Notes
Article history paragraph text
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 09/2001/19. The contractual start date was in September 2010. The final report began editorial review in May 2013 and was accepted for publication in November 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
During the MIA project, Monica Lakhanpaul was appointed as a National Institute for Health and Care Excellence (NICE) Fellow, member of the NHS Evidence advisory board, the Health Technology Assessment advisory panel and the Drugs and Therapeutics Bulletin editorial panel.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Lakhanpaul et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Overview and background of the Management and Interventions for Asthma project
The Management and Interventions for Asthma (MIA) project, carried out in a largely urban area in and around Leicester, UK, aimed to work with families from Indian, Pakistani and Bangladeshi ethnic backgrounds and healthcare professionals (HCPs) to collaboratively design interventions to improve management of childhood asthma in South Asian children. The MIA project consisted of three principal phases of work. The first phase consisted of a review of literature separately funded by Asthma UK, on barriers and facilitators to optimal management of asthma in South Asian families. In phase 2, exploration of community, family and HCPs’ perceptions of asthma and the asthma management pathway in South Asian families followed. This in turn led to the development of an asthma management intervention-planning framework and then a tailored focused, multifaceted, integrated programme to address one exemplar key issue identified. This chapter provides an overview of the background, aims and objectives of the integrated phases for the MIA project.
Introduction
The Management and Interventions for Asthma project
There is unacceptable variation across the country in the quality of care for children, e.g. in the treatment of long-term conditions such as asthma and diabetes. We want the NHS to do even more to improve care for children and young people. 1
While the burden of chronic illness (e.g. asthma and diabetes) continues to increase, the NHS is undergoing financial constraints. In children, it is noted that the outcomes for those with chronic disease are one of the worst in Europe, with death rates for illnesses that rely heavily on primary care services such as asthma being higher in the UK than in other countries. 2,3 The report also indicates that 75% of hospital admissions for children with asthma could have been prevented with better primary care. 2 Asthma is one of the most common chronic conditions in childhood, with inequalities existing in some ethnic minority groups. Children in South Asian communities, a group traditionally considered to be ‘hard to reach’, are known to suffer from under-recognition of symptoms/disease severity and increased attendance to the emergency department. The British Thoracic Society (BTS) guideline4 recommends that HCPs have a heightened awareness of the complex needs of minority ethnic groups among other named vulnerable groups. This is due to the recognition that care in minority ethnic groups is suboptimal and that there is a variation in the health care that they receive.
The Government White Paper5 recognises the importance of contextual factors and their contribution to maintaining good health, not only to the importance of employment and socioeconomic status (SES) but also to the environment and family relationships. An individual’s culture, beliefs and attitudes and those of their community also have an influence on behaviour towards their own health and their interaction with the health system. The Children’s Outcome forum report2 and Healthy Lives, Healthy People5 have not only recommended stronger partnerships between individuals, health, local authority and the voluntary sector to develop an integrated approach to health to tackle some of these issues, but have also delivered a strong recommendation to ensure that the voices of children, young people and their families are heard so that they can contribute to the improvements in services they will be accessing. Consequently, NHS HCPs, commissioners and policy makers are working more collaboratively with their communities so that services can be tailored to their needs. Tailoring, although recommended by a Cochrane review of 26 studies6 as an approach to intervention development, is, however, supported by little evidence on how the actual transition from evidence and theory to the design of the practical interventions should be made. Michie7 recommended that intervention developments use available evidence to inform and support the intervention. Michie7 noted that suggestions for intervention design tended to be evidence inspired rather than evidence based and that there is a need for studies of techniques, methods of delivery and implementation and use in a variety of target populations to identify the techniques and combinations that are needed to result in effective interventions. The Cochrane Collaboration ‘Equity’ group8,9 also noted that the evidence base for interventions to address inequalities is fundamentally flawed and recommended further research to inform intervention development.
The MIA project, therefore, chose asthma as an exemplar to demonstrate the processes aimed to enable collaboration between South Asian children, families, communities and HCPs to produce a multifaceted health intervention framework for asthma management tailored to the needs of South Asian children of primary school age, using a participatory, theory-based approach with an aim that the process could be transferrable to other chronic conditions and communities.
This introductory chapter explains, in more detail, why the MIA study focused on South Asian children with asthma and why the project adopted a participatory approach towards the development of the intervention framework.
Asthma
Asthma affects individuals of all ages. It is a disease characterised by recurrent attacks of breathlessness and wheezing, which vary in severity and frequency from person to person. In an individual, they may occur from hour to hour and day to day. 10
World Health Organization
Asthma produces a significant workload for general practice, hospital outpatient clinics and inpatient admissions. Asthma is responsible for 4 million general practitioner (GP) consultations, 70,000 hospital admissions and over 1000 deaths per year in the UK,11,12 and 1.1 million children are currently receiving treatment for asthma in the UK. 11 The total cost to the UK economy, including the use of primary and secondary care services, emergency services, medications and lost productivity from days off work/school, is estimated to be over £2.3B per year. 12 It is clear that much of this morbidity relates to poor management, particularly the underuse of preventative medicine. 4 While the patient with severe asthma is easy to recognise, patients with mild asthma merge imperceptibly with well people, with fluctuation between normal and asthmatic states. 13
Asthma and children
Childhood asthma is one of the most common chronic conditions of childhood. In the UK, current prevalence estimates suggest that 1.1 million children, or 1 in 11 children, will experience asthma at some point in their childhood. 11 Every year, 44,000 children are admitted to hospital, with between 40 and 50 children dying as a result of asthma. 11 In children under the age of 5 years, it is very difficult to differentiate, with any degree of certainty, wheezing attacks due to asthma from viral infections. Measurements of respiratory function is also known to be difficult, with very young children responding differently to many of the available drugs. 13 As a consequence, asthma places a substantial burden of care on families, communities and the health services. 11
Evidence suggests that UK children’s health services provide inferior care compared with equivalent European countries. 14 Wolfe et al. 14 acknowledged that, while there are pockets of good practice, there are also poor outcomes with services planned around the needs of organisations and providers rather than the children, young people and families. This ultimately means that services fail to recognise children and young people’s specific requirements, or acknowledge important recommendations for children’s health care. 15 Key recommendations from the Marmot Review16 indicate that investments in children’s services should be carefully planned and fit for purpose in order to improve care and reduce inequality while improving overall efficiency. The challenge for researchers, clinicians and policy makers is to understand what and why variations in care exist and to explore how these variations could be addressed.
Asthma management and control in children
Asthma management encompasses the whole pathway from awareness of asthma itself, recognition of symptoms, diagnostic, pharmacological, educational, clinical and preventative elements which reflect the diverse impact of asthma on a child’s life. This therefore includes both modifiable and non-modifiable factors, such as parental knowledge and compliance with medication (modifiable) and genetic variations in asthma phenotypes (non-modifiable). The asthma management pathway for the purposes of the MIA study has been defined by the research team as ‘stages of ideal care required to recognise, diagnose, treat and optimally manage asthma’.
In order to intervene in any condition, the issues present in its management must first be understood. The National Service Framework (NSF) for Children Asthma Exemplar17 highlights the many aspects of management along a patient journey from the onset of symptoms through to achieving asthma control and, while the mortality associated with asthma may be limited to acute asthma attacks, the morbidity associated with asthma is widespread. As a result, over the last 15 years HCPs have moved from a focus on treating acute asthma attacks to achieving overall asthma control. The US National Asthma Education and Prevention Programme (NAEPP) guideline defines control as ‘the degree to which the manifestations of asthma (symptoms, functional impairments, and risks of untoward events) are minimised and the goals of therapy are met’ (p. 36). 18 In contrast, the Global Initiative for Asthma (GINA), acknowledges that control can be defined in different ways and suggests that assessment of asthma control should include ‘control of the clinical manifestations (symptoms, night waking, reliever use, activity limitation, lung function), but also control of the expected future risk to the patient such as exacerbations, accelerated decline in lung function and side effects of treatment’ (p. 23). 19 The British Guidelines on the Management of Asthma state that the aim of asthma management is control. Complete control of asthma is defined as ‘no day time symptoms, no night-time awakening due to asthma, no need for rescue medication, no exacerbations, no limitations on activity including exercise, normal lung function and minimal side effects from medication’ (p. 37). 4 It also means that a child’s asthma will not interfere with his or her daily life including exercise and going to school, in addition to having normal breathing tests, for example peak flow and spirometry. 4 Having good asthma control therefore reduces the risk of children having asthma attacks. 4
Minority ethnic health and the UK
Minority ethnic groups often experience higher morbidity and mortality than majority populations for a range of chronic diseases. 20 Erickson et al. 21 indicated that minority ethnic groups frequently have poor outcomes for long-term conditions. Finding effective interventions to address these health inequalities is, therefore, important. The need to reduce inequalities in health outcomes between majority and minority groups is widely recognised by governments22,23 and physician groups. 24 There is a considerable body of evidence that indicates that some minority ethnic groups in the UK experience disproportionate levels of morbidity and mortality compared with the majority White European-origin population. 25 However, while there are significant differences in health outcomes between ethnic groups, it is important to note that there are also differences in health outcomes within minority ethnic groups. 26 Even where inequalities in health status are not present, there is evidence of inequity in access to health care and preventive services with worse patient experience. 27
The Independent Inquiry into Inequalities in Health Report28 highlighted both ethnic and class-related inequalities in health and recommended that minority ethnic groups be specifically considered in needs assessment, resource allocation, healthcare planning and provision. The 2010 White Paper Equity and Excellence focused on the need to address ethnicity and inequalities in health,29 with the Marmot Review16 identifying numerous influences on health inequalities and the urgent need to address them. While restructuring of NHS and Department of Health management has continued, a commitment to adhere to the equality and diversity objectives and the ‘Public Sector Equality Duty’ laid out in the Equality Act 2010 remains in Government policy and NHS pronouncements.
Asthma and South Asian children
In the UK, people of South Asian origin with asthma experience excess morbidity, with hospitalisation rates three times those of the majority White population. 30 There is evidence to suggest a disproportionate impact of asthma on minority ethnic children, with calls to urgently redress this imbalance. 31,32 A 13-trial meta-analysis30 reported lower prevalence of wheeze and asthma in South Asian children than in White British children, but the same prevalence of exercise-induced bronchospasm on objective testing. These findings suggested an underdiagnosis of asthma in South Asian children. The meta-analysis additionally reported that, once diagnosed with asthma, South Asian children were less likely to receive prescriptions for reliever and preventer medications than their White British counterparts.
Additionally, further UK data indicate that South Asian children with asthma are more likely to suffer uncontrolled symptoms and be admitted to hospital with acute asthma than White British children, with no evidence to suggest that South Asian children have more severe asthma. 30,31,33 There are numerous risk factors associated with asthma, some of which have been specifically highlighted in relation to South Asian children. Several reports identify being UK born (compared with being of the same ethnic origin but non-UK born) as a risk factor for developing asthma. 34,35 Gilthorpe et al. 36 and Rona et al. 37 both indicated that sex may be relevant. Furthermore, Gilthorpe et al. 36 reported that Pakistani and Indian boys tended to use emergency department (ED) services more than other groups or sexes, with Rona et al. 37 identifying that the male sex is a risk factor for developing asthma.
Socioeconomic status is an important determinant of asthma control for both South Asian and majority populations,31,36 as low SES is associated with poor access to primary health care and higher hospitalisation. However, even with adjustment for SES, there is still a correlation between South Asian ethnicity and poorer health outcomes for asthma. 36,38 Potential explanations include ethnicity-specific health beliefs and explanatory models of asthma,39–43 which in turn influence concordance and adherence to management plans. 44 In Leicester, the hospital admission rate for South Asian children is 4.6 times higher than for White British children. 33 Given the high number of families of Asian descent living in the UK, with the three largest groups being of South Asian origin (Indian, Pakistani and Bangladeshi),45 the inequalities experienced by South Asian children are of significant concern.
Barriers and facilitators to asthma management in South Asian children
An Asthma UK-funded review on the barriers and facilitators to asthma management in South Asian children was carried out by members of the MIA research team (see Appendix 1). 46 The review identified barriers including knowledge gaps and erroneous beliefs regarding the nature of asthma, underuse of preventer medications (due to underprescription and fears of overuse), non-acceptance and denial of asthma, reliance on EDs in preference to primary care, difficulties in perception of symptom severity, language barriers and use of complementary therapies.
The review highlighted the importance of not only establishing what a barrier might be, but also exploring why that barrier exists. For each barrier identified, there were various documented and theorised explanations; however, the majority of studies did not identify clear associations between a barrier, its explanations and management behaviour. Several key issues were identified as likely to be ethnic-specific in relation to South Asian families: the impact of parental and professional knowledge and beliefs; access to health services and preventer medication utilisation patterns; dietary modifications; and the presence and impact of prejudice and stigmatisation.
Given the large number of potential barriers and explanations that may impact upon asthma management, it is understandable that clinicians may be daunted by the prospect of attempting to address these barriers in everyday practice. Nonetheless, these findings highlight the importance of cultural and community beliefs. For example, there is minimal evidence to support the theory that dietary restrictions are an appropriate method for asthma management. As a consequence, they are often not considered a key factor in asthma management according to the BTS guidelines, used by the majority of British practitioners. 47 However, it was identified that beliefs and practices concerning food and asthma are prevalent among minority families in the UK. Thus, there is a need for clear and clinically applicable interventions that have considered the various barriers and explanatory factors, including the impact of cultural and community beliefs. While identifying ethnicity-specific barriers is important in developing ethnically tailored intervention programmes, academics and clinicians must guard against assuming too great a role for ethnicity. In exploring cultural difference, it is important not to ignore the commonalities in experience between ethnic groups. 48 The focus of research, therefore, needs to shift towards clearly linking ethnic-specific beliefs, barriers and management practices to development of interventions and improving clinical outcomes. A shift also needs to be made from a focus on deficit models of culture in minority ethnic groups as an explanation for health inequalities towards an approach which recognises the responsibility of healthcare systems to develop services which are sensitive and appropriate to the needs of their communities.
Interventions in asthma management
Asthma management and morbidity can be improved by effective interventions including increasing awareness of trigger factors, new ways of monitoring of symptoms, or the usage of newer medications and written self-management plans. 49 The BTS guideline for asthma4 and an Asthma UK systematic evidence synthesis carried out by the MIA research team (www.asthma.org.uk)46 regarded education as an important step in asthma management. A Cochrane review50 found that education-based strategies for improving self-management in children can reduce school absences and emergency visits. For primary school-aged children, a variety of educational interventions and techniques, including group or individual sessions at home, clinic or school, use of didactic teaching, written materials, role plays/problem-solving, artistic activities, games and puzzles, were all used to educate children, their families, their teachers and their doctors about asthma. 50 However, a subsequent systematic review51 concluded that information-only education resulted in very little improvement in any clinical outcome measure.
There have been several successful reported interventions with reference to children and asthma that focus on issues other than education. These have included a community-based programme to identify and address environmental triggers,52 a school nurse initiative to ensure correct use of inhalers through supervised monitoring,53 child-centred, psychology-based training to enhance self-belief and management,54 a web-based intervention using an online diary, interactive symptom manager and reminder system55 and a nurse-led outreach programme for practical advice, support and education. 56 However, while these and many other programmes report success in improving various aspects of asthma management, they either excluded minority ethnic groups, or were significantly less effective or successful in minority ethnic groups. This may, consequently, increase inequality. Even when language-appropriate educational materials are provided, educational interventions still provide better outcomes for White patients than for South Asian patients. 57 The development of cost-effective interventions to reduce morbidity in minority populations with asthma must, therefore, remain a high priority,58 with evidence suggesting that, while most interventions are focused on one particular domain, an effective asthma management needs to be multifaceted. The MIA project was based on the recognition that, when trying to understand health behaviour, it is important to explore not just the beliefs and attitudes of individual patients, but also the wider socioeconomic, cultural and environmental context. These must be integrated to develop multifaceted interventions which can support individuals across the whole pathway of care and wider health system.
Intervention design
A 2004 literature review regarding the design of interventions to change health behaviours7 concluded that many intervention evaluations were inconclusive due to research design limitations and, as a consequence, represented a waste of resources, time and effort. It has been suggested that health interventions are often developed without sufficient consideration given to their evidential or theoretical base, their fundamental design or appropriateness to the target population. 59
Tailored interventions
One important issue in intervention design thus concerns the need to tailor interventions to specific populations. The Medical Research Council (MRC)60 guidance on the design of complex interventions suggests that, rather than assume that standardised interventions designed for generic groups are applicable to all groups, interventions should be tailored to the needs of ethnic minority groups as these are more likely to succeed than generic approaches. The MRC argue that complex interventions may work best if tailored to local circumstances such as ethnicity or SES, rather than being completely standardised. 60 Three systematic reviews have addressed the question of whether or not culturally sensitive education programmes are more effective than generic ones;61–64 all three concluded that, while the reviews were limited by the small number of available trials for inclusion, culturally sensitive programmes were more effective with further study warranted.
A Cochrane review of interventions for improving asthma management in children demonstrated that interventions specifically tailored to address the needs of ethnic minority groups were more successful than those focusing on the generic population. 61 A further Cochrane review explored whether or not culture-specific asthma programmes, in comparison with generic asthma education programmes or care, improved asthma-related outcomes in children and adults with asthma who belonged to minority groups. 65 Interventions included individual asthma educational sessions focusing on relational and collaborative asthma management among children, parents, families, physicians and mental health specialists; and others on the optimisation of treatment and improving knowledge about disease severity and medication. The report noted that the use of culturally specific asthma education programmes for children from minority groups was effective at improving overall asthma-knowledge scores for children. However, it failed to note significant improvements in the number of participants with asthma exacerbations or its frequency, including ED visits. While the report noted a benefit of tailoring interventions to be culture-specific with regard to asthma knowledge in children, the evidence base was lacking and, as a result, these findings could not be confirmed.
Adaptation and tailoring
There remains some controversy over the relative merits of ‘adaptation’ and ‘tailoring’ and the difference between these. Based on a systematic review of the literature, a recent Health Technology Assessment review66 discussed this at great length in relation to minority ethnic groups. It noted that some intervention studies reported were based on generic interventions already operating for mainstream populations, which had been altered to meet the characteristics of the ethnic population that it was (intended to be) serving, as opposed to those that were designed from first principle for ethnic minority populations (e.g. using a community participatory-based approach). In strict terms, adaptation would refer to the former type of interventions; however, on reviewing the literature, there were no interventions demonstrated that were not in some way based on a generic intervention or principle (e.g. a smoking cessation intervention may be designed through a community participatory-based approach to target an ethnic minority population but still remained based on nicotine replacement therapy or counselling). We have, therefore, used this previous evidence to ensure that the intervention would incorporate both ‘tailoring’, based on community beliefs and preferences, and ‘adaptation’ of general principles. 67
There also remains some concern over the appropriateness of targeting investment in interventions on specific minority or high-risk groups, rather than focusing on a more ‘equitable’ distribution of resources through tailoring generic services. It appears that, while there is little strong evidence, there is a consensus suggesting that interventions that specifically target high-risk groups and seek, thereby, to reduce inequalities are relatively cost-effective, and may be more clinically effective than seeking to ensure that broader interventions also ensure inclusion of those most at risk. The arguments for reducing health inequality by targeted action, therefore, serve more than a political or a moral agenda: they can be justified on the basis that this type of action reduces the costs overall for society, and produces a higher return on investment in terms of improved health, than otherwise. 68–70 Targeted action without tailoring the intervention for the group being targeted, however, is unlikely to have any benefits.
User involvement in service design and improvement
Recent White Papers and other policy documents have emphasised the need to strengthen local communities by empowering people to influence the decisions that affect them. 71 It is argued that involving patients, clients and other service users directly in working alongside professionals to create and deliver services will have a more positive effect on people’s health and well-being than merely informing, advising or consulting them. 72 The Darzi report ‘High Quality Care for All’ stated that interventions should be effectively designed around the needs of children and families,73 indicating that their involvement in the design of interventions would be beneficial. In contrast, the Marmot Review16 recommended stronger engagement with minority ethnic groups in service design and improvement. The review suggested that there needed to be a more systematic approach to engaging communities, moving beyond often routine, brief consultations to effective participation in which individuals and communities define the problem and develop community solutions. It is argued that without such participation and a shift of power towards individuals and communities it will be difficult to achieve the penetration of interventions needed to impact effectively on health inequalities. That said, specific issues and complexities in incorporating the views of minority ethnic groups in this process remained, which the MIA project was specifically designed to address. 66
Intervention design approaches
Creating a Patient-led NHS74 highlighted the ambition of the government to create a NHS that moves away from doing things ‘to’ and ‘for’ patients, towards a NHS that works ‘with’ patients. However, there is little consensus on how this should be operationalised. Neither traditional deficit models of service development (where health professionals identify a deficit in service provision and develop/identify services to fill them) nor newer patient-led models of service development (where patients identify their needs and either they or service providers provide/adapt services for them) entirely address the needs of the NHS. 75 An exclusive focus on either the healthcare provider or the patient is, therefore, unlikely to be effective in the long term. It is argued by Bovaid76 that partnerships developed between health professionals/systems, patients, and the public will be the key to success in creating a new, more effective NHS. 76 Several approaches to intervention design are suggested. Evidence suggests that multifaceted interventions are more effective in improving clinical outcomes than those which take a single approach. 50,51,77,78 Research suggests that the more strategies are combined in one intervention, the more likely an improvement in clinical outcome will be found. 79 Equally, it remains true that the more complex an intervention, the harder it is to evaluate and to identify which elements are the most critical. 80
Participatory research
Working with individuals and communities to define problems and develop solutions is one of the fundamental principles of participatory research (PR). PR does not replace other forms of research, but instead defines how the research process is carried out. Green et al. 81 defined PR as systematic inquiry, with the collaboration of those affected by the issue being studied for purposes of education and taking action or effecting social change (p. 1927). PR is a way of addressing health issues in their social context, rather than in the traditional medical model where health issues are addressed in their clinical context. 82 PR is based upon effective information exchange and shared decision-making to respond to service users’ needs. 83
Community-based participatory research
Community-based participatory research (CBPR) is a collaborative approach to research. CBPR involves all partners in the research process equally and recognises the unique strengths that each brings. CBPR begins with identifying a research topic of importance to the community with the aim of combining knowledge and action for social change to improve community health and eliminate health disparities. 84 CBPR is, therefore, a collaborative research approach designed to ensure and establish structures for participation by communities affected by the issue being studied, representatives of organisations, and researchers in all aspects of the research process; the aim is to improve health and well-being through taking action, including social change, which has been widely recognised internationally as a core principle of equal participation. 85 It is an orientation to research that focuses on relationships between academic and community partners, with principles of co-learning, mutual benefit and long-term commitment, while incorporating community theories, participation and practices into research efforts. 84
Engaging minority ethnic communities in health research
People from minority ethnic groups are under-represented in UK research. This problem is particularly prevalent in the field of asthma. 30 This under-representation may be a result of a range of factors, including difficulties encountered by researchers or the deliberate exclusion of minority ethnic communities from clinical trials. 86 The involvement of people from minority ethnic backgrounds should therefore be considered at the outset of the research process. 87 Effective inclusive research can be argued to require specific forms of community engagement, consent and data collection methods,16,88,89 provision of interpreters,16 engagement with community leaders to build trust,87,90,91 utilisation of community facilitators (CFs)/lay researchers and dissemination of results to participants and communities. 87,92
Engaging children in research
Just as minority ethnic groups have been under-represented in research, children have similarly been excluded from research,93,94 yet engaging both children and parents in research is vital for the success of interventions and the production of interventions with positive outcomes. 95 Paediatric research has traditionally utilised parents and carers as the primary information source, based on the belief that children do not possess the necessary communication and recall skills to express themselves,96 or that adult carers ‘know best’. 93,97,98 However, there is an increasing view that the best source of information about a child’s experience is the child himself,99–101 with reports suggesting that children from age 3 years can give graphic but accurate descriptions and demonstrate good recall for experiences related to illness. 100,102–104
Ethical constraints have also often prevented children’s engagement in research. Adults have power over children and, as a consequence, children are vulnerable to exploitation, including from adult researchers; engaging with adult carers is, therefore, a way of protecting children from harm. 105 Practical considerations have also hampered children’s research participation. Children have their own language, concepts and understandings that are distinct from adult versions and can be difficult for adults to access and interpret. 97 As a consequence, engaging adult carers is seen as a practical measure to gain interpretable data. 97 Children’s participation in research has also been influenced by documentation of children’s rights, such as Article 12 of the United Nations (UN) convention on the Rights of the Child106 which recognises a child’s right to participate in making decisions that affect their lives. Glauser107 indicated that ‘it is inappropriate that international organisations, policy makers, social institutions and individuals who feel entitled to intervene in the lives of children with problems, do so on the basis of obviously unclear and arbitrary knowledge about the reality of these children’s lives’. Thus, there is an urgent need to improve children’s engagement with research, particularly in the field of intervention design and research. There are many potential benefits of including children in participatory research, in terms of both improving the relevance of the research and personal benefits for children. However, it must be noted that there are also potential risks in including children in PR, including raising unrealistic expectations and placing an unreasonable burden on them. 108
A child is defined by the UN as person under the age of 18 years;106 however, childhood is more complex than a simple number. Definitions, understandings and expectations of children and childhood vary between cultures and societies. 109,110 These differences affect the expectations of a child’s developmental level at a given age, and the perceived appropriateness of a child’s participation in various activities, including research. When working with someone under 18 years, not only is their ‘child’ status considered, but their race, ethnicity, social class, religion and various other influences need to be evaluated in parallel. It has been suggested that the complexity of taking all of these factors into consideration when developing research projects may be a factor in why the voices of minority ethnic children are often missing from research. 110
Use of the socio-ecological model in intervention design
Commitment to participatory research was one of the guiding principles of the MIA project. This was complemented by the use of a socio-ecological model of health and intervention design. Over the past 20 years there has been a shift from examination of determinants and interventions to address individual behaviour change towards broader, multilevel behaviour and social change models, not least because even the most effective individual interventions cannot address larger population-based health goals. 111 With the introduction of co-production and the necessary partnerships between service users and service providers, behaviour change models that link health planning with public health organisations, community and environmental organisations, policy makers and clinicians are rising in prominence and relevance. These are known as ecological models. 111
A basic tenet of the socio-ecological model is that any behaviour has multiple levels of influence, including biological, psychological, social, cultural, organisational, community, physical, environmental and policy. 111 Ecological models provide comprehensive frameworks for understanding multiple and interacting determinants of health behaviours and can be used to develop comprehensive intervention approaches that systematically target each level of influence. 112 In particular, in contrast to interventions that reach only individuals who choose to participate, ecological interventions can affect large populations. 113
The socio-ecological model (Figure 1) is a theoretical framework that considers the complex interplay between several factors, with particular focus on the influence of the social/community environment. 114 This model has been used successfully for the development of interventions in other conditions, such as obesity. 112 The model proposes that individual perspectives and opinions, with those of family, community and healthcare providers, integrate to form a healthcare system, such that all aspects must be addressed to bring about change. 115,116 It is argued that research that focuses on only one factor will underestimate the importance of the other levels. 115,116 The socio-ecological model provides a holistic approach for interventions as it ensures that structural, individual and interpersonal factors are considered.
FIGURE 1.
Socio-ecological model.

In view of the dominance of cultural influences and community perspectives in health behaviours in South Asian communities,117 it was decided that interventions should draw upon a socio-ecological perspective and be informed by relevant inputs through a process of co-production.
Intervention mapping as a structured process for intervention design
The socio-ecological model requires an intervention development programme which can address multiple levels of influence on behaviour. The MIA project used some of the principles of an approach to intervention design and evaluation known as intervention mapping (IM). 118,119 This approach insisted on the importance of programmes being guided by theories of health behaviour and behaviour change.
Intervention mapping is a stepwise, structured approach moving through an iterative process of assessing the current health and behavioural change needs, identifying health limiting behaviours and their determinants, identifying change objectives and programme outcomes, utilising psychological theories to identify the best means of delivering the programme to achieve these outcomes, implementing and subsequently evaluating the programme. 118,119 IM acknowledges the numerous levels implicit in healthcare delivery, their interwoven nature and the broader social and cultural context in which they exist: a fundamental requirement for successful knowledge translation. 120
Intervention mapping typically follows six iterative steps (Figure 2).
FIGURE 2.
Intervention mapping steps.
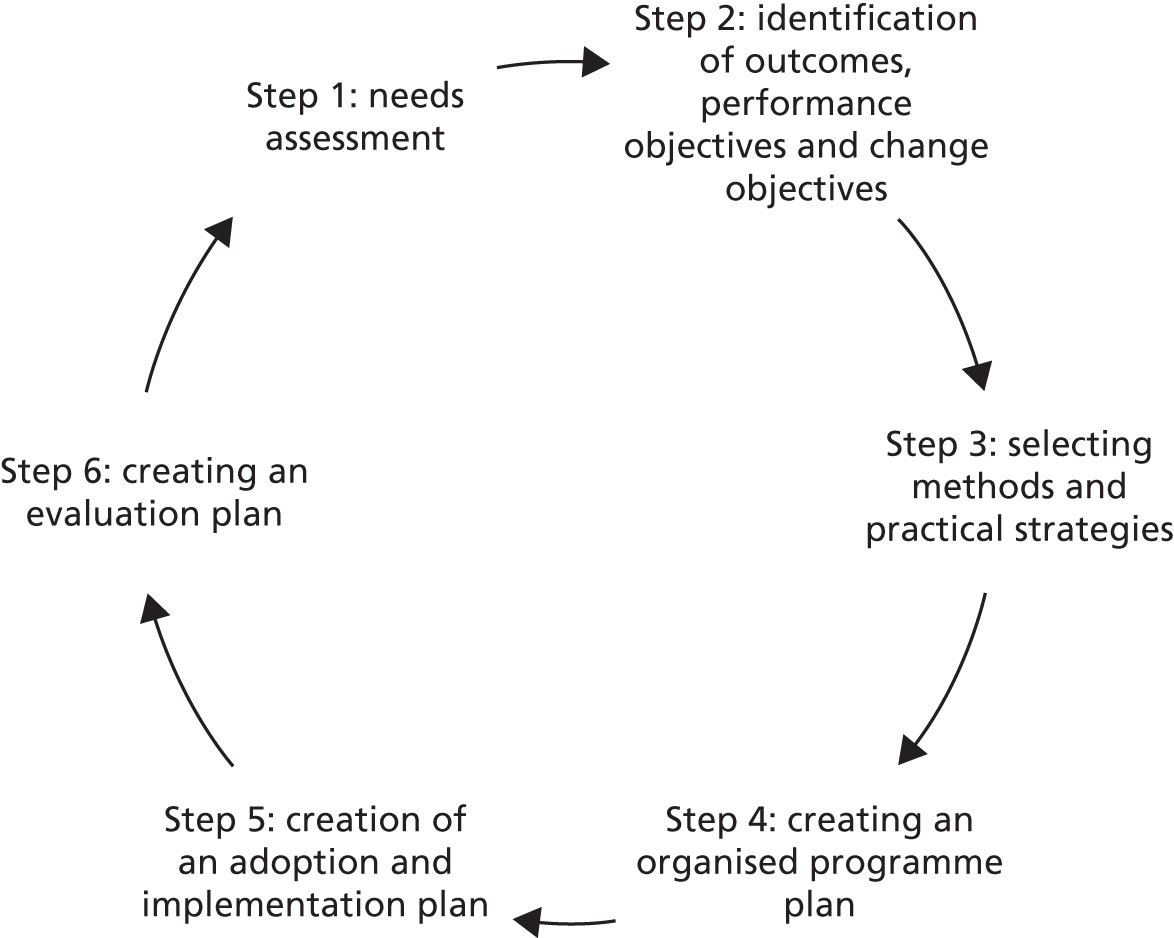
Intervention mapping has been used successfully to develop interventions for asthma, obesity, sexual health, mental health and healthy-eating programmes;121–124 however, it has been applied only a limited number of times to healthcare design in the UK124 for the development of a workplace physical activity promotion programme. Results concluded that, while IM was successful at generating a tailored intervention programme due to its structured, evidenced and needs-based iterative approach, it was resource and time intensive, in addition to being challenging to apply. The MIA team made a proactive decision to use a modified form of IM, adopting the principles of a structured, stepwise approach and the consideration of theory, but recognising that the framework could not be easily applied to our broad set of research questions. This application is described in Chapter 5. Using the principles of IM, the MIA study intended to enable collaboration between patients, carers, community members and health professionals to plan and design an intervention planning framework and then a tailored exemplar programme. It is an example of collaboration in health services research starting at the earliest stage. Though it is beyond the life of this particular project, it is anticipated that participation will continue as the intervention programme is commissioned, managed, delivered, monitored and evaluated.
The MIA study was based in Leicester, UK. Leicester has a diverse population consisting of a high proportion (35.8%) of the population categorised as South Asian (including Indian, Bangladeshi, Pakistani and other Asian). 125 South Asian, for the purposes of this project, refers to a person with ancestry in countries of the Indian subcontinent, including India, Pakistan, Bangladesh and Sri Lanka. The MIA study, therefore, used purposive sampling to ensure proportionate representation from the four largest South Asian religious/ethnic groups (Indian Sikh, Indian Hindu, Pakistani Muslim and Bangladeshi Muslim) and from four of the linguistic/ethnic groups (Bengali, Urdu, Gujarati and Punjabi). Participants were asked to self-assign their ethnicity. A comparator group of White British families and children were included in the study to identify commonalities and differences across groups in addition to generic recommendations.
The MIA project recruited primary school-aged children and their families, as the children were largely dependent on their parents for asthma management. As adolescents are encouraged to take a leading role in their management, an intervention targeted to adolescents would require a different approach. As a consequence, a proactive team decision was therefore made not to include them in this study. 17 Purposive sampling was used to identify children with a wide range of asthma severity within each ethnic group. Severity was defined by the BTS guidelines’ ‘stepwise approach to management’, which places a child’s asthma control in one of five steps or categories of asthma. 49
An examination of the literature on asthma and its management in South Asian children, consideration of approaches to participatory intervention design, and discussions with South Asian families and HCPs responsible for delivering asthma services in Leicester led to the following research aims and objectives.
Aims and objectives
Study aim
-
To use a collaborative method of designing healthcare interventions to develop an intervention programme for South Asian children with asthma.
Study objectives
The MIA project sought to explore and answer four key questions:
-
to test a participatory model of healthcare intervention development;
-
to provide an evidenced-based understanding of asthma and its management in South Asian children;
-
to provide a comparative analysis of understandings of asthma and its management in White British and South Asian children to account for geographical and sociocultural context; and
-
to produce a realistic and achievable intervention planning framework for asthma management.
Research questions
There were four key research questions that the MIA project sought to explore and answer:
-
What are the lay understandings and perceptions of asthma in South Asian communities?
-
How do health professionals perceive asthma and its management in South Asian children?
-
What is the knowledge and awareness of asthma, its triggers, and control among South Asian families and children with asthma and, correspondingly, what are the facilitators and barriers to good asthma management?
-
What interventions to optimise asthma management are effective, acceptable and feasible for children and parents from South Asian communities?
The following chapter discusses the methodological approach of the MIA project in more detail.
Chapter 2 Overview of project design, collaborative approach and methods
This chapter presents a brief overview of the project design as well as the collaborative approach taken to researching asthma within South Asian communities. The project was a community-based study designed with four main phases (see Figure 3) and utilised a participatory approach throughout. The design was informed by the socioecological model of health (see Figure 1) and drew on principles of qualitative inquiry and methods of IM (see Figure 2). Given the methodological complexity of the study, a more detailed description of the methods and the sampling that relate to each particular phase of the study is provided at the beginning of the appropriate chapters.
Overview of design and methods
The phased project structure was designed to enable the research team to build iteratively on findings from each stage and to use this to guide subsequent stages of the research. Iterative working requires flexibility and, thus, despite the apparently linear structure, there was a degree of overlap between the stages (Figure 3). A brief overview of the stages is described below.
FIGURE 3.
The stages of the MIA project.
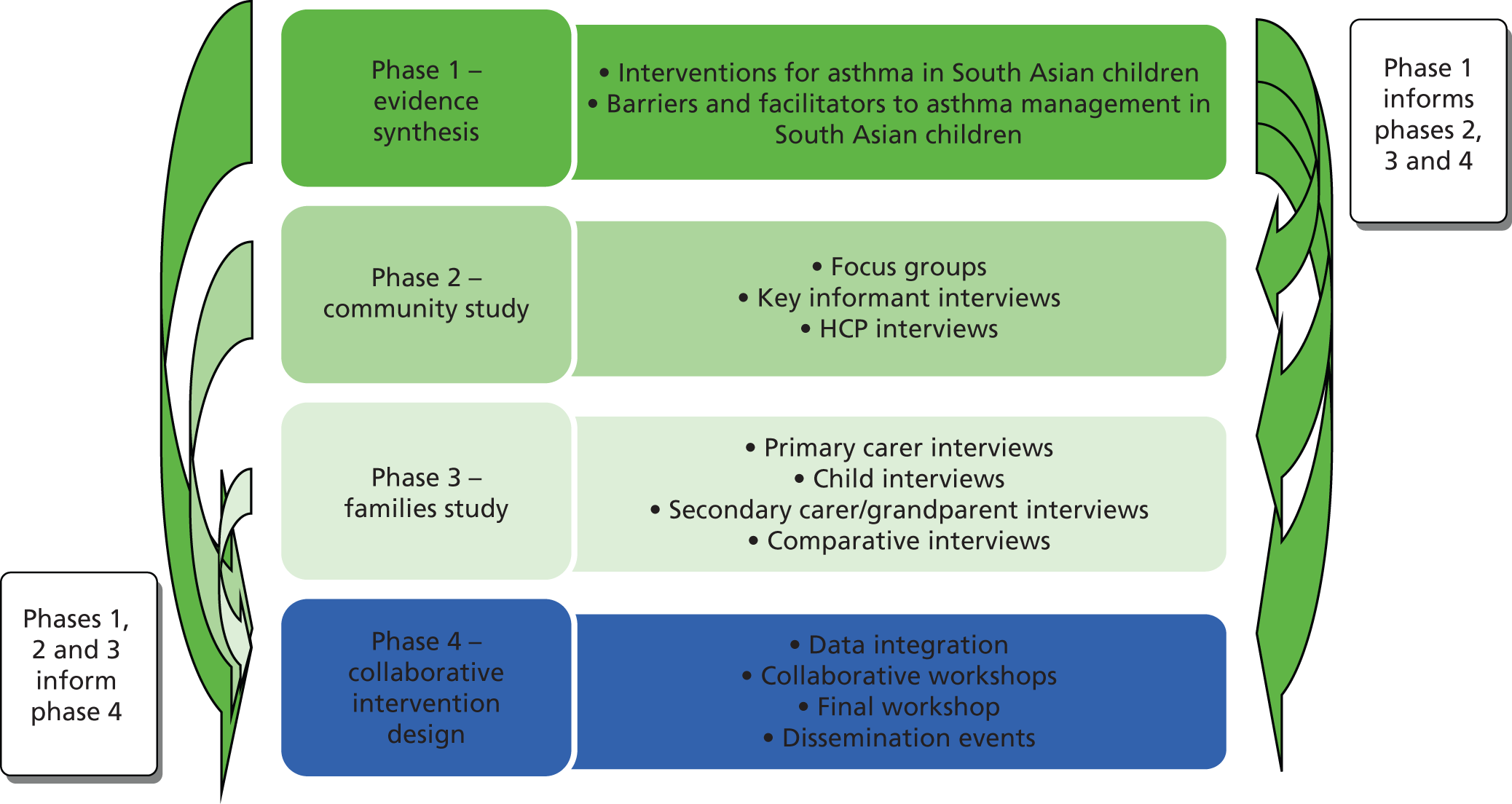
Phase 1: systematic evidence synthesis
Phase 1 was a systematic evidence synthesis of the barriers and facilitators to asthma management in South Asian children, funded by Asthma UK and conducted prior to the MIA project. While this review was an important prestudy activity which contextualised the subsequent phases, it was not funded as part of the MIA study and is therefore not discussed at length in the rest of this report. An overview can be found in Appendix 1 with a copy of the report available online (www.asthma.org.uk) later in 2013. 46
Phase 2: community study
Phase 2 of the MIA study was a study of community perceptions designed to explore lay understandings of asthma and its management in children. The objectives of phase 2 were to understand the South Asian community perceptions of asthma and to gain an understanding of the ways in which families of children with asthma are perceived and treated by the wider community. Community focus groups and key informant interviews were used to explore lay perceptions among a range of individuals and groups and to take into account the wider cultural, religious and socioenvironmental context of a potential intervention targeted at asthma. The research team, in partnership with CFs, developed interviews and focus group question schedules built on the findings from the review in phase 1.
Phase 3: families and healthcare professionals study
Phase 3 aimed to explore the perceptions and experiences of families living with childhood asthma (South Asian and White British) and experiences of healthcare providers who had supported or treated South Asian children living with asthma, with a particular focus in barriers and facilitators to its management. Semi-structured interviews were carried out with South Asian children and their parents or carers to discuss and explore perceptions and experiences of living with asthma. A subsample of White British families were also interviewed in order to further clarify the role of ethnicity in determining barriers to management by assessing the perceptions of the ‘majority’ White British population (see Chapter 4). Semi-structured interviews were carried out with HCPs involved in the management of children with asthma. As the primary aim of the study was to develop tailored interventions for South Asian children, HCPs were asked only to comment on their experiences and work with South Asian children and their families (see Chapter 4). No attempt was made, therefore, to ask HCPs about perceptions regarding the care of White British children. Interview schedules were developed in partnership between the research team and CFs in response to the initial findings from phases 1 and 2.
Phase 4: development of potential collaborative intervention strategies
The aim of this substantial and iterative phase was to synthesise the data from all previous stages and to develop an intervention planning framework and exemplar programme for South Asian children with asthma. The objectives were to enable collaborative intervention development, and produce an acceptable and achievable intervention plan for asthma management. Findings from the phase 1 review, the phase 2 community study and the phase 3 family and HCP study were integrated, discussed collaboratively at workshops with families, HCPs and community members and refined into the final intervention planning framework and exemplar programme. This complex process was guided by principles of intervention mapping and took place following the process described in more detail in Chapter 1. Following on from the collaborative intervention development, the research team gathered data on participants’ experiences of the methods of intervention development to feed into a reflection and review of the process of collaborative development. Short semi-structured interviews were conducted with a sample of study participants, team members and advisory group members to explore their experiences of this method of intervention development. The data from these interviews was used to contribute to the team’s reflection on the process; a component of the iterative approach adopted, with a view to improving the process when applied to future projects.
The research team and advisory group
The multidisciplinary research team included academics from the following disciplinary backgrounds: academic and clinical paediatrics (ML, DB), social science (MJ, LC and NH), clinical psychology (NR), nursing (MMcF), respiratory paediatrics (JG) and health psychology (CHW). A South Asian parent representative, (NJ), was also a member of the core research team and worked in partnership in each phase of the study, from the initial design of the protocol and research design, to managing the study, taking part in project activities such as team meetings, running workshops, discussions and reviewing related literature including the final report. Additionally, the core team were supported by a group of ‘community facilitators’: bilingual members of South Asian communities who were trained as lay researchers to assist with all stages of the research. This method was employed as part of the participatory, inclusive research design and is described in more detail below.
A multidisciplinary advisory group was set up in order to assist the team to carry out the research and to include the perspectives of those with a stake in the research. The group therefore included representation from the following areas: paediatrics, public health, general practice, commissioners and children’s services (including service managers, school nurses and paediatricians). South Asian parents of children with asthma were also represented on the advisory group. Both parent representatives on the project (NJ and SA) had children with asthma and were involved at all stages of the research. As part of her role in the advisory group, SA also participated in study recruitment, development of data collection tools and in the running of the children’s workshops.
Collaborative research engagement: the role of community facilitators
The communities which collectively constitute the category ‘British South Asian’ represent approximately 4% of the UK population, yet as with most minority ethnic groups, South Asians remain significantly under-represented in clinical research trials. 86,126 This tendency to exclude certain groups from research persists despite the fact that there is now a well-established and growing body of literature that describes how and why members of minority ethnic communities should, and can, be effectively engaged in research. 127,128 Researchers from the USA and the UK suggest that, to successfully recruit South Asian participants, developing a sense of trust between researchers and participants is of vital importance,128 in addition to consideration of specific language needs in securing informed consent. 127
The MIA project engaged community members as partners rather than subjects, involving them in all stages of research, from identifying research questions to recruitment, developing an intervention, interpreting research findings and disseminating results.
Engaging community members as collaborators is powerful on multiple levels. 129 Developing a research project from the bottom up and working with the community members to identify important issues and factors has the potential to improve a population’s participation and enthusiasm for a project, which can subsequently mobilise the community in addition to improving the effectiveness of the intervention.
Previous research has suggested that, to engage successfully with minority ethnic groups, earning the trust of potential study participants is important. 87 Strategies to achieve this include ensuring ongoing involvement with community groups, key community representatives and faith organisations, with emphasis placed on the employment or involvement of community representatives as study personnel. 66,127 Personal contact with key community representatives is also described as essential by those with positive previous experiences of recruiting minority participants. 87 A personal touch, including face-to-face contact, is seen as instrumental to building relationships between research staff and members of minority ethnic communities. 87 In the MIA study, this collaboration and engagement was achieved by tailoring recruitment, consent and participation in the study in a number of ways.
A team of male and female CFs were actively involved in all stages of the study. The inclusion of CFs in carrying out research is an approach adopted previously by members of the team130,131 and was designed to facilitate the engagement of participants from across a number of South Asian communities. This approach was designed to allow participation by those whose first language was not English; to provide participants with a choice of facilitator or interviewer in terms of sex and ethnicity; and to ensure that the research was relevant to the communities involved. 131 The CFs facilitated a relationship between the research team and the local communities, with many authors suggesting that the role community partners and liaisons play in recruitment may significantly improve the effectiveness and retention of minority participation in research. 129
All of the female CFs had previous experience of research involvement in studies with South Asian communities, while the male CFs were recruited following recommendations from the existing CFs. The facilitators were chosen based on their relevant language skills (Bengali, Gujarati, Punjabi and Urdu), sex, and identification with and knowledge of the four communities to which the study was being undertaken in. Linguistic skills alone were not considered adequate and, to ensure that a positive rapport was developed between the CFs and the participants, cultural and religious familiarity with the intended research participants was also essential. 131 Training on both research methods (e.g. refresher training) and asthma management was provided for the CFs by the research team.
The CFs utilised personal contacts and a snowball sampling method to recruit participants from within their respective communities. They provided verbal explanations of the research process and discussed the study information with potential participants in their preferred language. The CFs were instrumental in enabling verbal-consent procedures when English was not the participant’s preferred language, having been previously trained in this method in sessions with the research team. The use of spoken study information and verbal consent was essential as there were no agreed written consent forms in several South Asian languages, such as the Sylheti and Mirpuri dialects. Research indicates that literacy, even in a native tongue, can be very low among some South Asian communities. 132,133 While informed consent is considered preferable in written format, verbal consent was considered more appropriate at times when participants were non-literate134–137 (see Appendix 2).
The CFs were involved in the development of the data collection tools, organised and facilitated focus groups in the appropriate languages and assisted the research team in conducting family and key informant interviews when necessary. When focus groups or interviews were held in languages other than English, the CF also worked in partnership with the research team, asking questions in the chosen language and providing brief on-the-spot translations for the research team such that any follow-up questions could be asked spontaneously by either the research team or the participants, supporting an interactive, real-time dialogue between the two. At the study workshops, the CFs provided translations of the verbal presentations in five languages and facilitated table discussions. During the analysis process, the CFs attended group meetings to review and discuss the interim results, and to ensure correct understanding of translations and to ensure cultural sensitivity.
The CFs advised the research team throughout the study on how best to maximise community engagement. This was an iterative process and at different phases the research team sought advice from the CFs in order to ensure that engagement with the community was as successful as possible through the utilisation of appropriate financial and human resources. Examples of advice provided included profiles of key informants that they considered important to be approached for the study, venues for workshops that would be more appealing to the different groups, considerations required when choosing the day on which workshops should be held and considerations regarding cultural acceptance of food to be served at the workshops.
Participatory workshops were part of the collaborative design of the study. Dialogue between the research team and the participants at the workshops allowed the team to collect direct feedback on the processes involved. Members from the voluntary sector organisation, Asthma UK, also attended the workshops, providing an opportunity for families who attended to opportunistically learn more about asthma and the support available.
Several community-based organisations were actively involved in the recruitment or provision of key informants. These included Clarendon Park Temple (where study participants and key informants were recruited from); Bengali women’s groups (where Bangladeshi women were recruited for the focus groups); the Federation of Muslim organisations (aided with recruitment and provided several key informants); and Leicester Central Mosque (provided a key informant). A number of other local community centres were used for events and workshops as well as providing key informants.
Collaborative research engagement: the role of children
Children were involved in several aspects of the MIA study to enable us to effectively include their perspectives. It is considered good practice to engage children in decisions about their own health; however, parents are often invited to speak on behalf of their children. The age range of children included in the MIA study was 5–12 years and can be considered young. Research has demonstrated, however, that even young children can effectively respond to research participation. 97 A variety of approaches were utilised to encourage children to communicate with us, both in interviews and at the workshops. This encouraged the bidirectional sharing of information and enhanced the relevance of the whole research project. The children were actively involved in the workshops and contributed to the intervention design through helping to prioritise specific research areas. Teenage ‘peer’ facilitators (aged 14–16 years) were used to put the children at ease, to promote engagement between the research team and the children and, therefore, to enable meaningful participation by the children at the workshops. Further information regarding children’s involvement in the MIA study can be found in Chapter 4.
Recruitment
There were two avenues for recruitment in the MIA project: through the NHS or directly through the community. NHS recruitment drew on primary care research networks (PCRNs) and comprehensive clinical research networks (CLRNs) to recruit through pharmacies, GP surgeries, emergency primary care, and hospital and community paediatric clinics using standard NHS ethics and recruitment procedures (see Appendix 3). Community-based recruitment involved CFs who drew on methods such as snowballing, telephone and mail shots (for all recruitment methods see Appendix 3). The recruitment process used by the CFs (and throughout the study) was a standard three-step approach (see Appendix 2). In addition to through the CFs, the study was advertised using posters, flyers, and university and research websites. A study website (www.http://mia.ocbmedia.com) was designed to signpost individuals to study information in English and translated into the main South Asian languages relevant to our study, available in both written and audio formats to enable those with low literacy to still engage with the research project.
Ethical considerations
Ethical approval was gained through the local NHS ethics committee, university ethics and NHS research and development (R&D) approval. National Research Ethics Service (NRES) procedures were used throughout the study to minimise distress to participants and safeguard anonymity and confidentiality, as well as providing a guarantee for a continued standard of care (see Appendix 2 for further details regarding ethics and consent procedures).
Chapter summary
This chapter has given a brief overview of the research design, the methods used, the team structure and the overall participatory approach. Individual chapters provide a more detailed description of the methods as well as a breakdown of the resulting sample for each phase.
Chapter 3 The community study: perceptions of childhood asthma in South Asian communities (phase 2)
In line with recommendations to consider not only an individual’s attitudes and beliefs towards health but also the influence of the environment and community relationships,5 the first phase of the MIA project focused on exploring lay understandings and perceptions of asthma and its management in South Asian communities. This was regarded as an important contextual phase of the project, and was in accordance with the socio-ecological model underpinning MIA. The attitudes, beliefs and health behaviours of parents/carers and children living with asthma (and other health problems) do not exist in a social vacuum. 2 It is argued that the social context of the wider family and community understandings and attitudes may have a significant influence on parents and children living with asthma2 and this broader context merits further investigation if we wish to fully understand this setting. This phase was also regarded as an opportunity to identify any general community concerns regarding barriers to meeting the needs of the community so that they could be taken into consideration when developing the MIA asthma intervention planning framework. This phase enabled the research team to take the first steps to engaging with South Asian communities, an important starting point in participatory research (see Chapter 4). The focus group participants were, thus, recruited not on the basis of having direct experience of living with a child with asthma, but to gather data on the wider social meanings of childhood asthma within the communities engaged in the study, and to gather general suggestions on improvements in the health system that participants felt could contribute to improvements along the whole asthma management pathway.
This phase of the study was separated into two parts: focus groups representing the main South Asian communities and individual interviews with ‘key informants’ considered to be individuals of influence within their community. The ‘key informants’ were an important inclusion in this phase of the MIA project as they were seen as potentially helpful in assisting the team to interpret and contextualise the community understandings of asthma and its management emerging from the focus group data.
The aims of this phase of the study were therefore to understand lay perceptions of asthma and the potential impact that cultural, religious and wider socioenvironmental factors have on a child with asthma. In addition, this phase also provided an opportunity to engage with individuals who were invited and encouraged to contribute to phase 4 of the study. This phase was therefore designed to take account, as much as possible, of generational, sex and ethnoreligious differences within heterogeneous South Asian communities. As a consequence, the recruitment process, described below, reflected this approach.
Sampling and recruitment
Purposive sampling was used to ensure that at least one community focus group and key informant interview was carried out with participants from each of the main South Asian ethnic, religious and linguistic groups: Indian Gujarati Hindu, Indian Gujarati Muslim, Indian Punjabi Sikh, Indian Punjabi Hindu, Pakistani Muslim and Bangladeshi Muslim. We were also keen to recruit focus group participants from a wide age range, recognising the potential significance of generational differences, and held focus groups with both men and women (Table 1).
| Group | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Community focus groups | Adults aged 18+ years | None |
| South Asian descent | ||
| Key informant interviews | Adults in a position of authority or influence within South Asian communities | None |
Community focus groups consisted of between 6 and 10 participants. In some cases, these were divided by sex to take account of religious/cultural requirements. Key informants were interviewed individually.
Participants were recruited to the focus groups by CFs and members of the research team, using the three-step approach described in Appendix 2. Identification of key informants was predominantly carried out by direct recommendations from the community focus groups to identify persons of influence and tasking each CF to identify key people within their respective communities. All participants in the community focus groups and key informant interviews gave formal verbal or written consent (see Appendix 2).
Methods
Facilitation of community focus groups
A pre-set interview/discussion schedule was devised by the research team (see Appendix 4), informed by findings from the systematic evidence synthesis in phase 1 and consultation with the CFs, and the project advisory group. Discussions took place in both English and the appropriate South Asian language. The CFs were asked to convene eight focus groups: one Bengali female, one Bengali male, two Indian Gujarati, two Indian Punjabi, one Pakistani female and one Pakistani male. The language of the focus group was then a pragmatic choice based on the participants’ needs, for example both Pakistani groups were run in a mixture of English and Urdu with the CFs translating when necessary, one Indian Gujarati group was conducted in Gujarati, and the other Gujarati group was conducted predominantly in English. All discussions were recorded; those taking place in English were directly transcribed and interviews that took place in a South Asian language were translated into English by the CFs and subsequently transcribed.
Facilitation of key informant interviews
The key informant interviews used a semi-structured format with a question schedule informed by the findings of the systematic review and input from external advisors and the advisory group (see Appendix 4). Interviewees were offered their choice of language for the interview. The remaining interviews were conducted by a member of the research team in English. All interviews were digitally recorded, transcribed and translated where necessary. The data analysis utilised a framework based on the principles of IM (see Chapter 1, Intervention mapping as a structured process for intervention design). The themes from the data were extracted and transferred to standardised tables (charted) (see Appendix 5 for an example of the tables) used for phases 2 and 3 in preparation for the development of the intervention programme in phase 4. A narrative summary was also produced and is presented in this chapter.
Results
Participants
Seventy-five participants were recruited to the community study in total, of whom 63 participants attended a total of eight focus groups (Table 2).
Community focus groups
As part of best practice, individuals were allowed to self-assign their ethnicity.
| Focus group | Ethnicity | Sex | Religions | Age range | |||
|---|---|---|---|---|---|---|---|
| 18–34 years | 35–54 years | ≥ 55 years | Did not answer | ||||
| 1 | Indian Punjabi | Male, n = 2 | Sikh, n = 6 | 0 | 3 | 3 | 0 |
| Female, n = 4 | |||||||
| 2 | Indian Punjabi | Male, n = 4 | Sikh, n = 4 | 5 | 2 | 2 | 1 |
| Female, n = 6 | Hindu, n = 5 | ||||||
| Did not answer, n = 0 | |||||||
| 3 | Indian Gujarati | Male, n = 0 | Hindu, n = 7 | 1 | 4 | 3 | 0 |
| Female, n = 8 | Muslim, n = 1 | ||||||
| 4 | Indian Gujarati | Male, n = 5 | Hindu, n = 5 | 0 | 4 | 1 | 0 |
| Female, n = 0 | |||||||
| 5 | Pakistani (female group) | Male, n = 0 | Muslim, n = 6 | 1 | 2 | 1 | 2 |
| Female, n = 6 | |||||||
| 6 | Pakistani (male group) | Male, n = 9 | Muslim, n = 9 | 1 | 4 | 2 | 2 |
| Female, n = 0 | |||||||
| 7 | Bangladeshi (male group) | Male, n = 8 | Muslim, n = 8 | 2 | 6 | 0 | 0 |
| Female, n = 0 | |||||||
| 8 | Bangladeshi (female group) | Male, n = 0 | Muslim, n = 11 | 4 | 4 | 2 | 1 |
| Female, n = 11 | |||||||
| Totals | Eight groups | 63 participants | 14 | 29 | 14 | 6 | |
Key informant demographics
Twelve key informants were interviewed, comprising seven men and five women. Examples of their roles included religious leaders, community centre managers, community liaison officers, school–home liaison officers and support workers (Table 3).
| Ethnicity | Sex | Religion | Age range (years) |
|---|---|---|---|
| British Asian, n = 2 | Male, n = 7 | Hindu, n = 2 | 18–34, n = 0 |
| Indian, n = 7 | Female, n = 5 | Sikh, n = 1 | 35–54, n = 4 |
| Bangladeshi, n = 2 | Jain, n = 1 | ≥ 55, n = 2 | |
| Pakistani, n = 1 | Muslim, n = 3 | Did not answer, n = 6 | |
| Did not answer, n = 5 |
Community focus groups: key themes
One of the aims of this phase was to inform the development of the interview schedules for the family interviews as well as informing the development of the intervention planning framework and exemplar intervention programme. The interviews, therefore, focused on organisational issues within the health system as well as issues related to the community or families. Several key themes relevant to asthma and its impact on families were identified from the focus group data and are discussed briefly below: understandings of asthma; impact of having a child with asthma; expectations for a child with asthma; influence of community attitudes; diet and asthma; using inhalers and other medicines; perceptions of the NHS; and suggestions for interventions to help families.
Understandings of asthma
Public awareness is known to be a driver of optimal management, for example by encouraging early recognition and intervention. By identifying community understanding of asthma, the language used to describe it, the symptoms of asthma and what the management involves, an insight into the public awareness of the condition can be gained.
Understandings of asthma were similar across all groups regardless of religion, culture or sex. A key area of discussion included participants’ perceptions of the causes and symptoms of asthma.
Awareness of asthma symptoms
To identify the level of awareness of asthma in the community, participants were asked to discuss, very generally, their thoughts about asthma. Participants reported that they were unsure of the symptoms of asthma and that awareness of symptoms in the community was generally poor. The most commonly identified symptoms mentioned by the participants were difficulty with breathing and ‘being wheezy’.
There are different symptoms that I think a lot of people are not aware of.
FG4, Indian Gujarati
From the breathing you can tell that someone is suffering from asthma yeah – cos they’ll get a tight chest and they can feel their chest getting tight and then you know they struggle to breathe.
FG5, Pakistani female
I always thought asthma was when you can’t breathe properly. It’s not really just that . . . she has a very heavy cough.
FG4, Indian Gujarati
Language used to describe asthma and their relevance: asthma versus wheeze
‘Medical’ language is known to be a barrier to optimal management due to its contribution to communication difficulties between HCPs and patients/carers. Having knowledge of the presence of this barrier should lead HCPs to establish ways of overcoming it and improving communication. The terms ‘wheeze’ and ‘asthma’ are key terms used when communicating about asthma. The research team wished to explore participants’ understanding of these terms, what they meant to participants and the level at which they were used interchangeably.
Wheeziness is mostly related to asthma but I don’t think generally it’s always asthmatic.
FG5, Pakistani female
I wouldn’t say wheeziness was like having asthma; it could be due to chest infections . . .
FG2, Indian Punjabi
People have wheeziness if they have asthma, but some people are wheezy if their chest is weak.
FG1, Indian Punjabi
Some participants felt that asthma was an intermittent periodic condition or was present only when the individual had related symptoms, such as when the child was actually wheezing or having an acute asthma attack.
Sometimes my younger son has it [asthma].
FG3, Indian Gujarati
If they’ve got a cold or bad cough or chesty cough they will get wheeziness and perhaps that instance you can classify as asthma but they not asthmatic children.
FG5, Pakistani female
It’s not a constant thing like diabetes or heart trouble. Asthma is very periodic, your get it at certain times.
FG5, Pakistani Muslim female
While standard medical definitions describe a wheeze as a whistling noise heard on breathing as a result of narrowed airways in the lungs, many participants struggled to define ‘wheeze’ using various definitions, with many relating wheezing to coughing.
It’s a kind of cough you can hear in the chest. You know you have a bad cough and you are kind of chesty.
FG4, Indian Gujarati 2
I would say if anyone has a chest problem they would be wheezy.
FG1, Indian Punjabi
When it’s hard to breathe, the throat makes loud sound.
FG7, Bangladeshi male
There may be blockages in your arteries and you can’t breathe properly, infection swelling of that sort. There is some form of difficulty in breathing.
FG2, Indian Punjabi
It means the child is coughing. When the child has very chesty cough.
FG3, Indian Gujarati
In summary, participants highlighted a difficulty with the language used when describing asthma as a chronic illness and the medical terms commonly used to describe asthma symptoms.
Causes of asthma
Health professionals require a knowledge of the perceptions of an illness’s causes so that any myths or misunderstandings can be addressed; this would help to improve early diagnosis, increase the likelihood of the presentation of an individual suspected of asthma and disclosure of an illness within their community and, in turn, improve adherence to asthma management strategies.
When asked about the causes of asthma, participants either responded that they did not know or referred to either genetic/hereditary factors or factors relating to the weather and general environment.
I have no idea.
FG2, Indian Gujarati
Something to do with inheritance and a family history problem.
FG5, Bangladeshi female
It may be a genetical [sic] illness.
FG6, Bangladeshi male
The weather here [in the UK] is misty, cold due to which asthma is more severe here.
FG7, Pakistani male
I think it’s because of the damp weather here which . . . and it’s also hereditary.
FG8, Pakistani female
Asthma begins from dust and dirty house.
FG6, Bangladeshi male
Pollution also has an effect on this.
FG3, Indian Punjabi
Asthma as a contagious condition
Diagnosis related to ‘breathing difficulty’ can include pneumonia and other communicable diseases. Asthma, a condition that may present with breathing difficulty, may be wrongly aligned with such communicable diseases. As a consequence, individuals may believe that the transmission of asthma is similar to such illnesses as pneumonia and other communicable diseases. The research team wanted to explore this potential link and possible misunderstanding. The views regarding the possibility that asthma could be contagious were divergent but present among some of the participants and related to limited knowledge and awareness about asthma in general.
By going close to the child or breathing close to that child you might catch it and you’ll be like them. I don’t to what extent it’s true but there are people who believe that this is a true fact.
FG3, Indian Punjabi
The fear is that my healthy child might catch this from the other child [with asthma].
FG5, Bangladeshi female
Other parents won’t want their children playing [with] him as they may fear that their children might catch the condition.
FG3, Indian Punjabi
I’m not saying this but some parents might feel that if a child has asthma, their child might catch that condition if their child keeps friendship with this child. There is fear amongst other parents in the community.
FG3, Indian Punjabi
Asthma is like bacteria, it spreads from person to person. If someone stays with one with asthma they’ll get it.
It’s not true. It’s not a plague that it’s going to spread.
Sneezing spreads it.
Asthma doesn’t spread. It’s just gossip that it spreads one to other.
Excerpt from FG6, Bangladeshi male
They should keep their children away from that child [one with asthma] as they need to protect their children from catching the condition.
You can’t catch asthma like that, from one person to another . . .
So it doesn’t happen like that?
No, it’s only people’s thinking. You might think that if one child has got it the others might catch it, it doesn’t happen like that. We think like that but it’s not true in fact.
Yes, most of us think like that.
Excerpt from FG3, Indian Punjabi
This belief regarding the contagious nature of asthma was often related to a lack of knowledge about asthma itself, and a misunderstanding of the causes.
Because of lack of knowledge about asthma in our community, people can think it can affect other children as well . . . most people think every disease is a viral disease.
FG7, Pakistani male
Back in Bangladesh people would try to stay away from anyone who has asthma. That’s because our elder didn’t understand what asthma was . . . they thought it was a contagious illness. They didn’t go near them thinking they would get it.
FG6, Bangladeshi male
The solution is with awareness, as I didn’t know the facts; I thought you could pass this condition from person to person.
FG4, Indian Punjabi
There is a stigma attached that you don’t want to catch it from other children. This is because there is lack of awareness.
FG3, Indian Punjabi
When they have a lack of knowledge in this topic so people think what it may be in a negative way. And so they want to stay away from this and is afraid of it [asthma] and once they have understood what this is then they don’t bothered [not afraid] of this.
FG5, Bangladeshi female
Differential understanding of the causes and triggers of asthma
From a medical view, the causes of asthma (multifactorial with genetic, immunological and environmental elements) are distinct from asthma triggers which are amenable to modification and have an influence on asthma control (exposures to triggers cause acute asthma symptoms but not the underlying asthma itself). Identifying participants’ understanding of these two similar but distinct terms provides HCPs with guidance on further barriers to optimal control and may guide professionals in developing educational programmes and the key messages to include.
Some participants were able to draw distinctions between causes and triggers, while other participants found it difficult to distinguish between them. Commonly mentioned triggers included diet, UK weather (e.g. damp, cold and rain), other illnesses and environmental factors (e.g. dust and smoke); this provided the team with guidance on triggers to be discussed in the interviews with family.
Some are affected by smoking because they would inhale the fumes or cleaning around the house, inhaling the dust can affect as well.
FG1, Indian Gujarati
A person realise themselves that certain food is not good for them. They cannot take things like buttermilk, grapes or yoghurt. All these are cold food so it could set off asthma.
FG1, Indian Gujarati
Make sure she is wrapped her warm otherwise she will get her asthma.
FG2, Indian Gujarati
If people suffer with hay fever that will trigger your asthma.
FG8, Pakistani female
Summary of key points regarding understandings of asthma
Understandings of asthma were similar across all groups, regardless of religion, culture or sex. However, differences between groups were noted when discussing perceptions of causes and symptoms of asthma.
-
Many people were unsure of the symptoms of asthma, with symptom awareness within the community generally poor.
-
Asthma was described as ‘difficulty in breathing’ or ‘wheezing’.
-
The definition of a ‘wheeze’ varied between participants and groups.
-
Participants indicated they thought asthma was an intermittent periodic condition.
-
Groups suggested that asthma was a contagious illness.
-
Causes and triggers of asthma were discussed and while some participants could differentiate between causes and triggers, others found it more difficult.
-
Triggers discussed included diet, the UK weather, illness and environmental factors.
Perceptions of the impact for a child living with asthma
Community members were asked to discuss the perceptions of members of the community towards a child with asthma, their views on how the child may be treated and what issues they thought the child may encounter related to school, physical activity, future employment and relationships (e.g. marriage).
Social impact
Participants in all focus groups expressed concerns that a child who has been given a diagnosis of asthma would be socially isolated from their peers with consequential impacts on the child’s emotional and psychological well-being. This finding, shared by all the focus groups, is of importance when considering the integration of a child into the community and also public awareness of asthma to support this integration. It was also an aspect of asthma that the research team needed to consider when interviewing the families and, in particular, their children. Interventions tailored towards the well-being of a child with asthma rather than the medical management of asthma are less common within the health system and may require further consideration.
Parents of healthy children don’t let their children play with the asthmatic child.
FG2, Indian Gujarati
You know people from our community, the elderly people, they used to say oh my god so and so’s child has asthma. So they would say to keep the normal child away from that child [with asthma].
FG5, Bangladeshi female
I think community does isolate people having asthma.
FG7, Pakistani male
Yes they [friends] will leave them out.
FG5, Bangladeshi female
He’ll keep himself away from everyone, that he has this condition and that he is not good enough like everyone else.
FG3, Indian Punjabi
He will feel very isolated.
FG3, Indian Punjabi
[If you have a child with asthma] they may stop visiting you, they might give their children instructions not to mix with the asthmatic child. Partners might tell their husbands or wives that don’t let our child play with that child. They may limit the time the children play together and might instruct their partners to keep an eye on the playing children.
FG4, Indian Punjabi
It can affect the child psychologically. The thoughts of others being healthier than me can make one’s life challenging.
FG7, Pakistani male
To some extent they might even face social isolation as they don’t or can’t participate in activities.
FG3, Indian Punjabi
Impact on schooling and education
Community members were asked to discuss how they thought a child might think about having asthma, and what they thought their attitudes might be towards school and physical activity. Some participants reported that children might find having asthma disruptive to their daily life.
Difficulty in concentrating if you are constantly having asthma attacks. Their attention span tends to go.
FG2, Indian Gujarati
Impact on physical activity
Promotion of physical activity is a requirement for the well-being of all children and any barriers to this should be addressed. People in all focus groups reported a perception either that children with asthma would not be able to be as physically active as other children, or that parents or the child would feel that they could not or should not be as active. A minority, however, dissented from this view.
We tell them not to run and get out of breath.
FG2, Indian Gujarati
They have very little physical exercise/activities, maybe they are not encouraged . . . Unintentionally they are told that they shouldn’t do it, in case they get an asthma attack . . . When we talk about their well-being, their confidence might come into this, it’s not just physical aspect, and these children might lose confidence.
FG4, Indian Punjabi
I’d like to say that with asthma – you can have a perfectly normally life even if have it, there is a famous footballer, who plays for England, Paul Scholes, he has asthma and he is one of the best. It doesn’t matter, even if you have asthma you can do anything.
FG3, Indian Punjabi
Potential impact on future employment
All children with asthma need to transition through adolescence and into adulthood when they may seek employment. Enabling individuals to have equal opportunities for employment is of increasing interest to HCPs and has led to more partnerships between local authorities, employers and the health system. Community perspectives on the employment prospects for children with asthma are, therefore, of importance. Community members were asked whether or not they thought that having a diagnosis of asthma might affect future career prospects and whether or not they would have concerns about employing a young person with asthma. Many participants expressed a view that a child might have limited career options due to their asthma, often relating this to the practicalities of doing the job in question (e.g. ability to climb stairs or be around dusty environments), though others disagreed. Potential financial impacts for the employer were also raised as an issue.
I would think twice, as if, he was unwell then who will do his work, we’ll have to hire a replacement worker – it may be too costly.
FG3, Indian Punjabi
The job? Well if the job is very hard or industry type and they have to have an active body, then people will think twice before hiring. I would think what has he got and should I give him a job or not, so I would think twice.
FG5, Bangladeshi female
He will need office-based work. In clean places . . . He wouldn’t be able compete in all jobs because he has a problem, he need to try.
FG6, Bangladeshi male
They cannot do some activities . . . when my husband arrived in UK during 1970s, he applied for a job at [name of company] but he was told he could not do it . . . because there was spray (fumes) in the air.
FG1, Indian Gujarati
In my personal view I don’t think that there should be anything to be worried about. Support is available, but there may be some families that may think whether she’ll face problems when she grows up and has to work.
FG3, Indian Punjabi
I don’t think it stops you from doing anything [career options].
FG8, Pakistani female
Potential impact on social events
Attendance at social events was used as an indirect marker for stigmatisation or overprotectiveness of the child. Limiting integration in the community and limiting interaction with peers can have consequences for a child’s self-esteem and well-being. Working in partnership with families and understanding reasons for their actions can lead to health professions providing improved support for children and families. Participants reported that there might be practical problems that could affect the ability of a family to take a child with asthma to social events. Concerns were raised about the potential suitability of foods that might be available, how warmly dressed a child could be in ‘wedding’ clothing, or that people at such events might be smoking (which might trigger asthma).
If ice cream is served at the wedding, should not eat it!
FG1, Indian Gujarati
With our Asian wedding we have different clothes; you have to wear garments this way that way. They would think if we dress the child like this the child will catch cold or their asthma may exacerbate.
FG5, Bangladeshi female
You will naturally think that if you go there, it will be noisy, too much dust, it might be hot and you might be worried that your child doesn’t have an asthma attack.
FG3, Indian Punjabi
Need to have an extra eye. Such as he does not do something which can cause asthma and interfere with the family function.
FG7, Pakistani male
In family function some people might smoke so the child has to be away because it can badly affect the child.
FG7, Pakistani male
Potential impact on the rest of the family
A child with asthma may live in a wide family setting with either siblings or within the extended family. The ‘traditional’ health service approach is to focus on the individual child and parents with less of a focus on the impact on the rest of the family or on the parents themselves. In this study, this issue is explored more widely.
Participants were asked their views on the effect of being a parent of a child with asthma on wider family relationships, relationships between the child and their partners and between the child and the extended family. Participants raised a number of issues related to the family dynamics that need to be considered when holistically managing a child with asthma.
I think he might feel slightly inferior to his siblings because his siblings because they can do the things may be he can’t.
FG2, Indian Gujarati
In some families, yes it can affect . . . In my family my mum had it, I didn’t and then my daughter had it. This creates arguments and hostile environment at home. Especially in the Punjabi families: they blame it on the daughter-in-law, that because of you this problem has occurred in their house.
FG4, Indian Punjabi
Naturally parents are more alert about the child’s diet and take extra care of the child. They’ll give extra attention to the child, pay attention to hygiene and cleanliness and prepare food separately. I don’t think they’ll treat her any less but they will give more attention.
FG4, Indian Punjabi
It shouldn’t, but can have an effect. They may argue – it was because of your family [and vice versa], blaming each other’s families. If parents don’t think like this then the grandparents think about ‘blaming’ that because of such and such in his/her family that it has happened to our grandchild.
FG3, Indian Punjabi
Potential impact on marriage
When supporting children for adulthood, it is important to consider not only employment prospects but also future relationships such as marriage. Attitudes towards marriage prospects may be considered a surrogate marker of stigma but also of public awareness of the condition.
Individuals in groups varied in their opinions with regard to the perceived impact that asthma would have on a child’s future marriage prospects. Some individuals felt that there would not be any impact now in the UK, while others felt strongly that there would definitely be a problem for girls in particular. This was most pronounced in the Bangladeshi groups. The concerns related to a woman’s ability to manage a household and look after her children if she had asthma, in addition to the risk of heritability of asthma.
It would affect the marriage prospects as people will be concerned about the future of their marriage.
FG7, Pakistani male
When we arrange marriages, we are always worried that the groom’s side doesn’t get to find out that your daughter has asthma.
FG4, Indian Punjabi
If we knew [our future daughter-in-law] had asthma, most likely the wedding wouldn’t happen.
FG6, Bangladeshi male
It would be difficult for her marriage, because her children would have asthma. It will carry on from her that what people would think.
FG6, Bangladeshi male group
I know there will be an affect because if you want to get a son married one looks for a wife that is good and healthy if they know that there is an illness then she will be disregarded . . . One may think that if they bring this daughter-in-law would she be able to bear children and what if the child inherits this illness.
FG5, Bangladeshi female
I am sure if my son had this [asthma] then other people would not give their daughters to him.
FG5, Bangladeshi female
How we going to get marriage proposal for her, she got asthma, people won’t marry her.
FG4, Indian Punjabi
[Another participant] thinks it’s harder to find a wife for him, but I don’t think it matters.
FG4, Indian Punjabi
I was told to go and give up myself to a temple and not to ruin my life! [By marrying someone with asthma.] I am happy; I have not ruined my life.
FG1, Indian Gujarati
I think it doesn’t so much as it used to, I think it’s changing.
FG8, Pakistani female
Some participants felt that any potential impact on marriage was more pronounced for girls than for boys, while others felt that impacts were equal in boys and girls.
[When discussing impact on marriage] It affects the girls more; it is better for boys.
FG6, Bangladeshi male
They don’t want anyone to find out, especially if they girls as it may have some implications when it comes to marriage proposals.
FG4, Indian Punjabi
If a boy has it, that is accepted, but if a girl has it that generally isn’t accepted.
FG4, Indian Punjabi
[When asked if impact on marriage was different for girls and boys] No. That’s unbelievable.
FG2, Indian Gujarati
Summary of key points regarding perceptions of the impact for a child living with asthma
Community members were asked to discuss perceptions of the community towards a child with asthma and share their views on how the child may be treated. Issues that were discussed included school, physical activity, employment and social activities, as well as relationships.
-
Children with asthma may be socially isolated from their peers, and this may have subsequent impacts on the child’s emotional and psychological well-being.
-
Participants felt that having asthma may be disruptive to a child’s daily life and attendance at school.
-
Results suggested that participants thought that children with asthma would not be able to be as physically active as other children, or that either parents or the child would feel that they could not, or should not, be as active.
-
Participants thought that, in the future, children with asthma would have limited career options due to their asthma.
-
Concerns were raised over the impact that asthma would have on marriage prospects. This was particularly pronounced in relation to girls.
Expectations for a child with asthma
Asthma, health and normality
Interactions of children and support to reach their potential at school, at home and with peers and siblings can depend on perceptions towards what is ‘possible for them to achieve’. Awareness of what people living with asthma are able or expected to achieve will, therefore, potentially have an impact on the child and the family.
While some participants expressed views that children with asthma are ‘normal’ and healthy, and thus should be regarded in the same way as children without asthma, others disagreed. Health in a child was perceived to be linked to being ‘normal’, that is to say being active and happy. Children with asthma were perceived by participants as not healthy, having less energy and being less active and, therefore, not ‘normal’.
She must be healthy, active and should be eating well.
FG7, Pakistani male
Not in our community, they won’t be seen as normal.
FG3, Indian Punjabi
Compared with other ‘normal’ children they might be overweight.
FG4, Indian Punjabi
I think when children are playing and taking part in activities, they feel why can’t they run around and do things like other children. That child feels inside themselves that there is something wrong with her/him. She feels that she isn’t normal like other children.
FG4, Indian Punjabi
Perception of whether or not a child with asthma would be perceived as ‘normal’ was noted to be related to community familiarity and levels of knowledge about asthma.
If they have awareness they’ll think he is normal but if there isn’t awareness then they’ll think that there is a problem.
FG3, Indian Punjabi
We know people had it and you know they live perfectly normal life . . . it’s considered not being normal because they [older generations] did not know anybody who had it. It’s not having the knowledge that we [younger generations] all have.
FG2, Indian Gujarati
You got to maintain normality hundred per cent. Otherwise the child then know that I have got something wrong with me and that is sort of last thing you want the child to feel that I am being treated like this because there is something wrong with me. There is nothing wrong with you. No you are normal.
FG2, Indian Gujarati
Summary of key points regarding expectations for a child with asthma
-
Awareness of what people living with asthma are able to, or expected to, achieve may have an impact on the child and the family.
-
Children with asthma are perceived as not being healthy or ‘normal’, and as having less energy and being less active than children without asthma.
Influences, attitudes, knowledge and beliefs
As mentioned earlier, perceptions of a community towards a child with asthma are a marker of awareness. These perceptions and misunderstandings can affect an individual’s engagement with their management. The team wanted to explore the community’s views on the effect that coming from one of the South Asian groups chosen for this study might have on a child with asthma. This would support the BTS’s view that professionals should have heightened awareness to the needs of some vulnerable groups, such as some ethnic minority groups, in addition to demonstrating a need for increased awareness among the community itself.
When asked whether they thought that being Indian or Bangladeshi or Pakistani would influence, or make a difference to, how the child living with asthma would be treated, participants in the Indian groups felt strongly that negative traditional attitudes and beliefs which had persisted throughout the generations existed in relation to health and illness generally.
If we could move time and don’t have these ill-feelings based on lack of knowledge, we could have happier and fuller lives in our communities, it’s not just about asthma, there are a lot of views based on misunderstandings.
FG4, Indian Punjabi
Maybe in the older generations people used to think like that, it shouldn’t be like that nowadays.
It shouldn’t be – but it is . . .
We can never get rid of these things from our communities!
FG3, Indian Punjabi
There are people like that with more traditional views held dearly . . . I guess it would be about 10% . . . But there are things that held traditionally.
FG2, Indian Gujarati
I also think that within the Asian community, probably not in our generation but the generation above us has set ideas.
FG2, Indian Gujarati
Several traditional but persisting attitudes present among the represented South Asian communities were discussed, including a tradition of hiding illness within a family, an attitude of ‘fear of the unknown’, not wanting to know about conditions that they are not directly affected by, and apportioning blame. The Indian Punjabi groups expressed a cultural preference for families to keep the knowledge of an illness private within a family. This was often related to future marriage prospects and was also raised in the Bengali women’s group.
So we are not so open about things.
No I don’t think we are. We hide things.
FG3, Indian Punjabi 1
Families don’t share the information with anyone, not even with their close friends. They want to keep it in the family and don’t discuss it with anyone else.
You can’t hide anything especially this illness. The family will know anyway.
FG4, Indian Punjabi
I think is very true in our communities, in our communities, it’s not that they don’t want to share anything, they hide conditions such as these, they don’t want anyone to find out that their child is any less that other children, or he is ill.
FG4, Indian Punjabi
Say your son has asthma in childhood and then it goes away when older then you have to tell the other party the truth you cannot hide it away.
There are many who would not declare this. They will hide this.
Keeping it hidden will not matter because people will go and ask the neighbours and the community . . . People talk behind healthy people and surely people will talk about someone who is ill.
FG5, Bangladeshi female
Until something like this happens to us, our attitude is based on 40/50-year-old values and beliefs. We don’t try and learn. If someone in the family or friends circle, have a condition, we tend to think of it as it’s not our problem and try to ignore it. It becomes our problem when it happens to us directly. Only then our attitudes change.
FG4, Indian Punjabi
In our Punjabi community, so it’s easy to blame the women, for example that she didn’t look after the child, not feeding properly, or giving the child cold drinks etc. Instead of tackling the issue in the family set-up, we look at soft targets.
FG4, Indian Punjabi
They may argue – it was because of your family (and vice versa), blaming each other’s families. If parents don’t think like this then the grandparents think about ‘blaming’ that because of such and such in his/her family that it has happened to our grandchild.
FG3, Indian Punjabi
Summary of key points regarding influences, attitudes, knowledge and beliefs about asthma
Perceptions and misunderstandings from the community can affect an individual’s engagement with their management and prevent optimal asthma management.
-
Participants reported that negative traditional attitudes and beliefs, which were carried between generations, existed in relation to health and illness.
-
It was suggested that many families choose to hide a family illness, with a cultural preference for families to keep the knowledge of an illness private within a family.
Diet and asthma
The most recent update of the BTS guideline 20124 makes reference to the importance of diet in relation to asthma. However, evidence regarding specific diets acting as triggers for asthma is still very limited. The research team wished to explore the communities’ perceptions of the link between asthma and diet in order to provide further guidance as to whether or not further exploration was required when interviewing the families.
The impact of a child’s diet on asthma was of great interest to members of the focus groups, who discussed dietary restrictions in relation to both causes and treatments for asthma. Certain foods such as dairy and cold foods [both physically cold and those believed to have ‘cold’ (‘thanda’ – not cold in the English sense but in a sense based on ‘humoral’ classification) properties] were thought to be best avoided. However, participants recognised that this itself could have negative consequences for the child, for example in relation to the child being upset at being denied foods or being singled out as different from other children.
I would not give him cold drink from the fridge because I know soon as he has cold food he will get a cough and with the cough he will have the asthma.
FG5, Bangladeshi female
They cannot take things like buttermilk, grapes or yoghurt. All these are cold food so it could set off asthma.
FG8, Pakistani female
Must stop them from eating wrong foods, sugary stuff.
FG3, Indian Punjabi
You sometimes have to shout at the child if they eat the wrong food.
FG5, Bangladeshi female
You have to be firm with them that you can’t take things out of the fridge and eat anything . . . things like that. They [child with asthma] will not understand of course they would want to do things they have been told not to.
FG5, Bangladeshi female
I would have to make sure I give my children suitable food and I’ll have to explain to children why I can’t give certain food types to asthmatic child, obviously, it’s not good that I make the child cry but I’ll have to explain the situation carefully.
FG4, Indian Punjabi
Summary of key points regarding diet and asthma
The community members perceived a link that existed between asthma and diet, and suggested that certain foods should be avoided to prevent asthma attacks.
Using inhalers and other medicines
Asthma management involves a variety of treatments which can often cause confusion for the individual affected by asthma. The research team did not expect participants or the wider community to have a great amount of knowledge of individual treatments but still wished to explore what level of understanding existed, as many children require treatment while outside their home and may in fact require the support of peers or members of the community to make their treatment available to them. It was felt important, therefore, to explore community awareness of treatments.
Many participants in all of the focus groups professed a lack of knowledge about the different medicines for asthma. Even though some participants understood the need for a child to adhere to asthma medication, others expressed concern regarding side effects related to inhalers and other asthma medications, particularly steroids.
I have never used them therefore I don’t know.
FG7, Pakistani male
Taking steroids long term may cause certain problems possibly.
FG2, Indian Gujarati
Steroids and the side effects of taking steroids long term may cause certain problems possibly.
FG1, Indian Gujarati
The majority of participants did not perceive any problems with children using inhalers; however, there were some concerns raised regarding the perception of inhalers and the visibility of using an inhaler, despite some acknowledging inhalers as being a superior treatment to tablets or syrups.
It is sometimes awkward using them socially. People notice you using your inhalers. They would prefer tablets which are not noticeable. Something soluble – you place it on your tongue and it melts . . .
FG3, Indian Punjabi
Inhaler is the best option as in asthma you need to breath and it helps the lungs without affecting any other body parts. In medicine [tablets and syrups] will also go in blood stream and other parts of the body.
FG7, Pakistani male
Inhaler is the quick action, for sudden attacks, inhalers is the best for the quick relief.
FG7, Pakistani male
In addition to the concerns regarding side effects of steroids, there were concerns related to a fear of the child becoming addicted to inhalers or that the use of inhalers might further weaken the child.
If your doctors prescribes inhalers etc, they he/she may get addicted to using these medicines, like these inhalers.
FG3, Indian Punjabi
I was told not to give him regularly I was told not to give inhaler too much. I was told he is gonna get hooked on it I was told it’s really bad that he is on inhalers.
FG8, Pakistani female
I’ve been told by Homeopath practitioner that by taking inhaler airways gets weaker when it was given to my child. It was stopped by him unless he has severe attack; otherwise don’t take it.
FG8, Pakistani female
In actual fact you are ruining their health and not helping them. It [giving medicines] leads to weakness in children.
FG3, Indian Punjabi
Summary of key points regarding asthma medication
-
Community members showed a lack of knowledge about the different medicines for asthma.
-
Concerns were raised by participants about the side effects of asthma medication, in particular regarding the use of steroids.
-
There were negative perceptions related to the visibility of carrying and using an inhaler, which may prevent individuals from using their inhalers effectively.
Complementary therapies and religion
Complementary therapies are increasingly becoming an integral part of personal management strategies in all communities, be it in relation to asthma or to any other illness. Health professionals, therefore, need to be aware of the utilisation of these therapies and have an understanding of the reason behind their use.
In all focus groups, participants have stated that they would advise parents to seek traditional medical help with asthma; however, alongside this they perceive that alternative remedies would be helpful in the management of childhood asthma, with many expressing the view that they would recommend their use to parents. Dietary supplements and/or restrictions were the most popular recommendations, followed by the use of herbal remedies and homeopathy. Additionally, some participants mentioned taking advice from religious leaders about asthma, while others stated that families would seek advice from family or practitioners in the Indian subcontinent, in particular about potential complementary therapies.
There is another alternative: mushrooms. This clears glands and throat therefore it is easier to breath. How would you eat this? Make bhaji, fried or anyway you like it. There is form of water in the mushroom that clears it [asthma].
FG6, Bangladeshi male
I used to use home remedy: mix honey and ginger powder and give him before bed time.
FG8, Pakistani female
Dill seed, to warm them and she used to put on his chest and so it says that takes out all the cold out and prevent asthma and things like that.
FG8, Pakistani female
They’ll try ayurvedic medicines . . . homeopathic medicines and do yoga.
FG3, Indian Punjabi group
Most parents go to their doctors and then speak with people who’ve had this condition or seek alternative remedies. Some even go to places of worship and even black magic for curing the condition. They would travel as far as India to get medicine/treatment.
FG3, Indian Punjabi group
There were mixed views in all groups about why they would recommend alternative therapies, with the general approach adopted that there was a need to utilise all additional means to improve a child’s health if there was no obvious harm related to those means. In general, participants expressed the view that, in contrast with prescribed medicines for asthma, herbal remedies did not produce side effects.
Herbal remedies don’t give you side effects. I think that’s why sometimes people take them as they give them wanted effects without giving them unwanted effects.
FG2, Indian Gujarati
One is got stronger steroids in it, and that can affect the health. I mean there is a lady works with me, fifty five years old and she just found out from her optician because it’s [the inhaler] got strong steroids and she takes it on regular basis it’s affected her eyes and now she got cataract.
FG8, Pakistani female
The Indian and Bangladeshi participants additionally raised seeking support and guidance from religious leaders and religious ‘healers’.
Your condition has nothing to do with your religion but most people belonging a faith normally say, it’s God’s will and it was meant to be, or even think like a curse on that child or family, rather than thinking, okay, we know it’s with our child what we can do to move on.
FG4, Indian Punjabi
The priest might say to sacrifice a meal or something or do something once a week or on particular day or at a particular time or giving something up likes that . . . I think a lot of people who are not educated may well think that I go and do that as it would make my child better.
FG2, Indian Gujarati
I guess the traditional people listen to priest more than doctor. I think it does not apply to our generation. We believe into science first before religion and go to doctor.
FG2, Indian Gujarati
Summary of key points regarding complementary therapies for asthma
Complementary therapies are increasingly becoming an important part of personal management strategies, in relation to both asthma and other illnesses. Community members perceived that alternative remedies would be helpful in the management of childhood asthma. These remedies included:
-
dietary supplements and/or restrictions;
-
advice and support from religious leaders and religious ‘healers’;
-
herbal remedies and homeopathy; and
-
advice from HCPs in the Indian subcontinent.
Community members perceived that complementary therapies would be used because they did not produce the same concerning side effects as traditional asthma medications.
Perceptions of the NHS
For the NHS to be able to deliver a service to meet the needs of the people, it needs to hear their voices, be reflective and work in partnership to develop services that meet their requirements. In order to optimise management for children with asthma, understanding the organisational issues that need addressing in the health system is of equal importance to addressing issues around knowledge, understanding and beliefs of the individual or the community.
Participants were asked about the health service’s contribution to supporting a child with asthma and who they thought should be the lead professional for the child (GP or specialist). They were also asked to share their views on HCPs’ attitudes and service provision. Participants were also asked their views on perceptions and attitudes of HCPs to children from Indian/Bangladeshi/Pakistani backgrounds compared with other children. Additional discussions included the doctor’s ethnicity in relation to treatment and service provision for the child.
Participants in the focus groups did not perceive that HCPs held prejudiced views of South Asian children and families when treating them. However, where negative attitudes were experienced, it was often reported that this was a reflection of that specific HCP and their attitude or approach to their patients, and was not felt to be a result of prejudice from HCPs towards people of South Asian ethnicity per se.
The doctor will try his best to treat his patient no matter who the doctor or the patient is.
FG3, Indian Punjabi
Once the doctor diagnoses [in this case one has asthma], he will treat equally no matter what the ethnic background doctor has. The procedure might slightly vary but the treatment is same and leads to the same cure.
FG7, Pakistani male
If the doctor is good he’ll treat everyone in the same way regardless of their colour or creed. And if the doctor ‘isn’t good’ regardless whether he is black or white will not treat his patients in the appropriate way.
FG4, Indian Punjabi
Participants were also asked to discuss where they thought parents would go to access care or treatment, and to discuss their own experiences of accessing health care and the services provided. Participants reported various difficulties in accessing services and gaining the ‘right’ treatments. These included attitudes of individual professionals, GP opening hours, waiting times and language barriers.
Being who we are people don’t see us like the others. For example if you go to the doctors and you don’t speak English they may need to get an interpreter, which is a big hassle for them so the doctors just prescribe a medicine.
FG6, Bangladeshi male
We don’t get the right services because we don’t speak English, therefore we can’t ask for it.
FG6, Bangladeshi male
Sometimes you see the child has had an attack late at night but they would say you have to wait till eight in the morning until the doctor’s surgery is open.
FG5, Bangladeshi female
When I phone the GP for appointments then never answer and they do then there is no appointments. When I go to the surgery to make an appointment, they pay no attention to me the receptionists keep chatting amongst themselves.
FG6, Bangladeshi male
One area I was in, I found very helpful. As soon as you said you got asthma they let in straight away. Whereas now I find if I say I got asthma they say oh we are not treating you and you got to book in to come and see them. I got asthma and I am trying seeing someone and before it gets bad. I am trying to prevent it but you cannot do that, there is a stop. You know, it’s like you are stopped before you start.
FG3, Indian Punjabi
In the old days we did not have cars or telephones. We do have facilities now but if we need the help of the doctors for these children, they do not come for home visits anymore. At one time if we rang doctors used to visit at home, they do not do home visits anymore. We have to take the sick child by taxi to see the doctors. They should visit home for the children.
FG3, Indian Punjabi
Pakistani women in focus group 8 reported that there was still a cultural attitude among their community not to question doctors, and a tendency to be too frightened to ask questions to health professionals, suggesting that receiving further information from doctors or requesting additional appointments may be harder for some people in this community.
Specific issues were raised in relation to how asthma was diagnosed in children. Some participants reported that they thought that there was a lack of tests available, or provided, to help with diagnosing asthma.
When we ask the doctors what is wrong so they have to tell you something, half the time you don’t actually have the condition but the doctors just tell you it’s asthma just to give you a ‘condition’.
FG3, Indian Punjabi
When my son gets a cold the doctor prescribes inhaler for it, it’s not asthma.
FG6, Bangladeshi male
Sometimes doctors don’t diagnose it properly; even if they have cold they give them pumps straight away with steroids.
FG3, Indian Punjabi
I mean last week doctor prescribed the medicine over the phone without seeing my daughter. So there got be fair amount of guess work there. No checks or anything!
FG2, Indian Gujarati
When we take him to the doctor [GP] they would give him inhaler or give him cough medicine. They [GP] will not say to send him to the hospital and get him checked properly. He [GP] would not send him for any of this [investigation].
FG5, Bangladeshi female
Sometimes you will find that the doctor will not do anything about it or examine with anything he will just say go and give an inhaler.
FG5, Bangladeshi female
Some issues around cultural competence were raised, especially in relation to the role of the extended family in South Asian families.
When they are non-Asians [doctors] they don’t have the knowledge of the communities, their limitations etc.
FG5, Bangladeshi female
In general, however, participants in all groups felt that there was not a community preference for having a South Asian doctor. The technical skills, cultural competence, communication skills and accessibility of doctors were more important characteristics than ethnicity per se.
Please make a note that we don’t especially want Asian health care professionals assigned to us every time we go to the hospital.
FG3, Indian Punjabi
They must take it out of their systems that we want south Asians, we just want good professionals.
FG4, Indian Punjabi
Our doctors sometimes ignore you. I feel the white doctors care for you more. Our doctors are a bit proud of themselves. Some young doctors think really too big of themselves, just because they have qualified they think they are above everyone else.
FG3, Indian Punjabi
Indian doctors assume that their patients know nothing. They think you are idiots, they are going to prescribe medicine for you and they think they don’t need to explain anything to you.
FG4, Indian Punjabi
He was Indian [a GP], we are Indian but he didn’t know how to talk to his patients. His attitude used to let us down and we used to think we’d rather not have medicine from him if we have to deal with him.
FG4, Indian Punjabi
Many places it seem they [Asian doctors] are afraid to touch the patients in case they get the illness, they may have a problem, they don’t like to do their job but the white doctor does it properly.
FG6, Bangladeshi male
Whites see the child, they are happy to see them, when Indian doctor see them they seem to get fed up and you feel annoyed and you feel worse than before.
FG6, Bangladeshi male
Whites help you, Indians don’t.
FG6, Bangladeshi male
My friends and family they all moan about the doctor’s receptionists and I’m sorry to say they are the usually the Asian ones.
FG8, Pakistani female
Summary of key points regarding perceptions of the NHS
-
Participants discussed their perceptions of the NHS and how they felt that the NHS contributed to the support of a child with asthma, through both the structure of the NHS and the personnel available. Community members did not feel that HCPs held prejudice towards people of South Asian ethnicity, and they did not report specifically wanting South Asian doctors to treat them.
-
Participants reported experiencing difficulty accessing services and getting the ‘right’ treatments. This was a result of several factors:
-
GP opening hours
-
waiting times
-
language barriers.
-
-
Participants reported that some people are too frightened to ask questions of the HCPs and, as a result, getting further appointments or additional information may be harder for these people.
Accessing services and quality of services
Access to service and quality of services was a generic issue which was raised in all the focus groups, both in relation to asthma and more generally. Within the NHS, there is a tendency to assert that patients do not always use services ‘correctly’. For example, the number of attendances to the ED for South Asian children with asthma was higher than for those from other ethnicities,36 and this needs to be explained. Recognising how services can meet the needs of the individuals more effectively requires an insight into the barriers they are experiencing, in terms of an awareness either of what is available or of when to seek particular forms of medical advice. Even in the presence of such knowledge, additional problems with accessing appropriate care may exist.
Participants were asked where they thought that parents would go for treatment for their child with asthma, how they would access this care and service, and to discuss their own experiences of the NHS. Participants reported ‘annoyance’ at delays in treatment and at not being referred to specialists in a timely manner. These were noted as general perceptions of the healthcare system, and not just limited to experiences relating to asthma management. Participants felt that once asthma had been diagnosed it was very difficult to get a follow-up appointment with the GP, with specialist asthma clinics not regular enough to be able to be utilised effectively.
In the end I insisted I wanted to see a specialist . . . I had to push it twice before I got that far.
FG4, Indian Gujarati
They never give the appointments quick enough.
FG3, Indian Gujarati
Yes just once a year you get to see her. I needed to see her recently but was told I have to wait till November as I had [asthma] review in November. Otherwise I should see the GP. None of the doctors were available, that is very stupid.
FG3, Indian Gujarati
Participants also reported that while trying to make appointments with their GP or another specialist, they were often prevented from doing so in a timely manner, with the provision of available services lacking and unacceptable.
I got asthma and I am trying seeing someone and before it gets bad I am trying to prevent it but you cannot do that, there is a stop. You know, it’s like you are stopped before you start.
FG3, Indian Gujarati
The issue of accessing care and the quality of care provided is discussed in further detail in Chapter 4.
Summary of key points regarding access to care and quality of services
Community members discussed, if they had a child with asthma, where they would go for treatment, how they would access this care and service, and also their own experiences of the NHS. Key themes that were extracted from the data included:
-
‘annoyance’ at delays in treatment
-
not being referred to specialists in a timely manner
-
difficulty with getting follow-up appointments.
Suggestions for interventions to improve asthma management
Many participants felt that delays in accessing health care were a major issue for families of a child with asthma. Most suggested that families needed to have faster access to doctors during acute attacks, either at the general practice or at the ED.
I think if you take time from a specialist you get your turn after like six months or something, maybe this can be improved if you can get an appointment for the specialist quickly, like lesser duration time.
FG8, Pakistan woman
I think maximum should be one month. I got an appointment for my son it was not for asthma, but I went in March and I got an appointment for August – that was almost five months.
FG8, Pakistani woman
The importance of having access to good-quality information about asthma was emphasised by all participants. Participants reported that such information should be available for parents and children, and many participants felt that it should be available for wider community members, with the exception of one Indian Punjabi group who felt that people were already bombarded with too much information and therefore felt it would be best to focus on the families of children with asthma.
More workshops sessions should be conducted to make people aware.
FG7, Pakistani male
Leaflets should be provided in different languages and distributed to people in our community.
FG7, Pakistani male
There is need for more information on asthma and the effect it has on the families.
FG6, Bangladeshi male
I think the doctor should give some training to the parents . . . they need to educate the parents.
FG5, Bangladeshi female
Key informant data
Key informant data suggest the importance of several key themes, most of which reinforce the findings from the community focus groups.
Understanding asthma
Key informants frequently discussed environmental factors as ‘causing’ asthma, with 4 of the 12 interviewees providing a view that overcrowding, worsened by large and extended families within South Asian communities, was responsible. A minority of informants perceived parental knowledge of asthma or misconceptions regarding asthma as a barrier to the effective management of childhood asthma in South Asian families.
I think it’s a lack, I think, of knowledge, I think.
KO081
I know there’s a quite high percentage of asthma affecting kids within our community. But I think it’s seasonal.
KI078
I think when it’s like minorities sometimes what the child needs in the diets, the Asian diets are completely different.
KI078
Potential impact on marriage
Key informants supported the view related to the impact on marriage prospects for children with asthma and suggested that this impact would be more significant for girls than boys.
When I talk about this, I’m talking about the girls . . . So, if your child, if a girl had asthma, and it depends how severe her asthma is, if we look at the severe cases and they do talk about it, that might be a problem [for marriage].
KI079
Activity levels for the child with asthma
The community focus group participants reported that children with asthma would have reduced activity compared with children without asthma and noted that this may be due to exercise-induced asthma symptoms limiting their activity or an expectation that a child with asthma should not participate in physical activity. Six key informants expanded on this concept and reported that South Asian parents were more likely to restrict activities when compared with White families, regardless of asthma. They described South Asian parents as being more anxious and protective over children in many regards.
Using inhalers and other medicines
Key informants were asked how they thought one’s cultural background would affect the way they thought about asthma or whether or not it would create problems. Two key informants felt that inhalers were unpopular within South Asian communities due to the visibility of inhalers and their being an obvious sign that one has asthma. This reflects the focus group data.
There is that sense of embarrassment. I think there’s quite a bit of that in the Asian community.
KI078
Complementary therapies
Most key informants reported that families should seek advice from HCPs but they also felt that, in addition, families would advocate herbal remedies, homeopathic remedies or yoga.
A lot of people you see, they turn to homeopathic treatments because, from background thought from back home, whether you’re Bangladeshi, Indian or Pakistani, you know, sometimes you go I’ve tried all this and it’s not worked, let me try this [homeopathic treatment].
KI078
Concealing asthma
Two key informants suggested that the fear of getting asthma management wrong (in comparison with community norms or medical models) or being regarded as a ‘bad’ parent by their social peers encouraged families to conceal the presence of asthma within the family. Several key informants felt parents did not inform schools of asthma due to families being embarrassed by their child’s diagnosis.
But a couple of families that do have [children with] asthma but, you know, they don’t come forward [and inform].
Key informant
Community perceptions of NHS management
The focus group with Pakistani women suggested that there was still an attitude among their community not to question doctors in addition to being too frightened to ask questions to health professionals. This suggestion was confirmed by five key informants. Specific language needs were also raised by six key informants as particular problems for families in understanding health conditions and in accessing services.
That doesn’t happen because of the language problems, whether there are no language leaflets in those . . . and even if there are leaflets, whether the parents have seen them, understood them, whether the right terminology has been used for them to understand, it’s a huge problem you know, it’s a huge huge area that needs to be looked at in a way.
KI084
Communication is the main thing at the moment. And to breach that area, you know, first, and then it’d be much easier for the parents to understand one thing or the other.
KI078
Communication skills were highlighted as a vital area that can be very challenging, with key informants acknowledging the difficulties that language barriers can raise for both professionals and patients.
If you can’t talk to your doctor properly, they can’t communicate with the patient they get a little bit agitated or you could say frustrated and that sometimes shows up in their, the way they are dealing with a case.
KI085
Key informants also felt that a patient’s communication skills could impact on how professionals perceive, frighten and disempower a patient by not listening to them. They also felt that professionals’ overall communication skills could be improved through the use of simple and clear explanations.
I feel that they are vulnerable [Bangladeshi mothers]. I think, professionals know that they are a weak community and . . . if they’re not literate in their own language, let alone English, they’re in a no-win situation.
KI079
That’s another issue, the plain English. You know, people think that if you speak Queen’s English or difficult English that shows how educated you are, but the most difficult job is to speak in simple language. The message should be conveyed. That’s your quality. What’s the point if you’re talking and nobody understands what you talk, rubbish!
KI088
Three key informants reported that South Asian families may not feel that they can speak up regarding poor-quality services due to the fear of any resulting consequences or as a result of embarrassment.
If there are individuals who cannot speak the language, or have limited knowledge of English language tend not to complain if they do not get appropriate treatment. The reason they do not complain, in some cases, in fact I spoke to an elderly lady and you would not believe what she said to me but it may sounds ridiculous to you and me but, to her, it as a real fear. She said to me, son, you don’t understand. If I were to complain of the treatment that I’m getting in hospital, which is not very good, the nurse may just give me the wrong injection and kill me off.
KI081
Sometimes if Hindus go to the hospital and if they are not given good care or attention, sometimes people don’t ask questions maybe because they are embarrassed or something.
KI083
Key informants identified a number of problems with the NHS organisational structure, particularly the difficulties of getting and duration of appointments, overstretched or a shortage of NHS staff and disorganised follow-up arrangements.
If they do attempt to go to the doctors, and they get that barrier there: you can’t have an appointment, it’s busy.
KI079
The GP sometimes is closed and is going to be many hours before you can actually see a doctor, sometimes; it is not easy to get an appointment to see the doctor.
KI085
The [GPs] don’t listen. You know, you might be saying: ‘oh, come on, come to the point, what’s wrong with you? Yeah okay this is what you do’ before they give you the time of day and, as I understand now, people are coming back and saying it has gotten worse because there’s an overload of, like, patients in surgeries so they’re not getting the service that they should be.
KI079
Key informants reported that dissatisfaction with health services was largely, but not exclusively, directed towards GPs, as opposed to other NHS services and professionals. Receptionists were also perceived to be a barrier to good-quality care.
I find that nurses do try and be helpful, they do want to help the parents, um, they find GPs very hard but, um, they find that nurses open more doors for them, that they talk on behalf of them, they help them.
KI079
Sometimes receptionist . . . they really upset people before they even go to doctor. So, starting from receptionist to, you know, they go to doctors, attitude is very, very important.
KI088
Accessing services and quality of services
Particular concerns were raised by key informants around how the diagnosis of asthma is made, with two key informants reporting a perception that GPs are not undertaking sufficient tests and are ‘jumping to conclusions’.
You go and the GP will say, ‘okay, yes, I know and I’ll write out a prescription’ without even checking you.
KI084
They don’t assess you.
KI084
Professionals’ attitudes were perceived to impact on quality of care. Two key informants reported ethnicity-based prejudice experienced by South Asian families with negative attitudes felt to be present in South Asian professionals in comparison with White British professionals. As a consequence, some South Asians preferred to see White British professionals.
There is no attention being given, only one person, no more questions, the sort of attitude nowadays doctor give it to the patients. What’s next? What do you mean? They don’t want questions. One person, second person, come next time.
KI086
The way they treat, their attitude; one doctor can make you almost cry where the other doctor can make you feel assured.
KI085
[When asked if professionals might treat an Asian child differently from a White child] From my experience of living in this country, I cannot say no . . . I don’t want to call doctors racists and this and that, but I feel it depends on the kind of background you [the doctor] personally come from . . . unfortunately some doctors are different from others.
KI085
Three key informants related the problems with quality of care in the NHS to financial restrictions or waiting lists. Others suggested that a less detailed assessment was likely in a ‘free’ service compared with one for which patients were paying directly. As a consequence, some families preferred to travel overseas to pay for medical assessments and treatments to receive what they perceived as a superior assessment in a timely manner.
Some people may think that it is the result of the waiting list and that they’re not treating their asthmatic child enough. So there’s also this factor, they may go across to India or another part of the world to get treatment.
KI081
Like people may feel that the doctor is not giving me the correct medication, they are not responding, let’s go to another part of the world, maybe because it’s free in this country so they’re not taken as much care, let’s go to India, pay and get it done.
KI081
Preferences for which HCP families would feel most comfortable with and in which locations families would prefer to be treated were also discussed. One key informant felt that female doctors would be taken less seriously than male doctors as a result of the cultural perception of males and females in society. Another key informant felt that families would prefer to see doctors rather than nurses, with another highlighting the desire to be seen quickly as a driver for attendance at ED.
When an individual of that nature goes to see a doctor, and say it was a female doctor, I think there may be slight difference as to how they take advice as it would be if it were a male doctor. Not because one is superior to the other, it’s just that they may have come from that background where the man is the dominant factor in society and so a woman is not regarded in the same level.
KI081
If anything happens to my child, he obviously can’t breathe and this and that and it will come to asthma, taken straight away they go to A&E [accident and emergency] because they feel comfortable that at least someone is there to look after my child.
KI086
One key informant raised the issue of the difference between NHS services and herbalist services, perceiving that herbalists considered aspects of health not considered by doctors, such as diet.
Okay, if you go to herbalist, they will tell you want you can eat, what you can’t eat. Yet, doctor never tells you what to eat. Back home, doctor used to tell us what you eat, what you don’t eat for this condition, but here doctor never tells you.
KI088
Others felt that having an understanding of how South Asian communities function and are structured was important in managing South Asian children with asthma.
There’s the medical profession, nursing staff, doctors etc. They need to know the differences in communities, how different communities operate.
KI081
Key informants also discussed how best to address knowledge gaps and effect change within South Asian communities and the NHS by highlighting the importance of grassroots participation and the benefits of partnership in promoting and improving services. The impact of literacy on health promotion efforts was also recognised.
The top level and the grass root level needs to mix. I find that the top level and the bottom level, the gap in communication, it’s massive.
KI078
There should be some sort of input from community and the doctor’s forum in relation to how the public sees doctors, etc. And I think there is still a detach between provider and the client and I think that is to be reached somehow.
KI081
[When discussing how to reach out to communities and effect change] Other way of doing it also is to show partnership working. I’ve seen the benefit of partnership working . . . we need to sort of tap into more joined up working. Let’s move away from the person who sits in the ivory tower and says this is what I think is best for the community. Do this in consultation with the community, may be one way forward.
KI081
Discussion
Variations in the meaning of the words ‘wheeze’ and ‘asthma’ were common findings in phase 2. This was a result consistent with the findings from the systematic evidence synthesis (see Appendix 1) and has also been noted in relation to other minority ethnic groups. 138 Houle et al. 138 reported that the understanding and definition of the term ‘wheeze’ in African American children and carers could often be very different to the way the term was used by HCPs. Differing understandings of terminology, particularly where language barriers are also present, have been suggested to affect the rates of diagnosis for asthma. While Claudio et al. 139 demonstrated that the rate of underdiagnosis in English-speaking and Spanish-speaking Latino families in the USA were the same, Mosnaim et al. 140 found that, among Hispanic children classified as ‘at risk’ of asthma based on symptom questionnaires, only 36% of children with Spanish-speaking parents had been given a diagnosis of asthma compared with 55% of children with English-speaking parents. Previous studies, together with the findings from this phase, informed phase 3 of the MIA project. This resulted in communication – with particular focus on language barriers – being included as specific prompts for both parents and HCPs in phase 3.
In addition to variations in the meaning of terminology related to asthma, the data from the community focus groups highlight a range of beliefs on the causes of asthma, the transmission or heritability of asthma, the episodic nature of the illness, and the impact of medication. These findings highlight that community understandings often contrast with biomedical definitions. Similar findings have been identified in the Netherlands141 and the USA. 142
Both community members and key informants held strong beliefs of benefits of alternative remedies and treatments, reporting that they would advise parents to use them. Complementary medicine is widely practised in South Asian countries, with evidence suggesting that 9% of Pakistani parents visit a Hakim (traditional practitioner) and 11% visit a homeopath for treatment of childhood asthma, in conjunction with visiting a doctor. 143 Additional studies showed that 65% of Indian parents sought treatment outside hospital for asthma,144 with 79% of Indian parents using alternative therapies to manage their child’s asthma, including Ayurvedic treatments, homeopathy and yoga. 145 Despite evidence that suggests possible harm as a result of some treatments,146,147 complementary therapies were perceived among focus group participants as having no side effects or risks and were therefore promoted on the principle that they cannot hurt even if they do not help.
A Cochrane review of the efficacy and safety of herbal remedies for chronic asthma in children and adults148 identified 27 eligible studies. For primary outcomes (exacerbations, steroids use and lung function measurements), two out of six studies noted benefits. There were very little data available on the frequency of exacerbations, with the one study reporting this data noting negative findings. As study quality was often poor with considerable variation in the remedies studied and the outcomes measured, no overall conclusion could be drawn.
Similarly, a Cochrane review assessing the efficacy of breathing exercises for adults and children with asthma149 identified seven eligible studies. Two studies demonstrated significant reductions in bronchodilator use; three studies showed reductions in acute exacerbations and two studies showed significant improvements in quality of life measures. As before, while acknowledging that the results were encouraging, no overall conclusions could be drawn due to variations in the treatments used and outcomes measured.
Dietary modification was the most popular complementary therapy suggested. Research has previously identified beliefs that bananas, cold milk and ice cream should be avoided by asthma sufferers among Bangladeshi mothers,150 along with frustration that UK doctors do not discuss dietary restrictions as part of management. Similar beliefs regarding foods were found among Pakistani parents where certain types of rice, oil-rich foods and drinks were cited as asthma triggers by 89% of respondents. 143 Sixty-eight per cent of Southern Indian parents reported cool drinks, iced water and ice creams as triggers for asthma,151 with parents from Northern India frequently mentioning food items as triggers. 144 Beliefs regarding the role of foods in asthma are not limited to parents; 40% of general physicians in Delhi, India, believed that drinking milk increased mucus production in asthmatic children,152 with the same GPs believing that children with asthma should not eat bananas, chilled food, dairy products or sour food and should also not drink chilled liquids. 152 These beliefs were closely correlated to the length of time in practice, with more experienced (or older) GPs more likely to hold these beliefs than newer GPs. With the ease of international travel and communication, this raises the possibility of a continued influence of overseas practitioners on the management of children in the UK. 153 As a result of these findings, specific questions regarding diet, complementary therapies and advice-seeking from overseas were included in the parental question schedules used in the family study.
Results from the community study highlighted that the social impacts of asthma are, potentially, considerable. While the majority of participants did not report overt prejudice from the community towards families of a child with asthma, there were many indicators of potential impacts on children from wider social attitudes, such as marriage prospects, particularly for girls, limited future employment opportunities for boys and girls and reduced expectations regarding the type and levels of activity to which children could or should engage in. This suggests that there may well be stigma attached to asthma in some sections of some South Asian communities. Some of this potential stigma appears to relate to the fear of contagion, which would have a direct influence on social interactions for the child with asthma and thoughts on heritability of asthma.
Beliefs regarding the possible contagious nature of asthma have been previously noted. A sample of Bangladeshi mothers reported that ‘other’ people viewed asthma as contagious, but that they themselves did not. 150 Studies in Pakistan143 and India144,151 revealed that between 26% and 37% of parents believed asthma to be contagious. These beliefs may, therefore, be consistent across South Asian cultures in both South Asia and the UK, possibly perpetuated by international travel and communication. This is, therefore, an important belief that needs further exploration in the UK, as persistent beliefs in the contagious nature of asthma are likely to impact on community and parental expectations and management for a child with asthma and their integration into the community. Following discussion with the CFs, we also can hypothesise that the concern about ‘being able to catch’ asthma may stem from the more frequent diagnosis of chest problems such as pneumonia or tuberculosis rather than asthma.
The impacts of childhood asthma are not limited to the child, with noted impacts on the family including apportioning of blame for having caused the asthma. This issue was discussed in greater depth by several key informants, who suggested that the fear of being blamed by relations, friends or HCPs may be preventing parents from publicly admitting that their child has asthma and from seeking help and effectively managing their child’s asthma.
Poor provision of care and a lack of organisation within the NHS for asthma management were factors raised both by the community focus groups and by key informants. Problems surrounding appointments and the availability of GPs was also highlighted and seen as a key barrier to optimal asthma management by participants.
The discussion of organisational structures and the quality of care received from HCPs in the community study highlights that it is not just individual attitudinal factors or community knowledge deficits that are barriers to optimal asthma management. Indeed, there are factors external to the immediate control of the individual or family that interact with family knowledge and attitudes to influence management behaviour and service use. This is explored in more detail in Chapter 4, which discusses the experiences of families with a child who has asthma.
Conclusion
In line with the socio-ecological theory underpinning the MIA project, the community study identified broader social perceptions of asthma and its management in families. The focus group discussions suggested that, in many cases, lay understandings of asthma contrast with medical definitions of causes, triggers, symptoms, treatment and outcomes. This suggests a need for better public information about asthma within these communities to raise awareness of asthma. Such an educational project would improve recognition of symptoms of asthma, dispel myths of contagion and potentially reduce some of the stigmatising impact of an asthma diagnosis for children. This part of the MIA study highlights that community perceptions must be considered and addressed in any multifaceted intervention programme aimed at enhancing the management of childhood asthma, as broader cultural norms and attitudes are likely to impact on parents and children. It also suggests that involving community members in developing such an intervention provides a means of increasing community knowledge of asthma. The findings from this phase of the study also clearly highlight that both issues relating to community knowledge of, and attitudes to, asthma and problems pertaining to current service provision need to be addressed in developing an intervention programme.
How did phase 2 relate to subsequent phases of the Management and Interventions for Asthma project?
The data collected from the focus groups and key informant interviews directly informed the interview/discussion schedules for the family and healthcare providers in the family study. For example, evidence from the systematic review (see Appendix 1) identified that findings from India and Pakistan indicated the existence of stigma associated with asthma. The community study demonstrated that stigmatisation is also present in the UK, even if it is not overtly recognised as such, with the views of extended families likely to be of key importance in asthma management. While there was a suggestion among all groups that negative attitudes were receding, there remains a need to consider stigma, particularly for young girls, and how this might influence family management of asthma. Consequently, this topic was included as a specific prompt for interviews in the family study.
In developing the intervention described in Chapter 5, data from the focus groups and key informant interviews were reviewed to identify community and organisational behaviours and determinants within the IM framework. These data additionally contributed to the discussion of the impact of service organisation. Participants from the community study were invited to collaborate with the team in designing the intervention, with many of these participants taking part in subsequent parts of the project, which consequently added an important community perspective to the intervention development.
Phase 2 of the MIA project also demonstrated that engaging South Asian participants from a range of cultural, religious and linguistic backgrounds was possible. The utilisation of CFs ensured successful recruitment and full participation, with the phase 2 participants being an essential part of the research process. They assisted in recruitment for the study by suggesting additional recruitment avenues or by inviting friends and colleagues to join the study, an example of community engagement, mobilisation and participation.
This chapter has discussed the findings from the qualitative data in the community study of the MIA project via the examination of community members’ and key informants’ perceptions, thoughts and experiences regarding asthma and children in the South Asian community, and their experiences of accessing health care and services. The following chapter will examine the perceptions, thoughts and beliefs of families within the South Asian community who have children living with asthma.
Chapter 4 The management of childhood asthma: the perceptions of families and healthcare professionals (phase 3)
Phase 3 of the study had two broad aims: to explore perceptions of asthma among South Asian families and a smaller, comparative group of White British families [protocol amendment approved by the National Institute for Health Research (NIHR)]; and to understand how HCPs perceive asthma and its management in South Asian children. A comparative White British sample was included in this phase of the study in order to identify whether or not the management of asthma was subject to variation between communities and to consider ways in which a generic intervention to improve asthma management could be usefully tailored to meet the needs of South Asian families. The socio-ecological model requires a consideration of the organisational context of service delivery. It was considered important to understand the perceptions of those delivering services to South Asian families about the current organisation of asthma care for families. Professionals from a range of disciplines were interviewed to ascertain their perceptions of asthma in South Asian children, their view of issues relating to its effective management and their suggestions for the intervention programme plan. As described in Chapter 1, the study adopted a qualitative methodology, using semistructured interviews with parents/carers, children and HCPs. This chapter discusses the process of data collection for this phase of the study and presents the key findings from the interviews with parents/carers and children, followed by key themes from the health professional interviews.
Interviews with families
Sampling frame
Purposive sampling was used to ensure proportional representation from the main South Asian groups (as in phase 2), as well as to ensure inclusion of children with a broad range of asthma severity (judged by position on the BTS steps of asthma management; see Appendix 6) and from both sexes (Table 4). Purposive sampling was used to ensure participation of families from each of the six main religious-ethnic groups described previously: Indian Gujarati Hindu; Indian Gujarati Muslim; Pakistani Muslim; Bangladeshi Muslim; Indian Punjabi Sikh; and Indian Punjabi Hindu. The aim was to interview up to a maximum of 30 South Asian parents or carers and 30 South Asian children.
| Group | Inclusion criteria | Exclusion criteria |
|---|---|---|
| South Asian families | Child has at least one parent of South Asian descent | Child has a co-existing respiratory disorder, e.g. chronic lung disease, long-term ventilation |
| Child has asthma | ||
| Child aged 4–12 years | ||
| Parent or secondary carer of a child fulfilling the inclusion criteria | ||
| White British families | Child has at least one parent of White British descent | Child has a co-existing respiratory disorder, e.g. chronic lung disease, long-term ventilation |
| Child has asthma | ||
| Child aged 4–12 years | ||
| Parent or carer of a child fulfilling the inclusion criteria |
Purposive sampling was subsequently also used to select a sample of White British families broadly matched to the South Asian families. This strategy allowed sampling against previously identified, theoretically relevant variables. 154 The South Asian family data (see Appendix 7), along with the review of the existing literature (phase 1; see Appendix 1), identified that the sex of the child with asthma and the SES and education of parents might be of importance in shaping families’ experiences of managing asthma and access to services. In order to sample according to these characteristics, a simple sampling matrix was constructed to enable selection of potential participants from a cohort of volunteers on the basis of these predetermined attributes.
The required number of participants for each attribute category was determined by broadly matching to the proportion of cases already in the study. While this helped to develop a preferred model against which to sample the White British subgroup,155 the constraints of the voluntary and time-limited nature of recruitment meant that this model was not entirely achievable. However, the resulting sample was sufficient to allow confidence in the transferability and comparability of the data with South Asian families. Excessive geographical variation in the sample was restricted by recruiting all families (South Asian and White British) from the same region. This also ensured some consistency in terms of healthcare service provision. Parental employment status and occupation were used as proxy for SES. The research team did recognise, however, that this was an imperfect predictor, particularly in minority ethnic communities where equality of opportunity in education and employment had not been a typical experience. 156,157
Recruitment
Multiple recruitment avenues were used to identify and approach families in order to ensure variability of experience within the sample. 158 Table 5 identifies the numbers of families approached via the various recruitment avenues.
| Recruitment numbers | Recruitment methods | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Direct approach in the community | Letters | Telephone | Opportunistic recruitment | |||||||||
| Advertising | By CFs | By the research team | Community events | Mail shot | Letters to recent attendees | GPs | GPs | Pharmacies | A&E | Asthma clinic | Paediatric clinics | |
| Number of EoIs returned | 0 | 11 | 7 | 7 | 0 | 1 | 10 | 6 | 21 | 7 | 3 | 8 |
| Ineligible | 0 | 0 | 1 | 1 | 0 | 0 | 2 | 0 | 4 | 0 | 0 | 0 |
| Not recruited | 0 | 1 | 2 | 1 | 0 | 0 | 5 | 5 | 11 | 2 | 2 | 6 |
| Recruited | 0 | 10 | 4 | 5 | 0 | 1 | 3 | 1 | 6 | 5 | 1 | 2 |
Thirty South Asian families were interviewed in total. They comprised 44 parents (n = 29 mothers, n = 15 fathers), 5 secondary carers (n = 4 female, n = 1 male) and 33 children (n = 20 boys, n = 13 girls) with a total of 82 South Asian family participants. Families originated from a range of ethnic groups, identified by asking participants to self-assign their ethnicity and religion (Table 6).
| Family member | Religion | ||||||
|---|---|---|---|---|---|---|---|
| Indian Gujarati | Pakistani | Bangladeshi | Indian Punjabi | ||||
| Hindu | Muslim | Jain | Muslim | Muslim | Sikh | Hindu | |
| Mothers | 6 | 4 | 1 | 4 | 7 | 6 | 1 |
| Fathers | 4 | 3 | 1 | 2 | 1 | 3 | 1 |
| Secondary carers | 0 | 0 | 0 | 1 | 1 | 3 | 0 |
| Total | 10 | 7 | 2 | 7 | 9 | 12 | 2 |
There were 33 South Asian children recruited in to the study (n = 20 boys, n = 13 girls), aged between 5 and 12 years: seven were at BTS level 1, 17 at BTS level 2, six at BTS level 3, three at BTS level 4 and no children were at BTS level 5.
Fourteen White British families were recruited, comprising 17 parents (n = 13 mothers, n = 4 fathers) and 14 children (n = 8 boys, n = 6 girls).
The White British children were aged between 5 and 11 years: three were at BTS level 1, eight at BTS level 2, three at BTS level 3, and no children were at BTS level 4 or 5.
South Asian and White British children provided a proportionally good representation of asthma severity in the UK.
Methods
Data collection
Interview schedules for parents/carers and children were developed with the assistance of the CFs from the systematic evidence synthesis and from data generated in phase 2 (see Appendix 4). Interviews covered the following topics: understandings of asthma; family and community perceptions of asthma; day-to-day management; medical management; interactions with healthcare providers; and the quality of healthcare services and provision. Children were also invited to write statements or draw pictures relating to their asthma; these were then used to prompt discussion during the interviews. The pictures and statements were not compulsory and the drawings were not formally analysed (see Appendix 8 for examples). Demographic information was collected, with families given the choice whether they wished to be interviewed together or as individuals. The team were particularly sensitive to the children’s needs; some children preferred to voice their views independently and separately from their parents, while others chose to remain in close proximity to their parents. Interviews took place at the families’ homes, were digitally recorded and transcribed, and were translated by the CFs where required.
Data analysis
All interview data were analysed using standard methods of thematic analysis (described in the following paragraph) to identify key themes and facilitate comparison between South Asian and White British groups. In addition, data from the interviews with South Asian families were further organised according to principles of intervention mapping. As with phase 2, interview data were subsequently transferred to charts to facilitate the intervention design process (phase 4), described in detail in Chapter 5.
The South Asian and White British family interviews were analysed according to the principles of interpretive thematic analysis and facilitated by the use of NVivo (QSR International, Warrington, UK). 159 The analytic process for the family interviews began with coding of the South Asian data set using a process of open coding, followed by the development of emergent themes and the clustering of themes in an interpretive process. The basic codes were then elaborated into a framework of thematic categories within NVivo. All of the South Asian family interview transcripts were then coded using the resultant framework.
The White British interviews were subjected to an independent process of open coding by a second analyst in order to avoid undue influence from the existing South Asian coding framework. The emergent White British codes were then closely compared with the existing South Asian coding framework. Where existing codes were conceptually transferable, these were preserved in the framework (e.g. advice from HCPs). A small number of nodes were added (e.g. smoking during pregnancy and out-of-date medicine). Some nodes remained in use for South Asian data but were not used in analysing the White British data as no instances were found (e.g. taking a child abroad). Subsequently, some of the generic nodes were discussed by both analysts and were amended to ensure consistency of meaning and validity across both data sets (e.g. decisions about taking medication).
The existing framework was amended to allow applicability to the entire data set. This became the final, comprehensive MIA family-coding framework. The South Asian data were subsequently revisited by the first analyst at this stage to ensure that the integrity of the coding was maintained following the changes. All transcripts were systematically coded in NVivo using the resultant comprehensive framework. This allowed further case and cross-case analysis to be performed between and within subgroups. 159
Results
South Asian and White British comparative findings
Comparative findings from the South Asian and White British families are described below. Parents’ and carers’ data were explored using the following key themes: beliefs and understandings about asthma; the role of the extended family and community; medicines; non-medical management; asthma control; interaction with NHS services; and school and asthma. This is followed by key themes identified from the children’s data: understandings about asthma; interaction with healthcare systems; children’s self-management of asthma; perceptions of asthma; and school and friends.
Parents and carers
Beliefs and understandings about asthma
The major theme, beliefs and understandings about asthma, consists of two subthemes: aetiology and exacerbation, and previous knowledge and experience of asthma.
Aetiology and exacerbation of asthma
Both South Asian and White British families provided a number of possible explanations for their understanding about the origins of asthma. Aetiological ‘causes’ of asthma and exacerbations or ‘triggers’ for asthma, however, were often confused in the interviews in both groups (reflected also in the community study). The most commonly mentioned causes across all families were environmental (e.g. the weather, damp, dust, pollen or pollution), physiological and genetic causes (e.g. weak immune system, asthma being hereditary or mothers not breastfeeding). In addition, dietary and lifestyle causes and the idea that asthma was predestined or fated for a child were mentioned. While views about environmental, physiological and genetic causes of asthma were similar across the sample, South Asian families were much more likely than the White British families to discuss the possibility of asthma being in a child’s destiny or related to karma. Of the 18 South Asian families who discussed religion and fate relating to the origins of asthma, 10 noted that it was attributable to fate. When this was discussed further, belief in either God’s will (Muslim participants) or karma, i.e. their child’s asthma was destined to be (Hindu participants), was revealed. No White British families discussed asthma as related to fate or religious beliefs. They were also more likely to attribute its origins to environmental or hereditary ‘causes.’ Nine out of 30 (30%) South Asian families and 5 out of 14 White British families (35%) felt that the cause of asthma was either not known or not identified.
There’s no, there’s no sort of identifiable cause but it is very common, becoming more common.
128FM, mother, Indian Gujarati
South Asian families also differed in their perceptions that environmental factors such as pollution were specific to the UK context. They compared the environment in the UK with that of South Asia (India, Pakistan or Bangladesh), where it was felt that there were fewer environmental triggers for asthma.
Across all families, the expectation was that asthma improved with age and was something a child could outgrow. Twenty out of 30 South Asian families and eight out of 14 White British families expressed this expectation.
Previous knowledge and experience of asthma
Previous knowledge of asthma, in particular recognising its symptoms, was important for families in subsequently managing asthma. If someone else in the family already had asthma (sometimes the child’s parent or older siblings), the family was more likely to have some knowledge about asthma and its management. However, in the absence of this experience, South Asian families were less likely to have heard about asthma. White British families were more likely to know that asthma was a condition that existed even without previous familial experience of it (Table 7).
| Similarities | Differences |
|---|---|
|
|
Sources of knowledge
Many South Asian (n = 30) parents talked about their sources of knowledge about asthma. The types of interaction included advice from HCPs (n = 27); advice, knowledge or support from lay networks (n = 24; mixed views about its helpfulness dependent on complex factors); and the value of support groups (n = 4). A large number of parents (19 interviews) wanted more information or to ask HCPs more questions. Six talked about the knowledge they picked up ‘through life’. South Asian families also reported that their extended family was often a source of knowledge, as elders often influence the younger generation.
I’m not a doctor, if the doctor says she needs it, she needs it. Period.
063FD, Indian Gujarati
Yeah if we happen to talk to people at work about their child, we do talk about 123FC having asthma. Occasionally you get to hear good advice or stories about recovery or what to do and what not to do.
123FM, Indian Gujarati
[I]f there is a place where, it’s like a centre or something where there are other people who’ve got similar things and she can share it with other families, what they do with their children [. . .] sort of like a support group.
127FM, Indian Punjabi
I have not had any help but I have learnt things from observing. When my husband had asthma attack and ambulance people came, they asked for 2 quilts and kept him upright. I have learnt from situations like that.
125FM, Indian Gujarati
Who influences you like that? Are we talking about grandfather and grandmother or ‘other people’?
People who are elder to us and advise us we have to listen to them, grandfather and grandmother.
123FM, Indian Gujarati
The role of extended family and community
Few in either South Asian or White British families felt that their extended family, friends or community members were a central source of information about asthma and its management. However, families from across both ethnic groups reported that advice was often given, even if it was not adhered to. South Asian families were more likely to report advice giving by relatives than White British families, especially in relation to alternative remedies and management strategies. In some South Asian families, the grandparents lived with the family, and where this was the case they had a greater role to play in advising and decision-making around the health of the child with asthma:
. . . [Y]ou have this extended influence around you. There’s no doubt that clearly, living in the UK and obviously, born and raised here, that you’re far more accepting of different opinions. However, because you really do interfere quite heavily with an extended family, including quite generational so you have your parents and your grandparents, it’s not unusual where they all, just sometimes just say ‘Oh well, you want to go and see X, Y and Z,’ or ‘I know somebody, you know, somebody’s mentioned it to me’, so it’s not unusual for the family to give advice because they’ll see it as, oh yeah, you know, we just got, it’s one of their own, it’s not unusual.
120FD, father, Pakistani
In South Asian families, unlike in the White British families, the ‘advice giving’ from relatives in some cases extended to receiving advice from family members in South Asia. In White British families, advice most often came from family members who themselves had asthma.
In almost all families, the mother played the central role in managing the child’s asthma, although many fathers were also actively involved. Twenty-six South Asian parents talked about the member(s) of the family who made health decisions, and those identified as being involved included the mother (n = 12); the father (n = 8); both parents (n = 9); joint decision-making with the child (n = 7); the grandparents (n = 5); explicitly not the grandparents (n = 6); and the whole extended family (n = 1).
Well 110FD who takes the decisions mostly but he takes all my views, we decide silently, I can’t say ok yeah go with his decision but if I make a point then he will consider and change the plans so yeah.
110FM, Indian Gujarati
We both make the decision. Here we both take equal responsibility and decisions if it comes to children matters.
112FM, Bangladeshi female
Reaction from others
Across all families, telling others about the child’s asthma was sometimes a necessity because they might need to know what to do if there was an emergency. However, this sharing of information did not extend more widely, with a number of parents indicating that it was not necessary to discuss asthma with others beyond the immediate family context.
South Asian families were more likely to discuss the types of reactions that they had received from others about their child’s asthma; this included a small number of negative responses from others in the family or community (Table 8). These included the fear that asthma was ‘contagious’ or that it was caused by ineffective parenting. For a small number of South Asian families, mothers ‘felt blamed’ for their child’s asthma.
It might make a change because they blame me. [My extended family] just say, tell me that I don’t take care of her. That’s what they say to me. [Laughter] I’m not taking care of her . . . that’s what they think and then I just turn around and I say, what makes you think that? Is it because I’m working? Because I enjoy working? I’m not going to stop working because she’s ill, because that ain’t going to make her better. If I stop working, I can’t sit down with her twenty-four seven and say, Oh you feeling better? I can’t keep her from school and say Oh, don’t go to school, you’re going to get ill.
108FM, mother, Bangladeshi
| Similarities | Differences |
|---|---|
|
|
None of the White British families reported negative reactions from others about their child’s asthma, although one mother felt that she may have been to ‘blame’ because she smoked during her pregnancy.
Information about asthma
Both South Asian and White British families reported a lack of information giving by HCPs in relation to asthma, especially a lack of written information and written plans for asthma. Subsequently, many families (8 out of 14 White British families and 19 out of 30 South Asian families) reported a desire for more information about asthma and how to manage it in their child (Table 9). Families would prefer this to be given by the HCP responsible for their child’s care, at a relevant time when it is needed (e.g. while receiving an explanation of what asthma is upon its diagnosis). When this did happen (sometimes at emergency admission to hospital), parents welcomed it because it helped them to better understand subsequent asthma management and avoid repeat emergencies.
It would have been nice for someone to have come over and tells us from the initial start how to control it. Doctor to advise you, this is how you do, give more time to the patient in actually explaining. Maybe have follow-up appointments who deal with asthma, who specialise in asthma patients and actually help those families to enable them to, sort of, overcome that barrier, really. Overcome . . . understanding how to deal with it.
109FM, mother, Bangladeshi
| Similarities | Differences |
|---|---|
|
|
Families felt that it was important that this was information that could be shared with a child and was age-appropriate, but also that it was a consistent message given by all HCPs. Consistency of information was important for families in both groups, who reported feeling confused as a result of being given differing information by various HCPs at different times. This related, in particular, to guidance about when and how to take medicines. This inconsistency included differences between GPs in the same surgery, differences between the GP and practice nurse, and differences between the GP and the HCPs in ED.
The only advice our GP said to me is ‘increase the inhalers to try and prevent him from having a further incident.’ But it was very difficult at the time because at the [hospital] they had said ‘stop giving him the inhalers because he is so young, it might not even be asthma.’ So again it was a bit of a quandary with what to do . . . so it was difficult because we were told conflicting advice.
179FM, mother, White British
There were specific difficulties for families where the parents’ first language was not English. However, in these cases, families had addressed the potential problem by seeking access to HCPs (especially GPs) who spoke the same language as they did.
We try to go and see our Punjabi speaking doctor because we can understand what he is trying to tell us, but we have to see a white lady doctor as well, she is very nice but with her, we need someone’s help to get the information.
127FSC1, secondary carer, Indian Punjabi
The issue of language and understanding information from healthcare providers was not discussed frequently in the interviews. This could have been either because the families were fluent in, or could communicate in, English or because they had access to primary care staff with whom they could communicate in a South Asian language. As a result, they may not perceive this as a problem. However, several parents in the South Asian group reported that their first language was not English, with several interviews taking place in South Asian languages. One parent identified that this was something which needed to be improved for South Asian families.
But explaining, interpreting it in their language, as in speaking the same language and telling them, don’t know if that might help. It’s just an idea . . . Let parents know whether they can speak or not, they have to take interpreters. And that’s that question. Family member can go and discuss.
109FM, mother, Bangladeshi
Across all family interviews, there was little discussion about parents or children actively seeking information about their child’s asthma themselves. While a small number reported having heard things on TV or read things in the newspaper, no one reported looking up information for themselves. Additionally, no family in the study described having been given a written asthma plan.
Medicines
The major theme, medicine, consists of several subthemes: understanding medicines, taking and managing medicines, decisions about medicines, and side effects (Table 10).
| Similarities | Differences |
|---|---|
|
|
In both South Asian and White British families there was, or had in the past been, confusion about medicines for asthma. This related to the use of different inhalers: what they do and when to take them. Parents reported feeling confused about which inhaler to use, how frequently to give it and the dosage to administer. This related to the issue about inconsistency of information and lack of written information from HCPs.
Because, when the nurse at the hospital said, ‘Has she got an inhaler?’ And I said, ‘A blue one, we’ve been told twice a day,’ she didn’t say, ‘Oh okay, well, actually you can use it up to ten times, and you might find that might more be helpful.’ It was ‘Oh for goodness’ sake, that’s, that’s just a waste of time, it’s a waste of medication, that is’. You know, and that made me feel like ‘Oh great, so the doctor’s wasted my time and because of that, I’m here’. . . I don’t, well, we don’t know. So that would have been helpful. How we control it, and just, just consistent information about how often we should be using the blue inhaler. Not one person saying . . . twice and then two . . . two squirts in the evenings, as opposed to someone else [laughs] telling us that it’s well, you can do it up to ten times. That would have helped.
117FD, father, Indian Punjabi
Making decisions about when and how to use asthma medicines was an issue that a significant proportion of families discussed (11 out of 14 White British families and 26 out of 30 South Asian families). This related to their knowledge and beliefs about both asthma and the effectiveness of the medicine. Asthma medicines were not used consistently and this often related to the issue of diagnosis; if a child had not received a firm diagnosis, parents may be more reluctant to give medicines.
It’s still very much no one has ever said it’s asthma. And even to the extent when she was admitted I never said it was an asthma attack I just said she had a wheeze and she is short of breath. I never said it was an asthma attack. They have never said ‘oh it’s definitely asthma’. And because she is normally very well, this was her first episode where she has been that unwell that we’ve had to go into hospital, we tend to manage just with an inhaler. And we are rubbish, we don’t do them every day because most of the time, she is symptom free and it isn’t a problem. It tends to be the colder weather, gets a cold, a viral illness or whatever. She has been a little bit wheezy recently.
177FM, mother, White British
Five South Asian families discussed buying over-the-counter (OTC) medicines from South Asia, while a small number had travelled to India for treatment. Both South Asian and White British families described using OTC medicines in the UK, such as Vicks VapoRub®. Cough, cold and allergy medicines were mostly used either for comfort or for addressing other cold/flu/allergy symptoms.
Most families reported difficulties experienced with administering asthma medicines to children or remembering to take medicines, especially with younger children or children with learning difficulties. In general, in both White British and South Asian families, the parent took responsibility for the medicines until a child was considered old enough to take on this role. This often coincided with the child starting secondary school and needing to take charge of their own inhaler during the school day. A number of families described being unsure about whether or not the child’s inhaler technique was correct, and this was something that they would have liked more advice about. Spacers were often used to help with administering asthma medicines; this occurred particularly in younger children and where parents were concerned that they would otherwise not be getting the required dosage.
I don’t know if we are still using it right. When he is doing his inhalers he is getting smoke coming out and I am saying to him you can’t be doing it right because that shouldn’t be happening.
172FM, mother, White British
Strategies to help adherence, reported by both South Asian and White British families, included rewards and games, using reminders to make it routine, trying to disguise the taste, and having inhalers as part of a child’s usual ‘kit’ when out of the house.
Families gave a number of reasons for either why they chose to adhere to their medication or why they might decide to increase or decrease their use of medicines. Three White British families described using the medicines as prescribed for the fear of the consequences for their children’s health if they did not. Reasons for increasing the dosage mainly centred on instances of viruses and colds. Reasons for not adhering to the medicines were a lack of diagnosis, concerns about side effects, an absence of symptoms at certain times of the year, children refusing or deciding not to take their medicine, and misunderstandings about how to take the medicine. While families from both groups described making modifications to their child’s treatment regimen, South Asian families were more likely to discuss not giving medicines or reducing the dosage because of concerns about side effects or overdependence.
The possible side effects from asthma medicines was commonly discussed by families in both groups (22 out of 30 South Asian families and 11 out of 14 White British families); however, South Asian families mentioned a wider range of concerns about this compared with White British families. Side effects mentioned by South Asian families included concerns about children’s growth, stomach problems, heart problems, addiction, reduced immunity, oral thrush, mood or behavioural issues and reduced immunity to drugs. One South Asian parent believed that medicines made their child’s asthma worse. White British families talked mainly of general concerns about the long-term use of medicines, and steroids in particular. They also specifically mentioned effects of steroids on weight, fear of overdose, behavioural problems, bowel problems and dry mouth/cold sores. Concerns about the long-term use of steroids, particularly in relation to dependence caused by ‘over-reliance’, was a concern for both South Asian and White British families. This related to the decisions people made about using medications.
That stuff can actually, sort of [affect his] growth or his bones can be a bit thinner bones. We were more sort of thinking, that if he’s going to have steroids, we were not worried about the pumps, giving steroids the pink tablets, which we were concerned about, because he was given that, let’s say, every 4 weekly, every 3 weekly . . . Because his body, immune system, would not work if you keep feeding him steroids and his immunity will be so broken down he’ll have to rely on steroids for the rest of his life, which I wouldn’t want.
102FD, father, Indian Gujarati
Non-medical management of asthma
Both South Asian families and White British families described using non-medical management and OTC medicines to try to help control the symptoms of their child’s asthma (Table 11). This included home adaptations and changes around the house as well as dietary modifications, religious solutions and non-asthma medications. While both groups engaged in changes around the home, such as damp dusting, vacuuming, changing beds more frequently, improving ventilation, changing flooring and not having pets, South Asian families described taking additional direct measures involving the child. This included keeping them warm or indoors (n = 6) and rubbing, massaging or patting the back (n = 3). A small number of South Asian families talked about symptoms of asthma being reduced by taking the child into another environment. This was usually to a warmer country in South Asia (India, Pakistan or Bangladesh).
| Similarities | Differences |
|---|---|
|
|
While diet was mentioned by White British families (e.g. the importance of eating healthily, cutting down on junk food), South Asian families were much more likely to adapt their child’s diet in an attempt to control symptoms; all South Asian families alluded to this practice. Avoiding physically cold foods, such as ice cream, and giving warm foods was a common strategy. Additionally, there was the issue of the intrinsic ‘hot’ and ‘cold’ properties of different foodstuffs (based on the Ayurvedic system, where an individual can affect their physical or mental status by taking either more or less of a particular hot or cold food).
[My husband] and [doctor] don’t agree with it. Whereas I’ve experienced where she’s had it and it’s gave a cooling effect . . . I think grapes are cooling fruits. And the next day she does . . . not wheeze but she coughs.
063FM, mother, Indian Gujarati
But then I do keep alert, you know, to see how much ice cream they’re having or how much cold thing they’re having. Like, obviously, their ice cubes, and when they put in the glass, I see how much they put in the glass, because that might, it makes them worse sometimes.
031FG, mother, Bangladeshi
There was a small amount of reference to the use of religious remedies by South Asian families such as praying, blessings, reading Scriptures (n = 9), wearing talismans (n = 3) and bathing in Mecca water (n = 1). This was mainly by participants who identified themselves as Muslim.
And herbal remedies, I don’t trust most of the medicines here today. To use what my mother and my father give me from the ancient history to me it doesn’t sound right.
109FM, mother, Bangladeshi
Parents talked commonly about alternative therapies. These took the form of herbal or natural remedies, religious remedies, acupuncture, breathing exercises or Buteyko, or magnetic therapy.
Well I rather have her alternative method therapy, if it was acupuncture or a healing method you know those oil massages and everything like that.
106FM, Indian Gujarati
Yeah, this breathing exercise, it opens your lungs and you breathe out and it opens your lungs every time you breathe out. [. . .] Let’s say in the morning and at the night because at night sometimes I get chesty coughs and sometimes I get chesty cough in the morning so that’s what I do to help me.
106FC, Indian Gujarati
It was a magnetic one he did, it was a magnetic therapy or something? We paid for that one as well, [laughs] but it was anything to get them better [laughter].
122FM, Indian Gujarati
Families often mentioned herbal and natural remedies taking various forms: oral, inhalation or applications. These remedies included drinking warm water (n = 1); turmeric (n = 5); honey, lemon, ginger or linseed in water (n = 11); Ayurvedic medicine, ready-made herbal medicines bought from a shop and herbal drinks.
If he [child] wheezes then she would say to keep him well covered up and warm . . . To give him warm water to drink.
112FM, Bangladeshi
In Indian community, they give (hudhra) which is turmeric powder in the milk which cleans out the chesty cough out, so we just boil the milk and put some powder on [. . .] turmeric powder, and mix it and it doesn’t taste of, it doesn’t have any taste, just let the milk goes a bit yellow. You treat that, soon the cough kind of settles or it’s cleared out, so that was one thing as a child he has normally always get.
121FM, Indian Gujarati
I’ve always used it. You know, when you’ve got the flu or you’ve got a cold, Vicks and hot water and steam, lemon and honey and that sort of thing. It’s just . . . I’ve picked it up from somewhere. There in your head somewhere.
105FM, Punjabi Sikh
Yes. I give him honey in boiled milk three times a week as I don’t give him cold milk because it affects his asthma because I think it will keep him feel better.
103FM, Pakistani
And he’s started this one now. He’s taking it, it’s an Ayurvedic medicine and it’s helping, well, people say it helps with the asthma. And, you know, that’s why we’ve started him on, see if it helps him.
121FM, Indian Gujarati
Control of asthma
Both South Asian and White British families talked about keeping their child’s asthma under ‘control’; however, there is no one set definition of asthma control. It was not always clear whether or not these references related to formal measures of asthma control used by families’ healthcare providers. In some cases, the previously discussed non-medical management behaviours (see Non-medical management of asthma, above) were also described as being carried out in order to keep things ‘under control’. For example, in both groups there were various understandings and misunderstandings of the meaning of asthma control.
I don’t want to give him puffs all the time when he doesn’t need it. So I’m rather hopeful as he grows up, he grows out of it so as long as he is getting better and you are giving him when he needs it and as he gets old he doesn’t have this problem to just try and keep it in control.
104FM, mother, Pakistan
However, a number of parents related asthma control to the regular and appropriate use of asthma medications.
I think a lot of it is to do with the medication, if he came off his medication I think he would be quite a poorly child.
180FD, father, White British
Some families also reported feeling that, as a result of variability in asthma symptoms after some trial and error and tailoring of medication, they were now more able to achieve good control of their child’s asthma.
And the only times, really, she’s had to have an inhaler is when she’s been poorly. So I’ve just increased it, you know, I’ve just increased it on myself, because, I know, when she’s poorly, she gets linked, it triggers off her asthma, so I’ve just increased it at those times, until she’s been over her, she’s been feeling a lot better.
115FM, mother, Indian Punjabi
We reduced the dose but he became unwell after a week or two so we went back to normal.
123FM, mother, Indian Gujarati
Interacting with NHS services
Data demonstrated that, for families with a child with asthma, there were three key ‘moments’ when they might interact with the NHS. These were:
-
during the process of getting a diagnosis (mostly with the GP but in some cases with ED staff);
-
when the child had an acute asthma attack (NHS Direct, out-of-hours service, ED); and
-
during ongoing management (most likely to be the practice nurse or, for some South Asian families, the pharmacist).
Getting a diagnosis for asthma was experienced as difficult in both South Asian and White British families. Seven out of 14 White British families and 13 out of 30 South Asian families reported that they had not received a direct diagnosis of asthma, despite the fact that all of the families recruited in to the study had been prescribed asthma medicines (Table 12). Many South Asian and White British families described problems in getting a diagnosis which were common to both groups: undue delays in the process, feeling ‘fobbed off’ or not being taken seriously, repeat visits to the GP with recurring problems, and feeling that HCPs were reluctant to make a diagnosis. Not receiving a diagnosis led to feelings of frustration, upset and anger.
It’s just getting people to listen, that’s what used to get me so angry because nobody would listen to me. When I used to take him doctors I used to mention my nephew had the same symptoms and now he is on all these inhalers. Because your nephew has got these symptoms don’t mean to say you have got the same thing, it’s just chest infection, it’s just something it’s just common to him, that’s what I used to get. I used to go in there and come out upset all the time.
172FM, mother, White British
| Similarities | Differences |
|---|---|
|
|
There was a perception among families that HCPs (usually the GP) did not take their concerns seriously or were reluctant to diagnose their child with asthma and that this was related to a child’s age, the implication being that asthma is not or cannot be diagnosed in younger children. Some families reported having been told this directly by their HCPs, but then did not understand why they had been prescribed asthma medication.
Now we, that’s the funny thing, I just don’t know if I’m coming or going with them. I want to know if she has got it [asthma]. If she has, then, is it a permanent thing? Or is she going to get out the phase? So, when I did ask, he goes that ‘with kids, you can’t tell’. And I go, ‘What is the cause of it’. He goes ‘it could be many stuff’. He’s not given me a full diagnosis. He hasn’t told me, he hasn’t even confirmed she has got asthma.
108FM, mother, Bangladeshi
This experience was common to both South Asian and White British families. Not having a diagnosis for their child’s symptoms led to a great deal of uncertainty about the best course of action. Without an official ‘label’ of asthma, parents were unclear about whether or not to give medicines or how to manage symptoms. A small number of families reported ambivalence about the diagnosis when they did get it and, in some cases, they sought a second opinion (six South Asian and two White British families). Some parents were surprised that the symptom their child had (e.g. persistent coughing) was in fact a symptom of asthma. A number of families reported relief, with some reporting vindication on receiving the diagnosis. They felt that this conferred a status that gave them access to reviews and medications, in addition to making it easier to communicate the information about the condition to their child and to others, such as the child’s school.
Well the difference is that if; if you have got asthma then I can say that my child has got asthma. I mean if somebody ask me, I just say no, no, no the doctor hasn’t diagnosed it as asthma, I always say that.
106FM, mother, Indian Gujarati
In some cases, a diagnosis had been made or communicated by hospital staff following an acute attack and associated emergency visit to hospital. For those families, this had been a defining point in the process.
A significant proportion of families had experienced the need to access the NHS in an emergency or non-routine situation. This had involved decisions from the parents about two things: (1) the severity or usualness of the child’s symptoms, and (2) where to seek help. The general perception among both South Asian and White British families was that the GP was the first point of contact in managing their child’s asthma, where appropriate (see Table 12). However, when symptoms were perceived to be beyond the assistance or expertise, or if the practice was closed (in the evenings and at weekends), families needed to make a decision about where to take the child. White British families were more likely to report using their own doctor’s out-of-hours service when the practice was closed (9 out of 14, compared with 3 out of 30 South Asian families) and when compared with other options such as walk-in centres or NHS Direct. In contrast, South Asian families were more likely to self-refer to ED in an emergency (13 out of 30 families).
Seven out of 14 White British families and 15 out of 30 South Asian families had experienced one or more emergency visits to the ED. In seven White British families and three South Asian families this had occurred following advice from another HCP: the GP, NHS Direct, the out-of-hours service or the walk-in centre. In some cases, being ‘referred’ to the ED on the first occasion led families to independently follow this process on subsequent occasions.
I just went to my GP and say I’m seeing the same symptoms. They referred him to the hospital. And [we’ve] just been going from there.
114FM, mother, Pakistan
A small number of South Asian families reported having been worried enough to call an ambulance, whereas none of the White British families had taken this step (though some had had an ambulance called on their behalf by a HCP). Both South Asian and White British families described dissatisfaction in relation to the experience at the ED, which included long waiting times for getting to see a HCP or getting a bed.
When our son had breathing problems, we went to the hospital and waited a long time. Everything seems to take too long. We went to the hospital around 12 midnight and came back about 5 am in the morning.
118FD, father, Indian Punjabi
White British families were more likely to feel that the GP cannot be an expert in asthma and, as a consequence, a small number of families felt that there should have been a referral on to an asthma ‘specialist’. However, where South Asian families felt dissatisfaction with the GP, they were more likely to divert straight to the ED. Some South Asian and White British families had received information relating to diagnosis via the ED’s HCPs and in some cases this was interpreted as meaning that the staff at the hospital had more expertise and knowledge about asthma than the GP.
The ongoing management of a child’s asthma often required that families interacted with HCPs on a regular basis. Outside acute attacks or exacerbations, this usually took the form of the regular or annual asthma review with the practice nurse. Most families who described attending reviews (approximately one-third of South Asian families and two-thirds of White British families) were satisfied with this process (see Table 12). Here, the review was seen as a process which involved ‘checking’ things, such as inhaler technique and peak flow, rather than about getting a diagnosis or new information or for changes in medicines.
It’s more a question and answer session as to how they have been, but that’s not a review of their medication because it’s the doctor surely who has to sanction any new or alterations.
179F, father, White British
The nurses who provided this service were viewed positively by both South Asian and White British families. In the families who were not accessing the annual review (more likely South Asian families), this was often either because they did not consider it of much value or because they were seeking advice from other sources, such as pharmacists. Almost one-third of South Asian families specifically described accessing the pharmacist for advice about a child’s asthma and medications. Sometimes this was for a second opinion, sometimes for additional information about the medicines and in some cases the pharmacist demonstrated how to use inhalers or spacers. For parents who had difficulties with English, using a local pharmacist who spoke the same language meant that they could get clarity about the information given to them by the GP.
You see [my wife] want more information, probably haven’t got time or something so that’s why she went straight to the pharmacist . . . the pharmacist says the same language she speaks. Sometimes doctors do not speak the same language, the Gujarat language. So you see she tells me now, so that’s why sometimes she doesn’t understand what doctor say . . . She still don’t believe in the doctor, she will believe in doctor but not that much, not 100%, like 90% so she will always go for second opinion to the pharmacist.
101FD, father, Indian Gujarati
Only three White British families discussed the pharmacist and in all three cases it was in relation to trying to access medicines in an emergency without a prescription, and not about advice.
A larger proportion of South Asian families (21 out of 30) discussed negative experiences when interacting with HCPs than did White British families (6 out of 14). However, the concerns were broadly similar and included being given inconsistent or conflicting advice, feeling that HCPs were not doing their jobs properly and poor communication.
One concern expressed by both South Asian (7 out of 30) and White British (5 out of 14) families was about inconsistency of information and management by different HCPs. Families reported being given conflicting advice by nurses, GPs and HCPs, which caused confusion, particularly with regard to medicine use.
The only thing I am slightly confused about, which I don’t think information is good, I am not entirely clear about how she is supposed to take, I am sure I have had different guidance from [younger child] about how to use the inhaler as I am for [older child].
181FM, mother, White British
Both South Asian families and White British families had mixed opinions about the skills and quality of care provided by HCPs and this tended to relate less around the profession of the individual (nurse, GP or pharmacist) and more about how well they were felt to be doing their job. Complaints about professionals often related to things they were not doing: not treating asthma well or appropriately enough, not taking enough time to treat, ‘fobbing’ patients off, making incorrect diagnosis, not providing enough follow-up, not communicating well enough, or, in a small number of cases, acting in a ‘rude, patronising or unprofessional way’.
When we went to the GP surgery they were unhelpful. They never paid attention.
102FM, mother, Indian Gujarati
Both White British and South Asian families felt that there were communication issues relating to insufficient information giving, inadequate explanations about asthma and not having diagnoses communicated. As described above, a number of South Asian families also reported being unable to communicate directly in English with HCPs, and were therefore making decisions about who to access based on language needs.
Yes the main issue was about English language, there were difficulties about getting an interpreter.
123FM, mother, Indian Gujarati
As well as negative experiences, 6 out of 14 White British families and 27 out of 30 South Asian families described positive experiences with HCPs. In the White British families, these included feeling that HCPs were knowledgeable, keeping parents informed and giving explanations, being ‘life-savers’, not rushing appointments, being child-friendly and giving good demonstrations. For the South Asian families, this included being supportive and understanding, being thorough and knowledgeable, and being proactive and child-friendly.
One thing for sure [the asthma nurse] made us comfortable. She was honest, she was very understanding of our knowledge. And she knew what she was talking about. She knew how to communicate, that’s the vital and clear point I want to focus [on].
102FD, father, Indian Gujarati
School and asthma
Both White British and South Asian families reported that the management of asthma in their children’s school was variable. In some cases, schools were described as being very proactive and having systems for recording asthma and using medications in relation to each child. In contrast, in other schools, the process was perceived as being fairly haphazard. School staff (which included teachers, teaching assistants and school nurses) were described as having varying degrees of knowledge about asthma and associated medicines. There were concerns from many parents (8 out of 14 White British families and 10 out of 30 South Asian families) that school staff did not know enough about asthma and this led to feelings of uncertainty about how it would be managed when children were at school (Table 13).
But without being awful to them I don’t think they are that clued up on [asthma], which is another thing really. They have got a good system where they document when he has had the inhaler but I said just keep an eye on him because it’s his first day back. I kept him off for the rest of that week but you can’t keep them off forever can you. And I was on egg shells and I did come away thinking do they even know to use the [inhaler] . . . And you try to talk to them and they have got 30 children in a line trying to get in the room and the time is limited. But there is a school nurse there so presumably she would be . . . And [child] has told me before when he has needed his inhaler and it hasn’t been the teacher that gives it.
168FM, mother, White British
| Similarities | Differences |
|---|---|
|
|
Ensuring that medications were up to date, accessible and administered appropriately was discussed in two-thirds of White British families and more than three-quarters of South Asian families. Having a clear diagnosis of asthma and understanding how medicines should be used was also mentioned by a small number of White British families, who were concerned about what they should tell the school in the absence of having received a diagnosis.
Management of a child’s medication by school staff appeared to be more of a concern in relation to younger nursery and primary school-aged children. Once children were older or began secondary or high school, they were more likely to be responsible for carrying and administering their own medications. South Asian families were more likely to report children missing school because of their asthma (17 families) than White British families (three families).
Impact of asthma
Parents discussed the impact that asthma had on them, their families and their children. For parents and carers, the main impacts were around taking time off work (four South Asian parents, two White British parents) and the emotional impact, fear and worry caused by seeing their child ill or in distress (23 South Asian families and five White British families).
It’s quite shock . . . shocking really. I’m quite traumatised at times because it was . . . a couple of times we had to take her in and out, it wasn’t just once. It was like coming . . . straight after she was diagnosed it was so difficult and, on occasion, every 2–3 months, this was a couple of times we went to the hospital. The first thing it was go to A&E and I don’t think you’re allowed to go to A&E now for such things unless it’s really, really severe. Yeah, all we did for five hours in hospital or even longer, half the night in hospital we had to spend with her while she was on the bed and she’ crying and screaming and they put the nebulisers on . . . and it’s quite . . . she’s so small and tiny. Tiny little girl. Poor thing. She was screaming, she didn’t like the mask thing on her face, it was happening all the time and she was getting scared of hospitals, was thinking ‘what was going on?’.
109FM, mother, Bangladeshi
While many families felt that asthma should not impede a child’s life, six South Asian families and two White British families talked about children missing activities or sport because of their asthma. For some South Asian families, there was an additional concern and worry expressed in terms of what a diagnosis of asthma may mean for the child as they grew older. This included a possible impact on their future job prospects (n = 7) and, for a small number of families with a daughter, the possible impact on future marriage prospects was discussed. White British families, in contrast, were less likely to express concerns in this way (Table 14).
| Similarities | Differences |
|---|---|
|
|
Suggestions for service improvements
Families had many thoughts and ideas regarding future interventions or projects. These included developing a cure so that children do not have to be reliant on long-term medication, and offering a better diagnosis pathway so that a diagnosis of asthma is made clearer to parents through appropriate tests and relevant follow-up appointments, thus helping to remove ambiguity. Families reported wanting more information on the condition, the warning signs, how it should be managed and what the inhaler was prescribed for. It was suggested that a telephone advice service or advice centre for asthma, where people were trained and have knowledge on asthma, would be beneficial. Parents suggested that for acute attacks, when advice was required quickly, a telephone advice service would be very useful. There was a desire for more information about asthma from someone who is knowledgeable. Families felt that using schools to educate and provide information and to run courses would be useful, with nurses teaching schoolchildren using demonstrations also being seen as beneficial.
Parents felt that advice, such as in leaflets or on posters, needed to be given in multiple languages. It was reported, however, that families would prefer a bilingual person to help convey messages and give advice. Families reported that multilingual leaflets were available at the pharmacy but suggested that they could be placed in temples and other community venues to aid ease of access to the information as well as raising community awareness. Additionally, families suggested that HCPs could visit temples and schools to talk about asthma and the symptoms, in addition to offering advice. Families reported wanting somewhere to go where they could communicate with HCPs, such as a community centre. A community centre would enable parents to meet other parents who have children living with asthma, in addition to allowing nurses and doctors to run talks and presentations. Families indicated that getting information into the community was important and, in order to do this, it was suggested that using bilingual people and lay facilitators in local community centres that people knew, which were run by people and leaders in the community who they recognised, would be most effective.
Practical elements of asthma management were highlighted as important factors to consider for future service improvements, for example helping children to learn about their inhaler or spacers, where to put their lips and when to breathe. Families also suggested that alternative remedies such as yoga, exercise or massage therapies would be useful in order to manage asthma. Families perceived that there was an inconsistency of care and therefore suggested integrating medical health records so that all HCPs treating the children were aware of past medical history.
Children’s understandings and experiences
Children’s data were explored, collated and discussed separately from the adults’ data to ensure that the children’s perspectives were clearly identified and accommodated in the intervention design process in later phases.
Children’s understandings of asthma
Children talked about their understandings of what asthma is. This was mostly described as a ‘problem with breathing’. Some children gave reasons or causes of asthma (often confused with triggers), which were similar to those given by their parents (e.g. weather and environment, being hereditary, or caused by or related to colds and viruses).
I just think, I’m just born with asthma. As mum keeps saying over and over again, the damp weather, yes, it just, you know, some people get colds and coughs from the damp weather, you know, I may have caught asthma from the damp weather and it just carries on in that type of weather.
063C, Indian Gujarati
I know it runs in families and stuff because me and my mum have got it.
174FMC, White British
A number of children from both groups reported that they did not know what asthma was or what caused it.
Interactions with healthcare system
Children discussed what they could and could not remember about having visited the doctor, the nurse or the hospital. Their memories of these interactions depended largely on their age or how long ago the visit happened. Few children could remember getting a diagnosis, but several recalled recent visits to the GP or practice nurse. These experiences were of a broadly neutral or positive nature. Both South Asian and White British children described the visits to the nurse or GP and related it to the need for monitoring or checking their asthma and medicines.
They listen to my heartbeat and they just generally check me over.
177FMC, White British
He [doctor], he’ll tell you what’s happening, what’s wrong, and if you have asthma or if you don’t have asthma, and he’ll tell you if you need a, the stuff for the inhaler you when you put it in.
107FC, Pakistani
Recalling acute attacks and related visits to hospital often involved more emotive descriptions, such as feeling afraid or upset.
I sometimes worry about like . . . I remember when I had the asthma attack, I was so scared, I thought I was going to die or something. And my mum was like, ‘oh don’t be silly’ . . . Not now because I know that I won’t die. Because if I would die then I probably would have died at the asthma attack.
105FC, Indian Punjabi
Like, I didn’t like [staying in hospital]. I like, I like . . . I really missed my dad and my mum, and my brother and my sister and my little sister.
114FC, Pakistani
Young children often remembered specific details about the visit to the hospital, for example that there were toys to play with, or what they had to eat.
Just a little bit scary . . . because sometimes you have to have injections . . . At the hospital I had the yucky medicine and it was pink and I thought it was yummy at first, but it was yucky.
111FC, Indian Punjabi
I had to have a gas mask, and I had to have injections, and like, it hurt . . .
107FC, Pakistani
Children’s self-management of asthma
In the majority of cases, for South Asian and White British families, parents were responsible for reminding and instructing a child about her or his inhalers, particularly those who used medications regularly in the morning and evening. However, children did also actively take a role in their own asthma management, especially as they got older, and often with encouragement from parents. Families discussed systems they had devised to help children remember their medicines.
Like so . . . so always have two inhalers of the same colour, like. So, if like . . . say if like this was another blue inhaler, if this one ran out then I’d tell my Mum or Dad or sister to go to the chemist to get another one so I’ll always have two whether they’re full or not.
105FC, Indian Punjabi
I have got a brown one which I have to take two puffs morning and night, but then I have got a blue one which I take when it’s super bad.
174FMC, White British
Both South Asian and White British children talked about sometimes being ‘nagged’ by their parents when they refused or forgot to take their medicines. Children identified their mothers as being most likely to help, instruct, or remind them about needing and taking their medicines. This also related to managing acute attacks where it was often the parents who spotted symptoms and encouraged children to use their inhalers.
I just, just suddenly I thought I could choke differently and I just really started to cough and . . . I had to literally run to get my pump and . . . I couldn’t breathe properly. So I had to take one. Well, sometimes it’s me [who decided to take my medicine] . . . most of the time. Because sometimes it’s just a cough a normal, natural cough. But sometimes it might be mum, she can go ‘oh [name] I would take your pump if I were you’.
063FC, Indian Gujarati
Children’s perceptions of asthma
One of the biggest impacts of asthma described by children was the impact on their ability to take part in play activities, sports and physical education (PE). In these circumstances, breathlessness and coughing were the commonest symptoms, with children either sitting out or avoiding activities.
Well, if it’s bad Mum tells me to take my inhaler to school in case I end up coughing really bad. I have had to do it once before but it was sports day and I wasn’t feeling too good but I still did it.
174FMC, White British
Because you know when I run the wheeziness starts and make me cough so much I get puffed out and I really don’t like it. So that’s why I take the inhaler sometimes when we come back from sports or anything. Like in school when we have sports day and sometimes I get puffed out, sometimes I say to the teacher or head teacher if I am puffed out I just say that I need my inhaler because I am puffed out. So we take the inhaler and stay out for about five minutes and go back in and then I am fine.
106FC, Indian Gujarati
The most commonly mentioned emotion related to asthma among children was embarrassment. However, this was usually through the child explaining that, although asthma could be considered embarrassing, they themselves were not embarrassed. Instead, this embarrassment often related to the perceptions of friends and peers (further details in School and friends, below). Other common feelings expressed by the children were fear, feeling upset and unfairness.
Why can’t I live a normal life like the others?
114FM, Pakistani
That I have to cough when my sister doesn’t cough, or I have to have more medication than she has to have. It’s a bit annoying sometimes but you get used to it.
177FMC, White British
I wouldn’t say ‘oh, I’ve got asthma, I don’t want people to feel sorry for me’. I just want to, you know, forget about it, put it to one side and when it comes, we’ll deal with it and then, when it goes, that’s it. End of story. Get on with your life. And, when it comes, you know, just sort it out.
063FC, Indian Gujarati
School and friends
A child’s peers and friends were described as having an important role to play in their experiences. Having friends who understood about their asthma, and in some cases could help if needed, was deemed important for South Asian and White British children. In some cases, this included having friends who themselves had asthma. Although it was widely discussed in the interviews, few children felt that having asthma and having to use an inhaler caused embarrassment for them personally (three South Asian, three White British).
At school it doesn’t affect me much, people don’t tease me or anything, they treat me normally, their friends are aware of my asthma, some of them have asthma themselves and they help me.
120FC, Pakistani
Despite asserting that asthma did not make them feel embarrassed, asthma was a cause to feel different or ‘not normal’, and a small number of children described managing information about their asthma as a result. For some, this also meant having to explain to others what asthma was. Some children reported that only their close friends knew about their asthma. One girl felt that using her inhaler at school attracted unwanted attention and one South Asian child reported being teased about their asthma.
No, I told some of them but I didn’t want to tell anybody at first and then I told a couple of people and then it started spreading.
And why didn’t you want to tell them?
Because I was shy that they might laugh or something like that.
177FMC, White British
I don’t know anyone else at school who has it, none of my friends have it, I have to explain it a lot . . . they understand I have got it and I think they are alright because they know it’s not catching.
174FMC, White British
Children discussed the role of friendships and teachers as important in helping them to manage their asthma and medicine use while they were at school.
I was playing in the playground and I felt a bit wheezy, so I went to my teacher and said ‘[teaching assistant] I feel a bit wheezy’, and she said ‘Go inside and tell [teacher],’ so I went inside and told my teacher. She said ‘have a few puffs on your inhaler’ so I went to get it out of my book bag but I couldn’t find my pump, I could only find that little thing to shake. I felt a bit like, ‘where’d it go?’ and they rang up my dad and my dad got it from because I left it at home and then I did a couple of [puffs] and then I still felt wheezy so I went to the office and then they said I had to go home so I went home.
115FC, Indian Punjabi
What about at school, do your friends know you have got asthma?
Yes and they mostly help me, like they usually go get it [inhaler] for me.
175FMC, White British
Suggestions for service improvements
Some children, along with their parents, discussed ways in which they could increase their understanding of asthma and offered ideas for future interventions. Children reported wanting to speak to someone who had experience of asthma, whether it was someone living with asthma or a HCP.
Well, I would like to meet somebody who’s knows a lot about asthma, like, who has asthma, and like, is a doctor, to know more about asthma. Like, how they, have they helped the person like they had asthma and now they don’t, they live a normal life, like you, you don’t have asthma.
115FC, Indian Gujarati
Children also suggested that face-to-face demonstrations would be useful to learn inhaler techniques.
They should say it to you face-to-face or, you know, they should tell you in some way how . . . what’s it for, how it will help, how, you know . . . what it does and why I need it.
063C1, Indian Gujarati
Some children and their families also described ways in which information could be provided that they would find most useful.
[On the website there should be] what happens in like, the lungs, and what’s happening in your body, and like, and things to improve on it. Like, what to do to help it. And stop it.
128FC, Pakistani
Pictures maybe.
115FC, Indian Gujarati
A presentation about it to a group of people sit down and some of the teacher can present. [. . .] They tell you things that I did not know like in more detail. The effects of inhaler, what it does and how it affects you. [. . .] The chemist and the GP were ok but the school one explained it best and easy to understand.
125FC, Indian Punjabi
[B]ecause, at the Gurdwara, we do Punjabi school where you learn the alphabet. And we could do something like that at each Gurdwara so, and like, people like adults could come with them and they could learn about it as well if it, if their child has asthma and they haven’t been to a doctor yet, [. . .] know about it.
115FC, Indian Gujarati
The interviews with families and children provided an opportunity for those affected by asthma to offer their perceptions of the barriers and facilitators to optimal asthma management, in addition to providing them with the chance to discuss their own ideas and how improvements to services and quality of care could be improved. These data formed the basis of the intervention development (see Chapter 5), shaping the development of the content and the delivery methods. Following on from the interviews with families and children, HCPs who have had experience of working with South Asian children living with asthma were interviewed to discuss their perceptions of asthma management and ways in which services and quality of care could be improved.
Healthcare professional interviews
Healthcare professionals are key stakeholders in service improvement and as such they were included in the project in order to identify their perceptions of the barriers and facilitators to optimal asthma management in South Asian children.
Sampling
Purposive sampling was utilised to ensure representation from medical (primary, secondary and tertiary) and nursing professionals from acute and community services and from professionals at different stages in their careers (Table 15).
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
Data collection
All HCPs spoke English, enabling all interviews to be conducted by the research team. Participants were offered the option of one-to-one or group interviews if more than one person at a particular practice wished to participate. In recognition of their limited availability, flexibility in the approach to data collection with HCPs was crucial to securing their participation in the study. Methods of recruitment were amended to ensure that adequate HCPs could be recruited into the study and that interviews could be carried out at a time convenient for them. The interviews were conducted using a semistructured format with a question schedule based on the interim findings from phases 2 and 3 (see Appendix 4). Demographic data collection forms were completed at the end of each interview. All interviews were conducted face to face at the participant’s place of work and were digitally recorded and transcribed. There were 37 HCPs recruited: four GPs, one trainee GP, one health visitor, one inclusion manager, one nurse, two paediatric ED registrars, one paediatric respiratory consultant, two paediatricians, three community pharmacists, one paediatric intensive care unit consultant, one practice manager, three practice nurses, one research assistant, five school nurses, one senior hospital play specialist, two staff nurses, one student children’s nurse, one ward sister, three community children’s nurses, one foundation year 1 (FY1) doctor and one clinical operational lead. Data saturation (ensuring validity of the findings) was reached for the entire sample and gave particular confidence in relation to smaller, subpopulation numbers. Validation was ensured by checking back with the clinicians that their messages had been accurately represented and heard.
Analysis
The interviews were analysed using standard methods of thematic analysis to identify key themes. In addition, the data from the interviews were further organised according to principles of intervention mapping and were compiled into charts to facilitate the intervention design process (see Chapter 5). To maintain professional anonymity, the professional roles of the interviewees have not been disclosed in this report.
Results
The following key themes were identified and are discussed below: consultations with South Asian families; South Asian family barriers to asthma management; and professional and organisational barriers to asthma management.
Consultations with South Asian families
Time
All HCPs reported that having insufficient time to talk to children and their parents and carers was a major problem. GPs reported how they struggled to cover as much information as they would like in the already-brief appointments. This was made more difficult when there was a language barrier or multiple issues to be discussed. ED staff and pharmacists also discussed limitations on consultations imposed by time pressures.
I guess there are always the usual time pressures. There is not enough time, no asthma nurse.
Time – if I have the ability at a time that is convenient to me and we can talk and then discuss it then, I would have no problems in employing an interpreter with every family I see. However, the only practical way of doing it out of hours is by a language line which involves making a phone call, getting the family to the phone for a stilted two-way conversation which I usual only resort to for serious cases. I appreciate that this is not best practice but one of the limitations of working means that I simply cannot spend that amount of time with every family I see.
Communication
Language barriers were the biggest single issue raised by all HCPs. The presence of a language barrier impacted on the time taken for all types of consultations. The ability of the HCP to explain and give information in a language that was understood resulted in simplified and less detailed information. Where possible, interpreters including family or friends brought in by patients were used. Several HCPs mentioned concerns about the quality and veracity of interpretation when informal interpreters were used. The Language Line service was also used by professionals, but this was regarded as slow and difficult to use.
I think language can be a difficult barrier, although we use Language Line regularly, it is not an ideal situation to have.
Some HCPs felt that, in some instances, communication difficulties led South Asian patients to be less confident about asking questions and left professionals feeling unsure that the information had been fully understood. Although they recognised that it was their responsibility to ensure understanding, they felt frustrated that this was not always possible within the time constraints of a short consultation:
With a lot of the parents that come in with prescriptions when we start to counsel them and ask how the doctor has explained it to them they will be quiet and just say ‘Yes’. They won’t say too much. We will say take this and needs to be puffed four times day and they will just sort of nod their heads and we have to say ‘would you like me to explain it again/did you understand?’.
Some HCPs reported deliberately adopting a different approach for some South Asian families where English was not a first language – speaking more slowly, providing less detailed information, and providing simplified explanations in a more direct and matter-of-fact style. Most HCPs reported engaging with parents during a consultation rather than directly with the child.
It is just a question of mirroring the patient. It is not that ‘I act this way with a South Asian family’. It is basically reacting to an individual really. If there are more than two people there it may need a bit more time and effort.
Obviously I tailor the language and when you change the language I think your manner changes as well, especially as there is a Bangladeshi ethnic minority as well and I have to really explain things quite slowly to them, just to make sure that they understand it.
I give less information, because I have made the assumption that giving more information will just get lost due to the potential language barrier.
Healthcare professionals’ provision of information on asthma
Most HCPs felt that they did not have sufficient time to provide information to patients and families. They reported that they tended to focus on medicines and inhaler techniques, offering very little information on explaining what asthma is or the impact of lifestyle or diet. Information was largely delivered verbally, with half of HCPs routinely using leaflets in English because translated versions were not easily available. Demonstration devices were felt to be useful but not widely available as a result of recent recommendations that devices should be single-patient use only due to issues with infection control, with multiple devices being difficult to store.
My priority is making sure they understand what medication does and when to use it.
I make it very clear at the top what medication is and how often they should be taking it. That’s all I deal with.
We talk about food allergies and common triggers and get them to do food diaries – so that side of it I would be happy. The medical/cultural treatments – I wouldn’t understand and as I don’t know about them it would be hard to give professional advice on them.
Healthcare perceptions of South Asian family barriers to effective management
Healthcare professionals reported that most problems experienced by families (of all ethnicities) were due to a lack of knowledge or misunderstandings about asthma and that this was particularly relevant in South Asian families. HCPs reported that this was due to language barriers, maternal education levels, and general unfamiliarity with asthma.
My perception is that the parents cannot clearly say what is happening, that they don’t really understand what you are telling them.
Healthcare professionals felt that South Asian families’ understanding and expectations about asthma as a chronic condition could impact on a HCP’s ability to achieve effective consultations and overall management. HCPs felt that South Asian families compared the UK NHS and treatments received in the UK with health services in South Asian countries (e.g. India). Their perception was that families looked to doctors to ‘fix’ problems rather than engaging in long-term management strategies. HCPs also described differing styles of family structures and parenting in South Asian communities, with, for example, a different style of managing children, less expectation for children to take a role in self-management, and the role of extended family and community leader in directing management all being factors that influenced asthma management.
Healthcare professionals suggested that South Asian families relied more on ED services, were less engaged with preventative or primary care services, and were less likely to adhere to prescribed medication, in addition to expressing a higher level of related symptoms of ‘breathing difficulties’ than White British families.
I did find it a bit frustrating with the management, because I would give them a management plan and then they’d come back three months later and they’d done something completely different to what I’d said, and invariably they’d stopped all the medication.
I think the worst for me is when the parents say [in front of the child] ‘Well they won’t take their inhaler, so there is no point’. That is really quite then to show the child that it is not that bad and that actually yes it can be managed.
I have found that a couple of the parents expect you to have a cure for asthma.
Community knowledge and attitudes
Some HCPs felt that general awareness of asthma was low among South Asian communities, particularly among older generations. They felt that this impacted on symptom recognition, acceptance of asthma as a diagnosis and the understanding of asthma and its management.
Medications
Most HCPs felt that families of all ethnicities were often reluctant to use medicines, in particular inhaled and oral corticosteroids. In addition, several HCPs recognised an increased risk in South Asian families of stopping treatment despite advice to the contrary from HCPs.
There definitely appears to be a reluctance to stay on the steroid inhalers.
There seems to be a perception that there is a case when they don’t need it [medicine] but they fail to realise that it is because of [their medicine] that they are feeling ok and that it is not just the inhaler it is to do with the medicines as well.
Professional/organisational barriers to the management of asthma
Interprofessional communication
Most HCPs reported that communication between services and professionals was problematic, with several significant consequences for families. Examples include limited options for co-ordinated working; information about patients being lost; contradictory messages being given to patients; long-term management planning being impaired and effective; and timely follow-up being compromised.
Consequences of communication difficulties were magnified if patients moved house across city/county or across county borders and families changed their GP and/or hospital. In these circumstances, most professionals reported that they were reliant on parents to pass information between services. Referral pathways between services were similarly reported to be problematic. HCPs felt that pathways were unclear, involved multiple forms and were unduly restricted by location, a process contradictory to the vision of developing quality integrated services for children:
There’s a huge variation between the various GP practices and there’ll be some practices that you hardly ever get a referral from.
We rarely get to meet the GPs that manage patients from the other end, so we consider that a barrier.
Ideally I write a little note in the system, a letter gets printed and that goes to the GP, ideally the GP would read that letter, knows what I was thinking, the parents will present to the GP because I have told them to, the GP will read the letter and take action. That would be an ideal situation. Does that happen? Does the GP read the letter? Maybe not. Do the parents attend the GP? Maybe not. Do I chase that up? No.
Available services
All HCPs reported some confusion among South Asian families concerning the nature and availability of asthma services. Many were reported to experience difficulty with keeping track of the numerous NHS services for children with asthma, and as a result often were unsure where to refer children so that they received the optimal service. For example, it was reported to be difficult to identify whether or not primary care practices employed a trained asthma nurse. Several expressed the view that the multiplicity of services often resulted in a lack of continuity of care and resulted in families visiting different services at different times. Several HCPs expressed concern that South Asian families were less likely to attend annual asthma reviews provided by the primary care practices to particularly review the child’s medication and inhaler technique.
The down side is probably that they don’t want to come [to the review] and I think that is – asthma is particularly difficult . . . the patients need to come back for review.
Professional knowledge and training
All HCPs interviewed for the study had received some asthma training but few had undertaken any specific paediatric education for asthma. There was a diverse opinion on the need to pursue further training. Several suggested that further training would be helpful while others reported that the existing options for further training were sufficient and that further mandatory training would consequently impact on service delivery. Most professionals reported being familiar with either the BTS guideline or a local guideline for the management of asthma. However, adherence to the guidelines was reported as variable: half of HCPs interviewed perceived variations in training and knowledge among professionals as a barrier to effective management.
I think across the board, training is an issue. People don’t always get the right educational support to manage professionally in that role. You learn by dealing with them in the right way, but it is not always the correct way and that is where confusion arises in patients and parent’s minds.
Diagnosis of asthma
Healthcare professionals reported very few problems regarding diagnosis. They indicated that they did not perceive underdiagnosis or undertreatment to be issues in South Asian families, and stated that they were not aware of issues in accepting diagnosis in South Asian families. Participants reported that it was usual for HCPs to make a structured diagnosis using testing where possible, depending on the age of child, and that it was generally best practice for the GP to diagnose asthma as they are most likely to be aware of the child’s history. Asthma diagnosis in preschool children can be an issue with HCPs, with a reluctance to make a diagnosis unless there are strong features that increase the risk of asthma such as personal or family history of asthma. GPs indicated that they could not always make a clear diagnosis and they would suggest a review with a nurse. HCPs felt that South Asian families often did not return to these follow-up appointments, which may contribute to problems with diagnosis. HCPs did not suspect underdiagnosis in South Asian families as they described parents as ‘overanxious’ and as tending to be very quick to seek help. HCPs reported a general desire among parents to want tests or something concrete to be done, and this was particularly noted in South Asian fathers, but a number of interviewees went on to note that this was a general parental issue and not specific to South Asian families.
Have you had any difficulties around diagnosing asthma in South Asian families?
Not particularly. I don’t think this is necessarily related to Asian families. We always, I think the party line from paediatricians and GPs is, the age at which you make that diagnosis, given the very high prevalence of viral induced wheeze and then significant crossover between symptoms, so I don’t think it’s necessarily to do with South Asian families. They seem to be equally accepting of the diagnosis as Caucasian families are. I don’t think it would be an underdiagnosis because by and large, Asian families are quick to seek help.
Is that more noticeable in South Asian families versus white families or is that more normal for families generally?
I am not quite as sure about that distinction as I am about the families being concerned. I suspect probably more families want some clarity – fathers more actually. Definitely there are certain things that fathers want. They need to feel that their trip has been justified in some way and that just being sent home with a casual nod is not always to their liking. I am not quite sure about that as I am about the clear distance between accepting a fever on its own is not a matter of great concern.
School management
Despite children spending most of their day at school and, therefore, there being a need to ensure that they are being managed effectively when at school, few HCPs felt that they could comment on school management of asthma as they felt that this was outside their remit. However, the education professional interviewed for this study expressed a view that teachers and other members of staff in schools were provided with very limited training on the management of childhood asthma.
What about the rest of the teachers in the school, would they also be able to help the child with an inhaler?
I would say not all of the staff are trained. The main teachers are not trained.
This interviewee also felt that the limited availability of school nurses means that schools are reliant on parents to share information and provide their child’s medicines to school staff.
You are not getting letters from the GPs or the hospitals, I take it?
No.
So you are entirely reliant on what the parent tells you the GP said?
Exactly!
Sensitive issue there.
Yes, it is something that is not the ‘done thing’.
Suggestions for service improvements
Healthcare professionals had numerous thoughts and ideas regarding ways in which the quality of, and access to, care could be improved. These included the utilisation of an asthma nurse for follow-up appointments or the monitoring of children’s asthma, as well as being available for home visits. HCPs indicated that they thought this would be particularly useful for South Asian families. In an ideal scenario, asthma nurses were seen as linked to tertiary clinics, with regular contact with GPs still being necessary as the nurses should not provide an independent service. HCPs perceived that patients were more likely to attend specialist appointments than to attend a GP appointment, and therefore providing more access to appointments with asthma specialists was a further suggestion. The possibility of giving asthmatic children 48-hour open access to GPs, so that once a diagnosis has been made the child can be seen quickly to reduce anxiety for parents, and reduce unnecessary presentations at ED, was also suggested. A further option was to lengthen GP appointments specifically for asthma to ensure that information can be discussed in detail and so that both patients and GPs did not feel rushed and miss out vital information.
Healthcare professionals highlighted that inconsistency of care was a problem and suggested training for HCPs to be consistent across the region, so that everyone gives the same, consistent advice to families. It was suggested that asthma management should be added to regular, rolling education programmes for HCPs, with content regarding how ethnicity might impact management, or basic training in South Asian languages, though problems with the large number of languages this might involve were also highlighted. Following on from the discussion regarding language, HCPs felt that leaflets with asthma information in should be translated into multiple languages, or be written in simple terms or with a lot of diagrams in order to make information more accessible. HCPs also indicated that better access to interpreters would help with diagnosis or management strategies and would help improve parental understanding. To ensure, or aid, consistency of care, HCPs suggested that combined or shared patient medical notes should be available for all professionals involved in care so that they could automatically see any developments or changes such as hospital attendances or changes in medicine.
Healthcare professionals held the view that South Asian mothers do not drive, and therefore suggested that services need to be local and accessible, and also need to take into account school days or holidays. Having a drop-in centre or training evening in local pharmacies or community-based venues where a doctor or nurse is available to demonstrate inhaler techniques or discuss management plans was felt to be a way to overcome geographic and travel issues. HCPs also suggested that more information and education is needed in schools so that children learn basic ideas about asthma when they are young. Additionally, this may reduce any stigma associated with asthma and the use of inhalers, which may subsequently reduce non-adherence with treatment.
Anywhere, probably in GP surgeries where we are trying to get them in more: give them more time on appointments. The more educational devices in different languages the better. Use the things that the normal mother can understand. The mum can come and be a bit more involved in the child’s care rather than relying on the dad to come. But probably at the hospital – have an asthma specialist there.
I think that is general, but more so with South Asians, who do seem to like a home visit and then have a telephone – triage thing – because a lot don’t like to visit and it would be nice to have a number (if they have a problem) and be able to triage on the phone – or we could triage them on the phone. Then we need more interpreters, I think.
What’s worked quite well in the past with adults is we’ve sometimes had specialist asthma nurses coming into practice, and running clinics, (haven’t we?) and we’ve found that we’ve been quite successful with that, sending out the invitations and patients have come quite happily to have their inhaler, medication, whatever, reviewed. But, so, I don’t know if there was a specialist community paediatric nursing service available, whether patients would feel that that was something special, relating to their condition and a spec- a resource that they were able to tap into if necessary.
A follow-up person who would be employed solely to look at previous discharges from the day to ensure that the action plans for follow-up of those patients have been implemented.
Giving a training to the few pharmacists in that area would be helpful and literature resources would be really helpful possibly giving to the patients like are they new diagnosed with asthma to get the basic understanding of the basic issue and the facts and may be like we have blood pressure days, diabetes and do they have any national asthma day.
Discussion
This phase of the study provided an opportunity for parents, carers, children and HCPs to offer their perceptions regarding barriers to optimal asthma management in children. The Children’s Outcome Forum report recommends that, when considering strategies for improving outcomes for children, health professionals should work in close partnership among themselves, and that other agencies (developing an integrated approach with families, children and young people) must be placed at the centre of such initiatives. 2 As well as incorporating the perceptions of key stakeholders, the study was also designed to be sensitive to the needs of the NHS in providing solutions that are feasible and sustainable. The tailoring of generic services and the improvement of the cultural competence of existing organisations was one way this could be achieved. 160 This phase was, therefore, designed to explore ways in which existing services could be enhanced for a wider population by using a comparative White British sample in order to explore key issues that were similar for both White British and South Asian families which could be effectively addressed in a common, generic intervention programme. However, the analysis also revealed several issues that were specific to South Asian families which should be addressed by tailoring of interventions to meet these specific needs. The key findings from the families (parents, carers and children) and health professionals from this phase are summarised below. These findings were designed to be synthesised into the multifaceted tailored approach required to develop the asthma intervention framework and formed the basis of the next phase of the study (see Chapter 5).
Summary and discussion of key findings
Understanding asthma, including the recognition of symptoms, triggers and management strategies, is central to effective asthma management for children. Having this knowledge supports the development of a partnership between families and health professionals and increases the opportunity for the child and family to be fully involved in decision-making. Health professionals, therefore, have a responsibility to deliver information to families and to check the understanding of this information. The BTS guidelines4 recommend what information should be shared with patients, with the Scottish Intercollegiate Guidelines Network and Asthma UK (www.asthma.org.uk) having developed leaflets that are available for HCPs to provide to patients and families. Despite these resources being available and national recommendations instructing health professionals to take a role in providing education as part of their consultations and management plan, families in this study reported either that information had not been provided to them or that they had difficulty in understanding the information. None of the families recalled an asthma management plan being provided by any HCP, despite this being a national recommendation which has now been included as one of the national asthma quality standards. 4 Both South Asian and White British families also highlighted issues related to the consistency, timeliness and quality of the information provided which often lead to confusion about the different medications available and the techniques required to deliver them (e.g. how to use inhalers). The families requested that information be provided both face to face and in written format for later reference. Only half of the HCPs in our study provided South Asian families with information in a format other than verbal. This may not be a reflection of the quality of care received, but may be a result of lack of availability of information for non-English speaking families in written or other forms.
Understanding what asthma is and how it is managed was also found to be variable among South Asian and White British families (including children), with similar confusions and misconceptions regarding causes, triggers and nature of asthma in both groups. Both groups had similar views on issues such as the origins of asthma, role of genetics and the perception that one could ‘grow out’ of asthma. It is apparent that further efforts are required to check if the diverse ranges of healthcare providers delivering an asthma service understand and adhere to national guidance on information provision. This includes checking whether or not the children and families understand the information being provided to them.
This study revealed that, to some extent, all families, regardless of ethnicity, had to overcome barriers related to information provision or in understanding the information provided. However, these barriers were more pronounced for South Asian families because of language or translation issues. Where families had no previous exposure to asthma prior to diagnosis – South Asian families in particular – they tended to be less familiar with bio-medical definitions of the characteristics and management of the condition. HCPs should not, therefore, assume a level of understanding among families, something which should always be checked at the beginning of any consultation. Interestingly, the South Asian families did not directly raise language barriers as a major issue; however, the data suggest that this may because they had developed their own mechanisms to overcome these. Families reported that they used strategies such as seeking out GPs who could speak the same language, choosing to attend the ED where interpreters were more easily available or accessing their local pharmacist who was often of the same cultural background or could offer advice in a language other than English. 161 HCPs did raise language as a major barrier and felt that they had limited provisions to overcome it. HCPs also suggested that they required more time for their consultations with South Asian families in order to effectively utilise interpreters, talk slowly or use alternative ways of addressing the communication difficulties. They also raised concerns that, due to time constraints, they were not covering all of the issues which may affect South Asian families, such as dietary changes (see Suggestions for service improvements, below), and subsequently may provide those families for whom English was not their first language with less information than they would provide to White British or other English-speaking families.
Healthcare professionals reported that during consultations with families, their own focus was on addressing the medications required for treating asthma, with little attention given to a more holistic approach to management. This included the influence of the physical environment (e.g. rain, cold) and diet on asthma exacerbations, or the impact of asthma for the child as they move into adulthood, factors which were perceived as important by South Asian families. This was partly related to a lack of time to address additional issues but also, potentially, to a lack of cultural competence and awareness of the issues that may be important to South Asian families. Furthermore, this is complicated by the fact that South Asian families may be more likely to be given additional (and possibly contradictory) advice about asthma by members of the wider family and community (in the UK and overseas). For example, South Asian families were more likely to describe being advised about particular dietary inclusions or exclusions and about the use of complementary therapies of various kinds, or seeking support from religious leaders (supported by phase 2 data), issues often overlooked by HCPs. It is important, therefore, to encourage HCPs to positively engage these key individuals, some of whom may also be providing a caring role to the child, and to be aware of the types of information that is being shared within families and communities to better understand the context in which a child’s asthma is managed. Asthma education programmes within the UK, such as nurse-led asthma reviews, traditionally focus on the direct family unit of parents (often the mother) and child, with little acknowledgement of the need to include the wider family.
Accessing care
Accessing appropriate care is essential to ensure a timely diagnosis, optimisation of treatment and the prevention and management of acute attacks. Previous experience of contacts with the health service can influence future health-seeking behaviour,162 both positively and negatively. As with other chronic conditions, the aim for asthma management is to keep a child functioning at the optimal level, attending school and preventing hospital attendance. 162 Within the NHS, primary care services are available to initially provide a diagnosis of asthma and regular reviews to optimise management, with ‘out-of-hours’ services and emergency services being available for urgent care and acute severe attacks. In practice, however, emergency attendances for all clinical problems are increasing,14 with a higher attendance rate for South Asian children with asthma than for White British children. Drivers for this health-seeking behaviour need to be understood if families are to be encouraged and supported to manage their asthma and to choose primary care services in preference to emergency care. In this study, difficulties expressed by parents regarding the most appropriate place of presentation during an acute attack highlighted an important problem with current provision and access to the NHS. South Asian families in this study chose to access the ED if they were unable to access their GP. In contrast, White British families were more likely to use the out-of-hours service provided by the NHS. These differences were driven by previous experiences of using the health system (e.g. being referred to the ED during previous acute asthma attacks, or experiencing negative or delayed appointments with their GP) as well as difficulties in the recognition of the severity of symptoms and, as a consequence, this delayed timely access to treatment.
In the current study, none of the South Asian families and very few of the White British parents had any formal means of assessing their child’s symptoms. No parents had been provided with written asthma plans, while a minority of White British families reported using peak flow meters. No one reported employing any objective measure of severity. Without being able to assess severity, parents are unable to know at what point and where to access health care for early intervention. This may also lead to a quick deterioration in the child, with the need to seek urgent care from the ED and, in some cases, to call an ambulance for help.
Both White British and South Asian families expressed feelings of being ‘fobbed off’ within the healthcare system and described delays in getting a diagnosis, which subsequently led to feelings of frustration or anger. Despite this, all families described the need to use the GP as the first point of contact in a non-acute situation. In an acute situation, the patterns of presentation to primary care or emergency services differed between the groups. Despite their disappointment with ED waiting times, South Asian families would self-refer to the ED and bypass other services in the next event if they had previously been referred there via NHS Direct or the out-of-hours services; this reinforced the idea that South Asian families perceived hospital services as more expert or knowledgeable than primary care. They were also more likely to call an ambulance if they were concerned about their child.
Organisational discrimination
Despite a tendency for families to feel that they had not been discriminated against, the interviews with HCPs revealed the potential existence of problematic cultural stereotypes about South Asian families within the NHS. South Asian families were viewed as ‘difficult clients’ rather than being recognised in the context of the structural discrimination facing patients whose needs are not aligned with the majority White population. 163 A tendency to see South Asian families as inappropriate users of services (e.g. overuse of A&E services, non-attendance at follow-up) was present in our data; this reflects the stereotype of minority ethnic patients themselves being part of the problem of providing adequate services, a type of ‘victim-blaming’. However, HCPs did also recognise that services were not currently structured in a way which would enable them to meet the needs of South Asian patients, especially in relation to having the time to give more information and to use interpreters.
Children’s experiences
The team considered it important to engage children and to gain an insight into their perceptions of living with asthma. The children also provided suggestions for interventions. By involving them in this phase of the study, a partnership and relationship with them that supported their involvement in phase 4 of the study was developed.
This phase of the study found that there was considerable similarity in the experience of asthma described by South Asian and White British children. As with the adults interviewed, children from both groups expressed some confusion around either the causes or the triggers of asthma, and described not knowing what asthma was or why they had been diagnosed. These findings suggest inadequacies in the education of children about their condition. In their interviews, both groups of children focused on their experience of acute attacks and described the strong emotions they felt during or about these attacks. They reported often feeling frightened and upset. 164,165 However, when describing their interaction with HCPs, they could not recall discussions about why acute attacks might arise or what to do in this situation. This suggested that HCPs were not communicating these important messages adequately to children. In their recall of visits to the GP or practice nurse, children reported discussions of administering and monitoring medication. They could not recall any holistic discussion about school attendance or more general quality of life issues.
Previous evidence in health research has consistently demonstrated that ‘feeling normal’ is important to children. 165–167 A desire to be ‘normal’ was commonly expressed by children in the current study. This was sometimes in relation to the unfairness of restrictions associated with having asthma in comparison with siblings, or the embarrassment of having to use inhalers in public. Research has documented feelings of embarrassment about having asthma among teenagers, with those who felt embarrassed about their asthma significantly less likely to carry or use inhalers in front of others. 165 Feelings of embarrassment were expressed by children from both groups in this study. Parents and focus group members also described potentially negative reactions from members of the wider South Asian community if they were aware of a child having a diagnosis of asthma. This highlighted the possibility of children in South Asian communities having greater potential of experiencing asthma-related stigma.
One way in which children could be made to feel ‘different’ from other children, especially at school, was in relation to non-participation in sporting activities. Despite the fact that children with asthma are encouraged to participate in sport,168 children (and parents) reported a lack of engagement in these activities. This would appear to reflect a lack of appropriate guidance for parents, children and teachers about appropriate management of asthma. Parents, in particular, expressed concerns that schools were not always fully knowledgeable about medication and how to administer this. Nevertheless, in general, children acknowledged that friends and teachers were important agents in helping them to manage their asthma, indicating that schools can be important sites for delivering asthma interventions. 169
Suggestions for service improvements
Families, children and HCPs offered numerous suggestions for how the provision and quality of service could be improved. Families discussed how an advice centre or telephone service would be useful for when questions arose. Families, children and HCPs suggested working closely with and in schools to educate and inform children, not only those with asthma but also the wider community, to improve education and remove the stigma associated with asthma and inhalers. Families, children and HCPs also suggested that presentations or information centres at easily accessible local community venues, such as temples or community centres, might be places where doctors, nurses or people with experience of asthma could provide information or demonstrations of inhaler techniques. Children reinforced their desire for face-to-face demonstrations or meetings with people who had experience of asthma. Families and HCPs suggested the production of leaflets and posters in multiple languages to ensure that most people’s information needs could be catered for. Families reported that a better diagnosis system was favoured, as current difficulties with diagnosis caused stress and anxiety to families. HCPs had many suggestions for the improvement of care, including lengthening GP appointments, providing follow-up appointments with asthma nurses and the provision of education programmes for HCPs to ensure consistency of care. This consistency was something that both families and HCPs alluded to, with the suggestion of integrated medical health records between all HCPs. These suggestions fed directly into the next phase of the MIA project and helped to develop the intervention framework.
Conclusion
Building on the findings from phases 2 and 3, the study of families and HCPs identified the need for interventions that addressed multiple levels of influence on health outcomes at the patient, provider and system levels. This included understandings, beliefs and behaviours of all parties (parents, children, communities and HCPs), in addition to the impact of how healthcare services were organised. The findings also reinforce the importance of collaboration with service users and other stakeholders and the relevance of exploratory qualitative methods of inquiry. Listening to the voices of participants in this detailed way enabled the research team to understand the perceptions and experiences of parents, carers, children and HCPs. The project was thus able to reflect on issues considered important to those receiving and delivering care, and to work with both groups to design an intervention programme which includes those issues at its core. This work was subsequently taken forward into the fourth phase of the project, the collaborative intervention design which is discussed in the following chapter.
Chapter 5 The development of potential collaborative intervention strategies (phase 4)
Chapter summary
This chapter presents the structured, collaborative, step-by-step process, moving from the evidence gathered in phases 1 to 3, integrating this, prioritising and underpinning it with psychological theory to design an intervention planning framework for the asthma management pathway in children, and finally presenting an example of an integrated, multifaceted intervention programme for one priority area chosen: getting a diagnosis. As noted earlier, the process was informed and directed by the principles of IM and the application of this approach will be highlighted where applied.
Phase 4, based on the findings of phases 1 to 3, sought to produce an intervention planning framework to address the asthma pathway, with the ultimate aim to optimise asthma management and then to develop an acceptable and achievable evidence-based and theory-informed collaborative exemplar intervention programme focused on one key issue drawn from the planning framework. The systematic evidence synthesis in phase 1 provided the evidence base which guided the interview schedules for phases 2 and 3. The qualitative data from phases 2 and 3 identified the issues that the families, communities and HCPs perceived as needing to be addressed in relation to asthma and its management pathway. The data also provided the underpinning evidence and content for the intervention planning framework and final exemplar program. While the aim was to tailor the intervention plan and programme for the South Asian families, the White British families were included to identify if there were common problems that existed across groups, and to establish any issues that were specific to one group. An exemplar asthma programme (to optimise the initial steps in asthma diagnosis) was developed from the intervention planning framework. Only one key issue was identified to demonstrate the process used to move from the planning framework to a final, collaboratively developed, integrated, multifaceted intervention program. To do this, psychological theories were used as they provided structure for addressing the issues identified and the type of interventions that could then be utilised (both content and means of delivering the intervention) (see Appendix 17). To support this process, a rapid review of existing asthma interventions was conducted during this phase and provided the team with examples and ideas of when intervention prototypes for this study were being considered (the delivery mechanism for the intervention) (see Appendix 10). The information was integrated and presented to our collaborative participants for refinement so that a feasible tailored programme for one key issue could be finalised. The findings from the project were disseminated at local events, after which we explored participants’ experiences of being involved in participatory research with the view to improving or refining future collaborative activities.
Phase 4 comprised five sections and has been reported as sections A–E below. Owing to the integrative process used in this phase, overlaps exist among sections A to D.
Section A sought to combine and condense the charted data from phases 1 to 3 to identify 11 key themes that needed to be addressed to optimise asthma management and to develop an intervention planning framework based on these themes.
Section B reports how the 11 key themes were presented to the participants at workshops, a summary of who attended the workshops and the processes by which the themes were prioritised. The prioritisation process identified ‘getting a diagnosis’ as a key issue. As the participants were asked to consider the whole asthma pathway in this project and a socioecological approach was being used, ‘getting a diagnosis’ was approached from a socioecological and holistic perspective, covering a number of steps required within the diagnostic process. These steps included an awareness of asthma, recognition of symptoms, accessing health care and the investigative process to make the diagnosis of asthma, and not solely the narrow steps of investigating the child to confirm or refute a diagnosis. ‘Getting a diagnosis’ was used as an exemplar theme to demonstrate the step-by-step process used to achieve a programme for the themes. It was not feasible within the timescale to undertake this for each theme. This exemplar theme resulted in the development of outcomes and objectives for a proposed intervention programme generated using IM matrices (see Appendices 5 and 7; Chapter 1). This subsequently led to the proposal of a three-arm multifaceted integrated intervention programme, which was refined at collaborative finalisation workshops. The process used for this theme provided a model process which could be used for any of the other themes identified.
Section C outlines how the components of the proposed three-arm intervention were selected by members of the research team, advisory panel, CFs and external advisors. Specific considerations were given to the feasibility of implementing the intervention within the NHS.
Section D presents the iterative process through which the revised draft intervention was taken, returning to a combined professional and layperson workshop (including children) for further refinement and finalisation. As a result of this refinement, a fourth arm was subsequently added to the intervention and the proposed intervention programme was finalised.
Section E discusses the finalised intervention programme and how the dissemination was approached using events tailored specifically for the relevant audiences.
Figure 4 shows how sections A to D linked together to result in the production of an asthma management pathway intervention programme. The diagram shows that the qualitative data provided the content of the intervention and the specific areas that needed addressing with psychological theory giving the project a way of achieving change. The diagram shows the delivery mechanism through which these changes were achieved and implemented.
FIGURE 4.
Representation of phase 4: sections A to D. ACT on Asthma, Awareness, Context (cultural and organisational) and Training; IPF, Intervention, Planning Network.
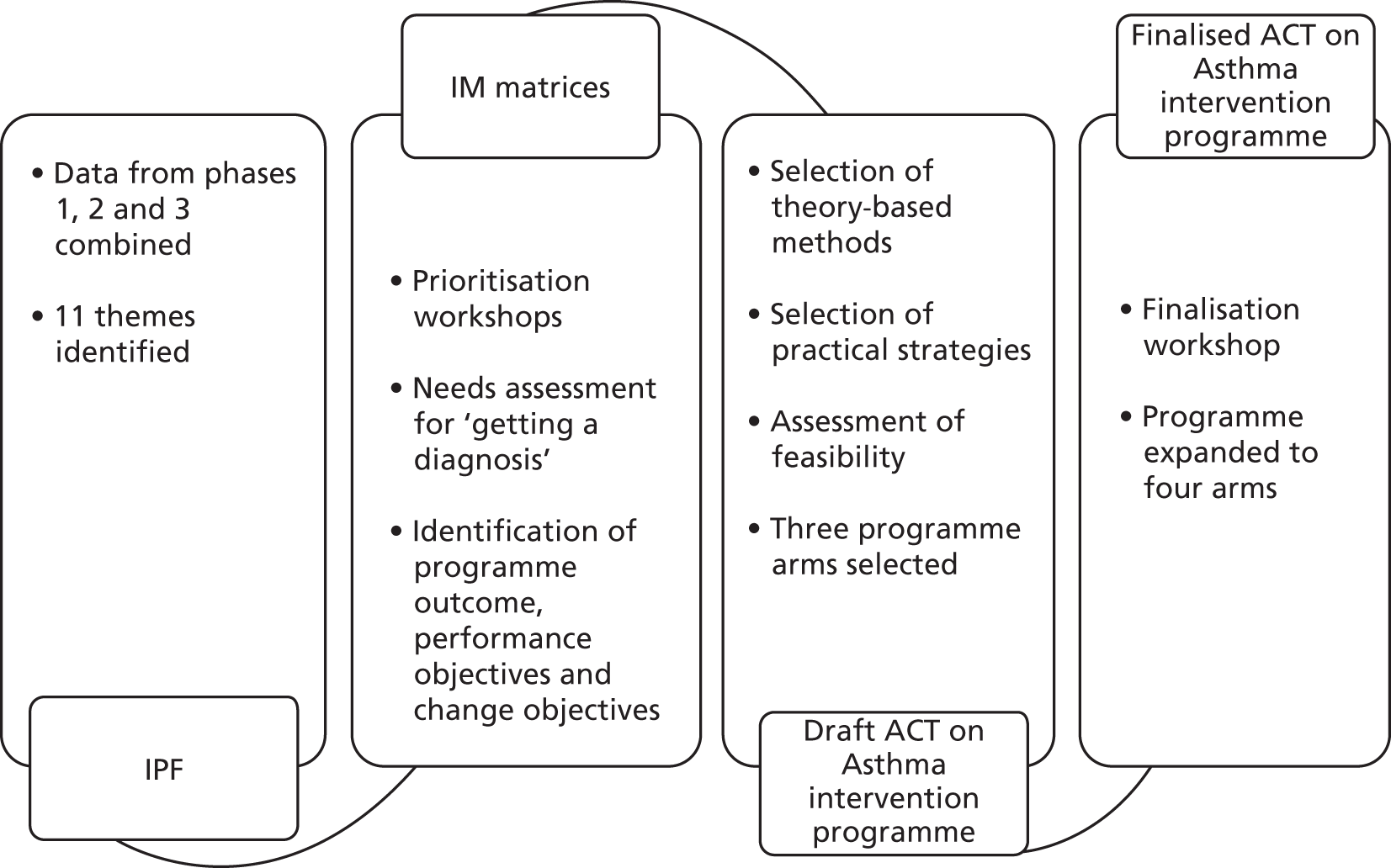
Section A: formatting the qualitative data
The qualitative data gathered from focus group attendees and key informants in phase 2 and from South Asian families and HCPs in phase 3 was subjected to a modified framework approach utilising the standard fields of IM to define actors, domains, behaviours and determinants (see Chapter 1 and Appendices 5 and 7 with examples), rather than a framework based on a priori themes. This permitted the streamlining of the process of data integration and, crucially, allowed behaviours or determinants of behaviours identified (e.g. attending the ED) in different data sets to be charted multiple times if they occurred in multiple domains. This allowed them to be easily viewed and combined (see Appendix 7).
Identifying themes
Identified behaviours and putative determinants were discussed and grouped inductively by the research team, using the constant comparison method to compare and consider each behaviour and determinant against other behaviours and determinants to allow the identification of similarities and differences. Behaviours, determinants and groupings were collated, compared and contrasted until data saturation was reached. This process resulted in the identification of 11 key themes (Table 16).
| Key themes | |
|---|---|
| 1 | Being able to talk to doctor and nurses |
| 2 | Being able to use the services |
| 3 | Community awareness of asthma |
| 4 | Getting a diagnosis |
| 5 | Having suitable information on asthma |
| 6 | Medicines for asthma |
| 7 | School and my child’s asthma |
| 8 | Types of services available for asthma |
| 9 | Quality of care |
| 10 | Understanding asthma |
| 11 | What to do day to day |
Creating an intervention planning framework
The 11 key themes, each corresponding to an aspect along the asthma management pathway and underpinned by evidence collected in previous phases of the study, were combined within an intervention planning framework. This enabled the examination of potential barriers and facilitators to asthma management identified within each theme (from phase 1 to 3 data), as well as behaviours and determinants within each theme potentially amenable to intervention.
Using the intervention-planning framework
The intervention planning framework presented an overview of the aspects of asthma management that required intervention, complete with the evidence base supporting that need and example interventions that had been applied in previous research (see Appendix 10) shown in the rapid review of existing asthma interventions. The intervention planning framework can be a valuable research tool, but moving from an evidence base to developing an effective intervention is challenging. Techniques based on steps 1 to 4 of IM were used as the basis for a structured approach to intervention design. Given the volume and complexity of data generated during phases 1 to 3 and the time and resource constraints of the project, a pragmatic decision that only one theme from the intervention planning framework would be selected for further development (see Finalisation workshops, below) was taken to demonstrate the translation of qualitative data into an evidence-based tailored intervention program. Expert advice was sought from K. Bartholomew, an expert on IM, for this plan in order to ensure that a comprehensive and holistic perspective could still be taken when designing the intervention framework with the inclusion of only one aspect. Collaborative workshops were thus carried out to enable the selection of a theme for further development (section B). Despite selecting only one theme, it can be argued that the methods employed to design the intervention programme for this theme provided a model process that could be applied to other themes.
Section B: collaborative workshops
Four workshops were held: three laypersons’ workshops (two targeted to South Asian families and one targeted to White British families) and one HCP workshop. Three layperson workshops were necessary due to the different preferences of communities among South Asian groups and between South Asian and White British families regarding venues, days and catering arrangements.
Collaborative workshops were used in order to facilitate the collaborative development of the intervention programme. Health promotion officers from Asthma UK were present and brought added value to the workshops. Children and families had the opportunity of meeting with the health promotion officers at the workshops, and therefore, even though the children and families were there to be part of the research study, they gained something additional at the workshops by having direct access to additional information on asthma and awareness of what Asthma UK could offer.
The workshops enabled the participants to review the findings and set priorities for intervention development. The analyses had identified 11 key themes that could be suitable for the development of an intervention programme. A modified nominal group technique (NGT), advocated to achieve group agreement,170 was used in the workshops. While NGT enables minority opinions to be heard, there is still a risk that minority opinions can be dismissed if quieter and less assertive group members are unable to vocalise their positions in a group discussion. The research team therefore decided to include discussion and revision elements of NGT but also opted for individual voting rather than table consensus (the latter being typical of NGT). This ensured that all participants were given the opportunity to be heard. The methods for enabling meaningful collaboration and prioritisation of these 11 themes by all participants over a series of workshops are detailed here.
Layperson workshops
-
The findings were presented orally, supported by PowerPoint displays and hard copies available at each table.
-
Participants were grouped according to language requirements.
-
CFs provided simultaneous whispered translations during the presentation in one of five languages as required by participants.
-
-
The ranking data sheets (see Appendix 9) were presented, along with examples of how to complete them.
-
A linear ranking was used, with no equal placing allowed.
-
-
Participants were asked to rank the 11 key themes based on the presentations they had just heard.
-
This was followed by a small group discussion of the 11 themes presented, which focused particularly on the level of need for an intervention to be developed for each of them. The team reassured the participants that all of the themes were recognised as important and would be presented in the report. A facilitator from the research team and a CF were present to support the groups and answer any questions that arose during the exercise.
-
The aim was not to achieve consensus but rather to share different views to provide participants an opportunity to consider their initial choices.
-
-
Participants were asked to use the second data sheet to rerank the themes.
-
A linear ranking was used, with no equal placing allowed.
-
-
Participants were asked to use the third data sheet to explain their reasoning or add any other aspects of managements that they felt had been omitted in the workshop.
-
The data from the first and second workshops were tabulated with the Borda approach used to calculate overall priorities (Table 17) for ranking results.
| South Asian community rankings (n = 62) | South Asian parents of children with asthma rankings (n = 22) | White British parents of children with asthma rankings (n = 2) |
|---|---|---|
| Getting a diagnosis | Getting a diagnosis | What to do day to day |
| Understanding what asthma is | Not all doctors and nurses treating asthma well enough | Getting a diagnosis |
| Types of services available for asthma | Types of services available for asthma | Medicines for asthma |
| Being able to talk to doctors and nurses | Being able to talk to doctors and nurses | Information and support for families |
| Not all doctors and nurses treating asthma well enough | Understanding what asthma is | School and my child’s asthma |
| Medicines for asthma | Medicines for asthma | Understanding what asthma is |
| Having suitable information on asthma | What to do day to day | Not all doctors and nurses treating asthma well enough |
| School and my child’s asthma | Having suitable information on asthma | Knowing about and using services for asthma |
| What to do day to day | School and my child’s asthma | Raising awareness and understanding about asthma |
| Community awareness of asthma | Being able to use the services | Knowing what to do in an emergency |
| Being able to use the services | Community awareness of asthma |
Children’s involvement in determining the research themes
Children’s workshop methods
The children participated in both the prioritisation and the finalisation workshops. The workshops were more successful in enabling children’s participation compared with interviews. Evidence suggests that to work effectively with children the research methods used need to engage children’s interest171 and take into account variations in age, understanding and ability. We therefore chose to use more discursive workshops and visual-based methods rather than the presentation and written methods used with adults.
The first workshop involved the children’s involvement in a prioritisation exercise using ranking tools. Diamond ranking is a method of ranking that has been used successfully with children. 171–173 Diamond ranking requires participants to arrange a set of nine statements in a diamond pattern (1–2–3–2–1 format, creating a diamond shape) according to their opinion of their relative importance to each other. Diamond ranking allows equal positioning of some items, which previous research suggests makes ranking exercises easier for children to complete. 174 We modified this approach into a 14-card diamond ranking using a 1–2–4–4–2–1 format, retained the clear top and bottom priorities and allowed equal ranking in the middle. To account for the different ages and abilities of the children present, we opted to allow children to conduct either a modified diamond ranking followed by a standard linear ranking (no equals allowed) or only a diamond ranking. The data from these exercises were tabulated and Borda approach175 used to calculate overall priorities (Table 18) for ranking results. In addition, the children were given the option of an alternative ranking method, Budget Pie. Each child was given £300 in toy money in small denominations and a board with the various aspects of management marked upon it with a plastic wallet affixed that could hold the toy money. Each child was asked to divide their money between the aspects of management (based on the 11 core themes identified), thinking about what was most important and, if tackled, would make the biggest difference to them. Facilitators were available to assist with placing money into the board but did not direct the children’s choices. The amounts allocated were totalled and the overall amount awarded was used to determine rank position.
| Linear ranking | Budget Pie ranking with overall amount | |
|---|---|---|
| South Asian children’s rankings (n = 21) | ||
| Having an asthma attack | Having an asthma attack (£1470) | |
| Being looked after well enough by doctors and nurses | Using pumps, inhalers and medicines for asthma (£630) | |
| Using pumps, inhalers and medicines for asthma | Being looked after well enough by doctors and nurses (£620) | |
| Being able to get the help I need | Being able to get the help I need (£530) | |
| Having information about asthma | Having information about asthma (£450) | |
| Understanding what asthma is | Understanding what asthma is (£420) | |
| Having someone tell me I’ve got asthma | Being able to talk to doctors and nurses (£380) | |
| Being able to talk to doctors and nurses | Having someone tell me I’ve got asthma (£300) | |
| Having asthma and being at school | Having asthma and being at school (£260) | |
| Being able to talk to my parents about asthma | Being able to talk to my parents about asthma (£260) | |
| Friends, family and neighbours knowing about asthma | Friends, family and neighbours knowing about asthma (£190) | |
| Different places and people I can go to get help for my asthma | Different places and people I can go to get help for my asthma (£190) | |
| Being embarrassed by having asthma | Doing different things to everyone else (£180) | |
| Doing different things to everyone else | Being embarrassed by having asthma (£120) | |
| White British children’s rankings (n = 1) | ||
| Knowing what to do in an emergency | Not all doctors and nurses treating asthma well enough (£110) | |
| Not all doctors and nurses treating asthma well enough | Knowing what to do in an emergency (£50) | |
| Medicines for asthma | What to do day to day (£30) | |
| Getting a diagnosis | Getting a diagnosis (£20) | |
| What to do day to day | Medicines for asthma (£20) | |
| School and my child’s asthma | Knowing about and using services for asthma (£20) | |
| Knowing about and using services for asthma | Understanding what asthma is (£20) | |
| Understanding what asthma is | School and my child’s asthma (£10) | |
| Information and support for families | Information and support for families (£10) | |
| Raising awareness and understanding about asthma | Raising awareness and understanding about asthma (£10) | |
Healthcare professional workshop methods
Healthcare professionals were also requested to participate in the ranking exercise described above. It was recognised, however, that securing their attendance at a workshop would be difficult and therefore an alternative process was designed.
-
An e-workshop format (sometimes referred to as a modified Delphi) was used for the HCPs in order to enable maximum participation. The questionnaire link was sent by e-mail to all participating HCPs.
-
The e-mail contained an overview of the 11 themes identified, how they had been identified and the aims of the e-workshop.
-
Participants were asked to rank the 11 themes based on the information provided by labelling the issues 1 to 11, with no equal placing allowed.
-
Participants were asked to explain their reasoning or add any other aspects of the management pathway that they felt had been omitted in the workshop.
-
The data from the questionnaires was tabulated with the Borda approach used to calculate final positions (Table 19) for ranking results.
| Healthcare professional rankings (n = 37) |
|---|
| Managing issues arising from language barriers |
| Informing South Asian families’ knowledge, expectations and understandings |
| Supporting professional education and training |
| Making time to deliver care |
| Improving information and education |
| Standardising the quality of management |
| Facilitating interprofessional working |
| Managing behaviours arising from South Asian cultures |
| Developing cultural competency |
| Facilitating management of asthma at school |
| Improving diagnostics |
Finalisation workshops
Workshop attendees
All participants from phases 2 and 3 who indicated agreement to be contacted were invited to attend the workshops. This was in addition to community members who had returned expression-of-interest (EoI) forms, but had not yet been recruited into the study. Participants were also encouraged to invite extended family members to the workshops in response to findings from phases 2 and 3. These phases argued for wider community inclusion in intervention development, with workshops an excellent opportunity to engage the wider community in developing asthma interventions and to raise the profile of research. The finalisation workshops brought together the South Asian and White British participants in order to help identify generic and specific components for the intervention programme. Bringing both groups together demonstrated a shared goal and helped to validate the findings.
One hundred and twelve South Asian participants (62 community members, 29 parents of children with asthma and 21 children) and six White British participants (four adults and two children) were involved in the workshops.
Selection of the exemplar theme to demonstrate the intervention programme development process
An exemplar theme was chosen for which a multifaceted intervention programme could be developed and process demonstrated following the review of the ranking data from the collaborative workshops by the CFs and research and advisory team. Workshop rankings indicated that the processes and procedures involved in ‘getting a diagnosis’ were a high priority for families, but not for HCPs, who ranked it much lower down. As mentioned previously, in relation to this project, ‘getting a diagnosis’ covered a number of steps required with the diagnostic process and not solely the narrow steps of investigating the child to confirm or refute a diagnosis. Data underpinning the ‘getting a diagnosis’ theme, therefore, overlapped, with some other themes identified that emphasised the need for a multifaceted integrated approach to tackling themes. The notable discrepancy in the ranked priorities between families and HCPs suggested that ‘getting a diagnosis’ was ideally placed to allow further dialogue between families and professionals; notably, highlighting the professionals’ suboptimal delivery, even where guidelines and procedures are in place. As the planned intervention programme would be designed around the needs of the children and families, this underscored one of the fundamental principles of the MIA project and current NHS policy,72 and was a further reason why this theme was considered a priority for further development. Data from phases 2 and 3 revealed that ‘getting a diagnosis’ underpinned all aspects of condition management, including access to asthma services, information and education, and knowledge of acute asthma attacks. By intervening in the diagnostic process, the educational aspects and knowledge of how to approach an acute asthma attack could also be incorporated into an intervention and thereby incorporate children’s voices.
Using techniques drawn from intervention mapping to develop intervention programme components
To develop the exemplar intervention programme, a structured approach to analyse available data was undertaken utilising techniques drawn from IM, which in turn draws upon psychological theories. The adapted process was developed in conjunction with K. Bartholomew, an international expert in IM. IM typically follows six iterative steps (see Chapter 1). However, the aim of the MIA project was not to implement and evaluate an exhaustive intervention programme, but rather to assess the collaborative methods used in enabling children, families, communities and professionals to work together to develop an intervention programme. As a consequence, an adapted IM approach was taken, utilising IM steps 1 to 4 (Table 20 and Figure 5). IM is an iterative process and, thus, each step was visited on more than one occasion.
| Step | Description |
|---|---|
| 1 | Needs assessment |
| 2 | Identification of outcomes, performance objectives and change objectives |
| 3 | Selecting methods and practical strategies |
| 4 | Creating an organised programme plan |
FIGURE 5.
Intervention mapping methods used. ACT on Asthma, Awareness, Context (cultural and organisational) and Training.
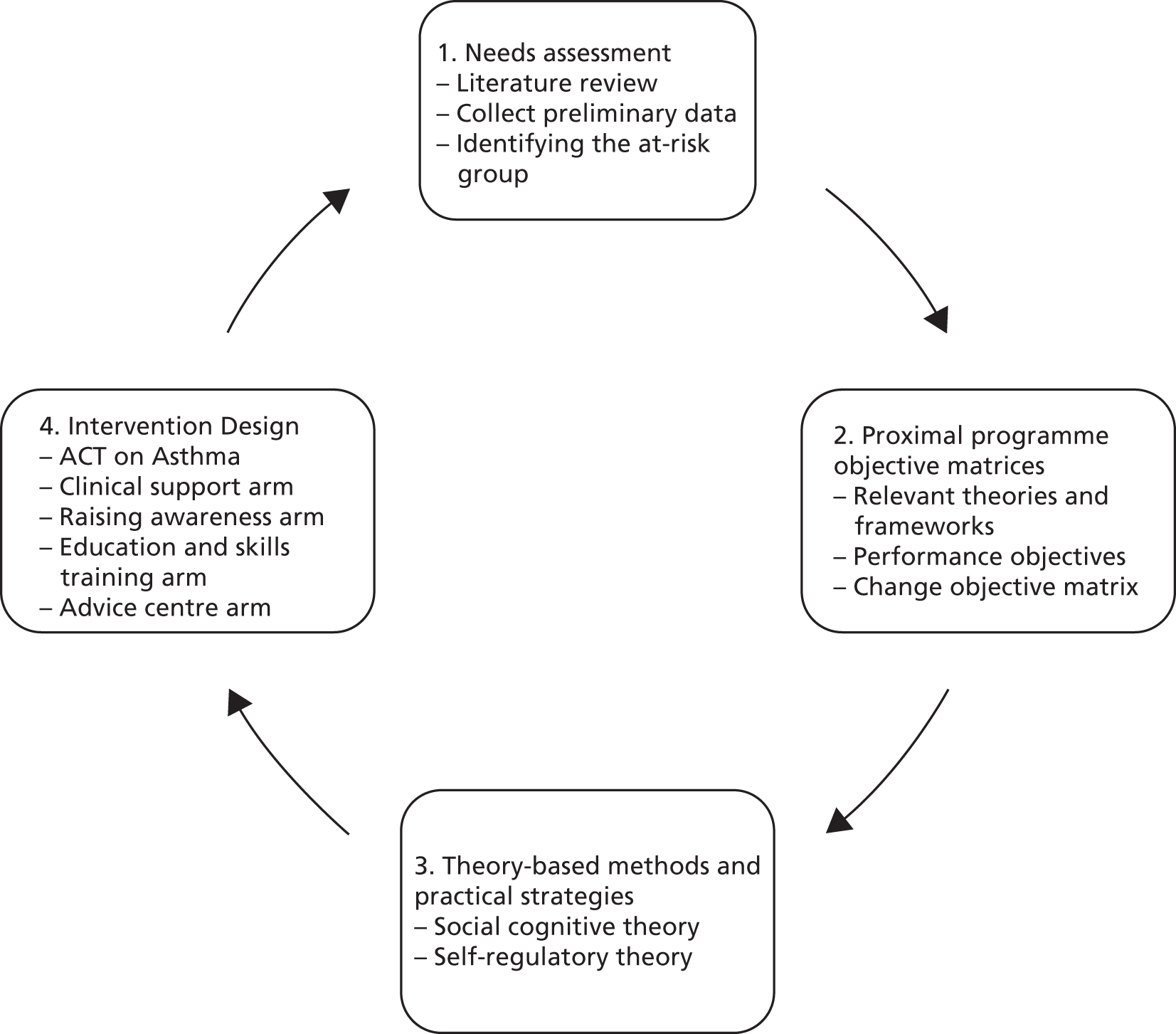
Needs assessment
The literature and scoping reviews of phase 1 and qualitative data collection of phases 2 and 3 comprised the needs assessment, which permitted the identification of the barriers and facilitators to achieving effective asthma management in South Asian children.
Identification of outcomes, performance objectives and change objectives
Following the selection of ‘getting a diagnosis’ as the exemplar, the main programme outcome focused on achieving a clear, accurate and timely diagnosis of asthma.
Performance objectives, which can be defined as specific sub-behaviours that feed into the overall programme objective, were constructed by answering two questions:
-
What do participants currently do?
-
What do participants need to do instead to achieve the desired programme outcome?
Members of the research team participated in a ‘brainstorming’ session to generate steps to articulate the performance objectives guided by the answers to the above questions. Additionally, the performance objectives were informed by salient theories from clinical and health psychology which explained determinants and maintainers of health-related behaviour (see Appendix 17).
Phase 1 indicated that achieving a diagnosis might be related to improved knowledge, high self-efficacy, outcome expectancies and perception of risk. As a consequence, self-regulation theory176 and social cognitive theory177 were used to enable the creation of change objectives. Change objectives result from merging performance objectives with theory.
Section C: draft intervention production with assessment of feasibility
Selecting methods and practical strategies to bring about change
Section C, mapping to step 3 of IM, ensured that change objectives were linked to practical, feasible strategies for behaviour change which were also theoretically embedded. When completing this phase to identify practical strategies and provide the team with examples and ideas, previous interventions that had met with success identified from the scoping review (see Appendix 10) were considered in conjunction with theory.
Scoping review
The scoping review identified 408 examples of asthma interventions trialled for, with or on children; four were targeted to South Asians. Three of these interventions focused on education and clinical support, with one including additional elements of raising awareness. The scoping review of interventions undertaken as part of this study (phase 4; see Appendix 10) demonstrated that the majority of current asthma interventions have been developed by professionals and then tested for effectiveness with a target population; in most cases, this was a majority ethnic population. The interventions identified in the review often lacked a multifaceted integrated approach, with most being delivered in one setting with little consideration of the experiences of patients across the whole pathway of care. Most interventions (whether universal or tailored) are developed from the perspective of service providers rather than including a detailed exploration of patient perspectives. Comprehensive asthma programmes were reported from the USA178 or Australia, with very few reported in the UK. Furthermore, very few culturally tailored interventions were identified by the review, with fewer still ‘generic’ interventions tested in minority populations.
The scoping review was useful in highlighting previously successful interventions and the delivery methods used to direct the research team to the most successful intervention methods. This scoping review informed subsequent sections of the project. In addition, to ensure that any practical strategies would be fitting and culturally tailored to the target population, the qualitative data from phases 2 and 3 were also considered, especially with data regarding ideas for future interventions (Figure 6; see Appendix 11).
FIGURE 6.
Process of selection methods and strategies to effect change in the MIA project. ACT on Asthma, Awareness, Context (cultural and organisational) and Training.
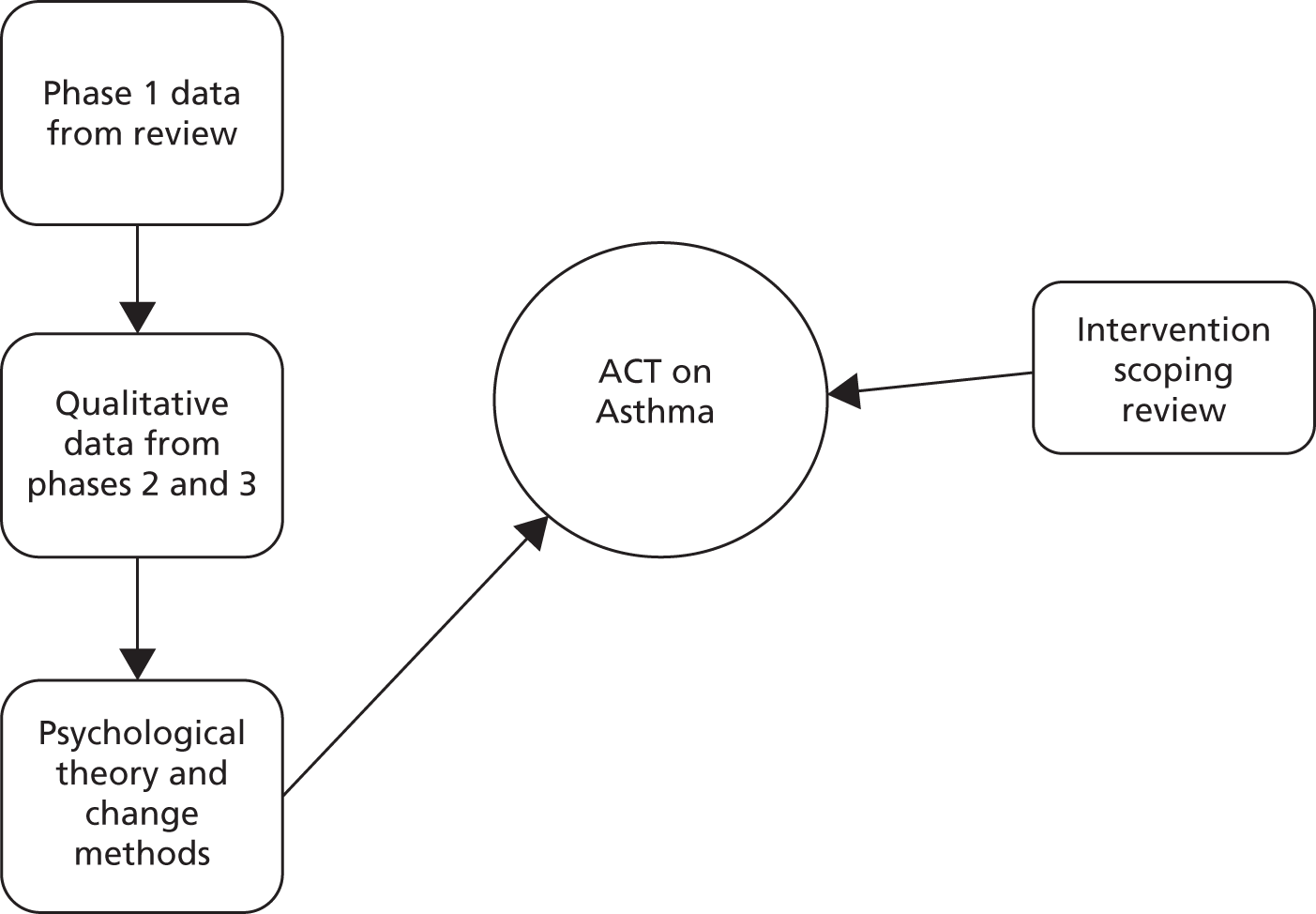
During the process of selecting methods and strategies to effect change, modelling was noted to be a recurring theory-based method which addressed a number of change objectives (i.e. to encourage parents to believe that going to the GP has value for them and their child; to enhance parents’ belief that they will be able to have an effective consultation with their GP; to encourage a child to believe that expressing their symptoms will be of benefit to them; and to enhance HCPs’ belief that improving consultations will improve management). Thus, from a theoretical perspective, the use of vignettes or role-model stories to demonstrate success in managing these objectives was deemed a very appropriate component of an intervention programme. Vignettes and stories were also attractive because they can be delivered in multiple contexts and formats and can be produced within a fixed budget.
The MIA project aimed to develop a feasible intervention programme with the subsequent step to consider the scope of the draft intervention. An expert steering group comprising L.K. Bartholomew, the CFs, the advisory group and external experts was consulted to evaluate core versus peripheral elements of the intervention. The steering group suggested a number of additions and considerations (see Appendix 12) to support feasibility. These suggestions are summarised below.
-
The impact on NHS workloads, including organisational capacity to cope, needs to be considered when raising awareness of asthma.
-
Integrated and secure information technology (IT) services were deemed essential for programme success.
-
Strong support from HCPs to enable behavioural change, encompassing education, skills training and organisational revisions would be necessary for implementation.
-
Lay and professional educator partnerships could be pragmatic and effective educational delivery systems.
By taking the above points into consideration in addition to the qualitative data from phases 2 and 3, the research team were able to identify salient components of an intervention programme aimed at improving ‘getting a diagnosis’ of asthma. Mindful of the IM model and the scoping review of interventions, it was concluded that awareness (addressing knowledge deficits), context (mindful of cultural and organisational parameters) and training (to enhance self-efficacy and encompass education) were essential components of the intervention program. This led to the coining of the name ‘ACT [Awareness, Context (cultural and organisational) and Training] on Asthma’ when making reference to the intervention programme. ‘ACT on Asthma’ recognises that achieving a diagnosis of asthma does not only rely on the medical investigations but starts with awareness of the symptoms, awareness of the services available for diagnosis and awareness of the procedures for diagnosis. These all require the involvement of children, parents, communities and HCPs. The context in which the programme was to be implemented was equally important. Within the UK, health service organisational barriers impede presentation to professionals, communication between families and professionals, and professionals’ ability to utilise existing asthma diagnostic pathways. Training enables children, families and professionals to achieve greater awareness and overcome organisational barriers.
Translating strategies into organised programme components
The process used to develop the ‘ACT on Asthma’ intervention programme resulted in a multifaceted intervention, simultaneously addressing several levels of the socioecological model. Each arm of the ‘ACT on Asthma’ intervention programme was translated into component parts. The programme was thus based on both the principles of participatory research – shared knowledge expressed by service users and providers, starting at grassroots level and building upwards – and the socioecological approach of moving the focus away from individual knowledge, attitudes and behaviours and towards the wider layers of influence that include the community and social context, environment and organisational systems.
The research team reviewed change objectives and strategies to identify key components that were encompassed by the majority of strategies. Consideration was also given to strategies that fit the theories we were drawing upon. It was during this process of developing and designing intervention components that the value of IM appeared most evident: intervention components and content of material was directed by previously noted strategies from the scoping review (see Appendix 10), and theory. For example, the suggestion of the use of layperson and professional educators was informed by social cognitive theory, with respect to role models who would be culturally and professionally acceptable. Similarly, the use of vignettes and stories woven into education and training modules was informed by modelling. This presented the opportunity to demonstrate effective coping or develop beliefs that particular strategies would have benefit.
The draft ‘ACT on Asthma’ intervention diagnostic programme
The intervention programme was underpinned by the findings from the qualitative research work carried out with communities, parents, children and the HCPs in phases 2 and 3 of the project and informed by the systematic evidence synthesis in phase 1. The proposed intervention programme represented an enhanced service for the management of paediatric asthma. The data from previous phases of the study highlighted the need for consistency within the NHS. Consideration by the team regarding the delivery of consistency across a range of services across an asthma pathway led to the draft programme being centred on a co-ordinating team with satellite arms reflecting the different elements of the programme, providing a multifaceted but integrated approach. The proposed arms of the intervention programme are the mechanisms for delivering the intervention, and these do not change regardless of the ethnicity of the families involved. However, the content for each arm comes from the data collected in the previous phases, and as such the content would need to be tailored for South Asian families based on differences reported in the data (see Tables 8–14). Each arm of the enhanced service linked into the others; however, by co-ordinating from one central team, consistency of message and the ability to effectively co-ordinate asthma management across the multiple services involved would be enhanced. The basis for each arm is presented below.
Clinical support arm
The aim of this arm of the programme was to ensure consistency and quality of diagnostic approach regardless of where the patient presents for diagnosis and management. The aim was not to take over all asthma management, but to offer additional support to GPs.
Supporting evidence for a clinical support arm from phases 2 and 3
-
Parents and professionals reported that inconsistent and contradictory advice, information and services are given by different professionals at different times and in different places. Furthermore, parents reported long delays in receiving any information regarding asthma, and that access to detailed, relevant information was difficult and reliant on having a diagnosis of asthma.
-
These variations caused confusion as to the correct management or correct avenues for regular and emergency care, in both families and professionals. These variations were found to diminish parental confidence in individuals and the NHS, and affected the seriousness with which asthma was taken. These variations also diminished professionals’ respect for colleagues. Parents perceived these variations to be particularly problematic when crossing between primary, secondary and tertiary care and this was because notes or child information were not always shared across different institutional boundaries. Professionals supported addressing this problem and highlighted that the lack of information sharing between sections of the NHS was a significant problem.
-
-
Families perceived that GPs did not test children for asthma due to time or financial constraints or a lack of interest in doing so.
-
HCPs reported that testing was not always needed and that clinical diagnosis often sufficed; however, HCPs also reported that at times where further testing or further patient education may be desired, they could not access such services due to either unclear referral pathways, lack of knowledge of available services or the inability to request only a one-off review from a tertiary service.
-
-
Parents reported that EDs were used for various reasons relating to service provisions.
-
GP services were shut or appointments were unavailable.
-
Parents also viewed EDs as appropriate for a child with difficulty breathing because GPs were not equipped to handle acutely unwell children, either in terms of equipment or knowledge.
-
Parents also indicated that knowledge of alternatives to ED presentation were low. This was more common for the South Asian families.
-
-
Schools reported that information regarding diagnosis of asthma was largely provided by parents. This indicated that a school’s ability to manage asthma in a child relies on parents’ understandings and acceptance of the diagnosis, as well as parental provision of information and inhalers to the school.
-
Parents and professionals specifically requested a more co-ordinated service across primary, secondary and tertiary care that would encompass not just children with diagnosed asthma, but also those with possible asthma or using an inhaler so that these families could access information and education in a timely manner.
Raising-awareness arm
The aim of this arm of the programme was to increase awareness of asthma among South Asian families, communities and professionals working with South Asian families as a means of enhancing the timeliness and accuracy of diagnosis of asthma in South Asian children. Our work recognised that this was more relevant for the South Asian families than the White British families; this highlighted the importance of the inclusion of this arm.
Supporting evidence for raising-awareness arm
-
Interview and focus group data identified that parents waited several years after the onset of symptoms or treatments before a clear diagnosis of asthma was made. Some did not receive a clear diagnosis at all. This was perceived to be due to numerous factors including:
-
a lack of familiarity among families and community members of asthma as a possible explanation for children’s symptoms
-
a perception of normality for children who are coughing or have reduced activity levels in response to UK living conditions and weather
-
misattribution of symptoms of asthma to other conditions which are then managed accordingly
-
a lack of familiarity among families and professionals in the varying presentations of asthma in young children
-
a perception that asthma cannot or should not be diagnosed in certain categories of child (e.g. those under 5 years or those without an acute attack)
-
a lack of importance attached to asthma by families, extended families, community members and professionals.
-
-
Parents found this delay in diagnosis distressing, as they were concerned that, without diagnosis, treatments may not have been implemented as quickly as needed, or at all. In contrast, HCPs felt that appropriate treatments could be offered without a clear diagnosis.
-
Interview data further identified that for parents, having a clear diagnosis of asthma increased the importance and significance that parents attached to asthma management.
-
South Asian families were influenced by extended family, key informants and general community members in varying ways:
-
Even though families did not necessarily perceive the influence, parents still echoed views and suggestions prevalent within the South Asian community.
-
Parents have competing priorities, particularly when caring for other family members in addition to children.
-
Although parents believed traditional attitudes to be changing, they had not changed yet.
-
-
Parents reported feeling that schools did not always understand their child’s asthma or medication needs, and may not always recognise asthma in children or have the capacity to act appropriately.
Education and skills training arm
The aim of this arm of the programme was to provide a multicomponent programme of education and skills training modules that would provide a shared and consistent platform for education and training for all. This would ensure consistency of messages across the service. This was an important arm for all families, both South Asian and White British, but as we see from previous phases (2 and 3), the content needs to be specifically tailored.
Supporting evidence for education and skills training arm
-
Families perceived long delays in receiving a clear diagnosis of asthma, which they felt impacted on the treatment received, the information and support provided and the importance the families then placed on the condition.
-
Families believed that GPs did not feel any need to confirm or diagnose asthma and were happy to prescribe antibiotics, cough medicines and inhalers without a diagnosis. Often they did not explain the diagnosis even if the term asthma was used.
-
HCPs also reported that time and language barriers prevented detailed explanations, or that detailed explanations were not necessarily part of their role or part of diagnosing asthma.
-
-
Interview data further identified that for parents, having a clear diagnosis of asthma increased the importance and significance that parents attached to asthma management.
-
Knowledge of asthma symptoms, signs, treatments and outcomes among families and communities, in specific relation to children, was limited.
-
Similarly, knowledge of how the NHS works, and specifically the roles of multiple HCPs and the diagnostic pathway for asthma, was very limited, particularly among individuals who were not UK born.
-
Among healthcare and educational professionals, confidence in management in specific relation to paediatric asthma was variable, with options for training and education reliant on individual choices for continued professional development rather than a co-ordinated programme with regular updates.
-
Parents highlighted the variable knowledge among GPs, hospital doctors, nurses and teachers as an area of particular concern.
-
-
The level of knowledge and skill in managing paediatric asthma varied between parents and between professionals.
-
The content of information and advice given to parents by professionals in different settings was variable. This caused considerable confusion and eroded faith in the healthcare service. Ensuring consistency of information and message was vital.
-
Modular education and training programmes can be effective in enhancing chronic disease management, for example DESMOND (Diabetes Education and Self-Management for On-going and Newly Diagnosed) for diabetes. 179
Working closely with healthcare practitioners and partners enabled the research team to discuss the feasibility of the proposed ‘ACT on Asthma’ intervention. The intervention was modified and refined with input from stakeholders. However, the research team made efforts to engage with commissioners, but this was largely unsuccessful. MIA was progressing at a time when there were many changes to the structure of the NHS. Commissioners’ time, attention and focus was therefore engaged with these very complex processes, which meant that their involvement in research was not prioritised. In addition, some commissioners approached at the outset of the study were not in their roles at the end stage of the study, which again influenced the strength of partnerships established in earlier phases of the study. The intervention could therefore not be assessed for feasibility from a commissioning perspective. Future research should further attempt to engage with commissioners to gain insight into the sustainability and likelihood of successful implementation of the intervention programme. Previous studies179 have shown that elements of the proposed intervention programme, such as the face-to-face and electronic training, can be successful and effective, further validating the proposed intervention. However, further research needs to be done to assess the practicality and feasibility of implementing the ‘ACT on Asthma’ intervention within the NHS. This should include further refinement of the intervention with commissioners.
Economic evaluation
A health economist was employed to review the programme in order to identify the key cost elements and in reference to specific examples, to assist in costing this intervention programme to the NHS. A scoping exercise, rather than a definitive economic analysis, was conducted. It was not a cost-effectiveness analysis and aimed to provide an indication of the resource items that might require costing should the proposal be implemented (see Appendix 13). The economic evaluation showed that full implementation of the ‘ACT on Asthma’ programme would be relatively costly. However, the MIA study has provided information that can be utilised in several contexts and offers insights into both substantive issues of asthma management and a process of working with communities, families and HCPs from which both parents and providers can draw a range of actions to improve the asthma management pathway for children.
Section D: finalisation workshop
Once the exemplar theme to be addressed in this study had been chosen and a draft exemplar intervention programme developed to address it, the draft programme was presented and collaboratively refined at the finalisation workshop by including both South Asian and White British adults, children and health professionals (see Appendix 14 for photographs of the workshops).
-
Participants were divided in advance into groups:
-
Children were kept with at least one parent, with parents potentially separated from each other.
-
Groups were intentionally mixed between adults, children and HCPs.
-
Those requiring interpretation were placed together according to language required, with interpreters available throughout the workshop.
-
-
The draft intervention programme was presented to all participants.
-
Small group discussions were used by each group to explore one particular aspect of the intervention programme.
-
Participants were asked to consider if they would or would not use this aspect, how they might improve it and what problems they could foresee in implementing it.
-
Tables were not asked to achieve consensus.
-
Where diverging opinions existed, tables were asked to note down both/all opinions.
-
Each group nominated one person to scribe and then summarise the group opinions to the workshop.
-
For each table, one child and one adult presented the table’s views.
-
Sampling and recruitment
All participants who indicated agreement to be contacted were invited to attend this workshop: no additional participants were recruited into the study at this stage. Thirty participants participated in the finalisation workshops (two HCPs, 15 parents with a child with asthma, 12 children and one key informant).
Methods
Participants were divided in advance into groups. Adults, children and HCPs were intentionally mixed; however, those with a need for interpreters were placed together according to language requirements. CFs were present to act as discussion facilitators and interpreters throughout the workshop. The draft intervention programme was briefly presented, followed by directed small group discussions to explore one particular aspect of the intervention programme. Group opinions were then fed back to the workshop. Within each group the facilitator was tasked to ensure that the tone and language remained accessible to the children present. This validation and revalidation process ensured that thoughts and feelings on the intervention from the communities involved could be heard and to ensure that participants’ messages had been heard and interpreted correctly. It was an iterative process whereby changes to the intervention programme were based on findings from this workshop to ensure that any changes were applicable and appropriate.
Workshop findings
The revisions were incorporated into the proposed intervention programme elements, with ‘ACT on Asthma’ modified to a four-arm programme, with the addition of an advice centre, based around a co-ordinating team.
Supporting evidence for the addition of an advice centre arm
From the finalisation workshop, it was evident that participants desired an advice centre, and they suggested a mobile unit where drop-in sessions, educational sessions and raising awareness could all occur. Parents felt that an advice centre would be useful, particularly if it was led by a trained layperson with bilingual staff. An advice centre could be a place for coffee mornings or to meet with other parents who live with a child with asthma, reducing any feelings of isolation that may exist within the community. In addition, many parents and HCPs in phases 2 and 3 suggested the utilisation of an advice centre.
The finalised ‘ACT on Asthma’ programme
As a result of the iterative process involved in programme modification, the final ‘ACT on Asthma’ programme comprised four arms. Each arm represented an intervention strategy. The four arms represented education and training, clinical support, advice centre and raising awareness. All arms were co-ordinated by a central team (Figure 7).
FIGURE 7.
Finalised ‘ACT on Asthma’ programme.
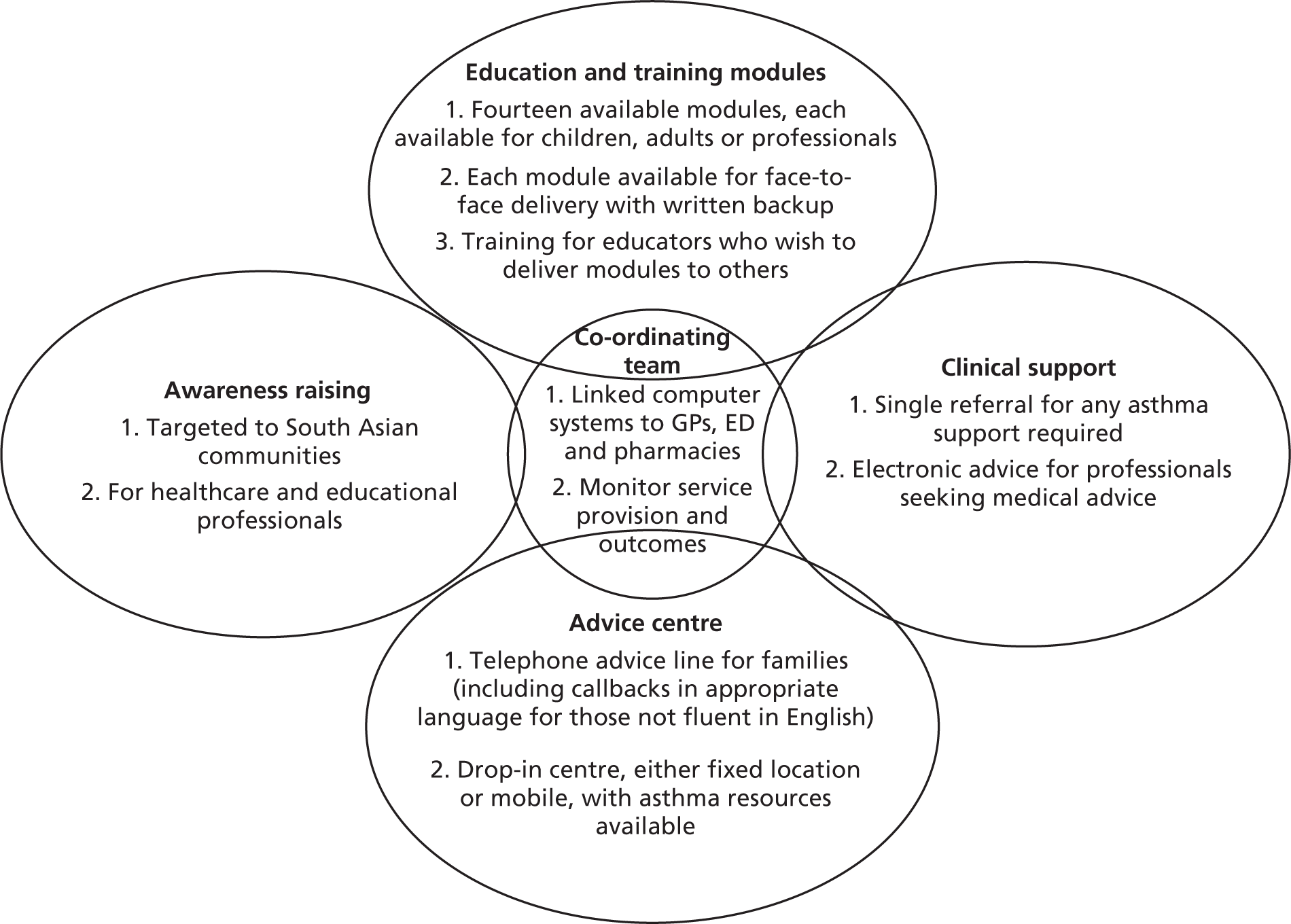
Education and training arm
The education and training arm would be presented as 14 modules, drawn from the qualitative data in phases 2 and 3. The content of the education modules was informed by the qualitative findings from previous phases alongside the understanding of the inter-related, multidimensional nature of problems that arise along the asthma pathway. This emerged from the family data in phase 3 and suggested that the issue of diagnosis inevitably impacts on other aspects of asthma management. This highlighted the necessity for the educational modules to incorporate other aspects of asthma management alongside getting a diagnosis. Some of the modules included were generic and relevant to all families; however, some were more relevant to the South Asian families and tailored to them to respond to the data reported in previous phases, particularly relating to complementary therapies and diet and asthma.
Modules selected were:
-
signs and symptoms – general knowledge of the symptoms of asthma or of asthma as a potential explanation for common symptoms
-
medicines for asthma – knowing what the different medicines are, what they are for and the benefits and negatives of taking them
-
inhaler skills training for children – specific ideas and tips for supporting children to take inhalers effectively
-
complementary therapies for asthma – advice and information on the evidence for or against the use of complementary therapies for asthma, including herbal treatments and breathing exercises
-
diet and asthma – specific advice on traditional dietary restrictions or encouragements within South Asian communities thought to be beneficial for asthma management
-
how to use the NHS – overview of NHS structure, what services are available and the importance of returning to seek further information and support, including the right to ask questions
-
acute versus preventative management – overview of why preventative management matters and the psychological principles of self-management
-
achieving effective consultations – communication skills training in how to achieve a successful consultation, with tailored advice according to whether it is being delivered for laypersons or for HCPs
-
mythbuster – common myths, ideas and suggestions in relation to asthma, with the evidence for and against each one
-
household adaptations and asthma – the current guidance on what changes to make around the home and why/why not
-
what to expect for a child with asthma – looking at what to expect from a child with asthma, levels of activity, strength and future careers
-
diagnosing asthma in children – explaining the diagnostic pathway for asthma
-
explaining asthma to children – skills and tools for explaining asthma
-
asthma and school – what parents should expect from schools, what schools should expect from parents, managing absence.
The modules would be grouped together and delivered as a fixed course. Completion of all modules would be necessary for completion of the course, although this could be achieved intensively (over a 2-day course) or gradually (by attending evening sessions over a period of weeks or months). The modules would be delivered face to face by a lay facilitator and a professional facilitator working together. There would also be a resource pack available online and given in hard copy to attendees. The modules would have three delivery formats: one for children, one for parents/laypersons, and one for professionals. Although presented differently, the content would remain broadly consistent regardless of delivery format.
Clinical support arm
The clinical support arm would be based on a linked computer system that could be used for referrals, for electronic advice and to monitor prescriptions for inhalers and audit data on paediatric asthma outcomes.
The IT package would include a computerised pro forma that prompts the professional to perform the required education, follow-up, referrals and tests, and monitors their completion. This pro forma would be the only referral needed to access any asthma service across the region, with the professional ticking which services are required and the co-ordinating team liaising with other service providers to fulfil the request.
The co-ordinating team would map all asthma resources in the local area, including the expertise and resources available at each GP practice in relation to diagnosis and management of asthma in children. This would enable the co-ordinating centre to receive referrals and advice/information requests from GPs or other HCPs and direct their queries to the appropriate resource.
Advice centre arm
An advice centre that anyone can attend, staffed by a mixture of volunteers and educators, would be set up. The advice centre would contain hard copy and electronic resources relating to asthma, functioning as a library. It would also be a centre for informal advice and conversation and a location for evening education and skills training modules to be held. The advice centre would also be available by telephone, with links to the Asthma UK advice line, such that local persons could ring the advice centre, and if their query could not be answered locally, Asthma UK could be contacted as needed.
Raising awareness arm
The raising awareness arm has two key elements to consider: greater awareness of the signs and symptoms of asthma in children and the strengths and limitations of the diagnostic pathway for asthma in children.
Section E: dissemination
The intervention programme and emergent findings have been disseminated to the participants and to relevant external organisations in targeted events to highlight specific components of the intervention to the relevant audiences. As a consequence, the nature of the dissemination activities varied significantly.
Dissemination activities have ranged from local presentations to wider dissemination events, including publications and conference presentations. A full list of dissemination activities can be found in Appendix 15.
Participant feedback
As the overall aim of the MIA study was to use a collaborative participatory approach to design an intervention to optimise the asthma management pathway for South Asian children with asthma, it was important to explore participants’ experiences of being involved in this type of research study to determine whether or not it was a beneficial process.
To assess participants’ views of their involvement in the MIA project, a sample were asked to take part in a short interview. While it was important to try to capture participants’ experiences of the project, the research team felt that this interview should be relatively brief given the considerable time and effort that many community-based participants had already committed to the project. The interviews thus covered three main areas:
-
experiences of taking part, including experiences of working relationships with other participants and their perceptions of partnership in the research
-
perceptions of the usefulness of involving families and professionals and whether or not they felt that their contribution was relevant to the study
-
whether or not participants felt that children gained from being involved in the study and how (see Appendix 16 for extended results).
The feedback from the participant interviews suggested that beneficial relationships between researchers and participants were developed. The majority of study participants reported positive experiences of participation, including beneficial working relationships with the research team and with other participants. Focus group and parent participants in particular valued the learning that they felt had occurred in the process of their participation in the project. An extended discussion of the feedback is given in Appendix 16.
Discussion
Phase 4 sought to develop an intervention programme based around ‘getting a diagnosis’, selected for the striking disparity between South Asian parents’ and HCPs’ rankings. ‘Getting a diagnosis’ was approached from a socio-ecological and holistic perspective, covering a number of steps required within the diagnostic process. These steps included an awareness of asthma, recognition of symptoms, accessing health care and the investigative process to make the diagnosis of asthma, and not solely the narrow steps of investigating the child to confirm or refute a diagnosis. In this way, a more collaborative approach was adopted, key to conducting health research with service users and providers.
The aim of phase 4, coupled with the overall aim of the MIA study, was to develop a tailored intervention planning framework and to draw from this a tailored, multifaceted, integrated asthma intervention programme. This was achieved and is presented as the ‘ACT on Asthma’ programme. ‘ACT on Asthma’ is a multifaceted, integrated programme, identifying multiple actors, behaviours and determinants that make up barriers to effective management. These data have already been, and will continue to be, made available to service providers and commissioners, from which further evidence-based intervention programmes can be developed. Throughout the study, a modified framework analysis was used to prepare the data for the data breakdown and integration of phase 4, section A. These techniques were drawn from IM (see Chapter 1) but modified to be more applicable to the broader-based approach of the MIA study. This modified data breakdown approach developed for use in the current study has both strengths and limitations. All data gathered during phases 2 and 3 were successfully tabulated in the same manner within a predefined framework, enabling the selection of appropriate social or psychological theories for each element in the table, thereby incorporating flexibility while ensuring a systematic and transparent approach. Additionally, tabulation permitted cross-comparison and identification of the same behaviour or determinant across multiple sources and domains. This allowed the research team to highlight key points where one intervention might be applicable to multiple groups or settings, yet still be able to identify unique behaviours and determinants where specific interventions are needed. This ensured that all needs could be considered in developing the programme. This is consistent with the principles of the socioecological model upon which this study is based, but also permits focus on core elements with potential to target the widest number of behaviours and determinants. This broad-based approach draws upon multiple sources of information which encompasses multiple issues that can be teased out, with each one worked up into an intervention programme as required. These advantages enable the development of an intervention programme that is multifaceted in terms of its evidence and theoretical base and capable of reaching the target audience. Furthermore, the use of explicit structured tables ensured that focus on programme objectives and reduction of subjective bias was enhanced, which was vital in the implementation and evaluation stages.
Chapter 6 contains further reflections, discussions and conclusions regarding the overall process of collaboration as used in the MIA project.
Chapter 6 Discussion, conclusions and future recommendations
Working with minority ethnic communities, engaging multiple organisations in a changing NHS and involving children in research brought many complex challenges to the MIA project, the overarching aim of which was to use a collaborative method of designing healthcare interventions to develop an intervention programme for South Asian children with asthma. Each of the earlier chapters in this report closes with a discussion and conclusion of each phase of MIA, all ultimately leading to the ‘ACT on Asthma’ intervention programme. This chapter will, firstly, critically reflect on the strengths and challenges of using a participatory approach to meet the methodological objective of the project in developing a multifaceted tailored intervention. This is followed by a discussion of the substantive findings relating to asthma management in South Asian families (asthma being used as an exemplar condition for this study) and an outline of the implications of this work for policy, practice and future research.
Critical reflections on the study approach, strengths and challenges
Intervention mapping provided the research team with the opportunity to utilise a process that was systematic, and ensured that the research was informed by theory and that the different levels involved in asthma management were considered. Through working in a multidisciplinary fashion, all team members were able to learn from different people and found the experience enriching.
Principles behind using a participatory research approach with South Asian participants
The MRC guidance for designing and evaluating complex interventions advocates a staged approach involving end users in the design process, and suggests that interventions that are tailored to the needs of minority ethnic groups are more likely to be successful. 60 The MIA study aimed to address both issues: tailoring for the needs of the South Asian community and also developing a participatory staged approach that could be translated to other communities and other clinical areas. The MIA team made a positive decision to test the approach on two groups considered to be ‘hard to reach’: minority ethnic groups and young children.
Despite the existence of ethnic variations in health and disease,25 minority ethnic groups are under-represented in medical research. 126 This is ethically questionable,180 introduces bias181 and limits generalisability by overlooking the influence of potential genetic predisposition, diet and environmental factors on responses to disease and medication. 87,126,182 Varying explanations for the under-recruitment of minority ethnic groups have been suggested, including investigator bias,183 misunderstandings regarding the aims of research among potential participants,183,184 the use of universal methods for recruitment, informed consent and data collection rather than those tailored to the community,134,136,185–188 language barriers with associated time and cost implications,86,91,183 the need to use CFs/lay researchers131 and additional efforts being required for the dissemination of results to participants and communities. 87 With an aim to overcome some of these perceived barriers, the MIA study adopted a participatory research approach utilising culturally sensitive methods such as working with CFs, using audio consent and identifying venues acceptable to the communities concerned (see Chapter 2). This approach enabled the researchers to take a broader perspective; not focusing solely on NHS-led strategies for asthma management, but accommodating a wide range of attitudes, beliefs and experiences with regard to asthma, and recognising the priorities of service users. The project was intended to provide a ‘proof of concept’ testing to establish the principle for tailoring interventions for use with South Asian communities.
Successes and challenges in using a participatory approach
Taking a participatory approach, and following IM methods, was extremely resource intensive, both financially but also in terms of staff time and staff engagement.
A challenge when using participatory research is that the scope of the project can grow, as it is not apparent from the outset what the needs and agendas of the participants might be. Given the volume of data generated in the study, it was not feasible to develop an entire intervention, but rather in developing this plan and demonstrating a methodology for development of a tailored intervention programme, we have laid the foundation and provided the data for intervention development addressing remaining themes within the plan to take place in the future.
Recruitment of South Asian participants
One of the key challenges in the MIA project was to successfully engage South Asian families and community members in the research. Despite exceeding recruitment targets throughout, the resources, energy and time required to sustain recruitment and retention of participants over the study period were significant. The study team had prior experience of working with CFs and recognised their value in supporting access to identified communities. CFs were, therefore, central to the success of the recruitment and retention of participants within the study. The snowball sampling method of recruitment adopted for the MIA study can lead to the positive selection of a limited subsection of society. It has many benefits, however, including enabling access to groups otherwise reluctant to engage with any forms of social or health research.
Research participation is known to be influenced by the manner and context in which participants are approached, as well as the role and position of the person recruiting them. 189,190 The CFs were selected from the participants’ ethnoreligious communities and it is assumed that they were more aware of cultural sensitivities and needs of participants. As a result, this increases the level of trust between participants and the university-based research team. The CFs also played a key role in assisting the academic team to interpret the qualitative data in a culturally sensitive way during the analysis phases of the project. The project followed an iterative process, with constant referral back to CFs and community members, supporting validation of the process and interpretation of the data and enabling them to guide the direction of the project. The success of these strategies suggests that the term ‘hard to reach’ needs to be reconsidered as a descriptor for minority ethnic communities. Successful engagement was determined by advice from the CFs and parent representatives involved in the study. Reflection, revalidation and endorsement of findings from the workshops reinforced the successful manner in which participants were engaged within the study. Parent representatives on the project steering group also assured the research team that the MIA project had explored different ethnic groups in a more thorough and comprehensive manner than other research projects they had been involved in. As the CFs had previously been involved in other research projects, they were able to comment on the new methods for recruitment and engagement used in the MIA project. Despite successful engagement methods, the challenges encountered must not be underestimated. Recruiting and training CFs is time-consuming.
Identification and recruitment of the CFs in the MIA study was eased by the fact that several had worked with members of the research team on previous community-based projects and, thus, were experienced in interviews and focus group facilitation. As a consequence, only minimal refresher training on issues such as consent and research ethics was required. This prior experience reduced the financial costs and time related to recruitment and training. Additional facilitators were needed to meet the specific language and cultural needs of MIA participants; however, this required further expenditure on training which was often outside normal working hours. In addition to being skilled, it is also important that CFs ensure that they have a good understanding of the particular topic they are involved in researching. The CFs in the MIA study were thus paid to attend a special briefing sessions on issues relating to asthma and its management in children. The cost of training community-based researchers in research methods and costs associated with the need to familiarise them with the context and content of the study need to be recognised and included in any research funding application.
One limitation of having the CFs centrally involved in recruitment to the community study and to the workshops was that they predominantly approached families or other community members drawn from an established group of contacts. This may have limited the demographic profile of available participants and, as a consequence, the research team regularly reviewed demographic data to try to overcome this possible limitation. Additionally, the repeated use of the same CFs, who drew on the same communities or contacts, may eventually result in ‘research fatigue’. Research fatigue, when individuals and groups become tired of engaging with research, can be found in all forms of research. 191 It can be particularly problematic in qualitative and participatory research, where a high degree of active personal involvement, constant thought and consideration and long-term involvement are required by participants. 191 Research fatigue manifests in a reluctance to engage further with existing research or a reluctance to engage with new research, and typically occurs in two contexts: projects that require participation over time192 and research groups where requests for participation are common, such as limited or ‘hard-to-reach’ populations. 193,194 Both contexts were relevant to the MIA project. Research fatigue was minimised by providing feedback on the outcomes of the research. This enabled participants to perceive the benefits of their involvement by clearly delineating expectations and requirements at initial engagement191 and included consideration of school and religious holidays. Awareness of research fatigue led to a request by the research team to extend the timeline for the study to reduce the intensity of the commitment requested from participants. Future participatory research studies may wish to consider ‘slowing the study’ to account for the ‘research fatigue’ described here and thereby enhance the retention of participants throughout the study period.
An additional successful, easily transferable strategy for including diverse perspectives was the inclusion of parents as members of both the research team and the advisory group. The parent research team member (and grant co-applicant) was present at each research meeting, allowing for direct and immediate feedback on research methods and data interpretation. The parent representative on the advisory group provided a second individual who was removed from the day-to-day running of the project, but continued to provide a valuable role in presenting a parental perspective to the overall management of the project in addition to contributing to design of interview schedules and data interpretation. Both parent advisors were also key players in the recruitment of participants.
Utilising workshops to facilitate community and parental engagement
Three participatory workshops were held in phase 4 of the study to prioritise key themes from earlier data and to review the proposed intervention (see Chapter 5). The benefits of participatory workshops are that they can provide participants with opportunities to engender shared ownership of research data in addition to opportunities to meet others, share perspectives and test ideas in a non-judgemental and informal forum. 195 During the MIA workshops, participants (including children) worked in partnership with the research team in setting priorities, determining the ongoing direction of the research and tailoring the intervention programme. However, it is also important to recognise the limitations of this process. One key issue involved the difficulty in achieving a balance between the depth and breadth of information presented. Furthermore, the participatory nature of MIA resulted in a diverse set of participants at the workshops with variable knowledge and experience of asthma, and diverse language needs. The finalisation workshop included children and adults working together, which also brought further diversity into play. This required intense preparation to ensure that all participants could access and understand the information being presented and to keep all participants effectively engaged. This planning and preparation required a significant investment of time for the research team and this needs to be fully recognised and costed in research funding bids.
Language differences within the workshops were addressed by having each CF provide simultaneous translation, with breaks to allow for differences in the speed of translation. In addition to providing direct translation, the CFs were able to provide context to the discussion for the participants. While largely successful in facilitating the use of five different languages during the workshops, this approach also has drawbacks as simultaneous translation can be disruptive for participants. 196 The investment of time and effort on the part of many MIA participants was significant as many were involved in both interviews and workshops. This was minimised by carrying out interviews in participants’ homes and workshops in venues local to the respective communities. These venues were accessible by public transport, with taxis made available for those with specific needs. Workshops were held either at weekends or in the evenings at times judged to be suitable to most participants. While convenient for community participants, this had likely reduced the level of engagement of HCPs. This highlighted an important dilemma in accommodating competing needs. Low-value vouchers for local shops were provided for workshop participants to thank them for their participation, and an on-site crèche was for provided for those who needed to bring along children not directly involved in the study. Additional considerations included providing refreshments (including full meals) for the participants and accommodating diverse dietary requirements. These practical and logistical challenges were minimised by working with established, community-run ‘South Asian’ centres and similar venues, many of which had expertise in catering for their local communities.
Collaborating with healthcare professionals
Engagement with HCPs was considered to be a crucial element in the study. A range of HCPs were invited to be members of the advisory board and take part as participants in phases 3 and 4. They were selected not only for their knowledge related to asthma but also for their experience in commissioning or providing local services. Access to HCPs for focus groups and individual interviews was facilitated by the PCRN and CLRN. HCP participants included frontline clinical staff in addition to service managers and commissioners. It was hoped that, in this way, further insight into the organisational and aspects of asthma could be gained. However, engaging and retaining HCP involvement in the study was often challenging. Attendance at workshops and at advisory group meetings proved particularly difficult for HCPs, despite the offer of financial reimbursement to employers to support their release from primary activities. Holding workshops at weekends and in the evenings was preferred by the family and community participants, but presented a barrier to the participation of healthcare providers. HCP engagement in the study was also negatively impacted by the concurrent reorganisation and reconfiguration of services being undertaken during the course of the study. This meant that not only did personnel in key positions change through the duration of the study, but also participation in research generally appeared to be a reduced priority, especially for those participants faced with uncertainty about their employment or those taking on significantly revised roles. Membership on the advisory team was also difficult to sustain. Changes within organisations meant that staff turnover was frequent, leading to individuals on the advisory panel leaving to take up positions elsewhere. This state of flux within the NHS thus had an impact on the conduct of research, requiring additional time and energy from the research team to attempt to recruit and sustain involvement of HCPs. While recruitment to interviews was eventually successfully achieved, with some HCPs attending community-based workshops, the research team decided to use electronic ‘workshops’ for HCPs, which were of value, but perhaps not as successful as engaging people in direct group interaction. In this study, therefore, the HCPs were found to be ‘harder’ to reach than the South Asian community.
Critical reflection on children’s involvement in the Management and Interventions for Asthma project
Research collaboration with children is encouraged and has been embedded in national policy. 2 However, the evidence supporting involvement generally and collaboration specifically is limited. This gives the impression that the drive towards collaboration is based on the assumption that collaboration is best practice, rather than on evidence of its effectiveness. 197 The MRC guidance for designing and evaluating complex interventions60 proposes involving end users in the design process and, clearly, within the context of this project, such users are children as well as parents. Collaborating with children requires additional time commitments by trained personnel and provision of child-friendly resources. As a consequence, this has a cost implication.
There are several reported benefits to collaborating with children. These include identifying different perspectives on research topics and methods; improving the suitability of research tools for use with other children; improving the quality and depth of interview data by enabling other children to be more relaxed and open; improving the dissemination and uptake of research by enabling target children to identify with a child of a similar age and characteristics; enhancing adults’ perceptions of children’s knowledge and value in research; increasing children’s self-confidence and self-esteem; and teaching children valuable skills. 110,198–200 The MIA study obtained informed consent and enrolled children into the study as interviewees in phase 3, but also directly engaged the children in prioritisation and intervention development through their active participation in the phase 4 workshops. It is important, therefore, to reflect on the strengths and challenges of this approach.
Interviews with young children
All children in the MIA study were of primary school age (aged 5–12 years). They were invited to be interviewed either with their parents or separately. Review of the interview transcripts and reflection by the study team has highlighted some of the challenges encountered when interviewing children at this young age, including limited depth of data. While qualitative experts have laid down internationally accepted standards for conducting good quality qualitative interviews,201–203 such as building rapport between the interviewer and interviewee, the use of open-ended questions and consideration of the location and space for the interview to optimise comfort and focus, a lack of specific guidance when conducting interviews with the 5- to 12-year-old age group has been noted. 204 Research has demonstrated that very young children can provide important information and insights regarding their health experiences. However, there has been relatively little research into the practicalities of applying standard qualitative techniques to young children. 205
Building rapport with children during the interviews for this study was at times challenging. To overcome this, several techniques were used; the use of first names only (thereby avoiding identifying the interviewer as a researcher or a medical doctor), asking the parents to be present at the beginning of the interview (or throughout if preferred) and the use of activities such as drawing, writing or games to engage the children. However, each of these techniques created additional challenges. Parents frequently introduced the interviewer to the child, for example ‘a doctor who wants to ask you questions about your asthma’, thus setting the tone of the interview. Additionally, parents invited to join the interview at the beginning found it difficult to then leave the interview, which changed the dynamics of the interview from a child-only interview to a family interview. Further problems included children not wishing to participate in the activities provided, such as drawing, and the activities themselves increasing the length of time required for the interviews, which placed additional burden on the child and interviewer.
Open-ended questions are recommended in qualitative research but are more difficult to adopt when interviewing young children. In this study, children struggled with answering hypothetical questions and responded more easily to closed questions, which limited the depth of the interviews. This experience was in line with Irwin and Johnson205 and Wilson and Powell206 who reported that closed questions were less taxing on a child’s linguistic and reasoning skills and less daunting. Considering the use of peer researchers or of alternative participatory methods of data collection such as games, especially with the younger children, may have been more effective methods of eliciting accounts of their experiences.
The timing and locations of the interviews were further relevant considerations. Interview dates, times and locations for the MIA study were all selected by the parents. Accessing children after school was more practical but meant that, as a result, some of the children were tired at the time of interview. Parental choice of time and venue may also not be one that is preferable to the child, demonstrating that in trying to overcome as many barriers as possible to increase recruitment of children by engaging with parents, the child’s choice of interview style may be overlooked. In addition, the length of question schedules should be adjusted to accommodate the additional time required to engage in any ‘creative’ or ‘relaxing’ activities and consideration should be given to whether or not multiple meetings may be required to enable a child to develop familiarity with the interviewer.
Workshops with children
The children participated in two styles of workshops: prioritisation workshops and finalisation workshops. Evidence suggests that to work effectively with children, the research methods used need to engage children’s interests174 and take into account variations in age, understanding and ability. There was greater scope to adapt methods to suit children within the workshops than in the interviews. It was possible to offer multiple methods of engagement within one event and, as a result, children were able to work together as a group. More discussion and visual/physical-based methods were adopted in place of the presentational and written methods used with adults.
Summary and discussion of key findings
One of the objectives of the MIA study was to use a participatory model of research with the South Asian community. The collaborative approach utilised in the study was successful in reaching its recruitment target and retaining participants throughout the project, despite the challenges faced. This illustrates that the South Asian community, including children, are not ‘hard to reach’ if appropriate techniques are adopted. The finalisation workshops brought together the South Asian and White British participants in order to help identify generic and specific components for the intervention programme. Bringing both groups together demonstrated a shared goal and helped to validate the findings. Participants were valuable partners in the decisions made throughout the process and were integral to shaping the final ‘ACT on Asthma’ intervention programme.
Asthma management in South Asian children
This section of the report addresses the achievement of the substantive objective of the MIA project, which was to explore the barriers and facilitators to effective management of childhood asthma in South Asian families, provide the evidence for the asthma intervention planning framework and produce the tailored, multifaceted MIA asthma intervention programme ‘ACT on Asthma’.
Each phase of the study is briefly described and discussed. Further information is provided in earlier report chapters.
In aiming to address the ethnic inequalities in asthma outcomes and management identified in Chapter 1, the MIA study aimed to understand the underlying reasons for the barriers to optimal asthma management for South Asian children across the whole pathway from diagnosis to treatment, from living with asthma at home and in the community to requiring admission from an acute attack. Furthermore, the project sought to gain insight into the perspectives and experiences of communities, families and HCPs.
The socio-ecological model which underpinned the project recognised the significance of considering issues that arise from the community context, the individual family and child, and the organisational/environmental context. An overarching evidence-based, integrated, needs-driven, multifaceted asthma intervention planning framework was then developed to address the barriers identified for both healthcare providers and families. The ‘ACT on Asthma’ intervention programme was devised for one of the key themes identified by families: ‘getting a diagnosis’ (see Chapter 4). This was achieved as the culmination of a phased approach involving a literature review, a community-based study of understandings of asthma, and interviews with parents and children in families living with childhood asthma and service providers, followed by the collaborative development of an intervention. Chapter 5 describes in detail the supporting evidence for each aspect of ‘ACT on Asthma’.
The community study: perceptions of childhood asthma in South Asian communities
Phase 2 of the MIA study aimed to address lay perceptions of asthma and the impact of cultural, religious and wider socioenvironmental influences and to form a holistic picture of the context of childhood asthma in South Asian communities.
This phase, often not included in similar studies, has time and financial implications and may require culturally sensitive research methods to be utilised (see Chapter 3). The additional benefit of including this phase in the study, therefore, needs to be justified. As demonstrated by the socio-ecological model, patients do not live in isolation but rather within the context of their family and the community all having an influence on behaviour. Understanding these influences can, therefore, enhance the effectiveness of an intervention and also provide evidence that health programmes need to target the wider community as well as that of the individual patient or family.
The focus group discussions with community members suggest that, in many cases, lay understandings of asthma contrast with medical perceptions of cases, triggers, symptoms, treatment and outcomes, suggesting a need for better public information about asthma within these communities. Key findings in this phase were the variations in the meaning and use of the words ‘asthma’ and ‘wheeze’, particularly where language barriers were also present, beliefs about the heritability of asthma, understanding of asthma as episodic rather than chronic, concerns about asthma as a contagious condition, concerns about the negative side effects of asthma medication, the presence of stigma related to an asthma diagnosis, and strong beliefs regarding the benefits of alternative remedies and treatments including dietary modification. These perceptions of asthma and its impact can affect parental expectations and management, as well as families or individuals’ relationships and interactions with their community. Data suggested that fear or embarrassment that one’s child is unwell, potentially due to reactions from community members, may be preventing parents from seeking help and managing their child’s asthma effectively. Findings from phase 3 (see Chapter 4) further confirmed the continued influence of community norms and attitudes and, thus, the importance of including community members in intervention development when working with South Asian communities. These influences were recognised by the children and families, and led to one of the arms of the exemplar intervention programme (‘ACT on Asthma’; see Chapter 5) focusing on raising awareness of asthma within the South Asian community. At the same time, community members identified a range of issues relating to access to healthcare provision and the quality of care such as poor provision and lack of organisation of care within the NHS. These deficiencies in health care must also be addressed if true improvements are to be seen.
The management of childhood asthma: the perceptions of families and healthcare professionals
In phase 3, children, parents/carers and HCPs were interviewed to identify key factors relating to optimal asthma management. The inclusion of the White British group in this phase enabled the research team to identify which interventions were amenable to a universal approach, and which required tailoring to specific communities. Many of the problems facing families of a child with asthma were common to all communities: lack of understanding and knowledge about the origins or triggers of asthma, poorly communicated information, a lack of a written asthma plan, inconsistent care between HCPs, and dissatisfaction with the health service. However, some issues, such as barriers relating to information provision, were present in both groups but were exacerbated for South Asian families because of language barriers or translation issues and due to limited provision of information. Issues particularly relevant to South Asian families included the use of complementary therapies or adjusting diet to manage their child’s asthma. South Asian families were more likely to use the emergency services if they could not access their GP. The findings indicate one of the reasons for this was difficulty in recognising the severity of symptoms, resulting in delayed access to treatment.
As we have seen, families prioritised the category of ‘getting a diagnosis’ for asthma as an important area of intervention. This category encompasses issues for both families and healthcare providers. Interview and focus group data identified that many parents waited several years after the onset of symptoms or, in some cases, treatment, before a clear diagnosis was given to them. Diagnosis was dependent on parental recognition of problematic symptoms and knowledge of what is ‘normal’ for children and, for a minority of parents, a desire to avoid the stigma of illness (factors at the individual/family/community level). Prior to diagnosis, many families were unaware of asthma as a possible explanation for children’s symptoms or misattributed the symptoms to other conditions. Timely diagnosis, however, was also related to the knowledge and practices of HCPs with whom parents and children came into contact and the way in which services were provided (factors at the organisational/environmental level).
Families perceived long delays in receiving a clear diagnosis of asthma from health professionals, which they felt impacted on the treatment received, the information and support given and the importance that they attached to asthma management. They also reported variable knowledge of asthma among GPs, hospital doctors, nurses and teachers and that the content of advice and information given to them, including around diagnosis, varied between professionals and individuals. Inconsistent, and what parents sometimes perceived as contradictory, advice added to their confusion about correct management, reduced their confidence in the NHS and, in some cases, affected the seriousness with which asthma was taken. HCPs often had a different perception of the need for objective tests for asthma but also reported that where additional testing or patient education was desired they were often unable to access services due to unclear referral pathways.
Children (White British and South Asian) expressed similar perceptions of asthma to those of their parents, including beliefs about the contagious nature of asthma, mixing up causes and triggers of asthma and not understanding what a diagnosis of asthma meant. Children also described a fear of an acute attack. These data are consistent with previous research findings166,207,208 and highlight the lack of effective education-based interventions or their effective implementation. Compared with the adults, children were more focused on acute attacks. Confirming previous research,164,165 both White British and South Asian children described experiencing strong emotions during acute attacks and often felt scared or upset. Other feelings described included embarrassment or feelings of not being ‘normal’.
Healthcare providers also identified several issues that led to poor asthma management for children. These included barriers that occurred during consultations with South Asian families such as time and communication issues as a result of language barriers, perceptions of barriers to asthma management for South Asian families and professional and organisational barriers to asthma management. HCPs acknowledged that their focus was often on addressing medication requirements for treating asthma and indicated that they gave less attention to more holistic approaches to asthma management. HCPs also acknowledged that services were often not structured in a way that would enable them to meet the needs of South Asian families adequately, especially in relation to having the time to give more information and to adequately address the additional communication support needs which some families required. Professionals were also aware that parents faced difficult decisions about accessing care during acute episodes. Parents often used the ED because GP surgeries were closed, or because they were not confident that GPs were equipped to handle acutely unwell children, in terms of equipment or knowledge. Parental knowledge of alternatives to ED presentation was limited. These environmental factors were thus clearly identified by both parents and professionals as major barriers to optimum management. Many of the professionals interviewed were aware that parents received variable information about asthma. Both professionals and parents specifically requested a more co-ordinated approach across primary, secondary and tertiary care that would encompass children with diagnosed asthma, but also those with possible asthma or those using an inhaler, so that these families could access information and education in a timely manner. Both parents and professionals felt that there was an important role for schools in disseminating information about asthma as well as in helping parents and children living with asthma.
Identifying barriers and facilitators to optimal management is important; however, MIA has been able to provide further insight into some of the factors underpinning these barriers and, just as importantly, provided further evidence on levers that could be used to bring about change. Organisational discrimination such as the existence of ‘cultural stereotypes’ (i.e. viewing South Asian families as ‘difficult clients’) was also apparent. 38 If change is to be successful, organisational barriers and culture within the NHS need to be addressed in combination with the health beliefs and attitudes of families and communities.
The development of a collaborative intervention
The integration of the primary qualitative data collected in phases 2 and 3 led to the identification of 11 key themes: being able to talk to doctors and nurses; being able to use services; community awareness of asthma; getting a diagnosis; having suitable information on asthma; medicines for asthma; school and my child’s asthma; types of services available for asthma; quality of care; understanding of asthma; and day-to-day management. These themes were needs led, addressed the whole pathway of the child and would each need to be addressed by an integrated intervention programme delivered by an integrated system to comprehensively address optimal asthma management for South Asian children. However, recognising resource constraints within the NHS and wider society, it is unrealistic to expect such a comprehensive programme to be implemented simultaneously, and so participants were asked to identify one priority theme for which an intervention programme could be developed which would be acceptable to families and HCPs for implementation.
From the 11 key themes identified, the South Asian families in this study prioritised ‘getting a diagnosis’, whereas the HCPs located this much lower down their order of priorities (see Tables 17–19). There was a further discrepancy noted when analysing the children’s data, with children prioritising acute asthma attacks. This discrepancy and perception in what matters to the family or child compared with what is important to the HCP supports the current view that patients should have greater control and power in their health care and decision-making. 71
Data from phases 2 and 3 (see Chapters 3 and 4) revealed that diagnosis of asthma underpinned all aspects of condition management, including access to asthma services, information and education, and knowledge of acute asthma attacks. By intervening in the diagnostic process, the educational aspects and knowledge of how to approach an acute asthma attack could also be incorporated into an intervention, thereby incorporating children’s voices. This led to the decision to use ‘getting a diagnosis’ as the exemplar for the current study. As we have seen, an intervention designed around this issue encompasses change in knowledge and behaviour for communities and families, change in the behaviour of healthcare providers and change in the organisation of asthma services.
A further important theme identified by both White British and South Asian parents was ‘what to do day to day’. However, despite both groups of families wishing to address what they could do ‘day to day’ (other than medication), South Asian families were more focused on home adaptations, diets and other complementary strategies, demonstrating an area where culturally specific tailoring could be beneficial. Despite national recommendations being available for HCPs on providing all children with information and written asthma plans,4 ‘lack of information’ was a frequently cited issue during both sets of interviews, leading to ‘having suitable information on asthma’ being a further priority theme recognised as requiring an intervention, not only for South Asian but also for White British families. This lack of provision of information needs to be considered by all HCPs; however, it was clear from the study that providing more information without checking for understanding would be insufficient. In addition, it was suggested that tailored information which addressed questions or concerns more commonly raised by South Asian families was more likely to be effective than totally generic information.
We have presented only a selection of the themes from the MIA study to demonstrate the disparity and divergent views held by the children, their families and the HCPs. These disparities provide potent targets for interventions and, consequently, demonstrate a need for a collaborative approach which will thereby prevent the development of interventions that are driven by the perceptions of healthcare providers and which fail to take into account issues of importance to parents and children living with asthma.
To develop the exemplar intervention programme for ‘getting a diagnosis’, the data from phases 2 and 3 were used in a modified intervention framework to identify multiple actors, behaviours and determinants that contribute to barriers to effective management. Through using methods drawn from IM (see Chapter 1), performance objectives were developed informally by salient theories from clinical and health psychology and were linked to practical, feasible strategies for behaviour change, which were also theoretically embedded. The multifaceted final ‘ACT on Asthma’ diagnostic programme consisted of four integrated arms, each of which represents an intervention strategy. The four arms represented a need for community awareness, education and training, clinical support and the provision of an advice centre, of which all would be centrally co-ordinated. Development of the tailored, multifaceted ‘ACT on Asthma’ diagnostic programme was one of the main outputs of the study. Integrated programmes for the management of asthma do exist but most have been developed in the USA or Australia. Culturally tailored programmes are less commonly available, with the MIA team unaware of any programmes for South Asian children that have been developed and implemented in the UK.
In summary
Phases 2 and 3 provided evidence from multiple perspectives influencing the overarching asthma intervention planning framework leading to the ‘ACT on Asthma’ programme developed in phase 4 and supporting the collaborative approach adopted by MIA. The diverse understandings and priorities of families and HCPs which emerged in the course of the study (see Chapter 4) support the need to engage children and their families and not rely solely on the perspectives of healthcare providers. The study illustrates the need for interventions to be integrated, developed and delivered at the patient, provider and system levels if they are to be effective.
Conclusions and recommendations for practice and future research
Recommendations for healthcare practice
The MIA project was a large, complex study raising many questions regarding asthma management, intervention design and collaboration with communities considered to be ‘hard to reach‘. Each chapter has discussed in detail the findings from each phase of the study. In this concluding section, we will present some key recommendations for consideration by practitioners, policy makers and researchers.
Marginalised communities have greater healthcare needs and inequality in health outcomes. Redressing this is central to many governments’ health policies. Patient and public involvement in health research is widely promoted, yet for minority ethnic communities there is a gap between rhetoric and reality: minority ethnic communities are viewed as hard to reach and, as a consequence, are under-represented in research and its translation into health service improvements. A similar picture exists with regard to children. Health outcomes within the UK, particularly for children, have been shown to be lagging behind those in other European countries. 14 This led to the launch of the Children’s and Young People Health Outcome Strategy in January 2012 and the publication of the Children’s Outcome Forum Report,2,3 which set out key recommendations to bring about change and improve health outcomes for children in the UK. Recommendations relevant to this report included the need for the wider health system to tackle inequalities in health, and for children, young people and their families to be more involved in decision-making and the development of interventions and services to meet their needs. The report2 recommended that organisations and those delivering care on the front line should not only listen to the voices of children, young people and their families but also set out and demonstrate ways in which they will do this. At the same time, it is increasingly being recognised that the health and social care delivery system has not led to improvements in health outcomes209 and that a much ‘bolder’ approach is required. An integrated system approach is being advocated to prevent individual organisations such as health, education and social care from delivering interventions in isolation. With this in mind, it will be necessary for feasible evidence-based services to be locally commissioned that can be implemented within this new NHS structure and that are tailored to the needs of their local community.
This study provides a template and an evidence-based methodology that can be followed by commissioners and providers of health and social care, who will need to engage with their local communities to develop innovative solutions to improve outcomes for a wide variety of problems, ranging from public health to non-communicable diseases. The model presented here provides not only a way forward for engaging with children and families (often not included in such activities) but also for engaging with the diverse communities for whom inequalities in health are evident. The study demonstrates how, within a new integrated system, evidence-based, needs-led interventions can be developed. Local detailed studies will, however, always be required to establish the local levels of acculturation, mixture and inherited tradition arising from localised outcomes of the patterns of migration. Policy makers may wish to consider and ensure methods are in place to engage with consumers to effectively shift the balance from interventions being driven by providers to more interventions being consumer led and ensuring that they are tailored to their needs.
Asthma is one of the most common chronic conditions of childhood and provides an example for the inequalities in outcomes mentioned above. The evidence suggests that the UK health services provides inferior care compared with services in Europe,14 despite the existence of national guidelines4 and National Institute for Health and Care Excellence (NICE) quality standards. Variation in outcomes exists210 with guidelines not consistently implemented. Outcomes for minority ethnic children, such as South Asian children, are recognised to be worse than those for the majority population, with the BTS asthma guidelines4 recommending ‘heightened awareness to the needs of asthma in vulnerable groups’ (p. 21) such as minority ethnic groups.
A new health inequalities duty created from the 2012 Health and Social Care Act has the duty to ‘have regard to the need to reduce inequalities between people of England with respect to the benefits that they can obtain from the health service’. To achieve this goal, services need to be planned and delivered to ensure that they reach the individuals who need them most, but equally to ensure a focus on whole pathways of care, building or strengthening of partnerships and evidence to lever the change. The MIA study provides the underlying evidence that will help to lever change across the asthma pathway. The findings from the study not only support previous research reporting on the barriers to asthma management in South Asian children but provide a deeper understanding of the factors underlying these barriers, with a tailored approach required to overcome them. Many factors identified by the study were generic and should be applied by practitioners to all children with asthma.
We recommend that greater effort be made to provide appropriate and timely education on asthma and its management to families, and to check the understanding of the information provided. This was rarely achieved among our study participants. In line with national guidelines, parents should be provided with an asthma plan in a format that is accessible and appropriate. Organisations such as the Academic Health Science Networks may be able to assist with supporting and measuring such activities. The role of the wider family in managing asthma also needs to be recognised and HCPs may wish to reconsider the traditional parent/child consultation and develop a more inclusive approach where appropriate.
As recommended by the BTS guidelines, a culturally sensitive holistic approach to management is required when addressing minority ethnic children. Public health policies have not traditionally considered asthma as a priority area for interventions. However, the South Asian community had less pre-existing knowledge of asthma, although children and families are known to be influenced by the communities in which they live. The MIA study findings suggest a key role for Public Health policy in addressing broader social perceptions of asthma and its management in families.
Communication barriers and lack of consistent information, for a variety of reasons, were identified by HCPs, parents/carers and communities in the MIA study. Effective management of childhood asthma is underpinned by effective communication. Further work is needed to address the problems created by a lack of communication support and the need for increased time for consultations with families who have a lower proficiency in English. Health providers need to consider innovative ways of communicating with children and families if improved outcomes are to be achieved. Information provided to children and families also need to be tailored, with South Asian families potentially wishing to address different issues from the majority population.
The cultural competence of the NHS workforce has been questioned in many research reports. The MIA study also demonstrates that further effort is needed in this area if organisational discrimination is to be overcome.
The procedures used in the MIA project can be adapted using the principles described, and applied in other settings with other South Asian and other culturally distinctive groups, with due attention to such local issues as the mix of ethnicity, language, religion and history. In particular, attention should be given to access to schooling, dietary preferences and family structure. Where ‘complete’ families have migrated, dynamics may differ from those places where family relationships are more fractured or conducted at a distance within the diaspora.
Recommendations for future research
The extensive remit of the MIA study has highlighted a number of gaps in current evidence, not only in respect of methodological approaches to collaborating with consumers of health care and intervention design in South Asian communities but which can be applied to other ethnic minority and White British communities. The MIA study focused on childhood asthma but consideration should also be given to other chronic illness pathways where management is suboptimal and which could be addressed by a similar process. The 11 key themes presented in the MIA study represent key points along the asthma pathway where research could be focused. Some additional examples of further research are suggested below.
-
The MIA project has highlighted how taking a collaborative multifaceted approach to intervention development can be a successful method of intervention development, but future research needs to explore the feasibility, practicality and success of such interventions. The four armed integrated multifaceted ‘ACT on Asthma’ intervention programme whose aim is to improve ‘getting a diagnosis’ by addressing community awareness, education and training, clinical support and the provision of an advice centre, each underpinned by tailored strategies and centrally co-ordinated, now needs to be tested for its feasibility and effectiveness.
-
The need to involve the wider family in asthma management and the most appropriate mechanisms for achieving this in diverse communities should be explored further. Studies should identify effective means of engaging the wider family and test the effectiveness of this strategy in reducing exacerbations, reducing hospital admissions and improving quality of life.
-
Community knowledge of asthma was found to be limited. Further research could explore the value and effectiveness of techniques such as social marketing to enhance public understanding of asthma in South Asian communities.
-
This study identified several challenges in involving children in participatory research and intervention design. If we wish children to be more involved in decision-making and we wish to ‘give children a voice’, then we need further methodological studies to guide the development of effective ways to fully collaborate with children in redesigning services.
-
Children prioritised fear of acute attacks as a theme they would like further attention being given to. Research with children to identify ways of improving understanding and the management of acute attacks but also the emotions related to them should be a priority for further work.
-
Little evidence is available to help inform parents whether dietary modification is effective in asthma management. Further research is required to investigate this issue and also the effectiveness of a range of complementary therapies that are commonly adopted by families.
-
Organisational discrimination requires further attention from researchers. Ethnographic research involving direct observation and event questioning as they unfold is likely to be needed to compare and contrast clinical management and expectations in children of different ethnic backgrounds.
-
The MIA study has demonstrated that, despite the existence of BTS guidelines, there are significant organisational barriers to effective management of childhood asthma. Further research is clearly needed to explore the barriers to the implementation of such guidelines and how system changes to improve the co-ordination and delivery of asthma services can be integrated into the new commissioning models of the NHS.
Acknowledgements
The authors would like to express their thanks to the following:
-
All families, children, community members and healthcare professionals who participated and took part in the focus groups, interviews and workshops.
-
All of our community facilitators: Shiria Bakht, Rita Saujani, Rukhsana Hanif, Gurpreet Santini, Saad Miah, Junaid Razaq, Rukhsar Tariq Mehmood and Hushara Begum.
-
The advisory committee: Dr Cath Pritchard, Mrs Suzanne Leatherland, Dr Judith West, Dr Leslie Borrill, Mrs Anne-Marie Olphert, Mrs Shaheena Ali, Mrs Kam Gill, Ms Jo Wilson and Wendy Desbrow.
-
Professor Jonathan Grigg, Professor of Paediatric Respiratory and Environmental Medicine, Queen Mary University London. Made contributions to the conception and design of the study and gave advice to the research team when needed throughout the project.
-
Our external advisor, Professor Mike Thomas, Professor of Primary Care Research, University of Southampton.
-
Maya Lakhanpaul, Chelsea Huddlestone and Aadil Ali, who were our youth facilitators.
-
Ms Gill Perkins and Jo Wilson who assisted with the reviewing of the literature for the systematic evidence synthesis in phase 1.
-
Dr Logan Manikam who assisted with the reviewing of the literature for the systematic evidence synthesis in phase 1, for the evidence review of the asthma interventions in phase 4 and for proofreading the report.
-
Emma Angell who helped with qualitative analysis.
-
Mrs Stephanie Langan, Mrs Elaine Huddlestone and Mrs Liz Knight.
-
University of Leicester, Leicester Royal Infirmary and the Children’s Assessment Unit (CAU), Leicester Community Child Health Services (now Leicester partnership trust), Bangladesh Youth and Cultural Shomiti (BYCS), Highfields Community Centre, Belgrave Neighbourhood Centre, Peepul Centre, Clarendon Park, East Park Road Gurdwara, Nuthon Aloh, BYCS, Highfields Community Centre, Belgrave Community Centre, Federation of Muslim Organisations, Leicester Centre for Ethnic Health Research (LCEHR), Guru Nanak Gurdwara, Shree Manatan Mandir and Community Centre, and Leicester Central Mosque.
-
Asthma UK for the support throughout the project, with particular thanks to Brigid Hall and Leanne Metcalf who, in addition to the support provided by Asthma UK, attended workshops and gave additional support at the workshops.
-
Scalliwags Mobile Creche for providing childcare to make interviews with families possible.
-
Janice Strand, Jane Robertson, Sukhjinder (Jennie) Uppal, Chris Abley and Claire O’Neill from the PCRN and CLRN.
-
Deb Wall, Gemma Ryan, Lynne Hartwell, Mark Randall and Joanne Wilson from Leicester Community Children’s Partnership.
-
Dr Jo Forster.
-
Dr Neena Lakhani, Senior Lecturer, Pharmacy and Pharmacy Practice, De Montfort University (DMU).
-
Dr Marian Carey, National Director of DESMOND.
-
Our recruitment sites: Abbey Primary School, CAU, East Leicester Medical Practice, East Park Road Gurdwara, HealthServe Pharmacy and Silverdale Pharmacy.
All of those who worked in partnership with us or families, children, community leaders and HCPs.
Contributions of authors
Professor Monica Lakhanpaul (Professor of Integrated Community Health; expertise in integrated child health, health service research and quality improvement) has made substantial contributions to the conception and design of the study, and was co-responsible for the overall direction of the project, the analysis and interpretation of data. She contributed to the systematic evidence synthesis, as well as to the participatory workshops. She contributed to the drafting of the report and has given final approval of this report.
Dr Deborah Bird (Specialist Registrar in Community Paediatrics/Clinical Research Fellow; expertise in general and community paediatrics with expertise in engaging and interacting with young children) has made substantial contributions to the conception and design of the study and was responsible for the day-to-day management of the study, as well as having a major role in the systematic evidence synthesis, interviews and focus groups, the analysis and interpretation of qualitative data and contributed to drafting the report, and has given final approval of this report.
Professor Lorraine Culley (Professor of Social Science; expertise in qualitative health sociology) has made substantial contributions to the conception and design of the study, the analysis and interpretation of data and systematic evidence synthesis, as well as to the participatory workshops. She substantially contributed to the drafting of the report and has given final approval of this report.
Dr Nicky Hudson (Senior Research Fellow; ethnicity and health, qualitative methods) has made substantial contributions to the conception and design of the study, the analysis and interpretation of data and systematic evidence synthesis, as well as to the participatory workshops. She contributed to the drafting of the report and has given final approval of this report.
Dr Noelle Robertson (Senior Lecturer/Consultant Clinical Psychologist; clinical and health psychology and implementation) has made substantial contributions to the conception and design of the study, and the analysis and interpretation of data, as well as to the participatory workshops. She contributed to the drafting of the report and has given final approval of this report.
Narynder Johal (parent representative) has made substantial contributions to the conception and design of the study, interpretation of the data and the participatory workshops and contributed to the drafting of the report and has given final approval of this report.
Melanie McFeeters (Consultant Nurse for Children’s Respiratory Diseases, Senior Lecturer; Care & Management of Paediatric Respiratory Diseases) has made substantial contributions to the conception and design of the study, the analysis and interpretation of data, the participatory workshops and contributed to the drafting of the report and has given final approval of this report.
Dr Charlotte Hamlyn-Williams (Research Fellow; Children’s Health and Exercise) has made contributions to the drafting of the report, analysis of data and has given final approval of this report.
Professor Mark Johnson (Professor of Diversity in Health & Care; Specialist in Equality and Diversity in Health & Social Care) has made substantial contributions to the conception and design of the study, the analysis and interpretation of data and systematic evidence synthesis, as well as to the participatory workshops. He substantially contributed to the drafting of the report and has given final approval of this report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Improving Children and Young People’s Health Outcomes: A System Wide Response. London: Department of Health; 2013.
- Report of the Children and Young People’s Health Outcomes Forum. London: Department of Health; 2012.
- Chief Medical Officer’s Annual Report 2012: Our Children Deserve Better: Prevention Pays. London: Department of Health; 2013.
- British Guidelines on the Management of Asthma: A National Clinical Guideline. Edinburgh: Scottish Intercollegiate Guidelines Network; 2012.
- Healthy Lives, Healthy People: Our Strategy for Public Health. London: HSMO; 2010.
- Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, et al. Tailored interventions to overcome identified barriers to change effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2010;3. http://dx.doi.org/10.1002/14651858.CD005470.pub2.
- Michie S, Abraham C. Interventions to change health behaviours: evidence-based or evidence-inspired?. Psychol Health 2004;19:29-4. http://dx.doi.org/10.1080/0887044031000141199.
- Tugwell P, Petticrew M, Kristjansson E, Welch V, Ueffing E, Waters E, et al. Assessing equity in systematic reviews: realising the recommendations of the Commission on Social Determinants of Health. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c4739.
- Welch V, Tugwell P, Petticrew MdMJ, Ueffing E, Kristjansson B, McGowan J, et al. How effects on health equity are assessed in systematic reviews of interventions. Cochrane Database Syst Rev 2010;12. http://dx.doi.org/10.1002/14651858.MR000028.pub2.
- World Health Organization . Asthma: Definition 2014. www.who.int/respiratory/asthma/definition/en/ (accessed 27 May 2014).
- Asthma UK . Key Facts 2008. www.asthma.org.uk/asthma-facts-and-statistics (accessed 27 May 2014).
- Asthma UK . Where Do We Stand? Asthma in the UK Today 2004. www.asmabronquica.com.br/medical/wheredowestand%5B1%5D.pdf?id=92 (accessed 27 May 2014).
- Pearson M GM, Coles J, Amess M, Cleary R, Fletcher J, Mason A, et al. Health Outcome Indicators: Asthma. Oxford: National Centre for Health Outcomes Development; 1999.
- Wolfe I, Cass H, Thompson MJ, Craft A, Peile E, Wiegersma PA, et al. Improving child health services in the UK: insights from Europe and their implications for the NHS reform. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d1277.
- Kennedy IS. Getting it Right for Children and Young People: Overcoming Cultural Barriers in the NHS so as to Meet their Needs. London: Department of Health; 2010.
- Marmot M. Fair Society, Healthy Lives (The Marmot Review). London: Marmot Review Team; 2010.
- National Service Framework for Children, Young People and Maternity Services; Asthma. London: Department of Health; 2004.
- Guidelines for the Diagnosis and Management of Asthma. National Institutes of Health; 2007.
- Global Initiative for Asthma . Global Strategy for Asthma Management and Prevention 2009. www.ginasthma.org (accessed 27 May 2014).
- Gill P, Kai J, Bhopalr, Wild S. Health Care Needs Assessment of Black and Minority Ethnic Groups. Oxford: Radcliffe Medical Press; 2003.
- Erickson S. Effect of race on asthma management and outcomes in a large, integrated managed care organisation. Arch Intern Med 2007;167:1846-52. http://dx.doi.org/10.1001/archinte.167.17.1846.
- Tackling Health Inequalities: a Programme for Action. Department of Health Publications; 2003.
- Better Health, Better Care and Better Value for All: Equality Objectives Action Plan September 2012–December 2013. London: Department of Health; 2012.
- Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002.
- Bhopal RS. Ethnicity, Race, and Health in Multicultural Societies: Foundations for Better Epidemiology, Public Health, and Health Care. Oxford: Oxford University Press; 2007.
- Nazroo J. The structuring of ethnic inequalities in health: economic position, racial discrimination, and racism. Am J Public Health 2003;93:277-84. http://dx.doi.org/10.2105/AJPH.93.2.277.
- Health Inequalities and Population Health. London: NICE; 2012.
- Acheson DS. Independent Inquiry into Inequalities in Health. London: The Stationery Office; 1998.
- Equity and Excellence: Liberating the NHS. London: HMSO; 2010.
- Netuveli, Hurwitz B, Levy M, Fletcher M, Barnes G. Ethnic variations in UK asthma frequency, morbidity, and health-service use: a systematic review and meta-analysis. Lancet 2005;365:312-17. http://dx.doi.org/10.1016/S0140-6736(05)17785-X.
- The Asthma Divide: Inequalities in Emergency Care for People with Asthma in England. London: Asthma UK; 2007.
- Speaking Up: Experiences of Asthma Care in Minority Ethnic Communities. London: Asthma UK; 2008.
- Kuehni CE, Strippoli MP, Low N, Brooke AM, Silverman M. Wheeze and asthma prevalence and related health-service use in white and south Asian pre-schoolchildren in the United Kingdom. Clin Exp Allergy 2007;37:1738-46. http://dx.doi.org/10.1111/j.1365-2222.2007.02784.x.
- Whitrow MJ, Harding S. Asthma in Black African, Black Caribbean and South Asian adolescents in the MRC DASH study: a cross sectional analysis. BMC Pediatr 2010;10. http://dx.doi.org/10.1186/1471-2431-10-18.
- Morrison-Smith J, Cooper SM. Asthma and atopic disease in immigrants from Asia and the West Indies. Postgrad Med J 1981;57:774-6. http://dx.doi.org/10.1136/pgmj.57.674.774.
- Gilthorpe, Lay-Yee R, Wilson RC, Walters S, Griffiths RK. Variations in hospitalization rates for asthma among black and minority ethnic communities. Respir Med 1998;92:642-8. http://dx.doi.org/10.1016/S0954-6111(98)90511-X.
- Rona RJ, Duran-Tauleria E, Chinn S. Family size, atopic disorders in parents, asthma in children, and ethnicity. J Allergy 1997;99:454-60.
- Griffiths C, Kaur G, Gantley M, Feder G, Hillier S, Goddard J, et al. Influences on hospital admission for asthma in south Asian and white adults: qualitative interview study. BMJ 2001;323:962-6. http://dx.doi.org/10.1136/bmj.323.7319.962.
- Hussein, Partridge M. Perceptions of asthma in South Asians and their views on educational materials and self-Smanagement plans: a qualitative study. Patient Educ Counsel 2002;48:189-94. http://dx.doi.org/10.1016/S0738-3991(02)00033-2.
- Chambers CV, Markson L, Diamond JJ, Lasch L, Berger M. Health beliefs and compliance with inhaled corticosteroids by asthmatic patients in primary care practices. Respir Med 1999;93:88-94. http://dx.doi.org/10.1016/S0954-6111(99)90296-2.
- Joseph CL, Williams LK, Ownby DR, Saltzgaber J, Johnson CC. Applying epidemiologic concepts of primary, secondary, and tertiary prevention to the elimination of racial disparities in asthma. J Allergy Clin Immunol 2006;117:233-40. http://dx.doi.org/10.1016/j.jaci.2005.11.004.
- Peterson JW, Sterling YM, Stout JW. Explanatory models of asthma from African-American caregivers of children with asthma. J Asthma 2002;39:577-90. http://dx.doi.org/10.1081/JAS-120014922.
- Handelman L, Rich M, Bridgemohan CF, Schneider L. Understanding pediatric inner-city asthma: an explanatory model. J Asthma 2004;41:167-77. http://dx.doi.org/10.1081/JAS-120026074.
- Smeeton NC, Rona RJ, Gregory J, White P, Morgan M. Parental attitudes towards the management of asthma in ethnic minorities. Arch Dis Child 2007;92:1082-7. http://dx.doi.org/10.1136/adc.2006.112037.
- Office for National Statistics . Ethnicity and National Identity in England and Wales 2011 2012. www.ons.gov.uk/ons/rel/census/2011-census/key-statistics-for-local-authorities-in-england-and-wales/rpt-ethnicity.html (accessed 27 May 2014).
- Lakhanpaul M, Bird D, Manikam L, Culley L, Perkins G, Hudson N, et al. A systematic review of explanatory factors of barriers and facilitators to improving asthma management in South Asian children. BMC Public Health 2014;14. http://dx.doi.org/10.1186/1471-2458-14-403.
- Michel G, Silverman M, Strippoli MPF, Zwahlen M, Brooke AM, Grigg J, et al. Parental understanding of wheeze and its impact on asthma prevalence estimates. Eur Respir J 2006;28:1124-30. http://dx.doi.org/10.1183/09031936.06.00008406.
- Chattoo SA, Atkin KM, Craig KA, Chattoo S, Flynn R. Understanding Race and Ethnicity: Theory, History, Policy and Practice. Bristol: Policy Press; 2012.
- British Thoracic Society Scottish Intercollegiate Guidelines Network . British guideline on the management of asthma. Thorax 2008;63:iv1-12. http://dx.doi.org/10.1136/thx.2008.097741.
- Wolf FM, Guevara JP, Grum CM, Clark NM, Cates CJ. Educational interventions for asthma in children. Cochrane Database Syst Rev 2003;1.
- Gibson PG, Powell H, Coughlan J, Wilson AJ, Abramson M, . Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev 2003;1.
- Seguinol-Medina S, Rivera-Rentas A. Risk assessment and community participation model for environmental asthma management in an elementary public school: a case study in Puerto Rico. Int J Environ Res Public Health 2006;3. http://dx.doi.org/10.3390/ijerph2006030009.
- Gerald LB, McClure LA, Mangan JM, Harrington KF, Gibson L, Erwin S, et al. Increased adherence to inhaled steroid therapy among schoolchildren: randomised, controlled trial of school-based supervised athma therapy. Pediatrics 2009;123:466-74. http://dx.doi.org/10.1542/peds.2008-0499.
- Tieffenberg JA, Wood EI, Alonso A, Tossutti MS, Vicente MF. A randomized field trial of ACINDES: a child-centered training model for children with chronic illnesses (asthma and epilepsy). J Urban Health 2000;77:280-97. http://dx.doi.org/10.1007/BF02390539.
- Wise M, Gustafson DH, Sorkness CA, Molfenter T, Staresinic A, Meis T, et al. Internet telehealth for pediatric asthma case management: integrating computerized and case manager features for tailoring a web-based asthma education program. Health Promot Pract 2007;8:282-91. http://dx.doi.org/10.1177/1524839906289983.
- Griffiths C, Foster G, Barnes N, Eldridge S, Tate H, Begum S, et al. Specialist nurse intervention to reduce unscheduled asthma care in a deprived multiethnic area: the east London randomised controlled trial for high risk asthma (ELECTRA). BMJ 2004;328:144-7. http://dx.doi.org/10.1136/bmj.37950.784444.EE.
- Partridge M. In what way may race, ethnicity or culture influence asthma outcomes?. Thorax 2000;55:175-6. http://dx.doi.org/10.1136/thorax.55.3.175.
- Taylor SJC, Bremner SA, Choudhury A, Cook V, Devine A, Eldridge S, et al. OEDIPUS: a cluster randomised trial of education for South Asians with asthma, and their primary and secondary care physicians, to reduce unscheduled care. J Epidemiol Community Health 2011;65.
- Mittal V, Khanna P, Panjabi C, Shah A. Subjective symptom perceptual accuracy in asthmatic children and their parents in India. Ann Allergy Asthma 2006;97:484-9. http://dx.doi.org/10.1016/S1081-1206(10)60939-8.
- Craig P, Dieppe P, Macintyre S, Mitchie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:979-83. http://dx.doi.org/10.1136/bmj.a1655.
- Bailey EJ, Cates CJ, Kruske SG, Morris PS, Chang AB, Brown N. Culture-specific programs for children and adults from minority groups who have asthma. Cochrane Database Syst Rev 2009;1. http://dx.doi.org/10.1002/14651858.CD006580.pub3.
- Beach MC, Gary TL, Price EG, Robinson K, Gozu A, Palacio A, et al. Improving health care quality for racial/ethnic minorities: a systematic review of the best evidence regarding provider and organization interventions. BMC Public Health 2006;6. http://dx.doi.org/10.1186/1471-2458-6-104.
- Chin MH, Walters AE, Cook SC, Huang ES. Interventions to reduce racial and ethnic disparities in health care. Med Care Res Rev 2007;64:7S-28. http://dx.doi.org/10.1177/1077558707305413.
- Fisher TL, Burnet DL, Huang ES, Chin MH, Cagney KA. Cultural leverage: interventions using culture to narrow racial disparities in health care. Med Care Res Rev 2007;64:243S-82. http://dx.doi.org/10.1177/1077558707305414.
- Cheater F, Baker R, Gillies C, Hearnshaw H, Flottorp S, Robertson N, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2005;3.
- Liu JJ DE, Bhopal RS, White M, Johnson MRD, Netto G, . Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis. Health Technol Assess 2012;16.
- Johnson M, Ingleby DCA, Devillé W, Kotsioni I. Inequalities in Health Care for Migrants and Ethnic Minorities (COST Series on Health and Diversity). Antwerp/Apeldoorn: Garant; 2012.
- Woodward A, Kawachi I. Why reduce health inequalities?. J Epidemiol Community Health 2000;54:923-9. http://dx.doi.org/10.1136/jech.54.12.923.
- Hallam A. The Effectiveness of Interventions to Address Health Inequalities in the Early Years: A Review of Relevant Literature. Scottish Government; 2008.
- Griffin S, Cookson R, Rice N, Asaria M, Claxton K, Culyer T, et al. Identifying Appropriate Methods to Incorporate Concerns about Health Inequalities into Economic Evaluations of Health Care Programme. York: University of York, Centre for Health Economics; 2012.
- Communities in Control: Real People, Real Power. London: HMSO; 2008.
- Coulter A. Engaging Communities for Health Improvement: A Scoping Study for the Health Foundation. London: The Health Foundation; 2009.
- Darzi A. High Quality Care for All: NHS Next Stage Review Final Report. London: The Stationery Office; 2008.
- Creating a Patient-led NHS. London: Department of Health; 2005.
- Dunston R, Lee A, Boud D, Brodie P, Chiarella M. Co-production and health system reform – from re-Imagining to re-making. Aus J Pub Health 2009;68:39-52.
- Bovaid T. Beyond engagement and participation: user and community coproduction of public services. Pub Admin Rev 2007;67:846-60. http://dx.doi.org/10.1111/j.1540-6210.2007.00773.x.
- Toelle BG, Ram FS. Written individualised management plans for asthma in children and adults. Cochrane Database Syst Rev 2004;2.
- Guevera JP, Wolf FM, Grum CM, Clark NM. Effects of educational interventions for self management of asthma in children and adolescents: a systematic review and meta-analysis. BMJ 2003;326:1308-9. http://dx.doi.org/10.1136/bmj.326.7402.1308.
- Bravata DM, Gienger AL, Holty JEC, Sundaram V, Khazeni N, Wise PH, et al. Quality improvement strategies for children with asthma. Arch Pediatr Adolesc Med 2009;163:572-81. http://dx.doi.org/10.1001/archpediatrics.2009.63.
- Shepperd S, Lewin S, Straus S, Clarke M, Eccles MP, Fitzpatrick R, et al. Can we systematically review studies that evaluate complex interventions?. PLOS Med 2009;6. http://dx.doi.org/10.1371/journal.pmed.1000086.
- Green LW, Mercer SL. Can public health researchers and agencies reconcile the push from funding bodies and the pull from communities?. Am J Public Health 2001;91:1926-9. http://dx.doi.org/10.2105/AJPH.91.12.1926.
- Macaulay A, Commanda LE, Freeman WL, Gibson N, McCabe ML, Robbins CM, et al. Responsible Research with Communities: Participatory Research in Primary Care. Leawood, KS: NAPCRG; 1998.
- Bettencourt L, Ostrom A, Brown S, Roundtree R. Client co-production in knowledge-intensive business services. Cali Manag Rev 2002;44:100-28. http://dx.doi.org/10.2307/41166145.
- Minkler M, Wallerstein N. Community Based Participatory Research for Health: Process to Outcomes. San Francisco, CA: Jossey Bass; 2008.
- Viswanathan M, Ammerman A, Eng E, Gartlehner G, Lohr KN, Griffith D, et al. Community-based Participatory Research: Assessing the Evidence. Rockville, MD: Agency for Healthcare Research and Quality; 2004.
- Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P. Involving South Asian patients in clinical trials. Health Technol Assess 2004;8.
- Stirlanda L, Halanib L, Bhopal R, Netuveli G, Partridge M, Card J, et al. Recruitment of South Asians into asthma research: qualitative study of UK and US researchers. Prim Care Respir J 2011;20:282-90. http://dx.doi.org/10.4104/pcrj.2011.00032.
- Balarajan R. Ethnic differences in mortality from ischaemic heart disease and cerebrovascular disease in England and Wales. BMJ 1991;302:560-4. http://dx.doi.org/10.1136/bmj.302.6776.560.
- Crane J, O’Donnell TV, Prior IA, Waite DA. The relationships between atopy, bronchial hyperresponsiveness, and a family history of asthma: a cross-sectional study of migrant Tokelauan children in New Zealand. J Allergy Clin Immunol 1989;84:768-72. http://dx.doi.org/10.1016/0091-6749(89)90307-2.
- Brown DR, Fouad MN, Basen-Engguist K, Tortolero-Luna G. Recruitment and retention of minority women in cancer screening, prevention, and treatment trials. Ann Epidemiol 2000;10:S13-21. http://dx.doi.org/10.1016/S1047-2797(00)00197-6.
- Areán PA, Gallagher-Thompson D. Issues and recommendations for the recruitment and retention of older ethnic minority adults into clinical research. J Consult Clin Psychol 1996;64:875-80. http://dx.doi.org/10.1037/0022-006X.64.5.875.
- Borde T, Johnson M, Culley L, Hudson N, van Rooij F. Marginalized Reproduction: Ethnicity, Infertility and Reproductive Technologies. London: Earthscan; 2009.
- Crivello G. How can children tell us about their wellbeing? Exploring the potential of participatory research approaches within young lives. Soc Indicat Res 2009;90:51-72. http://dx.doi.org/10.1007/s11205-008-9312-x.
- Powell M. Children’s participation rights in research. Childhood 2009;16:124-42. http://dx.doi.org/10.1177/0907568208101694.
- Evans D, Clark NM, Levison MJ, Levin B, Mellins RB. Can children teach their parents about asthma?. Health Educ Behav 2001;28:500-11. http://dx.doi.org/10.1177/109019810102800409.
- Faux, Walsh M, Deatrick JA. Intensive interviewing with children and adolescents. West J Nurs Res 1988;10:180-94. http://dx.doi.org/10.1177/019394598801000206.
- Boyden J, Ennew J. Children in Focus – a Manual for Participatory Research with Children. Stockholm: Save the Children; 1997.
- Docherty S, Sandelowski M. Focus on qualitative methods interviewing children. Res Nurs Health 1999;22:177-85. http://dx.doi.org/10.1002/(SICI)1098-240X(199904)22:2<177::AID-NUR9>3.0.CO;2-H.
- Deatrick JA, Faux SA, Morse JM. Qualitative Nursing Research: A Contemporary Dialogue. Rockville, MD: Aspen; 1989.
- Bearison D. They Never Want to Tell You: Children Talk about Cancer. Cambridge: Harvard University Press; 1991.
- Thompson RJ, Gustafson KE. Adaptation to Chronic Childhood Illness. Washington, DC: American Psychological Association; 1996.
- Alex MR, Ritchie JA. School-aged children’s interpretation of their experience with acute surgical pain. J Pediatr Nurs 1992;7:171-80.
- Woodgate R, Kristjanson LJ. My hurts: hospitalized young children’s perceptions of acute pain. Qual Health Res 1996;6:184-201. http://dx.doi.org/10.1177/104973239600600204.
- Yoos HL, McMullen A. Illness narratives of children with asthma. Pediatr Nurs 1996;22:285-90.
- Rottem M, Szyper-Kravitz M, Shoenfield Y. Atopy and asthma in migrants. Int Arch Allergy Immunol 2005;136:198-204. http://dx.doi.org/10.1159/000083894.
- Summary of the United Nations Convention on the Rights of the Child. London: UNICEF; 2009.
- Glauser B, James A, Prout A. Constructing and Deconstructing Childhood: Contemporary Issues in the Sociological Study of Childhood. London: Falmer Press; 1997.
- Bird D, Culley L, Lakhanpaul M. Why collaborate with children in health research: an analysis of the risks and benefits of collaboration with children. Arch Dis Child Educ Pract Ed 2013;98:42-8. http://dx.doi.org/10.1136/archdischild-2012-303470.
- James APA. Constructing and Reconstructing childhood: Contemporary Issues in the Sociological Study of Childhood. London: Falmer Press; 1997.
- Clavering EK, McLaughlin J. Children’s participation in health research: from objects to agents?. Child Care Health Develop 2010;36:603-11. http://dx.doi.org/10.1111/j.1365-2214.2010.01094.x.
- Glanz H, Rimer B, Viswanath K. Health Behaviour and Health Education: Theory, Research, and Practice. San Francisco, CA: Jossey Bass; 2008.
- Sallis JF, Owen N, Glanz K, Rimer BK, Viswanath K. Health Behaviour and Health Education: Theory, Research and Practice. San Francisco, CA: Jossey-Bass; 2002.
- Glanz K, Mullis R. Environmental interventions to promote healthy eating: a review of models, programs, and evidence. Health Educ Behav 1988;15:395-41. http://dx.doi.org/10.1177/109019818801500403.
- Sallis JF, Owen N, Fisher EB, Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research and Practice. San Francisco, CA: Jossey-Bass; 2008.
- Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot 1996;10:282-98. http://dx.doi.org/10.4278/0890-1171-10.4.282.
- Klein KJ, Tosi H, Cannella AA. Multilevel theory building: benefits, barriers, and new developments. Acad Manag Rev 1999;24:243-8. http://dx.doi.org/10.5465/AMR.1999.1893934.
- Liu J, Davidson E, Bhopal R, White M, Johnson MRD, Netto G, et al. Health Inequalities and Risk Factors among Migrants and Ethnic Minorities (COST Series on Health and Diversity). Antwerp/Apeldoorn: Garant; 2012.
- Bartholomew LK, Parcel GS, Kok G, Gottlieb NH. Planning Health Promotions Programs: An Intervention Mapping Approach. San Francisco, CA: John Wiley and Sons; 2006.
- Kok G, Schaalma H, Ruiter RA, van Empelen P, Brug J. Intervention mapping: protocol for applying health psychology theory to prevention programmes. J Health Psychol 2004;9:85-98. http://dx.doi.org/10.1177/1359105304038379.
- Graham ID, Tetroe J, Group KTTR. Some theoretical underpinnings of knowledge translation. Acad Emerg Med 2007;14:936-41. http://dx.doi.org/10.1111/j.1553-2712.2007.tb02369.x.
- van Oostrom SH, Anema JR, Terluin B, Venema A, de Vet HCW, van Mechelen W. Development of a workplace intervention for sick-listed employees with stress-related mental disorders: intervention mapping as a useful tool. BMC Health Serv Res 2007;7. http://dx.doi.org/10.1186/1472-6963-7-127.
- Brug J, Oenema A, Ferreira I. Theory, evidence and intervention mapping to improve behavioral nutrition and physical activity interventions. Int J Behav Nutr Phys Activity 2005;2. http://dx.doi.org/10.1186/1479-5868-2-2.
- Wolfers MEG, van den Hoek C, Brug J, de Zwart O. Using Intervention Mapping to develop a programme to prevent sexually transmittable infections, including HIV, among heterosexual migrant men. BMC Public Health 2007;7. http://dx.doi.org/10.1186/1471-2458-7-141.
- McEachan RRC, Lawton RJ, Jackson C, Conner M, Lunt J. Evidence, theory and context: using intervention mapping to develop a worksite physical activity intervention. BMC Public Health 2008;8. http://dx.doi.org/10.1186/1471-2458-8-326.
- 2011 Census: Key Statistics for Local Authorities in England and Wales. London: Office for National Statistics; 2012.
- Mason S, Hussain-Gambles M, Leese B, Atkin K, Brown J. Representation of South Asian people in randomised clinical trials: analysis of trials’ data. BMJ 2003;326:1244-5. http://dx.doi.org/10.1136/bmj.326.7401.1244.
- Lloyd CE, Johnson M, Sturt J, Collins GS, Barnett AH, Williamson A, et al. Researching with Communities: Grounded Perspectives on Engaging Communities in Research. Auckland: Muddy Creek Press; 2007.
- National Research Ethics Service . Information Sheets and Consent Forms: Guidance for Researchers and Reviewers Versin 3.6.1 2011. www.nres.nhs.uk/EasySiteWeb/GatewayLink.aspx?alld=338 (accessed 27 May 2014).
- De Las Nueces D, Hacker K, DiGirolamo A, Hicks LS. A systematic review of community-based participatory research to enhance clinical trials in racial and ethnic minority groups. Health Serv Res 2012;47:1363-86. http://dx.doi.org/10.1111/j.1475-6773.2012.01386.x.
- Morjaria-Keval A, Johnson M. Our Vision Too: Improving the Access of Ethnic Minority Visually Impaired People to Appropriate Services. Leicester: MSRC with Housing Corporation and Thomas Pocklington Trust; 2005.
- Culley L, Hudson N, Rapport F. Using focus groups with minority ethnic communities: researching infertility in British South Asian communities. Qual Health Res 2007;17:102-12. http://dx.doi.org/10.1177/1049732306296506.
- Baker P, Eversley J. Multilingual Capital: The Languages of London’s Schoolchildren and their Relevance to Economic, Social and Educational Policies. London: Battlebridge; 2000.
- Carr-Hill R, Passingham S, Wolf A, Kent N. Lost Opportunities: The Language Skills of Linguistic Minorities in England and Wales. London: Basic Skills Agency; 1996.
- Bhutta ZA. Beyond informed consent. Bull World Health Organ 2004;82:771-7.
- Lloyd CE, Sturt J, MRD Johnson, Mughal S, Collins G, Barnett AH. Development of alternative methods of data collection in South Asians with type 2 diabetes. Diab Med 2008;25:455-62. http://dx.doi.org/10.1111/j.1464-5491.2008.02401.x.
- Lloyd CE, Johnson MRD, Mughal S, Sturt JA, Collins GS, Roy T, et al. Securing recruitment and obtaining informed consent in minority ethnic groups in the UK. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-68.
- Roy T, Lloyd CE. Development of audio methods of data collection in Bangladesh. Divers Health Soc Care 2008;5:187-98.
- Houle CR, Caldwell CH, Conrad FG, Joiner TA, Parker EA, Clark NM. Blowing the whistle: what do African American adolescents with asthma and their caregivers understand by “wheeze?”. J Asthma 2010;47:26-32. http://dx.doi.org/10.3109/02770900903395218.
- Claudio L, Stingone JA. Primary household language and asthma care among Latino children. J Health Care Poor Underserved 2009;20:766-79. http://dx.doi.org/10.1353/hpu.0.0164.
- Mosnaim GS, Sadowski LS, Durazo-Arvizu RA, Sharp LK, Curtis LM, Shalowitz MU, et al. Parental language and asthma among urban Hispanic children. J Allergy Clin Immunol 2007;120:1160-5. http://dx.doi.org/10.1016/j.jaci.2007.08.040.
- van Dellen QM, van Aalderen WMC, Bindels PJE, Öry FG, Bruil J, Stronks K, et al. Asthma beliefs among mothers and children from different ethnic origins living in Amsterdam, the Netherlands. BMC Public Health 2008;8. http://dx.doi.org/10.1186/1471-2458-8-380.
- Rose D, Garwick A. Urban American Indian family caregivers’ perceptions of barriers to management of childhood asthma. J Pediatr Nurs 2003;18:2-11. http://dx.doi.org/10.1053/jpdn.2003.2.
- Hazir T, Das C, Piracha F, Waheed B, Azam M, Tam A. Carers’ perception of childhood asthma and its management in a selected Pakistani community. Arch Dis Child 2002;87:287-90. http://dx.doi.org/10.1136/adc.87.4.287.
- Lai AKL, Malhotra S. Knowledge of asthma among parents of asthmatic children. Indian Pediatr 1995;32:649-55.
- Singh V, Sinha HV, Gupta R. Barriers in the management of asthma and attitudes towards complementary medicine. Respir Med 2002;96:835-40. http://dx.doi.org/10.1053/rmed.2002.1368.
- Mazur LJ, De Ybarrondo L, Miller J, Colasurdo G. Use of alternative and complementary therapies for pediatric asthma. Tex Med 2001;97:64-8.
- Graham DM, Blaiss MS. Complementary/alternative medicine in the treatment of asthma. Ann Allergy Asthma Immunol 2000;85:438-849. http://dx.doi.org/10.1016/S1081-1206(10)62569-0.
- Arnold E, Clark CE, Lasserson TJ, Wu T. Herbal interventions for chronic asthma in adults and children. Cochrane Database Syst Rev 2008;1. http://dx.doi.org/10.1002/14651858.CD005989.pub2.
- Holloway E, Ram FS. Breathing exercises for asthma. Cochrane Database Syst Rev 2004;1.
- Cane R. Understanding childhood asthma in focus groups: perspectives from mothers of different ethnic backgrounds. BMC Fam Pract 2001;2. http://dx.doi.org/10.1186/1471-2296-2-4.
- Shivbalan S, Balasubramanian S, Anandnathan K. What do parents of asthmatic children know about asthma? An Indian perspective. Indian J Chest Dis 2005;47:81-7.
- Gautam VP, Shah A, Malhotra A, Dewanwala A, Taneja DK, Gupta VK, et al. General practitioners knowledge of childhood asthma in Delhi, India. Int J Tuberculosis Lung Dis 2008;12:677-82.
- Culley L, Hudson N, Baldwin K, Lakhanpaul M. Children travelling for treatment: what we don’t know. Arch Dis Child 2013;98:442-4. http://dx.doi.org/10.1136/archdischild-2012-303189.
- Seawright J, Gerring J. Case selection techniques in case study research: a menu of qualitative and quantitative options. Political Res Q 2008;61:294-308. http://dx.doi.org/10.1177/1065912907313077.
- Onwuegbuzie AJ, Leech NL. A call for qualitative power analyses. Int J Method 2007;41:105-21.
- Johnson M, Cross MEH. Lost Illusions. London: Tavistock; 1988.
- Karlsen S, Nazroo J. Fear of racism and health: research report. J Epidemiol Community Health 2004;58:1017-18. http://dx.doi.org/10.1136/jech.2004.020479.
- Cooley ME, Sarna L, Brown JK, Williams RD, Chemecky C, Padilla G, et al. Challenges of recruitment and retention in multisite clinical research. Cancer Nurs 2003;26:376-86. http://dx.doi.org/10.1097/00002820-200310000-00006.
- Silverman D. Interpreting Qualitative Data: Methods for Analysing Talk, Text, and Interaction. Thousand Oaks, CA: Sage; 2001.
- Fountain JaH. Delivering Race Equality in Mental Health Care: Report on the Findings and Outcomes of the Community Engagement Programme. Preston: International School for Communities, Rights and Inclusion, University of Central Lancashire; 2010.
- Szczepura A JM, Gumber A, Jones K, Clay D, Shaw A. An Overview of the Research Evidence on Ethnicity and Communication. Healthcare Report to the Department of Health. Coventry: Warwick Medical School (CEEHD); 2005.
- Scheppers E, van Dongen E, Dekker J, Geertzen J, Dekker J. Potential barriers to the use of health services among ethnic minorities: a review. Fam Prac 2006;23:325-48. http://dx.doi.org/10.1093/fampra/cmi113.
- Atkin K, Ali S, Atkin K. Primary Healthcare and South Asian Populations: Meeting the Challenges. Abingdon: Radcliffe; 2004.
- Eiser C. It’s OK having asthma . . . young children’s beliefs about illness. Prof Nurse 1991;6:342-5.
- Cohen R, Franco K, Motlow F, Reznik M, Ozoah PO. Perceptions and attitudes of adolescents with asthma. J Asthma 2003;40:207-11. http://dx.doi.org/10.1081/JAS-120017992.
- Ireland LM. Children’s perceptions of asthma: establishing normality. Br J Nurs 1997;6:1059-64.
- Callery P, Milnes L, Verduyn C, Couriel J. Qualitative study of young people’s and parents’ beliefs about childhood asthma. Br J Gen Pract 2003;53:185-90.
- Managing Asthma: A Guide for Schools. US Department of Health and Human Services, National Institute of Health; 2003.
- Lasserson TJ, McDonald VM. School-based self-management educational interventions for asthma in children and adolescents. Cochrane Database Syst Rev 2010;2.
- Allen, Dyas J, Jones M. Building consensus in health care: a guide to using the nominal group technique. Br J Community Nurs 2004;9:110-14. http://dx.doi.org/10.12968/bjcn.2004.9.3.12432.
- Bucknall S. Exploring Children’s Experiences of Carrying Out Their Own Research Studies. Milton Keynes: Open University; 2005.
- O’Kane C, Christensen P, James A. Research with Children: Perspectives and Practices. London: Falmer Press; 2000.
- Clark J. Using diamond ranking as visual cues to engage young people in the research process. Qual Res J 2012;12:222-37.
- Bucknall S. Exploring Children’s Experiences of Carrying Out Their Own Research Studies. Milton Keynes: The Open University; 2005.
- Ying Z, Zhang W, Pei J, Lin X, Lin Q, Li A. Consensus-based ranking of multi-valued objects: a generalized Borda count approach. IEEE Transact Knowledge Data Engin 2014;26:83-96. http://dx.doi.org/10.1109/TKDE.2012.250.
- Bohs KD, Baumeister RF. Handbook of Self-Regulation: Research, Theory and Applications. New York, NY: Guildford Press; 2007.
- Bandura A. Social Foundations of Thought and Action. Upper Saddle River, NJ: Prentice Hall; 1986.
- Clark N, Mitchell H, Rand C. Effectiveness of educational and behavioural asthma interventions. Pediatrics 2009;123:S158-92. http://dx.doi.org/10.1542/peds.2008-2233I.
- Khunti KGL, Skinner T, Carey ME, Realf K, Dallosso H, . Effectiveness of a diabetes education and self management programme (DESMOND) for people with newly diagnosed type 2 diabetes mellitus: three year follow-up of a cluster randomised controlled trial in primary care. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e2333.
- Ashcroft R, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL. Implications of socio-cultural contexts for the ethics of clinical trials. Health Technol Assess 1997;1.
- Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C. Threats to applicability of randomised trials: exclusion and selective participation. J Health Serv Res Policy 1999;4:112-21.
- Matthews HW. Racial, ethnic and gender differences in response to medicines. Drug Metabol Drug Interact 1995;12:77-91. http://dx.doi.org/10.1515/DMDI.1995.12.2.77.
- Sheikh A, Halani L, Bhopal R, Netuveli G, Partridge M, Car J, et al. Facilitating the recruitment of minority ethnic people into research: qualitative case study of South Asians and asthma. PLOS Med 2009;6. http://dx.doi.org/10.1371/journal.pmed.1000148.
- Hussain G, Atkin K, Leese B. Why ethnic minority groups are under-represented in clinical trials: a review of the literature. Health 2004;12:382-8.
- Newton SK, Appiah-Poku J. Perspectives of researchers on obtaining informed consent in developing countries. Dev World Bioeth 2007;7:19-24. http://dx.doi.org/10.1111/j.1471-8847.2006.00147.x.
- Helgesson G. How to handle informed consent in longitudinal studies when participants have a limited understanding of the study. J Med Ethics 2005;31:670-3. http://dx.doi.org/10.1136/jme.2004.009274.
- Collins G, Johnson MRD. Addressing ethnic diversity in health outcome measurement: a systematic and critical review of the literature. Health Technol Assess 2009.
- Hunt S, Bhopal R. Self-reports in research with non-English speakers. BMJ 2003;327:352-3. http://dx.doi.org/10.1136/bmj.327.7411.352.
- Karnieli-Miller O, Strier R, Pessach L. Power relations in qualitative research. Qual Health Res 2009;19:279-89. http://dx.doi.org/10.1177/1049732308329306.
- Peel E, Parry O, Douglas M, Lawton J. “It’s no skin off my nose”: why people take part in qualitative research. Qual Health Res 2006;16:1335-49. http://dx.doi.org/10.1177/1049732306294511.
- Clark T. ‘We’re over-researched here!’ Exploring accounts of research fatigue within qualitative research engagements. Sociology 2008;42:953-70. http://dx.doi.org/10.1177/0038038508094573.
- Thompson R, Holland J. Hindsight, foresight and insight: the challenges of longitudinal qualitative research. Int J Soc Res Method 2003;6:233-44. http://dx.doi.org/10.1080/1364557032000091833.
- Clark T, Sinclair R. The costs and benefits of acting as a research site. Evidence Policy 2008;4:105-20. http://dx.doi.org/10.1332/174426408783477855.
- Emmel N, Hughes K, Greenhalgh J, Sales A. Accessing socially excluded people: trust and the gatekeeper in the research–participant relationship. Sociol Res Online 2007;12. www.socresonline.org.uk/12/2/emmel.html (accessed 27 May 2014).
- Pathways through Participation . Research, Engagement and Impact 2011. http://pathwaysthroughparticipation.org.uk/wp-content/uploads/sites/3/2011/12/Research-engagement-and-impact.pdf (accessed 27 May 2014).
- Lightfoot J, Sloper P. Having a say in health: involving young people with a chronic illness or physical disability in local health services development. Chil Soc 2003;17:277-90. http://dx.doi.org/10.1002/chi.748.
- Staniszewska S. Patient and public involvement in health services and health research: a brief overview of evidence, policy and activity. J Res Nurs 2009;14:295-8. http://dx.doi.org/10.1177/1744987109106811.
- Skelton T. Research with children and young people: exploring the tensions between ethics, competence and participation. Child Geograph 2008;6:21-36. http://dx.doi.org/10.1080/14733280701791876.
- Kellett M. Small shoes, big steps! Empowering children as active researchers. Am J Community Psychol 2010;46:195-203. http://dx.doi.org/10.1007/s10464-010-9324-y.
- How to Involve Children and Young People in Research. London: National Children’s Bureau; 2009.
- Miller J, Glassner B, Silverman D. Qualitative Research: Theory, Method and Practice. London: Sage; 1997.
- Morse JM, Field PA. Qualitative Research Methods for Health Professionals. Thousand Oaks, CA: Sage; 1995.
- Mrazek DA, Klinnert M, Mrazek PJ, Brower A, McCormick D, Rubin B, et al. Prediction of early-onset asthma in genetically at-risk children. Pediatr Pulmonol 1999;27:85-94. http://dx.doi.org/10.1002/(SICI)1099-0496(199902)27:2<85::AID-PPUL4>3.0.CO;2-B.
- Greig A, Taylor J. Doing Research with Children. London: Sage; 1999.
- Irwin LG, Johnson J. Interviewing young children: explicating our practices and dilemmas. Qual Health Res 2005;15:821-31. http://dx.doi.org/10.1177/1049732304273862.
- Wilson C, Powell M. A Guide to Interviewing Children: Essential Skills for Counselors, Police, Lawyers, and Social Workers. London: Routledge; 2001.
- Gleeson C. Assessing children’s knowledge of asthma. Profess Nurse 1995;10:517-21.
- Kieckheffer G, Spitzer A. School age children’s understanding of the relations between their behaviour and asthma management. Clin Nurs Res 1995;4:149-67. http://dx.doi.org/10.1177/105477389500400203.
- Ham C, Dixon A, Brooke B. Transforming the Delivery of Health and Social Care: the Case for Fundamental Change. London: The King’s Fund; 2012.
- The NHS Atlas of Variation in Healthcare. London: Department of Health; 2012.
- Research Ethics Board McMaster University. Sample Assent for Children 2006.
- Levy MDL, Larcher V, Kurz R. Informed consent/assent in children. Statement of the Ethics Working Group of the Confederation of European Specialists in Paediatrics (CESP). Eur J Paediatr 2003;162:629-33.
- Moudgil H, Honeybourne D. Difference in asthma management between white European and Indian subcontinent ethnic groups living in socioeconomically deprived areas in the Birmingham (UK) conurbation. Thorax 1998;53:490-4. http://dx.doi.org/10.1136/thx.53.6.490.
- Oldam D. Nurse-led asthma clinic in an Asian community. Nurs Times 1997;93:58-9.
Appendix 1 Asthma UK systematic evidence synthesis abstract
Background
South Asian children with asthma are less likely to receive prescriptions, more likely to suffer uncontrolled symptoms and admitted with acute asthma compared with White British children. Understanding and addressing barriers are therefore vital in addressing health inequalities. We therefore undertook a systematic review to identify explanatory factors which underlie barriers and facilitators to asthma management in South Asian children.
Methods
Data sources – MEDLINE, HMIC, EMBASE, ASSIA, Web of Science, BNI, CINAHL, PsycINFO, OpenSIGLE, CRD, Scopus, NHS Evidence, Cochrane Library, Campbell Collaboration, RCPCH, ATS, ERS, Asthma UK, Google Scholar & Asthma Guidelines (BTS, GINA, ATS, Monash, NAEPP, Singapore & New Zealand) to May 2010.
Inclusion criteria – Qualitative, quantitative or mixed research with primary focus on identifying explanations for barriers and/or facilitators to asthma management in South Asian children aged 0–18 years with diagnosed/suspected asthma and/or carers and/or healthcare professionals.
Data extraction – Three authors independently reviewed selected & extracted eligible articles with disagreements resolved by research team discussion.
Results
Fifteen studies encompassing 25,755 children, 18,483 parents/carers and 239 healthcare professionals were included. The barriers and explanatory factors identified were:
-
lack of asthma knowledge in families and healthcare professionals.
-
under-use of preventer medications
-
non-acceptance/denial of asthma
-
over-reliance on Emergency Department management
-
communication problems
-
non-adherence to medication
-
use of complementary therapies.
Little information regarding asthma management facilitators was identified.
Conclusion
Several key issues were identified as likely to be ethnic specific to South Asian families, rather than a reflection of minority status: impact of parental and professional knowledge and beliefs, health service utilisation pattern explanations and the impact of prejudice and stigmatisation. Other explanations such as language barriers are not strictly ethnic specific but instead reflect a minority position.
Further research is required to move beyond only identifying what a barrier is and into identifying both what and why the barrier is and how it impacts on management. Furthermore, understanding the difference between barriers and explanations that are ethnic-specific and those related to being a minority will enable the application of generic system-wide interventions where ethnicity is not the issue and ethnically-tailored interventions where needed.
Appendix 2 Three-step approach for recruitment
Step 1: initial approach
Individuals and families were given a brief outline of the study and if interested in learning more or possibly taking part, completed an EoI form and were given the study information sheets. Completing an EoI form did not commit anyone to participation but was passed to the research fellow for step 2. The forms contained contact details as well some basic demographics used to enable the research fellow to identify the language required and to purposively select individuals and families who fulfilled the required criteria for different elements of the study. All individuals or families who completed EoI forms were contacted, either to be invited to participate in specific study activities or to be thanked but have it explained that persons with their particular characteristics had already been recruited into the study.
The initial approach could be made in one of three ways: face to face (direct), via telephone or via letter (mail shot).
-
Direct approach
-
During a face-to-face meeting (whether clinical or social or other), the study is introduced and explained in outline. If the individual or family is interested in learning more, an EoI is completed and signed and returned to the research fellow in the envelopes provided.
-
-
Telephone approach
-
Potential participants are contacted by telephone, identified via clinic lists or by a personal contact. The study is introduced and explained in outline. If the individual or family is interested in learning more, an EoI is completed and signed by the person making the call on behalf of the person they called. The EoI is then returned to the research fellow in the envelope provided.
-
-
Mail shot
-
Potentially eligible participants were sent a study pack in the post with a cover letter that briefly explained the purpose of the study and asked that the study information be read. If interested, individuals could either complete and return the EoI form using the envelope provided, or contact the research fellow directly.
-
In addition to the CFs, the study was advertised using posters, flyers and the university and research websites such that interested participants could contact the research team directly, and a study website, http://mia.ocbmedia.com, was designed to signpost individuals to study information in English and in the main south Asian languages, available in both written and audio formats.
Secondary contacts were made by telephone or face to face. These recruitment methods were in order to identify and approach potential participants, including CFs, the research and advisory team members, research participants and clinicians (including pharmacists, GPs, nurses and community and hospital-based paediatricians) involved with the study. Evidence from the UK and USA36,57 suggested that mail shot and advertising would be ineffective for South Asian participants. However, they were included as direct comparisons with the more personal face-to-face and telephone recruitment. The recruitment data reinforce these previous findings, with trusted people being a more effective method of engagement.
Step 2: secondary contact
In step 2, the research fellow (or appropriate community facilitator if English was not the preferred language) used the returned EoIs to contact individuals or families to explain the study in more depth and provide detailed study information sheets if not already provided in step 1. After leaving time to consider the study, individuals and families were contacted a second time to ask if they wished to participate. If no, they were not contacted further. If yes, a suitable research activity was identified (e.g. a family interview, a focus group, a workshop), and details of the activities provided and consent forms sent out.
Clear guidance on patient information sheets and consent forms has been given by the National Research Ethics Service of the National Patient Safety Agency since April 2007: see www.nres.npsa.nhs.uk. The study information was designed in accordance with the guidance contained in the national research ethics service documents: Explaining Research and Information Sheets and Consent Forms – guidance for researchers.
Step 3: formal consent
Step 3 involved taking formal consent to participate in the study. Adults consented for themselves, with parents also consenting on behalf of their children. Children were also asked for their assent to participate in the study.
Consent procedure
At the point of approach, potential participants were asked to provide some basic demographic information, which included the participant’s preferred choice of language (see EoI form). Study materials were then provided, either in English written format or in translated audio format. Where study materials have been provided in English written format, consent was taken in English in written format unless a participant who has received English study materials did not have sufficient literacy skills to read the consent form, in which case verbal audio-recorded consent was used. Where study materials were provided in translated audio format, consent was taken in the appropriate language following this process:
-
At initial approach, individuals were given or posted the patient information sheet and consent form in English and an audio recording of the patient information, or directed to the study website where information in minority ethnic languages was available.
-
At the follow-up telephone call, conducted in the appropriate language:
-
– Any questions concerning the study material were answered.
-
– Time/date/venue for focus group/interview were agreed.
-
-
Prior to the start of the focus group/interview, the researcher, aided by CFs, checked that the information had been read or audio recording had been listened to, and a further opportunity to ask and answer any questions was given.
-
The researcher, aided by community facilitators, explained how informed consent is taken as an audio recording and recorded.
-
The prospective participant was asked to state their name, the date and the time of giving their consent.
-
The consent form was read out by the CF in the relevant community language point by point and the participant asked to repeat the words and confirm that they understood and agreed with each point of the consent form. This process was recorded. If they wished, participants could also initial and sign the written consent form at the same time.
-
A copy of the audio-recorded consent was given to the participant to take away with them.
Assent from children
Article 12 of the United Nation Convention on the Rights of the Child recognises a child’s right to ‘form his or her own views; the right to express those views freely in all matters affecting the child; the views being given due weight in accordance with age and maturity’. Under UK law, the 1986 Gillick vs. West Norfolk and Wisbech Area Health Authority ruling determined that children under the age of 16 can give valid consent provided they are competent to understand the risks and benefits of the proposed therapy. 108 However, Gillick competency is rarely applied below the age of 10 years.
Informed assent, defined as ‘a child’s affirmative agreement to participate in research’,211 can and should be sought when involving children in research. The aim of the assent process is to listen to the opinion and wishes of the child, to promote and protect their dignity, privacy and confidentiality. 212 There is no agreed lower age limit at which assent should be sought, although age 7 is often taken as a cut-off for obtaining assent. 211 Children vary in their ability to understand and interpret information, and therefore to assent to participate in research. 108,211
In this study, the team sought assent from all children aged 7 years upwards. Children under the age of 7 years were judged by the research team as to their ability to provide assent, and where appropriate, assent was sought.
Ethics procedures
The process of project approval involved the following four stages:
-
NHS ethical approval
-
university approval (project sponsor)
-
NHS R&D approval
-
honorary contracts/research passports/letters of confidentiality.
NHS ethical approval
The Integrated Research Application System (IRAS) application was completed and sent to the Derbyshire Research Ethics Committee (REC) on 26 October 2009 (ref. 09/H0401/85). The ethics committee met on 17 November 2009 (chairperson Phil Hopkinson). We received a request for further information and revisions to study documentation on 30 November 2009 and responded on 8 December 2009. We received the REC decision letter confirming favourable ethical opinion (conditional on permission or approval granted by each host organisation) on 10 December 2009.
University approval (project sponsor)
Copies of the REC and R&D forms were sent to the University of Leicester Research and Governance Officer, Mr Graham Hewitt, for approval as research sponsor. Project sponsorship was granted on 19 November 2009.
NHS research and development approval
On 2 July, IRAS R&D forms were submitted to University Hospitals Leicester (UHL) and Leicester City primary care trust (PCT).
There were significant delays to the project at this stage due to changes of key members of staff and reorganisation of R&D procedures. R&D forms, study documents and site-specific information forms were completed and submitted to each trust for review in December 2009. Approval was granted by Leicester City PCT on 15 March 2010. Approval was granted by UHL NHS Trust on 20 July 2010.
As a later addition to the study, R&D approval was also sought from NHS Leicestershire County and Rutland (LCR). Approval was granted on 12 April 2011.
Honorary contracts/research passports/letters of confidentiality
There was a lack of clarity as to the requirement for research passports, honorary contracts and letters of access, particularly in relation to the CFs. After discussion between the R&D offices and the University of Leicester, it was agreed that the CFs would be employed by the University of Leicester on a temporary contracted basis, which included a clause on confidentiality and data protection.
Ethical considerations
National Research Ethics Service procedures were used throughout the study to minimise distress to participants, safeguard anonymity and confidentiality, as well as guaranteeing continuation of standard care.
Consent and voluntary participation
All participants were provided with accessible study information and asked for their informed consent/assent, using either written or verbal methods. All participants were informed that their consent was voluntary.
Data protection and confidentiality
All study staff endeavoured to protect the rights of the study’s participants to privacy and adhered to the Data Protection Act 1998. We collected only the minimum required information for the purposes of the study. Study data, including signed consent forms and recordings, are held securely in a locked cabinet. Access to the information was limited to the study staff and any relevant regulatory authorities. Computer-held data, including the study database, are held securely and password protected, with access further restricted by user identifiers and passwords.
All medical data revealed during-study activities were treated as confidential. A procedure for reporting a disclosure of any behaviour that could adversely affect a child’s health and well-being was in place during the study, although this was not required. This limitation to confidentiality was clearly stated on the study information forms.
Lone working
A large number of interviews and focus groups were attended solely by the research fellow, often in community centres or participants’ work/homes. The University of Leicester adheres to the Code of Practice for the Safety of Social Researchers.
Minimising distress
This was not an intervention study; however, in-depth interviews discussing health can be distressing. 102 Therefore, interviews were conducted in a professional and sensitive manner. Participants were reminded that they did not have to answer any questions that they considered too intrusive and interviews would be stopped at any time at the request of the parent or child. In addition, if the researcher felt that the child no longer wished to participate, even if no request to stop was made, the interview was ended. This was necessary at times during the study.
Separate child and adult workshops were planned, although in the same building at the same time. To ensure children’s well-being, if at any time a child became distressed during a workshop, they would be removed from the workshop and reunited with their parents or responsible adult. If a child became ill during a workshop, they would be reunited with their parents, and if necessary the emergency services would be contacted. These procedures were not necessary during the study.
Appendix 3 Recruitment avenues
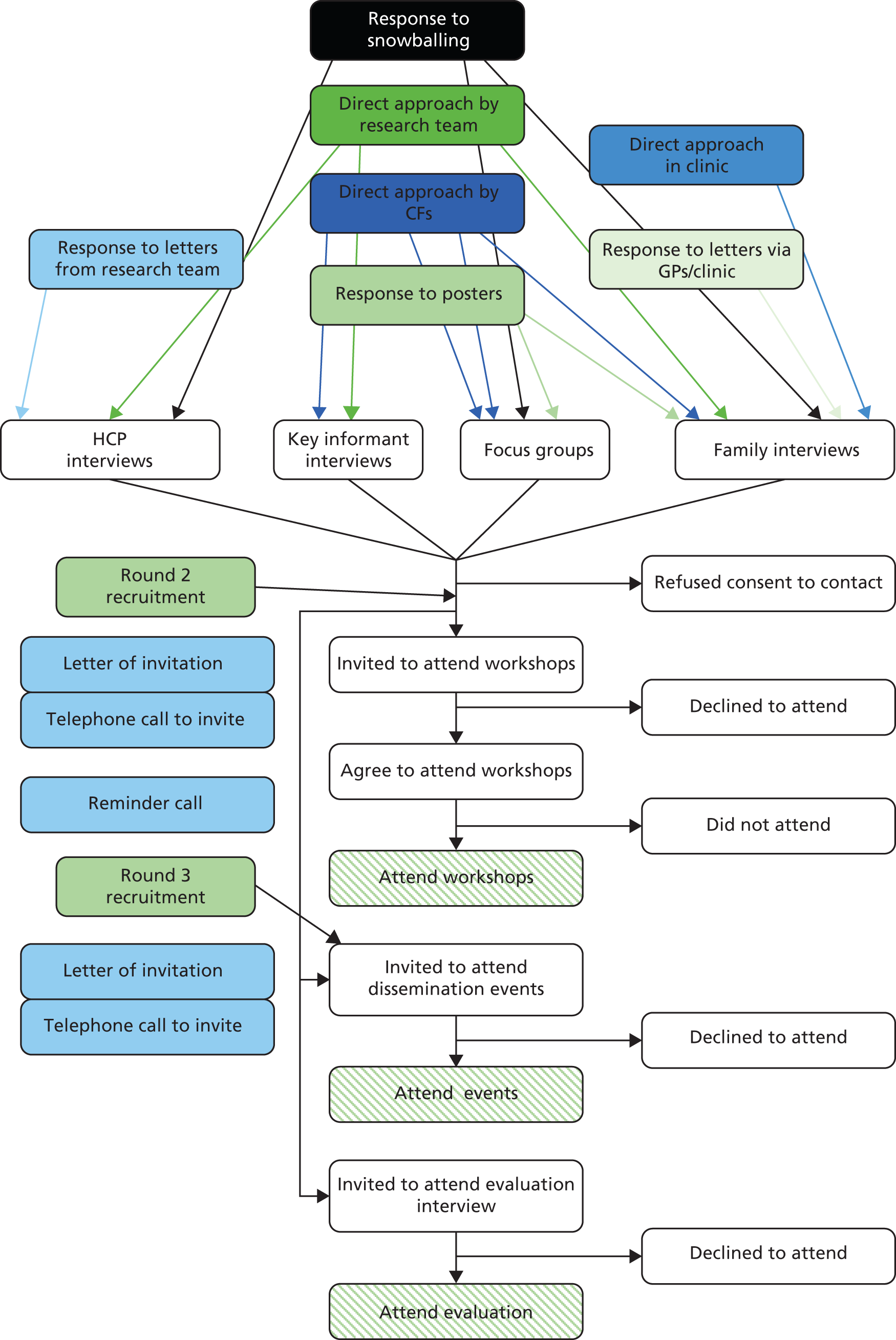
Appendix 4 Interview schedules
MIA: Management and Interventions for Asthma
Focus group question guide
Introduction
Firstly, I’d like to welcome you all to the group and thank you for agreeing to speak to us.
The reason we’re here is because a team of researchers from the University of Leicester, De Montfort University, and the NHS are trying to improve the care of Indian/Bangladeshi/Pakistani children with asthma. We would like to know what people think about children and families who have asthma, and to ask for your help in improving the lives and care for children with this problem. This is important because asthma affects lots of children and can be very difficult for children and parents.
Don’t worry if you think you don’t know anything about asthma – we have lots of different things to talk about and you might find that you know more than you think. We’ll also be using a story about a boy called Samir to discuss some of the different ideas. If you do know someone with asthma or have asthma yourself and would like to know more about the things we talk about today, we have some information leaflets that we can give out at the end of the session.
Before we begin I would like to remind you that whatever you say here will be kept confidential. I hope that you will feel free to express your views. Your names and personal details will not be mentioned in any report.
I am using a tape recorder to record our conversation because it is difficult for me to write down everything you say. Please try to speak one at a time so that I can follow what is being said.
-
Let’s start with everyone telling us their name and whereabouts they were born? I’ll go first . . .
-
Can everyone think of a child that they know? Can you describe them briefly? I’ll go first . . . (say one or two sentences about a child you know e.g. I’m thinking of my niece, she’s 6 years old and very lively, never sits still and never stops talking).
-
If I were to say ‘this is a healthy child’, what would this mean to you?
-
You may have heard the word ‘wheezy’ (in translation or in English if no translation) used to describe a child. What does wheezy mean to you?
-
Many of you may have heard about a condition called asthma. In your own words, can you describe a child with asthma?
-
Probe: Is wheezy the same as asthma?
-
Is asthma common?
-
How do you know if a child has asthma?
-
What kind of things can happen to someone who has asthma?
-
I’m going to tell you a bit about a boy called Samir. Samir is 6 years old. Samir’s always been prone to chesty coughs and often wakes up at night coughing. Samir often can’t keep up with his brothers and sisters when playing and gets out of breath very easily. Samir’s parents took him to their local GP, who said that Samir has asthma.
-
What do you think that Samir might think about having asthma?
-
Probe: Might he worry about anything?
-
What about his friends?
-
What about sports?
-
Might he be thinking about school?
-
What about going to see doctors?
-
-
If you were Samir’s mother or father, how would you feel about having a child with asthma?
-
Probe: Might it affect the relationship between you and your husband/wife?
-
Might it affect your relationships with other people in the community?
-
Might it affect your standing in the community?
-
Would you want to seek advice from anyone else?
-
Might it affect Samir’s future career prospects?
-
Might it affect Samir’s future marriage prospects?
-
-
How might having one child with asthma affect the rest of the family?
-
Probe: Might it affect going out to a family function, like a wedding?
-
Might it affect the relationships between Samir and his brothers and sisters?
-
What about the extended family?
-
Might the family change the way they treat Samir?
-
-
What do you think that an average person in the community might think about a child with asthma?
-
Probe: Does it matter?
-
Would they be seen as healthy?
-
Would they be seen as normal?
-
Would anyone treat the child differently because they have asthma?
-
Would anyone treat the family differently?
-
Is there a stigma attached to asthma?
-
Would anyone worry about having that child visit their house?
-
What about staying in their house?
-
Would anyone worry about their child marrying someone with asthma?
-
Would anyone worry about hiring a young person with asthma?
-
-
Do you think that being Indian/Bangladeshi/Pakistani means that you think differently about asthma to someone who is not from this background?
-
Do you think that being Indian/Bangladeshi/Pakistani influences the way people respond to a child or family with asthma?
-
Probe: (If yes or no) – why is that?
-
Does age make a difference to what people think?
-
Does being born in the UK or in India/Bangladesh/Pakistan make a difference?
-
Does religion make a difference?
-
Does being male or female make a difference?
-
Does your job/role in the community make a difference?
-
-
Do you think that doctors might respond differently to a child who’s from an Indian/Bangladeshi/Pakistani family, compared to a child who’s not from this background?
-
Probe: Does the doctor’s ethnicity make a difference?
-
What about nurses?
-
What about receptionists?
-
-
If parents want to get treatment for their child with asthma, how do they do this?
-
Probe: Where would most parents go to for treatment?
-
Who would most parents go to for treatment?
-
The GP gave Samir two inhalers to use; a brown one to take every day, and a blue one to take whenever he’s wheezy (hold up example inhalers).
-
What do you know about these medicines?
-
Probe: Do they work?
-
Are there any problems with them?
-
Are there any times or places that you can’t take them?
-
Would it be better to take the medicine in a different way?
-
If yes, why?
-
-
Are there any concerns about a child with asthma taking medicines every day, even if they seem OK?
-
Probe: Is it better to only take medicines when they’re wheezing? Why?
-
Does the type of medicine, e.g. steroid (show the brown inhaler again) make a difference?
-
Are there any alternatives to using medicines for asthma and wheezing?
-
-
Is there anything that the NHS could do to help children who have asthma?
-
Probe: What about making appointments with GPs?
-
What about going to see specialist children’s doctors?
-
What about going to see specialist asthma nurses?
-
Is it important whether you see a doctor or a nurse?
-
Is it important whether you see a GP or general paediatrician, or an asthma specialist doctor?
-
Do you think that where the clinics are held makes a difference?
-
-
Is there anything people could do to themselves?
-
Is there anything children could do for each other?
-
If there anything families could do?
-
Is there anything communities could do?
-
-
Is there any need for more information about asthma in children and families?
-
Probe: Do you think that people in the community understand what it’s like to have a child with asthma?
-
Do you think that people in the community understand what children with asthma can and can’t do?
-
What information is there already?
-
What kinds of things do you think people need to know about?
-
Why are these things important?
-
-
What is the best way of getting information to families and communities?
-
Is there anything else that you feel it would be useful for us to know about a child with asthma in your community?
Summary
The intention tonight was to talk about how the Indian/Bangladeshi/Pakistani community views asthma. We’ve talked about the symptoms of asthma, about where and how to get treatment, and how having asthma affects a child and their family. We’ve also talked about how this community might see a child with asthma and what the community could do to help. Have we missed anything?
Is there anything else you’d like to add before we finish?
Thank you very much for your time. You will be given a voucher for your involvement in this focus group. If you would like any further information about asthma, please stay behind for a minute and I will provide some.
Key informant topic guide
-
Could you tell me a little bit about your role in the community and what you do?
-
Probe: How long have you been working in this or a similar role?
-
What contact do you have with children/families?
-
-
In your experience, have you met or worked with any children with asthma or their families? Could you describe a typical child with asthma?
-
Probe: What are the key features of asthma?
-
Do you have any sense of the numbers of children with asthma in the community?
-
-
How do you think parents in your community might feel about their child having asthma?
-
Probe: Might they be self-conscious/embarrassed/worried about their standing in the community?
-
-
What do you think that the average person in the community thinks about children with asthma?
-
Probe: Would anyone treat the child or their family differently because they have asthma?
-
Do you think that people in the community understand what it’s like to have a child with asthma?
-
Do you think that people in the community understand what children with asthma can and can’t do?
-
-
Do you think that someone’s cultural background, being . . . has any effect on the way they think about asthma?
-
Probe: What about what causes asthma?
-
About treatments for asthma?
-
About what’s normal/expectations for a child with asthma?
-
In relation to how families are treated in the community?
-
-
Do you think that a person’s religion makes any difference to how they view asthma, or creates any problems?
-
Does being . . . have any impact on how the child is treated by others, including professionals?
-
Probe: Is there a perception of prejudice amongst doctors and nurses?
Research shows that sometimes parents find it very difficult to have a child with asthma.
-
What do you think might be some of the problems they face?
-
Probe: Within the family
-
Within the community
-
With professionals – at diagnosis, getting treatments
-
-
As far as you know, what kinds of treatments are there for asthma?
-
Probe: How are treatments viewed by the community?
-
Problems with western medicines, especially steroids?
-
What might stop someone from using their medicines?
-
Use of alternative medicines?
-
A very important part of this research is identifying ways that we can help young children with asthma and their families.
-
What information or support, if any, should be offered to parents and children if diagnosed with asthma?
-
What do you think the NHS – doctors and nurses – could do differently that might help families in your community?
-
What do you think the community might be able to do that could help?
-
What could someone in your position do that might be useful?
-
What do you feel is the best way to involve people in the community in any of these suggestions? (Depending on answer . . .) Why would that work?
Question schedule for parents
Hello. Thank you very much for agreeing to speak to me. We’re going to talk about you and your son/daughter (say name) and their breathing. I’d like to talk about when things first started, then we’ll move on to what things are like now. I’ll also ask some questions about what happens when he/she has a bad day, and about any treatments you use.
Please feel free to say whatever you’re thinking and please remember that everything you say will be kept confidential. If at any time you’d like to stop or take a break, just let me know and we’ll do just that.
Let’s start by talking a little bit about your family. How many children do you have? Who lives in your house? Does anyone else help you to look after your son/daughter?
-
When did (child’s name)’s breathing problems first start?
-
Initial symptoms/recognition
-
Who/how diagnosed
-
Information/support provided
-
Barriers to diagnosis
-
Seeking help
-
HCP attitude
-
Access to service
-
-
-
People have lots of different ideas about why children get wheezy. Why do you think children get wheezy?
-
Triggers vs. causes
-
Heritability
-
Contagion
-
Gods will
-
Diet
-
-
What do you think causes (child’s name)’s asthma/wheezing?
-
Could you describe what (child’s name)’s asthma is like on a day-to-day basis?
-
Symptoms
-
Impact on day-to-day life
-
Lifestyle restrictions
-
Time of work
-
Family life
-
Schooling
-
-
-
Who makes the decisions about day-to-day things?
-
Mum/dad
-
Child
-
Extended family
-
-
Could you describe a recent asthma attack? (substitute bad attack if little response)
-
Describe management
-
Use of health services
-
Use of tests/diagnostics
-
Role of extended family in management
-
-
-
Problems faced
-
Recognition of need to seek help
-
Access to service A&E/walk in/GP
-
Practicalities – finances, time of day, weekends, childcare
-
HCP communication/attitudes/ethnicity/gender
-
-
What worked well?
-
Good service
-
Good person
-
-
Information provided
-
What
-
From who
-
Useful/not
-
What else wanted
-
Timing
-
-
Solutions used/wanted
-
Let’s talk about treatments. What do you hope treatments will do for (child’s name)’s asthma/wheezing?
-
Personal goals of treatment
-
Management vs. cure
-
Concept of asthma control
-
What is good control?
-
-
Does (child name) take any medicines for his/her asthma? (substitute inhalers if no response) (go through medicines one by one)
-
When do you use this/how do you feel about it/any problems getting child to take it/how do you remember to take it/does everyone in family know about it/use in public
-
For preventer medicines: when do you stop/who makes decisions/side effects
-
Specific attitudes
-
Longterm med use
-
Inhaler vs. tablets
-
Steroids
-
-
-
Who has helped you learn about the wheezing/asthma?
-
Sources of knowledge
-
Skills
-
Overseas advice
-
Role of schools/community centres/religious centres
-
Use of written management plans
-
-
What do the rest of your family think about (child’s name)’s asthma?
-
Who knows/gets involved?
-
What does child think?
-
Does anyone offer advice/do you follow it?
-
Impact on management?
-
-
What about your friends?
-
Do you tell others/stigma?
-
Would you tell about another illness/specific to asthma
-
Would it be the same for an adult illness? Future marriage?
-
Common beliefs about causes
-
Common attitudes towards asthma/children with asthma
-
Advice offered/follow it?
-
Has anyone upset you?
-
Do cultural attitudes influence management?
-
-
Where do you go for help about (child’s name)’s asthma?
-
Usual source of care – GP/A&E/walk-in/family and friends/internet/religious leaders
-
Who do you go to?
-
What is the key issue – opening hours, location, relationship, gender, ethnicity
-
Problems faced getting help
-
Communication with HCPs
-
Getting prescriptions
-
-
-
-
What would help overcome these?
-
Is there anything that’s you’ve found particularly helpful in taking care of (child’s name)’s asthma?
-
What/why?
-
Alternative therapies used
-
What/why
-
Diet
-
Heating/furnishing changes
-
Barriers or facilitators to using different options
-
-
-
Is there anything else we could do to help you cope with (child’s name)’s asthma?
-
What/Why/How
-
Specific to your family
-
General suggestions for families and children
-
Specific points for Indian/Pakistani/Bangladeshi families
-
-
-
Question schedule for healthcare professionals
Hello. Thank you very much for agreeing to speak to me.
The MIA research group are investigating the barriers and facilitators to asthma management in south Asian children with a view to developing an intervention programme that will be both practical and suitable. We’ll be discussing your experiences of managing asthma with south Asian children and families, in particular, any barriers you’ve faced and if, how or why these issues have affected your management. Towards the end I will ask about elements you’d like to see improved and how we might work together to achieve this.
-
Please tell me about your experience working with South Asian children and families with asthma
-
Diagnosis
-
Use of testing
-
Acceptance
-
Discussion/information given
-
-
-
Communication
-
Language
-
Attitudes
-
-
Particular problems encountered
-
Particularly helpful aspects
-
How much do you feel you know about the lives of south Asian families?
-
Confidence in knowledge
-
Confidence in achieving working relationships
-
Particular issues or helps around achieving working relationship with South Asian families
-
-
Is there anything you do differently for south Asian families?
-
Modification to communication style, information given, choice of treatments
-
Why?
-
-
What barriers do you think parents of south Asian children with asthma face in managing their children?
-
Practical barriers
-
SES/education/place of birth
-
Cultural factors
-
-
Do you feel that there are any organisational barriers affecting how you manage asthma in south Asian children?
-
Resources
-
Time
-
Training needs
-
Interpreters
-
-
What would you like to see made better?
Appendix 5 Example of chartered data in intervention mapping tables
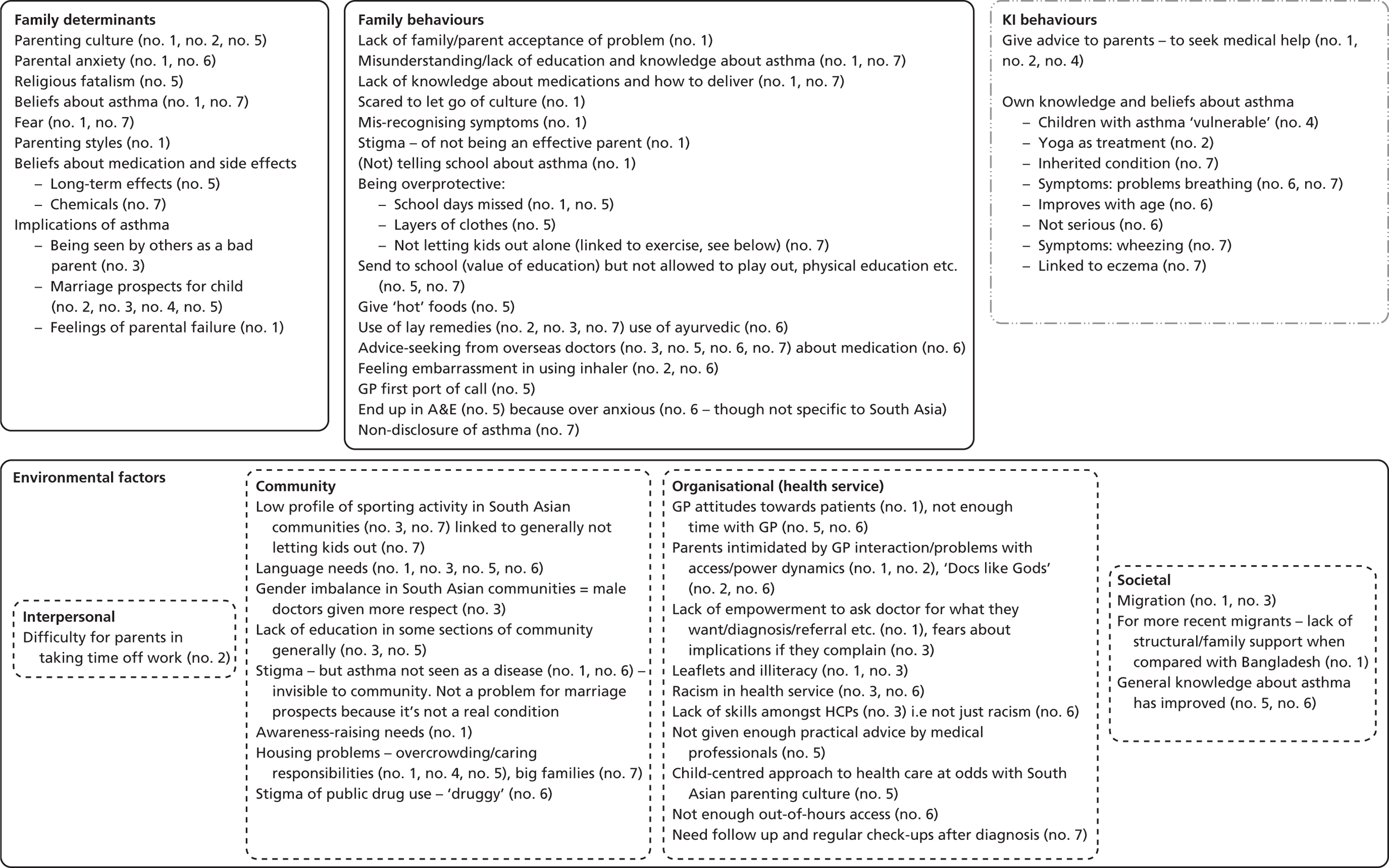
Appendix 6 British Thoracic Society steps of asthma management
Appendix 7 Behaviours and determinants from family interviews in intervention mapping tables
Eleven broad themes (no priority):
-
understanding asthma
-
community awareness of asthma
-
types of services available for asthma
-
getting a diagnosis
-
not all doctors and nurses treating asthma well enough
-
being able to talk to doctors and nurses
-
school and my child’s asthma
-
having suitable information on asthma
-
medicines for asthma
-
being able to use services
-
day-to-day management of asthma.
| Behaviours: parents being able to use the services | Determinants: being able to use the services | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
(1a) Conflicting roles at home Can be hard to women to get out/not good to out alone/have other kids or other responsibilities at home (109), lots of referrals to reviews disrupt household life (109). More of an immediate ‘if child is ill then take action’ but when seems well, have other things to do (109). This is most prominent in women new to UK, living with extended families (109), again if live with extended family hard to do all the trigger avoidance/managing asthma if caring for elderly relatives (104), hard to find time with mosque, school, other kids, etc. (108) Is difficult with other kids, who looks after them, have to divide between parents so can’t both go to hospital/doctors (111). Very hard if parent unwell as well, mobility problems (114) (1b) Don’t see the point Regular trips to GP but don’t do anything so what’s the point in going (104), has to be useful or why take time off work (128) Don’t want to go to endless round of doctors when child seems OK (105) Hospitals are seen as more important, going there or appointment there is OK, but clinics/children centres not important (109) Does go because see as useful, explain to child, practical demonstrations, gets peace of mind (126) (1c) Finances Perception of being denied treatment due to cost (103). Costs money to run a car but essential (104, 125), need money for taxis if don’t drive (129). Costs money in petrol and parking (108). Had to buy a car, needed to borrow money (114). Had to pay for lots of taxis (114). Financial barriers are minimal as NHS treatment is free (114), but there is a cost to adapting house (114). Costs in buying herbal remedies, all private, costs of going overseas to see if warmer, drier climate helped (114) (1d) Fear Some women may fear professionals/organisations, especially if new to country, associate with social services telling them not caring for child well enough and taking child away, so avoid clinics/doctors, etc. (109) Child gets upset and worried about asthma (111). Parents fear what will happen to child if parent ill, disabled (114) (1e) Practicalities Hard to get time off work when child ill repeatedly (106, 128, 110, 2, 128), can’t get appointments to fit in work schedule (128), can’t get to pharmacist when is open (128). Need help from family looking after other kids (119), or getting to appointments (119). Takes time to get appointments with GP (1), GP closed, is out of hours (124, 119). Easy to get appointments (129, 116). Receptionists generally perceived as rude, have to get past them to see a doctor (109, 108, 121) is off-putting, less private, can’t get around practice protocols for setting appointments, etc. (121) One symptom one appointment rule is annoying (121). Have to use up all annual leave on sick days, etc. (111) Not hard to get time off, do give (125, 111) (2a) Getting there Need to be able to drive (104, 121, 114, 108); hard to get to and from hospital – need another family member, can’t always get hold of them, or wait for transport but can be hours to get home (124, 119, 114); is hard to get kids to ED at night – cold, dark, they are tired and want to sleep (104, 108); not going to use public transport if your child can’t breathe (104). Mum called dad when saw breathing problem for first time for dad to take to hospital (112). Can’t then park when get home again (108). Would be better to go to local GP because of all of these problems but GP isn’t good enough (108). Don’t want to call ambulance in case other children are sicker (108) (3a) Children get scared
|
|||||||||
| Behaviours: having suitable information on asthma | Determinants: having suitable information on asthma | |||||||||
|
|
|||||||||
| Behaviours: not all doctors and nurses treating asthma well enough | Determinants: not all doctors and nurses treating asthma well enough | |||||||||
|
1. (a) Parents don’t differentiate between services (108) Parents don’t really distinguish between Children’s Assessment Unit, out-of-hours and ED, all ‘hospital’ or ‘emergency’ (108). Go to hospital, they then send you to ED or downstairs, etc. (104, 108). Happy with GP and pharmacist management (116) ED doctors generally viewed in better light in terms of treatment (b) Fear Get scared. Get annoyed. Don’t understand why not prioritised for breathing difficulties (104, 108). Don’t understand why not being given treatment (118). Can’t follow explanations as too worried (121), doctors don’t listen or don’t seem to take them seriously (121). Different doctors and nurses don’t take asthma seriously (108), don’t give enough nebulisers (108). Previous misdiagnosis or feelings of not being taken seriously affect all future interactions with GP, lack of trust (108) 2. (a) Training
|
|||||||||
| Behaviours: school and my child’s asthma | Determinants: school and my child’s asthma | |||||||||
|
Feel schools not very interested in child’s asthma (124, 122, 106, 117, 111, 114) inhalers common, not very interested. Others say do notice and care, check on his asthma regularly (121). No problems at school with other kids (125), no embarrassment (125), no problems at school (163). Easy access to inhaler at school (108). School more concerned, insist on multiple inhalers (126) School don’t have a lot of knowledge about asthma (114). Don’t believe parents word on severe asthma (114)
|
|||||||||
| Behaviours: being able to talk to doctors and nurses | Determinants: being able to talk to doctors and nurses | |||||||||
Parents don’t understand why doctor not explaining more, think doctors must know about asthma, must be doctors don’t care (106), withholding information (106) Think there is a cultural attitude to trust doctor, not question doctor (111) Asthma clinic – excellent communication, talk to the children, explain and say what have to do, do home visits and school visits, all help family to feel supported, confident (114) |
1a. Affects choice of who to see and who comes
Don’t perceive language or attitude as a problem (108)
|
|||||||||
| Behaviours: medicines for asthma | Determinants: medicines for asthma | |||||||||
|
1a. Choice/decision-making
d. Fear: fear addiction (104, 106, 128, 116, 108), accumulation (102, 126), but this is for all drugs
f. Advice from others/GP: Family say can’t give 10 puffs, will overdose child, makes mum scared especially if not working (104) |
|||||||||
| Behaviours: medicines for asthma | Determinants: medicines for asthma | |||||||||
|
2a. May choose to give as have seen them work in other kids (130) 2b. Use ideas from other illness – Olbas oil, Vicks, steam, etc. (104, 105, 121). Aim to release phlegm, good for cough. Use paracetamol and cough mixtures (106, 116), partly on GP advice or chemist advice. Use ideas from other conditions for asthma – chest physio (102), Vicks (130) Buy OTC preparations from Indian shops, don’t know what’s in them but herbal so must be OK (121) – Suduri (cough mixture) Dextromethorphan, hydrobromide menthol – so not actually herbal at all. But convinced that herbal medicines can’t have side effects (121) 3a. Some carry inhalers everywhere (2, 120, 112, 104, 105) but is a hassle or don’t as don’t get many symptoms (3, 119) 3b. Can’t get multiple inhalers or spacers, if want extras to give to school (127), other say GP gives out multiples (112) for school 3c. Child won’t use at school, gets embarrassed (128), thinks is waste of time/other things to do (128, 117) 3d. Not sure spacers work, how much is child getting, better to put in mouth (126) Spacer useful, child can use it on her own (111) 4a. Maternal knowledge Mum tells child when to use inhaler (130), child decides when to use (129), confusion between brown or blue – some think brown is when wheezing (104), not sure why two or what they are (129), know why is two but not sure which is which (126). Not sure what prednisolone is, maybe for infection (129) 5a. Children get scared of using inhalers, especially spacers (106, 103). Son doesn’t like prednisolone (104) therefore don’t give (104) but likes using spacer (104) so use it. Don’t understand the point of the spacer, seems more logical to use inhaler directly (163) Doctor said avoid fizzy drinks (119), doctor said all coughing would stop if they go to Bangladesh (119) Doctor said to avoid oranges, chocolate, bananas as they all trigger asthma (121) Given salbutamol syrup, didn’t work well, not sure why syrup not inhaler initially (121) Complementary therapies
Believe strongly (122, 123), don’t believe, don’t use (3, 108 – it’s herbal, it’s something they just make up, 110), desire to do something. Feels relief that is doing something (130) – go to practitioner as salbutamol ‘not working’ – recurring symptoms, missing school (122) feeling of guilt for not doing something (try a remedy or older sisters inhaler) – ‘anything to be them better really’ (122). Mostly treatments for cough, but use anyway (125). Tried it, didn’t work, cost a lot of money (114) b. Defining what is complementary therapy Some parents say no but are using (106), not sure what counts as complementary. Prayer – mostly say no, one mum says she’s been advice to use a line from Quran to make a tabiz (112), advised to wear camel skin around the neck (112, 129), put baby duck on the chest (129), but doesn’t do, prefers to listen to doctor c. Safety Parents do a bit of trial and error with complementary therapies, see if it works, one parent unsure about experimenting with child, so won’t, although would try themselves (115). If herbal cannot have side effects so may as well use them. (121) Bought OTC from Indian shops (122) or India (123). But Chinese herbs not used – concerns over side effects (122). Some prefer not to use. Best to stick to doctor advice (3, 127, 112, 119, 123) worried might do some harm (117), don’t know what they might contain (123) e. Tradition Complementary therapies used because older generation know them, (123,163), was their experience of local healers (120, 126) f. Might just be mind over matter/placebo effect (163) |
|||||||||
| Behaviours: getting a diagnosis | Determinants: getting a diagnosis | |||||||||
Nursery noted symptoms not parents (127) Relatives noted symptoms and suggest asthma (114) Parents notice symptoms at home – not sleeping/coughing at night (106, 109, 116, 119), getting out of breath when running a lot (127) Slow onset of symptoms (120) Parents had to take responsibility themselves (120), noticed increasing salbutamol use and asking for assessment Won’t believe diagnosis of asthma as dad is asthmatic and child doesn’t look same as dad when ill, so can’t be asthma (111) Getting clear diagnosis of asthma Using tests for asthma
|
1. Overlap and confusion with cough/upper respiratory tract infection/chest infection and repeated visits (130, 120, 112, 106, 109, 103, 126, 116, 118, 121, 108, 110, 111, 114) for doctors and parents, confusion with tonsils (118)
|
|||||||||
| Behaviours: what to do day to day | Determinants: what to do day to day | |||||||||
|
1a. Common sense My opinion: some of this is advice, some is what seems common sense to parents. Overlap between treatments for runny nose, colds, cough and asthma (121) 3a. ‘Why not’ View is other alternatives exist (like soya milk) so is no problem to avoid milk or children don’t need cheese in their diets to be OK (106). Don’t think dietary restrictions or treatments hurt, so why not do it (111) 5a. Fear of consequences If friends house not suitable for asthmatic might trigger attack (112), keep kids indoors for 4–5 days with a little cold to stop it from getting worse/developing asthma (112, 104) 6a. Expectations Deny impact on questioning, seen as normal consequence of asthmatic child (106, 109, 104) Overall Willing to spend money on treatments, even if not sure will work – try anything, feel need to do something. All is try it and see, no knowledge if will work or not. See a clear improvement with daily salt pipe, so stick to this (122) Herbalists say will treat – just one success story and everyone believes them |
|||||||||
| Behaviours: types of services available for asthma | Determinants: types of services available for asthma | |||||||||
|
2a. Parental assessment of symptoms is important (3, 1, 104). Parents get very worried by DiB, especially if had previous bad experience – intensive care unit or death (114)
|
|||||||||
| Behaviours: community awareness of asthma | Determinants: community awareness of asthma | |||||||||
|
Travel to India to get second opinion, confirm medicines are right or get herbal medicines (1, 110). Easier to get appointments with who you want to see in India (110). Others say why should I need to (106, 115). Influence of Indian health system is present, even though families know is different here. Diagnosed in Bangladesh (129). Symptoms better in India (118, 121). Compare Indian treatments with UK ones, feel India quicker treatment and service, one injection and problems sorted (123) 1b. Influence of community Don’t perceive that they influence them although might offer advice (104, 126, 110). Influence is stronger if born in India (126). Is an overall influence of community and upbringing, not specific to asthma (126). Do offer advice and does follow it (129, 121), feels people ask her why child got this (129, 121). Other people always want to give their opinion, not interested in listening to mums point of view (community and doctors) (106). Attitudes and beliefs persist in older generations (128) and in uneducated (128), but fading. Traditional Indian view to see everything as related to what you eat (126). Don’t accept there’s no answer, Indian tradition to find an answer, must be a solution. Extended family give advice – not to eat foods, not to inhale smoke from cooking (119) b. Cultural attitudes towards health and illness Recognise a cultural attitude not to tell others about any illness (112, 102, 101, 124, 122, 130, 109, 105, 118, 121, 125, 163, 108, 110) – but parents generally break this as feel is necessary, important to protect child as people need to know just in case (112, 102, 101, 124, 122, 130, 109, 105), or people see when they have attack so find out (118). Need to know what to do (109, 104, 112, 127, 106, 126), already in family so do tell (104), no hesitation about telling (117). If tell others can get useful advice and information (123). Don’t tell but just because feel it isn’t a big deal, minimise it, helps to manage it (163) don’t tell because people will gossip about them (108)
A person in a position of authority (even if not medical authority) still is influential, so if they don’t like steroids, has an influence (like teachers). Extended family do influence younger generation (129), even if younger generation don’t believe in same way. Grandparents don’t influence mum (118), don’t live together so no influence (117). Elders do influence, have to listen, make decisions with grandparents as a family (123). Not influenced by anyone, don’t know their opinion is right, decide for self (163, 108) but grandparents do offer opinions including how mum is managing children (108, 111), listen to bits and pieces c. Impact on marriage Not a problem now (126)/asthma not a big enough issue to have an impact on marriage. Still gets brought up around marriage (127, 118, 125, 123) cultural tradition to be wary if someone is poorly, poor marriage prospect, but is that people don’t know about asthma, don’t know what it is (115), don’t want an ill/weak wife (129), don’t want wife to pass on to daughters (not problem for man) (111). Have to mention it then up to families to decide (123). Particular problem for girls (125), girls judged more, taken into new family (126, 125, 118, 111), suggest shouldn’t have brought her into family if has asthma (118). Would be issue for child (118), not them but other families think like that. Don’t hide it though, other side will find out anyway after marriage then causes problems (123, 125). Recognise that some previous generation attitudes towards concerns over marriage, but is different for children now – they will be able to choose marriage partner more (106,129, 104, 126, 163,111). Is more an older generation thing (126, 123), younger children will choose for themselves now (123) d. Fear of contagion Some say contagious (130, 112, 124, 118, 125), others not (127, 115, 104,116, 119, 121, 123). Others may still object to asthmatic child being brought to their house (112, 118, 121) is fear of catching it (118). Sort of accept that it is right – asthma can be dangerous, wouldn’t wish that on someone else (118). Some may avoid family (130), ask not to bring child here suggest don’t share a glass of water, etc., not sit here (130). Won’t let child go to other people’s house or share a glass in case gives them asthma (124) e. Stigmatisation Feels communities have moved on from shunning someone with asthma (127, 106, 104), still present in India (111) although mums felt blame/mother did something wrong to cause this (106, 121, 126, 108) and some don’t accept within family – ‘not my family, my wife’s family’ (103) some shame (163), some gossip (111). Attitudes are and will change, but in another 30 years. Feel sympathy from community (129), no stigma now (128). Is moving on, still there in older members of community (126, 163). Still some shunning due to contagion, fear of death/very severe illness (163, 111). 108 dad doesn’t want to label daughter with asthma, not good to have any illness in body (108)
|
|||||||||
| Behaviours: understanding asthma | Determinants: understanding asthma | |||||||||
|
What is asthma
|
|||||||||
| Child management behaviours | ||||||||||
Acute attacks
Inhalers Don’t always take (114), don’t want to take medicines, just want to be normal (114), don’t want to waste it (103) forget to take (101, 123, 125), wants reminders – diary or wall planner or mum (106, 101, 123), try to use own systems to remember like keep next to bed (105). Can demonstrate technique well (115) but some confusion on timings. Reliant on mum to decide whether to use it or not (121, 111). Worried about side effects therefore tries to limit his own use (125) (echoed by mum). But feels worse when don’t take so gets annoyed as then does take (125) Don’t want parent to be angry for using inhaler too much (103). Don’t want to worry parent by telling them (108), or be taken to hospital (108) Some children keep it nearby to them (131). Some don’t know where kept (127). Really annoying to carry inhaler everywhere (126). Can’t give to teacher, has to keep it in case need it and teacher not free (126). Doesn’t want to have to carry it around. No problems getting inhaler in school, uses it herself (111), likes it, is fun (111) Use inhalers themselves (131, 163), especially at school (120, 163) but some schools the teacher keeps inhaler and gives to child (115, 123), parents might prompt her to take it (163) Can demonstrate technique fairly well (111), bit confused on timings (116), one child doesn’t like having to hold her breath/gets fed up (115) wants tablets instead (but mum things she wouldn’t take tablet either, doesn’t like taste, doesn’t like swallowing tablet). Child wants to choose each day depending on how she feels (115) or add something nice tasting to inhalers like Ribena (115). Not sure why two inhalers, what they do. Wants something that makes it go away, a tablet/medicines so don’t need inhaler (126). Has own understanding of why two inhalers but not in line with medical understanding (123) Symptoms/activity levels Experience and recognise wheezing (131, 111) then act on it themselves, especially at school (131, 111) or have to find a teacher themselves (115). Cough is big symptoms, chest tickling and feels funny (126, 123), pain in throat (111) Perception of severity: know it can be, but class self as moderate/mild (130), no set way to judge symptoms but loosely based on breathlessness on activity (131, 120, 124, 121, 125), decide herself (106) but liked child’s asthma action plan idea (106). If was serious problem then someone would do something serious (121) Don’t or can’t run around as much (131, 114), is noticeable that can’t play as much, run as much (114) but still are active and do sports (120) just use inhalers, active as per usual (119, 121, 125, 111, 123) Some use inhaler before sport to stop symptoms Is aware of limited activity tolerance at home (106). Is aware that can’t do as much as brother, not as tall as identical twin brother (104), not allowed out as much as sister (111) Can’t be PE teacher when grow up as too much running (131) Gets scared going to friends or family as has had attacks there (too cold, or too dusty) (114), so now doesn’t go (114) Spacers Don’t always use spacer – sometimes a choice (103), sometimes don’t know where is (111), don’t keep it at school (108 ), others do have at school (106, 115). Don’t need spacers any more (126), for little kids only. Others do use but don’t know why (106), have some understanding but not clear (123), mum said don’t need it anymore (108), don’t have a spare for school so stopped using it (108) Information Most not using internet to look up asthma (130), others are (105, 125 – neither found Asthma UK). Nurses can be good, explain to child (121) Chemist was ‘useful’, good at explaining to child (105, 116) Asthma nurse useful, good at explaining (105, 115 – told me lots about what was happening to me). Helped with symptoms like mouth ulcers, how to use inhalers so don’t get them (115) Want dad to know about management too, so he can take care of me (126). Want parents to have most explanations, doctors talk to them, then they take care of me (123). Asthma clinic excellent, listens to me, explains the things I want to know, helps me with the things I care about (114) Self-management Using some diet restrictions but decided by parents (106, 121) No bullying or negativity (106, 111, 121), friends not bothered (120), but doesn’t want friends to know, hides the asthma, thinks it’s private business (114). Get embarrassed (114) Gets brother to do things for him, says I can’t (when probably could) (104), likes saying he’s got asthma then doesn’t have to go to school (123). Feel sorry for parents as they get woken up, always having to run around after him with asthma, parents worry about my asthma (114). Get annoyed as think there are too many things can’t do due to asthma (114). Not sure what future careers can have due to asthma (114) Knowledge
|
||||||||||
| Child determinants | ||||||||||
| Nebulisers work better than inhalers (103) Hospitals
|
||||||||||
| Environmental factorsInterpersonalCommunitySocietalAsthma not always prioritised (secondary to other health conditions) (1), not significant, will grow out of itUsed to feel discrimination, but not now (3), not about being Asian (2)Other people have suggested daughter caught asthma (130)Information sharing between parents – if dad goes to doctor, then he explains to mum (127)Extended family and friends do offer opinions on management (1, 2, 3, 112), few participants live with extended families. Mums deny that this influences them. But then do own thing. People can be unkind (130) but most say no to this. Advice is usually about not eating cold, not going out in cold, dressing warmly (112)Might try herbal remedy, no harmDeny impact on marriage in ‘our family’ (3, 127, 130), only in ‘other families’ (3). Other interviews do think asthma is still mentioned in relation to marriage and that some areas of society would prefer not to mention it. But feel it is changingDeny impact on social life/limitations to family life (127)Deny impact of culture on management (3)Admit cultural attitude to hide illnessNot all classify asthma as an illnessPeople need to know so tell anyway – this is recurring, need to keep children safe, do what’s best for themAsthma not serious enough to be a problemWorse if eczemaPracticalities (no car, waiting for taxi) (103)Visit India, get treatments there. Intentional trip to India to get treatment, not for asthma, but seem to work, so erodes confidence in British healthcare system and medicines (1). Also visit Saudi Arabia (2) | Environmental factors | Interpersonal | Community | Societal | Asthma not always prioritised (secondary to other health conditions) (1), not significant, will grow out of it Used to feel discrimination, but not now (3), not about being Asian (2) Other people have suggested daughter caught asthma (130) Information sharing between parents – if dad goes to doctor, then he explains to mum (127) |
Extended family and friends do offer opinions on management (1, 2, 3, 112), few participants live with extended families. Mums deny that this influences them. But then do own thing. People can be unkind (130) but most say no to this. Advice is usually about not eating cold, not going out in cold, dressing warmly (112) Might try herbal remedy, no harm Deny impact on marriage in ‘our family’ (3, 127, 130), only in ‘other families’ (3). Other interviews do think asthma is still mentioned in relation to marriage and that some areas of society would prefer not to mention it. But feel it is changing Deny impact on social life/limitations to family life (127) Deny impact of culture on management (3)
|
Practicalities (no car, waiting for taxi) (103) Visit India, get treatments there. Intentional trip to India to get treatment, not for asthma, but seem to work, so erodes confidence in British healthcare system and medicines (1). Also visit Saudi Arabia (2) |
|||
| Environmental factors | ||||||||||
| Interpersonal | Community | Societal | ||||||||
| Asthma not always prioritised (secondary to other health conditions) (1), not significant, will grow out of it Used to feel discrimination, but not now (3), not about being Asian (2) Other people have suggested daughter caught asthma (130) Information sharing between parents – if dad goes to doctor, then he explains to mum (127) |
Extended family and friends do offer opinions on management (1, 2, 3, 112), few participants live with extended families. Mums deny that this influences them. But then do own thing. People can be unkind (130) but most say no to this. Advice is usually about not eating cold, not going out in cold, dressing warmly (112) Might try herbal remedy, no harm Deny impact on marriage in ‘our family’ (3, 127, 130), only in ‘other families’ (3). Other interviews do think asthma is still mentioned in relation to marriage and that some areas of society would prefer not to mention it. But feel it is changing Deny impact on social life/limitations to family life (127) Deny impact of culture on management (3)
|
Practicalities (no car, waiting for taxi) (103) Visit India, get treatments there. Intentional trip to India to get treatment, not for asthma, but seem to work, so erodes confidence in British healthcare system and medicines (1). Also visit Saudi Arabia (2) |
||||||||
| Possible interventions/ideas | ||||||||||
| Develop a cure (3c, 118, 125), medicine that cures asthma (3), so don’t have to be on long-term medications Better diagnosis system, be clearer (106), earlier trials of salbutamol with good follow up (110), clearer tests/diagnosis so can be sure (123, 110) Reduce waiting times in ED/walk-in for asthmatic children, faster treatments when ill (106, 104, 123, 108) Referral system, automatic if wheezy, place for all new diagnosed families. Want to see specialist for information, not to confirm diagnosis (1). If prescribed salbutamol, should be automatic trigger to think about asthma/test for asthma/education about possible asthma. Need to remove ambiguity. Do proper check-up Quicker referrals to a specialist/asthma nurse who can give good clear advice at the beginning, not 2 years later (115) Use schools to education, give out info, then get kids and parents. Could do classes or courses at schools for parents (112). If not this time, would need child-care arrangements otherwise can’t go to classes (112) Feel doctors should acknowledge how scared parents are at the beginning (106) Have a phone service, can call for advice, some kind of centre for asthma, place where people are trained, have knowledge, can be self-referral or via GP Letter of access: states diagnosis and gets them quick appointments (102) More spaces for asthmatic child to be put and oxygen level checked in GP/walk-in/ED (163) Mum wanted something written down (115, 109, 108) especially for emergency management. 104 says did get info from hospital but on emergency management Want info on what the condition is, the warning signs, and people that can sit down with just to talk, how it’s managed, what the inhalers are for, what the chambers are for, what the chemist can do . . . Practice helps children not be scared of inhalers/spacers, then know where to put lips, when to breathe, feel more confident (115). Learn from ED and nurses (104). Using rewards helps child to use spacer (106) then get used to it. Also back up from nurses/doctors reinforces parents (106) Desire for more information about asthma from HCPs (108)
Doctors need to explain how it’s part of life, need to live with it, community/friends need to understand it’s a way of life (106) Need to have advice in multiple languages (109, 116), leaflets but bilingual people better (109,163) use pictures/images (116, 163) Understand doctors can make firm diagnosis, so be clear about try this, then come back, then try this, work with parent (106 ) – phone advice or closer follow-up, especially at night when child coughing ++, get prepared in advance so know how to handle 2 a.m. cough/wheeze (106), other parents say not telephone, want face to face consult (163). Could be phone or written plan/booklet, some support when scared at night Need to raise community awareness, so can suspect it isn’t a cold (106, 123, 163, 108), so they know parents are doing it right (108) Would like something from hospital that’s for the children (after acute attack) so can explain, something for them to have (115) Suggest leaflets in right languages (123, 163) do have in chemist but have in temples, etc. (115). People coming into temples to talk is better (115), also to tell children in school or gurdwara (115), can use local radio to advertise symptoms of asthma (123) Suggest a register of patients with asthma, wherever present to, so can automatically get information and referred to nurses, etc. (115) |
||||||||||
| Possible solutions | ||||||||||
| Would like breathing exercises/yoga/ (117) massage therapies (106). Makes kids calmer. Some advice on what parents can do. (106) Even if doctors still saying not sure yet is asthma Need to promote parents right to ask questions, tell them is OK, doctor will be happy (109) – do this in multiple languages in surgeries Give free inhalers on a regular basis, don’t make people wait or ask for them (3c) Nurse teaching with demonstrations is useful (1, 112), especially school nurse teaching in school (125c). Let parents come too, helps them in school (125) Integrated records, so don’t have to repeat themselves (2) Access letter or card to allow quick treatment (2) Having staff who speak different languages to act as interpreters Regular monitoring – feels like they care, don’t brush me off, give me help (104) Good communication – listen to parents, clear explanations, practical advice for home management, honest with them (104, 2, 117, 108). Doctors talk to parent and child (130). Want doctors to be source of information (127). Chemist good source, best in private room with time to demonstrate and practice (116) Want to be treated politely and kindly by nurses in hospital. Given information they can understand (124, 112). Understand they are scared. GP take them seriously (108) Not sure that can educate whole community, won’t change. Perhaps can try to suggest that hiding asthma is not fair to children, but not sure any education can work Use clear words so children understand (130, 163) Explain to child what it is, is it serious (130) Use talking to explain to child (in preference to books, DVDs, etc.) (130, 115), although pictures might be OK (115, 163), books useful (163). Talking to other kids with asthma could be OK (115) Family help child to remember to take inhalers. Work in school on asthma (125), in lessons, whole school (125) Want somewhere to go where can communicate (112), wants to feel involved in child’s care (127), community centre, can meet other parents, what they do with their children, have doctors and nurses come into to do talks, etc., but not run by them. Local better but would go to one in central Leicester. Family doctor/consistent doctor, someone who can work with family regularly over a period of months Also for acute moments, want to be able to get advice quickly, maybe by phone (112). When do get there, quick response to settle breathing, then kept under observation until child better (104). Want nebulisers at home, home oxygen (104), feel it would reduce need to go to hospital – doctors will only give for really severe patients Transport, especially if have other kids, can’t leave them behind, need to get to and from clinic/hospital and be able to do something with siblings (112) Location of clinics not vital, referrals and availability more important Getting information to community and people who don’t engage is important, need face to face, bilingual people, lay facilitators – don’t trust unknown people (109), white people might be social services so don’t open door. Use local community centres that people know and leaders in community to promote research (109). Desire to know more about non-medical management (127) Encourage everyone to go to chemists and GPs, neighbours tell neighbours (116) A lot of oral traditions in South Asian community, need to use that to educate, be oral (109). Increase community awareness of symptoms, what do to in attack, is serious, etc. (118) Willing to take daily medicine if would totally remove symptoms/asthma (106) (but not steroid and no side effects). Want to know about non-medical options but don’t know who to ask (127) want to do something (130) Want someone to explain to her but is husband who goes to doctor (mum doesn’t speak English), wants explanations herself (112) Want a way to explain to child – simple, pictorial, actions. Can be leaflets that do this (126) Suggest leaflets in different languages (123, 125). Doesn’t have an asthma plan, would like it. Communication is hard for many South Asian people, language problem. Would like info, pictures for the child, to explain, simple literature for adults. Annual review very useful too. Needs basics of asthma, which inhalers to take, what to do in emergency. Simple pictorial, or videos or voiceovers. Use TV for awareness. (126). Books for children, to read with parents (123) |
||||||||||
| Agents | Health problem? | |||||||||
| Mum Dad Child Extended family Class teacher PE teacher GP Practice nurse Hospital doctors Hospital nurses Pharmacist |
Uncontrolled symptoms Quality of life |
|||||||||
| Notes | ||||||||||
| Male/female doctor not important (103) Parents chose to use ED, not just winding up there. Fear is big motivator. So is perception of it being right and GP not able to cope Same for choosing to accept symptoms in preference to regular medication use. If want to change this, need to prove effects of long-term failure to control asthma – parents believe kids will grow out of it, and most do Experiences in one illness are translated to asthma too Parents want to do SOMETHING, so will try remedies for colds or coughs even though they know isn’t asthma, but might help and sometimes does. It’s the ‘it won’t hurt them’ principle Cough is far more commonly reported by parents than wheeze Seasons – cough/colds in winter, go to GP a lot, but goes away in summer, so not diagnosed/forgotten about/not serious Want help, relevant to them, listen to them. Takes time and a relationship |
||||||||||
Appendix 8 Drawings by children
Appendix 9 Ranking data sheet
Appendix 10 Interventions scoping review
Using the same search strategies and approach as above, we identified 408 examples of asthma interventions trialled for, with or on children: four were targeted to South Asians, 22 were targeted to another ethnic minority group, 134 targeted to a specific group (but not an ethnic minority, e.g. inner-city children) and 252 were generic. In addition, we identified 15 systematic and non-systematic reviews of asthma interventions for children.
Of the four targeted to South Asians, three focused on education and clinical support. One included additional elements of raising awareness. All of the interventions targeted both adults and children; no studies with interventions specifically targeted at South Asian children alone were identified (see Table 21 for details).
Moudgil et al. 213 assessed the impact of a patient education and GP support programme for White and non-White groups in reducing asthma morbidity in 2000. This study included patients aged 11–60 years. Six hundred and ninety-eight patients were recruited, of whom 42% were of South Asian ethnicity; of those, 42% were born outside the UK (India, Pakistan, and East and Central Africa) and 34% spoke no or very little English. Patients received an individualised asthma education programme which was reinforced after 4 and 8 months, and GPs were given advice and equipment. The results showed that, overall, the active intervention group had reduced GP consultations, reduced accident and emergency attendance, reduced hospital admission, reduced prescriptions for rescue oral steroids and less antibiotics. However, when stratified by ethnicity, significant improvements were seen only in the White European group, not in the south Asian group. Asthma Quality of Life Questionnaire (AQLQ) scores demonstrated lower values associated with South Asian ethnicity, although there were small but significant changes in AQLQ scores recorded over the length of the study in both White European and South Asian groups, suggesting that both White and South Asian patients are responsive to the Hawthorne Effect, although the intervention itself was less effective in South Asians.
The ELECTRA study, Griffiths et al. ,56 tested a liaison model of specialist nursing in 2004 with asthmatic patients aged 4–60 years old. This study combined the education of patients after discharge with educational outreach and clinical support for primary care clinicians in the Tower Hamlets region of London. The study aimed to identify whether or not specialist nurses could reduce health service use, and do so equally in different ethnic populations. The intervention delayed time to first attendance with acute asthma, reduced the percentage of participants attending with acute asthma, and increased the percentage of patients with reviews in primary care but showed no effect on self-management skills, quality of life or frequency of symptoms. When analysed by ethnic group, the results were consistent with (but non-significant for) a greater benefit for white patients than for South Asian patients or those from other ethnic groups.
The OEDIPUS study continued on the work started in ELECTRA but focused exclusively on South Asian patients. An established educational programme from the USA (PACE – physician asthma care education) was adapted for use in the UK with South Asian patients aged 4–60 years. Practice nurses and GPs were trained using PACE and patients received either PACE-style management or standard management. The study found that while attendance at asthma reviews improved, there was no change in acute exacerbations.
The final study reports on a community-based nurse-led clinic for the assessment, diagnosis, education and treatment of asthma. Although not exclusive to South Asian participants, the location was established in an area with a predominantly South Asian population. In addition to intervening in service provision, the study reports that workshops and talks were held to raise awareness and acceptability of asthma. However, while the study reports that standards of care were improved (assessed by agreement with the BTS guidelines on asthma management), no clinical or personal outcomes were measured.
| Citation | Study type | Year/location | Intervention | Results |
|---|---|---|---|---|
| Griffiths: specialist nurse intervention to reduce unscheduled asthma care in a deprived multiethnic area: the east London randomised controlled trial for high-risk asthma (ELECTRA)56 | Cluster RCT | 2004 UK – London n = 319 |
2 × 1-hour visits to participating practices for discussion/education, and use of computer template or stamp to prompt patient review. The patients received a review by specialist nurse, and were given equipment and written plans with changes to medication plans as needed | Intervention delayed time to first attendance with acute asthma, reduced the percentage of participants attending with acute asthma and increased the percentage of patients with reviews in primary care No effect on self-management, quality of life or symptoms was found When analysed by ethnic group, the difference in effect on ethnic groups was not significant, but results were consistent with greater benefit for white patients than for South Asian patients or those from other ethnic groups |
| Moudgil: asthma education and quality of life in the community: a randomised controlled study to evaluate the impact on White European and Indian subcontinent ethnic groups from socioeconomically deprived areas in Birmingham213 | RCT implementing asthma education/medication management to White British and ethnic minority groups – whether or not morbidity rates can be reduced by implementation of such education interventions | 2000 UK – Birmingham |
An individual asthma education programme (initial session approximately 40 minutes) which was reinforced after 4 and 8 months; advice for GPs; peak flow meters; booklets | Active intervention reduced the number of hospital admissions, consultations, prescriptions of rescue oral steroids and antibiotics But when analysed by ethnicity, statistically significant changes occurred only in the White European group Lower Asthma Quality of Life Questionnaire values were associated with Indian subcontinent ethnicity Longitudinal changes (for 522 subjects) in the mean AQLQ scores were small but statistically significant for both ethnic groups, with scores improving in the active and worsening in the control groups |
| Oldam: nurse-led clinic in an Asian community214 | Pilot study | 1994–5 Bradford, UK |
A nurse-led community clinic with direct referrals from local GPs for assessment, diagnosis, education and treatment recommendation, plus roadshows and talks organised to raise awareness and acceptability of the diagnosis of asthma in the ethnic community | The evaluation demonstrated an improvement in the standard of care – not specified further and no comparison group, no fixed outcomes |
| OEDIPUS: can education for South Asians with asthma and their clinicians reduce unscheduled care? A cluster randomised trial and qualitative evaluation58 | Cluster RCT | 2011 London, UK n = 375 patients from 87 GP practices |
Modified PACE programme. Intervention group were seen in outpatient care by PACE-trained specialist nurses, provided with education and self-management advice, referred for follow-up by PACE-trained practices, invited to participate in asthma adaptation of Stanford Chronic Disease Self-Management Programme. Control patients were seen in outpatient care by specialist nurses providing usual care | The intervention did not change the time to first exacerbation with cough It did reduce time to first asthma review (i.e. better attendance at asthma reviews) Conclusion: intervention failed to reduce unscheduled care for South Asians with asthma but did improve follow-up in primary care |
Appendix 11 Ideas for future interventions from phases 2 and 3
| Key issues | Focus groups | Key informant interviews | Parents/carers | Children | HCPs |
|---|---|---|---|---|---|
| Time | Quick referrals to specialists, maximum 1 month More time with GP – ability to book longer session to discuss asthma |
For acute moments, want to be able to get advice quickly, maybe by phone When do get to ED/walk in, quick response to settle breathing, reduce waiting times, faster treatment times for asthma, then kept under observation until child better Want time in GP appointments for full physical assessment Quicker referrals to a specialist/asthma nurse who can give good clear advice at the beginning, not 2 years later Someone with time to sit down with just to talk |
Get treatment quickly, are scared | Having longer 30-minute appointments specifically for asthma education | |
| Access to clinics | Local clinics, specifically for ladies (PF) Not essential to have clinics locally but is nice Quick access to clinic is more important, i.e. getting appointments Ability to park important too |
Out-of-hours clinics Specialist clinics in ‘Asian’ areas |
Location of clinics not vital, specialist referrals and appointment availability more important Transport to help get to and from clinic, especially if have other kids, can’t leave them behind Be able to do something with siblings Local clinics better but would go to one in central Leicester, especially if was asthma centre/one-stop shop Self-referral into one-stop shop asthma centre |
One central asthma clinic, could base clinics in children’s centres but co-ordinated care between outreach/hospital/GPs/nurses essential Others suggest multiple clinics cited around Leicester but not all mums drive, need transport Give all asthmatic children 48-hour open access to GP or CAU (can just ring and show up) following an admission so can see HCP quickly, reduces anxiety and un-needed returns to hospital Need facilities to see more children and provide rapid assistance if do open-access Need to signpost existing PCT services for HCPS, no one sure what is offered by whom Set clinic hours around school day and school holidays, religious holidays Assist with transport |
|
| Diagnostics | Better diagnosis system, be clearer about the process, if can’t be sure, book follow-up, offer phone follow-up Need to remove ambiguity HCPs to give information and advice even if not confirmed asthma, help parents be prepared for possibilities If prescribed salbutamol, should be automatic trigger to think about asthma/test for asthma/education about possible asthma |
Clear diagnosis, helps me to understand why I’m wheezing | Quick and simple test for asthma Access to lung function testing but without formal referral to specialist, option for one-off ‘assess and return’ |
||
| NHS services | Dedicated asthma clinics in the community GP can diagnose, then straight to specialist clinic for information/testing, then yearly review |
Want nebulisers at home, home oxygen so can reduce need to go to hospital More spaces for asthmatic child to be put and oxygen level checked in GP/walk-in/ED Phone advice line, especially at night Integrated records, so don’t have to repeat themselves Access letter or card to allow quick treatment Suggest a register of patients with asthma, wherever present to, so can automatically get information and referred to nurses, etc. Offer more help to families having problems One-stop clinic Place for all new diagnosed families to go Provides information and one-off specialist assessment Automatic referral system, automatic if GP says wheeze or gives salbutamol Place where people have asthma training and knowledge Can offer quick appointments |
Playrooms in hospitals | Dedicated asthma clinic/asthma nurse service for closer follow-up/monitoring, family education, spirometry/lung function, visits to practices and home visits especially for South Asian families, needs to link to tertiary clinic with regular contact not an independent service, can act like children‘s rapid assessment and follow-up team (CRAFT) to review questionable patients, check on improvements, etc. More co-ordination between different specialties so can provide united service One front-door policy for ED/CAU to provide faster access and united management then education on ward Telephone advice service, with links to local services, can direct and advise Increase specialist asthma nurse reviews More space in clinics to accommodate large South Asian families Put diagnosis on prescriptions so pharmacist can reinforce message Joint management between hospital, GP and pharmacist, joint records and meetings |
|
| Other services | Local point of contact/facilitator | Helpline | Lay facilitators – face to face, bilingual people – don’t trust unknown people, white people might be social service Community centre, can meet other parents, what they do with their children, have doctors and nurses come into to do talks, etc., but not run by HCPs |
Some kind of tool to assess asthma but also their beliefs, attitudes, issues from community about asthma could be useful especially for non-compliant families Someone in ED to check all post-attendance management in community put in place and acted on Take onus off parents to co-ordinate systems and book appointments Use local pharmacies or GP surgeries for evening drop in service on asthma Could give updates on current advise on home management/alternative remedies/foods, etc., like pregnant women get on foods in pregnancy |
|
| Specialist care | Specialist can be nurse or doctor But not exclusive nurse management |
Specialist nurses | |||
| Medications and therapies | Syrup might be easier, more familiar too (BF) | Breathing exercises/yoga/massage A cure A daily medicine that completely stops symptoms (even if not a cure) but not if steroid based and no side effects Want to know about non-medical therapies, either from HCP or HCP advises where to go Give free inhalers on a regular basis, don’t make people wait or ask for them |
Help the family to remember to give inhalers/remind child Use diaries or wall-planners Mum should remember Develop a cure Medicines that taste better, can put in drinks, liquid or tablet Medicines that work better and stop the asthma |
||
| Review/monitoring | 6-monthly reviews for asthmatic children Yearly reminders on technique |
Better follow-up after diagnosis | Annual review Regular monitoring – feels like they care, don’t brush me off, give me help |
Use peak flows, are fun and shows how good or bad breathing is | Way for children to report their symptoms, pictorially, smiley faces, etc., no dependent on language skills |
| Information | More information (PM, PF) Practical help and training for inhalers Advice on home changes/management parents can do Kids to go to appointments, need education too Leaflets in own languages |
Education and information for parents/families Use real-life case studies/parents to spread message Definitely not leaflets! (Though no. 7 yes) |
Want info on:
Want information for children/to help parents explain to children/for children to keep as reference on asthma Leaflets in multiple languages, with pictures/simple language, in chemists, temples, gurdwaras, schools Verbal explanations better/should go with leaflets HCP to explain to child what it is, is it serious Use videos or voiceovers Want information from someone expert in asthma/specialist just for information Practice helps children not be scared of inhalers/spacers, then know where to put lips, when to breathe, feel more confident |
Want professionals to be source of information or parents, easier than using internet Given information they can understand, use clear words Use talking to explain to child (in preference to books, DVDs, etc.) Nurse teaching with demonstrations good, nurses good at explaining, although pictures might be OK Talking to other kids with asthma could be OK Want information when feeling better, not when ill |
GP should be primary source of information – when acutely ill not right time Others say increase role of asthma nurse or pharmacist in education as no one else has time:
Need to offer information quickly following acute illness Automatic alerts to GPs on arrival at ED with need to offer education appointment within 2 weeks Need to offer consistent advice and information from all sources Leaflets:
Simple animations for asthma management, what inhalers are, in different languages, how to use inhalers, more effective than leaflets which no one reads regardless of language DVDs to take home, can’t be for sale, has to be free, could be via pharmacy with prescriptions Use devices for training Use models/diagrams
|
| Communication with HCPs | Want somewhere to go where can communicate Overcome language barriers Having staff who speak different languages to act as interpreters Someone to explain to parent who doesn’t attend doctor appointment, usually not in English then HCPs to listen to parents HCPs to give information in clinic, give clear explanations, practical advice for home management Doctors talk to parent and child Want to be treated politely and kindly |
Should insist all families learn English and remove interpreting services Need clear and quick communication between GP/hospital Electronic discharge summary systems United computer system between all HCPs for quicker communication, can see prescriptions and admissions and education, etc. Would need to be able to flag new info or changes otherwise easily missed (paper more obvious) Offer basic training in South Asian languages, but hard to know which one to concentrate on Better access to interpreters, quickly available in multiple languages to allow mums to understand more, able to deliver education in acute settings |
|||
| Training | Training for medical professionals – GP forums Training for imams |
Training for HCPs:
Add asthma management to regular, rolling education programmes for HCPs with content regarding how ethnicity might impact management |
|||
| Awareness | Communities need to be more open, more matter of fact, treat kids normally, share knowledge themselves Need to address community myths about cold, foods, etc. Target parent places – Sure Start, children’s centres Have talks about asthma (like do for diabetes and heart disease), talks in own languages, workshops on asthma Use Indian radio and TV Advertising like the stroke advert |
Outreach with community groups and mosques by trained HCPs Groups for parents and separate groups for children – self-support groups Radio Public health campaign |
Raise community awareness, is a way of life, can be managed Use Asian TV Use Asian radio A lot of oral traditions in South Asian community, need to use that to educate, be oral Local community centres that people know and leaders in community to promote research People coming into temples/gurdwara/mosque to talk is better than leaflets |
Someone who can do health promotion/asthma at school parents evenings, school fair, assembly, in local pharmacies or clinic in pharmacies Need to incentivise people – food, money, free DVDs, goody bags Use local places so going is easy and socially acceptable Use key informants/facilitators to bring people into events Tie into local events so becomes culturally acceptable to attend |
|
| School | Need to train teachers better too, how to recognise attack (example of boy who died in school) Use school newsletters |
Raise awareness in schools | Talks in schools for children Talks in schools for parents is good time as child in school, otherwise need to provide childcare at workshops Schools provide information |
More education on asthma at young age for kids, may reduce stigma More education on medications generally at young age, may improve compliance when older |
|
| Parents | Self-help – encourage parents to use leaflets, look for information in library, internet | Promote parents right to ask questions, tell them is OK, doctor will be happy – do this in multiple languages in surgeries | Want parents to make decisions about asthma (primary school aged) Want parents to remind them about asthma and medications (older kids) Want parents not to get angry about them using inhaler too much |
Appendix 12 Steering group suggestions for additions and considerations to proposed intervention
| Issues and suggestions | Clinical and layperson advice centres | Education and training modules | Raising awareness |
|---|---|---|---|
| Feasibility: issues raised | The programme was felt to be ambitious but largely feasible, although the feasibility of achieving HCP change in practice was raised, in particular how liaison between the co-ordinating office and GPs will be provided | Overall, this arm was reported as ambitious and resource intensive, with potential difficult issues around recruiting and retaining educators | Broadly feasible to implement but risks of being too narrowly focused on one group and whether or not overworked NHS services can tolerate increased workloads |
| Suggestions | Good-quality and reliable computer system essential Need consortia buy-in from early stages |
To combine or condense the 14 modules into a shorter training course To offer yearly refresher training for lay educators, and partner lay educators with professional educators |
Need to ensure everyone relevant is included Use Asian TV and partner with other organisations and community groups |
| Barriers: issues raised | HCP resistance to change was reported as the most likely barrier, although other considerations such as the need for a secure and reliable computer programme to manage this were also raised | Too many modules People who think they know an area will opt out and miss vital knowledge Big time commitment for families or professionals |
Issues with HCPs’, teachers’ and parents’ lack of time, but also lack of knowledge and training or lack of interest in working this way |
| Suggestions | It was suggested that strong support from the new GP consortia and linking this arm closely to the education and training modules would assist in overcoming barriers | To offer whole course as a fixed set, not to allow people to choose which modules to take Sessions could be 30 minutes to 1 hour, whole programme about 4 hours |
Could integrate awareness into existing classes |
| Resources | Reviewers identified that the staff required to run the co-ordinating centre and the cost of increased service demands would need to be accounted for Concerns were raised over long-term sustainability without research funding |
Will need to develop electronic and hard-copy back-up resources for each module Resources to recruit and train lay educators, and pay for time spent on educating others, plus venues |
Will need to have resources and clinical ability to support any changes in expectations or behaviours, linked to term sustainability/resources to embed this |
| Suggestions | Will need expert medical backup to ensure content of modules up to date | Get buy in from right people, time and effort to get people on board |
Appendix 13 Economic evaluation
Cost assessment for education and training module
Costs of training the trainers
C1. Cost of developing evidence-based and/or consensus-based advice: details of the Education and Training intervention proposal imply that the module must be evidenced based or, if such evidence does not exist, must be consensus based. Little indication is given as to whether the project team have collated information on this evidence already, or whether this still needs to be done. If research is required in order to inform this process (i.e. a literature review to obtain information on what is effective) then the costs of this need to be considered. The most sensible way of going about this might be to specify what issues a review might consider, and then conduct a competitive tendering process to establish what the minimum cost might be of providing the information required to inform the training module (by researchers competent enough to do the job).
C2. Cost of training educators: the proposal envisages that educators ‘will need to complete all the modules themselves first, then take part in a 2-day training course to learn how to deliver the modules’. Personnel capable of providing training will be required. It is unclear from the proposal what pay scale and grade of personnel might be required in order to provide such a 2-day training course for each person who requires training. There is also the requirement that ‘each educator will be required to attend a yearly update support session’ which will mean accommodation will be required as well as personnel to deliver such sessions. This implies that an ongoing unspecified annual cost will need to be borne for the provision of education to educators.
C3. Costs of accommodation: training sessions will need to be provided using some form of daytime accommodation. This might range from temporary use of a primary care trust office, which might be provided free of charge, to having to hire out conference facilities at a hotel. Hotel conference facility costs do vary considerably and will depend upon location and quality of provision sought. Such costs ought to be considered, if applicable. If delegates have to stay in hotels overnight, this cost also needs also to be taken into account.
C4. Costs of handouts: when people are being trained, they will require handouts; some assumptions have to be made about the costs of providing these.
C5. Costs of refreshments: while being trained on a 2-day course, people attending for training will require refreshments including coffee breaks, lunch and an evening meal.
C6. Transport costs: if training sessions are provided by centrally based staff who travel to different regional locations to provide training sessions, then those providing training might have higher travel costs than those in attendance. The travel costs of those providing training and those receiving training both need to be considered.
C7. Costs of hotel for overnight stays: as this is a 2-day course, the cost of an overnight stay in a hotel needs to be considered.
Costs of training the trainers (refresher courses)
C8. Costs of refresher training (staff time): a 1-day course will be required every 3 years to ensure that those providing training retain up-to-date skills; the cost of staff time involved providing this needs to be considered.
C9. Costs of accommodation: the 1-day refresher training sessions need to be accommodated, and the cost of this needs to be considered.
C10. Costs of handouts: when people are on refresher training, they require handouts; some assumptions have to be made about the costs of providing these.
C11. Costs of refreshments: while being trained on the 1-day course, people attending for training will require refreshments, including coffee breaks and lunch.
C12. Transport costs: if refresher training sessions are provided by centrally based staff who travel to different regional locations to provide training sessions, then those providing training might have higher travel costs than those in attendance. The travel costs of those providing training and those receiving training both need to be considered.
C13. Central administration costs for the intervention: inevitably, a training intervention will require central administration. The proposal envisages that ‘the central programme office . . . will support and monitor the delivery of modules by observing module delivery’ by providing ‘specific information and advice in response to questions asked by educators (or module participants)’. This all implies that costs are incurred; the level of these will depend upon the level of support and monitoring required (and the wage costs of the people providing it), and also upon the extent of advice required by educators. The average costs of this will probably also tend to drop as the intervention becomes increasingly widespread.
Cost of delivering the intervention to patients
C14. Cost of staff who deliver the intervention.
C15. Costs of accommodation: the proposal assumes that there are 7 evening sessions, and the cost of accommodation for each of these evening sessions needs to be considered.
C16. Costs of handouts: when people attend the evening training sessions, they require handouts; some assumptions have to be made about the costs of providing these.
C17. Costs of refreshments: while attending evening training sessions, will refreshments such as drinks need to be provided?
C18. Costs of certificates and resource packs: the details of the ‘education and training proposal’ suggest that they will be run as a complete course with attendance at all modules required to gain a certificate of completion or a resource pack. Therefore, the cost of printing certificates and producing a ‘resource pack’ for each completing delegate needs to be considered.
| Nature of cost | Source of cost information | Cost and year cost figures relate to | Costs in 2013 prices |
|---|---|---|---|
| (A) Training the trainers costs | |||
| Training the trainers (Cost of trainers to train the trainers) Assume 2 days of training @ 7.5 hours per day, provided by a hospital consultant (asthma specialist) plus a Band 6 nurse |
PSSRU cost report 2011 | Hospital consultants at £162 per hour × 15 hours = £2430 Band 6 nurse at £51 per hour × 15 hours = £765 |
Hospital consultants at £171.87 per hour × 15 hours = £2578.05 Band 6 nurse at £54.11 per hour × 15 hours = £811.65 Total cost of staffing = £3,389.70 With eight attendees = £423.71 per delegate With 10 attendees = £338.97 per delegate |
| Cost of accommodation for training sessions | Assumed rather than actual cost | This will be variable, but decent accommodation should be available for £200 per day = £400 With eight attendees = £50 per delegate With 10 attendees = £40 per delegate |
|
| Cost of handouts for training sessions | Assumed rather than actual cost | Assume 200 pages at 5 pence per page = £10 per delegate | |
| Cost of refreshments (coffee breaks and lunch and evening meal) | Assumed rather than actual cost | Assume £20 per delegate per day = £40 | |
| Transport costs (we assume claim expenses for this) | Assumed rather than actual cost | Assume £50 per delegate + £100 for each of the two trainers With eight attendees = £75 per delegate With 10 attendees = £70 per delegate |
|
| Costs of hotel for overnight stay | Assume £39 (cost of some accommodation via Travelodge) | £39 per delegate | |
| Total cost of initial training for someone to provide training | £537.97 to £637.71 per person trained. Assuming each person trained trains 32 children + person accompanying them per year = £16.81 to £19.93 per child receiving the intervention |
||
| Cost of refresher training (cost of trainers to train the trainers every 3 years after initial training) Assume 1 days of training @ 7.5 hours per day, provided by a hospital consultant (asthma specialist) plus a band 6 nurse |
Assume 1 days of training @ 7.5 hours per day, provided by a GP plus a band 6 nurse | Hospital consultants at £162 per hour × 7.5 hours = £1215 Band 6 nurse at £51 per hour × 15 hours = £382.50 |
Hospital consultants at £171.87 per hour × 7.5 hours = £1289.03 Band 6 nurse at £54.11 per hour × 15 hours = £405.83 Total cost of staffing = £1,694.86 With eight attendees = £211.86 per delegate With 10 attendees = £169.49 per delegate |
| Cost of accommodation for training sessions | Assumed rather than actual cost | This will be variable, but decent accommodation should be available for £200 per day = £200 With eight attendees = £25 per delegate With 10 attendees = £20 per delegate |
|
| Cost of handouts for training sessions | Assumed rather than actual cost | Assume 200 pages at 5 pence per page = £10 per delegate | |
| Cost of refreshments (coffee breaks and lunch) | Assumed rather than actual cost | Assume £10 per delegate per day = £10 | |
| Transport costs | Assumed rather than actual cost | Assume £50 per delegate + £100 for each of the two trainers With 8 attendees = £75 per delegate With 10 attendees = £70 per delegate |
|
| Total cost of refresher training for someone to provide training | £279.49 to £331.86 per person given refresher training to train people Assuming the annual cost is only borne once every 3 years, and 32 trained per year = £2.91 to £3.46 per child receiving the intervention |
||
| (B) Cost of delivering intervention to patients | |||
| Cost of training per child given intervention | Costs from (A) above, assuming each person trained delivers intervention to 32 children (and their parent) per year | £16.81 initial + £2.91 annual cost for refresher course (one-third of annual cost, because refresher training only every 3 years) = £19.72 £19.92 + £3.46 annual cost for refresher course (one-third of annual cost, because refresher training only every 3 years) = £23.38 |
|
| Central administration costs for the asthma intervention | Assumed rather than actual cost | £6 per delegate | |
| Costs of delivering actual intervention sessions to patients Assume 14 modules @ 45 minutes, provided by a GP, plus a Band 2 lay worker Assume 14 modules @ 45 minutes, provided by a pharmacist, plus a Band 2 lay worker Assume 14 modules @ 45 minutes, provided by a Band 6 nurse, plus a Band 2 lay worker |
PSSRU cost report 2011 | GP @ £186 per hour for 10.5 hours & a Band 2 nurse at £20 per hour = £1953 + £210 = £2163 Pharmacist @ £53 per hour for 10.5 hours and a Band 2 nurse at £20 per hour = £766.50 Band 6 @ £50 per hour for 10.5 hours and a Band 2 nurse at £20 per hour = £735 |
GP @ £186 per hour for 10.5 hours and a Band 2 nurse at £20 per hour = £1953 + £210 = £2163 Four delegatesa = £540.75 per delegate; five = £432.60 per delegate Pharmacist @ £53 per hour for 10.5 hours and a Band 2 nurse at £20 per hour = £766.50 Four delegates = £191.62 per delegate; five = £153.30 per delegate Band 6 @ £50 per hour for 10.5 hours and a Band 2 nurse at £20 per hour = £735 Four delegates = £183.75 per delegate; five = £147 per delegate |
| Costs of accommodation Seven evenings at 90 minutes each |
Assume £30 for accommodation for each evening session = £210 for all seven sessions Four delegates = £52.50 per delegate; five = £42 per delegate |
||
| Refreshments Tea or coffee, or squash, provided during each evening session |
Assumed rather than actual cost | £7 for all seven evening sessions (covers cost of patient + legal guardian) | |
| Cost of handouts for training sessions | Assumed rather than actual cost | Assume 200 pages at 5 pence per page = £10 per delegate | |
| Total cost of delivering the intervention to patients (GP + Band 2 lay worker) | £517.32 to £639.64 per child enrolled (includes cost of guardian’s attendance) | ||
| Total cost of delivering the intervention to patients (pharmacist + Band 2 lay worker) | £238.02 to £290.51 per child enrolled (includes cost of guardian’s attendance) | ||
| Total cost of delivering the intervention to patients (Band 6 nurse + Band 2 lay worker) | £231.72 to £282.64 per child enrolled (includes cost of guardian’s attendance) | ||
Appendix 14 Photographs of the collaborative workshops
Appendix 15 Dissemination activities
Local dissemination events to participants
-
Dr Bird presented overview of MIA results to Leicester Royal Infirmary Emergency Department meeting to feedback to ED HCPs involved with the study.
-
A summary of key findings was placed in the CLRN and University Hospital Leicester newsletter to inform all the staff who were actively engaged in recruitment for the MIA project.
-
The research team held a community event at Highfield Community Centre, one of the main study venues, with interim findings available via leaflet. CFs were present for interpretation and members of the research team were available to respond directly to participants’ questions and comments regarding the study.
-
The research team held a community event at Braunstone Health Centre, one of the study recruitment sites, with interim findings available via leaflet. CFs were present for interpretation and members of the research team were available to respond directly to questions and comments regarding the study.
-
Children who participated in the study were approached by the team parental advisor, N Johal, to take part in school assemblies.
-
Interim findings were presented at a regional community pharmacy study evening, enabling direct feedback to participants and recruitment partners.
-
Members of the research team presented an overview of the MIA results at Trent Paediatric meeting to feedback to paediatric and primary care HCPs involved with the study.
Dissemination meetings
-
Meeting with Birmingham Collaboration for Leadership in Applied Health Research and Care (CLAHRC) to disseminate emergent findings.
-
Meeting with staff from Queen Mary’s London University to disseminate emergent key findings.
-
Meeting with North London Asthma Network to disseminate emerging key findings and to identify existing interventions and ongoing collaborations or projects of relevance.
-
Meeting with the Department of Health Respiratory Team to disseminate MIA findings.
-
Teleconference with the British Lung Foundation to share information regarding emerging MIA findings.
-
Meeting with Islington commissioners who agreed funding for the development of a multifaceted educational approach to improve asthma management in North London.
Wider dissemination events
-
Members of the research team discussed the study on Kohinoor Radio several times to both advertise the study and disseminate the community study findings.
-
Members of the research team, including the advisory group parental advisor, S Ali, presented the study’s emergent findings on BBC Asian Network as part of their Asthma Day.
-
Emergent findings were shared with Asthma UK throughout the project, leading to the submission of a bid called ‘Speaking Up’ to the Department of Health.
The CFs were offered the opportunity to take a greater role in the dissemination of the finding, but only two were able to work with the team for dissemination. They were involved in the development and organisation of the two community events.
Further research
The research team has begun seeking for further funding and searching for future collaboration opportunities to enable the findings of the MIA project to be taken forward and implemented.
-
Meeting with a Professor of Behaviour Medicine at University College London to discuss possible support in the development of a programme bid to develop and test the interventions.
-
A bid has been made to the Department of Health in collaboration with Asthma UK for a community asthma facilitator programme in London to reach children from black and minority ethnic (BME) families. The emerging evidence from the MIA project was used to inform and develop the bid.
-
A pharmacist has looked at the possibility of Regional Innovation Fund (RIF) funding from DeMontfort University to develop a proposal on culturally competent pharmacy care relating to advice on asthma in South Asian families.
-
Members of the research team have engaged in dialogue with the South Asian Health Foundation to learn from their experience, develop interest in the MIA project and assist in developing a community awareness campaign.
-
Contacts and discussions have been carried out with Asthma UK to discuss how findings from the MIA project could fit with Asthma UK’s long-term research strategy.
-
The MIA project provided some of the evidence base on which a proposal to Islington PCT for the development of multifaceted integrated educational modules for HCPs and families, particularly with an aim of outreach to the community, was based. The proposal was successfully funded and co-creation of this has begun.
-
A meeting with the Children’s Acute Asthma Research Programme (CAARP) was undertaken as they are currently reviewing the development of asthma outcomes. It was suggested that they extend their collaboration to include non-medicinal intervention studies and also consider outcomes tailored to BME groups.
-
The preliminary results are being directly fed into the pathway development projects related to Quality, Innovation, Productivity and Prevention (QIPP) in North London.
-
There is a potential collaboration with Naveen Mehotra in New Jersey, USA, who is currently involved in research on South Asian health and may replicate some of the MIA work in the USA.
-
Advice has been given to West London Research Network and West London Primary Care Research Network who are conducting a coping exercise on resources available to researchers for conducting research with ethnic health groups.
-
Discussions have been had with Warren Lenny with regard to the project with Gill Hall at Respiratory Education United Kingdom (REUK) on Asthma DVD – Improving Asthma Care: Effective Care – Effective Communication Educational Package.
Publications and conference presentations
| Title | Authors | Funder | Where submitted | Date submitted | Reference no. | Outcome |
|---|---|---|---|---|---|---|
| The influence of community perceptions on the management of childhood asthma in South Asian groups: initial data from the Management and Interventions for Asthma (MIA) research group | Bird D, Culley L, Lakhanpaul M | HSR | American Thoracic Society conference | 3 November 2010 | 18227 | Accepted – poster presentation |
| Perceptions of childhood asthma in British South Asian communities: consequences for health communication | Dr Deborah Bird, Professor Lorraine Culley and Dr Monica Lakhanpaul on behalf of the MIA research team | HSR | COMET (Communication, Medicine and Ethics Conference) | 12 February 2011 | Accepted – oral presentation | |
| The influence of community perceptions on the management of childhood asthma in South Asian groups: initial data from the Management and Interventions for Asthma (MIA) research group | Bird D, Culley L, Lakhanpaul M | HSR | Am J Respit Crit Care Med 2011;183 | A1898 | Publication | |
| A systematic review of underlying reasons for barriers to asthma management in ethnic minority children | Dr Deborah Bird, Dr Gill Perkins, Professor Lorraine Culley, Professor Jonathon Grigg, Professor Mark Johnson, Mrs Narynder Johal, Dr Logan Manikam, Mrs Melanie McFeeters, Dr Noelle Robertson, Mrs Joanne Wilson and Dr Monica Lakhanpaul | Asthma UK | European Respiratory Society (ERS) | 24 February 2011 | 850704 | Accepted – poster discussion session |
| A structured process of developing tailored and integrated healthcare interventions with, and for, seldom heard groups to reduce inequalities in health outcomes: the Management and Interventions for Asthma (MIA) project | Monica Lakhanpaul, Deborah Bird, Lorraine Culley, Nicky Hudson, Noelle Robertson, Narynder Johal, Melanie McFeeters, Charlotte Hamlyn Williams, Mark Johnson | HSR | UK Public Health Conference | Accepted – poster presentation | ||
| Management and Interventions for Asthma: Collaboration in Action | M Lakhanpaul, D Bird, Lorraine Culley, Nicky Hudson, Noelle Robertson, Jonathon Grigg, Melanie McFeeters, Narynder Johal and Mark Johnson | NIHR HSR | ERS | 850882 | Accepted – poster presentation | |
| Asthma Management in British South Asian Children: an application of the candidacy framework to an understanding of barriers to effective and accessible asthma care | Nicky Hudson, Lorraine Culley, Mark Johnson, Melanie McFeeters, Noelle Robertson, Deborah Bird, Monica Lakhanpaul | NIHR HSR | ISA | |||
| Patient centred care: involving parents/carers and children in developing healthcare interventions | L Culley, M Lakhanpaul, D Bird, N Hudson, M Johnson on behalf of the Management and Interventions for Asthma (MIA) research team | Qualitative Health Research Conference | Conference – oral presentation | |||
| Improving asthma management for South Asian children: whose priorities matter? | M Lakhanpaul, D Bird, L Culley, Management and Interventions for Asthma (MIA) research team | European Association of Paediatric Societies Congress | Oral presentation | |||
| Playing the game: working with young children to develop asthma interventions | D Bird, L Culley, M Lakhanpaul, Management and Interventions for Asthma (MIA) research team | European Association of Paediatric Societies Congress | Poster presentation | |||
| Management and Interventions in Asthma (MIA): Collaboration in Action | Professor Monica Lakhanpaul, Dr Deborah Bird, Professor Lorraine Culley, Dr Nicky Hudson, Dr Noelle Robertson, Narynder Johal, Melanie McFeeters, Dr Charlotte Hamlyn Williams and Professor Mark Johnson | IAP/RCPCH | Poster presentation |
Appendix 16 Participation evaluation
Introduction
The overall aim of the MIA study was to use a collaborative participatory approach to design an intervention programme to improve the management of South Asian children with asthma. To assess participants’ views of their involvement in the MIA project, a sample of participants were asked to take part in a short interview. While it was important to try to capture participants’ experiences of the project, the research team felt that this interview should be relatively brief, given the considerable time and effort that many community-based participants had already committed to the project. The interviews thus covered three main areas: experiences of taking part, including experiences of working relationships with other participants and their perceptions of partnership in the research; perceptions of the usefulness of involving families and professionals and whether or not they felt that their contribution was relevant to the study; and whether or not participants felt that children gained from being involved in the study and how.
Relatively few examples of research and development collaboration with children under 16 years of age exist in health services research, but some have involved children collaborating with a research team to formulate study design and data collection tools198–200 and working with 14- and 15-year-olds to identify the need for, and prioritise of, a research topic.
The children in the MIA study were aged between 4 and 12 years old. The MIA project, through participatory research, gave children the opportunity to be involved and, where possible, share their views on their asthma management. They were given the opportunity to collaborate at the workshops, either alongside but separate from the main workshop or by voicing their opinions as part of the main workshop, enabling them to share their views directly with the adult participants and, at the final workshop, to do so with the support of their parents/carers. The evaluation assessed children’s experiences of being involved in the MIA project, as well as evaluating parents’ experiences of their children’s involvement.
Methods
We aimed to include the perceptions of participants from each of the main stakeholder groups: focus group members, parent and child interviewees, key informants, HCPs and advisory group members. To reduce bias, interviews were carried out by the research administrator and one of the CFs. The interviews were conducted by e-mail (with interview schedules being sent via e-mail) or by telephone (according to participant preference). All telephone interviews were digitally recorded, translated if necessary and transcribed. E-mail interview schedules were reformatted into Microsoft Word (Microsoft Corporation, Redmond, WA, USA) and then transcribed. The interview data were entered into NVivo and a thematic analysis was carried out by a researcher independent of the immediate research team.
Findings
In total, 35 interviews were completed with participants of focus groups (7), parents of children with asthma (8), children with asthma (5), key informants from the community study (3), HCPs (5), advisory group members (3) and research team members (4). The findings are presented according to the following key themes:
-
overall experience of taking part
-
working relationships and partnerships
-
involving families and professionals
-
involving children.
Experience of taking part
Most participants reported a positive experience of taking part in the project. Positive experiences included emphasis on collaboration and problem solving, feeling confident, feeling valued and ‘good experiences’, as well as a perception of practical benefits.
I found it za good experience, obviously it’s to benefit my son, and I thought it was a good project to get involved with.
Parent
It was really a beautiful experience to get involved in such an actual thing, because there were so many good people who have got a very good knowledge about these things so it was really good for me.
Workshop attendee
My experience as a MIA advisory group member was positive. The advisory team projected a ‘can do’ approach with an emphasis on collaboration and problem solving.
Advisory group member
Negative experiences were related not to the participatory element of the study but to the role some individuals interviewed had in recruiting people to the study, which they had found difficult. One of the children, though not unhappy with the experience as a whole, did express some concern that being involved has made them aware of how little they understood about their asthma, and this made them feel uncomfortable.
I didn’t like it when they asked me a lot of questions about the inhaler . . . I was quite shocked, surprised that there were lots of things I didn’t know about.
Child with asthma
One parent was concerned that they had not received any feedback about the outcomes of the research at the time of interview.
Several interviewees mentioned challenging aspects of the project. Two people (a parent and an advisory group member) raised questions about the feasibility of embedding the methodology into NHS practice.
The project was time consuming and labour intensive and the results achieved were a result of the efforts of highly motivated facilitators. One could question the feasibility of embedding this methodology into NHS practices.
Advisory group member
Other challenging issues raised by individual participants included the perception that they had not learned anything personally and that by taking part in the study they discovered the quality of care for their child was suboptimal. One person commented that the second workshop was not ‘as good’ as the first group attended, while one felt that families could have been more involved in the actual study process itself, and a small number commented on the length and commitment required.
Where we might have done more was to have more involvement from families in the process of carrying out the study. I wonder whether we used the most appropriate methods to elicit data from the kids – perhaps using peer researchers might have helped . . . in the context of such an already complex project, it might have added an unmanageable amount of work.
Team member
I think every part of the project was valuable but only this gap I found it very long.
Key informant
Working relationships, partnerships and shared ownerships
Twenty-four interviewees spoke about the working relationships within the project, including perceptions of partnership and shared ownership. Twenty-three responses were positive; 22 reported a feeling of partnership.
Very friendly, friendly enrolment and warm welcome there. The main team, they were brilliant and they taught everyone in a warm and friendly environment.
Focus group participant
I felt that working relationships were positive and mutually supportive.
Advisory group member
Of course, I feel much better, I feel like somebody decides to talk to you and give you advice, it’s good to be a partner and visit other people.
Focus group participant
Well yes, by the simple fact that you asked questions and you contributed to the debate means that you have a buy into that project.
Key informant
Oh yes, it was very good because I sort of made my contribution but I think I got a lot out of it as well.
Parent
I didn’t feel any control or ownership but yes partnership. We all had different experiences of asthma and a different point of view but the outcome we wanted was the same for all of us.
Parent
The majority of interviewees described relationships within the project in a very positive manner, with one expressing a more mixed response. Several mentioned the value of sharing the experiences of other parents.
Involving families and professionals
The majority of participants spoke positively about the relevance and value of involving families and children in research.
I would think just the fact that the research has been done in itself is most valuable, because we don’t often hear about research into asthma, we hear about cancer, heart diseases etcetera.
Key informant
Most of the time people don’t get a chance or the opportunity to give feedback, I keep going back to the very first [focus group] because there was opportunity for people, or the participants, at that workshop to say, to share how they perceived things . . . their very personal experiences, what they felt about it.
Focus group participant
As a parent representative I feel involving families and professionals at this early stage was extremely valuable to the outcome of the study. I feel this ensured that we were on the right path from the start and if there was any uncertainties they were resolved early on. I feel the parents and children were very forthcoming with their trials and tribulations with their children’s asthma.
Parent member advisory group
The majority of those interviewed interpreted a question about benefits of participation in the project in terms of the learning that had occurred for participants during the project, and for parents and children in particular.
It’s the parents and children who are suffering. Professionals can tick boxes but parents’ views are important as they are the ones suffering.
Advisory group member
One parent remarked that HCPs also could learn from parents:
I think both [families and HCPs], both because as I say intervention is about parents following the advice that professionals give. And sometimes parents can actually help professionals occasionally.
Parent
Some interviewees mentioned the value of community members and parents being able to take the learning from the project and share this more widely.“
If you know this, this, and this then you can listen and carry on and pass on to the others, that is always valuable.
Focus group
The majority of interviewees considered that the time and effort of being involved in the project was worthwhile from their perspective, again often from the perspective of what they had learned in the course of being involved.
Yes of course it was worth it to learn new things, to learn how to protect my son from suffering so it was worth it.
Focus group
Yes 100% I say, because at the end of the day building confidence, to me I thought my son how do I, we used to do it this way, and now we have found a professional way of understanding that asthma can be controlled and also the prevention as well.
Parent
Oh yes definitely, not just for the food and the vouchers [given as an incentive for attending workshops], I don’t think you really need to have an incentive to go to places like this. If your child is suffering and someone wants to help you and somebody is doing some research you should be positive and say yes ok. Well I personally think that but some others might not think that.
Parent
It was definitely that, it was definitely things like, it made me think about, mainly it was the stuff about what I needed to find out, it highlighted what I needed to find out about how to manage [name]’s asthma, what I needed to tell other people who looked after her about how to manage it. And also it made me realise, I am a teacher, and it also made me realise that sometimes in schools we don’t find out properly how we need to manage children’s asthma. So I think for me it was quite interesting on a professional level as well.
Parent
Involving children
Of the 29 interviewees who expressed an opinion about the value of involving children, all responded positively. Although the children responded briefly to most questions asked, all interviewees expressed the view that children should be involved and one felt that they had learned important lessons from their involvement in the project.
Yes, I think it helps, yes, because then you get their point of view as well and how they feel and what they want to get out of these types of group meetings as well.
Focus group
Maybe, these days I think children are very clever, they are very intelligent from the start, so I think so, I think it’s a good thing if they want to be involved.
Focus group
Yes. [. . .] Because it’s affecting them so it’s really just taking on board their experiences, you know, and just by talking to the parents you won’t get the same picture.
Parent
Yes.
Child
Yes we need to take their opinion into account.
Health-care professional
The majority of those interviewed also felt that involving children was beneficial to the children themselves, and that they personally had benefited from children being involved.
Many children shared their experiences and it was good to find out how other children felt who were suffering the same. It’s easy to feel you are the only one.
Parent
Yes it just, you know, enables them to talk about something they’re dealing with and it makes them feel like they’re valued as well and their contribution is valued.
Parent
One participant reported a negative experience and level of frustration with the workshops and suggested that some attendees had lower levels of background knowledge and were more motivated by the food provided during the sessions rather than the improvement of services. These are important considerations when involving the wider community in intervention design and in offering incentives for attending events. Levels of background knowledge will vary between all participants: the data from phases 2 and 3 clearly demonstrated the low levels of community awareness of asthma and the potential lack of interest in exploring asthma further. Many factors are known to motivate research participation, including person interest in the research topic, a need to express oneself and be heard on the topic, altruism, willingness to help the specific researcher, interest in the research outcomes and implementations, and interest in financial gain. 227,230,234–237 Therefore, motivations are likely to be different for a parent with a child with asthma from those of a community member without. Attendees to workshops received a meal and £20 financial incentive; this may have influenced some individuals’ decision to attend. However, by attending the collaborative workshops, hearing the stories of parents and children with asthma and realising the barriers that families are facing, it could be argued that the level of awareness within the community could be increased and could potentially alter individuals’ motivation to attend future workshops or be involved with asthma research. Similarly, if parents realise how little others know, they may be able to speak out and advocate more strongly on behalf of their children. These potential benefits, personal empowerment, satisfaction and development, uniting people around a common cause and fostering social cohesion are key proposed benefits to participation in research and other service-building activities.
Conclusion
The evaluation interviews suggest that beneficial relationships between researchers and participants were developed. The majority of study participants reported positive experiences of participation, including beneficial working relationships with the research team and with other participants. Focus group and parent participants in particular valued the learning that they felt had occurred in the process of their participation in the project.
Appendix 17 Psychological theories
| The actor | What to people/organisation do? | Why do people do that? (Determinants) | Why does this matter? | What do we want them to do instead? (Performance outcomes) | Change objectives | How should we go about that? (Theoretical model) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| From parents perspective | From child’s perspective | From HCP perspective | From key informant perspective | From community perspective | Parents | Child | HCPs | Community | Knowledge and skills | Outcome expectations | Self-efficacy | Risk perception/fear | Interventions or theoretical model if no good example intervention | ||||
| Child | Child doesn’t tell parents about their symptoms | Get busy doing other things | Don’t want to have to go to doctor | Parents unable to take action | Respond positively to child raising symptoms | Recognise possible symptoms | Child: ability to know symptoms from normal | Child: expect that parents will listen and take action | Persuasion | Action plan/cues (for both parent and child) | |||||||
| Parents learn to view reduced activity as normal for that child | Speak to parents regarding symptoms | Memory chunking | Activate self-management | ||||||||||||||
| Parents | Don’t present to the GP with initial symptoms | Misattribution of symptoms: they think it’s a cough or cold and therefore suitable for home management; don’t think it’s something to be concerned about (think it’s normal for the child to cough or be tired), assume will go away | Communication barrier: some words don’t translate, not known in South Asian communities, parents don’t speak English | Misattribution: think parents don’t recognise the symptoms as possible asthma/illness | Misattribution: mixed up between cough/cold/chest infections; give other causes such as damp house, etc.; mixed up between asthma/hay fever/eczema | Chronic symptoms are being seen as normal or being attributed to the UK climate/housing conditions. Not being recognised as potential illness. Then exacerbated by overlap between colds/asthma attacks, families feel no value in attending GP as will be dismissed | To recognise potential symptoms from normal behaviour | Enable families to present repeatedly | Be aware of potential symptoms of asthma | Parent: ability to identify symptoms of asthma | Parents: believe that going to GP has value to them and their child | Parents: believe that they are able to have an effective conversation with their GP | Parents: perceive that without treatment, asthma could be dangerous to their child | Knowledge of asthma symptoms: modelling behaviour | Community vignettes | ||
| Knowledge: don’t recognise importance of wheeze: think it’s normal, not aware of association to asthma, not aware that asthma is important, don’t think could be asthma if no one else in family has asthma | Denial: don’t accept that child might have a problem | Knowledge: not sure what wheezing is; use wheeze to mean other sounds; not sure what asthma is | Some parents would have been quicker to act if they had recognised the symptoms, feel anger as delayed diagnosis exposes child to delayed management | To recognise symptoms as possible asthma | Take families’ concerns seriously | Support a parent’s decision to take child to GP | Parent: ability to identify symptoms in their child | Child: believe that going to GP will benefit them | To address knowledge, asthma as chronic, modelling, persuasion, implementation intent, social comparison, framing (PMT) | Vignettes and stories/action planning and cues/prompts, posters and media/tales of others success/emphasise advantages of help seeking | |||||||
| Don’t believe HCP can/will do anything: GP always dismisses colds so why keep going back; feel that they are not taken seriously by GP; can’t communicate with GP | Fear: parents frightened to question GP, to keep returning | Believe that they will be taken seriously by GP | Recognise symptoms in children | Community: have awareness of symptoms of asthma in children | Community knowledge: as above plus media/advocacy | Community organisers/media and communication intervention reinforced | |||||||||||
| Don’t feel able to keep returning, not appropriate to question doctor | Believe is appropriate to attend GP repeatedly | Recognise asthma symptoms in children | Community: acceptance that symptoms might be asthma | GP dismissive/outcome expectations: modelling | Role models/good consultations | ||||||||||||
| Communication barrier: can’t explain to HCP; don’t speak English; some words don’t translate into other languages | Believe that attending the GP is valuable | Don’t feel able to return: modelling and guided practice/feedback/mass media | Training/role play/stories of positive outcomes | ||||||||||||||
Glossary
- Asthma
- A chronic inflammatory condition presenting with one or more of wheeze, breathlessness, chest tightness and cough (according to British Thoracic Society guidelines). Asthma affects all age groups but often starts in childhood. It is a disease characterised by recurrent attacks of breathlessness and wheezing which vary in severity and frequency from person to person. In an individual, they may occur from hour to hour and day to day. This condition is due to inflammation of the air passages in the lungs and affects the sensitivity of the nerve endings in the airways so that they become easily irritated. During an attack, the lining of the passages swell, causing the airways to narrow and reducing the flow of air in and out of the lungs (according to the World Health Organization).
- Asthma management
- The process of treatment with the aim of achieving and maintaining asthma control.
- Asthma management pathway
- The asthma management pathway for the purposes of the Management and Interventions for Asthma study has been defined as ‘stages of ideal care required to recognise, diagnose, treat and optimally manage asthma’.
- Ayurvedic treatments
- Ayurvedic medicine is a system of healing that originated from ancient India. In Sanskrit, ayur means life or living, and veda means knowledge, so Ayurveda has been defined as the ‘knowledge of living’ or the ‘science of longevity’. Ayurvedic medicine utilises diet, detoxification and purification techniques, herbal and mineral remedies, yoga, breathing exercises, meditation and massage therapy as holistic healing methods. Ayurvedic medicine is widely practiced in modern India and has been steadily gaining followers in the West.
- Barriers
- Factors that impede the achievement and maintenance of asthma control, which include (but are not limited to) health beliefs, professional barriers, language and communication, prejudice and discrimination, delivery and organisational issues, issues around diagnoses and treatments offered.
- Borda approach
- A voting system in which voters rank items in order of preference and points are awarded to items based on these rankings. The winning item is one with the most points.
- Determinants
- The objects which are expected to change due to the programme: personal and external.
- External determinants
- In the immediate (interpersonal) environment (e.g. influence of parents/friends) and/or in the more remote environment (higher ecological levels).
- Getting a diagnosis
- ‘Getting a diagnosis’ was approached from a socioecological and holistic perspective, covering a number of steps required within the diagnostic process. These steps included an awareness of asthma, recognition of symptoms, accessing health care and the investigative process to make the diagnosis of asthma, and not solely the narrow steps of investigating the child to confirm or refute a diagnosis.
- Intervention mapping
- Iterative, structured approach in developing healthcare interventions. It is a protocol for developing theory-based and evidence-based health promotion programmes.
- Intervention-planning framework
- The overarching plan for all 11 themes identified across the asthma pathway.
- Intervention programme
- A description of a planned intervention strategy for a target population, a programme for the exemplar theme of ‘getting a diagnosis’.
- Minority ethnic
- A status that includes culture, language, religious traditions and geographical origins that differ from those of the majority population. It is important to recognise the flexibility of ethnic identities and the diversity within both minority and majority populations.
- Participatory research
- Systematic inquiry with the collaboration of those affected by the issue being studied, for the purposes of education and taking action or effecting social change.
- Performance objectives
- The specific behaviours that make up behaviour change.
- Personal determinants
- Predisposing factors, for example knowledge, attitudes, beliefs, values and perceptions.
- Socioecological model
- A theoretical framework which proposes a complex interplay between individual, community and societal factors influencing health status and access to health care.
- South Asian
- A person with ancestry in countries of the Indian subcontinent, including India, Pakistan, Bangladesh and Sri Lanka.
- Snowballing
- A non-probability method of sampling: recruited subjects nominate other potential subjects for inclusion in the study.
- Wheeze
- A whistling noise on breathing out.
List of abbreviations
- A&E
- accident and emergency
- ACT (on Asthma)
- Awareness, Context (cultural and organisational) and Training
- BTS
- British Thoracic Society
- CF
- community facilitator
- CLRN
- comprehensive local research network
- ED
- emergency department
- EoI
- expression of interest
- GINA
- Global Initiative for Asthma
- GP
- general practitioner
- HCP
- healthcare professional
- IM
- intervention mapping
- MIA
- Management and Interventions for Asthma
- MRC
- Medical Research Council
- NAEPP
- National Asthma Education and Prevention Programme
- NGT
- nominal group technique
- NIHR
- National Institute for Health Research
- NSF
- National Service Framework
- OTC
- over the counter
- PCRN
- primary care research network
- PR
- participatory research
- R&D
- research and development
- SES
- socioeconomic status
- UN
- United Nations