Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/1011/51. The contractual start date was in January 2011. The final report began editorial review in November 2012 and was accepted for publication in June 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Stuart Parker declares National Institute for Health Research (NIHR) grants for Health Services and Delivery Research 12/5003/02 and was Deputy Director for the NIHR South Yorkshire Collaboration for Leadership in Applied Health Research and Care.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Ariss et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Objective 1 To identify those patients most likely to benefit from intermediate care and those who would be best placed to receive care elsewhere
Chapter 1 Which patients are most or least likely to benefit from intermediate care?
Introduction to the chapter
This chapter begins with an exploration of the literature regarding patients who are most or least likely to benefit from intermediate care (IC) services. The chapter considers descriptions of some commonly found types of IC services and some specific clinical needs of service users. The review moves on to look at reported patient characteristics, including age and sex, cognitive impairment, living arrangements and functional status on admission and examines how these impact on outcome. This chapter then focuses on the secondary analysis of data from the two previous studies. 1,2
Background
If IC is to contribute to the current NHS agenda by using resources in the most effective way while maintaining service quality, then it is essential that it is offered to those patients who are most likely to benefit from these services.
In order to target services appropriately, evidence is clearly needed to inform the development of appropriate criteria in order to identify both those patients who are most likely to benefit from IC and to identify which patients are least likely to benefit in terms of both physical functioning and quality of life (QoL). The reasons for this are outlined below.
Introduction of intermediate care
The need to provide services to facilitate early discharge and to prevent admission to hospital has been identified in Department of Health guidance over two decades, with winter pressures resources being made available in 1997. 3 The concept of IC was first articulated as formal policy in the UK NHS Plan4 and National Service Framework (NSF) for older people. 5 A review of these policies can be found in the National Audit Report (2012). 6 The framework identifies the range of community-based services that should be used to prevent hospital admission, to facilitate timely discharge from hospital and provide active rehabilitation in the community following discharge. The concept arose from concerns about the unnecessary use of acute hospital inpatient care to meet the needs of older people. 7 More information to ensure that services are tailored to support the needs of those they support is required.
Demographics
The proportion of older people in the population continues to rise, leading to concerns about the appropriateness and sustainability of current models of care. The rising prevalence of long-term conditions, which are often multiple, concurrent and associated with the development of acquired disability and complications – such as acute exacerbations, cognitive decline and institutionalisation – has been associated with an intention to reorient health-care systems from acute hospital-based services to more care in the community. However, it is likely that some patients will respond better than others to the different forms of intervention available in the community.
Public policy to treat close to home
Public policy is to treat close to home; in England, the Department of Health has directed that more people with long-term conditions be supported to retain independence in the community, using innovations in health technologies and improved carer support. 8,9 It is recognised in policy that, within this context, services that function at the interface between primary and secondary care are crucial. They influence the setting in which acute care can be provided, the durations of stay in different compartments of the care system (home or other community setting, hospital emergency service, acute inpatient care, inpatient or home-based rehabilitation and reablement services) and can be constructed to influence capacity for self-management and community care. This in turn may affect demand for hospital bed use (influencing admissions, durations of stay and readmissions). Therefore, it is important to understand who benefits (and, crucially, who does not benefit) from service interventions that are targeted at people with care needs which fall between traditional hospital inpatient and community care needs.
Literature review
Review methods
Details of the literature search undertaken to support this chapter are located in Appendix 1. The review built on the reviews conducted as part of the costs and outcomes of older peoples’ services (COOP)1 and enhancing the effectiveness of interdisciplinary working (EEICC)2 studies, as well as a number of systematic reviews, specifically a review of the evidence for the effectiveness of IC conducted as part of the National IC evaluation10 and three Cochrane reviews of non-disease-specific IC services. Two of these focused on hospital at home (HAH) for admission avoidance11 or early discharge12 and one focused on rehabilitation of older people. 13 Relevant studies from a systematic review of HAH were also considered. 14
We drew on evidence from a number of sources to identify English-language studies published since 2000, in which the intervention or setting is IC (including descriptions of services offering similar provision) and for which the outcomes assessed were any measure of physical functioning or QoL. We defined IC services as community-based services provided mostly for older people, aiming at avoiding unnecessary admission to hospital and/or facilitating discharge from hospital and preventing admission to long-term residential and nursing care.
It should be noted that this review has focused on patients who may or may not currently benefit from IC. It was somewhat beyond the scope of the focus of this chapter to explore the clinical effectiveness and cost-effectiveness of IC services or to compare effectiveness with other forms of service delivery.
Findings from the literature
Seventy-two studies met the inclusion criteria for this review. Of these, six studies explore the patient characteristics associated with changes in physical functioning or QoL (Table 1). However, these six outcomes studies are heterogeneous in terms of type of intervention, country and care setting, and this limits the conclusions that can be drawn. What does emerge from them though is a consistent and clear message that not all patients benefit from IC.
| Study ID | Type of service | Objectives of care | Disease/condition | Country | Care setting | Study design | Relevant outcomes |
|---|---|---|---|---|---|---|---|
| Landi et al. 200215 | Community hospital rehabilitation | Post-acute rehabilitation | Frail older people | Italy | Geriatric hospital | Cohort study | The Minimum Data Set for Post Acute Care which includes physical and cognitive function and health status was assessed on admission, then every 2 weeks |
| Analysis and findings | Logistic regression. In the unadjusted mode, patients aged > 85 years with cognitive or sensory impairment were less likely to improve. After adjusting for age, sex, social and functional status, indicators of disease severity and ‘all possible negative factors affecting rehabilitation’ only cognitive impairment remained significant | ||||||
| Findings reported in Kaambwa et al. 200816 | Various forms of IC | Various including rehabilitation, supported discharge and rapid response | Elderly patients | UK | Various including patients homes, residential homes and day hospitals | Cohort study | EQ-5D and Barthel Index |
| Analysis and findings | Regression modelling. Mean improvement (SD): 0.16 (0.32) increase in EQ-5D score and 1.68 (2.89) increase in Barthel Index. For EQ-5D, a lower score on admission was associated with a greater improvement in EQ-5D score on discharge. Those who live alone were more likely to improve. Lower score on admission for Barthel Index and EQ-5D was associated with a greater improvement in independence on discharge. Older patients were less likely to improve. Those who live alone were more likely to improve. No effects for sex | ||||||
| Pereira et al. 201017 | Rehabilitation in a day hospital | Admission avoidance, rehabilitation | Frail older people | Canada | Day hospital | Cohort study | Barthel Index, instrumental ADLs using the Older Americans Resources and Services, EQ-5D, Timed Up and Go test for general mobility, 6-minute walk test, gait speed, Berg Balance Scale and grip strength |
| Analysis and findings | Logistic regression. Overall 58% (134 out of 233) patients achieved a ‘successful improvement’ (significant improvement in ≥ 3 tests). Patient characteristics associated with ‘successful improvement’ were lower admission score on Barthel Index, Older Americans Resources and Services, Timed Up and Go test, gait speed and 6-minute walk test, with a trend for lower scores on the Berg Balance Scale and EQ-5D. No significant differences for age or sex | ||||||
| Fusco et al. 200918 | Home-based rehabilitation | Rehabilitation | Frail older people | Italy | Home | Cohort study | Functional status was assessed using the Minimum Data set for Home Care at the end of treatment, 6 months and 12 months. One of the summary scales describes ADLs |
| Analysis and findings | Only 30% of patients improved significantly after 6 months. When adjusted for potential confounders, there were four ‘negative factors’: (1) cognitive impairment (OR 0.85, 95% CI 0.75 to 0.85); (2) urinary incontinence (OR 0.44, 95% CI 0.27 to 0.70); (3) bowel incontinence (OR 0.47, 95% CI 0.27 to 0.81); and (4) visual impairment (OR 0.55, 95% CI 0.32 to 0.92). Similar results when the main diagnoses were considered in the main model. After adjustment for baseline ADLs, impaired cognitive performance, depression, urinary and faecal incontinence and sensory impairment were associated with the outcome | ||||||
| Gitlin et al. 200819 | Home-based rehabilitation | Rehabilitation | Frail older people | USA | Home | RCT | Functional ability was assessed at 6 and 12 months using a self-report measure of difficulties in 17 areas including six IADLs, six ADLs and six mobility/transferring items. Each item was self-rated on a 1 to 5 scale. Mean difficulty was calculated across all items |
| Analysis and findings | Analysis of covariance. For ADLs at 6 months, sex, age and education moderated treatment outcomes with women, the oldest (aged > 80 years) and those with less education benefiting more. When all three interactions were entered into one model only age and sex remained significant. At 12 months, only age was significant. For mobility difficulties at 6 months, there were significant effects for age and sex only – women had a bigger decrease in mobility. At 12 months, age as well as education were significant. For IADLs, there were no differences at 6 months, but at 12 months, race was significant, with whites having less difficulty than non-whites | ||||||
| Comans et al. 201120 | Community rehabilitation service | Rehabilitation, admission avoidance | Frail elderly following falls or poor balance/functional decline | Australia | Home | RCT | EQ-5D and a visual analogue scale |
| Analysis and findings | Factors negatively impacting on QoL were depression, impaired hearing and vision and poor nutritional intake. EQ-VAS was positively associated with level of participation in normal activities and perceived HRQoL. Negatively impacting factors were depression, having poor reading vision and poor nutrition. Test of physical capabilities were not found to have significant associations with HRQoL. Age, sex, living alone and comorbidities were not associated with differences in QoL | ||||||
The Cochrane database of systematic reviews includes three highly relevant reviews of disease-unspecific services provided in the home and compared with hospital-based alternatives,11–13 and three reviews of disease-specific services providing home-based IC for patients with stroke21,22 and chronic obstructive pulmonary disease (COPD). 23
In a review examining HAH and comparing it with hospital inpatient care, a study found that early discharge in certain patients groups may reduce pressure on acute beds,11 but that there was insufficient evidence of economic benefit. A review of HAH for acute exacerbations of chronic obstructive airways disease shows that mortality and readmission rates are not significantly different between intervention and control groups and suggests that both patients and carers prefer the HAH services to inpatient acute care. 12,23 Few other outcomes were reported.
A review of services to help acute stroke patients avoid hospital admission concluded that there was no evidence from clinical trials to support a radical shift in the care of acute stroke patients from hospital into the community. 21 Whereas, a review of services for reducing duration of hospital care for acute stroke patients concluded that supported early discharge services for stroke have significant effects on inpatient length of stay (amounting to a reduction in length of stay of about 9 days). The risk ratios (RRs) for adverse outcomes, including death, institutionalisation and benefits (on functional outcome) and costs remain unclear. 22
Key point 1: a substantial number of randomised controlled trials (RCTs) have been conducted in populations including frail older people, for whom disease-specific inclusion criteria have not been set. These populations include older people at risk of adverse outcomes including delirium, polypharmacy and urinary complications. These trials demonstrate a reduction in pressure on acute beds and are preferred by patients.
Models of care
The main models of service delivery relevant to UK IC that have been researched are HAH, nurse-led clinical services and home-based rehabilitation. The trials fall naturally into two groups: those that have investigated the use of IC services in non-disease specific conditions, such as frail older people and elderly medical admissions, and those that have investigated specific service models in patients with particular diagnosed health conditions.
Recently reported trials have tended to focus on interventions in specific chronic diseases and some have demonstrated quite significant reductions in inpatient hospital stays. Early supported discharge services after stroke typically include rehabilitation and are associated with reduced length of inpatient stay. 24–27 Discharge support services in a range of other specific conditions which have been associated with significant reductions in inpatient length of stay including after surgery for breast cancer28 or coronary artery bypass graft (CABG),29 treatment for acute exacerbations of COPD30 or diabetes. 31 Interventions of specific relevance to frail older people that achieved significant reductions in inpatient length of stay included home-based rehabilitation for a range of conditions32,33 and after fractured neck of femur. 34
Key point 2: many RCTs of IC services have been conducted with patient groups with specific conditions, mostly medical conditions such as stroke, COPD and heart failure and demonstrate reduced length of stay.
Most studies have been conducted in the home setting, with some including patients in special facilities in acute hospitals. No studies were found which employed interventions in non-clinical institutions. One of the Cochrane Database reviews specifically addresses the use of residential care settings for rehabilitation for older people, but has not identified any trials that the met the inclusion criteria for this study.
Key point 3: RCTs investigating IC for frail older people have not investigated alternative non-clinical residential facilities such as nursing and residential homes. Nevertheless, these settings are routinely used by IC services.
The question of ’who may benefit from intermediate care’ has been tested in RCTs for the following main groups:
-
Patients with a medical condition including:
-
patients at risk of delirium
-
patients at risk of urinary tract complications
-
frail older people.
-
-
Patients in need of rehabilitation:
-
after stroke
-
after fractured neck of femur
-
after CABG
-
after breast surgery
-
with ischaemic heart disease.
-
-
Patients with exacerbation of specific long-term conditions:
-
COPD
-
heart failure.
-
It is worth noting that none of the trials contributing to the above list specifically included patients with cognitive impairment or dementia. There is current debate on assessment and rehabilitation for people with dementia and other comorbidities, but for now it is not an area that has been extensively investigated in controlled trials.
Key point 4: RCTs do not address the use of IC services for people with physical rehabilitation or recuperation needs, which are complicated by the presence of cognitive impairment.
Another important issue is related to whether or not IC and community rehabilitation can provide benefits for those coming to the end of their life.
Key point 5: the literature suggests that there is a case for integrating palliative care services for older people with IC/community rehabilitation as the complexity of cases being cared for in the community is increasing. However, no controlled trials have been conducted to evaluate the use of IC services (e.g. HAH, early supported discharge teams) in the provision of palliative and end-of-life care.
More recently, the notion that home-based care for a range of acute care needs may be superior to inpatient hospital care has begun to emerge. For example, RCTs of ‘hospital in the home’ (HITH) for acute care35 and rehabilitation36 suggest that home-based care which substitutes for, and meets, clinical care needs that would otherwise be provided in an inpatient hospital setting reduces the incidence of delirium and urinary tract complications, that may lead to further illness and/or admission. A recent and extensive meta-analysis of this concept, substitution of care at home for hospitalisation using HITH and similar schemes, included 61 RCTs that demonstrated reduced length of stay in hospital. 14 The authors of this review concluded that HITH is associated with reduced mortality, readmission rates, costs and increased patient and carer satisfaction. The effect sizes were not small. The odds ratios (ORs) pooled from 42 RCTs with 6992 subjects for mortality was 0.81 [95% confidence interval (CI) 0.69 to 0.95; p = 0.008; i.e. a 19% reduction in mortality in HITH] and for readmission was 0.75 (95% CI 0.59 to 0.95; p = 0.02; i.e. a 20% reduction in readmission). The number needed to treat to prevent one death was 50 patients. These effect sizes are similar to those found for many interventions that have been regarded as essential health technologies, for example Streptokinase® (CSL Behring UK Ltd, West Sussex, UK), for acute myocardial infarction.
Key point 6: admission avoidance by the use of HAH services that substitute for acute hospital admission have been shown to reduce the incidence of delirium and urinary tract complications with reductions in mortality and readmission. This indicates that patients who are particularly at risk of such complications should be considered for home management of their acute care episode, where the facilities are available.
A further seven studies meeting the inclusion criteria for this review did not include any exploration of the relationship between patient characteristics and treatment outcomes as one of the study aims, but did include reference to relevant analyses within the papers. These are summarised in Table 2.
| Citation | Type of service | Objectives of care | Disease/condition | Country | Care setting | Study design | Relevant outcomes |
|---|---|---|---|---|---|---|---|
| Fjaertoft et al. 201137 | ESD by multidisciplinary team | Discharge support | Stroke | Norway | At home or in a day clinic | RCT | mRS to measure independence, Frenchay Activity Index, Scandinavian Stroke Scale, Barthel Index |
| Analysis and findings | Logistic regression. Within the ESD group, predictors of good outcome (mRS score ≤ 2) after 5 years were lower age at stroke onset (median age 69.0 years for good outcome/76.6 years for bad outcome), a lower mRS score and cohabitation (living alone 26.4% for good outcome/48.5% for bad outcome) at baseline | ||||||
| Koh et al. (2012)38 | Community hospital rehabilitation | ESD and rehabilitation | Stroke | Singapore | Community hospitals followed by outpatient rehabilitation centre | Cohort study | Barthel Index |
| Analysis and findings | Mixed-model analysis. At all five time points (admission, discharge, 1 month, 6 months and 1 year post discharge) predictors of lower Barthel Index scores were increasing age, hypertension, greater cognitive impairment greater depressive symptoms and greater neurological impairment | ||||||
| Mallinson et al. (2011)39 | Rehabilitation in community or subacute settings | Early supported discharge and rehabilitation | Those aged > 65 years following knee or hip replacement | USA | Inpatient rehabilitation. Skilled nursing facility or Home Health Agency | Cohort study | Functionality using inpatient rehabilitation Facility Patient Assessment Instrument, Outcomes and Assessment Information Set and Minimum Data set 2.0 |
| Analysis and findings | Stepwise regression. Self-care function at discharge unaffected by age and sex, but significant factors were severity of procedure, number of comorbidities, urinary incontinence and level of self-care on admission. For mobility function, only urinary incontinence and mobility on admission were significant | ||||||
| Hogg et al. 200940 | Preventive primary care team | Admission avoidance | Those aged > 50 years at risk of experiencing adverse health outcomes | Canada | Home | RCT | SF-36, HRQoL scales, functional status (IADLs scale) |
| Analysis and findings | Multivariate regression performed for each outcome adjusted for a variety of patient characteristics. Results for QoL and functional status not reported | ||||||
| Courtney et al. (2009)41 | Home-based rehabilitation | Admission avoidance | Those > 65 years of age following an acute medical admission and at least one risk factor for readmission | Australia | Home | RCT | SF-12 at baseline, 4,12 and 24 weeks post admission |
| Analysis and findings | Analysis of covariance. For the intervention group, admission diagnosis had no effect on Physical Component Summary Score of the SF-12 | ||||||
| Allen et al. (2009)42 | Home-based rehabilitation | Discharge support | Stroke | USA | Home | RCT | Neuromotor function (Timed Up and Go test), QoL using stroke specific QoL scale |
| Analysis and findings | Multivariate modelling. For the intervention group, at 6 months, patients with a prior stroke/transient ischaemic attack/atrial fibrillation identified a substantial subgroup interaction benefit in terms of neuromotor function. Severity of stroke, comorbidities, age, sex and race were not significant | ||||||
| Carratala et al. (2005)43 | HAH following discharge from emergency department | Admission avoidance | Community-acquired pneumonia | Spain | Home | RCT | SF-36 |
| Analysis and findings | Multivariate analysis using age, sex, comorbidities and pneumonia severity index scores as confounders. Results not reported in detail | ||||||
Table 3 summarises the effects of patient characteristics on physical functioning and QoL across all the included studies that contained data pertinent to the research question (n = 13).
| Patient characteristic | Effect on physical functioning | Effect on HRQoL | ||||
|---|---|---|---|---|---|---|
| Improvement | No effect | Reduction | Improvement | No effect | Reduction | |
| Age (increasing) | Gitlin et al.19 | Landi et al.15 | Kaambwa et al.16 | Comans et al.20 | ||
| Pereira et al.17 | Fjaertoft et al.37 | |||||
| Fusco et al.18 | ||||||
| Allen et al.42 | ||||||
| Mallinson et al.39 | ||||||
| Sex (female) | Gitlin et al.19 | Landi et al.15 | Comans et al.20 | |||
| Kaambwa et al.16 | ||||||
| Pereira et al.17 | ||||||
| Fusco et al.18 | ||||||
| Allen et al.42 | ||||||
| Fjaertoft et al.37 | ||||||
| Mallinson et al.39 | ||||||
| Living alone | Kaambwa et al.16 | Fjaertoft et al.37 | Kaambwa et al.16 | Comans et al.20 | ||
| Sensory impairment | Landi et al.15 | Fusco et al.19 | Comans et al.20 | |||
| Cognitive status impairment | Landi et al.15 | Pereira et al.17 | Fusco et al.18 | |||
| Functional status on admission low | Kaambwa et al.16 | Fusco et al.18 | Pereira et al.17 | Comans et al.20 | ||
| Pereira et al.17 | ||||||
| Fjaertoft et al.37 | ||||||
| QoL on admission low | Kaambwa et al.16 | Kaambwa et al.16 | ||||
| Diagnosis/comorbidities | Fusco et al.18 | Mallinson et al.39 | Comans et al.20 | |||
| Allen et al.42 | Courtney et al.41 | |||||
| Incontinence | Landi et al.15 | Fusco et al.18 | ||||
| Mallinson et al.39 | ||||||
| Depression | Fusco et al.18 | Comans et al.20 | ||||
Evidence on the characteristics of patients who do not improve in IC is limited.
In a retrospective cohort study of 233 frail elderly patients undergoing a multidisciplinary rehabilitation programme in a geriatric day hospital in Canada,17 only 58% (n = 134) of patients achieved a ‘successful improvement’, which was defined as a significant improvement in ≥ 3 tests of functional status.
A study of rehabilitation in Italy identified the outcomes of 598 elderly patients undergoing a multidisciplinary home-care rehabilitation programme. 18 Only 30% of patients improved significantly after 6 months of rehabilitation when assessed using the Minimum Data set for Home Care which describes activities of daily living (ADLs).
Key point 7: there is scant evidence to indicate which patients are less likely to do well in IC in terms of physical functioning and QoL.
Age and sex
Five studies15,17,18,39,42 assessed the impact of age on physical functioning and found no effect. In three other studies,16,19,37 age was found to have an effect, but the direction of the effect was not consistent. A randomised trial by Gitlin et al. 19 of a home-based intervention in the USA included occupational and physical therapy visits and telephone follow-up for 319 frail older people (> 70 years of age). This found that age moderated treatment outcomes (using self-reported functional ability) at 6 and 12 months, with the oldest (> 80 years) benefiting more from the intervention in terms of both ADLs and mobility.
However, in a UK-based study of IC services for the elderly15 and a Norwegian study of early supported discharge for stroke patients,37 increasing age was associated with a reduction in benefit. The UK study found that older patients were less likely to improve their level of independence as detected by the Barthel Index. Similarly, a study by Fjaertoft et al. ,37 found that age at stroke onset predicted outcome as measured by the modified Rankin Scale. The median age was 69.0 years for good outcomes and 76.6 years for bad outcomes.
There was little indication of the effect of sex on physical functioning or outcome across any of the studies.
Cognitive impairment
There is also some indication that cognitive status may have an effect on physical functioning, although, again, the direction of the effect is not consistent across studies. Landi et al. 15 conducted a cohort study to identify predictors of rehabilitation outcomes in 244 frail older people in a geriatric hospital in Italy following admission to acute care. Cognitive impairment was the strongest predictor of recovery. People with dementia had a 64% reduction in their odds of recovery relative to patients with normal cognitive performance (OR 0.36, 95% CI 0.14 to 0.92). Conversely, in a cohort study to determine predictors of outcome in 598 elderly patients undergoing a multidisciplinary home-care rehabilitation programme, again conducted in Italy,18 cognitive impairment had a negative impact on physical functioning (OR 0.85, 95% CI 0.75 to 0.85).
Comans et al. 20 conducted a RCT of a community rehabilitation service in Australia, which received referrals from the emergency department or general practitioners (GPs) and explored the outcomes of 107 frail older patients presenting with falls or poor balance/functional decline, or QoL.
Living alone
Similarly, living alone had both a positive and negative effect on physical functioning. In Kaambwa et al. ,16 those who lived alone were more likely to improve but in Fjaertoft et al. ,37 those living alone were less likely to improve (26.4% for good outcome and 48.5% for bad outcome).
Key point 8: there is some indication that age, cognitive status and living alone may affect outcomes. However, the direction of this effect is inconsistent.
Functional status on admission
The literature indicates that those with lower functional status on admission improve more in terms of their physical functioning and, therefore, those whose scores are higher are less likely to improve. However, it is possible that this is as a result of a ceiling effect of most measures. This effect was clear in three studies,16,17,37 although baseline scores had no effect in another study. 18
There were suggestions that those with sensory impairment,18 more comorbidities,39 incontinence18,39 and depression18 do less well.
Key point 9: those who enter IC with higher levels of independence and health-related QoL improve less than those with lower levels. However, this is likely to be an artefact of the ceiling effect of most measures. The potential to demonstrate improvement on measures may be less for those starting with high scores. Those with sensory impairment, increased number of comorbidities, incontinence and depression may do less well in IC.
Discussion of the literature review
Few studies explicitly set out to answer the question ‘which patients are more or less likely to benefit from IC in terms of QoL and physical functioning?’
However, given that IC can include a wide range of community-based services, such as HAH and community rehabilitation, and can take place in a number of settings (e.g. patients’ homes, community hospitals or care homes) there is a substantial body of literature exploring the impact of IC. For example, within The Cochrane Library alone, there are three reviews of IC which are non-disease specific11–13 and three which are disease specific for stroke21,22 and COPD. 23 Within any single study of IC, there may well be secondary analyses, which have explored the characteristics of patients who are less likely to do well in IC in terms of physical functioning and QoL. This review has taken a pragmatic approach to exploring a selection of this literature since 2000, through a combination of database searches and incremental searching of reference lists of existing reviews of IC services that are non-disease specific. However, given the extensive volume of literature identified, relatively few studies were found.
Key point 10: few studies have aimed to explore which patient characteristics are associated with adverse or improved outcomes in terms of physical functioning or QoL.
Secondary analysis of data
Methods
The patient outcomes collected were the four domains from the therapy outcome measure (TOM) scale (impairment, activity, participation and well-being) and the European Quality of Life-5 Dimensions (EQ-5D) questionnaire. For each of the five scales [impairment, activity, participation and well-being (as measured by the TOM scale) and EQ-5D questionnaire], two outcomes were used:
-
the magnitude of improvement, defined as the change from score at admission to score at discharge
-
the presence or absence of improvement, defined as patient improved (an increase from admission score) or patient not improved (no change or worsened from admission score).
The relationship between these outcomes was assessed against the following patient characteristics: the value of the baseline score of the (EQ-5D or TOM) and each of age, sex, level of care (LoC) on admission, route of referral, the usual living arrangements and place where care was provided. As the last two variables were heavily correlated, it was not appropriate to include both in the model at the same time, instead, they were assessed in two separate models as described in Table 4. The first model assessed whether or not the patient’s residence during IC was associated with outcome, whereas the second was to investigate whether or not there was any additional impact among patients who had left their home in order to receive IC. The results are reported for the most parsimonious model, i.e. for model 1 unless there was an additional impact of leaving home, which was assessed by the likelihood ratio test.
| Model 1 | Model 2 |
|---|---|
| Included in both models: age, sex, LoC at admission, route of referral and baseline value of outcome (EQ-5D or TOM score) | |
| Place where care was provided | Usual living arrangements |
| Did patient leave a home residence to receive care? | |
| If left home to receive care, where was care provided? | |
Missing data
An important consideration for this reanalysis, and one that is also pertinent to Chapters 1–3, 5, 6 and 10, was how to handle patients with incomplete data. There were missing data in a substantial number of patient records, encompassing both baseline data (i.e. patient characteristics at admission) and, more commonly, outcome data at discharge. This presented a challenge, especially with missing outcome data; ignoring patients with missing data makes the strong assumption that these are a random subgroup of the study population (the so-called ‘missing completely at random’ assumption as described by Schafer). 44 This is unlikely to be true; for example, missing data were more common among patients discharged to acute settings or nursing homes, but it is clear (both from available data and from intuition) that these patients had worse outcomes than patients discharged to their own home. Moreover, even if the ‘completely at random’ assumption were met, the ability to detect a difference is compromised by losing a high proportion of data.
We addressed this by a multiple data imputation approach. 45 Missing data were multiply imputed to give a range of plausible values, the details of which are described at length in Appendix 2. In order to assess the extent to which the findings were robust to missing data, analyses were performed on both complete case data and data sets incorporating imputed data. Five augmented data sets were sufficient to ensure that the between-data set variance was negligible in the model coefficients.
Analyses of continuous outcomes (the magnitude of change in TOM and EQ-5D scores) were undertaken by fitting a generalised least square model in which the team was a random effect. An analogous approach was taken for binary (yes/no) outcomes, for which a random-effects logistic regression model was applied. All analyses were undertaken using version 12.1 of the Stata statistical software (2011; StataCorp LP, College Station, TX, USA), with analyses on imputed data sets incorporating adjusted standard errors as described by Schafer. 46
Results are presented as tables of coefficients (reflecting the difference in means) for magnitude of change and as predicted probabilities for any improvement. The graphs depicting mean change by patient characteristics are adjusted for other model parameters, in each case displaying least square means ± 95% CIs based on analyses of the imputed data.
Results
Remaining or returning home
In all 4556 out of 7620 patients (60%) remained or returned home following an episode of IC. The distribution of this outcome is presented in Figure 1.
FIGURE 1.
Frequency of patients remaining or returning home.
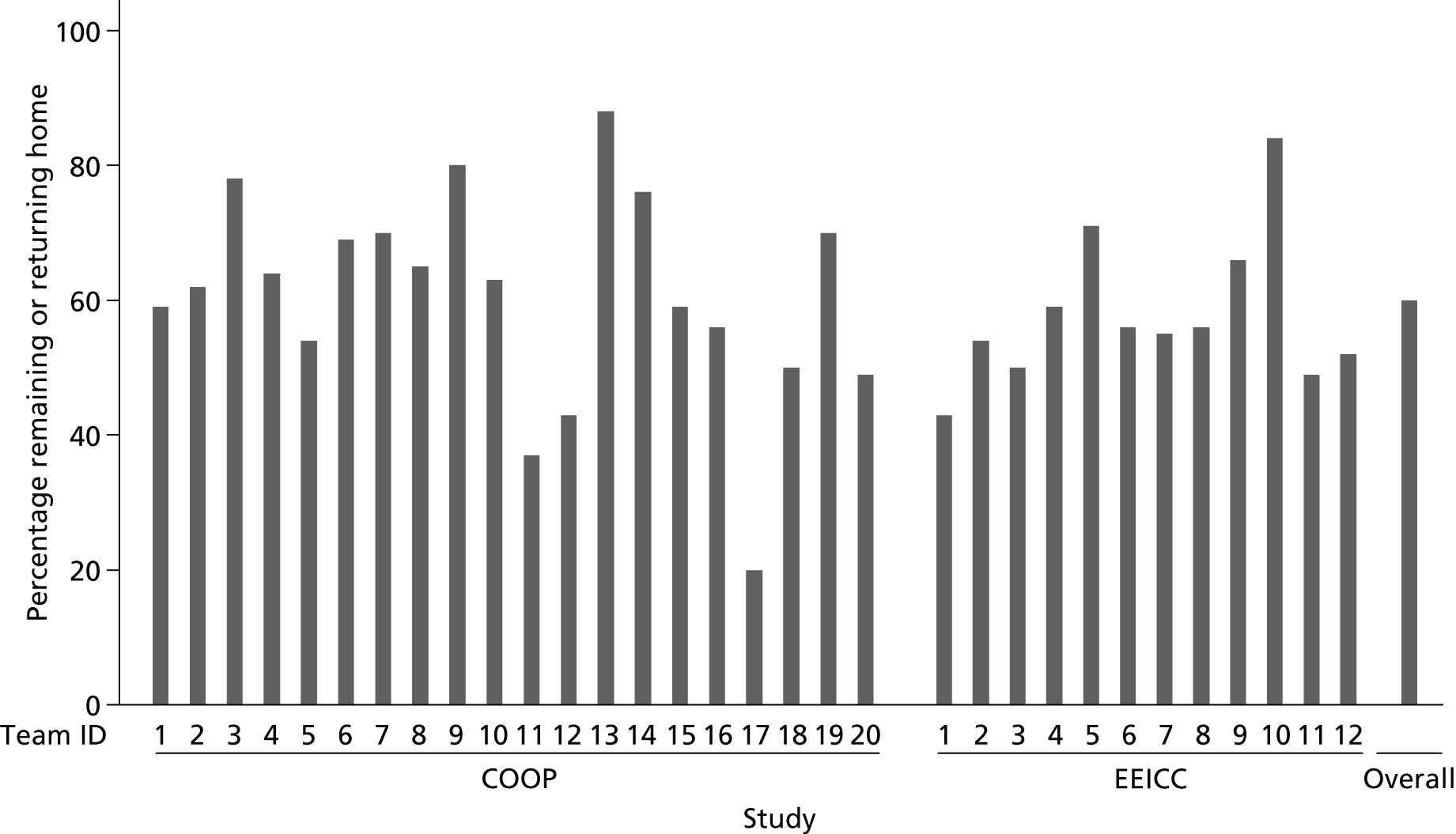
The likelihood of returning home shows a large amount of variation between teams. Team COOP PB had the greatest percentage of patients who remained or returned home, with 88% of their patients remaining or returning home. Team COOP SG had the smallest percentage of patients who remained or returned home, with 20% of their patients remaining or returning home.
Level of care at admission
The chance of remaining or returning home is greatest for patients with a LoC, at admission, of 4 (needs regular rehabilitation programme) and 3 (needs slow-stream rehabilitation). Patients with these LoCs, at admission, have a 66.0% and 63.7% chance of remaining or returning home, respectively.
The chance of remaining or returning home is lowest for patients with a LoC, at admission, of 0 (does not need any intervention) for which there was only a 20.4% chance of remaining or returning home. However, many of the patients with a LoC, at admission, of 0 were marked as being an inappropriate referral. Those with a LoC, at admission, of 7 (needs medical care and rehabilitation) had a 34.8% chance of remaining or returning home.
Key point 11: the likelihood of remaining or returning home is related to the LoC at admission to IC. It is greatest for levels 3 and 4 and is lowest (20.4%) for patients with a LoC, at admission, of 0 (does not need any intervention).
Age and sex
For every 10-year increase in age, there was a 6% decrease in the odds of returning home. The chance of returning home was greater for females than males. Females had a 51.8% chance of returning home and males a 47.4% chance.
Key point 12: for every 10-year increase in age there was a 6% decrease in the odds of returning home. The chance of remaining or returning home was greater for females than males.
Relationship between patient characteristics and therapy outcome measures
For all domains of the TOM scale, around half of all patients with outcome data did not improve or worsen. More patients showed improvement in TOM impairment and activity than in participation or well-being. In the imputed data set, the proportion of patients who failed to improve was slightly higher, as patients with missing outcomes had worse predicted outcomes than those for whom data were available. Table 5 summarises the improvement in these scores.
| Outcome | Complete case | After data imputation (n = 7291)a | |||
|---|---|---|---|---|---|
| Number of patients with data | Mean (SD) improvement | % (n) with any improvement | Mean (SD) improvement | % with any improvement | |
| TOM impairment | 5337 | 0.44 (0.71) | 50% (2659) | 0.28 (0.83) | 43.1% |
| TOM activity | 5339 | 0.46 (0.71) | 51% (2735) | 0.31 (0.84) | 44.4% |
| TOM participation | 5340 | 0.38 (0.71) | 43% (2279) | 0.22 (0.85) | 37.0% |
| TOM well-being | 5330 | 0.30 (0.68) | 37% (1975) | 0.13 (0.87) | 32.1% |
The magnitude of these changes is displayed graphically in Figure 2.
FIGURE 2.
Change in TOMs by domain.

Key point 13: nearly half of all patients with outcome data did not improve on any of the domains of TOM.
Baseline scores
Patients with higher TOM scores on admission were less likely to improve. The relative increase in odds of improvement per 1-point increase in score on admission ranged from 0.53 (TOM well-being) to 0.75 (TOM impairment) using imputed data (see Appendix 2). The extent that this is as a result of a ceiling effect (i.e. because the potential to improve is less for those who already have high scores) is not known.
Age
The magnitude of a TOM score increase was related to patient age, with smaller changes being observed in older patients. Although statistically significant, the decreases were modest. On average, the change in TOM scores decreased by 0.02–0.03 units per additional 10 years of age (see Appendix 2).
Sex
Fewer men than women improved for all domains of the TOM. However, the difference in mean scores between men and women was small, i.e. ≤ 0.1 units for all domains. The odds of improvement were significant for all domains except participation (see Appendix 2).
Level of care on admission
Level of care at admission was associated with change in all TOM domains. Fewer than 20% of patients with a LoC, on admission, of 0 improved their TOM scores for all domains (using imputed data). The patients most likely to improve were those with admission LoCs of 3, 4 or 5 [> 40% for impairment, activity and participation, > 30% for well-being (see Appendix 2)]. However, the magnitude of change was modest, with the average (adjusted) mean changes in the highest (levels 4 and 5) and lowest (levels 0 and 6) groups being within 0.06 units of each other. The probability of any improvement as calculated from the imputed data was between 64% (level 6) and 77% (level 4) (see Appendix 2).
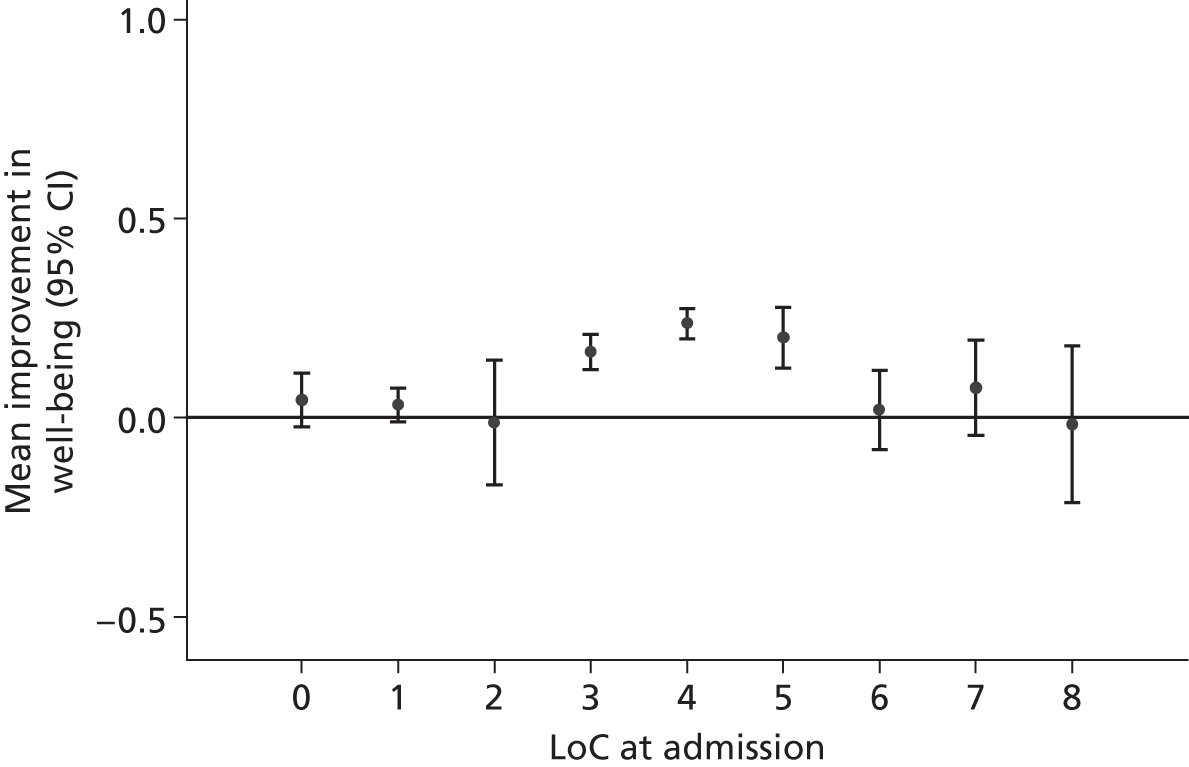
Compared with level 0, levels 1–8 all had a higher probability of having any improvement for impairment, activity and participation. The mean difference between the best and worst LoC group was around 0.3 to 0.4 TOM units. The magnitude of the changes in impairment, activity and participation and well-being, adjusted for other covariates, are illustrated graphically in Figures 3–6.
FIGURE 3.
Change in impairment by LoC at admission (model adjusted).

FIGURE 4.
Change in activity by LoC at admission (model adjusted).

FIGURE 5.
Change in participation by LoC at admission (model adjusted).
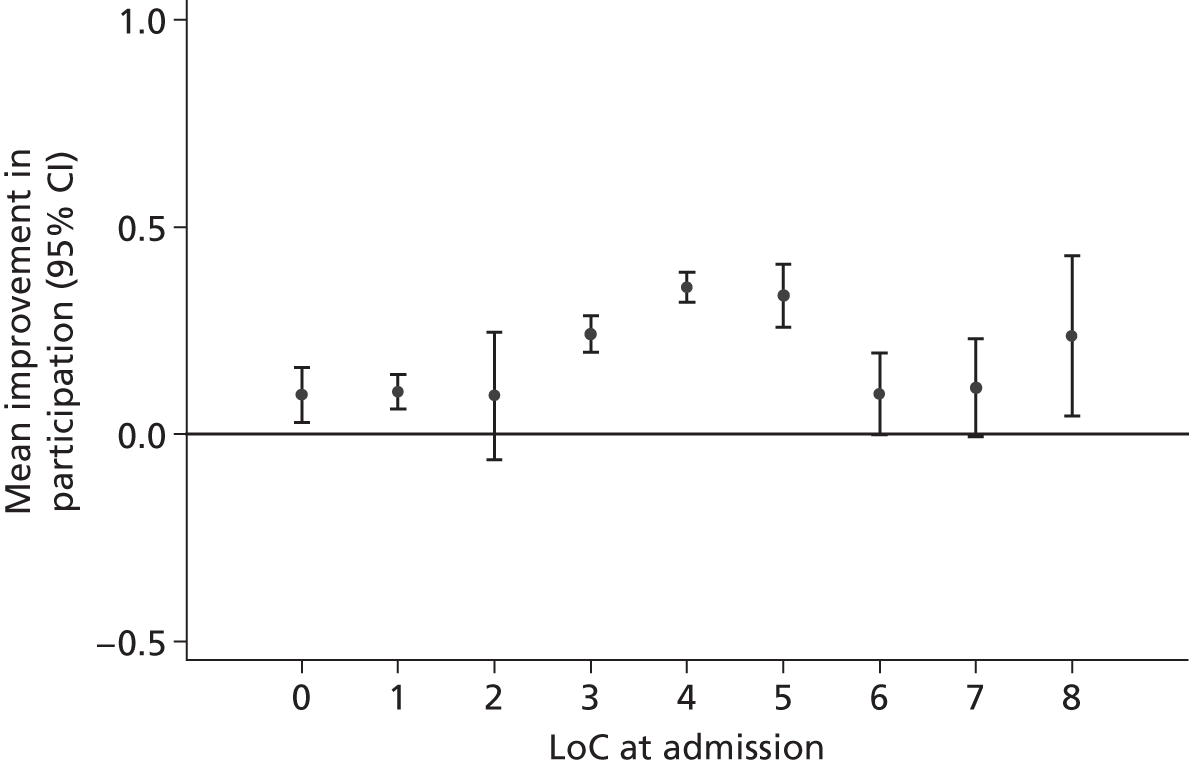
FIGURE 6.
Change in well-being by LoC at admission (model adjusted).
Key point 14: patients most likely to improve were those with admission LoCs levels of 3, 4 or 5 (> 40% for impairment, activity and participation; > 30% for well-being). The probability of any improvement as calculated from the imputed data was between 64% (level 6) and 77% (level 4).
Route of referral
Improvement was greatest among patients referred in from acute settings [accident and emergency (A&E), ambulance, rapid response, acute hospital, day clinics and fall clinics]. Of particular note is that baseline TOM scores in these subgroups were similar to those referred in from other settings and so these differences are not obviously an artefact of regression to the mean. Patients referred via a community nurse, social care or social work had the smallest improvements in TOMs. Again, despite statistical significance, the effects were modest with the highest and lowest group means being around 0.2 TOM units different.
Key point 15: improvement was greatest among patients referred in from acute settings (A&E, ambulance, rapid response, acute hospital, day clinics and fall clinics) despite similar baseline scores to those admitted from other settings.
Place of care
The patient location was also associated with outcome for TOM and EQ-5D scores, with better outcomes observed among those who initially live more independently (i.e. in their own home, an IC facility or resource centre), who have bigger changes than those admitted from residential or hospital settings.
As was found with the TOM data, the relationship between the EQ-5D score and different locations of care was affected by the fact that 3738 patients (46%) had missing data.
Smaller proportions of the patients in residential/nursing home or acute hospital settings improved than those receiving care in more independent care settings, such as at home or in an IC facility or resource centre. However, the percentage showing an improvement became more consistent across the groups when the imputed data set was analysed.
The proportion of patients showing any improvement was significantly lower among people receiving care in a residential/nursing home, A&E or acute hospital compared with those in other settings for all domains of the TOM (see Appendix 2). The magnitude of the changes was modest (< 0.4 units in all domains) and smallest for TOM well-being scores. Mean changes ranged from < 0.1 (residential/nursing) to 0.2 units (IC facility) (see Appendix 2).
The chance of remaining or returning home was greatest for patients receiving care at home who had previously lived at home unaided prior to their health complication; these patients had a 71.9% chance of returning home. This variable also suggests that the chance of returning home is smallest for patients receiving IC at residential or nursing homes; these patients had only a 10.1% chance of returning home.
Key point 16: smaller proportions of the patients in residential/nursing home or acute hospital settings improved compared with those receiving care in more independent care settings, such as at home or in an IC facility or resource centre.
Key point 17: the chance of returning home was greatest for patients receiving care at home who had previously lived at home unaided (71.9%).
Key point 18: the chance of returning home is smallest for patients receiving IC at residential or nursing homes (10.1%).
Usual living arrangements and changes during intermediate care
After data imputation, the patients’ usual living arrangements were found to be highly associated with level of improvement across all four TOM domains. Patients who normally live in their own home or in sheltered accommodation had greater improvements than those living with relatives, who in turn had greater improvements than those in residential, nursing or other settings.
The mean improvement in TOM impairment was > 0 for all subgroups, but ranged from 0.32 (patients living alone in their own home) to 0.01 (other settings). The association was stronger for TOM activity, ranging from 0.36 (own home) to –0.06 (nursing home). Changes in TOM participation and well-being were less pronounced, but patients living in their own home fared, on average, 0.4 units better than patients who are institutionalised prior to IC. The patterns observed in the complete case data were less clear cut, but broadly echoed these.
The greatest level of improvement was observed among patients who were transferred to IC facilities, followed by those who did not leave their own home during IC. Patients who were transferred to hospital or nursing home were the least likely to improve during IC. Figure 7 illustrates these changes, which account for health status.
FIGURE 7.
Change in activity by location of care (for those not institutionalised pre entry; model adjusted).

Key point 19: patients’ usual living arrangements were found to be highly associated with level of improvement across all four TOM domains. The greatest level of improvement was observed among patients who were transferred to IC facilities, followed by those who did not leave their own home during intervention.
Relationship between patient characteristics and European Quality of Life-5 Dimensions scores
The EQ-5D scores of 38% of patients did not improve during their episode of treatment. This is less than the proportion who did not improve on any of TOM domains. This may be a reflection of the fact that EQ-5D is effectively a continuous measure and is a patient-completed measure (reflecting the patient’s view their own health status), whereas the TOM scale has only 11 possible levels and reflects the health-care professional’s view. Improvements in EQ-5D scores were found to have statistically significant relationships with other variables. For instance, the greatest improvements were seen for LoCs 4, 5 and 7 (approximately 0.04 increase), patients receiving care in their own homes (0.06 increase), referrals from A&E/ambulance service or acute wards (0.05 increase) and lower baseline EQ-5D score (0.05-unit increase per 0.1-unit decrease in baseline). Tables 6 and 7 summarise the improvements in these scores.
| Outcome | Complete case | After data imputation (n = 7291)a | |||
|---|---|---|---|---|---|
| Number of patients with data | Mean (SD) improvement | % (n) with any improvement | Mean (SD) improvement | % with any improvement | |
| EQ-5D | 4332 | 0.18 (0.28) | 62% (2684) | 0.15 (0.25) | 66.4% |
| Characteristic | Relationship with TOM | Relationship with EQ-5D | ||
|---|---|---|---|---|
| Statistically significant? | Nature of relationship | Statistically significant? | Nature of relationship | |
| Age | Yes | Minimal: TOM reduced by 0.02–0.03 units per 10-year increase in age | No | |
| Sex | Yes | Minimal: on average, females had approximately 0.1 unit greater improvement than males | No | |
| LoC at admission | Yes | Levels 3, 4 and 5 improved greatest. Impairment and activity: levels 3–5 typically 0.2–0.3 units higher than lowest (0 and 6), with other levels between. Participation and well-being: levels 3–5 around 0.15–0.25 higher than other levels | Yes | Levels 7, 4 and 5 had greatest improvement, around 0.04 units more than the remainder |
| Normal living arrangements | Yes | Greatest improvement for patients receiving care in their own home, with an average increase of 0.15–0.3 units more than living in a residential home or relatives home (which showed the least improvement) | Yes | Greatest improvement for patients receiving care in their own home, with an average increase of 0.06 units more than other locations |
| Effect of leaving own home during IC | Yes | Greatest improvement for patients in IC facilities, showing an improvement of around 0.5 greater than acute hospitals, which show the smallest improvement. Patients remaining at home or transferred to resource centre have next greatest improvement overall | Yes | Greatest improvement among patients who transfer to IC facility, resource centres or remain in own home. Improvement approximately 0.05–0.15 greater than other locations. Those transferred to acute settings had least change |
| Who made the referral | Yes | Greatest improvement for wards in acute hospitals of around 0.1–0.25 units more than the remainder | Yes | Greatest improvement for A&E/ambulance service and wards in acute hospitals, this showed an increase of around 0.05 units more than the remainder |
| Baseline score | Yes | On average, improvement in TOM scores reduced by approximately 0.2 units per unit increase in baseline TOM score | Yes | Improvement in EQ-5D reduced by 0.05 units per 0.1-unit increase in baseline EQ-5D |
The magnitude of these changes is displayed graphically in Figure 8.
FIGURE 8.
Change in EQ-5D score.

Discussion
This chapter has explored which patients are most likely to benefit from IC and those which are least likely to benefit and, therefore, may be best placed to receive care elsewhere. A summary of the main findings is detailed in Table 7.
In order to use resources appropriately, it is important to select patients carefully to receive interventions that are most likely to be of benefit. The data presented here provide information to improve the selection of patients most likely to be assisted by IC. The analysis adds to the evidence in the literature review that the most very elderly patients may be less likely to benefit from IC in terms of rehabilitation outcomes. However, the differential benefits associated with reduced age were small and, therefore, the clinical significance of this is tenuous. The data analysis supports the findings of the literature review that neither age nor sex is likely to be useful criteria on which to select patients for IC.
However, both the literature review and analysis of these data indicate that severity of impairment and health-related QoL (HRQoL) appear to affect outcomes. Patients with higher scores on the TOM scale and EQ-5D questionnaire, on admission, are less likely to benefit, although this may be because patients with higher score are healthier to begin with and have less room for improvement. This assertion is supported by the finding in the data analysis that those with a LoC of 0 (‘client does not need any intervention’) showed less change than other levels. However, it is important to note that many of these clients were discharged on the same day that they had been admitted to the service as they were deemed as not requiring intervention. Patients considered ‘inappropriate referrals’ or who did not need the intervention that they had been referred for are a poorly described group and require further investigation.
Key point 20: the group of patients considered as ‘inappropriate referrals’, or not needing IC services after referral, are poorly understood and require further research.
A similar lack of change in TOM and EQ-5D scores was found for those who need relatively little care (convalescence/respite or prevention/maintenance) rather than those who need slow-stream, regular or intensive rehabilitation, indicating that use of the LoCs may be a useful tool for resource allocation.
The literature provides information about the types of patients included in studies evaluating IC service models using RCTs. The systematic reviews and meta-analyses essentially capture those models for which there has been extensive interest, leading to funding and the conducting of several RCTs.
A key message from the literature review is that RCTs include older people with specific medical [stroke, COPD, congestive heart failure (CHF)] and surgical conditions (fractured neck of femur, CABG). Trials have not included the general population of service users. There is evidence that the rates of improvement in patients admitted to IC are often modest, with two studies showing that only around one-third of patients improve at all. Given the frailty of most of the patients admitted to IC, it could be that no decline in health status is also a positive outcome and perhaps the parameters for success of IC services need to be reconsidered.
The literature review showed evidence that age, cognitive impairment, living alone at admission and functional status at admission may all have an influence on the outcomes of patients using IC; however, the strength and direction of these findings were not consistent enough to draw conclusions for this study.
Analyses of data from our two studies focus on two main sets of characteristics: the assessed need of the subjects in receipt of IC services and the location of care. Age and sex are also included in the analysis but the effects, although statistically significant, were numerically rather small.
For each of the five measures, the extent of change was negatively associated with the baseline score: higher scores at baseline tended to have smaller changes. Increasing age was associated with lower gains in all TOM scores, but the association was small in absolute terms (< 0.05 units of TOMs per 10-year increase). When compared with females, males had marginally higher improvements in impairment and activity, but lower improvements in participation and well-being. EQ-5D score was not associated with age or sex.
The overall outcomes of this study showed that, on average, 60% of patients remain or return home following an episode of IC. Rates of improvement varied according to the outcome measure. On average, 43% of patients improved on the measure of TOM impairment, 44% on TOM activity, 37% as measured by TOM participation and 32% on TOM well-being. Two-thirds of patients (66%) improved on the EQ-5D score measurement after data imputation.
Factors that were statistically associated with a change in TOM scores were patient age (improvement declines with age), sex (females more likely to improve), LoC at admission, living in own home, receiving care in own home or IC facilities, referrals made by acute hospitals and having a lower score at admission.
With respect to all the outcomes (return home, TOM score and EQ-5D score), the analyses generally support the same conclusion: those patients who are more likely to have the most positive outcomes (return to home, large improvement in TOM parameters and EQ-5D score) are more likely to have been assessed as in need of rehabilitation (according to LoC need) by the admitting team.
Levels of care 3, 4 and 5 provide the springboard for most improvement and these represent an assessment that the patient is in need of slow-stream, regular or high-intensity rehabilitation.
Those patients who are likely to do best receive the IC service in their own home. This implies that those who do worst receive IC elsewhere, although it should be noted from the literature review that residential and nursing home settings are largely unevaluated.
However, there are clear indications from the secondary data analysis that place of care is important and that those who improve the least are those who receive care in residential/nursing homes and acute hospital settings. This finding is not surprising given that the level of impairment tended to be more severe for these patients, indicating a higher burden of chronic disease.
Key point 21: those patients who are more likely to have the most positive outcomes (return to home, large improvement in TOM parameters and EQ-5D score) are more likely to have been assessed as in need of rehabilitation (according to LoC need) by the admitting team.
Conclusion
The literature review and data analysis can be seen to agree. Those patients for whom IC may be of benefit include older people with medical and selected long-term conditions for whom a needs assessment suggests that there is potential for rehabilitation, which should be provided, when possible, in the patient’s own home.
Gaps in the evidence base concern the location of care (specifically the use of residential and nursing home settings) and the specific clinical concerns of meeting the needs of patients with dementia, or palliative and end-of-life care needs.
Key point 22: those patients for whom IC may be of benefit include older people with potential for rehabilitation, which should be provided, when possible, in the patient’s own home.
Chapter 2 What factors are associated with increased hospital admissions for patients using intermediate care services?
Introduction
This chapter deals with the question of whether or not the use of IC services changes the use of hospital inpatient facilities by reducing hospital admissions and what factors (if any) are associated with increased rates of hospital admission (and/or readmission) during or after the use of IC services.
Background
In the first instance, there are some conceptual issues which need to be clarified. Admission to acute hospital care is an event that IC services are frequently designed to avoid completely. For example, HITH services can be constructed to bypass the acute hospital, providing substitute acute and/or subacute care in the community and resulting in the total avoidance of hospital admission. A person in receipt of such a service, whose condition deteriorated to require admission to hospital, would be experiencing a first admission to inpatient hospital care for the episode of care in question. Conversely, someone who deteriorated in an IC scheme designed to support early discharge from hospital will be readmitted to hospital (i.e. will experience a second period of inpatient care during the same episode of illness). For example, nurse-led, post-acute care for frail older people was set up to deliver quality transition care (rather than change episode duration). RCTs showed that the nurse-led inpatient units tended to increase the length of inpatient hospital stay. 46–48 However, the subsequent use of health-care resources was different between intervention and control.
In one unit, this was shown to be largely at the expense of community hospital transfers, i.e. total resource use was similar between the intervention group, who had longer inpatient stays, and the control group, who had shorter inpatient stays but made more use of community resources after discharge. These examples are given to illustrate the potential interdependence of the relationship between duration of inpatient stay and subsequent use of services after discharge. 49 Hospital length of stay has become a simplistic metric used as an indicator of efficiency with associated political overtones. Thus, there are incentives for patients to be moved out of hospital, or to avoid hospital, when in fact they may receive more efficient rehabilitation within a hospital setting.
For the purpose of this chapter, the notion of avoiding first admission and avoiding readmission will be conflated, so that we can consider the issue of reducing hospital admissions without worrying about somewhat arbitrary definitions concerning the type of hospital admission.
Admission/readmission as a policy focus
During the first decade of this century, policy-led initiatives focused on reducing recurrent hospital use by patients at risk of multiple admissions. Examples of this include the idea of case management in the community and using specialised nurses or health-care teams to identify at-risk individuals and provide them with additional support in the management of their long-term conditions. The aim of such interventions would be to reduce the use of secondary care and improve health and well-being through encouraging enhanced self-management and providing support in the community for acute or subacute episodes of deterioration.
Although there was some early enthusiasm for these forms of care in England, the potential for them to reduce secondary care use was somewhat overstated in the first instance. Evaluation of the potential for reductions in hospital admissions,50 and the impact of one form of enhanced nurse practitioner working with older people in England,51 was followed by a re-evaluation of the potential for case management to solve the problem of rising numbers of hospital admissions. Case management approaches have been shown to be appreciated by users and carers52 and, in some configurations, to impact on functional health and well-being of recipients. 53 Another approach to targeting interventions to help prevent hospital admissions has involved the use of predictive modelling to identify people at high risk of readmission54 and target additional support in the community. Both of these approaches (anticipatory case management in primary care and predictive modelling) have typically considered hospital admission risk over a 12-month period.
More recently, there have been a series of shifts in policy, directly and indirectly, addressing the issue of unplanned acute hospital readmissions in England. In particular this has included a focus on community care of chronic conditions,8 payment by results, practice-based commissioning55 and, more recently, the setting up of Clinical Commissioning Groups and alterations to the tariff concerning readmissions. 56 The current government has confirmed a policy of altering the remuneration available to NHS trusts (the tariff) for patients readmitted to acute care within a month of discharge. This has been applied to elective care, but in the future may include a proportion of acute care admissions. The key point about this change in policy is that the trust responsible for the initial episode of inpatient care becomes responsible for the cost of subsequent inpatient care if the patient is readmitted within 30 days of the initial discharge. This places the responsibility for managing discharge across the interface between secondary and primary care (i.e between hospital and community care) firmly in the domain of the acute trust and is probably intended to stimulate re-engineering of services at the crucial interface between primary and secondary care so that they become more closely integrated than they may have been in the past.
Literature review
In conducting this review of the relevant literature, we have focused on the evidence from RCTs, evidenced mostly from systematic literature reviews. These sources sometimes report on admission rates and sometimes report on readmission rates, depending on the objectives of the services being reviewed. We have treated these terms as interchangeable for our purpose of describing the literature evidence on interventions affecting hospital admission rates.
Review methods
In developing this literature review, we have drawn on previous systematic literature reviews of discharge arrangements and IC57–59 conducted as part of a series of studies investigating the influence of workforce factors on costs and outcomes in IC. 2,60,61 These reviews have been supplemented with additional literature searches (see Appendix 1) from 2008 to April 2012 and we have identified additional systematic61 and narrative62 reviews, trial protocols63,64 and reviews conducted for the Cochrane collaboration.
Findings from the literature: Cochrane reviews
The Cochrane database of systematic reviews includes three highly relevant reviews of disease-unspecific services provided in the home and compared with hospital-based alternatives. 11,13,65
One review of HAH admission avoidance services addressed the specific research question ‘do readmission rates, or transfers to hospital, differ for patients treated in admission avoidance hospital at home compared with patients who are treated in hospital and are discharged at the standard time?’13 The analysis, combining data from three trials (n = 423), showed a non-significant increase in admissions for patients allocated to HAH [hazard ratio (HR) 1.49, 95% CI 0.96 to 2.33] which persisted even after removing admissions occurring within 14 days of randomisation (HR 1.42, 95% CI 0.87 to 2.30).
A review of early discharge HAH examined services designed to care for patients discharged early from hospital and provide co-ordinated rehabilitation with specialist care. The aim of these services was to relieve the pressure on acute hospital beds. 12 The meta-analysis of the effect on readmission found no significant difference in readmission rates between those allocated to HAH rather than to inpatient care at the 3-month (RR 1.06, 95% CI 0.47 to 2.38) and 6-month follow-up (RR 1.00, 95% CI 0.63 to 1.60). No significant heterogeneity was seen.
In a review of trials of IC in nurse-led beds,65 the intervention was complex and involved professional substitution (nurse for doctor) and altered the case mix of the unit. The objective of care was to enhance the quality and quantity of nursing care received by patients in preparation for discharge. In this analysis, the impact of the intervention on resource use was complex and included alterations in duration of stay in the inpatient and community sectors. The impact on readmission (to 30 days) was considered separately and reported in five studies. Overall, odds of readmission were reduced for patients from the nurse-led units (NLUs) (OR 0.52, 95% CI 0.34 to 0.80). The effect size was maintained (but the statistical significance lost) when this analysis was repeated for the three methodologically stronger studies.
Key point 23: non-disease-specific IC schemes have not been shown to have a major impact on the numbers of hospital (re)admissions. A possible exception is nurse-led inpatient units, which also have complex effects on other resources used (e.g. skill mix).
A further three reviews from The Cochrane Database of Systematic Reviews are about disease-specific services providing home-based IC for patients with stroke21,22 and COPD. 23
A review of services aimed at helping acute stroke patients avoid hospital admission concluded that, overall, fewer patients who received the service were admitted to hospital than those who did not receive the service. 21
A review of HAH for acute exacerbations of chronic obstructive airways disease showed that readmission rates were not significantly different between intervention and control groups. In these schemes, patients who would usually be managed in hospital have most of their care undertaken by a specialist respiratory nurse who makes regular visits to the patient’s home. Further analyses suggested that both patients and carers prefer the HAH services to inpatient acute care. 23
A review of services in which stroke patients in hospital were offered an alternative to conventional systems of care through a policy of early discharge with community-based rehabilitation [early supported discharge (ESD)] concluded that supported early discharge services for stroke has significant effects on inpatient length of stay (amounting to a reduction in length of stay of about 9 days). 22 Five trials (663 patients) provided data on hospital readmission. Rates during scheduled follow-up (27% vs. 25%) were very similar between the patients who received the ESD services and controls.
Key point 24: services designed to reduce inpatient bed use (such as admission avoidance schemes and early discharge schemes) are likely to do so, but there are no consistent effects on readmissions from these types of intervention.
Findings from other systematic literature reviews
In a systematic review of discharge arrangements for older people (> 65 years of age),59 31 studies were identified for which formal synthesis of readmission data was possible. The results of readmission rates were reported in terms of the readmission rate ratio (RRR). A RRR of < 1 indicates that the intervention was beneficial in reducing the risk of readmission to inpatient hospital care. Overall, the RRR was 0.851 (95% CI 0.760 to 0.953; p < 0.001). Analysis of the RRR by the characteristics of the interventions showed that interventions that were implemented by either an individual or a team had similar effects on the reduction in the RRR. The trend to fewer readmissions in the intervention groups was most marked for those provided for both at hospital and at home. It was less marked among interventions delivered only in the hospital, or only in the home, either face to face or by telephone. Interestingly, analysis of readmission rates by service model (such as discharge planning protocols, use of comprehensive geriatric assessment or discharge support arrangements) did not reveal beneficial effects of specific service models on readmission rates. This observation was repeated in a systematic literature review conducted as part of a national evaluation of IC,10 with no particular benefit for readmission rates for discharge support arrangements, admission avoidance schemes or post-acute care.
A systematic review of complex interventions to improve physical function and maintain independent living in elderly people61 concluded that the interventions studied reduced hospital admissions by a small but significant amount (about 6%). Subgroup analysis found that the significant effects were attributable to performing a comprehensive geriatric assessment of frail older people (OR 0.90, 95% CI 0.84 to 0.98), and in community-based care after hospital discharge (OR 0.95, 95% CI 0.90 to 0.99).
Key point 25: working across the interface between hospital and community is a key characteristic of services that achieve reductions in readmissions to hospital inpatient care.
Key point 26: frail older people are less likely to be readmitted to inpatient hospital care if they have a comprehensive geriatric assessment and receive community-based care after hospital discharge.
Secondary analysis of data
Methods
Hospitalisation was defined as a patient being transferred to an acute hospital following IC. The methods used to analyse predictive factors for hospitalisation were similar to those used in the previous objective in Chapter 1, but with some modifications, which are described below.
The analysis of factors predicting hospitalisation was modelled using random-effects logistic regression in which the team was a random effect. Initially, the covariates considered were age, sex, LoC on admission and route of referral. Variables were chosen more sparingly for this analysis than the previous chapter, as regression models with binary outcomes and relatively low event rates are more prone to either ‘overfitting’66 (spurious associations with too many covariates) and ‘model non-convergence’66 (difficulties in fitting models with very low occurrences in some combinations) than regression models for continuous outcomes. 66 Hence only terms that were found to be statistically significant at the 5% level were included.
Following on from this, the usual living arrangements and place where care was provided were considered. As in Chapter 1, the model did not include both because of their collinear nature. Starting with the model chosen above, the patients’ location during IC was added and assessed for statistical significance using the likelihood ratio test. The model was then refitted, removing location during IC but adding the usual living arrangements, whether or not the patient had left this place for the duration of IC and, if so, where to. The best of these models was chosen based on the significance of the likelihood ratio test. All omitted terms were then tested one last time for inclusion and included terms vice versa, using the likelihood ratio test.
Additional analyses were undertaken to assess the impact of the five TOM and EQ-5D baseline assessments. Again, as these five measures are correlated, these analyses were undertaken by adding each of these five in turn, and separately.
Missing data
Missing covariate (i.e. baseline) data were imputed as detailed in Appendix 2, but outcome data were less commonly missing and no imputation was performed for this analysis.
Results
Table 8 provides information on the numbers of patients transferred back to hospital following admission to their service. In total, 628 patients were transferred to hospital. One team (COOP-D) did not transfer any patients to hospital. The EEICC-PB team had the greatest proportion of people transferred to hospital (21%).
| Team | Number transfered to hospital | % of total number of people transfered (to nearest integer) |
|---|---|---|
| COOP study | ||
| A | 27 | 10 |
| B | 8 | 10 |
| C | 1 | 6 |
| D | 0 | 0 |
| E | 1 | 2 |
| F | 7 | 14 |
| G | 18 | 11 |
| J | 12 | 16 |
| L | 2 | 7 |
| M | 13 | 13 |
| N | 5 | 5 |
| PA | 1 | 7 |
| PB | 1 | 6 |
| Q | 4 | 9 |
| SA | 6 | 10 |
| SB | 30 | 16 |
| SG | 2 | 4 |
| T | 7 | 13 |
| TA | 14 | 6 |
| U | 6 | 13 |
| EEICC study | ||
| B | 17 | 6 |
| D | 16 | 5 |
| DO | 7 | 4 |
| E | 27 | 6 |
| F | 17 | 10 |
| G | 128 | 10 |
| H | 78 | 8 |
| I | 71 | 9 |
| PB | 24 | 21 |
| Q | 8 | 5 |
| R | 58 | 12 |
| U | 12 | 7 |
The location following IC was known for 7084 patients, of whom 628 (9%) were hospitalised at the end of IC. Hospitalisation was found to be associated with age (p < 0.0001), sex (p = 0.004), LoC at admission (p < 0.0001) and the place receiving care (p = 0.002), but not with the route of initial referral (Table 9). In addition, the TOM and EQ-5D scores at admission were associated with hospitalisation as described below.
| Term | OR | 95% CI | p-value |
|---|---|---|---|
| Age (per 10-year increase) | 1.20 | 1.10 to 1.32 | < 0.0001 |
| Sex (male vs. female) | 1.36 | 1.12 to 1.62 | 0.004 |
| LoC at admission | |||
| 0 | Reference | < 0.0001 | |
| 1 | 1.34 | 0.85 to 2.09 | |
| 2 | 1.51 | 0.66 to 3.48 | |
| 3 | 1.43 | 0.91 to 2.27 | |
| 4 | 1.86 | 1.21 to 2.88 | |
| 5 | 2.87 | 1.72 to 4.77 | |
| 6 | 2.30 | 1.28 to 4.12 | |
| 7 | 6.54 | 3.84 to 11.14 | |
| 8 | 1.73 | 0.63 to 4.75 | |
| Care location | |||
| At home, alone | Reference | 0.002 | |
| At home, not alone | 0.90 | 0.71 to 1.12 | |
| Relatives home | 1.53 | 0.87 to 2.67 | |
| Residential/nursing home | 0.61 | 0.38 to 0.96 | |
| Sheltered housing | 1.18 | 0.68 to 2.06 | |
| Acute hospital | 2.74 | 0.51 to 14.66 | |
| A&E | 2.20 | 1.04 to 4.69 | |
| IC facility | 1.88 | 1.26 to 2.78 | |
| Day hospital or community hospital | 0.29 | 0.04 to 2.22 | |
| Resource centre | 1.18 | 0.39 to 3.57 | |
| Community hospital | 0.91 | 0.54 to 1.54 | |
| Other | 0.35 | 0.08 to 1.47 |
Level of care at admission
The probability of being transferred to hospital was greatest for a LoC of 7 (needs medical care and rehabilitation); for these patients the probability of being transferred to hospital is 25.4%.
The chance of being transferred to hospital is smallest for LoCs of 0 (does not need any intervention) and 1 (needs prevention programme); for these patients the chance of being transferred to hospital is 5.2% and 6.6%, respectively.
Location of care episode
Some IC service provision is within an acute setting. The chance of being transferred back to the non-IC wards (acute) hospital is unsurprisingly greatest for patients receiving IC within the acute hospital settings and these patients have a 20% chance of being transferred to hospital.
The chance of being transferred to hospital is smallest for patients receiving care at ‘other’ settings; these patients have a 3.5% chance of being transferred to hospital. Patients receiving care in residential or nursing homes are the second least likely, having a 5.1% chance of being transferred to hospital.
Age and sex
For every 10-year increase in age, there is a 20% increase in the odds of being transferred to hospital. The chance of being transferred to hospital is greater for males than females. Males are more likely to be transferred to hospital than females (OR 1.36, 95% CI 1.12 to 1.62) (see Table 9).
Key point 27: patients identified as having medical care needs on the LoCs had the highest probability of being hospitalised. Those identified as 0 on LoCs had the least chance of being transferred to hospital.
Key point 28: for every 10-year increase in age, there is a 20% increase in the odds of being transferred to hospital. The chance of being transferred to hospital is greater for males than females.
Therapy outcomes measures and European Quality of Life-5 Dimensions scores
Further modelling addressed the impact of the TOM and EQ-5D scores at admission. As these terms were highly correlated, they were assessed separately as opposed to in the same model. Adding each in turn to the above model improved the model fit for all five terms, suggesting that all were associated with hospitalisation, and higher scores were associated with a reduced probability of hospital admission (p < 0.001 for all five). Of the four TOM components, impairment and activity (both OR = 0.66 per unit change) had the highest magnitude of effect, with participation and well-being having ORs of 0.72 and 0.77 respectively. The odds of being admitted to hospital reduced by 8% for every 0.1-unit increase in EQ-5D score.
Discussion
The literature does not suggest that any particular IC model (admission avoidance, discharge support, community rehabilitation, community hospital or other clinical facility for rehabilitation or recuperation, or both, including nurse-led inpatient units) will achieve a specific and consistent impact on admission or readmission to inpatient hospital care.
However, recent changes in policy may have affected the viability of nurse-led discharge units. These hold the potential to transform the experience of discharge, but at the expense of somewhat increased hospital inpatient resource use. These schemes were shown to reduce readmission rates significantly in some analyses. Essentially, this was achieved by taking time to prepare patients for discharge, effectively managing the timing of discharge to suit their needs by increasing duration of inpatient stay. In the new policy environment, in which early readmission is becoming the financial responsibility of the discharging hospital, it is possible that the economics of such NLUs may be more favourable than when originally evaluated.
There is some evidence from analysis of the characteristics of interventions associated with reduced (re)admission rates that a key issue is the effectiveness of working across the interface between primary and secondary care,59 or providing community-based care after hospital discharge. 61 These observations imply that it is important, when transferring patients with complex care needs across the interface between inpatient hospital and community-based care, to transfer the capacity to meet their complex needs in the community.
Our data suggests significant variation between clinical teams in the rates of admission to hospital (range 0–21%). This is consistent with a view that factors other than the specific care model (such as the degree of integration across the acute and secondary care interface) may be important in determining (re)admission risk. The main patient characteristic associated with increased transfer to hospital was a complex presenting need as defined on LoCs, which included the requirement for both rehabilitation and elements of medical care.
The main patient characteristics associated with low rates of transfer to inpatient hospital care were low LoCs need (no need and preventive need only) and being resident in nursing home care. In the latter case, although care needs may be high, or complex, the surrounding environment and (possibly) care plans and policies, may be conducive to receiving such care in situ.
Conclusion
Taken together, a consistent message that emerges from the literature and the secondary analysis of the data from these two studies is that a central concept in minimising hospital admissions in IC in the community is the capacity of the service to meet the client’s, often complex, care needs. That is to say that hospital admissions will be minimised when the services are sufficiently integrated across the interface between hospital and the community that the patient’s care needs can be matched to the available service in the setting to which the client is assigned.
Key point 29: matching the needs of patients with a care setting in which the needs can be met is a potential unifying mechanism for reducing the risk of subsequent hospital (re)admission.
Chapter 3 Factors predicting admission to institutional care among intermediate care service users
Introduction
Making the transition into long-term care is difficult for many older people and is frequently associated with loss of identity, fractured social networks and discontinuity. The literature surrounding admission to long-term/institutional care for older people suggests that entry into a nursing or residential home often results from a crisis. In such situations, rather than managing the process and ‘making a decision’ about care, older people and their families are more likely to be find themselves ‘realising the inevitable’ and entering the care network with little information or choice. 67 Alongside the personal costs associated with admission to long-term care, considerable public costs have also been identified and a long-standing policy commitment has been made to prevention, with IC at its centre. 4,5,68 The downward trend in the numbers of people in care year on year might suggest some success in relation to this and other objectives. 69
Background
In recent years, a raft of community-based complex interventions has evolved to help prevent admission, with evidence to suggest that these, in part, may have contributed to delays in admission to care for some older people. Nevertheless, around 220,000 people are supported to live in residential or nursing home care in England on a long-term basis, with over three-quarters (77%) of those being aged ≥ 65 years, with over two-fifths (43%) being aged ≥ 85 years. 69 These figures do not include all of those individuals in private residential and nursing home facilities or those with continuing care requirements.
This chapter sets out to identify those factors associated with admission to institutional care for users of IC. This will be achieved through addressing three objectives. First, relevant literature concerning the role of IC in reducing the risk of admission to long-term care will be highlighted. Second, the evidence concerning those factors that have shown to predict admission to institutional care in older people will be presented. Finally, the findings that have emerged from the secondary analysis of the COOP1 and EEICC2 data sets and that address factors that predict admission to institutional care are presented.
Literature review
Review methods
A full copy of the search strategy used to support this chapter is provided in Appendix 1. The literature searches undertaken for the COOP1 and EEICC2 studies were also used, alongside hand searches. Systematic reviews and reports of meta-analyses are given prominence here, although individual studies are cited in isolation where appropriate. The results of pooled data analysis are presented using methods for each review and these vary. As such, HRs, ORs and RRs are used and CIs are used when available.
Intermediate care has, for some time, been promoted as a form of provision that may contribute to the range of services which, alongside family care, might mediate the impact of long-term illness and disability and prevent admission to long-term/institutional care. 5 Some evidence from the international literature is reviewed below in relation to this issue. The evidence presented here relies on one systematic review70 and one meta-analysis. 61 A further meta-analysis, relevant only to stroke, is also included. 71
Effectiveness of intermediate care in reducing risk of admission to care
Evidence from the Cochrane database includes one relevant systematic review. 70 The review evaluated the provision of HAH as an intervention when compared with acute inpatient care in the context of end-of-life care. As part of the review, HAH is defined as time-limited provision carried out by health-care professionals in the patient’s own home. For the purpose of this chapter, this definition is considered a legitimate representation of the UK interpretation of IC. The review is inclusive of patients over the age of 18 years, although excludes obstetric and mental health evaluations. As such, attention is given over to the effect of such interventions on outcomes for older people. Specific attention is also given to the effect of HAH for people who have had a stroke, possibly as a result of the relative strength of available evidence in this particular field. 12 The review12 highlights two relevant sets of findings here. First, the review included four trials evaluating HAH and risk of admission to forms of long-term care following stroke. Pooled data (n = 574) showed that fewer patients who had used HAH schemes were in residential care at follow-up (RR 0.6, 95% CI 0.40 to 0.98). Second, pooled data (n = 484) from three studies indicate similar findings with fewer older HAH patients with a range of medical needs admitted to residential care at follow-up (RR 0.69, 95% CI 0.48 to 0.99).
Beswick et al. 61 have undertaken a meta-analysis of the range of complex interventions aimed at maintaining independent living. Included within this study were geriatric assessment, falls assessment, falls prevention, community-based care after hospital and group education and counselling. Again, these were considered a legitimate representation of the UK interpretation of IC. Pooled data resulted in the inclusion of 89 studies and over 97,000 patients. Findings suggest that such interventions reduced the risk of admission to institutional care (RR 0.87, 95% CI 0.83 to 0.90). Of the five categories of complex intervention, only community-based care after hospital discharge and geriatric assessment demonstrated significant reduction in risk independently (RR 0.77, 95% CI 0.64 to 0.91 and RR 0.86, 95% CI 0.83 to 0.90 respectively). The authors note the diverse range of the type of interventions included within the study and the variation of intensity of provision within and between individual studies.
A further meta-analysis of similar evaluations in the field of stroke71 noted that ESD evaluations for stroke, including studies with rehabilitation at home, were less likely to result in admission to institutional care (OR 0.74, 95% CI 0.56 to 0.96). This meta-analysis also noted as a significant interaction between mild and moderate initial stroke and institutional care as an outcome.
Additional evidence supporting IC as an intervention which may assist in the prevention of nursing home care admission is provided in research not included in the above systematic review or meta-analysis. Garasen et al. 72 conducted a RCT of IC within a community hospital compared with usual discharge. Nursing home admission was more likely within the control group at 6 months (OR 2.19, 95% CI 0.51 to 9.40).
Key point 30: there is evidence to suggest that IC has some effect in reducing the risk of admission to long-term care for older people.
Evidence concerning predictors of admission to nursing and residential home
A number of reviews have been undertaken in this specific area. This includes a meta-analysis of US-based data73 and a systematic review including international data. 74
Gaugler et al. 73 identified a number of key predictors in a review of factors contributing to nursing home admission in the USA. Pooled data concerning over 178,000 older adults was included. Three primary predictors were identified: three or more ADLs dependencies (OR 3.25, 95% CI 2.56 to 4.09), cognitive impairment (OR 2.54, 95% CI 1.44 to 4.51) and prior use of nursing home facilities (OR 3.47, 95% CI 1.89 to 6.37).
Luppa et al. 74 also reviewed data relating to predictors of admission to care from the international literature and utilised a relatively inclusive methodology. Additionally, the Luppa et al. 74 review used a conceptual model segmenting contextual (predispositions) and individual (needs) as important independent variables. Contextual factors identified as strong evidence were increasing age (HR 1.06–7.72, OR 1.30–8.34) and not having one’s own home (HR 1.8, OR 2.61). Individual factors identified as strong evidence were low self-rated health status (HR 3.40, OR 1.48–1.67), poor functional ability (as indicated by ADLs; HR 1.32–3.70, OR 1.30–1.78); presence of a diagnosis of dementia (HR 1.54–5.09, OR 16.70), previous use of nursing home provision (OR 1.70–5.84) and a high number of prescriptions (HR 1.04–1.67, OR 1.15). It should be noted that these comprehensive reviews give rise to discussion about likely methods of measurement and prediction of admission, but do not help to explain which mechanisms are apparent in the process of admission.
Key point 31: poor ADLs, existence of cognitive impairment and increasing age are consistently associated with admission to long-term care.
Secondary analysis of data
Methods
This section investigates the factors that predict admission to institutional care among IC service users. For the purpose of the analyses, admission to institutional care is defined as those patients discharged to permanent residential or nursing home provision (Table 10). Study participants already living in institutional care were excluded for the purpose of this analysis. A total of 85 patients were newly admitted to institutional care under these circumstances. Given the scarceness of this outcome, a more descriptive statistical analysis was performed. The probability of institutionalisation was modelled using a random-effects logistic regression in which the team was a random effect, but only univariate models and summaries are presented, as there were too few events to enable model stability and convergence.
| Patient measures on admission | OR (95% CI) | p-value |
|---|---|---|
| Age (per 10-year increase) | 1.93 (1.48 to 2.51) | < 0.001 |
| TOM score at admission (per unit increase) | ||
| Impairment | 0.60 (0.47 to 0.75) | < 0.001 |
| Activity | 0.51 (0.41 to 0.62) | < 0.001 |
| Participation | 0.48 (0.38 to 0.59) | < 0.001 |
| Well-being | 0.55 (0.45 to 0.67) | < 0.001 |
| EQ-5D score (per 0.1-unit increase) | 0.84 (0.78 to 0.91) | < 0.001 |
Missing data
Missing covariate (i.e. baseline) data were imputed as detailed in Appendix 2, but outcome data were less commonly missing and no imputation was performed for this analysis.
Results
A total of 85 out of 6550 patients (1.3%) were discharged into permanent residential or nursing home care. Ten teams reported no institutionalisations, with only two teams reporting over 4% [COOP E, 3 out of 46 patients (6.5%); EEICC PB, 6 out of 109 patients (5.5%)]. Analyses based on complete case data were similar to those based on imputed data and, for simplicity, we present only the former.
The age of the patient, their usual living arrangements and leaving home for IC were all highly statistically significant (p < 0.001) predictors of institutionalisation on univariate analysis. Age was associated with a 93% increase in the odds of institutionalisation per 10-year increase (95% CI 48% to 151%; p < 0.001). All four TOM and EQ-5D scores at admission were also associated with a reduced probability of institutionalisation.
Out of all 1006 patients who received IC in an institutional setting, 56 (5.6%) were discharged to institutions. Out of all 5544 patients who received IC in their usual place of residence (excluding those whose usual residence was an institution), 29 (0.5%) were discharged to institutions.
As with the hospitalisation outcome, the TOM and EQ-5D scores at admission were entered into five separate models because of their collinearity. In each case, the baseline measurement added to the model and all four TOM scores had an associated OR of around 0.7, in other words, the relative odds of admission were reduced by 30% for each unit increase in TOM scores at admission. The gradient in the reduction of probability with increase in the TOM participation score at admission is illustrated in Figure 9. A higher EQ-5D score at admission also reduced the likelihood of being institutionalised following IC (OR 0.92 per 0.1-unit increase).
FIGURE 9.
Institutionalisation for TOM participation score.
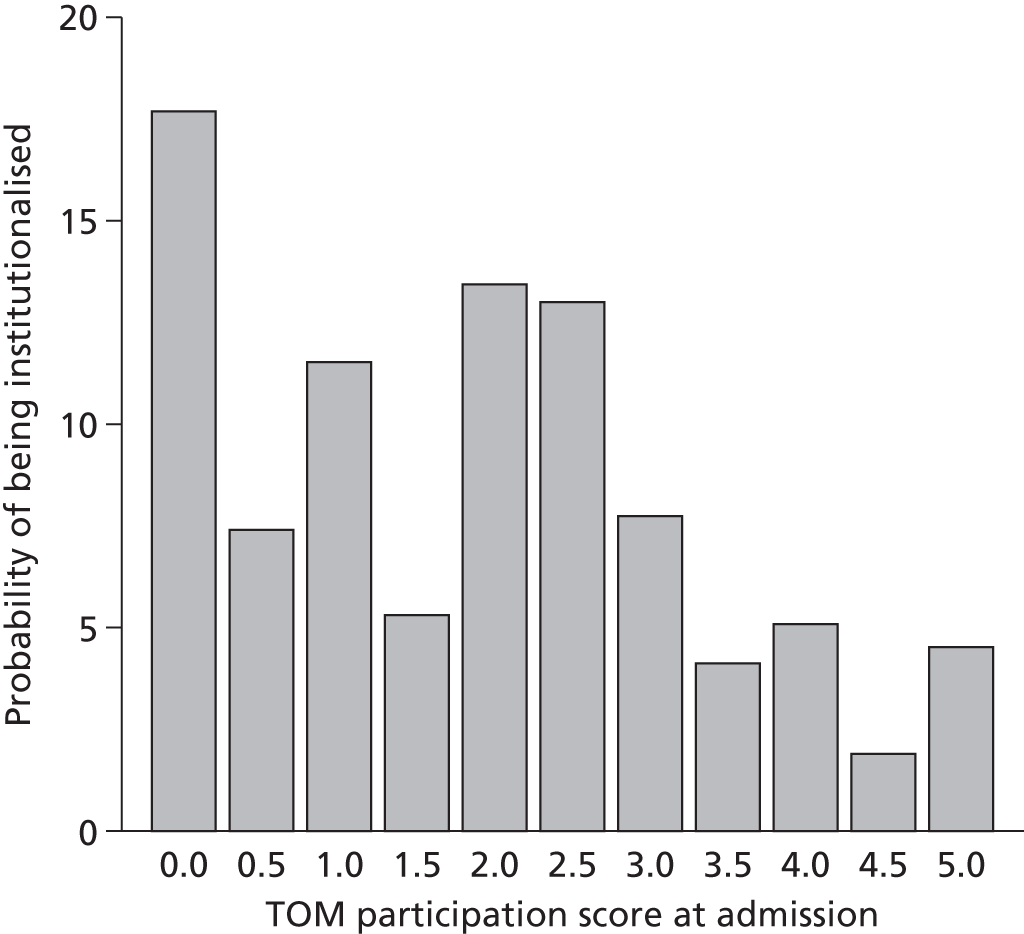
Key point 32: on average, for every 1-point increase in TOM participation score, at baseline, there is a 32.8% decrease in the likelihood of admission to long-term care (OR 0.67; p < 0.0001).
Key point 33: increasing age and poor TOM or EQ-5D scores at admission are associated with admission to care for IC service users. Receiving IC services at home is strongly associated with not being admitted to long-term care.
Discussion
This chapter addressed the question concerning those factors that might predict discharge from IC to long-term/institutional care. As such, it set out to review evidence concerning the effectiveness of IC in preventing admission, as well as literature that has highlighted factors, which might predict admission to care for older people. It should be noted that with the exception of Langhorne et al. 71 there exists little analysis on the interaction of the use of IC services, individual factors and admission to institutional care as an outcome.
Factors identified as being statistically significant include residential care home as a place of IC provision, increasing age and lower TOM participation score at admission.
Notable non-significant factors include LoCs of 6 and 2 and being female. It should be noted that discharge to a care setting was likely in only 2% of cases, adding credence to the potential for IC to provide a preventative service,61,70 particularly in the light of more recent UK research, which would suggest that living alone is a significant predictor of admission to long-term care. 75
Findings relating to increasing age concur with previous studies, which have explored those factors that predict admission to care. 73,74 There is a consistent theme within the existing evidence in relation to poor ADLs and admission to care. 74 TOM participation score on admission to IC is identified as a significant finding here, and although conceptually distinct to ADLs, the relationship between function and participation is clear.
Conclusion
Again, the findings here resonate with existing evidence. Langhorne et al.,71 in a review of the effectiveness of early supported discharge, noted that patients with poor ADLs scores at admission were more likely to enter long-term care. It is important, however, to note that by focusing on individual characteristics, the opportunity to explore the relationship between contextual factors and likely outcome is missed. The variations in team composition, setting, skill mix, size and integration and, in particular, the relationship with discharge destination are variables that could explain differences in the data. These areas of investigation demand further research.
Key point 34: although the findings linking individual characteristics to outcomes support previous evidence, the relationship with contextual factors demands further research.
Chapter 4 What factors are associated with increased risk of mortality for intermediate care patients?
Introduction
This question is significant because of substantial political and economic pressure for more elderly patients to be managed in their own homes, whereas previously they had been cared for in hospitals and other institutions. It is important that such changes (at the very least) do not put patients at an increased risk of adverse outcomes, such as death.
Background
There is evidence that IC and community rehabilitation is beneficial to many older people. However, it is important to be able to identify those who are at risk of deteriorating health who may benefit from hospitalisation or increased length of stay prior to discharge.
Intermediate care and rehabilitation should be available to those individuals who are likely to benefit from such services and palliative care services should be available to those who are likely to die. Although we recognise that prediction of death in the elderly is not a precise science, it is important to address this question and examine differences between different teams so we can determine whether or not patients are being correctly referred to appropriate services and whether or not changes have occurred over time.
Knowledge about survival and prognosis is important to clinicians, patients, family and other caregivers and for the planning of long-term facilities and home care. Indeed, in the acute care sector, NHS trusts regularly see their mortality statistics, appropriately corrected for case mix, as one of the routine metrics about them on public information systems. 76 Such data are not available for those receiving community-based NHS services.
Literature review
A copy of the search strategy used to support the literature review for this chapter is located in Appendix 1.
There have been several studies using different algorithms to identify the community-dwelling vulnerable older people who are more likely to die at an earlier point in time but none specifically studying those receiving IC. Therefore, we describe here some key studies that focus on those at increased risk of death in old age.
Key point 35: we identified little literature of direct relevance to the question: what factors are associated with increased risk of mortality for IC patients?
Saliba et al. 77 developed a screening tool that was tested on more than 6000 community-dwelling older people, who were defined as persons aged ≥ 65 years.
A complex data analysis investigated a method for identifying older people at risk of losing physical function and death. This was used to identify a vulnerable group that comprised 32% of the ≥ 65-year-olds studied. This group had a fourfold greater risk of death when compared with the rest of the population.
Unsurprisingly, increased mortality is associated with increased age and clinical instability. A study by Guerini et al. 78 provided a definition of clinical instability which used routine clinical measures (such as blood pressure and heart rate) to predict increased likelihood of death on admission to a rehabilitation and aged care unit.
Chronic kidney disease, which is more common in old age, was investigated by Roderick et al. 79 who showed that declining kidney function is significantly associated with an increase in all-cause and cardiovascular mortality in those > 75 years of age.
After a study of more than 9000 patients in the USA living in the community aged between 65 and 102 years of age, Kazanjian et al. 80 concluded that pulse pressure appears to be the best measure for predicting mortality in older people.
Key point 36: increased mortality is related to age, limitations in physical function, functional disabilities and clinical instability, which are all issues associated with requiring IC.
The many physiological and social factors that have been investigated to determine their contribution to mortality often give rise to symptoms which increase the likelihood of hospitalisation and may still be present on early discharge and transfer to IC.
The study by Kazanjian et al. 80 found that the odds of death increased with institutionalisation and with increasing cognitive and physical impairment. Although vision and hearing problems and the presence of heart disease, stroke and diabetes were all strongly related to 5-year mortality in univariate and unadjusted analyses, their contributions were minimal in the multivariate analyses. Increased body mass index was associated with lower mortality in both univariate and multivariate analyses.
Ostbye et al. ,81 in a similar population-based study in Canada, confirmed the importance of sex, age, functional status, cognition and health status in predicting 5-year mortality. Accounting for cognitive status, physical status and specific disease variables led to the difference in mortality between older people in the community and in institutions being reduced.
A population-based prospective study of more than 1000 older individuals (64–85 years) in Finland by Hirvensalo et al. 82 ranked participants into four groups: (1) intact mobility and physically active (mobile–active), (2) intact mobility and sedentary (mobile–sedentary), (3) impaired mobility and physically active (impaired–active) and (4) impaired mobility and sedentary (impaired–sedentary). The analysis adjusted for age, marital status, education, chronic conditions, smoking and physical exercise earlier in life. The study found a twofold increase in the risk of death in impaired–active and a three times greater risk in impaired–sedentary groups than in mobile–active groups. However, the risk of death did not differ between mobile–active and mobile–sedentary groups.
The authors concluded that mobility impairments predicted mortality and dependence. However, among people with impaired mobility, physical activity was associated with lower risks, whereas the risk did not differ according to activity level among those with intact mobility. Despite their overall greater risk, mobile-impaired people may be able to prevent further disability and mortality by physical exercise. Interestingly, increasing independent activity is one of the key aims of IC.
Key point 37: even when mobility is impaired, physical activity is associated with a lower risk of death.
Secondary analysis of data
The statistical methodology was undertaken as described in Appendix 2. Reported probabilities of mortality were calculated using a model, which included age, sex, LoC at admission, route of referral and the location where the patient was receiving care.
Results
The percentage of deaths in the first study (COOP)1 was 1.3% (n = 25) and 3.4% (n = 212) in the second study (EEICC). 2 Overall, 237 patients (3%) recruited to the two studies died during IC. In the seven teams participating in both studies, percentage of death was 1.4% (n = 281) in the first study and 2.1% (n = 1462) in the second. However, most teams show a low percentage of deaths with nine teams for which no recruited patients died. Team COOP-C had the greatest percentage of deaths (Table 11).
| Team | Number of deaths | % of total number of deaths in each of the teams (to nearest whole number) |
|---|---|---|
| COOP study | ||
| A | 4 | 1 |
| B | 3 | 4 |
| C | 2 | 11 |
| D | 0 | 0 |
| E | 3 | 4 |
| F | 0 | 0 |
| G | 2 | 1 |
| J | 0 | 0 |
| L | 1 | 3 |
| M | 1 | 1 |
| N | 0 | 0 |
| PA | 1 | 5 |
| PB | 0 | 0 |
| Q | 1 | 2 |
| SA | 1 | 1 |
| SB | 4 | 2 |
| SG | 1 | 1 |
| T | 1 | 2 |
| TA | 0 | 0 |
| U | 0 | 0 |
| EEICC study | ||
| B | 3 | 0.6 |
| D | 11 | 3 |
| DO | 3 | 1 |
| E | 14 | 3 |
| F | 3 | 2 |
| G | 82 | 6 |
| H | 53 | 5 |
| I | 38 | 4 |
| PB | 0 | 0 |
| Q | 0 | 0 |
| R | 2 | 0.5 |
| U | 3 | 2 |
Key point 38: there is an indication that patients in the more recent study (EEICC) had more complex conditions.
The results of the modelling are presented in Table 12. Mortality was higher among males than females (OR 1.23, 95% CI 1.07 to 1.44; p = 0.021) and increased with age (OR per 10-year increase 1.23, 95% CI 1.07 to 1.43; p = 0.004). Mortality was also higher among LoCs of 2 and 3, and lower when patients were receiving care in their own home.
| Term | OR | 95% CI | p-value |
|---|---|---|---|
| Age (per 10-year increase) | 1.26 | 1.11 to 1.43 | 0.004 |
| Sex (male vs. female) | 1.40 | 0.55 to 0.95 | 0.021 |
| LoC at admission | |||
| 0 | Reference | < 0.0001 | |
| 1 | 3.23 | 1.60 to 6.20 | |
| 2 | 5.36 | 2.00 to 14.22 | |
| 3 | 3.04 | 1.52 to 6.07 | |
| 4 | 1.79 | 0.88 to 3.63 | |
| 5 | 2.92 | 1.18 to 7.16 | |
| 6 | 3.19 | 1.28 to 7.95 | |
| 7 | 2.14 | 0.64 to 7.08 | |
| 8 | 1.68 | 0.35 to 8.04 | |
| Care location | |||
| At home, alone | Reference | < 0.0001 | |
| At home, not alone | 1.66 | 1.17 to 2.86 | |
| Relatives home | 2.46 | 1.14 to 5.33 | |
| Residential/nursing home | 3.71 | 2.47 to 5.57 | |
| Sheltered housing | 0.75 | 0.22 to 2.36 | |
| Acute hospital | 0.00 | Not estimablea | |
| A&E | 1.75 | 0.70 to 5.13 | |
| IC facility | 2.07 | 0.23 to 17.1 | |
| Day hospital or community hospital | 1.81 | 0.23 to 14.3 | |
| Resource centre | 2.76 | 0.34 to 22.62 | |
| Community hospital | 4.66 | 2.39 to 9.10 | |
| Other | 1.77 | 0.50 to 5.71 |
The literature suggests that older people in the community with increased number and severity of impairments have a higher probability of death. This is borne out when examining the severity of the TOM rating scale on admission and the numbers of deaths related to each scale point.
To assess the impact of TOM scores at admission, each was added in turn to the above model (separately). In each case, there was a significant association (p < 0.001) between the score at admission and probability of death. This is illustrated by Table 13, showing the relationship between each of the four TOM scores and death. Ninety-four patients with a score of less than three on impairment died, compared with 65 with a score of three or above (a scale point of three on the TOM scale is termed moderate/severe to severe).
| TOM admission score | Domain, number (%) deaths | |||
|---|---|---|---|---|
| Impairment | Activity | Participation | Well-being | |
| 0–1.5 | 41 (8.5%) | 33 (5.9%) | 35 (7.3%) | 17 (5.7%) |
| 2–2.5 | 53 (3.9%) | 58 (4.9%) | 47 (3.6%) | 34 (5.5%) |
| 3–3.5 | 50 (1.7%) | 53 (2.1%) | 42 (2.0%) | 54 (3.4%) |
| 4–5 | 16 (0.9%) | 17 (0.7%) | 37 (1.4%) | 56 (1.4%) |
Key point 39: those patients well enough to receive IC in their own home have the lowest probability of death. Those receiving these services in an institutional setting have the highest probability.
Discussion
There has been an increase in deaths of patients referred to intermediate/community care over time. This is associated with a greater number of patients receiving these services who have more complex and severe health and social care needs. These findings are in line with the literature related to deaths within the community of older people. However, this needs to be placed in the context of the evidence that even the best geriatric medical acute unit expects a mortality rate of around 15–20% of patients at 3 months after admission. 83 The determinants of death in inpatient care are the same as we found in these community studies (i.e. severity and complexity of health condition and previous functional health status). Although IC services may have seen a rise in mortality, they are receiving patients at a lower risk of death compared with the population they are likely to have come from (i.e. mortality rates in the region of 1–3% could be interpreted as indicating appropriate selection of patients for IC services).
Another important issue is related to whether or not IC and community rehabilitation are appropriate or inappropriate services in caring for those coming to the end of their life.
Conclusion
Many surveys have concluded that, generally, people would prefer to die in their own home,84 but unfortunately people with palliative and supportive care needs are generally explicitly excluded from the IC trials, so we have little or no evidence about providing palliative care in IC services to work with. However, there is a trend in developing services, which integrate rehabilitation and IC services with those of palliative care for older people with a broad range of disabilities and health-care challenges. Moving more of this care into the community may well be appropriate but it is important to consider that a recent meta-analysis (of more than 10,000 patients) indicated the value of comprehensive geriatric assessment to reducing deterioration of health, and yet costs increased. 85 Consideration needs to be given to the skill mix to support these patients appropriately.
Key point 40: there is a case for integrating palliative care services for older people with IC/community rehabilitation because the complexity of cases being cared for in the community is increasing.
Objective 2 To examine the effectiveness of different models of intermediate care
Chapter 5 What team-level factors are associated with the greatest benefits for patients in terms of health status?
Introduction
Over recent years, it has been recognised that about 85% of health-care expenditure is spent on treating 15% of the population. Much of this expenditure is focused on patients with chronic conditions, an increasing number of which are older patients. These patients are much more frequent users of all health services, but in particular, they are much more frequently admitted to hospital for episodes of acute care.
Background
As a result of the NHS Plan4 and NSF for older people,5 IC and rehabilitations services have been developed to rehabilitate patients more effectively after episodes of acute care, assist earlier discharge, promote the greater independence of older people with acute conditions and provide support in the community to prevent hospital readmissions. IC services are generally, but not always, community-based, interdisciplinary teams, which are staffed by a range of health and social care professionals. Some are located in NHS organisations and others in social care. The development of community rehabilitation and IC/services (CRAIC/S) service has followed no particular formula and, in reality, services across England and Wales differ enormously in their size, configuration and working practices. This has led to some researchers questioning whether or not IC really exists as a stable concept. 1 Furthermore, there is little real understanding about how most effectively to configure IC services for optimum impact. Knowledge about what team factors are associated with the greatest benefits for patients in terms of improving and maintaining their health status, and their independence, is therefore vital.
Literature review
Review methods
Two different literature searches were conducted for this review using health and social care databases. The search strategies (see Appendix 1) aimed to find studies published in 2008–12 to supplement the searches concluded in the COOP and EEICC reports. 1,2 A three-step search strategy was utilised in each component of this review. In the first instance, an initial scoping search was undertaken. This was followed by analysis of the text, words contained in the title and abstract, and of the index terms used to describe relevant articles. A second, more extensive search using all identified terms and index terms was then undertaken across all included databases. Third, the reference lists of all identified reports and articles were searched for additional studies.
Searches identified 473 unique papers of potential interest. After review at title and abstract level, 29 papers of possible interest remained. After examination of full texts, 20 further papers were excluded and two further papers were excluded as they were not deemed to be of sufficient quality. Seven full-text papers were reviewed in depth. However, it has to be stated that only five papers directly addressed the issues raised by this question. The remaining two considered services that fitted into the broad definition of IC proposed for this study, but the declared focus of research was not directly on IC and not primarily on team-level factors.
The review included published accounts of IC teamworking, regardless of study type, and considered studies that described and/or evaluated the interdisciplinary team-level factors that were associated with the greatest benefits for IC patients. For the review, the definition of interdisciplinary teamworking was defined as work groups that include more than two professional groups or disciplines. The review aimed to identify themes and conceptual models of team-level factors that were associated with better outcomes for patients. Within this, it considered studies that included any objective measure of change in patient outcomes resulting from a planned intervention aimed at either introducing interdisciplinary teamworking if it was previously not present or changing interdisciplinary teamworking methods.
Findings from the literature
Four studies directly addressed factors relating to the research question of focus in this chapter. 1,5,86,87 One further paper60 did not report a study that directly researched IC team delivery, but examined interdisciplinary teamworking with patients with chronic conditions. Generally, quantitative studies tended to compare the outcomes for patients of interdisciplinary team-based interventions with traditional care. Very few papers examined specific team-level factors that may be associated with better outcomes for patients.
Key point 41: very few studies examine specific team-level factors that may be associated with better patient care.
A non-randomised study by Blewett et al. 86 looked at improving transitional care through implementing interprofessional care teams. Patient outcomes were compared for both patients who received transitional care from an interprofessional team (n = 163) and patients who received care by a traditional single provider (n = 176). Patients who received care from an interprofessional team had significantly shorter lengths of stay (20.3 days) than patients receiving care by the traditional model (27 days). Analysis of costs also showed that care by the interprofessional team was significantly cheaper (interdisciplinary team = US$12,001 vs. traditional care = US$14,298). Several team-level factors were mentioned by the authors as contributing to these improvements:
-
team composition – it was important that the team was the right size and able to counteract negative effects of status differences
-
team tenure – a core of the interdisciplinary team had all worked together for several years
-
regular team meetings – to discuss patient care were held several times a week and a formal team meeting was held every 3 weeks
-
task allocation – tasks were matched between roles and responsibilities
-
cohesiveness – was actively promoted
-
open communication – interdisciplinary team members were willing to share large amounts of information about both progress and process.
However, although the text indicates that there was some formal evaluation of the team to reach these conclusions ‘communication was consistently listed as a positive aspect of the team’,86 it does not specify the methods used to qualitatively evaluate these team processes.
Key point 42: delivery of care by interprofessional care teams reduced average length of stay (27 vs. 20.3 days) and the cost of care (traditional care = US$14,298 vs. interdisciplinary team = US$12,001). Team factors contributing to these improvements were listed as team composition, team tenure, regular team meetings, task allocation, cohesiveness and open communication.
A study by Dixon et al. 87 assessed the relationship between skill mix, patient outcomes, length of stay and service costs in IC services in England, working primarily with older people. A multivariate analysis was conducted which analysed data from between 337 and 443 older people admitted to 14 IC teams. Independent variables included the numbers of different types of staff within a team and the ratio of support staff to professionally qualified staff within teams. Outcome measures included the Barthel index, EQ-5D score, length of service provision and costs of care. Increased skill mix (raising the number of different types of staff by one) was associated with a 17% reduction in service costs (p = 0.011). Weak evidence was found that that a higher ratio of support staff to qualified staff leads to greater improvements in EQ-5D scores of patients (p = 0.090).
Key point 43: increased skill mix (increasing the number of different disciplines in the team by one) in IC teams was associated with a 17% reduction in service costs. A higher ratio of support staff to qualified staff may be associated with greater improvements in EQ-5D scores.
Regen et al. 60 conducted a series of qualitative case studies, by interview (n = 61) and focus group (n = 21), to assess the ‘challenges, benefits and weaknesses’ of IC. The perceived benefits to patients of IC included flexibility, patient centeredness, promotion of independence, with the ‘home-like’ environment in which care was received being perceived as favourable to hospital care. At a structural level, workforce and funding shortages, poor collaboration between health and social care agencies and lack of support/involvement from clinicians were perceived as challenges. Weaknesses to services were perceived as insufficient capacity and problems of access and awareness between mainstream care and IC services. The conclusions were that IC might not be achieving its full potential to benefit services users because of these weaknesses and challenges. Service user benefits were not directly attributed to team-level factors in the study, other than the fact that all of the services operated as interdisciplinary teams. In fact, the staff identified interdisciplinary teamworking and the opportunities for role flexibility in terms of the benefits for themselves, rather than to patients.
Key point 44: perceived benefits of IC for patients were found to include flexibility, patient centeredness, promotion of independence and a ‘home-like’ environment.
Bird et al. 88 trialled the use of ‘integrated care facilitators’ for patients with COPD and CHF. The study was a collaboration between acute and community-based services to reduce hospital (re)admissions and improve health outcomes in patients who frequently presented to hospitals. The care model was designed by a multidisciplinary care team. It involved the co-ordination of care between different disciplines and agencies by the facilitator. Health facilitators undertook a comprehensive assessment of needs using established disease-specific assessment tools. The assessment results were discussed at a case conference and an individual care plan was developed from these discussions. The facilitator then provided information, education and advice to the patient and facilitated the patient’s access to the services they required, including making appointments and ensuring the care was delivered in a way appropriate for the client. For patients in the COPD intervention arm emergency readmissions presentations reduced by 10%, whereas for patients in the control arm they increased by 45%. For the CHF arm, emergency readmissions presentations reduced by 39%, compared with a reduction of 26% in the control group. Admissions were reduced by 25% (control +41%) in the COPD arm and 36% for CHF (control –20%). Length of stay decreased by 18% (control +51%) in the COPD arm and 36% (control +15%) in the CHD arm. Mortality for both intervention arms combined was 18% at 365 days compared with 36% in the non-intervention arms. Although care was delivered by a multidisciplinary team in community settings and co-ordinated by a single care facilitator, no team-level factors were tested in the trial.
Key point 45: the use of ‘integrated care facilitators’ to improve co-ordination of care reduced emergency readmission presentations by 10% (COPD) and 39% (CHF), admissions by 25% (COPD) and 36% (CHF) and length of stay by 18% (COPD) and 36% (CHF). Mortality at 365 days was 18% (COPD and CHF combined) compared with 36% in the control arm.
Burton et al. 89 examined the organisational features staff felt were important for the delivery of high-quality care. Although the paper was written from a nursing perspective, members of multidisciplinary stroke rehabilitation teams (in acute care settings) were interviewed. The following factors were identified as important. Teamworking was recognised as very important for effective care and rehabilitation, multidisciplinary rounds were identified as an important structure that supported teamworking, supervision and personal development reviews were identified as important to ensure continuous improvement and development and education and training was stated as being required for staff to access relevant training opportunities. Leadership is needed both internally and externally, a holistic approach to care in which staff get to know patients and understand family and social relationships is important, communication via multidisciplinary notes and bedside notices can be effective ways of ensuring all staff understand the therapy regime/plan; however, some professions also had their own notes. Informal communication was recognised as extremely important and strong interpersonal relationships were vital to ensure effective communication. Several factors were identified that appeared to act against effective interdisciplinary teamworking, these included rotation of staff, location of staff and risk aversion.
Key point 46: delivery of stroke rehabilitation using an interprofessional team approach was perceived to contribute to better care for patients. Contributing team-level factors included teamworking, multidisciplinary rounds, supervision and personal development reviews, education and training, leadership, a holistic approach to care, communication and strong interpersonal relationships. Rotation, colocation of team members and risk aversion of nursing staff were identified as potential confounding factors.
Very few papers have been published within the past 4 years that discuss the impact of team-level factors on patient outcomes in IC teams. Four papers were found that were directly relevant to IC. 58,84–86 Although these papers are consistent in their focus on interdisciplinary teams generally, none of them directly addresses the team-level factors specifically mentioned in the research question (i.e. team size, grade mix, team organisation and context). However, they do highlight other variables that are associated with better outcomes. These variables tend to be more oriented to work processes rather than team structure. There is generally not much overlap in the findings of the papers, although collectively they do reflect the wider body of literature on interdisciplinary teamworking in health and social care settings generally, as well as IC services in particular.
The study by Dixon et al. 87 does identify increased skill mix within teams as related to reduced service costs and finds weak evidence that a higher proportion of rehabilitation support workers is related to higher QoL for patients. Regular formal interdisciplinary team meetings and case conferences are mentioned as important,86 whereas the paper by Regen et al. 60 discusses multidisciplinary rounds as important. Effective communication is cited as very important by two papers and all other papers refer to formal communication mechanisms such as multidisciplinary, meetings, notes and rounds. The paper by Blewett et al. 86 mentions team tenure as an important factor in effective interdisciplinary teams. In keeping with this, the paper by Burton et al. 89 suggests that regular rotation of staff can inhibit effective interdisciplinary teams.
Secondary analysis of data
In keeping with the question aims, the available data set and the findings of the literature review, the relationships between a number of structural team-level variables and patient outcomes, hypothesised as potentially significant, were tested.
Method of analysis
The combined data set allowed investigation of the team characteristics listed in Table 14. The evaluation was undertaken as a two-stage analysis. In stage 1, the patient outcomes in each team were analysed using generalised least squares random-effects regression. The patient covariates assessed were the patient age, sex, LoC at admission, living arrangements prior to entering IC, living arrangements during IC and the profession or service referring into IC. The second stage of the analysis was to calculate, within each team, the residual effect (the observed mean change minus the expected mean change, as calculated by the stage 1 regression model) together with its standard error. These team-level means are therefore adjusted for differential case mix in respect to the model covariates. Finally, a weighted regression analysis was performed by regressing the mean residual change on the team characteristics, using a restricted maximum likelihood model in which weights are the inverse of the squared standard error, to establish whether or not the team’s average response (standardised for case mix) was associated with the team-level characteristics.
| Predictor variables (team level) | Outcome variables (patient level) |
|---|---|
| Number of different services referring in | Change in TOM impairment |
| Total number of staff in team | Change in TOM well-being |
| Total number of staff types in team (skill mix) | Change in TOM activity |
| Estimated number of patients per year | Change in TOM participation |
| Estimated number of patient-months per member of staff (case load)a | Change in EQ-5D |
| Number of clinical staff in team | Length of stay |
| Number of clinical support staff in team | |
| Number of management staff in team | |
| Number of social care staff in team | |
| Number of non-clinical support staff in team | |
| Number of domiciliary support staff in team | |
| % skilled workers in teamb | |
| Number of team leaders |
As described previously, a substantial number of missing data were encountered in the TOM and EQ-5D patient questionnaires. A multiple imputation approach was used to address the impact of this (see Appendix 2). In summary, two analyses were undertaken: a complete case data only (ignoring missing data) and an analysis incorporating imputations. The results of both are reported. All analyses were undertaken using version 12.1 of the Stata statistical package.
The evaluation of team characteristics in relation to duration of IC was undertaken in using the same two-stage analysis approach as used for questions in objective 1. As missing data were uncommon for this outcome, no imputation-based analyses were used.
The first stage was to derive mean durations adjusted for case mix (age, sex, LoC, referral route and place receiving IC), using the model described previously. The second stage of the analysis was to calculate, within each team, the residual effect (the observed mean change minus the expected mean change, based on the regression model) together with its standard error. Finally, a weighted regression analysis was performed by regressing the mean residual change on the team characteristics, using a restricted maximum likelihood model in which weights are the inverse of the squared standard error. The findings are reported in Results and full details of the results can be seen in Appendices 3–5.
Results
Skill mix
The full results of the analysis can be seen in Figure 10. Overall, the analysis of the combined data set found few significant relationships. The results do suggest that TOM impairment improves more among teams that have a higher skill mix (i.e. larger number of different disciplines), with TOM impairment change scores increasing by 0.029 units with each additional discipline represented in the team. This relationship is represented in the scatterplot in which the size of the circle represents the magnitude of the teams’ weight in the analysis.
FIGURE 10.
Scatterplot showing the relationship between skill mix and change in TOM impairment. Circles represent the individual teams, with the size of the circle representing the magnitude of the teams’ weight in the analysis.

Ratio of support staff to professionals
It was found that having more domiciliary or clinical support staff in teams was associated with a small improvement in TOM impairment scores. For every unit increase in clinical support staff, TOM impairment scores increased by approximately 0.01 units; this increase was consistent whether or not the complete case data set or a data set with imputed data was used. There was also a similar relationship between TOM impairment and number of domiciliary support workers but, unlike the other findings, this was heavily influenced by the data from one team. The largest standardised mean TOM impairment change (0.6 units greater than predicted by its case mix) was observed in the team with the highest number of domiciliary staff but, although interesting, removing this data point from the analysis resulted in a substantially reduced (and non-significant) relationship. The relationships are shown in the scatterplots Figures 11 and 12.
FIGURE 11.
Scatterplot showing the relationship between numbers of clinical support workers and change in TOM impairment. Circles represent the individual teams, with the size of the circle representing the magnitude of the teams’ weight in the analysis.
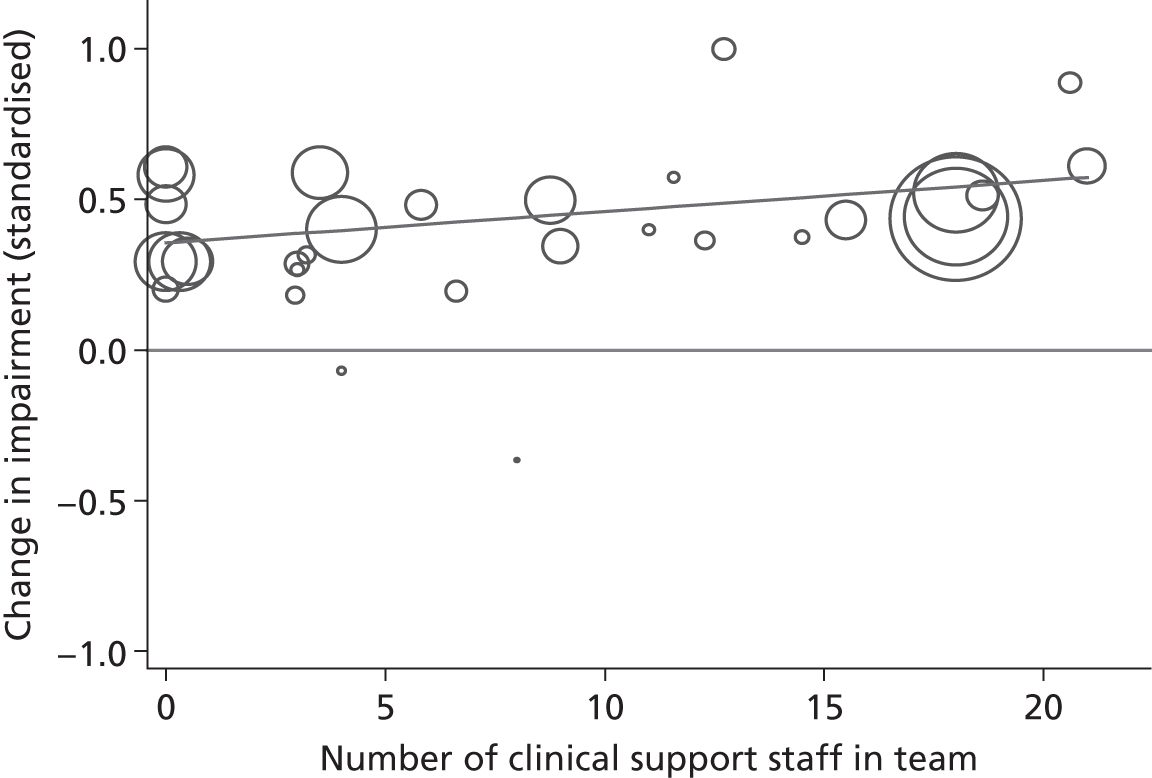
FIGURE 12.
Scatterplot showing the relationship between numbers of domiciliary support workers and change in TOM impairment. Circles represent the individual teams, with the size of the circle representing the magnitude of the teams’ weight in the analysis.
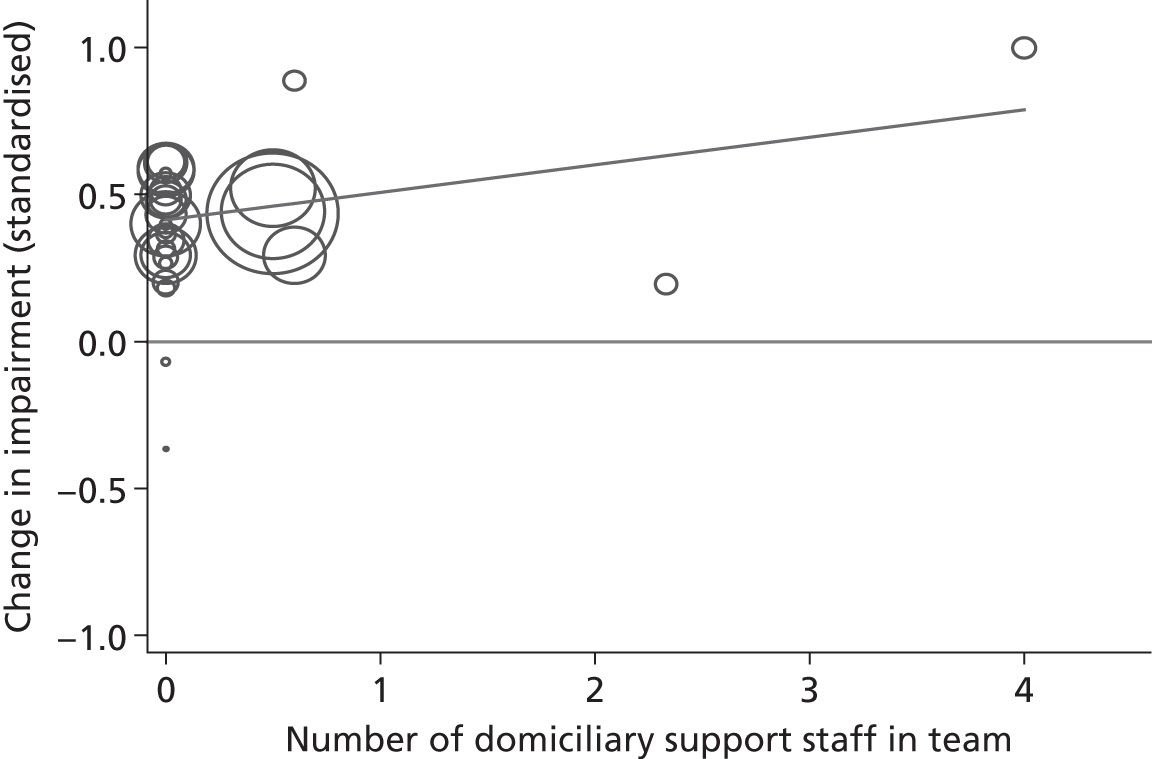
Key point 47: there is consistent evidence that more clinical support staff in teams were associated with a small improvement in TOM impairment scores. Similar results were found for domiciliary staff. However, this latter finding was heavily influenced by data from one team.
Discussion
A literature review was undertaken examining papers published between 2008 and 2012. Only five papers were found to be relevant to the question ‘what team-level factors are associated with the greatest benefits for patients in terms of health status?’. The results of the review showed that there was some empirical evidence that interdisciplinary teamworking in IC with older patients was more effective than usual care in reducing length of stay and costs. 86 Using integrated care facilitators to improve co-ordination between interdisciplinary team members proved effective with COPD and CHF patients in reducing emergency readmissions presentations, admissions and length of stay. 88 However, these studies do not directly examine team-level factors associated with better outcomes.
The study by Dixon et al. 87 did find that increased skill mix was significantly associated with a 17% reduction in service costs and a high proportion of support workers were associated with better improvement in patient QoL.
Qualitative studies in the review found indicative evidence that a number of team process variables contribute to better patient care. However, the variables identified were not within the scope of this study.
The results of the statistical analysis of this combined data set found some weak empirical evidence to support the findings of the above empirical study. Increased skill mix and higher proportions of clinical and domiciliary support workers in CRAIC/S teams were significantly associated with improvements in impairment scores using the TOM tool. However, it must be noted that the study by Dixon et al. 87 utilised one of the two original data sets which form the combined data set for this study. 1 In addition, owing to the number of hypothesis tests undertaken, there is a high possibility of at least one of the findings being a spurious association.
Key point 48: increased skill mix and higher proportions of clinical and domiciliary support workers in IC teams were significantly associated with improvements in impairment scores using the TOM tool. Given the number of hypothesis tests undertaken one cannot be confident that this result is anything more than a spurious association.
Conclusion
The literature review and secondary analysis of this combined data set does provide additional evidence that interdisciplinary teamworking in IC may be associated with better outcomes for patients. However, relatively few significant results were found overall and a relatively wide number of variables were analysed. Therefore, we urge that caution is taken when considering these results.
Key point 49: this study provides additional evidence that interdisciplinary teamworking in IC may be associated with better outcomes for patients, but care should be taken with overinterpretation.
Chapter 6 What is the cost-effectiveness of different models of care?
Introduction
Owing to limited resources, it is important that health care is provided in the most efficient way possible so that the health produced by those services that are provided is maximised. The standard framework by which this is investigated is cost-effectiveness analysis. This examines the costs and effects of different ways of treating patients and summarises this in an incremental cost-effectiveness ratio.
Earlier in the report, we described teams that have been involved in the two studies. Only two were integrated health and social care teams and the others had a broad range of different professional and support staff. The analysis here is restricted to examining the configurations of the teams involved, which may not represent all the different models of IC available.
Different skill mixes across IC teams can potentially have an effect on patient outcomes and costs. Therefore, for example, a greater number of professions and a greater number of professionally qualified staff could improve care by allowing a fuller range of therapies and support to be provided, but it could increase costs because of higher salaries and a greater number of visits.
Background
The simplest approach to cost-effectiveness analysis compares two randomised groups and then calculates the additional costs and additional benefits associated with the most effective treatment for each group. However, this is not possible here as different services have different patient groups. Controlling for these differences, in the presence of patient clustering and cluster-level costs, makes assessment of cost-effectiveness problematic. The analysis plan for this study starts with simple descriptive analysis, then adds in multivariate analyses of costs then ends with an exploratory analysis of cost-effectiveness. Specifically, we sought to produce:
-
descriptive analysis of mean resource use, costs and quality-adjusted life-years (QALYs) per patient for each team
-
multivariate analyses examining the relationship between skills mix and patient-level costs
-
mean costs and QALYs gained will be plotted for each team on the cost-effectiveness plane to highlight which teams are the most cost-effective
-
multivariate analysis examining the relationship between skills mix and team cost-effectiveness.
Literature review
The COOP study1 identified several important relationships between team characteristics and costs. Using a sample of 1167 patients, it was shown that the average cost per patient increased as the number of different practitioners increased, but fell with a rise in the proportion of qualified staff. Strong relationships were also identified relating to teamworking as measured by the Workforce Dynamics Questionnaire. Exploratory analyses showed no relationship between cost-effectiveness and skills mix variables across the 20 teams studied. However, another study of 403 patients produced different findings, which indicated the opposite effect with respect to the number of different practitioners and no effect relating to qualified staff. 1 No assessment of cost-effectiveness was undertaken in the latter study.
Key point 50: the COOP study1 showed that the average cost per patient increased as the number of different practitioners involved in their care increased but, counterintuitively, fell with a rise in the proportion of qualified staff.
The EEICC study2 did not include a formal evaluation of cost-effectiveness but did collect some of the same data as COOP. 1 Combining these two data sets is therefore possible and, with the greater number of patient observations and IC teams, it could give us a clearer picture of the relationship between team characteristics, costs and cost-effectiveness.
Secondary analysis of data
Our analysis undertaken within COOP1 and the subsequent study (EEICC)2 had different objectives and collected different sets of data. For example, within COOP1 we collected patient-level data on number and length of all patient contacts broken down by staff professional group. As such, we were able to estimate detailed costs for each patient and explain how these varied by patient and team characteristics. These data were not collected for EEICC,2 which looked more broadly at how overall cost changed with the implementation of an interprofessional management tool. 90 Consequently, the COOP1 analysis cannot be directly replicated using data from both studies. The analysis is necessarily restricted to data that were collected in both studies using the same methods.
Resource use and costs
Duration of care data were collected for each patient observed within both studies. The overall staff cost of the service was estimated using reported staffing levels multiplied by unit costs developed from Agenda for Changes scales uprated to include on-costs. 91 This was then divided by the annualised total number of patient days recorded in the study periods within each service to calculate a cost per day, then attributed to individual patients based on their individual duration of care within the service.
Outcomes
The EQ-5D was completed at initial assessment and discharge. EQ-5D scores (utilities) were then calculated using the UK tariff based on time-trade-off values. Baseline and discharge utilities were then combined with the length of time between initial assessment and discharge (assuming any change was linear) in order to produce QALYs as well as QALY change relative to baseline.
Cost-effectiveness
Two summary measures of cost-effectiveness were calculated for each team: the average cost-effectiveness ratio and the average net monetary benefit (NMB). The average cost-effectiveness ratio is calculated as the average cost per patient divided by the average QALY gain per patient. The NMB is calculated as the monetary value of health gain produced by the service minus the cost of the service. The monetary value per patient is calculated as the mean QALY gain per patient multiplied by £20,000. The NMB is preferred for explanatory analyses because of the problems with the measurement properties of ratios (i.e. the generation of extremely high ratio values in the presence of small values in the denominator).
It is important to note that the ratios and NMBs reported are not those typically reported in economic evaluations, which are based on incremental values. Incremental values require a counterfactual – what would have happened if an alternative service were provided? – which is not available in an observational study. With incremental figures, we can assess whether or not a particular service is cost-effective (i.e. benefits exceed costs) and those factors that influence cost-effectiveness. With the average figures produced in this study, we can only assess the factors that influence relative cost-effectiveness, we cannot assess whether or not a particular service is cost-effective in absolute terms. For example, using incremental costs and effects, a negative NMB implies that the increase in benefits for a particular service is exceeded by the increase in costs for the service (i.e. it is not cost-effective). In the study here, negative NMBs do not suggest this as we do not know the costs and health effects of alternative courses of action.
Key point 51: the analysis undertaken was to investigate the value of health gain compared with the cost of the service. This cannot demonstrate absolute cost-effectiveness, but allows for comparisons between teams.
Analysis
The initial analysis is descriptive in nature. Mean resource use, costs and QALYs per patient are reported for each team. No hypothesis testing was undertaken for these analyses. Following this, cost functions were estimated to examine the relationship between individual patient costs and skills mix. The dependent variable in these multivariate analyses (cost) will be log-transformed as the data are heavily skewed.
Within these multivariate analyses, skill mix is characterised in terms of the proportion of staff who have a professional qualification and the number of different professions involved in the care of patients. These two explanatory variables attempt to capture notions of substitution and specialisation. These variables are only available at the service level, for example proportion of qualified staff across the service.
Although the preceding analysis examines only costs, cost-effectiveness involves the simultaneous examination of costs and outcomes. A separate set of analyses had been undertaken to look at this issue. Firstly, mean costs and QALYs gained will be plotted for each team on the cost-effectiveness plane to highlight which teams are the most cost-effective. Secondly, a multivariate analysis of cost-effectiveness will be undertaken. The dependent variable will be the NMB of each service, which was described earlier. These analyses should be considered exploratory as they are based on only 33 observations (representing each of the teams) and, therefore, have limited power to identify any relationships. As such, simpler regression models are used which omit several of the explanatory variables used in the patient-level analyses.
Two sets of analyses were undertaken, based on complete cases (i.e. excluding cases with missing data) and an imputed data set (i.e. when missing data are estimated) (see Appendix 2). For the patient-based regression analyses, the team characteristics are incorporated within the multivariate analysis using a random-effects model in Stata.
Results
The teams show a wide variation in average duration of care (ranging from 1 to 138 days) and average cost per patient (ranging from £318 to £11,511) as shown in Table 15. All teams saw, on average, an increase in the health of their patients as shown by positive QALY gains.
| Team | Duration of care (mean days) | Mean cost per patient (£) | QALYs gained | Average cost-effectiveness ratio (£/QALY gained) | Mean NMB (£) |
|---|---|---|---|---|---|
| COOP study | |||||
| A | 18 | 1411 | 0.009 | 152,837 | –1226.63 |
| B | 60 | 2114 | 0.016 | 131,939 | –1793.39 |
| C | 138 | 5411 | 0.019 | 290,385 | –5038.29 |
| D | 41 | 482 | 0.018 | 27,048 | –125.51 |
| E | 41 | 482 | 0.018 | 27,048 | –125.51 |
| F | 32 | 5465 | 0.029 | 185,869 | –4877.06 |
| G | 30 | 1562 | 0.020 | 79,365 | –1168.58 |
| J | 1 | 318 | 0.000 | 2,900,372 | –316.26 |
| L | 45 | 3329 | 0.012 | 280,428 | –3091.41 |
| M | 38 | 610 | 0.018 | 33,077 | –241.25 |
| N | 10 | 860 | 0.004 | 208,212 | –777.33 |
| PA | 84 | 6325 | 0.015 | 421,271 | –6024.89 |
| PB | 28 | 9236 | 0.020 | 470,347 | –8843.29 |
| Q | 47 | 4142 | 0.012 | 355,707 | –3909.14 |
| SA | 60 | 3037 | 0.029 | 104,693 | –2456.72 |
| SB | 21 | 3174 | 0.015 | 214,828 | –2878.28 |
| SG | 64 | 3551 | 0.001 | 4,403,761 | –3535.07 |
| T | 22 | 2957 | 0.019 | 158,736 | –2584.26 |
| TA | 33 | 802 | 0.016 | 49,310 | –476.49 |
| U | 9 | 1065 | 0.007 | 163,412 | –934.76 |
| EEICC study | |||||
| B | 27 | 2600 | 0.016 | 159,386 | –2274.09 |
| D | 40 | 1014 | 0.021 | 48,017 | –591.54 |
| DO | 116 | 3069 | 0.044 | 69,456 | –2185.36 |
| E | 43 | 1261 | 0.022 | 56,468 | –814.22 |
| F | 37 | 2273 | 0.029 | 77,657 | –1687.35 |
| G | 41 | 860 | 0.016 | 53528 | –538.80 |
| H | 41 | 860 | 0.016 | 53,528 | –538.80 |
| I | 41 | 860 | 0.016 | 53,528 | –538.80 |
| PB | 36 | 11,511 | 0.039 | 296,529 | –10,734.66 |
| Q | 45 | 3176 | 0.015 | 208,088 | –2870.57 |
| R | 22 | 2360 | 0.015 | 153,168 | –2051.69 |
| U | 25 | 2060 | 0.015 | 138,614 | –1763.20 |
When patient-level costs are examined, clear relationships are seen with respect to HRQoL (as measured by the EQ-5D), impairment and activity (both as measured by the TOM) (Table 16). The nature of the relationship is the same for all three variables, i.e. costs initially increase with improving health (or reduced impairment) and then fall for higher levels of health improvement. Considering the staffing variables, there is only good evidence to suggest that increased numbers of different types of practitioners are associated with higher costs.
| Independent variable | Dependent variable ln (cost) parameter | Geometric means estimate |
|---|---|---|
| Sex (female) | 0.090a | 1.094 |
| Age (years) | 0.017 | 1.017 |
| Age squared | –0.000a | 1.000 |
| Baseline EQ-5D | 0.357b | 1.429 |
| Baseline EQ-5D squared | –0.716c | 0.489 |
| TOM impairment score | 0.293a | 1.340 |
| TOM impairment score squared | –0.067b | 0.935 |
| TOM activity score | 0.489c | 1.630 |
| TOM activity score squared | –0.088c | 0.916 |
| TOM participation score | 0.208 | 1.231 |
| TOM participation score squared | –0.034a | 0.966 |
| TOM well-being score | –0.033 | 0.967 |
| TOM well-being score squared | 0.004 | 1.004 |
| Number of practitionersd | 1.341a | 3.822 |
| Number of practitioners squared | –0.065 | 0.938 |
| Proportion skillede | –0.259 | 0.772 |
| Proportion skilled squared | 0.228 | 1.255 |
| Annualised total number of patient days within each team | 0.000 | 1.000 |
| Annualised total number of patient days within each team squared | 0.000 | 1.000 |
| Constant | –2.433 | 0.088 |
Key point 52: costs initially increase with improving health (or reducing impairment), then fall for higher levels of health improvement (or impairment). Increased numbers of different types of practitioners are associated with higher costs.
An examination of Figure 13 shows a massive variability in costs and outcomes. The three services depicted by the points joined by the kinked line are relatively more efficient than the others are. Points vertically above the three points defining this efficiency frontier are services that have higher costs for the same outcomes. The frontier represents combinations of the efficient services and, therefore, in theory, all services above the frontier are generating higher costs for patient outcomes than could be produced by the efficient services.
FIGURE 13.
Cost-effectiveness of the different teams. Note: data points represent mean cost and mean QALY gain for each of the teams. The slope of an imaginary line drawn from the origin to the data point equates to cost divided by QALY gain and represents the average cost-effectiveness ratio. The three teams linked by the two lines are relatively more cost-effective than the others.
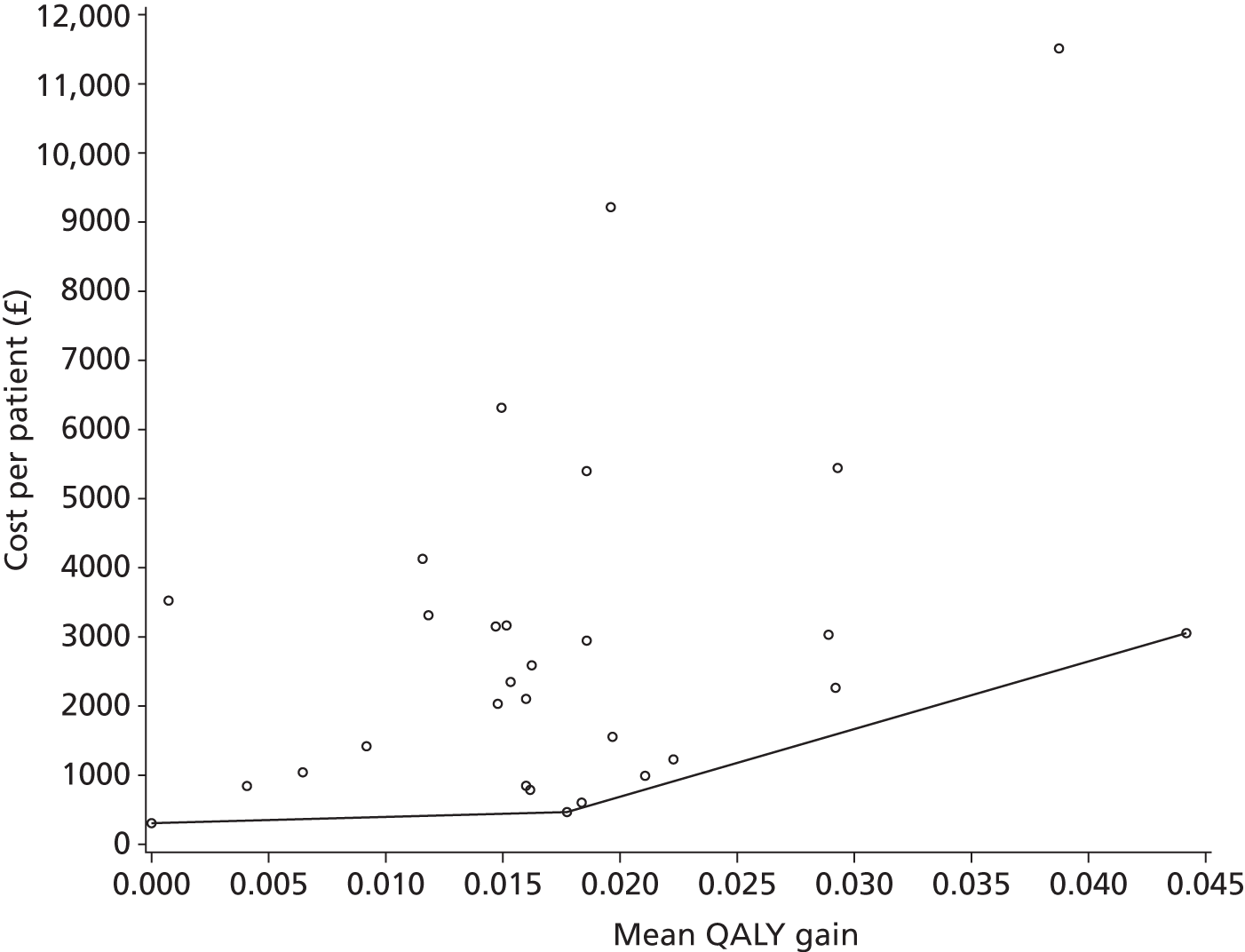
Key point 53: there is substantial variability in costs and outcomes between the IC teams being studied.
An explanation of this variability in statistical terms was undertaken using the multivariate analysis on average NMB, with the results shown in Table 17. These results show no clear explanatory effect of different staffing patterns (i.e. number of practitioners and proportion of skilled staff). However, there is weak evidence of economies of scale, with larger services (proxied by annualised patient days) generating a higher NMB.
| Independent variable | Dependent variable | |
|---|---|---|
| NMB parameter | p-value | |
| Age (mean age) | 173.83 | 0.1500 |
| Baseline EQ-5D | 3947.84 | 0.5080 |
| Number of practitionersa | –107.79 | 0.3782 |
| Proportion skilledb | 1281.54 | 0.5625 |
| Annualised total number of patient days within each team | 0.025 | 0.0505 |
| Constant | –18172 | 0.0904 |
Key point 54: there is no clear effect of different staffing patterns (i.e. number of practitioners and proportion of skilled staff) on NMB. There is weak evidence that larger services generate a higher NMB.
Discussion
The results indicate highly heterogeneous services. Costs per patient range from £318 to £11,511, with patient characteristics being the dominant explanatory effects. Cost-effectiveness is also highly variable with only size of service showing any sign of an explanatory effect. Staffing patterns as described by the proportion of qualified staff and number of different types of staff have little or no influence on costs and relative cost-effectiveness.
These results add to a growing body of literature that show highly variable costs, outcomes and inconsistent relationships relating to staffing patterns. 1,87 The massive heterogeneity of services is likely to have an impact on our ability to identify any relationships that exist. Indeed, the variability may also suggest that comparisons between all the services is not sensible and they appear to differ in terms of their purpose. A service with an average duration of care of 1 day cannot be designed to deliver the same care packages as a service with an average duration of care of 138 days. A further qualitative assessment of the different types of teams may be helpful to identify more useful comparisons; however, with only 33 teams, subdividing the sample will make any statistical exploration of differences problematic.
Key point 55: the purposes and composition of IC teams vary substantially and thus it may not be sensible to compare costs indiscriminately between all services. Costs per patient showed great variation and cost-effectiveness was highly variable, with the size of service being the only sign of explanatory effect.
Critique of the methods
There are limitations to the analysis and the comparison with the previous studies. The costs in the COOP1 and this study are based on staff costs only; full budget information was not available for around half of the services. It is possible that non-staff costs vary between services but these variations should not be expected to be related to staffing patterns.
This study did not have patient-level staffing data but, instead, the total staff costs were allocated to patients based on duration of care episode. This inconsistency could lead to different conclusions but this would only relate to patient-level costings; the team-level costings were generated in broadly similar ways. The team-level results are very similar between COOP1 and this study.
The calculation of QALY gains and, hence, monetary benefit assumes a linear change in health between the start and end of the care spell. Both the linear change and the implicit assumption of no health effects beyond discharge are open to question. However, in the absence of good evidence, we feel that further analyses based on alternative assumptions relating to the rate and duration of health changes would be highly speculative. This does, however, add further uncertainties to the results and the conclusions we are capable of making.
One final data problem present in both the EEICC2 and COOP1 study is the potential for missing data. As demonstrated in Chapter 7, there are discrepancies between the estimated throughput of the individual services and the throughput implied by their data returns for our research. These differences suggest either under-reporting within the study or overestimates of patient numbers. These differences could potentially explain some of the large variability in mean cost per patient (which requires an estimate of patient numbers), as seen in Table 1 and Figure 1.
Conclusion
This study represents the most comprehensive attempt to explain differences in costs and cost-effectiveness across different IC teams. This work, in tandem with other comparable studies, is unable to identify consistent and clear relationships relating to staffing. This suggests that efficiency savings are possible by many services by reducing staff costs to levels seen in comparable teams. However, the identification of comparable teams may be problematic, as there appear to be quite profound differences between them that are not readily explained quantitatively.
Key point 56: further studies of cost-effectiveness of IC services should consider mixed-methods approaches, as the identification of comparable teams might be problematic using quantitative methods alone. We suggest efficiency savings may be possible.
Objective 3 To explore the differences between intermediate care service configurations and how they have changed over time
Chapter 7 How have intermediate care services changed over time?
Introduction
There are two interrelated reasons why it is important to explore how IC services have changed over time. First, IC services are widely assumed to be flexible regarding the services they provide and how these are delivered as they need to respond to changes in national policy and to fit with local variations in health-care provision.
At a national level, they have been widely implemented as a mechanism to deal with policy changes, such as emergency care reform. 92,93 At a local level, IC entry thresholds are inconsistent and any entry guidance that does exist is locally determined. IC services often receive patients on the basis that there is ‘nowhere else for them to go’, rather than because they demonstrate a real potential for improvement in the IC setting. 1 IC is, therefore, uniquely sensitive to changes in the health-care system as a whole. Qualitative data arising from projects 1 and 2 found that IC teams perceive that they are under growing pressure to help meet hospital targets regarding lengths of stay and waiting times, by accepting patients with increasingly complex needs.
Second, service- and team-level characteristics have been associated with patient outcomes. Indeed, one national evaluation of IC found that service characteristics were a better predictor of service costs and patient outcomes than patient characteristics. 10 Therefore, in order to provide appropriate care it would be expected for services to change in line with the changing demands placed on them.
Background
There has been rapid growth in the use of support workers, rather than qualified practitioners, to deliver much of the care within IC. 94 Project 1 found that the level of patient impairment and patient needs were unrelated to skill mix. 1 Evidence is urgently needed to ensure that hospital avoidance schemes such as IC benefit the patient and that IC facilities have the appropriate skill mix to address the increasingly complex needs of the patients they take on. However, there has been little research to date to inform decisions regarding what constitutes appropriate staffing in IC in terms of staff type, skill mix and intensity. In the context of ongoing changes to case mix and workforce, commissioners and managers have a distinct lack of evidence to support decision-making regarding staffing of, or referrals to, IC.
The investigation of staff type and skill mix changes in IC services over time may demonstrate whether there are trends across the data set regarding a direction of development of these services, or whether local considerations continue to determine changes in the sector leading to increasing heterogeneity.
Literature review
Literature searches for this chapter (see Appendix 1) were undertaken on MEDLINE (via EBSCOhost) and Cumulative Index to Nursing and Allied Health Literature (CINAHL; via EBSCOhost) between December 2011 and June 2012. Articles were included as an update for an earlier set of extensive literature searches (COOP1 and EEICC2). The search used terms relating to IC and then facets relating to service models, for example, skill mix or management structures. These searches identified 2176 papers of potential interest.
These papers were explored to establish their relevance to the study. The main inclusion criteria were that they provided either empirical evidence or commentary on any of the following themes:
-
drivers for change in English community care
-
organisational and interorganisational models of community care in the UK
-
workforce planning and team configurations for community care in the UK
-
the effect of team configurations on patient outcomes for community care or rehabilitation in the UK.
Papers were excluded in cases in which findings were not transferable to the English health-care setting or if they were concerned with aspects of service configuration which were not recorded in the data for this study (for instance, methods of case management, non-mandatory training or details of leadership and supervision).
After titles were examined, 294 papers remained. The abstracts were read and further papers were eliminated, leaving 18 papers of possible interest. After examination of full copies, four further papers were excluded. These were concerned with models and methods for workforce planning, indicators of interorganisational integration, a qualitative study of stepped care and prevalence of mental health problems in IC patients. The remaining 14 papers were then reviewed in depth and a main aim of the review was to explore the range of evidence. Therefore, although the quality of studies was taken into consideration, papers were not excluded on the grounds of quality.
No papers directly addressed the issues raised by the study question (i.e. changes in IC service configuration over time). A main theme in the literature, with limited importance for this study, was models of services at a macro level including aims of the service, place of treatment or description of type of service (e.g. supported discharge or admission prevention, geriatric day hospital, community hospitals, NLUs, HAH, home-based rehabilitation). These papers rarely described the make up of such services, although it is recognised that staffing requirements for the specific aims of services (e.g. facilitated discharge and admission avoidance) should be distinct. 95 Papers describing drivers for change provide useful background information, as do snapshot descriptions of IC service configurations (including the relationship of configurations with patient outcomes).
Key point 57: no literature was found that directly addressed the issue of how IC services have changed over time.
Defining and organising intermediate care
Although some literature has a focus on configuration issues such as skill mix, size, team organisation, internal roles and responsibilities,1,87,94,96 much of the existing literature concentrates on defining IC in terms of the broader health-care economy. This work seeks to describe service models, criteria, objectives and the relationship of IC with other types of health care and different organisations. 97,98
However, there is a shortage of national outlines of the sorts of IC services that make it ‘difficult to ascertain representativeness, and thus, the extent to which . . . findings can be generalised to other intermediate care services’. 99
Other literature concentrates on methods of service delivery such as integrated case management (as promoted in recent Best Practice Guidance, ‘Delivering Care Closer to Home’). 100 An integrated case management approach might be beneficial to patients101,102 and reduce costs. 103 However, potential benefits are likely to be contingent on, for instance, the context, leadership, management and previous methods of service delivery (e.g. Anelay et al. , 2002). 104 For instance, Anelay et al. 104 state that there is evidence to suggest that staff appraisal has an effect on patient mortality rates. These are very complex service-development interventions, with many possible confounding factors, and compared with more straightforward structural changes, these are difficult to define and replicate.
Key point 58: intermediate care services and services to support/rehabilitate the elderly aiming to reduce admissions and facilitate early discharge have been developed in many and various ways across the country making it difficult to compare costs and outcomes.
Services for long-term or short-term treatment
The literature clearly draws a distinction between services providing chronic care and the shorter-term services usually associated with IC (e.g. Proudfoot et al. ). 105 However, in clinical practice, these divisions are often not maintained. This is most likely as a result of IC filling the gaps when there are no alternative services available to address patients’ needs (e.g. Martin et al. ). 106 There are ‘anecdotal reports of intermediate care becoming a “dumping ground” when other services lack the capacity to cope, even though the patients may not meet the strict definitions of intermediate care’. 95 Indeed, in the service pro forma returned by one of the teams participating in both studies, under ‘duration of care’ it was stated that, despite the service specification being for 6–8 weeks, the maximum stay was 194 days. This was reported to be due to having no suitable services to take over for patients with long-term conditions.
Key point 59: admission criteria and discharge arrangements are dependent on availability of other local services.
Qualitative evidence from project 2 supports this view, demonstrating a widespread lack of understanding at a practitioner level of the values that might define the services in which they worked. This was reflected in a lack of consistent entry requirements for patients and confusion around the vision and values of the service.
Key point 60: there is little evidence of commonly agreed vision and purpose for IC services.
Integrating intermediate care with other services
It is notable that service development work aimed at integrating older peoples’ services and improving interprofessional working has focused on integrating community and local authority services and excluded general practice. 98 The difficult relationship between general practice and IC (e.g. Young107 and Wilson and Parker108), has been described as a problem with communication and trust. 109 However, this perhaps highlights a broader issue in the NHS regarding the primacy of issues of responsibility and ownership rather than collaboration, co-operation and integration. 110 This view is supported by Weinberg et al. 111 who concluded that collaborative capacity is somewhat constrained by a rigid hierarchy of health-care occupations and division of labour.
Key point 61: intermediate care has variably been integrated with other services and these relationships are generally unstable.
The issue of conflict over the control of community health services was demonstrated by two services taking part in project 2. On completion of our work with the service [coinciding with the dissolution of the primary care trust (PCT) and initiation of a Clinical Commissioning Group], the service was disbanded and staff members were reassigned to work under the supervision of various district nurses based at general practices across the region. In other areas, IC services have moved to acute trusts. The permanence of these measures is yet to be discovered; however, the various local arrangements put in place to manage this transition have contributed to further heterogeneity of IC services and changing relationships in local health economies.
The effect of policy on intermediate care configurations
Few studies have explored the configuration of IC services and literature reviewed for this study failed to identify any explorations of changes over time. This is despite a range of policy initiatives and Department of Health guidance intended to influence the development of such services, particularly since the NHS plan of 2000. 4 It is notable that a qualitative study of the association between policy directives and community health service provision identified a gap between the rhetoric driving workforce change and the ‘reality of implementing change’. 112
Intermediate care services have not directly been defined by policy implementation. Rather than there being a single model of IC, IC policy has been variously applied and interpreted, depending on the local needs (Barton et al. 10 cited in McClimens et al. ). 113
Although ‘intermediate care has seen the rapid and, in some cases, engineered introduction of new roles, particularly “support worker” roles’,99 it is likely that the lack of incentives directed at the creation of new roles or spread of support workers means that the situation has stabilised somewhat.
Key point 62: there have been range of policy initiatives over the last decade relating to the development of IC services, but there remains a great variation in the interpretation of policy and models of service.
An additional feature leading to variability of services is the range of external pressures, which mean that workloads are rarely static. This includes an adapting policy environment that effects not only how care is provided but also where, as well as the conditions in which work is conducted and the pay provided. Varied population demands and needs of the client create additional external pressures. 95 Therefore, IC managers need to innovate to address requirements for service delivery while dealing with a limited and changing workforce.
Skill mix and workforce configurations
The importance of skill mix and configurations of staff types for achieving performance objectives such as quality, speed and efficiency has been demonstrated regarding the design of front/back office design114,115 and the mix of skilled and less skilled staff (Baldauf et al., University of Warwick, 2009).
Although ‘intermediate care demands that strict role boundaries are erased in favour of more flexible and generic skills’,113 this is not well reflected in job titles and, therefore, difficult to establish the extent to which role boundaries are maintained in individual teams. There is also a conflict with the increasingly hierarchical structure of health services, which, following the Agenda for Change initiative, could be ‘seen to reward specialisation rather than skill sharing’. 113
Key point 63: there is a tension between the specialisation and hierarchy seen in other areas of the NHS and the more generalised and collaborative approaches needed in multidisciplinary IC teams.
According to Baldauf et al. (University of Warwick, 2009) the 1990s saw the evolution of workforce innovations, through the introduction of nurse practitioners and health‐care assistants. The NHS Modernisation Agency (2001–5) has since been instrumental in promoting new ways of working (Changing Workforce Programme116). Moving care from hospitals to the community has involved redesigning care pathways, or simply delivering care in different settings. Drawing on a literature review, Sibbald et al. 117 have identified three different types of closer to home services: (1) transfer of services to primary care, (2) relocation of services into the community and (3) hospital redesign (Baldauf et al., University of Warwick, 2009).
In particular, workforce innovation has focused on delegating tasks from higher- to lower-qualified staff groups,118 suggesting a shift over time to less skilled staff types. The Pathology Workforce Reprofiling Project119 found that there was potential to use a higher proportion of band 2 and 3 staff and a smaller proportion at band 6 and 7 (Baldauf et al., University of Warwick, 2009). Pilot sites showed improvements in three areas: (1) better care for the patients, (2) better opportunities for staff and (3) better value for money. The final point contradicts findings from the COOP study. 1
Key point 64: there are potential drivers for shifting tasks from higher- to lower-qualified staff groups. However, the benefits of this strategy are not clear.
Secondary analysis of data
The purpose of these analyses was to investigate whether or not IC teams had undergone changes in their configuration or their patient’s characteristics over the time period between the first and second studies. A simplistic approach would be to compare the data collected for all the teams involved in study 1 with data for all the teams involved in study 2. The major drawback of this approach is that many of the teams were involved in only one of the two studies. As there is considerable heterogeneity among IC teams, any differences observed could be due to the underlying differences in the teams included in the two studies, as opposed to a temporal effect. Although we report these findings below, this caveat will need to be borne in mind when interpreting the figures. An alternative approach, and one which allows a more direct comparison, is to compare data taken from teams included in both studies. This is not without difficulty, as doing so still relies on a concept of unchanging, well-defined IC teams. Service evaluations carried out as part of study 2, demonstrated that members of IC teams often had disparate and poorly defined definitions of their work organisation. They were subject to almost constant change, with very little managerial focus on maintaining a cohesive approach to joint working. On occasions, it was found that while managerial definitions and aims of the service had changed substantially (including changes to admission criteria), these changes had not been communicated to staff members. Therefore, the assumption that comparing the same team at different time points is actually comparing like with like cannot be taken for granted and must be explored in some depth at various levels of the organisation.
It is notable that shortly following study 2, two of these teams were disbanded (with staff being allocated to GP practices over a large geographical area) and one team stopped working with clients in their homes. Many of the other teams had uncertain futures and were preparing for unpredictable changes. All teams were wholly or partly funded by PCTs, which are being rapidly dismantled as a result of the recent white paper. 56 The heterogeneity and instability of IC services presents the researcher in this field with a challenging environment, particularly regarding conducting longitudinal studies and in drawing conclusions and making generalisable recommendations.
However, although some teams changed beyond recognition owing to major service reorganisation, seven teams remained fairly stable between project 1 (COOP)1 and project 2 (EEICC). 2 The majority of the analyses focused on these seven teams.
Key point 65: heterogeneity, ambiguity and instability of IC services creates difficulties in conducting longitudinal studies and in drawing conclusions and making recommendations that can be generalised.
Results
Team characteristics
Table 18 and Figure 14 demonstrate some important differences between the ways that services are organised. Although most aim to prevent acute/long-term care admissions and facilitate discharge from acute services, there are some differences to priorities. Services range from medically focused nurse-led, community hospital-based teams funded by PCTs (e.g. EEICC team PB) to teams based in local authority establishments, jointly funded by social services and the NHS, with a focus on providing social care in clients’ own homes and small residential units (e.g. teams F and Q).
| Team | Service aim | Service description | Primary and secondary setting | Initial age of service | Background of team leader | Funding organisation | Organisation setting |
|---|---|---|---|---|---|---|---|
| 1 | Supported discharge | Multidisciplinary team | Resource centre, client’s home | 5 years | Social worker | PCT/support staff | Support staff |
| 2 | Admission prevention | Rapid response and community rehabilitation service | Client’s home, nursing home | 4 years | Nurse | PCT/LA | PCT |
| 3 | Admission prevention and facilitate early discharge | Step-up and step-down multidisciplinary team | Client’s home, hospital (inpatient/outpatient) | 3 years | Dietitian | PCT | PCT |
| 4 | Admission prevention and facilitate early discharge | Nurse-led step-down/step-up facility | Community hospital | 8 years | Nurse | PCT | PCT |
| 5 | Community stroke rehabilitation | Community multidisciplinary team | Client’s home, hospital outpatient | No data | Nurse | PCT/support staff | PCT |
| 6 | Admission prevention and facilitate early discharge | Primarily step down, social services assessment and co-ordination | Client’s home, reablement unit | 8 years | Social worker | PCT/support staff | Support staff |
| 7 | Admission prevention and facilitate early discharge | IC | Client’s home, hospital (inpatient) | 8 years | OT | PCT | PCT |
FIGURE 14.
Changes in team configurations. (a) Number of clinical staff; (b) number of clinical support staff; (c) number of management staff; (d) number of social care staff; (e) number of non-clinical support staff; (f) number of domiciliary support staff; (g) total number of staff; and (h) total number of staff types. a, The average of the six teams; and b, the average of all teams combined.
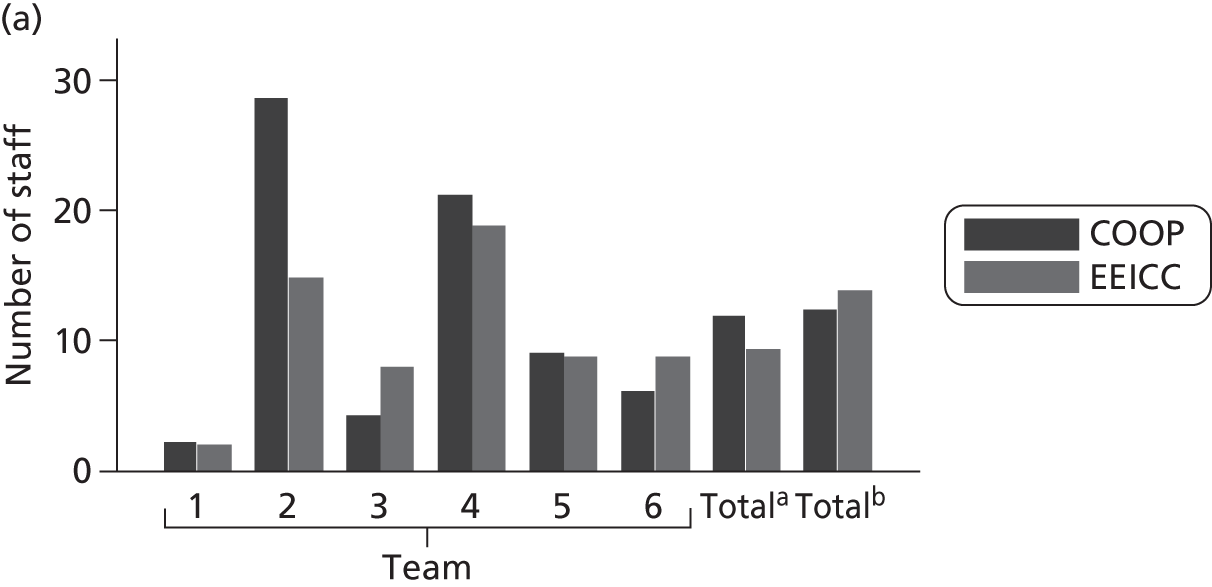


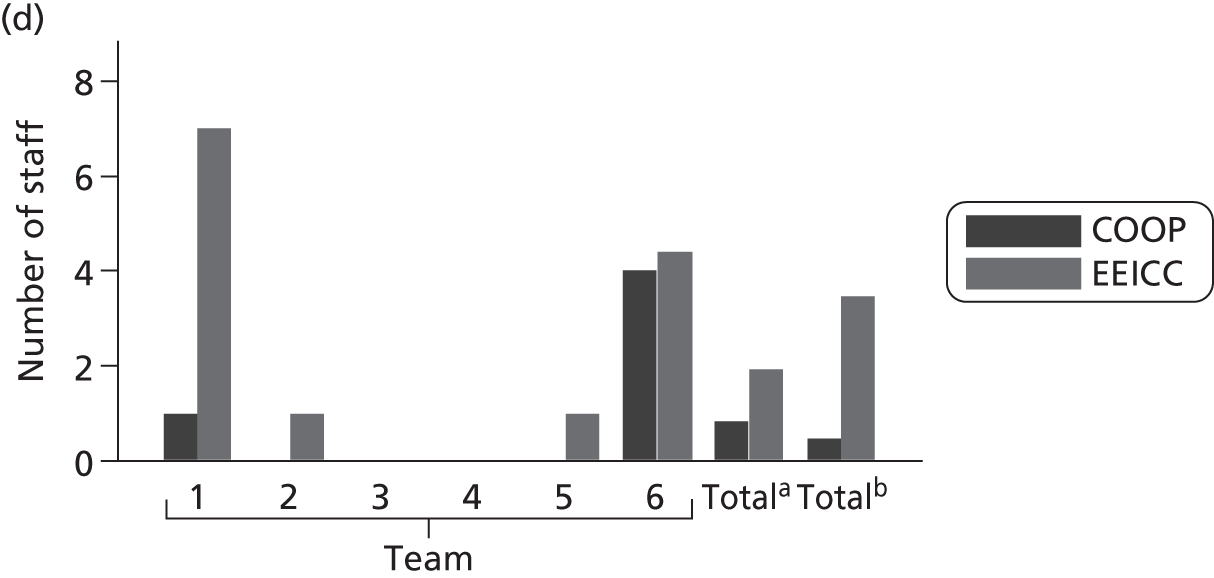


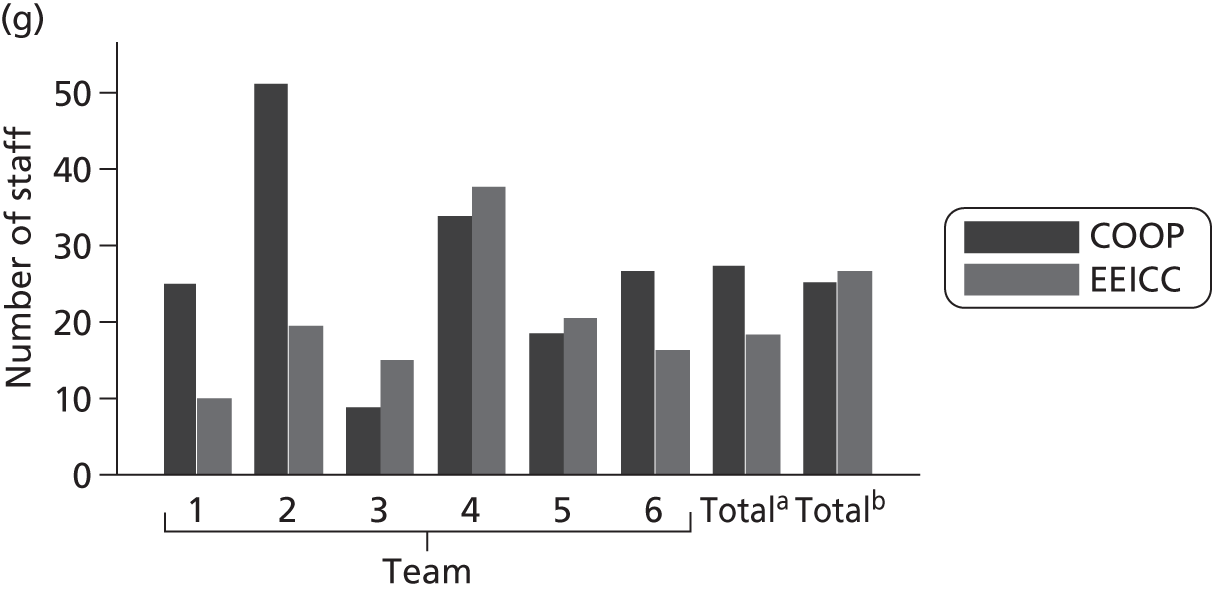
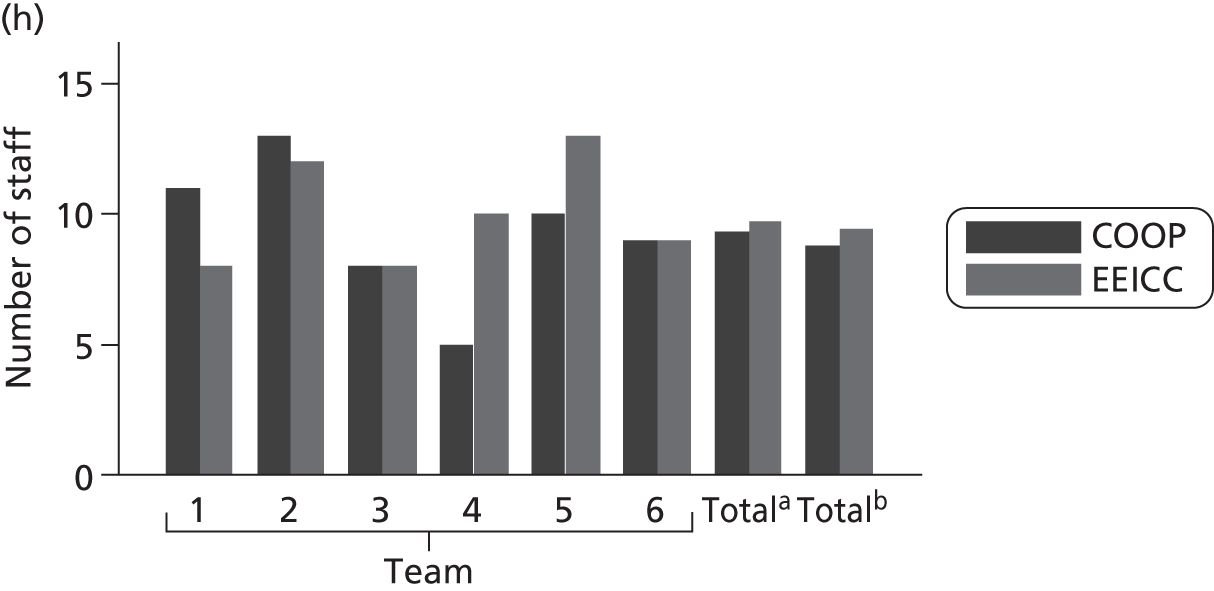
Team configurations
As can be seen in Figure 14, changes in team configurations reflect the general picture of team characteristics. There is some stability but also a wide range of changes in both directions for some teams, which are somewhat masked by the average changes. For two measures (number of clinical staff and total numbers of staff) this heterogeneity is reflected in declining numbers for the six teams involved in both studies who returned staffing information (information was not received from one team), while the numbers increase for the studies as a whole.
The following findings regarding team configurations are given in the number of whole-time equivalent (WTE) staff, rather than the number of actual staff members.
Clinical staff
Team 2 had a large decrease of clinical staff members by about 50%, while team 3 (a smaller team) showed a notable increase. Team 6 also increased its number of clinical staff and teams 1 and 5 showed very slight decreases. Overall, there was a large increase, although for six of the teams taking part in both studies, there was a decrease in numbers of clinical staff. These changes in staffing numbers and team size were associated with changes in boundaries and PCTs in local areas.
Clinical support staff
Teams 1 and 2 had no clinical support staff in study 2, despite having 21 and 16, respectively, in study 1. Team 6 had a similar reduction from 14 to < 1 WTE clinical support staff. Teams 3, 4 and 5 had slight increases. Overall, there was a large decrease in the average number of clinical support staff from eight to just over five. However, for six of the teams taking part in both studies the decline was greater – the mean average number of clinical support staff reduced by two-thirds (from 12 to 4).
Management staff
Team 4 had no management staff in study 1 and one WTE in study 2. Team 5 remained static (with one WTE) and team 1 saw a slight reduction from a very low baseline of < 0.5 WTE. Team 2 saw an increase of one WTE (from two to three), team 3 increased from 0.5 to one member of management staff and team 6 increased from one to 1.8. Overall, there was a slight increase in the number of management staff (1.5–1.9 WTE). However, for the teams taking part in both studies, the increase was minimal (0.1 WTE) and had a lower baseline (one WTE).
Social care staff
Only two teams (1 and 6) had any social care staff (care assistants and domiciliary support staff) in the first study, while in the second study four teams had social care staff. Team 1 increased from one to seven WTE social care staff and team 6 increased very slightly from four staff members (< 1 WTE increase). Teams 2 and 5 increased from zero to one WTE social care staff. For the teams taking part in both studies, there was a mean increase in the number of social care staff of one WTE. However, overall, the mean increase for the second study was larger (three WTEs) and had risen from a lower baseline.
Non-clinical support staff
Team 1 had no non-clinical support staff in either study. Teams 4 and 6 were static and team 5 had a very slight increase. Team 2 reduced the number of non-clinical support staff from four to < 2 WTE. Team 3 increased from one to two members of staff. Overall, there was a slight increase in the number of non-clinical support staff; however, for six of the teams taking part in both studies there was a decrease, from a lower baseline.
Domiciliary support staff
Teams 2, 3, 5 and 6 had no domiciliary support staff in either study. Team 1 was static at 0.5 WTE and team 4 saw a dramatic rise from zero to four domiciliary support staff. Overall, there was a slight increase in the mean number of domiciliary support staff. For the teams taking part in both studies, the average for the second study was greater, despite having a slightly lower baseline.
Total number of staff
The greatest change in total numbers of staff was seen in team 2, decreasing from 50 to 20 members of staff. Teams 1 and 6 also had a very large reduction in the total number of staff members, dropping from 25 to 10 and 27 to 16, respectively. Teams 4 and 5 saw a very slight increase and team 3 had the least number of staff members and increased from 8 to 15. For the teams taking part in both studies, there was a large decrease in the mean total number of staff (from 28 to 19). Overall, the total number of staff members in the second study was very slightly greater. However, it should be recognised that the increases in the size of teams could be as the result of extensive reorganisation, thereby reducing the relevance of comparing over time. A consistent identity of a team or service in longitudinal studies is important, which is complicated by the almost continual change in this sector.
Total number of types of staff
Teams 3 and 6 were static regarding the numbers of different types of staff members in the teams. Team 2 saw a very slight reduction and team 1 saw a greater reduction from 11 to 8 different types of staff. Teams 4 and 5 had an increase in the numbers of different types of staff members from, 5 to 10 WTE and 10 to 13 WTE, respectively. The mean numbers of different types of staff members rose by a similar amount overall, as it did for the teams taking part in both studies. However, the teams that took part in both studies had a slightly higher baseline and therefore a slightly higher final number of staff types.
Key point 66: regarding changes to team configurations there were some consistent trends between the data from the seven teams and the whole data set, but changes were small and variation from team to team meant that there was no discernible pattern of changes.
Sources of referrals
Table 19 shows the sources of referrals for the seven teams involved in both studies. Changes of ≥ 10% are in bold. It is notable that, apart from teams 1 and 3, these largest changes occupy categories that are not mutually exclusive [i.e. Allied Health Professionals (AHPs) and either acute or community hospital]. This indicates that these differences could possibly be as a result of inconsistent reporting between the two studies. For instance, an AHP referring from a community hospital could be reported as either.
| Referral route | Team 1 | Team 2 | Team 3 | Team 4 | Team 5 | Team 6 | Team 7 | Overall (seven common teams)a | Overall (all teams)b | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | |
| GP/doctor | 0.0 | 0.6 | 11.5 | 18.8 | 21.9 | 27.4 | 0.0 | 0.9 | 5.6 | 13.2 | 0.0 | 0.6 | 19.2 | 17.5 | 10.9 | 16.3 | 16.6 | 17.4 |
| Self/informal carer/friend/family | 3.9 | 7.4 | 0.3 | 0.4 | 3.1 | 0.7 | 0.0 | 0.0 | 0.0 | 0.0 | 2.2 | 5.4 | 3.9 | 1.8 | 1.5 | 1.4 | 1.4 | 1.9 |
| Community nurse/nurse | 9.6 | 1.2 | 8.5 | 11.0 | 7.8 | 4.7 | 0.0 | 6.1 | 0.0 | 0.9 | 4.4 | 6.0 | 15.4 | 8.6 | 8.3 | 7.3 | 8.7 | 11.1 |
| Social worker/social services | 30.8 | 21.5 | 4.1 | 3.1 | 3.1 | 1.2 | 0.0 | 0.0 | 0.0 | 0.0 | 26.1 | 19.1 | 3.9 | 0.9 | 8.1 | 4.4 | 9.9 | 6.2 |
| AHP | 13.5 | 7.4 | 51.4 | 11.0 | 9.4 | 14.7 | 0.0 | 1.8 | 16.7 | 5.3 | 23.9 | 5.4 | 13.5 | 29.1 | 34.2 | 12.5 | 26.9 | 21.7 |
| A&E/ambulance service/rapid response | 0.0 | 0.0 | 6.8 | 12.5 | 0.0 | 2.1 | 6.3 | 2.6 | 0.0 | 0.4 | 0.0 | 0.0 | 5.8 | 0.0 | 4.4 | 5.6 | 8.0 | 5.1 |
| Ward in acute hospital/day clinics/fall clinics | 23.1 | 33.1 | 13.2 | 40.5 | 4.7 | 10.7 | 93.8 | 86.0 | 77.8 | 50.2 | 17.4 | 18.5 | 13.5 | 8.9 | 18.0 | 32.0 | 18.8 | 24.1 |
| Community hospital | 19.2 | 28.8 | 4.4 | 2.6 | 50.0 | 38.6 | 0.0 | 2.6 | 0.0 | 29.5 | 26.1 | 44.6 | 23.1 | 33.1 | 14.5 | 20.4 | 14.2 | 14.2 |
| Other | 0.0 | 0.0 | 0.0 | 0.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.4 | 0.0 | 0.6 | 1.9 | 0.0 | 0.2 | 0.2 | 0.4 | 0.2 |
Number of referrals and staffing levels
Prior to each study, all teams provided an estimate of the annual throughput of patients. Table 20 shows the differences between estimated and actual annual throughput of patients. The actual throughput per annum for each team was derived from the number of patient records completed.
| Team | Study 1 (COOP)1 | Study 2 (EEICC)2 | % actual change | ||||
|---|---|---|---|---|---|---|---|
| Estimated throughput | Actual throughputa | Throughput as % of estimate | Estimated throughput | Actual throughputa | Throughput as % of estimate | ||
| 1 | 183 | 116 | 64 | 135 | 129 | 96 | 111 |
| 2 | 1800 | 1060 | 59 | 1650 | 875 | 53 | 83 |
| 3 | 320 | 274 | 86 | 350 | 329 | 94 | 120 |
| 4 | 166 | 86 | 52 | 160 | 104 | 65 | 121 |
| 5 | 400 | 82 | 20 | 225 | 184 | 82 | 224 |
| 6 | 460 | 175 | 38 | 380 | 174 | 46 | 99 |
| 7 | No data | 217 | – | 358 | 243 | 68 | 112 |
The potential inaccuracy of using the number of completed patient records as a proxy for patient throughput is shown in Table 21. During the EEICC study,2 it was recognised that the accuracy of data collection could be variable at each site and further information was requested. We requested their actual throughput taken from service records for the study period.
| Team | Duration of study (months) | Total admissions during study | Actual 12-month throughputa | Client records/per annum | 12-month estimate |
|---|---|---|---|---|---|
| 1 | 15 | 176 | 141 | 129 | 135 |
| 2 | 15 | 1712 | 1370 | 875 | 1650 |
| 3 | 15 | 491 | 393 | 329 | 350 |
| 4 | 15 | No data | – | 104 | 160 |
| 5 | 17 | 355 | 251 | 184 | 225 |
| 6 | 16 | 214 | 161 | 174 | 380 |
| 7 | 16 | 344 | 258 | 243 | 358 |
All teams gave a higher estimated annual total than the actual number of completed patients records received over 12 months. A large part of this discrepancy is most likely due to incompleteness of records and teams varied regarding the percentage of patients who were actually recorded for the study. All teams apart from team 3 reduced their estimates for the second study. However, team 3 increased its throughput as well as its estimate, with the result that the estimate was more accurate (94%) for study 2.
Key point 67: it is important to gain actual throughput figures from service records on completion of data collection, as the completeness of study-level data can vary.
According to completed patient records received, five of the seven teams increased their throughput (range 111–224% increase), one team reduced slightly (team 2 = 83%) and one team had almost the same throughput (team 6 = 99%). The overall increase for the seven teams is limited by the reduction in throughput of the largest team (team 2). Although the reduction is slight in terms of the team, the actual numbers have a disproportionally large influence over the total owing to this team having the largest throughput. Despite the majority of teams seeing an increase, the overall increase is only from 2010 to 2038 completed patient records received per annum. However, as demonstrated by Table 21, there are limitations to the accuracy of this calculated change.
All teams that we have data for, except team 3, experienced an increase in the ratio of patients to all staff, as shown in Table 22. There was a large variation in the patient-to-staff ratio, which ranged from 0.28 patients per member of staff (team 2) to 13.69 patients per member of staff (team 3). For the seven teams overall, the ratio of patients to staff rose from 1.2 to 2.1 patients for each full-time member of staff between study 1 and study 2.
| Team | Study | Average number of patients in the service at any time | Total staff (WTE) | Average number of patients per full-time member of staff |
|---|---|---|---|---|
| 1 | COOP | 24.0 | 24.9 | 0.97 |
| EEICC | 33.4 | 9.9 | 3.40 | |
| 2 | COOP | 14.1 | 51.1 | 0.28 |
| EEICC | 14.0 | 20 | 0.70 | |
| 3 | COOP | 119.1 | 8.7 | 13.69 |
| EEICC | 103.1 | 15 | 6.87 | |
| 4 | COOP | 13.4 | 33.7 | 0.40 |
| EEICC | 17.1 | 37.6 | 0.46 | |
| 5 | COOP | 18.9 | 18.5 | 1.02 |
| EEICC | 58.5 | 20.5 | 2.85 | |
| 6 | COOP | 27.9 | 26.6 | 1.05 |
| EEICC | 30.0 | 16.3 | 1.84 | |
| 7 | COOP | 13.0 | No data | – |
| EEICC | 14.1 | 9.1 | 1.55 | |
| Average for seven teams | COOP | 32.9 | 27.3 | 1.2 |
| EEICC | 38.6 | 18.3 | 2.1 |
Key point 68: these findings support the literature, demonstrating an increase in the ratio of patients to staff.
Patient characteristics
Demographics
The following patient characteristics changed slightly. Overall, patients were 1 year younger in the EEICC study2 than in the COOP study. 1 Although the majority of patients were females, the percentage of males rose by 4% from COOP1 to EEICC. 2 Comparisons for the seven teams involved in both studies are shown in Figures 15 and 16. These demonstrate a stable average age of patients and slightly less of an increase in the percentage of male patients for these teams.
FIGURE 15.
Changes in ages of patients. T1 represents the COOP study and T2 the EEICC study. a, The average of the seven teams; and b, the average of all teams combined.
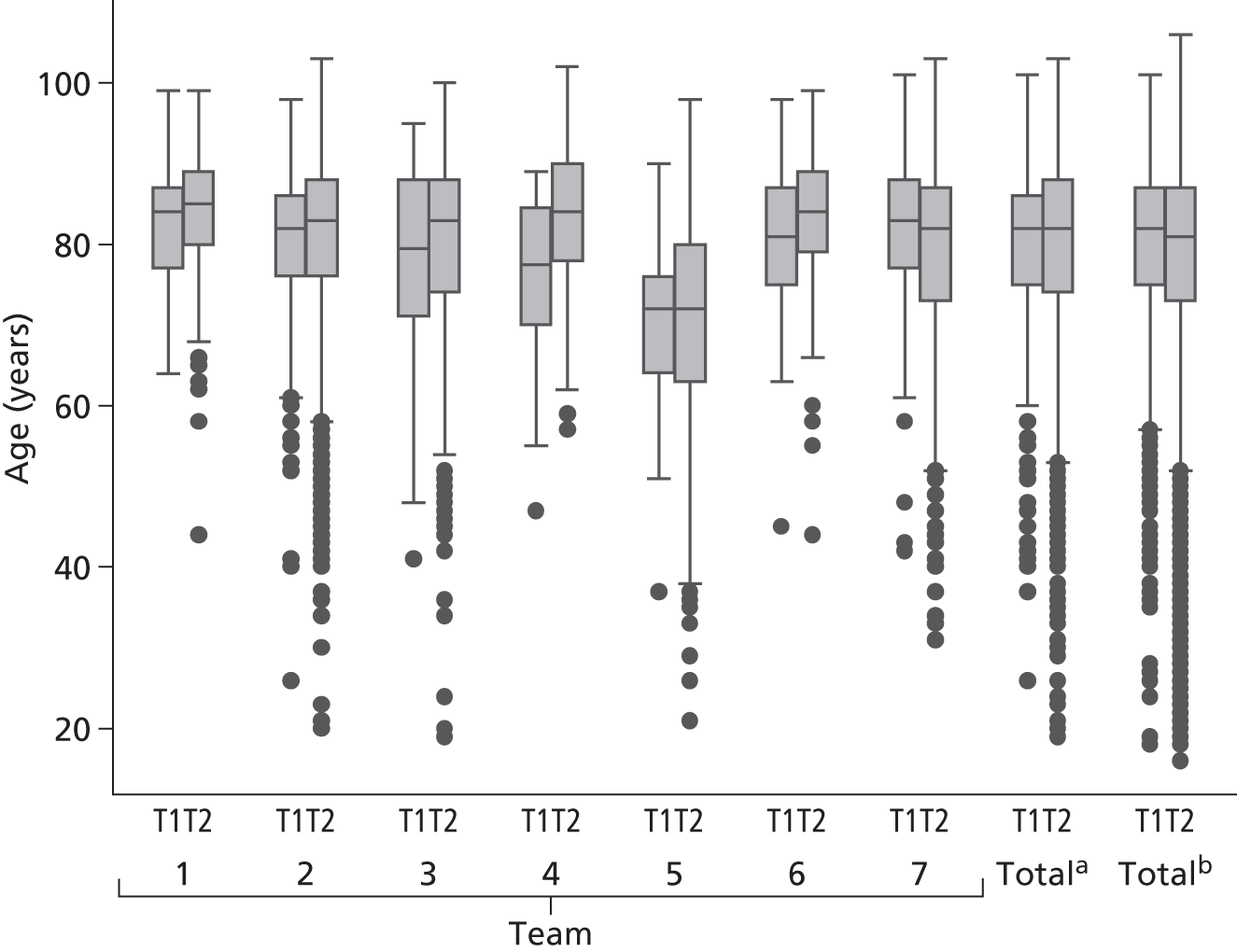
FIGURE 16.
Changes in sex of patients. T1 represents the COOP study and T2 the EEICC study. a, The average of the seven teams; and b, the average of all teams combined.
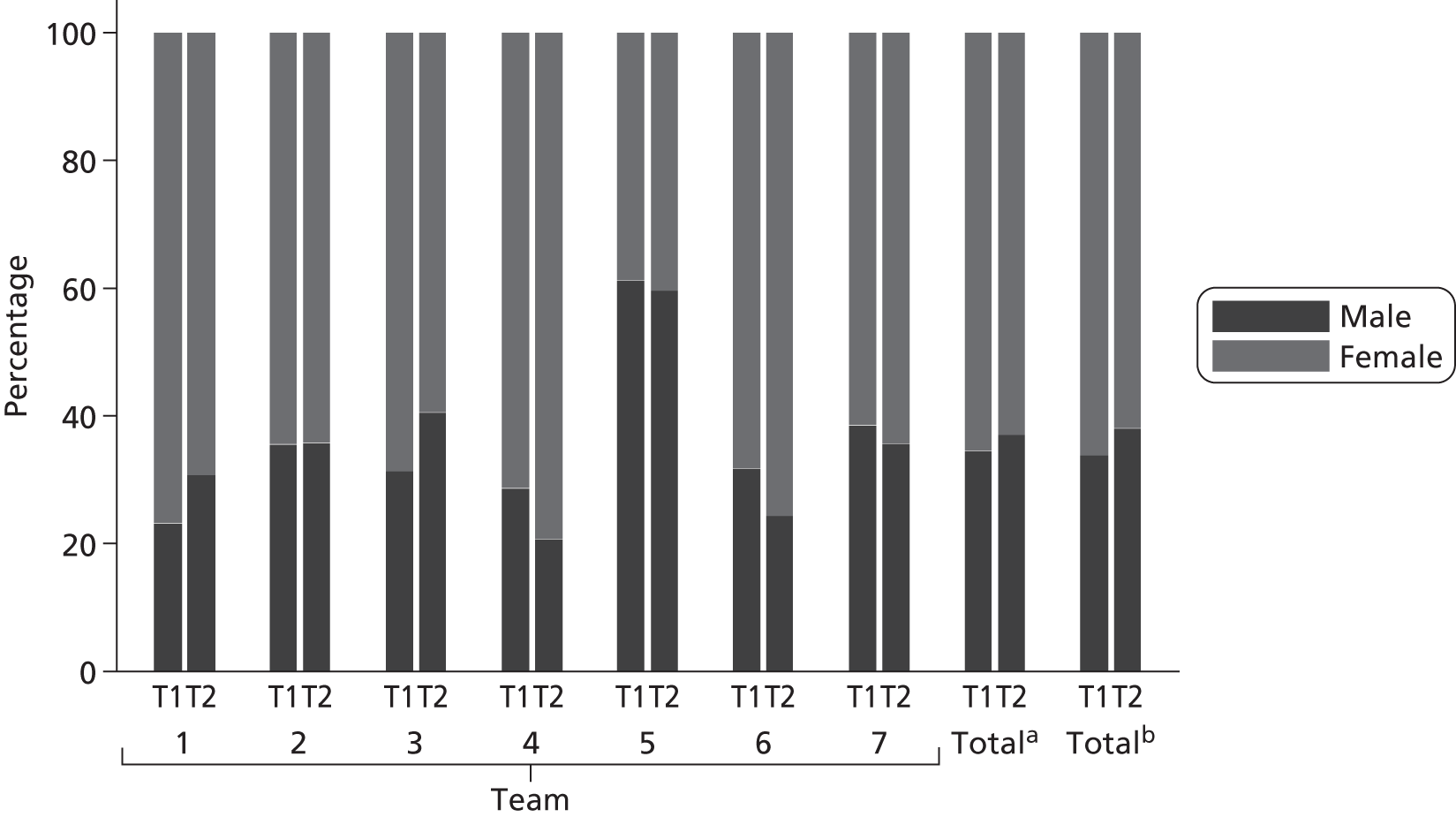
In the following summaries, data are presented for the seven teams that appeared in both COOP1 and EEICC,2 the average of these (‘Totala’) and the average of all teams combined (‘Totalb’).
Patient care needs
Level of care
A comparison of the LoC needs (Table 23) of admitted patients shows some large changes (> 10%) between study 1 and study 2 (bold text in Table 23). The LoC applicable to the highest percentage of patients for each team is also shown (italic text in Table 23). Level 4 is the most common; overall, this level shows a slight upward trend, whereas for the seven teams from both studies, the trend is in the opposite direction.
| LoC at admission | Team 1 | Team 2 | Team 3 | Team 4 | Team 5 | Team 6 | Team 7 | Average 1a | Average 2b | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | |
| 0 (does not need any intervention) | 2.0 | 0.0 | 7.6 | 8.5 | 1.9 | 8.0 | 0.0 | 0.0 | 14.3 | 11.2 | 0.0 | 0.0 | 0.0 | 20.1 | 5.0 | 8.5 | 6.7 | 9.5 |
| 1 (needs prevention/maintenance programme) | 2.0 | 0.0 | 14.1 | 12.2 | 7.7 | 16.1 | 6.3 | 0.9 | 0.0 | 25.9 | 5.1 | 1.8 | 9.8 | 15.7 | 10.3 | 12.3 | 15.2 | 25.9 |
| 2 (needs convalescence/respite) | 0.0 | 0.0 | 3.4 | 1.3 | 1.9 | 2.4 | 6.3 | 0.9 | 0.0 | 0.5 | 2.6 | 1.8 | 0.0 | 1.4 | 2.5 | 1.4 | 2.6 | 1.4 |
| 3 (needs slow-stream rehabilitation) | 7.8 | 1.3 | 9.1 | 19.5 | 34.6 | 28.9 | 0.0 | 6.9 | 14.3 | 16.8 | 35.9 | 27.7 | 24.4 | 20.1 | 15.1 | 19.8 | 19.3 | 20.3 |
| 4 (needs regular rehabilitation programme) | 64.7 | 56.7 | 46.8 | 37.1 | 32.7 | 37.8 | 81.3 | 83.6 | 64.3 | 38.6 | 38.5 | 32.5 | 51.2 | 38.9 | 48.5 | 41.0 | 29.9 | 31.3 |
| 5 (needs intensive rehabilitation) | 19.6 | 42.0 | 9.1 | 9.6 | 9.6 | 4.3 | 0.0 | 1.7 | 7.1 | 4.6 | 12.8 | 23.5 | 4.9 | 1.0 | 9.9 | 10.0 | 13.5 | 5.4 |
| 6 (needs specific treatment for individual acute disability) | 2.0 | 0.0 | 3.8 | 3.7 | 1.9 | 0.7 | 6.3 | 5.2 | 0.0 | 0.5 | 0.0 | 9.4 | 1.9 | 0.3 | 3.2 | 2.7 | 6.1 | 3.3 |
| 7 (needs medical care and rehabilitation) | 2.0 | 0.0 | 4.2 | 7.4 | 7.7 | 1.7 | 0.0 | 0.9 | 0.0 | 0.5 | 0.0 | 0.6 | 2.4 | 1.4 | 3.6 | 3.6 | 5.1 | 2.2 |
| 8 (needs rehabilitation for complex disabling condition) | 0.0 | 0.0 | 1.9 | 0.8 | 1.9 | 0.0 | 0.0 | 0.0 | 0.0 | 1.5 | 5.1 | 2.9 | 2.4 | 1.0 | 1.9 | 0.8 | 1.7 | 0.9 |
It is again noticeable that the average gives a misleading picture owing to the heterogeneity of IC services. There are no particularly large changes when the average of all teams is calculated, which masks substantial positive and negative individual team changes. For instance, team 7 has no patients with LoC = 0 (‘does not need any intervention’) in the first study. However, this has risen to > 20% of all patients for study 2. Team 5 had no patients with LoC = 1 (needs prevention/maintenance programme) in the first study,1 but this rose to almost 26% in the second study.
The most common LoC (in bold) for each team remained stable in all but one team – team 3. Team 3 changed from ‘slow-stream rehabilitation’ (level 3) to ‘regular rehabilitation programme’ (level 4) as the most common level. For all other teams level 4 (‘needs regular rehabilitation programme’) was the most common in studies 1 and 2. However, there were some rather large changes in the distribution of LoCs for some teams from one study to the next. Teams 1 and 6 increased the percentage of patients needing ‘intensive rehabilitation’ (level 5) from 19.6% to 42% and 12.8% to 23.5%, respectively.
Therefore, although patients’ needs on admission to each service are grouped around level 4 (‘needs regular rehabilitation programme’), there is a wide range between teams of the percentage of patients who fall into this category (range 32.5–83.6%). Additionally, although some teams remain quite stable regarding patients’ needs, others see quite drastic changes. This would indicate that changes to local services, for instance, in referral procedures, admission criteria and availability of alternative services, are influential in determining patients’ needs in IC services.
Key point 69: patients’ LoC needs on admission to each service are grouped around level 4 (‘Needs regular rehabilitation programme’). However, between teams there is a wide range of patients assessed at this level (range 32.5–83.6%). Small changes in LoC when the average of all teams is calculated mask substantial positive and negative individual team changes.
Inappropriate referrals
The extent to which teams had inappropriate referrals was measured through two routes. First, there was a response on the patient record form to indicate patients who were considered to have been inappropriately referred. Second, it can be assumed that patients who are assessed as having a LoC need of 0 (not requiring service) at admission have not been appropriately referred.
There was considerable overlap between patients considered as inappropriately referred when using both methods of identification as demonstrated in Table 24. Therefore, we have shown findings using both methods individually and also included findings that take the overlap into account.
| LoC at admission | Number (%) of inappropriate referrals |
|---|---|
| 0 | 252 (45) |
| 1 | 69 (4) |
| 2 | 8 (8) |
| 3 | 26 (2) |
| 4 | 35 (2) |
| 5 | 6 (1) |
| 6 | 11 (4) |
| 7 | 21 (11) |
| 8 | 3 (4) |
For teams that took part in both study 1 and study 2, LoC 0 at admission and inappropriate referrals both increased (from 5.0% to 8.5% and from 5.0% to 13.0% respectively). The increase in the mean for all teams was similar (LoC 0 = 6.7% to 9.5%, inappropriate referrals = 4.1% to 10.4%). The trend was upwards; some teams demonstrated a slight decrease or remained almost the same, while three teams showed large increases. There was no uniform increase across all teams (Figures 17 and 18).
FIGURE 17.
Changes in LoC = 0, patients not needing an intervention on admission. a, The average of the seven teams; and b, the average of all teams combined.

FIGURE 18.
Changes in patients indicated as inappropriately referred. a, The average of the seven teams; and b, the average of all teams combined.
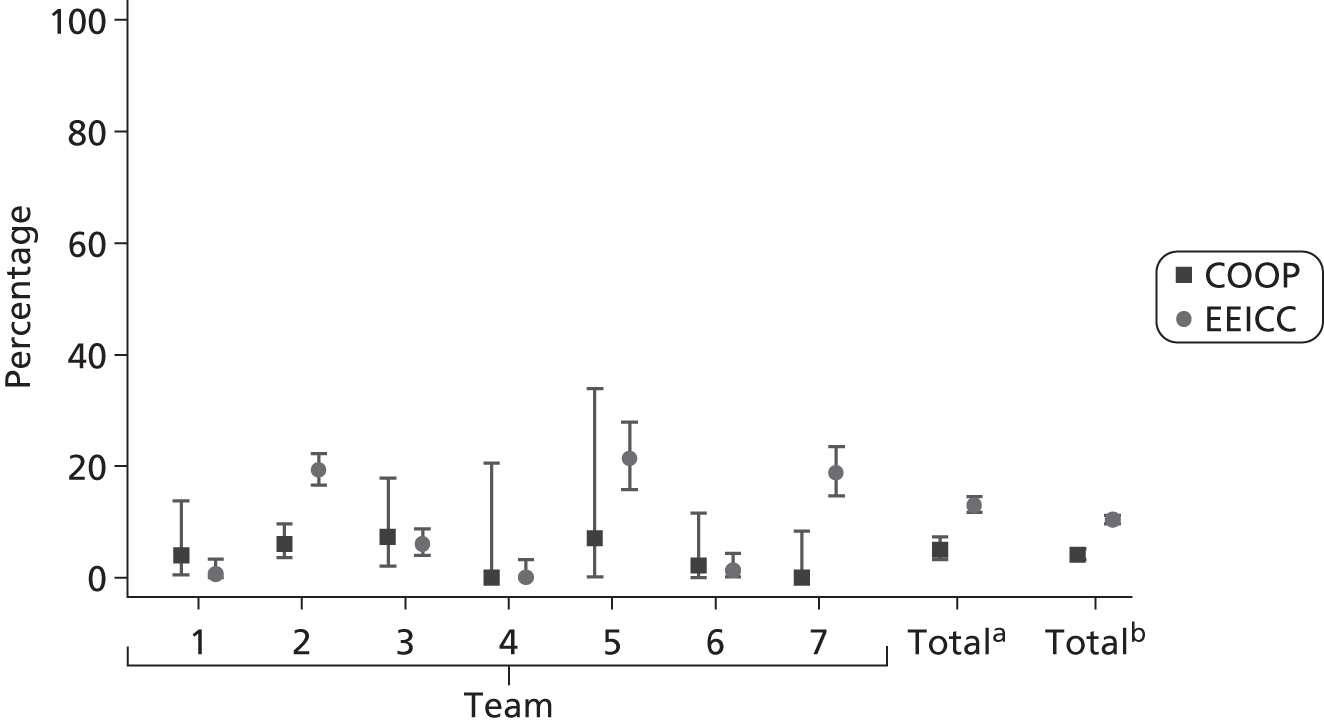
Teams 1 and 5 had a small reduction in LoC = 0. Team 7 had the highest LoC = 0 in study 2 and this rose considerably from 0% in study 1 to 20% in study 2.
Teams 1, 4 and 6 had very low numbers of inappropriate referrals in study 2. This represented a small reduction for team 1 and a nearly steady situation for teams 4 and 6. Teams 2, 5 and 7 saw large increases. Team 3 remained fairly steady, above the mean for study 1 and below the mean for study 2.
Although the variation between teams demonstrates that the specific reasons for the overall increase in inappropriate admissions are likely to be different for each team that contributes to the increase, the upward trend should be noted. Qualitative evidence from study 2 indicates that this may be due to a lack of alternative appropriate services for people with low-level needs or little rehabilitation potential. The lack of clear service identities and admission criteria may also be a contributing factor.
Key point 70: for the teams taking part in both studies, the percentage of patients deemed not to require the service (LoC = 0) or inappropriately referred rose (from 5.0% to 8.5% and from 5.0% to 13.0%). There were similar increases for all study data (from 6.7% to 9.5% and from 4.1% to 10.4%, respectively).
Figure 19 makes allowance for the overlap between patients identified as inappropriately referred and with a LoC of 0. Across the teams involved in both studies, the percentage of patients either identified as inappropriate referrals or with a LoC = 0 increased from 7.7% to 14.8%, and from 8.6% to 14.4% across all 22 teams. Although the trend is upwards, these averages mask the high variability between teams. Three of the teams (teams 2, 5 and 7) demonstrated a large increase, but a fourth (team 3) showed only very minor increase and the remaining three teams reported small decreases, albeit on very few inappropriate referrals, between COOP1 and EEICC. 2
FIGURE 19.
Patients either identified as inappropriate referrals or LoC = 0. a, The average of the seven teams; and b, the average of all teams combined.
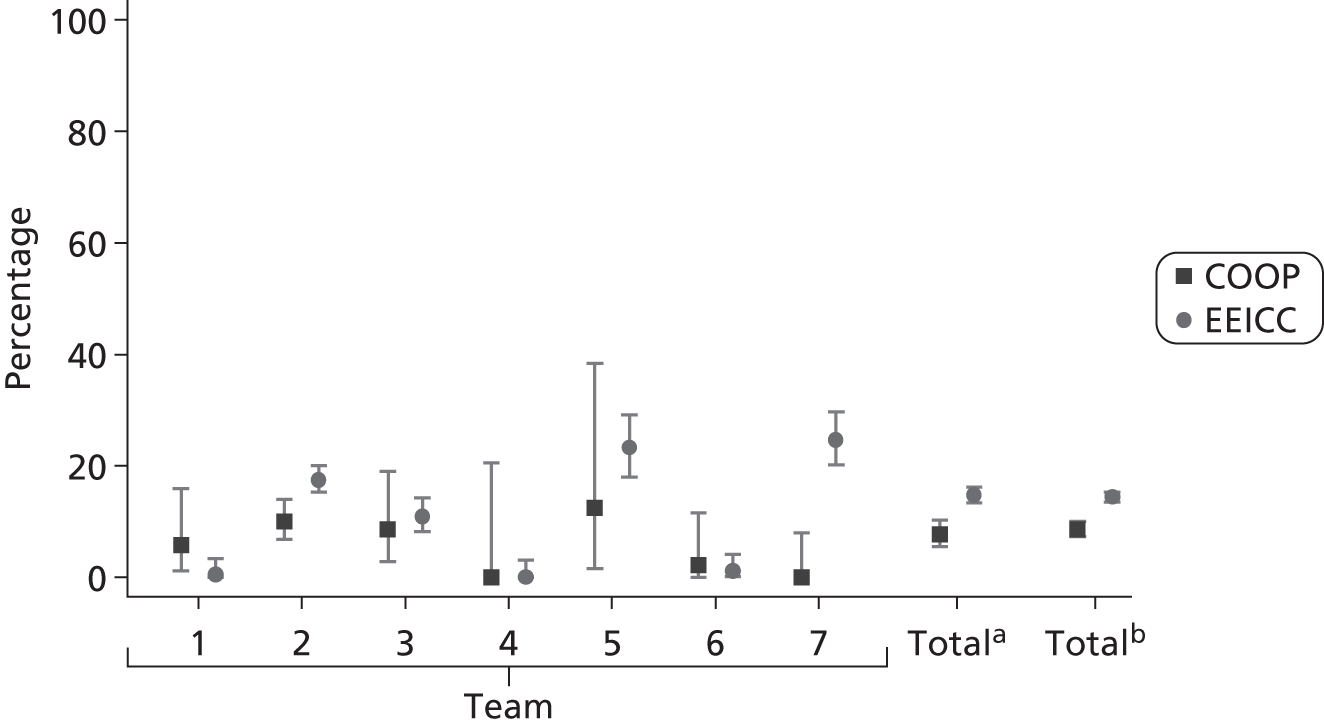
Location of care
The location where teams deliver care is an important predictor of patient outcomes, and has an important bearing on the culture of the team and the type of care they are able to provide. For the sake of comparison, the percentage of patients receiving care at home was compared with patients receiving care in hospital. Patients receiving care in other locations account for the differences between these.
Overall, the percentage of patients receiving care at home increased; however, when considering the teams that participated within both study 1 (COOP1) and study 2 (EEICC2), this decreased. Teams 1,3, 4 and 6 all had increases in the percentage of patients receiving care at home, while teams 2, 5 and 7 all had decreases. Regarding the number of patients receiving care in hospital, teams 1, 2, 5 and 6 were quite stable, whereas teams 3 and 7 saw large increases and team 4 had a large decrease. However, differences between teams varied by up to 100%.
Key point 71: perhaps the most striking feature of changes in the location of care is the variation between teams (up to 100%), rather than the variation over time.
Overall, comparing both studies, the number of patients receiving care at home increased (Figures 20 and 21). However, looking just at teams who participated within both study 1 and study 2, this decreased. A similar story is told by the changes in patients receiving care in hospital. Although there was a reduction for the study as a whole, for teams taking part in both studies there was a slight increase. These findings suggest that the teams themselves had different referral patterns and provided different types of services in a varying diversity of locations. The types of locations for which services are provided are mostly stable and, therefore, do not seem to be influenced by national issues such as changes in patients’ needs or policy directives. However, there seem to be strong local determinates incorporating structural changes, which redefine how the service is incorporated into the local health economy.
FIGURE 20.
Changes in patients receiving care at home. a, The average of the seven teams; and b, the average of all teams combined.
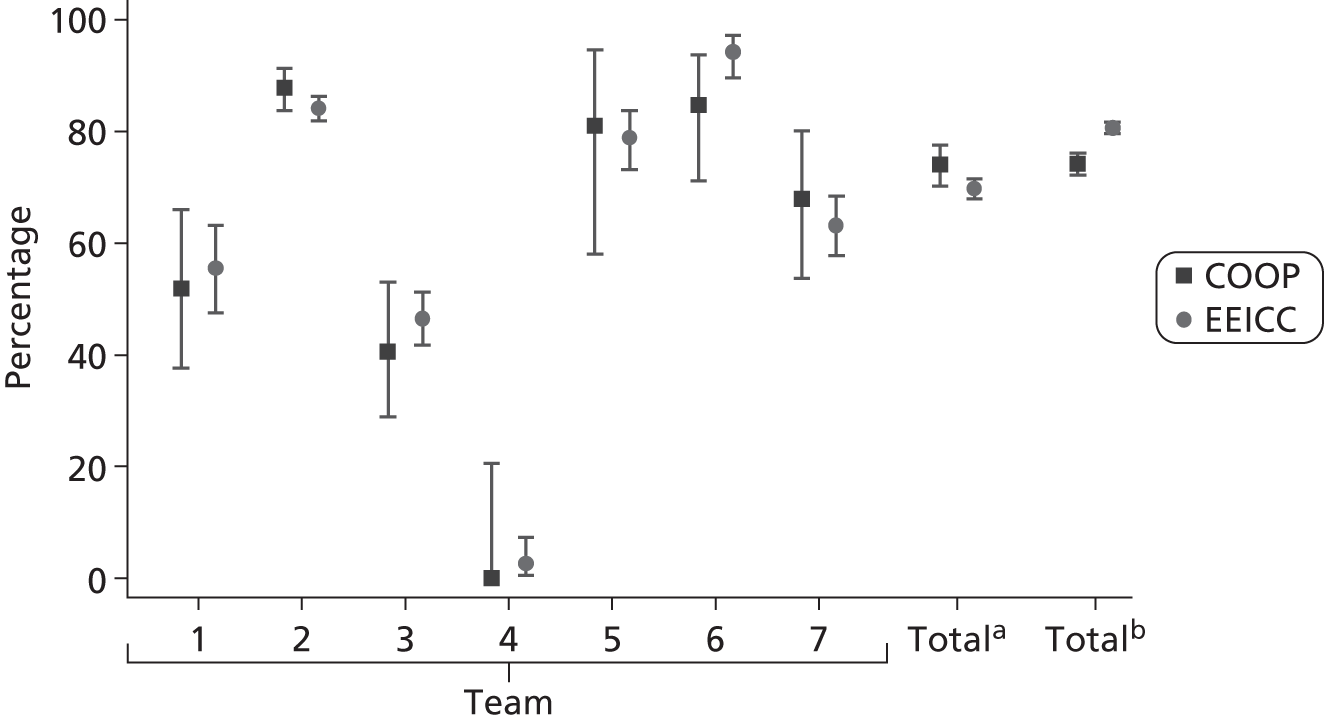
FIGURE 21.
Changes in patients receiving care at hospital. a, The average of the seven teams; and b, the average of all teams combined.

Teams 1, 3, 4 and 6 had a slight increase in the percentage of patients receiving care at home, but teams 2, 5 and 7 saw a slight decrease. Regarding the number of patients being treated in hospital, this increased for teams 3 and 7, reduced for team 4, and the other teams were stable.
Team 4 had a reduction in the amount of care provided in hospital from 100% in study 1 to a little over 80% in study 2. However, only a small amount of this is accounted for in providing care in patients’ homes. This ward-based service seems to have diversified to provide more care in other locations and, again, these findings do not demonstrate a uniform change. Instead, they suggest relative stability for the majority of teams and changes in both directions for a small number of teams, which (when data are aggregated) tend to suggest small trends.
Most teams provide care in a mix of locations, which makes the distinction between bed- and home-based care difficult to sustain at a service level. Teams also seem to be diversifying regarding their locations of care. Future studies would therefore benefit from the ability to distinguish between bed- and home-based care at a patient level rather than a service or team level. This would be particularly important for the purposes of benchmarking services.
Patient mortality
As stated in Chapter 8, patient deaths in IC are quite rare. This factor makes it difficult to interpret differences over time, as changes also tend to be rather small. The teams that had contributed to both studies showed no changes in mortality rates over time. Notable exceptions are teams 3 and 7 (Table 25), which are both hospital-based IC teams, managed by a PCT where the team leader is an AHP. They provide care mostly in clients’ homes, but also in a hospital setting.
Discussion
An interesting finding regarding patient characteristics is related to the age and sex of the patients across the two projects. It is widely accepted that the population of the UK is aging and that life expectancy is higher for females. Therefore, we would expect to see a slightly older mean patient age and slightly more females than males in the second project. However, across the whole data set, the reverse was observed. It is difficult to make assumptions about why it might be the case that patients admitted to these IC services do not follow demographic trends.
There were some consistent trends between the data from the seven teams and the whole data set, for example increased management and social care staff, decreased clinical support staff and increased total number of staff types. However, these changes were small and variation from team to team meant that there was no discernible pattern of changes for team characteristics.
Overall, and for the teams that took part in both projects, there were increases in management, social care and domiciliary support staff. Clinical support staff saw drastic reductions for the teams that took part in both studies and for the studies overall.
The total number of staff increased slightly for the studies as a whole, but decreased substantially for the teams that took part in both studies. The total number of different types of staff increased overall and for teams from both studies. These findings would suggest that, on the whole, team size is increasing slightly, the number of management staff is increasing slightly and there are a greater variety of roles and increased skill mix in IC services. The number of social care staff increased from a very low baseline, while clinical support staff numbers were noticeably reduced. However, when viewed on a team-by-team basis, the picture is much more complicated. Although some teams remained quite stable on these measures, others changed drastically and not in a uniform direction. Therefore, slight mean increases shown in the aggregated data sets disguise the radical and unpredictable changes experienced by some individual teams.
Conclusion
The changes highlighted in the teams that took part in these projects continue to reflect the diversity of the delivery of care through IC services. Far from being any uniformity regarding models of service organisation, there is not even any coherent direction of service development. The large variation in this small sample hints at the difficulty of categorising IC services and the complexity of predicting how they might develop. A useful area for further investigation would be to investigate the complex drivers for change: what evidence (if any) informs decisions about the development of IC services, how are these decisions taken, who do they involve, what are the triggers for change and what are the impacts for service users and members of staff?
Chapter 8 How have referral patterns changed over time and what is the relationship with patient outcomes?
Introduction
Earlier in this report detail was given on the number of policy changes and directives published over the last 10 years by the Department of Health aimed at promoting and influencing the character of IC. These changes are likely to directly influence the nature and types of patients admitted to IC.
Background
Our qualitative data from the two studies suggests that IC services are receiving referrals of more chronically ill and dependent patients in recent years. This needs further interrogation as it has important resourcing implications. It is known that there are many influences associated with referring patients to particular services. Those who refer to services are often seen as the gatekeepers to the services. Investigating these issues provides insight into issues associated with policy change, equity of access and local provision.
Literature review
The systematic reviews of the literature (derived from the search strategy in Appendix 1 for the COOP1 and EEICC2 studies) did not elicit any studies relating to changes in referral patterns to community-based health-care provision for older people over time. However, studies of referral patterns to hospital-based services and mental health care services at particular points in time identify issues affecting local variation. For example, Bickell et al. 120 identified a sex bias in referral patterns for coronary heart disease treatment, which had increased over time and led to more appropriate referral for females than males.
Key point 72: although policy has changed over the last decade, we have not found any literature examining the impact of this on referral patterns to IC.
The impact of change in style of service delivery having an effect on referrals was identified by Beck et al. 121 who established that the shift from an inpatient- to an outpatient-based service resulted in fewer patients being investigated and treated in hospital and more patients treated as outpatients. This had the impact of reducing inpatient related costs, while outpatient-related costs increased. The overall contribution of drug costs to the total cost had increased greatly over time.
Clinical practice often diverges from clinical practice guidelines. Espeland and Baerheim’s122 study of GP referrals for plain radiography of the lumbar spine in different countries found that 60% did not conform to documented guidelines. The factors that affected their decisions included clinical ordering criteria, patient wishes, the practitioner’s response, uncertainty, professional dignity, access to services, perception of patient needs, sense of pressure from other health-care providers and expectations about the consequences. The authors suggested that there are several attitude-related and external barriers, which change over time.
A longitudinal observational study123 of a tertiary care psychiatric service over a 10-year period (1988–97), including 4429 consecutive referrals, exposed significant changes during the study period. Not only were changes in the diagnosis of patients observed over time (e.g. levels of psychosocial and somatic functioning of referred patients decreased), but management recommendations were also altered. Interestingly, these authors note that owing to a decrease in length of stay over the 10-year observation period, the correlation of lag time (the time from admission to the hospital until referral to community psychiatry service) and length of stay decreased.
Key point 73: although the literature does not give us much information of direct relevance to IC, it does suggest that referral patterns change over time and these are affected by a broad range of factors.
Secondary analysis of data
Seven teams were involved in both studies (COOP1 and EEICC2). In general, these teams showed small increases in the number of referrals over the period of the two studies. It is important to remember when considering these results that the referral agent was not noted on the records of all patients.
For the seven teams taking part in both studies, the most notable changes are the decrease in referrals from AHPs (from 34.2% to 12.5%) and the increase in referrals from acute settings (from 18% to 32%). Referrals from GPs over the two study periods rose slightly (from 10.9% to 16.3%) and there has been a reduction in referrals by social workers (from 8.1% to 4.4%). There has been little change in referral patterns from informal carers, friends and family and A&E (see Table 19).
When considering teams as a whole, i.e. including data from teams that were not in both studies, referrals from acute settings remain fairly stable (from 18.8% to 24.1%). Referrals from AHPs are slightly decreased (from 26.9% to 21.7%) and there is a slight increase in referrals from community nurses (from 8.7% to 11.1%). One referral route that showed similar changes to the data from the seven teams was social workers. Referrals through this route declined (from 9.9% to 6.2%) (see Table 19).
Comparing teams exposes the great variation in referral rates and demonstrates that these have not changed in a similar fashion over the period. Some teams show greater changes in referral routes between the two study periods. For example, team 2 shows a referral rate from acute hospitals changing from 13.2% to 40.5% as compared with team 3, which changed from 4.7% to 10.7%. Team 1 shows an increased referral rate, again from acute hospitals, from 23.1% to 33.1% (see Table 19) and team 5 shows the opposite trend with a reduction in referral rates from acute hospitals (from 77.8% to 50.2%). Most teams have shown a broadening of referral routes between the two study periods; team 5 showed only three referral routes in the first study and this had broadened to seven referral routes in the second study.
Key point 74: the majority of teams (four out of seven) have shown an increase in the percentage of referrals from acute hospital wards and a decrease (four out of seven) in referrals from AHPs to IC over the period studied.
Key point 75: all teams, except teams 4 and 5 (which remained on 0%), showed a decline in referrals from social services.
Key point 76: the number of referral routes to IC has increased over time.
We investigated whether or not the referral route has an impact on patient outcome. It is possible that some referrers will be able to refer patients who would be more likely to benefit from IC, whereas others may not be identifying patients who would be the most appropriate for these services.
Figure 22 relates the referral route with changes in impairment on the TOM. This indicates that referrals from A&E and acute hospitals benefit most with the least benefit coming from those directly referred by nurses and social services.
FIGURE 22.
Change in TOM impairment by referral route.

This finding is confirmed by examining referral routes against the EQ-5D (Figure 23).
FIGURE 23.
Change in EQ-5D score by referral route.

Key point 77: there are small differences in impairment and health-related QoL related to referral routes into IC services.
Changes in patient characteristics at admission
Table 23 in Chapter 7 shows the percentage of patients with each LoC at admission for each of the two studies. This is shown individually for each of the seven teams, that were in both studies, the average of the data from the teams, that were in both studies and for all the data.
Key point 78: the nature of referrals has changed over time in different ways for different teams.
The average LoC at admission, when considering the teams that were included in both studies (see Table 23), indicates a slightly higher percentage not requiring IC and more requiring slow-stream rehabilitation. However, when reviewing the data from all teams in both studies, it is noticeable that there has also been an increase in the numbers of patients not needing any intervention (but from a higher baseline) which may lead one to consider whether or not there has been an increase in the number of inappropriate referrals over time. Across the whole data set, there is also a large increase in LoC = 1 (needs prevention/maintenance programme).
Key point 79: there is some indication of an increase in inappropriate referrals to IC in more recent years.
Therapy outcome measures
Despite this increase in inappropriate referrals, there is some indication from the two studies that the proportion of patients being referred to IC who have more severe impairments has increased over time with 23% having scores of 2.5 or lower in COOP1 and 29.7% having scores of 2.5 or lower in EEICC2 (Table 26). Many patients with severe impairments would not be seen as likely to benefit from enablement or rehabilitation; their needs being judged as requiring more social care support alone.
| TOM impairment score on admission | Study | |
|---|---|---|
| COOP,1 % (n) of patients (N = 456) | EEICC,2 % (n) of patients (N = 2172) | |
| 0–2.5 | 23 (105) | 29.7 (645) |
| 3–5 | 77 (351) | 70.3 (1527) |
However, these averages fail to demonstrate the complexity at an individual team level, as demonstrated in Figure 24. Although patients in some teams (teams 2, 3, 4 and 5) show more impairment in the second study, patients in teams 1, 6 and 7 are (on average) less severely impaired.
FIGURE 24.
Therapy outcome measures impairment at admission for study 1 and 2. a, The average of the seven teams; and b, the average of all teams combined.
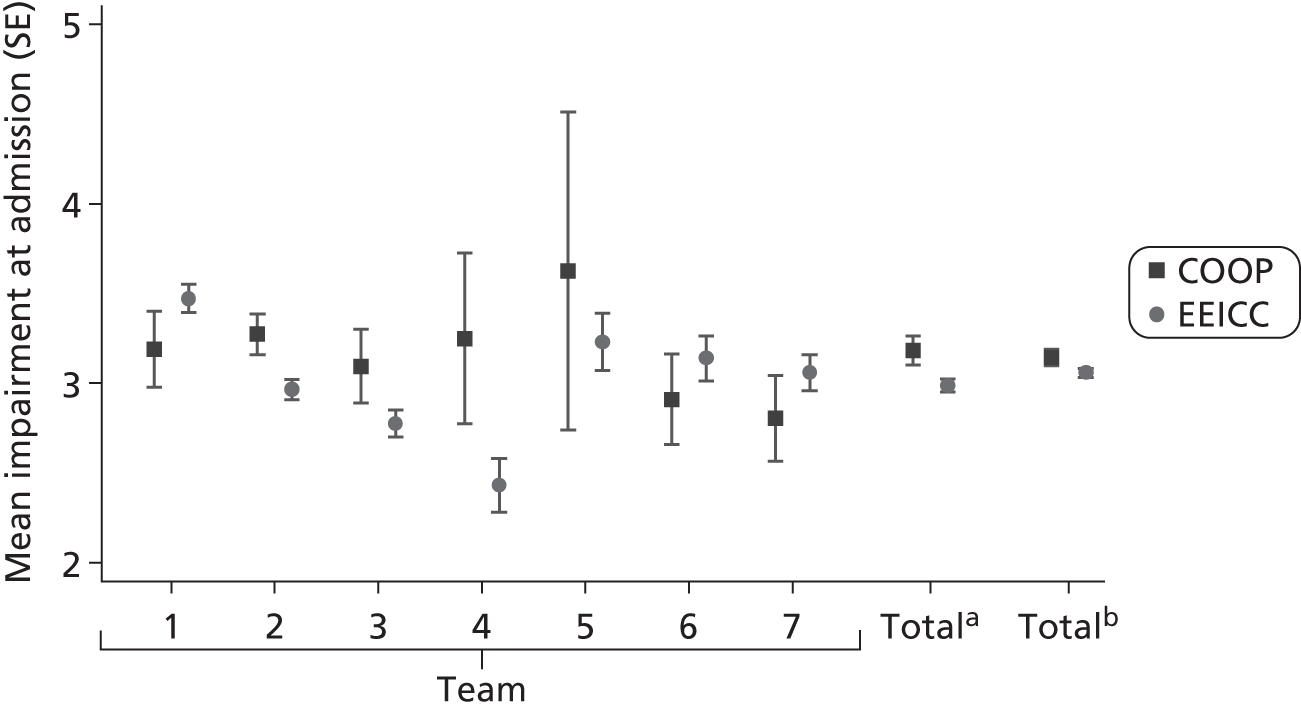
Although the trend is towards more severely impaired patients, the activity scores of the TOM do not show much difference between the studies (Table 27).
| TOM activity score on admission | Study | |
|---|---|---|
| COOP,1 % (n) of patients (N = 460) | EEICC,2 % (n) of patients (N = 2172) | |
| 0–2.5 | 25.2 (116) | 27.9 (605) |
| 3–5 | 74.8 (344) | 72.1 (1567) |
Key point 82: a higher proportion of patients with more severe impairments are being referred to IC.
EQ-5D
There is little overall change between the studies for the health-related QoL measure on admission for patients from the seven teams included in both studies. However, for data from the whole study, there is a slight improvement (Figure 25). Three of the seven teams show an improvement in the health status of their patient population on admission for this measure, whereas four teams show a decline over time.
FIGURE 25.
The EQ-5D score at admission. a, The average of the seven teams; and b, the average of all teams combined.
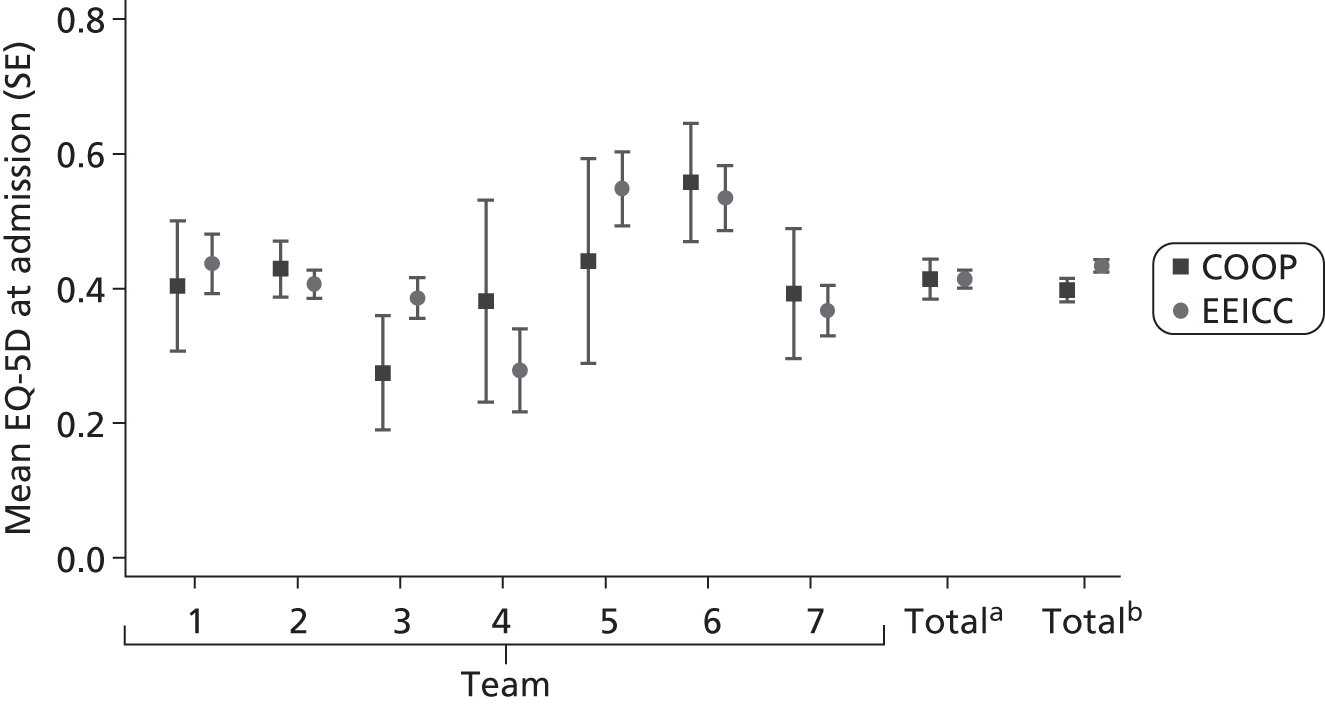
Discussion
We were surprised that so little research had been conducted into the impact of health policy on service provision for care of the elderly. There is a lot to be learned from monitoring change over time in service provision and its impact on outcomes.
All new services take some time to be integrated into the cohesive structure of integrated care so it is not overly surprising that the numbers of referrals to IC have increased over time. Furthermore, this trend has been encouraged by explicit Department of Health policy and NHS incentives to care for the frail elderly within the community. However, there remains substantial variation between IC teams in the number of referrals they receive through different routes and the increase in numbers over time. The greatest change has been in referrals from acute hospitals and we suspect that this was associated with greater emphasis on reducing length of stay. This could be one of the reasons why a greater percentage of more impaired patients are being referred to IC.
The number of referral routes to IC has increased, which is likely to be associated with greater recognition of the services provided by a broader community of health- and social-care professionals.
The finding that those referred by A&E and hospital departments improved to a greater extent than those referred directly by nurses, many of whom would be community based, is not surprising. It is likely that these patients would have had acute disabling conditions, whereas a greater proportion of those referred from the community would have chronic/frail and declining conditions.
Objective 4 Service toolkit
Chapter 9 Development of a service toolkit to guide providers and commissioners of services
Research that this team has conducted over the last decade has convinced us that collecting routine data and feeding the results back to IC teams facilitates improved service delivery. The two forms of formalised methods are health dashboards and benchmarking tools.
A dashboard is a tool, primarily for internal service use, which is used as a summary display for ongoing performance/outputs. It is largely a tool for internal, comparative use allowing comparison of changes in performance over time or over different population groups. They are often presented on a single page and have different graphical displays of related data sets. The idea is that looking at different visual displays of related data enables clear representation of relationships between the internal data.
Benchmarking is often used for both internal and external audiences and allows comparison of performance between different organisations. It does not lend itself to the one-page dashboard display, but provides more complex information.
Combining the two data sets from the projects has allowed us to examine the utility, validity and reliability of the data collection tools. Literature searches (see Appendix 1) were also undertaken to explore the use of toolkits in IC settings. Based on this research, we are confident that these tools can be used to populate both tiers of monitoring approaches for use in the IC environment. The first is a clinical dashboard, which could be used in the clinical context as a summary display aiming to monitor ongoing performance and outputs relative to population type. The second is a benchmarking tool, which could be used to compare performance and activity across different IC services.
The clinical dashboard will provide a real-time, visual display of the key patient characteristics, which may be associated with outcomes (age, sex, normal living arrangements, referral source, LoC at admission), staffing inputs (staff-to-bed-day ratio, total number of staff and qualified-to-support staff ratio) and outcomes data (length of stay, discharge destination, death, admission to higher-level care/hospital). This would allow a service to monitor change over time and identify issues related to their performance.
The benchmarking framework will provide a basis for comparison between services, for example the specific service performance as compared with amalgamated ‘all team’ performance against the following criterion. For example, Figure 26 illustrates the referrals from a particular trust over different periods of time to compare patient needs referred with different services.
FIGURE 26.
Illustration of dashboard of quarterly referrals.
Whereas Figure 27 compares the LoC of patients related with different IC services.
FIGURE 27.
Comparison of the LoC of patients admitted to 11 IC services.

To make valid comparisons in benchmarking, it is important that services collect similar information at the same point in time. We would suggest that the data in Box 1 are considered for the purposes of benchmarking.
Age (mean and bar chart).
Sex (pie chart or % female).
LoC need at admission and discharge (pie chart showing proportions).
TOM scores on admission and discharge.
EQ-5D score on admission.
Place where care provided (% home/institution, bed vs. home).
Staffing ratiosAmount of input from support staff, qualified staff (breakdown by discipline type by hours).
Referral sources (pie chart).
Outcomes of careLength of stay (mean and tabulated by LoC on admission).
Discharge destination.
Change in health status.
The data in Box 2 would be more appropriate for use in a dashboard.
Age (mean and bar chart).
Sex (pie chart or % female).
LoC need at admission and discharge (pie chart showing proportions).
Therapy outcome measure and discharge (pie chart showing proportions).
Place where care provided (% home/institution, bed vs. home).
Staffing ratiosAmount of input from support staff, qualified staff (breakdown by discipline type by hours).
Referral sources (pie chart).
Outcomes of careLength of stay (mean and tabulated by LoC on admission).
Discharge destination.
Change in health status.
Having established the data collection tools for developing a dashboard and benchmarking, we have entered an arrangement with an industrial partner to test methods of data collection from different services, the requirements for analysis and establish the different needs for styles/format of results and feedback. This pilot study will result in the industrial partner being able to provide services, which can be marketed to providers.
Chapter 10 Discussion
This secondary analysis came from two studies, the first involving 20 teams incorporating 158 team members and the second 11 teams incorporating 253 team members. Seven of these teams took part in both studies. A total of 8070 patients had been referred to these teams for IC at two different time points. The purposes of combining the data from these studies were threefold. First, to identify those patients most likely to benefit from IC; second, to examine the effectiveness of different models of IC; and third, to explore the differences between IC service configurations and how they have changed over time. We have used the findings to provide evidence to guide service commissioning and monitoring.
When considering patients most likely to benefit from IC, we found from the updated literature reviews (2008–11) that there was little new evidence in some areas, but what was available supported the secondary data analysis. A key message from the literature review is that RCTs mostly study older people with specific medical (stroke, COPD, CHF) and surgical conditions (fractured neck of femur, CABG). Most trials are related to specific conditions and do not include the general population of service users, which are for the frail elderly who have several medical and social problems. However, the literature provides evidence that the rates of improvement in patients admitted to IC are often modest, with two studies showing that only around one-third of patients improve in any measurable way. Given the frailty of most of the patients admitted to IC, it could be that no decline in health status is also a positive outcome and the definition of success of IC services may need to be considered further.
Studies reported in the literature review showed evidence that age, cognitive impairment, living alone at admission and functional status at admission have an influence on the outcomes of patients using IC; however, the strength and direction of these findings was not consistent enough to draw conclusions. Gaps in the evidence base concern the best place to provide care for this population (specifically the use of residential and nursing home settings) as well as meeting the combined health and social care needs of patients with dementia, palliative and end-of-life care needs.
The overall outcomes of the secondary analysis showed that, on average, 60% of patients remain at or return home following an episode of IC. On average, 43% of patients improved on the measure of TOM impairment, 44% on TOM activity, 37% on TOM participation and 32% on TOM well-being. Two-thirds of patients (66%) improved on the EQ-5D measurement after data imputation.
Factors that were statistically associated with a change in TOM scores were patient age (improvement declines with age), sex (females more likely to improve), LoC at admission, living in own home, receiving care in own home or IC facilities, referrals made by acute hospitals and having a lower TOM (impairment) score at admission.
Our data indicate that the patients most likely to make the greatest improvements were those with acute onset medical conditions being referred from A&E for acute hospitals identified as requiring rehabilitation on the LoC tool. Those with long-term chronic conditions incorporating several different impairments did less well, i.e. they showed fewer positive improvements in EQ-5D and TOM scores, and chronicity was more important than age or sex in indicating benefits.
Patients who entered IC with high scores on EQ-5D and TOMs appeared to do less well, but we suspect that this is due to the ceiling effect of the measures. This assertion is supported by the finding that those with LoC of 0 (‘client does not need any intervention’) showed less change than other levels. A considerable number of patients referred to IC were identified as inappropriate referrals and did not need the intervention that they had been referred for. The findings indicate that the percentage of these patients is increasing over time. There are many possible reasons for the high number of inappropriate referrals, including referrers being unfamiliar with other community services, which may be more appropriate.
A consistent message emerges from the literature and the secondary analysis of the data when considering which factors are associated with preventing hospital admission on reducing length of stay of patients requiring IC. This is the capacity of the IC service to meet the client’s (often complex) care needs. Hospital admissions will be minimised when the services are sufficiently integrated across the interface between hospital and the community, ensuring that the patient’s care needs can be matched to the available service in the setting to which the client is best suited and that transitions of care between different levels of services can be managed seamlessly.
Our data indicate significant variation between clinical teams in the rates of admission to hospital (range 0–21%) from IC. This is consistent with the literature that factors other than specific care model (such as the degree of integration and ease of access across the acute and secondary care interface) may be important in determining (re)admission risk. The main patient characteristic associated with increased transfer to hospital in our study was LoC of 7, a complex presenting need, which included the requirement for both rehabilitation and elements of medical care.
The main patient characteristics associated with low rates of transfer to inpatient hospital care were low LoC need (no need and preventive need only) and being resident in nursing home care. In the latter case, although care needs may be high, or complex, the surrounding environment and (possibly) care plans and policies, may be conducive to receiving such care in situ.
When considering factors that predict discharge from IC to long-term institutional care, for example nursing home, our study identified the following factors as being significant: residential care home as a place of IC provision, increasing age and lower TOM participation score at admission. It should be noted that < 5% of cases in our study were discharged to a long-term care setting, adding credence to the potential for IC to provide a preventative service.
In particular, the significance of TOM participation score on admission to IC as a predictor of discharge to long-term institutional care is a significant finding. Furthermore, these findings resonate with existing evidence. Langhorne et al. ,71 in a review of the effectiveness of early supported discharge, noted that patients with poor ADL scores at admission were more likely to enter long-term care. Although conceptually distinct to ADLs, the relationship between function and participation is clear.
However, it is important to note that by focusing on individual characteristics, the opportunity to explore the relationship between contextual factors and likely outcome is missed. The variations in team composition, setting, skill mix, size and integration and, in particular, the relationships with discharge destination are variables that could explain the differences in the data. These areas of investigation require further research.
The literature does not suggest that any particular IC model (admission avoidance, discharge support, community rehabilitation, nurse-led inpatient units or other clinical facility for rehabilitation or recuperation) will achieve a consistent impact on admission or readmission to inpatient hospital care. There is evidence that there has been an increase in nurse-led discharge units, which have the potential to transform the experience of discharge, but at the expense of somewhat increased hospital inpatient resource use. These have been shown to reduce readmission rates significantly in some analyses. Essentially, this was achieved by taking time to prepare patients for discharge and effectively managing the timing of discharge to suit their needs by increasing duration of inpatient stay. In the new policy environment, in which early readmission is becoming the financial responsibility of the discharging hospital, it is possible that the economics of such NLUs might be more favourable than when originally evaluated.
This secondary analysis indicates an increase in the death rate of patients referred to intermediate/community care over the time of the two studies. This is associated with a greater number of patients receiving these services who have more complex and severe health and social care needs in more recent years. These findings are in line with the literature related to deaths within the community of older people but needs to be placed in the context of the evidence that the average inpatient geriatric medical acute unit expects a mortality rate of around 20% of inpatients and higher. The determinants of death in inpatient care are the same as we found in these community studies (i.e. severity and complexity of health condition and previous functional health status). However, although IC services may have seen a rise in mortality, they are receiving patients at a relatively lower risk of death than the population they are likely to have originated from. As more ill and needy patients are receiving IC the question arises whether or not palliative care services should be integrated to meet those needs. Although surveys consistently find that people would prefer to die in their own home,83 people with palliative and supportive care needs are often explicitly excluded from IC trials, thus leaving little supportive evidence. There is a trend towards integrating rehabilitation and IC services with those of palliative care for older people. Although community provision of this care may well be appropriate, a recent meta-analysis (of more than 10,000 patients) indicated that comprehensive geriatric assessment reduces deterioration of health, yet increases costs. 84 The trend for more palliative care in the community suggests a need for more active medical engagement in the provision of more integrated care in community settings. Skill mix is an important consideration for the appropriate support of these patients.
There is little in the literature on the economics of IC. The updated literature review indicated some empirical evidence that interdisciplinary teamworking in IC working with older patients was more effective than usual care in reducing length of stay and costs. 85 However, none of the studies directly examine which team-level factors were associated with better patient outcomes. The study by Dixon et al. 87 did find that increased skill mix was significantly associated with a 17% reduction in service costs and a high proportion of support workers were associated with better improvement in patient QoL.
The results of the statistical analysis of this combined data set found further weak empirical evidence to support the findings of the above study. Increased skill mix and higher proportions of clinical and domiciliary support workers in CRAIC/S teams were significantly associated with improvements in impairment scores using the TOM tool. However, it must be noted that the study by Dixon et al. 87 utilised one of the two original data sets that formed the combined data set for this study. 89
Although this study represents the most comprehensive attempt to explain differences in costs and cost-effectiveness across different IC teams, it has its limitations and is unable to identify consistent and clear relationships relating to staffing. This suggests that efficiency savings are possible by many services by reducing staff costs to levels seen in comparable teams. However, the identification of comparable teams is problematic as there are profound differences between the teams and their contexts that are not readily explained quantitatively.
Our results, although tenuous given the data, indicate highly heterogeneous services with costs per patient ranging between £318 and £11,511, with patient characteristics being the dominant explanatory effects. Cost-effectiveness is also highly variable with only size of service showing any sign of an explanatory effect. Staffing patterns as described by the proportion of qualified staff and number of different types of staff have little or no influence on costs and relative cost-effectiveness.
These results add to a growing body of literature that show highly variable costs, outcomes and inconsistent relationships relating to staffing patterns. 1,86 The massive heterogeneity of services, which is likely to be associated with different referral criteria and alternative associated support services as well as staffing and methods of delivery of care, is likely to have an impact on our ability to identify any relationships that exist. Indeed, the variability may also suggest that comparisons between the services are not sensible. A service with an average duration of care of 1 day cannot be designed to deliver the same care packages as a service with an average duration of care of 138 days.
This study highlights the need for funding high-quality studies that attempt to examine which specific team-level factors are associated with better outcomes for patients. Within this, there are strong indications in qualitative studies that, rather than definitive (quantitative) team outcome variables, many softer (qualitative) team process variables may contribute to better patient outcomes. These findings reflect the general focus within wider teamworking literature on process-level variables. It is, therefore, important that studies in the future attempt empirically to examine which process-level team variables are associated with patient outcomes.
The combined data sets incorporated studies over a decade, which allows examination of change of the services over time. However, only a small number of teams124 were included in both studies. Interestingly, the total number of staff within teams increased slightly for the studies as a whole, but decreased substantially for the teams that took part in both studies. The total number of different types of staff increased overall and for teams from both studies. These findings would suggest that the overall team size is increasing slightly, the number of management staff is increasing slightly and there are a greater range of roles and increased skill mix in IC services. Numbers of social care staff increased from a very low baseline, while clinical support staff numbers were noticeably reduced. However, when viewed on a team-by-team basis, the picture is much more complicated. Although some teams remained quite stable on these measures, others changed drastically and not in a uniform direction. Therefore, slight mean increases shown in the aggregated data sets disguise the radical and unpredictable changes experienced by some individual teams.
The changes highlighted in the teams that took part in these projects continue to reflect the diversity of the delivery of care through IC services. Far from there being any uniformity regarding models of service organisation, there is no coherent direction of service development. The large variation in this small sample hints at the difficulty of categorising IC services and the complexity of predicting how they might develop.
All new services take some time to be integrated into the cohesive structure of care so it is not surprising that the numbers of referrals to IC have increased over time. Furthermore, this trend has been encouraged by explicit Department of Health policy and NHS incentives to care for the frail elderly within the community. There remains substantial variation between IC teams in the number of referrals they receive through different routes and the increase in numbers over time. The greatest change has been an increase in referrals from acute hospitals and we suspect that this was associated with greater emphasis on reducing length of stay. This could be one of the reasons why a greater percentage of more impaired patients are being referred to IC.
The number of referral routes to IC has increased over time, which is likely to be associated with greater recognition of the services provided by a broader community of health and social care professionals.
The teams show substantial differences in size and composition while the complexity of the patients being referred are remarkably similar reinforcing our view that benchmarking services would be valuable. This should be helped by using tools chosen for use in our studies and the work we are undertaking on data capture and rapid, flexible analysis.
Implications for clinicians, purchasers and researchers
For clinicians
Adoption of the collection of consistent information would assist in monitoring change over time and benchmarking practice. The tools used in this study have been found to be reliable, valid and easy to use.
The aims and objectives of IC services should be explicit and agreed by team members and approved by purchasers and referrers.
For purchasers
Determining the skill mix required within an IC team is important. An increased range of professional disciplines within the team was associated with reduced costs and better outcomes. An increased number of non-professional support staff was associated with better outcomes but increased costs. Appropriate management structure and good management practices are associated with better interdisciplinary working.
Consideration should be given to the issue of incorporating palliative care into IC.
Many referrers appeared to be unclear as to which services are available for them to refer patients to on discharge from hospital or to consider in the prevention of admission. This led to many inappropriate referrals to IC teams, which are time-consuming, and delayed access to appropriate services.
For researchers
There are many different models of IC. Direct comparison of these is difficult without a randomised trial. Comparing community-based IC with bed-based IC is required. A randomised study of patients receiving care from teams staffed with different professional groupings would be valuable.
Acknowledgements
We thank the following for their contribution to this report:
The authors would like to thank all of the staff members, managers and commissioners at the study sites who gave valuable time effort and support for the two original projects. Particular thanks go to the administrative staff and clinicians who co-ordinated data collection, staff training and research meetings. Additionally, we appreciate the contribution to the projects by many patients and their carers.
Adele Blinston was the project administrator for EEICC 1. 2 She also helped to compile this report and assisted with proof reading and formatting.
Andrew Booth and Anna Cantrell conducted the original literature reviews for COOP1 and EEICC. 2
Data input and data management assistance was provided by various casually employed staff. Particular thanks go to Poppy Roworth and Sam Cooke who worked on the EEICC 1 project. 2 Sam Cooke also contributed to data preparation and to preliminary analyses of quantitative and qualitative data.
Contributions of authors
The authors of this report are listed in agreed order related to their contribution. The following were involved in the construction of the original bid, including the research design: Pamela Enderby, Ann McDonnell, Tony Smith, Susan Nancarrow, Stuart Parker, Michael Campbell, Steven Ariss, Mike Bradburn and Anthony Ryan.
All authors were part of the project-working group, who met regularly throughout the project. A Project Management Committee consisted of Professor Pamela Enderby, Dr Steven Ariss and Mr Mike Bradburn and was responsible for the day-to-day management of the project. Professor Pamela Enderby was the chief investigator, Dr Steven Ariss was the project manager and Mr Mike Bradburn managed the data cleaning and statistical analyses.
The specific contribution of each author is listed below.
Dr Steven M Ariss (research fellow, Health Service Research) was the project manager for this project (EEICC 2) and for study 2 (EEICC). 2 He led the analysis and writing of Chapter 7. He led the collection and analysis of qualitative data and managed the quantitative data for study 2 (EEICC). 2 He carried out the initial data cleaning of the EEICC2 data set, prior to input to Stata. He also assisted Professor Pamela Enderby in compiling and editing this final report.
Professor Pamela M Enderby (Professor of Community Rehabilitation) was the chief investigator of this project. She contributed to both previous projects (COOP1 and EEICC). 2 She assisted with data cleaning, analyses and interpretation of the findings. She provided leadership to the working group and compiled the final report. She was lead author on Chapter 8.
Dr Tony Smith (senior lecturer, Health and Social Care Leadership) was a codesigner of the proposal for EEICC 12 and project manager, and a contributor to the EEICC 2 proposal. He led the analysis and writing of Chapter 5. He led the collection and input of qualitative data (EEICC 1). 2 He also assisted Professor Pamela Enderby in compiling and editing this final report.
Professor Susan A Nancarrow was the principal investigator on the COOP1 project. She reviewed and edited two drafts of the final compiled report, reformatted and restructured Chapter 1 (combined two original sections into one) and developed an outline of the proposed benchmarking framework.
Mike J Bradburn was the lead statistician. He undertook the merger of the databases and data manipulation, led the quantitative analysis and contributed to the writing of the report.
Deborah Harrop co-ordinated and carried out the literature reviews and was responsible for the citations and references in this report.
Professor Stuart G Parker was the joint lead author of Chapter 1 and lead author of Chapter 2.
Professor Ann McDonnell (Reader in Health and Social Care Research) led the literature review and the analysis of data to explore the characteristics of patients whose health does not improve or declines in IC. She led the writing up of this work and was joint lead for Chapter 1.
Professor Simon Dixon was responsible for the economic analysis and was the lead author for Chapter 6.
Dr Tony Ryan was the lead author of Chapter 3.
Alexandra Hayman undertook additional quantitative analyses and contributed to the writing of the report.
Professor Michael Campbell (Professor of Medical Statistics), was a co-applicant and attended management meetings and advised on data collection, form design and statistical analysis.
Project advisory group
The research advisory group was chaired by David Quinney and included representatives with extensive experience of care service management, service delivery, statistical analysis and a lay member. Members were Fiona Shield, Stuart Parker, Michael Campbell and Christine Allmark. This group provided valuable direction for the project and a knowledgeable external perspective.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Nancarrow SA, Enderby PM, Moran AM, Dixon S, Parker SG, Bradburn MJ, et al. The Relationship Between Workforce Flexibility and the Costs and Outcomes of Older Peoples’ Services (COOP). Southampton: NIHR SDO; 2010.
- Nancarrow SA, Enderby PM, Ariss SM, Smith T, Booth A, Campbell MJ, et al. The Impact of Enhancing the Effectiveness of Interdisciplinary Working (EEICC). Southampton: NIHR SDO; 2012.
- Whitfield L. Feeling the Chill. Health Serv J 1997;107.
- The NHS Plan: A Plan for Investment, A Plan for Reform. London: Department of Health; 2000.
- National Service Framework for Older People. London: Department of Health; 2001.
- National Audit of Intermediate Care Report 2012. London: NHS Benchmarking Network; 2012.
- Inpatient Admissions and Bed Management in NHS Acute Hospitals. London: The Stationery Office; 2000.
- Supporting People With Long Term Conditions: An NHS and Social Care Model to Support Local Innovation and Integration. London: Department of Health; 2005.
- End of Life Care Strategy: Promoting High Quality Care for All Adults at the End of Life. London: Department of Health; 2008.
- Barton P, Bryan S, Glasby J, Hewitt G, Jagger C, Kaambwa B, et al. A National Evaluation of the Costs and Outcomes of Intermediate Care for Older People. Birmingham and Leicester: University of Birmingham and University of Leicester; 2005.
- Shepperd S, Doll H, Angus RM, Clarke MJ, Iliffe S, Kalra L, et al. Hospital at home admission avoidance. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.CD007491.
- Shepperd S, Doll H, Broad J, Gladman J, Iliffe S, Langhorne P, et al. Hospital at home early discharge. Cochrane Database Syst Rev 2009;1. http://dx.doi.org/10.1002/14651858.CD000356.pub3.
- Ward D, Drahota A, Gal D, Severs M, Dean TP. Care home versus hospital and own home environments for rehabilitation of older people. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.CD003164.pub2.
- Caplan GA, Sulaiman NS, Mangin DA, Ricauda NA, Wilson AD, Barclay L. A meta-analysis of ‘hospital at home’. Med J Aust 2012;197:512-19. http://dx.doi.org/10.5694/mja12.10480.
- Landi F, Bernabei R, Russo A, Zuccalà G, Onder G, Carosella L, et al. Predictors of rehabilitation outcomes in frail patients treated in a geriatric hospital. J Am Geriatr Soc 2002;50:679-84. http://dx.doi.org/10.1046/j.1532-5415.2002.50162.x.
- Kaambwa B, Bryan S, Barton P, Parker H, Martin G, Hewitt G, et al. Costs and health outcomes of intermediate care: results from five UK case study sites. Health Soc Care Community 2008;16:573-81. http://dx.doi.org/10.1111/j.1365-2524.2008.00780.x.
- Pereira S, Chiu W, Turner A, Chevalier S, Joseph L, Huang A, et al. How can we improve targeting of frail elderly patients to a geriatric day-hospital rehabilitation program?. BMC Geriatr 2010;10. http://dx.doi.org/10.1186/1471-2318-10-82.
- Fusco D, Bochicchio GB, Onder G, Barillaro C, Bernabei R, Landi F. Predictors of rehabilitation outcome among frail elderly patients living in the community. J Am Med Dir Assoc 2009;10:335-41. http://dx.doi.org/10.1016/j.jamda.2009.02.004.
- Gitlin LN, Winter L, Dennis MP, Hauck WW. Variation in response to a home intervention to support daily function by age, race, sex, and education. J Gerontol A Biol Sci Med Sci 2008;63:745-50. http://dx.doi.org/10.1093/gerona/63.7.745.
- Comans TA, Currin ML, Brauer SG, Haines TP. Factors associated with quality of life and caregiver strain amongst frail older adults referred to a community rehabilitation service: implications for service delivery. Disabil Rehabil 2011;33:1215-21. http://dx.doi.org/10.3109/09638288.2010.525288.
- Langhorne P, Dennis M, Kalra L, Shepperd S, Wade D, Wolfe CDA. Services for helping acute stroke patients avoid hospital admission. Cochrane Database Syst Rev 1999;3.
- Early Supported Discharge Trialists . Services for reducing duration of hospital care for acute stroke patients. Cochrane Database Syst Rev 2005;2.
- Ram F, Wedzicha J, Wright J, Greenstone M. Hospital at home for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2003;4.
- Anderson C, Rubenach S, Mhurchu CN, Clark M, Spencer C, Winsor A. Home or hospital for stroke rehabilitation? Results of a randomized controlled trial I: health outcomes at 6 months. Stroke 2000;31:1024-31. http://dx.doi.org/10.1161/01.STR.31.5.1024.
- Fjaertoft H, Indredavik B, Lydersen S. Stroke unit care combined with early supported discharge: long-term follow-up of a randomized controlled trial. Stroke 2003;34:2687-91. http://dx.doi.org/10.1161/01.STR.0000095189.21659.4F.
- von Koch L, Widen Holmqvist L, Kostulas V, Almazan J, de Pedro-Cuesta J. A randomized controlled trial of rehabilitation at home after stroke in Southwest Stockholm: outcome at six months. Scand J Rehab Med 2000;32:80-6. http://dx.doi.org/10.1080/003655000750045596.
- Mayo NE, Wood-Dauphinee S, Côté R, Gayton D, Carlton J, Buttery J, et al. There’s no place like home: an evaluation of early supported discharge for stroke. Stroke 2000;31:1016-23. http://dx.doi.org/10.1161/01.STR.31.5.1016.
- Wells M, Thompson A, Harrow A, Donnan P, Davey P, Devereux S, et al. Patient, carer and health service outcomes of nurse-led early discharge after breast cancer surgery: a randomised controlled trial. Br J Cancer 2004;91:651-8.
- Penque S, Petersen B, Arom K, Ratner E, Halm M. Early discharge with home health care in the coronary artery bypass patient. Dimens Crit Care Nurs 1999;18:40-8. http://dx.doi.org/10.1097/00003465-199911000-00007.
- Ojoo JC, Moon T, McGlone S, Martin K, Gardiner ED, Greenstone MA, et al. Patients’ and carers’ preferences in two models of care for acute exacerbations of COPD: results of a randomised controlled trial. Thorax 2002;57:167-9. http://dx.doi.org/10.1136/thorax.57.2.167.
- Wong FKY, Mok MPH, Chan T, Tsang MW. Nurse follow-up of patients with diabetes: randomized controlled trial. J Adv Nurs 2005;50:391-402. http://dx.doi.org/10.1111/j.1365-2648.2005.03404.x.
- Cunliffe AL, Gladman JRF, Husbands SL, Miller P, Dewey ME, Harwood RH. Sooner and healthier: a randomised controlled trial and interview study of an early discharge rehabilitation service for older people. Age Ageing 2004;33:246-52. http://dx.doi.org/10.1093/ageing/afh076.
- Miller P, Gladman JRF, Cunliffe AL, Husbands SL, Dewey ME, Harwood RH. Economic analysis of an early discharge rehabilitation service for older people. Age Ageing 2005;34:274-80. http://dx.doi.org/10.1093/ageing/afi058.
- Crotty M, Whitehead C, Miller M, Gray S. Patient and caregiver outcomes 12 months after home-based therapy for hip fracture: a randomized controlled trial. Arch Phys Med Rehabil 2003;84:1237-9. http://dx.doi.org/10.1016/S0003-9993(03)00141-2.
- Caplan GA, Ward JA, Brennan NJ, Coconis J, Board N, Brown A. A hospital in the home: a randomised controlled trial. Med J Aust 1999;170:156-60.
- Caplan GA, Coconis J, Board N, Sayers A, Woods J. Does home treatment affect delirium? A randomised controlled trial of rehabilitation of elderly and care at home or usual treatment (The REACH-OUT trial). Age Ageing 2006;35:53-60. http://dx.doi.org/10.1093/ageing/afi206.
- Fjaertoft H, Rohweder G, Indredavik B. Stroke unit care combined with early supported discharge improves 5-year outcome: a randomized controlled trial. Stroke 2011;42:1707-11. http://dx.doi.org/10.1161/STROKEAHA.110.601153.
- Koh GCH, Saxena SK, Ng TP, Yong D, Fong NP. Effect of duration, participation rate, and supervision during community rehabilitation on functional outcomes in the first poststroke year in Singapore. Arch Phys Med Rehabil 2012;93:279-86. http://dx.doi.org/10.1016/j.apmr.2011.08.017.
- Mallinson TR, Bateman J, Tseng H-Y, Manheim L, Almagor O, Deutsch A, et al. A comparison of discharge functional status after rehabilitation in skilled nursing, home health, and medical rehabilitation settings for patients after lower-extremity joint replacement surgery. Arch Phys Med Rehabil 2011;92:712-20. http://dx.doi.org/10.1016/j.apmr.2010.12.007.
- Hogg W, Lemelin J, Dahrouge S, Liddy C, Armstrong CD, Legault F, et al. Randomized controlled trial of anticipatory and preventive multidisciplinary team care: for complex patients in a community-based primary care setting. Can Fam Physician 2009;55:76-85.
- Courtney M, Edwards H, Chang A, Parker A, Finlayson K, Hamilton K. Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: a randomized controlled trial to determine the effectiveness of a 24-week exercise and telephone follow-up program. J Am Geriatr Soc 2009;57:395-402. http://dx.doi.org/10.1111/j.1532-5415.2009.02138.x.
- Allen K, Hazelett S, Jarjoura D, Hua K, Wright K, Weinhardt J, et al. A randomized trial testing the superiority of a postdischarge care management model for stroke survivors. J Stroke Cerebrovasc Dis 2009;18:443-52. http://dx.doi.org/10.1016/j.jstrokecerebrovasdis.2009.02.002.
- Carratala J, Fernandez-Sabe N, Ortega L, Castellsague X, Roson B, Dorca J, et al. Outpatient care compared with hospitalization for community–acquired pneumonia: a randomized trial in low-risk patients. Ann Intern Med 2005;142:165-72. http://dx.doi.org/10.7326/0003-4819-142-3-200502010-00006.
- Schafer JL. Analysis of Incomplete Multivariate Data. London: Chapman & Hall; 1997.
- van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat Meth Med Res 2007;16:219-42. http://dx.doi.org/10.1177/0962280206074463.
- Griffiths P, Wilson-Barnett J, Richardson G, Spilsbury K, Miller F, Harris R. The effectiveness of intermediate care in a nursing-led in-patient unit. Internat J Nurs Stud 2000;37:153-61. http://dx.doi.org/10.1016/S0020-7489(99)00061-9.
- Griffiths P, Harris R, Richardson G, Hallett N, Heard S, Wilson-Barnett J. Substitution of a nursing-led inpatient unit for acute services: randomized controlled trial of outcomes and cost of nursing-led intermediate care. Age Ageing 2001;30:483-8. http://dx.doi.org/10.1093/ageing/30.6.483.
- Steiner A, Walsh B, Pickering RM, Wiles R, Ward J, Brooking JI, et al. Therapeutic nursing or unblocking beds? A randomised controlled trial of a post-acute intermediate care unit. BMJ 2001;322:453-9. http://dx.doi.org/10.1136/bmj.322.7284.453.
- Roland M, Dusheiko M, Gravelle H, Parker S. Natural history of emergency admission in older people: analysis of routine admission data. BMJ 2005;330:289-92. http://dx.doi.org/10.1136/bmj.330.7486.289.
- Gravelle H, Dusheiko M, Sheaff R, Sargent P, Boaden R, Pickard S, et al. Impact of case management (Evercare) on frail elderly patients: controlled before and after analysis of quantitative outcome data. BMJ 2007;334:31-4. http://dx.doi.org/10.1136/bmj.39020.413310.55.
- Sheaff R, Boaden R, Sargent P, Pickard S, Gravelle H, Parker S, et al. Impacts of case management for frail elderly people: a qualitative study. J Health Serv Res Policy 2009;14:88-95. http://dx.doi.org/10.1258/jhsrp.2008.007142.
- Steiner WA, Ryser L, Huber E, Uebelhart D, Aeschlimann A, Stucki G. Use of the ICF model as a clinical problem-solving tool in physical therapy and rehabilitation medicine. Phys Therapy 2002;82:1098-107.
- Melis RJF, van Eijken MIJ, Teerenstra S, van Achterberg T, Parker SG, Borm GF, et al. A randomized study of a multidisciplinary program to intervene on geriatric syndromes in vulnerable older people who live at home (Dutch EASYcare Study). J Gerontol A Biol Sci Med Sci 2008;63:283-90. http://dx.doi.org/10.1093/gerona/63.3.283.
- Billings J, Dixon J, Mijanovich T, Wennberg D. Case finding for patients at risk of readmission to hospital: development of algorithm to identify high risk patients. BMJ 2006;333:327-30. http://dx.doi.org/10.1136/bmj.38870.657917.AE.
- Creating a Patient Led NHS – Delivering the NHS Improvement Plan. London: Department of Health; 2005.
- Equity and Excellence: Liberating the NHS. London: The Stationery Office; 2010.
- Parker G, Lindesay J, Shepperdson B, Wilson A, Bhakta P, Katbamna S, et al. Best place of care for older people after acute and during subacute illness: a systematic review. J Health Serv Res Policy 2000;5:176-89.
- Parker SG, Jones DR, Peet SM, McPherson A, Cannaby AM, Abrams K, et al. A systematic review of discharge arrangements for older people. Health Technol Assess 2002;6.
- Parker SG. Do Current Discharge Arrangements from Inpatient Hospital Care for the Elderly Reduce Readmission Rates, the Length of Stay or Mortality, or Improve Health Status?. Copenhagen: World Health Organization Regional Office for Europe (Health Evidence Network Report); 2005.
- Regen E, Martin G, Glasby J, Hewitt G, Nancarrow S, Parker H. Challenges, benefits and weaknesses of intermediate care: results from five UK case study sites. Health Soc Care Community 2008;16:629-37. http://dx.doi.org/10.1111/j.1365-2524.2008.00788.x.
- Beswick AD, Rees K, Dieppe P, Ayis S, Gooberman-Hill R, Horwood J, et al. Complex interventions to improve physical function and maintain independent living in elderly people: a systematic review and meta-analysis. Lancet 2008;371:725-35. http://dx.doi.org/10.1016/S0140-6736(08)60342-6.
- Woodford HJ, George J. Intermediate care for older people in the UK. Clin Med 2010;10:119-23. http://dx.doi.org/10.7861/clinmedicine.10-2-119.
- Buurman BM, Parlevliet JL, van Deelen BAJ, de Haan RJ, de Rooij SE. A randomised clinical trial on a comprehensive geriatric assessment and intensive home follow-up after hospital discharge: the Transitional Care Bridge. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-296.
- Fleischer S, Roling G, Beutner K, Hanns S, Behrens J, Luck T, et al. Growing old at home – a randomized controlled trial to investigate the effectiveness and cost-effectiveness of preventive home visits to reduce nursing home admissions: study protocol. BMC Public Health 2008;8. http://dx.doi.org/10.1186/1471-2458-8-185.
- Griffiths PD, Edwards MH, Forbes A, Harris RL, Ritchie G. Effectiveness of intermediate care in nursing-led in-patient units. Cochrane Database Syst Rev 2007;2.
- Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996;49:1373-9. http://dx.doi.org/10.1016/S0895-4356(96)00236-3.
- Nolan M, Davies S, Grant G. Working with Older People and their Families. Buckingham: Open University Press; 2001.
- Intermediate Care. London: Department of Health; 2001.
- Community Care Statistics 2010/2011: Social Services Activity Report. Leads: Health and Social Care Information Centre; 2012.
- Shepperd S, Wee B, Straus SE. Hospital at home: home-based end of life care. Cochrane Database Syst Rev 2011;7. http://dx.doi.org/10.1002/14651858.CD009231.
- Langhorne P, Power M, Rodgers H, Ronning OM, Rudd A, Suwanwela N, et al. Early supported discharge services for stroke patients: a meta-analysis of individual patients’ data. Lancet 2005;365:501-6. http://dx.doi.org/10.1016/S0140-6736(05)17868-4.
- Garåsen H, Windspoll R, Johnsen R. Intermediate care at a community hospital as an alternative to prolonged general hospital care for elderly patients: a randomised controlled trial. BMC Public Health 2007;7. http://dx.doi.org/10.1186/1471-2458-7-68.
- Gaugler J, Duval S, Anderson A, Kane R. Predicting nurse home admission in the US: a meta-analysis. BMC Geriatr 2007;7.
- Luppa M, Luck T, Weyerer S, König H-H, Brähler E, Riedel-Heller SG. Prediction of institutionalization in the elderly. A systematic review. Age Ageing 2010;39:31-8. http://dx.doi.org/10.1093/ageing/afp202.
- McCann M, Donnelly M, O’Reilly D. Living arrangements, relationship to people in the household and admission to care homes for older people. Age Ageing 2011;40:358-63. http://dx.doi.org/10.1093/ageing/afr031.
- Dr Foster Intelligence . Your Mortality Rate Is Your Pulse 2014. http://myhospitalguide.drfosterintelligence.co.uk/#/mortality (accessed 12 February 2014).
- Saliba D, Sloss EM, Wenger NS, Elliott M, Rubenstein LZ, Solomon DH, et al. The vulnerable elders survey: a tool for identifying vulnerable older people in the community. J Am Geriatr Soc 2001;49:1691-9. http://dx.doi.org/10.1046/j.1532-5415.2001.49281.x.
- Guerini F, Frisoni GB, Morghen S, Speciale S, Bellelli G, Trabucchi M. Clinical instability as a predictor of negative outcomes among elderly patients admitted to a rehabilitation ward. J Am Med Dir Assoc 2010;11:443-8. http://dx.doi.org/10.1016/j.jamda.2009.10.005.
- Roderick PJ, Atkins RJ, Smeeth L, Mylne A, Nitsch DDM, Hubbard RB, et al. CKD and Mortality Risk in older people: a community-based population study in the United Kingdom. Am J Kidney Dis 2009;53:950-60. http://dx.doi.org/10.1053/j.ajkd.2008.12.036.
- Kazanjian RK, Drazin R, Glynn MA. Creativity and technological learning: the roles of organization architecture and crisis in large-scale projects. J Eng Technol Manage 2000;17:273-98. http://dx.doi.org/10.1016/S0923-4748(00)00026-6.
- Ostbye T, Hill G, Steenhuis R. Mortality in elderly Canadians with and without dementia. A 5-year follow-up. Neurology 1999;53:521-32. http://dx.doi.org/10.1212/WNL.53.521.
- Hirvensalo M, Rantanen T, Heikkinen E. Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. J Am Geriatr Soc 2000;48:493-8.
- Baztan JJ, Suarez-Garcia FM, Lopez-Arrieta J, Rodriguez-Manas L, Rodriguez-Artalejo F. Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta-analysis. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b50.
- Barclay S, Case-Upton S. Knowing patients’ preferences for place of death: how possible or desirable?. Br J Gen Pract 2009;59:642-3. http://dx.doi.org/10.3399/bjgp09X454052.
- Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d6553.
- Blewett LA, Johnson K, McCarthy T, Lackner T, Brandt B. Improving geriatric transitional care through inter-professional care teams. J Eval Clin Prac 2010;16:57-63. http://dx.doi.org/10.1111/j.1365-2753.2008.01114.x.
- Dixon S, Kaambwa B, Nancarrow S, Martin GP, Bryan S. The relationship between staff skill mix, costs and outcomes in intermediate care services. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-221.
- Bird S, Noronha M, Sinnott H. An integrated care facilitation model improves quality of life and reduces use of hospital resources by patients with chronic obstructive pulmonary disease and chronic heart failure. Aust J Prim Health 2010;16:326-33. http://dx.doi.org/10.1071/PY10007.
- Burton CR, Fisher A, Green TL. The organisational context of nursing care in stroke units: a case study approach. Internat J Nurs Stud 2009;46:85-94. http://dx.doi.org/10.1016/j.ijnurstu.2008.08.001.
- Smith T, Cross E, Booth A, Ariss S, Nancarrow S, Enderby P, et al. The Interdisciplinary Management Tool–Workbook 2009. www.nets.nihr.ac.uk/__data/assets/pdf_file/0020/81551/A2-08-1819-214.pdf (accessed 11 December 2014).
- The NHS Staff Council . NHS Terms and Conditions of Service Handbook, Annex B n.d. www.nhsemployers.org/SiteCollectionDocuments/AfC_tc_of_service_handbook_fb.pdf (accessed 12 February 2014).
- Developing Intermediate Care to Support Reform of Emergency Care Services. British Geriatrics Society; 2003.
- Revision to the Operating Framework for the NHS in England 2010/11. London: Department of Health; 2010.
- Moran A. A Study to Examine the Contribution of Support Workers to the Delivery and Outcomes of Community Rehabilitation and Intermediate Care Services in England. Sheffield: University of Sheffield; 2009.
- Nancarrow S. Promoting flexibility in the intermediate care workforce. J Integr Care 2003;11:25-30. http://dx.doi.org/10.1108/14769018200300055.
- Nancarrow S, Moran A, Freeman J, Enderby P, Dixon S, Parker S, et al. Looking inside the black box of community rehabilitation and intermediate care teams in the United Kingdom: an audit of service and staffing. Qual Prim Care 2009;17:323-33.
- Young J. The development of intermediate care services in England. Arch Gerontol Geriatr 2009;49:S21-5. http://dx.doi.org/10.1016/S0167-4943(09)70008-1.
- Goodman C, Drennan V, Scheibl F, Shah D, Manthorpe J, Gage H, et al. Models of inter professional working for older people living at home: a survey and review of the local strategies of English health and social care statutory organisations. BMC Health Serv Res 2011;11. http://dx.doi.org/10.1186/1472-6963-11-337.
- Nancarrow SA, Shuttleworth P, Tongue A, Brown L. Support workers in intermediate care. Health Soc Care Community 2005;13:338-44. http://dx.doi.org/10.1111/j.1365-2524.2005.00563.x.
- Delivering Care Closer to Home. London: Department of Health; 2008.
- Manthorpe J, Goodman C, Drennan V, Davies SL, Masey H, Gage H, et al. Nurse-led case management in the National Health Service: bridging clinical and social worlds. Primary Health Care Res Dev 2012;13:153-64. http://dx.doi.org/10.1017/S1463423611000533.
- Banihashemi B, Goodman SG, Yan RT, Welsh RC, Mehta SR, Montalescot G, et al. Underutilization of clopidogrel and glycoprotein IIb/IIIa inhibitors in non-ST-elevation acute coronary syndrome patients: the Canadian global registry of acute coronary events (GRACE) experience. Am Heart J 2009;158:917-24. http://dx.doi.org/10.1016/j.ahj.2009.09.016.
- Dodd J, Taylor CE, Bunyan P, White PM, Thomas SnM, Upton D. A service model for delivering care closer to home. Primary Health Care Res Dev 2011;12:95-111. http://dx.doi.org/10.1017/S1463423610000356.
- Anelay S, West MA, Carter M, Borrill C, Patterson MG, Waring J, et al. The link between the management of employees and patient mortality in acute hospitals. Internat J Human Resource Manag 2002;13:1299-310. http://dx.doi.org/10.1080/09585190210156521.
- Proudfoot JG, Bubner T, Amoroso C, Swan E, Holton C, Winstanley J, et al. Chronic care team profile: a brief tool to measure the structure and function of chronic care teams in general practice. J Eval Clin Pract 2009;15:692-8. http://dx.doi.org/10.1111/j.1365-2753.2008.01085.x.
- Martin GP, Peet SM, Hewitt GJ, Parker H. Diversity in intermediate care. Health Soc Care Community 2004;12:150-4. http://dx.doi.org/10.1111/j.0966-0410.2004.00481.x.
- Young S. Professional relationships and power dynamics between urban community-based nurses and social work case managers: advocacy in action. Prof Case Manag 2009;14:312-20. http://dx.doi.org/10.1097/NCM.0b013e3181b5de1c.
- Wilson A, Parker H. Intermediate care and general practitioners: an uncertain relationship. Health Soc Care Community 2003;11:81-4. http://dx.doi.org/10.1046/j.1365-2524.2003.00406.x.
- Harris MF, Chan BC, Daniel C, Wan Q, Zwar N, Davies GP. Development and early experience from an intervention to facilitate teamwork between general practices and allied health providers: the Team-link study. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-104.
- Plamping D. Change and resistance to change in the NHS. BMJ 1998;317:69-71. http://dx.doi.org/10.1136/bmj.317.7150.69.
- Weinberg DB, Cooney-Miner D, Perloff JN, Babington L, Avgar AC. Building collaborative capacity: promoting interdisciplinary teamwork in the absence of formal teams. Med Care 2011;49:716-23. http://dx.doi.org/10.1097/MLR.0b013e318215da3f.
- Hamilton S, Huby G, Tierney A, Powell A, Kielmann T, Sheikh A, et al. Mind the gap between policy imperatives and service provision: a qualitative study of the process of respiratory service development in England and Wales. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-248.
- McClimens A, Nancarrow S, Moran A, Enderby P, Mitchell C. ‘Riding the bumpy seas’: or the impact of the Knowledge Skills Framework component of the Agenda for Change initiative on staff in intermediate care settings. J Interprof Care 2010;24:70-9. http://dx.doi.org/10.3109/13561820903078124.
- Broekhuis M, de Blok C, Meijboom B. Improving client-centred care and services: the role of front/back-office configurations. J Adv Nurs 2009;65:971-80. http://dx.doi.org/10.1111/j.1365-2648.2009.05014.x.
- de Blok C, Meijboom B, Luijkx K, Schols J. Demand-based provision of housing, welfare and care services to elderly clients: from policy to daily practice through operations management. Health Care Anal 2009;17:68-84. http://dx.doi.org/10.1007/s10728-008-0095-7.
- NHS Modernisation Agency . Introduction to Role Redesign n.d. http://collections.europarchive.org/tna/20070306013213/http:/www.wise.nhs.uk/cmsWISE/Workforce+Themes/Using_Task_Skills_Effectively/roleredesign/Introduction/Introduction.htm (accessed 12 February 2014).
- Sibbald B, Pickard S, McLeod H, Reeves D, Mead N, Gemmell I, et al. Moving specialist care into the community: an initial evaluation. J Health Serv Res Policy 2008;13:233-9. http://dx.doi.org/10.1258/jhsrp.2008.008049.
- Wanless D. Securing Our Future Health: Taking a Long-Term View. London: HM Treasury; 2002.
- Pathology: Towards a Competence Based Workforce. A Report of the Pathology Profiling Project. London: Department of Health; 2008.
- Bickell N, Pieper K, Kerry L, Mark D, Glower D, Pryor D, et al. Referral patterns for coronary artery disease treatment: gender bias or good clinical judgement?. Ann Intern Med 1992;15:791-7. http://dx.doi.org/10.7326/0003-4819-116-10-791.
- Beck ES, Kennelly J, McKevitt C, Whitaker L, Wadsworth J, Miller DL, et al. Changing use of hospital services and costs at a London AIDS referral centre, 1983–1989. AIDS 1994;8:367-7. http://dx.doi.org/10.1097/00002030-199403000-00012.
- Espeland A, Baerheim A. Factors affecting general practitioners’ decisions about plain radiography for back pain: implications for classification of guideline barriers – a qualitative study. BMC Health Serv Res 2003;3. http://dx.doi.org/10.1186/1472-6963-3-8.
- Diefenbacher A, Strain JJ. Consultation-liaison psychiatry: stability and change over a 10-year-period. Gen Hosp Psychiatry 2002;24:249-56. http://dx.doi.org/10.1016/S0163-8343(02)00182-2.
- Enderby P, Stevenson J. What is intermediate care? Looking at needs. Managing Community Care 2000;8:35-40.
Appendix 1 Search strategies
-
Chapters 1–4 (1, 3 and 4 searches completed 21 December 2011, Chapter 2 searches completed 12 April 2012).
-
Chapter 1: intermediate care, older people and quality of life.
-
Chapter 2: intermediate care, older people and EQ-5D/TOMs.
-
Chapter 3: intermediate care, older people and institutionalisation.
-
Chapter 4: intermediate care, older people and home care.
-
Chapter 4: intermediate care, older people and mortality.
-
-
Chapter 5 (search completed 23 March 2012).
-
Chapters 7 and 8 (searches completed 10 April 2012).
-
Chapter 9 (searches completed 21 December 2011).
-
Chapter 9: intermediate care and toolkits.
-
The following databases were searched:
-
MEDLINE (via EBSCOhost)
-
CINAHL (via EBSCOhost)
-
ASSIA (via ProQuest) Chapter 4 only.
Results summary
| Chapter | CINAHL | MEDLINE | ASSIA | No duplicates |
|---|---|---|---|---|
| Chapter 1 | 828 | 981 | N/A | 1560 |
| Chapter 2 | 712 | 1512 | N/A | 1884 |
| Chapter 3 | 837 | 30 | N/A | 859 |
| Chapter 4 | 299 | 408 | N/A | 633 |
| Chapter 4 | 387 | 332 | N/A | 624 |
| Chapter 5 | 165 | 293 | N/A | 404 |
| Chapter 5 (additional search) | 57 | 44 | N/A | 93 |
| Chapter 7 | 1308 | 1552 | N/A | 2176 |
| Chapter 8 | 11 | 14 | N/A | 16 |
| Chapter 9 | 768 | 1413 | 72 | 1516 |
| Chapter 9 (UK only) | 81 | 150 | 27 | 208 |
All searches have been written up for MEDLINE using the EBSCOhost interface.
Explanation of search terms used: / = medical subject heading (MeSH); exp = exploded MeSH; * = denotes any character/s; ? = denotes any character; ti = title word; ab = abstract word; N = adjacency of words; N3 = adjacency within 3 words; "" = phrase search
Chapter 1 search strategy
Numbers in brackets are the number of hits.
-
intermediate care.ti,ab. (1402)
-
patient* N5 hotel*.ti,ab. (111)
-
transition* N3 car*.ti,ab. (13,142)
-
halfway N3 home*.ti,ab. (11)
-
halfway house*.ti,ab. (192)
-
subacute N3 care.ti,ab. (365)
-
community N5 rehabilitation.ti,ab. (1533)
-
rehabilitat* N5 cent*.ti,ab. (4794)
-
home* N5 hospital*.ti,ab. (7991)
-
facilitat* N3 discharge*.ti,ab. (504)
-
support* N3 discharge*.ti,ab. (700)
-
expedit* N3 discharge*.ti,ab. (55)
-
earl* N3 discharge*.ti,ab. (3758)
-
home* N3 car*.ti,ab. (2283)
-
home* N3 treatment*.ti,ab. (4359)
-
communit* N5 hospital*.ti,ab. (20,421)
-
communit* N3 care.ti,ab. (7703)
-
intermediate care facilities/ (594)
-
subacute care/ (701)
-
exp rehabilitation centers/ (10,711)
-
hospitals, community/ (9603)
-
exp home care services/ (36,693)
-
or/1-22 (71,742)
-
old* N3 people.ti,ab. (16,058)
-
old* N3 person*.ti,ab. (10,293)
-
elder* N3 people.ti,ab. (12,278)
-
elder* N3 person*.ti,ab. (7412)
-
old* N3 generation*.ti,ab. (811)
-
elder* N3 generation*.ti,ab. (115)
-
pensioner*.ti,ab. (709)
-
geriatric*.ti,ab. (27,648)
-
exp aged/ (2,026,009)
-
geriatrics/ (25,588)
-
or/24-33 (2,056,204)
-
therap* N3 outcome* N3 measure*.ti,ab. (758)
-
quality N2 life.ti,ab. (114,333)
-
qaly*.ti,ab. (3666)
-
benefi*.ti,ab. (417,322)
-
return* N3 home*.ti,ab. (2386)
-
exp outcome assessment (health care)/ (547,012)
-
exp treatment outcome/ (510,872)
-
quality-adjusted life years/ (5185)
-
or/35-42 (998,477)
-
23 and 34 and 43 (3503)
-
publication date 20080101-20110131 (981)
Chapter 2 search strategy
Numbers in brackets are the number of hits.
-
intermediate care.ti,ab. (1402)
-
patient* N5 hotel*.ti,ab. (111)
-
transition* N3 car*.ti,ab. (13,142)
-
halfway adj3 home*.ti,ab. (11)
-
halfway house*.ti,ab. (192)
-
subacute N3 care.ti,ab. (365)
-
community N5 rehabilitation.ti,ab. (1533)
-
rehabilitat* N5 cent*.ti,ab. (4794)
-
home* N5 hospital*.ti,ab. (7991)
-
facilitat* N3 discharge*.ti,ab. (504)
-
support* N3 discharge*.ti,ab. (700)
-
expedit* N3 discharge*.ti,ab. (55)
-
earl* N3 discharge*.ti,ab. (3758)
-
home* N3 car*.ti,ab. (2283)
-
home* N3 treatment*.ti,ab. (4359)
-
communit* N5 hospital*.ti,ab. (20,421)
-
communit* N3 care.ti,ab. (7703)
-
intermediate care facilities/ (594)
-
subacute care/ (701)
-
exp rehabilitation centers/ (10,711)
-
hospitals, community/ (9603)
-
exp home care services/ (36,693)
-
or/1-22 (71,742)
-
old* N3 people.ti,ab. (16,058)
-
old* N3 person*.ti,ab. (10,293)
-
elder* N3 people.ti,ab. (12,278)
-
elder* N3 person*.ti,ab. (7412)
-
old* N3 generation*.ti,ab. (811)
-
elder* N3 generation*.ti,ab. (115)
-
pensioner*.ti,ab. (709)
-
geriatric*.ti,ab. (27,648)
-
exp aged/ (2,026,009)
-
geriatrics/ (25,588)
-
or/24-33 (2,056,204)
-
tom.ti,ab. (1888)
-
toms.ti,ab. (230)
-
"therapy outcome measure*".ti,ab. (71)
-
EQ5D.ti,ab. (358)
-
"quality of life".ti,ab. (115,094)
-
qaly*.ti,ab. (3832)
-
"quality adjusted life years".ti,ab. (2513)
-
exp outcome assessment (health care)/ (565,906)
-
exp treatment outcome/ (528,785)
-
quality-adjusted life years/ (5408)
-
or/35-44 (662,574)
-
23 and 35 and 45 (5024)
-
publication date 20080101-20120431(1512)
Chapter 3 search strategy
Numbers in brackets are the number of hits.
-
intermediate care.ti,ab. (1402)
-
patient* N5 hotel*.ti,ab. (111)
-
transition*N3 car*.ti,ab. (13,142)
-
halfway N3 home*.ti,ab. (11)
-
halfway house*.ti,ab. (192)
-
subacute N3 care.ti,ab. (365)
-
community N5 rehabilitation.ti,ab. (1533)
-
rehabilitat* N5 cent*.ti,ab. (4794)
-
home* N5 hospital*.ti,ab. (7991)
-
facilitat* N3 discharge*.ti,ab. (504)
-
support* N3 discharge*.ti,ab. (700)
-
expedit* N3 discharge*.ti,ab. (55)
-
earl* N3 discharge*.ti,ab. (3758)
-
home* N3 car*.ti,ab. (2283)
-
home* N3 treatment*.ti,ab. (4359)
-
communit* N5 hospital*.ti,ab. (20,421)
-
communit* N3 care.ti,ab. (7703)
-
intermediate care facilities/ (594)
-
subacute care/ (701)
-
exp rehabilitation centers/ (10,711)
-
hospitals, community/ (9603)
-
exp home care services/ (36,693)
-
or/1-22 (71,742)
-
old* N3 people.ti,ab. (16,058)
-
old* N3 person*.ti,ab. (10,293)
-
elder* N3 people.ti,ab. (12,278)
-
elder* N3 person*.ti,ab. (7412)
-
old* N3 generation*.ti,ab. (811)
-
elder* N3 generation*.ti,ab. (115)
-
pensioner*.ti,ab. (709)
-
geriatric*.ti,ab. (27,648)
-
exp aged/ (2,026,009)
-
geriatrics/ (25,588)
-
or/24-33 (2,056,204)
-
institutionali*.ti,ab. (9711)
-
exp institutionalization/ (7391)
-
or/35-36 (15,212)
-
23 and 34 and 37 (252)
-
publication date 20080101-20110131(30)
Chapter 4 search strategy
Numbers in brackets are the number of hits.
-
intermediate care.ti,ab. (1402)
-
patient* N5 hotel*.ti,ab. (111)
-
transition* N3 car*.ti,ab. (13,142)
-
halfway N3 home*.ti,ab. (11)
-
halfway house*.ti,ab. (192)
-
subacute N3 care.ti,ab. (365)
-
community N5 rehabilitation.ti,ab. (1533)
-
rehabilitat* N cent*.ti,ab. (4794)
-
home* N hospital*.ti,ab. (7991)
-
facilitat* N discharge*.ti,ab. (504)
-
support* N discharge*.ti,ab. (700)
-
expedit* N discharge*.ti,ab. (55)
-
earl* N discharge*.ti,ab. (3758)
-
home* N3 car*.ti,ab. (2283)
-
home* N3 treatment*.ti,ab. (4359)
-
communit* N5 hospital*.ti,ab. (20,421)
-
communit* N3 care.ti,ab. (7703)
-
intermediate care facilities/ (594)
-
subacute care/ (701)
-
exp rehabilitation centers/ (10,711)
-
hospitals, community/ (9603)
-
exp home care services/ (36,693)
-
or/1-22 (71,742)
-
old* N3 people.ti,ab. (16,058)
-
old* N3 person*.ti,ab. (10,293)
-
elder* N3 people.ti,ab. (12,278)
-
elder* N3 person*.ti,ab. (7412)
-
old* N3 generation*.ti,ab. (811)
-
elder* N3 generation*.ti,ab. (115)
-
pensioner*.ti,ab. (709)
-
geriatric*.ti,ab. (27,648)
-
exp aged/ (2,026,009)
-
geriatrics/ (25,588)
-
or/24-33 (2,056,204)
-
"meals on wheels".ti,ab. (113)
-
community N4 nurs*.ti,ab. (7804)
-
neighbo*rhood N4 nurs*.ti,ab. (55)
-
district N4 nurs*.ti,ab. (1682)
-
public N4 health N4 nurs*.ti,ab. (5120)
-
home* N4 nurs*.ti,ab. (24,661)
-
home* N4 car*.ti,ab. (30,147)
-
domicil* N3 therap*.ti,ab. (210)
-
home* N3 therap*.ti,ab. (3682)
-
home* N3 rehabilitat*.ti,ab. (1272)
-
food services/
-
community health nursing/
-
home care services/
-
house calls/
-
or/35-48
-
follow*.ti,ab. (1,997,134)
-
after*.ti,ab. (2,993,989)
-
subsequent*.ti,ab. (466,724)
-
or/50-52 (4,494,480)
-
23 and 34 and 49 (8019)
-
53 and 54 (1721)
-
publication date 20080101-20120131 (408)
Chapter 4 search strategy
Numbers in brackets are the number of hits.
-
intermediate care.ti,ab. (1402)
-
patient* N5 hotel*.ti,ab. (111)
-
transition* N3 car*.ti,ab. (13,142)
-
halfway N3 home*.ti,ab. (11)
-
halfway house*.ti,ab. (192)
-
subacute N3 care.ti,ab. (365)
-
community N5 rehabilitation.ti,ab. (1533)
-
rehabilitat* N5 cent*.ti,ab. (4794)
-
home* N5 hospital*.ti,ab. (7991)
-
facilitat* N3 discharge*.ti,ab. (504)
-
support* N3 discharge*.ti,ab. (700)
-
expedit* N3 discharge*.ti,ab. (55)
-
earl* N3 discharge*.ti,ab. (3758)
-
home* N3 car*.ti,ab. (2283)
-
home* N3 treatment*.ti,ab. (4359)
-
communit* N5 hospital*.ti,ab. (20,421)
-
communit* N3 care.ti,ab. (7703)
-
intermediate care facilities/ (594)
-
subacute care/ (701)
-
exp rehabilitation centers/ (10,711)
-
hospitals, community/ (9603)
-
exp home care services/ (36,693)
-
or/1-22 (71,742)
-
old* N3 people.ti,ab. (16,058)
-
old* N3 person*.ti,ab. (10,293)
-
elder* N3 people.ti,ab. (12,278)
-
elder* N3 person*.ti,ab. (7412)
-
old* N3 generation*.ti,ab. (811)
-
elder* N3 generation*.ti,ab. (115)
-
pensioner*.ti,ab. (709)
-
geriatric*.ti,ab. (27,648)
-
exp aged/ (2026009)geriatrics/ (25,588)
-
or/24-33 (2,056,204)
-
mortalit*.ti,ab. (373,017)
-
death.ti,ab. (380,908)
-
dying.ti,ab. (21,582)
-
mortality/ (31,253)
-
death/ (10,887)
-
or/35-39 (717,348)
-
23 and 34 and 40 (1548)
-
publication date 20080101-20110131 (332)
Chapter 5 search strategy
Numbers in brackets are the number of hits.
-
interdisciplinary.ti,ab. (16,908)
-
interprofessional.ti,ab. (2059)
-
multiprofessional.ti,ab.(663)
-
multidisciplinary.ti,ab. (34,399)
-
inter-disciplinary.ti,ab. (290)
-
inter-professional.ti,ab. (393)
-
co-operat*.ti,ab. (8157)
-
multi-professional.ti,ab. (459)
-
multi-disciplinary.ti,ab. (2574)
-
"inter disciplinary".ti,ab. (290)
-
"inter professional".ti,ab. (393)
-
"multi disciplinary.ti,ab. (2574)
-
"multi professional".ti,ab. (459)
-
cooperat*/ti,ab. (83,511)
-
collaborat*.ti,ab. (64,743)
-
or/1-15 (202,352)
-
team*.ti,ab. (74,350)
-
patient care team/ (47,188)
-
or/18-19 (107,956)
-
team* N1 size*.ti,ab. (59)
-
grade* N1 mix*.ti,ab. (190)
-
skill* N1 mix*.ti,ab. (577)
-
intensity.ti,ab. (208,889)
-
workload*.ti,ab. (14,122)
-
leadership.ti,ab. (16,538)
-
satisf*.ti,ab. (181,055)
-
role* N2 flexibility.ti,ab. (247)
-
integrat*.ti,ab. (226,942)
-
team* N2 work*.ti,ab. (4199)
-
management.ti,ab. (575,321)
-
"career progression".ti,ab. (159)
-
quality.ti,ab. (435,142)
-
empower*.ti,ab. (9366)
-
communicat*.ti,ab. (14,2904)
-
"sense of direction".ti,ab. (139)
-
uncertainty.ti,ab. (31,353)
-
culture*.ti,ab. (701,693)
-
conflict*.ti,ab. (63,560)
-
training.ti,ab. (197,867)
-
workload/ (13,250)
-
leadership/ (23,694)
-
communication/ (55,282)
-
conflict psychology/ (13,018)
-
culture/ (24,064)
-
or/20-44 (2,573,427)
-
treatment* N1 outcome*.ti,ab. (31,821)
-
mortality.ti,ab. (377,671)
-
"length of stay".ti,ab. (22,662)
-
patient* N1 admission*.ti,ab. (8163)
-
patient* N1 discharge*.ti,ab. (17,686)
-
patient* N1 readmission*.ti,ab. (580)
-
patient* N1 transfer*. ti,ab. (5271)
-
"quality of health care".ti,ab. (2419)
-
outcome* N1 assessment*.ti,ab. (4605)
-
treatment* N1 fail*.ti,ab. (22,580)
-
"cause* of death*".ti,ab. (43,437)
-
"child mortalit*.ti,ab. (1577)
-
fatal* N1 outcome*.ti,ab. (6508)
-
"fetal mortalit*".ti,ab. (1171)
-
hospital* N2 mortalit*.ti,ab. (22,155)
-
"infant mortalit*".ti, ab. (5952)
-
"maternal mortalit*". ti,ab. (5111)
-
"perinatal mortalit*". ti,ab. (7125)
-
surviv* N1 rate*.ti,ab. (87,735)
-
patient* N1 admitted*.ti,ab. (37,601)
-
patient* N1 readmit*.ti,ab. (966)
-
patient* re-admit*.ti, ab. (147)
-
patient* re-admission*.ti,ab. (56)
-
length of stay/ (49,269)
-
patient admission/ (163,82)
-
patient discharge/ (16,155)
-
patient readmission/ (6227)
-
patient transfer/ (4987)
-
quality of health care/ (50,269)
-
outcome and process assessment/ (19,442)
-
treatment failure/ (22,713)
-
cause of death/ (31,025)
-
child mortality/ (921)
-
fatal outcome/ (43,961)
-
fetal mortality/ (190)
-
hospital mortality/ (17,663)
-
infant mortality/ (23,300)
-
maternal mortality/ (7059)
-
perinatal mortality/ (474)
-
survival rate/ (107,386)
-
quality of health care/ (50,269)
-
process assessment (health care)/ (2570)
-
or/46-87 (852,356)
-
"intermediate care".ti,ab. (902)
-
patient* N3 hotel*.ti,ab. (71)
-
transition* N3 car*.ti,ab. (13,149)
-
halfway N3 home*.ti,ab. (11)
-
"halfway house*".ti,ab. (191)
-
subacute N3 care.ti,ab. (367)
-
community N3 rehabilitation.ti,ab. (1210)
-
rehabilitat* N3 cent*.ti,ab. (4298)
-
home* N4 hospital*.ti,ab. (7155)
-
facilitat* N3 discharge*.ti,ab. (506)
-
support* N3 discharge*.ti,ab. (702)
-
expedit* N3 discharge*.ti,ab. (56)
-
earl* N3 discharge*.ti,ab. (3758)
-
home* N3 car* N3 service*.ti,ab. (2283)
-
home* N3 treatment*.ti,ab. (4359)
-
communit* N3 hospital*.ti,ab. (17,855)
-
communit* N3 care.ti,ab. (7705)
-
primary N3 care.ti,ab. (70,690)
-
"general practitioner*".ti,ab. (32,292)
-
GP*.ti.ab. (97,306)
-
"family physician*".ti,ab. (10,135)
-
community N3 nurs*.ti.ab. (7058)
-
"post acute care".ti,ab. (234)
-
"step up".ti,ab. (1367)
-
"step down".ti,ab. (195)
-
community N3 rehab*.ti,ab. (1260)
-
home* N3 nurs*.ti,ab. (24,072)
-
home* N3 car*.ti,ab. (27,538)
-
neighbo*rhood N3 nurs*.ti,ab. (52)
-
district N4 nurs*.ti,ab. (1681)
-
public N3 health N3 nurs*.ti,ab. (4935)
-
domicil* N3 therap*.ti,ab. (210)
-
home* N3 therap*.ti,ab. (3682)
-
home* N3 rehabilitat*.ti,ab. (1275)
-
care N3 home* N3 manager*.ti,ab. (4)
-
nursing N3 home* manager*.ti,ab. (2)
-
commission*.ti,ab. (21,902)
-
provider* N3 care*.ti,ab. (28,430)
-
nursing homes/ (25,961)
-
primary health care/ (45,727)
-
physicians, family/ (14,001)
-
general practitioners/ (599)
-
intermediate care facilities/ (594)
-
subacute care/ (702)
-
rehabilitation centers/ (6051)
-
hospitals, community/ (9603)
-
exp home care services/ (36,767)
-
hospitals, community/ (9608)
-
community health nursing/ (17,613)
-
home nursing/ (7642)
-
house calls/ (2035)
-
health personnel/ (18,038)
-
community health services/ (24,665)
-
community health centers/ (5352)
-
or/89-142 (480,040)
-
16 and 19 and 45 and 88 and 143 (922)
-
publication date 20080101-20120331 (293)
Chapter 5 (additional) search strategy
Numbers in brackets are the number of hits.
-
support* N2 staff*.ti,ab. (379)
-
support* N2 worker*.ti,ab. (200)
-
non-professional*.ti,ab. (43)
-
or/1-3 (613)
-
4 N5 30 (41)
-
professional*.ti,ab. (17,637)
-
management.ti,ab. (33,065)
-
leader*.ti,ab. (5364)
-
leadership/ (23,694)
-
or/6-9 (75,679)
-
5 N5 10 (91)
-
10 N5 30 (6664)
-
team* N1 size*.ti,ab. (59)
-
grade* N1 mix*.ti,ab. (190)
-
skill* N1 mix*.ti,ab. (577)
-
or/13-16 (1243)
-
length of stay/ (49,269)
-
patient admission/ (16,382)
-
patient discharge/ (16,155)
-
"length of stay".ti,ab. (22,662)
-
patient* N1 admission*.ti,ab. (8163)
-
patient* N1 discharge*.ti,ab. (17,686)
-
patient* N1 readmission*.ti,ab. (580)
-
patient* N1 transfer*. ti,ab. (5271)
-
dur* N3 stay*.ti,ab. (2303)
-
or/17-25 (37,350)
-
or/16, 26 (38,518)
-
patient*.ti,ab. (138,013)
-
patients/ (146,346)
-
or/27-28 (271,334)
-
16 N10 30 (28)
-
staff* N10 ratio*.ti,ab. (829)
-
patient* N10 ratio*.ti,ab. (8422)
-
interdisciplinary.ti,ab. (16,908)
-
interprofessional.ti,ab. (2059)
-
multiprofessional.ti,ab.(663)
-
multidisciplinary.ti,ab. (34,399)
-
inter-disciplinary.ti,ab. (290)
-
inter-professional.ti,ab. (393)
-
co-operat*.ti,ab. (8157)
-
multi-professional.ti,ab. (459)
-
multi-disciplinary.ti,ab. (2574)
-
"inter disciplinary".ti,ab. (290)
-
"inter professional".ti,ab. (393)
-
"multi disciplinary.ti,ab. (2574)
-
"multi professional".ti,ab. (459)
-
cooperat*/ti,ab. (83,511)
-
collaborat*.ti,ab. (64,743)
-
or/34-48 (202,352)
-
or/ 5, 11, 12, 32, 33, 31 (15,676)
-
27 and 49 and 50 (57)
-
publication date 20080101-20120331 (44)
Chapter 7 search strategy
Numbers in brackets are the number of hits.
-
team* N1 size*.ti,ab. (59)
-
grade* N1 mix*.ti,ab. (190)
-
skill* N1 mix*.ti,ab. (577)
-
work* N1 distribut*. ti,ab. (765)
-
role* N1 distribut*.ti,ab. (395)
-
“role* structure*”.ti,ab. (43)
-
team* N2 distribut*.ti,ab. (81)
-
team* N2 organi?*.ti,ab. (902)
-
team* N2 structur*.ti,ab. (378)
-
team* N1 model*.ti,ab. (421)
-
team* N2 style*.ti,ab. (34)
-
team* N2 strategy* (89)
-
team* N2 strategies* (199)
-
team* N2 plan*.ti,ab. (586)
-
service* N2 distribut*.ti,ab. (680)
-
service* N2 organi?*.ti,ab. (4767)
-
service* N2 structur*.ti,ab. (1061)
-
service* N1 model*.ti,ab. (1951)
-
service* N2 style*.ti,ab. (122)
-
service* N2 strategy*.ti,ab. (252)
-
service* N2 strategies.ti,ab. (540)
-
management* N1 style*. ti,ab. (518)
-
management* N1 strategy*. ti,ab. (4078)
-
“management* strategies.” ti,ab. (9601)
-
management* N1 structur*.ti,ab. (1207)
-
management* N1 model*.ti,ab. (1538)
-
manager* N2 style*.ti,ab. (112)
-
manager* N2 strategy*.ti,ab. (50)
-
manager* N2 strategies.ti,ab. (164)
-
manager* N2 structur*.ti,ab. (110)
-
manager* N1 model*.ti,ab. (120)
-
leadership N1 style*.ti,ab. (520)
-
leadership N1 strategy*.ti,ab. (49)
-
leadership N1 strategies.ti,ab. (95)
-
leadership N1 structur*.ti,ab. (137)
-
leadership N1 model*.ti,ab. (218)
-
“service provision*”.ti,ab. (3106)
-
service N2 goal*.ti,ab. (217)
-
service N2 aim*.ti,ab. (395)
-
service N2 vision*.ti,ab. (101)
-
service N2 mission*.ti,ab. (117)
-
“organi?ation* provision*”.ti,ab. (30)
-
organi?ation* N2 goal*.ti,ab. (734)
-
organi?ation N2 aim*.ti,ab. (466)
-
organi$ation N2 vision*.ti,ab. (180)
-
organi$ation N2 mission*.ti,ab. (334)
-
service* N2 commission*.ti,ab. (575)
-
service* N2 “policy driver*”.ti,ab. (2)
-
service* N2 re-organi$*.ti,ab. (26)
-
service* N2 reorgani$*.ti,ab. (346)
-
service* N2 fund*,ti,ab. (1446)
-
service* N2 restructur*.ti,ab. (224)
-
service* N2 re-structur*.ti,ab. (3)
-
organi?ation* N2 commission*.ti,ab. (159)
-
organi?*ation* N2 re-organi$*.ti,ab. (576)
-
organi?ation* N2 reorgani$*.ti,ab. (99)
-
organi?ation* N2 fund*,ti,ab. (827)
-
organi?ation* N2 restructur*.ti,ab. (188)
-
organi?ation* N2 re-structur*.ti,ab. (2)
-
organi?ation* N2 style*.ti,ab. (123)
-
organi?ation* adj2 strategy*.ti,ab. (494)
-
“organi?ation* stategies*”.ti,ab. (272)
-
organi?ation* N2 structur*.ti,ab. (12,489)
-
organi?ation* N1 model*.ti,ab. (1238)
-
“financial policy*”.ti,ab. (23)
-
“financial policies”.ti.ab. (25)
-
“economic policy*”.ti,ab. (168)
-
“economic policies”.ti,ab. (154)
-
/or 1-68 (31,734)
-
"intermediate care".ti,ab. (902)
-
patient* N3 hotel*.ti,ab. (71)
-
transition* N3 car*.ti,ab. (13,149)
-
halfway N3 home*.ti,ab. (11)
-
"halfway house*".ti,ab. (191)
-
subacute N3 care.ti,ab. (367)
-
community N3 rehabilitation.ti,ab. (1210)
-
rehabilitat* N3 cent*.ti,ab. (4298)
-
home* N4 hospital*.ti,ab. (7155)
-
facilitat* N3 discharge*.ti,ab. (506)
-
support* N3 discharge*.ti,ab. (702)
-
expedit* N3 discharge*.ti,ab. (56)
-
earl* N3 discharge*.ti,ab. (3758)
-
home* N3 car* N3 service*.ti,ab. (2283)
-
home* N3 treatment*.ti,ab. (4359)
-
communit* N3 hospital*.ti,ab. (17855)
-
communit* N3 care.ti,ab. (7705)
-
primary N3 care.ti,ab. (70,690)
-
"general practitioner*".ti,ab. (32,292)
-
GP*.ti.ab. (97,306)
-
"family physician*".ti,ab. (10,135)
-
community N3 nurs*.ti.ab. (7058)
-
"post acute care".ti,ab. (234)
-
"step up".ti,ab. (1367)
-
"step down".ti,ab. (1957)
-
community N3 rehab*.ti,ab. (1260)
-
home* N3 nurs*.ti,ab. (24,072)
-
home* N3 car*.ti,ab. (27,538)
-
neighbo*rhood N3 nurs*.ti,ab. (52)
-
district N4 nurs*.ti,ab. (1681)
-
public N3 health N3 nurs*.ti,ab. (4935)
-
domicil* N3 therap*.ti,ab. (210)
-
home* N3 therap*.ti,ab. (3682)
-
home* N3 rehabilitat*.ti,ab. (1275)
-
care N3 home* N3 manager*.ti,ab. (4)
-
nursing N3 home* manager*.ti,ab. (2)
-
provider* N3 care*.ti,ab. (28,430)
-
nursing homes/ (25,961)
-
primary health care/ (45,727)
-
physicians, family/ (14,001)
-
general practitioners/ (599)
-
intermediate care facilities/ (594)
-
subacute care/ (702)
-
rehabilitation centers/ (6051)
-
hospitals, community/ (9603)
-
exp home care services/ (36,767)
-
hospitals, community/ (9608)
-
community health nursing/ (17,613)
-
home nursing/ (7642)
-
house calls/ (2035)
-
health personnel/ (18,038)
-
community health services/ (24,665)
-
community health centers/ (5352)
-
or/70-122 (460,761)
-
69 and 123 (4192)
-
publication date 20080101-20120431 (1552)
Chapter 8 search strategy
Numbers in brackets are the number of hits.
-
"intermediate care".ti,ab. (902)
-
patient* N3 hotel*.ti,ab. (71)
-
transition* N3 car*.ti,ab. (13,149)
-
halfway N3 home*.ti,ab. (11)
-
"halfway house*".ti,ab. (191)
-
subacute N3 care.ti,ab. (367)
-
community N3 rehabilitation.ti,ab. (1210)
-
rehabilitat* N3 cent*.ti,ab. (4298)
-
home* N4 hospital*.ti,ab. (7155)
-
facilitat* N3 discharge*.ti,ab. (506)
-
support* N3 discharge*.ti,ab. (702)
-
expedit* N3 discharge*.ti,ab. (56)
-
earl* N3 discharge*.ti,ab. (3758)
-
home* N3 car* N3 service*.ti,ab. (2283)
-
home* N3 treatment*.ti,ab. (4359)
-
communit* N3 hospital*.ti,ab. (17,855)
-
communit* N3 care.ti,ab. (7705)
-
primary N3 care.ti,ab. (70,690)
-
"general practitioner*".ti,ab. (32,292)
-
GP*.ti.ab. (97,306)
-
"family physician*".ti,ab. (10,135)
-
community N3 nurs*.ti.ab. (7058)
-
"post acute care".ti,ab. (234)
-
"step up".ti,ab. (1367)
-
"step down".ti,ab. (1957)
-
community N3 rehab*.ti,ab. (1260)
-
home* N3 nurs*.ti,ab. (24,072)
-
home* N3 car*.ti,ab. (27,538)
-
neighbo*rhood N3 nurs*.ti,ab. (52)
-
district N4 nurs*.ti,ab. (1681)
-
public N3 health N3 nurs*.ti,ab. (4935)
-
domicil* N3 therap*.ti,ab. (210)
-
home* N3 therap*.ti,ab. (3682)
-
home* N3 rehabilitat*.ti,ab. (1275)
-
care N3 home* N3 manager*.ti,ab. (4)
-
nursing N3 home* manager*.ti,ab. (2)
-
provider* N3 care*.ti,ab. (28,430)
-
nursing homes/ (25,961)
-
primary health care/ (45,727)
-
physicians, family/ (14,001)
-
general practitioners/ (599)
-
intermediate care facilities/ (594)
-
subacute care/ (702)
-
rehabilitation centers/ (6051)
-
hospitals, community/ (9603)
-
exp home care services/ (36,767)
-
hospitals, community/ (9608)
-
community health nursing/ (17,613)
-
home nursing/ (7642)
-
house calls/ (2035)
-
health personnel/ (18,038)
-
community health services/ (24,665)
-
community health centers/ (5352)
-
or/1-53 (460,761)
-
team*,ti,ab. (75,913)
-
patient care team/ (47,188)
-
or/55-56 (109,851)
-
refer*.ti,ab. (446,319)
-
pattern*.ti,ab. (786,253)
-
structur*.ti,ab. (1,247,720)
-
decision*.ti,ab. (126,552)
-
behav*.ti,ab. (677,616)
-
decision*.ti,ab. (171,876)
-
or 58-63 (2,625,621)
-
57 N1 64 (4191)
-
54 and 57 and 64 (42)
-
publication date 20080101-20120431 (14)
Chapter 9 search strategy
Numbers in brackets are the number of hits.
-
"intermediate care".ti,ab. (902)
-
patient* N3 hotel*.ti,ab. (71)
-
transition* N3 car*.ti,ab. (13,149)
-
halfway N3 home*.ti,ab. (11)
-
"halfway house*".ti,ab. (191)
-
subacute N3 care.ti,ab. (367)
-
community N3 rehabilitation.ti,ab. (1210)
-
rehabilitat* N3 cent*.ti,ab. (4298)
-
home* N4 hospital*.ti,ab. (7155)
-
facilitat* N3 discharge*.ti,ab. (506)
-
support* N3 discharge*.ti,ab. (702)
-
expedit* N3 discharge*.ti,ab. (56)
-
earl* N3 discharge*.ti,ab. (3758)
-
home* N3 car* N3 service*.ti,ab. (2283)
-
home* N3 treatment*.ti,ab. (4359)
-
communit* N3 hospital*.ti,ab. (17,855)
-
communit* N3 care.ti,ab. (7705)
-
primary N3 care.ti,ab. (70,690)
-
"general practitioner*".ti,ab. (32,292)
-
GP*.ti.ab. (97,306)
-
"family physician*".ti,ab. (10,135)
-
community N3 nurs*.ti.ab. (7058)
-
"post acute care".ti,ab. (234)
-
"step up".ti,ab. (1367)
-
"step down".ti,ab. (1957)
-
community N3 rehab*.ti,ab. (1260)
-
home* N3 nurs*.ti,ab. (24,072)
-
home* N3 car*.ti,ab. (27,538)
-
neighbo*rhood N3 nurs*.ti,ab. (52)
-
district N4 nurs*.ti,ab. (1681)
-
public N3 health N3 nurs*.ti,ab. (4935)
-
domicil* N3 therap*.ti,ab. (210)
-
home* N3 therap*.ti,ab. (3682)
-
home* N3 rehabilitat*.ti,ab. (1275)
-
care N3 home* N3 manager*.ti,ab. (4)
-
nursing N3 home* manager*.ti,ab. (2)
-
commission*.ti,ab. (21,902)
-
provider* N3 care*.ti,ab. (28,430)
-
primary health care/ (45,727)
-
physicians, family/ (14,001)
-
general practitioners/ (599)
-
intermediate care facilities/ (594)
-
subacute care/ (702)
-
rehabilitation centers/ (6051)
-
hospitals, community/ (9603)
-
exp home care services/ (36,767)
-
hospitals, community/ (9608)
-
community health nursing/ (17,613)
-
home nursing/ (7642)
-
house calls/ (2035)
-
health personnel/ (18,038)
-
community health services/ (24,665)
-
community health centers/ (5352)
-
or/1-53 (437,544)
-
benchmark*.ti,ab. (12,724)
-
service* N2 configur*.ti,ab. (137)
-
service* N2 audit*.ti,ab. (390)
-
"performance indicator*".ti,ab. (1401)
-
performance* N2 measure*.ti,ab. (17,460)
-
monitor* N2 service*. ti,ab. (937)
-
compar* N2 service*.ti,ab. (2355)
-
quality N2 indicator*.ti,ab. (5274)
-
benchmarking/ (8670)
-
clinical audit/ (438)
-
exp quality indicators, health care/ (9573)
-
or/56-65 (52,354)
-
tool N3 kit*.ti,ab. (360)
-
toolkit*.ti,ab. (1488)
-
guide*.ti,ab. (276,818)
-
checklist*.ti,ab. (14,962)
-
"check list*".ti,ab. (1988)
-
guidance.ti,ab. (46,127)
-
referral*.ti,ab. (54,407)
-
recommendation*.ti,ab. (113,722)
-
checklist/ (858)
-
practice guidelines as topic/ (64,122)
-
referral and consultation/ (45,783)
-
or/68-77 (527,630)
-
54 and 66 and 78 (1413)
Chapter 9 (with UK specification) search strategy
Numbers in brackets are the number of hits.
-
"intermediate care".ti,ab. (902)
-
patient* N3 hotel*.ti,ab. (71)
-
transition* N3 car*.ti,ab. (13,149)
-
halfway N3 home*.ti,ab. (11)
-
"halfway house*".ti,ab. (191)
-
subacute N3 care.ti,ab. (367)
-
community N3 rehabilitation.ti,ab. (1210)
-
rehabilitat* N3 cent*.ti,ab. (4298)
-
home* N4 hospital*.ti,ab. (7155)
-
facilitat* N3 discharge*.ti,ab. (506)
-
support* N3 discharge*.ti,ab. (702)
-
expedit* N3 discharge*.ti,ab. (56)
-
earl* N3 discharge*.ti,ab. (3758)
-
home* N3 car* N3 service.ti,ab. (2283)
-
home* N3 treatment*.ti,ab. (4359)
-
communit* N3 hospital*.ti,ab. (17,855)
-
communit* N3 care.ti,ab. (7705)
-
primary N3 care.ti,ab. (70,690)
-
"general practitioner*".ti,ab. (32,292)
-
GP*.ti.ab. (97,306)
-
"family physician*".ti,ab. (10,135)
-
community N3 nurs*.ti.ab. (7058)
-
"post acute care".ti,ab. (234)
-
"step up".ti,ab. (1367)
-
"step down".ti,ab. (1957)
-
community N3 rehab*.ti,ab. (1260)
-
home* N3 nurs*.ti,ab. (24,072)
-
home* N3 car*.ti,ab. (27,538)
-
neighbo*rhood N3 nurs*.ti,ab. (52)
-
district N4 nurs*.ti,ab. (1681)
-
public N3 health N3 nurs*.ti,ab. (4935)
-
domicil* N3 therap*.ti,ab. (210)
-
home* N3 therap*.ti,ab. (3682)
-
home* N3 rehabilitat*.ti,ab. (1275)
-
care N3 home* N3 manager*.ti,ab. (4)
-
nursing N3 home* manager*.ti,ab. (2)
-
commission*.ti,ab. (21,902)
-
provider* N3 care*.ti,ab. (28,430)
-
primary health care/ (45,727)
-
physicians, family/ (14,001)
-
general practitioners/ (599)
-
intermediate care facilities/ (594)
-
subacute care/ (702)
-
rehabilitation centers/ (6051)
-
hospitals, community/ (9603)
-
exp home care services/ (36,767)
-
hospitals, community/ (9608)
-
community health nursing/ (17,613)
-
home nursing/ (7642)
-
house calls/ (2035)
-
health personnel/ (18,038)
-
community health services/ (24,665)
-
community health centers/ (5352)
-
or/1-53 (437,544)
-
benchmark*.ti,ab. (12,724)
-
service* N2 configur*.ti,ab. (137)
-
service* N2 audit*.ti,ab. (390)
-
"performance indicator*".ti,ab. (1401)
-
performance* N2 measure*.ti,ab. (17,460)
-
monitor* N2 service*. ti,ab. (937)
-
compar* N2 service*.ti,ab. (2355)
-
quality N2 indicator*.ti,ab. (5274)
-
benchmarking/ (8670)
-
clinical audit/ (438)
-
exp quality indicators, health care/ (9573)
-
or/56-65 (52,354)
-
tool N3 kit*.ti,ab. (360)
-
toolkit*.ti,ab. (1488)
-
guide*.ti,ab. (276,818)
-
checklist*.ti,ab. (14,962)
-
"check list*".ti,ab. (1988)
-
guidance.ti,ab. (46,127)
-
referral*.ti,ab. (54,407)
-
recommendation*.ti,ab. (113,722)
-
checklist/ (858)
-
practice guidelines as topic/ (64,122)
-
referral and consultation/ (45,783)
-
or/68-77 (527,630)
-
54 and 66 and 78 (1383)
-
UK*.ti,ab. (56,026)
-
united kingdom*.ti,ab. (21,109)
-
england*.ti.ab. (27,344)
-
"northern ireland*.ti,ab. (3061)
-
scotland*.ti,ab. (10,036)
-
wales*.ti,ab. (13,984)
-
english*.ti,ab. (40,592)
-
britain*.ti.ab. (11,214)
-
british.ti.ab. (31,370)
-
scottish.ti,ab. (5387)
-
"northern irish”.ti.ab. (149)
-
welsh.ti.ab. (1216)
-
or/81-91 (189,972)
-
54 and 66 and 78 (1410)
-
54 and 66 and 78 and 92 (150)
Appendix 2 Details of multiple imputations
Two distinct types of missing data were encountered: missing admission (baseline) data and missing discharge (outcome) data. The data imputation was conducted for baseline and outcome data separately as follows.
Missing patient characteristics data
Of the 8070 patients included, 3731 (46%) had missing data for at least one of the data items in the table above. The most common missing fields were the baseline questionnaires for EQ-5D (29%) or one of the four TOM items (16%). Of the remaining factors, 2024 (25%) patients had one missing data item and a further 724 (9%) had two or more missing. A total of 225 patients (3%) were excluded as a result of having excessive missing data (including age or sex), as there was too few observed data to base imputations on.
The remaining patients had missing data imputed by multiple imputation incorporating chained estimation. 45 Convergence issues were encountered when fitting models based on multiple logistic regression and as a result the number of predictive covariates had to be limited for the LoC, usual living arrangements, place receiving care and referral route. Although the four TOM domains were highly correlated, these were generally all present or all absent and so the domains could not be used to predict each other. Furthermore, although EQ-5D outcomes tended to be associated with the TOM outcomes they were more frequently missing and so TOM scores (when present) were used to predict EQ-5D but not vice versa.
Missing outcome data
Outcome data were imputed independently of the patient characteristic data, with the exceptions of the IC team and the baseline score (the latter was itself imputed when necessary). Along with these, additional data concerning the destination of the patient at discharge were also used to predict the missing TOM or EQ-5D outcome scores. Patients with missing data were categorised as having either died, discharged home, discharged to residential/nursing home or similar, admitted to hospital or an inappropriate referral. This categorisation was particularly relevant, as discharge to nursing home was associated with worse outcomes than patients discharged to their own home among patients for whom data were available. Patients who died were assigned a TOM or EQ-5D score of 0 at discharge; otherwise, the missing items were predicted based on the above along with the (possibly imputed) baseline score and team. Other covariates (e.g. age, sex) were deliberately omitted from the imputation of the outcome data, as the aim of the study was to assess whether or not there was an association and their inclusion would directly influence this.
Change between baseline and outcome measures
The relationship between baseline characteristics and change in the TOM and EQ-5D scores was assessed in two ways. First, by the magnitude of change in each of the TOM dimensions and EQ-5D scores and, second, by whether or not there was a positive or negative change in those scores. These analyses were done with complete case data and with a data set in which the missing values were imputed. A comparison of the analyses of the complete case data set and the imputed data set demonstrated that the results were generally in agreement.
| Covariate | Method | Predictors |
|---|---|---|
| Covariate data (as measured at admission) | ||
| LoC | Multiple logistic regression | Age, sex |
| Usual living arrangements | ||
| Place receiving care | ||
| Referral route | ||
| TOM (all domains) | Ordered logistic regression | Team, age, sex, referral route |
| EQ-5D | Linear regression | Team, age, sex, referral route, LoC at admission, usual living arrangements, TOM scores at baseline |
| Outcome data | ||
| TOM (all domains) | Ordered logistic regression | Team, baseline score, reason for missing data |
| EQ-5D | Linear regression | |
Model coefficients for therapy outcome measures change: impairment
| Covariate | Complete case data (n = 5337) | Imputed data (n = 7291) | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| Baseline TOM impairment score | –0.218 | –0.240 to –0.197 | < 0.001 | –0.188 | –0.214 to –0.162 | < 0.001 |
| Age (per 10-year increase) | 0.001 | –0.014 to 0.016 | 0.900 | –0.019 | –0.036 to –0.001 | 0.036 |
| Sex (female vs. male) | 0.072 | 0.032 to 0.111 | < 0.001 | 0.100 | 0.059 to 0.141 | < 0.001 |
| LoC at admission | < 0.001 | < 0.001 | ||||
| 0 | Reference category | Reference category | ||||
| 1 | 0.124 | 0.031 to 0.217 | 0.051 | –0.036 to 0.139 | ||
| 2 | 0.224 | 0.040 to 0.408 | 0.031 | –0.150 to 0.212 | ||
| 3 | 0.279 | 0.184 to 0.373 | 0.185 | 0.098 to 0.271 | ||
| 0.367 | 0.274 to 0.459 | 0.292 | 0.210 to 0.373 | |||
| 5 | 0.317 | 0.206 to 0.429 | 0.234 | 0.129 to 0.340 | ||
| 6 | –0.024 | –0.151 to 0.102 | 0.002 | –0.128 to 0.132 | ||
| 7 | 0.156 | 0.004 to 0.308 | 0.079 | –0.079 to 0.236 | ||
| 8 | 0.002 | –0.189 to 0.193 | 0.078 | –0.168 to 0.323 | ||
| Who made the referral | < 0.001 | < 0.001 | ||||
| GP/doctor | Reference category | Reference category | ||||
| Self/informal carer/friend/family | 0.023 | –0.105 to 0.152 | 0.001 | –0.150 to 0.152 | ||
| Community nurse/nurse | –0.039 | –0.105 to 0.027 | –0.094 | –0.169 to –0.020 | ||
| Social worker/social services | –0.111 | –0.191 to –0.031 | –0.051 | –0.139 to 0.036 | ||
| AHP | 0.057 | 0.001 to 0.113 | –0.025 | –0.089 to 0.038 | ||
| A&E/ambulance service/rapid response | 0.088 | –0.008 to 0.185 | 0.102 | –0.012 to 0.217 | ||
| Ward in acute hospital/day clinics/fall clinics | 0.121 | 0.058 to 0.184 | 0.158 | 0.088 to 0.229 | ||
| Community hospital | –0.058 | –0.144 to 0.029 | 0.011 | –0.097 to 0.118 | ||
| Other | 0.066 | –0.259 to 0.391 | 0.141 | –0.232 to 0.515 | ||
| Living arrangements | 0.005 | < 0.001 | ||||
| Lives alone in own home (owned or rented) | Reference category | Reference category | ||||
| Lives with other(s) in own home (owned or rented) | –0.035 | –0.077 to 0.007 | –0.032 | –0.086 to 0.023 | ||
| Lives in relative’s home | –0.079 | –0.209 to 0.052 | –0.142 | –0.283 to –0.002 | ||
| Lives in residential/nursing home | –0.125 | –0.209 to –0.040 | –0.310 | –0.403 to –0.216 | ||
| Lives in sheltered housing | –0.127 | –0.214 to –0.039 | –0.071 | –0.172 to 0.030 | ||
| Other | –0.124 | –0.336 to 0.088 | –0.231 | –0.448 to –0.015 | ||
| If patient left own home for service, where to: | < 0.001 | 0.004 | ||||
| Residential/nursing home | –0.181 | –0.348 to –0.014 | –0.180 | –0.349 to –0.011 | ||
| Acute hospital | –0.292 | –0.870 to 0.286 | –0.348 | –0.837 to 0.140 | ||
| A&E | –0.258 | –0.429 to –0.086 | –0.149 | –0.366 to 0.068 | ||
| IC facility | 0.154 | 0.066 to 0.241 | 0.163 | 0.058 to 0.267 | ||
| Day hospital | –0.221 | –0.417 to –0.025 | –0.073 | –0.317 to 0.171 | ||
| Resource centre | 0.038 | –0.227 to 0.304 | –0.022 | –0.327 to 0.282 | ||
| Community hospital | 0.065 | –0.033 to 0.164 | –0.025 | –0.159 to 0.109 | ||
| Other | 0.029 | –0.230 to 0.289 | –0.123 | –0.345 to 0.100 | ||
Model coefficients for therapy outcome measure change: activity
| Covariate | Complete case data (n = 5339) | Imputed data (n = 7291) | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| Baseline TOM activity score | –0.195 | –0.215 to –0.175 | < 0.001 | –0.176 | –0.200 to –0.153 | < 0.001 |
| Age (per 10-year increase) | –0.014 | –0.029 to 0.002 | 0.079 | –0.023 | –0.042 to –0.005 | 0.013 |
| Sex (female vs. male) | 0.073 | 0.034 to 0.112 | < 0.001 | 0.095 | 0.050 to 0.139 | < 0.001 |
| LoC at admission | < 0.001 | < 0.001 | ||||
| 0 | Reference category | Reference category | ||||
| 1 | 0.135 | 0.042 to 0.228 | 0.063 | –0.019 to 0.144 | ||
| 2 | 0.248 | 0.064 to 0.433 | 0.086 | –0.089 to 0.262 | ||
| 3 | 0.297 | 0.202 to 0.391 | 0.204 | 0.117 to 0.292 | ||
| 4 | 0.399 | 0.307 to 0.492 | 0.325 | 0.232 to 0.417 | ||
| 5 | 0.386 | 0.275 to 0.498 | 0.302 | 0.192 to 0.412 | ||
| 6 | 0.071 | –0.055 to 0.197 | 0.078 | –0.047 to 0.202 | ||
| 7 | 0.174 | 0.022 to 0.326 | 0.104 | –0.056 to 0.265 | ||
| 8 | 0.095 | –0.096 to 0.287 | 0.159 | –0.087 to 0.405 | ||
| Who made the referral | < 0.001 | < 0.001 | ||||
| GP/doctor | Reference category | Reference category | ||||
| Self/informal carer/friend/family | 0.047 | –0.081 to 0.176 | 0.045 | –0.104 to 0.193 | ||
| Community nurse/nurse | –0.027 | –0.093 to 0.040 | –0.105 | –0.179 to –0.031 | ||
| Social worker/social services | –0.066 | –0.146 to 0.014 | –0.035 | –0.128 to 0.058 | ||
| AHP | 0.091 | 0.035 to 0.147 | –0.008 | –0.072 to 0.055 | ||
| A&E /ambulance service/rapid response | 0.127 | 0.030 to 0.224 | 0.118 | 0.002 to 0.234 | ||
| Ward in acute hospital/day clinics/fall clinics | 0.157 | 0.093 to 0.220 | 0.177 | 0.102 to 0.252 | ||
| Community hospital | 0.046 | –0.041 to 0.133 | 0.089 | –0.011 to 0.189 | ||
| Other | 0.136 | –0.190 to 0.463 | 0.178 | –0.203 to 0.558 | ||
| Living arrangements | < 0.001 | < 0.001 | ||||
| Lives alone in own home (owned or rented) | Reference category | Reference category | ||||
| Lives with other(s) in own home (owned or rented) | –0.035 | –0.077 to 0.008 | –0.040 | –0.088 to 0.008 | ||
| Lives in relative’s home | –0.097 | –0.228 to 0.034 | –0.171 | –0.311 to –0.030 | ||
| Lives in residential/nursing home | –0.264 | –0.351 to –0.177 | –0.416 | –0.510 to –0.323 | ||
| Lives in sheltered housing | –0.148 | –0.236 to –0.060 | –0.089 | –0.190 to 0.011 | ||
| Other | –0.150 | –0.364 to 0.063 | –0.183 | –0.405 to 0.039 | ||
| If patient left own home for service, where to: | < 0.001 | < 0.001 | ||||
| Residential/nursing home | –0.217 | –0.385 to –0.049 | –0.217 | –0.396 to –0.038 | ||
| Acute hospital | –0.152 | –0.732 to 0.429 | –0.369 | –0.824 to 0.086 | ||
| A&E | –0.381 | –0.553 to –0.209 | –0.276 | –0.490 to –0.062 | ||
| IC facility | 0.194 | 0.106 to 0.282 | 0.186 | 0.075 to 0.298 | ||
| Day hospital | –0.299 | –0.496 to –0.102 | –0.181 | –0.441 to 0.079 | ||
| Resource centre | 0.058 | –0.208 to 0.325 | 0.000 | –0.283 to 0.283 | ||
| Community hospital | 0.001 | –0.098 to 0.100 | –0.083 | –0.196 to 0.030 | ||
| Other | –0.009 | –0.275 to 0.256 | –0.189 | –0.412 to 0.035 | ||
Model coefficients for therapy outcome measure change: participation
| Covariate | Complete case data (n = 5340) | Imputed data (n = 7291) | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| Baseline TOM participation score | –0.193 | –0.212 to –0.174 | < 0.001 | –0.191 | –0.217 to –0.164 | < 0.001 |
| Age (per 10-year increase) | –0.022 | –0.037 to –0.006 | 0.006 | –0.026 | –0.043 to –0.008 | 0.005 |
| Sex (female vs. male) | 0.036 | –0.003 to 0.075 | 0.069 | 0.068 | 0.022 to 0.114 | 0.004 |
| LoC at admission | < 0.001 | < 0.001 | ||||
| 0 | Reference category | Reference category | ||||
| 1 | 0.078 | –0.014 to 0.171 | 0.008 | –0.091 to 0.107 | ||
| 2 | 0.166 | –0.018 to 0.350 | –0.002 | –0.188 to 0.184 | ||
| 3 | 0.248 | 0.154 to 0.341 | 0.147 | 0.060 to 0.233 | ||
| 4 | 0.333 | 0.241 to 0.425 | 0.260 | 0.167 to 0.352 | ||
| 5 | 0.323 | 0.213 to 0.434 | 0.240 | 0.121 to 0.358 | ||
| 6 | –0.004 | –0.129 to 0.122 | 0.003 | –0.131 to 0.137 | ||
| 7 | 0.048 | –0.103 to 0.199 | 0.018 | –0.148 to 0.183 | ||
| 8 | 0.108 | –0.082 to 0.299 | 0.143 | –0.063 to 0.348 | ||
| Who made the referral | < 0.001 | < 0.001 | ||||
| GP/doctor | Reference category | Reference category | ||||
| Self/informal carer/friend/family | 0.070 | –0.058 to 0.199 | 0.063 | –0.093 to 0.218 | ||
| Community nurse/nurse | –0.041 | –0.107 to 0.025 | –0.112 | –0.200 to –0.024 | ||
| Social worker/social services | –0.082 | –0.162 to –0.001 | –0.044 | –0.137 to 0.050 | ||
| AHP | 0.076 | 0.019 to 0.132 | –0.009 | –0.077 to 0.058 | ||
| A&E/ambulance service/rapid response | 0.116 | 0.019 to 0.213 | 0.120 | 0.004 to 0.237 | ||
| Ward in acute hospital/day clinics/fall clinics | 0.152 | 0.088 to 0.215 | 0.170 | 0.092 to 0.248 | ||
| Community hospital | 0.028 | –0.058 to 0.115 | 0.067 | –0.044 to 0.178 | ||
| Other | –0.290 | –0.616 to 0.036 | –0.173 | –0.566 to 0.219 | ||
| Living arrangements | < 0.001 | < 0.001 | ||||
| Lives alone in own home (owned or rented) | Reference category | Reference category | ||||
| Lives with other(s) in own home (owned or rented) | –0.033 | –0.075 to 0.009 | –0.043 | –0.090 to 0.005 | ||
| Lives in relative’s home | –0.049 | –0.180 to 0.082 | –0.116 | –0.274 to 0.042 | ||
| Lives in residential/nursing home | –0.329 | –0.415 to –0.243 | –0.467 | –0.571 to –0.364 | ||
| Lives in sheltered housing | –0.145 | –0.233 to –0.057 | –0.086 | –0.190 to 0.017 | ||
| Other | –0.301 | –0.514 to –0.087 | –0.336 | –0.557 to –0.114 | ||
| If patient left own home for service, where to: | 0.003 | 0.034 | ||||
| Residential/nursing home | –0.196 | –0.363 to –0.028 | –0.205 | –0.386 to –0.024 | ||
| Acute hospital | –0.267 | –0.847 to 0.312 | –0.201 | –0.750 to 0.348 | ||
| A&E | –0.283 | –0.455 to –0.111 | –0.192 | –0.412 to 0.029 | ||
| IC facility | 0.172 | 0.084 to 0.259 | 0.168 | 0.064 to 0.273 | ||
| Day hospital | –0.129 | –0.326 to 0.067 | 0.002 | –0.251 to 0.256 | ||
| Resource centre | –0.094 | –0.360 to 0.172 | –0.109 | –0.417 to 0.199 | ||
| Community hospital | 0.008 | –0.091 to 0.106 | –0.084 | –0.214 to 0.047 | ||
| Other | –0.069 | –0.329 to 0.190 | –0.228 | –0.445 to –0.011 | ||
Model coefficients for therapy outcome measure change: well-being
| Covariate | Complete case data (n = 5330) | Imputed data (n = 7291) | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| Baseline TOM well-being score | –0.254 | –0.273 to –0.236 | < 0.001 | –0.236 | –0.261 to –0.212 | < 0.001 |
| Age (per 10-year increase) | –0.018 | –0.033 to –0.004 | 0.014 | –0.028 | –0.046 to –0.009 | 0.003 |
| Sex (female vs. male) | 0.040 | 0.003 to 0.077 | 0.034 | 0.082 | 0.037 to 0.127 | < 0.001 |
| LoC at admission | < 0.001 | < 0.001 | ||||
| 0 | Reference category | Reference category | ||||
| 1 | 0.042 | –0.045 to 0.129 | –0.013 | –0.096 to 0.070 | ||
| 2 | 0.092 | –0.082 to 0.265 | –0.057 | –0.256 to 0.142 | ||
| 3 | 0.186 | 0.098 to 0.275 | 0.120 | 0.030 to 0.210 | ||
| 4 | 0.232 | 0.146 to 0.319 | 0.191 | 0.104 to 0.279 | ||
| 5 | 0.210 | 0.106 to 0.314 | 0.157 | 0.048 to 0.265 | ||
| 6 | –0.027 | –0.146 to 0.091 | –0.025 | –0.164 to 0.115 | ||
| 7 | 0.047 | –0.096 to 0.190 | 0.030 | –0.119 to 0.179 | ||
| 8 | –0.193 | –0.373 to –0.014 | –0.061 | –0.279 to 0.157 | ||
| Who made the referral | 0.004 | < 0.001 | ||||
| GP/doctor | Reference category | Reference category | ||||
| Self/informal carer/friend/family | 0.066 | –0.055 to 0.187 | 0.024 | –0.137 to 0.185 | ||
| Community nurse/nurse | –0.010 | –0.073 to 0.052 | –0.101 | –0.185 to –0.017 | ||
| Social worker/social services | –0.056 | –0.132 to 0.019 | –0.039 | –0.139 to 0.061 | ||
| AHP | 0.069 | 0.015 to 0.122 | –0.015 | –0.092 to 0.061 | ||
| A&E/ambulance service/rapid response | 0.039 | –0.053 to 0.130 | 0.076 | –0.030 to 0.181 | ||
| Ward in acute hospital/day clinics/fall clinics | 0.076 | 0.017 to 0.136 | 0.118 | 0.036 to 0.201 | ||
| Community hospital | 0.005 | –0.077 to 0.087 | 0.065 | –0.042 to 0.172 | ||
| Other | 0.111 | –0.197 to 0.418 | 0.201 | –0.186 to 0.589 | ||
| Living arrangements | < 0.001 | < 0.001 | ||||
| Lives alone in own home (owned or rented) | Reference category | Reference category | ||||
| Lives with other(s) in own home (owned or rented) | –0.040 | –0.080 to –0.001 | –0.045 | –0.094 to 0.003 | ||
| Lives in relative’s home | –0.104 | –0.228 to 0.019 | –0.187 | –0.339 to –0.035 | ||
| Lives in residential/nursing home | –0.322 | –0.403 to –0.242 | –0.469 | –0.563 to –0.375 | ||
| Lives in sheltered housing | –0.089 | –0.172 to –0.006 | –0.033 | –0.134 to 0.067 | ||
| Other | –0.304 | –0.508 to –0.100 | –0.331 | –0.556 to –0.105 | ||
| If patient left own home for service, where to: | < 0.001 | < 0.001 | ||||
| Residential/nursing home | –0.230 | –0.387 to –0.072 | –0.220 | –0.391 to –0.050 | ||
| Acute hospital | –0.417 | –0.964 to 0.129 | –0.318 | –0.794 to 0.158 | ||
| A&E | –0.144 | –0.306 to 0.018 | –0.089 | –0.309 to 0.132 | ||
| IC facility | 0.125 | 0.042 to 0.208 | 0.125 | 0.014 to 0.236 | ||
| Day hospital | –0.073 | –0.259 to 0.112 | 0.038 | –0.226 to 0.302 | ||
| Resource centre | 0.097 | –0.154 to 0.348 | 0.015 | –0.305 to 0.334 | ||
| Community hospital | 0.087 | –0.006 to 0.180 | –0.038 | –0.164 to 0.087 | ||
| Other | 0.272 | 0.027 to 0.518 | –0.043 | –0.285 to 0.199 | ||
Model coefficients for change in European Quality of Life-5 Dimensions score
| Covariate | Complete case data (n = 4332) | Imputed data (n = 7291) | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| Baseline score | –0.493 | –0.516 to –0.470 | < 0.001 | –0.493 | –0.509 to –0.477 | < 0.001 |
| Age (per 10-year increase) | 0.006 | –0.001 to 0.012 | 0.076 | 0.001 | –0.003 to 0.005 | 0.618 |
| Sex (female vs. male) | –0.001 | –0.016 to 0.015 | 0.908 | 0.008 | –0.002 to 0.018 | 0.106 |
| LoC at admission | < 0.001 | < 0.001 | ||||
| 0 | Reference category | Reference category | ||||
| 1 | –0.002 | –0.049 to 0.045 | 0.002 | –0.017 to 0.021 | ||
| 2 | 0.055 | –0.025 to 0.135 | 0.008 | –0.033 to 0.050 | ||
| 3 | 0.033 | –0.015 to 0.080 | 0.025 | 0.005 to 0.045 | ||
| 4 | 0.055 | 0.009 to 0.102 | 0.051 | 0.032 to 0.070 | ||
| 5 | 0.048 | –0.004 to 0.100 | 0.046 | 0.019 to 0.072 | ||
| 6 | –0.034 | –0.093 to 0.025 | –0.010 | –0.039 to 0.019 | ||
| 7 | 0.059 | –0.008 to 0.126 | 0.028 | –0.005 to 0.062 | ||
| 8 | –0.032 | –0.119 to 0.055 | 0.009 | –0.042 to 0.059 | ||
| Who made the referral | < 0.001 | < 0.001 | ||||
| GP/doctor | Reference category | Reference category | ||||
| Self/informal carer/friend/family | 0.013 | –0.036 to 0.063 | 0.015 | –0.020 to 0.050 | ||
| Community nurse/nurse | –0.016 | –0.042 to 0.011 | –0.023 | –0.040 to –0.006 | ||
| Social worker/social services | –0.010 | –0.043 to 0.022 | –0.004 | –0.025 to 0.017 | ||
| AHP | 0.018 | –0.004 to 0.041 | –0.004 | –0.019 to 0.010 | ||
| A&E/ambulance service/rapid response | 0.091 | 0.053 to 0.129 | 0.063 | 0.039 to 0.087 | ||
| Ward in acute hospital/day clinics/fall clinics | 0.039 | 0.014 to 0.063 | 0.041 | 0.024 to 0.057 | ||
| Community hospital | –0.003 | –0.035 to 0.030 | 0.011 | –0.013 to 0.035 | ||
| Other | –0.023 | –0.151 to 0.104 | –0.011 | –0.103 to 0.081 | ||
| Living arrangements | < 0.001 | < 0.001 | ||||
| Lives alone in own home (owned or rented) | Reference category | Reference category | ||||
| Lives with other(s) in own home (owned or rented) | –0.020 | –0.036 to –0.004 | –0.013 | –0.024 to –0.002 | ||
| Lives in relative’s home | –0.067 | –0.118 to –0.016 | –0.050 | –0.085 to –0.014 | ||
| Lives in residential/nursing home | –0.107 | –0.156 to –0.058 | –0.108 | –0.130 to –0.085 | ||
| Lives in sheltered housing | –0.061 | –0.096 to –0.027 | –0.032 | –0.055 to –0.008 | ||
| Other | –0.115 | –0.214 to –0.017 | –0.082 | –0.133 to –0.031 | ||
| If patient left own home for service, where to: | < 0.001 | 0.004 | ||||
| Residential/nursing home | –0.096 | –0.167 to –0.025 | –0.068 | –0.108 to –0.028 | ||
| Acute hospital | –0.085 | –0.348 to 0.178 | –0.070 | –0.173 to 0.033 | ||
| A&E | –0.150 | –0.228 to –0.072 | –0.101 | –0.154 to –0.047 | ||
| IC facility | 0.074 | 0.041 to 0.107 | 0.056 | 0.031 to 0.081 | ||
| Day hospital | –0.091 | –0.164 to –0.018 | –0.069 | –0.130 to –0.007 | ||
| Resource centre | 0.031 | –0.072 to 0.133 | 0.007 | –0.062 to 0.077 | ||
| Community hospital | –0.022 | –0.059 to 0.014 | –0.045 | –0.072 to –0.017 | ||
| Other | 0.082 | –0.018 to 0.182 | –0.011 | –0.059 to 0.037 | ||
Predicted probabilities of improvement in therapy outcome measure impairment (any improvement compared with no improvement)
| Covariate | Complete case data (n = 5337) | Imputed data (n = 7291) | ||||
|---|---|---|---|---|---|---|
| Predicted % improving | 95% CI | p-value | Predicted % improving | 95% CI | p-value | |
| Sex | 0.001 | 0.001 | ||||
| Male | 43 | 39 to 48 | 37 | 32 to 42 | ||
| Female | 48 | 44 to 53 | 42 | 37 to 47 | ||
| LoC at admission | < 0.001 | < 0.001 | ||||
| 0 | 7 | 4 to 11 | 17 | 14 to 22 | ||
| 1 | 35 | 31 to 40 | 33 | 28 to 38 | ||
| 2 | 42 | 29 to 55 | 34 | 25 to 44 | ||
| 3 | 53 | 48 to 58 | 46 | 40 to 52 | ||
| 4 | 61 | 57 to 65 | 53 | 48 to 59 | ||
| 5 | 55 | 48 to 61 | 46 | 39 to 53 | ||
| 6 | 27 | 21 to 34 | 28 | 22 to 35 | ||
| 7 | 38 | 29 to 49 | 32 | 25 to 40 | ||
| 8 | 35 | 23 to 48 | 36 | 25 to 48 | ||
| Who made the referral | < 0.001 | < 0.001 | ||||
| GP/doctor | 45 | 39 to 50 | 38 | 33 to 44 | ||
| Self/informal carer/friend/family | 42 | 32 to 53 | 37 | 28 to 47 | ||
| Community nurse/nurse | 39 | 34 to 45 | 35 | 30 to 41 | ||
| Social worker/social services | 34 | 28 to 40 | 33 | 27 to 39 | ||
| AHP | 48 | 43 to 53 | 41 | 35 to 46 | ||
| A&E /ambulance service/rapid response | 53 | 45 to 61 | 44 | 36 to 51 | ||
| Ward in acute hospital/day clinics/fall clinics | 54 | 49 to 60 | 48 | 42 to 53 | ||
| Community hospital | 47 | 40 to 54 | 43 | 36 to 51 | ||
| Other | 33 | 14 to 59 | 36 | 18 to 60 | ||
| Where receiving care | < 0.001 | < 0.001 | ||||
| Own home, lives alone | 48 | 43 to 52 | 42 | 37 to 47 | ||
| Own home, doesn’t live alone | 47 | 43 to 52 | 42 | 37 to 47 | ||
| Relative’s home | 47 | 36 to 58 | 37 | 28 to 47 | ||
| Residential/nursing home | 35 | 29 to 42 | 30 | 24 to 36 | ||
| Sheltered housing | 37 | 29 to 47 | 36 | 28 to 45 | ||
| Acute hospital | 32 | 7 to 75 | 24 | 9 to 50 | ||
| A&E | 22 | 10 to 40 | 30 | 17 to 49 | ||
| IC facility | 51 | 42 to 60 | 42 | 34 to 51 | ||
| Day hospital | 34 | 20 to 51 | 36 | 22 to 53 | ||
| Resource centre | 55 | 32 to 76 | 38 | 23 to 57 | ||
| Community hospital | 52 | 42 to 62 | 41 | 32 to 50 | ||
| Other | 43 | 27 to 60 | 35 | 25 to 46 | ||
Predicted probabilities of improvement in therapy outcome measure activity (any improvement compared with no improvement)
| Covariate | Complete case data (n = 5339) | Imputed data (n = 7291) | ||||
|---|---|---|---|---|---|---|
| Predicted % improving | 95% CI | p-value | Predicted % improving | 95% CI | p-value | |
| Sex | 0.030 | 0.009 | ||||
| Male | 47 | 41 to 52 | 41 | 35 to 47 | ||
| Female | 50 | 45 to 56 | 44 | 38 to 50 | ||
| LoC at admission | < 0.001 | < 0.001 | ||||
| 0 | 8 | 5 to 13 | 18 | 14 to 24 | ||
| 1 | 38 | 32 to 44 | 35 | 29 to 42 | ||
| 2 | 54 | 41 to 68 | 44 | 33 to 55 | ||
| 3 | 56 | 50 to 61 | 49 | 43 to 56 | ||
| 4 | 61 | 56 to 67 | 54 | 48 to 61 | ||
| 5 | 59 | 51 to 66 | 50 | 42 to 58 | ||
| 6 | 32 | 24 to 40 | 32 | 25 to 40 | ||
| 7 | 44 | 33 to 55 | 38 | 29 to 47 | ||
| 8 | 35 | 23 to 49 | 36 | 25 to 49 | ||
| Who made the referral | < 0.001 | < 0.001 | ||||
| GP/doctor | 44 | 38 to 50 | 39 | 33 to 46 | ||
| Self/informal carer/friend/family | 52 | 41 to 63 | 46 | 36 to 56 | ||
| Community nurse/nurse | 41 | 35 to 48 | 37 | 31 to 44 | ||
| Social worker/social services | 41 | 33 to 48 | 37 | 30 to 45 | ||
| AHP | 51 | 45 to 57 | 43 | 37 to 50 | ||
| A&E/ambulance service/rapid response | 55 | 46 to 63 | 47 | 39 to 56 | ||
| Ward in acute hospital/day clinics/fall clinics | 57 | 50 to 63 | 50 | 43 to 57 | ||
| Community hospital | 51 | 43 to 59 | 47 | 39 to 55 | ||
| Other | 40 | 18 to 66 | 40 | 20 to 64 | ||
| Where receiving care | < 0.001 | < 0.001 | ||||
| Own home, lives alone | 52 | 46 to 58 | 46 | 39 to 52 | ||
| Own home, doesn’t live alone | 51 | 45 to 57 | 45 | 39 to 52 | ||
| Relative’s home | 47 | 35 to 58 | 38 | 29 to 49 | ||
| Residential/nursing home | 31 | 25 to 39 | 29 | 23 to 36 | ||
| Sheltered housing | 37 | 28 to 48 | 36 | 27 to 45 | ||
| Acute hospital | 57 | 17 to 89 | 39 | 17 to 65 | ||
| A&E | 16 | 6 to 36 | 24 | 12 to 44 | ||
| IC facility | 50 | 40 to 60 | 43 | 34 to 52 | ||
| Day hospital | 35 | 20 to 53 | 34 | 19 to 51 | ||
| Resource centre | 63 | 38 to 83 | 45 | 27 to 63 | ||
| Community hospital | 50 | 39 to 61 | 40 | 31 to 50 | ||
| Other | 53 | 36 to 70 | 36 | 25 to 48 | ||
Predicted probabilities of improvement in therapy outcome measure participation (any improvement compared with no improvement)
| Covariate | Complete case data (n = 5340) | Imputed data (n = 7291) | ||||
|---|---|---|---|---|---|---|
| Predicted % improving | 95% CI | p-value | Predicted % improving | 95% CI | p-value | |
| Sex | 0.464 | 0.213 | ||||
| Male | 41 | 36 to 45 | 35 | 30 to 41 | ||
| Female | 42 | 37 to 46 | 37 | 32 to 43 | ||
| LoC at admission | < 0.001 | < 0.001 | ||||
| 0 | 10 | 7 to 16 | 18 | 14 to 23 | ||
| 1 | 30 | 26 to 35 | 29 | 24 to 34 | ||
| 2 | 44 | 31 to 57 | 35 | 25 to 45 | ||
| 3 | 48 | 43 to 53 | 43 | 37 to 49 | ||
| 4 | 53 | 48 to 58 | 47 | 41 to 53 | ||
| 5 | 50 | 43 to 57 | 43 | 36 to 50 | ||
| 6 | 25 | 19 to 32 | 25 | 19 to 32 | ||
| 7 | 32 | 23 to 42 | 29 | 22 to 37 | ||
| 8 | 34 | 22 to 48 | 34 | 23 to 46 | ||
| Who made the referral | < 0.001 | < 0.001 | ||||
| GP/doctor | 38 | 33 to 44 | 34 | 29 to 40 | ||
| Self/informal carer/friend/family | 45 | 35 to 56 | 40 | 30 to 50 | ||
| Community nurse/nurse | 33 | 27 to 38 | 30 | 25 to 36 | ||
| Social worker/social services | 33 | 27 to 39 | 30 | 24 to 36 | ||
| AHP | 45 | 40 to 51 | 39 | 34 to 45 | ||
| A&E/ambulance service/rapid response | 42 | 34 to 50 | 37 | 30 to 45 | ||
| Ward in acute hospital/day clinics/fall clinics | 49 | 43 to 54 | 42 | 37 to 49 | ||
| Community hospital | 43 | 36 to 50 | 39 | 32 to 46 | ||
| Other | 20 | 7 to 46 | 20 | 8 to 43 | ||
| Where receiving care | < 0.001 | < 0.001 | ||||
| Own home, lives alone | 45 | 40 to 50 | 40 | 34 to 45 | ||
| Own home, doesn’t live alone | 43 | 38 to 48 | 38 | 33 to 44 | ||
| Relative’s home | 44 | 33 to 55 | 35 | 26 to 45 | ||
| Residential/nursing home | 23 | 17 to 29 | 21 | 17 to 27 | ||
| Sheltered housing | 31 | 23 to 41 | 29 | 21 to 38 | ||
| Acute hospital | 17 | 2 to 67 | 26 | 10 to 54 | ||
| A&E | 8 | 3 to 22 | 15 | 6 to 32 | ||
| IC facility | 46 | 37 to 55 | 37 | 29 to 45 | ||
| Day hospital | 38 | 23 to 56 | 38 | 23 to 55 | ||
| Resource centre | 57 | 34 to 77 | 42 | 26 to 60 | ||
| Community hospital | 46 | 36 to 56 | 38 | 30 to 47 | ||
| Other | 34 | 20 to 51 | 26 | 17 to 38 | ||
Predicted probabilities of improvement in therapy outcome measure well-being (any improvement compared with no improvement)
| Covariate | Complete case data (n = 5330) | Imputed data (n = 7291) | ||||
|---|---|---|---|---|---|---|
| Predicted % improving | 95% CI | p-value | Predicted % improving | 95% CI | p-value | |
| Sex | 0.001 | 0.001 | ||||
| Male | 30 | 26 to 35 | 26 | 22 to 31 | ||
| Female | 33 | 29 to 38 | 29 | 25 to 34 | ||
| LoC at admission | < 0.001 | < 0.001 | ||||
| 0 | 6 | 3 to 10 | 13 | 10 to 17 | ||
| 1 | 25 | 21 to 30 | 23 | 19 to 29 | ||
| 2 | 31 | 20 to 45 | 25 | 17 to 35 | ||
| 3 | 37 | 32 to 43 | 33 | 27 to 38 | ||
| 4 | 43 | 38 to 48 | 37 | 31 to 43 | ||
| 5 | 38 | 32 to 46 | 32 | 26 to 39 | ||
| 6 | 22 | 16 to 29 | 23 | 17 to 30 | ||
| 7 | 22 | 15 to 32 | 20 | 14 to 27 | ||
| 8 | 17 | 10 to 28 | 19 | 12 to 30 | ||
| Who made the referral | < 0.001 | < 0.001 | ||||
| GP/doctor | 30 | 25 to 35 | 26 | 21 to 32 | ||
| Self/informal carer/friend/family | 35 | 26 to 46 | 29 | 21 to 38 | ||
| Community nurse/nurse | 26 | 21 to 32 | 24 | 19 to 29 | ||
| Social worker/social services | 27 | 21 to 33 | 24 | 19 to 30 | ||
| AHP | 36 | 31 to 42 | 31 | 25 to 36 | ||
| A&E/ambulance service/rapid response | 31 | 24 to 39 | 26 | 20 to 34 | ||
| Ward in acute hospital/day clinics/fall clinics | 37 | 31 to 42 | 32 | 27 to 38 | ||
| Community hospital | 32 | 26 to 40 | 30 | 23 to 37 | ||
| Other | 20 | 7 to 45 | 22 | 9 to 46 | ||
| Where receiving care | < 0.001 | < 0.001 | ||||
| Own home, lives alone | 37 | 32 to 42 | 32 | 27 to 37 | ||
| Own home, doesn’t live alone | 33 | 28 to 38 | 28 | 24 to 34 | ||
| Relative’s home | 32 | 23 to 44 | 24 | 17 to 33 | ||
| Residential/nursing home | 13 | 9 to 17 | 14 | 10 to 18 | ||
| Sheltered housing | 28 | 20 to 37 | 25 | 18 to 34 | ||
| Acute hospital | a | 16 | 4 to 44 | |||
| A&E | 4 | 1 to 18 | 12 | 4 to 31 | ||
| IC facility | 35 | 27 to 45 | 29 | 22 to 37 | ||
| Day hospital | 28 | 15 to 45 | 28 | 15 to 45 | ||
| Resource centre | 49 | 27 to 71 | 34 | 19 to 54 | ||
| Community hospital | 38 | 29 to 49 | 30 | 22 to 39 | ||
| Other | 44 | 28 to 62 | 28 | 19 to 40 | ||
Model coefficients for improvement in European Quality of Life-5 Dimensions score (any improvement compared with no improvement)
| Covariate | Complete case data (n = 4332) | Imputed data (n = 7291) | ||||
|---|---|---|---|---|---|---|
| Predicted % improving | 95% CI | p-value | Predicted % improving | 95% CI | p-value | |
| Sex | 0.585 | 0.871 | ||||
| Male | 65 | 62 to 68 | 72 | 69 to 75 | ||
| Female | 64 | 61 to 67 | 72 | 69 to 75 | ||
| LoC at admission | < 0.001 | < 0.001 | ||||
| 0 | 26 | 18 to 38 | 69 | 64 to 74 | ||
| 1 | 55 | 51 to 60 | 69 | 65 to 72 | ||
| 2 | 56 | 41 to 70 | 70 | 60 to 79 | ||
| 3 | 66 | 62 to 70 | 72 | 68 to 75 | ||
| 4 | 72 | 69 to 75 | 77 | 74 to 80 | ||
| 5 | 67 | 61 to 73 | 74 | 68 to 78 | ||
| 6 | 49 | 40 to 57 | 64 | 56 to 70 | ||
| 7 | 61 | 49 to 71 | 74 | 65 to 80 | ||
| 8 | 57 | 40 to 72 | 74 | 61 to 84 | ||
| Who made the referral | < 0.001 | < 0.001 | ||||
| GP/doctor | 62 | 58 to 66 | 71 | 67 to 74 | ||
| Self/informal carer/friend/family | 63 | 53 to 73 | 71 | 62 to 78 | ||
| Community nurse/nurse | 57 | 51 to 62 | 68 | 63 to 72 | ||
| Social worker/social services | 57 | 50 to 63 | 69 | 63 to 74 | ||
| AHP | 66 | 62 to 70 | 73 | 69 to 76 | ||
| A&E/ambulance service/rapid response | 75 | 68 to 81 | 79 | 74 to 84 | ||
| Ward in acute hospital/day clinics/fall clinics | 71 | 67 to 75 | 77 | 73 to 80 | ||
| Community hospital | 59 | 53 to 66 | 71 | 65 to 76 | ||
| Other | 52 | 25 to 77 | 62 | 37 to 82 | ||
| Where receiving care | < 0.001 | 0.002 | ||||
| Own home, lives alone | 66 | 63 to 69 | 74 | 70 to 77 | ||
| Own home, doesn’t live alone | 64 | 61 to 68 | 73 | 69 to 76 | ||
| Relative’s home | 63 | 51 to 74 | 72 | 63 to 80 | ||
| Residential/nursing home | 47 | 38 to 57 | 69 | 63 to 74 | ||
| Sheltered housing | 54 | 43 to 64 | 67 | 59 to 74 | ||
| Acute hospital | 34 | 4 to 86 | 66 | 38 to 86 | ||
| A&E | 19 | 8 to 36 | 50 | 33 to 67 | ||
| IC facility | 77 | 69 to 83 | 78 | 71 to 83 | ||
| Day hospital | 45 | 30 to 62 | 56 | 39 to 72 | ||
| Resource centre | 76 | 48 to 91 | 78 | 59 to 89 | ||
| Community hospital | 62 | 53 to 71 | 64 | 55 to 72 | ||
| Other | 85 | 64 to 95 | 79 | 69 to 86 | ||
Appendix 3 Results of the data analysis for therapy outcome measures by team composition
Results of the data analysis for therapy outcome measure: impairment
| Outcome: change in TOM impairment | Complete case | Imputed | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| Number of different services referring in | –0.009 | –0.057 to 0.039 | 0.703 | –0.001 | –0.056 to 0.053 | 0.959 |
| Total number of staff in team | 0.001 | –0.001 to 0.004 | 0.231 | 0.001 | –0.001 to 0.004 | 0.315 |
| Total number of staff types in team | 0.029 | –0.000 to 0.057 | 0.052 | 0.032 | –0.000 to 0.065 | 0.050a |
| Estimated number of patients per year | 0.000 | –0.000 to 0.000 | 0.734 | 0.000 | –0.000 to 0.000 | 0.974 |
| Number of patients per member of staff | –0.002 | –0.006 to 0.001 | 0.199 | –0.003 | –0.007 to 0.001 | 0.089 |
| Number of clinical staff in team | 0.002 | –0.002 to 0.007 | 0.348 | 0.002 | –0.003 to 0.007 | 0.473 |
| Number of clinical support staff in team | 0.010 | 0.001 to 0.019 | 0.025a | 0.011 | 0.001 to 0.021 | 0.040a |
| Number of management staff in team | 0.010 | –0.025 to 0.045 | 0.554 | 0.007 | –0.033 to 0.047 | 0.719 |
| Number of social care staff in team | 0.000 | –0.013 to 0.014 | 0.951 | 0.000 | –0.015 to 0.015 | 0.995 |
| Number of non-clinical support staff in team | 0.010 | –0.027 to 0.048 | 0.584 | 0.008 | –0.035 to 0.051 | 0.700 |
| Number of domiciliary support staff in team | 0.094 | 0.010 to 0.178 | 0.030a | 0.108 | 0.016 to 0.199 | 0.023a |
| % skilled workers in team | –0.002 | –0.006 to 0.002 | 0.305 | –0.003 | –0.008 to 0.001 | 0.160 |
| Number of team leaders | 0.005 | –0.039 to 0.049 | 0.823 | –0.001 | –0.052 to 0.049 | 0.957 |
Results of the data analysis for therapy outcome measure: activity
| Outcome: change in TOM activity | Complete case | Imputed | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | 95% CI | Coefficient | p-value | |
| Number of different services referring in | –0.009 | –0.060 to 0.042 | 0.716 | –0.003 | –0.059 to 0.053 | 0.906 |
| Total number of staff in team | 0.001 | –0.002 to 0.003 | 0.703 | 0.000 | –0.003 to 0.003 | 0.762 |
| Total number of staff types in team | 0.015 | –0.018 to 0.047 | 0.362 | 0.018 | –0.017 to 0.053 | 0.308 |
| Estimated number of patients per year | 0.000 | –0.000 to 0.000 | 0.895 | 0.000 | –0.000 to 0.000 | 0.744 |
| Number of patients per member of staff | –0.002 | –0.006 to 0.002 | 0.264 | –0.003 | –0.007 to 0.001 | 0.146 |
| Number of clinical staff in team | 0.001 | –0.004 to 0.006 | 0.777 | 0.000 | –0.005 to 0.006 | 0.864 |
| Number of clinical support staff in team | 0.006 | –0.005 to 0.016 | 0.272 | 0.006 | –0.005 to 0.018 | 0.279 |
| Number of management staff in team | 0.000 | –0.038 to 0.038 | 0.985 | –0.004 | –0.046 to 0.038 | 0.859 |
| Number of social care staff in team | –0.002 | –0.016 to 0.012 | 0.741 | –0.003 | –0.019 to 0.013 | 0.711 |
| Number of non-clinical support staff in team | –0.003 | –0.044 to 0.037 | 0.866 | –0.005 | –0.050 to 0.040 | 0.829 |
| Number of domiciliary support staff in team | 0.055 | –0.038 to 0.149 | 0.233 | 0.067 | –0.033 to 0.167 | 0.182 |
| % skilled workers in team | –0.001 | –0.006 to 0.003 | 0.586 | –0.002 | –0.007 to 0.003 | 0.357 |
| Number of team leaders | –0.006 | –0.053 to 0.042 | 0.808 | –0.012 | –0.064 to 0.041 | 0.653 |
Results of the data analysis for therapy outcome measure: participation
| Outcome: change in TOM participation | Complete case | Imputed | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| Number of different services referring in | –0.026 | –0.064 to 0.012 | 0.167 | –0.022 | –0.068 to 0.024 | 0.329 |
| Total number of staff in team | 0.000 | –0.002 to 0.002 | 0.915 | 0.000 | –0.002 to 0.003 | 0.849 |
| Total number of staff types in team | 0.003 | –0.023 to 0.030 | 0.799 | 0.008 | –0.023 to 0.039 | 0.585 |
| Estimated number of patients per year | 0.000 | –0.000 to 0.000 | 0.812 | 0.000 | –0.000 to 0.000 | 0.672 |
| Number of patients per member of staff | –0.001 | –0.004 to 0.002 | 0.628 | –0.002 | –0.006 to 0.001 | 0.234 |
| Number of clinical staff in team | 0.000 | –0.004 to 0.004 | 0.923 | 0.000 | –0.004 to 0.005 | 0.862 |
| Number of clinical support staff in team | 0.003 | –0.006 to 0.011 | 0.532 | 0.003 | –0.007 to 0.013 | 0.506 |
| Number of management staff in team | –0.003 | –0.032 to 0.027 | 0.863 | –0.004 | –0.040 to 0.032 | 0.825 |
| Number of social care staff in team | –0.003 | –0.014 to 0.007 | 0.538 | –0.003 | –0.016 to 0.010 | 0.608 |
| Number of non-clinical support staff in team | –0.002 | –0.033 to 0.030 | 0.905 | –0.001 | –0.039 to 0.037 | 0.971 |
| Number of domiciliary support staff in team | 0.053 | –0.022 to 0.128 | 0.159 | 0.071 | –0.013 to 0.155 | 0.095 |
| % skilled workers in team | –0.000 | –0.004 to 0.003 | 0.959 | –0.001 | –0.005 to 0.003 | 0.678 |
| Number of team leaders | –0.010 | –0.047 to 0.027 | 0.579 | –0.015 | –0.059 to 0.030 | 0.508 |
Results of the data analysis for therapy outcome measure: well-being
| Outcome: change in TOM well-being | Complete case | Imputed | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| Number of different services referring in | –0.002 | –0.037 to 0.033 | 0.898 | 0.002 | –0.037 to 0.041 | 0.915 |
| Total number of staff in team | 0.000 | –0.002 to 0.002 | 0.883 | 0.000 | –0.002 to 0.002 | 0.922 |
| Total number of staff types in team | 0.008 | –0.014 to 0.031 | 0.446 | 0.009 | –0.016 to 0.034 | 0.450 |
| Estimated number of patients per year | 0.000 | –0.000 to 0.000 | 0.838 | 0.000 | –0.000 to 0.000 | 0.725 |
| Number of patients per member of staff | –0.001 | –0.004 to 0.001 | 0.251 | –0.002 | –0.005 to 0.001 | 0.140 |
| Number of clinical staff in team | 0.000 | –0.003 to 0.003 | 0.965 | 0.000 | –0.004 to 0.004 | 0.973 |
| Number of clinical support staff in team | 0.002 | –0.004 to 0.009 | 0.476 | 0.003 | –0.005 to 0.011 | 0.488 |
| Number of management staff in team | –0.001 | –0.026 to 0.024 | 0.937 | –0.002 | –0.030 to 0.026 | 0.870 |
| Number of social care staff in team | –0.001 | –0.010 to 0.007 | 0.756 | –0.002 | –0.012 to 0.008 | 0.731 |
| Number of non-clinical support staff in team | –0.002 | –0.027 to 0.024 | 0.894 | –0.003 | –0.032 to 0.027 | 0.847 |
| Number of domiciliary support staff in team | 0.037 | –0.035 to 0.110 | 0.303 | 0.050 | –0.024 to 0.123 | 0.176 |
| % skilled workers in team | –0.001 | –0.004 to 0.002 | 0.651 | –0.001 | –0.004 to 0.002 | 0.424 |
| Number of team leaders | –0.006 | –0.036 to 0.025 | 0.706 | –0.009 | –0.044 to 0.026 | 0.618 |
Appendix 4 Results of the data analysis for European Quality of Life-5 Dimensions score change by team composition
Results of the data analysis for European Quality of Life-5 Dimensions score change
| Outcome: change in EQ-5D | Complete case | Imputed | ||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| Number of different services referring in | 0.000 | –0.009 to 0.009 | 0.988 | 0.000 | –0.011 to 0.011 | 0.983 |
| Total number of staff in team | 0.000 | –0.000 to 0.000 | 0.796 | 0.000 | –0.001 to 0.000 | 0.782 |
| Total number of staff types in team | 0.005 | –0.000 to 0.010 | 0.070 | 0.004 | –0.002 to 0.011 | 0.185 |
| Estimated number of patients per year | 0.000 | –0.000 to 0.000 | 0.921 | 0.000 | –0.000 to 0.000 | 0.623 |
| Number of patients per member of staff | 0.000 | –0.001 to 0.001 | 0.500 | –0.001 | –0.001 to 0.000 | 0.232 |
| Number of clinical staff in team | 0.000 | –0.001 to 0.001 | 0.676 | 0.000 | –0.001 to 0.001 | 0.583 |
| Number of clinical support staff in team | 0.000 | –0.001 to 0.002 | 0.575 | 0.001 | –0.001 to 0.003 | 0.464 |
| Number of management staff in team | –0.001 | –0.007 to 0.004 | 0.681 | –0.002 | –0.009 to 0.005 | 0.547 |
| Number of social care staff in team | –0.001 | –0.002 to 0.001 | 0.548 | –0.001 | –0.003 to 0.002 | 0.611 |
| Number of non-clinical support staff in team | –0.001 | –0.007 to 0.005 | 0.802 | –0.002 | –0.009 to 0.006 | 0.641 |
| Number of domiciliary support staff in team | 0.003 | –0.016 to 0.022 | 0.752 | 0.008 | –0.014 to 0.029 | 0.468 |
| % skilled workers in team | –0.000 | –0.001 to 0.000 | 0.224 | –0.001 | –0.011 to 0.007 | 0.060 |
| Number of team leaders | –0.001 | –0.008 to 0.006 | 0.796 | –0.002 | –0.011 to 0.007 | 0.590 |
Appendix 5 Results of the data analysis for length of stay by team composition
Results of the data analysis for length of stay
| Characteristic | Coefficient | 95% CI | p-value |
|---|---|---|---|
| Probability of short duration of ICa | |||
| Number of different services referring in | –0.013 | –0.034 to 0.009 | 0.226 |
| Total number of staff in team | –0.001 | –0.002 to 0.001 | 0.361 |
| Total number of staff types in team | –0.012 | –0.026 to 0.003 | 0.123 |
| Estimated number of patients per year | 0.000 | –0.000 to 0.000 | 0.660 |
| Number of clinical staff in team | –0.001 | –0.003 to 0.001 | 0.300 |
| Number of clinical support staff in team | –0.001 | –0.006 to 0.004 | 0.561 |
| Number of management staff in team | 0.002 | –0.015 to 0.020 | 0.781 |
| Number of social care staff in team | –0.003 | –0.009 to 0.004 | 0.389 |
| Number of non-clinical support staff in team | –0.007 | –0.025 to 0.012 | 0.455 |
| Number of domiciliary support staff in team | –0.011 | –0.055 to 0.032 | 0.594 |
| % skilled workers in team | 0.058 | –0.655 to 0.539 | 0.845 |
| Number of team leaders | 0.001 | –0.021 to 0.023 | 0.908 |
| Length of ICb | |||
| Number of different services referring in | –0.761 | –7.610 to 6.089 | 0.821 |
| Total number of staff in team | –0.056 | –0.448 to 0.337 | 0.774 |
| Total number of staff types in team | 2.738 | –1.637 to 7.113 | 0.211 |
| Estimated number of patients per year | –0.024 | –0.053 to 0.004 | 0.095 |
| Number of clinical staff in team | –0.050 | –0.773 to 0.672 | 0.888 |
| Number of clinical support staff in team | –0.295 | –1.810 to 1.221 | 0.694 |
| Number of management staff in team | –2.944 | –8.216 to 2.328 | 0.263 |
| Number of social care staff in team | –0.026 | –2.120 to 2.068 | 0.980 |
| Number of non-clinical support staff in team | –1.133 | –7.001 to 4.735 | 0.696 |
| Number of domiciliary support staff in team | 0.580 | –12.505 to 13.666 | 0.928 |
| % skilled workers in team | 0.001 | –0.001 to 0.003 | 0.445 |
| Number of team leaders | –2.760 | –9.454 to 3.934 | 0.406 |
Appendix 6 Level of care at admission: change over time
The tables below show the percentage (and number) of patients with each LoC at admission for each of the two studies. This is shown individually for each of the seven teams that were in both studies, the average of the data from the teams that were in both studies and for all the data.
The totals at the top of each column are the total number of patients per team/study, but not all patients have data for LoC at admission.
Team 1
| LoC at admission | % (n) of patients | |
|---|---|---|
| COOP1 (N = 52)a | EEICC2 (N = 166)b | |
| 0 (does not need any intervention) | 2.0 (1) | 0.0 (0) |
| 1 (needs prevention/maintenance programme) | 2.0 (1) | 0.0 (0) |
| 2 (needs convalescence/respite) | 0.0 (0) | 0.0 (0) |
| 3 (needs slow-stream rehabilitation) | 7.8 (4) | 1.3 (2) |
| 4 (needs regular rehabilitation programme) | 64.7 (33) | 56.7 (89) |
| 5 (needs intensive rehabilitation) | 19.6 (10) | 42.0 (66) |
| 6 (needs specific treatment for individual acute disability) | 2.0 (1) | 0.0 (0) |
| 7 (needs medical care and rehabilitation) | 2.0 (1) | 0.0 (0) |
| 8 (needs rehabilitation for complex disabling condition) | 0.0 (0) | 0.0 (0) |
Team 2
| LoC at admission | % (n) of patients | |
|---|---|---|
| COOP1 (N = 313)a | EEICC2 (N = 1116)b | |
| 0 (does not need any intervention) | 7.6 (20) | 8.5 (77) |
| 1 (needs prevention/maintenance programme) | 14.1 (37) | 12.2 (110) |
| 2 (needs convalescence/respite) | 3.4 (9) | 1.3 (12) |
| 3 (needs slow-stream rehabilitation) | 9.1 (24) | 19.5 (176) |
| 4 (needs regular rehabilitation programme) | 46.8 (123) | 37.1 (335) |
| 5 (needs intensive rehabilitation) | 9.1 (24) | 9.6 (87) |
| 6 (needs specific treatment for individual acute disability) | 3.8 (10) | 3.7 (33) |
| 7 (needs medical care and rehabilitation) | 4.2 (11) | 7.4 (67) |
| 8 (needs rehabilitation for complex disabling condition) | 1.9 (5) | 0.8 (7) |
Team 3
| LoC at admission | % (n) of patients | |
|---|---|---|
| COOP1 (N = 69)a | EEICC2 (N = 437)b | |
| 0 (does not need any intervention) | 1.9 (1) | 8.0 (33) |
| 1 (needs prevention/maintenance programme) | 7.7 (4) | 16.1 (67) |
| 2 (needs convalescence/respite) | 1.9 (1) | 2.4 (10) |
| 3 (needs slow-stream rehabilitation) | 34.6 (18) | 28.9 (120) |
| 4 (needs regular rehabilitation programme) | 32.7 (17) | 37.8 (157) |
| 5 (needs intensive rehabilitation) | 9.6 (5) | 4.3 (18) |
| 6 (needs specific treatment for individual acute disability) | 1.9 (1) | 0.7 (3) |
| 7 (needs medical care and rehabilitation) | 7.7 (4) | 1.7 (7) |
| 8 (needs rehabilitation for complex disabling condition) | 1.9 (1) | 0.0 (0) |
Team 4
| LoC at admission | % (n) of patients | |
|---|---|---|
| COOP1 (N = 16)a | EEICC2 (N = 116)b | |
| 0 (does not need any intervention) | 0.0 (0) | 0.0 (0) |
| 1 (needs prevention/maintenance programme) | 6.3 (1) | 0.9 (1) |
| 2 (needs convalescence/respite) | 6.3 (1) | 0.9 (1) |
| 3 (needs slow-stream rehabilitation) | 0.0 (0) | 6.9 (8) |
| 4 (needs regular rehabilitation programme) | 81.3 (13) | 83.6 (97) |
| 5 (needs intensive rehabilitation) | 0.0 (0) | 1.7 (2) |
| 6 (needs specific treatment for individual acute disability) | 6.3 (1) | 5.2 (6) |
| 7 (needs medical care and rehabilitation) | 0.0 (0) | 0.9 (1) |
| 8 (needs rehabilitation for complex disabling condition) | 0.0 (0) | 0.0 (0) |
Team 5
| LoC at admission | % (n) of patients | |
|---|---|---|
| COOP1 (N = 21)a | EEICC2 (N = 250)b | |
| 0 (does not need any intervention) | 14.3 (2) | 11.2 (22) |
| 1 (needs prevention/maintenance programme) | 0.0 (0) | 25.9 (51) |
| 2 (needs convalescence/respite) | 0.0 (0) | 0.5 (1) |
| 3 (needs slow-stream rehabilitation) | 14.3 (2) | 16.8 (33) |
| 4 (needs regular rehabilitation programme) | 64.3 (9) | 38.6 (76) |
| 5 (needs intensive rehabilitation) | 7.1 (1) | 4.6 (9) |
| 6 (needs specific treatment for individual acute disability) | 0.0 (0) | 0.5 (1) |
| 7 (needs medical care and rehabilitation) | 0.0 (0) | 0.5 (1) |
| 8 (needs rehabilitation for complex disabling condition) | 0.0 (0) | 1.5 (3) |
Team 6
| LoC at admission | % (n) of patients | |
|---|---|---|
| COOP1 (N = 46)a | EEICC2 (N = 173)b | |
| 0 (does not need any intervention) | 0.0 (0) | 0.0 (0) |
| 1 (needs prevention/maintenance programme) | 5.1 (2) | 1.8 (3) |
| 2 (needs convalescence/respite) | 2.6 (1) | 1.8 (3) |
| 3 (needs slow-stream rehabilitation) | 35.9 (14) | 27.7 (47) |
| 4 (needs regular rehabilitation programme) | 38.5 (15) | 32.4 (55) |
| 5 (needs intensive rehabilitation) | 12.8 (5) | 23.5 (40) |
| 6 (needs specific treatment for individual acute disability) | 0.0 (0) | 9.4 (16) |
| 7 (needs medical care and rehabilitation) | 0.0 (0) | 0.6 (1) |
| 8 (needs rehabilitation for complex disabling condition) | 5.1 (2) | 2.9 (5) |
Team 7
| LoC at admission | % (n) of patients | |
|---|---|---|
| COOP1 (N = 53)a | EEICC2 (N = 329)b | |
| 0 (does not need any intervention) | 0.0 (0) | 20.1 (59) |
| 1 (needs prevention/maintenance programme) | 9.8 (4) | 15.7 (46) |
| 2 (needs convalescence/respite) | 0.0 (0) | 1.4 (4) |
| 3 (needs slow-stream rehabilitation) | 24.4 (10) | 20.1 (59) |
| 4 (needs regular rehabilitation programme) | 51.2 (21) | 38.9 (114) |
| 5 (needs intensive rehabilitation) | 4.9 (2) | 1.0 (3) |
| 6 (needs specific treatment for individual acute disability) | 4.9 (2) | 0.3 (1) |
| 7 (needs medical care and rehabilitation) | 2.4 (1) | 1.4 (4) |
| 8 (needs rehabilitation for complex disabling condition) | 2.4 (1) | 1.0 (3) |
Average using data from teams that were in both studies
| LoC at admission | % (n) of patients | |
|---|---|---|
| COOP1 (N = 670)a | EEICC2 (N = 2722)b | |
| 0 (does not need any intervention) | 5.0 (24) | 8.5 (191) |
| 1 (needs prevention/maintenance programme) | 10.3 (49) | 12.3 (278) |
| 2 (needs convalescence/respite) | 2.5 (12) | 1.4 (31) |
| 3 (needs slow-stream rehabilitation) | 15.1 (72) | 19.8 (445) |
| 4 (needs regular rehabilitation programme) | 48.5 (231) | 41.0 (923) |
| 5 (needs intensive rehabilitation) | 9.9 (47) | 10.0 (225) |
| 6 (needs specific treatment for individual acute disability) | 3.2 (15) | 2.7 (60) |
| 7 (needs medical care and rehabilitation) | 3.6 (17) | 3.6 (81) |
| 8 (needs rehabilitation for complex disabling condition) | 1.9 (9) | 0.8 (18) |
Average using all data
| LoC at admission | % (n) of patients | |
|---|---|---|
| COOP1 (n = 1880)a | EEICC2 (n = 6190)b | |
| 0 (does not need any intervention) | 6.7 (109) | 9.5 (520) |
| 1 (needs prevention/maintenance programme) | 15.2 (248) | 25.9 (1412) |
| 2 (needs convalescence/respite) | 2.6 (43) | 1.4 (74) |
| 3 (needs slow-stream rehabilitation) | 19.3 (315) | 20.3 (1106) |
| 4 (needs regular rehabilitation programme) | 29.9 (488) | 31.3 (1709) |
| 5 (needs intensive rehabilitation) | 13.5 (220) | 5.4 (296) |
| 6 (needs specific treatment for individual acute disability) | 6.1 (99) | 3.3 (180) |
| 7 (needs medical care and rehabilitation) | 5.1 (83) | 2.2 (118) |
| 8 (needs rehabilitation for complex disabling condition) | 1.7 (27) | 0.9 (48) |
Appendix 7 Protocol
Glossary
- Allied Health Professional
- This refers to professions aligned to medicine, excluding nurses. These professions include arts therapists, chiropodists, dieticians, occupational therapists, orthoptists, paramedics, physiotherapists, prosthetists and orthotists, psychologists, psychotherapists, radiographers, and speech and language therapists.
- Care provider
- Any person employed in formal care delivery for a service user, either professionally trained staff or non-professional staff.
- Community rehabilitation
- Community-based services including a range of professions and support workers (physiotherapists, occupational therapists, nurses, speech and language therapists, dieticians, psychologists and pharmacists, etc.) aimed at increasing and promoting the independence and autonomy of persons with disabilities.
- European Quality of Life-5 Dimensions
- A generic, patient-reported, standardised health-related quality-of-life measure, formerly called the EuroQoL.
- Extended-scope practitioner
- These are general practitioners, nurses, therapists and other health professionals with special interests who develop an additional expertise that enables them to expand their clinical practice in a defined area.
- Interdisciplinary
- A team of individuals including professionals and support workers frequently from different agencies (health and social care) working with common policies and approaches focused on a clear goal.
- Interdisciplinary working
- The interactive effort and contribution of various disciplines, which implies a high level of communication, mutual planning, collective decisions and shared responsibilities. These independent contributions have to be co-ordinated.
- Intermediate care
- Community-based services that are provided, mostly for older people, and aim to avoid unnecessary admission to hospital and/or to facilitate early discharge from hospital and prevent admission to long-term residential and nursing care.
- Interprofessional team
- A group of professionals working closely together with blurred boundaries of their roles.
- Interprofessional working
- Team collaboration that involves co-ordination of expertise to optimise the care of the service user. An interprofessional team will have regular meetings, formalised systems for the exchange of information and work to a joint treatment plan with common goals for the service user.
- Multidisciplinary team
- A group of practitioners with different training who meet regularly to co-ordinate their work providing services to one or more service users in a defined area. Each team member brings expertise to address problems separately.
- Multidisciplinary working
- In multidisciplinary teams, members of different professions or disciplines assess or treat a client/patient independently and share only information with each other. The team is focused on the task, not the collective working process, and contributions are made either in parallel or sequentially to each other with minimum communication. Each contribution stands alone and can be performed without input from others.
- Multiprofessional team
- A group of professionals working closely alongside each other but maintaining professional boundaries.
- Professional
- An individual belonging to a group that has a clear definition of the elements of work over which the individual has autonomy or control. There is legislative recognition of the profession by the state, protecting the profession from encroachment by another profession, and ownership over an exclusive body of knowledge and skills and a code of ethics that protects their legitimacy.
- Role
- A function designed to achieve a defined output or outcome.
- Role substitution
- The ability of a worker from one discipline to adopt the roles of a worker from another discipline.
- Service user
- A recipient of health or social care services. Depending on the context, the service user may include the family and/or carers of the person directly receiving the service.
- Skill
- A level of knowledge or competence that is required to successfully perform a work-related function or role.
- Skill mix
- Can refer to the mix of disciplines involved in care, the mix of skills within a disciplinary group or the skills possessed by an individual worker.
- Support worker/support staff
- An individual who works with professionally qualified staff who may have health and/or social care training such as National Vocational Qualifications but who do not have tertiary or equivalent qualifications and who does not have legislative recognition of professional status by the state. Titles included under this category are technical instructors, rehabilitation assistants, social work assistants, physiotherapy assistants, rehabilitation technicians, psychology assistants, occupational therapy technicians, carers, intermediate care technicians, care management assistants, therapy assistant, technician and home enablers.
- Transdisciplinary working
- The transdisciplinary team operates at the opposite end of the continuum compared with the multidisciplinary team. The team uses an integrative work process and disciplinary boundaries are partly dissolved.
- Workforce configuration
- The combination of skill mix, training, delegation, substitution and specialisation and role overlap.
- Workforce development
- Activities that increase the capacity of individuals to participate effectively in the workplace. It incorporates components of workforce planning, education and training and management.
- Workforce planning
- A component of workforce development that aims to ensure that there are sufficient staff with the appropriate skills to deliver quality care to patients and also to predict and plan for the future workforce needs.
List of abbreviations
- A&E
- accident and emergency
- ADL
- activity of daily living
- AHP
- Allied Health Professional
- ASSIA
- Applied Social Sciences Index and Abstracts
- CABG
- coronary artery bypass graft
- CHF
- congestive heart failure
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- COOP
- costs and outcomes of older peoples’ services
- COPD
- chronic obstructive pulmonary disease
- CRAIC/S
- community rehabilitation and intermediate care/services
- EEICC
- enhancing the effectiveness of interdisciplinary working
- EQ-5D
- European Quality of Life-5 Dimensions
- ESD
- early supported discharge
- GP
- general practitioner
- HAH
- hospital at home
- HITH
- hospital in the home
- HR
- hazard ratio
- HRQoL
- health-related quality of life
- IC
- intermediate care
- LoC
- level of care
- MeSH
- medical subject heading
- NLU
- nurse-led unit
- NMB
- net monetary benefit
- NSF
- National Service Framework
- OR
- odds ratio
- PCT
- primary care trust
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- RCT
- randomised controlled trial
- RR
- risk ratio
- RRR
- readmission rate ratio
- TOM
- therapy outcome measure
- WTE
- whole-time equivalent