Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/1007/01. The contractual start date was in June 2011. The final report began editorial review in June 2013 and was accepted for publication in November 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Waring et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
The challenge of patient safety
Patient safety remains a health policy priority. Over the last two decades, and following the publication of To Err is Human1 and An Organisation with a Memory,2 advances in patient safety research and policy have been significant. In the UK, for example, a dedicated portfolio of research led the development and application of new theories, research methods and improvement interventions to enhance patient safety. 3 This body of work has transformed thinking about the sources of unsafe care and the possibilities for safety improvement. In particular, a new conceptual approach has emerged that draws attention to the ‘upstream’ risk factors located within the wider organisation of care and how these can influence the ‘downstream’ safety of clinical practices. These ideas have provided the conceptual basis for many safety-enhancing interventions that aim, for example, to improve team communication, simplify complex activities and foster a culture of safety.
Despite advances in ‘systems thinking’, research continues to highlight worryingly routine levels of substandard care and patient harm. 4 The recent public inquiry into Mid-Staffordshire NHS Trust again highlights the complex social, cultural and organisational factors that influence the quality and safety of patient care. 5 The study presented here addresses recent calls for research to examine the more complex sociocultural and organisational context of patient safety. 6,7 Elaborating this need, the study suggests that patient safety research to date has tended to focus on the sources of safety and risk located within clinical domains, such as the operating room or the emergency room, but with less attention to the sources of safety and risk located between care settings, such as between health and social care. 3 The sociology of organisational failure shows how catastrophes and errors are often ‘rooted’ within complex intra- and interorganisational processes. 8,9 Such complex structures and processes are often recognised by current ‘systems approaches’ as applied to patient safety, but they are not fully developed in the sense of complex systems of interdependencies that cut across or between care settings and processes. As such, this study suggests that the delivery of high-quality patient-centred health care requires the co-ordination and collaboration of multiple professionals, agencies and organisations working and interacting in the manner of a complex system.
This study aims to extend theory in patient safety through elaborating and understanding the complex interdependencies that frame the safe delivery of patient care across occupational and organisational boundaries.
In line with this aim, the study suggests that the co-ordination of health-care professionals, organisations and other agencies is enhanced where there is shared understanding, common values and aligned ways of working. In other words, system complexity can be mitigated, in part, by system actors knowing how to integrate their distinct activities to meet common goals. Research suggests that such collaboration is typically based upon enhanced patterns of communication and, importantly, knowledge sharing. 10 Knowledge sharing is more than the communication of information, relating instead to how meanings, beliefs, values and ‘know-how’ are shared with and used by groups or networks of actors to support collaborative working. 10–12 Knowledge sharing might therefore be interpreted as a source of system safety, which can support system-level integration through helping different actors to co-ordinate and align discrete practices. Research highlights a number of sociocultural factors that facilitate and inhibit knowledge sharing, including the extent of difference in the forms of knowledge, cultural values and norms, and organising factors that support knowledge sharing. 10–13
This study aims to identify interventions and practices that support knowledge sharing across organisational and occupational boundaries, which in turn can support collaboration and mitigate systems complexities.
The challenge of hospital discharge
The study takes as its focus the complex patterns of care organisation associated with hospital discharge. Specifically, hospital discharge exemplifies the problems of interorganisational dependencies within a complex health and social care system. National policies suggest that timely, integrated transition of care from hospital to a community setting is integral to patient recovery, quality of life, independence and longer-term care. 14 Inappropriate or poorly planned hospital discharge can introduce risks to safety and additional resource costs, inhibit recovery and lead to readmission. 14,15 Data provided by the former National Patient Safety Agency16 indicate that ‘transfer/discharge of patient and infrastructure’ accounted for 7%–8% of reported safety incidents in 2009. This figure is likely to be a significant underestimate given that reporting systems are not well utilised across health and social care boundaries. In their study of 400 patients discharged from hospital, Forster et al. 17 found that nearly 20% experienced some form of adverse event, with those related to drug reactions being the most common. The range of threats to safety in hospital discharge is diverse, often linked to the needs of individual patients. Common risks include the management of medicines, the provision of appropriate health and social care, the fitting and use of home adaptation to support recovery, and the risks of falls, infections or sores. 13–26 Hospital discharge is therefore interpreted as a ‘vulnerable stage’ in the care pathway that exemplifies the opportunities for ensuring patient safety located between care settings.
Research repeatedly highlights communication as integral to the quality and safety of hospital discharge. 14,27,28 Returning to NPSA data, ‘notifying and organising external services’ was identified as the most common category related to hospital discharge. 16 Kripalani et al. ’s (2007) systematic review29 of information transfer between hospital and primary care, and the links to patient safety, found that communication was often rare, piecemeal and poorly timed. Communication and information sharing, particularly in the processes of referrals and discharge planning, are consistently seen as underpinning the quality of hospital discharge. 14,27–31 In line with the above theoretical approach, this study examines how knowledge sharing can be a source of quality and safety in the context of organising hospital discharge.
This study aims to identify interventions and practices that support knowledge sharing across care settings, and thus promote safe hospital discharge by mitigating systems-level complexity.
Research objectives
-
To determine the stakeholders and agencies involved in discharge, including their distinct roles, responsibilities and relationships, as elaborated in terms of (a) their specific knowledge and practice domains; (b) their prevailing cultural norms and assumptions; and (c) organisational context.
-
To determine the patterns, media and content of knowledge sharing between stakeholders with a particular focus on interventions to facilitate communication, including (a) multidisciplinary teams(MDTs); (b) guidelines and toolkits; (c) co-ordinators; and (d) information communication technologies (ICTs).
-
To determine stakeholders’ relative perceptions of the threats to ‘safe’ discharge, with a particular focus on known risks and sources of readmission, including (a) falls and (b) medicines management, as well as other perceived risks.
-
To determine how knowledge sharing represents a latent threat to patient safety and source of delayed discharge, including known factors such as ‘delayed’, ‘missing’, ‘fragmented’ or ‘repetitious’ communications and the persistence of communication ‘boundaries’.
-
To explain the patterns of knowledge sharing as threats to patient safety based upon the heuristic categories of knowledge, cultural and organisational factors.
-
To identify lessons and interventions that support knowledge sharing and, in turn, integrated, efficient and safe hospital discharge and reduced readmission.
The clinical context
The study focuses on the discharge of stroke and hip fracture patients. These represent high-demand areas of NHS care and national priorities for service improvement. Although the majority of patients in both tend to be elderly, they offer an opportunity for comparison in terms of how services might be organised differently, or indeed how resources could be shared across the two areas.
Stroke discharge
Stroke is the third leading cause of death in the UK and the single largest cause of disability in community settings, where over 50% of strokes result in some form of permanent disability. 32 The annual cost to the NHS of providing stroke care is over £2.8B. 33 The threats to safe discharge for stroke patients are considerable, including falls, the use of take-home medicines, psychological distress and cognitive recovery, access to and use of therapists, and the associated complications of personal care, such as incontinence. 19,21,22 Highlighting the contribution of ‘systems’ thinking, such risks often have their origins in the wider organisation and integration of stroke services. 34
For the last decade, health policies have promoted standards in the organisation and delivery of stroke care, culminating in the National Stroke Strategy. 35,36 These include the introduction of dedicated stroke units, thrombolisation pathways, specialist rehabilitation services and early supported discharge (ESD) services in the community. Each aims to diminish long-term disabilities and promote improved outcomes for patients and families. Evidence suggests, however, that there remain many inequalities in stroke care provision and subsequent outcomes related to age, location, professional skills, organisational strategies and service provision. 37,38 A growing body of research demonstrates the potential benefits of initiatives to support safe and timely discharge, including the use of ESD models. 39 Such techniques bring together service providers and users located in different settings to plan discharge. The National Stroke Strategy,36 for example, sets out the aspirations for ‘life after stroke’ by emphasising the importance of integration between stakeholders to plan and support the transfer of patient care. Similarly, it emphasises the importance of ‘working together’ through stroke networks that bring together stakeholders to review, organise and deliver services. Linked to this, the National Clinical Guideline for Stroke40 suggests stroke rehabilitation should include a MDT of relevant agencies to plan care needs after hospital.
Hip fracture discharge
Each year in the UK around 310,000 patients, the majority of whom are elderly, present to hospital with fractures. Around a quarter of these, up to 80,000, are hip fractures. 41 Projections suggest that, if this continues, numbers will rise from the current figure of approximately 80,000 to 101,000 in 2020. The average age of hip fracture patients is 81 years; 74% are female and they are among the most vulnerable groups to be admitted to hospital. Many have multiple comorbidities, including cognitive and physical impairment, which leads to longer lengths of stay, more complex discharge planning and higher readmission rates. 42 More than 60% have diagnosed dementia. 43 The median length of stay in acute hospital is 26 days, probably an indication of the general frailty of the patients, increased survival rates and increased longevity.
Care of fragility fractures is expensive. Direct medical costs to the UK health-care economy have been estimated at £1.8B in 2000, with most of these costs relating to hip fracture care. 41,42,44 Patient frailty is reflected in the outcome of hip fracture: 10% of people die in hospital within a month, and one-third are dead at 1 year. The fracture is responsible for less than half of deaths,44 but patients and families will often identify the hip fracture as playing the central part in a final illness. Hip fracture can seriously damage quality of life for survivors, of whom only half will return to their previous level of independence. Most can expect long-term discomfort and half will suffer deterioration in mobility, such that they will need an additional walking aid or physical help. Between 10% and 20% of people admitted from home will move to residential or nursing care. Length of hospital stay varies considerably between units, reflecting variability in service structures and provision, such as in early rehabilitation and the availability of downstream beds. After discharge, additional costs for health and social aftercare average £13,000 in the first 2 years.
Like stroke patients, hip fracture patients experience many potential threats to patient safety around hospital discharge, including the risks of falls, social and personal care planning, and management of medicines. Also in common with stroke care, there remains little evidence of the latent sources of risk manifest in these interagency patterns of interaction and knowledge sharing. Many specialities and agencies are involved in hip fracture care, and when discharge is planned and co-ordinated effectively through interagency working, this is shown to reduce length of stay and improve patient recovery. 45–47 Again, this requires effective and timely knowledge sharing between agencies. Alternatively, ‘offsite’ rehabilitation units are commonly aimed at frailer patients who require further rehabilitation; however, the complexities around discharge planning are often more significant given the additional level of care introduced before the patient is ultimately returned home.
Taking the discharge of stroke and hip fracture care as its focus, the study investigates the patterns of knowledge sharing across occupational and organisational boundaries and relates these to the perceived and observed threats to patient safety.
Report structure
Following this introduction, Chapter 2 reviews contemporary policies, practices and interventions for hospital discharge, and relates these to research and theory on organisational safety, complexity and knowledge sharing. Chapter 3 describes the study design and methods. Chapters 4 and 5 present the main empirical findings from the study. Chapter 4 provides a comparative ethnographic analysis of discharge planning and care transition, focusing on the main ‘situations’ or opportunities for knowledge sharing that structure the discharge process. Chapter 5 describes the threats to safe discharge as perceived by stakeholders and attempts to explain these with reference to the observed patterns of knowledge sharing discussed in Chapter 4. Chapter 6 draws out the learning from the study to tentatively outline those aspects of discharge planning and care transition that promote knowledge sharing and mitigate the threats to safety in hospital discharge, on which future interventions might be based. It also discusses the limitations of the study, summarises the main contributions to theory and research and offers suggestions for future research.
Chapter 2 Hospital discharge and patient safety: reviews of the literature
Introduction
This chapter reviews the two literatures that inform this study. The first addresses the safety challenge of hospital discharge, elaborating this as a problem of co-ordination and collaboration among various health and social care agencies. Attention is given to major policy changes and interventions aimed at enhancing discharge, as well as research evidence on clinical risk and patient safety. The second literature develops the analysis of patient safety as applied to hospital discharge, suggesting that the transition from acute hospital to community care might be interpreted as a complex system with vulnerable connections between multiple actors. The chapter draws together these literatures to explore how knowledge sharing might be a source of system safety through helping to co-ordinate and integrate the activities of different agencies and, in turn, reducing system complexity.
Understanding hospital discharge
Locating hospital discharge
Hospital discharge describes the point at which inpatient hospital care ends, with ongoing care transferred to other primary, community or domestic environments. Reflecting this, hospital discharge is not an end point, but rather one of multiple transitions within the patient’s care journey. 14,48 The organisation and provision of this transitional care typically involves multiple health and social care actors, who need to co-ordinate their specialist activities so that patients receive integrated and, importantly, safe care. The inherent complexity of co-ordinating a large number of actors, often based in distinct organisations, leads to the view that hospital discharge can be a vulnerable, time-dependent and high-risk episode in the patient pathway.
A prominent example of this complexity is ‘delayed discharge’, where the patient remains in hospital because of the failure to appropriately co-ordinate care between agencies. 27,48 According to Victor et al. ,49 nearly 30% of older people experience some delay in their hospital discharge, which is known to expose patients to additional hospital-related risks, create emotional and physical dependency, incur additional hospital costs and restrict the availability of inpatient beds. In parallel, premature discharge or discharge without appropriate arrangements for onward care can also lead to complications for patient recovery. For example, the 28-day readmission rate for older people has doubled from 103,000 in 2001–2 to 201,000 in 2010–11,50,51 suggesting that more needs to be done to support patient recovery following acute care.
The problems of delayed or poorly planned discharge illustrate the broader challenge of integrating health and social care. 27 Analysing the causes of these delays, Tierney et al. 31 point to a range of common factors, including (a) poor communication between health and social care; (b) lack of assessment and planning for discharge; (c) inadequate notice of discharge; (d) inadequate involvement of patient and family; (e) over-reliance on informal care; and (f) lack of attention to the special needs of vulnerable groups. Reflecting this and other evidence,27 policies have repeatedly sought to improve discharge planning, especially the integration of health and social care agencies. A review of these initiatives is outlined below.
Discharge planning
Improved ‘discharge planning’ has been a consistent recommendation of policy and research. 27,52–54 Over the last two decades, the precise form of discharge planning guidelines has varied to reflect wider health and social care reforms, changing economic imperatives and emerging concerns about care quality. 55–58 Furthermore, they have been developed both locally, by individual care organisations, and nationally, for example by the NHS Institute for Innovation and Improvement, and there is no commonly agreed model. Despite efforts to promote discharge planning, the recent European HANDOVER study found that health-care professions still did not prioritise discharge planning or interagency communication as supporting enhanced discharge. 59 In 2010, the Department of Health published its new discharge workbook, Ready to Go? Planning the Discharge and Transfer of Patients from Hospital and Intermediate Care,30 which outlined 10 ‘steps’ to ensuring a timely, safe and patient-centred transition from hospital, including:
-
effective communication with individuals and across settings
-
alignment of services to ensure continuity of care
-
efficient systems and processes to support discharge and care transfer
-
clear clinical discharge management plans
-
early identification of discharge or transfer date
-
identified named lead co-ordinators
-
organisational review and audit
-
7-days-a-week proactive discharge planning.
Effective discharge planning is usually associated with a number of common activities and procedures along the care pathway:14,30
-
On admission Prepare detailed and accurate patient record; review assessment information and estimate date of discharge with reference to standard care pathway and complexity of patient circumstances.
-
During admission Undertake regular multidisciplinary assessment of patient condition to identify and assess opportunity for discharge; discuss with patient and family ongoing and continuing needs.
-
At least 48 hours prior to discharge Inform MDT about estimated date of discharge and review assessment criteria; initiate referrals to community health-care providers and social care agencies; contact agencies responsible for ordering and/or installing patient equipment or home modification; social work/care assessment and referrals; complete referral for social care; finalise care package; order take-home medicines; arrange transport.
-
Day of discharge Contact family and carers to confirm follow-up care arrangements; check documentation completion; issue discharge letter to general practitioner (GP); reinforce patient behaviour recommendations and rehabilitation; confirm and finalise transport.
-
Follow-up care Initiate social care package and continuing health-care package, where relevant in consultation with GP.
As these policies suggest, a number of specialist roles and activities are promoted as supporting the integration of different agencies. A longstanding objective has been to promote the use of MDTs in discharge planning. 14,53 These are normally organised as formal, usually weekly, meetings between relevant health and social care specialists with the aim of supporting timely communication, inclusive decision-making and continuity of care. Research often describes MDTs as comprising a core team including the named doctor and nurse, occupational therapists (OTs) and physiotherapists (PTs), and representatives from community and social care agencies, as well as family representatives, GPs and other specialist therapists. According to Bull and Roberts,52 MDTs help break down barriers between professional groups and foster a sense of common purpose and trust. Importantly, MDTs provide an opportunity for communication, first between professionals, second with patient and family, and third with community health-care providers. Furthermore, MDTs can help make clear the lines of responsibility for different tasks and create opportunities for individuals to take the lead in co-ordinating the planning process. In practice, however, convening all representatives for individual patients can be challenging in terms of time or resources. 27
A further initiative has been the introduction of discharge co-ordinators. 14,30 These are individuals, usually experienced nurses, who take lead responsibility for both strategic planning and co-ordination of discharge at the interorganisational level. 60 Research suggests that discharge co-ordinators can improve hospital discharge through supporting the integration of different professionals, overseeing and directing planning and addressing emergent problems in a more responsive way. 61 In particular, co-ordinators acquire both deeper understanding of and extended relationships with a wider range of care agencies that help them better navigate and align divergent ways of working that usually delay or undermine discharge. 52,61,62
Integrating care services
In line with the developments in discharge planning, policies have also introduced new or extended statutory powers, financial opportunities and penalties to support more integrated discharge pathways. For example, the Health Act 199963 enabled health and social care agencies to pool resources to codeliver rehabilitation services. Similarly, in 2005, delayed discharge grants were made available to social service authorities across England to develop reablement services. In contrast, the Community Care (Delayed Discharges) Act (CCDDA) 200364 addressed the problems of integration by allowing hospitals to claim financial reimbursements from local authorities where they delayed discharge by not providing timely services. Against this backdrop, a variety of integrated services and new care pathways have emerged to support the transition from hospital to community, but in doing so have extended (and made more complicated) the range of services involved in discharge planning.
One significant development has been the introduction of ESD. ESD is often associated with the care and rehabilitation of mild-to-moderate stroke patients. It enables patients to return home early with a dedicated package of rehabilitation and reablement of a similar intensity to that provided by inpatient care. ESD is shown to reduce the burden on acute providers and support patient recovery. 65 The funding of ESD through joint commissioning between the acute NHS providers, GPs, social services and central government highlights the role of joint working and resource pooling, but there remain variations across the UK, especially in rural areas, where a lack of funding can limit provision. 66,67
Intermediate services provide transitional, ‘step-down’ care between acute hospital and the domestic environment (usually for 30 days). Patients are typically declared as ‘medically fit’ but requiring ongoing care or rehabilitation, for example those at risk of readmission or with complex care needs. Rather than receiving rehabilitation at home or in hospital, intermediate care offers a form of residential, hospital-like care, but with a focus on rehabilitation. Research suggests that intermediate care services have been effective in both reducing financial costs and improving patient outcomes. 68 Owing to their close proximity to patients’ homes and relatives, community (NHS) hospitals or nursing homes are often used for intermediate and post-discharge rehabilitation. Stays in such units can be longer than in other intermediate care services, yet research suggests patient outcomes are generally favourable. 69 The recent Cochrane reviews of long-term rehabilitation in care homes show no evidence of negative health outcomes. 65,70
A similar initiative is the introduction of reablement services. These usually involve a dedicated package of social care to support daily living in the immediate period following discharge (e.g. personal care, cooking and cleaning). They are usually managed and provided by local authority social services, although in some cases they are funded through both health and social care budgets. In 2012, the Department of Health allocated £150M for reablement linked to hospital discharge,30 to be allocated through primary care commissioners working in partnership with social care authorities. Significantly, these services are normally arranged and provided by social services to ease transition from hospital for a period of 4–6 weeks, with the expectation that ongoing social care will be reassessed and provided by other agencies.
A further example of service innovation, with particular reference to end-of-life care, is the introduction of ‘fast-track’ discharges. This normally relates to supporting early discharges from hospital for those patients wishing to spend the last days of life in the community with palliative support. This end-of-life discharge can exemplify effective joint working and rapid prioritisation, whereby the patient can be discharged within 48 hours with all specialist support and medications in place. 71 For example, funding decisions are established post discharge to remove delays; the needs of the patient and family are met by deliberate use of a continuous dialogue with one specialist co-ordinator; and the emphasis is on timely collaborative working to ensure the patient gets home as requested. 72
The threats to ‘safe discharge’
Multiple sources of evidence suggest that care quality can be suboptimal in, or as a consequence of, hospital discharge. 28 In a major telephone survey of 400 patients following discharge, Forster et al. 17 found that nearly 20% reported some form of adverse event, of which 6% were preventable and 6% ameliorable. Research highlights a number of common discharge-related risks associated, for example, with the management of medicines, the provision of appropriate health and social care, incomplete tests and scans, the fitting and use of home adaptation, and the risks of falls, infections or sores. 17–28 The underlying sources of these risks can range from factors related to the patient’s condition or comorbidities, to the assessment of patient need, the availability of specialist resources in the community, and wider organisational and cultural factors. For example, research shows that the patient’s condition, such as hip fracture, and other comorbidities, especially cognitive function and fragility, can represent a cluster of risks, particularly for older patients, that can complicate the discharge process. 73,74 Research also suggests that time of day, week or year can also have an impact on discharge planning and quality. In particular, discharges during the weekend have been shown to increase the likelihood of death compared with those taking place between Tuesday and Friday, accounting for 34% of all post-discharge deaths. 75,76
Although studies highlight the importance of clinical risk in discharge planning, it is not always clear how ‘risk’ is measured. Moreover, the causal analysis of risk is often implicit or an emergent feature of wider trial research. Reviewing the recent literature (Table 1), a number of risks (direct threats to safety) and identified causes (suggested or inferred) are catalogued.
| Study | Identified risks | Identified causes |
|---|---|---|
| Lankshear et al.77 (Research) |
Anti-coagulant medication risks: non-compliance, polypharmacy, lack of monitoring | Poor documentation, communication between acute and primary care providers, accessibility of clinics |
| Hansen et al.78 (Research) |
Rehospitalisation and link with quality of discharge documentation | No direct association found except in patients with follow-up and larger number of medications |
| Laugaland et al.28 (Review) |
Transitional care safety risks among older people | Lack of discharge planning and post-discharge support |
| Hagino et al.79 (Research) |
Risk factors for hip fracture patients: a prognostic approach | Age (over 85 years), chronic disease, dementia, mobility prior to fall (walking disability) |
| Howard et al.80 (Review) |
Identification of drugs and underlying drug-related issues most likely to cause readmissions | Four groups of medicines account for 50% of drug-related readmissions. Three underlying causes related to patient adherence, monitoring and prescribing errors |
| Romagnoli et al.81 (Research) |
Discharged patients with unmet information and communication needs | Limited medication information, non-medication issues about care/safety/follow-up, functional limitations, severity of condition and communication problems |
| Clarke et al.82 (Research) |
Experience of risk in ESD scheme | Lack of patient consent, patients not ready for discharge, feeling unsafe, medication supply problems, transport home problems, lack of home nursing |
| Goulding et al.83 (Interview study) |
Patient safety among patients on clinically inappropriate wards | Placement of patients on to clinically inappropriate wards poses a latent threat towards safe discharge planning; specifically, patients are more likely to be deemed medically fit before they actually are |
| Härlein et al.73 (Systematic review) |
Risk factors for patients with dementia | Identified eight risk factors for falls in older people with dementia on discharge from hospital, which could be used prospectively on admission |
| Courtney et al.84 (Research) |
Risks of readmission for individualised 24-week post-discharge programme of rehabilitation and telephone support. Randomised controlled trial | Intervention group had lowered readmission rates, lowered emergency GP contact and improved quality-of-life indices |
| Coffrey85 (Research summary) |
Discharging older people and risks | Summary of evidence about discharge risks among older people |
Although the sources of these risks can be complex and variable, research frequently highlights incomplete, inaccurate and inaccessible information as undermining collaborative workings and contributing to unsafe patient discharge. 27–29,86,87 A systematic review conducted by Kripalani et al. 29 found that communication between hospital and family doctor was often partial or missing, relying primarily upon discharge summaries which were often incomplete, lacking in detail and not provided in a timely manner. Similarly, poor communication between the hospital and social care providers is a long-standing risk factor in adverse events. 27,29,88 There remains little extensive research, however, examining the causes of poor communication and adverse events. 29,89 Less is known about how communication breakdowns and patient safety are experienced by patients and carers. 54 A number of studies propose, and in some cases evaluate, interventions to support communication and information transfer at discharge, including structured communication tools, discharge planning guides, discharge checklists, medicine reconciliation guides and patient education strategies. 84,90–94 These suggest that effective discharge planning depends upon effective communication and collaboration between health and social care agencies. 28,86,95 In his analysis of the factors that support or hinder such communication and collaboration, Glasby27 highlights three dimensions:
-
occupational factors related to the particular knowledge, cultures and practices of different professionals
-
organisational factors related to the working patterns, capabilities and resources of different agencies
-
compatibility and co-ordinating factors related to how occupational and organisational factors are aligned, or differences reconciled.
Attention to these and other factors is needed to better understand and enhance communication and collaboration in discharge planning and care transition. Furthermore, greater appreciation is needed of how communication might undermine not only co-ordination but, in turn, safety. In this sense, communication might be seen as a latent (or active) factor that influences the safety of hospital discharge. The next section develops this idea through relevant theory and research on organisational complexity and safety.
Understanding discharge safety
The quality and safety of hospital discharge is framed by a variety of contextual and system-level factors related to the type of discharge, the configuration of different providers, the availability of resources and, importantly, the relationships between actors in terms of communication, decision-making and joint planning. These issues, as identified in the research literature,27–29,86,87 represent possible upstream sources of risk, for example where the failure to communicate and jointly plan services can lead to reduced integration of care agencies and substandard patient care. To better understand this, the present chapter considers relevant patient safety literatures.
The systems approach to patient safety
Current thinking in patient safety is largely informed by theories and research within the fields of ergonomics and human factors. In broad terms, this suggests that performance mistakes are not necessarily brought about by individual negligence, malice or incompetence, but more often by pressures located within the work environment. 96 This line of reasoning makes the distinction between ‘active’ and ‘latent’ errors. The former refers to individual slips, mistakes or omissions that lead to patient harm; the latter to the unsafe conditions that create, enable or exacerbate the potential for active error or patient harm. This can include poorly designed working arrangements, poor defence and early-warning mechanisms or an over-reliance on automation. This approach suggests that risk reduction should attend, not to individual performance alone, but to the upstream factors that make performance error prone, for example by standardising task design, improving team cohesion and communication, alleviating situational ambiguity and recognising the influence of resource management and culture. 96
This ‘systems approach’ to patient safety has been articulated through policies such as To Err is Human1 and An Organisation with a Memory,2 and developed through major programmes of applied health research. 3 For example, it has been used to highlight how a range of ‘task’, ‘team’, ‘situational’ and ‘organisational’ factors contribute to front-line clinical safety. 97 Of specific relevance to this study, this conceptualisation of safety draws attention to the way health care is organised and delivered through a system of interdependent elements interacting to achieve a common goal. 1 Based upon these ideas, various strategies have been promoted to better understand and address the threats to patient safety. These include, for example, the use of incident reporting procedures to enable clinicians to share their experiences of clinical risk and engender system-wide learning of the root causes;98,99 the creation of a safety culture that is mindful of danger, blame free and responsive to organisational learning;100 and a variety of safety-enhancing interventions, such as ICTs or single-use devices which limit unsafe behaviour; checklists, guidelines and the standardisation of practices to reduce variability; and staff training and culture change activities. 3 The ‘human factors’ approach provides a framework (drawing on Vincent101) for conceptualising and investigating the threats to safe discharge (Table 2).
| Dimension | Risk-producing/enabling factors | Discharge risks |
|---|---|---|
| Patient characteristics | Complexity, severity, personality, demographics | Comorbidities and complexity of patient need; cognitive impairment, cultural and language barriers to engagement |
| Task factors | Clarity, complexity, standardisation | Clarity of the discharge pathway and the steps involved in organising and arranging discharge |
| Individual factors | Knowledge, skills, motivation | Clinical understanding of discharge requirements, attitude towards discharge in context of wider care process |
| Team factors | Communication, decisions, supervision, structure | Communication breakdowns between health and social care teams, limited joint decision-making |
| Work environment | Staffing, skill mix, workload, support structures | Demand for inpatient beds, social care staffing changes and health-care workload placing pressure on discharge arrangement |
| Organisational and management factors | Resources, policy/strategy, culture | Extent of resource sharing and joint working between health and social care agencies |
| Institutional context | Socioeconomic and regulatory systems | Changing policies and regulatory arrangements for discharge, such as compensation for delayed discharge placing pressure on social care staff |
Extending the systems approach
Despite the enormous advances in patient safety research, it has been suggested that the distinctive sociocultural and political dimensions of health care are sometimes overlooked. 6 A related view suggests that the human factors approach tends to, although does not always, focus on what might be considered the ‘clinical micro-system’ or local work environment. Take, for example, the emphasis on team skills, communication aids, decision-support tools and checklists. This approach considers less frequently (and in less detail) the wider cultural, institutional or system factors related to workplace practice. Similarly, research has tended to focus within clinical specialities, departments or units, such as operating theatres, care homes or emergency departments, with less attention to the interconnections between these areas and the wider organisation. 3 Although organisational and societal factors are recognised,96,101 they are not well developed theoretically or empirically as distinct and interconnected levels of analysis.
Attention to the sources of risk and safety between care settings and processes is important for hospital discharge as relates directly to broader organisational and interorganisational factors. It calls for attention to the nature of the relationships and interdependencies between care organisations as patients pass from hospital to community care. These interdependencies constitute ‘system-level’ (latent) sources of safety, and where research does attend to these interdependencies it shows that the organisation of health care is often so complex and non-linear that the idea of creating a reliable, standardised and safe system remains a ‘wicked problem’. 102–106 Extending this line of thinking, Hollnagel107 suggests that although the human factors approach goes beyond a simple (single agent) model of error causation to identify instead environmental causation, it too often neglects the non-linear and more complex dynamic coupling involved in many organisational or system processes.
Developing this perspective, a ‘system’ describes a collection of actors, units or parts that together, and through their various connections, form the basis of a structured and relatively bounded entity. Through combining these constituent elements, systems produce particular effects; in many instances these are positive, but they can also be unpredictable, unanticipated or unsafe. 108 Broadly speaking, ‘complex systems’ have emergent properties that result from the non-linear or complex connections between their heterogeneous units, subsystems, variables or actors. 108,109 Furthermore, complex systems can produce effects that are not always evident from the actions or attributes of the individual parts, owing to the potential for the actions of one component to transform the contexts and actions of others. 108 More than this, complex systems are characterised by the absence of structural design and by patterns of self-organising and adaption. For example, the constituent parts within a system interact according to local rules (e.g. customs or cultures) without any overarching direction or control (e.g. leader). 110
Health-care systems are increasingly identified as complex systems. 102,111–114 The organisation and delivery of health care typically involves a vast number of agencies that span different economic sectors (public, private, voluntary), health domains (primary, secondary, tertiary) and care domains (health, social, personal), with distinct roles and responsibilities (commissioners, providers, regulators) and caring specialities. Moreover, the interactions between these actors are not always well defined, but remain dynamic, non-linear and multifaceted, from micro-level clinical interactions, to the meso-level interactions of service planning or commissioning and the macro-level interactions of policy-making and professional associations. As such, health-care systems can change in ways that are not always easily anticipated by policy-makers or service leaders. Extending this line of thinking, hospital discharge might have been conceived as a complex system involving a network of diverse, often heterogeneous actors, interacting in dynamic and non-linear ways that over time produce unpredictable and unanticipated behaviours or outcomes, both positive and negative.
One seminal analysis of organisational complexity that specifically demonstrates the potential for negative consequences is Charles Perrow’s study of Normal Accidents. 8 This was developed through an investigation of the system failures that contributed to the Three Mile Island nuclear disaster. His analysis suggests that organisational accidents might be interpreted as inevitable for complex organisational systems, not simply because of the high-risk nature of the work or potential for ‘operator error’, but because of the way organisational processes are configured. In particular, his research elaborates how relatively small, isolated or ‘discrete failures’ that occur in one part of a complex system can cascade and escalate into more substantial disasters. In other words, risks do not develop through linear causal chains but through unpredictable interactions. Where organisational activities are ‘tightly coupled’ there are higher levels of interdependence between work processes, meaning that what happens in one area is influenced by, or influences, the work of others. In health care, research has demonstrated how errors and failures from one department have consequences in other tightly coupled activities across the health-care system. 106,115
Although health policies call for greater attention to, and learning about, the systemic threats to patient safety,2 research has largely centred on the latent threats located within discrete and often localised parts of the health-care system. 3 There remains limited understanding or evidence of the threats to, and opportunities for, patient safety located within the wider health-care system, especially in the complex interdependencies and non-linear interactions that exist between care providers located in diverse occupational, organisational and sectoral domains.
Applying these ideas to the problem of hospital discharge, it becomes apparent that the complex interdependencies and non-linear couplings between health and social care agencies can be the latent source of poorly timed, inappropriate or unsafe transition from hospital to community care. Policies to support integrated discharge planning have repeatedly looked to introduce improved or more stable couplings between these agencies through, for example, resource pooling and MDTs, and more routine and robust methods of information sharing. 30 There remain, however, enduring compatibility factors27 that inhibit co-ordination, and hence discharge safety, given the persistence of heterogeneous, tightly coupled and interdependent working practices.
Integration and safety through knowledge sharing
The above literatures show that hospital discharge is a vulnerable or unsafe stage in the care pathway, often because of the challenges of co-ordinating different health and social care agencies. Extending this idea, this study suggests that hospital discharge might be thought of as a complex system, whereby interdependencies and couplings between caring professionals and agencies can be a source of and threat to patient safety, depending on how they are co-ordinated. The literature repeatedly emphasises communication as helping to reduce this complexity and support co-ordination, for example, in discharge planning or the use of checklists. 27–29,86,87,94 Extending this idea, we propose the concept of knowledge sharing as a way of supporting the co-ordination and integration of health and social care agencies and mitigating the uncertainties inherent within complex health-care systems.
Knowledge sharing involves more than the communication of information, but instead denotes the exchange and use of meanings, assumptions, practices and know-how between different groups to engender shared understandings and collaborative practices. 11 For many improvement strategies, such as knowledge management and evidence-based medicine, knowledge is conceived as an explicit, abstract and tangible resource that can be accessed, codified and exchanged, for example in the form of formal policies or incident reports. In other words, it is an explicit ‘thing’ to be shared with others in the form of documents or evidence. This contrasts with the idea that knowledge or know-how is often tacit, experiential and situated in practice. 116 In this sense, knowledge is difficult to share and is typically acquired and developed through participation in communities of practice. 117 In short, knowledge is not a ‘thing’ that a community ‘has’, but rather it is what they ‘do’ and who they ‘are’. 117 This distinction is important because efforts to understand and indeed promote knowledge sharing should not only focus on the formal assemblages of knowledge, but also the more informal and unarticulated manifestations of know-how. Knowledge sharing is therefore more than the communication of information; it refers to how the meanings, ‘know-how’ and practices of one group or organisation can be shared and integrated into the practices of another. 10
The research literature highlights a range of factors that facilitate or inhibit knowledge sharing. 10–12,118 This includes the characteristics of both ‘donor’ and ‘recipient’ actors, such as their motivations, accessibility, levels of trust, values, hierarchies and absorptive capacity. 119–121 For example, competitive pressures can inhibit knowledge sharing where it threatens competitive advantage. 11 The ‘structural configuration’ of relationships can also channel knowledge flows through ‘central actors’ or knowledge brokers, rather than between peripheral actors. 122 Similarly, power hierarchies and cultural difference between actors can have an impact on knowledge sharing, especially where powerful actors assume control of knowledge to advance their own interests. 12,123 For professional work, these issues are exacerbated where expert knowledge is closely linked to sociolegal jurisdiction within the division of labour. 124 In this context, knowledge sharing can threaten professional boundaries and identities. 13,125 The research literature highlights a number of key dimensions that shape the potential for knowledge sharing. 117,122,126–128 Drawing together this literature, three inter-related factors are identified as shaping knowledge sharing and collaboration within and between health-care organisations:
-
Knowledge Related to differences in epistemology, cognition and sense-making, for example how actors make sense of discharge; the types of knowledge that guide practice; and whether or not knowledge represents a competitive resource.
-
Culture Related to the shared norms, attitudes and values that guide practices, for example when knowledge should be shared and with whom; how identities and trust reinforce knowledge hoarding; the different philosophies of care that guide work organisation.
-
Organisation Related to the influence of (inter/intra)organisational structures, processes, regulatory factors and management priorities that shape knowledge sharing, such as sociolegal rules, professional jurisdictions, organisational connections and resource constraints.
Knowledge sharing for safe discharge
Applying the above literatures to hospital discharge, this study investigates how patterns of knowledge sharing among health and social care agencies influence discharge planning and care transition. Developing this view, knowledge sharing is conceptualised as a latent source of safety that, through shaping the patterns of co-ordination, shared decision-making and integrated working, can mitigate system complexity. As such, understanding the barriers to and drivers of knowledge sharing can contribute to the development of new knowledge on the possibilities for improved integration and safety in hospital discharge. These lines of analysis are tentatively outlined in Table 3.
| Dimension of knowledge sharing | Examples in context of hospital discharge |
|---|---|
| Knowledge |
|
| Culture |
|
| Organisation |
|
Summary
This chapter has reviewed research literatures on hospital discharge and patient safety to suggest that discharge from hospital to community is located within a complex and vulnerable system, involving a diverse range of heterogeneous actors interacting in dynamic and non-linear ways. Policy and research highlight the need for improved integration, especially in discharge planning and care transition; however, given the complex, dynamic patterns of interaction and the variable institutional environments in which caring professionals work, this integration remains problematic. The idea of communication and collaborative decision-making is frequently cited as a basis for integration. 27–29,86,87 The study extends this idea by suggesting that knowledge sharing can support enhanced integration and collaboration among system actors, based upon the exchange and alignment of different meanings, assumptions and know-how, as well as more explicit knowledge and information. Knowledge sharing is therefore presented as a source of (and threat to) safety within the complex systems involved in hospital discharge, and requires further empirical understanding.
Chapter 3 Study design and methods
Study aims and objectives
This exploratory study investigates how knowledge sharing, as a latent factor, contributes to discharge planning and the transition of care, with the broad aim of identifying interventions and practices that support knowledge sharing and thus mediate system complexity and promote patient safety. As outlined in Chapter 1, the study focuses on the discharge of stroke and hip fracture patients as two comparator groups, but with the intention of developing broader lessons for improving care transitions. In line with this, the research objectives include:
-
to determine the stakeholders and agencies involved in discharge, including their distinct roles, responsibilities and relationships, as elaborated in terms of (a) their specific knowledge and practice domains; (b) their prevailing cultural norms and assumptions; and (c) organisational context
-
to determine the patterns, media and content of knowledge sharing between stakeholders with a particular focus on interventions to facilitate communication, including (a) MDTs; (b) guidelines and toolkits; (c) co-ordinators; and (d) ICTs
-
to determine stakeholders’ relative perceptions of the threats to ‘safe’ discharge, with a particular focus on known risks and sources of readmission, including (a) falls and (b) medicines management, as well as other perceived risks
-
to determine how knowledge sharing represents a latent threat to (sources of) patient safety, including known factors such as ‘delayed’, ‘missing’, ‘fragmented’ or ‘repetitious’ communications and the persistence of communication ‘boundaries’
-
to explain the patterns of knowledge sharing as threats to patient safety based upon the heuristic categories of knowledge, cultural and organisational factors
-
to identify lessons and interventions that support knowledge sharing and, in turn, integrated, efficient and safe hospital discharge and reduced readmission.
Methodological considerations
The proposed study methodology combined two complementary approaches for identifying, analysing and understanding patterns of knowledge sharing within complex social systems. This included social network analysis (SNA) and ethnography. SNA is an approach for identifying, mapping and measuring social systems and relational processes through analysing the relationships (ties) between people, groups and organisations (nodes). 129–132 Despite a resurgence of interest in more qualitative approaches to understanding social networks,132,133 quantitative approaches for measuring and statistically analysing social relationships remain dominant in organisational research. 131 Although the study obtained a range of qualitative data to describe and understand the patterns of knowledge sharing involved in hospital discharge, these data have not been analysed in the form of SNA, i.e. looking for structural relationships, actor centrality or network density. 131 Through consultation with methodological advisors, and reflecting the comments of the study reviewers, it was determined that, although a range of qualitative data on the patterns of knowledge sharing were collected, these were not of a consistent format and character to enable more standardised SNA. As such, the report draws upon these qualitative data to develop a ‘thick’ description and interpretative understanding of the patterns of knowledge sharing involved in discharge planning and care transitions. 132,133
In broad terms, ethnography is concerned with developing a rich description and interpretative understanding of how different peoples, communities or cultures ‘experience, interpret and structure their lives’. 134 Ethnography is particularly suited to organisational research,135 providing insight into how knowledge is constructed through intersubjective and culturally informed sense-making; how beliefs and assumptions are shared among different groups or communities; the importance of shared language and stories in expressing and reinforcing shared values; how ceremonies and rituals guide interaction and convey shared meaning; how social activities occur and unfold in context; and how wider sociocultural and institutional pressures shape everyday life. 136–138 The ethnographic approach is associated with specific methods for understanding social and cultural processes, especially observations that allow for an emic or insider’s perspective. 136
With reference to this study, ethnography affords exploratory understanding of hospital discharge as a situated social activity involving the sharing of knowledge between multiple actors, each with distinct cultures and modes of social organisation. Ethnography facilitates the identification and analysis of the distinct knowledge and practice domains that characterise different groups involved in hospital discharge; how their distinct cultural norms, values and identities have an impact on their discharge practices; and how wider social and organisational customs frame social practices. As well as providing a detailed and holistic understanding of the social and cultural world of health and social care professionals,138 ethnographic research is well suited to investigating issues of patient safety,139,140 including how latent factors located within this wider sociocultural fabric interact with and make clinical practice potentially (un)safe. 106
Sampling and selection
The study was designed as two system (and two patient group) case studies of discharge planning and care transition. The case study approach enables in-depth and contextual insight within cases, but also comparison and theoretical generalisation between cases. 141 In line with the case study approach, the selection of care systems and patient groups purposively aimed to investigate known differences between these cases.
System and organisational selection
The primary unit of analysis was the local care ‘system’, within which patient discharge is planned and organised. This ‘system’ is conceptualised as comprising an acute NHS hospital around which other primary, community, rehabilitation and social care services are arranged. Discharge is seen as the planning and transition of care from the acute NHS hospital to community-based health and social care. In line with this view, the study was undertaken in two geographically distinct English care systems, broadly defined by county boundary. Each has a principal administrative city and conurbation (Farnchester and Glipton), with smaller towns, and villages located in rural areas. For the purpose of maintaining anonymity of participating organisations and individuals, the city, country and organisational names have been changed. Sampling of these geographical areas took into account their relative size, ethnic diversity and urban/rural balance (Table 4). Sampling also considered variations in the configuration of the care systems in these counties. Each was served by a single NHS acute trust; one was a large teaching and research-active health-care provider, operating over three large organisational units (Glipton), and the other was a smaller district general hospital with limited teaching and research activities (Farnchester). Sampling also considered the geographic spread of community-based care services, the proportion of single-handed GPs and structure of social care services. These differences are summarised in Table 4 [data were obtained through National Health Profiles143 and the Office for National Statistics (ONS)142 from 2010 to 2012].
| Study site | Population (n) (2011142) | Geography (square miles) | Ethnic diversity | Life expectancy, male (years) | Life expectancy, female (years) | Life expectancy variance between most deprived and least deprived city areas (years) | Number of GP practices | Hospital arrangements | Community services | Social services | Ambulance service |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Glipton city | 307,000 | 60% white | 75.4 | 80.1 | Male, 9.4 Female, 5.0 |
65 | Three large city acute and specialist hospitals with extensive teaching and research (NHS acute trust) | Dedicated rehabilitation centres, ESD services, intermediate care, mental health care and large number of private care providers | City providers | Single NHS provider for acute response; private provider for planned discharges | |
| Farnchester city | 90,000 | 95% white | 76.5 | 81.2 | Male, 10.6 Female, 5.8 |
24 | Two medium-sized district general hospitals with limited teaching (NHS acute trust) | Limited range of generic rehabilitation services with small range of private care homes | Single care provider | Single NHS provider for acute response and planned discharges | |
| Glipton county | 649,000 | 823 | 80% white | 79.8 | 81.2 | Male, 6.2 Female, 5.7 |
145 | Two general community hospitals (NHS community health-care trust) | Large number of private providers and approximately six social service-run homes with registered dementia care units | County providers | Single NHS provider for acute response; private provider for planned discharges |
| Farnchester county | 703,000 | 2350 | 98% white | 78.7 | 82.4 | Male, 7.3 Female, 4.9 |
102 | One general community hospital in remote town | Limited range of private providers with no registered dementia care homes | One single care provider | Single NHS provider for acute response and planned discharges |
| England average | n/a | n/a | 86% whitea | 78.6 | 82.6 | n/a | n/a | n/a | n/a | n/a | n/a |
Farnchester NHS Trust comprises two medium-sized district general (acute) hospitals, one located in the administrative city of the county and the other in another market town (Farnchester and Fallow), and a third, smaller community hospital located in a remote small town (Ribble). The hospitals were merged in 2000 under the management of a single NHS trust, with headquarters based at Farnchester Hospital. According to available records, the Trust employs over 7500 staff and treats more than 180,000 emergency patients, 500,000 outpatients and 100,000 inpatients every year. Farnchester Hospital is the main provider of specialist services across the majority of the county, including stroke and hip fracture patients. At the time of data collection, two primary care trusts (PCTs) (east and west of the county) commissioned specialist and acute services. Following the Health and Social Care Act 2012, services are commissioned by four Clinical Commissioning Groups (CCGs) (north, south, east and west), which operated in shadow form during the last year of the study. The Trust works closely with Farnchester Community Healthcare NHS Trust, which was formerly managed by one of the PCTs but became a separate provider of health care. It also works closely with a single unitary local authority for the county, whose social service department assesses and provides social and personal care, or contracts care provisions from private or third sector agencies.
Glipton NHS Trust comprises three distinct hospitals (City, General and District), located in different areas of the same city and also brought under the management of one NHS trust in the early 2000s. The Trust employs over 10,000 staff and provides services to over 1 million residents in the local population. It is an established site for health education, with strong links to the local universities, and the site of an extensive portfolio of clinical research. At the start of the research, the Trust worked closely with two NHS PCTs (city and county), who commissioned the majority of its acute and elective services. Following the Health and Social Care Act 2012, three new CCGs operated in ‘shadow’ form until assuming responsibility for commissioning in April 2013. Two community NHS trusts (city and county) provide continuing health care, rehabilitation and home-based care, including the management of two community hospitals. The social services departments of the city and county local authorities were involved in assessing, providing or commissioning social care through a mixed market of public, private and third sector organisations. This includes a specialist reablement service for immediate postdischarge care. The regional NHS ambulance trust supports the transition of patients both to and from Glipton and Farnchester NHS Trusts, and a private transportation firm is also contracted to provide patient transports from hospital.
Sampling started with the two acute NHS hospitals, and included other primary, community and social care agencies. It was anticipated that the variety and number of agencies involved in discharge planning and care might be considerable, and variable according to patient need. Reviewing the literature, a range of common agencies was identified. Although many of these groups could be identified in advance of the study, such as social services, it was difficult to determine the exact profile for each county. As such, a snowball sampling strategy was used to identify agencies and organisations involved in hospital discharge. This group included:
-
GPs and primary care administrative and commissioning units (PCTs, now CCGs)
-
community health-care services (some formerly managed by PCTs)
-
specialist community in-reach/outreach services (possibly managed by PCTs)
-
community pharmacies
-
local authority, social services
-
social care providers working in private, public or third sector (including reablement)
-
intermediate care and rehabilitation services
-
residential and nursing homes
-
ambulance and transportation services
-
voluntary sector support groups.
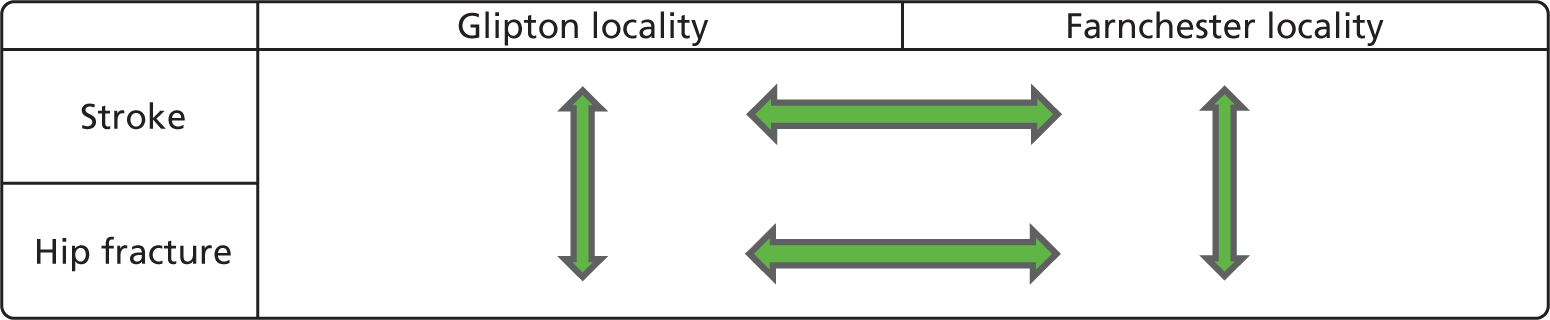
Through purposively selecting differences in health system configuration and patient group (stroke and hip fracture patients), it was possible to develop comparison along four dimensions: between different hospital types and system properties (e.g. single site vs. multisite), where some degree of control is obtained through looking at the same patient group, and between different patient groups (e.g. stroke and hip fracture patients) within the same hospital (Figure 1).
FIGURE 1.
Selection and basis of analytical comparison.
Patient selection
The research used ‘patient tracking’ to develop a patient-centred understanding of hospital discharge (see Patient tracking). This involves focused observations and interviews with patients and families as they experienced discharge planning and care transitions. To facilitate representation across patient groups, a sampling strategy was devised in consultation with clinical specialists on the project team, patient and public involvement (PPI) representatives and clinical leaders at each site. This recognised key variables and comorbidities known to influence discharge activities, such as cognitive impairment or family situation. Sampling included participants with and without cognitive capacity to reflect the general adult hospital population.
Essential criteria
-
Treated in acute hospital for hip fracture (non-elective) or stroke.
-
Expected day of discharge within 7 days of initial information giving by researcher.
-
Lives within the study site boundary.
-
Aged over 18 years.
-
Able to hear and speak to respond to interview questions or has family member able to assist with communication.
Additional selection criteria for each study site
-
Ages: 1 × over 85, 3 × over 65 and 1 × under 65 years.
-
Cognition: at least two patients with recognised confusion or cognitive difficulties (as determined by care team).
-
Place of discharge: 2 × living in residential or nursing home, 1 × home alone, 1 × sheltered housing, 1 × with family.
-
Fast-track can be included but must fit essential criteria and researcher to have made direct contact with family prior to discharge.
Based on these criteria, the study aimed to recruit eight patients within each service area (a total of 32 across all four sites). Selection involved identification of potential participants in consultation with senior members of the care team around the time of admission, before inviting patients and families to take part in the research. This technique proved to be highly successful within three sites. In the Farnchester hip fracture service, difficulties were experienced in sustaining the required number of participants because of frequent transfers between wards, staff shortages and ‘out of area’ patients. In total, across all sites a total of 32 patients were recruited (see Table 7). Reasons for withdrawal during the data collection periods included death, deterioration of condition, loss of discharge destination information, discharge out of the study area, readmission, transfer to a new location and patient or family not wishing to continue.
Research methods and data collection
Data collection involved two sustained periods of data collection within each local care system (Glipton and Farnchester), starting in the respective stroke and hip fracture services of each hospital before moving to the wider health and social care system. Data collection typically involved 2–3 months of research in and around each stroke and hip fracture service (i.e. 5–6 months of research in each hospital) and a further 2–3 months of research in the local community health and social care sector, including patient tracking (i.e. approximately 8 months of research within each health-care system). Patient tracking commenced around the same time that community health and social care agencies were involved in the research.
Qualitative interviews
Semistructured qualitative interviews were used to understand how hospital discharge is planned, organised and experienced from the perspectives of different health and social care professionals, patients and family members. Interviews were especially important for identifying the roles and responsibilities of actors within the discharge process, the patterns of knowledge sharing between actors and how actors’ knowledge domains, cultures and organisational context shaped their interactions. The interviews were designed to be conducted in a semistructured, conversational style, giving participants the opportunity to explore emergent issues. All semistructured interviews were guided by a topic guide developed to reflect the study objectives. Draft questions were developed by the project team and representatives from the PPI group and piloted at one research site with three clinicians. These topics (see also Appendix 1) included:
-
career biographies and backgrounds
-
details of roles and responsibilities, with a specific focus on discharge activities
-
an account of the discharge process, including the broad process, planning issues, and working with patients and families
-
the role of communication and knowledge sharing in discharge processes
-
identification of individuals or groups contacted during discharge activities
-
exploratory accounts of knowledge-sharing relationships with identified individuals
-
perceptions and experiences of risk and safety
-
recommendations and improvements.
A modified guide was developed for patients, family members and carers, based on the advice and feedback from the PPI representatives. This included:
-
ways in which discharge plans were discussed and planned with patient and carer
-
how the discharge was expected and experienced
-
whether or not the plan met the needs of the patient
-
ways in which discharge can be improved.
An important feature of the interview questions was that they were structured to generate participant narratives, or stories of discharge processes. These stories were not read necessarily as ‘truths’ but rather as analytical windows into how participants make sense of and give meaning to discharge, thereby highlighting differences in knowledge and culture. These narratives were particular insightful when exploring how participants make sense of the discharge process, and especially the sources of safety and risk. A further feature of the interviews was that they were used to inform snowball sampling, that is, to help identify other potential, unanticipated actors or groups involved in the discharge process and the patterns of knowledge sharing with these actors. For example, all participants were asked to describe the different people, groups or organisations they communicate and share knowledge with in the processes of discharge planning and care transition.
Most participants were invited in writing to participate in the study. This invitation included a participant information sheet and an opportunity to contact the project team for further information. Other participants were recruited during ethnographic observations; for example, where an individual was observed as having an important role they would be asked to participate in the study and provided with a participant information sheet. All participants were asked to confirm that they had understood the participant information sheet and give written consent. The majority of interviews were digitally recorded with the consent of participants and all were transcribed verbatim for the purpose of subsequent data analysis. Table 5 details the interview participants according to location and number, and Table 6 further details the interview participants by their occupational background.
| Organisational location | Number of interviews |
|---|---|
| Glipton system total | 98 |
| Glipton Hospital: stroke unit | 45 |
| Glipton Hospital: hip unit | 16 |
| Glipton Hospital: management | 2 |
| Glipton community hospitals | 7 |
| Glipton Community NHS Healthcare | 9 |
| Glipton social care | 6 |
| Glipton community health care | 7 |
| Primary care/CCG/GP | 6 |
| Farnchester system total | 64 |
| Farnchester Hospital: stroke unit | 17 |
| Farnchester Hospital: hip unit | 20 |
| Farnchester Hospital: management | 2 |
| Farnchester community health care | 7 |
| Farnchester social care | 5 |
| Farnchester community others | 10 |
| Primary care/CCG/GP | 3 |
| Ambulance service (regional) | 2 |
| National organisations | 5 |
| Total interviews | 169 |
| Group | Glipton | Farnchester | Total |
|---|---|---|---|
| Medical (hospital) | 10 | 8 | 18 |
| Nursing | 18 | 15 | 33 |
| HCAs | 5 | 2 | 7 |
| OTs | 10 | 10 | 20 |
| PTs | 16 | 8 | 24 |
| Other therapists (speech, dieticians) | 2 | 3 | 5 |
| Pharmacists | 1 | 2 | 3 |
| Ambulance (regional) | n/a | n/a | 2 |
| Administrative | 2 | 2 | 4 |
| Managerial/leadership | 3 | 3 | 6 |
| Social work | 9 | 5 | 14 |
| Social care | 2 | 2 | 4 |
| Community nursing | 2 | 7 | 9 |
| GPs | 1 | 2 | 3 |
| GP/CCG administration | 2 | 0 | 2 |
| Support group/voluntary | 4 | 2 | 6 |
| Patients (interview stage 1) | 16 | 14 | 30 |
| Carers/family (unpaid) | 12 | 11 | 23 |
Alongside semistructured interviews, the research involved more informal ethnographic-type interviews with participants, normally as part of observations. These ranged from small interactions or ‘chats’ to clarify an observed occurrence or activity (i.e. asking a participant what they are doing or to explain a technical procedure) to more open, unstructured and lengthy exchanges (i.e. to explain a series of events or a particular situation in greater detail). Many of these interviews occurred when shadowing participants or in other informal settings, such as rest areas or cafés. As such, it was not always feasible to digitally record these interactions and most were recorded as handwritten notes in field journals.
Observations
Ethnographic observations of discharge activities provided the main source of data. Observations focused on how discharge was planned, organised and supported as a series of complex interactions between various health and social care agencies. These involved non-participatory or passive observations144 of everyday practices; that is, the research team did not have a formal, legitimate membership role in discharge activities, but they did build rapport and shared understanding with participants through interacting and engaging in other forms of participatory engagement, such as conversations and non-clinical (technical) interactions. The observations combined different activities to build rapport and understanding:
-
Guided tours and structured familiarisation Undertaken at the start of the research over a period of 3–5 days, including ‘walking tours’ with service leaders, introductory meetings with stakeholder groups, informal presentations at weekly meetings and collection of relevant documents, policies and procedures.
-
Work process observations More in-depth workplace observations undertaken over a period of 1–6 weeks (depending on the location). These included mapping the temporary and spatial organisation of daily work (schedule of ward rounds, meetings, handovers, discharge times); identifying key events and activities (MDTs, drug rounds); identifying key individuals or groups (discharge co-ordinators, clinical leads); and drawing together these data into a complex descriptive account of the social setting. For the main research settings, i.e. hospital wards, observations were undertaken on a daily basis (3–4 days per week, including evenings and weekends) for 4–6 weeks; in other settings, such as community hospitals or care homes, they were undertaken over 1–2 weeks, and in more dispersed or peripheral settings, such as social service departments, they were undertaken over a shorter time period, i.e. day visits. Some settings were not amenable to observation given the diversity and demands of their workload, such as GP surgeries and community pharmacies, where interviews provided the primary source of data.
-
In-depth observations of situational activities, tasks and settings Prolonged follow-up observations of key knowledge-sharing activities, tasks and settings. These observations were usually conducted concurrently with other research activities, including shadowing or interviews. Each setting was observed at least three times and some settings, such as weekly MDTs, were observed up to 10 times. This included observations of:
-
daily/weekly planning and decision-making meetings (MDTs)
-
trauma and assessment ward rounds
-
patient and family consultation meetings
-
community hospital reception
-
nurses’ station ambulance handover
-
social services assessment
-
use of ICT and manual records relating to discharge planning
-
pharmacy ward checking of medications to take out (TTO) on discharge
-
fast-track planning and handovers
-
referrals to multiple agencies by phone.
-
-
Shadowing of individuals To deepen understanding of the roles and contributions of certain individuals or groups, shadowing observations were also undertaken with key individuals (leaders or discharge co-ordinators) or representatives from professional groups (nurses or therapists). These ranged from several hours (ward clerks) to several days (discharge co-ordinators) of observing individuals as they went about their day-to-day work. These individuals included:
-
discharge co-ordinators
-
ward nurses
-
junior doctors
-
consultants
-
hospital social workers
-
ward clerks and administrators
-
OTs
-
PTs.
-
Using these techniques, it is estimated that the research involved over 180 hours of direct observations and many more opportunistic observations, in a variety of health and social care settings. All observations were recorded, first in handwritten field journals including rich description and separate interpretations. These were later typed up electronically as corresponding text and interpretation, as well as a summary overview of key points.
Patient tracking
A key feature of the research design was the use of ‘patient tracking’ to understand the first-hand experiences of patients and their families/carers as they were discharged from hospital to a community setting. This involves a series of short semistructured interviews (up to five), with patients both before and after discharge, focused observations of their discharge planning and arrangements, and the collection of patient diaries (where possible) (see Appendix 2 for extracts of patient diaries). These activities led to the collection of rich and diverse data that enabled the research team to construct a picture of how patients and family members experience hospital discharge.
In the first instance, patients/families were approached in hospital after admission, usually when an initial date of discharge had been set (within 72–48 hours of planned discharge). Each patient was asked to participate in a series of short follow-up interviews, starting in hospital and then at 1, 2, 4 and 6 weeks post discharge. Although every effort was made to schedule interviews at these times, in some instances they needed to be moved ± 1 week owing to other appointments. Furthermore, not all patients were able to participate in the full series of interviews because of withdrawal (their health had worsened), readmission to hospital or death. Observations were also undertaken with patients, families and carers, on the wards and at home or in a care setting (nursing home) to understand how care was organised and provided. Patients were also invited to keep diaries about their discharge experiences (Table 7). In consultation with PPI representatives, a short, open-text diary was designed and printed and given to each participant with a short description explaining its voluntary use. The diary had a minimal structure and allowed for open text. Specifically, it stated that:
The purpose of this diary is to give the researchers a way of understanding how you are living your life since leaving hospital. The team are interested in what happens each day, especially when you have contact with health and social care workers. Please spend at least 10 minutes each day writing in your diary, but don’t worry if you miss a day.
| Patient participant numbers | Farnchester stroke | Farnchester hip | Glipton stroke | Glipton hip | Total |
|---|---|---|---|---|---|
| Pre-discharge interview | 7 | 9 | 8 | 8 | 32 |
| Interview one | 6 | 6 | 8 | 7 | 27 |
| Interview two | 4 | 3 | 5 | 3 | 17 |
| Interview three | 2 | 0 | 4 | 2 | 8 |
| Withdrawals | 2 | 5 | 1 | 0 | 8 |
| Deaths | 1 | 3 | 2 | 0 | 6 |
| Readmissions | 1 | 0 | 1 | 2 | 4 |
| Diaries | 2 | 2 | 2 | 2 | 6 |
It also included a number of prompts asking participants to consider which health and social care providers they had interacted with, what they talked about, what kind of decisions were made and who else helped with their care. Participants were asked to keep the diaries for up to 30 days. Diaries were collected following the last interview or earlier if patients needed to withdraw from the study. In most instances, patients withdrew from the study because of continuing illness or moving out of area, in most cases around the time of the second interview.
Focus groups and validation workshops
The research involved a number of focus groups and workshops at each research site, together with a validation workshop at a third hospital site. The focus groups aimed to explore similarities and differences in staff members’ understandings of the discharge process. Each involved structured activities with representatives from professional groups in ward or community settings. Each started by asking participants to individually visualise and draw what they saw as the key stages or activities involved in hospital discharge. These were used to prompt reflection and to gather insight into how discharge was understood by different groups (see Appendix 6). Each group was then tasked with collectively drawing the discharge process on large sheets of A2 paper, using pens and Post-it notes. These usually took the form of flow diagrams, but varied as they were revised and amended. Throughout this process, a member of the research team asked probing questions to clarify the choices made, differences between participants and to surface shared or divergent reasoning. Finally, each focus group involved an open discussion about the sources of risk and breakdowns within the discharge process. Although focus groups were organised with all four sites, the Farnchester hip fracture service was unable to participate in the activity owing to staff shortages and workload pressures. As such, only three of these focus groups were undertaken. Table 8 details the numbers and staff representatives involved in the focus groups.
| Glipton stroke | Glipton hip | Glipton community | Farnchester stroke | Farnchester community | Regional |
|---|---|---|---|---|---|
| OTs PTs SaLTs ESD services (n = 11) |
OTs PTs (n = 6) |
Rehabilitation nurses Stroke support group (n = 17) |
PTs OTs Ward nurses (n = 15) |
OTs PTs Social services (n = 4) GP and PCT leads (CCG) (n = 4) |
End-of-life group (n = 4) Ambulance service (n = 3) |
At each research site a feedback (validation) workshop was organised after data collection to outline preliminary findings, raise any unresolved questions and seek validation on emerging interpretations. These were organised in consultation with service leaders to include staff representatives and clinical leads, usually involving between five and 10 people. They each involved a short visual presentation and provided a written report about the study aims and design, data collection and key findings, including a list of anonymised recommendations from participants for service improvement. These workshops were particularly useful for validating and confirming the early analysis.
An extended ‘validation workshop’ was organised with an additional acute care provider of hip fracture services, not involved in data collection. This aimed to further validate and confirm the research findings through exploring relevance and similarity with professionals and managers from another locality, thereby helping to develop more generalisable lessons. This workshop was organised after all data collection and early analysis was complete. It was attended by the hip services clinical leader and representatives from different professional groups, including nursing, occupational therapy, physiotherapy, and administrative and support staff. The workshop was structured with an overview of the research design and data, including the main points of convergence and divergence across the research sites, and analysis of the common barriers to and facilitators of hospital discharge. Participants were asked to discuss the relevance of the findings to their own service, the growing complexity of patient comorbidities, resource demands in the acute and community settings and the challenges of meeting increased patient expectations. This workshop helped to identify additional lines of analysis to test emerging conclusions.
Overall, the validation workshops identified and help clarify the following issues:
-
the range and number of actors involved
-
discharge pathways and structure of interactions
-
communication and knowledge-sharing problems
-
the main perceived threats to patient safety
-
contextual factors, i.e. staffing, resource constraints, targets
-
wider contextual changes, i.e. CCG priorities
-
recommendations for future interventions.
Documents, policies and routine data
Through the study, various documents were collected from each research site. These included formal policies and pathways for discharge planning, patient leaflets and guides, and pictures of posters, fact sheets and other information. These were used to contextualise observational and interview data and provide a point of comparison between expected or planned discharge and observed discharge. The research also aimed to gather routinely collected performance data related to hospital discharge at each site, including data about staffing, bed usage, safety incidents, number of patients, average length of stay and number of readmissions. In three participating sites much of this information was made available by service leaders, and with additional third-party data, specifically health profiles and ONS data. As with the focus groups, however, one site was reported as too busy to help provide these data and, as such, only third-party data were collected. These statistical data were used to help contextualise the organisation and performance of each site, and were not used for formal statistical analysis. The range of data collected included:
Data management and analysis
All data were managed in accordance with NHS and university research governance frameworks. All interview transcripts were anonymised with pseudonyms, and all identifying information such as contact details was securely filed. Handwritten ethnographic notes did not include identifiable names or locations and were archived within 48 hours in locked cabinets. Electronic data were stored within encrypted and secure external drives and backup copies kept within a locked location within the university. The following sections detail the data analysis techniques.
Interpretative qualitative data analysis145–147 was undertaken to develop descriptive and contextualised understanding of the knowledge-sharing relationships and their contribution to discharge planning and care transition across each of the research sites. This involved an iterative process of close reading of data, coding, constant comparison, elaboration of emerging themes and re-engaging with wider literature. In the first instance, three members of the research team (JW, FM, SB) independently reviewed a sample of five transcripts and three observations records to devise an agreed coding strategy that reflected the over-riding research objectives. At this point, one researcher (FM) took responsibility for ongoing data coding and categorisation using the computer package NVivo 10 (QSR International, Warrington, UK), into which all transcribed interviews, focus groups and observational records were entered. This involved systematic coding of all data records. To assure the reliability of the coding process, codes and categories were reviewed on a weekly basis by the wider team to ensure the accuracy of interpretation and internal consistency of codes. As the coding process progressed, family codes and categories of data were identified, as well as thematic relationships. Through this iterative process a number of common themes were developed in relation to:
-
knowledge-sharing roles
-
knowledge-sharing relationships
-
knowledge-sharing situations
-
ethos and cultures
-
materials and resources
-
service organisation and management
-
perceptions of risk
-
sources of risk.
The aim of the analysis was to understand the relationship between knowledge sharing and discharge safety. In the first stage, it aimed to develop an in-depth and comparative analysis of the knowledge-sharing relationships by ‘zooming in’ and comparing between key activities, situations or interactions, drawing on observations records, interview narratives, diaries and informal accounts. This centred on a comparison between Glipton and Farnchester sites, and between stroke and hip fracture services. In the second stage, the analysis aimed to identify and elaborate research participants’ perceptions of the threats to patient safety associated with hospital discharge, drawing on in-depth narratives to identify actual safety events and underlying risk factors. These perceived risks were reanalysed with reference to observational data to understand how the patterns of knowledge sharing might explain these perceived risks. Further analysis aimed to look across the discharge process, knowledge-sharing relationships and perceptions of discharge safety to identify thematic categories that would help explain similarities and differences between research sites and how discharge safety might be enhanced through activities or interventions that reduce discharge complexity and increase knowledge sharing. This led to the identification of four broad areas where strategies and interactions might be developed to promote knowledge sharing, reduce system complexity and enhance patient safety (Figure 2).
FIGURE 2.
Thematic categorisations towards learning points.
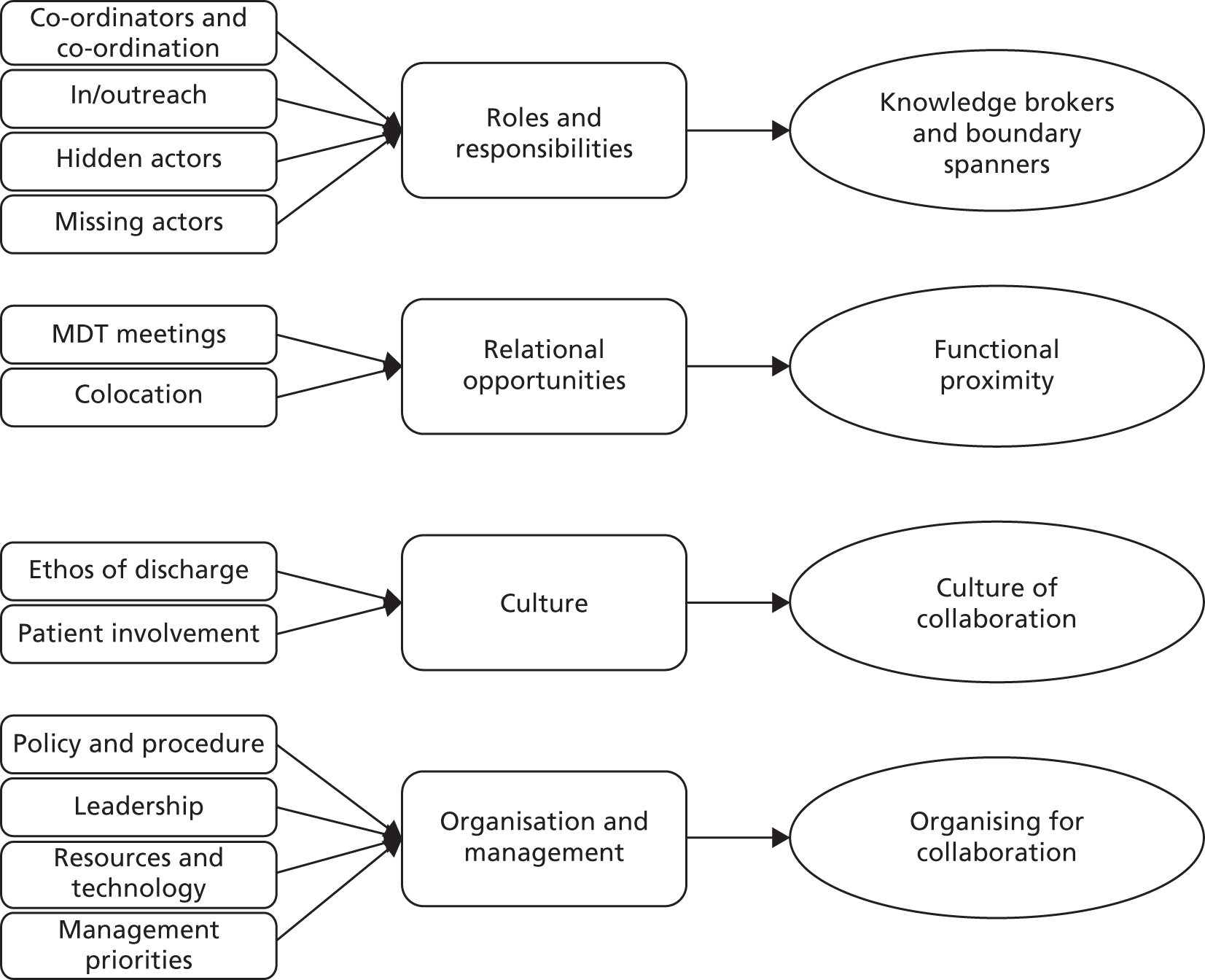
Public and patient involvement
Given the complex nature of hospital discharge and the pivotal role of the patients and their relatives at the centre of the discharge process, the study gave particular attention to understanding the views and experiences of patients and families, and of patient advocacy and support groups, throughout study design, conduct and analysis. At the study design stage, PPI representatives working in association with the National Institute for Health Research Collaborations for Leadership in Applied Health Research and Care (CLAHRC) Nottinghamshire, Derbyshire and Lincolnshire were consulted to understand the issues pertinent to patients and to develop the patient tracking exercise. This helped clarify, for example, the rich source of data likely to be collected during patient tracking and the importance of focusing on quality, not quantity of participants.
During the study period, an initial PPI group was formed to advise the study. Despite recruiting eight individuals to participate in this group, including representatives from the regional Stroke Association, Age UK and specialist PPI representatives working through Nottingham University Hospitals, it proved difficult to convene this meeting with full attendance. For example, at the first meeting only the chairperson and the study team attended. Therefore, the decision was made to form two smaller PPI groups within each of the communities being researched, based upon the contacts and groups involved in the study. As such, meetings were organised at the midpoint and end point of the study with local support groups, faith-based groups and local representatives from the Stroke Association and Age UK operating within each of the study areas. These smaller PPI groups were attended by between three and six people and were convened to fit with existing meetings and information sessions provided in each area. In each meeting the study aims and objectives, methods and plan of work were presented, and participants were invited to question and offer recommendations about the study focus, design and emerging findings. These meetings were particularly important in helping to determine the sampling criteria and methods for patient tracking, especially the time points at which to conduct interviews, the best ways of approaching patients and families, the design of the diaries and ways of keeping in touch with participants. Through the use of the patient tracking exercise, the study worked extremely closely with patients and their relatives, with the experienced researcher (FM) developing strong relationships with most participants, including high levels of trust, rapport and shared understanding. The nature of these relationships meant that participants not only provided data towards the study, but also an important source of timely feedback and guidance on the design and conduct of the study.
Ethical approval and research governance
The study received a favourable ethical opinion in May 2011 from the National Research Ethics Service Committee, East Midlands: Nottingham 1. The study also received research and development approval from each participating NHS trust, including letters of access for all researchers.
Presentation of findings
The main findings of the study are presented in the following two chapters. Chapter 4 develops a comparative analysis of the ways in which knowledge sharing contributes to discharge planning and care transition. In line with the research objectives 1 and 2, it identifies the range of actors involved in hospital discharge, including their distinct roles, responsibilities and relationships, and the patterns of knowledge sharing between them, including attention to the different forms of knowledge, media and materials. Chapter 5 describes and elaborates the perceived sources of safety and risk within discharge planning and care transition, and builds upon the previous chapter to consider how similarities and differences in the patterns of knowledge sharing can explain these threats to (and sources of) patient safety. In line with the research objectives 3 and 4, it draws primarily on the views and experiences of participants to describe the perceived threats to safety in relation to hospital discharge, and in analysing these accounts the chapter draws upon Chapter 4 to interpret and explain the relationship between the perceived risk and knowledge sharing. Chapter 6 draws together the preceding chapters to identify and elaborate the activities and interventions that might promote knowledge sharing, mitigate system complexity and promote safer discharge. In line with research objectives 5 and 6, it identifies tentative lessons for enhancing patient safety through understanding and addressing the barriers to knowledge sharing.
It is worth acknowledging that the presentation of the findings was particularly challenging given the enormous complexity involved in discharge planning and care transition. Broader still, the proposed research underestimated the enormous complexity involved in hospital discharge. In short, hospital discharge remains a highly complex social and technical process, with a myriad of contributing activities and factors, many of which exist in parallel, duplicate one another or run counter to one another, in the true sense of a complex system. As such, the report has struggled, at times, to convey this complexity and still maintain a coherent line of analysis and interpretation. The following chapters highlight many similar or repeated issues, and as such may appear at times repetitive, but this illustrates the sheer difficulty of trying to describe and analyse a complex system, as well as emphasising those particular issues that, time and again, appeared to influence knowledge sharing and discharge safety.
Chapter 4 Discharge planning and care transition
Introduction
This chapter develops a comparative analysis of the ways in which knowledge sharing contributes to discharge planning and care transition. In line with the research objectives 1 and 2, it identifies the range of actors involved in hospital discharge, including their distinct roles, responsibilities and relationships, and the patterns of knowledge sharing between them, including attention to the different forms of knowledge, media and materials. The premise of this analysis is that variations in the observed patterns of knowledge sharing can help explain differences, including discrepancies, inconsistencies and potentially unsafe practices, in discharge planning and care transition.
Hospital discharge does not occur as a single or isolated event, but rather as a complex series of linked incremental activities involving a diverse range of occupational groups and spanning organisational boundaries. It is also the case that no two patient discharges are identical, inasmuch as each patient experiences a relatively unique care journey and discharge destination. That being said, the study found that discharge planning and care transition was organised through a number of broadly common ‘situations’ whereby actors interact to make decisions, complete tasks and organise care. Many of these situations were routine in day-to-day care, such as the ward round, whereas others were designated for discharge planning, such as referral to social services. These ‘situations’ are analytically significant because they provide the primary sites or opportunities for knowledge sharing within the discharge process. This does not mean that other, less regular or ad hoc opportunities were not identified at the margins or outside these situations, but this study focuses on a number of common situations. Through attending to these more common situations, the chapter elaborates the complexity of hospital discharge, showing how discharge planning and care transition occurs through a series of linked temporarily stable and spatially bounded knowledge-sharing networks. That is, localised groups of actors and resources come together at a particular time and place to exchange and use knowledge in the processes of addressing a given decision or task. The connections or links between these groups or clusters contribute to the planning and progression of care transition.
This chapter ‘zooms in’ on these situations to describe and compare the different patterns of knowledge sharing and to determine their contribution to discharge planning and care transition. Despite the commonality of these situations across the research sites, it highlights important variations in terms of (a) the number and range of actors sharing knowledge; (b) the forms of knowledge shared; (c) the methods and media of knowledge sharing; (d) how knowledge is used in relation to discharge; and (e) the wider organisational context. Chapter 5 relates these patterns of knowledge sharing to the quality and safety of the discharge. The chapter proceeds with a brief overview of the common situations and ‘zooms in’ on each to describe the observed variations in knowledge sharing, including the range of actors, materials and resources involved, the forms of knowledge shared and how knowledge is used in relation to discharge. The chapter concludes with a visualisation of the knowledge-sharing networks within each phase, revealing how discharge planning and care transition unfolds. Extracts of qualitative data can be found in Appendix 4 and four patient ‘journeys’ or narratives can be found in Appendix 3, both of which support the account developed in the chapter.
The situations of discharge planning and care transition
The study acknowledges that for many patients the care journey is not linear, but involves a complex trajectory of false starts, delays and repeated steps. The patient stories presented in Appendix 3 demonstrate this complexity and variability. As suggested above, however, the study found that discharge planning and care transition was organised through a number of relatively common ‘situations’. These situations are conceptualised as temporarily stable and spatially bounded knowledge-sharing networks, which combine or link together across the patient journey to progress hospital discharge and onward care. Elaborating this idea, these situations involve a particular grouping of actors who come together around a given task or activity, and at a particular time and place, and through their interaction they share knowledge that either directly or indirectly relates to hospital discharge. Some of these situations only occur once within the care pathway (admission) whereas others occur through routine clinical interactions (ward rounds), or in situations that are more explicitly linked to discharge (social care referrals). However, hospital discharge usually depends upon the combination of patterns of knowledge sharing within and across these situations. The chapter zooms in on the following situations or opportunities for knowledge sharing, while also showing how the distribution and contribution of these situations to hospital discharge varied across the research sites:
-
admission
-
ward round
-
ward-based interactions
-
MDT meetings
-
family meetings
-
internal care transfers (to an alternative ward)
-
health care referrals and assessment
-
social care referrals and assessment
-
equipment requests
-
day of discharge.
The study also found important differences in ‘discharge destination’, which reflect variations in local service configuration. For example, one hospital had access to a number of community hospitals to support care transition, whereas the other relied more upon residential (nursing) homes. These variations in ‘discharge destination’ inevitably influence discharge planning and care transitions and therefore frame the pattern of knowledge sharing and decision-making. For example, transfer to a community hospital involves a different pattern of interaction from discharge home. The main ‘discharge destinations’ observed included:
-
early supported discharge (stroke only)
-
home with social care reablement
-
community hospital for longer-term rehabilitation or end-of-life care
-
residential and nursing home (including intermediate care bed)
-
home with primary and community care.
The distribution of these ‘situations’ and ‘discharge destinations’ across the four research sites is summarised in Table 9, while Figures 3–6 illustrate the links between these situations in diagrammatic form, acknowledging that such processes are rarely linear. Using these situations and destinations as a framework for analysing the patterns of knowledge sharing, the research highlights important differences in the number and range of actors involved (occupational groups or agencies); the forms of knowledge shared; the methods and media of knowledge sharing; and how knowledge was used to inform hospital discharge. These variations were found to shape the general coherence and quality of discharge planning and the quality of care transition. The chapter describes and compares the patterns of knowledge sharing observed at each research site.
| Situations and destinations | Farnchester stroke | Farnchester hip | Glipton stroke | Glipton hip |
|---|---|---|---|---|
| Admission | • | • | ||
| Ward round | • | • | • | |
| Ward-based interactions | • | • | • | • |
| MDT meetings | • | ◦ | • | • |
| Ward transfers | • | • | ||
| Family meetings | • | ◦ | ◦ | ◦ |
| Social care referrals | • | • | • | • |
| Health-care referrals | • | • | • | • |
| Equipment requests | • | • | • | • |
| Day of discharge | • | • | • | • |
| ESD | • | • | ||
| Social care (home reablement) | • | • | • | • |
| Community hospital | • | • | ||
| Nursing care (intermediate) | • | • | • | • |
FIGURE 3.
Farnchester stroke unit knowledge-sharing situations and discharge destinations.
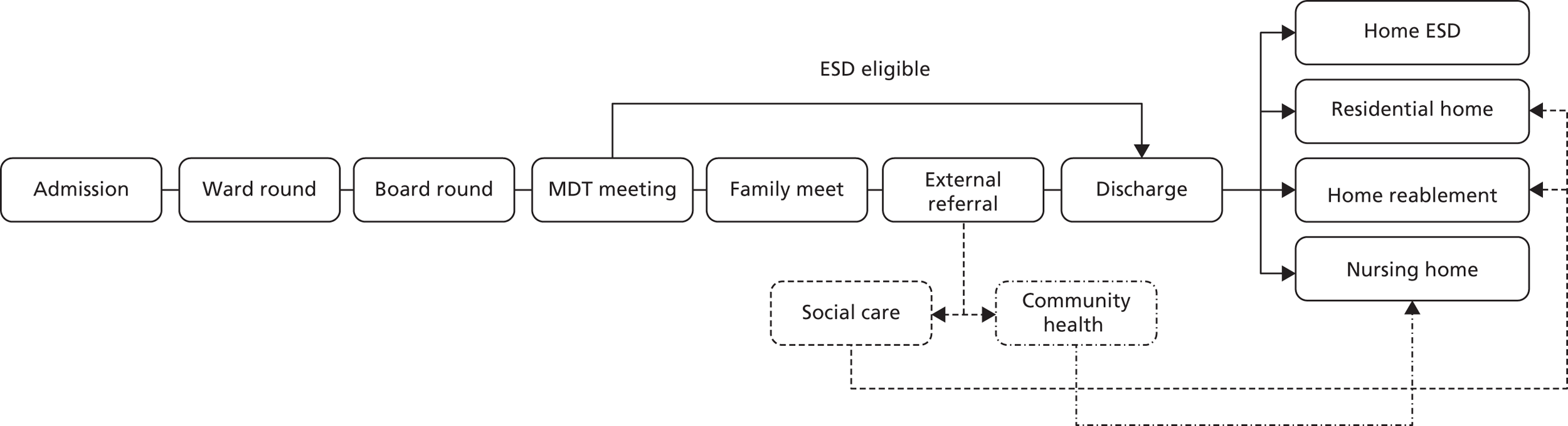
FIGURE 4.
Farnchester trauma orthopaedic unit knowledge-sharing situations and discharge destinations.
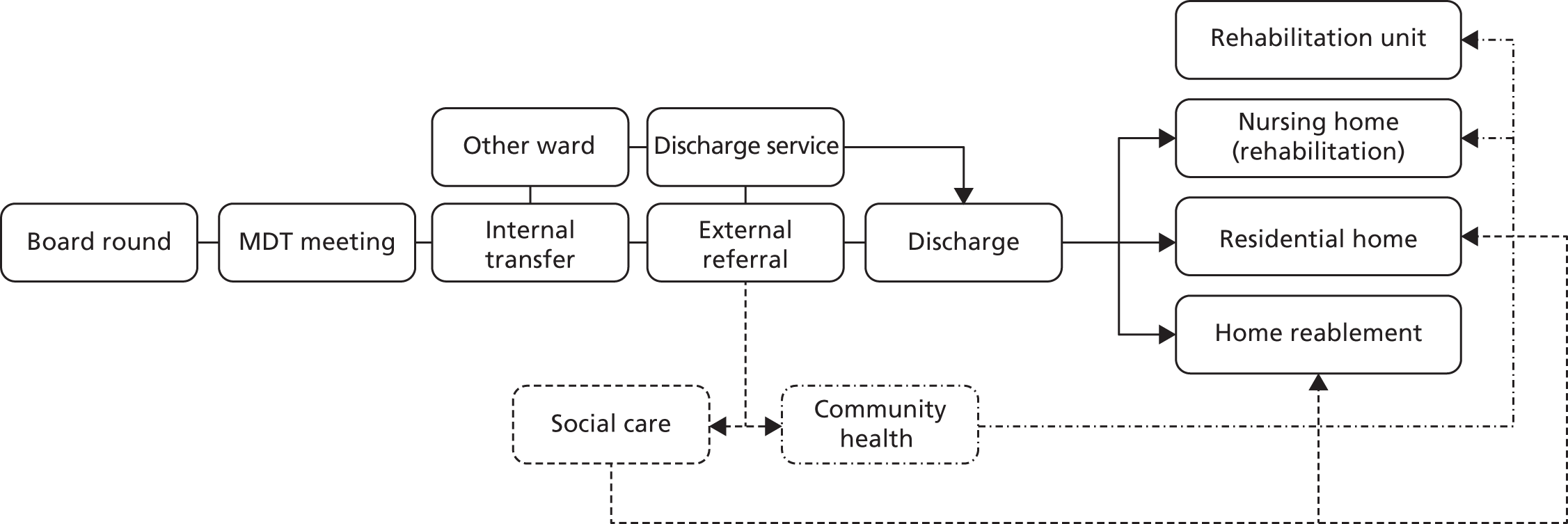
FIGURE 5.
Glipton stroke unit knowledge-sharing situations and discharge destinations.
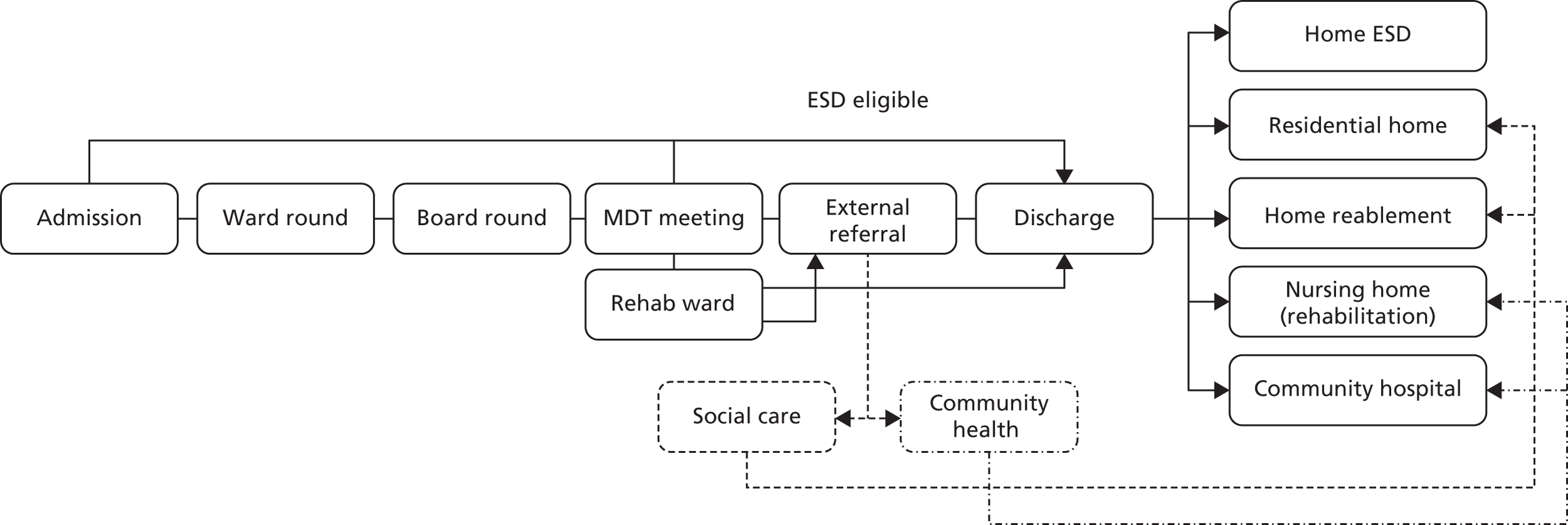
FIGURE 6.
Glipton trauma orthopaedic unit knowledge-sharing situations and discharge destinations.
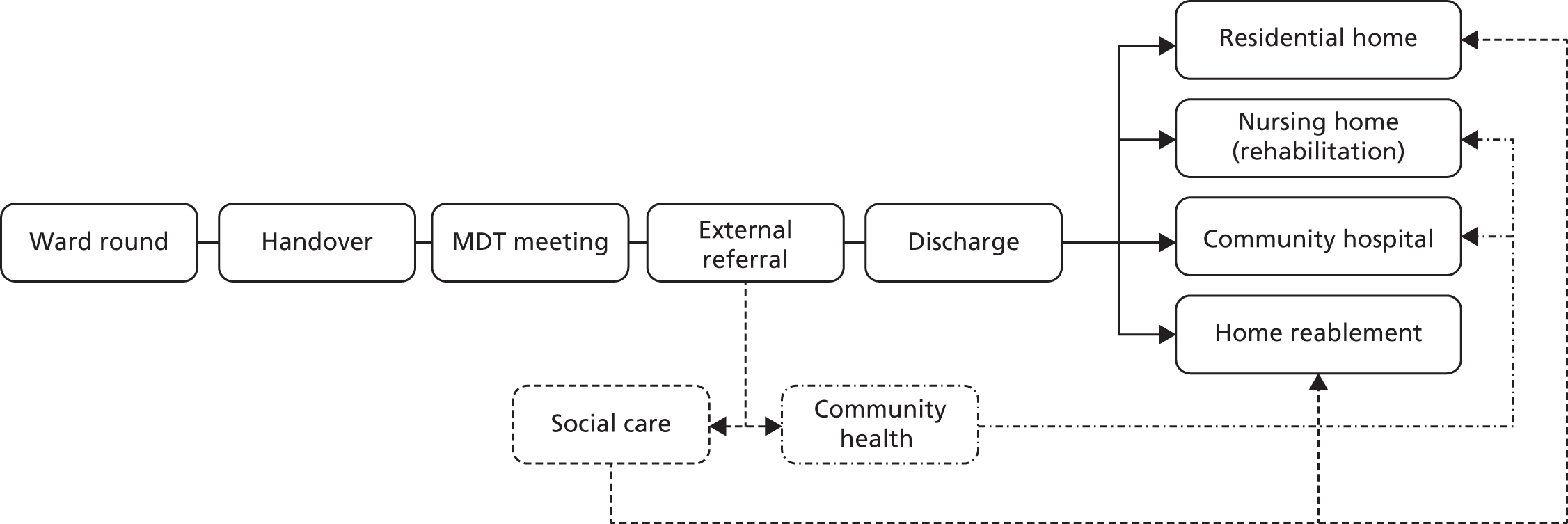
Admission
At admission, patient care is overwhelmingly concerned with determining an accurate diagnosis, stabilising the patient and commencing initial treatment, with patients usually assessed in the emergency department before being transferred to either the stroke or orthopaedic trauma units. Despite this over-riding focus, the admission stage provided an early opportunity for gathering knowledge related not only to the patient’s immediate care needs, but also to his or her onward care and possible discharge arrangements. In particular, it was an opportunity for clinicians to gather information related to the patient’s wider health and personal circumstances to consider the length of admission, need for rehabilitation and likely discharge arrangements.
At the Farnchester stroke unit, patients were usually admitted by a stroke consultant, junior doctor and ward nurse who would interact with the patient and family to gather and combine knowledge about his or her comorbidities (other health complaints), wider personal circumstances (employment and activities) and domestic arrangements (residence). This line of questioning extended beyond informing initial care planning, to help the medical team determine the level of longer-term rehabilitation and anticipated discharge destination, according to the severity of the stroke and available support structures. A similar pattern was observed at the Glipton stroke unit, but here it was also common for a representative from ESD to join the admitting team (if available), with the aim of identifying more quickly whether or not the patient was suitable for ESD. This was seen as avoiding potential delays in accessing ESD where decisions about patient suitability were primarily made at weekly MDTs rather than at admission.
In contrast, there was little attention to discharge planning during admission at the two orthopaedic units. Rather, patients were usually admitted on to the orthopaedic trauma units by a junior doctor and ward nurse. At this time, clinicians, patients and relatives would interact to determine the cause of the hip fracture, comorbidities and pre-existing health-care interventions. This information would not be explicitly used to inform discharge planning; rather, its primary purpose was to inform surgical decision-making. For example, it was customary for the junior doctor to present each patient at the next orthopaedic trauma meeting, thereby enabling the surgical consultant to determine and schedule surgery. These activities showed almost no attention to issues of discharge, with the primary emphasis on surgical decision-making. At Glipton, it was usual for an orthogeriatrician to meet with the patient prior to surgery. Through a short bedside consultation they would gather information related to the patient’s general health and social circumstances to inform postsurgical care planning, such as palliative care decisions, but there was no clear evidence that this led to early discharge planning.
Ward rounds
In general, the ward round enables the medical team to systematically review the care of each admitted patient through assessing their current health state and recovery; determining ongoing care needs; deciding upon necessary tests or therapies; allocating tasks to the wider care team; and supporting learning. In the course of these routine activities, the ward round represented a significant opportunity for progressing patient care towards discharge, i.e. facilitating the patient’s recovery; allocating tasks directly related to discharge, i.e. ordering TTOs; and, importantly, determining the patient’s readiness or ‘fitness’ for discharge. In other words, the ward round was a major knowledge-sharing and decision-making opportunity in the routine organisation of care.
At the Farnchester stroke unit, ward rounds were led by the lead consultant and involved the participation of junior doctors, the patient’s designated nurse and OT, a ward-based pharmacist and, significantly, patient relatives (if the patient agreed to their involvement). In addition to assessing and reviewing each patient’s ongoing care needs, it was usual for issues of patient discharge and onward care to be explicit (as a standing item) at each ward round. This largely centred on determining the patient’s likely date of discharge and, as this approached, the necessary tasks and activities required to ensure their onward care. This involved a relatively open exchange of knowledge whereby the consultant would lead a process of question and answer with the expectation that others would contribute according to their knowledge and practice domains. For example, the nurse would comment on the patient’s overall well-being and recovery, the OT on his or her rehabilitation, the pharmacists on the patient’s medicines regime, and relatives on their expectations for recovery. Although this pattern of exchange supported a combined and shared understanding of patient recovery, the primary purpose of the ward round still seemed to be to inform medical decision-making. As such, the consultant would use this information to lead decision-making and allocate tasks, i.e. he or she was the primary user of the knowledge.
A similar arrangement was observed at the Glipton stroke unit, with medical-led ward rounds used on a daily basis to inform overall care planning, but also the planning of care towards discharge. However, it was not usual for relatives to be in attendance, and as such there were fewer opportunities to include information about the patient’s personal circumstances. It was more usual for a speech and language therapist (SaLT) and a dedicated discharge liaison nurse to participate in the ward rounds, thereby providing additional insight. The discharge liaison nurse played a particularly important role, being responsible for recording and co-ordinating agreed tasks related to progressing hospital discharge, as well as providing daily feedback on their completion.
At the Glipton orthopaedic unit, the ward round was structured differently, being split between ‘surgical’ and ‘orthogeriatric’ rounds. Following surgery, each patient’s surgeon, junior doctors and designated ward nurse would conduct a relatively standard daily ward round. Significantly, these tended to focus on surgical recovery, for example wound care, infection and mobilisation, with little or no consideration of onward care or discharge. As the patient recovered from the surgical procedure, the junior doctor, under the supervision of the consultant surgeon, would declare the patient as ‘surgically’ fit. This, however, did not necessarily mean the patient was ready for discharge; rather, this would trigger non-surgical clinical and therapeutic interventions with the explicit aim of preparing the patient for care transition. In line with this approach, each patient received a distinct daily ward round from an additional team made up of an orthogeriatrician, PT and OT. This second team would be tasked with supporting physical recovery and rehabilitation towards an estimated date of discharge, often with reference to meeting the unit’s prescribed fractured neck of femur (NoF) pathway. These additional ward visits provided a more discharge-centred set of daily interactions which would be addressed in weekly MDT meetings, where more formal discharge planning decisions would be reached.
In contrast to all other sites, the arrangements for ward rounds at Farnchester orthopaedic unit were even more fragmented, with no clear structure or pattern of daily ward rounds. Instead, patients were visited intermittently by the surgical consultants according to their ‘clinical days’, with no clear fixed schedule. As such, these meetings provided little opportunity for knowledge sharing with or to the wider clinical team. Instead, the surgeon would usually interact with nursing staff during daily board rounds and conduct relatively ad hoc ward rounds.
Ward-based interactions, board rounds and handovers
In the course of their inpatient stay, both stroke and hip fracture patients experienced a wide range of bedside interactions with clinicians, therapists and health-care assistants (HCAs). These were integral to the general provision of inpatient care, including personal care tasks such as feeding, washing or toileting; the completion of routine observations and assessment; dispensing of medicines; and the delivery of specialised rehabilitation or therapeutic interventions. These routine daily interactions were important because they provided a unique opportunity for clinicians to build rapport and trust with patients through the often intimate processes of direct caregiving. In doing so, clinicians and patients often become able to share more tacit or sensitive information about patient well-being, mental health and expectations for the future that might often be overlooked or difficult to articulate in a more formal setting, such as the ward round. This knowledge would then be relayed, in a way that protected patient confidences or trust, within these other, more formal meetings or situations, thereby enriching decision-making. Although this knowledge often seemed trivial or inconsequential, it could often be integral to developing more personalised or robust discharge plans, for example where the therapist could understand more about the patient’s fears of being left alone at home, or HCAs could identify problems with toileting.
Across all research sites, these interactions were common features of day-to-day care. It was also apparent, however, that where clinical work was more time pressured, or where there were staff shortages, these opportunities were dominated by functional task completion, with less potential to adopt a more holistic approach to patient care. Despite being widely common there were some important differences in the local organisation of care that also seemed to frame differences in these patterns of knowledge sharing. A relatively obvious finding related to the general sense of teamwork or integrated working on the ward. At the two stroke units, ward nurses, HCAs and therapists had a relatively strong and close working relationship. For example, they had co-ordinated working patterns, participated in daily team briefings, shared common office areas, and interacted regularly and routinely in the everyday patterns of hospital work, i.e. in reception areas, rest areas and corridors. More than this, their working patterns were overtly patient centred, with their co-ordinated activities primarily focused on advancing patient recovery, and the patient was often at the centre of their collective interactions. These patterns of daily working appeared to further facilitate rapid and timely knowledge sharing across occupational boundaries and led to more joined-up planning activities around hospital discharge.
At the Glipton orthopaedic unit, there were also close working practices between nurses, HCAs and therapists, but this also appeared to be framed by an implicit division of labour in ward-based care. As described above, in the initial days following surgery much of the patient’s care was centred on surgical recovery; as such, ward nurses were more attentive to issues of wound care and less so towards rehabilitation, and there was relatively little involvement of therapists until the patient was declared surgically fit. Therefore, there seemed to a staggered approach to integrated working. That being said, once therapists started work with patients, the pattern of interaction with ward nurses and HCAs did appear to become close and more integrated, like that observed in the stroke units.
The main difference was at the Farnchester orthopaedic unit, where there was little evidence of integrated or team-based working. In general, ward nurses appeared primarily concerned with the patient’s surgical recovery and then with managing the transition of care to other actors. Therapists at this site were not based on or colocated with the ward but rather worked across the entire hospital with an office based away from the orthopaedic wards. There was also little evidence that therapists and nurses tried to co-ordinate their work, except where therapists attended nurse-led handovers and MDT meetings; however, they did so primarily as observers. This led to a situation whereby nurses and therapists would develop close working relationships with their patients, but with few opportunities to share knowledge with each other. There was also found to be little stability or continuity in the provision of rehabilitation, with frequent changes in staffing making it difficult to build interprofessional relationships on the ward.
An important example of the differences in daily ward-based interaction could be seen with the organisation and use of daily handovers and board rounds. These were routine features of day-to-day care planning, and often helped to allocate and plan the types of daily activities described above. In these situations, ward-based clinicians would come together, usually at the start and end of the day, to identify, allocate and review tasks. These relatively formal meetings could have a particularly important role in co-ordinating and prioritising shared activities related to hospital discharge, such as arranging tests, completing assessments, initiating external referrals, ordering medicines or arranging transportation. At the Glipton orthopaedic unit, ward staff followed a traditional morning handover meeting. This was led by the shift ‘nurse in charge’ and was attended by other nurses, HCAs, an OT and a PT representative (who would feedback to their teams) and the discharge liaison nurse. The lead nurse would read from a printed sheet that detailed each patient’s overall care plan and outstanding tasks to be completed during the next shift. It was expected that each patient’s nurse and therapists would provide additional information to offer a more developed account of patient progress, and would also agree to relevant tasks and co-ordinate their activities. As such, these handover meetings became an important situation for sharing knowledge, especially at the beginning of the day, to help identify and manage issues related to care progression and transition.
Similar daily activities were observed at the two stroke units, but here knowledge sharing and decision-making was co-ordinated through the use of large wall-mounted whiteboards, hence ‘board round’. These boards provided an important knowledge-sharing resource for co-ordinating daily clinical activities. They displayed each patient’s basic details (name and date of birth), his or her location on the ward, and also other handwritten annotations or abbreviations, with the expectation that each professional group uses a different-coloured pen. It was also found that magnet tokens and symbols were used to denote certain procedures or tasks, such as ‘close observations’, ‘awaiting test results’, ‘ready for discharge’ or ‘collect TTOs’. These boards contributed to the co-ordination of day-to-day knowledge sharing as they provided an open, visible and real-time picture of ward-based work. In both stroke units, they were used to co-ordinate daily tasks, for example informing therapists that the patient was ready to start rehabilitation or for junior doctors to order prescriptions. They were both managed by the senior nurse in charge and updated by a wide range of other ward-based therapists and support workers. Although ward staff continued to use other records and documents to co-ordinate daily work, the whiteboard remained a centralised point of reference around which staff would regularly congregate to review progress and share knowledge.
At the Farnchester orthopaedic unit, board rounds were also a regular feature of daily care management. Given the absence of more customary ward rounds, the board round was used by the consultant surgeon to review patients with the lead nurse and, where possible, the patient’s designated nurse and junior doctors. As the consultant did not keep a regular schedule of ward visits it was not always feasible for other clinicians to leave other duties to attend the board round. In this interaction, the surgeon would usually request an update from the nursing staff about the patient’s surgical recovery and review patient progress in much the same way as a ward round, but in the absence of the patient. Notably, many nurses showed a reliance on scrap paper to note tasks rather than relying upon the whiteboard. The primary focus of these meetings was to assess postoperating wound care, patient stability and early mobilisation. A significant watershed in these meetings occurred when the surgeon declared that the patient was ready to start mobilisation, at which point the nursing staff would be asked to instruct the therapist team to assess and treat the patient, and the level of surgical input gradually decreased.
Multidisciplinary team meetings
A major knowledge-sharing situation across all research sites was the weekly MDT meeting. Where daily ward activities supported incremental care planning, the weekly MDT meeting was widely seen as the main decision-making forum, especially with regard to hospital discharge. These meetings facilitated a range of clinicians and stakeholders to review the care plan for each patient and, in doing so, to contribute to the general management of workflow and service management. In line with national policies, MDT meetings were found at all sites, but they also varied in terms of the way they were organised and how they contributed to discharge planning.
At the Farnchester orthopaedic unit, MDT meetings were led by the nurse in charge and were attended by two or three senior nurses from different ward bays, and representatives from the hospital’s OT and PT teams. It was customary for the junior doctors to attend the meeting, but in an observer capacity, and it was expected that the orthogeriatrician should attend, although this was intermittent owing to staff shortages. It was not expected that consultant staff should attend the meetings. Within the MDTs each patient’s surgical recovery was rapidly reviewed. The typical format was for the nurse in charge to introduce each patient according to his or her designated bed (not name or date of birth). This in itself caused confusion if the patient had been moved. The nurse in charge would then review the decisions made by the consultant surgeon, usually in relation to surgical recovery and readiness for discharge planning. It was expected that the ward nurses would offer additional input into outstanding tasks, but there was no expectation that therapists should contribute information, and when some did it was observed that the nurse in charge would quickly close off discussion. As such, these weekly meetings appeared to be dominated by managing nursing work in relation to surgical recovery, based upon the senior nurse issuing instruction for onward care planning. For example, it was usual for the lead nurse to inform the therapist team to start rehabilitation or to prepare the patient for care transition, but not to engage in shared decision-making.
In contrast, the other three sites had more developed and inclusive MDT meetings. At the Farnchester stroke unit, the MDT meeting was led by the lead consultant and was attended by other doctors, the nurse in charge and nurse representatives, the lead HCA, the ward manager, OT, PT and SaLT representatives, the ESD service lead, the community stroke nurse and representatives from the local Stroke Association. This provided a broad spectrum of contributions to care planning. Each patient was introduced with a detailed medical summary and summary of the existing care plan. This introduction alone was normally longer in duration than the entire discussion for each patient in the same hospital’s orthopaedic unit. The ward nurse and therapists would be invited to add to the medical account, for example describing the patient’s psychological and emotional state, and his or her general health and level of rehabilitation. In the early stages of the admission, these discussions tended to focus on initial recovery, and included direct reference to the patient’s suitability for ESD. At this point the ESD representative would talk through his or her assessment. Even at this early stage, the MDT meeting would consider patient discharge and set precise goals for therapist activity. As patients neared the point of discharge, the focus of decision-making would turn to the wider personal and domestic circumstances of the patient, drawing upon the knowledge acquired through day-to-day ward-based interactions. This would include attention to the need for additional therapy or rehabilitation in a nursing home, or whether or not the patient could be cared for at home with suitable support. It was usual for both the community stroke nurse and the Stroke Association representative to offer a view on the level of follow-up care. This input seemed important because hospital-based staff had limited appreciation of the available support services in the community. An important contribution was made by the community stroke nurse who provided detailed knowledge on the range of available services, housing issues and issues of accessibility related to the need for home adaptations. A significant feature of these MDT meetings was that all information and decisions were recorded in a single patient record, rather than in separate files, which resulted in a collective record rather than a medical or nurse record.
A similar pattern of interaction was observed at the Glipton stroke unit. However, two interesting features made it different from the Farnchester unit. First, the meeting was not led by the consultant physician; rather, it was expected that a different member of ward staff would lead the discussion of different patients. The consultant had introduced this format in the hope that it would foster greater appreciation among the team of the contribution of different actors and encourage shared ownership of clinical decision-making. Following this format, each patient was introduced by his or her designated spokesperson, who would review the patient’s history and care plan before similarly inviting contributions from other specialists. A further difference at these meetings was the role played by the discharge liaison nurse, who would provide specialist problem-solving expertise for each patient’s discharge plan. For example, he or she would often clarify legal or housing issues. Although the tasks required for care transition would be delegated to specific individuals, such as ward nurses and OTs, the discharge nurse would also act as a key reference source, for example advising on the availability of social care providers in certain areas or whether or not a suitable nursing home or community hospital was available. A similar issue addressed in these meetings was whether or not patients with mild strokes were suitable for ESD, and whether or not those with more severe strokes needed to be transferred to a community hospital or specialist rehabilitation ward in the hospital. However, as an ESD representative was usually present at the point of admission, the involvement of this representative at meetings normally centred on confirming the ESD service’s proposed care plan.
A similar format was found at the Glipton orthopaedic unit’s weekly MDT meeting, where a discharge liaison nurse was also active in discharge planning. However, there were other subtle differences in the composition and format of these meetings. For example, the meeting was usually led by the nurse in charge, who similarly reviewed each case and invited contributions from other actors. Interestingly, this nurse tended to focus her knowledge sharing on matters related to supporting the patient’s ward-based (postsurgical) recovery, whereas the patient’s readiness for discharge and wider health state tended to be discussed by the orthogeriatrician and the discharge nurse. As such, a tight subgroup was evident that seemed to lead decision-making and discharge planning. For example, it was usual for the discharge nurse to provide recommendations of the proposed discharge destination and the activities needed to facilitate transition, whereas the orthogeriatrician was responsible for determining medical suitability for discharge. An important variation at this site was the explicit use of a discharge checklist, which was held by the discharge nurse to list key activities required to progress discharge. This was regularly used within the meetings to progress unfulfilled activities, and outside the meetings to enable the discharge nurse to identify those staff members who might need assistance. There was some concern from participants that the emphasis within these MDT meetings was on determining the earliest possible opportunity for discharge so as to meet performance targets, i.e. percentage of patients meeting the 10-day pathway, and to free up acute care beds.
Internal transfers
Although the primary focus of the study was to investigate the transition of care to a community destination, the frailer patients with complex care needs were often transferred to another hospital unit or ward where their other comorbidities would be attended to before discharge. These transfers of care did not necessarily relate to the recovery from either stroke or hip fracture, but rather to wider health issues that prevented ongoing recovery in the community. This process was more of an intermediate step or diversion of care, but it involved a particular type of interface with internal rather than external agencies. This type of transfer was more common at Farnchester orthopaedic unit and Glipton stroke unit.
At Farnchester, internal transfers usually occurred where patients with complex care needs were seen as ‘problem cases’ and outside the normal remit of care provided on the orthopaedic unit. This transfer process was normally triggered when the patient’s surgeon declared the hip surgery successful but the orthogeriatrician believed the patient remained too frail to be discharged. These decisions were usually communicated via the senior nurse, i.e. in the weekly MDT meeting. The orthogeriatrician would also consult with the patient’s OT and often family members before recommending that the patient be transferred to the care of the elderly ward. In a daily board round, the senior nurse would then delegate responsibility for organising the transfer to the patient’s designated nurse, who would contact a relevant care-of-the-elderly or general medical ward by telephone to request a bed based upon a summary of the patient’s care needs. When a bed space was confirmed, the patient would be transferred by porter to the new ward, where the patient’s nurse would provide a verbal handover or summary of the nursing record, noting any specific health-related issues. The receiving nurse would then reclerk the patient on the new ward and prepare the patient for the next available ward round. It was recorded that the patient’s therapist team would not normally be informed of this transfer, which meant they would often need to search for their patient across different wards. Once transferred, there was also considerable duplication of assessment and care planning, for example repeated tests and consultations with family members. The patient’s discharge planning was therefore transferred to the other ward where an entirely separate planning process was involved.
At the Glipton stroke unit, patients with complex recovery needs would often be transferred to a specialist long-stay rehabilitation ward. This decision was made at the weekly MDT meeting through discussion between the consultant and the patient’s OT, where it was acknowledged that further hospital-based rehabilitation was needed before transition to a community setting. The transfer of care was usually initiated by the patient’s OT, who would telephone the rehabilitation ward to initiate a transfer. At this time, they would give a detailed summary of patient condition and the existing rehabilitation plan. During the transfer of care the OT would also accompany the patient to the new ward and conduct a more thorough handover to the new rehabilitation team. For example, the patient’s existing therapists would introduce the patient directly to the new nursing and therapy staff, assuring them that they would be well looked after. It was also common for the new rehabilitation team to telephone the stroke unit to enquire about additional issues that might be detected later in their work. Despite being based on different wards and having a different emphasis in their care plans, the two stroke care teams work as part of a larger combined service. As such, there was a greater sense of collaboration and integration across the entire service, whereby knowledge and know-how gathered in the acute care unit would be shared and made available to those in the rehabilitation ward.
Family meetings
Across all sites, family members, friends and carers made a significant contribution to diagnosis, clinical decision-making and longer-term care planning. They had a unique insight into the patient’s wider circumstances and often acted as mediators or translators between the patient and the wider clinical team, especially if the patient did not speak English or where there were pre-existing speech and cognitive difficulties. With regards to planning a patient discharge and onward care, family members were often invited by ward nurses and therapists to help assess the patient’s ability to cope at home, providing specific details about his or her domestic, personal and financial circumstances, such as layout of the home, eligibility for benefits and availability of support networks. It was also the case that at the point of discharge, family members were integral to supporting care transition through enabling carers to access the home, accompanying their relative from the hospital and supporting him or her to attend outpatient appointments. Those patients without relatives or carers not only had limited options for ongoing care, but their discharge arrangements were often underspecified, subsequently requiring urgent home visits from social workers or OTs on discharge. Equally, it was often reported that where family members were absent or unco-operative it could be difficult to transfer patient care. Illustrating the role of family members, visiting hours were commonly used by the patient’s nurse or therapist to speak directly to relatives. Here he or she would explain the patient’s care arrangements and often discuss postdischarge care needs. At the same time, he or she would actively gather additional information about the patient’s wider personal circumstances to enrich care planning. A significant pattern of knowledge sharing at all sites took place between the patient, family member and OT. The OTs often focused more explicitly on post-hospital care, discussing the patient’s rehabilitation plan, ongoing care needs and the ways in which relatives could support recovery outside hospital. In particular, OTs would often work with family members to explain the use of certain equipment or therapeutic exercises. The OT would normally ask additional questions about the patient’s home layout, number of steps, toileting arrangements and bedroom options to develop the rehabilitation plan.
An important variation was found at the Farnchester stroke unit, where the lead consultant had introduced a more family-centred approach to care planning. For example, family members were invited to be present during ward rounds and the consultant would also be available during visiting hours to speak with family members. Also at this site, a formal family meeting had been introduced to enable more structured knowledge sharing and shared decision-making with relatives and/or carers. These were usually scheduled when the patient’s recovery was underway with the express purpose of supporting discharge planning and communicating ongoing care needs. These were also opportunities for giving and receiving information among clinical staff and family members. Family meetings were usually initiated by the consultant or ward nurse, who would give a short, non-technical account of the patient’s condition and care before asking if family members or carers had any questions. The meeting was used by the clinical team to further clarify the information they had gathered to date and to understand more about the patient’s domestic circumstances. Prominent topics of discussion related to the patient’s general health condition prior to the stroke; his or her home arrangements and layout, including toilets and stairs; his or her work expectations or general activities; and the availability of relatives or carers to support recovery. This interaction provided additional knowledge about the patient’s wider circumstances which helped to determine the most appropriate care pathway given his or her home circumstances, i.e. nursing or home-based care, and enabled family members to better understand the responsibilities and tasks they might need to address after discharge.
Referrals and assessment for social care
For the majority of stroke and hip fracture patients, the discharge planning process involved referral to the local authority social services department to initiate an assessment for social care following care transition. In line with the CCDDA 2003, hospital staff initiated the referral to social services by completing a Section 2 request (notifying local social services that a patient requires assessment for social care) and a Section 5 request (confirming that the patient is ready for transfer of care). The Section 2 request would trigger social care assessment, usually undertaken by a local authority social worker who would organise and commission a package of social care according to the patient’s assessed needs, home circumstances and financial arrangements. The Section 5 request is significant because it relates to current regulations which stipulate that a social care package should be in place and ready to receive the patient 24 hours from the notification; delays in the provision of this care can result in financial reimbursement to the hospital. Despite awareness of these broad parameters among service leaders and discharge co-ordinators, it was often the case that ward nurses and therapists were not altogether clear about this process, which might explain the frequent complications and errors in completing these referrals.
At the Farnchester orthopaedic unit, social care referrals were usually initiated by the patient’s OT, following the weekly MDT meeting where the nurse in charge would inform the OT that the patient was approaching discharge. The referral would be completed in the therapist department (not on the ward), where the OT would review the patient’s therapist record and request, where necessary, additional information from the patient’s nurse. The Section 2 referral was faxed to the local authority social care contact centre, which acted as a centralised referral point to validate and process social care referrals for the county. Where a patient with more complex health or personal circumstances was being discharged, the OT might contact the hospital’s discharge liaison service, which could provide specific guidance on legal and financial assessment criteria and the types of services available to different patient groups. The referral would then be reviewed by the social care contact centre, at which point referrals could be returned owing to missing or inaccurate information. Where accurate, the referral would be forwarded to the patient’s locality social work team, determined by his or her place of residence.
A similar process of social care referral was observed at the Glipton stroke unit, where the patient’s OT also took responsibility for making referrals to a similarly centralised social care contact centre. At this site, referrals would usually be made on the ward, because stroke therapists were colocated on the stroke unit. This had the advantage of providing easier access to nursing and medical records and information detailed on the whiteboard, and also for making direct enquiries with nursing and medical staff. In comparison with Farnchester, this seemed to enable more detailed and accurate referrals, where multiple information sources were combined and included into a single referral. It was also found that the unit’s discharge liaison nurse would routinely provide additional support and guidance, especially for more novice staff, and take overall responsibility for more complex patient discharges. A further difference was that the referral form would be telephoned through to the Glipton contact centre, often with a fax sent as a basis of confirmation. This direct contact made it more possible to address any potential inaccuracies and missing information, thereby reducing delays, but also depended upon referrals being made during office hours.
At the Glipton orthopaedic unit and the Farnchester stroke unit, social care (and health-care) referrals were completed by the patient’s designated ward nurse, during normal working hours. The process broadly followed the above interaction, with referrals made in both cases by fax to the social services contact centre. Although the patient’s nurses often had a good understanding of the patient’s care plan, they did not always have details of his or her current rehabilitation plan and general home circumstances. As such, ward nurses at both sites usually worked closely with the patient’s OT to draw together information to complete the referral. This normally occurred after the daily handover meeting at Glipton or the board round at Farnchester, when clinicians were usually available on the ward. A significant problem faced by nurses at both sites related to the difficulties of completing social care (and health-care) referrals alongside their other clinical duties. It was observed that nurses would set aside time each day to complete patient referrals and other administrative tasks, but they were often interrupted or required to give direct patient care. As such, many referrals were completed in a fragmented and disjointed way which seemed to reduce the coherence and timeliness of some referrals. At the Glipton orthopaedic unit, the dedicated discharge liaison nurse would often step in to assist nurses at this time by checking information and completing documentation. It was also usual for the discharge nurse to assume general responsibility for discharges during busy periods or where there were staff shortages, and always for more complex discharges that required more engaged knowledge sharing and negotiation with both social and health-care agencies. Significantly, where both health and social care referrals were made by the same person, i.e. the patient’s nurse, there was less duplication of work and less need to pass on or share patient records. A further observation from the Farnchester orthopaedic unit was that Section 2 and Section 5 referrals were made simultaneously. It was described how delays in the time between requesting social care assessment and initiating social care transfer meant that the unit often over-ran its 10-day care pathway, and by submitting both referrals together it placed pressures on the locality social work teams to respond quickly.
For all sites, social care assessments were completed by a locality social worker selected according to the patient’s place of residence. Previously, social work teams were based in each hospital, not in the community, which participants described as making it easier to complete assessments (i.e. no need to travel to the hospital), and as fostering closer working between hospital and social work teams. With recent local authority changes, social workers were no longer located in hospital but instead in locality teams, which many participants believed had degraded the relationship between health and social care. At both stroke units and the Farnchester orthopaedic unit, social care assessments were completed through direct interaction between the social worker, the patient and family members at the patient’s bedside. The social worker would usually spend time speaking with the patient to complete the necessary assessment documentation, and also with the patient’s designated nurse. At both stroke units the patient’s OT would also join these discussions to share additional insights or to prompt the patient, as they tended to have a more detailed and intimate knowledge of the patient’s personal or home circumstances. This was possible because they were colocated on the stroke unit. At Farnchester orthopaedic unit this was more difficult as therapists visited hospital wards on scheduled rotation. As such, there were often some discrepancies in the breadth of information used to inform the social care assessment.
In contrast, social care assessments at the Glipton orthopaedic unit were completed by telephone. Here it was usual for the social worker to first speak to the patient’s designated nurse or nurse in charge to check the basic patient details and then to speak to the patient. Although this made for a relatively speedy referral, care packages were often basic in design and requiring modification once the patient was transferred to the community setting. Developing this observation, the focus of the social care referral seemed to be on completing referrals quickly, rather than thoroughly, in order to avoid financial penalties. At all sites, the social work team would complete their preliminary assessment and invariably organised a package of 6-week reablement to address the immediate personal and social care needs following discharge, or a short-term placement in a residential home for those with more complex needs. In most cases, it was expected that a further social work assessment would be completed after discharge to determine the patient’s longer-term care needs. As such, the social care referral and assessment process seemed predominately concerned with facilitating a short-term or transitional package with the expectation that further and more detailed assessments would be completed later.
Referrals and assessment for health care
For ongoing health and community-based care a similar process of referral was undertaken, but this could vary according to the configuration of local health-care services, such as the availability of intermediate care beds or community hospitals. For both hospitals, intermediate or step-down services were funded by the local PCT (now CCG) and provided by a local NHS community trust or private sector provider. This often involved a fixed package of 30-day care for specialist rehabilitation provided in a community hospital or a nursing home with dedicated rehabilitation beds. For patients with more complex needs and comorbidities, it was also possible to make a referral for continuing health care at home or end-of-life care.
Across all sites referrals for ongoing health care were completed by the patient’s designated nurses. At the Farnchester site, this involved an initial fax request to the community rehabilitation team, colocated on the hospital site. This colocation made assessment at the patient’s bedside relatively easy, with a community nurse or OT attending to the patient within 24 hours of referral. Being colocated also fostered a close working relationship between acute and community staff and, despite some tension points around workload and timing, the interaction between ward and community staff was based on shared knowledge and understanding of their respective working practices. At the Farnchester stroke unit, fax referrals were usually made mid-morning after the morning board and ward rounds. The rehabilitation team would receive the fax and contact the ward in person or by telephone, with a view to determining the most appropriate rehabilitation care package, typically within a privately run nursing home. The community rehabilitation team would then assume responsibility for liaising with the local nursing homes to arrange an appropriate bed, thereby reducing the demand on ward staff. In contrast, health-care (and some social service) referrals from the Farnchester orthopaedic unit were made during the night shift, on the assumption that there would be less demand for direct patient care and more opportunity for completing routine administration. Although this appeared to be an effective use of nursing time, it was often difficult for nurses to obtain all the necessary information to complete some referrals, because they had no access to the therapist records and were not able to speak with family members. As such, many referrals remained incomplete and were passed on to the day shift. It was also found that many faxed referrals were lost or incomplete because of problems using the fax machine. This was also exacerbated by the lack of administrative support at night (e.g. no ward clerk) and also the inability to contact the community rehabilitation team to check that they had received the referral. As such, many referrals were delayed while the day shift and community rehabilitation service interacted by telephone to remedy problems experienced at night.
At the Glipton site, referrals for continued health care were usually made to one of the local community hospitals or on occasion to nursing/residential homes with rehabilitation beds (usually because of patient residence). Where it was felt that no rehabilitation was possible, patients would be referred directly to nursing/residential homes for longer-term places. Community hospitals provided an extension to both stroke and hip fracture care, having dedicated rehabilitation units for both patient groups. Referrals to the community hospitals were usually made by the patient’s nurse (or discharge liaison nurse), who would book a bed by telephone, providing a brief overview of the patient’s condition, recovery and ongoing care needs. A ward nurse would receive and log the request, which would be reviewed by the nurse in charge or ward manager to assess bed availability and level of care. A similar process would be undertaken with nursing/residential homes, but here it was usual for the discharge liaison nurses to negotiate with care home managers about bed availability and care plans. This would often involve lengthy discussions about clinical risk and patient need before agreeing on a placement; for example, it was usual for nursing homes to turn away patients if they were too sick.
Requests for home adaptations and equipment
An additional external referral related to the ordering of home adaptations or equipment for postdischarge recovery and rehabilitation. This included, for example, commodes, hand/grab rails, stair lifts or ramps, bedding and mattresses, wheelchairs or frames, and tables, chairs and other assistive devices. Across all sites, the general expectation was for the patient’s OT to order this equipment, usually when the discharge date had been confirmed and the level of need assessed. The ordering process varied, however, between sites. At Glipton an electronic (e-mail-based) ordering system was used, whereby the OT would complete an online order form. At Farnchester, the OT would contact the equipment supplier relevant to the patient’s residence via telephone and place an order. Although there were no significant differences between these approaches, telephone-based orders had the benefit of enabling staff to provide more detailed responses to queries, but these also seemed to take longer and relied upon the availability of staff in the supplier agencies.
A number of additional issues seemed to have an impact upon the ordering of equipment. The first related to equipment availability, where it seemed that certain more complex or specialist items, such as a type of brace or mattress, would not be in stock. This would create delays in patient transfer or lead to a situation where the patient returned home without equipment. The second related to whether or not suppliers and fitters had access to the patient’s house to fit certain grab rails or ramps. This therefore involved an additional line of communication with family and relatives to arrange a home visit. The third related to the level of funding for home adaptation and whether certain changes should be funded by health or social care. Again, a prominent example was grab rails and ramps; these were often seen as social care issues, but the delays in assessing patients for financial eligibility often meant that health-care workers ordered the equipment without confirming the details. Fourth, at both sites there had been a recent change of supplier, with new IT systems that were uniformly described as undergoing teething problems. Staff at both sites were learning to deal with new processes for ordering and frequently identified that equipment was currently delayed. Finally, there was fragmentation in the process of ordering equipment, with some responsibility for authorising equipment orders residing with the OT and some with the district nurse (particularly for pressure mattresses). This took significant co-ordination and was identified as a point of daily difficulty in preparing patients’ home environment for discharge.
Day of discharge
In general, the day of discharge involves a frantic series of linked activities that escalate in pace and intensity as care is transitioned. Across all sites, this usually involved the following activities:
-
At the start of the day, the patient’s nurse would confirm whether or not the patient was still deemed medically fit and ready for discharge, usually by enquiring with the consultant or junior doctor as a part of the morning ward round. The ward round would also be used to confirm the patient’s take-home medicines, which would then be ordered by the junior doctor for collection or delivery.
-
The patient would then be reviewed as a part of the morning board round (handover) where further tasks would be described and allocated to the patient’s nurse, HCAs and the ward clerk.
-
Following this, the ward nurse would contact the locality social work or health-care provider to confirm that the care package was in place and to give a final verbal handover of the patient’s current health state, medicines and ongoing care needs.
-
The ward clerk would order transportation from the regional ambulance trust, or possibly a taxi, requesting an appropriate time slot. When confirmed, the ward clerk would contact the patient’s family to notify them of the transfer time. The ward clerk or nurse would also follow up on the patient’s medicines and have them ready along with any other personal items.
-
Before he or she was collected by the transport service, the HCA and nursing team would prepare the patient by removing any catheters or monitoring equipment, completing the patient’s observations and health checks and, where used, completing a discharge checklist with the patient.
-
If the patient was mobile, he or she would be moved to the waiting area, but more often patients would remain near or on their beds. Both hospitals had discharge lounges for patients to wait for transport, but these were only used for patients not requiring regular supervision or care. At around this time the nurse in charge would contact the bed bureau or manager to notify them that a bed would be available later in the day.
-
The patient’s nurse would complete and sign off the nursing care documentation and request that discharge letters be issued by the ward clerk.
-
Upon arrival of transportation, the patient would be taken to his or her community destination.
Within this common pattern of activity, a number of important variations were detected. First, there were variations in the extent of consultant or medical involvement. At both orthopaedic sites there was relatively limited interaction with the designated consultant because they did not operate a usual ward round (Farnchester) or because the orthogeriatricians operated a variable pattern of ward visits. As such, there was greater reliance on junior doctors to confirm patient readiness for discharge. In instances where a junior doctor was uncertain about the patient’s condition, i.e. where a new blood test showed some anomaly or the patient was reporting new symptoms, it was customary for discharge arrangements to be delayed until the consultant could be contacted. The alternative was that the patient was discharged with potential health issues remaining and requiring further medical attention in the community.
Second, there were frequent problems with the timely ordering, dispensing and completion of TTOs. Across all sites these were completed by junior doctors with varying levels of medical supervision. At the Glipton stroke unit, for example, the stroke consultant closely supervised and monitored these processes, leading to more accurate and timely procedures. In other sites, we found nurses and ward clerks were often required to ‘chase up’ the junior doctors to complete the prescriptions. At Farnchester this was made relatively easier as the hospital utilised an electronic prescribing system that communicated prescriptions to the pharmacy, which then dispensed medicines via an internal delivery service. At the stroke unit, this was further supported by two additional variations: an expectation that all medicines would be ordered the day before anticipated discharge so that medicines were ready in the morning, and the availability of a pharmacist on the stroke unit, meaning that TTOs could be checked and amended before leaving hospital. That being said, it was not uncommon for patients to leave hospital without the complete range of medicines or with prescriptions to be completed in a community pharmacy.
Third, it was also found that in the processes of progressing patient discharge a number of tests and procedures were reallocated to be undertaken on an outpatient basis. For example, the patient would be asked to visit his or her GP in the subsequent 48 hours to request a particular blood test, and would be given a letter of instruction for the GP. Alternatively, he or she would be requested to return to the hospital over the next week for further tests. Although this was not found to cause any significant health-related problems, it did appear to transfer the burden of care to both the community sector and the patients themselves. This was especially problematic for patients living in rural areas and some distance from the hospital, who would need to organise taxis or family assistance to return to the hospital for follow-up tests.
Fourth, an important activity was the organisation and scheduling of ambulance services. A single ambulance provider operated across both areas and utilised a standardised booking system for patient transfers. Across all sites it was usual for the ward clerk to complete this booking by providing each patient’s details and destination, general care needs, specific requirements with regards to mobility issues (for example hip precaution) and the desired time for transfer. The booking clerk would enter this information into a computerised system to identify a suitable time slot for the patient reflecting his or her condition and locality. In the vast majority of patient transfers this system tended to work, but with regular delays in collection and drop-off due to time slippages. As such, patients tended to be collected on time earlier in the day and with delay later in the day. This created particular complications for community hospitals, especially for Glipton orthopaedic patients; here it was reported that patients might not arrive until the evening, at which point there were limited staff to fully admit the patient. As such, the patient would be stabilised on the ward but no detailed care could be initiated.
Fifth, there were variations in the involvement of the patient’s family at the point of discharge. At both stroke sites, it was an expectation of the medical team that relatives be closely involved in helping to prepare and ready the patient on the day of discharge, at which time the opportunity would be taken to provide further information or education to relatives about ongoing care needs. At the orthopaedic sites, however, there was relatively limited family involvement, other than a telephone call to provide notification of the time of transfer. A major concern among medical staff related to the difficulties of contacting family members, especially where they were contacted at the last minute or not given sufficient warning to prepare their relative’s home, and therefore excluded from supporting the transition process.
Finally, there were differences in how discharge documentation and letters were distributed at the point of handover. At all sites, the ward clerk would usually collate the necessary information to complete a generic discharge summary to be sent to the patient’s GP. At Glipton this issued electronically, together with a summary of the changes in the patient’s medicines and other diagnostic test results. In Farnchester, this remained a paper-based summary sheet sent via post. As such, GPs in the Glipton area had a more comprehensive and immediate overview of their patient’s care and transition. In addition, the consultants at each site also reported writing an additional letter to each GP (dictated to and typed by their secretary), which provided a separate medical overview of the patient’s care. For transfers to community hospitals or nursing care homes, the main handover was by telephone between the ward nurse and the service provider, but it was also expected that a similar summary record be issued with the patient and taken with the transport service. This record would be completed by the patient’s nurse providing further details about ongoing care needs and medicines regime. Those in the community hospitals often reported that the quality of these summaries was poor and that they provided limited information about ongoing care needs, requiring additional telephone contact with the acute hospital. As noted previously, however, where this involved an evening transfer this contact could not be made.
Returning home with early supported discharge
Early supported discharge provides a comprehensive package of home-based rehabilitation and support for patients with mild to moderate strokes. ESD is provided by a dedicated team of therapists, nurses, HCAs and social care workers who together provide a range of services to support patient recovery outside hospital and to prepare patients for a return to the activities of daily living, including employment. As the title suggests, it is initiated relatively early within the patient’s care pathway because of the reduced need for acute medical care. As described above, the decision to refer a patient for ESD is typically made within the weekly MDT meeting and involves interaction between the medical team and an ESD representative.
When a patient was transferred home with the ESD team it was expected that the local ESD representative would have devised an appropriate care plan that provided a degree of continuity with hospital-based rehabilitation. Although this package of care can be relatively generic, ESD leads attempted to tailor services to individual needs, for example if a patient required speech and language support or had an employment-related issue. Across both stroke research sites, the broad process of initiating ESD care involved a particular pattern of knowledge sharing between the patient and family, ESD therapists, community nurses and HCAs, and other support groups, especially the Stroke Association. It was typically the case that few community-based professionals had had contact with the patient or relatives prior to discharge and a significant proportion of early interactions involved building trust and developing a shared understanding through exchanging both health-related and more personal information. This would then help nuance and refine the more generic care plan. It was also found that there was limited knowledge sharing between the stroke unit and the ESD team in terms of formal records. Instead, there was greater reliance upon the community stroke nurse (Farnchester) and the discharge liaison nurse (Glipton) in facilitating more personal and direct knowledge sharing between the acute and community sectors based upon their well-developed working relationships with both groups. These actors not only supported the continuity of care or assisted with problem-solving but helped to establish a broader shared understanding, or at least a set of operating expectations, between hospital and community, based upon providing feedback and sharing lessons.
It was also found that both ESD services utilised a relatively standardised and centralised patient record that captured the information sources, decisions and activities of multiple professional groups in a single knowledge resource. This was particularly important for supporting the continuity of care where the roster of therapists and community staff changed. In general terms, there were few reported concerns with either ESD service, and patients found them both to provide a supportive and patient-centred package of care that supported early recovery from stroke. A key consideration was the ability of ESD representatives to accurately determine patient suitability for ESD and follow a relatively rigid assessment procedure in order to reduce potential risks, whereby the patient required more extensive hospital care. Again, this decision-making process seemed to benefit from the strong connections between ESD and stroke units earlier in the care pathway.
Returning home with social care reablement
For both stroke and hip fracture patients, the provision of local authority reablement care was a common occurrence. Reablement usually involves a 6-week package of general personal and social care that supports adjustment to home life and activities of daily living, with the expectation that more therapeutic or rehabilitation activities are provided on an outpatient basis. This included, for example, help with dressing and toileting, domestic chores, shopping, the use of braces or other devices and some rehabilitation. A feature of all reablement services was that they were designed to provide an initial period of intensive and close personal support with the expectation that this would reduce in line with patient recovery and with the patient taking more responsibility for their own care. Two factors regularly seemed to influence this model. The first was where patient recovery and independence did not increase in line with the reduced need for reablement care, because of more complex social and personal care needs. The second was where family members were not available or forthcoming in providing additional care both during and after this initial 6-week period. These circumstances would require additional social work assessment of patient need and financial eligibility for ongoing social care.
For both Farnchester and Glipton localities, the provision of reablement was well received and seen as well organised by patients and families. The provision of reablement relied upon an initial period of intense knowledge sharing and decision-making between the patient, family members and reablement team (usually the team leader) immediately after the patient arrived home. It was common for the team leader to review with the patient the package of care that had been scheduled and authorised by his or her social worker. This schedule of care usually took the form of a three- to four-side document providing basic personal information, an account of the patient’s recent inpatient treatment, the outcome of the social care assessment and details about his or her ongoing care need. It was rare for the reablement service to have access to additional information. Through the interaction with the patient it was often found that the proposed care package was poorly specified or inaccurate. For example, for a number of patients the proposed care plan provided limited information about their complex personal care needs, such as the use of a hip brace or feeding aids, which required specialist skills among the reablement team. Given deficiencies in the proposed care plan, it was usual for the reablement team to initiate a more detailed assessment through close interaction with the patient and his or her family members, and also through assessing the home environment and other domestic arrangements. This pattern of knowledge sharing was therefore important for ensuring patients had a more bespoke package of care that fitted their recovery needs, and which was then documented more thoroughly and reviewed daily by each reablement team.
Given the requirement to undertake a thorough review of patient needs when commencing reablement, an issue that occasionally appeared to complicate care transition was discharge from hospital on a Friday or over the weekend. As was common across all research sites, there was a general desire to discharge patients towards the end of the working week, especially after the mid-week MDT meeting. This could sometimes place pressure on social care agencies as they were expected to process and manage new patients before the weekend. The consequence of this during busy times was that team leaders would struggle to complete a thorough patient assessment and the initial package of care provided, over the weekend, would be generic and not tailored to individual care needs. This led to the possibility that staffing levels or expertise would not always be to the level required by patients with complex needs.
A more common issue experienced by patients returning home, and often managed by the reablement service, related to problems associated with the delivery, fitting and use of home adaptions and other equipment. As outlined above, OTs would often order specialist equipment to facilitate home rehabilitation but there were frequent problems with availability of these in advance of the patient’s transition. Some prominent examples included missing commodes, beds, grab rails and hoists. It often fell upon the reablement team, family or social worker to chase up these items and arrange time for them to be fitted, while patient recovery would often be limited in their absence.
Transfer to a community hospital
At Glipton hospital it was usual for more frail patients and those needing longer-term rehabilitation to be transferred to the community hospital for intermediate care. Upon receiving the patient at the community hospital, ward staff in the respective stroke and orthopaedic units would seek to clerk the patient, admit them to the ward and devise an appropriate care plan. However, at the point of transition there had usually been only limited knowledge sharing between acute and community hospitals. As described above, this took the form of an initial telephone enquiry about patient need and bed availability, and a follow-up call to conduct a telephone handover of the patient happened at a later stage. The patient was also transferred to the community hospital with a short discharge summary of their care and treatment regime.
For those working in the community, this care transition was widely seen as problematic. In particular, staff often reported concerns about the timing of discharge, especially where patients arrived in the community later in the afternoon or in the early evening when staff were generally wrapping up the end of the working day or dealing with shift handovers. As such, there were often limited time or staff resources to admit and clerk the patient onto the ward, which in broad terms functioned at a different pace compared with acute hospitals. A significant concern was the transfer of patients later in the evening, when the available ward staff could often lack the necessary skills or experience to admit and continue the programme of care for patients with complex needs.
A more common issue related to the lack of opportunity for thorough handover or knowledge sharing between acute and community staff. As described above, a telephone conversation and summary record represented the main sources of knowledge sharing, and ward staff often had too little information from which to continue supporting patient recovery. For example, the information provided often detailed the patient’s medications, broad treatment plan and current levels of rehabilitation, but gave little detail about how they had responded to care, their wishes or preferences, or their wider personal circumstances. There was a general sense of community staff ‘flying blind’ as they worked to provide continuity of care. In many instances, this necessitated a series of repeated interactions to determine the most appropriate plan of care. In such circumstances, the lead nurses would contact the acute ward to request further information, but this was regularly complicated by not knowing the name of the patient’s nurse or because the relevant clinician was not on duty. As such, there was a general lack of familiarity between the community and acute hospitals with little shared understanding of their respective needs. For those in the community hospital it often seemed that the community was regarded as a dumping ground to free up acute beds. The discharge liaison nurses at both the Glipton stroke and orthopaedic units recognised that there were often demands on the community hospitals and often seemed to act as mediators and problem-solvers. In particular, they were found to be on first name terms with the ward managers and senior nurses in the community and would often be contacted by telephone to discuss particular patients. However, not all nurses within the community had this type of relationship and the discharge liaison nurses were not always available to fill the knowledge gaps, especially in the later afternoon and evening.
Transfer to a residential and nursing home (including intermediate care bed)
The transfer of care to a residential and nursing home was evident across all research sites, but was particularly common in the Farnchester area given its lack of community hospitals and the enhanced availability of city-located nursing homes. There were distinctive challenges in securing nursing home placements in rural or registered dementia homes because of a lack of capacity to meet the demand in Farnchester. These provided multiple levels of support for patients leaving hospital, from step-down intermediate health-care support, where a patient would receive a 30-day package of specialist rehabilitation, to more residential care to support personal and social needs, where the expectation might be that the patient might not be able to care for him or herself at home. For many elderly patients, admission to hospital was often from one of these nursing or residential homes where they were already receiving some level of nursing care or assisted living due to a pre-existing condition. For others, their discharge to a nursing home was an alternative to their own home or other domestic setting.
As with other forms of discharge, the transfer of care to a care home was usually arranged by the patient’s designated nurse. As described above, this would usually be initiated after the anticipated date of discharge was confirmed and following instruction from a senior nurse during the daily board round or handover. The patient’s nurse would usually incorporate this within his or her daily tasks and as a part of completing other referral requests. In the stroke and orthopaedic units at Glipton, the discharge liaison nurse provided a key resource in this process through providing information about the available nursing and residential homes, including the types of patients they cared for, the levels of care they could provide and their location within the wider county. At the Farnchester orthopaedic unit this process was typically assisted or taken up by the dedicated community health (rehabilitation) team, who had a more detailed knowledge of the local nursing homes and the services they provided for rehabilitation. At the Farnchester stroke unit a similar support service was provided by the community stroke nurse, who would advise the patient’s designated nurse. However, it was also common for social workers to organise residential care placements where less demanding nursing care was needed but the patient was still not able to return home.
In most cases, the exchange of information largely centred on this initial telephone interaction between the patient’s nurse and the residential/nursing home manager. This conversation involved a broad overview of the patient’s details, primary health condition (stroke or hip fracture), wider health state and comorbidities, and the continuing needs for his or her recovery and rehabilitation. The nursing home manager would usually question and probe this review to determine whether or not the patient was suitable for their specific nursing home; for example, whether or not he or she needed intensive personal care as well as rehabilitation, or specific forms of speech and language rehabilitation. This interaction seemed to focus on whether or not the nursing home had both availability and the necessary skills to care for the patient. This assessment of need and service provision appeared complicated and protracted. Although both relied upon formal hospital records and patient eligibility criteria to assist their decision-making, it also seemed that decision-making relied upon the judgement and experience of the nurse and the nursing home manager.
At the point of transfer, there was also evidence of a lack of knowledge sharing between hospital and care home, especially about the patient’s care plan and personal circumstances. Some nursing homes had tried to remedy this by initiating their own transfer-of-care checklist, which required information regarded as necessary to continue care. For those nursing homes providing intermediate care and rehabilitation, it was also common for community therapists to telephone the acute hospital to obtain further information about the patient’s rehabilitation plan, expectations and activities of daily living. Although they would normally complete their own assessment and care plan, it was seen as important to check the accuracy of their records and to ensure continuity of care. In general, it seemed that the acute rehabilitation teams at both hospitals tended to have relatively positive relationships with the community therapist teams based upon these almost daily telephone interactions. For the hospital therapists this was seen as promoting patient recovery based upon the continuation of their care plan. In the Farnchester area, stroke patients also benefited from the work of the community stroke nurse who would attempt to visit patients in the nursing home following discharge to support their adjustment and recovery. As the community nurse regularly visited the acute ward and worked closely with patients and families prior to discharge, this provided an important source of continuity in the discharge process and often enabled discussion of important information about the patient’s stroke, care plan and recovery. Notably, the Glipton ESD service was resourced to continue care in both residential and nursing homes as part of the rehabilitation plan. This liaison provided opportunities to build strong relationships with certain private providers and share expert knowledge of equipment use with staff.
Primary care support
For all patients leaving hospital, the local medical practice and GP was an important provider of ongoing care and recovery. Across all sites, GPs were notified about their patients’ hospital treatment and discharge back to the community, usually with details about their ongoing care and changes in medicines. Although it was difficult to recruit GPs to take part in the study (see Chapter 3), those who did participate talked about the variable quality of discharge letters and summaries. For example, whereas some of these provided limited descriptive information about the surgical procedure and care plan, others offered more detail about the patient’s general recovery and ongoing needs. This often depended on the individual consultant who completed the letter and suggested a lack of uniformity in completing discharge letters. It was also reported that there were often delays in receiving discharge letters, and often the first a GP would hear about a patient’s admission and discharge was when he or she was contacted by the patient, family member or nursing home manager following care transition. This suggests significant delays and time lags in the knowledge-sharing process between acute and primary care.
General practitioners, and community nurses working in GP practices, were described by most patients as providing an important source of ongoing security and support following discharge, especially in relation to the more medical aspects of recovery and medicines management which other carers might not be able to address. GPs were generally described as helping to explain and manage the ongoing plan of care, especially changes in medicines. For many patients, the GP was often ‘called out’ to address significant changes in the patient’s health, especially where there appeared to be infection or general decline in well-being. However, some patients reported difficulties in accessing their GPs, especially those who lived in rural areas, and greater reliance upon the community nurse for support. An additional source of support for many patients, especially stroke patients, was provided by community pharmacists, who were also described as explaining changes in medicines and reviewing medicines management as the patient progressed.
Community nurses provided an important level of ongoing support for patients, especially when transferred home. In general, they not only attended to ongoing care needs, such as wound care, but were found to act as ‘problem-solvers’, helping to track down missing equipment, ordering additional supplies and providing essential instruction and guidance to family members on how best to support their relative’s recovery. In many ways, community nurses picked up the responsibility of care where ward nurses left off. However, the availability of community nursing support was limited across all sites and visits to the patient were usually limited to two or three per week. Moreover, it was not always clear to the community nurses what levels of support were needed, as there was no standard handover between hospital and community nurses. As such, the community nurses would often need to contact the acute ward to make additional enquiries, which was generally facilitated where there was a designated discharge liaison nurse who would act as the primary point of contact. Further, it seemed that ward-based discharge liaison nurses, where in place, had a relatively positive relationship with these community nurses and the exchange of knowledge between them was generally supportive and enabled continuity of care.
Conclusion: comparing the knowledge-sharing networks
This chapter describes the patterns of knowledge sharing involved in discharge planning and care transition. It shows how hospital discharge does not involve a single or isolated period of decision-making but rather relies upon complex situations of knowledge sharing (gathering, exchange and use) across the entire care journey, from admission through to post-hospital care in the community. Specifically, it develops the idea that hospital discharge involves a linked series of temporarily stable and spatially bounded knowledge-sharing networks. Rather than portraying the interactions between actors and resources as one large network, this helps unpack the way in which hospital discharge relies upon a number of smaller subnetworks or clusters of interaction, where a particular group of actors and resources come together at a given time and place to address specific decisions or tasks. It is through these linked subnetworks or ‘situations’ that actors exchange and use knowledge to plan and progress hospital discharge.
Looking across the research sites, the chapter also shows variation not only in the distribution of these situations or opportunities for knowledge sharing but, more significantly, in the range of actors involved, the forms of knowledge sharing, the methods and media used and how knowledge contributes to discharge, in relation to other organisational or clinical priorities. With specific reference to the research objectives, the chapter therefore shows how a range of different stakeholders are involved in discharge planning and care transition, each with distinct roles and responsibilities (objective 1), and how discharge planning and care transition is dependent upon the particular patterns of knowledge sharing between these stakeholders (objective 2). In addressing these objectives, nine specific issues are highlighted as influencing the patterns of knowledge sharing and how knowledge sharing contributes to hospital discharge.
First, the findings show differences in the range of groups involved in discharge planning and care transition; not so much the total number of groups, but more when and how these groups were involved. Across the research sites, the total range of groups involved was broadly similar – for example doctors, nurses, HCAs, therapists, patients, relatives, social workers, social care workers, community nurses, GPs, pharmacists, et cetera – yet they were involved to a lesser or greater extent in the different situations. In all hospitals, discharge planning was led by a core group of nurses, OTs and patients, with whom other actors (junior doctors, social workers and pharmacists) would interact at different times. At the two stroke units, it was usual to find more frequent involvement of consultants in discharge planning, through both daily ward rounds and weekly MDT meetings. In the orthopaedic unit, there was less involvement of medical groups, except around dedicated tasks such as confirming readiness for discharge. At the stage of making external referrals and care transition, a range of additional actors (social workers, community nurses, equipment suppliers) came into contact with hospital staff, but there were variations in these processes. For example, at the Glipton orthopaedic unit social work interaction with the ward was primarily mediated by telephone, whereas at other sites it involved ward visits. Meanwhile, at the Farnchester stroke unit it was usual for the community stroke nurse to attend weekly MDT meetings and participate closely in care transition. Also significant at this site was the closer involvement of relatives and carers, which enabled more thorough knowledge sharing and holistic decision-making.
Second, and extending the first point, the sharing of knowledge was greatly influenced not only by the range of actors, but also the way in which they interacted. The research sites varied according to whether actors were more integrated and collaborative, or conversely more siloed and sequential. Again, the two stroke units showed clearer evidence of integrated working, whereby the entire team of doctors, nurses and therapists was seen as contributing to patient recovery and discharge planning. At these sites there was also a strong desire, even expectation, for external agencies to work more closely with the ward staff to facilitate collaborative decision-making. In contrast, the orthopaedic sites showed more fragmented working. This was exemplified by the divide between surgery and orthogeriatric input; the first phases of the patient journey were, in most cases, dominated by surgical decision-making with almost no attention to discharge, and only after surgical care did other clinicians become more active in discharge planning. This was particularly evidenced at the Farnchester hospital, where all hip fracture patients remained under the primary care of the surgeon. At Farnchester, these divisions were further reflected in the (low) levels of interaction between therapists and nurses, with nurses tending to focus more on surgical recovery and marginalise therapists from overall decision-making.
A significant factor that might compound this finding, and help to explain the enhanced levels of integration at the stroke services, was whether or not therapist teams were colocated on the given unit. For both stroke services, therapists were dedicated to the units, which facilitated integrated working; in contrast, at Farnchester orthopaedic they were organised through a centralised department that serviced the entire hospital on a rotational basis. Similar issues of colocation were also evident for social workers and community health-care teams. The past system of social workers being colocated in the hospitals was strongly missed by virtually all groups. Where there was a degree of colocation, for example within Farnchester community health care, there seemed to be greater familiarity, integrated working and knowledge sharing. In summary, the lack of colocation or ‘functional proximity’ between different stakeholders not only led to more fragmented, sequential-like and siloed working, but also limited opportunities to develop shared understanding and integrated practices. Where relations were limited or strained then discrepant views were difficult to resolve, often leading to some form of stand-off, for example between ward nurses and social workers.
Taken together, the first two concluding observations might explain whether discharge planning is based upon a relatively narrow or more holistic understanding of the patient’s medical, physical, psychological and social circumstances. The sites that regularly brought together multiple professional and stakeholder perspectives within and across different situations appeared able to generate more comprehensive discharge plans, shared points of understanding about the patient and better co-ordinated working, including handovers and transitions of care. Where multiple perspectives were brought together, especially early in the care pathway, decision-making and subsequent discharge planning appeared to be more robust; for example, staff would not need to chase information, there would be less duplication and discharge plans would consider more health-related and domestic issues. In other words, different professional groups more easily recognised, valued and took into consideration the contributions that others make to care planning. As such, they developed more collaborative working practices based upon shared understanding and collective learning. Where clinical activities were more fragmented or sequential, decision-making was often narrow or rudimentary in quality, lacking the depth of detail to support robust care transition.
Third, the findings suggest an important interplay between the more formal, designated situations for decision-making, and the more informal, ad hoc opportunities for knowledge sharing. There is a tendency in policies to promote more formal settings for discharge planning, such as weekly MDT meetings, but the study suggests that the more routine, daily interactive encounters between patients, clinicians and therapists often provide a more situated and contextualised opportunity for sharing tacit know-how about patient recovery or personal circumstances. Moreover, this knowledge is shared close to the action or at the point of care and can directly inform immediate decision-making, as well as wider discharge planning. However, it is arguably the interplay between the informal and formal that underpins hospital discharge. That is, know-how appears to be gathered through everyday ward-based interactions but is then relayed and shared in more formal settings, such as a ward round or MDT meeting, to inform collective decision-making, with subsequent actions or tasks undertaken in the more informal settings. Again, the stroke units not only seemed to offer more opportunities for both informal and formal knowledge sharing, but explicitly sought to utilise knowledge gathered through informal interactions in more formal settings. At the orthopaedic sites, there was more of a separation between these types of settings where, for example, the know-how acquired by therapists was not always used to enrich decision-making.
Fourth, the study suggests that the knowledge-sharing relationship between acute and community care providers can be based on instances of ‘push’ and ‘pull’ knowledge sharing. ‘Push’ relates to the idea that knowledge is proactively transmitted or shared by the hospital sector with external agencies to support ongoing care planning and recovery. Across all sites, there was seemingly little explicit push from hospital teams, except in the form of referrals, discharge summaries or letters. As such, those receiving the patient, and assuming responsibility for patient care, often had a partial or incomplete picture of ongoing care. ‘Pull’ describes the need for those in the community to reach back into the acute sector to acquire knowledge relevant to continuing care. As shown, however, those in the community often struggle to know which groups or actors to contact within the hospital. For example, nurses within the Glipton community hospitals were often unable to identify the relevant ward nurse when looking to progress the care of patients recently transferred to the community. As such, more targeted push of knowledge, or appreciation of where to pull knowledge, might support enhanced care transition. Alternatively, the study suggests that having actors who mediate push and pull across organisational boundaries can be beneficial.
Fifth, and following on from the above, the findings suggest that within three of the study sites certain actors were identified with distinct roles and responsibilities that involved working across established occupational and organisational boundaries, often with the express purpose of supporting hospital discharge. At the Glipton stroke and orthopaedic units, clearly designated discharge liaison nurses helped co-ordinate ward-based planning activities, and also carried out an ‘outreach’ role by acting as a point of contact and knowledge sharing with external agencies. At the Farnchester stroke unit, the community stroke nurse provided a similar ‘in-reach’ role by liaising with ward-based staff and families to provide more appropriate care following discharge. These key actors made two significant contributions to the patterns of knowledge sharing and hospital discharge. First, they acted as ‘boundary spanners’ and ‘knowledge brokers’, working across and helping to close the gaps between occupational groups. In Glipton, this involved co-ordinating the work of doctors, nurses and therapists in everyday decision-making processes and weekly MDTs, where they often took leadership or oversight for discharge processes. They also helped co-ordinate the interactions between health and social care agencies through mediating and reconciling the distinct modes of working or bureaucratic procedures, and acting more directly as a go-between in complex decision-making processes. In other words, they provided an important knowledge-brokering role by helping to get the right knowledge to the right people, at the right time. Through these roles, these actors became important repositories of knowledge or ‘knowledge resources’. For example, the community stroke nurse at Farnchester had a developed appreciation of local housing issues or support services and the discharge liaison nurses at Glipton were skilled in navigating the local arrangements for community care. As such, they provided essential know-how and experiential knowledge for the wider constellation of actors and agencies about how to plan and progress hospital discharge. Looking at the range of situations and opportunities for knowledge sharing, these individuals often had an integral role in the discrete patterns of knowledge sharing and decision-making and, more importantly, acted as a link and source of continuity between these different situations.
Sixth, the study found important variations in the way in which knowledge and decisions were recorded across the four study sites. In everyday clinical practice, clinicians used a range of electronic and paper-based recording systems. There remains widespread interest in the benefits of electronic care records, and the study found that clinicians often used electronic resources to order tests, scans and prescriptions, and to receive and review results. However, the study also found that each site retained more traditional paper-based records. The form and use of these paper records varied significantly across sites, which appeared to influence the opportunities for knowledge recording and sharing, and hence hospital discharge. At all but one site there were separate medical, nursing and therapist ‘notes’, which together made up the patient record. At Glipton these were managed by the respective clinical group, but importantly they were all stored or colocated on the respective stroke and orthopaedic units. This meant that each professional group was responsible for updating and managing their distinct patient records, but these records remained accessible to other groups who might want to check or clarify issues. As such, it provided a material resource or basis of knowledge sharing in the absence of direct contact. For example, at the Glipton stroke unit it was common to find records regularly passed between therapists and nurses as each group sought to progress patient care, in the understanding that each would be able to provide additional insight, for example when making external referrals. Conversely, at Farnchester orthopaedic unit the separate records were not colocated but were stored in distinct offices on the ward and in the therapists department. This not only prohibited easy access when, for example, making external referrals, but illustrated the underlying demarcation and disparate modes of working between occupational groups. At Farnchester stroke unit, a different system was found, whereby a single patient record was used that included different sections for each professional group and a common care summary or narrative. Although this could make it difficult for professionals to complete certain tasks when, for example, the record was held by another group, it did provide a shared record of collective activity. There was no sense that this was controlled by any one group, and it further illustrated the integrated way of working in this unit. Notwithstanding the differences in recording systems, it was universally believed that handwritten systems were problematic, and issues such as legibility often framed the ease of use and accuracy.
Seventh, knowledge sharing in relation to hospital discharge was influenced by a range of other technological and material resources and media. As suggested above, written patient records remained a prominent resource and medium of connecting activities and decisions through providing a documentary source of knowledge. Although ICTs might not have equalled these paper records in this sense, they were used in a number of other areas, such as ordering tests, scans and prescription. In addition, ICTs were often used when contacting external suppliers of equipment. Where these were not used, a range of other media devices were used, including telephones and fax, especially for referrals to social care. These technologies all shared common problems with use, accessibility and timing, for example telephone calls were often limited to normal working hours, whereas e-mails and faxes could be sent at almost any time; however, the impersonal nature of these in comparison with telephone could mean that potential ambiguities or problems were unresolved until later in the care pathway. There were also identified problems with staff skills in using certain resources such as computers and faxes, especially where multiple complex steps were involved. In addition to ICTs, whiteboards also played a significant role in providing ‘live’ representations of ward-based activities. Again, there were marked differences in how and whether or not these were used, but in general they appeared to provide an important level of additional knowledge to guide everyday activities.
Eighth, medical leadership across the research sites also varied and appeared to influence the pattern of knowledge sharing. At the two stroke units, there was relatively strong and visible leadership from the respective stroke consultants who tended to lead most decision-making processes or delegate responsibility to a senior nurse or other representative. In both cases, however, these consultants worked to create an open and participatory culture in which others were encouraged to participate in both formal and less formal knowledge-sharing situations. For example, in MDT meetings different actors would be actively invited to contribute; similarly, during ward rounds nurses and HCAs would be encouraged to contribute to decision-making. At the Glipton orthopaedic unit, there was a form of distributed leadership where the surgical consultant would lead initial care processes but then pass on responsibility for ongoing care and discharge planning to the orthogeriatrician team and other therapists. At the Farnchester orthopaedic unit, the orthopaedic surgeon again held leadership responsibility in the initial period of surgical and postsurgical care, but this gradually diminished as the patient recovered from surgery and moved into a rehabilitation phase. At this time there was little overall leadership in care planning, with the senior ward nurse seeming to acquire this responsibility despite an apparent conflict with other clinical duties. Leadership was important for the overall organisation of patient care, but especially in terms of the range of actors and types of knowledge that were permitted or encouraged to shape discharge planning and care transition.
Ninth, and often shaped by the style of leadership, there were significant differences in the ethos of care, especially the value placed on hospital discharge and the patterns of decision-making required to facilitate discharge. An initial difference between research sites was whether care was primarily focused on the immediate diagnosis and treatment of a specific clinical issue, or included a broader and more holistic concern with patient recovery and longer-term care. The orthopaedic sites, for example, showed a strong and clear emphasis on attending to the immediate surgery, with relatively little thought for discharge or longer-term care until after surgical recovery, at which point care was handed over to another clinical team. In contrast, the stroke sites showed a greater appreciation of the wider recovery and longer-term care of the patient early in the care pathway. These distinct models of care might simply reflect differences in the nature of the disease, whereby stroke care is inherently more concerned with longer-term recovery following stabilisation whereas treatment for hip fractures has a very precise focus on surgical intervention. However, these differences also carried forward into the general organisation of care and the relationships between different clinical groups, with the orthopaedic services revealing relatively fragmented working in comparison with the stroke services.
Moreover, these differences shaped the general priority given to discharge in day-to-day work; the stroke services tended to see ‘care transition’ as one step in a complex and ongoing pathway, whereas the orthopaedic services tended to see ‘discharge’ as an end point and the handing over of responsibility. In particular, the influence of organisational targets at Glipton, where service leaders were encouraged to meet the established 10-day NoF pathway, meant that discharge decisions often seemed to be driven by a need to meet this target rather than consideration of ongoing patient care; hence the frequent use of community hospital to facilitate the transfer of care and compliance with the target. Similarly, there were marked differences in the ethos and meaning of discharge between health and social care organisations. Hospital staff, including those in stroke services, typically saw discharge as an ‘end point’ of acute care and, as such, tended to organise care transition for the end of the day or week. In contrast, social and community care agencies saw it as a ‘starting point’ for care and tended to organise their work for the beginning of the day or week. This subtle difference in how discharge was seen framed many of the operational and planning tensions between health and social care, often leaving patients with a break or gap in their care. Moreover, it framed the patterns of interaction between groups, with situations or opportunities for knowledge sharing often ‘out of step’ or mistimed. This could be seen, for example, in the organisation of MDT meetings in the middle of the week, which gave less time for social care agencies to participate in discharge planning before the end of the week.
Chapter 5 The threats to safe discharge
Introduction
This chapter describes and elaborates the perceived sources of safety and risk within discharge planning and care transition, and builds upon the previous chapter to consider how similarities and differences in the patterns of knowledge sharing can explain these threats to (and sources of) patient safety. In line with research objectives 3 and 4, it draws primarily on the views and experiences of participants to describe the perceived sources of and threats to safety in relation to hospital discharge, and in analysing these accounts the chapter draws upon the previous chapter to interpret and explain the relationship between perceived risk and knowledge sharing.
In line with current thinking in patient safety research, and reflecting the language of study participants, the chapter makes a distinction between perceived ‘safety events’ (a situation, occurrence or adverse event involving patient harm) and ‘risk factors’ (actions or inactions that might cause a safety event), with knowledge sharing being both an active and latent source of safety and risk. As shown in the previous chapter, hospital discharge is not an isolated event, but relies upon a complex and incremental series of temporarily stable networks of knowledge-sharing activities, such as decision-making and responses to new information. The analysis considers how knowledge sharing can represent both an active and latent source of safety, as well as a positive and negative influence upon safety, i.e. how the patterns of knowledge sharing can either bring about or mitigate risk. In developing this analysis, the chapter seeks to extend this ‘systems approach’ to show how the system, in this case the patterns of knowledge sharing involved in hospital discharge, are potentially more complex and non-linear than current thinking allows.
The chapter proceeds with a reflective analysis of participants’ safety narratives, which elaborates the challenges and sensitivities involved in using a narratological perspective for patient safety. This reveals how sociocultural and political influences often frame sense-making and perceptions of safety events. The chapter then provides an analysis of the main types of risk or threats to safe discharge as perceived and described by participants, based primarily upon interview and documentary data. This analysis does not comprise a formal observation (counting) study of the frequency or severity of risk; rather it seeks to describe the common issues, concerns or safety events as seen by participants and, where relevant, highlight differences in perception between groups. For each type of safety event and risk factor, the chapter draws upon the findings presented in the previous chapter to interpret and explain the potential influence of knowledge sharing that indirectly conditioned or directly shaped these threats to patient safety. As such, it seeks to link participants’ interpretations and meanings of discharge safety to the wider social, cultural and organisational framing of patient care, especially the observed patterns of knowledge sharing.
Reflections on the analysis of safety narratives
The chapter draws primarily on the safety narratives of participants, that is, participants’ accounts, descriptions and stories of safety and risk in relation to hospital discharge and care transition, as developed through interviews, in conversations during observation, or in diaries or other documented form. These narratives reveal how actors make sense of, give meaning to and try to explain safety events. At the same time, they highlight differences in perception, interpretation and understanding which are shaped by each actor’s, or group of actors’, position within the care process, together with their prevailing cultural norms and assumptions. As suggested above, the narrative approach does not aim to establish an objective count or taxonomy of risk, although participants’ perception of frequency and significance can be detected; rather it aims to explore differences in sense-making and to reveal underlying cultural and organisational differences between participants. These shared perceptions and meanings can then be linked to the wider sociocultural and organisational context of hospital discharge as a basis of interpretation and explanation.
Undertaking this line of analysis is complicated by the difficulty that participants had in detecting safety events within complex care processes and, further, in understanding the causal relationship between safety outcomes and perceived risk, especially where a decision or action does not have an immediate or obvious impact. For example, a patient fall might easily be identified as a safety event or incident, but it is not always possible to attribute this to a specific causal factor, especially as the relevant knowledge-sharing issue may have occurred several weeks prior to the incident, when ordering equipment. At the same time, participant narratives often focused on general risk factors, such as problems with prescribing or delays, without always being able to relate these to specific incidents of harm or as perceived factors capable of mitigation. For example, delay was seen as creating risk conditions in general, but few participants described specific examples of how delay directly led to harm. A challenge for the interviewers, therefore, was teasing out the link between seemingly mundane general risks, without resort to extreme memorable events. A particular problem in relation to hospital discharge is that the patient journey crosses multiple occupational, organisational and sector boundaries, making it difficult for those in one location to understand the work of others. For example, safety events observed in the community setting often have their roots in the precursory acute sector. As such, it is difficult for those in the acute sector, or ‘upstream’, to appreciate the outcomes of their actions because they cannot easily see them. Equally, it is difficult for those in the community setting, or ‘downstream’, to understand the source of many safety events because these originate in the acute setting. As such, some described risks are broad and poorly specified, for example delay or timing, and it was the task of the research team to trace or track risks through the system.
To elaborate this issue, the study develops the idea of narrative ‘sight lines’. This describes the idea that actors tend to construct safety narratives from their particular position or location within the patient pathway, from where they can look backwards to help explain why something has happened, or alternatively forwards to consider what might happen. Moreover, participants’ narratives tend to follow or mirror their own involvement in the care pathway, starting and ending at around the time of their interaction with the patient. As such, these sight lines have ‘horizons’ that make it difficult to understand what might be beyond the ‘edge’ of their perceived process. Multiple actors are involved in patient care, discharge planning and care transition, and this leads to the existence of multiple, overlapping narratives, but few span the entire care pathway except those of the patient and their relatives, which are likely themselves to be limited in other ways. As noted above, those in the acute sector tend to have a detailed appreciation of what happens on the ward, for instance, but not within community settings (except some discharge liaison nurses or in-reach workers who span these boundaries). As such, multiple narratives were developed through interview according to participants’ position in and sight line with the patient pathway (Figure 7).
FIGURE 7.
Illustration of different safety narratives (story arcs) along the care pathway.
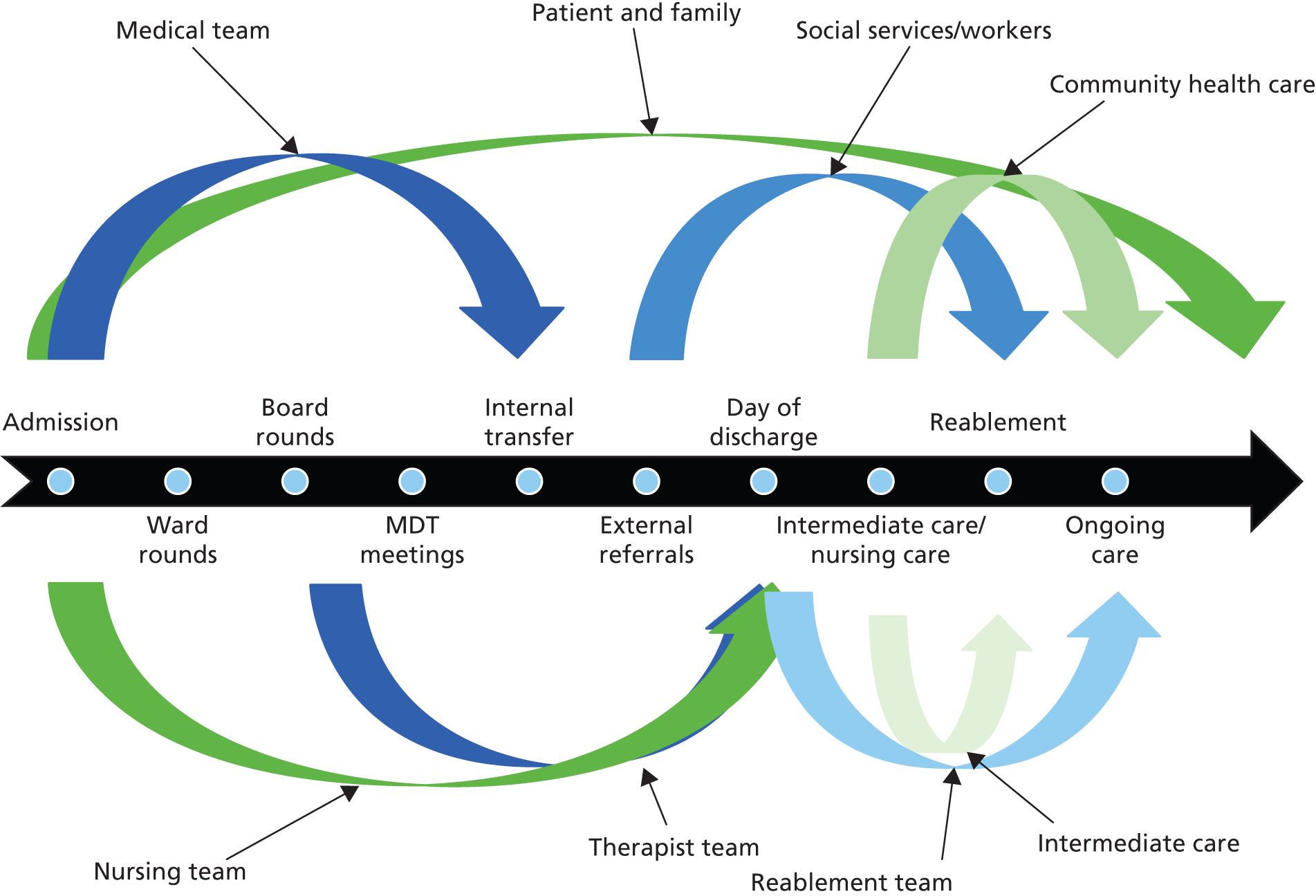
Developing this idea, the study found that participants tended to develop similar safety narratives according to their position within the pathway and, more significantly, their occupational background and organisational role. For example, the narratives of ward nurses generally coalesced around a number of common issues, such as delays associated with the availability of ongoing care. As suggested above, these occupational narratives can overlap, but they can also highlight conflicting views about the sources of risk. For example, ward nurses and social workers would offer different accounts of why delays might occur. Rather than interpreting these discrepant views as errors of judgement or bias, the study takes the view that these reflect underlying cultural differences that frame sense-making and perception, and which can themselves be a source of risk. For example, where two clinical groups perceive or assess a clinical risk in different ways it not only offers a site for conflict, but also infers divergent rather than integrated practices. From this perspective risks are not seen as real or objective but constructed according to shared cultural meanings. As such, what one group sees as a risk is not just a reflection of their position or sight line, but also their shared cultural assumptions about risk, uncertainty and danger.
Given that discharge planning and care transition is so complex and involves a myriad of interconnected decisions and processes, it is entirely understandable that those involved often find it difficult to understand with any certainty the sources of risk. In order to accommodate this uncertainty, occupational and organisational groups developed shared cultural scripts or stories, which are used to help make sense of these inconsistencies and breakdowns. Importantly, these cultural scripts often have enduring or underlying assumptions about risk and the causes of risk that frame sense-making. In particular, they help attribute causation in the absence of more concrete or direct knowledge. In other words, where an actor’s sight line makes it difficult to perceive system complexity, his or her occupation’s or organisation’s shared cultural ‘frames of reference’ help the actor develop a coherent explanatory account that can be articulated, confirmed and shared with colleagues and coworkers in a meaningful way. Significantly, these cultural frames of references assist both individual actors and occupational groups in explaining and mitigating many safety events through the ‘responsibilisation of risk’ or allocation of blame, i.e. patients fall at home because ‘someone’ in the hospital did not order the appropriate equipment. This not only helps provide a coherent explanatory account of patient harm and system complexity, but also mitigates the actor’s own responsibility in the process. Importantly, analysis of these narratives reveals underlying tensions or conflict between different groups, which are manifest in their cultural norms about why discharge fails or becomes complicated, especially where health and social care agencies tend to blame one another. As such, these narratives need to be ‘read’ carefully to appreciate the limits or horizon of sense-making and how they are used to allocate responsibility according to underlying cultural assumptions.
Notwithstanding these reflections, safety narratives provide a powerful lens for understanding the incident and sources of safety in hospital discharge as culturally scripted views, which are imbued with notions of responsibility and blame. They provide a detailed guide to understanding the variety of perceived risks and, when used in conjunction with observations and documentary analysis, can help develop a more nuanced, multidirected understanding of the sources of safety and risk in complex care processes. As noted above, the chapter draws on the ethnographic observational data to interpret and explain participants’ perceptions and meanings of risk and to relate these to the wider patterns of knowledge sharing that frame discharge planning and care transition.
Perceived risks and safety events
As outlined above, participant narratives helped identify potential adverse safety events (involving harm) as well as active and latent ‘risk factors’ (producing, enabling or conditioning the possibility for harm). In all cases, this analysis was limited to activities, situations and, importantly, knowledge-sharing processes related to discharge planning and care transition, i.e. where safety events were described in relation to other care-related activities, they were not considered in the analysis. Analysis of participants’ narratives led to the identification of seven broad categories or types of safety events and/or risk factors associated with discharge planning and care transition, with extracts of supporting data provided in Appendix 5. To support the coherence of this analysis, these categories were cross-referenced with the World Health Organization’s International Classification for Patient Safety148 conceptual framework. These include:
-
falls
-
medicines
-
infection
-
clinical procedure
-
equipment
-
timing and scheduling
-
communication.
Before elaborating these risks, it is worth noting that ‘falls’, ‘infection’ and ‘medication’ risks were typically associated with more direct threats to patient safety, but each was also associated with a range of wider contributory or latent factors, i.e. ‘falls risks’ or ‘medication risks’. In contrast, ‘clinical procedure’, ‘equipment’ and ‘timing and scheduling’ were all described as more contextual or latent risks that framed or conditioned patient safety, i.e. where the immediate impact on safety was less clear or direct. As the analysis shows, these risks often overlap or combine in the context of patient safety, for example where medication risks relate to infection and together lead to a fall. This is especially the case for ‘communication’, which was widely described as a systemic or latent source of risk that often framed or explained many of the other identified risks. Given the centrality of communication or, more precisely, knowledge sharing to the overall analysis, this theme is discussed through the chapter in relation to these other risks. Each described risk category is illustrated and data presented in the previous chapter are used to interpret the link between participants’ perceived threats to discharge safety and the observed patterns of knowledge sharing.
Falls
Falls, including slips, trips and collapses, were described by almost all participant groups as a common safety event in relation to discharge. Falls can occur at almost any time within a patient’s care journey and have a range of causes. It was usual for those in hospital and community settings to describe different situations where falls occurred, but in general these related to falls from the patient’s bed, when using a chair, the toilet or other bathroom facilities, when ascending or descending stairs or steps, and when being mobilised during therapy. It is important to note, however, that many of these accounts described falls as part of general care management, and not with specific reference to discharge planning and care transition. With specific reference to the falls and falls risk factors associated with discharge planning and care transition, a number of specific issues were identified. These were broadly related to processes of ‘transportation’ and ‘resettlement and adjustment’, with the second group also associated with the use of equipment and devices (see Equipment).
In terms of ‘transportation’, two issues were raised by patients and/or family members. First, it was described how falls could happen when being moved or handled between hospital, vehicle and community location. For example, the process of helping patients into the ambulance or back into their own home was often described by patients as challenging because they were still adjusting to their mobility constraints and because carers were seen as unsure how best to move the patient or were unfamiliar with the home layout. This suggested underlying concerns about the knowledge and skills of some support groups, i.e. porters and ambulance crews, to appropriately and safely move patients. Second, it was also described how, on occasion, ambulances used for transportation might not be suitable for certain types of patients in terms of seating arrangements, availability of chairlifts or having the necessary devices to support the care of frail patients. A number of patients on hip precaution following hip replacement described how the wrong type of ambulance was provided as there were no high-seats or supports to enable safe transfer between hospital and home. A number of ward clerks also described how inappropriate ambulances were provided when transferring very frail, bed-bound patients to community hospital, because they could not accommodate a bed. In such cases, it was usual for participants to describe unnecessary delay, rather than an actual fall, but where alternative transportation could not be arranged then the risk of fall remained. In general, patients and their relatives reflected negatively on the transportation process and often referred to falls and other risks associated with both the physical movement of patients and the suitability of the vehicle. When describing these risks it was common for hospital-based participants (doctors, nurses, HCAs, ward clerks) to highlight deficiencies in the regional ambulance service, especially where bookings for a particular time, location and ambulance type were not fulfilled. For some participants, this reflected a communication problem between the wards and the ambulance service, especially where booking systems and the ambulance control did not accurately record or meet provided instructions. Representatives from the ambulance service acknowledged these problems but also described themselves as overburdened by the demands of emergency care and often struggling to manage service provision. It is also important to recognise the potential for missing information at the time of booking, for example if the ward clerk had not been informed about specific needs and could not therefore relay this to the ambulance service.
More prominent were falls associated with ‘resettlement and adjustment’ within a domestic setting, usually home. Three safety events were described within patient and family narratives. The first group comprised trips, slips and falls within the home that seemed, in general, to be associated with everyday activities, such as using furniture, tripping over rugs and internal steps, ascending or descending stairs, using bathroom facilities or getting in or out of bed or a chair. For many participants, these were associated with patient confidence following discharge and the need to readjust to the home setting after prolonged hospitalisation. It was also described how certain aspects of the home layout could be taken for granted rather than moved to reduce the risk of fall, such as the position of rugs and tables. A widely understood risk related to the use of bathroom facilities, which were especially problematic for hip fracture patients. For example, patients often described minor slips or falls when sitting or rising from a toilet seat or when entering the bath. A range of possible risk factors were described as increasing the likelihood of falls around the time of discharge, including cognitive impairment, medicines use or adverse effect, infection [especially urinary tract infection (UTI)], patients’ understanding of their ability to mobilise, lack of support from carers and the use of equipment or devices (see Equipment). It seemed that, for many, these risks were accepted as normal for patients needing to readjust to their home or care home and, as such, extra vigilance was needed in the early days following discharge. However, some also raised the possibility that these risks were heightened by a lack of thoroughness in, or poor communication of, clinical assessments, i.e. where cognitive impairment was not adequately determined, or information on the use of medicines or equipment was incomplete (see Equipment).
The second group of resettlement-related falls risks were associated with the provision and use of home adaptations and equipment to support recovery and mobilisation around the house (see also Equipment). Both hip fracture and stroke patients were commonly provided with a range of grab rails, seat and bed risers, steps, frames, walking sticks and wheelchairs to support their recovery outside hospital. Two specific issues were associated with this equipment. First, patients and carers (including reablement teams) described problems with the availability and appropriateness of equipment and devices. A common example described essential equipment, such as grab rails, walking frames, commodes, steps/ramps, beds and mattresses, being delivered or fitted after the patient had arrived home. In such situations, patients were at risk of fall or accident because everyday activities, such as washing, toileting or walking, were not appropriately supported. As explained below, these delays were often linked to problems in the ordering of equipment, especially in contacting suppliers, or disagreements between nurses and OTs about whose responsibility it was to order commodes, or between health and social care about who should fund certain adaptions, especially steps and ramps. Second, patients, relatives and carers also experienced complications in the use of certain devices, such as hoists or pressure mattresses. For example, one patient described a fall when using the toilet because he did not realise that his weight needed to be evenly distributed on the support frame. These risks are elaborated below, but again participants described shortcomings in supporting patients and carers in the use of equipment.
The third group of falls risks relate, in very general terms, to the quality and appropriateness of the domestic settings to which the patient is transitioned. A number of city-centre patients were discharged to Victorian-era homes with several steps between pavement and door, narrow and steep staircases and relatively small bathroom facilities. In contrast, a number of other patients were discharged to more rural settings, to small cottages or farms. These property types were commonly described by community nurses or other social carer workers as poorly suited to patient recovery, some with outside toilets, making it difficult to accommodate necessary home adaptations and requiring patients to take unnecessary risks. The failure of social work and community health-care teams to recognise and consider these issues in discharge planning was seen by community nurses as putting patients at risk. In many instances, it was suggested that patients needed further rehabilitation at an intermediate facility before returning to these home settings.
In general, falls and falls risks featured more often in the narratives of patients and families, but they were also included in those of community-based carers (reablement teams, community nurses, OTs) following hospital discharge. It was more usual for community nurses to discuss the link between falls and cognition, medicines use or infection, reflecting their enhanced clinical understanding of the possible causes. It was more usual for community stroke nurses (Farnchester) and the discharge liaison nurses (Glipton) to mention property type in relation to discharge planning. There were no variations between sites in terms of perceptions of risk associated with falls as it seemed a general issue related to postdischarge recovery. Drawing on participant narratives and, where possible, cross-referencing these with observational data, falls and falls risks associated with discharge planning and care transition are summarised in Figure 8.
FIGURE 8.
Illustration of falls-related risks.
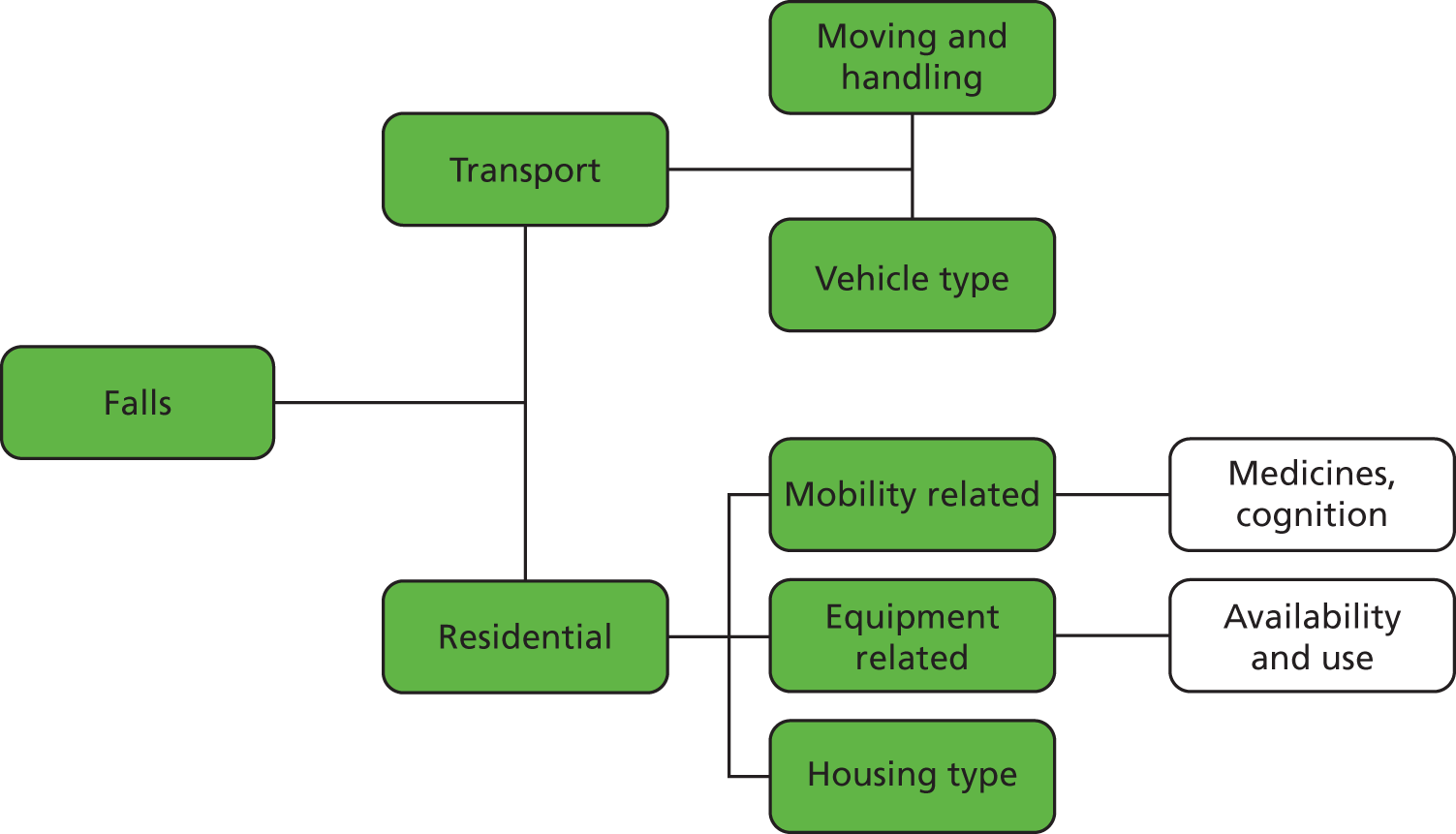
The above paragraphs describe how participants understood the risk of falls. Relating this to the patterns of knowledge sharing explicated in the previous chapter, we can begin to make a number of suggestions about how knowledge sharing contributed to the source of risk. Although falls can be brought about by a range of local and environmental factors, a number of knowledge-sharing dynamics condition or mitigate this potential. In relation to hospital transportation, the booking process involved an important opportunity for knowledge sharing between ward clerk, ambulance control and ambulance crews. The study found that this could be complicated, i.e. missed or incorrect, when the ward clerk was not on duty and other ward staff would be required to arrange transportation, for example nurses or HCAs. Although booking transport was relatively straightforward, the ward clerks appeared to have a developed understanding of the types of transportation available and an interpersonal relationship with staff at the ambulance service. As such, they were often more accurate in booking ambulances or appreciating the daily demands and schedules of the ambulance service. The absence of the ward clerk and reliance upon other staff could, on occasion, lead to the dispatch of inappropriate transportation or lead to delays. As such, the ward clerk provided an important knowledge-sharing resource on the day of discharge.
In relation to the patient’s general well-being and mobility, and also his or her use of equipment, a key knowledge-sharing dynamic was found in the interaction between the patient, his or her relatives and the ward-based therapist team. Specifically, OTs and PTs had an essential role in assessing the patient’s overall mobility, ability to undertake activities of daily living and cognitive function. They also provided individualised information and training to patients and relatives on the use of specific equipment and devices to be used after discharge. These types of activities relied upon relatively detailed, close and personalised knowledge-sharing relationships in day-to-day ward-based interaction across all sites, for example explaining to patients how best to use walking aids or climb stairs. At some sites, however, this pattern of interaction and knowledge sharing could become more fragmented, less patient-centred and not integrated into other ward-based activities. At Farnchester, for instance, therapist teams worked across the entire hospital and had sessional visits to the orthopaedic unit (note that the stroke unit had a dedicated therapist team). It was observed how OTs and PTs often had limited time with individual patients, could not always co-ordinate their sessions with family visits and were often marginalised from ward-based decision-making, such as MDT meetings. As such, the opportunities for both giving and receiving knowledge to and from patients and ward staff were limited. A similar format of therapist input was observed at the Glipton orthopaedic unit, but here there was closer involvement of therapists in ward-based activities. The two stroke units, however, featured dedicated therapist teams which facilitated closer, regular and more timely interaction with patients and families, and thereby more continuous exchange of knowledge. A related feature at Farnchester stroke unit was the explicit emphasis on family-centred care, including the use of family meetings, which enabled closer working with family members so that they were better aware of their relative’s ongoing needs and use of equipment. A further issue related to the provision of equipment related to ordering and supply, which is discussed below.
A further knowledge-sharing issue was the involvement in discharge planning of specialist staff who could provide knowledge about specific devices, medicines or housing. In particular, a key contribution was made by discharge liaison nurses at Glipton, and also the community stroke nurse at Farnchester, who had detailed, even ‘encyclopaedic’, knowledge of local housing quality, including steps from pavement to door, layout and bathroom arrangements. Their involvement in discharge planning could often avoid the need for home visits, but more commonly enhanced the decision-making processes of therapists, for example when ordering equipment (see Equipment) or supporting patient use of devices. A similar contribution was also found in the role of both hospital- and community-based pharmacists, who could inform patients and family members about the potential medicine-related complications that might reduce stability (see Medicines). Where these actors were not present, or were marginal, it seemed that discharge planning was often more generic and less specific to the needs of individual patients.
Infection
As with falls, infections were identified as a patient safety concern for both stroke and hip fracture patients, especially where both patients and staff were attentive to the problems of hospital-acquired infections, such as methicillin-resistant Staphylococcus aureus (MRSA). Notwithstanding these broader infection risks, two types of infection risk were discussed in relation to hospital discharge, usually by ward and community nurses. The first was associated with ‘extended admission’, where patients would be exposed unnecessarily to hospital-acquired infections because of delayed discharge. For example, ward nurses talked of the risks of contracting pneumonia and Clostridium difficile, especially for frail older patients. As outlined below, clinicians describe a ‘window of opportunity’ for care transition, which once missed could lead to patients being ‘trapped’ within a cycle of infection and recovery, which could have little direct connection to their stroke or hip fracture but reflect other comorbidities and the general risks of admission. Similarly, the risk of pressure sores was discussed for extensive inpatient admissions, where a lack of mobilisation and extended confinement to bed could lead to sores and chest problems. This was usually related to problems with ongoing patient monitoring after delayed discharge, when the patient was seen as ready for discharge and hence levels of direct active medical care were reduced, but monitoring and mobilisation were still required. As such, infection risks were often related to delays in discharge and the changing patterns of care giving (see Timing and scheduling).
The second group of infection risks were associated with ‘follow-up care’, when infection developed or was identified immediately after discharge. A prominent concern, for example, was UTI, which was seen as relatively common among both patient groups. Community nurses, in particular, described the need to monitor patients for signs of increased temperature and confusion in case of UTI, and also the need to involve the patient’s GP to prescribe antibiotics. An additional, but less common, infection risk related to sepsis, again following surgery, which might not develop until the patient was discharged into a community setting. This was raised by community nurses and ward nurses in community hospitals; for example, one Glipton hip fracture patient was found to have developed sepsis due to a surgical clip being left undetected at the time of care transition. A more common problem was with wound care and whether or not the reablement teams had the appropriate nursing skills to thoroughly clean and bandage surgical wounds or to detect potential problems. A more general concern for community nurses was the patient’s adherence to prescribed medicines after leaving hospital. It was described by one pharmacist, for example, that patients often attend the community pharmacy confused about their changed medicines regime (see Medicines). Such confusion and lack of adherence to prescribed antibiotics was seen as contributing to the potential risk for infection.
It was more usual for nurses within community hospitals to highlight the potential for postoperative infection after hip fracture patients were transferred from the Glipton hospital. This seemed to suggest a belief that patients could be transferred too quickly or without a more thorough assessment of need. It was also more common for community nurses in the rural Farnchester area to describe the problems of regularly monitoring patients dispersed across a large geographical area, where it could also be difficult to access GP services. Drawing on participant narratives the infection risks associated with discharge planning and care transition are summarised in Figure 9.
FIGURE 9.
Illustration of infection-related risks.
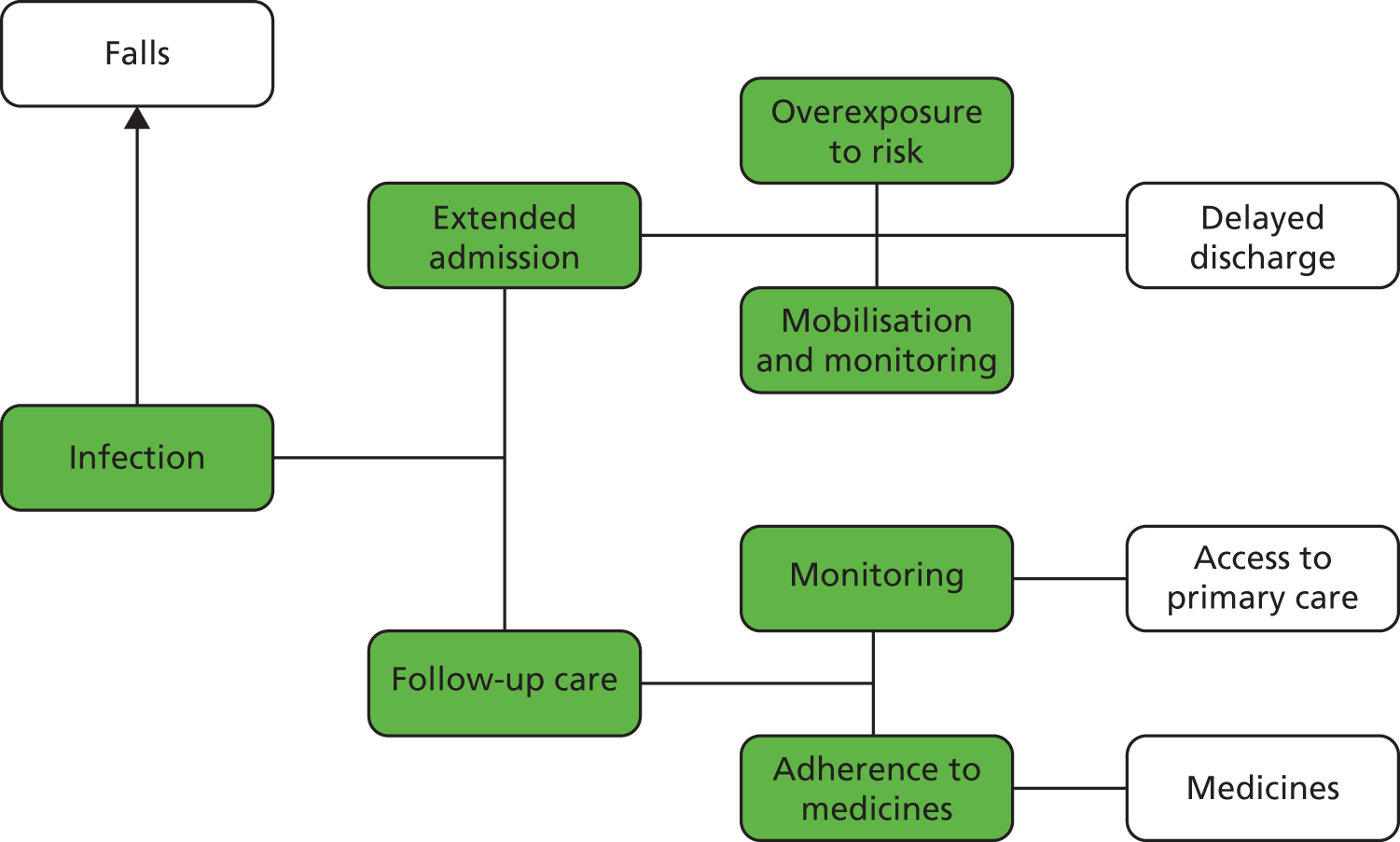
The above paragraphs describe how participants understood the risk of infection. Relating this to the findings described in the previous chapter, we can begin to make a number of suggestions about how knowledge sharing could frame or mitigate infection risk, often in relation to other risk issues discussed below, such as reducing delays, improving adherence to medicines or identifying at-risk patients. For patients on the ward awaiting discharge, and with delayed discharge, knowledge sharing between ward nurses and other therapists was observed as important for identifying and managing bed sores or pneumonia. Where ward-based activities were more integrated (i.e. in both stroke services) there were more opportunities to share knowledge between clinical groups about the need for therapeutic intervention, such as turning, to limit infection risk. For patients transferred to community hospital and nursing homes, the sharing of knowledge between ward nurses and carers was also important for maintaining monitoring and therapeutic interventions. As shown in Glipton, the sharing of knowledge between these sectors could often be limited or fragmented, leading to subsequent complications in ongoing care following transfer. In care homes and other residential homes, support staff routinely assessed and monitored infection risks and, as such, problems were usually detected early.
For patients transferred home, access to primary health-care services was particularly important, for example GPs, community nurses and pharmacists. In general, where patients had easier access to their GP, community nurse and community pharmacy, often due to colocation of services and proximity to home, it was easier to share knowledge about potential infection concerns and seek advice or treatment. Where patients lived in rural areas, for example around Farnchester, it seemed that patients had more fragmented and partial relationships with their community health-care team. That being said, across all sites community nurses fulfilled a proactive role in monitoring infection risks and other care issues, such as nutrition, continence, wound care or medicines adherence. However, where community nurses were stretched in workload, especially in rural Farnchester, there was less opportunity for patients or family members to share their concerns in more immediate, direct and personal ways. Interestingly, it was found that GPs had a more reactive involvement in monitoring infection risk, in that their intervention was usually prompted by a community nurse or family member once infection concerns were identified. It was seen as rare for GPs to take a more proactive role in postdischarge care, often because they received little detailed or timely information about patient need from the acute hospital.
Medicines
Medicines were one of the most discussed risk issues across all participant groups. Although these were highlighted across the entire care pathway, specific problems with prescription, dispensing and adherence were also described in relation to discharge planning and care transition. These broadly fell into two categories: first, those related to organising and providing take-home or TTO medicines before discharge, and second, those related to medicines use and safety following discharge.
The perceived risks associated with TTOs resemble more common safety issues associated with prescribing and dispensing medicines, but highlight particular issues associated with hospital discharge. Prescribing errors are well recognised within the wider patient safety literature and occur when, for a variety of reasons, the prescriber (usually a medical doctor) requests, for example, an inappropriate medicine, the wrong dosage or the wrong combination of medicines. At discharge, such prescribing issues were often discussed in relation to the work of junior doctors, who tended to be responsible for prescribing TTOs. A number of accounts were given where the wrong medicines were prescribed; where medicines were prescribed that were unsafe for certain patients, i.e. those with pace makers or allergic reactions; where insufficient medicines were ordered, i.e. the patient would run out after discharge; or where medicines were not ordered in sufficient time to be ready for discharge. A very common situation, for example, was for relatively standard or regular medicines, such as furosemide, not to be prescribed because it was assumed that an existing prescription existed and the records were not checked.
A number of common accounts were given for why TTOs might be incorrect or unsafe. First, junior doctors could find it difficult to access all the relevant information about often unfamiliar patients, especially their previous history of medicines, because patient records were poorly documented. This made it difficult to find relevant information or meant that the information was simply not available. Second, it was common for other staff groups, including ward nurses, clerks and hospital pharmacists, to highlight poor handwriting or ineffective channels of communication as a problem with prescribing. Thirdly, junior doctors may not have the necessary prescribing knowledge to accurately prescribe oxygen and pre-emptive palliative care drugs, leading to delays in managing fast-track patients. At Farnchester hospital electronic prescribing was seen to greatly improve the quality of prescribing and communication between departments. Finally, there were the broader error-creating pressures associated with the wider organisation of work, especially excessive workload, limited work planning and the general lack of support and guidance. For example, junior doctors often seemed to be thrust into new prescribing roles with relatively little guidance, and expected to rush TTOs ‘urgently’ to facilitate a last-minute discharge, with little time for reviewing records in detail or seeking support. At the Glipton stroke unit all TTOs completed by junior doctors were checked by the stroke consultant prior to being issued as a basis for quality control and also to support learning.
Risks were also described in relation to the dispensing of medicines within hospital, especially the checking, transporting and storage of medicines before being issued to the patient. A prominent narrative at the Farnchester orthopaedic unit was for patients to be given incomplete medicines or even the medicines of a different patient. It was explained that TTOs were ‘dropped off’ at the ward in large batches, and stored in a general side room before being sorted according to patient name. This made it possible for multiple packages and dosset boxes to become mixed up or separated. At the point of discharge it was observed that ward nurses would enter this side room to obtain patient medicines, but because of poor storage, limited handover within the pharmacy department and time pressures, medicines would often be missed or mixed up. A further problem occurred when large dosset boxes were requested late on Thursday in advance of a Friday or Saturday morning discharge. Although the prescribing information was usually accurate, there was insufficient time to complete these orders, suggesting that ward staff were not knowledgeable about the work schedules and demands in the pharmacy department; in turn, this would delay discharge until the Monday or require the patient to leave hospital with incomplete medicines. More generally, it was described how ‘last-minute’ prescribing would often mean that discharge could be delayed or, again, patients might have incomplete medicines. At Farnchester hospital the use of electronic prescribing and 24-hour dispensing seemed to enable more balanced workload planning and reduce the pressure on dispensing at the point of discharge.
Medicines risks were also discussed in relation to postdischarge recovery at home or in a nursing home. First, participants described possible adverse physical (side) effects associated with inappropriate medicines use, i.e. where contraindications existed or where medicines were missing. Some examples included TTOs containing antibiotics despite penicillin allergy, or aspirin despite the patient also taking warfarin. If these errors in prescribing and dispensing were not identified in the hospital prior to discharge, the potential side effects would invariably be detected in the community by nurses, pharmacists, GPs and care home staff. This was often complicated by polypharmacy where patients were prescribed multiple medicines to deal with complex health needs; this made it difficult for community staff to understand health-related problems associated with medicines, for example confusion or decline in health or well-being.
Second, community nurses and GPs also described problems with patient adherence to prescribed medicines. Common examples were failure to complete the prescribed course of antibiotics, reverting to medicines regimes used prior to admission or not taking certain medicines in the expected way. For example, community nurses reported concerns about their patients not taking calcium medicines as required because of the complex instructions; they were not sitting for sufficient time to allow absorption on empty stomachs. Problems with adherence were linked to a range of factors, including lack of instruction or guidance by hospital staff, difficulty in remembering what medicines to take and when, and physical complications in opening medicines (dosset box) or being able to swallow (after stroke). Importantly, adherence appeared to be based upon key knowledge-sharing interactions between patients (and relatives) and ward nurses at the point of discharge, and with community nurses following discharge. Where these interactions were rushed, there was often an absence of knowledge sharing and therefore adherence could be incomplete.
Third, risks were associated with the reconciliation of new and old medicines in the community and the extent to which medicines use was monitored and supported. Patients’ and family members’ narratives revealed a burden of responsibility to follow a prescribed medicines regime, but often with limited understanding of the medicines prescribed. A significant factor, therefore, was whether or not patients, family members and other carers felt supported by community and primary care professionals. Community nurses were often described as providing essential support in explaining ongoing patient care needs and in monitoring the provision, use and physical effects of medicines. Similarly, GPs were often described by patients as providing essential support in reviewing new medicines and altering existing medicines regimes after leaving hospital. Further still, community pharmacists were seen as a readily available source of information to describe new medicines and support adherence. However, participant narratives also highlight common problems with accessing these specialists, especially in rural areas where access to a GP or pharmacist was difficult. As described above, it was also suggested that GPs often took a reactive, rather than proactive approach to managing patient medicines, i.e. attending to the patient after problems were detected. Again, GPs related this to a lack of communication at the point of discharge, especially in terms of receiving timely or complete summaries following discharge, and relying upon the medicines held by patients to determine the new medicine regime (which could be inaccurate if not all medicines were dispensed).
As with other aspects of patient care, medicines were seen as a significant source of risk and potential unsafe care, especially in relation to the processes of prescribing, dispensing, use and adherence. At the time of discharge, however, these processes were seen as potentially exacerbated by a general lack of continuity of care, where medicines are prescribed and dispensed in one setting but taken and monitored in another. The handover of medicines management between secondary and primary care professionals appears integral to patient safety, but across all sites there was relatively limited direct communication between these groups; instead, the patient and his or her medicines became the primary basis for knowledge sharing. These processes are also often complicated by the very nature of discharge itself, which, as shown in the previous chapter, can be a complex process involving lots of last-minute activities undertaken by a multitude of actors, and not always well co-ordinated. Medicines-related risks were common to all sites, but problems of follow-up care and adherence were particularly marked in more rural areas, especially Farnchester; at the same time, however, this hospital also benefited from more accurate dispensing of TTOs because of its electronic prescribing system. Drawing on participant narratives these medicines-related risks are summarised in Figure 10.
FIGURE 10.
Illustration of medicines-related risks.
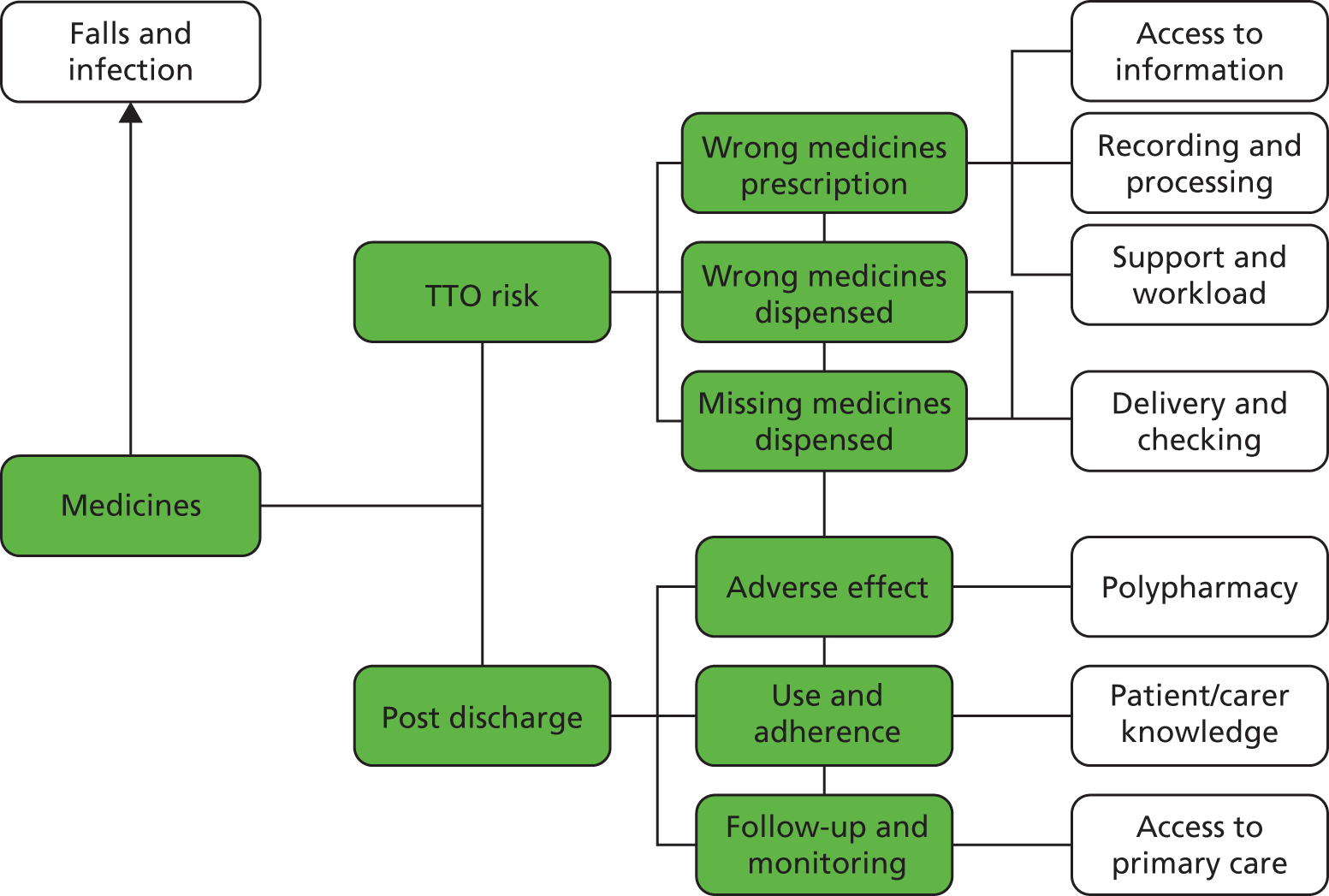
As indicated above, effective knowledge sharing before and after discharge is essential for medicines safety. For example, accurate and complete prescribing of TTOs is based upon the ability of junior doctors to effectively access, understand and use recorded knowledge about patients’ pre-existing medicines, allergies, contraindications and ongoing care needs (which is itself dependent upon the accuracy of record keeping throughout patient admission). At hospitals with multiple and fragmented care records, i.e. the orthopaedic units, the initial prescribing process seemed more complicated than that observed where a single patient record was used, i.e. the stroke units. The prescribing process then relies upon knowledge sharing between prescriber and hospital pharmacy, where timely and accurate exchange is essential. At Farnchester, the use of an electronic prescribing system appeared to facilitate this process over and above the use of more traditional, paper-based prescriptions at Glipton. These ICTs also enabled prescriptions to be made 24 hours a day, and so potential delays in the process could be avoided. In contrast, at the Glipton stroke unit it was found that a senior doctor would usually check TTO prescriptions for their accuracy and handwriting, thereby providing an additional level of quality control. The study found, therefore, that the availability and distribution of knowledge materials (records) and also knowledge systems (ICTs) could enhance the quality of TTOs.
Knowledge sharing was also important at the point of dispensing medicines, especially when deliveries were made to the ward or medicines were issued to patients. At all sites, there were no rigorous methods or systems for checking medicines at the time of delivery, often because of time and work pressures. It was customary for medicines to be checked at the time of giving them to the patient, which could create further delays if items were missing or incorrect. More significant, however, was the level of knowledge sharing with patients and relatives prior to discharge. At all sites, for example, it was usual for the patient’s designated nurses to explain medicines use. The study found that this interaction could easily become fragmented or piecemeal during busy times or when discharge had been delayed. This would lead to patients being discharged with relatively poor understanding of their medicines and would lead to potential problems with adherence. Following discharge, it was also found that access to a GP or, more often, community pharmacy was important for providing patients with additional information about their medicines and medicines use. As described above, those living in more rural and remote areas usually had limited access to these services and sources of knowledge.
Clinical procedures
In the days and hours leading up to hospital discharge it was usual for patients to undergo a range of assessments, procedures and tests to confirm readiness for care transition and inform onward care planning. Common examples included blood tests to clarify the absence of infection, electrocardiograms to confirm the patient’s cardiovascular health, and scans to provide a final image of the patient’s hip to facilitate subsequent comparison and analysis of follow-up scans after discharge. Although concerns about these clinical procedures and tests featured less than those regarding other safety issues, such as medicines, they were identified by clinicians and patients as relatively common in occurrence if not significant in impact. In broad terms, the failure to complete these procedures was seen as allowing possible underlying health concerns to go undetected, leading to complications following discharge. A major concern, for example, was stroke patients discharged without a computerised tomography (CT) scan or, more commonly, other comorbidities not thoroughly investigated prior to discharge. For example, several ward nurses commented that certain blood tests might not be completed on the day of discharge because the patient was already confirmed as leaving and it was assumed the test would be completed in the community. Similarly, one SaLT described how patient swallowing tests were not always reassessed prior to discharge, and so the proposed care plan might not be accurate. More commonly, it was described that patients were regularly discharged in need of almost immediate appointments for outpatient scans or tests, as these could not be completed on an inpatient basis within the time frame available prior to completing discharge (for example, because of delays in booking scans on the day of discharge).
Similar issues were identified by patients and relatives following discharge, normally in relation to follow-up outpatient appointments. A number of participants described not receiving appointment letters, which necessitated that they contact the hospital directly to arrange an appointment. A particular problem concerned patients whose first language was not English, who could not easily understand appointment letters without translation. More specific problems were found among patients accessing community orthopaedic physiotherapy, where it seemed that bookings often went astray, especially in the Farnchester area. It was also found that patients would sometimes present at outpatient clinic to find that not all tests could be completed on the same day, especially where they involved specific diagnostic imaging, thereby requiring a second hospital visit. This was especially draining for frail patients who relied upon the hospital ambulance service, where additional risks were incurred (see Falls), and for those who lived in more remote rural areas. In contrast, clinicians also talked about the problems of patients not attending follow-up clinics and putting their own health at risk.
Failure to complete clinical procedures, tests or scans, or to attend follow-up appointments, did not necessarily constitute a direct threat to patient safety, but created the possibility that health concerns or problems might go undetected or without sufficient medical intervention. There were no clear indications that missed tests had led to patient harm, although one patient did restroke after discharge and had missed a scan before discharge. Furthermore, outpatient appointments were often an important opportunity for patients to discuss their progress and to seek additional guidance on recovery. As such, failure to maintain a follow-up relationship could undermine adherence to clinical instruction and recovery. Drawing together the patient narratives, the risks associated with clinical procedures are summarised in Figure 11.
FIGURE 11.
Illustration of risks associated with clinical procedures.
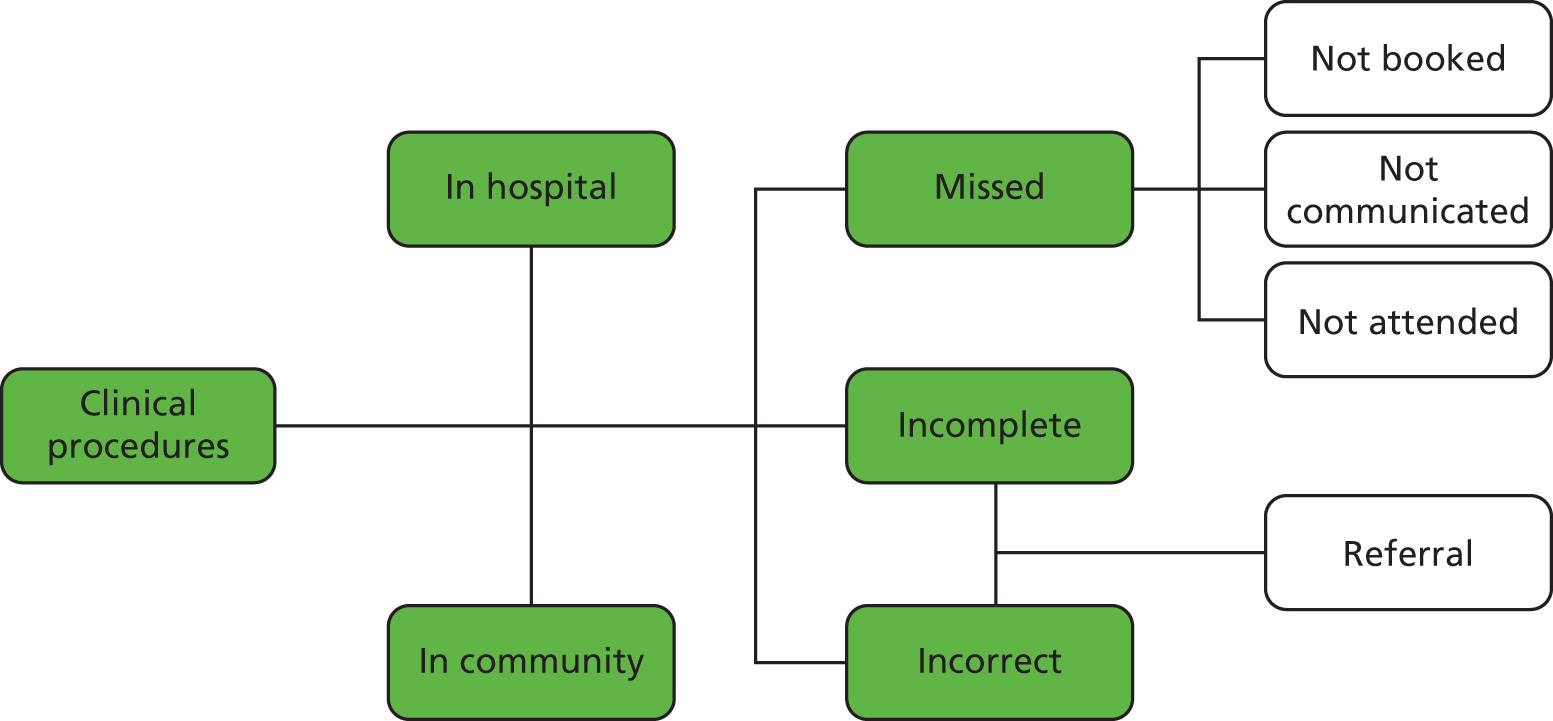
The planning and completion of clinical procedures, tests and scans either before or after discharge was framed by a number of knowledge-sharing issues. First, the decision to initiate or request a specific test or assessment was often taken as part of daily ward-based interaction, such as the ward round, or alternatively in weekly MDTs. Variations in how these decisions were communicated and recorded could determine how quickly and thoroughly requests were actioned. During the initial period of inpatient care, it seemed that these tests were escalated in priority, but as the patient neared discharge, especially after a date was set and readiness confirmed, the priority given to completing tests seemed to decline. It seemed that staff assumed these patients were healthy and ready for discharge and, as such, clinical attention could be given to more frail patients. This would mean that some more routine tests or scans would be overlooked in daily planning activities, such as ward and board rounds. For example, they might be recorded in the patient notes, but the allocation of responsibility might be left unsaid or vague. In other words, it seemed that the cultural value of diagnosis was absent, as these tests usually dealt with confirming readiness for discharge, and therefore there was less emphasis on or importance attached to these requests.
A range of more obvious knowledge-sharing issues was identified in relation to daily ward-based planning activities, especially handovers and board rounds. As described in the previous chapter, these helped to co-ordinate routine activities, such as ordering and completing tests. In sites where these interactions were more inclusive of different staff groups and based upon shared decision-making, i.e. in both stroke units, it seemed that staff worked together to identify and complete tasks, thereby reducing the potential for procedures to be overlooked. In other sites, clinical interactions seemed more fleeting or fragmented. Moreover, there were seemingly important differences in how requests for clinical procedures were recorded during these interactions. At the Glipton orthopaedic unit, for example, staff often relied upon scraps of paper or memory to record activities, which seemed to explain why certain tasks were overlooked until the last minute. In contrast, the use of whiteboards, for example, helped staff record and monitor task completion and could be reviewed regularly and easily throughout the day. The availability and use of ICTs also shaped the booking and provision of tests and scans. At all sites, ICTs were increasingly used to request appointment slots and to receive test results. In general, this appeared to facilitate the process, but it was also observed that interpersonal skills and the ability to negotiate were also important determinants of the successful booking of requests. In particular, ward clerks and some experienced ward nurses at Glipton would often contact the pathology or radiology department, for instance, to request a different slot or to rush requests. These interactions were facilitated by personal connections and familiarity which enable the ward staff to circumvent the procedures prescribed by ICTs, and expedite test results to enable discharge. Furthermore, the Farnchester stroke unit had recently procured several imaging and specialist computer terminals to reduce dependence on shared hospital resources. Finally, arrangements for outpatient tests and procedures often relied upon the quality of record keeping at the time of discharge and the detail of the discharge summary. At Glipton, it was customary for all ward clerks to independently log requests for outpatient appointments (in addition to the discharge summary) and to action these on the day of discharge. At Farnchester, however, the consultant’s discharge letter and nurse’s discharge summary provided the primary triggers for onward requests for appointments and often became delayed as they were processed alongside other competing tasks by the medical secretary or the patient’s nurse.
Equipment
Equipment and other devices are integral to the continuing recovery and rehabilitation of hip fracture and stroke patients before and after discharge. For the vast majority of patients they provided invaluable support, yet, linked to the discussion of falls, equipment availability and use were widely described as a source of risk following discharge. In terms of the availability of equipment, a common occurrence was for patients to arrive home without essential items being delivered in advance of care transitions, especially commodes, wheelchairs, walking frames and foot stools. In some cases, items were delivered up to 48 hours after discharge, meaning that patients lacked appropriate support, and either resulting in confinement to bed or increasing the possibility of a fall. A significant concern for patients was toileting and the desire to avoid using pads or bedpans, or soiling the bed. In other instances, equipment was delivered in a staggered or fragmented way. A common example was for a bed frame and mattress to be delivered several days apart. In one instance, a patient bed was delayed by over 9 days, requiring the patient to sleep in an armchair; he passed away in his armchair before the bed could be delivered. A linked concern was the delivery of incorrect equipment, for example a walking frame supplied when the patient required a wheelchair. A common problem was for grab rails and other handles to be fitted after the patient had returned home.
A second set of issues related to equipment use by both patients and their carers. Clearly, inappropriate use of equipment runs the risk not only of falls, but of additional health hazards such as trapped fingers. Common, but seemingly trivial, examples included not locking brakes on wheelchairs, not using walking sticks appropriately or not being able to use adjustable beds. Although hospital OTs described their efforts to prepare patients for recovery outside hospital, including advising them on how to use basic equipment such as walking sticks or wheelchairs, it was felt that some patients did not thoroughly understand or value the importance of lessons provided. Cognitive impairment was often highlighted as making it difficult to explain equipment use. A further concern was patient reliance on relatives or carers who were also not adequately trained or experienced in the use of certain devices. For example, relatives or carers were often required to assist with certain feeding tubes and bathing aides, but typically had little or no training. Moreover, some reablement teams described how they had not been trained in performing certain moving and handling tasks or in the use of certain equipment, such as rotundas. Inappropriate use of such devices introduced additional risk to patient recovery.
Equipment risks were often pre-empted by OTs, ward nurses and other therapists in both the stroke and hip fracture units, but it tended to be community nurses, patients, relatives and reablement staff who described incidents of actual or potential harm. The problems with equipment supply and fitting were generally more common in rural areas where there was usually a longer delay compared with city or urban locations. The use of electronic systems seemed to be associated with reduced delay in supply and fitting, possibly because of the benefits of electronic stock control and workload management. Drawing on participant narratives, equipment-related risks associated with discharge planning and care transition are summarised in Figure 12.
FIGURE 12.
Illustration of equipment-related risks.
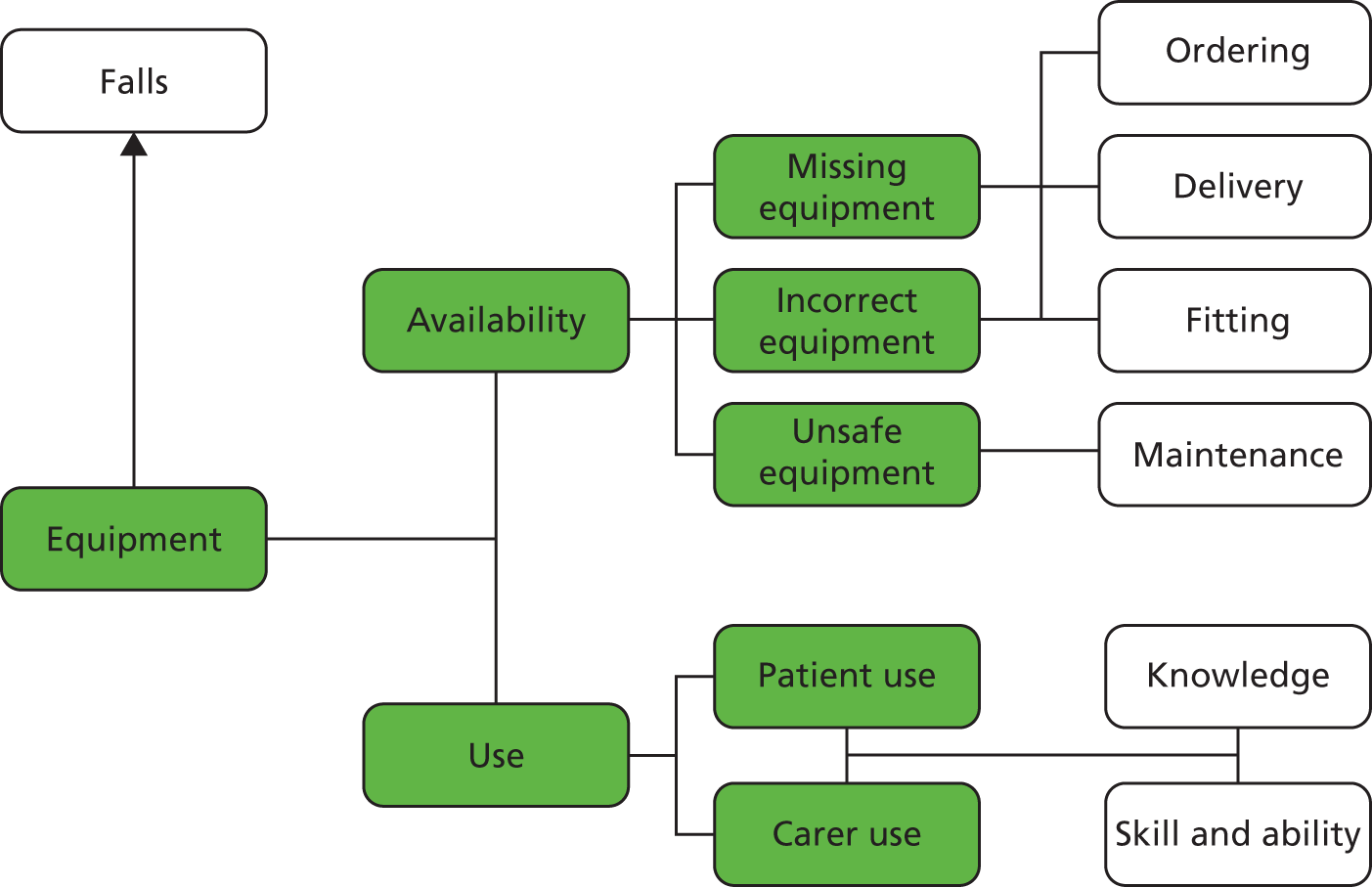
As above, drawing upon the issues described in the previous chapter, knowledge sharing played a significant role in the provision and use of equipment. As described, the ordering, delivery, fitting and even maintenance of equipment was dependent on the patterns and quality of knowledge sharing between hospital staff (OTs and ward nurses), equipment suppliers (private firms), fitters and delivery drivers (often another private firm) and relatives and carers (to provide access to the home). Although the interaction between these groups was often effective, there were common breakdowns across all sites. In particular, the interaction between the hospital staff and the suppliers could be complicated by whether or not the ordering and booking system could accommodate bespoke needs or requests. At Glipton it was usual for staff to use computer-based ordering systems which made ordering possible across a wider time frame and supported more rapid ordering, so equipment could easily be ordered at the last minute despite increased costs. At Farnchester, urgent orders were not supported by the hospital, despite costing less than the resulting delay in discharge. However, the computer system could make it difficult to address complex or unique needs or specialist equipment. At Farnchester, the use of a telephone service made it easier to address and explain specialist requests, but the process was often protracted and dependent upon the working hours of the equipment suppliers. A further knowledge-sharing issue related to the level of experience and knowledge of the person ordering the equipment. It was found that discharge liaison nurses and most OTs were highly skilled at navigating the ordering process, but some relatively new nurses often struggled to understand the process. This was especially the case for more complicated and unusual devices, where a discharge liaison nurse would usually know a specialist supplier who served the region.
In terms of patients’ and carers’ use of equipment, the ward-based and therapeutic relationship between the OT and the patient was integral. In all sites, OTs worked closely with patients to support their onward recovery, but it was not always possible to involve relatives or carers in this process. At the two stroke units this was more common because the therapist teams were dedicated to the units and could be available to meet with family members. As such, they could more easily share knowledge on the use of equipment to support use in the community setting. In the orthopaedic sites, however, this was less common and there were few formal opportunities to explain to family members how they might support their relatives following discharge. It was also found that where therapist teams rotated between different wards and were not dedicated to an area, there was generally less time to build familiarity and work closely with patients. As such, there was less instruction on how to use equipment. In general, there was no direct communication between the hospital OTs and the social care reablement teams, which meant that any guidance or instruction on the use of specialist equipment was missed.
Timing and scheduling
Turning to risks associated with the broader organisation and planning of care, participants often talked of problems broadly related to whether or not discharge occurred at ’the right time’ or during what some called the ’window of opportunity’. For example, participant narratives highlighted both ‘premature’ and ‘delayed’ discharge as potential threats to patient well-being, where a patient can either be discharged while requiring acute care or remain in hospital despite the possibility that his or her recovery might be better supported in the community. Reflecting on these narratives, it often seemed that delayed discharge, in particular, was invoked as a risk perhaps because it was a wider organisational priority that had penetrated the wider culture of health and social care, especially given legislation and financial inducements to reduce delays. As such, it was not always clear whether descriptions of delayed discharge were directly or necessarily related to patient safety, but the coming together of these two organisational priorities seemed significant for participants.
Where patients were discharged prematurely, participants described how patients could return home still requiring more extensive rehabilitation, without which recovery would be compromised and patients could, theoretically, be placed at increased risk of fall or relapse. Community nurses and some reablement teams commented that some severely sick and frail patients were discharged and the level of care needed was often beyond their skills or abilities. Another common concern was situations where patients seemed to have recovered sufficiently from their primary stroke or hip replacement, but other comorbidities were not sufficiently addressed prior to discharge. More broadly, premature discharge framed or conditioned many of the other, more direct risks discussed above. In other words, where discharge was brought forward or seen as too early, it often reflected a situation in which staff felt unable to complete the range of necessary tasks to assure a safe discharge, such as ordering equipment, TTOs or clinical tests. As such, premature discharge was a latent risk conditioning factor. For participants, premature discharge was often related to wider organisational priorities and demands, especially bed shortages. As observed at Glipton, service managers and bed bureau representatives would often attend daily board rounds to review bed availability and encourage the transition of care. In these interactions, more senior clinicians would often need to share complex patient-related and clinical information to explain why certain patients should not be discharged early. Similarly, weekly MDTs were often used to balance different clinical opinions to ensure that relevant comorbidities and health issues were addressed when setting the date of discharge, but where these meetings were more limited or exclusive, i.e. within the Farnchester orthopaedic service, there were fewer opportunities to draw together these different views.
As described above, delayed discharge featured prominently in the narratives of virtually all participants. Delays were described as creating the opportunity for patients to be exposed to additional risks such as infection, or to become anxious, depressed or even institutionalised. Again, it was not always clear how delayed discharge had a direct impact upon patient safety, but it did represent a contextual factor that complicated the co-ordination of care. More experienced participants, especially consultants, sisters and social work managers, described how patients could easily become depressed through prolonged hospital stay, leading to general lowering of independence, increased incontinence, agitation and immobility. A number of stroke consultants talked of the risks associated with prolonged stay which had relatively little direct association with the primary medical condition, such as hospital-acquired infections, delirium, incontinence and weight loss. More broadly, it was described how progressive rehabilitation and recovery, in particular with respect to activities of daily living, would be stalled owing to delayed discharge, potentially leading to lower-than-anticipated longer-term outcomes of recovery and rehabilitation.
The sources of delay were wide-ranging and highlight the complexity of the discharge process. At the point of making an external referral, for instance, OTs discussed a tendency for social services contact centres to question relatively trivial documentary inconsistencies, thereby holding up the discharge process. Similarly, social workers would comment that referrals were often inadequate because of missing information or difficulty in accessing ward-based staff to clarify information. At the point of care transition, further issues were identified as creating delay. It was common, for example, for health-care teams to blame social services for holding up discharge by not putting in place necessary provision or for querying referral notices; in turn, social services described limited capacity for providing social care or reablement because of increased demand (and diminished funding). It was suggested that patient discharge could be delayed because essential home adaptations and equipment had not been delivered. In these instances, the community nurse or social worker would request that transition be paused while the supplier was contacted to expedite the delivery and fitting of devices. Similarly, the transition of care to community hospital could be blocked because of limited capacity, which could cause acute services to miss pathway targets, especially the orthopaedic unit. At the same time, community hospitals and nursing homes often described the larger acute hospital as pushing patients out to the community without completing necessary checks or sharing information.
The risks associated with timing were therefore more indirect and less obvious than those associated with other identified safety issues, such as medication or equipment. That being said, it seemed that timing issues framed these other risks. Where patient discharge was delayed owing to problems with ordering equipment or planning social care, for instance, this created two broader changes in the provision of care. First, it framed a wider shift in clinical emphasis whereby acute patient care was regarded as complete, with little need for further care. In these cases, the patient was often seen as ‘bed blocking’ for more urgent cases and, in parallel, clinical attention or care seemed to diminish because ward staff seemed to feel that their responsibilities had been transferred. As such, changes in patient condition, such as new illness or relapse, were not always detected as readily as during the early stages of admission. Second, when these delayed patients did reach the point of discharge there seemed to be greater urgency to transition their care, and less attention given to the thoroughness or completeness of this discharge. Again, it seemed that staff had figuratively almost discharged the patient and therefore gave less attention to this process. This was more common for the two orthopaedic units and less so for the stroke services, possibly because of the stroke patient’s ongoing need for direct care.
Broader still, the risks associated with the timing of discharge also appeared to reflect differences in the discharge means for different groups. National policies suggest that discharge should not be seen as an end point, but rather a transition of care. For many participants, however, discharge meant very different things, which framed underlying tensions in the planning and scheduling of care. Specifically, for many hospital staff hospital discharge signalled the end of their direct involvement in patient care, and the passing on of responsibility to other, more relevant, agencies. As such, hospital discharge seemed to be located, in terms of both work planning and cultural norms, towards the ‘end’ of both the working day and the working week. It seemed, for example, that work planning was geared towards Friday discharge to make space for admissions over the weekend and new cases to be discussed at the ‘start’ of the following week. This could be seen with the weekly MDT which, for all research sites, was in the middle of the week, with the intention of reviewing new admissions and planning the discharge of existing patients. In contrast, for those in the community setting, hospital discharge signalled the start of their clinical or caring activities with the patient and was generally preferred to start at the beginning of the working day or week.
The mismatch in preferences and perceived meanings of discharge, as either the end or beginning of care, seemed to frame many of the issues outlined above. For example, discharge delays often came about because social care services were not ready to accept new patients on Friday afternoons or over weekends. More importantly, this created the possibility of relatively minimal or poorly specified care immediately following discharge where many of the required assessments or start-up meetings for organising ongoing care were delayed, usually over a weekend. Many patients and family members described feeling coerced and abandoned immediately following discharge because the community nurse, social care team or GP was not ready to support the patient until the start of the following week. Drawing on participant narratives, the risks associated with timing of discharge are illustrated in Figure 13.
FIGURE 13.
Illustration of timing-related (latent) risks.
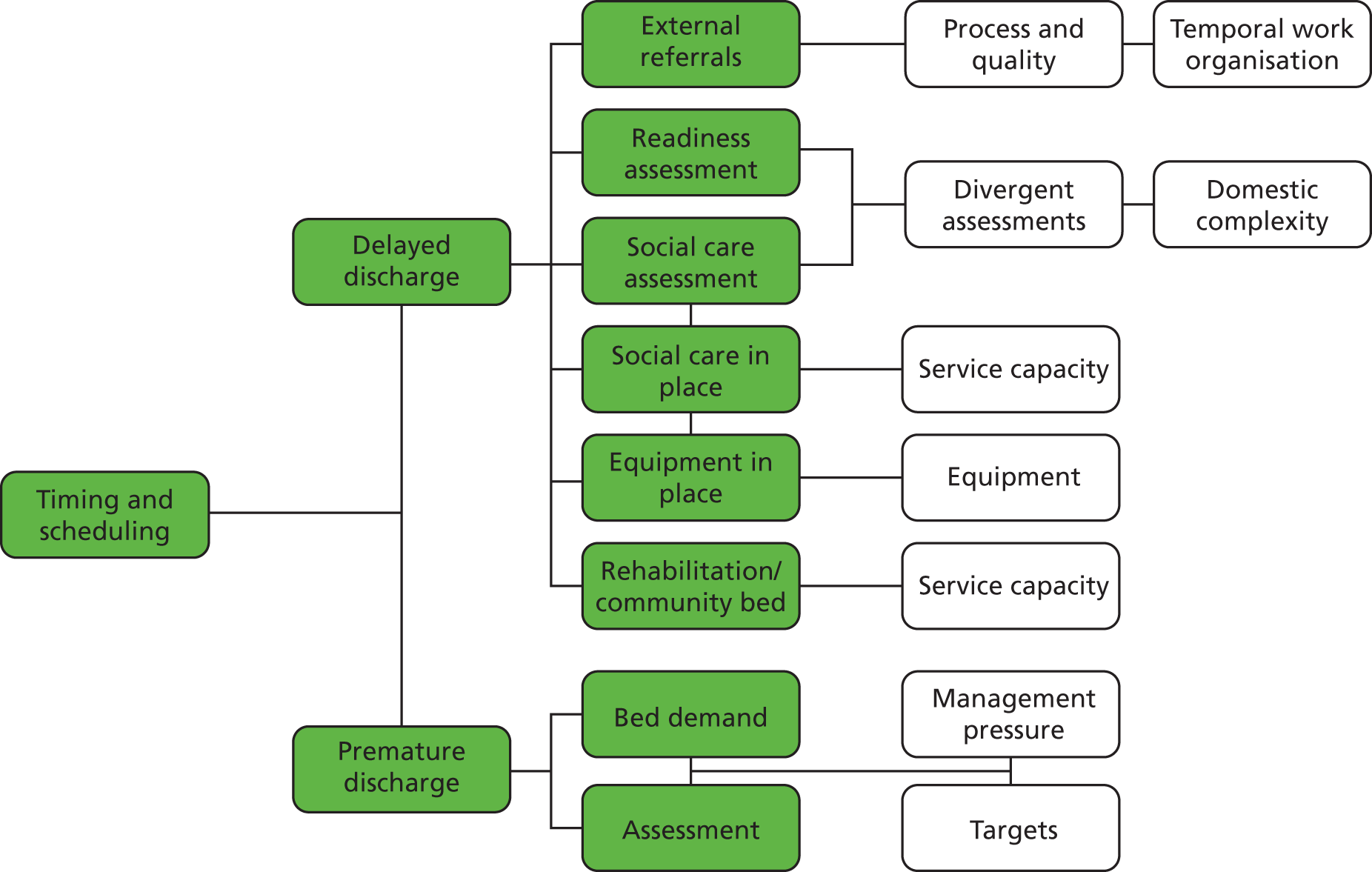
As outlined above, knowledge sharing was integral to determining and supporting timely care transition. Three specific knowledge-sharing dynamics stand out, which broadly correspond to the three phases of patient care outlined in the previous chapter.
In the acute care phase, the planning and scheduling of patient discharge was shaped by a range of cultural and organisational factors, such as at which stage a date of discharge should be set, but also by the range of actors involved in determining these decisions. At both stroke units, decision-making was broadly inclusive, with initial decisions made at the point of admission and regularly reviewed in daily and weekly meetings. At the orthopaedic units (especially Farnchester) discharge decisions were largely made by the surgical team in consultation with nursing staff, with limited involvement of others. Such differences appeared important when determining the patient’s readiness for discharge and the level of care needed following discharge. Where divergent views and perspectives were regularly brought together, decision-making seemed more thorough and robust; this helped to guard against premature discharge, in particular, but also allowed co-ordination with external services, whereby OTs or liaison nurses could relay difficulties in ordering or arranging ongoing care. Where decision-making was more fragmented and carried out by a limited range of clinicians, issues or problems associated with specific tasks or activities were not always adequately addressed. An important issue was whether or not these sites had the opportunities, and also the collaborative patterns of working, to address discrepant views between nurses, therapists and doctors.
A further set of problems related to the patterns of knowledge sharing between health and social care agencies. As described in the previous chapter, these processes were often protracted and complicated and revealed underlying cultural and organisational differences between these sectors. A challenge for social workers was meeting the growing demand for rapid referrals and the limited opportunities and time available for making robust assessments and care planning. A significant issue described at all sites was the shift from hospital- to locality-based social work teams. Although this made it easier for social workers to visit patients following discharge at home or in residential care, it made it difficult to assess need when in hospital or to meet with family members. As such, the opportunities for knowledge sharing with social workers seemed to have reduced. Furthermore, hospital staff described social workers as having limited regular and sustained contact with ward-based staff and rarely attending weekly MDTs. As such, the sharing of knowledge between health and social care was difficult and often fractious, leading to misunderstandings and accusations of delay. At Glipton, hospital staff described a strategy of issuing both referral notices simultaneously, therefore requiring social services to respond more quickly in order to avoid penalties. However, this also seemed to have encouraged further queries at the point of referral as a strategy to delay the process. Where services utilised a discharge liaison nurse, it seemed that many of these issues or tensions were resolved as these nurses acted as a regular contact point for social work teams to clarify issues or to arrange patient visits.
A third knowledge-sharing issue related to the involvement of family members and other community-based carers in the decision-making process. Where services had a more explicit and formal approach to involving patients and their relatives in decision-making, it was more possible to identify and address wider complicating factors associated with patients’ domestic or personal circumstances. Some significant issues related to family disputes, access to housing, the levels of support available and the financial arrangements for onward care. Involvement of relatives early and regularly within the planning process not only enabled more thorough knowledge sharing, but also increased trust and family involvement in care. As described above, helping relatives to understand the use of equipment or adherence to medicines was important. Equally, building trust with family members and gaining their involvement in care planning ensured that often crucial basic issues were addressed by the day of discharge, such as having the home prepared, providing access to equipment suppliers, enabling fitters to access the house to fit steps or grab rails, and being available at the time of discharge to support transition. One problem much discussed among nursing staff was that of family members going on vacation during their relative’s hospitalisation, which could delay discharge.
Communication
Notwithstanding the more direct or manifest safety events, such as medication errors, or the more ubiquitous concern with delays, communication problems and breakdowns featured widely across the narratives of participants. In part, this is arguably a reflection of the type of questions asked during interview and the over-riding focus of the study. That being said, three specific communication issues were widely described by participants as framing discharge safety, while the broader challenges of knowledge sharing are discussed below.
The first, and very broad, communication issue related to the quality of interpersonal relations and teamwork both within and across different care settings. Most participants talked of the importance of an open and inclusive approach to everyday clinical activities and discharge planning. It was described how the quality (safety, timeliness and completeness) of clinical assessments, care planning and task allocation depended upon the quality of face-to-face and interpersonal interactions. Where services had more regular and inclusive opportunities for interaction and communication, for example ward rounds, board rounds or weekly MDT meetings, participants usually described more possibilities for communication, which also framed a clearer understanding of what others contributed to the care process, a greater sense of teamwork and co-ordinated working practices. For example, daily board rounds were widely seen as providing a structured opportunity for people to come together and participate in shared decision-making by carving out time not typically found amidst daily tasks and activities. This opportunity was absent at the Farnchester orthopaedic unit, where clinical groups remained more isolated and independent, and where communication and teamwork were seen as problematic by all participant groups. Similar issues were also noted in relation to the interaction between health and social care teams, where the opportunities for communication and collaboration appeared to have been lessened by recent changes in social work organisation. Additionally, the reliance upon telephone consultations and regular changes in social work staff meant that it was difficult to build lasting and mutually beneficial relationships between these different communities. Looking across the research sites, there were marked differences in local cultures and the importance or value given to teamwork. In the stroke units, there was a clearer sense that teamwork and open communication were essential for patient care and discharge planning, whereas in the orthopaedic units there was a clearer distinction, and lack of communication, between surgical and non-surgical groups. Across all sites, however, staffing pressures, shift patterns and also the wider workload pressures were frequently described as undermining the potential for teamwork and robust communication.
A second and more specific communication issue was linked to the quality of handovers between clinical shifts, between organisational units and between care agencies. Participants described how handovers should provide the key information necessary to maintain and advance patient care, but too often involved relaying basic information which lacked necessary accuracy or clinical detail. Prominent examples of handover failure included the transfer of daily tasks or observation duties between ward shifts at the Farnchester orthopaedic unit; communication during the transfer of care of patients to community hospitals at Glipton; and, more broadly, the handover of care to reablement services. In each of these common examples, participants – usually those receiving the responsibilities for care – described how it was usual for communication to be problematic, with many gaps in their understanding of patient need, including highly important information related to observations or infection risks, as well as more general plans for onward care and rehabilitation. The use of standardised handover checks at all sites appeared to have improved daily communication patterns, and the regular use of board rounds, especially at the two stroke units, was described as improving general communication, task allocation and teamwork. Discharge checklists were used at the Glipton research site, but these seemed to be reserved for more complex patients, when managed by the discharge co-ordinator. There were no checking or documented procedures for supporting communication commonly used during care transition.
The third broad communication issue relates to the quality of documented knowledge, which could influence a variety of discharge planning activities, from prescribing to ordering equipment. A range of documents were regularly used during discharge planning and care transition, yet they were described as being variable in quality, with subsequent implications for the safety of discharge. Discharge letters often featured in the narratives of consultants and GPs as a formal basis for communication between the two. Although these were described as offering a clear, usually medically focused summary of the patient’s care in hospital, anticipated care needs, medication changes and future appointments, they were widely described as a problematic and limited form of communication. For GPs, they were seen as patchy or variable in quality, often providing limited detail, and were usually received long after the patient had left hospital. Some GPs seemed to regard them as a record of past activity, whereas others did seem to use them as a basis for ongoing care planning. Hospital consultants also described a sense of dissatisfaction with discharge letters which were, for some, an outdated and outmoded basis for interactions where instead shared or integrated ICTs should be used. As such, discharge letters were commonly seen as offering limited benefit to the advance of patient care.
Hospital (patient) records varied considerably between sites, which in turn seemed to shape a number of safety-related issues, such as the ease of sharing knowledge between clinical groups, making referrals or ordering equipment. At most sites, patient details and clinical activities were detailed in more than one document or record, usually a ‘medical record’, a ‘nursing record’ and a ‘therapist record’. This arrangement reflects the distinct knowledge requirements and recording procedures of different clinical groups. However, it meant that the knowledge contained within these different sources was typically dispersed and not easily reconciled as a basis for communication or shared decision-making. In MDT meetings, for example, it was usual for different clinical participants to read from their distinct records. A further issue was whether these records were colocated or stored in different hospital locations. At Glipton, therapists were permanently based on the stroke unit and stored their records in a shared office, making it easier for other clinicians to access this information. At the Farnchester orthopaedic unit, however, therapist records were stored in a hospital therapists’ department, making it difficult for ward staff to access relevant information when contacting, for example, external agencies. The main difference was at the Farnchester stroke unit, where a single patient record had been introduced that compiled the different records of each specialist. Although this could make it difficult for staff to simultaneously access the often bulky document, it ensured that all relevant information was recorded in one place.
Information communication technologies are widely described as enabling safer working through more detailed and accurate management of knowledge. A range of ICTs were described across all research sites, including general summary records, prescribing systems, equipment ordering and discharge summaries. Although these were usually described in positive ways, there were reported problems associated with accessing computers in order to complete prescriptions or update records, and in terms of whether or not different ICT systems were integrated. For example, GPs talked about the lack of integration with hospital systems, while one ward clerk described how she needed to use at least five separate computer packages to process one hospital discharge.
A further documentation issue related to the process of making referrals, both within the hospital for tests or scans and, more commonly, to external agencies such as social services. As described above, these issues represented common concerns related to delayed discharge or missing assessments. The problems described often related to underlying differences in understanding about care, or indeed the patient. Those in the health-care setting, for example, tended to talk about the need for detailing information relevant to the patient’s ongoing care needs, whereas those in the social care setting talked more about information required to understand his or her home, personal and financial circumstances. Referral letters generally offered little opportunity to provide sufficient detail of either type of knowledge, and therefore became a focal point for blame, requiring more personal or direct interaction between health and social care staff. For virtually all participants, referral processes were described as unsatisfactory and not enabling a robust or well-developed assessment of patient care needs. Drawing on participant narratives, the communication risks associated with hospital discharge are illustrated in Figure 14.
FIGURE 14.
Illustration of communication risks associated with hospital discharge.
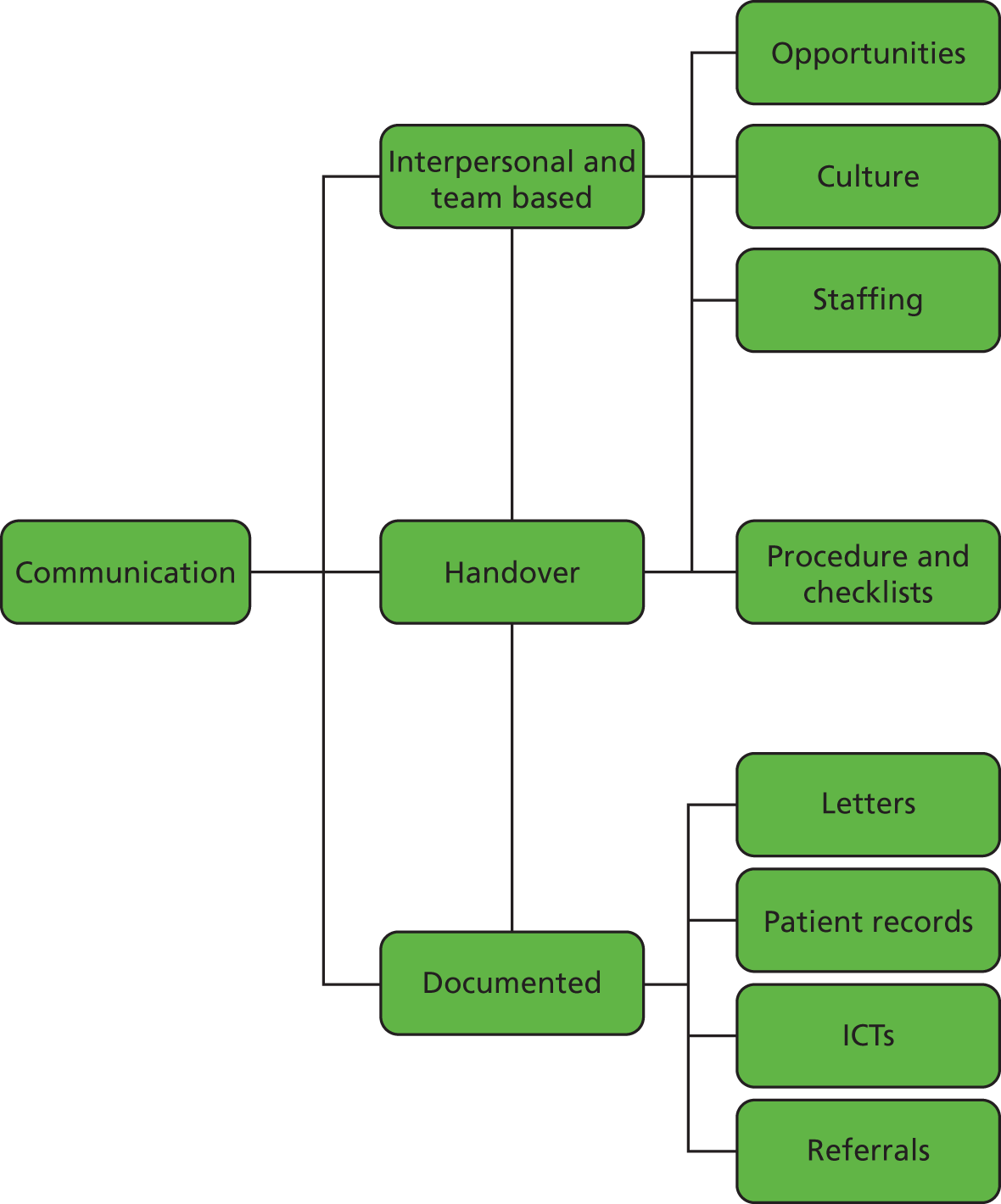
As suggested above, communication features as a risk concern more broadly across the care pathway and often as a less explicit risk issue or one that is taken for granted. As such, participants often talked of communication breakdowns more in relation to other risks, such as in ordering equipment or making referrals. Moreover, the underlying dynamics or patterns of knowledge sharing were also revealed as framing or conditioning many of these risks (or sources of safety).
Conclusion: the contribution of knowledge sharing
This chapter details the threats to patient safety associated with discharge planning and care transition, as perceived and described by study participants. In particular, it highlights seven main categories or types of unsafe patient care. Some are seen by participants as more directly leading to patient harm, such as falls, infection and medicines, while others are interpreted as more latent risk factors, such as equipment, clinical procedures, scheduling and communication. As discussed at the start of the chapter, it is recognised that these narratives are not objective or complete, but reflect the particular roles and positions of participants within the patient journey and their prevailing cultural norms and assumptions about discharge and patient safety. This list is unlikely to be inclusive of all possible safety issues and it does not intend to provide a formal count or taxonomy of risk, but rather to explore the perceptions of different stakeholders. For each of these categories of risk, the chapter draws upon the ethnographic research data presented in the previous chapter to understand how participants’ perceptions, understandings and meanings of risk might be related to and explained by the observed, and variable, patterns of knowledge sharing. In particular, it shows how a range of common social, cultural and organisational factors that are associated with discharge planning and care transition, especially the flows of knowledge involved in these processes, might explain the perceived threats to safe discharge. With specific reference to the research objective, the chapter therefore develops a descriptive account of the perceived threats to patient safety associated with discharge planning and care transition (objective 3) and also shows how the observed patterns of knowledge sharing might represent a latent (and more active) threat to safety (objective 4).
Returning to the overarching theme of the study, the chapter shows how communication and knowledge sharing can play a pivotal role in discharge planning and care transition, representing both an active and a latent source of safety. For example, where knowledge is not shared at an appropriate time, the integration of clinical activities and continuation of patient care can be compromised. Take, for example, the transition of patient care to community hospitals and the common problems of insufficient handover which appeared to frame associated risks of infection. Similarly, problems with knowledge sharing between health and social care teams, and with families, often seemed to frame problems with the scheduling or timing of discharge which could, in turn, lead to problems with ordering clinical tests or medicines. Comparing across the study sites, six significant aspects, indeed variations, in the patterns of knowledge sharing might explain many of the perceived risks identified in this chapter.
First, the chapter highlights the importance of key actors or roles in facilitating discharge planning and care transition, and ensuring that knowledge is effectively shared to promote overall care quality. Discharge liaison nurses, and similar boundary-spanning roles, were commonly found to hold together the complex networks involved in hospital discharge and mitigate against many of the potential complexities and threats to safety that often escalate in routine care. However, alongside these more obvious key actors, the above analysis also shows the importance of other, more taken-for-granted or hidden actors, such as ward clerks and some porters, who complete many of the small tasks, such as ordering ambulances or chasing TTOs, that enable discharge to happen.
Second, the chapter shows how the quality and integration of everyday clinical activities on the ward, especially when providing direct therapies and care to patients, provides an important site for knowledge sharing, where many small tasks and complications can be addressed through rapid and localised knowledge sharing and problem-solving. Those involved rarely seem to appreciate the importance of these interactions, but small conversations and chats, around the patient, at reception areas or in daily board rounds, are integral to the overall continuity of care and highlight the importance of integrated multiprofessional working on the ward to discharge planning and care transition.
Third, the findings also reveal the importance of patient and family involvement in discharge planning and care transition. Relatives often represent the primary source of care outside hospital and patients can also have an important contribution in self-management, whether through adhering to medicines or using equipment. Linked to the above, the involvement of relatives and patients in daily ward-based interactions, such as ward rounds, or during routine care, not only helps to build rapport and trust with clinicians, but also makes for a basis for knowledge sharing from which to educate patients about their ongoing care and enable relatives to play a fuller role.
Fourth, the chapter shows that the interaction between acute and community-based health and social care agencies was one of the most important knowledge-sharing relationships that could frame potential risk. The exchange of knowledge between hospital-based staff (and also patients) and social services, community health-care providers, GPs and even social care agencies was generally found to be problematic and a source of uncertainty. In particular, the link between hospitals and GPs seemed especially precarious, with GPs often having little early warning or knowledge about potential patients-at-risk. Similarly, social care providers received almost no detailed knowledge about the necessary package of care and were usually required to initiate or repeat patient assessments. More significantly, the general relationship between health and social care seemed strained and fractured, with generally low levels of communication and integrated working, which resulted in parallel and disconnected forms of patient care.
Fifth, the chapter also shows how material resources and media, especially ICTs, could support knowledge sharing and reduce the threats to safety, if appropriately developed and used. Whiteboards, patient records and computers played a pivotal role in everyday care, but there were clear variations in how they were used and whether or not they supported knowledge sharing and safety. In some instances, for example medical prescribing or equipment ordering, ICTs were useful, possibly because they involved a relatively linear process of direct knowledge sharing or request. In other, more complex and multiprofessional contexts, ICTs appeared less able to cope with the dynamic and changing flow of knowledge, and as such whiteboards and patient records appeared to provide more adaptable resources. Significantly, however, the use of these resources was linked to the extent of integrated working in general, and where they were embedded within and integral to collaborative working, they were more likely to support knowledge sharing, unlike those settings where these resources reinforced more sequential, linear and siloed working.
Finally, the analysis further shows how the influence of wider differences in knowledge, culture and organisation frame knowledge sharing and discharge safety. The chapter shows, for example, how those involved in discharge planning and care transition operate within distinct knowledge or epistemic communities, where discharge can mean very different things and patient-related knowledge can be used in different ways. Common examples were discrepant views between hospital staff about patient readiness for discharge, and between social care teams and families concerning the levels of care needed. Cultural differences also framed the patterns of knowledge sharing, especially in relation to the norms and customs associated with hospital discharge; this includes, for example, whether discharge was seen as the start or end of care and, more importantly, to what extent collaboration and integration was seen as meaningful or valued by different groups. Finally, the chapter shows how organisational constraints and factors also influence knowledge sharing, whether in the availability of human resources, the use of checklists or, further still, management priorities and targets for patient throughput.
Chapter 6 Conclusion
Introduction
The study supports the view that hospital discharge is a complex and vulnerable stage in the patient’s journey. It develops the idea that knowledge sharing, especially between health and social care agencies but also others in both acute and community settings, can help mitigate this complexity and promote safe discharge. Knowledge sharing is defined as the sharing of both implicit ‘know-how’ (the meanings, beliefs and practices that characterise individual groups) and more explicit knowledge (evidence, assessments, reports) which, when shared and used by others in the same system of activity, can foster more co-ordinated or collaborative practices. 10–12 Knowledge sharing is therefore interpreted as a source of safety within complex systems,111 helping to integrate dynamic and tightly coupled interactions based upon shared understanding and integrated working. In the case of hospital discharge, knowledge sharing can help those in health and social care, for instance, better understand their distinct contributions and roles within discharge planning and care transition, and thereby foster joined-up working, in terms of ongoing rehabilitation and recovery.
The preceding chapters show how hospital discharge does not occur as a single or isolated event, but rather through a complex series of linked incremental situations of knowledge sharing. It also shows how variations in these patterns of knowledge sharing (frequency, range of actors, media of sharing and use of knowledge) might be interpreted as latent factors that bring about or mitigate the possible threats to patient safety. In line with the study objectives, this concluding chapter develops the learning from the previous two chapters by identifying and elaborating factors, strategies and interventions that might promote or be associated with enhanced knowledge sharing in the context of discharge planning and care transition. This learning is grouped according to the (a) roles, (b) relational opportunities, (c) culture and ethos and (d) organisational factors that support (or hinder) knowledge sharing. These strategies and interventions are not formally evaluated or appraised; rather, the study evidence suggests that these might be developed through subsequent research as the basis of new or modified discharge interventions. This concluding chapter also outlines the study’s broader contributions to theory and research in the area of patient safety, especially the idea that complex system processes operating in different care settings represent a significant latent threat to patient safety. It also discusses the limitations of the study and areas for future research.
Towards safer discharge
The study develops the idea that hospital discharge depends upon a complex series of linked incremental activities and situations, where groups of actors and resources come together, at a given time and place, to exchange and use knowledge in the processes of discharge planning and care transitions. It also suggests that the inherent complexity of these situations, including the patterns of knowledge sharing within them as well as the interdependencies between them, represent latent threats to patient safety. Specifically, where knowledge sharing is missing, incomplete or not appropriately timed, there is a greater possibility that aspects of patient discharge and ongoing care will not be adequately planned or arranged, thereby leading to delays or harm related, for example, to falls, infection or the use of equipment. As shown in the previous chapters, a range of factors inhibit or promote knowledge sharing, which stem from underlying differences and tensions in stakeholders’ knowledge, culture and organisational contexts. Building on these findings, the study identifies a number of learning points from which future strategies or interventions might be developed to promote knowledge sharing, mitigate system complexity and enhance patient safety. These are categorised according to the (a) roles, (b) relationships, (c) cultures and (d) organisational factors that enable, support or frame knowledge sharing and hospital discharge.
Roles
First, the study shows how certain key actors or observed roles made significant contributions to discharge planning and care transition, not necessarily in terms of their input into individual tasks, but rather through helping to co-ordinate the entire process, mitigate system complexity and facilitate knowledge sharing. In particular, discharge liaison nurses, community stroke nurses and ESD teams worked across occupational and organisational boundaries, often in the form of in-reach or outreach services. 53,61 Their contribution to discharge safety can be summarised along four lines. First and foremost, they supported the sharing of knowledge within and across different boundaries, helping actors in one setting to recognise and use the knowledge of another. This could be seen, for example, in the way community stroke nurses reached into the hospital setting to provide knowledge about community services, or discharge liaison nurses reached out to community health-care teams to co-ordinate onward care. Second, these actors often became, in themselves, repositories of knowledge, whereby they accumulated and recombined different bodies of knowledge found dispersed across the wider system. Operating as repositories of knowledge, they were often sought out by other actors for the purpose of rapid problem-solving and for guiding decision-making. For example, discharge liaison nurses were often sought out by others to navigate complex discharge processes. Third, through their developed knowledge of the wider care system and its stakeholders, these key actors often assumed a co-ordinating role by supporting the work of others. For example, discharge liaison nurses often supervised other ward nurses and therapists when organising discharge, or administered key paperwork. As such, they became informal or distributed leaders of discharge who would direct, supervise and monitor the work of others. Finally, these actors became the champions or advocates of the patient. They worked to develop a combined or holistic view of each patient, through pooling the knowledge and experience of different actors and working closely with patients and families. They also provided a sense of continuity for patients, working with them early in admission, through discharge planning and often providing follow-up care in the community (this was especially true of the community stroke nurse). This proximity to the patient provided a further level of insight or know-how, but meant that patients also had a source of knowledge or guidance when confronted with difficult decisions.
As well as the more obvious discharge liaison roles, the study found that other ‘hidden’ or backstage actors made similar contributions in discharge planning and care transition. This was exemplified by the taken-for-granted work of ward clerks, porters, voluntary workers, domestic staff and ambulance drivers. These actors also supported routine information exchange between groups, for example retrieving records, passing on memos or chasing up referrals. More than this, they acted as a repository of knowledge and contextual know-how of the wider care system. They also performed hidden ‘repair’ work, by double-checking referrals, chasing up missing documentation, reminding clinicians to complete tasks and dealing with the consequences of delayed or inaccurate communications. These hidden actors represented the ‘small cogs’ that ensured the overall operational performance of the system.
Elaborating the significance of these roles, knowledge brokers and boundary spanners are those actors who ‘get the right information, to the right people, at the right time’. 117,149 Knowledge brokers are able to work within and across engrained occupational and organisational boundaries, either through their roles within more than one group or by having extended social relations with a wider range of groups. 149 Through these relationships, knowledge brokers can identify, translate and support the use of knowledge between groups, thereby supporting learning and integration. As such, they are effective translators of knowledge as they are able to recognise, articulate and reframe the knowledge and working practices of one group, so it can be understood and acted upon by others. In the context of this study, these key actors possessed a form of ‘architectural’ knowledge of hospital discharge, i.e. they recognised how the wider system and its inter-related parts fit together, unlike other stakeholders who tended to have a more ‘component’ view of their individual contributions within the system. This architectural knowledge was integral to how they co-ordinated different activities, mediated gaps between staff groups and developed more collaborative practices. This enabled these actors to co-ordinate the complex discharge process, ensuring that decisions were reached, recorded and acted upon. As such, they reinforced the standards of effective discharge through promoting good practices and, in particular, placing the longer-term needs of the patient at the centre of their activities.
During the course of the research, the study found evidence of these roles being scaled back or discontinued as a result of funding constraints, leading to more fragmented knowledge sharing, reduced co-ordination and growing uncertainty in discharge planning. Although the reduced dependence on single actors can promote more shared and collective responsibility for hospital discharge, it seemed to reduce the overall co-ordination and coherence of discharge planning, limited active problem-solving and inhibited knowledge sharing across boundaries. As such, the study cautions against the loss of knowledge brokers and supports the creation of further opportunities for actors to bridge the gaps between acute and community care.
The study suggests that formally designated discharge co-ordinators or similar in-/outreach teams might be introduced or extended to foster knowledge sharing across organisational and occupational boundaries, with clearly designated and protected responsibilities for co-ordinating discharge planning and care transition.
The study also found that a number of seemingly important groups were often marginal or had limited involvement in collective discharge planning and care transition. These groups included social workers, some community health-care services and GPs. Social workers, for example, appeared to have a highly limited, narrow or technical role in assessing ongoing care needs, checking the patient’s eligibility and arranging a package of care. There was little evidence, however, of social workers actively working with others in the hospital or community setting to produce more comprehensive or joined-up decision-making. Similarly, GPs were largely decoupled from the planning of patient discharge, despite having primary responsibility for patient well-being and continuity of care in the community. Few agreed to participate in the study, but those who did suggested that the existing patterns of communication with the local hospital provided only a partial and descriptive understanding of ongoing patient care needs. Moreover, they suggested that such information was often communicated after the patient had returned home, thereby placing the GP in a reactive position. As such, community nurses often acted as the primary contact point and conduit of information between the patient and the GP following discharge.
The study suggests that greater attention is needed to the timing, detail and accuracy of communication between hospital, GP and social workers both before and at the time of hospital discharge. This might include notifications of discharge, opportunities to (remotely) participate in decision-making and extended use of ICTs.
Relational opportunities
Second, the study found that discharge planning and care transition occurred through a complex series of linked activities and situations. These temporarily stable and spatially bounded situations or networks provided the primary opportunities for knowledge sharing, and together provided the framework or constellation of activities through which hospital discharge was progressed. Despite many of these activities and situations being informed by discharge planning policies,14,30 the study found significant variations in their form and function as well as the connections between them. In particular, it finds a number of interesting differences in the use of both formal and informal opportunities for knowledge sharing and, more broadly, the importance of physical or functional proximity in enabling knowledge sharing.
The study shows how formal situations, such as weekly MDTs and ward rounds, greatly facilitated knowledge sharing. In general, these represented a designated opportunity or ‘hub’ for sharing knowledge, addressing relatively common or regular tasks (i.e. agreeing the date of discharge or initiating referrals),47 formulating decisions and allocating resources. In short, these formal meetings were often the key decision-making points around which other activities or decisions were organised. That being said, the potential for these formal situations to contribute to discharge planning and care transition depended upon the range of actors involved, how they interacted with one another and the assumed purpose and ethos of the meeting. Specifically, knowledge sharing and shared decision-making was more apparent where these meetings were organised as more open and discursive opportunities to explore different perspectives, and where the over-riding purpose was to inform more comprehensive and patient-centred care planning. This was particularly evident in the stroke service. In contrast, others involved only a limited range of actors, were centred on information-giving and were primarily used to co-ordinate uniprofessional activities. This was exemplified by the Farnchester orthopaedic MDT meetings. Such differences explain the relative contributions of MDTs, for instance, to overall discharge planning, and where these situations offer limited opportunities for knowledge sharing, they also fail to contribute to the overall progress of hospital discharge. In such circumstances, stakeholders need to find alternative means of sharing knowledge. As such, the study suggests that MDTs should remain an important feature of discharge planning but based upon some form of inclusive representativeness of the wider workforce and on the assumption of collective decision-making.
Notwithstanding the contribution of weekly MDT meetings to discharge planning, a universal finding related to their position or timing within the weekly flow of care. In all sites, they were organised towards the middle of the week, for example Wednesday afternoon, on the assumption that this enabled more comprehensive assessment of newly admitted patients and the planning of care for those about to be discharged. However, this could make it difficult to escalate, arrange and complete discharge planning for patients by the end of the week, while creating time pressure on both ward staff and social work teams to complete tasks. Furthermore, it led to the increased likelihood that patients would be discharged on Friday with limited weekend care or would be kept in hospital until the following week. This not only highlighted a mismatch in the timing of work scheduling between health and social care but, more broadly, a mismatch between the standard working week (Monday to Friday) and the complexity of patient care, which not only spanned more than 10 days, but remained relatively constant over weekends and bank holidays. Aligning clinical decision-making to the patient pathway, and reducing reliance upon one midweek MDT meeting might alleviate these pressures, especially where more informal and daily knowledge-sharing opportunities are available.
Alongside these more formal situations, the study therefore highlights the contribution of more informal and daily knowledge-sharing opportunities. These included everyday encounters during ward-based care, handover, at reception areas, in corridors and during rest breaks. In these less structured situations, clinicians, patients and families often appeared to develop a sense of rapport and understanding that enabled the free flow of experiential know-how, related, for example, to psychological well-being, personal care or domestic circumstances. For example, it was often during the intimate acts of toileting or personal hygiene that patients would share apprehension about the ability of their relatives to provide this level of care. In other words, through these situations clinicians were able to develop a richer understanding or awareness of patients and their relatives concerning their ongoing care needs and, in particular, the use of certain devices and equipment to support their recovery outside hospital. These informal situations became a basis for experiential learning or education which then supported self-management and adherence. 150 These situations also enabled the flow of know-how between clinicians, whether working together in direct patient care or interacting during board rounds or other handovers. Through these everyday interactions, clinicians came to appreciate the expertise, practices and contributions of others and, consequently, more collaborative practices could emerge. The contributions of these informal knowledge-sharing opportunities to everyday knowledge sharing and integrated practice were reinforced in settings where they were absent or less common, i.e. where board rounds were infrequent or clinicians worked in a more sequential and siloed way, because these sites exhibited less shared understanding of discharge processes and more fragmented working.
The study suggests, therefore, that both formal and informal relational opportunities contribute to hospital discharge, but more significantly, it suggests that the interplay or connection between these formal and informal situations is integral to overall discharge planning and care transition. Specifically, the research shows how more routine and informal day-to-day interactions between clinicians, patients and families enabled the sharing of more tacit and experiential know-how about the patient’s personal circumstances. This experiential know-how was typically used to inform immediate decision-making and clinical care, but it was also relayed or shared within other, more formal situations, such as the ward round or the weekly MDT meeting, to enrich other forms of explicit knowledge and to enhance overall decision-making. In other words, the recombination of explicit information and experiential know-how was made possible through actors’ participation in multiple formal and informal situations. This suggests that where actors are confined to only the informal (or formal) situation, and not permitted to participate in both, there is less scope to draw together and use both the implicit and explicit forms of knowledge.
Developing this line of analysis, the study suggests that knowledge sharing relies upon open and reciprocal interaction where stakeholders are colocated or have ‘functional proximity’ in formal or, more often, informal situations. This everyday proximity enables actors to share their unique know-how, develop mutual understanding and common working practice, build trust and rapport and, in general, work more collaboratively. 117,126 This could be seen, for example, where therapists were permanently based on the acute wards, had routine interactions with other clinical groups, and more easily shared knowledge and collaborated with coworkers. Problems associated with a lack of colocation could be seen where hospital-based social workers had been transferred to community localities, which not only restricted opportunities for more routine interactions between health and social care teams, but fractured the sense of trust and understanding between these groups. Similarly, where therapists were based within a central hospital department, rather than on the given ward or unit, there was less evidence of knowledge sharing and collaboration with ward nurses. Although periods of service reconfiguration inevitably require adjustments, the loss of this functional proximity in discharge planning seemed to exacerbate the tensions between health and social care. As such, the study encourages the promotion of more routine and regular contact or functional interaction between different agencies around common problems, including the introduction of both formal and informal settings.
The study suggests that increasing the colocation and functional proximity of different stakeholders throughout the discharge planning process is likely to support knowledge sharing and collaborative working. More formal knowledge-sharing opportunities, especially MDTs and ward rounds, should be used to promote the structured involvement of different stakeholders at key decision-making points, and more informal opportunities for interaction and knowledge sharing should be promoted in day-to-day practice, especially through the colocation and integration of different clinical tasks.
The study suggests that increasing the colocation and functional proximity of different stakeholders throughout the discharge planning process is likely to support knowledge sharing and collaborative working. More formal knowledge-sharing opportunities, especially MDTs and ward rounds, should be used to promote the structured involvement of different stakeholders at key decision-making points, and more informal opportunities for interaction and knowledge sharing should be promoted in day-to-day practice, especially through the colocation and integration of different clinical tasks.
Culture and ethos
The study shows how each of the occupational groups and organisational units involved in discharge planning and care transition appeared to have, to varying degrees, a distinct culture or ethos of discharge. That is, they had distinct ways of making sense of discharge, prioritising or valuing discharge, allocating or taking up responsibilities for discharge and involving the patient in discharge planning. Differences and similarities in these cultures inherently framed the possibility for knowledge sharing and integrated working; for example, where actors held different priorities for discharge they were less likely to place the same value on key activities in the discharge planning process. This culture, or the ethos of discharge, is important because it frames the possibility for integration and knowledge sharing. Elaborating this idea, four specific features are emphasised as framing knowledge sharing.
The first relates to the way different groups made sense of or gave meaning to hospital discharge. A key area of difference was whether discharge was understood as an ‘end point’, a ‘beginning point’ or an ‘ongoing’ feature of patient care. Many hospital staff, for example, saw discharge as an end point that was positioned at the ‘end of the day’ or the ‘end of the week’. In contrast, community-based groups saw it as the beginning of patient care, which was reflected in the assumption that it should start at the ‘beginning of the day’ or the ‘beginning of the week’. This simple mismatch in understanding explained many complications in the integration and co-ordination of acute and community care, including when knowledge should be shared and when discharge should be scheduled. These mismatches often seemed to frame many of the breakdowns in communication and delays in care transition. Where different groups saw discharge in similar ways, often as a single stage in an ongoing care process, there was greater emphasis on working together to share knowledge and hand over responsibility.
The second cultural feature relates to the relative priority or value given to hospital discharge within the work and organisation of different care providers. Some groups, especially surgeons, appeared to prioritise the initial period of acute patient care, including diagnosis and surgery, but placed less emphasis on planning for onward care. For others, hospital discharge was a high priority that triggered or determined the pattern of their work, and was central to their overall work and identity, i.e. discharge co-ordinators and social workers. These differences did not simply reflect when or how discharge planning should commence, but rather the underlying significance or value of discharge to both the patient and the wider care system. When clinicians valued discharge highly as a key stage in the overall care pathway, they were more likely to value knowledge sharing that supported discharge planning and care transition. Further, a mismatch in the priority given to discharge helps explain some of the tensions observed between different groups, especially in regards to their lack of interaction or involvement in discharge planning.
Following on from the above, the third feature reflects whether discharge was regarded as ‘somebody’s business’ or ‘everybody’s business’. In some sites, it was apparent that discharge planning was a shared responsibility of the entire health and social care team, with the expectation that all groups participate in knowledge sharing and shared decision-making. In other settings, discharge responsibilities were delegated to individuals or subgroups, with the expectation that this freed up the work of the wider clinical team. Where discharge responsibilities were devolved or delegated it seemed to signal to others that there was little or limited need to participate in decision-making, and as such it reflected a less integrated or collaborative workplace. This could mean that knowledge gathered through informal situations was not valued as important or worthy of sharing in other, more formal situations. Although the delegation of discharge responsibilities to a single group (discharge co-ordinators) can help with workload management, a more inclusive approach seemed to support more collaborative working and mutual learning.
The fourth cultural feature relates more broadly to the relative value given to patient (and family) involvement in discharge planning. Arguably, patients are at the centre of their own care journeys and represent the only point of continuity between different care settings. In other words, they can be both the focus and medium of knowledge sharing. Where stakeholders actively involved patients and relatives in care planning, knowledge sharing allowed not only for a more bespoke and patient-centred care transition, but also for learning among clinicians where different members of the care team co-ordinated their distinct activities rather than addressing sectional or uniprofessional concerns. Although all sites claimed to recognise and value the contribution of the patient and family to discharge planning, only one site appeared to proactively involve these stakeholders in formal situations, including the use of designated family meetings and the routine use of daily clinical encounters to engage patients in the planning of their own care. The importance given to the patient at this site reflected a broader culture of inclusive and integrated working that supported knowledge sharing and discharge planning.
Together, these four cultural features highlight how a ‘culture of collaboration’ frames discharge planning and care transition. An ethos of discharge based on collaboration was more evident where actors shared broadly common understandings or meanings of discharge and similarly valued the importance of discharge – not just within their own work, but also for the wider service and individual patients – and where there was an assumption that all stakeholders, including patients, should participate in supporting discharge planning and care transition. Looking across the research sites, it is doubtful that such a culture of collaboration was evident across the wider care system, yet there was evidence of this culture in different organisational pockets. Furthermore, it seemed that where services utilised designated discharge co-ordinators, had enhanced levels of functional proximity and actively involved the patient in discharge planning, they also exhibited a strong sense of collaboration and integration based upon a broadly shared ethos of discharge.
The study suggests that efforts should be made to foster shared understandings, values and priorities around collaborative discharge planning, based upon aligning divergent meanings, enhanced exposure to and functional proximity with divergent practices and involvement of the patient in discharge planning and care transition.
Organisation factors
Finally, the study highlights the wider significance of organisational and interorganisational factors as influencing both the patterns of knowledge sharing and hospital discharge. Although each study site had a particular organisational and system-wide configuration, including systems of commissioning and governance, the study suggests that four common factors appeared to have an impact upon knowledge sharing and relate more broadly to the extent of integration and collaboration in discharge planning and care transition.
First, the discharge policies, procedures and pathways can have an important structuring influence on the patterns of knowledge sharing, especially through stipulating when decisions should be reached and communicated, and in some cases defining the anticipated pathway of patient care. 14,24,30,47,53,30,62,94 In general, the recommended use of MDT meetings and national guidelines for initiating social care referrals were strongly followed in all sites. 47,30 At the same time, the findings suggest that slavish adherence to such policies can potentially compromise the ability of stakeholders to work flexibly or to adapt to complex cases, especially patients with comorbidities or complicated personal circumstances. That being said, two particular policies or procedural features appeared to be particularly beneficial in supporting knowledge sharing. The first was the use of a discharge checklist or summary. 94 Although all sites had developed discharge summaries, these were rarely used, and often seemed to be completed post hoc as a bureaucratic exercise. 94 At the Glipton orthopaedic unit, however, such checklists had been modified by the discharge co-ordinator and were regularly used prospectively to collate key information, record outstanding tasks and co-ordinate the discharge process. It appeared that national frameworks and tools require some degree of translation and modification to fit with local practices and, more importantly, need to be valued by a local champion in order for them to be taken up.
The second procedural feature related to the setting and use of an expected date of discharge (EDD) to direct and co-ordinate discharge planning activities. 30 The study found that where an EDD was set, usually within 48 hours of admission, clinical work appeared to be more explicitly directed towards discharge planning, in the sense that it brought together and galvanised disparate groups towards a shared or common target. When adopted and made visible, for example on whiteboards, a preliminary EDD acted as a shared goal and point of reference against which different groups could focus their work. Sites that set an EDD tended to use it as a flexible rather than hard target, given that patient needs often changed, but it still helped to focus attention. For example, in daily interactions or weekly MDTs, the EDD became an important marker and point of reflexive assessment, i.e. ‘are we still on target?’. EDD setting can be seen as triggering consequential collective activities and knowledge sharing when embedded as part of the cultural norms of practice. At the same time, pressures to meet more formal organisational or managerial targets, such as the 10-day NoF pathway, were frequently considered as compromising professional practice. Although national policies and procedures can structure and guide discharge planning, the most significant contributions to knowledge sharing appeared to be the use of MDTs, the potential use of discharge planning tools and setting an EDD.
Second, and linked to the above, the study found that the availability, design and use of various technological and material resources strongly influenced the potential for knowledge sharing. This included more traditional paper-based records, as well as a large variety of information technologies, such as telephone, fax machine, computer software and hospital bleeper, which were all used on a daily basis for communicating between groups. In general, well-co-ordinated, easily accessible and legible patient records were integral to knowledge sharing. Where such records were developed along uniprofessional lines or in duplicate, or were stored within different organisational units, the sharing of knowledge became difficult. Conversely, where records were colocated and treated as an open resource, i.e. as a single care record, knowledge sharing was more apparent and discharge planning more co-ordinated. Furthermore, the excessive demands of completing paperwork were frequently described as delaying discharge activities, creating confusion and leading to communication breakdowns. As such, fewer and more straightforward methods of documentation might further simplify discharge planning. A significant resource was the use of whiteboards to help share knowledge and co-ordinate daily activities. These provided more real-time access to information and helped to structure daily planning of work. More than this, they acted as a type of departure board whereby each patient’s progress, date of discharge and outstanding tasks could be easily monitored and updated. Although these lacked the detail of patient records or ICTs, they often provided the primary ‘go-to’ source of information about a patient before seeking additional sources of knowledge either by referring to the records or consulting with other members of staff. In short, records and materials need to provide timely, rapid and robust access to knowledge within the parameters of routine day-to-day practice.
With particular regard to the use of ICTs, the study found no consistent approach. Where systems were used, i.e. for prescribing or ordering equipment, they generally supported less personalised but more timely knowledge sharing. For example, it was possible to request scans, medicines or equipment ‘out of hours’. However, a problem across all research sites was the fragmentation and duplication of computer programmes. For example, ward-based staff often needed to switch between different systems to prescribe drugs, order equipment, complete letters, gain access to hospital information or bring up referral forms for community health services. This took time and also required staff to retain different sets of login information. In some locations there was limited access to computer terminals, and queues and interruptions were a common occurrence. Furthermore, focusing on the processes of information technology could be seen as taking attention away from the content of communication, increasing the communication workload and the possibility of confusion or inaccuracy. This could be seen to contribute to errors in record keeping that were subsequently passed around the system.
Third, the study found that patterns of leadership influenced the general pattern of discharge planning and care transition. At all sites, there was an over-riding sense of medical leadership where doctors led MDTs, ward rounds and other key decision-making situations. In general, this type of medical leadership was important when drawing together and completing different sources of knowledge around more complex or ambiguous issues. 151 In many instances, the medical doctors provided a level of authority for decision-making, as well as for structuring the overall process. However, where doctors were less active in daily activities and offered less support for collaborative working, there also appeared to be less overall structure and coherence to discharge planning, for example within the Farnchester hip fracture service. Medical leaders could also have a strong influence on the ethos and culture of patient care in general, and discharge in particular. As noted above, services were characterised by different assumptions and customs around the importance of collaborative working, which often stemmed from the approach fostered by the senior medical leaders; this was particularly evident at the stroke units. A further example of medical leadership was seen where doctors interacted, and sometimes came into conflict, with service managers or administrators in regards to escalating ‘early’ patient discharges in order to meet service-level targets, for example to reduce delayed discharges or increase bed availability. Here, medical leadership was found to articulate the continuing needs of acute care, thereby countering the demands of bed managers or ward managers.
In less formal ways, examples of distributed leadership were also observed in day-to-day problem-solving around discharge. 152 For example, discharge co-ordinators and more experienced nurses provided support and guidance to more junior colleagues when they struggled to understand discharge procedures. In other settings, more ‘reluctant leaders’ (ward clerks, social workers, ESD leads) were found to ‘step up’ and ‘fire-fight’ in situations that seemed to be spiralling out of control, especially when a series of activities had not been completed on the day of discharge, for example organising TTOs, ordering transportation and contacting the family. The patterns of knowledge sharing supported by these informal leaders not only supported the discharge of individual patients but, more broadly, promoted collaborative learning and shared understanding among the wider care team. In the community settings, however, leadership seemed particularly absent. Although different social work teams, social care agencies and health-care teams had designated ‘team leaders’, these roles seemed either administrative in focus (social workers) or focused on localised clinical care. As such, there was little over-riding sense of leadership for ongoing care planning, except by some community stroke nurses, and knowledge sharing tended to remain isolated within individual care teams with no over-riding sense of collaborative or joined-up care.
Finally, the study highlights the influence of wider organisational priorities and resource constraints in shaping (both positively and negatively) discharge planning and care transition. Across all sites, there was pressure to improve performance in line with measures enshrined in national audit documents, chiefly the National Sentinel Stroke Audit (NSSA) and the NHFD. These identified factors such as length of stay, timeliness of treatment, involvement of relevant professionals and other best practice guidelines by which the organisation’s performance on particular conditions would be judged, with future financial implications for the organisation. These measures appeared to shape the broader organisation and management of ward-based priorities and planning; for example, skill mix, care pathways and availability of resources were partially linked to the priorities set out in the national measures. Such targets framed discharge planning and could, in many instances, help focus activities towards a common goal in much the same way as an EDD. However, this seemed to depend upon the type of medical leadership, for example where leaders could translate organisational targets into more clinical-facing priorities, and where they would mediate tensions between organisational and professional goals.
There was also important variation in priorities between health and social care organisations. Whereas hospital priorities were focused on progressing individual patients along a particular pathway, social services viewed discharges on a more collective level, with generic population-based guidelines relating to response time, fulfilment of care preferences and funding levels. As a result of this, social workers placed a greater value on assessment of ongoing need rather than patient pathway targets. This meant that there was a lack of shared understanding around the urgency or requirements of particular cases. In general, there was little evidence that health and social care agencies really appreciated the local pressure and organisational constraints that each faced, and which made integrated working complicated.
There were also pronounced financial and staffing constraints across all health and social care settings as a consequence of current spending restraints. This framed changes in the provision of social care services and the funding of specialist roles, especially discharge co-ordinators. More broadly, it was observed that staff levels placed considerable demands on routine working practices and limits on the opportunities for different staff groups to work openly and in collaboration around discharge activities. This is an inherent feature of contemporary health-care organisation, and calls for creative ways of using scarce resources to better co-ordinate the networks of activity necessary for effective care delivery.
The study suggests that knowledge sharing might be supported through (a) relatively standardised discharge planning procedures, checklists and the use of EDDs, if they can accommodate unanticipated change; (b) the use of accessible and shared patient records; (c) ICTs that are streamlined and simplified into a single discharge system; (d) strong professional leadership which promotes collaborative working, but also more distributed leadership which supports everyday problem-solving; and (e) the use of service-level targets and EDDs to foster collaboration towards a share goal, rather than as an assessed (or punitive) expectation.
Summary of key learning points
Knowledge sharing is likely to be enhanced, system complexity mitigated and discharge safety improved where:
-
discharge co-ordinators, and other boundary spanners, are appointed to co-ordinate discharge planning and facilitate the exchange and use of knowledge across organisational and occupational boundaries between otherwise disconnected groups
-
different health and social groups, and other stakeholders, are colocated and/or afforded functional proximity in day-to-day work, and local (informal) learning is actively utilised in more formal decision-making settings
-
different stakeholders share the view that hospital discharge is an ongoing but crucial stage in a complex care pathway and it is everybody’s business, including the patient’s, to support and contribute to discharge planning and care transition
-
locally adapted discharge procedures and checklists are used in conjunction with simplified, streamlined and shared record keeping and ICT systems
-
formal and distributed leadership supports integrated working, and goals and targets are aligned to changeable patient- and service-level needs.
Contributions to theory
The study offers a number of potential contributions to contemporary theory and debate in the field of patient safety. At the outset, it was suggested that the reconceptualisation of patient safety, based upon theories and frameworks developed in the fields of social psychology and human factors, had made a significant contribution to policy and practice. 1,2,96,101 This approach suggests that patient harm is not necessarily brought about by individual negligence, malice or incompetence, but rather is conditioned, enabled or exacerbated by wider environmental or upstream factors. Despite the important contribution of ‘systems thinking’ to patient safety research and practice, the study also suggests that this approach might be extended in a number of areas. First, the application of systems thinking to health care, and possibly other settings, often appears to be too linear, focusing on causal chains or relationships between latent factors and active errors. This often downplays the inherent complexity of health organisation and delivery, especially the persistence of non-linear relationships. Second, the application of systems thinking often remains at the level of the local work environment or clinical microsystems, without fully acknowledging the influence of broader organisational, cultural or institutional factors. This includes the influence of wider regulatory procedures, professional powers and broader sociocultural institutions. Third, and linked to this, patient safety research tends to focus within care settings, such as the operating theatre or pharmacy, without giving equal attention to the sources of safety located between care settings and processes, as exemplified by hospital admission and discharge.
Taking hospital discharge as its focus, this study directly addresses these three issues to highlight the inherent complexity of health-care systems, especially the interdependencies between heterogeneous actors, and where the sources of risk are located within these complex patterns of interaction and dependancy. 111,112 Specifically, it shows how discharge planning and care transition involves non-linear, dynamic and recursive interactions between heterogeneous actors working within and across various organisational settings. From this perspective, safety is located not only within the components of the system, but in the interdependent couplings of system actors, which represent a latent, non-linear threat to patient safety. It also suggests that system complexity, and therefore the threats to patient safety, might be mitigated through enhanced knowledge sharing and collaboration, so that different parts of the system have a better appreciation of how other parts contribute to the whole, leading to more integrated and safer working. The analysis further demonstrates how particular forms of knowledge sharing seem effective at promoting collaboration and reducing system complexity. It therefore encourages further research on the relevance and application of complex system theories to understanding health-care service and delivery in general, and patient safety in particular.
Contributions to methodology
The study develops the use of patient tracking as a means of foregrounding and recognising the unique perspective of the patient as he or she passes through different care settings. As suggested above, the patient is often the only point of continuity across complex care systems. As such, the patient becomes a rich source of insight and understanding for research on complex care systems. Qualitative health research has long valued the patient’s perspective, and research increasingly collects narratives of patient and carer experience. This study has developed a ‘real-time’ and longitudinal account of care processes as they are experienced by the patient. This patient tracking approach is yet to be developed into a coherent methodology, but it involves close collaboration with patients and families throughout their care journey, starting in hospital and moving to the community or home setting. It involves a combination of first-hand observations of patient–carer interactions as well as patient–family interactions; small conversations and regular updates; and the use of other techniques to capture patient experience, such as diaries, voice memos or video diaries. Integral to this research approach is building a strong rapport and trust with patients through open and frank discussion of the research process, recognising the demands of data collection, and providing opportunities for patients and families to ‘tell their stories’. The patient narratives developed through this study are not easily represented in this report, but instead add detail and insight to the analysis presented in previous chapters (see Appendix 3). The study recommends further development and refinement of this technique as a basis for more patient-centred and holistic data collection over complex care pathways.
Limitations
It is important to acknowledge the limitations of this study. The first limitation relates to the generalisability of the findings beyond the selected case study sites. The purposive selection of the two health-care systems (Farnchester and Glipton) and two patient groups (stroke and hip fracture) was made to examine how variations in local demographics, health and social care configurations and patient need might have an impact on discharge planning and care transition. The potential for difference within and between these cases was seen as offering novel empirical insight from which tentative theoretical elaborations and propositions might be developed. 141 As such, selection was not intended to be representative of all health and social care systems and it is acknowledged that other regional systems, especially major metropolitan areas, are likely to have distinct patterns of hospital discharge. This raises questions about the extension of the study findings beyond these two care systems and patient groups, and whether or not more general statements can be made about hospital discharge and care transition. That being said, each service revealed common features from which broader lessons can be inferred and more general statements induced. In particular, they highlight the general complexity of hospital discharge, the central roles played by certain individuals and the contribution of knowledge-sharing activities such as MDT meetings. Similarly, the study might have focused only on the discharges of two patient groups, thereby limiting a more general account of hospital discharge, but these represent major areas of health-care demand where both sets of patients tend to be elderly. As such, the study reveals common points of learning from the shared experiences of these patient groups.
The second limitation relates to the proposed use of SNA as a method of analysing the patterns of knowledge sharing. As discussed in Chapter 3, the rich body of ethnographic data enabled detailed insight into the complex patterns of knowledge sharing involved in discharge planning and care transition, but this was not of a form or consistency needed to undertake more quantitative SNA, including statistical measures of centrality and density. 131 Specifically, there was no standardised or validated method of collecting participant ratings of their relationships with other actors. Although the qualitative data afforded the opportunity to present diagrams and visualisations of knowledge sharing, these were seen to add little empirical or analytical value without additional descriptive commentary, for which there is little scope within the report. As such, the decision was made to utilise the qualitative data in line with a more traditional ethnographic tradition.
The third limitation relates to the use of patient narratives as an explicit and stand-alone source of data. As described above, this method powerfully brought to life the first-hand, patient-centred experiences of hospital discharge. At the same time, the depth and richness of data was not easily presented in the report, partly as a result of word limits and also because of the sheer complexity of these accounts. Appendices 2 and 3 illustrate the richness obtained and also the level of detail needed to tell an individual story. The expectation is that this data will be used for dedicated publications. For this report, however, it was combined with and used to develop the descriptive accounts presented in Chapters 4 and 5.
The fourth limitation relates to the challenge of gaining participation from certain stakeholder groups. In particular, it was difficult to recruit GPs to the study. The GPs of patients involved in the tracking exercise were contacted in writing to notify them of their patient’s involvement, and to invite them to take part in the study. After receiving no responses from the first 15 GPs, a more proactive approach was taken by contacting GP practices by telephone, following written correspondence, to invite their participation. At the same time, PCT and new CCG leads in each area were contacted, which led to further recruitment of GPs as well as one focus group (see Chapter 3). However, the lack of GP recruitment remains a limitation of the study and possibly presents a limited picture of the contribution of GPs to discharge planning and care transition.
The final limitation reflects the lack of consideration given to readmission, as outlined in the initial proposal. Although all participating hospitals collected variable sources of data on admissions, discharges and readmissions, this was found to be universally incomplete and inconsistent across the participating research sites. Where patients were discharged, it was common for notes and records to be misplaced and no robust method of data collection was found. Even those patients involved in patient tracking often ‘went missing’ between interviews with health-care providers who were unsure as to where they had moved. Although readmission remains a significant problem, the study was unable to acquire sufficient data for it to remain a part of the study design.
Recommendations for future research
Finally, the study highlights potential areas for future research. First, and with regards to the role of knowledge brokers and boundary spanners in supporting knowledge sharing and collaboration, further research is needed to understand and appraise the contribution, economic costs and clinical outcomes of discharge co-ordinators. This might also include closer attention to how discharge co-ordinators vary in terms of their position within and between health and social care agencies, their professional background and legitimacy, levels of training and organisational support. Such variables are likely to influence whether or not and how brokers are successful in supporting knowledge sharing and collaboration.
Second, and addressing the importance of colocation and functional proximity as a basis for collaboration, more research is needed to understand and assess the relative contributions of both formal and informal interactions. Currently, a multitude of interactive situations or opportunities frame hospital discharge, but there has been limited appraisal of their costs (time and resources), processes (shared knowledge and decision-making) and outcomes (enhanced patient care). Further comparative research on these multi-agency arenas and opportunities for interaction might provide lessons for other instances of health and social care interaction. Particular attention might be given, for example, to the role of ward rounds in supporting more regular discharge planning, rather than weekly MDT meetings.
Finally, the study highlights the opportunities to investigate further how cultural differences and tensions between health and social care agencies might be mediated through nurturing shared values around commonality or convergence in their areas of activity. Although a range of financial incentives and legislative levers have been used to engender integration, the issue of cultural difference remains under-researched and difficult to change. As such, research might explore best practice examples of integrated working to identify underlying antecedents and contingencies for other care settings.
Acknowledgements
The study team would like to acknowledge and express thanks for the support and participation of the NHS trusts and local authorities involved in this study, as well as all individuals and groups who agreed to take part. Special mention is needed for the local Stroke Association representatives and voluntary support groups who greatly supported the study and helped with local PPI arrangements. In addition, further acknowledgement is needed for the patients and families who shared with the study team their personal and often protracted experiences of hospital discharge. The study team would also like to express thanks for the support of Tara Lamont, Joanne Cooper, Jon Glasby, Mark-Alexander Sujan and Emma Rowley, who provided advisory support and guidance to the study team.
Contributions of authors
Professor Justin Waring (lead and corresponding author) designed and led the research project, conducted qualitative research, collected data from interviews and observations, and managed data analysis and report writing.
Dr Fiona Marshall conducted qualitative research, collected data from interviews, observations and patient tracking, and contributed to data analysis and report writing.
Dr Simon Bishop codesigned the project, conducted qualitative research, collected data from interviews and contributed to data analysis and report writing.
Professor Opinder Sahota, Professor Marion Walker, Professor Graeme Currie, Dr Rebecca Fisher and Professor Tony Avery codesigned the research project and provided valuable advice and guidance throughout the study.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Kohn LT, Corrigan JM, Donaldson MS. ‘To Err is Human’. Building a Safer Health System. Washington, DC: National Academies Press; 1999.
- An Organisation with a Memory. London: The Stationery Office; 2000.
- Waring J, Rowley E, Dingwall R, Palmer C, Murcott T. A narrative review of the UK Patient Safety Research Portfolio. J Health Serv Res Policy 2010;15:26-32. http://dx.doi.org/10.1258/jhsrp.2009.009042.
- Landrigan CP, Parry GJ, Bones CB, Hackbarth AD, Goldmann DA, Sharek PJ. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med 2010;363:2124-34. http://dx.doi.org/10.1056/NEJMsa1004404.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry: Executive Summary. London: The Stationery Office; 2013.
- Rowley E, Waring J. A Socio-Cultural Perspective on Patient Safety. Aldershot: Ashgate Publishing; 2012.
- Hollnagel E. FRAM: the Functional Resonance Analysis Method-Modelling Complex Socio-Technical Systems. Aldershot: Ashgate Publishing; 2012.
- Perrow C. Normal Accidents. Princeton, NJ: Princeton University Press; 1984.
- Vaughan D. The dark side of organizations: mistake, misconduct, disaster. Annu Rev Sociol 1999;25:271-305. http://dx.doi.org/10.1146/annurev.soc.25.1.271.
- Cabrera A, Cabrera EF. Knowledge-sharing dilemmas. Organ Stud 2002;23:687-710. http://dx.doi.org/10.1177/0170840602235001.
- Easterby-Smith M, Lyles M, Easterby-Smith M, Lyles M. Handbook of Organizational Learning and Knowledge Management. Oxford: Blackwell; 2005.
- McDermott R, O’Dell C. Overcoming cultural barriers to sharing knowledge. J Knowledge Manag 2001;5:76-85. http://dx.doi.org/10.1108/13673270110384428.
- Currie G, Waring J, Finn R. The limits of knowledge management for public sector modernisation: the case of patient safety and quality. Public Adm 2008;86:363-85. http://dx.doi.org/10.1111/j.1467-9299.2007.00705.x.
- The Way to Go Home: Rehabilitation and Remedial Services for Older People. London: The Stationery Office; 2000.
- Managing Patients’ Medicine after Discharge from Hospital. London: CQC; 2009.
- National Reporting and Learning System Quarterly Data Summary – England. London: NPSA; 2009.
- Forster A, Murff H, Peterson J, Gandhi T, Bates D. The incident and severity of adverse events affecting patients after discharge from hospital. Ann Intern Med 2003;138:161-7. http://dx.doi.org/10.7326/0003-4819-138-3-200302040-00007.
- Haworth R. Use of aids during the first three months after total hip replacement. Br J Rheumatol 1983;22:29-35. http://dx.doi.org/10.1093/rheumatology/22.1.29.
- Levesque J. Assessing the foreseeable risks in discharge planning: the challenge of discharging the brain-injured patient. Social Work Health Care 1988;13:49-63. http://dx.doi.org/10.1300/J010v13n04_05.
- Mahoney J, Sager M, Dunham NC, Johnson J. Risk of falls after discharge. J Am Geriatr Soc 1994;42:269-74.
- Moreland J, Depaul V, Dehueck AL, Pagliuso SA, Yip DW, Pollock BJ, et al. Needs assessment of individuals with stroke after discharge from hospital stratified by acute Functional Independence Measure score. Disabil Rehabil 2009;31:2185-95. http://dx.doi.org/10.3109/09638280902951846.
- Nosek M. Personal assistance; its effect on the long-term health of a rehabilitation hospital population. Arch Phys Med Rehabil 1993;74:127-32.
- Rosenblatt D, Campion E, Mason M. Rehabilitation home visits. J Am Geriatr Soc 1986;34:441-7.
- Simmons W. Planning for discharge with the elderly. Qual Rev Bull 1986;12:68-71.
- Tansley K, Gray J. Ensuring safe and appropriate discharge for people who are homeless or in housing need. Nurs Times 2009;105:14-7.
- Utzolino S, Kaffarnik M, Keck T, Berlet M, Hopt UT. Unplanned discharge from a surgical intensive care unit: readmission and mortality. J Crit Care 2009;25:375-81. http://dx.doi.org/10.1016/j.jcrc.2009.09.009.
- Glasby J. Hospital Discharge. Integrating Health and Social Care. Abingdon: Radcliffe Medical Press; 2003.
- Laugaland K, Aase K, Barach P. Interventions to improve patient safety in transitional care – a review of the evidence. Work J Prevent Assess Rehabil 2012;41:2915-24. http://dx.doi.org/10.3233/WOR-2012-0544-2915.
- Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA 2007;297:831-41. http://dx.doi.org/10.1001/jama.297.8.831.
- Ready to Go? Planning the Discharge and Transfer of Patients from Hospital and Intermediate Care. London: The Stationery Office; 2010.
- Tierney A, Gloss J, Hunter H, MacMillian MS. Experiences of elderly patients concerning discharge from hospital. J Clin Nurs 1993;2:179-85. http://dx.doi.org/10.1111/j.1365-2702.1993.tb00158.x.
- National Sentinel Stroke Clinical Audit 2010 Round 7. London: Royal College of Physicians; 2011.
- Reducing Brain Damage: Faster Access to Better Stroke Care. London: Stationery Office Books; 2005.
- Hart E. Systems induced setbacks in stroke recovery. Sociol Health Illn 2001;23:101-23. http://dx.doi.org/10.1111/1467-9566.00243.
- National Service Framework for Older People. London: The Stationery Office; 2001.
- National Stroke Strategy. London: The Stationery Office; 2007.
- Hickey A, Horgan F, O’Neill D, McGee H. Steering Committee of the Irish National Audit of Stroke Care . Community-based post-stroke service provision and challenges: a national survey of managers and inter-disciplinary healthcare staff in Ireland. BMC Health Serv Res 2012;12. http://dx.doi.org/10.1186/1472-6963-12-111.
- Aziz N, Leonardi-Bee J, Phillips MF, Gladman J, Legg LA, Walker M. Therapy-based rehabilitation services for patients living at home more than one year after stroke. Cochrane Database Syst Rev 2008;2. http://dx.doi.org/10.1002/14651858.CD005952.pub2.
- Longhorne P. Early supported discharge: an idea whose time has come?. Stroke 2003;34:2691-2. http://dx.doi.org/10.1161/01.STR.0000101665.18062.21.
- National Clinical Guideline for Stroke. London: Royal College of Physicians; 2008.
- Torgerson DJ, Iglesias CP, Reid DM, Barlow D, Francis RM, Miles A. The Effective Management of Osteoporosis. London: Aesculapius Medical Press; 2001.
- The National Hip Fracture Database National Report 2012. London: British Geriatrics Society; 2012.
- Giusti A, Barone A, Razzano M, Pizzonia M, Pioli G. Optimal setting and care organization in the management of older adults with hip fracture. Eur J Phys Rehabil Med 2011;47:281-96.
- Parker M, Anand J. What is the true mortality of hip fractures?. Public Health 1991;105:443-6. http://dx.doi.org/10.1016/S0033-3506(05)80614-6.
- O’Cathain A. Evaluation of a hospital at home scheme for the early discharge of patients with fractured neck of femur. J Public Health 1994;16:205-10.
- Farnworth MG, Kenny P, Shiell A. The costs and effects of early discharge in the management of fractured hip. Age Ageing 1994;23:190-4. http://dx.doi.org/10.1093/ageing/23.3.190.
- Tierney AJ, Vallis J. Multidisciplinary team working in the care of elderly patients with hip fracture. J Interprof Care 1999;13:41-52. http://dx.doi.org/10.3109/13561829909025534.
- Ellins J, Glasby J, Tanner D, McIver S, Davidson D, Littlechild R, et al. Understanding and improving transitions of older people: a user and carer centred approach 2012.
- Victor CR, Healy J, Thomas A, Seargeant J. Older patients and delayed discharge from hospital. Health Social Care Community 2000;8:443-52. http://dx.doi.org/10.1046/j.1365-2524.2000.00270.x.
- Department of Health . Emergency Readmissions Data n.d. www.gov.uk/government/publications/emergency-readmissions (accessed 10 May 2013).
- Sentif Intelligence . Hospital Readmissions on the Increase 2013. www.ssentif.com/archive/13_feb2013.shtml (accessed 10 May 2013).
- Bull MJ, Roberts J. Components of a proper hospital discharge for elders. J Adv Nurs 2001;35:571-81. http://dx.doi.org/10.1046/j.1365-2648.2001.01873.x.
- Summerton H. Discharge planning: establishing an effective coordination team. Br J Nurs 1998;7:1263-7. http://dx.doi.org/10.12968/bjon.1998.7.20.5565.
- Cornwell J, Levenson R, Sonola L, Poteliakhoff E. Continuity of Care for Older Hospital Patients. London: The King’s Fund; 2012.
- Working for Patients. London: Her Majesty’s Stationery Office; 1989.
- The New NHS. London: Her Majesty’s Stationery Office; 1997.
- The NHS Plan. London: The Stationery Office; 2000.
- Equity and Excellence: Liberating the NHS. London: The Stationery Office; 2010.
- Hesselink G, Schoonhoven L, Plas M, Wollersheim H, Vernooij-Dassen M. Quality and safety of hospital discharge: a study on experiences and perceptions of patients, relatives and care providers. Int J Qual Health Care 2013;25:66-74. http://dx.doi.org/10.1093/intqhc/mzs066.
- Nazarko L. Continuity of care for older people. Nurs Stand 1998;16:42-5.
- Houghton A, Bowling A, Clarke KD, Hopkins AD, Jones I. Does a dedicated discharge coordinator improve the quality of hospital discharge?. Qual Health Care 1996;5:89-96. http://dx.doi.org/10.1136/qshc.5.2.89.
- Bauer M, Fitzgerald L, Haesler E, Manfrin M. Hospital discharge planning for frail older people and their family. Are we delivering best practice? A review of the evidence. J Clin Nurs 2009;18:2539-46. http://dx.doi.org/10.1111/j.1365-2702.2008.02685.x.
- Health Act 1999. London: The Stationery Office; 1999.
- Community Care (Delayed Discharges etc.) Act 2003. London: The Stationery Office; 2003.
- Crotty M, Unroe K, Cameron ID, Miller M, Ramirez G, Couzner L, et al. Rehabilitation interventions for improving physical and psychosocial functioning after hip fracture in older people. Cochrane Database Syst Rev 2010;1. http://dx.doi.org/10.1002/14651858.CD007624.pub3.
- Imison C, Poteliakhoff E, Thompson J. Older People and Emergency Bed Use: Exploring Variation. London: The King’s Fund; 2012.
- Stroke Association . Life After Stroke Services. n.d. www.stroke.org.uk/professioanals/life-after-stroke-services/index.html (accessed 10 May 2013).
- Kaambwa B, Bryan S, Barton P, Parker H, Martin G, Hewitt G, et al. Costs and health outcomes of intermediate care: results from five UK case study sites. Health Social Care Community 2008;16:573-81. http://dx.doi.org/10.1111/j.1365-2524.2008.00780.x.
- Griffiths PD, Edwards M, Forbes A, Harris RL, Ritchie G. Effectiveness of intermediate care in nursing-led in-patient units. Cochrane Database Syst Rev 2012;2.
- Crocker T, Forster A, Young J, Brown L, Ozer S, Smith J, et al. Physical rehabilitation for older people in long-term care. Cochrane Database Syst Rev 2013;2. http://dx.doi.org/10.1002/14651858.CD004294.pub3.
- Coventry PA, Grande GE, Richards DA, Todd CJ. Prediction of appropriate timing of palliative care for older adults with non-malignant life-threatening disease: a systematic review. Age Ageing 2005;34:218-27. http://dx.doi.org/10.1093/ageing/afi054.
- Aneurin Bevan Health Board . Fast Track and End of Life Initiative. 2012. http://nliah.com/compendiums/Articles.aspx (accessed 10 May 2013).
- Härlein J, Dassen T, Halfens RJ, Heinze CT. Fall risk factors in older people with dementia or cognitive impairment: a systematic review. J Adv Nurs 2009;65:922-33. http://dx.doi.org/10.1111/j.1365-2648.2008.04950.x.
- Mukadam N, Sampson EL. A systematic review of the prevalence, associations and outcomes of dementia in older general hospital inpatients. Int Psychogeriatr 2011;23:344-55. http://dx.doi.org/10.1017/S1041610210001717.
- Freemantle N, Richardson M, Wood J, Ray D, Khosla S, Shahian D. Weekend hospitalization and additional risk of death: An analysis of inpatient data. J R Soc Med 2012;105:74-8. http://dx.doi.org/10.1258/jrsm.2012.120009.
- Monacelli F, Aramini I, Odetti P. For debate: the August sun and the December snow. J Am Med Direct Assoc 2010;11:449-52. http://dx.doi.org/10.1016/j.jamda.2010.01.013.
- Lankshear A, Lowson K, Weingart SN. An assessment of the quality and impact of NPSA medication safety outputs issued to the NHS in England and Wales. BMJ Qual Saf 2011;20:360-5. http://dx.doi.org/10.1136/bmjqs.2010.040287.
- Hansen LO, Strater A, Smith L, Lee J, Press R, Ward N, et al. Hospital discharge documentation and risk of rehospitalisation. BMJ Qual Saf 2011;20:773-8. http://dx.doi.org/10.1136/bmjqs.2010.048470.
- Hagino T, Ochiai S, Eiichi S, Yoshiyuki W, Senga S, Haro H. Prognostic prediction in patients with hip fracture: risk factors predicting difficulties with discharge to own home. J Orthopaed Traumatol 2011;12:77-80. http://dx.doi.org/10.1007/s10195-011-0138-y.
- Howard R, Avery A, Slavenburg S, Royal S, Pipe G, Lucassen P. Which drugs cause preventable admissions to hospital? A systematic review. Br J Clin Pharmacol 2007;63:136-47. http://dx.doi.org/10.1111/j.1365-2125.2006.02698.x.
- Romagnoli KM, Handler SM, Ligons FM, Hockheinser H. Home-care nurses’ perceptions of unmet information needs and communication difficulties of older patients in the immediate post-hospital discharge period. BMJ Qual Saf 2013;22:324-32. http://dx.doi.org/10.1136/bmjqs-2012-001207.
- Clarke A, Sohanpal R, Wilson G, Taylor S. Patients’ perceptions of early supported discharge for chronic obstructive pulmonary disease: a qualitative study. Qual Saf Health Care 2010;19:95-8. http://dx.doi.org/10.1136/qshc.2007.025668.
- Goulding L, Adamson J, Watt I, Wright J. Patient safety in patients who occupy beds on clinically inappropriate wards: a qualitative interview study with NHS staff. BMJ Qual Saf 2012;21:218-24. http://dx.doi.org/10.1136/bmjqs-2011-000280.
- Courtney M, Edwards H, Chang A, Parker A, Finlayson K, Hamilton K. Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: a randomized controlled trial to determine the effectiveness of a 24-week exercise and telephone follow-up program. J Am Geriatr Soc 2009;57:395-402. http://dx.doi.org/10.1111/j.1532-5415.2009.02138.x.
- Coffey A. Discharging older people from hospital to home: what do we know?. Int J Older People Nurs 2006;1:141-50. http://dx.doi.org/10.1111/j.1748-3743.2006.00023.x.
- Cameron A, Lart R, Bostock L, Coomber C. Factors that Promote and Hinder Joint and Integrated Working Between Health and Social Care Services. London: Social Care Institute for Excellence; 2012.
- Johnson, Batalden P, Sollecito W, Johnson J. Continuous Quality Improvement in Health Care: Theory, Implementations, and Applications. London: Jones and Bartlett Learning; 2013.
- Hesselink G, Schoonhoven L, Barach P, Spijker A, Gademan P, Kalkman C, et al. Improving patient handovers from hospital to primary care. Ann Intern Med 2012;57:417-28. http://dx.doi.org/10.7326/0003-4819-157-6-201209180-00006.
- Shepperd S, Lannin NA, Clemson LM, McCluskey A, Cameron ID, Barras SL. Discharge planning from hospital to home. Cochrane Database Syst Rev 2013;1. http://dx.doi.org/10.1002/14651858.CD000313.pub4.
- Lees L, Lees L. Timely Discharge from Hospital. London: M&K; 2012.
- Coleman E, Smith J, Raha D, Min S. Posthospital medication discrepancies: prevalence and contributing factors. Arch Intern Med 2005;165:1842-7. http://dx.doi.org/10.1001/archinte.165.16.1842.
- Coleman E, Parry C, Chalmers S, Min S. The care transitions intervention: results for a randomised control trial. Arch Intern Med 2006;166:1822-8. http://dx.doi.org/10.1001/archinte.166.17.1822.
- Jack B, Chetty V, Anthony D, Greenwald J, Sanchez G, Johnson A. A reengineered hospital discharge programme to decrease hospitalization: a randomized trial. Ann Intern Med 2009;150:178-87. http://dx.doi.org/10.7326/0003-4819-150-3-200902030-00007.
- Soong C, Daub S, Lee J, Majewski C, Musing E, Nord P, et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med 2013;8:444-9. http://dx.doi.org/10.1002/jhm.2032.
- Philibert I, Barach P. The European HANDOVER Project: a multi-nation program to improve transitions at the primary care–inpatient interface. BMJ Qual Saf 2012;21:1-6. http://dx.doi.org/10.1136/bmjqs-2012-001598.
- Reason J. Human error: models and management. BMJ 2000;320:768-70. http://dx.doi.org/10.1136/bmj.320.7237.768.
- Vincent C, Reason J, Rosenthal M, Mulcahy L, Lloyd-Bostock S. Medical Mishaps. Buckingham: Open University Press; 1999.
- Waring J. Beyond blame: the cultural barriers to medical incident reporting. Social Sci Med 2005;60:1927-35. http://dx.doi.org/10.1016/j.socscimed.2004.08.055.
- Seven Steps to Patient Safety. London: NPSA; 2003.
- Pronovost P, Sexton B. Assessing safety culture: guidelines and recommendations. Qual Saf Health Care 2005;14:231-3. http://dx.doi.org/10.1136/qshc.2005.015180.
- Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ 1998;316. http://dx.doi.org/10.1136/bmj.316.7138.1154.
- Braithwaite J, Clay-Williams R, Nugus P, Plumb J, Holnagel E, Braithwaith J, et al. Resilient Health Care. Aldershot: Ashgate; 2013.
- Debono DS, Greenfield D, Travaglia JF, Long JC, Black D, Johnson J, et al. Nurses’ workarounds in acute healthcare settings: a scoping review. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-175.
- Rittel H, Webber M. Dilemmas in a general theory of planning. Policy Sci 1973;4:155-69. http://dx.doi.org/10.1007/BF01405730.
- Waring J, McDonald R, Harrison S. Safety and complexity: the inter-departmental threats to patient safety in the operating department. J Health Organ Manag 2006;20:227-42. http://dx.doi.org/10.1108/14777260610662753.
- Waring J. Getting to the ‘roots’ of patient safety. Int J Qual Health Care 2007;19:257-8. http://dx.doi.org/10.1093/intqhc/mzm035.
- Hollnagel E. Proactive Approaches to Safety Management. London: The Health Foundation; 2012.
- Byrne D. Complexity Theory and the Social Sciences. London: Routledge; 1998.
- Waldrop MM. Complexity: the Emerging Science and the Edge of Order and Chaos. New York, NY: Simon & Schuster; 1992.
- Stacey RD. Complexity and Creativity in Organizations. San Francisco, CA: Berrett-Koehler Publishers Inc.; 1996.
- Plsek PE. Crossing the Quality Chasm: a New Health System for the 21st Century. Washington, DC: National Academies Press; 2001.
- Plsek PE, Greenhalgh T. Complexity science: the challenge of complexity in health care. BMJ 2001;323:625-8. http://dx.doi.org/10.1136/bmj.323.7313.625.
- Sweeney K, Griffiths F. Complexity and Healthcare: an Introduction. Oxford: Radcliffe Publishing; 2002.
- Trenholm S, Ferlie E. Using complexity theory to analyse the organisational response to resurgent tuberculosis across London. Soc Sci Med 2012;93:229-37. http://dx.doi.org/10.1016/j.socscimed.2012.08.001.
- Tamuz M, Harrison MI. Improving patient safety in hospitals: contributions of high-reliability theory and normal accident theory. Health Serv Res 2006;41:1654-76. http://dx.doi.org/10.1111/j.1475-6773.2006.00570.x.
- Blackler F. Knowledge, knowledge work and organizations: an overview and interpretation. Organ Stud 1995;16:1021-46. http://dx.doi.org/10.1177/017084069501600605.
- Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge: Cambridge University Press; 1991.
- Argote L, McEvily B, Reagans R. Managing knowledge in organizations: An integrative framework and review of emerging themes. Manag Sci 2003;49:571-82. http://dx.doi.org/10.1287/mnsc.49.4.571.14424.
- Cohen W, Levinthal D. Absorptive capacity: a new perspective on learning and innovation. Adm Sci Q 1990;35:128-52. http://dx.doi.org/10.2307/2393553.
- Bartol K, Srivastava A. Encouraging knowledge sharing: the role of organizational reward systems. J Leadership Organ Stud 2002;9:64-76. http://dx.doi.org/10.1177/107179190200900105.
- Van Wijk R, Jansen JJ, Lyles MA. Inter- and intra-organizational knowledge transfer: a meta-analytic review and assessment of its antecedents and consequences. J Manag Stud 2008;45:830-53. http://dx.doi.org/10.1111/j.1467-6486.2008.00771.x.
- Owen-Smith J, Powell W. Knowledge networks as channels and conduits: the effects of spillovers in the Boston biotechnology community. Organ Sci 2004;15:5-21. http://dx.doi.org/10.1287/orsc.1030.0054.
- Addicott R, McGivern G, Ferlie E. Networks, organizational learning and knowledge management: NHS cancer networks. Public Money Manag 2006;26:87-94. http://dx.doi.org/10.1111/j.1467-9302.2006.00506.x.
- Abbot A. The System of Professions. Chicago, IL: University of Chicago Press; 1988.
- Waring J, Currie G. Managing expert knowledge: organizational challenges and managerial futures for the UK medical profession. Organ Stud 2009;30:755-78. http://dx.doi.org/10.1177/0170840609104819.
- Brown J, Duguid P. Knowledge and organization: a social-practice perspective. Organ Sci 2001;12:198-213. http://dx.doi.org/10.1287/orsc.12.2.198.10116.
- Phelps C, Heidl R, Wadhwa A. Knowledge, networks, and knowledge networks: a review and research agenda. J Manag 2012;38:1115-66. http://dx.doi.org/10.1177/0149206311432640.
- Sorenson O, Rivkin JW, Fleming L. Complexity, networks and knowledge flow. Res Policy 2006;35:994-1017. http://dx.doi.org/10.1016/j.respol.2006.05.002.
- Granovetter M. Network sampling: some first steps. Am J Sociol 1976;81:1287-303. http://dx.doi.org/10.1086/226224.
- Granovetter M. The strength of weak ties: A network theory revisited. Sociol Theory 1983;1:201-33. http://dx.doi.org/10.2307/202051.
- Knoke D, Yang S. Social Network Analysis. London: Sage; 2008.
- Scott J. Social Network Analysis. London: Sage; 2000.
- Crossley N. The social world of the network. Combining qualitative and quantitative elements in social network analysis. Sociologica 2010;4.
- Burgess RG. In the Field: an Introduction to Field Research. London: Routledge; 1984.
- Bate SP. Whatever happened to organizational anthropology? A review of the field of organizational ethnography and anthropological studies. Hum Relat 2004;50:1147-75. http://dx.doi.org/10.1177/001872679705000905.
- Fetterman DM. Ethnography: Step by Step. London: Sage; 1998.
- Hammersley M, Atkinson P. Ethnography. London: Routledge; 1995.
- Pope C, Mays N. Qualitative Research in Health Care. London: Blackwell; 2006.
- Dixon-Woods M. Why is patient safety so hard? A selective review of ethnographic studies. J Health Serv Res Policy 2010;15:11-6. http://dx.doi.org/10.1258/jhsrp.2009.009041.
- Finn R, Waring J, Walshe K, Boaden R. Patient Safety: Research into Practice. Maidenhead: Open University Press; 2005.
- Yin R. Case Study Research: Design and Methods. London: Sage; 1994.
- Office for National Statistics . Ethnicity and National Identity in England and Wales 2011 2012. www.ons.gov.uk/ons/dcp171776_290558.pdf (accessed May 2013).
- Public Health England . National Public Health Profiles 2011 n.d. www.apho.org.uk/default.aspx?RID=49802 (accessed May 2013).
- Spradley JP. Participant Observation. Wadsworth Town: Wadsworth Publishing; 1980.
- Lincoln Y, Guba E. Naturalistic Inquiry. London: Sage; 1985.
- Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. London: Sage; 1990.
- Charmaz K. Constructing Grounded Theory. London: Sage; 2006.
- Conceptual Framework for the International Classification for Patient Safety. Geneva: WHO; 2009.
- Hargadon A, Staw B, Kramer R. Research in Organizational Behaviour. Greenwich: JAI Press; 2002.
- Waring J, Bishop S. ‘Watercooler learning’: knowledge sharing at the clinical backstage and its contribution to patient safety. J Health Organ Manag 2010;24:325-42.
- Hartey J, Bennington J. Leadership for Healthcare. Bristol: Policy Press; 2010.
- Martin G, Currie G, Finn R. Leadership, service reform and public service networks: the case of cancer-genetic pilots in the English NHS. J Public Adm Res Theory 2009;19:769-94. http://dx.doi.org/10.1093/jopart/mun016.
Appendix 1 Interview topic guide
1. Professional background
Can you tell me a little about your occupational background and role?
What does a typical day involve for your work?
What do you like about your job?
What are the main work issues or problems you face on a day-to-day basis?
How do you try to work through them?
P1. Patient or family background
Can you tell me a little about yourself, so we can get a sense of who you are and how you came to be in hospital/you have been supporting your relative?
P [Patient] ONLY: And who do you see as your primary carer?
F [Family] ONLY: And how long have been providing this support?
2. Staff: the discharge process
Overview . . .
Can you help me understand the discharge process? Maybe talk me through what you see as the steps for patients on your ward/you see in the community?
When do you start thinking about discharge plans?
Which main factors do you consider?
What happens when delays occur?
Are there any particular days which are more difficult? Why?
Are there any particular times of day which are more tricky? Why?
Are there any particular ways in which you work around these anticipated difficulties?
What happens when patients are all ready to go but have to wait for transport?
Do you get to hear if a patient is readmitted soon after discharge? If so how does that make you feel?
Planning issues . . .
And in your day-to-day work, what input or responsibilities do you have in terms of patient discharge?
Can you identify a point during the discharge process at which you have completed your task?
How do team meetings, staff briefings or other group activities help with the discharge planning? What do they help to do?
It seems like there are lots of forms and paperwork in the discharge process? What do they aim to do? How do they support you? Are these easy to complete or use?
Do you follow the guidelines to the letter?
Are there any parts of your job which don’t fit into any of the discharge guidelines?
Do you have your own way of doing things?
What kinds of technologies or computer systems are used during the discharge process? What do they aim to do? Are they easy to use? Does everybody use them in the same way?
Patients and families . . .
Do families understand their role once a patient is fit to go home?
Do patients understand that they are fit to go home?
What about immobile end-of-life patients? Are they accompanied by a nurse?
What happens when a patient self-discharges?
The wider context . . .
In addition to yourself, who do you see as the main people involved in facilitating or managing the discharge process? How do they go about their work and what do they contribute to the process?
What are the key organisational factors that shape the discharge process, such as management approaches or resources? Can you give me an example?
As far as you know, what interventions or changes have been used to improve the way people work with each other across the hospital?
As far as you know, what interventions or changes have been used to improve the way people work with each across between the hospital and the community?
P2a/3a. Communication processes
We are particularly interested in the way in which people communicate with each other during the discharge process, what do you think makes for effective communication? Can you give an example?
Do you feel there are communication breakdowns in the discharge process, can you give an example?
Why do you think these communication problems arise?
From your perspective, what do you think are the essential pieces of information you need to know, or share with others to make sure the discharge process works?
P2b/3b. Communication networks
We would like to ask a bit about the typical people you would normally share knowledge with to make the discharge process work.
If you think about the usual or typical discharge process, who are the most important people you share knowledge with, either because they give you essential information or you have to pass on essential information to them?
Why are these people important? What specific pieces of information do they give you?
When do you normally try to contact them?
How often do you communicate with them in the discharge process?
As they are going through, also ask them to explore (where necessary – it may be often self-evident or explored elsewhere in the interview):
-
formal meetings
-
informal conversations
-
notes
-
e-mails
-
others.
What is your relationship like with them and how easy is it to communicate any information you need?
Are there any challenges or frustrations you have with communicating with these people?
If there are any new people also ask about if/how we can contact them.
Are there other people who you think it would be important to share information with but currently find it difficult?
3c. Communication in general
Thinking more generally, how would you describe the communication between different professional groups?
Do status differences or hierarchies influence who communicates with you?
Can you think of an instance where someone from a different professional background didn’t understand what you were trying to tell, maybe because they have different words or terms?
In what ways do the different groups involved in the discharge processes share similar values and priorities for how to support the discharge process? Or do they have different cultures?
How do organisational or managerial factors influence the way in which people communicate with each other, for example, do people work on different shifts or schedules?
What are the communication problems that are specifically related to working across organisations and sectors, for example between health and social care?
From your experience what is it like communicating with those based in:
-
other hospital wards
-
primary care
-
pharmacies
-
care homes
-
family members.
P4/5. Patient safety
Reflecting on what we have been talking about, what do you think are the main threats to the patient’s safety during the discharge processes? Can you give an example?
What are the risks of discharging a patient too early?
What are the risks of discharging a patient too late?
We have been told that there are particular risks associated with medication and take-home medicines. How do you see this problem and how might improved communication make it less risky?
We have been also told that there are particular risks associated with falls either in hospital or at home. How do you see this problem and how might improved communication make it less risky?
What do you think brings about these threats to safety? What might be their underlying causes?
Have you ever reported discharge-related incidents? What happened?
When things seem to go wrong or not the way they should be, who seems to take responsibility for getting things back on track?
If you were concerned that a patient discharge was not appropriate what would you try to do, who would you turn to?
What are the safety checks to ensure that discharge is appropriate?
Can you think of any instances where people or teams have learnt from past experiences and tried to change the way they work?
What might service leaders do to improve communication and the safety of hospital discharge?
P5a. Family member questions
Are you satisfied with discharge plans?
What is a good discharge?
If you could change one thing what would it be?
Who made the most difference?
Do you think (insert name) was ready to go home? If not why not (explore this fully)?
Did you have enough information?
Were you able to cope?
When did the discharge happen? Time of day/day of week.
When did you know about the discharge? Were you prepared practically? E.g. food/heating on?
Were you given any paperwork?
Were you expected to give any medications? If so what?
Were you expected to give any intimate care? If so can you tell me what? Were you happy to do this?
Any other comments?
P5b. Patient questions
Do you worry about your plans for discharge?
Are you able to discuss these? Who with?
What do you want to happen?
Do you manage your own medicines? Have you been able to self-medicate whilst in hospital?
Do you understand your medication and what it is for?
Did you have enough medication when you came out of hospital?
Did you have any problems reading the labels?
Did you have any problems getting your medicines ready to take?
Does somebody have to help you? Is somebody around to help you?
Do you have any difficulties with:
Hearing, seeing, getting around, keeping clean, making a warm drink, answering the door, the phone, keeping warm, keeping warm at night, going to the toilet, feeling safe?
Do you have any daily help from family, friends or neighbours?
If you could change one thing what would it be?
Who has helped you the most? How? Did they make you feel safe?
Did you worry when you got home? Were you home alone? For how long? (does not matter if not accurate)
If you could change one thing about your discharge from hospital what would it be?
Did you think you were ready to go home? Did you feel able to cope?
Did you feel able to tell somebody how you felt?
Looking back do you think you were discharged home at the right time?
Tell me about how it went? Did you feel safe?
Did you lose any items?
Were you aware of your condition when you came home? Did you agree?
Appendix 2 Patient diary extract
Sample 1
Sample 2
Appendix 3 Patient narrative accounts
Please note that for the purposes of maintaining anonymity, all names have been changed.
Thelma’s story: Glipton hip fracture patient
Seventy-nine-year-old Thelma lived in a residential area on the outskirts of Glipton city centre. She had lived there since the early 1950s and had been an active member of the local Irish Catholic community, and raised seven children. She had a well-established network of family and community support and a history of falls that had resulted in several home adaptations to support her mobility, initiated by her local GP and district nurse. These support systems would become essential to her recovery after she fractured her neck of femur in mid-June 2012 while getting on to a bus during a shopping trip. After being attended to by a local shopkeeper and first responder, she was transferred to the Glipton emergency department, where one of her daughters joined her after being called by the paramedic.
On attending the emergency department, Thelma was given more pain relief and helped with her personal care by her daughter. After being assessed by the on-call orthopaedic registrar, she was transferred to the trauma orthopaedic unit, where she was further assessed by the consultant surgeon and clerked on the ward by the nursing staff. At this time, she had the necessary pre-operation checks, including blood matching and tests in the emergency department. Her verbal history and patient records indicated that she had moderately severe arthritis and normally mobilised with one stick. In the evening of her first visit, Thelma was briefly seen by an OT, who explained that she would need rehabilitation and that one of the dedicated trauma therapists would visit her in a few days to plan her care. Thelma received surgery the next day (Saturday) in the late evening, and appeared to recovery remarkably well.
On Monday morning, Thelma was reviewed as a part of the morning surgical ward round, where the consultant surgeon recommend that she start early rehabilitation given her positive response. He also requested that the ward nurse contact the orthogeriatrician team to assess her care needs and her suitability for early discharge. Later that day, her designated PT and OT attended her bedside and made their initial assessments of need by asking about her activities of daily living, expectations for recovery, and mobility and pain, and recording information about her domestic arrangements. The PT initiated therapy by focusing on her managing steps and getting in and out of her chair. After visiting time, her daughters and son sought out the OT and nursing staff and asked to be kept informed of any plans for discharge; at this time her relatives informed the OT that she already had several home adaptations and that a home assessment would probably not be necessary. Her family remain active in the discharge planning process, with at least one family member visiting each day and providing emotional and personal care.
The following morning Thelma was reviewed at her bedside by her orthogeriatrician, who assessed her for any cognitive difficulties, her general well-being and comorbidities. The initial review of her progress suggested that she was responding well to therapy and was unlikely to need longer-term care or rehabilitation.
Two days after starting rehabilitation, Thelma’s recovery was reviewed at the weekly MDT meeting. The orthogeriatrician summarised Thelma’s surgical procedure and care plan, referring to the main medical record, and then asked the ward nurse to comment on her general recovery. The nurse was very positive about Thelma’s progress and suggested that she might start to show frustration with being on the ward if her care was not progressed in a timely manner. This was also confirmed by the HCA representative, who described Thelma as lively. The OT then added that her rehabilitation was progressing well and that she already had home adaptations and would not be a complicated referral. The only addition would be a commode to reduce the need for extended travel to the toilet. The unit’s discharge liaison nurse asked if this had been confirmed with the family and what level of support she might receive. Both the OT and ward nurse agreed that Thelma would be well looked after by her large family, who had been very proactive and supportive in her recovery. The orthogeriatrician ended the discussion by setting a date in early July as the EDD, leaving sufficient time to continue rehabilitation and confirm reablement.
At the following morning’s handover, the staff were informed about Thelma’s EDD. At around this time, the OT initiated a referral to social services for reablement to support Thelma’s personal care at home, ordered a commode from the external suppliers and also referred Thelma for continuing OT to support her mobility. As the date of Thelma’s planned discharge approached, her case was again reviewed at the following week’s MDT meeting, where the final arrangements for her discharge were very briefly confirmed. The discharge liaison nurse had a more active role at this stage, saying that she had spoken with family members and also confirmed that a standard package of community rehabilitation had been arranged with the PCT. The OT reported that the social worker had spoken with Thelma and her family and decided that a reablement package would not be necessary as several of her children had committed to providing ongoing care. Later that day, Thelma’s TTOs were ordered by a junior doctor and the ward clerk booked patient transport.
The following day Thelma was discharged from hospital. In the morning, the discharge liaison nurse rang two of her daughters to inform them that she was coming home, as requested at a previous meeting. This enabled the daughters to prepare their mother’s home by buying groceries and putting the heating on. The discharge nurse also contacted the ambulance service to confirm the timing of the transport and to request that they contact another of Thelma’s daughters before pick-up so that she could meet the ambulance crew with keys and help settle her mother. This daughter had also agreed to move into the home to support Thelma’s recovery. However, the daughter did not receive a phone call notifying her that Thelma had been collected, and by lunchtime telephoned the ward to be told that, according to the computer system, her mother had been discharged. The daughter then drove to the hospital to find her mother sitting on a chair on the ward, next to her stripped bed. She was very angry with the ward nurse and explained that Thelma was supposed to have been transported home earlier and that the ward clerk had said that she had already left the hospital. The discharge liaison nurse then attended to Thelma and her daughter and explained that there must have been a mix-up with the ambulance crew. She apologised for the confusion and arranged for another ambulance to transport Thelma. Given the mistake made by the ambulance service, an emergency ambulance was used to transfer her home.
When Thelma arrived home she also found that her commode had not been delivered and some of her medications were incomplete; the dispensed content did not match the prescribed list. The next day, her daughter contacted the ward to speak to the OT and explained that the commode had not arrived. The OT suggested that she could collect one directly from the hospital to save waiting for the supplier. The same day, another daughter phoned the GP to sort out Thelma’s medication, especially pain relief, and discussed the problems with her discharge. The GP did not have all the details from the hospital but agreed to send the district nurse to the home that afternoon and to arrange pain relief.
Thelma’s recovery steadily progressed with the support of the community rehabilitation team who visited her twice a week. She was also provided with a wheelchair by the local church group, which she used to get around outside the house. However, she was also adamant that she wished to walk, and 2 weeks after returning home she attempted to walk to the local shop with the aid of a frame. On the way, she fell on an uneven pavement slab, which pulled her wound site. Neighbours took her home and her daughter was contacted at her local workplace. The GP was called by the daughter and a home visit requested. The GP examined her in the home and declared that she had strained herself with no serious issues.
Over the next 3 days Thelma appeared to worsen, with her wound site looking infected, and the GP was called. The community nurse visited her and found she had a severe fever and possible infection. The GP prescribed a course of antibiotics without directly examining Thelma. Three days later Thelma started to respond to the antibiotics and her overall recovery continued. The community nurse again visited Thelma at home over the next week and suggested she have an eye test to check if her vision was affecting her mobility, and also that she buy a stronger pair of slippers to reduce the risk of falling in the home. Ten weeks after surgery, Thelma seemed very upbeat and discussed wanting to maintain her independence and the pressure from her daughters to take things easier. Despite a clearly loving relationship, this interview highlighted the tensions involved in caring, perceptions of risk-taking and the ways in which older adults navigate risk in their lives.
Ahmad’s story: Glipton stroke patient
Ahmad was unsure of his age but believed himself to be 86 years old. He lived in the centre of Glipton with his wife and extended family, including his son and daughter-in-law and their new baby. Ahmad and his wife had recently emigrated from Pakistan to the Glipton area to be closer to their extended family and grandchildren. Ahmad had a severe stroke in early May 2012, which left him with problems with his speech, swallowing, walking and continence. He was transferred by ambulance to the emergency department and then transferred to the stroke unit, where he was examined by Dr Wood, who ordered tests (blood and CT scan) and took a patient history. Ahmad spoke little English and he relied upon his daughter-in-law to translate for him. Ahmad was not suitable for thrombolisation because he had missed the 4-hour window, and so the consultant and the admission nurse decided to admit him on to the hyperacute pathway.
Over the next 48 hours he was closely monitored and stabilised on the ward by nursing staff. On the day following his admission, Ahmad was reviewed as a part of the daily ward round. This was led by Dr Wood, accompanied by two junior doctors, a physician assistant, the senior nurse for the hyperacute bay, the unit’s SaLTs and a specialist stroke PT. Ahmad’s family were invited to join the meeting as this was customary on the stroke unit, but also because his daughter-in-law could translate between Urdu and English. At the meeting, Dr Wood also invited Sandy, the SaLT, to comment on his swallowing and to complete a formal assessment later that day. The PT also suggested that Ahmad might benefit from some physiotherapy to prevent him from getting chest infections. Through talking with Ahmad and his daughter-in-law, Dr Wood established that he been quite active prior to his stroke and that he had recently retired and moved to the area from Pakistan. Through the interaction, it was also established that he had no registered GP in the area, which would complicate discharge planning, and Dr Wood decided to refer his case to the hospital’s specialist discharge nurse who could look into his wider social needs and determine who might act as his GP. These decisions were noted concurrently in Ahmad’s medical record by the junior doctor; this was then reviewed by the consultant for consistency, thoroughness and legibility before being signed.
Later that day, the SaLT assessed Ahmad’s swallowing and coughing to decide whether or not he could take food, and determined that he should remain nil by mouth. Over the next 24 hours Ahmad’s condition appeared to improve, and he became progressively agitated and frustrated, especially with being catheterised given his incontinence. In consultation with the nursing staff, the senior nurse asked one of the ward clerks, Deepa, to act as a translator for Ahmad as it was not feasible to rely upon his daughter-in-law. She was asked to explain to Ahmad about the importance of not interfering with his catheter. Deepa would remain the primary translator for Ahmad during his stay.
On his third day in hospital, Ahmad’s case was reviewed at the weekly MDT meeting. This took place in the designated meeting room on the stroke unit, and included OT and PT representatives, the SaLT, the unit’s discharge nurse, a palliative care nurse, a senior ward nurse, the lead stroke consultant and two junior doctors. The meeting was initiated by the consultant, but the review of each patient was led by a different member of the meeting, with the aim of reducing hierarchy within the unit, promoting shared decision-making and encouraging multidisciplinary participation. Ahmad’s case was presented by the OT representative, who reviewed his care on the ward, and noted that he was becoming frustrated with his illness and limited mobility and that he had a strong family support network. The SaLT contributed to this review by raising the possibility of using a nasogastric tube to enable feeding and the possibility that he might not regain the ability to swallow. She also recommended referring his case to a hospital dietician. These decisions were discussed by the wider group but confirmed by the stroke consultant. The PT and OT also outlined their weekly targets for Ahmad’s rehabilitation on the ward, including that he be able to sit up on the edge of the bed. A significant feature of this meeting was that his care plan was discussed with a view to his suitability for ESD, on the basis that communication in his own home would be easier, and therefore rehabilitation would be better suited to his needs. However, while he still required a nasogastric tube it was decided this would not be possible. The group decided to informally approach the ESD team during their routine ward visit to discuss the options for Ahmad’s care outside hospital. They set his EDD at 6 weeks from admission to allow sufficient time for his rehabilitation, but pending discussion with the ESD team.
Based upon the care plan agreed in the MDT, Ahmad received a package of care including daily medical ward rounds and daily sessions with the OT and PT to support his rehabilitation. He also met weekly with the SaLT and the dietician. His progress and care was reviewed again at weekly MDTs for 4 weeks. Concurrent with his ward-based care and rehabilitation, the stroke unit’s specialist discharge nurse liaised with the hospital’s dedicated discharge support team to find and register Ahmad with a GP. This then made it possible to start considering external referrals for continuing health care and ESD. At around week 4, Ahmad’s swallowing improved considerably, raising the possibility that he could be discharged earlier if he did not need the nasogastric tube. The stroke unit invited Ahmad’s wife and daughter-in-law to attend an education programme on the management of thickened fluids which would assist his recovery at home.
At the week 5 MDT, his case was again reviewed and the possibility of ESD was again discussed. The OT representative described the progress made in his mobility, i.e. his ability to stand, and the SaLT indicated that he no longer needed the nasogastric tube and might therefore be suitable for earlier discharge. However, the ward nurse informed the group that his wife had left the country for a short period and there was limited family support at home. It was still decided to refer his case for continuing health and social care, which was to be undertaken by the specialist discharge nurse given the complexities surrounding his residential and legal status. Later that day, the specialist discharge nurse initiated external referrals for social care using a computer-based referral system. Social services reviewed and declined the request for social care on the grounds that he was not formally registered as a local resident and did not have appropriate legal status within the UK. The social care referral stalled at this point and remained unresolved. His referral for ESD was also made later that day by the OT. A member of the ESD team attended to Ahmad the following day, when he was assessed by a specialist OT who was able to speak Urdu. The ESD OT completed the standard assessment form with the support of the ward OT and nurse and used Google Earth to determine the location and type of Ahmad’s house.
The ESD OT presented the findings of their assessment to Ahmad and discussed the options for his care with the ESD manager, who decided that there would not be capacity to provide Ahmad’s care package for another 5 days. Following this meeting, the ward-based OT initiated a request for additional equipment and adaptations for Ahmad’s home. This was completed using an online ordering service whereby specific items of equipment, such as a commode and a wheelchair, were ordered for direct delivery to the patient’s home.
At the next week’s MDT, the decision to accept Ahmad for ESD was reviewed and the discussion turned to consideration of his discharge plan. This was guided by a standardised discharge checklist that detailed the steps required for transportation, medication, discharge letter, equipment, GP contact and emergency contact numbers. The discharge nurses completed this document, which also structured the discussion among the MDT. A major point of discussion related to Ahmad’s medication, with the consultant requesting that Ahmad leave hospital with a dosset box to manage his medicines regime, for example making it easier for his daughter-in-law to provide his daily medicines. The consultant also requested that he leave hospital with additional thickened fluid packs and pictorial instructions for their use for his family members. The SaLT noted that she would contact the local pharmacist to provide additional instructions on ordering the thickened fluid packs. The OT reported in the meeting that they had already ordered a wheelchair, a Zimmer frame and a commode. Following the MDT, one of the junior doctors completed the TTO for Ahmad’s medicines, which was reviewed by the consultant. When this had been checked by the consultant, the ward clerk would issue the TTO to the hospital pharmacy via a dedicated computer programme.
Two days after the MDT Ahmad was transferred home, where his care was taken up by the ESD team. He went home by ambulance, which had been ordered by the ward clerk, who also checked that he had his medicines and his personal property, and then issued a discharge letter to his GP via a shared computer system. Later that afternoon, Ahmad was visited and reviewed at home by the ESD OT, who reviewed the accuracy of his care records and plan. The OT spoke at length with Ahmad and his family about his care, benefiting from being able to speak Urdu. Ahmad then started an 8-week package of home-based rehabilitation provided by a team of five specialists, including PTs, OTs and community nurses. Over this time he regained his ability to walk independently, and started to talk more clearly, to eat softened food and to use his hands. However, Ahmad and his family reported that he remained incontinent and required considerable personal care to address his toilet needs. They also reported that his wheelchair arrived a week late because of delays with the equipment supplier. Although this limited his immediate mobility, Ahmad remained adamant that he did not want it because he wanted to recover his walking. Ahmad also missed his outpatient appointment with the neurologist because he and his family could not understand the paperwork.
Ahmad did not receive any social care as he was deemed ineligible because his residential status could not be finalised. As such, his personal and social care was provided by his daughter-in-law, who reported feeling extremely tired because she was required to look after her mother-in-law and her own baby, in additional to Ahmad. She requested help through the ESD team but was informed that this package of care would end soon and that it was a social care issue. The GP did not attend to Ahmad and at the end of our involvement with Ahmad he remained unaware who his GP was. At the point where Ahmad’s ESD care ended, he reported being in much improved health and appeared extremely grateful for the care he had received.
Charles’s story: Farnchester Hip Fracture Patient
Charles was a 96-year-old man who lived with his 98-year-old wife in the centre of Farnchester. He had a history of cerebral vascular accidents and chronic obstructive pulmonary disease, and fractured his neck of femur on a Monday in October 2012, while walking in his garden. He was assessed at home by the ambulance service and transported to Farnchester’s accident and emergency department. He was further assessed by the medical team, who ordered X-rays and other diagnostic tests and confirmed his hip fracture, and requested attendance from the trauma orthopaedic team. A junior doctor from the trauma team visited Charles in the emergency department and agreed to the transfer of his care. Simultaneously, the dedicated orthopaedic trauma admissions nurse started a new patient record for Charles, including patient identifiable data, using existing hospital records; however, this was done before he had arrived on the ward where his details could be confirmed. This led to several areas of incomplete data that were not always rectified and meant that Charles’s record in hospital continued to have inconsistencies and missing data.
While on the orthopaedic trauma ward, Charles was further assessed by the junior doctor and also visited by one of the anaesthetic team. The anaesthetist raised concerns about his medications and requested that a pharmacist visit to change his prescription for warfarin so as to enable surgery. The next morning Charles’s history and case was presented at the trauma intake meeting, where all orthopaedic trauma cases are reviewed, surgical procedures decided and the operating schedule agreed. The junior doctor presented his case, whereupon the specialist consultant asked questions about his X-rays and comorbidities, as much for teaching purposes as for decision-making. Following discussion with the anaesthetic representative, it was agreed that a hip replacement would be performed the following day to allow for his change in medicines; this was recorded by the theatre staff (for scheduling), the trauma nurse (for the hospital record) and the junior doctor (for the surgical record). At no point was any mention made of Charles’s onward care needs or rehabilitation, and the views or wishes of Charles were not shared. On his second full day in hospital, Charles received his hip replacement operation and returned to the orthopaedic ward for surgical recovery.
Charles stayed on the orthopaedic ward for a total of 15 days before being transferred to a general rehabilitation ward for older people. Throughout his time in Farnchester hospital, Charles was not visited by his wife because of her health-related problems and he reported feelings of loneliness and isolation. For the first 6 days following his operation, Charles’s recovery from the surgery was managed by the surgical and nursing team. This involved personal care on the ward, where his wounds and general health were monitored by ward nurses and HCAs. His recovery was reviewed in a daily board round by his consultant surgeon, junior doctors, the trauma nurse and the lead ward nurse. This involved a relatively short (3- to 5-minute) case review led by the surgeon and involving requests for further information from the ward nurse. The primary focus of the interaction was to assess Charles’s surgical recovery, but with no explicit regard to his rehabilitation or discharge. On a number of occasions the surgeon attended to Charles at his bedside to ask about his recovery and mobility, but generally he had limited involvement in decision-making; instead, nursing staff tended to represent Charles’s views. On the sixth day post surgery, the consultant requested that the orthogeriatrician be asked to review his care needs, presumably with a view to onward care. The (part-time) geriatrician visited Charles the following day and noted his comorbidities, reviewed his medicines and requested further blood tests, and visited him once more 5 days later to again monitor the results. The consultant surgeon also declared on this sixth day that Charles was ready to start mobilisation and instructed the nursing staff to notify the hospital’s therapist team.
At about this time, the surgeon’s involvement in Charles’s care reduced dramatically; for example, in board rounds he tended only to acknowledge that his care was progressing and that no significant changes had occurred. In many ways it seemed that the responsibility for Charles’s care had been transferred to the rehabilitation team as there was little surgical interest in his case. This decision was in no way formally recorded or communicated, but seemed to be taken for granted by the surgical team, with the general sense that no group had responsibility for his care.
Following the lead nurse’s internal referral for rehabilitation, a pair of OTs and PTs attended to Charles on the afternoon of the sixth day post surgery. Working together, they assessed his recovery, usual activities of daily living, current range of mobility and wider personal and domestic circumstances. From this preliminary knowledge they designed a broad package of hospital rehabilitation and noted further enquiries in relation to his discharge. This was the first formal record of discharge planning recorded in both his medical and therapist records. Significantly, the therapists reported both duplication and discrepancy between their own records and the medical records. On the seventh day, the therapist team again attended to Charles to progress his rehabilitation and discussed with him the possibility that he might struggle to manage at home. He felt that he was familiar with his home layout and could easily manage, but through discussion agreed to the provision of a commode and other home adaptations.
On the seventh day post surgery, Charles’s care was also reviewed at the weekly MDT meeting within the orthopaedic trauma unit. This was led by the nursing team and involved a very short review of his current condition and nursing needs and acknowledgement that the therapist team was now leading on his care. The therapists were not asked to elaborate on their work or to contribute to the discussion; rather, they acknowledged their involvement. At this meeting there was no mention of onward care or discharge. Later the same day, Charles’s care plan was discussed at the weekly therapist review meeting where the OT described his proposed care plan and sought guidance from therapist colleagues with specific reference to his need for reablement or more intensive rehabilitation.
On day 8, the OT initiated a referral to social services for social care reablement at home, in line with Charles’s wishes. This involved using both his medical and therapist records to complete the county-wide referral form, which was then faxed to the social service assessment contact centre. This form was then passed on to the locality social work team, but there was no acknowledgement of receipt for a further 2 days. Two days later, the referral for social care was returned to the therapist team because it contained missing information related to his family circumstances and relatives. This might have been because Charles had had no visitors by this stage and had mentioned that his wife was also ill. On the twelfth day post surgery, the OT completed another referral form, noting her inability to complete the information, and requested further social work involvement.
The referral for social care was verbally shared with the lead nurse, who also, on the seventh day post surgery, instructed the night-shift nurses to initiate a continuing health-care request. This referral was made during the quieter hours of the night, again referring to Charles’s medical record. However, the referral form contained no logical sequencing of events and had prospective entries, as well as many missing data; for example, the nurses reported that his commode had been ordered when there was no confirmation of this, and details related to his housing arrangement were missing. This seemed to reflect the lack of detail contained within his medical record and the lack of access to therapist records. The fax to the community health-care and rehabilitation team (who happened to be located within the hospital grounds) was not received owing to an error in the use of the fax machine, and there was no policy of issuing fax receipts. This created a 4-day delay until the lead nurse followed up the rehabilitation assessment at a morning board round. The ward clerk was asked to resend the fax. The rehabilitation team visited Charles at his bedside on day 12 to assess his need for a specialist rehabilitation place.
At 13 days post operation, Charles’s son rang the ward to raise a concern about his father’s and mother’s ability to cope at home. This was the first record of any family contact in his medical record but there was no report that this information was used to inform decision-making. On day 15 post surgery, the decision was made in the morning board round to transfer Charles’s care to the general rehabilitation ward for older people, as his recovery was now related not to his hip replacement but rather to comorbidities, and he was using an orthopaedic bed. His transfer to this ward involved only a short handover between ward staff and the reallocation of his medical records. He was then assessed again by the general and orthopaedic care team, including a different doctor and nursing staff. At this point he was diagnosed with a severe chest infection and then pneumonia. The only point of continuity in Charles’s care was his OT, who was not directly informed about his internal ward transfer and had to ‘search for him’ across the hospital. On this new ward, there was a dedicated discharge liaison nurse who specialised in supporting discharge planning. Working with his OT, the decision was made that Charles might be better in a rehabilitation bed, rather than at home with reablement, because of his broader health concerns. This was discussed with Charles; it was explained that he would struggle at home and that this would place an extra burden on his wife. Charles agreed to this plan of action. On day 25 post surgery, Charles was again referred to the community rehabilitation team, who agreed with the decision to find him a specialist rehabilitation bed for 30 days.
On day 26, the geriatrician decided that Charles would be fit for discharge when his blood results stabilised for 2 days. Thirty-four days after his operation Charles was discharged to an intermediate care facility. This transfer involved an ambulance, booked by the ward clerk. At the point of discharge, Charles’s medicines had not been fully reviewed and no TTOs were issued. Charles’s rehabilitation bed was located in a local nursing home, where he was admitted and reviewed by the dedicated nursing and therapist team. When he was visited in the home 6 days later he was found to be severely unwell with the possibility that he might be readmitted; he was not readmitted. A week later Charles reported that he was feeling better and was hoping to return home. His rehabilitation and general recovery was further supported in the nursing home, and at around day 21 of his placement the therapist made a referral to the social care assessment centre for a social work assessment. To facilitate this process, the OT visited Charles’s home to record a more accurate picture of his needs, which was used to inform the care plan devised with his designated social worker. This included a period of reablement and home adaptation, and a specialist mattress to cope with his severe continence issues. On day 58 post surgery Charles was transferred home, where a further period of personal and social care was provided. In the final visit with Charles, his community nurse reported that he was receiving twice-weekly visits from his GP, and daily visits from both social care and community nursing to support his recovery. However, it was also reported that Charles was starting to suffer with pressures sores and ulceration because he had not been provided with a new mattress. This seemed to be related to a problem with the referral to social care, but this was not confirmed. At this stage, the research team in consultation with Charles and the community nurse decided to stop data collection as his condition seemed to be deteriorating. In a follow-up telephone call with Charles’s community nurse, it was reported that she had initiated an end-of-life care package as Charles was not recovering well from his comorbidities.
Ralph’s story: Farnchester stroke patient
Seventy-three-year-old Ralph had a stroke in September 2012. It happened at his home, a small rural cottage 30 miles from Farnchester, where he lived with his daughter and an elderly friend. Ralph was assessed by a paramedic and transported by ambulance to Farnchester emergency department. He was assessed by the medical team and transferred to the stroke unit. Dr White, the specialist stroke consultant, assessed Ralph’s physical condition and requested further diagnostic tests. He enquired about his history and reviewed his medical records, including previous transient ischaemic attacks (TIAs) and strokes. Dr White asked Ralph about changes in his general health and medicines use since his last stroke, and made an initial assessment to determine the extent of the stroke, the likely pathway he was to follow and ongoing care needs. These were recorded in his medical records together with instructions to stabilise and monitor the patient overnight. Ralph was clerked on to the stroke unit by a ward nurse where additional physical, personal and domestic information was recorded in a shared hospital record.
The following morning Ralph’s status was briefly reviewed as a part of the morning board round. Like all patients on the unit, Ralph’s basic details were recorded and reviewed on a wall-mounted whiteboard in the reception area, which listed his general condition, any instructions for observation and any outstanding tasks in relation to his care. The lead ward nurse, a therapist representative and a HCA quickly reviewed this information; the therapist noted Ralph’s admission to the unit and made a note to obtain any pre-existing care records and to visit him later in the day.
Later that morning, Ralph was reviewed as a part of the daily ward round. This was led by Dr White and Ralph’s ward nurse, together with four junior doctors and an OT and PT designated to that ward area. These clinicians congregated around his bedside to review his care progression; the results obtained from diagnostic tests; his speech, mobility and cognition; and options for his discharge (‘what shall we do with you next?’). Dr White verbally asked that his OT (Mandy) and PT (Theresa) commence rehabilitation and mobility exercises, and clarify his domestic circumstances in preparation for discharge planning. Dr White also requested that Ralph’s medication be reviewed by the stroke unit pharmacist.
Later that day, Ralph commenced intensive rehabilitation on the ward with Mandy and Theresa. Theresa focused more on his physical mobility, standing and walking, whereas Mandy asked questions about his home environment, activities of daily living and general well-being. The three-way interaction helped established a more nuanced understanding of his expected needs and recovery. The close and personal interaction also enabled Ralph to express his anxieties about his general health. The therapists used this opportunity to reassure Ralph about his recovery. The OT and PT spent over 30 minutes with Ralph and recorded a summary of their activities in the shared patient record, including a plan of action for future mobilisation. This also included a note to discuss his home circumstances with his family, either by telephone or during a hospital visit. On the same day, Ralph was also visited by the stroke unit pharmacist, following a request from the ward nurse. The pharmacist reviewed his medicines and endorsed the decision of Dr White to reduce his medication load.
At the end of the day shift, another board round was conducted to record general changes on the ward and to identify any outstanding tasks. This was attended by the junior doctors, nurses, OT and PT leads, HCAs and SaLTs. At this meeting, Mandy asked the evening OT (Sally) to contact Ralph’s family members either by telephone or in person. As they did not visit Ralph on this day, Sally contacted Ralph’s daughter by telephone to explain his condition and arrange a meeting the following day.
On the second day, Ralph’s daughter and Mandy met briefly before she visited him on the ward. Meeting without Ralph seemed to provide an opportunity for his daughter to raise concerns that she might not be able to raise in front of her father. It also enabled Mandy to gather a more detailed understanding of Ralph’s home environment. Following this, Ralph met with both his daughter and OT at his bedside to review similar issues and to consider his preferred domestic arrangements.
For the next 3 days, Ralph’s care generally followed the same pattern of being reviewed and assessed through board rounds and ward rounds, and having regular therapeutic input. On day 4, Ralph’s case was reviewed at the weekly MDT. This was led by Dr White and involved input from the nurse in charge, representatives from the therapist team, the specialist community stroke nurse and a stroke association representative. Ralph’s case was introduced by Dr White, who summarised his diagnosis and care plan, followed by the OT and PT leads, who gave a summary of their involvement using the shared record. The ward nurse also reviewed his progress and suggested rapid discharge home, given that he seemed to be responding well to recovery and that he was generally anxious about staying in hospital. Through the meeting, the decision was made to discharge Ralph the following day, and to consider his transport arrangements, medicines and follow-up care. These decisions were recorded in both Ralph’s medical notes and the shared care record. No direct instructions were given to any one individual or group, but the different professionals involved made separate notes for actions to be followed.
Later that day, Ralph’s progress was again reviewed as a part of the evening board round, where the nurse in charge allocated relevant tasks for his forthcoming discharge, including arrangements for his medicines and transportation. Following this review, one junior doctor consulted Ralph’s medical records and made arrangements for his TTOs, using the hospital’s electronic prescribing system. Later the same day, one of the OTs (Sally) met with Ralph and his family to review his discharge arrangements. It was decided that a hospital taxi would be more convenient to transport him back to his rural home rather than waiting for the ambulance service. No other arrangements were made with the community health-care provider and no referrals were made with social care providers because the OT believed he was not eligible for support.
On the morning of his fifth day in hospital Ralph was discharged home. This commenced with the daily board round, where the final tasks for his discharge were allocated. The taxi was booked in the morning by the ward receptionist, who also advised Ralph that he would have his follow-up appointment sent by post. Ralph’s medicines were ready for him on departure after being delivered to the unit by the 24-hour pharmacist service. Before Ralph was discharged home, the junior doctor told him that he still needed a heart scan but that this could not be arranged until the next morning. As such, he could either delay the discharge or return to the hospital the next day. Ralph decided to return the next day. The junior doctor also informed Ralph that a discharge letter would be sent to his GP by Dr White within the week.
After arriving home, Ralph was extremely tired and later felt that the hospital therapy ‘was too much exercise’ for him. His daughter looked after him that evening and reported that Ralph experienced a fall when using his toilet on his own. There were no evident physical consequences from this fall, but he later felt it was too difficult for him to get upstairs. The next morning, Ralph and his daughter returned to the hospital for his heart scan; he was told that he had a slight murmur but nothing significant. Later in the afternoon he visited his GP to review his care, and the GP arranged a commode to be delivered later that day after Ralph explained his difficulties in getting around the house.
The following morning Ralph restroked. The paramedic service attended to him at home before an ambulance transported him back to hospital. Upon readmission, he was told by Dr White that it was an extension of his previous stroke, and he was admitted for a further 4 days. This time Ralph had more severe physical and speech impairments from his stroke and required additional therapist input. Ralph believed that he had had another stroke because he was given too much extensive therapy in hospital and because his medicines had been changed. Meeting with Ralph at his home 4 weeks later, he reported that he had made some recovery from his stroke, including improved mobility. However, he had received no support from the community stroke nurse because she did not cover his area. Ralph managed to obtain a wheelchair, walking aids and hand rails around his home, but he said that these were provided by a community specialist heart nurse who was looking after his elderly lodger, and were not strictly for his use. As his daughter explained, they lived outside of the catchment area for the community stroke service so were lucky to benefit from these other services. His daughter also thought that the GP was very supportive, making regular home visits to check up on him, and the local pharmacist had reviewed his medicines to help him follow his prescription. She also said that he relied upon his neighbours to help transport him to subsequent hospital appointments.
Appendix 4 Extracts of data on knowledge sharing and discharge planning
Tabulated illustrative quotes
| Stages of the discharge planning and care transition process | Farnchester hip | Farnchester stroke | Glipton stroke | Glipton hip |
|---|---|---|---|---|
| Admission |
|
|
|
|
| Board/handover |
|
|
|
|
| Ward round |
|
|
|
|
| MDT meeting |
|
|
|
|
| Family meeting |
|
|
|
|
| Social care referral |
|
|
|
|
| Health-care referral |
|
|
|
|
| Internal care transfer |
|
|
||
| Day of discharge |
|
|
|
|
|
||||
| Social care |
|
|
|
|
| Health care |
|
|
|
|
Appendix 5 Extracts of data on safe discharge and knowledge sharing
| Risk | Interview evidence | Observed knowledge-sharing actions |
|---|---|---|
| Falls |
|
Referrals to PTs and community falls clinics by telephone, fax, letter Referrals by nursing and residential homes to community physiotherapy, via GP, by telephone and direct contact (waiting times varied from 6 to 14 weeks) ESD service and specialist community nurses (stroke) providing falls advice to patients in own home Community nurses and reablement staff suggesting changes to environment as part of falls advice Patient raising awareness of broken pavements by writing a letter to the council Evidence of patients masking falls from family carers and reablement staff by minimising the number and types of falls |
| Falls and medication |
|
Discussions with patients before discharge about medications, with nurse, pharmacy and OT Checking ability to physically and cognitively manage medications by OT Provision of dosset boxes for medicines for patients on discharge Requests by pharmacy and nurses for old medicines to be disposed of by hospital Detailed written instructions for patients and carers about medicine management |
| Falls and equipment |
|
Missed or poorly timed equipment led to loss of independence and patients adapting their own homes or borrowing equipment (e.g. frames), which limited rehabilitation potential and safety Gaps in community OT services and confusion over who pays for what between social services and health led to delays in supply of essential equipment such as commodes Limited transfer of knowledge information about safe use and monitoring of use resulted in abandonment of equipment or open interpretation of use by social care staff and family carers Allied health professionals worked hard to ensure equipment was identified, sourced and delivered prior to delivery Items such as dressings, continence pads and hygiene items were more likely to be missed or require duplication of assessment on discharge, as acute continence and community continence supplies separated in funding arrangements. Informal sharing of items between some wards and nursing homes, as staff known to each other Little provision for equipment checking or follow-up once delivered by professionals |
| Infections, urinary tract infections, pneumonia, pressure sores, wounds and septicaemia |
|
Patients poorly informed of the signs of infection on day of discharge and consequent delays in accessing GP care if an infection developed Documentation often poor with little information about infection status for community staff Access to primary care may be compromised by rural location, leading to potential deterioration before medical help sought Tendency for acute nursing staff to assume that family carers and patients have knowledge to seek assistance as required once discharged Little capacity for proactive monitoring of patients on discharge unless package of care in place and social and/or health staff in regular contact as part of ongoing health needs Specialist community nurses, community pharmacists and GPs tended to be used as a service to provide reactive responses to concerns about deterioration in health status |
| Medicines contributing towards deterioration of health, infections and falls |
|
Proactive pharmacy actions in both community and acute settings helped to mitigate the medication risks by increasing the knowledge of patients and close liaison with junior medics and GPs Support for junior doctors by expert interventions by pharmacist and checking of prescriptions by senior medics greatly valued by health professionals OT input to identify any potential cognitive and physical difficulties helped inform decisions about type and mode of dispensing Nursing staff expected to give verbal handover of medications on day of discharge but variable in ways of communicating this effectively to patient Ward clerks tended to make sure patient had medication bag on discharge; weekend discharges could lead to missed medications Location of community pharmacy and provision of free delivery of medications ensured continuity of supply in community and opportunity for patient to raise concerns Specialist community nurses frequently advised GPs, community professionals and patients about medications |
| Discharge planning is marginalised as part of health-care provision in acute settings |
|
Discharge planning may not commence until the patient is declared fit for discharge by medical team within hip sites Stroke sites used daily reviews, MDT meetings, technologies and setting of expected discharge date from admission as a way of centralising planning as a core remit of patient care Distinctive professional cultures tended to cause tensions with knowledge-sharing activities, especially among social service staff, nurses and ward clerks. OTs tended to mediate and work proactively to ensure verbal and written communications clear, with goal and review setting. PTs provided support and used positive coercion to maintain pace of discharge planning, especially between medical and nursing staff Nursing and junior medical staff tended to minimise discharge activities to task-orientated care, with minimal exploration of patient or family issues Changing policies and services led to sense of resignation that appropriate follow-up care was not available, so knowledge of referrals and procedure incomplete among acute staff |
| Timing of care planning and transition |
|
Maintain pace of the planning by daily reviews, accurate record keeping, allocation of dedicated person for each patient, 7-day working, knowledge of various discharge pathways and procedures not confined to distinctive professional groups or grades of staff. Tendency for OT and PT groups to maintain momentum and keep timely accurate records of progress Nursing groups (except discharge co-ordinators) relied on own pocket-held jottings or word of mouth rather than comprehensive record keeping of discharge activities Liaison between community and acute hospital providers by in-reach/outreach services tended to be more comprehensive and personalised communications via specialist nurses, ESD service and social workers Maintain communication with family, care provider and patient about planning for discharge, primarily by nursing and OT staff Regular and comprehensive MDT meetings, attended by all relevant professionals and led in a structured goal and review manner Fragmentation and stalling of the process during weekends, school holidays and bank holidays except on 7-day working sites because key staff (including ward clerks) not available Notable delays around winter crisis and Christmas time because of lack of panel meetings in social services for funding and community capacity issues Bed crises lead to increased outliers and early discharges when plans may not have been comprehensively completed |
| Care transition; period of rapid consolidation of all prior arrangements and transfer of patient. Risks of gaps in planning, timing and failure to achieve safe discharge |
|
Majority of discharges did happen on the date specified However, a proportion of discharges did not meet the longer-term support needs and so patient and family left to sort problems out, most commonly by seeking help from GP and community health services Discharge lounges a cause for concern for those patients requiring regular care assistance such as pressure area care, feeding, medication and emotional support because of the lack of comprehensive handover to staff Transport policies and providers changed during the study, leading to difficulties booking transport in advance and subsequent delays in waiting for transport home for many rural patients Ward clerks and discharge nurses key to maintaining pace and securing transport, ensuring patient goes home with all necessary transfer information and medications Blaming cultures between acute care staff and social services often led to the persistent eroding of effective communication; lack of dedicated social workers in units limited opportunities for developing sustainable knowledge exchange in the patients’ best interests Sense of pride and achievement apparent when managing end-of-life fast-track discharges among acute and community care professionals across the health and social service providers. These discharges tended to foster cohesive knowledge exchanges and a commitment to achieving rapid discharges |
| Clinical procedures and follow-up in hospital and community settings as part of medical care being missed, incomplete or incorrect |
|
Early discharges can lead to reliance on patient and family to return to hospital to complete further tests such as bloods and heart scans Ward clerks key to ensuring follow-up appointments are booked and communicated to patient accurately; direct information sharing across departments Some referrals missed, especially over weekends and during periods of high bed movements when documentation suboptimal Lack of consideration by hospital staff about how patient and family will physically attend appointments, so some not attended Specialist community nurses able to undertake specific tests such as titrations in patient home, thereby avoiding hospital attendance (stroke) |
Appendix 6 Sample of staff illustration of hospital discharge
List of abbreviations
- CCDDA
- Community Care (Delayed Discharges) Act
- CCG
- Clinical Commissioning Group
- CT
- computerised tomography
- EDD
- expected date of discharge
- ESD
- early supported discharge
- GP
- general practitioner
- HCA
- health-care assistant
- ICT
- information communication technology
- MDT
- multidisciplinary team
- NHFD
- National Hip Fracture Database
- NoF
- neck of femur
- ONS
- Office for National Statistics
- OT
- occupational therapist
- PCT
- primary care trust
- PPI
- patient and public involvement
- PT
- physiotherapist
- SaLT
- speech and language therapist
- SNA
- social network analysis
- TTO
- to take out (of hospital upon discharge)
- UTI
- urinary tract infection