itself is accepted at ward level by team members it runs the risk of still being marginalised.
The impact of pursuing the final objective, developing the AP role as a new leadership position, on boundaries at the nurse–support worker interface proved more difficult to assess. This objective was articulated in only one of our cases: the roll-out trust. It was underpinned by quite a strong organisational rationale. Given increasing public policy attention on direct care delivery and RNs’ drift away from the bedside, the trust felt that there was scope to develop an AP role with dedicated responsibility for direct bedside care, through co-ordinating and managing the band 2 and 3 HCAs on any given shift. Indeed, this leadership role was envisaged as broadening to take on more general line management responsibility for HCAs such as on-ward induction, mentoring and performance appraisal.
The effect of such an AP leadership role would clearly have been to reinforce or exacerbate the RN departure from the bedside. However, and in doing so, it begged a number of different questions. For example, where did accountability lie in instances where a non-registered support worker directed other support workers in care delivery? What, if any, authority would the AP have in directing nurses, not least given that nurses were still often involved in some aspects of the fundamentals of care?
In the event, this AP leadership role at the roll-out case gained limited traction, rendering it difficult to gauge nurse responses. The failure of such a leadership role to make headway at the trust might well reflect the concerns highlighted above, but more profoundly it can be linked to the dilemmas faced by a trust in using the AP role to pursue various, often conflicting, goals. Thus, it can be seen above that the roll-out case trust was seeking to use the AP role to address a range of objectives: nurse recruitment difficulties; cost reductions; and improved bedside leadership. These goals were not necessarily compatible, with the former two arguably driving out the latter. If the AP role is being used to fill nurse posts and dilute skill mix, it has to be carrying out tasks traditionally performed by nurses, such as MM. These are the very tasks likely to take the AP away from the bedside and prevent the post from being used to lead and direct bedside care. If the AP role is to be used in this leadership capacity, it has to be based on additional staffing, that is to say a new AP post, rather than as a replacement for a RN.
The bands 2 to 4 interface
Our study suggests that the RN–support worker boundary is not the only one to generate jurisdictional issues. There remains some debate on the boundaries between support roles at pay bands 2, 3 and 4. This debate was evident in the scoping phase of our innovation theme and during our four regional engagements workshops. Thus, it was clear from both sources that trusts were often unclear about whether or not there was a meaningful substantive difference between support roles at these different levels. In general, the band 4 AP role was seen as distinguishable from bands 2 and 3; it was qualitatively different in terms of the tasks performed. While unregistered, the AP role was nevertheless rooted in a robust training programme: a 2-year FD, underpinned by workplace learning and the acquisition of appropriate competencies. While residual concerns remained about the delivery and substance of this training, not least related to its sensitivity to specific trust needs and circumstances, the training provided some confidence in, and assurance about, the capabilities of APs. In the context of a much more uneven approach to the training of band 2 and 3 HCAs, and a traditionally less ordered approach to the development and use of workers at these levels, trusts were finding it much more difficult to differentiate between band 2 and 3 HCA roles and to establish sharp boundaries between them.
The blurring of the boundary between bands 2 and 3 was highlighted in our four regional engagement workshops, with views varying on the steps to be taken to address it. The ‘future nurse support role’ model, embracing emerging standard practice (see Figures 11 and 13), included the clarification of band 2 and 3 role boundaries. Indeed, at these workshops, attempts were made to hammer out differences between band 2 and 3 roles on the basis of autonomy, capacity to recognise and respond to care needs, and level of skill. In practice, some trusts were seeking to formalise and reinforce the distinction between these bands by developing distinct sets of band 2 and 3 competencies. There were, however, other trusts less convinced about the substantive difference between band 2 and 3 HCA roles, in particular whether or not any such difference was significant enough to justify fine-tuning the grade mix to reflect it. For such trusts, the band 3 support role was increasingly becoming a redundant grade, with their nurse support workforces solely comprising workers at bands 2 and 4.
Institutional approaches to change
The final theoretical perspective drawn upon to interpret our study’s findings is the institutional approach to organisational change. While it is clearly beyond the scope of the report to examine this approach in detail, this section concentrates on the three prominent features of, or debates within, institutionalism and relates them to the use and management of nurse support workers:
-
institutionalist assumptions about the nature of change;
-
the role played by different actors in institutional change; and
-
the change processes in which these actors engage.
Each is considered in turn.
The nature of change and the support worker
Institutional theorists have traditionally found organisational change problematic. Institutions are, after all, enduring systems and structures which shape behaviour on a recurring basis. More precisely, Scott defines institutions as consisting of:
. . . cultural-cognitive, normative and regulative elements that . . . provide stability and meaning to social life. . . Institutions are transmitted by various carriers, including symbolic systems, relational systems, routines and artefacts. . . They operate at multi levels. 75
p. 11
A few features of Scott’s definition are worth stressing for our purposes. First, the definition identifies various ‘elements’ as the source of stability and meaning: a regulative element, which might be viewed as formal rules, often grounded in means–ends rationality; a normative element, apparent in less formal rules, typically rooted in non-rational values and beliefs; and cultural-cognitive element allowing actors to interpret or give meaning to such rules. Second, the definition acknowledges that these elements might operate at different levels, including various organisational levels. Finally, Scott’s emphasis on ‘stability’ might be seen to reflect a traditional bias in institutionalism towards inertia: actors are deeply embedded in institutions, which constrain their behaviour and render change difficult. 39
It has long been acknowledged that acute health-care trusts are remarkably complex organisations in these institutional terms. They operate at myriad levels and display considerable vertical and horizontal differentiation, the latter reflecting the diverse clinical needs addressed by any given trust. Indeed, in dealing with a range of patient conditions, these various clinical areas have often developed their own institutional logic and set of institutional practices. Of course, the situation is even more challenging for trusts, given that such diversity is managed under a single trust governance structure, accountable for all of its activities.
Nurse support workers are particularly deeply embedded in the distinctive institutional practices at the level of the clinical area and, indeed, the individual ward. This might be seen as in part related to the unregistered status of such workers. The use and management of support workers is not subject to the standardisation of training, expected behaviours and discipline typically wrought by a national model of statutory regulation. Falling beyond this form of regulation, the treatment of nurse support worker becomes much more malleable and sensitive to the needs and circumstances not only of the trust, but of the clinical area and the ward in which they work. Less formal, normative mechanisms on the use of support workers at these levels come to complement, and sometimes subvert, more formal national and trust regulatory mechanisms on the use and management of this group of workers.
This diversity of institutional practice between clinical areas and wards in the same trust helps to account for the difficulties highlighted by a number of our case study organisations in implementing support worker initiatives, particularly top-down and across the whole of a trust. Often, such initiatives simply ‘bounced back’ and were not perceived as sensitive enough to local ward practices. This was particularly the case with the HCA beginner competencies initiative. A number of wards had already developed starters’ competencies more attuned to their needs, and felt that the trust-wide initiative was either unnecessary for them or not sensitive to their own competency frameworks. Similarly, in the AP roll-out case, the trust encountered difficulties in gaining acceptance for the AP role, especially in general wards, where it was perceived as not easily accommodated within established routines. Indeed, it might be argued that the introduction of the MCA within the context of a broader service reorganisation represented a determined senior management attempt to break through the traditional institutionalisation of workforce practices in maternity services at the trust, an attempt which elicited a strong backlash by staff and considerable demoralisation.
A more specific example of the power of ward-based institutions to shape the use and management of nurse support workers was the nurse–support worker skill-mix ratio on any given shift. In a number of our trusts, this regulative mechanism had not been modified to account for the development and presence of an AP(s) on a shift: as we have seen, APs are unregistered but often highly trained and capable of performing extended roles. In the absence of this modified approach to skill mix, the tasks performed by the AP on a shift were determined not by the capabilities of the AP but by whether or not he or she was included in the nurse or the support worker skill-mix numbers: counted in the former, clearly the AP was in a nurse ‘slot’ with the scope to perform an extended role; counted in the latter, the AP was classified as a carer and restricted to undertaking more routine tasks.
Institutional entrepreneurs
Our study has highlighted the importance of various individuals willing and able to break through institutional constraints to facilitate and drive change in the use and management of nurse support workers. The research literature has referred to these figures as institutional entrepreneurs. 40 In our innovation theme, two of the cases centred on such IEs: the HCA development nurse at UCLH and the CSW trainer at OUH. More broadly, such figures emerged in a number of our other cases: the AP project co-ordinator in the roll-out case; the consultant dermatologist involved with the SAP at OUH; the key figure in the Torbay ED; and the nurse consultant so prominent in developing the C-SW role at Hillingdon. Indeed, the ubiquity of such figures is testament to their importance in attempts to change the use and management of support workers.
Drawn from our cases, these IEs appeared to have a number of characteristics, capabilities and resources.
Characteristics: credible and approachable
Changing the use and management of support workers often involved the IE dealing with a range of different actors: the support workers themselves, their line managers, more senior decision-makers and, in some cases, such as the nurse consultant at Hillingdon, external funders. The IE needed to be credible to these actors: that is to say knowledgeable, competent and authoritative. Such credibility might well have come from the ‘insider status’ of the IE; many of our IEs had considerable experience within the trust and were therefore known and trusted by staff members. However, this was not invariably the case; the CSW trainer, for example, was new to the OUH but quickly established credibility through her competence.
Institutional change generates uncertainty, pressure and stress. IEs were typically accessible to others, helping them to deal with such difficulties. The project co-ordinator at our roll-out case, for example, was available to TAPs who had difficulties with their studies, and was usually able to help them out. It might be argued that a geographically compact trust facilitated staff access to the IE, and, indeed, the capacity of the IE to navigate her way through trust systems. Again, however, this was not necessarily the case. In larger, more dispersed trusts, IEs were often proactive in making themselves available; for example, in OUH and UCHL, both multisite trusts, the CSW trainer and the HCA-DN had respectively set up drop-in sessions and road shows on a rolling basis on different sites, providing spaces for staff to approach them.
Capabilities: networking and advocating
Institutional change in the use and management of support workers typically involves not only initial engagement with the ‘right’ people in and sometimes beyond the trust, but also sustaining that engagement. This requires networking capabilities on the part of the IE. These capabilities were evident in the case of the ED at Torbay, reaching out to different clinical areas to hammer out whether or not and how the AP role might address service needs. Similarly, the HCA-DN at UCLH had to connect with clinical facilitators in developing ward-based HCA training packages. Indeed, it was arguably the absence of a networking IE at the MM case trust which contributed to the difficulties in launching the MM pilot: such a figure was needed to connect interested parties in the trust’s staff development section, its midwifery service and in its pharmacy department as a means of building agreement and ensuring that they were all moving forward on the same basis.
The IEs in our case study trusts were, typically, strong advocates of the innovation or initiative in question. They were not only passionate in presenting it and tenacious in pursuing it, but also skilful in doing so. Indeed, they were particularly capable of navigating their way through the trust’s decision-making structures, ensuring that issues were dealt with in a timely and appropriate manner.
Resources: time and power
As roles dedicated to developing new support worker policies and practices, a number of the IEs in our cases had the time to devote to the task: the AP project co-ordinator at the roll-out case, the HCA-DN and the CSW trainer. However, there were also instances where the IE created his or her own time for the initiative: the consultant dermatologist at OUH was, for example, prepared to devote time teaching the SAP new skills on the job.
Institutional entrepreneurs were not invariably powerful, hence the importance of their capacity to network with those with authority. Nonetheless, there were powerful IEs in our cases, able to push through institutional change. The most obvious example was again the consultant dermatologist in relation to the SAP role at OUH. This was our only example of a clinician-led innovation or initiative, and highlighted how status could facilitate change. It was reflected in the alacrity with which the trust’s senior nurse managers came on board with the change and the efficacy and effectiveness with which clinical governance issues were handled.
Institutional work
The institutional change literature has moved on from what some have viewed as an over-reliance on the ‘heroic actions’ of the IE. The notion of ‘institutional work’41 is designed to draw attention in part to the wide variety of actors working alongside, often in support of, the IEs in bringing about change. However, this notion also highlights the wide variety of techniques used by such actors, often on a sustained and routine basis, to disrupt, create and maintain institutions. 41
Attention has already been drawn to the range of actors involved in seeking to change the use and management of nurse support workers. Emphasis has been given, in particular, to the importance of partnerships between different functions. Two additional actors are worth highlighting in this context. The first such actor is the trust’s support worker education lead, often crucial in developing the training and education programmes needed to extend the nurse support role. The importance of these education leads was clearly illustrated in the case of the SAP, with the education lead at OUH able to translate the consultant dermatologist’s aspirations for the role into a viable training programme through the design of the FD. The education lead at Torbay was similarly important, developing a strong relationship with the local college to devise a FD well suited to the trust’s needs.
More generally, it can be argued that RNs working alongside the nurse support worker also play a crucial, but often overlooked, part in institutional change. We have seen that change often rests on training up support workers to perform new tasks in order to extend their roles. This training is, in turn, heavily dependent on workplace learning and the willingness and ability of RNs to provide and supervise such learning and to sign off competencies once acquired by the support worker. Findings from our three themes suggested that supervision and sign-off were often problematic. Nurses did not have the time, the opportunity and, in some instances, the inclination to supervise support workers. Certainly, these difficulties were apparent in the MCA case as well as in attempts to develop the beginner competencies in one of our ECs. Indeed, recognition of these difficulties was encouraging some trusts to seek more efficient and effective ways of supervising support workers, whether through the creation of protected time on shift or through the development of roles dedicated to such supervision.
This is not the place to explore the wide range of techniques associated with institutional work, and used to disrupt, create and maintain institutional practices associated with the use and management of nurse support workers. 42–44 It is sufficient to say that central to the application of these techniques is the search for legitimacy, seen by institutional theorists as the basis for such practice being accepted or taken for granted at the workplace. 76,77 There are grounds for arguing that many of the practices presented in our IC studies had become legitimised and embedded in local routines; certainly this was apparent in relation to the C-SW and the SAP roles. Both cases were small scale – involving single post-holders – and their incremental or organic development allowed them to mould themselves around established ward/departmental practices and to become trusted by colleagues. It was also stressed that the establishment of these roles rested on a confluence of organisational need and the availability of a person well suited to meet this need. This tight ‘organisation need–available person’ nexus raises some interesting questions about the sustainability of such roles: if their legitimacy rests so much on who performs them, it remains open to debate as to whether or not they will survive when the current post-holder leaves.
More generally, the one process which consistently emerged as crucial to the legitimacy of changes in the use and management of support workers was involvement, and the degree to which institutional change was inclusive of different stakeholders. Given the range of actors with a stake in support roles, legitimate change would seem to require a process which builds consensus on the nature of the change and the ways to progress it. Despite the difficulties of implementation highlighted in our EC study, the CF was founded on this premise, seeking to heighten awareness among and engage workplace actors in the different stages seen as underpinning the redistribution of nursing tasks and responsibilities.
Indeed, in a number of ECs, the trusts acknowledged shortcomings in communicating with and involving key stakeholders. In the roll-out case, there was a general view that the nature of the AP role and the reasons for its introduction were not fully understood at ward level. In the new 2-week HCA induction case, matrons had been consulted about the design of the programme but ward managers had not, while the downgrading of many band 7 midwifery roles in the MCA case dissipated any support for broader organisational change in the midwifery services and any willingness to engage in the implementation of this change.
Limitations and the future
This has been an ambitious project, covering a diffuse range of issues and adopting a variety of research techniques. Indeed, during a 24-month fieldwork period, we carried out and processed data from scoping discussions with over 100 participants; a survey of chief nurses and HR directors in all trusts in England; 12 case studies with eight different trusts, a number involving large-scale surveys of staff; and four regional workshops. The result has been some unevenness in the quality of the research process and in the data generated by the study. Our survey of innovative practice was unable to elicit a high response rate from trust HR directors to match that received from nurse directors, limiting the scope to compare and contrast functional views on innovative practice. There was a tantalising glimpse of functional differences in perspective, which we were unable to explore more fully. The six ICs were always designed to be retrospective snapshots of the development of new practices within a trust from the perspective of a vertical slice of respondents. However, given the small scale of these cases, in terms of both numbers interviewed and research techniques used, there were limits to how far we were able to delve into the detail of these innovative practices, for example the problems faced, how they were overcome and how the practices were impacted. In naming these trusts, we have sought to provide some justification for claims of naturalistic generalisation, and more detailed case reports can be accessed from the project’s website.
In the engagement theme, the regional workshops did not attract as diverse a range of stakeholder as hoped for. In particular, we were seeking a stronger patient voice at these events. Moreover, while the workshops allowed us to map the form of a management toolkit on support workers, there is still scope to develop such a toolkit on a sustainable basis.
The main limitations emerged in relation to the evaluation theme. The tight timescale for the fieldwork meant that we had to commit to the ‘before’ and ‘after’ evaluation of nascent trust initiatives whose roll-out sometimes proved to be problematic in practice. There were cases where the planned implementation was delayed as unforeseen problems arose, or the take-up of the initiative was lower than envisaged by the trust. In some of the cases, this presented difficulties in undertaking the follow-up or ‘after’ research, limiting the scope to compare it with the ‘before’ material. The range of research methods used in the ECs was also limited. In the main, we relied upon interviews, surveys and documentary material, with little, if any, use of observation to assess how initiatives were being implemented and impacting. In addition, the problems faced by our case trusts in delivering on their initial commitment to facilitate patient involvement in the formative stage of our evaluation work dissipated the level of service user involvement.
Recommendations for future research
Against the backdrop of these limitations, a number of recommendations on future research in the field of health-care support workers in acute care can be presented:
-
Further research is required into different functional views on, and approaches to, the management and use of health-care support workers. Our research has found that the efficacy of trust attempts to innovate and develop support roles is crucially dependent on partnership working between functions: for example, nursing, HR and pharmacy. However, such partnership working has also been revealed as often problematic, not least reflected in differences of perspective on whether or not and how health-care support workers might be developed. More research is needed to explore such differences of perspective – their nature and intensity – and how they might be reconciled.
-
There is a need for more research on the resistance faced at ward level as new support roles and ways of working are introduced. Our research has suggested that, regardless of how well support workers are trained and however well planned their introduction, new roles and practices can still be contested by members of the ward team. Unless new health-care roles and practices are accepted by colleagues, the investment made in them might well be wasted. Our work indicated that this resistance in part stemmed from uncertainty about whether or not and in what sense RNs were accountable for support workers, a particular concern given the growing pressure on nurses to delegate tasks. A focused piece of research on perceived nurse accountability for support workers might contribute to attempts to address these uncertainties. More generally, there would be considerable value in undertaking ethnographic studies on how new support roles are viewed, developed and used at ward level, as a means of exploring and then addressing resistance to them.
-
Public policy developments are likely to create a new but still uncertain training agenda for support workers, related not least to the Skills for Health minimum training standards64 and the Cavendish Review’s65 call for a care certificate. Given the uneven development of training for support workers, trusts are likely to vary in their need and capacity to meet the challenges associated with this new agenda. A research project working closely with trusts, and adopting a training needs analysis approach, would help these organisations to address the new training agenda, and generate a deeper understanding of how they approached the development of their support workers to deliver higher-quality health care.
Acknowledgements
Our thanks go to the considerable number of people who contributed to and supported this project. We are particularly grateful to those who helped us set up the ICs and ECs and to those HCAs, nurses, ward managers, matrons and senior managers who participated in the interviews, focus groups and surveys (often on more than one occasion). We are also grateful to all those involved in the four regional workshops and the end-of-project conference, and to the members of our advisory group. There are a number of people we would particularly like to thank: Cathy Barrett, Pat Black, Lucy Connolly, Jane Connor, Sue Crew, Katie Croisdale, Andrea Doherty, Sam Donohue, Jane Gidman, Richard Griffin, Diana Last, Lisa Nobes, Linda Taylor, Cathy Skilbeck, Claire Wardle, Trish Whale, Teresa Wright and Richard Turner. There are more we would have liked to thank by name, but we are keen to ensure the anonymity of our EC study trusts.
This report presents independent research commissioned by the NIHR. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS; the NIHR; NIHR Evaluation, Trials and Studies Coordinating Centre (NETSCC); the Health Services and Delivery Research (HS&DR) programme or the Department of Health. The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
Contributions of authors
Ian Kessler (Professor in Public Service Policy and Management, Department of Management) led the study, contributed to all elements of the study, provided expert knowledge in qualitative methods, undertook interviews and analysis of qualitative data, led the overall synthesis of findings, wrote stakeholder case study feedback and drafted the final report.
Karen Spilsbury (Professor in Nursing, Department of Health Sciences) contributed to all elements of the study, led on development of the toolkit and data collection and analysis of the Calderdale Framework evaluation. She prepared results for the final report and also contributed important intellectual content to revisions of the final report.
Paul Heron (Senior Research Associate, Saïd Business School) project managed the study. He contributed to all elements of the study, undertook scoping and case study interviews, provided expert knowledge in quantitative methods and led on the data collection and analysis of the national survey and all evaluation surveys. He prepared results for the final report and stakeholder case study feedback and contributed intellectual content to revisions of the final report.
Acknowledgements of the contributions of others to the study
Alison Wells (Registered Nurse, independent consultant) managed, facilitated and was responsible for the data collection of the regional workshops. She also managed and facilitated the end-of-project conference.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Kessler I, Heron P, Dopson S, Magee H, Swain D, Askham J. The Nature and Consequences of Support Workers in a Hospital Setting. Final Report 2010.
- Kessler I, Heron P, Dopson S. The Modernization of the Nursing Workforce. Oxford: Oxford University Press; 2012.
- Francis R. Independent Inquiry into Care Provided by Mid Staffordshire NHS Foundation Trust January 2005 to March 2009. London: The Stationery Office; 2010.
- Stokes J, Warden A. The changing role of the healthcare assistant. Nurs Stand 2004;18:33-7. http://dx.doi.org/10.7748/ns2004.09.18.51.33.c3684.
- Spilsbury K, Adamson J, Carr-Hill R, McCaughan D, McKenna H, Wakefield A, et al. Evaluation of the Development and Impact of Assistant Practitioners Supporting the Work of Ward-Based Registered Nurses in Acute NHS (Hospital) Trusts in England. Final Report 2010.
- Hardie M. Nursing Auxiliaries in Health Care. London: Croom Helm; 1978.
- Thornley C. The Invisible Workers: An Investigation into the Pay and Employment of Health Care Assistants in the NHS. London: UNISON; 1997.
- Project 2000: A New Preparation for Practice. London: UKCC; 1986.
- Beardshaw V, Robinson R. New for Old? Prospects for Nursing in the 1990s. London: King’s Fund Institute; 1990.
- Thornley C. A question of competence? Re-evaluating the roles of the nursing auxiliary and health care assistant in the NHS. J Clin Nurs 2000;9:451-8. http://dx.doi.org/10.1046/j.1365-2702.2000.00398.x.
- Department of Health . Nursing Set to Become All Graduate Entry by 2013 n.d. http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/MediaCentre/Pressreleasesarchive/DH_108359 (accessed 4 July 2013).
- Delivering HR in the NHS Plan. London: Department of Health; 2003.
- Hansard . House of Commons Debate: Health Care Assistants 1999. www.publications.parliament.uk/pa/cm199899/cmhansrd/vo990224/debtext/90224-16.htm#90224-16_head0.
- Malhorta G. Grow Your Own. London: King’s Fund; 2006.
- Langlands A. The Gateways to the Professions Report. London: Department for Education and Skills; 2005.
- Cox A, Grimshaw D, Carroll M, McBride A. Reshaping internal labour markets in the National Health Service: new prospects for pay and training for lower skilled service workers?. Hum Resource Manag J 2008;18:347-65. http://dx.doi.org/10.1111/j.1748-8583.2008.00073.x.
- Working Together, Learning Together: A Framework for Life Long Learning in the NHS. London: Department of Health; 2001.
- Agenda for Change: Final Agreement. Leeds: Agenda for Change Project Team, Department of Health; 2005.
- Just a Little Respect. London: UNISON; 2008.
- James N. Care = organisation + physical labour = emotional labour. Sociol Health Illn 1992;13:270-5.
- Jack B, Brown J, Chapman T. Ward managers’ perceptions of the role of health care assistants. Br J Nurs 2004;13:270-5. http://dx.doi.org/10.12968/bjon.2004.13.5.12400.
- Daykin N, Clarke B. ‘They’ll still get the bodily care.’ Discourses of care and relationships between nurses and health care assistants in the NHS. Sociol Health Illn 2000;22:349-63. http://dx.doi.org/10.1111/1467-9566.00208.
- Ford P. The role of support workers in the department of diagnostic imaging: service managers’ perspective. Radiography 2004;10:259-67. http://dx.doi.org/10.1016/j.radi.2004.03.009.
- Knibb W, Smith P, Magnusson C, Bryan K. The Contribution of Assistants to Nursing: Report for the RCN. Guildford: University of Surrey; 2006.
- Spilsbury K. Who Cares? A Case Study to Explore HCAs’ Jurisdiction in a Hospital Setting 2004.
- Workman BA. An investigation into how the health care assistants perceive their role as ‘support workers’ to the qualified staff. J Adv Nurs 1996;23:612-19. http://dx.doi.org/10.1111/j.1365-2648.1996.tb00026.x.
- Nancarrow S, Borthwick A. Dynamic boundaries in the healthcare workforce. Sociol Health Illn 2005;27:897-919. http://dx.doi.org/10.1111/j.1467-9566.2005.00463.x.
- Abbott A. The System of Professions: An Essay on the Division of Expert Labour. Chicago, IL: University of Chicago Press; 1988.
- Larson M. The Rise of Professionalism. Berkeley, CA: University of California Press; 1977.
- Witz A. Professions and Patriarchy. London: Routledge; 1992.
- Carr-Hill R, Dixon P, Gibbs I, Griffiths M, Higgins M, McMaughan D, et al. Skill Mix and the Effectiveness of Nursing Care. University of York: Centre for Health Economics; 1992.
- McKenna H. Nursing skill mix substitutions and quality of care – an exploration of assumptions from the research literature. J Adv Nurs 1995;21:452-9. http://dx.doi.org/10.1111/j.1365-2648.1995.tb02727.x.
- McKenna H, Hasson F, Keeney S. Patient safety and quality of care: the role of the health care assistant. J Nurs Manag 2004;12:452-9. http://dx.doi.org/10.1111/j.1365-2834.2004.00514.x.
- Saks M, Allsop J. Social policy, professional regulation and health support work in the UK. Social Policy Soc 2007;6:165-77. http://dx.doi.org/10.1017/S1474746406003435.
- British Broadcasting Corporation . RCN: NHS Healthcare Assistants’ Training ‘Unacceptable’ 2011. www.bbc.co.uk/news/health-15016634 (accessed 8 July 2013).
- Griffiths P, Robinson S. Moving Forward with Healthcare Support Workforce Regulation. A Scoping Review: Evidence, Questions, Risks and Options. London: National Nursing Research Unit, King’s College London; 2010.
- Hayes J. The Theory and Practice of Change Management. Basingstoke: Palgrave; 2010.
- Burns B. Managing Change. Harlow: Pearson Education; 2009.
- Dacin M, Ventresca M, Beal B. The embeddedness of organizations: Dialogue and directions. J Manag 1999;25:317-56. http://dx.doi.org/10.1177/014920639902500304.
- DiMaggio P, Zucker L. Research on Institutional Patterns and Organizations: Culture and Environment. Cambridge, MA: Ballinger; 1988.
- Lawrence T, Suddaby R, Leca B. Institutional work: refocusing institutional studies of organization. J Manag Inqu 2011;20:52-8. http://dx.doi.org/10.1177/1056492610387222.
- Currie G, Lockett A, Finn R, Martin G, Waring J. Institutional work to maintain professional power: recreating the model of medical professionalism. Organ Stud 2012;33:937-62. http://dx.doi.org/10.1177/0170840612445116.
- Kitchener M, Mertz E. Professional projects and institutional change in healthcare: the case of American dentistry. Soc Sci Med 2012;74:327-80. http://dx.doi.org/10.1016/j.socscimed.2010.10.005.
- Reay T, Golden-Biddle K, Germann K. Legitimizing a new role: small wins and micro processes of change. Acad Manag J 2006;49:977-98. http://dx.doi.org/10.5465/AMJ.2006.22798178.
- University of Oxford . Support Worker Research in Acute Healthcare 2013. www.sbs.ox.ac.uk/ideas-impact/health-care/support-workers-research (accessed 8 July 2013).
- Levy C. Making the Most of Public Services: A Systems Approach to Public Innovation. London: Work Foundation; 2011.
- Innovation Health and Wealth: Accelerating Adoption and Diffusion in the NHS. London: Department of Health; 2011.
- Baregheh A, Rowley J, Sambrook S. Towards a multidisciplinary definition of innovation. Manag Decis 2009;47:1323-39. http://dx.doi.org/10.1108/00251740910984578.
- Van de Ven AH. Central problems in the management of innovation. Manag Sci 1986;32:590-607. http://dx.doi.org/10.1287/mnsc.32.5.590.
- HCA-DN Job Description. London: UCLH; n.d.
- Clinical Support Worker Trainer Job Description. Oxford: Oxford Universities Hospitals; n.d.
- Smith R, Duffy J. Developing a competent and flexible workforce using the Calderdale Framework. Int J Ther Rehabil 2010;17:254-9. http://dx.doi.org/10.12968/ijtr.2010.17.5.47844.
- Administration of Medicine Experiences from the Northwest. York: Firefly Research & Evaluation; 2012.
- Vaughan P. A WiPP toolkit for healthcare assistants: what’s it all about?. Br J Healthcare Assist 2007;1:20-1. http://dx.doi.org/10.12968/bjha.2007.1.1.23230.
- NHS East Midlands . Assistant Practitioner Toolkit n.d. www.nhsemployers.org/∼/media/Employers/Publications/Assistant-Practitioner-Toolkit.pdf (accessed 8 July 2013).
- NHS Education for Scotland . Healthcare Support Workers Toolkit n.d. www.hcswtoolkit.nes.scot.nhs.uk (accessed 8 July 2013).
- West Yorkshire Lifelong Learning Project . Assistant Practitioner Toolkit n.d. www.jayconsulting.co.uk/our-clients/west-yorkshire-lifelong-learning-network-wylln (accessed 8 July 2013).
- NHS Tayside . Assistant Practitioner Project 2012. www.nhstayside.scot.nhs.uk/files/AP-%20Final%20Report.pdf (accessed 8 July 2013).
- NHS Employers . Support Workers n.d. www.nhsemployers.org/your-workforce/retain-and-improve/standards-and-assurance/developing-your-support-workforce (accessed 8 July 2013).
- Royal College of Nursing . HCAs &Amp; APs 2013. www.rcn.org.uk/development/health_care_support_workers (accessed 8 July 2013).
- Francis R. Mid Staffordshire NHS Foundation Trust Public Inquiry: Final Report. London: The Stationery Office; 2013.
- Delivering Dignity: Securing Dignity in Care for Older People in Hospitals and Care Homes. London: NHS Confederation, the Local Government Association and Age UK; 2012.
- Dignity and Nutrition Inspection Programme: National Overview. Newcastle: CQC; 2011.
- National Minimum Training Standards and Code of Conduct for Healthcare Support Workers and Adult Social Care Workers. London: Skills for Health; 2013.
- Cavendish C. The Cavendish Review: An Independent Review into Healthcare Assistants and Support Workers in the NHS and Social Care Settings. London: HMSO; 2013.
- Stake R, Trumbull D. Naturalistic generalizations. Rev J Philos Soc Sci 1982;7:1-12.
- Melrose S, Mills A, Durepos G, Wiebe E. Encyclopaedia of Case Study Research. London: Sage; 2010.
- Burns T, Stalker G. The Management of Innovation. London: Tavistock; 1961.
- Mintzberg H. The Rise and Fall of Strategic Planning. New York, NY: Free Press; 1994.
- Abel-Smith B. A History of the Nursing Profession. London: Heinemann; 1960.
- Hughes E. The Sociological Eye. London: Transaction; 1993.
- Etzioni A. The Semi Professionals and their Organization: Teachers, Nurses and Social Workers. New York, NY: Free Press; 1969.
- Maxi Nurses: Advanced and Specialist Nursing Roles. London: RCN; 2005.
- Mullaly S. Keynote Address. Presented at CNO Conference 2003. http://webarchive.nationalarchives.gov.uk/20040216034425/doh.gov.uk/cno (accessed 30 November 2013).
- Scott W. Institutions and Organizations. Thousand Oaks, CA: Sage; 2001.
- Ray AT, Golden-Biddle K, Germann K. Legitimizing a new role: small wins and microprocessors of change. Acad Manag J 2006;49:977-98. http://dx.doi.org/10.5465/AMJ.2006.22798178.
- Nelsen B, Barley S. For love or money? Commodification and the construction of an occupational mandate. Adm Sci Q 1997;42:619-53. http://dx.doi.org/10.2307/2393652.
- List of NHS Foundation Trusts. London: Monitor; 2011.
- List of Trust by Type. London: NHS National Patient Safety Agency; 2011.
- Workforce Statistics. London: NHS Information Centre; 2011.
- Financial Statements by NHS Trust. London: Audit Commission; n.d.
Appendix 1 Research advisory group
| Name | Job titlea | Organisation |
|---|---|---|
| Gail Adams | Head of Nursing | UNISON |
| Robin Arbuthnot | Senior Learning and Development Manager | HPMA |
| Stephen Bach | Professor of Employment Relations | King’s College London |
| Sue Dopson | Professor of Organisational Behaviour | University of Oxford |
| Vicki Finlay | Professional Officer for Nursing | Department of Health |
| Helen Green | Director of Practice | University of Leeds |
| Peter Griffiths | Professor of Health Services Research | University of Southampton |
| Roswyn Hakesley-Brown | Trustee | Patients Association |
| Tanis Hand | Healthcare Assistant Adviser | Royal College of Nursing |
| Helen Kilgannon | Assistant Director – Workforce Modernisation | NHS North West |
| Katerina Kolyva | Acting Director of Policy and Standards | NMC |
| Dorothy McCaughan | Research Fellow | University of York |
| Rob McSherry | Professor of Nursing and Practice Development | Teeside University |
| Susan Nancarrow | Professor of Health Sciences | Southern Cross University, NSW, Australia |
| Don Redding | Director of Policy | National Voices |
| Jo Rycroft-Malone | Professor in Health Services and Implementation Research | Bangor University |
| Robert Standfield | Divisional Manager | Skills for Health |
| Elaine Strachan-Hall | Chief Nurse | Oxford Radcliffe Hospitals NHS Trust |
| Caroline Waterfield | Deputy Head of Employment Services | NHS Employers |
| Kate Webb | Senior Policy Analyst | Council for Healthcare Regulatory Excellence |
| Ian Wragg | Workforce Modernisation Manager | NHS Yorkshire and the Humber |
Appendix 2 Patient and public involvement
The current project was very much rooted in how patients and the public viewed support workers in acute care settings. Our previous NIHR project had surveyed patients in four trusts and, along with observational and focus group work involving patients, had picked up aspects of the patient–support worker relationship in need of further study. The attempt to engage patients in the current project as a means of addressing these issues took various forms. Our advisory group comprised representatives from two patient/user groups: the Patients’ Association and National Voices. Members of the advisory group were involved throughout the project: findings were regularly fed back to them and they were given opportunities to comment on the design of research instruments (e.g. the innovation survey). Representatives from both organisations attended the single face-to-face meeting of the advisory group, and the end-of-project conference.
We had hoped to engage patients and service users in the ECs, providing them with an opportunity to feed into the process. This occurred in one of our evaluation sites, involving two of the six evaluations: one related to an ADP for MCAs and another to the administration of medicine by APs. A working group of stakeholders from the trust met on two occasions: at the outset of the research and to feed back and to discuss initial findings. At both meetings, a patient representative was present and contributed to deliberations. Determined attempts to set up similar groups involving patient at the other evaluation trusts unfortunately proved less successful.
Our regional workshops were also designed to involve patient and the public involvement. Again, the level of such involvement was not as high as we had hoped. However, the discussions at these workshops were very much geared towards exploring how support worker roles were perceived and impacted on patients. Indeed, the ICs and ECs also concentrated on a number of patients of outcomes in exploring new approaches to the use and management of support workers.
Appendix 3 Scoping: topic guide
General developments
Our interest concentrates on nurse support roles in AfC pay bands 2–4 in an acute care setting:
-
How are trusts seeking to develop roles at these band levels?
-
What is prompting them to develop these roles and how far are they being driven by the current financial context (are developments in these accelerating)?
-
In terms of band levels 2, 3 and 4, where is most of the activity concentrated, and why at these levels?
-
To what extent are these developments linked to skill-mix reviews, and what is prompting these reviews?
-
How, and in what ways (if at all), are developments being supported and prompted by SHAs and the Department of Health?
-
In which clinical areas are such developments likely to be found, and how does the use of support roles vary in these areas?
-
Is it possible to talk about leading edge trusts and/or SHAs when it comes to the development of nurse support roles? Or to refer to innovative developments?
-
If so, what does leading edge or innovative developments mean in this context? Provide examples?
Band 4/assistant practitioners
Focusing on specific bands, and starting with band 4, AP and like roles:
-
What progress has been in different trusts in developing these roles?
-
What explains uneven progress between trusts: why are some trusts being more proactive than others?
-
How strategic are trusts being in the development of APs: formal working groups, workforce planning, support systems, evaluation?
-
How are band 4 roles being developed:
-
What tasks are they taking on?
-
Are newly labelled roles emerging?
-
In what clinical areas are they found?
-
What forms of training are being used – foundation degrees/apprenticeships?
-
-
What impact are these AP roles having on outcomes and stakeholders – variously defined?
-
Are attempts being made to assess outcomes and if so in what ways?
Bands 2–3
-
Repeat band 4 questions.
-
Compare and contrast development with those among band 4s.
-
Consider any integration of band 2–4 developments.
Appendix 4 National survey: questionnaire
Appendix 5 Cluster analysis
Rationale
Cluster analysis is a tool used to find natural groupings within a data set. A cluster represents a group of respondents that is relatively homogeneous on a set of observations, yet distinct from other respondents within other clusters. This method of using survey data to group our responding trusts, rather than the more traditional grouping of variables that occurs in factor analysis, is particularly useful to our inquiry and allows us to explore any meaningful patterns that may exist between trusts themselves in terms of the support worker practices they are using.
Method
The 15 practices used in the analysis included how trusts were managing support workers, their managerial infrastructure and any new support worker roles or ways of working. The categorical response to each of the 15 practices was recoded into a dichotomy to indicate if the practice was used by the trust. Cluster analysis is a list-wise procedure: there were 50 trusts which had provided details to each of the 15 practices and thus were included in the analysis. There were no significant differences found between those trusts included in the analysis versus those excluded due to missing data on the key background variables described in Chapter 2 (see Focus and methods).
The sample was analysed using the hierarchical cluster analysis procedure. Following investigation of the dendogram and the agglomeration coefficient, it was determined that five clusters using the Ward method with the Jaccard measure for dichotomous data produced the most acceptable solution. The five-cluster solution is presented in Table 31, and also included for interest are the four AP-related practices. Significant differences exist among the five clusters for the majority of practices. The profiles of the clusters are discussed in the main body of the report. Table 32 provides background information on the five clusters.
| Innovative practice | Non-innovator (n = 8) | Regulatory innovator (n = 9) | Grounded innovator (n = 13) | Focused innovator (n = 11) | Full innovator (n = 9) | χ2 |
|---|---|---|---|---|---|---|
| All band 2 candidates screened for numeracy and literacy | 63 | 100 | 69 | 100 | 100 | 11.48a |
| Recruit all new band 2 staff to an apprenticeship programme | 50 | 33 | 0 | 0 | 78 | 22.44b |
| Off-ward induction programme for new band 2 staff (3+ days) | 63 | 100 | 85 | 64 | 100 | 8.59a |
| New band 2 recruits must achieve training targets to be confirmed in post | 38 | 44 | 54 | 55 | 89 | 5.59 |
| On completion of training APs guaranteed a band 4 rolec | 60 | 43 | 75 | 17 | 57 | 5.95 |
| A forum/support group at division/trust level attended by NSWs | 0 | 0 | 54 | 64 | 100 | 26.75b |
| A designated NSW champion at divisional/trust management level | 13 | 33 | 69 | 55 | 78 | 10.23a |
| An established support worker strategy group | 13 | 44 | 39 | 18 | 44 | 3.89 |
| A written nurse support workforce strategy | 13 | 0 | 92 | 9 | 11 | 32.88b |
| Revised job descriptions for bands 2 or 3 in the last 2 years | 50 | 100 | 62 | 73 | 78 | 6.28 |
| A code of conduct for NSWs | 0 | 67 | 39 | 36 | 100 | 19.46d |
| A critical care support worker role with patient care duties | 13 | 22 | 77 | 100 | 100 | 28.89b |
| A health-care support worker role that spans different professional boundaries | 13 | 44 | 92 | 100 | 67 | 22.33b |
| A maternity support worker role with direct care duties | 75 | 100 | 92 | 100 | 89 | 5.00 |
| A NSW role that includes administration of medication | 0 | 11 | 23 | 36 | 11 | 5.08 |
| Guidelines for delegation of tasks to NSWs | 0 | 100 | 100 | 9 | 78 | 39.73b |
| An annual revalidation of AP competencea | 0 | 14 | 42 | 20 | 43 | 5.12 |
| A formal evaluation of AP rolesa | 50 | 25 | 92 | 60 | 57 | 10.11a |
| A preceptorship programme for newly qualified APse | 50 | 44 | 67 | 33 | 71 | 3.03 |
| Background characteristics | Non-innovator (n = 8) | Regulatory innovator (n = 9) | Grounded innovator (n = 13) | Focused innovator (n = 11) | Full innovator (n = 9) | Statistical validity |
|---|---|---|---|---|---|---|
| Foundation trust statusa (%) | 54 | 22 | 55 | 88 | 67 | χ2 = 7.84, p = 0.10 |
| SHA clusters (%) | χ2 = 15.21, p = 0.23 | |||||
| North | 63 | 33 | 31 | 18 | 11 | |
| Midlands | 0 | 22 | 31 | 9 | 56 | |
| London | 13 | 22 | 8 | 36 | 11 | |
| South | 25 | 22 | 31 | 37 | 22 | |
| Trust categoryb (%) | χ2 = 10.37, p = 0.24 | |||||
| Specialist | 13 | 0 | 0 | 0 | 0 | |
| Teaching | 13 | 11 | 23 | 45 | 11 | |
| District general hospital (large, medium and small) | 75 | 89 | 77 | 55 | 89 | |
| Number of RNsc (mean) | 1175 | 1363 | 1433 | 1602 | 1473 | F = 0.42, p = 0.80 |
| In receipt of financial supportd (%) | 13 | 0 | 0 | 27 | 33 | χ2 = 8.00, p = 0.09 |
Appendix 6 Evaluation case 1: questionnaire
Appendix 7 Evaluation case 1: survey results
| Itema | Band 2 | Band 5+ |
|---|---|---|
| I am able to do my job to a standard I am personally happy with | 4 | 4 |
| I am satisfied with the quality of care I give | 4 | 4 |
| I am able to deliver the patient care I aspire to | 4 | 4 |
| I cannot meet all the conflicting demands on my time | 4 | 4 |
| I have adequate materials . . . | 4 | 4 |
| I have some say over the way I work | 4 | 4 |
| There are enough staff | 3 | 2 |
| I do not have time to carry out all my work | 3 | 3 |
| Relationships at work are strained | 3 | 3 |
| I get help and support I need | 4 | 4 |
| My team members are willing to listen | 4 | 4 |
| My line manager encourages me | 4 | 4 |
| I look forward to going to work | 4 | 4 |
| I am enthusiastic about my job | 4 | 4 |
| Time passes quickly when I am working | 4 | 5 |
| I am clear what is expected of me at work | 4 | 5 |
| I have a choice in deciding how I do my work | 4 | 4 |
| I can rely on my line manager | 4 | 4 |
| There is friction or anger | 3 | 3 |
| I am clear what my duties are | 5 | 5 |
| Staff are always consulted | 4 | 4 |
| I have sufficient opportunities | 4 | 4 |
| When changes are made at work | 4 | 3 |
| Considering all aspects of my job | 4 | 4 |
| I often think of leaving | 2 | 2 |
| I will probably look for a new job | 2 | 2 |
| As soon as I can find another job | 2 | 1 |
| In general most HCAs keen to extend role | 4 | 4 |
| Most HCAs have ability to carry out more complex tasks | 5 | 4 |
| I am concerned about HCAs | 2 | 3 |
| I feel there is still considerable scope | 5 | 4 |
| I am confident that HCAs know what they are doing | 4 | 3 |
| Gender | Frequency (%) |
|---|---|
| Male | 1 (4.3) |
| Female | 22 (95.7) |
| Total | 23 (100.0) |
| Age range (years) | Frequency (%) |
|---|---|
| 21–30 | 2 (8.7) |
| 31–40 | 9 (39.1) |
| 41–50 | 5 (21.7) |
| 51–65 | 7 (30.4) |
| Total | 23 (100.0) |
| Bands | Frequency (%) |
|---|---|
| Band 2 | 8 (34.8) |
| Band 5 | 9 (39.1) |
| Band 6 | 4 (17.4) |
| Band 7 | 1 (4.3) |
| Band 8a | 1 (4.3) |
| Total | 23 (100.0) |
| Years worked | Frequency (%) |
|---|---|
| 1–2 years | 2 (8.7) |
| 3–5 years | 3 (13.0) |
| 6–10 years | 11 (47.8) |
| 11–15 years | 2 (8.7) |
| > 15 years | 5 (21.7) |
| Total | 23 (100.0) |
| Years worked | Frequency (%) |
|---|---|
| < 1 year | 1 (4.3) |
| 1–2 years | 4 (17.4) |
| 3–5 years | 8 (34.8) |
| 6–10 years | 5 (21.7) |
| 11–15 years | 3 (13.0) |
| > 15 years | 2 (8.7) |
| Total | 23 (100.0) |
| Hours | Frequency (%) |
|---|---|
| Up to 29 hours per week | 4 (17.4) |
| > 30 hours per week | 19 (82.6) |
| Total | 23 (100.0) |
Appendix 8 Evaluation case 3: baseline questionnaire
Appendix 9 Evaluation case 3: survey results
| Scales | Baseline (2012) | Follow-up (2013) | ||
|---|---|---|---|---|
| Cohort 1 (n = 17) | Cohorts 2–4 (n = 46) | Cohort 1 (n = 4) | Cohorts 2–4 (n = 17) | |
| Intention to leave | 2.04 | 1.93 | 2.00 | 2.23 |
| Caring behaviours | 3.78 | 3.31b | 4.05 | 3.76 |
| Induction programme | 4.29 | 4.06 | – | – |
| CSW activity confidence | 3.21 | 3.22 | 3.44 | 3.43 |
| Psychological contract (owed) | 4.24 | 4.29 | – | – |
| Psychological contract (importance) | 4.50 | 4.30 | – | – |
| Psychological contract (provided) | – | – | 3.83 | 3.44 |
| Post-induction programme evaluation | – | – | 3.56 | 3.60 |
| Organisation-based self-esteem | – | – | 4.05 | 4.39 |
| Propensity to extend the role | – | – | 4.06 | 3.04 |
| Job satisfaction | – | – | 4.00 | 3.67 |
| Trusted by colleagues | – | – | 4.06 | 4.14 |
| Work role | – | – | 4.38 | 4.50 |
| Motivated to do best for employer | – | – | 4.25 | 4.19 |
| Recommend workplace to others | – | – | 4.25 | 3.80 |
Appendix 10 Evaluation case 4: phase 1 questionnaire
Appendix 11 Evaluation case 6: phase 1 questionnaire
Appendix 12 End-of-project conference: delegates
The end-of-project conference took place at King’s College London on 25 July 2013. Delegates from the following organisations were to attend:
-
Bangor University
-
BMI Healthcare
-
Burton Hospitals NHS Foundation Trust
-
Council of Deans of Health
-
Great Western Hospitals NHS Foundation Trust
-
Guy’s and St Thomas’ NHS Foundation Trust
-
Health Education North West London
-
Health Education South West
-
Health Education Wessex
-
Heart of England NHS Foundation Trust
-
Institute of Vocational Learning and Workforce Research
-
King’s College London
-
Middlesex University
-
National Voices
-
NHS Employers
-
North Bristol NHS Trust
-
North West Workforce Modernisation Hub
-
NMC
-
OUH NHS Trust
-
University of Oxford
-
Patients Association
-
Professional Standards Authority for Health and Social Care
-
Royal College of Midwives
-
RCN
-
Skills for Health
-
The Hillingdon Hospitals NHS Foundation Trust
-
The Royal Wolverhampton NHS Trust
-
UNISON
-
United Lincolnshire Hospitals NHS Trust
-
University Campus Suffolk
-
UCLH NHS Foundation Trust
-
University of York
-
West Suffolk Hospital NHS Foundation Trust
-
Yeovil District Hospital NHS Foundation Trust
-
York Hospitals NHS Foundation Trust.
Appendix 13 Regional workshops: tasks by pay band
| Task | Pay band | ||
|---|---|---|---|
| 2 | 3 | 4 | |
| Completion of patient menus | ✗ | ||
| Support patients and carers | ✗ | ||
| Basic nursing care | ✗ | ||
| Housekeeping activities | ✗ | ||
| Essential patient care around the activities of daily living | ✗ | ||
| Hydration and nutrition | ✗ | ||
| Feeding | ✗ | ||
| Deliver essential basic care | ✗ | ||
| Close supervision | ✗ | ||
| Checking skin for sores | ✗ | ||
| Simple dressings | ✗ | ||
| Manual handling | ✗ | ||
| Help position patient on operating table | ✗ | ||
| Washing | ✗ | ✗ | |
| Dressing | ✗ | ✗ | |
| Feeding | ✗ | ✗ | |
| Hair and teeth, etc. | ✗ | ✗ | |
| Support qualified practitioner: patient care within scope of practice | ✗ | ✗ | |
| End-of-life care | ✗ | ✗ | ✗ |
| Continence care | ✗ | ✗ | ✗ |
| Catheter care | ✗ | ✗ | ✗ |
| Assess ‘some’ patients | ✗ | ||
| Assist in more procedures | ✗ | ||
| Essential patient care | ✗ | ||
| Task | Pay band | ||
|---|---|---|---|
| 2 | 3 | 4 | |
| Assist qualified practitioners | ✗ | ||
| Cannula care | ✗ | ||
| Record fluids | ✗ | ||
| Supervise patients taking medication | ✗ | ||
| Ear syringing | ✗ | ||
| Removal of urethral catheters, i.v. cannulae, NG tubes | ✗ | ||
| Perform early warning scores | ✗ | ||
| Give TENS machines under supervision on ‘ad hoc’ basis | ✗ | ||
| Work within boundaries of competence and accountability | ✗ | ✗ | ✗ |
| Observations, BP, TPR MEWS | ✗ | ✗ | ✗ |
| Physiotherapy/rehabilitation | ✗ | ✗ | ✗ |
| Venepuncture | ✗ | ✗ | ✗ |
| ECG | ✗ | ✗ | ✗ |
| Risk assessment/screening | ✗ | ✗ | ✗ |
| Midwifery HCA/hearing department/birth centre/neurophysiology clinic/catheter lab assistant/renal dialysis | ✗ | ||
| Discharge patients (except medications) | ✗ | ||
| Pre-operation screening | ✗ | ||
| Writing/reporting observation anomalies | ✗ | ||
| Assist surgeon with identified low-risk procedures | ✗ | ||
| Take histories | ✗ | ||
| Continence assessments | ✗ | ||
| Circulate in theatre | ✗ | ||
| Set up theatre for list/instruments | ✗ | ||
| Peg feeding | ✗ | ✗ | |
| Wound care | ✗ | ✗ | |
| Interpret information | ✗ | ✗ | |
| Provide scrub support to the surgeon/team | ✗ | ✗ | |
| Basic wound care, sutures and clip removal | ✗ | ✗ | |
| Care for groups of patients | ✗ | ✗ | |
| Cannulation | ✗ | ||
| Insertion of male/female catheters | ✗ | ||
| Scrub for minor procedures | ✗ | ||
| Protocol-driven assessment, e.g. falls risk, MUST, etc. | ✗ | ||
| Instil eye drops prior to examination | ✗ | ||
| Retrieve patients from theatres | ✗ | ||
| Assessment of OPD under supervision of band 6 | ✗ | ||
| Interpret observations and initiate appropriate treatment | ✗ | ||
| Assess patients in transdisciplinary way | ✗ | ||
| Complex dressings | ✗ | ||
| Task | Pay band | ||
|---|---|---|---|
| 2 | 3 | 4 | |
| Administrative support to senior nurses | ✗ | ||
| Report to trained nurses | ✗ | ||
| Access services and facilities | ✗ | ✗ | ✗ |
| Link practitioners | ✗ | ✗ | ✗ |
| Chaperoning NVQ assessors bands 2–4 | ✗ | ✗ | ✗ |
| Order stock | ✗ | ✗ | ✗ |
| Escort patients between areas | ✗ | ✗ | ✗ |
| Link between patient and nurse/doctor | ✗ | ✗ | ✗ |
| Responsibility to top up patient information leaflets | ✗ | ||
| Organise clinics in conjunction with administrative staff | ✗ | ||
| Documentation of perioperative journey | ✗ | ||
| Supervise/mentor band 2 | ✗ | ||
| Document in electronic patient records | ✗ | ||
| Assessment of bands 2–3 | ✗ | ||
| Conduct audits | ✗ | ||
Appendix 14 Regional workshops: improvements
| Area | Leeds | London | Birmingham | Taunton |
|---|---|---|---|---|
| Recruitment | Education of potential recruits prior to application – provide insight into role | Literacy test prior to interview linked with local college for those who fail | Opportunity to shadow prior to AP application | Good recruitment process. Applicants need clear understanding of the role |
| Use competence and values for recruitment and selection | Robust screening of numeracy/literacy before interview | Step in work (recruitment and induction) | ||
| Central recruitment | Basic skills testing | |||
| Minimum entry standards to post | Values-based recruitment | |||
| Induction | Excellent induction programme (practical and online) | Training and development relevant on induction | Induction and development at band 4 with local FE | Induction programme |
| Recognised induction for all HCAs that address role and competencies | Structured induction in line with the QCF apprenticeship programme | Band 3 induction plus departmental | ||
| More robust induction than previous year | All HCAs undergoing a robust induction on joining the trust | Structured induction for band 2s | ||
| Good induction and mandatory training | Comprehensive induction programme and focus days | |||
| Consistent induction to working area and consistent training | ||||
| Enhancing induction of HCAs through extended training | ||||
| Development | Appraisal and PDR opportunities | Education development for new HCAs which are APEL to NVQ level 2 | Competency portfolio and a mentor allocated to new HCAs | |
| PDR for registered staff re: HCA | Competency assessments | Role models | ||
| Portfolios for HCAs | Progression pathway | Champions | ||
| Supervision and appraisal and one-to-ones | Development pathway from recruitment to enable lifelong learning | Progression routes | ||
| Competency-based appraisal and development | Diploma in health for those wanting to progress | Skill audits | ||
| IPR using competency frameworks | Identified education needs | Offer education | ||
| Career pathway for ambitious candidates | Encouraged to go to higher education | Ward managers using 1 : 1 appraisal to develop staff competency | ||
| Support local economy by providing innovative career pathway | Different roles being developed with a clear career pathway to support CPD | |||
| Structured PDP/review process for HCAs | Dedicated HCA pathways co-ordinator | |||
| Have bands 2 and 3 so can develop | Extended skills | |||
| Some opportunity to continue nurse studying | ||||
| Good practice greater clarity of role within health care | ||||
| Training | Accreditation of work-based learning | Role specific training (renal and midwifery) | 12-month HCA training programme | Dedicated training team for bands 1–4 |
| Training of support staff in generic re-enablement skills to NVQ level 3 | All HCAs encouraged to complete NVQ (now apprenticeship) | Structured development programme for band 3s during first year with national accreditation | Training and development team HCA champions | |
| Quality assured training for HCAs | Preceptorship for band 4s once qualified | Offer CPD for HCAs with educational sessions | Clear and supportive education pathways | |
| Innovation of education provision | Secondments for HCAs to nurse training | Commissioning for further development of APs | Defined job description linked to training to do the job | |
| Competency training programme ‘Prepare to Care’ | Encouraged to go to nurse training via secondment | Supernumerary time for band 3s while training | On ward training of specialist procedures | |
| Apprenticeship scheme | Access to the apprenticeship framework | Regular training with dedicated mentor | Good QCF delivery | |
| Work-based training and development for role competencies | Opportunities to undertake professional training, e.g. nursing, physiotherapy | Formal preparation for band 4s for AP role with work-based learning and local workshops | ||
| Competency booklet for training | ||||
| In-house study days for band 4s | ||||
| Band 2 competencies recognised by RCN linked to KSF and reflect trust and national standards | ||||
| Study leave (1 day per week) for band 3s while training | ||||
| New ways of working within speciality competency-based band 4 FD | ||||
| Development of AHP care competency framework | ||||
| Use of apprentice framework to feed into career pathway | ||||
| Band 2 monitoring by senior band 2–3 staff while learning role | ||||
| Making use of e-learning | ||||
| Supervision and support | Effective supervision | Cautious delegation of care duties | Support worker code of conduct | |
| Clinical supervision | Training support ‘buddy’ mentor | |||
| Clear understanding when to stop | Band 2–3 code of conduct | |||
| Probationary periods | Local code of conduct (bands 3–4) | |||
| Code of practice | Freedom to practice (some) | |||
| Team understand the role of their support staff at different bands | Knowing who you are accountable to | |||
| Clearly delegated tasks with an understood escalation framework | Commitment of money to support development of AP role | |||
| System of clinical supervision and reflective practice in place | Bank HCA ‘buddy shifts’ to promote time to complete competencies | |||
| Provide a support network | ||||
| Empowering band 2–3s by introducing extended practice competencies | ||||
| Code of conduct, delegation protocol, local registration, competency framework, change management, peer support | ||||
| Roles and ways of working | Clarifying responsibilities between bands | Developing competencies broader than just the ‘normal’ HCA | Academic support for developing staff | |
| Locally agreed skills/competencies across bands 3–4 to improve employability across local trusts | Developing AP role | Specialist practice role development in NICU | ||
| Team and manager to know the skill sets and competence of their HCAs | Integration of profession specific roles delivered at trust level bands 2–4 | |||
| Development of a competency framework for key skills and to distinguish between roles and grades | Piloted induction of rehabilitation support workers in key areas | |||
| Use of CF to identify role, develop competencies, develop training and governance | Dementia support workers | |||
| Use of national occupational standards | Rehabilitation practitioners for the AHPs | |||
| Develop HCA role to work across health and social care and across community and acute to reflect integrated care agenda | Link with local HEI for development of curriculum for integrated physiotherapy and OT roles bands 2–8 | |||
| Deliver extended clinical care within defined competencies | ||||
| Role evaluation | ||||
| Clear role boundary in terms of when to stop and when to seek help | ||||
| Extended roles and responsibilities | ||||
| More holistic approach to create a blended physiotherapy role | ||||
| Champions of new roles | ||||
| Effective handovers | ||||
| Audit of practice of HCA and registered practice | ||||
| HCAs as discharge co-ordinators | ||||
| Other | Listening and engagement, i.e. care process | Recognition/credit for role | ||
| Listening to those who experience the role | Development team website | |||
| Rewarding HCAs who are doing good work/roles | Bands 2–4 dedicated website area |
Appendix 15 Regional workshops: visioning
FIGURE 14.
Leeds workshop model 1 of the future HCA role.
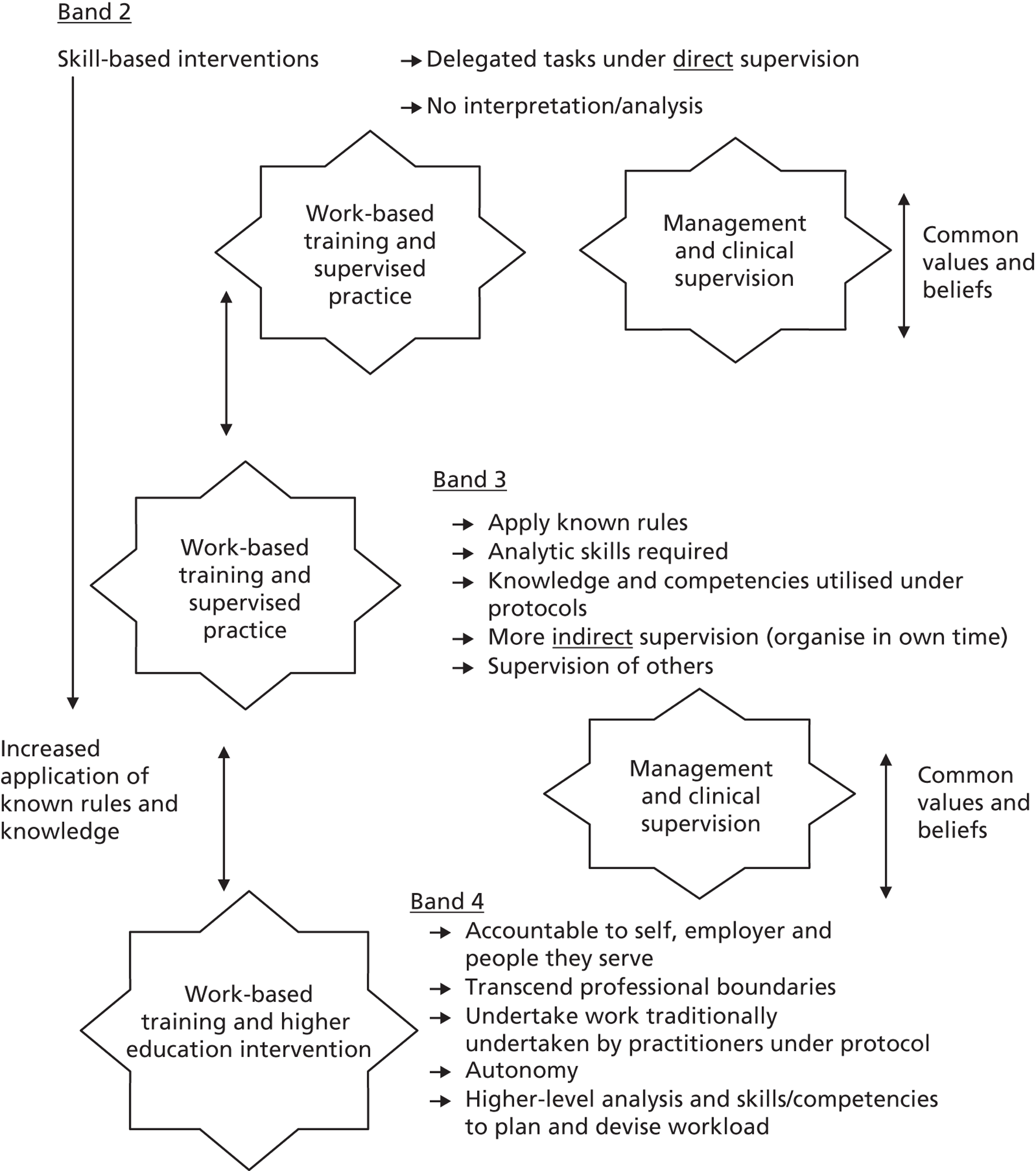
FIGURE 15.
Leeds workshop model 2 of the future HCA role. A&P, anatomy and physiology.
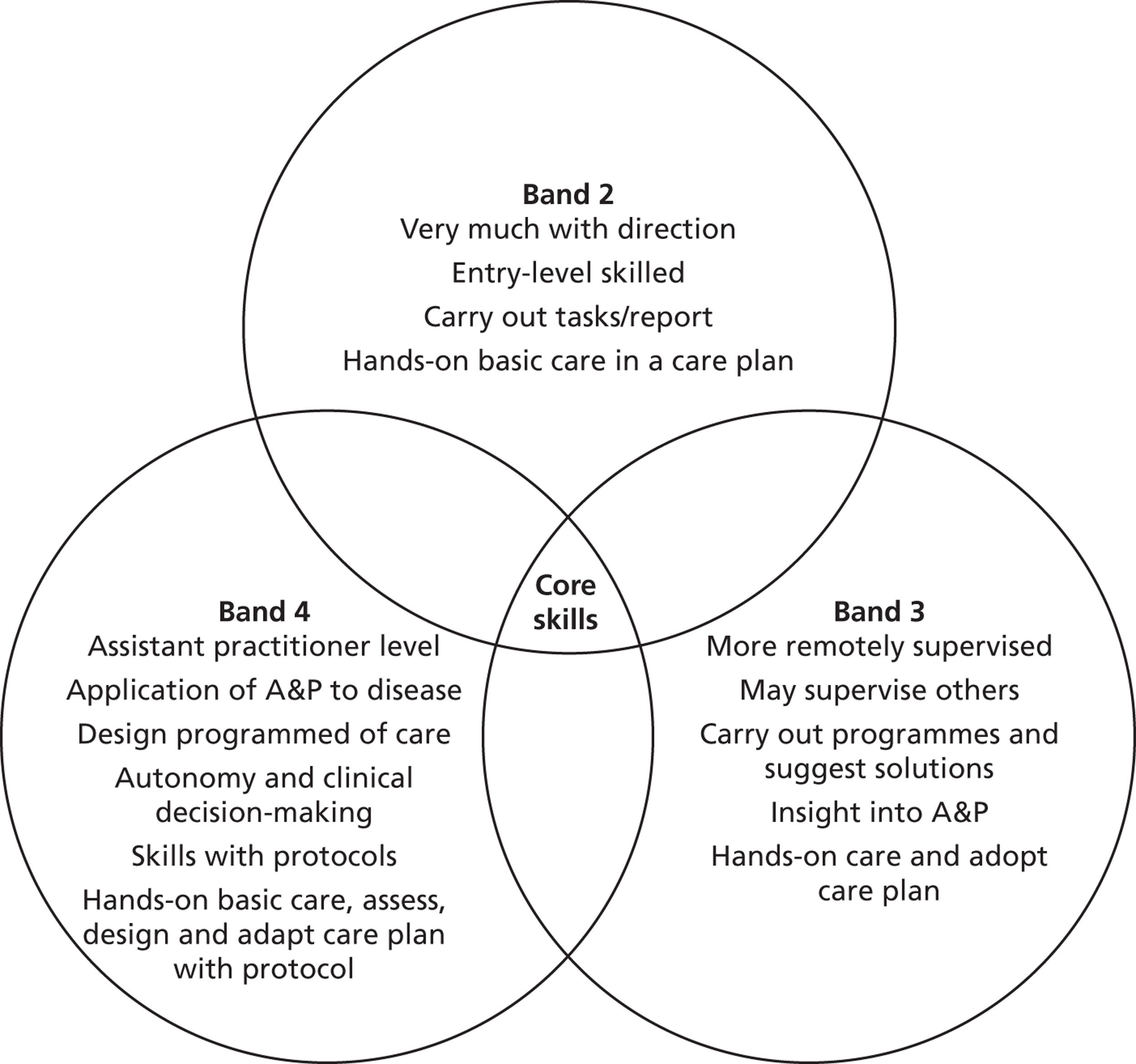
Appendix 16 Toolkit development presentation
Glossary
- Acute trust
- Hospitals in England are managed by acute trusts, of which there are currently 166. Acute trusts are commissioned to provide secondary health services by NHS England and Clinical Commissioning Groups.
- Agenda for Change
- The 2004 collective agreement which established the current NHS grading and pay system for NHS staff. It harmonises their pay scales and career progression arrangements across traditionally separate pay groups. There are nine new numbered pay bands subdivided into points, similar to the old alphabetic Whitley Council ‘grades’ pay scales.
- Apprenticeship in health care
- An apprenticeship provides work-based training and experience for hospital support workers and leads to a nationally recognised qualification.
- Care Quality Commission
- Formerly the Healthcare Commission, it is a non-departmental public body established in 2009 to regulate and inspect health and social care services in England.
- Clinical Commissioning Groups
- These are clinical-led NHS organisations responsible for commissioning health-care and NHS services in local geographical areas.
- Clinical governance
- The systematic approach to improve the quality of service and standard of care within the NHS.
- Department of Health
- The department of the UK government with responsibility for government policy for England on health, social care and the NHS.
- Foundation trust
- A NHS trust that is part of the NHS in England and has gained a degree of independence from the Department of Health. All acute trusts are expected to attain foundation trust status by 2014.
- Knowledge and Skills Framework
- A competence framework to support personal development and career progression within the NHS, introduced as part of Agenda for Change.
- National Health Service
- The publicly funded health-care system in England.
- National Vocational Qualification
- Work-based awards in England, Wales and Northern Ireland that are achieved through assessment and training. Now superseded by the Qualifications and Credit Framework model.
- Nursing and Midwifery Council
- The body set up by Parliament to regulate the nurse and midwifery professions.
- Performance Development Review
- Integral to Knowledge and Skills Framework, performance development review is the approach for assessing individual performance.
- Personal identification number
- This is a unique identifier issued by the Nursing and Midwifery Council as part of the nurse registration process. In order to work as a registered nurse in the NHS, it is a legal requirement to have a valid personal identification number from the Nursing and Midwifery Council.
- Project 2000
- A scheme, introduced in 1989, which formed the basis for the academic education of all nurses and midwives.
- Qualification and Credit Framework
- A new award for recognising skills and qualifications in the workplace. Qualification and Credit Framework was introduced in 2011 to replace the National Vocation Qualification system.
- Royal College of Nursing
- A membership organisation representing nurses and nursing.
- Secondary health care
- The service provided by medical specialists who generally do not have first contact with patients. The term is usually synonymous with ‘hospital care’.
- Skill mix
- The profile of different categories of workers in the nursing workforce.
- Skills escalator
- An approach to career progression in the NHS that dates back to 2002, often used as a visionary metaphor by the Department of Health whereby a porter could become a consultant. More commonly seen as a structure to help encourage staff to participate in workplace learning and thereby develop and extend their skills.
- State enrolled nurse
- Prior to the implementation of Project 2000, state enrolled nurse students used to follow the first 12 months training of the state registered nurses (now known as level one nurses), and then had another 12 months of training before sitting state enrolled nurse exams and becoming registered nurses.
- Strategic Health Authority
- Until 31 March 2013, Strategic Health Authorities were part of the NHS structure in England and responsible for enacting the directives and implementing fiscal policy as dictated by the Department of Health at a regional level. They have been replaced by NHS England and Clinical Commissioning Groups.
- UNISON
- The main union representing support workers in health care.
List of abbreviations
- AAU
- acute assessment unit
- ADP
- accelerated development programme
- AfC
- Agenda for Change
- AP
- assistant practitioner
- CDS
- central delivery suite
- CF
- Calderdale Framework
- CPF
- clinical practice facilitator
- C-SW
- colorectal support worker
- CSW
- clinical support worker
- EAU
- emergency assessment unit
- EC
- evaluation case
- ED
- education department
- ERP
- enhanced recovery programme
- FD
- foundation degree
- HCA
- health-care assistant
- HCA-DN
- health-care assistant development nurse
- HEI
- higher education institution
- HPMA
- Healthcare People Management Association
- HR
- human resources
- HS&DR
- Health Services and Delivery Research
- HSJ
- Health Service Journal
- IC
- innovation case
- IE
- institutional entrepreneur
- MCA
- maternity care assistant
- MM
- medicines management
- NETSCC
- NIHR Evaluation, Trials and Studies Coordinating Centre
- NIHR
- National Institute for Health Research
- NMC
- Nursing and Midwifery Council
- NVQ
- National Vocational Qualification
- OUH
- Oxford University Hospitals
- PDN
- practice development nurse
- QCF
- Qualification and Credit Framework
- RCN
- Royal College of Nursing
- RN
- registered nurse
- SAP
- surgical assistant practitioner
- SDC
- South Devon College
- SEN
- state enrolled nurse
- SHA
- Strategic Health Authority
- SOP
- standard operating procedures
- TAP
- trainee assistant practitioner
- UCLH
- University College London Hospitals
- WTE
- whole-time equivalent