Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/1010/08. The contractual start date was in August 2011. The final report began editorial review in February 2014 and was accepted for publication in July 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Steve Goodacre is Deputy Chairperson of the National Institute for Health Research Health Technology Assessment Clinical Trials Evaluation and Trials Board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by O’Cathain et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Context of increasing emergency admissions
Provision for emergency hospital admissions is a necessary and important role for the NHS in England. The NHS has faced a large increase in emergency admissions, with a 12% increase between 2004 and 2008. 1 The aging population accounts for at most 40% of this increase, with the increase largely occurring in short-stay admissions of under a day. 1 Not all emergency admissions are necessary. They may even be harmful because they can result in hospital-acquired infections, distress to patients and their families, difficulties for service providers trying to balance elective and emergency care, and unnecessary high-cost intervention in a resource-limited health service. As a consequence, reducing unnecessary admissions has been a focus of policy-makers, commissioners and service providers for many years.
Unnecessary emergency admissions
Definitions of unnecessary emergency admissions focus on either ‘preventability’ or ‘avoidability’. ‘Ambulatory or primary care sensitive conditions’ (ACSCs) have been identified, where emergency admissions are prevented through intervention in primary care. 2 For example, primary care asthma nurses monitor asthma patients regularly to ensure optimum health and thus prevent exacerbations which might lead to an emergency admission. Problems have been identified with this set of conditions, with a recommendation for clarification of what admissions can be prevented. 3 An alternative approach focuses on avoidability; that is, when a person has an acute health problem, or an exacerbation of an existing health problem, it is dealt with without resort to emergency admission. For example, an asthma attack is dealt with immediately in a walk-in centre or general practice before it becomes serious enough to require emergency admission. Responsibility for preventability tends to be focused on primary care, while the responsibility for avoidability lies with the range of services in the wider system of emergency and urgent care that respond to patients suffering an acute health problem. 4
Admissions avoidable by emergency and urgent care systems
In England the range of services that could respond to an acute health problem includes same day appointments in general practice, general practitioner (GP) out-of-hours (OOH) services, walk-in centres, telephone helplines such as NHS Direct/NHS 111, community services such as district nursing, emergency departments (EDs) and emergency ambulances. Some health problems are accompanied by a need for social care and, therefore, social services can be included within an emergency and urgent care system. These services can be viewed as an emergency and urgent care system because patients living within a geographical area seeking emergency or urgent care will make decisions about which service to contact first and will often have pathways of care involving a number of services. 4,5 The availability, accessibility and quality of services within any system, as well as the co-ordination and integration between services, may affect emergency admission rates.
Defining and measuring the avoidable admissions is difficult but is an essential prerequisite to any study of the effect of services on avoidable admissions. Direct measurement would involve detailed analysis of individual admission and a judgment of whether or not the patient benefited from admission. It would not be feasible to undertake such an analysis on sufficient numbers of admissions to support a national study. An indirect measure of the avoidable admission rate is therefore required. In a previous study we used a Delphi exercise to identify health conditions, defined by ICD-10 (International Classification of Diseases, Tenth Edition) code, where experts believed that exacerbations could be managed by a well-performing emergency and urgent care system without admission to an inpatient bed. 6 We combined these conditions to develop a system performance indicator of ‘hospital emergency admission rates for acute exacerbation of urgent conditions that can be managed out of hospital or in other settings without admission to an inpatient bed’. This indicator identifies the rate of potentially avoidable emergency admissions for a given population through calculation of an age- and sex-adjusted rate of admissions from conditions rich in avoidable admissions, rather than a direct measure of avoidable admissions. This allows us to estimate the avoidable admission rate using routinely available administrative data. Although it is not a direct measure of avoidable admissions, it has clear advantages over an unselected analysis of all hospital admissions, which would include many substantial disease categories in which most admissions are unavoidable.
Research is needed on how characteristics of the emergency and urgent care system – its configuration, integration and accessibility – affect avoidable emergency admissions. There is a need to understand more about why some emergency and urgent care systems have lower avoidable emergency admission rates than others. It would be useful to identify the rate of avoidable emergency admissions, consider whether there is variation in rates between different systems and identify system-wide factors explaining variation in order to identify modifiable factors for decreasing these rates.
Conceptual framework
The conceptual framework for this study is that patients, health professionals and health services operate within an emergency and urgent care system. 4,5 General systems theorists have suggested that a system can be understood as an arrangement of components, and their interconnections, that come together for a purpose. 7 In the context of an emergency and urgent care system, the parts are the range of services available with a purpose of treating or managing acute health problems quickly. If the availability, accessibility and quality of services in the emergency and urgent care system are good then avoidable admission rates will be low. However, systems are about more than their components. Services are linked by the pathways patients take through a number of services when they need acute care. For example, a patient may call an emergency ambulance, be transported to an ED and be discharged home with support from district nursing, physiotherapists and social care. Co-ordination between services can be as important as the presence of individual services. Mingers and White8 recommend that systems thinking should involve:
-
viewing the situation holistically as a set of diverse interacting elements within an environment
-
recognising that the relationships or interactions between components are as important as the parts themselves in determining the behaviour of the system
-
recognising a hierarchy of levels of systems; for example, an ED operates within the larger system of an acute trust
-
accepting that people within a system will act in accordance with differing purposes or rationalities; that is, services may have differing priorities which are at odds with each other.
Defining emergency and urgent care systems in England
We used two definitions of an emergency and urgent care system in this study. Health-care systems operate at a national level and at a local level. Local emergency and urgent care systems can be virtual entities defined by their shared administration, or physical entities defined by geography. At the time this study was designed, local emergency and urgent care systems could be defined as primary care trusts (PCTs) which commissioned services for a defined geographical population. 9 That is, the geographical boundaries of PCTs identified 152 local emergency and urgent care systems in England in operation between 2006 and 2013. Each of these 152 PCTs managed an emergency and urgent care system, ensuring that their population had access to emergency and urgent care, and that the system of care – as well as individual services – met the needs of their population. PCTs ceased to operate in April 2013 but their geographical basis has historical relevance that is likely to persist in affecting patient pathways in current configurations of health and social care commissioning and provision. Therefore we used PCT resident populations to define 152 geographically based systems in our study. General acute trusts are the focus of emergency admissions. Therefore we used a secondary definition of a local emergency and urgent care system as the catchment population of general acute trusts (acute trust-based systems).
Factors affecting emergency admissions
Many researchers have explored the factors affecting emergency admission rates overall, or for specific conditions, through studying variation between general practices in the UK10–19 and internationally,20 commissioning organisations in the UK12,21–23 or hospitals internationally. 24,25 Factors explaining variation were related to the population, particularly in terms of deprivation and health (Table 1). Much of the focus on health service-related factors affecting variation in emergency admissions has been on primary care (Table 2), for example the quality and supply of,10,12,14,17 and access to, primary care. 10,12,15,16 There is some evidence that factors within hospitals can affect emergency admissions, such as bed numbers and availability,16 physical space24 and clinical decision-making. 25
| Factor | All emergency admissions | Condition-specific | Preventable, avoidable or ambulatory set of conditions |
|---|---|---|---|
| Deprivation | General practice10,11,13,15,18 PCT21 |
General practice: COPD,12,16 asthma,16 MI,17 angina,17 stroke19 PCT: COPD,12,23 diabetes,21 asthma21 |
General practice20 PCT23 Hospital,24 local authority22 |
| Ethnicity | General practice10,15 | General practice: diabetes14 PCT23 |
General practice20 |
| Vulnerability, e.g. living alone | General practice: lone parenthood18 | PCT23 | |
| Urban/rural status | General practice: COPD,16 asthma,16 angina17 | Hospital24 | |
| Distance to hospital | General practice10,15 | General practice: COPD, asthma,16 angina17 | Hospital24 |
| Morbidity and mortality | General practice10,18 PCT21 |
General practice: COPD12,16 asthma,16 MI,17 angina,17 diabetes,14 stroke19 PCT: COPD,23 diabetes21 |
|
| Prevalence of health behaviours such as smoking | General practice: COPD,12,16 asthma,16 MI,17 angina,17 diabetes,14 stroke19 PCT: COPD12 |
||
| Agea | General practice10,11,13,15 | GP: diabetes14 | General practice20 |
| Sexa | General practice10,11,15 | GP: diabetes14 |
| Factor | All emergency admissions | Condition-specific | Preventable, avoidable or ambulatory set of conditions |
|---|---|---|---|
| Quality of primary care | General practice: COPD,12 diabetes,14 angina17 PCT: diabetes23 |
||
| Supply of primary care (i.e. GPs/primary care staff per head of population) | General practice: COPD,12 MI,17 stroke19 PCT: COPD12 |
||
| Access to primary care (single handed GPs, practice size) | General practice10 | General practice: asthma16 | |
| Perceptions of access to general practice | General practice10,15 | General practice: COPD12 | |
| Amount of floor space in hospitals | Hospital24 | ||
| Total bed number/availability | General practice: COPD,16 asthma16 | ||
| ED doctor | Hospital25 | ||
| Hospital variation | General practice18 Hospital25 |
||
| Prescribing | General practice: angina17 | ||
| GP fundholding | General practice18 |
Research has also been undertaken on factors affecting variation in use of a common gateway to emergency admission – EDs. Some studies have found that perceived access to general practice affects ED attendance. 26,27 Less research has been undertaken on system-related factors, such as integration of health and social services. Two limited case studies suggested integration of services was associated with reduced increase in emergency admissions. 1
We designed a study to address gaps in the evidence base. We focused on avoidable rather than all emergency admissions, and on all services in the emergency and urgent care system rather than primary care and hospitals only.
Aim and objectives
Aim
To identify system-wide factors explaining variation in potentially avoidable emergency admissions in different emergency and urgent care systems.
Objectives
-
Calculate the ‘age- and sex-adjusted potentially avoidable emergency admission rate’ for each emergency and urgent care system in England.
-
Explain variation in the ‘age- and sex-adjusted potentially avoidable emergency admission rate’ in different systems using routine data on population, health and system characteristics.
-
Undertake in-depth research in systems with high and low ‘age- and sex-adjusted potentially avoidable emergency admission rate’ to identify further factors which may be influencing variation.
-
Identify modifiable factors which affect potentially avoidable emergency admissions to help policy-makers, commissioners and service providers implement changes to reduce avoidable admissions.
Chapter 2 Overview of methods
Design
We calculated an age- and sex-adjusted potentially avoidable emergency admission rate, that is a standardised avoidable admission rate (SAAR), for emergency and urgent care systems in England in 2008–11. We defined these systems in two ways: geographically based systems (populations of 2006–13 PCTs) and acute trust-based systems (the catchment populations of acute trusts).
The study design was a three-phase mixed-methods design known as ‘ethnographic residual analysis’28 or ‘qualitative residual analysis’. 29 The first phase of this approach involves a regression to identify factors affecting variation between a large set of cases. The second phase involves qualitative research on some cases that the first-phase regression fails to predict well. That is, the qualitative research focuses on cases that are likely to identify factors not already included in the regression model. The third phase involves reassessing the regression in phase 1, in particular looking for variables which measure the additional factors identified in the qualitative research. The strength of this approach is that qualitative research generates hypotheses for testing in the quantitative component as well as helping to explain how factors in the regression affect the outcome of interest. For this study:
-
Phase 1 was quantitative, involving a regression to identify factors that explained variation in the SAAR. We identified routinely available data on the characteristics of these systems and tested whether they explained variation in the SAAR. We then identified systems with large residuals within our analysis, that is systems that had SAARs which could not be explained by the system characteristics in our regression.
-
Phase 2 was largely qualitative. We identified six geographically based systems with large residuals in our phase 1 regression and used in-depth case studies to identify further more complex system characteristics which might explain variation in the SAAR.
-
Phase 3 was quantitative, building on the phase 1 regression by identifying routine data on factors from phase 2 and attempting to explain further variation in the SAAR.
Integration between the quantitative and qualitative components of this mixed methods study was built into the design. The first quantitative component (phase 1) helped to identify the sample for the qualitative component (phase 2) so that the case studies were more likely to offer additional factors rather than simply repeat those found in phase 1. The qualitative component (phase 2) helped to identify further factors for testing in a second quantitative component (phase 3). Further integration took place by displaying the findings from different components together and considering the convergence, complementarity and disagreement between the findings from each component. 30 The design was superior to an alternative design of a regression followed by case studies of high and low SAARs in which the case studies might identify only similar issues to the regression. The design is displayed in Figure 1, which also shows where the methods and findings are reported.
FIGURE 1.
Design of study.

Patient and public involvement
The Sheffield Emergency Care Forum (SECF) is an independent group of members of the public with an interest in emergency care. A member of this group (Enid Hirst) was a coapplicant on the proposal for this study, and an active member of the study management group, contributing to operationalising the study proposal and interpreting the emerging findings. For example, as a member of the public with an interest in emergency care she identified a list of factors to test in phase 1 from the perspective of the general public. Another member of this group (Beryl Darlison) was a member of the Project Advisory Group for this study, offering advice on emerging findings and interpretation. A subset of SECF met with the team at three key points in the study to contribute to the selection of factors for testing in phase 1, the selection of the six case studies, the development of the case studies and interpretation of overall findings.
Chapter 3 Calculation of potentially avoidable admission rate
Based on fourteen conditions
A consensus group of 48 senior clinicians, researchers and health-care commissioners with a special interest in emergency and urgent care identified 14 health conditions where exacerbations could be managed by a well-performing emergency and urgent care system without admission to an inpatient bed. 6 Consensus group members included patient representatives, pharmacists, NHS Direct staff, GPs, pre-hospital care staff, paediatricians, public health officials, psychiatrists, emergency medicine doctors and nurses, acute medicine doctors and nurses, walk-in centre nurses and PCT commissioners. The 14 conditions are displayed in Table 3.
| Condition | ICD-10 codes | Numbers (%) | % aged > 75 years |
|---|---|---|---|
| Non-specific chest pains | R07.2, 7.3, 7.4 | 731,758 (22) | 21 |
| Non-specific abdominal pains | R10 | 660,438 (20) | 10 |
| Acute mental crisis | F00–F99 | 340,826 (10) | 15 |
| COPD | J40–J44 | 322,747 (10) | 44 |
| Angina | I20 | 186,394 (6) | 38 |
| Minor head injuries | S00 | 100,178 (3) | 32 |
| UTIs | N39.0 | 356,814 (11) | 54 |
| DVT | I80–I82 | 74,914 (2) | 29 |
| Epileptic fit | G40–G41 | 111,697 (3) | 13 |
| Cellulitis | L03 | 164,499 (5) | 31 |
| Pyrexial child aged under 6 years | R50 | 33,562 (1) | 0 |
| Blocked urinary catheter | T83.0 | 20,277 (< 1) | 61 |
| Hypoglycaemia/diabetic emergencies | E10.0, E11.0, E12.0, E13.0, E14.0, E15, E16.1, E16.2 | 40,299 (1) | 43 |
| Falls not elsewhere classified | W00–W19 cause and diagnosis (based on DIAG_01) S00, S10, S20, S30, S40, S50, S60, S70, S80, S90, T00, R | 128,992 (4) | 100 |
| All avoidable admissions | 3,273,395 (100) | 29 | |
There were a total of 15 million emergency admissions in the 3-year period 2008–11, approximately 5 million in each year and increasing over time. Twenty-two per cent (3,273,395 of 14,998,773) of these admissions were for the 14 conditions identified as rich in potentially avoidable admissions. That is, our avoidable admissions accounted for one fifth of all emergency admissions in this time period. Chest pain, abdominal pain, urinary tract infections (UTIs), acute mental crisis and chronic obstructive pulmonary disease (COPD) accounted for over two-thirds of these potentially avoidable emergency admissions (see Table 3). Twenty-nine per cent occurred in people aged over 75 years old. Admissions came from a number of sources: EDs, GPs, bed bureaus, outpatients and other.
Calculation of avoidable admission rate
Geographically based systems
Numbers of emergency admissions for the set of 14 conditions for each emergency and urgent care system were calculated using Hospital Episode Statistics (HES) for the 3 financial years April 2008 to March 2011. Admissions from all sources were included. The most common admission route was EDs, with an average of 69% of avoidable admissions through this route, although this varied by system between 44% and 92%.
The condition code for the first finished consultant episode was used. PCT mid-2009 resident populations were then used as the denominator to calculate the rate of potentially avoidable emergency admissions per 100,000 population. The directly age- and sex-standardised admission rates per 100,000 per year were calculated for each PCT for the 3-year period using seven age groups (0–4, 5–14, 15–44, 45–64, 65–74, 75–84, 85+ years), standardised to the whole population for England in 2009. A 3-year period was selected to ensure that the effect of annual variability in emergency admission rates at a system level was minimised. It is important to understand that this rate is an indicator of avoidable admissions. It is based on conditions rich in avoidability; that is, not all admissions from these conditions were avoidable in practice. For shorthand, we call this the SAAR even though it was a directly standardised rate.
Acute trust-based systems
Catchment populations for acute trusts were needed to calculate admission rates for the 14 conditions. There are different ways of calculating catchment populations for hospitals, with debates about which approach is best. 31,32 We used estimates of acute trust catchment populations for emergency admissions in 2009 calculated by Public Health Observatories in England. 33 These catchment areas were defined as the number of people in each sex and age group who live in the catchment of the acute trust. They were calculated using HES data between April 2006 and March 2009 to count the number of patients in each age and sex group admitted from small areas called Middle Super Output Areas. These areas have a minimum population of 5000, with an overall mean of 7200. Mid-year population estimates for 2009 were supplied by the Office for National Statistics (ONS). Within each 5-year age and sex group, the proportion of patients who went to each acute trust as a proportion of patients who used any acute trust was calculated. For each small area, this proportion was multiplied by the resident population in that age and sex group to give the small area catchment population for each acute trust. Then the small area catchment populations for each acute trust were summed to give the total catchment population for each acute trust.
We calculated the SAARs per 100,000 per year for each acute trust for the 3-year period April 2008 to March 2011 using seven age groups (0–4, 5–14, 15–44, 45–64, 65–74, 75–84, 85+ years) standardised to the whole population for England in 2009. A 3-year period was selected to ensure that the effect of annual variability in emergency admission rates was minimised.
Some specialist acute trusts offer care to specific age, sex or condition groups only. We wanted to compare similar types of acute trusts and focused on general acute trusts because they account for the majority of emergency admissions. 1 We included any acute trusts where the estimated population in each age and sex group was > 1000. This was an arbitrary cut-off point which successfully excluded children’s hospitals, women’s hospitals and condition-specific hospitals. It also excluded some general acute trusts located near children’s hospitals because they did not admit children.
Variation in the standardised avoidable admissions rate
Geographically based systems
There were 152 geographically based systems (based on PCT populations). The reliability of the HES data was checked by looking for consistency between numbers of emergency admissions per year within each system. The only large differences between years for any system were two systems with zero emergency admissions for 2010–11. We excluded them from the analysis, leaving 150 systems.
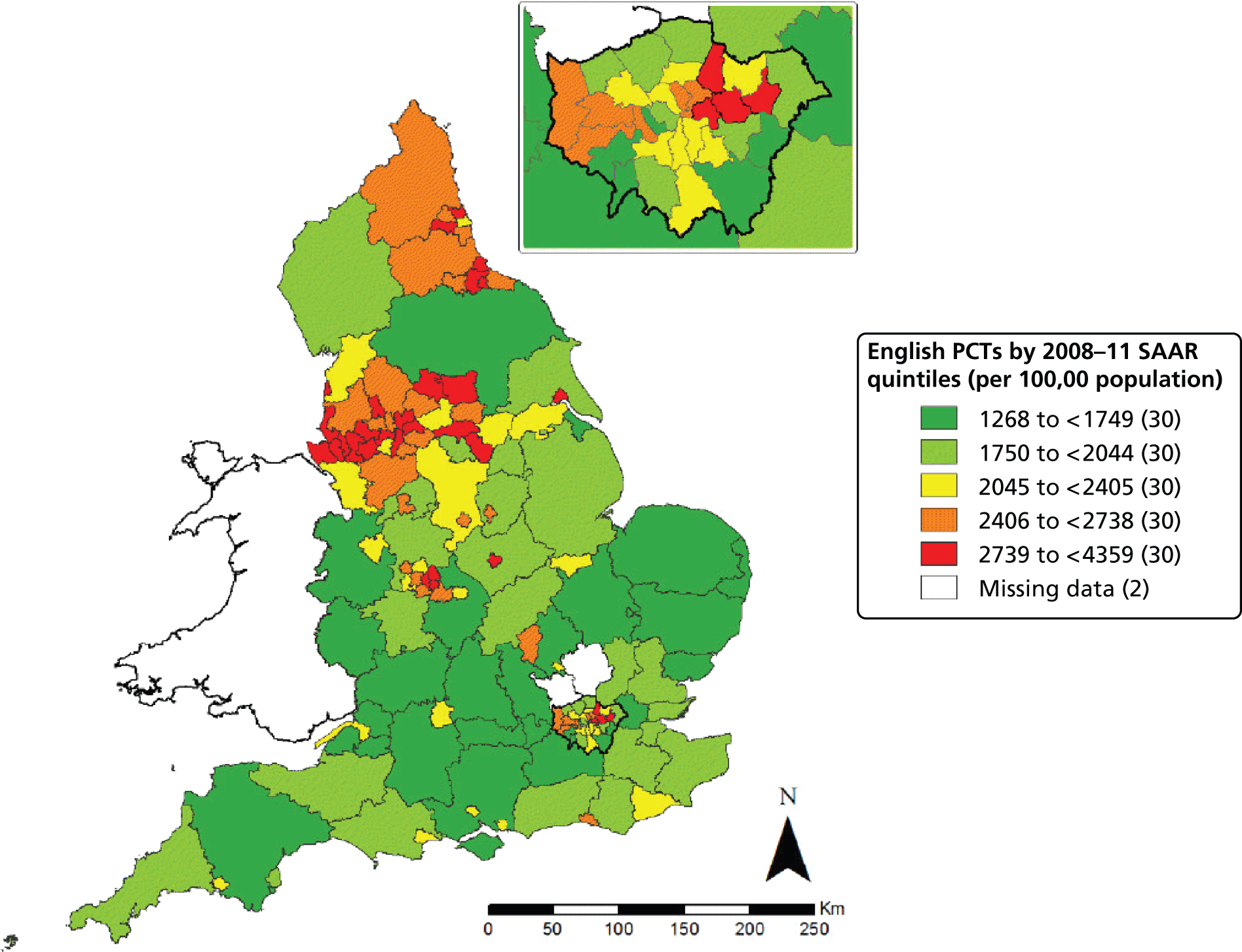
The median SAAR was 2258 [interquartile range (IQR) 1808–2662], with a 3.4-fold variation between systems ranging from 1268 to 4359, and a 1.9-fold variation between the 10th and 90th percentiles. Geographical variation in the SAAR was apparent, with highest rates clustering in the north-west of England, the north-east of England and east London (Figure 2).
FIGURE 2.
Variation in SAAR in 150 geographically based systems in England.
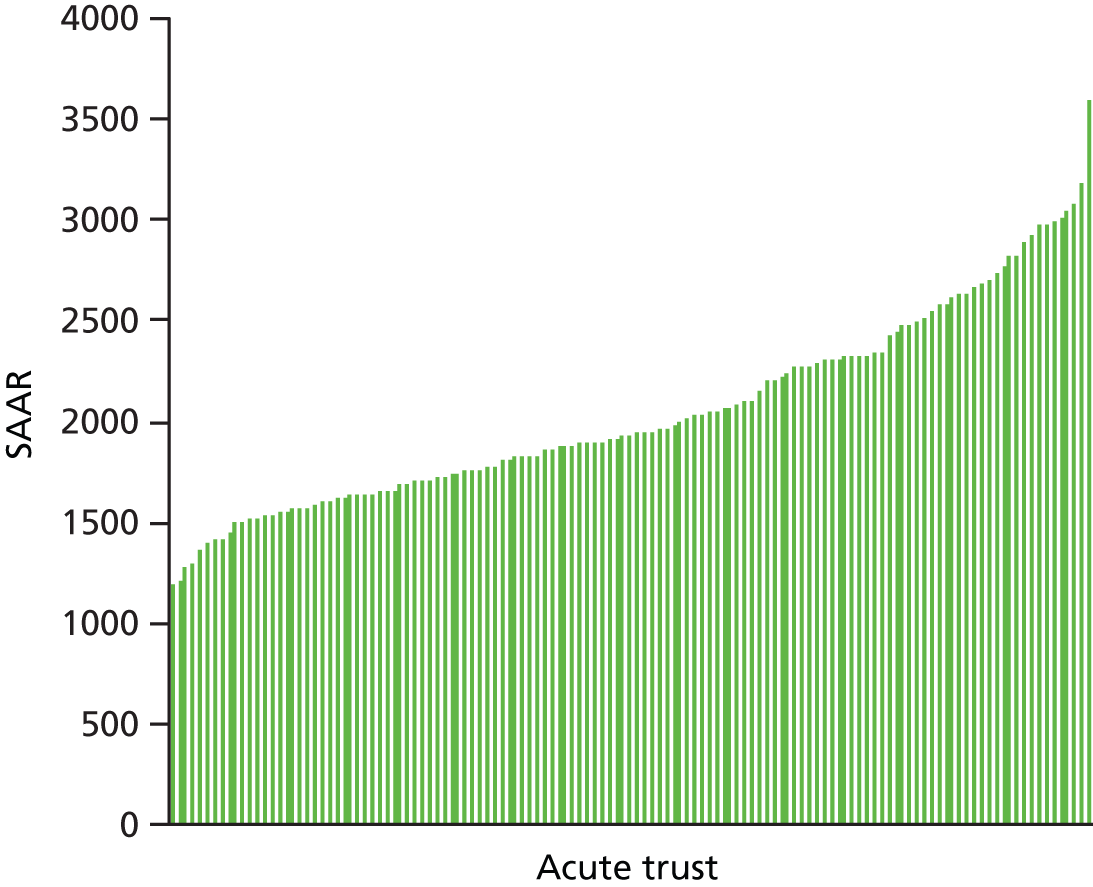
Acute trust-based systems
There were 131 acute trusts after exclusion of specialist hospitals. Two acute trusts had missing data for admissions in 2010/11 and were removed, leaving 129 acute trusts. The median SAAR was 1939 (IQR 1676–2331) per 100,000 population per year, with threefold variation between acute trusts ranging from 1194 to 3601, and a 1.8-fold variation between the 10th and 90th percentiles (Figure 3).
FIGURE 3.
Variation in SAAR in 129 acute trust-based systems in England.
Relationship between the standardised avoidable admissions rate and similar measures
It is useful to understand the relationship between the SAAR and other related emergency admission rates. Other indicators are available for PCTs and, therefore, we compared our geographically based system SAAR with other measures.
Standardised avoidable admissions rate and all emergency admissions
There was a strong association between the SAAR (2008–11) and the directly standardised rate for all emergency admissions for geographically based systems (2009–10) (Figure 4). Systems with high SAARs tended to have high rates of emergency admissions (Pearson’s r = 0.88, p < 0.001).
FIGURE 4.
Relationship between SAAR and directly standardised rate of all emergency admissions rate by geographically based systems. DSR, directly standardised rate.
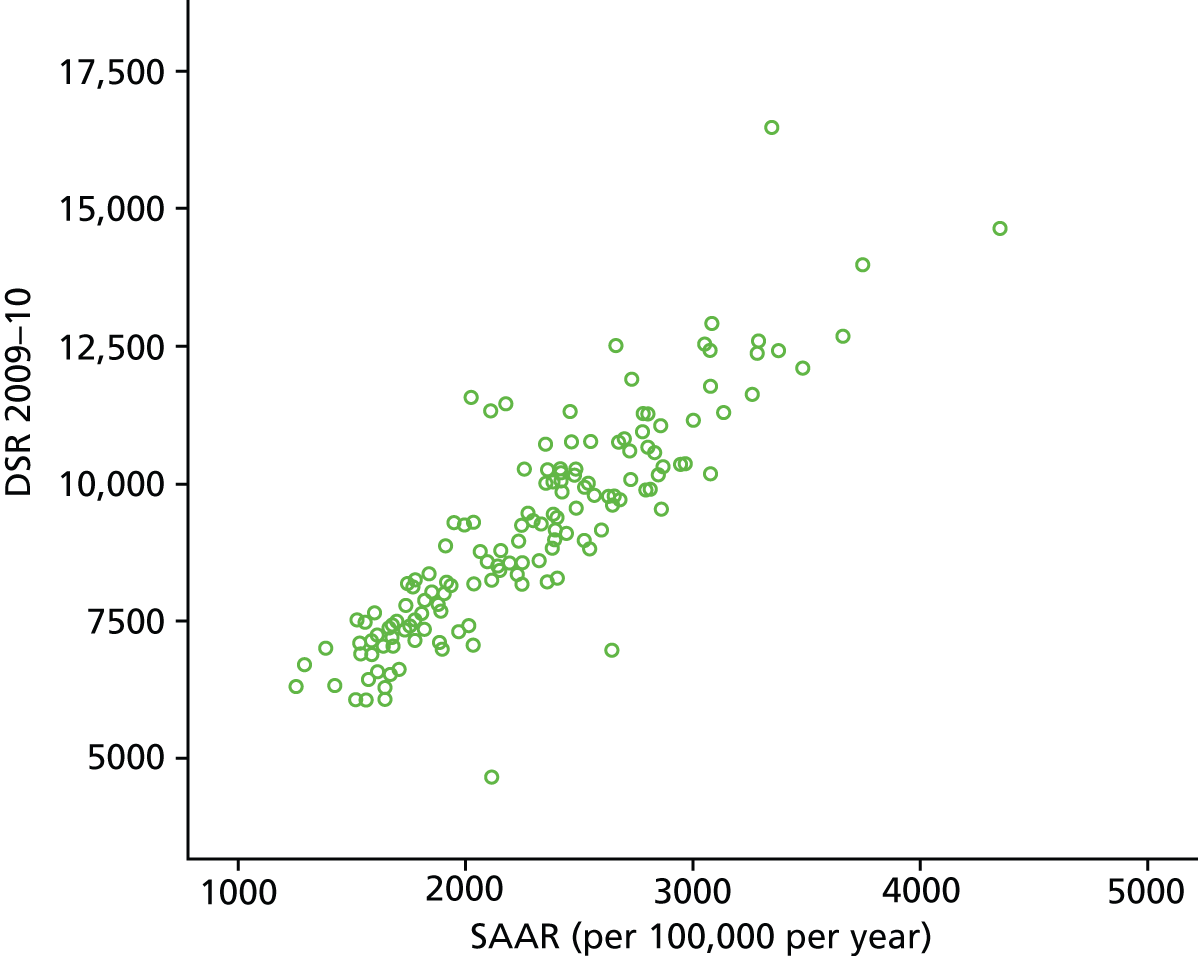
It is also worth noting that five of the conditions in our SAAR appeared in the top 10 diagnostic groups contributing to an increase in emergency admissions over recent years. 1
Standardised avoidable admissions rate and ambulatory emergency admissions
Ambulatory or primary care sensitive conditions are conditions for which hospital admission could be prevented by interventions in primary care. There are various definitions34 but the King’s Fund list is the most frequently used in England. 22 There is some overlap between these 19 ACSCs and our 14 conditions (indicated by * below):
-
influenza and pneumonia
-
other vaccine-preventable conditions
-
asthma
-
congestive heart failure
-
diabetes complications*
-
COPD*
-
angina*
-
iron-deficiency anaemia
-
hypertension
-
nutritional deficiencies
-
dehydration and gastroenteritis
-
pyelonephritis
-
perforated/bleeding ulcer
-
cellulitis*
-
pelvic inflammatory disease
-
ear, nose and throat infections
-
dental conditions
-
convulsions and epilepsy*
-
gangrene.
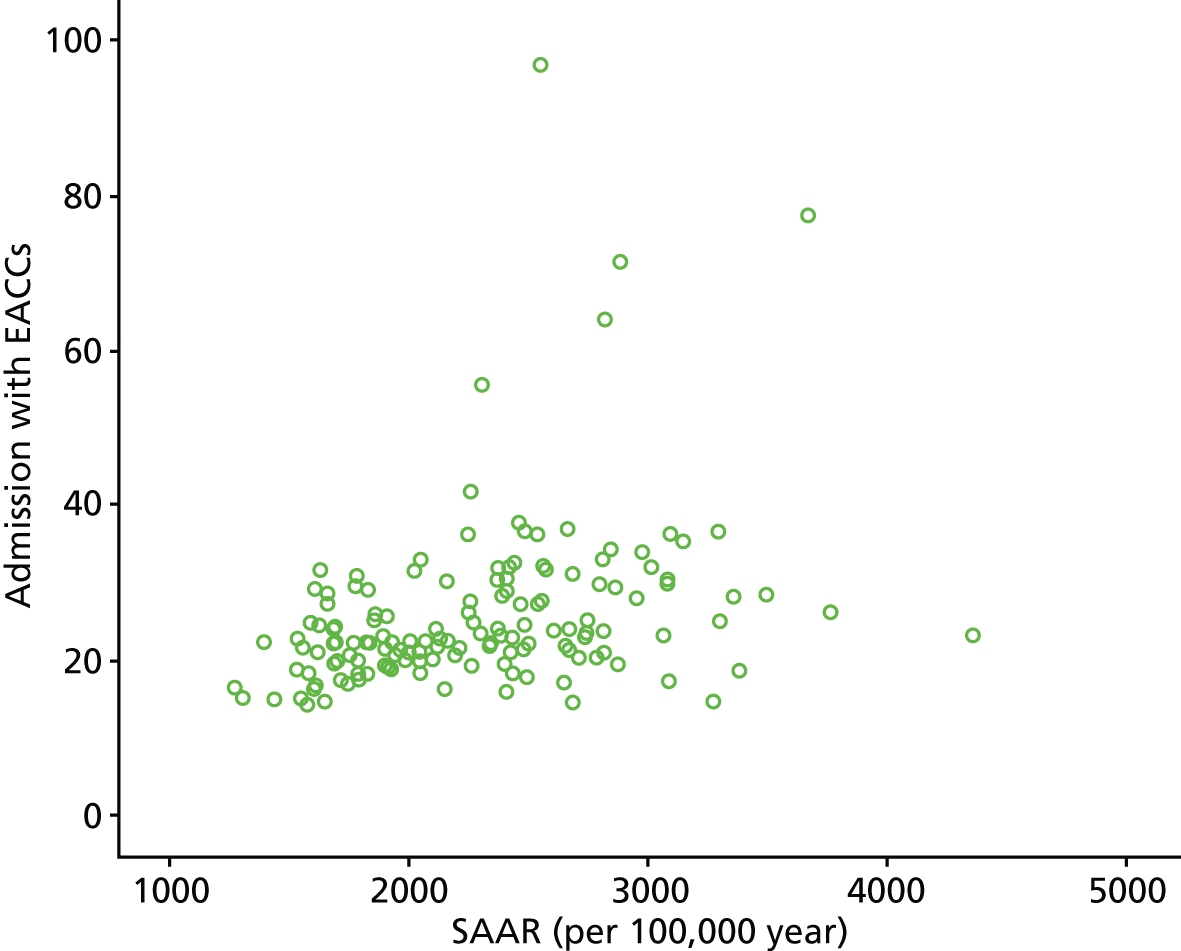
Our SAAR is based on injuries as well as illness and includes mental as well as physical health problems. We could not locate ACSC rates for our systems but we did locate the rate of admissions with emergency ambulatory care conditions (EACCs) per population by PCT. 35 This is a directly age-, sex- and deprivation-standardised admission rate based on 49 emergency conditions with the potential to be managed on an ambulatory basis. The 49 conditions were developed by the National Institute for Improvement and Innovation. Figure 5 shows that there is correlation between our SAAR and the EACC (Pearson’s r = 0.34, p < 0.001) but that it is weaker than that between our SAAR and all emergency admissions.
FIGURE 5.
Relationship between SAAR and admissions with EACCs by geographically based systems.
Conclusion
Over one fifth of all emergency admissions in England between 2008 and 2011 were accounted for by 14 conditions that are likely to be rich in avoidable admissions. There was considerable variation in an age- and sex-adjusted rate of potentially avoidable admissions – the SAAR – for emergency and urgent care systems defined in two different ways, with high rates clustering in the north of the country and east London. There was correlation between the SAAR and other types of emergency admission rates.
Chapter 4 Phase 1: explaining variation in potentially avoidable admissions rates for geographically based systems
Objective
In this chapter we present the methods and findings of a regression to explain variation in the SAAR for geographically based systems. This was published during the course of the study. 36
Methods
Identification of factors
Based on previous research on variation in emergency admission rates, and the focus here on the emergency and urgent care system, it was necessary to locate factors relating to the population, geography, health and range of emergency and urgent health services for the 150 geographically based systems. We searched national databases of routinely available data for relevant data on factors reported at PCT level. Where factors were available by financial year, we selected 2009–10, which was the mid-point year of the SAAR, or the calendar year 2009, or summed quarterly data for 2009. The source of data for factors is reported in Appendix 1.
Population factors
The SAAR was adjusted for age and sex, using 5-year age groups. We attempted to locate data on social deprivation, minority ethnic groups, density of elderly people and social isolation. The Index of Multiple Deprivation has often been identified as an explanatory factor for variation in emergency admissions. We used two domains of this index – employment and income deprivation – because the index itself includes standardised emergency admission rates. 37 The employment deprivation domain reports the proportion of the working age population unable to work because of unemployment, sickness or disability. The income deprivation domain reports the proportion of the population in families who are out of work or have low earnings. We included a factor on the percentage of the population aged over 75 years old even though the SAAR was adjusted for age in case the density of older people in an area created pressure on services.
Geography
We tested one geographical factor, which was a six-category urban–rural scale. We started the analysis with a three-category scale. A patient and public involvement (PPI) representative drew attention to the effect of geography on the SAAR when we presented preliminary findings. We then sought out a more detailed scale to represent geographical differences between systems.
Health
The standardised mortality ratio has been shown to explain variation in emergency admissions overall (see Table 1). We decided not to include it because it may be an indicator of both health status of a population and performance of services for that population. Instead we used indicators of morbidity: we found data on the prevalence of three conditions included in the 14 conditions in the SAAR.
Services in an emergency and urgent care system
We located factors about key services in the emergency and urgent care system: general practice, GP OOH, EDs, acute trusts and ambulance services. We wanted to locate data on the availability, accessibility and quality of all services but could locate data on only some aspects of these services.
The Atlas of Variation was a source of health service-related factors but the authors have expressed concerns that some variation may be accounted for by data management problems. 35 We replaced very high values with the median value for two factors: ED attendance rate (replaced two high values) and admissions from nursing homes rate (replaced five high values).
We calculated two factors using HES data. The first was the percentage of all emergency admissions staying less than 1 day because this had been identified as explaining the recent increase in emergency admission rates. We felt that this factor could indicate one of two things: either (1) coding differences between hospitals, for example, with patients waiting in the hospital for a few hours without using a bed coded as admissions in some hospitals and as ED discharges in another, or (2) different ways of managing patients within the hospital; for example, some hospitals may have been able to put community services in place to discharge ED attendances while others admitted patients to a hospital bed to arrange community services to allow discharge. Second, we calculated the percentage of all emergency admissions referred by GPs to identify the direct influence of general practice on emergency admissions.
Two factors about the emergency ambulance service – percentage of incidents not transported to hospital (non-conveyance) and the percentage of incidents meeting the 8-minute response target – were available only for ambulance services rather than PCTs. We allocated the ambulance service rate to each of the PCTs nested within that ambulance service, an underestimate of the variation at PCT level.
Services we could find no data for
We found no routine data for community/intermediate care, social care or system integration.
Analysis
We undertook general linear modelling in SPSS version 20 (IBM Corporation, Armonk, NY, USA) weighted for the size of the system population to account for larger uncertainty of estimates for smaller systems. The dependent variable was the SAAR for 150 systems. The independent variables were tested in a hierarchical multiple regression in two blocks, using forward stepwise regression within each block. Variables were included if the p-value for the t-test was < 0.05. The blocks were determined by the extent to which service providers could affect a factor. Block 1 was population-related factors. We used the residuals from block 1 as the dependent variable in block 2 and then tested the effect of service-related factors.
After we had completed the analysis and moved on to phase 2 of the study, we felt that this regression did not capture enough of the conceptual framework of the study. Although our conceptual framework led us to include factors which other researchers had not – that is those from services other than primary care and hospitals – we had ignored the fact that factors might operate in sequence. That is, services outside the hospital would affect numbers who turned up at the hospital. For example, difficulty getting a GP appointment has been shown to explain higher rates of attendance at EDs. 26,27 We undertook a three-block analysis to reflect this:
-
block 1: population-related factors: population, geography, health
-
block 2: out of hospital service-related factors – GP access, GP quality, ambulance service performance, GP OOH service
-
block 3: in hospital service-related factors: ED attendance, conversion rate at ED, short length of stay in hospital.
Findings
Univariate linear regression
We display descriptions of the variables tested in the multiple regression (Table 4). It is interesting to note that two factors explained a very large amount of variation in the SAAR. Both were population factors related to deprivation: income deprivation and employment deprivation, explaining 60% and 72% of variation respectively. These are likely to be correlated. We explore correlation between factors in the next section.
| Factor | Sourcea | Median (IQR) | Range | Pearson’s r2 (%) | p-value | Direction of correlation |
|---|---|---|---|---|---|---|
| Population | ||||||
| INCOME: % population in an area that live in income-deprived families | IMD 2010 | 15 (11–19) | 7–33 | 60 | < 0.001 | + |
| EMPLOYMENT: % population with employment deprivation | IMD 2010 | 6 (5–8) | 3–12 | 72 | < 0.001 | + |
| ETHNICITY: % population minority ethnic | ONS | 9 (5–20) | 3–63 | 9 | < 0.001 | + |
| OVER75: % population aged 75 or over | ONS | 7 (7–9) | 3–13 | 18 | < 0.001 | – |
| ALONE: % pensioners living alone | ONS | 6 (5–6) | 3–8 | < 1 | 0.547 | + |
| Geography | ||||||
| URBAN/RURAL | ONS | No PCTs (%) | 29 | < 0.001 | – | |
| Major urban | 58 (39%) | |||||
| Large urban | 19 (13%) | |||||
| Other urban | 23 (15%) | |||||
| Significant rural | 26 (17%) | |||||
| Rural 50% | 22 (15%) | |||||
| Rural 80% | 2 (1%) | |||||
| Healthb | ||||||
| CHD: prevalence of coronary heart disease | QOF | 4 (3–4) | 1–5 | 3 | 0.032 | + |
| COPD: prevalence of COPD | QOF | 2 (1–2) | 1–3 | 20 | < 0.001 | + |
| DIABETES: prevalence of diabetes | QOF | 5 (5–6) | 3–9 | 18 | < 0.001 | + |
| Hospital | ||||||
| MANAGEMENT/CODING: % emergency admissions with length of stay < 1 day | HES | 28 (24–30) | 14–41 | 16 | < 0.001 | + |
| MANAGEMENT: % population waiting 4 or more weeks for elective admission | Department of Health | 62 (53–68) | 35–98 | 1 | 0.198 | – |
| EDs | ||||||
| EDUSE: directly age-, sex- and deprivation-standardised rate of ED attendances per 100,000 population | NHS Atlas of Variation 2011 | 275 (241–324) | 149–909 | 15 | < 0.001 | + |
| EDCONVERSION: directly age-, sex- and deprivation-standardised rate of conversion from ED attendance to emergency admissions | NHS Atlas of Variation 2011 | 100 (88–112) | 70–148 | 7 | 0.001 | + |
| Community | ||||||
| CAREHOME: admission rate for people aged >74 from nursing home or residential care home settings per 10,000 | NHS Atlas of Variation 2011 | 12 (6–29) | 1–193 | 4 | 0.013 | + |
| General practice | ||||||
| GPSUPPLY: GPs per 100,000 population | London Health Observatory | 69 (64–75) | 54–99 | 0 | 0.855 | + |
| GPACCESS1: % GP single handed | Information Centre | 13 (7–23) | 0–48 | 17 | < 0.001 | + |
| GPACCESS2: % practices offering extended opening hours | Department of Health | 75 (69–86) | 39–100 | 0 | 0.901 | – |
| GPACCESS3: % able to see GP in 48 hours | GP survey | 80 (77–83) | 71–89 | 25 | < 0.001 | – |
| GPADMISSION: % admissions from general practice | HES | 18 (7–26) | 0–44 | 11 | < 0.001 | – |
| GP QUALITY: QOF indicators | QOF | Six indicators tested | 0–9 | < 0.001–0.570 | –c | |
| General practice OOH | ||||||
| GPOOH1: % know how to contact GP OOH | GP survey | 66 (62–69) | 48–79 | 10 | < 0.001 | – |
| GPOOH2: % of GP OOH users reporting ‘very easy’ to contact by phone | GP survey | 38 (34–42) | 20–55 | 1 | 0.231 | – |
| Ambulance service | ||||||
| AMBRESPONSE: % category A response within 8 minutesd | Information Centre | 75 (73–75) | 71–78 | 13 | < 0.001 | – |
| AMBTRANSPORT: % not transported to hospitald | Information Centre | 21 (16–30) | 8–34 | 35 | < 0.001 | – |
Correlations between factors
Some of the factors were correlated with others. It is important to describe these correlations to facilitate interpretation of the final multiple regression. Employment deprivation was positively correlated with income deprivation and the prevalence of some of the 14 conditions (Table 5). Urban/rural status was positively correlated with a number of factors including the proportion of elderly people in a system and some access to general practice factors.
| Factors in multiple regression | Factors correlated with | Pearson’s r |
|---|---|---|
| EMPLOYMENT | INCOME | +0.87 |
| COPD | +0.55 | |
| DIABETES | +0.42 | |
| AMBTRANSPORT | –0.44 | |
| URBAN/RURAL | ETHNICITY | –0.60 |
| OVER75 | +0.62 | |
| CHD | +0.42 | |
| GPACCESS3 | +0.66 | |
| GPOOH1 | +0.61 | |
| GPADMISSION | +0.59 | |
| AMBTRANSPORT | +0.45 | |
| GPACESS3 | INCOME | –0.54 |
| ETHNICITY | –0.63 | |
| OVER75 | +0.71 | |
| ALONE | +0.43 | |
| URBAN/RURAL | +0.66 | |
| CHD | +0.44 | |
| GPACCESS1 | –0.46 | |
| GPOOH1 | +0.62 | |
| GPADMISSION | +0.52 |
Factors affecting standardised avoidable admissions rate in a multiple linear regression
We then undertook multiple linear regression to identify the combination of factors which predicted the SAAR (Table 6). We undertook the block 1 analysis – which tested population-related factors – and identified two factors which predicted the SAAR: employment deprivation and urban/rural status. The more deprived populations and more urban populations had higher SAARs. These two factors together predicted 75% of the variation. In the block 2 analysis – which tested service-related factors – those related to EDs, hospitals, emergency ambulance services and primary care explained further variation (r2 = 85% in a non-hierarchical analysis). Systems with higher SAARs had higher attendance rates at EDs, higher rates of conversion of ED attendances to admissions, higher proportions of very short-stay patients, higher rates of ambulance calls transported to hospital and better perceived access to general practice (see Table 6). This last factor was in the opposite direction from the univariate linear regression and counterintuitive in the context of the conceptual framework of the study. We discuss this in Chapter 10.
| Block | Predictorsa | Unstandardised coefficient | 95% CI | Standardised coefficient | p-value |
|---|---|---|---|---|---|
| 1: population, geography, health | EMPLOYMENT | 203 | 179 to 227 | 0.78 | 0.001 |
| URBAN/RURAL | –0.17 | 0.001 | |||
| Major urban | 536 | 138 to 934 | |||
| Large urban | 437 | 23 to 850 | |||
| Other urban | 452 | 38 to 867 | |||
| Significant rural | 386 | –14 to 787 | |||
| Rural 50% | 322 | –81 to 725 | |||
| 2: services | EDUSE | 0.9 | 0.4 to 1.3 | 0.30 | 0.001 |
| EDCONVERSION | 7.3 | 5.1 to 9.4 | 0.46 | 0.001 | |
| MANAGEMENT/CODING | 18.4 | 10.1 to 26.6 | 0.29 | 0.001 | |
| AMBTRANSPORT | –5.6 | –10.2 to –0.9 | –0.18 | 0.02 | |
| GPACCESS3 | 16.6 | 6.5 to 26.8 | 0.24 | 0.001 | |
Regression metrics are reported in Appendix 2, showing that the model was a good fit. There was no evidence of multicollinearity in block 2: variance inflation factors varied between 1.1 and 1.4. Some of the factors in the multiple regression were correlated with each other even though there was no multicollinearity: employment deprivation was negatively correlated with the proportion of ambulance callers not transported to hospital; urban/rural status was correlated with perceptions of access to general practice and the proportion of ambulance callers not transported to hospital (see Table 5). Because of the large amount of correlation between factors, it is likely that a number of regressions would fit the data equally well, so there is some uncertainty about the model presented here.
Test of a stronger system-based theoretical model
The first block was the same as block 1 in the primary analysis reported above. In block 2 – out-of-hospital factors – ambulance performance was the only factor adding to the regression. That is, factors about availability of, access to and quality of primary care did not explain further variation at this stage. In block 3 – in-hospital factors – the factors explaining further variation were those in the two-block analysis reported earlier. That is, this approach made little difference to our findings.
Conclusion
Variation in potentially avoidable emergency admissions was explained mainly by population factors. Health-care providers can reduce avoidable emergency admissions by investigating why some populations attend EDs more than others, why some EDs convert more attendances to admissions than others and why some ambulance services transport more of their calls to hospital than others. The greatest potential for reduction in avoidable emergency admissions lies with understanding more about how services can best provide care to deprived communities in ways that avoid emergency admission.
Link with phase 2: identifying residuals and potential case studies
A residual is the difference between the dependent variable for a case and its value predicted by the multiple regression. The description of qualitative residual analysis is brief28,29 and there is no guidance on which type of residual to measure or the size of a large residual. The histogram of standardised residuals from our earlier regression shows that they were normally distributed (see Appendix 2). We identified large standardised residuals as > 1.5 or < 1.5. We noted that some systems with large residuals were in geographical clusters, in that neighbouring systems had similar SAARs and similar residuals. We changed our definition of a large residual to > 1.3 or < 1.3 to include systems within each of these geographical clusters. Twenty-seven systems had large residuals (Table 7).
| Type | System grouped by cluster | Residual | SAAR | Predicted SAAR | Rank | Predicted rank |
|---|---|---|---|---|---|---|
| High SAAR (overpredicted) | HO | –2.51 | 2669 | 3238 | 115 | 147 |
| High SAAR (underpredicted) | HU1 | 1.55 | 3493 | 3172 | 147 | 144 |
| HU | 2.41 | 4359 | 3637 | 150 | 148 | |
| HU | 1.31 | 3295 | 3029 | 143 | 138 | |
| HU | 1.72 | 3383 | 3016 | 146 | 136 | |
| HU | 2.16 | 3272 | 2767 | 142 | 127 | |
| HU | 3.07 | 2861 | 2363 | 130 | 87 | |
| HU | 1.85 | 2808 | 2580 | 124 | 107 | |
| HU | 1.43 | 2860 | 2534 | 129 | 103 | |
| Medium SAAR (overpredicted) | MO3 | –1.47 | 2481 | 2710 | 100 | 118 |
| MO | –1.50 | 2432 | 2731 | 96 | 121 | |
| MO | –1.74 | 2427 | 2742 | 94 | 122 | |
| MO | –1.34 | 1961 | 2299 | 53 | 81 | |
| MO | –2.03 | 2116 | 2572 | 65 | 106 | |
| MO6 | –1.45 | 2421 | 2748 | 93 | 123 | |
| MO | –1.32 | 2108 | 2430 | 63 | 92 | |
| Medium SAAR (underpredicted) | MU | 2.10 | 1821 | 1441 | 39 | 2 |
| MU4 | 1.39 | 1905 | 1690 | 48 | 22 | |
| MU | 1.57 | 2270 | 1949 | 77 | 42 | |
| MU | 1.70 | 2661 | 2312 | 113 | 84 | |
| MU | 1.43 | 2530 | 2204 | 104 | 66 | |
| Low SAAR (overpredicted) | LO5 | –2.67 | 1776 | 2300 | 32 | 82 |
| LO | –2.23 | 1754 | 2232 | 31 | 72 | |
| LO2 | –2.98 | 1572 | 1950 | 9 | 43 | |
| LO | –2.02 | 1607 | 2113 | 14 | 55 | |
| LO | –1.66 | 1656 | 2128 | 20 | 59 | |
| LO | –1.78 | 1268 | 1553 | 1 | 8 | |
| Low SAAR (underpredicted) | None | – | – | – | – | – |
We used purposive sampling to identify six systems for our in-depth case studies. We wanted to select cases with high, medium and low SAARs in case the way in which systems operated differed by size of SAAR. The median SAAR was 2258 with an IQR of 1808–2662. We labelled any system in the highest quartile ‘high SAAR’, any system in the lowest quartile ‘low SAAR’ and all others ‘medium SAAR’. We also wanted to select systems where the residual was positive and negative, indicating over- and underprediction of the SAAR. Some systems had predicted SAARs that were higher than the actual SAAR (overpredicted) and some had predicted SAARs that were lower than the actual SAAR (underpredicted). We categorised the 27 cases by size of SAAR and direction of residual (see Table 7). We then grouped geographical neighbours together with the intention of selecting only one case from a cluster in order to maximise variation of selected cases.
Our intention had been to select one case from each ‘type’ (see column 1 in Table 7). However, ‘low SAAR underpredicted’ did not have any cases and ‘high SAAR overpredicted’ was very similar to the ‘medium SAAR overpredicted’. Instead we selected cases that could represent a cluster of systems distributed across the types. We labelled selected cases using H for high SAAR, M for medium SAAR, L for low SAAR, U and O for under- and overpredicted, and 1–6 to indicate case number. Selected cases HU1, LO2, MO3, MU4, LO5 and MO6 are indicated in bold in Table 7.
Chapter 5 Phase 1: explaining variation in potentially avoidable admissions rates for acute trust-based systems
Objective
The majority of emergency admissions occur in general acute trusts. 1 These trusts are a key part of any emergency and urgent care system. How they manage admissions may affect rates of avoidable emergency admissions, and indeed acute trusts can be the focus of efforts to address avoidable admissions. In Chapter 4 we found routine data on a limited number of hospital characteristics for the geographically based systems studied. We found that three of these hospital characteristics explained variation in the SAAR: the conversion rate of ED attendances to admission, the proportion of all emergency admissions with length of stay < 1 day, and the use of EDs. Another characteristic we tested did not explain variation in the SAAR: waiting time for planned admission. Some hospital characteristics are routinely available by acute trust that are not available by PCT, for example numbers of acute beds. Our objective was to test whether or not hospital characteristics explained variation in the SAAR. This work was published towards the end of the study. 38
Methods
Characteristics of acute trusts
We searched databases for routinely available data on the characteristics of acute trusts in England. Ideally we wanted to include characteristics of the acute trust catchment populations because these were important when explaining variation in the geographically based SAAR (see Chapter 4). The best variable we found was the deprivation level of the population in the geographical area in which the acute trust was located. We used the postcode of the ED of each acute trust and identified the percentage of households in poverty in the area around the postcode using the ONS data on Middle Super Output Areas. Where there were two or more EDs based at different geographical sites, we took the mean of these percentages. We found routine data on 11 acute trust characteristics including demand, supply, accessibility and management variables.
Analysis
We undertook linear regression in IBM SPSS Statistics version 20 weighted for acute trust catchment population to account for larger uncertainty of estimates for smaller populations. The dependent variable was the SAAR for 129 acute trusts. The independent variables were tested in a hierarchical multiple regression in two blocks, using forward stepwise regression within each block. Variables were included if the p-value for the t-test was < 0.05. These blocks were determined by the extent to which the factors tested were modifiable by acute trust managers. In block 1 we tested population-related factors: percentage of household poverty in the area in which the hospital was located and demand for the ED in terms of attendance rate. We then used the residuals from block 1 as the dependent variable in block 2 and tested the additional effect of acute trust characteristics.
Findings
Univariate linear regression
We display descriptions of the factors that were tested in the multiple regression in Table 8.
| Factor | Source | Rationale for inclusion | Expected direction of relationship | Median (IQR) | % for variable | Range | Pearson’s r2 (%) | p-value | Direction of effect |
|---|---|---|---|---|---|---|---|---|---|
| Location | |||||||||
| POVERTY: % households in poverty in location of hospital | ONS 2007–8 | Emergency admissions are higher in deprived areas and areas at short distance to hospital | The higher the deprivation, the higher the admission rate | 22 (17–27) | – | 9–52 | 13 | < 0.001 | + |
| Demand | |||||||||
| EDUSE: number of first attendances at EDs per head of population | Health and Social Care Information Centre 2009–10 | People are more likely to be admitted if they attend an ED | The more attendances, the higher the admission rate | 0.29 (0.23–0.33) | – | 0.13–0.53 | 27 | < 0.001 | + |
| Supply | |||||||||
| ACUTEBEDS: number of acute beds per 1000 population | Department of Health website KHO3 2009–10 | Supply-induced demand OR demand-driven supply | The more beds, the higher the admission rate | 1.8 (1.5–2.1) | – | 1.0–2.9 | 16 | < 0.001 | + |
| EDNUMBER:a number of type 1 or type 2 EDs within an acute trust | QMAE Q1 2009–10 | Use of EDs increases when distance is shorter and patients are more likely to be admitted if they attend the ED | The more EDs, the higher the admission rate | – | 1, 56%; 2, 24%; 3+, 20% | – | 0 | 0.994 | + |
| Hospital management | |||||||||
| FT: foundation trust statusb | Name of trust | Foundation Trust status is given to hospitals able to manage services independently | Foundation trusts have lower admission rates | – | FT, 53%; not FT, 47% | – | 1 | 0.199 | – |
| Accessibility | |||||||||
| ACUTEOCC: % acute beds occupancy | Department of Health website KHO3 2009–10 | High occupancy rates cause EDs to look for alternative to admission OR lots of emergency admissions keep acute bed occupancy high | The higher the occupancy rate, the lower the admission rate OR the higher the occupancy rate, the higher the admission rate | 0.86 (0.83–0.89) | – | 0.72–0.97 | 3 | 0.054 | – |
| OPWAIT: % waiting 1 month or less from primary care referral to outpatient appointment | Health and Social Care Information Centre Outpatient statistics 2009–10 | The higher the proportion waiting less than a month, the less likely it is that health will deteriorate and lead to emergency admission | The higher the proportion, the lower the admission rate | 51 (45–56) | – | 34–88 | 5 | 0.009 | + |
| EDWAIT: mean duration in ED (minutes) | Health and Social Care Information Centre 2009–10 | Long waits create pressure in ED to admit OR short waits increase accessibility, which increases demand, which leads to more admissions | The longer the wait, the higher the admission rate OR the longer the wait, the lower the admission rate | 131 (124–149) | – | 98–203 | 5 | 0.015 | – |
| ELECTIVE: mean time waiting for elective admissions (days) | Health and Social Care Information Centre Provider level analysis for admitted care 2009–10 | People waiting longer for elective care may deteriorate and increase the rate of emergency admissions OR a high rate of emergency admissions causes long elective waits | The longer the wait, the higher the emergency admission rate | 47 days (42–51) | – | 20–79 | 6 | 0.005 | – |
| ED management | |||||||||
| LOS0: % admissions which stay less than 1 day in hospital | Calculated from HES 2008–2011 | Hospitals which cannot provide rapid discharge from ED admit people briefly | The higher the percentage of short stays, the higher the admission rate | 28 (23–31) | – | 17–42 | 9 | < 0.001 | + |
| CONVERSION: % ED attendances admitted | Health and Social Care Information Centre AE 2010–11 | Hospitals which convert more of their attendances to admissions will have a higher admission rate | The higher conversion rate, the higher the admission rate | 24 (21–27) | – | 14–39 | 0 | 0.712 | + |
Correlation between factors
Use of the ED and poverty levels around the acute trust were correlated (Pearson’s r > 0.4). There was a negative correlation between use of the ED and the conversion rate (Pearson’s r > 0.4): as use of the ED increased, the percentage of attendances converted to admissions decreased.
Multiple regression
In block 1, only demand for the ED was statistically significant because of the correlation between this factor and poverty levels around the acute trust (Table 9). The residuals from block 1 were used as the dependent variable to then test the added effect of acute trust characteristics. Five factors explained some variation in block 2: supply determined by the number of acute beds per 1000 population, management or coding of admissions determined by percentage of admissions with length of stay < 1 day, management within the ED determined by the conversion rate from ED attendance to emergency admission, the management of the hospital determined by its foundation trust status, and access to planned care determined by percentage of people waiting less than 1 month for a hospital outpatient appointment. Regression metrics are reported in Appendix 2, showing that the model was a good fit. The variance inflation factor for block 2 was approximately 1 for each factor so there was no indication of collinearity. The final multiple regression explained 53% of the variation in the SAAR when all the factors in Table 9 were entered in a single block. Because of the correlation between some factors, it is likely that a number of regressions would fit the data equally well so there is some uncertainty about the model presented here.
| Block | Predictorsa | Unstandardised coefficient | 95% CI | Standardised coefficient | p-value |
|---|---|---|---|---|---|
| 1: population | EDUSE | 2566 | 1608 to 3524 | 0.445 | < 0.001 |
| 2: acute trust related | ACUTE BEDS | 0.80 | 0.40 to 1.20 | 0.30 | < 0.001 |
| LOS<1 | 0.06 | 0.04 to 0.09 | 0.34 | < 0.001 | |
| CONVERSION | 0.06 | 0.04 to 0.09 | 0.31 | < 0.001 | |
| FT | –0.31 | –0.59 to –0.02 | –0.16 | 0.035 | |
| OPWAIT | 1.56 | 0.16 to 2.97 | 0.16 | 0.031 |
Conclusion
Avoidable admission rates were higher for acute trusts with higher ED attendance rates, higher numbers of acute beds per 1000 catchment population and higher conversion rates from ED attendance to admission. Hospital managers may be able to reduce avoidable emergency admissions by reducing supply of acute beds and by reducing conversion rates from ED attendance.
The factors which explained variation in the SAAR for acute trust-based systems were very similar to those found for geographically based systems in Chapter 4: ED attendance rates, short length of stay and the conversion rate from ED attendance to admission explained variation. One difference was that deprivation levels explained a much lower amount of variation between acute trust-based systems. This is probably to do with the poor quality of the deprivation factor we obtained for acute trust catchment areas. Other differences were related to the availability of data for different definitions of systems. For acute trust-based systems we were able to test the new factor of the number of acute beds per 1000 population and this explained some variation: the higher the number of beds, the higher the SAAR. The model was a good fit (see Appendix 2). There is uncertainty about this model, and other models are likely to exist which explain the SAAR equally well.
Link with phase 2
We identified the large residuals for the regression reported in Table 9. Only two of the acute trusts associated with the six case studies had large residuals in this analysis (emboldened in Table 10). That is, the variables included in this regression predicted the SAAR well for most of the acute trusts in our case studies.
| Case study system | Acute trust | Residual | SAAR | Predicted SAAR |
|---|---|---|---|---|
| HU1 | A | 1.27 | 2985 | 2516 |
| B | 2.17 | 3601 | 2807 | |
| LO2 | A | –0.49 | 2105 | 2310 |
| B | –1.02 | 1287 | 1555 | |
| MO3 | A | 0.99 | 2446 | 2158 |
| MU4 | A | –0.35 | 1814 | 1946 |
| B | –0.40 | 1912 | 2106 | |
| LO5 | A | –1.19 | 1511 | 1943 |
| B | –1.35 | 1719 | 2115 | |
| MO6 | A | 0.15 | 2314 | 2259 |
Chapter 6 Phase 2: case studies of six emergency and urgent care systems – methods and overarching themes
Aim and objectives
The aim was to explore six emergency and urgent care systems in depth to identify further factors that explain variation in potentially avoidable admission rates. A secondary aim of the case studies was to help explain how factors identified in phase 1 affected potentially avoidable admission rates.
The objectives were to:
-
describe each system configuration in terms of services available and relationships between services
-
obtain perceptions of key stakeholders about what worked within their system and what needed to be improved.
Design: multiple case studies
For this component of the study we used Yin’s multiple case study approach. 39 Yin’s post-positivist perspective was suitable for our use of case studies within a mixed-methods study. The cases were emergency and urgent care systems defined by our geographically based systems. Yin identifies three types of case studies: exploratory, descriptive and explanatory. Our case studies were both descriptive and explanatory, describing six systems and offering further possible explanation of variation in the SAAR.
Numbers of cases
There is a need to balance selecting a large enough number of case studies to allow patterns to be determined across cases and a small enough number to make full use of the strength of the case study approach to explore issues in depth. Yin points out that ‘A fatal flaw in doing case studies is to conceive of statistical generalisation as the method of generalising the results of the case study’ (p. 32). 39 Rather, analytic generalisation is important, where a theory is generated within one case study and replication – or not – of the theory is considered in the other case studies. We selected six case studies to offer a balance of pattern identification and depth of understanding.
Selection of case studies
The regression undertaken in phase 1 identified 27 candidate systems for in-depth case study, that is with SAARs which could not be fully explained by the factors in the regression reported in Table 5. We explained in Chapter 4 (section Link with phase 2) how we selected the case studies, whereby we purposively selected a mix of high, medium and low SAARs and over- and underprediction by the phase 1 regression. Early in the study the health-care commissioners in two selected cases did not want to participate in the study or did not respond to our invitation. At the time we felt that commissioners were an essential stakeholder because they helped us to define the services providing care to the population of the system. Therefore, we replaced each system with another system within the same geographical cluster. When this occurred again later in the study we kept the original systems because we realised that we could make use of the commissioner’s website to obtain the information we needed about service use by their population.
Data collection
Case studies can draw on six key sources of evidence: documents, records, interviews, direct observation, participant observation and physical artefacts. 39 Because of the complexity and size of each system, observation was difficult. Therefore, within each case we used three types of data: documents, routine data and interviews. The interviews were central to the case studies, with support from documents and routine data.
Interviews
We undertook semistructured face-to-face and telephone interviews with key stakeholders in the system to describe the system configuration and perceptions of issues affecting avoidable emergency admissions within their service and the wider emergency and urgent care system. Our intention had been to undertake one case at a time, visiting the site two or three times to undertake most of the interviews face to face. However, permissions were needed for access to multiple organisations within each system; procedures were time-consuming and occurred at different speeds for different organisations. We made a decision early in the data collection period to undertake interviews for an organisation as soon as the permissions were given and we considered that telephone interviews offered a more efficient approach. EK visited each site once for 1–2 days to undertake as many face-to-face interviews as possible and then conducted the majority of interviews by telephone.
It was important that a wide variety of stakeholders were interviewed to offer different perspectives of the system in which they worked. The sample we attempted to recruit in each case study was informed by our conceptual framework, drawing on commissioners, service providers and patient representatives. Services included the wide range of services within an emergency and urgent care system. Within any acute trust serving a large proportion of the system population, we included parts of the trust responsible for emergency admissions such as EDs, medical admission units and bed managers. Our planned sample included health-care commissioners, ED staff (consultant, lead nurse, manager), acute trust bed manager/medical admissions unit, GP, GP OOH service, ambulance trust operations manager and paramedic, community health service providers, social care staff, nursing/residential care home manager and the Healthwatch lead. We did not attempt to interview patients and their families, so an important set of voices was missing from our work.
A local collaborator was identified in each organisation of our six systems, who helped to identify relevant staff within the local area. Each potential interviewee was contacted by email and formally invited to take part in the study. Non-responders to our initial invitation were contacted again within 1 month. Our intention was to undertake around 15 interviews per case, totalling around 90 interviews across the six case studies.
Emma Knowles began the interviews by being clear about the geographical area we were interested in and the services we included in any emergency and urgent care system. She then read out a list of the 14 conditions rich in avoidable admissions. This ensured that each interviewee was clear about the territory being addressed by our study. The interviews covered key drivers of potentially avoidable admissions within the interviewees’ organisation and the wider system. We clarified when initiatives were in operation, because interviewees liked to discuss new services and future plans whereas we were more interested in services operating in 2008–11. We did not tell interviewees whether their system had a high or low SAAR, or why we had selected their system, until near the end of the interview. A topic guide was developed based on our research objectives (see Appendix 3) and piloted in the first few interviews. The topic guide worked well and few adjustments needed to be made for later interviews. Written informed consent was gained. Interviews were digitally recorded with permission and lasted around 60 minutes. We offered £77 to the organisation (not the individual) for the time given for the interview.
Documents
We searched the websites of commissioners and service providers for information that would help us to describe the system configuration and relationships between services. We also searched for key documents to identify initiatives in operation that might affect avoidable admissions during our SAAR time period. In particular we searched for the annual reports from each PCT, acute trust, community health trust, ambulance service trust, local authority commissioner and Local Involvement Networks (LINks) published between 2008 and 2013, and the annual public health report in each system. We paid particular attention to any references made to major changes to the structure of the organisations or workforce; emergency care; emergency admissions; and our 14 clinical conditions.
Routine data
We had planned to request from the services within each case study any local data on use of key services within the system during the previous financial year. However, as our interviews progressed we became more interested in the routine data about the case in our phase 1 regression and focused on this instead because it was measured consistently for all of our cases.
Operationalising the definition of a case
Each case was an emergency and urgent care system defined by the main services used by a population served by the health-care commissioning bodies known as PCTs at the time of the data collection (2011–13). Services included in a case could be within or outside the geographical boundaries of the geographically based systems in the phase 1 regression. We relied on local commissioners and their websites to identify key services to include in a case.
Context in which cases were operating
We were interested in 2008–11, for which the SAAR was calculated. We interviewed stakeholders in 2012 and 2013. As stated earlier, we asked interviewees to clarify when initiatives they discussed were in operation so we could relate these to the findings in the phase 1 regression.
The interviews were undertaken at a time of major NHS reorganisation. PCTs were in the process of being disbanded to make way for Clinical Commissioning Groups (CCGs). Patient representation structures were also changing, with Healthwatch introduced in April 2013, taking over the function of LINks. This made it difficult to identify some stakeholders for interview because they were in the process of leaving their job or had yet to be appointed.
The subject of emergency admissions and their reduction was high on the political and commissioning agenda. Tariffs were in operation nationally which reduced payments to service providers for emergency admissions occurring over the rate of previous years.
Analysis
Analysis of interviews
Interviews were transcribed verbatim. We analysed the data in a number of stages:
-
Alicia O’Cathain selected a case and read 6–10 transcripts from a variety of stakeholders to identify themes based on issues common to the set of transcripts. These themes were written up in conjunction with the quantitative data from the phase 1 regression for that case. The aim was to describe the case and to identify some hypotheses about factors affecting potentially avoidable admissions that we had failed to measure in phase 1 and reasons why we had over- or underpredicted the SAAR for that case. We called these our ‘case personalities’. These documents were read by our research team and discussed at our management meetings and at SECF meetings, where the content was questioned and challenged. This focus on one case at a time helped with analytical generalisation, as subsequent cases were compared and contrasted with previous cases.
-
When we had completed our six case personalities we analysed all the interviews using the first four stages of framework analysis. 40 The framework approach was appropriate because it allows for the exploration of both a priori and emergent issues. The first stage of familiarisation had already occurred during the development of the case personalities. The second stage of developing a thematic framework was based on the issues we identified in our case personalities. These themes were mainly descriptive, based on the key services within the emergency and urgent care system. We had some conceptual themes, such as incentives within the system related to avoiding emergency admissions and how easy it was perceived to be to admit a patient. The third stage involved EK and COK systematically coding transcripts to the themes using NVivo 10 (QSR International, Warrington, UK). During this process, AOC, EK and COK discussed the process of coding to facilitate consistency. The fourth stage involved EK and AOC taking data extractions related to a theme or subtheme and analysing these for three purposes:
-
We identified stakeholder perceptions of an issue without paying attention to the cases.
-
We identified within-case perceptions of that issue in preparation for the multiple case analysis, focusing on summarising the issue for each case in comparison with the other cases.
-
We rewrote our case personality documents to ensure that they reflected the more systematic approach to our interview analysis.
-
Analysis of documents
We extracted data from documents by making summary notes of issues related to emergency and urgent care, documenting date and source. Data extraction was undertaken by a researcher who had not been involved in the interviews (RC), who was therefore not focused on finding issues to support the interviews. After writing up a preliminary case personality based on the interviews, we used this documentary extraction to add to the case personalities by offering context; verifying, contradicting or clarifying interview content; and identifying gaps in the interviews.
Analysis of multiple case studies
After developing full case personalities, and a matrix summarising findings for each case for each theme, we undertook a multiple case study analysis by using ‘pattern matching logic’39 to look for cross-case patterns, particularly issues that appeared distinctly in one type of case (e.g. underpredicted SAAR) and not another (e.g. overpredicted SAAR). The matrix displayed subthemes (rows) for each case (columns) and we used it to identify hypotheses for testing in phase 3.
Validity
There can be concerns about the validity of data collected within interviews in terms of whether or not it represents ‘the truth’. For example, interviewees can give accounts of a situation to show themselves or their service in a good light, while finding fault with others; or they may repeat beliefs that are held within a community of health and social care professionals, which may not be supported by data. Construct validity can be increased by using multiple sources of evidence, and chains of evidence, within a case. 39 Our multiple sources were the interviews, the phase 1 regression and documents. We took the views of interviewees as valid individual perceptions of a system, but we also cross-referenced the views of one stakeholder with those of other stakeholders in the system. Sometimes stakeholders described the service provision differently and we put more weight on the view of the stakeholder providing the relevant service.
Findings
The findings are reported in this chapter and Chapters 7 and 8 for ease of reading:
-
We start by describing the cases and interviewees in the case studies (next section).
-
We consider some overarching themes emerging from the case studies (following section).
-
We describe each case in detail (see Chapter 7).
-
We undertake multiple case study comparison to attempt to explain variation between the six emergency and urgent care systems and develop hypotheses for testing in phase 3 (see Chapter 8).
We chose this order of presentation even though the primary focus of the case studies was the multiple case study comparison. We felt that it was helpful to the reader to lead up to the primary analysis by first understanding the overarching themes emerging from the case studies and then seeing how they played out in the six different cases.
Description of cases and interviewees
Cases
We summarise the findings from the phase 1 regression for each of the cases in Table 11. Some key issues to notice are:
-
HU1 had a high SAAR; it was one of the highest in England.
-
LO2 and LO5 had low SAARs; LO2 had one of the lowest in England.
-
Three cases had medium SAARs, although MU4’s SAAR was rather low.
-
HU1 and MU4 had actual SAARs that were higher than their predicted SAARs (underpredicted) and four had actual SAARs that were lower than their predicted SAARs (overpredicted). One interpretation of this is that HU1 and MU1 performed worse than predicted and the others performed better than predicted in our phase 1 regression. We use the terms ‘better’ and ‘worse’ here for ease of communication, rather than necessarily suggesting that a lower than predicted SAAR is good. The premise of the study suggests that services should aim for a low SAAR, but this involves a value judgement and various assumptions.
-
Three cases were rural (LO2, MO3 and MU4).
-
One case had an exceptionally high ED attendance rate (HU1).
| HU1: high SAAR, underpredicted | LO2: low SAAR, overpredicted | MO3: medium SAAR, overpredicted | MU4: medium SAAR, underpredicted | LO5: low SAA, overpredicted | MO6: medium SAAR, overpredicted | |
|---|---|---|---|---|---|---|
| SAAR | 3493 | 1572 | 2481 | 1905 | 1776 | 2421 |
| Rank SAARa | 147 | 9 | 100 | 48 | 33 | 93 |
| Predicted SAAR | 3172 | 1950 | 2710 | 1690 | 2300 | 2748 |
| Predicted rank | 144 | 43 | 118 | 22 | 82 | 123 |
| Deprivation (%) | 9 | 5 | 9 | 4 | 5 | 8 |
| Rural status | Urban other | Rural 50% | Rural 50% | Rural 50% | Urban major | Urban major |
| ED attendance rateb | 426 | 175 | 218 | 349 | 319 | 284 |
| Conversion rateb | 94 | 125 | 105 | 74 | 108 | 94 |
| % LOS < 1 day | 32 | 27 | 29 | 27 | 35 | 31 |
| % non-conveyance | 8 | 34 | 20 | 31 | 16 | 8 |
| % able to see GP in 48 hours | 80 | 81 | 82 | 89 | 79 | 77 |
Interviewees
We invited 186 individuals to be interviewed. We undertook 82 interviews with all those who agreed (Table 12). We had representation from each acute, ambulance and community NHS trust, and each of the local authorities identified within our systems. GPs were represented in five of our systems (no GP representation from HU1). We had representation from four PCTs/CCGs (no representative could be identified in LO2, and MO6 did not respond to our request to engage with the study). In our early selection of cases we replaced cases if the commissioner did not agree to be interviewed. We were unable to undertake interviews with Healthwatch representatives in four systems (HU1, MO3, LO5 and MO6) because some of them were not fully in operation at the time of our interviews. A nursing/residential care home manager was identified in each system and invited to take part in an interview; there was no response to these requests.
| Organisation | Role | HU1 | LO2 | MO3 | MU4 | LO5 | MO6 |
|---|---|---|---|---|---|---|---|
| Commissioning | Emergency/urgent care | 2 | 0 | 1 | 1 | 1 | 0 |
| General practice | GP | 0 | 1 | 1 | 1 | 1 | 1 |
| GP OOH | 0 | 1 | 1 | 0 | 0 | 1 | |
| Community | Trust manager/director | 1 | 1 | 1 | 1 | 1 | 0 |
| District nurse/lead | 0 | 0 | 1 | 0 | 0 | 0 | |
| Community matron/practitioner | 0 | 1 | 1 | 1 | 1 | 1 | |
| MIU/WIC/UCC | Manager/practitioner | 1 | 0 | 1 | 1 | 1 | n/a |
| Ambulance | Operations manager | 1 | 1 | 1 | 1 | 1 | 1 |
| Paramedic | 1 | 1 | 1 | 1 | 1 | 1 | |
| Acute trust A | Strategic manager | 1 | 1 | 0 | 0 | 0 | 0 |
| Bed manager | 1 | 0 | 0 | 0 | 1 | 1 | |
| Medical admissions unit/clinical decisions unit practitioner | 0 | 0 | 1 | 1 | 0 | 1 | |
| ED A | Clinical lead/consultant | 0 | 0 | 1 | 1 | 1 | 2 |
| Senior nurse/matron/practitioner | 0 | 2 | 1 | 1 | 1 | 0 | |
| Manager | 0 | 1 | 1 | 1 | 0 | 1 | |
| Acute trust B | Strategic manager | 0 | 1 | n/a | 1 | 0 | n/a |
| Bed manager | 1 | 0 | n/a | 1 | 1 | n/a | |
| Medical admissions unit/clinical decisions unit practitioner | 0 | 1 | n/a | 0 | 1 | 0 | |
| ED B | Clinical lead/consultant | 1 | 0 | n/a | 1 | 0 | n/a |
| Lead nurse/matron | 0 | 0 | n/a | 0 | 1 | n/a | |
| Manager | 1 | 0 | n/a | 0 | 1 | n/a | |
| Healthwatch | 0 | 1 | 0 | 1 | 0 | 0 | |
| Local authority A | Adult care director/manager/practitioner | 2 | 1 | 1 | 1 | 1 | 2 |
| Local authority B (if applicable) | Adult care director/manager/practitioner | 1 | n/a | n/a | n/a | n/a | n/a |
| Nursing/residential care | Home manager | 0 | 0 | 0 | 0 | 0 | 0 |
We undertook between 11 and 17 interviews in each system (see Table 12). The system with the fewest interviewees was MO6 because this had only one acute trust with a single ED, whereas the other five systems each had two EDs. At the time of the interviews for MO6, there were negative media reports about the acute trust and staff redundancies. Some potential interviewees did not take part because they were in the process of leaving their jobs, or were no longer employed by the trust. Overall, we felt that we achieved a reasonable balance of views across all the case studies and within the cases. We paid attention during the analysis to the voices that were missing within each case.
Overarching themes
As well as helping to identify differences between the six systems, the case studies identified general issues about emergency and urgent care systems and avoidable admissions. The cases were selected because they were more likely to identify issues we had not measured in the phase 1 regression. These cases could also identify issues that might be common to all systems. We report the overarching themes below before describing how these issues occurred within each case. We selected quotes which illustrated the issues we found, labelling them by type of stakeholder but not by case in order to protect the anonymity of our interviewees.
The standardised avoidable admissions rate includes the right conditions
Most of our interviewees agreed that the 14 conditions we had included in our SAAR as rich in avoidable admissions should not be admitted to a hospital bed. That is, our SAAR had credibility among key stakeholders in the emergency and urgent care systems in our sample.
A lot of things can be dealt with very well in primary care as long as the team’s set up to deal with them. I mean just from what you’ve told me, 75% of them [patients with the 14 conditions] could be dealt with face to face [in primary care] and that’s the end of the story.
GP
A few interviewees had some interesting reflections on the list of 14 conditions. One GP noted that some of the conditions were preventable from a primary care perspective, for example exacerbations of COPD, whereas others simply had to be dealt with when they occurred, such as head injury. Some interviewees felt that, although they could see why abdominal pain was on the list, uncertainty about this condition in practice meant that admission was likely. Other interviewees wanted to add further conditions, including some trauma, alcohol-related admissions, dementia, heart failure, end-of-life care and ‘off their legs’. A counterargument was raised by a few interviewees – illustrated by the quote below – that admissions from these conditions were not as avoidable as one might think because minor illness is more complicated than it appears. This drew attention to the point that we made earlier in the report, that these conditions may be rich in avoidable admissions rather than all admissions with these conditions being avoidable.
The thing about all of these conditions you list, I mean on the face of it they’re quite straightforward but actually each and every one of them has got a huge list of differential diagnoses and they all exist within a specific context. There are different patients with a lot of different backgrounds and if you think about it, critical illness is actually very simple to deal with most of the time but minor illness is more of an academic game to make decisions and the critical thing is about information and so actually although straightforward in many ways it can also be quite complicated.
Ambulance service
Population characteristics drive avoidable admissions
Interviewees considered population characteristics to be a major driver of admission rates and of health-care use in general. This concurred with our findings in the phase 1 regression, where employment deprivation explained a large amount of variation in the SAAR. This was also visible in our six case studies, where there was a clear relationship between high SAAR and high levels of deprivation. Interviewees identified four interlinked population-related factors relevant to avoidable admissions.
Social deprivation and morbidity
Interviewees perceived that people from socially deprived areas used health services more and were admitted more than people from affluent areas. This was supported by our phase 1 regression, where deprivation explained 72% of variation in the SAAR. Interviewees’ perceptions offered some insight into why this might occur. They felt that these populations had more health problems. This was also apparent in our phase 1 regression, where the prevalence of health problems such as COPD explained 20% of variation in the SAAR in the univariate regression (see Table 4) (interviewees from areas described as having high COPD prevalence caused by their industrial history saw this as a significant driver of avoidable emergency admissions. COPD admissions made up 10% of our 14 conditions), and deprivation and morbidity were highly correlated (see Table 5). Health problems mentioned as contributors to avoidable admissions included COPD, coronary heart disease, dementia and alcohol-related illness.
In our phase 1 regression, there was a correlation between prevalence of health problems and deprivation, but deprivation had an effect over and above morbidity levels because it explained far more variation than any disease prevalence variables we tested. The views of interviewees helped to identify possible explanations for this. They described issues associated with deprivation other than morbidity, such as people not making use of health promotion services or not engaging in healthy activities, which they often described as ‘not looking after themselves’, people using health care inappropriately, a lack of car ownership causing people to use the emergency ambulance service or stay in a hospital bed once they were taken to an ED, and low morale in these communities, with accompanying mental health issues. They also perceived that comorbidities within this group made it difficult to discharge them from an ED. In addition, they felt that the level of acuity of the condition when people turned up at the ED could affect admission; some older people and people from rural communities did not contact services until their situation was very serious and therefore were more likely to need an admission. Affluent populations were not simply the opposite of this but were described as sometimes having alternatives to the NHS available to them such as seeking private health and social care.
Ethnicity and immigration
Interviewees described how the ethnicity of their population could affect avoidable admissions. In our phase 1 regression we tested the percentage of the population from ethnic minority groups. We found that it explained 9% of variation in the SAAR in the univariate regression but that it was no longer significant once deprivation was included in in the regression. The reason for this was apparent in the case study interviews, where interviewees described many people within ethnic minority groups as socially deprived. However, interviewees also described how ethnic minority groups were extremely diverse. Some communities were described as making less use of NHS services because they had support structures within their communities, and in one system some groups were described as less likely to have avoidable admissions because they had their own health services or were more likely to use private health care.
When ethnic minority groups were described as high users of health services, this was in relation to EDs rather than hospital bed use. This high use of EDs was related to recent immigrants whose English was poor, or recent immigrants from Eastern European countries where people used health services in a very different way from how policy-makers and service providers wanted people to use health care in England. This latter issue was described as a recent problem and might not have been applicable to the time period of our SAAR.
Elderly people
The increasing numbers of elderly people were seen as driving increases in admissions. Interviewees perceived that the increases were due both to elderly people living alone and thus not having someone to look after them on discharge from an ED, and to elderly people in nursing homes being sent to EDs inappropriately. Dementia and confusion, and comorbidities, increased their chances of being admitted once in contact with the health service. Interviewees from our rural systems were acutely aware of their large elderly population, whom they saw as either vulnerable or having high expectations (depending on their wealth). When calculating the SAAR we adjusted for age, so any variation in age between systems was considered in our phase 1 regression. Our standardisation was based on a number of older age groups including > 85 years old, so we took very elderly people into consideration. We also tested for the density of older people within a system population in the phase 1 regression and found that, although this explained 18% of variation in the SAAR in the univariate regression, it no longer explained variation once deprivation was included. The percentage of pensioners living alone did not explain any variation the phase 1 univariate regression and this may be because of the dual effect of elderly people living alone and living in nursing homes.
Culture, expectation, stoicism
Interviewees talked about two problem subgroups of the population: people who did not contact services until their problem was very serious (described as stoic) and people who contacted services for very minor problems. The former group were described as coming from rural and elderly populations, using health services in the way people had used them in the past. This was sometimes viewed as a problem because, instead of seeking help when a problem was minor, they waited until it was serious and so were more likely to need hospital admission when they presented with their problems. The latter group were described as younger people and people in urban areas who were used to a 24-hour culture, people from socially deprived communities and wealthy elderly in rural areas. Interviewees referred to a changing culture of entitlement and people not wanting to wait for any service beyond a few hours: ‘I think again that people are perhaps impatient’ (Healthwatch). This culture was described as affecting demand for EDs and then once people got to an ED they were more likely to be admitted because of the way EDs were run (see later section on EDs). Given the relationship between culture/expectation and other population characteristics such as age, geography and social deprivation, it is likely that we measured this in our phase 1 regression without explicitly intending to. Indeed, because of the link interviewees made between culture and social deprivation, this was possibly another issue wrapped up in the deprivation variable in our phase 1 regression. Many interviewees regarded this increase in expectations and impatience for access to services as a national problem, and indeed noted it occurring in all of the case studies.
Relentless demand . . .
These population characteristics, and changing characteristics, caused a heartfelt perception from some interviewees in all six systems that demand for emergency and urgent care services was relentless, regardless of the amount of effort made to establish new ways of dealing with it. The language used was emotive and we show quotes from interviewees from a range of services across our six systems to illustrate the sense of helplessness expressed by some interviewees in the face of this demand:
We do have this almost relentless tide of – don’t take this the wrong way – relentless tide of human misery we have to deal with. And it’s going to keep coming whatever we do. I don’t particularly think the self-patient education is a worthwhile thing. I think we just have to deal with what we have to deal with, and you can try and educate patients until you’re blue in the face and it won’t make much difference.
GP
The number of patients attending is getting bigger, the number of ambulance attendances is getting bigger and despite everything that everybody appears to be doing we’re not making an impact in getting the numbers down.
ED
We have all these systems in place. We don’t know why people keep [. . .] going to these horrible A&Es [accident and emergency].
Commissioner
Sometimes it feels like we’re on the edge of a cliff [laughs]. And we’re about to sort of step into the unknown because actually we can’t hold back the tide. I’m mixing all my metaphors here aren’t I [laughs]. We can’t hold back the tide any more. We are seeing for some reason this year we have seen unprecedented increase in demand and in emergency admissions [. . .] we can’t just play with initiatives any more; we have to do something that’s more radical.
Commissioner
Interviewees from cases with relatively low SAARs described high demand for their services. This highlights that the SAAR includes only one fifth of the emergency admissions within a system, is adjusted for age and does not take supply/resources within a case into consideration.
. . . but is educating the population a solution?
Interviewees in all six systems described how people were confused about the choice of services available or were not aware of many of the newer services within emergency and urgent care systems. Their default was to use familiar services such as the GP, ED or 999. Interviewees suggested educating people about the range of services available, and what services do, for example the availability of X-rays. They suggested using marketing campaigns or individual-level education when someone attended an ED. However, not everyone agreed, thinking that people did know about services or that they had tried a number of marketing education approaches already with varying degrees of perceived success.
Supply-induced demand may be at play
The phase 1 regression for acute trust-based systems indicated the possibility of supply-induced demand whereby, the more acute beds a hospital had, the higher the SAAR was. There was some explanation of how the number of beds affected practice in one system: the acute medical consultant went down to the ED to help to discharge patients when the beds were almost all full but did not do this otherwise. In other systems some interviewees expressed concerns about the potential to increase demand by increasing supply. For example, placing more services in EDs would simply result in higher attendances, sending ambulances to everyone would increase the likelihood of admission, and increasing capacity in social services would simply result in that capacity being filled. The quotes we use below are from commissioners but this view was also expressed by a range of service providers.
Because the more we put into the acute end the worse it has got.
Commissioner
I think one of the reasons that we’re not as low [avoidable admission rate] as we potentially could be is we’ve got so many beds. You know we have the equivalent of a DGH [district general hospital] out there in our community hospital [. . .] some health communities hardly have any or have none and when you have beds they get filled you know. It’s a very strange thing but it happens . . . even if they weren’t counted as emergency admissions, you would get a high percentage of transfers from acute hospitals to community hospitals which releases more [beds in the acute trust to fill].
Commissioner
Urban and rural areas face different challenges
Interviewees described the different challenges faced by systems based in urban and rural areas. In urban areas, populations were described as more likely to be deprived and have expectations of instant access to services, whereas in rural areas they were described as more likely to be elderly and stoical. Both of these descriptions included factors associated with high rates of emergency admissions, although age was adjusted for in our SAAR. In our phase 1 regression, urban areas had higher SAARs than rural areas, even after adjusting for deprivation levels. However, interviewees in rural areas described how difficult it could be to provide services such as GP OOH, home-based community services and emergency ambulance services because of the distance these services needed to travel:
If people choose to live in deepest darkest [X] to a certain extent they’re making a choice about being kind of further away from services generally. [. . .] We have responsibility to make sure that everyone gets acceptable high quality health care but when you’re in such a rural county how can you ensure that that happens when you have you know people who are living miles away from anywhere.
GP
The geography of rural areas appeared to be an incentive for services to focus on care provided by general practices and non-conveyance of patients to EDs by the ambulance service. Indeed the three rural systems in our sample had higher rates of ambulance non-conveyance than our three urban systems (see Table 11).
Acute trusts
Emergency admissions occur in acute trusts, making them an extremely important part of any emergency and urgent care system. Acute trusts were situated centrally within some of our six geographically based systems, or on the boundary where they offer care to populations from a number of geographically based systems. The source of admissions can be through the ED, directly from GPs into an admission unit, or from other sources within the acute trust such as outpatients. We interviewed health professionals and managers from medical admission units (or similar), EDs and wards within these acute trusts. Admissions were mainly through EDs in our six cases (52% to 77%). A later theme describes EDs but some of the subthemes described here were also relevant to EDs within the acute trusts.
Hospital-centric systems
Interviewees in one case described their system as hospital-centric, with resources focused on the acute trust rather than the community services. This case had the highest SAAR in our case studies. This issue was not raised by interviewees in the other five cases.
Coding of admissions
Interviewees in two of our case studies offered starkly different views on how admissions were coded within their acute trusts. In one acute trust any patient moved from the ED to one of the ‘holding areas’ such as the clinical decision unit, in order to limit breaching of the 4-hour wait target for EDs, was coded as an admission. This trust had a high SAAR and it was higher than predicted. In an acute trust in another system, a number of ‘holding units’ were available and people were not coded as admissions even if they stayed overnight in a bed in one of these areas. This trust had a medium SAAR that was lower than predicted. In our phase 1 regression we included a factor of the percentage of admissions staying less than 1 day; this was significant in the multiple regression and might represent variation in coding of admissions.
Senior review
Interviewees from all cases identified junior doctors (across hospital specialities) as being more likely to admit patients than their more experienced colleagues. In EDs junior doctors were also described as more likely to order diagnostic tests. This could lead to an increased likelihood of admission in two ways. First, patients had to wait for tests, with the potential then for breaching the 4-hour waiting target and being admitted to prevent this. Second, diagnostic tests could create more rather than less uncertainty by identifying something that needed further investigation before a patient could be discharged from the ED.
Early senior input into a patient pathway was perceived by many interviewees as the key to reducing avoidable admissions. This input could come from ED consultants or their colleagues in medicine and surgery. Senior review could occur within EDs by having their own consultants available 7 days a week or being actively on admission avoidance duty by assessing attendees as soon as they arrived. Consultants could then start the discharge process early or identify those needing diagnostic tests early. In our phase 1 regression, the conversion rate from ED attendance to admission explained variation in the SAAR, and variation in senior review might possibly underlie this.
Interviewees described initiatives they had put in place whereby medical – and to a lesser extent surgical – consultants were easily available to ED doctors to offer advice about the need for admission. This senior review was described as being offered to GPs as well as EDs in some of our cases.
If you talk to A&E places they are fed up to the back teeth of when they have an admission they ask for an opinion from say the surgical team and the F1 House Officer comes down and what you need is senior decision makers, seeing the patient as early in the journey as possible. That’s the only way you can avoid unnecessary admissions.
Hospital
When we’ve got consultants, I think the decision making’s pretty good [. . .] the more junior doctors [. . .] will not take the same risk as a consultant [. . .] my experience is the more senior person you get to see the patient, the quicker you get a decision, the quicker you often get them discharged and turned around [. . .] but as soon as you start putting junior doctors in they tend to take longer, they over assess, over investigate [. . .] and find something else.
Hospital
Proactive about early discharge or admission avoidance
Acute trusts in the six cases were described differently in terms of the emphasis they placed on admission avoidance. In one system (high SAAR and higher than predicted), interviewees discussed initiatives in place to facilitate early discharge even though we were interviewing them about admission avoidance. In the other systems, the acute trusts had initiatives to deal with admission avoidance which were sometimes described as taking a very proactive approach to their work. Schemes included increasing the use of senior review (see above) and use of multidisciplinary teams to facilitate discharge from attendance (see later theme ‘Proactive initiatives to avoid admissions’ for details). In our case studies, these systems had medium and low SAARs that were lower than expected.
Emergency departments: extremely busy places
A strong theme running across five of the systems was the busyness which acute trust and ambulance interviewees reported within the EDs. There was also some perception that this had increased over time:
busy is not always the right word, it can be quite hectic it can be, extremely, extremely busy with an awful lot going on [. . .] there can be several ambulances waiting, all the rooms can be full and you think, if there was a major incident to happen, anything major that can be you know, several people just in a row of accident one two cars and you just think we just seem sometimes to be right at that capacity point and you think what would happen if something was to happen.
Ambulance service
The hospital and the A&E has been red [busy] quite a lot. It feels more so this year than it has been in other years.
Community services
One reason offered for this busyness was having too few consultants. Two cases reported significant shortage and both of these had higher SAAR than predicted in our regression. Other reasons were the need for senior review and the lack of access to services OOH. In addition, some interviewees also noted that their EDs were physically small in terms of the space available to accommodate demand and that this added to the sense that the department was busy. The relentless demand theme described earlier was highly relevant to EDs because they were seen as attractive to the general population (see following quote). In the phase 1 regression, use of EDs explained variation in the SAAR for the acute trust-based systems.
I think sometimes people are confused but they know A&E is there 24/7. So they’ll just turn up [. . .] everyone knows A&E so why are we trying to put other things in and we still know they are going to turn up in A&E anyway, so why don’t we just put it in one place and then stream?
Hospital
Ambulance services: relying on other services
Interviewees described ambulance services as helping to avoid admissions. In the phase 1 regression, there was considerable variation between the non-conveyance rates of different ambulance services, and this explained some variation in the SAAR. Interviewees from services other than the ambulance service wanted ambulance services to do more non-conveyance, even in systems with high levels of non-conveyance.
Emergency care practitioners: good in theory
Interviewees described a number of current or past initiatives in their systems where emergency care practitioners (ECPs; this was the terminology used by our interviewees) worked in different settings such as ambulance services, GP OOH, urgent care centres (UCCs) or general practices. We focus here on their use in ambulance services, where their job was to keep people out of hospital appropriately by treating them at home or referring them to community based services. ECPs were described by interviewees as having the potential to reduce avoidable admissions but as meeting problems in practice: they were often few in number and this could affect their ability to show an impact, or affect their availability when needed; the service faced competing priorities around admission avoidance and helping their organisation to meet response time targets; and although ECPs could administer antibiotics they could not prescribe drugs and thus needed to involve other health professionals in a patient’s care. Five of the six systems had ECPs in the ambulance service at some point during the SAAR period but only two systems had active ECPs at the time of the interviews; initiatives had been stopped in other systems because of financial constraints or the view that they had not been cost-effective. Interviewees in systems with active ECPs wanted more ECPs and wanted them to do more in terms of prescribing and testing. Interviewees from ambulance services described a move towards training paramedics to do more rather than increasing numbers of ECPs.
Need to rely on other services
The ambulance service interviewees described efforts to avoid admission, many of which required collaboration with other services in the system. They described using some type of tool/service to help ambulance crews to take patients to services other than EDs, such as decision software, a clinical controller or a directory of services. Because of the need to use a range of services, ambulance service interviewees had connections with other services through regular meetings of managers to discuss problems and solutions, through formal pathways for managing specific conditions or through informal referrals to different services such as walk-in centres, GPs and GP OOH. Interviewees from the ambulance services discussed the risk involved in leaving people at home and the need to have responsive services to refer to or discuss patients with, such as GP, GP OOH and social care. This ability to communicate easily and quickly with other services was identified as key to admission avoidance but often lacking:
one of the issues my staff talk to me about is social patients . . . Now people think that the stress of being in the ambulance service comes from attending multi-vehicle road accidents where there’s carnage. The biggest stress faced by my staff is you have a patient that is not looking after their self, the A&E department is not the appropriate place but you can’t get hold of social services to come in and intervene at an early stage . . . We don’t have access to them . . . They won’t accept referral from the ambulance service.
Ambulance service
Community services
Community beds: available but not accessible
While community beds were described as being available as an admission avoidance option, there was a sense among interviewees from some systems that community beds were predominantly used for ‘step down’ rehabilitation from hospital rather than as a ‘step up’ from the community. Despite beds being available in each system, there was widespread discussion regarding the problems in accessing such beds for admission avoidance purposes. Issues described were strict access criteria, a lack of bed availability on a daily basis, and complicated and time-consuming processes in obtaining beds. Some interviewees felt that it was sometimes easier to admit to an acute bed than a community bed (see the later theme of ‘easy option’).
Community nursing
The role of community nursing was discussed with regard to avoiding admissions, specifically community matrons, district nurses and specialist nurses, for example for COPD. In some systems, interviewees were not explicit about the numbers of community matrons within their system. Where there was discussion, there appeared to be a large variation in the numbers of community matrons operating within systems: between 2 and 35. The focus of our interviews was avoiding acute admissions and this was reiterated throughout each interview. The lack of discussion of community matrons by interviewees in some systems may have indicated that they were not seen as a significant stakeholder in emergency admissions avoidance work locally. However, in some systems they were highly valued for the work they did in keeping people at home. The work that community matrons and specialist community nursing teams did in relation to respiratory patients was discussed frequently as effective at admission avoidance.
District nurses were also discussed more in some systems than others, particularly for their work during OOH. In some systems they were seen as a valuable and accessible resource in general, and specifically for avoiding admissions relating to catheter issues:
if we have a catheter problem, I mean I don’t even go out to see the patients, I just ring up the district nurse and I tell them to sort the catheter out, and that is the same boat for out of hours as well as in hours.
GP
Primary care, in and out of hours
Access to general practitioners in hours
A number of interviewees perceived that patients attended EDs because they could not access a GP appointment quickly. They also described scenarios whereby patients were recommended to attend the ED by general practice staff because of a lack of appointments. In the phase 1 regression, there was an association between patient-reported access to their GP within 48 hours and the SAAR in the univariate analysis. This factor explained 25% of the variation in the SAAR. However, in the multiple regression this factor contributed in the opposite direction and this is discussed in relation to the wider literature in Chapter 8.
There were also very positive comments about the general high quality of GPs in the six cases, and recognition of the variability of GP care within a system. For example, while the GP below was clearly passionate about reducing avoidable admissions, he acknowledged that some of his colleagues were not as enthusiastic:
Anything that you think you could do differently?
Well I would tell some of my [GP] colleagues off. You know do not send people to A&E as a way of passing the buck and getting rid of the problem.
The quality of general practitioner out-of-hours services
The views expressed about GP OOH services by interviewees in all six systems were generally negative. The service was viewed as a problem nationally since the time when GPs could opt out of providing care OOH. The problems described with provision included an inability to engage local GPs in providing the service because it was not paid well compared with in-hours work and GPs wanted a work–life balance. In some systems this led to shifts where no GPs were available to cover some localities. There was reliance on locums from outside the area, and sometimes outside the country, who were described as not knowing local patients, services or systems and having no incentive to keep people out of hospital. This was perceived as particularly a problem in our case study with a medium SAAR which was higher than predicted:
they do struggle to fill the shifts. In particular [locality A] and often [locality B] can’t get anybody to come. Some, most weekends there’s 2 or 3 shifts that haven’t been filled.
GP
Patient access to GP OOH services was viewed as poor because of a lack of capacity, and a lack of patient confidence in the service, which was perceived as leading to increased use of EDs OOH. Indeed one system had introduced a GP into their ED OOH to deal with this type of demand, and another had tried but failed to attract GPs to do this. The ambulance service, as well as patients, sought contact with GP OOH services. In one system the interviewee from the ambulance service felt that if the GP OOH service were more responsive to contacts from the ambulance service they could leave more people at home rather than transport them to hospital. In the phase 1 regression we tested awareness of how to contact the GP OOH service and ease of making contact. The first factor explained 10% of variation in the SAAR but neither factor contributed to the multiple regression.
Walk-in centres
All six systems had walk-in centres at the time of the SAAR, although the walk-in centre in one system had been closed by the time we undertook our interviews in that system. Some interviewees valued walk-in centres and could see their role in keeping patients away from EDs and offering an alternative to general practice. Interviewees not from walk-in centres were more likely to express negative views. The closure of a walk-in centre was reported as making no discernible difference to demand for the local ED or primary care. Where a walk-in centre was close to an ED in another system, interviewees in the acute trust questioned its value in terms of alleviating ED workload.
Clinical Commissioning Groups: a positive development
Commissioning was rarely mentioned by interviewees. A few interviewees who did discuss it were positive about CCGs because they perceived that this encouraged GPs to take a greater interest in the wider system of emergency and urgent care.
Social care: under-resourced
Interviewees in different services in the emergency and urgent care system described examples of close relationships with social services, including working within the same team as them and colocation of health and social teams. However, a common request was for more responsive social care input to allow the timely discharge of patients from EDs. There was also a perceived need to strengthen links between social care and the ambulance service. In contrast, the local authority staff interviewed described a proactive and responsive culture within their organisations:
And we do everything we can to keep people at home wherever possible because that’s where they want to be. Don’t get me wrong, there are times that people do have to be admitted. My team goes out and sees many, many people who have gone off their feet for one reason or another. And you know we put hoists in, we do everything we can to keep them at home, but there are times that people do need medical intervention that can’t be maintained at home. You know and I have said that to people [staff]: do your utmost but you know we can’t prevent everything really.
Local authority
Even interviewees from health services who were positive about the responsiveness of their social care colleagues found it difficult when social care was not available OOH. Local authority interviewees described a lack of resources to offer all the services required by health services to avoid admissions.
Access to mental health services a problem
Mental health conditions made up a tenth of the admissions in our SAAR. While interviewees discussed successful pathways for dealing with many of the conditions in our SAAR, mental health was usually highlighted as a problem. Mental health services were organised in different ways across our six case studies. Mental health and community services were delivered by the same NHS trust in some systems (HU1, MU4, LO5) whereas in others they are delivered by a separate mental health NHS trust (LO2, MO3, MO6). In some systems one aspect of mental health services was spoken about positively, for example the psychiatric team in an ED in one system. However, in the main, concern was expressed about access to mental health services to avoid admissions. Pathways were described as unwieldy, there appeared to be a lack of integration between mental health services and other services, and interviewees from a range of services within and outside acute trusts felt that responsiveness was a problem. As with social care, a lack of resources was highlighted by some interviewees.
What else is really bad is mental health services. They’re absolutely appalling, we don’t have a mental health service I don’t think. What we actually need is some sort of mental health liaison team. [. . .] We don’t have anything in the A&E department, we have to refer in to it . . . it’s appalling, it’s one of the worst services that there are I think.
ED
Care homes: education and community support needed to keep people in the home
Care home patients were viewed by interviewees as potentially a problem because they were more likely to be admitted and more likely to stay in hospital for longer. Interviewees from a range of health services discussed the tendency for nursing and residential home staff to call an ambulance to transport their elderly residents to hospital when this was not necessary. While interviewees sometimes described how social services could be bypassed through hospital admission when a residential home patient required a ‘step up’ to nursing home care, they also described how more support for care homes was needed, particularly from general practice, both in and out of hours. In five of the case studies there was some discussion of schemes that had been put in place to educate staff in nursing homes about when hospital care was needed, or general practices were attached to nursing homes to offer personal primary care. Interviewees across systems described the potential such initiatives had for making substantial reductions in emergency admissions.
Lack of out-of-hours provision
Some interviewees in some systems praised the OOH availability of experienced district nurses facilitating admission avoidance. However, most of the interviewees in all six systems expressed concern about the lack of OOH provision of support services causing avoidable admissions. Interviewees reported a lack of community and social care provision, diagnostic testing and multidisciplinary teams based in EDs. In some systems these services were available weekdays 09.00 to 17.00, in others they were available weekdays 08.00 to 10.00 and in some they were also available at weekends. Even the system with weekend services available wanted services available for longer to help avoid more admissions. In three systems, perceptions of OOH provision were particularly poor, with references made to a Monday-to-Friday mentality. These included the two systems where the SAAR was higher than predicted.
I mean everything is pretty much 09.00 to 16.30, and barely existent at weekends . . . I think I guess things like DVT [deep-vein thrombosis] clinics, cellulitis clinics, work at the weekend. The access to community hospitals is non-existent at weekends. Anyone who needs packages of care, intermediate care for discharge, supported discharge teams don’t seem to work at weekends and I think we need to move towards a 7-day service if we’re going to cope with the increase in numbers of attendances.
Acute trust
Interviewees from the ambulance service appeared particularly frustrated by the lack of options available to them OOH:
Services are still predominantly available in hours of working, so when old Mrs Jones has a chest infection, that needs dealing with quite quickly, there is no pathway for us to feed into at 02.00 in the morning. If they phone their GP, their GP might not be able to get out there for several hours. Yet you’re met with a patient who maybe needs to start on a course of antibiotics and to be treated in some way but within the community. I’ll give you an example, with the COPD patients their service closes basically at 6 p.m. so it doesn’t work over the weekends either. The majority of calls that we get are either in the evening or they are at the weekend. And the majority of them will be because old Mrs Jones has waited through the weekend, and would much rather go and see her own doctor on a Monday, and she just can’t manage any longer. Whereas that patient could have a COPD nurse that would come out and see them, but there is no access to that service at the weekend.
So the only alternative is to take Mrs Jones to ED?
That is correct, yes.
Integration is a way of working, not simply a scheme
So far, we have discussed individual services within systems. Our interviewees felt that admission avoidance required co-ordination between these services. Integration could take a number of forms which we discuss below, and could face a number of facilitators and barriers.
Colocation of services
One way of offering an integrated service is to locate services in the same space. This colocation occurred for some services in some of the six systems. For example, social services and specialist nurses shared an office, or a walk-in centre or the GP OOH service was located next door to the ED. There was a view among interviewees that more colocation was needed, even in systems that had more of it than the other systems. Some interviewees had a vision of a full range of emergency and urgent services on the same site – GP, social services, ED, minor injury unit and walk-in centre – with a front door directing patients to the most appropriate place. This vision was driven by the need to be both efficient from a service point of view, and patient-friendly so that patients did not feel they had gone to the wrong place or had to choose where to go. Although colocation could occur for services run by different organisations, it could also occur for services within a single organisation. In particular, one acute trust interviewee felt that the different admission routes into the hospital were not co-ordinated and that colocation would help. The ED was seen as the focus of some colocation because patients were seen to gravitate there anyway: ‘I think people will naturally, we’re like a magnet, a big flashing beacon’ (ED). The downsides of colocating services with EDs were also put forward: a lack of space in EDs and, if the ED was not situated centrally, the need for patients to travel large distances for care.
Interviewees in one system spoke positively about the colocation of health and social services, which allowed informal communication between staff who needed to offer a co-ordinated approach to admission avoidance:
When you’re talking about like an admission avoidance [. . .] I can walk out of my office [. . .] the first desk outside my office is the manager of the social workers. But then my [. . .] community health staff sit next to the social workers and the social workers’ assistants and if you’ve got somebody that you’re particularly concerned about all parts of the jigsaw need to come together and that’s how we do it here.
District nurse
However, colocation did not necessarily mean integration because one service might not be able to refer to another (if a contract had not been established for this to happen). Interviewees with colocated services could also identify ways of improving on integrated working by sharing managerial structures and information databases as well as premises.
Formal and informal relationships
Some systems had joint posts and joint working practices such as multidisciplinary teams within health, and between health and social services. ‘We have a social worker within the team as well, so we have got three stakeholders within one service’ (rapid assessment team). These teams often had a remit of admission avoidance. Relationships between services could be formalised through these specific posts and specific teams, but could also have built up over the years as professionals in different organisations, or parts of the same organisation, got to know each other. Interviewees who noted the presence of informal relationships facilitating integration were aware that this was dependent on personalities and wanted to see more formal processes of integration in place.
Pathways
A common approach to formalised integration was the development of pathways for specific conditions. A number of those discussed in the interviews were for conditions in our SAAR: falls, DVT, cellulitis and COPD. Different agencies involved in the care of patients with the specific condition signed up to a process for treating the condition efficiently and in a way that avoided admission unless this was necessary. Interviewees described pathways within their systems, both ones which they perceived as effective and others which were not. Interviewees describing effective pathways highlighted the need to develop the initial pathway on a small scale, get full sign-up across the system and ensure effective communication between different professionals:
what works well [in terms of developing an effective pathway] is when the system all works together essentially so you’ve got clear pathways of care that’s actually everyone is signed up to in the system instead of having a pathway of care that people aren’t signed up to because then they don’t work. So you’ve got to have clear pathways of care. You’ve got to have really good interfaces between all of the organisations and you’ve got to make sure that it’s getting the systems to work together because if you don’t you’re almost like it’s never going to work really.
GP
Facilitators and barriers to integration
Interviewees identified the need for frequent meetings between different agencies to facilitate integration. These allowed people to talk about problems and look for solutions together. The meetings described took place at different levels: senior management met to consider strategy and frontline workers met to facilitate integration at an operational level. These meetings could help professionals understand what services outside their own organisations provided, and could facilitate them making joint decisions about individual patients when needed:
because what we could do there was we all worked together and because we all sat around the table every Tuesday afternoon, we all got to know each other very well, discussing cases that sometimes were relevant and sometimes weren’t relevant but because we actually got to know each other we struck up I wouldn’t say friendship but certainly professional support if you like. So if there’s an issue, I know I can contact somebody who was part of that team and vice-versa.
Local authority
If one service needed to pass a patient onto another to avoid an admission then they needed to have confidence that the service could deliver safe care. Interviewees described how confidence came through building knowledge about each other’s skills, and trust in each other. The necessity of trust to integration was brought up by many interviewees. This trust built up over time through communication and understanding the expertise within different organisations. Colocation could help by allowing professionals to get to know each other.
I think that some of it is just the fact the people get to know you, and what you’re providing and get to know how your service, what your service does . . . Some may get to see the stats so they see that they are an effective service, and those things. Sometimes it is just the fact that they see what the referrals are like, and are generally happy with the referrals.
Walk-in centre
Poor experience of another service on one occasion could result in bypassing it in the future. This was particularly pointed out by ambulance service interviewees, who stated that ambulance crew would not transport patients to an alternative to an ED if that service had failed to deliver care on a previous occasion.
To actually ensure that the need for communication and we can be confident in the support that there is in the community when we discharge these patients back. Too often we are obliged to admit because we don’t have enough information and we’re not confident enough of what exists in the community to support the discharges.
ED
Interviewees described how different services worked to different timescales and this could prevent integration. Ambulance service and ED interviewees needed help from other services within minutes and hours, whereas other services – such as social services – were viewed as working on a basis of days and weeks. Responsiveness could also be about willingness to help and ease of asking for help, for example a single telephone number.
Interviewees described how integration took time. Some systems seemed to have a history of integrated practices, whereas others had recently introduced schemes to help integration. The history of integration could pervade the system, or simply relate to a single pathway around COPD, for example.
I just don’t think there’s been a culture of working together.
Commissioner
Quite often they’re not used as well as they should be because our A&Es have got a culture of once somebody’s in there, particularly somebody with support needs, because of the lack of understanding of what goes on in the community they default to admission.
ED
A stable workforce was identified by interviewees as allowing different organisations to build trust in others needed to support admission avoidance. ‘But some of that again is because I know the people because I’ve been here for a long time’ (local authority).
Interviewees described how information about a patient was required to offer confidence about a decision not to admit. Some sharing of patient-level information occurred, which facilitated admission avoidance. Some of this was paper copy, but some interviewees described information technology systems which talked to each other. For example, in two systems the acute trust staff could access GP notes for residents of a particular CCG to check on medication. However, it was mainly the case that the records of other organisations such as GPs and social services could not be accessed because of the perceived reluctance of that organisation to do so, or the lack of information technology compatibility between relevant organisations.
Interviewees recognised that they needed to communicate with a range of agencies and departments to avoid an admission if a patient had complex needs. An issue we identified within the interviews, rather than interviewees themselves raising this, was the sheer number of groups and organisations that needed to operate in an integrated way to help avoid admissions. The ambulance service needed to work closely with the ED, walk-in centres, GPs, GP OOH and community services. The acute trust needed to work with GPs, community and social services. Departments within the acute trust had to work with each other: the medical admissions unit and consultants from different specialties had to work with staff in the ED; for example, a pathway within a hospital was reported as ensuring that diagnostics were undertaken quickly enough to send patients home rather than into a hospital bed. Some systems focused on one or two of these integrations only, and indeed interviewees reported the breaking up of some integrated working in order to prioritise other integrated working. For example, teams within primary and community care were dismantled to create integrated teams between health and social care:
we had many years ago modernised the way that they worked and did a lot of stuff that again helped keep people out of hospital. And then in the name of integration many of those nurses were removed from practices. [. . .] They were down-graded. They were merged with Social Services [. . .] kind of disintegration of primary care began then.
Commissioner
There were many aspects to integration; the variation between our six case studies is explored in detail in Chapter 8 but the cases with the lowest SAARs had the best integration practices within our six cases.
Geographical boundaries
The geographical boundaries of different services in the system could make avoiding admissions extremely difficult. Some EDs took patients from a number of localities, each with different community services and local authorities. Interviewees in hospitals described the difficulty of not admitting patients if they resided in a neighbouring area because of the need to know about the provision of primary, community and social services which could help to avoid an admission:
the referrals are different, the assessments are different, the you know what I mean everything is very different and that is just something very simple but that does happen with a lot of services you know trying to get through [to] even the district nurse, everything.
ED
In five of our geographically based systems, the population had an acute trust of which they were the largest users. Therefore, the acute trust had an incentive to integrate with community and social services within that locality. Patients living outside that locality would not necessarily have the same level of admission avoidance available to them because of the challenges of integrating with a large number of agencies in different localities. One ED employed a health professional to get to know the services available in the localities it dealt with. One system population faced extreme difficulties on this front because they were not the main population for either of the two acute trusts they used (high SAAR which was higher than predicted).
Proactive initiatives to avoid admissions: multidisciplinary teams
Interviewees described schemes for bringing different disciplines together to help to avoid admissions. A common scheme was a rapid assessment team. These had different names in different places but were made up of multiple disciplines such as nurses, physiotherapists, occupational therapists (OTs) and social workers (sometimes) as well as access to equipment. These were often seen as highly successful at admission avoidance by services in touch with them, particularly if they were described as proactively seeking patients within the system to help avoid admission. They could run from the acute trust or ED, actively seeking attendances at medical admission units or EDs to facilitate discharge.
Other schemes involved senior clinicians proactively assessing patients for discharge from the ED, GPs in EDs, creating pathways, and helping GPs to access community beds with one telephone call. All systems described some schemes that were present during our SAAR period or had been recently introduced. An important aspect of these schemes for generating a local perception of success at admission avoidance appeared to be their proactive approach: actively looking for patients in the ED, or actively checking on vulnerable patients who were in their own homes. The importance of being proactive was highly apparent in one system with two acute trusts which ran the same type of scheme. One scheme was described as successful and the other not because ‘[name of acute trust] as an organisation were not as proactive’ (community service).
A hospital bed is the easy option, the safe option and the only option
Interviewees used the terms ‘easy option’ and ‘safe option’ to describe emergency admission to a hospital bed, or direction to an ED. Hospital-based interviewees described services outside the hospital as not taking responsibility for the care of patients and taking the easy option of calling an ambulance or sending patients to EDs. Interviewees from outside the hospital described why the hospital was an easy option: they had difficulty in locating an alternative service because of the time it would take or because it was not available. Examples included a GP spending an hour attempting to locate a team who might (or might not) prevent an individual patient being admitted, a paramedic experiencing a lack of community diagnostics and timely GP advice during the OOH period, and a community matron highlighting that it was easier for staff to admit a patient rather than identify which community services were available in a particular locality. Within the hospital, ED staff also discussed admission to a hospital bed as an easy option. Sometimes discharging from an ED required contact with numerous community and social care providers, or locating the relevant one for a patient’s postcode. It was quicker and easier to admit to a hospital bed, and this option inspired more confidence in ED staff worried about whether community services would be available if they sent a patient home:
and often the easy option the safe option is to send people into hospital, although we know that’s not often the safest option ha! for patients to go into hospital these days.
Commissioner
Incentives to avoid admissions: winter pressures
Some references have been made within earlier themes to incentives to avoid admissions. For example, there was some indication from our interviews with ambulance service managers and paramedics that non-conveyance could help to meet response time targets in rural areas as well as avoid admissions. There was an example of a possible incentive within one system to keep avoidable admissions high: the local private finance initiative was viewed by interviewees as needing high admission rates because these generated money to pay the debt. Other incentives within systems were described which could serve to keep avoidable admissions high because different services needed to address their own targets – the 4-hour target in EDs – or protect their own limited resource – social services. An active incentive to keep avoidable admissions low was winter pressures or ‘escalation’ when hospital beds were full. Interviewees described initiatives put in place temporarily to deal with these pressures, for example senior review in hospital, frequent communication between services and integrated working. This required resources in terms of money and time, which appeared to make it unsustainable all year round. Interviewees also described their incentives to improve integration and thus avoid admissions: wanting to put patients at the centre of care, encouragement from the Department of Health, the vision of their strategic management cascading down, that it was part of people’s job descriptions, and a desire to reduce duplication. Incentives also worked in the opposite direction: ‘At the moment the system’s being incentivised in silos, so the acute trust, the community trust, social care and they’re all about slightly different priorities’ (acute trust).
Resources available within a system
Interviewees referred to reductions over the years in some service provision that focused on admission avoidance, such as reductions in ECPs in ambulance services and the variety of disciplines within a rapid assessment team. Local authority interviewees highlighted a lack of resources to reduce avoidable admissions by meeting social care needs and that therefore there was a need to consider who pays for any integrated working:
I don’t think that in this climate we’ve got the staffing still haven’t got the staffing levels right to meet the demand to best prevent emergency admissions.
Local authority
They’re not going to commission the same services any more. There are going to be less around, so integration actually probably [will] get a little bit worse, because things are going to start being withdrawn. So you can’t integrate with something that’s not there.
Walk-in centre
The documentary analysis confirmed perceptions that job losses and funding reductions had been made during the SAAR period in all six systems. No measure of the variability of resources available within systems was included in our phase 1 regression; this was a significant gap in our quantitative analysis.
Chapter 7 Individual case studies
We report the individual case studies in the order we wrote the preliminary case personalities. We do not label quotes in this chapter at all to maintain anonymity.
HU1 (high standardised avoidable admissions rate, underpredicted)
-
A complex system with two acute trusts outside the boundary and two local authorities within the boundary.
-
A population with high use of EDs.
-
Reported shortage of consultants in the ED.
-
A hospital-centric system with coding of attendances into admissions, and reportedly few community services available particularly out of hours.
-
Reported fragmentation rather than integration of services within the system.
Why HU1 was selected: a really high standardised avoidable admissions rate
This case was part of a geographical cluster of two systems with very high SAARs which were underpredicted by our phase 1 regression (H = high, U = underpredicted). It is helpful to have HU1 in the case studies because:
-
It is a system with a very high SAAR. At 3493 it was ranked at 147 out of the 150 systems. The other system in this geographical cluster also had one of the highest SAARs.
-
It had an underpredicted SAAR in our regression. The predicted SAAR in our regression was 3172, ranked at 144 out of 150, so it was still one of the highest predicted SAARs. The other system in the cluster shared the underprediction and both had two of the worst ranked predicted SAARs.
Description of factors in the phase 1 regression
Its SAAR was ranked at 147 out of 150. It was ranked high for most factors in the regression in phase 1 (Table 13). It had low rankings for two factors: it was ‘other urban’ and had a low conversion rate.
| Factor | HU1 score | Median (range for 150 systems) | HU1 rank |
|---|---|---|---|
| Employment deprivation (%) | 9 | 6 (3–12) | 139 |
| Rural status | Other urban | n/a | 62 |
| ED attendance rate | 426 | 275 (149,909) | 144 |
| Conversion rate | 94 | 100 (70–148) | 56 |
| % length of stay < 1 day | 32 | 28 (14–41) | 131 |
| % ambulance calls not transported to ED | 8 | 21 (8–34) | 138 |
| % able to see GP in 48 hours | 80 | 80 (71–89) | 78 |
Condition-specific standardised avoidable admissions rates: a system-wide problem
HU1 ranked 147 out of 150 overall for the SAAR and generally ranked highly for all conditions with the exception of ‘pyrexial child’ (Table 14). That is, the high avoidable admission rate was likely to be system-wide rather than related to some parts of the system specific to dealing with some conditions. There was some possibility that the system might operate differently for children and adults but the numbers of ‘pyrexial child’ admissions were small compared with other conditions and small numbers may account for the different ranking of this system. There was no obvious relationship between the SAAR and interviewees’ views of pathways for these conditions (see Table 14). In the documentary analysis, COPD and mental health were identified as priorities within the system, with initiatives aiming to improve COPD care in primary care and the early identification of mental health symptoms.
| Condition | Rank of condition-specific SAAR | Interviewees’ perceptions of pathways for condition |
|---|---|---|
| Minor head injury | 148 | |
| Chest pain | 143 | Positive |
| DVT | 87 | Positive |
| Angina | 147 | |
| COPD | 122 | Mixed. Negative: referral route from ambulance service to community not open |
| Mental health | 146 | Negative: pathways, quality, unresponsive but recent improvements |
| Abdominal pain | 143 | Negative |
| Cellulitis | 101 | Negative: no intravenous therapy pathway from walk-in centre |
| Blocked catheter | 110 | |
| Hypoglycaemia | 130 | |
| UTI | 122 | |
| Epilepsy | 93 | |
| Falls | 148 | Mixed. Positive: integrated multidisciplinary team |
| Pyrexial child | 38 |
System configuration: a complicated system
The population of the system is approximately 300,000 people. The services used by the system population are shown in Figure 6, based on information provided during the interviews and the documentary analysis. The system is unusual in our six case studies because the two main acute trusts used by the population are located outside the geographical boundaries of the system. The system also has two local authorities and two GP OOH services. There are two walk-in centres provided by the community trust and one minor injury unit provided by an acute trust, two of which offer radiography.
FIGURE 6.
Emergency and urgent care system configuration for HU1. LA, local authority; MIU, minor injuries unit; WIC, walk-in centre.

Acute trusts: both high standardised avoidable admissions rates, particularly acute trust B
Emergency admissions from this population went to two acute trusts with EDs, both of which were outside the geographical boundaries of the system. In the documentary analysis we identified that one of these acute trusts opened a new hospital building with a new ED at the early part of the SAAR period. Interviewees mentioned this too. One acute trust (A) had a lower SAAR than the other (B), but both had the highest SAARs in our sample of 129 acute trusts (Table 15). The SAARs were similar to the geographically based SAAR of 3493. Acute trust B – with the highest SAAR – was used by the other system in this geographical cluster of two systems with high unexplained SAARs.
| Factor | Acute trust A (rank out of 129) | Acute trust B (rank out of 129) |
|---|---|---|
| SAAR | 2985 (123) | 3601 (129) |
| Predicted SAAR | 2516 (117) | 2807 (127) |
| Acute beds per 1000 population | 1.64 (47) | 2.12 (101) |
| % population attending ED | 32 (91) | 34 (105) |
| % ED attendance converted to admission | 27 (97) | 35 (125) |
| % length of stay < 1 | 34 (117) | 35 (120) |
| % outpatient wait < 1 month | 71 (120) | 67 (117) |
| Foundation trust | Yes | No |
There were differences between the two acute trusts for the factors included in the phase 1 regression (see Table 15) in that acute trust A’s factors tended to be ranked lower than acute trust B’s. Nonetheless, both acute trusts had higher SAARs than predicted by the regression. Note in particular the conversion rate from ED to admission, which was one of the highest in the country. This did not tally with the conversion rate for the geographically based system in Table 13 which was of middling rank and calls into question the accuracy of the conversion rate for the geographically based systems given interviewees’ perceptions of a high rate. The low ranking for percentage of households in poverty identifies a problem with this factor in that it is based on the small geographical area in which the ED is located rather than the catchment population of the acute trust.
Population factors
A sick, deprived and needy community
Interviewees described the population as having high levels of health problems, especially respiratory problems and heart disease relating to its industrial history. It was also a socially deprived population. This system had one of the highest rates of employment deprivation in the country (see Table 13). An annual public health report related the high emergency admissions rate in this area to deprivation. Interviewees described the population as stoic, whereby people approached services late when a health problem was severe rather than attending early for more proactive treatment. However, they also described a ‘culture of dependency’, whereby people wanted to have their health problems checked unnecessarily and did not want to wait for GP appointments.
A lack of awareness of services
Although some interviewees saw this as a national problem, a wide range of interviewees in this area were exercised by the lack of awareness of service provision of their local population, with some evidence that more of them were concerned about this than in the other five systems.
Historical use of services
In contrast to the other five systems, numerous interviewees discussed historical cultural divisions within the population. Interviewees felt that these divisions affected the population’s use of services in that people would attend services only in a specific locality:
Certain people in certain areas will not access services in other areas. [Area A] people will not access healthcare in [Area B]. There’s a mind set in [Area A] that once you get into [Area B] it is a whole different area and we don’t want to be associated. The same will be with [Area C] and [Area D]. [. . .] you might call the whole area [name of HU1] but people will still stick to their roots. [. . .] there’s a boundary that they’re not necessarily willing to cross.
Geographical factors: poorly located services affect demand
Interviewees described how the geographical location of services affected their inappropriate use. First, the area had two walk-in centres and one minor injury unit for a population of 300,000. However, interviewees noted that the distribution of services across the geography incentivised use of the EDs because people in some communities needed to drive past an ED to get to their nearest walk-in centre or tackle a geographical barrier of a bridge. Interviewees also discussed how the acute trusts were distant from many communities so if people travelled to them then they tended to stay or be admitted, especially from deprived communities with low car ownership. In phase 1 we did include a factor about the urban/rural status of a system but this factor did not address the location of services.
Incentives to keep admissions high
A brand new hospital creates supply-induced demand . . .
Interviewees described a hospital in acute trust B as a newly opened private finance initiative which attracted patients to it and which needed to be paid for. They felt that admissions created the money needed to fund the new build and created an incentive for high admissions. We had no evidence that this occurred in practice; this was the perception of a number of interviewees. The following interviewee was not one who said this explicitly but it was there in the way they described the challenges of admission avoidance:
so what we can do is have conversations around tariffs and make sure the hospital doesn’t lose its vital funding in terms of what it relies on in terms of its footfall [. . .] and shift that tariff around so the hospital doesn’t lose out, [. . .] and the people who are shifted out don’t affect the hospital’s finances.
The hospital was not open throughout the whole of our SAAR period of 2008–11. However, one interviewee said that the financial impact of the new build had been felt by the area from 2006 onwards.
. . . and creates a hospital-centric system . . .
A related view was that investment had been hospital-centric in this system, resulting in a lack of investment in community services. The community-based interviewees felt that the balance of investment was of a bygone age when health care was focused on acute beds rather than community beds and there needed to be more emphasis on community beds within the system. In our phase 1 regression, the number of acute beds per 1000 catchment population for acute trust B was high (ranked 101 out of 129), which fits with the picture held by community interviewees that the area was acute bed heavy.
So they have put the money in the wrong place frankly. They have not tried to design a system, just created a very big hospital for the population rather than thinking about a system.
. . . focused on early discharge, not admission avoidance . . .
Interviewees described the existence of intermediate care beds and some initiatives involving integration between different services, but these tended to focus on early discharge rather than admission avoidance. Interviewees with roles to improve integration between services recognised this:
I think when we look to try to avoid admissions from A&E I think it’s quite difficult. We have social work teams in the hospitals around discharge at the back, but we don’t really have a systematic approach to social work or multidisciplinary teams in A&Es [. . .] our A&Es have got a culture of once somebody’s in there, particularly somebody with support needs, because of the lack of understanding what goes on in the community they default to admission. [. . .] we need more of a proactive approach [. . .] there should be that proactive assessment but there isn’t.
. . . with the result that at acute trust B everything gets coded as an admission
Our access to acute trust A for interviews was limited. We managed to undertake only one interview in that trust compared with three at acute trust B. All three interviewees from acute trust B described how patients who were moved from the ED to ‘holding areas’ within the hospital were coded as admissions even if they stayed for only a few hours:
all our patients that stay in the [emergency] department beyond 4 hours are called admissions. So some of these cases quite rightly to work up and exclude a diagnosis requires more than 4 hours, but they would still count on a trust basis as an admission, although they would be a less than 24 hours stay. [. . .] [pause], you’ve avoided admission into the main hospital but you haven’t avoided a nominal admission.
In our phase 1 regression, this system had one of the highest-ranking percentages of people staying less than a day for both acute trusts. This may have been associated with the coding practice in these trusts. Interviewees identified an incentive to generate money to pay for the new hospital. However, there also seemed to be another issue affecting this; a lot of people who needed to be moved to holding units within acute trust B related to 4-hour target breaches in the ED.
Ambulance service
In the phase 1 regression the ambulance service providing care to this system had the lowest non-conveyance rate in the country. The interviewees from the ambulance service were interested in non-conveyance and discussed the positive relationships they had with some health services. However, they were concerned about the lack of consistent provision of services, which limited their ability to keep people in their own homes or take them somewhere other than hospital. The ambulance service annual reports described missed response targets and plans to enable crews to make more use of community-based facilities such as district nursing and walk-in centres.
The emergency department of acute trust B struggled to deal with high demand
High demand for the emergency department
Interviewees identified high demand for both EDs in this system, as interviewees did in our other case studies. This was highlighted in the documentary analysis within annual reports for both acute trusts, with acute trust B describing itself as having one of the busiest EDs in the region. They wondered if this was caused by the location of services, poor access to GPs or an attractive new hospital. Table 15 shows that both acute trusts in this system had high ED attendance.
Lack of senior cover in the emergency department in acute trust B
Two acute trusts in our case studies identified considerable problems with recruitment of consultants within the ED and this was one of them. The ED was identified as having a shortfall of three consultants so patients were reviewed by junior doctors, who were perceived to request lots of diagnostic tests and were risk averse. The view was that there seemed to be little OOH senior cover and even when consultants were present they were not necessarily reviewing patients. Acute trust A was not really described but what few data we had within the interviews identified it as using senior review of attendances. Both acute trusts had high conversion rates from attendances to admissions, with acute trust B having one of the highest in the country (ranked 125 of 129, see Table 15). However, the conversion rate for the geographically based system was surprisingly low (see Table 13) and did not tally with the acute trust data or the interviews, suggesting that it might be incorrect.
Slow diagnostic testing in the emergency department
A second problem identified by interviewees within acute trust B was that diagnostic testing took a long time in the ED and anyone who waited for tests risked breaching the 4-hour wait target so was admitted.
Out-of-hours provision was poor
Interviewees identified that admission avoidance services (delivered in the acute and community sectors), which were available 5 days a week, worked well but needed to be available 7 days a week and in the evening as well as daytime. For example, the ambulance service described how they could not contact a district nurse to come out at 02.00 to unblock a catheter when they could do this at 14.00 on weekdays. This was a common complaint made by a wide range of stakeholders about community, social and mental health services. This was despite both local authorities describing intermediate care services delivered 7 days a week. The community trust interviewees were aware of gaps in community provision and were willing to provide OOH services but identified commissioner unwillingness to fund this. Some interviewees expressed concerns about the lack of availability of GP OOH services locally and how this led to patients attending the EDs. The CCG wanted to place a GP in the ED OOH as a solution but had struggled to find GPs to do this.
Lack of access to intermediate beds
Interviewees discussed the need for community beds for patients who did not need a hospital bed but were admitted for social reasons. There are 30 intermediate care beds available in this area but these were seen as inaccessible because they took patients with only some health problems. In addition, it was highlighted that the geographical location of these beds served a distinct part of the population, and these beds were underutilised, with an interviewee describing them as ‘40% full’. Some interviewees described how these beds were seen as early discharge beds rather than admission avoidance, fitting in with the sense that admission avoidance was not a priority in the area.
There is limited capacity and the acute trusts tend to use the limited capacity for step down, because they would prefer to step down than avoid an admission, because of the step down they have generated an in-patient spell which comes with a finance package associated with it. Whereas a step up they avoid the patient being admitted in the first place.
You’ve got to be fitter than Linford Christie to get a bed in Intermediate Care.
It was a joke, because basically you could only be admitted if you were very well.
In the documentary analysis we identified that acute trust A had opened, and closed, an intermediate care facility with approximately 40 beds during the SAAR period. No mention was made of this during the interviews.
Difficulties accessing primary care
Walk-in centres
There are two walk-in centres and one minor injury unit in the system. Two were identified as offering diagnostic services such as radiography and being able to complete assessments. Interviewees discussed the need to have more diagnostic facilities in the community (which might be related to the perception of having slow diagnostic services in the ED). Even a centre with diagnostic facilities was seen as presenting problems because the facilities might not be available during the centre’s operational hours. Patients could get frustrated, as could ambulance services, which after one or two problems would decide not to divert someone to a centre but take them to the ED, where they were guaranteed to have diagnostics available.
Radiography cover is only part of the opening hours, which is again seems bonkers . . . Some of the time it is there and some of the time it is not . . . when [the centre] is open it needs to be a standard offer I think. It is far too complicated and confusing to have it open as a partial facility some of the time and a full facility at other times.
Although we invited GPs to take part in the interviews, this was the only one of the six systems where we did not undertake a GP interview. Interviewees in all six systems suggested that poor access to general practice might cause high ED attendances. However, here there were hints of a primary care service which had historically built barriers around itself and felt threatened by the introduction of new (and competing) initiatives:
It’s better [the relationship with GPs] than it used to be. Years ago it was a bit of a problem because they were concerned that we might be taking their patients off them. They didn’t really know what to expect of us and therefore they were dubious about us . . . as the years have gone by they’ve realised they’re not as concerned about us as they thought they were. They became more concerned about the . . . Darzi Centres that were being set up.
Fragmentation but determination to integrate
Interviewees described new initiatives, meetings, an urgent care board and a general willingness of service providers to work together. Progress was described, for example recently seeing social services and mental health support available onsite in the EDs. However, this progress was recent, sometimes focused on early discharge rather than admission avoidance, and described by some interviews as ‘add-on’ rather than integrated:
[. . .] the District Nursing team and the Rapid Response Team do a good job. [. . .] I think lots of the teams are working well. I think where the difficulty sits for them is they’re working well in isolation, and they need to start to look at it a little bit more holistically, and that’s kind of the area that we are now embracing really.
An enthusiastic social care sector but a lack of connection with health
Two local authorities served this system; staff were interviewed from both of these organisations. Both interviewees enthusiastically described their involvement in admission avoidance and highlighted some positive relationships between themselves and health care colleagues. In one local authority there was a feeling that social services were being more proactive in admission avoidance than their health colleagues:
I’m really struggling to think of a positive example that helps prevent unnecessary admissions that the council doesn’t lead . . . it’s ploughing through the constant reasons for not doing things because in health there’s always a reason why you shouldn’t do it.
Interviewees from social care and community services acknowledged that the relationship between these two sectors could be improved. A community interviewee perceived these barriers as driven by a lack of colocated working, and working with performance indicators which put health and social care at odds with each other.
Explanatory analysis
The interviews were highly supportive of the results of the phase 1 regression and appeared to explain some of the findings. None of the interviewees was surprised to hear that the system had a high avoidable admission rate. They raised issues about the deprived unhealthy population, the high attendance at the ED and the high conversion rate at the ED. The conversion rate was seen to be caused by consultant shortages and slow diagnostics. Another issue was coding, in that one acute trust needed to fund their new hospital, so it had a perceived incentive to code people as admissions if they were using alternatives to staying in the ED. The SAAR might be higher than predicted because of:
-
poor availability of services OOH
-
a needy sick population
-
acute trust coding of people in ‘holding areas’
-
geographical layout of services
-
lack of senior review in ED
-
lack of integration
-
a hospital-centric system with little access to community beds
-
a focus on early discharge, not admission avoidance.
LO2 (low standardised avoidable admissions rate, overpredicted)
-
A large rural population.
-
Two systems within one, focused around each acute trust.
-
Integration embedded, particularly between community and social services.
-
Proactive approach to admission avoidance.
-
Good GPs.
Why this case was selected
It is helpful to have LO2 in the case studies because:
-
It is a system with a very low SAAR. At 1572 it was ranked at ninth lowest out of the 150 systems.
-
It had an overpredicted SAAR in our regression. The predicted SAAR in our regression was 1950, ranked at 43 out of 150, so it was still low.
-
It is one of two systems in a geographical cluster and also one of six systems following a similar pattern.
Description of factors in the phase 1 regression
Its SAAR was ranked as ninth out of 150. Its ranking was low for many factors in the phase 1 regression but it had a high ranking for the conversion rate from ED attendance to admission, employment deprivation, short length of stay in hospital and access to GP (Table 16).
| Factor | LO2 score | Median (range for 150 systems) | LO2 rank |
|---|---|---|---|
| Employment deprivation (%) | 5 | 6 (3–12) | 47 |
| Rural status | Rural 50% | n/a | 13 |
| ED attendance rate | 179 | 275 (149–909) | 8 |
| Conversion rate | 125 | 100 (70–148) | 135 |
| % length of stay < 1 day | 27 | 28 (14–41) | 65 |
| % ambulance calls not transported to ED | 34 | 21 (8–34) | 6 |
| % able to see GP in 48 hours | 81 | 80 (71–89) | 65 |
Condition-specific standardised avoidable admissions rates
LO2 ranked ninth out of 150 overall for the SAAR and generally ranked low for all conditions with the exception of blocked catheters, angina and falls (Table 17). That is, the low avoidable admission rate was likely to be system-wide rather than related to some parts of the system specific to dealing with some conditions. On the whole, positive interviewee perceptions of specific conditions correlated with the quantitative data: chest pain, cellulitis and UTI were ranked lower in this system than in other systems and management of these conditions was viewed positively by interviewees in various parts of the system. An exception was mental health, which was ranked low in comparison with other systems, but there were negative interviewee perceptions regarding the mental health pathway. In addition, a local public health report during the early part of the SAAR period highlighted the need to develop NHS mental health services in partnership with the voluntary sector and other providers to ensure an integrated service was provided in the community.
| Condition | Rank of condition-specific SAAR | Interviewees’ perceptions of pathways for condition |
|---|---|---|
| Minor head injury | 14 | |
| Chest pain | 13 | Positive: pathway at acute trust B |
| DVT | 32 | Positive: pathway at acute trust B. Mixed view at acute trust A |
| Angina | 76 | |
| COPD | 14 | Positive: effective community nursing pathway. Negative: no ambulance service referral pathway to specialist nurses |
| Mental health | 21 | Negative: inappropriate GP referrals to acute trust A, difficulty for GPs getting same day assessment |
| Abdominal pain | 39 | |
| Cellulitis | 6 | Positive: effective acute, community and ambulance service pathway |
| Blocked catheter | 79 | |
| Hypoglycaemia | 35 | |
| UTI | 11 | Positive: effective community and ambulance service pathway |
| Epilepsy | 35 | |
| Falls | 65 | Positive: effective acute and ambulance service pathway |
| Pyrexial child | 5 |
System configuration
The population is approximately 750,000 people across a very large geographical area. The services used by the system population are shown in Figure 7. The system has two acute trusts in different parts of the area, and a large number of community units indifferent localities. The ambulance service provides the GP OOH service.
FIGURE 7.
Emergency and urgent care system configuration for LO2. LA, local authority; MIU, minor injuries unit; WIC, walk-in centre.
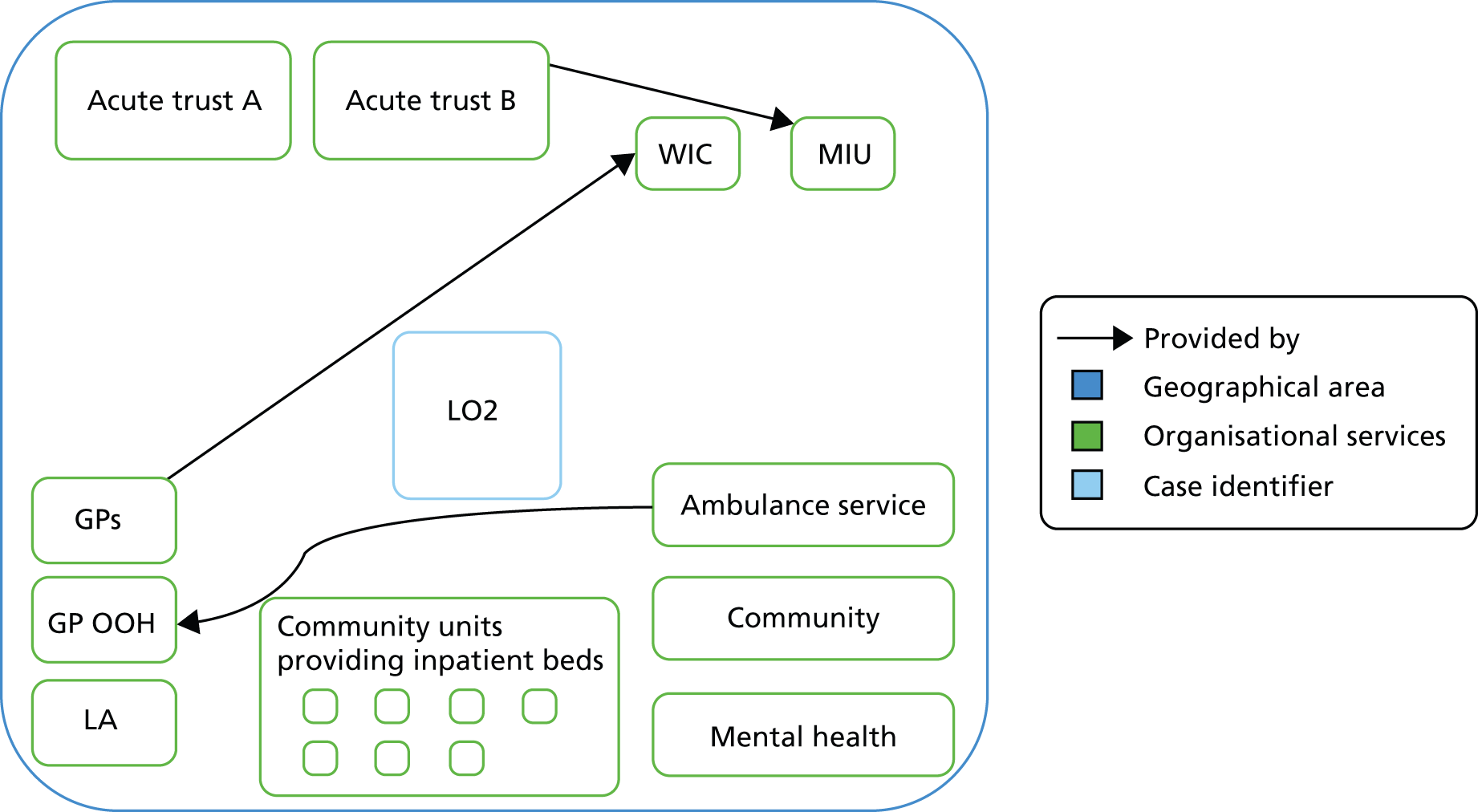
A tale of two acute trusts
Emergency admissions from this population go to two acute trusts with EDs. One acute trust (B) has a considerably lower SAAR than the other trust (A). The population within which each trust is based is very different, with acute trust A located in a much poorer area than B. Acute trust B has one of the lowest SAARs in the country and neighbours the other system in this geographical cluster. Two-thirds of the population of the geographically based system go to this hospital, so it has a considerable effect on the SAAR. The conversion rate is much higher than expected given the SAAR for both of the acute trust-based systems.
Population: two very different areas within the system
In this geographical area there was a sense of two systems in operation, one focused around each acute trust. The catchment population around each trust was described as very different. One side of the area (west) was described by interviewees as having a population which needed or used emergency care more than others: elderly people, deprived communities and immigrant communities. The second area (east) was less well described by interviewees but was seen as having a stable community. These two very different populations were apparent in the acute trust data in Table 18, where the poverty levels around each hospital were very different, as were all the statistics for each trust.
| Factor | Acute trust A (rank out of 129) | Acute trust B (rank out of 129) |
|---|---|---|
| SAAR | 2105 (81) | 1287 (4) |
| Predicted SAAR | 2310 (102) | 1555 (7) |
| % households in poverty | 24 (81) | 11 (5) |
| Acute beds per 1000 population | 2.2 (108) | 1.3 (10) |
| % population attending ED | 26 (51) | 16 (3) |
| % conversion rate | 35 (127) | 26 (87) |
| % length of stay < 1 | 27 (63) | 28 (66) |
| % outpatient wait < 1 month | 48 (51) | 50 (59) |
| Foundation trust | Yes | Yes |
Geography
Rural area
The area is geographically large and mainly rural. Interviewees noted how this made it difficult to travel to offer care in the community. For example, GP OOH and emergency ambulance services were described as difficult to provide. Community services offered more community care because of the distance to travel to hospitals. Interviewees felt that distance affected hospital use in that people living far away would not go to hospital or the ED. There was some suggestion that the rural status of the system encouraged services to take a community focus, yet some interviewees also noted there were other rural areas close by which did not offer the same community services focus as their system.
We’re really lucky in this locality, we have 12 community matrons. Now whilst we’re a very rural patch, which is the rationale for having so many, [. . .]
Separate localities
Interviewees described the different localities within the system, each with very different service configurations and resources. An interviewee based in one locality might describe lots of community beds where another would describe lots of community matrons but no community beds. Indeed the provision of community services was described as a ‘postcode lottery’ by one interviewee. This made it difficult to analyse the interviews and we had to pay detailed attention to where interviewees worked. We had limited access to acute trust B for interviews so the views expressed were largely about the west side of the system. Differences between services in different localities were seen by some interviewees as a problem in terms of ED staff not knowing what was available in each locality and taking the easy option of admitting to a hospital bed.
A strong community service focus
Some interviewees noted a lack of acute beds in their area, although they were in the locality served by an acute trust with a relatively high rate of acute beds per 1000 population. Some interviewees said this was made up for by having lots of community beds available to them and others by the use of community matrons and home care packages:
We have good access to spot purchase beds, and we have access to social care beds, planning beds, rehabilitation beds, intermediate care, domiciliary home care. We have access to therapy, voluntary, mental health.
Proactive approach to admission avoidance
There was a contrast between this case and HU1 in that interviewees described a large, proactive and accessible set of services focused on admission avoidance. There was a rapid assessment team in acute trust A which worked within the ED proactively identifying people who could be discharged. This team was seen by four interviewees as having the single most positive impact on avoiding admissions. Community matrons and district nurses were highly valued by others in the system. District nurses were also highlighted as being ‘excellent’ during the OOH period. There were a dozen community matrons in one locality who were known by and respected by the other interviewees, who viewed them as key to avoiding admissions. Overall, there was a sense that they were proactive about admission avoidance:
as a Trust, admission avoidance has always been, in the 8 years I have been doing this team, it’s just been at the forefront all the time and I think that’s because we are a small, it’s a small acute trust, it’s very small, we have got few community beds so I think there has always been that keep-at-home ethos embedded in the Trust really.
Interviewees also described good community nurse-led services focused on specific conditions: falls service, COPD service, continence and palliative care at home.
Good-quality primary care
The view that LO2 provided good-quality GP care was described by interviewees across the system (acute trust B, ambulance service, GPs and Healthwatch). Interviewees alluded to the geography, population demographic and workforce stability within the area, which contributed to this. These factors were also highlighted in MU4, the only other system that stood out because interviewees discussed high-quality GP care.
The average quality of a GP in [area] is actually very good [. . .] the link-up between the patients and the GPs is still quite 18th century; you know where the patients they think about the GPs as their GPs, my GP, you know. It’s not, let’s say I have got certain old elderly population, they will not see anybody else besides me . . . there’s a good continuity of care.
One connection that appeared well established was that between GPs and paramedics. In the regression analysis, LO2 had high rates of ambulance non-conveyance and this relationship between GPs and the ambulance service was described as facilitating non-conveyance:
you know most GPs if you make a reasonable case to them [are happy with a referral]. And sometimes we don’t even if we’re phoning a GP surgery in hours quite often we don’t even speak to the doctor. Quite more often than not the receptionist will make an appointment for us on our say so . . . I think probably most GPs are used to getting phone calls from the ambulance service and it just becomes part of the way things are done.
A strong emphasis on admission avoidance, out-of-hours service provision and integration
Historical emphasis on admission avoidance
Some interviewees described an ethos of admission avoidance, which contrasted with HU1, where there was emphasis on use of hospital beds and early discharge from those beds. There had been a multidisciplinary health and social services team focused on admission avoidance for many years, which had been stopped to create a different set of integrated health teams and a new team had been created to continue admission avoidance.
Out of hours: normal
When describing services, interviewees communicated the OOH availability of community services (weekend in particular) in a way that suggested this was normal. Extended opening hours for GP practice in the urban areas was described as common. District nurses were available 24/7 and were described as being ‘excellent OOH’. Interviewees wanted an expansion of OOH for some services in some localities but this contrasted with HU1, where there was a sense of little OOH availability and the interviewees wanted some OOH provision. Here in LO2 they felt that social services offered some good services but were not available OOH.
Integration: normal
Interviewees described a range of integration activities embedded in work practices historically, and new initiatives to expand it. The system had participated in early work on integration as part of a national initiative. One locality had community matrons and these were described as working with GPs, community services, hospitals and social services. However, the move to integrate some groups in health in this area had resulted in the dismantling of other groups that integrated health and social care. A health and social services integrated team had been in operation at the time our SAAR was calculated.
Colocation of services occurred and was important to interviewees. There were lots of descriptions of services based in the ED: a proactive rapid assessment team trying to discharge people from the department, as well as newer services such as acute GPs trying to discharge people, mental health team based there as pilot, and social services. Attention was also being paid to improving informational continuity. Colocation in the same office rather than department was viewed positively:
I think we bring in a different mindset into the team and it’s like cross-pollination if you like. It stops the team being just acutely focused. It stops the blame culture that I described earlier around you know it’s because the community didn’t do something that the patient got to us. And I think it’s cohesive. It brings the managers together as well. I mean the teams I don’t think probably see the boundary issues that we see between organisations at a more senior level. We probably pick up on it a bit more because we’ve got more to lose and it’s who’s going to get the hardest beating in a meeting. So it is that we’ve got a different level of responsibility, but it definitely helps with that because it brings us together in a room.
Ambulance service could do more
In an ambulance service annual report the ambulance service regarded itself as having made a significant contribution to reducing hospital admission within this system, and indeed had this as a priority. Good performance in non-conveyance was evident in the quantitative data. Surprisingly, interviewees wanted the ambulance service to do more to keep people at home and away from EDs. Community services wanted a better relationship with the ambulance service and wanted ECPs to offer more widespread services. However, this seemed to be about wanting more, that is expansion, because there were examples given of the ambulance service making direct referrals to community services. There was a falls pathway to allow ambulance services to refer directly to community services, but the community felt more could be done around falls. There was a sense of connection between services and the ambulance service but frustration expressed that that more could be done.
Explanatory analysis
The effect of population and geographical make-up on the SAAR is very large (based on phase 1 regression). This area had low employment deprivation and large distances to travel to a hospital, which were likely to produce low avoidable admissions. This area had a high rate of non-conveyance of ambulance calls and this may fit with the large range of community-based services that the ambulance service could make use of both in and out of hours. The regression may have overpredicted the SAAR because of:
-
integration between services in this system
-
the emphasis on community services
-
proactive approach to admission avoidance
-
availability of services OOH.
MO3 (medium rate, overpredicted)
-
Rural area.
-
Busy EDs.
-
Range of GP-led UCCs in addition to EDs.
-
Integrated health and social care in the community.
Why this case was selected
It is helpful to have MO3 in the case studies because:
-
It is a system with a medium SAAR. At 2481 it was ranked at 100 out of the 150 systems.
-
It had an overpredicted SAAR in our regression. The predicted SAAR in our regression was 2710, ranked at 118 out of 150, making it high.
-
It is one of two systems in a geographical cluster.
Description of factors in the phase 1 regression
Its SAAR was ranked as 100 out of 150. It had this ranking for most factors in the regression in phase 1 (Table 19). It had a low ranking for attendance at EDs.
| Factor | MO3 score | Median (range for 150 systems) | MO3 rank |
|---|---|---|---|
| Employment deprivation (%) | 9 | 6 (3–12) | 130 |
| Rural status | Rural 50% | n/a | 13 |
| ED attendance rate | 218 | 275 (149–909) | 20 |
| Conversion rate | 105 | 100 (70–148) | 93 |
| % length of stay < 1 day | 29 | 28 (14–41) | 98 |
| % non-conveyance | 20 | 21 (8–34) | 90 |
| % able to see GP in 48 hours | 82 | 80 (71–89) | 50 |
Condition-specific standardised avoidable admissions rates
MO3 ranked 100th out of 150 overall for the SAAR and generally ranked in this medium to high area for most conditions with the exception of mental health, blocked catheters and pyrexial child, where it had relatively low admission rates (Table 20). That is, the medium to high avoidable admission rate was likely to be system-wide rather than related to some parts of the system specific to dealing with some conditions. There was some correlation between the rank of the condition and interviewee perceptions; for example blocked catheter, falls and hypoglycaemia, which ranked relatively low in this system (that is low avoidable admissions) and were highlighted by interviewees as having effective pathways. Documentary analysis also highlighted that the ambulance service had improved its links with the falls team and identified a reduction in elderly fallers in the middle part of the SAAR period. There were mixed perceptions of mental health, so it was surprising that this was the second lowest-ranked condition within this system.
| Condition | Rank of condition-specific SAAR | Interviewees’ perceptions of pathways for condition |
|---|---|---|
| Minor head injury | 124 | |
| Chest pain | 90 | |
| DVT | 123 | Mixed. Positive: effective acute and community pathway. Negative: no community pathway open to ambulance service |
| Angina | 107 | |
| COPD | 112 | Positive: effective community pathway |
| Mental health | 33 | Mixed. Positive: effective liaison in ED. Negative: problems for ambulance service OOH |
| Abdominal pain | 120 | Negative: limited access to surgeons in ED |
| Cellulitis | 102 | |
| Blocked catheter | 32 | Positive: effective community pathway |
| Hypoglycaemia | 78 | Positive: effective community pathway |
| UTI | 95 | |
| Epilepsy | 74 | |
| Falls | 61 | Positive: effective community pathway |
| Pyrexial child | 54 |
System configuration
The population is approximately 500,000 people across a large geographical area. The services used by the system population are shown in Figure 8. A key difference between this system and the others so far (HU1 and LO2) is the number of UCCs. During 2008 the emergency and urgent care system closed a number of EDs and opened GP-led UCCs around the geographical area. It also introduced telephone access to urgent advice around the same time to direct people to appropriate levels of care and transport them to the UCCs.
FIGURE 8.
Emergency and urgent care system configuration for MO3. LA, local authority.
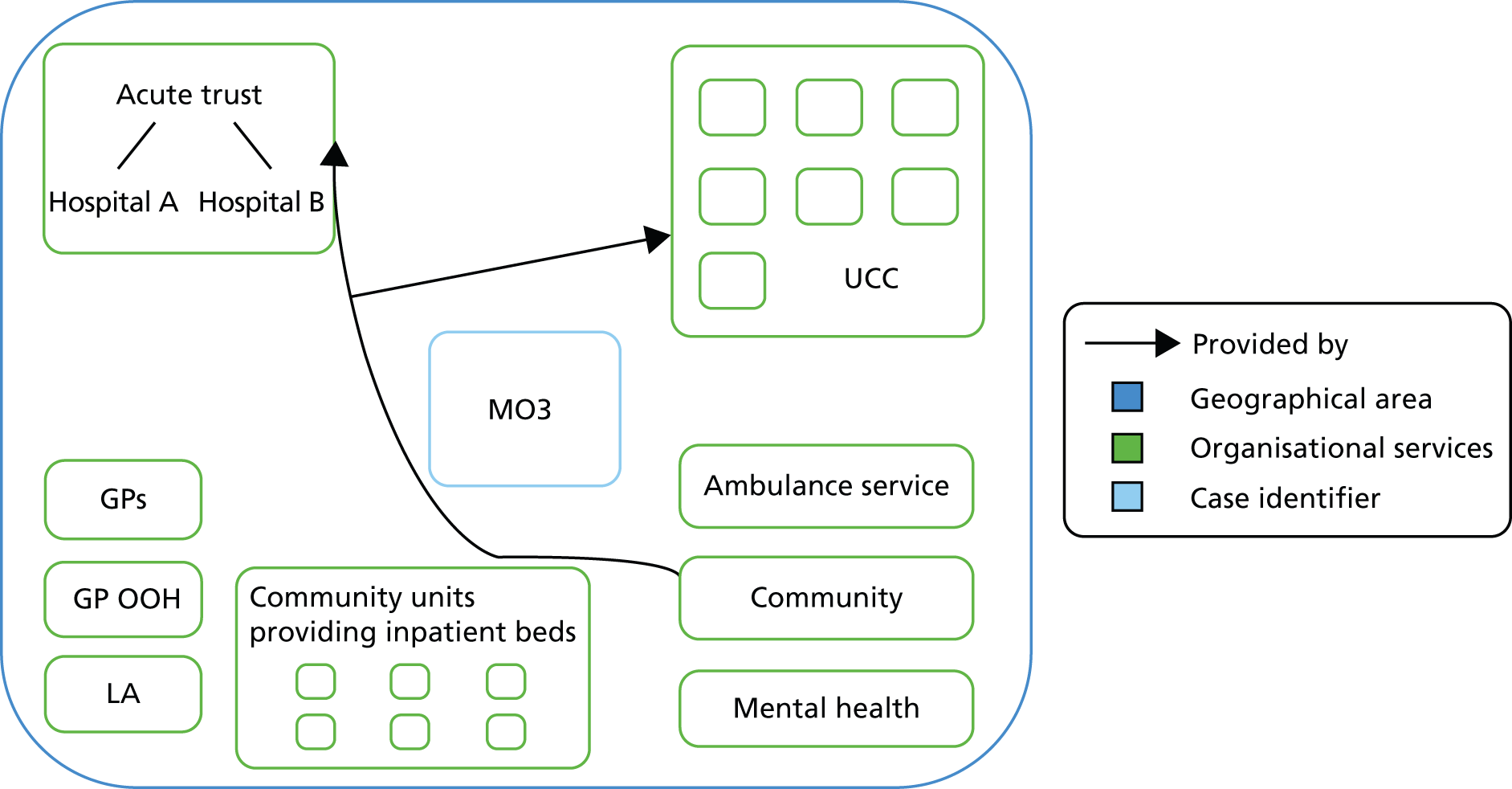
Acute trust
Emergency admissions from this population go to two hospitals with EDs, both of which are managed by a single acute trust. The data are available nationally only at trust level. The community and acute trust merged two years before our interviews, after the time period of the SAAR. The trust had a high ranking of number 102 of the 129 acute trusts included in our phase 1 regression and its SAAR was considerably higher than predicted in our regression (Table 21). This is the opposite of the situation for our geographically based system analysis. Few of the factors we included in the regression aligned with this high-ranked SAAR.
| Factor | Rate (rank) |
|---|---|
| SAAR | 2446 (102) |
| Predicted SAAR | 2158 (83) |
| % households in poverty | 20 (55) |
| Acute beds per 1000 population | 1.71 (53) |
| % population attending ED | 27 (55) |
| % conversion from ED to admission | 24 (69) |
| % length of stay < 1 day | 32 (100) |
| % outpatient wait < 1 month | 46 (104) |
| Foundation trust status | Yes |
Population
The population was described by interviewees as diverse in terms of health, socioeconomic status and age. One subgroup described was a stoic rural population suffering from COPD caused by mining. This group did not use health services until their condition was really serious. A number of interviewees referred to the elderly population and the high number of nursing homes in the area, which they felt impacted on demand for emergency services.
Interviewees felt that demand for their services was extremely high, especially for the EDs, and that nothing they did seemed to impact on this. This was a very surprising view given the low rate of demand for the ED shown in Table 21 compared with other acute trusts in England. This may be due to time differences between our data in Table 21 (2009–10) and our interviews (2012–13), or it may be about capacity versus demand in the ED.
I think we put a lot of effort into stopping people coming into hospital and for all our effort it doesn’t seem to me that it bears much fruit.
Geography
The area is largely rural with one city and a number of smaller towns. The difficulties in accessing care in rural areas identified in rural LO2 were also highlighted for this system. However, interviewees felt that services were in the right place and in particular that the UCCs were based in the right localities. One of the EDs was in the town centre and therefore considered to be easily accessible.
Rapid assessment teams in the hospitals avoid admissions
Interviewees within and outside both hospitals spoke highly of the rapid assessment teams in each hospital. One team had been available for 4–5 years, and one for only 2 years, so only one was available in our SAAR timeframe. These teams were described as having senior doctor and nurse cover, fast access to diagnostics and some OOH availability in that they worked up until 20.00 5 days per week. These services were described as high-volume, seeing 140 patients in a busy week. Interviewees felt that there was a need to extend these services more into weekends and have the diagnostics support available OOH. Interviewees viewed these services as successful at avoiding admissions, describing them as accessible and responsive and turning people round the same day:
rapid response people are really good and what they do is they come and they make an assessment, decide that that person can go home with x, y and z and then they just organise the x, y and z. They sort it all out, they book the transport, they’re brilliant, they’re absolutely brilliant.
A crowded emergency department
Interviewees across the system described the EDs as busy, with many highlighting one of hospitals as being particularly busy:
they [the hospitals] are overwhelmed and often closing their doors saying they’ve got no beds left . . . and A&E, always look busy and bursting at the seams, in [named hospital] in particular.
Interviewees described how they had put a lot of effort in recently to sort out problems with patients backed up in their ED by setting up systems to streamline minor cases to nurse practitioners and the UCC which was nearby. The really busy hospital had also recently implemented a senior review model for all patients to deal with the fact that junior doctors were making decisions to admit and were requesting lots of tests to support their decisions. Even though the statistics show that attendance at the ED was relatively low compared with other parts of England (see Table 21), interviewees working in the ED described it as normal to have ambulances queuing up outside. These new schemes were established after our SAAR time period and it may be that the need to find solutions in recent years indicates problems occurring during our SAAR time frame.
Primary care
The UCCs are GP led, with some accessible 24 hours a day, so this system appeared to have high levels of access to GPs. This was not apparent in the quantitative data in Table 19, where patient-perceived access was average. GPs appeared to have good connections with other providers across the system. Community nurses were aligned to GP practices (rather than being centralised), which contributed to relationship building, GPs were active in providing weekly education for community nurses, district nurses described ‘open-door’ access to GPs, and paramedics described telephone contact with GPs regarding patients.
A range of community services
Urgent care centres
Interviewees described this area as having a lot of GP-led UCCs with strong clinical input and a culture of discharging people rather than admitting.
Do they [UCC] play a role in admission avoidance?
Oh absolutely because the alternative to go to an urgent care centre is either a GP or an A&E department so you know and again I do think that it goes back to and I don’t want it to sound glib but it goes back to I think it is about the primary care focus, the people that work in the urgent care centres are primary care nurses, they’ve evolved from community nurses and therefore their focus is out rather than in.
However, interviewees felt that availability of diagnostics within some of these centres, especially OOH, could be difficult and this caused people to attend EDs. There was also some concern expressed that their accessibility generated demand.
Beds exist but difficulty accessing them
The hospital-based staff expressed difficulty in knowing which community services were available in different localities. Confusion was also related to the large number of new services introduced as pilots and beginning and ending at different times. Interviewees described the existence of a range of services, including community beds, but interviewees in one hospital felt that the beds were not accessible because they were full or criteria for entry were strict:
some mostly you would try to, but sometimes you abandon it on a busy Saturday afternoon, where you have got numerous other cases to see you can think ‘I can admit this with one phone call or I can spend the next hour trying to track down this team who may or may not keep them out of hospital’.
District nurses
Interviewees described a district nursing service which was available 24/7, with the majority of nurses able to provide intravenous antibiotics. The service appeared well regarded and was described as having a high level of experience within the team.
Nursing homes
Interviewees described a large number of nursing homes in the area and the need to prevent inappropriate attendance at the ED. There was a local initiative offering training and education to these homes.
Integration is partial and informal
The main formal integration described was the merger between the acute trust and the community trust, which occurred 2 years before our interviews (after our SAAR time frame). This had offered an opportunity to manage the ED and UCCs together, with an emphasis on taking the pressure off the ED. It also raised the issue for hospital-based staff that they needed to know what was in the community so they could refer to these services. There was also some colocation of services in the EDs which facilitated integrative working. However, much of the integration described was more informal than that, relying on relationships between individuals and services. Indeed some of the interviewees felt that there were many opportunities to talk to other services, which they appreciated, but that actions were needed too. Documentary analysis highlighted much discussion regarding integration. Acute trust annual reports, during the SAAR period and beyond, iterated a desire to maximise integrated pathways and care. Such integration was seen as desirable in improving access to unscheduled care but was also seen as a factor in reducing avoidable admissions.
An integrated health and social care system with a community focus
Views of social care in this system were generally positive. Interviewees from community settings and the local authority described effective cross-working relationships with each other. Social workers were colocated with district nurses and community matrons and this was viewed positively by interviewees across the community and social care sector. This was a contrast to the lack of integration between the acute trust and community services.
Explanatory analysis
Possible explanations for the SAAR being lower than predicted:
-
use of UCCs as a central part of the emergency and urgent care system; however, the low use of the EDs – which may be due to the high use of these centres – is already in the regression
-
rapid response team
-
the integrated health and social care teams in the community
-
the difference between the acute trust and the geographically based system.
MU4 (medium rate, underpredicted)
-
Large rural area.
-
One ED short of consultants.
-
Large number of minor injury units.
-
Perceived poor GP OOH service.
-
High levels of perceived access to GPs in hours.
Why this case was selected
It is helpful to have MU4 in the case studies because:
-
It is a system with a medium SAAR. At 1905 it was ranked at 48 out of the 150 systems.
-
It had an underpredicted SAAR in our regression. The predicted SAAR in our regression was 1690, ranked at 22 out of 150, making it a low SAAR.
-
It is one of three systems in a geographical cluster.
Description of factors in the phase 1 regression
Its SAAR was ranked at 48 out of 150. The population factors were also ranked low but the ED factors were not (Table 22). This system had very high demand for EDs and a very low conversion rate to admission. It has the highest perceived access to GPs in 48 hours. At the beginning of the SAAR period (2008–9), documentary analysis identified that the PCT set out a 5-year framework aimed at reducing avoidable emergency admissions, and reported in the same year that reductions in hospital admissions had been achieved by the commissioning of new services, better social care and GPs working with community hospital matrons.
| Factor | MU4 score | Median (range for 150 systems) | MU4 rank |
|---|---|---|---|
| Employment deprivation (%) | 4 | 6 (3–12) | 33 |
| Rural status | Rural 50% | n/a | |
| ED attendance | 349 | 275 (149,909) | 128 |
| Conversion rate | 74 | 100 (70–148) | 5 |
| % length of stay < 1 day | 27 | 28 (14–41) | 68 |
| % ambulance calls not transported | 31 | 21 (8–34) | 16 |
| % able to see GP in 48 hours | 89 | 80 (71–89) | 1 |
Condition-specific standardised avoidable admissions rates
MU4 ranked 48th out of 150 overall for the SAAR and generally ranked in this medium to low area for most conditions with the exception of DVT and abdominal pain, where it had relatively high admission rates (Table 23). That is, the medium to low avoidable admission rate was likely to be system-wide rather than related to some parts of the system specific to dealing with some conditions. There was extensive discussion of condition specific pathways in this system. On the whole, pathways for the lower-ranked conditions (i.e. COPD, hypoglycaemia and UTI) were viewed positively by interviewees.
| Condition | Rank of condition-specific SAAR | Interviewees’ perceptions of pathways for condition |
|---|---|---|
| Minor head injury | 63 | |
| Chest pain | 48 | Mixed. Positive: effective specialist nurses in acute trust A. Negative: slow diagnostics in acute trust B |
| DVT | 118 | Negative (during SAAR period): inconsistent sign-up to community pathways among GPs, ineffective pathway in both of the acute trusts and community services |
| Angina | 74 | |
| COPD | 24 | Positive: effective specialist nurses and ECPs |
| Mental health | 39 | Mixed. Positive: mental health crisis pathway, responsive crisis team in acute trust A. Negative: OOH assessment, links to ambulance service |
| Abdominal pain | 90 | Negative: poor historic links between acute trust B ED and surgery, GPs experiencing delays in accessing acute surgical advice |
| Cellulitis | 73 | Mixed. Positive: effective pathway in acute trust A. Negative: inconsistent sign-up to community pathways among GPs |
| Blocked catheter | 23 | Mixed |
| Hypoglycaemia | 12 | Positive: effective ambulance service pathway |
| UTI | 28 | Positive: effective ECP pathway, integrated social and community health pathway |
| Epilepsy | 52 | Positive: effective pathway in acute trust A |
| Falls | 48 | Mixed: effective multidisciplinary team in acute trust A but not available OOH, minor injuries unit pathway |
| Pyrexial child | 61 | Positive: GP in acute trust A |
Although our interviewees did not mention it, the documentary analysis identified investment (just prior to the SAAR period) in mental health services to reduce admissions. During the same period the ambulance service also reported the introduction of 24/7 access to advice from mental health specialists. This fitted with the relatively low SAAR for mental health but did not tally with ambulance service interviewee perceptions of difficulties in accessing mental health services.
System configuration
The population is approximately 500,000 people across a large geographical area. The system has two acute trusts (Figure 9). There are a large number of minor injury units and community bed units within this system. The ambulance service provides the GP OOH service.
FIGURE 9.
Emergency and urgent care system configuration for MU4. LA, local authority; MIU, minor injuries unit; WIC, walk-in centre.
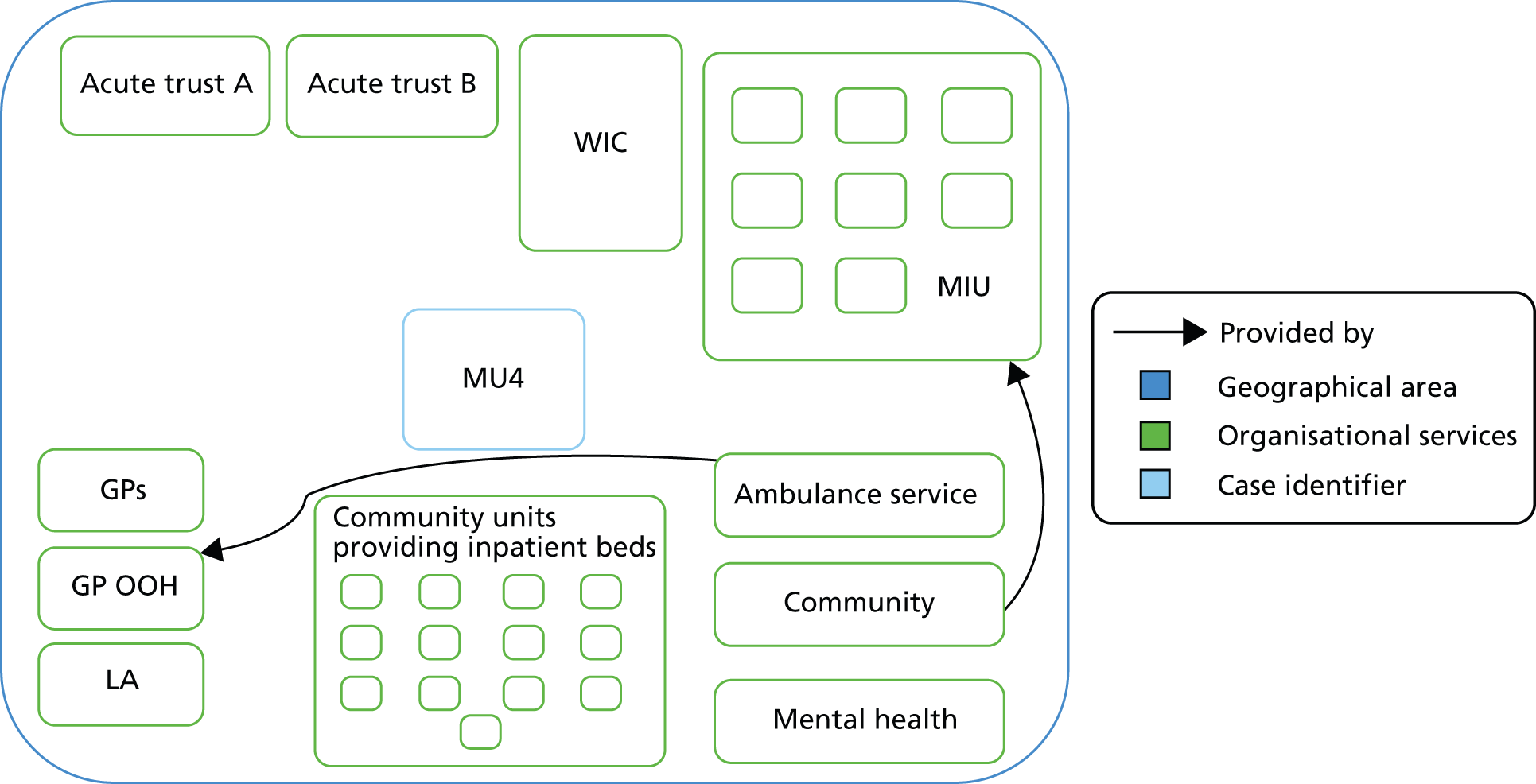
Acute trusts
Emergency admissions from this population go to two acute trusts with EDs within the system boundary. A further two acute trust in other areas were mentioned during the interviews, which a minority of the population was described as attending. The two local acute trusts are based in two towns of equal size, accounting for only 20% of the population of the system. That is, a large part of the population lives at a distance from the acute trusts.
The two acute trusts had a similar SAAR, which was similar to the geographically based SAAR. However, the two hospitals acted quite differently in the regression. The regression underpredicted acute trust A’s SAAR, similar to the geographically based SAAR, but overpredicted acute trust B’s SAAR.
This acute trust-level data did appear to relate to the geographically based system data (Table 24). In the geographically based system regression the use of EDs was very high (see Table 22) but there was no sign of this for the acute trusts (Table 24). This may indicate incorrect data about EDs in the geographically based system regression, as suspected for some of our other case studies, or it may be related to the large number of minor injury units (which are classed as type 3 EDs in routine data), which may have been included in some routine data sources and not others. This lack of consistency was also apparent for the conversion rate in the ED. The conversion rate was very high for each acute trust.
| Factor | Acute trust A (rank out of 129) | Acute trust B (rank out of 129) |
|---|---|---|
| SAAR | 1814 (47) | 1912 (62) |
| Predicted SAAR | 1946 (57) | 2106 (73) |
| % households in poverty | 13 (10) | 25 (88) |
| Acute beds per 1000 population | 1.90 (80) | 1.94 (85) |
| % population attending ED | 17 (6) | 25 (42) |
| Conversion rate | 29 (101) | 31 (113) |
| % length of stay < 1 day | 32 (110) | 24 (32) |
| % outpatient wait < 1 month | 46 (57) | 49 (54) |
| Foundation trust status | Yes | No |
Services for admission avoidance
Multidisciplinary teams were well regarded by interviewees in acute trust A, but these were recent additions and had not been around at the time of the SAAR. There was discussion of the need to expand ambulatory care pathways in acute trust B in contrast to other systems, which appeared more developed in this area. Acute trust B described recently initiating pathways for conditions such as DVT/cellulitis/UTI:
I think [the introduction of these pathways] will make a big change within the next probably 6 months, how a, how a lot of those conditions are managed whereas currently a lot of them just are admitted.
Population
Contrasting populations: elderly and stoic
A number of different groups of the population were mentioned, each with different needs and demand levels. Demand from rural localities was described as low because of a stoic population which does not attend services unless their condition is very serious. On the other hand, interviewees drew attention to a large elderly population who required a lot of care. This area was described as a holiday destination with an influx of visitors during the summer with minor health-care problems.
Relentless demand
Interviewees felt that there was a lot of demand for emergency and urgent care and described it as relentless. This is a theme that occurs across the case studies, even in systems with relatively low avoidable admissions.
There seems to be more and more coming to be honest. As I say we’ve got more patients.
And those are the, that’s the difficulty I think, and maybe for all providers, is how you demonstrate that interventions are reducing admissions because they just they always increase.
Educating people about services
A couple of interviewees felt that a lot had been done in this area to educate the population about available services but more interviewees drew attention to the lack of awareness of services available and how to use them.
Geography
This is a very rural area and its rurality was seen as causing difficulties similar to those raised in the other rural cases of LO2 and MO3. Interviewees felt that the population living outside the two major towns had some distance to travel to an acute trust. However, the distribution of minor injury units throughout the system led one interviewee to describe how the population was not further than a 30-minute drive from a unit or an ED. Interviewees discussed the need to balance putting care close to people and not so close that it generated demand. Similarly to HU1, the large distance to the hospitals was seen as causing increases in avoidable admissions because once people got to the ED they could not get home so they were admitted. That is, they raised a reason working in the opposite direction from another reason for distance to ED affecting admission rates: people living close to EDs being more likely to attend and perhaps then more likely to be admitted. The large distances created a need to find ways of providing care over a large geography such as using ECPs in the ambulance and GP OOH services.
Good chronic obstructive pulmonary disease care
A number of interviewees discussed the range of initiatives that prevented and avoided COPD admissions. They offered this information without prompting and also in response to us pointing out a low SAAR for COPD. They described their outreach hospital team, a good respiratory network, a good pathway and the use of telehealth. This did not seem as if interviewees were trying to find a reason for a low SAAR, because when we mentioned the low UTI admission rate they could think of no reason for it. The documentary analysis showed emphasis on avoiding emergency admissions for long-term conditions.
Emergency departments
Some issues that arose in other cases also arose here around lack of space within the EDs and the need for more consultants. Some services were available within the EDs such as psychiatric liaison and professions allied to medicine offering assessments. Interviewees were keen on having GPs in the EDs to discharge attendances and had tried a scheme that they felt had created demand because it was not integrated within the ED. Now they had a new approach and felt positive about it. For all the similarities with other cases, there was no sense of crisis here; in fact one interviewee described how ambulance queues were less common here so ambulances were more likely to take patients to these EDs. There was also a sense that, while interviewees acknowledged that there had been issues within EDs, they were very much moving forward, identifying problems and implementing solutions, including extending the ED in acute trust A. Nothing interviewees said explained the high demand for EDs in our geographically based system quantitative data in Table 22. One of the EDs (acute trust B) was described as having had problems with consultant presence at the time of our SAAR, although nothing in Table 24 supported this as a problem affecting avoidable admissions.
Confusion about assessment versus admission
Interviewees described confusion about the role of the medical assessment unit in acute trust A because it admitted people to its assessment beds. Scenarios were described whereby social care packages for patients attending the unit were cancelled by family or social care because there was an assumption that the patient was taken to the unit to be ‘admitted’ rather than ‘assessed’. This arose only within MU4.
The medical assessment unit haven’t really got a clear identity, because we call it a medical assessment unit but really it’s a ward and it’s got beds. The staff use a ward routine and I think their mentality to a certain extent isn’t an assessment unit, it’s an admissions unit. So some people call it an assessment unit, some people call it admissions unit so I think in some ways it needs some work, you know, because it’s only, we’ve only got 20, 22 beds, but we know that we get between either 40 and 60 admissions a day.
Out of hours is problematic
There was a general feeling among a range of service providers in this system that there were problems with OOH provision: ‘some of the services we access during the day aren’t available at night either’. Some services such as the minor injury units were described as providing a 7 days a week service but interviewees felt that too many services stopped running at 17.00 and later provision of support services was needed. Indeed, of the eight minor injury units, one was operational overnight, with none offering X-ray facilities beyond 17.00. While overnight opening of another unit had been trialled, it was acknowledged by others in the system that this was not financially viable in a rural community. This system had an urgent referral telephone service open to any health-care professional to facilitate the referral of patients to community hospitals, nursing/residential care and minor injury units. It was operational 7 days a week but was not open overnight (which interviewees wanted):
it [telephone referral service] suddenly stops at half past seven and you’re left on your own again and you have to try and sometimes make do and mend it until the next day . . . I’d love it if they kept [the referral service] open overnight . . . I think would make our job easier in my mind . . . having somebody to refer to on the path when you’ve finished your shift would certainly help in my mind and I would certainly feel more confident about leaving people at home. The referral service should be open 24 hours.
Poor general practitioner out-of-hours service
The GP OOH service was described as problematic by most interviewees. The service providers were described as having difficulty staffing the service, relying on locums from other countries who did not know the local services, and this did not inspire confidence in users. The service was seen as one which admitted patients as the easy option.
We have lots of problems. There are lot of unfilled shifts, it’s very difficult to get GPs to work in the service. We get lots of locums working in the service and if they’re not familiar with the systems or they aren’t able to access information in a timely way then patients get admitted. And a lot of our, I would say, our unnecessary admissions happen in the out-of-hours period.
A well-connected ambulance service focusing on non-conveyance
A number of interviewees described working closely with the ambulance service. The service was described as treating people at home and had a directory of services to allow them to refer and transport to services other than the ED. Some of this was attributed to the rural nature of the system:
In the rural area you tend to spend a little bit more time seeing if the GP could manage that . . . which probably costs more resources, [but is] ultimately better for the patients. But they tend to happen in the more rural areas where it costs more to transport.
Indeed the phase 1 regression in Table 22 shows that this service had high non-conveyance rates compared with its counterparts. The documentary analysis supports this. Ambulance service annual reports throughout the SAAR period highlighted the achievements made in non-conveyance.
Primary care
Good general practitioners but are they engaged with the wider system?
Some interviewees felt that rural areas attracted good GPs and that this area had good-quality GPs, despite primary care feeling that they were ‘under pressure’. They also felt that people relied more on GPs care in rural areas because of distance from other services. This matched the quantitative data presented in Table 22, where this system had one of highest percentages of perceived good access to GPs. A frequent complaint was that GPs visit their patients late in the day and, by the time they get to the hospital, admission is the only option.
There was a sense that connections between GPs and other providers were not well established. A GP described how it was difficult to know what’s going on in the community, while a community provider described GPs as ‘a really difficult group, they often can’t be bothered to access things’. GPs were not seen as facilitators in terms of reducing avoidable admissions.
The walk-in centre has created demand in the system
There is one walk-in centre in this system, located in close proximity to acute trust B. Historically the walk-in centre had offered a walk-in facility, but interviewees described the centre as now accessed by appointment only. While one interviewee felt that the walk-in centre alleviated pressure on the nearby ED, this view was not shared by others in the system. One interviewee pointed out that the use of the walk-in centre was of the same order as the ED (40,000 attendances per year), with little change in the use of the ED before and after the opening of the walk-in centre.
A lot of community services
Lots of community beds but not necessarily accessible
Interviewees acknowledged that there were a lot of community beds in their system (around 340 according to data we received from the trust), but that accessing them was not easy. Demand came from a number of sources including GPs, community staff, ED and acute wards. Interviewees described strict admission criteria, seen by social care as a step-down resource from the acute trust rather than a step-up service. The beds were located across the geographical area so might not be available in the locality needed. There was a sense that these beds were not working well for the system:
The pathway [to obtaining a community bed] is just horrific . . . so the default becomes, I mean to be honest we do still try to get people into [community] beds because the [acute] beds here are so bad. But we had a Monday 2 weeks ago, we had our worst ever day in this trust with back-logs of patients, we couldn’t move them through we were full. And at the end of that day when we’ve been in absolute crisis the whole day it turned out there were 41 community beds in the county which had not been made available.
Social care: a hindrance to admission avoidance?
While there were some positive comments regarding social care, these were offered by the interviewee from the local authority. On the whole, negative views regarding social care were offered from the acute setting. As in HU1, there were references to the difference in the speed of decision-making within social care from health, and different organisational cultures. Interviewees in both acute settings described scenarios whereby they felt that social care potentially hindered admission avoidance:
my concern would be once you start to get social services and that sort of people involved it can delay discharge sometimes rather than necessarily speed things up . . . so I’m not convinced that having social workers in the [emergency] department necessarily would add great benefit to our patients . . . I think they tend to work on a slightly different timescale too, to the way we do. You know, they haven’t worked in an environment where they have had to make those rapid decisions as much as we do.
More integration needed
There were mixed views about how much integration occurred in this system. Here, it seemed patchy with plans to improve it.
I think we’ve got lots and lots of work going on but sometimes it’s not very joined up.
We’re just creating an urgent and emergency care strategy in [system] the idea of which is to pull all the organisations together so we do have a shared vision and purpose for the whole community.
Coding of admissions
Some interviewees described how attendances were coded as admissions once they left the ED and moved to other parts of the hospital, such as the clinical decision unit:
the system doesn’t allow us to code as an ambulatory care patient or whatever. They get admitted. And then that causes us a problem particularly if we bring them back the next day because then they are classed as a readmission.
Explanatory analysis
This case was very similar to LO2 in terms of the population and geography yet MU4 had a much higher SAAR (MU4 = 1900 versus LO2 = 1600). Possible reasons for a higher SAAR than predicted are:
-
a lack of proactiveness of the rapid response team seen in LO2
-
the lack of integration described in LO2
-
the perception of poor OOH provision, particularly GP OOH service.
LO5 (low rate, overpredicted)
-
Metropolitan area with significant boundaries with other systems.
-
Described as an affluent population.
-
One acute trust offers proactive approaches to admission avoidance and the other does not.
-
Concerns about lack of integration between health and social care.
Why this case was selected
It is helpful to have LO5 in the case studies because:
-
It is a system with a low SAAR. At 1776 it was ranked at 33 out of the 150 systems.
-
It had an overpredicted SAAR in our regression. The predicted SAAR in our regression was 2300, ranked at 82 out of 150, so it was still medium but considerably higher than the actual SAAR.
-
It is one of two systems in a geographical cluster.
Description of factors in the phase 1 regression
Its SAAR was ranked as 33 out of 150. It had very high ranking for most factors, which was not in line with the low SAAR (Table 25).
| Factor | L05 score | Median (range) | LO5 rank |
|---|---|---|---|
| Employment deprivation (%) | 5 | 6 (3–12) | 38 |
| Rural status | Major urban | n/a | 121 |
| ED attendance | 319 | 275 (149–909) | 107 |
| Conversion rate | 108 | 100 (70–148) | 101 |
| % length of stay < 1 day | 36 | 28 (14–41) | 144 |
| % ambulance non-conveyance | 16 | 21 (8–34) | 111 |
| % able to see GP in 48 hours | 79 | 80 (71–89) | 80 |
Condition-specific standardised avoidable admissions rates
LO5 ranked 33rd out of 150 overall for the SAAR and generally ranked in this low area for most conditions with the exception of blocked catheters and pyrexial child, where it had relatively high admission rates (Table 26). That is, the low avoidable admission rate was likely to be system-wide rather than related to some parts of the system only. Pathways in acute trust A for the 14 SAAR conditions were generally viewed positively within the interviews. COPD and falls were low-ranking conditions where perceptions were positive across the emergency and urgent care system. Documentary analysis indicated that the ambulance service had been working with GPs regarding the management of falls during the SAAR period, and highlighted successes in referring more falls patients to GPs following this.
| Condition | Rank of SAAR | Interviewees’ perceptions of pathways for condition |
|---|---|---|
| Minor head injury | 58 | |
| Chest pain | 30 | Mixed. Positive: pathway acute trust A and B |
| DVT | 28 | Positive: ambulatory pathway (both acute trusts) |
| Angina | 30 | |
| COPD | 32 | Positive: community and acute trust pathways |
| Mental health | 65 | Positive: pathway from WIC to mental health services. Negative: ineffective in acute trust B |
| Abdominal pain | 15 | Positive: acute trust A access to surgeons |
| Cellulitis | 94 | Positive: ambulatory pathway (both acute trusts) |
| Blocked catheter | 103 | |
| Hypoglycaemia | 53 | |
| UTI | 94 | |
| Epilepsy | 63 | Positive: acute trust A pathway |
| Falls | 21 | Positive: effective across acute trusts, community and ambulance service |
| Pyrexial child | 106 | Positive: WIC can assess and treat babies |
A number of interviewees discussed the range of initiatives that prevented and avoided COPD admissions. They offered this information without prompting and also in response to us pointing out a low SAAR for COPD. They described a valued outreach hospital team providing hospital at home, good specialist community nurses and a good respiratory network which linked acute and community care. These initiatives were in place during the time period of the SAAR.
System configuration
The system has a population of 350,000 within a metropolitan area. The services used by the system population are shown in Figure 10. One acute trust is within the geographical boundaries of the system and the other is in another system. The community trust was contracted to deliver community services in this system towards the later part of the SAAR period.
FIGURE 10.
Emergency and urgent care system configuration for LO5. LA, local authority; WIC, walk-in centre.
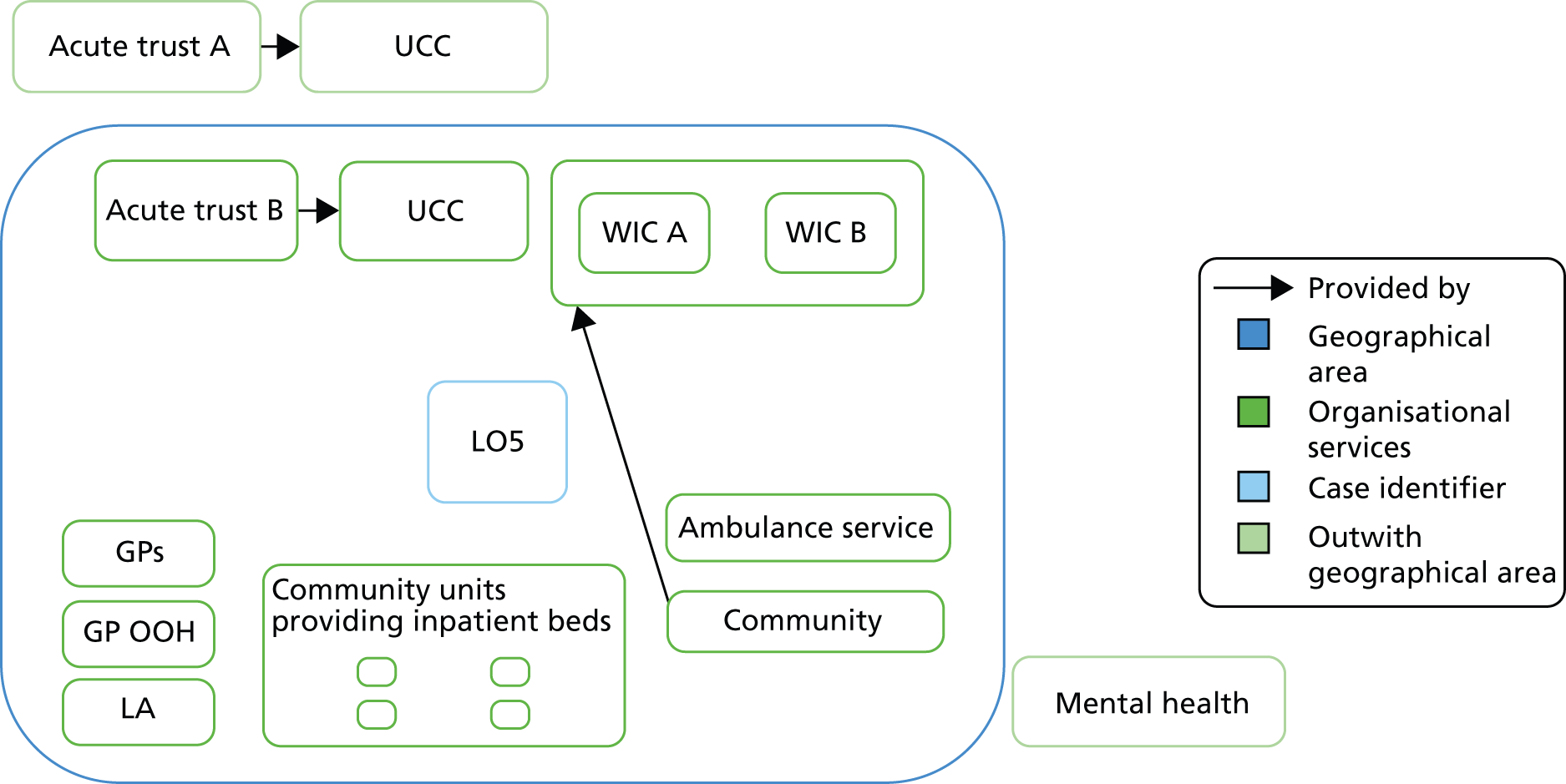
Acute trusts: another tale of two trusts
The population uses two acute trusts mainly but has access to a range of trusts because it is situated in a large city with many hospitals. The catchment populations of the two main trusts are 300,000 (acute trust A) and 450,000 (acute trust B). These acute trusts are used by populations other than our system population but B is located within the system boundaries and interviewees reported that two-thirds of the system population used it. Both acute trusts had low SAARs, but one had a very low SAAR (acute trust A). Both SAARs were overpredicted by the phase 1 regression. They showed a similar pattern for factors to that of the geographically based analysis, with higher ED attendance and conversion rates than expected given their SAARs. Acute trust B was based in an area with higher poverty levels and had fewer acute beds than acute trust A (Table 27).
| Factor | Acute trust A (rank) | Acute trust B (rank) |
|---|---|---|
| SAAR | 1511 (12) | 1719 (38) |
| Predicted SAAR | 1943 (56) | 2115 (76) |
| % households in poverty | 13 (11) | 22 (65) |
| Acute beds per 1000 population | 1.91 (82) | 1.44 (17) |
| % population attending ED | 29 (69) | 33 (95) |
| Conversion rate | 22 (45) | 24 (66) |
| % length of stay < 1 day | 26 (50) | 40 (128) |
| % outpatient wait < 1 month | 55 (84) | 34 (1) |
| Foundation trust status | Yes | No |
During the interviews, acute trust A was described in much more positive terms than acute trust B for admission avoidance. It was described as proactive, engaging with community services and offering senior decision-making in the ED. This was supported by the acute trust A annual reports, which used phrases such as ‘integrated working’, ‘working together’ and ‘productive relationships with other organisations’. Acute trust B adopted services established in acute trust A after a number of years and not in the time frame of our SAAR. This stark difference described by interviewees was not fully apparent in Table 27, where we might expect to see much lower conversion rates in acute trust A than B. However, the difference was extreme for the percentage of short-stay admissions, with acute trust B having the highest percentage in the country.
Population
An affluent population with access to private health care
This case was unusual in our six case studies because interviewees described the population as affluent. This was supported by our quantitative data, according to which the area had low levels of employment deprivation (see Table 26), especially around one of the acute trusts (see Table 27). The population was described as stable, with some established minority ethnic groups using private health care and their own private services run specifically for their communities. There was a lack of comment on expectations driving demand for emergency and urgent care that was present for the other systems. However, there were recent immigrants who were described as using EDs more than the established population.
Lots of nursing homes
Most interviewees drew attention to the large number of nursing homes in the area and the need for nursing home staff to be educated about avoiding admissions.
Primary care
Perceived poor access to general practitioners
Interviewees described the GPs as a stable workforce, living locally, so it was surprising that they were criticised for their knowledge of local community services, which was deemed to be poor. The perception of access to GPs was that it was poor. This was not supported by quantitative data in the phase 1 regression, where patient-perceived access to their GP was average for the nation (see Table 25).
The GP doesn’t work well in the fact that we can never get them an urgent appointment. So we’re trying to plug them into the GP but there’s never any appointments to see them, even though they’re emergencies in hours and obviously out of hours . . . there doesn’t seem to be enough GPs around . . . It’s been going on now for a long time, since they changed the GPs providing out-of-hours services. For some reason, I don’t know why. But also they can’t get an appointment for 10 days.
Good provision of walk-in services
The area has two walk-in centres as well as a colocated UCC at acute trust A and a GP-led centre. These centres were well regarded by the interviewees and perceived to be busy services. Their value came from the perception that they were embedded within the system: they had been established for over 10 years, were open ‘long hours every day’, ‘had a good range of diagnostics’, utilised ‘high-level nursing’, assessed children and ‘issued antibiotics to children’. In one of the centres, radiography was available during the entire operational hours; this was in contrast to other systems, where if radiography was available it did not cover the entire operational hours of the centre. The centres were viewed as ‘different’ from other walk-in centres, with one interview describing the centres as ‘urgent care centres cum walk-in centres’.
Poor services: out-of-hours provision and social services
Many of the interviewees described how services which were good for admission avoidance did not operate at weekends or overnight. These included overnight cover at walk-in centres and the community rapid response teams. Community beds were theoretically available 24/7 but described as difficult to access OOH. There was a vast difference in the provision of OOH described by interviewees for the two acute trusts. Acute trust A (with a very low SAAR) operated 7-day access to admission avoidance schemes and urgent radiology. In contrast, acute trust B did not describe 7-day working practices and vocalised more negative views about the OOH period:
I think not having OT, physio, social worker input particularly out of hours is a big problem . . . the last referral for OTPT is 4 o’clock which is not adequate, it’s not good enough.
Interviewees from acute trusts A and B, and the community trust, offered negative views about the local social care sector. The service was described as being under pressure and criticisms focused on the ‘long-winded’ process to get care, and the lack of staff available at weekends to discharge patients from the ED:
Well there’s a lot of bad feeling with the social services because social services don’t provide a good service. Whatever the reason that is we don’t feel they provide a good service so in general you have to speak to a social worker out of hours for example you ring them up and you have to leave a message with somebody at the civic centre and then you might get a call back in 2 hours and it may be that you’ve got a patient that is being discharged medically fit but they haven’t . . . their house is in a state or the door’s been broken into because the neighbours broke the door down because they were worried about them. You can’t do anything about it, you can’t get anybody to help you at that time . . . It’s not responsive I mean whether it’s because of how many staff they’ve got I don’t know.
Social care themselves acknowledged that, historically, integration between themselves and health had not been strong but the impetus towards making these connections was under way.
Evidence of integration for one acute trust only
Acute trust A proactive about admission avoidance
There were mixed views on integration within the system. Some interviewees felt that it was very good and others that services worked in silos. There was a definite difference between the two acute trusts, with acute trust A interviewees describing initiatives that functioned in-house, that is care and follow-up care that was delivered in or around the ED in an integrated way, which reduced avoidable admissions. Both acute trusts operated rapid response teams available in the ED targeting older people. Acute trust B had only recently introduced this. In acute trust A, a consultant geriatrician-led team included occupational therapy, physiotherapy and social care input to keep people in their own homes. It was described by interviewees as a highly successful admission avoidance scheme operational since late 2010. This service operated a 7-day service. The success of the scheme was attributed to an ethos of discharge, proactive targeting of specific patients with a multiskilled workforce, senior clinician input at an early stage and being well integrated:
it is just a matter of talking to them you know do you mind having a look and call out if everything’s fine. It’s that communication, the communication it’s all about communication, communication is quite important there but yes in theory they [the team] will be triaging these people early on.
Another initiative valued in LO5 was a post-discharge scheme operated by the community but based in acute trust A. This was seen to complement the older person rapid response scheme described above, with integration seen as a key to its success:
It [post discharge scheme] works beautifully with [the rapid response scheme] and [hospital A] say [the rapid response scheme] would have not been as successful if they hadn’t had the [post-discharge scheme] service underpinning it. Because they can then get the patient out within 2 to 4 hours, back home. Being seen immediately since they get home, and, and then being managed er, with you know whatever on going care they need . . . [it involves] loads of team working.
A lot of good pathways
Interviewees described a number of pathways for keeping people out of hospital and these were for conditions on our SAAR list. The falls referral pathway was spoken about positively between the ambulance and the community service. These pathways gave people confidence about referring on or leaving people in their own home. Some pathways were new and not around during our SAAR. Communication was important to making these pathways work; for example, GPs may not use pathways because they are not aware of them. The ambulance service was part of these pathways but the data in the phase 1 regression did not indicate large use of non-conveyance.
Colocation of services
Both acute trusts have a colocated UCC and ED, although acute trust B has only recently introduced this. This colocation was generally discussed in positive terms as a good way of managing demand. For example, the ambulance crews liked this model because if they made the wrong decision about taking someone to an UCC then the consequences of doing so were minor. However, one interviewee was concerned that this model simply made access easier and, therefore, increased demand.
Health professionals’ awareness of services
The usual statements were made by interviewees about the population needing to be more aware of services available to them but a much more dominant view was that health professionals were not aware of services available. In this system, the population used services from many areas so health professionals had to know the service configurations within many areas, and have confidence that they would work.
Explanatory analysis
This case was unusual in that it was described not only as affluent – and this was evident from its low employment deprivation level in the phase 1 regression – but also as having minority ethnic populations making use of private health care. Reasons why the system had a lower SAAR than predicted are:
-
One acute trust had proactive rapid assessment teams.
-
Use of private care was described as high.
MO6 (medium SAAR, overpredicted)
-
A simple system.
-
Similar population and same ambulance service as HU1.
-
Proactive medical consultants avoiding admissions.
-
Holding areas where attendances are not coded as admissions.
Why this case was selected
This case was geographically close to a set of systems with high SAARs but had a medium SAAR of 2421, ranked at 93 out of the 150 systems. The predicted SAAR was 2748, ranked at 123 out of 150. It offered some useful contrasts with some of our other six cases. It was covered by the same ambulance service as HU1 but had a different SAAR. It had a similar SAAR to MO3, offering the opportunity to compare and contrast two systems that appeared to perform the same.
Description of factors in the phase 1 regression
Its SAAR was ranked as 93 out of 150 but it had a low conversion rate from ED attendance to admission (Table 28).
| Factor | MO6 score | Median (range) | MO6 rank |
|---|---|---|---|
| Employment deprivation (%) | 8 | 6 (3–12) | 119 |
| Rural status | Urban major | n/a | 121 |
| ED attendance rate | 284 | 275 (149–909) | 88 |
| Conversion rate | 94 | 100 (70–148) | 55 |
| % length of stay < 1 day | 31 | 28 (14–41) | 116 |
| % ambulance non-conveyance | 8 | 21 (8–34) | 138 |
| % able to see GP in 48 hours | 77 | 80 (71–89) | 112 |
Condition-specific standardised avoidable admissions rates
MO6 ranked 93 out of 150 overall for the SAAR but had very low ranks for some conditions (DVT, cellulitis, blocked catheters, UTI, falls) and high ranks for others (angina, mental health, abdominal pain, pyrexial child). The low-ranking conditions were issues dealt with by community services (Table 29). Interviewees had positive perceptions of community pathways.
| Condition | Rank | Interviewees’ perceptions of pathways for condition |
|---|---|---|
| Minor head injury | 74 | |
| Chest pain | 96 | |
| DVT | 23 | Positive: ED pathway |
| Angina | 128 | |
| COPD | 87 | Positive: community pathway |
| Mental health | 121 | Positive: GP access to crisis teams. Negative: social service access to teams |
| Abdominal pain | 123 | Negative: historical issues in accessing senior surgeons in ED |
| Cellulitis | 5 | Positive: ED and community pathway. Negative: GP use of community pathway |
| Blocked catheter | 8 | |
| Hypoglycaemia | 74 | Positive: ambulance service pathway |
| UTI | 31 | |
| Epilepsy | 69 | |
| Falls | 28 | Positive: community pathway. Negative: GP use of community pathway |
| Pyrexial child | 136 |
System configuration
The system has a population of 265,000, most of which is served by a single acute trust. The services used by the system population are shown in Figure 11. It is a very simple system with one acute trust. During the SAAR period this system had an NHS walk-in centre, which has since closed.
FIGURE 11.
Emergency and urgent care system configuration for MO6. LA, local authority.
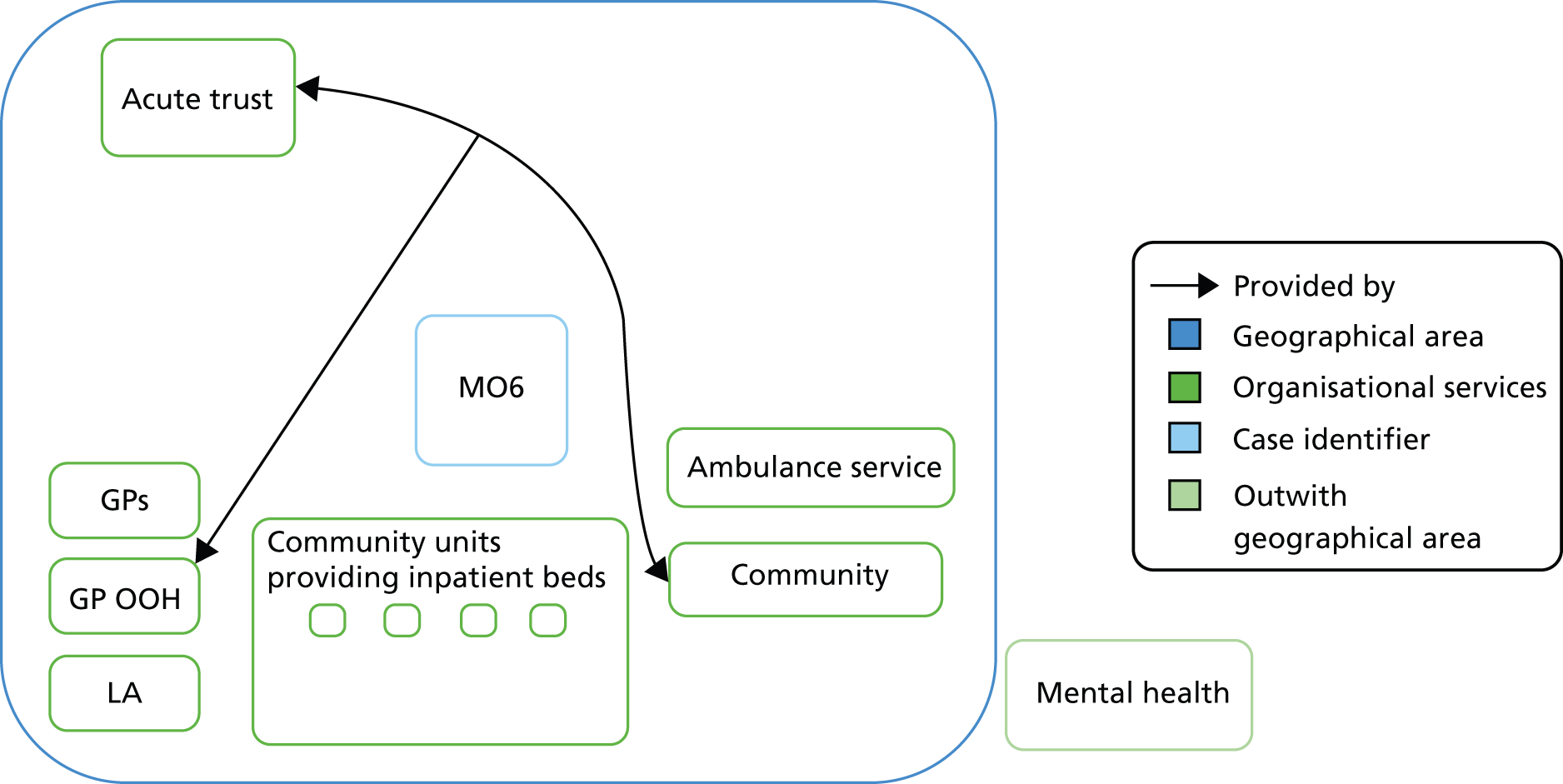
Acute trusts: low conversion rate
The acute trust SAAR was ranked 94th out of 129 trusts, with a very similar SAAR to the geographically based system (Table 30). The SAAR was underpredicted in the phase 1 regression in contrast to the overprediction for the geographically based system. The conversion rate from ED attendance to admission was very low for the acute trust, that is similar to the geographically based system.
| Factor | Rate (rank) |
|---|---|
| SAAR | 2314 (94) |
| Predicted SAAR | 2259 (99) |
| % households in poverty | 23 (79) |
| Acute beds per 1000 population | 1.69 (52) |
| % population attending ED | 36 (112) |
| % conversion | 20 (19) |
| % length of stay < 1 day | 31 (95) |
| % outpatient wait < 1 month | 57 (87) |
| Foundation trust status | Yes |
Population
Interviewees described a deprived population with high prevalence of health problems and expectations of quick access to urgent care, as well as stoic older people. The high deprivation levels could be seen in the quantitative data presented in Table 28. One would expect a much higher SAAR given these deprivation levels.
Coding of admissions
An issue that stood out in this system compared with the other six was the way in which attendances at the ED could be placed temporarily, including overnight, in units where they did not count as admissions. There were a number of these units, including the clinical decision unit. The most long-standing of these units was for PCT residents only and designed specifically for admission avoidance. This offered an explanation for the low conversion rate from ED to admission.
And they specifically set up [the unit] for admission avoidance. Now they are admitted in the traditional sense, they are on a ward, but [. . .] not on the mainstream hospital, not in the investigation part, they’re there purely for the purpose of getting them back where they came from.
Proactive management of avoidable admissions
Interviewees consistently described services, units and teams in the hospital and community that GPs and others could contact to avoid an admission. Some of the services established, which interviewees believed reduced avoidable admissions, were GP access to medical and surgical advice, a senior medical physician proactive within the ED, a GP admissions unit to which GPs could refer directly, a hospital-based unit established for residents of the area only and a rapid response team to which GPs referred. The community rapid response team, made up of nurses, OTs, physiotherapists and social care, with access to equipment, worked in a highly responsive mode to offer short-term care to keep people in their own home and was perceived as avoiding ‘an awful lot of admissions’. It had been established in some form for many years, and dealt with frail elderly, cellulitis and UTIs – conditions which had low SAARs in this system (see Table 29). Some of these services had been set up in the previous 2 years and would not have affected the SAAR, but one unit was a long-established unit with beds, which was highlighted as an asset in a public health annual report and highly valued by interviewees within the system:
one of our biggest assets is [unit], a unit which was set up specifically to admit people for a few hours and then return them to their own homes. So admission in the very loosest sense of the word because they’re there to be seen by social workers and by physiotherapists and OTs and then returned to their own homes. Generally we’ll send them from the ED there so if they’re waiting for transport, waiting for relatives, they’ve got outstanding things that need doing, [. . .] which avoids about 14 admissions a day.
Interviewees described not access to community beds but rather a focus on helping people to return to their own homes from the ED. The number of initiatives described was large and indeed one interviewee commented that this issue needed to be addressed on a number of fronts: ‘it’s multi-faceted [. . .] I don’t think there’s one thing because [unit 1] works, [unit 2] works, some of the internal pathways we’ve got work.’
A busy emergency department
The ED was described as busy by both its staff and the ambulance service interviewees. Interviewees in all six of our systems described busy EDs and increasing demand but the language used to describe this department was more emotive, suggesting an extreme situation. The quote below is from an interviewee from the ambulance service who was likely to have experienced a number of other EDs:
it’s really busy . . . always at full capacity in terms of the major areas/bays . . . I think that the department is not big enough [for the number of patients attending] . . . there’s quite a lot of stress within the staff. I don’t know how they’ve stayed there for so long in comparison to other A&E departments, with the work load or with the way it’s managed and managed to stay sane [. . .] it is a good department, it’s just basically at breaking point! . . . [it’s been overloaded] for a long time.
There was some quantitative evidence of high demand for this ED because it had one of the highest attendance rates for an acute trust catchment area (see Table 30). It did not have a particularly high attendance rate for its geographically based system (see Table 28). There was some explanation for this within the interviews in that some of the demand was seen to be exacerbated by the location of the acute trust (on the geographical periphery of the system) and the good transport links around it, making it a popular destination for ambulance crews. More than one interviewee described that one-fifth of ED attendances came from populations residing in neighbouring systems, impacting on the ability to discharge patients from the ED. The low conversion rate seems all the more surprising given this context.
Good out-of-hours provision but wanting more
The ED in this system was unique among our six case studies because it had access to a hospital-based 24/7 admission avoidance service which was described as operating consistently over the 24-hour period. The ED also utilised GPs in the department 7 days a week, which was viewed positively by interviewees. Even so, ED interviewees wanted more access to OOH provision for community services.
A financially challenged acute trust
The positively viewed units and initiatives described earlier were based in the acute trust. Yet we had initially had problems with access to interviewees in this system because the acute trust was receiving adverse media attention. The interviewee below describes it as ‘a failing trust’, yet there did not seem to be evidence of this in our routine data or interviews.
You’ve hit us at a very good time you see, because as you know [we have] been a failing trust until recently. We’ve got Monitor with us all the time. Because we’ve failed financially and we’ve failed all our A&E targets last year, so we’re on red, both for our clinical targets and for our finances. And we’ve got a turnaround team at the moment trying to put us back on track. We know the only way to turn around the trust is to reduce hospital admissions.
Explanatory analysis
One would expect a system with this level of deprivation, demand for its ED and a ‘failing acute trust’ to have a much higher SAAR. Reasons why it might have an overpredicted SAAR were:
-
having many proactive admission avoidance initiatives, some of which were available OOH
-
having a rapid response team accessible by GPs and the ED
-
coding of admissions that was the opposite of that in case study HU1 because ‘holding areas’ did not code people as admissions.
Chapter 8 Comparison of multiple cases
While compiling the case personalities above, we identified issues in earlier cases which we compared and contrasted with later cases. We identified some hypotheses to test more formally within a multiple-case comparison. We display the hypotheses below and investigate them by considering:
-
the extent to which we had tested each hypothesis in the phase 1 regression
-
whether or not variation between the six cases supported the hypothesis.
Population characteristics have not been adequately adjusted for in phase 1
Interviewees identified a range of population characteristics as important factors driving avoidable admissions. They mentioned very elderly people, deprivation, comorbidities, recent immigrants, high expectations of quick access to care and lack of awareness of how to use emergency and urgent care services. To a large extent these were included in the phase 1 regression. Age was adjusted for in the SAAR, including > 85 years old, and deprivation was the most explanatory factor in the phase 1 regression. The interviews helped to explain how deprivation may also be measuring other factors such as morbidity and high expectations of fast access. There seems little utility in pursuing further measurement of any population characteristics because these were measured in phase 1.
Conclusion: deprivation in phase 1 regression is likely to have captured these issues already.
Acute trusts have different coding practices for admissions which affect variation in the standardised avoidable admissions rate
Some acute trusts have assessment units or ‘holding areas’ where patients can wait for tests or be prepared for discharge without staying in the ED and breaching the 4-hour wait. There was evidence in our six case studies that different coding practices were applied to these patients. This was explicit and extreme in two cases. In HU1, with a very high avoidable admission rate which we underpredicted, interviewees from one of the acute trusts were explicit that any attendances to their assessment units were classed as admissions, even though some junior staff did not realise this. In contrast, in MO6, with a medium admission rate which we overpredicted, interviewees in the acute trust were explicit that attendances to their assessment units were not classed as admissions, even if they stayed overnight. This distinction was less clear for the other four case studies. Even so, it appears that coding practices could explain further variation in the SAAR.
In the phase 1 regression two factors were included in the multiple regression which might be related to coding practices: conversion rate and percentage of short-stay patients. Looking at factors in the phase 1 regression for the acute trusts in HU1 and MO6, we can see little difference in poverty and the population use of their EDs (Table 31). However, there is a stark difference in the conversion rates from attendance to admissions, suggesting that this variable may be capturing coding practices as well as issues such as differences in presence of senior review at an acute trust. Surprisingly, there is not much difference in the proportion of emergency admissions staying for less than a day between these two acute trusts; both trusts have high rates of short-stay patients. Short stays can be influenced by approaches to early discharge as well as coding practices, but nevertheless a larger difference between the two trusts would be expected.
| Factor | HU1 acute trust | MO6 acute trust |
|---|---|---|
| SAAR | 3601 | 2314 |
| Predicted SAAR | 2807 | 2259 |
| % households in poverty | 20 | 23 |
| Acute beds per 1000 population | 2.12 | 1.69 |
| % population attending ED | 34 | 36 |
| Conversion rate (%) | 35 | 20 |
| % length of stay < 1 day | 35 | 31 |
Conclusion: different coding practices are likely to be captured in the phase 1 regression by the variables ‘conversion rate’ and ‘length of stay < 1’.
Integrated systems have lower standardised avoidable admissions rates
Integration of different services was identified by interviewees as important for avoiding admissions. Interviewees in each of the six cases identified some integration within their system and some problems they perceived there to be with integration. We did not measure integration in the phase 1 regression. In our case studies there was evidence of considerable variation in integration, based on interviewees’ perceptions of their systems. We ordered the six systems by level of integration from best to poorest, a subjective assessment based on the interviews (Table 32). If integration is likely to explain further variation in the SAAR, the pattern we would expect to see is the two systems with underpredicted SAARs at the poor end of the spectrum. This pattern was not consistent in that MO6 is at the poor end of integration. However, the pattern is strong enough to support the hypothesis and we will test this in the phase 3 regression.
| Factor | LO2 | LO5 | MO3 | MU4 | MO6 | HU1 |
|---|---|---|---|---|---|---|
| Integration | History of integrated working. Lots of examples of joint working | One acute trust excellent at integration while the other is problematic | Community and social services integrated but disconnect between acute trust and community | Lots going on but concerns about it not being joined up. One acute trust disconnected | Relies on informal relationships | Interviewees gave accounts of working hard at it but sense it was recent and focused on early discharge |
| Colocation of services | Social services and nursing | Social services and nursing | Social services and nursing | Social services and nursing | Little | Little |
| Joint working | Rapid assessment team at acute trust | Rapid assessment team | Joint working in teams | New team focused on community beds only | Rapid assessment team | No evidence |
| Working relationships | Systems thinking and communication. Only ED feels negative | Good relationships and communication in some areas | Good relationships and communication | Partial | Good relationships and communication but informal | GP lack of trust |
| Summary | Embedded | Good for one acute trust only | Mixed | Weak | Weak | Fragmented |
| SAAR | 1572 | 1776 | 2481 | 1905 | 2421 | 3493 |
Conclusion: integration may explain further variation in the SAAR so test it in phase 3.
Proactive approach to admission avoidance gives low standardised avoidable admissions rate
Some systems had initiatives with a remit of admission avoidance which were described by interviewees as proactive and in operation during the time of the SAAR. These involved proactive senior review by medical staff, multidisciplinary teams actively seeking out hospital attendances who could be safely sent home with support, or teams actively checking on vulnerable people at home. We ordered the cases by the level of proactiveness around admission avoidance (Table 33). Again, this was a subjective assessment. There was a pattern of systems with underpredicted SAARs lacking proactive admission avoidance initiatives.
| Factor | LO2 | MO6 | LO5 | MO3 | MU4 | HU1 |
|---|---|---|---|---|---|---|
| Focus on avoidable admissions | Yes: strong focus on avoidable admissions by rapid access stream and community matrons | Yes: strong focus on avoidable admissions but there had been more historically, plus proactive senior review | Partial: proactive in one acute trust | Some: some focus with a rapid assessment service in the hospital that is well regarded | Some: team is community focused rather than acute trust linked and is new | No: focused on early discharge so intermediate beds used for this, not admission avoidance |
Conclusion: proactive approach to admission avoidance could explain further variation in the SAAR so test this in phase 3.
Hospital-centric systems have higher standardised avoidable admissions rates
One system was described as hospital-centric by interviewees (HU1), with little investment in community services. Interviewees did not describe others systems in this way. One way of avoiding admissions is to offer community support in community beds or patients’ own homes. There seemed to be variation in the amount of community services available in different systems in terms of community beds and community matrons, based on interviewees’ views. We had partial information about numbers of community services so we recontacted interviewees and searched websites to obtain these numbers (Table 34). In the phase 1 regression the number of acute beds per 1000 population was included in the acute trust-based analysis but not the geographically based analysis. This factor explained variation in the final multiple regression. In the geographically based system case studies, systems could have two acute trusts with very different numbers of acute beds. We took the average of these and found that our cases did not differ very much by this factor. When we compared community bed and matron numbers in each system, they were low in HU1 compared with the other five systems, supporting the interviewees’ perceptions in HU1. However, if this were another explanatory factor of the SAAR then we would expect both HU1 and MU4 to have low numbers, and this was not the case (Table 34).
| Factor | HU1 | LO2 | LO5 | MO6 | MO3 | MU4 |
|---|---|---|---|---|---|---|
| Population size | 300,000 | 750,000 | 350,000 | 265,000 | 500,000 | 500,000 |
| Acute beds per 1000 population, average (acute trust A, acute trust B) | 1.9 (1.6, 2.1) | 1.8 (2.2, 1.3) | 1.7 (1.9, 1.4) | 1.7 | 1.7 | 1.9 (1.9, 1.9) |
| Community beds numbers per 1000 population | 0.1 (30 beds in 1 unit) | 0.3 (235 beds in 7 units) | 0.24 (83 beds in 4 units) | 0.3 (80 beds in 4 units) | 0.3 (150 beds in 6 units) | 0.7 (340 beds in 13 units) |
| Community matrons per 1000 populationb | 0.06 (17.2 wte including vacancies) | 0.02 (13) | < 0.01 (2) | 0.03 (8 wte long-term conditions practitioners) | 0.03 (17 current reduced from 35) | 0.02 (11.3 wte) |
| Perception of community nursing | Improving | Highly valued | COPD nursing singled out as highly valued | Mixed | High valued | Generally positive |
Conclusion: there is not enough support for hospital-centric systems explaining further variation in SAAR.
Systems with support services out of hours have lower standardised avoidable admissions rates
Interviewees described how having community nursing, mental health and social services available OOH (in evenings, at night and at weekends) could help to avoid admissions. Interviewees in every system wanted more services available for longer regardless of the amount of OOH availability they had. Nonetheless, some systems appeared to have more services available OOH than others, based on the interviews. Perceptions of OOH services differed by system, with a pattern that systems with underpredicted SAARs were perceived to have poorer access (Table 35).
| Limited criticism | Perception of lack of OOH provision across health and social care |
|---|---|
| LO2 MO3 MO6 |
HU1 MU4a LO5 |
The GP OOH service is a significant service in the system and one on which we had few data in the phase 1 regression. We were able to test the population’s knowledge of how to access this service and their perceptions of how easy it was to access. However, we had no data on availability or quality. In the case studies, the views about this service differed by system. Interviewees in both rural systems felt that covering a large geographical area exacerbated problems with filling shifts and providing a good-quality service (LO2, MU4). In one system a much larger number of interviewees expressed negative views, particularly expressing concerns about the extent to which the service failed to cover shifts (MU4).
We searched websites and documents for information on the opening times of different services relevant to avoiding admissions. We included availability of radiography because access to diagnostics OOH had been raised by a number of interviewees. We mapped these onto the system configuration diagrams, shading services darkest where they were open longer. It was not possible to see a pattern between different systems that supported the perceptions in Table 35 (see Figures 12–17).
Conclusion: there is conflicting evidence that availability of services OOH may explain more variation in the SAAR. We should try to measure OOH availability and test it in phase 3.
FIGURE 12.
HU1 OOH service opening hours and radiography availability. MIU, minor injuries unit; WIC, walk-in centre.
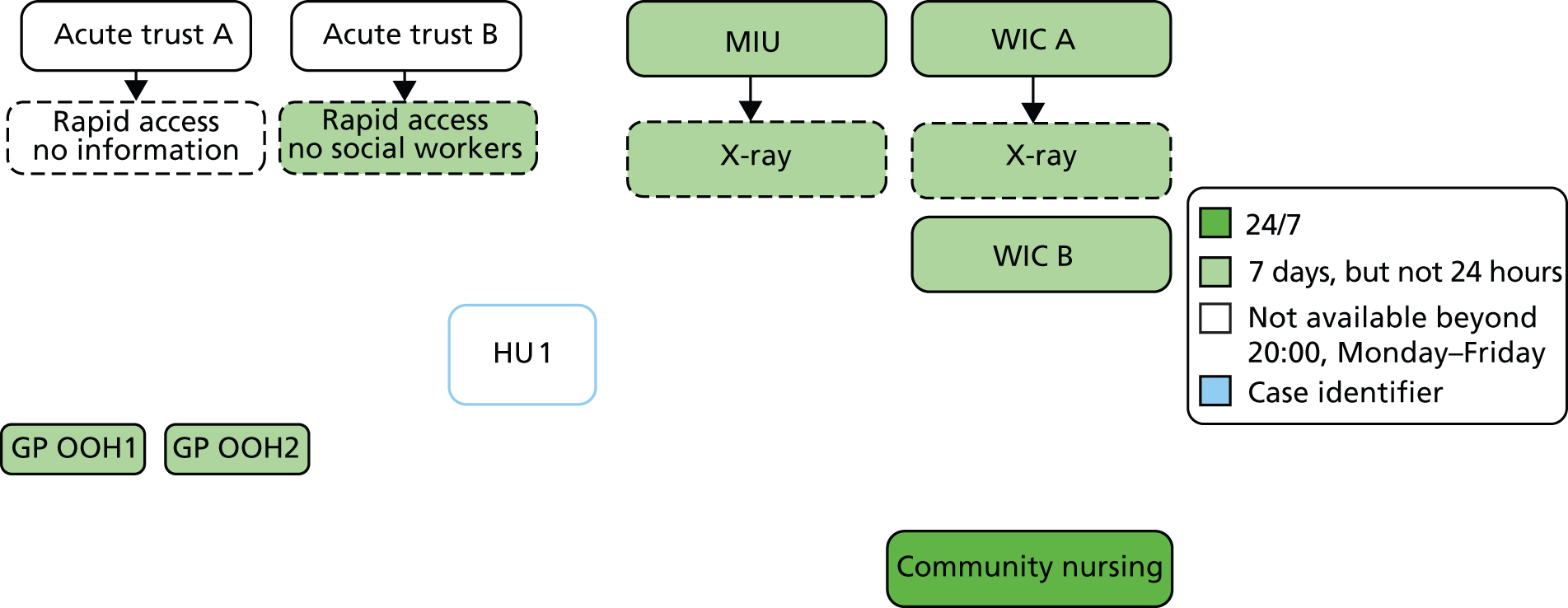
FIGURE 13.
LO2 OOH service opening hours and radiography availability. MIU, minor injuries unit; WIC, walk-in centre.
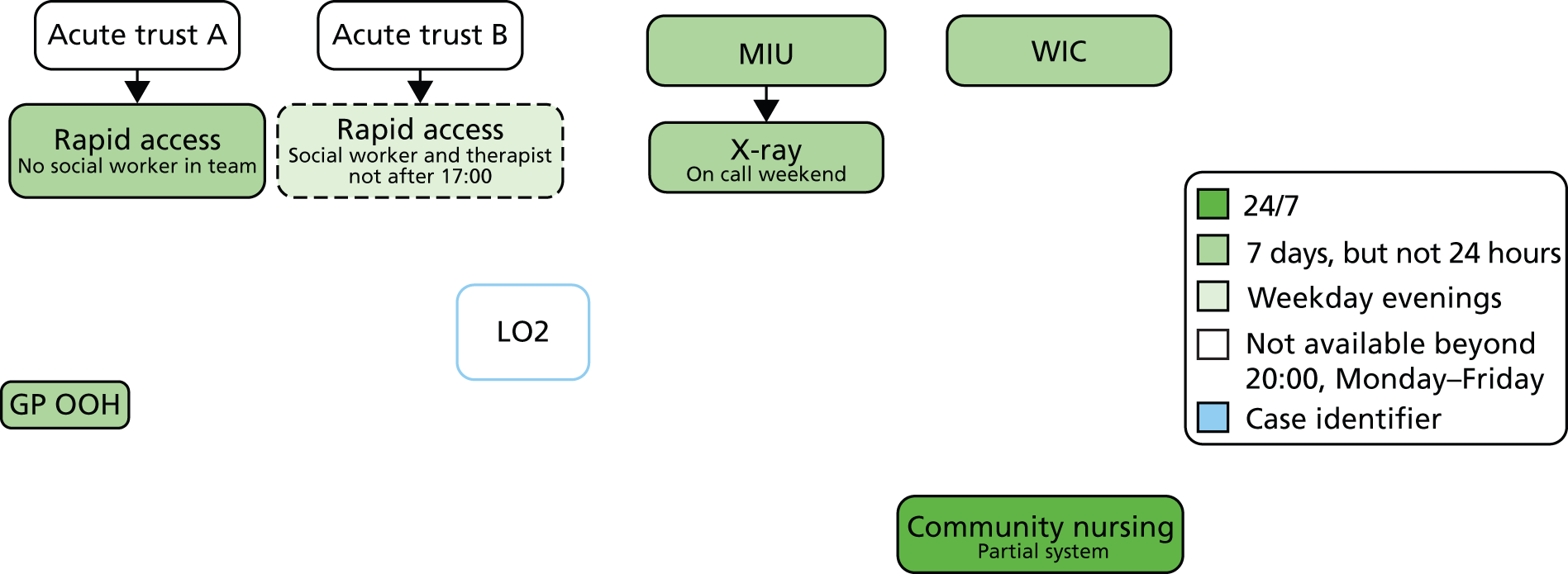
FIGURE 14.
MO3 OOH service opening hours and radiography availability. MIU, minor injuries unit.
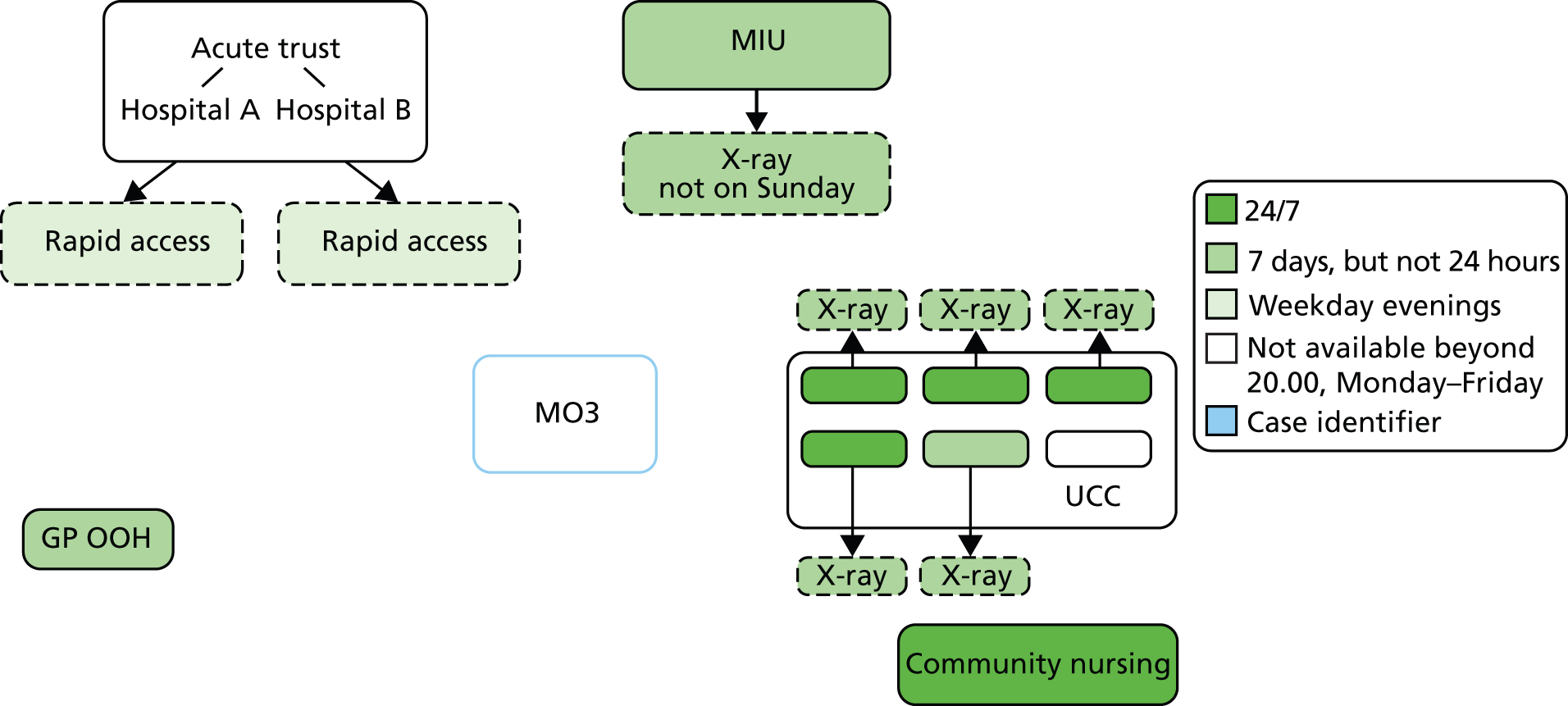
FIGURE 15.
MU4 OOH service opening hours and radiography availability. MIU, minor injuries unit; WIC, walk-in centre.
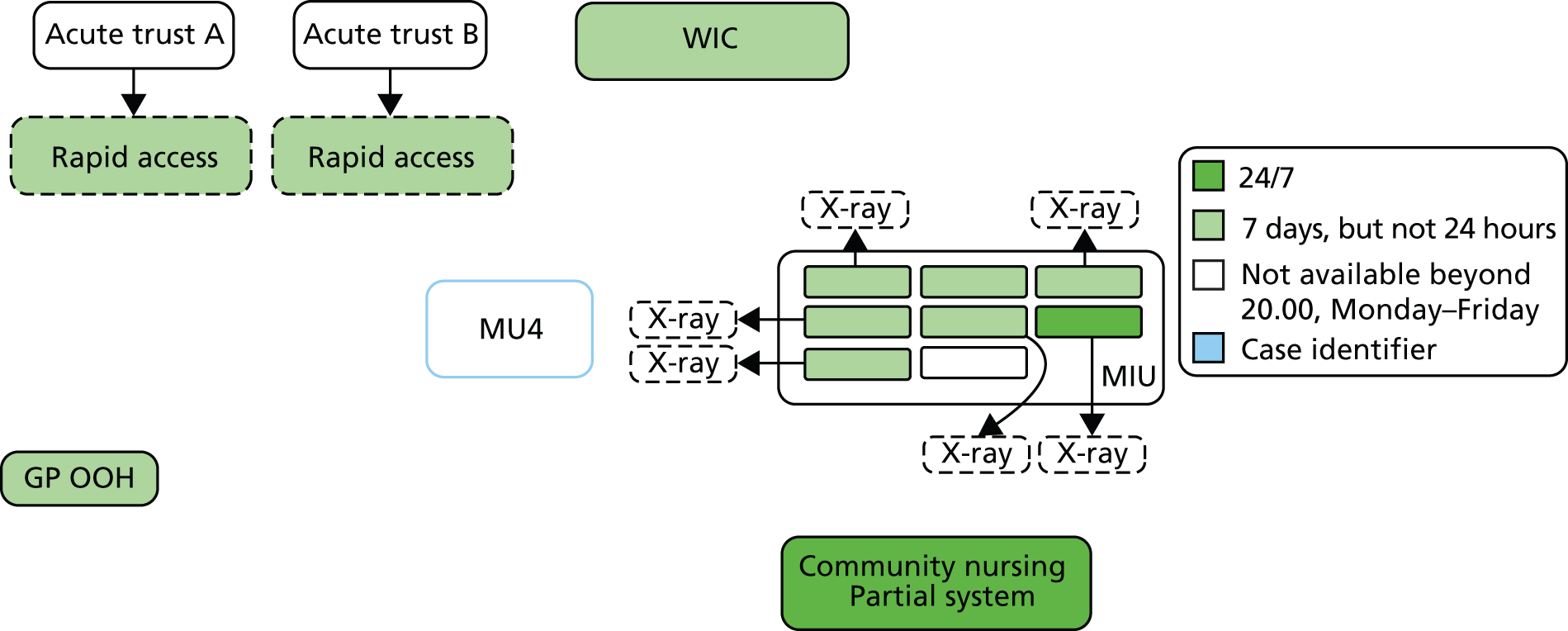
FIGURE 16.
LO5 OOH service opening hours and radiography availability. WIC, walk-in centre.
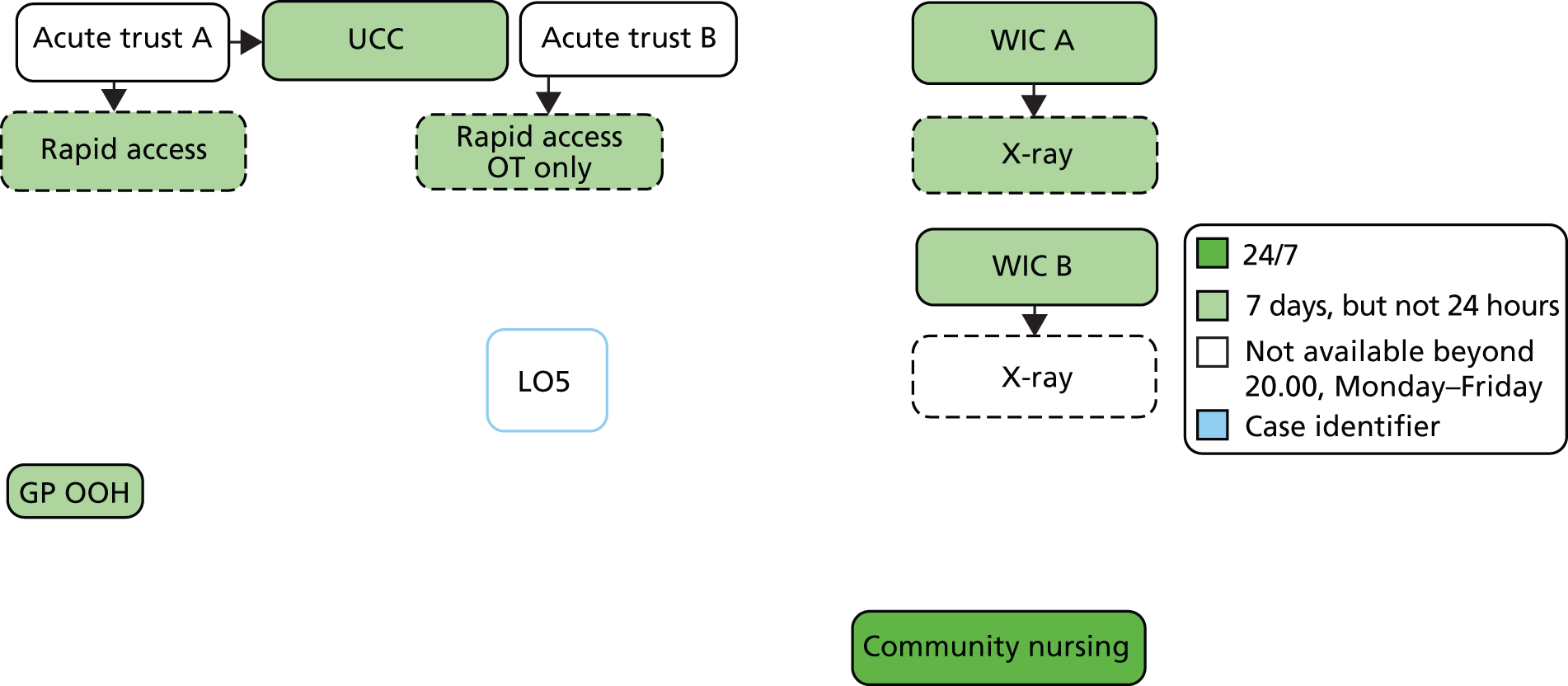
FIGURE 17.
MO6 OOH service opening hours and radiography availability.

Well-functioning emergency departments can help to avoid admissions
In the interviews there was some evidence that EDs with relationships with services within their hospital and in the community could avoid admissions, as could those which were not suffering from low ED consultant presence. No ED interviewees said that they were fully staffed and had the full complement of support services they needed. However, in one ED in each of our underpredicted systems (HU1 and MU4) there was discussion about significant difficulties recruiting consultants. We did have some variables in the phase 1 regression that are likely to capture what happens in the ED, particularly the conversion rate from attendance to admission and the length of stay < 1 day.
Conclusion: if how EDs function affects admission rates this is probably measured in the phase 1 regression already.
The conversion variable in the geographically based system phase 1 regression may be incorrect
As we developed the case personalities we started to doubt the data used about EDs for the geographically based systems. The data for geographically based systems sometimes looked very different from those for acute trust-based systems and did not tally with interviewees’ comments. We specifically wondered if systems with large numbers of UCCs, walk-in centres and minor injury units (known as type 3 and 4 EDs in national data sets) had sometimes been incorporated with EDs led by consultants (type 1 and type 2). The data for the two variables about ED use and conversion rates had come from the Atlas of Variation,35 which had issued a caution about the quality of its variables. Therefore we used HES A&E 2009/10 data to calculate the demand for EDs (types 1 and 2 only) and the conversion rate for our six geographically based systems. The data from the two sources were different for some of our cases (emboldened), but especially for HU1, where only 47% of the attendances in HES A&E were for type 1 and 2 EDs compared with over 90% for the other five cases (Table 36). The new data were more in line with interviewees’ comments and the acute trust data. The data were also different for MO6 ED attendance rates.
| Case | % type 1 or 2 | Original conversion rate (rank out of six) | New conversion rate % (rank) | Original ED attendance rate (rank) | New ED attendance rate % (rank) |
|---|---|---|---|---|---|
| HU1 | 47 | 94 (2) | 42 (6) | 426 (6) | 24 (2) |
| LO2 | 94 | 125 (6) | 29 (5) | 179 (1) | 17 (1) |
| MO3 | 98 | 105 (4) | 21 (3) | 218 (2) | 24 (2) |
| MU4 | 99 | 74 (1) | 19 (1) | 349 (5) | 28 (3) |
| LO5 | 99 | 108 (4) | 23 (4) | 319 (4) | 29 (4) |
| MO6 | 99 | 94 (2) | 19 (1) | 284 (3) | 33 (6) |
Conclusion: there is evidence to support the hypothesis that two variables we tested in phase 1 were based on inaccurate data. We will use the new variables in the phase 3 regression.
Systems which are not the primary population for an acute trust struggle with integration and therefore have high standardised avoidable admissions rates
HU1 had a population which was not the primary population of either of the two acute trusts it used. This appeared to mean that integration between the acute trusts and community services was difficult. This may have been the case for one acute trust in LO5.
Conclusion: there was not enough evidence to support this hypothesis.
Systems with low resources cannot fund services to avoid admissions
The case studies highlighted that our phase 1 regression did not take into account the resources available within systems. There was some evidence that systems facing financial difficulties reduced their admission avoidance schemes. We did not include a resource variable in the regression because the one on which we found data – resource allocation – was based on emergency admission rates.
Conclusion: even though there was no evidence that resources were lower in our two underpredicted systems, the non-testing of a resource factor in the phase 1 regression was a gap and efforts are needed to find a resource-related variable to test in phase 3.
Conclusions
The 14 conditions on which the SAAR was based had credibility among our interviewees. Interviewees offered views which supported and explained some of the findings in the phase 1 regression. For example, social deprivation was identified as driving avoidable admissions and the reasons for this were high levels of morbidity but also how people from deprived communities used services. There was also some indication of why rural areas might have lower SAARs: that the difficulty in offering services over a large geographical was an incentive to keep people out of hospital. The conversion rate from ED attendance to admission could indicate the use of proactive initiatives such as senior review or rapid assessment teams, or the way in which admissions were coded. The case studies also identified further factors that might explain variation in the SAAR, for example the level of integration within a system or the availability of support services OOH.
Factors to test in phase 3
-
Level of integration between services in the system.
-
Amount of proactive admission avoidance initiatives.
-
New data on attendance and conversion rates at EDs.
-
Availability of services OOH.
-
Amount of resource within systems.
Chapter 9 Phase 3 integration of regression and case studies
Introduction
Qualitative residual analysis offers a formal approach to integrating the qualitative and quantitative components of a study. Once issues are identified from the qualitative component for further testing in the quantitative component (see last section of Chapter 8), the next stage is to identify the relevant routinely available data. We expected to find limited data availability at this phase, perhaps identifying three or four extra variables for testing within the phase 3 regression. In addition, further insights about the variation in potentially avoidable admission rates may be available through comparison of findings from the regression and the case studies.
Methods
We identified five potential factors that might offer further explanation of variation in the SAAR (see last section of Chapter 8). Then we looked for data available at PCT or acute trust level which measured these factors or acted as proxies for them. Further integration took place by displaying the findings from different components together and considering the convergence, complementarity and disagreement between these findings as well as silence. 30
Finding and testing new variables
Level of integration between services in the system
We found no variable to measure the level of integration between services in different systems.
Amount of proactive admission avoidance initiatives
We found no variable to measure the amount of proactive admission avoidance initiatives in systems.
New data on attendance and conversion rates at emergency departments for geographically based systems
We used the HES A&E 2009–10 data for type 1 and 2 EDs only, to recalculate attendance rates and conversion rates for EDs for geographically based systems. We repeated the phase 1 regression with these two new variables and found that the regression results were similar but not identical to phase 1: length of stay < 1 day, the conversion rate and the ambulance non-transport rate still explained variation in the SAAR in the multiple regression. However, attendance rate at the ED and seeing a GP within 48 hours were no longer significant predictors within the multiple regression. The residuals from this new regression for our six case studies were still large enough to be selected as cases (< 1.3 or > 1.3), and still in the same direction, with the exception of HU1. HU1 had a very small residual because its new conversion rate was extremely high. This was supported by perceptions of interviewees from that case study who reported that ED attendances were coded as admissions and problems within the ED with consultant availability.
Availability of services out of hours
We would expect systems with poor OOH availability to have higher rates of avoidable admissions OOH. Ideally we wanted to test the ratio of admissions in hours (Monday to Friday, 09.00 to 17.00) to those OOH, but time of admission is not available in HES. Instead we created a proxy variable of the percentage of admissions occurring at the weekend. If there is a uniform distribution of admissions by day of week, we would expect 29% of avoidable admissions to occur at the weekend, with this percentage higher in systems with poor OOH support services. The mean was 24% for our geographically based systems, ranging from 20% to 26%. That is, the admission rate was lower at the weekend than week days, which does not support the conceptual framework that access to services in the wider system may avoid admission. There was also little variation between systems in the percentage of weekend avoidable admissions. This variable explained a small amount of variation in the SAAR in the univariate linear regression (Pearson’s r2 = 4%, p = 0.019) but did not add to the multiple regression once deprivation and geography were included.
Amount of resource within systems
We used routine data we had obtained for another study about the amount of surplus or deficit a PCT had in 2006–7. 41 We used this as a proxy for financial status in 2008–11. This factor explained a large amount of variation in the SAAR in the univariate linear regression (r2 = 14%, p = 0.001) but did not add to the multiple regression once deprivation and geography were included.
Opportunity to test further emergency department-related factors for acute trust-based systems
One of our authors (SG) is an expert in chest pain research and worked with a medical student, Tom Bidmead, to explore variation in admissions for chest pain between acute trusts using the HES data from our study and a survey of how EDs deal with chest pain. We added two general issues to the questionnaire which we felt were relevant to our study: the amount of senior cover in EDs and the perceptions of the amount of support services available to EDs for dealing with social admissions. The response rate to the survey was 105 of the 142 trusts (74%), with data available for 94 of the 129 acute trusts in our analysis in Chapter 5.
Senior cover
A question in the survey was about weekday cover in the ED: on a typical weekday, how many hours of the day is a consultant present in the department? This explained no variation in our SAAR in the univariate linear regression (r2 = 0%, p = 0.607).
Support services
There were two questions about support services for social admissions: Do you have a service which you can make use of to avoid ‘social admissions’, that is patients who are medically fit but require support for social issues? How many hours a day is it available on a typical weekday? We created a four-category variable of ‘not available’, ‘available < 8 hours a day’, ‘available 8–23 hours’ and ‘available 24 hours a day’. This explained no variation in our SAAR in the univariate linear regression (r2 = 2%, p = 0.592).
Comparing findings from each component
We displayed findings from each component in a matrix (Table 37). Then we looked for:
-
convergence of findings from different components (where findings agreed)
-
complementarity (usually where findings from the case studies explained or expanded on findings from the regressions)
-
discrepancy or disagreement (where findings from different components appeared to contradict each other)
-
silence (where findings from the case studies offered insights not available from the regression because of a lack of data availability for inclusion in the regressions).
| Factor | Regressions phases 1 and 3 | Case studies phase 2 | Relationship |
|---|---|---|---|
| SAAR | |||
| 14 conditions | Based on 14 conditions. SAAR generally consistent for different conditions | Credible set of conditions for admission avoidance. Some successful pathways or services existed for specific conditions | Convergence. Not consistent – some pathways for conditions highly regarded but still had high SAAR |
| Variation | Threefold variation in SAAR | – | Silence |
| Population | |||
| Deprivation | Strongest predictor | Big influence on avoidable admissions. Includes neediness for immediate access, lack of awareness of services, morbidity and some ethnic groups | Convergence and complementarity (case studies explain why deprivation is important in regressions) |
| Elderly | SAAR adjusted for age but % over 75 in population still explained 18% of variation in univariate regression. No longer explains variation when deprivation in regression. % elderly living alone does not explain variation in univariate regression. % nursing and residential home admissions explained 4% of variation in univariate regression. No longer explains variation when deprivation in regression | Both elderly living alone and in nursing homes increase avoidable admission rates | Convergence and complementarity (regression shows that deprivation subsumes some of these age-related factors) |
| Ethnicity | Explains variation in univariate regression (9%) but not once deprivation is in the regression | Can vary by ethnic group. Correlation between deprivation and ethnic groups. Effect of recent immigrants is on ED attendances, not admissions | Convergence and complementarity (case studies show it is not as simple, as ‘ethnic groups have higher admissions’) |
| Morbidity | Prevalence of individual diseases explains 20% of variation in univariate regression but not once deprivation is in the regression. Deprivation and morbidity correlated | Morbidity affects avoidable admission rates. COPD is a key condition for this | Convergence |
| Neediness | – | Modern consumerist society expects instant access and this is more likely in deprived communities | Silence – not measured in regression but also complementarity in that this may explain why deprivation explains so much variation in the regression |
| Awareness of services | Awareness of how to contact GP OOH services explains 10% of variation in univariate regression but not once deprivation is in the regression | People not aware of range of services available nationally. More likely in deprived communities | Convergence |
| Geography | |||
| Urban/rural | Rural areas have lower SAARs | Distance to hospital is an incentive to offer more services at home and in the community even though this is difficult because of distances to travel for service providers. GPs are better in rural areas. People may be more stoical in rural areas and more impatient for access in urban areas | Complementarity: case studies explain why urban and rural areas have different SAARs. Also highlights a relationship between perceived access to GP and rurality |
| Location of services | – | Some MIUs/WICS/UCCs may be in the wrong place | Silence (case studies identify factor for which there are no quantitative data) |
| Primary population for an acute trust | – | Some systems have an acute trust that considers them to be their primary population so makes efforts to create integration and offer proactive services around admission avoidance for that population | Complementarity (case studies identify factor for which there are no quantitative data) |
| Services | |||
| Ambulance | The more non-transport to ED undertaken by an ambulance service, the lower the SAAR | If ambulance services can contact support services such as social services, mental health, community nurses, WICs, GP, GP OOH, then they can keep people at home | Complementarity (case studies explain how ambulance can increase non-conveyance) |
| Acute trust | |||
| Supply | High rate of acute beds per 1000 population means high SAARs | When beds are full, services work in integrated way to avoid admissions so bed numbers act as ceiling | Complementarity |
| Coding | Short length of stay and conversion rate explained variation in the multiple regression | ED attendances can be coded as admissions or not when in holding areas | Complementarity (explains what some variables in regression might represent: different approaches to coding may be measured by short length of stay and conversion rate) |
| Outpatients | Short wait for outpatients explains higher SAARs, which is counterintuitive | – | Silence |
| Proactive with senior review, rapid assessment team etc. | Not measured in regression but may have been measured by length of stay < 1 and conversion rate | Some acute trusts very proactive with admission avoidance by offering senior review by medical staff and within ED, GPs in EDs and proactive multidisciplinary rapid assessment teams | Complementarity |
| Quality of acute trust | Foundation trust status explained variation in SAAR | – | Silence |
| ED | |||
| Shortage of consultants | Not measured in phase 1 but variable about senior cover in phase 3 did not explain variation | Shortage of ED consultants can affect functioning of department in relation to hospital and community. Junior staff request more diagnostics, which breaches 4-hour wait and increases likelihood of admission | Disagreement |
| Busyness | Not measured | Very busy departments feel chaotic and may admit to deal with this | Silence |
| GP OOH | |||
| Supply | Not measured | No doctors to run some sessions | Silence |
| Quality | Ease of contact with GP OOH did not explain variation in the univariate regression | Use of locums produces low-quality service in which general public loses faith. We would expect to see ease of contact variable explain variation | Disagreement. On reflection, people may stop using GP OOH due to loss of faith so do not complete questions about ease of access |
| General practice | |||
| Supply | Does not explain variation in univariate regression | – | Silence |
| Access | Perceived access to GP explained 25% of variation in univariate regression. Remains in the multiple regression but in counterintuitive direction. Demand for EDs explains variation in univariate and multiple regression | Belief that poor access to GPs causes people to attend EDs. Once people get to the ED they are seen by junior doctors who run tests and admit | Convergence and disagreement. The relationship between GP access and ED attendance may explain counterintuitive finding. Complementarity |
| WICs | Not measured | People can be taken to WICs by ambulance instead of EDs. People use these instead of GP in general practices | Silence |
| Community services | Not measured | Community matrons, district nurses and multidisciplinary teams can offer admission avoidance support | Silence |
| Social services | Not measured | Social services under-resourced and hard to access for admission avoidance support | Silence |
| Mental health | Prevalence of mental health problems explains variation in SAAR in univariate regression but not in multiple regression | Mental health services under-resourced and hard to access in order to avoid admission | Complementarity |
| Nursing homes | Admission rate from nursing homes explained 4% of variation in SAAR in univariate regression only | Nursing homes send patients to hospital unnecessarily | Convergence |
| System | |||
| Availability of OOH services | Explained 4% of variation in SAAR in univariate regression but not in multiple regression. Tested in phase 3 by proxy variable and did not add to the regression | Support services not available at weekends and evenings | Disagreement. This may have been due to use of a proxy quantitative variable in phase 3 or because a variable already in the regression accounted for this e.g. length of stay < 1 |
| Integration | Not measured | Integration could occur between the acute and community services, or between health and social services. Aspects of integration were colocation, joint posts, communication and condition-specific pathways | Silence |
| Hospital-centric | Not measured | Some systems had a lot of community beds and services to keep people at home | Silence |
| Proactive avoidance | Not measured | Some systems had initiatives proactively focused on admission avoidance | Silence |
| Resources available | Surplus/deficit status explained 14% of variation in SAAR in the univariate regression but not in the multiple regression | Some services were described as under-resourced and others as being cut because of financial constraints | Convergence but correlation with deprivation in the regression |
We expected to see more complementarity than convergence because we had selected the cases for the qualitative component that were not well predicted by the regression in phase 1. Findings from the different components of the study mainly agreed or offered complementary information (see Table 37). We considered where there appeared to be disagreement. The comparisons drew attention to the number of issues raised in the case studies on which we did not have routine data in our regressions. This matrix helped us to draw conclusions from the whole study, which are reported in Chapter 10.
Chapter 10 Discussion
Summary of findings
There were 3,273,395 potentially avoidable admissions in 2008–11, accounting for 22% of all emergency admissions. The mean age- and sex-adjusted admission rate was 2258 per year per 100,000 population, with a 3.4-fold variation between systems (1268 to 4359). Characteristics of the population explained the majority of variation: employment deprivation rates explained 72% of variation, with urban/rural status explaining 3% more. Systems serving populations with high levels of deprivation and in urban areas had high rates of potentially avoidable admissions. Interviewees highlighted the complexity of deprivation, which may include high levels of morbidity, low awareness of alternative services to EDs and a desire for immediate access to urgent care. Factors related to a range of services in the emergency and urgent care system explained a further 10% of variation: EDs, hospitals, emergency ambulance services and general practice. Systems with high potentially avoidable admission rates had high rates of acute beds (suggesting supply-induced demand), high rates of attendance at EDs, high rates of conversion from ED attendances to admissions, and low rates of non-conveyance by emergency ambulances. The six case studies revealed further possible explanations of variation. There was variation in how hospitals coded admissions; some systems focused proactively on admission avoidance (in particular using multidisciplinary rapid assessment teams and senior review in acute trusts) whereas others were more interested in hospital discharge; there appeared to be different levels of integration between different services such as health and social care, and acute and community trusts; and some systems faced more challenging problems around geographical boundaries than others. The system with the highest SAAR in our six case studies appeared to have a combination of these issues: it focused more on discharge than admission avoidance, coded people who did not use hospital beds as admissions, described shortages of ED consultants, was not the primary catchment area for any acute trust and appeared to have lower levels of integration between services.
Comparison with other research
Variation in admission rates
We found a large amount of variation in potentially avoidable admission rates between geographically based systems and acute trust-based systems. The order of variation found is not unusual for emergency admissions overall11,13,18 and for ambulatory care-sensitive conditions in England22 and in the USA. 24
Deprivation affects admission rates
Employment deprivation explained a very large amount of variation in our study and this is not unusual. Deprivation has been identified as an important explanatory factor of variation in emergency admissions within multiple regressions exploring variation between PCTs,12 general practices10,12,13,18–20 and hospitals. 24 For example, age and deprivation explained 64% of variation between practices,13 and age, sex, ethnicity and deprivation explained 64% of preventable hospital admission variation between practices. 20 Researchers have used different indicators of deprivation such as receipt of social security benefits,21 the Index of Multiple Deprivation12 and the Carstairs score. 11 The type of indicator may not be important given that the two we used (employment and income deprivation) were highly correlated and both explained large amounts of variation. Not all studies have found a relationship between deprivation and emergency admissions. 15
Interviewees in our case studies proposed that deprived communities had higher levels of morbidity, poor access to transport and high expectations of immediate access to emergency care. The reasons proposed for deprivation explaining so much variation in other studies were that people in deprived areas may be more ill, may present later for treatment or may not have social support at home. 18 Recent evidence shows a strong association between deprivation and multimorbidity. 42 Researchers also suggest that people from deprived communities may have difficulty negotiating access to services when they are ill. 43 In the context of our study, this may result in underuse of alternatives to EDs and community-based services which could help people to avoid a hospital admission. A study of variation in health-care utilisation in the USA related high use to low social capital. 44
Supply-induced demand
We found that the number of acute beds per 1000 population was associated with emergency admission rates. This is supported by other research. The supply of acute beds has been shown to be related to admissions overall45 and for terminally ill people. 46 Numbers of beds in these studies were considerably higher than in our study, varying between 2.1 and 4.3 per 1000 population compared with our variation of 1 to 2.9 beds per 1000 population. This relationship between supply and demand has not been found consistently. 24 Our finding may be explained by supply-induced demand. There was some support for this in our interviews, because interviewees described initiatives put in place in times of high demand and full beds to avoid admission. Supply-induced demand has been put forward as affecting evaluations of interventions to reduce emergency admissions. 47 In a discussion of variation in health care more widely, Wennberg discusses variations in supply-sensitive care and how clinicians find it hard to believe that the capacity of their health-care system affects their practice. 48
What does the large percentage of short length of stay patients mean?
The percentage of all emergency admissions staying less than a day explained variation in our multiple regression. In the UK, these short-stay admissions have been shown to be responsible for some of the recent increase in emergency admission rates. 1 It is unclear what this factor represents in our study. We surmised from our case studies that variation in this factor might be associated with different hospitals coding attendances differently. ED attendances that are moved to another part of the hospital to avoid breaching the 4-hour wait target in EDs may be coded as attendances or admissions depending on the hospital. Standardisation of coding might help to understand how best to avoid admissions appropriately by allowing researchers, commissioners and service providers to focus on actual admissions.
Conversion rate in emergency departments
The conversion rate from ED attendance to admission explained variation in potentially avoidable admissions in our study. Based on our case study findings, this factor may have been representing the availability of ED consultants or the use of admission avoidance schemes such as senior review or multidisciplinary teams offering rapid assessment within EDs. There are studies showing considerable variation in admission rates between doctors in EDs which was not related to illness severity or associated with higher mortality rates. 49 The conversion rate has been increasing in England over recent years. 50
Busy emergency departments
Our interviewees described relentless demand for emergency services and very busy EDs. These departments can be busy because lots of patients arrive or because it takes a long time to admit or discharge patients, resulting in crowding. On the issue of use of this service, a number of research studies have reported on why patients choose to attend EDs rather than alternatives. 51,52 Qualitative interviews with ED attenders have identified lack of access to general practice, anxiety about the presenting problem, perceptions of the availability of treatments in the ED and a lack of alternative pathways as important predictors of attendance rates. 52 On the issue of crowding, our interviewees identified that junior doctors are more likely to use diagnostic tests which patients have to wait for. A US group of researchers studied change in occupancy in an ED over recent years and identified that intensity of practice, whereby patients had more tests and treatments than in previous years, accounted partly for increased crowding. 53 This intensity of treatment has been related to increased admission rates from EDs over recent years. 54
Four-hour target
Our interviewees who were based in EDs described the effect of the 4-hour target on their practice. They were keen not to breach the 4-hour waiting time and moved patients out of the ED to facilitate this. In some hospitals this resulted in ED attendances being coded as emergency admissions, while this did not occur in other hospitals. Concerns have been expressed about the potential adverse effects of this target but research evidence does not support the potential for it to increase short-stay emergency admissions; in fact it decreased short-stay admissions. 55
Improving access to primary care?
We found that, in our univariate regression, perceived access to general practice explained variation in potentially avoidable admission rates, with poor access associated with high SAARs. This fitted with our conceptual framework. Additionally, our interviewees perceived this to be the case, identifying that patients would attend the ED for immediate care rather than their general practice and thus increase their likelihood of admission. Our univariate analysis concurred with other studies which showed that perceived poor access to primary care was associated with high admission rates. 10,12,15 Aspects included patients reporting being able to see a particular GP and having access to a GP within 2 days, which are relevant to avoidable emergency admissions because people with acute exacerbations may not be able to access urgent appointments at their general practice or may perceive this to be a barrier. However, in our multiple regression the relationship reversed, with good perceived access associated with high SAARs. We may have found a reverse relationship with access to general practice because of the other variables included in our regression. We included ED attendance rates, which in other studies were predicted by perceived access to general practice. 26,27 Therefore, the ED attendance rate may have been a measure of access to general practice in our regression. It is also worth noting that the relationship between poor perceived access to general practice and high use of EDs has not always been found. 56 This is also true for its relationship with emergency admissions. 20
Effective interventions for reducing emergency admissions
In our case studies, managers and clinicians had introduced schemes or initiatives to avoid admissions and our interviewees spoke highly of some of them. These included multidisciplinary rapid assessment teams available to the acute trust or ED to facilitate discharge from EDs mainly and medical admission units sometimes; condition-specific pathways which allowed a co-ordinated approach to managing patients; senior review in EDs by medical or emergency consultants; GPs in EDs; easy access to community beds for hospital and primary care staff; education or individual GP for nursing homes; and rapid response teams or community matrons in the community stopping patients getting to the hospital in the first place. Our PPI coapplicant viewed these as examples of good practice to promote to the rest of the NHS. However, before recommending them, it is important to explore the research evidence base about their effectiveness. We could reference positive and null findings from a number of studies evaluating some of the schemes in use within our case studies. However, this should be done in the context of a systematic review which pays attention to use of robust evaluative designs and systematic searching. Purdy et al. 57 published a series of systematic reviews of interventions to reduce unplanned admissions and concluded that the majority of interventions tested did not reduce admissions. They also highlighted insufficient evidence on some types of initiatives. This concurred with a non-systematic review on a wide range of approaches aimed at reducing emergency admissions in people with long-term conditions and frail elderly. 58 It is interesting to note that few of the schemes/initiatives being used in practice within our six case studies have been found to be effective, or evaluated at all with randomised controlled trials in this comprehensive systematic review. 57 Pathways had an evidence base but the conclusion was that there was no convincing evidence that they worked. 57 There was a lack of studies of ED interventions, including GPs in EDs. 58
More recent research has been published about some of the schemes discussed by our interviewees. For example, the effectiveness of a team of allied health professionals offering co-ordinated care to older people in EDs (similar to our rapid assessment teams) found a very small reduction in emergency admissions albeit using a non-randomised design. 59 The use of geriatric assessment in an ED (a type of senior review initiative) identified a lower conversion rate to admission, again using a non-randomised design. 60 However, it is important to evaluate robustly some of the types of schemes discussed in our study, using randomised controlled designs if possible.
Is integration the way forward?
It is important to remember what we have been unable to include in our regression analysis. There were no routinely available data on availability and quality of community/intermediate/social care services, or integration between services, so we could not assess the effect of these potentially important factors. Integration of different types of services (health and social care, acute and community care) was described differently in our six case studies. Our interviewees felt that integrated practice could facilitate admission avoidance. The evidence base is less positive than our interviewees. Bardsley et al. 61 reflected on the 30 integrated and community-based interventions aimed at reducing emergency admissions that the Nuffield Trust had evaluated over time. These included the integrated care pilots which used structured care for at-risk older people. The results of their work were overwhelmingly negative in terms of reducing emergency admissions, including the integrated care pilots. They concluded that structural change does not necessarily deliver integration in practice. This aligns with other research on structurally integrated health and social care for mental health which showed that it was not sufficient for integrated care in practice and did not necessarily lead to better outcomes. 62 Evans et al. 63 undertook a review of the literature on integration in health care and discussed the belief that integration can offer better quality of care, efficient care and higher patient satisfaction. Their conclusion was that we do not necessarily know what integration is (even though many definitions and models exist) or how to achieve it. The literature does not support enforced structural integration but points more to integration in terms of shared vision and trust. 62 Evans concurs with this, recommending a move from a focus on structure to one on culture. Indeed our study highlighted the complexity of integration and the importance of communication and knowledge to build up trust between services.
There was some indication in our study that integration was easier between an acute trust and the main PCT population they served. There is some support for this in the literature where emergency bed use for older people was found to be lower in PCTs with a high proportion of their population going to a single acute trust. 64
Is 7-day working the way forward?
Our interviewees wanted more OOH provision of services that help to avoid admissions such as mental and social services. Two recent national reviews of emergency care in England have supported consideration of 7-day working. 50,65 There would be a substantial cost to the NHS of providing this and cost-effectiveness studies would be required.
Will educating the general public about how to use urgent care help?
Our interviewees wanted to see more education of the general public about which services to use under different circumstances when they had perceived urgent health needs. Our previous research showed that recent users of emergency and urgent care had a lack of awareness of alternatives to GPs and EDs and were confused about when to use newer services. 4 Research focusing on people with long-term conditions suggests that they understand which services are available and choose those that suit them most. 66 They see newer services such as walk-in centres as not offering the technological input of the ED or the established relationship of general practice. The permeability or ease of access of a service affects their choice, with EDs viewed as more permeable than general practice. 66 For people with long-term conditions, simply educating them on choices available would not work. However, it might be useful to explore whether any approaches to educating the general public about how to use emergency and urgent care services have been effective. It would also be useful to review the literature on why people use emergency and urgent care services and how this might affect avoidable emergency admissions, as well as to interview patients and their families about factors affecting avoidable emergency admissions.
Non-conveyance by ambulance services
We found that the large variation in non-conveyance rates by ambulance services explained some variation in avoidable admissions. This is a unique and important finding. Non-conveyance rates have increased considerably in recent years in England and there is support for it nationally as a way of managing demand for emergency care. 65 A review recommended that research be undertaken into how best to deliver appropriate and safe non-conveyance;67 some of this research is ongoing. 68
Easy and safe option
A prominent theme throughout our interviews was hospital admission or ED attendance as the easy or safe option. This is supported by a study of non-conveyance in the ambulance service for epilepsy, where ambulance crew were concerned about litigation and therefore transported people to hospitals. 69 Additionally, hospital admission has been seen as the only option for ED management of people with mental health problems in rural areas in Australia. 70
Reflecting on incentives
It is worth considering how incentives in the emergency and urgent care system appeared to affect the behaviour of staff within it. We heard in our case studies about the perceived incentive to admit to make money for an acute trust in need of financial support; the incentive to save time by admitting patients because of the workload involved in finding alternatives; the incentive to meet targets such as 8-minute response for ambulance services and 4-hour waiting at EDs leading to admission or coding as admission; and the incentive to avoid winter crises in bed use through schemes to avoid admission. Making alternatives to hospital admission the easy and safe options could act as an incentive for staff to avoid some admissions.
Resources
We could not use resource allocation data in our regression because they include emergency admission rates. The data we located about PCT surplus and deficit were limited in terms of their age and focus, so we could not measure the effect of variation in resources available in different systems. Lack of resources was raised in our case studies, however, with discussions about how it affects the input of social services and the loss of some disciplines from multidisciplinary teams providing proactive admission avoidance schemes.
Strengths and limitations
Strengths
The strengths of the study were that it focused on admissions for conditions rich in avoidable admissions rather than all admissions; it moved beyond previous research which has focused on either primary care or hospital factors explaining emergency admissions; and the design used a combination of quantitative and qualitative research to understand the factors affecting avoidable emergency admissions.
Limitations
Interpretation of the standardised avoidable admissions rate
The 14 conditions upon which the SAAR was based were identified by an expert panel as rich in avoidable admissions. It is important to note that some admissions would not have been avoidable even in the best of systems and therefore the SAAR exaggerates the extent of avoidable admissions. This exaggeration did not affect our study because we were interested in variation in the SAAR between systems.
Missing factors in the regression
Factors could only be tested in our quantitative component if the data were available routinely by PCT or acute trust. There were factors potentially affecting admission that we were unable to include. Importantly some factors may be related to the population, such as severity of illness. A key missing variable was distance to hospital, because this has been shown to explain variation in emergency admission rates between general practices, with higher emergency admissions for practices close to a hospital. 10 We could not generate a distance variable because PCT populations often use not a single hospital but a number of hospitals within or outside the PCT boundaries. However, the geographical variable in our analysis may have addressed some of this issue in that distance to hospital is likely to be longer in rural than urban areas. Other important missing variables were related to social services, nursing homes, intermediate care and system-level variables such as integration between services and resources available. Although other researchers have tested some of these variables, for example the numbers of community beds available, they have collected these data themselves and expressed concerns about the quality of the data used. 64
A lack of clarity about exactly what factors in the regression measure
The final regression was dependent on the variables that were tested. For example, at an earlier stage of the study we included length of stay < 2 days rather than < 1 day because we were concerned that coding differences might account for variation. Later, we decided that length of stay < 2 days might reflect discharge policy rather than admission policy so we changed it to < 1 day. By making this decision, we made the rate of attendance at EDs a statistically significant addition to the regression. This highlights that it was not clear exactly how the factors we included in the regression affected the SAAR. For example, the short length of stay might indicate coding differences between hospitals for the same types of cases, or different management practices related to the ED, or simply that avoidable admissions tend to stay in hospital for less than a day. In addition, high ED attendance rates might indicate a lack of availability or accessibility of alternative sources of urgent care in systems, for example minor injury units or walk-in centres, or that an ED was located in a densely populated area with a short travel distance. Higher conversion rates from ED attendance to admissions might be caused by risk-averse decision-making in the ED or lack of access to alternative services to admission at the ED. The phase 2 case studies threw some light on the meaning of some of these factors but did not fully explain how these factors affected emergency admissions in the regression.
Uncertainty of findings of the regression
Stepwise linear regression was used but it has limitations. First, the model identified is dependent on the selection algorithm used. We used forward selection rather than backward elimination; there is no consensus about which is best. Because of the amount of correlation between variables, our final model is likely to have differed using backward elimination. Second, the aim of linear regression is to identify the ‘best model’ and suggests a level of confidence in the specific regression model that is not justified. An alternative approach – an information-theoretic approach – might show that no one model could be relied upon for inference because a number of models describe the data equally well, resulting in averaging these models for a final regression model. 71 Third, linear regression overestimates the fit. Finally, it inflates the probability of a type I error, where some variables are identified as statistically significant by chance. A large number of predictors were tested in our regression (n = 30) for the number of subjects (n = 150). This can result in some factors being significant by chance and an overoptimistic regression with regard to goodness of fit. Therefore, there is uncertainty about the findings from the regression.
We could have used Poisson regression instead of linear regression because numbers of admissions are counts. We selected linear regression because the assumption of normality is usually robust (and was robust in our study) and variation is usually greater in practice than estimated by Poisson, requiring attention to extra-Poisson variation.
Inaccurate data
There may have been data errors in the routine data used. Our case studies highlighted that the ED data we used in the geographically based system analysis were likely to be inaccurate. When we tested a variable based on different routine data we found that it slightly changed the results of the regression but that most of the factors identified in the original regression were statistically significant.
Catchment populations for acute trusts
The regression relied on the calculation of hospital catchment areas for emergency admissions. There is debate about the best way to calculate catchment areas. The type of proportional flow model used here has been shown to work well32 but can give smaller catchment areas than more sophisticated approaches. 31 This should not have been a problem because any underestimate would affect all the estimated catchment populations.
Overestimate of correlation
Regressions can overestimate correlation if the dependent and independent variables share the same denominator. Many of our variables were based on the PCT population. Taking the logarithm of the independent variables removes this problem. This made little difference to the findings. For example, employment deprivation explained 70% rather than 72% of variation in our geographically based regression.
Implications of sampling six cases purposively
The six cases were purposively sampled to identify high, medium and low SAARs and over- and underprediction by the phase 1 regression. There is always the question of what issues might have emerged had we sampled differently. The strength of the approach we took was that having identified a regression model with good fit, a focus on residuals was more likely to lead us to further issues rather than identification of the same issues as the regression. We did not include well predicted cases and so have been unable to reflect on the extent to which our six cases identified issues over and above cases chosen simply because they had high medium or low SAARs.
The cases we selected often represented a cluster of cases with similar SAARs and levels of prediction so they were not unusual cases in the context of the 27 cases with large residuals.
Interview-focused case studies
Our aim was to engage with the breadth of stakeholders within each system. This was at the cost of some depth that we could have achieved through use of non-participant observation and immersion in the field. We relied on accounts and perceptions of the system rather than direct observation. Originally we felt that observation of a whole system would be too challenging to undertake, requiring spending time in EDs, ambulance services, general practice, GP OOH, walk-in centres, and community and social services. In hindsight, observation within an ED in each system would have been helpful because this is the route through which the majority of admissions occur.
Breadth of system emerged over time
We started the study with a view of the stakeholders to include. During interviews, key people to interview emerged, for example leaders of rapid assessment teams. Some important stakeholders emerged late in the process and we did not include them, in particular managers from mental health trusts. We attempted to include heads of nursing and residential homes because these emerged as important from early interviews, but did not get responses to our requests for interviews.
Lack of patient voice
We included Healthwatch in our case studies to offer a patient viewpoint. However, because this organisation was being set up during our study we only managed to undertake two interviews in the six case studies. Therefore the study is very much focused on the health and social care professional voice, with little understanding of how patients and their families view factors affecting avoidable admissions. Our PPI coapplicant would have preferred the inclusion of patients’ voices within the study. Indeed a study of older people and emergency admissions followed the patient journey and identified issues that did not appear in our study such as carer burden. 72
Reflection on qualitative residual analysis
Qualitative residual analysis was a helpful approach to take because it went beyond a sequential mixed-methods approach of a regression followed by a qualitative study. We believe that the sampling of the case studies helped us to identify factors such as differing coding practices that might not have been identified using another approach to sampling. Even though the phase 3 regression did not explain further variation, this may have been a result of the large amount of variation already explained in phase 1 and the complexity of deprivation as a factor. In practice the approach was more art than science because there is little guidance on the specifics of undertaking this approach, for example types of residual to use or what is a large residual.
Generalisability, transferability and reflexivity
The study was undertaken in England using quantitative data from 2008–11 and qualitative data from 2012–13. National health systems differ so the findings may not be transferable to other countries. However, the literature we reference on variation in health care from the USA and Australia suggests that the findings may be transferable to those countries. Although emergency admissions continue to rise, and PCTs have disappeared, the findings are likely to remain highly relevant to today’s health-care system.
The research team consisted of health researchers and viewed social care as a component of the emergency and urgent care system rather than central to it. Social care researchers might have adopted a different perspective. Most of our team are social scientists with experience of researching the emergency and urgent care system rather than seeing care from a single perspective such as general practice, EDs or ambulance services. Our PPI team member took a wide perspective of the topic.
Patient and public involvement
Our PPI team member, our PPI Project Advisory Group member and SECF members commented on findings as the study progressed. Their views were embedded in the study and the report. Towards the end of the study, they offered guidance on dissemination so that findings could have an impact. They recommended we inform ministers, local and national politicians, and the general public through local radio and existing charities such as Age UK. They were also interested in the research being used to educate people about how to use emergency and urgent care services through use of televisions in health-care facilities and pharmacies.
Challenging the conceptual framework
We began the study with a strong conceptual framework: emergency and urgent care systems that performed well would have lower avoidable admission rates. We meant by this that, if patients were able to seek help from services outside the hospital when they had an urgent care need, they would be less likely to end up in a hospital bed. As the study progressed, our understanding of our framework expanded to include explicitly the ability of health professionals as well as patients to seek appropriate care outside the hospital. We identified two separate aspects to avoidable admissions:
-
avoiding attendance at the acute trust
-
avoiding admission once patients attended the acute trust.
For the first aspect, the focus was on patients themselves seeking care from services other than EDs, and being able to obtain that care when needed. The focus was also on the ambulance service, primary care and community services maintaining patients at home or using alternatives to a hospital attendance. The acute trust could affect this aspect by offering advice on individual patients to health professionals outside the hospital, such as GPs and nurses in walk-in centres. For the second aspect, the focus was on the decision-making of clinicians in acute trusts, particularly in EDs but also in medical admission units, who needed to work in partnership with GPs, community and social services to discharge patients home instead of using hospital beds. How EDs operated within the acute trust, and with services which supported discharge home, became much more central to our study as our analysis progressed.
On the whole our conceptual framework was supported by the data we collected. In our quantitative component we identified that variation in services in the wider emergency and urgent care system explained variation in potentially avoidable admission rates. Our interviewees appeared to believe in the conceptual framework, identifying how services provided by the ambulance service and community, social and primary care affected admissions. One issue did not support our conceptual framework. Our interviewees described how the lack of availability of community and social services OOH severely limited their ability to avoid admissions. This led us to expect that more avoidable admissions would occur at weekends but this was not the case; avoidable admission rates were lower at weekends than weekdays.
Impact on national reviews of emergency care
During our study there was considerable national interest in emergency care, with a review of emergency admissions50 and a major review of the emergency and urgent care system. 65 We spoke to both of these groups about the early results from this study as well as our previous emergency and urgent care studies.
Conclusions
Our conceptual framework was that some admissions are avoidable if services in the wider emergency and urgent care system operate well. Much of what we found supported this but we also found that practice within the micro-system of an ED and acute trust was extremely important, for example variation in conversion rates from ED attendances to admissions. Social deprivation, associated with high levels of illness and possibly high expectations around service access, explained a large amount of variation in avoidable admissions. Some variation appeared to be related to different coding practices in acute trusts. Health-care staff perceived admission to be the easy or safe option when faced with time constraints. Some admission avoidance schemes, and integrated working, were well regarded by staff, for example rapid assessment teams, but the research evidence base on the effectiveness of these schemes is limited.
Implications for health care
All health and social services have a role to play in admission avoidance. Given the large impact of deprivation on variation in avoidable admissions, there is a need to develop admission avoidance initiatives tailored to deprived communities. There is a need to standardise coding practices so that hospital attendances staying a few hours in ‘holding areas’ are not coded as admissions. There is a need to evaluate schemes/initiatives that health-care staff perceive to offer easy and safe alternatives to a hospital bed, for example rapid assessment teams, because the research evidence base is too limited to recommend that these approaches be adopted nationally.
Recommendations for research (in order of priority)
-
Better understand how deprivation affects admissions to facilitate the development of effective interventions to avoid admissions for deprived communities.
-
Robustly evaluate the different types of admission avoidance schemes used by some systems, in particular the use of multidisciplinary teams/rapid assessment teams available to acute trusts to facilitate discharge from EDs and medical admission units.
-
Understand why ambulance services have such different percentages of calls dealt with, without transport to an ED.
-
Understand avoidable emergency admissions from the viewpoint of patients and their families.
-
Understand the decision-making processes and the perceptions of decision-makers in terms of the risks and benefits of hospital admission (both to themselves and to the patients), with an emphasis on differences between junior and senior doctors.
-
Address evidence-light relevant issues such as the cost-effectiveness of 24/7 availability in the emergency and urgent care system and unintended consequences of the 4-hour target in EDs.
Acknowledgements
Contribution of authors
Alicia O’Cathain (Professor of Health Services Research) designed and led the study, analysed the quantitative and qualitative data and wrote the first draft of the report.
Emma Knowles (Research Fellow) was project manager, led the case studies, wrote parts of the first draft and contributed to interpretation of the study.
Janette Turner (Senior Research Fellow) contributed to management and interpretation of the study, bringing expertise in pre-hospital care research.
Ravi Maheswaran (Reader in Public Health) led the calculation of variables using HES data and contributed to management and interpretation of the study.
Steve Goodacre (Professor of Emergency Care) contributed to management and interpretation of the study, bringing expertise in ED research.
Enid Hirst (Co-ordinator and Founder of SECF) led the PPI and contributed to management and interpretation of the study.
Jon Nicholl (Professor of Health Services Research) contributed to management and interpretation of the study, bringing expertise in the performance indicators for emergency and urgent care.
Acknowledgement of other contributions
Project Advisory Group
We would like to thank members of the Project Advisory Group who offered support, encouragement and evaluations of the content and progress of the study: Dr Sarah Purdy (Chair, GP, researcher at the University of Bristol), John Soady (Sheffield Clinical Commissioning Group/Public Health), Beryl Darlison (PPI).
Patient and public involvement
We would like to thank members of the SECF for providing a patient and public perspective on the design, findings and interpretation of the study over and above the input from Enid Hirst as management team member and Beryl Darlison as Project Advisory Group member.
Researcher support
Colin O’Keefe helped to code the qualitative data within NVivo.
Robin Chatters contributed to the documentary analysis.
Tim Pearson calculated the SAAR and other variables using data from the HES.
Tom Bidmead undertook a survey of management of chest pain in EDs in England and shared his data with us for phase 3 of our study.
Administrative support
Susan Proctor offered administrative support to the project.
Marc Chattle and Richard Campbell managed data for phases 1 and 3.
Participation in the study
We would like to thank all the interviewees who spent time out of their extremely busy work days to share their views of their emergency and urgent care systems.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
Publications
O’Cathain A, Knowles E, Maheswaran R, Pearson T, Turner J, Hirst E, et al. A system-wide approach to explaining variation in potentially avoidable emergency admissions: national ecological study. BMJ Qual Saf 2014;23:47–55.
O’Cathain A, Knowles E, Maheswaran R, Turner J, Hirst E, Goodacre S, et al. Hospital characteristics affecting potentially avoidable emergency admissions: national ecological study. Health Serv Manag Res 2013;26:110–18.
References
- Blunt I, Bardsley M, Dixon J. Trends in Emergency Admissions in England 2004–2009. London: The Nuffield Trust; 2010.
- Bindman AB, Grumbach K, Osmond D, Komaromy M, Vranizan K, Lurie N, et al. Preventable hospitalizations and access to health care. JAMA 1995;274:305-11.
- Purdy S, Griffin TP, Salisbury C, Sharp D. Prioritising ambulatory care sensitive hospital admissions in England for research and intervention: a Delphi exercise. Prim Health Care Res Dev 2010;11:41-50. http://dx.doi.org/10.1017/S1463423609990211.
- O’Cathain A, Coleman P, Nicholl J. J Health Serv Res Policy 2008;13:19-25. http://dx.doi.org/10.1258/jhsrp.2007.007097.
- Knowles E, O’Cathain A, Nicholl J. Patients’ experiences and views of an emergency and urgent care system. Health Expect 2012;15:78-86. http://dx.doi.org/10.1111/j.1369-7625.2010.00659.x.
- Coleman P, Nicholl J. Consensus methods to identify a set of potential performance for systems of emergency and urgent care. J Health Serv Res Policy 2010;15:14-8. http://dx.doi.org/10.1258/jhsrp.2009.009096.
- von Bertalanffy L. General System Theory: Foundations, Development, Applications. New York, NY: George Braziller; 1968.
- Mingers J, White L. A review of the recent contribution of systems thinking to operational research and management science. Eur J Operational Res 2010;207:1147-61. http://dx.doi.org/10.1016/j.ejor.2009.12.019.
- Nicholl J, Coleman P, Knowles E, O’Cathain A, Turner J. Emergency and Urgent Care Systems. Sheffield: Medical Care Research Unit; 2009.
- Bankart MJ, Baker R, Rashid A, Habiba M, Banerjee J, Hsu R, et al. Characteristics of general practices associated with emergency admission rates to hospital: a cross-sectional study. EMJ 2011;28:558-63. http://dx.doi.org/10.1136/emj.2010.108548.
- Blatchford O, Capewell S, Murray S, Blatchford M. Emergency medical admissions in Glasgow: general practices vary despite adjustment for age, sex, and deprivation. Br J Gen Pract 1999;49:551-4.
- Calderón-Larrañaga A, Carney L, Soljak M, Bottle A, Partridge M, Bell D, et al. Association of population and primary healthcare factors with hospital admission rates for chronic obstructive pulmonary disease in England: national cross-sectional study. Thorax 2011;66:191-6. http://dx.doi.org/10.1136/thx.2010.147058.
- Duffy R, Neville R, Staines H. Variance in practice emergency medical admission rates: can it be explained?. Br J Gen Pract 2002;52:14-8.
- Dusheiko M, Doran T, Gravelle H, Fullwood C, Roland M. Does higher quality of diabetes management in family practice reduce unplanned hospital admissions?. Health Serv Res 2011;46:27-46. http://dx.doi.org/10.1111/j.1475-6773.2010.01184.x.
- Gunther S, Taub N, Rogers S, Baker R. What aspects of primary care predict emergency admission rates? A cross sectional study. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-11.
- Purdy S, Griffin T, Salisbury C, Sharp D. Emergency respiratory admissions: influence of practice, population and hospital factors. J Health Serv Res Policy 2011;16:133-40. http://dx.doi.org/10.1258/jhsrp.2010.010013.
- Purdy S, Griffin T, Salisbury C, Sharp D. Emergency admissions for coronary heart disease: a cross sectional study of general practice, population and hospital factors in England. Public Health 2011;125:46-54. http://dx.doi.org/10.1016/j.puhe.2010.07.006.
- Reid FD, Cook DG, Majeed A. Explaining variation in hospital admission rates between general practices: cross sectional study. BMJ 1999;319:98-103. http://dx.doi.org/10.1136/bmj.319.7202.98.
- Soljak M, Calderon-Larrañaga A, Sharma P, Cecil E, Bell D, Abi-Aad G, et al. Does higher quality primary health care reduce stroke admissions? A national cross-sectional study. Br J Gen Pract 2011;61:e801-7. http://dx.doi.org/10.3399/bjgp11X613142.
- Barnett R, Malcolm L. Practice and ethnic variations in avoidable hospital admission rates in Christchurch, New Zealand. Health Place 2010;16:199-208. http://dx.doi.org/10.1016/j.healthplace.2009.09.010.
- Majeed A, Bardsley M, Morgan D, O’Sullivan C, Bindman AB. Cross sectional study of primary care groups in London: association of measures of socioeconomic and health status with hospital admission rates. BMJ 2000;321:1057-60. http://dx.doi.org/10.1136/bmj.321.7268.1057.
- Tian Y, Dixon A, Gao H. Emergency Hospital Admissions for Ambulatory Care-Sensitive Conditions: Identifying the Potential for Reduction. London: The King’s Fund; 2012.
- Saxena S, George J, Barber J, Fitzpatrick J, Majeed A. Association of population and practice factors with potentially avoidable admission rates for chronic diseases in London: cross sectional analysis. J R Soc Med 2006;99:81-9. http://dx.doi.org/10.1258/jrsm.99.2.81.
- Finegan MS, Gao J, Pasquale D, Campbell J. Trends and geographic variation of potentially avoidable hospitalizations in the veterans health-care system. Health Serv Manag Res 2010;23:66-75. http://dx.doi.org/10.1258/hsmr.2009.009023.
- Abualenain J, Frohna WJ, Shesser R, Ding R, Smith M, Pines JM. Emergency department physician-level and hospital-level variation in admission rates. Ann Emerg Med 2013;61:638-43. http://dx.doi.org/10.1016/j.annemergmed.2013.01.016.
- Baker R, Bankart MJ, Rashid A, Banerjee J, Conroy S, Habiba M, et al. Characteristics of general practices associated with emergency-department attendance rates: a cross-sectional study. BMJ Qual Saf 2011;20:953-8. http://dx.doi.org/10.1136/bmjqs.2010.050864.
- Cowling TE, Cecil EV, Soljak MA, Lee JT, Millett C, Majeed A, et al. Access to primary care and visits to emergency departments in England: a cross-sectional, population-based study. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0066699.
- Fry G, Chantavanich S, Chantavanich A. Merging quantitative and qualitative research techniques: toward a new research paradigm. Anthropol Educ Q 1981;12:145-57. http://dx.doi.org/10.1525/aeq.1981.12.2.05x1889q.
- Onwuegbuzie AJ, Teddlie C, Tashakkori A, Teddlie C. Handbook of Mixed Methods in Social and Behavioural Research. London: Sage Publications; 2003.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c4587.
- Gilmour SJ. Identification of hospital catchment areas using clustering: an example from the NHS. Health Serv Res 2010;45:497-513. http://dx.doi.org/10.1111/j.1475-6773.2009.01069.x.
- Jones S, Wardlaw J, Crouch S, Carolan M. Modelling catchment areas for secondary care providers: a case study. Health Care Manag Sci 2011;14:253-61. http://dx.doi.org/10.1007/s10729-011-9154-y.
- Edmonson-Jones M. Acute Hospital Catchment Populations 2009 2011. www.erpho.org.uk/viewResource.aspx?id=21919 (accessed 25 March 2013).
- Purdy S, Griffin T, Salisbury C, Sharp D. Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians. Public Health 2009;123:169-73. http://dx.doi.org/10.1016/j.puhe.2008.11.001.
- South East Public Health Observatory . Atlas of Variation n.d. www.sepho.org.uk/extras/maps/NHSatlas/atlas.html (accessed 1 February 2013).
- O’Cathain A, Knowles E, Maheswaran R, Pearson T, Turner J, Hirst E, et al. A system-wide approach to explaining variation in potentially avoidable emergency admissions: national ecological study. BMJ Qual Saf 2014;23:47-55. http://dx.doi.org/10.1136/bmjqs-2013-002003.
- Department for Communities and Local Government . The English Indices of Deprivation 2010: PCT Summaries n.d. www.gov.uk/government/publications/english-indices-of-deprivation-2010 (accessed 29 January 2013).
- O’Cathain A, Knowles E, Maheswaran R, Turner J, Hirst E, Goodacre S, et al. Hospital characteristics affecting potentially avoidable emergency admissions: national ecological study. Health Serv Manag Res 2013;26:110-18. http://dx.doi.org/10.1177/0951484814525357.
- Yin RK. Case Study Research: Design and Methods. London: Sage Publications; 2003.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analysing Qualitative Data. London: Routledge; 1994.
- Sampson F, O’Cathain A, Strong M, Pickin M, Esmonde L. JHSPR commissioning processes in primary care trusts: a repeated cross-sectional survey of health care commissioners in England. J Health Serv Res Policy 2012;17:31-9. http://dx.doi.org/10.1258/jhsrp.2011.010191.
- Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37-43. http://dx.doi.org/10.1016/S0140-6736(12)60240-2.
- Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 2006;6. http://dx.doi.org/10.1186/1471-2288-6-35.
- Williams J. Geographic variations in health care utilization: effects of social capital and self-interest, and implications for US Medicare policy. Socio-Econ Rev 2012;10:317-42. http://dx.doi.org/10.1093/ser/mwr018.
- Fisher ES, Wennberg JE, Stukel TA, Skinner JS, Sharp SM, Freeman JL, et al. Associations among hospital capacity, utilization, and mortality of US Medicare beneficiaries, controlling for socio-demographic factors. Health Serv Res 2000;34:1351-62.
- Wilson DM, Truman CD. Does the availability of hospital beds affect utilization patterns? The case of end-of-life care. Health Serv Manag Res 2001;14:229-39. http://dx.doi.org/10.1258/0951484011912735.
- Roland M, Abel G. Reducing emergency admissions: are we on the right track?. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e6017.
- Wennberg J. Unwarranted variations in healthcare delivery: implications for academic medical centres. BMJ 2002;325:961-4. http://dx.doi.org/10.1136/bmj.325.7370.961.
- Dean NC, Jones JP, Aronsky D, Brown S, Vines CG, Jones BE, et al. Hospital admission decision for patients with community-acquired pneumonia: variability among physicians in an emergency department. Ann Emerg Med 2012;59:35-41. http://dx.doi.org/10.1016/j.annemergmed.2011.07.032.
- National Audit Office . Emergency Admissions to Hospital: Managing the Demand 2013.
- Penson R, Coleman P, Mason S, Nicholl J. Why do patients with minor or moderate conditions that could be managed in other settings attend the emergency department?. Emerg Med J 2012;29:487-91. http://dx.doi.org/10.1136/emj.2010.107276.
- Agarwal S, Banerjee J, Baker R, Conroy S, Hsu R, Rashid A, et al. Potentially avoidable emergency department attendance: interview study of patients’ reasons for attendance. Emerg Med J 2012;29. http://dx.doi.org/10.1136/emermed-2011-200585.
- Pitts SR, Pines JM, Handrigan MT, Kellermann AL. National trends in emergency department occupancy, 2001 to 2008: effect of inpatient admissions versus emergency department practice intensity. Ann Emerg Med 2012;60:679-86. http://dx.doi.org/10.1016/j.annemergmed.2012.05.014.
- Schuur JD, Venkatesh AK. The growing role of emergency departments in hospital admissions. N Engl J Med 2012;367:391-3. http://dx.doi.org/10.1056/NEJMp1204431.
- Freeman J, Croft S, Cross S, Yap C, Mason S. The impact of the 4 hour target on patient care and outcomes in the emergency department: an analysis of hospital incidence data. Emerg Med J 2010;27:921-7. http://dx.doi.org/10.1136/emj.2009.085431.
- Harris MJ, Patel B, Bowen S. Primary care access and its relationship with emergency department utilisation: an observational, cross-sectional, ecological study. Br J Gen Pract 2011;61:e787-93. http://dx.doi.org/10.3399/bjgp11X613124.
- Purdy S, Paranjothy S, Huntley A, Thomas R, Mann M, Huws D. Interventions to Reduce Unplanned Hospital Admission: A Series of Systematic Reviews 2012. www.bristol.ac.uk/media-library/sites/primaryhealthcare/migrated/documents/unplannedadmissions.pdf (accessed 15 October 2014).
- Ham C. Reducing Unplanned Hospital Admissions: What Does the Literature Tell Us?. Birmingham: Health Services Management Centre, University of Birmingham; 2006.
- Arendts G, Fitzhardinge S, Pronk K, Donaldson M, Hutton M, Nagree Y. The impact of early emergency department allied health intervention on admission rates in older people: a non-randomized clinical study. BMC Geriatr 2012;12. http://dx.doi.org/10.1186/1471-2318-12-8.
- Conroy SP, Ansari K, Williams M, Laithwaite E, Teasdale B, Dawson J, et al. A controlled evaluation of comprehensive geriatric assessment in the emergency department: the ‘Emergency Frailty Unit’. Age Ageing 2013;43:109-14. http://dx.doi.org/10.1093/ageing/aft087.
- Bardsley M, Steventon A, Smith J, Dixon J. Evaluating Integrated and Community-Based Care. London: The Nuffield Trust; 2013.
- Reilly S, Challis D, Donnelly M, Hughes J, Stewart K. Care management in mental health services in England and Northern Ireland: do integrated organizations promote integrated practice?. J Health Serv Res Policy 2007;12:236-41. http://dx.doi.org/10.1258/135581907782101633.
- Evans JM, Ross Baker G, Whitney B, Barnsley J, Goes J, Savage GT, et al. Annual Review of Health Care Management: Revisiting the Evolution of Health Systems Organization. Bingley: Emerald Group Publishing Limited; 2013.
- Imison C, Poteliakhoff E, Thompson J. Older People and Emergency Bed Use: Exploring Variation. London: The King’s Fund; 2012.
- NHS England . Transforming Urgent and Emergency Care Services in England: Emergency and Urgent Care Review 2013.
- Hunter C, Chew-Graham C, Langer S, Stenhoff A, Drinkwater J, Guthrie E, et al. A qualitative study of patient choices in using emergency health care for long-term conditions: the importance of candidacy and recursivity. Patient Educ Couns 2013;93:335-41. http://dx.doi.org/10.1016/j.pec.2013.06.001.
- Snooks HA, Dale J, Hartley-Sharpe C, Halter M. On scene alternatives for emergency ambulance crews attending patients who do not need to travel to the accident and emergency department: a review of literature. Emerg Med J 2004;21:212-15. http://dx.doi.org/10.1136/emj.2003.005199.
- Snooks H, Anthony R, Chatters R, Cheung WY, Dale J, Donohoe R, et al. Support and assessment for fall emergency referrals (SAFER 2) research protocol: cluster randomised trial of the clinical and cost effectiveness of new protocols for emergency ambulance paramedics to assess and refer to appropriate community-based care. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2012-002169.
- Burrell L, Noble A, Ridsdale L. Decision-making by ambulance clinicians in London when managing patients with epilepsy: a qualitative study. Emerg Med J 2012;30:236-40. http://dx.doi.org/10.1136/emermed-2011-200388.
- Jelinek G, Weiland TJ, Mackinla C, Hill N, Gerdtz MF. Perceived differences in the management of mental health patients in remote and rural Australia and strategies for improvement: findings from a national qualitative study of emergency clinicians. Emerg Med Int 2011. http://dx.doi.org/10.1155/2011/965027 (accessed 13 February 2014).
- Whittingham MJ, Stephens PA, Bradbury B, Freckleton RP. Why do we still use stepwise modelling in ecology and behaviour?. J Anim Ecol 2006;75:1182-9. http://dx.doi.org/10.1111/j.1365-2656.2006.01141.x.
- Henderson C, Sheaff R, Dickinson A, Beech R, Wistow G, Windle K, et al. Unplanned Admissions of Older People: The Impact of Governance. Final Report. NIHR Service Delivery and Organisation programme; 2011.
Appendix 1 Sources of information for regressions
Atlas of Variation. URL: www.sepho.org.uk/extras/maps/NHSatlas/atlas.html (accessed 1 February 2013).
GP Extended Opening Hours Results for July 2009. URL: www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/PrimaryCare/DH_089459 (accessed 29 January 2013).
GP Survey April 2009 to March 2010 Unweighted. www.gp-patient.co.uk/results/archive_unweighted/sha/ (accessed 1 February 2013).
HES. URL: www.dh.gov.uk/en/Publicationsandstatistics/Statistics/HospitalEpisodeStatistics/index.htm (accessed 31 January 2013).
Mid-2009 Population Estimates for Primary Care Organisations in England by Quinary Age Groups and Sex. URL: www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77–250425 (accessed 29 January 2013).
Information Centre. Number of Primary Care Professionals (GPs) per 100,000 Population (2009). URL: www.lho.org.uk/viewResource.aspx?id=9319 (accessed 1 February 2013).
ONS. URL: www.ons.gov.uk/ons/index.html (accessed 31 January 2013).
Pensioners in Households: Percent, by Age Group, P. Census 2001. URL: https://indicators.ic.nhs.uk/webview/ (accessed 29 January 2013).
Population Estimates by Ethnic Group Mid-2009. URL: www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-50029 (accessed 13 August 2012).
Provider Based Inpatient Waiting Lists 2009/10. URL: www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/HospitalWaitingTimesandListStatistics/index.htm (accessed 1 February 2013).
Quality and Outcomes Framework. Compendium of Public Health Indicators, Illness or Condition (COPD/Diabetes/CHD). URL: https://indicators.ic.nhs.uk/webview/ (accessed 29 January 2013).
Rural/Urban Primary Care Classification. URL: www.ons.gov.uk/ons/guide-method/geography/products/area-classifications/rural-urban-definition-and-la/rural-urban-local-authority--la--classification--england-/index.html (accessed 29 January 2013).
Information Centre. Single Handed Practitioners. 2010. URL: www.lho.org.uk/viewResource.aspx?id=9319 (accessed 1 February 2013).
The English Indices of Deprivation 2010: PCT Summaries. URL: www.gov.uk/government/publications/english-indices-of-deprivation-2010 (accessed 29 January 2013).
The Information Centre. Ambulance Services – England, 2009–10. URL: www.ic.nhs.uk/article/2021/Website-Search?productid=173&q=Emergency+calls+resolved+through+telephone+advice+only%2c+by+ambulance+service+2009-10&sort=Relevance&size=10&page=1&area=both#top (accessed 1 February 2013).
Appendix 2 Performance of regressions
Chapter 4 Geographically based systems
The regression was a good fit (F = 116, p < 0.001). The histogram of standardised residuals shows they were normally distributed (see first graph below). The normal probability–probability (P–P) plot of the residuals was the expected straight line (see second graph below).

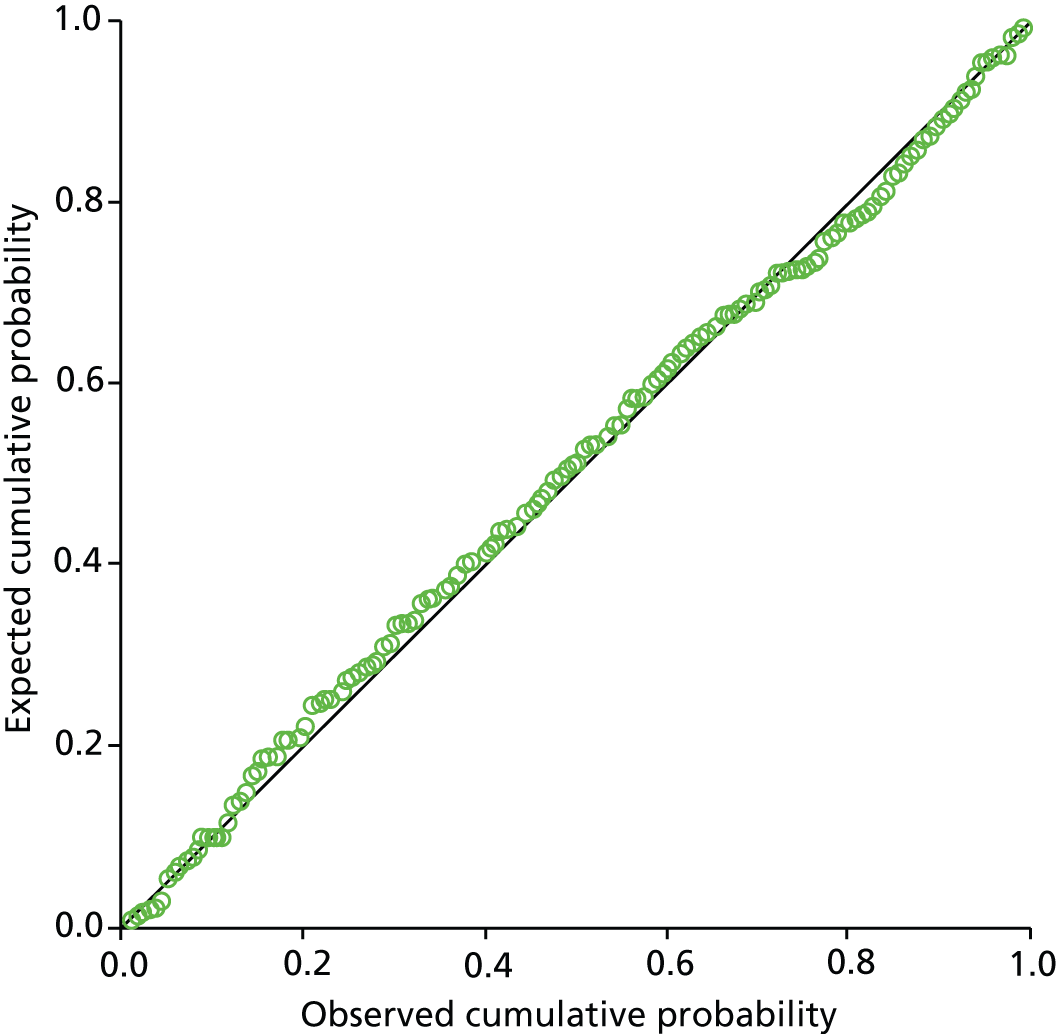
Chapter 5 Acute trust-based systems
The regression was a good fit (F = 23, p < 0.001). The histogram of standardised residuals showed they were normally distributed (see first graph below). The normal P–P plot of the residuals was the expected straight line (see second graph below).
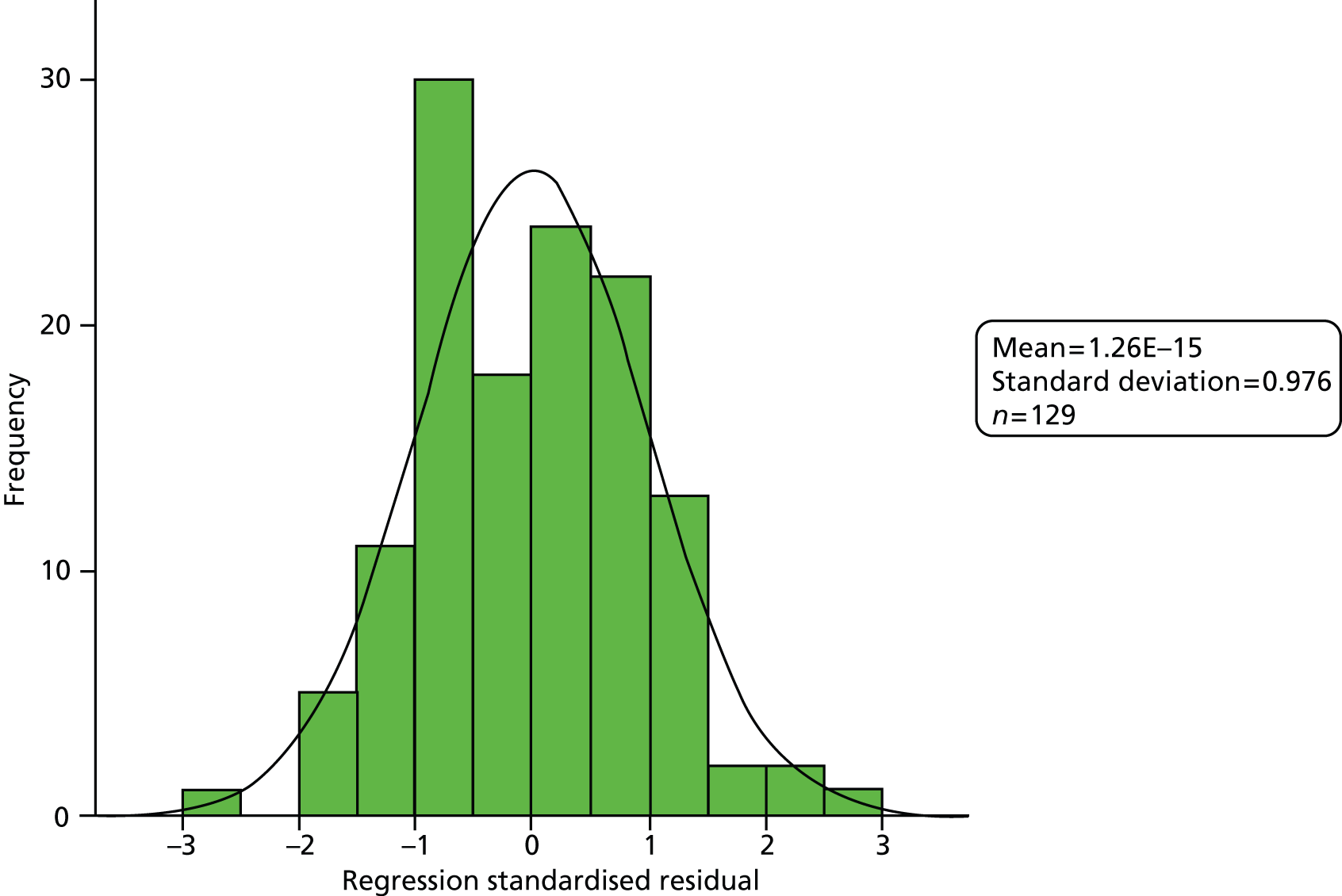
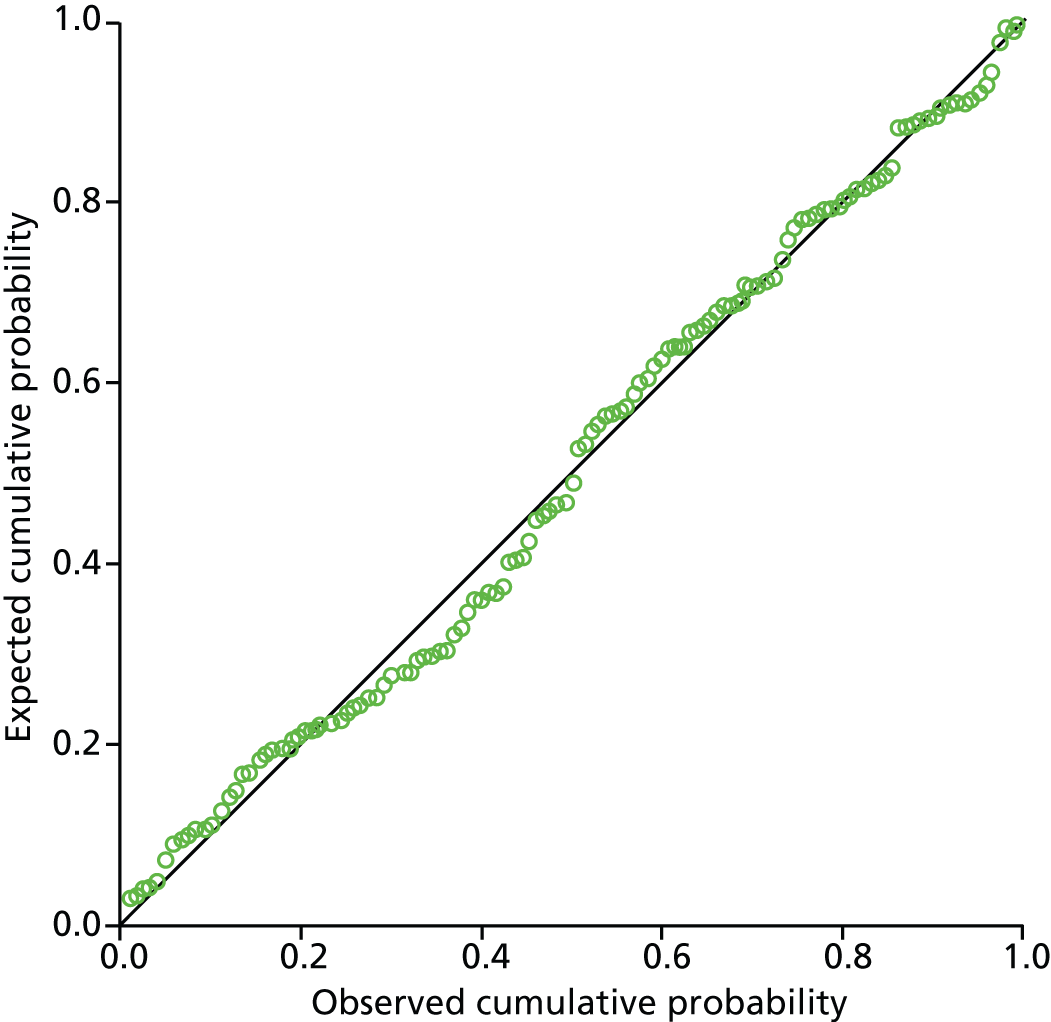
Appendix 3 Topic guide for interviews
I want you to think about emergency admissions that can be avoided if an emergency and urgent care system works well. By that I mean that the right services are in place, working in a coordinated and integrated way, to ensure that people experiencing an acute episode who don’t need to be admitted to hospital are not admitted. Services might include GP, GP OOH, ambulance, social services, EDs, community health services, NHS Direct – I would like you to think widely.
1. Here’s a list of conditions that have been identified by an expert panel as sometimes avoidable if a system is working well. Prompt with a card listing conditions. Do you have any comments about this list . . . are these the types of conditions that you would expect to see?
2. Thinking about helping people with an acute episode of these conditions to avoid a hospital admission
(i) What works well in the area you serve (i.e. PCT or hospital catchment area)
Prompts:
Presence of services (services that help reduce avoidable admissions)
Well performing services (services that meeting targets/operate safely)
Service integration or coordination (services that work together well)
Awareness of services by doctors/nurses or patients/public
Good accessibility to services (opening hours, location, capacity)
(ii) What does not work well in your locality?
Prompts:
Missing services (e.g. any services that you feel are important but are not currently operational in your locality)
Poor services (e.g. underperforming services, unsafe services)
Integration of services (e.g. services that could, but don’t work together)
Poor awareness of services by health professionals or patients
Lack of accessibility to services (opening hours, location, capacity)
3. Thinking about your organisation (prompt with appropriate term)
(i) What works well in avoiding emergency admissions?
(ii) What does not work well in avoiding emergency admissions?
4. You have discussed a range of issues (problems/solutions) affecting avoidable emergency admissions in your locality/service.
(i) Which solution has had the most impact?
(ii) Which solution could have the most impact?
5. Is there anything else that you’d like to say about avoidable emergency admissions?
The study is due to be completed in February 2014. If you would like to see a summary of the findings I would be happy to forward them on to you. Would you like me to do this?
Thank you for your time.
List of abbreviations
- A&E
- accident and emergency
- ACSC
- ambulatory or primary care sensitive condition
- CCG
- Clinical Commissioning Group
- COPD
- chronic obstructive pulmonary disease
- DVT
- deep-vein thrombosis
- EACC
- emergency ambulatory care condition
- ECP
- emergency care practitioner
- ED
- emergency department
- GP
- general practitioner
- HES
- Hospital Episode Statistics
- HU
- high standardised avoidable admission rate, underpredicted
- ICD-10
- International Classification of Diseases, Tenth Edition
- IQR
- interquartile range
- IT
- information technology
- LINk
- Local Involvement Network
- LO
- low standardised avoidable admission rate, overpredicted
- MO
- medium standardised avoidable admission rate, overpredicted
- MU
- medium standardised avoidable admission rate, underpredicted
- ONS
- Office for National Statistics
- OOH
- out of hours
- OT
- occupational therapist
- PCT
- primary care trust
- PPI
- patient and public involvement
- SAAR
- standardised avoidable admissions rate
- SECF
- Sheffield Emergency Care Forum
- UCC
- urgent care centre
- UTI
- urinary tract infection