Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/1011/01. The contractual start date was in September 2011. The final report began editorial review in June 2013 and was accepted for publication in April 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Disclaimer
this report contains transcripts of interviews conducted in the course of the research and includes language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Greenhalgh et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background and literature review
The problem of ‘failed’ information and communication technology programmes in health care
The history of information and communication technologies (ICTs) in health care includes some expensive disasters. For example, England’s National Programme for Information Technology (NPfIT) was established in 2006 with a projected cost of £12.7 billion over the ensuing 8 years,1 but after numerous delays and difficulties, most of its component technologies were abandoned in 2011–12, and expensive penalties were incurred for breach of commercial contracts. 2–5 To accompany the release of a damning summary of the programme’s failures in May 2011, the head of the National Audit Office wrote:
The original vision for the National Programme for IT [information technology] in the NHS will not be realised. The NHS is now getting far fewer systems than planned despite the Department paying contractors almost the same amount of money. This is yet another example of a department fundamentally underestimating the scale and complexity of a major IT-enabled change programme. The Department of Health needs to admit that it is now in damage-limitation mode. I hope that my report today, together with the forthcoming review by the Cabinet Office and Treasury, announced by the Prime Minister, will help to prevent further loss of public value from future expenditure on the Programme.
Amyas Morse, head of the National Audit Office, 18 May 20116
In 2007–10, our team evaluated the introduction of two components of the NPfIT: the Summary Care Record (SCR) and a linked patient portal, HealthSpace (see Chapter 3, The primary data sets). Policy-makers had predicted that these technologies would be widely adopted and would lead to rapid improvements in the quality, safety and efficiency of care as well as empowering patients, promoting choice and reducing health inequalities. 7 Lack of realisation of their hoped-for benefits was attributed mainly to the fact that they were not being used. 8–11 Similar findings were documented by the evaluators of the implementation of hospital records within the NPfIT. 3,12–14 At the time of writing, most of the technologies in the NPfIT (including hospital-based records and HealthSpace) had been withdrawn because of delays in supply and/or non-uptake by clinicians, and a new policy emphasising local development and/or procurement introduced. 15 The SCR was still Department of Health policy but its use in clinical practice remained limited. 16
Both we and other research teams have described numerous other instances of non-adoption, limited adoption or adoption followed by abandonment of ICTs by clinicians, especially when they were introduced as part of a large, top-down change programme. 3,17–19 As one study concluded, ‘Most [healthcare ICT] implementations fail because, despite high investments in terms of both time and financial resources, physicians simply do not use them’ (p. 309). 20
The literature on resistance to ICTs in health care is extensive. In the next few sections, we summarise that literature and introduce our own chosen approach. Immediately below, we consider the (broadly) behaviourist approach taken by many cognitive psychologists and health services researchers to ‘resistance’ to ICTs, which is still the dominant framing taken by many academics or policy-makers. In the section Multilevel models of resistance to information and communication technologies, we review multilevel models of resistance in which group and organisational factors are added to individual ones. Next (see Interactional models of resistance: the sociotechnical perspective), we consider theoretical approaches that take an organic or interactional view of how individuals in organisations use technologies (or not), focusing in particular on Lynne Markus’s classic study from 1983 on technology-system fit, Albert Cherns’ work on sociotechnical systems theory, computer-supported co-operative work (CSCW) and Carl May’s normalisation process theory.
In the section Critical studies of organisational power relations, we outline the literature from critical management studies (and, more specifically, from critical information systems studies) that considers people’s resistance to ICTs in the workplace in terms of the play of power between dominant and ‘dominated’ groups. We then briefly explain actor–network theory (ANT: Bruno Latour) and related perspectives (see Actor–network theory), including important extensions of this approach in the work of Ole Hanseth and colleagues from Norway on standardisation and Marc Berg from the Netherlands on the agency as a product of the network. We introduce the sociological work of Anthony Giddens (see Giddens’ work on structuration, modernity and technology), including structuration theory and its links to modernity and technology. Finally, we explain how an empirically-oriented extension of structuration theory developed by one of us (RS) and known as ‘strong structuration theory’ (SST) can be further enhanced for the study of technologies using selected elements of ANT (see Strong structuration theory). When we originally planned this study, we were drawing on our work on this ‘ANT–SST hybrid’, though as we explain in the Discussion (see Chapter 5), we modified our stance somewhat as our thinking developed and data analysis progressed.
The technology acceptance model
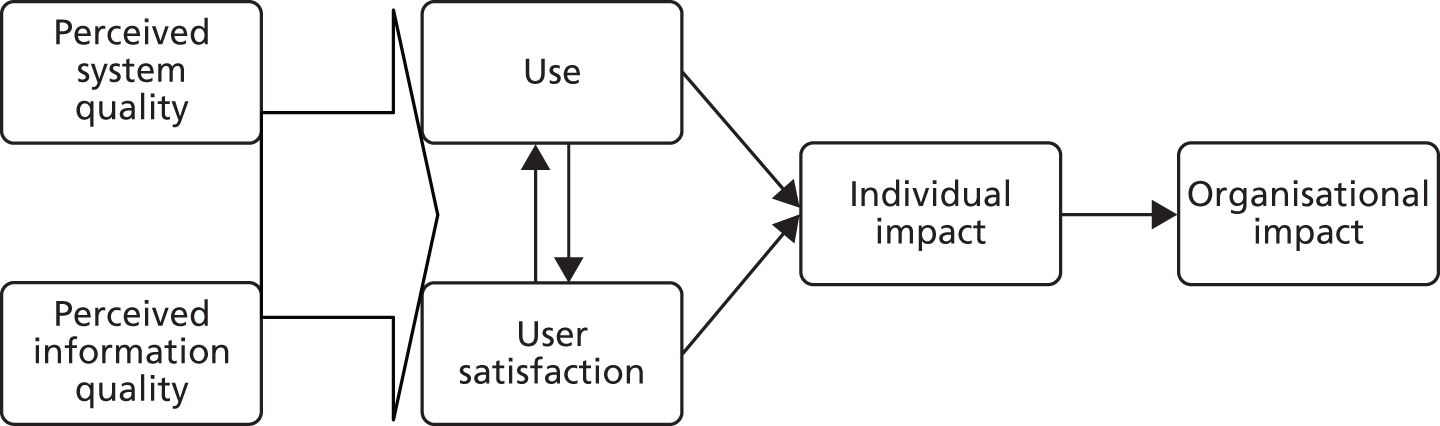
The most widely used model for considering ICT adoption in organisations is probably Davis’ ‘technology acceptance model’ (TAM), located in the cognitive psychology/human–computer interaction literature and cited by over 2000 studies since. 21 It states that a technology is more likely to be adopted by a potential user if it scores highly on a set of attributes including ‘usefulness’ (e.g. the degree to which it helps someone do their job and improves their productivity) and ‘ease of use’ (e.g. features such as user-friendliness, speed and ‘clunkiness’). The TAM, which was originally derived as an adaptation of Rogers’ diffusion of innovation theory, was subsequently extended to produce a model of information system success, seen as determined by user uptake, which in turn was determined by users’ perceptions of the quality of the system and the quality of the information it contained. 22 All of these variables are seen as interconnected and interdependent; the strength of the relationship between any of them, and the influence of particular mediating or moderating variables, will vary with the situation, but according to the model, they can (in theory at least) be measured and quantified.
Delone and McLean later added a third component (perceived service quality, such as helpdesk support) to the first column in Figure 1. 23 They also unpacked the dependent variable (‘organisational impact’) into four dimensions: task productivity (the extent to which an application improves the user’s output per unit of time); task innovation (the extent to which an application helps users to create and try out new ideas in their work); customer satisfaction (the extent to which an application helps the user ‘create value’ for customers); and management control (the extent to which the application helps to regulate work processes and performance). Although their model rests on positivist assumptions (i.e. it assumes an objective reality ‘out there’ that can be measured and whose behaviour can potentially be predicted), Delone and McLean emphasised (drawing implicitly on contingency theory) that it should not be used in a simplistic, deterministic way, as different systems will have different independent variables that impact on the dependent variable.
FIGURE 1.
The Delone–McLean model of information system success. Adapted with permission from Delone WH, McLean ER, Information systems success: the quest for the dependent variable, Information Systems Research, volume 3, number 1, March 1992. 22 Copyright 1992, the Institute for Operations Research and the Management Sciences, 5521 Research Park Drive, Catonsville, Maryland 21228, USA.
A 2010 review by Holden and Karsh of the applicability of the TAM in health care considered 16 data sets analysed in over 20 studies of clinician use of health information technology (IT) for patient care across a range of settings. 24 Certain TAM relationships (e.g. between perceived usefulness and the behavioural intention to use) were consistently found to be significant, whereas others (e.g. between perceived ease of use and behavioural intention to use) were inconsistent. The authors concluded that TAM predicts a substantial portion of the use or acceptance of health IT, but that the theory may benefit from several additions and modifications – specifically, with more attention to norms and beliefs of potential adopters of the technology.
A citation track of Davis’ original paper and Holden and Karsh’s later review showed that hundreds of empirical studies of user resistance to technology have been based on the TAM and that several dozen of these relate to ICTs in health care. 25–31 These studies invariably conceptualise the individual user of an ICT as a rational actor who seeks control over his or her work and weighs up constructs such as ‘usefulness’, ‘ease of use’ and the ‘costs’ and ‘benefits’ of change. Indeed, most such studies implicitly or explicitly combine the TAM with the Theory of Planned Behaviour. 32 They depict user resistance as an individual deficit, usually comprising a combination of parochial self-interest, misunderstanding, lack of trust, a belief that change is worthless and low tolerance for change,33 and emphasise measures through which resistance (thus defined) can be overcome – for example, via ‘engagement’ activities, incentives or punishments, firm leadership of the change project and ensuring that staff feel ‘in control’ during implementation. 34 All place a central emphasis on the individual user of an ICT, and all see user acceptance – and its converse, user resistance – as a key focus of enquiry (especially in explaining ‘failed’ ICT projects).
One author in this tradition articulated the problem of resistance thus:
. . . the major challenges to system success are often more behavioral than technical. Successfully introducing such systems into complex healthcare organizations requires an effective blend of good technical and good organizational skills. People who have low psychological ownership in a system and who vigorously resist its implementation can bring a ‘technically best’ system to its knees. However, effective leadership can sharply reduce the behavioral resistance to change--including to new technologies--to achieve a more rapid and productive introduction of informatics technology.
p. 1135
As the following sections show, many researchers have rejected such overt behaviourist framings. However, this section has shown that un-nuanced and uncritically pro-innovation applications of the TAM remain popular in some parts of the research literature. In such studies, the adoption and use of new technologies is seen as a necessarily positive step linked to the promise of greater procedural efficiency (and, implicitly, clinical effectiveness). In such traditions, research has assumed a ‘rational actor’ and been directed mainly at ‘overcoming resistance’ using behaviourist methods. Reflecting this rationalist emphasis, policy measures for introducing ICTs in health care often focus largely or exclusively on ‘overcoming [individual] resistance’ (e.g. see the Department of Health’s consultation36).
Multilevel models of resistance to information and communication technologies
A number of authors have extended the focus of the TAM by nesting it within a multilevel conceptual framework. Sabherwal et al. ,37 for example, propose context-related constructs (top management support for the system, facilitating conditions); user-related constructs (user experience with an information system, user training, user attitudes, user participation in the development of the system); and system constructs (system quality, perceived usefulness, user satisfaction, system use).
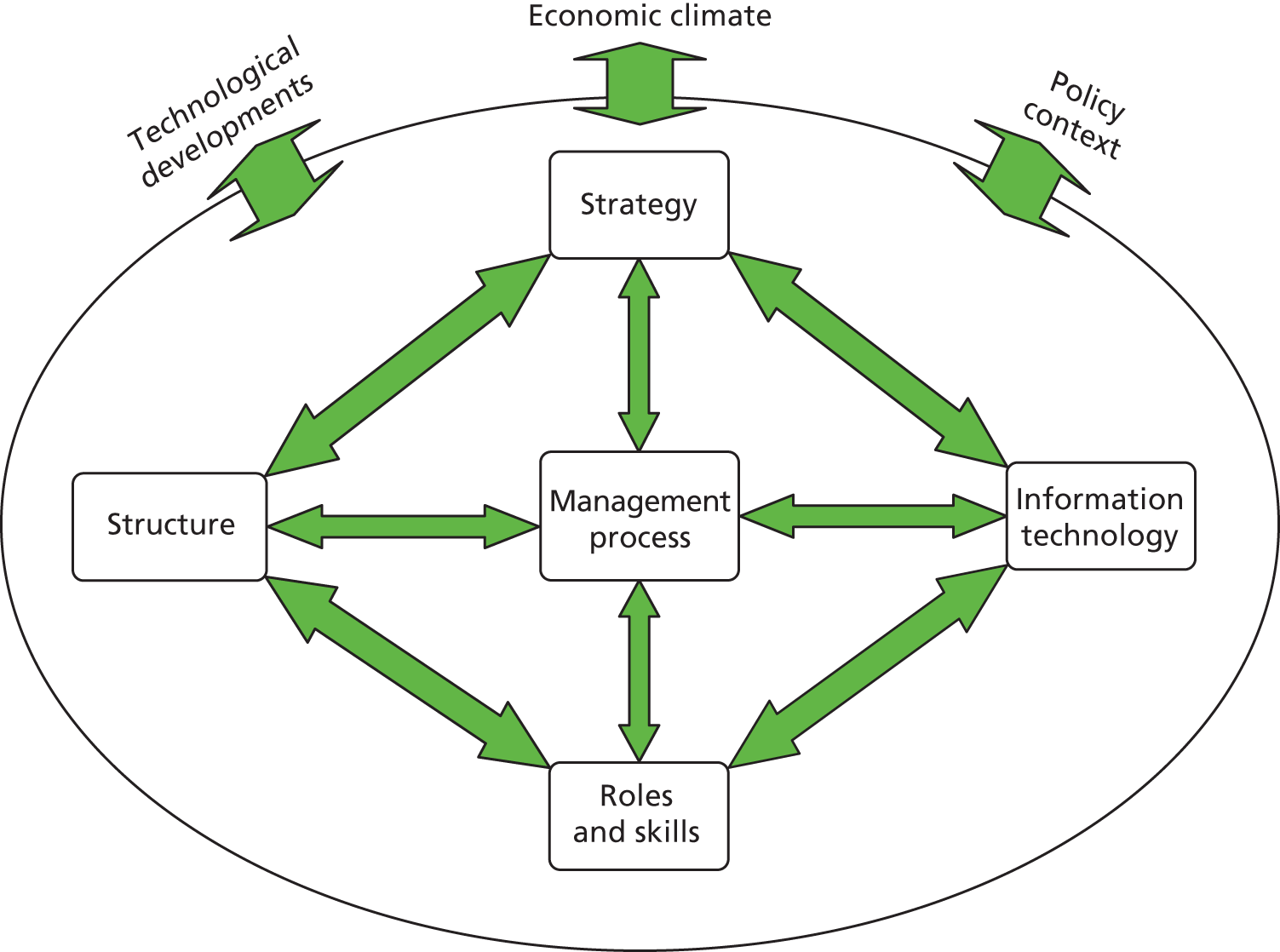
Yusof et al. 38 suggest that the Delone–McLean model lacks attention to certain factors that are particularly important in the healthcare setting – specifically, the ‘soft’ human and organisational factors such as culture, buy-in and so on. They offer a model of ‘fit’ between information systems, organisational factors, and external influences (Figure 2).
FIGURE 2.
‘Fit’ between information technology, internal organisation factors and external factors. © 2014 IEEE. Reprinted and adapted, with permission, from Yusof MM, Paul RJ, Stergeoulas L. Towards a framework for health information systems evaluation. HICSS ’06 Proceedings of the 39th Annual Hawaii International Conference on System Sciences. IEEE Digital Library; 2006. 38
Based on a series of studies of the differing fortunes of ICT systems in different hospitals,39–41 an interdisciplinary group of researchers developed a ‘triple-level’ model of resistance comprising individual (people’s perceptions of the technology), group (the extent to which the new system reinforces or threatens a group’s power base) and organisational (the extent to which the innovation aligns with organisational strategy and goals). This model is shown in Figure 3.
FIGURE 3.
Triple-level model of information system implementation, based partly on Markus. Adapted with permission from Lapointe L, Rivard S, A triple take on information system implementation, Organization Science, volume 18, number 1, 2007. 41 Copyright 2007, the Institute for Operations Research and the Management Sciences, 5521 Research Park Drive, Catonsville, Maryland 21228, USA.
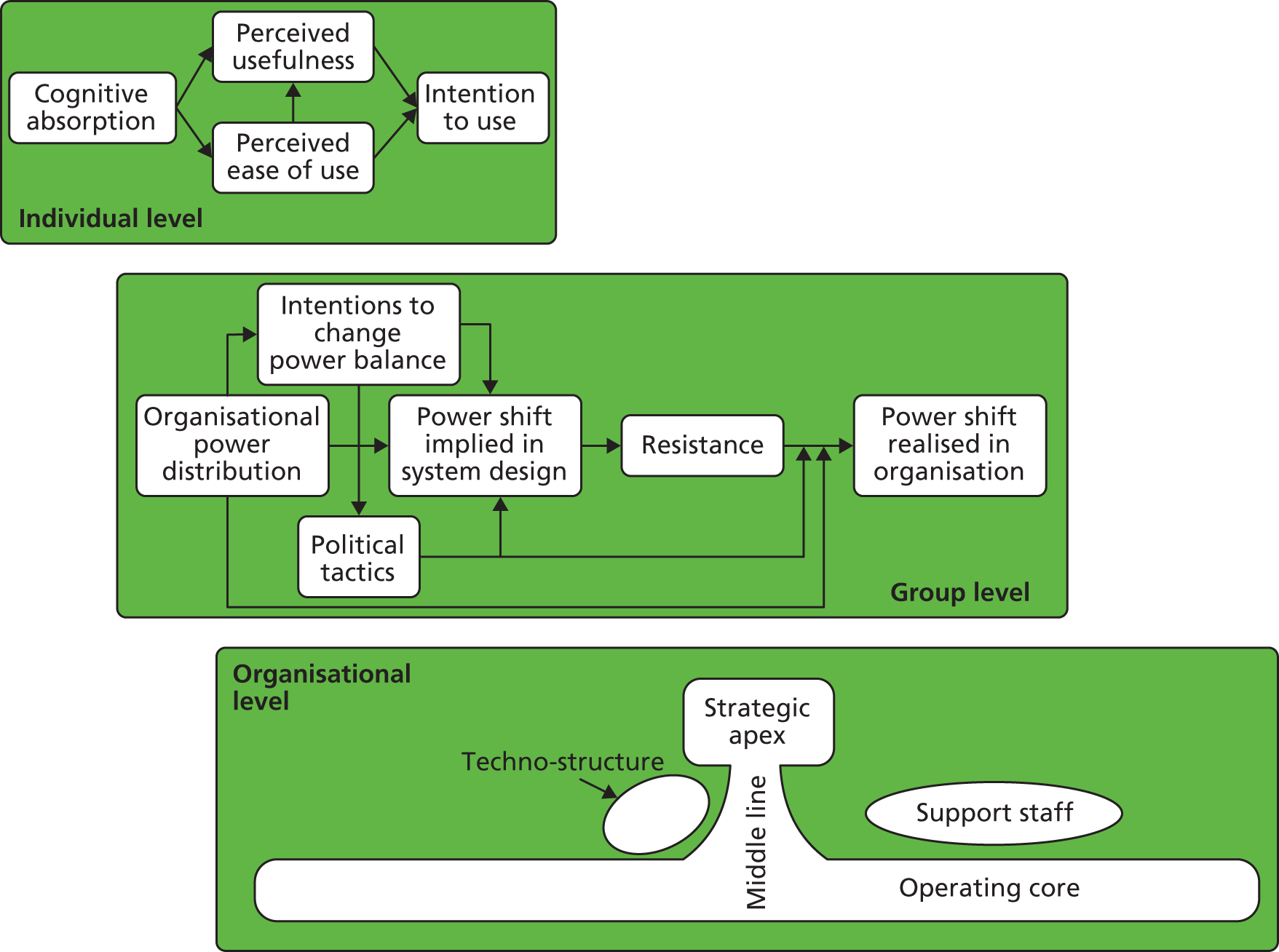
In this ‘triple model’, resistance is seen not simply as a psychological deficit (obstinacy, indolence, ignorance and irrational fear of change) that needs to be overcome (e.g. via top management mandate or the psychological tactics for increasing engagement). Rather, it is a phenomenon that develops over time as users interpret the alignment (‘fit’) between a new technology and individual, group and organisational context. According to this model, when resistance generates conflict and consumes time and attention, it tends to have negative impact, but resistance may also have a positive impact when it stops organisations from investing in systems that would lead to losses in productivity and stress among staff. This is true of any organisation, but Lapointe and Ricard suggest that it may be particularly apposite in health care, where ‘fit’ between an information system and the internal properties of the organisation may be particularly poor.
While this stream of research marks an important step forward from individual-focused models, it remains uncritical of the place of technology in health care and is relatively uninterested in the external forces (political, economic, technological, professional) that give rise to ICT programmes or in the subtle but potentially important ways in which ICTs may influence the nature of clinical work and the quality of the clinical interaction.
Interactional models of resistance: the sociotechnical perspective
Back in 1983, Lynne Markus published a classic review paper in a US management journal of barriers to implementation of information systems in organisations. In it, she divided theories and models into ‘people-determined’ (resistance is explained by people’s personalities, goals, capabilities and so on); system-determined (resistance is explained by features of the technology itself and how it is implemented); and interactional (resistance is explained by what we would now call sociotechnical issues, i.e. the interaction between people and technologies). 42 ‘People-determined’ theories, said Markus, depicted the solution to resistance in terms of education, training, incentives, policies and user participation (to achieve commitment). ‘System-determined’ theories saw the solution in terms of better technical and ergonomic design, better protocols and procedures, and user participation (to achieve better design). Interactional theories suggested that the organisational problems should be addressed before the system is introduced (or even designed), and that the relationships between users and designers were all-important.
At around the same time as Markus’s paper on ‘Power, Politics and Information Systems’ was published in the USA,42 British researchers based at the Tavistock Centre in London, UK (which specialises in the study of organisational dynamics from an interpersonal perspective), were developing sociotechnical systems theory. This proposes that technologies and work practices are best codesigned using participatory methods in the workplace setting, drawing on such common-sense guiding principles as staff being ‘able to access and control the resources they need to do their jobs’, and insisting that ‘processes should be minimally-specified (e.g. stipulating ends but not means) to support adaptive local solutions’. 43 Sociotechnical theory frames resistance to ICTs in terms of poor fit between the micro-detail of work practices and the practicalities of using technology.
Sociotechnical theory, developed in the 1980s, has more recently been taken forward in a number of ways. It inspired the interdisciplinary field of inquiry known as CSCW, in which one key concept is the social–technical gap. 44 A fundamental tenet of CSCW is that the interaction between people and technologies in the workplace is, with few exceptions, far more complex than would initially appear. A key reason for this, argued Ackerman, is that there is a gap between the nuanced, flexible and often unpredictable nature of human activity and what it is possible to deliver technically. 44 This is an inherent problem and can probably never be fully ‘designed out’. It links to a more general mismatch between formal work procedures (as in a manual) and the informal routines that actually occur. Grudin, cited by Symon et al. ,45 put it thus:
Work processes can be described in two ways: the way things are supposed to work and the way they do work. Software that is designed to support standard procedures can be too brittle
p. 2545
Technical solutions, argue the CSCW community, tend to be designed to align with an idealised, formal map of work processes, which may bear limited relation to what actually happens (especially in non-standard and emergency situations). Two partial solutions to this problem are recognised by CSCW: articulation and co-evolution. Gerson and Star (cited by Goorman and Berg46) define articulation as follows:
All tasks involved in assembling, scheduling, monitoring and co-ordinating all of the steps necessary to complete a production task (patient trajectory). This means carrying through a course of action despite local contingencies, unanticipated glitches, incommensurable opinions and beliefs or inadequate knowledge of local circumstances. Every real world system is an open system . . . No formal description of a system (or plan for its work) can thus be complete . . . every real world system thus requires articulation to deal with the unanticipated contingencies that arise. Articulation resolves these inconsistencies by packaging a compromise that ‘gets the job done’ that is, that closes the system locally and temporally so that the work can go on.
p. 2046
‘Articulation’ includes both temporal co-ordination (sequencing the inputs of different actors over time) and spatial co-ordination (ensuring that the right people and artefacts are in the right place). ‘Co-evolution’ refers to the parallel and reciprocal evolution of technologies and work roles or routines. 44,47 It might be a largely unintended consequence of introducing a technology (i.e. it is inadvertently found that work roles and practices have to change), or there might be a deliberate plan for such evolution to occur (i.e. the technology is introduced along with a plan for new roles and routines). This begs the question of when the introduction of a technology can justify prospective job redesign and when it is better for technologies to be closely designed around people’s current jobs. As Pratt et al. 48 put it:
At one extreme, developers carefully design the application to fit the specific work practices of its users. Under this model, users do not change their work practices at all, because the technology accommodates their specific needs and work styles. The alternative extreme is to reshape the processes of the organization around the new application. [. . .] most applications fall in a middle ground: a mixture of supporting some existing work practices and attempting to change others.
p. 13348
It follows from these principles that ‘resistance’ to ICTs by staff in any organisation may be explained by the subtle contingencies – and inherent messiness – of work. One of the leading researchers to apply these principles to the healthcare setting is Marc Berg, who also draws on ANT (see Actor–network theory, below). Berg talks, for example, of ‘growing’ rather than ‘building’ information systems in health care and working to achieve synergy between three fundamental (re)design tasks: the technical system, the primary work process (e.g. clinical care), and the secondary work process (e.g. audit, management). 49 It is perhaps worth commenting that critiques of the NPfIT have (naively, in our view) tended to emphasise poor planning, poor contracting and lack of vision but not the inherently organic nature of information system design. 4
In a contrasting development of sociotechnical theory, Brown and Duguid50 have shown how technologies in the workplace are embedded in networks of social relationships that make their use meaningful. The detail of how to use, adapt, repair or work round technologies is learned through membership of a community of practice; this social infrastructure, local and specific to an organisation, strongly influences whether or not and how particular technologies ‘work’ in particular conditions of use.
Another broadly interactional theory of technology adoption in organisations is Carl May’s normalisation process theory, which he developed to explain the uptake (or non-uptake) of ICTs, especially telemedicine, in healthcare organisations. 51 This theory comprises four constructs: interactional workability (to what extent does the technology fit with the micro-environment of the clinical encounter?); relational integration (to what extent does it fit with the network of relationships within which the clinical encounter sits, and, especially, how does it impact on issues such as interpersonal trust?); skill-set workability (to what extent does it fit with the formal and informal division of labour between staff?); and contextual integration (to what extent does the organisation understand the innovation and agree to allocate material and human resources to its implementation?).
An interview study of NHS clinicians and managers using normalisation process theory identified that Choose and Book referral software was unpopular and little used, and suggested that the main barrier to uptake was poor interactional workability, defined as ‘the impact that a new technology has on interactions, particularly . . . consultations’; in contrast, Picture Archiving and Communication System (PACS; a digital image storage and retrieval package), was popular and widely used because it scored highly on all of the four constructs listed in the previous paragraph. 19 Normalisation process theory is presented very explicitly as a ‘rational’ model for considering the uptake (and non-uptake) of complex technology-based interventions. 52 The theory recognises the complex nature of healthcare work and the human relationships on which that work depends, but it lacks a theoretical perspective on the technology itself and remains explicitly couched in assumptions of ‘rationality’ rather than in normative concerns about what constitutes good clinical practice. 52
Critical studies of organisational power relations
Some researchers, especially those aligned with critical management studies, have emphasised the network of power relations in which the introduction and use of technologies is embedded, and especially how ICTs affect domination and power struggles in organisations. The use of ICTs to monitor work, they suggest, inevitably opens the performance of organisational members to administrative surveillance – and it makes them aware that managers may be checking up on them. Drawing on Foucault’s powerful metaphor, Doolin53 describes the impact of this ‘panopticon’ in the healthcare setting:
. . . representational, inscriptional and computational techniques associated with information systems render individuals calculable, and thus knowable and governable. Some activities are given existence and attention, while others remain unrecognized, enabling managerial knowledge to make stronger truth claims and engendering compliance in those subject to such scrutiny.
p. 34553
In such situations, staff may have only limited possibilities to resist the introduction of pervasive ICT systems. Indeed, Doolin suggests that, as suggested by Foucault’s theory of governmentality, staff may come to internalise and hence fail to question the managerialist discourse that is built into, and perpetrated by, the system.
Others, however, have proposed that in such situations, resistance may take subtle forms. In a paper called ‘The failed panopticon’, for example, Timmons describes how hospital managers colluded with nurses to resist a new information system for monitoring nursing work. 54 The system’s abstracted work plans, while in theory producing ‘action at a distance’ (i.e. the quantification and control of nursing work), were recognised by managers as failing to reflect the real work of nursing. When the system appeared to reflect poor performance on a particular ward, the lead nurse was given no more than a sham telling-off by senior managers.
In an ethnographic study in UK general practice, Winthereik55 studied how general practitioners (GPs) managed two potentially conflicting agendas: accountability to external scrutiny [e.g. via the Quality and Outcomes Framework (QOF) and other government-imposed audits and incentive schemes]; and professional autonomy (the need to feel in control of their own clinical practice). Many GPs were largely negative about the new external controls and expectations, and felt that the standards against which they were being judged were arbitrary and sociopolitically driven. Despite this, they engaged actively with accountability tools (e.g. by complying with the use of codes through which their work was being audited), and they were keen to make their work visible and demonstrate good performance against the standards. Winthereik concluded that there was no simplistic zero-sum relationship between being rendered accountable and retaining clinical autonomy. Rather, accountability and autonomy appeared to co-evolve such that new, positive forms of autonomy emerged alongside the accountability agenda.
There is a small but important literature that uses a critical feminist lens to study resistance to new technology in nursing and midwifery. Henwood and Hart,56 for example, conducted a large, multisite case study of the introduction of electronic records in maternity units from the perspective of midwives. They found that in fewer than half of the units had midwives been consulted at all about the nature of their work or the design of the IT system. In interviews and focus groups, there was a marked disinterest among many midwives, who saw the new system as something introduced by management, ‘boring’, or something they might engage with when ‘it’s all sorted out’. This resistance was palpable and widespread; midwives appeared to be actively participating in their own exclusion by defining the electronic record as part of a techno-medical world, imposed by (male) doctors, marginal to the ‘real’ work of midwifery, and detrimental to client care. One interviewee is quoted thus:
I just think it would totally ruin the whole point of being a midwife. You’re supposed to be with the woman, looking after the woman. To have a computer in the corner, where you’re away and typing into it, it’s just not part of what having a baby’s all about, to me. Because that would take over what you’re actually there for, I’m sure . . . So I wouldn’t want there to be any more technology involved – it’s supposed to be a normal process. So all this hi-tech stuff is just not what I think it’s about.
Senior midwife; p. 25756
Having first positioned the ICT as ‘masculine’ and as interfering with the ‘normal’ process of birth, this interviewee went on to distance herself (and midwifery in general) from the low-status administrative work of ‘data entry’. In her symbolic world, technology was either about ethereal, unreal aspects of care or not about care at all. This example of resistance from feminist nursing studies has some resonance with our own findings, described below.
Actor–network theory
One increasingly popular approach to incorporating the material properties of technology in a sociological analysis of ICTs is Latour’s ANT,57 which shares some of its intellectual roots with CSCW (see Interactional models of resistance: the sociotechnical perspective). We have described the key concepts and assumptions of ANT relevant to this topic in more detail elsewhere. 58 Briefly, ANT considers networks that are made up of both people and technologies. A key focus is what people and technologies become as a result of their position in a network, and the power that emerges from dynamic configurations of human and non-human actors. A nurse who takes a job in a 24-hour call centre dealing with ‘emergency’ calls from the public takes on particular characteristics and develops particular skills; his or her role is shaped, enabled and constrained by the (human and technological) properties of the telephone network – and also by the other technologies to which the system is connected (e.g. access to the electronic records of the patients who call in). In such a situation, the electronic patient record becomes a part of this particular enactment of unscheduled care.
Critics of ANT are quick to point out that technologies do not have agency, but its protagonists depict agency as a product of the network, not as something internal to either a person or a technology. In Berg’s59 words:
The elements that constitute these networks should not be seen as discrete, well-circumscribed entities with pre-fixed characteristics. Rather, those entities acquire specific characteristics, roles and tasks only as part of a network. A ‘physician’ is only a ‘physician’ in the modern western sense because of the network of which s/he is a part and which makes his/her work and responsibilities a reality. [. . .] Because of this tight interrelation between elements in a network, the introduction of a new element or the disappearance of an element (as when a hospital stops training junior residents) often reverberates throughout the healthcare practice.
p. 8959
Actor–networks (that is, networks of people and technologies) are typically highly dynamic and inherently unstable. They can be stabilised to some extent when people, technologies, standards, procedures, training, incentives and so on are aligned. When introducing a new technology, this alignment is achieved (or, at least, attempted) through what Latour called ‘translation’, which involves the four stages of problematisation (defining a problem for which a particular technology is a solution), interessement (getting others to accept this problem-solution), enrolment (defining the key roles and practices in the network), and mobilisation (engaging others in fulfilling the roles, undertaking the practices and linking with others in the network). 60
Studies of resistance to ICTs from an ANT perspective tend to focus on two main issues: the efforts made by human actors to achieve (or thwart the achievement of) particular alignments of people and technologies; and the tendency of the inbuilt properties of software (e.g. access controls or pull-down menus) to shape and constrain the possibilities open to organisational actors. 61 While other research traditions have also addressed these issues, ANT offers a novel way of theorising them. Efforts made by groups of actors to influence the codes, architecture and algorithms inscribed into particular ICTs, for example, are interpreted as political moves rather than simply attention to clinical and technical standards. 62–64
Latour has suggested, for example, that if usage of a new technology that aligns with designers’ intentions is a ‘program’, resistant individuals seek to mobilise others into enacting and stabilising an ‘anti-program’ (in which the technology may be used differently for different purposes), and this wider program–anti-program dynamic across the network should be the focus of analysis when studying resistance to any technology. 65
Studies in the ANT tradition have also shown that the tension between standardisation (which helps to stabilise the network) and contingency (which reflects and responds to local needs and priorities) can never be resolved once and for all; rather, it must be actively and creatively managed – and this gets harder as the network gets bigger. 62,66,67 In this framing, ‘resistance’ may simply reflect the practical impossibility of resolving the tension between standardisation and contingency. Hanseth and Monteiro,68 for example, have used ANT to consider the institutionalisation of technology standards – whether in health care or in other fields such as transport, telecommunications or education. Infrastructure is built on an installed base (hardware and software); the (increasingly) large installed base attracts complementary production and makes the standard cumulatively more attractive. As the installed base expands, complementary products and components emerge and this in turn increases the credibility of the standard among the key groups of human actors on which its adoption and sustainability depends. This promotes adoption, which further increases the size of the installed base. Thus, a particular network of technologies and the people who (necessarily) use them emerges and becomes progressively more stable.
Actor–network theory’s framing of resistance is perhaps best illustrated with a detailed example. Constantinides and Barrett69 drew on ANT to address what they called ‘networks of power’ [‘the close interdependencies between institutional arrangements, people, ICTs, and work practices and how these mobilize (spread and extend) each other’s strength and durability, for example, how ICTs can become standardized in organizational practices’ (p. 77)] in the introduction of a region-wide health information network in Crete. They were interested in how particular tools and activities become ‘filtered’ in the habits and routines of different communities, either by becoming integrated into everyday work practice or by being discarded as impractical. The ‘surviving’ tools and activities would become parts of large, sociotechnical systems and influence, in turn, other tools and activities. They were also interested in ‘body politics’ – that is, how different institutions, people and technologies are brought together to form different versions of the diseased body and exercise politics through different rules and resources. 70
The authors interviewed senior managers and IT professionals from the private IT company that initiated the project, healthcare professionals, and senior management from the regional health authorities. They found that political negotiations between these parties were complex and protracted, with multiple competing efforts at problematisation. One early move by the IT company was to recruit three GP enthusiasts (who were already high users of other IT solutions and champions for electronic records) and, through them, engage a ‘community of users’ of fellow GPs (what Latour would call ‘interessement’ and ‘enrolment’). This positive move was to some extent outweighed, however, by the limited interest of the Ministry of Health in the project (hence use of the system remained voluntary for GPs) and also by a large denominator of undertrained GPs whose interest in the project was at best lukewarm (lack of enrolment). Despite having recruited some influential clinical champions, the company’s power was limited to offering ‘free’ computers; it did not extend to enforcing the use of these technologies. The demise of the system was linked to two key events: an acrimonious intellectual property rights dispute between the IT company and a GP who felt that he had contributed to the design of the system, and a key clinical champion who reverted to using paper records.
At the time of that study’s publication, the actor–network was fragile and the authors were unsure whether the electronic record system (which was widely seen as ‘state of the art’ and had won an international e-health award) would be taken up further or abandoned. They conclude (a) that networks of power are key to success – and especially that an IT company should seek to mobilise the enthusiasm and influence of its clinical user base; (b) that large-scale ICT innovation requires access to heterogeneous resources, the control of which can externally influence the process of translation; and (c) that the network is fragile and dynamic [‘large-scale ICTs have distributed and multiple effects on participant organisations and need to be managed over time as use may be transformed into nonuse, resources initially gained may be later lost, and collaboration with key stakeholders may turn into conflict’ (p. 89)]. This example illustrates how individual ‘resistance’ to a particular ICT can be conceptualised as emerging as a product of the actor–network rather than as originating within the person’s ideas, beliefs, competences and so on.
As we have argued previously, some concepts from ANT, notably the notion of a fluid and potentially unstable network involving people and technologies, are extremely useful in theorising large-scale ICT systems in health care. 58 However, ANT does not include a sophisticated theory of either human agency (e.g. embracing a detailed analysis of what actors ‘know’ and how they assess particular small-scale situations) or the macro social structures in which human action is nested. The quote from Berg earlier in this section, for example, suggests that a physician is a physician ‘only’ because of his or her position in the sociotechnical network – a framing that minimises the importance of such things as professional identity, values and virtues (what some sociologists would call ‘agency’). In the next section, we consider an alternative theorisation of people, society and technology, in which the concepts of social structure and human agency are key.
Giddens’ work on structuration, modernity and technology
The theory of structuration links the macro of the social environment (‘social structures’) with the micro of human action (‘agency’) and considers how this structure–agency relationship changes over time as society becomes ‘modernised’. 71 On the one hand, agents are influenced by the context in which they operate (and also, historically, by the contexts in which they were brought up, educated and trained). On the other hand, human action has consequences (intended and unintended) that influence (and, therefore, gradually change) the external social context. People can be thought of as ‘social actors’ who are, to a greater or lesser extent, knowledgeable and reflexive. They contemplate any action by taking account of social structures such as norms (‘structures of legitimation’ – what they see as reasonable and ethical, such as assumptions about the nature of clinical excellence that underpin professional practice), meaning-systems (‘structures of signification’ – the symbolic meanings and significance which they attach to people, experiences and artefacts) and rules and regulations (‘structures of domination’ – what they see as following protocol or obeying external authority). 71
In developing structuration theory, Giddens sought to bring together two apparently contradictory traditions within sociology: on the one hand, that of interpretative scholars such as Goffman and Garfinkel, who emphasised human interpretations and action, and on the other hand, the work of structural sociologists such as Durkheim and Marx, who were more interested in the wider social forces that shape and define society. Far from being mutually exclusive or incommensurable, proposed Giddens, these two perspectives are intimately and dynamically related: structure shapes agency, and agency, in turn, shapes structure.
Giddens’ application of structuration theory focused mainly on four large-scale systems: the world capitalist economy, the international division of labour (and the role of industrialisation in this), the world military order (including the industrialisation of war), and the nation-state system (including the modern revolution in administrative techniques, surveillance and the control of information). 72 The system of medical practice, supported by technological artefacts and shared guidelines and standards, represents another large-scale social system which, while operating semiautonomously and to its own logic, also depends on and interfaces with these four systems.
Giddens also proposed that, as a result of modernity and globalisation, connections between different social contexts become networked, such that local happenings are shaped by events on the other side of the world, and vice versa. Globalised disease surveillance networks linked to national public health systems allow for co-ordinated international responses to potential pandemics, but such responses – typically dictated by distant committees – inevitably restrict the freedom of individuals to attend work, school or leisure activities locally. Similarly, guidelines and protocols developed by distant committees (and, increasingly, standardised at national or international level) restrict the capacity of clinicians to tailor their practice to local needs and circumstances.
Giddens proposed that humans, both individually and collectively, continually reflect on their predicament and try to control their future. However, because they are unable to control the reflexive responses of others, they generate new forms of risk and uncertainty, from financial instability to the threat of nuclear accidents and environmental catastrophe. To this list, we might add the inability of doctors to control the exponential increase in ‘lifestyle’ diseases linked to obesity and inactivity, the failure to date of the expanding industry of ‘risk scores’ (designed to identify high-risk individuals at a sufficiently early stage to intervene and prevent disease) to translate into tangible and scalable gains in health or life expectancy, and the numerous examples of large-scale ICT programmes in health care that have generated recurring technical glitches and operational confusion rather than the predicted efficiency gains. All these disappointments undermine trust in the ability of globalised institutions (the economy, nation-states, industry, the military – and medical science) to create the structural conditions for what Giddens called the ‘ontological security’ of individuals. 73
Social practices (everything from parenting to conducting a job interview or a clinical consultation) depend in part on actors’ personal knowledge of the local context and the network of relationships in which they live and work. Social structures are reproduced because (and to the extent that) people know how to ‘go on’ in a particular social setting. However, in the modern world, social practices become disembedded as a result of the twin social forces of modernity and globalisation, which produce (among other things) ‘expert systems’ – defined by Giddens as ‘[a] system of technical accomplishment or professional expertise that organize[s] large areas of the material and social environments in which we live today’ (p. 27) – that manipulate abstract, impersonal knowledge using new technologies. 74
Social practices are now, in large part, removed from the immediacies of context, with the relations they involve typically being stretched over large tracts of time and space. Local experiences and events are shaped by processes taking place on the other side of the world, and vice versa. These are processes, moreover, that are primarily impersonal and abstract. [. . .] Each of these abstract systems plays a part in coordinating social relations between distant and absent others. Local contexts are cross-cut and ‘emptied out’ by the power and authority of these stretched relations.
pp. 449–5075
A closely related sociological concept is that of distanciation, originally defined by Giddens as ‘[t]he stretching of social systems across time-space, on the basis of mechanisms of social and system integration’ (p. 377). 71 By ‘system integration’, Giddens is referring to the different ways in which the parts of a social system are combined and co-ordinated – activities which increasingly happen at a distance and on the basis of technologically mediated and abstracted forms of information. 76 Global disease surveillance networks replacing (or substantially augmenting) the localised monitoring and management of disease outbreaks are a good example of distanciation: in the 19th century, public health physician John Snow plotted cases of cholera by hand on a street map and thereby traced their source to the Broad St. water pump; removal of the handle of that single pump successfully curtailed the outbreak. Today’s GP or public health physician typically takes action in response to an e-mail from an authorised source that conveys the recommendations of senior experts, derived in turn from calculations undertaken on regionally, nationally or internationally-aggregated data sets. While these data sets are built from locally collected data, the direct link between documenting local cases and taking local action is replaced with an indirect one based on abstracted and distantly processed data.
Another social change characteristic of modernity is the replacement of reason with rationality. As Sayer77 (drawing on various scholars including Aristotle) has argued, rationality is distinguishable by its formal and instrumental character, its abstraction from concrete situations, and its focus on means rather than ends. For example, it is concerned with identifying the most efficient method of getting a job done (‘doing the thing right’) but is not centrally engaged with the appropriateness and reasonableness of the job itself (‘doing the right thing’). In contrast, phronesis (practical reason) is characterised by its concern with the concrete and the particular; its practical, embodied and tacit character; its focus on ends rather than means (in particular, whether the ends are ethically justified); and its focus on people rather than things.
A reasonable person is someone who takes account of the specificities of the people they interact with, their particular capacities, needs and vulnerabilities, as well as other specificities of the situation. [. . .] When we talk of having ‘reasonable expectations’ of people, we mean expectations that take into account their particular characteristics, constraints and resources, including their vulnerability and fallibility, and ‘reasonable behaviour’ also suggests some degree of emotional sensitivity to others. Further, to be a reasonable person is to be able to imagine things from other people’s standpoints – in other words, to be willing to take the standpoint of the other. [. . .] Hence to call someone ‘a reasonable person’ in such contexts suggests an ethical judgement of them.
p. 65, emphasis in original77
Despite the increasing tendency for expert systems to ‘empty out’ the significance of local events and relationships by invoking general rules that apply everywhere and anywhere, the processes of system integration must necessarily be animated by local actors working in specific local situations and dependent on local contextualities. These will include physical and material constraints (such as the availability and cost of broadband) as well as symbolic ones (such as the extent to which doctors are trusted in a particular society). While the general rules governing the expert system might reflect the impersonal logic of rationality, local actors will, to a greater or lesser extent, seek to act reasonably – that is, ethically and practically with regard to the situation at hand and their (perceived) obligations towards their fellow human beings.
Giddens famously said very little about technology in his original formulation of structuration theory apart from recognising that technologies are key components of social systems, and particularly of expert systems. Other scholars, particularly in the information systems tradition, have attempted to theorise technology from within structuration theory. Notably, Barley proposed that the introduction of a new technology provides an ‘occasion for structuring’ – that is, it creates new possibilities for changing the taken-for-granted routines and patterns of interacting (‘scripts’) between actors, potentially allowing new institutional logics (i.e. patterns of interacting that are culturally and cognitively taken for granted) to emerge. 78 However, as Barley emphasised, the technology does not determine these logics since a key component of structuration is the interpretation that human actors place on the technology and the work they choose to do with it. Barley’s early work on the introduction of computerised tomography (CT) scanners in hospitals informed Orlikowski’s ‘technology structuration theory’, which considers how organisational actors, working collaboratively around common tasks, engage in a process of adapting the meaning, properties and applications of technologies to a particular context, and a parallel process of adapting the context to accommodate the technology. 79 Both Barley and Orlikowski are organisational scholars and so have focused their research efforts at the assimilation of technologies in organisations rather than considering issues of national policy.
In sum, structuration theory offers potential to analyse human action (including the use and non-use of technologies) as social practice, influenced by – and, in turn, influencing – the norms, meaning-systems and rules of a particular social system. It potentially allows us to study the fortunes of planned change efforts either as broadly aligned with prevailing social structures (and, in particular, with actors’ internalised norms, meaning-systems and rules) or as cutting across these structures and creating the preconditions for ontological insecurity.
Strong structuration theory
Whereas Giddens formulated structuration theory in a somewhat abstract way (e.g. focusing on ‘structure’ and ‘agency’ as theoretical concepts), Stones has sought to give the theory a more empirical slant in what he has called ‘strong structuration theory’, focusing on the interpretations and actions of particular people in particular circumstances, and especially on their assessment of particular situations and their efforts to act reasonably in those situations. 80,81
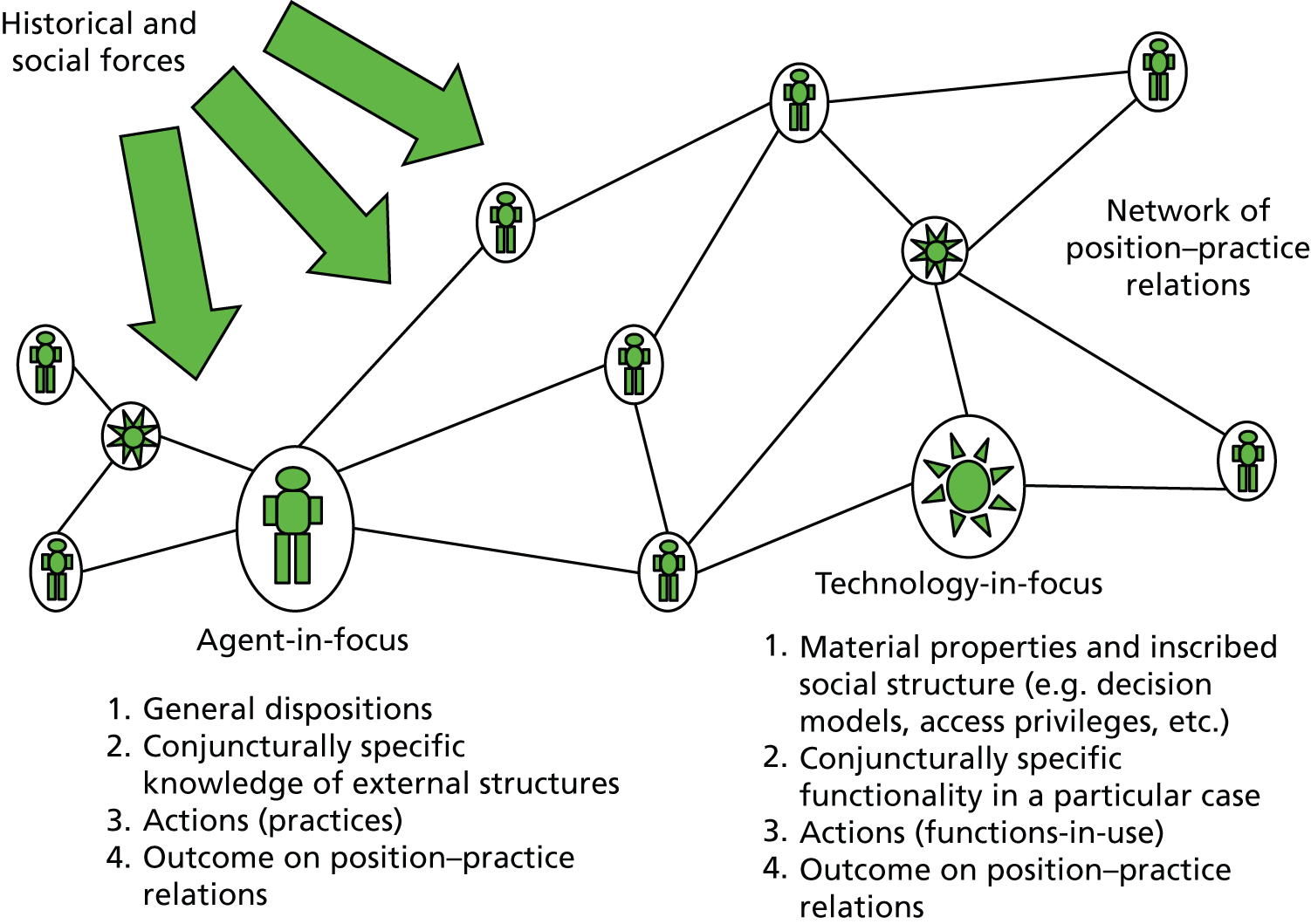
Strong structuration theory’s focus on empirical cases in which individuals are considered as situated in webs of networked relations (Figure 4) resonates with ANT’s focus on dynamic and unstable networks of people and technologies described in the previous section. However, in contrast with ANT’s ‘flat ontology’, SST holds that the recursive (i.e. mutually influencing) relationship between structure and agency remains a useful concept.
FIGURE 4.
Networks of position–practice relations along with technologies in SST. Reproduced with permission from Greenhalgh and Stones. 58
Stones’ quadripartite approach to structuration theory, depicted in Figure 5, considers not only external structures (the macro-level structures that form the contextual conditions of action in any situation) but also internal structures (what agents ‘know’, albeit sometimes imperfectly and even incorrectly, about the external world), actions (observed behaviour) and outcomes (how observed behaviour in a given scenario feeds back to reinforce and/or change internal and external structures). To get an empirical handle on the structure–agency relationship, SST considers the conjuncture (defined as a critical combination of events or circumstances), of which ‘the clinical encounter’ is one example.
FIGURE 5.
Stones’ quadripartite theory of structuration, adapted to encompass a technology dimension. Reproduced with permission from Greenhalgh and Stones. 58
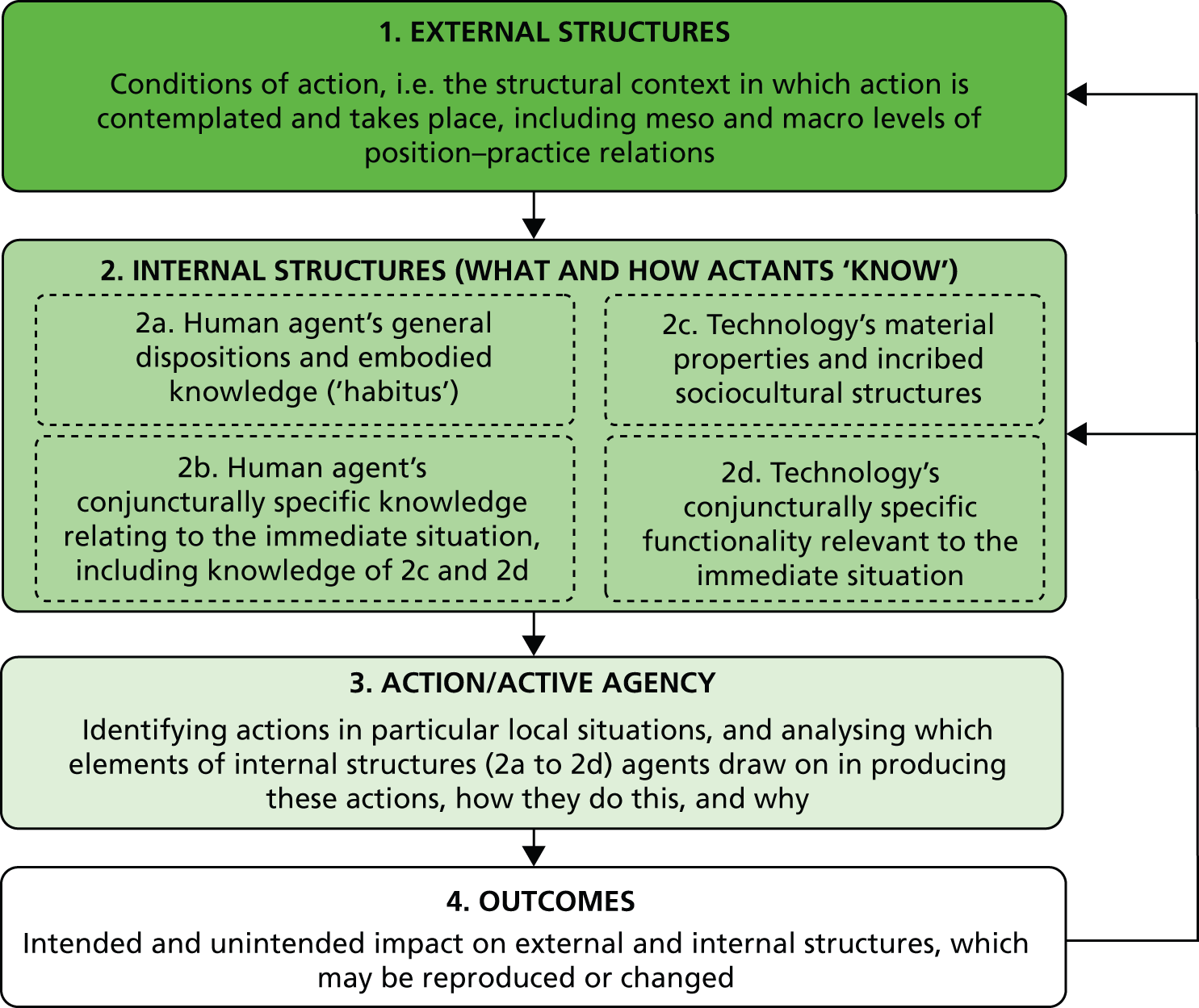
Strong structuration theory proposes that external structures are mediated largely through position–practices (defined as a social position and associated identity and practice), together with the network of social relations that recognise and support it (‘position–practice relations’). Agents’ internal structures may be divided into:
-
general dispositions, which include such things as sociocultural schemas, discourses and world-views, moral and practical principles, attitudes, ambitions, technical and other embodied skills, and personal values – roughly what Bourdieu82 called ‘habitus’; and
-
particular (‘conjuncturally specific’) knowledge of the strategic terrain and how one is expected to act within it, based on one’s hermeneutic understanding of external structures.
Within a particular conjuncture, action occurs when the human agent draws actively and more or less reflexively on his or her internal structures.
To study active agency, SST incorporates theories from phenomenology (the study of agents’ shifting fields and horizons of action arising from the focused activity at hand83), ethnomethodology84 and symbolic interactionism (the study of the subjective meaning and interpretation of human behaviour85).
Strong structuration theory emphasises that while each of us brings generic capabilities, dispositions and strategic knowledge to any particular conjuncture, what we actually do in that situation will depend on a host of specificities including our horizon of action and particular features of context.
The healthcare setting is heavily institutionalised: behaviour in healthcare organisations is strongly influenced by such things as regulations and other governance measures, norms, professional codes of practice and deeply-held traditions (all of which are embodied and reproduced by human agents including clinicians, administrators and patients) rather than exclusively by business concerns like efficiency and profit. The agent’s knowledge of these institutional structures (in the language of SST, the ‘strategic terrain’) may be more or less accurate and more or less adequate. Outcomes of human action in any situation may be intended or unintended, and will feed back on both external and internal structures – either preserving them faithfully or changing them as they are enacted.
As we have argued previously, SST can be enhanced by selected concepts from ANT. 58 First, technologies and human actors might usefully be conceptualised as part of the same network, and both may be thought of as having a ‘position–practice’ in that network (see Figure 5). SST can accommodate ANT’s emphasis on studying the complex and dynamic alignments in the network, including efforts by commercial companies (marketing, lobbying) to influence uptake of technologies, coalition-building within and across stakeholder groupings, and local reinterpretation of objects-in-use. However, SST rejects ANT’s assumption of ‘ontological symmetry’ between people and technologies. Humans and technologies ‘act’ in different ways, and a technology can only ever have a limited and qualified form of agency. Secondly, SST can accommodate ANT’s notion that aspects of the social order can be inscribed in technologies and this may to some extent ‘freeze’ certain position–practice relations within the technology. Thirdly, human behaviour will be shaped and constrained by complex forces in the sociotechnical network and hence may in some senses be an ‘effect’ rather than a ‘cause’ of what we are studying, though SST contends that human agency cannot be reduced entirely to network effects. Indeed, from a SST perspective, what ANT theorists call ‘the sociology of translation’ (interpreting the moves of different actors as they seek to build and stabilise a network of human actors and technologies) is likely to be productively enhanced by considering agency as sited within the human actor rather than merely as a product of the network.
Technological orientations of structuration theory have only recently begun to theorise how the material properties of technologies are coconstituted along with the social practices in which they are used. 86 Conversely, ANT has been criticised for overemphasising the material aspects of technologies at the expense of the lived relationship between humans and material objects. 87 Dant’s notion of ‘material interaction’, informed by phenomenology, in which human agents meaningfully experience, perceive and manipulate objects to achieve a task, has some parallels with the notion of sociomateriality which Barley and Orlikowski’s group have latterly begun to embrace. 88,89 It also resonates with SST’s emphasis on how active agency occurs when the actor draws on phenomenological and embodied dispositions and capabilities (see boxes 2a and 2b in Figure 5).
Figure 4 summarises the broad conceptual model for considering ICT programmes, comprising a network of position–practices (humans and technologies), which evolves over time and is influenced by macro historical and social forces (which exist more or less independently of the agents on which a particular empirical study might focus), and they contribute to the external conditions of action in any given conjuncture. Social structures are embodied and reproduced by both human agents (when they use technologies for meaningful social action) and technologies (when external structures, built into the technology, are instantiated when humans choose to use the technologies – or find they cannot use them as intended).
Having developed the above adaptation of SST using insights from ANT, we drew up a provisional list of questions to guide the study of resistance to ICTs:
Macro-level questions
-
What is the prevailing macro-level context within which the (changing) social practice is undertaken and the ICT has been or is being introduced?
-
What does the sociotechnical network consist of (key people and technologies, position–practices, relationships)?
-
To what extent has stability of the network been achieved – and why?
Micro-level questions focused on specific conjunctures
-
Which human(s) and ICTs are ‘in focus’ in this conjuncture?
-
What are the relevant general dispositions of the human agent, and what does he or she know (perhaps imperfectly) about relevant external structures? In particular, how does he or she think other agents view the world; and what does he or she know or believe about the ICT?
-
What are the relevant material properties and inscribed social structures of the ICT(s)?
-
What does the human agent do (i.e. how do they draw on their general dispositions and conjuncturally specific knowledge to produce action)?
-
How do the social structures inscribed (deliberately or inadvertently) in the ICT enable, influence or constrain the human agent?
-
What are the consequences of the use or non-use of the ICT, and how do these feed back on the wider system?
These questions were subsequently refined and focused as set out in Chapter 2 (see Research questions) and also in the more specific questions outlined at the start of each main findings section.
Chapter 2 Aims, approach and research questions
Aims
Our aim was to help policy-makers and change agents move beyond the commonly used (but, we believe, impoverished) rational actor models of the (non-)uptake of ICTs and un-nuanced conceptualisations of clinicians’ resistance to them. We sought, through literature review and secondary analysis of data (collected for previous empirical studies by our team8–10,16,90–95) and building on our previous preliminary theoretical work to link SST and ANT,58 to produce a sociologically informed model that would explain ICT adoption and use. In particular, we sought to account for its non-adoption and non-use in certain social and organisational situations. Our starting position was the assumption that clinical work is a social practice, shaped and constrained by wider social influences including norms, meaning-systems and rules, and that ‘resistance’ to ICTs would be explained at least partially in terms of professionals’ ethically-motivated efforts to do their job well and deliver excellence in clinical practice – and that administrative staff in healthcare organisations were also driven, at least in part, by these ethical and professional concerns.
We wished to produce a multilevel model of resistance that unpacked this notion of excellence and which also incorporated the influence of institutional changes in the healthcare field; the meanings people attach to technologies in the workplace; the complex, situated and unpredictable nature of clinical work; the material properties and affordances of ICTs and how these create possibilities and limit what is possible for the user; and the potential for creative human action to overcome the limitations of technology and bridge the ‘model-reality gap’. We were particularly interested in how nationally mandated ICTs were adopted (or not) by local actors.
A normative anchor: what is excellence in clinical practice?
As the literature review above illustrates, many, but by no means all, previous approaches to ICTs in health care begin with the index technology and ask ‘is this technology being used by its intended adopters, and if not, how can we increase or optimise its use?’. Interactional models consider the fit between the technology, organisational routines and individual capability. ANT considers dynamic changes in, and stability of, the sociotechnical network. In this study, framed in SST, we sought to take a different starting point: the internal structures of human agents – in other words, what people know. By ‘know’, we include what they believe and what they value – and how these beliefs and values are influenced by past experience and by the norms, meaning-systems and rules of society described in the section on SST (see Chapter 1, Strong structuration theory). Thus, we sought to shift the focus from means (the use or non-use of a particular technology) to ends (the purpose for which technology is used – or for which it may be more appropriate not to use a technology).
We begin, therefore, not with a focus on technology or even on the system or network, but by depicting the clinician as a social agent and considering clinical practice primarily from a normative (i.e. professional and ethical) perspective. Professionals are strongly influenced by socially shared notions of what good practice consists of and how they should behave towards patients and towards one another.
Accordingly, a key guiding question in this study was, ‘what is excellence in clinical practice and how is the use and non-use of ICTs influenced by (changing) notions of excellence?’. In this section, we summarise the literature on good clinical practice mainly in relation to doctors (because most of the relevant studies have been done on doctors and their work). We also refer to the nursing literature where available.
Much has been written about good doctoring. Perhaps the pithiest statement of its essence is the motto of the UK Royal College of General Practitioners – cum scientia caritas (‘loving care with expert knowledge’: see www.rcgp.org) – which depicts the professional ideal of delivering the highest-quality bioscience while also attending to the human needs of the patient. While the ‘scientia’ component of good doctoring is often equated with evidence-based medicine (EBM), the original definition of EBM actually incorporates ‘caritas’ too. This definition is reproduced in full below, though only the first sentence is generally quoted.
Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research. By individual clinical expertise we mean the proficiency and judgment that individual clinicians acquire through clinical experience and clinical practice. Increased expertise is reflected in many ways, but especially in more effective and efficient diagnosis and in the more thoughtful identification and compassionate use of individual patients’ predicaments, rights, and preferences in making clinical decisions about their care. By best available external clinical evidence we mean clinically relevant research, often from the basic sciences of medicine, but especially from patient centred clinical research into the accuracy and precision of diagnostic tests (including the clinical examination), the power of prognostic markers, and the efficacy and safety of therapeutic, rehabilitative, and preventive regimens.
p. 7196
Evidence-based medicine was acknowledged by its early protagonists as being dependent on clinical judgement and contingent on patient choice (i.e. the ‘best’ treatment is not necessarily the one shown to be most efficacious in randomised controlled trials but the one that fits a particular set of individual circumstances and aligns with the patient’s preferences and priorities). Unsurprisingly, given its disciplinary roots in clinical epidemiology, the early research literature on EBM focused on the scientific component and sought to build an evidence base of randomised controlled trials and other ‘methodologically robust’ research designs. Later, a tradition of ‘evidence-based patient choice’ emerged in which the patient was assumed to be a (more or less) rational chooser and the clinical challenge was framed as how to convey the research evidence about different treatment options in a way that supported informed patient choice. 97 However, the third component of EBM – individual clinical judgement – has not been extensively theorised within that tradition.
The US bioethicist Kathryn Montgomery, drawing on Aristotle’s notion of praxis, considers clinical practice to be an example of case-based reasoning. 98 Medicine is governed not by hard and fast laws but by competing maxims or rules of thumb; the essence of judgement is deciding which (if any) rule should be applied in a particular circumstance. Clinical judgement incorporates science (especially the results of well-conducted research) and makes use of available tools and technologies (including guidelines and decision-support algorithms that incorporate research findings). However, rather than being determined solely by these elements, clinical judgement is guided both by the scientific evidence and by the practical and ethical question ‘what is it best to do, for this individual, given these circumstances?’.
The dual commitment to ‘scientia’ and ‘caritas’ has been analysed from a philosophical perspective by the Norwegian doctor and philosopher Edvin Schei. ‘Scientia’ requires the practitioner to consider the ‘objective patient’ (i.e., the patient as expressed in terms of measurements and standardised procedures, for which objectively-assessed diagnostic tests and treatments are then considered), whereas ‘caritas’ requires attention to the ‘existential patient’ (i.e. the patient’s subjective experiences and human needs). 99 The notion of evidence-based patient choice can be incorporated in the former (objective) component of good clinical practice but there are also subjective (and intersubjective) aspects of the interaction to consider.
Unlike disease, which can be defined in terms of a typical constellation of symptoms, signs and test results, illness is a personal, lived experience that is both emotionally laden and socially meaningful (e.g. it may come with various connotations of shame and blame100). The good clinician engages reflexively with this lived experience and acts not merely as diagnostician or technical expert but also as active listener101 and professional witness. 102 Using Schei’s definition, good doctoring is ‘a relational competence, where empathic perceptiveness and creativity render doctors capable of using their personal qualities, together with the scientific and technologic tools of medicine, to provide individualized help attuned to the particular circumstances of the patient’ (p. 394). 99 This definition has obvious parallels in nursing and allied professions.
The personal qualities referred to by Schei are strongly aligned with what Aristotle called virtues – character traits that strike a balance between undesirable extremes (such as courage, which lies between the extremes of recklessness and cowardice). 103 Toon has challenged principle-based medical ethics (in which clinical practice is guided by a set of core principles such as beneficence, non-maleficence, autonomy and justice) and argued that above all else, doctors must develop their professional virtues through reflection and peer support. 104 Similarly, good nursing practice has also been defined in terms of personal virtues. 105 The UK General Medical Council acknowledges the importance of virtues in the opening paragraph of its guidance ‘Good Medical Practice’: ‘Patients need good doctors. Good doctors make the care of their patients their first concern: they are competent, keep their knowledge and skills up to date, establish and maintain good relationships with patients and colleagues, are honest and trustworthy, and act with integrity’ (p. 1). 106
Whereas the objective dimension of clinical practice has often been tightly defined (and frequently redefined) in terms of adherence to best evidence guidelines, the subjective dimension is something of a mystery107 – depending as it does on a form of knowledge that is tacit, experiential and difficult to codify. 108 The judgements made by virtuous, wise clinicians entail ethical and practical considerations not just about what to do in relation to the particular circumstances of this patient but also about how to balance the competing demands of advocacy (addressing the needs of the individual patient) and distributive justice (balancing this patient’s needs or wants against the wider needs of the population in the context of limited resources) – for example, in relation to the questions of whether or not to prescribe, whether or not to operate, whether or not (and where and how urgently) to refer, and so on. 107
Critical scholars have voiced concerns that the essence of good clinical practice is being lost as society moves from a traditional era in which medicine and nursing were viewed as vocations, health care as a public good and the sick patient as a vulnerable citizen who had a right to care (and to whom the doctor has a duty of care) to a new era of market values where medicine is a business, health care a transaction and the sick patient a customer. In this latter era, informed choice by ‘empowered’ patients is seen as the driving force for achieving excellence, as clinicians (and health services) that do not produce ‘satisfaction’ will quickly go out of business. The doctor’s role is defined either as seller of specialist services or as an information purveyor. It follows from these assumptions that a good consultation is one in which the patient or their nominated advocate has been given sufficient balanced information to make a well-informed choice. 109 The empowerment of the patient is assumed to exist, more or less, in a zero-sum relationship with the disempowerment of the doctor – with the caveat that many patients do not wish to be completely autonomous (and some do not even seek ‘shared’ decision-making).
However, in the vocational model, patient empowerment and ethical practice are all defined differently. For one thing, it is illness itself, and not medical paternalism, that makes patients vulnerable. 99 Doctors’ specialist knowledge has symbolic significance; in many cases, power is not so much seized by doctors as conferred by society (doctors symbolise hope, trust, agency and authority, making possible a powerful therapeutic alliance of reciprocal interpretation and projection110). This ‘cognitive institution’ facilitates doctor–patient interaction and produces a ‘legitimate hierarchy of domination and subordination, recognized by all participants’ (p. 397)99 – though this hierarchy is rightly renegotiated and redefined more progressively as society evolves. In this hierarchy, patients are doubly vulnerable – because they opt (or are compelled) to rely on the doctor’s skill and judgement in potentially life-threatening situations, and because they expose themselves to the potential for shame or loss of dignity as intimate secrets and body parts are revealed (with the risk of loss of face if this is met with ridicule, disbelief or indifference).
For another thing, as Mol has argued, decision-making (shared or otherwise) is only part of the challenge. 111 As health problems increasingly involve chronic, non-communicable diseases which require ongoing effort by both patients (self-management) and health professionals (periodic surveillance, management of exacerbations and long-term support of disability and impairment), so the ‘logic of choice’ (episodic, decision-focused, objective, predictable – as in a decision tree) becomes less relevant than the ‘logic of care’ (continuous, relationship-focused, intersubjective, unpredictable). The logic of care includes the role of the doctor or nurse as witness and active listener – but it also includes the practicalities of care such as the effectiveness of medication in controlling symptoms, the accessibility of the clinician at times of need, and whether or not tools and technologies introduced with the aim of supporting the process of care are usable and useful in particular situations. In this framing, ‘care’ has a substantial physical and material component as well as a socioemotional one.
Good clinical practice is thus – arguably – less about achieving equal distribution of power (as in shared decision-making) than it is about ensuring that doctors draw on their personal virtues (integrity, honesty and so on) to build a healing relationship, wield their socially conferred power and use technologies pragmatically and judiciously in the patient’s best interests. Patients are also influenced by social norms: they will conform to a greater or lesser extent with expectations of what they understand to be the ideal of a good patient – for example, constructing an account of conscientious self-care, acknowledging the needs of other patients (hence not taking up too much of the doctor’s time), deferring to the doctor (or, perhaps, exerting what seems to be a reasonable level of autonomy) and seeking to demonstrate an appropriate level of knowledge and curiosity about their condition. 112 These small acts of deference contribute further to sustaining the established power differential.
In sum, the clinical consultation is not merely an informational transaction or a set of decisions. Rather, it is a complex social encounter in a heavily institutionalised environment. It has symbolic as well as scientific and practical significance. Good clinical practice involves judgement and attention to the particularities of the patient and their situation (the ‘existential patient’) as well as up-to-date knowledge and incorporation of best scientific evidence (the ‘objective patient’). It follows – and this is the point of this discursion into professional practice – that technologies that support the latter at the expense of the former are likely to be experienced by clinicians as interfering with excellent care.
We recognise that this focus on excellence in professional practice is a radical departure from most approaches to the use and non-use of technologies in health care, but it is very resonant with the ‘moral turn’ in contemporary sociology, which rejects the widespread focus on means (e.g. the efficiency of processes) and exhorts researchers and practitioners to make ends (what the processes are oriented to achieving) their primary focus. 113,114 The emphasis of SST on values and norms within the internal structures (or ‘habitus’) of actors means that humans are viewed not only as rational actors, nodes in a network or members of a sociotechnical system but as moral beings who have commitments, desires and values, both personal and professional. It views work – especially the work of doctors – not merely as a series of co-ordinated tasks but as having symbolic significance in society. In Sayer’s words, ‘things matter to people’ – objects, actions, experiences and relationships have personal and moral significance as well as economic or instrumental worth. 77
With this in mind, our analysis set out to explore the tensions between professional morals and values (inculcated by medical education, professional identity and professional communities of practice) on the one hand and the demands made on healthcare staff in the here and now by the nationally mandated technology on the other. The nexus of ethical values embedded within the habitus of a healthcare professional is not static or unproblematic. Indeed, it may be variously ambivalent, fragmented or conflicting, reflecting the ethical tensions and inherent conflicts of healthcare practice. 99 In this study, we considered that an understanding of these values and how they inform professional notions of excellence would be a useful point of departure for illuminating those practices that are framed as ‘resistance’.
Research questions
Our research questions were:
-
How does the dynamic relationship between the macro (external social structures), meso (organisational routines and logics) and micro (individual understandings, dispositions and frontline actions) explain situations in which clinicians and other actors appear to resist the use of nationally mandated ICTs in health care?
-
What can we learn from the detailed analysis of small-scale episodes of resistance that will inform the design, delivery and ongoing support of health-related ICT programmes and the development of health policy?
-
To what extent is ‘resistance’ a useful framing – and how might the issue of low uptake and use of ICTs be better framed?
-
Where should further research effort be directed?
This generic framing of our research questions was modified as needed to match the particular practice and technology under consideration, as described in the case studies in Chapter 4.
Chapter 3 Method
Study design
This study had two linked components. One was a review of the literature, focusing mainly on the social sciences, on topics relevant to adoption and non-adoption of ICTs and, more widely, the phenomenon of resistance as sociologists see it. This review focused in particular on the sociology of clinical practice, especially the contemporary ‘moral turn’ (which emphasises what matters to people and what drives them in terms of ‘doing the right thing’) and on the sociology of expert systems, and is presented in the first two chapters.
In parallel with this literature review, and feeding iteratively into it, we undertook a secondary analysis of qualitative and quantitative data gathered for three previous in-depth case studies of computer use in the English NHS, all gathered in the time period 2007–10. In each of these cases, we began with a much larger primary data set and selected for detailed analysis both background material (e.g. policy documents, business plans) and small-scale examples (e.g. video capture or ethnographic field notes on real consultations) relevant to ‘compliance with’ or ‘resistance to’ the index technology.
In order to develop our theoretical model of resistance, and as the main focus of our empirical analysis, we considered a data set on the practice of referral to hospital by GPs, for which the index technology was Choose and Book. This technology had been introduced in 2004 by the English Department of Health to help GPs and their patients to book hospital outpatient appointments remotely. It was anticipated that remote booking would become standard practice once technical challenges were overcome. However, despite political pressure and financial incentives, Choose and Book remained unpopular and was used reluctantly or not at all by many practices. Policy-makers framed this as a problem of ‘clinician resistance’.
We considered Choose and Book as an expert system. Our data set comprised background documents, field notes, interviews, clinical consultations (directly observed and videotaped) and naturally occurring talk relating to referral to hospital in four general practices. We used SST, Giddens’ conceptualisation of expert systems and sensitivity to other sociological perspectives on technology, institutions, the professions and values to examine the relationship between the external environment, the evolving technology and the decisions and actions of human agents (GPs, administrators, managers and patients).
We subsequently applied this theoretical model to two further data sets. One addressed chronic disease management in general practice, for which the index technology was electronic templates built into the local GP record and linked to the pay-for-performance QOF. 115 These were used extensively by practice nurses but rarely by GPs. The other data set was from a national case study of emergency and unscheduled care encounters, for which the index technology was the SCR, a centrally stored extract drawn from a patient’s general practice record. At the time, the SCR was rarely accessed, for complex reasons (again attributed by policymakers to ‘clinician resistance’116).
The secondary analysis of empirical data progressed alongside the literature review, each feeding into the other, as explained in more detail below.
The primary data sets
We used data from two primary studies. Healthcare Electronic Records in Organisations (HERO) was a 30-month study (2007–10), funded by the Medical Research Council (MRC), which sought to explore how work practices and organisational routines were shaped and constrained by electronic patient records in four UK general practices. 91 We studied the local detailed record in use, including the clinical interaction between GPs and patients;92 template-supported chronic disease management;117 and the organisational routine for repeat prescribing. 94 We also studied the use – and, significantly, non-use – of ‘networked’ technologies introduced into general practices as part of national IT policy, notably the Choose and Book online booking system for outpatient appointments. 58
The HERO data set included 50 videotaped consultations, some but not all of which were transcribed in full, and most of which also had contemporaneous screen capture of the dynamic entries onto the electronic record (e.g. it was possible to see, in real time, what the clinician typed onto the record, including entries that were erased before the record was saved), as well as ethnographic field notes, documents (e-mails, letters, business plans, protocols, practice leaflets) and naturalistic interviews. It should be noted that the original aim of the HERO study was to explore the introduction of a much wider range of networked ICTs including electronic transfer of prescriptions between GPs and pharmacies and the SCR (see Chapter 4), but because of severe slippage these programmes did not become active in the study sites within the lifetime of the study.
Our second primary data set was Summary Care Record Independent Evaluation (SCRIE), a 3-year study funded by the Department of Health. We used a mixed-methods case study design to map the multiple stakeholders and complex story of government’s attempt to introduce a centrally stored electronic summary record for every citizen in England. 118 Creation of SCRs was slow because many GPs refused to participate in the programme or allow their patients’ data to be uploaded to the central database. Analysis of a large quantitative data set on out-of-hours encounters showed that even when SCRs were available as a one-click option, clinicians working in unscheduled care settings accessed them in only one case in five. 8 Other findings included strong opposition by a minority of citizens and health professionals to the idea of centrally held medical records,90 ignorance and confusion among the lay public,10 and conflicting interpretations of the programme by clinicians, service users, policy-makers, industry and technical designers. 8,11 The SCRIE data set included ethnographic field notes on 235 unscheduled (emergency and/or out of hours) consultations in primary and secondary care (in which the patient’s SCR was accessed in only 35) as well as field notes, national and local documents, and interviews with staff.
Selecting data sets for secondary analysis
The purpose of this secondary analysis was to draw on both the raw empirical data from the above studies and the analyses already undertaken to develop a robust and detailed theoretical approach to studying what is typically described as ‘resistance’ to ICTs by clinicians and other healthcare staff. However, rather than making the technology the focus of our analysis (arguably, a modernist bias), we chose to focus on particular social practices – referral, chronic disease surveillance and unscheduled care – and consider how the technologies linked to those practices – respectively, Choose and Book, electronic templates on the GP-held record and the SCR – were used (or not) to support that practice.
The data set for each social practice consisted of (a) background documents (e.g. national and local policies, patient information materials, training materials, correspondence, minutes of meetings, press coverage); (b) clinical consultations (observed directly or video/audio recorded); (c) other observed activities (e.g. ‘backstage’ work done by administrative staff on referrals or audits); and (d) interviews with organisational staff about their work. We did not seek to classify the clinician on a unidimensional scale as ‘complying with’ or ‘resisting’ the technology in question, as interaction (and non-interaction) with technology from the perspective of the actor might take many forms including being unaware of its existence, considering it irrelevant, being unable to access it, using it minimally, using it creatively (and not as the designers intended), and so on. Our focus in each case was to understand what the actor ‘knew’, what perceptions and dispositions they brought to the encounter and the actor’s own explanations for how the technology was used (or not).
We had already published a number of papers on technology-supported chronic disease surveillance in general practice90,91,93,119 and technology-supported unscheduled care. 8,9,11,90,116 All had covered the theme of resistance as an integral aspect of the non-adoption, partial adoption, reinvention (or customisation) and abandonment of the index technologies (electronic templates and the SCR, respectively). One publication in particular included substantial excerpts from ethnographic field notes and quotes from interviews, and an extended analysis of why clinicians chose not to use (or sometimes, found that they were unable to use) the SCR,116 though we felt that this analysis would benefit from further theorising.
In addition, we had a large number of raw data, not previously analysed in detail, which covered the practice of referral and use and non-use of the Choose and Book technology. The final data set for our secondary analysis is listed in Table 1. Overall, we placed more emphasis on analysing the Choose and Book secondary data set because this had not been previously analysed for other publications and our resource did not allow us to analyse all three data sets to the same level of detail.
| Original data set from HERO study 2007–10 | Raw data selected for secondary analysis | First-order interpretations | Higher-order theoretical categories |
|---|---|---|---|
| Field notes from ≈ 200 directly observed clinical consultations | 25 observed consultations in which the GP offered or discussed a referral |
|
External social structures
GPs’ professional identity, values, morals Administrative staff’s perceptions about ‘doing a good job’ Skills and techniques for using the technology Social structures inscribed in Choose and Book technology
|
| 54 videotaped clinician–patient consultations, including screen capture from computer | Six video excerpts in which a GP offered a referral. Striking ‘silence’ in the data: no examples of GPs directly accessing Choose and Book with patient present | ||
| Field notes from directly observed administrative work by GPs (≈ 40 hours) and practice staff (≈ 330 hours), including naturalistic interviews: total 800 pages of typewritten notes | One case in which a GP attempted to make a Choose and Book referral without the patient present; three where referral letters were dictated with no such attempt. Fifty-eight cases of administrator processing referrals manually (n = 12) or via Choose and Book (n = 46). Forty-five examples of naturally occurring talk where referral was mentioned (13 GPs, 31 administrators, one practice manager) |
|
|
| Field notes from practice meetings (≈ 20 hours) | Notes from one meeting between supplier and practice staff (Elm) | ||
| Fifteen national policy documents on electronic records. Information for professionals and public on these. National audits and surveys on electronic record use | Seven policy documents in which electronic referral was mentioned. Sections of ‘NHS Choices’ website relating to referral. Referral guidelines and DVD for GPs. Annual surveys on ‘choice’ and Choose and Book use |
|
|
| > 30 semistructured interviews with local policy-makers on use of electronic records | One (joint) interview with two PCT managers charged with implementing Choose and Book locally |
|
|
| Local documentation on electronic record use | Four practice protocols, 10 newsletters, one PCT patient choice survey, one letter from PCT to GPs | ||
| Correspondence and e-mails among clinicians in field sites on electronic record use | E-mail exchange among GPs and PCT leads (one thread, 15 participants) including doctors from Beech and Clover practices |
|
Theoretical framework: strong structuration theory
As set out in detail in the literature review above, our starting position was structuration theory, originally developed by Anthony Giddens and focusing centrally on the reciprocal (mutually-shaping) relationship between social structures and human agency. 71 The original version of this theory has been widely cited, but also criticised in some circles for its alleged rigidity and relatively limited empirical application. It was subsequently extended and refined by one of us (RS) as SST, an empirically grounded refinement of Giddens’ original theory which focuses on micro-level interactions between human agents and considers how these are influenced by (and how they, in turn, influence) wider social structures and relational networks. 80 We enhanced this position using selected elements from ANT, as previously described. 58
Modernity, rationalism and the expert system
Sociologists contend that the forces of modernity include an inexorable drive for change and technological innovation (both of which tend to be viewed in a positive light as representing progress) and a growing tendency to rationalise and formalise tasks and interactions, thereby making these transparent and open to scrutiny. In this study, we were interested to apply SST to the introduction of large-scale technology systems in the NHS, many of which were explicitly linked to policy changes.
NHS policy changes in the early 2000s were strongly influenced by the mind-set of late modernity, with its various commissions and omissions. These included an overwhelmingly rationalist frame of reference; a prevailing belief that innovation and change represent progress; a perception that expert systems (see Chapter 1 for definition) will almost inevitably increase efficiency and save human labour; a failure to think seriously about the possible negative consequences of such technical systems, including their impact on valuable forms of social interaction; and a powerful orientation to a vaguely imagined ‘proximate future’ – that is, a time that is almost but not quite upon us when the index technology is fully functional and all practical, technical, ethical and political challenges have been smoothed out. 74,120
While expert systems may be designed to encapsulate professional expertise, they are nevertheless characterised by an impoverished conception of the professions. An important defining feature of expert systems is their capacity to deploy impersonal knowledge, classificatory systems and procedures to shape, monitor, standardise and render calculable the work they support. Anthropologist Mary Douglas, developing earlier insights from the sociologist Emile Durkheim, set out the argument that the production of lists, rankings and other classification systems helps to establish and then sustain social institutions by introducing conventions which serve to ‘describe the way things are’ in the social world. 121 Classification systems are fiercely negotiated and defended for precisely this reason. 122 They have long been combined with those bureaucratic forms of instrumental rationality which the sociologist Max Weber carefully described and explored. 123
The expert system is a relatively recent phenomenon, resulting from the powerful triad of classificatory systems, bureaucracy and information technology in the age of globalisation. 73,124 Such systems are driven by impersonal and abstract rules, and procedures designed to co-ordinate social relations across large distances.
Giddens proposed that these expert systems, using technology to encode information and store formal knowledge, have an inherent tendency to ‘empty out’ the content of local interactions because the technical knowledge they contain is assumed to have validity independently of any particular interaction, and to have the authority to override situational contingencies. 73 The goals and characteristics of the sociotechnical network in which Choose and Book was introduced and implemented, for example, are typical of such systems,125 and the same is true for chronic disease management templates in general practice,93 though it applies less to our third case of the SCR. The prompts and sanctions embedded within this system marginalise and downplay the in situ characteristics and contingencies of particular cases and encounters. Their ability to exert control and order – measurable, quantifiable – over distance relies on removing (or, at least, attenuating) the ability of distinctive people, relations and contexts to upset the uniform application of the rules and classificatory system embedded in the system. There is a powerful momentum towards general and universalising rules and processes, and away from the application of practical wisdom (what Aristotle called phronesis) in specific contexts.
The ‘rational chooser’ assumption
The assumption behind cognitive models of ICT adoption and use (see Chapter 1, The technology acceptance model) is that the indented user rationally weighs up the pros and cons of the technology and decides if adoption is ‘worthwhile’. This user is assumed to focus in particular on whether or not the technology is easy to use and likely to make a task more effective, efficient or profitable. Such models are often explicitly behaviourist in their framing. As we shall argue in case 2, incentive schemes oriented around paying NHS clinicians or organisations to use a new technology linked to a policy (of which the chief example is the QOF for chronic disease surveillance), for example, are known as ‘pay-for-performance schemes’,115 suggesting that the professional ‘performs’ in order to get the (financial) reward. Likewise, schemes in which organisations or clinicians are financially penalised or subjected to public release of performance data (‘named and shamed’) for not using a particular technology, implicitly rest on what are arguably simplified, behaviourist ‘rational actor’ assumptions.
In our own analysis, we deliberately did not seek to classify the clinician on a unidimensional scale as ‘complying with’ or ‘resisting’ the technology in question (or, to express this slightly differently, as having more or less ‘resistance’ to the technology), as this would have bought into a naively cognitive and rationalist view of the phenomenon.
In the case of Choose and Book, the classificatory rules and procedures driving, and embedded in, the software and its networks were informed by another oversimplified modernist image – of the sick patient as a rational chooser, able and willing to weigh up information about the range of potential options for outpatient referral and decide between them (or as potentially capable of this if provided with high-quality information and decision support). The picture assumes that managing illness consists, more or less, of making a series of objective decisions based on a limited number of decontextualised indicators and then following through on these. It follows from these assumptions that provision of statistical information on the ‘quality’ of services in a standardised format (such as a table of comparisons using star ratings on key metrics) will prompt the ‘right’ choices and that these choices will lead to the ‘best’ services winning out in a competitive market. The policy ideology was that by adjusting the regulatory structures of the NHS through the coercive introduction of choice, government would be able to engineer a shift in professional norms (from ‘doctor knows best’ to ‘informed decisions by empowered patients’) and the cultural logics that define expected behaviour (supporting informed patient choice would become ‘business as usual’ throughout the NHS). 126
The sociotechnical system of the Choose and Book initiative was also heavily influenced by the ideology of competition, and by the salutary effects that competition was said to have on cost-efficiency, patient satisfaction and patient outcomes. It is appropriate to use the term ‘ideology’ here, as Choose and Book seems to have been driven quite forcefully by faith in a hybrid which saw the well-worn belief in competition as a social mechanism allied to the novel facilitating conditions of expert systems. This was ideological in that a policy of enforced competition between hospital providers – driven, it was assumed, by the rationally-choosing patient – was pushed forward with considerable confidence, deflecting attention away from that strategy’s limited evidence base (in particular, its lack of anchoring in the demonstrable conditions, processes, possibilities and consequences relevant to its assumed success). There was no detailed surfacing or exploration of the meso- and micro-level interactions and processes that would convert the policy idea (of hospitals competing to attract outpatient referrals) into the reality of a more efficient, effective and responsive healthcare system that improved patient satisfaction and outcomes.
It was with a view to countering this misleading degree of abstraction that we sought to develop a new, more empirically grounded theory of resistance to Choose and Book (and to nationally mandated ICTs more generally) that rested far less on naive rationalist assumptions.
Applying the normative anchor: medicine’s ‘internal goods’
We began by adopting MacIntyre’s conception of the internal goods and notions of excellence intrinsic to a set of practices. 127 By ‘internal goods’, we include the Aristotlean virtues, along with the dispositions and capacities, that are valued by clinicians and which they believe are necessary to sustain standards of excellence in their profession (see Chapter 2, A normative anchor: what is excellence in clinical practice?). We then use these internal goods as a benchmark against which to judge not merely the means by which an action is taken (e.g. a referral to hospital is made either via traditional letter or the Choose and Book technology) but also the ends that are in mind when that action is taken. Importantly, much of the knowledge and judgement of healthcare professionals, particularly in primary health care, relies on being rooted in the immediacies of context.
A GP’s judgements about the referral of a patient to hospital, for example, have traditionally been informed by (a) knowledge of the patient’s personal history (both medical and social), (b) knowledge of the workings of their own practice (including the various incentives, disincentives and practicalities of different options), and (c) knowledge of local social relations, including the character of local hospitals and the clinical interests and personal style of particular consultants. The ‘expert system’ character of Choose and Book militates against using such knowledge, thus impoverishing the scope and quality of judgements. We expand on this argument using empirical examples in Chapter 4.
Medicine’s internal goods are clustered, broadly speaking, around the themes of caring, curing and comforting, and are embedded in the formal and informal codes of practice of the medical, nursing and other related professions. It has long been argued by sociologists that because they bear a commitment to the refined knowledge, ethics and values of their specialised community, professionals act as a bulwark against the impersonal march of capitalist and bureaucratic forces. 128 More recently, French sociological theorist Luc Boltanski has called for policy-makers to go beyond ‘neomanagerialism’ and engage with the moral and normative positions taken by individuals and groups on particular issues, notably the ethically motivated concerns of professionals and lobbyists. 113
Given that medicine’s professional norms are built on shared and deeply held assumptions and values, which differ significantly from the assumptions behind ‘rational economic man’ or from the narrow values of efficiency and cost-effectiveness, nationally mandated ICTs were always likely to encounter problems if their design did not (at the very least) acknowledge what could be lost if these technologies were widely implemented. While economic and resource issues need to be taken seriously, so do professional norms and the internal goods of health care.
Choose and Book, like all expert systems, will necessarily impose abstract and generalised protocols that have limited capacity to take account of local circumstances and contingencies. Similarly, templates for chronic disease management that are built around national guidelines and a pay-for-performance system will tend to impose a highly standardised structure and set of priorities on the consultation. This leads to a tendency to greatly oversimplify the nature of, and to downplay the significance of, local situations and interactions. In an area such as health care, this can have highly negative effects, as medicine is inherently exception-filled (most cases differ in some way from the ‘textbook case’) and medicine’s internal goods are not, in large part, reducible to formulaic rules and nostrums. 98,99
The problem is that abstract systems uproot social relations from their previous grounding in the immediacies of context; they are unable to take account of all that derives, in terms of well-being and the quality of relationships, from the embeddedness and indexicality of social interactions in local contexts. The intended effect is the remote co-ordination and control of healthcare interactions through a promotion of their abstract, quantifiable and divisible characteristics. However, the (partially intended but partially unrecognised) by-product is a downgrading of practitioners’ skills of responsive interaction and situated judgement, and a corresponding emptying out of the space and time in which these skills used to be deployed. This threatens to subvert highly valued internal goods intrinsic to the activity of general practice, which rely on certain kinds of ‘socially established co-operative human activity’ (p. 175)127 between doctors, nurses and administrators, in their relations both with each other and with patients.
The professional framing of medical work sees doctors (and other clinicians) as wielding their symbolic power with integrity and commitment with the patient’s best interests in mind. While these professional norms are shifting to incorporate, to varying degrees, the ideal of the active and empowered patient, they also assume that there are aspects of the unequal relation between doctors and patients whose legitimacy is socially conferred, due largely to the fact that illness makes people (in a range of ways) vulnerable and in need of society’s help. 99 To the extent that the clinician’s role includes making decisions (perhaps on a shared basis with the patient), these are not merely ‘rational’ (i.e. based on the best available medical evidence) but also practical and ethical – that is, they take account of the situated details of individual cases, including a serious engagement with ‘what matters to people’ to particular flesh-and-blood patients. 77
The issue of patients’ needs and well-being is a complex one that needs to be subjected to much more scrutiny than is given to it in the policy literature on technologies such as Choose and Book, the QOF or the SCR. Neither technologies nor the policies and processes in which they become embedded are ethically neutral, and in order to be able to judge the appropriateness and adequacy, the strengths and the shortcomings, of particular policy initiatives, it is necessary to be able to assess their impact on patient well-being. Having a clear sense of the criteria of well-being relevant to particular cases is the final piece in the toolkit necessary to begin to open up policies and their sociotechnical networks to qualitative critical scrutiny. What do patients care about? What matters to them? These questions will be foregrounded in the analysis so as to focus on ends rather than means.
Analysis of cases and development of theory
Development of theory and analysis of data from our principal data set on referral (Choose and Book) occurred concurrently, each feeding into the other. Two of the authors (TG and DS) are medical doctors with an interest in the sociology of professional practice and clinical interaction; the third (RS) is a professor of sociology who is an acknowledged expert on the work of Anthony Giddens80,129,130 and has applied Giddens’ work on expert systems to the study of cultural, political and economic phenomena outside health care. 131,132 Both the literature review and the empirical analysis were informed mainly by a series of regular discussions among the three authors, grounded in the study’s objectives, research questions and contracted deliverables and informed by the policy background and emerging empirical findings. For these meetings, TG and DS selected illustrative examples of the empirical data to share with RS, and RS in turn selected sociological texts that he felt would inform the analysis of particular items of data. DS was particularly crucial in selecting the cases for discussion as she had undertaken a PhD nested within the HERO study that had entailed close reading and analysis of transcripts selected from 54 video-recorded consultations, and hence was very familiar with this data set. 95
This iterative process drew particularly on the principles of interpretivist information systems research, especially the notion of the hermeneutic circle (constantly comparing each new item of data or theoretical insight with an emerging picture of the whole). 133,134 Using a small subsample of three or four detailed examples, we developed a preliminary analytic framework which we revised as we applied it successively to all the referrals in the relevant secondary data set (see Selecting data sets for secondary analysis). Having produced a theoretical model of resistance to ICT that explained our empirical findings on Choose and Book, we then considered the extent to which the same model also explained our previously published findings on resistance to electronic templates and the SCR.
The methodology of SST applied to the use and non-use of ICTs has been described previously,58 and is summarised above (see Chapter 1, Strong structuration theory). Applying this methodology, we focused on the conjuncture – that is, a critical combination of events and circumstances in which the human agent draws on both habitus (i.e. their internal dispositions, beliefs, values, norms and so on) and knowledge of the here-and-now situation (i.e. their assessment of the particular strategic terrain and how they are expected to act within it), and is supported or constrained by the available technologies, to inform, execute and justify a particular course of action.
For the purposes of our study on referral, we considered two kinds of conjuncture: clinical consultations in which outpatient referrals were initiated and administrative activities in which staff sought to follow through on such referrals. In both types of conjuncture, the actor (clinician or administrator) either used or chose not to use (or, sometimes, was prevented from using) Choose and Book to support the referral. For each conjuncture, we considered how the actor’s habitus (e.g. the doctor’s professional identity and code of practice, or the administrator’s efforts to do a good job) combined with their assessment of external circumstances (including the incentives and reward systems linked to Choose and Book and their perception of what would happen if they did or did not use this technology). The purpose of this was to focus in detail on the extent to which, and the ways in which, the actors in particular situations felt enabled and constrained by the material properties and capabilities of Choose and Book (including the role assumptions, categories, values and other social structures inscribed in the software).
Having developed our preliminary theoretical model on the referral (Choose and Book) data set, including a set of questions to ask of a nationally mandated healthcare technology, we then considered our two other data sets – chronic disease management (QOF templates linked to the GP record) and unscheduled care (SCR). We applied the model to relevant parts of the large empirical data sets. Because of resource constraints on this project, we did not undertake exhaustive analysis of raw data on these two further cases. Rather, we used published versions of these case studies along with unpublished interim summaries, and also returned to selected segments of raw data to check particular aspects of our analysis. In these two additional cases, we were particularly vigilant to seek disconfirming data (i.e. examples that did not fit the explanatory model of resistance developed on the referral data set) and to extend our theorisation to explain such examples.
In the presentation of results that follows, we have offered a narrative synthesis of each case using conventional case study notation and formatting,135 illustrated by quotes and extracts that were selected to illustrate theoretical points derived from analysis of the wider data set.
Chapter 4 Main findings and case-specific discussions
Description of data set
As described above, our final data set was selected from a much larger combined data set of two large empirical studies, HERO and SCRIE, conducted between 2007 and 2010. It consisted of raw data (not previously analysed or written up) pertaining to one technology-supported practice (referral) and completed reports along with interim summaries and selected data extracts from two other practices (chronic disease surveillance and unscheduled care). The material used in the three case studies is listed in Table 1 (referral – Choose and Book), Box 1 (chronic disease surveillance – QOF templates) and Box 2 (unscheduled care – the SCR).
PhD thesis linked to HERO study95 on use of computers in general practice, containing the following relevant material:
-
Overview of policy background, especially in relation to local detailed records in general practice and QOF.
-
Extensive field notes from observation of administrative and clinical work, including 30 directly observed consultations of chronic disease management by nurses.
-
Fifty-four video-recorded consultations along with dynamic screen capture of the electronic record, selected sections of which were transcribed and analysed in depth using linguistic ethnography. Of these, 24 were chronic disease surveillance consultations undertaken by nurses (GPs did not formally follow the chronic disease templates but sometimes collected and entered data for these in the course of the consultation).
-
Theoretical analyses (drawing on symbolic interactionism) on use and non-use of templates; authority and voice in the consultation; and ‘backstage’ work in the administrative areas of the practices.
Project report (235 pages) from SCRIE study containing extended data extracts, plus linked interim data summaries, containing the following relevant material:116
Summary and synthesis of 214 observed clinical consultations, 26 in which a SCR was known to exist (and was accessed in 15) and 188 in which a SCR did not exist or was not accessible. Original field notes from the 26 cases with a SCR.
Contextual summary based on:
-
observation of approximately 100 boards, committees working groups and meetings about the SCR at national, regional and local level, including Department of Health, PCTs, professional bodies and patient/community groups
-
129 semistructured interviews with clinicians, project managers, IT suppliers, policy-makers, patient interest group members and service users
-
Department of Health policy and strategy documents on SCR (including risk register), correspondence between Department of Health, professional bodies and Information Commissioner
-
project initiation documents and benefits realisation plans for SCR local implementation.
PCT, primary care trust.
In the sections that follow, we first present a worked-up analysis of our main case study (referral, for which the index technology was Choose and Book). We give a brief narrative of the policy background to Choose and Book, and then describe the material properties of the technology, how it was intended to be used, how it was actually used in both clinical and administrative settings (and/or why it was not used as intended by its designers and policy-makers), and what the consequences were. We then offer a new theorisation of the non-use of Choose and Book technology using our adaptation of structuration theory, and suggest that it would be fruitful to move beyond the term ‘resistance’ to conceptualise and (where appropriate) overcome the non-use of ICTs in healthcare settings.
We then apply our theoretical model to the two supplementary case studies. We describe these cases (chronic disease surveillance and unscheduled care) briefly, and suggest how and to what extent the model may be transferable to other policy-driven technology projects in healthcare. We have deliberately placed most emphasis on case study 1 in this write-up because this was where most of our analytic effort was directed.
Case study 1: referral (‘Choose and Book’)
Specific research questions
Our specific research questions in relation to the use and non-use of Choose and Book for referring patients to hospital were: (1) In the practice of referral, how does the tension between the systemic demands of Choose and Book as an expert system and the application of local (patient-, practice- and community-specific) knowledge through professional judgement play out? (2) To what extent can ‘resistance’ to the use of Choose and Book by GPs and their staff be explained in terms of sociological theories of professional practice and medicine’s core norms and values?
The policy context
The policy background to the shift in referral procedure supported by Choose and Book has been described in detail by others. 125,136,137 The first government commitment to providing patients with a choice over the time and date of their hospital appointment was in 2001 with the Labour government’s landmark ‘NHS Plan’;138 choice of hospital was promised a year later in a ‘Next Steps’ follow-on to this policy. 139 At the time, these changes were accompanied by more specific policies in two disease areas: coronary heart disease patients nationally who had been waiting more than 6 months and those waiting for elective surgery in London for more than 8 months were offered the option of changing to an alternative provider. The assumption behind this policy was that patient choice would reduce overall waiting times and use NHS capacity more efficiently.
In 2004, the same government published the direct policy announcement of the Choose and Book system, The NHS Improvement Plan, which promised all patients a choice of hospital at the time of referral. 140 It was predicted that expansion of ‘choice’ would not only reduce waiting times but also make the service more responsive to patients’ needs, promote quality improvement and increase efficiency (and, therefore, cost-effectiveness). The same policy document sought to introduce competition between providers via a new reimbursement system that paid a fixed tariff price per case.
According to the NHS Improvement Plan, since January 2006 all NHS patients referred to hospital for elective care should have been offered a choice of four or five ‘clinically appropriate’ local providers. In April 2008, patients became eligible to choose any provider nationally who offered care at the national tariff rate and who met standards set by the Care Quality Commission (the government’s independent regulator of quality). 141 These ‘rights’ became enshrined in law via the NHS constitution in 2009. 142
The assumption underpinning the introduction of choice in hospital referral was that the possibility that patients might take their custom elsewhere (what Le Grand calls ‘the power of exit’), which was a significantly more effective driver for quality improvement than the possibility that they might complain (‘the power of voice’) – and indeed, that the potential for ‘exit’ added weight to ‘voice’. 137,143
The technology to support the introduction of patient choice at the point of referral in England was an electronic booking system called ‘Choose and Book’, whose development and implementation was funded in 2003 via a 5-year, £64.5M contract to the commercial supplier ATOS. 144 National implementation of Choose and Book was the responsibility of a designated lead within the Department of Health. Its local implementation was formally the responsibility of primary care trusts (PCTs), which were charged with ensuring that patients were offered the choice of being treated at any clinically appropriate hospital. 140,142
This technology was viewed by policy-makers as something more than a tool for delivering choice at the point of referral. It was also anticipated that by replacing the traditional paper system (in which referral letters were typed, printed and then either faxed, posted or collected on a daily courier round) with an ‘integrated’ electronic system, Choose and Book would also (a) be more convenient for patients and GPs; (b) reduce the number of referral-based enquiries GPs and their staff had to deal with; (c) lessen the bureaucracy associated with referrals; (d) reduce ‘did not attend’ (‘DNA’) and cancellation rates (on the grounds that if patients had chosen the provider and the time slot they would have less reason to default on the appointment); and (e) encourage a more standardised format for referrals. 137,140 All this, it was anticipated, would increase the speed and efficiency of referrals, and help achieve the target of the ’18-week wait’ for first outpatient appointment.
Recognising that ‘choice’ would only be effective if patients were informed of the key differences between local (and national) providers in a particular service, the Department of Health also introduced a website, NHS Choices, giving details of these services to allow comparison between providers prior to referral, launched in June 2007. 145 A ‘Choosing Your Hospital’ booklet was produced with a view to it being supplied to patients by the referring GP, and was also downloadable from the NHS Choices website. This booklet emphasised patients’ right to choice and encouraged them to report services to their GP if they were not satisfied. The interactive NHS Choices website, which has expanded and evolved over time, offered three types of comparative information on providers: performance against published indicators, patient experiences (bulletin-board postings in similar format to travel experience websites) and distance from the patient’s postcode. The format of the website was mostly question and answer – for example:
How can I compare hospitals?
The Find and Choose Hospitals function [hyperlink] is the most sophisticated hospital comparison system in the UK. It allows you to compare hospitals on a wide and growing range of factors, including:
-
overall quality of service (judged by the regulator),
-
mortality rates,
-
other patients’ views,
-
waiting times,
-
infection rates,
-
food quality,
-
parking facilities, and
-
disabled access.
The system allows you to limit your search according to the operations, treatments and specialities [sic] that the hospitals offer. For example, you could search for hospitals within 50 miles of your home that offer hip replacements. You can then compare them in an easy-to-read table, according to the factors above and many more.
Extract from ‘NHS Choices’ website, accessed 15 September 2012
The website also contained photographic images depicting various kinds of choices (showing pictures of GP and hospital consultations, treatment options and various depictions of healthy lifestyles). Patients were advised how they could ‘find out what choice means in the 21st century NHS and learn how you can take control of your health and treatment’. The assumption behind this invitation was that health is something a person can manage effectively by selecting a health-promoting lifestyle, a preferred treatment option and a particular GP or hospital. Images on the website tended to depict smiling, well-groomed and mostly young and apparently healthy patients, enjoying the outdoors on sunny days or using computers competently in clean contemporary surroundings. Another image (accessed August 2008) showed colourful air balloons floating up in an orderly fashion into the blue sky, conjuring up the idea of gently reaching new heights, not alone but together. This imagery resonates strongly with modernist discourse – of rationally organised activity made more efficient and delivering happiness through the use of smoothly working technology. 146
Another element of the Department of Health’s choice policy was that the performance of different localities and provider units would be monitored and that data on key metrics would be collected and published on a quarterly basis. These metrics included the proportion of eligible patients who said that they were aware of the possibility of choosing their provider, the proportion who recalled being offered such a choice and the proportion recalling being offered the ‘Choosing Your Hospital’ booklet. For example, in 2007, 237,000 questionnaires were sent out by Ipsos Mori on behalf of the Department of Health; 32% of 237,000 patients returned a valid questionnaire. Of these, 37% said that they were aware of ‘choice’, 48% said that they had been offered a choice of provider and 17% (36% of this 48%) said that they had been offered the ‘Choosing Your Hospital’ booklet. 147 By 2010, the proportion of patients surveyed who recalled being offered choice remained similar at 49%. 148 Despite the strong policy push to provide objective and standardised information to support choice, 72% of people surveyed in 2010 cited their GP, their own experience or the experience of family and friends as the most important influence on their choice of hospital. Only 6% cited the ‘Choosing Your Hospital’ booklet – and this figure had fallen steadily year on year since the survey began. 148 The patient choice survey was abandoned after 2010, though no reasons were given for this.
Use of Choose and Book in participating practices
At the time that data collection for this study began (2007), Choose and Book had been available for a little over 2 years. Many practices had invested in training and additional staff and begun to use it for referrals but had subsequently reduced their use of it. Of the four GP practices we observed, anonymised as Dale, Beech, Elm and Clover, the percentage of referrals being submitted via Choose and Book was reported to us as 50–60%, 0%, 25% and 80–90%, respectively. We never saw a GP use the Choose and Book system directly during a consultation – even in Clover practice, which described itself as ‘top of the [local] league table’ for percentage of referrals made using the system.
In Beech practice, initial cautious enthusiasm for the Choose and Book system had waned rapidly after attempts to use it. This practice had received a local incentive payment to support the introduction of Choose and Book but had stopped engaging with the system when the (non-recurrent) funding ceased. The decision to do so had been made formally at a partners’ away day, and none of the GPs or administrative staff had used the system since. Similarly, our observations and interviews in Elm practice suggested that the practice had initially been keen to introduce Choose and Book but had gradually reduced the number of referrals made using the system because it was perceived as technically complex, time-consuming and provided no clear advantage over traditional referral, though in this practice there had not been a formal change of practice policy.
While GPs in all four participating practices in our sample expressed personal reservations about the Choose and Book system, most of those in Dale and Clover sought to help their practice reach its ‘targets’ in this area. In some of the referral-related consultations we observed in these two practices, the GP generated an artefact (usually, an internal form) that prompted administrative staff to complete a Choose and Book referral and send details of this to the patient, thereby allowing the referral to ‘count’ towards the percentages quoted above even when the GP did not actively use the system.
Our secondary analysis revealed four analytically distinct but empirically overlapping foci of resistance: to the policy of choice that Choose and Book symbolised and purported to deliver; to the technology’s sociomaterial constraints and implications (including its cost); to interference with doctors’ contextual judgements; and to the altered social relations consequent on its use. After briefly introducing the technology and illustrating the resistance by quoting from e-mail exchanges, we offer a more analytic discussion of these four foci of resistance.
The material properties of Choose and Book
Choose and Book software, developed to deliver a policy promise, was materially accessible from the desktops of GPs and administrative staff in the practices we studied. One or two computers could link to Choose and Book directly from the practice electronic record system. From most, however, the system was accessible only indirectly by entering the patient’s NHS number into the Choose and Book portal. This could be done by cutting and pasting from the GP record (hence by minimising one window and maximising the other) or by manually copying the number down from one window and retyping it into a box on a different window. The patient’s NHS number enabled the hospital patient administration system (PAS) to link to the Personal Demographic Service (the patient’s centrally stored demographic details) on the NHS Spine (a national database holding demographic data and the SCRs of non-dissenting citizens).
The software design assumed that the Choose and Book system would be used one of two ways. In one option, a member of practice staff (the GP, or, as was almost invariably the case in the practices we studied, an administrator) would access the hospital system through Choose and Book to see what appointments were available. In the other option, the patient would be given printed instructions, including a unique identifier and password, allowing them to access this information themselves (typically in the privacy of their own home) either by telephone to a dedicated call centre or via the internet using the ‘HealthSpace’ personal portal to the NHS Spine.
If the GP accessed the system direct (ideally, in the policy vision, with the patient in the room), they could allocate a level of priority (at the time of our data collection, this was restricted to ‘routine’ or ‘urgent’, though it later became possible to request a ‘2-week wait’ if cancer was suspected) before selecting the specialty and clinic type from a series of pull-down menus. It was technically possible, but usually not available in practice (because the function was rarely enabled locally), for a named consultant also to be selected. Having set the parameters of the referral (a particular clinic, a particular level of urgency), the GP or administrator could search for possible providers using one of three criteria: (1) distance from the patient’s postcode, (2) key word (such as the name of a provider) or (3) indicative waiting time (based on the last 20 appointments in the system). A list of providers, clinics (with distance from the postcode entered), and indicative waiting time would then appear. Clicking on any of the providers on the list would (in theory) call up information about them from a directory of services (supplied by providers), including the sort of clinical conditions for which the clinic is intended.
If the patient accessed the system using the ‘HealthSpace’ portal (for which they needed to register in advance and receive a password), they would see the same or similar information. In addition, HealthSpace contained a link to the ‘NHS Choices’ website described above.
The above steps allowed the user (GP, practice administrator or patient) to view and compare different providers, thereby supporting the ‘choose’ component of Choose and Book. The ‘book’ component required a further step. In most cases (‘directly bookable’ appointments), booking could be achieved electronically by clicking the preferred provider in the list offered by the system. Directly bookable appointments were possible only when the provider hospital’s PAS or alternative service provider system was compliant with the Choose and Book software and able to connect to it. If it was not (yet) compliant, the patient was given the hospital’s telephone number and appointment request form with a booking reference number and a password. In such circumstances, the provider booked the appointment in the hospital PAS when the patient telephoned in, and then entered the date and time manually in the Choose and Book software.
Thus, at the time of data collection for our study, the Choose and Book technology was far from seamlessly interoperable with either the GP record system or the hospital system. Even when working as intended, it required a number of additional manual steps (supported by telephone calls and/or paper printouts) to achieve the goals of choosing a hospital and booking an appointment.
Whichever way the booking was made, GPs (or their staff) were required to upload a referral letter onto the Choose and Book software within a defined time limit that could be set on the system (usually a few days). Many booking requests were handled not by the hospital but by an intermediate service called a Referral Management Centre, where a designated individual (e.g. booking clerk working to an eligibility protocol) decided whether or not the referral was appropriate and either confirmed or rejected it accordingly. If necessary, the booking clerk would also contact the patient to change the appointment time (e.g. to take account of staff holidays).
The above might be considered the ‘intended use case’ for Choose and Book. Below, we present the four forms of resistance identified in our secondary analysis. However, before doing this, we set the scene for the story of resistance to Choose and Book by reproducing excerpts from an e-mail thread.
Resistance articulated: some examples of correspondence and publications
Resistance to Choose and Book was particularly well illustrated by an e-mail correspondence involving the co-chair of the Professional Executive Committee (PEC) of the PCT and over 20 local GPs in the locality covering Beech and Clover practices. This exchange (of which selected parts are reproduced with the written consent of the relevant contributors) had been triggered when a letter had been sent from the co-chair of the PEC to all GPs in 2009, and several had hit ‘reply to all’ to put their views. The original letter informed the GPs that this PCT had fallen even further down the national league tables for Choose and Book usage, and exhorted them to make one or two attempts to send every referral using the system. It continued:
Our failing performance in both Choice and Choose and Book is unfair to patients and compromises our service significantly. This, in turn, is affecting the negotiations over brokerage and other issues, as our areas of more modest underperformance are examined ever more critically and our justifications are subjected to time consuming enquiry.
In many other areas we are performing well in [this locality] and the excellent results from the Quality and Outcomes Framework show that our patients receive good quality primary care. We must do everything possible to uphold these standards in all aspects of our healthcare service.
Extract from letter from GP lead for Choose and Book at PCT
This call to action drew a number of responses by return of e-mail, pointing out that the system remained slow, cumbersome to use, technically unreliable and ‘pointless’. As these GPs put it:
Our surgery has tried extremely hard to work with this system but it is totally unreliable. It is very embarrassing to suggest to a patient that I can give them an ENT [ear, nose and throat] appt and then find the only appts on the system are in S--- [40 miles away]! The hospital locally has been very erratic in its supply of appts and we cannot refer to named consultants which is hopeless if you are arranging a follow up on someone who his been seen previously.
In my view the failure of local take-up is testament to the good judgement of our local GP colleagues. I was a pioneer user in my surgery but I no longer use it at all.
we should not use C&B [Choose and Book] because to do so would be to collude in a lie with the government that choice was actually being given . . .
The frustration factor is too great. I tried (once again) to use C&B to refer a patient to gynaecology at [local] Hospital. 2 days later I was told that the referral should be faxed and the C&B request cancelled. No explanation. I may be just unlucky but almost every time I have tried to use the system, something has gone wrong. I would very much like it to work but I’m afraid it doesn’t and it is just easier to use a quill, papyrus and carrier pigeon. (I would add that I am not a technophobe – I happily book my holidays/flights/car hire on-line, without a problem).
Responses in reply-to-all e-mail among local GPs
A single contributor to the e-mail thread pointed out a number of features that they liked about the Choose and Book system (e.g. shifting responsibility for booking to the patient meant that the practice received fewer queries about the referral’s progress). However, even they agreed that the Choose and Book system was a very cumbersome and expensive way of achieving this goal.
When we interviewed the PCT lead in this locality, that individual referred in vague terms to ‘some people’ who were using the system ‘100%’ with ‘no problems’ (‘they love it’). This mismatch between the PCT story and the GPs’ collective story was only highlighted when the reply-to-all function revealed how widespread and deep the strength of feeling was.
Up to now, my practice and many others have had a warped view of Choose and Book because we have relied on the PCT as the sole source of information. We have been told that Choose and Book has been working well. Relying on only one source of information gives you a different answer to the one obtained from an open and democratic forum.
Response by GP in reply-to-all e-mail among local GPs
This heartfelt correspondence appeared to produce no change of policy within the PCT. On the contrary, the managers persisted in seeking to ‘improve performance’. The following is a typical automated e-mail that continued to be sent out on a monthly basis to practices:
Dear [name of practice manager]
The Central C&B data collection office sends out information on appointments that have been Chosen & Booked.
I have mapped these against a report we receive from [the three nearest hospitals] which informs the PCT the number of referrals made into these hospitals on a monthly basis.
In order to get a feel for the accuracy of the C&B data I wondered if you could look at the data below and confirm – or otherwise if you think it reflects the bookings you have made to [these three hospitals].
| April- | May- | |||||
|---|---|---|---|---|---|---|
| Practice Code | Practice Name | Post Code | Number of GP Referrals | Number of C&B | Number of GP Referrals | Number of C&B |
| Dxxxxx | THE [NAME] SURGERY | X00 X0 | 114 | 12 | 93 | 8 |
Many thanks
[PCT administrator]
The correspondence we captured locally was reflected in documents, letters and articles published nationally over a similar time period. The Department of Health continued to produce reports and electronic updates purporting that Choose and Book was working well and producing the intended impact on ‘choice’. 149 These were countered by letters and articles published by doctors in academic journals that documented increased workload and a rise in ‘DNA’ rates following the introduction of Choose and Book,150,151 patients referred under Choose and Book who had no recollection of being offered a choice of provider,119 and a widespread perception that the technology was inefficient, inflexible, complicated and politically driven. 152–156
‘Trade’ publications for GPs depicted the Choose and Book initiative in overtly political terms as an attempt by government to reduce GPs’ power base. They also highlighted that power was explicitly shifting from GPs to their hospital colleagues, as expressed in this e-mail sent out by the medical newspaper ‘Pulse’:
Dear [GP’s name],
How are you getting on with Choose and Book? Some GPs are big fans, while it’s no exaggeration to say others would prefer to catch the norovirus bug than use it. Our lead story that hospitals across the country are abusing C&B to clamp down on referrals will certainly not improve GPs’ views of the system.
A Pulse investigation has found that 90% of hospitals have cut their so-called ‘polling ranges’, thereby increasing dramatically the number of slots listed as unavailable. And the reason they’re doing it? As usual, it’s to hit a Government target. In this case, the 18-week wait.
E-mail sent by Pulse newspaper to subscribing GPs, 27 February 2008
It is hard to recall a technology introduced in the NHS that has drawn such heartfelt and longstanding opposition despite financial incentives for using it. In the analytic sections that follow, we consider four foci of resistance – that is, four different issues towards which the resistance of GPs and other staff was being directed.
Resistance to the policy of ‘choice’
One of our most consistent findings when observing GP–patient consultations was that choice of hospital either was not offered at all or was presented to the patient as an external requirement (something the GP ‘had’ to do), with GPs often highlighting the perceived absurdity of the situation by expressing humour or exasperation [‘we’re supposed to offer you St. [X]’s [hospital 20 miles away] or Timbuktu’ (GP, Beech practice)]. The following example illustrates a typical exchange:
I’ll refer you up to gynaecology. Have you got any preference where you’d like to go, choose and book-wise?
No, just wherever.
So I if I say that you’d like to go anywhere, you might end up going to D--- [30 miles away] or places or do you want to go to C--- [local hospital]?
Ah, I see what you’re saying. No, I would rather go to C---.
That’s what I thought. That’s why I said it more clearly. He he he.
Yeah, sorry.
We’re supposed to offer everybody anywhere, you see.
I’d prefer to go to C---.
Yeah, that’s fine – C--- preference and, uhm, you’ll get an outpatients appointment through.
Transcription of video-recorded consultation, Beech practice
We observed a number of examples in which the offer of choice introduced a distinct note of confusion into an otherwise smooth conversation, as the patient could not understand why they were being given the option of travelling to a distant and unfamiliar hospital. Indeed, GPs appeared to invoke ‘the government’ or ‘the computer’ as a third party in an attempt to reduce this confusion. In all cases where choice of provider was offered, it was recorded on the electronic record using a distinct code that could later be used to audit the practice’s performance.
Our informal discussions and naturalistic interviews with GPs suggested that this recurring pattern appeared to be driven by three things that GPs ‘knew’: first, that the overwhelming majority of patients wished to attend their local hospital (hence there was no genuine reason to offer them choice); second, that the government was mistaken in assuming that choice of hospital would act as an effective mechanism to promote competition and efficiency in the NHS (they described the policy as ‘pointless’ and ‘political’); and third, that offering choice was linked to a financial incentive, embedded within the technology, for the practice (hence there was a perverse reason for offering it). Thus, GPs were ‘resisting’ the policy of choice by presenting it to patients as an absurd demand of the system, at odds with their judgement, and refraining from the active investment of energy that its design relied upon, while most were also ‘complying’ with it at a superficial, pragmatic level in order to gain the financial reward.
Many GPs when observed directly simply did not comply with the policy requirement to offer ‘choice’, as the following excerpt from our field notes shows:
Patient has gynaecological condition for which a referral is needed. Dr Y says: ‘I’ll get onto them . . . I’ll write a letter and they will send you an appointment’. He also took her BP [blood pressure] and entered this. Interestingly his notes read ‘choice and book – enh serv admin’. There was no discussion whatsoever about choice of hospital or C+B.
. . . Between patients Dr Y asked me: ‘Are you in on this Choose and Book palaver? . . . it’s bollocks’
Field notes from direct observation of consultation (practice identifier removed to maximise anonymity of participant)
General practitioners’ perceptions were, broadly speaking, borne out by our data. We did not encounter a single example of any patient choosing to go anywhere except their local hospital, and only one example of a member of staff who recalled (on a single occasion) such a choice being made. Neither did we encounter any examples of either doctors or patients seeking or using comparative performance data when considering their referral preferences. Tellingly, the capacity of the technology to generate ‘personalised’ lists of options depending on whether patients wished to choose by distance, car parking, food quality and so on was never instantiated. Beech practice stopped using Choose and Book when financial incentives ceased. A facility for patients to access such data in their local library in the district where Dale and Elm practice were located had no takers in 6 months. This facility had been established with high hopes of the PCT managers, who depicted sick patients very explicitly as rational choosers selecting on the basis of standardised, abstracted information on the limited range of indicators described in the NHS Choices quote earlier in this chapter (see The policy context):
. . . with the libraries they can do comparisons, can’t they? If they look up three hospitals that they are thinking about they can pick out the most important things and it would compare and give you points so if you want to go to the best one for hygiene or the best one for parking . . .
. . . Or the best one for food . . .
PCT managers in locality covered by Beech and Clover practices
In terms of the wider social structures impacting on choice of hospital, our data set included substantial evidence of attempts to lever political authority. Locally, PCT managers described the PCT as being ‘beaten up’ by the strategic health authority, which in turn was (they said) being ‘hammered’, ‘bashed’ and ‘kicked’ by the Department of Health. Monthly bulletins from the Department of Health reported on progress in implementing the policy, and annual large-scale national patient choice surveys were commissioned by the Department of Health in an attempt to demonstrate that the technology had been instrumental in achieving the policy goal. 148 In these, around half of responding individuals recalled being offered ‘choice’, but the response rate was very low.
A particularly striking finding on our data was that neither local managers nor national policy-makers engaged with the arguments put by the GPs against the choice policy. They did not feel that they had to justify the ‘rightness’ of the policy itself (i.e. the ends); rather, they saw the policy as a given and their own role as maximising compliance with it (i.e. the means). We return to this important distinction between means and ends in the Discussion section for this case.
Resistance to the sociomateriality of Choose and Book
Almost all the activity we observed relating to Choose and Book took place in the administrative areas of the practice. This was partly because even those GPs who had tried using it in real time during the consultation had found the technology (and the explanations the patient needed to engage with its use as a ‘choice’ tool) too time-consuming to fit into a 10-minute consultation.
The following is a typical description of use of Choose and Book in the administrative area:
JJ [secretary] had just been given a C+B referral by Dr X and asked if I would be interested in seeing this. There was no paperwork in the brown wallet used for C+Bs and she said that Dr X would have given it to the patient; she would know for sure when she listened to the tape on which the letter was dictated. Inside the brown wallet there was a small notebook in which the name of the patient was written. JJ had difficulty reading Dr X’s writing and it took several attempts to identify the correct patient. She opened the patient’s record and found the entry relating to the referral and wrote the UBRN [unique booking reference number] number on a post-it note. She clicked on the icon for C+B, which brought up the referral screen. From a drop down menu she selected it as a C+B referral and then clicked on another icon, which generated an outpatient referral letter. At the top of the letter she inserted the URBN and underneath ‘Choose and Book’ and then the department – in this case Gynaecology. The referral was for a routine appointment for a patient who had [details of clinical symptoms/signs removed].
JJ listened to the tape and typed the referral letter. She said she couldn’t make out one of the words on the tape and entered a few possibilities in the Read code field in an attempt to identify the correct one, using [detail removed] as the key word. After three attempts she gave up and took a medical dictionary from the bookcase behind her – still no luck. She decided to email Dr X to ask her and just as she opened Outlook she noticed that the C+B page which she had minimized had disappeared and she had lost her connection to the server. [description of how this lost connection was explored, ending with discovery that someone had accidentally unplugged a network cable]
Dr X came into the office and JJ asked her about the term she couldn’t make out. Dr X listened to the tape and said it was [detail removed]. JJ logged back in and opened the referral letter she had working on and inserted the word and saved the changes. Dr X had already Read coded ‘Choice and booking enhanced service administration’ but had not coded ‘Choice of provider’ – JJ added this Read code. She clicked on an icon which brought up a screen message box ‘Do you want to send this referral?’ and clicked ‘yes’. Once the booking had been sent she wrote the name of the patient and C+B in the column ‘type of referral’ in the ledger where all referrals are recorded, highlighting the C+B with a fluorescent pen.
Field notes from observation of administrative staff in Dale practice
In the above example, the GP had already begun the Choose and Book referral on the system (either in a consultation with the patient or, more likely, in a subsequent administrative session). The following example from Clover practice shows how such a referral was done in cases when the GP had not initiated anything on the system:
XY explained that their use of Choose and Book had evolved over the time they had been using it. She said that the doctors had all ‘washed their hands of it’ and wanted nothing to do with it. She said that at the beginning Dr N was keen, but now he was the most negative about it. She explained that to get into C+B they use an ‘integrated’ system, meaning the C+B software can be accessed via the EMIS [local GP] system. She said that she goes into ‘consultation mode’ to access it. I watched her select ‘referral for further care’ then chose the referring doctor’s name from a pick list in EMIS. She said that when she clicked f8 the patient’s information is pulled into C+B from EMIS and she is taken straight to the ‘referral’ screen. She remarked that it is slow today. This integrated system meant that she didn’t need to copy and paste the NHS number from EMIS into C+B nor search for the patient. The name, address, DOB [date of birth] and NHS number are imported automatically. However the telephone number is not, so she has to add that manually every time.
The referral she was dealing with was to the musculoskeletal preliminary assessment service MPAS. This is an intermediate service between primary and secondary care. She typed MPAS into the ‘keyword’ field, selected the local option (rather confusingly called ‘Primrose Building’ [the name of PCT building] although the clinics actually take place at ‘Rosedale Clinic’) then had to choose a clinic type. She commented that this was new and she hadn’t been asked to select a clinic type for MPAS referrals before. The pick list identified different parts of the body and she selected ‘knee’. A UBRN is generated (unique booking reference number).
Field notes from observation of administrative staff, Clover practice
While the Choose and Book referral itself was always submitted electronically, the system was far from ‘paperless’. Practices invariably sent patients a letter confirming that their referral letter had been sent, enclosing the instructions for contacting the booking service (including the UBRN and password), and reminding the patient to make the telephone call to book their appointment. An example of such a letter is shown below:
Dear
Following your recent consultation with [name of doctor], a referral letter to [name of department] via Choose and Book has been sent today.
I have enclosed the computer generated paperwork for your use, which gives the reference number, the telephone number and a password.
I have highlighted the important pieces of information you will need at your fingertips when you phone.
You MUST phone and book your appointment within 2 weeks or my application for your Outpatient Appointment will no longer be valid.
Yours sincerely
Dr [X] and Partners
Standard covering letter, Elm practice
The examples above illustrate several material features of the Choose and Book technology-in-use that we saw commonly and across all participating practices in the HERO study. Choose and Book referrals were more complex, more time-consuming and consisted of many more steps than a traditional referral. None of the referral bookings was completed within the consultation, and the subsequent steps almost always included work for the patient.
While Choose and Book is an electronic system, it was invariably implemented with the help of numerous paper and other material artefacts. In the first of the examples above, six artefacts were described (or implied) in addition to the tape on which the referral letter has been recorded: a ‘wallet’ (the folder in which the internal referral from GP to administrator was placed); a ‘notebook’ (a paper record of which patients have been referred and identifying details for these); the printed-out details of the UBRN, password and instructions for the patient; sticky notes to support transfer of information from one electronic package to another (if the integrated system is not used); a paper ledger; and a highlighter pen. In the third example, a printout and covering letter amounting to several pages in total was posted to the patient.
Other examples of Choose and Book referrals in our data set described the following additional artefacts: internal structured form for GP to prompt administrator to initiate Choose and Book referral (sometimes accompanied by a printout of the consultation); printed lists of in-progress Choose and Book referrals; ‘pending’ boxes in which part-completed or ‘problem’ referrals were placed; a paper ledger of the financial claims for Choose and Book incentive scheme; a printed-out urgent referral which was faxed ‘just in case’; and a file of troubleshooting instructions. Of particular note was the fact that three of the four participating practices kept a paper log of every Choose and Book referral and the fourth entered all details on a Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) file.
At the time of our fieldwork, the Choose and Book technology was far from ‘plug and play’. On the contrary, administrative staff often spoke of having to get to know the system through accumulated experience and trial and error. We observed many examples of staff helping one another across a shared office in this regard. They also spoke of not trusting the electronic system (or the organisations and/or individuals with whom it connected), and of being unable to navigate the system comfortably even when highly experienced in using it. Because the work of practice administration was complex and fragmented (e.g. part-completed referrals were often put aside for hours or days pending a response to a query), paper artefacts such as notebooks, scribble pads and sticky notes were widely used. One secretary in Elm practice, who kept a personal notebook in which she recorded referrals and other tasks she did, commented: ‘I don’t know if it’s a bit of a girly thing to do but I’d be lost without it’. Clover practice had a large lever-arch file known as the ‘idiot guide’ to Choose and Book with detailed explanations of the different steps and troubleshooting guidance; it had been considered necessary to develop this despite an official users’ manual.
The Choose and Book system was predictably unreliable – indeed, staff described it using terms such as ‘hopeless’, ‘like flogging a dead horse’, ‘a minefield’, ‘a complete shambles’, ‘the bane of my life’ and ‘Creak and Break’. Errors and glitches which we noted while directly observing the technology-in-use (or observing people attempting to use it) included website ‘down’ centrally, server ‘down’ locally, system running slowly, failure of system to supply a password, options listed contained no free appointments (or none locally), incorrect telephone number supplied on computer-generated printout and automated reminders sent to patients from the ‘wrong’ clinic. Administrative staff spent considerable time on the telephone to a helpdesk or to their counterparts in the hospital service trying to over-ride or work around the system to fix these various glitches. Compared with the near-100% reliability of placing a letter in an envelope and sending it to the hospital, the Choose and Book system was almost universally viewed as unpredictable and failure-prone.
Many staff interviewed for our research felt that the most significant aspect of the ‘unreliability’ of the Choose and Book system was not the technical aspects but the lack of booking slots. They also bemoaned the power of a service to ‘reject’ a referral even after the booking had been made (e.g. a referral for paediatric urology was rejected because it had been incorrectly sent to ‘paediatrics’) and the relatively common problem of services contacting patients to cancel bookings that had been made using the system. Indeed, some staff were convinced that the hospitals were taking advantage of the Choose and Book system to control the number of referrals – as absence of a booking slot meant that the referral could not be made (except by bypassing the Choose and Book system entirely).
There was also the problem of ‘cancelled UBRNs’. The following extract from a naturalistic interview with an administrator in Clover practice illustrates this problem:
The hospital will cancel the UBRN if there are no appointments available. This happens frequently. [XY] added that usually the referral seems to get lost in this instance and the next she hears is that the patient phones to say they have not heard about their appointment. What is happening at C--- hospital is that they [patients] are taken out of the Choose and Book system and will be sent an appointment in the (old fashioned) way, generated manually and sent in a letter to the patient. From the practice’s point of view this is still counted on their figures for C+B. From the patients’ point of view this is no different to the system that existed before C+B came into being. Whatever system is used with C+B, if there are no appointments available (and often there are not) then it will ultimately end up ‘manual’.
Cancelled UBRNs were perceived as likely to get lost in the system. Although the Choose and Book portal offered the practice a list of cancelled UBRNs on its patients, this was unwieldy for staff to navigate as there were many such cancellations and they remained on the system for 6 months. In practice, they waited to hear from the patient.
Our empirical observations consistently showed that the Choose and Book system greatly reduced the potential for local control over the referral process. This was particularly evident when a relatively minor procedural or technical glitch occurred.
LC explained one problem they had had recently where a clinician had saved his changes to the master template on a referral form. This had resulted in a particular box remaining checked for all subsequent referrals being made from the practice. This had resulted in lots of queries from the RMC [referral management centre] who deals with these. Furthermore she explained that they had not been able to tell them just to ignore that box for the referrals they had submitted but they had had to re-do all the referrals, submitting a newly completed form for each patient.
Field notes from observation of administrative staff, Clover practice
The secondary care service, too, had lost some local control – for example, the ability to control workflow as referrals came in (perhaps to an intermediate booking service), by making fine adjustments to the number of clinic slots allocated in any particular week. With Choose and Book, the slots were ‘in the system’ and the booking of slots was one step removed from the week-on-week planning of the clinics.
Another finding from our observations of the technology-in-use was that because Choose and Book was linked to a high-profile national policy to promote ‘choice’ (see previous section), use of the system required the collection of secondary data for audit and payment purposes. All Choose and Book referrals had to be coded as such on the practice administration system; the practice manager had to produce monthly returns on the proportion of referrals done using Choose and Book; and the PCT was required to monitor use of the system by all practices and explore the role of incentives in increasing uptake.
In contrast to this complex, technically unreliable and difficult-to-use system, traditional referrals were materially much simpler and smoother. The following is a typical example of a directly observed traditional referral (demographic details have been omitted for confidentiality reasons):
After listening to the patient Dr X said it sounded like [. . .] vertigo and as she had been experiencing symptoms for a while he would refer to her an audiologist. He made a note on the pad next to him to complete a referral form and as he did so he asked her about the second problem. [. . .] After the patient left Dr X said he could have used Choose and Book for the referral to ENT but it was just as easy to do it in the traditional way.
Field notes from direct observation of consultations, Elm practice
In sum, the detailed descriptions above of the complexity and unreliability of the ‘automated’ referral system contrast markedly with the policy expectation (and the explicit promise on the Choose and Book website) of greater reliability and efficiency because ‘most of the communication is done via computers’. 157 We pick up on this dramatic model-reality gap in the Discussion section for this case.
Administrative staff considered Choose and Book highly temperamental and spoke of having to get to know the system through accumulated experience and trial and error. We observed many examples of staff helping one another across a shared office in this regard. They spoke of not trusting the electronic system (or the organisations and/or individuals with whom it connected), and of being unable to navigate the system comfortably even when highly experienced in using it. They spent considerable time on the telephone to a helpdesk or to their counterparts in the hospital service trying to over-ride or work around glitches in the system.
An aspect of this sociomateriality was resistance to the expense of the Choose and Book system and the opportunity cost of using the money for this rather than alternative potential uses. A recurring complaint was that using the technology diverted both clinicians and administrative staff away from time that could be spent on direct patient care. Importantly, the cost of the system was particularly resented given that it was perceived to reduce the quality of care that it was possible to provide:
Perhaps [this locality] is at the bottom of the list because we realise what a waste of time and effort it is and our intention is to utilise resources to provide the best possible care for our patients despite the PCT’s best efforts to reduce these resources, all in the name of efficiency i.e. cost cutting!
GP in reply-to-all e-mail to PCT Choose and Book lead
In this focus of resistance, the key external structures impacting on human actors were, on the one hand, the modernist ideal of a reliable, touch-of-a-button automated system and, on the other, the reality of technologies-in-use: invariably messy, expensive to install and maintain, and (in numerous ways) less than ideally fit for purpose. 50
Resistance to interference with the doctor’s contextual judgement
In all of the GP consultations we observed directly, the practice of referral to hospital was what a sociologist would describe as ‘locally embedded’. In other words, when considering whether or not and where to refer the patient, the GP drew on his or her personal knowledge of the patient (clinical and social) and of local services (including the scope of particular clinics in particular localities, the patient’s own history of being treated at a particular hospital, transport services and the patient’s ability and willingness to use these, the expertise and interests of local consultants, personal experience of referring patients to that service previously, and even personal experience of being treated by local consultants themselves).
The choice policy for which the Choose and Book system had been developed assumed that in different localities, similar service models with similar names would be available for a limited menu of diseases or conditions, allowing the ‘best’ service to be selected easily using a dashboard of performance metrics. The reality was that patients invariably presented not – or not merely – with a ‘textbook’ clinical condition but with a unique illness along with a unique set of comorbidities, personal priorities and social circumstances. Services in other localities were typically organised differently (e.g. they called the ‘same’ clinic by a different name or subdivided the work of the specialty in a different way), so a GP was typically very knowledgeable about a local hospital service but much less knowledgeable about comparable services in other localities.
Importantly, the kind of knowledge the GP needed to select the best option for the patient (personal, relationally situated and professional knowledge such as the trust and regard which this GP held for a particular consultant and how that consultant was likely to manage this condition in this patient) was not the kind available on the ‘NHS Choices’ website (which provided formal, regularised knowledge such as scores that had been allocated by a distant third party for ‘food’, ‘parking’, ‘infection rates’, ‘mortality’ and so on). This is a good example of the delocalisation of social practices, which Giddens described as an inevitable consequence of expert systems. 74
The following example, collected during observation of a GP doing an administrative session, illustrates the mismatch between the knowledge that was available (e.g. infection rates, distance from patient’s home – see The policy context) and the knowledge that was needed to make a professionally appropriate referral that was in the patient’s best interests and the best use of NHS resources:
He accessed the [Choose and Book] website and said the referral was for a hearing test. As he waited for the page to come up he asked me ‘you can do C+B referrals for hearing tests, can’t you?’. I said I wasn’t sure. When the page opened he entered ‘ENT’ as the department and ‘hearing test’ in ‘service’. Nothing came up for any local hospitals, the nearest was C--- hospital which is more than 20 miles away. Dr X said, ‘that’s no good’ and tried searching under audiology – still nothing. He said he would have one more attempt and entered ‘ear problems’ (I think) – this brought up a match for P--- hospital but Dr X said he was worried that the patient would end up in a clinic for people needing surgical procedures or the like and this would be a waste of the consultant’s time. At this point he decided to give up and said as there was nothing satisfactory using C+B he would make an old fashioned referral. He dictated a message onto his machine to the secretary, indicating that he had intended to make a C+B referral for this patient but it would now be a traditional one.
Field notes from Dale practice
In the above example, the GP sought to make a straightforward appointment for his patient to have a routine hearing test. It is unclear here whether he had offered the patient the option of other providers or simply assumed (on the basis of his local knowledge of the service, his knowledge of the patient or both) that there would be no advantage in attending a distant provider for a standard ENT investigation. While the system did offer ‘choice’, there was ambiguity about which listed clinic was likely to offer the particular service needed, and there was also the possibility of inconvenience (to the patient – if they ended up in a clinic that was poorly matched to their needs) and inefficiency (if a relatively minor problem took up space in a specialist clinic). Having made several attempts to find a suitable local option using the Choose and Book technology, the GP bypassed the Choose and Book system and initiated an ‘old-fashioned’ referral to the local hospital.
As in the above example, trying and failing to identify any available local appointments for the particular clinic of interest was one of the main frustrations voiced by GPs who had tried (and given up on) Choose and Book. As noted in the section on materiality above, a common complaint from clinicians was that the hospital was (allegedly) not releasing appointments onto the system (i.e. the GPs knew the service was available locally but it did not appear on the system when they looked for it).
The commonest reason cited to us by GPs for bypassing the Choose and Book system and doing a traditional referral instead was that, as in the example cited above, ‘patients don’t want a choice of where they are seen, they just want to attend the hospital nearest to them’ (naturalistic interview with GP, Elm practice). In some such cases, the GP gave the patient information based on personal knowledge of the individual consultant. For example, a patient newly diagnosed with an eye condition was advised by their GP: ‘I suggest you go to Mr Z because I have [same eye condition] too and he looks after my eyes’ (field notes from observation of consultations, Dale practice). Many local referrals were made to a known consultant with whom the GP was on familiar (and perhaps first-name) terms.
Applying our theoretical framework, the abstract systems inscribed within Choose and Book served to subvert and efface the local knowledge and contextual judgement that enabled the referral to be truly personalised and aligned with professional care as defined in Chapter 3 (see Applying the normative anchor: medicine’s internal goods). As phenomenology and ethnomethodology teach us, individual professionals draw skilfully and with wisdom (Aristotle’s phronesis) on this background knowledge to respond to unfolding contingencies. The abstracted criteria embedded in the Choose and Book software and NHS Choices website were far less nuanced. As one GP in the e-mail exchange reported above put it, ‘the choice is only of the crudest kind’.
In terms of external structures, this locus of resistance reflected a wider mismatch between what we have called ‘medicine’s internal goods’ (the emphasis on professionals drawing skilfully and with wisdom on personal and contextual knowledge to make practical, ethical judgements) and neoliberal policy (in which the choices offered are ‘rational’ but lack granularity). The pressure from policy-makers on the medical profession to comply with a restricted taxonomy of readily classifiable disease states that map unproblematically to particular investigations or treatments reflects the kind of technology-work mismatch described by Brown and Duguid50 in a range of work settings. In a more layered sociological analysis, such mismatch in relation to medical work is depicted as having political origins and been termed ‘conceptual commodification’:
External control over medical care requires something more than literal commodification. Rather, it requires conceptual commodification of the output of the medical labour process: that is, its conceptualization in a standardized manner. Such commodification facilitates control over the production of services, not just over the arrangements for their exchange . . . The basic strategy of commodification is to establish a classification system into which unique cases can be grouped in order to provide a definition of medical output or workload.
p. 190158
Resistance to the altered social relations consequent on use of Choose and Book
In the consultations we observed directly, most discussions about referral took a traditional format, with the GP suggesting a consultant and a course of action and the patient accepting the suggestion. One reason why they did not use Choose and Book during consultations was a reluctance to take on what they viewed as a more technical (and less professional) role. As one GP put it on the e-mail exchange shared with us about Choose and Book, ‘We seem to be moving away from curing, caring and comforting to robotic automata’.
As with the other forms of resistance described above, this can be explained in terms of internal social structures – specifically, professional identity. GPs considered it their professional duty to recommend a clinically appropriate outpatient clinic, including any necessary dialogue with the patient about their needs and preferences. However, they defined the technicalities of booking appointments as outside their scope of practice and associated these with a loss of status and autonomy that was often deeply held and strongly expressed (as in the quote above).
This resistance was played out at locality level, between GPs (largely opposed to Choose and Book) and PCT staff (who were responsible for implementing the technology locality-wide). PCT managers did not question the ends of Choose and Book but presupposed that it was fit for purpose, attributing its low uptake to Luddism and even ‘to be spiteful to the PCT’ (direct quote from interview with PCT manager, who alleged that GPs’ resistance to the system was to punish the PCT for financial cuts elsewhere). However, when the PCT sent GPs a letter that spoke of ‘failure’ against the ‘standard’ of Choose and Book and described low uptake as a ‘threat to good quality care’ (see Resistance articulated: some examples of correspondence and publications), the GPs responded vociferously by challenging this definition of quality and the legitimacy of the metrics being applied. On the contrary, they claimed, they had abandoned Choose and Book because it was a threat to professional standards.
Our observational data revealed that the tension between the professional and the technical was perceived by some administrative staff as well as by most doctors. One administrator in Clover practice, BN, told us that she had decided to take early retirement as a direct result of Choose and Book. She associated professionalism in her role with qualities such as knowledge of the services available locally, and with the ‘family doctor’ relationship that was built between patients and particular staff through continuity of care: ‘The patients have always been my main concern here. I don’t know where patients are these days – lost under piles of paper and in the Choose and Book system’.
BN was concerned that patients often telephoned the practice because they did not understand instructions for booking their appointment. She bemoaned the introduction of a standard accompanying letter sent to patients with Choose and Book paperwork (which began ‘Dear Patient’ and was signed ‘Practice Secretary’) as impersonal (‘I could be anyone’), and insisted on adding her own name and signature to it, but the new system discouraged such personal touches. As BN commented while doing a Choose and Book referral: ‘I need to save this [letter] in Choose and Book . . . now what I’m going to do in my capacity as “absolutely nothing”, I’m going to attach it. . .’.
A few administrative staff, however, were positive about Choose and Book. The lead administrator at Clover practice, XY, for example, was a ‘super user’ of the system: skilled, confident and keen to help others learn it. She saw Choose and Book’s technical idiosyncrasies as a challenge (‘I won’t be beaten by it’) and felt that its complexity made her job more interesting (‘not just mindless typing’). She took particular pride that the practice was outperforming all other practices locally for use of Choose and Book. When some GPs in the practice had advised her to ‘hold off a bit’ on using the Choose and Book technology because of its questionable cost-effectiveness, her response was ‘I can’t do my job 50%’.
In terms of dispositional values, BN aligned strongly with the values of the traditional family doctor service (reflecting the wider social structure of ‘medicine’s internal goods’ described above). In contrast, XY had positioned herself as a bureaucratic cog within the expert system, reflecting the ‘new professionalism’ of what Harrison has called scientific-bureaucratic medicine,158 overly detached from the professional values of the locally embedded general practice and focused primarily on the efficiency of means rather than the value of the ends.
Both national and local policy-makers were characterised by a striking lack of engagement with the values, identities and relationships of general practice. The PCT managers we interviewed, for example, saw referral as the same administrative process whether achieved via Choose and Book or a traditional referral (‘it’s just two or three more mouse clicks’). This framing did not take account of the wider changes in roles, responsibilities or identities associated with the Choose and Book system.
Means versus ends
In an interview held (jointly) with two managers from the PCT covering Beech and Clover practices, who were joint leads for Choose and Book implementation, they made passing reference to GPs’ perception of the pointlessness of discussing ‘choice’ and the technical limitations of the technology:
They [GPs] see it as a waste of their time, a waste of the patient’s time and not good for the patient. They actually feel that, that what they are being asked to do is just hit a government target.
In their [GPs’] words, it fails, it freezes, it takes them time, the patient wants to go to the local hospital. It’s in their opinion pointless.
PCT managers
However, while the managers acknowledged these perceptions, they did not appear to consider them legitimate. For example, they challenged the claim that Choose and Book takes more time:
They think it’s going to take more time, but our argument is that if there’s a paper referral they have to process that paper referral and type it all up and all the rest of it, and send it off, whereas, so whatever they have to do to achieve the Choose and Book referral probably doesn’t take any longer than processing a paper referral, but they see it as extra work and we haven’t managed to convince them that it’s just changing the way you work, it’s not extra work.
PCT manager
As described above, our own observations indicated that Choose and Book referrals required many more steps and represented a significant shift in responsibility – partly because the task of finding an appointment slot fell to the practice rather than the hospital, and partly because the patient became responsible for telephoning the booking centre and often needed support to do this. However, the managers’ argument was that the Choose and Book referral process was no more complex or difficult than a traditional referral.
. . . for them [practice administrators] to produce a UBRN is just two or three more mouse clicks, then print the UBRN and they would, whatever the practice is, would be to either get the patient back or telephone the patient, post it to the patient, it’s all instructions on the UBRN for the patient what next to do, but it’s no different for them printing that referral letter putting it into an envelope and posting it to the hospital or referral management centre or whatever they do now, and they can’t seem to grasp that it’s all the same process.
PCT manager
The managers’ argument that Choose and Book and traditional referrals are the ‘same’ process centred on comparing the sequence of technical and procedural tasks involved (‘two or three more mouse clicks’, ‘putting a letter in an envelope’). It did not take account of the wider changes in roles, responsibilities or identities associated with the Choose and Book system. Indeed, when pushed by the researcher to consider these, they depicted a misconception by practice staff that needed to be corrected.
They obviously see it as quite a significant change in their role, for some reason . . .
Yes, yes, they do.
If only I could get to their computers with them and just say look this is what you do, and it is just two or three more clicks, isn’t it?
Interview with PCT managers
Note that here, as elsewhere, staff whose identity and perceived role aligned closely with the structure and processes of the expert system focused entirely on the means of achieving the task and did not question the ends.
Ironically, the managers’ main concern in this interview appeared to be precisely what they thought was an (implicitly, incorrect) ‘opinion’ of the GPs – that the PCT was not hitting its assigned target for Choose and Book. This particular PCT had recently been named and shamed by publication of national comparative figures, on which it had scored towards the bottom.
The managers’ approach to the practices was oriented to ‘improving performance’ (i.e. increasing the number of referrals undertaken via Choose and Book). To that end, they considered that GPs could ask their administrative staff to do the referral rather than encroach into consultation time, and had even developed a ‘proxy’ system in which many of the steps of the referral could be initiated and processed in the traditional way. Practices using the proxy system were allowed to count such referrals as ‘Choose and Book’, allowing the PCT to meet its targets and reduce its risk of getting ‘hammered’. The metaphors used by these PCT managers to describe the pressure they were under from the Department of Health (see Resistance to the sociomateriality of Choose and Book) illustrates the coercive pressure behind some nationally mandated technologies linked to policy priorities.
Discussion
This case study of referral to hospital in the English NHS between 2007 and 2010 has revealed a contested social practice driven by national policy and linked to the use and – more significantly – non-use of a new, nationally mandated technology. The combination of SST, Giddens’ conceptualisation of expert systems, and a hermeneutic and ethical sensitivity to professional values has allowed us to do the following. Firstly, we have been able to theorise this phenomenon in relation to wider social changes in late modernity. Specifically, we have reanalysed the non-use and abandonment of Choose and Book as resistance to an expert system. Secondly, it has allowed us to construct an ideal typical conception of the professional values of those involved in general practice that articulates the moral basis for their resistance. Thirdly, it has allowed us to explore the tensions between these value-dispositions on the one hand and the specific forces and pressures introduced by the abstract system of Choose and Book on the other.
The various hierarchical orderings (e.g. lists, ratings and rankings) inscribed within the Choose and Book system and on the NHS Choices website, to the extent that they were accepted and used, created the potential for policy-makers to influence social relations and practices beyond immediate face-to-face interaction. In particular, Choose and Book helped produce ‘action at a distance’ by supporting policy-makers’ efforts to control and co-ordinate the referral activities of frontline GPs and the choices of patients – or at least, it may have done so had the GPs and/or patients used the system as intended.
When expert systems are used, knowledgeable actors draw on the knowledge inscribed in them, thereby disseminating it and integrating it into local practices and embodied knowledge. This was illustrated in our data by the administrator XY in Clover practice who had become a ‘super user’ of the Choose and Book system and was reluctant to revert to traditional referral methods. One interpretation of this data is that in so doing she had – perhaps unwittingly – embodied and reproduced the assumptions and value hierarchies inscribed in the technology, though there are other interpretations. However, expert systems can produce ‘action at a distance’ only if and to the extent that the people who are intended to use them actually do so. If they refuse to use them (e.g. because a professional engagement with the activity depends on embedded knowledge or because they contest the legitimacy of the expert system), or if they are prevented from using them (e.g. when the system does not ‘work’ or its functionality does not fit the time or space constraints of the social situation), the intended ‘action at a distance’ does not occur.
Our findings suggest a significant mismatch between the model of clinical work underpinning the ‘choice’ policy and inscribed in the Choose and Book technology, and the much more complex, granular and exception-filled nature of real-world clinical practice. For one thing, the ‘choice’ policy introduced and pursued by the English Department of Health depicted clinical care in transactional rather than relationally situated terms: it emphasised the episodic, bounded nature of doctors’ input and used the term ‘quality’ mainly in relation to discrete, abstractly conceived, structures, processes and procedures. A contextual and professional framing, in contrast, would emphasise the quality of the relationship between patient and doctor, and between GP and consultant (including such things as trust and positive regard) and the continuity of these relationships over time.
A striking finding in this study was the limited understanding by either policy-makers or PCT managers of the detail of clinical work or the nature of the knowledge that informed referral practice. Both national policy-makers and local PCT managers appeared to consider that GPs would be incentivised to use the system through two behaviourist mechanisms: (1) financial incentives and (2) disclosure of performance data (‘naming and shaming’). They were either unaware of, or dismissed, the influence of institutional structures such as the norms of professional practice, which defined quality in ethical and relational terms rather than in terms of a state-imposed metric of compliance with a policy. They also underestimated the extent to which the material properties of the technology would prove limiting.
The framing of Choose and Book use as a ‘quality standard’ by PCT staff, and their refusal to engage with the GPs’ concerns about threats to quality, is an example of the silencing effects that the French sociological theorist Luc Boltanski writes about in criticising neo-managerialism’s concerted, ill-advised constriction of the space for meaningful conversation and debate about the role of normative values in guiding policy. 113 The PCT managers’ perspective reflects a situated frame of meaning, in which their role is defined in such a way that they deal solely with implementing means. Theirs is a bureaucratic form of professionalism, refusing to question ends and the values that inform these. 123
We conclude from this case study that the challenge of reducing resistance to ICTs by health professionals cannot be addressed purely with behaviourist approaches – and neither is the solution entirely to do with improving the fit between the technology and the practical micro-detail of work tasks. Rather, resistance to such technologies and the expert systems of which they are part would be reduced if there was, firstly, a greater recognition and dialogue with the world of professional values within its design and implementation, and secondly, a greater willingness to seek degrees of balance between such virtual, remote systems and the exigencies of the local sites in which professional values are performed.
Choose and Book is one of many expert systems currently being introduced, top down, in the English NHS. The findings in this case study suggest that it is time for academics and policymakers to heed Boltanski’s call to open up debate with a view to managing the tension between normative values and forms of order and authority (p. 155). 113
It is important to emphasise that while the technology in this study (Choose and Book 2007–10) has evolved (e.g. it may be faster, less ‘clunky’, more intuitive to use and so on), the fundamental theorisation of actors’ concerns about this technology and their reasons for being reluctant or unable to use it remains (we believe) valid.
Case study 2: chronic disease surveillance (templates linked to Quality and Outcomes Framework)
Specific research questions
Our specific research questions in relation to the use and non-use of chronic disease management templates were: (1) In the practice of chronic disease surveillance, how does the tension between the systemic demands of the QOF as an expert system and the application of local (especially patient-specific) knowledge through professional judgement play out? (2) To what extent can compliance with, and ‘resistance’ to, the use of these templates by practice nurses and GPs be explained in terms of sociological theories of professional practice and the core norms and values of nursing and medicine? We also sought to validate and refine the theoretical approach that we had developed in relation to the Choose and Book case described above.
Brief summary of the case
We have described and analysed this case study in detail elsewhere. 58,92,93,95 Electronic local detailed records emerged within UK general practice decades before the government-led NPfIT began. They were developed and refined largely by technically-oriented GPs who wanted to make tasks such as repeat prescribing, patient recall (for check-ups) and item-of-service claims easier.
The national pay-for-performance policy for general practice was developed and introduced as part of in the 2004 General Medical Services Contract via the QOF, which used data from the local GP record to calculate a percentage of GPs’ income. It was to a large extent professionally (and academically) led, though its architects liaised closely with the Department of Health to negotiate funding (and in later years it was incorporated into the National Institute for Health and Care Excellence). The QOF aligned with wider efforts from within general practice to improve the quality of clinical practice through structured, template-driven, evidence-based care linked to financial incentives. 115,159 It was couched in the professional values of EBM and quality improvement, and aspired to reflect best evidence about important clinical outcomes and the processes likely to achieve these. While the QOF was rapidly embraced by politicians as a potentially powerful tool for improving quality and cost-efficiency in general practice, it was not initiated by politicians. In that sense, it differed from the Choose and Book example, which was much more explicitly politically driven.
At the micro level of the clinical consultation, the GP in the surgery had little scope to alter the assumptions about good clinical practice that had been inscribed into QOF software. He or she was typically (and understandably) influenced by the financial rewards that came with compliance with completing the data fields and following the management recommendations inscribed in the QOF templates. GPs were not, of course, compelled to act in these ways by the technology, but they could not prevent those networked external structures from imposing a material cost on their ‘resistance’. At a broader strategic level, the situation was different. There was (and, at the time of writing, still is) an annual round of negotiation that fed into the redesign of both the QOF targets (what actions GPs were rewarded for) and the linked software templates. GPs collectively had considerable scope to negotiate changes in the topic areas, decision models and financial reward systems linked to these.
The existence of the QOF, and its material intrusion into the clinical consultation by way of pop-up prompts and template-driven surveillance of chronic diseases (such as ischaemic heart disease, diabetes, asthma and depression), became increasingly controversial among GPs after its introduction, not least because the proportion of their income accounted for by ‘QOF points’ rose steadily year on year and the amount of time that needed to be spent gathering and entering data to ensure that the record was complete (and hence eligible for QOF payments) also rose. While inscribing evidence-based guidelines in technology may not be a bad thing, the range of quality indicators in the QOF is far more limited than the breadth of conditions seen in general practice, and it became increasingly apparent that technology-driven prompts for this limited range of indicators occurred frequently and were materially and socially intrusive. They had the unintended effect of making consultations awkward and shifting attention from what the patient wished to talk about. 160
Like Choose and Book, the QOF fulfils the description of an expert system. The evidence-based guidelines that underpin it are a good example of a classification system that describes ‘the way things are’121 and is linked to a set of performance criteria, a financial reward scheme and a set of technological prompts that (to the extent that clinicians use them) enables action at a distance, prompting opportunistic check-ups and data capture during routine consultations. 71
The ambivalence of many GPs towards the QOF reflects controversy about the extent to which it captures the essence of professional practice set out earlier (see Chapter 2, A normative anchor: what is excellence in clinical practice and Chapter 3, Applying the normative anchor: medicine’s internal goods). The academic GPs who were instrumental in developing and implementing the QOF were convinced that it did. 115 However, other academic GPs argued forcefully that the QOF brought major risks to the quality of patient care by imposing distant rules and protocols in a way that could not be sensitive to the unique psychological and social elements of a particular patient’s predicament and the unfolding nuances of a real-time consultation. 161–163 As one pair of authors argued in an editorial entitled ‘What Have You Done to Yourselves?’:
By following a medicine-by-numbers, pay-for-performance path under the QOF, the profession cannot lay claim to its own knowledge base and priorities. There is a real risk that general practice will lose its ability to deconstruct evidence and apply it critically in a biopsychosocial model. The systematic mistrust of general practice implied in paying for performance, and in care driven by ‘one size fits all’ treatment guidelines, undermines the moral imperative of beneficence. Evidence shows that using external incentives to drive behaviour decreases internal motivation. [. . .] QOF by its nature promotes simplicity over complexity and measurability over meaningfulness. Unfortunately, these latter dimensions are usually inversely related.
pp. 435–6161
Empirical data on use and non-use of chronic disease templates
Our data set of 54 video-recorded consultations (12 of them chronic disease management reviews by practice nurses), together with field notes from many hours of additional observation of clinical encounters, contained numerous examples of chronic disease surveillance. Practice nurses tended to follow these templates more or less as they were intended to be used, working through the relevant template for each successive patient in a designated ‘asthma clinic’, ‘diabetes clinic’ and so on. In contrast, we never saw a GP start at the top of an electronic template and work methodically and in a structured way through to the end of it, though we did observe many examples of the GP asking opportunistically about lifestyle or offering to take a patient’s blood pressure or weigh them when they had attended for a different problem, and entering data in the relevant field.
As we have illustrated in detail elsewhere,93 consultations for chronic disease surveillance invariably centred on the ‘evidence-based’ protocols inscribed in the QOF templates. Importantly, templates did not simply identify tasks for completion but contributed to defining what chronic diseases were (the patient’s condition became defined in terms of the particular variables that made up the template), how care was delivered (the consultations were usually conducted in a linear fashion, oriented to completing each box in turn), what it meant to be a patient (an individual was a ‘patient’ if they were part of a denominator population who were recalled for regular check-ups, whether or not the initial diagnosis had been an accurate and firm one) and what it meant to be a professional (nurses were defined in terms of the disease they were employed to monitor, as in ‘the asthma nurse’, and their role was defined not merely as managing and monitoring patients but as managing and monitoring QOF data).
The example in Box 3 illustrates how the patient’s agenda is systematically suppressed as the nurse remains focused on collecting the data needed for the QOF template. ‘Professionalism’ is evident to the extent that this equates with efficiency of the process of data collection, but the nurse (either consciously or unconsciously) repeatedly fails to pick up on the various problems that are concerning the patient (immobility, deafness, diarrhoea). As with other manifestations of scientific-bureaucratic medicine described in case 1, above, the nurse appears to pursue the means (efficient completion of the data fields) at the expense of the patient-centred ends (dealing with the actual problems he has).
A frail-looking 86-year-old man struggled in to the clinic, barely able to walk. He was very deaf. He hung his walking stick over his chair and grimaced as he sat down, looking as if he was in pain.
The nurse said loudly ‘We’ve called you in to look at you from the heart point of view. I know you have a lot of other things going on but we’ve called you in to look at your heart.’
She then asked ‘How often do you use the angina tablet under your tongue?’
The patient replied in a way which made his most pressing concern clear: ‘Not much . . . for the simple reason that I can only crawl like a tortoise’.
Nurse: ‘and the simvastatin?’
Patient: ‘no . . . I stopped that. I think it’s giving me diarrhoea. These hearing aids are not very good you know. I’ve had it adjusted several times but I’m really disappointed. I had hoped for better than this’.
As Box 1 shows, through the ‘efficient’ pursuit of template-defined items, patients’ stories morphed into data bytes; the particular became generalised; the complex was made discrete, simple and manageable; and uncertainty became categorised and contained (as many of the items required a binary response such as ‘present’ or ‘absent’ and equivocal responses were invariably classified firmly as one or the other). As in this example, many consultations had characteristics of overtly bureaucratic encounters, primarily oriented to ensuring that data fields were complete and lacking coherence for the patient. We identified a tension, sharpened by the electronic template, between different framings of the patient – as ‘individual’ (a person with a unique and perhaps idiosyncratic illness) or as ‘one of a denominator population for disease X’ (e.g. as ‘moderately severe asthma’ or ‘grade 2 heart failure’).
It might be expected that nurses always ‘complied’ with the templates and GPs (who never formally followed them) always ‘resisted’ them, but the picture is far more complex. Some nurses enacted conversationally disjointed (and, for the patient, frankly confusing) encounters as illustrated in Box 1, and persisted in steering the conversation rapidly back to the agenda set by the template whenever the patient embarked on a wider narrative. However, other nurses were highly skilled in managing the tension between the patient as unique individual and the patient as a ‘case of disease X’, responding creatively to prompts within a dialogue constructed around the patient’s narrative. One described herself explicitly as a ‘paper person’ though conceded that her work was also ‘template driven’.
Another nurse, also clearly a ‘paper person’, ignored the computer entirely during the consultation. Instead of taking a linear route through the template questions, she consulted across the corner of her desk with her back to the computer, and allowed the consultation to flow in an open-ended and patient-led way. She used inclusive, conversational prompts such as ‘tell me about . . .’ and ‘what have we got here?’ (emphasising the interactional aspect of the encounter), rather than put a series of narrow, bureaucratic questions about particular symptoms or behaviours (as illustrated in Box 3). Only when the patient had left the room did this nurse open the computer template and complete the fields.
This particular nurse went to great lengths to minimise her need to look at the computer during her consultations, seizing brief opportunities as they arose (e.g. as patients removed socks). She often placed one hand on the patient’s arm as she rotated her chair to look at the screen, keeping it there as she typed with her other hand – an awkward posture, but one that allowed her to maintain a physical connection to the patient as she attended to the template. She always went into surgery 30 minutes before her clinic was due to start, to prepare a written page of notes for each patient in her notebook. She meticulously studied the record of each patient she was due to see, and copied blood results and other information she thought she might need to refer to. She ‘knew’ the template, and would frequently anticipate the next field in the template before displaying it on the screen, weaving it into the consultation while keeping it backgrounded to the patient. Importantly, this nurse had negotiated a longer consultation time (30 minutes rather than 15) per patient with her GP employers as she had found it impossible to attend to both the patient’s agenda and the template’s data requirements in the shorter time window.
General practitioners, in contrast, did not overtly work through templates. Rather, when faced with a patient with a chronic illness, most GPs asked questions and conducted selected elements of a physical examination (such as checking a patient’s blood pressure) to satisfy their own real-time clinical concerns. In addition, and to a greater or lesser extent for different GPs and in different consultations, they responded to point-of-care prompts from the electronic record to complete particular data fields. Typically, this took the format of including ad hoc questions or comments such as ‘Could I just ask you if you’re still smoking?’ or ‘It looks like you’re overdue for your flu jab, would you like to make an appointment?’ towards the end of the consultation.
Video and screen capture data revealed that some requests to which GPs responded in real time were actively prompted by the software (e.g. when the patient’s record was opened, a pop-up window appeared saying ‘overdue for cervical smear’). Others, however, were pursued more surreptitiously. The example in Table 2 shows the GP–patient conversation (third column) and GP’s entries on the electronic record (fourth column) for a patient who had made an appointment to review a recent respiratory problem. The extract begins after the doctor has checked the patient’s chest and the patient has begun to speak about wider issues that are troubling him, including planning for his own death and providing for his children, one of whom has learning difficulties.
| Time | Speaker | Words spoken | Doctor’s actions on electronic record |
|---|---|---|---|
| 5.22 | Patient |
|
Enters ‘136’ in template box for
‘systolic blood pressure’ Enters ‘78’ in template box for ‘diastolic blood pressure’ |
| 5.45 | Doctor |
|
|
| 5.45 | Patient |
|
Holds cursor on ‘target systolic BP’ (bypassed). This box has never been completed |
| Doctor |
|
||
| Patient |
|
Leaves empty template boxes for ‘target diastolic
BP’, ‘target weight’ and
‘target height’ Holds cursor on ‘urine glucose’ and range of options for this item |
|
| 5.59 | Doctor |
|
|
| Patient |
|
||
| 6.03 | Doctor |
|
|
| 6.25 | Patient |
|
|
| 6.26 | Doctor |
|
|
| 6.29 | Patient |
|
|
| Doctor |
|
||
| 6.44 | Patient |
|
Keystrokes bypassing ‘urinary glucose’, ‘urinary protein’ and ‘diet advice’ |
| 6.46 | Patient |
|
Cursor on template item ‘smoking status’
(response “never” has been entered 9 months
earlier). Enters ‘Never’ Holds cursor briefly on items ‘smoking advice’, ‘alcohol intake’, ‘alcohol advice’ before bypassing each Holds cursor on ‘depression screen’. Selects ‘Y’. Enters free text: ‘recently low, with anxiety’. Hits return key |
| 7.08 | Doctor |
|
Holds cursor on ‘serum cholesterol’, bypasses item |
| 7.14 | Patient |
|
Bypasses items ‘creatinine’,
‘digoxin’, ‘12 lead ECG’,
‘exercise ECG’ Item ‘exercise grading’. Selects ‘light exercise’ from pick list (same as last entry from 2 years ago). Other options were ‘exercise impossible’, ‘avoids exercise’, ‘enjoys moderate exercise’, ‘enjoys heavy exercise’, Bypasses ‘exercise advice’, ‘echocardiogram’, ‘max tolerated therapy’ |
| Doctor |
|
||
| 7.25 | Patient |
|
Item ‘Aspirin’. Enters ‘salicylate prescribed’ (same as 4 years ago) |
| Doctor |
|
||
| 7.28 | Patient |
|
Item ‘Warfarin’. Selects ‘not
indicated’ (same as 4 years ago) Selects ‘beta blocker contraindicated’ (same as 9 months earlier) |
| 7.38 | Doctor |
|
|
| Patient |
|
Selects ‘ACE not indicated’ (same as 5 years
ago). Then selects ‘Angio II’ not indicated
(same as 4 years ago) Selects ‘clopidogrel not indicated’ (same as 4 years ago) |
|
| 7.52 | Doctor |
|
|
| 7.53 | Patient |
|
|
| 7.56 | Doctor |
|
|
| 7.57 | Patient |
|
Selects ‘statin not indicated’ (same as 5
years ago), then returns to this box and cursor sits on it
for several seconds Bypasses ‘diabetes screen’, ‘standard CXR’, ‘cardio referral’. Bypasses ‘flu vaccination’ and ‘pneumococcal vaccination’ Item ‘medication review’. Enters ‘Y’. System returns message ‘invalid format, enter date or e.g. 2D = 2 Days. 1M = 1 month 3Y = 3 Years’. Enters ‘6m’ (which results in a date 6 months hence appearing). Item ‘next review due’; enters ‘6m’, hits return. Template ‘completed’, returns to consultation screen. Screen shows ‘coronary heart disease annual review due in 6m’ Selects ‘medication screen’, scrolls down to look at second page |
In this example, an alert box showing in one corner of the computer screen displays all the relevant missing QOF data fields for the diseases in which the patient will count as part of the denominator population. A significant focus of his attention, as shown by the screen capture, is completing the ‘QOF boxes’ that are now revealed, though the patient is not aware of this. While doing so, the doctor also manages to attend to the patient’s poignant narrative but in a way that falls short of full conversational engagement.
Analysis: foci of resistance
In this section, we consider how well the four foci of resistance identified from the data in our Choose and Book case study – resistance to policy, to the material properties of the technology, to the ability to respond to local contingencies and to altered roles and relations – apply to the case of QOF templates for chronic disease management.
Our first observation in relation to this case is that there was less resistance overall to both the policy and the technology, hence (in this respect) this is a less extreme example than case 1. The introduction of pay-for-performance for chronic disease management (via QOF templates) as a national policy contrasts with the introduction of ‘choice’ (via Choose and Book) in that it was clinically led and strongly supported by doctors’ leaders, who worked to persuade politicians of its value. Their efforts were positively received, as the electronic templates made two things possible: first, point-of-care prompting of clinicians to collect the necessary data and offer the recommended interventions, and, second, the aggregation of data on clinicians’ performance so as to monitor and reward the delivery of ‘evidence-based’ care. In this sense, the QOF was strongly aligned with the new managerialism being introduced by the New Labour government in the early 2000s – a policy of ‘transparency’ (i.e. the collection and public release of performance data) and close monitoring of this performance towards nationally set targets. 164
Our data did not suggest major adverse perceptions of the material properties of the QOF templates. We encountered no examples of the templates crashing, running excessively slowly or freezing during routine use (though a system crash that required staff to work without computers for a morning caused particular confusion in the chronic disease management clinic because templates were unavailable). Unlike Choose and Book, the software was easily and seamlessly accessible from the screens routinely used by clinicians, and the fields were relatively quick to complete. They were also customisable by those with a moderate level of technical knowledge (e.g. additional fields could be added and the order in which the items appeared could be changed). Indeed, clinicians typically found the templates the quickest and easiest way to collect the required data in a way that allowed them to be audited and submitted for payment. This, in direct contrast to Choose and Book, which was costly to the practices because they had had to hire additional staff to deliver it, was extremely lucrative for most practices if they complied with it. The clinicians in our data set perceived QOF to be a highly efficient way of covering a large population of at-risk individuals and preventing expensive-to-treat complications. GPs in particular (who were usually in a profit-share arrangement) went to great lengths to use the technology to its maximum potential, as illustrated by the example in Table 2. This example thus affirms cost as a key element of resistance by illustrating, perhaps, how financial benefit can lead to extreme forms of compliance. In sum, few clinicians were resistant to the material and practical aspects of the QOF technology.
There was a great deal of resistance, however, to the intrusion of the template – and the QOF data collection process – into the local, unfolding detail of individual consultations. Just because it is good clinical practice to collect a standard set of data and offer a particular set of treatments for chronic diseases does not mean that these issues should always and inevitably dominate over the patient’s current priorities and concerns – either when attending for an invited check-up or (even more so) when attending for a different problem. The editorial ‘What Have You Done to Yourselves’, written by academic GPs from outside the UK commenting on the UK system, articulated this paradox well. 159 The issue is not that the policy is wrong in principle, or that the QOF produces role conflict for the GP, but that the sheer number of QOF items and the pervasive intrusion of prompts and reminders in almost every adult consultation makes it impossible for the consultation to follow a traditional interaction around the ‘presenting problem’.
The nurse who made little or no direct use of the template until the patient had left the room was actively resisting this intrusion of the standardised protocol into the granularity of local clinical care while at the same time complying closely with the policy of evidence-based chronic disease management. By physically distancing herself from the computer, and by copying out selected data items onto paper to use when they were needed in the unfolding consultation, the nurse creatively resisted the institutionalised, scientific-bureaucratic role that had been defined for her and achieved a more traditional nurse–patient interaction in which she was able to elicit, attend to and respond to the patient’s concerns (as her first priority) while also later completing the template’s data fields (as her second). Again, this nurse stood out as someone who had an unusual level of skill and sensitivity; her colleagues in similar roles were much less able to make their consultations patient-focused.
In relation to roles and relationships, the QOF template technology aligned with a wider shift in the role of the practice nurse towards surveillance and preventative care of chronic diseases. This in turn reflected the steady rise in prevalence of chronic conditions and corresponding decline in acute conditions in the UK over the past two decades. In this sense, the policy of financially rewarding proactive surveillance of such conditions and the technology that enabled this to be done systematically and in a structured way were all resonant with shifts in professional roles (especially that of the practice nurse) that were occurring anyway. It is perhaps for this reason that relatively few nurses saw the use of the templates as interfering with their professional role. The GPs in our data set were also very comfortable with the role for them as implied in the policy and inscribed in the technology: to oversee the proactive, evidence-based management of chronic diseases.
It is worth noting, however, that while the completion of evidence-based template is consistent with the traditional role of the primary care clinician, it does not constitute that role. The nurse who had negotiated a longer consultation time for her chronic disease management appointments was quite prepared to complete the templates – but she was not prepared to forego all other aspects of her role. In particular, she saw it as crucial to be able to respond to the patient’s own agenda and to let that agenda unfold in a spontaneous, largely unstructured way, allowing her (the nurse) to enact the traditional components of the nursing role: listener, empathiser, adviser and educator. That most nurses observed in our study did not resist the overshadowing of these human components by that of ‘follower of evidence-based protocol’ is perhaps of some concern, and perhaps reflects the limited negotiating power held by many practice nurses.
Discussion
This example illustrates how the expert system developed for chronic disease surveillance encountered far less resistance than that developed for referral to hospital. The lower levels of resistance could be explained by greater acceptance of the policy of chronic disease surveillance; greater alignment of this policy with professional norms, values and traditional roles; greater material performance and reliability; scope to use the technology in a way that did not completely ‘empty out’ local, contingent detail (in particular, the option, used by some nurses, of filling out the template after the patient has left the room or when they are getting changed, and also the technical facility, used by all the GPs, of entering coded data in an ad hoc way but with this appearing as structured entries if the template view is called up); and a positive financial benefit rather than a cost to the user.
The brief coverage of this example here does not, however, do justice to the numerous and subtle ways in which the QOF-driven templates influenced both administration and clinical practice in our four sites. Dr Swinglehurst’s PhD and associated papers describe how the expert system of the QOF constructs the patient in a particular, standardised and institutionalised way; embodies a voice of distant authority that is hard to ignore; and contributes to a bureaucratisation and managerialisation of care. 92,95 Why an expert system with such far-reaching effects on practice was not resisted to any significant degree by most practitioners (despite critics’ cry of ‘What have you done to yourselves?’161) is a question that might be explored in further study.
Case study 3: unscheduled care (the Summary Care Record)
Specific research questions
Our specific research questions in relation to the use and non-use of the SCR for emergency and unscheduled care were: (1) In the practice of creating and/or using extracts from patients’ medical records for unscheduled care, how does the tension between the systemic demands of the SCR national database as an expert system and the application of local (especially patient-specific) knowledge through professional judgement play out? (2) To what extent can ‘resistance’ to the creation and use of SCRs by GPs and other primary care staff be explained in terms of sociological theories of professional practice and the core norms and values of clinical practice?
Brief summary of the case
A detailed account of this case is available as a 235-page report116 and series of academic papers. 8,10,16,90 Briefly, the SCR is an extract from the local GP-held electronic record for NHS patients in England, whose main data fields are current drugs and allergies. It was introduced as part of the NPfIT via a complex governance structure sited within Connecting for Health (the IT arm of the Department of Health). The technology, and the policy of ‘placeless’ record access that it was introduced to support, were strongly politically led. Indeed, getting every citizen a universally-accessible electronic record was an election promise of the Labour government in 1997. 116 The SCR implementation was driven by a detailed national implementation plan and a centrally co-ordinated monitoring scheme driven by Connecting for Health. SCRs were introduced in two ‘early adopter’ localities from 2007; national roll-out of the programme began in 2009.
One of the issues on which the SCR’s success turned was confidentiality. Medical records are highly sensitive and it is a traditional professional duty of doctors to keep all patient details strictly confidential. This principle conflicted directly with the (perhaps equally important) principle of making data accessible to the clinician treating the patient in an urgent care situation in order to support informed clinical decision-making. Most patients, especially those with chronic conditions (such as epilepsy or diabetes) that could present as acute emergencies, saw the balance between protecting privacy and sharing data to lie in favour of having a SCR. 90
A large-scale public information programme led by Connecting for Health sought to inform people about the SCR, the balance of benefits (improved care) and harms (threats to privacy), and their right to opt out. Its success in raising awareness of the SCR was limited. 10 Despite this, fewer than 1% of citizens actively opted out, and because the default option was to create a SCR for anyone who had not opted out, the high level of public ignorance about the scheme was not seen in policy circles as a barrier to the roll-out. However, there was significant opposition to the SCR from the British Medical Association, many of whose members considered the programme unethical because personal medical data were to be uploaded to the national Spine without patients’ explicit consent. In 2008–10, many GP practices refused to join the scheme. However, their reservations appeared gradually to lessen as more and more practices joined. 16
If reluctance to be part of the SCR scheme was occurring in many GP practices, there was also very limited awareness or adoption of it in the settings for which it had been designed. Use of SCRs by clinicians was low in most, though not all, emergency and unscheduled care settings for a variety of reasons, including non-availability of records (referred to as the ‘low hit-rate’), technical glitches (e.g. slowdowns, ‘bugs’ leading to partial or complete incompatibility between software packages, temporary loss of access to Spine), low levels of training and motivation, information governance issues (such as forgotten passwords and lost smart cards) and fear of surveillance by staff (especially junior nurses and pharmacists). Protests from civil liberties groups and negative press coverage exacerbated the programme’s political sensitivity, which was associated in the minds of many citizens with a wider ‘surveillance state’ [e.g. it was explicitly linked to the contemporaneous debate about universal identity (ID) cards165].
Our independent evaluation report published in June 2010 raised a number of concerns, including the high complexity of the programme, slow overall pace of progress, alleged scope creep, persistent technical challenges, greater-than-anticipated workload for frontline staff, and whether or not the ambitious information governance plans were workable and sustainable. 116 By the end of 2012, over 40 million of England’s 51 million population had been sent a letter about the SCR and over 18 million records had been created, with new records being created at a rate of approximately 1 million per month. 16 While this was considerably slower than the pace of progress originally anticipated by policy-makers, the programme appears to have become less politically contentious over time and the opt-out rate has remained low at around 1%.
The NPfIT was formally withdrawn in late 2011 in favour of locally developed electronic record systems, but at the time of writing the SCR remains national policy and efforts continue to create one for every consenting NHS-registered citizen in England. However, a previously linked programme to create a patient portal (HealthSpace) for the SCR was abandoned in 2012 because of very low uptake. Data on how much the SCR is currently accessed and used in unscheduled care settings are difficult to obtain – but in any case our analysis relates to the data set we collected in 2010 and pertains to the enactment of resistance at that time.
Empirical data on use and non-use of the Summary Care Record
For the purposes of this short case study, we have selected two small sections of data – one to illustrate reluctance to create SCRs on the part of GPs and their staff in the early pilot period of 2007–10, and the other to illustrate reluctance to access and use the SCR on the part of clinicians in unscheduled care settings at the same time.
From the GP practices that chose not to join the pilot in the early adopter sites, a number of reasons were given. The most common and strongly expressed was data protection. The GPs felt strongly that their role was to ‘protect’ their patients’ data rather than ‘pass it to the government’. They depicted the SCR programme as a ‘political’ initiative and felt that security issues had been skated over in the pursuit of the (then) explicit government policy of large-scale national databases.
Dissenting GPs described the government-driven Public Information Programme (known as ‘PIP’) as ‘propaganda’, as they viewed it as one-sided (setting out the benefits of SCRs but not their risks). Indeed, one GP used the word ‘Orwellian’ to refer to a scene in the waiting room of a neighbouring surgery, in which a slide presentation on the benefits of the SCR was playing on a plasma screen in a continuous loop – and (allegedly) neither patients nor staff could switch off the programme or even turn down the sound. Our observations confirmed that this continuous-loop ‘educational presentation’ was indeed playing in local surgeries, though we did not confirm that staff were unable to turn it off. GPs were also concerned that if a patient changed their mind about having a SCR, the record could not be deleted. Rather, the best that could be done was to toggle a function key centrally so that local staff could no longer access the patient’s SCR. The GP who described the ‘Orwellian’ scene also commented that ‘it [the SCR] is apparently ours for life and we haven’t got the ability to change it’. 116
A related concern was that the ‘implied consent’ model (in which citizens were sent a letter informing them that if they did nothing, a SCR would be created using extracts from their GP-held medical record) did not actually lead to informed consent in most people because the letter tended to be interpreted as junk mail and binned (frequently unopened). They did not feel that the low opt-out rate could be interpreted as meaning that patients had received the letter, understood it and made an informed decision. One practice manager expressed this concern well: ‘I think the elderly were more confused about what it was all about. We haven’t had any elderly patients ask me questions or opt out. I think they just put it [the letter] to one side and ignored it. I went to see my mother, she’s 86, she got her letter, I saw it open on the table and I asked her “have you read that?” and she replied “can’t be bothered”. . . she just ignored it’.
A minority of dissenting GPs took an explicitly ideological stance and aligned with formal civil liberties campaigns. ‘The Big Opt-Out’ campaign (see www.nhsconfidentiality.org), for example, warned the public that once their SCR had been created, ‘everything you tell your GP . . . will be sent to BT [the commercial supplier of parts of the NHS Spine]’ and exhorted them to download a pro forma letter to opt out of having a SCR. The website of one GP practice opposed to the SCR, and linked to the Big Opt-Out stated: ‘EVERY SINGLE PATIENT SHOULD OPT OUT OF THE NHS DATABASE WITHOUT DELAY’ (emphasis in original).
An early solution proposed for the question of data protection was the facility for patients to designate certain items of data [e.g. anti-human immunodeficiency virus (HIV) medication] as ‘not for sharing’. This solution was later abandoned as unworkable and also inappropriate, mainly because for individuals with ‘sensitive’ information on the SCR, the key choice appeared to be not whether any particular item of information (or indeed, the record as a whole) was classified as ‘share’ or ‘don’t share’ but whether or not they trusted any particular individual with access to their record at a particular point in time. If they trusted the clinician (or indeed a receptionist or administrator), they were usually happy for all information to be viewed as part of their care, but if they did not trust that individual, they did not want them seeing any part of their record. 116
Another common concern of dissenting GPs was that the clinical data on the SCR was not adequately matched to the pressing information needs in emergency and unscheduled care settings. The SCR extracted current drugs, allergies and adverse reactions, but dissenting GPs felt that such information in the absence of any specific clinical detail (e.g. key diagnoses such as diabetes or HIV) could be inadequate and even prove misleading or dangerous in some instances. However, despite numerous committees and working groups to define a ‘minimum data set’ of core clinical information, no agreement was reached as members disagreed on, for example, the balance between minimal summary information and additional clinical detail. In the early days of the SCR programme, many GPs expressed a wish to wait until such issues were ‘sorted out’ before committing their practices to join the scheme – yet at national level, the idea of a formally defined minimum data set had been abandoned as ‘too difficult’.
There was much clinical interest (strongly supported by an interest group within the Royal College of General Practitioners) in an ‘enriched’ clinical record created in a bespoke way for individual patients by their own GP. The idea was that, instead of an automated upload of a standard minimum data set of clinical information, the GP and patient would have a conversation about which data fields in their particular case would be useful to have in an emergency. When this decision had been made jointly, and consent for the upload given in real time, the GP would ‘drag and drop’ this personalised information into a zone from which would be uploaded to the SCR. This facility created considerable technical challenges, however, and did not materialise in the lifetime of our study (nor, incidentally, did it become available between the end of our study in mid 2010 and the submission of this report at the end of 2013).
A further concern by dissenting GPs related to workload. An extract is only as complete and accurate as the record from which it is created, and so practices seeking to join the SCR programme had to meet stringent data quality standards – a task that often involved several weeks of ‘cleaning’ the GP-held records in preparation for the upload. In addition, explaining to patients about the forthcoming go-live and the options for opting out was time-consuming, especially if the clinician took a position of equipoise and sought to set out arguments both for and against having a SCR. Furthermore, after the first few practices went live with the SCR, word soon spread that ‘go-live’ was not simply a matter of flipping a switch. Rather, uploads took anything from several hours to a week, and on-site technical support was necessary to troubleshoot minor glitches in the system so that the ‘automated’ upload from thousands of records progressed relatively smoothly. This phase tended to be highly disruptive for practices as the system was slow or inoperable for clinical consultations for the duration of the upload period. While the inconvenience was temporary, the practice gleaned few, if any, benefits from creating SCRs, as the technology was designed to be accessed by other NHS staff in other settings.
A final concern from GPs was that in order to be actively participating in the SCR programme, the GP practice had to be more or less continuously connected to the central NHS Spine. This was because records on the Spine were updated twice every day to take account of new data added. If the practice only connected (say) once per week, the data on patients’ SCRs would often not reflect their most recent encounter. However, as GPs found, being connected to the Spine brought material problems. Many local GP systems had been bought several years previously and designed for far fewer data than they currently held. There was simply not enough slack in the system to accommodate a further demand on their running capacity. GPs described screens freezing, crashing and running perceptively more slowly. This was particularly irritating for local GPs because, as explained above, they themselves did not benefit directly from the existence of SCRs for their own patients.
As a result of these various concerns, fewer than half of the GP practices in participating sites agreed to upload any patient details to the central Spine to create SCRs in the early adopter phase. Connecting for Health had an active programme of ‘GP engagement’ led by respected GP leaders who were paid a daily rate to visit their fellow GPs and champion the new technology – an initiative that met with some (albeit limited) success. 116
If these were the ‘resistance’ issues at the supply end of the SCR technology, there were also problems at the demand end. One of our main (and most controversial) findings was very low use in unscheduled care settings in the early adopter phase in 2007–10. This appeared to be for several reasons: SCRs were not easy to access; clinicians did not always trust the information they provided; even when they did trust it, they found it useful some but not all of the time; and some clinicians did not like asking for consent to view the record.
Apart from the early days when the system for accessing the SCR was not integrated with the software being used (and hence required manual access to a completely separate system), the biggest problem initially was what was known as the ‘low hit-rate’. Doctors in accident and emergency (A&E) departments would click on the icon to call up the patient’s SCR, but would get a message saying, ‘this patient does not have a SCR’ or ‘this patient’s SCR is blank’. Repeated low hit-rate quickly led to a change in behaviour pattern – the doctors no longer even tried to call up patients’ SCRs. For this reason, and very sensibly, several participating unscheduled care centres had decided ‘not to push’ use of the SCR until the hit-rate had risen. Even when the hit-rate rose significantly as more SCRs were created, some records that should have been accessible still came up as ‘blank’. All of this probably reflected inevitable technical teething problems in making a nationally stored record accessible locally – and may have been largely temporary.
A more significant problem in the longer term was that, as clinicians told us and as our own observations confirmed, the information on the SCR often conflicted with the patient’s own account. We encountered several examples of patients claiming a penicillin allergy that was not recorded on their SCR – and vice versa. In contrast to the assumption of a ‘complete and accurate’ electronic record that represented the final truth, clinicians had to make a judgement between the trustworthiness of the patient’s account and the information on the record – and this played out differently in different cases. The SCR became one of many sources of information, and was weighed against other sources including the patient, their relatives and any material evidence presented in the here-and-now (such as a printout of a repeat prescription or the packaging of a medicine).
An interesting finding from our interviews with staff working in unscheduled care settings was that almost everyone interviewed felt that the SCR would be useful – but only for someone else, not for them. Many doctors, for example, felt that the SCR would be particularly helpful for nurse practitioners working in walk-in centres, but walk-in centre nurses themselves said they would use the SCR only ‘if I was going to prescribe anything, which isn’t very often’. The mismatch was that the doctors were usually unaware of the clinical caseload in walk-in centres, which tended to be minor injuries or illnesses that rarely required prescribed medication. Nurses working in call centres doing telephone consultations commented that ‘Often there’s nothing much on there. [. . .] It’s more useful for the doctors’ and ‘If someone has chest pain, we just call the ambulance, there’s not time to look at the SCR’.
General practitioners who did not work in out-of-hours centres thought that the SCR would be very useful to those who did, but the GPs working in that setting felt it would be much more useful in ‘major’ A&E settings (e.g. if a person was admitted with a heart attack), as their own work tended to involve patients who were well enough to give a good account of their medication and allergies and/or who were attending for reasons that were not primarily clinical (e.g. to get a certificate to sanction sick leave or confirm that their child was not contagious). 116
Accident and emergency doctors, in contrast, said that the information on the SCR tended to be irrelevant to their clinical concerns (and this was borne out by our own observations). For example, the SCR was designed to give information on ‘current medication’ and hence reflected what a patient had been prescribed many days previously, and on allergies and adverse reactions that their GP knew about. However, it was not necessarily accurate about what they had been prescribed the night before (because their GP system had not synchronised with the Spine or because this had been given in an out-of-hours centre) and which was more likely to account for a new adverse reaction for which they were attending A&E. If the patient was unconscious (e.g. in diabetes or epilepsy), the key information need was not the current medication but rapidly changing physiological variables such as blood glucose or oxygen saturation levels.
Summary Case Records were also of limited use in overdoses – partly because someone accompanying the patient usually knew what they had taken (and ambulance staff were trained to bring in any empty bottles or packets), and partly because patients were as likely to overdose on someone else’s medication or stockpiled over-the-counter tablets (such as paracetamol) as they were to take their own prescribed medication. Thus, even when the SCR contained a ‘complete and accurate’ list of current GP-prescribed medication, this still did not reflect what some of the sickest patients were actually taking. The most complete and accurate account of the medication tended to come not from the SCR (whose information was distant in time and place) but from the patient, or from a close relative or friend who knew their here-and-now circumstances. Interestingly, one pharmacist told us that even when a patient’s SCR was present, she always telephoned the GP surgery ‘because we get better information by phoning the GP’ – meaning, perhaps, that the personalised response of a doctor or other staff member who knew the patient and could select as-needed information from the full electronic record was far more useful than a ‘standardised’ data set, accessed remotely.
A final issue accounting for resistance to accessing the SCR was reluctance to ask the patient for consent to view the record. Because of the civil liberties protests and concerns detailed above, the consent model for the SCR was changed in 2009 to ‘implied consent to create, point-of-care consent to view’. In other words, in order to reassure GPs that no patient’s record would be accessed without true informed consent (hence gain their co-operation in creating SCRs and increasing the hit-rate), Connecting for Health made it an information governance requirement that explicit verbal consent be obtained from the patient before any clinician viewed their SCR. All accesses were logged automatically and a proportion of them audited. In practice, this meant that any staff member who accessed a patient’s SCR could expect to be called to account for their actions by a line manager some days or weeks later.
Some staff were comfortable seeking consent to view. Others saw such requests as pointless, as they had clinical responsibility for the patient (hence, they argued, implied consent to access relevant clinical information). There was an emergency ‘break glass’ facility where a clinician could over-ride this requirement in the best interests of the patient, and some doctors used this routinely without asking the patient directly. Other staff (especially non-doctors) were anxious about the possibility of being accused of inappropriately accessing SCRs, and so erred on the side of not doing so [‘Before, we could look at records without worrying, now we have to worry about generating alerts. Nobody wants to get into trouble for breaking confidentiality’ (nurse in out-of-hours call centre)]. 116
It is worth commenting that the SCR was accepted and accessed far more in primary care settings (out of hours and walk-in centres) than in A&E departments. This may be because of how trust played out differently in these settings. In the unscheduled primary care encounter, both GP and nurse consultations occurred in the context of a clear, readily understood, one-to-one clinical relationship (albeit brief and transient), and also in a culture where patients were routinely told (or expected to be told) what was happening to them and why. In this context, trust was high and staff responsibilities were clear. The patient’s consent to view the SCR was relatively easily sought and readily given, though it was perceived as a hassle by frontline staff and some felt that the disadvantages of asking patients outweighed the advantages. Staff were aware of the possibility of access alerts but were not, in general, put off by them. However, in secondary care, the typical ‘major’ patient was being attended to by multiple clinicians (often working to a sophisticated division of labour where everyone knew their role in a wider routine) and moved from one physical location to another, often very rapidly. Care was more fast-paced and ‘technical’ in nature, involving blood tests, procedures and other interventions, and the various individuals caring for the patient had less clear direct responsibility for care (hence, perhaps, a greater chance of perceiving, rightly or wrongly, that they could be breaching information governance rules by accessing the patient’s SCR).
Analysis: foci of resistance
Below, we consider the reluctance (and sometimes inability) of staff to create and/or use SCRs, using the framework for resistance developed for the Choose and Book case study and described above. There was certainly strong resistance to the policy of creating a national database containing extracts from patients’ medical records. This took two forms. One was a vocal and visible (but small minority) civil liberties protest, led by citizens but including some clinicians who tried to draw their own patients into the ideological cause of resisting a ‘database state’. The other was a more subtle, broad-based and clinically focused concern, led by doctors, about the release of patients’ data without their consent. This second protest against the policy was not aligned with wider concerns about a database state; rather, it was rooted in professional norms and values about the doctor’s duty of confidentiality. Interestingly, whereas the minority civil liberties protests continued, professional resistance lessened noticeably with time – due partly to a change in the consent model to include point-of-care consent to view, and partly to the gradual shift in professional norms over time to define the electronic sharing of information as part of good professional practice. 16
There was marked resistance by some GPs to the material aspects of SCR creation, as linking to the Spine often caused significant slow-down of the local system. There was also resistance at the demand side in the early days when the SCR could only be accessed manually through a separate piece of software. The former difficulty was partially overcome as systems were upgraded and/or through after-hours synchronisation of systems, and the latter was resolved when an integrated system was developed. By the end of our data collection period, materiality was rarely the rate-limiting issue. Resistance to the cost of the SCR was evident, in particular, at the supply end of the relationship, with GPs asking whether or not the effort and resource of joining the SCR programme and remaining linked to it was worthwhile. In the early adopter sites where our fieldwork was done, GP practices were fairly generously remunerated for participating, though none felt that they had made a profit. As the scheme was rolled out nationally, the amount of funding per practice diminished – but the technical and operational challenges also reduced with accumulated experience. Whether or not the cost of the national system will be viewed as worthwhile in the long term, particularly given the relatively low use of the SCR, remains to be seen.
In relation to the tension between the rules and categories of the expert system tending to ‘empty out’ the granularity of local detail, the model applies to some but not all aspects of practice. The SCR differs in an important respect from the other two technologies in this study in that it does not contain a clinical algorithm or other decision support function, hence there is not ‘action at a distance’ (or any attempt to produce this by the policy-makers or software designers) in relation to the clinical aspects of care. There was, however, an attempt to do this for administrative reasons: surveillance of professional practice. The resistance of hospital nurses and pharmacists to access the SCRs of patients with whom they clearly had a legitimate clinical relationship was readily explained in terms of fear of being accused of inappropriate access. The introduction of ‘automated’ surveillance via a set of inbuilt alerts meant that when contemplating viewing a record, the clinician was influenced not only by local, immediate clinical concerns but also by distant managerial ones. Understandably, this had a particularly powerful effect on staff in more junior roles and in more hierarchical professions.
Use of SCR at point of care required considerable shifts in some professional roles and relationships. In particular, the requirement to formally ask the patient’s permission to access their SCR was a new departure from any other information access associated with clinical care. Arguably, and as some A&E doctors argued in interviews with our team, the care relationship rests on implied consent from the patient to view their record. To ask permission to access felt (for some of these doctors) inappropriate, because such access went with the job and in the fast-paced world of A&E, developing a close dialogue with the patient often did not. This was why some doctors (especially the senior ones) never asked explicit consent but routinely used the emergency over-ride ‘access for the purposes of urgent clinical care’. In contrast, GPs and nurses working in unscheduled primary care settings appeared to find it unproblematic to seek consent at point of care, and our analysis suggested that this was because such settings already had many of the preconditions for dialogue and trust (such as closed rooms and a one-to-one clinical relationship).
Discussion
This example raises the additional question of whether or not the model developed for Choose and Book, which certainly explains some of our findings, is sufficient to explain all of them. There is, perhaps, an additional dimension of resistance at play here – resistance to the formalisation and abstraction of knowledge. Our data illustrate the need to interpret the coded and possibly inaccurate, possibly incomplete data of the SCR in the light of other information given by the patient or generated by clinical tests in the here-and-now (and/or obtained by moves such as telephoning the patient’s GP). In the idiosyncratic, unpredictable, exception-filled world of acute clinical care, ‘expert’ knowledge can never be equated with standardised data fields entered onto a computer in some other place and time. Rather, expert knowledge is the ability to make judgements about the significance and trustworthiness of partial and conflicting pieces of information – some of which consist of coded entries on the record but which also include the patient’s narrative, phenomenological knowledge (what the patient – and the clinician – feel at the time) and real-time observations and tests. We suggest that this dimension of resistance is best captured in our model by expanding the fourth dimension of resistance (resistance to ‘emptying out’ of the local situation by the expert system) to specifically include consideration of the different forms of knowledge.
Chapter 5 Discussion and conclusions
This secondary analysis of three data sets collected in 2007–10 on three different ICTs in health care has allowed us to develop and test a new theorisation of ‘resistance’ – and, more generally, to further develop and test our previously developed theoretical approach to studying ‘big IT’ in the healthcare setting. 58 Below, we first consider the practical implications of our findings, then suggest avenues for further research and finally reflect on the ‘theoretical’ success of the ANT–SST hybrid.
Practical questions for studying resistance in real-world settings
The academic outputs from this study include a contribution to social theory and will be published mainly in medical sociology journals. 166 However, in addition, we wish to contribute to efforts by policy-makers and change agents to reduce (what are perceived as) inefficiency and waste in healthcare organisations by overcoming the widespread phenomenon of ICTs that clinicians do not use. We do not share the assumption that health systems would be maximally efficient and effective if clinicians never resisted ICT use, but that position has not prevented us from developing a preliminary set of questions that should be asked when staff ‘resist’ using nationally mandated technologies.
First, what is the nature and justification of the policy that this technology was introduced to support? Our three case studies illustrate widely different professional positions on this question from near-universally in favour (of systematic, structured chronic disease surveillance) to near-universally opposed (to the ‘choice’ policy in hospital referral), as well as a profession divided over whether or not extracts from patients’ records should be made accessible on a national remotely accessible database.
Second, what are the material properties and limitations of the technology under conditions of expected use and how do these properties shape and constrain the possibilities for action? Again, our case examples illustrate wide variation in the extent to which this factor impacted on practice – from extreme material mismatch between the technology and the task it had been introduced to support (Choose and Book) to close alignment between these (chronic disease templates), and a somewhat middle position for the SCR. An aspect of materiality is cost – including the question of opportunity cost (from where is resource diverted to fund the technology and the expert system to which it is linked?). Choose and Book was costly but not cost-effective for participating GP practices, and financial incentives cut little ice in this context. The technology to support the QOF, in contrast, cost practices little or nothing to install (or at least, it came as part of a standard software package), and promised lucrative benefits if used as intended. The cost equation for the SCR was unbalanced as those who did the work (GPs and their staff creating records) were not the ones to benefit if SCRs were used – a fact that may well have contributed to reluctance to participate in the scheme.
Third, to what extent, and in what way, are local, contextual judgements attenuated or compromised when the technology is used? This question encompasses the more specific question: to what extent does use of the technology require the user to place undue emphasis on generic, abstracted forms of knowledge and/or knowledge that has been generated at another time or place over the local, particular and of-the-moment knowledge in the clinical encounter? In this regard, all the technologies studied produced this difficulty. At the most extreme level, use of Choose and Book inevitably required a profound ‘emptying-out’ of the local situated detail of the encounter, leading to awkwardness and even absurdity in negotiating referral decisions. Chronic disease surveillance templates ‘configured the patient’ and produced pop-up prompts that were intrusive to the flow of the consultation, and the SCR offered ‘objective’ information on drugs and allergies that sometimes conflicted with the patient’s here-and-now account (and, perhaps, the bottle of medication they held in their hand) – and its defined data fields may or may not have accorded with the data needed clinically or with what the patient themselves wished to share or keep private.
Finally, what changes in social roles and relations are required or made possible when the technology is used? In particular, how does the technology ‘configure the user’ and what are the implications for professional identity and the delivery of high-quality, ethical care? Again, Choose and Book stood out as requiring GPs to adopt roles that were perceived as professionally demeaning and even unethical. Some GPs also viewed uploading SCRs as a breach of their professional code of conduct. In contrast, the roles expected by the QOF and inscribed in the chronic disease surveillance templates produced relatively minor conflicts in this regard (although they did result in new distributions of work between doctors, nursing and administrative staff).
Upstream of these questions about resistance to the technology is a preliminary, overarching question about means versus ends: have professionals’ concerns about the ends (the achievement of high-quality, ethical practice) been fully acknowledged and addressed, or have these concerns been dismissed in the pursuit of means (‘efficiency’)? Again, the means-versus-ends tension played out most dramatically in relation to Choose and Book, though it was also illustrated by both of the other case examples.
An anonymous reviewer of a previous draft of this report made the following perceptive comment, which aptly sums up the implications of the above for the frontline clinician:
Perhaps the strongest message I am taking away from [this] study is a renewed conviction that professionals need to understand a system, to learn it, and then to use it to enhance their practice rather than substitute for it.
To this we would add the following caveat: that this ‘enhancement’ of practice may only be fully realised if the design of systems becomes sufficiently customisable by professionals in their particular context of use that it becomes possible to align the technology with the professional and ethical concerns of clinicians and the needs of their patients.
Some avenues for further research
Our findings imply that if policy-makers and change agents seek to reduce ‘resistance’ to centrally mandated IT systems, there are huge potential benefits to seeking a genuine dialogue with the world of professional values at the stage of design and implementation. Efforts to strike a balance between such virtual, remote, systems and the exigencies of the local sites in which professional values are performed are likely to be rewarded by the emergence of technologies and systems that support excellent professional practice rather than – whether by accident or design – cut across the granular details of such practice. If there is one overarching conclusion to our three case studies, it is that when (and to the extent that) the design and introduction of nationally mandated IT systems fails to take account of deeply held professional norms, values and social roles, such technologies will receive (at best) limited interest and (more likely) active opposition from professionals and the people who support them in their work.
While this study has illustrated potential synergies between SST and ANT and identified some important preliminary findings (see previous paragraph), it has raised more questions than it has answered about how such things as ‘professional virtues/standards’, ‘good clinical care’ and the symbolic role of the health professions in society might be placed more centrally in research on new technologies in health care. We propose a number of additional avenues for further research.
The first avenue is methodological. While small-scale ethnographic studies undoubtedly provide a useful window into the micro-level detail of clinical practice and the material reality of frontline technology use,167 and while such ethnographic studies can also illuminate the meso level of organisational life, reviewers of an earlier draft of this report were less convinced that the data sets used in the three case studies had allowed us to gain maximum purchase on the various external (‘macro-level’) social structures that we conceptualised as influencing the human actors we had observed. As with all research that offers a significant shift in paradigm, methodology is only roughly specified in early studies and becomes more systematised and sophisticated as the paradigm develops. 168
A specific aspect of methodology that might be developed is how to achieve in-depth study of large-scale networked systems in use. A limitation of the main case study in this report (Choose and Book) was that we did not study the hospital ‘end’ of that technology (because the research was funded from a MRC grant to look at the use of electronic records in general practice, and so did not ‘follow the technology’ beyond that setting). This and similar case studies would of course be more complete if they pursued all of the different types of local setting that a networked technology reached. In an untitled online paper, Star has written powerfully on the challenges of using a small-scale technique such as ethnography to study a large-scale networked infrastructure. 169 Elsewhere, she suggests a methodology for undertaking such an ‘ethnography of infrastructure’. 170
The second avenue is further theory development. Professional identities and practices are increasingly complex, fragmented and interdependent. The three practices we studied in this secondary analysis were all relatively discrete; they all involved one individual working with the technology in a fairly autonomous way (though see DS’s previous work on the complex ‘voices’ in even these relatively simple use cases95). Many technologies in healthcare support (or, at least, are intended to support) multidisciplinary team working in which multiple professionals, as well as the patient, carer(s) and staff from beyond the healthcare sector, interact in complex ways over time. In a different study, for example, we have begun to theorise the use and non-use of assisted living technologies using a social practice lens and drawing on the theoretical insights from the present study. 171
The third avenue is application of findings. Surfacing such things as the dispositions, values, virtues and concerns of both patients and professionals and seeing how these explain the use (or not) of existing technologies may be an important starting point. However, the definitive phase of any such programme of research will be assessing how these findings can be used to inform the design of new technologies and systems that are (a) more likely to support good clinical practice and (b) less likely to be resisted. We anticipate that a codesign or corealisation approach will prove particularly helpful here. 47
Finally, there is the question of the ‘generalisablity’ of our theory of resistance raised by reviewers of this report. The three cases (three contrasting social practices linked to three very different technologies) all ‘fitted’ the theory – but this study is preliminary and was not designed or resourced to provide a definitive theoretical framework that has been fully tested across the full range of possibilities. We tentatively hypothesise that the approach we developed is likely to align with examples where resistance (e.g. by doctors, nurses, pharmacists and those working to support their practice) is rooted in professional identity and values, but that there may be other forms of resistance whose underlying drivers are not captured by this conceptual approach.
Reflections on the ‘structuration theory/actor–network theory hybrid’
We began by rejecting a conceptualisation of resistance to technology adoption that is common in the health informatics literature and policy documents (though it is by no means universally held in the academic literature more widely), in which resistance is framed in cognitive–behaviourist terms. Instead, we began from the position adopted by social scientists that the clinical consultation is a complex social encounter in a heavily institutionalised environment. From this, it follows that ‘resistance’ to ICT use is a complex phenomenon with both normative and sociomaterial components; it is unlikely to be overcome using atheoretical behaviourist measures, nor would attempts to do this be desirable.
The two coapplicants for this study, TG and RS, had met when TG, excited by the potential of ANT to theorise large-scale IT projects but also frustrated by its limitations, contacted RS, whose reading of Giddens’ structuration theory included mapping networks and how these networks changed over time (see Chapter 1, Strong structure theory). When we applied for funding for the present study, we had recently published a paper in Social Science and Medicine entitled ‘Theorising big IT programmes in healthcare: strong structuration theory meets actor–network theory’. 58 We had planned to develop our new ‘hybrid’ of SST and ANT in more detail. Here, we consider how successful that attempt was, both in general and as applied to each of our three cases.
We spent most of our time on the first case study (referral to outpatients by GPs, using – or not using – the Choose and Book technology). Let us first consider how a ‘pure’ ANT approach to this case might have unfolded. It would probably have focused on the ‘sociology of translation’, specifically on efforts by different interest groups to achieve the stages of problemisation, interessement, enrolment and mobilisation in Chapter 1 (see Actor–network theory). We would have considered Choose and Book as a ‘program’ and the efforts of detractors [such as the GPs in the e-mail correspondence we described in Chapter 4 (see Resistance articulated: some examples of correspondence and publications)] as attempting to mobilise an ‘anti-program’. 65 The focus of the analysis would have been on the network of ‘actants’ (people and technologies) and how it changed over time, and especially on interactions and artefacts that helped (or failed) to stablise the network. For example, the efforts by PCT managers to impose a particular set of ‘quality standards’ of performance rankings in the use of Choose and Book could have been presented as an attempt to use this artefact to stabilise the actor–network.
In ANT, irreversibility of a network is viewed as being achieved through ‘black boxes’ – that is, through configurations of actors (human and non-human) that are taken for granted as the way things are, and hence no longer questioned. A key contributor to this is what Latour called immutable mobiles – inscription devices (such as maps, graphs, quality standards, rankings and so on, as well as the codes and categories inscribed in software) that move within a network and its nodal points of passage, but which retain the same essential properties in different contexts, thereby allowing relations to be performed in the same way in a variety of different settings and locations. 172
Our empirical data set was small-scale, qualitative and based largely on ethnographic observation. This was because we sought to study social practices. We could have done this from an ANT perspective, as ANT is a performative theory – that is, it seeks to study what people do, and what is brought into being through practice(s). Indeed, had we wished merely to reject ANT’s controversial notion of symmetry between human actors and technologies (all of whom are ‘actants’ in the network), we could have aligned with Schatzki’s widely-used ‘practice theory’, which similarly views humans and technologies as linked in networks and studies practices, and actions as effortful, collective accomplishments. 173 Nicolini, for example, has studied the introduction of, and (indirectly) resistance to, telemonitoring using a Schatzkian practice theory lens along with ANT’s notion of the sociology of translation. 174,175
For actor–network theorists and practice theorists, stability of the network (and hence successful implementation of a big IT programme) is seen as being achieved through both people (who argue rhetorically for particular viewpoints or truth statements) and things (such as graphs, diagrams, lists and other inscriptions as well as the hidden infrastructure of hardware and software). As Bowker and Star put it:
Marx referred to technology as ‘frozen labor’ – work and its values embedded and transcribed in transportable form. Modern information technologies similarly embed and inscribe work in ways that are important for policy-makers, but which are often difficult to see. . . . Arguments, decisions and uncertainties and the processual nature of decision-making are hidden away inside a piece of technology or in a complex representation. Thus, values, opinions, and rhetoric are frozen into codes, electronic thresholds and computer applications. Extending Marx, then, we can say that software is frozen organizational and policy discourse.
p. 135122
Importantly, an ANT analysis of Choose and Book would necessarily have embraced the theory’s ‘flat ontology’ – the notion that the distinction between social structures and human agency does not exist (or, perhaps, is an unhelpful way of conceptualising reality). Rather, ‘layers’ in society are viewed as consisting of (usually, inherently unstable) ‘black boxes’ which tend to need continual effort to be maintained. ANT holds that there are no pre-existing layers but only ‘a single plane of endlessly entangled translations’ (p. 173). 176 The nearest a hard-line actor–network theorist will get to admitting the existence of social structures is the notion of the ‘black box’ (see above) – though even the latter represents only a set of stable-for-now relations that could change at any time. Callon and Latour, for example, produced the widely quoted statement back in 1986 that ‘macro-actors are micro-actors seated on top of many (leaky) black boxes’. 177 Nicolini’s notion of understanding practice by repeatedly ‘zooming in’ and ‘zooming out’ on the various ‘black boxes’ resonates with this metaphor. 175
Harris has summed up ANT’s treatment of social institutions:
. . . institutions are loci of methods of ordering, whose essential operation resides in the recurrent patterns by which the relations between humans (subjects) and non-humans (objects) are generated and maintained. These patterns are not architectonic, they do not precede or exceed the site of their operation: organizations (noun) are sustained by organization (verb).
p. 165176
In our analysis of the social practice of referral and the use and non-use of the Choose and Book technology, we returned, somewhat unfashionably perhaps, to the layered ontology of structuration theory and the concept of social institutions in the way Giddens (and others such as Bourdieu) conceptualised them. In particular, our theorisation of the practice of referral placed central emphasis on the social significance of medicine as a profession, the question of medicine’s ‘internal goods’ (MacIntyre) and the normative expectations on both clinicians and patients of how they ‘should’ behave.
As we argued early on in this report:
it is illness itself, and not medical paternalism, that makes patients vulnerable. 99 Doctors’ specialist knowledge has symbolic significance; in many cases, power is not so much seized by doctors as conferred by society (doctors symbolise hope, trust, agency and authority, making possible a powerful therapeutic alliance of reciprocal interpretation and projection110). This ‘cognitive institution’ facilitates doctor–patient interaction and produces a ‘legitimate hierarchy of domination and subordination, recognized by all participants’ (p. 397)99 – though this hierarchy is rightly renegotiated and redefined more progressively as society evolves.
This document, Chapter 2, A normative anchor: what is excellence in clinical practice?
And furthermore:
Good clinical practice is . . . less about achieving equal distribution of power (as in shared decision-making) than it is about ensuring that doctors draw on their personal virtues (integrity, honesty and so on) to build a healing relationship, wield their socially conferred power and use technologies pragmatically and judiciously in the patient’s best interests. Patients are also influenced by social norms: they will conform to a greater or lesser extent with expectations of what they understand to be the ideal of a good patient – for example, constructing an account of conscientious self-care, acknowledging the needs of other patients (hence not taking up too much of the doctor’s time), deferring to the doctor (or, perhaps, exerting what seems to be a reasonable level of autonomy) and seeking to demonstrate an appropriate level of knowledge and curiosity about their condition. 112 These small acts of deference contribute further to sustaining the established power differential.
This document, Chapter 2, A normative anchor: what is excellence in clinical practice?
This explicitly professional and normative framing of practice allowed us to begin our analysis of the referral/Choose and Book case study by considering the habitus of the doctor, nurse or other member of the healthcare team, how that habitus (the ‘internal structures’ of the individual – knowledge, attitudes, virtues, dispositions and so on) was shaped and influenced by external social structures (in particular, professional norms about what good medical practice and good nursing practice consist of and what Schei99 called the ‘cognitive institution’ of society’s expectations about health professionals), and how action resulted from the interplay of internal structures and the unfolding of here-and-now events in any conjuncture.
As set out in the discussion section for this case (see Chapter 4), this focus on structures (internal and external) thus allowed us to study ‘resistance’ to Choose and Book through the lens of ethical, professional practice (at least as perceived by its practitioners) and link with the ‘moral turn’ in sociology as set out by (among others) Sayer and Boltanski. 113 The empirical data in the Choose and Book case revealed that doctors’ (and managers’ and patients’) actions are strongly influenced by their normative perceptions of how they are expected to behave by virtue of their social position – and that these perceptions (which some have termed ‘scripts’178) are an excellent starting point for studying ‘resistance’.
As we explored the case of referral/Choose and Book, the concept of the expert system [defined and explained in detail in Chapter 1 (see Giddens’ work on structuration, modernity and technology)] became central to our analysis. In particular, this case illustrated what was, potentially, a more general phenomenon: ‘resistance’ playing out as a clash between the abstracted, generalised knowledge and ‘frozen discourses’ (see quote above, this section) of the expert system and the situated, case-based ‘ethical practices’ that doctors, nurses and even non-clinical staff felt driven to provide for their patients. The concept of expert systems also allowed us to highlight the difference between means-oriented and ends-oriented practice – a source of much tension in this particular case.
Our second case, which considered the social practice of chronic disease surveillance and the technology of ‘QOF templates’, also highlighted to some extent the tension between an expert system (in this case, ‘evidence based’ guidelines for chronic disease management linked to a national pay-for-performance scheme) and the exigencies of the local situation (in this case, the fact that patients do not behave as textbook disease cases or come with one problem at a time). Again, much of this tension could be explained in terms of internal social structures and the scripts about ‘good practice’ that guided health professionals’ behaviour.
The last case study – the social practice of unscheduled care and the SCR technology – is slightly different in that the SCR was not an ‘expert system’ in the same sense as Choose and Book or the QOF templates. Every SCR contained different data because those data were patient-specific. To some extent, however, it did inscribe a body of (more or less contested) expert knowledge – for example, knowledge about what constituted ‘immediate and necessary’ data about a patient in an emergency, what the ‘minimum data set’ of sharable fields within any GP-held record should be, or which diseases or risk states should be classified as ‘private’ or ‘sensitive’ (and, therefore, not to be shared).
At the time of our study on the adoption and non-adoption of the SCR, there was much debate about all these issues at national level (within Connecting for Health and also within the Royal Colleges – as illustrated by the attempt by the Royal College of General Practitioners to define the fields relevant for an ‘enriched’ record). 116 Arguably, committees charged with sharpening the definitions and clarifying the classification system (defining what Douglas called ‘the way things are’121) continually failed to resolve their internal disagreements precisely because such knowledge can never be generic and context-free. Rather, a data item (‘rash on penicillin’, ‘attention-deficit disorder’ – or even the person’s home address) acquires the qualities of relevance, urgency, sensitivity and so on only in relation to particular scenarios and particular contexts. In the sense that the SCR contained inscribed knowledge about which data fields were to be made available and which were irrelevant or ‘private’ (hence not to be uploaded onto the nationally accessible SCR), it was an expert system – and the reluctance of doctors and others to help create it stemmed at least partly from a lack of confidence in that expert system.
Having placed social structures so central to our analysis and used SST as our primary analytic lens, the question arises: did we draw on ANT to any significant extent? This is a question on which actor–network theorists are unlikely to agree, as ANT is a broad church whose protagonists range from purists who would consider ANT to be a ‘post-social’ (i.e. to exclude any possibility of theorising such things as social roles and identities179) to those who use its concepts eclectically and pragmatically180 and others who describe themselves as ‘post-actor–network theorists’. 181,182
We believe that ANT influenced our analysis in three ways but that each of those influences had limits. First, it gave us the general orientation towards sociotechnical networks: networks of people and technologies that are complex and (to a greater or lesser extent) unstable, and which may be stabilised through the efforts of people and/or the substance afforded by material things. However, we treated the people and the technologies very differently (as illustrated in Figure 5). We considered human agency to be important in its own right, and not to be merely a product of the network; unlike the stance taken by ANT, we viewed that agency as profoundly influenced by, and reciprocally linked to, social structures.
The second way in which ANT allowed us to extend and enhance SST was the notion that people become particular actors as a result of their position in the sociotechnical network. This is perhaps best illustrated by our second case: chronic disease management supported by QOF templates. The nurses whose work we observed became, to a significant extent, the fillers-out of the templates. Chronic disease management was perhaps not reduced to the entry of data onto the template but it was certainly oriented around that task – not least because so little time was available to address other aspects of the nurse’s work or the spontaneously-raised symptoms and concerns of the patient. However, we found the notion of a professional role as purely the product of all the relationships in the network (as with the quote from Berg in Chapter 1) inadequate to explain all of our findings. A good example of this is the nurse who negotiated with her GP employers to allocate 30 rather than 15 minutes per patient. This change was achieved through human agency, driven by dispositions and professional values: the nurse had insisted that her ‘job’ was not merely completing the templates, important and evidence-based though these were. Good nursing practice was also about providing empathic listening to the patient’s concerns and dealing with whatever issues the patient wished to raise. The actions of this nurse are, we contend, thus better explained using a layered ontology than a ‘single plane of endlessly entangled translations’.
Third, because of its focus on the materiality of technology, ANT allowed us to explore how these material properties interacted with clinicians’ internal structures (dispositions and professional values, especially in relation to the uniquely confidential nature of sensitive information about patients’ illnesses), influenced in turn by external structures (professional norms and the ‘internal goods’ of medicine and nursing) to shape and/or constrain action in any given situation – and to produce unintended consequences that fed back to influence the wider network. For example, in relation to the SCR, the very idea of a source of complete and accurate data on a patient’s medication and allergies, available ‘at the touch of a button’ to someone with appropriate authorisation, depends heavily on the button providing reliable access to the promised data fields when it is touched. Our data revealed how, even when accessing the SCR resonated with the script of good professional practice, the SCR sometimes provided nothing more than an error message. In relation to Choose and Book, the technology sometimes offered up no available outpatient slots for the desired referral. In both cases, even when the technology supported rather than conflicted with ‘good professional practice’ (and especially when it did not), its physical unreliability and/or sheer material complexity tended to generate unintended consequences for the clinician, patient or organisation. However, we found that ANT did not allow us to theorise these unintended consequences adequately, as a key finding in our data set was how these unintended consequences grated uncomfortably with clinicians’ perceptions of their professional role, their duties to their patients and their definition of excellent, ethical practice.
Conclusion
This study has confirmed the findings of previous researchers who have studied healthcare practices through a social science lens: the clinical consultation is a complex social encounter in a heavily institutionalised environment. ‘Resistance’ to ICT use is a complex phenomenon with both normative and sociomaterial components. It is, of course, unlikely to be overcome using atheoretical behaviourist measures, nor would attempts to do this be desirable. Rather, we suggest a number of questions that should be asked when staff ‘resist’ using nationally mandated technologies: (1) what is the nature and justification of the policy that this technology was introduced to support?; (2) what are the material properties and limitations of the technology under conditions of expected use (including its cost and the opportunity cost of introducing and supporting it) and how do these properties shape and constrain the possibilities for action?; (3) to what extent, and in what way, are local, contextual judgements attenuated or compromised when the technology is used?; and (4) what changes in social roles and relations are required or made possible when the technology is used? In particular, how does the technology ‘configure the user’ via inbuilt expectations for roles and behaviours, and what are the implications for professional identity and the delivery of high-quality, ethical care?
Upstream of these questions about resistance to the technology is a preliminary, overarching question about means versus ends: have professionals’ (and other staff’s) concerns about the ends (the achievement of high-quality, ethical practice) been fully acknowledged and addressed, or have these concerns been dismissed in the pursuit of means (efficiency of tasks and processes)?
Our findings are consistent with the conclusion that those who seek to reduce ‘resistance’ to centrally mandated IT systems should seek a dialogue with the world of professional values at the stage of design and implementation and show willingness to strike a balance between such virtual, remote systems and the exigencies of the local sites in which professional values are performed. However, a potential danger of this theoretical framing pointed out by reviewers of this report is that it could be mistakenly read as suggesting a somewhat naive dualism: ‘professionals’ (local) perspective good, policy-makers’ (distant) perspective bad’. It is clear that professionals, too, have their vested interests, which should be approached critically, and national policy-makers may in other cases be more flexible and biddable than the examples in this study suggest. Another way in which this research could be taken forward is to explore, in a more nuanced way, how the tension between mandated policy (introduced through technology) and professional resistance plays out.
Acknowledgements
Thanks
We thank the study participants, the members of the HERO-2 steering group, and four anonymous peer reviewers for helpful comments on earlier drafts of this report.
Funding
This secondary analysis of data was funded by the National Institute for Health Research (study no. 10/1011/01). The primary studies that produced the empirical data sets were funded by the MRC (Methodology Research Programme 07/133) and the National Institute for Health Research (CFHEP002 and CFHEP007).
Ethical approval
Ethical approval for the empirical work was obtained from Thames Valley Multicentre Research Ethics Committee in January 2007 (06/MRE12/81 and subsequent amendments) and North West 8 Multicentre Research Ethics Committee in September 2009 (09/H1013/36 and subsequent amendments).
Contributions of authors
Trisha Greenhalgh was the principal investigator on both of the primary studies that produced the empirical data sets for this secondary analysis.
Deborah Swinglehurst was the lead fieldworker on one of those studies (HERO); her PhD included data collection for the first case study (Choose and Book) and a detailed analysis of the second (chronic disease management templates in general practice), excerpts and adaptations of which are included in this report.
Rob Stones provided theoretical input, especially but not exclusively in relation to the conceptualisation of expert systems, the analysis of medicine and nursing from a normative perspective and the application of structuration theory to the empirical data.
Trisha Greenhalgh and Rob Stones conceptualised the study. All authors contributed to the data analysis and production and refinement of the theoretical model.
Trisha Greenhalgh took overall responsibility for drafting the final report and Deborah Swinglehurst and Rob Stones drafted sections and contributed to revisions.
All authors approved the final manuscript.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Connecting for Health: A guide to the National Programme for Information Technology. London: The Stationery Office; 2005.
- Kreps D, Richardson H. IS success and failure – the problem of scale. Polit Q 2007;78:439-46. http://dx.doi.org/10.1111/j.1467-923X.2007.00871.x.
- Robertson A, Cresswell K, Takian A, Petrakaki D, Crowe S, Cornford T, et al. Implementation and adoption of nationwide electronic health records in secondary care in England: qualitative analysis of interim results from a prospective national evaluation. BMJ 2010;34. http://dx.doi.org/10.1136/bmj.c4564.
- The National Programme for IT in the NHS: an Update on the Delivery of Detailed Record Systems. London: The Stationery Office; 2011.
- Programme Assessment Review of the National Programme for IT. London: Cabinet Office; 2011.
- Morse A. The National Programme for IT in the NHS: an Update on the Delivery of Detailed Care Records Systems (press release). London: National Audit Office; 2011.
- Beale P. NHS Summary Care Record Implementation Strategic Outline Case. London: NHS Connecting for Health; 2007.
- Greenhalgh T, Stramer K, Bratan T, Byrne E, Russell J, Potts HWW. Adoption and non-adoption of a shared electronic summary record in England: a mixed-method case study. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c3111.
- Greenhalgh T, Hinder S, Stramer K, Bratan T, Russell J. Adoption, non-adoption and abandonment of an Internet-accessible personal health organiser: case study of HealthSpace. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c5814.
- Bratan T, Stramer K, Greenhalgh T. ‘Never heard of it’– understanding the public’s lack of awareness of a new electronic patient record. Health Expect 2010;13:379-91. http://dx.doi.org/10.1111/j.1369-7625.2010.00608.x.
- Greenhalgh T, Russell J, Ashcroft RE, Parsons W. Why national eHealth programs need dead philosophers: Wittgensteinian reflections on policymakers’ reluctance to learn from history. Milbank Q 2011;89:533-63. http://dx.doi.org/10.1111/j.1468-0009.2011.00642.x.
- Sheikh A, Cornford T, Barber N, Avery A, Takian A, Lichtner V, et al. Implementation and adoption of nationwide electronic health records in secondary care in England: final qualitative results from prospective national evaluation in ‘early adopter’ hospitals. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d6054.
- Cresswell KM, Worth A, Sheikh A. Integration of a nationally procured electronic health record system into user work practices. BMC Med Inform Decis Mak 2012;12. http://dx.doi.org/10.1186/1472-6947-12-15.
- Cresswell K, Ali M, Avery A, Barber N, Cornford T, Crowe S, et al. The Long and Winding Road . . . an Independent Evaluation of the Implementation and Adoption of the National Health Service Care Records Service (NHS CRS) in Secondary Care in England. Edinburgh: University of Edinburgh Department of Primary Health Care; 2011.
- The Power of Information: Putting All of Us in Control of the Health and Care Information We Need. London: The Stationery Office; 2012.
- Greenhalgh T, Morris L, Wyatt JC, Thomas G, Gunning K. Introducing a nationally shared electronic patient record: case study comparison of Scotland, England, Wales and Northern Ireland. Int J Med Inform 2013;82:e125-38. http://dx.doi.org/10.1016/j.ijmedinf.2013.01.002.
- Greenhalgh T, Potts H, Wong G, Bark P, Swinglehurst D. Tensions and paradoxes in electronic patient record research: a systematic literature review using the meta-narrative method. Milbank Q 2009;87:729-88. http://dx.doi.org/10.1111/j.1468-0009.2009.00578.x.
- Shekelle PG, Goldzweig CL. Costs and Benefits of Health Information Technology: an Updated Systematic Review. London: Health Foundation on behalf of the Southern California Evidence-based Practice Centre, RAND Corporation; 2009.
- Murray E, Burns J, May C, Finch T, O’Donnell C, Wallace P, et al. Why is it difficult to implement e-health initiatives? A qualitative study. Implementation Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-6.
- Rodriguez C, Pozzebon M. APROS 11: Asia-Pacific Researchers in Organization Studies: 11th International Colloquium, Melbourne, Australia, 4–7 December 2005. Melbourne: Asia-Pacific Researchers in Organization Studies; 2006.
- Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q 1989;13:319-40. http://dx.doi.org/10.2307/249008.
- Delone WH, McLean E. Information systems success: the quest for the dependent variable. Inform Syst Res 1992;3:60-95. http://dx.doi.org/10.1287/isre.3.1.60.
- Delone WH, McLean EH. The DeLone and McLean model of information systems success: a ten-year update. J Manag Inform Syst 2003;19:9-30.
- Holden RJ, Karsh BT. The technology acceptance model: its past and its future in health care. J Biomed Inform 2010;43:159-72. http://dx.doi.org/10.1016/j.jbi.2009.07.002.
- Holden RJ. What stands in the way of technology-mediated patient safety improvements? A study of facilitators and barriers to physicians’ use of electronic health records. J Patient Saf 2011;7. http://dx.doi.org/10.1097/PTS.0b013e3182388cfa.
- Chen R-F, Hsiao J-L. An investigation on physicians’ acceptance of hospital information systems: a case study. Int J Med Inform 2012;81:810-20. http://dx.doi.org/10.1016/j.ijmedinf.2012.05.003.
- Aggelidis VP, Chatzoglou PD. Hospital information systems: measuring end user computing satisfaction (EUCS). J Biomed Inform 2012;45:566-79. http://dx.doi.org/10.1016/j.jbi.2012.02.009.
- Ketikidis P, Dimitrovski T, Lazuras L, Bath PA. Acceptance of health information technology in health professionals: an application of the revised technology acceptance model. Health Inform J 2012;18:124-34. http://dx.doi.org/10.1177/1460458211435425.
- Dünnebeil S, Sunyaev A, Blohm I, Leimeister JM, Krcmar H. Determinants of physicians’ technology acceptance for e-health in ambulatory care. Int J Med Inform 2012;81:746-60. http://dx.doi.org/10.1016/j.ijmedinf.2012.02.002.
- Venkatesh V, Sykes TA, Zhang X. What the Doctor ordered’: A Revised UTAUT for EMR System Adoption n.d.
- Holden RJ. Social and personal normative influences on healthcare professionals to use information technology: towards a more robust social ergonomics. Theor Issues Ergon 2012;13:546-69. http://dx.doi.org/10.1080/1463922X.2010.549249.
- Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980.
- Kotter JP, Schlesinger LA. Choosing strategies for change. Harv Bus Rev 1979;57:106-14.
- Baronas AM, Louis MR. A sense of control during implementation: how user involvement leads to system acceptance. MIS Q 1988;12:111-23. http://dx.doi.org/10.2307/248811.
- Lorenzi NM, Riley RT. Managing change: an overview. J Am Med Inform Assoc 2000;7:116-24. http://dx.doi.org/10.1136/jamia.2000.0070116.
- Liberating the NHS: an Information Revolution. London: The Stationery Office; 2010.
- Sabherwal R, Jeyaraj A, Chowa C. Information system success: individual and organizational determinants. Manag Sci 2006;52:1849-64. http://dx.doi.org/10.1287/mnsc.1060.0583.
- Yusof MM, Paul RJ, Stergeoulas L. Towards a Framework for Health Information Systems Evaluation 2006.
- Desjardins GA, Lapointe L, Pozzebon M. La Resistance des Utilisateurs Face aux TI: Un Processus de «Sensemaking». Montréal: HEC (ISSN 0832–7203); 2006.
- Lapointe L, Rivard S. A multilevel model of resistance to information technology implementation. MIS Q 2005;29:461-91.
- Lapointe L, Rivard S. A triple take on information system implementation. Organ Sci 2007;18:89-107. http://dx.doi.org/10.1287/orsc.1060.0225.
- Markus ML. Power, politics, and MIS implementation. Commun ACM 1983;26:430-44. http://dx.doi.org/10.1145/358141.358148.
- Cherns A. Principles of sociotechnical design revisted. Hum Relations 1987;40:153-61. http://dx.doi.org/10.1177/001872678704000303.
- Ackerman MS. The intellectual challenge of CSCW: the gap between social requirements and technical feasibility. Hum-Comput Interact 2000;15:179-203. http://dx.doi.org/10.1207/S15327051HCI1523_5.
- Symon G, Long K, Ellis J. The coordination of work activities: cooperation and conflict in a hospital context. Comput Support Cooperative Work 1996;5:1-31. http://dx.doi.org/10.1007/BF00141934.
- Goorman E, Berg M. Modelling nursing activities: electronic patient records and their discontents. Nursing 2000;7:3-9.
- Hartswood M, Procter R, Rouncefield M, Slack R, Voss A. Working IT out in medical practice: IT systems design and development as co-realisation. Methods Inf Med 2003;42:392-7.
- Pratt W, Reddy MC, McDonald DW, Tarczy-Hornoch P, Gennari JH. Incorporating ideas from computer-supported cooperative work. J Biomed Inform 2004;37:128-37. http://dx.doi.org/10.1016/j.jbi.2004.04.001.
- Berg M. The search for synergy: interrelating medical work and patient care information systems. Methods Inf Med 2003;42:337-44.
- Brown JS, Duguid P. The Social Life of Information. Boston, MA: Harvard Business Review Press; 2002.
- May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54.
- May C. A rational model for assessing and evaluating complex interventions in health care. BMC Health Serv Res 2006;6. http://dx.doi.org/10.1186/1472-6963-6-86.
- Doolin B. Power and resistance in the implementation of a medical management information system. Inform Syst J 2004;14:343-62. http://dx.doi.org/10.1111/j.1365-2575.2004.00176.x.
- Timmons S. A failed panopticon: surveillance of nursing practice via new technology. New Technol Work Employ 2003;18:143-53. http://dx.doi.org/10.1111/1468-005X.00116.
- Winthereik BR, van der Ploeg I, Berg M. The electronic patient record as a meaningful audit tool: accountability and autonomy in general practitioner work. Sci Technol Hum Values 2007;32:6-25. http://dx.doi.org/10.1177/0162243906293884.
- Henwood F, Hart A. Articulating gender in the context of ICTs in health care: the case of electronic patient records in maternity services. Crit Soc Policy 2003;23:249-67. http://dx.doi.org/10.1177/0261018303023002007.
- Latour B. Reassembling the Social: An Introduction to Actor–Network-Theory. Oxford: Oxford University Press; 1992.
- Greenhalgh T, Stones R. Theorising big IT programmes in healthcare: strong structuration theory meets actor–network theory. Soc Sci Med 2010;70:1285-94. http://dx.doi.org/10.1016/j.socscimed.2009.12.034.
- Berg M. Patient care information systems and health care work: a sociotechnical approach. Int J Med Inform 1999;55:87-101. http://dx.doi.org/10.1016/S1386-5056(99)00011-8.
- Callon M, Law J. Power, Action, and Belief: A New Sociology of Knowledge. London: Routledge; 1986.
- Walsham G, Lee AS, Liebenau J, DeGross JI. Information Systems and Qualitative Research: Proceedings of the IFIP TC8 WG 82 International Conference on Information Systems and Qualitative Research, 31st May–3rd June 1997, Philadelphia, Pennsylvania, USA. New York, NY: Springer; 1997.
- Ellingsen G, Monteiro E. Seamless integration: standardisation across multiple local settings. Comput Support Coop Work 2006;15:443-66. http://dx.doi.org/10.1007/s10606-006-9033-0.
- Jaeger JF, Monteiro E. Proceedings of Continuity of Care, HelsIT, September 2005, Trondheim, Norway. Trondheim: HelsIT; 2005.
- Obstfelder A, Moen A. The electronic patient record in community health services--paradoxes and adjustments in clinical work. Stud Health Technol Inform 2006;122:626-31.
- Latour B. Technology is society made durable. Sociol Rev 1991;S1:103-31.
- Hanseth O, Jacucci E, Grisot M, Aanestad M. Reflexive standardization: side effects and complexity in standard making. MIS Q 2006;30:563-81.
- Oborn E, Barrett M, Davidson E. Unity in diversity: electronic patient record use in multidisciplinary practice. Inform Syst Res 2011;223:547-64. http://dx.doi.org/10.1287/isre.1110.0372.
- Hanseth O, Monteiro E. Changing irreversible networks. European Conference on Information Systems (ECIS) 1998 Proceedings 1998:1123-39.
- Constantinides P, Barrett M. Large-scale ICT innovation, power, and organizational change: the case of a regional health information network. J Appl Behav Sci 2006;42:76-90. http://dx.doi.org/10.1177/0021886305284291.
- Berg M, Bowker G. The multiple bodies of the medical record: toward a sociology of an artefact. Sociol Q 1997;38:513-37. http://dx.doi.org/10.1111/j.1533-8525.1997.tb00490.x.
- Giddens A. The Constitution of Society. Berkeley, CA: University of California Press; 1984.
- Stones R, Ritzer G. The Wiley-Blackwell Encyclopaedia of Globalization. Oxford: Blackwells; 2012.
- Giddens A. Modernity and Self-Identity: Self and Society in the Late Modern Age. Cambridge: Polity Press; 1991.
- Giddens A. The Consequences of Modernity. Cambridge: Polity Press; 1990.
- Stones R, Ritzer G. The Wiley-Blackwell Encyclopaedia of Globalization. Oxford: John Wiley & Sons; 2012.
- Stones R, Ritzer G. The Wiley-Blackwell Encyclopaedia of Globalization. Oxford: John Wiley & Sons; 2012.
- Sayer A. Why Things Matter to People. Cambridge: Cambridge University Press; 2011.
- Barley SR. Technology as an occasion for structuring: evidence from observations of CT scanners and the social order of radiology departments. Admin Sci Q 1986;31:78-108. http://dx.doi.org/10.2307/2392767.
- Orlikowski WJ, Barley SR. Technology and institutions: what can research on information technology and research on organizations learn from each other?. MIS Q 2001;25:145-65. http://dx.doi.org/10.2307/3250927.
- Stones R. Structuration Theory. Basingstoke: Palgrave-Macmillan; 2005.
- Stones R, Ritzer G. The Wiley-Blackwell Encyclopedia of Globalization. Oxford: John Wiley & Sons Ltd; n.d.
- Bourdieu P, Richardson JG. Handbook for Theory and Research for the Sociology of Education. Slough: Greenwood Press; 1986.
- Habermas J. The Theory of Communicative Action. Boston, MA: Beacon; 1987.
- Garfinkel H. Studies in Ethnomethodology. Engelwood Cliffs, NJ: Prentice-Hall; 1967.
- Goffman E. The Presentation of Self in Everyday Life. Edinburgh: University of Edinburgh, Social Sciences Research Centre; 1958.
- Orlikowski WJ. The sociomateriality of organisational life: considering technology in management research. Camb J Econ 2010;34:125-41. http://dx.doi.org/10.1093/cje/bep058.
- Dant T. Materiality and Society. Maidenhead: Open University Press; 2004.
- Orlikowski WJ, Scott SV. Sociomateriality: challenging the separation of technology, work and organization. Acad Manag Ann 2008;2:433-74. http://dx.doi.org/10.1080/19416520802211644.
- Leonardi PM, Barley SR. Materiality and change: challenges to building better theory about technology and organizing. Inform Organ 2008;18:159-76. http://dx.doi.org/10.1016/j.infoandorg.2008.03.001.
- Greenhalgh T, Wood GW, Bratan T, Stramer K, Hinder S. Patients’ attitudes to the summary care record and HealthSpace: qualitative study. BMJ 2008;336:1290-5. http://dx.doi.org/10.1136/bmj.a114.
- Swinglehurst D, Greenhalgh T, Myall M, Russell J. Ethnographic study of ICT-supported collaborative work routines in general practice. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-348.
- Swinglehurst D, Roberts C, Greenhalgh T. Opening up the ‘black box’ of the electronic patient record: a linguistic ethnographic study in general practice. Commun Med 2011;8:3-15. http://dx.doi.org/10.1558/cam.v8i1.3.
- Swinglehurst D, Greenhalgh T, Roberts C. Computer templates in chronic disease management: ethnographic case study in general practice. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2012-001754.
- Swinglehurst D, Greenhalgh T, Russell J, Myall M. Receptionist input to quality and safety in repeat prescribing in UK general practice: ethnographic case study. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d6788.
- Swinglehurst D. The Electronic Patient Record: a Linguistic Ethnographic Study in General Practice. London: Queen Mary University of London; 2012.
- Sackett DL, Rosenberg WC, Gray JAM. Evidence based medicine: what it is and what it isn’t. BMJ 1996;312:71-2. http://dx.doi.org/10.1136/bmj.312.7023.71.
- Edwards A, Elwyn G. Shared Decision-Making in Health Care: Achieving Evidence Based Patient Choice. Oxford: Oxford University Press; 2009.
- Montgomery K. How Doctors Think: Clinical Judgement and the Practice of Medicine. Oxford: Oxford University Press; 2006.
- Schei E. Doctoring as leadership: the power to heal. Perspec Biol Med 2006;49:393-406. http://dx.doi.org/10.1353/pbm.2006.0048.
- Scambler G. Health-related stigma. Sociol Health Illn 2009;31:441-55. http://dx.doi.org/10.1111/j.1467-9566.2009.01161.x.
- Frank A. Just listening: narrative and deep illness. Families Syst Health 1998;16:197-216. http://dx.doi.org/10.1037/h0089849.
- Berger J, Mohr J. A Fortunate Man: the Story of a Country Doctor. London: Vintage; 1997.
- Nichomean Ethics. London: Penguin; 1996.
- Toon P. Towards a Philosophy of General Practice: a Study of the Virtuous Practitioner. London: Royal College of General Practitioners; 1999.
- Bradshaw A. The virtue of nursing: the covenant of care. J Med Ethics 1999;25:477-81. http://dx.doi.org/10.1136/jme.25.6.477.
- Good Medical Practice. London: GMC; 2012.
- Heath I. The Mystery of General Practice. London: Nuffield Provincial Hospital Trust; 1997.
- Polanyi M. Personal Knowledge: Towards a Post-Critical Philosophy. Chicago, IL: University of Chicago Press; 1958.
- Barry MJ, Edgman-Levitan S. Shared decision making – the pinnacle of patient-centered care. N Eng J Med 2012;366:780-1. http://dx.doi.org/10.1056/NEJMp1109283.
- Balint M. The Doctor, His Patient and the Illness. London: Routledge; 1957.
- Mol A. The Logic of Care: Health and the Problem of Patient Choice. London: Routledge; 2008.
- Goffman E. The Presentation of Self in Everyday Life. New York, NY: Penguin; 1969.
- Boltanski L. On Critique. Cambridge: Polity Press; 2011.
- Sayer A. The Moral Significance of Class. Cambridge: Cambridge University Press; 2005.
- Roland M. Linking physicians’ pay to the quality of care--a major experiment in the United Kingdom. N Eng J Med 2004;351:1448-54. http://dx.doi.org/10.1056/NEJMhpr041294.
- Greenhalgh T, Stramer K, Bratan T, Byrne E, Russell J, Hinder S, et al. The Devil’s in the Detail: Final Report of the Independent Evaluation of the Summary Care Record and HealthSpace Programmes. London: University College London; 2010.
- Swinglehurst D, Greenhalgh T, Roberts C. Computer templates in chronic disease management: ethnographic case study in general practice. BMJ 2012;2. http://dx.doi.org/10.1136/bmjopen-2012-001754.
- Greenhalgh T, Stramer K, Bratan T, Byrne E, Mohammad Y, Russell J. Introduction of shared electronic records: multi-site case study using diffusion of innovation theory. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1786.
- Green J, McDowall Z, Potts H. Does Choose and Book fail to deliver the expected choice to patients? A survey of patients’ experience of outpatient appointment booking. BMC Med Inform Decis Mak 2008;8:36-8. http://dx.doi.org/10.1186/1472-6947-8-36.
- Dourish P, Bell G. Divining a Digital Future: Mess and Mythology in Ubiquitous Computing. Cambridge, MA: MIT Press; 2011.
- Douglas M. How Institutions Think. Syracuse, NY: Syracuse University Press; 1986.
- Bowker GC, Star SL. Sorting Things Out: Classification and its Consequences. Cambridge, MA: The MIT Press; 1999.
- Weber M. Economy and Society. Los Angeles, CA: University of California Press; 1978.
- Stones R, Ritzer G. Encyclopedia of Social Theory. Thousand Oaks, CA: Sage; 2005.
- Jones L, Mays N. Systematic Review of the Impact of Patient Choice of Provider in the English NHS. London: Health Services Research Unit, Department of Public Health and Policy, London School of Hygiene and Tropical Medicine; 2009.
- Scott WR. Institutions and Organizations. Thousand Oaks, CA: Sage; 2001.
- MacIntyre A. After Virtue: a Study in Moral Theory. London: Duckworth; 1981.
- Parsons T, Parsons T. Essays in Sociological Theory: Pure and Applied. New York, NY: Free Press; 1949.
- Stones R, Ritzer G. The Wiley-Blackwell Encyclopedia of Globalization. Oxford: John Wiley & Sons; 2012.
- Stones R, Ritzer G. The Wiley-Blackwell Encyclopedia of Globalization. Oxford: John Wiley & Sons; 2012.
- Stones R, Tangsupvattana A. Social theory, current affairs, and Thailand’s political turmoil: seeing beyond reds vs. yellows. J Polit Power 2012;5:217-38. http://dx.doi.org/10.1080/2158379X.2012.698900.
- Stones R, Clegg S, Haugaard M. The SAGE Handbook of Power. London: Sage Publications Ltd; 2009.
- Klein HK, Myers MD. A set of principles for conducting and evaluating interpretive field studies in information systems. MIS Q 1999;23:67-93. http://dx.doi.org/10.2307/249410.
- Greenhalgh T, Russell J. Why do evaluations of eHealth programs fail? An alternative set of guiding principles. PLOS Med 2010;7. http://dx.doi.org/10.1371/journal.pmed.1000360.
- Stake R. The Art of Case Study Research. London: Sage; 1995.
- Coulter A. Do patients want a choice and does it work?. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c4989.
- Dixon A, Robertson R, Bal R. The experience of implementing choice at point of referral: a comparison of the Netherlands and England. Health Econ Policy Law 2010;5:295-317. http://dx.doi.org/10.1017/S1744133110000058.
- The NHS Plan: a Plan for Investment, a Plan for Reform. London: The Stationery Office; 2001.
- Delivering the NHS Plan: Next Steps on Investment, Next Steps on Reform. London: The Stationery Office; 2002.
- Choose and Book – Patient’s Choice of Hospital and Booked Appointment: Policy Framework for Choice and Booking at Point of Referral. London: The Stationery Office; 2004.
- Choice at Referral – Guidance Framework for 2007/8. London: The Stationery Office; 2007.
- National Health Service England. The Primary Care Trusts (Choice of Secondary Care Provider) Directions 2009. London: The Stationery Office; 2009.
- Le Grand J. The Other Invisible Hand. Delivering Public Services Through Choice and Competition. Princeton and Oxford: Princeton University Press; 2007.
- Department of Health: The National Programme for IT in the NHS. London: The Stationery Office; 2006.
- NHS . NHS Choices n.d. www.nhs.uk/Pages/HomePage.aspx (accessed 7 September 2014).
- Greenhalgh T, Procter R, Wherton J, Sugarhood P, Shaw S. The organising vision for telehealth and telecare: discourse analysis. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2012-001574.
- Report on the National Patient Choice Survey – July 2007. London: The Stationery Office; 2007.
- Report on the National Patient Choice Survey – February 2010. London: The Stationery Office; 2010.
- Report on the National Patient Choice Survey – September 2007. London: The Stationery Office; 2008.
- Modayil PC, Hornigold R, Glore RJ, Bowdler DA. Patients’ attendance at clinics is worse with choose and book. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b396.
- Beckingsale TB, Wallace IW. Orthopaedic attendance also worse with choose and book. BMJ 2009;338:674-5. http://dx.doi.org/10.1136/bmj.b1060.
- Rashid M, Abeysundra L, Mohd-Isa A, Khan Y, Sismeiro C. Two years and £196 million later: where is Choose and Book?. Inform Prim Care 2007;15:111-19.
- Rabiei R, Bath PA, Hutchinson A, Burke D. The National Programme for IT in England: clinicians’ views on the impact of the Choose and Book service. Health Inform J 2009;15:167-78. http://dx.doi.org/10.1177/1460458209337423.
- Pothier D, Awad Z, Tierney P. ‘Choose and book’ in ENT: the GP perspective. J Laryngol Otol 2006;120:222-5. http://dx.doi.org/10.1017/S0022215106000132.
- Pothier DD, Repanos C, Awad Z. Analysing GP referral priorities: the unforeseen effect of choose and book. Clin Otolaryngol 2006;31:327-30. http://dx.doi.org/10.1111/j.1749-4486.2006.01180.x.
- Midgley AK. ‘Choose and book’ does not solve any problems. BMJ 2005;331. http://dx.doi.org/10.1136/bmj.331.7511.294-b.
- NHS . Choose and Book n.d. www.chooseandbook.nhs.uk/patients/whatiscab (accessed 8 June 2013).
- Harrison S. Co-optation, commodification and the medical model: governing UK medicine since 1991. Public Admin 2009;87:184-97. http://dx.doi.org/10.1111/j.1467-9299.2009.01752.x.
- Campbell SM, Reeves D, Kontopantelis E, Sibbald B, Roland M. Effects of pay for performance on the quality of primary care in England. N Eng J Med 2009;361:368-78. http://dx.doi.org/10.1056/NEJMsa0807651.
- Starfield B, Mangin D. An international perspective on the basis for payment for performance. Qual Prim Care 2010;18:399-404.
- Mangin D, Toop L. The Quality and Outcomes Framework: what have you done to yourselves?. Br J Gen Pract 2007;57:435-7.
- Gillam S. Pay for Performance in UK General Practice – the Ambiguous Impact of the Quality and Outcomes Framework 2011. www.qualitymeasures.ahrq.gov/expert/expert-commentary.aspx?id=25658&search=Primary+Health+Care+ (accessed 6 June 2013).
- Gillam S, Siriwardena AN, Gillam S, Siriwardena AN. The Quality and Outcomes Framework: QOF Transforming General Practice. Oxford: Radcliffe Publishing Ltd; 2010.
- Harrison S. New Labour, modernisation and the medical labour process. J Soc Policy 2002;31. http://dx.doi.org/10.1017/S0047279402006694.
- Anderson R, Brown I, Dowty T, Inglesant P, Heath W, Sasse A. Database State. York: Joseph Rowntree Reform Trust; 2009.
- Greenhalgh T, Stones R, Swinglehurst D. Choose and Book: a sociological analysis of ‘resistance’ to an expert system. Soc Sci Med 2014;104:210-19. http://dx.doi.org/10.1016/j.socscimed.2013.12.014.
- Greenhalgh T, Swinglehurst D. Studying technology use as social practice: the untapped potential of ethnography. BMC Med 2011;9. http://dx.doi.org/10.1186/1741-7015-9-45.
- Kuhn TS. The Structure of Scientific Revolutions. Chicago, IL: University of Chicago Press; 1962.
- Star SL. Short Contribution from Susan Leigh Star, University of California, San Diego, for Paris Conference, Distributed Communities of Practice, September 2000 n.d. www.limsi.fr/Individu/turner/DCP/Paris2OOO/star-pcd.pdf (accessed 7 September 2014).
- Star SL. Infrastructure and ethnographic practice: working on the fringes. Scand J Inform Syst 2002;14:107-22.
- Greenhalgh T, Wherton J, Sugarhood P, Hinder S, Procter R, Stones R. What matters to older people with assisted living needs? A phenomenological analysis of the use and non-use of telehealth and telecare. Soc Sci Med 2013;93:86-94. http://dx.doi.org/10.1016/j.socscimed.2013.05.036.
- Latour B, Lynch M, Woolgar S. Representations in Scientific Practice. Cambridge, MA: MIT Press; 1990.
- Schatzki TR. The social bearing of nature. Inquiry 2000;43:21-37. http://dx.doi.org/10.1080/002017400321352.
- Nicolini D. Medical innovation as a process of translation: a case from the field of telemedicine. Br J Manag 2010;21:1011-26. http://dx.doi.org/10.1111/j.1467-8551.2008.00627.x.
- Nicolini D. Zooming in and out: studying practices by switching theoretical lenses and trailing connections. Organ Stud 2009;30:1391-418. http://dx.doi.org/10.1177/0170840609349875.
- Harris J. The ordering of things: organization in Bruno Latour. Sociol Rev 2005;53:163-7. http://dx.doi.org/10.1111/j.1467-954X.2005.00548.x.
- Callon M, Latour B, Knorr-Cetina K, Cicourel AV. Advances in Social Theory and Methodology. London: Routledge & Kegan Paul; 1986.
- Pentland BT. Grammatical models of organizational processes. Organ Sci 1995;6:541-56. http://dx.doi.org/10.1287/orsc.6.5.541.
- Knorr Cetina KD. Sociality with objects. Theory Cult Soc 1999;14:1-30. http://dx.doi.org/10.1177/026327697014004001.
- Cresswell KM, Worth A, Sheikh A. Actor–network theory and its role in understanding the implementation of information technology developments in healthcare. BMC Med Inform Decis Mak 2010;10. http://dx.doi.org/10.1186/1472-6947-10-67.
- Mol A. The Body Multiple: Ontology in Medical Practice. Durham, NC: Duke University Press; 2002.
- Law J, Singleton V. Object lessons. Organisation 2005;12:3-331.
List of abbreviations
- A&E
- accident and emergency
- ANT
- actor–network theory
- CSCW
- computer-supported co-operative work
- DNA
- did not attend
- EBM
- evidence-based medicine
- ENT
- ear, nose and throat
- GP
- general practitioner
- HERO
- Healthcare Electronic Records in Organisations
- HIV
- human immunodeficiency virus
- ICT
- information and communication technology
- IT
- information technology
- MRC
- Medical Research Council
- NPfIT
- National Programme for Information Technology
- PAS
- patient administration system
- PCT
- primary care trust
- QOF
- Quality and Outcomes Framework
- SCR
- Summary Care Record
- SCRIE
- Summary Care Record Independent Evaluation
- SST
- strong structuration theory
- TAM
- technology acceptance model
- UBRN
- unique booking reference number