Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/2002/03. The contractual start date was in March 2012. The final report began editorial review in December 2013 and was accepted for publication in May 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Hassan et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
In the UK, the number of people in prison with mental illness is higher than ever, and likely to increase; therefore, a continuing high level of need for psychotropic medication in prisons is inevitable. 1 International studies have shown that prescriptions for psychotropic medicines, such as antidepressants and antipsychotics, are elevated in incarcerated populations in comparison with the community. 2–5
Few UK-based studies have explicitly addressed prescribing patterns in prisons. A large survey of psychiatric morbidity among prisoners in England and Wales carried out in 1997 by the Office for National Statistics (ONS)6 found that one-fifth of men and half of women interviewed were prescribed medication acting on the central nervous system (CNS), including drugs to treat mental health disorders and substance dependence. However, the study did not assess prescription costs, doses or the appropriateness of prescribing, nor did it make any comparisons with prescribing rates or appropriateness in the community.
Aim
The aim of this study was to undertake a comprehensive and robust examination of psychotropic prescribing patterns in prisons across England and Wales.
Objectives
The study had five objectives:
-
To establish rates of prescribing for psychotropic medications in prisons in England and Wales with respect to (a) medication type, (b) dose and (c) cost.
-
To compare prison psychotropic prescribing patterns with those in the wider community, accounting for demographic and clinical characteristics.
-
To compare prescribing patterns between different prison types and specific demographic groups.
-
To determine the appropriateness of psychotropic prescribing patterns in prisons.
-
To determine the perceived satisfaction and acceptability of psychotropic prescribing decisions to patients and general practitioners (GPs) in prisons.
Method
The study included two distinct components:
-
a cross-sectional survey of psychotropic prescribing patterns in prisons; and
-
a questionnaire survey to measure acceptability and levels of satisfaction with prescribing decisions to patients and GPs in prisons.
Research approvals
Ethical approval for the study was obtained from NHS National Research Ethics Service (NRES) Committee North East – York (09/HO903/54). Approval to access patient clinical records without consent was granted by the Ethics and Confidentiality Committee, on behalf of the National Information Governance Board (NIGB), under Section 251 of the NHS Act 2006. 7 Other relevant approvals required to conduct the research were obtained from local NHS organisations, the National Offender Management Service (NOMS) Research Committee, the Independent Scientific and Advisory Committee for the Clinical Practice Research Datalink (CPRD), and individual prison governors.
The prevalence of mental illness in prison
Research has consistently indicated that prisoners have poorer health than the general population and suffer from disproportionately high rates of psychiatric disorder. Several large-scale studies of psychiatric morbidity have been conducted in the England and Wales prison estate over the years in order to estimate demand for mental health services and to identify unmet treatment needs. 8–14 Table 1 provides a summary of the key studies since 1990, the measures used and the prevalence rates reported for different psychiatric disorders.
| Authors | Study population | Sample size, n | Diagnosis, % | ||||
|---|---|---|---|---|---|---|---|
| Psychosis | Neurosis | Personality disorder | Substance misuse | Any psychiatric disorder | |||
| Gunn et al.9 | Sentenced adult men | 1365 | 2 | 6 | 9 | 23 | 40 |
| Sentenced young men | 404 | < 1 | 6 | 14 | 19 | 33 | |
| Sentenced women | 258 | 1 | 15 | 16 | 31 | 56 | |
| Maden et al.11 | Remand adult men | 544 | 6 | 28 | 11 | 39 | 66 |
| Remand young men | 206 | 2 | 19 | 12 | 36 | 53 | |
| Remand women | 245 | 5 | 44 | 16 | 42 | 77 | |
| Brooke et al.8 | Remand adult/young men | 750 | 5 | 18 | 11 | 38 | 63 |
| Birmingham et al.14 | Remand adult men | 528 | 5 | N/A | 7 | N/A | 62 |
| Singleton et al.6 | Sentenced men | 1250 | 7 | 40 | 64 | 63 – alcohol; 43 – drugs | 90 |
| Remand men | 1121 | 10 | 59 | 78 | 58 – alcohol; 51 – drugs | ||
| Sentenced women | 584 | 14 | 63 | 50 | 39 – alcohol; 41 – drugs | ||
| Remand women | 187 | 76 | 41 – alcohol; 54 – drugs | ||||
| Senior et al.13 | Remand/sentenced men/women | 3482 | 4 | N/A | N/A | 66 | 71 |
In the early 1990s, a series of studies were undertaken by researchers at the Institute of Psychiatry to establish rates of psychiatric disorder and treatment needs among prisoners. 8–12 Large, representative and random samples of prisoners from prisons in England and Wales participated in clinical interviews with psychiatrists (see Table 1 for details). Overall, psychiatric disorders were diagnosed in 40% of adult and 33% of young sentenced men. The most common disorders were substance misuse, personality disorders and neurosis. The highest rates of psychiatric disorder were seen among women (56–77%) and remand prisoners (53–77%). Among sentenced prisoners, it was estimated that 44% of women and 23% of men required some form of treatment, most commonly on an outpatient basis, within prison or as part of a therapeutic community. 9,10,12
In the 1990s, the ONS conducted a series of surveys to establish the point prevalence of psychiatric morbidity in a range of different settings, including households,15,16 psychiatric institutions17 and prisons. 6 In 1997, a sample of 3142 prisoners (stratified by sex and legal status), from all prisons throughout England and Wales, participated in the ONS prison survey. 6 Singleton et al. 6 found that rates of psychosis were 10% and 7% among male remand and sentenced prisoners, respectively, and 14% among female prisoners. The prevalence of neurotic disorders [such as depressive, generalised anxiety (GAD), panic and obsessive–compulsive disorders (OCD)] was particularly high; 59% of remand and 40% of sentenced men, and 76% of remand and 63% of sentenced women had at least one neurotic disorder. They concluded that 90% of prisoners had a diagnosable mental illness, personality disorder and/or a substance misuse disorder. The ONS study, though now over a decade old, is still often referred to by researchers and policy-makers today. 1,18 The study by Senior et al. is the most recent of those considered in Table 1;13 the authors reported that, overall, 71% of prisoners were estimated to have a serious mental illness, a substance misuse problem, or both.
In summary, the increased prevalence of mental illness among prisoners has been well established by studies in the UK. 6,8–12,14,19 When comparing these figures, however, there are some important methodological differences to bear in mind, in particular the heterogeneity of clinical assessments and tools used (see Table 1) and the differences in training and qualifications of the interviewers.
The problem of increased prevalence of mental disorder in prisons is not uniquely a UK phenomenon. Fazel and Danesh20 conducted a systematic review and meta-analysis of 62 studies across 12 western countries, comprising 22,790 prisoners. The authors reported that, overall, 4% of male and female prisoners were diagnosed with psychosis and 10% of men and 12% of women in prison were diagnosed with major depression. The study concluded that one in seven prisoners had psychosis or major depression, which, after accounting for age differences, meant that rates of psychosis and major depression were two to four times higher in prison than in the community. A recent update of this systematic review,21 which included data from 33,588 prisoners worldwide, found no substantial changes in rates of psychosis and depression since the 2002 review. While pooling findings in this manner might have masked considerable heterogeneity in the time periods, methodologies and findings of individual studies, they do confirm a substantial level of mental health need in prisoner populations.
Health-care services for mentally ill prisoners
Prisoners in England and Wales should have access to the same quality and range of health-care services that they would expect to receive in the wider community. 22 This is known as the ‘principle of equivalence’ and has been the driving force behind the most recent wave of prison health-care reforms. 23
In terms of the delivery of mental health-care services in prison in recent times, the Department of Health document Changing the Outlook24 outlined the roles of primary and secondary care services in treating prisoners with mental illness. The document outlined development needs for primary care mental health services in prisons, including the need to diagnose mental health problems and facilitate access to further care; to provide wing-based support; to develop prisoners’ coping strategies and provide anxiety management; to refer to specialist psychiatric services for further assessment and/or support; and to provide chronic disease management.
Additionally, Changing the Outlook announced multidisciplinary mental health ‘in-reach’ teams, modelled on Community Mental Health Teams (CMHTs), as the main vehicle for delivering specialist mental health care services in prisons. CMHTs provide multidisciplinary, community-based care for adults, using a wider range of interventions. In-reach teams, like CMHTs, were set up to perform a range of tasks including identifying and assessing those with mental illness, improving access to appropriate treatment, discharge planning and facilitating effective through care on release. Like CMHTs,25,26 in-reach teams were initially intended to focus on severe and enduring mental illness, although there was recognition that others may also benefit from such services. 24
Since the publication of Changing the Outlook, major changes have taken place in the delivery of prison-based mental health services, but deficits in care remain. A national evaluation of the operation of in-reach teams reported that services still struggle to identify their key client group, i.e. those with severe and enduring mental health. 13 The study found that only 25% of those with psychosis were assessed by in-reach services, and only 13% were accepted onto teams’ caseloads. In-reach caseloads were identified as containing people presenting a range of needs much more diverse than the core group with severe and enduring mental illness, including those with substance misuse, common mental health problems, personality disorder and those who present with complex issues associated with imprisonment in the absence of a clearly defined clinical diagnosis. 13 The delivery of mental health services in prisons is additionally challenged by high rates of dual diagnosis, especially drug and alcohol issues. Most recently, developments in the area of primary care mental health services have occurred, including the setting up in prisons of improving access to psychological therapies (IAPT) services. IAPT services initially started in the wider community to provide rapid access to ‘talking therapies’ for common mental health problems. Their introduction into prisons is a welcomed development, although a full evaluation of their efficacy and impact is required.
Psychotropic medicines
Psychotropic medication has been a mainstay of mental health care since the mid-20th century and is widely cited as instrumental in the decreased need for the long-term hospitalisation of people with severe and enduring mental illness. The range of available drugs has evolved over time as a result of research and development in the pharmaceutical industry. Prescribing guidelines and advice to clinicians regarding the management of psychotropic medication regimes are also under constant review by a number of national bodies, such as the National Institute for Health and Care Excellence (NICE).
For the purposes of this study, psychotropic medicines are defined as any medicine listed in subchapters 4.1–4.4 of the British National Formulary (BNF), which includes:
-
hypnotics and anxiolytics (4.1)
-
drugs used in psychoses and related disorders, including mood stabilisers (4.2)
-
antidepressant drugs (4.3)
-
CNS stimulants and drugs used for attention deficit hyperactivity disorder (ADHD) (4.4).
In the following sections, an overview of the drugs included within each of these four categories, and their clinical uses, is provided.
Hypnotics and anxiolytics (4.1)
Hypnotics are generally used to relieve insomnia, while anxiolytics are effective in the relief of acute anxiety, tension and agitation. The group of drugs known as the benzodiazepines are the most commonly used hypnotics and anxiolytics. 27 The main difference between different benzodiazepine drugs is the variation in the half-lives (the period of time for the blood concentration of a substance to decrease by half). Half-lives are clinically relevant, as longer-acting benzodiazepines (e.g. diazepam) are commonly used as anxiolytics, whereas those with shorter half-lives are more often used as hypnotics (e.g. temazepam).
Though benzodiazepines are clinically effective, they carry the risk of physical and psychological dependence. Users can rapidly develop tolerance, meaning that greater doses are required to achieve the same effects. Furthermore, after longer periods of continuous use (> 4 weeks), withdrawal symptoms have been reported, including insomnia, anxiety, flu-like symptoms, stiffness or weakness and possibly seizures. 27,28 Users may misinterpret discontinuation symptoms as signs of relapse. 29 Furthermore, benzodiazepines can be misused for recreational purposes, either alone or in combination with street drugs such as opiates or stimulants. 28,30
In consideration of these risks, NICE has recommended that benzodiazepines are indicated only in cases where symptoms are severe, disabling or causing extreme distress, and then only after non-pharmacological methods have been considered. 31 Benzodiazepines are not recommended for chronic conditions, such as GAD, post-traumatic stress disorder (PTSD) or OCD, except as a short-term measure during crises. 32–34 In particular, it has been suggested that repeat prescriptions should be avoided in patients with a history of substance misuse or marked personality disorder. 27,28 Certain long-acting benzodiazepines (usually chlordiazepoxide) are also used in the management of alcohol withdrawal in primary care. 30
Drugs used in psychoses and related disorders (4.2)
Antipsychotic drugs, also referred to as neuroleptics, are used in the treatment and prophylaxis of schizophrenia, bipolar disorder and other psychoses. They also have a calming effect on agitated or disturbed patients. Antipsychotic drugs have been grouped according to both the pattern and the mechanism of clinical action. 34 The BNF identifies four categories of neurological ‘extrapyramidal’ side effects (EPSEs) associated with older, first-generation (‘typical’) antipsychotic medications (e.g. chlorpromazine or haloperidol): parkinsonian symptoms (e.g. tremors); abnormal face and body movements (dystonia); restlessness; and tardive dyskinesia, a potentially irreversible condition characterised by involuntary facial contortions, commonly involving the tongue, face and jaw. 27 Subsequently, second-generation (‘atypical’) drugs were launched in the 1990s, which avoided EPSEs, making antipsychotics more tolerable. While first-generation antipsychotic drugs are thought to work by interfering with dopaminergic transmission in the brain, second-generation drugs have a ‘rich pharmacology’, meaning that they act on multiple receptors. 35,36 More recently, a third generation of antipsychotic drugs, with different pharmacological properties, has been introduced. 37 For the purpose of this research, second- and third-generation antipsychotic drugs have been grouped together and will be referred to as atypical antipsychotics. NICE has recommended that atypical antipsychotics should normally be used as first-line treatment with newly diagnosed schizophrenia. 38
Clozapine is the only atypical drug found to be superior in efficacy to typical antipsychotics. 39 Though not a first-line response to psychosis, clozapine has emerged as the gold-standard treatment for patients with ‘treatment resistant schizophrenia’,38,40 defined as those whose illness has not responded to at least two different antipsychotic drugs, including an atypical antipsychotic agent. 38
Mood stabilisers are used in the treatment of hypomania, mania and bipolar disorder to reduce the severity of symptoms, to stabilise mood and as a preventative measure. In the UK, lithium, sodium valproate and certain antipsychotics (olanzapine, quetiapine and risperidone) are licensed for the treatment of acute mania. NICE recommends valproate as a first-line treatment for acute episodes of mania, characterised by periods of overactive, disinhibited behaviour. 41 In such cases, randomised controlled trials have shown that valproate has a response rate of 50%. 28 Potential side effects include weight gain and gastric irritation; it is also teratogenic and should not normally be prescribed for women with child-bearing potential. 41 Lithium has a slower onset of action than valproate and antipsychotics, but is regarded as a useful treatment for moderate symptoms of mania. Side effects of certain medicines used to treat mania include tremors, weight gain and gastric irritation. 27
Antidepressant drugs (4.3)
Antidepressants are used mainly to treat symptoms of depression and anxiety and can also be used in combination with antipsychotics and drugs to treat mania, bipolar disorder and psychotic depression. While antidepressants have been found to be beneficial in the treatment and prophylaxis of moderate to severe depression, they are not recommended for mild depression. 42 Unfortunately, the risk of recurrent depression is high; over half of patients who have a depressive episode will go on to have a second episode. 43
In the BNF, antidepressant drugs are divided into four classes: selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs), monoamine-oxidase inhibitors, and other drugs. 27 TCAs were the first antidepressants to be introduced. There is little difference in terms of efficacy between the different groups of antidepressants. 27 A flexible approach is recommended when choosing antidepressant drugs, taking into account risk of interactions, side effect profiles and patient preferences. NICE has recommended that the newer SSRI drugs (e.g. fluoxetine, citalopram and sertraline) should normally be used first-line as they are safer in overdose and more tolerable than other antidepressants. 42 However, a series of case reports published two decades ago sparked concerns regarding a possible link between SSRIs and suicidal thoughts and behaviour, though this remains to be conclusively proven or disproven. 44–48 While antidepressants are not addictive, it has been known for years that patients may experience unpleasant effects such as dizziness, mood changes, gastrointestinal disturbances and insomnia on reducing/missing or stopping them. 49
Central nervous system stimulants and drugs used for attention deficit hyperactivity disorder (4.4)
This subchapter of the BNF includes amphetamines and other stimulant medicines, mainly used to treat ADHD. In the Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (DSM-IV), ADHD has been defined as a ‘persistent pattern of inattention and/or hyperactivity–impulsivity that is more frequently displayed and is more severe than is typically observed in individuals at comparable level of development’ (p. 85). Methylphenidate, atomoxetine and dexamfetamine are normally the drugs of choice with regard to ADHD. ADHD is normally diagnosed in childhood; however, adult ADHD is a recognised condition. 50–52 Drugs within this class have a high propensity for diversion, abuse and dependence. 53 Indeed, the effects of methylphenidate have been compared to those of cocaine, although there are distinct pharmacological differences between the two. 54 Thus, where there is a history of substance misuse, prescribers should be cautious about prescribing, and additional monitoring may be required. 27
The use of psychotropic medicines in prison
Historical perspectives
Although psychopharmacology is central to contemporary mental health care, the use of psychotropic drugs in prison has, historically, been controversial. In prisons in England and Wales during the 20th century, as in psychiatric hospitals, psychotropic drugs became an important new tool in doctors’ ‘medical armoury’. 55 The ability of drugs to manage difficult behaviour and create ‘a quiet prison’ was not lost on prison doctors or discipline staff. For many years, doctors were open about using drugs to help make prisoners more manageable and amenable to the regime; for example, as late as 1978, a prison doctor wrote a paper concerning the use of the antipsychotic drug Depixol® (Flupentixol, Lundbeck) to ‘treat’ individuals with a psychopathic disorder. 55 However, as prisons became more open to external scrutiny, reports began to surface from prisoners and ex-prisoners who claimed to have been drugged against their will, or who had apparently accepted treatment only as a result of coercion and threats. 55 Increasingly, critics of prison health care and patient pressure groups questioned whether or not drugs were prescribed in prisons for disciplinary purposes to control difficult individuals, rather than to treat mental illness. 55
In 1980, the prison service published data concerning the use of psychotropic medicines in prisons as part of its annual report. 56,57 Unfortunately, the style of analysis and presentation of figures made it difficult to derive meaning from the data. 58 The lack of clarity regarding how drugs were categorised, absence of data on dose and aggregation of data across multiple prisons were some of the problems noted; some went as far as to say that the figures were purposely designed to be ‘as misleading as possible’ (p. 250). 59 Notwithstanding their limitations, the data did highlight the wide variation in dosage rates between prisons.
Current approaches and policy
Today, prescribing psychotropic medication in prison remains a complex topic in current clinical practice, undertaken at the boundary of the care/custody interface. In accordance with the principle of equivalence, prisoners are entitled to access pharmacy services and appropriate medicines, as they would do in the wider community. Nonetheless, health-care professionals have argued that certain aspects of prison-based health care, notably around medicines management, may need to be altered in prisons in order to mitigate risk and to safely discharge the prison’s duty of care to prisoners.
Part of the problem is that staff commonly believe that a minority of prisoners may present with exaggerated or fictitious symptoms in order to attempt to acquire medication to misuse or sell. 60–62 This presents a number of safety and security risks, both to individuals taking illicitly obtained medicines and to vulnerable individuals with genuine mental health needs, who may come under pressure to share prescribed medication with others.
Currently, there is no national agreed formulary in operation in prisons in England and Wales. However, in 2011, the Royal College of General Practitioners (RCGP) Secure Environments Group issued Safer Prescribing in Prison, which evaluated the suitability of individual medicines for use in prison. 61 Written from the position that prescribers in prisons need to balance security and safety risks against individual health needs, this document introduced a traffic-light system for medicines based on risk for harm. It classified medicines as either green, indicating lower-risk and first-choice options (including SSRI antidepressants); amber, suggesting that these may be used with caution, or after other choices have been unsuccessful (e.g. antipsychotics); and red, for medicines considered inappropriate in prisons (e.g. temazepam, a short-acting benzodiazepine).
Although a welcome and useful contribution to the literature, the RCGP guidance was written from a prescriber viewpoint and strongly focused on risk management and drug choice. Although this and other policy guidance documents have acknowledged the values of equivalence and patient-centred care, there are indications that achieving the optimum balance between health care and security remains a significant challenge. For example, while medicines are meant to be held in the possession of prisoners as a matter of principle, research has suggested that staff remain cautious about the risks of allowing this. 5,60
In qualitative research studies, patients have complained about discontinuity of prescribing between the community and prison, preoccupation with security and inadequate access to medicines. With reference to mental health in particular, policy clearly states that medication for mental disorder should not be automatically withdrawn on entry into prison without proper clinical assessment. 24 Yet studies have reported that prisoners experience problems with continuing established medication regimes on entry into prisons, causing significant frustration and distress. 62–66 These reports are corroborated by a records-based study in five English prisons, which found that half of all psychotropic medicines prescribed in the community were discontinued in prison, often without evidence of clinical review or other justification recorded in the notes. 67
The inherent complexities associated with medicines management in prisons are further compounded by a lack of access to robust prescribing data. Unlike in the community, high-quality prescribing data are not routinely available from prison-based prescribers. 5 In a thematic report on mental health, the Chief Inspector of Prisons expressed concern that psychotropic medicines may be overused in prisons, in comparison with non-pharmacological interventions such as ‘talking therapies’. 68 Without robust data, however, questions like these are unlikely to be answered.
Research on psychotropic prescribing in prisons
The Office for National Statistics study
The 1997 ONS survey of psychiatric morbidity in England and Wales provided detailed, high-quality data on rates of psychotropic prescribing in prison. 6 Table 2 provides a summary of the psychotropic prescribing rates reported by the ONS for adult men and women in prisons and young people in young offender institutions (YOIs).
| Study | Study population | Subgroup | Type of drug, % | |||
|---|---|---|---|---|---|---|
| Hypnotics and anxiolytics | Antipsychotics | Antidepressants | Any CNS druga | |||
| Singleton et al.6 | Prisoners | Sentenced men | 3 | 2 | 6 | 18 |
| Remand men | 7 | 4 | 8 | 23 | ||
| Sentenced women | 12 | 8 | 21 | 48 | ||
| Remand women | 29 | 14 | 23 | 56 | ||
| Lader et al.69 | Young offenders | Sentenced men | 2 | 2 | 3 | 10 |
| Remand men | 2 | 2 | 3 | 10 | ||
| Women | 14 | 8 | 12 | 40 | ||
One-fifth of men in prison were prescribed some form of medication acting on the CNS, which included psychotropic medicines and also analgesics, antiepileptics and drugs for substance dependence. Among this group, the most commonly prescribed medicines were antidepressants, followed by hypnotics and anxiolytics, and antipsychotics. Rates of prescribing were higher in remand prisoners than in sentenced prisoners.
Prescribing among women in prison followed a similar pattern, though rates were even higher: women were twice as likely as men to be prescribed CNS medicines. Overall, half of women were prescribed CNS drugs, one in five women received antidepressants and one in 10 received antipsychotics. In YOIs, 10% of young men were prescribed CNS drugs. For young men, unlike for adult men, rates of prescribing were the same among remand and sentenced individuals. In line with those for adult prisoners, rates of prescribing were much higher among young women than among young men; overall, 40% of young female prisoners were prescribed CNS drugs, with hypnotics and anxiolytics being the most commonly prescribed types of drug (14%).
While the ONS study provided some useful data, a number of limitations are noteworthy. First, the data were collected 15 years ago. Owing to a variety of factors, it is likely that psychotropic prescribing will have changed during this time. Second, the ONS surveys were focused on determining the prevalence of psychiatric morbidity, rather than on medicines use. Inevitably, this gives rise to a number of methodological limitations. There is a limited level of detail provided on medicines use, including a lack of data on drug types, individual drugs and doses prescribed. Certain aspects of the study design and analysis could also be seen to create difficulty in interpreting data. For instance, psychotropic drugs used to treat mental illness are often pooled together with other CNS drugs, which have quite different clinical indications (e.g. drugs for substance dependence, epilepsy and analgesics).
Furthermore, the use of antipsychotic medication was used as an indicator of probable psychosis; as the authors acknowledge, this means that associations between diagnosis and medication use are inevitable, but not necessarily accurate. While there is some consideration of prescribing patterns within particular diagnostic groups, this is complicated due to comorbidity. For example, if an individual has more than one diagnosis, it might be unclear which condition is being treated by a particular medication. Such factors prevent us from drawing any firm conclusions regarding the appropriateness of prescribing patterns from these data.
Finally, one of the purported strengths of the study was that, as one of a series of national psychiatric morbidity surveys with similar methods and measures, comparisons could be drawn between different groups, for example with the general population. 70 However, comparing crude prescribing rates does not take into account the substantial differences in the age and sex mixes between prison and community populations (prisoners are, on average, younger and more likely to be male). Furthermore, the way in which the data are presented makes certain comparisons difficult: for example, it is not easy to compare relative rates of psychotropic prescribing and mental illness in prisons and communities.
The east of England study
Until recently, the ONS study was the only published source of robust research data available on psychotropic prescribing patterns in prisons in England and Wales. One major difficulty which has impeded efforts to investigate prescribing has been information technology. Until recently, prisons relied on paper-based clinical records and adopted varied pharmacy data management systems. Thus, previous attempts to collect pharmacy data were time-consuming, small-scale and impractical. 5 In 2011, the roll-out of a single health-care information technology (IT) system (SystmOne, The Phoenix Partnership, Leeds, UK), in common use in community primary care settings, was completed throughout the prison estate, creating a novel opportunity to link prescriptions with individual patients.
In 2010, researchers from the Offender Health Research Network (OHRN) at The University of Manchester conducted a study which tested the feasibility of extracting data from patient clinical records held in SystmOne to establish psychotropic prescribing patterns in prisons. 71 The research was completed in four prisons in the east of England, covering the counties of Bedfordshire, Cambridgeshire, Essex, Hertfordshire, Norfolk and Suffolk. This particular region of the UK was chosen largely for practical reasons: several prisons in the region had already adopted SystmOne and the enthusiasm and support from the local offender health and medicines management team guaranteed access to prisons and resources. Of the four prisons recruited to the study, two accepted both adult and young men, one accepted adult and young women and one accepted adult men only. Three of the prisons recruited accepted both convicted and unconvicted prisoners and the fourth accepted only convicted prisoners.
On census days, local health-care staff used SystmOne to identify and collect prescribing and demographic data on all prisoners with current, valid prescriptions for hypnotic, anxiolytic, antipsychotic, antimanic, antidepressant and/or stimulant medication, as listed in subchapters 4.1 to 4.4 of the BNF. For comparison purposes, we also obtained a large data set on a random sample of CPRD patients in the community, under a free-licence scheme funded by the Medical Research Council (MRC) (now expired).
The findings of the study indicated that one-fifth (20%) of men and almost half (44%) of women in prison were prescribed at least one psychotropic medication. After adjusting for age differences, rates of psychotropic prescribing in prison were 5.5 and 5.9 times higher than in community-based men and women, respectively. We also found marked differences in the individual psychotropic drugs prescribed in prison and community settings.
The study had a number of limitations. Only prisons in the east of England were sampled, a region which accounted for approximately 10% of prisons in England and Wales at the time, thereby limiting generalisability. Furthermore, while the study attempted to collect data on indications for medicines, these were of questionable reliability, having been collected by several different health-care staff. Analyses on costs, doses or drug interactions were not completed; thus, it was difficult to make inferences regarding the appropriateness of prescribing. Despite these limitations, the study allowed us to develop and refine a data extraction methodology and proved the feasibility of using SystmOne for research purposes. It also enabled us to obtain a valuable community data set and provided some interesting preliminary data on prescribing patterns in prisons in one region of England.
Evidence from international studies
Aside from the UK-based literature, a number of studies have been published describing psychotropic prescribing in prison populations internationally, particularly in Europe and the USA. For example, in 2004, a national cross-sectional study of Norwegian prisons reported that 34% of men and 44% of women in prison were in receipt of medication acting on the CNS. 72 No significant sex differences were found with regard to prescribing. Overall, they concluded that the rate of prescribed psychotropic drug use in prison was higher than in the general population but lower than that observed in psychiatric hospital units.
A Swiss study73 compared prescribing outcomes among a sample of prisoners (n = 179) attending primary care consultations over a 3-week period in 1997. The study showed that psychotropic drugs (mostly anxiolytics and hypnotics) accounted for about half of drugs (46%) prescribed at these appointments. Female prisoners were significantly more likely to be prescribed psychotropic drugs than men (77% vs. 56%), although it should be noted that the female sample was very small (n = 22). Notably, the study also recruited a group of community-based patients (n = 701), who attended an ambulatory care clinic (outpatients only) at a local hospital in an urban area over the same period, for comparison purposes. In an effort to control for age-related differences between the populations, comparisons were limited to male patients in prison and the community aged < 39 years of age. An analysis of this subgroup showed that psychotropic medication was prescribed five times more often at appointments in prison than at the hospital clinic.
Several studies have been completed in the USA reporting the prevalence of psychotropic prescribing in prisons. In response to concerns about rising pharmacy costs, Lund et al. 74 undertook a longitudinal analysis of prescribing trends in the Iowa Department of Corrections prison system. The study utilised a combination of prison population data and drug expenditure records over the years 1990–2000 to determine trends in annual expenditure per inmate. Overall, annual expenditure on psychotropic drugs increased dramatically from $291 per 100 inmates in 1990 to $8138 in 2000, a 28-fold difference. Both the volume and the costs of antidepressants, mood stabilisers, hypnotics and anxiolytics all increased. However, while the overall volume of antipsychotic prescriptions showed a slight decrease, expenses increased ninefold. The authors concluded that a shift towards newer (and safer) drugs was largely responsible for the increase in costs, placing additional strain on already scarce resources.
Baillargeon et al. 2,75,76 and Williams et al. 77 conducted a series of studies in Texas Department of Criminal Justice (TDCJ) prisons. Unlike most of the studies discussed previously, these studies focused on prescribing patterns within two particular diagnostic categories, namely prisoners with depressive disorders and prisoners with psychosis. Retrospective data on prescribing patterns were collected from the clinical records of a large sample of TDCJ inmates with depressive disorders (n = 5305) in 1998–9. 2,76 Data were also collected on 3750 TDCJ prison inmates who were (a) diagnosed with schizophrenia and/other psychotic disorders and (b) receiving antipsychotic medication. 75 In TDCJ prisons, medication prescription and compliance data are maintained within computerised medical records systems on all inmates receiving prescribed medication. Individual-level data on prescriptions, clinical characteristics and sociodemographic data were obtained for all participants.
A detailed analysis of the antidepressant prescribing patterns showed that, overall, 47% of inmates with depressive disorders were prescribed SSRIs, 31% received TCAs and 22% received no antidepressant medication. The researchers found that:
-
Men and older prisoners (aged > 50 years) diagnosed with depression were less likely to be prescribed antidepressants than their female and younger counterparts.
-
Women, young people (aged < 30 years) and white inmates were more likely to be prescribed SSRIs.
-
Male sex, older age and being prescribed TCAs were all positively associated with ‘compliance’ scores (i.e. the number of doses taken divided by the number of doses prescribed during the study period).
Furthermore, among prisoners with schizophrenia treated with antipsychotics:
-
Eighty-five per cent received first-generation (typical) antipsychotics; this rose to 89% for other forms of psychoses.
-
Women, black men and non-violent prisoners were less likely than their counterparts to be prescribed second-generation (atypical) drugs.
The authors concluded that these findings were reflective of both the increased costs of atypical antipsychotics and newer SSRI drugs costs, and also TDJC prescribing policies; at the time, local formularies stipulated that first generation antipsychotics should be attempted first-line. The authors also noted that SSRI use appeared to be lower among prison inmates than among USA community and inpatient populations (no equivalent community data were available for antipsychotics).
Griffiths et al. 78 recently conducted a systematic review of the literature on prescribing psychotropic drugs to prisoners. This included qualitative and quantitative research on prisoners located in a variety of settings, including forensic hospitals, high-security psychiatric wards, prisons and jails. The review generated a final sample of 32 papers. The studies included in the review examined topic areas such as polypharmacy, prescribing errors, high-dose antipsychotic prescribing and prescribing in older prisoners. Eighteen papers originated in the UK: of these, most (n = 12) were from secure forensic hospitals. The key themes identified from the reviewed studies were polypharmacy, high-dose therapy, duration of treatment, documentation and monitoring, and issues associated with the prisoners’ environment. The authors concluded that polypharmacy, use of high doses and poor continuity of care were common among prisoners prescribed psychotropic medicines. Nonetheless, the authors noted that, owing to the heterogeneity of settings in which studies were conducted, these issues might not apply equally to all settings. They also noted that research to date had focused on antipsychotics, rather than on the broader category of psychotropic medicines. Furthermore, where prevalence studies had been conducted, these often lacked comparisons between key population subgroups, such as between sexes, age groups and ethnicities.
Overall, the evidence from international studies of prescribing in prisons is useful, yet far from comprehensive. Studies appear to indicate elevated use of psychotropic medication among prisoners in comparison with the communities from which they are drawn, a finding which could reflect the increased rates of psychiatric morbidity generally observed in such populations globally. 8–12,20,21,79 Some studies also reported noticeable sex differences in psychotropic use. 2,6,73,77 In such instances, women were generally more likely than men to be prescribed psychotropic drugs, which is consistent with the increased psychiatric morbidity in this group.
The most obvious gap in the existing literature relates to studies which provide comparison data between the general prison population and the community or other settings. 72,73 Community data are arguably useful as they allow us to consider the extent to which there is equity and continuity of prescribing between settings. Unfortunately, neither of the studies which made such comparisons adequately accounted for age and sex differences between populations.
A second limitation concerns the use of drug volume and expenditure data in some studies. 72,74 While making use of readily available data is a simple and efficient strategy, prescriptions cannot be matched to individuals; therefore, this method relies on using mean dosages to calculate use/costs per head. Use of individual-level data, as in the TDCJ studies,2,75,76 while more time-laborious, is far superior as it has the potential to better account for the full range of pharmacological, clinical and demographic factors.
The relationship between psychotropic prescribing and psychiatric morbidity
A key issue that is relevant to research in this area, and indeed to this study, is the extent to which patterns of psychotropic prescribing are mediated by the presence of mental illness. More specifically, a question pertinent to the current study is as follows: if rates of psychotropic prescribing are higher among prisoners, is this simply due to increased rates of psychiatric morbidity?
For a number of reasons, this relationship is not straightforward. While it is likely that underlying patterns of mental illness exert an influence on patterns of psychotropic prescribing, we would not expect complete correspondence between the two rates. The first reason for this is that not all patients with mental illness will be treated with psychotropic medicines, or indeed treated at all. Secondly, patients prescribed psychotropic drugs may not necessarily have a mental illness. Psychotropic medications may be prescribed ‘off label’, outside the narrow terms of their licences, to treat conditions other than mental illness. Thus, while we can expect rates of psychiatric morbidity to exert an influence, this is unlikely to fully account for any variation observed in rates of psychotropic prescribing.
Summary
Mental illness is significantly more common among prisoners than in the general population. UK policy entitles prisoners to the same standard of health care as that available in the community, including access to appropriate medications for mental illness. Ideally, imprisonment should offer an opportunity to engage a hard-to-reach population with high levels of physical and mental health morbidities with NHS services, to improve individual health outcomes, improve engagement with services and contribute to wider public health targets. Psychotropic medicines are widely used in the community to treat mental illness. However, the equity, consistency and safety of prescribing for mental illness in prisons have been questioned.
Robust research on prescribing in prisons is scarce. The limited evidence base available suggests that prescribing practices in prisons are different from those in the community, both in terms of the way medicines are managed and with respect to the particular types, combinations, doses and formulations of medications that are prescribed. Health-care professionals have argued that some aspects of prison-based health care have to be altered from those commonly practised in the wider community in order to mitigate risk and to safely discharge the prison’s duty of care to prisoners. However, prisoner-patients have complained about discontinuity of prescribing between the community and prison, and have reported that prescriptions are frequently contested, changed or withdrawn. They have also expressed dissatisfaction with the arrangements for accessing psychotropic medicines once in custody.
Access to psychotropic medication in prison is a particularly controversial and challenging area, with tensions between policy and practice. Health-care staff working with mentally ill prisoners, while remaining mindful of the particular risks within a secure setting, work within the policy context of equivalence of care. Medicines research in prisons in England and Wales has been limited by the lack of centralised, comprehensive prison pharmacy data, and the most robust research study in this area6 is now out of date. Robust data on prescribing in prisons are essential to determine whether or not prisoners receive equitable access to medications and to ensure that medicines are used in a way that is safe, cost-effective and minimises the risk of harm to patients while promoting positive health outcomes for individuals.
Preliminary research by the OHRN proved the feasibility of using a newly introduced clinical health-care IT system to measure the prevalence of psychotropic prescribing in prisons and to compare rates with those of the wider community. 71 However, the survey was limited to prisons in one region of England and did not robustly assess prescribing appropriateness. In the current study, we aimed to use a refined version of this methodology to undertake a comprehensive and robust examination of the prevalence and appropriateness of psychotropic prescribing in prisons across England and Wales.
Chapter 2 Methods
Overview
Three research questions were defined to guide the study:
-
What are the patterns of psychotropic medication prescribing in prisons in England and Wales, and how do these compare with those in the wider community?
-
How appropriately are psychotropic medications prescribed in prisons?
-
How acceptable are psychotropic medication prescribing decisions to patients and GPs in prisons?
Design
The study comprised two discrete components: (1) a prevalence survey of psychotropic prescribing patterns, using a cross-sectional design, and (2) an acceptability study of patients and GPs in prisons to determine expectations and levels of satisfaction with prescribing decisions. Table 3 shows how the research questions and methods correspond directly to five objectives.
| Research question | Objective | Method |
|---|---|---|
| 1 |
|
Cross-sectional prevalence survey of psychotropic prescribing (the ‘prevalence survey’) |
| 2 |
|
Cross-sectional prevalence survey of psychotropic prescribing (the ‘prevalence survey’) |
| 3 |
|
Prescribing decision acceptability study of patients and GPs in prisons (the ‘acceptability study’) |
Research approvals
Ethical approval for the study was obtained from NHS NRES Committee North East – York (09/HO903/54). To access Her Majesty’s Prison Service establishments, governance approval was obtained from the NOMS Research Committee and from individual prison governors. Site-specific approval was obtained from each of the relevant NHS or management organisations responsible for the delivery of health care at participating prisons. Approval to access patient clinical records without consent was granted by the Ethics and Confidentiality Committee, on behalf of the NIGB, under Section 251 of the NHS Act 2006. 7 The Independent Scientific and Advisory Committee approved the use of data from the CPRD for comparison purposes.
Patient and public involvement
In order to provide ongoing patient and public involvement, we established an ex-prisoner research advisory group. We achieved this by collaborating with colleagues at The University of Manchester who established a similar group for a National Institute for Health Research (NIHR), Research for Patient Benefit-funded research project. 80
Several members of this group, plus additional members recruited separately, formed an additional group called the Medication, Access, Care and Equality (MACE) group to advise on the current project. The MACE group met on a monthly basis throughout the life of the project and included seven regular members (men and women), all of whom had experience of (a) imprisonment and (b) accessing health services in prison. Some members have also received treatment for mental health problems and/or taken psychotropic medicines in prison.
The MACE group provided representatives to attend project steering group meetings and helped to inform aspects of the study design, procedures and plans for dissemination. Specifically, the group contributed towards the following activities:
-
deciding which types of prison should be sampled as part of the prevalence survey
-
reviewing and adapting patient questionnaires previously used in the community for use in prisons
-
reviewing and adapting patient information sheets for the acceptability study
-
designing posters to advertise the acceptability study in prison
-
drafting and editing summaries of findings for patients, including the plain English summary in this report; and
-
identifying audiences and organisations to be informed about the results of the study (e.g. charities, prisoner newspapers and local media).
The MACE group also delivered a presentation describing their role in the study at a dissemination event in February 2014.
The cross-sectional prevalence survey of psychotropic prescribing
A cross-sectional prevalence survey was designed to establish rates of psychotropic prescribing in prisons. Cross-sectional designs involve collecting data on exposures and outcomes in a population at a single point in time. 81 This approach was chosen as the most appropriate design for establishing point-prevalence rates, the primary goal of the study. A point-prevalence approach was selected, meaning that prescribing rates would be determined on a single day. This method was most effective for ascertaining population denominators (needed to calculate rates of prescribing) in busy, local prisons with transient prisoner populations. To compare prison-prescribing rates with rates in the general population, a comparative two-sample design was used with a sample of patients in prison and a control group of community patients.
Prison sample
Based on our preliminary work in the east of England,71 we expected the overall point-prevalence of psychotropic prescribing in prisons and the community to be approximately 26% and 8%, respectively.
In a comparative study of percentages, the minimum sample size needed to have a 90% chance of detecting this difference as significant (p = 0.05, two-sided) is 90 per group. However, to perform the detailed subgroup analyses needed for this study (e.g. the proportion of atypical vs. typical antipsychotic prescriptions among black male prisoners), a much larger sample is required. Based on our preliminary work, we aimed to recruit 12 average-sized prisons (n = 500) to ensure that the study was adequately powered, even for detailed subgroup analyses. On this basis, we expected to generate prescriptions for 360 hypnotics/anxiolytics, 360 antipsychotics and 840 antidepressants (Table 4).
| BNF subchapter | Medication type | Estimated prevalence (%) of prescribinga | Estimated number of patients prescribed medications in 12 prisonsb |
|---|---|---|---|
| 4.1 | Hypnotics and anxiolytics | 6 | 360 |
| 4.2 | Antipsychotics | 6 | 360 |
| 4.3 | Antidepressants | 14 | 840 |
| 4.4 | Stimulants and ADHD | No figures available due to low numbers | |
| 4.1–4.4 | Any | 20 | 1200 |
In total, 11 prisons were recruited to the study. A range of prisons in England and Wales were invited to participate in the study. Following the preliminary work in the east of England, a number of sites had already expressed interest in participation. Others were recruited via direct e-mail enquiries to health-care managers. Recruited prisons were geographically spread across northern England, the south-west of England, London and the Midlands. The sample included three local prisons, three training prisons, two women’s prisons, two prisons for young offenders and an open prison. Each prison type is further explained in Box 1.
Women’s prisons operate to the same standards as men’s prisons but with additional sex-specific requirements. Women account for only 5% of the prison population. Prisons for women are either closed or open. Women present particular challenges from a mental health perspective, as they are more likely to have pre-existing psychiatric, self-harm and substance misuse problems. 6
Young offender institutionsYoung men aged between 18 and 21 years old are dealt with separately from adult male prisoners, either in separate prisons (known as young offender institutions) or in wings (in prisons with a mixed adult/YOI function). Young male offenders constitute approximately 10% of the prison population and have different mental health-care needs from adult prisoners, in particular an increased prevalence of ADHD. 82
Local prisonsLocal prisons house those awaiting trial, those serving short sentences and those at the beginning of longer sentences. They make up approximately half of the prison estate. Local prisons house highly transient prisoner populations, with high rates of admission and discharge. Newly received prisoners are often dependent on illicit drugs and/or alcohol and may require detoxification.
Training prisonsTraining prisons accept convicted and sentenced individuals. They are designed to offer work and rehabilitation-oriented regimes for men serving substantial sentences.
Open prisonsOpen prisons house prisoners who require minimal supervision and are considered a low risk to the public. They are designed with a focus on rehabilitation and permit prisoners to take up employment in the community, returning to prison in the evenings.
Data collection procedure
For logistical reasons, it was not possible to use a single census day across all prisons; therefore, a census day was identified for each individual prison. Census days were dependent on the timing of approvals and site access arrangements; all census dates were between 30 November 2012 and 30 July 2013.
On census days at participating prisons, population figures (stratified by age, legal status and ethnicity) were obtained from each individual establishment using Prison National Offender Management Information System (P-NOMIS) for use as denominators for calculating prevalence rates. At each prison, SystmOne was used to select all patients who met the following inclusion criteria: (1) aged 18 years or over; (2) in prison custody; and (3) in receipt of a valid, current prescription for psychotropic medication. At three prisons, SystmOne was not used for all prescribing. At these prisons, drug charts were searched manually for patients who met the inclusion criteria. For each patient who met the inclusion criteria, a researcher then extracted the relevant demographic, clinical and prescription data from their clinical record and recorded this on a data extraction pro forma.
For each patient, the following data were collected:
-
demographic data, including prison, sex, legal status, ethnicity and year of birth
-
physical and mental health diagnoses, as recorded on the standard prison health-screening assessment tool.
For each psychotropic prescription identified, the following data were collected:
-
drug name
-
dose
-
formulation
-
indication.
To measure the appropriateness of prescribing, we applied the prescribing appropriateness indicator (PAI) to each psychotropic prescription. The PAI is a set of nine standardised, validated indicators83,84 that are designed to be applied to prescribing data held in medical records. For the current study, we used a subset of five of the indicators deemed to be applicable to psychotropic prescribing (see Appendix 4 for PAI operational guidance):
-
The indication for the drug is recorded and upheld in the BNF.
-
The reason for prescribing a drug of limited value is recorded and valid (according to the BNF, the drug is of limited or no clinical value if it is considered by the Joint Formulary Committee to be less suitable for prescribing. The use of the drug may be justifiable under certain circumstances, which should be clearly documented in the patient medical records).
-
A generic (non-branded) product is prescribed if one is available.
-
If a potentially hazardous drug–drug combination is prescribed, the prescriber shows knowledge of the hazard.
-
If the total daily dose is outside the range stated in the BNF, the prescriber gives a valid reason.
In addition, we reviewed relevant NICE guidelines on anxiety, depression, bipolar disorder and schizophrenia34,38,41,85 to identify other appropriate, measurable standards that may be applied to prescribing. As a result, the following measures were also used:
-
the proportion of antipsychotic prescriptions prescribed for GAD
-
the proportion of patients prescribed more than one antipsychotic medication, without it being documented as a changeover period
-
the proportion of benzodiazepine prescriptions issued for longer than 4 weeks, excluding those prescribed for detoxification purposes
-
the proportion of benzodiazepine prescriptions prescribed for GAD or panic disorder.
Prison data set preparation
Using Stata version 12 software (StataCorp LP, College Station, TX, USA), the data were entered into two separate data sets (one for patients and one for prescriptions), linked by an anonymised unique patient identifier generated for the purposes of this research. Data were checked for errors made during data collection/entry. Duplicates were identified and excluded. Range checks were performed to identify impossible numerical values. Consistency checks were used to check for invalid combinations of values (e.g. pregnancy and male sex). Where necessary, continuous (e.g. daily dose) or ordinal variables (e.g. ethnicity) were transformed to form additional categorical variables (e.g. under/over BNF maximum; white/non-white).
Community (Clinical Practice Research Datalink) comparison data
For comparison purposes, we used a data set on a random sample of GP-registered patients in the community from the CPRD. This had been obtained at the time of the preliminary east of England study under a free-licence scheme funded by the MRC (which closed in 2011), and hence the data were from 2010.
The CPRD (www.cprd.com) is a computerised database of anonymised longitudinal medical records from primary care. It is the largest and most representative primary care database in the UK, containing health data on over 4 million active patients from around 488 UK primary care practices. A well-regarded and powerful research tool, it has been used extensively for observational research in primary care, generating over 700 peer-reviewed publications to date. Data are collected using routinely collected data via GP electronic clinical records systems. Data sets available to researchers comprise anonymised patient records, including clinical data on diagnoses, prescribing, comorbidity and demographic details.
Clinical Practice Research Datalink data sets are restricted to general practices and patient records that consistently meet predefined thresholds for levels of quality and completeness, supplying data that are fit for use in research. Only patient data from practices that are ‘up to standard’ are included in research data sets. Individual patient records are also checked for validity issues that would render them ineligible for use in research. Previous population comparisons have indicated that CPRD patients are representative of the general UK population with respect to age and sex. 86
Figure 1 provides an overview of the method used to sample CPRD patients. All CPRD patients who were (a) alive, (b) aged ≥ 18 years and (c) registered with a GP throughout 1 February and 30 July 2010 were eligible for inclusion in the study. CPRD provided total patient counts detailing the number of patients prescribed at least one medicine from each of the following medication groups at any time within the 6-month period specified: hypnotics and anxiolytics, antipsychotics, antimanic drugs, antidepressants and CNS stimulants, and/or medicines for ADHD. All counts, including denominators, were stratified by age, sex and UK region.
FIGURE 1.
Clinical Practice Research Datalink sampling flowchart. a, Sample size calculated on the basis of the mean proportion of the total sample represented by other regions of England and Wales (7.3%).
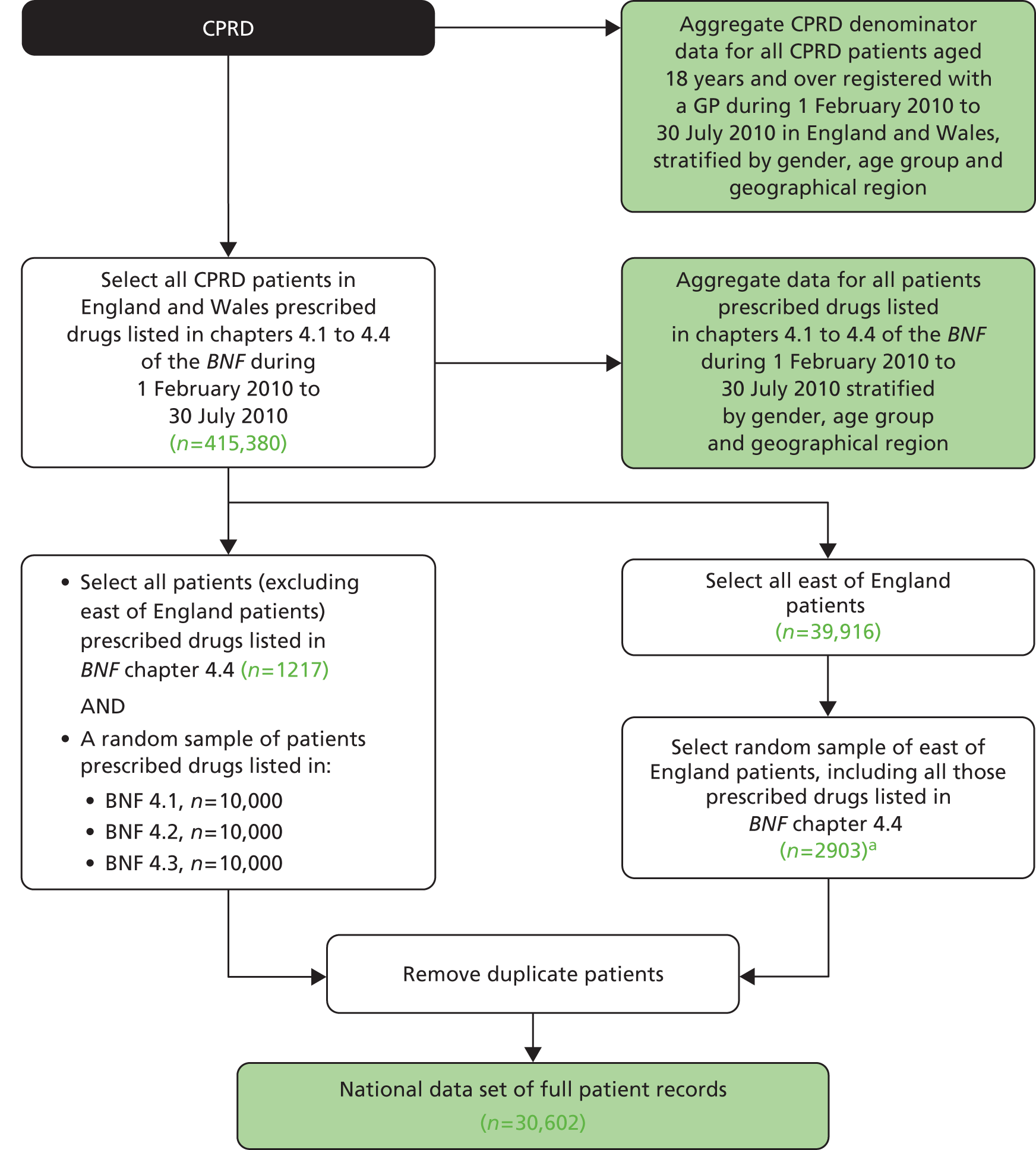
In addition, CPRD supplied anonymised individual patient-level data for a random sample of 30,602 patients who were prescribed psychotropic medicines. We could not obtain individual-patient-level data (prescription details, demographics, etc.) on all patients prescribed psychotropic medicines in the 6-month period specified, as this exceeded the 100,000 case limit set by the CPRD under the terms of the MRC licence. Thus, we obtained aggregate data on all CPRD patients and individual-patient-level data on a randomly sampled subset of CPRD patients prescribed psychotropic medicines for this purpose; we deliberately included all CPRD patients prescribed CNS stimulants listed in BNF 4.4. This sample included:
-
10,000 patients prescribed hypnotics and anxiolytics (4.1)
-
10,000 patients prescribed antipsychotics and drugs for the psychoses (4.2)
-
10,000 patients prescribed antidepressants (4.3)
-
all patients prescribed CNS stimulants or drugs used for ADHD (4.4).
Data analysis
Statistical analyses were performed using Stata software version 12. As the CPRD provided individual-patient data on only a sample of patients prescribed psychotropic medicines, the population denominators supplied (total CPRD counts) had to be adjusted (reduced) accordingly. To generate appropriate denominators for calculating point-prevalence rates, the following calculation was applied to each age/sex stratum (by BNF subchapter):
Period prevalence (6-month) counts and adjusted denominators for CPRD point-prevalence prescribing rates are reported in Appendix 5.
Sex-specific point-prevalence psychotropic prescribing rates [percentage and 95% confidence intervals (CIs)] were generated for prison and community samples for each BNF subchapter, i.e. hypnotics and anxiolytics (4.1); antipsychotics and antimanic drugs (4.2); antidepressants (4.3); and stimulants and drugs used for ADHD (4.4). Rates were indirectly standardised for age where appropriate, using the CPRD data set as the standard population.
Subgroup analyses were performed to examine heterogeneity in prescribing rates (percentage and 95% CIs) among particular subgroups, including (a) sex; (b) prison type (e.g. local, training, open); (c) age group; (d) legal status; and (e) ethnicity. Prevalence ratios (PRs) and appropriate univariate analyses were used to test group differences for statistical significance. Chi-squared tests were used for categorical data and t-tests were used for continuous data.
Key outcomes included the proportion of prescriptions issued in prison that met each of the indicators in the PAI. We also identified the drugs most frequently associated with an inappropriate or no recorded indication, hazardous drug–drug interactions and prescribed daily doses outside the range stated in the BNF.
The mean total cost of psychotropic prescriptions per patient was calculated using prices in the most current version of the BNF. 87 As actual purchasing costs were not available, we calculated the cost for a 28-day prescription for each drug at the dose nearest to the World Health Organization’s defined daily dose (DDD). 88 The DDD has been defined as ‘the assumed average maintenance dose per day for a drug used for its main indication in adults. . . It should be emphasised that the defined daily dose is a unit of measurement and does not necessarily reflect the recommended or Prescribed Daily Dose’. 88
The prescribing acceptability study
The prescribing acceptability study aimed to measure the perceived satisfaction with and acceptability of psychotropic (vs. non-psychotropic) prescribing decisions to patients and their doctors. This part of the study centred on primary care consultations in prison (GP clinics).
Sample
Three prisons participated in this part of the study, comprising one local prison for adult men, one training prison for adult men and a women’s prison. All three prisons had also taken part in the prevalence survey. At selected GP clinics at each prison, researchers aimed to recruit approximately one in four patients who had booked appointments with the GP. To be eligible to participate, patients had to be:
-
aged ≥ 18 years
-
able to consent for themselves (if in doubt, the prison health-care team would be consulted)
-
suitable to be interviewed by a researcher alone (no risk markers); and
-
able to understand spoken English.
In total, data on 156 consultations were generated, which represented 78% of the original target (n = 200).
Procedure
At each prison, researchers worked with participating doctors (n = 6) to identify sessions suitable to sample patients (‘research clinics’). These sessions were all within standard primary care clinics, delivered by GPs (akin to GP consultations in community settings). Standard primary care clinics, rather than dedicated clinics for mental health issues, were sampled to ensure opportunities to recruit prisoners with a wide range of health problems, including common mental illnesses and physical health problems (for comparison purposes). To ensure a more representative sample, sessions were sampled from wings housing remand, convicted and vulnerable prisoners (including clinics on dedicated wings for prisoners who, for safety reasons, need to be segregated).
All doctors had received a participant information sheet and had given formal written consent to participate in the study. All clinics took place over the period July 2013 to October 2013. Once rules had been established for choosing suitable clinics (e.g. one doctor requested that no research should be conducted on days where student doctors were in attendance), the days which would be sampled were not always known in advance to the doctor.
Subsequently, a member of the local health-care team with access to clinic appointment lists identified all eligible patients with appointments booked to see the doctor at these sessions. Patients from each session (approximately one in four) were then selected and approached to participate in no particular order, often depending on availability on the wing. Potential participants were each given a participant information sheet to read or, where preferred, this was explained to them verbally. Written consent was obtained from all patients who agreed to participate.
Over the study period, researchers attended prison GP clinics and asked recruited patients to complete pre- and post-consultation questionnaires (see Appendices 1 and 2), either themselves or as a structured interview if preferred/indicated, for example in cases where participants had literacy problems.
Questionnaires were based on those used by Britten et al. 89 in a similar study based in community primary care settings. Pre-consultation questionnaires aimed to collect basic demographic data, and to identify the nature of the main health problem to be discussed and any secondary health problems. In addition, patients were asked about their expectations and the types of help they wished to receive from the doctor. This was achieved by asking them to indicate their agreement with a series of statements on a three-point scale (agree, uncertain, disagree). Statements addressed areas such as diagnoses, prescribing, medication advice, communication and referrals. After the consultation, each patient was asked to complete a post-consultation questionnaire. These aimed to measure help received and satisfaction with outcomes, including any new prescriptions or changes to medicines.
Following consultations, the doctor was also asked to complete a post-consultation questionnaire for each participating patient in the study (see Appendix 3). In all cases, doctors were not aware which patients were participating in the study until after their consultation. This questionnaire was aimed at measuring understanding of patients’ health problems, perceived pressure to prescribe and satisfaction with prescribing decisions. Doctors were also asked to provide details of drugs prescribed, and whether or not they were strictly indicated.
Data analysis
Key outcome measures included:
-
the proportion of patients who, prior to the consultation, wish to start, change or stop a psychotropic prescription
-
the proportion of patients who, following the consultation, received a prescription; were satisfied with the consultation; and were happy with the prescribing decision
-
the proportion of doctors who, following the consultation, were satisfied with the consultation; felt pressured to write a prescription; and felt comfortable with the prescribing decision (including the decision to prescribe nothing)
-
the proportion of prescriptions that were unwanted (by the patient); and not strictly indicated (in the doctor’s opinion).
Descriptive statistics (percentages, frequencies and means) were used to analyse questionnaire responses. Differences between consultations involving psychotropic versus other types of medication were also compared using prevalence ratios (PRs). Predictors of prescribing outcomes, satisfaction and pressure to prescribe were also identified.
Chapter 3 Results
All percentages reported are valid percentages, unless otherwise stated. Total counts may not be equal to the sum of row counts as a result of missing data.
Rates of psychotropic prescribing in prison
Sample characteristics
Table 5 provides an age and sex breakdown of the samples drawn from prisons and the wider community (via the CPRD). Overall, 6052 male prisoners and 785 women prisoners were included in the survey. Based on available prison population statistics dated 26 July 2013 (the week of the final census day), this sample represented 7.5% of the male prisoner population and 20.5% of the female prisoner population.
| Sample | Age group (years), % (n) | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| 18–24 | 25–34 | 35–44 | 45–54 | 55–64 | 65–74 | 75+ | ||
| Prisoners | ||||||||
| Men | 30.5 (1847) | 28.4 (1718) | 19.0 (1148) | 13.0 (785) | 5.3 (323) | 2.8 (169) | 1.0 (61) | 100 (6052) |
| Women | 20.9 (164) | 33.5 (263) | 30.4 (239) | 11.7 (92) | 2.2 (17) | 1.0 (8) | 0.0 (0) | 100 (785) |
| Community: whole CPRD counts | ||||||||
| Men | 10.6 (150,059) | 16.1 (227,956) | 19.1 (270,532) | 18.8 (266,973) | 15.8 (223,495) | 11.1 (157,767) | 8.6 (121,565) | 100 (1,418,347) |
| Women | 9.8 (143,783) | 15.6 (228,765) | 17.8 (261,060) | 17.6 (257,306) | 15.3 (224,179) | 11.5 (168,266) | 12.3 (180,489) | 100 (1,463,848) |
| Community: random sample of patients prescribed psychotropic medicines | ||||||||
| Men | 7.0 (770) | 10.5 (1149) | 16.4 (1802) | 18.0 (1981) | 18.6 (2047) | 14.1 (1549) | 15.3 (1682) | 100 (10,980) |
| Women | 4.4 (868) | 9.9 (1934) | 15.0 (2946) | 17.7 (3465) | 17.0 (3338) | 14.7 (2889) | 21.3 (4182) | 100 (19,622) |
The CPRD supplied aggregate denominator data for all patients who met the inclusion criteria, which totalled 1,418,347 men and 1,463,848 women (see Table 5). Counts of patients prescribed psychotropic medication within a 6-month period in 2010 were also supplied, broken down by age and sex. In addition, we obtained individual-level patient and prescription data on a random subsample of 10,980 men and 19,622 women prescribed psychotropic medication (see Table 5). Figure 2 provides an illustration of the age differences among the prison and community samples. Individuals in the prison sample were clearly younger: 91% of men and 97% of women in prison were aged ≤ 54 years, compared with 52% of men and 47% of women in the community (CPRD) sample.
FIGURE 2.
Sample characteristics, by age and sex.
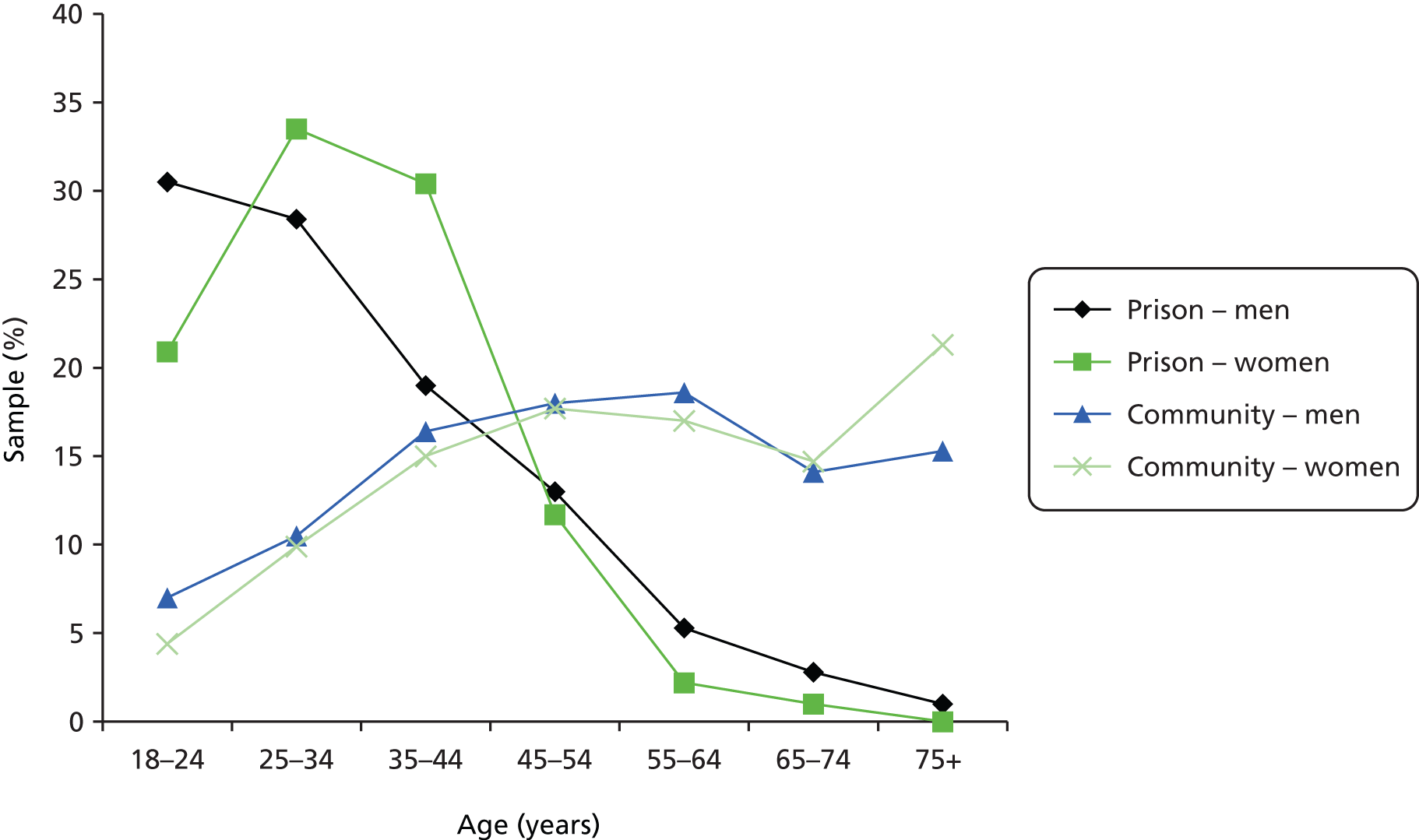
Table 6 provides a detailed breakdown of the characteristics of the prisoner sample. Eleven prisons were included in the study. Among the nine participating male prisons, three were category C training prisons, three were adult local prisons, two were institutions for young offenders and one was a category D open prison. Two closed women’s prisons were included. Among the prisoners included in the sample, 88.5% were male, 86.3% were sentenced and 82.9% were of white ethnicity. In 10 prisons, primary health-care services were delivered by NHS providers; in one prison, services were delivered by a social enterprise.
| Characteristics | n (%) |
|---|---|
| Sex | |
| Male | 6052 (88.5) |
| Female | 785 (11.5) |
| Prison type | |
| Local | 2192 (32.1) |
| Young offender | 1074 (15.7) |
| Female-only | 785 (11.5) |
| Open | 598 (8.7) |
| Legal status | |
| Sentenced | 5898 (86.3) |
| Unsentenced | 924 (13.5) |
| Othera | 15 (0.2) |
| Ethnicity | |
| White | 5620 (82.9) |
| Black | 574 (8.5) |
| Asian | 348 (5.1) |
| Mixed | 182 (2.7) |
| Other | 57 (0.8) |
| Age group (years) | |
| 18–24 | 2011 (29.4) |
| 25–34 | 1981 (29.0) |
| 35–44 | 1387 (20.3) |
| 45–54 | 877 (12.8) |
| 55–64 | 340 (5.0) |
| 65–74 | 177 (2.6) |
| 75+ | 61 (0.9) |
| Total | 6837 (100) |
Rates of psychotropic prescribing in prison and the community
Table 7 describes psychotropic medicine point-prevalence prescribing rates for patients in the community, stratified by age and sex. Overall, 5.8% of men and 11.8% of women were in receipt of at least one prescribed psychotropic medication on 30 July 2010. Antidepressants were the most commonly prescribed type of medication, prescribed to 4.6% of men and 10.0% of women. Overall rates of psychotropic prescribing were significantly higher among women than men (PR 2.03, 95% CI 1.98 to 2.09); this was a consistent finding across all medication types, except CNS stimulants/medicines for ADHD. Rates of prescribing increased with age across all medication types, except CNS stimulants/medicines for ADHD, which (as expected) were highest among the 18–24 age group.
| Sample | Age group (years), % (n) | |||||||
|---|---|---|---|---|---|---|---|---|
| 18–24 | 25–34 | 35–44 | 45–54 | 55–64 | 65–74 | 75+ | All | |
| Men | ||||||||
| Hypnotics and anxiolytics | 0.3 (62) | 0.6 (138) | 0.9 (274) | 1.3 (366) | 1.6 (383) | 2.3 (377) | 4.2 (482) | 1.4 (2082) |
| Antipsychotics | 0.5 (133) | 0.8 (272) | 1.1 (414) | 1.2 (486) | 1.3 (442) | 1.5 (322) | 2.1 (361) | 1.1 (2430) |
| Antidepressants | 1.2 (117) | 2.7 (395) | 4.2 (758) | 5.1 (876) | 6.3 (911) | 6.0 (570) | 7.2 (566) | 4.6 (4183) |
| CNS stimulants | 0.1 (203) | 0.0 (54) | 0.0 (50) | 0.0 (54) | 0.0 (48) | 0.0 (28) | 0.0 (20) | 0.0 (457) |
| Any | 2.1 (401) | 3.4 (630) | 5.3 (1083) | 6.4 (1269) | 7.7 (1327) | 8.3 (977) | 11.4 (1094) | 5.8 (6781) |
| Women | ||||||||
| Hypnotics and anxiolytics | 0.3 (43) | 0.7 (161) | 1.3 (339) | 2.0 (525) | 2.8 (653) | 4.2 (718) | 7.4 (1317) | 2.5 (3756) |
| Antipsychotics | 0.4 (70) | 0.6 (209) | 1.1 (433) | 1.7 (659) | 1.7 (562) | 2.1 (515) | 3.2 (847) | 1.6 (3295) |
| Antidepressants | 3.3 (266) | 5.8 (803) | 9.7 (1464) | 11.7 (1767) | 12.1 (1637) | 11.8 (1244) | 13.5 (1677) | 10.0 (8858) |
| CNS stimulants | 0.0 (53) | 0.0 (44) | 0.0 (79) | 0.0 (63) | 0.0 (51) | 0.0 (26) | 0.0 (19) | 0.0 (335) |
| Any | 3.6 (366) | 6.2 (995) | 10.4 (1781) | 12.9 (2213) | 13.7 (2141) | 14.7 (1828) | 19.6 (2822) | 11.8 (12,146) |
Table 8 describes psychotropic medicine point-prevalence prescribing rates for prisoner patients, stratified by age and sex. Overall, 16.9% of men and 47.9% of women were in receipt of at least one prescribed psychotropic medication. As with the community sample, antidepressants were the most common type of psychotropic medication prescribed in prison, prescribed to 13.2% of men and 41.1% of women. Antipsychotics were prescribed to 11.7% of women and 4.3% of men. Rates of psychotropic prescribing were significantly higher among women than men (PR 2.84, 95% CI 2.52 to 3.20); this was a consistent finding across all medication types, except CNS stimulants/medicines for ADHD. Rates of prescribing appeared to be lowest in the youngest age group (18–24 years), with the exception of CNS stimulants/medicines for ADHD, which (as expected) were highest among this group.
| Sample | Age group (years), % (n) | |||||||
|---|---|---|---|---|---|---|---|---|
| 18–24 | 25–34 | 35–44 | 45–54 | 55–64 | 65–74 | 75+ | All | |
| Men | ||||||||
| Hypnotics and anxiolytics | 0.5 (9) | 1.1 (19) | 1.8 (21) | 1.0 (8) | 0.3 (1) | 1.2 (2) | 1.6 (1) | 1.0 (62) |
| Antipsychotics | 3.2 (59) | 5.1 (87) | 5.3 (61) | 4.3 (34) | 3.7 (12) | 1.2 (2) | 0.0 (0) | 4.3 (258) |
| Antidepressants | 6.0 (111) | 13.3 (228) | 19.9 (228) | 16.2 (127) | 22.6 (73) | 16.0 (27) | 6.6 (4) | 13.2 (801) |
| CNS stimulants | 2.2 (41) | 0.2 (3) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.7 (44) |
| Any | 10.3 (191) | 17.3 (297) | 23.3 (267) | 19.2 (151) | 24.1 (78) | 17.8 (30) | 8.2 (5) | 16.9 (1024) |
| Women | ||||||||
| Hypnotics and anxiolytics | 3.0 (5) | 9.5 (25) | 10.9 (26) | 6.5 (6) | 0.0 (0) | 0.0 (0) | N/A | 7.9 (62) |
| Antipsychotics | 8.5 (14) | 12.5 (33) | 13.4 (32) | 10.9 (10) | 17.6 (3) | 0.0 (0) | N/A | 11.7 (92) |
| Antidepressants | 21.2 (35) | 43.7 (115) | 46.4 (111) | 55.4 (51) | 41.2 (7) | 25.0 (2) | N/A | 41.1 (323) |
| CNS stimulants | 1.8 (3) | 0.0 (0) | 0.4 (1) | 0.0 (0) | 0.0 (0) | 0.0 (0) | N/A | 0.5 (4) |
| Any | 26.8 (44) | 49.8 (131) | 55.6 (133) | 62.0 (57) | 41.2 (7) | 25 (2) | N/A | 47.9 (376) |
Figure 3 shows the relationship between psychotropic prescribing and age among patients in prison and the community (the data for these figures can be found in Tables 7 and 8). Among prisoners, psychotropic prescribing appears to peak in the middle age bands. In the community, however, psychotropic prescribing appears to show a linear increase with age.
FIGURE 3.
Prison and community psychotropic point-prevalence prescribing rates, by age group and sex.
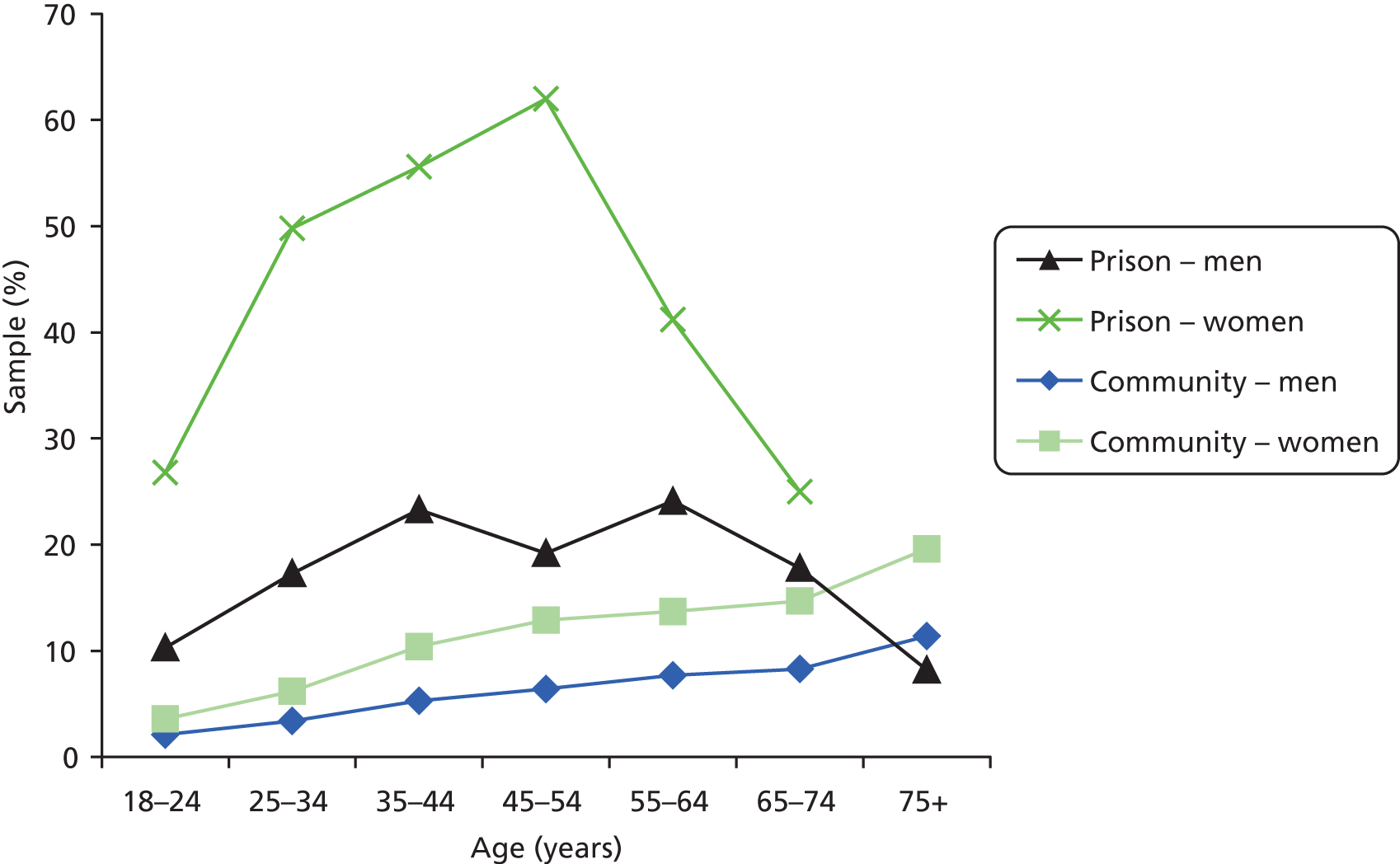
Table 9 compares psychotropic prescribing rates in prison and in the community. After adjusting for age differences, overall rates of psychotropic prescribing in prison were four times higher among men (PR 4.02, 95% CI 3.75 to 4.30) and almost six times higher among women (PR 5.95, 95% CI 5.36 to 6.61) than among patients in the community. Even after adjusting for age differences, rates of CNS stimulant prescribing, in particular, were much higher in prisons: 13 times higher among men (PR 12.99, 95% CI 9.48 to 17.80) and 19 times higher among women (PR 19.01, 95% CI 7.07 to 51.10). Women in prison were over seven times more likely to be prescribed hypnotics and anxiolytics than women in the community (PR 7.3, 95% CI 5.6 to 9.4); in comparison, men in prison were only slightly more likely to be prescribed these drugs than men in the community (PR 1.3, 95% CI 1.0 to 1.6). Rates of antipsychotic prescribing were at least 12 times higher among women in prison (PR 12.74, 95% CI 10.30 to 15.76) and almost five times higher among men in prison (PR 4.81, 95% CI 4.21 to 5.50) than among community patients.
| BNF subchapter | Community (reference group) | Prisoners | PR (95% CI) | |||
|---|---|---|---|---|---|---|
| n (%) | 95% CI | n (%) | 95% CI | Crude | Adjusted | |
| Men | ||||||
| Hypnotics and anxiolytics | 2082 (1.4) | 1.3 to 1.4 | 62 (1.0) | 0.8 to 1.3 | 0.74 (0.56 to 0.96) | 1.27 (0.97 to 1.64) |
| Antipsychotics | 2430 (1.1) | 1.1 to 1.2 | 258 (4.3) | 3.8 to 4.8 | 3.67 (3.21 to 4.18) | 4.81 (4.21 to 5.50) |
| Antidepressants | 4183 (4.6) | 4.4 to 4.7 | 801 (13.2) | 12.4 to 14.1 | 2.87 (2.66 to 3.10) | 4.16 (3.84 to 4.50) |
| CNS stimulants | 457 (0.0) | 0.0 to 0.0 | 44 (0.7) | 0.5 to 9.7 | 22.57 (16.17 to 30.79) | 12.99 (9.48 to 17.80) |
| Any | 6781 (5.8) | 5.7 to 5.9 | 1024 (16.9) | 16.0 to 17.9 | 2.90 (2.71 to 3.10) | 4.02 (3.75 to 4.30) |
| Women | ||||||
| Hypnotics and anxiolytics | 3756 (2.5) | 2.5 to 2.6 | 62 (7.9) | 6.1 to 10.0 | 3.11 (2.38 to 4.00) | 7.40 (5.73 to 9.55) |
| Antipsychotics | 3295 (1.6) | 1.5 to 1.6 | 92 (11.7) | 9.6 to 14.2 | 7.49 (6.01 to 9.22) | 12.74 (10.30 to 15.76) |
| Antidepressants | 8858 (10.0) | 9.8 to 10.2 | 323 (41.1) | 37.7 to 44.7 | 4.09 (3.65 to 4.58) | 5.55 (4.96 to 6.22) |
| CNS stimulants | 335 (0.0) | 0.0 to 0.0 | 4 (0.5) | 0.0 to 0.1 | 22.29 (6.04 to 57.61) | 19.01 (7.07 to 51.10) |
| Any | 12,146 (11.8) | 11.6 to 12.0 | 376 (47.9) | 44.4 to 51.5 | 4.05 (3.65 to 4.49) | 5.95 (5.36 to 6.61) |
Summary: rates of psychotropic prescribing in prison and the community
-
Overall, 17% of the men and 48% of the women we surveyed in prison were prescribed at least one psychotropic medicine.
-
After adjusting for age differences, psychotropic prescribing rates were four times higher among men and six times higher among women than in the community.
-
As in the community, antidepressants were the most common type of psychotropic medication prescribed to prisoners. Overall, 13% of men and 41% of women prisoners surveyed were prescribed antidepressants.
-
Rates of CNS stimulant prescribing for ADHD were particularly high among prisoners of both sexes when compared with patients in the community.
-
Prescribing rates for hypnotics and anxiolytics were much higher among women in prison, but were only slightly higher among men in prison, than in the community.
Drug type
In total, 1400 (out of 6837) of the prisoners surveyed were prescribed at least one psychotropic medicine on census days. These prisoners were in receipt of 1740 separate prescriptions for psychotropic medicines. In the community sample, 18,927 patients were prescribed at least one psychotropic medicine, generating a total of 27,621 prescriptions. Thus, among individuals prescribed at least one psychotropic medicine, prisoners were prescribed a mean of 1.2 prescriptions (range 1–5), compared with 1.5 prescriptions among patients in the community (range 1–8). Community patients were more likely than patients in prison to be prescribed more than one psychotropic medicine concurrently (33.0% vs. 20.1%; PR 1.64, 95% CI 1.48 to 1.83).
Table 10 describes the breakdown of these prescriptions by BNF subchapter. This shows that two-thirds (67.5%) of all psychotropic prescriptions in prison were for antidepressants, one-fifth (22.1%) were for antipsychotics, 7.5% were for hypnotics and anxiolytics and 2.8% were for CNS stimulants. Antipsychotic and CNS stimulant prescriptions accounted for a similar proportion of all psychotropic prescriptions in prisons and the community. Antidepressants accounted for a larger proportion of prescriptions in prisons, while hypnotics and anxiolytics accounted for a lower proportion, than in the community.
| BNF subchapter | Community, n (%) | Prison, n (%) |
|---|---|---|
| Hypnotics and anxiolytics | 6395 (23.2) | 131 (7.5) |
| Antipsychotics | 6404 (23.2) | 385 (22.1) |
| Antidepressants | 14,028 (50.8) | 1175 (67.5) |
| CNS stimulants/ADHD | 810 (2.9) | 49 (2.8) |
| Total | 27,621 (100) | 1740 (100.0) |
Table 11 describes which individual medicines were most frequently prescribed in prison, compared with the wider community. In prison, diazepam accounted for half (53.4%) of all hypnotic and anxiolytic prescriptions. Among individuals prescribed hypnotics and anxiolytics, prisoners were twice as likely as patients in the community to receive diazepam (PR 2.48, 95% CI 2.10 to 2.93). In the community, temazepam was the third most frequently prescribed hypnotic and anxiolytic and accounted for 18.5% of these prescriptions, but was prescribed only twice in prison. The most frequently prescribed antipsychotic drugs in prison were olanzapine and quetiapine; both of these drugs were more commonly prescribed in prison than in the community (PR 2.12, 95% CI 1.80 to 2.49; PR 2.25, 95% CI 1.90 to 2.67). There were 49 instances of CNS stimulant prescribing in prison. Methylphenidate accounted for 75.5% (n = 37) of prescriptions, while atomoxetine accounted for the remaining 24.5% (n = 12).
| Rank | 4.1: hypnotics and anxiolytics, % (n) | 4.2: antipsychotics, % (n) | 4.3: antidepressants, % (n) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Drug | Prison | Community | Drug | Prison | Community | Drug | Prison | Community | |
| 1 | Diazepam | 53.4 (70) | 21.5 (1376) | Olanzapine | 30.9 (119) | 14.6 (935) | Mirtazapine | 35.2 (413) | 8.3 (1157) |
| 2 | Zopiclone | 16.0 (21) | 32.3 (2067) | Quetiapine | 28.6 (110) | 12.7 (812) | Citalopram | 18.2 (214) | 27.3 (3826) |
| 3 | Chlordiazepoxide | 13.7 (18) | 0.9 (55) | Risperidone | 10.1 (39) | 9.0 (573) | Sertraline | 13.0 (153) | 7.4 (1043) |
| 4 | Promethazine | 9.2 (12) | 2.6 (164) | Carbamazepine | 9.4 (36) | 21.2 (1355) | Fluoxetine | 11.2 (132) | 12.8 (1801) |
| 5 | Melatonin | 2.3 (3) | 0.8 (48) | Chlorpromazine | 2.6 (10) | 2.9 (186) | Amitriptyline | 8.8 (104) | 16.7 (2338) |
| All | 100 (131) | 100 (6395) | 100 (385) | 100 (6404) | 100 (1175) | 100 (14,028) | |||
Collectively, SSRIs accounted for the greatest percentage of antidepressant prescriptions in prison (45.1%), TCA drugs accounted for 14.9% and other antidepressants constituted the remainder (40.0%). TCAs accounted for a lower proportion of antidepressant prescriptions in prison than in the community (14.9% vs. 26.5%; PR 0.56, 95% CI 0.49 to 0.65). Mirtazapine was the most frequently prescribed antidepressant in prison (35.2%), but accounted for just 8.3% of community antidepressant prescriptions (see Table 11). Among individuals prescribed antidepressants, prisoners were four times as likely as patients in the community to receive mirtazapine (PR 4.26, 95% CI 3.87 to 4.69).
Table 12 shows the median prescribed daily doses for the most frequently prescribed medications in prison. The median prescribed dose for diazepam, the most popular hypnotic/anxiolytic drug, was 10 mg. This represented one-third of the maximum daily dose identified in the BNF for anxiety (30 mg) and 100% of the World Health Organization’s DDD. Median prescribed doses for the two most popular antipsychotics, olanzapine and quetiapine, were 10 mg and 300 mg, respectively. For olanzapine, this represented 50% of the BNF maximum dose and 100% of the DDD. For quetiapine, this represented 37.5% of the BNF maximum dose and 75% of the DDD. The median prescribed dose for mirtazapine, the leading antidepressant, was 30 mg. This represented two-thirds (66.7%) of the BNF maximum dose and equalled the DDD. In all cases except for melatonin, the median dose prescribed in the community was equal to or lower than the median dose prescribed in prison.
| Rank | 4.1: hypnotics and anxiolytics, median dose (% of BNF maximum) | 4.2: antipsychotics, median dose (% of BNF maximum) | 4.3: antidepressants, median dose (% of BNF maximum) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Drug | Prison | Communitya | Drug | Prison | Communitya | Drug | Prison | Communitya | |
| 1 | Diazepam | 10 mg (33.3) | 5 mg (16.7) | Olanzapine | 10 mg (50.0) | 10 mg (50.0) | Mirtazapine | 30 mg (66.7) | 30 mg (66.7) |
| 2 | Zopiclone | 7.5 mg (100.0) | 7.5 mg (100.0) | Quetiapine | 300 mg (37.5) | 100 mg (12.5) | Citalopram | 20 mg (50.0) | 20 mg (50.0) |
| 3 | Chlordiazepoxide | 25 mg (10.0) | 5 mg (2.0) | Risperidone | 3 mg (18.8) | 2 mg (12.5) | Sertraline | 100 mg (50.0) | 100 mg (50.0) |
| 4 | Promethazine | 25 mg (50.0) | 25 mg (50.0) | Carbamazepine | 400 mg (20.0) | 200 mg (10.0) | Fluoxetine | 20 mg (33.3) | 20 mg (33.3) |
| 5 | Melatonin | 2 mg (100.0) | 3 mg (150.0) | Chlorpromazine | 87.5 mg (8.8) | 50 mg (5.0) | Amitriptyline | 25 mg (12.5) | 25 mg (12.5) |
Summary: individual drugs
-
Patients in the community were more likely than prisoners to be prescribed more than one psychotropic medicine concurrently.
-
Antidepressants accounted for a larger proportion of prescriptions in prisons than in the community, while hypnotics and anxiolytics accounted for a smaller proportion.
-
Diazepam accounted for half (53.4%) of all hypnotic and anxiolytic prescriptions in prison. While temazepam was the third most frequently prescribed drug in the community, it was prescribed only twice in prison.
-
Prisoners prescribed an antidepressant were at least four times as likely to receive mirtazapine as patients prescribed an antidepressant in the community.
-
Prisoners prescribed an antipsychotic were twice as likely as patients in the community to be prescribed olanzapine and quetiapine.
-
The median doses of antipsychotics prescribed in prison were all ≤ 50% of the BNF maximum dose.
-
Median doses of psychotropic drugs prescribed in the community were usually equal to or lower than median doses prescribed in prison.
Costs
Table 13 describes monthly prescription costs for drugs in each BNF subchapter for men and women. Across prisoners as a whole, the mean overall psychotropic prescription cost per patient was £1.47 for men and £12.98 for women; therefore, costs were almost nine times higher among women. Among women, hypnotics and anxiolytics accounted for the highest proportion of total drug costs; in part, this was due to increased use of the liquid form of diazepam in female-only prisons compared with male-only prisons (80% vs. 25%), which is a more costly preparation than standard tablets (93 pence for 28 tablets vs. £133.63 for the oral solution). Indeed, psychotropic prescriptions issued to women were almost 10 times more likely than those issued to men to be for non-standard preparations, for example liquid, depot and/or orodispersible tablets (19.33% vs. 2.0%; PR 9.8, 95% CI 6.38 to 15.19).
| BNF subchapter | Men | Women | ||
|---|---|---|---|---|
| £/patient | Rangea | £/patient | Range | |
| Hypnotics and anxiolytics | 0.18 | 0.93–133.63 | 5.61 | 0.93–160.57 |
| Antipsychotics | 0.50 | 1.21–143.51 | 3.83 | 1.21–353.08 |
| Antidepressants | 0.42 | 0.95–29.33 | 3.31 | 0.95–128.47 |
| CNS stimulants | 0.35 | 15.29–83.28 | 0.20 | 32.67–47.95 |
| Any | 1.45 | 0.93–143.51 | 12.95 | 0.93–353.08 |
Table 14 describes monthly prescription costs for different prison types (male prisons only). The highest mean overall psychotropic prescription cost was in prisons for young men, at £15.40 per patient. This appears to be attributable to the relatively high cost per patient of CNS stimulants (£11.81 per patient): these drugs were relatively expensive compared with other psychotropics and were prescribed more frequently in these establishments. Costs for adult male local and training prisons were relatively similar overall (£6.74 vs. £5.81); while local prisons spent more on hypnotics and anxiolytics (£1.83 vs. £0.04), training prisons spent more on antipsychotics (£3.18 vs. £2.09). The lowest costs were observed in the open male establishment, with an overall cost of £3.97 per patient.
| BNF subchapter | Local male | Training male | Young male (YOI) | Open male | ||||
|---|---|---|---|---|---|---|---|---|
| £/patient | Range | £/patient | Range | £/patient | Range | £/patient | Range | |
| Hypnotics and anxiolytics | 1.83 | 0.93–133.63 | 0.04 | 0.93–2.33 | 0.57 | 2.33–26.94 | 0.03 | 1.29–1.29 |
| Antipsychotics | 2.09 | 1.21–137.23 | 3.18 | 1.21–143.51 | 1.88 | 1.21–98.52 | 1.22 | 1.21–27.21 |
| Antidepressants | 2.00 | 0.95–28.67 | 2.38 | 0.95–29.33 | 1.14 | 0.95–28.38 | 2.73 | 0.95–28.38 |
| CNS stimulants | 0.82 | 15.29–83.28 | 0.21 | 15.29–83.28 | 11.81 | 15.29–83.28 | 0.00 | N/A |
| Any | 6.74 | 0.93–137.23 | 5.81 | 0.93–143.51 | 15.40 | 0.95–98.52 | 3.97 | 0.95–28.38 |
Summary: costs
-
The mean overall psychotropic prescription cost per patient was £1.47 for men and £12.98 for women: costs were almost nine times higher among women.
-
Increased drug costs among women were partly due to the increased use of the liquid form of diazepam in female prisons compared with male prisons, which is a more costly preparation than standard tablets.
-
Prisons housing young men had the highest mean overall psychotropic prescription costs, at £15.40 per patient.
-
The lowest costs were observed in the open male establishment, with an overall cost of £3.97 per patient.
Subgroup analyses
In the following sections, psychotropic prescribing rates will be stratified by sex, legal status, prison type and ethnicity.
Sex
Table 15 compares rates of psychotropic prescribing among men and women in prison. Women in prison were nearly three times as likely as men in prison to be prescribed psychotropic medication (PR 2.65, 95% CI 2.35 to 2.99). In particular, women were relatively more likely to be prescribed hypnotic and anxiolytic drugs (PR 7.84, 95% CI 5.42 to 11.36).
| BNF subchapter | Men (reference group) | Women | PR (95% CI) | |||
|---|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | Crude | Adjusted | |
| Hypnotics and anxiolytics | 62 | 1.0 (0.8 to 1.3) | 62 | 7.9 (6.1 to 10.0) | 7.84 (5.42 to 11.36) | 6.73 (4.68 to 9.69) |
| Antipsychotics | 258 | 4.3 (3.8 to 4.8) | 92 | 11.7 (9.6 to 14.2) | 2.78 (2.17 to 3.55) | 2.56 (2.01 to 3.26) |
| Antidepressants | 801 | 13.2 (12.4 to 14.1) | 323 | 41.1 (37.7 to 44.7) | 3.10 (2.72 to 3.54) | 2.87 (2.51 to 3.28) |
| CNS stimulants | 44 | 0.7 (0.5 to 9.7) | 4 | 0.5 (0.0 to 1.3) | 0.70 (0.18 to 1.92) | 0.97 (0.35 to 2.70) |
| Any | 1024 | 16.9 (16.0 to 17.9) | 376 | 47.9 (44.4 to 51.5) | 2.83 (2.51 to 3.19) | 2.65 (2.35 to 2.99) |
Legal status
Table 16 compares rates of psychotropic prescribing in convicted and unconvicted prisoners. Among men, rates of psychotropic prescribing were higher among unconvicted prisoners (PR 1.33, 95% CI 1.15 to 1.54). Among women, rates of psychotropic prescribing were similar among convicted and unconvicted prisoners.
| BNF subchapter | Legal status, n (%) | |
|---|---|---|
| Convicted | Unconvicted | |
| Men | ||
| Hypnotics and anxiolytics | 43 (0.8) | 16 (2.0) |
| Antipsychotics | 207 (3.9) | 49 (6.3) |
| Antidepressants | 670 (12.7) | 127 (16.2) |
| CNS stimulants | 40 (0.8) | 3 (0.4) |
| Any | 853 (16.2) | 169 (21.6) |
| Women | ||
| Hypnotics and anxiolytics | 47 (7.3) | 15 (10.7) |
| Antipsychotics | 67 (10.4) | 21.0 (15.0) |
| Antidepressants | 260 (40.4) | 55 (39.3) |
| CNS stimulants | 4 (0.6) | 0 (0) |
| Any | 300 (46.7) | 69 (49.3) |
Prison type
Table 17 compares rates of psychotropic prescribing in different types of prison for adult and young men. Overall, rates of psychotropic prescribing were lowest at the open prison. Prisons for young men also had relatively low rates of psychotropic prescribing; this was consistent across all medication types except CNS stimulants. Local male prisons had the highest rates of psychotropic prescribing, with 22.3% of men prescribed psychotropic drugs overall.
| BNF subchapter | Type of prison, n (%) | |||
|---|---|---|---|---|
| Local male | Training male | Young male (YOI) | Open male | |
| Hypnotics and anxiolytics | 42 (1.9) | 14 (0.6) | 5 (0.5) | 1 (0.2) |
| Antipsychotics | 122 (5.6) | 92 (4.2) | 35 (3.3) | 9 (1.5) |
| Antidepressants | 385 (17.6) | 332 (15.2) | 51 (4.7) | 33 (5.5) |
| CNS stimulants | 10 (0.5) | 2 (0.1) | 32 (3.0) | 0 (0.0) |
| Any | 489 (22.3) | 402 (18.4) | 101 (9.4) | 38 (6.4) |
Ethnicity
Rates of prescribing were compared across different ethnic groupings (Table 18). Overall, rates of prescribing were highest in prisoners who reported being of white ethnic origin. White prisoners were twice as likely as prisoners from black and minority ethnic (BME) groups to be prescribed psychotropic medication (22.2% vs. 9.3%; PR 2.38, 95% CI 1.98 to 2.87).
| BNF subchapter | Ethnicity, n (%) | ||||
|---|---|---|---|---|---|
| White | Black | Asian | Mixed | Chinese/other | |
| Hypnotics and anxiolytics | 117 (2.1) | 2 (0.3) | 0 (0.0) | 3 (1.6) | 0 (0.0) |
| Antipsychotics | 302 (5.4) | 20 (3.5) | 10 (2.9) | 3 (1.6) | 2 (3.5) |
| Antidepressants | 1017 (18.1) | 28 (4.9) | 22 (6.3) | 15 (8.2) | 5 (8.8) |
| CNS stimulants | 38 (0.7) | 6 (1.0) | 2 (0.6) | 0 (0) | 1 (1.8) |
| Any | 1247 (22.2) | 49 (8.5) | 32 (9.2) | 20 (11.0) | 7 (12.3) |
Summary: subgroup analyses
-
Among prisoners, women were nearly three times as likely as men to be prescribed psychotropic medication. In particular, women were more than seven times as likely to be prescribed hypnotic and anxiolytic drugs.
-
Among prisoners, psychotropic prescribing appears to peak in the middle age bands and decline in older age. In the community, however, psychotropic prescribing appears to show a linear increase with age, with the highest rates in the older age bands.
-
Local male prisons had the highest rates of psychotropic prescribing, with 22.1% of men prescribed psychotropic drugs overall. Overall, rates of psychotropic prescribing were lowest in the open prison. Prisons for young men also exhibited lower prescribing rates; this was consistent across all medication types except CNS stimulants.
-
Lower rates of psychotropic prescribing were observed in BME groups in prison.
The appropriateness of psychotropic prescribing in prison
In total, 1400 of the prisoners surveyed were prescribed at least one psychotropic medicine on census days. These prisoners were in receipt of 1740 separate prescriptions for psychotropic medicines. The PAI was applied to each individual prescription to determine different aspects of appropriateness. Table 19 describes the proportion of psychotropic prescriptions that met each of the indicators on the PAI.
| PAI | BNF subchapter, n (%) | ||||
|---|---|---|---|---|---|
| 4.1 | 4.2 | 4.3 | 4.4 | All | |
| 1: The indication for the drug is recorded and upheld in the BNF | 111 (88.1) | 196 (51.6) | 774 (66.2) | 45 (91.8) | 1126 (65.3) |
| 2: The reason for prescribing a drug of limited value is recorded and valid | 119 (98.4) | 379 (100) | 1147 (98.9) | 49 (100) | 1710 (99.1) |
| 3: A generic product is prescribed, if one is available | 130 (99.2) | 377 (97.9) | 1175 (100) | 49 (100) | 1731 (99.5) |
| 4: If a potentially hazardous drug–drug combination is prescribed, the prescriber shows knowledge of the hazard | 118 (96.7) | 290 (77.5) | 1000 (86.2) | 46 (93.9) | 1454 (85.3) |
| 5: If the total daily dose is outside the range stated in the BNF or SPC, the prescriber gives a valid reason | 114 (95.0) | 308 (80.6) | 1130 (96.5) | 46 (94.8) | 1598 (92.9) |
Prescribing appropriateness indicator 1: indication for the drug
Overall, the indication for the drug was recorded and upheld in the BNF in 65.3% of cases (see Table 19). Compared with other psychotropic medications, antipsychotic prescriptions were the least likely to be accompanied by a valid indication in the patient notes, with 51.6% of these prescriptions meeting the PAI standard (PR 0.75, 95% CI 0.67 to 0.83).
In 21.1% of cases (n = 364), an invalid indication was recorded for a psychotropic drug (Table 20). Antipsychotic prescriptions were more likely than prescriptions for other psychotropic medications to be accompanied by an invalid (not indicated) diagnosis in the patient notes (35.4% vs. 17.2%; PR 2.03, 95% CI 1.70 to 2.44). The most common invalid indications recorded for antipsychotic prescriptions were personality disorder (n = 50), anger/aggression (not associated with psychosis; n = 16) and anxiety (n = 12). Invalid indications recorded for antidepressant prescriptions included low mood (n = 96), insomnia (n = 25), anxiety (n = 24) and personality disorder (n = 22).
| BNF subchapter | Valid indications (licensed and unlicensed), as listed in the BNFa | Indicated, n (%) | Not indicated, n (%) | No diagnosis, n (%) | Total, N (%) |
|---|---|---|---|---|---|
| Hypnotics and anxiolytics | Anxiety, insomnia, alcohol dependence, benzodiazepine dependence and allergies | 111 (88.1) | 1 (0.8) | 14 (11.11) | 126 (100) |
| Antipsychotics | Schizophrenia, psychosis, bipolar disorder, epilepsy, severe aggression or agitation | 196 (51.6) | 133 (35.0) | 51 (13.4) | 380 (100) |
| Antidepressants | Depression, anxiety, bipolar disorder, OCD and PTSD | 774 (66.2) | 230 (19.7) | 165 (14.1) | 1169 (100) |
| CNS stimulants | ADHD | 45 (91.8) | 0 (0) | 4 (8.2) | 49 (100) |
| All | 1126 (65.3) | 364 (21.1) | 234 (13.6) | 1724 (100) |
A greater proportion of quetiapine (46.0% vs. 19.4%; PR 2.39, 95% CI 1.91 to 2.99) and olanzapine (35.6% vs. 20.0%; PR 1.78, 95% CI 1.37 to 2.31) prescriptions were accompanied by an invalid diagnosis than all other psychotropic medicines.
Prescribing appropriateness indicator 2: drugs of limited value
In 99.1% of cases, drugs of limited value either were not prescribed or were justified with a valid reason in the notes (see Table 19). Overall, there were 17 cases in which limited drugs were prescribed; the most common drug was amitriptyline for depression (n = 14).
Prescribing appropriateness indicator 3: generic prescribing
Overall, generic (non-branded) drugs were prescribed in 99.5% of cases (see Table 19). In total, 62 prescriptions were issued for branded medications. The most common of these was Concerta® XL (Janssen) (a modified release preparation of methylphenidate, a drug prescribed for ADHD), which was prescribed on 27 occasions. In 14.5% of cases in which a branded product was prescribed, a generic alternative was available.
Prescribing appropriateness indicator 4: drug–drug interactions
Overall, a serious (BNF ‘black dot’) drug–drug interaction involving a psychotropic medication was noted in 15.7% of prescriptions (n = 267). In a minority of cases (6.4%), the prescriber recorded the interaction in the notes, thereby showing knowledge of the hazard. In 85.3% of cases, PAI 4 was met, i.e. either there were no potentially serious drug–drug interactions involving psychotropic medicines or the prescriber had shown knowledge of the hazard (see Table 19). Listed below are the most frequently observed interactions and their potential adverse outcomes, as stated in the BNF: note that not all of these potential hazards would necessarily apply to every patient. For example, if the patient did not have epilepsy, lowering of the convulsive threshold would not be hazardous.
-
antipsychotics and antiepileptics (convulsive threshold lowered)
-
SSRI and non-steroidal anti-inflammatory drugs (increased risk of bleeding)
-
SSRI and antiepileptics (convulsive threshold lowered)
-
antipsychotics and methadone (increased risk of ventricular arrhythmias due to QT interval prolongation).
Prescribing appropriateness indicator 5: prescribed daily dose
In 92.9% of cases, the total daily dose was within the range specified in the BNF, or, if not, a valid reason was provided. Note that if there was an indication, we used the dose range for that indication (as described in the BNF). If the indication was invalid, or if there was no indication, we used the smallest minimum and largest maximum dose provided of all indicated conditions listed for the drug in the BNF. The standard was less likely to be met if the drug was an antipsychotic rather than another psychotropic drug (80.6% vs. 96.3%; PR 0.84, 95% CI 0.80 to 0.88).
In 7.2% cases (n = 123), the standard was not met. Among these cases, 95% of the doses prescribed were too low (subtherapeutic). By far the most common drug to be prescribed at subtherapeutic doses was quetiapine (36.8%). In over half (57.1%) of cases where quetiapine was prescribed at subtherapeutic doses, it was for an invalid indication. Other drugs commonly prescribed at subtherapeutic doses included trazodone (15.4%) and risperidone (10.3%).
Other standards
In addition, we measured the extent to which standards derived from relevant NICE guidelines on anxiety, depression, bipolar disorder and schizophrenia33,37,40,84 were met. In summary:
-
Overall, 9.7% of all patients prescribed antipsychotic medication in prison were prescribed more than one antipsychotic concurrently (compared with 10.7% of community patients). In four of these cases (11.8%), this was documented as a changeover period. By far the most common drug used in combination was olanzapine (n = 17).
-
Overall, 2.1% (n = 8) of antipsychotics were prescribed for GAD.
-
Overall, 54.2% (n = 71) of prescriptions for hypnotics and/or anxiolytics were issued for longer than 4 weeks. However, in 70.4% of such cases, the drug was prescribed as part of a benzodiazepine detoxification regime.
-
Four prescriptions were prescribed for GAD or panic disorder (3.1% of all hypnotic and anxiolytic prescriptions).
Summary: the appropriateness of psychotropic prescribing in prison
-
Valid (BNF-listed) indications for psychotropic drugs were recorded in 65.3% of cases.
-
The most common invalid indication recorded for antipsychotic prescriptions was personality disorder.
-
The most common invalid indication recorded for antidepressant prescriptions was low mood.
-
In 92.9% of cases, the total daily dose was within the range specified in the BNF, or, if not, a valid reason was provided. However, one in five (19.4%) antipsychotic prescriptions were prescribed at a subtherapeutic dose too low to treat psychoses.
-
Generic (non-branded) drugs were prescribed in 99.5% of cases.
-
A serious (BNF ‘black dot’) drug–drug interaction involving a psychotropic medication was noted in 15.7% of prescriptions.
-
One in 10 (9.7%) of patients prescribed antipsychotics in prison was prescribed two or more antipsychotic medicines concurrently.
The acceptability of psychotropic prescribing decisions to patients and doctors in prison
This section of the analysis describes the findings of the questionnaire survey, which focused on GP consultations in three prisons.
Sample characteristics
In total, 183 prisoners across three prisons were approached to take part in the questionnaire survey. Of these, 156 prisoners agreed to take part, yielding a response rate of 85.2%.
Table 21 describes the characteristics of the 156 patients recruited to the questionnaire survey. Almost two-thirds (62.8%) of the sample were male and the majority of prisoners were sentenced (87.6%). The mean age was 36 years, and almost half (48.3%) of the sample had been in custody at the current prison for < 6 months. Six GPs were recruited to the study, with an equal split of men and women.
| Characteristics | n (%) |
|---|---|
| Sex | |
| Male | 98 (62.8) |
| Female | 58 (37.2) |
| Prison | |
| A (category B local) | 57 (36.5) |
| B (category C training) | 41 (26.3) |
| C (female) | 58 (37.2) |
| Legal status | |
| Sentenced | 118 (87.6) |
| Unsentenced | 34 (22.4) |
| Time in prison | |
| < 1 month | 33 (21.9) |
| 1–3 months | 40 (26.5) |
| 3–6 months | 20 (13.3) |
| 6–12 months | 22 (14.6) |
| > 1 year | 36 (23.8) |
| Ethnicity | |
| White | 142 (93.4) |
| BME | 10 (6.6) |
| Age (years) | |
| Mean, SD | 36.2, 12.6 |
| Range | 18–79 |
| Total | 156 (100) |
Table 22 shows that, out of the 156 consultations considered as part of the study, the patient pre-consultation questionnaire was completed in 152 (97.4%) cases, the patient post-consultation questionnaire was completed in 134 (85.9%) cases, and the post-consultation doctor questionnaire was completed in 137 (87.8%) cases. In 100% of cases, at least one of these questionnaires was completed, and in 80.8% of cases, all three were completed. Reasons for non-completion of patient questionnaires included patient non-attendance at the appointment, patient refusal and the patient being missed by the researcher. The main reasons for non-completion of doctor questionnaires were patient non-attendance at the appointment and lack of time.
| Prison | Recruited, N (%) | Patient A (pre consultation), n (%) | Patient B (post consultation), n (%) | Doctor B (post consultation), n (%) | All, n (%) |
|---|---|---|---|---|---|
| A | 57 (100) | 57 (100) | 49 (86.0) | 49 (86.0) | 49 (86.0) |
| B | 41 (100) | 38 (92.7) | 38 (92.7) | 37 (90.2) | 35 (85.4) |
| C | 58 (100) | 57 (98.3) | 47 (81.0) | 51 (87.9) | 42 (72.4) |
| All | 156 (100) | 152 (97.4) | 134 (85.9) | 137 (87.8) | 126 (80.8) |
Before the consultation
Presenting problem
Before the consultation, patients were asked to state the main health problem that they wished to raise with the doctor. Almost one-quarter (23.8%) of patients identified a mental health problem as their main reason for seeing the doctor (Table 23).
| Health problem | n (%) |
|---|---|
| Mental health | 36 (23.8) |
| Musculoskeletal | 32 (21.2) |
| Cardiovascular | 7 (4.6) |
| Lump | 7 (4.6) |
| Skin | 7 (4.6) |
| Sleep | 6 (4.0) |
| Headaches | 6 (4.0) |
| Substance misuse | 6 (4.0) |
| Gastrointestinal | 5 (3.3) |
| Other | 38 (25.2) |
| Total | 151 (100.0) |
Patients were also asked to define secondary reasons for seeing the doctor, if they had any. Taking this into consideration, 29.1% of patients (n = 44) identified a mental health problem as one of their reasons (primary and/or secondary) for seeing the doctor.
Patient expectations
Patients were asked about the types of help they wanted, by indicating their level of agreement with a series of pre-prepared statements. Table 24 describes the proportion of patients who agreed with these statements.
| Rank | Statement | Proportion of patients who agreed, n (%) |
|---|---|---|
| 1 | I want the doctor to talk with me about my problem | 130 (85.5) |
| 2 | I want the doctor to listen to what I think is wrong | 125 (82.2) |
| 3 | I would like to participate in decisions about treatment | 115 (75.2) |
| 4 | I want the doctor to hear my views on the treatment I think I need | 103 (67.8) |
| 5 | I want the doctor to explain the treatment to me | 98 (64.5) |
| 6 | I want the doctor to diagnose what is wrong with me | 96 (63.2) |
| 7 | I want a prescription for some medicationa | 94 (61.8) |
| 8 | I want to know what services I can access | 94 (61.8) |
| 9 | I would like the doctor to offer me a choice of treatmentsa | 92 (60.5) |
| 10 | I want the doctor to explain the nature of my problem, and any side effects | 89 (58.6) |
| 11 | I want advice about medical treatment | 83 (54.6) |
| 12 | I want to be examined for the cause of my conditiona | 76 (50.0) |
| 13 | I want advice on medication/medicines | 73 (48.0) |
| 14 | I would rather not have a prescription unless it is really necessary | 67 (44.1) |
| 15 | I want to be referred to a specialist | 67 (44.1) |
| 16 | I want some tests done to find out what is wrong with me | 67 (44.1) |
| 17 | I have emotional problems for which I would like helpa | 60 (39.5) |
| 18 | I want to be reassured that nothing is wrong with me | 59 (38.8) |
| 19 | I would like emotional support from the doctora | 50 (32.9) |
| 20 | I want to change the medication I am takinga | 46 (30.3) |
| 21 | I would like to be taken off some medication I am taking | 26 (17.1) |
Overall, two-thirds (69.7%) of patients wished to start, stop and/or change their medication (as indicated by agreement with any of the following three statements: I want a prescription for some medication; I want to change the medication I am taking; I would like to be taken off some medication I am taking). Patients who identified mental health as their primary problem were more likely than patients who identified other types of health problems to want to start, stop and/or change their medication (91.7% vs. 62.6%; PR 1.46, 95% CI 1.23 to 1.74). Patients who identified mental health as their primary problem were also more likely to agree with the following statements:
-
I want a prescription for some medication (80.6% vs. 56.1%; PR 1.45, 95% CI 1.15 to 1.82).
-
I would like the doctor to offer me a choice of treatments (75.0% vs. 55.7%; PR 1.35, 95% CI 1.05 to 1.73).
-
I would like emotional support from the doctor (52.8% vs. 26.1%; PR 2.02, 95% CI 1.31 to 3.13).
-
I have emotional problems for which I would like help (77.8% vs. 27.0%; PR 2.89, 95% CI 2.04 to 4.09).
-
I want to change the medication I am taking (47.2% vs. 25.2%; PR 1.87, 95% CI 1.17 to 2.99).
They were less likely to agree with the following statement:
-
I want to be examined for the cause of my condition (27.8% vs. 56.5%; PR 0.49, 95% CI 0.28 to 0.85).
After the consultation
Help received
Patients were asked about the types of help that they actually received, by indicating their level of agreement with a series of pre-prepared statements.
Table 25 describes the proportion of patients who agreed with these statements overall, and, among those, patients who indicated agreement pre consultation. Overall, 60.9% of patients reported a change in their medication post consultation. Of these, 71.8% were happy with the prescribing decision. Where patients had wanted a change in their medicines, rates of satisfaction with prescribing decisions appeared higher when changes were subsequently made (70.5% vs. 50.0%); however, this was statistically non-significant [χ2(1) = 3.34, p = 0.07]. Patients who wished to start, stop and/or change their medication in some way before the consultation were more likely than other patients to report a prescription change (70.1% vs. 32.6%; PR 2.15, 95% CI 1.37 to 3.38). Of those who wanted advice on medicines before the consultation, half (51.6%) reported having received it. Half (51.5%) of all patients agreed that they had participated in decisions about their treatment, although this represented only half (52.5%) of those who wanted to be involved prior to the consultation.
| Rank | Statement | Pre consultation, n (%) | Post consultation, n (%) | |
|---|---|---|---|---|
| All patients | Those who wanted | |||
| 1 | The doctor talked with me about my problem | 130 (85.5) | 105 (79.6) | 89 (79.5) |
| 2 | The doctor listened to what I think is wrong | 125 (82.2) | 99 (75.6) | 83 (76.9) |
| 3 | I got a new medicine, or my medicine was stopped or changed in some waya | 106 (69.7) | 78 (60.9) | 61 (70.1) |
| 4 | The doctor gave me advice on medication/medicinesa | 73 (48.0) | 72 (54.6) | 32 (51.6) |
| 5 | The doctor explained the treatment to me | 98 (64.5) | 69 (52.7) | 42 (49.4) |
| 6 | The doctor listened to my views on the treatment I think I need | 103 (67.8) | 69 (52.3) | 50 (56.2) |
| 7 | I participated in decisions about my treatment | 115 (75.2) | 68 (51.5) | 52 (52.5) |
| 8 | The doctor diagnosed my problem | 96 (63.2) | 62 (47.0) | 37 (45.1) |
| 9 | The doctor gave me emotional support | 50 (32.9) | 50 (38.5) | 20 (51.3) |
| 10 | The doctor explained the nature of my problem, and any side effects | 89 (58.6) | 50 (37.9) | 26 (33.8) |
| 11 | The doctor told me about services I could access | 94 (61.8) | 48 (36.4) | 38 (46.3) |
| 12 | The doctor helped me with my emotional problemsa | 60 (39.5) | 32 (24.4) | 17 (36.2) |
| 13 | I was reassured that nothing is wrong with me | 59 (38.8) | 29 (22.0) | 14 (26.9) |
| 14 | I was offered a choice of treatments | 92 (60.5) | 27 (20.5) | 17 (20.0) |
Over one-quarter (26.9%) of patients who wanted help with emotional problems reported having received it. Patients who identified mental health as their primary problem were more likely than patients who identified other types of health problems to report having received the following from the doctor:
-
some kind of change in their medication (75.0% vs. 52.9%; PR 1.42, 95% CI 1.07 to 1.88)
-
advice on medication (71.4% vs. 49.0%; PR 1.46, 95% CI 1.07 to 1.98)
-
help with emotional problems (39.3% vs. 19.6%; PR 2.00, 95% CI 1.09 to 3.67).
Patient satisfaction
Patients were asked to rate their level of satisfaction with the consultation. Figure 4 shows that, in total, 83% of patients reporting being very satisfied (40%) or fairly satisfied (43%) with the consultation. Seventeen per cent of patients reported being fairly dissatisfied (8%) or very dissatisfied (9%).
FIGURE 4.
Patient satisfaction with the consultation.
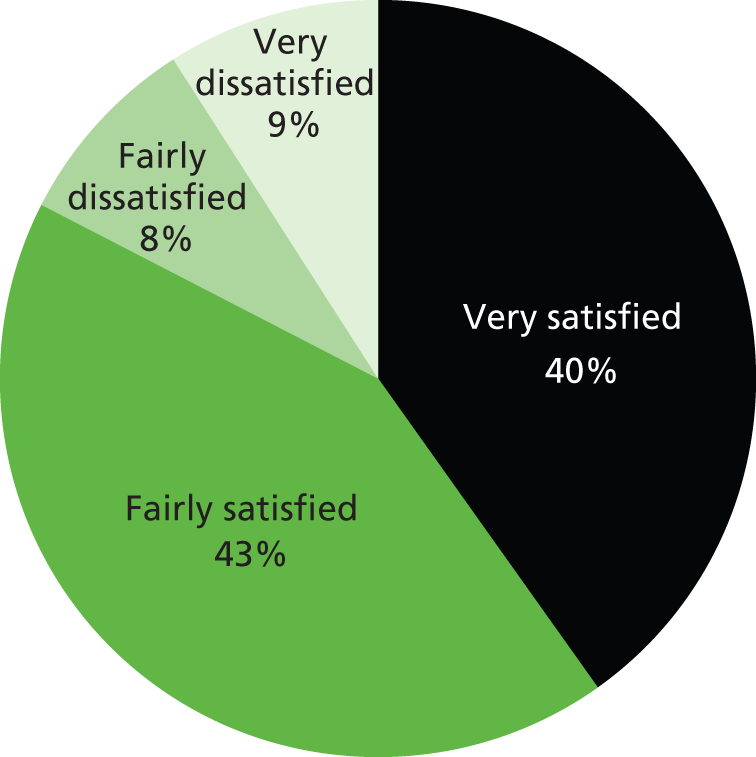
There were no significant differences in satisfaction rates between the different prisons or doctors. A greater proportion of individuals who identified mental health as their primary problem reported being fairly/very dissatisfied than other patients, although this was a statistically borderline result (34.9 vs. 19.8; PR 1.76, 95% CI 1.01 to 3.08).
Doctor perceptions
Perception of problem
Doctors were asked to record the main and, if applicable, secondary health problems for each patient participating in the study.
Table 26 shows that in two-thirds (63.2%) of cases in which the patient reported a mental health problem (primary or secondary), the doctor also recorded a mental health problem (primary or secondary). In the case of problems other than mental health problems, there was a higher level of agreement between patients and doctors (91.7% vs. 63.2%; PR 1.45, 95% CI 1.13 to 1.86). In eight cases, the patient reported problems other than mental health issues, while the doctor noted a mental health problem.
| Patient | Doctor | |
|---|---|---|
| Mental health | Other | |
| Mental health | 63.2 (24) | 36.8 (14) |
| Other | 8.3 (8) | 91.7 (88) |
| Total | 23.9 (32) | 76.2 (102) |
Prescribing decisions
Overall, doctors recorded 176 separate health problems and issued a prescription for half of these (49.71%). In 62% of cases, doctors thought that patients definitely (41.5%) or probably (20.5%) wanted a prescription (Figure 5). In 26.7% of cases, doctors reported feeling definitely pressured (5.1%) or a little pressured (21.6%) to prescribe (Figure 6). In 94.0% of cases, doctors reported feeling definitely comfortable (72.0%) or fairly comfortable (22.0%) with their prescribing decision, which included decisions not to prescribe (Figure 7).
FIGURE 5.
Did you think the patient wanted a prescription for this health problem?
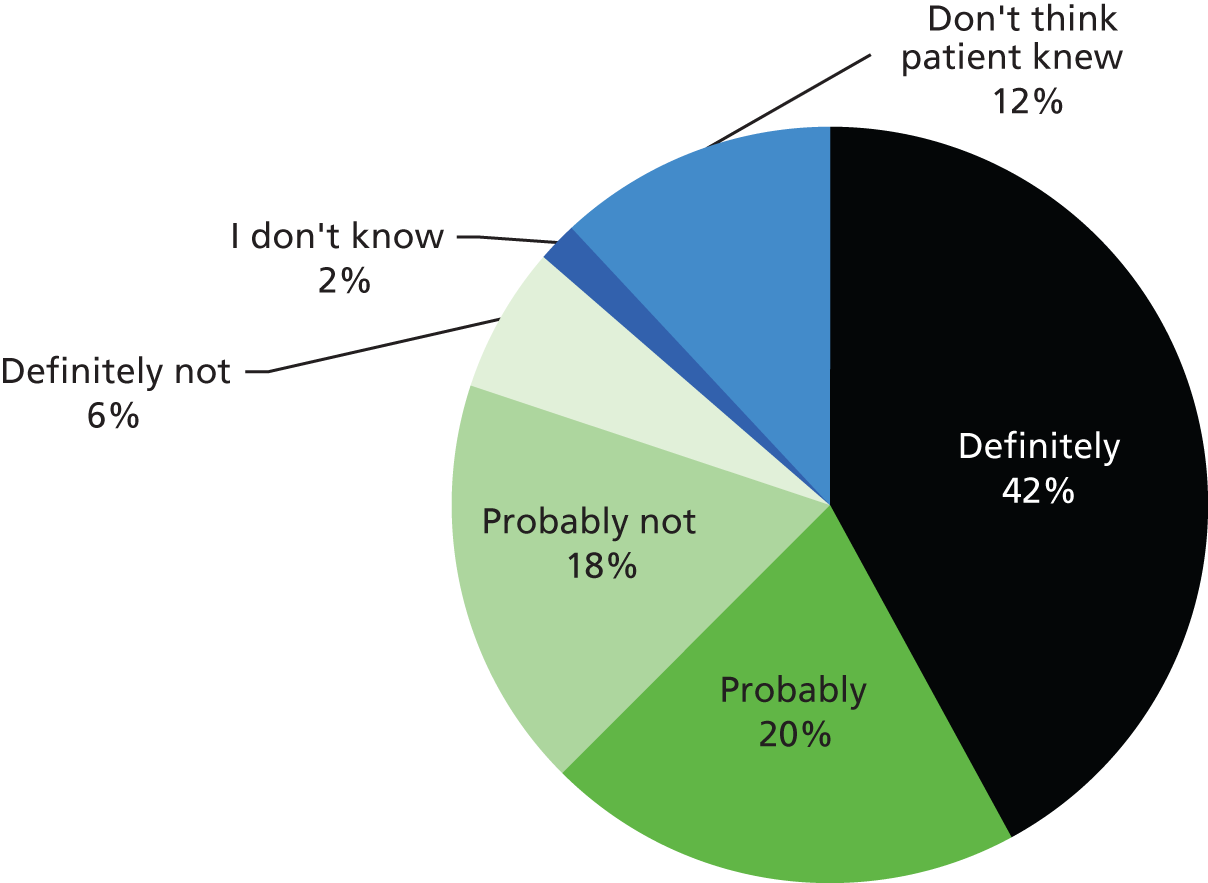
FIGURE 6.
Did you feel pressured by the patient to write a prescription for this problem?
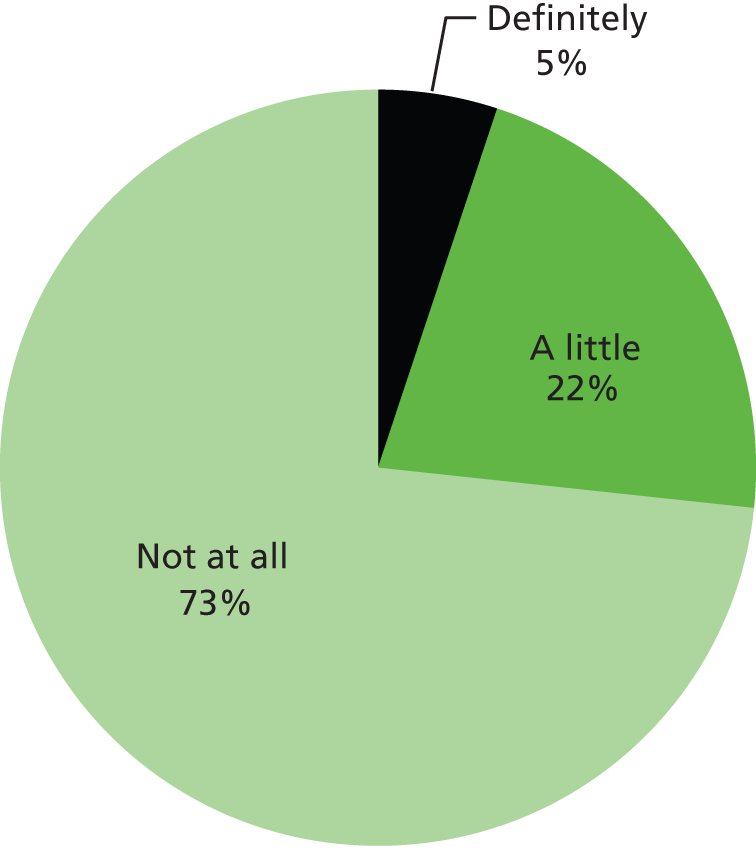
FIGURE 7.
Did you feel comfortable about this prescribing decision?
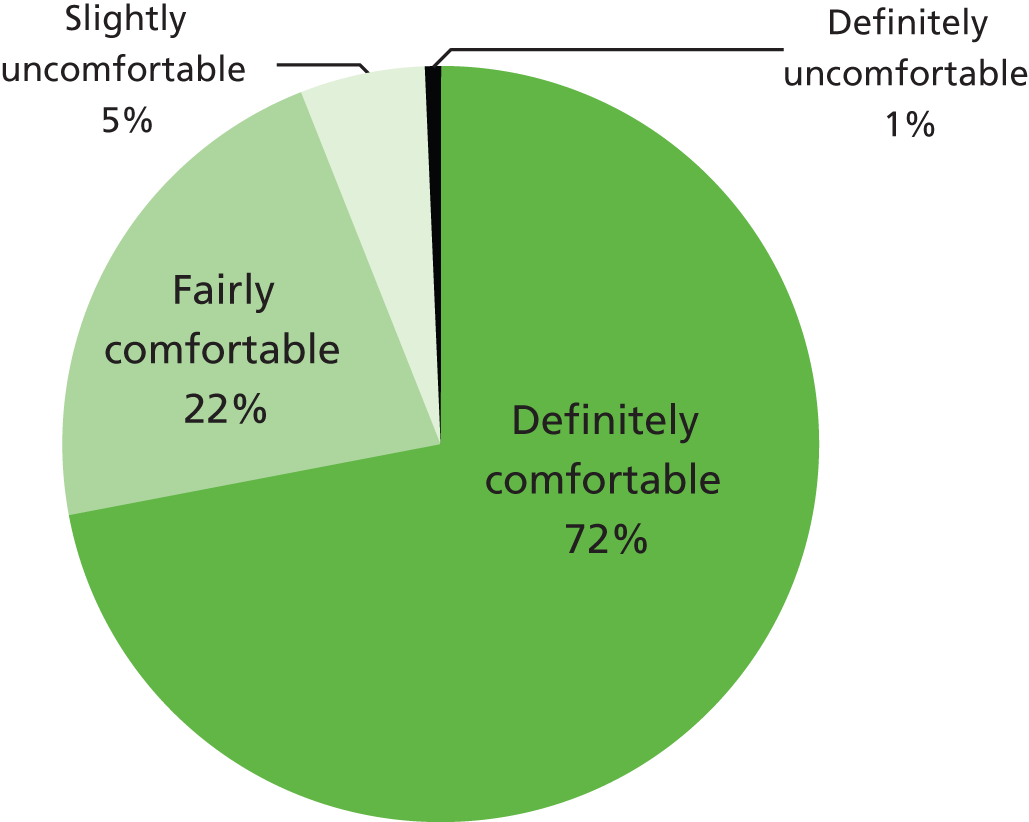
In 5.7% of cases (n = 10), doctors stated that prescriptions were not strictly indicated. In all cases, the prescriptions were wanted by the patient.
Doctors were more likely to issue a prescription when:
-
They thought that the patient definitely/probably wanted a prescription (69.7% vs. 16.7%; PR 4.2, 95% CI 2.41 to 7.28).
-
They felt definite/a little pressure to prescribe (70.2% vs. 42.2%; PR 1.66, 95% CI 1.26 to 2.19).
-
They thought that the problem was a mental health problem (73.5% vs. 44.0%; PR 1.67, 95% CI 1.27 to 2.20).
Doctors were more likely to be comfortable with prescribing decisions when:
-
They issued a prescription (100.0% vs. 51.06%; PR 1.96, 95% CI 1.67 to 2.30).
-
They did not think that the patient definitely/probably wanted a prescription (100.0% vs. 91.0%; PR 1.10, 95% CI 1.03 to 1.17).
-
They did not perceive definite/a little pressure to prescribe (98.1% vs. 83.7%; PR 1.2, 95% CI 1.02 to 1.34).
Doctor satisfaction
Doctors were asked how the consultation went. In 96% of cases, the consultation went OK (62%) or very well (34%). In 4% (n = 5) of cases, doctors reported that the consultation had not gone particularly well. There were no significant differences in satisfaction rates between the different prisons or doctors.
Summary: the acceptability of prescribing decisions
-
One-quarter (23.8%) of patients identified a mental health problem as their main reason for seeing the doctor.
-
Two-thirds (69.7%) of all patients wished to start, stop and/or change their medication. Patients who identified mental health as their primary problem were more likely to want to change their medication in some way.
-
The vast majority (83%) of patients were very or fairly satisfied with the consultation.
-
Half (51.5%) of all patients agreed that they had participated in decisions about their treatment.
-
One-quarter (26.9%) of patients who wanted help with emotional problems reported having received it.
-
Patients who identified a mental health issue as their primary problem were more likely to report having received some kind of change in their medication.
-
A greater proportion of individuals who identified mental health as their primary problem reported being fairly/very dissatisfied than other patients.
-
In 26.7% of cases, doctors reported feeling at least a little pressured to prescribe.
-
There were no cases were prescriptions were not strictly indicated or wanted by the patient.
-
Doctors were more likely to issue a prescription when they thought that the patient wanted a prescription, they perceived pressure to prescribe and/or the problem was a mental health problem.
Chapter 4 Discussion and conclusions
The overall aim of the study was to establish the prevalence, appropriateness and acceptability of psychotropic prescribing in prisons.
Rates of psychotropic prescribing in prison
A cross-sectional survey of patient records was used to establish patterns of psychotropic medication prescribing in prisons, and to compare to these with the wider community. Overall, 17% of men and 48% of women in prison were prescribed at least one psychotropic medicine. After adjusting for age differences, psychotropic prescribing rates were four times higher among men and six times higher among women than among the community.
The findings of this study are consistent with those of previous studies, which have reported higher rates of psychotropic prescribing in prisons, particularly among women. 2,4,6,72,73,75,90 On the surface, the overall rates of psychotropic prescribing reported in the current study are notably similar to those reported in a large study of psychiatric morbidity in prisons in England and Wales undertaken by the ONS study;6 the ONS study found that about one-fifth of men and half of women in prison were prescribed at least one drug acting on the CNS. In comparison with the current study, however, the ONS included a much wider range of drugs (any drug listed within BNF chapter 4), which included analgesics, antiepileptics and drugs for substance dependence. Thus, it would appear that psychotropic prescribing rates in prisons have increased since 1997.
In particular, there appears to have been a marked increase in antidepressant prescribing in prison. In the current study, 13% of men and 41% of women in the prisons surveyed were prescribed antidepressants. Thus, since the last UK-based study to consider psychotropic prescribing in prisons,6 rates have doubled among men and have increased by 50% among women. Although we cannot be certain, this apparent increase in antidepressant prescribing in prisons would appear to mirror the more general long-term, upwards trend in antidepressant prescribing in the wider UK population. 91 Several explanations have been proposed for increased antidepressant prescribing rates, including improved recognition of depression, increased help-seeking behaviour among patients and lower thresholds for prescribing. 91,92 Such factors may have also accounted for the apparent increase in prescribing observed in prisons, suggested by this study. Nonetheless, antidepressants accounted for a larger proportion of psychotropic prescriptions in prisons than in the wider community. It is also possible that antidepressants have partially displaced the use of drugs with higher potential for abuse and dependence, such as hypnotics and anxiolytics (which accounted for a lower proportion of psychotropic prescriptions in prison). This is consistent with previous qualitative research, which found that psychotropic prescribing was thought to serve multiple purposes in prisons. 93
There were particularly high rates of psychotropic prescribing among the women sampled in this study. A variety of clinical and situational reasons may account for the patterns observed in this study. Firstly, women typically have higher levels of ‘imported vulnerability’. 94 In prison, as in the wider community, women have higher rates of mental illness. 6,20 Secondly, imprisonment affects women differently from and disproportionately to men. 95 Corsten has argued that imprisonment can be harsher on women because prison regimes and practices have been designed for men. 95 Imprisonment can also be greatly disruptive to family life: one-third of women lose their homes and only 5% of children remain in their own home once their mother has been imprisoned. 96 The disproportionate impact of imprisonment on women has been backed up by recent research. In a prospective cohort study, Hassan et al. 97 measured changes in psychiatric symptoms among prisoners with and without mental illness. The authors reported that while symptoms among men showed a significant linear decline, they did not among women.
Despite the high levels of mental health need among women in prison, the fact that almost half of the women in this study were prescribed at least one psychotropic drug is, arguably, concerning. Psychotropic drugs can cause unpleasant side effects and are not without physical health risks. Although the relationship is complex, links have been made between certain prescribed psychotropic medicines and conditions such as diabetes, obesity, stroke and early mortality. 98 We have no reason to believe that the two prisons sampled were any different from other female-only establishments; indeed, preliminary work in the east of England reported similar rates of prescribing among women prisoners. 71 Rather, this appears to be a long-standing and widespread phenomenon. Historically, there has been a tendency to overmedicalise the problems of women who offend. 55 More recently, in 2007, the Chief Inspector of Prisons expressed concern that psychotropic medicines may be overused in prisons, particularly among women. 68 This echoed the concerns raised in a Prison Reform Trust report in 2003:99
There is anecdotal evidence that this increase in medication is not a result of careful exploration of the mental health needs of women in prison but rather a response by undertrained staff who resort to medication to contain a ‘problem’. Some of these medications are addictive and have unpleasant side effects, and would normally be prescribed outside prison only after careful professional judgement, and with proper supervision.
Reproduced with permission from the Prison Reform Trust. Justice for Women: The Need for Reform. London: Prison ReformTrust; 2000. p. 23
A common argument in the policy literature is that women in the criminal justice system require distinct and women-centred responses. In terms of mental health care, increased access to non-pharmacological interventions, such as ‘talking therapies’, and other forms of support for vulnerable individuals may be one way to avoid medication becoming the ‘default treatment’. 68
Lower rates of psychotropic prescribing were observed among BME groups in the current study. This is contrast to studies conducted in the USA, which have indicated increased rates of prescribing among BME groups. 100,101 There is no reason to suspect that rates of mental illness are lower among BME groups. However, studies in community settings have suggested differences in service provision for BME communities. 102,103 Such factors are significant, even for prisoners, as prior contact with services is an important predictor of mental health assessment in prisons. 13 Thus, any gaps in service provision for BME groups, or patterns of help-seeking among such populations, in the community may also be mirrored in prison. Such factors may explain the differences observed in the current study.
Drug choice
We found discernible differences in the individual psychotropic drugs prescribed in prison and community settings. In particular, the following three patterns emerged: diazepam accounted for a higher proportion of prescriptions for hypnotics and anxiolytics in prison than in the community; among patients prescribed antidepressants, prisoners were less likely to be prescribed TCAs than community-based patients; and there was a significant preference for certain antidepressant and antipsychotic drugs in prison, compared with the community.
Diazepam accounted for half of all hypnotic and anxiolytic prescriptions in this study and accounted for twice as many prescriptions in this group as it did among patients in the community. Dependence on benzodiazepines (both illicit and prescribed) is common among prisoners entering custody. Short-acting benzodiazepines (e.g. temazepam), though commonly prescribed in the community, are discouraged in prison owing to their potential for dependence and misuse. 61 This could explain why there were only two instances of temazepam prescribing in prison, despite it being the third most frequently prescribed hypnotic/anxiolytic in the community. Indeed, prisons in England and Wales commonly operate a policy of routine benzodiazepine detoxification on entry to custody. 61,104 To minimise withdrawal symptoms, benzodiazepine detoxification should be gradual. As diazepam is a longer-acting anxiolytic, the BNF recommends that this drug is most suitable for detoxification purposes. 27 This would explain its increased use in prison: indeed, benzodiazepine detoxification was the most commonly recorded indication for diazepam prescriptions. It might also explain why rates of hypnotic and anxiolytic prescribing were lower among sentenced men, as such prisoners would have been more likely to have completed detoxification.
Prisoners prescribed antidepressants were less likely than community-based patients to be prescribed TCAs. TCAs have similar efficacy to other classes of antidepressant drugs, but are more dangerous in overdose. 27 For such reasons, certain TCA drugs (e.g. dosulepin and amitriptyline) are no longer recommended for the treatment of depression. The high rates of suicide and self-harm among prisoners105 present added risks when prescribing such drugs. These concerns may have accounted for the reduced use of TCA drugs in prisons, and this could, therefore, be interpreted as a positive finding. Furthermore, where TCA drugs were prescribed, the doses were low and they were usually prescribed for indications other than depression, for example neuropathic pain. Prisoners prescribed an antidepressant were more than four times as likely as patients in the community to receive mirtazapine. Anecdotal evidence suggests that mirtazapine is valued by prisoners for its sedative effects. In a prison setting, where sleep problems are common,106 sedative side effects may be viewed as desirable and therapeutically beneficial; unfortunately, hypnotic effects also increase the value of such drugs and potential for diversion among prisoners without mental illness. Such factors, combined with the reluctance to prescribe benzodiazepines in secure environments, may have contributed towards the increased frequency of mirtazapine prescriptions in prisons observed in this study. Recent guidance issued on safer prescribing in prisons61 has reiterated that mirtazapine should not be prescribed as a sleeping tablet and should be prescribed second or third line for major depression only, in line with NICE guidance. 42
Among individuals prescribed antipsychotic drugs, olanzapine and quetiapine were prescribed twice as often in prison as in the community. Both medicines have a propensity for sedation and weight gain; the latter is associated with olanzapine in particular. 107 As with mirtazapine, sedative effects may be viewed as a desirable effect among prisoners. This could provide an added incentive for patients to adhere to antipsychotic medication regimes. Nonetheless, while patient preferences should be taken into account, the propensity for weight gain and adverse effects on physical health associated with these drugs should not be overlooked. Indeed, there is increasing evidence that certain prescribed psychotropic medicines can increase metabolic and cardiovascular risks, thereby increasing the risk of morbidity (e.g. diabetes, obesity and stroke) and early mortality. 98
The appropriateness of psychotropic prescribing in prison
It has been proposed that psychotropic prescribing rates reflect the prevalence of psychiatric morbidity in prison. 4 We did not measure the prevalence of mental illness in the current study. However, higher rates of mental illness in prisons have been consistently reported in the wider research literature. 6,8,11,12,14,20,21,79 A large meta-analysis estimated a two- to fourfold increase in psychosis and major depression in prison populations, compared with the community, after accounting for age differences. 20 Comparatively, the prescribing ratios generated in the current study for antipsychotics and antidepressants were much higher (four to six times higher). However, without knowing the rates of mental illness in the particular prisons sampled in the current study, it is not possible to draw any firm conclusions regarding whether or not the prescribing of psychotropic medicines is wholly appropriate and proportionate to the level of need.
Unfortunately, the largest and most robust study to provide psychiatric morbidity data for English and Welsh prisons was conducted over 15 years ago:6 since then, the prison population and health-care systems have changed considerably. Without current and robust data on the prevalence of mental illness in prison, it is difficult to fully assess the appropriateness of psychotropic prescribing. In a more recent study, Senior et al. 13 estimated the prevalence of mental illness in a large sample drawn from five English prisons (n = 3871). This reported approximate rates of psychosis and major depressive disorder as 4% and 19%, respectively, among the sample. On the basis of a crude comparison against the antipsychotic and antidepressant rates reported by the current study, these rates also appear low. However, it is important to note that the primary purpose of the study was to measure contact with secondary mental health services, rather than psychiatric morbidity. While the sample was large, it was not wholly representative of the prison estate; for example, YOIs and open prisons were not included. Thus, the sample is not directly comparable with that in the current study. Furthermore, as the authors themselves note, estimates of mental illness can vary according to aspects of the study design and methodology, including sampling techniques, definitions of mental illness, the way mental illness was assessed (e.g. the particular diagnostic tools used), and the characteristics of those conducting assessments (e.g. lay or clinical researchers).
Notwithstanding methodological differences, the relationship between psychotropic prescribing rates and rates of psychiatric morbidity in prison is complex, meaning that any comparisons would have to be made cautiously even if reliable data were available. While it is likely that underlying patterns of mental illness exert some degree of influence on patterns of psychotropic prescribing, complete correspondence between rates is unlikely in any setting. The first reason for this is that not all patients with mental illness will be treated with psychotropic medicines, or indeed treated at all. While psychotropic medications are commonly used to treat mental illness, non-pharmacological alternatives, such as counselling, cognitive–behavioural therapy and psychological therapies, have also been recommended, especially for common mental illnesses. 34,42 Furthermore, some cases of mental illness may go undetected. Senior et al. 13 found that just one-quarter of prisoners with serious mental illness were assessed by prison mental health services during their first month in custody; follow-up analyses revealed that the levels of mental health interventions received by prisoners were not consistently linked with diagnoses or symptom severity. 108 Such evidence would appear to suggest that prisons do not consistently identify and target mental health needs with appropriate treatments. The second reason for differences between psychotropic prescribing and mental illness rates is that patients prescribed psychotropic drugs may not necessarily have a mental illness. Psychotropic medications have, over time, been prescribed ‘off label’, outside the narrow terms of their licences, to treat conditions other than mental illness. 109 For example, the antidepressant amitriptyline is commonly used to treat neuropathic pain, while carbamazepine can be used to treat both epilepsy and bipolar disorder; all of these indications are listed in the BNF. 27 Furthermore, in line with the findings of the acceptability study, doctors in prison may perceive pressure to prescribe psychotropic drugs for genuine or perceived needs, or for subclinical symptoms. Indeed, symptoms of anxiety, depression and distress are common in prisoner populations during the early period of custody, even among those without a formal mental illness. 97
In the current study, the diagnoses recorded for individual psychotropic medicines prescribed in prison were noted and compared against the indications listed in the BNF. Overall, a ‘valid’ diagnosis (i.e. one that was recorded and upheld in the BNF) was recorded for 65% of psychotropic prescriptions. In a further 21% of cases, a diagnosis was recorded that was not upheld in the BNF; this proportion was significantly higher among antipsychotic medicines (35%). Personality disorder was the most common invalid indication recorded for antipsychotic drugs, most commonly borderline personality disorder. A proportion of antidepressants were also prescribed off-licence for personality disorder. Currently, no drugs are licensed for the treatment of personality disorder and there is little evidence in the literature to justify the use of any medicines in particular. NICE guidelines110,111 state that, outside short-term crises, drug treatment should not be used specifically for borderline or antisocial personality disorders or for associated symptoms (e.g. repeated self-harm, psychotic/pseudopsychotic symptoms). Nonetheless, the treatment of personality disorder is a complex and contentious area. Personality disorders are often comorbid alongside mental illnesses and substance misuse, presenting a complex clinical picture. Thus, it is possible for symptoms to be confused. Furthermore, comorbidity and negative interactions between symptoms (e.g. emotional dysregulation and excess alcohol use) may increase pressure on clinicians to act. While currently drug interventions lack a clear rationale and evidence base, there has been a lack of good-quality clinical trials in this area. It is possible that psychotropic medicines are being prescribed to prisoners with personality disorder to control adverse behaviours, to placate individuals or in the hope that something might work. This scenario might not necessarily be unique to prisons: one survey of patients on a CMHT caseload found that four-fifths of patients with a primary diagnosis of personality disorder were prescribed psychotropic medication. 112 As with individuals in the wider community, there is a need to understand the reasons for prescribing for personality disorder.
Prisoners were less likely to be prescribed two or more psychotropic medicines concurrently. This is an interesting and positive finding given that research has shown that concomitant use of certain psychotropic medicines may increase the risk of mortality. 113 It is possible that prisons are more averse to polypharmacy (the concurrent prescribing of medicines). It should be noted that polypharmacy is not always problematic and may be beneficial where treatment is optimised and evidence-based. However, it does increase the risk of drug–drug interactions and adverse effects, in some cases without empirical evidence for improved clinical outcomes. 114 In the current study, a potentially hazardous drug–drug interaction involving a psychotropic medication was noted in 16% of all psychotropic prescriptions. In particular, interactions involving SSRI antidepressants and antipsychotics were common. In many cases, harmful effects of adverse interactions can be reduced if the prescriber is aware of the hazard and takes appropriate precautions (e.g. by increased monitoring, prescribing additional drugs or switching medicines). However, in the vast majority of cases in this study, we found no written evidence that prescribers were aware of hazardous interactions. Though polypharmacy was less likely in prisons than the wider community, the possibility that some prisoners prescribed psychotropic drugs may be experiencing preventable iatrogenic effects should not be overlooked.
We also considered the dosages of psychotropic medicines prescribed to prisoners. In the vast majority of cases in this study, doses were prescribed within an acceptable range. Antipsychotics were, however, less likely to meet this criterion. One in five antipsychotics prescribed in prison were prescribed at subtherapeutic doses, at a level too low to treat the conditions for which they are currently licensed. Median doses for the most frequently prescribed antipsychotics were also low, compared with the maximum dosages listed in the BNF. This finding is consistent with the previous discussion regarding the use of antipsychotics for conditions other than psychoses. The use of lower dosages than recommended provides further support for the notion that, in prisons, antipsychotics are sometimes being prescribed outside the current evidence-base. It should be noted that median doses for antipsychotics were similar between the prison and the community; thus, it should not necessarily be assumed that these practices are unique to prisons.
In the current study, generic (non-branded) medicines were prescribed in over 99% of cases. Branded products were very rarely prescribed, except where there were no alternatives. Thus, it appears that, in prisons, full use is being made of generic substitutions to minimise costs. We did, however, note differences in estimated costs between different prison types. The highest mean costs were observed in prisons for young offenders. This is likely to be due to the increased use of drugs for ADHD, which are relatively expensive. Furthermore, owing to use of modified release preparations and differences in bioavailability among medicines for ADHD, branded products cannot always be substituted for cheaper generic drugs. 27 It was notable that, while psychotropic prescribing rates were three times higher among women, mean costs of psychotropic prescriptions were almost nine times higher. The increased drug costs among women were largely due to increased use of oral solutions (particularly for diazepam) in female-only prisons, which are significantly more costly than standard tablets. For example, liquid diazepam solution is 144 times more costly than tablet formulations; 1 month’s supply of diazepam tablets at 10 mg would cost 93 pence per patient, whereas the equivalent oral solution would cost £133. Anecdotally, clinician respondents to this, and our earlier related research, indicated that they felt under pressure, or indeed, had received clear instructions from prison partners to routinely prescribe liquid formulations, rather than only in exceptional circumstances. This is completely opposite to the wider community, and thus does not represent equivalence of care. Alternative formulations, such as oral solutions, may contribute towards making diversion and misuse of medicines more difficult,61 and it is known that women in prison have higher rates of substance misuse than their male counterparts,6 which may, in turn, further increase the risk of diversion. The RCGP has recognised that, while alternative formulations may carry cost implications, this should not prevent the prescription of medicines which are clinically necessary. 61 However, further work is required to examine whether or not the additional expense is justified, proportional to risk, and based on sound principles of risk management rather than blunt risk aversion.
The acceptability of psychotropic prescribing decisions in prison
A questionnaire survey was used to determine the acceptability of prescribing decisions to patients and GPs in prisons. Medication and mental health problems were high on the agenda among patients in prison. Seventy per cent of all patients who were visiting the doctor wished to start, stop and/or change their medication. About one in four (24%) patients identified a mental health problem as their main reason for seeing the doctor.
Overall, the majority of patients were very or fairly satisfied following their consultation with the doctor and the prescribing decision (including a decision not to prescribe). Though satisfaction rates were high in prison, it is notable that an equivalent study in the community using the same questionnaires found that none of the 186 patients they sampled reported dissatisfaction following the consultation generally, or with the prescribing decision. 89 Although patients in prison were satisfied overall, the specific expectations and perceived needs of individuals were frequently not met. As with patients in the community,89 most prisoners wanted to participate in treatment decisions and emphasised the importance of active listening and communication. Nonetheless, following consultations, only half of patients in this study felt that they had participated in decisions about their treatment and only half reported that the doctor had explained the treatment to them. Research on patients’ experiences of prison health care in the wider literature has also highlighted problems with communication, lack of input into decision-making and poor access to medicines. 62,93,115
In particular, this study revealed that patients who identified mental health as their primary problem had different needs and experiences from patients with other health problems. Patients who identified mental health as their primary problem were more likely to want emotional support, new prescriptions and/or changes to their medications. After consultations, they were more likely to receive new prescriptions and changes to their medications. However, patients who identified mental health as their primary problem were less likely to be satisfied with the outcomes of the consultation. The latter finding is concerning, but arguably consistent with the wider literature, which reports an ongoing disparity between mental and physical health care. 116 While 65% of the patients who identified mental health as their primary problem were satisfied with their care, focusing on certain aspects of their experience may highlight areas for improvement. For example, only one-third of patients who wanted help with emotional problems and half of patients who wanted emotional support reported having received this.
In the current study, doctors thought that patients wanted a prescription in 62% of cases, although they felt pressure to prescribe in only 27% of cases and were comfortable with the vast majority of prescribing decisions. These findings appear to be broadly similar to those of Britten et al. 89 Thus, while doctors can feel pressure to prescribe in prison, this may not necessarily be particularly intense, frequent or disproportionate to community settings. Nonetheless, doctors in prison were more likely to issue a prescription when they thought that the patient wanted a prescription, they perceived pressure to prescribe and/or they thought that the problem was related to mental health. Doctors rarely thought that the drugs they prescribed were not strictly indicated. Furthermore, there were no cases in which drugs were prescribed that were not wanted by the patient or strictly indicated, which is considered to be an indicator of ‘unnecessary prescribing’. 89
Methodological strengths and limitations
This study is the first in-depth analysis of psychotropic prescribing in prisons in the UK on a national scale since 1997. 6 Internationally, relatively few studies2,4,72,73,75,90 have described rates of psychotropic prescribing in prisons. Furthermore, few have included a large, robust community comparison group and none has adequately controlled for age differences. For this reason, the relative differences between prescribing rates in prisons and the community are likely to have been underestimated.
The current study builds on our initial work in the east of England, which demonstrated the feasibility of our methodology. While the east of England region represents just 10% of the total prison population, the current study included 11 prisons from throughout England. Recruited prisons were geographically spread across northern England, the south-west of England, London and the Midlands. This increased coverage and sample size will have further improved the precision and generalisability of our estimates, while allowing us to undertake novel analyses. We were not able to include any Welsh prisons in the study. One was invited, but unfortunately did not respond in time to complete the survey. While this is disappointing, we achieved our target sample (5–10% of the prison population) and included a good range of prison types in the study (female-only, YOI, training, open and local prisons). Although we recruited no Welsh prisons, it is likely that a significant number of Welsh prisoners are likely to have been included in the study owing to their residing in prisons that did participate in the study (in particular, prisons in the north-west and south-west). We have no reason to believe that prescribing practices in Welsh prisons would have been substantially different from those in England. Thus, while not all regions of the prison estate in England and Wales were sampled, we are confident that we obtained a sufficiently representative and robust sample upon which to base our analyses.
The cross-sectional survey of prescribing was records-based and no direct assessments of mental state were made. Clinical records are the only available source of routine data linking clinical information with prescribing for individual patients. Good record-keeping is essential to the quality and continuity of health care and it is reasonable to expect that information on medicines and clinical diagnoses should be available in patient notes. Nonetheless, it is possible that some prescriptions, diagnoses or information were missed. These factors could have limited the precision of our estimates and our assessments of prescribing appropriateness.
It is important to acknowledge that assessing prescribing appropriateness is a complex endeavour. We received only aggregate denominator data from prisons and the CPRD, broken down by demographic, but not clinical, factors. We only adjusted for age in comparisons between prisons and the community. Thus, we could not adjust for mental illness prevalence (or other possible health-related confounding factors) in the analysis. This is a limitation of the analysis. In addition, the PAI was applied only to prison data; while assessing the appropriateness of psychotropic prescribing in the community was outside the scope of the current study, it remains unclear how prisons compare with community settings in this respect. Furthermore, in using the PAI, the records-based study was largely limited to assessing pharmacological appropriateness; arguably, however, patient needs, expectations, prescriber perspectives and the greater good should also be taken into consideration. 89 While the latter two dimensions of appropriateness were addressed in the acceptability study, it was not possible to do this in the much larger, records-based cross-sectional survey. One area for further work may be to develop measures that can be routinely applied, yet capture more fully the complexity of prescribing appropriateness.
The CPRD only includes prescription data for drugs prescribed in primary care; therefore, psychotropic drugs prescribed in secondary care (e.g. hospital outpatient appointments) were excluded from the estimates provided in this study. This may have resulted in an underestimate of community psychotropic prescribing rates; however, the majority of prescribing in the UK takes place in primary care, and thus the impact is likely to be small.
While we arguably accounted for the most important demographic and clinical factors in our analyses, it is possible that other measured and unmeasured variables may have influenced psychotropic prescribing patterns, including adherence to local formularies (lists of approved medicines), the type of health-care provider (NHS vs. non-NHS), criminological characteristics (e.g. offence) and individual prescriber characteristics and/or behaviour. Owing to the number of data collected as part of the study, the most essential analyses were prioritised. It was not possible to provide equivalent community statistics for every analysis we performed on psychotropic prescribing in prison. Some of these data were unavailable for CPRD patients (e.g. ethnicity). However, it may be possible to follow up some of these areas as part of secondary analyses or future projects.
There are some limitations to the cost analyses undertaken in the current study. Costs were based on published BNF costs and average doses, rather than on actual purchasing costs. This approach was adopted partly for pragmatic reasons, to reduce complexity, and partly to make relative comparisons fairer between different prisons and demographic groups. Use of BNF costs and DDDs are common in the wider research literature. Nonetheless, while this may have been the most pragmatic approach, it could have resulted in a lack of precision in terms of budget estimates for psychotropic medicines. Prisons may have access to different wholesale suppliers, which may be cheaper. Thus, caution should be taken in applying these estimates elsewhere or attempting comparisons with data from other sources.
The acceptability study allowed us to determine the acceptability of prescribing to patients and doctors, thereby complementing our assessment of the pharmacological appropriateness of prescribing. The survey achieved a final sample of 156 patients, which was 78% of our original target (n = 200). The main reason for this was that major organisational changes to the NHS during the study resulted in a lack of clarity regarding research approval processes and prompted renegotiations over resources to support research. This had the effect of delaying access to participating prisons and reducing the resources available to support data collection. While the descriptive analyses should have been relatively unaffected, it is possible that the reduced sample size may have been too small to detect some group differences (known as a type II error). In particular, the sample of patients who identified mental health as their main health problem was relatively small (n = 36) and would have benefited from being larger. Nonetheless, several statistically significant differences were detected between this group and patients with other health problems. Furthermore, few of the major analyses were of borderline significance (close to p = 0.05), which suggests that the sample size was adequate.
Overall, satisfaction with consultations and prescribing were high in this study, which somewhat contradicts previous prisoner reports,117 research findings62–64 and, anecdotally, popular opinion. It is possible that individual patients were unwilling to disclose negative views to a researcher. Although the response rate was high (85.2%), it may have been the case that individuals who refused had more negative views. Anecdotally, however, patients who refused commonly gave reasons such as lack of time (e.g. expecting a visit or not wanting to miss association) or unwillingness to disclose their personal health issues.
Only six doctors participated in the study. While these doctors ran the majority of primary care clinics within their respective establishments, their views are not necessarily generalisable. In particular, it would be useful to compare the views of doctors with different characteristics, training and experiences of working in prisons. Although doctors were not told in advance which patients were participating in the study, sometimes they would have known that the researcher was sampling from that particular clinic. This may have influenced their practices. Furthermore, doctors may have been unwilling to identify prescriptions as not strictly indicated or to admit to feeling pressure or discomfort when prescribing.
Patient and public involvement
Ongoing patient and public involvement was achieved via the MACE research advisory group. Historically, service user involvement in offender health research has been challenging and uncommon. Challenges noted in the literature have been identifying and recruiting suitable individuals, managing payments, identifying resources and ensuring meaningful engagement. 118 However, we proved that it is possible to recruit a group of ex-offenders and engage them throughout the lifetime of the project.
Initially, we encountered difficulties in recruiting individuals. Advertising in standard public involvement research forums and networks (e.g. People in Research, the Mental Health Research Network) for individuals was unsuccessful. This delayed progress with some key project tasks, including questionnaire adaptation and ethics approvals. A successful resolution to the problem was found when we discovered colleagues in the psychology department at The University of Manchester who had assembled a group of ex-prisoners for a suicide prevention research project. The group agreed to collaborate with us on the current project and additional members were recruited via members’ acquaintances. Where possible, meetings for the two research projects were run consecutively on the same day and venue to accommodate the schedules of group members and to make attendance easier. This arrangement worked well for the group members and researchers on both projects, as resources and skills could be pooled for mutual benefit (e.g. travel expenses and individuals trained in research methods).
Once the MACE group was established, members assisted with adapting questionnaires, reviewing participant information sheets for readability and developing study advertisements (posters). The advice of members was also invaluable in advising on recruitment strategies and the workings of prison health-care systems (e.g. appointment application processes), allowing researchers to more effectively plan and execute the acceptability study. Members also took turns in attending project steering group meetings, thereby impacting on decision-making at steering-group level. One example of this was the suggestion to include an open prison in the prevalence survey, which came from a MACE group member attending a steering group; this was subsequently taken up and acted upon. The group have also been, and will continue, taking part in dissemination activities. Members assisted in preparing the lay summary in this report and they participated in a presentation at a seminar which took place in February 2014. Members have also reported personal benefits from participation including improved communication skills, access to research training, enhanced social and professional networks and increased confidence.
Although there were many advantages and positive impacts from involving ex-offenders in the management of this project, gaining and managing this type of input was not without its challenges. Although some members had previously worked together, changes in membership and working with a new set of researchers inevitably altered group dynamics. Thus, at times, conflict resolution strategies were needed to resolve disagreements. In such situations, we were glad to have established clear terms of reference and rules of conduct in collaboration with the group at the outset. While in some cases these had to be revisited, clarified and amended, they provided everyone with a clear reference point. Another challenge was dealing with different levels of ability, skills, confidence and experiences. Researchers had to adopt open and clear communication styles to ensure that members could understand research processes, and they had to be ready to explain or elaborate where necessary. Lastly, the time and resources needed to plan, facilitate and administer patient and public involvement for this project exceeded our expectations, and, with hindsight, dedicated input from an administrator or specialist facilitator would have been beneficial.
Chapter 5 Implications and recommendations for future research
In this concluding chapter, we discuss the potential implications of our findings for practice, and make recommendations for future research.
Implications for practice
The relationship between rates of mental illness and rates of psychotropic prescribing is, undoubtedly, complex. This, together with the lack of up-to-date data on the prevalence of mental illness in prisons, limits the extent to which we can draw any firm conclusions regarding whether or not the prescribing of psychotropic medicines is wholly appropriate and proportionate to the level of need. Nonetheless, what is clear from our study is that psychotropic medicines were prescribed frequently in prisons, and for a wider range of indications than those for which they are currently recommended. Furthermore, the acceptability study highlighted potential shortcomings in relation to support for mental illness and/or emotional problems. Set in the context of the wider evidence base in this area, this suggests that prisons may lack the precision and range of responses required when distinguishing between and responding to mental illness, challenging behaviours and distress. Greater access to psychological therapies, non-health activities and support for vulnerable individuals in custody could be possible ways to reduce reliance on psychotropic medication. This may be especially important to address in women’s prisons, where rates of psychotropic prescribing are particularly high.
We found evidence that psychotropic medicines were used in prisons to treat a broad range of illnesses and symptoms, not all of which have an established evidence base. Where medicines are prescribed for unlicensed uses, it is important for prescribers to justify their use and document this clearly. In particular, it would appear that doctors in prison are continuing to prescribe drugs for personality disorder, against the recommendations of NICE. This phenomenon might not be unique to prisons; indeed, personality is a contested and complex area. However, in the absence of an established evidence base, there remains a need to review such practices and, where possible, identify alternative treatment options.
The current study indicated there were discernible differences in drug choice between prisons and the community. In particular, certain antidepressant and antipsychotic medicines with propensity for sedation and weight gain were more likely to be prescribed in prison. There are a number of reasons why sedative effects may be viewed as desirable among prisoners, thereby increasing pressure on prescribers. Nonetheless, while patient preferences should be taken into account, the increased risk of adverse effects on physical health associated with these drugs cannot be overlooked. Given these risks, prisons should ensure that there are robust and integrated systems in place to monitor and manage the physical health of prisoners receiving such treatment. This is especially important among prisoners who commonly have multiple health problems (and medications), adding to the complexity of care. While we did not formally investigate this as part of the current study, anecdotally there appeared to be variation between prisons in terms of frequency of monitoring, the measures used and how the workload was distributed. It may, thus, be beneficial for prisons to consider offering medicines use reviews to provide advice on medicines, optimise medicines use and help to identify drug–drug interactions.
During the process of conducting this research, we noticed that some prisons were still not using electronic clinical record systems for issuing prescriptions. We consider this an unnecessary hindrance to information sharing between prescribers and other health-care professionals in prison. If prescribers cannot easily access up-to-date and accurate information on prescriptions, this increases the risk of polypharmacy, hazardous drug–drug interactions and iatrogenic effects. Therefore, using electronic prescribing when it is available, would improve transparency, patient safety and to provide effective and integrated health care. There may be a need to provide training to enable individuals to competently use these new systems.
Recommendations for future research
The findings and issues raised by the current study indicate several possible avenues for future research.
The first and most important priority is to develop and test a series of indicators for safe and appropriate prescribing, suitable for integration within clinical IT systems in prison. The current study used a combination of methods to extract the relevant demographic and prescribing data from each prison and convert them into meaningful information, requiring considerable time, effort and skill. If an automated system could be integrated within clinical IT systems capable of summarising prescribing activity, this would facilitate regular self-monitoring, review and benchmarking of a crucial area of practice. It could also allow commissioners and health-care providers to access (and act upon) data in ‘real time’ without the need for separate research. Harnessed correctly, data held in clinical IT systems in prisons could also be used, either alone or in combination with other data sets, in epidemiological studies to determine associations between psychotropic drug treatment in prison and a range of outcomes relating to mental and physical health, reoffending and social outcomes, both in custody and post release.
Another worthwhile direction for future research would be to determine the frequency and type of treatment responses (including prescriptions for psychotropic medicines and alternatives) among prisoners presenting with common mental health problems. This could be conducted alongside clinical trials to measure the impact of introducing alternative interventions (e.g. psychological therapies) on outcomes such as the prevalence of psychotropic prescribing, changes in psychiatric symptoms and patient satisfaction. It would also be important to include a health economics component to understand the relative costs of psychotropic prescribing versus other interventions. Research in this area could also consider whether or not the use of more costly formulations of medicines in prison (e.g. liquid diazepam) is justified and represents an effective balance between cost-effectiveness, safety and security.
The evidence from this study showed that doctors in prison are continuing to prescribe drugs for personality disorder. While this practice may be against national clinical guidance, there is arguably a need for research to explore the reasons and circumstances in which drugs are prescribed for personality disorder, not only in prison but in the wider community. A qualitative, exploratory approach may be an appropriate starting point for this type of study.
Finally, this study revealed important differences in prescribing patterns among demographic subgroups, in particular women and BME groups. Yet from the limited data we collected in the current study, it is unclear why exactly these differences were observed. For example, do the higher rates of psychotropic drug treatment among women in prison represent overprescribing or an appropriate response to increased clinical need? Are the lower rates of psychotropic prescribing among BME groups evidence of undertreatment of mental illness? Furthermore, we did not have the opportunity to explore in detail psychotropic prescribing among older prisoners, who are an important and rapidly growing group with complex health and medication needs. Further research in these areas would answer such questions and help to inform the future planning and commissioning of services for important demographic groups.
Acknowledgements
We would like to thank all of the staff and prisoners who participated in this research and assisted in its organisation. We are grateful to Liz Andrew, Becca Bishop and Suzanne Jakeman for assisting with prison data collection and Heather Noga for assisting with report preparation. We also thank Jolanta Shields, Njabulo Skhosana and Richard Poole for entering the data. The contribution of the MACE research advisory group was invaluable in helping to design the research, interpret findings and prepare the plain English summary.
This study is based in part on data from the Full Feature CPRD obtained under licence from the UK Medicines and Healthcare products Regulatory Agency. However, the interpretation and conclusions contained in this study are those of the author(s) alone. Access to the CPRD database was funded through the MRC’s licence agreement with Medicines and Healthcare products Regulatory Agency [Ref: 10_048R].
Contributions of authors
Dr Lamiece Hassan (research associate, offender mental health and epidemiology) helped to design the study, collect the data, perform the analysis and draft the final report.
Dr Martin Frisher (reader in health services research, psychology and epidemiology) helped to design the study, perform the analysis and review the final report.
Dr Jane Senior (research fellow, offender mental health) helped to design the study, supervise the researcher and draft the final report.
Dr Mary Tully (clinical senior lecturer, pharmacy) helped to design the study, performed the analysis and reviewed the final report.
Dr Roger Webb (senior research fellow, psychiatric epidemiology) helped to design the study, perform the analysis and review the final report.
Dr David While (research fellow, statistician) helped to design the study, perform the analysis and review the final report.
Professor Jenny Shaw (Professor, forensic psychiatry) was the principal investigator who took overall responsibility for the supervision and management of the study, and helped to design the study and review the final report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Bradley K. The Bradley Report: Lord Bradley’s Review of People with Mental Health Problems or Learning Disabilities in the Criminal Justice System. London: Department of Health; 2009.
- Baillargeon J, Black SA, Contreras S, Grady J, Pulvino J. Anti-depressant prescribing patterns for prison inmates with depressive disorders. J Affect Disord 2001;63:225-31. http://dx.doi.org/10.1016/S0165-0327(00)00188-9.
- Elger BS, Bindschedler M, Goehring C, Revaz SA. Evaluation of drug prescription at the Geneva prison’s outpatient service in comparison to an urban outpatient medical service. Pharmacoepidemiol Drug Saf 2004;13:633-44. http://dx.doi.org/10.1002/pds.907.
- Kjelsberg E, Hartvig P. Can morbidity be inferred from prescription drug use? Results from a nation-wide prison population study. Eur J Epidemiol 2005;20:587-92. http://dx.doi.org/10.1007/s10654-005-8156-9.
- A Pharmacy Service for Prisoners. London: Department of Health; 2003.
- Singleton N, Meltzer H, Gatward R. Psychiatric Morbidity Among Prisoners: Summary Report. London: Office for National Statistics; 1998.
- National Health Service Act 2006. London: The Stationery Office; 2006.
- Brooke D, Taylor C, Gunn J, Maden A. Point prevalence of mental disorder in unconvicted male prisoners in England and Wales. BMJ 1996;313:1524-7. http://dx.doi.org/10.1136/bmj.313.7071.1524.
- Gunn J, Madden A, Swinton M. Mentally Disordered Prisoners. London: Home Office; 1991.
- Gunn J, Maden A, Swinton M. Treatment needs of prisoners with psychiatric disorders. BMJ 1991;303:338-41. http://dx.doi.org/10.1136/bmj.303.6798.338.
- Maden A, Taylor C, Brooke D, Gunn J. Mental Disorder in Remand Prisoners. London: Home Office; 1996.
- Maden T, Swinton M, Gunn J. Psychiatric disorder in women serving a prison sentence. Br J Psychiatry 1994;164:44-5. http://dx.doi.org/10.1192/bjp.164.1.44.
- Senior J, Birmingham L, Harty MA, Hassan L, Hayes AJ, Kendall K, et al. Identification and management of prisoners with severe psychiatric illness by specialist mental health services. Psychol Med 2013;43:1511-20. http://dx.doi.org/10.1017/S0033291712002073.
- Birmingham L, Mason D, Grubin D. Prevalence of mental disorder in remand prisoners: consecutive case study. BMJ 1996;313:1521-4. http://dx.doi.org/10.1136/bmj.313.7071.1521.
- Meltzer H, Gill B, Pettigrew M. The Prevalence of Psychiatric Morbidity Among Adults Aged 16–64, Living in Private Households in Great Britain. London: Office of Population Censuses and Surveys; 1995.
- Singleton N, Bumpstead R, O’Brien M, Lee A, Meltzer H. Psychiatric Morbidity among Adults Living in Private Households, 2000. London: HMSO; 2001.
- Meltzer H, Gill B, Hinds K, Petticrew M. The prevalence of psychiatric morbidity among adults living in institutions. Int Rev Psychiatry 2003;15:129-33. http://dx.doi.org/10.1080/0954026021000046047.
- Appleby L. Offender health: the next frontier. Psychiatrist 2010;34:409-10. http://dx.doi.org/10.1192/pb.bp.110.032037.
- Shaw J, Senior J, Lowthian C, Foster K, Clayton R, Coxon N, et al. A National Evaluation of Prison Mental Health In-Reach Services. Manchester: Offender Health Research Network, The University of Manchester; 2009.
- Fazel S, Danesh J. Serious mental disorder in 23000 prisoners: a systematic review of 62 surveys. Lancet 2002;359:545-50. http://dx.doi.org/10.1016/S0140-6736(02)07740-1.
- Fazel S, Seewald K. Severe mental illness in 33,588 prisoners worldwide: systematic review and meta-regression analysis. Br J Psychiatry 2012;200:364-73. http://dx.doi.org/10.1192/bjp.bp.111.096370.
- The Provision of Mental Health Care in Prisons. London: Prison Service; 1997.
- Exworthy T, Samele C, Urquia N, Forrester A. Asserting prisoners’ right to health: progressing beyond equivalence. Psychiatr Serv 2012;63:270-5. http://dx.doi.org/10.1176/appi.ps.201100256.
- Changing the Outlook: A Strategy for Developing and Modernising Mental Health Services in Prison. London: Department of Health; 2001.
- Simmonds S, Coid J, Joseph P, Marriott S, Tyrer P. Community mental health team management in severe mental illness: a systematic review. Br J Psychiatry 2001;178:497-502. http://dx.doi.org/10.1192/bjp.178.6.497.
- Thornicroft G, Becker T, Holloway F, Johnson S, Leese M, McCrone P, et al. Community mental health teams: evidence or belief?. Br J Psychiatry 1999;175:508-13. http://dx.doi.org/10.1192/bjp.175.6.508.
- British National Formulary. No. 64, 2012. London: BMA and RPS; 2012.
- Taylor D, Paton C, Kapur S. Maudsley Prescribing Guidelines. Informa Healthcare; 2009.
- Chadwick H, Bressington D, Harris N, Baker J, Gray R. Medicines Management in Mental Health Care. Chichester: Wiley-Blackwell; 2009.
- Drug Misuse and Dependence: UK Guidelines on Clinical Management. London: Department of Health; 2007.
- Guidance on the Use of Zaleplon, Zolpidem and Zopiclone for the Short-Term Management of Insomnia. London: NICE; 2004.
- Obsessive–Compulsive Disorder. London: NICE; 2005.
- Post-Traumatic Stress Disorder (PTSD): The Management of PTSD in Adults and Children in Primary and Secondary Care. London: NICE; 2005.
- Anxiety. London: NICE; 2011.
- Bymaster FP, Calligaro DO, Falcone JF, Marsh RD, Moore NA, Tye NC, et al. Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology 1996;14:87-96. http://dx.doi.org/10.1016/0893-133X(94)00129-N.
- Roth BL, Sheffler DJ, Kroeze WK. Magic shotguns versus magic bullets: selectively non-selective drugs for mood disorders and schizophrenia. Nat Rev Drug Discov 2004;3:353-9. http://dx.doi.org/10.1038/nrd1346.
- Mailman RB, Murthy V. Third generation antipsychotic drugs: partial agonism or receptor functional selectivity?. Curr Pharm Des 2010;16:488-501. http://dx.doi.org/10.2174/138161210790361461.
- Schizophrenia. London: NICE; 2009.
- Wahlbeck K, Cheine M, Essali A, Adams C. Evidence of clozapine’s effectiveness in schizophrenia: a systematic review and meta-analysis of randomized trials. Am J Psychiatry 1999;156:990-9.
- McEvoy JP, Liebermann JA, Stroup TS, Davis SM, Meltzer HY, Rosenheck RA, et al. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry 2006;163:600-10. http://dx.doi.org/10.1176/appi.ajp.163.4.600.
- Bipolar Disorder. London: NICE; 2006.
- Depression: The Treatment and Management of Depression in Adults. London: NICE; 2009.
- Anderson IM, Ferrier IN, Baldwin RC, Cowen PJ, Howard L, Lewis G, et al. Evidence-based guidelines for treating depressive disorders with antidepressants: a revision of the 2000 British Association for Psychopharmacology guidelines. J Psychopharmacol 2008;22:343-96. http://dx.doi.org/10.1177/0269881107088441.
- Healy D. Lines of evidence on the risks of suicide with selective serotonin reuptake inhibitors. Psychother Psychosom 2003;72:71-9. http://dx.doi.org/10.1159/000068691.
- Healy D, Langmaak C, Savage M. Suicide in the course of the treatment of depression. J Psychopharmacol 1999;13:94-9. http://dx.doi.org/10.1177/026988119901300110.
- Khan A, Khan S, Kolts R, Brown WA. Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports. Am J Psychiatry 2003;160:790-2. http://dx.doi.org/10.1176/appi.ajp.160.4.790.
- Report of the CSM Expert Working Group on the Safety of SSRI Antidepressants. London: MHRA; 2004.
- Teicher MH, Glod C, Cole JO. Emergence of intense suicidal preoccupation during fluoxetine treatment. Am J Psychiatry 1990;147:207-10.
- Dilsaver SC, Greden JF. Antidepressant withdrawal phenomena. Biol Psychiatry 1984;19:237-56.
- Diagnostic and Statistical Manual of Mental Disorders. Arlington, VA: American Psychiatric Association; 2013.
- Attention Deficit Hyperactivity Disorder. London: NICE; 2013.
- The International Classification of Disease. Geneva: World Health Organization; 1992.
- Morton WA, Stockton GG. Methylphenidate abuse and psychiatric side effects. Prim Care Companion J Clin Psychiatry 2000;2:159-64. http://dx.doi.org/10.4088/PCC.v02n0502.
- Volkow ND, Ding YS, Fowler JS, Wang GJ, Logan J, Gatley JS, et al. Is methylphenidate like cocaine? Studies on their pharmacokinetics and distribution in the human brain. Arch Gen Psychiatry 1995;52:456-63. http://dx.doi.org/10.1001/archpsyc.1995.03950180042006.
- Sim J. Medical Power in Prisons: The Prison Medical Service in England 1774–1989. Bury St Edmunds: Open University Press; 1990.
- Report on the Work of the Prison Department 1980. London: HMSO; 1980.
- Report on the Work of the Prison Department 1979. London: HMSO; 1980.
- Gunn J. Report on the work of the prison department 1979. Psychiatr Bull 1981;5. http://dx.doi.org/10.1192/pb.5.2.31.
- Owen T, Sim J, Scraton P, Gordon P. Cause for Concern: British Criminal Justice on Trial. Reading: Penguin Books Ltd; 1984.
- Hassan L, Weston J, Senior J, Shaw J. Prisoners holding their own medications during imprisonment in England and Wales: a survey and qualitative exploration of staff and prisoners’ views. Crim Behav Ment Heal 2012;22:29-40. http://dx.doi.org/10.1002/cbm.822.
- Safer Prescribing in Prisons: Guidance for Clinicians. RCGP; 2011.
- Bowen RA, Rogers A, Shaw J. Medication management and practices in prison for people with mental health problems: a qualitative study. Int J Ment Health Syst 2009;3. http://dx.doi.org/10.1186/1752-4458-3-24.
- Douglas N, Plugge E, Fitzpatrick R. The impact of imprisonment on health: what do women prisoners say?. J Epidemiol Community Health 2009;63:936-42. http://dx.doi.org/10.1136/jech.2008.080713.
- Plugge E, Douglas N, Fitzpatrick R. Patients, prisoners or people. Women prisoners’ experience of primary care in prison: a qualitative study. Br J Gen Pract 2008;58:e1-8. http://dx.doi.org/10.3399/bjgp08X330771.
- Doing Time: The Experiences and Needs of Older People in Prison. London: Prison Reform Trust; 2008.
- Senior J, Hayes AJ, Bowen A, Foster K, Clayton R, Humber N, et al. Evaluation of the ‘Care of At-Risk Prisoners Project’. Manchester: University of Manchester; 2005.
- Hassan L, Senior J, Edge D, Shaw J. Continuity of psychiatric medicines’ supply for newly received prisoners. Psychiatrist 2011;35:244-8. http://dx.doi.org/10.1192/pb.bp.110.031757.
- Unjust Deserts: A Thematic Review by HM Chief Inspector of Prisons of the Treatment and Conditions for Unsentenced Prisoners in England and Wales. London: Her Majesty’s Inspectorate of Prisons for England and Wales; 2000.
- Lader D, Singleton N, Meltzer H. Psychiatric morbidity among young offenders in England and Wales. Int Rev Psychiatry 2003;15:144-7. http://dx.doi.org/10.1080/0954026021000046074.
- Coid J, Bebbington P, Jenkins R, Brugha T, Lewis G, Farrell M, et al. The national survey of psychiatric morbidity among prisoners and the future of prison healthcare. Med Sci Law 2002;42:245-50.
- Hassan L, Senior J, Frisher M, Edge D, Shaw J. A comparison of psychotropic medication prescribing patterns in East of England prisons and the general population. J Psychopharmacol 2014;28:357-62. http://dx.doi.org/10.1177/0269881114523863.
- Kjelsberg E, Hartvig P. Too much or too little? Prescription drug use in a nationwide prison population. Int J Prison Health 2005;1:75-87. http://dx.doi.org/10.1080/17449200500156871.
- Elger BS, Goehring C, Revaz SA, Morabia A. Prescription of hypnotics and tranquilisers at the Geneva prison’s outpatient service in comparison to an urban outpatient medical service. Soc Prev Med 2002;47:39-43. http://dx.doi.org/10.1007/BF01318404.
- Lund BC, Flaum M, Adam LA, Perry PJ. Psychiatric prescribing trends and practices in Iowa’s prisons. Psychiatr Serv 2002;53:1023-4. http://dx.doi.org/10.1176/appi.ps.53.8.1023.
- Baillargeon J, Contreras SA. Antipsychotic prescribing patterns in the Texas prison system. J Am Acad Psychiatry Law 2001;29:48-53.
- Baillargeon J, Contreras S, Grady JJ, Black SA, Murray O. Compliance with antidepressant medication among prison inmates with depressive disorders. Psychiatr Serv 2000;51:1444-6. http://dx.doi.org/10.1176/appi.ps.51.11.1444.
- Williams BA, Baillargeon JG, Lindquist K, Walter LC, Covinsky KE, Whitson HE, et al. Medication prescribing practices for older prisoners in the Texas prison system. Am J Public Health 2010;100:756-61. http://dx.doi.org/10.2105/AJPH.2008.154591.
- Griffiths EV, Willis J, Spark MJ. A systematic review of psychotropic drug prescribing for prisoners. Aust N Z J Psychiatry 2012;46:407-21. http://dx.doi.org/10.1177/0004867411433893.
- Steadman HJ, Osher FC, Robbins PC, Case B, Samuels S. Prevalence of serious mental illness among jail inmates. Psychiatr Serv 2009;60:761-5. http://dx.doi.org/10.1176/appi.ps.60.6.761.
- Pratt D. Prevention for Suicide in Prisons (PROSPeR) 2013. www.ukctg.nihr.ac.uk/trialdetails/ISRCTN59909209 (accessed 3 August 2014).
- Cresswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Sage; 2003.
- Young S, Thome J. ADHD and offenders. World J Biol Psychiatry 2011;12:124-8. http://dx.doi.org/10.3109/15622975.2011.600319.
- Cantrill JA, Sibbald B, Buetow S. Indicators of the appropriateness of long-term prescribing in general practice in the United Kingdom: consensus development, face and content validity, feasibility, and reliability. Qual Health Care 1998;7:130-5. http://dx.doi.org/10.1136/qshc.7.3.130.
- Tully MP, Cantrill JA. The validity of explicit indicators of prescribing appropriateness. Int J Qual Health Care 2006;18:87-94. http://dx.doi.org/10.1093/intqhc/mzi084.
- Depression: The Treatment and Management of Depression in Adults. London: NICE; 2009.
- Key Health Statistics from General Practice 1998. London: Office for National Statistics; 2000.
- British National Formulary. London: BMA and RPS; 2013.
- World Health Organization Collaborating Centre for Drug Statistics Methodology . Defined Daily Dose: Definition and General Considerations 2009. www.whocc.no/ddd/definition_and_general_considera/ (accessed 3 August 2014).
- Britten N, Jenkins L, Barber N, Bradley C, Stevenson F. Developing a measure for the appropriateness of prescribing in general practice. Qual Health Care 2003;12:246-50. http://dx.doi.org/10.1136/qhc.12.4.246.
- Harcouët L. L’exercice pharmaceutique hospitalier en milieu carcéral. Ann Pharm Françaises 2010;68:286-90. http://dx.doi.org/10.1016/j.pharma.2010.05.003.
- Middleton N, Gunnell D, Whitley E, Dorling D, Frankel S. Secular trends in antidepressant prescribing in the UK, 1975–1998. J Public Health Med 2001;23:262-7. http://dx.doi.org/10.1093/pubmed/23.4.262.
- Moore M, Yuen HM, Dunn N, Mullee M, Maskell J, Kendrick T. Explaining the rise in antidepressant prescribing: a descriptive study using the general practice research database. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b3999.
- Hassan L, Edge D, Senior J, Shaw J. Staff and patient perspectives on the purpose of psychotropic prescribing in prisons: care or control?. Gen Hosp Psychiatry 2013;35:433-8. http://dx.doi.org/10.1016/j.genhosppsych.2013.01.012.
- Liebling A, Tait S, Durie L, Stiles A, Harvey J. The Safer Locals Programme. Prison Serv J 2005;162:8-23.
- Corsten J. The Corsten Report. London: Home Office; 2007.
- Justice for Women: The Need for Reform. London: Prison Reform Trust; 2000.
- Hassan L, Birmingham L, Harty MA, Jarrett M, Jones P, King C, et al. Prospective cohort study of mental health during imprisonment. Br J Psychiatry 2011;198:37-42. http://dx.doi.org/10.1192/bjp.bp.110.080333.
- Newcomer JW. Antipsychotic medications: metabolic and cardiovascular risk. J Clin Psychiatry 2007;68:8-13.
- Troubled Inside: Responding to the Mental Health Needs of Women in Prison. London: Prison Reform Trust; 2003.
- Flaskerud JH, Hu LT. Racial/ethnic identity and amount and type of psychiatric treatment. Am J Psychiatry 1992;149:379-84.
- Szarek BL, Goethe JW. Racial differences in use of antipsychotics among patients with bipolar disorder. J Clin Psychiatry 2003;64:614-15. http://dx.doi.org/10.4088/JCP.v64n0518g.
- Connolly A. Race and prescribing. Psychiatrist 2010;34:169-71. http://dx.doi.org/10.1192/pb.bp.109.026435.
- Delivering Race Equality in Mental Health Care: An Action Plan for Reform Inside and Outside Services and the Government’s Response to the Independent Inquiry into the Death of David Bennett. London: Department of Health; 2005.
- Drug Misuse and Dependence: UK Guidelines on Clinical Management. London: Department of Health; 2007.
- Fazel S, Benning R, Danesh J. Suicides in male prisoners in England and Wales, 1978–2003. Lancet 2005;366:1301-2. http://dx.doi.org/10.1016/S0140-6736(05)67325-4.
- Elger BS. Insomnia in places of detention: a review of the most recent research findings. Med Sci Law 2007;47:191-9. http://dx.doi.org/10.1258/rsmmsl.47.3.191.
- Newcomer JW. Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs 2005;19:1-93. http://dx.doi.org/10.2165/00023210-200519001-00001.
- Hassan L, Rahman MS, King C, Senior J, Shaw J. Level of mental health intervention and clinical need among inmates with mental illness in five English jails. Psychiatr Serv 2012;63:1218-24. http://dx.doi.org/10.1176/appi.ps.201100344.
- Baldwin DS, Kosky N. Off-label prescribing in psychiatric practice. Adv Psychiatr Treat 2007;13:414-22. http://dx.doi.org/10.1192/apt.bp.107.004184.
- Borderline Personality Disorder: Treatment and Management. London: NICE; 2009.
- Antisocial Personality Disorder: Treatment, Management and Prevention. London: NICE; 2009.
- Baker-Glenn E, Steels M, Evans C. Use of psychotropic medication among psychiatric out-patients with personality disorder. Psychiatrist 2010;34:83-6. http://dx.doi.org/10.1192/pb.bp.108.021758.
- Joukamaa M, Heliövaara M, Knekt P, Aromaa A, Raitasalo R, Lehtinen V. Schizophrenia, neuroleptic medication and mortality. Br J Psychiatry 2006;188:122-7. http://dx.doi.org/10.1192/bjp.188.2.122.
- Mojtabai R, Olfson M. National trends in psychotropic medication polypharmacy in office-based psychiatry. Arch Gen Psychiatry 2010;67:26-3. http://dx.doi.org/10.1001/archgenpsychiatry.2009.175.
- Douglas N, Plugge E. A Health Needs Assessment for Young Women in Young Offender Institutions. London: Youth Justice Board; 2006.
- Whole-Person Care: From Rhetoric to Reality. Achieving Parity Between Mental and Physical Health. London: Royal College of Psychiatrists; 2013.
- Mellor PA. The inside story on prison health care. BMJ 2003;326. http://dx.doi.org/10.1136/bmj.326.7379.59.
- Service User Involvement: For Organisations Working with Offenders, Ex-Offenders and their Families. London: Clinks; 2010.
Appendix 1 Patient questionnaire A
Appendix 2 Patient questionnaire B
Appendix 3 Doctor questionnaire B
Appendix 4 Prescribing appropriateness indicators
Appendix 5 Additional tables
| Sample | Age group (years), % (n) | |||||||
|---|---|---|---|---|---|---|---|---|
| 18–24 | 25–34 | 35–44 | 45–54 | 55–64 | 65–74 | 75+ | All | |
| Men | ||||||||
| Hypnotics and anxiolytics | 1.0 (1516) | 1.9 (4266) | 2.8 (7544) | 3.1 (8334) | 3.7 (8174) | 4.8 (7546) | 7.3 (8876) | 3.3 (46,256) |
| Antipsychotics | 0.9 (1352) | 1.4 (3162) | 1.8 (4865) | 2.0 (5265) | 2.3 (5079) | 2.7 (4322) | 4.0 (4891) | 2.0 (28,936) |
| Antidepressants | 2.5 (3768) | 4.3 (9898) | 6.3 (16,910) | 7.3 (19,533) | 8.5 (19,005) | 8.3 (13,167) | 10.0 (12,127) | 6.7 (94,408) |
| CNS stimulants | 0.2 (353) | 0.0 (84) | 0.0 (74) | 0.0 (74) | 0.0 (68) | 0.0 (42) | 0.0 (27) | 0.1 (722) |
| Any | 4.0 (5932) | 6.3 (14,299) | 8.8 (23,676) | 10.0 (26,735) | 11.9 (26,571) | 13.2 (20,779) | 17.5 (21,244) | 9.8 (139,236) |
| Women | ||||||||
| Hypnotics and anxiolytics | 1.8 (2564) | 3.1 (7054) | 4.4 (11,437) | 5.5 (14,211) | 6.4 (14,420) | 8.5 (14,230) | 12.1 (21,890) | 5.9 (85,806) |
| Antipsychotics | 1.4 (2082) | 1.9 (4446) | 2.5 (6592) | 3.1 (8088) | 3.6 (8084) | 4.5 (7622) | 6.8 (12,221) | 3.4 (49,135) |
| Antidepressants | 6.5 (9352) | 9.4 (21,448) | 13.8 (36,103) | 16.2 (41,699) | 16.2 (36,415) | 16.0 (26,909) | 18.0 (32,476) | 14.0 (204,402) |
| CNS stimulants | 0.1 (95) | 0.0 (63) | 0.0 (113) | 0.0 (86) | 0.0 (67) | 0.0 (46) | 0.0 (25) | 0.0 (495) |
| Any | 8.6 (12,315) | 12.1 (27,699) | 17.1 (44,700) | 20.3 (52,114) | 21.4 (47,901) | 23.2 (39,079) | 29.0 (52,336) | 18.9 (276,144) |
| Sample | Age group (years), n | |||||||
|---|---|---|---|---|---|---|---|---|
| 18–24 | 25–34 | 35–44 | 45–54 | 55–64 | 65–74 | 75+ | All | |
| Men | ||||||||
| Hypnotics and anxiolytics | 18,807 | 25,008 | 28,975 | 28,607 | 23,897 | 16,120 | 11,587 | 153,000 |
| Antipsychotics | 26,527 | 35,109 | 37,090 | 39,602 | 33,883 | 22,157 | 17,249 | 211,618 |
| Antidepressants | 10,036 | 14,624 | 17,822 | 17,057 | 14,547 | 9466 | 7819 | 91,371 |
| CNS stimulants | 150,059 | 227,956 | 270,532 | 266,973 | 223,495 | 157,767 | 121,565 | 1,418,347 |
| Any | 19,478 | 18,317 | 20,590 | 19,782 | 17,218 | 11,761 | 9625 | 116,772 |
| Women | ||||||||
| Hypnotics and anxiolytics | 14,075 | 23,285 | 26,683 | 25,928 | 23,133 | 17,051 | 17,835 | 147,991 |
| Antipsychotics | 19,958 | 32,416 | 38,098 | 38,462 | 32,945 | 24,085 | 26,554 | 212,519 |
| Antidepressants | 7979 | 13,866 | 15,062 | 15,143 | 13,513 | 10,587 | 12,399 | 88,548 |
| CNS stimulants | 143,783 | 228,765 | 261,060 | 257,306 | 224,179 | 168,266 | 180,489 | 1,463,848 |
| Any | 10,134 | 15,973 | 17,205 | 17,108 | 15,622 | 12,439 | 14,422 | 102,904 |
Appendix 6 List of drugs in the British National Formulary (chapter 4)
Hypnotics and anxiolytics (4.1)
Hypnotics
-
Chloral hydrate.
-
Clomethiazole.
-
Flurazepam.
-
Loprazolam.
-
Lormetazepam.
-
Melatonin.
-
Nitrazepam.
-
Promethazine hydrochloride.
-
Sodium oxybate.
-
Temazepam.
-
Zaleplon.
-
Zolpidem tartrate.
-
Zopiclone.
Anxiolytics
-
Alprazolam.
-
Buspirone hydrochloride.
-
Chlordiazepoxide hydrochloride.
-
Diazepam.
-
Lorazepam.
-
Meprobamate.
-
Oxazepam.
Drugs used in psychoses and related disorders (4.2)
Antipsychotics
-
Amisulpride.
-
Aripiprazole.
-
Benperidol.
-
Chlorpromazine hydrochloride.
-
Clozapine.
-
Flupentixol.
-
Haloperidol.
-
Levomepromazine.
-
Olanzapine.
-
Paliperidone.
-
Pericyazine.
-
Perphenazine.
-
Pimozide.
-
Prochlorperazine.
-
Promazine hydrochloride.
-
Quetiapine.
-
Risperidone.
-
Sulpiride.
-
Trifluoperazine.
-
Zuclopenthixol.
-
Zuclopenthixol acetate.
Drugs used for mania and hypomania
-
Asenapine.
-
Carbamazepine.
-
Lithium carbonate.
-
Lithium citrate.
-
Valproic acid.
Antidepressant drugs (4.3)
Tricyclic and related antidepressant drugs
-
Amitriptyline hydrochloride.
-
Clomipramine hydrochloride.
-
Dosulepin hydrochloride.
-
Doxepin.
-
Imipramine hydrochloride.
-
Lofepramine.
-
Mianserin hydrochloride.
-
Nortriptyline.
-
Trazodone hydrochloride.
-
Trimipramine.
Monoamine-oxidase inhibitors
-
Isocarboxazid.
-
Moclobemide.
-
Phenelzine.
-
Tranylcypromine.
Selective serotonin reuptake inhibitors
-
Citalopram.
-
Escitalopram.
-
Fluoxetine.
-
Fluvoxamine maleate.
-
Paroxetine.
-
Sertraline.
Other antidepressant drugs
-
Agomelatine.
-
Duloxetine.
-
Flupentixol.
-
Mirtazapine.
-
Reboxetine.
-
Tryptophan.
-
Venlafaxine.
Central nervous system stimulants and drugs used for attention deficit hyperactivity disorder (4.4)
-
Atomoxetine.
-
Dexamfetamine sulfate.
-
Lisdexamfetamine dimesylate.
-
Methylphenidate hydrochloride.
-
Modafinil.
Glossary
- Acute care
- Short-term treatment for illnesses that start quickly and have distressing symptoms.
- Antidepressants
- Antidepressants aim to relieve the symptoms of depression. There are almost 30 different kinds of antidepressants available today, including tricyclic and selective serotonin reuptake inhibitors. They are commonly prescribed for the treatment for moderate to severe depression, severe anxiety, panic attacks, obsessive–compulsive disorders, chronic pain, eating disorders and post-traumatic stress disorder.
- Antipsychotics
- Antipsychotics are a range of medications that can be prescribed for some types of mental disorders, mainly schizophrenia and manic depression (bipolar disorder).
- Attention deficit hyperactivity disorder
- A common neurodevelopmental disorder, occurring in around 2–5% of children and characterised by inappropriate levels of inattention, hyperactivity and impulsivity associated with the development of long-term negative outcomes.
- British National Formulary
- The British National Formulary provides UK health-care professionals with authoritative and practical information on the selection and clinical use of medicines. It is updated and published biannually by a joint formulary committee.
- Central nervous system stimulants
- Central nervous system stimulants are agents that increase physical activity, mental alertness and attention span.
- Clinical Practice Research Datalink
- The Clinical Practice Research Datalink contains over 3 million active patient records drawn from approximately 400 primary care practices in the UK. It is the world’s largest database of anonymised longitudinal primary care medical records.
- Clinician
- Someone who provides care and treatment to patients, such as a nurse, psychiatrist or psychologist.
- Complex needs
- A combination of medical needs (e.g. diagnosis, treatment and rehabilitation) and social needs (e.g. housing, social care and independent living).
- Depression
- A common mental disorder characterised by feelings of extreme sadness, loss of interest, low self-worth, fatigue and/or diminished concentration. Depression can be long lasting and can impair an individual’s ability to function or cope with daily life, in severe cases leading to suicide.
- Diagnosis
- Identifying an illness or problem by its symptoms and signs.
- Diagnostic and Statistical Manual of Mental Disorders
- Produced by the American Psychiatric Association and updated periodically, the Diagnostic and Statistical Manual of Mental Disorders defines and standardises diagnostic categories for mental disorders. The categories used in the manual are accepted by most official organisations, including hospitals, insurance companies and other institutions.
- Dual diagnosis
- Refers to a person who has been diagnosed with more than one mental health issue. The term usually refers to having a mental illness with an accompanying substance misuse and/or personality disorder.
- Epidemiology
- The study of the incidence, distribution and possible control of diseases and other factors relating to health.
- General practitioner
- A doctor working in primary care who will usually be the first person seen for a physical illness or emotional problem. They can help directly or make onward referral for specialist care or assessment.
- Hypnotic/anxiolytics
- Often referred to as sedatives, most hypnotic/anxiolytics induce sleep at night or sedate during the day. Benzodiazepines are the most commonly prescribed hypnotic/anxiolytics.
- Local prisons
- Local prisons routinely house those on remand, awaiting trial, those who have been recently convicted or those serving short sentences. They make up approximately half of the prison estate.
- National Health Service
- Provides health care for everyone in the UK, based on need, not on the ability to pay. It is made up of a wide range of health professionals, support workers and health-care organisations.
- National Institute for Health and Care Excellence
- Provides clinical staff and the public in England and Wales with guidance on current treatments. It co-ordinates the National Collaborating Centres from whom it commissions the development of clinical practice guidelines.
- Patient and public involvement
- A way of involving people who use services, and the wider public, in how NHS services and research studies are planned and delivered.
- Pharmacology
- The study of drugs, their uses and their effects.
- Primary care
- A patient’s first contact with NHS health-care services. Services typically include those provided by general practitioners, dentists, pharmacists, opticians, community nurses, physiotherapists and social workers.
- Prison National Offender Management Information System
- A database operated by the National Offender Management Service. Those imprisoned are allocated a life-long unique identifier, which allows the totality of their offence and sentencing history to be stored as a single record.
- Psychopharmacology
- The management of mental illness using medication such as antidepressants or antipsychotics.
- Psychotropic medicine
- Medication usually prescribed for mental health problems. For the purposes of this study, this is defined as any medication listed in subchapters 4.1–4.4 of the British National Formulary,which cover hypnotic and anxiolytic (4.1), antipsychotic and antimanic (4.2), antidepressant (4.3) and central nervous system stimulant (4.4) medications.
- Schizophrenia
- A mental health condition that causes a range of different psychological symptoms, including hallucinations (hearing or seeing things that do not exist) and delusions (believing in things that are untrue).
- Secondary care
- Specialist health care, usually accessed following referral from a primary care clinician. Specialist mental health services are included in secondary care.
- Selective serotonin reuptake inhibitor
- A type of commonly prescribed antidepressant medication (e.g. fluoxetine) which boosts levels of serotonin in the brain to help lift mood.
- SystmOne
- A clinical information technology system used by health-care professionals in the UK. The system is commonly used in primary care and by prison-based health-care services.
- The prescribing appropriateness indicators
- A standardised, validated tool for measuring the appropriateness of long-term prescribing by doctors. It comprises a set of explicit indicators designed for use against prescribing data held in medical records.
- Training prisons
- Training prisons accept convicted and sentenced individuals. They are designed to offer work and rehabilitation-oriented regimes for men serving substantial sentences.
List of abbreviations
- ADHD
- attention deficit hyperactivity disorder
- BME
- black and minority ethnic
- BNF
- British National Formulary
- CI
- confidence interval
- CMHT
- Community Mental Health Team
- CNS
- central nervous system
- CPRD
- Clinical Practice Research Datalink
- DDD
- defined daily dose
- EPSE
- extrapyramidal side effect
- GAD
- generalised anxiety disorder
- GP
- general practitioner
- IAPT
- improving access to psychological therapies
- IT
- information technology
- MACE
- Medication, Access, Care and Equality
- MRC
- Medical Research Council
- NICE
- National Institute for Health and Care Excellence
- NIGB
- National Information Governance Board
- NOMS
- National Offender Management Service
- NRES
- National Research Ethics Service
- OCD
- obsessive–compulsive disorder
- OHRN
- Offender Health Research Network
- ONS
- Office for National Statistics
- PAI
- prescribing appropriateness indicator
- PR
- prevalence ratio
- PTSD
- post-traumatic stress disorder
- RCGP
- Royal College of General Practitioners
- SSRI
- selective serotonin reuptake inhibitor
- TCA
- tricyclic antidepressant
- TDCJ
- Texas Department of Criminal Justice
- YOI
- young offender institution