Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/2002/49. The contractual start date was in January 2012. The final report began editorial review in March 2013 and was accepted for publication in November 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by McLean et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Against the backdrop of monumental efficiency challenges facing health and social care, the NHS needs to achieve up to £20B of efficiency savings by 2015 through a focus on quality, innovation, productivity and prevention (QIPP). 1 The QIPP programme was developed to ensure value for money through cost efficiencies and improved productivity, while simultaneously working towards better patient outcomes. 1 Missed health-care appointments are a major source of potentially avoidable cost and resource inefficiency that impact on the health of the patient and treatment outcomes.
Since 1999, the cost of missed appointments to the NHS has tripled, and in 2009 was estimated to be more than £600M for that year. 2,3 A recent report by the Department of Health, England, reported that, of the 15 million appointments offered at consultant-led clinics between October and December 2012, around 1.5 million patients did not attend. 4 In the UK, more than 12 million general practitioner (GP) appointments are missed each year, costing the tax payer in excess of £162M. 2,5 There has been little research into the costs of missed appointments at outpatient clinics led by Allied Health Professionals (AHPs) and nurses; however, Gleeson et al. 6 reported that the average annual cost of missed appointments to one occupational therapy department was equivalent to a full-time member of staff. In addition, several studies indicate that non-attendance rates at physiotherapy clinics are frequently between 6% and 30%7–9 and could be as high as 46% in some services. 10 Nursing studies have found similarly high non-attendance rates. 11,12
In addition to the costs identified above, non-attendance may lead to increased waiting times for appointments,5,13 increased cost of care delivery,11,12 under-utilisation of equipment and personnel,12 reduced numbers of appointments available for all patients,5,11 reduced patient satisfaction14,15 and negative relationships between the patient and staff. 5,13 The delay in presentation at health-care departments and consequent lack of monitoring of chronic conditions may predispose patients to exacerbations of their condition and its related complications, leading to unnecessary suffering and possible costly hospital admission. 12,16 In addition, the impact of patient non-attendance, coupled with pressure from referring agents to manage waiting list length, can potentially increase health-care practitioners’ stress, anxiety and fatigue levels. 17
Reducing the rate of missed appointments may lead to many benefits, including reduced NHS costs and improved treatment outcomes. 18 At an estimated cost of around £100 per appointment,3 a 1% reduction in missed appointments could result in savings of £6M per year on consultant clinics in England and in excess of £16M per year in savings to GP practices. Potential cost savings to AHP and nursing clinics are also considerable. Reducing the number of missed appointments may be a relatively inexpensive way to support the intentions of the NHS to treat patients within 18 weeks of GP referral,19 while simultaneously supporting the NHS QIPP agenda.
In an attempt to manage the negative effects and improve the efficiency of appointment systems, many health-care organisations are increasingly investing in short message service (SMS), telephone and e-mail reminder systems. Many patients welcome the use of reminders, and patients who did not attend their appointment report that they would have been more inclined to attend if they had received a reminder. 20 However health-care organisations frequently employ a ‘one-size-fits-all’ approach, with little evidence of differential effectiveness or acceptability for particular populations or subgroups. This research systematically examined the published evidence around different models of patient reminders and their effectiveness for, and acceptability to, particular population groups who use outpatient clinical services. Identification of those reminder strategies that are most appropriate for particular subgroups of patients may help health-care organisations to improve attendance at outpatient clinic appointments. The output of this study is a practice guide to help managers identify which approaches are likely to be most effective for reducing non-attendance rates for their service and client groups.
Chapter 2 Objectives
The aim of the project is to explore the differential effect of alternative types of reminders (written and automated) for scheduled health service encounters for different segments of the population on fulfilled or rescheduled appointments, substitutions and satisfaction. In order to achieve this, the following questions will be addressed:
-
Which types of reminder systems are most effective in improving the uptake of health service appointments?
-
Do any systems effectively support the cancellation of appointments?
-
-
Do different reminder systems have differential effectiveness for particular subgroups of the population (e.g. by age group, ethnic group, socioeconomic status, gender, etc.)?
-
What factors influence the effectiveness of different reminder systems for particular population subgroups?
-
How do the perceptions and beliefs of patients, their carers and health professionals regarding specific types of reminder systems, and patient/carer resources and circumstances, influence their effectiveness?
-
How do external factors (e.g. content, delivery, setting, frequency, notice period) influence the effectiveness of reminder systems?
-
How do organisational factors (e.g. person sending the message, perceived status, proximity to delivery of care, et cetera) influence the effectiveness of reminder systems?
-
-
What factors or possible disadvantages should be considered when introducing reminder systems for specific populations for health care and health services?
-
Can potential economic impacts of any interventions be identified?
Chapter 3 Methods
Overall rationale
We performed an effectiveness review following conventional systematic review methodology [i.e. Centre for Reviews and Dissemination (CRD) guidelines] utilising systematic reviews and randomised controlled trials (RCTs). 21 As the scoping review revealed an overall pattern that reminder interventions are effective in many circumstances, albeit to varying degrees, we complemented this with a review informed by realist principles supplementing effectiveness information with non-randomised and qualitative research and engaging with specific and general theory. This review was informed by a conceptual review of relevant theories; thus, the overall project comprised three components:
-
conceptual review of relevant theories (review 1)
-
systematic review of effectiveness studies (systematic reviews and RCTs) (review 2)
-
review informed by realist principles (review 3).
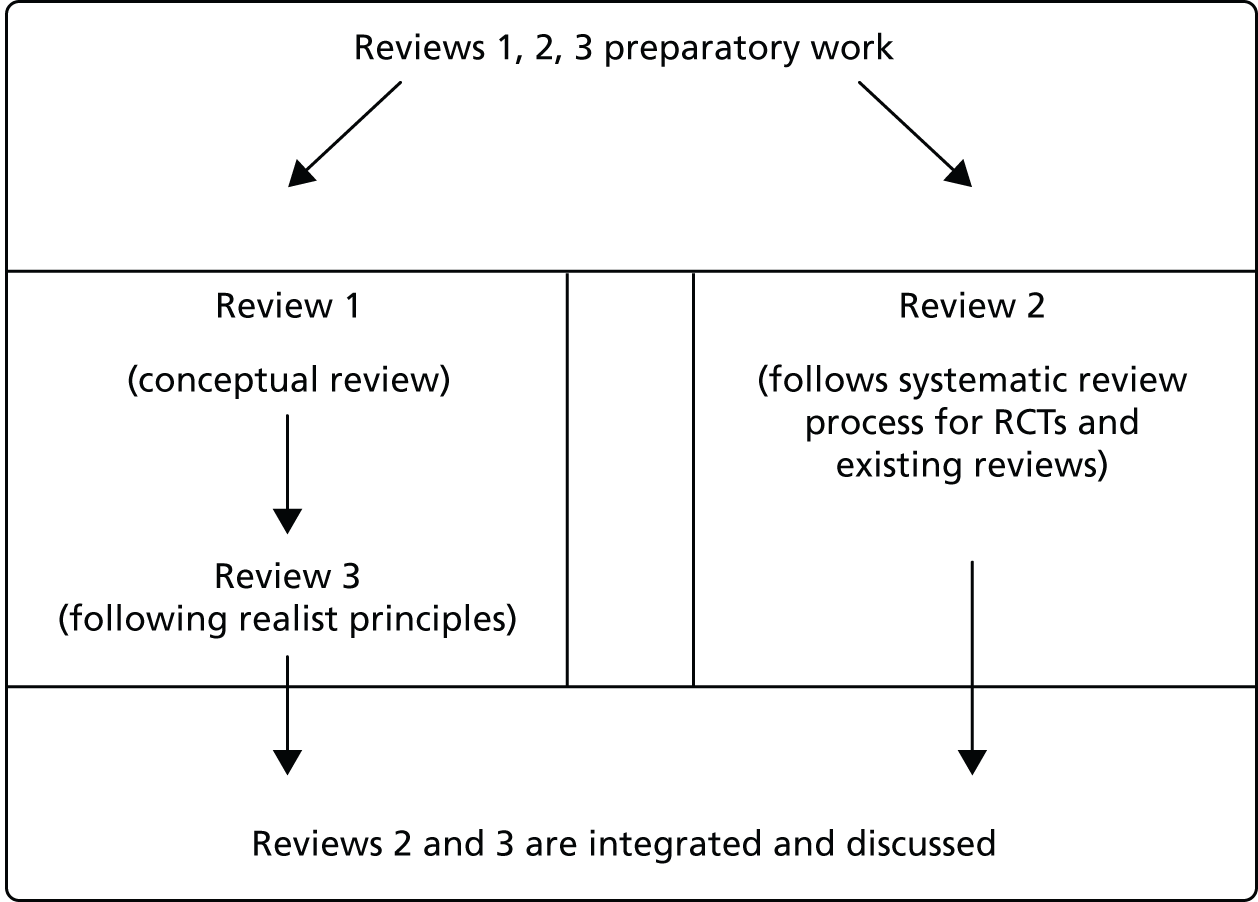
Figure 1 outlines the chronological process by which the three reviews were conducted, their relationship to each other and their overall contribution to the project.
FIGURE 1.
Flow chart summarising the review process.
Review questions
The review question for review 1 (the conceptual review) was: how has appointment non-attendance been characterised and explained in existing considerations of behavioural and sociological theory?
The review question for review 2 (the systematic review of effectiveness) was: what is the differential effectiveness (in terms of such outcomes as attendance/non-attendance, cancellation, rebooking, patient satisfaction and cost, etc.) of various appointment reminder systems (interventions and comparators) for users of health services and specific user groups (e.g. populations) when examined through RCTs and systematic reviews (study types)?
The review question for review 3 (the review informed by realist principles) was: which mechanisms are most able to explain the differential effectiveness (outcomes) of various appointment reminder systems (interventions) in different contexts and populations?
For ease of navigation, the relevant review components are indicated alongside the section headings below.
Literature searches (reviews 2 and 3)
Preliminary searches
The objective of the preliminary searches was to identify published studies and reviews relating to outpatient appointment reminder systems. A broad search strategy was used to capture relevant papers reporting the outcomes of the use of reminder systems or exploring attitudes, barriers or facilitators to their use, but not in technical papers describing reminder systems per se. However, technical papers describing reminder systems could be readily identified and eliminated at the title/abstract stage.
Searches were conducted on the following databases: Allied and Complementary Medicine (via Ovid, 1 January 2000 to 15 February 2012), Cumulative Index to Nursing and Allied Health Literature (CINAHL) Plus with Full Text (via EBSCOhost, 1 January 2000 to 11 January 2012), The Cochrane Library (1 January 2000 to 15 February 2012), EMBASE (via NHS Evidence, 1 January 2000 to 15 February 2012), Health Management Information Consortium database (via NHS Evidence, 1 January 2000 to 15 February 2012), Institute of Electrical and Electronics Engineers digital library Xplore (1 January 2000 to 15 February 2012), The King’s Fund Library catalogue (1 January 2000 to 8 February 2012), Maternity and Infant Care (via Ovid, 1 January 2000 to 15 February 2012), MEDLINE (via EBSCOhost 1 January 2000 to 11 January 2012), Physiotherapy Evidence Database (1 January 2000 to 8 February 2012), PsycINFO (via ProQuest, 1 January 2000 to 8 February 2012), SPORTDiscus (via EBSCOhost, 1 January 2000 to 11 January 2012), Web of Science (1 January 2000 to 2 February 2012).
The strategy used the concepts of reminders, prompts or alerts in proximity to appointments. If supported, appropriate database headings/thesaurus terms were also used. The search terms considered and investigated but rejected (as they did not yield any additional items of relevance but did return several irrelevant papers), included appointment recall and follow-up. The results were limited to papers published in or after 2000 and to English-language articles. See Appendix 1 for the search strategy for CINAHL Plus with Full Text, MEDLINE and SPORTDiscus (which were searched concurrently). The references were managed in a RefWorks database, version 2.0 (ProQuest, Ann Arbor, MI, USA).
Supplementary searches
Forward citation searches in Google Scholar were carried out for papers citing the RCTs about reminder systems selected for inclusion and alerts were set up to capture additional citing references. A cut-off publication date of 30 June 2012 was used for new primary studies, but there was no cut-off date for new reviews (i.e. all reviews published up to 28 February 2013 that cite any included RCTs about reminder systems, were screened for inclusion). The team checked reference lists of reviews selected for inclusion to identify additional post-2000 RCTs relating to reminder systems. The reference lists of RCTs selected for inclusion were checked for papers relating to the same named study or by at least one of the same authors and for papers that provided further theoretical material to supplement/inform the development of the conceptual framework. The reference lists of other studies selected for inclusion were checked for papers by at least one of the same authors and for papers that provided further theoretical material to supplement/inform our conceptual framework. Additional references were uncovered from general current awareness.
Sifting/categorisation of search results (reviews 2 and 3)
Title/abstract screening and categorisation of studies
Following removal of duplicate citations, all records were reviewed for initial inclusion and categorisation based on their titles and abstracts. The purpose of this initial screening and categorisation was to eliminate obviously irrelevant records and to start to map out and prioritise the relevant literature. The project team agreed screening and categorisation criteria following a pilot activity in which a test set of 150 randomly selected records were screened by five reviewers (AB, MG, SMc, SN and SS). This activity proved essential in reaching consensus among the team members as to what is meant by ‘appointment reminders’ and what would definitely fall outside this remit. As a result, the team agreed to exclude reminders sent to a patient to book an appointment, e.g. the type of ‘reminder’ prevalent in vaccination or screening. To be considered in this review as an ‘appointment reminder’, a reminder would need to be in respect of an appointment that had already been booked.
For review 2 (the systematic review of effectiveness studies), RCTs and systematic reviews about reminder systems, in any geographical context, published in or later than 2000 (as operationalised by the search strategy) were included.
For review 3, which utilises realist synthesis principles, the inclusion/exclusion criteria were less clear-cut. The team decided to be broadly inclusive, in recognition of the wider contribution from the evidence needed by the realist-based approach. Considering relevance as more of a continuum than a straightforward ‘in or out’, the analogy of an onion was invoked in moving outwards from a ‘core’ set of records that addressed exactly our research question, towards further outer ‘layers’ likely to be informative but perhaps less directly so. Thus, included papers comprised studies examining the effectiveness of outpatient appointment reminders in a UK context, studies of various quantitative and qualitative designs around appointment attendance behaviour in the UK and elsewhere, studies of adherence to treatment (including appointment attendance behaviour) in the UK and elsewhere, and theories/models/frameworks relating to appointment attendance. Included papers were categorised accordingly to aid focus for data extraction and synthesis. An ‘include other’ category was also applied to records that were felt to inform the review but did not necessarily fall within any of these categories. All included papers were published from 2000 onwards (as per the search strategy).
Five reviewers (AB, MG, SMc, SN and SS) performed the screening using Microsoft Excel 2010 (Microsoft Corporation, Redmond, WA, USA). The records were randomised and divided between the reviewers, with overlap sets of 20 records being double reviewed to explore inter-reviewer reliability. Discrepancies were resolved with reference to a third reviewer (SMc).
During the screening process, ‘included’ records were categorised to specify, for reminder system interventions, the reminder system technology used (e.g. letter/telephone/SMS, etc.) and whether or not the paper related to reminder effectiveness/acceptability/cost-effectiveness/factors influencing effectiveness. Studies were also categorised according to patient age, target population (gender and ethnic minority/social deprivation, etc.), the purpose of the appointment, study type and country. These data were used to populate a ‘PopInS’ (population/intervention/study-type) matrix to help visualise the ‘landscape’ of the literature.
Full-text screening
Full-text screening took place in conjunction with data extraction and is described below, see Production of draft conceptual framework and draft propositions (review 1).
Production of draft conceptual framework and draft propositions (review 1)
The multidimensional nature of health problems, health service settings and their interactions with individual service users implies that the mechanisms supporting or undermining patient attendance at outpatient appointments following receipt of a reminder are likely to be varied, complex and context dependent. Therefore, we sought to develop a comprehensive conceptual framework that could guide our review of the available literature systematically in order to explore the wide range of contextual and mechanistic factors that may influence reminder effectiveness. To construct this framework, we initially conducted a rapid review of our available literature base to identify any prior conceptual models or frameworks that had been employed to explain why and how reminder systems do, or do not, work. It was established early in this process that the majority of the reminder-focused literature was theory light, with a noticeable lack of attention within the identified RCTs to process evaluation that could explain why, how and in what circumstances reminders are effective and there were few and limited theories being advanced by authors to explain reminder system functioning. Indeed, it was apparent that much of the literature was framed very narrowly around the notion that reminders simply remind forgetful patients, with little consideration of the broader range of factors that could be at play.
We identified only one conceptual model specifically about appointment reminder systems. This model, developed by Coomes et al. ,22 proposes that communication functionality of SMS reminders (e.g. single or multicomponent, interactivity, frequency of reminder, timing of reminder and tailoring of the message) and patient psychosocial factors (e.g. patient involvement, social support, medication adherence, risk behaviours, and health and well-being) could mediate the impact of SMS reminders on health-care quality and health outcomes for people living with a human immunodeficiency virus (HIV) infection. 22 For the purposes of the current project, this model was limited in two regards: first, it dealt only with SMS reminders rather than the spectrum of available reminders; and, second, it dealt with mechanisms leading to health-care outcomes rather than considering the mechanisms leading to appointment attendance. However, it did identify features of SMS functionality that were potentially useful to consider within our own framework, which aimed to be more comprehensive.
Given the limited theoretical understanding available from the prior literature on reminder systems, it was decided to conduct a focused review of the conceptually close topic area of medical compliance and adherence. It was known to the team that at least some of the research in this area had been theoretically driven and it was decided that this literature could therefore yield conceptual insight of relevance to the topic of the current review. From this literature, we identified a number of conceptual models specifying factors that can explain medical adherence (including appointment attendance behaviour). These were:
-
theory of planned behaviour,23 which had been adapted to explain attendance at screening appointments,24 adherence with psychological therapies25 and attendance at a cardiac rehabilitation programme26
-
transtheoretical model (also known as ‘stages of change’),27 which had been adapted to explain adherence with psychological therapies25 and attendance at dental check-ups28
-
self-determination theory,29 which had been used to explain adherence with psychological therapies25 and dental clinic attendance30
-
health-care utilisation model,31 which has been adapted for use to explain medication adherence. 32
A further three models which appeared to have some relevance to our topic of enquiry were also identified during this stage of our work, although they had not been used to guide empirical work on adherence/attendance specifically. These were:
-
protection motivation theory,33 which contends that how a person behaves will be broadly explained by a person appraisal of the threat and an appraisal of how to cope with that threat and can, therefore, potentially be related to health behaviours such as making and attending appointments
-
rational choice theory, a development of William Glasser’s choice theory34 that has been discussed in relation to the role of message framing to motivate healthy behaviours35
-
complexity theory,36 which provides a scientific framework for understanding complex phenomena in the natural, biological and human sciences.
Although none of the above models specifically dealt with our topic, they provided a useful starting point for mapping out the contextual factors, mechanisms and outcomes that were important to consider in any attempt to explain how reminder systems work, for whom and in which circumstances. In addition to these behavioural models, which were predominantly informed by psychological theory, we also engaged with relevant sociological literature. This approach was in keeping with our desire to develop a comprehensive conceptual framework that mapped the range of influences operating at different levels, thereby seeking to understand the functioning of reminder systems within a broad psychosocial-systems perspective, rather than locating the phenomenon entirely at the individual level. Although our review did not identify any sociologically driven research papers that dealt specifically with responses to appointment reminders, a number of contributions were felt to be useful in relation to expanding our conceptual framework to encompass a broader range of potentially important factors. First, we noted earlier work on the uptake of screening interventions that highlighted the way in which attendance can be understood as a response to normative expectations about what constitutes responsible and legitimate action – a form of moral obligation – rather than an individual choice or decision (e.g. Griffiths et al. 37 on breast screening). 38 This strand of work can be seen to be influenced by Pierre Bourdieu’s concept of habitus:39 the embodiment of social rules, values and dispositions. Individuals, he argues, acquire a ‘sense of one’s place’ within hierarchically structured society and include/exclude themselves from goods, persons and places that are inside/outside their social group. 39 Understanding differential patterns of appointment behaviour between ‘groups’ may be enhanced by considering the way in which such behaviours may be supported or undermined by other taken-for-granted ‘ways of being’ or ‘sticky habits’ that exist within particular groups or communities. 39 Second, we identified work that seeks to highlight the roles of concrete, situated contingencies that shape and constrain behaviours, such as the practical demands of daily living, including health-related adherence/attendance. For instance, Rosenfield and Weinberg38 alert us to the need to counter the tendency for adherence research to focus on thought processes, knowledge and beliefs, thereby overlooking the importance of ‘the contours and rhythms of situated domestic practices’. 37 Understanding more about the day-to-day lives of patients can potentially throw light on how people respond to appointment reminders. Finally, we saw value in critical sociological contributions that take a more macro focus seeking to explore and expose the linkages between the health-care system and the broader political, economical and social systems of society in historical perspective. Critical theory has enriched various bodies of work exploring patient experiences of health care, revealing the ways in which medical ideology helps to maintain and reproduce class structure (as well as other social divisions, e.g. gender, race/ethnicity). These perspectives tend to challenge the way in which health-related behaviours and their promotion are frequently presented as unproblematic by health professionals and health researchers, while downplaying the complex costs and benefits that may be involved for the patient, particularly patients from more marginalised groups. These sociological contributions complemented the more individualistic focus of the psychological models and allowed us to usefully expand our conceptual framework.
At an operational level, team members drew on this wide-ranging theoretical literature together with evidence gathered during early data extraction and synthesis to develop a series of internal concept notes that were then discussed in team meetings. The multidisciplinary make-up of the project team meant that different members were well placed to engage with different literatures and to produce summaries for the rest of the team to consider. Deliberative discussions were combined with visual tools to iteratively consider alternative ways of representing reminder system functioning, considering:
-
Process maps of attendance charting patient decisions, appointment attendance/cancellation/rescheduling behaviour and consequent outcomes, looking at the day of initially receiving the appointment, the day of receiving a reminder closer to the appointment (if applicable) and, finally, the day of the appointment itself.
-
Balance-sheets focusing on patient decision(s) to attend or not, in terms of a weighing-up of the advantages of attending compared with the advantages of not attending. It was felt that, overall, the balance would tend to be weighed heavily in favour of not attending (as this is the easier option for the patient in the short term), but that various factors, including reminder interventions, may help tip the balance the other way.
-
A ‘tumblers in a safe’ model whereby various factors need to align if a patient is to attend the appointment. Such factors include individual patient characteristics, the wider social system (including norms, expectations and enablers such as transport) and the health service system (including flexibility of the appointment system and the effectiveness of the reminder system). Similarly, for an appointment reminder system to be effective, various elements must ‘line up’, namely the reminder should be received in time and its content should be accurate, the patient should be receptive and genuinely not forget and the service should be sufficiently flexible to enable cancellation/rebooking.
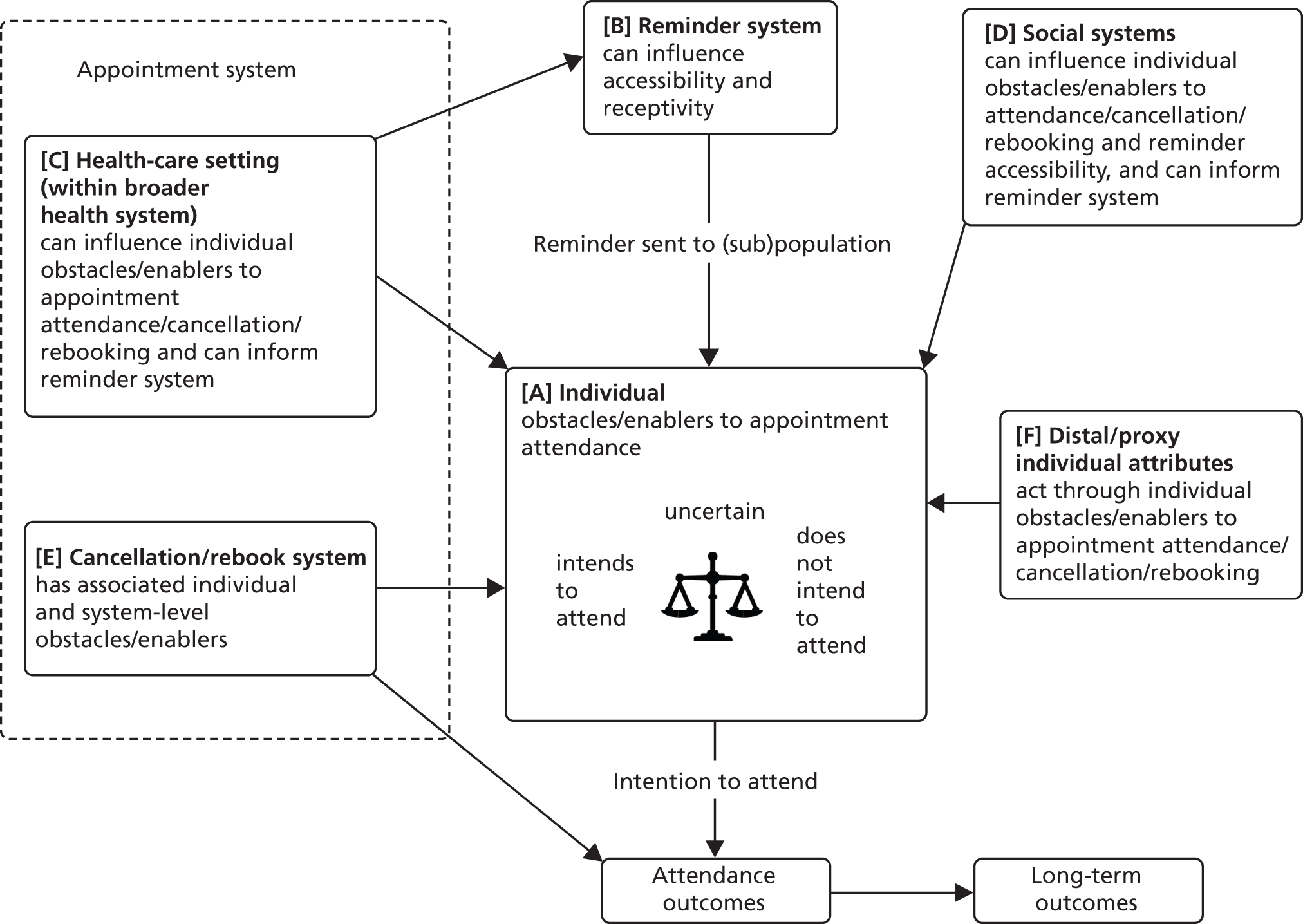
This process enabled the development of our conceptual framework, which is depicted in its final iteration in Figure 2. In this framework, propositions A–F identify various important contextual elements that are hypothesised to contribute to attendance outcomes. The individual (proposition A) is placed at the centre to convey the centrality of the patient role in deciding whether or not he or she will attend (or at least intends to attend). Each patient can be perceived as mentally constructing a balance sheet by which they weigh up perceived obstacles to attendance against enablers. The centrality of the patient interaction with the reminder system further indicates its central importance within this review. There are different factors that will influence the ‘baseline’ of where the patient is ‘at’ with respect to attendance obstacles or enablers when he or she receives an appointment notification. These include various social factors (proposition D) and health-care setting factors (proposition C), with the appointment system located at the heart of the latter. The model shows some possible ‘distal/proxy attributes’ (proposition F) – attributes that could be used to characterise a patient (or patient group) that may tend to give that patient or group a certain ‘baseline’ or which may predict the effectiveness of different types of reminder system. The reminder system (proposition B), depending on its characteristics and depending on where the patient weights the balance of obstacles/enablers before receiving the reminder, may tip the balance in favour of enablers so that the patient intends to attend. Other factors outside the reminder system per se, but within the control of the health-care system, may be modifiable in order to tip the balance in favour of intention to attend. Finally, the model recognises that there may be individual- and system-level obstacles and enablers to cancellation and rebooking (proposition E) that warrant consideration. An accompanying articulation document expands/explains the elements of the conceptual framework and highlights possible causal pathways between them (see Appendix 2). These propositions form the basis of our evidence statements and discussions in Chapters 4 and 5.
FIGURE 2.
Targeting the Use of Reminders and Notifications for Uptake by Populations (TURNUP) conceptual framework.
Preliminary data extraction: randomised controlled trials (review 2)
Full-text screening took place in conjunction with data extraction. The team prioritised RCT studies of appointment reminder interventions in order to draw out effectiveness data to address the objective concerning which types of reminder systems are most effective in improving the uptake of health service appointments. These data fed into review 2, to identify whether or not any studies conducted subgroup analyses, and to start to identify (if possible) any trends in terms of ‘what works’ and in ‘which context’. We mapped the studies to the draft propositions derived from the conceptual framework (Table 1 and see Figure 2). A data extraction tool was designed, piloted, refined and ultimately used in Google Forms (Googleplex, Mountain View, CA, USA) to extract data from included RCTs. Google Forms allowed the five reviewers to use the extraction tool concurrently and to view interim patterns from the data as soon as each study was submitted. Preliminary analysis of these data was used formatively by the review team to identify contextual patterns that might influence the effectiveness of reminder systems and, therefore, to support the development of the preliminary conceptual framework [see Production of draft conceptual framework and draft propositions (review 1)].
| Proposition | Hypothesised association with attendance |
|---|---|
| [A] The reminder–patient interaction | A reminder increases intention to attend (and, therefore, likelihood of attendance) when it (1) reduces patient-specific obstacles to attendance and/or (2) increases patient-specific enablers to attend. The patient will intend to attend when the enablers outweigh the obstacles |
| [B] Reminder accessibility | The aggregate impact of a reminder will vary between service settings because of variations in the patient population profile and the accessibility of the reminder to patients in different patient subgroups |
| [C] Health-care setting | The aggregate impact of reminder systems on intention to attend (and, therefore, likelihood of attendance) will vary between service settings (and patient subgroups) because health-care system factors and patient-/procedure-specific factors can influence patient-level obstacles/enablers (i.e. the ‘baseline’ of obstacles/enablers that are potentially modifiable by the reminder) |
| [D] Wider social systems | The aggregate impact of reminder systems on intention to attend (and, therefore, likelihood of attendance) will vary between service settings (and patient subgroups) because the wider social systems within which patient subgroups are situated vary and elements of these can influence reminder accessibility and patient-level obstacles/enablers (i.e. the ‘baseline’ of obstacles/enablers that are potentially modifiable by the reminder) |
| [E] Cancellation and rebooking | Intention to attend may not result in attendance because additional obstacles can arise for patients who would otherwise intend to attend. This will include patients whose intention to attend has been influenced by the reminder (i.e. whose obstacles–enablers balance has been shifted by the reminder) and those who already intended to intend but for whom the timing/location was not convenient |
| [F] Distal/proxy attributes | A range of factors can act as markers/proxies for proximate individual factors that are enablers or obstacles to attendance |
Testing the draft propositions: further data extraction (reviews 2 and 3)
Testing of the draft propositions (see Table 1) and populating them with evidence for the review informed by realist principles required further exploration of the included studies. Previously extracted data from the included RCTs about reminder systems were augmented with fields for data to be extracted directly against the contextual factors and potential explanatory variables identified in the preliminary conceptual framework (propositions A–F in Table 1). Other fields included gender, age, other population categories, description of study population, country, setting, stated underlying purpose of the study and, for each reminder intervention described, description of reminder intervention(s), reminder timing, reminder medium, reminder interactivity, reminder content, reminder source/bearer, reminder intensity, comparison/control, reported outcomes, economic analysis and disadvantages of introducing reminder systems. This process was also extended to papers reporting other study designs (both qualitative and quantitative), again utilising the same fields, to allow mapping against the research questions addressed by each study (see Review questions). The propositions are expanded in the results section (from Proposition A: the reminder–patient interaction onwards), with evidence statements demonstrating the strength of the findings for each proposition.
The extraction forms also provided a facility for memoing by each reviewer, including identification of any relevant references for follow-up and a field for noting any quality issues. See Quality appraisal (reviews 2 and 3) for a discussion about this.
From the outset, the team recognised that they would not be extracting from all eligible papers; therefore, the papers were prioritised for extraction, based on study type and likely relevance to a UK NHS context. All RCTs about reminder systems were prioritised for full extraction, as they could be seen to contribute to both the systematic review (review 2) and the review informed by realist principles (review 3). We also prioritised all reviews (systematic and otherwise) about reminder systems and appointment systems. We then turned to qualitative, mixed-methods and non-RCT quantitative studies about reminders and appointments for the UK, Ireland, Europe, Australia and New Zealand. In accordance with realist principles, we did not extract data from all possible studies. Having extracted from a sizeable number of the above categories of paper, we found that we were not routinely uncovering new ideas and concepts. Thus, during synthesis we focused on identifying potentially ‘rich’ sources of data from the remaining studies. The methodological justifications for this approach, predicated on considerations of data saturation, were subsequently endorsed by our project steering group (see Involvement of patient steering group).
Data extraction was carried out independently by six reviewers (AB, MG, SB, SMc, SN and SS). Although the team did not undertake double data extraction, individual reviewers were able to refer back to the original articles when interpreting their assigned section, thus corroborating the initial extraction process.
Synthesis (reviews 2 and 3)
Thematic synthesis
The extracted data from the RCTs and other study designs were exported from Google Forms into a single Microsoft Excel spreadsheet that was shared between four of the reviewers (AB, MG, SMc and SS). Each reviewer examined different propositions from the conceptual framework, in order to perform a thematic analysis of the evidence in respect of the different propositions. As described above [see Preliminary data extraction: RCTs (review 2)], the data extraction forms included fields for extracting directly to the different framework factors. A complete list of the different framework factors can be found in Appendix 3. One example of the different framework factors is item B.4 which refers to ‘the format of the reminder may or may not compromise the delivery of the content to the patient’; however, in most instances, it was necessary for the reviewer to ‘read across’ the extraction row in order to contextualise the excerpt or observation. The reviewers formulated evidence statements for each of the six areas of the model using the summary categories for bodies of evidence laid out in Table 2.
| Category | Factor type | Definition | Recommendation options |
|---|---|---|---|
| I. Strong consistent evidence (for/against) |
|
Studies pointing in the same direction (either for or against factor) with a general pattern of statistical significance | Factor must definitely be taken into account when planning change |
| II. Strong equivocal evidence |
|
Studies divided with statistical significance shared between positive and negative effects | Alternatives for practice tailored to local context. Factor may be of local importance and, if so, should be taken into account when planning change. Ongoing evaluation required |
| III. Weak consistent evidence (for/against) |
|
Studies pointing towards a general trend (either for or against factor) without statistical significance | Further sufficiently powered studies supplemented by local data. No basis for change in practice unless initiated by local considerations |
| IV. Weak equivocal evidence |
|
Studies divided between positive and negative effects without statistical significance | Further sufficiently powered studies required. No basis for change in practice except in the context of rigorous evaluation |
| V. Indicative evidence |
|
Studies suggesting that a factor may be considered important (e.g. results from isolated quantitative study or findings from qualitative studies/surveys) | Need for well-designed studies exploring putative factor as hypothesis. No basis for change in practice except in the context of rigorous evaluation |
| VI. Confounded evidence |
|
Studies include factor but have not been designed to isolate its importance | Need for well-designed studies specifically isolating factor. No basis for change in practice except in the context of rigorous evaluation |
| VII. No evidence |
|
No empirical studies | Need for well-designed studies exploring putative factor as hypothesis. No basis for change in practice except in the context of rigorous evaluation |
Consideration of meta-analysis
Following data extraction of all the included RCTs, the reviewers were in a position to examine the heterogeneity of this body of evidence. Identification of existing systematic reviews had revealed limited previous instances for which studies had been combined in meta-analysis. However, these previous meta-analyses were characterised by having very tightly specified population–intervention characteristics (i.e. a specific reminder technology being used in a specific clinical context). There is widespread recognition that uncritical use of meta-analysis is unhelpful – a review team should not perform a meta-analysis simply because it is technically possible. In the case of review 2 the commonality of a limited number of attendance outcomes (i.e. attendance/non-attendance, cancellation, rebooking, patient satisfaction, et cetera) was not to be allowed to determine the appropriateness of meta-analysis.
Two principal considerations must be taken into account when examining heterogeneity: clinical heterogeneity and statistical heterogeneity. Typically a qualitative examination of clinical heterogeneity (i.e. is combining results together statistically a clinically meaningful exercise?) precedes, and may indeed obviate, the need for a quantitative analysis (i.e. is combining results together statistically a valid statistical exercise?). The reviewers identified significant areas of clinical heterogeneity relating to the clinical context of the reminder, the purpose and timing of the appointment, the technology used, the content of the reminder message, the ’dosage’ and timing of the reminder, the patient’s relationship with the health-care provider, the credentials of the one delivering the reminder, the patient’s relationship with the one delivering the reminder as well as variations in definitions of non-attendance [e.g. whether rebooking was treated as a negative outcome (i.e. non-attendance) or as a positive outcome (eventual attendance)]. Therefore, the team decided that it would be unhelpful to mask these significant areas of variation either within a single meta-analysis display or within a series of ostensibly comparable displays.
Notwithstanding this decision not to employ formal meta-analysis, the team did map and investigate relationships between areas of clinical variation and attendance outcomes in order to inform the qualitative synthesis and analysis that was to follow. So, for example, the team arranged intervention and control attendance rates for each trial in a single display, from high to low, which revealed several clusters of studies with shared characteristics. To cite two such patterns, studies of blood donors tended to have relatively low overall ceilings of attendance and studies in paediatric populations shared high overall rates of attendance. Although such patterns were not conclusive, they did help to inform discussion about such important issues as symptomatic compared with asymptomatic attendance rates, the characteristics of attendance for ‘universal’, generalised health contacts, and the role of agency (of parents, partners or carers) in affecting the receipt of the reminder and/or subsequence attendance at an appointment and/or adherence to a programme of treatment.
Narrative synthesis
The reviewers also developed a narrative synthesis explaining the volume and strength of evidence underpinning the evidence statement and the potential mechanisms influencing how reminders support attendance, cancellation and rebooking. In addition, reviewers also provided a supplementary synthesis of evidence to explore emergent factors that might possibly explain patient attendance behaviours. This was not one of the original objectives of the review; however, owing to a relative absence of literature surrounding the contextual and mechanistic factors that influence the effectiveness of reminders, it was considered relevant to review our included studies for these explanatory factors because understanding why patients do and do not attend appointments may lead to useful insights and explanations about the differing circumstances in which different types of reminder systems may be more effective.
The final stage of synthesis involved bringing together the findings of the review. This synthesis will be used to support production of practice guidelines (see Development of materials for health service users).
Quality appraisal (reviews 2 and 3)
The data extraction forms included a field for the reviewer to memo any methodological quality issues noted, flagged up either by the author of the paper being reviewed or by the reviewer. Quality appraisal was not used as a mechanism for study inclusion or exclusion, as realist review principles (review 3) recognise that it is perfectly acceptable to use informative ‘nuggets’ from a methodologically flawed paper. 40 For the RCTs included in the systematic review (review 2), full formal quality appraisal was carried out using the Critical Appraisal Skills Programme (CASP) appraisal tool for those RCTs that had not already been quality assessed by a previous systematic review. 41
Review complexity
The sequential process outlined in this chapter belies the complexity of the project. Two specific areas of complexity were identified: complexity at a macro level, evident in the inter-relationship and interdependency of the three reviews with their methodologies; and complexity at a micro level, relating to the numerous factors that interact to impact upon appointment behaviour, a complexity acknowledged in the choice of a methodology informed by realist principles.
This complexity was explored, and largely resolved, through team discussions and by drawing on advice from the project steering group. The steering group drew on its experience of realist synthesis methodology, and of systematic reviews more generally, to help refine details of the review procedures. Group members facilitated fruitful discussion on the complementary strengths of the systematic review and the review informed by realist principles. They advised on strategies for managing and stratifying large volumes of qualitative literature and deciding when to stop pooling literature. The steering group confirmed the team’s perception that theoretical saturation was likely to occur with fewer new ideas and concepts being likely to emerge as extractions progressed. This served to inform the subsequent prioritisation and process of the remaining identified articles. The review team were, therefore, able to proceed with their more selective approaches utilising theoretical sampling, as mandated by realist synthesis methodologies. As a consequence, the team decided to scan the remaining papers for conceptual richness and to prioritise papers with particular richness or that offered unique perspectives on an issue, while proceeding with the thematic synthesis described above.
Furthermore, the steering group acted as a sounding board for theories identified from review 1, which sought to explain why patients do not attend appointments and the mechanisms by which reminder systems work to improve appointment attendance. Such discussions informed the subsequent development of the candidate propositions.
Development of materials for health service users
The findings of reviews 1, 2 and 3 were finally synthesised to support the development of materials for use by health service managers to support decision-making regarding the management of non-attendance at outpatient departments. The materials have been developed in three parts:
-
an outline of all known reasons for patient non-attendance and incorporating potential reminder and wider solutions for managing those reasons for not attending
-
clinical scenarios that focus on the managing attendance, cancellations and rescheduling
-
advantages and disadvantages of different reminder systems.
Involvement of patient steering group
In February 2013, two members of the project team (SMc and MC) met with a group of six patient representatives at Sheffield Teaching Hospital. These representatives were invited from a group of public governors from Sheffield Teaching Hospitals. They were presented with a draft of the clinical scenarios for managing attendance, cancellations and rescheduling, and were asked to review this from a patient perspective (see Chapter 6, Other emergent interpretations for a fuller explanation). Each scenario was discussed openly and frankly, with the patient representatives providing comments about the draft document and additional information around each scenario and suggesting additional clinical scenarios for inclusion in the document. These comments were utilised to refine our final clinical scenarios document.
Chapter 4 Results
In this chapter we report the results of the search process and the findings of the systematic review of effectiveness studies (review 2, see Figure 1 and Chapter 3, Review questions). When relevant, the findings of these systematic reviews and RCTs are supported by evidence from other study types. The findings from systematic reviews and RCTs are reported separately.
Results of searches
The preliminary database searches and supplementary searches are described in Chapter 3, Literature searches (reviews 2 and 3).
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart (Figure 3) shows the numbers of papers included at each stage of reviews 2 and 3. The preliminary database searches yielded 1200 records and, after duplicates were removed, 638 records proceeded to screening. Citation and reference searching yielded 86 and 49 additional references, respectively, that were deemed relevant after screening by title and abstract. Four additional references were added from the team’s general current awareness activities.
FIGURE 3.
The PRISMA flow chart. SR, systematic review.
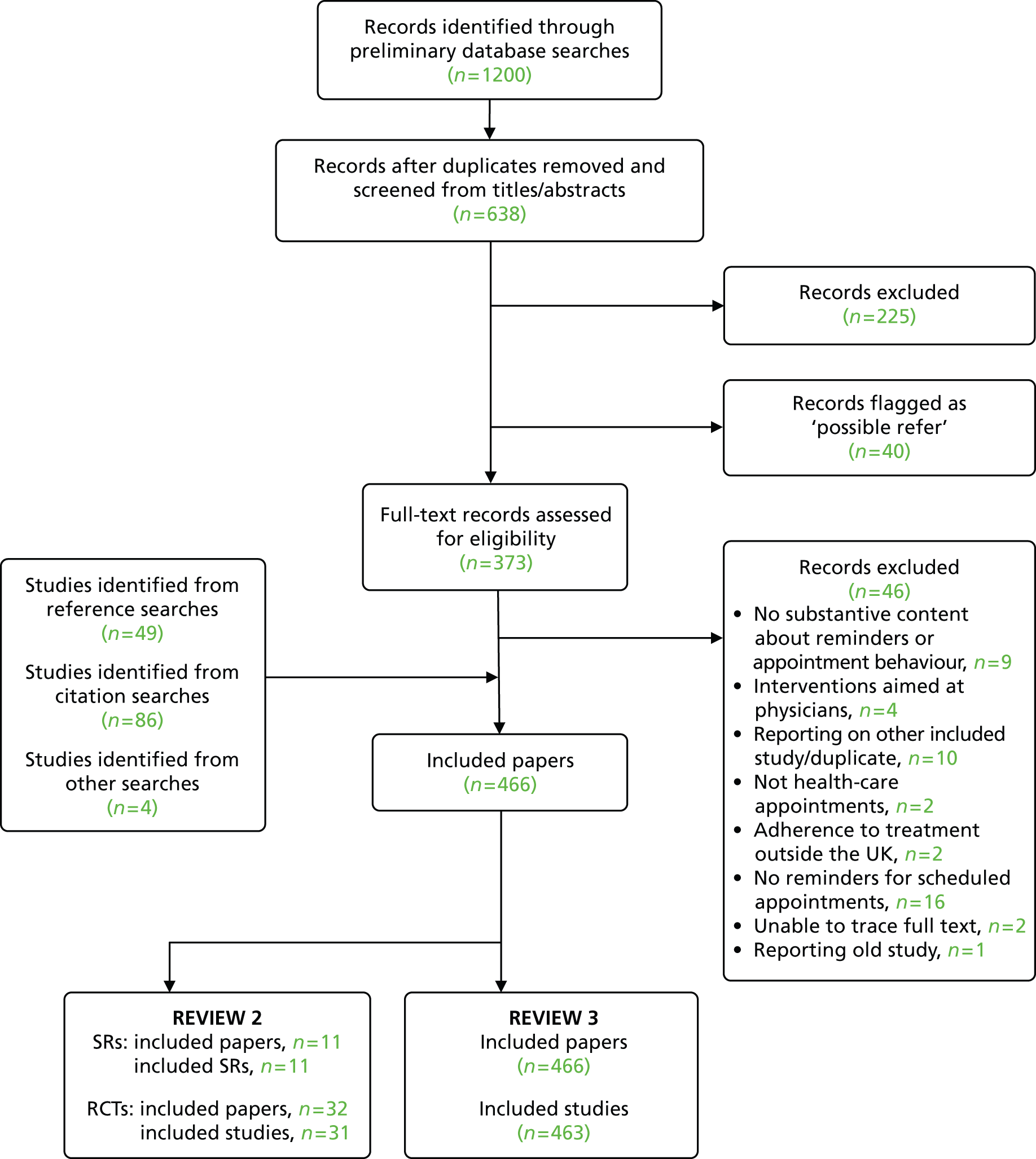
A total of 225 records were excluded at the title/abstract screening stage and a further 40 were placed in a ‘holding’ category (‘possible refer’) for reconsideration during the realist stage of the review (review 3). A further 46 records were excluded at the full-text screening/extraction stage. Thus, 466 records were included for reviews 2 and 3. Of these, 31 RCTs and 11 systematic reviews were included for review 2 (see Appendix 4). An additional 424 papers were identified for potential inclusion for review 3. See Appendix 5 for a list of studies excluded at the full-text screening/extraction stage.
In addition to items included from the formal bibliographic searches as documented, the review team drew on a wider evidence base when seeking to understand or explain the possible mechanisms impacting on appointment attendance. In accordance with agreed methods for reviews employing realist synthesis principles these items, which are primarily incorporated and referenced within Chapter 6, are not formally documented within the PRISMA flow diagram, as they do not constitute ‘included studies’ in the accepted sense of the phrase.
Evidence from systematic reviews
Our literature searches (see Chapter 3) identified 11 systematic reviews42–52 that met our inclusion criteria, namely systematic reviews that:
-
partially or completely examined appointment reminder systems, and
-
included studies published since 2000.
The identified reviews tended either to examine a single technology, e.g. a systematic review of SMS reminder systems (e.g. Guy et al. 44), or to explore the role of information technologies for multiple aspects along a patient care pathway, one of which might be appointment reminder systems (Table 3). As a consequence, existing systematic reviews did not match our own review question, being either narrower in terms of technology or health condition or including only a limited number of eligible studies within their broader inclusion criteria.
| Study | Letter | Manual telephone | Automated telephone | Mobile/SMS | Voice messaging | Other | |
|---|---|---|---|---|---|---|---|
| Atherton et al., 201242 | ✓ | ||||||
| Car et al., 201243 | ✓ | ||||||
| Free et al., 201345 | ✓ | ✓ | |||||
| Glynn et al., 201046 | ✓ | ✓ | ✓ | ||||
| Guy et al., 201244 | ✓ | ||||||
| Hasvold and Wootton, 201147 | ✓ | ✓ | ✓ | ||||
| Henderson, 200848 | ✓ | ✓ | ✓ | ||||
| Jacobson Vann and Szilagyi, 200949 | ✓ | ✓ | |||||
| Krishna et al., 200950 | ✓ | ||||||
| Reda and Makhoul, 201051 | ✓ | ✓ | ✓ | ✓ | ✓ | Personal visit | |
| Stubbs et al., 201252 | ✓ | ✓ | ✓ | ✓ | ✓ | Open-access scheduling |
Characteristics of included systematic reviews
Reviews were published in the period 2008–13. Four of these are Cochrane reviews on mobile phone messaging for general health-care appointments,43 use of e-mail for appointment reminders42 and for immunisation specifically. 49,51 Several of the other reviews, although using elements of systematic review methods, did not meet the criteria used by the Database of Abstracts of Reviews of Effects (DARE) for selecting systematic reviews for more detailed appraisal. 42,47
Quality of included systematic reviews
The quality of the included systematic reviews was assessed against the criteria used by the CRD when evaluating reviews for inclusion in the DARE. 53 Potential systematic reviews are independently assessed for inclusion by two researchers using the following criteria:
-
Were inclusion/exclusion criteria reported?
-
Was the search adequate?
-
Were the included studies synthesised?
-
Was the quality of the included studies assessed?
-
Are sufficient details about the individual included studies presented?
To be included in the DARE database, reviews must meet at least four criteria, with the first three criteria being considered mandatory. Our own pragmatic approach focused on the need to address our review questions and did not exclude any reviews on the basis of quality alone. Instead, we use judgements on quality to moderate our interpretation of review findings.
As can be seen from Appendix 5, the quality of included reviews was very variable. Two very recent reviews42,43 and two earlier reviews49,51 are Cochrane reviews and are therefore scrutinised against the highest quality standards. Four reviews44,45,50,52 all passed the CRD systematic review quality threshold. The review by Hasvold and Wootton,47 although an extremely informative source for our subsequent review, did not pass the minimum essential criteria for systematic reviews required by the CRD. The main limitation of this review lies in its incomplete coverage of possible database sources. The reviewers searched only PubMed in seeking to locate relevant studies. The implications of this relate to possible location bias in that, although PubMed typically approaches coverage of 70–80% included studies in a wide range of systematic reviews,54 it is possible that studies not identified could be substantively different in their findings from those discussed by the reviewers. Another useful review48 also fell short of the CRD criteria having been performed by a single reviewer and, therefore, open to possible reviewer bias.
Evidence from randomised controlled trials
Our literature searches (see Chapter 3) identified 31 RCTs55–86 that met our inclusion criteria for our review 2, namely they included RCTs that investigated the use of appointment reminder systems for a health-related outpatient appointment and were published in English between 2000 and 2012. For the purpose of this review, appointment reminders had to prompt patients to attend a health-related appointment that had already been scheduled; studies investigating reminders to make an appointment were excluded.
Characteristics of included randomised controlled trials
The majority of the included RCTs examined either the use of automated telephone reminders (15/31) or the use of SMS texting services (12/31). Seven out of 31 examined personalised telephone calls and 9 out of 31 studies examined postal (letter/postcard) reminders. In most studies, the comparator was no intervention. Tables 4–7 provide a breakdown of the interventions investigated. A variety of attendance-related outcomes were measured, including attendance, cancellation, rescheduling and patient satisfaction (see Table 7).
| Study | Letter | Personalised telephone | Automated telephone | Mobile/SMS | Voice messaging | Other | Comparator | |
|---|---|---|---|---|---|---|---|---|
| Bos et al., 200555 | ✓ | ✓ | ✓ | No reminder | ||||
| Can et al., 200356 | ✓ (plus reply slip) | No reminder | ||||||
| Chen et al., 200857 | ✓ | ✓ | No reminder | |||||
| Chiu, 200558 | ✓ | No reminder | ||||||
| Cho et al., 201059 | ✓ | ✓ | No reminder | |||||
| Christensen et al., 200160 | ✓ (telephone at 24 hours and 48 hours) | No reminder | ||||||
| Comfort et al., 200061 | ✓ | No engagement | ||||||
| Costa et al., 2008;62 Costa et al., 201063 | ✓ | No reminder | ||||||
| Fairhurst and Sheikh, 200864 | ✓ | No reminder | ||||||
| Goldenberg et al., 200365 | ✓ [telephone (doctor) and telephone (secretary)] | No reminder | ||||||
| Griffin et al., 201166 | ✓ | ✓ IVR (IVR at 3 and 7 days) | No reminder | |||||
| Hashim et al., 200167 | ✓ | No reminder | ||||||
| Irigoyen et al., 200068 | ✓ (postcard and postcard/telephone) | ✓ | No reminder | |||||
| Kitcheman et al., 200869 | ✓ | No reminder | ||||||
| Koury and Faris, 200570 | ✓ | ✓ | No reminder | |||||
| Kwon et al., 201071 | ✓ | No reminder | ||||||
| Leong et al., 200672 | ✓ | ✓ | No reminder | |||||
| Liew et al., 200973 | ✓ | ✓ | No reminder | |||||
| Maxwell et al., 200174 | ✓ | ✓ | No reminder | |||||
| Nelson et al., 201175 | ✓ (SMS) | Mobile | ||||||
| Oladipo et al., 200776 | ✓ | No reminder | ||||||
| Parikh et al., 201077 | ✓ | ✓ | No reminder | |||||
| Perron et al., 201078 | ✓ | ✓ | ✓ | No reminder | ||||
| Prasad and Anand, 201279 | ✓ | No reminder | ||||||
| Reti, 200380 | ✓ (telephone from hospital and telephone from GP) | No reminder | ||||||
| Ritchie et al., 200081 | ✓ | No reminder | ||||||
| Roberts et al., 200782 | ✓ | Usual care | ||||||
| Rutland et al., 201283 | ✓ | SMS plus health promotion message and no reminder | ||||||
| Sawyer et al., 200284 | ✓ | ✓ | No reminder | |||||
| Taylor et al., 201285 | ✓ | No reminder | ||||||
| Tomlinson et al., 200486 | ✓ (postal reminder and leaflet) | Standard information – no reminder |
| Study | Sample size | Country | Setting |
|---|---|---|---|
| Bos et al., 200555 | Four groups (N = 301) | Netherlands | Orthodontic clinic |
| Mail (n = 85) | |||
| Telephone (n = 73) | |||
| SMS (n = 51) | |||
| No reminder (n = 92) | |||
| Can et al., 200356 | Two groups (N = 231)a | UK | Orthodontic clinic |
| Mail plus reply slip (n = 115) | |||
| No reminder (n = 116) | |||
| Chen et al., 200857 | Three groups (N = 1859) | China | Health promotion centre |
| SMS (n = 620) | |||
| Telephone (n = 620) | |||
| No reminder (n = 619) | |||
| Chiu, 200558 | Two groups (N = 311) | Hong Kong | Radiology outpatients |
| Telephone (n = 154) | |||
| No reminder (n = 157) | |||
| Cho et al., 201059 | Three groups (N = 918) | Republic of Korea | Hospital-based family practice outpatients |
| SMS (n = 327) | |||
| Mail (n = 294) | |||
| No reminder (n = 297) | |||
| Christensen et al., 200160 | Three groups (N = 232) | USA | Children’s dental clinic |
| Telephone (24 hours) (n = 77) | |||
| Telephone (48 hours) (n = 71) | |||
| No reminder (n = 84) | |||
| Comfort et al., 200061 | Two groups (N = 102) | USA | Substance abuse treatment |
| Engagement (n = 51) | |||
| No engagement (n = 51) | |||
| Costa et al., 2008;62 Costa et al., 201063 | Two groups (N = 3362) | Portugal | Outpatients clinics |
| SMS (n = 1685) | |||
| No reminder (n = 1677) | |||
| Fairhurst and Sheikh, 200864 | Repeated non-attenders;b 2 groups (N = 418) appointments | UK | Inner-city general practice |
| SMS (n = 191) | |||
| No reminder (n = 227) | |||
| Goldenberg et al., 200365 | Three groups: (N = 723) | USA | Teaching clinic |
| Telephone – doctor (n = 193) | |||
| Telephone – secretary (n = 200) | |||
| No reminder (n = 330) | |||
| Griffin et al., 201166 | Three groups (N = 2381) | USA | Colposcopy |
| Interactive voice reminder 7 days (n = 797) | |||
| Interactive voice reminder 3 days (n = 794) | |||
| No reminder (n = 790) | |||
| Hashim et al., 200167 | Two groups (N = 930) | USA | Urban family practice |
| Telephone (n = 479) | |||
| No reminder (n = 451) | |||
| Irigoyen et al., 200068 | Four groups (N = 1273) | USA | Paediatric Vaccination Clinic |
| Postcard (n = 314) | |||
| Telephone call (n = 307) | |||
| Postcard and telephone call (n = 306) | |||
| No reminder (n = 346) | |||
| Kitcheman et al., 200869 | Two groups (N = 764) | UK | Inner-city outpatients |
| Prompt letter and appointment card for clinic (n = 388) | |||
| Appointment card for clinic only (n = 376) | |||
| Koury and Faris, 200570 | Two groups (N = 291) | UK | ENT clinics |
| Mobile phones (n = 143) | |||
| No reminder (n = 148) | |||
| Kwon et al., 201071 | Two groups (N = 404) | USA | Electrodiagnostic laboratory |
| Telephone (n = 223) | |||
| No reminder (n = 181) | |||
| Leong et al., 200672 | Three groups (N = 993) | Malaysia | Primary care clinics |
| SMS (n = 329) | |||
| Telephone (n = 329) | |||
| No reminders (n = 335) | |||
| Liew et al., 200973 | Three groups (N = 931) | Malaysia | Primary care clinics |
| Telephone (n = 314) | |||
| SMS (n = 308) | |||
| No reminder (n = 309) | |||
| Maxwell et al., 200174 | Three groups (N = 2034) | USA | Inner-city clinics |
| Automated telephone reminder (n = 700) | |||
| Postcard reminder (n = 664) | |||
| No reminder (n = 670) | |||
| Nelson et al., 201175 | Two groups (N = 318) | USA | Paediatric dental clinics |
| SMS (n = 158) | |||
| Mobile (n = 160) | |||
| Oladipo et al., 200776 | Two groups (N = 189) | UK | Colposcopy clinic |
| Telephone (n = 111) | |||
| No reminder (n = 78) | |||
| Parikh et al., 201077 | Three groups (N = 9835) Telephone from clinic staff (n = 3266) Automated telephone message (n = 3219) No reminder (n = 3350) |
USA | Academic outpatient clinics |
| Perron et al., 201078 | Two groups (N = 2123) | Switzerland | HIV/primary care clinics |
| Telephone call (fixed or mobile) reminder then if no telephone response: a SMS reminder; then if no mobile phone number a postal reminder (n = 1052) | |||
| No reminder (n = 1071) | |||
| Prasad and Anand, 201279 | Two groups (N = 206) | India | Dental preventative care |
| SMS (n = 96) | |||
| No reminder (n = 110) | |||
| Reti, 200380 | Three groups (N = 109) | New Zealand | Hospital outpatients department |
| Hospital (n = 37) | |||
| GP (n = 35) | |||
| No reminder (n = 37) | |||
| Ritchie et al., 200081 | Two groups (N = 400) | Australia | Hospital outpatients department |
| Telephone call (n = 200) | |||
| No reminder (n = 200) | |||
| Roberts et al., 200782 | Two groups (N = 504) | UK | Respiratory clinics |
| Telephone reminder (n = 246) | |||
| Usual care (n = 258) | |||
| Rutland et al., 201283 | Three groups (N = 252) | UK | GUM clinic |
| SMS notification of defaulted appointment and invitation to attend clinic (n = 88) | |||
| As per group 1 plus health promotional message about Chlamydia (n = 79) | |||
| No reminder (n = 88) | |||
| Sawyer et al., 200284 | Two groups (N = 53) | Australia | Adolescent clinics |
| Mail (n = 29) | |||
| Telephone (n = 24) | |||
| Taylor et al., 201285 | Two groups (N = 679) | Australia | Physical therapy clinic |
| SMS reminder (n = 342) | |||
| No reminder (n = 337) | |||
| Tomlinson et al., 200486 | Two groups (N = 500) | UK | Colposcopy clinic |
| Postal reminder and leaflet (n = 267) | |||
| No reminder (n = 233) |
| Interactivity | Frequency | Timing | Tailoring of message | |
|---|---|---|---|---|
| Bos et al., 200555 | ||||
| None | Single reminder | 1 day before | No details | |
| Telephone | No details | Single reminder | 1 day before | No details |
| SMS | No details | Single reminder | 1 day before | No details |
| Can et al., 200356 | ||||
| Mail with confirmation slip | Stamped-addressed postcard – reply required | Single reminder | 2 weeks before | No details |
| Chen et al., 200857 | ||||
| SMS | None | Single reminder | 72 hours before | Participant’s name and appointment details |
| Telephone | None | Single reminder | 72 hours before | Participant’s name and appointment details |
| Chiu, 200558 | ||||
| Telephone | No details | Single reminder – three attempts | Within 3 working days before | No details |
| Cho et al., 201059 | ||||
| SMS | None | Single reminder | Week 16 after enrolment |
|
| Telephone | No details | Single reminder | Week 16 after enrolment |
|
| Christensen et al., 200160 | ||||
| Telephone | No details | Single reminder | 1 working day before | No details |
| Telephone | No details | Single reminder | 2 working days before | No details |
| Comfort et al., 200061 | ||||
| Engagement (including telephone reminders) | Opportunity to ask questions about the program | No details | No details | Remind clients of intake appointments, to brief them on what to expect and to follow-up on missed appointments |
| Costa et al., 2008;62 Costa et al., 201063 | ||||
| SMS | None | Single reminder | 2 working days before | Messages written/sent by informatics department of hospital. Characteristics included name of institution, patient’s name, type of episode, date and hour. When necessary, included advice to arrive earlier |
| Fairhurst and Sheikh, 200864 | ||||
| SMS | None | Single reminder | Between 08.00 and 09.00 for morning appointments; and between 16.00 and 17.00 for afternoon appointments. Reminders for Monday morning sent on Friday afternoon |
|
| Goldenberg et al., 200365 | ||||
| Doctor call | No detail | Single reminder – two attempts | Within 48 hours before | No details |
| Secretary call | No detail | Single reminder – two attempts | Within 48 hours before | No details |
| Griffin et al., 201166 | ||||
| Nurse phone call | No data on whether or not patients spent more time engaged with nurses during telephone calls than they spent receiving IVR messages. Nurses answered any questions during call | Single reminder – two attempts | 7 days before procedure | Appointment reminder, information about preparation for examination and encouragement to prepare for and attend examinationa |
| IVR system call | None | Telephone calls programmed for morning. If answering machine picked up on initial call, IVR system left general message about purpose of call. System programmed to call again in afternoon and then again in evening until patient answered. Messages left only on first attempt. If IVR not completed that day, process repeated following day. Patients answering call had option for IVR call back at later time | 7 days before procedure | Appointment reminder, information about preparation for the examination and encouragement to prepare for and attend examination |
| IVR system call | None | Same call protocol as for 7-day reminder above | 3 days before procedure | Appointment reminder, information about preparation for the examination and encouragement to prepare for and attend examination |
| Hashim et al., 200167 | ||||
| Telephone | No details | Single reminder | 1 day before | No details |
| Irigoyen et al., 200068 | ||||
| Postcard | No details | Single reminder | 1 week before | No details |
| Telephone | Bilingual clerk | Single reminder – three attempts | Weekday evening before | No details |
| Postcard and telephone | No details | Single reminder – three attempts | 1 week before and weekday evening before | No details |
| Kitcheman et al., 200869 | ||||
| Orientation letter | No details | Single reminder | Sent out 72 hours before; received 24–48 hours before | Letter very short, taking 30 seconds to read. Written on headed paper: time of appointment, name of doctor, short description of clinic and its routine, a map, request to bring medication and a friend or family member |
| Koury and Faris, 200570 | ||||
| No details | No details | No details | No details | |
| Kwon et al., 201071 | ||||
| No details | No details | 1 day before | No details | |
| Leong et al., 200672 | ||||
| SMS | None | Single reminder – maximum of three attempts | 24–48 hours before | No details |
| Mobile | No details | Single reminder – maximum of three attempts | 24–48 hours before | Mobile phone conversation similar to SMS reminder. No clinical or laboratory information included |
| Liew et al., 200973 | ||||
| SMS | None | Single reminder | 24–48 hours before | No details |
| Telephone | To avoid caller bias, research assistant trained to deliver same message as in SMS group. Further enquiries from patient redirected to appointment counter | Single reminder – up to three further attempts made at 4-hourly intervals. | 24–48 hours before | No details |
| Maxwell et al., 200174 | ||||
| Automated telephone | None | Single reminder | 1 day before | No details |
| Mailed postcard | None | Single reminder | 5 days before | No details |
| Nelson et al., 201175 | ||||
| SMS | None | 48 hours before |
|
|
| Mobile | No details | No details | 48 hours before | No details |
| Oladipo et al., 200776 | ||||
| Telephone | No details | No details | 12–24 hours before | No details |
| Parikh et al., 201077 | ||||
| Clinic telephone | Appointment confirmed or rescheduled at patient’s request | 3 days before | No details | |
| Automated telephone | Recipient had option of confirming or cancelling appointment | System attempted to reach patient each night for three nights before appointment. After three attempts if appointment not confirmed, patient remained registered for appointment | 3 days before | Practice-customised computerised or live voice recording played after telephone call was answered |
| Perron et al., 201078 | ||||
| Phone call (fixed or mobile) plus SMS plus postal reminder | Languages used by research assistant for telephone calls were French, English or Spanish | Three ‘escalating’ reminders includes three attempts on telephone | 48 hours before. Postal reminder to reach patient on next day | SMS sent in French. Included name of physician, day and time of appointment, but no medical information |
| Prasad and Anand, 201279 | ||||
| SMS | Successful delivery assumed when indication showing that message had been sent. | Two reminders | 24 hours before and also on day of appointment | Included dentist’s name, date, time and location of the appointment. Reminders in local language for non-English language patients. Picture message of institution sent to seven patients |
| Reti, 200380 | ||||
| Hospital | Hospital waiting-list clerk | No details | 24 hours before | No details |
| GP | Patient’s GP | No details | 24 hours before | No details |
| Ritchie et al., 200081 | ||||
| Telephone | Telephoned by one of authors or research nurse | Single reminder | 1–3 days after attendance at A&E | To remind patient about appointment (and importance for medical follow-up) if one had been made and to offer to make an appointment if one had not been made. General enquiry made about their health and importance of medical follow-up explained in general terms |
| Roberts et al., 200782 | ||||
| Telephone | By researcher | Single reminder – two attempts. If patient not available, no message left | Between 09.00 and 17.00 during week prior to appointment | No details |
| Rutland et al., 201283 | ||||
| No details | No details | 1 week after defaulted appointment | No details | |
| Sawyer et al., 200284 | ||||
| No details | Single reminder | 5 days before | No details | |
| Telephone | Single administration officer made all telephone calls | Three attempts before contact deemed not to have occurred (leaving message on answering machine deemed as contact). Number of calls required and time required for each call noted | 1 day before | No details |
| Taylor et al., 201285 | ||||
| SMS reminder | Sent using automated system at clinic 1; manually by administration assistant at clinic 2 | No details | 2 days before if appointment made more than 3 days before, or day before appointment for appointment within 2 days. Timed to allow appointment slot to be offered to another patient and filled in event of cancellation | Reminder
|
| Tomlinson et al., 200486 | ||||
| Postal reminders | No interactivity | Single reminder | 7–10 days before | Detailed explanatory leaflet on implications of abnormal cervical smear, description of colposcopy, outpatient treatment using sensory information and detailing importance of follow-up (available in summary in most common ethnic languages) |
| Study | Attendance outcomes | Overall effect |
|---|---|---|
| Bos et al., 200555 | Standardised failure rate; respondents attitudes to receiving reminder; respondent’s reminder preferences | No-show rate reduced by 4.5% |
| Can et al., 200356 | Attendance rates | No-show rate reduced by 4.2% |
| Chen et al., 200857 | Attendance rates; cost per attendance of interventions | No-show rate reduced by 7% |
| Chiu 200558 | Attendance rates | No-show rate reduced by 9.4% |
| Cho et al., 201059 | Attendance rates; cost per attendance | No-show rate reduced by 3.4% (SMS) and by 1.1% (telephone) |
| Christensen et al., 200160 | Punctuality for appointment (15 minutes); rate of broken appointments | No-show rate reduced by 21% (48 hours) and by 26% (24 hours) |
| Comfort et al., 200061 | Engagement with services | No statistically significant differences |
| Costa et al., 2008;62 Costa et al., 201063 | Non-attendance rate | No-show rate reduced by 3.5% |
| Fairhurst and Sheikh 200864 | Non-attendance rates | No-show rate reduced by 5.3% |
| Goldenberg et al., 200365 | Attendance (show) rates | No-show rate reduced by 10% |
| Griffin et al., 201166 | Appointment non attendance; patient perceptions about the call | 38%, 42% and 41% did not attend in IVR7, IVR3 and nurse delivered call groups, respectively; 33% (FS) and 38% (colonoscopy) non-attendance at baseline |
| Hashim et al., 200167 | Outcome of call (confirmed, unable to leave message, appointment cancelled by patient/family, appointment rescheduled by patient/family or no active telephone number); cost of reminders | No-show rate reduced by 6.9% (95% CI 1.5% to 12%) |
| Irigoyen et al., 200068 | Appointment rates; cancellation coverage; cost of reminders | No-show rate reduced by 6.7% |
| Kitcheman et al., 200869 | Attendance at first appointment; continuing attendance; hospitalisation, transfer of care, discharge, presentation at A&E and death by 1 year | No-show rate reduced by 6.5% |
| Koury and Faris, 200570 | Non-attendance rate; willingness to receive SMS | No-show rate reduced by 8% |
| Kwon et al., 201071 | Non-attendance without prior notification | Non-attendance reduced by 2.6% but not significantly. For appointments of particular test, e.g. electromyography (EMG), non-attendance rate reduced by 21.7% |
| Leong et al., 200672 | Attendance rates; costs of interventions. | No-show rate reduced by 10.9% (SMS); no-show rate reduced by 11.5% (mobile); cost of SMS reminder lower than mobile phone reminder |
| Liew et al., 200973 | Non-attendance rates | No-show rate reduced by 9.3% (telephone); no-show rate reduced by 7.4% (SMS) |
| Maxwell et al., 200174 | Appointment adherence rates | No-show rate reduced by 3.2% (mailer); no-show rate reduced by 2.1% (phone) |
| Nelson et al., 201175 | Attendance rates | 8.97% improvement in voice over text |
| Oladipo et al., 200776 | Attendance rates | No-show rate reduced by 22% |
| Parikh et al., 201077 | No-show rate; cancellation rate; patient satisfaction | No-show rate reduced by 9.5% (personalised); no-show rate reduced by 5.8% (automated) |
| Perron et al., 201078 | Rate of missed appointments, cost of intervention and profile of patients missing their appointment | No-show rate reduced by 3.6% |
| Prasad and Anand, 201279 | Attendance rate | No-show rate reduced by 43.7% |
| Reti, 200380 | No-show rates | No-show rate reduced by 22% |
| Ritchie et al., 200081 | Making the recommended appointment; attendance at scheduled appointment; and reasons for non-attendance at scheduled appointment | No-show rate reduced by 16.2% |
| Roberts et al., 200782 | Attendance rate; cost of intervention | No-show rate reduced by 15% compared with control (71%, n = 258) and with patients who could not be contacted (68%, n = 142) (p = 0.007; p = 0.004) |
| Rutland et al., 201283 | Reattendance rates | Non-reattendance rate reduced by 3.7% for text reminder only. Non-reattendance rate reduced by 10.7% when reminder accompanied by health promotional message |
| Sawyer et al., 200284 | Clinic non-attendance, reason for non-attendance and satisfaction with the booking system | No-show rate reduced by 12% |
| Taylor et al., 201285 | Rate of non-attendance without cancellation; cancellation and attendance rates; factors associated with non-attendance | No-show rate reduced by 5% |
| Tomlinson et al., 200486 | Attendance and default rates | No-show rate reduced by 17% |
The majority of studies have been conducted in the USA (10/32), UK (8/32) and Australia (3/32), with New Zealand (1) and Canada (1) also being represented. Other European countries include the Netherlands (1), Portugal (1) and Switzerland (1). More recent years have seen the emergence of an active research agenda in Asia, including India (1/32), Malaysia (2/32), Republic of Korea (1/32) and China (including Hong Kong) (2/32).
Several settings are particularly well represented. Not surprisingly, general practice/primary care clinics (5/32) and outpatient departments (8/32) figure prominently given their prevalence; however, dental/orthodontic (5/32) and colposcopy clinics (3/32) are disproportionately represented.
The principal functions of the various reminder systems were reminder only, reminder requiring confirmation,56 reminder plus orientation, and reminder plus supporting clinical information.
Quality of included trials
Included trials uniquely identified by the review team were individually assessed for quality (see Appendix 6), using the CASP checklist for RCTs, and combined with the summary judgements of quality made by the authors of included systematic reviews to provide an overall assessment of comparative quality. In contrast to our approach to systematic review evidence, in which we used quality assessments to moderate and not exclude studies, for the RCTs we required all included RCTs to meet minimum quality standards. Studies not meeting these criteria were excluded from the effectiveness review. However, excluded studies still had the opportunity to contribute to the review informed by realist principles. In many cases, qualitative or epidemiological data from such studies contributed to the evidence base for our very specific review questions.
The biggest overall weakness of the studies as a group was that studies frequently used ownership of a particular technology as a selection criterion. Obviously, ownership of a technology is also strongly associated with a patient preference for that technology. The fact that such studies are, in essence, efficacy studies and not effectiveness studies is barely commented on in existing reviews. In order to assess the performance of such technologies in the real world, patients would need to be randomised before ownership, for example of a mobile phone, is established. It seems that the simplistic assessment that forgetfulness is the major reason for non-attendance has been a strong determinant of the research agenda, meaning that it is not considered acceptable for those in the randomised group to not receive a message. This is paradoxical given that the most frequent comparator in the identified studies is ‘no reminder’, meaning that it is considered acceptable for this group to not receive any reminder.
The implications of such a design flaw have been profound for our review. There is a strong likelihood that those groups in which we are particularly interested may have been excluded from our included RCTs prior to randomisation. This strong selection bias would result, for example, in those of lower socioeconomic status or older persons (for whom the ownership demographic is relatively low by comparison with younger persons) being excluded in the findings from the studies. Ironically, this design flaw does offer a degree of future proofing to existing studies in that they can be interpreted as once a population has access to the technology, then this is the likely effect of the reminder system. However, this relates only to applying findings to the population in general and does not address the particular focus on specific populations required for this review. Only by conducting trials in particular populations could we draw conclusions specific to that population.
For ease of reference, findings from the effectiveness review are discussed under each proposition supplemented with reference to other supporting evidence. These statements build on the preliminary propositions identified in Table 1.
Proposition A: the reminder–patient interaction
It is our proposition that a reminder increases intention to attend (and, therefore, likelihood of attendance) when it (1) reduces patient-specific obstacles to attendance and/or (2) increases patient-specific enablers to attend. The patient will intend to attend when the enablers outweigh the obstacles. The following evidence statements relate to this proposition.
Evidence statement (A.1): there is strong consistent evidence that simple reminders that provide details of timing and location of appointments are effective at helping a (forgetful) patient to attend their appointment (evidence category Ia)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
Free et al. 45 reported that the pooled effect on appointment attendance using text message (SMS) reminders compared with no reminder was increased, with a relative risk (RR) of 1.06 [95% confidence interval (CI) 1.05 to 1.07]. Car et al. 43 provides moderate-quality evidence showing that mobile text message reminders improved the rate of attendance at health-care appointments compared with no reminders (RR 1.10, 95% CI 1.03 to 1.17). These findings suggest that a small percentage of individuals (estimated variously at between 3% and 17%) do genuinely forget and, therefore, benefit from receipt of a reminder.
The overwhelming pattern from the systematic reviews and included trials is that reminder systems reduce non-attendance rates. However, there are differences in what investigators perceive as a meaningful difference (figures such as a 10% or 15% reduction are cited when calculating a sample size) and so some studies fail to reach statistical significance.
Stubbs et al. 52 conclude that telephone, mail and text/SMS interventions all improved attendance modestly, but at varying costs. Similarly, Jacobson Vann and Szilagyi49 found that reminding people over the telephone, sending a letter or postcard, or speaking to them in person increased vaccinations. Hasvold and Wootton47 undertook a systematic review of 33 independent studies pertaining to telephone, SMS or automated telephone reminders found that all but one reported a benefit from sending reminders and suggested a weighted mean relative change of 34% from the baseline non-attendance rate.
Bos et al. 55 tried three different types of reminder system and failed to confirm the hypothesis that a reminder would reduce the failed attendance rate. The explanation for this finding was that the clinic had a very high attendance rate with both a high perceived importance of the clinic and high levels of satisfaction with the orthodontist and the services being provided. Perron et al. 78 report that being part of a stepped approach intervention (telephone, text, mail) significantly decreased the risk of missing an appointment for all categories of patients found at risk [odds ratio (OR) 0.63, 95% CI 0.43 to 0.89]. A useful reminder function is served by whatever means is at a service’s disposal.
In their systematic review, Free et al. 45 report no difference in attendance using SMS reminders compared with other reminders; however, these findings did not reach statistical significance (RR 0.98, 95% CI 0.94 to 1.02). Car et al. 43 identified two studies of moderate quality that showed that mobile phone text message reminders and telephone call reminders had a similar impact on health-care attendance (RR 0.99, 95% CI 0.95 to 1.03). This suggests that patient compatibility/preference, not the inherent advantage of any technology per se, should determine selection of the candidate reminder system. In contrast, Bos et al. 55 found no differences between SMS, telephone and mail reminder when compared with no reminder. The authors concluded that the form of the reminder is irrelevant.
Findings from other studies
No additional studies.
Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ is more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
There is weak consistent evidence from two reviews that show that reminders providing additional information (e.g. orientation information, health information, etc.) over and above details of timing and location (reminder plus) are more effective than simple reminders, which provide information about time date and location of an appointment.
In their Cochrane review, Reda and Makhoul51 investigated the effects of reminders to encourage attendance at clinics for those with suspected serious mental illness. Of the four trials included in review, only one study87 (n = 120) compared a standard letter prompt with a letter ‘orientation statement’. The results of this study favoured the orientation statement approach rather than the simple letter prompting attendance, but the results did not reach conventional levels of statistical significance (RR of missed appointment 1.6, 95% CI 0.9 to 2.9). There is a chance of type II error in this particular study and simply increasing the number of participants in this study may have resulted in a more favourable result. This review provides very weak evidence that a simple orientation-type letter may be more effective than a telephone prompt at promoting attendance at mental health clinics.
A systematic review48 to assess the effectiveness of reminder systems as a means of increasing attendance and reducing ‘did not attend’ rates at all new outpatient appointments identified limited evidence, based on three studies, that ‘reminder plus’ were more effective than standard reminders. Postal reminders that offered a reward for attendance, threatened sanctions for non-attendance or provided orientation information about the clinic appeared to be more effective than standard reminders. In this review ‘warning reminders’ contained warnings that patients would fall to the bottom of the waiting list following failure to attend (FTA), ‘reward reminders’ contained the offer of rewards should patients attend and ‘orientation reminders’ contained information describing the clinic. There was an indication in this review, based on the findings of one study, that warning reminders were more effective than reward reminders. 88
Can et al. 56 describe an intervention that requested that patients return a stamped addressed postcard, so that the appointment could be confirmed. It could be hypothesised that the action of returning the postcard might be construed as a symbolic ‘contract’ between patient and provider, reducing the subsequent likelihood of non-attendance. Whatever the reasons, return of the postcard resulted in an attendance rate of 83% compared with only 48% if the card was not returned.
This evidence indicates that ‘reminder plus’ may be more effective than simple reminders; however, as a result of the small number of studies which have systematically investigated this hypothesis, it is not possible to be conclusive about this. There is no evidence to show in what way the receipt of additional information as part of the reminder will shape patients’ intentions to attend or their perceptions about the appointment. Further high-quality research is required to investigate these areas.
Findings from other studies
Several studies have utilised orientation strategies to apparent good effect. Kitcheman et al. 69 incorporated letter reminders on headed paper in their RCT explaining the time of the appointment, name of the doctor, description of the clinic and its routine, a map and a request to bring a list of medication and a friend or family member. This significantly reduced the numbers of people failing to attend a mental health clinic appointment. Booth and Bennett89 conducted a comparative study utilising telephone reminders incorporating information about appointments, directions to the clinics and other relevant information that reduced non-attendance at first appointments at a specialist alcohol treatment clinic. However, neither of these studies incorporated control groups receiving a simple reminder only and, therefore, it is not possible to determine from these studies the additive effect of orientation information.
Proposition B: reminder accessibility
It is our proposition that the impact of a reminder varies between service settings because of variations in the patient population profile and the accessibility of the reminder to patients in different patient subgroups. The following evidence statements relate to this proposition.
Evidence statement (B.1): there is strong consistent evidence that the reminder may not be received by the patient (evidence category Ia)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
Strong consistent evidence from multiple high-quality studies indicates that reminders may not be accurately received by a substantial proportion of patients for whom they were intended. This will contribute to suboptimal effectiveness of reminders. The extent to which patients do not receive their reminder varies depending on the technology, with telephone reminders demonstrating the lowest success rates for making contact with the patient.
Telephone reminders
The evidence suggests that successful contact rates for telephone reminders ranging from around 30–60% would be normal for a UK health-care context. Seven RCTs57,58,66,72,80,82,90 employed telephone reminders and followed a similarly standardised protocol consisting of up to three attempts to contact the patient before deeming the participant as uncontactable; if there was an answer machine or another person answered the telephone call, no message was left. Three RCTs58,72,90 provided no information about contact rates; however, four of the RCTs57,66,80,82 did provide relevant data indicating that between 0% and 58% of patients allocated to receive an appointment reminder by telephone could not be contacted. Roberts et al. 82 randomly allocated 504 patients to receive either a telephone reminder or usual care to investigate the impact on attendance at respiratory outpatient clinics in the English NHS. The telephone reminder group received a reminder telephone call between 9.00 and 17.00 hours during the week prior to their appointment. Of the 246 patients who were allocated to the telephone reminder group, 58% were not contactable. In their RCT, Griffin et al. 66 investigated whether or not an interactive voice response (IVR) system telephone call was equally effective as a nurse-delivered telephone call at educating and preparing patients (n = 2610) for flexible sigmoidoscopy and colonoscopy examinations in a US health-care setting. They found that between 44% and 54% of patients were not contactable and, therefore, did not receive their reminder; however, other RCTs have reported higher contact rates. Reti80 investigated the effectiveness of telephone reminders compared with no reminder to reduce non-attendance at hospital outpatient clinics in New Zealand and achieved contact rates of 79% in the telephone reminder group. One reason for the higher contact rates in this study could be ‘call-back’ requests that were left on patients’ messaging services, whereby patients were asked to call the clinic in order to receive their reminder. 80 In addition, this study was conducted over a short space of time (3 months) and included only 109 patients in total; such high intensity of inputs, sustainable in such a small trial over such a short space of time, may not be maintained over all patients, attending all clinics over a longer period of time, simply by utilising a ‘call-back’ request. In their RCT comparing the efficacy of a SMS text messaging, telephone reminders or control (no reminder) to improve attendance rates at a health promotion centre in China, Chen et al. 57 found that telephone reminders were received by 619 out of 620 subjects; 614 of these were completed by landline telephone and the remaining five were completed by mobile phone when patients were not contactable on their landline. This study of telephone reminders appears to be unique in its success at making contact with clients to remind them of their appointments, suggesting that something very different is happening in this study. The fact that contact rates are very high via landline suggests that these are more regularly available in the home than is the case in the UK context. Another unique element of the Chinese health service is that it provides a very popular health check-up programme; the visitors are predominantly middle- or high-income employees of local companies, owners of private enterprises and their spouses who tend to be more attentive to their health status and undergo health check-ups more often than other people of the same age range. In this study, an 80% attendance rate was observed in the control group, which received no reminder, indicating the apparent enthusiasm to attend, and this population may, therefore, also be very willing to engage with reminders. This is dissimilar to the UK NHS context that is more frequently explored in reminder studies, for which patients are more likely to come from less socioeconomically advantaged populations. Five other reviews and primary studies25,48,91–93 also report particularly poor contact rates using telephone reminders, ranging from 30% to 61%.
Short message service reminders
Thirteen RCTs reviewed in this study investigated SMS reminder and employed fairly standard protocols consisting of delivering a brief message 1–2 days prior to the appointment. In the majority of studies, successful contact was assumed when the mobile phone indicated ‘message sent’ in the SMS group. 57,72,79 There are few figures to show the failure rates of sending SMS reminders to patients. In an Irish audit of non-attendance rate at ear, nose and throat outpatients clinics following the introduction of a text reminder system, Geraghty et al. 94 reported that only 2–3% of people failed to receive their text message reminder as a result of incorrect data entry. Similarly, in an Australian study95 to evaluate the operational and financial efficacy of sending SMS text message reminders to the mobile telephones of parents of young children with scheduled outpatient clinic appointments, only 0.4% of recipients contacted the outpatient services stating that they had no knowledge of the scheduled appointment. This suggests that successful contact rates with SMS reminders are very high, although it is not possible to be conclusive about this.
E-mail reminders
None of the RCTs reviewed in this study utilised e-mail as a reminder technology. A recent high-quality Cochrane review42 found no good-quality research studies to determine the effectiveness of using e-mail for co-ordinating health-care appointments and attendance reminders. Further high-quality research is required to examine the use of e-mail for this purpose.
Findings from other studies
No additional studies.
Evidence statement (B.2): there are no studies investigating whether or not reminder factors (such as language, information provided, framing of information) influence the accessibility/comprehensibility of the reminder message for particular patient groups (evidence category VIIa)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
None of the included studies explicitly explored the extent to which factors such as language or the way in which a reminder is framed influences its comprehensibility and, therefore, the effectiveness of reminders. None of the included studies investigated the extent to which factors such as cognitive impairments, literacy and health literacy might influence the comprehensibility and subsequent effectiveness of the reminder. However, it is self-evident that comprehensibility of the reminder is an important determinant of the effectiveness of the reminder.
Very few trials of reminder systems specifically examine the content of the reminder. A notable exception is seen in recent interest in use of an ‘orientation statement’ specifically in the context of patients with severe mental illness [see Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)]. In fact, several trials exhibit a preoccupation for controlling against variation in content rather than exploring its variety. So, for example, in the trial by Chen et al. ,57 staff members making telephone calls were required by a trial protocol to follow as closely as possible the same format of words as used in the SMS group. Here we encounter a direct tension between rigorous research and pragmatic exploration of multiple alternative solutions.
Findings from other studies
No other studies investigate whether or not reminders address patient obstacles to attendance.
Evidence statement (B.3): there are no studies to show that the content of the reminder may effectively address the obstacles/enablers experienced by the patient in question (evidence category VIIa)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
No effectiveness studies investigate whether or not reminders address patient obstacles to attendance.
Findings from other studies
In the section Quality of included trials, we demonstrate that there is weak consistent evidence that reminders which provide additional information over and above details of timing and location (‘reminder plus’) are more effective than simple reminders which provide information about the time, date and location of an appointment. However, it is not known whether providing patients with additional information acts to reduce perceived obstacles to attending or by maximising enablers. This is an area that requires more research.
Evidence statement (B.4): there is controvertible evidence, based on multiple good-quality studies, that personal reminders have a greater impact on attendance rates than automated reminders (evidence category IIa)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
A systematic review by Clough and Casey25 investigating technological adjuncts to increase client adherence to psychological therapies found, based on two RCTs, that reminders with direct client and therapist contact were more effective at increasing appointment attendance than indirect reminders, such as letters, recorded messages, or reminder calls made by the clinic secretary. Similarly, a systematic review by Hasvold and Wootton47 on the effectiveness of personal or automated telephone calls or SMS message reminders for patients attending a variety of hospital outpatient appointments found that the effect of reminders on did-not-attend rates was higher for manual reminder calls than for automated calls. Based on data from 29 studies, reporting a total of 33 estimates of reminder effectiveness, 18 of the interventions were based on manual reminders (i.e. telephone calls made by health staff) and 15 were based on automated reminders (i.e. automated telephone messages or SMS messages). Taking into account the quality of the studies, the pooled estimates of the weighted means (using study quality as the weighting factor) showed that manual reminders can achieve a reduction in the did-not-attend rate of 39% of the baseline value, while automated reminders can achieve a reduction of 29% of the baseline value. This indicated that personal reminders are more effective than those sent automatically by a computer.
Two additional RCTs66,73 investigated the differences between personal and automated reminders, but neither found any difference between the direct contact reminder and the automated reminder. In a Malaysian RCT73 comparing the effectiveness of text messaging reminder (n = 308), telephone reminder (n = 314) and control (no reminder) (n = 309) in increasing appointment attendance in patients with chronic diseases requiring long-term follow-up, the absolute non-attendance rate for telephone reminders (13.7%) was 2% lower than with the text messaging group (15.6%). This study is limited in two regards. First, the person delivering the telephone reminder message was to deliver the same standardised message that was delivered by the SMS reminder and if patients had any further queries about their appointment they were directed to contact the appointment desk, thus minimising the personalised nature of the personal contact. Second, the study was powered to detect an absolute difference of 10% between the two reminder groups. Because of the risk of a type II error, it is not possible to conclude that there is no difference in effectiveness between the direct contact reminder (telephone) and the automated reminder (SMS). An appropriately powered study with greater personalisation of the telephone reminder would be required in order to reach a conclusion.
Griffin et al. 66 undertook a three-arm RCT (n = 3610) to test whether or not an IVR system telephone call was equally as effective as a nurse-delivered telephone call at educating and preparing patients for flexible sigmoidoscopy and colonoscopy examinations. The three study conditions were nurse telephone call 7 days before the procedure, an IVR system call 7 days before the procedure and an IVR system call 3 days before the procedure. All calls included an appointment reminder, information about preparation for the examination and encouragement to prepare for and attend the examination. There was no statistically significant difference in appointment attendance between automated, interactive telephone reminders and personal telephone reminders in the context of fluoroscopy and colonoscopy clinics. Significantly more patients in IVR conditions reported neutral perceptions about the telephone calls and more patients receiving nurse calls reported very positive perceptions about the telephone calls. Of particular note is that this automated IVR system was dissimilar to many other automated systems in that it was interactive and, thus, allowed patients to request that information be repeated. The system provided patients with cues to action for appointment attendance and procedure preparation, including targeted educational information about susceptibility and severity of colorectal cancer and motivational messages that addressed risks, benefits, barriers and self-efficacy associated with preparation and procedures. The interactive nature allowing flexible access to the information about the appointment may explain its relative success compared with the personal contact provided by the nurse.
Findings from other studies
No additional studies.
Evidence statement (B.4): the format of the reminder will compromise the amount, and type, of information that can be delivered to the patient (self-evident)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
Most examples from the effectiveness review indicate that the amount of text that can be delivered in a SMS text message is fairly limited. When described, many trials simply specified participant’s name and appointment details. However, the majority of the studies did not provide any details of the message content, making it difficult to analyse their content and intent. Cited examples of actual content include:
[Name] Your apt. is at [Time] on [Day]. See you then! To end reply STOP. 75
Dear Mr/Ms [. . .] Have you taken the prescribed lipid lowering medication as scheduled? I hope to see you at your next visit on [0000 year] [00 month] [00 day], at [000 hospital], from [doctor 000]. 59
You have an appointment at [name of practice] [today/tomorrow] at [time]. Please call [number] if you can’t make it. 64
Findings from other studies
It is self-evident that the format (medium) in which a reminder message is delivered will dictate, to some extent, how long and informative the reminder message can be. By their nature, SMS messages are length restricted and, in line with guidelines around confidentiality, usually contain minimal information. 96 Accordingly, SMS reminders can serve as memory joggers, but little more. Other reminder technologies, such as e-mail, letters and personal telephone calls, lend themselves to the provision of additional information that may facilitate appointment attendance (see Quality of included trials).
Evidence statement (B.4): very few studies investigated whether or not the reminder preferences of the patient may influence the impact a reminder has on the patient’s appointment behaviour (evidence category VIIa)
As the primary purpose of RCTs is to explore effectiveness, the reviews did identify instances in which supplementary and opportunistic data on patient preferences had been collected, alongside a trial. This was particularly likely when service delivery challenges are amenable to solutions that involve the introduction of relatively and comparably cheap technologies.
Findings from effectiveness review (systematic reviews and randomised controlled trials)
None of the included studies directly explore the relationship between patient reminder preferences and the effectiveness of the reminder on patient appointment behaviour. Parikh et al. 77 conducted a survey in conjunction with their study comparing personalised or automated telephone calls with no intervention. The personalised intervention was regarded as helpful by 85% of survey respondents, compared with 48% in the automated group. Perron et al. 78 report, from a satisfaction survey with 241 patients conducted alongside their RCT, that 93% were not bothered by the reminders and 78% considered them to be useful. Bos et al. 55 reported that most interviewed participants felt positive or very positive about receiving a reminder; however, no less than 20% of interviewed participants felt negative or very negative about the reminders and considered them to be a waste of time and money.
If patients are already disposed to using mobile technology and text messaging, then they are very highly (98%) in favour of using SMS as a mechanism for delivering reminders. 70 Participants in the RCT by Bos et al. 55 demonstrated a significant preference for a reminder by mail (56.3%), followed by a telephone reminder (26.0%) and a reminder by SMS (17.7%).
Findings from other studies
No additional studies.
Evidence statement (B.5): there is strong consistent evidence that the timing of a reminder, between 1 and 7 days prior to the scheduled appointment, has no effect on patient attendance behaviour (evidence category Ia)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
There is strong consistent evidence from six studies47,48,60,66,96,97 that the timing of the appointment reminder has no bearing on the effectiveness of the reminder. This evidence indicates that a reminder can be sent any time between 1 and 7 days without obvious reduction in the effectiveness of the reminder. It is possible that reminders sent up to 2 weeks before the appointment may also be effective.
A recent good-quality systematic review47 of 29 studies providing an appointment reminder by telephone, SMS or automated telephone calls for patients attending general hospital outpatient appointments investigated the relationship between appointment attendance and the time at which the reminder was issued (varying between 1 and 7 days). There was no significant relationship between attendance and the time at which the reminder was issued (Spearman’s rank-order correlation r = 0.18). This finding is supported by a systematic review investigating the effectiveness of postal and telephone reminder systems for first-time appointments in predominantly psychiatric settings. 48 Based on two RCTs, the author found that there was no significant difference in the effectiveness of either telephone reminders or postal reminders delivered 1 day or 3 days prior to the appointment. In a literature review and cross-sectional survey describing the effect of a postal reminder system on UK adult psychiatry clinic attendance, Magnes97 reaches the conclusion that a reminder sent at 14 days seems to work as well as prompts 3 days prior to the appointment. The author provides weak evidence from his literature review and a small very low-quality cross-sectional survey to support this claim.
In their recent three-arm RCT, Griffin et al. 66 investigated whether an IVR system telephone call at 3 days or 7 days was equally effective as a nurse-delivered telephone call 7 days before the procedure at educating and preparing patients (n = 3610) for flexible sigmoidoscopy and colonoscopy examinations in a US health-care setting. All calls included an appointment reminder, information about preparation for the examination and encouragement to prepare for and attend the examination. The authors found no statistically significant differences across the three study arms in appointment attendance, indicating that timing of the IVR message did not influence appointment attendance. Christensen et al. 60 conducted a prospective and randomised controlled study to evaluate whether confirmation calls made 1 or 2 working days before scheduled appointments reduce the percentage of broken appointments in a children’s hospital dental clinic. A total of 313 patients were randomly assigned to three groups: (1) confirmation call made 1 working day before appointment, (2) confirmation call made 2 working days before appointment and (3) control group (no confirmation call). Overall, there was a 62% reduction in non-attendance at appointments among patients who received a confirmation call compared with the control group and there was no significant difference between confirmation calls placed 1 or 2 working days prior to the appointment (p = 0.51). Finally, in a non-randomised comparative study, Sims et al. 96 examined the effect of SMS, or text message, reminders on the attendance of appointments at four community mental health clinics in London. Attendance of outpatient appointments was examined between March and June of 2008 (n = 648), 2009 (n = 1081) and 2010 (n = 1088). Reminder messages were sent 7 and 5 days before an appointment in 2009 and 7 and 3 days before an appointment in 2010; patients in the 2008 sample received no reminder messages. Appointment attendance during the sample periods was compared by using multiple logistic regression analysis and adjusting for sociodemographic and clinical confounders. There was no difference in attendance behaviours between the two different reminder schedules, indicating that the 7- and 5-day and the 7- and 3-day reminder systems were similarly effective. 96
A limited number of trials explore and directly compare different notification periods; for example, Griffin et al. 66 compare the same reminders sent at 7 days and 3 days. In other cases, the comparison periods are determined not by the optimal notification period but by the inherent limitations of the technologies, e.g. assumptions regarding postal delivery times. 74,84,86 As a consequence, technology and notification period variables are frequently confounded making isolation of their effect even more challenging.
Hasvold and Wootton47 found no apparent difference in the non-attendance rate whether the reminder preceded the appointment by a day or a week. One important implication of assuming equivalence for different notification periods is that, in the event of no period favouring patient preference, the decision on when to transmit the reminder becomes bound up with considerations that relate to the capacity of the service to reschedule patients into vacant time slots. Furthermore, parity between different notification periods questions assumptions regarding the importance of reminders as a response to ‘forgetting’. The implication is that, with no direct relationship between notification period and likelihood of forgetting, other obstacles or commitments, perhaps seen by the patient as non-negotiable, are equally likely to impair the likelihood of attendance.
However, the main focus of the research agenda is on comparing the technologies with the associated implications that (1) the main task is to deliver the reminder to the patient and (2) the quest is for a single technology (a ‘magic bullet’) that caters for the needs of the average patient and, by association, for the needs of all patients. Perhaps the only trials that recognise a ‘horses for courses’ approach are the trials by Perron et al. ,78 which used a progressive escalation procedure, and by Rutland et al. ,83 which employed multiple complementary approaches. Car et al. 43 identified one low-quality study that showed that mobile text message reminders with postal reminders, compared with postal reminders alone, improved rate of attendance at health-care appointments (RR 1.10, 95% CI 1.02 to 1.19).
Findings from other studies
No additional studies.
Proposition C: health-care settings
It is our proposition that the impact of a reminder on intention to attend (and, therefore, likelihood of attendance) will vary between service settings (and patient subgroups) because health-care system factors and patient-/procedure-specific factors can influence patient-level obstacles/enablers. The following evidence statements relate to this proposition.
Evidence statement (C.1–C.6): there are no studies investigating whether or not factors about health-care settings influence the effectiveness of the reminder (evidence category VIIa)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
The aforementioned emphasis on comparison of technologies has also constrained the degree of variation in exploring whether or not the source of the message is an important variable. We might hypothesise, for reasons associated with the therapeutic relationship, that a patient is more likely to attend if invited personally by a clinician. This is apparently supported by the findings of Nelson et al. ,75 who indicated that those receiving text reminders are less likely to attend than those receiving telephone calls from clinic staff. They hypothesise that this may relate to personal relationships between clinical staff and patients; greater interactivity is offered by personal telephone calls and text messages are easier to ignore. However, such conclusions may be driven by certain assumptions that themselves need to be questioned.
Findings from other studies
Evidence from non-randomised studies presented later in the report (see Chapter 6) suggests that doctors may, perversely, give the impression that attendance at a particular appointment is not that important. In contrast, reception staff who are directly inconvenienced by non-attendance, having to revisit schedules to reallocate the cancelling patient and to seek replacements to utilise vacant slots, may view cancellation much more seriously. Adding a further layer of complexity is that, if patients anticipate an unfavourable or unfriendly reaction from administrative or clinic staff when cancelling, they may be less likely to notify the service at all, leading to arguably more uncertainty, inconvenience and expense.
Proposition D: wider social systems
It is our proposition that the impact of a reminder on intention to attend (and, therefore, likelihood of attendance) will vary between service settings (and patient subgroups) because the wider social systems within which patient subgroups are situated vary and elements of these can influence reminder accessibility and patient-level obstacles and enablers. The following evidence statements relate to this proposition.
Evidence statement (D.1–D.9): there are no studies investigating whether or not wider social systems influence the effectiveness of the reminder (evidence category VIIa)
None of studies investigate whether or not reminders address patient obstacles to attendance.
Proposition E: are there any systems that effectively support the cancellation of appointments?
It is our proposition that intention to attend may not result in attendance because additional obstacles can arise for patients who would otherwise intend to attend. This will include patients whose intention to attend has been influenced by the reminder (i.e. whose obstacles–enablers balance has been shifted by the reminder) and those who already intended to attend but for whom the timing/location was not convenient. It should be noted that the included studies did not distinguish between those patients who intend to attend and, therefore, cancel and rebook, and those who do not intend to attend and cancel. Cancellation rates, rather than cancellation/rebook rates, are typically reported and, thus, in much of the analysis below these outcomes have necessarily been grouped together.
Evidence statement (E): there is strong consistent evidence that reminder systems will promote cancellation of appointments (evidence category Ia)
There is strong evidence that a reminder will increase patient cancellation/rebooking rates; however, the success may depend to some extent on the nature of the reminder (personal vs. automated contact) and the timing of the reminder. Reminders sent very close to the appointment date, as is frequently the case with SMS reminders, will allow the patient very little opportunity to cancel and the health service very little time to reallocate the appointment.
Telephone reminders (evidence category Ia)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
There is strong evidence from thee RCTs67,77,80 that a personal telephone reminder will increase patient cancellation rates. Parikh et al. 77 studied patient acceptance, no-show and cancellation rates among patients receiving a clinic staff reminder, an automated appointment reminder and no reminder in an academic outpatient practice. Patients were randomly assigned to one of three groups: clinic staff reminder (n = 3266), automated reminder (n = 3219) or no reminder (n = 3350). Patients in the clinic staff reminder group were called 3 days in advance by front-desk personnel, patients in the automated reminder group were reminded of their appointments 3 days in advance by an automated, standardised message and cancellation rates in the automated reminder and clinic staff reminder groups were significantly higher than in the no-reminder group (p < 0.004). Another study examined whether telephone reminders from GPs are more effective than those made from hospitals. 80 Outpatient department appointments for three GPs in New Zealand over a 3-month period were randomised into three groups: hospital, GP and control. Patients in the hospital and the GP groups were reminded of their appointment by telephone 24 hours beforehand by a hospital waiting-list clerk or their GP (n = 37 and n = 35, respectively). Patients were more likely to cancel or reschedule their appointment if they had received a reminder from the GP (7/35 = 20%) or the hospital (8/37 = 22%) than patients in the control group (3/37 = 8%). A RCT67 investigating telephone reminders 1 day before the scheduled appointments (n = 423) compared with no reminder (n = 403) in an urban family practice residency clinic in the USA found that the proportion of patients who cancelled was significantly higher (p = 0.0065) in the group that received a telephone reminder before their visit (70/423 = 17%) than in the group that received no reminder (40/403 = 10%). The practice was able to fill about 40% of cancelled appointment slots by the next day, yielding additional revenue. Perron et al. 78 report that in a Swiss urban primary care clinic, 7.4% of patients who were reminded of their appointment by telephone 48 hours previously cancelled their appointments during the telephone call and, of these cancelled appointments, 27.8% were reallocated to other patients. Cancellation data were not provided for the control group.
Findings from other studies
An audit of a personal telephone reminder system in a dental practice in an area of low socioeconomic status in the UK91 reported a statistically significant increase in cancellation rate among those patients who received telephone reminder (34/131 = 26%) compared with those who did not (12/95 = 13%) (p < 0.001).
SMS reminders
Findings from effectiveness review (systematic reviews and randomised controlled trials)
Free et al. 45 established that the pooled effect of using SMS text reminder compared with no reminder on the number of cancelled appointments was not significantly increased (RR 1.08, 95% CI 0.89 to 1.30). Taylor et al. 85 found that the cancellation rate for patients receiving a SMS reminder (20%) was higher than that for patients not receiving a reminder (15%). This observed difference in cancellation rates approached statistical significance (OR 0.70, 95% CI 0.47 to 1.05). The authors suggested that a key benefit of sending SMS reminders was in prompting patients to cancel their appointment rather than failing to attend.
Findings from other studies
Two non-randomised comparative studies98,99 did not report a statistically significant increase in cancellation rate when a SMS reminder was implemented. In a third non-randomised comparative study,100 13.4% of patients who received a SMS cancelled, compared with 11.2% of those who did not receive a reminder. There was no significant difference between the two groups (RR of cancellation 1.26, 95% CI 0.98 to 1.61; p = 0.068), but this could be as a result of the small numbers of cancellations in each group. A larger sample size in this study may have resulted in the results reaching significance.
Evidence statement (E.1 and E.4): there is indicative evidence to suggest that whether or not a patient cancels and rebooks will be influenced by patient perceptions of how easy it is to rebook (evidence category Va)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
None of the included studies explored the relationship between reminder systems and patient perceptions of the ease of rebooking or cancellation. The assumption is that a reminder system will facilitate cancellation and/or rebooking by offering the patient an opportunity and mechanism to cancel or reschedule the appointment.
There are suggestions that services sometimes select reminder technologies because of a perception that they will make it easier for patients to cancel or reschedule. Specifically, in two RCTs78,84 the choice of reminder method was based on the perception that this method would facilitate increased cancellation or rescheduling. Sawyer et al. 84 used telephone reminders to allow increased interaction with adolescents to allow them to cancel or reschedule within a tertiary public adolescent health-care service at the Centre for Adolescent Health, Melbourne, VIC, Australia. Clinic bookings of adolescents were randomly assigned to either a telephone reminder 1 day prior to their appointment or a routine booking (no reminder). The use of reminders (intention-to-treat analysis) significantly reduced the non-attendance rate from 20% to 8% (OR 0.35; p = 0.03). Non-attendance was three times more likely for a new appointment than for review appointments. A total of 79% of parents reported that telephone reminders were helpful at prompting attendance. It was concluded that telephone reminders greatly improved attendance at these adolescent clinics.
Similarly, Perron et al. 78 used a staged personal telephone/SMS/letter reminder design in which patients booked in a primary care or HIV clinic at the Geneva University Hospitals were sent a reminder 48 hours prior to their appointment according to the following sequential intervention: (1) telephone call (fixed or mobile) reminder; (2) if no telephone response, a SMS reminder; and (3) if no available mobile phone number, a postal reminder. This design was selected specifically to reach the maximum number of patients through different reminder systems, while giving the opportunity to a majority of patients to immediately cancel or postpone an appointment, allowing the service to reallocate consultations.
Findings from other studies
The ease of access to technology to cancel or reschedule appointments was addressed by only one qualitative study101 of attendance behaviour from the patient viewpoint at a young adult diabetes outpatient clinic in the UK. Attendance rates for 231 clinic appointments over 19 months for 102 patients were calculated. Semistructured interviews with 17 patients explored the routines, thoughts and feelings around clinic appointments. The study found that long waiting times on the telephone was a deterrent to cancellation. An audit of the cancellation system revealed that as many as 17 patients might be waiting in the queuing system on the telephone at any one time, with waiting times of more than 20 minutes, to contact an operator. In some cases, telephone calls were disconnected with no chance to wait or leave a message. Patients stated that they had also been told by friends or staff not to call the central cancellation line because of difficulties in getting through. Clearly, in this study, patients had a well-justified perception that cancellation/rebooking would not be simple and may even not be worth trying to do at all.
Evidence statement (E.2 and E.5): there is strong evidence that whether or not a patient cancels and rebooks will be influenced by reminder system factors that facilitate/hamper patient intentions to rebook (e.g. nobody answers the telephone) (evidence category Ia)
Interactivity of reminders
Reminder systems can be designed to facilitate patient intentions to cancel and rebook, to a variable degree, depending on the reminder technology, i.e. personal telephone reminder (maximum facility), SMS reminder with the opportunity to reply by SMS (good facility), SMS or other form of reminder providing a telephone number to call (some facility – the patient does not have to look elsewhere for the number).
Findings from effectiveness review (systematic reviews and randomised controlled trials)
There is strong evidence that a reminder will increase patient cancellation and rebook rates [see Evidence statement (E): there is strong consistent evidence that a reminder systems will promote cancellation of appointments (evidence category Ia)], indicating that reminder technology facilitates patient intentions and their subsequent cancellation and rebooking behaviour. In particular, the evidence shows that telephone reminders fare better in this regard than SMS reminders. Reti80 suggests that one dominant benefit of telephone reminders may be the ‘promotion of suitable cancellation behaviours’. The evidence on the effectiveness of SMS reminders to increase cancellation or rebooking rates is less clear, but one reason for this is that SMS reminders are frequently sent 1–2 days prior to the appointment, allowing very little time for patients to engage with cancellation or rebooking behaviours. A second reason may be that when patients receive a reminder they frequently are asked to phone a telephone number rather than simply replying to the text. Taylor et al. 85 found that the cancellation rate for patients receiving a SMS reminder that asked them to telephone a cancellation line if they were unable to attend was observed to be higher (20%) than that for patients not receiving a reminder (15%), and this observed difference in cancellation rates approached statistical significance (OR 0.70, 95% CI 0.47 to 1.05). The authors suggested that a key benefit of sending SMS reminders was in prompting patients to cancel their appointment rather than failing to attend.
Findings from other studies
In a survey of patients who had failed to attend a general surgical outpatient clinic appointment, Hogan et al. 20 report that a ‘text message reminder would have encouraged 51% (n = 49) to have either attended the appointment or contacted the hospital to cancel’. However, the way that SMS reminders are delivered varied across studies, hence influencing the way that they are used to cancel or reschedule. Most SMS reminder systems provided a telephone number for the patient to call to cancel in the body of the reminder message. 70,85 In some studies, the patient could also reply by SMS;78,98,102 however, few of these studies reported cancellation rates. Two non-randomised comparative studies98,99 did not report a statistically significant increase in cancellation rate when the reminder was implemented. In a third non-randomised comparative study,100 patients who received the reminder were able to either call a telephone number or reply to the text in order to cancel their appointment. The cancellation rates among patients who received a SMS was 13.4%, compared with 11.2% among those who did not receive a reminder. The difference between the two groups was not significant (RR of cancellation 1.26, 95% CI 0.98 to 1.61; p = 0.068), but this could be as a result of the small numbers of cancellations in each group. A larger sample size in this study may have resulted in these results reaching significance.
Although it has already been acknowledged above that the evidence for SMS as a means of promoting cancellations is not very clear [see Evidence statement (E): there is strong consistent evidence that reminder systems will promote cancellation of appointments (evidence category Ia)], none of the studies reported in this section or in the section titled Evidence statement (E): there is strong consistent evidence that reminder systems will promote cancellation of appointments (evidence category Ia) was powered to investigate the effectiveness of reminder systems to promote cancellations. Therefore, it is not possible to reach a conclusion about whether or not there would be a difference in effectiveness if a patient has to call a telephone number to cancel compared with responding by SMS.
Evidence statement (E.2 and E.5): strong consistent evidence indicates that system factors related to appointment systems will hamper patient intentions to cancel/rebook (evidence level Ib)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
There is no evidence from the effectiveness review that particular systems facilitate cancellation.
Findings from other studies
Good evidence from other types of studies indicates that whether or not a patient cancels/rebooks will be influenced by system factors that facilitate/hamper patient intentions to cancel/rebook. Four studies18,101,103,104 acknowledge potential system difficulties hampering cancellation by telephone, outside the context of a reminder system. Problems included:
-
difficulties faced by patients accessing the central booking line (long waiting times, call disconnecting with no option to wait or leave a message, phone engaged)18,101,103,104
-
poor reputation regarding access to the central booking number for the reasons outlined above, discouraging patients from making contact101
-
internal hospital communication problems resulting in cancellations and changes of address not being passed on to the clinic. 101
A systematic review on primary care appointment attendance behaviour (i.e. not on appointment systems per se)18 cites several studies indicating that busy telephone lines or administrative problems around the cancellation process are significant issues. This is acknowledged in a survey of primary care staff in Yorkshire: ‘When asked specifically how easy it was for patients to cancel . . . It was acknowledged that phone lines could be busy, making it difficult to cancel . . .’. 104 Similarly, in another study that explored patients reasons for failure, 14 out of 75 participants stated that they had telephoned or written to cancel their appointment already, indicating possible difficulties in the cancellation system. 103 The convenience of e-mail for cancellation, in so far as there is no need to wait to get through to a receptionist, is proposed by Atherton et al. 42
Evidence statement (E.3 and E.6): there is indicative evidence that for patients who intend to take up the offer of an appointment, whether or not a patient cancels and rebooks will be influenced by structural factors that facilitate/hamper patient intentions to rebook (e.g. has to be done online and no internet access) (evidence level Va)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
There is no evidence from the effectiveness review that structural factors may hinder rebooking.
Findings from other studies
Only one study91 explicitly examined the structural barriers to rebooking and cancellation. This study looked at the effectiveness of a telephone reminder on attendance and cancellation for dental appointments in a deprived community in Sheffield, UK. The authors observed that many patients in the community did not have telephones, or their telephones had been disconnected. This limited access to reminders and the ability of the patient to cancel, but many patients who were contacted did cancel. The authors assumed it likely that, if other patients had been contactable, they may have also cancelled if given the opportunity. Self-evidently, the requirement to telephone and cancel an appointment might present difficulties for those populations with higher levels of mobility or deprivation and, thus, less likely to have access to a telephone.
Evidence statement (E.7): there is no evidence that whether or not a patient cancels the appointment will be influenced by patient perceptions that cancelling the appointment is the morally right thing to do (evidence category VIIa)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
There is no evidence to explore whether or not receiving an appointment reminder will increase patient perceptions that cancelling the appointment is the morally right thing to do, if the patient has no intention of taking up the offer of the appointment.
Findings from other studies
The issue of the morality of cancellation and rebooking was not explored directly. The issue was explored peripherally in one qualitative study105 included in one systematic review18 and two surveys. 103,104 Two included studies suggest that cancellation is not given a high priority by patients, suggesting that they forget to cancel or do not think to do so in the first place. A study105 exploring dental appointment attendance reported ‘Well, a person has a lot more to think about than . . . just sitting around making a bunch of phone calls, so much is going on in my life, . . . you must have kids, and schools to deal with, and parent’s meetings and work . . .’.
Primary care staff surveyed by Hussain-Gambles et al. 104 did not perceive patients to have a sense of moral duty to cancel. In this study, some staff suggested that some patients may be too embarrassed or ashamed to cancel, many staff felt that patients were disrespectful or irresponsible. Similarly, in a study of appointment attendance for a surgical clinic serving a deprived population,103 the authors speculate that the patients may have a negative public attitude towards the NHS, with a corollary that this may influence whether or not patients are prepared to cancel appointments.
Proposition F: distal/proxy individual attributes
It is our hypothesis that a range of factors can act as markers/proxies for proximate individual factors that are enablers or obstacles to attendance. At a service setting level, this information could be used to judge the likely effectiveness of a particular reminder approach given the patient population profile or to explain the impact of a reminder system differs from that observed in other settings.
Do different reminder systems have differential effectiveness for particular subgroups of the population (e.g. by age group, ethnic group, socioeconomic status, gender, etc.)?
Evidence statement (F.1): there is sufficient weak equivocal evidence to suggest that age does not have a differential effect, over and above pre-existing appointment behaviour, on reminder effectiveness (in terms of attendance, cancellations or rebooking) (evidence category IVa)
Findings from effectiveness review (systematic reviews and randomised controlled trials)
In a recent systematic review, Guy et al. 44 performed subgroup analyses by age. They found no significant subgroup differences in reminder effectiveness by broad target age groups (i.e. paediatric, adult, older) (Table 8). However, their age classification was a relatively crude construct based on the median age of patients receiving SMS reminders, or specification of clinic type, e.g. as paediatric.
| Paediatric | Adult | Older |
|---|---|---|
| Downer et al., 2005106 (non-RCT) | Fairhurst and Sheikh, 200864 (RCT) | Chen et al., 200857 (RCT) |
| Downer et al., 200694 (non-RCT) | Leong et al., 200672 (RCT) | Cho et al., 201059 (RCT) |
| Foley and O’Neill, 200997 (non-RCT) | Liew et al., 200973 (RCT) | |
| Geraghty et al., 200893 (non-RCT) | Macpherson and Alpsten, 2008107 (non-RCT) | |
| Milne et al., 2006108 (RCT) | ||
| Stott and Gray, 2009109 (non-RCT) |
In six papers94,95,98,106,108,109 in this systematic review,44 the SMS reminders targeted patients attending paediatrics clinics. In paediatric settings, the SMS reminder was sent to the young patient or their parent/carer; in the non-randomised study by Stott and Gray,109 SMS reminders were sent directly to the young people. In two RCTs, the target population were adults (mean ages of 38 years64 and 33 years72). In four papers (three RCTs57,59,73 and one non-RCT107), the target group was older (mean age of 58 years57 or 50 years,59 aged 50–70 years3 or 68% > 50 years107), and in five others the age of the target group was not specified.
The systematic review of RCTs by Guy et al. 44 also demonstrated that SMS reminders are effective in a wide range of age groups from paediatric to older clients. Mobile phone usage data demonstrate that in many countries more than 90% of the population own mobile phones, but uptake is higher in younger people. 109 Neal et al. 110 postulate that because younger patients have higher non-attendance rates at clinical services, SMS reminders may be more beneficial in this group; however, this is not supported by any empirical findings.
Evidence statement (F.2–F.11): few studies investigate whether or not a range of distal/proxy individual attributes have a differential effect, over and above pre-existing appointment behaviour, on reminder effectiveness (in terms of attendance, cancellations or rebooking) (evidence category Va or VIIa)
There is minimal or no evidence that a range of individual attributes has a differential effect on reminder systems, including gender, deprivation status, employment status, substance abuse, ethnicity, mental health, other health problems, symptomatic compared with non-symptomatic health status, diagnostic stage, and perceived severity of the patient’s health condition.
For a trial to address these questions requires baseline measurement of population characteristics on inception and measurement of the same characteristics in the multiple arms of the trial. The informativeness of many trials is limited by (1) not having any baseline measurements against which to measure the effectiveness of the intervention (therefore any differences may simply reflect differences in appointment behaviour not the effect of the reminder system), or (2) reporting the population characteristics aggregated across all interventions making, it impossible to isolate a differential effect of particular technologies, or (3) not reporting population characteristics at all. Studies are further limited by (1) data dredging, i.e. measuring multiple characteristics and reporting those that achieve statistical significance, and (2) imputing a cause-and-effect relationship when the study has not been specifically constructed to examine that particular variable. For example, Can et al. 56 report differential attendance for boys over girls and the affluent over those with higher Townsend deprivation scores. However, they analyse these differences across study arms making it impossible to draw conclusions about differential population effects. They conclude from non-causal evidence that if a clinic has a catchment area in which there is a high level of social deprivation, then the use of reminders will not be as effective as in more affluent areas. They then assert that the main reasons for non-attendance of people who live in deprived areas are, therefore, likely to be more complex than simply forgetting an appointment. As the above implies, the circumstances that may impair either access to the reminder or access to the health-care appointment are not particularly suited to exploration through a RCT design. As a consequence, we pick up and explore many of these more qualitative factors following realist principles through examination of a wider body of evidence in the subsequent synthesis sections (see Chapter 5).
Chapter 5 Patterns and influences on health-care attendance behaviour: a narrative overview of key themes and issues
Having synthesised the evidence relating to reminder systems in the preceding chapters, we turn to provide a narrative overview of literature generated by our review on attendance behaviour more generally (review 3; see Figure 1 and Chapter 3, Review questions). Given that our review has identified significant gaps in current understanding regarding how reminder systems operate in different service settings and for different population subgroups, there is value in exploring the identified literature from this wider perspective. Specifically, looking beyond the evidence directly related to reminder systems to examine what is known about patterns and influences on attendance behaviour more generally may:
-
prompt ideas for how attendance/reminder interventions should be designed in future (for instance, in terms of particular barriers to attendance that they might seek to overcome or enablers they might seek to enhance)
-
provide insight into the reasons why reminders have greater/lesser impact in particular patient groups or in particular services settings
-
highlight aspects of the wider health-care setting that require particular attention if the impact of reminder/attendance interventions is to be maximise
-
suggest issues to consider, or areas where caution may be warranted, in introducing reminder interventions in relation to potential differential impacts of reminder interventions across patient subgroups
-
flag up specific areas requiring further research in relation to reminders.
It is important to highlight, however, that our project did not set out to provide a comprehensive review of the literature on patterns and determinants of health-care appointment attendance. The information presented here is necessarily limited. We have drawn primarily on sources generated from our review and, when possible, supplemented these with highly cited papers that provide further information in support of the key issues and themes that emerge. We also signpost additional literature, outside the scope of our review, that may usefully inform future work on reminder systems and associated interventions aimed at improving attendance levels.
Appointment attendance behaviour has been investigated extensively in both the UK and other contexts, with a wide variety of putative factors – relating to the health-care setting, the nature of the appointment, the characteristics of the individual patient and the wider social setting – having been explored through both qualitative and quantitative research methodologies. Although some studies simply report on the reasons that patients cite for not attending appointments, others have involved comparative analyses between different subgroups of patients and/or more detailed investigation of the processes that support or hinder appointment attendance. Some consistent findings emerge, but the relationships between many of these factors and attendance behaviour are inconsistent across studies, suggesting that context is important in moderating their influence.
In keeping with the conceptual framework presented in Chapter 4, we organise the material into the following subsections:
-
reported reasons for non-attendance
-
factors linked to the health-care setting (conceptual framework domain C)
-
factors linked to the wider social system (conceptual framework domain D)
-
distal/proxy patient attributes (conceptual framework domain F).
Reported reasons for non-attendance
Given that simple reminders are effective across a wide range of settings, it is not surprising that many studies identified ‘forgetfulness’ as the most common reason given by patients for not attending a health-care appointment. 20,111–114 Studies also suggest that health-care professionals perceive forgetfulness to be one of the most important reasons for non-attendance. 104 However, the evidence from multiple studies indicates that forgetting to attend accounted for between 8%112 and 45% of the patients who did not attend their appointments,74 suggesting that other factors are also in operation in many settings. Furthermore, other reasons for non-attendance cited by patients across a range of studies include:
-
health-related factors: hospitalisation115 (as cited by Horstmann et al. 116), feeling too sick to attend,72,84 had more important medical concerns117 and anxiety104
-
timing and (in)compatibility issues: having several appointments in various hospitals,20,72 effort (distance, transportation, parking),113,115,118 presence of a sick child or relative113 (as cited by Horstmann et al. 116), lack of child care113 (as cited by Horstmann et al. 116), conflicts with work schedules115 (as cited by Horstmann et al. 116), other commitments,69,84 overslept113 and having ‘lot on their mind’104
-
administrative errors and miscommunication: misunderstanding about appointment time and date,118,119 scheduling problems,80,113,119 hospital administrative problems (around 60%)120
-
financial reasons113
-
perceptions of the (dis)benefits of attending: fear of seeing a junior doctor,12 not understanding the importance or purpose of the appointment74 and because the appointment was no longer required. 69,84
These numerous reported reasons for not attending appointments suggest that non-attendance at appointments is a highly complex and multifactorial problem. The following sections throw further light on the processes operating to shape attendance behaviour.
Factors linked to the health-care setting
Perhaps unsurprisingly, a wealth of research suggests that attendance behaviour is linked to various aspects of the health-care setting. A variety of factors have been explored and yet many of these have received little attention within research focused on reminder interventions as reviewed in the preceding sections. For convenience, we organise this material under three broad themes: characteristics of the appointment system, patient–provider ‘alliance’ and ‘engagement’, and other features of the service/care. It is important, however, to recognise that these different arenas are not distinct but inter-relate, each being elements of the fundamental interplay between the patient and the health care on offer.
Characteristics of appointment systems
Our review examined six characteristics of appointment systems that appear important in relation to attendance behaviour: administrative (in)accuracy [a significant problem in some contexts, already discussed above – see Chapter 4, Evidence statement (B.1): there is strong consistent evidence that the reminder may not be received by the patient (evidence category Ia)], source of the appointment, timing of the appointment, time to wait for the appointment, patient involvement in appointment initiation and/or scheduling and whether the appointment is a first or follow-up.
The source of the original appointment
Only two studies25,80 were identified that explored the differential impact of reminders delivered by different sources and these produced equivocal findings. In addition, limited and inconsistent evidence was yielded on the effect of source of appointment on attendance behaviour. Just two UK papers89,121 reviewed included quantitative analyses addressing this hypothesised relationship and these related to contrasting settings and employed inconsistent categorisation of sources.
A UK-based study in a gynaecology clinic121 compared 105 non-attenders with 105 attenders at the same index clinics and concluded that referrals from primary care were more likely to be missed than interspecialty or referrals from the accident and emergency (A&E) department. In contrast, a study of attendance at a specialist alcohol treatment centre in the UK89 undertook multivariate analysis of patient characteristics of non-repliers (n = 100), non-attenders (n = 100) and attenders (n = 100) and found no statistically significant association between source of referral and attendance. A study in a paediatric dermatology clinic in Hong Kong122 found that non-attendance was significantly higher among referrals from the emergency department than among referrals by private practitioners (p = 0.05).
A qualitative study exploring attendance for breast screening by women in Turkey123 provided some support for the hypothesis that invitations/recommendations for screening received from family doctors might be important in encouraging attendance. Respondents in the study reported ‘if we face a genial approach, we wouldn’t hesitate going to a doctor, even if it is a male doctor’, ‘we might be ignorant, but our doctor should enlighten us in detail, we need information’. 123
Despite the limited information in the review, a scan of the wider literature (including citations in our reviewed papers) indicates that the hypothesis that the source of the appointment/invitation can influence attendance has received some attention in both research and practice, particularly in relation to screening interventions. A key contrast of interest has been between GP/primary care referral and referral from a hospital clinic or central administrative unit. For instance, in relation to attendance for breast screening, some UK interventions have involved letters of endorsement or telephone calls from the woman’s local GP practice in addition to standard screening invitations and leaflets, but the reported impact on uptake has been disappointing. 124,125
Explanations and implications for reminders
Several potential mechanisms might explain variations in levels of attendance by source of original appointment. First, the identity of the person/department/service that initiates the making of an appointment (invites the patient to the appointment) may influence patient perceptions that attendance at the appointment will positively contribute to well-being and/or that non-attendance will result in negative consequences. It may also be hypothesised that the source of the original appointment could influence patient perceptions that attendance is the morally ‘right thing’ to do, for instance if the appointment invitation comes from a health-care professional with whom the patient has a pre-existing relationship.
In addition, however, associations between the source of a referral/original appointment and attendance may relate to differences in the knowledge level of the practitioner about how likely a patient is to attend, perhaps related to knowledge of personal circumstances and/or readiness to engage with the particular treatment/care on offer. For example, Booth and Bennett89 in their study of a specialist alcohol treatment centre in the UK suggest that ‘it is possible that since GPs tend to have a longer-standing professional relationship with their clients than other referral sources, they may be better placed to assess patient readiness to seek help for an alcohol problem’. In this way, some practitioners may act as gate-keepers/demand managers by not offering referrals to patients they believe will not turn up anyway.
Differential attendance rates by source of referral may also reflect a higher degree of involvement of the patient in the decision to seek the appointment and the scheduling of that appointment. For instance, hospital referrals made by a GP are likely to result from a consultation initiated by a patient in response to some perceived need and may also allow for involvement of the patient in the scheduling of the appointment, whereas referrals between departments may not involve the patient to the same degree.
In addition, higher attendance rates associated with appointment invitations emanating from general practices may reflect more up-to-date and far-reaching patient contacts, so that the appointment information may simply be received by more patients when it comes from some sources rather than others.
The available evidence does not allow a detailed exploration of these various potential mechanisms and does not provide consistent evidence to inform decisions regarding the source of reminders that are likely to be most effective.
Timing of the appointment
The review identified several studies that had explored patterns of attendance by appointment timing, looking at both the day of the week and time of day. Explanation for higher non-attendance at particular times or on particular days has centred on the incompatibility of the appointment with employment commitments, with some discussion of caring commitments also.
Time of day
Three studies, all with reasonable designs and sample sizes – a RCT including 3899 patients, a prospective study and a case–control design – reported no evidence that the time of day of the original appointment has an effect on attendance.
A RCT in Portugal63 included 3899 patients of various ages across various outpatient clinics and found that looking at the overall attendance data (for reminder and control groups) the time of day (morning or afternoon) was not a statistically significant variable with respect to non-attendance (p > 0.05). A UK study based in a specialist alcohol treatment centre89 undertook multivariate analysis of patient characteristics of non-repliers (n = 100), non-attenders (n = 100) and attenders (n = 100), and also included a trial element that examined the effect of a telephone reminder. The authors found that the time of the appointment (morning or afternoon) was not an independent predictor variable associated with attendance and was the last to emerge from the logistic regression equation. In addition, it was not significant over and above age and distance. The authors were somewhat surprised by this finding and speculated that there may have been a chance combination of older patients with shorter distances to travel to morning appointments. A UK study121 exploring attendance behaviour at a gynaecology clinic with an ethnically diverse and deprived patient population employed a case–control design to explore the association of morning compared with afternoon clinic attendance (compared characteristics of 105 attenders with 105 non-attenders) and did not find evidence of a statistically significant difference (p > 0.05).
In contrast, one study112 – a prospective study of non-attendance in a physiotherapy outpatient department in Ireland – reported a statistically significant association between time of day of the appointment and did-not-attend rate. This study categorised attendance into three time periods – morning, early afternoon and late afternoon – in contrast to the studies above that simply used ‘morning compared with afternoon’. Late afternoon appointments produced a non-attendance rate of 6%, compared with 10% and 13% in the morning and early afternoon, respectively. A study126 in the USA reported that morning appointments were significantly more likely to be kept (72.1%) than afternoon appointments (65.8%).
It may be that the cruder classification employed by the first three studies reported above – grouping early and later afternoon appointments – failed to identify time of day that is associated with higher attendance. If the main obstacle to attendance is conflicting work commitments, then it would seem likely that late afternoon (or evening, if offered) appointments would be more likely to be attended.
Day of the week
The available studies identified in our review produced equivocal evidence regarding the link between day of the week and appointment attendance. One UK study based in a specialist alcohol treatment centre reported no evidence of a relationship between day of appointment and attendance. Authors undertook multivariate analysis of patient characteristics of non-repliers (n = 100), non-attenders (n = 100) and attenders (n = 100) and found day of appointment (Monday to Thursday; clinics did not run on Friday) did not have any significant bearing on patient attendance in response to referrals. 89 Similarly, a study126 in the USA reported no association between attendance level at a family practice residency clinic and day of the week (65.8%).
However, three studies (two RCTs63,85 and a case–control analysis121) reported a statistically significant association between day of appointment and attendance rates, but the findings were inconsistent in terms of which days produced the best level of attendance.
A RCT in Portugal63 included 3899 patients of various ages across various outpatient clinics and found that looking at the overall attendance data (for reminder and control groups) patients were more likely to not attend in the middle of the week (Wednesday). In fact, the non-attendance rate increased from Monday to Wednesday and decreased from Wednesday to Friday. The authors suggest that this pattern can be explained by the fact that people going to appointments on Monday or Friday can skip their jobs and have an extended weekend.
A UK study121 exploring attendance behaviour at a gynaecology clinic, with an ethnically diverse and deprived patient population, employed a prospective case–control design to explore the association of day of appointment with attendance (105 attenders compared with 105 non-attenders). In contrast to the Portuguese study, the non-attendance rate was significantly higher on Mondays and Fridays than on other days (non-attendance rates on Monday and Friday were 17.6% compared with 15.1% on the other three days; p = 0.009).
Similarly, a RCT85 involving 679 patients invited for an appointment at two physical therapy outpatient departments in metropolitan acute public hospitals in Australia found higher non-attendance on Mondays and Fridays. The non-attendance rate on Mondays was 16% and on Fridays was 24%, compared with 10–13% on other days of the week. They also found that younger patients were more likely to not attend and speculated that this may be to do with difficulty attending during normal working hours.
Subsequently, a large-scale UK data analysis has produced some noteworthy results. Ellis and Jenkins127 conducted two related studies. In the first they examined attendance records for 4,538,294 outpatient hospital appointments across Scotland between 1 January 2008 and 31 December 2010. The did-not-attend rate was highest on Mondays (11%), lowest on Fridays (9.7%) and decreased monotonically over the week. In their second study, they analysed attendance records for 10,895 appointments at a single GP clinic in Glasgow, Scotland. Here again, did-not-attend rate was highest on Mondays (6.2%), lowest on Fridays (4.2%) and decreased monotonically over the week. A further observation was that this weekly decline was found in male and female patient groups of all ages, but was steeper for younger age groups. They conclude that the did-not-attend rate could be significantly reduced by preferentially loading appointments onto high-attendance days.
In addition to these studies that employed quantitative analyses to compare attenders and non-attenders, several descriptive qualitative and quantitative studies report, perhaps not surprisingly, the importance of appointments being compatible with other commitments. Again, employment commitments featured prominently.
A qualitative study in the UK115 exploring attendance behaviour among asthma patients reported that the inability to schedule appointments at a convenient time was considered a barrier to attendance. In another UK study,128 the authors reported that they had previously shown that 63% of patients attending the cardiorespiratory outpatient clinics would like out-of-hours clinics, largely because they are in employment during the day. A discrete choice experiment among 1200 patients presented respondents with trade-offs between two hypothetical, yet realistic, health conditions: an acute, low-worry condition and an ongoing, high-worry condition. For both conditions, one of the four valued components of appointment systems was a convenient time of day.
Explanations and implications for reminders
Higher levels of non-attendance at particular times and on particular days may primarily be explained by incompatibility with other commitments, particularly employment.
Several qualitative and descriptive quantitative studies identify incompatibility with other commitments as a reason for non-attendance. For example, in a qualitative study investigating the perspectives of young adults attending diabetes outpatient clinics in the UK,101 some respondents reported that the available hours at the clinic were not compatible with unsympathetic employers’ demands and that time booked off work for an appointment could sometimes be cancelled at very short notice. Addressing this aspect of non-attendance would clearly require attention to the appointment systems and clinic opening hours, rather than to reminder interventions. 101
Addressing this aspect of non-attendance would clearly require attention to the appointment systems and clinic opening hours, rather than to reminder interventions.
However, available evidence suggests that the proportion of patients who actually miss appointments because they are unable to secure appointment times that are convenient varies considerably between settings. For example, in a UK study129 based in a genitourinary clinic, no patients reported that clinic opening hours prevented their attendance. Wilkinson and Daly130 report a small retrospective and prospective audit of 142 patients who did not attend their appointment at Care Plus and diabetes clinics in a large general practice in New Zealand, finding that work commitments or being unable to take time off work were cited by only four participants (although they identified the patient population as being predominantly > 65 years and highly deprived; therefore, potentially high numbers were unemployed). A descriptive US study of pregnant women (from a deprived and ethnically diverse patient population) found that 12% of no-show patients who were surveyed said that their reason for non-attendance was that their appointment was at an inconvenient day or time. Casey et al. 131 conducted a small (n = 76) telephone survey over a 1-month time frame to determine reasons for non-attendance in patients who had missed their urology outpatient appointment and found that approximately 10% were unable to attend because of work commitments.
Thus, although it seems reasonable to assume that having an appointment time that is compatible with other commitments is important for all patients (albeit that some patients will consider that they have more competing commitments than others), available evidence does not suggest that large proportions of patients in different settings are unable to ensure such compatibility when the original appointment is made. The extent to which this is an important contributory factor to non-attendance will clearly relate to the appointment system and patient involvement in identifying the timing of the initial appointment (see Time to wait to the appointment).
Furthermore, incompatibility of appointment timing will translate into consistent patterns of higher non-attendance at certain times of day or on certain days of the week only if a significant proportion of people have commitments that are hard to shift on those particular times/days and are nevertheless offered appointments at those times. Again, it seems likely that this will be a more significant issue when appointments are allocated rather than booked in conjunction with the patient. It is also likely that any such patterns would be context specific, as daily and weekly work patterns vary between settings, thus reducing the transferability of findings across settings and highlighting that clinic managers and practitioners need to be aware of local schedules.
Aside from incompatibility issues, some studies have suggested that at least part of the explanation for higher non-attendance on certain days may be greater forgetfulness. For instance, a UK study121 exploring attendance behaviour at a gynaecology clinic found that a majority of patients cited ‘forgetting’ and family and work commitments as reasons for FTA and the authors postulated that patients are more likely to default on days falling after and before the weekend, as their daily routine is less regular. The authors also reported that these reasons might also be partly explained by the fact that the defaulters are, on average, 8 years younger than those who are compliant (38.93 vs. 46.44 years; p = 0.002) and, thus, may have school-aged children.
If people do indeed forget their appointments more when they coincide with certain days, then clearly reminders would be particularly important for patients with appointments on those days.
Time to wait to the appointment
The review generated strong consistent evidence that a longer time between the date of the appointment being made and the date of the appointment taking place is associated with higher non-attendance. Multiple primary quantitative comparative studies (across a range of contexts and patient groups) found a statistically significant association between time between appointment scheduling and appointment date and non-attendance. No studies were found that reported a lack of association between the time between booking and appointment and attendance behaviour.
In a UK RCT study based in a respiratory clinic,82 authors employed linear regression to explore predictors of non-attendance. They demonstrated that each increase in wait time for initial patient visits of 30 days resulted in a 25% increase in the no-show rate. Similarly, a study in a UK eating disorders clinic serving young adults and adults132 reported that the adjusted OR of attending an appointment was 2.4 times greater for those with short waiting times (≤ 4 weeks) than for those with long waiting times (≥ 5 weeks). A logistic regression model in which waiting time (in weeks) was entered as a continuous variable suggested that the odds of attendance at an appointment falls by 15% per week (OR 0.85, 95% CI 0.770 to 0.945; p = 0.002). A UK study121 in a gynaecology clinic serving an ethnically diverse and relatively deprived population also reported that the longer the interval between hospital appointment letter and the actual appointment date, the more likely patients were to default on their appointments (p = 0.001). Another UK study,89 based in a specialist alcohol treatment centre, also found that attendance was less likely with longer delays between referral and an appointment invitation being sent by the clinic. However, in this context the authors also noted that delays could result from both patient- and agency-originated factors contributing to the total waiting time and that patient delays might indicate greater ambivalence about their alcohol problem.
A review paper133 employing hand searches and forward citation searching focused on mental health services in the UK and also reported that waiting time to appointments was a factor that is consistently linked to higher non-attendance.
In addition to the UK studies, numerous studies from other settings report a negative relationship between attendance and time to wait for the appointment. A US study based at a veterans outpatient clinic134 found that missed appointments increased with time between scheduling and appointment up to 13 days, with the rate of missed appointments being between 10% and 20% when the interval was 1 day and between 16% and 25% for an interval of 13 days; however, they found no further rise thereafter. In contrast, for cancellations, the authors found that the rate continues to rise with time interval up to and beyond 1 month. A study of adult primary care in Geneva79 reported that having a follow-up appointment of more than 1 year was significantly associated with missed appointments. Similarly, an Australian study in a general hospital setting93 reported that those with a waiting time of more than 21 days until their appointment were significantly less likely to attend than those with a shorter waiting time (OR 2.8; p = 0.002).
Explanations and implications for reminders
Several papers identified through the review provided some insight into the reasons why a longer delay to appointment is associated with lower attendance.
First, unsurprisingly, forgetfulness is implicated as the cause of the association in several studies. For instance, in a study of adolescent outpatients in Switzerland,135 the authors reported that forgetting the appointment was a common cause and suggested that the higher non-attendance for appointments with a long delay probably reflects the greater risk of forgetting the appointment. Similarly, a study in a dermatology clinic in Italy136 concluded that as long delays to appointments were common; this explains why the most frequent reason given for non-attendance is forgetting the appointment.
However, other factors are also identified as potentially contributing to lower attendance when appointments are scheduled further in advance. First, it has been suggested that other issues are more likely to arise that mean the appointment timing becomes incompatible. 135
It has also been suggested that when appointments are scheduled a long time in advance, patient symptoms may be resolved, either because they resolve themselves or because the patient (or referring health-care professional) opts to seek alternative care. For instance, an Irish study that examined appointments in a general surgical outpatients department20 revealed that resolution of symptoms accounted for almost one-third of missed appointments. The authors suggested that this finding questions the appropriateness of some referrals and suggests that many patients might be managed in the primary care setting. They suggest that in the absence of a quick referral, GPs may be forced to institute treatment measures as intermediate solutions and that these may often these prove sufficient to alleviate symptoms. In the Italian study,136 the authors also reported that a common reason for non-attendance was that the patient had been able to consult a private dermatologist in a shorter time.
However, some authors suggested that under particular circumstances, a long delay could result in reduced motivation on the part of the patient despite continued need. In the context of an eating disorders clinic, Bell and Newns132 noted that their clients ‘. . . may be at a motivational juncture and delaying their appointment on a treatment programme may mean that by the time their appointment is due, they are less ready to address change . . . All patients waiting for mental health care are potentially at risk of failing to engage’. Similarly, this association, also found in a study by Booth and Bennett89 in a specialist alcohol treatment centre in the UK, seems unlikely to be explained by patient symptoms/need having been resolved and more likely by a loss of motivation, which raises concerns about long appointment waits contributing to poor health. It may be that scheduling an appointment a long time in advance can convey the impression to the patient that the appointment is unimportant.
One study suggested an alternative explanation for the association between time to appointment and non-attendance. The authors of a study in a US veteran’s clinic134 speculated ‘it is known that clinicians vary widely in their selection of return visit interval, it is possible that characteristics of clinicians who choose shorter intervals affect these rates [of non-attendance and cancellation] rather than the interval itself’. However, the consistency of this relationship across contexts suggests that this mechanism, even if present, is unlikely to explain the observed patterns in their entirety.
It seems likely that the association between time to appointment and attendance rates will also depend on the nature of the appointment, in particular whether it is a one-off (or first) appointment or rather a regular (repeat) appointment that is scheduled at regular (familiar) intervals of some considerable duration. However, the available evidence did not provide any such exploration.
Keeping waiting times down remains a government priority with patient rights to receive non-emergency treatment within a maximum waiting time being enshrined in the NHS constitution. 137 A short waiting time is also shown to be an important criterion for patients seeking care in many contexts. For instance, a discrete choice experiment128 among 1200 patients in which respondents were presented with making trade-offs between different levels of attributes for two hypothetical, yet realistic, health conditions: an acute, low-worry and an on-going, high-worry condition found that for both conditions one of the four key components of appointment systems that were of value was an appointment sooner rather than later (fourth out of four – behind choice of doctor, a convenient time of day and a doctor rather than a nurse).
Nevertheless, some appointments will necessarily be scheduled at longer intervals than others either because of constraints in appointment slots or because the patient’s treatment demands such an interval. The available evidence suggests some issues for consideration in relation to reminder systems:
-
Reminders will be particularly important when appointments are scheduled well in advance.
-
It may be useful to explain to patients why they are having to wait and why the appointment is, nevertheless, important.
-
It is particularly important to provide easy ways to cancel when appointments are scheduled long in advance given that a proportion of patients will no longer need the appointment or no longer be able to attend.
-
Keeping waiting times to a minimum is important (as already recognised) in clinics that deal with patients with serious conditions that are unlikely to resolve themselves, particularly mental health conditions that result in the patient’s readiness to engage with services fluctuating over time.
Patient involvement in the initiation and scheduling of the appointment
Several studies support the hypothesis that when patients make their own choice of appointment time and date, attendance is better. A US-based study of elderly patients attending a veterans clinic138 explored the effects of advanced clinic access on patient appointments. Patients were sent a letter advising them to call and make an appointment a month before their next anticipated visit. Advanced clinic access (or open-access scheduling system) worked for elderly veteran patients and indicated that they would prefer to schedule their next appointment than to use the previous system. A UK study in a paediatric hospital108 discusses ‘partial booking’, whereby patients are sent a letter inviting them to call and make an appointment. The authors report that the rate of non-attendance for first appointments was significantly lower for those who experienced partial booking than those who did not regardless of whether or not a reminder was sent (5.2% vs. 15.3% among those with no SMS reminder and 3.4% vs. 9.8% among those who did receive SMS). Murdoch et al. 12 refer to an earlier study139 in which they achieved a reduction in non-attendance by asking patients to make their own appointments and confirm their intention to attend.
Closely linked to the above discussion is the issue of whether the appointment is patient or provider initiated. Service-initiated appointments will often be screening-type appointments for which most patients will not recognise any current symptoms or prompts. However, service-initiated appointments may also be referrals between departments. In both these cases, some studies suggest lower levels of attendance than when patients initiate the appointment themselves in response to some perceived need (see First versus follow-up appointments for a discussion of evidence on this).
Explanations and implications for reminder/attendance interventions
Better attendance rates when patients are engaged in initiating and scheduling their own appointment may reflect numerous different mechanisms. First, and perhaps most obviously, the timing is more likely to be convenient for the patient. Second, patients may be less likely to forget if they have made the booking themselves (and perhaps entered a note of it into a diary at the same time). Third, patients may be more likely to feel obliged to attend if they have booked it themselves (and may, therefore, take steps to overcome obstacles to attendance that arise, etc.). There is some evidence that asking patients to enter into an agreement by sending back a confirmation of attendance or contracting to attend may act to compel patients to attend their appointment. 56,140,141 A more recent study142 adopted three specific mechanisms aimed at increasing attendance at primary care appointments, two of which can been seen to relate to engaging the patient more closely in the scheduling process with a view to reducing the likelihood of forgetting and increasing the feeling of obligation to attend: patients calling for an appointment were asked to repeat back the time and date of their appointment before the call ended and when booking follow-up appointments; patients were asked to write down the time and date on an appointment reminder card rather than health-care or reception staff doing it for them.
If patient involvement in appointment booking has an effect on causal pathways that a reminder intervention is also intended to address (e.g. prompting a forgetful patient, appealing to moral obligation) then, ceteris paribus, we would expect to find the baseline level of attendance to be higher and the reminder effect size to be lower in contexts in which patients are engaged in original booking than when they are not (because there would be fewer patients within the patient population who experienced the obstacle to attendance that the reminder seeks to overcome). The UK-based study by Milne et al. 108 did indeed find a smaller absolute reduction in non-attendance, from 5.2% to 3.8% (i.e. a difference of 1.4%) among those who experienced partial booking, than among those who did not, for whom non-attendance fell from 15.3% to 9.8% (i.e. a difference of 5.5%).
A shortcoming of some of the studies of the effectiveness of reminder interventions is that the pre-existing appointment system into which the reminder intervention is introduced is not always adequately described nor taken into consideration as a factor that might influence the effectiveness of the reminder in the current or other contexts.
Greater involvement of patients in the scheduling of their appointments appears to be beneficial in increasing attendance rates. However, it is worth noting a recent evaluation141 of the UK ‘Choose and Book’ initiative aiming to involve patients in the scheduling of their hospital care has reported that patients did not, in practice, experience the degree of choice over date, time and location that Choose and Book was designed to deliver.
If appointments are necessarily service initiated rather than patient initiated, efforts will often be needed to increase patient perception that attendance at the appointment will positively contribute to their health/well-being and will not imply any significant risks, downsides or inconvenience. Reminder systems in relation to such appointments will likely also need to address these issues rather than simply serve as a prompt for the date and time of the appointment.
First compared with follow-up appointments
As discussed above, a small number of studies48,89 have examined whether reminder effectiveness varies according to whether or not an appointment is a first or a follow-up, but findings are rather inconsistent. The review also identified several studies that explored attendance behaviour more generally in relation to first compared with follow-ups and, again, the findings were equivocal.
Five quantitative papers74,98,108,121,135 reported higher no-show rates for follow-up appointments in comparison with initial appointments, with most speculating that this is because initial appointments are more likely to be prompted by the patient rather than the provider (see Patient involvement in the initiation and scheduling of the appointment).
However, four quantitative comparative studies59,82,84,85 reported higher no-show rates for initial rather than for follow-up appointments. Suggested explanations related to patient–provider relationships and perceived value of the appointment (see Patient–provider ‘alliance’, communication and ‘engagement’). A UK study based in a respiratory clinic82 found that the overall no-show rate was significantly higher for new patients than for established patients. A study of a general adolescent clinic in New Zealand84 reported that 22% of new appointments were not attended compared with 9.5% of review appointments (OR 2.7, 95% CI 1.1 to 6.8; p = 0.034), although this no longer reached significance in a multivariate analysis.
Furthermore, some studies63,112 report no significant differences between first and follow-ups in non-attendance.
Explanations and implications for reminders
Clearly, the results of studies comparing first and follow-up appointment attendance are equivocal. It seems likely that more sophisticated study designs are needed to fully understand the processes that are in operation. Indeed, explanations for the results presented have largely been speculative in studies reported to date.
Foley and O’Neill,98 in their study of a UK dental clinic, reported that there was a significant cohort of patients who attend as casual patients with dental pain or facial swelling and who, having received symptomatic relief of their symptoms, do not attend for further appointments that are often booked with the non-specialist dentists. Similarly, in their study of antenatal care among a deprived US population, Maxwell et al. 74 speculate that higher no-show rates for follow-up visits relate to the ‘crisis-oriented health care-seeking behaviours’ of the patient population and the fact it is often the patient who identifies the need for an initial visit, while the provider often identifies the need for follow-up care. Therefore, follow-up visits may not be as highly valued by the patient.
In contrast, Roberts et al. 82 suggest that higher attendance among established patients compared with new patients is explained by established patients feeling a connection with their provider and, therefore, being more likely to attend the appointment to maintain the relationship and continuity of care. Similarly, in their study of physiotherapy in New Zealand, Taylor et al. 85 speculate that higher attendance for review appointments may be because of ‘developing an understanding of benefits of attending and establishment of a relationship with the treating therapist’.
The above findings suggest that reminder interventions are appropriate for both first and follow-up appointments, but that the distribution of reasons for non-attendance among those who do not attend may differ between these two scenarios as well as across service contexts and may therefore warrant different types of reminder input.
Patient–provider ‘alliance’, communication and ‘engagement’
The review yielded some evidence on the issue of whether or not the degree of provider–patient ‘alliance’ or patient ‘engagement’ with the treatment process affects levels of appointment attendance. Five descriptive qualitative studies from contrasting UK service settings provided evidence that the relationship between the patient and the service can impact on attendance behaviour.
A study143 employing focus group discussions and interviews with 43 drug users identified various barriers to treatment uptake, including perceptions of long waiting times, stigma and a perceived lack of understanding among providers. A qualitative study115 involving 50 patients with asthma illustrates how the patient’s perception of his or her relationship with the doctor and the treatment received was an important factor shaping attendance. In this study, patients reported that a desire not to jeopardise what was seen as an important relationship with their doctor was a factor that could influence their attendance behaviour. In contrast, an existing poor relationship with the doctor would deter some patients from attending an appointment with that doctor.
Similarly, a qualitative study101 explored the reasons for attendance behaviour from the patient viewpoint at a UK young adult diabetes outpatient clinic. Semistructured interviews were conducted with a purposive sample of 17 patients. An important theme linked to attendance was the behaviour of health-care professionals. The authors noted that, while previous studies of non-attendance assume a causal connection between missed appointments and associated higher HbA1c, results from this study indicated that fear of being ‘told off‘ for failing to reach biomedical targets was an important factor in the decision not to attend. In other words, health professionals’ negative reactions to patients exhibiting poor control of glucose levels encouraged non-attendance. The respondents valued friendly, positive behaviour among both reception and clinical staff.
In another qualitative study144 investigating the perspectives of 12 long-term non-attending adults with diabetes, several respondents reported feeling fearful and anxious about attending the diabetes clinic and identified the counterproductive use of ‘fear arousal tactics’ employed by some health professionals.
. . . I can honestly say that there’s a type of depression when I go out there [the diabetic clinic]. Every time I go in . . . all I hear is . . . ‘You’re gonna go blind, you’re gonna have your legs amputated, your arteries are gonna clog up’ . . .
Patient called Liam144
Lawson et al. 144 also identified that the main differences between groups of patients who seek structured care and those who do not is that those who seek structured care appear to need the support and reassurance that can be offered by health-care professionals.
In another UK study,145 focus groups and semistructured interviews were used to explore communication experiences of 30 pregnant women from diverse social and ethnic backgrounds affiliated to a large London hospital. The authors concluded that poor communication and lack of empathy among providers could act to discourage patients from attending appointments. They further noted that constructive communication styles, characterised by empathy, openness, time to talk through problems and proactive contact such as reminders or text messages, were more likely to reassure patients, facilitate information exchange, foster tolerance in stressful situations and improve attendance at appointments. They identified features of poor communication as including insufficient discussion and discourteous styles of interaction. The authors also concluded that providers require communications training to encourage empathic interactions that promote constructive provider–user relationships and better use of technologies to improve communication with patients.
The review also identified a qualitative study123 employing focus group discussions with 43 women in Turkey exploring attendance for breast screening that reported similar findings. Authors reported that women demanded a friendly and tolerant approach from health personnel who were making recommendations for screening programmes. One of the women participating in the study suggested that she would not hesitate to attend an appointment with a male doctor provided the interaction was genial and enlightening.
As well as supportive and respectful behaviour, ‘navigational support’ – which provides information and guidance regarding how the health system works and what to expect from treatment/care – has also been suggested as important. 145
Thus, several studies identified through the review concluded that a supportive, non-judgemental attitude of the health-care professional and a responsive service more generally is considered important by patients who are considering attending their clinic appointments. These review findings echo those reported in the much wider body of research literature that explores issues related to the relationship between patients and the service on offer, employing such concepts as ‘therapeutic alliance’, ‘(dis)engagement’ and ‘trust’. 146,147
In addition to the research literature, the importance of developing a close service–patient relationship has been recognised in several practice settings, particularly those dealing with long-term conditions and more vulnerable patients. For instance, Comfort et al. 61 highlight the many strategies that have been tried out in substance abuse treatment settings to improve patient engagement and patient–service alliance, although they note that few have been carefully evaluated.
Explanations and implications for reminders
The studies highlighted above suggest that, when there is a poor relationship between the patient and the service (or particular providers within the service), the patient will tend to perceive the likely costs of attending an appointment to outweigh any anticipated benefits, for instance because interactions with staff will be unpleasant or stressful or because the care/treatment on offer is perceived to be inappropriate, unhelpful or even risky/harmful.
These findings suggest several implications for reminder systems and wider intervention to support attendance. There may be some, relatively simple, measures that can be taken to ensure that reminder systems do not have a negative effect on patient engagement and patient–provider relationships, for instance ensuring that patients receive reminders in the format of their preference and do not receive reminders that they find irritating or stressful. 55 It is worth noting that several of the reviewed studies highlighted the fact that many patients view regular communication from their health professional positively, so that reminders may actually contribute to a more positive patient–service relationship.
High levels of non-attendance are likely to reflect obstacles to attendance over and above forgetfulness and may be reflective of poor patient experiences and low levels of therapeutic alliance, such that reminder systems alone are unlikely to be sufficient to achieve high levels of attendance.
Although many patients indicate that they are happy to receive a reminder (see Chapter 6, Other reminder characteristics), there is a risk of antipathy from a sizeable percentage of patients who feel negative or very negative about reminders. Those who were disturbed by the reminder gave the following reasons: telephone call too early in the morning, they were waiting for other important results, they were contacted at work, felt that were being treated as senile or felt that the reminder was unnecessary. 79
Service features
In addition to the engagement/alliance issues discussed above, the review highlighted two other service-related features that have been explored in relation to attendance behaviour: service location and related transportation/access issues, and seniority/identity of the health-care practitioner providing the appointment.
Service location and transport difficulties
The review indicated that service location and transport difficulties have been implicated in non-attendance in both research and practice interventions across a variety of settings. However, the available evidence regarding the impact of service location on attendance levels appears somewhat limited and equivocal, suggesting that the importance of transportation issues is likely to vary importantly between service settings and patient groups.
Several descriptive studies identified transport difficulties as a reason given for non-attendance in diverse settings. For example, a US study118 reported that the main reasons associated with missed appointments in paediatric clinics were effort (waiting time, distance, transportation, parking), communication (misunderstanding about appointment time and date) and forgetting. Hamilton and Gourlay148 conducted 120 face-to-face survey interviews with women who had missed maternity appointments in the London Boroughs of Richmond and Newham. Almost 70% considered transport the main reason for their missing an appointment and more than half the women had dependent children and reported difficulties travelling with their children to hospital, especially where this travelling was on public transport. In a qualitative Turkish study123 focused on breast screening attendance, respondents noted that receiving the screening procedures in a familiar institution would be more convenient. Those women who discussed transportation facilities as something they were concerned about shared lower socioeconomic status.
However, in contrast, one descriptive study130 of diabetes patients in New Zealand (n = 142) reported that transport difficulties/location issues affect only a small proportion of patients and are not a major reason for non-attendance, with just 2 out of 142 patients giving this as the reason for missing their appointment. Furthermore, the available quantitative studies in the review produced equivocal evidence on the relationship between travel distance and appointment attendance.
Three quantitative studies explored the association between travel distance and attendance. One quantitative study89 indicated that location of the clinic may affect attendance, but only for patients who live very close to the clinic. This UK study based in a specialist alcohol treatment centre undertook multivariate analysis of patient characteristics of non-repliers (n = 100), non-attenders (n = 100) and attenders (n = 100) and found that patients who had a very short distance to travel were more likely to attend their appointment. The distance variable was calculated from patient postcodes. These were divided into four bands on the basis of distance from the clinic (with band 1 being the immediate surrounding area). Patients living in distance band 1 were more likely to attend than patients living at all other distances [OR vs. distances 2, 3 and 4: 4.41 (p < 0.001), 3.12 (p < 0.01) and 3.32 respectively (p < 0.05)]. Further from the clinics, there was no difference between attenders and non-attenders and there was also no effect of distance on the likelihood of replying to the appointment invitation. The authors speculated that, although the clinics were easily accessible by public transport, the cost of travelling probably reduced attendance by some patients. They cited previous observations, from a US treatment manual,149 that problems arising from lower socioeconomic status, including lack of transportation and a telephone (which would, in addition, make it unlikely that patients would cancel their appointments), may lead to decreased chances of attendance specifically for treatment of alcohol problems. Other research150 had previously demonstrated that distance travelled is also correlated with non-attendance at a specialist alcohol clinic.
One small RCT in the USA,61 that sought to explore whether or not a series of interventional supports could improve attendance levels among substance abuse patients, found no significant effect overall, but reported that van transportation was the most frequently used element of the package of support that was on offer. However, two quantitative comparative studies60,82 concluded that service location is not related to attendance; and one study113 suggested that patients living closer to the clinic were more likely not to attend.
A US study60 of attendance at a paediatric dental clinic serving a deprived population reported that 85% or more of patients travelled < 1 hour to the appointment and that only 3 of the 28 long-distance patients (> 1 hour) failed to show up for their scheduled appointment. The authors also reported that the long-distance patient group demonstrated better punctuality than the study group as a whole. They speculated that this may reflect the greater degree of planning required for the long-distance drive or the practice of co-ordinating multiple health care. Similarly, a UK study82 of respiratory outpatients, employing a randomised controlled design and involving 504 patients, reported that travel distance was not associated with attendance.
Interestingly, findings from a UK service evaluation113 of a genitourinary clinic involving telephone interviews with 182 non-attenders contradict the hypothesis that easier/closer appointments are more likely to be attended. Patients were significantly more likely not to attend if they were unemployed, resident within the local catchment population area (i.e. Southampton Primary Care Trust area) and had previously accessed genitourinary medicine (GUM) services. The authors speculate that as such patients do not have competing employment demands, live close to the clinic, have previously made and kept GUM appointments and do not cite clinic opening hours, or similar, as a reason for not attending, their non-attendance does not reflect problems of accessibility.
A brief scan of the wider literature also suggests some varying degrees of success for interventions that have sought to overcome transport difficulties and, thereby, improve attendance at appointments. For example, Ogilvie and Mayhew151 report on a carefully conducted audit in the UK and conclude that holding appointments for school-aged children at schools rather than clinics was an effective way to increase attendance by parents and children. In contrast, Bell et al. 125 evaluated an intervention through which private transport was provided to minority ethnic women, but found no increased uptake of breast screening appointments.
Explanations and implications for reminder/attendance interventions
The variable findings across different studies examining the association between travel distance/accessibility and attendance highlight several complexities and considerations.
First, varied measurement approaches between studies can compromise their comparability; for instance, while some studies use travel time, others use travel distance. Furthermore, the qualitative studies indicate that clinic accessibility is composed of multiple components not simply being a function of distance or travel time. Potentially, these include travel costs, ease/difficulty of parking and public transport availability on the route. It is possible that such dimensions vary between patients who are grouped according to travel distance or travel time and also between clinic contexts that appear to have similar patient profiles in terms of travel times/distances. For example, the ability to park near to the facility may be more of an issue for parents bringing small children to an appointment than for young adults, who may be more likely to travel by public transport. These factors do not seem to have been tested rigorously in the current research base.
Second, it seems likely that transport issues (however measured) are more significant for some groups of patients than for others. The literature suggests that patients who are more socioeconomically deprived may experience transport-related obstacles to attendance more often than more advantaged patient populations, for instance because travel costs are more prohibitive or because they are more reliant on public transport (see Deprivation). Transport issues may also be more relevant to patients with young children and the elderly.
Third, Swarbrick et al. 129 suggest that more readily accessible clinics can actually encourage non-attendance, noting of non-attenders that ‘such patients appear capable of accessing GUM clinic services without difficulty, and may be prepared to miss appointments precisely because alternative access (whether through new appointments, or via “walk-in” services) is known to be equally accessible’. This suggestion alerts us to the fact that travel distances/durations and other aspects of physical accessibility may also inter-relate with appointment availability and booking systems, as well as patient motivations, to influence attendance behaviour.
It seems clear that further research is needed to fully understand the relationships between clinic location/transport issues and appointment attendance, but in relation to reminder/attendance interventions, the following implications can be drawn from the existing evidence base.
-
Services should consider whether or not they can include within any reminder useful information that could aid patients’ journey to their appointment.
-
Different groups of patients will experience the same journey differently.
-
For some groups of patients in some settings, reminders will be insufficient to prompt attendance because transport difficulties over-ride the incentives to attend.
Seniority/identity of the health-care provider
Findings from the review were equivocal in relation to the effect of health-care provider identity/seniority on attendance. Three descriptive quantitative studies with adequate sample sizes reported a positive association between seniority/qualification level of the provider and attendance rate.
A UK study based in a dentistry clinic98 reported that significantly more patients failed to attend their appointment with non-specialist dentists and a similar pattern was observed at clinic level, with the non-attendance being low at specialist staff clinics but high at non-specialist staff clinics, although the difference did not attain statistical significance. Similarly, a study135 in Switzerland of adolescent attendance at outpatient clinics explored the characteristics of non-attenders (n = 2193, women = 1873) and found that the intended provider being a member of the paramedical staff (vs. a physician) significantly increased the risk of missing appointment for females with a somatic diagnosis but not for those in the psychiatric model. The risk of missing an appointment was also increased among those who had consulted a paramedical provider at the last appointment. The most prominent factor predicting non-attendance was the intended provider, with a non-weighted probability of non-attendance of 6% for physician appointments compared with 17% for paramedics. In another Swiss study,79 the authors examined attendance at a primary care and ambulatory HIV clinic in a deprived Genevan population and studied the characteristics of 2123 patients included in a RCT and found that being cared for by a junior doctor rather than a senior doctor was significantly associated with missed appointments. Analysis of predictors of non-attendance showed an OR of 0.5 (senior vs. junior; 95% CI 0.27 to 0.93).
In addition to these primary studies, the review identified a study by Magnes97 that included a limited review of earlier work on psychiatry outpatient attendance. This study identified a paper by McIvor et al. 152 in which non-attendance rates were examined by cross-sectional survey of 482 patients seen by psychiatrists of different grades and a consultant clinical psychologist over a 21-month period. The clinical psychologist’s patients had the lowest rate of non-attendance (7.8%), followed in turn by those of consultant psychiatrists (18.6%), specialist registrars (34%) and senior house officers (37.5%).
However, in contrast to the findings reported above, a study of physiotherapy in Ireland112 reported higher non-attendance for appointments with senior grade staff and suggested various reasons why this might be the case. This prospective study found that non-attendance rates were significantly higher for senior grade (12.7%) than staff grade (8.9%) physiotherapists. A survey by Murdock et al. 12 found that fear of being seen by a junior doctor rated fifth on a list of reasons for non-attendance alongside more common explanations.
Explanations and implications for reminders
Several mechanisms are suggested for differences in attendance behaviour by type of provider to be seen. Differential attendance may relate to patient perceptions of the importance of attending the appointment and/or to the quality of care they expect to be received.
A study128 using a discrete choice experiment among 1200 patients in which respondents were presented with trade-offs between two hypothetical, yet realistic, health conditions – an acute, low-worry condition and an on-going, high-worry condition – found that, for both conditions, the two of the four key components of appointment systems that were of value were being offered a choice of doctor and a doctor rather than a nurse.
Magnes97 suggested that factors such as continuity of care, perceived clinical competence and the provision of non-medical interventions might have an impact on attendance rates.
Chariatte et al. 135 observed that the risk of missing an appointment was also increased among those who had consulted a paramedical provider at the last appointment, suggesting that expectations for a subsequent appointment may well be shaped and modified by past experience. However, differential allocation of more serious cases to higher-grade staff could also affect the rates of attendance. This could be because less serious cases may resolve themselves before the appointment or patients with less serious cases may be more likely to forget their appointment or to prioritise other commitments over appointment attendance. In a mental health context, there is specific concern that more serious cases are more likely to be those that do not attend.
French et al. 112 cite an earlier study by Brookes153 that reported a perceived increase in the rate of non-attendance for the senior therapist as a result of such factors as leave and transfer of patients from other staff. However, these anecdotal reasons lacked detailed analysis. In this study, it was noted that one senior therapist who was specialised in one particular area with a complex group of patients had a did-not-attend rate of 45%.
It is unclear what implications can be drawn from these findings in terms of reminder systems. It could be argued that reminders should not indicate which health-care professional will be seen; for instance, the practice in some clinics is always make the appointment under the name of the senior provider, even if the practitioner to be seen will be another member of staff. However, this could potentially be counterproductive for those patients who have established a positive relationship with a practitioner whom they would like to see again.
More generally, it would seem important to monitor attendance patterns by individual members of staff as well as grades of staff in order to identify any patterns indicative of issues to be addressed, such as poorer engagement/alliance achieved by particular staff, while recognising that attendance levels will be influenced by such factors as the types of cases referred to different providers within a team.
Wider social system (conceptual framework domain D)
Our conceptual framework hypothesised that factors operating at the level of the wider social system including norms of behaviour, values, attitudes and prevailing understandings, as well as structural factors, could act as enablers or obstacles to attendance and might, therefore, be of relevance to how reminder interventions operate in different contexts or for different population subgroups. In general, however, our review did not generate very much information on this area. This reflects the fact that most reminder-related research has taken a rather narrow focus. Nevertheless, we highlight key themes flagged up by our review for which there are wider bodies of research evidence that warrant consideration by those seeking to enhance attendance levels.
Norms, attitudes and understandings regarding the (dis)benefits of health care on offer
The prevailing norms, attitudes and understandings within a ‘community’ might be hypothesised to shape attendance behaviour because they could influence patient perceptions that attendance at the appointment will positively or negatively contribute to his/her well-being. However, while our review yielded evidence to suggest that how an individual rates the health care on offer is a factor that influences attendance (see Seniority/identity of the health-care provider), we did not identify evidence that related to factors operating at the level of the wider social setting or ‘community’.
Nevertheless, it is important to note that prior literature covering a range of care settings has identified the relevance of shared norms, values and meaning systems within ‘communities’ in shaping individual health-care behaviour, including appointment attendance, particularly for marginalised groups of patients. For example, the meta-synthesis of qualitative work by Downe et al. 154 on antenatal care uptake identified several shared perceptions among marginalised groups relating to quality of care, the trustworthiness and cultural sensitivity of staff and feelings of mutual respect that shaped attendance. Similarly, Manderson and Allotey155 report of the ‘story-telling’ about health services that takes place within immigrant communities in Australia and shapes their uptake of health care.
Indeed, evidence that patient behaviour is influenced by the values and attitudes of their immediate peers has underpinned various recent interventional approaches aimed at enhancing health-care engagement, including appointment attendance. For example, Turner et al. 156 compared the effectiveness of a telephone call by a peer coach compared with an informational brochure in increasing attendance for colonoscopy among 275 patients who had a poor attendance record in primary care and found that the peer coach had a greater impact. Greenhalgh et al. 157 have developed interventional approaches using story-telling techniques that are grounded in the finding that patients from some minority ethnic and cultural backgrounds often learn about health and the health system through informal interactions with other members of their communities through which shared meanings and norms are established.
Norms, attitudes and understandings regarding condition/symptoms
In our conceptual framework we also hypothesised that norms, attitudes and understandings relating to particular conditions or symptoms might also shape attendance behaviour.
One study143 found that the behaviours and attitudes of the wider population (significant others) around certain health conditions may influence patient attendance at health-care appointments. In this qualitative study of ‘hard-to-reach’ heroin users who were not currently in structured treatment, subjects reported that the experience of stigma within individual relationships (e.g. GP, family or friends) and social groups impacted on either their intention to attend or actual attendance at appointments related to their substance abuse.
Furthermore, Ambrose and Beech17 observe that primary care psychiatric nurses have tended to schedule client appointments in the community setting, usually in GP surgeries or health centres, with the intention of minimising stigma and easing accessibility, a factor with a positive impact on attendance. A further study158 observing attendance behaviour among patients attending a Spanish allergy clinic, 3 years after setting up and launching telephone reminders for patients’ first appointments, suggested that one possible reason for continued non-attendance could be related to cultural factors related to certain pathologies.
Clearly, these findings from the review were rather limited and it would of interest to explore the wider literature on stigma and how this relates to appointment attendance (see, for example, Scambler159).
Norms, attitudes and understandings regarding whether or not attendance is the morally right thing to do
We hypothesised that prevailing norms and attitudes might influence attendance through the way they construct attendance as (in)appropriate or (il)legitimate or indeed the morally right or wrong thing to do. However, none of the included studies generated information on this aspect.
However, wider literature does relate to these issues. So, for example, there is work that shows that non-attendance at health-care appointments can, in some cases, be explained by patients (usually women) prioritising the care of their children or husbands over their own health because they perceive this to be what is expected of them by significant others and to behave otherwise might bring condemnation. 160 There is also past work on patterns of screening uptake that has linked attendance to patient perceptions of moral obligation to perform this health behaviour. 161
A recent study focused on non-attendance has sought to use social influence to reduce no-shows at primary care appointments in the UK. As well as other interventions, Martin et al. 142 replaced signs in the clinics that had communicated the number of patients who did not attend appointments in previous months with signs that conveyed the much larger number of patients who do turn up.
Explanations and implications for reminders
Whether and how societal/community-level norms, attitudes and understandings shape attendance behaviours among different groups of patients deserves greater investigation and there is greater scope to consider how these factors might be relevant to the design of reminder interventions.
Structural factors
As discussed above, the review generated quite a large amount of evidence to indicate that structural factors can influence whether or not reminders are accessible to particular groups of patients (see Chapter 4, Proposition B: reminder accessibility). In addition, several studies highlighted the ways in which structural factors affecting particular communities can result in higher levels of non-attendance. We discuss these factors under Patient characteristics as they relate to groups of patients with particular characteristics.
Patient characteristics
Our review indicated that various studies have explored whether or not levels of attendance vary between groups of patients identified by particular individual characteristics, but that findings are inconsistent. These studies have not always been designed to support such comparative analyses and sampling design and sample sizes may, therefore, compromise the results in some cases and provide partial explanation for the inconsistency in findings across studies. Nevertheless, the inconsistent findings are also suggestive of the importance of factors, perhaps related to the practice setting, nature of the appointment or wider social setting, that moderate the associations between patient characteristics and attendance. This is, of course, not surprising as each of these distal factors must operate through some more proximate mechanisms which, as discussed in the sections above, are sensitive to a range of factors. Here we provide an overview of the findings that emerged from our review organising the materials into three main sections: demographic and socioeconomic characteristics (age, gender, ethnicity and deprivation), health- and well-being-related patient characteristics (substance misuse, mental health, co-morbidity and severity of illness) and past attendance behaviour. While not completely exhaustive, we felt that these patient characteristics are those that are most likely to have potential utility in identifying categories of patients or constructing patient population profiles that might inform clinic managers or clinicians designing interventional approaches to improving attendance levels.
Demographic and socioeconomic characteristics
Age
Our review indicated that age has been found to be associated with attendance behaviour in a large number of studies across varied geographical and clinic settings. Despite the fact that differences in the categorisation of age groups complicates comparisons across studies, a largely consistent pattern is reported among adult patient populations of higher levels of non-attendance among younger patients than older patients.
Sharp and Hamilton162 provide an informal review of the evidence on non-attendance and report that youth is frequently found to be associated with hospital non-attendance. Parikh et al. ,77 in their study of outpatients from 10 clinics in the USA, used linear regression modelling to demonstrate that, for every 1-year increase in age, the absolute no-show rate decreased by 2.4% (p < 0.0001). Similarly, Costa et al. 63 found a decreasing level of non-attendance rate with increasing age in their study of outpatient attendance at a district hospital in Portugal. In their study in primary care of patients receiving lipid-lowering therapy in the Republic of Korea, Cho et al. 59 noted age differences in attendance, with older adults being more likely to attend than younger adults. In a study of primary care attendance in urban Geneva,79 missed appointments were significantly associated with younger age. Similarly, Booth and Bennett89 found that older patients were more likely than younger patients to attend their assessment appointments at an alcohol treatment clinic. Waller and Hodgkin163 examined attendance patterns across nine general practice clinics in the UK and reported that non-attendance rates were highest among young adults. The investigation by Moore et al. 126 of over 4000 appointments at a family practice centre in the USA found that older patients were less likely to fail to show than younger patients and that appointment keeping increased with age. Thus, an older person was 1.18 times more likely to keep an appointment than a person 10 years younger (OR 1.18, 95% CI 1.13 to 1.23). Neal et al. 108 also report higher non-attendance rates at clinical services among younger patients in the UK general practice context.
Patterns of attendance for children across ages or in comparison with adults are less clear and, as in the UK context they are often attending specialist paediatric clinics, it is difficult to draw direct comparisons. In their study of appointment attendance in a Scottish general dental clinic, Patel et al. 164 reported the highest rate of non-attendance among the 21–30 year age group, followed by 31–40 years and then 11–20 years. Clearly, this study focused on younger patients and grouped children with young adults, which may explain why the observed pattern was not similar to the patterns presented in previous studies. Bos et al. 55 examined attendance at an orthodontic clinic in the Netherlands and found similar levels of non-attendance in patients aged under 12 years and 12–18 years (around 3.4%) but higher non-attendance in those aged greater than 18 years (8.1%), although numbers included in the study were small.
Explanations and implications for reminders
Numerous explanations have been advanced for the positive association between patient age and attendance. First, it is postulated that older people may have fewer competing commitments than younger people77 and that children in particular may have high rates of non-show because of their dependence on other people (usually working-age adults) to accompany them to an appointment. 63 No studies were identified that explored the age group of parents/carers in relation to children’s attendance at appointments.
A second line of argument, however, is that older patients may be more likely to attend scheduled appointments because of the nature of their health condition and being more likely than younger patients to have multiple conditions necessitating appointment attendance77 or less likely to have symptoms that resolve themselves before the appointment date. 89 Parikh et al. 77 also speculated that older patients may be more cognisant of their own health care.
To date, there has been little detailed exploration of these alternative potential explanations. Nevertheless, as discussed in Chapter 4, Evidence statement (F.1): there is sufficient weak equivocal evidence to suggest that age does not have a differential effect, over and above pre-existing appointment behaviour, on reminder effectiveness (in terms of attendance, cancellations or rebooking) (evidence category IVa), there is good evidence that reminders are effective at improving attendance among all age groups. Furthermore, although rates of non-attendance are higher among younger patients, it is older patients who make up the majority of appointments, often at outpatient clinics where non-attendance costs the UK NHS an estimated £790M per year. 165 Therefore, the findings reported provide no support for the suggestion that the use of reminder systems should be restricted to certain patient age groups. Furthermore, the findings here confirm the importance of reminder systems enabling patients to cancel and, if necessary, rebook their appointment with ease. However, as discussed above, there are important considerations to be made in relation to the type of reminder technology that may be most appropriate for different age groups (e.g. mobile phones remain less commonly used by older populations108).
Gender
Our review indicated that there is inconsistent evidence regarding differential attendance behaviour between male and female patients, but that researchers often confidently state that male patients are more likely than female patients to default on appointments.
Several studies reported higher levels of non-attendance among male patients than females. Sharp and Hamilton162 provide an informal review of the evidence on non-attendance and report that being male is one of the main associations with hospital non-attendance. Moore et al. 126 investigated over 4000 appointments at a family practice centre in the USA and found that females tended to be less likely to miss appointments than males, although the effect was of borderline statistical significance in a multivariate analysis (OR 0.8, 95% CI 0.7 to 1.0; p = 0.06). Hon et al. 122 report on a study of non-attendance at a paediatric dermatology clinic in Hong Kong and found that 67% of non-attenders were male and that males were more than twice as likely as females to fail to attend clinic (p = 0.010).
However, in contrast, Sims et al. 96 found that gender was not a significant predictor of attendance at four adult community mental health outpatient clinics in London. Similarly, Bos et al. ,55 in their study of attendance at an orthodontic clinic in the Netherlands, including both adult and child patients, reported no significant difference between males (n = 109) and females (n = 153). Meanwhile, Can et al. 56 reported that females were twice as likely as males to not attend their appointment in their study of 232 new patients referred to an orthodontic clinic in England. Furthermore, Waller and Hodgkin163 examined attendance patterns across nine general practice clinics in the UK and reported that women were disproportionately represented among the group of patients who were frequent defaulters (defined as missing an appointment five or more times per year).
Explanations and implications for reminders
Given that the reasons behind any observed gender differential in attendance behaviour are likely to be shaped by gender-related factors, it is unsurprising that contrasting results are reported across geographical and cultural contexts. In general, however, the available studies that reported on attendance patterns did not explore in any detail the reasons behind any observed gender differentials.
Instead, authors have speculated about the underlying causes of observed gender differences in attendance. For example, when it was found that females were less likely to attend a dental appointment than males, Can et al. 56 suggested ‘. . . that dentists may be more willing to refer a girl when the malocclusion is mild and following the referral the patients then change their mind about attending. This, however, is purely conjecture.’.
Some authors have suggested that differentials could arise because of different patterns of disease and symptomology between male and female patients. For example, Hon et al. 122 were unable identify the exact reasons for higher non-attendance among male patients in their paediatric dermatology clinic in Hong Kong, but speculated that female referrals may involve more serious dermatological conditions. However, as noted above (see Sex), it is also recognised that differential patterns of referral for male and female patients, as well as differential responses by patients (and their carers/parents in the case of children), could also contribute to the patterns of attendance observed.
In relation to reminders, the available evidence on attendance rates does not suggest that reminder systems should be differentially employed for male and female patients, but clearly this is an area that warrants further investigation.
Deprivation
Our review indicates that there is weak but consistent evidence to suggest that deprivation status is a factor in attendance. Although the use of a variety of measures of deprivation or low socioeconomic status makes aggregation of evidence across studies difficult, as does variation in the economic context across geographical settings, there is nevertheless evidence from a range of studies that patients with higher levels of deprivation are more likely to miss appointments than those who are more affluent/advantaged.
Several studies employing individual measures have reported a negative association between deprivation or low socioeconomic status and the likelihood of appointment attendance. Sharp and Hamilton162 provide an informal review of the evidence on non-attendance. They report that deprivation is one factor that is commonly associated with hospital non-attendance. Ramm et al. 166 compared attenders and non-attenders at a cardiac rehabilitation programme in New Zealand using simple univariate statistics and found lower levels of attendance among patients categorised as having a low socioeconomic status on the basis of their occupational grouping. In a study of colposcopy attendance in Cornwall, Oladipo et al. 76 reported that younger, unmarried women of lower socioeconomic status were less likely to attend than more affluent patients. Another colposcopy clinic study,86 in Manchester, reported a similar association with deprivation. In their study of 232 new patients referred to an orthodontic clinic in England, Can et al. 56 reported that patients living in an area of high social deprivation were 2.7 times more likely to fail to attend an appointment than people who were resident in more affluent areas (95% CI 1.1 to 6.5). A study167 (as cited by Dixon-Woods et al. 168) of management of women with cancer found that significantly more patients from deprived areas failed to attend hospital appointments, although the difference was small.
A study that employed analysis at the aggregate clinic level also documented this association. Waller and Hodgkin’s UK study,163 in 2000, found that levels of non-attendance at general practice level showed a high correlation (Pearson’s r = 0.72; p = 0.028) with the score at each practice on the Townsend Index of Deprivation (attributed to practices according to the practice population in each enumeration district).
In contrast, a smaller number of studies report no difference in attendance levels between patients categorised by measures of deprivation or socioeconomic status, for example a study by Conduit et al. 169 of attendance at a university-based psychology clinic in Australia. However, when no difference was reported, the results are often compromised by small sample sizes, questionable measures of socioeconomic status or low levels of socioeconomic diversity within the patient population.
Explanations and implications for reminders
A range of explanations have been advanced for why non-attendance is often higher among the more deprived sections of patient populations, as well as at clinic level for those clinics serving deprived areas. However, there has been little detailed exploration of these causal pathways in the literature that has focused on appointment attendance behaviour.
Several authors draw attention to the potential influence of structural factors, such as poor transport options,89,123,148,166 low ownership of landline telephones,89 low levels of social support and difficulties in arranging child care. 86 A systematic review by George and Rubin18 identifies that the appointment systems themselves can prove a barrier to care. They may be particularly challenging to use for members of communities in areas of social deprivation, because such systems require resources and competences that are not readily available. People in these groups may have less predictable, chaotic lives that are not consistent with structured systems. They conclude that non-attendance can be viewed as the manifestation of a critical level of unsuitability in the agreed arrangements for an access episode. This perspective that problematises the rigid system rather than a perceived ‘difficult’ population is to be welcomed. 168 As Dixon-Woods et al. 168 point out, services that use appointments systems rely on people being able to read and require people to present themselves in particular places at particular times. Such services include immunisation and screening programmes, outpatient clinics and elective procedures, and these encounter very high rates of ‘default’ by more deprived people.
Higher levels of non-attendance may also in part be explained by the mobility of people in deprived populations. People who are in rented accommodation rather than owner occupation may change address much more frequently, and this puts them at risk of not receiving invitations (or reminders). 103,168 The Fourth National Survey of Morbidity in General Practice170 found that 8% of people registered with practices were not at their stated addresses and were not contactable. At the more extreme end, people who are homeless or who live in travelling communities may not be sent or receive invitations to appointments at all171 while asylum seekers may face similar obstacles to receiving appointments and navigating the health-care system, resulting in high levels of non-attendance. 78
Heath172 argues that all barriers to consultation should be examined to ensure that those on low incomes are not disadvantaged, giving the highly pertinent example of those without a telephone, who may be easily disadvantaged if appointment systems are rigidly enforced and largely organised by telephone, or if there is increased use of e-mail. Another concern regarding text messaging reminders is their possible impact on health inequalities, as people in higher socioeconomic groups, who are more likely to own a mobile phone, will be less likely to miss appointments. 173 However, this concern may not be realised given mobile phone ownership statistics and other unpublished studies regarding mobile phone use and socioeconomic status. 174,175 The availability of same-day compared with advance appointments and the potential for such appointment mixes to affect different groups of patients differentially has also been raised. 176–178 It has been suggested that patients in deprived areas are more likely to use same-day appointments. 177 A recent study found that patients receiving same-day care were likely to be in work and have a higher educational status. 176 Sampson177 found differential levels of satisfaction with appointment mixes by age and by deprivation of practice population and concluded that it is important to accommodate the requirements of different patient groups by allowing both pre-bookable and same-day appointments; Sampson’s conclusions echo those of earlier studies. 176,178
A further line of explanation for lower levels of attendance among deprived patient groups relates closely to the issues of patient–provider communication, therapeutic alliance and engagement discussed in section Patient–provider ‘alliance’, communication and ‘engagement’. One study103 has suggested the possibility that deprived groups are more likely than the better-off to hold a negative perception of health services on offer. Hussain-Gambles et al. 104 report on the attitudes of health-care providers who perceived patients living in more deprived areas as lacking responsibility and missing more appointments, and suggests that these negative attitudes may not be beneficial to improving attendance. Patel et al. 164 suggest that single parents and low-wage earners find dental treatment a low priority.
Associations between employment status and appointment attendance are also important to consider, since the most common reasons cited for missing an appointment, after forgetting it, are family and work commitments. However, the findings across studies are inconsistent and difficult to interpret because of the complex of causal pathways that may be in operation. First, as discussed above under Reported reasons for non-attendance, incompatibility of appointment timing with work commitments is commonly cited as a reason for appointment non-attendance. For instance, Roberts and Partridge179 had previously shown that 63% of patients attending their cardiorespiratory outpatient clinics would like out-of-hours clinics, largely because they are in employment during the day. However, the degree to which employment status presents a barrier to appointment attendance is likely to depend on both the type of employment and the appointment system on offer. It is suggested that people in lower occupational groups may have less flexibility at work and, therefore, face greater problems in negotiating time off work for health-care appointment attendance. 168 However, people who are unemployed have been found in some cases to have higher rates of non-attendance than those who are employed (see, for instance, Patel et al. 164) and they may face a different set of obstacles to appointment attendance that are linked to lack of income and structural factors.
The available literature tends to suggest that deprived populations face multiple obstacles to health-care appointment attendance. Thus, while simple reminders may be effective at prompting attendance among those who are at risk of forgetting their appointment, it seems likely that more sophisticated attendance interventions will be needed to achieve high levels of attendance. Clinics that achieve high levels of attendance despite serving patient populations with high levels of socioeconomic deprivation would warrant close investigation, as they may have introduced ways of working that could be transferable to other settings. Furthermore, as discussed above, reminder systems are very dependent on accurate and stable data from patients and so deprived populations with unstable contact details (either address or telephones) may mean these patients are disadvantaged. 103
Ethnicity
Race and ethnicity are complex, contingent and contested biosocial concepts that have been operationalised in diverse ways in health-related research, making any attempt to compare and synthesise findings across studies fraught with difficulties. 180 It is not, therefore, surprising to find that our review yielded rather inconsistent evidence on the association between (minority) ethnicity and attendance behaviour. Furthermore, compared with measures of deprivation, race/ethnicity appears to have been less often considered in attendance research, particularly outside the USA.
Patel et al. 164 explored attendance at dental clinics in the UK and reported that Asian patients had higher non-attendance rates than English patients in an outpatient setting. In a study130 of non-attendance at Care Plus and diabetes clinics in New Zealand, the ethnic breakdown showed that New Zealand European people were under-represented as non-attendees in proportion to the enrolled population, while Pacific people were over-represented, accounting for 13% of non-attendances while constituting 3% of the enrolled population. Maori non-attendance (13%) was slightly higher than the enrolled population of 11%. An audit study181 of paediatric outpatients in a hospital in the West Midlands of England found differences in the appointment-keeping behaviour of patients by ethnicity. An original 1995 study had shown that non-attendance for clinic visits was around 33% for Europeans compared with 50% for Asian patients. 182 A subsequent follow-up study in 1998, following interventions, showed a fall to 12.0% and 13.5%, respectively, with an overall rate of 12.3%. 183
There is a much wider body of evidence that reports on the health-care experiences of minority ethnic patients in different settings, often highlighting issues of cultural (in)competence, lack of trust and in some cases inappropriate or abusive treatment. Some of this work has made direct connections to low levels of attendance and poor uptake of health-care interventions among minority ethnic groups as compared with majority populations (see, for example, Greer184).
Explanations and implications for reminders
Ethnic (and racial) categories are proxy markers for a host of inter-related factors that may affect attendance behaviours. In particular, the interplay of minority ethnic status and socioeconomic deprivation requires careful consideration. However, studies of attendance behaviour have largely failed to unpack ethnicity to examine causal pathways in any detail. Nevertheless, various potential explanations for lower levels of attendance among minority ethnic (or racial) groups have been suggested.
First, several studies identify language difficulties as contributing to lower attendance among some minority ethnic patients. For example, Maxwell et al. 74 found, in a US multiethnic population, that reasons for non-attendance included a lack of understanding of the purpose of the appointment related to language difficulties. Similarly, a study in inner London148 suggested that language difficulties may result in problems in accessing available facilitators for attendance, specifically hospital transport. It is worth noting that one study reported no differences in attendance levels by language competency and has drawn attention to the fact that availability of translator services and advocacy for immigrant communities can help to ensure that there is no disparity in the delivery of services in this respect. 121
Second, higher levels of mistrust and lower degrees of therapeutic alliance or engagement with services have been noted for minority ethnic patients across several studies (see, for example, Mir and Sheikh185).
Third, as minority ethnic populations often experience high levels of individual and neighbourhood deprivation, the structural factors identified above – such as transport difficulties, high levels of residential mobility and low access to telephones – frequently apply to these groups of patients. Interestingly, however, US observers have remarked that cellular phones are the first technology with a documented trend towards more use by other ethnicities than Caucasians. African Americans and English-speaking Latinos were identified among the most active users of cell phones. 186,187 According to the Pew Report,186 more African Americans and Latinos than Caucasians own a cell phone (87% vs. 80%) and minority cell phone owners use a greater range of the features on their phones. Denizard-Thompson et al. 187 found, in their study of low-income patients in an adult medicine clinic, that SMS messaging was more common among African Americans than Caucasians, and was more common among females and patients aged < 50 years. Although we must be cautious in translating such trends to a UK population, it is important to consider that the overall effect of mobile phone access may be to ‘leapfrog’ other technologies such as landlines, thereby widening access to services. Clearly, wireless mobile technology holds significant potential to improve communication regarding appointments and reminders and increase utilisation in certain underserved populations provided that patients have a mobile phone, can afford a mobile tariff and are able to utilise the full range of features available on their mobile phone. However, caution should be exhibited in recognition that Denizard-Thompson et al. 187 observe that clinicians typically overestimated the usage of mobile phone technologies by their population.
Fourth, some studies have recognised that cultural factors may influence attendance behaviour for particular groups of patients in particular contexts. For example, in the study by Gatrad,181 various cultural practices found among the local Asian Muslim population were identified as potentially affecting attendance patterns and, therefore, requiring accommodation within the appointment-making system, such as lunchtime Friday prayers.
Patient indicators of health and well-being
Substance abuse
Our review yielded indicative evidence to suggest that substance abuse can be a factor in non-attendance. A study188 of patients with schizophrenia found that those who missed 20% or more of their appointments were more likely to abuse drugs and alcohol and manifested lower levels of community functioning. Clearly, the proportion of a patient population who are substance abusers will vary greatly between service contexts and geographical areas, with mental health services being the most likely to have large numbers of patients with this characteristic.
Mental health
Our review yielded indicative evidence to suggest that mental health status can be a factor in attendance. One study188 showed that patients who missed more than 20% of appointments in mental health clinics were more likely to abuse drugs and alcohol and exhibited lower levels of community functioning. Sims et al. 96 reported percentages of missed appointments of 36% (in 2008), 26% (in 2009) and 27% (in 2010). The reduction in RR of failed attendance following a text message intervention was 28% between the 2008 and 2009 samples and 25% between the 2008 and 2010 samples.
Donaldson and Tayar189 conducted a feasibility study of use of SMS messages in mental health outpatients. They encountered some unexpected difficulties, for example, despite mobile phone ownership matching that expected for the national average (76%), only 74% of these could remember their telephone number and only 53% were agreeable to being contacted by text message. The authors concluded that although SMS appointment reminders appear to be a potentially useful and cost-effective method of improving psychiatric outpatient clinic attendance rates, it is ‘unlikely that psychiatric clinics would provide as impressive results as those reported in other settings’. 189
Pennington and Hodgson190 conducted a non-randomised study of non-attendance to assessment for clients referred for psychological therapy in relation to invitation type. The study concluded that telephone invitations followed by a telephone prompting reminder significantly reduced non-attendance to initial assessment appointments. Limitations of the study included key variables being omitted or not being controlled which may have biased the findings, together with the small effect size.
Physical illness/comorbidity
Our review yielded evidence to suggest that poor health status or perceived poor health status can be a factor in attendance.
Roberts et al. 111 used a questionnaire-based study to explore reasons for non-attendance among 204 outpatients at neurology clinics in Ireland and found that, after simply ‘forgetting’, being ‘too ill’ to attend was one of the most frequent explanations for missed appointments.
Killaspy et al. 191 is one of several studies8,192,193 that demonstrates that non-attendance at psychiatric services is related to increased pathology and greater need, and serves as a corrective to suggestions that non-attenders may self-select because they do not need to be seen.
Alexandre et al. 8 conducted an exploratory prospective cohort study in New Yorkers with low back pain. Part of their study investigated predictors of attending. Following multivariate analysis, the authors identified that the presence of other comorbidities, such as diabetes and hypertension, was associated with poor attendance at scheduled physical therapy sessions. As part of their RCT, Resnick et al. 192 evaluated attendance at treatment visits among older women post hip fracture. At 6- and 12-month follow-ups, physical health (measured by evidence of comorbidities or overall physical health status) and mental health (measured by evidence of depressive symptoms or mental health status) directly influences attendance at treatment visits. Whitmarsh et al. 193 investigated psychological variables predicting poor attendance or non-attendance at cardiac rehabilitation. Using multivariate analysis they found that poor/non-attenders at cardiac rehabilitation were distinguished by illness representations, distress and usage of coping strategies.
Explanations and implications for reminders
Although low levels of attendance among patients experiencing the above health and well-being-related characteristics, i.e. substance misuse, poor mental or physical health, and/or low levels of social support, may in part be explained by forgetfulness, it seems likely that other factors are also in operation that are unlikely to be overcome by simple reminder systems.
These characteristics are likely to be clustered within particular clinic populations, particularly clinics serving those with mental illnesses and elderly populations. Such clinics will need to consider more sophisticated interventions to support attendance. In addition, however, within any clinic setting, managers should be alert to the fact that patients exhibiting these characteristics may be particularly vulnerable to non-attendance and that simple reminder systems may further disadvantage them when compared with the general patient population.
Symptomatology and severity
In contrast to the tendency for some patients to be ‘too ill’ to attend their appointment, the review highlights the fact that attendance at appointments may also be less likely when patients do not recognise symptoms that warrant the appointment on offer. Several studies suggest, perhaps not surprisingly, that patients are less likely to attend when asymptomatic (for instance, when being called for a screening check) or when the symptoms they have are perceived to be minor or unconcerning.
Oladipo et al. 76 report that patients referred to colposcopy are mainly symptom free and, therefore, exhibit some inertia to keep their appointments. Booth and Bennett89 similarly observed that patient contact with the referrer may be initiated after concerns about physical symptomatology or other crises, specifically within the context of alcohol disorders. Roberts et al. 111 reported that when patients were ‘happy’ with their neurological symptoms they were more likely to be non-attenders. In her study of respiratory outpatient clinics in the UK, Roberts et al. 82 cited Grufydd-Jones et al. ,194 who showed that the main reason for non-attendance in an asthma clinic in primary care was low perception of severity. Parikh et al. 77 report, within the context of the US health system, that if a patient thought an appointment was unnecessary (either the condition had resolved or the patient was able to self-manage the symptoms), he/she was less likely to show. As discussed above under Time to wait to the appointment, the higher levels of non-attendance with longer wait to appointment have been explained in part by the resolution of symptoms in the interim period. A study20 in a general surgical clinic in Ireland revealed resolution of symptoms to account for almost one-third of missed appointments. The authors questioned the appropriateness of referral, suggesting that many patients might be managed in the primary care setting. It may also be a function of delays in obtaining a specialist opinion. GPs may be forced to institute treatment measures as intermediate solutions, and often these prove sufficient to alleviate symptoms. This could be viewed as a successful outcome provided that the patients (or GP) contact the hospital to let them know of the resolution of symptoms in sufficient time to reallocate the appointment slot.
However, as Martin et al. 142 observe, ‘one cannot assume that a did not attend is a medical condition resolved’. They further point out that ‘patients still present, but at less convenient times, in less appropriate care settings, with the additional health and financial implications that frequently accompany a worsened condition’. Being too ill to attend was discussed in the previous section (see Physical illness/comorbidity).
Explanations and implications for reminders
When patients do not recognise the need to attend an appointment, or see little value/benefit in attending, simple reminders are unlikely to encourage attendance, although they could be useful in encouraging people to cancel. Non-attendance in this context could be seen as a positive sign of resolution of symptoms without clinical intervention, a marker of inappropriate referral as judged by the patient or a warning sign of unacceptable delays in receiving an appointment. Clearly, when attendance is important, even for those who are asymptomatic or experiencing only minor symptoms, attendance interventions will need to enhance patients’ perception that attendance at the appointment will contribute positively to their health and well-being. There are, for example, studies focused on screening appointments that have evaluated the impact of different approaches to increasing patient perception of the importance of attendance that could provide useful insights for other health-care contexts for which low attendance is a problem, such as ‘stepped reminders’46,195 and patient navigators. 196,197
Previous patterns of non-attendance
Our review indicated that whether non-attendance at health-care appointments can be predicted on the basis of past attendance patterns has been the subject of some interest in past research. For instance, several studies categorise patients into ‘high non-attenders’ or ‘frequent defaulters’ and try to isolate the characteristics of these patients. However, several studies suggest that patterns of attendance behaviour are unpredictable and that patients do not necessarily display consistent patterns of poor or good attendance over time.
Snow and Fulop101 reported that diabetic patients in their study could not be divided into ‘attenders’ and ‘non-attenders’ as many showed a complex record of attendance, non-attendance and cancellations. Non-attendance can thus be viewed as ‘the manifestation of a critical level of unsuitability in the agreed arrangements for an access episode, either from the outset or as a result of change in circumstances’. 101 Within the study sample, participants could be grouped into those who made a cost–benefit analysis of the obstacles and benefits of going to clinic and those who did not think about it at all. However, some patients moved from one group to another over time. Waller and Hodgkin163 similarly concluded that it was difficult to predict non-attendance on the basis of past behaviour. They noted that most people who defaulted missed one appointment and did not default again. In addition, they found that, among those categorised as ‘frequent defaulters’ (missing five or more appointments in 1 year), most ceased to be frequent defaulters in the following year. The authors suggest that many of these patients may be ‘experiencing a life crisis of some form, or living a chaotic phase of their lives. They will have more pressing problems to deal with than their tendency to default.’163 They further suggest that prioritising the clinical management of the underlying health problem may be more effective in reducing non-attendance than the application of administrative processes to attempt and alter their behaviour.
However, Chariatte et al. 135 found that in an adolescent outpatient clinic, the probability of missing an appointment was explained in their statistical models in part by having missed or cancelled the next to last appointment and having missed the antepenultimate appointment. Having missed the next to last appointment was found to be the most important of these factors, providing 39% of the total explanation.
At least two of the RCTs64,83 examined in review 2 were targeted at defaulters rather than at a general clinic population. The study by Rutland et al. 83 included all patients aged from 16 to 30 years who did not attend a booked GUM appointment during a 6-month study period. In the study by Fairhurst and Sheikh,64 only patients who failed to attend two or more appointments in preceding 12 months were included. Rutland et al. 83 recorded a reduction in non-reattendance of 3.7%, while Fairhurst and Sheikh64 demonstrated a reduction in the non-attendance rate of 5.3%. These rates appear fairly modest compared with some of those achieved in the general clinic population. This may suggest that, for this particular group, it is factors other than ‘forgetting’ that have acted as barriers to attendance.
Explanations and implications for reminders
Included studies were ambivalent with regard to whether or not previous non-attendance may predict future non-attendance. It seems largely intuitive that most people can find themselves in circumstances which mean that they may not be able to attend an appointment from time to time and that they may need to cancel an appointment;101 therefore, at a general level, it would seem sensible to send all patients a reminder which includes a message about cancelling an unwanted appointment and rescheduling for a future appointment if treatment is still required. For health services that do find that in their population there is a clear relationship between previous non-attendance and future non-attendance, and that there is a relatively high rate of ‘frequent defaulters’, more intensive reminder strategies such as the sequential reminder intervention described by Perron78 could be initiated. First, a telephone call to either landline or mobile; second, a SMS if participants do not answer the telephone after three attempts and have a mobile phone and, finally, a postal reminder if participants did not answer the telephone, had no mobile phone for SMS, or had no phone at all. Such a design, although labour intensive, would reach the maximum number of participants and may increase attendance rates while still being cost-effective.
Chapter 6 Discussion
Main findings
The objective of this project was to explore the differential effect of alternative types of reminders for scheduled health service encounters for different segments of the population on fulfilled or rescheduled appointments, substitutions and satisfaction. This study has presented the findings of three separate reviews in order to answer the more specific research questions outlined in this project (see Objectives). A brief discussion of the literature as it relates to each of the questions is outlined below.
Which types of reminder systems are most effective in improving the uptake of health service appointments?
Simple reminders
All reminders are effective at improving attendance at appointment. Simple reminders, which provide details of timing and location of appointments, are effective at increasing attendance at appointment [see Chapter 4, Evidence statement (A.1): there is strong consistent evidence that simple reminders which provide details of timing and location of appointments are effective at helping a (forgetful) patient to attend their appointment (evidence category Ia)]. Forgetfulness is reported by patients and by health professionals as the most common reasons for not attending a health-care appointment and accounts for between 8% and 44.8% of patients who did not attend their appointments, indicating that this is a substantial problem (see Chapter 5, Reported reasons for non-attendance). Forgetfulness or confusion over date, time or location of the appointment appears to act as the theoretical basis for many reminder systems identified in this review. 59,63,70,76,78,79,98,99,102,106,198–200 It has been suggested that simple reminders may be effective because they act as cues to counteract prospective memory failures. 25 Numerous studies suggest that as many as 80–90% of patients have a positive attitude to receiving a reminder that jogs the memory. 55,79,145,200 The evidence presented indicates that the use of simple reminders is both acceptable and feasible across a wide array of health-care settings. Although very few studies have investigated the influence of preference on reminder effectiveness [see Chapter 4, Evidence statement (B.4): very few studies investigated whether or not the reminder preferences of the patient may influence the impact a reminder has on the patient's appointment behaviour (evidence category VIIa)], it may provide some indication about a patient’s ability to access the reminder, which may ultimately influence the effectiveness of the reminder [see Chapter 4, Evidence statement (B.1): there is strong consistent evidence that the reminder may not be received by the patient (evidence category Ia)]. Therefore, the choice of reminder system remains an important consideration for health services. In an acquired immunodeficiency syndrome (AIDS) clinic serving young adult patients, a high percentage of whom were mobile phone users, SMS was the preferred option. 200 In a different study of adolescents attending dental clinics, participants reported a significant preference for letter reminders (56.3%), followed by telephone reminders (26.0%) and SMS reminders (17.7%). 55 Patient preferences for reminders appear to vary considerably, and we hypothesise that this may be related to sociodemographic factors such as age, employment status, etc. or possibly in relation to the health setting; patients attending sensitive health-care appointments may prefer a very confidential reminder, although this needs to be confirmed through research.
Although simple reminders are effective memory joggers for people who might otherwise forget, this does not explain why, in settings where reminders have been used, forgetfulness continues to be a commonly cited reason for non-attendance. 74,136 Forgetfulness may also be a reason that is offered by patients, as it may be more convenient and easier than the truth. Murdock et al. 12 have suggested that the underlying reason may be apathy; however, the truth may be considerably more complex and uncomfortable than that. Patients may be uncomfortable stating that they did not find the treatment helpful or that they did not like their doctor, etc. The implication of this is that ‘true forgetfulness’ may be over-rated, whereas other reasons may be under-rated or even unaccounted. Numerous other reasons have also been reported (see Chapter 5 for an account of these reasons). It has been suggested that, for patients who receive, or expect to receive, some benefit from attending their appointment, reminders will be effective in increasing appointment attendance. 25 Reminders will be effective in increasing appointment attendance provided the clients receive some benefit from their attendance, such as useful information, alleviation of symptoms or emotional support. 201 If patients no longer find the treatment sessions rewarding, then the prompts will eventually be ignored by the client;201 therefore, clients may fail to attend after the initial appointment because the treatment is simply not meeting their expectations or needs. 25 This suggest that reminders, even simple reminders, have a more complex mechanism than simply ‘jogging the memory’.
Reminder plus
There is currently weak evidence (category IIIa) that ‘reminder plus’, which provides additional information over and above the date, time and location of the appointment, are more effective than simple reminders at helping a patient to attend their appointment [see Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)]. Many authors have suggested that the provision of additional information may reduce the number of perceived obstacles to patient attendance and, in this way, increase patient intentions to attend, thereby enhancing the effectiveness of a reminder system.
Gain-framed compared with loss-framed reminders
Specifically, it has been suggested that the provision of information that increases patient perceptions that attendance is important and will contribute positively to his/her well-being will be effective in increasing appointment attendance (gain-framed reminders). 59,89,164 Alternatively, it has been suggested that the provision of information that increases patient perceptions that non-attendance will contribute negatively to his/her well-being will be effective in increasing appointment attendance (loss-framed reminders). 86,89,202 Ersin et al. 123 recommend a combination of the two. Patients themselves stated that they felt reassured and more confident about attending the appointment if they had received information that emphasised the importance or the benefit of the health check. 203
The use of additional information as a way of increasing appointment uptake is supported in different contexts. Rutland et al. 83 conducted a prospective randomised control study to determine whether or not SMS follow-up of patients who had not attended a booked GUM appointment would improve subsequent reattendance rates and to assess the impact of inclusion of a health promotional message on reattendance rates. Participants (n = 252) who did not attend a booked GUM appointment during the 6-month study period were randomised to (1) no intervention, (2) SMS notification of the defaulted appointment and invitation to attend clinic or (3) SMS notification of the defaulted appointment, invitation to attend clinic and a health promotional message about Chlamydia. All SMS messages were sent 1 week after the defaulted appointment. The reattendance rate was 4.5% in the control group compared with 8.2% in the group receiving a text reminder (p = 0.36) and 15.2% (12/79) in the group receiving a text reminder with a health promotional message (p = 0.032). In this study, SMS messages with a health promotional message improved subsequent reattendance rates of clinic defaulters. However, not all studies support this finding. Marteau et al. 204 found no significant difference in the uptake of appointments for diabetic screening appointments in their RCT when they compared an invitation letter promoting informed choice for screening presenting diabetes as a serious potential problem and providing details of possible costs and benefits of screening and treatment in text and pie charts, with a standard invitation describing diabetes as a serious potential problem.
There may be a contextual element around whether messages should be gain-framed, emphasising the advantages of adherence with recommendation, or loss-framed, emphasising the disadvantages of non-adherence. A meta-analytic review205 of 93 studies (n = 21,656) found that gain-framed messages advocating dental hygiene behaviours were effective, whereas there appeared to be less difference between gain- and loss-framed messages concerning other preventative actions such as safer gender behaviours, skin cancer prevention behaviours or diet and nutrition behaviours. More research is required to consider the influence of message framing.
Orientation information
There is weak evidence that reminders that provide orientation information (e.g. provision of maps, information about clinics and procedures, transport, etc.) may be more effective at increasing appointment attendance than simple reminders. It has been suggested69,89 that reminders of this nature may decrease patient perceptions that attendance at the appointment will be difficult and help patients to feel more confident about attending their appointment. Some authors25,140 have further speculated that orientation information is specifically effective for improving attendance at specific types of appointments, for example new patient appointments or screening appointments for which patients are likely to be attending the clinic for the first time.
Creating a positive perception of the appointment and health-care provider
Providing information that increases patient perceptions that the appointment will be a positive experience may increase appointment attendance. The act of simply sending a reminder may increase patient perceptions of the value of the appointment. 80,145 Patients have also reported that receiving a reminder felt like a proactive, positive contact with the health-care provider, which left them feeling that their health-care provider was genuinely concerned about their health problem. 145,203 The degree of alliance and quality of communication between patients and the health-care provider and health services impacts on patient attendance behaviour (see Chapter 5, Patient–provider ‘alliance’, communication and ‘engagement’) and a positive communication through reminder systems may lead to positive patient action to attend, cancel or change their appointment. 80,203 However, if reminders are handled badly, some patients may feel disinclined to engage with health-care providers and appointments. 145
Moral obligation to attend
Our review identified examples from the attendance literature to indicate that patients may not attend appointments if they feel morally obligated to undertake a higher-priority activity such as child care; or that they will attend an appointment if the patient feels morally obligated to perform that health behaviour (see Chapter 5, Norms, attitudes and understandings regarding whether or not attendance is the morally right thing to do). It has been suggested that providing information that increases patient perceptions that attending the appointment is morally the right thing to do will be effective at increasing appointment attendance. 104 Some authors102,123 suggest that the receipt of a reminder or influential wording of the reminder may compel some patients to attend their appointment. Some patients recognised and valued the extra time and effort taken by health services to send a reminder and, consequently, felt compelled to attend their appointment. 115,203 Asking patients to enter into an agreement by sending back a confirmation of attendance or contracting to attend may further compel patients to attend their appointment. 56,140,141
Although there is strong evidence to support the use of reminders, there is a need for high-quality studies investigating the differential influence of providing additional information as part of the reminder system in different contexts (first vs. follow-up appointment), particularly the use of loss-framed compared with gain-framed messages and orientation information for facilitating attendance behaviours.
Are there any systems that effectively support the cancellation of appointments?
Currently, there is strong evidence that a personal telephone reminder will increase patient cancellation/rescheduling rates [see Chapter 4, Evidence statement (E): there is strong consistent evidence that reminder systems will promote cancellation of appointments (evidence category Ia)]. Reti80 suggests that one of the dominant benefits of telephone reminders may be the ‘promotion of suitable cancellation behaviours’. Telephone reminders carry the inherent advantage that patients who are unable to attend can cancel their appointment at the time of contact from staff. This advantage is further heightened if the same telephone interchange can be used either to rebook the appointment or to establish that the appointment is no longer required. There is less evidence to support the use of SMS messages to promote cancellation and rebooking [see Chapter 4, Evidence statement (E): there is strong consistent evidence that reminder systems will promote cancellation of appointments (evidence category Ia)]; however, this may be because SMS reminders are frequently sent very close to the appointment time, which may leave insufficient time for patients to act on the prompt. 78 A second reason that SMS may not optimise cancellations could be that when patients receive a reminder they are frequently asked to phone a telephone number rather than simply replying to the text [see Chapter 4, Evidence statement (E.2 and E.5): there is strong evidence that whether or not a patient cancels and rebooks will be influenced by reminder system factors that facilitate/hamper patient intentions to rebook (e.g. nobody answers the telephone) (evidence category Ia)]. There is strong evidence that patients frequently encounter heath-care system factors such as difficulties accessing cancellation lines, which can hamper patient attempts and intention to cancel and rebook [see Chapter 4, Evidence statement (E.2 and E.5): strong consistent evidence indicates that system factors related to appointment systems will hamper patient intentions to cancel/rebook (evidence level Ib)]. Better administrative processes in support of SMS may support cancellation more effectively.
Reminder systems are often employed with increased attendance rates in mind and relatively little attention is given to cancellation and/or rescheduling of appointments. Cancellation of appointments may be considered a desirable outcome, especially when the cancellation occurs in time for the appointment to be reallocated to another patient. Even under time-constrained conditions, cancellation without reallocation of the appointment may still be viewed as a favourable outcome as it reduces uncertainty about whether or not the patient will attend, allows clinical staff to assign the equivalent freed time to other patients or to alternative activities and, therefore, reduce the pressure on crowded appointment schedules. Rescheduling of appointments may also be a desirable outcome, especially when the health need of the patient is great. As there is strong evidence that the timing of a reminder, between 1 and 7 days prior to the scheduled appointment, has no effect on patient attendance behaviour [see Chapter 4,Evidence statement (B.5): there is strong consistent evidence that the timing of a reminder, between 1 and 7 days prior to the scheduled appointment, has no effect on patient attendance behaviour (evidence category Ia)], it would seem appropriate to send all reminders with more time to allow patients to cancel their appointments and for health services to reallocate appointments to other patients. Although there are no studies investigating the framing of reminders [see Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)], it is recommended that the reminder should be framed with cancellation and/or rescheduling in mind. How the request is framed may increase a patient’s sense of moral obligation to cancel;102 however, more robust structures to support cancellation are also required. Cancellation procedures that are easy and require minimal effort from the patients are important, e.g. automated responses to SMS messages rather than the patient having to phone a telephone number, or cancellation and rescheduling telephone lines with adequate administrative support so that patients can quickly leave a message. E-mail may also be a convenient cancellation medium for many patients, as there is no need to wait to get through to a receptionist. 42 Automated methods of cancellation may be perceived as easier than methods that require direct contact, as they offer flexibility to cancel at a time convenient to the patient and also reduce the need to provide explanations for cancellation. 42,206 Following cancellation of appointments, rescheduling of the appointment, if it has not occurred synchronously, also needs to be easy for the patient. For example, it may be sensible to have central booking lines which are open 24 hours a day.
Kitcheman et al. 69 observed that an effective reminder system will increase the ‘already heavy workload of psychiatric out-patient clinics’. The authors note that ‘even when appointments are missed clinicians do not, as a rule, waste their time’. Alternative activities include the fact that ‘patients are double-booked, dictation is completed, telephone calls made and colleagues consulted’. 69 This highlights that increased attendance at appointments may be welcomed more by managers, primary carers and patients than by those working in outpatient clinics. As a consequence, each service faces the challenging dilemma of whether to build in assumptions of non-attendance without opportunity for appointment cancellation or reallocation or to build in processes that optimise cancellation and rescheduling. If building in processes to optimise cancellation and rescheduling, then services will also need to consider the impact on staff that frequently utilise non-attendance at appointments as an opportunity to catch up on other health-care-related activities.
Although reminder systems will increase attendance, full appointment attendance is unlikely to be an achievable outcome; therefore, cancellation and rescheduling of appointments should be seen as a desirable outcome. Reminders would appear to have considerably more potential for promoting cancellation of unwanted appointments to allow reallocation of cancelled appointments than the current evidence indicates. Researchers and health services seeking to optimise attendance should not only consider reminder solutions, but should also consider the supporting resources that would be required to facilitate patient cancellation and rescheduling, reallocation of appointments to other patients while simultaneously supporting hard-pressed clinicians to manage administrative tasks that are routinely carried out when a patient misses an appointment.
Do different reminder systems have differential effectiveness for particular subgroups of the population (e.g. by age group, ethnic group, socioeconomic status, gender, etc.)?
There is very little good-quality evidence investigating whether or not reminder systems have differential effectiveness for population subgroups (e.g. gender, socioeconomic status, ethnicity, employment status, mental health, other comorbidities, presence of symptoms, diagnosis, severity of condition) (see Chapter 4, Proposition F: distal/proxy individual attributes). The majority of included studies have not been designed to perform secondary analysis to identify subgroups who are more or less likely to respond to reminders.
Age
There is weak evidence that age does not have a differential impact on the effectiveness of reminders [see Chapter 4, Evidence statement (F.1): there is sufficient weak equivocal evidence to suggest that age does not have a differential effect, over and above pre-existing appointment behaviour, on reminder effectiveness (in terms of attendance, cancellations or rebooking) (evidence category IVa)], indicating that reminder systems can be employed across all age groups. Further investigation of wider attendance literature (see Chapter 5, Age) indicates that there is largely consistent evidence, across health and geographical settings, that higher rates of non-attendance is related to younger age, although this may not hold for paediatric patients who have greater parental involvement in the health care. However, older people tend to have multiple health problems or conditions that may be less likely to resolve and therefore take up the bulk of outpatient appointments. There is speculation surrounding the reasons why younger patients are at greater risk of not attending; however, there has been little solid exploration of the reasons. Therefore, there is little theoretical basis to inform reminder selection so we contend that there is no reason not to employ reminder systems equitably across all age groups. However, as discussed under Accessibility, there are important considerations to be made in relation to the type of reminder technology that would be most appropriate or acceptable for different age groups. Accessibility is a key issue in selection of reminder technology, and older populations are likely to have lower levels of accessibility to mobile phones and, therefore, SMS than younger people108 (see Accessibility). Patient preferences for reminders are another key issue as it may be a proxy for acceptability, with patients unlikely to prefer reminder systems that they cannot access (see Other reminder characteristics).
Gender
There are no studies indicating that gender has a differential impact on the effectiveness of reminders [see Chapter 4, Evidence statement (F.2–F.11): few studies investigate whether or not a range of distal/proxy individual attributes have a differential effect, over and above pre-existing appointment behaviour, on reminder effectiveness (in terms of attendance, cancellations or rebooking) (evidence category Va or VIIa)], suggesting that reminder systems can be employed regardless of gender (see Chapter 5, Gender). There is conflicting evidence, across health and geographical settings, that gender predicts non-attendance at appointments. Half of the studies searched find that women are more likely to miss appointments and the other half find that women are more likely to attend their appointment. On this basis, we can see no reason for employing reminder systems differentially for male and female patients.
Deprivation
There are no studies indicating that deprivation has a differential impact on the effectiveness of reminders [see Chapter 4, Evidence statement (F.2–F.11): few studies investigate whether or not a range of distal/proxy individual attributes have a differential effect, over and above pre-existing appointment behaviour, on reminder effectiveness (in terms of attendance, cancellations or rebooking) (evidence category Va or VIIa)]. There is weak but consistent evidence that deprivation is a factor in non-attendance (see Chapter 5, Deprivation). This section reveals an array of suggested reason why patients from deprived backgrounds may not attend appointments and reveals a potentially complex set of circumstances that could make it difficult to engage with health-care systems in general, or appointment and reminder systems in particular. Although there has been little exploration of these circumstances in relation to appointment attendance behaviours, these circumstance explain why this group of patients may struggle to engage with complex appointment systems that require a relatively high degree of health literacy;207 they may also not receive appointment information or reminders and subsequently may find it difficult to attend, cancel or reschedule appointments. The available literature suggests that deprived populations face multiple obstacles to health-care appointment attendance. 86,89,123,148,166 Health services providing care to deprived populations have a wide range of complex issues to consider in addition to thinking about strategies for improving attendance. Clinics that achieve high levels of attendance despite serving patients populations with high levels of socioeconomic deprivation would warrant close investigation, as they may have introduced ways of working that could be transferable to other settings. Reminder systems are likely to be indicated although, as discussed above, reminder systems are very dependent on accurate data from patients and so deprived populations with unstable contact details may be disadvantaged. 103 Health services will need to give careful attention to having robust procedures for keeping patient contact details up to date and for providing easy to use systems for patients to make, cancel and reschedule appointments.
Ethnicity
There are no studies indicating that ethnicity has a differential impact on the effectiveness of reminders [see Chapter 4, Evidence statement (F.2–F.11): few studies investigate whether or not a range of distal/proxy individual attributes have a differential effect, over and above pre-existing appointment behaviour, on reminder effectiveness (in terms of attendance, cancellations or rebooking) (evidence category Va or VIIa)]. Our evidence suggests that there may be a link between ethnicity and non-attendance, although this is not completely consistent. On the whole, studies in this review have failed to examine ethnicity and to understand the causal pathways that link ethnicity to non-attendance. Ethnicity is itself an umbrella term that covers multiple potentially relevant and inter-related factors that, by themselves, may be linked to non-attendance, e.g. socioeconomic or deprivation status (see Deprivation), language barriers (see Other reminder characteristics), health literacy (see Deprivation), issues of trust, mutual respect and cultural competency (see How do the perceptions and beliefs of patients, their carers and health professionals regarding specific types of reminder systems, and patient/carer resources and circumstances, influence their effectiveness?). Several factors could interact to create difficulties with patient engagement and therapeutic relationships (see Characteristics of the appointment system). Ethnic groups face multiple potential obstacles to health-care appointment attendance. Health services providing care to ethnic groups have a wide range of complex issues to consider in addition to thinking about wider strategies for improving attendance in this group. Reminder solutions are one possible way forward; however, owing to the likelihood of concurrent deprivation status, similar issues around accuracy of contact details and general accessibility of patients to reminder technologies are likely to exist. In addition, health services need to give consideration to having reminder systems, cancellation procedures and rescheduling procedures that suit the language requirements of their particular ethnic groups and are easy for this group of patients to understand and engage with.
Substance abuse/mental health/comorbidity and physical illness
There are no studies indicating that substance abuse, mental health or comorbidity has a differential impact on the effectiveness of reminders [see Chapter 4, Evidence statement (F.2–F.11): few studies investigate whether or not a range of distal/proxy individual attributes have a differential effect, over and above pre-existing appointment behaviour, on reminder effectiveness (in terms of attendance, cancellations or rebooking) (evidence category Va or VIIa)]. High levels of non-attendance are found in patients who abuse drugs and alcohol (see Chapter 5, Substance abuse), patients with mental health problems (see Chapter 5, Mental health) and patients with comorbidities and illness (see Chapter 5, Physical illness/comorbidity). Although forgetfulness may occur, it is likely that other, more substantial, problems may be acting as the obstacle to attendance. Non-attendance at the appointment is an indicator that there may be a deterioration of the mental health, drug and alcohol problems. In such cases, patients may need active follow-up in order to support them through their relapses and to re-engage them in their treatment programmes. Patients with other co-morbidities or illness may find themselves too ill to attend, too ill to cancel or may even be admitted to hospital. Health services serving large numbers of these patients need to be aware that this group are at high risk of not attending and to be aware that non-attendance may indicate an increased health need and will have a wide range of complex issues to consider in relation to finding wider strategies for improving attendance in this group. Simple reminders and automated reminders to attend may be ignored or overlooked, particularly when patients are experiencing an increased level of illness or substance abuse. In fact, the use of simple reminders may put these patient groups at a disadvantage compared with general outpatient populations. Reminders with direct personal contact might be appropriate in these groups (see Other reminder characteristics, Format of the reminder). To facilitate attendance, a sequential reminder intervention such as that described by Perron et al. 78 could be initiated: first a phone call to either landline or a mobile phone; second, a SMS message if participants do not answer the telephone after three attempts and have a mobile phone; and, finally, a postal reminder if participants do not answer the telephone, have no mobile phone for SMS, or had no phone at all. Such a design, although labour intensive, would reach the maximum number of participants and may increase attendance rates while still being cost-effective. A further consideration is how to re-engage patients with treatment after they have missed their appointment. Intensive approaches, such as ‘stepped reminders’46,195 and patient navigators,196,197 have been effective at increasing attendance at screening and immunisation programmes in disadvantaged and vulnerable populations and might also be effective at re-engaging similar groups of patients who have dropped out of treatment.
Symptomatology and severity
There are no studies indicating that symptoms or severity of a condition have a differential impact on the effectiveness of reminders [see Chapter 4, Evidence statement (F.2–F.11): few studies investigate whether or not a range of distal/proxy individual attributes have a differential effect, over and above pre-existing appointment behaviour, on reminder effectiveness (in terms of attendance, cancellations or rebooking) (evidence category Va or VIIa)]. Our review does suggest that patients who have no symptoms, improved symptoms or low perception about the severity of the condition are more likely to not attend a scheduled appointment (see Chapter 5, Symptomatology and severity). However, there will be patients in this bracket who do not have a life- or function-threatening condition who can manage their health condition satisfactorily for many years and for whom continued attendance is unnecessary. In this case, a reminder system could be used to promote cancellation without rescheduling leading to a negotiated discharge. Conversely, there may be patients or people in this bracket who do have a potentially serious health problem but who are either unaware of its potential severity and impact if it remains untreated or who do not know it because they have not attended a screening appointment. There is a huge amount of literature, which has not been investigated in this review, investigating strategies for increasing uptake of screening appointments. Some of these strategies, including stepped reminders and patient navigation, are labour intensive but might be relevant to consider for re-engaging patients with health-care procedures if they have dropped out (see Substance abuse/mental health/comorbidity and physical illness). The end point of these kinds of processes is either rescheduling of further health-care appointments or a negotiated discharge.
Previous patterns of non-attendance
Previous patterns of attendance are often cited as indicators of future attendance; however, the evidence in this review presents a more unpredictable picture than this (see Chapter 5, Previous patterns of non-attendance). In some studies, patterns of attendance and non-attendance can be variable, with no clear picture emerging of those patients who are ‘attenders’ or those who are ‘non-attenders’. In this review we have already identified that people may not attend for many different reasons and these may be variable over time. For anyone at any time, the appointment can be unsuitable from the outset or can become unsuitable because of a change of circumstances,101 indicating that all patients are likely, at some point, to be unable to attend an appointment. We recommend sending all patients reminders that include a message about cancelling an unwanted appointment and rescheduling for a future appointment if treatment is still required.
What factors influence the effectiveness of different reminder systems for particular population subgroups?
We have added no further comments to this section as we have discussed this under Previous patterns of non-attendance in the context that understanding patient non-attendance can provide insights into how reminder systems could be designed and deployed.
How do the perceptions and beliefs of patients, their carers and health professionals regarding specific types of reminder systems, and patient/carer resources and circumstances, influence their effectiveness?
In general, our review did not generate much information on the perceptions and beliefs of patients regarding specific reminder systems, as opposed to their preference for particular technologies, and we cannot say how perceptions and beliefs of patient or health professionals about reminder systems influence their effectiveness. This reflects the fact that most reminder-related research takes a rather narrow focus. There is evidence to suggest that a personalised interaction with a member of practice staff is perceived as more useful than an automated reminder system. However, there is also conflicting evidence as to whether this would make a patient more or less likely to communicate a cancellation than a less personalised method of delivery. Our review has also identified that an individual’s perception about health-care systems and professionals will influence patient attendance (see Chapter 5, Patient–provider ‘alliance’, communication and ‘engagement’). This could be related to an individual’s view of the quality of care provided, trustworthiness, empathy and cultural sensitivity of staff and issues of mutual respect. However, individuals’ views may also be shaped by the surrounding community in which they live, through a process of ‘storytelling’ whereby negative storylines will contribute to the individual’s negative perceptions of the health system or health professionals. 155 Patients may experience stigmatisation within individual relationships, such as those with family, GPs or other health professionals, which may directly influence an individual’s intention to attend or further colour the individual’s perception of the health service. 143 This is a difficult area to manage, and wider solutions must also be considered, but there is greater scope to consider how these factors might influence the effectiveness or design of reminder systems interventions. The role of reminder systems in this context is potentially limited given the negative publicity that British health services and health professionals have received through the media. However, the small role that reminder systems might play here in positively influencing individual-level perceptions of health-care services is via their contribution to patient engagement and therapeutic alliances (see Characteristics of the appointment system). Positively framed reminder messages, delivering appropriate and helpful information, could help to counter an individual’s negative perceptions of a health service.
How do external factors (e.g. content, delivery, setting, frequency, notice period) influence the effectiveness of reminder systems?
There are few studies that directly investigate the extent to which characteristics of the reminder system can influence the effectiveness of the reminder system; however, two characteristics stand out as being important. There is strong evidence that factors such as accessibility to the reminder will influence the effectiveness of the reminder and that the timing of the reminder, between 1 and 7 days prior to the appointment, will not influence the effectiveness of the reminder and we suggest that there are good reasons for sending reminders earlier than usual, i.e. 3–7 days prior to the appointment (see Timing of the reminder).
Accessibility
There is strong consistent evidence that the reminder may not be received by the patient [see Chapter 4, Evidence statement (B.1): there is strong consistent evidence that the reminder may not be received by the patient (evidence category Ia)]. It is largely intuitive that if the patient does not receive the reminder, this may contribute to suboptimal effectiveness of the reminder. Several reasons for non-receipt of reminders are discussed in the literature. There appears to be a consistent amount of either technology error or human error associated with all reminder systems, and consequently many patients report not receiving a reminder or receiving it late. The reminder systems will be most effective when contact details are accurate and patients receive the reminder. It is therefore important for the health-care organisation to have systems in place to ensure that patient contact details are current and that reminders are successfully received by the patient. 95,208
Telephone reminders (automated or manual)
One of the reasons that patients may not receive telephone reminders is that landline calls are often made during business hours, when it is most likely that patients will be out of the house. 25 In our review, all the RCTs that reported procedures for making telephone contact attempted to contact patients within usual working hours (09.00–17.00 hours) during the working week (Monday to Friday) in a 1–7 day window prior to the clinic appointment. 57,66,80,82,90,179 Many other reasons have also been frequently reported that further explain why patients may not be contactable using a telephone reminder system, e.g. the patient either did not have a telephone or had been disconnected, the patient never answers the telephone or the contact number provided was incorrect. 91,92 Some patient groups, e.g. deprived populations and homeless groups, may not have equitable access to landline systems or mobile phone technology. Other groups may not answer the telephone and may let the telephone run to the answerphone, e.g. patients with mental health problems, deaf patients or those with poor mobility. However, for reasons of confidentiality, most telephone reminder systems do not leave messages on answerphones. Despite the relatively low contact rates reported, ranging from 30% to 60% [see Chapter 4, Evidence statement (B.1): there is strong consistent evidence that the reminder may not be received by the patient (evidence category Ia)], there are also considerable potential advantages of interactive telephone calls, including allowing patients to verify and confirm their appointment, respond to instructions about logistics, request additional preparation materials, answer queries about their current health, request that information is repeated and ask for a summary of instructions. 80 There is also an opportunity for receptionist or health-care professionals to resolve any misunderstandings, or to deliver educational information about procedures, as well as motivational messages that address the risks, benefits, barriers and self-efficacy associated with health-care procedures. 80 If telephone reminder systems are to be the reminder of choice, then clinics using such systems should consider using both landline and mobile telephones in combination57 or out-of-hours reminder calls to maximise the contact rate. 82
Short message service reminders
The recognised advantages of SMS reminders over telephone messages are that SMS reminders can be automated and the technology allows large batches of text messages to be delivered almost instantly, minimising labour costs. 57 They do not require the mobile phone to be active or within range, messages can be sent after normal business hours and it does not matter whether the patient is at home or at work. 53,57 A high rate of successful contact is assumed with SMS reminders, as indicated by most included RCTs for which success is based on a ‘message sent’ response being received by the sender. However, this does not recognise that many patients either may not receive their SMS reminder or may receive and ignore a reminder that was not intended for them as a result of incorrect data entry on hospital systems. 95,100 However, some clients may not receive their text message until after their scheduled appointment because of delays in delivery of the text, because their telephones were switched off or because, in the case of individuals from poorer economic groups, they may have delayed purchase of pay-as-you-go tariffs at financially challenging times. 119 One disadvantage of using SMS reminders is that patient groups are not equally likely to have a mobile phone. Although very popular among the young British population,101 mobile phone ownership declines sharply with increasing age;108 however, the total number of people > 60 years of age with a mobile phone is increasingly annually. In addition, patients with mental health problems appear to have a higher level of distrust of SMS, which means that they have a lower preference rate for SMS reminders than other patient groups. 209 If SMS is considered to be the reminder of choice, then services that provide health care to older patients, patients from deprived backgrounds, patients with mental health problems or the homeless should carefully consider whether or not mobile phone technology is an appropriate medium for sending out reminders.
E-mail reminders
Although not yet rigorously tested, e-mail has been proposed as a suitable medium for appointment reminders. 42 Bespoke secure e-mail programmes can incorporate special features such as standard forms guiding the use and content of the e-mail sent and the capacity to show read receipts (in order to confirm the patient has received the correspondence). However, they are costly to set up and may require a greater degree of user skill than standard, unsecured mail. 42 In addition, technological issues may occur, such as recipients having a full mailbox causing e-mails to bounce back to the sender. 210 Systems may be at risk of failure owing to the loss of the link to a central server, delay in transmission of e-mails, power failure or, in worst-case scenarios, natural disasters. There is also potential for human error, which can lead to unintended content or e-mails being sent to incorrect recipients. Future research is required to consider the likely usefulness/availability/accessibility and practical implications of e-mail reminders.
The importance of successfully contacts through reminder systems is largely intuitive but should not be underestimated. For example, in their RCT secondary analysis, Chiu58 identified that non-attendance rates for successful and failed reminders were 3.86% and 18.68%, respectively. With any reminder system, there is likely to be a level of unsuccessful contact; however, poor selection of reminder systems will exacerbate this problem in to hard-to-reach groups, e.g. substance abusers,211 older patients108 and homeless populations. 212
Timing of the reminder
There is strong evidence that the timing of a reminder, between 1 and 7 days prior to the scheduled appointment, has no effect on patient attendance behaviour [see Chapter 4,Evidence statement (B.5): there is strong consistent evidence that the timing of a reminder, between 1 and 7 days prior to the scheduled appointment, has no effect on patient attendance behaviour (evidence category Ia)]. SMS or telephone reminders are typically sent either the day before or on the day of the health-care appointment. 64,70,71,73,76,78,84,89,100,108 Reminders of this nature appear to be sent to benefit those patients who have genuinely forgotten about their appointment [see Chapter 4, Evidence statement (A.1): there is strong consistent evidence that simple reminders which provide details of timing and location of appointments are effective at helping a (forgetful) patient to attend their appointment (evidence category Ia)]. For this reason, the reminder is not sent too far in advance as this may allow that patient to forget again. 102 It might be supposed that if a reminder mainly serves as a memory prompt for the genuinely forgetful patient, then it is more likely to be effective at increasing attendance behaviour the closer it is to the date of the appointment. Although the evidence from our included studies does support the use of reminders for supporting forgetfulness [see Chapter 4, Evidence statement (A.1): there is strong consistent evidence that simple reminders which provide details of timing and location of appointments are effective at helping a (forgetful) patient to attend their appointment (evidence category Ia)], it further indicates that reminders can be sent any time between 1 and 7 days, with no diminished effectiveness of the reminder at facilitating attendance at appointments. The evidence does not determine whether or not effectiveness of reminders is diminished beyond 7 days, but presumably a 1- to 7-day window is plenty of time in which to operate any kind of reminder system, e.g. SMS, telephone, letter, etc., with any kind of outcome in mind, e.g. attendance, cancellation, rescheduling, information sending, etc.
There are several advantages of sending out earlier reminders. First, there is strong evidence that reminders, particularly telephone reminders, increase cancellation and rescheduling of appointments [see Chapter 4, Evidence statement (E): there is strong consistent evidence that reminder systems will promote cancellation of appointments (evidence category Ia)]. Earlier discussion also suggests that other types of reminders have the potential to increase cancellation and reallocation of appointments to other patients with the commensurate benefits that this can bring (see Are there any systems which effectively support the cancellation of appointments?). Because the timing of appointment reminders makes no appreciable difference to the scale of attendance behaviour, it is sensible to send out reminders that are received by patients a minimum of 2–3 days prior to the appointment in order to take advantage of the efficiencies that can be gained through patient cancellations and health service reallocation of appointments. Second, earlier reminders allow for the patients to be provided with information leaflets about appointments or procedures, orientation information such as maps, etc. that patients can read prior to attending their appointment, which may also help to increase the effectiveness of the reminder [see Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa) and Chapter 6, Reminder plus for more detailed about provision of additional information].
Other reminder characteristics
There is either no evidence, weak evidence or conflicting evidence that a range of other reminder characteristics influence the effectiveness of the reminder. This includes language and framing of information [see Chapter 4, Evidence statement (B.2): there are no studies investigating whether or not reminder factors (such as language, information provided, framing of information) influence the accessibility/comprehensibility of the reminder message for particular patient groups (evidence category VIIa)], content of the reminder [see Chapter 4, Evidence statement (B.3): there are no studies to show that the content of the reminder may effectively address the obstacles/enablers experienced by the patient in question (evidence category VIIa)], personal reminders compared with automated reminders [see Chapter 4, Evidence statement (B.4): there is controvertible evidence, based on multiple good-quality studies, that personal reminders have a greater impact on attendance rates than automated reminders (evidence category IIa)], the format of the reminder [see Chapter 4, Evidence statement (B.4): the format of the reminder will compromise the amount, and type, of information that can be delivered to the patient (self-evident)] and patient reminder preferences [see Chapter 4, Evidence statement (B.4): very few studies investigated whether or not the reminder preferences of the patient may influence the impact a reminder has on the patient's appointment behaviour (evidence category VIIa)].
Language and framing of information
None of the included studies explored the extent to which the language in which a reminder is framed influences its comprehensibility, although the scale of this potential problem would depend on the language demographic of the population served. One of the included RCTs based in Switzerland used a multilingual research assistant who spoke French, English and Spanish to make telephone calls;78 however, two RCTs81,141 involving telephone reminders excluded patients who did not speak English fluently. The majority of RCTs were silent on the issues of language. Health-care services do not have the luxury of being able to exclude sectors of the population based on English language and, therefore, should consider different suitable language options for their reminder systems. There is scope for catering for different languages with reminder systems. 53,78 For a discussion about framing of information see Reminder plus.
Cognitive ability/literacy level will further determine whether or not a patient will understand the reminder, irrespective of format. These are important considerations for health services serving older populations, travelling communities and inner-city deprived populations, for example. The included studies did not explore this factor and were silent on this point, although two RCTs explicitly excluded those patients with dementia100 or with significant cognitive impairment. 141 Boll et al. 213 describe alternative ways in which reminders may be presented in users’ homes, e.g. using non-speech sound, ambient light and tactile feedback.
Content of the reminder
The addition of different types of content (e.g. orientation, etc.) may be appropriate as part of the reminder system in order to alleviate concerns, fears and anxieties that patients may have about attending an appointment [see Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)] and Chapter 6, Reminder plus. SMS reminders have a limited amount of space in which to convey information and may, therefore, be better suited to simple reminders for follow-up appointments. 59 E-mails and postal reminders may be well suited to encouraging attendance at first appointment reminders as these reminders can be automated and can contain extra orientation information at no extra, or minimal extra, cost. 52,214 Personal telephone reminders have the advantage of being interactive such that specific information can be exchanged between patient and sender. 80 There is little evidence to indicate what patients would find helpful by way of reminder content; however, it is likely that this will depend on the nature of the health service. Patient preferences for the type of information that would be helpful will potentially dictate the choice of reminder system.
Format of the reminder
The appointment reminder immediately prior to a first appointment may also be an appropriate time for patients to receive additional information, e.g. directions to the clinic, or information/reassurance about the procedure. 69 Consequently, reminder systems that support the provision of extra information, e.g. personal telephone calls, e-mail and letter, may be most useful for supporting new patient attendance. Simple reminders, e.g. SMS, automated telephone calls, etc., may most useful for follow-up appointments.
There is generally inconsistent evidence that personal reminders are more effective than automated reminders [see Chapter 4, Evidence statement (B.4): there is controvertible evidence, based on multiple good-quality studies, that personal reminders have a greater impact on attendance rates than automated reminders (evidence category IIa)]. However, on balance, the evidence appears to favour the use of personal reminders. In the larger of the reviews, based on data from 29 studies reporting a total of 33 estimates of reminder effectiveness, the difference between personal versus automated reminders in absolute reduction of non-attendance compared with baseline is around, on average, 10%. 47 It is not known whether or not specific groups of patients, e.g. patients with mental health problems, etc., would show a greater differential increase in attendance as a specific result of the reminder system, but there is evidence to suggest that patients report greater positive perceptions to (and may prefer) personal contact, which may explain the increased level of attendance. 66 It has been suggested by that patients may associate ‘a [personal] clinic staff reminder [compared with an automated reminder] with respect for their own time and higher quality of care’. 77 But the authors continue that ‘. . . according to our survey results, patients found an appointment reminder helpful, but they could not accurately differentiate between a clinic staff reminder and an automated reminder.’77 A comparatively novel feature of reminder systems is the development of interactive automated reminders. 66 This technology offers some of the features of direct contact reminders, e.g. patients can ask for information to be repeated, patients may be able to select from a range of options about specific types of information that they may want to hear about (e.g. appointment procedures or health service location), etc. Given that there is a considerable cost saving in using automated technologies compared with personal reminder technologies (see What are the likely economic impacts of reminder systems?), it would seem that interactive reminder technologies are worth further investigation.
Patient reminder preferences
The included studies do not directly explore the relationship between patient reminder preferences and the effectiveness of the reminder in impacting on patient appointment behaviour [see Chapter 4, Evidence statement (B.4): very few studies investigated whether or not the reminder preferences of the patient may influence the impact a reminder has on the patient's appointment behaviour (evidence category VIIa)]. However, it can readily be postulated that the degree to which a patient is comfortable with the reminder technology used may have an impact on how well the reminder message is ‘received’ and, thus, whether or not the patient chooses to act on it. For instance, some population groups may not regularly use mobile phones and so SMS messages would not be welcome or useful. 208 One study209 found that ‘the reported rates of mobile phone ownership and of the ability to use text messaging were significantly lower in patients with psychotic illness than in those with non-psychotic disorders.’ Therefore, preferences for SMS may be low in this group. A survey of patients attending a neurological outpatients clinic reported that ‘over half of the participants (55 per cent) said they would like a pre-appointment reminder by text message; 19 per cent said they would prefer a telephone reminder while another 19 per cent said they would prefer a reminder by e-mail’. 111
How do organisational factors influence the effectiveness of reminder systems?
No studies investigating whether or not factors about health-care settings influence the effectiveness of reminder systems were identified from this review [see Chapter 4, Evidence statement (C.1–C.6): there are no studies investigating whether or not factors about health-care settings influence the effectiveness of the reminder (evidence category VIIa)]. However, there is a wealth of research that shows that attendance behaviours are linked to health-care settings; however, often the findings are conflicting, indicating that contextual issues may contribute to complexity. Exploration of this evidence offers possible insights into how reminder systems and supporting processes should be designed in order to optimise attendance at outpatient appointments. This section will focus on specific organisational factors that impact on attendance and for which a reminder-based solution might contribute to reducing non-attendance. For clarity, this material is organised into four inter-related themes: (1) administrative errors, (2) characteristics of appointment systems, (3) patient–provider alliance and engagement and (4) clinic accessibility.
Administrative errors
There is strong evidence that reminders are not always received by patients [see Chapter 4, Evidence statement (B.1): there is strong consistent evidence that the reminder may not be received by the patient (evidence category Ia)]. In Accessibility we focused primarily on patients’ ability to access reminder technology; however, health-care systems frequently have incorrect or out-of-date contact details for their patients. 95,208 It is largely intuitive that incorrect patient contact details will lead to suboptimal reminder effectiveness and that the reminder system will be most effective when contact details are accurate and patients receive the reminder. This is a greater problem for health services that are dealing with less geographically stable communities, e.g. populations consisting mainly of students, young adults or socioeconomically deprived groups, who may frequently change address, mobile phones or landline telephone numbers. 103 However, this population is also greatly at risk of non-attendance at appointments (see Chapter 5, Demographic and socioeconomic characteristics). Although the use of reminders can be justified in all health services, there appears to be a particular need in health services dealing with geographically unstable populations. Nevertheless, the use of reminders could be considered redundant unless there are also robust processes in place that regularly check to ensure the accuracy of their patient contact details.
Characteristics of the appointment system
Although several characteristics of appointment systems were discussed in detail in Chapter 5, Characteristics of appointment systems, three main issues affecting appointment attendance are discussed because they are potentially modifiable through the use of reminder systems.
Compatibility of appointments with other commitments
The date and time of the appointment have been shown to be potentially less important than the compatibility of the appointment time and date with other commitments such as employment commitments or child care commitments (see Chapter 5, Timing of the appointment). Such issues exist at an individual patient level and indicate that flexible appointment systems that can accommodate a variety of patient lifestyles are likely to have a lower rate of non-attendance. In this regard, flexibility may mean negotiated appointments for which patients have a say in the day and time of their appointment (e.g. partial booking systems, Choose and Book) or out-of-hours clinics, which may be popular with employed patients who may struggle with work commitments or carers who may then be able to find an alternative carer. Better engagement of patients with the health-care system allows patients to negotiate appropriate appointment dates and times and simultaneously to develop a positive relationship with the health service, which is likely to result in higher levels of attendance at appointments (see Chapter 5, Patient–provider ‘alliance’, communication and ‘engagement’). It is difficult to envisage a justification of a system in which appointments are simply allocated to patients, as this does not recognise the important starting point that a reminder might have for promoting patient engagement and a therapeutic alliance (see Characteristics of the appointment system). However, when this is the case, non-attendance is also likely to be particularly high and, therefore, robust procedures for reminders, cancellations and rescheduling will be warranted.
Long waiting times
There is strong consistent evidence that long waiting times for appointments are associated with higher non-attendance. The long wait could be between the date the appointment was scheduled and the date of the appointment or it could be a long delay between patient referral and the invitation to make an appointment (see Chapter 5, Time to wait to the appointment). The longer the wait, the greater is the likelihood of the patient not attending. A variety of things may happen to patients while they are waiting for their appointment: they can forget, improve or recover, seek help elsewhere, lose motivation to attend or become committed to other more pressing issues. While the government’s priority is to provide non-emergency treatment within a maximum wait137 and, while patients report that short waiting times for treatment are important to them, it is likely that most health-care appointment systems will be exposed to the degrading effects of time on attendance. Therefore, reminder systems that promote attendance are warranted for all health-care appointments. For health-care systems that do have longer waits, particularly when patients have no symptoms (e.g. screening) (see Chapter 5, Symptomatology and severity), are likely to recover (e.g. acute injury and post-surgery clinics) or seek care elsewhere from an alternative health-care provider, we would suggest that reminders that encourage cancellation of unwanted appointments and rescheduling of inconvenient appointments would be useful. This would allow the health service to reallocate cancelled appointments to other patients. It would also be sensible to explain to patients why they have to wait and why the appointment is important.
First appointment compared with follow-up appointments
The studies investigating attendance at first appointment compared with follow-up appointment attendance are inconclusive. Approximately equal numbers of studies show higher non-attendance rates for first appointments or follow-up appointments (see Chapter 5, First versus follow-up appointments). Whether or not patients attend their first appointment may depend on a variety of contextual factors, such as whether or not the appointment was prompted by the patient or the presence of symptoms. Follow-up appointments may not be as highly valued once the symptoms have been alleviated or the concerns dealt with and, therefore, non-attendance can result. However, continued treatment benefits, continuity of care and a valued relationship with the health-care provider may drive continued attendance at follow-ups. On balance, the findings in Chapter 5, First compared with follow-up appointments suggest that the use of reminders is equally valid for first appointments and follow-up appointments, although the reasons for non-attendance may vary between the two groups and may vary by health service. In the section Reminder plus, we suggest that the provision of additional information as part of the reminder system (or as part of appointment scheduling) may be beneficial for facilitating attendance at first appointments, particularly when such information addresses concerns about well-being, anxieties about procedures, concerns about location of the health service, etc. A simple reminder to attend, cancel unwanted appointments or to reschedule inconvenient appointments may be appropriate for follow-up appointments. However, this hypothesis remains untested at this time.
Patient–provider alliance and engagement
There is good evidence that the relationship between the patient and the health service may impact on patient attendance at appointments (see Chapter 5, Patient–provider ‘alliance’, communication and ‘engagement’). Patients are less likely to attend appointments when they feel that staff are being judgemental or lack empathy. 101,145 One interesting difference between patients who seek structured health care and those who do not is the apparent need for the support and reassurance that can be offered by health-care professionals. 145 The provision of orientation information or ‘navigational support’, which is information and guidance regarding the way that the health service works and what to expect from treatment/care, is viewed by many patients to be a positive interaction that would encourage attendance at appointments. 145 This has direct implications for utilisation of reminder systems and the simple act of sending a reminder may increase patient perceptions of the value of the appointment and of the interaction with the health service. 80,145 The provision of information through automated systems is an opportunity to build on that (see Reminder plus). It could be argued that the provision of individualised information to patients through direct regular patient contact would be specifically beneficial for some patients, such as those with long-term health problems and more vulnerable patients. 61 The findings presented here would suggest that reminder messages which are gain-framed would be more welcome than those which are loss-framed and that may be perceived as pressurising, stressful or irritating (see Reminder plus for a brief discussion about message framing).
Clinic accessibility
The available evidence regarding the impact of service location and transport on attendance levels is equivocal and suggests clinic accessibility is not simply a function of travelling time or distance to the clinic (see Chapter 5, Service location and transport difficulties). Some of the reported difficulties faced by patients trying to access clinics were difficulties with getting transport, parking, availability of public transport and cost of travelling, and the impact of these factors is likely to vary between service settings and within patient groups. The impact of transport issues is potentially greater for patients who are more socioeconomically deprived because they may be more reliant on public transport, which may be relatively and prohibitively expensive. Transport difficulties may also be more pertinent to patients with young children or for the elderly who may have problems negotiating public transport systems. Many of the issues discussed here require a broader solution to tackle the problems of patient accessibility in order to increase attendance. However, health services should consider whether or not they can include useful information that could aid the patient journey to an appointment within any reminder, e.g. availability and cost of parking, bus routes, etc., that may encourage patients to make the journey (see Reminder plus for information regarding orientation information). In many cases, patients may know in advance that they will not be able to attend their appointment because of transport difficulties and a reminder that is framed to support cancellation of appointments and rescheduling to a more convenient time may reduce a proportion of travel-related non-attendance (see Are there any systems which effectively support the cancellation of appointments?). It is unlikely to make much difference for patients who encounter travel difficulties while they are en route to their appointment.
What disadvantages (or challenges) should be considered when introducing reminder systems for specific populations for health care and health services?
The principal technologies should not only be considered in terms of their principal characteristics. Technologies may possess additional functionalities that, if activated, may have a differential effect on the effectiveness of the reminder. To take just two examples, SMS technology can be used to deliver a message (one way), to reply with a confirmation of attendance or, in some cases, to effect a cancellation and/or a rebooking. When evaluating text messaging reminders, Leong et al. 72 did not require participants to confirm receipt of reminders. This carried the implication of uncertainty whether or not all participants had received the text messages. In this circumstance, they assumed that those who did not receive messages were more likely to be non-attenders and, therefore, concluded that their study would probably underestimate the effectiveness of text messaging reminder. Similarly, the effectiveness of a telephone-based reminder system, whether personal or automated, will depend on factors such as whether or not a patient possesses an answering machine and whether or not it is acceptable policy to leave a message without speaking to the patient themselves or to a nominated next of kin. Again, Leong et al. 72 made no attempt to leave messages on the answerphone/voicemail, stating that the ‘investigators were of the opinion that most people do not check their voice-mail and there is no way to check if the participants had retrieved their messages’.
Accuracy of patients contact details/clerical errors
Reminder systems rely on accurate and stable data from their patients. Our review has highlighted that contact details of patients are frequently not up to date, incorrectly entered into the database or wrong contact details were given by patients [see Chapter 4, Evidence statement (B.1): there is strong consistent evidence that the reminder may not be received by the patient (evidence category Ia)]. In addition, there can often be clerical errors in the sending out of appointments whereby a patient may receive a reminder intended for another patient. This raises possible implications for patient confidentiality, appointment non-attendance and increased cost and time implications of dealing with errors. Health services need to work hard to ensure that they have robust procedures for updating patient records in order to optimise attendance and cancellation/rebooking systems. 103 An effective reminder system with appropriate cancellation and reminder systems will almost certainly increase attendance and utilisation of health-care appointments (see Are there any systems which effectively support the cancellation of appointments?), which will increase the workload of health-care clinicians. 69 Health services will also need to consider the impact on staff that frequently use unattended appointments as an opportunity to catch up on other health-care-related activities (see Are there any systems which effectively support the cancellation of appointments?).
Inequitable access to reminder technologies
With any reminder system there is likely to be a level of unsuccessful contact; however, some patient groups, e.g. deprived populations and homeless groups, may not have equitable access to landline systems or mobile phone technology. Other groups may not answer the phone and may let the phone run to the answerphone, e.g. patients with mental health problems, deafness or those with poor mobility. Our review illustrates that reminder interventions are not being developed specifically to address inequalities in access to services between population subgroups, nor is consideration being given to whether or not interventions may actually serve to increase disparities (so-called intervention-generated inequalities). Henderson48 observes that the impact of implementing initiatives on inequalities in access to services was not considered by any of the studies included in his review. Health services need to bear in mind the sociodemographic status of the population that they are serving and consider issues of accessibility to reminder technologies of all their patients otherwise they run the risk of increasing inequalities in access.
Reminder preferences
Although many patients indicate that they are happy to receive a reminder (see Other reminder characteristics), there is a risk of antipathy from a sizeable percentage of patients who feel negatively or very negatively about reminders. 55 Those who were disturbed by the reminder gave the following reasons: telephone call too early in the morning, they were waiting for other important results, they were contacted at work, felt that were being treated as senile or felt that the reminder was unnecessary. 78 Evaluations of reminders do not typically examine any inherently harmful effects of reminder systems and it is unclear how reminder preference might influence the effectiveness of the reminder [see Chapter 4, Evidence statement (B.4): very few studies investigated whether or not the reminder preferences of the patient may influence the impact a reminder has on the patient's appointment behaviour (evidence category VIIa)]. We have postulated that how comfortable the patient is with the reminder technology used may have an impact on how well the reminder message is ‘received’ and, thus, whether or not the patient chooses to act on it. If the reminder is irritating, demeaning or badly done, then this could lead to a loss of faith or trust in the health-care service and for some patients, the effect of the reminder could be counter-productive. Potential negative impacts of reminders and reminder preferences should be considered in future evaluations.
Ceiling effects
Several studies suggest the presence of a ceiling effect, i.e. when the baseline attendance rates are already high the potential for improvement is correspondingly reduced. 63 In such cases, the use of complex reminders may simply not be required. Recognising that all patients across all health services will occasionally forget or find that the appointment is no longer convenient, it is likely that simple reminders that encourage cancellation of unwanted appointments and rescheduling to a more convenient time may be all that is warranted in health services with an already high attendance rate.
What are the likely economic impacts of reminder systems?
A full economic analysis of reminder systems is beyond the scope of this review. In the majority of included studies, there is either no or minimal data capture on health economics. However, 11 studies25,43,47,53,57,72,100,102,108,208,215 discussed the cost of reminder systems, using different methods of calculating cost savings and providing sufficient data to create a picture of possible economic impacts. All 11 studies support the view that SMS messaging is a cheaper option than other type of reminders. Hasvold and Wootton47 conducted a systematic review of 14 studies and found that the mean cost of SMS reminders, although it varied from country to country, was €0.14 per patient, compared with €0.90 for telephone reminders. The cost-effectiveness analysis showed that the cost per attendance for the SMS group (¥0.31) was significantly less than that for telephone group (¥0.48). 57 Leong et al. 72 found that text messaging was the cheaper option, as suggested by the total costs, i.e. 87.66 Malaysian ringgit for text messaging reminders and 160.33 Malaysian ringgit for mobile phone reminders’ for clarity. When the authors compared the two reminder systems, the ratio of the cost of text messaging versus mobile phone was 0.55. 72 A US trial in a physiotherapy setting calculated that 19 SMS reminders needed to be sent to prevent one missed appointment. 85 The authors suggest that this system of sending reminders to patients may lead to economic savings when the relatively low cost of each SMS reminder is balanced against the cost of employing a physical therapist for the time of a non-attended appointment. However, they do point out that a formal economic evaluation is needed. Milne et al. 108 calculated that the cost of SMS to reduce non-attendance was £7.50 (US$13.13, €10.88) per ‘no-show’ avoided. Based on number needed to text (NNT) analysis, approximately 14 people would need to be sent a SMS reminder to prevent one non-attendance. 100 Perry et al. 208 stated that the cost of the SMS reminder is minimal, considering the loss of revenue generated by failed appointments. Text reminders on a large scale would be a cost-effective strategy that could be improved. Battistotti et al. 102 calculated costs on an annual basis and estimated that for 500 SMS/day at a unitary cost of €0.0065, the first-year cost will be €11,500, while next-year cost will be about €8200, accounting for SMS and maintenance. They calculated that this would average out at around €35 per day once the SMS system was established. As the average monetary loss of a dropout is €20 per appointment missed, recovering two dropouts per day would be to sufficient to pay for the system. The annual cost of missed appointments in England is estimated to be close to £575M and the use of SMS reminders could save £55.6–83.5M a year. 165
Reminders over the telephone may be expensive when compared with other approaches. 49 In a recent systematic review,47 the average estimated costs from 14 studies reporting phone reminders was €0.90 compared with €0.14 for SMS messages; however, costs of telephone calls vary from country to country. 47 Chiu58 similarly found that with an absolute reduction in non-attendance rate of 9.4–14.82% as a result of telephone reminders, 7–11 telephone reminders were required to prevent one non-attendance. Computing the cost for each telephone reminder by clerical staff at HK$7.44–15.33, Chiu58 estimated that it cost HK$109.37–296.79 for clerical staff to prevent one non-attendance using telephone reminders. In his specific context of radiological procedures, Chiu58 estimated that the cost of wasted computerised tomographic scan appointments offset the cost for the delivery of telephone reminders. This cost–benefit ratio would naturally be less favourable for less expensive interventions. 58 Robert et al. 82 estimated that the cost of telephoning 200 patients could be offset by preventing one non-attendance.
Perron et al. 78 reported results from a stepped approach to reminders, comprising telephone call, text and then postal reminders, and demonstrated that this generated 55 additional consultations. The intervention proved to be cost-effective in providing a total net benefit of €1846 per 3 months once the cost of the intervention had been deducted. Bech215 concludes that very few studies include more than one intervention. This, combined with the fact that very few report information on the cost of the intervention, enables only vague conclusions about the cost-effectiveness of the interventions to be made.
Charging a fine for missing appointments is unlikely to be cost-effective as the cost of charging and collecting a fine includes personnel time, setting up information technology (IT) facilities and accounting systems, postal and reminders cost. 215 These costs have recently been estimated in Denmark to be around 40 Danish krone per fine at 2003 prices. At first glance this appears to be more costly per unit than letter and telephone reminders; however, these administrative costs are generated only for non-attendees whereas letter and telephone reminders by their very nature generate a cost for every scheduled patient; therefore, fines may very well be cost-effective because of their low average cost per patient. However, these estimates would need to be tested in various UK settings in order to determine whether such a system is feasible or, indeed, acceptable. Whether or not charging a fine is cost-effective would depend partly on the cost of the appointment and partly on whether or not non-attendances decrease. As non-attendances decrease, so the unit cost of administering the fine increases.
Methods: strengths and limitations of the review
When discussing the strengths and limitations of our review, it is necessary to highlight three complementary aspects. First we need to consider the strengths and limitations of the systematic review method, then we need to consider the strengths and limitations of the review informed by realist principles and, finally, by recognising that any review will only be as good as its included studies, we encounter the collective limitations of the evidence base. As the last of these has important implications, both for current practice and for future research, we have highlighted the limitations of the evidence base separately, in Limitations of the evidence base.
Strengths and limitations of the systematic review
Generally speaking, the systematic review method seeks to provide a precise answer to a tightly focused question. Such reviews tend to be most useful when there is a high degree of homogeneity around the five PICOS elements: the population, intervention, comparison, outcomes and study types. As can be seen from our description of findings in Chapter 5, such homogeneity is not present in this particular review. A wide range of population types is included within the RCTs we identified. This variation by population is seen in the clinical settings, countries and age groups studied in the included studies. Some populations are recruited completely randomly, increasing our confidence in the applicability of results in a real-world setting. However, others either established technology preferences prior to the study or excluded those who did not have a particular technology (e.g. mobile phones). The reader should, therefore, carefully examine the number and nature of participants exiting the study prior to randomisation before drawing conclusions on real-world effectiveness. In addition, two studies targeted non-attenders, but not in comparison with a general population. 64,83 As a consequence, we are unable to advise on specific strategies for the non-attending population – an otherwise viable decision alternative to blanket coverage.
Further variation is observable in the interventions. Although it is not unusual for a systematic review to examine, for example, different drugs within the same therapeutic class, this is quite different from appointment reminder systems for which different technologies employ vastly different mechanisms. Such variation is not simply evidenced in the technologies themselves [e.g. synchronous (SMS text) vs. asynchronous (letter); interactive (personalised telephone call) vs. non-interactive (e.g. automated calls); or mobile (SMS/mobile) vs. ‘static’ (letter/landline)]. Different studies use different features of the technologies, for example reply slips (post),56 acknowledgements/confirmations (SMS)56 or answerphones (for landlines). 66,84 Included studies also follow different protocols with regard to, for example, the number of attempts to be made and whether or not leaving a message on an answerphone constitutes successful contact. Such heterogeneity makes it extremely challenging to attribute success to a particular technology and/or to a specific component feature.
Notwithstanding a fairly plentiful body of studies, the number of different interventions being compared and, in addition, the number of supplementary questions they simultaneously seek to answer (e.g. comparing nurse calls with doctor calls, 3-day with 7-day intervals, etc.) adds a vast array of comparators with only single studies occupying many of the intervention–comparator matrix cells. Some interventions compare adjunct interventions, e.g. postal reminder plus SMS text reminder, while one intervention in particular has a stepped approach proceeding through telephone, SMS then post. 78
The domain probably experiencing least heterogeneity is that of outcomes. Attendance rate (expressed alternatively as its converse, the no-show rate) is ubiquitous among the studies. A limited number of studies report cancellations, and an even lower number examine rebookings. Clearly, all three are required for an understanding of interactions and ‘knock on’ effects. This commonality of outcome did help our review team in performing some preliminary comparisons that showed, for example, that attendance rates for non-diagnosis specific situations, such as blood donation, are generally lower and that paediatric studies tend to report higher attendance rates than other populations, particularly compared with adolescents. However, such apparent conformity belies variation in how attendance or cancellations are actually defined. In some cases, actual attendance is collected while, in other cases, an operational definition depends on the timeframe within which a particular service can respond.
With regard to study type, this particular area of investigation is well travelled by systematic reviews but is complicated by differential inclusion of study types. Our systematic review included only RCTs and, as a consequence, it became challenging to compare our included studies with those in several existing systematic reviews.
It is important to note that the scope of the review required a specific focus on appointment reminder systems. While this opened up a fairly substantial body of evidence, it did restrict the team by excluding studies about appointment behaviour. The focus on RCTs further restricted the number and types of question that these studies could address.
Our systematic review has numerous strengths, including a structured search protocol requiring thorough searches of electronic databases, reference lists and citations. As a consequence, we believe that we have assembled the widest possible body of relevant knowledge. Comparison with other systematic reviews demonstrates the improved currency and coverage of our review combined with a sole reliance on properly conducted RCTs, which led to increased rigour and robustness of studies. To extend our coverage in a field that is rapidly changing, we conducted various internet searches to identify new developments. While we acknowledge that innovation must be accompanied by evaluation, this at least ensured that the team was aware of the main directions for future travel. The rigour of the process was ensured by various mechanisms such as the use of multiple reviewers, regular consensus processes and checking of newly identified studies against original sift criteria.
There are also limitations to our review. Our review was limited to English-language literature, but we consider this acceptable given the intended audience for this review. However, it should be noted that published, non-English reports are not identified in our report. Our reporting and assessment of each study was limited to data in each published article with no attempt made to contact the authors for additional information or missing data. Assessments of quality are based on the reporting of study details, which is regarded as an adequate surrogate but may not equate to the quality of the conduct of each study. An additional limitation to this review stems from the potential for publication bias whereby studies that demonstrate positive results in favour of a particular technology are more likely to be published.
We can conclude that the systematic review component followed accepted guidelines for conducting such reviews. It utilised a clearly focused question that was easily operationalisable in terms of inclusion and exclusion criteria. However, as we freely acknowledge, the topic area itself possessed several complexities. Decisions we made at the systematic review stage therefore carry associated ‘knock on’ implications for the review informed by realist principles as discussed below under Strengths and limitations of the review informed by realist principles.
Strengths and limitations of the review informed by realist principles
Methods for realist review (also known as realist synthesis) are still in their relative infancy and standards for conduct and reporting are still subject to ongoing development. Our review team recognised the value of exploring the complexity of appointment behaviour as it determined interaction with appointment reminder systems. However, we had concerns that our overarching aim was to inform practical recommendations for appointment reminder systems, not only to generate explanatory theory. We followed realist principles by starting from outcomes and then seeking to identify upstream determinants that may have influenced appointment behaviour. We consider context to be informed by four principal considerations (personal, organisational, trial and problem context). 216 Personal context includes personal characteristics such as age, gender, sociodemographic and employment status. These attributes can variously act as ‘baffles’ to damp down the signals from the appointment reminder or as ‘amplifiers’ to give a reminder additional urgency and/or importance. Health-care organisations can create a culture within which attendance, or indeed non-attendance, becomes the norm. Paradoxically, flexibility of appointment systems may be misinterpreted as either a ‘couldn’t care less’ or an ‘it’s not that important’ mentality and could aggravate non-attendance trends. All staff, clinical and administrative, have an influence in creating and/or communicating this culture. The trial context relates to some of the decisions that may be taken in the context of a trial protocol that might not be carried through in a real world situation. This might include the number of attempts that is reasonable or feasible to make to contact a patient via telephone or counting patients as non-attendances when they have actually used the opportunity to rebook. Finally, the problem context refers to the way in which the nature, scale and cause of the problem may shift (with varying and sometimes unknown impact on its size and frequency). Other national and/or local policy factors may determine patterns of attendance, which may result in oversimplification of the mechanisms of effect. Even using the tools suggested by realist synthesis methods such contextual challenges continued to pose a significant challenge.
Realist synthesis itself poses a challenge to systematicity in that its processes are iterative, intuitive and often defy audit and transparency. We used the systematic review principles described above to ensure that we constructed a transparent and well-defined sampling frame. Characteristics of identified studies were plotted on our ‘PopInS’ matrix to map the landscape for our question; however, once we had extracted and analysed all systematic reviews and RCTs to address the questions relating to effectiveness, we faced a decision as to how to prioritise the remaining studies. We decided to focus on UK studies and, in particular, to pay closest attention to those studies that supplied data against the various aspects of the conceptual framework.
Several decisions made in connection with the earlier systematic review had implications for the subsequent review informed by the realist principles. These included:
-
Appointment systems for screening programmes for which a patient is required to respond by booking an appointment. These were characterised as ‘recall’ systems not ‘reminder’ systems and were therefore, excluded from the review. We argue that the action of booking indicates the presence of some extrinsic motivation for fulfilling the appointment thus making attendance atypical from appointments in general. However, such an exclusion may seem arbitrary alongside such systems as Choose and Book, which are included in our review, and indeed the extra interactions required by, for example, systems requiring postcard and/or reply-paid confirmations. It is possible, however, that an exploration of recall systems might contribute to our further understanding of motivations for appointment attendance and how these might be harnessed within a reminder system.
-
Interventions that include not simply a ‘reminder’ but also some therapeutic interaction, typically via the telephone. Clearly there is a substantive difference between a member of administrative staff telephoning with factual details of a time and location of appointment and a clinically qualified staff member offering reassurance, advice and treatment options, etc., along with an exhortation to attend a forthcoming appointment. Such therapeutic interactions may be particularly important in the contexts of counselling, health promotion and psychological therapies, etc. However, it is methodologically challenging to isolate the reminder component from the therapeutic component and, therefore, we chose to exclude such studies from our systematic review. Nevertheless, our review informed by realist principles identifies ‘engagement’ with treatment, service or health provider as a likely contributor to attendance behaviour. It is again possible that an exploration of therapeutic communication may contribute further insights and offer value added services that can be easily integrated with the basic reminder function. Indeed, such a distinction becomes even more blurred where health promotion information is included with a SMS reminder or when an orientation statement is included with a postal reminder (both included).
-
The content of SMS text messages, telephone calls and letters is poorly described in many included studies. Little attention is given to the ‘framing’ of any spoken or written communication. Framing is a significant area of research in disciplines such as psychology and information science and it is likely that assumptions on what is the default position (assume to attend or assume not to attend), to use one example, will have an effect on the effectiveness of reminder systems. We highlight the impact of such framing in our discussion on ‘nudge theory’ (see Nudge theory and custard creams), but only in connection with the collective behaviour of a practice population. However, there is clearly significant potential for further exploration in terms of effects on individual behaviour, both in terms of theory-building and subsequent empirical inquiry.
The strengths of our review informed by realist principles include the strong embedding of our propositions in the extracted data. This stems from the practical orientation of our review and facilitates the production of implications for practice.
A weakness of our review, and yet a corresponding strength, is the fact that, unlike realist synthesis, we did not settle on a single theory as an overarching explanation for what can be observed in the very complex situation of appointment attendance and non-attendance. We engaged with a full range of theory operating at different levels and originating from different disciplines, in a sense problematising the literature as a collective evidence base, analogous to critical interpretive synthesis methods. It is, therefore, not entirely coincidental that we discovered resonance with the work of Dixon-Woods et al. 168 nor, indeed, that those authors chose appointment attendance as one case by which they explained their own findings. Our steering group encouraged us to identify a leading candidate theory in the quest to simplify the subsequent review process. However, the review team strongly believed that no single theory served to explain all aspects of the phenomenon of attendance and the effect of appointment reminder systems. To the contrary, we sincerely considered multiple theories, in total or in part, to stimulate our interpretation of the problem. This is but one reason why we prefer to describe our review as being ‘informed by realist principles’.
Scope
The scope of our review was limited by both practical and conceptual constraints. Our original intention was to characterise the response to appointment reminders by different population groups. We hoped to find RCTs that measured population differences at baseline and then again following completion of the intervention. Subsequently, it became clear that the research agenda privileged investigation of the technologies and of the reminder processes over and above exploration of population differences. We encountered numerous instances when investigators chronicled the baseline differences in attendance, but did not examine the differential effect of the intervention. As a consequence, we have gained valuable insights into what challenges exist for particular populations without being able to select the best candidate solutions. Such a finding leads us to a null hypothesis that there are no population-specific differences in the effect of an intervention other than those already observed in the population at baseline. A more sophisticated variation of this line of thought might suggest that rather than certain reminder interventions improving appointment attendance for particular groups, the reverse perspective is true, namely that these technologies carry intrinsic properties that impair the achievement of the full potential effectiveness achieved by the population on average. If this is indeed the case, then one might envisage that removal of such barriers, unless differentially targeted, would also benefit the population in general, thereby perpetuating, rather than removing, inequalities in access to health care.
When it became clear that our principal review question would not be answered by rigorously conducted RCTs, we faced the challenge of accessing a wider evidence base. However, clearly there is an expectation that we summarise the findings of systematic reviews and trials. As a consequence, we found ourselves expending significant resources exploring the trial literature with a reduced prospect of such sources answering our questions of principal interest. In turn, this had a cumulative effect on the review informed by realist principles for which, again, we prioritised studies of appointment reminder systems but increasingly found that useful insights were being generated by other bodies of literature (i.e. appointment behaviours, behavioural economics, communication and framing of health messages, interactions and consultations with health professionals, operational research and modelling, etc.). We intend to continue making such productive connections over and above the resources of this project by exploring alternative funding for research projects and fellowships.
Limitations of the evidence base
It is a truism in review methodology that a systematic review is only as good as its included studies, and this has been our collective experience in relation to this review. On the positive side, interventions relating to appointment reminder systems are relatively straightforward to undertake as they typically involve either offering alternative routes for communication (a relative advantage model) or providing a system when one had not previously existed (a service enhancement model). As a consequence, and partly because this particular form of experimentation is often integrated with routine administration, several included trials have succeeded in recruiting large study populations. However, motivation for change is frequently a ‘technical fix’, and this has several implications for the research evidence. There is little evidence of a systematic and priority-based pursuit of the research agenda, or even of a close-knit research community within this area, with most contributions being locally focused and opportunistic. Scant attention has been paid to those who are typically excluded from population-based solutions to attendance. For example, Neal et al. 110 are among the few who observe the difficulty of studying attendance behaviour, specifically in the context of unmet mental health problems. They recommend that ‘more work needs to be done to engage people who miss appointments with research in a more meaningful way’. 110 This requires creativity in the use of research methodologies, in recruiting participants and, subsequently, in devising appointment reminder or service solutions. There is a particular role for qualitative methods given the review team’s experience of the value of such studies to our understanding of appointment behaviour. Rather than the ‘averaging effect’ documented so thoroughly by systematic reviews and trials, there is a need to extend such work to ‘other “disengaged” or potentially vulnerable groups of patients’. 110
Therefore, it is particularly worth highlighting additional complexity in that those who fail to engage with appointment systems, and, indeed, health services in general, will also represent those informants who are most challenging to access when performing observational (i.e. non-representative) or research studies (i.e. uneven recruitment) of appointment behaviour. Commissioners of health services, and specifically those designing appointment systems, should therefore be aware that, even if they take steps to investigate non-attendance behaviour, there is still a danger of creating solutions predicated on the views of a vocal ‘more easily researchable’ minority.
The most significant omission from all the effectiveness studies was contextual detail on the working assumptions under which each clinic or service scheduled its appointments. In applying the findings of research studies to their own practice, service managers would find it helpful to know whether the clinic was designed to operate at overcapacity, thereby bringing the actual rate down to 100% once non-attendances have been taken into account, or whether appointments were booked at 100% capacity with the consequence of underutilisation or scheduling of alternative activities in the light of subsequent no-shows.
Another important limitation of the evidence base relates to mobile phone ownership. Some studies, for example the RCT by Leong et al. ,72 randomised patients after establishing mobile phone ownership. This is the technological equivalent of an efficacy trial that overestimates the effect of an intervention when compared with its real-world performance. To adequately explore the impact of reminder technologies in a health service setting, it is necessary to employ an intention-to-treat analysis approach for which patients are randomised before ascertaining mobile phone ownership. This would be analogous to taking lack of compliance into account when planning pharmaceutical trials; however, this creates both ethical and practical issues. As a result, the effect sizes achieved by many of the trials are seen to be artificially inflated.
Other emergent interpretations
In the absence of evidence on the differential impact of particular appointment reminder systems on different populations, aside from factors already present in the population preintervention, what valuable insights might we offer from the course of our review? Our own thinking has been enhanced with regard to the following:
-
That factors apparently indicated in leading to patients being more likely to attend their appointments are perceptions of importance, severity, timeliness, engagement with the service, clinician and/or clinical problem, and the perception of an appointment being an ‘event’ rather than something routine or mundane.
-
That ‘forgetting’ includes both genuine forgetting and forgetting as a non-judgement-laden excuse.
-
That conventional characterisation of attendance as an optimal outcome and non-attendance as a poor outcome are challenged by adopting and attempting to reconcile different perspectives, in particular those of the clinicians, the administrative staff and the patients.
-
That rather than problematising patients as being particularly poor attenders, those managing and delivering services could view non-attendance rates as key indicators of such aspects as lack of flexibility, inadequate allaying of anxiety or unwelcoming staff or premises. The challenge is diagnosing which of these pathologies is predominant in a particular setting.
-
That length of delay in appointments is a critical consideration that impacts across multiple aspects of attendance, including self-resolution of symptoms, perception of non-urgency or non-importance, inappropriate referral and disengagement from the service, clinician and/or clinical problem. Actual length of delay is exacerbated by undesirable connotations associated with periodic (i.e. non-patient determined) follow-up intervals bearing little relation to patient needs.
-
That patients may be encouraged to attend by employing principles from ‘nudge’ theory that includes reinforcing positive norms, use of service-enhancing not service-limiting defaults and memory retention strategies.
-
That feasible solutions to attendance problems may be best re-engineered if tackled within the overall context of integrated service delivery and not simply within the relatively stand-alone subroutine of appointment reminders.
The appointment as an event
Ambiguity: importance of appointment as an event will increase the likelihood that patients attend, up to a point. However, beyond this point it may simply increase anxiety. Similarly on the one hand doctors want to appear supportive, reassuring and alleviate anxiety; however, they may want to stress the importance of attending the appointment.
Lest we forget – or forget about forgetting
Forgetting consistently features as the most commonly cited reason for missing an appointment. However, results on reminders, e.g. 24-hour or 48-hour reminders, show no significant differences in effectiveness for these intervals. This suggests that the reminder function is not the most important consideration for the communication between service and patient. If timing of the message is not significant from a patient viewpoint then we can reverse the direction of the imperative and determine the reminder interval by the time period within which a service can best accommodate cancellations and rebooking. Such an approach does seem to fly contrary to the literature, which almost unanimously confirms the orthodoxy that reminder systems are for the express benefit of the forgetful patient. In fact, it is the service that stands to benefit most, not from the reminder itself but from the response that it triggers either in terms of notifying the service of cancellations or initiating rebooking at a more convenient time. However, such a response becomes useful only if notification is received in sufficient time for the service to reallocate the vacant slots to other areas of clinical need.
Further support for this counter-narrative that appointment reminders systems are primarily determined by considerations of service scheduling, not of assisting the forgetful patient, is seen by attitudes to late arrival, which were seen as more disruptive than non-attendance. In the study by Martin et al. ,5 professionals felt that it was, in fact, even more disruptive if patients turned up late for an appointment than it was if they did not attend at all.
However, from a patient perspective it seemed that patients were unaware of the implications of turning up late for the practice. The impression, from previous experience, of waiting past their appointment time for their actual appointment had misled them into thinking that the practice would be quite relaxed to their late arrival. This reinforces the idea that norms around attendance may be either consciously or subconsciously reaffirmed by health service staff as much as by fellow patients. At this point it should be emphasised that health services staff working in the same service or at the same location will not necessarily communicate unambiguous messages regarding the values associated with attendance. For example, in the study by Martin et al. ,5 receptionists were more concerned than GPs about missed appointments, possibly because of the greater disruptive effect that non-attendance had on reception staff. Hussain-Gambles et al. 104 also found that receptionists felt that they were most affected by non-attendance and wanted GPs to address this in consultations with patients. GPs were more guarded about this, being more fearful of damaging the doctor–patient relationship. 104
What are desirable outcomes?
Our review informed by realist principles yielded some interesting insights on what might be considered a good or bad outcome. First cancellation, although an irritation to administrative staff, could be seen as a desirable outcome provided that the system has the flexibility to compensate for the non-attendance of the particular patient and the welfare of the patient is not impaired, e.g. there is no disease window of opportunity that is missed by deferral.
A key variable that is not addressed by any of the studies is the underlying assumption around clinic capacity, i.e. is the clinic booked at 100% capacity with cancellations providing much needed respite or is a clinic booked at overcapacity to allow for 100% attendance following the inevitable withdrawals. All recommendations and planned interventions should be moderated by an understanding of this underpinning service rationale.
Such ambivalence could also be observed from the viewpoint of the individual clinician. 5 Missing appointments may be seen to offer some respite from an often relentless stream of appointments and offered clinicians the chance to catch up with note writing or other administrative tasks. 5
However, reception staff themselves found missed appointments more frustrating and irritating than GPs. They talked about how hard they had worked to find patients an appointment slot. If this appointment was then wasted, there were fewer appointments available to other patients. 5
Reaction to a reminder in terms of cancellation can be considered a valuable trigger of a service response by reducing the uncertainty of whether or not the patient is going to attend. A system of telephone reminders, particularly because it offers interactivity, not only reduces the non-attendance rate, but also decreases the uncertainty associated with non-attendance. Therefore, health-care managers become more able to control the workload, plan duty rosters and allocate health-care resources.
There is some evidence to suggest that ‘forgetting’ is readily adopted as a ‘blame-free’ explanation for non-attendance and may therefore be used as an avoidance strategy against articulating other priorities or reasons that may not be so readily accepted. 5,12,56 Qualitative evidence suggests that ‘forgetfulness’ is used as an umbrella explanation for non-attendance when subsequent explanation reveals other more tangible factors. 5,12 For example, Martin et al. 5 observed that, following an initial explanation of forgetfulness, numerous patients identified a variety of employment and family-related factors which might become a higher priority than attending the appointment.
Nevertheless, figures from our effectiveness review demonstrate a consistent effect of any reminder suggesting that genuine forgetfulness does indeed play a significant, if less prominent, part. Such a ‘smoke screen’, perhaps in response to perceived or actual judgemental behaviour from clinicians or administrative staff, ironically performs a disservice when it comes to understanding appointment behaviours and developing effective reminder strategies. Only if candour, in a non-judgemental blame-free context, can be elicited by researchers and replicated in interactions with health service staff will service managers be able to devise appropriate patient-focused solutions to problems of non-attendance. In the course of our review informed by realist principles we have found that the observations of Dixon-Woods et al. 168 resonate with our own work, namely that attendance behaviour research displays a consistent tendency to problematise the patient, not the service. The phenomenon of ‘convenient forgetting’ should not be allowed to mask the fact that certain sections of the community are particularly prone to genuine forgetting, for example the elderly or those experiencing symptoms of dementia. Clearly it would be retrograde to imprint suspicion of the explanation of forgetting too vigorously in the minds of those managing appointment rescheduling.
Voting with their feet
Non-attendance rates can be viewed as a way of patients expressing their reaction to the perceived inaccessibility or inflexibility of the service. If cancellation is easy (and does not subject a patient to disapprobation), then a service will gain valuable opportunities to reschedule other patients or for clinicians to plan to utilise downtime effectively. If services are flexible in terms of good availability of clinical services then cancellations and rebookings will be low. Very little attention is paid in the literature to attendance and cancellation rates as a diagnostic indicator for a service manager in assessing how their service performs with regard to access and availability. Instead, the research literature focuses on ‘fixing’ the problem rather than on understanding it and re-engineering innovative service solutions.
Another way in which poor attendance rates can be seen as a diagnostic indicator relates to inappropriate referral. Patients may fail to attend an appointment because they no longer consider it necessary, a condition may be self-resolving, a crisis point may have passed and been successfully negotiated or a patient may have arrived at a view that their referral is no longer desirable or necessary. In health-care systems that maximise patient choice, through availability of other health-care providers, a patient may simply have gone elsewhere for resolution of their condition.
Inappropriate referral and self-resolution of symptoms are two possible explanations for the commonly reported phenomenon of high non-attendance for appointments located in the distant future from onset of symptoms. Another factor, which itself may lead to patients concluding that their visit to a clinician is not entirely necessary, relates to signals that conflict with a sense of urgency. As a result of our review informed by realist principles, we hypothesise that any single factor or combination of factors that attributes importance or significance to attendance at a particular appointment serves to create a sense of that appointment being an ‘event’ rather than being routine or mundane. These signals may emanate from the individual patient (e.g. the severity of the symptoms), from the disease trajectory (e.g. the sense of a limited ‘window of opportunity’), from the service (e.g. a battery of tests or procedures in close succession) or from the health staff (e.g. how urgently they treat scheduling of an appointment or how they react to cancellation of an appointment). This ‘event’ hypothesis possesses explanatory power in terms of the frequent use of forgetfulness as a reason for non-attendance – in general, we are less likely to forget those occurrences that have acquired the status of an ‘event’.
A further hypothesis relates to the importance of creating a sense of ‘engagement’, whether this be engagement with the service, the treatment or the therapeutic relationship. Patients who are more engaged are more likely to prioritise their attendance at appointments and to take such appointments seriously. In terms of appointment reminder systems, various degrees of engagement are possible. These include speaking to a member of health service staff rather than an automated message, speaking to the clinician handling your case and interactively acknowledging that you will attend an appointment – the ‘symbolic contract model’ mentioned in Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminders plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa).
Within the specific context of help-seeking for mental health problems, commentators have described the interplay of approach–avoidance conflict whereby an appointment holds both the potential of resolution of symptoms and exposure to a stressful situation. 217 This tension neatly captures some of the ambiguities encountered in the course of the review informed by realist principles whereby an appointment can be seen as both a positive and a negative event leading to markedly alternative ‘futures’.
Carrots, sticks and sermons
It has been suggested that a three-part classification of carrots, sticks and sermons is one way of characterising three different approaches to changing behaviour. This classification could be applied to the content of the reminder messages and how they are framed. Carrots can refer either to financial or other tangible incentives or to positive ‘strokes’ aimed at appealing to personal reward (you will be treated in a timely fashion, you will reduce your uncertainty promptly, etc.) or social good. Sticks can again be tangible (as in financial penalties) or affective (e.g. if you don’t attend then . . .), perhaps in provoking a guilt response. In a health education context, sermons refer to information that tells patients why reminders are good for them. Appointment reminder messages would tell you the health consequences of missing the appointment, particular if there is a relatively narrow window of opportunity with regard to the particular condition. It is our perception that there is a considerable body of literature on these phenomena in a health education context and yet, except when health promotion messages are included with appointment reminders, this evidence is largely divorced from the reminder context.
Do I really need to go?
Except in a mental health context for which patients may have an impaired sense of determining their need for treatment, it may be reasonable to expect patients, particularly those with a chronic self-managed condition, to be able to judge when they need an appointment. However, certain conditions may have a brief and critical window of opportunity which, if missed, can lead to severe consequences in terms of patient health and/or health-care resource utilisation. In addition, if members of health service staff endorse inappropriate over-utilisation they may perpetuate such a situation. Alternatively, if they appear too judgemental, they may discourage utilisation all together. Regular, unmediated appointment intervals may be viewed as an alternative to more sophisticated communication and interaction between patient and clinician and to facilitate informed patient self-determination in decision-making. It also may be viewed as a defensive procedure to minimise risk of negligence. As mentioned under Carrots, sticks and sermons, patients may receive ambiguous messages about the importance of the appointment particularly if there is a juxtaposition of a ‘task-focused’ view from the administrative staff with a ‘person-focused’ perspective of the clinical task. Of course, these roles are equally problematic if the perspectives are reversed.
Nudge theory and custard creams
Current thinking on mechanisms for effecting behavioural change is heavily influenced by the so-called ‘nudge theory’. Nudge theory has its origins in behavioural psychology and economics and is currently being promoted by the ‘behavioural insights team’ at the UK Cabinet Office. Nudge theory suggests that making it easier for people to take a healthier or more socially acceptable course can prove more effective than introducing legislation or penalties. Of particular relevance to the problems associated with appointment attendance are experiments being trialled with regard to payment of taxes or fines. Initiatives, such as sending personalised text messages urging people to pay fines and including images of untaxed vehicles in demands for payment of duties, have demonstrated initial success. Other suggestions include highlighting key information in bold or ‘strong’ colours, using lotteries or prize draws as an incentive for prompt payment of taxes and sending ‘thank you’ letters to people. Clearly some, although not all, of these approaches have direct implications for appointment behaviour and appointment reminder systems. For example, Hayes et al. 218 describe how they initiated a behavioural contract to increase appointment keeping among low-income families in a child and family therapy programme. Such families received US$30 in coupons at attendance at four consecutive appointments with costs offset against the potential cost of broken appointments.
This potential for social influence or ‘nudge’ theory has recently been explored in the specific context of those who did not attend appointments. Martin et al. 142 describe three interventions tested in GP surgeries in NHS Bedfordshire that could be implemented quickly and appear to be cost neutral.
-
Patients calling for an appointment should be asked to repeat back the time and date of their appointment before the call ends.
-
When booking follow-up appointments, patients should write down the time and date on an appointment reminder card rather than health-care or reception staff doing it for them.
-
Replacing common signs that communicate the number of patients who did not attend appointments in previous months with signs that conveyed the much larger number of patients who do turn up.
These first two interventions correspond to our ‘engagement’ hypothesis in that they seek to increase patient participation, thereby either reducing did-not-attends or at least increasing a sense of responsibility such that those subsequently unable to attend would call and cancel. Surgery staff booking appointments over the telephone asked patients to repeat back the time and date of their appointment before ending the call. This led to a 3.5% reduction in did-not-attends, which is comparable to the minimum gains made by moving from no reminder to using any form of appointment reminder system. The second intervention, asking patients to write the time and date of their follow-up appointment with a nurse on the appointment card themselves, rather than the nurse doing so, led to a reduction in did-not-attends of 18%. This figure equates to some of the highest gains made when introducing reminder systems.
Finally, Martin et al. 142 turned their attention to the idea that publicising the number of patients who did not attend via posters on waiting room walls or TV monitors might increase rather than decrease did-not-attends. By drawing attention to the regrettable frequency of unwanted behaviours they understood that this would be likely to normalise such behaviours thereby resulting in increased occurrence. They replaced these signs with posters that conveyed the much larger number of patients who did attend. When this intervention was combined with the verbal and written commitment-led interventions described above, this resulted in a 31.7% reduction in did-not-attends compared with the average of the previous 12 months. While caution should be expressed at the use of relative, rather than absolute, figures for improvement, particularly when there is no way of knowing what the baseline rates were and whether they are high or low when compared with typical practices, it is clear that low-cost behavioural interventions should at least merit as prominent place in the future research agenda as high-technological ‘fixes’.
Service inertia
One of the attractions of the approaches by Martin et al. 142 is involvement of practice staff in the diagnosis and resolution of problems associated with non-attendance over a coffee break, hence the ‘custard creams’ of the article title. This is particularly to be welcomed given that there is some evidence to suggest that health service staff may act as a barrier to the development of innovative patient-friendly solutions that overcome obstacles to their attendance. In the study by Martin et al. ,5 patients described difficulties in getting through to the surgery by telephone, as lines were often busy. Interestingly patients did express the perception that getting through to the surgery might have enabled others to take advantage of a cancellation slot, although there was no evidence that the practice offered such flexibility. This suggests that if services were able to actively demonstrate that they were able to reutilise slots freed by cancellations, an ‘altruistic’ subset of patients might choose to phone in to cancel, providing that the structural barriers, such as engaged telephone lines, were removed. However, there was evidence from this particular study site that the surgery problematised the patients, not the service. This attitude may explain an apparent inertia from this surgery in response to the suggestion concerning a dedicated cancellation line or facility to use SMS text messaging as a means of cancelling an unwanted appointment. In fact, staff expressly rejected these suggestions from patients as being impractical to implement or difficult for existing staff to manage. 5
Clinical implications
General implications
In this section we provide an overview of findings that are potentially relevant for all health services. All reminders are effective at improving attendance at appointment. Simple reminders which provide details of timing and location of appointments are effective at increasing attendance at appointments and would appear to be useful for all patients, across all health-care settings, who are at risk of forgetting their appointment [see Chapter 4, Evidence statement (A.1): there is strong consistent evidence that simple reminders which provide details of timing and location of appointments are effective at helping a (forgetful) patient to attend their appointment (evidence category Ia)]. There is also weak evidence that ‘reminder plus’, which provides additional information over and above date, time and location of the appointment, is more effective than simple reminders at helping a patient to attend their appointment [see Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)]. Orientation information and information about health services and procedures may be helpful at reducing perceived obstacles to attendance, although more high-quality research is required to confirm this. We speculate that ‘reminder plus’ may be particularly useful to facilitate first appointment attendance and attendance at screening appointments, and that simple reminders may be appropriate thereafter for most patients and most health services, most of the time (see Reminder plus), although this hypothesis requires further testing.
Appointments can be scheduled at inconvenient times, become inconvenient owing to a change of circumstances or no longer be required for very many reasons that have been discussed in this review. This indicates that all patients are likely to be unable to attend an appointment (whether it is a new appointment or a follow-up) at some point (see Previous patterns of non-attendance). Unless patients indicate that they do not want to receive a reminder, we recommend that all patients should receive a reminder or ‘reminder plus’, which recognises this as true and actively encourages patients who are unable to attend to cancel their appointment and to reschedule if further appointments are required (see Are there any systems which effectively support the cancellation of appointments?). We further recommend sending the reminder around 3 days in advance because although timing of a reminder between 1 and 7 days prior to the scheduled appointment has no effect on patient attendance behaviour, this will allow sufficient time for patients to cancel and health services to reallocate the cancelled appointment to another patient [see Chapter 4, Evidence statement (B.5): there is strong consistent evidence that the timing of a reminder, between 1 and 7 days prior to the scheduled appointment, has no effect on patient attendance behaviour (evidence category Ia)] or allow the clinician to undertake care-related administrative tasks, e.g. telephone calls, discharge letters, etc. (see Are there any systems which effectively support the cancellation of appointments?).
We found many examples in the literature of inefficient reminder activity (e.g. poor patient accessibility to reminder technology, incorrect patient contact details and human error) leading to suboptimal reminder effectiveness (see Accessibility) and poor resourcing of reminder systems. To optimise attendance, cancellation and rescheduling, there needs to be robust procedures to ensure that patient contact details are up to date. There needs to be easy-to-use, probably multiple, systems for cancelling appointments that suit the needs of the patients and not just the needs of the service, e.g. automated SMS cancellation, answerphone, e-mail, etc. Robust rescheduling procedures need to be in place to allow easy rescheduling of appointments for patients, both within and outside normal working hours to provide patients with flexible opportunities. Finally, an effective reminder system will increase the workload on clinical staff and services will need to build in alternative administrative time for staff that frequently utilise non-attendance at appointments as an opportunity to catch up on other health-care-related activities (see Are there any systems which effectively support the cancellation of appointments?).
We found few studies investigating the differential effectiveness of reminder systems for population subgroups. Consequently, we have provided a narrative overview of literature generated by our review, to identify groups who are at higher risk of non-attendance. In general, contrary to the popular view, our review provides no evidence that age, gender and previous attendance patterns predicts non-attendance but it does show that key groups at high risk of non-attendance are related to deprivation status, ethnicity, substance abuse and comorbidity/illness (see Chapter 5, Patient characteristics). Our findings suggest that reminder system choices need to be carefully considered in order to maximise accessibility for these key patient groups. Simple reminders and automated reminders to attend may be ignored or overlooked and may put these patient groups at a disadvantage compared with general outpatient populations. Reminders with direct personal contact might be appropriate in these groups (see Other reminder characteristics, Format of the reminder). To facilitate attendance in the most at risk, vulnerable groups we have suggested that reminder systems of increasing intensity and interactivity could be introduced to ensure that disparities in health-care opportunities are not compounded. We have introduced the concept of a sequential reminder intervention in order to reach the most number of patients and maximise attendance78 (see Substance abuse/mental health/comorbidity and physical illness). The re-engagement of patients with treatment after they have missed their appointment may be important if they have particular health problems that need ongoing treatment. Intensive approaches, such as ‘stepped reminders’ and patient navigators, have been effective at increasing attendance at screening and immunisation programmes in disadvantaged and vulnerable populations and might also be effective at re-engaging similar groups of patients who have dropped out of treatment [see Do different reminder systems have differential effectiveness for particular subgroups of the population (e.g. by age group, ethnic group, socioeconomic status, gender, etc.)?].
Specific implications
The general implications above should be considered by all health-care services; however, this review also identifies various reminder or appointment-related issues that may be relevant to specific health services. Therefore, along with the ideas outlined above, health service managers should consider the following issues that will add a layer of decision making to their choices about reminders. In essence, reminder systems are a complex intervention,219 because of the potential number of interacting components within the interventions, and so owing to the requirement for tailoring of the intervention to the health service and the number of difficulties and behavioural changes from those receiving and delivering the reminder to facilitate decision-making, we developed:
-
a conceptual framework (see Figure 2)
-
a set of clinical scenarios (see Appendix 7)
-
reasons for non-attendance and possible reminder solutions and wider solutions (see Appendix 8)
-
advantages/disadvantages for various reminder systems (see Appendix 9).
Conceptual framework: implications for practice
We examined existing conceptual frameworks to identify models that explain reasons for FTA appointments. No existing models explored the complexity of the different interactions between the patient, the service, the reminder system and the factors that support or inhibit attendance. Consequently, we developed a conceptual framework exploring FTA. This framework places patients at the centre, to convey their centrality in forgetting or deciding whether or not they will attend (or at least intend to attend). The framework examines patient status when they receive the appointment notification in terms of obstacles or enablers to their attendance, ‘distal/proxy’ attributes that could characterise a patient group to predict the effectiveness of different types of reminder systems and the characteristics of the reminders.
Our study proposes five possible outcomes relating to appointment attendance, cancellation, rebooking and FTA (see Appendix 2):
-
outcome 1 – patient attends the original appointment
-
outcome 2 – patient does not attend the original appointment but rebooks and attends
-
outcome 3 – patient does not attend the original appointment, cancels, but does not rebook and attend
-
outcome 4 – patient does not attend the original appointment and does not cancel
-
outcome 5 – patient does not attend the original appointment and does not cancel, but is rebooked by the clinic.
The conceptual framework was further developed to propose a series of hypotheses with respect to the interaction between the patient and the reminder system (see Appendix 3). These explore the patient–reminder interaction [A] and the attributes associated with increasing the likelihood of attendance, including reminding the forgetful patient to attend [A.1], providing information that attending the appointment will positively affect his/her well-being [A.2], providing information that non-attendance will negatively affect his/her well-being [A.3], that attendance will not be difficult [A.4], the experience will be positive [A.5], attendance is compatible with other commitments [A.6] and is morally the right thing to do [A.7].
The hypotheses further explored the relationship between the accessibility of the reminder [B] and the outcomes for the patient. In particular, the outcomes are more likely to be detrimental for the service if the reminder is not received [B.1] or understood [B.2] by the patient, does not overcome potential obstacles experienced by the patient [B.3], is not formatted appropriately [B.4] or timed appropriately to allow cancellation or rebooking [B.5].
Several components of the reminder can be varied to impact on the effectiveness of the reminder, specifically, the medium (e.g. telephone, SMS, letter, multiple modalities), timing, content, interactivity and intensity.
Further, we hypothesised that the impact and effectiveness of reminder systems vary by health-care settings [C], including the source of the original appointment [C.1], service location [C.3] and initial or follow-up appointment [C.5].
The study also hypothesised that the wider social systems in which the appointment is situated impacts on the likelihood of attendance [D] and that obstacles to attendance and rebooking impact on attendance [E].
Clinical scenarios: implications for practice
In response to the findings from this study, we have developed a series of clinical scenarios relating to the use of reminder systems (see Appendix 7) that synthesise the evidence presented into this report to address specific scenarios for service providers, outlined below:
-
if you want to optimise the likelihood of the patient attending the appointment
-
if you want to optimise the likelihood of attendance at an initial appointment
-
if you want to increase the rates of attendance at screening appointments
-
if you want to optimise the likelihood of attendance at follow-up appointments
-
if you want to optimise the likelihood of attendance of specific population groups
-
if you want minimise the number of unfilled, non-attendances on any one day (i.e. minimise unused capacity)
-
if it is a high priority that patients cancel then it is important that health-care services make it as easy as possible for patients to cancel
-
if it is a high priority that patients reschedule their unwanted appointment in order to receive priority treatment
-
if you want to make it easy for the patient to cancel or reschedule
-
if the health service has to reschedule an appointment.
Reasons for non-attendance
In addition, we have summarised below the major reasons proposed for missing appointments (see Appendix 8). In particular, we propose solutions to address each of these issues based on the evidence presented in the report.
-
problems with appointment system
-
patient illness
-
patient perceptions and fears regarding the importance or value of appointment
-
timing and incompatibility of the appointment: planned (avoidable)
-
timing and incompatibility issues: unplanned (unavoidable)
-
issues to do with patient: practitioner relationship or interaction
-
issues to do with the accessibility of the appointment
-
patient attributes.
Advantages and disadvantages of different reminder systems
The advantages and disadvantages of the range of reminder systems are presented in Appendix 9, including a discussion of the costs and implications for cancellation and rebooking.
Practice guidelines
In our original proposal, we identified that one of the outcomes of the project would be a stand-alone practice guide based on the information provided in Appendices 7–9. Owing to the complexity of the information, we propose to create a web-based practice guide which will allow health service managers to negotiate the information more readily. A brief outline proposal of this is provided in Appendix 10.
Research implication
The gaps in the evidence point to three clear research priorities that could lead to increased effectiveness of reminder systems, more efficient use of appointment resources while simultaneously recognising the needs of specific patient groups who may be at higher risk of missing appointments. These research priorities are identified below:
-
Although there is strong evidence to support the use of reminders, there is a need for high-quality studies investigating the differential influence of providing additional information as part of the reminder system in different contexts (first vs. follow-up appointment, particularly the use of loss- vs. gain-framed messages and orientation information for facilitating attendance behaviours) (see Which types of reminder systems are most effective in improving the uptake of health service appointments?).
-
Reminder systems would appear to have considerably more potential for promoting cancellation of unwanted appointments to allow reallocation of cancelled appointments than the current evidence indicates. To optimise attendance, cancellation and rescheduling there needs to be robust procedures to ensure that patient contact details are up to date and that there are easy-to-use, probably multiple, systems for cancelling appointments that suit the needs of the patients, e.g. automated SMS cancellation, answerphone, e-mail, etc. Robust 24-hours-per-day rescheduling procedures should allow easy rescheduling of appointments for patients. Finally, an effective reminder system will increase the workload on clinical staff and alternative time will need to be scheduled for staff to undertake health-care-related administration. Further research is required to investigate the differential effectiveness and cost-effectiveness of an ‘optimised’ reminder system over and above usual reminder systems.
-
This study set out to examine whether certain types of reminder systems are more effective for specific population subgroups; however, there was a lack of research in this area. Specifically, we have identified patient groups who are higher than average risk of non-attendance. For these groups, we have introduced the concept of a sequential reminder intervention in order to reach the maximum number of patients and to maximise attendance; however, the effectiveness of these reminders in this context needs to be established. The re-engagement of these patient groups with treatment after they have missed their appointment may be important if they have particular health problems that require ongoing treatment. Intensive approaches, such as ‘stepped reminders’ and patient navigators have been effective at increasing attendance at screening and immunisation programmes in disadvantaged and vulnerable populations; however, their effectiveness in this context also needs to be investigated.
Current and future developments (innovations)
Bech215 suggests the following interventions to combat non-attendance: information given to patients before appointments, reminder letters, telephone reminders, punishing non-attendees by discharging them from the waiting list or by assigning them to the bottom of the waiting list, and charging non-attendees a monetary fine. Some of these suggestions have been examined in the systematic review section of this report. Within our review team we have expanded the range of possible alternatives, as shown in Box 1. It should be emphasised that such potential solutions have been identified through narrow specific searches of the literature and are not intended as a systematic mapping of the area. Nevertheless, we are confident that we have identified the main choices available to those managing services.
Modify current ways of delivering appointment reminders.
Utilise new ways of delivering appointment reminders.
Utilise new ways of appointment booking.
For example:
-
over the internet.
Utilise new ways of managing appointment systems.
For example:
-
charging for non-attendance
-
open-access systems
-
Choose and Book
-
patient-initiated appointments.
Utilise alternative ways of delivering health care.
For example:
-
teleconsultations e.g. via Skype™ (Skype Ltd, Rives de Clausen, Luxembourg)
-
changes to appointment opening times.
Modify current ways of delivering appointment reminders
A study carried out last year at two Bedfordshire practices142 revealed how three simple and cost-effective measures could significantly reduce the number of appointments missed by patients. Asking patients to write down their appointments cut did-not-attends by 18% compared with the average of the previous 6 months. Asking patients who booked over the phone to repeat back the time and date of their appointments cut did-not-attends by 3.5% compared with the previous month. Displaying posters stating how many patients had attended their appointments in the previous month, in combination with the other two measures, cut did-not-attends by a total of 31% in comparison with the average for the previous 12 months.
Further recommendations about how services can cut did-not-attend rates are outlined in the ‘did not attends – Reducing Did Not Attends’ Quality and Service Improvement Tool from the NHS Institute for Innovation and Improvement. 220
Another alternative is to integrate appointment reminders within a more wide-reaching approach to caring for the client by utilising other features of the chosen reminder technology. For example, NHS Bolton supplemented a text-based appointment reminder system within the context of an alcohol relapse prevention programme. 221 In addition to allowing clients to confirm whether or not they will be attending their aftercare appointments, clients were contacted a few times a week via text message with simple questions about their feelings and emotional state. The response from the clients triggered, in turn, an appropriate service response depending on the answers given. This innovative use of mobile technology as an engagement strategy is concordant with our earlier observations and seeks to enhance self-sufficiency for clients through reminder and feedback on treatment success.
Utilise new ways of delivering appointment reminders
Intensive reminders
We have identified that high levels of non-attendance are found in patients who abuse drugs and alcohol (see Chapter 5, Substance abuse), patient with mental health problems (see Chapter 5, Mental health) and patients with comorbidities and illness (see Chapter 5, Physical illness/comorbidity). For these groups, simple reminders and automated reminders to attend may be ignored or overlooked particularly when experiencing an increased level of illness or substance abuse. In fact, the use of simple reminders may put these patient groups at a disadvantage compared with general outpatient populations. Reminders with direct personal contact might be appropriate in these groups (see Other reminder characteristics, Format of the reminder). To facilitate attendance, a sequential reminder intervention such as that described by Perron et al. 78 could be initiated. First, a phone call to either landline or mobile; second, a SMS if participants do not answer the phone after three attempts and have a mobile phone and, finally, a postal reminder if participants did not answer the phone, had no mobile phone for SMS, or had no phone at all. Such a design, although labour intensive, would reach the maximum number of participants and may increase attendance rates while still being cost-effective. A further consideration is how to re-engage these groups with treatment after they have missed their appointment. Intensive approaches, such as ‘stepped reminders’46,195 and patient navigators,196,197 have been effective at increasing attendance at screening and immunisation programmes in disadvantaged and vulnerable populations, and might also be effective at re-engaging similar groups of patients who have dropped out of treatment.
E-mail reminders
E-mail has been proposed as a suitable medium for sending appointment reminders42 (see Accessibility). Bespoke secure e-mail programmes can incorporate special features such as standard forms guiding the use and content of the e-mail sent and the capacity to show read receipts (in order to confirm the patient has received the correspondence). However, they are costly to set up and may require a greater degree of user skill than standard unsecured mail. 42 E-mail may also be a suitable medium for many patients to cancel appointments that are no longer convenient or no longer required. It is unlikely to be suitable for all patients, but does provide an automated mechanism for quick and easy cancellation. Future research is required to consider the likely usefulness/availability/accessibility and practical implications of e-mail reminders.
Utilise new ways of appointment booking
Booking/cancellation over the internet
Derby Hospitals NHS Foundation Trust uses online cancellation forms to make it easier for patients who do need to cancel to get in touch with the trust. This addresses difficulties, such as those identified by Martin et al. ,142 in accessing, or indeed providing, staffing for a cancellation telephone line. A Department of Health press release222 indicates that because of projects to reduce missed appointments, the number of missed appointments in Derby between April and December 2011 fell by over 12,000 (2%) compared with the same period the previous year. A 2011 survey of 1700 patients by www.patient.co.uk showed that 85% wanted to book GP appointments online. 223 Nearly half of patients surveyed (47%) were over 55 years of age and, therefore, challenged assumptions about the demographics for users of such technologies. 223
Integrated care including appointment booking
University College London Partners has been working on an internet-based solution that allows a pregnant woman to automatically receive all the information she needs about her forthcoming 12-week scan. Appointments can be made online with the content being tailored to individuals (e.g. according to age group or language spoken). 224
Utilise new ways of managing appointment systems
Charging for non-attendance
In their qualitative study, Martin et al. 142 discuss the ramifications of charging for non-attendance. They describe how some patients held the view that that financial penalties for patients who did not attend appointments was justified. If this measure had an effect on attendance then it might seem justified; however, some patients indicated that this would not have prevented the non-attendance in their particular case. They further indicated that, in this context, a fine would not be an intervention to reduce non-attendance but would simply provide a financial reimbursement for the NHS or a penance for patients who did not attend.
They go on to compare this with the USA, where most appointments actually do involve a financial cost to the patient, and non-attendance rates are similar. They report an association with lack of insurance cover and Medicaid for which individuals often have to make some contribution to costs and are, by definition, poor. They conclude, as does Bech,215 that financial penalties would have some effect in reducing non-attendance, but that it would not be substantial.
Resistance to a system of financial penalties came from medical staff who were not only opposed to the system but who emphasised that implementation would prove difficult. 142 A contrary view comes from the Developing Patient Partnerships Survey and Hussain-Gambles et al. 104 qualitative study of primary care team members. However, there was common recognition of the administrative pitfalls and approval of fining was not universal. Martin et al. 142 conclude by proposing that an evaluation of such a policy on health service efficiency, administrative staff burden, costs and patient–clinician relationships would be an important first stage that should precede any implementation of monetary penalties. We were unable to establish whether or not such a pilot has actually taken place.
The effectiveness of charging a fine for non-attendees was been debated in Denmark and the UK in the middle of the last decade, but has been investigated in very few studies. 215 These studies225,226 reveal that a fine will, as most economists expected, reduce the non-attendance rate. The literature of non-attendance discloses ‘a significant need for studies addressing the non-attendance problem applying economic theory and standards of analysis’. 215
Open access systems
A recent innovation, adopted by many primary care clinics, is the advanced or open-access system, credited to Murray and Tantau. 227 In this approach, physicians attempt to accommodate patient requests for appointments on the day they call; this is not to be confused with walk-ins who do not call in advance. Future appointments at a time that is more convenient for the patient are also permitted. Service providers vary available capacity to meet the demand of each day. The ability of a patient to book an appointment on the day he or she calls is no longer a function of his/her medical condition and, in contrast, clinics that do not offer advanced access often employ a triage nurse to assess the urgency of medical need of a caller who requests an appointment without delay. Only callers whose need is deemed urgent are offered a slot reserved for urgent requests.
The impetus for adopting advanced access comes from the desire to make clinic practices more patient focused, to accommodate faster access for patients with urgent needs and to gain competitive advantage. St Levan Surgery in Plymouth won the Health Service Journal (HSJ) Award for a patient access system whereby patients phone the surgery and receptionists record all requests for doctor contact on the computer screens of the GPs. 228 The GP phones the patient back, usually within an hour, to agree a plan. Options may include an appointment at a time convenient to the patient (70% of patients choose to be seen on the day), phone advice, investigations, appointments with other practice staff or directions to other services. Follow-ups are also often carried out by phone. However, the implementation of advanced access systems remains a challenge.
First, providers are limited in their capacity to absorb variations in daily demand. It may not be possible to accommodate all appointment requests on the day they originate. This leads to demand spill over to a future day, limiting the clinics ability to meet the demand of that future day.
Second, true demand for same-day service is not captured by the appointments data because it is difficult to tell whether a patient actually preferred to book an appointment on a future date or (s)he did so because a same-day appointment was not available. Same day services may prove particularly challenging for those managing appointment services who seek to determine approximately how much capacity should be available at the start of each day for the demand.
Third, in many clinics, different physicians’ patient list compositions and sizes are significantly different, with the result that some physicians have fewer available slots to accommodate same-day demand. 228,229
The open-access policy that calls for ‘meeting today’s demand today’ has been demonstrated to be a reasonable choice when the patient load is relatively low. 230
Luo et al. 231 have shown that appointment scheduling policies that ignore interruptions for emergency requests perform quite badly in relation to patient waiting times, especially when the number of appointments to be scheduled is also a decision variable. They also found that policies requiring equally spaced appointments perform reasonably well when the interruption rate is constant; however, their performance worsens significantly when the interruption rate is time dependent.
Choose and Book
An important component of enhancing patient experience of care is to provide more flexibility to patients regarding how, when and where to receive treatment. In pursuit of this objective, the NHS in the UK launched its electronic booking system, Choose and Book, for outpatient appointments in January 2006. 232 However, there is some evidence, mainly anecdotal, to suggest that this system will impair outpatient practice233 and, in particular, patient attendance is worse under a Choose and Book service. 234 Commentators have suggested that part of the problem is that patients are given only one chance for booking with one phone call with the implication that a three contact system, at different times, of the day would prove more successful. 235
Patient-initiated appointments
Patient-initiated appointments offer patients the opportunity to self-manage their disease by requesting specialist reviews at times of need instead of clinician-scheduled appointments. Claimed benefits for patient-initiated care, in comparison with traditional clinician-driven care, include reduction of unnecessary medical reviews, greater satisfaction to patients and staff and maintenance of the patient’s physical and psychological status. 236 In a 2-year RCT, subsequently extended to 6 years, 209 consecutive patients with rheumatoid arthritis were assigned to either a direct access group or a control group receiving regular clinician-initiated care. 236 Patients in the direct access group expressed significantly higher satisfaction and confidence in the system and also had significantly fewer (38%) hospital appointments (median 8 vs. 13 hospital appointments; p < 0.0001) than patients in the control group. This approach is regarded as particularly promising for other chronic diseases.
Systematic overbooking
Each service faces a challenging dilemma, i.e. whether to build in assumptions of ‘non-attendance without opportunity to reassign’ into their appointment schedules (i.e. overbooking) or whether to expect clinical staff to redeploy the freed time (with a consequent risk of underutilisation). Flexibility to redeploy the time to the benefit of other patients will also be limited by factors relating to those patients themselves, i.e. if a patient turns up early (or is invited to turn up early) for their appointment, he or she may be able to occupy a previous slot. However, such patterns then drive future appointment behaviour with being seen early on one occasion being likely to modify expectations for future appointments and, conversely, perceived ‘idle time’ experienced by turning up early but being seen at the appointed time being likely to lead to presentation closer to the scheduled time on subsequent occasions. While service providers such as airlines respond to uneven attendance patterns by offering stand-by opportunities, they risk losing significant good will when overbooking flights. 237 They similarly face a vicious cycle whereby a customer’s previous experience of the convenience of standby may modify their expectations that this option will then be available on a repeat occasion, thereby increasing demand and making such provisions less likely for the particular individual. In an award-winning paper, LaGanga and Lawrence237 show that a simple solution is to shorten the time between appointments relative to the average rate of no-shows. For example, if the average no-show rate is 30% and the average time allotted per visit is 15 minutes, a practice could reduce that 15 minutes by 30% and allow only 10.5 minutes per appointment, resulting in more appointment slots.
Utilise alternative ways of delivering health care
Teleconsultation
Newham University Hospital NHS Trust has reportedly started seeing diabetes patients who do not need a physical examination via Skype™ (Skype Ltd, Rives de Clausen, Luxembourg). Results from a pilot suggest that this has caused missed appointments to fall by 11% because of the time saved in travelling, waiting and fewer patients attending A&E. Importantly, feedback from patients suggests that the quality of care was the same as with face-to-face appointments. 222 The project had a significant impact on patients, particularly those who have difficulty accessing care because of their busy lifestyles or multiple commitments and those with limited mobility or who are housebound. For staff, it encouraged more focused consultations and better use of face-to-face time for clinical activities. 238
Patient decision aids
There are also early indications that patient decision aids, given at an initial meeting with a nurse and followed up by a telephone consultation, may reduce the need for face-to-face appointments. A follow-up appointment is required only when the patient is struggling to make a decision. However, the need to respect patient choice means that such provision can only be offered as an alternative and not as a standard default. 239
Changes to appointment opening times
Experience from the Royal Bolton Hospital NHS Trust,240 which responded to perceived capacity issues by holding extra outpatient clinics out of normal hours, at high cost, indicates the importance of a sophisticated understanding of appointment behaviours in using poor performance as an indicator of systemic issues. The trust encountered a significant number of cancellations and rescheduling of appointments, with the consequence that some clinics were under-running. Furthermore, it identified waste within the appointments themselves. As a consequence, the trust has been working with the Health Foundation to apply innovative ‘lean’ methods to the outpatient setting.
Chapter 7 Conclusions
These three associated reviews have found strong, consistent evidence to support the use of all reminder systems for all patients in any outpatient setting for increasing attendance, cancellation or rescheduling. There is additional evidence that ‘reminder plus’, which provides additional information over and above date, time and location of the appointment, may be more effective than simple reminders at reducing non-attendance, particularly at first appointments. However, there is a need for high-quality studies investigating the differential influence of providing additional information as part of the reminder system in different contexts (first compared with follow-up appointment, the use of loss- compared with gain-framed messages and orientation information for facilitating attendance behaviours).
There was strong evidence that:
-
the timing of reminders, between 1 and 7 days prior to the scheduled appointment, has no effect on attendance
-
a substantial number of reminders may not be received by patients
-
reminders promote cancellation of appointments
-
patients find difficulty with cancelling appointments because of structural factors affecting reminder systems (e.g. busy telephone line, nobody answers the telephone).
This leads to the conclusion that, unless patients indicate otherwise, all patients should receive a reminder or ‘reminder plus’ that actively encourages patients who are unable to attend to cancel their appointment and to reschedule if further appointments are required. The reminder should be sent around 3 days in advance of the appointment as timing of a reminder, between 1 and 7 days prior to the scheduled appointment, has no effect on patient attendance behaviour. This will allow sufficient time for patient cancellation and health service reallocation of the appointment to another patient or allow the clinician to undertake care-related administrative tasks. To optimise attendance, cancellation and rescheduling there needs to be robust procedures to ensure that patient contact details are up to date and that there are easy to use, probably multiple, systems for cancelling appointments that suit the needs of the patients, e.g. automated SMS cancellation, answerphone, e-mail, etc. Robust 24-hours-per-day rescheduling procedures should allow easy rescheduling of appointments for patients. Finally, an effective reminder system will increase the workload on clinical staff and alternative time will need to be scheduled for staff to undertake health-care-related administration. Further research is required to investigate the differential effectiveness and cost-effectiveness of an ‘optimised’ reminder system over and above usual reminder systems.
There were few studies investigating the differential effectiveness of alternative types of reminders for different segments of the population and this we believe is a key area for further research. Nevertheless, we have used the findings of our review to suggest possible reminder alternatives for key groups of patients who appear to be at higher risk of not attending appointments, namely deprived, ethnic, substance abusers, and those with comorbidities and illness. Simple reminders and automated reminders to attend may be ignored or overlooked and may put these patient groups at a disadvantage compared with general outpatient populations. Reminders with direct personal contact might be appropriate in these groups. To facilitate attendance in the most at risk, vulnerable groups we have suggested that reminder systems of increasing intensity and interactivity could be introduced to ensure that disparities in health-care opportunities are not compounded. We have introduced the concept of a sequential reminder intervention in order to reach the most number of patients and maximise attendance, although their effectiveness in this context needs to be established. The re-engagement of these patient groups with treatment after they have missed their appointment may be important if they have particular health problems that need ongoing treatment. Intensive approaches, such as ‘stepped reminders’ and patient navigators have been effective at increasing attendance at screening and immunisation programmes in disadvantaged and vulnerable populations, although their effectiveness in this context needs to be investigated.
Reminder systems are a complex intervention, because of the potential number of interacting components within the interventions, the requirement for tailoring of the intervention to the health service and the number of difficulties and behavioural changes from those receiving and delivering the reminder. Therefore, in addition to following the general recommendations provided above, health service managers will need to tailor their reminder systems to meet the needs of the service and the patient population that it serves. This review provides a range of findings that will inform health service managers’ decision-making processes. To this end, we are producing a practice guide to help health service managers consider specific issues that may be relevant to the design of reminder systems for their health service.
Acknowledgements
The contributions of the different authors were as follows:
Sionnadh McLean (Senior Lecturer in Physiotherapy), co-principal investigator and project manager, was responsible for the strategic and day-to-day management of the research project. She was involved in all stages of the review, particularly in relation to developing conceptual frameworks, data extraction and synthesis, and managed steering groups and the patient group. She also provided expert topic advice and contributed to the development of practice guidelines and was involved in drafting, revising and editing the report.
Melanie Gee (Information Scientist) developed and conducted the literature searches, document delivery and reference management. She was involved in all stages of the review, including development of conceptual frameworks and data extraction, and provided input to the steering groups. She was also involved in drafting, revising and editing the report.
Andrew Booth (Reader in Evidence-based Information Practice) designed the original review stages. He provided expert methodological advice on the systematic review and the review informed by realist principles. He provided expert input to ensure the delivery of the searches and was involved in all stages of the review, particularly in relation to developing conceptual frameworks, data extraction and synthesis. He provided input to the steering groups and was involved in drafting, revising and editing the report.
Sarah Salway (Senior Research Fellow), co-principal investigator, was involved in all stages of the review, particularly in relation to development of conceptual frameworks, data extraction and synthesis. She provided input to steering groups and was involved in drafting, revising and editing the report.
Susan Nancarrow (Professor of Health Sciences) conceived the idea for the original project. She was involved in all stages of the review, particularly in relation to developing data extraction, synthesis. She provided expert topic advice and contributed to the development of practice guidelines. She was also involved in drafting, revising and editing of the report.
Mark Cobb (Director of Clinical Service at Sheffield Teaching Hospital Foundation Trust) provided contextual ideas at all stages of the project to ensure the clinical relevance and local application of the project. He was involved in managing the patient representative group and in editing the report.
Sadiq Bhanbhro (Researcher) was involved in screening of articles, data extraction, and drafting and editing the report.
We are grateful for the involvement of Joanne Greenhalgh, Mark Pearson and Peter Allmark for their involvement in the Project Steering Group and for six patient representatives from Sheffield Teaching Hospitals for their contribution to the development of the Practice Guidelines.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- The NHS Quality, Innovation, Productivity and Prevention Challenge: An Introduction for Clinicians. London: Department of Health; 2010.
- Beecham L. Missed GP appointments cost NHS money. BMJ 1999;319.
- Kennard J. UK: Missed Hospital Appointments Cost NHS £600 Million 2009. www.digitaljournal.com/article/277529 (accessed 3 August 2013).
- Department of Health . Quarterly Hospital Activity – Published Data 2012. http://transparency.dh.gov.uk/?p=19701 (accessed 9 March 2013).
- Martin C, Perfect T, Mantle G. Non-attendance in primary care: the views of patients and practices on its causes, impact and solutions. Fam Pract 2005;22:638-43. http://dx.doi.org/10.1093/fampra/cmi076.
- Gleeson R, Chant A, Cusick A, Dickson N, Hodgers E. Non-compliance with occupational therapy outpatient attendance: a quality assurance study. Aust Occup Ther J 1991;38:55-61. http://dx.doi.org/10.1111/j.1440-1630.1991.tb01681.x.
- El-Tantawy C, Re AD, Frare G. The challenge of managing patient cancellation and non-attendance in an outpatient physiotherapy clinic. Physiother Can 2000;52:163-7.
- Alexandre NMC, Nordin M, Hiebert R, Campello M. Predictors of compliance with short-term treatment among patients with back pain. Rev Panam Salud Pública 2002;12:86-95. http://dx.doi.org/10.1590/S1020-49892002000800003.
- Kolt GS, McEvoy J. Adherence to rehabilitation in patients with low back pain. Man Ther 2003;8:110-16. http://dx.doi.org/10.1016/S1356-689X(02)00156-X.
- Funch DP, Gale EN. Predicting treatment completion in a behavioral therapy program for chronic temporomandibular pain. J Psychosom Res 1986;30:57-62. http://dx.doi.org/10.1016/0022-3999(86)90066-8.
- Weinger K, McMurrich SJ, Yi JP, Lin S, Rodriguez M. Psychological characteristics of frequent short-notice cancellers of diabetes medical and education appointments. Diabetes Care 2005;28:1791-3. http://dx.doi.org/10.2337/diacare.28.7.1791.
- Murdock A, Rodgers C, Lindsay H, Tham TCK. Why do patients not keep their appointments? Prospective study in a gastroenterology outpatient clinic. J Roy Soc Med 2002;95:284-6. http://dx.doi.org/10.1258/jrsm.95.6.284.
- Gucciardi E. A systematic review of attrition from diabetes education services: strategies to improve attrition and retention research. Can J Diabetes 2008;32:53-65. http://dx.doi.org/10.1016/S1499-2671(08)21011-7.
- Lloyd J, Dillon D, Hariharan K. Outpatient clinics. Down the line. Health Serv J 2003;113:22-3.
- Taylor S, Ellis I, Gallagher M. Patient satisfaction with a new physiotherapy telephone service for back pain patients. Physiotherapy 2002;88:645-57. http://dx.doi.org/10.1016/S0031-9406(05)60107-1.
- Karter AJ, Parker MM, Moffet HH, Ahmed AT, Ferrara A, Liu JY, et al. Missed appointments and poor glycemic control: an opportunity to identify high-risk diabetic patients. Med Care 2004;42:110-15. http://dx.doi.org/10.1097/01.mlr.0000109023.64650.73.
- Ambrose J, Beech B. Tackling non-attendance for outpatient appointments. Ment Health Pract 2006;9:22-5. http://dx.doi.org/10.7748/mhp2006.02.9.5.22.c1900.
- George A, Rubin G. Non-attendance in general practice: a systematic review and its implications for access to primary health care. Fam Pract 2003;20:178-84. http://dx.doi.org/10.1093/fampra/20.2.178.
- The NHS Constitution: A Consultation on New Patient Rights. London: The NHS Confederation; 2009.
- Hogan AM, McCormack O, Traynor O, Winter DC. Potential impact of text message reminders on non-attendance at outpatient clinics. Ir J Med Sci 2008;177:355-8. http://dx.doi.org/10.1007/s11845-008-0187-2.
- Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. York: CRD, University of York; 2009.
- Coomes CM, Lewis MA, Uhrig JD, Furberg RD, Harris JL, Bann CM. Beyond reminders: a conceptual framework for using short message service to promote prevention and improve healthcare quality and clinical outcomes for people living with HIV. AIDS Care 2012;24:348-57. http://dx.doi.org/10.1080/09540121.2011.608421.
- Ajzen I, Kuhl J, Beckmann J. Action-Control: From Cognition to Behavior. Heidelberg: Springer; 1985.
- Cooke R, French DP. How well do the theory of reasoned action and theory of planned behaviour predict intentions and attendance at screening programmes? A meta-analysis. Psychol Health 2008;23:745-65. http://dx.doi.org/10.1080/08870440701544437.
- Clough BA, Casey LM. Technological adjuncts to increase adherence to therapy: a review. Clin Psychol Rev 2011;31:697-710. http://dx.doi.org/10.1016/j.cpr.2011.03.006.
- Wyer S, Earll L, Joseph S, Harrison J, Giles M, Johnston M. Increasing attendance at a cardiac rehabilitation programme: an intervention study using the theory of planned behaviour. Coron Health Care 2001;5:154-9. http://dx.doi.org/10.1054/chec.2001.0131.
- Prochaska JO, Norcross JC, DiClemente CC. Changing for Good: The Revolutionary Program that Explains the Six Stages of Change and Teaches You How to Free Yourself from Bad Habits. New York, NY: W. Morrow; 1994.
- Coulson NS, Buchanan H. Students attendance at dental checkups: an application of TTM. Health Educ J 2002;61:309-19. http://dx.doi.org/10.1177/001789690206100404.
- Deci EL, Ryan RM, Ryan RM. The Oxford Handbook of Human Motivation. Oxford: Oxford University Press; 2012.
- Munster Halvari AE, Halvari H, Bjørnebekk G, Deci EL. Motivation and anxiety for dental treatment: testing the SDT model of self care behaviour and dental clinic attendance. Motiv Emotion 2010;34:15-33. http://dx.doi.org/10.1007/s11031-010-9154-0.
- Phillips KA, Morrison KR, Andersen R, Aday LA. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res 1998;33:571-96.
- Murray MD, Morrow DG, Weiner M, Clark D, Tu W, Deer MM, et al. A conceptual framework to study medication adherence in older adults. Am J Geriatr Pharmacother 2004;2:36-43. http://dx.doi.org/10.1016/S1543-5946(04)90005-0.
- Rogers RW. A protection motivation theory of fear appeals and attitude change. J Psychol 1975;91:93-4. http://dx.doi.org/10.1080/00223980.1975.9915803.
- Glasser W. Choice Theory: A New Psychology of Personal Freedom. London: Harper Collins; 2009.
- Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behaviour: the role of message framing. Psychol Bull 1997;121:3-19. http://dx.doi.org/10.1037/0033-2909.121.1.3.
- Cooper HC, Geyer R. What can complexity do for diabetes management? Linking theory to practice. J Eval Clin Pract 2009;15:761-5. http://dx.doi.org/10.1111/j.1365-2753.2009.01229.x.
- Griffiths F, Bendelow G, Green E, Palmer J. Screening for breast cancer: medicalization, visualization and the embodied experience. Health 2010;14:653-68. http://dx.doi.org/10.1177/1363459310361599.
- Rosenfield D, Weinberg D. Domestic practice, situated contingency and adherence to medical directives: a call for research. Soc Theory Health 2012;10:42-60. http://dx.doi.org/10.1057/sth.2011.9.
- Bourdieu P. Outline of a Theory of Practice. Cambridge: Cambridge University Press; 1977.
- Pawson R. Digging for nuggets: how ‘bad’ research can yield ‘good’ evidence. Int J Soc Res Methodol 2006;9:127-42. http://dx.doi.org/10.1080/13645570600595314.
- Guyatt HH, Sackett DL, Cook DJ. User’s guide to the medical literature. II How to use an article about therapy or prevention. JAMA 1994;271:59-63. http://dx.doi.org/10.1001/jama.1994.03510250075039.
- Atherton H, Sawmynaden P, Meyer B, Car J. E-mail for the coordination of healthcare appointments and attendance reminders. Cochrane Database Syst Rev 2012;8. http://dx.doi.org/10.1002/14651858.CD007981.pub2.
- Car J, Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Atun R. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Syst Rev 2012;7. http://dx.doi.org/10.1002/14651858.CD007458.pub2.
- Guy R, Hocking J, Wand H, Stott S, Ali H, Kaldor J. How effective are short message service reminders at increasing clinic attendance? A meta-analysis and systematic review. Health Serv Res 2012;47:614-32. http://dx.doi.org/10.1111/j.1475-6773.2011.01342.x.
- Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLOS Med 2013;10. http://dx.doi.org/10.1371/journal.pmed.1001363.
- Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev 2010;3. http://dx.doi.org/10.1002/14651858.CD005182.pub4.
- Hasvold PE, Wootton R. Use of telephone and SMS reminders to improve attendance at hospital appointments: a systematic review. J Telemed Telecare 2011;17:358-64. http://dx.doi.org/10.1258/jtt.2011.110707.
- Henderson R. Encouraging attendance at outpatient appointments: can we do more?. Scott Med J 2008;53:9-12. http://dx.doi.org/10.1258/rsmsmj.53.1.9.
- Jacobson Vann JC, Szilagyi P. Patient reminder and recall systems to improve immunization rates. Cochrane Database Syst Rev 2005;3.
- Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E Health 2009;15:231-40. http://dx.doi.org/10.1089/tmj.2008.0099.
- Reda S, Makhoul S. Prompts to encourage appointment attendance for people with serious mental illness. Cochrane Database Syst Rev 2010;4.
- Stubbs ND, Geraci SA, Stephenson PL, Jones DB, Sanders S. Methods to reduce outpatient non-attendance. Am J Med Sci 2012;344:211-19. http://dx.doi.org/10.1097/MAJ.0b013e31824997c6.
- The Centre for Reviews and Dissemination . About the Databases – About DARE n.d. www.crd.york.ac.uk/CRDWeb/AboutPage.asp (accessed 27 June 2014).
- Booth A. How Much Searching Is Enough? Towards a Beyond Medline Index (BMI) of Topic-Specific Differences n.d.
- Bos A, Hoogstraten J, Prahl-Andersen B. Failed appointments in an orthodontic clinic. Am J Orthod Dentofacial Orthop 2005;127:355-7. http://dx.doi.org/10.1016/j.ajodo.2004.11.014.
- Can S, Macfarlane T, O’Brien KD. The use of postal reminders to reduce non-attendance at an orthodontic clinic: a randomised controlled trial. Br Dent J 2003;195:199-201. http://dx.doi.org/10.1038/sj.bdj.4810443.
- Chen Z, Fang L, Chen L, Dai H. Comparison of an SMS text messaging and phone reminder to improve attendance at a health promotion center: a randomized controlled trial. J Zhejiang Univ Sci B 2008;9:34-8. http://dx.doi.org/10.1631/jzus.B071464.
- Chiu SH. The Effect of Telephone Reminders on the Attendance for CT Scan: A Randomized Control Trial 2005.
- Cho SJ, Kim YS, Shin HC, Sung EJ, Kim DH, Lee S, et al. A randomized controlled trial of SMS text messaging versus postal reminder to improve attendance after lipid lowering therapy in primary care. Korean J Fam Med 2010;31:284-93. http://dx.doi.org/10.4082/kjfm.2010.31.4.284.
- Christensen AA, Lugo RA, Yamashiro DK. The effect of confirmation calls on appointment-keeping behavior of patients in a children’s hospital dental clinic. Pediatr Dent 2001;23:495-8.
- Comfort M, Loverro J, Kaltenbach K. A search for strategies to engage women in substance abuse treatment. Soc Work Health Care 2000;31:59-70. http://dx.doi.org/10.1300/J010v31n04_04.
- Costa J, Lima M, Sousa D, Cunha A, Viana S, Tinoco M, et al. Impact of Appointment Reminders via Short Message Service in a District Hospital RID A-2756–2009 2008. http://medicina.med.up.pt/im/trabalhos06_07/ppt/Turma4/IntroMed_Annual_Assignment_-_Class_4_-_Presentation_Slides.ppt (accessed 27 June 2014).
- Costa J, Lima M, Sousa D, Cunha A, Viana S, Tinoco M, et al. Impact of Appointment Reminders via Short Message Service in a District Hospital. Porto: Universidade do Porto; 2010.
- Fairhurst K, Sheikh A. Texting appointment reminders to repeated non-attenders in primary care: randomised controlled study. Qual Saf Health Care 2008;17:373-6. http://dx.doi.org/10.1136/qshc.2006.020768.
- Goldenberg S, DeLuca J, Sacajiu G, Paccione G. Effect of reminder calls on new patient appointment adherence. J Gen Intern Med 2003;18:131-2.
- Griffin JM, Hulbert EM, Vernon SW, Nelson D, Hagel EM, Nugent S, et al. Improving endoscopy completion: effectiveness of an interactive voice response system. Am J Manag Care 2011;17:199-208.
- Hashim MJ, Franks P, Fiscella K. Effectiveness of telephone reminders in improving rate of appointments kept at an outpatient clinic: a randomized controlled trial. J Am Board Fam Pract 2001;14:193-6.
- Irigoyen MM, Findley S, Earle B, Stambaugh K, Vaughan R. Impact of appointment reminders on vaccination coverage at an urban clinic. Pediatrics 2000;106:919-23.
- Kitcheman J, Adams CE, Pervaiz A, Kader I, Mohandas D, Brookes G. Does an encouraging letter encourage attendance at psychiatric out-patient clinics? The Leeds prompts randomized study. Psychol Med 2008;38:717-23. http://dx.doi.org/10.1017/S0033291707001766.
- Koury E, Faris C. Mobile phones and clinic appointments: the start of a beautiful new friendship?. Br J Health Comput Inf Manage 2005;22:18-20.
- Kwon SB, Hong SS, Kang SY, Jung S, Hwang SH. Telephone call reminders and attendance in an electromyography laboratory. J Neurol 2010;257.
- Leong KC, Chen WS, Leong KW, Mastura I, Mimi O, Sheikh MA, et al. The use of text messaging to improve attendance in primary care: a randomized controlled trial. Fam Pract 2006;23:699-705. http://dx.doi.org/10.1093/fampra/cml044.
- Liew SM, Tong SF, Lee VK, Ng CJ, Leong KC, Teng CL. Text messaging reminders to reduce non-attendance in chronic disease follow-up: a clinical trial. Br J Gen Pract 2009;59:916-20. http://dx.doi.org/10.3399/bjgp09X472250.
- Maxwell S, Maljanian R, Horowitz S, Pianka MA, Cabrera Y, Greene J. Effectiveness of reminder systems on appointment adherence rates. J Health Care Poor Underserv 2001;12:504-14. http://dx.doi.org/10.1353/hpu.2010.0766.
- Nelson TM, Berg JH, Bell JF, Leggott PJ, Seminario AL. Assessing the effectiveness of text messages as appointment reminders in a pediatric dental setting. J Am Dent Assoc 2011;142:397-405. http://dx.doi.org/10.14219/jada.archive.2011.0194.
- Oladipo A, Ogden S, Pugh S. Preclinic appointment telephone contact: an effective intervention for colposcopy clinic nonattendance. J Lower Genital Tract Dis 2007;11:35-8.
- Parikh A, Gupta K, Wilson AC, Fields K, Cosgrove NM, Kostis JB. The effectiveness of outpatient appointment reminder systems in reducing no-show rates. Am J Med 2010;123:542-8. http://dx.doi.org/10.1016/j.amjmed.2009.11.022.
- Perron NJ, Dao MD, Kossovsky MP, Miserez V, Chuard C, Calmy A, et al. Reduction of missed appointments at an urban primary care clinic: a randomised controlled study. BMC Fam Pract 2010;11. http://dx.doi.org/10.1186/1471-2296-11-79.
- Prasad S, Anand R. Use of mobile telephone short message service as a reminder: The effect on patient attendance. Int Dent J 2012;62:21-6. http://dx.doi.org/10.1111/j.1875-595X.2011.00081.x.
- Reti S. Improving outpatient department efficiency: a randomized controlled trial comparing hospital and general-practice telephone reminders. N Z Med J 2003;116.
- Ritchie PD, Jenkins M, Cameron PA. A telephone call reminder to improve outpatient attendance in patients referred from the emergency department: a randomised controlled trial. Aust N Z J Med 2000;30:585-92. http://dx.doi.org/10.1111/j.1445-5994.2000.tb00860.x.
- Roberts N, Meade K, Partridge M. The effect of telephone reminders on attendance in respiratory outpatient clinics. J Health Serv Res Policy 2007;12:69-72. http://dx.doi.org/10.1258/135581907780279567.
- Rutland E, Roe H, Weaver A. O11 Health promotional messages in short message service (SMS) follow-up of GU medicine clinic defaulters; a tool to improve subsequent attendance rates?. Sex Transm Infect 2012;88:A4-5. http://dx.doi.org/10.1136/sextrans-2012-050601a.11.
- Sawyer SM, Zalan A, Bond LM. Telephone reminders improve adolescent clinic attendance: a randomized controlled trial. J Paediatr Child Health 2002;38:79-83. http://dx.doi.org/10.1046/j.1440-1754.2002.00766.x.
- Taylor NF, Bottrell J, Lawler K, Benjamin D. Mobile telephone short message service reminders can reduce nonattendance in physical therapy outpatient clinics: a randomized controlled trial. Arch Phys Med Rehabil 2012;93:21-6. http://dx.doi.org/10.1016/j.apmr.2011.08.007.
- Tomlinson A, Kyrgiou M, Paraskevaidis E, Kitchener H, Martin-Hirsch P. Does improving communication and information for women increase attendance at colposcopy in an inner city clinic? A randomised controlled trial. Eur J Gynaecol Oncol 2004;25:445-8.
- Swenson TR, Pekarik G. Interventions for reducing missed initial appointments at a community mental health center. Community Ment Health J 1988;24:205-18. http://dx.doi.org/10.1007/BF00757138.
- Parrish JM, Charlop MH, Fenton LR. Use of a stated waiting list contingency and reward opportunity to increase appointment keeping in an outpatient paediatric psychology clinic. J Paediatric Psychol 1986;11:81-9. http://dx.doi.org/10.1093/jpepsy/11.1.81.
- Booth PG, Bennett HE. Factors associated with attendance for first appointments at an alcohol clinic and the effects of telephone prompting. J Subst Use 2004;9:269-79. http://dx.doi.org/10.1080/14659890410001711715.
- Watt BD, Hoyland M, Best D, Dadds MR. Treatment participation among children with conduct problems and the role of telephone reminders. J Child Fam Stud 2007;16:522-30. http://dx.doi.org/10.1007/s10826-006-9103-4.
- Blankenstein R. Failed appointments – do telephone reminders always work?. Clin Governance Int J 2003;8:208-12. http://dx.doi.org/10.1108/14777270310487011.
- Mariotto A. Reminder calls help waiting-lists’ management and fairness. Internet J Healthc Adm 2001;2.
- MacDonald J, Brown N, Ellis P. Using telephone prompts to improve initial attendance at a community mental health center. Psychiatr Serv 2000;51:812-14. http://dx.doi.org/10.1176/appi.ps.51.6.812.
- Geraghty M, Glynn F, Amin M, Kinsella J. Patient mobile telephone ‘text’ reminder: a novel way to reduce non-attendance at the ENT out-patient clinic. J Laryngol Otol 2008;122:296-8. http://dx.doi.org/10.1017/S0022215107007906.
- Downer SR, Meara JG, Da Costa AC, Sethuraman K. SMS text messaging improves outpatient attendance. Aust Health Rev 2006;30:389-96. http://dx.doi.org/10.1071/AH060389.
- Sims H, Sanghara H, Hayes D, Wandiembe S, Finch M, Jakobsen H, et al. Text message reminders of appointments: a pilot intervention at four community mental health clinics in London. Psychiatr Serv 2012;63:161-8. http://dx.doi.org/10.1176/appi.ps.201100211.
- Magnes RM. Out-patient appointments: a necessary evil? A literature review and survey of patient attendance records. Psychiatr Bull 2008;32:458-60. http://dx.doi.org/10.1192/pb.bp.108.020065.
- Foley J, O’Neill M. Use of mobile telephone short message service (SMS) as a reminder: the effect on patient attendance. Eur Arch Paediatr Dent 2009;10:15-8. http://dx.doi.org/10.1007/BF03262661.
- Nair VR, Butt A, Baguley S. Text reminders are reducing non-attendance rate significantly. Int J STD AIDS 2008;19. http://dx.doi.org/10.1258/ijsa.2008.008131.
- Koshy E, Car J, Majeed A. Effectiveness of mobile-phone short message service (SMS) reminders for ophthalmology outpatient appointments: observational study. BMC Ophthalmol 2008;8. http://dx.doi.org/10.1186/1471-2415-8-9.
- Snow R, Fulop N. Understanding issues associated with attending a young adult diabetes clinic: a case study. Diabetic Med 2012;29:257-9. http://dx.doi.org/10.1111/j.1464-5491.2011.03447.x.
- Battistotti A, Quaglini S, Cuoco E. Reducing dropouts in outpatient care through an SMS-based system. Stud Health Technol Inform 2006;124:935-40.
- Corfield L, Schizas A, Noorani A, Williams A. Non-attendance at the colorectal clinic: a prospective audit. Ann R Coll Surg Engl 2008;90:377-80. http://dx.doi.org/10.1308/003588408X301172.
- Hussain-Gambles M, Neal RD, Dempsey O, Lawlor DA, Hodgson J. Missed appointments in primary care: questionnaire and focus group study of health professionals. Br J Gen Pract 2004;54:108-13.
- Hallberg U, Camling E, Zickert I, Robertson A, Berggren U. Dental appointment no-shows: why do some parents fail to take their children to the dentist?. Int J Paediatr Dent 2008;18:27-34.
- Downer SR, Meara JG, da Costa AC. Use of SMS text messaging to improve outpatient attendance. Med J Aust 2005;183:366-8.
- Macpherson S, Alpsten T. Mobile Health Promotion Campaign to Increase Attendance at Breast Screening Appointments. London: Tower Hamlets Primary Care Trust; 2008.
- Milne RG, Horne M, Torsney B. SMS reminders in the UK national health service: an evaluation of its impact on ‘no-shows’ at hospital out-patient clinics. Health Care Manag Rev 2006;31:130-6. http://dx.doi.org/10.1097/00004010-200604000-00006.
- Stott S, Gray C. SMS Appointment Reminders: An Innovation in Youth Health Research and Practice n.d. www.caah.chw.edu.au/resources/speaker_notes/200909/Sam%20Stott.pdf (accessed 27 June 2014).
- Neal RD, Hussain-Gambles M, Allgar VL, Lawlor DA, Dempsey O. Reasons for and consequences of missed appointments in general practice in the UK: questionnaire survey and prospective review of medical records. BMC Fam Pract 2005;6. http://dx.doi.org/10.1186/1471-2296-6-47.
- Roberts K, Callanan I, Tubridy N. Failure to attend out-patient clinics: is it in our DNA?. Int J Health Care Qual Assur 2011;24:406-12. http://dx.doi.org/10.1108/09526861111139214.
- French H, McGrane E, Cooke G. A prospective study of non-attendance to a physiotherapy outpatient department. Physiother Ireland 2005;26:16-22.
- Campbell JD, Chez RA, Queen T, Barcelo A, Patron E. The no-show rate in a high-risk obstetric clinic. J Womens Health Gend Based Med 2000;9:891-6. http://dx.doi.org/10.1089/152460900750020928.
- Hamilton W. Non-attendance in general practice: a questionnaire. Prim Health Care Res Dev 2002;3:226-30. http://dx.doi.org/10.1191/1463423602pc106oa.
- van Baar J, Joosten H, Car J, Freeman GK, Partridge MR, van Weel C, et al. Understanding reasons for asthma outpatient (non)-attendance and exploring the role of telephone and e-consulting in facilitating access to care: exploratory qualitative study. Qual Saf Health Care 2006;15:191-5. http://dx.doi.org/10.1136/qshc.2004.013342.
- Horstmann E, Brown J, Islam F, Buck J, Agins BD. Retaining HIV-infected patients in care: where are we? Where do we go from here?. Clin Infect Dis 2010;50:752-61. http://dx.doi.org/10.1086/649933.
- Orton E, Forbes-Haley A, Tunbridge L, Cohen S. Results of a health equity audit to increase uptake of diabetic retinopathy screening in Derbyshire. Diabetic Med 2011;28.
- Halpern V, Grimes DA, Lopez L, Gallo MF. Strategies to improve adherence and acceptability of hormonal methods for contraception. Cochrane Database Syst Rev 2006;1.
- Judson G, Blain D, Taranaki A, Adamson S, Schroder RN, Sheridan J. New Zealand Addiction Treatment Research Monograph. 2012.
- Hull AM, Alexander DA, Morrison F, McKinnon JS. A waste of time: non-attendance at out-patient clinics in a Scottish NHS trust. Health Bull 2002;60:62-9.
- Pillai R, Bhangu N, Narayanan M, Yoong W. A demographic study to profile non-attenders at a gynaecology outpatient clinic. J Obstet Gynaecol 2012;32:156-8. http://dx.doi.org/10.3109/01443615.2011.635228.
- Hon KL, Leung T, Ma K. Issues regarding nonattendance at a paediatric dermatology centre. Clin Exp Dermatol 2002;27:711-13. http://dx.doi.org/10.1046/j.1365-2230.2002.01163.x.
- Ersin F, Bahar Z. Inhibiting and facilitating factors concerning breast cancer early diagnosis behavior in Turkish women: a qualitative study according to the health belief and health development models. Asian Pac J Cancer Prev 2011;12:1849-54.
- O’Connor AM, Griffiths C, Underwood MR, Eldridge S. Can postal prompts from general practitioners improve the uptake of breast screening? A randomised controlled trial in one east London general practice. J Med Screen 1998;5:49-52. http://dx.doi.org/10.1136/jms.5.1.49.
- Bell TS, Branston LK, Newcombe RG, Barton GR. Interventions to improve uptake of breast screening in inner city Cardiff general practices with ethnic minority lists. Ethn Health 1999;4:277-84. http://dx.doi.org/10.1080/13557859998056.
- Moore CG, Wilson-Witherspoon P, Probst JC. Time and money: effects of no-shows at a family practice residency clinic. Fam Med 2001;33:522-7.
- Ellis DA, Jenkins R. Weekday affects attendance rate for medical appointments: large-scale data analysis and implications. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0051365.
- Hole AR. Modelling heterogeneity in patients’ preferences for the attributes of a general practitioner appointment. J Health Econ 2008;27:1078-94. http://dx.doi.org/10.1016/j.jhealeco.2007.11.006.
- Swarbrick C, Foley E, Sanmani L, Patel R. Do ‘do not attends’ at a genitourinary medicine service matter?. Int J STD AIDS 2010;21:326-8. http://dx.doi.org/10.1258/ijsa.2009.009349.
- Wilkinson J, Daly M. Reasons for non-attendance: audit findings from a nurse-led clinic. J Prim Health Care 2012;4:39-44.
- Casey RG, Quinlan MR, Flynn R, Grainger R, McDermott TED, Thornhill JA. Urology out-patient non-attenders: are we wasting our time?. Ir J Med Sci 2007;176:305-8. http://dx.doi.org/10.1007/s11845-007-0028-8.
- Bell L, Newns K. What factors influence failure to engage in a supervised self-help programme for bulimia nervosa and binge eating disorder?. Eur Eat Disord Rev 2004;12:178-83. http://dx.doi.org/10.1002/erv.554.
- Hawker DSJ. Increasing initial attendance at mental health out-patient clinics: opt-in systems and other interventions. Psychiatr Bull 2007;31:179-82. http://dx.doi.org/10.1192/pb.bp.105.007377.
- Whittle J, Schectman G, Lu N, Baar B, Mayo-Smith M. Relationship of scheduling interval to missed and cancelled clinic appointments. J Ambul Care Manag 2008;31:290-302. http://dx.doi.org/10.1097/01.JAC.0000336549.60298.1d.
- Chariatte V, Berchtold A, Akre C, Michaud PA, Suris JC. Missed appointments in an outpatient clinic for adolescents, an approach to predict the risk of missing. J Adolesc Health 2008;43:38-45. http://dx.doi.org/10.1016/j.jadohealth.2007.12.017.
- Cusini M, Auxilia F, Trevisan V, Visconti U, Castaldi S. A telephone survey on the reasons for non-attendance in a dermatological clinic. G Ital Dermatol Venereol 2008;143:353-7.
- The NHS Constitution for England (2012 Edition). London: Department of Health; 2012.
- Cherniack EP, Sandals L, Gillespie D, Maymi E, Aguilar E. The use of open-access scheduling for the elderly. J Healthc Qual 2007;29:45-8. http://dx.doi.org/10.1111/j.1945-1474.2007.tb00224.x.
- Garton M, Torgerson D, Donaldson C, Russell I, Reid D. Recruitment methods for screening programmes: trial of a new method within a regional osteoporosis study. BMJ 1992;305:82-4. http://dx.doi.org/10.1136/bmj.305.6845.82.
- Myers EF, Heffner SM. Solution center. Strategies for improving follow-up client appointment-keeping compliance. J Am Diet Assoc 2001;101:935-9. http://dx.doi.org/10.1016/S0002-8223(01)00232-2.
- Zanjani F, Bush H, Oslin D. Telephone-based psychiatric referral-care management intervention health outcomes. Telemed J E Health 2010;16:543-50. http://dx.doi.org/10.1089/tmj.2009.0139.
- Martin SJ, Bassi S, Dunbar-Rees R. Commitments, norms and custard creams – a social influence approach to reducing did not attends (Dnas). JR Soc Med 2012;105:101-4. http://dx.doi.org/10.1258/jrsm.2011.110250.
- Notley C, Maskrey V, Holland R. The needs of problematic drug misusers not in structured treatment – a qualitative study of perceived treatment barriers and recommendations for services. Drugs Educ Prev Policy 2012;19:40-8. http://dx.doi.org/10.3109/09687637.2011.570384.
- Lawson VL, Lyne PA, Harvey JN, Bundy CE. Understanding why people with type 1 diabetes do not attend for specialist advice: a qualitative analysis of the views of people with insulin-dependent diabetes who do not attend diabetes clinic. J Health Psychol 2005;10:409-23. http://dx.doi.org/10.1177/1359105305051426.
- Raine R., Cartwright M., Richens Y. A qualitative study of women’s experiences of communication in antenatal care: identifying areas for action. Matern Child Health J 2010;14:590-9. http://dx.doi.org/10.1007/s10995-009-0489-7.
- O’Brien A, Fahmy R, Singh SP. Disengagement from mental health services. Soc Psychiatry Psychiatr Epidemiol 2009;44:558-68. http://dx.doi.org/10.1007/s00127-008-0476-0.
- Greenhalgh T, Heath I. Measuring quality in the therapeutic relationship – part 2: subjective approaches. Qual Saf Health Care 2010;19:479-83. http://dx.doi.org/10.1136/qshc.2010.043372.
- Hamilton K, Gourlay M. Missed Hospital Appointments and Transport. London: University of East London; 2002.
- Zweben A, Barrett D, Carty K, McRee B, Morse P, Rice C. Strategies for Facilitating Protocol Compliance in Alcoholism Treatment Research (NIAAA Project MATCH Monograph Series Vol 7). Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1998.
- Jackson KR, Booth PG, McGuire J, Salmon P. Predictors of starting and remaining in treatment at a specialist alcohol clinic. J Subst Use 2006;11:89-100. http://dx.doi.org/10.1080/14659890500143614.
- Ogilvie D, Mayhew R. Addressing low clinic attendance by making them school-based. Br J Sch Nurs 2012;7:143-5. http://dx.doi.org/10.12968/bjsn.2012.7.3.143.
- McIvor R, Ek E, Carson J. Non-attendance rates among patients attending different grades of psychiatrist and a clinical psychologist within a community mental health clinic. Psychiatr Bull 2004;28:5-7. http://dx.doi.org/10.1192/pb.28.1.5.
- Brookes C. Loss of treatment time due to non-attendance for physiotherapy out-patient appointments in a district general hospital: a pilot study. Physiotherapy 1992;87:349-52. http://dx.doi.org/10.1016/S0031-9406(10)61485-X.
- Downe S, Finlayson K, Walsh D, Lavender T. ‘Weighing up and balancing out’: a meta-synthesis of barriers to antenatal care for marginalised women in high-income countries. BJOG 2009;116:518-29. http://dx.doi.org/10.1111/j.1471-0528.2008.02067.x.
- Manderson L, Allotey P. Storytelling, marginality, and community in Australia: how immigrants position their difference in health care settings. Med Anthropol 2003;22:1-21. http://dx.doi.org/10.1080/01459740306767.
- Turner BJ, Weiner M, Berry SD, Lillie K, Fosnocht K, Hollenbeak CS. Overcoming poor attendance to first scheduled colonoscopy: a randomized trial of peer coach or brochure support. J Gen Intern Med 2008;23:58-63. http://dx.doi.org/10.1007/s11606-007-0445-4.
- Greenhalgh T, Collard A, Begum N. Sharing stories: complex intervention for diabetes education in minority ethnic groups who do not speak English. BMJ 2005;330. http://dx.doi.org/10.1136/bmj.330.7492.628.
- Pacheco RR, Alvarez JMN, Lopez FJC, Orenesr FP, Aleman TM, Santose ES, et al. Non-compliance with appointments amongst patients attending an allergology clinic, after implementation of an improvement plan. Allergol Immunopathol 2007;35:136-44. http://dx.doi.org/10.1157/13108224.
- Scambler G. Health-related stigma. Sociol Health Illn 2009;31:441-55. http://dx.doi.org/10.1111/j.1467-9566.2009.01161.x.
- Piercy H, Chowbey P, Soady J, Dhoot P, Willis L, Salway S. A care pathway approach to identifying factors that impact on diagnosis of heart disease in British Pakistani women. Ethn Inequal Health Soc Care 2012;5:78-8.
- Orbelli S. Cognition and affect after cervical screening. The role of previous test outcome and personal obligation in future uptake expectations. Soc Sci Med 1996;43:1237-43. http://dx.doi.org/10.1016/0277-9536(95)00443-2.
- Sharp DJ, Hamilton W. Non-attendance at general practices and outpatient clinics. BMJ 2001;323:1081-2. http://dx.doi.org/10.1136/bmj.323.7321.1081.
- Waller J, Hodgkin P. Defaulters in general practice: who are they and what can be done about them?. Fam Pract 2000;17:252-3. http://dx.doi.org/10.1093/fampra/17.3.252.
- Patel P, Forbes M, Gibson J. The reduction of broken appointments in general dental practice: an audit and intervention approach. Prim Dent Care 2000;7:141-4. http://dx.doi.org/10.1308/135576100322578889.
- Atun RA, Sittampalam SR, Mohan A. Uses and Benefits of SMS in Healthcare Delivery. London: Imperial College London; 2005.
- Ramm C, Robinson S, Sharpe N. Factors determining non-attendance at a cardiac rehabilitation programme following myocardial infarction. N Z Med J 2001;114:227-9.
- Macleod U, Ross S, Twelves C, George W, Gillis C, Watt GC. Primary and secondary care management of women with early breast cancer from affluent and deprived areas: retrospective review of hospital and general practice records. BMJ 2000;320:1442-5. http://dx.doi.org/10.1136/bmj.320.7247.1442.
- Dixon-Woods M, Kirk D, Agarwal S, Annandale E, Arthur T, Harvey J, et al. Report for the National Coordinating Centre for NHS Service Delivery and Organisation R&D (NCCSDO). London: NCCSDO; 2005.
- Conduit T, Byrne S, Court J, Stefanovic S. Non-attendance at a university-based psychology clinic: telephone appointment reminders versus no reminders. Aust Psychol 2004;39:68-75. http://dx.doi.org/10.1080/00050060410001660362.
- Martin R, Sterne J. Social and economic variation in general practice consultation rates amongst men aged 16–39. Health Stat Q 2001;9:29-36.
- Van Cleemput P. Health care needs of travellers. Arch Dis Child 2000;82:32-7. http://dx.doi.org/10.1136/adc.82.1.32.
- Heath I. The Role of the NHS in Tackling Health Inequalities. UK Health Equity Network n.d. www.publications.parliament.uk/pa/cm200809/cmselect/cmhealth/286/28609.htm (accessed 4 September 2014).
- Fahey D. Reminding patients by text message: text reminders could lead to increased health inequalities. BMJ 2003;327. http://dx.doi.org/10.1136/bmj.327.7414.564-e.
- Ellenbogen J. Preference for text message reminders may be greatest in lower socio-economic groups. BMJ 2003;327:564-6. www.bmj.com/rapid-response/2011/10/30/preference-text-message-reminders-may-be-greatest-lower-socio-economic-gro (accessed 22 September 2014).
- Vernon S. Families in poor socio-economic areas and mobile phones. BMJ 2003;327:564-6. www.bmj.com/rapid-response/2011/10/30/families-poor-socio-economic-areas-and-mobile-phones (accessed 22 September 2014).
- Stoddart H, Evans M, Peters TJ, Salisbury C. The provision of ‘same-day’ care in general practice: an observational study. Fam Pract 2003;20:41-7. http://dx.doi.org/10.1093/fampra/20.1.41.
- Sampson F. Impact of same-day appointments on patient satisfaction with general practice appointment systems. Br J Gen Pract 2008;58:641-3. http://dx.doi.org/10.3399/bjgp08X330780.
- Pascoe SW, Neal RD, Allgar VL. Open-access versus bookable appointment systems: survey of patients attending appointments with general practitioners. Br J Gen Pract 2004;54.
- Roberts NJ, Partridge MR. Telephone consultations in secondary care. Respir Med 2007;101:1665-9. http://dx.doi.org/10.1016/j.rmed.2007.03.003.
- Salway SM, Higginbottom G, Reime B, Bharj KK, Chowbey P, Foster C, et al. Contributions and challenges of cross-national comparative research in migration, ethnicity and health: insights from a preliminary study of maternal health in Germany, Canada and the UK. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-514.
- Gatrad A. A completed audit to reduce hospital outpatients non-attendance rates. Arch Dis Child 2000;82:59-61. http://dx.doi.org/10.1136/adc.82.1.59.
- Gatrad AR. Comparison of Asian and English non-attenders at a hospital out-patient department. Arch Dis Child 1997;77:423-6. http://dx.doi.org/10.1136/adc.77.5.423.
- Gatrad AR. A Study of Asian and English Out-Patient Attendance 1998.
- Greer TM. Perceived racial discrimination in clinical encounters among African American hypertensive patients. J Health Care Poor Underserved 2010;21:251-63. http://dx.doi.org/10.1353/hpu.0.0265.
- Mir G, Sheikh A. ‘Fasting and prayer don’t concern the doctors . . . they don’t even know what it is’: communication, decision-making and perceived social relations of Pakistani Muslim patients with long-term illnesses. Ethn Health 2010;15:327-42. http://dx.doi.org/10.1080/13557851003624273.
- Smith A. Mobile access 2010: Pew Internet Reports. Washington, DC: Pew Research Centre; 2010.
- Denizard-Thompson NM, Feiereisel KB, Stevens SF, Miller DP, Wofford JL. The digital divide at an urban community health center: implications for quality improvement and health care access. J Community Health 2011;36:456-60. http://dx.doi.org/10.1007/s10900-010-9327-5.
- McDowell I, Lindsay J, Sykes E, Verreault R, Laurin D, Hendrie HC, et al. Patient factors associated with missed appointments in persons with schizophrenia. Can J Psychiatry 2004;49:145-8.
- Donaldson A, Tayar Z. Mobile telephone text messaging of clinic appointments in psychiatry. Psychiatr Bull 2009;33. http://dx.doi.org/10.1192/pb.33.1.39a.
- Pennington D, Hodgson J. Non-attendance and invitation methods within a CBT service. Ment Health Rev J 2012;17:145-51. http://dx.doi.org/10.1108/13619321211287256.
- Killaspy H, Banerjee S, King M, Lloyd, M. Prospective controlled study of psychiatric out-patient non-attendance characteristics and outcome. Br J Psychiatry 2000;176:160-5. http://dx.doi.org/10.1192/bjp.176.2.160.
- Resnick B, D’Adamo C, Shardell M, Orwig D, Hawkes W, Hebel JR, et al. Adherence to an exercise intervention among older women post hip fracture. J Clin Sport Psychol 2008;2:41-56.
- Whitmarsh A, Koutantji M, Sidell K. Illness perceptions, mood and coping in predicting attendance at cardiac rehabilitation. Br J Health Psychol 2003;8:209-21. http://dx.doi.org/10.1348/135910703321649178.
- Gruffydd-Jones K, Nicholson I, Best L, Connell E. Why don’t patients attend the asthma clinic?. Asthma Gen Pract 1999;7:36-8.
- Hambidge SJ, Phibbs SL, Chandramouli V, Fairclough D, Steiner JF. A stepped intervention increases well-child care and immunization rates in a disadvantaged population. Pediatrics 2009;124:455-64. http://dx.doi.org/10.1542/peds.2008-0446.
- Battaglia TA, Kronman A, Beaver K, Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population: a patient navigation intervention. Cancer Prev Res 2010;3:CN03-4. http://dx.doi.org/10.1158/1940-6207.PREV-10-CN03-04.
- Percac-Lima S, Grant RW, Green AR, Ashburner JM, Gamba G, Oo S, et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med 2009;24:211-17. http://dx.doi.org/10.1007/s11606-008-0864-x.
- Peffers G, Foubister E, Rai A, Takavarasha T, Cartwright J. Improving rheumatology outpatient attendance using short message service text reminders: results of a clinical service evaluation assessing did not attend rates in patients offered the short message service. Rheumatology 2011;50.
- Knight V, Lu H, McNulty A. Automatic SMS reminders decrease waiting time and non-attendance rate at a sexual health centre. Sex Health 2009;6:352-3.
- Cohen CE, Coyne KM, Mandalia S, Waters A, Sullivan AK. Time to use text reminders in genitourinary medicine clinics. Int J STD AIDS 2008;19:12-3. http://dx.doi.org/10.1258/ijsa.2007.007149.
- Martinez KK, Wong SE. Using prompts to increase attendance at groups for survivors of domestic violence. Res Soc Work Pract 2009;19:460-3. http://dx.doi.org/10.1177/1049731508329384.
- Silberstein N. Reducing no-shows. Podiatry Manag 2008;27:71-4.
- Sinclair A, Alexander H. Using outreach to involve the hard-to-reach in a health check: what difference does it make?. Public Health 2012;126:87-95. http://dx.doi.org/10.1016/j.puhe.2011.11.004.
- Marteau TM, Mann E, Prevost AT, Vasconcelos JC, Kellar I, Sanderson S, et al. Impact of an informed choice invitation on uptake of screening for diabetes in primary care (DICISION): randomised trial. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c2138.
- O’Keefe DJ, Jensen JD. The relative persuasiveness of gain-framed and loss-framed messages for encouraging disease prevention behaviors: a meta-analytic review. J Health Commun 2007;12:623-44. http://dx.doi.org/10.1080/10810730701615198.
- Car J, Sheikh A. E-mail consultations in health care: 1 – scope and effectiveness. BMJ 2004;329:435-8. http://dx.doi.org/10.1136/bmj.329.7463.435.
- Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int 2000;15:259-67. http://dx.doi.org/10.1093/heapro/15.3.259.
- Perry JGW. A preliminary investigation into the effect of the use of the short message service (SMS) on patient attendance at an NHS dental access centre in Scotland. Prim Dent Care 2011;18:145-9. http://dx.doi.org/10.1308/135576111797512810.
- Sanghara H, Kravariti E, Jakobsen H. Using short message services in mental health services: assessing feasibility. Ment Health Rev J 2010;15:28-33. http://dx.doi.org/10.5042/mhrj.2010.0369.
- Virji A, Yarnall KSH, Krause KM, Pollak KI, Scannell MA, Gradison M, et al. Use of e-mail in a family practice setting: opportunities and challenges in patient-and physician-initiated communication. BMC Med 2006;4. http://dx.doi.org/10.1186/1741-7015-4-18.
- Bamford Z, Booth PG, McGuire J, Salmon P. Maximizing patient follow-up after alcohol treatment: the effect of a three-step reminding system on response rates. J Subst Use 2004;9:36-43. http://dx.doi.org/10.1080/14659890410001665069.
- Brady S. A recent survey of drug clinics in the south western area suggests that text messages may help to reduce non-attendance. World Ir Nurs Midwifery 2006;14:24-5.
- Boll S, Heuten W, Meyer EM, Meis M. Development of a multimodal reminder system for older persons in their residential home. Inform Health Soc Care 2010;35:104-24. http://dx.doi.org/10.3109/17538157.2010.528651.
- Kane B, Sands DZ. Guidelines for the clinical use of electronic mail with patients. J Am Med Informat Assoc 1998;5:104-11. http://dx.doi.org/10.1136/jamia.1998.0050104.
- Bech M. The economics of non-attendance and the expected effect of charging a fine on non-attendees RID G-2588–2011. Health Policy 2005;74:181-91. http://dx.doi.org/10.1016/j.healthpol.2005.01.001.
- Wells M, Williams B, Treweek S, Coyle J, Taylor J. Intervention description is not enough: evidence from an in-depth multiple case study on the untold role and impact of context in randomised controlled trials of seven complex interventions. Trials 2012;13. http://dx.doi.org/10.1186/1745-6215-13-95.
- Paige L, Mansell W. To attend or not to attend? A critical review of the factors impacting on initial appointment attendance from an approach-avoidance perspective. J Ment Health 2013;22:72-8. http://dx.doi.org/10.3109/09638237.2012.705924.
- Hayes RA, Efron LA, Richman GS, Harrison KA, Aguilera EL. The effects of behavioural contracting and preferred reinforcement on appointment keeping. Behav Change 2000;17:90-6. http://dx.doi.org/10.1375/bech.17.2.90.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing and evaluating complex interventions: the new medical research council guidance. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1655.
- NHS Institute for Innovation and Improvement . DNAs: Reducing Did Not Attends 2008. www.institute.nhs.uk/quality_and_service_improvement_tools/quality_and_service_improvement_tools/dnas_-_reducing_did_not_attends.html (accessed 24 June 2014).
- The Health Foundation . NHS Bolton: Alcohol Relapse Prevention Programme n.d. www.health.org.uk/areas-of-work/programmes/shine-eleven/related-projects/nhs-bolton/ (accessed 17 March 2013).
- Department of Health . NHS Hospitals Using Innovative Solutions to Prevent Missed Appointments 2012. www.dh.gov.uk/health/2012/08/do-not-attends/ (accessed 18 March 2013).
- Riddle S. The race to get the NHS online. Health Serv J 2012. www.hsj.co.uk/resource-centre/best-practice/it-e-health-and-e-medicine-resources/the-race-to-get-the-nhs-online/5048506.article# (accessed 27 June 2014).
- The Health Foundation . M(Ums)-Power: Putting Women at the Centre of Antenatal Care n.d. www.health.org.uk/areas-of-work/programmes/closing-the-gap-through-changing-relationships/related-projects/putting-women-at-the-centre-of-antenatal-care/ (accessed 18 March 2013).
- Mantyjarvi M. No-show patients in an opthalmological outpatient department. Acta Ophthalmol 1994;72:284-9. http://dx.doi.org/10.1111/j.1755-3768.1994.tb02760.x.
- Lesaca T. Assessing the influence of a no-show fee on patient compliance. Adm Policy Ment Health 1995;22:629-31. http://dx.doi.org/10.1007/BF02254826.
- Murray M, Tantau C. Same-day appointments: exploding the access paradigm. Fam Pract Manag 2000;7:45-50.
- Neve H, Brimacombe L. GP, phone home. Health Serv J 2012. www.hsj.co.uk/HOME/INNOVATION-AND-EFFICIENCY/GP-PHONE-HOME/5052766.ARTICLE# (accessed 27 June 2014).
- Gupta D, Denton B. Appointment scheduling in healthcare: challenges and opportunities. IIE Trans 2008;40:800-19. http://dx.doi.org/10.1080/07408170802165880.
- Liu N, Ziya S, Kulkarni VG. Dynamic scheduling of outpatient appointments under patient no-shows and cancellations. Manufacturing Serv Op Manag 2010;12:347-64. http://dx.doi.org/10.1287/msom.1090.0272.
- Luo J, Kulkarni VG, Ziya S. Appointment scheduling under patient no-shows and service interruptions. Manufacturing Serv Op Manag 2012;14:670-84. http://dx.doi.org/10.1287/msom.1120.0394.
- Green J, McDowall Z, Potts HWW. Does choose & book fail to deliver the expected choice to patients?: a survey of patients’ experience of outpatient appointment booking. BMC Med Inform Decis Mak 2008;8. http://dx.doi.org/10.1186/1472-6947-8-36.
- Wood J. Patients get four choices for NHS treatments: choose and book will hinder development of good outpatient services. BMJ 2006;332.
- Modayil PC, Hornigold R, Glore RJ, Bowdler DA. Letter: choose and book update: patients’ attendance at clinics is worse with choose and book. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b396.
- The Press Association . One in 10 NHS appointments missed. Health Serv J 2012. www.hsj.co.uk/news/acute-care/one-in-10-nhs-appointments-missed/5048704.article (accessed 18 March 2013).
- Paudyal P, Perry M, Child S, Gericke CA. Evaluation of a patient-initiated review system in rheumatoid arthritis: an implementation trial protocol. BMC Musculoskelet Disord 2012;13. http://dx.doi.org/10.1186/1471-2474-13-120.
- LaGanga LR, Lawrence SR. Clinic overbooking to improve patient access and increase provider productivity. Decis Sci 2007;38:251-76. http://dx.doi.org/10.1111/j.1540-5915.2007.00158.x.
- The Health Foundation . Newham University Hospital NHS Trust: Web Based Outpatient Consultations in Diabetes n.d. www.health.org.uk/areas-of-work/programmes/shine-eleven/related-projects/newham-university-hospital/ (accessed 18 March 2013).
- The Health Foundation . Newcastle Urology: Changing Attitudes With Information for Patients n.d. www.health.org.uk/areas-of-work/programmes/shared-decision-making/case-studies/newcastle-urology-changing-attitudes-with-information-for-patients/ (accessed 18 March 2013).
- The Health Foundation . Innovation to Improve Outpatient Clinic Efficiency n.d. www.health.org.uk/areas-of-work/programmes/innovation-to-improve-outpatient-clinic-efficiency/the-programme/ (accessed 18 March 2013).
- Krishna S, Boren SA. Diabetes self-management care via cell phone: a systematic review. J Diabetes Sci Technol 2008;2:509-17. http://dx.doi.org/10.1177/193229680800200324.
- Oldham M, Kellett S, Miles E, Sheeran P. Interventions to increase attendance at psychotherapy: a meta-analysis of randomized controlled trials. J Consult Clin Psychol 2012;80:928-39. http://dx.doi.org/10.1037/a0029630.
- Välimäki M, Kauppi K, Hätönen H, Kuosmanen L, Warwick-Smith K, Adams CE. Information and communication technology based prompting for treatment compliance for people with serious mental illness (protocol). Cochrane Database Syst Rev 2012;7.
- Satiani B, Miller S, Patel D. No-show rates in the vascular laboratory: analysis and possible solutions. J Vasc Interv Radiol 2009;20:87-91. http://dx.doi.org/10.1016/j.jvir.2008.09.027.
- Koury E, Faris C. Mobile phones and clinic appointments: the start of a beautiful new friendship?. Br J Healthc Comput Inf Manage 2005;22:18-20.
- Liew SM, Tong SF, Lee VK, Ng CJ, Leong KC, Teng CL. Text messaging reminders to reduce non-attendance in chronic disease follow-up: a clinical trial. Br J Gen Pract 2009;59:916-20. http://dx.doi.org/10.3399/bjgp09X472250.
- Leong KC, Chen WS, Leong KW, Mastura I, Mimi O, Sheikh MA, et al. The use of text messaging to improve attendance in primary care: a randomized controlled trial. Fam Pract 2006;23:699-705. http://dx.doi.org/10.1093/fampra/cml044.
- Chen ZW, Fang LZ, Chen LY, Dai HL. Comparison of an SMS text messaging and phone reminder to improve attendance at a health promotion center: a randomized controlled trial. J Zhejiang Univ Sci 2008;9:34-8. http://dx.doi.org/10.1631/jzus.B071464.
- Matsuoka Y, Fukai K. What Is Keeping Appointments? 2010. www.fihs.org/volume10_1/article3.pdf (accessed 27 June 2014).
Appendix 1 Example search strategies
Example search strategy
Cumulative Index to Nursing and Allied Health Literature Plus with Full Text, MEDLINE, SPORTDiscus
Searched via EBSCOhost 2000 to 11 January 2012.
| Search strategy | Citations |
|---|---|
| S1 (MH "Reminder Systems") | 2850 |
| S2 TI reminder* OR AB reminder* | 8104 |
| S3 TI appointment* OR AB appointment* | 18,257 |
| S4 (MH "Appointments and Schedules") | 10,007 |
| S5 s3 or s4 | 25,901 |
| S6 s5 and s1 | 409 |
| S7 s1 or s2 | 9797 |
| S8 s7 and s4 | 452 |
| S9 s6 or s8 | 543 |
| S10 TI remind* n5 appointment* OR AB remind* n5 appointment* | 277 |
| S11 TI prompt* n5 appointment* OR AB prompt* n5 appointment* | 34 |
| S12 TI alert* n5 appointment* OR AB alert* n5 appointment* | 6 |
| S13 S10 or S11 or S12 | 316 |
| S14 S9 or S13 Limiters - Published Date from: 20000101- | 470 |
NB. Ten records eliminated because not in English, leaving 460.
Appendix 2 Articulation of possible causal pathways between elements of the conceptual framework
Patient categories
At the time the original invitation for appointment is received, the patient may intend to attend, be uncertain whether to attend or not, or not intend to attend, depending on how the patient’s personal ‘balance sheet’ is weighed up. As the appointment day/time approaches, the patient’s position may alter. We hypothesised that the reminder system had a part to play for each of these categories of patient:
If the patient initially intends to attend, reminders could
-
guard against patient forgetting/going to wrong place – simple reminder
-
guard against intention waning in intervening period – information that supports intention.
If the patient is initially uncertain about attending, reminders could
-
enable patients to cancel and rebook (if the primary obstacle is timing/location)
-
provide information that addresses obstacles and/or supports enablers.
If the patient does not intend to attend, reminders could
-
enable patient to cancel and rebook (if the primary obstacle is timing/location)
-
provide information that addresses obstacles and/or supports enablers
-
enable and encourage patient to cancel (if the obstacles are insurmountable).
Attendance outcomes
There are five attendance outcomes and it is important to recognise that their potential implications for (1) the patient, (2) the immediate service and (3) the wider health-care system, are varied:
[O.1] Patient attends the original appointment.
[O.2] Patient does not attend the original appointment but rebooks and attends.
[O.3] Patient does not attend the original appointment, cancels, but does not rebook and attend.
[O.4] Patient does not attend the original appointment and does not cancel.
[O.5] Patient does not attend the original appointment and does not cancel but is rebooked by the clinic.
Further, long-term, outcomes (with associated costs) apply for those patients falling into attendance outcome categories O.3 and O.4, i.e. those who do not attend and do not rebook themselves or are not rebooked by the clinic:
-
self-recovery
-
deterioration/later (less favourable) presentation.
It is important that these outcomes and their associated costs are recognised, but they lie beyond our remit.
Appendix 3 Hypotheses associated with different elements of the conceptual framework
[A] The reminder–patient interaction
A reminder increases intention to attend (and, therefore, likelihood of attendance) when it (1) reduces patient-specific obstacles to attendance and/or (2) increases patient-specific enablers to attend. The patient will intend to attend when the enablers outweigh the obstacles.
We hypothesised that a reminder will tend to increase intention to attend (and, therefore, likelihood of attendance) when it:
[A.1] Reminds a ‘forgetful’ patient of the timing and location of the appointment.
[A.2] Provides information that increases the patient’s perception that attendance at the appointment will positively contributes to his/her well-being (i.e. importance).
[A.3] Provides information that increases the patient’s perception that non-attendance at the appointment will negatively impact on his/her well-being (e.g. for screening appointments, if the patient is asymptomatic).
[A.4] Provides information that reduces the patient’s perceptions that attendance at the appointment will be difficult (e.g. transport issues, navigation of the hospital).
[A.5] Provides information that increases the patient’s perception that his/her experience of the appointment and associated procedures will be positive (e.g. fear, pain, communication difficulties, approachability of clinic/professional).
[A.6] Provides information that increases the patient’s perception of the compatibility between attending the appointment and his/her other commitments (e.g. OK to bring children).
[A.7] Provides information that increases the patient’s perception that attendance at the given appointment is the morally right thing to do.
[B] Reminder accessibility
The impact of a reminder varies between service settings because of variations in the patient population profile and the accessibility of the reminder to patients in different patient subgroups.
We hypothesised that characteristics of the reminder system can influence the accessibility of the reminder for particular patients because:
[B.1] The reminder may or may not be received by the patient.
[B.2] The reminder may or may not be understood by the patient.
[B.3] The content of the reminder may or may not effectively address the obstacles/enablers experienced by the patient in question.
[B.4] The format of the reminder may or may not compromise the delivery of the content to the patient (‘acceptability’, ‘receptivity’, e.g. personalised message from GP may be more effective at allaying fears than a standardised message for some groups).
[B.5] The timing of the reminder may or may not give patient time to address obstacles to attendance.
We identified the following modifiable factors within the reminder system:
-
timing of reminder
-
medium of reminder
-
reminder interactivity
-
content of reminder (message, language, framing, tone, etc.)
-
source/bearer of reminder
-
reminder intensity (frequency, content, ‘reminder plus’/patient navigation).
[C] Health-care setting
The impact of reminder systems on intention to attend (and, therefore, likelihood of attendance) varies between service settings (and patient subgroups) because health-care system factors and patient/procedure-specific factors can influence patient-level obstacles/enablers (i.e. the ‘baseline’ of obstacles/enablers that are potentially modifiable by the reminder).
We hypothesised that:
[C.1] The source of original appointment can influence the patient’s perception that attendance at the appointment will positively contribute to his/her well-being.
[C.2] The timing of the original appointment can influence the patient’s perception of (in)compatibility with other commitments.
[C.3] Service location can influence the patient’s perception that attendance at the appointment will be difficult (e.g. transport issues).
[C.4] Features of the service that impact on patient experience (procedure itself, wait times, provider–patient communication, provider attitudes, etc.) can influence the patient’s perception that his/her experience of the appointment and associated procedures will be positive [and (in)compatibility with other commitments].
[C.5] Whether the appointment is a first appointment or a follow-up appointment can influence the patient’s perception that attendance at the appointment will positively contribute to his/her well-being.
[C.6] A patient’s previous appointment attendance behaviour may predict future attendance at similar appointments.
We identified the following modifiable factors:
Within the reminder system
-
content reinforcing the benefits of attending the appointment for first or follow-up appointments as applicable
-
content reinforcing the benefits of attending the appointment for patients with a poor attendance history.
Without the reminder system
-
identity of sender of original appointment invitations
-
procedure for setting timing of original appointment, e.g. patient involvement, consideration of patient characteristics including past attendance patterns – mobile clinics, outreach services, drop-ins
-
staff training reduces wait times; ways in which procedures delivered (discomfort, etc.).
[D] Wider social systems
The a impact of reminder systems on intention to attend (and, therefore, likelihood of attendance) varies between service settings (and patient subgroups) because the wider social systems within which patient subgroups are situated vary and elements of these can influence reminder accessibility and patient-level obstacles/enablers (i.e. the ‘baseline’ of obstacles/enablers that are potentially modifiable by the reminder).
We hypothesised that:
[D.1] Prevailing norms of behaviour and attitudes can influence patient perceptions that attendance at the appointment will positively contribute to his/her well-being (e.g. understandings of the condition and potential for intervention by mainstream health care).
[D.2] Prevailing norms of behaviour and attitudes can influence the patient’s perception that non-attendance at the appointment will negatively impact on his/her well-being (e.g. understanding of the condition and its severity, general trust in medical intervention vs. other ways of managing the condition).
[D.3] Prevailing norms of behaviour and attitudes can influence the patient’s perception that attendance at the appointment will be difficult (e.g. general attitudes to moving outside own locality, wider experiences of discrimination in society, etc.)
[D.4] Prevailing norms of behaviour and attitudes can influence the patient’s perceptions that experience of the appointment and associated procedures will be positive/negative (e.g. stories circulating of other people’s bad experiences).
[D.5] Prevailing norms of behaviour and attitudes can influence the patient perceptions that attending the appointment is compatible with other commitments [e.g. (il)legitimacy of a wife attending an appointment if she is caring for a sick husband].
[D.6] Prevailing norms of behaviour and attitudes can influence patient perceptions that attending the appointment is the morally right thing to do (e.g. local understandings of entitlements, responsible behaviour, state funding, etc.)
[D.7] Structural factors (e.g. transport links, availability of child care, availability of someone to go with patient) can influence the patient’s perception that attendance at appointment will be difficult and/or incompatible with other commitments.
In recognising that the wider social system can influence the accessibility of the reminder to some patients, we hypothesised that:
[D.8] Prevailing norms of behaviour and attitudes can influence the accessibility of the reminder to the patient (e.g. high levels of mistrust of government may mean that patients are not receptive to a reminder delivered by the health-care system – perhaps thrown away, fear of technology).
[D.9] Structural factors can influence the accessibility of the reminder to the patient (e.g. lack of landline phones, mobile populations).
We identified the following modifiable factors:
Within the reminder system:
-
careful framing of content of reminder to address specific attitudes/understandings known to be prevalent within particular communities/patient groups
-
interactivity of reminders that allow patients to seek answers/information that address their own concerns/obstacles
-
careful choice of medium of reminder so that it reaches the intended recipient
-
careful choice of source/bearer of reminder to ensure receptivity
-
careful presentation of content so that it is comprehensible to the intended recipient.
Without the reminder system:
-
wider communications campaigns
-
interventions within health-care system to address issues of quality of care, cultural competence, etc.
[E] Cancellation and rebooking
Intention to attend may not result in attendance because additional obstacles can arise for patients who would otherwise intend to attend. This will include patients whose intention to attend has been influenced by the reminder (i.e. whose obstacles–enablers balance has been shifted by the reminder) and those who already intended to intend but for whom the timing/location was not convenient.
We hypothesised that, in the case of patients who intend to take up the offer of an appointment, whether or not they cancel and rebook will be influenced by:
[E.1] The patient’s perception of how easy it is to rebook.
[E.2] System factors that facilitate/hamper the patient’s intention to rebook (e.g. nobody answers the phone).
[E.3] Structural factors that facilitate/hamper the patient’s intention to rebook (e.g. has to be done online and no internet access).
We hypothesised that, in the case of patients who have no intention of taking up the offer of an appointment, whether or not they cancel the appointment will be influenced by:
[E.4] The patient’s perception of how easy it is to cancel.
[E.5] System factors that facilitate/hamper the patient’s intention to cancel (e.g. nobody answers the phone).
[E.6] Structural factors that facilitate/hamper the patient’s intention to cancel (e.g. has to be done online and no internet access).
[E.7] The patient’s perception that cancelling the appointment is the morally right thing to do.
We also recognised that elements of the health-care system, wider social system and reminder system will influence the likelihood that a patient will cancel or rebook.
[F] Distal/proxy attributes
A range of factors can act as markers/proxies for proximate individual factors that are enablers or obstacles to attendance.
We hypothesised that, at a service setting level, this information could be used to judge the likely effectiveness of a particular reminder approach given the patient population profile, or to explain why the impact of a reminder system differs from that observed in other settings.
Appendix 4 Included and excluded systematic reviews and randomised controlled trials for review 2
Included systematic reviews
Atherton et al. , 2012. 42
Car et al. , 2012. 43
Free et al. , 2013. 45
Glynn et al. , 2010. 46
Guy et al. , 2012. 44
Hasvold and Wootton, 2011. 47
Henderson, 2008. 48
Jacobson Vann and Szilagyi, 2009. 49
Krishna et al. , 2009. 50
Reda and Makhoul, 2010. 51
Stubbs et al. , 2012. 52
Included randomised controlled trials
Bos et al. , 2005. 55
Can et al. , 2003. 56
Chen et al. , 2008. 57
Chiu, 2005. 58
Cho et al. , 2010. 59
Christensen et al. , 2001. 60
Comfort et al. , 2000. 61
Costa et al. , 2008. 62
Costa et al. , 2010. 63
Fairhurst and Sheikh, 2008. 64
Goldenberg et al. , 2003. 65
Griffin et al. , 2011. 66
Hashim et al. , 2001. 67
Irigoyen et al. , 2000. 68
Kitcheman et al. , 2008. 69
Koury and Faris, 2005. 70
Kwon et al. , 2010. 71
Leong et al. , 2006. 72
Liew et al. , 2009. 73
Maxwell et al. , 2001. 74
Nelson et al. , 2011. 75
Oladipo et al. , 2007. 76
Parikh et al. , 2010. 77
Perron et al. , 2010. 78
Prasad and Anand, 2012. 79
Reti, 2003. 80
Ritchie et al. , 2000. 81
Roberts et al. , 2007. 82
Rutland et al. , 2012. 83
Sawyer et al. , 200284
Taylor et al. , 2012. 85
Tomlinson et al. , 2004. 86
Excluded systematic reviews
Krishna and Boren, 2008:241 no eligible Included studies.
Oldham et al. , 2012:242 presents no analysis of reminders alone as a strategy for increasing appointment attendance.
Välimäki et al. , 2012:243 study protocol only, no results.
Excluded randomised controlled trials
Watt et al. , 2007:90 on basis of quality of reporting, cannot see how many patients in each study arm or effect size.
Appendix 5 Reviews included in this review with an assessment of their quality
| Study ID | Review question/aims | Overall review quality | Implications for technologies | Implications for specific populations |
|---|---|---|---|---|
| Atherton et al., 201242 | To assess effects of using e-mail for co-ordination of health-care appointments and attendance reminders, compared with other forms of co-ordinating appointments and reminders, on outcomes for health professionals, patients and carers, and health services, including harms | Cochrane Empty Review with no eligible studies. A limitation of this review is the date of the search. The search was conducted in January 2010. Length of time between search date and publication of review means it is possible that relevant studies have been published in interim period | Not applicable | Not applicable |
| Car et al., 201243 | To assess effects of mobile phone messaging reminders for attendance at health-care appointments. Secondary objectives include assessment of patient and health-care provider evaluations of intervention, costs and possible risks and harms associated with intervention | Cochrane review. Included studies were of varying methodological quality; most provided insufficient information to accurately assess risk of bias. Sequence generation for randomisation considered adequate (although randomisation method unclear in one study) but in two studies it was not clear whether or not, and how, allocation was concealed. Lack of blinding in all studies can be partly explained by interactive nature of text message interventions, which does not permit blinding of participants or health-care providers. Potential bias from apparent lack of blinding of outcome assessors | Included four RCTs involving 3547 participants. Three studies with moderate quality evidence showed that mobile text message reminders improved rate of attendance compared with no reminders (RR 1.10, 95% CI 1.03 to 1.17). One low-quality study reported that mobile text message reminders with postal reminders, compared with postal reminders, improved rate of attendance at health-care appointments (RR 1.10, 95% CI 1.02 to 1.19). However, two studies of moderate quality showed that mobile phone text message reminders and phone call reminders had a similar impact on health-care attendance (RR 0.99, 95% CI 0.95 to 1.03). Costs/attendance of SMS lower compared with phone reminders. No studies reported harms or adverse effects of the intervention, nor health outcomes or user perception of safety related to the intervention | Further research should focus on older patients, given that this population has, on average, more health-care appointments and uses mobile phones less frequently than the younger population |
| Free et al., 201345 | To quantify effectiveness of mobile technology-based interventions delivered to health-care providers or to support health-care services, on any health or health-care service outcome | Identified as meeting CRD criteria. No full evaluation yet available | Pooled effect on appointment attendance using text message (SMS) reminders vs. no reminder increased, with RR of 1.06 (95% CI 1.05 to 1.07, I2 = 6%). Pooled effects on number of cancelled appointments was not significantly increased RR 1.08 (95% CI 0.89 to 1.30). No difference in attendance using SMS reminders vs. other reminders (RR 0.98, 95% CI 0.94 to 1.02). SMS reminders no more effective than postal or phone call reminders, and texting reminders to patients who persistently missed appointments did not significantly change number of cancelled appointments. SMS appointment reminders have modest benefits and may be appropriate for implementation | This review presents no findings or implications for specific subgroups |
| Glynn et al., 201046 | To evaluate the effectiveness of reminders on improving the follow-up of patients with hypertension | Cochrane review. Included RCTs with a contemporaneous control group. The methodological quality of included studies was generally poor to moderate with 40% of included articles describing their randomisation processes and only 19% describing adequate concealed allocation processes | Included eight RCTs investigating appointment reminder systems. All but one of the RCTs was associated with improved outcomes. The pooled results favoured appointment reminder systems for follow-up of patients (OR of being lost to follow-up 0.4, 95% CI 0.3 to 0.5) | This review presents no findings or implications for specific subgroups |
| Guy et al., 201244 | To assess the effectiveness of SMS reminders at increasing the uptake of appointments in health-care settings | Although searched grey literature still possible some evaluations not identified, particularly those with negative outcomes. Unable to assess possibility of effect according to clinical reasons for attending, as few papers present this information. Clinical presentation could affect priority placed by patients on need for keeping an appointment. To maximise value of future evaluations, studies should collect and report information on clinical reason for attendance as well as the visit status (new and follow-up) | Summary effect from RCTs was 1.48 (95% CI 1.23 to 1.72). No significant subgroup differences by clinic type (primary care clinics, hospital outpatient clinics) or message timing (24, 48, and 72 + hours before scheduled appointment). SMS reminders substantially increase likelihood of attending clinic appointments. SMS reminders appear to be simple and efficient option for health services to improve service delivery, as well as bringing health benefits for patients who receive the reminders | No significant subgroup differences by target age group (paediatric, adult, older). Age classification based on median age of patient receiving SMS reminders, or specification of clinic type as paediatric. RCTs demonstrated SMS reminders effective in wide age range from paediatric to older. Mobile usage data demonstrate that over 90% of population in many countries own mobile phones, but uptake is higher in younger people.108 As younger patients have higher non-attendance rates at clinical services,110 SMS reminders may be more beneficial in this group. However, older patients have considerably more health appointments each year, often at outpatient clinics where non-attendance costs UK NHS estimated £790M per year162 |
| Hasvold and Wootton, 201147 | (1) What is best estimate of effect of sending reminders on non-attendance rates? (2) Are there any differences in non-attendance when using reminders sent manually (i.e. from phones operated by a human) or automatically (i.e. by SMS text messages or by automated voice recordings)? (3) Does time at which reminder is sent influence effect on non-attendance rates? (4) What are costs and benefits of using reminders? | Not classed as systematic review by DARE (CRD). PubMed only searched | Weighted mean relative change in non-attendance was 34% of baseline non-attendance rate. Automated reminders less effective than manual phone calls (29% vs. 39% of baseline value). No difference in non-attendance rate, whether reminder sent day before or week before. Cost and savings not measured formally, but almost half included cost estimates. Average cost of using either SMS, automated telephone calls or telephone calls was €0.41 per reminder | All studies except one244 showed positive effect from using reminders. (Patients themselves chose in advance whether they wished to receive reminder or not – potential bias in intervention group.) Overall no-show rate (outpatients in vascular laboratory) was 12% (average 7.6 missed appointments/week: gross annual revenue loss of US$89,107 based on ultrasound costs). Of 8766 patients offered automated reminders, only 53% agreed to receive calls. No-show rate significantly greater for patients choosing automated reminders (8.9% vs. 5.9%; p < 0.0001) |
| Henderson 200848 | To assess the effectiveness of appointment reminders as a means of increasing attendance and reducing ‘Did not Attend’ rates at new outpatient appointments | Not classed as systematic review by DARE (CRD). Undertaken by single reviewer, with possibility of reviewer bias. Hand-searching not performed. Non-English language papers not included. Relevant material may have been missed. Methodological quality of evidence base generally poor. Several trials failed to describe randomisation. In many studies blinding was poorly addressed, study participants were inadequately described and only a small number of participants were recruited | Telephone reminders, if received, can have positive impact on attendance and did-not-attend rates. Postal reminders found to be effective. Although limited, literature suggests that impact of ‘standard’ reminders is similar to that of telephone reminders. Suggests that ‘reminders +’ are more effective than ‘standard’ reminders | Impact of implementing initiatives on inequalities in access to services not considered by any studies included in review. Majority of included studies conducted in psychiatric settings outside the UK, raising issues of generalisability |
| Jacobson and Szilagyi, 200949 | To assess overall effectiveness of patient reminder or recall systems, or both, in improving immunisation rates. Compare effectiveness of different types of reminder or recall interventions (e.g. postcard, letter, telephone), or combination of both reminder and recall | Cochrane Review | Reminding people over telephone, sending a letter or postcard, or speaking to them in person increased vaccinations. Providing numerous reminders was more effective than single reminders. Reminding people over telephone more effective than postcard or letter reminders. Reminders over telephone may be expensive compared with alternative approaches. Reminders worked whether from private doctor’s office, medical centre, or public health department clinic. Studies all from developed countries | Reminding people to have vaccinations increased the number of people vaccinated, whether the people were due or overdue for vaccinations. Increases were observed in both children and adults for all types of vaccines, but not among urban adolescents in one study |
| Krishna et al., 200950 | To investigate role of cell phones and text messaging interventions in improving health outcomes and processes of care | Research question supported by inclusion criteria for study design, intervention and outcomes. Authors did not report searches of unpublished data. Only studies published in English/English-language abstracts eligible for inclusion. Publication/language bias could not be ruled out. Authors did not report review process, so not known whether or not steps taken to reduce possible error and bias (such as performing processes in duplicate). Study quality not assessed, so unknown whether or not results of included studies were reliable. Many studies had small sample sizes. Narrative synthesis was appropriate given diversity of included studies. Owing to possibility of bias and error in review process and unknown quality of included studies, authors’ conclusions may not be reliable | Text messaging associated with fewer days to diagnosis. Failure-to-attend rates significantly improved in two studies, but did not differ significantly between intervention/control groups in two other studies. Mobile phone reminder, disease monitoring and management and education can improve health outcomes and care processes | Text messaging associated with improved communication in participants with disabilities |
| Reda and Makhoul, 201051 | To estimate the effects of simple prompting by professional carers to encourage attendance at clinics for those with suspected serious mental illness | Cochrane review | No clear difference between those prompted by telephone 1 or 2 days before appointment and those given standard appointment management system (two RCTs, n = 457, RR missed appointment 0.84, 95% CI 0.7 to 1.1). Text-based prompts as a letter, a few days before the appointment day, may increase clinic attendance vs. no prompt (three RCTs, n = 326, RR missed appointment 0.76, 95% CI 0.43 to 1.32). One small study (n = 61) compared combined telephone/text-based prompts vs. no prompt; no real difference between groups (RR missed appointment 0.7, 95% CI 0.4 to 1.2). Telephone prompts vs. text-based prompts (one RCT, n = 75), the latter, as an ‘orientation statement’ may be more effective than telephone prompt (RR missed appointment 1.9, 95% CI 0.98 to 3.8). One study (n = 120) compared standard letter prompt with a letter orientation statement. Overall, results tended to favour orientation statement vs. simple letter but not statistically significant (RR missed appointment 1.6, 95% CI 0.9 to 2.9). For prompts regardless of type, results of greater significance suggesting increased attendance (RR missed appointment 0.80, 95% CI 0.65 to 0.98) | Indication for serious mental illness it may be important to provide textual reminder plus orientation statement (a short paragraph, taking about 30 seconds to read, explaining the programme of care, the fee system, and providing gentle encouragement).66 Contrasts with general trend in favour of telephone reminders |
| Stubbs et al., 201252 | To compare telephone, mail, text/ SMS, e-mail and open-access scheduling to determine which is best at reducing outpatient non-attendance and providing net financial benefit | Review addressed broad research question to evaluate impact of all methods for reducing outpatient non-attendance. Methods used to identify and select studies for inclusion generally clear, but publication bias cannot be ruled out. No attempts to assess study quality or minimise errors and bias in review process mentioned. Included studies extremely diverse in populations, settings and research methods. Analysis based on simple weighted average for each approach (telephone, text, post or open access). Influence of other relevant factors on non-attendance not explored. Authors acknowledge that only more recent studies (electronic rather than paper reminders), likely to be relevant now. Potential publication bias notwithstanding, authors conclude that most included interventions modestly improved attendance. Appears reliable, but did not investigate factors that might influence effectiveness of these interventions in different populations and settings. Different reminders not compared with each other. Conclusion that telephone reminders were better than text and post reminders may not be reliable. No formal evaluation of cost-effectiveness, so conclusion on relative cost-effectiveness of interventions also may not be reliable | Telephone, mail and text/SMS interventions all improved attendance modestly but at varying costs. Text messaging most cost-effective of the three, but its applicability may be limited. Few data available regarding e-mail reminders, whereas open-access scheduling is area of active research | This review presents no findings or implications for specific subgroups |
Appendix 6 Judgement on quality of included trials (not already covered in included reviews)
| Study ID | Review question/aims | Overall review quality | Implications for our model | Implications for technologies | Implications for specific populations |
|---|---|---|---|---|---|
| Comfort et al., 200061 | To examine the effect of the provision of ‘tangible’ engagement services during the intake period to women’s outpatient substance abuse treatment on rates of admission, retention and service utilisation. The engagement group received additional services such as transport and child care to help with the uptake and sustainability of service use | Poor quality of reporting of the study design makes it difficult to judge quality. No reporting of blinding; allocation to groups; follow-up of all participants. The sample size was very small, which may have led to the lack of significant result | The engagement group used more services (specifically transport services) than the control group – in other words, they had a higher rate of uptake of services. They did not have high rates of utilisation of child care when provided. Fits with D7, see Chapter 4, Evidence statement (D.1–D.9): there are no studies investigating whether or not wider social systems influence the effectiveness of the reminder (evidence category VIIa); and see Appendix 3 | Nil | This was a study about women participating in outpatient substance abuse programmes, but did not produce any significant findings |
| Costa et al., 2008,62 Costa et al., 201063 | Reduce rates of FTA by sending SMS 2 days before due appointment. Sent by IT department. Personalised to extent, they included name of institution, patient name, type of episode, date and hour. When necessary, included advice to arrive earlier | Lack of reporting on allocation to intervention groups, blinding of participants, and lack of reporting on follow-up of all participants. Sample size calculations undertaken. Seems reasonably robust study, but not well reported | Confirms that Wednesday is the day with highest rate of FTA. Confirms that time of day is a significant indicator of attendance (higher rates of FTA in the morning). (Fits with C.2 in Appendix 3) | SMS improves attendance rates compared with no reminder | Rates of non-attendance highest in younger age groups (< 15 years and decreases with age); in males; people attending for the first time; people attending for tests; highest on Wednesdays; higher in the morning; varies by mobile phone network; and is higher for medical than surgical specialties, but even higher in ‘others’ (and specialty is the most significant difference). All p < 0.5 relevance for section F (see Chapter 4, Proposition F: distal/proxy individual attributes; and see Appendix 3) |
| Goldenberg et al., 200365 | Improve adherence to new patient appointments, assess effectiveness of telephone reminders on compliance, and to identify other factors affecting patient adherence to appointments | Conference abstract only, so lacks detail, RCT, sample size n = 393, intention to treat used. Unable to comment on blinding or process of randomisation | Patients were called by doctor, secretary or not called 48 hours prior to appointment. High rates of attendance (67%) when person spoken to directly compared with leaving message with person (55%), 51% if message left on machine, or 41% if patient not reached. No difference when the call was made by the doctor or the secretary | Direct personal contact with patient increases likelihood of attendance | Privately insured patients more likely to attend than Medicaid patients (61% vs. 46%). This fits with D.9 (see Appendix 3) – more deprived communities less likely to attend |
| Prasad and Anand, 201279 | To evaluate the efficacy of appointment reminders, sent as SMS text messages to patient mobile telephones, in comparison with no reminders given to patients, at outpatient clinics at the ITS Centre for Dental Studies and Research, Muradnagar, Ghaziabad, Uttar, Pradesh, India | Randomised at departmental, rather than patient level, so differences may be due to different treatment type/patient groups. No blinding, no ‘intent to treat’ analysis provided | Implication is the need to tailor the message appropriately to the audience. Fits with theme B.3. May also fit with D.9 (language barrier) and B.2 (see Appendix 3) | SMS may improve attendance rate in comparison with no reminder (although evidence weak) | When appointment reminders were being scheduled, 22 patients stated that they did not understand the English language. Reminders for these subjects were sent in the local language on the mobile phone [relevance for B.2, see Chapter 4, Evidence statement (B.2): there are no studies investigating whether reminder factors (such as language, information provided, framing of information) influence the accessibility/comprehensibility of the reminder message for particular patient groups (evidence category VIIa); and see Appendix 3]. In addition, a picture message of the institution was sent to seven patients |
| Taylor et al., 201285 | To determine whether or not SMS reduces rates of non-attendance in physiotherapy outpatient appointments. Secondary aims were to evaluate effect of SMS reminders on cancellation and attendance rates and explore factors associated with non-attendance | Good-quality, well-powered, well-conducted RCT | Every 19 SMS messages sent prevents one FTA | Strong evidence to show that people who were not sent a SMS were 1.77 times more likely not to attend their appointment (includes adjusting for other factors) | Other statistically significant contributors to the model were health condition/diagnosis of neck and trunk musculoskeletal disorder (OR 2.86, 95% CI 1.53 to 5.32), neuromuscular disorder (OR 3.27, 95% CI 1.17 to 9.17), and age (OR 0.98, 95% CI 0.97 to 0.995). |
| Griffin et al., 201166 | To test whether an IVR system phone call was equally as effective as nurse-delivered phone call at educating and preparing patients for flexible sigmoidoscopy and colonoscopy examinations. Outcomes were appointment non-attendance and preparation non-adherence. Non-attendance defined as cancelling appointment or not attending appointment. Appointments cancelled by clinic as not considered as non-attendance. Preparation non-adherence assessed whether or not patients had adequately prepared to complete procedure | Well-constructed study with sample size calculation and intent to treat, randomisation not specified | No significant difference between three study arms in terms of attendance or adherence outcomes. Significantly more patients in IVR conditions reported neutral perceptions about phone calls, and more patients receiving nurse calls reported very positive perceptions about phone calls. Fits with D.7 (see Appendix 3) – better information about the procedure did not lead to better adherence or attendance | Three arm RCT: nurse phone call 7 days before procedure, IVR system call 7 days before procedure, and IVR system call 3 days before procedure. All calls included an appointment reminder, information about preparation for examination, and encouragement to prepare for and attend the examination. IVR system was effective at reminding patients of their appointments. IVR system can effectively deliver complex information, e.g. preparation information, equally effectively as phone calls from clinic nurses at delivering information; patients receiving IVR messages reported more ‘neutral’ perceptions about phone calls; patients receiving nurse calls reported more ‘very positive’ perceptions about phone calls |
Appendix 7 Clinical scenarios
Clinical scenario 1
If you want to optimise the likelihood of the patient attending the appointment:
Forgetfulness is one of the major reasons for non-attendance (A1).
-
Use a reminder system to improve attendance rates: all reminders improve attendance [see Chapter 4, Evidence statement (A.1): there is strong consistent evidence that simple reminders which provide details of timing and location of appointments are effective at helping a (forgetful) patient to attend their appointment (evidence category Ia)].
-
Use of a simple reminder will help to reduce the risk of forgetting [see Chapter 4, Evidence statement (A.1): there is strong consistent evidence that simple reminders which provide details of timing and location of appointments are effective at helping a (forgetful) patient to attend their appointment (evidence category Ia), and Appendix 3, theme A.1]; however, reminders that provide additional information (such as orientation information and health information) are more effective than simple reminders [see Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)].
-
The content of the reminder is important. The reminder should at least contain details of the timing and location of the appointment [see Chapter 4, Evidence statement (A.1): there is strong consistent evidence that simple reminders which provide details of timing and location of appointments are effective at helping a (forgetful) patient to attend their appointment (evidence category Ia)]. Patients have also expressed a preference for a standardised format, so they know that it is a reminder and, for clear content, using plain English (e.g. eye clinic instead of ophthalmology). (Public Governors’ Comments, see Chapter 3, Involvement of patient steering group.)
-
Use a reminder technology that is appropriate for the audience. Have an awareness of the preferences and needs of the patient, including speech, language and hearing difficulties [see Appendix 3, theme B.4, and Public Governors’ Comments (see Chapter 3, Involvement of patient steering group)].
-
The effectiveness of different reminder systems is influenced by whether or not the patient receives the reminder [see Appendix 3, theme B.1, and Chapter 4, Evidence statement (B.1): there is strong consistent evidence that the reminder may not be received by the patient (evidence category Ia)]. Issues include accessibility to the reminder (homeless or travelling communities, does the patient have the available technology); structural barriers to the reminder being received, for instance not aligning the address with the window on a reminder envelope; and patient understanding of the reminder if they do receive it (mobility, hearing difficulties speech difficulties, language, etc.). Carers may need to take delivery of the reminder.
-
The service should ensure that the contact details for patients are accurate and check these on a regular basis (especially telephone numbers) [see Appendix 3, theme B.1, and Chapter 4, Evidence statement (B.1): there is strong consistent evidence that the reminder may not be received by the patient (evidence category Ia)].
-
Send a reminder before the appointment; however, the timing of the reminder, up to 1 week before the appointment date, does not appear to influence attendance behaviour [see Appendix 3, theme B.5, and Chapter 4, Evidence statement (B.5): there is strong consistent evidence that the timing of a reminder, between 1 and 7 days prior to the scheduled appointment, has no effect on patient attendance behaviour (evidence category Ia)].
-
Do not make the appointment too far ahead of the appointment date. Reminders sent between 1 and 7 days prior to the appointment are equally as effective as each other and reminders sent up to 2 weeks before the appointment may be effective [see Appendix 3, theme B.5, and Chapter 4, Evidence statement (B.5): there is strong consistent evidence that the timing of a reminder, between 1 and 7 days prior to the scheduled appointment, has no effect on patient attendance behaviour (evidence category Ia)]. If the appointment has been scheduled several months in advance, a preliminary reminder should be sent a few weeks in advance of the appointment.
-
Patients perceive that the appointment cannot be important if it is cancelled or rescheduled multiple times by the service [see Appendix 3, theme E, and Public Governors’ Comments (see Chapter 3, Involvement of patient steering group)].
-
Consider the time and day of the appointment and potential obstacles to attendance. For instance, although highly variable, some studies show that the times at highest risk of non-attendance are the mornings and Wednesdays112,162 (see Chapter 5, Timing of the appointment).
-
Consider the flexibility of times for appointments for the audience, e.g. after work, to fit with transport access, such as senior citizens bus pass constraints (Public Governors’ Comments, see Chapter 3, Involvement of patient steering group).
-
Provide information that increases the patient’s perception that attendance at the appointment will positively contribute to their well-being [see Appendix 3, theme A.2–6, and Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)].
Clinical scenario 2
If you want to optimise the likelihood of attendance at an initial appointment:
Considerations from clinical scenario 1 plus:
-
Much may depend on the person making the referral explaining the need of the referral to the patient, so that the patient understands the importance of the appointment and agrees that attending the appointment would be important for them (Public Governors’ Comments, see Chapter 3, Involvement of patient steering group).
-
Consider the nature and the location of your service. How easy is it for patients to find or get to and whether the procedures that patients are undergoing invasive, worrying or anxiety provoking. Provide information that increases patient perceptions that attendance at the appointment will positively contribute to their well-being (see Appendix 3, theme A.2).
-
Patients may need to overcome anxieties about going to a new (unknown) place (see Appendix 3, theme A.5). There may be issues of access/parking difficulties/patient mobility. Patients may also be anxious about specific procedures (e.g. colonoscopy, cervical screening, breast screening, etc.). Patients may benefit from the provision of materials that may influence their intention to attend (see Appendix 3, themes A.2–6, and Chapter 4, Quality of included trials). Consider what type of information would be most beneficial to provide; orientation information, such as location, parking, transport, the department may be beneficial for some clinics. Information about procedures, such as benefits of attending and consequence of not attending, may be helpful for patients by providing reassurance and motivation. How information is provided should be carefully considered, e.g. written direction vs. map, gain-framing or loss-framing of messages [see Appendix 3, themes A.2–6, and Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)].
-
The provision of additional information at the first appointment may be specifically relevant and important to increase attendance [see Appendix 3, themes A.2–6, and Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)’.
Clinical scenario 3
If you want to increase the rates of attendance at screening appointments:
Considerations from clinical scenario 1 plus:
-
Is the health service screening symptomatic or asymptomatic patients? If the patient is asymptomatic and the health service is calling patients in for routine screening, patients may be less motivated to attend than if the patient is symptomatic and has been referred for a screening appointment [see Chapter 5, Norms, attitudes and understandings regarding the (dis)benefits of healthcare on offer]. Provide information to highlight the importance of the appointment. Consider whether the message should be gain-framed (benefits of attending) (see Appendix 3, theme A.2) or loss-framed (consequences of non-attendance) (see Appendix 3, theme A.3, and Chapter 6, Reminder plus).
-
Provide full information about the screening programme, including details of how and when the results will be reported to the patient (Public Governors’ Comments, see Chapter 3, Involvement of patient steering group).
-
Provide information that increases patient perceptions that the appointment will be positive (see Appendix 3, theme A.5).
-
Provide a follow-up reminder to patients who reschedule their appointment (Public Governors’ Comments, see Chapter 3, Involvement of patient steering group).
Clinical scenario 4
If you want to optimise the likelihood of attendance at follow-up appointments:
Considerations from clinical scenario 1, plus:
-
First consider whether patients’ non-attendance is unintentional (e.g. forgetfulness, slept in, missed bus) or intentional (no longer wished to attend).
-
You may reduce the risk of unintentional non-attendance through the use of simple reminder systems (see Clinical scenario 1).
-
Patients who no longer wish to continue with their treatment may not openly choose to discuss this issue with service providers. Consider the most likely reasons why patients may decide they no longer wish to attend (see Appendix 8) and understand whether or not this is something that the health service can address.
-
Ensure reminders contain appointment cancellation requests and procedures. Let patients know that the appointment can be given to someone else (see Appendix 3, theme E, and Chapters 5–7).
-
Make cancellation and rebooking easy (partly through the use of appropriate reminders) (see Appendix 3, theme E; Chapter 4, Proposition E: are there any systems which effectively support the cancellation of appointments?; and Clinical scenarios 7–10).
-
Patients should be told how long the outpatient appointment takes and informed of known or likely delays to the service (Public Governors’ Comments, see Chapter 3, Involvement of patient steering group).
Clinical scenario 5
If you want to optimise the likelihood of attendance of specific population groups:
Considerations from clinical scenario 1 plus:
-
Consider whether or not the health service deals with populations subgroups who are traditionally at a higher risk of non-attendance [see Chapter 5, Demographic and socioeconomic characteristics, for risk factors (refugees, mental health, young men, very old people, deprived populations, homeless people)] [see Appendix 3, theme F.3; Chapter 4, Evidence statement (F.2–F.11): few studies investigate whether or not a range of distal/proxy individual attributes have a differential effect, over and above pre-existing appointment behaviour, on reminder effectiveness (in terms of attendance, cancellations or rebooking) (evidence category Va or VIIa); and Appendix 8].
-
Consider the appropriateness of different technologies (e.g. SMS, phone uptake).
-
Language needs to be considered and pictorial messages may be appropriate in some circumstances [see Appendix 3, theme B.2, and Chapter 4, Evidence statement (B.2): there are no studies investigating whether or not reminder factors (such as language, information provided, framing of information) influence the accessibility/comprehensibility of the reminder message for particular patient groups (evidence category VIIa)].
-
For service users with severe mental health problems, it may be important to provide additional information such as orientation information or information that increases patient intention to attend, e.g. that attendance will contribute to patient well-being (see Appendix 3, themes A.2 and A.3).
-
Consider issues to do with accessibility, such as child care, transport, work commitments (see Appendix 3, theme A.6 and the table reasons for not attending).
-
Consider multimodal packages of reminders (these might be more interactive, personalised styles of reminders). In groups with extreme difficulties in attendance, sequential reminder intervention or patient navigation services could be considered. Such highly intensive and personalised services might, therefore, be targeted at supporting those patients with the greatest difficulties (see Chapter 5, Demographic and socioeconomic characteristics, and Chapter 6, Substance abuse/mental health/comorbidity and physical illness).
Clinical scenario 6
If you want minimise the number of unfilled, non-attendances on any 1 day (i.e. minimise unused capacity):
-
Optimise the likelihood of attendance by sending a reminder (see Clinical scenario 1).
-
Understand likely barriers to attendance in the health service (see Appendix 8).
-
Make it easy for people to attend/reduce barriers to attendance (see Clinical scenario 1).
-
Make it easy for patients to cancel and/or reschedule (see Clinical scenarios 9 and 10).
-
Install notices in clinic waiting areas to inform patients about delays.
-
Consider whether or not overbooking clinics is right for the health service; however, also consider the possible disadvantages of in-clinic waiting times, which can be off-putting for patients and could lead to increased non-attendance rates [see Chapter 6, Current and future developments (Innovations)].
Clinical scenario 7
If it is a high priority that patients cancel then it is important that health-care services, make it as easy as possible for patients to cancel:
-
Health-care services and staff should consider taking a non-judgemental approach to cancellation and recognise that cancellations (and rescheduling) of appointments is a desirable outcome. This recognises that patients are people with busy lives, various commitments and shifting priorities that need to be juggled around health care. It recognises that patients can sometimes be too embarrassed/fearful to phone and say that they cannot attend (see Appendix 3, themes A.1, A.7 and D.3).
-
Reminders need to be sent well in advance, but not more than 7 days in advance. Patients should be asked to cancel an unwanted appointment and reminders should contain a request regarding cancellation. The language and framing of the reminder should be checked to ensure that it is not alienating (see Appendix 3, theme E). This will allow the service to reallocate the appointment to a different patient.
-
Some reminder systems that are more interactive, such as personal telephone calls, have the advantage that cancellations (and rescheduling) can occur concurrently [see Appendix 3, theme E, and Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)]. This may particularly helpful in health services with very high non-attendance rates.
-
Patients should know the mechanism for cancelling an unwanted appointment. Reminders should make it clear what the cancellation procedures are and thereby offer several possible options. Wider advertisement of cancellation procedures should also be considered, for instance by including information on cancellation procedures in standardised patient information, as part of routine appointment-making processes (Public Governors’ Comments, see Chapter 3, Involvement of patient steering group).
-
Patients should be informed that using the mechanism will be quick and easy and this should be made clear in the reminder [see Appendix 3, themes E.1 and E.4, and Chapter 4, Evidence statement (E.1 and E.4): there is indicative evidence to suggest that whether or not a patient cancels and rebooks will be influenced by patient perceptions of how easy it is to rebook (evidence category Va)].
-
Unhelpful or difficult cancellation mechanisms will lead to patient frustration, lack of engagement with the cancellation mechanisms and poor levels of cancellation [see Appendix 3, themes E.2 and E.5, and Chapter 4, Evidence statement (E.2 and E.5): strong consistent evidence indicates that system factors related to appointment systems will hamper patient intentions to cancel/rebook (evidence level Ib)].
-
Health services should have quick and easy cancellation procedures in place, such as dedicated phone lines (with answerphones, if required), SMS reply in order cancel, e-mail facilities, etc., which means that patients can make a brief contact any time, day or night, in order to cancel. It may be helpful to offer a variety of ways to support cancellation by patients, which could all be automated, so that patients can cancel at any time that is convenient to them [see Appendix 3, themes E.1 and E.4, Chapter 4, Evidence statement (E.1 and E.4): there is indicative evidence to suggest that whether or not a patient cancels and rebooks will be influenced by patient perceptions of how easy it is to rebook (evidence category Va)].
-
Health services need to ensure that there are sufficient resources in place to make a cancellation system work [see Appendix 3, themes E.2 and E.5, and Chapter 4, Evidence statement (E.2 and E.5): strong consistent evidence indicates that system factors related to appointment systems will hamper patient intentions to cancel/rebook (evidence level Ib)].
-
Patients should be informed about the costs to the service of FTA and the opportunity costs to other patients of lack of access to appointments. This may also increase a patient’s sense of obligation to cancel an unwanted appointment [see Appendix 3, theme E.7, and Chapter 4, Evidence statement (E.3 and E.6): there is indicative evidence that for patients who intend to take up the offer of an appointment, whether or not a patient cancels and rebooks will be influenced by structural factors that facilitate/hamper patient intentions to rebook (e.g. has to be done on line and no internet access) (evidence level Va)].
Clinical scenario 8
If it is a high priority that patients reschedule their unwanted appointment in order to receive priority treatment:
-
Make cancelling and rescheduling easy (see Clinical scenario 9).
-
Consider initiating contact with the patient in order to reschedule the appointment. For groups who find it difficult to engage with health services, consider more intensive/or individualised support systems to encourage attendance, e.g. patient navigation systems (see Chapter 6, Utilise new ways of managing appointment systems).
-
If it is important that the patient attends a further appointment, then consider whether or not it would be relevant to send out a reminder asking the patient to reschedule when he or she is better.
-
Offer flexibility to overcome those barriers to attendance; this is likely to be service specific in relation to important contextual issues.
-
Provide clear explanations of how the patient can overcome the barriers.
Clinical scenario 9
If you want to make it easy for the patient to cancel or reschedule:
-
A personal telephone call will increase the likelihood of the patient cancelling or rescheduling the appointment.
-
Short message service reminders do not increase the likelihood of the patient cancelling or rescheduling, but work better when the patient can respond directly to the SMS and does not have to call a telephone number given within the body of the message (see Appendix 3, themes E.3 and E.6, and Chapter 4, Evidence statement (E.3 and E.6): there is indicative evidence that for patients who intend to take up the offer of an appointment, whether or not a patient cancels and rebooks will be influenced by structural factors that facilitate/hamper patient intentions to rebook (e.g. has to be done on line and no internet access) (evidence level Va)].
-
Ensure that the systems to enable cancellation or rebooking are easily accessible by the patient. For instance, patients will not wait for long periods on a telephone. Consider having several automated options for cancelling, e.g. SMS reply, answerphone, e-mail. Consider rescheduling systems that also work outside conventional working hours and are, therefore, accessible [see Appendix 3, themes E.1, E.2, E.4 and E.5, and Chapter 4, Evidence statement (E.3 and E.6): there is indicative evidence that for patients who intend to take up the offer of an appointment, whether or not a patient cancels and rebooks will be influenced by structural factors that facilitate/hamper patient intentions to rebook (e.g. has to be done on line and no internet access) (evidence level Va)].
-
Ensure that the internal systems are able to capture, record and relay the cancellation information to the service provider for fast action, which will allow health services to reallocate appointments [see Appendix 3, themes E.1 and E.4, and Chapter 4, Evidence statement (E.1 and E.4): there is indicative evidence to suggest that whether a patient cancels and rebooks will be influenced by patient perceptions of how easy it is to rebook (evidence category Va)].
-
Provide patients with clear information about how to and how easy it is to cancel or reschedule an appointment. Cancellation and rescheduling systems need to be adequately resourced to prevent patients giving up on cancelling [see Appendix 3, themes E.1 and E.4, and Chapter 4, Evidence statement (E.1 and E.4): there is indicative evidence to suggest that whether a patient cancels and rebooks will be influenced by patient perceptions of how easy it is to rebook (evidence category Va)].
Clinical scenario 10
If the health service has to re-schedule an appointment:
-
First be aware that patients may perceive that the appointment cannot be important if it is cancelled or rescheduled multiple times by the service (Public Governors’ Comments, see Chapter 3, Involvement of patient steering group).
-
Letters need be sent in time, and with sufficient priority that they reach the patient before the appointment date/time. If an appointment is cancelled in writing, then the message needs to be clearly laid out and prominently display the new appointment date/time (as the letter includes the old date/time as well) (Public Governors’ Comments, see Chapter 3, Involvement of patient steering group).
-
Ensure that rescheduling is easy and convenient for patients (see Clinical scenario 9).
Appendix 8 Reasons for missing appointments
| Reason | Reminder solutions | Other possible solutions | Implications for attendance, cancellation and rescheduling |
|---|---|---|---|
| Problems with appointment system | |||
| Appointment not received or received too late; being unable to cancel or reschedule; did attend (clerical error); did cancel (clerical error); scheduling of appointments with long delay (perception of importance of appointment) | Sending a reminder between 1 and 7 days in advance would provide patients with an opportunity to rearrange their schedule or to cancel and reschedule to a more convenient appointment (CS 7–9) | Send appointment letters/information letter in advance. Up to 2 weeks in advance is potentially adequate. Procedures for updating patient contact details are important to prevent patients from not receiving appointment information. Dedicated telephone lines. Link on web site. Improved clerical systems. Provide appointments in the near future | Having correct contact details would ensure that appointment information arrives with more patients in a time frame that allows patients to attend, or cancel and reschedule if the appointment is inconvenient. Receipt of a reminder up to 7 days in advance of the appointment will allow patients to attend, cancel or reschedule |
| Patient illness | |||
| Too ill to attend | Reminder systems which promote cancellation and rescheduling | Cancellation and rescheduling procedures need to be in place especially when rescheduling of appointments is an important priority | A reminder which encourages cancellation and rescheduling would reduce wasted appointments and allow the service to reallocate the appointment (CS 9,10) |
| Too ill to cancel | Reminders could be sent, but it is quite likely that patients and relatives/carers may not receive or respond to reminders | Easy cancellation for patients’ relatives to navigate (e.g. automated SMS reply). Consider whether or not it is very important for a patient to reschedule their health appointment when they are feeling better (CS 10). Send a reminder asking patients to reschedule when they are feeling better | In this case, it seems likely that the appointment will be missed, and that cancellation will not occur. A reminder (SMS, letter) could be effective at encouraging rescheduling behaviour when the patient is better |
| In hospital at time | For planned hospital admissions, a reminder shortly before the appointment could trigger cancellation/rescheduling. In the case of unplanned (emergency) hospital admissions, cancellation or rescheduling is unlikely to occur | Cancellation and rescheduling procedures in place (CS 7, 8). Linked record keeping | A reminder that encourages cancellation and rescheduling would reduce wasted appointments and allow the service to reallocate the appointment (CS 9,10). In the case of emergency admission, it is unlikely that cancellation will occur |
| Patient perceptions and fears regarding the importance or value of appointment | |||
| Anxiety about procedures | Provision of information that reduces anxiety (see Appendix 3, themes A.3 and B.3) (CS 3) | Provide full information about the screening program, including details of how and when the results will be reported to the patient (Public Governors’ Comments, see Chapter 3, Involvement of patient steering group). Provide information that increases patient perceptions that the appointment will be positive (see Appendix 3, theme A.5). Provide a follow-up reminder to patients who reschedule their appointment (Public Governors’ Comments, see Chapter 3, Involvement of patient steering group) | Likely to increase attendance |
| More important health concerns (comorbidities) (see Appendix 3, theme F.8) | When health services are dealing with populations with multiple health problems, e.g. older patients, reminder systems that encourage cancellation and rebooking might be an appropriate way to manage non-attendance (CS 7–9) | Open recognition that other health problems can get in the way of attending the current health appointment, may alleviate concerns or embarrassment about cancelling (see Chapter 5, Physical illness/comorbidity). Easy cancellation for patients or relatives/carers to navigate (e.g. automated SMS reply). Consider whether or not it is very important for a patient to reschedule their health appointment when they are feeling better (CS 8). Send a reminder asking patients to reschedule when they are feeling better.83 Assuming that patients are actually well enough to attend, consider batching of health-care appointments for people who are receiving treatment for multiple health problems simultaneously | A reminder may prompt an individual or carer to cancel an unwanted appointment that they might have forgotten about. A reminder (SMS, letter) could be effective at encouraging rescheduling behaviour when the patient is better.83 Batching of appointments may make it easier for patient to attend appointments |
| Asymptomatic health status, e.g. screening appointments or symptom resolution following treatment; not understanding the importance of the appointment; could not be bothered; patients do not find the appointments helpful or rewarding, etc. | Provide information that reinforces the importance of continued treatment through reminder systems (CS 3). Reminder systems should also positively promote cancellation (and rescheduling if it is indicated). Provision of information that increases understanding (reminder plus) (see Appendix 3, themes A.3 and B.3) | Provision of information that reinforces the importance of the screening procedure through appointment letters (see Appendix 3, theme A.2, and Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)]. Health-care providers check whether or not patients would like to continue with appointments or not or discuss the importance of continuing with treatment if this is indicated or negotiate a discharge if patients no longer want to continue with treatment | Promotes attendance at follow appointments through provision of information (see Appendix 3, themes A.2 and A.3). Good communication with patient to encourage attendance at appointments if this is required or self-management without wasted appointments if that seems more appropriate for the patient. Patients may feel reassured, more confident about attending |
| Low perceived severity of condition | This is likely to result in higher than usual non-attendance, consider using reminder plus or more intensive reminders (see Chapter 6, Symptomatology and severity). Consider whether or not the message should be gain-framed (benefits of attending) or loss-framed (consequences of non-attendance) (CS 3) | When patients actually have non-severe health conditions are self-managing or have reduced symptoms and no longer wish to attend, provision of information that reinforces the importance of relevant self-management strategies and what to do when/if the patient relapses negotiated discharge [see Appendix 3, theme A.2, and Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)]. When patients actually have severe health conditions and low level of symptoms, provision of information about management processes that reinforces the importance of continued treatment may be helpful to promote attendance [see Appendix 3, theme A.2, and Chapter 4, Evidence statement (A.2–A.6): there is weak consistent evidence that ‘reminder plus’ are more effective than simple reminders at helping a patient to attend their appointment (evidence category IIIa)]. Reminder systems should promote attendance and the importance of rescheduling to maximise positive outcomes and minimise negative outcomes, and to address fears that are relevant to the health service, etc. (see Appendix 3, theme A – several may be relevant; and see Appendix 3, theme E). Negotiate a discharge if patients no longer want to continue with treatment | Patients with actual low severity conditions could be encouraged to self-manage for as long as possible and encouraged to reschedule via appropriate scheduling mechanisms when they feel that they need further input. May facilitate attendance and may lead to an informed decision to stop treatment. May also facilitate cancellation or rescheduling |
| Lower actual severity of condition (see Appendix 3) | Simple reminders are potentially useful in promoting attendance. Consider reminders that incorporate messages to cancel if patient no longer intends to attend treatment, and reminders to reschedule if patient simply unable to attend but wishes to continue with treatment | Prepare patients for self-management of condition as a part of the overall management strategy | Promotes attendance: allows patients to self-manage beyond the period of treatment decreasing the requirement for patients to attend. Promotes cancellation: promotes rescheduling for patients who do wish to continue with treatment. Patients can be referred for treatment if the patient feels that they need further treatment |
| Timing and incompatibility of the appointment: planned (avoidable) | |||
| Employment status – work commitments; inconvenient time; unable to get time off work | Reminder systems which promote cancellations and rescheduling | Easy cancellation and rescheduling procedures (CS 9); more flexible scheduling (see Appendix 3, theme F.4); provision of evening clinics; consider issues to do with accessibility, such as child care, transport, work commitments (see Appendix 3, theme A.6) (CS 4, 5) | A reminder that encourages cancellation would reduce wasted appointments and allow the service to reallocate the appointment (CS 8, 9). It is possible that more patients will be able to attend their appointments if there is greater flexibility in the appointments system. There is some evidence that patients would welcome this179 (see Appendix 3, theme F.4) |
| Timing and incompatibility issues: unplanned (unavoidable) | |||
| Other family commitments – sick child | Reminder systems which promote cancellations and rescheduling | Easy cancellation procedures (CS 9), more flexible scheduling (see Appendix 3, theme F.4) (CS 8) | A reminder that encourages cancellation would reduce wasted appointments and allow the service to reallocate the appointment (CS 8, 9). It is possible that more patients will be able to attend their appointments if there is greater flexibility in the appointments system. There is some evidence that patients would welcome this179 (see Appendix 3, theme F.4) |
| Forgetting | Send a simple reminder, it does not appear to matter what type of reminder is sent in this situation. Send reminder 1–7 days in advance | Cancellation and rescheduling procedures need to be in place, especially when rescheduling of appointments is an important priority (CS 7–9) | Simple reminders are effective at helping forgetful patients to attend (see Appendix 3, theme A.1) (CS 1). A reminder that encourages cancellation and rebooking would reduce wasted appointments and allow the service to reallocate the appointment (CS 8, 9) |
| Overslept | Reminder unlikely to be effective unless on same day, prior to appointment | Consider whether or not it is very important for a patient to reschedule their health appointment when they are feeling better (CS 8). Send a reminder asking patients to reschedule.83 Consider making appointments later in the day; evening clinics | A reminder (SMS, letter) could be effective at encouraging rescheduling behaviour when the patient is better.83 An appointment later in the day would prevent similar problems arising in the future |
| Issues to do with patient: practitioner relationship or interaction | |||
| Appointment not with doctor of choice; poor therapeutic relationship with HCP (see Appendix 3, theme C.4); accessing alternative health provider (e.g. doctor shopping in Hong Kong) | Ensure reminders contain appointment cancellation requests and procedures. Let patients know that the appointment can be given to someone else (see Appendix 3, theme E, and Chapters 5–7) | More flexible scheduling; constructive, open, non-judgemental communication and behaviour from HCP; provide option of appointment with alternative HCP | Allow rescheduling with other practitioner. Encourage resolution of issue |
| Issues to do with the accessibility of the appointment | |||
| Unable to get transport; unable to park; distance to clinic | Include information about transport and accessibility in reminder/appointment invitation: ‘reminder plus’ (see Chapter 6,Reminder plus) | Transport provision; provide health care in more accessible location | No strong evidence from the literature around reminder systems |
| Financial reason: cost of transport (costs of health care not so relevant in a UK context) | Privately insured patients more likely to attend than Medicaid patients65 | ||
| Patient attributes | |||
| Age (adolescents and young adults) (see Appendix 3, theme F.1) | Reminders are indicated for all age groups but for different reasons; younger people more likely to miss appointments, but older patients take up the bulk of the appointment. Consider reminder accessibility (see Chapter 6, Accessibility) | Age appropriate technologies could be considered – no evidence to support or describe this | The evidence strongly suggests that reminders will impact upon attendance62 and that this is likely to be the case regardless of age. We do not know how age impacts the effectiveness of reminders to increase cancellation figures |
| Too embarrassed to call clinic to cancel | Provide solutions that reduce patient: clinic interaction, such as SMS, answerphone (CS 7, 8) | Facilitates cancellation/rebooking without need for explanation or interaction | |
| Gender | There is no evidence that gender influences a person’s attendance at appointments therefore a reminder solution does not need to consider gender | No general recommendations can be offered, consider local health service needs | |
| Deprivation status (or problems arising from deprivation status) | Provide multiple methods of cancelling and rescheduling appointments. Consider a range of reminder technologies appropriate to the audience | Accuracy of contact details; ease of understanding health-care literature; easy and inexpensive ways to make, cancel, reschedule appointments (CS 1, 5, 7–9); transport; appointment batching (see Appendix 3, theme F.3) | Inability to access a population (for instance, owing to lack of telephones) makes cancellation and rebooking less likely and more difficult |
| Ethnicity: there is no clear evidence to suggest that ethnicity influences attendance; there is also equivocal evidence that language difficulties may lead to non-attendance | Consider the appropriateness of different technologies (e.g. SMS, phone uptake). Language needs to be considered and pictorial messages may be appropriate in some circumstances (see Appendix 3, theme B.2, and Chapter 5, Ethnicity) | It is hypothesised that sending appointment letters and reminders in a language that is understood by the patient would be an appropriate thing to do; although there is no evidence to suggest that this increase attendance, cancellation or rebooking | |
| Substance abuse: see Appendix 3, themes F.6 and D.3 and Chapter 5, Substance abuse) | Simple reminders and automated reminders to attend may be ignored or overlooked particularly when are experiencing an increased level of illness or substance abuse. In fact, the use of simple reminders may put these patient groups at a disadvantage as compared with general outpatient populations. Reminders with direct personal contact might be appropriate in these groups (see Chapter 6, Other reminder characteristics, Format of the reminder). A sequential reminder intervention78 would reach the maximum number of participants but may increase attendance rates and still be cost-effective (CS 5) (see Chapter 6, Substance abuse/mental health/comorbidity and physical illness) | A further consideration is how to re-engage patients with treatment after they have missed their appointment. Intensive reminder approaches might also be effective at re-engaging similar groups of patients who have dropped out of treatment (C8) (see Chapter 6, Substance abuse/mental health/comorbidity and physical illness) | Maximise attendance in a generally low-attending group. Re-engage patients following non-attendance |
| Mental health service users | As above in row Substance abuse | As above in row Substance abuse | Maximise attendance in a generally low-attending group. Re-engage patients following non-attendance |
Appendix 9 Advantages and disadvantages of reminder systems
| Simple reminder | Reminder plus (brief orientation) | Other reminder systems 1 | Other reminder systems 2 | |
|---|---|---|---|---|
| Examples | SMS/letter: provides details of time, date, venue | Letter/e-mail/telephone plus orientation information | Reminder plus encouragement to cancel/reschedule | Telephone calls |
| Advantages | Most people will get SMS reminder provided contact details have not changed or are inaccurate – delays in text are possible (see Appendix 3, theme B.1). Can encourage attendance in those who simply forget (see Appendix 3, theme A.1). SMS is popular and most widely welcomed mode of reminder amongst adolescents and young adults.101 There is strong consistent evidence that mobile text message reminders improved rate of attendance compared with no reminders (RR 1.10, 95% CI 1.03 to 1.17).43,85 IVR system can deliver complex information and is equally as effective as nurses at delivering information; however, patients who receive nurse phone calls report more positive interactions than those receiving IVR.66 SMS software allows large batches of text messages to be delivered almost instantly, minimising labour costs. SMS messages do not require the mobile phone to be active nor necessarily within range and can be held for a number of days until the phone is active or within range. Furthermore, SMS is also private in a way that voice calling is often not57 | The review by Car et al.43 finds conflicting evidence that favours the effectiveness of ‘reminder plus’. They report that one low-quality study245 reported that mobile text message reminders with postal reminders, compared with postal reminders, improved rate of attendance at healthcare appointments (RR 1.10, 95% CI 1.02 to 1.19). However, three studies of moderate quality showed that mobile phone text message reminders and phone call reminders had a similar impact on health-care attendance (RR 0.99, 95% CI 0.95 to 1.03)246–248 | Can encourage attendance in those who simply forget (see Appendix 3, theme A.1). Can encourage patients who can no longer attend or no longer want to attend their appointment to cancel their appointment, making the appointment available for others (see Appendix 3, themes E.1 and E.4). Can encourage those patients who need to reschedule to make another appointment (see Appendix 3, theme E.1). Multimodal reminders (e.g. written invitation, phone call, reminder, home visit) increase attendance for disadvantaged populations with diabetes in comparison with standard reminder (written invitation and two reminders) | Personal telephone calls have a higher rate of attendance in comparison with leaving a message or not reaching the patient at all65 |
| Disadvantages | Does not encourage cancellation or rescheduling in patients who cannot attend or who no longer wish to attend. Some patients reported that they never received a SMS reminder. It is possible that mobile phone numbers were entered incorrectly on patient records, or that those patients changed their phone numbers during the study.208 Patients may not receive the SMS reminders due to incorrect data entry. Older patients were considerably less likely to own a mobile phone, making them harder to access using reminder technology.100,108 People may not be willing to disclose their mobile phone numbers and record them in patient notes.91 High rate of 10% of clerical errors.111 Some clients expressed concern over having received a copy of a referral letter of another patient in ‘error’; therefore, negatives associated with this approach include the possible implications for client confidentiality, and the increased cost and time implication. One-third of patients gave incorrect contact details when booking the appointment.129 Inner city populations may have less stable contact details (either address or phones) and this may put these patients at a specific disadvantage.103 A potential disadvantage of the system was that 2–3% of people failed to receive their text reminder as a result of incorrect data entry. Patients with mobile phones are most likely to change their contact number.94 Use of this emerging technology disadvantages those who do not have a mobile telephone. 35% patients of this study did not give their mobile phone number.106 Problem in retrieving mobile phone numbers of the citizens, only 12% of the registered citizens did have a mobile phone; thus the initial sample of people eligible for reminders was 66,000 out of 544,000. Wrong phone numbers can result in the SMS reaching someone other than the patient.102 A limitation in the application of this reminder process to the wider hospital community is the degree to which different patient groups are familiar with SMS messaging.106 Issues with SMS: incidence of incorrect mobile telephone numbers; 92 (0.4%) of the 22,658 recipients contacted outpatient services stating that they had no knowledge of the scheduled appointments in the reminder message. It is possible that this value was higher but the recipients did not take any action. The high prevalence with which consumers change their mobile telephone and or mobile telephone service is another issue with SMS.95 Patients with mental health problems have a lower preference rate for SMS reminders than other patient groups.209 Older age groups are less likely to own mobile phone: 61% of 71- to 90-year-olds reported ‘no mobile’.198 90% of the population in many countries own mobile phones, but the uptake is higher in younger people.108 A concern often cited by both patients and physicians is the security of e-mail messaging206 and so this should be addressed specifically (by future research) to allay or confirm fears that may be influencing its use42 | E-mail is a relatively untested reminder method42 | May not promote attendance who are anxious about the intervention or who are not sure how to access the health-care service. Computerised appointment system: a disadvantage to this system is the automated call does not specify the clinic in which the patient has an appointment. Hard for some patients to understand and operate practice computer appointment systems249 | Telephone reminders have particularly poor contact rates – need to consider when calls are made (see Appendix 3, theme B.1). Need to ensure patient records are up to date. Telephone reminders are problematic for groups of the population who have no telephone or who have been disconnected (i.e. deprived populations). Of people in this audit, 23% did not have a telephone or their telephone was disconnected.91 The disadvantage of telephone reminder is that several calls may be needed and this increases the cost of this type of intervention215 |
| Cost | The cost of the SMS reminder is minimal, considering the loss of revenue generated by failed appointments. Text reminders on a large scale would be cost-effective strategy could be improved.208 Annual cost of missed appointments in England is estimated to be close to £575M. The use of SMS reminders could save £55.6–83.5M a year.165 Costs/attendance of mobile phone text message reminders have been shown to be lower compared with phone call reminders.43 Based on NNT analysis, approximately 14 people would need to be sent a SMS reminder to prevent one non-attendance.100 The average estimated costs in these 14 studies was €0.41 per patient. The mean cost of phone reminders was €0.90, while the mean cost of SMS or automated phone call reminders was €0.14. The three highest reported costs were from phone reminders.47 This study found that the impact is modest, but also is the cost about £7.50 (US$13.13, €10.88) per ‘no-show’ avoided.108 Considering 500 SMS/day at a unitary cost of €0.0065, the first year cost will be €11,500 while next year cost will be about €8200, accounting for SMS and maintenance. Reasoning on a daily basis, this amounts to €35 in the future. As the average monetary loss of a dropout is €20, it’s sufficient to recover 2–3 dropouts/day to amortise the system.102 The cost of sending the SMS reminder during the trial period amounted to 5164 Australian dollars. Attendance rate achieved estimated 11.5% (273,993 Australian dollars).95 Although the attendance rate was similar, the cost-effectiveness analysis showed that the cost per attendance for SMS group was significantly less than that for telephone group. The ratio of cost per attendance of SMS text messaging to that of phone was 0.65 : 1.57 Text messaging reminder is cheaper than mobile phone reminder. The ratio of cost per unit attendance of text messaging vs. mobile phone was 0.55 : 172 | |||
| Implications for attendance | One systematic review conducted by Car et al.43 found moderate-quality evidence showing that mobile text message reminders improved the rate of attendance at health-care appointments compared with no reminders (RR 1.10, 95% CI 1.03 to 1.17). [See Chapter 4, Evidence statement (A.1): there is strong consistent evidence that simple reminders which provide details of timing and location of appointments are effective at helping a (forgetful) patient to attend their appointment (evidence category Ia)] | |||
| Implications for cancellation and/or rebooking | There is strong evidence that a personal phone reminder will increase patient cancellation rates,67,77,80 but can be problematic when people do not have phone access. SMS can increase cancellations in comparison with no reminder.100 Telephone reminders are more effective than SMS reminders at facilitating cancellation and rebooking.80 The convenience of e-mail for cancellation, insofar as there is no need to wait to get through to a receptionist, is discussed by Atherton et al.42 The evidence for different technologies on rebooking is weak; however, the evidence suggests that cancellation and rebooking will be influenced by the simplicity ease of access to cancellation/rebooking systems101 |
Appendix 10 Outline proposal for a web-based practice guide
List of abbreviations
- A&E
- accident and emergency
- AHP
- Allied Health Professional
- CASP
- Critical Appraisal Skills Programme
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CRD
- Centre for Reviews and Dissemination
- DARE
- Database of Abstracts of Reviews of Effects
- FTA
- failure to attend
- GP
- general practitioner
- GUM
- genitourinary medicine
- HIV
- human immunodeficiency virus
- IT
- information technology
- IVR
- interactive voice response
- NNT
- number needed to text
- OR
- odds ratio
- PopInS
- Population/Intervention/Study type
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QIPP
- quality, innovation, productivity and prevention
- RCT
- randomised controlled trial
- RR
- relative risk
- SMS
- short message service