Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 09/1002/05. The contractual start date was in March 2011. The final report began editorial review in September 2013 and was accepted for publication in April 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Currie et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
General background
Patient safety is a global concern. Research suggests that, in line with the USA and Australia, around 10% of patients admitted to acute hospitals in the UK experience an adverse event, of which half are identified as preventable, costing the NHS around £1B a year in terms of additional bed-days. 1 Empirically, our study focuses on the brokerage of patient safety knowledge (PSK) by hybrid middle-level managers (H-MLMs) for quality improvement in the care of older people in a hospital, a knowledge domain considered to be ineffectively mobilised for continuous improvement in clinical frontline care. Data captured via the UK’s National Reporting and Learning System (NRLS, released September 2012) identify inpatient falls within hospitals as the largest single type of patient safety incident (26%), followed by medication incidents (11%), and incidents relating to treatment and/or procedures (11%). This trend remains consistent with previous data releases. Such patient safety issues are the subject of intense policy focus across developed countries, particularly with ageing patient populations, where older patients take up increasing hospital resources to the extent that their care may be characterised as ‘mainstream business’ rather than specialist. Linked to this, older patients may remain in hospital longer than intended (e.g. because they have fractured their hip following a fall), or be discharged but quickly return to hospital (e.g. because the social care package is inadequate in the light of cognitive impairment, such as dementia), both of which are very costly.
Learning from safety events and clinical risks is recognised as vital to enhance patient safety,2 yet the brokering of PSK to the clinical front line remains problematic. The brokering of PSK related to the care of older people represents a high-profile and visible topic to examine more general matters of knowledge brokering by H-MLMs in health-care and social care organisations beyond hospitals, and in service domains beyond elderly care.
The knowledge-brokering role of the hybrid middle-level manager
Knowledge brokering across organisational and professional boundaries is particularly crucial for high-quality health-care delivery. Learning from PSK derived from ‘exogenous’ sources [e.g. National Institute for Health and Care Excellence (NICE) guidelines, National Patient Safety Agency (NPSA) alerts, and scientific research and publications], and ‘endogenous’ sources (e.g. experiential knowledge from the clinical front line, and patient safety incidents) is central to enhancing patient safety. 2
A knowledge broker is defined as an individual who uses their in-between vantage position to support innovation through connecting, recombining and transferring to new contexts otherwise disconnected pools of ideas, i.e. they get the right knowledge into the right hands, at the right time. 3,4 Middle-level managers (MLMs) play an important brokering role in understanding the functionality of the knowledge (i.e. for what purposes knowledge may be used) and how they can match the knowledge to potential opportunities. 5 In health-care organisations, a significant number of MLMs are ‘hybrid’, i.e. they hold responsibility for clinical service delivery as well as conduct a managerial role. 6 On the basis that H-MLMs have credibility with their clinical communities and, thus, enjoy legitimacy to broker knowledge within health-care organisations – more so than their generalist counterparts – H-MLMs are uniquely placed within organisations to broker the flows of exogenous and endogenous sources of PSK to improve the overall quality of care in four ways.
We highlight that H-MLMs are able to broker exogenous knowledge ‘downwards’ from external producers and disseminators of evidence – e.g. NPSA ‘safety alerts’ and NICE guidelines – and broker endogenous knowledge ‘upwards’ from within the organisation, for example through incident reporting and investigation, such as framed by the NRLS. 7–9 Further to this, we suggest that H-MLMs span the boundary between managerial structures for brokering PSK, such as clinical governance structures, and frontline clinical practice. They are, thus, uniquely positioned to fuse their understanding of local context (endogenous knowledge) with the more generic evidence base that constitutes exogenous knowledge, to ensure continuous development and implementation of high-quality service delivery that is patient-safe. Finally, if the necessary antecedents for H-MLM knowledge brokering are in place, such as H-MLM interaction with the external environment, then H-MLMs can effectively broker knowledge across organisations, as well as within organisations,10 to influence global best practice. We revisit our conceptualisation of the knowledge-brokering role of the H-MLM in Chapter 2.
Aims and objectives
Our research study examines the role of the H-MLM in brokering PSK relating to the care of older people within hospitals, between hospitals and other health-care organisations, and between hospitals and producers/disseminators/auditors of exogenous PSK and health-care context. We aim to identify contingent factors framing a more strategic role for H-MLMs, which is predicated on knowledge brokering.
The key dimensions of the knowledge-brokering process we analyse are shown in Box 1.
-
DIMENSION 1: The brokering of patient safety knowledge from external sources to inform service development within their local employing organisation.
-
DIMENSION 2: The brokering of patient safety knowledge from internal sources to inform service development within their local employing organisation.
-
DIMENSION 3: The fusing of external and internal knowledge within organisations, to ensure that service enhancement is aligned with global best practice, and simultaneously locally contextualised.
-
DIMENSION 4: The brokering of patient safety knowledge across the constituent organisations of a local health and social care delivery system for service development.
Our research will generate a deep understanding of the processes through which H-MLMs broker knowledge, grounded in the larger social context, aligned with the following RQs (as stated in our original protocol):
-
RQ1. What expectations and perceptions do external regional and national producers/disseminators/auditors of PSK have regarding the brokering of top-down knowledge (‘safety alerts’, broadly defined) through MLMs and risk management structures to influence clinical practice?
-
RQ2. Which MLMs are more likely to enact a knowledge-brokering role within organisations and across the system, and why: e.g. more ‘senior’ or more ‘junior’ MLMs; more or fewer H-MLMs; those affiliated to certain more powerful professional groups, notably doctors?
-
RQ3. What is the contribution of MLMs towards brokering PSK, e.g. when do they broker knowledge, of what type, how, within or across organisations, and qualitative description of outcomes?
-
RQ4. How do expectations and perceptions of knowledge-brokering patterns held by external national and regional producers/disseminators/auditors of PSK diverge or converge from knowledge-brokering patterns at local organisational or system levels?
-
RQ5. How do patterns of brokering associated with top-down PSK differ from knowledge-brokering patterns associated with bottom-up PSK?
-
RQ6. What prescriptions can our analysis of knowledge brokering offer for policy and practice, e.g. how can MLMs be enabled to broker PSK more effectively?
RQ, research question.
Research context
Knowledge brokering
The nature of knowledge, and knowing, is an important starting point for any research that aims to understand how knowledge is mobilised. This has been covered extensively in a recent scoping review of the literature by Crilly et al. for the National Coordinating Centre for the Service Delivery and Organisation (NCCSDO). 11 In essence, we regard knowledge as a resource applied by social actors in an attempt to solve problems. It can never be removed from its context, as it is bound to its use and its user within the organisation. 12 We position the concept of knowledge brokering as one solution to the challenge of knowledge mobilisation.
Our review of the strategic role of the H-MLM in brokering PSK draws upon the knowledge-based view (KBV) of the firm. KBV focuses upon knowledge as the most strategically important resource for any organisation. 13 In this study, we adopt a practice-based view of knowledge,14 distinguishing, first, between knowledge which is tacit (personal) or explicit (can be codified),15,16 and, second, between that which derives externally to the organisation (exogenous knowledge, more likely explicit) or internally (endogenous knowledge, more likely tacit). In complex organisations, and where the dominant core of the organisation is characterised by professional knowledge as in health care, knowledge mobilisation is inherently problematic. 17 Specificity of context, combined with the personal nature of knowledge,18 engenders knowledge that is ‘sticky’ and, thus, difficult to broker within and across organisations. Evidence suggests that clinical professionals privilege more contextualised, endogenous knowledge over and above exogenous knowledge which is explicitly presented and accessible to the whole health-care community,19 a phenomenon that Gabbay and Le May20 have termed ‘mindlines, not guidelines’. Attempts at brokering both explicit and tacit knowledge for patient safety face considerable challenges. 21,22 Generating a deep understanding of the processes through which explicit and tacit PSK is brokered within and across health-care organisations, grounded in the larger social context, is critical to inform quality improvement in health-care delivery.
Strategic management
Strategic management literature considers MLMs to be well placed as brokers because they provide a unique ‘linking pin’ between operational and strategic contexts. 23 Despite this, the role of the MLM has been under scrutiny in the private and public sector since the late 1970s. An increasingly globally competitive environment encouraged senior organisational management to delayer MLMs on the basis that the latter did not add value to the organisation’s activities. 10,24–27 However, organisations have found that the expected reduction in costs has not been realised, in large part explained by the loss of ‘tacit’ knowledge as MLMs ‘walk out of the door’, and management consultants are hired to fill the knowledge gap. 10,28 This highlights that the value of MLMs is linked to their role as a knowledge resource, which may be ‘hidden’ in more populist prescriptions for delayering.
In particular, where they have a relevant professional background, MLMs act as ‘hybrid’ managers10,29 who bridge managerial and clinical contexts, i.e. some MLMs may be better placed than others to enact a strategic knowledge-brokering role. Llewellyn6 describes the hybrid concept using a metaphor of a ‘two-way window’. In the context of health care, H-MLMs with a clinical background act as ‘mediating persons’ capable of working through sets of ideas belonging to management and sets of ideas belonging to clinical practice. The strategic role of the H-MLM lies in their ability to look through a ‘two-way window’, to ‘broker’ tacit as well as explicit PSK across clinical and managerial knowledge domains for service improvement. 4–6,19,30
Summary of research context
In summary, the research brings the following literatures together to frame analysis of the processes through which H-MLMs broker PSK in health care: strategic management literature about KBV of the firm and the role of MLMs; organisation studies literature about knowledge mobilisation and brokering; and a more specific health-care policy and management literature about MLMs and knowledge mobilisation. Our study seeks to understand the external and internal contextual influences that impact the ability and disposition of H-MLMs to broker exogenous and endogenous PSK within the organisation and across the wider elderly care pathway to improve the quality of health-care delivery for older people specifically and other patient groups more generally.
Research approach and report structure
The research adopted a mixed-methods approach incorporating interviews, observation, document analysis, tracer studies, focus groups and social network analysis (SNA). The rationale for a mixed-methods approach follows that of other National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) projects. There is general agreement in the literature that the combination of such methods yields results that are both robust and significant,31 and further that a mixed methods approach is particularly useful in health-care settings. 32,33
The main data-gathering method was semistructured interviews. In total, 127 semistructured interviews were conducted, mostly with H-MLMs, who broker PSK within three hospitals, but also with those involved in the external production/dissemination/auditing of PSK (henceforth referred to as ‘external producers’). Details of respondents and their organisations can be found in Chapter 3.
All interviews were semistructured, allowing for broad exploration of H-MLMs’ brokering of exogenous and endogenous PSK in line with our research questions (RQs). Interviews were conducted in line with work packages 1, 2 and 3 as outlined below.
Work package 1
Seventeen semistructured interviews were conducted with external, national- and regional-level producers, disseminators and auditors of PSK around falls, medication and transition, as outlined in our original proposal and in accordance with our research protocol. The primary purpose of interviews in work package 1 was to ascertain the expectations and perceptions of external producers of PSK regarding knowledge-brokering transfer from the ‘external producers’ to the ‘internal users’ of PSK.
Work package 2
Fifty-four interviews were conducted with individuals on and outside the main clinical governance structure, the Clinical Risk Committee (CRC), across three health-care organisations (two hospitals, cases A and B, and one mental health-care organisation, case C, with which the first two link around cognitive impairment of older patients in hospitals). These interviews focused, firstly, upon knowledge brokering of exogenous PSK produced or disseminated by external parties (e.g. in the form of ‘safety alerts’, broadly defined, or best practice guidelines) into clinical practice, by H-MLMs who are members of the CRC within a hospital. Then, secondly, we analysed the brokering of exogenous PSK from the CRC to the clinical front line. This provided an illuminating counterpoint to the expectations and perceptions of those producing and disseminating external evidence, who are interviewed in work package 1. Work package 2 examines, in detail, the social structures that impact upon knowledge-brokering roles.
We employed SNA to help us to identify key knowledge brokers and their characteristics. However, while our preliminary SNA data concur with our qualitative data in highlighting H-MLMs as key knowledge brokers, we found the ‘network’ to be very difficult to define. Questions about structural relations in the brokering of PSK yielded a range of answers regarding who was encompassed within the elderly care pathway through which PSK was brokered, commonly veering between ‘everyone’ and ‘no one’. While we do not present a specific SNA within this report, given the difficulties of defining any network in relation to PSK, our more qualitative assessment of the network following SNA, applied to interview transcripts, informs our analysis of relationships between H-MLMs at different levels within the organisation, and between H-MLMs and other actors within our hospital cases, and outside to external producers of PSK.
Supplementing interviews and SNA, we carried out observation of the CRC, and other relevant committees, such as the Inpatient Falls Committee (IPFC) and the Falls Operational Group, in hospital A. This amounted to approximately 20 hours’ observation of discussions related to PSK in elderly care, and helped to contextualise our research analysis.
Work package 3
Work package 3 focused upon the brokering of bottom-up or endogenous PSK. We traced knowledge brokering from serious untoward incidents (SUIs) related to falls, medication management and/or transition that resulted in unexpected patient harm (or death), anticipating that learning and quality improvement ensues. Recognising the importance of this work, one case study organisation, hospital A, requested an evaluation of the effectiveness of root cause analysis (RCA: a systematic investigation technique that looks beyond the individuals concerned and seeks to understand the underlying causes and environmental context in which the incident happened22) as a vehicle for learning and service improvement from patient safety incidents. Subsequently, the research team were asked to conduct focus groups with wards in order to work through problems and devise a plan for improvement. Work package 3 was consequently modified to involve more junior members of clinical staff located closer to clinical practice than participants in work packages 1 and 2 – i.e. registered and non-registered nurses, ward managers, matrons and junior doctors – in order to evaluate whether or not knowledge had been brokered to the clinical front line following a patient safety incident. Data collected in work package 3 provided a valuable insight into the importance of knowledge brokering to facilitate learning from endogenous PSK directly back to the ward where the incident occurred, and the challenge of brokering such knowledge upwards (and across) for wider learning across the hospital and to linked health and social care providers. Following this work, the research team conducted an evaluation of learning and service improvement from SUIs following RCA in a second case study organisation, hospital Z. This second evaluation allowed the research team to consider the generalisability of emergent research findings at hospital A about the brokering of PSK from RCAs for learning and service improvement in elderly care. Within work package 3, 56 interviews were conducted in total, supported by approximately 20 hours of observation of the day-to-day running of the wards and departments related to the SUI.
Feedback and engagement with user groups
Maximising and harnessing research impact is a major objective of our study, facilitated by the coproduction of data and the involvement of stakeholder groups across the health-care organisations. This was facilitated in the following way:
-
holding of three meetings of the Study Advisory Board across the project duration
-
presentation of emergent research findings to the IPFC and the Falls Operational Group (chaired by the chief executive) at hospital A, and to the patient safety team at hospital Z
-
facilitation of focus groups to share findings and work with stakeholders, to improve learning from bottom-up patient safety knowledge, within hospital A
-
presentation of emergent research findings at Health Services Research Network (HSRN) (June 2013)
-
employment of a professional corporate communications company to codevelop high-impact accessible lessons from study for health-care managers, professionals and policy-makers
-
facilitation of national dissemination via end-of-study report and a website, including video presentation (in place October 2013).
Relevance to National Institute for Health Research Health Services and Delivery Research programme
Our research fills a knowledge gap that is timely given initiatives in the Next Stage Review,34 which highlighted a need for locally driven innovation located nearer the front line of service delivery, impending constraints on NHS expenditure, and the concerted efforts around innovation adoption by the NIHR. A recent review of the Patient Safety Research Programme, funded by the Department of Health Policy Research Programme,9,35 highlights a need for system-level analysis and research on older people. The NPSA identifies the following PSK domains relevant to the care of older patients: (i) falls – a major and highly reported area of patient safety; (ii) medication-related safety – a prominent area of concern which exemplifies the challenge of brokering across jurisdiction, for example general practitioner (GP) or pharmacy to acute; and (iii) transition – as an elderly patient moves from one care provider to another, information may be absent, delayed, lost, distorted, misinterpreted or repeated.
The health-care literature about knowledge brokering is relatively normative,36 although there is anecdotal evidence about the effectiveness of knowledge brokering in improving the quality and use of evidence in health-care decision-making. 36–38 There is a particular need to understand how social context impacts upon brokering of evidence for service innovation. 11,39 Prescriptions around effective brokering of PSK by H-MLMs could save the NHS billions of pounds and prevent reputational damage. Finally, we link to the NIHR HSDR commissioning document around the Knowledge Transfer and Innovation (KT&I) programme of research (KM259), the systematic review of Ferlie et al. ,11 its follow up (Crilly et al. 40) and other ongoing research about knowledge mobilisation funded by the NIHR, particularly the study led by Waring, which focuses upon safe discharge and hospital readmission. 41 Regarding our focus upon H-MLMs, this relates to a number of previous studies commissioned by NIHR Service Delivery and Organisation examining the role of middle managers, specifically Annandale et al. ,42 Buchanan et al. ,43 Checkland et al. ,44 Dopson et al. 45 and Hyde et al. 46
Chapter 2 Literature review
This chapter reviews literature pertaining to the knowledge-brokering role of the MLM as a contribution to strategy. Our approach to reviewing literature represents a narrative synthesis,47 one which has previously been used in management sciences. Drawing on the interpretivist approach, adhering to the same principles of organisation, transparency and replicability as standard systematic review approaches in the field of health sciences, and with both quality and relevance as the organising matrix, narrative synthesis is a flexible method that allows the reviewer to be reflexive and critical through their choice of organising narrative. By developing a critical narrative, an evidence synthesis seeks to generate an understanding of the evidence and provide new insights that would not otherwise be apparent, either by focusing on individual or small clusters of studies or by including only certain types of data (e.g. quantitative). Through its emphasis on ‘evidence’ as opposed to ‘statistical significance’, an evidence synthesis thus looks to the nature and scale of the effects in practice but without compromising on quality (i.e. validity) or relevance. It highlights the importance of the social (contextual) as well as the scientific nature of evidence and emphasises the need for reflexivity in conducting evidence reviews. It also emphasises credibility to denote an approach which yields results that are meaningful at both objective (reliable) and subjective (trustworthy) levels. The literature review focused upon those concepts most relevant to our a priori objectives, specifically ‘knowledge brokering’ and ‘the role of hybrid middle managers’. Readers might note, however, that within our empirical sections we draw in other concepts, specifically ‘absorptive capacity’. We highlight analysis that applies the concept of absorptive capacity ensued as a consequence of inductive reasoning derived from thematic coding of data. As later detailed in research design, themes not anticipated in the literature review may emerge during the coding process; thus, ‘absorptive capacity’ did not represent an original search term in our narrative literature review. Such a more inductive or iterative approach to literature review and thematic coding is consistent with academic practice in social science. 48
Following our narrative synthesis, we begin by outlining the ongoing debate concerning the role and value of the MLM in the generic literature and specifically in relation to health care. Following this outline, we draw upon strategic management literature to illustrate the strategic role of the H-MLM as uniquely capable of brokering knowledge to influence and implement strategy in a manner that fuses exogenous sources of knowledge with the organisation’s endogenous knowledge base. Aligned to this, we review literature that adopts a more nuanced view of knowledge brokering and delineates between types of knowledge-brokering roles enacted by individuals within organisations and highlights the influence of context.
We then review the knowledge-brokering literature in health care, which we describe as normative and focusing mostly on external knowledge brokering. On this basis, we extend our review to consider the nature of knowledge in a health-care environment, and compare and contrast two approaches to brokering knowledge: a managed system-based approach (the NRLS) and an informal people-based approach [communities of practice (CoPs)]. We conclude that both approaches have strengths and weaknesses. Finally, we summarise the literature, highlighting key findings that guide our study.
The role and value of the middle-level manager
The role of the MLM has been under scrutiny in the private and public sector since the late 1970s, when an increasingly globally competitive environment encouraged senior organisational management to delayer MLMs on the basis that the latter did not add value to the organisation’s activities. 10,24–27 However, organisations have found that the expected reduction in costs has not been realised, in large part explained by the loss of ‘tacit’ knowledge as MLMs ‘walk out of the door’, and management consultants are hired to fill the knowledge gap. 10,28 This highlights that the value of MLMs is linked to their role as a knowledge resource, which may be ‘hidden’ in more populist prescriptions for delayering.
Cognisant of the hidden value of MLMs, since the early 1990s a less pejorative view of MLMs has emerged among academic commentators, highlighting the importance of their strategic contribution to organisational performance, although this has translated slowly to practice. The less pejorative view highlights the capacity of MLMs to develop, as well as implement, organisational strategy in a way that adds value to, rather than subtracts value from, organisational activities, through both upwards and downwards strategic influence, and which may diverge from, as well as converge with, the strategic intentions of executive management. 28 Central to this notion of strategic influence is the capacity of the MLM to ‘broker’ knowledge from one domain to another, given their position at the ‘nexus’ of the organisation to support innovation through connecting, recombining, and transferring to new contexts otherwise disconnected pools of ideas, i.e. they get the right knowledge into the right hands, at the right time. 3,4
Despite such a view of the more productive MLM, the efficiency drive to target MLMs continues to escalate. A recent column published in Harvard Business Review entitled ‘The end of the middle manager’49 proposes that ‘Technology itself is now the great general manager . . . thanks to the internet and search engines, everyone now knows or can know something about everything’ (p. 36). The underlying suggestion is that those with general management skills are vulnerable, as they no longer have knowledge that is considered valuable to the firm. The ensuing dissension among the ranks of academics and practitioners in response to this article was captured online and was swiftly picked up on in the Financial Times. 50 The general thread of the revolt against the argument by Gratton49 is centred on the increased complexity and velocity of change in modern organisations that require the more contextualised knowledge of those in the middle to shape, as well as to execute, strategy. In response to Gratton,49 Massachusetts Institute of Technology (MIT) professor, Steven Spear, employs the analogy of the human body to emphasise the crucial role of the MLM:
The human body has layer after layer of middle management, across cells, tissue, organ, leading up to the brain. Remove any one of those layers and ask the brain to talk directly to cells and you have something quite different and less efficient.
Steven Spear, cited in Broughton50
Reinforcing such a view, Wooldridge et al. 51 state that ‘Organisations require distributed and interactive leadership throughout the organisation with middle managers as important mediators between levels and units’ (p. 1191). In a related literature, that of distributed leadership, we note similar calls for a more influential role for those actors located at the middle levels of the organisation. 52
Returning to the crux of Gratton’s argument, that technology will supplant the role of the general manager, Dopson and Stewart27 trace this prediction back more than half a century to Leavitt and Whisler. 53 Other commentators followed similarly, from 1960 through to the middle of the 1980s,54–57 yet there was little evidence to support these assertions. 58,59 During the mid 1980s, research was published that suggested that rather than information technology (IT) shrinking the role of the MLM, it was actually reshaping and enhancing their strategic role,60,61 with evidence highlighting a variety of changes to the work of the MLM that had, almost without exception, enriched jobs, with reports of widespread upskilling and increased responsibility and autonomy. 25,58,62 In attempting to make sense of these competing views of the interaction of IT and the role of MLMs, Pinsonneault and Kraemer63 argue that the latter will continue to perform tasks where they have comparative advantage and renounce those tasks that are best performed by IT, ‘Hence IT takes over most informational and structured decisional activities, but few (if any) interpersonal and unstructured decisional activities’ (p .279). The authors also argue that the numbers of MLMs vary according to the degree of centralised decision-making in the organisation. In organisations where decision-making is decentralised (a characteristic of health-care organisations), MLMs are crucial to the synthesis of information to bestow it with meaning and purpose,10,24,63,64 in turn permitting the MLMs to influence strategy and decision-making at a strategic level of the organisation. 28,65–67 In such a situation, the numbers of MLMs may even be likely to increase rather than diminish. 63 Finally, Pinsonneault and Kraemer63 argue that factors other than IT can cause a decay or enhancement of the numbers of MLMs, specifically environmental triggers such as a cost-efficiency drive or changes in the policy environment. These triggers are apparent in the English NHS, as follows.
Middle management and the NHS
The efficiency drive to target MLMs has continued to escalate, with the current coalition government (elected in 2010) pledging a reduction in management costs in the English NHS by more than 45% by 2014. This drive to reduce management costs is reflected in recent figures published by the NHS Information Centre (March 2011), which highlights a decrease in the number of managers and senior managers by 6.2% between September 2009 and September 2010, alongside an overall expansion in the size of the workforce during this time. In their report to the King’s Fund, Walshe and Smith68 suggest that the widely professed rise of bureaucracy may actually be exaggerated. Their report concludes that ‘There is no persuasive evidence that the NHS is over-managed, and a good deal of evidence that it may be under-managed’ (p. vii). Further, they caution policy-makers: ‘the denigration of managers and the role they play in delivering high-quality health care will be damaging to the NHS and to patient care in the short and long term’ (p. vii).
Reflecting the bifurcated debate in generic literature, in the English NHS the attack on the utility of the MLM goes hand in hand with policy drives to reduce organisational costs. 10 We highlight that the justification for reducing the numbers of MLMs appears emotive, linking a strong emblematic association of the NHS with national values, and a need to reduce management costs and distribute savings to safeguard frontline care. 69 Provocative and captivating headlines in the popular press expose the evocative language employed by high-profile politicians in their efforts to reduce the numbers of MLMs in health care. 68 Disparaging terms have emerged to describe MLMs in health care within daily printed media and online communities, such as ‘faceless bureaucrats’, ‘idle pen pushers’ and ‘men in grey suits’. The depth of negative feeling about MLMs in health care is evidenced in the use of satirical language; for example, see ‘nhsmanagerturnedtrader.blogspot.com’ (last accessed 21 March 2013), describing one ex-NHS manager’s journey from ‘faceless bureaucrat to bad-assed trader’ [sic], and the ‘idlepenpusher.blogspot.com’, where the writer describes himself as ‘a public sector nobody’.
At the same time, from a strategic perspective, reflecting the more generic literature, arguments that MLMs should be delayered in health care lack an empirical evidence base. Rather, it may be that an enhanced role for MLMs is required. Developing this line of argument further, we now review the strategic management literature in line with a reconceptualisation of the MLM role as strategic. Our assertion is that MLMs, specifically H-MLMs, are central to the brokerage of PSK, meaning that they play a crucial role in enhancing service quality.
The strategic role of the middle-level manager
The classical view of strategy suggests strategy formulation is an isolated, planned and deliberate process. The senior manager formulates strategy and the MLM executes the strategy. 70,71 During the past 25 years, the scope of strategy process research has expanded to include not only senior managers but also MLMs. 51 Quinn72 was among the first to challenge the classical view with his concept of ‘logical incrementalism’, suggesting that strategy is gradually adapted over time through experimentation and learning. 73 Since 1980, strategic management theorists have agreed that strategy is neither completely deliberate nor completely emergent. Instead, the two approaches represent polar ends of a continuum upon which ‘real world strategies would fall’ (p. 259). 74 Thus, to varying degrees, strategy is as much emergent as it is planned. 66,74 Reflecting this, Nonaka75 describes the process of strategy at Honda using the term ‘compressive management’. The author explains that this ‘middle up–down’ style of management involves the translation of senior management vision to resolve the contradiction between their visionary (but abstract) concepts and the experientially grounded concepts originating from the ‘shop floor’. Thus, by virtue of their structural location at the nexus of the organisation, the MLM acts as a linking pin between senior management vision and bottom-up reality. 23 This suggests that the MLM is an important catalyst for change, as opposed to being a passive recipient. 24 Specifically, the MLM has an important strategic role of mediating and resolving the knowledge gap between the top and bottom layers of the organisation, as strategic change emerges.
In common with Nonaka’s75 findings, empirical research conducted by Floyd and Wooldridge28,65,67,76 has shown a positive relationship between MLM involvement in strategy and organisational performance. 26 Based on this research, Floyd and Wooldridge65 developed a typology of MLM roles that illustrates their ability to influence strategy through their upwards and downwards relations. MLMs influence strategy upwards through interpreting information and channelling this information upwards to senior management (synthesis). Upwards influence may also occur through the championing of strategic alternatives as a result of divergent activities that combine the experience of the ‘shop floor’ (i.e. those at an operational level) with the strategic intentions of the top. Championing alternatives closely aligns to Nonaka’s15 view of the MLM role in mediating the conceptual knowledge at the top with the experiential knowledge on the shop floor (a ‘middle up–down’ style of management, in Nonaka’s terms75). In influencing strategic implementation (downwards influence), the MLM fuses their knowledge of top-down strategic objectives with bottom-up situated knowledge to facilitate adaptability, preparing the bottom for change,24 as well as the more traditional role of merely implementing deliberate strategy. 70
Floyd and Wooldridge23 conceptualise the process of influencing and implementing strategy as an iterative process that involves the conversion of new ideas into strategic initiatives. Over time, this process develops into organisational capabilities. They state that ‘Information flows and patterns of social influence that transform ideas and initiatives into new capabilities have their nexus at middle levels of management hierarchy. . . This is “where the action is” in a capability-based view of strategy’ (p. xvi). Floyd and Wooldridge imply that the role of the MLM is more than a ‘linking pin’. The MLM has the capability to fuse divergent ideas that arise at an operational level with top-down strategic issues based on their knowledge and experience, to shape strategy and influence change. 23 Such a view aligns with KBVs of the firm that have emerged in the strategic management literature. 13,77,78
The knowledge-based view and the strategic role of the middle-level manager
Grant13 argues that organisations exist because they are more efficient at integrating and applying specialised knowledge than markets are. The KBV of the firm is an innovation within the resource-based view (RBV) of the firm. 13,79–81 Underpinning KBV is an assumption that knowledge is the most important resource of any organisation and, thus, strategy should be concerned with the development, protection and transfer of knowledge. 77,78 In many ways, KBV, with its emphasis on knowledge development and transfer, may be thought of as the link between the traditional static conceptualisation of the RBV and more recent developments surrounding dynamic capabilities theory,82 combinative capabilities83 and absorptive capacity. 84 As such, KBV suggests a significant role for MLMs in the management of an organisation’s knowledge for improving quality through the successful transformation of new knowledge for service improvement. To explain, MLMs, given a set of knowledge resources, play an important brokering role in understanding the functionality of the knowledge (i.e. for what purposes knowledge may be used) and how they can match the knowledge to potential opportunities. In doing so, ‘knowledge broker’ MLMs bridge multiple domains, learn about the knowledge resources within those domains, link that knowledge to new situations, and finally build new networks around the innovations that emerge from the process. To emphasise, a knowledge broker is defined as an individual who uses their in-between vantage position to support innovation through connecting, recombining and transferring to new contexts otherwise disconnected pools of ideas, i.e. they get the right knowledge into the right hands, at the right time. 3,4
The hybrid middle-level manager
Strategic management literature argues that MLMs are well placed as knowledge brokers because they provide a unique ‘linking pin’ between operational and strategic contexts and are capable of shaping strategic change. 23 Particularly where they have a relevant professional background, MLMs act as ‘hybrid’ managers10,29 who can bridge managerial and clinical contexts, i.e. some MLMs may be better placed than others to enact a strategic knowledge-brokering role. 85 ‘Hybrid’ refers to MLMs who are skilled in an alternative profession, hereafter referred to as ‘H-MLMs’. Llewellyn6 describes the hybrid concept using a metaphor of a ‘two-way window’. In the context of health care, for example, H-MLMs with a clinical background act as ‘mediating persons’ capable of working through sets of ideas belonging to management and sets of ideas belonging to clinical practice. 6 This dual sense-making activity requires skills of ‘discursive competence’,86 described as the ability to ‘perform the conversation’ and ‘set the scene’, skills which Rouleau and Balogun86 assert go beyond the capacity to speak the right words to the right people, additionally involving the use of language to trigger linkages and build acceptance of their position among others.
The two-way window implies greater communication between clinical practice and management, which were previously opaque to each other, i.e. constituted as one-way windows. On the basis that there are now both people and organisational tasks that cross the boundary between clinical practice and management, management within health care is no longer about ‘oiling the wheels’. 87 Instead, management represents an organisational arena where difficult and contentious clinical management decisions are required, which H-MLMs are well placed to make. H-MLMs command credibility within their clinical communities and, thus, enjoy a legitimacy to broker knowledge within health-care organisations – more so than their generalist counterparts – and, further, have a zeal for service improvement. 24,88,89
In health care, professionals value and pursue local and tacit knowledge in making clinical decisions about patient care. Indeed, clinical professionals may privilege more contextualised knowledge over and above knowledge which is explicitly presented and accessible to the whole health-care community, a phenomenon that Gabbay and Le May20 have termed ‘mindlines, not guidelines’. Consequently, any attempt at managing professionalised and tacit knowledge in health care through the mobilisation of explicit and codified knowledge faces significant challenge. 21,22 The significance of tacit knowledge in the professionalised setting of health care leads us to assert that IT is unlikely to supplant the role of the H-MLM. We posit that the strategic role of the H-MLM lies in his or her ability to look through a ‘two-way window’, to ‘broker’ tacit, as well as explicit, clinical and managerial knowledge domains for service improvement. 4–6,19,30,90 Conceptually, based on the extant literature, we characterise the potential knowledge-brokering role of the H-MLM in relation to PSK for service improvement in the following way. Firstly, H-MLMs are able to broker exogenous knowledge ‘downwards’ from external producers and disseminators of evidence, for example, in England, from NPSA ‘safety alerts’. Secondly, H-MLMs are able to broker endogenous knowledge ‘upwards’ from the clinical front line to inform learning and improvement at a systems level, for example through incident reporting and investigation. 9 Thirdly, H-MLMs who hold responsibility for clinical service delivery span the boundary between managerial structures for brokering PSK, such as clinical governance committees and frontline clinical practice. Thus, they are uniquely positioned to fuse their understanding of local context (endogenous knowledge) with the more generic evidence base that constitutes exogenous knowledge, so as to ensure continuous development and implementation of high-quality service delivery that is patient-safe. Fourthly, H-MLMs can effectively broker knowledge across organisations, as well as within organisations, where they interact with the environment.
Having reviewed at length the literature with regards to the strategic role of the H-MLM, we now turn to a more nuanced discussion related to the range of knowledge-brokering roles enacted by the H-MLM.
A typology of knowledge-brokering roles
Fernandez and Gould91,92 delineate a typology of knowledge-broker roles: ‘liaison’, where knowledge is brokered across a triad of individuals each belonging to different groups, in which contact between sender and ultimate receiver is only indirectly reached through an intermediating party;93 ‘representative’, where the knowledge broker transfers knowledge received from an actor within his own professional group to an actor in another professional group, representing his own group to the outside; ‘gatekeeper’, where the broker screens knowledge to distribute within their own group; ‘co-ordinator’, where all of the actors are in the same group, and an individual brings two persons from his own divisions into contact with each other; and the ‘cosmopolitan’ broker, who mediates between actors in the same professional group, but where the broker is not part of this group. Shi et al. 85 extend this typology of brokerage roles, through considering how the knowledge-brokering roles relate to Floyd and Wooldridge’s typology of MLM strategic roles. 28,65–67 Like Fernandez and Gould,91,92 Shi et al. 85 conceive the knowledge broker sitting within a triad consisting of one knowledge broker and two ‘alters’ (i.e. lower, peer or more senior managers). However, they extend the number of brokerage types identified by Fernandez and Gould91,92 from five to eight, incorporating the notion that some roles (cosmopolitan, gatekeeper and liaison) involve different subgroups within the cadre of MLMs. To clarify, the authors explain: ‘In a cosmopolitan role, the middle-manager broker can have relationships either with two lower-level managers or with two top managers . . . such alternate scenarios [create] different brokerage roles because they involve different subgroups (the group of lower-level managers and the group of top managers) and consequently, they dictate different contexts’ (p. 1461). It is context, they argue, that impacts a broker’s strategic agency to engage a ‘union’ or ‘disunion’ strategy. A ‘disunion’ strategy refers to the bridging of a structural hole between two ‘alters’, i.e. for a H-MLM to keep them apart while brokering knowledge between them on a continuous basis. Conversely, a ‘union’ strategy94 refers to the joining of two previously isolated actors, and might occur where there may be more value in closing the structural hole and bringing the ‘alters’ together than in keeping them apart. This is more akin to blurring organisational and professional boundaries, and hints at an approach to knowledge brokering aimed more at developing community-like tendencies across disparate professional or managerial groups.
The work of Fernandez and Gould91,92 assumes that there is no potential linkage between the two alters, and, thus, the role of the broker is always to bridge a structural hole, rather than to close the hole altogether. Shi et al. 85 consider this view to be flawed. They argue that there may be instances where a ‘union’ strategy (bringing two alters together and closing the structural hole) may bring more benefits than a ‘disunion’ strategy (bridging the structural hole). The contention is based on two scenarios. The first is a straightforward situation where more value can be created through bringing two alters together rather than mediating information flows. The second situation may arise where the strategic intention of the broker is viewed with suspicion by the alters and reflects the ability of the alters to set up their own linkage, cutting out the broker altogether. The contribution of Shi et al. ’s85 work lies in the assertion that context surrounding the alters’ ability and desire to close the structural hole will also impact upon the broker’s intention to bridge or close it. In short, the strategic role of the knowledge broker is more complex than a mere linking of actors to broker knowledge. Consideration of context is vital to our understanding of the processes of knowledge brokering within professional organisations where more powerful actors may work together to ‘shut down’ a knowledge broker’s role in bridging a structural hole, or where an individual may benefit from closing a structural hole in a bid to conjure credibility and legitimacy to broker knowledge across professional groups and influence strategy.
In summary, the work of Shi et al. 85 supports the view of the knowledge broker as more than a ‘linking pin’ between senior and other managers/professionals and alerts us to the MLM’s potential to broker between two actors at higher levels of status than him or her.
Knowledge brokering literature and health care
Literature about knowledge brokering in health care resonates with strategic management literature, in emphasising the potential for MLMs to add significant value to organisations. 3,36,95–103 However, we suggest that the literature about knowledge brokering in health care is relatively normative regarding the role of MLMs. Further, it focuses mostly on external knowledge brokering (i.e. between research and practice), suggesting that health services are not very well organised or receptive to the application of exogenous knowledge for service development. 101 While this is relevant for our study, we highlight that brokering of endogenous knowledge remains under-researched, yet crucial where evidence is ‘complex’, i.e. not easily codified. Furthermore, the political dimension of knowledge brokering remains relatively unexplored, with a particular need to understand knowledge brokers’ legitimacy claim to carry out their activity, and also how others respond to brokerage activity, i.e. to shut it down where their interests are threatened. 85
In the next section, we build upon The hybrid middle-level manager in our discussion of the nature of knowledge and how this relates to the brokerage of PSK in the NHS.
The nature of ‘knowledge’ and approaches to broker patient safety knowledge in the NHS
What constitutes knowledge and the appropriate mechanisms for brokering knowledge both across and within occupational and organisational boundaries has been widely debated in academic circles. The debate is polarised around whether knowledge is an objective or a more subjective phenomenon. Those who hold an objective view of knowledge tend to privilege technological or structural aspects of storing and retrieving knowledge. 59 Those holding a more subjective view of knowledge focus on the conduciveness of the environment, emphasising human factors of trust, learning ability and information sharing among communities. 104,105 For those holding an objective view of knowledge, it is conceivable that technology may supplant the role of the MLM. However, for those holding a more subjective view which characterises knowledge as ‘fluid’ – i.e. cannot be stored as ‘stock’106,107 – then the concept of ‘knowledge management’ becomes something of a paradox, as how can knowledge be formally managed when it resides in practice and is a contextualised phenomenon?104 Bridging diverse views of knowledge, Styhre107 argues that such a division between objective and subjective views of knowledge is not helpful, as ‘Tacit and explicit knowledge are not discrete categories, but always co-exist in one another. All explicit knowledge pre-supposes some tacit skills, and tacit knowledge is always based on the use of explicit knowledge’ (p. 183). In short, we might consider how exogenous knowledge, which is explicit, fuses with endogenous knowledge, which is more contextualised and tacit.
Mobilising patient safety knowledge across the NHS
Reflecting the competing views of knowledge, as above, which coexist in health care, the problem of mobilising knowledge in this environment can also be conceptualised as one of two extremes. At one end, there exists a professionalised body of knowledge that develops increasing degrees of tacitness over time. This knowledge is localised, specialised and closely guarded within professions. 108 At the other extreme, there is a body of explicit knowledge, commonly presented as formal evidence, which is vast, expanding at a phenomenal rate and is ubiquitously accessible. 21 A literature review of knowledge management in health care by Nicolini et al. 21 finds that the highly fragmented and dispersed nature of clinically related knowledge lends itself well to electronic storage and retrieval to support the clinical decision-making process. The use of IT-based tools is considered important to enable health-care clinicians to access the vast array of scientific knowledge that is relevant to managing their practices and delivering quality of care to patients. 105 Perhaps paradoxically, the extant literature also portrays compelling evidence that professionals value and pursue local and tacit knowledge in making clinical decisions about patient care (e.g. Gabbay and Le May20). One might conclude that any attempt at brokering professionalised and tacit knowledge in health care through its conversion into explicit and codified knowledge is unlikely to succeed. 21 Overall, managing knowledge at the extremes is wrought with difficulty. Knowledge that is tacit-dominant tends to remain isolated in select circles with knowledge brokering ‘retarded’. 109 Knowledge that is explicit-dominant tends to be too voluminous, and so, despite its universal accessibility, the ability to first identify such knowledge and then broker it to the right person(s) in order to impact service is a formidable challenge.
The following section outlines two approaches to brokering knowledge across health-care organisations, which highlight this challenge. The first represents a structural solution designed to extract and codify ‘situated’ PSK (i.e. embedded in context) from individual health-care organisations in order to generate new PSK that is then brokered back to hospital organisations as ‘safety alerts’, usually prescribing remedial action regarding a patient safety issue. It exemplifies the challenge of pulling endogenous PSK upwards through a health-care system and converting this to exogenous PSK, which is then pushed back into health-care organisations for service improvement. The other approach is a much more informal arrangement, whereby tacit or endogenous knowledge is shared within CoPs110,111 to inform ongoing service improvement locally, but which remains insulated from other parts of the health-care organisation and system.
National Reporting and Learning System: a national approach to brokering knowledge across occupational and organisational boundaries
Following the publication of the Department of Health’s report entitled An organisation with a memory,2 in which it was estimated that around 10% of hospital admissions lead to the occurrence of an adverse event, i.e. unintended harm or near harm, a NRLS was implemented in England and Wales. The NRLS comprises a dedicated system for incident reporting throughout the health service. NRLS requires frontline clinicians to systematically report patient safety incidents (or near incidents) that they have experienced in order to generate national guidance and learning in the form of patient safety alerts. Patient safety alerts are issued to all NHS Trusts and are received through a central alert system, i.e. they represent exogenous sources of PSK for learning and service action to improve patient safety. Trusts are duly required to respond to alerts and to indicate when they have completed the actions required, or else to confirm that no action is required.
After a decade of incident reporting in England and Wales through the NRLS, the increasing number of incidents reported year on year by hospitals, and by other health-care providers, suggests that a responsible culture of incident reporting is being cultivated in the NHS England and Wales. Correspondingly, empirical research by Sheldon112 and Lankshear et al. 113 suggests that hospitals and other health-care providers are willing to follow guidance of this type. However, Lankshear et al. 113 find that, while health-care providers in the NHS England and Wales have succeeded in setting up systems to disseminate alerts to MLMs, implementation of recommendations by doctors is suboptimal. In a later study, the same authors found that medical directors were much less likely to be aware of medication-related alerts and rapid response reports (RRRs) than their nursing and clinical governance colleagues. Furthermore, around half of health-care providers in the NHS England and Wales reportedly struggle to communicate effectively and reliably with their junior doctors. 114,115 Such research raises questions about the efficacy of a national agency that systematically codifies knowledge from patient safety incidents across the NHS for transfer into practice and, correspondingly, the ability of MLMs to broker patient safety knowledge effectively to inform service action or influence strategy.
In summary, the NRLS comprises a dedicated system for incident reporting throughout NHS England and Wales, which requires frontline clinicians to systematically report patient safety incidents (or near incidents) that they have experienced. NRLS pulls endogenous and tacit-dominant PSK from the clinical front line as a basis for generating exogenous sources of PSK for brokerage across NHS England and Wales as a whole. It represents an approach that attempts to convert tacit knowledge into explicit for durable improvements for patient safety.
Conceptually, the efficacy of the NRLS as a vehicle for brokering PSK is challenged on the basis that the system is founded on a number of assumptions that violate both the nature of knowledge and the nuances of a professionalised context. For example, the first assumption is that incident-related PSK can be meaningful when codified and extracted from nuances of context. Second, that risk is a unified concept shared across professional occupations. Third, there is a misperception that doctors are amenable to being managed (and conceivably monitored) in a technocratic and managerial manner. 7,9,116,117 Waring and Currie9 subsequently report the unintended consequences of this approach as the strengthening (or blurring) of professional and managerial boundaries, as doctors seek to circumvent the NRLS through offering bespoke situated responses, which begin to cohere around a CoP110,111 and which limit management control over knowledge and reinforce claims to medical autonomy.
Communities of practice
Dopson and Fitzgerald88 are not entirely positive regarding the effects of CoPs upon knowledge brokering. The authors emphasise that professionalised contexts, such as health care, have differentiated knowledge domains, which are decoupled, and that this inhibits knowledge brokering. 85,88,109 So, there exist uniprofessional communities, which are self-sealing and highly institutionalised. These shut out neighbouring communities, and defend their professional jurisdiction, so creating a ‘cognitive lock-in’ to members of that community, and community ‘lock out’ to non-members. 85,88 In short, the challenge remains to join up self-sealing CoPs, so that a community of practitioners or interest is developed.
Oborn and Dawson118 offer a more optimistic view of the ability of CoPs to broker knowledge in a specialist health-care setting, where they encompass multidisciplinary activity. The authors initially observe the type of barriers to knowledge brokering typically associated with CoP, as outlined by Dopson and Fitzgerald. 88 However, they assert that the ability to broker knowledge across CoPs was gradually learned. Such learning was assisted by the development of boundary objects and processes such as the use of ‘ambassadorial’ brokers, who facilitated ‘a level of transparency into the knowledge held by the various CoPs’ (p. 853), enabling others to make sense and personalise the knowledge presented by the various CoPs.
In essence, Oborn and Dawson118 echo the knowledge-brokering role of the H-MLM as described earlier (see The hybrid middle-level manager). The ability of the H-MLM to broker clinical and managerial knowledge domains for service improvement is afforded not just by their epistemic ‘two-way’ window, but also in their ability to conjure credibility and legitimacy among others for their role to fuse knowledge from multiple perspectives in a multidisciplinary clinical setting.
To reiterate the value of two approaches to brokering knowledge, those that assume an objective view of knowledge, such as the NRLS, appear insufficiently contextualised. 9 Meanwhile, those assuming a subjective view of knowledge, such as CoPs, may suffer from ‘cognitive lock-in’ and the potential isolation of members from other knowledge perspectives. 88 Both approaches may be deficient, with potentially significant implications for the quality of care to service users and, ultimately, the long-term sustainability of the organisation, unless H-MLMs play a knowledge brokering role.
Our next section builds upon the KBV of the firm to explore literature relating to ‘combinative capabilities’. We consider how brokering of knowledge by H-MLMs is framed by the organisation’s ability to process knowledge for service improvement. Our focus upon combinative capabilities allows us to surface features of organisational context and its environment that represent contingencies that frame H-MLM’s knowledge brokering.
Combinative capabilities and knowledge brokering
Combinative capabilities refer to the knowledge-processing activities of an organisation to generate, synthesise and apply new knowledge. 83,119 Van den Bosch et al. 119 distinguish three types of combinative capabilities: systems capabilities, socialisation capabilities and co-ordination capabilities. Systems capabilities refer to formal knowledge exchange mechanisms, such as written policies, procedures and manuals, that are explicitly designed to facilitate the transfer of codified knowledge. Socialisation capabilities refer to cultural mechanisms that promote a shared ideology and collective interpretations of reality within an organisation. Co-ordination capabilities refer to lateral forms of communication such as education and training, job rotation, cross-functional interfaces and distinct liaison roles.
Regarding their effects upon knowledge brokering, combinative capabilities work in different ways. The shared culture or ideology that socialisation capability represents can transform and exploit new knowledge quickly, but may also represent a ‘mental prison’ that leaves little room for absorbing outside sources of knowledge that contradict shared beliefs. We see this in the example of CoPs outlined in the previous section. An organisation’s systems capabilities provide a memory for staff handling routine situations in an organisation, and mean that staff know what to do and can react very quickly. Like socialisation capabilities, they therefore increase the efficiency of knowledge exploitation, while narrowing the search for new external knowledge and the scope for information processing. In contrast, co-ordination capabilities increase the scope of external knowledge acquired and assimilated, and flexibility in knowledge absorption. In essence, managers might attend to organisational mechanisms associated with co-ordination capability to enhance the brokering of new knowledge for service improvement. 119,120
However, despite the burgeoning literature examining combinative capabilities, it remains unclear how to impact knowledge-brokering activity for service improvement. 121,122 From the literature, we can discern the following. First, organisations do not absorb knowledge without effort; rather, it is dependent upon deliberate will and individual agency. Second, the absorption of new, external knowledge proves easier where it is linked to that knowledge already embedded within the organisation, rather than representing a significant departure from pre-existing knowledge. Third, knowledge is more likely to be transferred between those within the organisation where they have common knowledge in terms of expertise, training or other background characteristics, i.e. socialisation capability effects. 121 Finally, powerful groups of actors, both within and outside an organisation, may influence knowledge absorption processes to achieve their own goals. 123,124 The implication is that employees need to be exposed to diverse knowledge sources, but these need to have complementarity with existing knowledge sources. 122 Organisational managers need to establish ties with external sources of new knowledge and support this through establishing dense networks of ties within the organisation. 120 However, mediating socialisation capability to allow this to happen is likely to prove challenging, as employees and managers may not ‘see’ or ‘understand’ the potential value of new, external knowledge. 124 They may be encouraged to do so in the presence of ‘activation triggers’, such as internal crises or performance failures. 121,122 This is more likely where co-ordination capabilities are developed in the domain of ‘social integration mechanisms’, such as boundary-spanning or liaison mechanisms, CoPs, and decentralising authority and decision-making. 84,120,121,125 Based upon this analysis, H-MLMs would appear to represent co-ordination capability, but may need to be supported through other social mechanisms to mediate the effects of systems capabilities and socialisation capabilities within health-care organisations.
In the next section, we consider how individual, organisational and interactional antecedents, linked to combinative capabilities, bound the brokering of PSK for service improvement within health-care organisations.
Brokering new knowledge for service improvement
Health-care organisations exemplify the professional bureaucracy archetype,126 within which professional organisation is likely to represent a key influence upon socialisation capability, limiting knowledge brokering in the following ways. Firstly, knowledge brokering interacts with strong organisational cultures and structures, so that socialisation capability restricts the development of critical review capacity in the organisation important for such knowledge brokering. 119 Power and status linked to professional roles are likely to impact an organisation’s ability to exploit new knowledge. 127–129 For example, Berta et al. 130 note the role of doctors in subverting an organisation’s learning capacity in relation to the adoption of clinical guidelines and the assimilation of new knowledge into practice. Similarly, Ferlie et al. 109 note that deeply ingrained organisational structures and social networks engender institutionalised epistemic CoPs, which exist in silos, relatively decoupled from one another. This stymies the search for new knowledge that lies outside current ways of thinking among powerful professional groups.
Secondly, public service organisations (PSOs), such as those in health care, are subject to New Public Management reform, which frames performance through financial incentives and regulation. Reflected in systems capability, such government policy affords access to external resources, and directs and formalises knowledge acquisition and assimilation. However, it narrows the search for new knowledge and the scope for information processing, as managers in health-care organisations ‘game play’ to ensure compliance with policy requirements around their governance. 131–133 Volberda et al. 121 highlight the importance of the ‘classical’ managerial logic, which portrays organisations as tools to achieve pre-set ends, and so limiting the level of knowledge brokering for service improvement. Knowledge brokering within health-care organisations towards patient safety appears particularly directed towards compliance with government regulation and performance management,22 in a way likely to limit external knowledge search and utilisation, hence limiting the level of brokering for service improvement.
Thirdly, in mediating the effects of socialisation and systems capabilities, Hotho et al. 134 highlight a health-care organisation must attend to co-ordination capabilities, particularly social mechanisms for bridging the gap between sources of exogenous knowledge and brokering of the knowledge for service improvement. Confirming assertions in the more generic management literature, commentaries on the development of combinative capabilities in health care highlight the following specific social mechanisms which engender co-ordination capabilities: they are the development of learning relationships through establishing internal and external networks; staff development and training; appropriate leadership; organisational strategy; investment in information support systems; and participation in decision-making. 128,129
In summary, extant literature suggests that systems and socialisation capabilities act to reduce knowledge brokering at the operational front line119,120 in a more pronounced way in health-care organisations. This highlights the need for health-care organisations to develop co-ordination capabilities, to offset the effects of systems and socialisation capabilities, and support knowledge brokering for service improvement in elderly care.
Summary of literature review
We highlight that health-care organisations are characterised by professional hierarchy, with power and status linked to professional roles likely to impact an organisation’s ability to exploit new knowledge. 127–129 Knowledge brokerage and learning interact with strong organisational cultures, systems and structures to restrict the brokering of knowledge for service improvement. 119 Deeply ingrained organisational structures and social networks engender institutionalised epistemic communities of professional practice that exist in silos, relatively decoupled from one another. 109 Of further relevance, systems capabilities such as pre-existing policy in the realm of organisational incentives, legislation and system-level dissemination mechanisms or initiatives, which afford access to external resources and influencers, formalise knowledge acquisition, but may restrict brokering of knowledge across organisational and professional boundaries within health-care systems. 130 In mediating the effects of the above, co-ordination capabilities, incorporating social processes and mechanisms, seem most influential within a health-care context, particularly for bridging the gap between the acquisition of new exogenous knowledge and service action. 84,122,128,129,134,135
In summary, in adopting a KBV of the organisation, we posit that the H-MLM has a pre-eminent strategic role as knowledge broker. However, aligned with Berta et al. ,130 our literature review highlights that the knowledge brokerage process is one that is highly complex and iterative, with considerable but variable agency for actors to affect the process. Aligned to this, we adopt a critical, social and political examination of approaches and mechanisms to broker knowledge for quality improvement in the care of older people.
Chapter 3 Methods
The research study was conducted across three sequential research phases. Phases 1 and 2 were exploratory, using semistructured interviews to help to develop a deep understanding of the knowledge-brokering activity of H-MLMs in relation to PSK and the care of older people. Phase 3 was more a validation phase regarding earlier findings, which we sought to elaborate at the same time, through a tracer study: this involved tracing the brokerage of PSK from the ‘ward to the board’ and back onto the ward for service improvement through the brokering activity of H-MLMs. Work packages 1, 2 and 3 (outlined below) align to each of research phases 1, 2 and 3, respectively. Permission to conduct field research was obtained in accordance with the recommendations of the UK’s National Research Ethics Committee. In line with such permission, readers should note that we were required to obtain voluntary consent from individuals where we wanted to interview or observe them. All individuals approached for interview and observation consented to our request.
Data collection
The main data-gathering technique was that of interview. All interviews were audio recorded and transcribed (except in two instances where respondents declined to be recorded). See our original research protocol for indicative interview schedules that relate to work packages 1, 2 and 3.
Work package 1 (17 interviews)
Work package 1 was particularly concerned to identify what PSK was generated and disseminated by external stakeholders and their expectations and perceptions of how that knowledge was brokered and by whom, thus linking to RQ1, RQ3 and RQ4. We also asked respondents in work package 1 about their perceptions of the contingencies of the knowledge-brokering process, i.e. what (do you perceive) are the limiting and facilitating contextual features for H-MLM knowledge brokering, and how can H-MLMs be enabled to broker PSK more effectively in older persons’ care? Thus, work package 1 also contributes to RQ6.
We conducted 17 semistructured interviews with external, national- and regional-level producers, disseminators or auditors of PSK around falls, medication and transition, as outlined on our original full proposal. Representatives from the following organisations were interviewed:
-
Department of Health (three respondents)
-
NPSA (two respondents)
-
National Professional Applied Research Network (three respondents)
-
strategic health authority (one respondent)
-
local government commissioners of health and social care (two respondents)
-
Royal College of Nursing Institute (one respondent)
-
Age Concern (one respondent)
-
university-based health-care professors (four respondents)
-
GP representative on regional commissioning and quality structures (one respondent).
To summarise, in the interviews with external stakeholders, our aim was to elicit their expectations and perceptions (expectations and perceptions may differ) of how exogenous knowledge is brokered, and who they perceive is likely to broker knowledge into the local organisation, and onwards to clinical practice.
Work package 2 (54 interviews)
Work package 2 aligns to RQ1–6. We conducted 54 semistructured interviews with H-MLMs, from lower-status MLMs such as ward managers through to more senior MLMs such as directorate managers and patient safety governance managers, in order to examine the brokerage of exogenous and endogenous sources of PSK. These respondents helped us to identify further respondents for interview, based on their knowledge-brokering role within our case-study organisations. These interviews took place across three separate health-care organisations: two hospital trusts (cases A and B) and one mental-health-care provider (case C). We asked what knowledge gets brokered, to whom, how and why. We began by conducting interviews with more senior H-MLMs who are members of the CRC within our case-study hospital organisations in order to ascertain details about the brokering of PSK produced or disseminated by external parties (e.g. in the form of ‘safety alerts’, broadly defined, or best practice guidelines) into clinical practice, and details of endogenous PSK at the clinical front line brokered upwards into the clinical governance system. Table 1 outlines who we interviewed and whether or not they were members of the CRC. Within Table 1, we also identify where H-MLMs were research active (i.e. held a research grant in last 5 years), as well as delivering and managing clinical services.
| Role | Committee: yes/no | Hybridity and manager level |
|---|---|---|
| Hospital A | ||
|
Yes | Hybrid senior manager |
|
Yes | H-MLM |
|
Yes | H-MLM |
|
Yes | H-MLM |
|
Yes | H-MLM |
|
No | Academic H-MLM |
|
No | Academic H-MLM |
|
Yes | H-MLM |
|
Yes | Academic H-MLM |
|
Yes | H-MLM |
|
No | H-MLM |
|
No | H-MLM |
|
Yes | H-MLM |
|
Yes | H-MLM |
|
Yes | H-MLM |
|
No | Academic H-MLM |
|
No | H-MLM |
|
No | H-MLM |
|
No | H-MLM |
|
No | H-MLM |
|
Yes | Senior manager |
|
Yes | H-MLM |
|
Yes | H-MLM |
|
Yes | H-MLM |
|
No | H-MLM |
|
No | H-MLM |
|
Yes | H-MLM |
| Hospital B | ||
|
Yes | Hybrid senior manager |
|
Yes | Senior H-MLM |
|
Yes | Senior H-MLM |
|
Yes | H-MLM |
|
No | H-MLM |
|
No | H-MLM |
|
No | H-MLM |
|
No | Senior H-MLM |
|
Yes | H-MLM |
|
Yes | H-MLM |
|
No | H-MLM |
|
No | H-MLM |
|
Yes | H-MLM |
|
Yes | General MLM |
|
No | H-MLM |
|
Yes | H-MLM |
| Mental health provider C | ||
|
Yes | Senior manager |
|
Yes | Senior MLM |
|
No | H-MLM |
|
No | H-MLM |
As a precursor to SNA, we concluded our interviews by asking our respondents to identify who they discussed PSK with, who they sought out to discuss issues in relation to falls, medication and/or transition in relation to the care of older people, and who would come to them for advice or to broker knowledge regarding these issues. Many of our respondents found these questions difficult to answer, with answers frequently veering between ‘everyone’ and ‘no one’. In the light of this, establishing a bounded network was difficult. This data collection did, however, identify exceptional actors and supplemented our qualitative data regarding which H-MLMs broker PSK to influence strategy and service action. We include an illustration of SNA in Appendix 1.
So that readers have some understanding of the relationships across the stakeholders we interview, we direct them to an organogram (Figure 1), which identifies how we conceive the relationship between external stakeholders, H-MLMs in clinical governance structures, such as CRC, those H-MLMs managing service delivery, and the front line of clinical practice, as they relate to older persons’ care in a typical hospital.
FIGURE 1.
An organogram to illustrate relationships between external stakeholders, H-MLMs in governance structures and H-MLMs managing service delivery. NHSLA, NHS Litigation Authority.
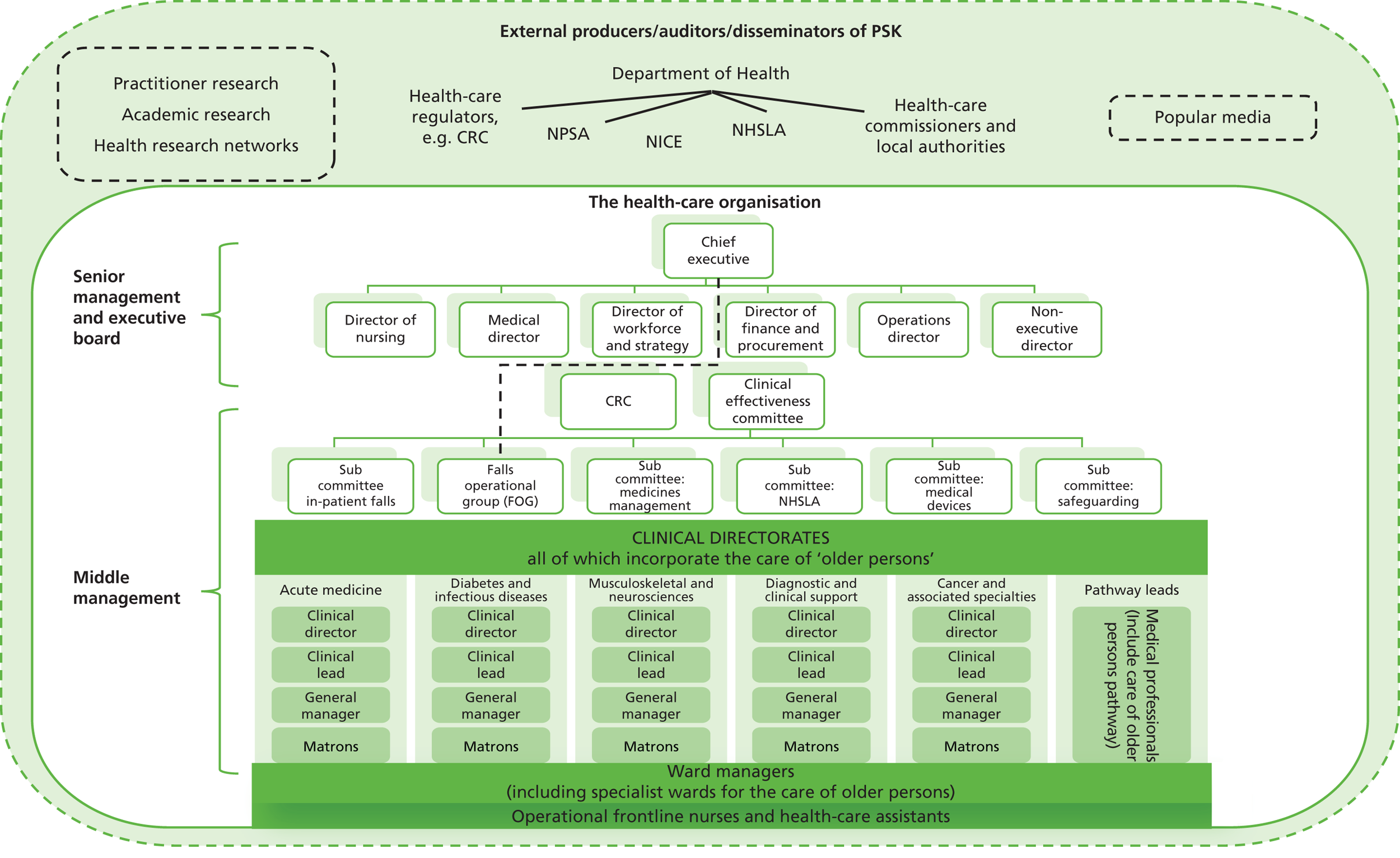
Work package 3 (56 interviews)
Work package 3 took place on the ward where the incident occurred to establish whether or not staff were familiar with the incident; how they heard of the incident/from whom; whether or not they were familiar with the action and learning that is connected to the incident in question; and whether or not they knew if the actions had actually taken place. Our interviews were semistructured and took place with ward managers, deputy ward managers, registered nurses and non-registered nurses, who were selected on the basis that they were available on the day we conducted interviews. A total of 21 interviews were conducted at hospital A. Table 2 lists our respondents’ roles at hospital A.
| Case number | Date of incident | Interviewees | Total number of interviewees |
|---|---|---|---|
| 1 | March 2012 | Ward manager, deputy ward manager, registered nurse × 2 | 4 |
| 2 | January 2012 | Ward manager, registered nurse, non-registered nurse | 3 |
| 3 | October 2011 | Ward manager, registered nurse, non-registered nurse | 3 |
| 4 | January 2012 | Ward manager, deputy ward manager, non-registered nurse | 3 |
| 5 | March 2012 | Ward manager, deputy ward manager | 2 |
| 6 | May 2012 | Ward manager, registered nurse, non-registered nurse | 3 |
| 7 | July 2012 | Ward manager, non-registered nurse | 2 |
| 8 | April 2012 | Ward manager | 1 |
Following analysis of data derived from the interviews described above, we were invited to convene focus groups at the request of one of our respondents (a geriatrician) in hospital A. The focus groups were established with staff working in areas where falls were identified by the organisation as an ongoing problem. Both doctors (e.g. surgeons as well as geriatricians) were invited. The objective was, first, to authenticate our emerging analysis, elaborate upon insights gleaned from fieldwork, and with a view to making practical impact, discussing ongoing (if any) organisational learning and service improvement. As readers might note, despite being invited, most doctors did not attend. As apparent later in empirical presentation, many doctors outside the ranks of geriatricians did not view patient safety related to older persons’ care as relevant for doctors. In total, two doctors and 41 ward managers, matrons and nurses attended four focus groups in July 2013. Our synthesis of outcomes from the focus groups was presented to hospital A in July 2013 (see Appendix 2).
At hospital Z, we studied one SUI involving a medication error, and interviewed 27 respondents working on the acute medical unit (AMU) where the incident occurred. Again, we studied the organisation’s high-level report prior to conducting semistructured interviews with the staff involved, following the same protocol employed at hospital A. A total of 27 interviews were undertaken with staff members in the AMU. The following roles and grades of staff were interviewed:
-
three band 8 registered nurses
-
three band 7 registered nurses
-
three band 6 registered nurses
-
eleven band 5 registered nurses
-
five band 2 non-registered nurses
-
two ‘F1’ doctors.
Within work packages 1 and 2, alongside interviews, our research design involved collecting archival data and observational field notes, in order to triangulate sources of evidence. 136 First, we observed relevant meetings, such as risk and governance committees and action groups (approximately 20 hours in total), concerned with reducing falls amongst frail older people in the hospital, and ward meetings concerned with service improvement for the care of frail older people. In work package 3, a further 20 hours were spent observing wards and departments (total observation = 40 hours). During the observations, the researchers took detailed notes and then wrote up a more expansive commentary post observation, where they reflected on what they had witnessed. The notes were written up on the day of the visit. Where available, we collected minutes of the meetings we observed, and similar meetings that preceded these over the previous 12 months, as well as documents that were submitted to the CRC to transfer data where information related to service quality from subcommittees. Second, we examined relevant government White Papers137 and associated publications (e.g. National Service Framework for Older People,138 Living Well with Dementia139). Third, at the organisational level, we collected strategy papers concerned with quality of care for frail older people and noted real-time data related to service quality at the level of individual wards and departments. In Gephart’s140 terms, we were able to collate ‘a substantial archival residue’ (p. 1469).
Data analysis
In advance of the analysis, we assembled all of the documents, interview transcripts and observational field notes for each of the cases into a single data file. We began with a fine-grained reading of the data,141 and then inductively created a list of first-order codes from the case evidence. We then consolidated all of our codes across the three cases, progressing with axial coding, structuring the data into second-order concepts and more general aggregate dimensions. 141,142 In doing so, we engaged in deductive reasoning whereby we linked our inductive codes with existing concepts and frameworks, derived from our literature review. 143 While we accept that our accounts are one of many potential interpretations,144 we worked to ensure that we did not retro-fit the data to service our theorising145 in two ways. First, we triangulated between data types; then, second, we triangulated across analysts. 146 Our approach follows Pratt147 and Gioia et al. ,48 who represent exemplars for the analysis of qualitative data in social sciences, and is designed to move from the ‘raw’ data to the theoretical and thematic interpretation of that data. Table 3 presents a snapshot example of how, within our analysis, we moved from respondent-centred, more empirical codes to researcher-centred, more theoretical codes, to arrive at the main themes within this report.
| First-order code: what influences the brokerage of exogenous PSK by H-MLMs | Second-order code | Emergent theme |
|---|---|---|
|
Externally derived financial pressures and incentives influence knowledge brokering | External regulatory context has a predominant influence upon what knowledge is brokered |
|
Externally imposed performance measures influences what knowledge is brokered and how |
Preface to research findings
As data were collected across the duration of the study, a number of themes emerged regarding the mechanisms, barriers and enablers for brokering both exogenous and endogenous sources of knowledge within health-care organisations. Collecting data regarding ‘who’ brokers knowledge, ‘how’ and ‘why’ was somewhat challenging, given the often unconscious nature of knowledge-brokering activity by individual actors. Subsequently, SNA analysis was particularly challenging in the light of brokering relationships that ostensibly veered between ‘everyone’ and ‘no one’. Our difficulty in reliably bounding a brokering network around PSK related to the care of older people mirrors the contrasting views of our respondents where more generalist professionals (e.g. geriatricians, matrons, nurses) view elderly care as ‘mainstream business’, recognising the very high proportion of older people who occupy hospital beds, and those more specialist clinicians (often more senior H-MLMs, and non-hybrid senior managers) who neglect to recognise the more general applicability of PSK relating to the care of older people to their own patients (many of whom are older people). Despite this context, our SNA does identify some exceptional actors within our data set who are capable of brokering PSK upwards, downwards and across the organisation. These actors are more senior H-MLMs who are connected to the organisation’s most senior committee and correspond with our more qualitative findings of work packages 2 and 3. SNA data can be found in Appendix 1.
Reflecting the literature, we find responses to our ‘who’, ‘how’ and ‘why’ questions vary according to the nature of knowledge that is to be brokered; for example, where PSK is predominantly explicit and codified, systems of co-ordination and policy appear dominant methods for brokering knowledge and targeting persons to whom such knowledge is valuable. However, brokering knowledge beyond the initial targeted person(s) for wider dissemination and diffusion into practice (e.g. from the hospital’s governance committee to the doctors and nurses on the ward) was much harder to evidence, suggesting a lack of knowledge brokering between organisational structures that are designed to co-ordinate and communicate activity across the organisation (such as the clinical risk committee) and the clinical front line.
Aligned to this, we find that health-care organisations design systems in response to external influences which determine what PSK is brokered into the organisation, by whom and how. We present our analysis of data relating to the brokering of exogenous knowledge in Chapter 4.
Where PSK is predominantly endogenous (i.e. from internal sources), our data highlight the challenge of brokering such knowledge upwards to shape strategy and influence service change. Again, our findings reflect the literature with regard to the need for legitimacy and status for the H-MLM’s ability to broker knowledge upwards and across professional groups. However, we also evidence effective knowledge brokering across professions and from lower- to higher-status H-MLMs. These data, which run counter to professional organisation, are presented in Chapter 5.
Work package 3 evaluates knowledge brokering for learning and service improvement following an adverse incident in our two hospital cases (A and Z). These findings are presented in Chapter 6, and evidence a lack of knowledge brokering at a local level, as well as across the top and middle tiers of the health-care organisation.
Our over-riding finding is that PSK is frequently not brokered across the organisation with the objective of service action to improve patient care. Individual agency to broker knowledge is frequently linked to a managerial orientation which favours compliance and assurance in line with external pressure for performance management and measurement via a process of organisational targets and financial incentives. Further, professional hierarchy narrows the scope and range of knowledge brokering. The resultant pattern of knowledge brokering can be characterised as a ‘broken chain’ where linkages do not exist across professional groups to enable the brokerage of PSK upwards or downwards for service change. However, our study is not entirely pessimistic in this regard, and through focus upon ‘combinative capabilities’ and descriptions of H-MLMs adopting various brokering roles and strategies for brokering PSK upwards and across health-care organisations, we offer prescriptions to enhance the development of a ‘brokering chain’, which mediates top-down policy pressure and professional hierarchy.
Throughout Chapters 4–6, we endeavour to offer a brief synopsis of our analysis at the end of each data section in order to highlight key findings to the reader. Further to this, each chapter concludes with a clear and concise depiction of the ‘research contribution’.
Chapter 4 Brokering exogenous patient safety knowledge
We begin with an empirical analysis of the exogenous knowledge environment, from the perspective of our internal users of PSK (H-MLMs), followed by examples of how such knowledge was identified and brokered by H-MLMs to others in the organisation.
Chapter 4 is structured around our emergent themes of context, the role of IT and combinative capabilities. The following section presents the perceptions of the exogenous PSK environment by H-MLMs working within our case-study hospital organisations. This section describes a ‘knowledge competition’, where the pursuit of PSK for service improvement, implicit in everyday professional work, has to compete with externally imposed performance measures and incentives. This competition has an attenuating effect upon the knowledge-brokering role of more senior H-MLMs, their focus being deflected from clinical roles and allegiances in favour of satisfying the requirements of managerial and external stakeholders. The search for new PSK by H-MLMs is tapered to conform with that which is necessary to demonstrate the organisation’s compliance to external regulatory bodies.
Aligned to the strategic management literature, The role of information technology outlines the significant role of IT in directing exogenous sources of PSK to the clinical front line in a way that can be managed by H-MLMs acting as gatekeepers and more junior clinicians who utilise IT to pull PSK as and when they need it. Overall, our analysis suggests that IT supports the role of the H-MLM as knowledge broker rather than supplanting it.
Combinative capabilities and patient safety knowledge: an examination of the knowledge-processing activities of an organisation utilises combinative capability theory to help us understand how the health-care organisation processes exogenous PSK, adding further insight into ‘who’ brokers knowledge, to whom, and why (or why not). Building on the first section (Context: the exogenous knowledge environment), we show how the health-care organisation designs system capabilities in response to PSK that is pushed into the organisation aligned to performance targets and incentives, and in the guise of safety alerts, data collection tools and initiatives (such as Dr Foster and the Global Trigger Tool). Aligned to the literature, we show how system capabilities are an insufficient mechanism for facilitating the brokerage of PSK to the clinical front line. In contrast, we outline the socialisation capabilities of our case-study organisations, in nurturing professional behaviours early in the careers of junior doctors and nurses who either rebel or conform to external sources of PSK that require service change. We conclude this section with identification of co-ordination capabilities employed by organisations and health-care professionals to facilitate the brokering of exogenous PSK beyond what is necessary for compliance to instigate service action and improvement.
Finally, we conclude Chapter 4 with a synopsis of our research contribution, reminding readers of the RQs that formed part of our original protocol, which we seek to address.
Context: the exogenous knowledge environment
A knowledge competition: targets and money versus professional interest
At an individual level, external sources of PSK are considered so profuse that a ‘knowledge competition’ ensues with the individual recipient’s prior knowledge, experiences and special interest as key factors determining what is acquired and assimilated.
The big problem here is, of course, in terms of external guidance. There is simply far too much of it. I couldn’t possibly keep up with everything that NICE puts out. You don’t read every textbook, you don’t read every paper. People talk about the policy environment, but there is also the knowledge environment that it is impacted on by your own thinking, by stuff you come across, by experiences you have . . . it competes with an awful lot of other stuff and you tend to seek out what you are interested in.
Professor H, geriatrician and H-MLM, hospital A
The macro context, however, reveals a wider competition at the organisational level, where the geriatricians in our study perceive a trade-off between ‘risk and safety’ and ‘targets and money’:
There is another sort of competition, or tension, really. We work in an organisation, we work in a structure. The organisation has its policies, procedures, standing orders and so on and so forth. To an extent what we do is governed by that. If they say, ‘You will not use drug X, you will use drug Y, although we are not going to stop drug X’, but the amount of effort it will take to get drug X simply isn’t worth, you know, ‘We are going to do certain things, we are not going to do operations unless you have X, Y and Z, A, B and C signed off’.
Professor H, geriatrician and H-MLM, hospital A
I get an email every few days about how many patients the hospital has discharged and so on. I never get any information about how many times we’ve harmed anyone . . . but what we do have is traffic lights to tell us whether we’ve discharged patients from hospital quickly enough, because the length of stay is what they’re interested in.
Professor G, geriatrician and H-MLM, hospital A
The importance of targets and money has a significant influence upon the role of H-MLMs. H-MLMs operate across two worlds – a managerial world and a clinical world. However, sometimes, the reconciliation of managerial with clinical objectives was regarded as problematic. The following quotations imply a balancing act between clinical goals of quality of care on the one hand, and managerial performance-driven goals on the other, with the latter frequently dominating the former.
In theory, when the modern matron initiative was launched, their objective was to look at quality issues, which is actually my passion. Having said that, once I got into this role, it’s a lot more to do with looking at finance, what your establishments are, what your overheads are, which although interest me, it’s not my passion.
Modern matron, H-MLM, hospital A
My role is the operational and strategic management and development of geriatric medicine and acute stroke services in the Trust . . . targets like infection control, they’re all driven, aren’t they, from a political bent rather than a clinical bent? It’s targets because targets are money. I have a little bit of difficulty with that as a nurse; not as a manager, as a nurse. As a manager, I understand that it creates the internal market because we are a business now, and it doesn’t matter how much we say as an NHS we’re not.
Head of Nursing for Geriatrics, H-MLM, hospital B
You’re not here as a business to make money. Yet finance generally is the first item on the agenda and then everything else follows it.
Patient safety manager, H-MLM, hospital B
Similarly, external producers of PSK perceive the wider problem to be one of ‘prioritisation, not knowledge’ (NPSA, respondent H, external knowledge producer).
Overall, the maxim ‘what gets measured, gets managed’ transpires into performance management rather than knowledge brokerage by H-MLMs with the aim of improving quality of care. This view is supported by a number of interviews with internal users:
There’s a general sort of truism in the NHS, and certainly in this organisation, which is that effectively what gets measured, gets managed. So the things that feature on the Trust Board’s monthly reports are, for example, healthcare associated infections. This has obviously been a massive issue in the NHS for the last number of years. Every month the Trust is seeing real-time data on MRSA infection and C. Diff infection. Because it’s been such a national priority, they take that very seriously. So there are very significant and well-established mechanisms for communicating back into the organisation ‘you must do better’. As a result, the levels of infection rates have steadily declined and, now, we perform very well.
Senior general manager, hospital A
A lot of stuff managers do have often nothing to do with safety or risk at all. They’re mainly charged . . . I mean the managers, you know, all they talk about here is meeting targets and coming in under budget.
Professor G, geriatrician and H-MLM, hospital A
I think the problem is that a lot of knowledge brokering is driven by policy from top-down. People who have influential, managerial capability tend to only work with the agenda that they’re given rather than any other interests about safety issues. For example, a manager may be interested in VTE [venous thromboembolism] about length of stay, but not about inpatient falls because it’s not a clinical agenda that we’ve been asked to deal about . . . because falls is not a big priority at Trust Board level, it’s not driven with the same importance as other issues.
Professor S, geriatrician and H-MLM, hospital A
How the NHS organisation responds to the exogenous patient safety knowledge environment
In both hospital A and hospital B, questions concerning the acquisition of exogenous sources of PSK led to the respondent identifying ‘patient safety’ as ‘someone else’s job’. This ominous and surprisingly frequent response reflects the organisation’s response to exogenous PSK: it is there to be managed. Thus, patient safety is viewed as the role of person X. The following quotes highlight the division between patient safety as understood by senior managers of the organisation and as viewed by H-MLMs and those on the clinical front line.
The medical director’s very clearly identified as the patient safety lead and champion for the organisation. It’s very prominent at the Board, which I think’s always important because effectively it shows that there’s top-level, absolutely top-level commitment to patient safety in the organisation. Where it starts to get more tricky, and I guess which is where your questions kind of come into their own is, at the end of the day there is a bureaucratic process that sits around all of this. Somebody at the Department, or in one of the agencies nationally, writes something and says, ‘Right, this needs to change,’ or ‘This is dangerous,’ or this is whatever, sends it out to the service and in many instances, bureaucratic processes in the NHS are kind of people just go, ‘Oh, another piece of paper. Another instruction, another bit of work to do’. Actually that’s not necessarily a motivating and empowering thing.
Senior general manager, non-hybrid MLM, hospital A
Certainly the Trust governance structure, such as audits, incidents, Clinical Risk Committee, is heavily influenced by government or regulatory/CQC [Care Quality Commission] requirements. They talk about safety and risk, but in clinical practice, safety is seen in a more holistic sense; for example, in assessing cognition and insight, in decision-making, and in day-to-day practice. This involves the whole multidisciplinary team, other doctors, nurses, OTs [occupational therapists] physios, speech therapists, social workers, as well as patients and families.
Professor H, geriatrician and H-MLM, hospital A
Reflecting the comment above, that formal patient safety structures and processes may be fragmented or narrow, respondents with a dedicated role for ‘patient safety’, many of whom carry ‘patient safety’ in their professional title (e.g. the following titles are identified in our data set: ‘patient safety lead’, ‘patient safety manager’, ‘head of patient safety’, ‘clinical quality, risk and safety manager’) are predominantly focused upon outward- and upward-facing governance-based activities and explicit PSK. Examples include the ‘global trigger tool’ (a methodology for sampling patient records to identify harm and the root cause of that harm), submitting and analysing data through systems such as Dr Foster (a provider of health-care information solutions in England, and a joint venture with the Department of Health), Datix (web-based patient safety software for health-care risk management applications, used for submitting and analysing safety incident data) and the NHS Litigation Authority (NHSLA: provides indemnity cover for legal claims against the NHS. Accreditation is correlated to the amount of premium NHS organisations have to pay). However, we note that it seems to have a positive effect upon quality improvement, albeit in a restricted domain.
The number one priority for the Trust at the minute is the financial position. I think the CQC come hotly after that in terms of quality and accreditation visits. For me the other next priority is NHSLA accreditation . . . The other thing I do for the executive medical director is I administer and support him in running a mortality group. So I support him in putting the meetings in, putting the agendas together, getting the data together for Dr Foster from a mortality point of view. So reactively, we look at the areas that are alerting. The other work that we’re doing currently is we’re proactively looking at the areas where we think we should be a bit better, but it’s not actually ‘pinging’ an alert off [via Dr Foster]. So we look at the data. So I prepare the data and present it at those meetings, then we discuss it and we decide who’s going to take it forward, who’s going to do the work around that diagnosis basket. Then I get the data off and my team get the case notes if we want to do a case-note review. So that’s been on-going for a while. So that’s sort of like a patient safety improvement project really, because it pulls out particular diagnosis groups.
Patient safety manager, non-hybrid, hospital B
Patient safety managers in our study represent more senior MLMs than a geriatrician, for example. They report directly to senior governance managers such as the medical director and participate on the CRC. However, they are not necessarily H-MLMs, and may have a generalist rather than a clinical background. These more senior MLMs appear to have limited engagement with the operational front line, typically relying upon others (mostly nurses) to broker strategy ‘down’ through the organisation as liaison knowledge brokers.
When patient safety initiatives come from external sources into the Trust . . . let’s take Safety Express, for example. How do you communicate Safety Express within the Trust? How do make people at the frontline aware of it?
It’s mostly nursing. So we take it down through the operational nursing route through the heads of nursing down onto the main wards.
The governance infrastructure represents the central vein for downwards knowledge brokering. The infrastructure comprises a complex network through which external knowledge should get brokered down and across the whole organisation:
So, in terms of external sources of patient safety knowledge and the elderly, how does knowledge about patient safety get cascaded across the organisation?
The structure we have in terms of a governance structure is probably the main way we do it. So I go to the clinical risk committee normally, and there are other committee meetings that different members of the directorate and the management team go to. So, at the moment in the Trust, there’s the quality and safety operational group and then under that there’s the clinical risk committee, the clinical effectiveness committee and organisation risk committee. So from a Directorate point of view, we have representation on each of those. We have our own directorate governance meeting monthly, which all the speciality leads come to. Then each speciality has their own governance meeting. So healthcare of the older person speciality will be coming to that and they have their own governance meeting. So, in terms of spreading information about patient safety, that’s probably the structure we have to do it.
Our data highlight how exogenous sources of PSK are brokered downwards by nursing professionals enacting H-MLM roles as part of a hierarchical infrastructure that forms a tightly linked chain. However, their role does not extend to brokering knowledge across the medical ‘side’ of the organisation, i.e. external sources of PSK are considered more challenging to broker across to medical professions by nurses due to the latter’s subordinate status to the former.
There are very different structures between the medical and nursing side. I’m much, much more reassured that if I had an important message, I can cascade it through the nursing side. I’m less confident that I would cascade it effectively through the medical side. That’s why many of those communications come with my name or the medical director’s name on it just to give it a little bit more impetus when it’s being progressed through the Trust.
Head of CRC, senior H-MLM, hospital A
The difference between nurses and doctors is, with nurses you can lead them, you can make them do it if you want. It’s not my style, but you can. Nursing is very hierarchical and if I say ‘jump’. . . I wouldn’t want to, but people could say ‘how high?’ You can influence. It’s not the right way, but you can. That’s renowned in nursing. You can’t do that with medics. They’re seen very much as individual, professional, very senior experts and you have to therefore use different tactics.
Director of Nursing, senior H-MLM, hospital B
In terms of fusing exogenous PSK with endogenous PSK, there appears little upwards flow of PSK to those who undertake a ‘patient safety manager’ role. Respondents in two of our case-study organisations suggested that the patient safety role is significantly under-resourced. This limits their ability to fuse of endogenous PSK with exogenous sources, as they are required to focus on the outward-facing priorities of the organisation, i.e. to evidence performance to external regulators.
My substantive post is patient safety manager, but I’m actually doing three jobs at the moment because of the way that the NHS is in saving money. I’m managing the research staff. I’m managing the clinical audit staff, the clinical effectiveness staff, the risk management staff. We haven’t got a clinical risk manager in post, so I’m picking that up as well. I’m driving NHSLA as part of that. I’m being pulled into gathering evidence for CQC compliance visits. I’m also the lead for emergency planning.
Patient safety manager, non-hybrid MLM, hospital B
Do you see yourself as able to influence the executive team in terms of their understanding of risk and how they perceive it?
Only responding to their concerns, so it is reactive rather than proactive at the moment. I do think the Trust could invest more in their own risk management team at corporate level. They are a very, very, small team which tells me a lot about the organisation and how they view risk and its importance. We did have a Risk M for the organisation that has got 7000 staff and God knows how many patients. That is a huge job for one person. I think that speaks volumes. They expect it to be done but I think they need to invest at Trust level a bit more and they need bums on seats to get work done and to raise awareness.
In hospital A, one patient safety manager’s previous nursing role allows her to span the boundary between senior management and the operational levels of the organisation. She was thus able to broker exogenous PSK that is fused with endogenous knowledge, in order to implement strategy:
People will regularly ring me and say, ‘Something’s happened. I need to talk to you about it.’ I kind of supervise and manage people with their investigations into serious incidents and high-level incidents. You will have heard my name kind of round and about because people will go, ‘I’ll just ask [Patient Safety Manager W] about that.’ So they’ll just say, ‘I’ve had this thing happen. Can I just tell you about it?’
Patient safety manager W, H-MLM, hospital A
However, organisational priorities have led to the distancing of this hybrid patient safety manager from endogenous sources of PSK knowledge, in order to focus upon outward-looking data for the NHSLA. NHSLA are insurers for NHS organisations, paying all of the Trust’s litigations, and the Trust pays them a premium in return. What ‘level’ of risk the Trust is judged to be at by the NHSLA determines the discount they get:
My big corporate role is to look after the Clinical Risk Committee. My other corporate role is I look after on-line incident reporting. So, for clinical incidents, we generally look after a couple of directorates each and we provide governance support to the directorates and then we have a couple of committees. Now I used to support the Falls Committee [IPFC] and the Transfusion Committee. Currently I’m not, because I’ve been taken out of some of my work to concentrate on NHSLA.
Patient safety manager W, senior H-MLM, hospital A
Summary of section
Data presented in this section have highlighted the distinction between the organisation’s view of PSK as something explicit, that must be managed and complied with, and the more abstracted clinical professional view of PSK as ‘implicit in everything we do’. Consequently, the NHS organisation’s response is to build systems and infrastructure in order to manage PSK and demonstrate compliance externally. However, we find that PSK from exogenous sources is not brokered ‘down’ or ‘across’ the organisation – the exception being national patient safety initiatives that are nursing orientated, which are ‘pushed’ down the nursing hierarchy in a tightly linked broker chain from senior nurse manager to matron, then on to the ward manager and finally to the ward.
In terms of brokering PSK more generally, we find that patient safety managers (including those with a clinical background) are not likely to be as clinically engaged as we might expect, because their priorities are shaped by external influences in the form of targets and money. Patient safety managers are unlikely to enact a downwards knowledge-brokering role, as their primary concern is to satisfy external regulators, by evidencing performance and compliance through policies, protocols and procedures. Thus, unlike the linked ‘broker chain’ that characterises the nursing profession, we evidence broken linkages between more senior hybrid managers and the clinical front line.
Hybrid middle-level managers maintaining close allegiance to their profession (e.g. heads of nursing, matrons and geriatricians), continuing to deliver aspects of a clinical role and remaining in clinical-facing positions (i.e. they interact with medical and nursing staff) perceive two separate but interdependent worlds: a managerial world that is orientated towards targets and money, and a clinical world which is focused on patient care.
The role of information technology
National Institute of Health and Care Excellence issues clinical guidelines and recommendations based upon ‘a rigorous process that is centred on using the best available evidence and includes the views of experts, patients and carers, and industry’. 148 NICE guidelines in particular appear highly regarded sources of PSK by medical professionals. PSK providers, such as NICE, will adopt a multimodal approach to push guidance directly towards clinical professionals delivering care to patients, rather than necessarily relying upon organisational systems to do this for them. However, technologically savvy MLMs (commonly younger clinicians) prefer to pull knowledge down into their practice, ‘as and when needed’, through IT systems.
I get stuff via email from NICE. We look at the NICE guidelines on the intranet and everything. If we can’t find them, we will Google them. Google works for everything really [laughs].
Mental health nurse H, H-MLM, hospital A
Increasingly, hospitals are supporting knowledge pull by more junior clinicians and H-MLMs. Our data revealed examples of guidelines and protocols placed onto intranet websites and the development of mobile phone applications where junior doctors are able to download guidelines ‘24/7’ without the need to rely on the presence of a more senior doctor to impart their knowledge.
To summarise all our core guidelines, we’ve just released as an app, an iPhone app, largely for internal consumption. We have had 2000 downloads so far. You get your iPhone out, two clicks and, you know what to do with delirium in older patients. It is there in your face! So the availability, the ability to access information rapidly is important. I mean, the test I always apply to is: ‘What is the information you need to produce for the junior doctor who’s never worked in your hospital at 2 in the morning and it needs to work for him?’ I think it’s just (a) so important, crucial for older persons’ care, and (b) done badly. In fact, it had just been deleted from the intranet so there was no guideline, but what they had was a 44-page document on dementia care and that was their guideline. It’s not much use to the junior doctor at 2 in the morning.
Professor H, geriatrician, H-MLM and National Professional Applied Research Network Member, external body
When the nature of knowledge that is required is urgent and clinical, IT can provide rapid access to guidelines to inform service action. The development of an iPhone app in the above example was an attempt to align with the technological capabilities and lifestyles of younger people. Below is an example of junior doctors using their mobile phones to co-ordinate laterally across professions to rapidly access the required expertise.
I’ll be with a patient and sometimes the guys and girls will be sort of either texting their friend about the patient care. So I’d say, ‘We need to get a cardiologist to see them,’ and they’d be sending a text to their friend in cardiology because the pager system is [xxxx] and doesn’t work because they all move so much in real time. Or they’ll be Googling information about the case you’re seeing. So, they’d say, ‘Do you know this?’ So there are all sorts of process stuff going on quite rapidly there. So when we meet the junior doctors, we say, ‘Well, this seems great. Carry on doing it,’ and yes, we need to abolish our bleep system because it doesn’t work.
Professor H, H-MLM, geriatrician & National Professional Applied Research Network Member, hospital A
However, the challenge of brokering PSK across to junior doctors was one that was frequently mentioned by H-MLMs, particularly geriatricians:
You get many more instances of where the ball gets dropped amongst junior doctors because they’ve no knowledge and they’re very transient. But lots of issues are tasked to junior doctors. So the junior doctor’s tasked to prescribe Warfarin, yet he or she is the lowest rank of an F1 and they have no idea. I mean, if there’s no guideline they might pick it out of the air or they might ask an SHO [SHO (senior house officer) is a junior doctor undergoing training within a certain speciality] who’s no idea either and says, ‘Oh, give them 3 milligrams’.
Professor K, geriatrician and National Professional Applied Research Network Member, external body
The use of IT in a bid to align with the lifestyle of more junior clinicians, who need to be able to access guidance and protocols quickly and easily, is not universally accepted. Many young clinicians prefer to learn in a more ‘situated’ way from their senior colleagues, and on a more gradual basis:
Facebook and Twitter don’t work. Mobile phones don’t work because a lot of the trainees say they don’t want us to have their phone number for work purposes. E-mail doesn’t work because many of them don’t have an organisational or NHS address.
Senior hybrid manager, anaesthetist and chair of CRC, hospital A
These days the students come to us, and I say to them, ‘So which clinical methods books are you using?’ and they don’t use them any more. They expect us to teach them entirely, start to finish, how to take a history and examine patients when actually that’s what their Clinical Practice 1 course is all about. I tell them all, ‘Get a book and read about this because you will not come across all the symptoms and all the myriad different clinical presentations just by listening to me. You need to read something’.
Geriatrician, H-MLM, hospital A
Thus, developing mechanisms that chime with the lifestyles of junior doctors, where rapid access to protocols and guidelines, appears effective for brokering PSK. However, such methods are insufficient in isolation as they rely upon individual agency of the knowledge user to pull exogenous knowledge from pre-existing knowledge repositories. The knowledge-brokering role of the H-MLM is critical for pushing new sources of knowledge across professions and levels, and is achieved via more lateral and personal forms of co-ordination.
Communication with staff is primitive in some ways. We’ve done many things with newsletters and the intranet site and obviously e-mail and then verbal cascades. We do that a lot in theatre, where there are clear, verbal cascades of information. However, in other parts of the Trust it’s not so well embedded. Actually getting information down to trainee doctors does rely on lots of things working properly, which I don’t have great control of. One of them is the engagement of the consultant or senior medical staff in progressing information which they’ve received. So it’s quite primitive and it’s one of the challenges of the NHS.
Chair of CRC, hybrid senior manager, hospital A
Moreover, the sheer volume of exogenous sources of PSK provides a distinct and important role for IT as a vehicle for pulling new PSK to the attention of H-MLMs, who then perform a gatekeeping role, brokering knowledge as they see relevant to their more junior counterparts.
The National Library of Medicine does a digest and it is a beautiful thing. The UK Medicines Information (UKMI) is a network of all the pharmacists, so hospital pharmacists have departments called medicines information to answer queries for patients. UKMI links to something called the National Electronic Library for Medicines, so there is a national electronic library and there is one for medicine and these guys do a daily digest. So I get a digest of medicines-related literature that has general stuff, and then medicines, and then something else. I skim it looking for ideas and I spread it out to my kids, but I don’t spread most of that out to this lot because they wouldn’t know what to do with it. I have got stroke specialists, I have got care of the elderly. I have got somebody else who is renal so I can cascade it to them to make sure they have got it.
Pharmacist, H-MLM, member of National Professional Applied Research Network, external body
I rely on my own systems. I sign up for e-mail alerts from NICE and I regularly visit the DH [Department of Health] website, ombudsman, HSJ [Health Service Journal] the HTA [Health Technology Assessment] site, you know for research and stuff like that. So I have my own system for scanning, if you like, and I am aware that other managers do the same. If anything comes out that I think is relevant, I will pass it round or take it to a meeting, you know that kind of thing, even down to newspaper reports on court cases, that kind of thing . . . I get weekly alerts and those are the most useful – info.gov and NICE, those are the ones I tend to cascade.
Clinical governance manager, non-hybrid MLM, hospital C
Where knowledge is brokered within a profession, but towards more junior counterparts, it often takes place via a teaching model. In the instance below, a H-MLM adopted a gatekeeping role to broker PSK that they deem valuable to whom they deem appropriate and when they deem appropriate:
A ward round is multifaceted and one of the purposes of it is to teach and to develop. If there is time, then they [H-MLM] will create a knowledge transfer and teaching environment. Then, if you have got the right pharmacist on the ward, when they review something the consultant will say, ‘Tell us more’ and it will become knowledge transfer.
Pharmacist, H- MLM, member of National Professional Applied Research Network, external body
I like to think that I use any opportunity to teach somebody something even if they probably know it in the first place, and I always say to them, ‘If I’m telling you something that you know, please tell me’.
Ward manager, H-MLM, hospital B
Hybrid middle-level managers rely upon their own agency to manually navigate the knowledge environment in the hope of identifying PSK that may be transformed and exploited for improved patient safety. One matron describes how she came across some potentially important guidance regarding staffing levels to help address patient safety in her area:
I’ll go and have a look on various websites and see what’s new and what’s happening. It’s like with this RCN [Royal College of Nursing] . . . I mean I wasn’t a member of the RCN, but actually I’ve just joined because I didn’t realise that they’d got an older person’s forum because I hadn’t joined it . . . But I used to always look on their site and see what they were up to, and they’ve brought out these new staffing guidelines for older people. So that’s great. For me, I’m thinking, ‘If I want to stop falls and I want to stop pressure ulcers and I want everybody to be hydrated and nourished, then I need more hands basically’. So I was quite delighted when I spotted this.
Matron, H-MLM, hospital A
However, an exploratory approach to navigating the ostensibly infinite exogenous PSK environment is not an activity that is supported by the organisation:
One of our problems is the funding of ongoing education, the Trust is actually meant to fund approved study leave. We are meant to have 10 days’ study leave a year and that is written into our contracts, but they have put a cap on that and they have done for 20 years and it is wholly inadequate. So most people fund their education by drug companies and, surprise surprise, the drug companies are not neutral parties.
Professor H, geriatrician, H-MLM, hospital A
Summary of section
Information technology is shown to be a valuable tool for enabling H-MLMs to identify and pull exogenous sources of PSK that are operationally relevant, and to broker knowledge within their professional groups. In particular, our data suggest that more junior H-MLMs use IT to ‘pull’ exogenous sources of PSK that are relevant to their clinical work on an ‘as and when needed’ basis, while more senior H-MLMs develop their own systems to automatically scan the exogenous environment PSK according to their individual knowledge interests, and then broker that knowledge across to their subordinate peers. We highlight in this section that H-MLMs, who are predominantly clinical facing, broker PSK to more junior counterparts on an ‘as and when’ basis, and via a teaching model, i.e. they adopt a gatekeeping role, navigating the profuse exogenous knowledge environment, sifting through evidence and sharing what they deem as relevant within their professional cohorts.
Our next section builds upon the first to examine in greater detail the influence of context upon the brokerage of exogenous PSK, and how the organisation transforms and exploits exogenous sources of PSK for organisational learning and service improvement. To frame contextual influences, we structure our findings around combinative capabilities83 to further examine the ‘how’ and ‘why’ (or ‘why not’) of knowledge brokerage relating to exogenous PSK.
Combinative capabilities and patient safety knowledge: an examination of the knowledge-processing activities of an organisation
Combinative capabilities refer to the knowledge-processing activities of an organisation to generate, synthesise and apply new knowledge. 83,119 We employ the theory of combinative capabilities to further examine the ‘who’, ‘how’ and ‘why’ (or ‘why not’) of knowledge brokerage relating to exogenous PSK and the care of older people. To reiterate the literature presented in Chapter 2, Van den Bosch et al. 119 distinguish three types of combinative capabilities: systems capabilities, socialisation capabilities and co-ordination capabilities. The authors119 describe systems capabilities as formal knowledge-exchange mechanisms such as written policies, procedures and manuals that are explicitly designed to facilitate the transfer of codified knowledge. Socialisation capabilities are described as cultural mechanisms that promote a shared ideology and collective interpretations of reality within an organisation, and co-ordination capabilities are identified as lateral forms of communication such as education and training, job rotation, cross-functional interfaces and distinct liaison roles.
We structure this section as follows. Firstly, we use our data to illustrate how systems capabilities are shaped by external influences, most notably targets and financial incentives, and how these attenuate the knowledge-brokering role of more senior MLMs, imposing a focus upon compliance in line with the demands of external regulators. Secondly, we examine the influence of socialisation capabilities in order to establish the knowledge-brokerage gap between organisational strategic goals (supported by systems capabilities) and the goals of the professional core (supported by socialisation capabilities). Finally, we depict mechanisms for mediating this gap and co-ordinating knowledge brokerage of PSK for improving elderly care.
System capabilities
Aligned to the literature, our data highlight the influence of government policy upon performance management. Specifically, we highlight emphasis upon financial incentives and targets in those performance systems imposed upon health-care organisations, i.e. these shape systems capabilities in a health-care organisation. As one geriatrician complained, ‘Important areas of risk and safety for elderly care have to fight against things which are far bigger – targets and money’ (geriatrician G, H-MLM, hospital A). This argument is supported by an ‘admission’ from one (non-hybrid) member of hospital A’s executive board that ‘what gets measured gets managed’. Consequently, the health-care organisation designs system capabilities to evidence compliance. The following quotes demonstrate the dominant influence of performance management and financial incentives as antecedents to the design of systems capabilities, and the impact of this influence on the acquisition of new PSK:
If the hospital stands to lose money either directly or indirectly as a consequence of compliance, then you comply.
Director of Strategy, non-hybrid senior manager, hospital A
Sometimes the order and the priority in which that [service action] has come about have been rather skewed by some of the financial targets.
Geriatrician G, H-MLM, hospital A
The knowledge that organisations seek becomes limited to:
How do you do it? How do you shunt them? What do you do? How do you get round this problem? That was the knowledge they [executive management] wanted, not safety knowledge. Because they want to hit our targets and get money and don’t want to be penalised.
Geriatrician G, H-MLM, hospital A
To emphasise, systems capabilities are shaped by ‘political’ incentives, with proof of compliance as the organisation’s priority, as opposed to the pursuit of quality improvement:
If the government says, ‘You’ll treat everybody within 18 weeks’, then you create an industry that makes sure that not only do you treat them within 18 weeks, but you can demonstrate that you treated them within 18 weeks . . . everybody’s running around making a computer system that can record and demonstrate it.
Director of Strategy, non-hybrid senior manager, hospital A
Aligned to this, our data suggest that an organisational focus upon compliance deflects some (more senior and managerial facing) MLMs away from brokering PSK for service improvement in favour of outward-facing activity to evidence performance, to satisfy regulators and, at the same time, reduce the financial costs of the organisation. As discussed in Chapter 5 (see Power differentials impact the brokerage of patient safety knowledge), we see that respondents with a dedicated role for ‘patient safety’ in particular, many of whom carry ‘patient safety’ in their professional title (e.g. patient safety lead, patient safety manager, head of patient safety) are predominantly focused upon a myriad of outward- and upward-facing governance-based activities.
The clinical effectiveness locomotive is so enormous, and is so worked up that it predominates above and beyond anything relating to patient safety, anything about the patient experience.
Geriatrician R, H-MLM, hospital B
Our data suggest that systems capabilities neglect the brokerage of PSK downwards and across the organisation for service action. To further evidence this, we use the example of a patient safety ‘alert’ released by the NPSA to signal action to prevent inpatient falls. The following excerpt describes the implementation of the NPSA bed-rails safer-practice policy that made recommendations for preventing falls within a health-care setting during 2007. Only half of hospitals in England adopted the recommendations, and so in January 2011 a RRR was issued, which dictated that all hospitals in England must have implemented a bed-rails policy by July 2011. Following the deadline for the RRR, all hospitals in England signalled compliance, i.e. they formally confirmed that they had devised a policy to explicitly describe the use of bed-rails. However, an automatically generated news feed set up by one of our respondents (a representative of NPSA), via Google, identified a patient death following a fall at a hospital where it was revealed that no policy was actually in existence, despite the hospital signalling its compliance:
I keep a Google alert for bed rails, which brings up inquests. On paper, every Trust in the country is compliant with bed rail policy . . . [but] an elderly lady falls out of a bed in August in a hospital where nothing was documented on bed rails, no policy on bed rails, no documentation format to prompt the nurses to think about whether bed rails are good or not, no observation after she hits her head.
NPSA H, external body
In the above example, we see that a formalised process (a ‘systems capability’) to demonstrate ‘compliance’ did not result in PSK being brokered to the frontline to improve patient safety. Thus, while we identify external political pressure and targets as primary antecedents of systems capabilities, we highlight that such systems capabilities are designed to react to external regulators with the aim of compliance, and not with the intention of brokering PSK to the front line for service improvement. The following quote from a chief hospital pharmacist (H-MLM) supports this.
I am going to have to write a guideline that I put on the intranet that says, ‘When you give medicines we are supposed to do this,’ which will make no difference at all, I can meet the requirement it is not a problem, [but] it is not worth doing.
Pharmacist, H-MLM, member of National Professional Applied Research Network, external body
Conversely, and reflecting a more positive effect of performance management policy, we find that exogenous sources of PSK linked to financial incentives can represent a lever for more powerful health-care professionals, such as doctors, to galvanise the organisation towards service action and innovation beyond the pursuit of compliance. Financial incentives emerge from our empirical data as a potential ‘co-ordination capability’ that can successfully mediate between externally orientated managerial goals, as dictated by the external political environment, and internally orientated clinical goals as derived from practice. One example of this professional ‘lever’ in action is the Commissioning for Quality and Innovation (CQUIN) payment framework. This framework enables commissioners to reward excellence by linking a proportion of the providers’ income to the achievement of local quality improvement goals. In short, CQUINs combine target-based incentives that secure the attention of managers at the top of a health-care organisation, while providing the resources and incentive for professions to acquire and transform new PSK for quality improvement at the front line.
We will put a CQUIN in that says you have got to do it better and there is money if you do it better, and then of course you galvanise an organisation to do it better because there is money behind it.
Pharmacist, H-MLM, member of National Professional Applied Research Network, external body
The external drivers are all pretty much financial pressures that we are feeling as a trust . . . but also there is a pot of money to work with. So the right drivers are in there.
Geriatrician H, H-MLM, hospital A
The critical role of financial incentives to mediate between the top-down, externally orientated goals of the organisation, which are driven by policy, and bottom-up, professional clinical goals, is further demonstrated in the example of the National Dementia Strategy. 139 In implementing the National Dementia Strategy, the Department of Health held a substantial consultation process across 2 years, holding over 50 stakeholder events attended by 4000 individuals. The draft strategy was reportedly ‘very well received by the public and professionals alike . . . the recommendations it set out were seen as being the right ones if dementia services are to fully meet the needs of people with dementia and their carers’ (p. 11). 139 However, the ability of the National Dementia Strategy to transform PSK into service action was reportedly hampered by a lack of financial incentive. One respondent, a commissioner of care services for older people, recalls the arrival of the National Dementia Strategy as a ‘damp squib’:
There was an expectation that the dementia strategy was going to revolutionise care for older people with dementia. Then, when it happened, there was no money attached to it really because the economic situation had changed practically overnight.
Commissioner, local authority, external body
In summary, our findings suggest that systems capabilities of health-care organisations are predominantly shaped by the external operating environment, in particular performance measures and targets. MLMs, who undertake a predominantly managerial role (regardless of hybrid status), are compelled to develop systems capabilities to evidence compliance, rather than brokering PSK downwards and across the organisation for improving the quality of care. Our data present evidence that systems capabilities in isolation do not broker PSK effectively to the operational front line for service action. Ultimately, our data imply that, at a managerial level, evidencing compliance is perceived to be more pertinent than brokering PSK for service improvement at the front line. On a more positive note, financial incentives that can be leveraged by those who make up the professional core of the organisation emerge as an important co-ordinating capability for the brokerage of exogenous PSK for improving patient safety in elderly care.
Socialisation capabilities
In the first section, and aligned to the sociology of professions literature, we evidence the role of status and power as a continuing and pre-eminent characteristic of medical and surgical professions that governs an individual’s legitimacy to broker knowledge. Our data suggest that junior doctors and nurses are socialised into the behaviours of their respective professions early on in their careers, which negatively impacts the ability of PSK to reach the clinical front line and improve practice. The following example describes a F2 (second-year graduate) junior doctor training event, where junior doctors were discouraged by their more senior counterparts from reporting PSK, arising from adverse events:
Hands up who’s made a report last year of any adverse event – that is, you know, a near miss or an actual harm event. How many put their hands up? It was extraordinary – none. It’s worse than you can think and one of them said in their hospital they were told, ‘Don’t bother your barney.’
Geriatrician M, H-MLM, hospital A
The following excerpt from interview highlights the preservation of professional silos through the shaping of socialisation capabilities, prior to professional registration, as part of professional education and training:
Classically, the relationship that’s most fundamental in the NHS, is the consultant’s relationship with everybody else. They decide what happens or, as you heard [the clinical manager] say off-line, if the consultants aren’t behind the clinical manager who’s a medic, then what she’s trying to do will just fall apart. Too often, consultants have been allowed to destroy or break up or compromise change for petty or non-petty reasons. So I think in our institution our belief is having co-location will break down the tension that exists in all hospitals between doctors and nurses. I think in our hospital there’s now a strong tension, but a healthy one, between doctors and nurses as professional groups. We should all be one team and I myself say this phrase, ‘One team’. We’re in it together. [But regardless,] people will view their professional identity in their own vision. So a nurse will have the right to question a consultant. Of course their professional society, their training, their education, their ethical duty is to ensure that, but lots of nurses don’t do that. They don’t feel able to do it and they don’t feel empowered to because of that mainly hierarchical structure. I mean you won’t get rid of hierarchy overnight, but having one team’s very good.
Geriatrician K, H-MLM, hospital A
The above respondent implies that a multidisciplinary approach, working across professions as ‘one team’, is continually impeded by the organisational structure, which is shaped by power and status. In our empirical case study, a hierarchical infrastructure is the health-care organisation’s formal ‘co-ordination capability’ for brokering knowledge across the organisation. Health-care organisations typically operate via an infrastructure comprising a myriad of committees, each reporting into a clinical risk committee and/or a clinical effectiveness committee. A committee infrastructure may act as a conduit for the brokering of PSK from external sources into the organisation. However, the effectiveness of such committees, in terms of acquiring and mobilising new external knowledge, depends on the linkages with members of the organisation who are located outside of the committee infrastructure:
You can have a committee with no local advocates – it doesn’t work. You can have people with a great interest, but no support in the local committee or in the infrastructure – that doesn’t work. You need local advocates outside the committee working with the committee, being empowered by the committee, but the advocates go at a fairly, you know, front-end level – talk to people, raise awareness. You can’t just do it with e-mails.
NPSA, C, external body
Legitimacy to broker knowledge does not necessarily go hand in hand with a position on a committee, particularly within medical and surgical professions. In hospital A, the chair of the CRC, a hybrid senior manager, observed a distinction between the organisation’s ability to cascade new knowledge through the ‘nursing side’, where hierarchy imparts power and status and a tightly linked broker chain ensues, and the ‘medical side’, where hierarchy is more ambiguous and knowledge brokerage is impeded:
If you were to look at a Directorate which has a clinical lead, every nurse in that directorate will in some way be in a structure which is below that clinical lead – either near the top of the structure or near the bottom of the structure, it doesn’t matter. There will be a pathway through that lead. In medical staff that is not the case because there’s not that recognised hierarchy that the heads of service are some way superior . . . they’re seen as equals. One of them happens to be head of service, but in no way are they in an elevated position. So that makes it complex.
Surgeon A, hybrid senior manager, hospital A
Thus, the intraprofessional hierarchy of the nursing profession supports the downward brokerage of PSK into service action. We see this in the successful implementation of numerous nurse-led interventions to improve patient safety in hospitals; for example, reducing health-care-acquired infections, reducing pressure ulcers, implementing ‘patient safety express’ [Safety Express is the name of the QIPP (Quality, Innovation, Productivity and Prevention) Safe Care work stream test pilot programme which ran in 2011], ‘care round the clock’ (an implementation of hourly ward rounds based on a US model by hospital A) and the ‘productive ward’ (Productive Ward is a national initiative developed by the NHS Institute for Innovation and Improvement, designed to improve the efficiency and effectiveness of the day-to-day running of the ward), to name but a few recent initiatives.
In order to broker PSK for service change across professional groups, however, committees need to be governed by individuals with the most senior power and status. For example, in hospital A, the formation of an operational group (OG) was the organisation’s response to more serious concerns that required a step change in management. An OG is generally chaired by an executive director and was, thus, able to enforce service action through strict performance management processes. With this in mind, one of our respondents describes his personal pursuit of a falls ‘OG’ with executive leadership, in a bid to drive the transformation of PSK into service improvement for patient safety:
Through the Inpatient Falls Committee [IPFC], we’ve made some progress. We’ve certainly got some of the structures and the infrastructure in place that we need to be able to monitor performance and indeed to try and disseminate the organisational learning from individual events, which is good, but I haven’t got the clout. I haven’t got one of the hammers if you like. [Interviewer: What would give you the clout?] Well, I’d say the executive director needs to be on my Inpatient Falls Committee. In fact they need to chair it. . . very few people would not go to a meeting which is chaired by either the chief executive, the medical director or the director of nursing, whereas they feel they can do that to me and, you know, what can I do?
Geriatrician M, H-MLM, hospital A
In another attempt to mediate the organisational infrastructure, one H-MLM, with a clinical-facing and academic policy-orientated role, explains how participation in policy writing can enable him and policy-makers to push PSK through the organisation’s infrastructure top-down because it is clinically relevant.
In summary, the organisational infrastructure, at first glance, represents a co-ordination capability because it is a formal mechanism for cascading knowledge across the organisation. However, ‘hierarchy’, and associated power and status, is the characteristic that appears to govern legitimacy to broker knowledge; thus, professional behaviours can impede knowledge brokerage for service action. The infrastructure itself, made up of committees, is perhaps more reflective of a procedural systems capability designed to service the organisation’s priority to comply with regulations, targets and financial incentives. As already discussed, systems capabilities alone narrow the scope and breadth of PSK, and often lack the ability to transform PSK into service action at the front line. Ostensibly, the organisation’s response to this known deficiency is to introduce further procedural checks as part of the senior committee meeting. For example, during our observation of the CRC, we noted the recurrence of the following question: ‘Can we be reassured, that “said” alert/incident/policy has been dealt with?’ One respondent describes the use of terms such as ‘assurance’ to echo the language of the NHS regulator, the CQC:
When they [CQC] come into a Trust they’ll say, ‘Well where’s your assurance? If you’re sat on a Board where’s your assurance?’ And that’s what we’re working on a lot and I think every NHS Trust is doing that . . . And why you’re hearing that is because of CQC because that’s their terminology. How are you assured? How are you reassured? What mechanisms do you use to make sure you are assured? It’s all that kind of language.
Head of nursing, H-MLM, hospital B
Mediating between system and socialisation capabilities to facilitate knowledge brokering between organisations
Earlier, in System capabilities, we identified financial incentives as a potential co-ordination capability that mediates between system and socialisation capabilities to instigate service action aligned to improving patient care. Alternatively, our data reveal how some individuals are better able to broker exogenous PSK than others by virtue of their diverse professional background and experiences. We see this in our interviews with representatives from external organisations, as well as those on the clinical front line. Applied researchers at the NPSA explained how they are able to exploit prior knowledge, relationships and linkages derived from their own professional background to nurture a network of ‘friendly hospitals’, and in turn to inform the development of exogenous PSK in the form of ‘patient safety alerts’. In another example, a H-MLM describes how she combines her existing role (commissioning health care), with her prior knowledge and relationships in a different but related professional area (social work), to inform others unofficially about necessary service changes that draw upon external PSK. This enables the respondent to develop mutually beneficial relationships across health and social care organisations to facilitate a two-way flow of knowledge across these organisations and commissioning:
I see this role as ‘in the middle’, because I come from a social work background, have been a social worker, been a team manager, been an operational manager. So I’ve got that experience, but also can see what’s coming from above. I might have an idea about developing something or how something’s going to work, and then I need to go and talk to my [prior] colleagues, often in an informal way and say, ‘I’ve got this idea. What do you think? How will it work?’ and they’ll say, ‘Well that’s a good idea, but it won’t work quite like that because of this or that,’ or, ‘We could tweak that and that’ll work’.
Commissioning manager, primary care organisation, external body
A geriatrician in hospital A explains how he furthers his own patient safety interest through his involvement with the Department of Health. In recognition that target-based guidelines attached to exogenous PSK enter the organisation top-down with greater velocity and veracity than PSK that is endogenous, the geriatrician effectively bypasses the limitations posed by socialisation capabilities, transforming PSK related to the care of older people into a format that will be prioritised in the same way that other target-based initiatives and guidelines are prioritised, i.e. the organisation will respond with the introduction of system capabilities to illustrate compliance.
Policies that move down quicker are probably those that are attached with targets and financial incentives, whereas those about good practice and essence of care tend to sort of move down a bit sort of slower. Hence, a lot of my efforts recently, in the years I’ve been working at Department of Health level, have been about influencing policy and writing guidelines informed by my clinical practice.
Geriatrician S, academic H-MLM, hospital A
The brokering of exogenous sources of PSK across professional groups within health-care organisations was evident between (hybrid) mental health nurses not employed by, but working within, the hospitals, and clinicians working on the hospital wards. Many doctors and nurses who care for older people are not skilled in treating patients suffering from forms of cognitive impairment, such as dementia, and this can compromise the quality of care provided. We spoke to mental health nurses working on a temporary basis (as part of a funded research pilot) within hospital A. Successful brokering of new exogenous sources of PSK occurred as a result of nurturing socialisation capabilities within the organisation, specifically via mental health nurses working alongside doctors and nurses in a situated way to build team-based relationships and trust:
They [mental health nurses] spent quite a long time embedding themselves to become credible within the team. The way they did that, by and large, was by working as auxiliaries, health-care assistants to start with, to show that they could wash a patient and they were happy to sit with somebody who was very agitated and so on. We also wanted them influencing the ward culture, in terms of policies and procedures and defining a role for themselves.
Geriatrician H, academic H-MLM, hospital A
The quote above highlights the need for ‘diversity of background knowledge’ at a team level as a co-ordination capability, with socialisation mechanisms facilitating the brokering of external PSK for service improvement at the middle levels of the organisation. This approach allowed the mental health nurses to cultivate legitimacy for their knowledge brokerage from one profession to another, initially becoming valued members of the clinical care team, before seeking to influence ward practice and culture. In hospital B, mental health nurses did not spend time ‘embedding’ themselves on the ward. Rather, they adopted the role of itinerant broker,91 distributing knowledge on a peripatetic basis, as and when needed. These mental health nurses were also afforded legitimacy, but on the basis they were imparting scarce, valuable knowledge as and when required:
I had two major concerns. First, how is a doctor going to react to being given advice by a nurse? However, it has been 99.9% arms open, thank you for coming! My other concern was to do with the ward staff. I thought that what we would get would be, ‘Why are you coming to tell us our job, don’t teach your grandmother to suck eggs, we know the basics,’ and all this. However, it was the exact opposite: ‘Thank God, the cavalry is here. We have been crying out for this for so long, thank you’.
Mental health nurse, H-MLM, hospital B
We discuss the brokerage of knowledge from mental health nurses across professions in greater detail in Chapter 5.
Summary of section
In this section, our empirical data have presented system capabilities and socialisation capabilities as two juxtaposing worlds. The first is driven primarily by compliance towards external stakeholders. The second is driven by locally generated PSK and innovation for service improvement, but narrowly orientated towards distinct professions. Each stymies the brokerage of exogenous sources of PSK to the clinical front line. While we make no suggestion that the intention of external providers of PSK is for organisations to focus upon compliance over and above improving health-care delivery for patient safety, our data do suggest that systems capabilities are primarily shaped to focus the role of more senior MLMs upon evidencing compliance to meet targets and reduce financial operating costs, as opposed to brokering PSK to the clinical front line for service action. We deduce co-ordination capabilities from our data that play a role in mediating between these two worlds, most notably the use of financial incentives by more senior H-MLMs who use incentives as a lever to galvanise the organisation towards service action and improvement, and the benefit of diverse knowledge and experience to mediate limitations of system and socialisation capabilities with regard to the brokering of exogenous PSK. In essence, we see that antecedents of systems and socialisation capabilities, such as financial incentives and professional hierarchy, can also be recast as shaping co-ordination capability to enhance the brokering of exogenous PSK. Meanwhile, the role of H-MLMs as a co-ordination capability for brokering exogenous PSK is significant. Finally, hybridity, in the form of MLMs’ understanding of, if not experience across, professions and organisations, engenders the diverse perspective helpful for brokering exogenous PSK.
Overall, our application of combinative capabilities theory presented in this section have highlighted how senior management solicit system capabilities primarily for evidencing compliance to the requirements of external regulators. The external political environment represents a dominant influence upon the shaping of system capabilities. In parallel, socialisation capabilities that characterise the professional core of the organisation stymie the top-down brokerage of exogenous sources of PSK across professions, exacerbating the knowledge-brokering gap between senior management and the clinically engaged professional cadre of the organisation. This finding echoes that of the recent Francis Report,149 where a managerially led ‘culture of assurances’ towards external targets is thought to have prevailed over improving the quality of care, suggesting that the problems encountered at Mid-Staffordshire NHS Trust, which led to many hundreds of avoidable deaths, may also be encountered in other health-care organisations. To highlight a particularly significant section of the report for our study:
[Within Mid-Staffordshire NHS Foundation Trust] this culture of assurances was operating in a structure where identifying systems and processes and meeting targets were the main measures of performance. Outcomes-based performance and risk-based, intelligence-informed regulation were still developing concepts.
Francis Report, paragraph 1.114149
Research contribution of Chapter 4
This section depicts the following contributions to our RQs:
RQ1. What expectations and perceptions do external regional and national producers/disseminators/auditors of PSK have regarding the brokering of top-down knowledge (‘safety alerts’, broadly defined) through MLMs and risk management structures to influence clinical practice?
External national producers of PSK expect organisations to develop system capabilities such as protocols and guidance, based on exogenous sources of PSK, and that such PSK will be brokered down to the clinical frontline for service action. Their perception is that to change behaviours is a slow and often ineffective process. To mediate, this requires systems capabilities:
Changing behaviours, convincing people to change behaviours is one thing, but actually having a system which just enables them to change their behaviour because it’s the path of least resistance, sending medicines which are better labelled or ready diluted or . . . It’s just simpler to do it that way.
NPSA, C, external body
Some patient safety interventions, however, are not easily changed and rely on early adopters and their networks to diffuse new PSK across the organisation through a mix of system and socialisation capabilities. This is recognition, however, from external producers of the critical role of power and status in relation to brokering PSK:
I would glibly expect that chief pharmacists in a hospital environment, for example, will take this [new exogenous PSK] seriously and use their governance and professional networks locally to influence how policy making is made at a local level. If they are not doing that, then I would like to know why. However, I am being very idealistic. Eventually, I suspect it will come down to getting into some of the levers in the system, such as a strong leader, you know, if you need a new system of making sure information gets moved about.
Department of Health representative, external body
Aligned with external regulators, national producers of PSK rely upon an organisation’s system capabilities to communicate PSK down and across the organisation. They pay little attention to the knowledge-brokering role of the H-MLM to implement strategy, or their role in fusing existing knowledge, held endogenously, with new, exogenous knowledge to improve patient safety.
RQ4. How do expectations and perceptions of knowledge-brokering patterns held by external national and regional producers/disseminators/auditors of PSK diverge or converge from knowledge-brokering patterns at local organisational or system levels?
The creation of performance targets and financial incentives by external regulators compel NHS organisations to focus on the target, often redirecting resources away from brokering PSK down and across the organisation. So, while more senior MLMs, such as patient safety managers, whether hybrid or non-hybrid, have managerial legitimacy to broker knowledge and span the boundaries of professions, only one of our four respondents in such positions was engaged with the clinical front line. Instead, they focused upwards towards executive managers. Even the patient safety manager who engaged with the clinical front line observed that she had been removed from tasks that had brought her in connection with clinicians, in order that she could focus on NPSA.
Further, our data suggest that an organisation which signals compliance may not actually be compliant, as they have neglected to broker PSK from executive management to the front line. Targets and incentives might actually encourage a gap between executive management/senior MLMs and the rest of the organisation, reflecting a culture of what one respondent described as ‘hitting the target but missing the point’ (geriatrician R, H-MLM, hospital A).
Having stated this, we suggest that the ‘CQUIN’ incentive payment framework from the Department of Health does appear to mediate the gap between more senior managers and the professional core. Through the creation of locally agreed quality improvement schemes, commissioners reward excellence by linking a proportion of the health-care provider’s income to the achievement of local quality improvement goals. This focuses attention away from a data-collecting exercise or policy-writing exercise that accompanies other targets set by external regulators, and places the responsibility for service action and innovation at the frontline. The power, therefore, lies with the professional core to galvanise the organisation towards service action and innovation towards clinical goals of patient safety rather than the mere pursuit of a target. In short, the CQUIN payment framework acts as a co-ordinating capability that draws H-MLMs into quality improvement.
RQ2. Which MLMs are more likely to enact a knowledge-brokering role within organisations and across the system, and why, e.g. more ‘senior’ or more ‘junior’ MLMs; more or fewer H-MLMs; those affiliated to certain more powerful professional groups, notably doctors, etc.?
RQ3. What is the contribution of MLMs towards brokering PSK, e.g. when do they broker knowledge, of what type, how, within or across organisations, and qualitative description of outcomes?
Based on our analysis of empirical data presented in Chapter 4, we can begin to consider RQ2 and RQ3 in relation to the brokerage of exogenous sources of PSK.
1. Top-down knowledge brokering of exogenous PSK by H-MLMs is influenced by professional power and status.
Power and status can determine whether or not knowledge gets brokered within and across professions. Across the nursing profession, power and status is clearly established in the nursing chain of command, and, thus, PSK is brokered down the nursing chain to implement nursing-led initiatives designed to improve patient safety. Across medical professions, however, power and status is much more ambiguous. There is no clearly demarcated chain of authority. Therefore, legitimacy to broker PSK top-down is much harder to establish. Top-down knowledge brokerage across the medical profession must, therefore, be driven by the most senior managers in the organisation, who may or may not be hybrid managers, but who are predominantly managerial facing rather than clinical facing. Even then, we note that general managers, in particular, may struggle to gain traction with doctors.
We characterise knowledge brokering of top-down exogenous PSK by H-MLMs in two ways, when comparing it across nursing and medical professions. We delineate between a ‘brokered chain’ within the nursing profession, and a ‘broken chain’ within the medical profession. Further, the ‘broken chain’ analogy applies to any attempt to broker top-down exogenous PSK across professions, as we discuss further below; however, this can be mediated.
2. Brokerage of exogenous PSK across professional groups is influenced by professional legitimacy.
Our empirical analysis reveals that legitimacy is not just attributed to those individuals with status and power. Individuals can establish legitimacy to broker exogenous knowledge across professions in innovative ways that support clinical goals of delivering high-quality care to patients. Within our empirical case, for example, mental health nurses in H-MLM roles, who may be considered relatively low status inter- and intraprofessionally, held knowledge that was pertinent to the care of older patients with cognitive impairment. Such knowledge was relevant to higher-status doctors, as well as to nurses on the ward. Mental health nurses were, thus, afforded legitimacy to broker exogenous knowledge that cut across professional hierarchy.
3. Regarding exogenous knowledge that is not centrally imposed, H-MLMs employ IT-based systems to scan the research environment and pull exogenous PSK directly to their desk. Adopting a gatekeeping role, H-MLMs typically broker PSK to their junior counterparts via situated learning.
Acquisition of exogenous PSK (that has not been centrally imposed, and therefore pushed top-down through the organisation) is commonly achieved via IT. This allows H-MLMs to scan the exogenous PSK environment and pull relevant knowledge to their desktops. Given the magnitude of the exogenous knowledge environment, H-MLMs subscribe to websites, which conduct research scans and deliver a ‘digest’ of new knowledge based upon specific, signalled areas of interest. Adopting a ‘gatekeeping’ type of knowledge-brokering role, such new knowledge is then fused with the existing, endogenous knowledge of H-MLMs, and if deemed relevant, the new knowledge will be brokered to others, such as junior doctors, for example, through situated teaching.
4. H-MLMs of traditionally lower professional status may seek to shape exogenous PSK through developing allegiances beyond their organisation in order to influence the organisation’s response to endogenous PSK.
Our empirical analysis reveals how H-MLMs of traditionally lower status may broker endogenous knowledge outside the organisation, in order to influence and shape what and how exogenous PSK enters their organisation top-down (reflective of a cosmopolitan type of brokering role). Examples include a geriatrician working laterally with external knowledge-producing organisations such as the British Geriatrics Society and writing policy and guidelines for NICE and the Department of Health to influence national practice (geriatrician S, hospital A); participating in regional networks to influence care in the community aligned to the service provided within the hospital (by geriatrician ALS, hospital B); and finally, as in the case of mental health nurses, working in situ on loan from hospital C for a fixed period of time (mental health nurses in hospitals A and B).
RQ6. What prescriptions can our analysis of knowledge brokering offer for policy and practice, e.g. how can MLMs be enabled to broker PSK more effectively?
Based on our findings presented in this chapter, we deduce the following prescriptions for policy and practice:
-
Hybrid middle-level managers with explicit and organisationally designated roles for patient safety, for example patient safety managers, are increasingly managerially orientated. To broker PSK, such actors should be encouraged to develop and maintain clinical relationships in order to broker exogenous sources of PSK outside of committees and into service action at the front line (see How the NHS organisation responds to the exogenous PSK environment).
-
Hybrid middle-level managers should adopt IT solutions to automatically scan the research environment and deliver a regular digest of relevant exogenous PSK. Adopting a gatekeeping role, H-MLMs can broker relevant knowledge across to peers and more junior colleagues (see The role of information technology).
-
Financial incentives that are accessible to H-MLMs who maintain allegiance to their clinical roles and colleagues facilitate the brokerage of PSK to the clinical front line for service action. Financial incentives reflect a ‘co-ordination capability’ that mediates between clinical and strategic goals for service action aligned to the organisation’s priorities. More senior H-MLMs who maintain allegiance to their clinical roles, for example chief pharmacists and academic hybrid geriatricians, appear most capable of influencing service action at the clinical front line at the same time as galvanising the organisation as a whole towards service improvement aligned to external influences. With the availability of financial resources aligned to service improvement at the front line, clinical and managerial objectives align for organisational change (see System capabilities).
-
Professional behaviours are nurtured early in the careers of junior doctors and nurses. Junior doctors and nurses should receive dedicated training during this time to promote a culture where PSK related to the care of older people is regarded universally relevant across all professions. This action may begin to break down persisting barriers related to professional power and status that currently impede the brokerage of PSK into service action (see Socialisation capabilities).
-
Legitimacy to broker exogenous PSK downwards and across professional groups is related to power and status. Organisational infrastructure is not a sufficient mechanism for brokering PSK across an organisation because a lack of formal hierarchy across the medical side of the organisation means that legitimacy to broker PSK is hard to establish. A brokering chain from the committees into professional groups requires the organisation’s most powerful doctor to enact a knowledge-brokering role (see Socialisation capabilities).
-
Hybrid middle-level managers with a diverse professional background are able to exploit prior relationships and nurture networks that can inform policy in a way that is aligned to both policy and practice, aiding the brokerage of PSK into service action by virtue of their access to knowledge which is both rare and valuable (see Mediating between system and socialisation capabilities to facilitate knowledge brokering between organisations).
Chapter 5 Brokering endogenous patient safety knowledge
In this chapter, we examine the knowledge-brokering role of H-MLMs in relation to endogenous sources of PSK. In our analysis, we highlight social structures that impact upon knowledge-brokering roles. 39,85 In particular, we examine the impact of professional power upon knowledge-brokering roles in health-care organisations, and how lower-status professionals in H-MLM roles are able to mediate this.
Chapter 5 is structured as follows. Power differentials impact the brokerage of patient safety knowledge illustrates how power differentials, associated with professional status, impact upon legitimacy for knowledge brokering, so that peer-to-peer knowledge brokering is more likely than that which crosses professional boundaries. Within this section, we highlight a paradox between those with a diverse knowledge base, such as junior doctors, who lack the legitimacy to broker knowledge, and individuals who have legitimacy to broker knowledge, but limited disposition to do so.
Mediating power differentials to broker endogenous patient safety knowledge across professions examines the different ways in which H-MLMs might mediate power differentials to broker endogenous knowledge across professions. Within this section, we depict the different knowledge-brokering roles aligned to those depicted in the literature.
Building further on the work of Shi et al. ,85 Research contribution of Chapter 5 argues that agency to broker endogenous PSK upwards and across professions to influence strategy is a matter of disposition of actors, commonly less powerful in the professionalised organisation. Disposition of H-MLMs, particularly those of lower status, towards knowledge brokering across professions, is a consequence of social connectedness they develop, where motivation, agency and opportunity150 coincide to enable knowledge brokering from lesser- to higher-status groups. Over time, we show that some lower-status H-MLMs develop an appreciation of others’ component knowledge that informs the delivery of health care, and then build up trust and reciprocity across professional boundaries.
Power differentials impact the brokerage of patient safety knowledge
Extending findings from work package 1 concerning the brokerage of exogenous PSK, in work package 2, we highlight the influence of professional hierarchy, both interprofessionally and intraprofessionally. In particular, we suggest that professional specialisation, particularly related to higher doctors, appears to have an adverse impact upon the quality and safety of care of the elderly. This is because elderly patients are more likely to suffer from comorbidities, including cognitive impairment, and this requires a more holistic approach to patient care.
It’s a complicated evidence base for falls. With falls you’ve got about 400 risk factors. Further, the evidence of what works isn’t sexy and exciting. I mean the evidence for what works is really multidisciplinary, back-to-basics stuff, such as: work out why they’re falling, work out if it’s the medication, have they got mild dementia starting you haven’t diagnosed, have they got a urinary tract infection, have they got a corn that makes them hobble when they’re walking and then they’re off balance, is their osteoarthritis being treated as well as it could so their joints are more flexible? It’s just loads and loads of bread-and-butter stuff, and I think that’s always been the challenge. People who are interested in falls are geriatricians, matrons and specialist nurses from an elderly care background, usually. So they’re quite good at being holistic, I would say. Geriatricians, more than any other doctors, are very, very good at ‘swings and roundabouts’ thinking: ‘Well okay, this might solve their chest infection, but if it does that to them is it worth it? You know, how does it all add up together?’ So I think in the context of falls and older people, no one is interested in falls as a single issue. They may care passionately about falls, but they can see all the other issues that could harm patients too.
NPSA H, external body
In general, those who are considered more ‘literate generalists’, i.e. non-specialists, such as geriatricians, matrons and specialist nurses, see themselves as representing the ‘underdog’ of medicine (geriatrician K, H-MLM, hospital B), and the ‘Cinderella’ of nursing (director of nursing, hospital B). They view themselves fighting a cause that is not traditionally considered ‘sexy’ by those with power and status, but the knowledge domain around that cause is increasingly important for quality of care.
20 years ago, most geriatricians in this country were failed something-elses. They couldn’t get a job in Respiratory Medicine, couldn’t get a job as a cardiologist and therefore did Elderly Medicine because that’s all they could do and didn’t want to be a GP. But 60% to 70% of what this Trust does is older people. It needs geriatricians and we are under-doctored from a geriatrician point of view. The evidence for that is slowly mounting now. Certainly this Trust recognises that and at every opportunity – so at the directors’ group, which is the highest operational group in the Trust – at every opportunity, I will challenge the appointment of an oncologist or an anaesthetist or a surgeon, asking, ‘Why are we not employing a geriatrician?’
Geriatrician M, H-MLM, hospital A
Dementia’s not very sexy. I’m a geriatrician and I’ve only got one chip on one shoulder, but most geriatricians have a chip on both. So how do you get orthopaedic doctors or surgeons to engage with all of this? And the problem is, if you set up one-to-one training, they just sort of switch off and do nothing. People aren’t interested and as a geriatrician I understand this. You can’t make people interested in things that they’re not interested in. You know, an orthopod is never going to find it interesting however inspirational the speaker. So that’s the challenge, isn’t it? How?
Geriatrician R, H-MLM, hospital B
Most of us do Geriatrics because we enjoy being personally the underdog but also, if you like, voicing the position of the underdog. So it amuses me that I am the medical establishment, when the medical establishment hasn’t even discovered this condition (delirium) that is one of the most important drivers for, if you like, variance and quality problems in health care. But it’s core business. If you’re in Geriatrics you know about delirium. You can’t avoid it.
Geriatrician K, H-MLM, hospital B
Without a generalist approach to the care of older patients, decisions by specialists are not typically based on a holistic approach to health and well-being. More generalist knowledge concerned with older patients needs to be brokered across professions to ensure the highest quality of patient care. Without a holistic and multidisciplinary approach to the care of the elderly, a diagnosis can be missed. The following excerpt from an interview with a mental health nurse (H-MLM) presents an example of a delirium diagnosis, which differs from a dementia diagnosis because it is ‘temporary, acute and treatable’. However, without rapid treatment, patients can die:
To the untrained eye (delirium) looks the same (as dementia), but it clearly isn’t. It is probably one of the most prevalent things in a general hospital and probably one of the fewest diagnosed, particularly in the elderly. It is a really, really poor prognosis for a patient with an untreated delirium, very, very poor.
Mental health nurse, H-MLM, hospital B
Brokering PSK from mental health nurses across to other professions has been shown to be effective in both hospitals A and B, as already discussed in Chapter 4 and further elaborated upon in the following section. Despite this success, some high-status professionals, such as surgeons, remain introspective and difficult to broker PSK into.
Surgery is still carpentry. ‘You have got a broken bone, we (surgeons) fix the broken bone, you have rehab, you go home, the rest is nothing to do with us’. That is how surgery works. The view is, ‘We are surgery: we fix the bone, if there is a problem beyond that we will transfer them to the healthcare of the older person’s wards’. They are the most difficult to change because they approach everything like that.
Mental health nurse, H-MLM, hospital B
We’ve got surgeons who have no clue about medicine, let alone the complexity of co-morbidity and frailty among older people. Yet we ask them to look after older people. Why would you do that?
Geriatrician, M, H-MLM, hospital A
There are still a lot of people working within a hospital that don’t see elderly care as part of their business . . . or they see abnormalities as part of normal ageing. So it’s okay that an older person is delirious, that’s what they’re like, and they won’t treat the delirium actively.
Geriatrician A, H-MLM, hospital B
This view extends to other specialities and wards that reportedly resist the admission of patients who are cognitively impaired.
With a lot of these patients, actually all people want to do is get them off their ward. People aren’t interested. As a geriatrician, I understand this.
Geriatrician R, H-MLM, hospital B
If there is a problem beyond [our specialty] we will transfer them to the health care of the older person’s wards. We won’t tell the rehab wards they are confused, because the rehab wards won’t accept them if they are confused.
Mental health nurse, H-MLM, hospital B
This view extends into community-based general practice. The following example was relayed to us by a geriatrician who was offered a partnership in a local general practice whose aim was to channel the care of older people across to a geriatrician. While this is a plausible idea, the majority of patients using the GP tend to be elderly, potentially leaving the respondent deluged and unsupported.
They [the GPs] said, ‘Name your dream team, who do you want to work with?’ But actually when it came down to it, and we started talking about what would be the nitty-gritty, because I thought I might as well explore it, actually it was about me doing all of the older people [laughs]. I thought, ‘Hang on a minute – that means you will be doing nothing then!’ It was significant of the attitude of the GPs that older people aren’t their problem somehow, or at least they are somebody else’s problem.
Geriatrician M, H-MLM, hospital A
One might expect clinical governance infrastructure to mediate tendency towards professional hierarchy and introspection, but this does not prove the case. In hospital A, subcommittees, all of which report into the CRC, which is situated at the apex of the governance infrastructure, intend to foster peer-to-peer knowledge brokerage among ‘interested parties’. Subcommittees appear ineffective, however, in brokering PSK beyond the committee itself. In describing the role of the subcommittees, the chairperson of the CRC (a senior manager and consultant anaesthetist) highlights how a lack of power and status at the level of the subcommittee precludes effective knowledge brokerage across professional groups.
The committees are groups of interested people, particularly at a lower level of the [organisation] as regards to management status, developing tool kits for trying to communicate with the rest of the organisation about the best way to manage . . . but without the teeth to make strong representation to every clinical department and every ward that they must take notice of this and make changes. They will be there forever because they will always be doing the audits and modifying the guidelines, modifying the policy and modifying the communication.
Chair of CRC, hybrid senior manager, hospital A
This lack of power to broker knowledge across professional groups is acutely recognised by the chairperson of the IPFC (a geriatrician). Bemoaning a lack of representation from certain professional groups across the organisation, ‘for example, diagnostics and clinical support, only 18% of meetings attended, yet we know there is at least one fatal fall in Diagnostics,’ he commented:
I have no stick to beat them with. All I can say is, ‘You should have come to my meeting and you didn’t,’ and they go, ‘What are you going to do about it?’ They wouldn’t say that to an executive director. I need some more teeth in my committee. Specifically, I want an executive director to lead it.
Geriatrician M, H-MLM, hospital A
Similarly, in hospital B, a geriatrician (H-MLM) laments an inability to engage higher-status professionals in learning.
It’s very interesting that you can get nursing staff to go to mandatory training things, but you can’t get doctors to. The problem is if you set up one-to-one training, they [doctors] just sort of switch off and do nothing.
Geriatrician A, H-MLM, hospital B
In short, some professionals may be unable, as well as unwilling, to broker knowledge across professional boundaries. Regulatory and normative processes shape the perspectives of health-care practitioners in such a way that professional affiliation adversely affects the likelihood of finding the ‘common ground’ for collaboration across professions.
I think brokering PSK upwards is way more challenging than across [peer to peer] because it’s often very difficult to find people going up who have common interests. Their pressure is performance targets and the financial incentives.
Geriatrician S, academic H-MLM, hospital A
Divergent education, training, socialisation and career structures for professional groups adversely influence knowledge brokering because the various professionals delivering health care may not share perspective, or language, through which to do this. The following example illustrates how a professionally orientated disposition to ‘fix’ the patient, in this case, by a cardiothoracic surgeon, led the patient’s family to expect a recovery far greater than was realistic:
I have been involved with a patient who has had a series of heart operations that have gone really badly. Because the cardiothoracic surgeon is not used to working with a multiprofessional team or actually talking to people, actually talking to families and being honest with them instead of being upbeat, this has gone really badly wrong. The elderly patient has been left paralysed and can’t walk. I have said, ‘He is not going to walk.’ I was the first person in 3 and a half months in hospital who said, ‘This is crazy. What are you doing? He is not going to walk again, so we need to start making plans’. They are not used to working in multiprofessional teams, where you can’t work without that honesty. If we are all telling different stories and being glass-half-full or whatever you like, it doesn’t work.
Geriatrician M, H-MLM, hospital A
Further, junior doctors are rotated throughout the hospital and across different hospitals. Therefore, they are the ones who are rapidly acquiring a diversity of clinical and operational knowledge, participating in decision-making across professional and organisational boundaries and developing extensive networks of social connections, all of which are crucial for brokering knowledge. Yet they are not in a social position to broker their knowledge – no one talks to them.
At another hospital I visited, which was struggling with their acute medicine unit, I just went for a day and told them, ‘Well, the most useful people to talk to are the junior doctors. They’re the people who actually do the work’. So I had lunch with about 20 of them and just asked, ‘How is it? What works? What doesn’t work? How could you do better?’ The beauty of the junior doctors is they all work in lots of different hospitals, so I always say they’re your built-in management consultants. For a hospital that was struggling and being pilloried in the local and national press and being heaved over the coals by the Department of Health, no one had talked to the junior doctors from that hospital ever about what was happening. And I did think, ‘Organisationally, this is mad’.
Professor H, external knowledge producer
Ultimately, as junior doctors develop their knowledge base and consolidate their experiences as their careers advance, the majority of them develop specialist skills. The implication is that, by the time they have developed legitimacy to broker knowledge related to professional status, their diverse knowledge base, experiences and network connections, gleaned in early training, are not maintained:
Just when they get potentially good at understanding patient safety, they get specialised and bracketed off into different areas.
Chief pharmacist, H-MLM, hospital A
The benefits and opportunities for knowledge brokerage by early career professionals, such as junior doctors, are not leveraged by the organisation towards improving patient quality. So, we have a paradox – individuals in possession of a diverse knowledge base, but with no legitimacy to broker knowledge; and individuals who have legitimacy to broker knowledge, but limited disposition to do so.
Summary of section
Through our empirical data, we have shown how power and status can prove a challenging matter for brokering endogenous PSK. We begin by highlighting the nature of PSK in relation to brokering knowledge across professions. We suggest that PSK related to elderly care is generalist and, therefore, not interesting or ‘sexy’ to higher-status professionals, who specialise in a single issue. We also highlight the prevalence of the ongoing division between generalist and specialist professionals and how this is nurtured as part of education and early career socialisation. To summarise our findings, our data reveal some very specific characteristics of knowledge brokerage linked to power, status and hierarchy that create a challenging environment for upwards knowledge brokerage by lower-status actors. Peer-to-peer knowledge brokering is common among lower-status actors, and this may take place in various committees. However, these actors lack ‘teeth’ to broker knowledge across professional groups, due to power and status differentials.
In the next section, we illustrate how H-MLMs seek to mediate power and status differentials, to broker knowledge upwards and across professional groups to shape organisational strategy.
Mediating power differentials to broker endogenous patient safety knowledge across professions
The ‘representative’ knowledge broker
In order to broker patient safety knowledge across the organisation, lower-status actors may enlist the help of a higher-status H-MLM to present endogenous PSK on their behalf. Thus, the H-MLM acts as a representative knowledge broker, often brokering knowledge on behalf of others marginal within the organisational or professional hierarchy. For example, a geriatrician (often a H-MLM themselves) wants to galvanise the organisation towards proactive falls prevention for patient safety – an issue that is not just pertinent to the care of older people, but relevant right across the organisation to young patients, new mothers, cardio patients, stroke patients and so on. In order to influence strategy across the whole organisation and broker endogenous PSK across professional groups, the issue of inpatient falls needs to be raised at the apex of clinical governance: the CRC. The representative broker in this case was a senior H-MLM, with a nursing background, whose role as ‘clinical quality, risk and safety manager’ requires her to participate in the CRC, working closely alongside the CRC chair. Working collaboratively with the geriatrician, and acting as a representative broker, translates the falls issue, so that it attains priority status, by presenting data in a format which conveyed in managerial terms the relevance of the issue to the senior members of the CRC. In the excerpt below, the clinical quality, risk and safety manager described how she brought falls to the attention of executive managers and directly influenced organisational strategy via a ‘representative’ type of knowledge-brokering role.
We used to know that people fell. We used to know that they might have had a fracture. However, we didn’t know that they then went on to die because we stopped at that point. We didn’t gather any more data. Now we’ve measured it, which enabled us to increase our risk score for falls. It’s now up the agenda and we can have something done about it.
Clinical quality, risk and safety manager, senior H-MLM, hospital A
The above example demonstrates two specific techniques employed by a lower-status actor, in this case a geriatrician, himself a H-MLM, to broker knowledge ‘upwards’ effectively across professional groups and the organisation to influence strategy. First, the lower-status actor enlists the help of a higher-status ‘representative’ broker, a senior H-MLM, who is a member of the organisation’s most influential committee, the CRC, and is therefore positioned structurally to broker knowledge to the right people (senior managers) in the right place (CRC) at the right time (at meetings of the CRC) and in a way that registers shared interest (avoidable patient deaths which can lead to regulatory intervention and penalties). In response to the presentation of data by way of a representative knowledge broker, the organisation was motivated to launch an ‘operational group’ to actively broker knowledge about falls prevention across the whole organisation. The issue was regarded as so important that the Falls Operational Group was set up and led by the chief executive himself, ensuring that the issue was a priority interest on everybody’s agenda.
The Falls Operational Group is a realisation that we have a big problem with people falling and that our activity to date is suboptimal. The beauty of the operational group is that they are generally chaired by an executive director, so they’ve got great power in that respect and they are therefore well attended.
Chair of CRC, hybrid executive manager, hospital A
In another example, a respondent of relatively low status intraprofessionally, a GP describes her own endeavour to broker PSK across professional groups in a way that would influence organisational strategy. The respondent conducted lengthy and detailed audits to determine the cause of high levels of patient readmission. The data revealed that a large number of patient readmissions were related to a miscommunication of patient medication (both intradepartmental and interorganisational) and that more than 50% of such readmissions were preventable. The respondent describes her frustration as attempts to broker important PSK across professional groups were stymied by a lack of knowledge mobilisation outside subcommittees at the middle levels of the organisation. As above, the subcommittees are made up of lower-status groups of ‘interested people’ who have limited ability to broker knowledge effectively across professional groups in a way that will influence strategy and improve practice. Faced with this obstruction, the respondent enlisted the help of a representative broker (a fellow GP, academic H-MLM) to publish the data in the British Medical Journal in order to gain the attention of senior hybrid managers and translate the data into financial repercussions in order to establish priority.
I naively thought that once you’d said something [at a committee], that would be it, and knowledge would flow and something would happen. But I realised after a period of time, it was not enough to say something once, you have to keep repeating it and putting it in different contexts. The Medicines Safety Group and the Medicines Management Committee are very supportive, and [representative knowledge broker] helped me get that audit to the point of publication. Then I got a paper published with more robust data, so I was able to do more presentations based on more robust evidence, supported by [representative knowledge broker]. I thought, ‘OK, I’ve got doctors thinking in numbers and managers thinking in numbers and they like to know percentages of this and that.’ So the result of that was we did [eventually] make some progress . . . it wouldn’t have happened without the links that I’d made with [representative knowledge broker].
Discharge team member and part-time GP, hospital A
In contrast, without a representative knowledge broker of sufficiently high status and social position, senior management can resist attempts by lower-status actors to raise issues of importance at the apex of the organisation. Our data revealed examples of such resistance in hospitals A and C.
We have lots of things in place to manage and reduce falls, but on our risk register we rate it as highly likely, fatal, as elderly people quite often die as a result of a fall later on. With our particular client mix (elderly patients with cognitive impairment), you concentrate that risk tremendously. Our Risk Management Committee didn’t agree and asked us to reduce the risk. This is where you get tensions between the tail wagging the dog rather than the other way round.
Clinical governance manager, non-hybrid MLM, hospital C
I manage the risk register for acute medicine. I took an issue to the governance lead for acute medicine, which is a consultant, and we talked through what the risk was, and it was agreed that this needed to go on the risk register. So I went through the right process, put it on the risk register and it created mayhem because I recorded it as a 15, which is a high risk. This means it has to be then escalated through the organisation. Then I got, ‘Well, have you told this person? And what about this person? Then, well, you know, we need to come and re-evaluate this risk,’ because they wanted to downgrade it. I refused to allow them to downgrade it. So it stayed as a 15, which is a high risk, and they keep telling me, ‘But a 12’s still high’. I went, ‘So if 12’s still high, I’ll leave it at 15. It doesn’t matter, does it?’ So they had no argument. So at the moment it still sits there as a 15, although they still want to come and review it.
Matron A, H-MLM, hospital A
In hospital A, the ‘practice development matron’ (H-MLM) plays a key representative type brokering role, spanning several trust-wide groups to facilitate the brokerage of PSK to acute medicine wards.
The role of [the practice development matron is] developing staff and getting the knowledge and the information out there to the staff, doing the training and the education and the development of the staff. It’s also about writing the policies and the guidelines and the procedures that help staff to do what they do. And also our job from an acute medicine point of view is being involved in a lot of Trust-wide groups, so that we can represent acute medicine and bring back to acute medicine what’s happening from developments such as dementia strategy, nutrition group, the falls group, all those sorts of things. We will bring all the information about what’s happening back down to our directorate and the staff that work within our directorate.
Matron A, H-MLM, hospital A
The liaison knowledge broker
Hierarchical relations are considered an aspect of social capital. Across the nursing profession, we see many levels of the hierarchy, encompassing and facilitated by H-MLMs, creating a neatly linked broker chain, where each actor is connected to someone who is of higher status and of lower status. Those in the nursing profession enact a liaison type of knowledge-brokering role, capable of cascading PSK down the ranks of nurses to align service action to externally derived PSK and to implement new initiatives for patient care.
We take [PSK] down through the operational nursing route, through the heads of nursing down onto the main wards. In terms of Safety Express (an external and national patient safety initiative), there’s the safety thermometer data collection that happens every month. It now has to happen on exactly the same day everywhere and we’ve just done that last week.
Patient safety manager, H-MLM, hospital B
This very linear structure creates a linked broker chain across which a liaison type of knowledge brokerage is enacted from top to bottom, which, as outlined in Chapter 4, is useful for brokering exogenous PSK to the clinical front line. However, while hierarchy aids the brokering of PSK downwards into clinical practice, hierarchy appears to impede the upwards flow of PSK between nurses at an operational level and nurses at a more strategic level.
I went onto a ward a few months ago and one of the non-registered nurses asked me if I wanted a Mars bar. She stopped me and said, ‘Have you had anything to eat today?’ I said, ‘No’. She said, ‘Do you want my Mars bar?’ She had just bought it off the trolley as I was standing there. I joked with her and said something like, ‘Oh gosh, I’m at Weight Watchers. I can’t eat that. I’d love to, but I can’t’. It was a really nice conversation. When I went back to that ward later on, she came over and said, ‘I’m really sorry if I offended you on the Mars bar’. The Ward Sister had told her that it was inappropriate to talk to me that way. I tell this story to illustrate communication blockages when we are disseminating knowledge. Ward Sisters don’t want me to hear things, because that’s a reflection on them. So I have to circumvent and go round and look at the data, and I imagine every director of nursing would have that problem really. You know, I was the same when I was at that level in the organisation. I did not want my boss to know everything, because that it might reflect failure on me.
Director of nursing, hybrid senior manager, hospital B
We find similar behaviour in hospital A, where the clinical nurse lead for the Acute Medicine Directorate acknowledges that nursing staff are unlikely to raise issues directly with her.
When I came into my post as clinical lead it was like, ‘Oh she’s a senior manager, don’t talk to her!’ As a change agent I need to be part of the team as well as a senior [middle] manager.
Clinical lead T, H-MLM, hospital A
To circumvent behaviour linked to such cultural norms, senior H-MLMs conduct ‘patient safety rounds’ in an attempt to pull PSK directly from the nurses on the ward.
The problem with the hierarchy we have is that with more junior nursing staff, for example, it would really be a very big deal for them to knock on the door or email me. It does happen occasionally, but from that point of view it’s much more me [going] to find them. We have patient safety rounds and the director of nursing walks around quite a lot in the Directorate. What we are trying to move towards really is that kind of shared governance thing really of visible leadership, I suppose, in terms of people at all levels – in terms of directors and people like me – being visible to people on the wards talking about issues, not just safety, but safety would definitely be one part of it.
Clinical lead M and senior nurse, H-MLM, hospital A
In hospital B, the director of nursing deploys a similar tactic to pull PSK from frontline nurses:
I go out and work on the wards. We have ‘back to the floor’ on Friday, so all the senior nurses are expected to be out on the floor on Friday on the wards in their uniform. For me, that’s about building the relationship, so that when I’m working with somebody, they’ll provide me those little bits that I start to think, ‘Hmmm’. Because, I’ll be honest, I don’t think many people are going to knock on my door and tell me. I don’t think they’d come to me with the minutiae, but the minutiae is important because it builds a picture, if you see what I mean. So that’s really the balance.
Director of nursing, hybrid senior manager, hospital B
The above examples highlight the strategic role of these more senior managers, including those senior in the ranks of H-MLM, synthesising knowledge from the operational front line with knowledge from above. This approach reflects a Liaison II type of knowledge-brokering role, where knowledge is brokered upwards from junior staff via a specific mediating intervention (see Shi et al. 85).
The cosmopolitan broker
A cosmopolitan-type brokerage role has been shown to be effective at brokering PSK across professions in elderly care. Within mental health issues in particular, our data reveal two approaches to broker mental health knowledge across professions. In hospital A, the cosmopolitan broker is localised and situated on a specialist dementia ward environment, while in hospital B, the cosmopolitan broker is an itinerant broker, working on a peripatetic basis across the organisation.
In hospital A, a geriatrician, who was positioned as an academic H-MLM, established a specialist dementia ward within the Medical and Mental Health Unit (MMHU), where mental health nurses from a major provider of specialist mental health services for older people were subcontracted to work on the ward. The aim of the intervention was to broker knowledge about dementia across organisations and professions. The following excerpt from interview describes the knowledge-brokering approach enacted by the academic geriatrician – what we characterise as a cosmopolitan type of knowledge-brokering role. This highlights the challenge of brokering knowledge to the clinical front line in ward environments, where many professionals outside the core nursing team come ‘in and out’ of the ward, which necessitates a need for a ‘situated’ approach:
In our experiment, which is strictly in a research context, we have parachuted in some extra expertise [mental health nurses]. That is not to say it is not a two-way relationship. They have had to learn things about the speed of acute hospitals. All the mental health staff we talked to and asked what their first impression was, and they were like, ‘The pace, the franticness, we never knew that you worked at this pace’. Nursing teams can be quite close knit at ward level, and then there are professionals, who are related, but on the periphery like the doctors and the occupational therapists. The occupational therapists have a department somewhere else and they come in and do their bit and they go away again. They may be there every day, but they are not part of that very close-knit core team. So that was what they had to infiltrate. The way they did that, by and large, was by working as health-care assistants to start with, to show that they could wash a patient and they were happy to sit with somebody who was very agitated and so on. We then began to say to them and others, ‘Well, we didn’t employ three relatively expensive people as health-care assistants’. We wanted them to give opinions, to make assessments of your hard cases and so on. We also wanted them to educate through modelling, co-working, coaching, on-the-job sort of training stuff.
Geriatrician, academic H-MLM, hospital A
The early results of this approach are promising with nurses operating on the ward observed to be ‘completely different to nurses on other wards . . . they’ve just absorbed the learning’ (matron A, H-MLM, hospital A).
In hospital B, a mental health liaison team, specifically their H-MLM, brokers knowledge on a peripatetic basis. The team have built credibility across the organisation and across professions based on the distinctiveness, the value and accessibility of their knowledge base with regard to caring for patients presenting with acute cognitive impairment.
Until the [mental health liaison team] service was up and running, the management of these people [older people with cognitive impairment] was just completely haphazard. 50% of the elderly inpatients are going to have cognitive problems of one sort or another. So it’s a huge population and we miss them. There is a more consistent approach to the way that they’re managed that’s evidence based. We complement formal evidence with the sort of anecdotal stuff in terms of feedback both from patients and relatives, but also from staff on wards.
Geriatrician R, H-MLM, hospital B
With us actually being based here, we now practically know everybody on the health care of the older people’s ward. Around the hospital, I think that one of the things about doing this type of job is because you are doing something slightly different, everybody knows you. They get to know you much quicker because you are the unusual. You are the celebrity visitor, if you like.
Mental health nurse, H-MLM, hospital B
He’s [mental health nurse and H-MLM] very good. We can manage things and he knows that when we get to that stage of referring to him that his input is needed. He’ll come and give practical advice around managing patients. Once a patient’s referred to him he comes and says, ‘This is what the diagnosis is. This is what we need to do with them’. So there’s a lot of interaction that way. So there’s that sort of learning.
Ward manager C, H-MLM, hospital B
In hospital B, unlike the local situated approach to a cosmopolitan-type of brokering role portrayed in hospital A, the itinerant approach has the benefit of accruing ‘social capital’ by virtue of the mental health nurse’s peripatetic approach. This gives rise to diverse network connections across the organisation, which is facilitated by his position as H-MLM. Further, the nature of mental health knowledge plays a part in facilitating a knowledge-brokering role for the relatively low-status H-MLM that the mental health nurse represents. Mental health knowledge is described in stark contrast to the more scientific status of medical knowledge more generally: ‘Psychiatry is a huge grey fog and we are somewhere in the grey fog. We don’t go for certainty, we go for potential’ (mental health nurse, H-MLM, hospital B).
Despite this, a ‘cosmopolitan/itinerant’-type of knowledge brokerage in a context where resources (i.e. knowledge) pertaining to that brokered are in high demand, yet of scarce availability (a high-value resource, in market terms), affords traditionally lesser status actors the opportunity and ability to build many ‘weak’ social ties across the whole organisation, based on shared interests.
In contrast, the localised approach to cosmopolitan brokerage exhibited at hospital A closely resembles a CoP, which coheres around the patient cohort, i.e. older patients with likelihood of cognitive impairment, such as dementia. Perhaps unfortunately in this case, the driver for such an arrangement is a funded research study. Consequently, the knowledge generated by the research is ‘guarded’ in line with the need for academic rigour. While applicable to other localised settings within hospital A, the tendency of the prototype CoP is more insular than might be expected, with the H-MLM leading the research study not predisposed towards brokering knowledge more widely. The characteristic downside of this approach is a failure to broker learning beyond the CoP to exploit best practice across the organisation. To demonstrate, we present an example of an elderly patient at hospital A with a diagnosis of both dementia and delirium who falls five times during a 6-week hospital stay. The patient in question had suffered a stroke and, while recovering on the stroke specialist ward, was reportedly exhibiting challenging behaviour that was both verbally and physically aggressive. A high-level enquiry was launched at hospital A due to a concern that the patient had fallen as a result of excessive sedation. However, the report concluded that this was not the case; instead, it highlighted the impact of poor levels of knowledge brokering in relation to the management of patients with cognitive impairment across the hospital. Specifically, the report highlights that junior nurses, having received no specific training with regards to the management of such patients, reported feeling ‘out of their depth’, and that there was inadequate use of the MMHU where specialist dementia nurses and a wealth of mental health expertise were available for consultation, specifically connected to the research described above. Reflecting on this last point, the ward manager stated that she was told that the MMHU would not be able to outreach their services because the ward was situated on another site approximately 4 miles away:
There was a suggestion that we should have sort of had an outreach from them for them to oversee. I actually know the ward manager on there and I spoke to her and asked, ‘Is it feasible for that to happen?’ and she said, ‘Well, no’. They struggled even when they were doing some research to actually outreach to that campus, let alone over to this campus.
Ward manager D, H-MLM, hospital A
In this case, the ward manager for MMHU conducted a gatekeeping role, preventing an itinerant cosmopolitan brokerage role being enacted. However, this conversation between ward managers was not included in the final report following the patient’s final fall. The report prescribed system-based changes to prevent a recurrence and to try to broaden access to expertise on the ward:
The availability of specialist nursing expertise in the Medical Mental Health Unit should be publicised, and contact details circulated to all charge nurses on both campuses.
Anonymous RCA report, hospital A
Other examples of cosmopolitan-type knowledge brokering by H-MLMs can be seen where geriatricians broker knowledge outside the organisation. As described in Chapter 4, one geriatrician describes how he has positioned himself as an academic hybrid, brokering academically orientated clinical knowledge through national committees to influence policies coming into the Trust top-down from the Department of Health.
Nationally, I work with NICE for hip fracture and I sit on the NICE inpatient falls working group. I’m chair of the British Geriatrics Society and I sit on Department of Health falls and fragility fracture board which is about improving health-care services . . . the success of the hip fracture care has been because one’s been able to input to the different committee levels nationally, and I think that does help bring things on quite quickly.
Geriatrician S, H-MLM, hospital A
Another geriatrician in a H-MLM role positions herself as a cosmopolitan and representative knowledge broker on regional committees to influence the approach to preventing falls both in the community and in the hospital, thereby brokering knowledge across organisations in a bid to manage the flow of elderly patients into the hospital.
I’ve established close links with the different forms of [falls] prevention teams that are community based. I got to know some of the therapists, just by being there and speaking with them. This is how I opened up the communication. I was part of the county-wide steering group and that steering group had representation from the commissioner, and I asked for direct referrals of patients to myself [cutting out doctor] to be formally agreed.
Geriatrician A, H-MLM, hospital B
A co-ordinator knowledge-brokering role
The need to develop new roles to co-ordinate across the structural holes of a fragmented care pathway for elderly patients has been recognised in both hospitals A and B. One example at hospital B illustrates how the need for architectural knowledge relating to the transition of patients from the hospital to the community creates an opportunity for lower-status actors to develop social capital. This facilitates the development, by H-MLMs, of a liaison type of knowledge brokerage role across professional groups. In short, H-MLMs do not need to necessarily broker PSK themselves, but can instead strategically respond to the need to bridge structural holes. In this example, the low-status knowledge broker, who was formerly employed as a ‘housekeeper’ for the ward, had developed a reputation for being indispensable, with several respondents commenting on the value of this employee’s vast knowledge and connections with providers of social care in the surrounding area. The H-MLM, ward manager in her area, developed a specific role that leveraged the value of the housekeeper’s social capital. This allowed the Integrated Discharge Team ‘to form that link between social care or the community that is not actually seen,’ but which ensures patient safety:
We’ve developed a role on here called patient pathway facilitator. I found a lot of my trained staff were spending time chasing Social Services and chasing occupational therapists to support safe transition. So we developed the role that [former housekeeper] is doing. She does all the ward rounds. So physiotherapists, occupational therapists and social workers, everybody goes to her. She knows everything.
Ward manager B, H-MLM, hospital B
A gatekeeper-type knowledge-brokering role
In Chapter 4, we identified H-MLMs, such as geriatricians and pharmacists, as gatekeepers of exogenous sources of PSK. They manage the knowledge environment to prevent deluge at the front line, at the same time as brokering knowledge that they deem relevant to their subordinate peers. In terms of endogenous knowledge sources, ward managers are also identified as enacting a gatekeeping knowledge-brokering role. At the level of the ward manager, we see they prevent an upward flow of PSK from nursing staff, as well as limiting the downwards flow of PSK to nurses on the ward. The ward managers are at the lower end of the H-MLM spectrum and the closest operationally to the patients. Ward managers have responsibility for balancing and managing resources, and are subject to a number of operational procedures and targets, at the same time as managing the daily minutiae of the ward. Given the busy nature of their role operationally, their knowledge-brokerage role is necessarily on a ‘need-to-know basis’. The extent to which they broker PSK varies, dependent upon their disposition. Some ward managers exhibit proactive brokering of PSK, others less so.
Individual leadership on wards is sometimes what is missing from all of the safety episodes. The truth is that the systems are in place. This means it is very much something that ward managers need to own. Each time there is a [patient safety] incident, it’s that much more pressure on their time. They often want to stop incidents, but don’t have time, so the systems don’t work.
Geriatrician M, H-MLM, hospital A
Another geriatrician describes a randomised controlled trial of bed sensors to alert nursing staff when high-risk (of falls) patients attempt to leave their beds. The project appeared to be successful, with particularly good use of technology on show for the management of localised knowledge. However, the trial was later abandoned when it transpired that the initiative would not succeed without strong ward leadership, i.e. knowledge brokering required leadership from H-MLMs.
In the pilot work there was a lot of leadership from myself, the ward manager and deputy ward manager saying every day, ‘We’ve got to do it, it’s best for patients’. However, on some wards, there was no leadership and the nurses were saying, ‘Oh, we hate this alarm going off. It’s another alarm,’ and equipment would be taken off beds, pagers would be left lying on their desk, batteries taken out, equipment would be sabotaged. That’s real-life NHS.
Geriatrician S, H-MLM, hospital A
When ward managers are leading change, remarkable improvements can happen. The following example relates to the work of a ward manager to reduce inpatient falls from 42 per month to nearly zero:
We have a ward here that takes pretty much all of the people with alcohol problems, but on that ward they’ve virtually reduced the fall risk to zero, by a set of tailored interventions. It is about one to one, providing nursing care on an individual basis, or at the very least, cohorting two or three people at very high risk together. So there’s something about the leadership that she [ward manager] provided there. It’s fantastic. She won’t accept when people say, ‘We’re not going to stop this,’ or ‘There’s nothing we can do here’. She won’t accept that and it’s about her leadership in the ward team that matters.
Geriatrician M, H-MLM, hospital A
The ward manager describes her approach as a ‘whole team’ effort that includes doctors, from whom she selected a consultant to act as a representative broker to engage junior doctors:
Looking back, our highest falls one month was 41. We just accepted that, that was normal. So we set the target at four a week and probably achieved it one week out of the month, if that, and the rest of the month we were always well over it at six, seven, eight per week. We had a meeting. I picked one consultant particularly because I’ve known his character. I knew that he would back me up and he would challenge the medical staff. So, in this instance, you have me as the ward manager leading the nursing staff and challenging them in their behaviour, but you also need somebody from the medical side that will challenge them because I don’t feel it’s my role and necessarily that they would listen to me. They may do because they’re juniors, but they’re going to take it more from a consultant as their peer and their senior than they are from me, even though I’ve been nursing for donkey’s years. It’s not just me making the target, it’s not just me saying we have to have less than so many falls a month, it is everybody’s job to stop people from falling.
Ward manager E, H-MLM, hospital A
So, as well as brokering commitment to the cohorting intervention through others, more powerful in the professional hierarchy, we see the ward manager also moving away from top-down imposition of targets. This seems a relatively straightforward intervention that might be brokered more widely across hospital A. To achieve this, the ward manager took an opportunity to broker her experience directly to the chief executive (a cosmopolitan brokering role) in order to shape strategy in relation to falls prevention across the whole organisation. She claims to have been responsible for co-opting the chief executive into leadership of the Falls Operational Group at hospital A. The following excerpt from interview recounts the story of how the ward manager above challenges the chief executive to address falls more seriously across the organisation:
I joined the Inpatient Falls Committee meeting [IPFC], in which I happened to say to the chair, ‘No disrespect to you as the Chairperson, but why is it you are the only consultant that attends this meeting?’ We listen to all the RCAs, the fractures and all the rest of it and why does nobody from the Board come? If you get an incident related to infection, for example, on your ward, you’ve got to go and answer to it in front of the Board and say what have you done, what are you not doing, slap on the wrist, go beat the staff up and all that sort of stuff. I said, ‘Why is it falls are not seen as a major issue? People die from falls’. Then I did the RCN leadership course last year, where you had to pick a topic, so of course mine was obvious – let’s pick falls. And during that course you have to present to your director of nursing and your chief executive. I said, ‘I’ve got a question for you. Why does nobody from the Board think it’s important to attend the Inpatient Falls Committee meeting [IPFC]?’ Two months later, the Falls Operational Group was in place, with the chief executive as chair.
Ward manager H, hospital A
Asked to reflect upon her actions as a nurse, the ward manager stated, ‘I’m a very mouthy person. I’m the sort of person that gets the bit between my teeth and I’ll go with it and if I feel very strongly about something I’ll just cut the middle man out and go straight to the top’. Based on this example, and the example of knowledge brokering by mental health nurses, we conclude that an individual’s ‘social capital’ comprising motivation, agency and opportunity150 can mediate power to broker PSK across professions and even directly to the organisation’s most influential actor, the chief executive. However, at the same time, we highlight the specific intervention of cohorting proved slow to spread throughout hospital A. During focus groups facilitated by the authors at the request of hospital A, it was noted that some wards were still not aware of the benefits of cohorting patients according to their falls risks.
Summary of section
Our data reveal how lower-status actors seek to mediate power and status differentials, so as to broker knowledge upwards and across professional groups and help to shape organisational strategy. Mental health nurses, particularly when enjoying H-MLM status, for example, are shown to be capable of enacting cosmopolitan knowledge-brokering roles by virtue of their knowledge being in high demand across disparate professions. Lack of knowledge relating to mental health across the organisation creates an opportunity for knowledge brokerage across structural holes, and the growing need for mental health knowledge creates motivation in other professional groups to solicit such knowledge. However, this may take place in very specific circumstances. At hospital A, for example, the mental health nurses do not extend social ties outside of the research environment (the ward), to broker knowledge effectively into other clinical areas. In contrast, within hospital B, the mental health nurse (H-MLM) and his team appear less constrained. Treated by other professionals ‘like a celebrity’, he is not constrained to work within a specific clinical area, and works on a peripatetic basis across the whole hospital, thus brokering mental knowledge more widely. We also highlight that geriatricians are similarly extending their social ties outside of their local areas, and attaining similar success in employing representative, liaison and cosmopolitan-type knowledge-brokering roles across professional groups to improve patient care and shape organisational strategy across hospitals A and B.
Research contribution of Chapter 5
This section depicts the following contributions to RQs 2, 3 and 5:
RQ2. Which MLMs are more likely to enact a knowledge-brokering role within organisations and across the system, and why, e.g. more ‘senior’ or more ‘junior’ MLMs; more or fewer H-MLMs; those affiliated to certain more powerful professional groups, notably doctors?
To summarise our findings in relation to RQ2, we find that it is more senior H-MLMs, connecting to executive management, who are the most influential knowledge brokers. In Chapter 4, we see that these more senior H-MLMs are often compelled to collate data and develop system capabilities to satisfy external regulators in line with performance targets and financial incentives. These more senior H-MLMs are predominantly managerial facing. To engage them with a view to soliciting a representative type of knowledge-brokering role, the lower-status H-MLM must be able to co-opt them into championing their cause as relevant to managerial concerns about compliance.
Outside the ranks of H-MLMs, we note that junior doctors do not have managerial or clinical legitimacy to broker endogenous PSK in the health-care organisation, despite their exposure to different wards and professions in the course of their training. Similarly, more junior nurses do not have legitimacy to broker PSK, as nursing is organised along strictly hierarchical lines, and, further, nurses remain subordinate to doctors.
RQ3. What is the contribution of MLMs towards brokering PSK, e.g. when do they broker knowledge, of what type, how, within or across organisations, and qualitative description of outcomes?
Looking more specifically at who brokers endogenous PSK, how, and for what outcome (RQ3), we highlight the following.
Upwards knowledge flow
Brokering endogenous PSK upwards in the organisation from lower status to higher status professionals is particularly challenging. Chapters 4 and 5 illustrate how the attention of executive managers and correspondingly more senior MLMs (hybrid and non-hybrid) is framed by external performance pressures in the form of targets and financial incentives. Brokering endogenous PSK upwards and across the organisation relies upon establishing shared interest between professional and managerial groups. Lower-status MLMs achieved this by:
-
Co-opting a senior H-MLM as a representative broker. Our data present examples of lower-status H-MLMs co-opting a more senior H-MLM, affiliated to the organisation’s most senior committee, to represent PSK for them by championing their cause as relevant to managerial concerns about compliance (see The ‘representative’ knowledge broker). The representative broker combines their knowledge of how to frame the attention of those on the organisation’s senior committee and engage them in the patient safety issue with reference to the clinical frontline. In this way, the lower-status H-MLM can push PSK upwards to executive management through a senior H-MLM. The outcome was to highlight falls as a significant risk factor to the organisation and one that required strategic attention.
-
Enacting a liaison type of knowledge-brokering role. This represents the reverse of soliciting a representative type of knowledge broker described above. More senior H-MLMs, with a nursing background, conduct ‘patient safety rounds’ and ‘back-to-the-ward Fridays’, where senior H-MLMs work alongside lower-status nursing staff to pull the ‘daily minutiae’ of the operational frontline environment (see The liaison knowledge broker). The outcome is that more senior H-MLMs understand issues on the ward that might impact patient safety, which otherwise, lower-status nurses feel disempowered to broker upwards. This enables senior H-MLMs to fuse their knowledge of the frontline operation with top-down strategy in order to implement strategy or champion alternatives to current organisational thinking and action around patient safety.
-
A cosmopolitan type of knowledge-brokering role. This describes the action by a lower-status H-MLM, in our example, a ward manager, to broker PSK directly to the most senior individual in the organisation for service change (see A gatekeeper-type knowledge-brokering role). Ward managers are identified in our data set as predominantly ‘gatekeepers’, preventing a deluge of PSK onto the clinical front line, while also controlling the brokering of PSK upwards. However, the cosmopolitan type of knowledge-brokering role enacted by one ward manager in our study was inconsistent with the more subservient character of the nursing profession. Further research should consider what makes this lower-status H-MLM exceptional. For example, our analysis suggests that this might be a matter of the disposition of the H-MLM towards service change which, in turn, relates to social connectedness she developed during her career in hospital A. In this case, the ward manager was motivated to reduce falls because they were so high on the ward, and because she had the agency and opportunity to broker knowledge directly to the chief executive (because of a leadership course she was participating in).
Knowledge flow across occupational boundaries
Similar to above, brokering knowledge across occupational boundaries is also challenging given that legitimacy to broker knowledge is usually associated with power and status, thus potentially constraining such knowledge brokering to certain individuals and professions. Our data reveal that, where individual actors have developed ‘social capital’, either through their position in the hierarchical structure (e.g. senior nursing H-MLMs) or through possession of diverse knowledge, which is distinctive and valuable, those H-MLMs of lower status interprofessionally (e.g. mental health nurses, geriatricians, matrons and ward managers) broker PSK across professions in the following ways:
-
Co-opting assistance of a more senior H-MLM to conduct a representative knowledge-brokering role on behalf of the lower-status H-MLM. For example, senior H-MLMs, such as clinical leads (nurses with directorate managerial responsibility), collaborate with other H-MLMs to broker knowledge vertically across occupational boundaries within the organisation (see The ‘representative’ knowledge broker).
-
Conducting a representative knowledge-brokering role. Through their involvement with many subcommittees, the H-MLM can raise issues laterally across occupational boundaries in the organisation (e.g. the practice development matron at hospital A).
-
Enacting a cosmopolitan knowledge-brokering role. For example, mental health nurses, who are H-MLMs, may work in a hospital, even though they are employed by a different organisation (see The cosmopolitan broker). They possess knowledge that is distinctive and valuable to other professions. This distinctive knowledge claim affords them legitimacy to broker knowledge across professions. Our empirical analysis reveals that these cosmopolitan knowledge brokers can work in one of two ways. Firstly, they may broker knowledge on an itinerant basis, with both doctors and acute-based nurses pulling knowledge towards them as and when they need it. Secondly, they may enact their knowledge-brokering role on a situated and localised basis, where knowledge is absorbed by others within daily work routines as mental health nurses and ward staff work side by side.
Knowledge flows across organisations
The most prevalent form of knowledge brokerage across organisations is via a cosmopolitan role. We see this in the example of mental health nurses, as described above (see The cosmopolitan broker). Our empirical data also identify geriatricians, who are H-MLMs, adopting a cosmopolitan type of knowledge-brokering role. Working in allegiance with external organisations, the strategic objective of these H-MLMs, who may be lower status interprofessionally or intraprofessionally, is to influence how knowledge is brokered into the organisation top-down by writing guidelines and policy for the Department of Health and related organisations (see The cosmopolitan broker).
RQ5. How do patterns of brokering associated with top-down PSK differ from knowledge-brokering patterns associated with bottom-up PSK?
Research question 5 requires a comparison of patterns of brokering associated with top-down PSK, with knowledge-brokering patterns associated with bottom-up PSK. In Chapter 4, exogenous flows of PSK are attenuated by the organisation’s prioritisation of compliance with performance targets. The organisation designs system capabilities to meet the demands of external regulators, producers and auditors of exogenous patient safety data such as the CQC, Doctor Foster, the NHSLA and agencies such as NICE and NPSA. Consequently, brokerage of PSK top down tends to be in the form of performance targets, rather than service improvement for patient safety, with more senior H-MLMs diverting their attention to performance related data in line with targets and financial incentives.
Where specific patient safety interventions have been designed for national implementation, and are primarily nursing led, the implementation on the ward is usually successful. This is because knowledge is brokered across a tightly linked hierarchical nursing chain, where legitimacy to broker knowledge for service action is the realm of the more senior nurse across the chain from director of nursing to heads of nursing/clinical leads to matrons and then ward managers. This neat knowledge-brokering chain is characteristic of the nursing profession.
Brokering top-down PSK through the medical side of the organisation is more challenging, as it is difficult to establish a hierarchy among doctors. There is not the same ‘neat’ knowledge-brokering chain as evident in nursing. ‘It’s not as established as it is in nursing hierarchy because all doctors, in theory, are seen as equals. One of them happens to be head of service, but in no way are they in an elevated position’ (chairperson of CRC, hospital A). Brokering knowledge to junior doctors is especially troublesome, as they move around a lot and often do not have an organisational e-mail address, thereby relying on their senior colleagues to broker PSK across to them. This method is unlikely to be effective given that those who do not specialise in the care of the elderly fail to see PSK related to elderly care as their business. In our empirical data, one junior doctor was reportedly told, ‘Don’t bother your barney,’ when attempting to submit incident data relating to a patient fall. There seems some necessity in these situations for a H-MLM with a medical background to ensure that PSK is pushed down to the clinical front line for their junior colleagues.
We see that brokering PSK top down related to elderly care has the added complexity of a lack of interest and engagement among many doctors, who perceive issues such as patient falls and cognitive impairment as the realm of those who specifically care for older patients, i.e. the Health Care of Older People wards in the hospital, and their consultant geriatricians. This is a significant problem, given that approximately 65% of patients entering hospitals in England are aged over 65. 151
In summary, Chapter 4 highlights that the knowledge which gets brokered top-down is primarily determined by performance targets and financial incentives. In terms of who brokers knowledge, we see that the nursing hierarchy facilitates an effective brokering chain from most senior H-MLM to the least senior H-MLM and onto the wards. In contrast, brokerage of PSK down the medical profession is far more challenging. We might characterise the latter as a ‘broken chain’ rather than a ‘broker chain’.
In contrast to the top-down brokerage of PSK, medically trained H-MLMs are more likely to attempt to broker knowledge bottom-up, while nurses are less likely. However, brokering knowledge upwards is challenging, as PSK going up has to ‘fight against’ money and targets coming down. Exemplifying this, geriatricians in hospital A and B describe a competition between targets and money and PSK related to the care of older patients. H-MLMs, particularly those involved with care of the elderly, adopt a range of knowledge-brokering roles primarily based upon a ‘union’ strategy, which bridges structural holes, in order to influence service improvements. These knowledge-brokering roles are wide ranging, encompassing cosmopolitan, representative and liaison roles, all intended to shape PSK in a way that engages the attention of senior managers.
RQ6. What prescriptions can our analysis of knowledge brokering offer for policy and practice, e.g. how can MLMs be enabled to broker PSK more effectively?
Building on Chapter 4 and the prescriptions presented in Research contribution of Chapter 4, we deduce the following prescriptions for policy and practice from Chapter 5:
-
Some H-MLMs have greater legitimacy to broker PSK than others (see Power differentials impact the brokerage of patient safety knowledge). The care of older people has traditionally been perceived as unattractive, with some consequences for geriatricians’ influence upon others. However, given the high percentage of inpatients classified as ‘older people’, it could be argued that the care of older people is increasingly ‘mainstream business’, cutting across the majority of specialities in a hospital. Therefore, new ways to co-opt H-MLMs who are aligned to more specialist clinical roles into brokering PSK in relation to the care of older people should be proactively encouraged and sought.
-
Hybrid middle-level managers undertaking an organisationally dedicated ‘patient safety’ role, for example a ‘patient safety manager’, have the ability to broker endogenous PSK from the operational front line as a representative knowledge broker in order to influence and shape organisational strategy. However, in order to do this more effectively, such H-MLMs need to maintain relationships at a clinical level as well as at a managerial level (see The ‘representative’ knowledge broker).
-
While the strict hierarchal structure of the nursing profession facilitates a broker chain from more senior nursing H-MLMs to more junior H-MLMs and into practice, brokering endogenous knowledge upwards from the ward along the nursing hierarchy is not facilitated in the same way. As a consequence, senior nursing managers in our study devised ways of pulling endogenous PSK from the front line through regularly immersing themselves in clinical activities on the ward and building relationships with ward staff in order to establish routes to broker PSK directly to senior managers. In this way, the senior managers are mediating the socialisation capabilities of the nursing profession in order to mobilise endogenous PSK that they might not have accessed without intervention. In this instance, senior nursing managers (hybrid) should act as a liaison knowledge broker to extract endogenous PSK and broker this upwards to influence strategy (see The liaison knowledge broker).
-
Hybrid middle-level managers of a lower status need to frame PSK in a manner that aligns with organisational priorities. Co-opting more senior H-MLMs who have established legitimacy with the organisation’s most senior committee to champion PSK is an effective mechanism to broker knowledge upwards and across the organisation (see The ‘representative’ knowledge broker).
-
Hybrid middle-level managers with valuable but rare knowledge (e.g. mental health and dementia expertise) are able to broker exogenous and endogenous PSK across professional groups. Our findings suggest that brokering PSK on a peripatetic basis is considered particularly valuable across professional groups, as in the case of hospital B (see The cosmopolitan broker).
-
While a pilot research setting in hospital A engenders successful knowledge brokerage between mental health nurses and nurses on the ward, consideration should be given to the extrapolation of this PSK through, for example, developing system and co-ordination capabilities to support the delivery of care to older people in other areas of the organisation without compromising the need for academic rigour associated with a research setting (see The cosmopolitan broker).
-
A cross-organisational cosmopolitan and representative knowledge-brokering role enables H-MLMs to broker PSK into linked community services to improve the delivery of care to older people. H-MLMs should seek to establish lateral and cross-organisational relationships to broker PSK in order to improve the care of older people outside as well as inside their hospital organisation (see The cosmopolitan broker).
-
Hybrid middle-level managers should consider the development of new roles for junior and non-clinical staff who specialise in lateral and non-clinical knowledge required to deliver a continuation of care outside of the hospital. Discharge co-ordinator roles were created in hospital B where individuals developed tacit and explicit knowledge regarding the care services available to older patients following discharge. This relieves pressure on ward staff and provides a better quality of service to older patients (see A co-ordinator knowledge-brokering role).
Ward managers are gatekeepers of exogenous and endogenous PSK brokered to and from the ward. In order to pull endogenous PSK upwards, more senior managers and H-MLMs need to engage with ward staff directly on the ward, as already discussed in point 3, above. In a similar vein, our research highlights the power of a lower-status H-MLM in brokering PSK upwards and across professional groups when faced with a combination of opportunity, motivation and agency. Our findings evidence that a relatively low-status H-MLM (a ward manager) can directly shape service action through bypassing the links in the nursing broker chain to broker PSK directly to the highest-status actor; therefore, organisations should create the opportunity for this type of knowledge brokering to occur between low-status H-MLMs and senior managers (see A gatekeeper-type knowledge-brokering role).
Chapter 6 Root cause analysis evaluation: a tracer study of knowledge brokerage
In previous empirical chapters, we have examined brokering of exogenous knowledge and endogenous knowledge by H-MLMs. We examined such brokering more generally around issues of quality improvement related to falls, medication management and transition. The top-down brokering of exogenous knowledge is primarily determined by performance targets and financial incentives. The bottom-up brokering of endogenous knowledge is impacted by professional hierarchy, which may prove challenging to overcome. To examine such issues in more depth, in particular to generate prescriptions for how H-MLMs might more effectively broker knowledge for service improvement around patient safety in the care of older people, we follow a tracer issue: service improvement following RCA. Where a SUI occurs that requires addressing, we might expect clinical governance systems and frontline practice to come together for a service improvement effect. Relatedly, we might expect a chain of knowledge brokering to be enacted through H-MLMs, so that exogenous knowledge and endogenous knowledge are likewise brought together for a service improvement effect. Our examination of the tracer issue within work package 3, service improvement following RCAs, aimed to provide insight into contingencies connected to the role of H-MLMs that mediate effective brokering of exogenous and endogenous knowledge so that they fused for a service improvement effect following RCAs. Combined with insight revealed in Chapters 5 and 6, we develop understanding of these contingencies around the knowledge-brokering role of H-MLMs more generally in making recommendations within our final chapter. We reviewed RCA data for eight separate falls-related incidents (many with associated problems of transition) on eight individual wards in hospital A; in the other (hospital Z), we reviewed one SUI related to a medication error (also with associated problems of transition) on the AMU.
This chapter presents our analysis for hospital A and hospital Z separately in Knowledge brokering following an incident of patient harm from a fall in hospital A and Knowledge brokering following an incident of patient harm from medication management and transition in hospital Z, respectively. The final section draws the data together to highlight contingencies related to the knowledge-brokering role of H-MLMs following an incident of patient harm.
Knowledge brokering following an incident of patient harm from a fall in hospital A
Challenge of brokering patient safety knowledge upwards
Root cause analysis investigation was commonly undertaken, written and presented to the IPFC by ward managers, or in two of our eight cases, by the deputy ward manager. Junior and non-registered nurses were not involved in most cases, although, in several instances, ward managers did identify the potential value of involving junior members of staff in the process. One ward manager (H-MLM, SUI no. 8, hospital A) described the potential value of junior staff being involved in RCA investigations:
I feel that it’s good experience to get people to write them and to do the investigating. When it’s just the ward managers or the practice development matrons, or the other senior staff, you don’t often get the trickling of the message downwards that you want to get. If one of the Band 5s looked into it more in depth, the information would get out there more.
Another ward manager agreed, but suggested that junior staff would need to be supported in attending, for example, the IPFC:
I don’t want them to panic and to have that fear of going . . . I think they’d probably think, ‘Oh, I’m in trouble and I’m going to have to go and present this.’
H-MLM, SUI no. 7, hospital A
This opinion is supported by junior nurses’ views of the IPFC:
I think it’s quite tense because obviously if you’re in the position to be presenting the RCA you don’t want to admit error.
Registered nurse band 5, SUI no. 1, hospital A
Apparently they can be quite scary.
Non-registered nurse, SUI no. 1, hospital A
While ward managers took responsibility for actions, and were able to give examples of ways in which they brokered knowledge downstream after attending the IPFC, frontline staff interviewed were often less clear on where learning and changes to practice had originated:
No, I don’t think I did [relate a change in ward practice to the RCA] because I think it was a little while after the incident. We’re always being introduced to new changes, so I don’t think I put it down to that in particular.
Non-registered nurse, SUI no. 2, hospital A
A lack of accountability for the implementation of service actions following presentation at the IPFC does little to establish the brokering of PSK as a priority between the IPFC and the ward for service improvement. As one ward manager highlights:
Because you have so many things to do and then once you feel like you’ve done the initial thing, then I suppose some of the other actions could get a bit put on the back-burner.
Ward manager, H-MLM, SUI no. 3, hospital A
Our data suggest that there is a knowledge-brokering gap between the level of the subcommittee (IPFC) where the incident and remedial actions are discussed and the ward where the incident occurred. This gap relates to several areas, notably, first, where RCA learning is being brokered by ward managers, it is often in a non-specific and informal manner, and so staff may not make the connection between IPFC recommendations and changes in practice. Second, actions set out during the RCA process are not necessarily being followed up at a later date, and knowledge brokering for service improvement may not occur at all.
Root cause analysis as compliance rather than learning?
The RCA process was viewed in various ways by ward managers who had completed investigations. For some, the completion of the documentation was seen as a ‘chore’:
The amount of time invested in sort of trawling through the notes and seeing what was done and what wasn’t done and so on and so forth, I’m not necessarily convinced is value for money, so to speak.
Ward manager, H-MLM, SUI no. 4, hospital A
For others, the documentation seemed very ‘black and white’, and risked decontextualising the incident:
Because filling it in is just a timeline, isn’t it, and anyone could really [do that], you know.
Deputy ward manager, H-MLM, SUI no.1, hospital A
However, for others, completion of the RCA document was considered a logical and valuable process:
It’s quite long, but to be fair, with the falls RCA, they’re very structured, so you can give a yes or no answer, or it’s not applicable. You’ve not got masses of variability, which I do think helps you then come to an outcome at the end of it, or a root cause at the end of it, rather than it be airy-fairy.
Ward manager, H-MLM, SUI no. 7, hospital A
Completion of RCA documentation was seen as a potential learning tool for more junior members of staff:
I think they would learn more doing that than me saying to them afterwards.
Ward manager, H-MLM, SUI no. 7, hospital A
While writing RCA documents was not seen as a particularly useful part of the process, presenting to the IPFC did hold value for ward managers, and this element of the RCA process appeared to represent an opportunity for brokering PSK for service improvement:
It’s not the most pleasant experience because you are under the spotlight . . . [but] it is still a good thing to do because sometimes when you work in an area you can’t see the wood for the trees and other people help you see better. Then you move on to discussing solutions. Action plans are discussed and I find that a really positive thing to do.
Ward manager, H-MLM, SUI no. 2, hospital A
From the ward managers’ perspective, the RCA process seems to be a mixture of compliance (paperwork) and brokering knowledge for learning at the ward manager and subcommittee level (presenting and discussing at IPFC). However, the required actions appear largely around compliance with the falls prevention policy in hospital A, rather than service improvement. The majority of actions revolved around issues of staff compliance with, for example, the falls training policy, and risk assessment and care plan documentation. However, less clear was evidence of any structured mechanism for ensuring that these actions were completed. This finding mirrors that of Chapter 4, where the implementation of system capabilities results in compliance but not necessarily service action.
Linked with this issue of compliance is the brokering of RCA learning and actions after the Falls Committee meeting (IPFC). Our findings suggest an unstructured process of brokering, decoupled from the RCA process itself.
Examples of this can be found in SUI no. 2. One of the actions was that the RCA author (a band 6 nurse, who also presented to the IPFC) should feed back findings and actions to all staff on the ward. However, the ward manager, who had been proactive in enabling the band 6 nurse to write and present the RCA, admitted that this was yet to happen:
I mean I know it was February and we’re now July. However, there are so many other things going on . . . I would have liked this to have been presented sooner to staff.
Band 6 nurse, SUI no. 2, hospital A
The non-registered nurse interviewed from this clinical area believed that it would be useful to have the RCA findings presented at a ward meeting ‘sooner rather than later’:
I think that would perhaps be an opportunity to discuss issues like this. I think that would be good. However, we don’t seem to have many ward meetings now.
Non-registered nurse, SUI no. 2, hospital A
It should be noted that this non-registered nurse is the one referred to earlier, who did not believe that changes to ward practice had come about as a direct result of this RCA. This adds support to our contention that the learning from the RCA process is not brokered through to frontline staff.
On the other hand, respondents in some clinical areas were able to give examples of changes to ward practices, which had come about following the RCA process:
We’ve been very focused on falls since [the RCA]. I can’t remember specifically what she [the ward manager] said about what happened with that lady, but obviously we’ve had a lot of things highlighted and changed a few things on the ward since then.
Registered nurse, SUI no. 3, hospital A
Staff have been told about the root cause analysis. They have been given the information. It has been cascaded to them. So they do have an awareness of what happened and why it happened and what we can try to learn from it.
Deputy ward manager, H-MLM, SUI no. 4, hospital A
It’s a bit of paper exercise that’s completed and no one’s really thought about it seriously and put into place what needs to be put into place, such as the evidence that a falls care plan should have been done. But I think recently due to this [fall], it’s been highlighted as a problem and now the staff have certainly been aware of what we can do.
Registered nurse, SUI no. 6, hospital A
When looking at the mechanisms used by ward managers in brokering knowledge from RCA, no clear picture emerges. A wide variety of methods are employed, with varying degrees of success and adoption at ward level. Methods might be described as indirect or direct.
Indirect methods include blanket e-mails to ward staff reminding them of the need to adhere to hospital policy, poster displays in the clinical area and in staffrooms, notices on the staffroom board, and the practice of leaving important documents, which are expected to be read by all staff, in the off-duty folder. More direct methods include cascading of information at time-out days designed to capture all ward staff, ward meetings, falls training sessions, and, most commonly, shift handover.
Managers and frontline staff had varying opinions on the value of the various knowledge-brokering methods, and no single ‘best practice’ emerged from the data. The ward manager linked to SUI no. 5 summed up the principal theme seen throughout the interviews:
I think it’s very difficult because not everybody reads their e-mails, you can’t get everybody there at a staff meeting. We have to try and use as many mediums as possible in order to filter that information down and pass it on.
Ward manager, SUI no. 5, hospital A
Committee culture: learning versus punishment
Ward managers, and their deputies, who presented the RCA to the IPFC described the experience as ‘threatening’:
They really come down on you, you know. It wasn’t nice presenting it at all . . . I wouldn’t present it again.
Deputy ward manager, H-MLM, SUI no. 1, hospital A
Some people made you feel a bit stupid really and were a bit condescending. It was a bit punitive in a way. They were generally just quite sarcastic about things you’d said, and it just felt a bit intimidating.
Ward manager, SUI no. 3, hospital A
While these experiences were described in fairly negative terms, those who had presented RCAs to the IPFC were generally understanding of the process and the necessity to investigate in depth:
It was my first ever RCA I’d presented as well, and I was petrified. I hated it because it’s horrible that it happened in the first place and then you’ve got to say what was missed and your heart just sinks that it should never have happened really. I felt responsible because it was my shift. I was sweating. But they have to ask their questions, don’t they? I think they were fair because they have to get to a point and find out how it happened. They’ve got to be direct about it. It was just nerve-racking really.
Deputy ward manager, H-MLM, SUI no. 5, hospital A
Where there was a more positive view of presenting to the IPFC, this was linked to the process being perceived as non-punitive:
I think they make quite an effort at all of these things that it’s not about blame, it’s about learning. I’m not one for feeling intimidated by things like that anyway. But you go, you’ve already looked at it, so you already know your failings as it were, and they’re not in the game of beating you up about it.
Ward manager, H-MLM, SUI no. 6, hospital A
The ward manager in SUI no. 8 echoed this point, suggesting that the IPFC is there to expand on points raised during the RCA document completion process:
It’s quite daunting . . . [but] I think it’s good. I think it’s a really good learning experience because things that you may not have thought about while you’re writing your RCA are often brought up, picked up, questioned. So for me, I always think they’re a good learning curve.
Ward manager, SUI no. 8, hospital A
Of note in the RCA writing and presenting experience is the lack of involvement by doctors in the process. In only one case was a consultant involved in writing the RCA, and no consultant attended IPFC in all eight cases examined. The ward managers interviewed did not express any opinion about the lack of medical involvement, but a striking point from the RCA documents is that, in every case seen, the required medical post-fall sticker was not completed. This is reflected in the separation of nurses and doctors in relation to falls prevention training, where there is no co-ordinated approach.
Is root cause analysis really root cause analysis?
The RCA process may be seen as more of a ‘signing off’ exercise than an example of knowledge brokering for in-depth organisational learning aimed towards service improvement. While there is evidence of learning and change at ward level, some interviewees question whether or not the root cause of incidents has been properly addressed. While actions post RCA addressed issues such as adequate falls training for staff, or adherence to hospital policy on timely and appropriate risk assessment and subsequent care planning, it could be argued that a deeper issue was missed.
I just think rather than it saying, ‘The staff are not filling in the paperwork correctly,’ the learning might be that, ‘they weren’t filling it in correctly because they were so stretched and they’d been really pulled so paper thin at that stage that something had to give and unfortunately in this case it ended up being detrimental’.
Ward manager, H-MLM, SUI no. 5, hospital A
While actions are largely confined to ensuring staff compliance post RCA, there was little evidence of actions reflecting deeper issues mentioned in interviews.
The [risk assessment] paperwork was a paperwork exercise. So people were doing the assessments, but it does not mean anything. It’s not changing their practice. And then, so a patient falls and you do all the checklists and stuff after that, but it’s not actually influencing how they look after the patient.
Ward manager, H-MLM, SUI no. 6, hospital A
To emphasise, RCA in hospital A appears to be more about compliance than learning, and that system-level issues at a deeper level are not being addressed during the RCA process. Actions are largely confined to easily manageable, tangible areas of care, rather than the more nebulous, and systemic, problems described by interviewees.
Pockets of good practice
From the evidence presented so far, it is apparent that good practice relies on individual H-MLMs, rather than structures in relation to knowledge brokering after RCA in these cases. Dissemination of actions and learning is often unco-ordinated and happens on an ad hoc basis. However, it should be noted that there are pockets of good practice visible in many of the RCAs in hospital A. As identified in Chapter 5, leadership by H-MLMs appeared crucial to this, with ward managers and, in some cases, their deputy ward managers, central to the involvement of others in knowledge brokering, and in fusing exogenous knowledge and endogenous knowledge for service improvement. Examples of these pockets of good practice include:
-
The ward manager in SUI no. 4 took a proactive approach to improving falls prevention awareness after undertaking RCA. She encouraged her deputy ward manager to undertake a project around falls in their clinical area, and, subsequently, the deputy ward manager was made Falls Champion for the ward. The ward manager also uses time out days to disseminate learning and actions from RCA, utilising her deputies to capture any staff not attending the time-out day. She describes the thinking behind her approach, which involves encouraging staff to think ahead rather than a culture of retrospective learning: ‘They’re focused on what happened after the fall whereas I’m trying to push them to think about, “Well, you know, Fred’s been with us 2 weeks now and when he gets agitated that’s usually a sign that he wants a wee. So look for signs of agitation and then consider using a bottle or going to the toilet or whatever so that he’s not getting so agitated he tries to stand up and ends up having a fall”‘.
-
In SUI no. 2, the ward manager encouraged one of the band 6 nurses to complete and present the RCA, with her support: ‘Actually as you do them [RCAs] it’s a really good way of joining the dots, finding out why, and I use them really quite constructively and think of them constructively now. So [the band 6 nurse] did this one. It was the first time she’d done one and presented it and she was able to connect the dots and she found it really useful to do’. This manager also encourages staff to view RCA as an effective learning tool: ‘When I talk to staff about them I do put it in a positive light. You know, it is an investigative tool. We need to find out what happened, but it’s not all about you’ve done wrong and it’s not punitive.’
-
The ward manager in SUI no. 5 described how best practice in relation to falls prevention is being dealt with at directorate level: ‘It’s basically the senior nurses. We meet as a directorate and it is all band 7s off the ward, band 6s if they can be released as well. Personally I like my band 6s to go. Not all of them because that wouldn’t be okay, but they take it in turns to go. Practice development matrons, matrons, health and safety matrons, anybody who kind of might have to get the information together, but it’s just like the nine wards specifically.’ This shared learning is then communicated back to the ward: ‘And we report back to them here via staff meetings, forwarding e-mails, and we also have a board which we update for more regular information.’
These examples of good practice are evidence of effective leadership at ward manager level. They show H-MLMs making a personal investment in changing practice and developing staff, and peer-level learning and information sharing.
In contrast, there are also examples of less than ideal practice apparent across the cases. The main areas for criticism include:
-
An ad hoc, unstructured approach to knowledge brokering. This is particularly evident in interviews where members of staff have observed changes to ward practice, but are unaware of the basis for the alterations. For example, one non-registered nurse describes a change in practice that happened while she was on leave: ‘I’ve just been off for a fortnight where I haven’t got a clue what’s happened in the last fortnight while I’ve been away. Nobody’s sort of said, “Oh, this has happened and this has changed” sort of thing and I’ve just suddenly found that there’s all these yellow stars everywhere on the backs of boards and people have got yellow bands on and I’ve had to ask, “Well, what are they for?” “It’s for the falls risks.” Okay, well it would have been nice to be told that things like this have changed because if you’re not told then you don’t know’ (non-registered nurse, SUI no. 6).
-
A lack of direct communication of RCA findings and actions, particularly in relation to staff not having access to the RCA report itself. In SUI no. 6, the Falls Champion for the ward had not seen the RCA report until it was shown to her during the interview, and had never attended a Falls Committee meeting either.
Evidence from the interviews suggests that while there are pockets of good practice, these are often based on the individual actions of particular H-MLMs, specifically some ward managers. More often, knowledge brokering after RCA is lacking in co-ordination, and undertaken on an ad hoc basis, with the result that knowledge is not being brokered effectively downstream to the clinical front line for a service improvement effect. Meanwhile, knowledge brokered upwards through clinical governance structures has little strategic impact; rather, it shows ‘mere’ compliance with the need to show that SUIs have been dealt with.
The Falls Champion
The role of Falls Champion was prominent throughout the interviews in hospital A. Once again, there was evidence of a lack of co-ordination in the development and enactment of the role:
-
Falls Champion selection happened via two mechanisms. There were cases where an individual had embraced the role, or had actively sought it out. However, there was also evidence that the role was being ‘given’ to band 5 nurses. The deputy ward manager in SUI no. 5 described how the Falls Champion on her ward came about the role: ‘So at the time a lot of staff nurses had got their own link nurse roles and [xxx] had come in without anything and this role needed filling, so [xxx] sort of fell into it really, which happens sometimes’.
-
While the role of Falls Champion was seen as an opportunity for knowledge to be brokered at peer level, with the majority of Falls Champions being a relatively low-status band 5 or 6, there was evidence of a lack of support for them in effectively enacting the role. This was apparent at ward and organisational level. In SUI no. 5, the deputy ward manager seemed unsure as to what exactly the Falls Champion did: ‘Now I’m talking to you, it’s made me think about things that I need to discuss with [her] about what she’s teaching and what data and making sure she’s putting current data on the board’. Similarly, in SUI no. 6, there was evidence of a lack of cohesion, with the Falls Champion not having seen the RCA report, despite her name appearing against some of the actions. This Falls Champion also described the difficulties of achieving her allotted protected time to undertake the role effectively: ‘I’m supposed to be given 6 hours a month which I’ve not actually had, so it’s been difficult’.
The Falls Champion role seems ideally suited to enhancing knowledge brokering in the clinical area, and there is potential for the role to be developed in this way. However, evidence from these cases suggests an underutilisation of Falls Champions, with patchy and sporadic approaches seen across clinical areas. Some respondents suggested that it may be best if the role falls to H-MLMs, such as deputy ward managers, with some legitimacy in the nursing hierarchy to ‘make things happen’.
Knowledge brokering following an incident of patient harm from medication management and transition in hospital Z
In hospital Z, we examined a single SUI related to a medication error involving an older patient undergoing end-of-life care. We provide a summary of the SUI as follows. The patient was admitted to hospital and placed on AMU, pending transfer to a nursing home where he had chosen to spend the last days of his life. Nurses on AMU had tried in vain to transfer the patient to a nursing home owing to the time of admission being after 5 p.m., when the bed manager in the nursing home had finished for the day. Dialogue between a nurse and the patient’s family led to a discussion about what was described as a ‘blue box’ given to the patient by the community nursing team, containing end-of-life drugs. The nurse asked the patient’s family to bring the blue box into the hospital. The patient and the patient’s family were keen for the patient not to die in hospital, leading the nurses to arrange for the patient to be transferred home for the night to be cared for by the district nursing team. Communication between nurses on AMU and the district nursing team was reportedly difficult to establish, with a number of teams covering different areas and operating in slightly different ways; however, it was agreed with the district nursing team that the patient should be returned home, with a syringe driver administering therapeutic end-of-life drugs. The nurse set up the syringe driver from the patient’s blue box, believing this to be the correct protocol. However, the syringe driver from the ‘blue box’ was different from hospital Z’s syringe drivers, and was set to deliver drugs over a 1-hour period instead of a 24-hour period as intended. The patient died.
An investigation revealed that the dose delivered accidently across a 1-hour period was within the therapeutic range and so, in this instance, the error did not directly cause death. However, the root cause of the medication error was:
-
administering drugs from non-hospital owned equipment.
More than 12 months after this incident occurred, our research team interviewed 25 nurses and non-registered nurses working on AMU, along with two junior doctors. The findings reveal that the incident was known to all but one respondent; however, the learning from the incident was very poor due to a lack of formal knowledge brokering. Our findings highlight that lessons have not been learned and transformed into service action to improve care for older people; furthermore, nurses have learned to be fearful of syringe drivers, avoiding their use despite the fact that the error occurred because it was an external syringe driver that was used. This case highlights the importance of formal knowledge brokering between H-MLMs and the ward, and the implications of a lack of knowledge brokering upon quality of care.
The limitations of knowledge brokering via informal conversation
With the exception of one registered nurse band 6 (who had no knowledge of the SUI), all respondents across all nursing bands stated that they had heard about the SUI, but that they had heard about it informally through conversations with colleagues. In many cases, the conversations were prompted by withdrawal of drug administration duties for two registered nurses, which consequently increased the workload for their colleagues on shift. While many respondents referred to ‘an open communication culture’ among their peers, it was evident that little knowledge had been brokered within nursing that placed the incident into context, i.e. that the nurses involved were under pressure from the patient’s family to get the patient home to die, but experienced difficulties of communication between the family and the community district nursing team. Instead, the focus of conversation about the medication/transition incident was on the SUI being a result of using a syringe driver. The resultant learning from the incident appeared to be restricted to the correct and careful use of a syringe driver, with many respondents reporting a heightened sense of fear, with some even admitting that they would avoid its use.
I remember the first time I actually found out about it. Two of the staff that were involved were on shift and a colleague from another zone asked me to come and check how to set up a syringe driver. Although I’d had the initial training, I’d never physically used the driver myself, so I said, ‘Oh, I haven’t been here for a year. I’m not the best person. I’d want to watch it a few times’. Then I said, ‘Why don’t you ask [xxx]? She replied, ‘I can’t ask her because she isn’t allowed to do it any more’. There was fear in everybody’s face. It was so scary. You would come into work and you could be working with three or four people that couldn’t do drugs. That made your workload go up 10 times and I felt more at risk of my own PIN number [nursing registration] and me making mistakes because you were having to do double your workload for somebody else and, to be perfectly honest, I think it was very poorly managed.
Registered nurse band 5, hospital Z
Owing to the lack of formal detail disclosed about the incident, combined with the very visible consequence for two members of staff (the removal of drugs responsibility), the learning from the incident is consistently reported by nurses across all bands as one of ‘fear’ and caution. This finding is supported by band 7s and 8s:
From my point of view, I don’t feel that the changes are completely embedded yet because staff are still fearful of using the syringe driver.
Registered nurse band 8, hospital Z
The following excerpt from interview reveals how a registered nurse equates the use of a pump brought into the hospital by the patient to the use of a patient’s own drugs and inhalers as encouraged by pharmacy:
If a box came in from the community like that, would you administer the drugs from it?
Patients come in with their own medications all the time and, yes, we do administer from those. We’re actually told by pharmacy that if a patient has their own drugs, then we should use these drugs. If they run out, that’s when we order. So because of the expense of the medications and things like inhalers and any kind of unusual medications that we wouldn’t ordinarily have in stock, we use the patient’s own. So I suppose if it’s all in date, if it is the correct dose and you’re familiar with that pump, I wouldn’t see why it wouldn’t be used.
It’s actually against policy [to use external equipment].
Really?
Registered nurse band 8, hospital Z
Conversely, other nurses express surprise that a registered nurse would use equipment from outside the Trust. Meanwhile, they also exhibited that they had gleaned little knowledge of the details of the SUI, other than that via informal conversations among colleagues.
I’m surprised though that they would use equipment that’s come from outside of the Trust. [Interviewer: Yes, that was the mistake – that it shouldn’t have been used.] However, I don’t know the full incident. I assumed that we [hospital Z] had two different syringe drivers and we’d used the wrong one, not that we had used one from the community.
Registered nurse band 5, hospital Z
Confusion remained in AMU about syringe drivers. A matron on AMU recalls the following recent incident:
There was an incident the other day and somebody said, ‘Oh, this patient’s on this syringe driver (one provided by the community)’. I said, ‘You need to speak to the doctor and ask him to prescribe something in the interim whilst you set up one of our syringe drivers’. And she said, ‘Why?’ I asked, ‘Do you not recall the incident?’ She went, ‘Well yes’. I said, ‘So they don’t stay on it’. She knew about the previous incident, but didn’t relate it to the similar situation she faced.
Registered nurse band 8, hospital Z
There also appears little or no attempt to formally rectify the situation and embed learning locally, other than H-MLMs ‘telling off’ staff when they see them doing the wrong thing. Clearly, while this may rectify the immediate behaviour of the individual, this relies on H-MLMs, such as matrons and ward managers, ‘watching’ staff at all times. The feeling of being ‘watched’ is a theme that emerged from a number of interviews, with adverse consequences for staff in terms of confidence in their own practice:
Because this [SUI] has happened, they’re [H-MLMs] picking up on every single thing and it is making people paranoid that you’re being watched. Then, because you’re being watched, you doubt your own practice and your own skills, because there’s that pressure, if you get one thing wrong, then . . .
Registered nurse band 6, hospital Z
Many staff viewed the decision to suspend two nurses linked to the SUI from drug administration as ‘punishment’, which was deemed humiliating to the individuals concerned.
I really felt for those two nurses suspended from drug administration. Yes, there was an error, but they were humiliated. I know obviously you have to go through certain protocols, but it was very demoralising.
Registered nurse band 5, hospital Z
While punishment has sent a very clear message that a SUI has occurred, it does not effectively promote or enable learning from the incident. Reflecting upon the learning gained from the SUI, two senior nursing respondents discuss how things could have been done differently in order to learn from the incident for improving the quality of care:
I think if we were to do it again, if I was the manager, I’d be talking to the individuals more and saying, ‘Can we discuss it? It could have happened to any of us under that pressure. We need to talk about it and let everybody know. You haven’t failed’. However, I think they think they’ve failed and they feel guilty, don’t they, and they’re frightened.
Registered nurse band 7, hospital Z
In summary, an absence of formal knowledge brokerage by H-MLMs about the SUI has created an environment where nurses have been forced to rely upon informal conversations between colleagues to understand why their colleagues have been suspended from administering drugs. The consequence of such informally based conversations is the evolution of what was frequently referred to by nursing staff in AMU as ‘Chinese whispers’, where certain details are incorrect and/or progressively exaggerated. Rather than learning about the dangers of using drugs and equipment originating from outside the Trust, staff learned to be fearful of using the Trust equipment, compromising the quality of care to patients. In short, in this SUI, we see the effects of H-MLMs not enacting a knowledge-brokering role for service improvement. Not only did service improvement not occur, but the quality of care seemed to actually get worse. This was exacerbated by top-down pressure from managers to move patients.
I just see the managers coming in to push people out, get people in, push people out, but they’re not concerned about what we have to do with the patients while they’re here.
Registered nurse band 5, hospital Z
A number of registered nurses state that they feel unsupported by management, creating a situation of low morale:
Management are more interested in the way things look, than the way they are.
Registered nurse band 6, hospital Z
In summary, pressures in AMU to move patients shaped the way that H-MLMs enacted their role. At the same time, we note that those H-MLMs applying pressure to staff on AMU were doing so because other H-MLMs situated on wards are slow to take in patients, often because they too faced similar pressures. Again, the metaphor of a ‘broken chain’ seems apt.
Because of the uniqueness of the unit, you’re under pressure. A lot of the wards can say, ‘No, we’re not ready yet’. We don’t have that privilege here. Our doors are always open. We have them queued up down the corridors and you’ve just got to keep on top of it.
Registered nurse band 5, hospital Z
Knowledge brokering at the system level
While there was some variability among nurses with regards to their awareness of hospital Z’s policy about drugs and equipment originating from outside the organisation, when informed of the context in which the SUI occurred (that the patient was at ‘end of life’, and did not wish to die in hospital), many understood the pressures faced by the nurses, and were not certain that it would not occur again.
People don’t do end-of-life 9 to 5. It’s a 24-hour service. However, community service tends to be 9 to 5, when patients can be discharged at 7 or 8 o’clock. I know people are desperate to get home, and if a patient’s wish is that they want to get home . . .
Registered nurse band 5, hospital Z
As intimated above, the patient was unable to get a bed at the hospice, as was his wish, due to the bed manager in the hospice working only daytime hours. The patient thus expressed his wish to return home to die, rather than to wait in hospital overnight, with the aim of transfer to the hospice in the morning.
They [the hospice] were basically saying, ‘Well, you’ll have to call back at 9 o’clock tomorrow morning’. I was like, ‘He has to go tonight. What do I do?’ No help at all. And then the family were adamant that he wasn’t to die in hospital, and so was he. Then we contacted district nurses, but it was out of hours again, and there was only a messaging service.
Registered nurse band 5, hospital Z
Once aware of the wider context surrounding the SUI, we asked whether or not the report findings and recommendations had been shared with the community. While hospital Z policy does recommend ‘Learning from the incident should be shared with the community services to raise awareness and minimise the potential of a similar incident occurring’, there was no knowledge among our respondents that this has been achieved. A band 8 registered nurse suggests that the community nurses involved in the incident have failed to co-operate:
My understanding is that there wasn’t very much co-operation in the initial stages of the investigation and obtaining statements from those individuals with a community perspective. They denied any knowledge of discussions (about the patient in AMU). Then there was a lot of, ‘We’re not getting involved. It’s nothing to do with us. We’re not providing statements’. In the end, when the first individual that was doing the investigation left and the second took over, they bypassed the community because they weren’t getting anything from the manager at all.
Registered nurse band 8, hospital Z
In summary, not only is brokering of knowledge absent within the organisation, but around medication management, and more notably transition of patients, there exists a significant challenge of brokering knowledge between organisations. At least in hospital Z and this particular SUI, no H-MLM is able to enact the necessary knowledge-brokering role for service improvement.
Mechanisms for knowledge brokering
Like much of the knowledge brokering discussed in previous empirical sections, across all our hospital cases, there was a strong sense from those on the clinical front line that managerial diktat was imposed from above, often via e-mail. The use of e-mails as a mechanism for brokering knowledge was generally met with disdain, with all staff stating that they did not have time to read e-mails, many even claiming that they often did not get a break:
You know, on a shift, when do you get a chance to check your e-mails? I’ve got hundreds and honestly I don’t have time to delete them.
Registered nurse band 6, hospital Z
One band 8 registered nurse, however, has a very different view from all other respondents. H-MLMs may need to engender a stronger learning culture among frontline staff should they want to broker knowledge for service improvement.
But they [registered nurses and non-registered nurses] have time to go for breaks, they have time to go to cigarette breaks and they have time to go and have a break. If an individual wanted to access information from e-mails, they can. There are several computer points throughout the wards that they can access because they access their e-roster from those points on a frequent basis. Time is not an issue. They are busy, I’m not disputing that at all, but if you can go for a break, go for a cigarette and you can access your e-roster, why can’t you access your e-mails?
Registered nurse band 8, hospital Z
Similarly, time constraints are cited as preventing staff from looking at the noticeboard in the staffroom, and time for completing online training assessments was limited.
On a more positive note, there was considerable support across all nursing bands, including non-registered nurses, for home access to e-mails and online training modules. However, while the option to access e-mails and online training modules during personal time was welcomed, some respondents were wary of being held accountable for home-based learning in excess of their working hours. This raises the spectre of work–life balance.
I’m all up for learning at the end of the day, but obviously if it was at home, as long as it didn’t become too regular that it became a lot of homework, as long it was out of your own choice, and as long as you don’t get punished for not looking at certain things at home.
Non-registered nurse, hospital Z
A number of staff recalled a time when the noticeboard was kept up to date and colour-coded with information, creating a visual display that was deemed valuable for brokering knowledge, with emphasis on the positive rather than a punitive approach to improving the quality of care.
It went from being all these different colours, which does draw you in. Then it was serious things, such as, ‘We didn’t reach 100% in this audit, so we need to try better’. It had a positive spin; now it’s almost like a ‘how poor we’re doing’ board. We didn’t do this well. You didn’t do this. We’re all rubbish’. Everything’s just very negative at the minute.
Registered nurse band 5, hospital Z
As at hospital A, there was considerable support for ‘link’ roles, where someone has responsibility for championing specific issues, representing a knowledge broker between the H-MLM with formal responsibility for patient safety and learning and the clinical front line. The role of champion or link worker was welcomed by all, but always with the caveat of ‘protected time’ for individuals. Many appeared sceptical that this would happen, highlighting the low morale among nurses on AMU with regard to feeling supported in their training needs. So, even if health-care professionals are able to enact the H-MLM role, they may be unwilling to do so because they might feel that they are not sufficiently resourced:
You’ve got to look at it and say, ‘Okay, if we’re going to do this, we need somebody to be given time to go away from this and do this role’.
Registered nurse band 6, hospital Z
Teaching sessions led by one H-MLM (a medical doctor) were mentioned frequently by respondents across all nursing bands, including non-registered nurses. The description of (a doctor’s) teaching highlights that he attempts to broker the right knowledge, to the right people, in the right way, at the right time.
He did actually do teaching sessions specifically for nurses, stuff we actually use. He actually started those again before he actually went on sick leave. I don’t know whether he has plans to restart them, but they’d be a fantastic help because, as I say, he does provide so much information. He makes sure that your knowledge is correct to actually receive the information in the first place. He actually starts with a question-and-answer thing, and then tells you more about what he wants you to know.
Registered nurse band 6, hospital Z
There were, however, mixed feelings regarding the usefulness of ward meetings for brokering knowledge. Many suggested that the ward meetings tend to be used to ‘air frustrations’. The following quote suggests that tensions between non-registered nurses and registered nurses come to surface at ward meetings:
Some of the higher bands blame the lower bands [Interviewer: Could it get a bit heated?] Yeah, it has done in the past.
Non-registered nurse, hospital Z
In contrast, there was considerable support for the idea that knowledge could be brokered formally and on a daily basis at handover.
During your handover you get a quick 5-minute session about anything, but nothing’s discussed in depth [by H-MLMs]. You’re given a brief overview of any incidents, or any kind of new issues that we’re dealing with now, and that’s it. If we could spend 5 or 10 minutes just going over particular issues that have come up, if it was communicated and cascaded down to the staff that way, I think that would be very beneficial.
Registered nurse band 5, hospital Z
The handover could also be used in a similar vein to broker knowledge upwards from the nurses themselves to more senior managers, through H-MLMs, although again it is not currently felt to be effective:
Well we’re quite vocal to our managers. They’re quite good. They’re really good ward managers as in we can go up and I can say anything to them, as in, ‘I don’t think this is right,’ and we can moan and say what we want about it and a lot of the time they do agree with us. They know that there’s certain points of this unit it just doesn’t work, but then it seems to . . . I mean I’m pretty sure that they will tell the matron and they will tell their bosses because that’s the kind of people they are, but it seems to stop there, do you know what I mean, and it feels like nothing goes further.
Registered nurse band 5, hospital Z
In summary, there is a range of potentially useful mechanisms for knowledge brokering highlighted by respondents. However, the organisation does not take full advantage of these, specifically supporting the role of H-MLMs for knowledge brokering. At some point, in brokering knowledge upwards, the chain appears to break.
Research contribution of Chapter 6
This section depicts the following contribution to RQ6 in particular:
RQ6. What prescriptions can our analysis of knowledge brokering offer for policy and practice, e.g. how can MLMs be enabled to broker patient safety knowledge more effectively?
Ward managers represent important H-MLMs in hospitals A and Z with respect to knowledge brokering around RCAs following a SUI. Ward managers agree that RCA is an opportunity for learning and reflection, and ultimately a chance to make significant service improvements. However, the process of undertaking a RCA investigation is challenging, particularly with respect to presentation at the relevant clinical governance committees. Ward managers are generally undertaking RCA report writing alone, often with no involvement by medical staff. There is some evidence of knowledge brokering by ward managers after RCA investigation aimed at service improvement in the care of older people, but there is often an unstructured approach, with much brokering happening on an ad hoc basis, particularly in the form of brief and informal discussions at shift handover. In hospital Z, despite the clear learning to be absorbed from the SUI that would prevent a recurrence of the incident, a lack of formal knowledge brokering led to confusion among nurses regarding the nature of the incident, and this reduced their confidence in using medical equipment, altering behaviour in a way that could compromise the delivery of high-quality care.
In some cases, there appears to be a decoupling of knowledge brokering as it moves downstream following RCA investigation, with frontline staff at times unaware that service changes are a direct result of the investigations. Sometimes, RCA investigations can result in tangible and achievable actions, but it appears that issues associated with deeper organisational or systems change are being ignored. There is also evidence that actions may not be completed following RCA, and the degree of follow-up to RCAs by clinical governance committees is unclear in such cases.
Regarding our understanding of the contingencies that underpin an effective knowledge-brokering role for H-MLMs, we remind readers of the definition of a knowledge broker as an individual who uses their in-between vantage position to support innovation through connecting, recombining and transferring to new contexts otherwise disconnected pools of ideas, i.e. they get the right knowledge into the right hands, at the right time. 3,4 Bearing these positives in mind along with our perception of the knowledge-brokering chain as ‘broken’, we need to consider how the latter might be ‘mended’.
As evident in other empirical chapters, clinical governance systems and frontline clinical practice appears decoupled. Brokering knowledge downwards from management only goes so far, as clinical governance systems, including those concerned with RCAs following SUIs, are more concerned with compliance rather than service improvement. The knowledge-brokering role of H-MLMs follows accordingly. Rather than engage clinical frontline staff in service improvement through their knowledge brokering, H-MLMs, such as ward managers, are fearful of encountering blame for mistakes, and so they themselves comply in the more bureaucratic process of showing that a RCA has taken place. Their energies are directed upwards rather than downwards towards brokering knowledge to, and engaging, frontline clinical staff in service improvement. At the same time, frontline clinical staff are concerned that they are blamed for SUIs, and so do not effectively broker knowledge upwards through H-MLMs for service improvement effect. In short, one of the most significant contingencies shaping the knowledge-brokering role of the H-MLM is that of an all-pervasive ‘blame culture’ rather than a ‘learning culture’. Link roles appear significant in ensuring that H-MLMs, such as ward managers, perceiving themselves to ‘walk on the tightrope’ of accountability and blame, broker downwards to frontline clinical staff. Given that legitimacy and status are important to allow such link roles to be effective, a more junior H-MLM, such as a deputy ward manager, might be co-opted to enact such a role.
Influenced by perceptions of a ‘blame’ culture, the analogy of a ‘broken chain’ applies particularly to relations between the hospital and community care providers; the latter, on a prosaic yet significant note, offer their services only on a 9-to-5 basis, excluding weekends, while seeming to buffer themselves against any expectation they might do otherwise. Hence they only reluctantly engage in any knowledge brokering for learning and service improvement, if engaging at all. This seriously limits the sphere of knowledge-brokering influence for H-MLMs to improve the care of older people.
Timelines also prove problematic regarding the workings of the clinical governance process around RCAs. H-MLMs often broker knowledge for service improvement following RCAs, except with a significant time lag after the original SUI. In part, this seems due to the ‘slow-turning wheels’ of the clinical governance structures and the time-consuming nature of the investigation and report writing that follows a SUI. However, it also relates in part to the passion of the H-MLM to prioritise knowledge brokering for service improvement following the SUI. Indeed, knowledge brokering and service improvement depends too greatly on the agency of the H-MLM, particularly their disposition for patient safety and service improvement. Hence, knowledge brokering tends to be ad hoc and unstructured, rather than systematic. A key challenge is how we might engender a widespread disposition among H-MLMs for knowledge brokering towards service improvement following RCAs.
Regarding who brokers knowledge, it is important how others perceive the legitimacy of any actor. Doctors appear absent in accounts of knowledge brokering for service improvement, yet these are high-status actors. Indeed, the power of high-status H-MLMs to more effectively broker knowledge was revealed in the lauding of the teaching contribution of a doctor in hospital Z around patient safety. If knowledge brokering by H-MLMs is limited to the nursing profession, then service improvement is likely to remain partial. Such a tendency was also highlighted in Chapter 6, in our analysis of the brokering of endogenous knowledge upwards from frontline nurses, but there were also glimpses of the more widespread influence of H-MLMs with a nursing background beyond their own ranks. Doctors proved hard to engage in our research around RCAs (e.g. they did not turn up for focus groups, despite being invited by one of their peers), so it is difficult to ascertain why they show particular reluctance to engage in RCAs. However, our earlier empirical chapters suggest that they do not see ‘patient safety’ as core activity. Perhaps the label itself is dismissed, even as they practice safely and try to improve this ‘safe’ practice. Perhaps their reluctance is linked to the particular managerial preoccupation with compliance they perceive around RCAs. Certainly, there seems to be work to do here around the contingency of managerial–medical or nurse–medical relations for knowledge brokering to be more widespread across the hospital and, potentially, beyond to community care providers.
Regarding how knowledge is brokered, in line with the very definition of knowledge brokering, it needs to be in a ‘situated way’, so that it fits with work routines and locations. At the same time, it needs to go beyond, and indeed sometimes counter, knowledge that is brokered by informal conversation at the local level. Left to informal conversation, the ‘wrong’ knowledge may be brokered, with deleterious consequences for service improvement. Careful thought needs to be given to the timing of knowledge brokering, with daily handover representing a potential golden opportunity for situated learning to drive service improvement. Effective visual management of knowledge, given time and space pressures during handover and other ‘downtime’, may engender a greater knowledge-brokering influence. Use of IT, specifically e-mail, may be varied in its uptake, and so needs to be complemented by other mechanisms for brokering PSK.
Chapter 7 Conclusion
The 1990s provided an ostensible turning point in our conceptual understanding of the role of the H-MLM, from one that was task orientated and operational to one that was more strategic. 28 Since then, a burgeoning body of literature has evolved which presents a compelling argument for the unique knowledge-based capability of hybrid MLMs to positively influence the ongoing development and implementation of strategy in an organisation. 13,82 Yet in the face of the recent global downturn, and specific financial challenges in health-care organisations, there remain continuing tensions around the strategic role of the H-MLM – specifically, whether or not they add value to health-care organisations. 68 Our study extends the understanding of the strategic influence of H-MLMs through a consideration of their knowledge-brokering role,4,5 and illustrates how they are capable of brokering both exogenous and endogenous PSK within and across professions, departments and organisations for service development.
We begin our conclusion by addressing our conflated RQs 1–4 which represent a paraphrasing of our original six RQs in order to draw conclusions that are more simply stated, and, therefore, of practical significance.
Research questions 1 and 3 are interlinked, as follows:
-
RQ1. Which H-MLMs broker what type of PSK (exogenous or endogenous), and why?
-
RQ2. How do H-MLMs broker exogenous and endogenous PSK?
-
RQ3. What are the limiting and facilitating contextual features for H-MLM knowledge brokering?
-
RQ4. How can H-MLMs be enabled to broker PSK more effectively in older persons’ care?
Who brokers what patient safety knowledge, and why?
RQ1. Which H-MLMs broker what type of PSK (exogenous or endogenous), and why?
Our study confirms assertions linked to strategic management literature that the value of MLMs’ value lies, at least in part, in their character as a knowledge resource,28,51,65–67 and their ability and willingness to broker exogenous and endogenous knowledge for organisational improvement. 85 Our study contributes towards the more nuanced understanding of the strategic role of MLMs called for in the generic literature, and within health-care organisations in particular. 10 H-MLMs are of strategic significance in health-care organisations, due to their ability to understand and respond to both professional and managerial concerns. 6 Further, through our study, focusing upon H-MLMs, we delineate, in line with RQ1 and RQ3, which H-MLMs are more able and willing to enact knowledge brokering for service improvement. Our study shows considerable variation regarding which H-MLMs broker PSK. Indeed, as evident in the recent high-level inquiry in the NHS about the appalling conditions of care in Mid-Staffordshire Hospital, and the associated large number of avoidable deaths,149 there is considerable variation, not just across hospitals but even within a single hospital, regarding quality and safety of care. Given this, a more detailed and theorised examination of the contingencies that frame the strategic role of H-MLMs, as we identify which H-MLMs broker PSK, is relevant. Specifically, we address a research gap in understanding social structures that impact knowledge brokering. 39
We highlight that clinical governance delivers managerial legitimacy against externally imposed requirements of performance, but there remains the challenge of ensuring a more productive relationship between clinical governance and service improvement, which requires knowledge brokering by H-MLMs, particularly those located nearer the clinical front line. 152,153 To realise a more productive relationship requires that we move beyond a naive understanding of knowledge brokering, and consider how various factors – the nature of knowledge that one is seeking to leverage; politics and power around sharing knowledge; and cultural frames of reference around knowledge sharing154 – impact the relationship between clinical governance and knowledge brokering for service improvement. From this perspective, firstly, clinical governance relies upon explicit, rather than local tacit, knowledge; secondly, there exists considerable power and politics around clinical governance as doctors and managers struggle over professional autonomy; and thirdly, management and clinicians hold different world-views, with the information requirements of managerially led clinical governance systems opaque to clinicians. 9,22,117
Considering the nature of PSK in health-care organisations, we note that much of the policy emphasis is upon external producers/disseminators/auditors ‘pushing’ exogenous knowledge, such as safety alerts and guidelines, into frontline practice through clinical governance systems. 2 The decontextualised nature of such PSK means that it may be acquired by health-care organisations, but is not subsequently applied for service improvement. Such PSK appears stuck with those H-MLMs, more senior in the managerial hierarchy, and who are orientated towards compliance rather than service improvement. For those more junior H-MLMs, closer to the front line of clinical care, such PSK will be ‘pulled’ in only where they perceive its relevance to the practice and operations of their local area. 90 Linked to this, much of the PSK likely to impact service improvement is endogenous. The endogenous knowledge is experiential or practice-based, often tacit, embedded in communities of practitioners, and not amenable to codification. 14 In Gabbay and le May’s20 terms, it may represent ‘mindlines’, rather than ‘guidelines’. As such, to pull such PSK up through clinical governance systems that encourage codification is problematic. Taking account of these two challenges to the brokering of PSK, fusing top-down exogenous knowledge with bottom-up endogenous knowledge represents a challenge. Rather than a knowledge-brokering chain upwards and outwards, inwards and downwards, we characterise the chain of knowledge as ‘broken’, rather than brokered.
How do hybrid middle-level managers broker knowledge?
RQ 2. How do H-MLMs broker exogenous and endogenous PSK?
Through drawing upon Fernandez and Gould’s typology of knowledge-brokering roles,91,92 as developed by Shi et al. ,85 we are able to address RQ2: how do H-MLMs broker exogenous and endogenous PSK?
The effect of power differentials upon knowledge-brokering roles for H-MLMs is very visible. 85 Within the nursing hierarchy, senior H-MLMs are co-opted by their lower-status peers to act in a representative brokering capacity. Meanwhile, senior H-MLMs and senior hybrid managers with a nursing background also enact a liaison knowledge-brokering role, as they pull endogenous knowledge upwards from lower-status H-MLMs, such as ward managers, into the clinical governance system in the course of situated interaction with those on the clinical front line of the organisation. Examining power differentials further, we might characterise H-MLMs concerned with the care of older people as mid-status actors, as they are relatively less influential either interprofessionally (nurses) or intraprofessionally (geriatricians), yet they do have legitimacy organisationally because they are higher in the managerial hierarchy. So, they may be relatively peripheral within power structures either interprofessionally or intraprofessionally, but they do exert some influence. Moreover, their relatively peripheral position disposes them towards service improvement. In short, it seems that those H-MLMs in mid-status positions who have some power and are pre-disposed towards service improvement enact a knowledge-brokering role that transcends professional hierarchy. 155 In our study, this involved co-opting more senior H-MLMs close to the most senior committee to champion their cause in a representative knowledge-brokering role. More intriguingly, our study shows that some lower-status H-MLMs enact a cosmopolitan knowledge-brokering role. For example, H-MLMs with a mental health nursing background may bring valuable, rare knowledge to other professionals, both nurses and doctors, to help the latter to care for an increasingly aged patient cohort with attendant cognitive impairment problems. This explains how such lower-status H-MLMs are able to transcend organisational and professional hierarchy. For other lower-status H-MLMs, notably ward managers, the reasons behind their ability to enact a cosmopolitan knowledge-brokering role are less clear. It seems more about their disposition for service improvement, which combines with the development of social connectedness. 156 We discuss this further below.
In connection with different knowledge-brokering roles in the context of organisational and professional hierarchy, we can discern disunion and union strategies. 94 Given that formal managerial and professional structures are institutionalised, the blurring of organisational and professional boundaries (a union strategy) is likely challenging, even more so in the face of top-down policy performance management pressures, which cause managerial demands and frontline clinical practice to decouple. The prevalence of a disunion strategy, where H-MLMs attempt to bridge disconnected actors, is perhaps unsurprising. However, as evident above, some thought needs to be given to the legitimacy and disposition of H-MLMs towards brokering PSK in any disunion strategy, as they may be ‘shut out’ by those more powerful between whom they are trying to broker. 85 We do not exclude possibilities for a union strategy; however, given the tendency within the health-care organisation towards professional and managerial insularity, communities are self-sealing, and so this is likely to represent a major challenge. 109
As with a disunion strategy, some thought needs to be given to legitimacy and disposition of H-MLMs towards brokering PSK. Our study illustrates H-MLMs, who are also geriatricians, make attempts to broker exogenous and endogenous knowledge across self-sealing communities, through engendering shared interests and practice in elderly care, i.e. a community of practitioners where organisational and professional boundaries are blurred. Attention to teaching PSK to junior doctors is one mechanism employed by geriatricians to transcend professional boundaries and to mediate the impact of socialisation upon attitudes and behaviours related to patient safety issues such as falls and medication management. Holding multiprofessional focus groups in areas where an adverse event has led to serious harm or the death of a patient is one approach employed by a geriatrician in hospital A, who sought to engender a ‘team’ approach to patient safety on the ward. In this instance, the research team observed doctors engaging in discussion for the first time because the incident was fatal and involved a patient they had treated. This represents the type of bottom-up intervention aligned with professional organisation and practice, which Oborn and Dawson118 encourage. Geriatricians, acting as H-MLMs, would seem to be well positioned for brokering through a union, as well as a disunion, strategy. They have the legitimacy to broker PSK across boundaries because they are high status interprofessionally. Their holistic approach to the care of older people allows them to see how different professional and managerial groups might come together for service improvement. In their practice, they interact with a wide range of clinical and managerial practitioners, and so are likely to develop social connectedness. 156 Finally, they are less powerful intraprofessionally, but this is likely to predispose them towards change. 155 However, unless H-MLMs engaging in such union strategies are able to engage those in senior H-MLM positions who are embedded in clinical governance systems, managerial systems and clinical practice remain decoupled. In its absence, the union strategy affects only those different professional groups nearer the clinical front line, with PSK brokered only in a more localised fashion. In short, despite aspiration otherwise, the knowledge-brokering chain remains ‘broken’.
Regarding media for brokering, our study emphasises that this needs to be situated on the basis that the nature of expert knowledge in health-care organisations is that which is practice-based and often tacit. 19 For this reason, producers, disseminators/auditors of PSK may face considerable challenge in ‘pushing’ such explicit knowledge through to the H-MLMs nearer the clinical front line if it is perceived as irrelevant to, and decontextualised from, clinical practice. There remains considerable challenge to ensure that the ‘right’ exogenous PSK is delivered to the ‘right’ professional experts, at the ‘right’ time, for service improvement. IT represents a partial solution to brokering exogenous PSK into health-care organisations;9 though arguably it is effective only when applied in a very situated manner, such as clinicians pulling in PSK through tailored ‘applications’ and automated customised research scans.
Conversely, those H-MLMs nearer the clinical front line, looking to push endogenous knowledge upwards to their senior H-MLM counterparts, are likely to succeed only where they recognise the situated nature of management demands for compliance with externally imposed measures of performance. RCAs carried out through the committee structure associated with clinical governance represent such a situated forum, where managerial demands for compliance and endogenous knowledge ‘pulled’ from practice could fuse more effectively. However, RCAs were variably used in such a manner, with a ‘blame culture’ rather than ‘learning culture’ prevalent. 22 We suggest that this represents a missed opportunity for situated brokering of exogenous and endogenous PSK, and present prescriptions for remedying this below.
Contingencies for knowledge brokering
RQ3. What are the limiting and facilitating contextual features for H-MLM knowledge brokering?
We highlight the effect of how a health-care organisation is structured managerially and professionally. The interests and perspectives of managers and health-care professionals are potentially at odds with each other, specifically with respect to knowledge brokering. 9 In particular, managerial concerns around PSK may be seen, by health-care professionals, to emphasise bureaucratic compliance, and so to represent a ‘managerial sideshow’ to ongoing clinical practice. 22 Our empirical cases, presented in Chapters 4–6, highlight that H-MLMs are indeed key to brokering PSK for a service improvement effect in elderly care around falls, medication management and transition, which bridges managerial and clinical boundaries. However, the level at which H-MLMs are positioned appears crucial to effective knowledge brokering, with the potential value of lower-level H-MLMs located nearer the clinical front line lost, unless they are able to broker through senior H-MLM peers. Further, we note that the need for hybridity extends beyond bridging managerial and clinical structures and practices, as follows.
The professional organisation is itself differentiated, structured interprofessionally so that similar occupations work together, and then stratifying further intraprofessionally around specialist practices,108,157,158 which commonly cohere into CoPs, as members are socialised towards shared interests and practice. 109 This engenders professionally-based knowledge around PSK, which may prove difficult to broker across boundaries as perspectives and interests diverge. Those H-MLMs with rare, valued PSK in others’ eyes, such as knowledge in the mental health domain, appear able to broker knowledge more effectively across boundaries. So, legitimacy may be attributed not just to those individuals with status and power, but also to those who hold knowledge that is considered distinctive and valuable. 84
Literature highlights that not all professional communities are equal. Professional organisation is hierarchical, and the associated status and power of those in H-MLM positions significantly dictates the legitimacy and hence the ability of H-MLMs to broker knowledge. This is a matter of both interprofessional and intraprofessional hierarchy. 157 So, doctors are better able to broker PSK, both upwards and downwards beyond their professional boundaries, than nurses. At the same time, within the medical profession, some doctors, such as geriatricians, may struggle to broker PSK to their peers, such as surgeons, because the latter are more narrowly focused in their role and less concerned about more holistic dimensions of care. We also suggest that some specialties, such as geriatrics, are perceived as less attractive than others, and so have traditionally been perceived as lower status within the medical community. 19 Further, we note that power and status can be used to block knowledge brokering, even by those in H-MLM positions. 85 For example, we find that some doctors In H-MLM positions adopt a gatekeeping role91,92 to broker knowledge to junior doctors as they themselves deem appropriate, sometimes even encouraging their junior counterparts to ignore PSK. Meanwhile, brokering of PSK by nurses is less bound by specialism difference, and more by rigid hierarchy. 159 Such hierarchy may, however, prove helpful in brokering PSK. Those more senior nurse H-MLMs may find it easier to broker PSK upwards and downwards, compared with H-MLMs further down the nursing hierarchy, particularly where the former H-MLMs are embedded in formal clinical governance structures. However, we note that in so doing they have some dependency upon their more junior H-MLM counterparts closer to the clinical front line to broker PSK for service improvement. Meanwhile, we highlight that junior H-MLMs are ideally situated for brokering practice-based knowledge upwards; however, the rigidity of the nursing hierarchy can impede an upwards knowledge flow to the extent that more senior managers need to engage with junior H-MLMs to pull PSK from the front line rather than relying upon a knowledge push.
Even within nursing, more formal, exogenous knowledge proves hard to fuse with the more contextualised, endogenous knowledge, given managerial emphasis upon compliance with external demands of performance management. 22 In short, performance management demands appear decoupled from the need for service improvement, with a consequent deleterious effect upon knowledge brokering upwards and downwards by H-MLMs, so that the brokering chain is somewhat ‘broken’. More ‘savvy’ H-MLMs, both doctors and nurses, recognise the need to align with managerial concerns around compliance for the effective brokering of endogenous knowledge upwards. Their ‘savvy-ness’ may be engendered by greater exposure to, perhaps even engagement in, the development of measures of compliance, i.e. their hybrid activity may encompass policy development as well as organisational management.
Finally, the knowledge-brokering chain might be characterised as more visibly ‘broken’, with respect to any brokering of PSK upwards and downwards, encompassing external producers/disseminators/auditors of PSK, through the medical profession, and across the different occupational communities of doctors, managers, nurses and other health-care professionals. One might expect clinical academic H-MLMs to enjoy a three-way window/prism of hybridity, which crosses exogenous knowledge, clinical practice and management responsibility, and allows them to effectively broker PSK across disparate communities. Where their research is situated, and they enjoy power and status as specialist doctors, we might expect a brokering chain from research through to practice across occupational communities; however, evidence is limited to one instance in hospital A, where academic demands determined that knowledge could not be brokered by the H-MLM in a timely manner, i.e. formative input into service improvement across hospital A.
Implications for practice
RQ4. How can H-MLMs be enabled to broker patient safety knowledge more effectively in older persons’ care?
Above, we acknowledge variation in knowledge brokering by H-MLMs, framed by power differentials. 85 Paradoxically, it is those relatively low-status staff in interprofessional or intraprofessional terms, enacting H-MLM roles closer to the front line of health service delivery, who hold practice-based knowledge (endogenous knowledge) with which to relate any strategic intention. 10 Thus, first, we need to consider how we might mediate status differentials to engender strategic influence from hybrid MLMs. Second, we need to consider how to mediate the dominant influence of the external political environment, which causes organisational management to focus upon compliance with external regulation and scrutiny requirements, rather than quality improvement. Finally, academic commentary argues that the presence of knowledge brokers is a necessary, though not sufficient, condition for knowledge brokering to be enacted. 19 Within a large, complex organisation, such as a local health-care system, individual knowledge brokers are likely to have limited impact unless the system is receptive to their efforts.
Through drawing upon the concept of combinative capabilities, and considering the interaction of systems capability, socialisation capability and co-ordination capability,83,119 we are able to derive theoretical generalisation around prescriptions to mediate professional and policy pressures, so that there is organisational support for the ability and willingness of H-MLMs to broker exogenous and endogenous PSK. Literature argues that the development of co-ordination capability counters the deleterious effect of system capabilities (managerial structures and processes geared towards knowledge brokering for compliance) and socialisation capabilities (knowledge brokering that is rather introspective as a result of professional differentiation and hierarchy) upon knowledge brokering by H-MLMs.
A first significant facet of combinative capability is that of the way system capabilities are orientated towards compliance. 9,22 External demands around performance represent antecedents to the way that health-care organisations set up their system capabilities. One obvious prescription might be that external targets and incentives change to better fit with the need for service improvement on the clinical front line. More local discretion might reduce the deleterious effect system capabilities have upon applying PSK for service improvement. However, such is the political profile of patient safety and quality in the NHS, particularly around elderly care, that policy-makers may rightly prove reluctant to reduce central control. In any case, no matter how much emphasis policy-makers place upon ‘steering rather than rowing’,160 academic commentators highlight that health-care organisations ‘game play’ to ensure compliance with targets in a way that may not necessarily improve service. 132,133,161 A more realistic route for enhancing combinative capabilities is to enhance the co-ordination capability represented by the knowledge-brokering role of H-MLMs, in order to mediate the deleterious effect of external demands, and to ensure that clinical practice and such demands align more effectively. The fusing of exogenous PSK and endogenous PSK through H-MLMs through a knowledge-brokering chain across the managerial and professional hierarchies seems crucial to ensuring a service improvement effect, which complies with political demands for high-quality elderly care.
A second significant facet of combinative capability is that of socialisation of H-MLMs. We have highlighted variability around H-MLMs’ disposition for knowledge brokering for service improvement. Some do and some do not, but this seems to transcend a mere structural explanation regarding H-MLMs’ position in the professional or managerial hierarchy. This seems a particularly intriguing matter with those lower-status H-MLMs, such as ward managers. Analysing such variability further, we highlight, in theory, H-MLMs may be socialised in a way that engenders a lack of will to broker PSK across professional and organisational boundaries, i.e. they may behave in a less proactive manner because of their position in the professional and managerial hierarchy. Academic commentators highlight how H-MLMs variably orientate towards the demands of their role, which is linked to socialisation capability. The importance of maintaining professional credibility and collegiality among colleagues is often a paramount concern, and responses to this inherent tension appear to vary. 162 Some professionals, when placed in a H-MLM role, may merely enact the role as a ‘representative’ of their professional peers in line with professional interest and traditional professional bureaucracy structures. 126 Some moving into H-MLM roles may attempt to protect or ‘buffer’ professional interests from managerial encroachment by taking on senior administrative positions in professional organisations and, in so doing, change hierarchical relations within the profession, i.e. they use the hybrid role to elevate themselves above their peers. 163 Others, meanwhile, may blend their clinical and managerial identities to claim that they sustain their focus upon patient care, and a managerial role allows them best to do this. 164 To emphasise our point, even where enjoying legitimacy among the professional organisation to enact a strategic role, H-MLMs may prove unwilling to do so. They may prove more reluctant than their general manager counterparts,165 or unable to look both ways through the two-way window of professional and management perspectives,6 in support of a knowledge-brokering role for service improvement within health-care organisations.
We also note that socialisation capability is manifested in the tendency of the health-care system to fragment when faced with adverse incidents. Our empirical findings highlight that a ‘blame culture’ pervades health care in a situation of adverse incidents. 166 Information processing and learning is inhibited in organisational contexts in which individuals feel pressure of accountability to hierarchical superiors. 167,168 To move from a ‘blame culture’ towards a ‘learning culture’ is challenging, but it is a process in which H-MLMs are central.
To mediate such socialisation capability at the individual and system levels, health-care organisations should develop co-ordination capabilities that link to social mechanisms. Bureaucratic clinical governance structures prove insufficient as a co-ordination capability. Our study highlights the potential co-ordination capability that H-MLMs represent. Even where H-MLMs may not broker knowledge themselves, they represent a resource to co-ordinate others’ brokering of knowledge. This is evident in the case of junior doctors, who, during training, come under line management by H-MLMs at ward level. Junior doctors, by virtue of their ‘Cook’s tour’ of different clinical areas in the hospitals, can put people and component knowledge together in pursuit of safer care for older people. H-MLMs can leverage junior doctors’ contacts and their knowledge for service improvement at the local level. To emphasise, by virtue of their position in the organisation, H-MLMs cross managerial and professional boundaries, and, thus, represent co-ordination capability. However, their structural position as hybrids is insufficient in isolation of social mechanisms for knowledge-brokering influence. We note that H-MLMs are well connected with others, and this engenders the type of social mechanism prescribed to support more effective knowledge brokering within and across organisations. 156 This is borne out in other studies. Recent studies highlight the ability of lower-status professions to mediate professional hierarchy and exert strategic influence through brokering knowledge, which follows the development of social connectedness. 19,169 For example, Finn et al. 169 demonstrate the ability of nurses to transform practices where collegial relationships between doctors and nurses are nurtured to engender a ‘mentality’ where consultants were reportedly ‘open to suggestions’ (p. 1087), describing a nurse as ‘top dog’ and emphasising her role as a valued member of the team. Similarly, Currie and White19 highlight that development of collective identity engendered the necessary understanding, trust and reciprocity that supports a knowledge-brokering contribution from nurses and others, which transcended status differentials.
Linked to collective identity, the development of communities of practitioners enhances co-ordination capability. Returning to our earlier conceptual distinction between IT-based systems such as NRLS, and socially based interventions such as CoPs, our prescriptions veer towards the latter. However, we suggest that the development of such CoPs, which cross organisational and professional boundaries, is not likely to be amenable to formal managerial intervention. 110 Instead, their development is best left to those H-MLMs positioned closer to the clinical front line, but with some power and status to bring different professional and managerial communities together. Policy-makers and senior managers may consider how they cultivate such community tendencies, rather than build them into formal structures of the organisation. On a prosaic level, a resource buffer for such community building, in terms of time and less pressurised operational environments, is helpful, but in the current parsimonious climate may prove difficult to engender.
Bringing the above together, we set out Figure 2, which highlights the oppositional pull of systems capabilities and socialisation capabilities, while co-ordination capabilities mediate between external objectives that focus the organisation towards compliance and professional norms and behaviours that privilege professional stratification. Indeed, systems capabilities represent a relatively fixed response to the external environment, as compliance might be deemed necessary for the organisation’s survival (as it relates to the financial steering of the organisation as a whole). Socialisation capabilities are also difficult to influence as they are entrenched in professional tradition. 19 Legitimacy, synonymous with hierarchy, power and status, is identified as a necessary condition for knowledge brokering, yet more generalist H-MLMs are typically viewed as lower status both inter- and intraprofessionally. Given this, we need to enhance the ability and disposition of H-MLMs to broker knowledge. Their ability to broker knowledge is enhanced through social connectedness, CoPs and IT, while their disposition is more difficult to enhance. Enhancing disposition, in part, may be a matter of supporting their transition from a purely clinical role to one of hybrid manager where they are expected to be more strategic. Commentators90 have suggested that this represents an identity transition. Within our study, it is apparent that some H-MLMs struggle more than others to adapt to expectations that they are more strategic. We encourage more research in this area.
FIGURE 2.
Enhancing knowledge brokerage in the health-care organisation.
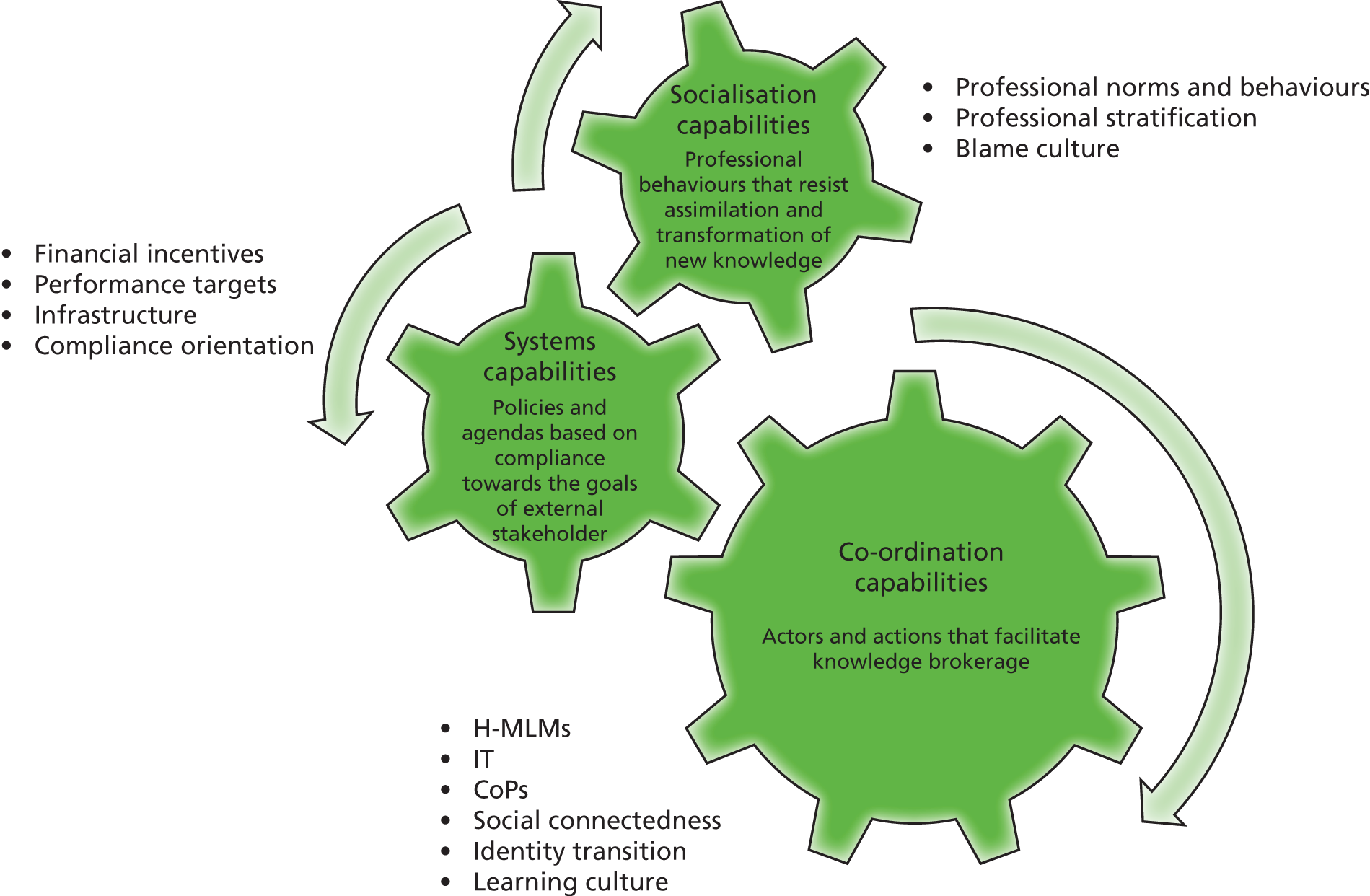
Limitations and future research
The doctors’ voice
The doctors’ voice is evident in our study, but relates mainly to those geriatricians positioned in H-MLM roles and who brokered PSK. The voice of other doctors is notable by its absence. Indeed, when running focus groups in work package 3 around organisational learning and service improvement following RCAs, most did not attend. Outside the ranks of geriatricians, doctors did not appear to see patient safety as a domain that they sought to impact (although we assume that they took it seriously in their professional practice). Thus, while we were able to interview geriatricians relatively easily, we interviewed few doctors beyond their ranks (e.g. GP, consultant acute medicine, doctors in senior clinical governance roles). As they are major actors in delivery of older person’s care, the lack of a medical perspective beyond the ranks of geriatricians is significant. Consequently, we encourage more research to examine doctors’ interaction with the issue of patient safety beyond their immediate clinical practice, which addresses the challenge of drawing them more into the patient safety domain as potential knowledge brokers.
Focus on falls
In work package 1, we explored falls, medication management and transition, with those external disseminators of PSK; for example, two of the three respondents from the Department of Health focused upon medication management as the issue of main concern. However, in work packages 2 and 3, falls came to the fore. To a large extent, our focus here was driven by managers and clinicians’ emphasising the importance of falls as an issue to which they had to respond, and was, therefore, of strategic priority for them, i.e. falls represented the area to which gatekeepers in the hospital cases were prepared to give privileged access. In part, the patient safety issue of falls represented a more bounded area to empirically investigate, i.e. there was an element of pragmatism in our choice. However, we suggest both that falls is an exemplary issue for our theoretical and empirical concerns, and that falls, medication management and transition are interdependent; for example, a fall may result from an older person transitioning into a general medical ward, where there is less expertise in this domain of patient safety, and the prospect for a fall may be fuelled by a complex medication regime. Nevertheless, we sought to counter the emphasis upon falls, when examining the SUI in hospital Z. This we categorised as a medication management issue, but we highlight that it also encompassed transition across hospital accident and emergency department, primary care and social care settings.
Comparative sample sizes
Hospital case A proved the site in which the most interviews, observation and documentary analysis ensued. Mental health case C was a specialist provider of care and staff, working into the hospital, specifically to support care for those older persons that were cognitively impaired (and may suffer more than most from falls, for example), hence we undertook a smaller number of interviews. Hospital Z, we used as a validation case for our emerging analysis, and within which we focused on a medication management (encompassing transition) patient safety issue. Readers may, however, question the relatively smaller number of interviews carried out in hospital case B (n = 16) than in hospital case A (n = 27), during work package 2. That there was a difference in number of interviewees is revealing of one our analytical themes, which relates to the effect of external performance management to which health care organisations are subjected. Hospital case B had been subject to external scrutiny from a government body, focused on inadequacies in older persons’ care, in the course of our research. This had a ‘suppressant effect’ upon their disposition to learn from failure, and gatekeepers failed to respond to communication via e-mail to continue their identification and accessing of relevant respondents for interview. Thus, we withdrew from the site of hospital B, recognising the situation faced by our gatekeepers and other managers and clinicians within hospital case B that caused them to indirectly withdraw support. We suggest that each organisation may have different structures and cultures, which impact brokering of PSK by H-MLMs, which may necessitate a need to unpick such local-level contingencies. Nevertheless, institutional level antecedents related to policy pressure and professional hierarchy are likely to play out in a similar way across all health-care organisations around the brokering of PSK by H-MLMs. 90
Use of social network analysis
Social network analysis proved particularly challenging in the light of brokering relationships that ostensibly veered between ‘everyone’ and ‘no one’ across the pathway for older persons’ care. Our difficulty in reliably bounding a brokering network around PSK related to the care of older people mirrors the contrasting views of our respondents where more generalist professionals (e.g. geriatricians, matrons, nurses) view elderly care as ‘mainstream business’, recognising the very high proportion of older people who occupy hospital beds, and those more specialist clinicians (often more senior H-MLMs, and non-hybrid senior managers) who neglect to recognise the more general applicability of PSK relating to the care of older people to their own patients (many of whom are older people). Given this, we report SNA not within the main body of our report, but within Appendix 1. Our purpose in reporting within an appendix is to illustrate the type of data generated by SNA, which in the case of this study, however, we warn is not sufficiently robust to include as part of our central analysis. For an exemplar of use of SNA in health-care research, which combines well with the type of qualitative data that formed the bulk of this study, we refer readers to Currie and White’s study of knowledge brokering in paediatric nephrology. 19 We note increasing use of SNA in health-care research, including that commissioned by NIHR HSDR, but also that others have also reported it as challenging regarding bounding the network and generating the necessary sociometric data. 170,171 Consequently, we suggest that SNA should be used with care, relevant to particular settings, and this may represent a pragmatic decision. Nevertheless, we highlight, our SNA does identify some exceptional actors within our data set, who are capable of brokering PSK upwards, downwards and across the organisation. These actors are more senior H-MLMs who are connected to the organisation’s most senior committee and correspond with our more qualitative findings of work packages 2 and 3. SNA data can be found in Appendix 2.
Moving onwards from inductive theory development
Our study approach has been one derived from a more qualitative organisational science tradition, which privileges as procedural assessment criteria the importance of theory development. Our study develops theory to (i) render visible why some H-MLMs are more disposed, and more able than others, to broker PSK for service improvement; (ii) understand how the chain of knowledge brokering might be enhanced so that exogenous and endogenous knowledge is better fused for service improvement effect. Nevertheless, we recognise that other disciplines, specifically clinician-scientists,172,173 might privilege more positivist, deductive approaches to addressing the problem of brokering of PSK by H-MLMs. With this in mind, we suggest that other, more positivist researchers might derive more testable propositions from our model of knowledge brokering presented in Figure 2.
Acknowledgements
The users of our research study are hybrid and general managers (rather than necessarily those patients and carers on receipt of clinical services) within and beyond our empirical case sites. We hope that our analysis informs safe clinical services for older persons. We thank those hybrid and general managers who participated in our study, including those who gave up time beyond interviews, to inform the ongoing development of our study, including commentary on our unfolding analysis in the course of advisory meetings. We also thank those interviewees from external bodies that produce and disseminate patient safety evidence.
Contributions of authors
Professor Graeme Currie designed and led the research project, conducting qualitative research, collecting data from interviews, conducting observation of various governance committees, data analysis and report writing.
Dr Nicola Burgess conducted qualitative research, collecting data from interviews, conducting observation of various governance committees, data analysis and report writing.
Professor Leroy White co-designed the research project and provided valuable advice and guidance throughout the project duration. Professor White conducted social network analysis and assisted with report writing.
Professor Andy Lockett co-designed the research project and provided valuable advice and guidance throughout the project duration, and assisted with report writing.
Professor John Gladman co-designed the research project and provided valuable advice and guidance throughout the project duration.
Professor Justin Waring co-designed the research project and provided valuable advice and guidance throughout the project duration.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
Publications
Burgess N, Currie G. The strategic role of the middle level manager (MLM): the case of healthcare. Br J Management 2013;24:S132–42.
References
- Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: preliminary retrospective record review. BMJ 2001;322:517-19. http://dx.doi.org/10.1136/bmj.322.7285.517.
- An Organisation With a Memory. London: Department of Health; 2000.
- Hargadon A, Sutton R. Building an innovation factory. Harvard Bus Rev 2000:157-66.
- Verona G, Prandelli E, Sawhney M. Innovation and virtual environments: towards virtual knowledge brokers. Organ Stud 2006;27:765-88. http://dx.doi.org/10.1177/0170840606061073.
- Hargadon AB. Brokering knowledge: linking learning and innovation. Res Organ Behav 2002;24:41-85. http://dx.doi.org/10.1016/S0191-3085(02)24003-4.
- Llewellyn S. ‘Two-way windows’: clinicians as medical managers. Organ Stud 2001;22:593-62. http://dx.doi.org/10.1177/0170840601224003.
- Waring J. A qualitative study of intra-hospital variations in incident reporting. Int J Qual Health Care 2004;16:347-52. http://dx.doi.org/10.1093/intqhc/mzh068.
- Waring J, Bishop S. Watercooler learning: knowledge sharing at the clinical backstage and its contribution to patient safety. J Health Organ Manag 2011;24:325-42.
- Waring J, Currie G. Managing expert knowledge: organizational challenges and managerial futures for the UK medical profession. Organ Stud 2009;30:755-78. http://dx.doi.org/10.1177/0170840609104819.
- Currie G, Procter SJ. The antecedents of middle managers’ strategic contribution: the case of a professional bureaucracy. J Manag Stud 2005;42:1325-56. http://dx.doi.org/10.1111/j.1467-6486.2005.00546.x.
- Ferlie E, Jashapara A, Crilly T, Peckham A. Research Utilisation and Knowledge Mobilisation – a Scoping Review of the Literature. London: National Institute for Health Research Service Delivery and Organisation; 2010.
- Blackler F. Knowledge, knowledge work and organizations: an overview and interpretation. Organ Stud 1995;16:1021-46. http://dx.doi.org/10.1177/017084069501600605.
- Grant RM. Toward a knowledge-based theory of the firm. Strateg Manag J 1996;17:109-22. http://dx.doi.org/10.1002/smj.4250171110.
- Orlikowski WJ. Knowing in practice: enacting a collective capability in distributed organizing. Organ Sci 2002;13:249-73. http://dx.doi.org/10.1287/orsc.13.3.249.2776.
- Nonaka I. A dynamic theory of organizational knowledge creation. Organ Sci 1994;5:14-37. http://dx.doi.org/10.1287/orsc.5.1.14.
- Polanyi M. The Tacit Dimension. London: Routledge; 1966.
- Elwyn G, Taubert M, Kowalczuk J. Sticky knowledge: a possible model for investigating implementation in healthcare contexts. Implement Sci 2007;2.
- Tsoukas H, Vladimirou E. What is organizational knowledge?. J Manag Stud 2001;38:973-93. http://dx.doi.org/10.1111/1467-6486.00268.
- Currie G, White L. Inter-professional barriers and knowledge brokering in an organizational context: the case of healthcare. Organ Stud 2012;33:1333-61. http://dx.doi.org/10.1177/0170840612457617.
- Gabbay J, Le May A. Evidence based guidelines or collectively constructed ‘mindlines?’ Ethnographic study of knowledge management in primary care. BMJ 2004;329. http://dx.doi.org/10.1136/bmj.329.7473.1013.
- Nicolini D, Powell J, Conville P, Martinez-Solano L. Managing knowledge in the healthcare sector. A review. Int J Manag Rev 2008;10:245-63. http://dx.doi.org/10.1111/j.1468-2370.2007.00219.x.
- Nicolini D, Waring J, Mengis J. Policy and practice in the use of root cause analysis to investigate clinical adverse events: mind the gap. Soc Sci Med 2011;73:217-25. http://dx.doi.org/10.1016/j.socscimed.2011.05.010.
- Floyd SW, Wooldridge B. Building Strategy from the Middle: Reconceptualizing Strategy Process. Thousand Oaks, CA: Sage; 2000.
- Balogun J. From blaming the middle to harnessing its potential: creating change intermediaries. Br J Manag 2003;14:69-83. http://dx.doi.org/10.1111/1467-8551.00266.
- Thomas R, Dunkerley D. Careering downwards? Middle managers’ experiences in the downsized organization. Br J Manag 1999;10:157-69. http://dx.doi.org/10.1111/1467-8551.00117.
- Currie G. The influence of middle managers in the business planning process: a case study in the UK NHS. Br J Manag 1999;10:141-55. http://dx.doi.org/10.1111/1467-8551.00116.
- Dopson S, Stewart R. What is happening to middle managers in Europe? Problems and promises associated with their changing roles and responsibilities. Int Exec 1994;36:55-78. http://dx.doi.org/10.1002/tie.5060360105.
- Floyd SW, Wooldridge B. Dinosaurs of dynamos? Recognizing middle managers strategic role. Acad Manag Exec 1994;8:47-5.
- Currie G, Brown AD. A narratological approach to understanding processes of organizing in a UK hospital. Hum Relat 2003;56:563-86. http://dx.doi.org/10.1177/0018726703056005003.
- Delmestri G, Walgenbach P. Mastering techniques or brokering knowledge? Middle managers in Germany, Great Britain and Italy. Organ Stud 2005;26:197-220. http://dx.doi.org/10.1177/0170840605049464.
- Newman I, Benz C. Qualitative–Quantitative Research Methodology: Exploring the Interactive Continuum. Carbondale, IL: Southern Illinois Press; 1998.
- Steckler A, McLeroy KR, Goodman RM, Bird ST, McCormick L. Integrating qualitative and quantitative methods – an introduction. Health Educ Q 1992;19:1-8. http://dx.doi.org/10.1177/109019819201900101.
- Greene J, Caracelli V. Advances in Mixed-Method Evaluation: the Challenges and Benefits of Integrating Diverse Paradigms. San Francisco, CA: Jossey Bass; 1997.
- High Quality Care for All. London: Department of Health; 2008.
- Dingwall R, Palmer C, Rowley E, Waring J, Murcott T. Synthesis of the Outputs Commissioned Under the Patient Safety Research Portfolio. Nottingham: Institute for Science and Society, University of Nottingham; 2009.
- Dobbins M, Robeson P, Ciliska D, Hanna S, Cameron R, O’Mara L, et al. A description of a knowledge broker role implemented as part of a randomized controlled trial evaluating three knowledge translation strategies. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-23.
- Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual Health Care 1998;7:149-58. http://dx.doi.org/10.1136/qshc.7.3.149.
- Lyons R, Warner G. Demystifying Knowledge Translation for Stroke Research: A Primer on Theory and Praxis. Halifax, NS: Atlantic Health Promotion Research Centre, Dalhousie University; 2005.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. http://dx.doi.org/10.1111/j.0887-378X.2004.00325.x.
- Crilly T, Jashapara A, Trenholm S, Peckham A, Currie G, Ferlie E. Knowledge Mobilisation in Healthcare Organisations: Synthesising Evidence and Theory Using Perspectives of Organisational Form, Resource Based View of the Firm and Critical Theory. London: National Institute for Health Research Service Delivery and Organisation; 2013.
- Waring J, Sahota O, Avery A, Currie G, Walker M, Bishop S, et al. Knowledge Sharing Across the Boundaries Between Care Processes, Services and Organisations: The Contributions to Safe Hospital Discharge and Reduced Emergency Readmission. London: National Institute for Health Research Service Delivery and Organisation; 2013.
- Annandale E, Harvey J, Goode J, Kuhlmann E, Loan-Clarke J, Parker M, et al. Mobilizing Identities: the Shape and Reality of Middle and Junior Managers’ Working Lives. London: National Institute for Health Research Service Delivery and Organisation; 2013.
- Buchanan D, Denyer D, Jaina J, Kelliher C, Moore C, Parry E, et al. How do they manage? A qualitative study of the realities of middle and front-line management work in healthcare. Health Serv Deliv Res 2013;1.
- Checkland K, Snow S, McDermott I, Harrison S, Coleman A. Management Practice in Primary Care Organisations: the Roles and Behaviours of Middle Managers and GPs. London: National Institute for Health Research Service Delivery and Organisation; 2011.
- Dopson S, Bennett C, Fitzgerald L, Ferlie E, Fischer M, Ledger J, et al. Healthcare Managers’ Access and Use of Management Research. London: National Institute for Health Research Service Delivery and Organisation; 2013.
- Hyde P, Granter E, Hassard J, McCann L, Morris J. Roles and Behaviours of Middle and Junior Managers: Managing New Organizational Forms of Health Care. London: National Institute for Health Research Service Delivery and Organisation; 2013.
- Briner R, Denyer D, Rousseau DM. Handbook of Evidence-based Management: Companies, Classrooms and Research. New York, NY: University Press; 2012.
- Gioia D, Corley KG, Hamilton AL. Seeking qualitative rigor in inductive research: notes on the Gioia methodology. Organ Res Methods 2012;16:15-31. http://dx.doi.org/10.1177/1094428112452151.
- Gratton L. The end of the middle manager. Harvard Bus Rev 2011;89.
- Broughton P. Time to Stand Up for Middle Managers 2011. www.ft.com/cms/s/0/bc3be534-1cea-11e0-8c86-00144feab49a.html (accessed 12 August 2014).
- Wooldridge B, Schmidt T, Floyd S. The middle management perspective on strategy process: contributions, synthesis, and future research. J Manag 2008;34:1190-221. http://dx.doi.org/10.1177/0149206308324326.
- Currie G, Lockett A. Distributing leadership in health and social care: concertive, conjoint or collective?. Int J Manag Rev 2011;13:286-300. http://dx.doi.org/10.1111/j.1468-2370.2011.00308.x.
- Leavitt H, Whisler T. Management in the 1980s. Harvard Bus Rev 1958:41-8.
- Drucker P. The coming of the new organization. Harvard Bus Rev 1988;66:397-428.
- Hicks RL. Developing the top management group in a total systems organization. Personnel J 1971;50:675-93.
- Hoos IR. When the computer takes over the office. Harvard Bus Rev 1960;38:102-12.
- Simon H, Leavitt HaLRP. Readings in Managerial Psychology. Chicago, IL: Chicago University Press; 1960.
- Dopson S, Stewart R. What is happening to middle management?. Br J Manag 1990;1:3-16. http://dx.doi.org/10.1111/j.1467-8551.1990.tb00151.x.
- Currie G, Kerrin M. The limits of a technological fix to knowledge management. Manag Learn 2004;35:9-29. http://dx.doi.org/10.1177/1350507604042281.
- Millman Z, Hartwick J. The impact of automated office systems on middle managers and their work. MIS Q 1987;11:479-91. http://dx.doi.org/10.2307/248977.
- Polakoff JC. Will middle managers work in the factory of the future?. Manag Rev 1987;26:50-1.
- McCann L, Morris J, Hassard J. Normalized intensity: the New Labour process of middle management. J Manag Stud 2008;45:343-71. http://dx.doi.org/10.1111/j.1467-6486.2007.00762.x.
- Pinsonneault A, Kraemer KL. The impact of information technology on middle managers. MIS Q 1993;17:271-92. http://dx.doi.org/10.2307/249772.
- Schwarz M, Nandhakumar J. Conceptualizing the development of strategic ideas: a grounded theory analysis. Br J Manag 2002;13:67-82. http://dx.doi.org/10.1111/1467-8551.00223.
- Floyd SW, Wooldridge B. Middle management involvement in strategy and its association with strategic type: a research note. Strategic Manag J 1992;13:153-67. http://dx.doi.org/10.1002/smj.4250131012.
- Floyd SW, Lane PJ. Strategizing throughout the organization: managing role conflict in strategic renewal. Acad Manag Rev 2000;25:154-77.
- Floyd SW, Wooldridge B. Middle managements strategic influence and organizational performance. J Manag Stud 1997;34:465-85. http://dx.doi.org/10.1111/1467-6486.00059.
- Walshe K, Smith L. The NHS Management Workforce 2011. www.kingsfund.org.uk/leadershipcommission (accessed 12 August 2014).
- Ghobadian A, Viney HP, Redwood J. Explaining the unintended consequences of public sector reform. Manag Decis 2009;47:1514-35. http://dx.doi.org/10.1108/00251740911004664.
- Chandler A. Strategy and Structure. Cambridge, MA: MIT Press; 1962.
- Whittington R. What is Strategy – and Does it Matter?. London: International Thomson Business Press; 1993.
- Quinn JB. Strategies for Change: Logical Incrementalism. Homewood, IL: Irwin; 1980.
- Whittington R. What is Strategy – and Does it Matter?. London: Thomson Learning; 2001.
- Mintzberg H, Waters J. Of strategies, deliberate and emergent. Strateg Manag J 1985;6:257-72. http://dx.doi.org/10.1002/smj.4250060306.
- Nonaka I. Towards middle up/down management: accelerating information creation. Sloan Manag Rev 1988;29:9-18.
- Wooldridge B, Floyd SW. The strategy process, middle management involvement, and organizational performance. Strateg Manag J 1990;11:231-41. http://dx.doi.org/10.1002/smj.4250110305.
- Henderson R, Cockburn I. Measuring competence? Exploring firm effects in pharmaceutical research. Strateg Manag J 1994;15:63-84. http://dx.doi.org/10.1002/smj.4250150906.
- Liebeskind JP. Knowledge, strategy, and the theory of the firm. Strateg Manag J 1996;17:93-107. http://dx.doi.org/10.1002/smj.4250171109.
- Barney J. Firm resources and sustained competitive advantage. J Manag 1991;17:99-120. http://dx.doi.org/10.1177/014920639101700108.
- Penrose E. The Theory of Growth of the Firm. Oxford: Blackwell; 1959.
- Wernerfelt B. A resource-based view of the firm. Strateg Manag J 1984;5:171-80. http://dx.doi.org/10.1002/smj.4250050207.
- Teece D, Pisano G, Shuen A. Dynamic capabilities and strategic management. Strateg Manag J 1997;18:509-33. http://dx.doi.org/10.1002/(SICI)1097-0266(199708)18:7<509::AID-SMJ882>3.0.CO;2-Z.
- Kogut B, Zander U. Knowledge of the firm, combinative capabilities, and the replication of technology. Organ Sci 1992;3:383-97. http://dx.doi.org/10.1287/orsc.3.3.383.
- Cohen WM, Levinthal DA. Absorptive capacity: a new perspective on learning and innovation. Admin Sci Q 1990;35:128-52. http://dx.doi.org/10.2307/2393553.
- Shi W, Markoczy L, Dess GG. The role of middle management in the strategy process: group affiliation, structural holes, and tertius iungens. J Manag 2009;35:1453-80. http://dx.doi.org/10.1177/0149206309346338.
- Rouleau L, Balogun J. Middle managers, strategic sensemaking, and discursive competence. J Manag Stud 2011;48:953-83. http://dx.doi.org/10.1111/j.1467-6486.2010.00941.x.
- Harrison S, Pollitt C. Controlling Health Professionals. Milton Keynes: Open University Press; 1994.
- Dopson S, Fitzgerald L. The role of the middle manager in the implementation of evidence-based health care. J Nurs Manag 2006;14:43-51. http://dx.doi.org/10.1111/j.1365-2934.2005.00612.x.
- Fitzgerald L, Ferlie E. Professionals: back to the future. Hum Relat 2000;53:713-39. http://dx.doi.org/10.1177/0018726700535005.
- Burgess N, Currie G. The strategic role of the middle level manager (MLM): the case of healthcare. Br J Manag 2013;24:S132-S42. http://dx.doi.org/10.1111/1467-8551.12028.
- Fernandez RM, Gould RV. A dilemma of state power: brokerage and influence in the national health policy domain. Am J Sociol 1994;99:1455-91. http://dx.doi.org/10.1086/230451.
- Gould RV, Fernandez R. Structures of mediation: a formal approach to brokerage in transaction networks. Sociol Methodol 1989;19:89-126. http://dx.doi.org/10.2307/270949.
- Aalbers R, Dolfsma W, Koppius K. On And Off The Beaten Path: How Individuals Broker Knowledge Through Formal And Informal Networks. Rotterdam: Erasmus Research Institute of Management (ERIM); 2004.
- Obstfeld D. Social networks, the tertius iungens orientation, and involvement in innovation. Admin Sci Q 2005;50:100-30.
- Clark G, Kelly L. New Directions for Knowledge Transfer and Knowledge Brokerage in Scotland: Office of Chief Researcher Knowledge Transfer Team Briefing. Edinburgh: Scottish Executive Social Research; 2005.
- The Theory and Practice of Knowledge Brokering in Canada’s Health System. Ottawa, ON: Canadian Health Services Research Foundation; 2003.
- Davies H, Nutley SM. Developing learning organisations in the new NHS. BMJ 2000;320:998-1001. http://dx.doi.org/10.1136/bmj.320.7240.998.
- Denis J-L, Lehoux P, Hivon M, Champagne F. Creating a new articulation between research and practice through policy: the view and experience of researchers and practitioners. J Health Serv Res Policy 2003;8:44-50. http://dx.doi.org/10.1258/135581903322405162.
- Hargadon AB. Firms as knowledge brokers: lessons in pursuing continuing innovation. Calif Manag Rev 1998;40:209-27. http://dx.doi.org/10.2307/41165951.
- Landry R, Amara N, Lamari M. Utilization of social science research knowledge in Canada. Res Policy 2001;30:333-49. http://dx.doi.org/10.1016/S0048-7333(00)00081-0.
- Lomas J. The in-between world of knowledge brokering. BMJ 2007;334:129-32. http://dx.doi.org/10.1136/bmj.39038.593380.AE.
- Martin G, Currie G, Finn R. Reconfiguring or reproducing intra-professional boundaries? Specialist expertise, generalist knowledge and the ‘modernization’ of the medical workforce. Soc Sci Med 2009;68:1191-8. http://dx.doi.org/10.1016/j.socscimed.2009.01.006.
- Pawlowski S, Robey D. Bridging user organizations: knowledge brokering and the work of information technology professionals. MIS Q 2004;28:645-72.
- Alvesson M, Kärreman D. Odd couple: making sense of the curious concept of knowledge management. J Manag Stud 2001;38:995-1018. http://dx.doi.org/10.1111/1467-6486.00269.
- Orzano AJ, McInerney CR, Scharf D, Tallia AF, Crabtree BF. A knowledge management model: implications for enhancing quality in health care. J Am Soc Info Sci Technol 2008;59:489-505. http://dx.doi.org/10.1002/asi.20763.
- Fahey L, Prusak L. The eleven deadliest sins of knowledge management. Calif Manag Rev 1988;40:265-76. http://dx.doi.org/10.2307/41165954.
- Styhre A. Rethinking knowledge: a Bergsonian critique of the notion of tacit knowledge. Br J Manag 2004;15:177-88. http://dx.doi.org/10.1111/j.1467-8551.2004.00413.x.
- Freidson E. Profession of Medicine: a Study of the Sociology of Applied Knowledge. Chicago, IL: University of Chicago Press; 1970.
- Ferlie E, Fitzgerald L, Wood M, Hawkins C. The nonspread of innovations: the mediating role of professionals. Acad Manag J 2005;48:117-34. http://dx.doi.org/10.5465/AMJ.2005.15993150.
- Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge: Cambridge University Press; 1991.
- Wenger E. Communities of Practice. Cambridge: Cambridge University Press; 1998.
- Sheldon TA. Basing decisions on better quality routine clinical data. Qual Saf Health Care 2003;12:327-8. http://dx.doi.org/10.1136/qhc.12.5.327.
- Lankshear AJ, Lowson KV, Wright D, Jones A, Saxby R, Lowson P, et al. Evaluation of Patient Safety Observatory Reports. National Patient Safety Agency; 2008.
- Haller G, Myles P, Taffé P, Perneger T, Wu C. Rate of undesirable events at beginning of academic year: retrospective cohort study. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b3974.
- Lankshear A, Lowson K, Weingart SN. An assessment of the quality and impact of NPSA medication safety outputs issued to the NHS in England and Wales. BMJ Qual Saf 2011;20:360-5. http://dx.doi.org/10.1136/bmjqs.2010.040287.
- Waring J. Beyond blame: cultural barriers to medical incident reporting. Soc Sci Med 2005;60:1927-35. http://dx.doi.org/10.1016/j.socscimed.2004.08.055.
- Currie G, Waring J, Finn R. The limits of knowledge management for UK public services modernization: the case of patient safety and service quality. Public Admin 2008;86:363-85. http://dx.doi.org/10.1111/j.1467-9299.2007.00705.x.
- Oborn E, Dawson S. Learning across communities of practice: an examination of multidisciplinary work. Br J Manag 2010;21:843-58. http://dx.doi.org/10.1111/j.1467-8551.2009.00684.x.
- Van den Bosch FAJ, Volberda HW, de Boer M. Coevolution of firm absorptive capacity and knowledge environment: organizational forms and combinative capabilities. Organ Sci 1999;10:551-68. http://dx.doi.org/10.1287/orsc.10.5.551.
- Jansen JJP, Bosch FAJVD, Volberda HW. Managing potential and realized absorptive capacity: how do organizational antecedents matter?. Acad Manag J 2005;48:999-1015. http://dx.doi.org/10.5465/AMJ.2005.19573106.
- Volberda HW, Foss NJ, Lyles MA. Absorbing the concept of absorptive capacity: how to realize its potential in the organization field. Organ Sci 2010;21:931-51. http://dx.doi.org/10.1287/orsc.1090.0503.
- Zahra S, George G. Absorptive capacity: a review, reconceptualization, and extension. Acad Manag Rev 2002;27:185-203.
- Easterby-Smith M, Graça M, Antonacopoulou E, Ferdinand J. Absorptive capacity: a process perspective. Manag Learn 2008;39:483-501. http://dx.doi.org/10.1177/1350507608096037.
- Todorova G, Durisin B. Absorptive capacity: valuing a reconceptualization. Acad Manag Rev 2007;32:774-86. http://dx.doi.org/10.5465/AMR.2007.25275513.
- Lane PJ, Koka BR, Pathak S. The reification of absoptive capacity: a critical review and rejuvenation of the construct. Acad Manag Rev 2006;31:833-63. http://dx.doi.org/10.5465/AMR.2006.22527456.
- Mintzberg H. The Structuring of Organizations: a Synthesis of the Research. Englewood Cliffs, NJ: Prentice-Hall; 1979.
- Ferlie E, Crilly T, Jashapara A, Peckham A. Knowledge mobilisation in healthcare: a critical review of health sector and generic management literature. Soc Sci Med 2012;74:1297-304. http://dx.doi.org/10.1016/j.socscimed.2011.11.042.
- Harvey G, Skelcher C, Spencer E, Jas P, Walshe K. Absorptive capacity in a non-market environment. Public Manag Rev 2009;12:77-9. http://dx.doi.org/10.1080/14719030902817923.
- Walshe K, Harvey G, Jas P, Skelcher C. Responding to Evidence of Poor Performance: Explaining Public Organisation’s Capacity to Deal With Failure 2009.
- Berta W, Teare GF, Gilbart E, Ginsburg LS, Lemieux-Charles L, Davis D, et al. Spanning the know-do gap: understanding knowledge application and capacity in long-term care homes. Soc Sci Med 2010;70:1326-34. http://dx.doi.org/10.1016/j.socscimed.2009.11.028.
- Lavertu S, Moynihan D. Agency political ideology and reform implementation: performance management in the Bush administration. J Public Admin Res Theory 2013;23:521-49. http://dx.doi.org/10.1093/jopart/mus026.
- Moynihan DP. Managing for results in state government: evaluating a decade of reform. Public Admin Rev 2006;66:77-89. http://dx.doi.org/10.1111/j.1540-6210.2006.00557.x.
- Moynihan DP, Hawes D. Responsiveness to reform values: the influence of the environment on performance information use. Public Admin Rev 2012;72:95-105. http://dx.doi.org/10.1111/j.1540-6210.2012.02653.x.
- Hotho JJ, Becker-Ritterspach F, Saka-Helmhout A. Enriching absorptive capacity through social interaction. Br J Manag 2011;23:383-401. http://dx.doi.org/10.1111/j.1467-8551.2011.00749.x.
- Ward V, Smith S, House A, Hamer S. Exploring knowledge exchange: a useful framework for practice and policy. Soc Sci Med 2012;74:297-304. http://dx.doi.org/10.1016/j.socscimed.2011.09.021.
- Jick TD. Mixing qualitative and quantitative methods: triangulation in action. Admin Sci Q 1979;24:602-11. http://dx.doi.org/10.2307/2392366.
- The NHS Plan: a Plan for Investment, a Plan for Reform. London: Department of Health; 2000.
- National Service Framework: Older People. London: Department of Health; 2001.
- Living Well With Dementia: A National Dementia Strategy. London: Department of Health; 2009.
- Gephart RP. The textual approach: risk and blame in disaster sensemaking. Acad Manag J 1993;36:1465-514. http://dx.doi.org/10.2307/256819.
- Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Newbury Park, CA: Sage Publications Inc.; 1990.
- Corley KG, Gioia DA. Identity ambiguity and change in the wake of a corporate spin-off. Admin Sci Q 2004;49:173-208.
- Walsh IA, Bartunek JM. Cheating the fates: organizational foundings in the wake of demise. Acad Manag J 2011;54:1017-44. http://dx.doi.org/10.5465/amj.2008.0658.
- Van Maanen J. Tales of the Field: On Writing Ethnography. Chicago, IL: University of Chicago Press; 1988.
- Wodak R, Seale C, Gobo G, Gubrium JF, Silverman D. Qualitative Research Practice. London: Sage; 2004.
- Mantere S, Schildt HA, Sillince JAA. Reversal of strategic change. Acad Manag J 2012;55:172-96. http://dx.doi.org/10.5465/amj.2008.0045.
- Pratt MG. For the lack of a boilerplate: tips on writing up (and reviewing) qualitative research. Acad Manag J 2009;52:856-62. http://dx.doi.org/10.5465/AMJ.2009.44632557.
- National Institute for Health and Care Excellence . Developing NICE Clinical Guidelines n.d. www.nice.org.uk/aboutnice/howwework/developingniceclinicalguidelines/developing_nice_clinical_guidelines.jsp (accessed 8 July 2013).
- Francis. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Adler PS, Kwon S-W. Social capital: prospects for a new concept. Acad Manag Rev 2002;27:17-40.
- Cornwell J, Levenson R, Sonola L, Poteliakhoff E. Continuity of Care for Older Hospital Patients: A Call for Action. London: The King’s Fund; 2012.
- Degeling PJ, Maxwell S, Iedema R, Hunter DJ. Making clinical governance work. BMJ 2004;329:679-82. http://dx.doi.org/10.1136/bmj.329.7467.679.
- Dent M, Van Gestel M, Teelken C. Introduction to symposium on changing modes of governance in public sector organisations: action and rhetoric. Public Admin 2007;85:1-8. http://dx.doi.org/10.1111/j.1467-9299.2007.00630.x.
- Currie G, Suhomlinova O. The impact of institutional forces upon knowledge sharing in the UK NHS: the triumph of professional power and the inconsistency of policy. Public Admin 2006;84:1-30. http://dx.doi.org/10.1111/j.0033-3298.2006.00491.x.
- Lockett A, Currie G, Waring J, Finn R, Martin G. Institutional entrepreneurship in healthcare: developing pathways of care in cancer treatment. Acad Manag J 2014.
- Nahapiet J, Ghoshal S. Social capital, intellectual capital, and the organizational advantage. Acad Manag Rev 1988;23:242-66.
- Freidson E. Professionalism Reborn: Theory, Prophecy and Policy. Cambridge: Polity Press, in association with Blackwell Publishers; 1994.
- Larkin G. Occupational Monopoly and Modern Medicine. England: Tavistock Publications; 1993.
- Allen D. The Changing Shape of Nursing Practice: The Role of Nurses in the Hospital Division of Labour. London: Routledge; 2001.
- Osborne D, Gaebler T. Reinventing Government: How the Entrepreneurial Spirit is Transforming the Public Sector. Reading, MA: Addison-Wesley; 1992.
- Moynihan DP, Landuyt N. How do public organisations learn? Bridging cultural and structural perspectives. Public Admin Rev 2009;69:1097-105. http://dx.doi.org/10.1111/j.1540-6210.2009.02067.x.
- Witman Y, Smid G, Meurs PL, Willems DL. Doctor in the lead: balancing between two worlds. Organization 2011;18:477-95. http://dx.doi.org/10.1177/1350508410380762.
- Freidson E. Profession of Medicine: A Study of the Sociology of Applied Knowledge. Chicago, IL: University of Chicago Press; 1988.
- Bolton S. Changing faces: nurses as emotional jugglers. Sociol Health Illn 2001;23:85-100. http://dx.doi.org/10.1111/1467-9566.00242.
- Scase R, Goffee R. Reluctant Managers: Their Work and Lifestyles. London: Routledge; 1989.
- Weick KE, Sutcliffe KM. Hospitals as cultures of entrapment. Calif Manag Rev 2003;45:73-84. http://dx.doi.org/10.2307/41166166.
- Morris MW, Moore PC. The lessons we (don’t) learn: counterfactual thinking and organizational accountability after a close call. Admin Sci Q 2000;45:737-65. http://dx.doi.org/10.2307/2667018.
- Lerner JS, Tetlock PE. Accounting for the effects of accountability. Psychol Bull 1999;125:255-75. http://dx.doi.org/10.1037/0033-2909.125.2.255.
- Finn R, Currie G, Martin G. Team work in context: institutional mediation in the public-service professional bureaucracy. Organ Stud 2010;31:1069-97. http://dx.doi.org/10.1177/0170840610376142.
- Scarborough H, Evans S, Newell S, Swan J. Networked Innovation in the Health Sector: Comparative Evaluation of the Role of CLAHRCs. Health Serv Deliv Res 2014.
- Sheaff R, Benson L, Boyd A, Charles N, Doran T, Dowling B, et al. The Management and Effectiveness of Professional and Clinical Networks 2011.
- Albert M, Laberge S, Hodges B, Regehr G, Lingard L. Biomedical scientists’ perceptions of social sciences in health research. Soc Sci Med 2008;66:2250-531. http://dx.doi.org/10.1016/j.socscimed.2008.01.052.
- Albert M, Laberge S, Hodges S, Biran D. Boundary work in the health research field: biomedical and cliniciain scientists’ perception of social science research. Minerva 2009;47:171-94. http://dx.doi.org/10.1007/s11024-009-9120-8.
- Marsden P, Lin N. Social Structure and Network Analysis. Beverley Hills, CA: Sage; 1982.
- Scott J. Social Network Analysis: a Handbook. Beverley Hills, CA: Sage; 2000.
- Kilduff M, Brass DJ. Organizational social network research: core ideas and key debates. Acad Manag Ann 2010;4:317-57. http://dx.doi.org/10.1080/19416520.2010.494827.
Appendix 1 Illustration of social network analysis
Background
There are different terms for actors in a network that facilitate transactions and the flow of knowledge/information/resources between people or groups who have no physical or cognitive access to one another, or, alternatively, who have no basis on which to trust each other. These terms include bridges, brokers and boundary spanners. Bridges, brokers and boundary spanners are just three of the most common descriptors in a lengthy list of synonyms for these roles reflecting the highly nuanced nature of the connectivity function. We use the term brokerage to refer generally to this activity. Marsden defines brokers as ‘intermediary actors who facilitate transactions between actors lacking access to or trust in one another’. 174 In other words, a broker must be seen as a trustworthy intermediary by the two being brokered. Brokers are considered key players in that their loss from a network would greatly affect its function and viability.
Social network analysis techniques allow these actors to be identified and the structure of the network to be empirically described, graphed and analysed. 175 Network analysis can provide information on such processes as flows and gatekeeping, which in turn may suggest interventions to enhance function. 176
Social network analysis measures of brokerage can vary. Most studies use the betweenness centrality to identify the brokerage positions. Other studies adopt the typology of ideal types of brokerage roles of Gould and Fernandez. 92 Both of these were used in the present analysis.
The health-care sector is a context that is rich in isolated clusters, such as silos and professional ‘tribes’, in need of connectivity. It is a key challenge in health service management to understand the role of key agents who have the capacity to connect disparate groupings in larger systems. Brokers are key players in the sense that they can be vital to the integrity and viability of the network. The importance of the non-medics as a knowledge broker was revealed in previous studies. 19
Method and data
As useful as SNA is to describe brokerage patterns and identify key actors, data collection through surveys or interviews can involve a significant time investment for already-stretched clinicians, and achieving a high response rate from health professionals can be difficult. The current study has shown that qualitative methods such as observation and the use of interviews are also useful and may be preferred.
The data were collected via a snowball sampling,175 but due to restrictions this was conducted at only the first level. It was used to identify key actors in the network. It was estimated that the sample represented about 60–70% of the full network. The respondents were asked who they would go to discuss patient safety, and details of their profession and affiliation were also elicited. The data were then recorded in a binary matrix for analysis.
Analysis
Descriptive analysis was conducted using the standard methods implemented in UCINET (Harvard Analytic Technologies, Boston, MA, USA). Centrality scores were calculated, as well as the Fernandez and Gould91 typology analysis. This calculates how many times every actor in a network plays these brokerage roles between groups, also giving the total number of brokerage roles. Profession as the grouping category was used for the analysis.
Results
Overall, the network is connected around a few key players. From the diagram, it is evident that there are a number of two-step brokerage paths, with doctors and nurses playing mainly gatekeeper and liaison roles. From the diagram, it appears that H-MLM M CL and H-MLM M B are exceptional actors. From the table with the centrality results, the analysis confirms their status in the network as brokers.
FIGURE 3.
Network showing professional category.
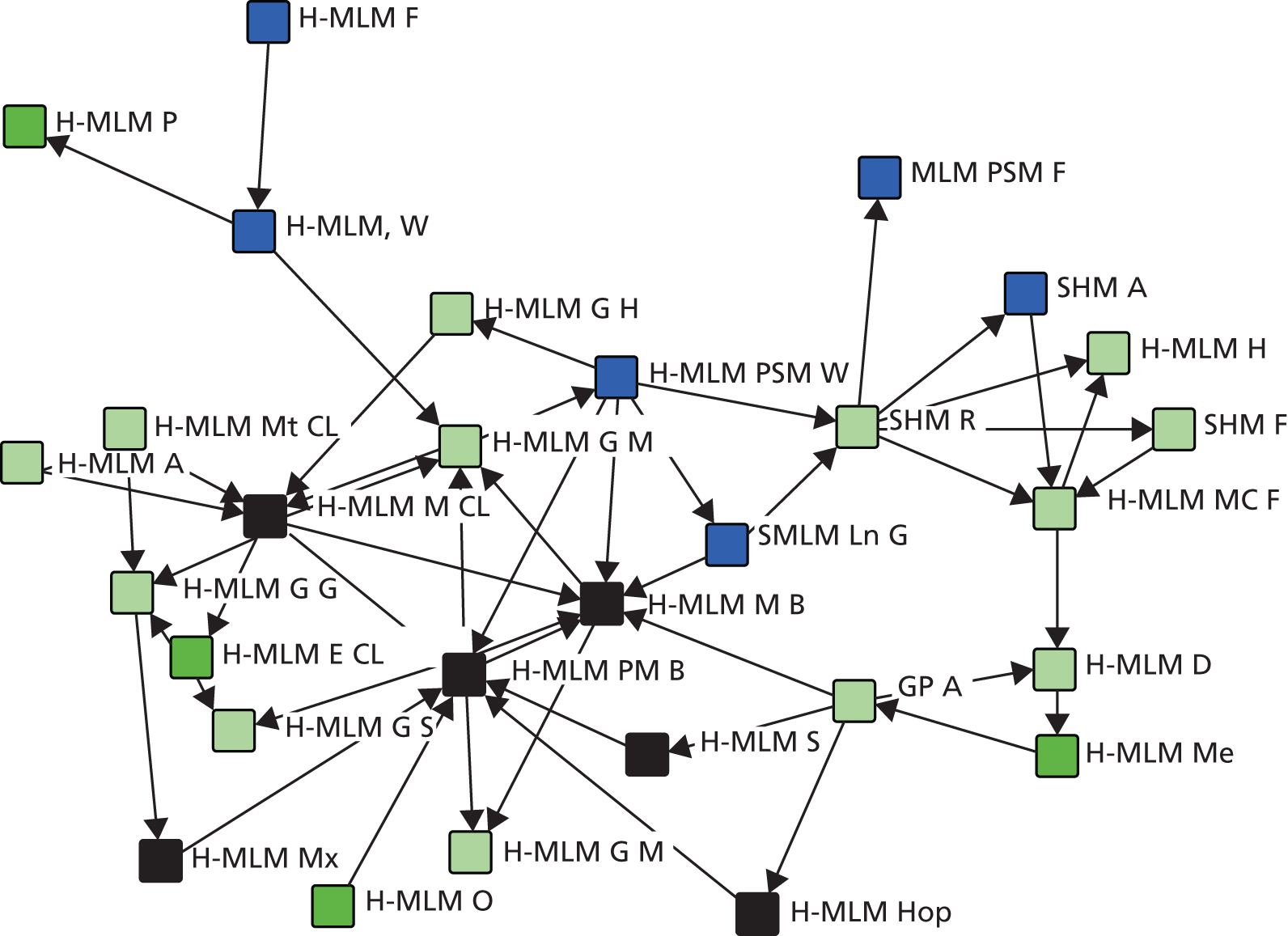
FIGURE 4.
Network showing MLM category.
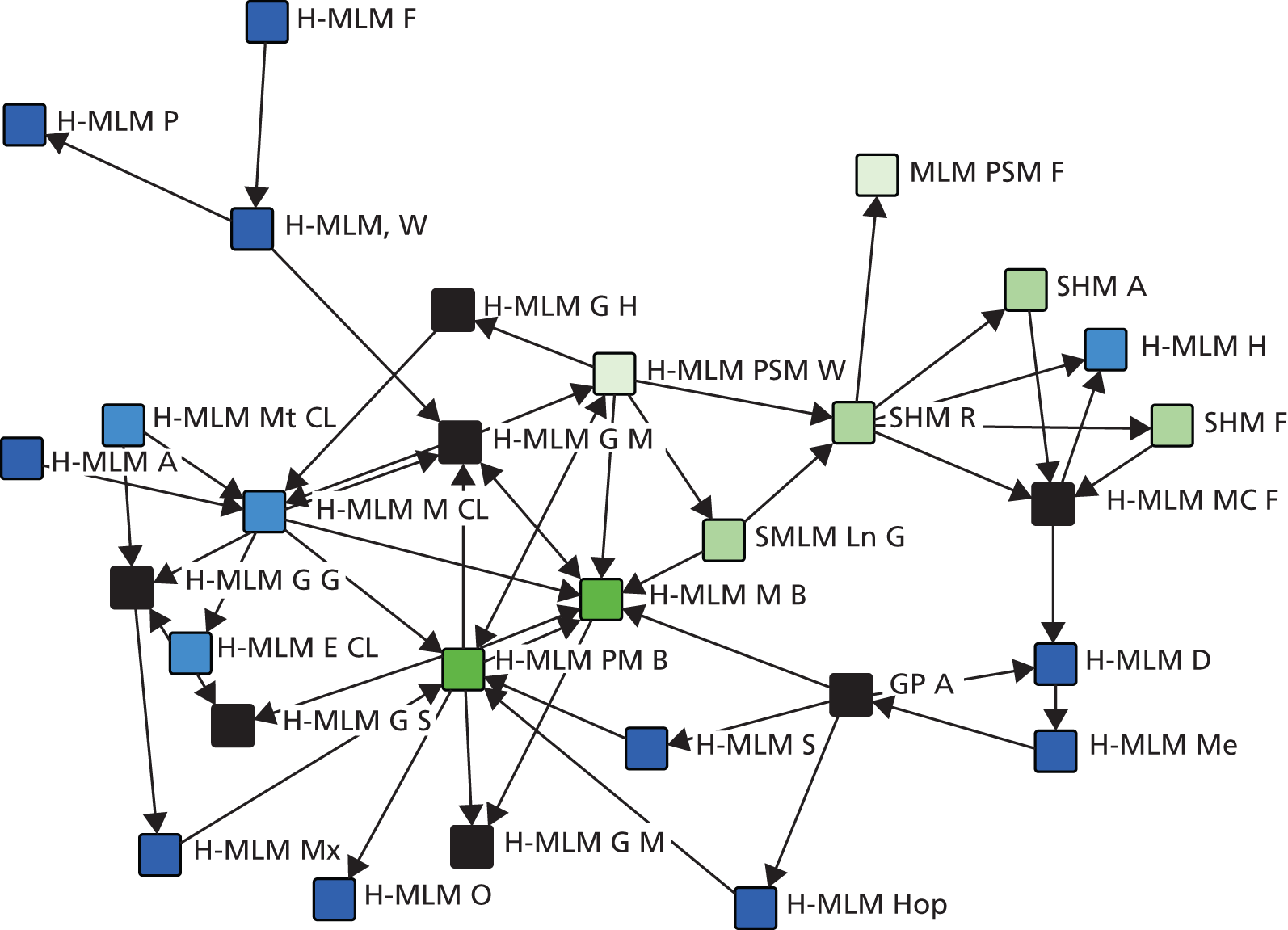
| In degree | Betweenness | |
|---|---|---|
| SHM F | 0.036 | 0.000 |
| H-MLM A | 0.000 | 0.000 |
| H-MLM MC F | 0.107 | 0.189 |
| H-MLM F | 0.000 | 0.000 |
| H-MLM PM B | 0.286 | 0.134 |
| SMLM Ln G | 0.036 | 0.000 |
| H-MLM E CL | 0.036 | 0.000 |
| H-MLM H CL | 0.071 | 0.000 |
| H-MLM M CL | 0.179 | 0.141 |
| H-MLM Mx | 0.036 | 0.002 |
| H-MLM Mt CL | 0.036 | 0.004 |
| H-MLM M B | 0.250 | 0.193 |
| H-MLM P | 0.036 | 0.000 |
| SHM A | 0.036 | 0.000 |
| SHM R | 0.107 | 0.288 |
| H-MLM, W | 0.036 | 0.033 |
| H-MLM G S | 0.107 | 0.017 |
| H-MLM O | 0.000 | 0.000 |
| H-MLM S | 0.036 | 0.002 |
| MLM PSM F | 0.036 | 0.000 |
| H-MLM G G | 0.107 | 0.035 |
| H-MLM Me | 0.036 | 0.153 |
| H-MLM G M | 0.214 | 0.129 |
| H-MLM G H | 0.036 | 0.005 |
| H-MLM Hop | 0.036 | 0.002 |
| H-MLM D | 0.071 | 0.000 |
| H-MLM G M | 0.071 | 0.000 |
| GP A | 0.036 | 0.152 |
| H-MLM PSM W | 0.214 | 0.354 |
The Gould and Fernandez brokerage routine output is recorded in Tables 5 and 6. These provide detailed scores about which groups every actor plays a specific role between. The most standout results are in terms of professional background (see Table 5), that mainly the nurses group covers the gatekeeping role. All members of this group play a form of gatekeeping role. Most members of the group show high values on gatekeeping, indicating their strategic position in this regard within the network. We notice that there are low values on co-ordination roles for every group: this is expected, as nodes are well embedded within their groups. However, H-MLM MC F and H-MLM G G (medics) are the strong co-ordinators in the network. H-MLM G H and GP A play the liaison role. Finally, H-MLM Me stands out as the highest scoring actor in the consultant role.
| 1 2 3 4 5 |
| Coordinat Gatekeepe Represent Consultan Liaison |
| 1 SHM F | 0 0 0 0 0 |
| 2 H-MLM A | 0 0 0 0 0 |
| 3 H-MLM MC F | 4.152 1.313 1.313 0 0.370 |
| 11 H-MLM Mt CL | 0 5.250 0 0 0 |
| 26 H-MLM D | 0 0 0 0 0 |
| 27 H-MLM G M | 0 0 0 0 0 |
| 21 H-MLM G G | 6.327 0 2.250 0 0 |
| 8 H-MLM H CL | 0 0 0 0 0 |
| 23 H-MLM G M | 0 2.019 1.212 0.808 0.682 |
| 24 H-MLM G H | 0 0 0 0 2.956 |
| 28 GP A | 0 1.313 0 0 2.217 |
| 15 SHM R | 0 3.150 0 2.100 0 |
| 17 H-MLM G S | 0 3.500 1.750 0 0 |
| 9 H-MLM M CL | 0 1.670 0.477 1.432 0.941 |
| 5 H-MLM PM B | 1.186 0.375 2.625 0 0.950 |
| 19 H-MLM S | 0 5.250 0 0 0 |
| 25 H-MLM Hop | 0 5.250 0 0 0 |
| 10 H-MLM Mx | 0 5.250 0 0 0 |
| 12 H-MLM M B | 0.443 1.680 0.420 1.890 0.591 |
| 6 SMLM Ln G | 0 0 0 0 0 |
| 4 H-MLM F | 0 0 0 0 0 |
| 29 H-MLM PSM W | 0 1.250 0.750 1.000 1.267 |
| 20 MLM PSM F | 0 0 0 0 0 |
| 14 SHM A | 0 0 0 0 0 |
| 16 H-MLM, W | 0 0 5.250 0 0 |
| 18 H-MLM O | 0 0 0 0 0 |
| 13 H-MLM P | 0 0 0 0 0 |
| 7 H-MLM E CL | 0 0 0 0 0 |
| 22 H-MLM Me | 0 0 0 5.250 0 |
In terms of MLM status, the picture is somewhat different. The gerontologists play a liaison role with regard to MLM status. The matrons (H-MLM M B, H-MLM PM B) mainly enact a gatekeeping role. H-MLM, W is the highest scorer on the co-ordination role in the network.
| 1 2 3 4 5 |
| Coordinat Gatekeepe Represent Consultan Liaison |
| 1 SHM F | 0 0 0 0 0 |
| 15 SHM R | 2.989 1.749 1.312 0.875 0.535 |
| 6 SMLM Ln G | 0 0 0 0 0 |
| 14 SHM A | 0 0 0 0 0 |
| 23 H-MLM G M | 0 2.523 1.514 0 0.772 |
| 3 H-MLM MC F | 0 0 0 0 2.008 |
| 24 H-MLM G H | 0 0 0 0 2.008 |
| 21 H-MLM G G | 6.405 1.874 1.874 0 0.287 |
| 28 GP A | 0 0 0 4.920 0.502 |
| 27 H-MLM G M | 0 0 0 0 0 |
| 17 H-MLM G S | 0 4.373 2.187 0 0 |
| 9 H-MLM M CL | 1.019 2.386 1.193 0.298 0.730 |
| 11 H-MLM Mt CL | 0 0 6.560 0 0 |
| 8 H-MLM H CL | 0 0 0 0 0 |
| 7 H-MLM E CL | 0 0 0 0 0 |
| 19 H-MLM S | 0 0 0 0 2.008 |
| 4 H-MLM F | 0 0 0 0 0 |
| 26 H-MLM D | 0 0 0 0 0 |
| 2 H-MLM A | 0 0 0 0 0 |
| 13 H-MLM P | 0 0 0 0 0 |
| 18 H-MLM O | 0 0 0 0 0 |
| 22 H-MLM Me | 0 0 0 6.560 0 |
| 16 H-MLM, W | 11.209 0 3.280 0 0 |
| 10 H-MLM Mx | 0 0 0 0 2.008 |
| 25 H-MLM Hop | 0 0 0 0 2.008 |
| 12 H-MLM M B | 0 1.050 0.262 2.362 0.883 |
| 5 H-MLM PM B | 0 1.171 0 0 1.649 |
| 20 MLM PSM F | 0 0 0 0 0 |
| 29 H-MLM PSM W | 0 0 0 0.625 1.816 |
Appendix 2 Focus groups
List of abbreviations
- AMU
- acute medical unit
- CoP
- community of practice
- CQC
- Care Quality Commission
- CQUIN
- Commissioning for Quality and Innovation
- CRC
- Clinical Risk Committee
- GP
- general practitioner
- H-MLM
- hybrid middle-level manager
- HSDR
- Health Services and Delivery Research
- IPFC
- Inpatient Falls Committee
- IT
- information technology
- KBV
- knowledge-based view
- MLM
- middle-level manager
- MMHU
- Medical Mental Health Unit
- NHSLA
- NHS Litigation Authority
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NPSA
- National Patient Safety Agency
- NRLS
- National Reporting and Learning Service
- PSK
- patient safety knowledge
- PSO
- public service organisation
- RBV
- resource-based view
- RCA
- root cause analysis
- RQ
- research question
- RRR
- rapid response report
- SHO
- senior house officer
- SNA
- social network analysis
- SUI
- serious untoward incident