Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 09/2000/43. The contractual start date was in June 2011. The final report began editorial review in December 2013 and was accepted for publication in April 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Roberts et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
This study tested a British Sign Language (BSL) version of the Strengths and Difficulties Questionnaire (SDQ) and so by its nature recruited participants who use sign language as a part of their lives. However, as discussed in later chapters, many children who regularly use sign language as a main language also have experiences of living in hearing families or attending mainstream hearing schools and many also use oral English, Sign Supported English (SSE: signs from BSL following English grammar structures) or other languages in their everyday lives, alongside their sign language. This diversity in multimodal use of language and the heterogeneous backgrounds of these young people means that it is not always possible to capture this diversity by the simple use of conventions to describe Deaf cultural experiences. However, for the purposes of this report we use ‘deaf’ to describe the majority of deaf people. We will use the word ‘Deaf’ with a capital D when referring to Deaf culture or Deaf identity.
This chapter outlines the main focus of the present research study, with particular reference to the key issues faced by deaf young people, and how the additional risk factors that they face lead to increased risk of mental health problems. We highlight how these issues would be identified earlier if there were better access to a mental health screening tool that is linguistically and culturally appropriate. We describe the process that this team followed in translating a mental health screening instrument for children and young people.
Finally, the validation process is outlined, whereby deaf young people, deaf parents and deaf teachers across England completed the newly developed screening questionnaire. Their responses were compared with a ‘gold standard’ clinical assessment by clinicians experienced in working with deaf children and young people who have child mental health problems. These clinicians were experienced at working over several years with deaf children who have mental health problems and they always worked with qualified interpreters who also had experience of working in the deaf child mental health field. We refer to this as the gold standard. Currently there is no validated tool which we can use to compare the SDQ’s responses from each group. It would be standard research practice to validate any standardised instrument against a clinical interview with experienced clinicians, as this interview will give the best way of detecting mental disorders.
Background: review of literature
Mental health in deaf children
Prevalence of mental health disorders
In Great Britain, the reported prevalence of mental health disorders in children and young people is 12–20%. 1 Various studies across the world have suggested that the prevalence of mental health problems is higher in deaf children than hearing children2–8 and that when deaf children receive care they need more resources and spend longer in treatment than hearing children and young people. 9 For example, in studies using the parent/carer version of the Child Behaviour Check List in both Holland (n = 238)5 and England (n = 84)6 deaf children and adolescents had two to three times the rates of mental health problems (about 40% in the samples studied) compared with hearing children.
Another English study using screening instruments followed by a structured diagnostic interview using a sign language interpreter found that 50.3% of 11- to 16-year-old deaf adolescents had a psychiatric disorder (42% of those in a school for deaf children and 61% in a hearing-impaired unit in a mainstream school). 2 Forty-one deaf boys (aged 6–11 years) had more internalising and externalising problems than hearing boys10 and the younger boys had more behaviour problems.
A sample of 111 Swedish deaf children also had higher levels of mental health problems using the SDQ11 in written English forms. Of 120 deaf children in Canada, 23% were thought to have moderate to severe psychiatric problems. 12 In the USA, deaf 4- to 17-year-olds receiving outpatient care had higher rates of attention deficit hyperactivity disorder (ADHD), conduct disorder, autism spectrum disorder (ASD) and bipolar disorder than hearing children. 9
There are several problems in interpreting this literature. First, the research shows large variations in rates across studies. Second, most studies are in small or selected samples or very heterogeneous samples with no analysis of subgroups. Third, in all studies, the instruments are not validated in deaf children and are inaccessible to many children, as they are not in their first language (where BSL is their first or main language). There is evidence in the study by Cornes that screening of deaf young adults using a questionnaire in BSL picked up higher rates of mental health difficulties than using the written English version13 although the translation methodology for that study did not follow accepted standards. 14
In summary, researchers tend to study heterogeneous samples with instruments not fit for purpose and this may partly explain the wide differences in findings between studies.
Why are mental health problems more common in deaf children?
There are various factors that are proposed to influence mental health negatively in deaf children, including degree of deafness, age at onset, and the presence of additional neurological difficulties. 15 Factors that are purported to increase the likelihood of behavioural and emotional problems include low intelligence quotient (IQ) and comorbid physical7 and neurological problems, severe or profound deafness,16 poor development of language and communication,17 and poor parent–child communication. 5 Factors that increase risk of ADHD are lower intelligence, acquired deafness (compared with hereditary deafness)18 and significant communication difficulties. 19 ADHD is thought to be more common in deaf children. 18 It has been suggested that people who are deafened by rubella infection have five times the likelihood of experiencing subsequent psychosis. 20
Physical problems, learning disability and syndromes
Children with glue ear (otitis media with effusion)21 and rubella (German measles)22 have higher rates of behaviour problems. There is considerable research showing that children with physical illness, chronic illness or chromosomal syndromes have higher rates of mental health problems23 and, as it is estimated that up to 40% of deaf children have some additional needs, with approximately 6% having complex syndromes,24,25 they are found to have higher rates of mental health problems. 22,23,26–30 Children with high-frequency, mild or unilateral deafness (sometimes grouped together and called minimal sensorineural hearing loss) have more problems with behaviour, anxiety and self-esteem than hearing children. 28 In CHARGE syndrome [coloboma of the eye, central nervous system anomalies; heart defects; atresia of the choanae; retardation of growth and/or development; genital and/or urinary defects (hypogonadism); ear anomalies and/or deafness], which is a chromosomal condition involving heart, kidney and visual problems as well as sensorineural deafness, many young people will have severe repetitive behaviours. 29 Usher syndrome, which can involve visual and balance problems as well as deafness, is associated with affective disorders,30 self-injury and aggression. 31 About two-fifths can be aggressive to self or others31 and about one-third in one study had received a psychiatric diagnosis, with 47% on some kind of psychotropic medication32 for problems including anxiety disorders, ADHD, obsessive–compulsive disorder (OCD) and ASD. Some have suggested increased risk of psychosis in deaf people33 and there have been case reports of psychosis in Usher syndrome. 34,35 However, there is no clear systematic evidence for an increased likelihood of psychotic disorders in deaf people. 36 Although many deaf children (especially those with no neurological deficits or neurological damage, and with healthy cultural and linguistic experiences) have an IQ similar to hearing counterparts,37,38 many deaf children with neurological damage have learning disabilities32,39,40 and there is ample research to show that children with learning disabilities have higher rates of mental health problems than those without. 41
Diagnosis of deafness and adjustment of family
Currently in the UK there is a well-established New Born Hearing Screening Programme, which is picking up 1 in 1000 children as having a significant hearing loss. 42 This enables early detection and support from professionals, but also generates potential anxiety around parenting and how to interact with a deaf baby. 43
Some families find it difficult to accept their deaf infant and may treat their deaf child as hearing. Other families may struggle to accept the feelings of loss and overcompensate for this by engaging in increasingly ‘professional parenting’. This may hamper development in many ways including communication, social learning, emotional literacy, and social and emotional development. 44
It is now well established that early social and emotional learning is a complex process that relies heavily on communication. Much vicarious learning45 and communicative reciprocity is absent for deaf children in early life46 because over 90% of deaf children are born to hearing families unprepared for the communicative challenges that they face.
High levels of stress in parents are associated with more emotional problems in the young person,44 although the direction of the association is unclear. Behaviour problems are seen less where positive family support is available. 47,48
In one sample of 86 children, whose deafness was identified late, there were more behaviour problems, as rated using the parent and teacher report Rutter Scales,49 than in hearing children,50 and there were also increased rates where those with low levels of loss were not using hearing aids. 28
Educational experiences and life choices
For families where a child is identified as deaf, there are a number of difficult choices to make, most significantly with respect to education. Parents receive early support from the peripatetic teacher of the deaf (ToD), who advises them on early communication and education. The advised approach often depends on the views and beliefs in the local authority education department. Some areas promote bilingual language development and education, whereas others recommend a strongly oral approach where signed communication is discouraged. Most deaf children are now educated within mainstream provision, with or without a hearing-impaired resource unit. 51 In some areas, families and children are encouraged to have access to Deaf adults and the Deaf community, but this is by no means the norm. Families who find it difficult to accept that their child is deaf may not be discerning about school choice, and there is tentative evidence that schooling has a stronger effect on outcomes for deaf children than in hearing children. 52 Good in-school support is particularly important. 53,54
More than one-third of deaf pupils have additional educational needs beyond communication needs,55 and deaf children consistently achieve less in school than their hearing counterparts. 56–58 They experience delays in written language, vocabulary, grammar, syntax, reading59–62 and verbal intelligence on testing,63 although the process of assessment disadvantages deaf young people in itself because tools are inadequate and the oral assessment process is in English. Typical reading delay on leaving school is approximately 5 years. 64,65 All of these educational and learning challenges lead to lower levels of self-esteem, satisfaction and achievement, all of which are associated with poorer mental health outcomes. 66
Emotional development and theory of mind
Socioemotional developmental delay has been shown to correlate with delay in the ability to infer the thoughts or feelings of others. 67 This has been shown to be significantly delayed in deaf children from hearing families,60,68–71 but not usually delayed in fluent signers in deaf families. 70,72,73 This is the case even when attempts are made to test it in their first language and in culturally sensitive ways68,74–78 or if the child has a cochlear implant. 79,80 This is important because it maps on to empathy skills, which in turn affect social and emotional development and potential emotional or psychological problems in the future. Although deaf children appear to catch up later, early delays create significant problems for deaf children socially and emotionally. 81,82
Abusive experiences
Surveys of adults in Norway and North America suggest that deaf children are between two and three times more likely to be sexually abused than hearing children, and less likely to disclose their abuse. 83 These experiences may lead to subsequent substance misuse behaviours and negative mental health outcomes,84 and abuse is in general associated with higher rates of negative mental health outcomes. 85
Social anxiety and social skills
A review of over 30 studies concludes that children who are deaf are delayed in the development of their social skills. 86 Many deaf children experience anxiety related to social difficulties in communication with hearing children. 87
When researchers have used quality-of-life measures such as the Child Health Questionnaire,88 which is a parent-report measure, there are significant differences between deaf and hearing children. 50 For example, some deaf children in mainstream schools face social difficulties89,90 and may not feel as accepted as their hearing peers even when losses are mild or moderate,91 although many do as well as hearing peers. 92 Fellinger and colleagues found that parents/carers viewed their children’s quality of life more positively than their deaf children, who reported higher levels of dissatisfaction when using a self-report questionnaire in German and Austrian Sign Language. 93
Other factors
Some specific problems are more common in deaf children for reasons that are not fully understood and have not been fully researched. For example, autism appears to be more common in deaf children94,95 and is more likely to be diagnosed later than in hearing children. 96,97 However, it remains unclear whether this is related to high rates of neurological problems, comorbidities or common pathways in deaf children or it is an artefact of the autism assessment process, as many of the behaviours associated with deafness in young children can be mistaken for those seen in autism (e.g. differences in eye and lip gaze, not being responsive to their name being called). 82
Resilience factors
Mental health problems are generally less frequent in deaf children who have greater intelligence,5 are good at sport (boys) and have good peer relationships (girls). 98 As with all children, social successes are likely to be related to resilience factors including intelligence, personality, developmental pathways (e.g. social problem-solving skills), good communication at home and school, support from key adults,48 supportive peers and school ethos.
Cochlear implantation
Cochlear implants are increasingly offered to deaf children as standard. They consist of an internal and external component. The receiver is surgically implanted in the mastoid bone behind the ear, with electrodes inserted into the inner ear (cochlea). The microphone and speech processor, sited externally, convert sound into an electrical signal which is sent to the electrodes in the inner ear. These then send the signal through the auditory nerve to the brain, where it is perceived as sound. Parents have to make a choice about implantation at a very young age, because of concerns around critical stages of language acquisition. Given this, the average age of implantation is 12–18 months. The trend is now for bilateral cochlear implants,99 which offer access to sound to both ears.
There is little consistent evidence about the impact of cochlear implantation on mental health and well-being, but Dammeyer noted that, although some studies suggested that those with an implant had fewer mental health difficulties than those deaf children who were not implanted, the evidence is far from convincing, and the studies were of poor quality. 100 It is certainly true that having an implant can enable speech development and the ability to manage in face-to-face individual conversations. 101 However, for others, group situations are more difficult; people often do not make allowances for good communication, as they do not understand the impact of the deafness and consider the person to be ‘hearing’. This gives rise to several complex issues around participation, identity and belonging. 92
Long-term outcomes
In deaf children, mental health is associated with long-term psychological morbidity, poor educational attainment, increased unemployment, increased crime and delayed social skill development. 58,86
The rates of mental disorder in the adult deaf population are higher than for hearing people. This is particularly true for diagnoses of personality disorders102 and emotional disorders,103 which are unlikely to receive treatment in their early stages for lack of access to appropriate interventions.
Deaf people are more likely to enter the criminal justice system and are overrepresented in the prison population. 104 It has been reported that over 30% of offenders have significant hearing loss, with suggestions that this may be related to the increased risks in deaf people of school-related failure, limited social relationship networks, poverty and unemployment. 105
As a result, many organisations have highlighted the need for better access to mental health services for deaf children and young people. To identify difficulties at the earliest opportunity, in order to be able to intervene to alter the trajectory of these young people, we need to have a valid screening instrument.
Early-intervention programmes for deaf children benefit parents and their deaf children63,106–111 but most of them are focused on language development and communication. Identification of mental health problems earlier would allow clearer understanding of need, proactive development and assessment of support or therapeutic programmes, and potentially better outcomes.
Difficulties identifying mental health problems in deaf children
There is very little research with high-quality methodologies in the area of mental health in deaf children, partly because of the lack of any suitable screening or outcome measures. The research reported here will provide a foundation on which further research studies can build both in terms of translation methodologies (from spoken to visual language) and in validating a mental health instrument with deaf people, and using it in the future. It is important to identify mental health problems in deaf children for the multitude of reasons already outlined.
However, the mapping of need is not accurate because, at present, we do not have an appropriate tool to screen deaf young people for mental health problems, nor are we able to evaluate whether the specialist National Deaf Child and Adolescent Mental Health Service (NDCAMHS) in England generates positive outcomes for clients or not. Deaf children may communicate in a range of different ways: 78% of children use spoken English only, 14% speak another spoken language either on its own or in combination with spoken English and 8% use sign language either on its own or alongside spoken English. 51
Until the development of this questionnaire, there was no instrument or questionnaire that focused specifically on those young people who use BSL as their first or main language. Within child and adolescent mental health service assessments, it is standard for parents and teachers also to complete proxy questionnaires to contribute to the assessment. The BSL questionnaire resulting from this research will support clinicians in making more accurate clinical screening and assessments. It will also enable future researchers to map out the prevalence of various mental health problems in deaf young people, therefore allowing NHS services to target interventions and spending where it is most needed and most likely to be of benefit. It will allow us to measure outcomes more effectively and will lead to improved skills in developing screening and assessment instruments that are accessible to deaf children.
Strengths and Difficulties Questionnaire
The SDQ is a multi-informant mental health questionnaire that can be used as a screening tool and a treatment evaluation measure. The ‘informant-rated’ version of the SDQ can be used for children and young people aged 4–16 years, and is completed by either a parent or a teacher; the ‘self-report’ version can be completed by young people aged 11–16 years. 112 Each version of the questionnaire comprises 25 questions. All questions are scored on a three-point Likert scale, which can be divided into five subscales measuring:
-
emotional symptoms
-
conduct problems
-
hyperactivity–inattention
-
peer problems and
-
pro-social behaviour.
This last subscale is a ‘strength’ subscale. The first four are ‘difficulties’ subscales. 113 The SDQ11 has been translated into over 60 spoken languages (www.sdqinfo.com) but not BSL. It is a self-report questionnaire, initially developed to improve the detection of child psychiatric disorders in the community. 1 There are three versions: one for children and young people, one for parents/carers and one for teachers. Together, the three SDQs show good sensitivity (63.3%) and specificity (94.6%). 114 The SDQ can be completed at the beginning and end of treatment to assess treatment efficacy115 and it is frequently used to evaluate Child and Adolescent Mental Health Services (CAMHS). 116 The SDQ has a satisfactory internal consistency (Cronbach’s alpha ranging from 0.80 to 0.87) and specificity ranging from 94% to 95% and sensitivity ranging from 23% to 47% for each version (parent, teacher and child). 113
Barriers to developing or validating screening instruments for deaf children
Generic CAMHS have only relatively recently started prioritising the measurement of outcomes. In the UK, the SDQ is recommended for national use within NHS mental health services by the CAMHS Outcome Research Consortium (CORC) guidelines117 and is a core part of the new national CAMHS data set required by commissioners of services and the UK government to evaluate services across the country, as from April 2013. 118 The newly funded CAMHS Increasing Access to Psychological Therapies (IAPT) initiative119 also requires better outcome monitoring. Local CAMHS often report that deaf children go to services in smaller numbers than expected. 120 There are several apparent reasons for this, including deaf families having a poor experience of services designed for hearing people with often limited understanding of Deaf culture and deaf developmental issues as well as limited and inconsistent availability of appropriately trained interpreters.
Research funding has not been sought or granted very often for deaf child mental health over the last 20 years in the UK. There are also considerable practical and theoretical boundaries to translating and validating screening instruments in a visual language, with no well-developed methodologies. 13,121
Few widely used mental health instruments are available in a format that is culturally and linguistically relevant to the Deaf population. 122 ‘Inappropriate tests, unsatisfactory administration, and the unrealistic norm referencing of results’123(p. 249) remain the biggest challenges to overcome in mental health research with deaf people.
Although sign language versions of the SDQ have been produced previously,124,125 they have not been fully and rigorously translated or validated. The methodology that this study has adapted was developed for translation of spoken and written languages, which outlines the process of translation/back-translation. 14 This methodology is widely used to translate mental health questionnaires by organisations such as the World Health Organization (WHO). Additional methodological considerations that pay close attention to cultural and linguistic differences126 can result in questionnaires and screening tools that are more meaningful to deaf participants as long as this is conducted rigorously and systematically.
In clinical practice, sign language interpreters may be called upon to do on-the-spot translations of diagnostic and screening instruments, but this process can present problems. Interpreters make a linguistic and conceptual leap based on the experience of a deaf person to relay information that is contextually relevant to a hearing mental health professional. 127 Each interpreter will bring something different to this interaction, based on their own experiences, background or training, so the information given may not be consistently expressed. Working with interpreters means that variability in the translation and meaning of questionnaires is inevitable. The other reality is that deaf young people and deaf parents are likely to meet these BSL interpreters in other areas of their life, such as education meetings, financial or social care appointments. The impact of this is that it is likely that clients will not communicate as openly or as honestly as they might, because of confidentiality concerns. There is significant value in a self-report measure.
Such inconsistency could be overcome by using a validated instrument. Arguably the best way of achieving culturally sensitive instruments is to develop them empirically from first principles. However, this process is expensive and time-consuming. An alternative solution is to translate existing instruments into BSL, but the current evidence base outlining best practice is small. Rogers and colleagues gave an in-depth account of the issues regarding translation of standardised mental health assessments into BSL. 128 These issues included the direction of the signing; influence of modality; emotional state in BSL; confirmation of statements; and statements in a social context. Cornes and colleagues13 have noted that pencil/paper tests tend to underestimate prevalence of common mental health difficulties in deaf people, particularly emotional problems, hypothesising that this is partly because of the written language gap often present in deaf people in hearing environments. Linguistic delays, particularly in younger children, may invalidate standardised instruments validated for their hearing peers. For clinicians this presents additional difficulties, particularly those who have little knowledge of deafness or Deaf culture in assessment and diagnosis. The consequences of this may be that many deaf young people do not receive appropriate treatment or they may develop more complex, long-term difficulties.
Previous research has highlighted the difficulties translating into sign languages128–131 but few studies give detailed descriptions of the translation process from English to sign language, and its challenges. We describe here the process employed in translating the SDQ into BSL.
The policy context for deaf children
A National Audit of Families Support listed lack of specific support for mental health issues as one of the areas of most concern to deaf children and their families. 132 Standard 8 of the National Service Framework for children requires all children to ‘have equal access to CAMHS’ and Towards Equity & Access133 highlighted the importance of improving provision and access to mental health services for deaf people. The Human Rights Act and Disability Discrimination Acts mean the inaccessibility of such services is hard to defend. Voluntary organisations such as the Royal National Institute for Deaf People (RNID, now Action on Hearing Loss), UK Council on Deafness,134 the Social Research with Deaf People (SORD) unit at Manchester University135 and the Social Policy Research Unit at York University136 have called for improved services and research in this group. The National Deaf Children’s Society (NDCS) sees it as one of its priorities. Improving screening instruments enables tier 1 professionals such as GPs, health visitors, school nurses and paediatricians to have an adequate tool to identify children with mental health problems. This research therefore provides an accessible tool for deaf children, deaf parents or deaf teachers whose main language is BSL to participate in the identification of individual or population needs of deaf children and young people.
What is the service context in the NHS?
In October 2009 the NDCAMHS was set up in England, specifically to target the needs of deaf children and young people with mental health problems. Its ethos is to be accessible to all service users no matter what their cultural or linguistic background. There are four main bases for NDCAMHS across the country: York, London, Dudley and Taunton. As a national research project, recruitment was led from these sites.
The outcome of this research was a validated translated questionnaire, which was then used both in practice for clinical screening and for research to determine prevalence and types of psychiatric morbidity in deaf young people.
This research involved the collaboration of a comprehensive network of national centres (in four main centres and six outreach centres that map onto the 10 old strategic health authority regions in England). This allowed us to screen children from across England. The research will, therefore, be generalisable nationally. One of the NDCAMHS’s aims is to improve accessibility of services to deaf children and this will be a vital tool in furthering this aim. It will enable better and earlier identification of deaf children with emotional and behavioural problems.
How could a new screening instrument be used?
The development of this screening instrument for those whose first or main language is BSL will become a routine part of the NDCAMHS’s ability to screen for mental health problems and to monitor mental health outcomes. This will be part of a set of outcome measures that will meet the government’s target that high-quality services should have good measures that monitor outcomes routinely. This has been prioritised in the National Services Framework, through CORC137 and through CAMHS IAPT119 and the new ways of working in the NHS.
With more accurate estimates of the prevalence and types of psychiatric morbidity in deaf young people, the organisation and delivery of CAMHS for deaf young people can better reflect the needs of this population. This could enable the development of appropriate care pathways for deaf children, which necessarily and appropriately involve professionals at tier 1 (e.g. social workers, teachers, youth workers), tier 2 (e.g. educational psychologists, mental health workers), tier 3 (e.g. specialist mental health teams including child psychologists, clinical psychiatrists) and tier 4 (e.g. residential units). Currently, deaf children find accessing mental health support difficult,138 and more accurate mapping of mental health needs will enable more appropriate targeting of services. It will also enable the NDCAMHS teams to monitor the outcome of their interventions and build up the evidence base of what works with this population, as there is very little evidence at the present time.
Summary
In summary, deaf children have higher rates of mental health problems, they do not easily access mental health services, and services or commissioners have no mechanisms (such as questionnaires or tools) for screening deaf children or monitoring outcomes.
This study set out to translate the SDQ into BSL and to validate its use in England.
Study aims and objectives
The overarching aim is to create a valid BSL translation of the SDQ for children, parents/carers and teachers.
There were two main objectives of the study:
-
To translate the SDQ into BSL.
-
To use the BSL version of the translated SDQ with a cohort of BSL-using deaf children, deaf parents and deaf teachers sampled across England and to validate it by comparing it with a gold standard clinical interview assessment to elicit true psychological morbidity in the children and young people.
Chapter 2 Stage 1: cross-cultural translation of a screening tool for mental health in deaf children
This chapter describes the translation of the most commonly used mental health screening questionnaire for children and young people into BSL. We took a cross-cultural perspective to accommodate the differences between spoken and signed languages. In order to do this, representation from the Deaf community was sought consistently throughout the study. This section also summarises some of the challenges faced throughout this translation work and how all the final materials for the study were produced and agreed.
Aims
The aim for this phase of the study was to create a valid BSL translation of the SDQ for children, parents/carers and teachers.
Methodology
This study was reviewed and approved by Leeds West Ethics Committee on 7 March 2011 (reference number 09/2000/43).
This study followed the translation model provided by Beaton and colleagues,14 which provides guidance for written translations. However, there are issues that make the current evidence base on translation less well-equipped for sign languages. This is not to say that sign language itself is a problem, rather that the problem is that the guidance outlined by Beaton and colleagues is designed for written languages. BSL is a language with its own syntax, morphology and prosodic features differentiating it from written languages. For example, BSL syntax uses three-dimensional space and, as distinct from written or oral languages, several morphemes can be signed at the same time. Prosody presents in visual space through eye gaze, facial expression, sign production and other visual features. Additionally, the difference in using visual media (i.e. videos) means that the respondent will be watching an actual person on the screen and the questions are being signed, which can have potential implications on understanding to whom the question is referring. In the written questionnaire, the questions do not involve having a person reading out the question. Finally, as BSL is a visual language, this means that substantial modifications need to be made to the standard model of translating for written languages. These differences are well illustrated through the use of words in the English version of the SDQ which represent aspects of frequency: words such as ‘often’ and ‘frequently’, or verb forms which express regularity such as simple present tense forms (‘steals’, ‘shares’) are most naturally expressed in BSL through inflections to manual signs, such as repetition of the sign or aspects of its articulation. Therefore, what is expressed by separate words in English is often expressed through prosodic features in BSL, as part of a complex morphological system that expresses meanings differently from English. 127
Identifying translation teams
Stage 1 was built around the structure of translation/back-translation methodologies, requiring a forward translation team and a back-translation team, independent of each other. The translation teams were made up of bilingual BSL/English professionals who had experience of translation work. Beaton and colleagues14 suggested that there should be two people each in the translation and back-translation teams. We included three in each team because several factors affect variation in BSL (or differences in BSL production, including age, educational background, previous communicative and linguistic experiences, and family history of deafness139–141) and it was important to have geographical diversity in the translation and back-translation groups. BSL varies dialectically across regions. Whereas English dialect varies largely according to accent and syntax, BSL variation is more related to lexical differences. It was therefore important to find more widely used signs and phrases where possible. 142 As there are questionnaire versions of the SDQ for young people, parents, and teachers, having a range of ages represented within the translation groups was essential.
Consultation with professional deaf researchers suggested that there was benefit to having Deaf translators on both teams, as Deaf and hearing cultures are very different. We utilised the skills of bilingual deaf translators as they could more readily discriminate the sign meanings, which was more useful for translation purposes.
Beaton and colleagues suggested that having a balance of expert and lay members on a translation team assists in retaining focus on both the academic aspects of translation (e.g. reliable knowledge of the constructs being measured) and the meaning of the language as it would be perceived by a wider population. 14 This was reflected in the construction of the translation teams, which comprised equal numbers of clinical psychologists and those experienced in translation work across the teams. Equally, members of an expert panel overseeing the translation process were selected on their ability to comment on the different psychological, linguistic, psychometric and cultural aspects of the translation. This group comprised the project leaders (two psychiatrists working in the field of deaf child mental health), a linguist with sign language expertise and a range of deaf professionals experienced in mental health, research and translation work.
The team also considered the issue of agency, in that sign language has to be signed by someone, whereas a written questionnaire involves no other person. This carries with it potential transference143 issues that may resonate in terms of perceptions or feelings, and attributions or unconscious feelings about the signer. For example, a questionnaire signer that reminds a child of their critical mother may affect responses and emotions. There may be a preference of adults/young people for certain types of signers. Separate versions of the SDQ were filmed, presenting different characteristics of the signers (male/female, younger/older, etc.) with a final version chosen by the focus groups of young people. A written test is neutral in this respect.
The translation methodology
The translation process is illustrated in Figure 1. Initially, three forward translation team members each filmed independent BSL translations of the SDQ materials, resulting in an initial unbiased signed translation. The translations were collated, presented and then discussed among the three forward translators as a group. The decision-making followed a systematic process of discussion and consideration of alternatives and appropriateness for the target audience (whether young person, parent or teacher). As a result, each item was filmed again, by one of the translators at the meeting, after agreement was reached on the best version. These final versions were then passed to the back-translation team.
FIGURE 1.
The translation process.
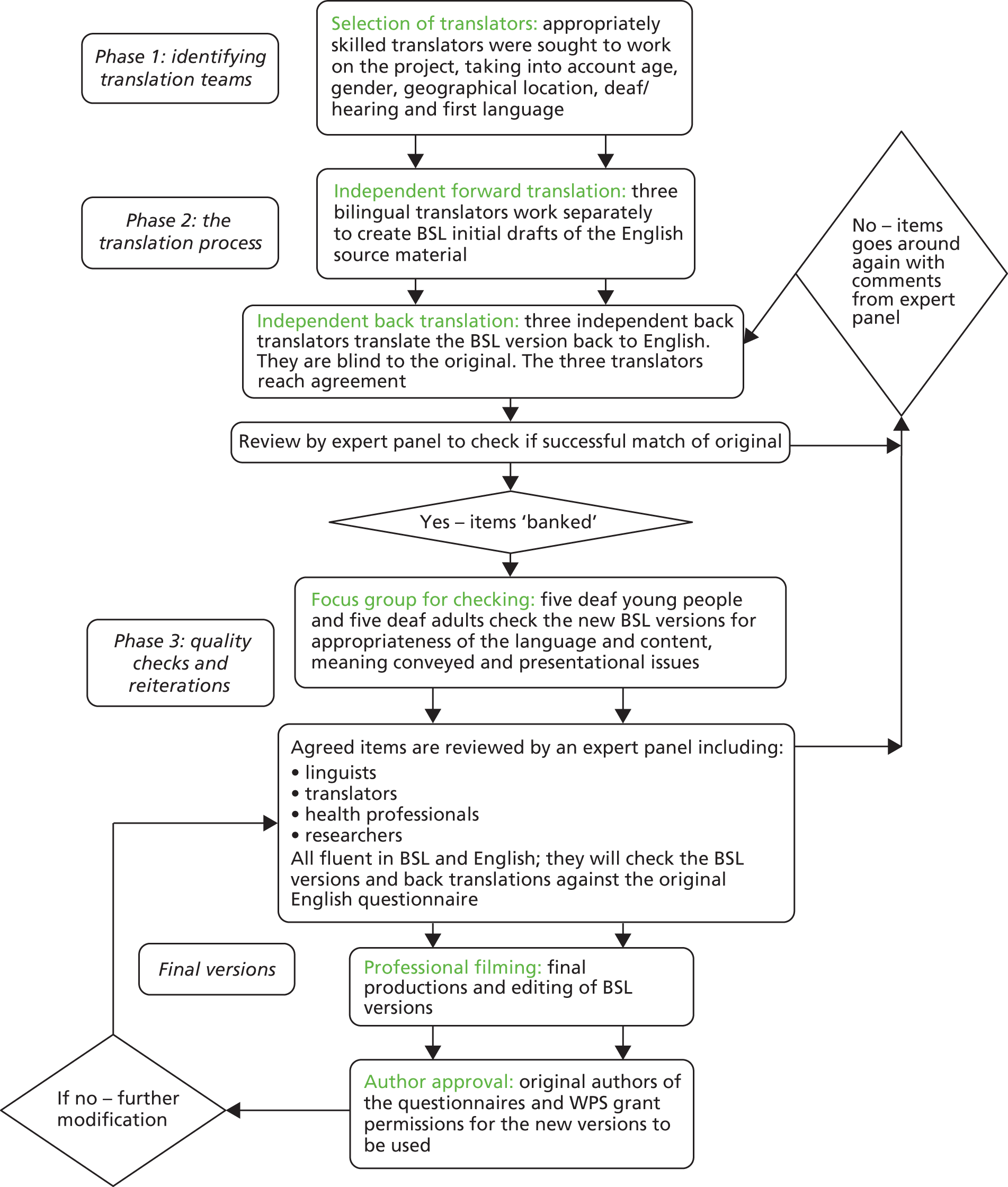
The back-translation team, three bilingual translators who were blind to the original versions, each individually produced English translations from each BSL item. These are called back-translations because they are taking the translated versions (now in BSL) and translating them back into English. The back-translations were collated and presented to all three translators for discussion as a group, where the appropriateness of each English word and phrase selection was scrutinised, and a final version agreed. This differs from the recommended process whereby independent back-translations are used only as a validity check for ‘gross inconsistencies’. 14 However, because sign languages are visual languages using the hands, face and body, it is possible for several meanings to be conveyed simultaneously. 144,145 Translating these meanings from signs into words is challenging because some elements that may be represented by words in spoken languages are expressed in sign languages through timing, aspects of sign articulation or facial expression.
Quality checks
The emphasis on service user involvement is highly important in the context of translation work; although efforts were made in order to balance the translation teams, as the Deaf community is such a heterogeneous group, the translators may not be representative of the population as a whole. Their linguistic ability in both BSL and English may mean they selected signs from a wider and more complex vocabulary than the average deaf person. In particular, this applies to young deaf people, whose exposure to sign language is likely to be limited compared with the exposure of a hearing English young person’s exposure to English. As many deaf young people are born to hearing families, their exposure to fluent sign language may be delayed, and potentially restricted. Often these young people will develop their sign language skills when they enter a deaf peer group within education, and the language is developed in a naturalistic and not necessarily grammatically correct way.
On completion of a full translation/back-translation cycle, the expert panel reviewed the equivalence of each back-translation to the original English SDQ in terms of meaning, linguistic structure and cultural/experiential sensitivity. 14,129 Translations that were agreed by the team as faithful and appropriate were judged as accepted (or ‘banked’), meaning no further translation of that item would be necessary. Where there were disparities, the questions were sent back to the forward translation group with comments on specific relevant issues. Versions of the items where the translation needed further iterations (the ‘un-banked items’) were translated again to make the meaning clearer. These items went round the translation/back-translation cycle again. The process was reiterated until all items were successfully banked.
This process was carried out for the young person’s SDQ, the parent’s/carer’s SDQ and the teacher’s SDQ. The BSL questionnaires produced were visual (e.g. available on a DVD and computer screen). The online computer version included both the questionnaire and an online method of providing an answer to each question on the SDQ explained in BSL and inputted interactively. We also produced a DVD version, which had a paper ‘fill in’ corresponding to the visual display.
Following this process, the newly translated SDQs were shown to two focus groups. The young person version was shown to five deaf young people and the parent and teacher versions were shown to five deaf adults (deaf parents/carers and deaf teachers) who all use BSL as their first language. These participants were approached through existing networks of the NDCAMHS throughout the country. This ensured that a variety of dialects and levels of BSL were represented in the focus group. We sought to utilise common mainstream signing forms. We also asked about the accessibility and cultural sensitivity of the delivery of the SDQ. This included presentational issues including characteristics of the presenter (e.g. gender, age, clarity of signing and pace).
Young people involved in the discussion group were given a £10 voucher for their contribution and adults were given a £50 voucher as a thank-you gift for giving their time. The focus groups were held at a geographically appropriate location at one of the NDCAMHS bases. Because of the visual nature of BSL we recorded the focus group on video. This has been discussed with deaf young people and parents (patient and public involvement, PPI) in the research team and it was felt that the full meaning of the discussion could not be captured using audio recording or process notes alone. Videoing allowed us to capture the language of the deaf people whom we are working with and provided us with rich qualitative data. A DVD of this session was produced and filed, as further evidence of the translation and discussion processes. This was destroyed at the end of the study.
Professor Robert Goodman, the original author of the SDQ, was then asked for feedback on the translated SDQ. He approved items and made suggestions for those not approved. These went back through the translation cycle until final and complete approval was achieved.
Results
The outcome was an instrument translated into BSL with versions that were understandable to both young people and adults whose first or main language was BSL.
Versions were successfully translated for:
-
11- to 16-year-old young people
-
parents or carers (adults)
-
teachers.
They could view it at their preferred location with a researcher’s work laptop hosted on an online forum, or play it on DVD.
Discussion
The translation process posed many unique challenges, which had to be overcome to ensure valid translation. These are discussed below, as are the study limitations with regard to translation.
Signer characteristics
As discussed, the characteristics of the signer were considered by the focus groups and expert panel. It had been hypothesised that a male signer would elicit lower response rates for emotional disorders, whereas a female signer might cause a young person to respond to questions about conduct or aggression less readily. Despite our initial belief that there may be preferences or biases in this area, both the young people and adult groups stated that, as long as the presenter was comfortable and clear in their signing, age and gender were of limited relevance to them. It is the content of what is being said that is of most relevance. (This was qualitative feedback and was not tested in any quantitative way.)
Culture, experience and language level
Deaf people’s experiences are very different. This includes differences in family background and makeup, differences in educational experiences, and changes across time and development. 146–148 They may be part of a Deaf culture, a hearing culture or both, and this may change over time. 149,150 For example, there is a question in the self-report SDQ about ‘playing alone’. This does not capture the fact that a deaf child might play alone because they struggle to communicate with their peers, rather than play alone because they do not have the necessary social skills to play with others. Thus, they might play alone at a school where they have only hearing peers, but play quite happily with other deaf children with whom they can communicate in their home environment. This may have the effect of creating disparities between parent and teacher responses. Another example of this is the question about whether or not the child is nervous in new situations; commonly deaf children will be nervous in situations with hearing groups, but will be much more confident at the Deaf club. This makes it very important for the clinician using the screening questionnaire to understand why any particular child might answer in any particular way and to have a good understanding of that child and the deaf experience.
A major point of discussion during the initial filming and reiteration of the young person informant version of the SDQ was around the level of signing in 11- to 16-year-olds. The discussion group was carried out with deaf young people, where the level of signing ability varied within the group. The translation strategy used to overcome this was to pre-pilot the SDQ in focus groups of young people. This allowed a ‘road test’ of the BSL SDQ, highlighting issues in vocabulary choice and structure of sentences. By including bilingual deaf signers as well as two psychologists on the forward translation team, the translators were able to adjust to an appropriate language level, as they had an understanding of the types of language that young people used in real-world environments.
Feedback from the focus groups highlighted a range of issues reflecting diversity of needs in the Deaf community. Whereas, in spoken language translations, questionnaires would be piloted in the hearing population, deaf young people often grow up with a mixture of language experiences, and may use many multimodal strategies in order to gain maximal information from messages. Though the fluent signers among the young person’s focus groups understood the items with relative ease, those from oral English families found this more difficult, despite using sign language as their main mode of communication. Despite ‘successful’ back-translation before the focus groups, it became apparent that the focus group did not understand some of the more complex BSL constructions in the questionnaire. Discussion with the focus groups led the team to believe that the level of language was inappropriate for this group, and therefore some BSL items were retranslated to simplify the language, though care was taken to preserve meaning.
Non-manual features
Non-manual features of sign languages (such as facial expression) can change meaning or imply hidden meaning. This may influence the answer given or alter how a person interprets a question, similar to the way that tone of voice in a spoken language can convey different meanings. This was the case in one of the items on the SDQ, which asked ‘do you take things that are not yours?’ The first translation of this was produced with non-manual features for a question, but with a facial expression indicating that, if the respondent were to choose ‘certainly true’, there would be a negative judgement made on the person answering the questionnaire. It is important at all times for the signer to produce sentences in an attitudinally neutral and non-leading way using only obligatory grammatical features; paralinguistic features should be avoided as much as possible, unless they are required to convey clear meaning, in order not to bias responses.
However, in the translation/back-translation process these features make it harder to obtain total linguistic fidelity. For example, the English SDQ response set for the main test items is on a scale of ‘certainly true’, ‘somewhat true’ and ‘not true’. In BSL, the degree of truthfulness is expressed on a continuum by facial expressions. These represent degrees of certainty simultaneously articulated with the sign ‘TRUE’. Facial expression thus inflects the sign and alters its meaning in the way that the modifiers ‘certainly’, ‘somewhat’ and ‘not’ change meaning. Selecting a sign-for-word substitution, as in SSE, would also be to negate a natural linguistic feature of BSL production. Content-for-content translation is common in interpreting scenarios but this elaborative process means that psychometric properties of a standardised questionnaire may be compromised if not done with great care. 127 In terms of finding suitable translations, we worked according to procedures outlined in previous research. 129 Discussions about the exact meaning and context of each statement were considered first by the bilingual translation terms, then by the expert panel and the focus groups and finally by the author. This process presented a range of checks and balances to obtain cultural and linguistic fidelity in our translation that was not without difficulty, but was thorough.
Statements as questions
The original English SDQ is formatted as a series of statements with which the respondent does or does not agree. In this way, the statement reads ‘I . . .’ In BSL the sentence must instead be produced in the second person, as the presenter and the respondent are not the same person. This, therefore, means that the sentence must also be interrogative, or something to be agreed or disagreed with, in order to elicit a response. This means that there are two key changes to the statement’s linguistic structure: a change of pronominal deixis, and a change of sentence format from declarative to interrogative.
Previously, sign language translation studies have made this reference to the self clear by using a technique of finishing each statement with the index finger pointing outward with head tilted to indicate questioning. 20,24 This might be glossed as ‘YOU WHAT?’ Using this second person singular pronoun denotes that the item is referenced to the test taker, rather than the person signing on screen, and the sign glossed as ‘WHAT’ makes it clear that the sentence is designed to elicit a response. Despite this, feedback from focus groups indicated that this format of questioning seemed unnecessary and was, in some cases, confusing.
Based on this, forward translators attempted to further clarify the distinction between the presenter and the respondent. For parent and teacher statements, asking about the child, ‘THIS CHILD’ was placed at the beginning of each statement. At the end of a sentence, an appropriate sign more related to the question was chosen (such as ‘YOU HAVE?’, ‘YOU BEEN?’ or ‘YOURS?’) rather than the more generic ‘YOU WHAT?’ Although it is not then standardised throughout the questionnaire, it fits more closely with the natural characteristics of BSL sentence structure.
Sign placement
The English version of the SDQ contains the item ‘nervous or clingy in new situations, easily loses confidence’. Many signs in BSL require the location to be marked. For example, in a class of verbs known as ‘directional verbs’, the location of the subject and object determine the start and end point of the sign when articulated. This is known as placement.
In translating ‘clingy’, the forward translators had to show that a young person might be clingy to a parent or guardian. In English this might be implicit, but in BSL needs to be referenced as the sign is visual and clinginess is directional towards somebody.
General and specific wording in oral English and British Sign Language
Having an understanding of Deaf culture within the core research team is highly important, in order to understand the functional ways in which BSL is commonly used. Category words or words with ambiguous meaning can be difficult to translate without further concrete explanation of what that word or concept might include (e.g. in BSL the signing for ‘considerate of other people’s feelings’ might include noticing those feelings in others, thinking about them and moderating one’s actions based on this observation). The SDQ tends to give examples where this has been felt to be necessary. Where examples are not given in the English version, the challenge is to avoid choosing signs that narrow the options too greatly (e.g. considerate of a specific person’s feelings). Research has shown this to be a key problem for interpreting in mental health settings. 127 An additional complication here is that lack of access to situational cues and incidental learning may mean that deaf young people struggle to ‘get the gist’ or understand when context is general as opposed to specific. Without a certain degree of openness to the statement, they may believe that the question relates only to a very specific context. To overcome this, translators must be aware of how they are contextualising situations in their sign choices and placements, and try to strike an appropriate balance between clarity and scope. Having psychological and psychiatric expertise within the research and translation teams allowed choices to be made based on the original intent behind each item.
This also links with an additional concern that any concrete explanation may be a judgement by the translator that goes beyond the meaning that is intended in the original. This is a particular concern between spoken and sign languages, as some English words have a more general sense than their BSL equivalents. The SDQ has an item in the parent version ‘Often complains of headaches, stomach-aches and sickness’. The word ‘sick’ in English can be translated into BSL with two different signs, which can also be glossed as ‘VOMIT’ (which is more specific than ‘SICK’) or as ‘ILL’ (which refers to more general illness or malaise). The English word ‘sick(ness)’ is ambiguous between these two meanings, but in BSL, as in other languages, one is explicitly forced to make a choice because there is no sign that covers both meanings in the way that ‘sick’ does in English. Thus, within the translation process it was important to consult with the author as well as mental health professionals, to understand how intended meaning is received, so that it is clear to the respondent; hence the need for culturally aware translation and focus groups.
Structural characteristics of the questionnaire
A key structural difference between a language presented in writing and one presented on film/video such as BSL is that, in responding to a written test, instructions are always present at the top of the page, and a respondent can keep checking back. However, with a visual questionnaire, this may need to be reiterated within the content or technical solutions sought to readily access instructions. Time frames, scales and instructions may need to be reinforced, and it may be necessary to give a specific contextual placement in each case rather than assuming that the information will be retained through several items.
Limitations
As discussed above there were a number of limitations inherent within the translation element of the study.
British Sign Language, like English, has numerous dialects. A commonly given example of dialectal variation within BSL is the numbering systems, which vary around the country. Variation in English is typically at the phonological or morphological level, and occasionally at the level of syntax; in BSL, the commonest variation is lexical. Typical semantic fields for variation in BSL are numbers, colours and some signs for family members: relatively common signs. This poses some difficulties in terms of intelligibility across the whole of the country. One way we tried to address this was by including translators and back-translators from different geographical regions to try and ensure that we used widely recognised signs to make the material intelligible to as wide a group of users as possible. Clearly, as the translation group had three bilingual adults within it, as did the back-translation group, it was not possible to cover all geographical regions and all possible dialects. This represents a limitation to both the trial methodology but also perhaps the very possibility of having a signed version in BSL that is universally accessible. As a way of attempting to overcome some of these issues, there was extensive discussion within both the translation teams and expert panels about the most commonplace or widely understood signs. For example, the London numbering system was felt to be more widespread and therefore was used throughout the videos. However, some of the qualitative feedback given by participants within the research suggested that throughout the questionnaire they had a strong preference for the signs common to their region. Providing local or regional forms in the video is not practical, so the team took the pragmatic decision to use signs that they believed would be most widely understood.
Another issue is that many deaf children are now in mainstream schools in the UK and, as it is estimated that around 90% of deaf children are born to hearing families,51 many deaf children do not have early life experiences that expose them to BSL from birth and through infancy. This means that many deaf children who do use BSL as their main language as teenagers or adults have learned the language late. Some may have a language impairment in sign language151 and this may be influenced by linguistic experiences in early life. 152 This in turn means that it may be more difficult for deaf people to understand a questionnaire in sign language.
Translation is not an exact science in that meaning may not be fully preserved even when the translation is considered accurate across both forward and back-translation. In this way back-translation may achieve literal equivalence but may struggle to convey full conceptual equivalence or achieve full comprehension of meaning in the target audience. 153 It is important to consider cultural usage, syntax and concept interpretation. 154 There is no gold standard method for translation of scales in cross-cultural research, and many of the issues apply across any two languages and cultures. 155,156 The need to make translations culturally appropriate is important in translations between any two languages157,158 and this is no different in cross-modal translations,159 although translating cross-modally from oral/written language forms to visual forms adds additional complexity. 150
The use of representatives of the Deaf community alongside a research team has been recommended as enhancing the process. 160 We applied additional measures such as focus groups of deaf parents and deaf young people and expert panel review (including a linguist) to review the work of the teams of bilingual translators and back-translators.
Summary
There are relatively few studies translating mental health instruments or questionnaires into sign languages, and fewer still focusing on the additional difficulties this presents when applied to deaf young people. There is a great need for further research in this area, and consideration of the impact of the circumstances of deaf young people in undertaking translation work. As an inclusive process, it is imperative to involve deaf people in the construction and assessment of the translation. The UK population of signing deaf people is comparatively small and tight knit, and encouraging deaf people to lead in the development of the study and early on in the process can be important to the overall success of such a pursuit.
Deaf culture embraces information sharing, and international collaboration on sign language translation processes could improve the quality and efficacy of mental health questionnaires, allowing services to more accurately map the prevalence rates of mental health in this population. Equally, it will allow the National Deaf Children, Young People and Family Service, and its collaborators, to better understand the needs of deaf children and young people.
Chapter 3 Stage 2: validation of the screening tool
Following approval of the translated questionnaires, the research proceeded to a validation stage.
Aims
To validate the new assessment tool, external validity was applied by testing the BSL SDQ version against a clinical interview assessment of parent and child together by an experienced hearing clinician from NDCAMHS with a qualified BSL/English interpreter. We refer to this henceforth as the ‘gold standard’ for assessment of mental health morbidity. All of these clinicians had level 3 BSL or above but always worked with a qualified interpreter.
We also carried out measures of internal consistency: exploratory factor analysis (EFA) to check dimensionality, test–retest reliability and cross-informant validity. Finally, structural validity was tested by analysing the fit of the data to the subscales of the questionnaire through a confirmatory factor analysis (CFA).
After this, the Rasch measurement model was used to see if the data from the BSL satisfied current measurement standards for invariant measurement, including invariance by gender. 161
Methodology
This study was reviewed and approved by Leeds West Ethics Committee on 7 March 2011 (reference number 09/2000/43).
Power calculations
Proposed sample size
Before the study, power calculations suggested that to have data that were comparable to normative SDQ data in the general population we would require 138 young people aged 11–16 years to participate. This was based on estimating the mean within a 95% confidence limit of ±1.0. This calculation was based on the standard deviation (SD) of 6 found in a normative population using the SDQ. 162
With regard to using clinical interviews of children in validation, a sample size of 80 in each category (young people, parents and teaching staff) achieves 80% power to detect a difference of 0.20 between the null hypothesis correlation of 0.70 and the alternative hypothesis correlation of 0.50 using a two-sided hypothesis test with a significance level of 0.05.
Based on the sample size for this study, we expected that we would be able to recruit enough parents (of children aged both 4–11 years and 11–16 years) and teachers to meet the numbers required in power calculation estimates, with 80 in each group (but recognising limitations in the availability of practising deaf teachers). With respect to the validation of the BSL teacher’s version of the SDQ, we were aware that the sample size would be small. This was because we were constrained by the very limited number of deaf teaching staff in England. To combat this we sought to add deaf teaching assistants to the sample. Deaf teaching assistants often know deaf young people very well and we would be able to tentatively explore the reliability of teaching assistants filling out SDQs, in comparison with teachers.
Inclusion/exclusion criteria
Three main groups we sought to include were:
-
Deaf 11- to 16-year-old young people who are BSL users compared with the clinical interview and the SDQs from their parents and teachers (deaf and/or hearing).
-
Deaf parents who are BSL users (with 4- to 16-year-old children) compared with the clinical interview and the SDQs from the young people and teachers (deaf and/or hearing).
-
Deaf teachers or teaching assistants who are BSL users (teaching 4- to 16-year-old children) compared with the clinical interview and the SDQs from the young people and parents (deaf and/or hearing).
Where additional disabilities were felt to affect the language of the young person, as determined by Deaf bilingual BSL researchers, they were excluded from the study. An example of this is when a young person requested to take part in the study at school but when the Deaf researcher met him it was clear he was unable to understand BSL because of his learning difficulties. Participants currently experiencing an active episode of psychosis were also excluded, but those with an existing diagnosis of psychosis without active symptoms were included in the research.
Procedure and recruitment
To recruit the clinical sample, staff from the 10 NDCAMHS outreach centres and the residential unit Corner House in London identified which children or young people had BSL as a main language. Their clinician then sent each of these families information leaflets about the study.
To recruit from the community we used a variety of strategies. Since each child in England with a loss of more than 40 dB has been routinely referred to a ToD, each locality keeps a register of such children. Using this, teachers passed an information pack containing consent forms and an information sheet about the study to children and their parents/carers. These information packs were available in plain English and BSL on DVD.
Researchers also visited all deaf schools across the country, as well as large hearing-impaired units in mainstream schools, and known youth clubs. Information about the study was posted on NDCS newsletters. It was established very quickly that prospective participants preferred face-to-face contact to sending out letters or advertising online. This may be because of a number of factors that the team considered. These included a possible preference of the Deaf community to converse directly with researchers whom they met and recognised and were able to ask as many questions as they would like. It also may have been that, because of the delay in English language comprehension, sending letters without having first made contact to explain the research may have been confusing for several families.
In order to recruit deaf teaching staff, we actively approached all the deaf educational establishments across the country. Many centres were extremely receptive to the aims and needs of the research team and were very happy to facilitate recruitment within the school environment. This made a marked difference in levels of recruitment and emphasised the importance of getting educational establishments on board with research of this nature. Deaf education is a hotly debated area, and many schools have different stances on the promotion of BSL or sign languages, inhibiting possibilities for successful recruitment in some areas. However, collaborative relationships with staff members who understood the relevance of mental health research to the well-being of their students and a clear understanding of the commitments involved in taking part in the study was of vital importance to the recruitment of deaf young people to this study.
Once consent was obtained, young people, parents/carers and teachers were asked to complete the SDQ. All parents and young people were also asked to complete a screening questionnaire confirming their eligibility to participate in the trial, and provide basic demographic information about themselves.
For completion of the SDQ, young people were asked to complete the BSL online version or the BSL DVD version with paper fill in. Depending on their preferred language, parents/carers and teachers were able to choose between the standard version of the SDQ and the BSL online version or the BSL DVD version with paper fill in. Where necessary a clinician or researcher fluent in BSL was available to support the process, but did not influence the answering of the questions or interpret them in any way. They gave gentle prompts and encouragement.
Young people were given a £10 gift voucher in order to thank them for their participation.
To produce the online version, we used the software Select Survey version 3 (Atomic Design, Kansas City, MO, USA), which enabled us to develop an interactive online video questionnaire. The software had been used in the past by experienced Deaf researchers from the SORD unit, who are collaborators on this study. We were able to upload the final BSL translations, and participants were able to select and input corresponding answers online. This program also allowed us to obtain consent online; the personal identifiable information from this was stored separately from any questionnaire data provided for the initial test. All data were stored centrally by the University of Manchester, and only members of the research team had password-protected access. The university is an established research centre with many years of experience in research methods and information governance, and we were confident that this was a secure method of retaining our data. This method of consent was visual and preferred by deaf people who use BSL.
Validation against a ‘gold standard’
In order to ensure that the new questionnaires were successfully eliciting true psychological morbidity, the newly translated BSL versions of the SDQ were validated by comparison with a blinded clinical interview administered by experienced deaf child mental health clinicians making use of research diagnostic criteria using the WHO’s International Classification of Diseases version 10. 163
These interviews generally happened in the young person’s home. The interview process involved a hearing clinician, working with a qualified BSL interpreter experienced in working with child mental health teams. As would be the process in clinical practice, the interview involved both the parent and the young person.
Validation of the young people’s (11–16 years) self-report Strengths and Difficulties Questionnaire
Eighty randomly selected deaf young people and their parents were seen for a structured clinical interview for validation purposes, as described above.
The children’s parents and teachers (hearing or deaf) also completed the appropriate version of the SDQ about their child.
Validation of the parent (4–16 years) Strengths and Difficulties Questionnaire
We aimed to interview the children of all deaf parents taking part in the study. Their children could be deaf or hearing. A clinical interview was completed involving the deaf parent and their child as described above.
The deaf or hearing teachers of these children and young people were also asked to complete the SDQ, and the 11- to 16-year-olds completed a self-report SDQ in whichever language (English or BSL) was appropriate for them.
Validation of the teacher (4–16 years) Strengths and Difficulties Questionnaire
Deaf teachers and teaching assistants completed the BSL SDQ with respect to children and young people. As deaf teachers are almost always involved in the teaching of deaf children, we minimised the number of validation interviews by seeking to recruit as participants the deaf children taught by the deaf teachers.
The parents of the young people were asked to complete an SDQ and the 11- to 16-year-olds completed a self-report version. Deaf and hearing parents of the young people involved were recruited when they gave informed consent.
Test–retest reliability
We sought to recruit 65 participants in an evaluation of test–retest reliability. This sample size was based on the following calculation for estimating the intraclass correlation coefficient (ICC). When the sample size is 65, a two-sided 95% confidence interval (CI) for an ICC for the test–retest will extend about 0.157 from the observed ICC when the expected ICC is 0.600. The ICC coefficient provides the test–retest reliability estimates in a sample of 50% of the children chosen randomly to complete the questionnaire on two occasions. (A sample size of 65 subjects with two observations per subject within 3 weeks achieves 81% power to detect an ICC of 0.70 under the alternative hypothesis when the ICC under the null hypothesis is 0.50 using an F-test with a significance level of 0.050.)
Contacting clinicians to recruit the clinical sample
We circulated information to all the clinicians working within the NDCAMHS including child psychiatrists, clinical psychologists, community mental health nurses, child mental health occupational therapists, family support workers, deaf clinical advisors, deaf child mental health social workers and other therapists. These clinicians passed on information leaflets to families who were eligible.
Contacting schools
In an attempt to recruit participants across England, the following educational establishments were approached:
-
11 deaf residential schools (nine with primary/secondary provision and two with secondary provision)
-
two deaf secondary schools (day pupils)
-
four deaf primary schools (day pupils)
-
54 mainstream secondary schools with hearing-impaired units
-
two mainstream secondary schools without hearing-impaired units
-
50 mainstream primary schools with hearing-impaired units
-
two mainstream primary schools without hearing-impaired units
-
five colleges with deaf services
-
five specialist schools for children with complex needs (four of which have residential provision).
Contact with deaf schools and hearing impaired units enabled us to identify deaf ToDs who were also eligible to participate, meaning that we were able to validate the deaf teacher version of the SDQ whilst simultaneously recruiting deaf children and young people. We had already developed good links with many of these schools through the NDCAMHS and built upon our existing relationships. Many ToDs were already aware of the research.
Initial contact with deaf schools and mainstream schools with units was made through telephone calls and letters. Once the rapport was established, we supplied information in accessible formats to parents and families through the schools. We were aware that accessibility issues might arise if too much written information were sent, so we encouraged teachers to make families aware of the study. Teachers provided families with information leaflets and consent forms, and noted which families were approached. All potential participants were given the option to contact a member of the research team for further information. Teachers and clinicians maintained records of those contacted, those who had been sent follow-up information and those who consented to participate in the study.
Contacting teachers of the deaf and other professionals working with deaf children
There were some independently located ToDs and professionals who were not based at any one particular school. They were contacted through either telephone calls or e-mails. We supplied information packs to ToDs and professionals working with deaf children and encouraged them to make families aware of the study. They acted as a third party between the research team and families to provide and collate the consent forms. A visit was arranged if they provided consent to either the ToDs or other professionals. ToDs maintained records of those who were contacted and we collated information about who consented to be involved in the study.
Advertising
We had good PPI support in thinking about advertising and recruitment, as well as the presentation and content of materials.
We advertised the study at national meetings of the British Association of the Teachers of the Deaf (BATOD), in its magazine, and on the NDCAMHS and NDCS websites. We also advertised on the Deaf Children with Deaf Parents website and the Ear Foundation website. We also sent materials to local support groups such as Lollipop and CHSWG (Children’s Hearing Services Working Groups). Materials were posted to schools, and leaflets were handed out in Deaf clubs and to Ear Foundation teenage groups. The NDCS also emailed information about the study to its parents’ groups, and the research team attended Deaf Day in London and events at the annual Deaf Awareness week. Information leaflets were available in DVD form in BSL. Presentations were given in BSL at some Deaf clubs on request.
Recruiting within the Deaf community
To recruit parents to the study, we advertised widely within the British Deaf Association, in Deaf social media and through contacts at Deaf clubs and support organisations. We went to talk about the study at various events and meetings. We were also able to advertise the study through the interpreter community. We sought and used PPI advice on how best to involve the Deaf community.
The NDCAMHS also employs several Deaf Service consultants, who were instrumental in providing ways to recruit within the Deaf community. Their advice was sought throughout the recruitment process, with several meetings set up to review recruitment and how we could reach more deaf people within the community. They were also able to provide deaf professional contacts throughout the country who in turn could promote the studies through their own organisations, encouraging recruitment throughout England.
One helpful aspect of PPI advice was alerting the research team to minority groups within the Deaf community that have less access to internet resources and are unlikely to have any access to information regarding current affairs and support within their regions. These groups needed face-to-face meetings in order to introduce the concepts of research, translation and mental health services. It was deemed important to spend the extra time on building a rapport with these groups in order to elicit sufficient trust for them to engage in the research. This targeting method provided access to both deaf adult participants as well as deaf children, and included travelling families.
In consultation with and on advice from our PPI colleagues, researchers visited youth clubs, parents’ groups, Deaf clubs and both deaf and mainstream schools along with visits to individuals, either at home or at their preferred locations, to raise awareness of the project and its aims. These visits also provided researchers with the opportunity to meet deaf teachers, deaf children and deaf parents, face to face, in environments that were familiar and comfortable. Potential participants were encouraged to ask questions and/or express concerns. FaceTime and Skype were also used to make contact and recruit participants if this was identified as their preferred method of communication.
Information governance
We used established International Committee on Harmonisation Good Clinical Practice guidelines164 for our research throughout, and all research staff had up-to-date training.
The use of Select Survey software presented some challenges for the team around security and storage of data to meet participating institutions’ extremely high standards. In the event we identified named approved gatekeepers.
Although we planned to have a facility for participants to upload video feedback using webcams, this was never used, as it was not possible to enable its use in time. Researchers noted comments in writing.
Statistical methodology
Validity and reliability analysis
To compare the SDQ scores with the clinical gold standard measures, analysis of variance (ANOVA) tests were undertaken.
A computerised algorithm predicts child psychiatric diagnoses from the symptom and impact scores derived from SDQs completed by parents, teachers and young people. The predictive algorithm generates ‘unlikely’, ‘possible’ or ‘probable’ ratings for four broad categories of disorder, namely conduct disorders, emotional disorders, hyperactivity disorders and any psychiatric disorder. This was used in some analyses to compare with the gold standard clinical interviews (see Appendix 1).
All analyses were undertaken using Statistical Product and Service Solutions (SPSS; version 21, IBM, Delaware, PA, USA). A p-value of < 0.05 was considered to indicate statistical significance. No adjustments were made for multiple significance testing based on current suggested practice. 165
The analysis for validity and reliability was undertaken individually for deaf children, deaf parents and deaf teachers.
The SDQ scores are described using means, SDs and number of respondents.
The internal consistency of the total score and the subscales were assessed using Cronbach’s alpha because it was important to know how close together a set of items are as a group and it gave insight into the questionnaire’s internal reliability. If items are used to form a scale, they need to have internal consistency; thus the items should all measure a similar construct, so they should be highly correlated with one another. Cronbach’s alpha166 is a measure of internal consistency. A high value of alpha is often seen as evidence that the items measure a construct. George and Mallery provide the following rules of thumb for interpretation: > 0.9 = excellent, > 0.8 = good, > 0.7 = acceptable, > 0.6 = questionable, > 0.5 = poor and < 0.5 = unacceptable. 167 A high alpha for the total score does not imply that the measure is unidimensional. So, in addition to measuring internal consistency, EFA was performed as a method of checking dimensionality. A Varimax rotated factor analysis was undertaken. This is the most popular orthogonal rotation method. It enables a simple structure by maximising variance of loadings within factors across variables. It makes large loadings larger and small loadings smaller. It also spreads the variance from first (largest) factor to other, smaller, factors. A five-factor model was chosen to mirror that of the scale (the impact was excluded in line with the original validation). 113 The number of factors extracted will ensure that all factors have eigenvalues > 1. The best factor solution is chosen from the factor structure with the highest number of loadings (≥ 0.3), lowest number of cross-loadings, highest number of stable factors (i.e. more than two items per factor) and lowest number of communalities (the amount of variance accounted from that item to the factor) below 0.4.
To measure test–retest reliability the ICCs were calculated. ICC values can be interpreted as follows: > 0.75 was excellent, 0.40–0.75 was fair to good and < 0.40 was poor. 168 The retest data were collected for a subsample of the deaf children, deaf parents and deaf teachers. Sixty-five participants were sought to take part in an evaluation of test–retest reliability for all three versions of the SDQ. There was an interval of 1–2 weeks between SDQ completions. Seventy-one young people, 131 parents and 47 teachers did the test–retest.
To further test validity, comparisons of the child, parent/carer and teacher versions were undertaken to test equivalence of correlations with versions of the SDQ. This was undertaken by a paired t-test and correlations between the scores.
Rasch analysis methodology
Adaptation of a scale requires evidence that the new version has the same structure as the original, measures one trait at a time and is invariant across key groups. That is, the scale works in the same way as designed and, at any given level of the trait being measured, responses to items will be the same (within error) irrespective of group membership. Classically, most of these attributes would be identified within a factor analytical framework, testing the unidimensionality structure(s) of the data. A hierarchy of invariance can be determined under these circumstances. 169 Group invariance can also be tested in this way. In the current study a CFA was undertaken using a polychoric matrix as a base. This technique was chosen because the self-reports used in this project consisted of rating scales ranging from ‘strongly disagree’ to ‘strongly agree’ (Likert scale) on the five domains, and the second-order factor obtained by summing the 20 items from four domains (omitting pro-social). As local dependency of items is common in health and psychological instruments, correlation of errors will be allowed within domains. We should expect a non-significant chi-square for confirmation of the CFA, and auxiliary fit statistics comparative fit index (CFI) and Tucker–Lewis index (TLI) to be > 0.95, and root-mean-square error of approximation (RMSEA) < 0.06. Should this fail, an EFA will be used to determine a possible revised factor structure.
Increasingly, modern psychometric approaches are being used to provide a comprehensive framework for scale development and review. These typically come under the rubric of item response theory (IRT), of which the Rasch measurement model is pre-eminent. 170,171 It is so because, in a probabilistic manner, it satisfies the rules (axioms) for creating fundamental measurement. 172,173 It has various properties which set it apart from other IRT models, but mostly it is the property of invariance that is crucial. 174,175 Here, the ratio of distance between any two questions on the trait remains the same, irrespective of how much of the trait is held by the person responding to those questions. It is this property of invariance that provides the means by which ordinal latent estimates, derived from questionnaires, can be transformed to interval-level scaling. 176 Group invariance can also be tested for through differential item functioning (DIF) within the framework of the Rasch model. 171,177 The property of sufficiency is also closely related to invariance. 176,178 In this case the simple summed raw score is all that is needed to ascertain the magnitude of the attribute. Where scales are used with cut points, as with the SDQ, this property becomes a requirement.
In the current study the data will be fitted to the Rasch model to test if it conforms to the requirements for achieving such measurement. The partial credit parameterisation of the model, developed by Masters, will be used. 179 A sample size of 250 will provide an estimate of item difficulty (location on the trait) consistent with high-stakes testing (e.g. clinical decision-making) with 99% confidence. 180 A number of model assumptions will be tested, including unidimensionality and local independence of items. The former is tested by comparing two estimates from sets of items loading positively and negatively on the first principal component of the residuals. 181 If fewer than 5% of such estimates are significantly different, then unidimensionality is supported. The latter is tested through an examination of the correlation of item residuals. Where items have a residual correlation of 0.2 above the average residual correlation (which may be negative with small scales) then a breach of the local independence assumption is observed. 182 In some instances it is possible to adjust for this by creating testlets, which are simply ‘super items’ where locally dependent items are summed together. 183 In a scale such as the SDQ, where there are predefined domains, local dependency may be expected within domains. Consequently the domains may be analysed as ‘super items’. Under these circumstances, a bi-factor solution is obtained, whereby the latent estimate is based upon the first dominant factor. 184,185 A value ‘A’ is obtained which indicates the proportion of non-error variance that is common under such a solution, and thereby indicates the amount of unique variance that has been discarded to achieve this solution.
The assumption of stochastic ordering is also tested through a series of fit statistics, either chi-squared based, requiring Bonferroni adjusted non-significance, or residual-based, requiring standardised residuals to be within the range ± 2.5 (99% CI). A Bonferroni adjustment was used because of the number of statistical tests applied. It requires a higher level of significance to be achieved. Group invariance was tested through DIF, based upon centre, gender and type of respondent (e.g. parent, teacher or child) and BSL-based completion or not. Finally, the category structure of items was examined to see if the transition from one category to the next is consistent with an increase of the underlying trait (threshold ordering). Further details of the process of Rasch analysis can be found elsewhere. 186
Results
Overall recruited sample
Figure 2 shows the planned (and actual) recruitment in the validation process. We recruited 144 deaf children (aged 11–16 years) and their parents/carers and teachers (both hearing and deaf) to validate the deaf young person version (11–16 years) of the SDQ.
FIGURE 2.
Design of the planned (and actual) validation procedure.

We recruited 191 deaf parents who had deaf or hearing children ranging from 4 to 16 years old. We sought deaf parents of deaf children or young people but we also recruited deaf parents with hearing children or young people (because only 5% of deaf children in the general population have at least one deaf parent).
We recruited 77 deaf teachers and teaching assistants to validate this version of the SDQ.
Young people sample description
We needed 138 young people for statistical power. We recruited a total of 144 young people aged 11–16 years who completed the SDQ in BSL. The majority (116, 80%) were recruited from the community through schools, youth groups and Deaf community contacts. A further 27 (19%) were recruited from the NDCAMHS (a clinical sample). We do not have this information for one participant.
Of the schools we approached we recruited from:
-
10 of the 11 (91%) deaf residential schools (nine with primary/secondary provision and one with secondary provision)
-
one of the two (50%) deaf secondary schools (day pupils)
-
three of the four (75%) deaf primary schools (day pupils)
-
15 of the 54 (28%) mainstream secondary schools with hearing-impaired units
-
one of the two (50%) mainstream secondary schools without a hearing-impaired unit
-
eight of the 50 (16%) mainstream primary schools with hearing-impaired units
-
one of the five (20%) colleges with deaf services
-
one of the five (20%) specialist schools for children with complex needs (residential school)
-
two mainstream primary schools without hearing-impaired units.
The main reasons for not wishing to take part included (1) not having a child or young person whose first or main language was BSL (e.g. the school reported their deaf young people used oral English); (2) that it would be too demanding for the staff; (3) that the school was too busy at the end of the school year (some were contacted in June/July); (4) not wanting to take a child out of their class; (5) having no deaf children within the age range; and (6) that there were no deaf children in their school any more.
Of the 144 deaf young people who completed the self-report BSL SDQ, 56% were male (n = 81) and 44% were female (n = 63) (Table 1).
| Gender | Community (%) | NDCAMHS (% clinical cases) |
|---|---|---|
| Male | 68 (59) | 11 (41) |
| Female | 48 (41) | 16 (59) |
As shown in Figure 3, the young people were aged between 11 and 16 years.
FIGURE 3.
Number of deaf young people in each age group completing the self-report SDQ.
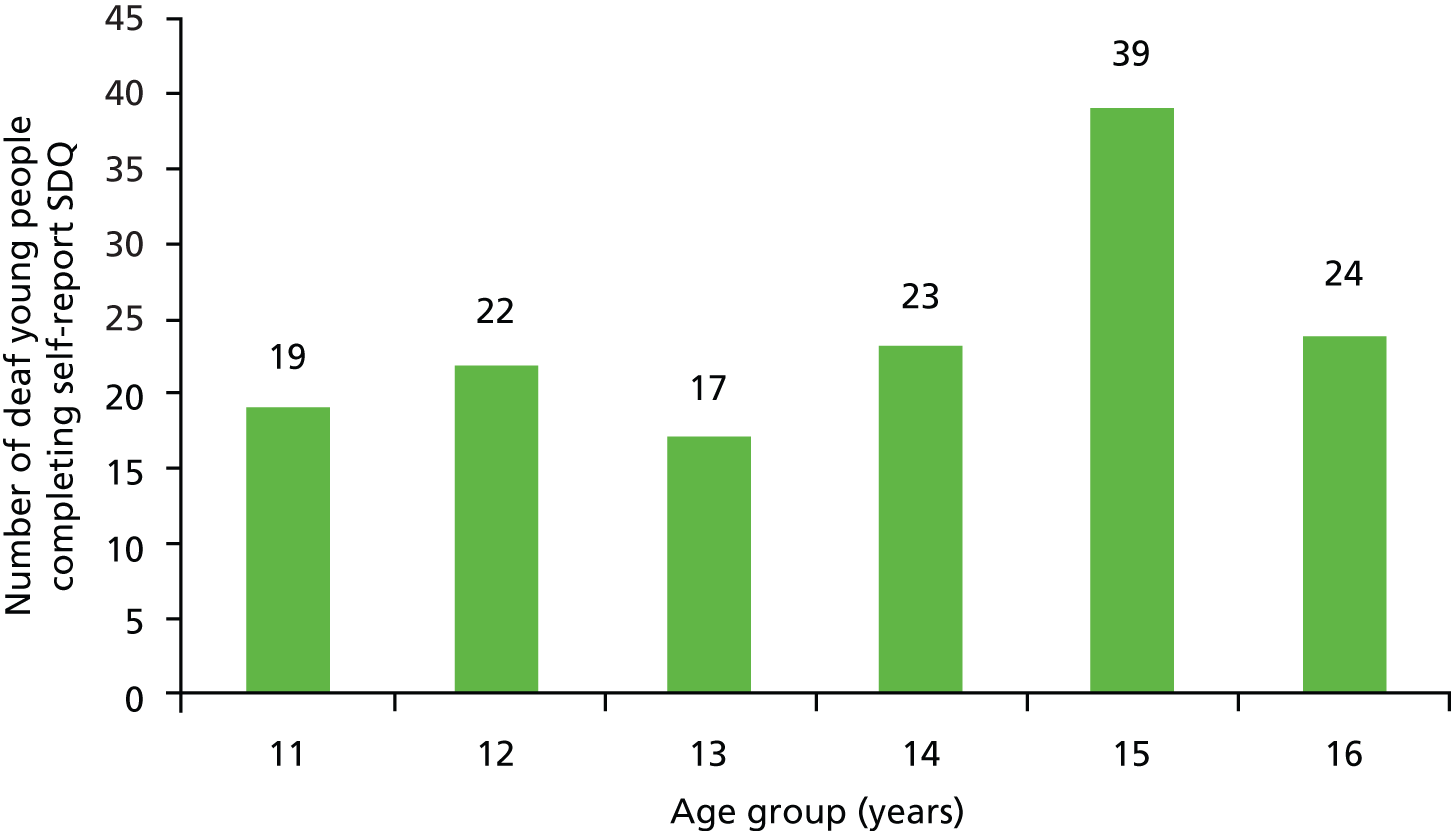
The majority of the young people (87, 60%) were white British. Twelve (8.3%) were white non-British; 26 (18%) were Asian, mainly of Pakistani (n = 16) or Bangladeshi origin (n = 6); 8 (6%) regarded their ethnicity as black (black British, black African, black Caribbean or black other) and 7 (5%) as mixed. Four did not declare their ethnicity.
The majority of the young people (115, 80%) described themselves as profoundly deaf, 16 (11%) as severely deaf, 7 (5%) as moderately deaf and 6 (4%) were not certain or did not declare.
Approximately one-third of the young people (50, 35%) used cochlear implants, 66 (45.8%) used behind-the-ear hearing aids, 14 (10%) indicated that they did not use either and were choosing not to wear hearing aids and 7 (5%) stated that they were unable to wear hearing aids. Seven (5%) did not answer the question.
One-quarter (37, 26%) had at least one deaf parent, with 21 (15%) having two deaf parents.
Overall, 30 (21%) described their family as a deaf family with BSL as their main language, 25 (17%) said that they were from a hearing family that was fluent in BSL, 53 (37%) were from a hearing family that knew some BSL and 30 (21%) described their family as hearing and oral in its use of language with them learning and using BSL at school and/or in the community. Six young people (4%) were not clear about what language their family usually used.
Two-thirds of young people (93, 66%) said that they had no learning difficulties or disability, while 28 (19%) declared at least some learning difficulties. The remainder (23, 15%) did not declare whether or not they had learning difficulties.
All participants understood that the responses were confidential and gave fully informed consent.
Clinical interview data for community sample
A clinical interview was completed for young people recruited in the community sample. It showed a range of diagnoses within the spectrum of the following disorders.
Twenty-two young people were diagnosed with a significant mental disorder. No young people met the criteria for an affective disorder. Six met the criteria for a diagnosis of an anxiety disorder, five of generalised type. One had OCD. Two met the criteria for a diagnosis of ADHD. Six met the criteria for a diagnosis of oppositional defiant/conduct disorder. No young people met the criteria for the diagnosis of an attachment disorder. Four had a diagnosis of an ASD. Four young people met the criteria for a less common disorder: two with serious sleep difficulties, one with a feeding disorder and one with a tic disorder.
Of those who were detected as having significant mental health problems as a result of the interview, a number (15) were already involved in other local services and receiving care. Four young people were referred for services as a result of involvement in the project, and three had been involved with services but were discharged and did not need active care.
Clinical interview data for clinical sample
A clinical review was completed by the responsible clinician for 28 young people recruited as the clinical sample actively in treatment. This showed a range of diagnoses within the spectrum of the following disorders.
Seven young people had a diagnosis of affective disorder, all of depressive type. Eight had a diagnosis of an anxiety disorder, all of generalised type. Five had a diagnosis of ADHD. Ten had a diagnosis of oppositional defiant disorder/conduct disorder. Twelve young people had a diagnosis of an attachment disorder or difficulties. One young person had anorexia nervosa.
Scores and validation of the self-report Strengths and Difficulties Questionnaire
Young people’s Strengths and Difficulties Questionnaire scores
This section describes the SDQ results for the deaf young people who have used the self-report SDQ scale in BSL.
Table 2 shows the mean (SD) for the total score and for the subscales.
| SDQ subscale | Mean | SD | n |
|---|---|---|---|
| Total difficulties | 14.4 | 5.6 | 136 |
| Emotional symptoms | 3.8 | 2.6 | 142 |
| Conduct problems | 3.1 | 1.9 | 138 |
| Hyperactivity | 4.2 | 1.8 | 136 |
| Peer problems | 3.5 | 1.7 | 138 |
| Pro-social behaviour | 7.1 | 1.8 | 142 |
| Impact | 2.1 | 2.5 | 135 |
Table 3 shows the SDQ scores by sample group. There were significant differences between the groups for the total difficulties (p = 0.011), emotional symptoms (p = 0.005) and conduct problems (0.005). In each case the NDCAMHS group had a higher mean score.
| SDQ subscale | Community | NDCAMHS (clinical case) |
|---|---|---|
| Total difficulties | 13.8 (5.5) 113 | 17.2 (5.4) 22 |
| Emotional symptoms | 3.4 (2.4) 114 | 5 (3) 27 |
| Conduct problems | 2.9 (1.8) 114 | 4.1 (1.8) 23 |
| Hyperactivity | 4.1 (1.8) 113 | 5 (1.6) 22 |
| Peer problems | 3.4 (1.7) 114 | 4 (1.6) 23 |
| Pro-social behaviour | 7.3 (1.7) 114 | 6.7 (2.1) 27 |
| Impact | 2.1 (2.5) 112 | 2.1 (2.8) 23 |
Table 4 shows the SDQ scores by gender. There were significant differences between the groups for the total difficulties (p = 0.002) and emotional symptoms (p < 0.001). In each case the females had higher mean scores than the males.
| SDQ subscale | Male | Female |
|---|---|---|
| Total score | 13.2 (4.9) 78 | 16.1 (6.1) 58 |
| Emotional symptoms | 3 (2.1) 78 | 4.7 (2.8) 64 |
| Conduct problems | 2.9 (1.8) 78 | 3.4 (2) 60 |
| Hyperactivity | 4 (1.8) 78 | 4.5 (1.8) 58 |
| Peer problems | 3.4 (1.6) 78 | 3.8 (1.8) 60 |
| Pro-social behaviour | 6.9 (1.7) 78 | 7.4 (1.8) 64 |
| Impact score | 2.4 (2.7) 76 | 1.7 (2.3) 59 |
Table 5 shows a descriptive summary of the self-report SDQ scores by whether they were from the community sample or NDCAMHS and by gender. There was a significant difference between males and females in the community sample for total score [12.7 (5) vs. 15.5 (5.8)] and the emotional symptoms score [2.9 (2.1) vs. 4.2 (2.6)] (p < 0.05). In the NDCAMHS group there was a significant difference between males and females for the emotional symptoms score [3.3 (2) vs. 6.2 (3)] (p < 0.05). Comparing the community sample with the NDCAMHS, there was a significant difference for the emotional symptoms score for females [4.2 (2.6) vs. 6.2 (3)] (p < 0.05). There was a significant difference for the conduct score for males [2.7 (1.7) vs. 4.1 (1.8)] (p < 0.05).
| SDQ subscale | Community | NDCAMHS (clinical case) | ||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| Total difficulties | 12.7 (5) 66 | 15.5 (5.8) 47 | 15.8 (3.5) 11 | 18.5 (6.7) 11 |
| Emotional symptoms | 2.9 (2.1) 66 | 4.2 (2.6) 48 | 3.3 (2) 11 | 6.2 (3) 16 |
| Conduct problems | 2.7 (1.7) 66 | 3.2 (2) 48 | 4.1 (1.8) 11 | 4.1 (1.8) 12 |
| Hyperactivity | 3.9 (1.9) 66 | 4.3 (1.8) 47 | 4.7 (1.3) 11 | 5.1 (1.9) 11 |
| Peer problems | 3.3 (1.5) 66 | 3.6 (1.9) 48 | 3.7 (1.7) 11 | 4.2 (1.6) 12 |
| Pro-social behaviour | 7.1 (1.6) 66 | 7.5 (1.7) 48 | 6.2 (1.8) 11 | 7.1 (2.2) 16 |
| Impact | 2.3 (2.7) 65 | 1.7 (2.1) 47 | 2.5 (2.8) 11 | 1.8 (2.9) 12 |
Classification of self-report Bristish Sign Language Strengths and Difficulties Questionnaire scores using existing coding frame
Table 6 shows a breakdown of the SDQ scores using the existing SDQ coding frame to categorise young people as normal, borderline or abnormal. On the total score 18% were classified as abnormal, 21% borderline and 61% as normal.
| SDQ subscale | Normal (%) | Borderline (%) | Abnormal (%) | Total |
|---|---|---|---|---|
| Total difficulties | 83 (61) | 28 (21) | 25 (18) | 136 |
| Emotional symptoms | 107 (75) | 10 (7) | 25 (18) | 142 |
| Conduct problems | 85 (62) | 23 (17) | 30 (22) | 138 |
| Hyperactivity/inattention | 108 (79) | 13 (10) | 15 (11) | 136 |
| Peer problems | 74 (54) | 42 (30) | 22 (16) | 138 |
| Pro-social behaviour | 121 (85) | 9 (6) | 12 (9) | 142 |
Concurrent validity
Table 7 shows the summary of the self-report SDQ scores by the clinical gold standard measures. There were significant differences in the total SDQ score between whether or not the clinical assessment identified the child as having an anxiety disorder, conduct disorder and attachment disorder. There were higher mean SDQ scores when the clinical assessment identified a disorder than for borderline or no disorder. For example, where the clinical assessment identified the child as having an anxiety disorder the mean score was 21.3 (3.4), for borderline it was 14.1 (6.5) and for no anxiety disorder it was 13.5 (5.5).
| Question | Response and significance | Total score | Emotional symptoms | Conduct problems | Hyperactivity/inattention | Peer problems | Pro-social behaviour | Impact score |
|---|---|---|---|---|---|---|---|---|
| Does the child have an affective/mood disorder? | p-value | 0.098 | 0.810 | 0.385 | 0.036 | 0.208 | 0.040 | 0.477 |
| No | 13.7 (5.7) 66 | 3.5 (2.8) 70 | 3.2 (2) 66 | 3.8 (1.7) 66 | 3.5 (1.6) 66 | 7.4 (1.5) 70 | 1.9 (2.5) 66 | |
| Borderline | 15 (6.6) 5 | 4.0 (2.1) 6 | 3.2 (1.9) 6 | 4.4 (1.7) 5 | 4.0 (1.8) 6 | 5.7 (2.9) 6 | 0.7 (0.8) 6 | |
| Yes | 22.5 (0.7) 2 | 4.5 (3.5) 2 | 5.5 (2.1) 2 | 7.0 (1.4) 2 | 5.5 (2.1) 2 | 6.0 (5.7) 2 | 1.5 (0.7) 2 | |
| Does the child have an anxiety disorder? | p-value | 0.034 | 0.170 | 0.274 | 0.201 | 0.100 | 0.944 | 0.097 |
| No | 13.5 (5.5) 59 | 3.5 (2.7) 64 | 3.1 (2) 60 | 3.8 (1.8) 59 | 3.6 (1.6) 60 | 7.3 (1.6) 64 | 1.8 (2.4) 60 | |
| Borderline | 14.1 (6.5) 10 | 3.0 (2.8) 10 | 3.5 (2.3) 10 | 4.4 (1.5) 10 | 3.2 (1.8) 10 | 7.2 (2.5) 10 | 0.9 (1.2) 10 | |
| Yes | 21.3 (3.4) 4 | 6.0 (3.2) 4 | 4.8 (1.7) 4 | 5.3 (1.7) 4 | 5.3 (1) 4 | 7.0 (3.2) 4 | 4.0 (4.5) 4 | |
| Does the child have a hyperkinetic disorder (or ADHD)? | p-value | 0.393 | 0.432 | 0.553 | 0.179 | 0.847 | 0.454 | 0.112 |
| No | 14.0 (5.9) 65 | 3.6 (2.8) 70 | 3.2 (2) 66 | 3.8 (1.8) 65 | 3.7 (1.7) 66 | 7.3 (1.8) 70 | 1.7 (2.4) 66 | |
| Borderline | 12.3 (3.5) 3 | 2.0 (1) 3 | 2.7 (2.1) 3 | 4.3 (1.5) 3 | 3.3 (2.1) 3 | 6.0 (3.5) 3 | 2.3 (2.5) 3 | |
| Yes | 17.8 (5) 4 | 4.8 (2.6) 4 | 4.3 (2.1) 4 | 5.5 (1.7) 4 | 3.3 (1.7) 4 | 7.5 (1.7) 4 | 4.3 (2.2) 4 | |
| Does the child have a conduct/oppositional defiant disorder? | p-value | 0.046 | < 0.001 | 0.265 | 0.291 | 0.946 | 0.208 | 0.093 |
| No | 13.3 (5.6) 56 | 2.9 (2.3) 57 | 3.1 (2) 57 | 3.8 (1.8) 56 | 3.6 (1.7) 57 | 7.4 (1.8) 57 | 1.5 (2.2) 57 | |
| Borderline | 18.2 (5.8) 9 | 6.8 (2.4) 13 | 3.9 (2.5) 9 | 4.8 (1.9) 9 | 3.8 (1.3) 9 | 7.5 (1.9) 13 | 2.9 (3.4) 9 | |
| Yes | 15.4 (5.8) 7 | 3.4 (2.8) 7 | 4.1 (1.9) 7 | 4.1 (1.1) 7 | 3.7 (1.7) 7 | 6.1 (1.9) 7 | 3.1 (2.6) 7 | |
| Does the child have any attachment difficulties or an attachment disorder? | p-value | 0.002 | < 0.001 | 0.079 | 0.030 | 0.062 | 0.584 | 0.203 |
| No | 13.0 (5.4) 59 | 2.8 (2.3) 60 | 3.1 (2) 60 | 3.8 (1.7) 59 | 3.4 (1.7) 60 | 7.3 (1.8) 60 | 1.7 (2.3) 60 | |
| Borderline | 18.8 (5.4) 8 | 5.1 (3) 8 | 4.5 (2.1) 8 | 4.3 (1.8) 8 | 4.9 (1.1) 8 | 7 (2.5) 8 | 3.3 (3.5) 8 | |
| Yes | 23 (0) 2 | 8.3 (1) 6 | 5.0 (1.4) 2 | 7.0 (1.4) 2 | 4.0 (0) 2 | 8.0 (1.5) 6 | 1.0 (1.4) 2 | |
| Does the child have an adjustment disorder? | p-value | 0.648 | 0.339 | 0.706 | 0.882 | 0.403 | 0.848 | 0.743 |
| No | 14.0 (5.8) 66 | 3.6 (2.7) 71 | 3.2 (2) 67 | 3.9 (1.8) 66 | 3.6 (1.6) 67 | 7.2 (1.8) 71 | 1.7 (2.3) 67 | |
| Borderline | 12.8 (4.1) 5 | 2.4 (0.9) 5 | 3.6 (2.4) 5 | 3.8 (1.1) 5 | 3 (1.6) 5 | 7.4 (2.4) 5 | 1.4 (2.1) 5 | |
| Yes | n/a | n/a | n/a | n/a | n/a | n/a | n/a | |
| Does the child have any uncommon disorders? | p-value | 0.123 | 0.210 | 0.014 | 0.695 | 0.497 | 0.385 | 0.036 |
| No | 13.4 (5.6) 63 | 3.4 (2.7) 68 | 3.0 (1.9) 64 | 3.9 (1.8) 63 | 3.5 (1.6) 64 | 7.3 (1.8) 68 | 1.7 (2.3) 64 | |
| Borderline | 20.5 (0.7) 2 | 6.0 (1.4) 2 | 7.0 (0) 2 | 3.0 (0) 2 | 4.5 (0.7) 2 | 9.0 (0) 2 | 5.5 (0.7) 2 | |
| Yes | 17.3 (7.6) 3 | 5.3 (1.5) 3 | 4.3 (2.5) 3 | 3.3 (1.5) 3 | 4.3 (2.3) 3 | 7.0 (1) 3 | 0.3 (0.6) 3 | |
| Does the child have an ASD? | p-value | 0.815 | 0.644 | 0.549 | 0.790 | 0.866 | 0.987 | 0.104 |
| No | 14.1 (5.9) 68 | 3.6 (2.8) 73 | 3.2 (2) 69 | 4 (1.8) 68 | 3.6 (1.7) 69 | 7.3 (1.8) 73 | 1.7 (2.3) 69 | |
| Borderline | 11 (–) 1 | 1 (–) 1 | 2 (–) 1 | 5 (–) 1 | 3 (–) 1 | 7 (–) 1 | 3 (–) 1 | |
| Yes | 15.3 (5.7) 3 | 3.7 (2.3) 3 | 4.3 (2.5) 3 | 3.3 (1.5) 3 | 4.0 (1.7) 3 | 7.3 (1.5) 3 | 4.7 (4.2) 3 |
Test–retest reliability
Test–retest data were available for 73 young people. Table 8 shows the descriptive summary of the retest scores.
| SDQ subscale | Mean | SD | n |
|---|---|---|---|
| Total difficulties | 12.8 | 5.6 | 72 |
| Emotional symptoms | 3.0 | 2.4 | 73 |
| Conduct problems | 2.9 | 1.7 | 72 |
| Hyperactivity/inattention | 3.8 | 1.5 | 73 |
| Peer problems | 3.2 | 1.7 | 73 |
| Pro-social behaviour | 7.0 | 2.2 | 73 |
| Impact score | 1.7 | 2.7 | 69 |
To compare the two scores using an ANOVA, the ICCs were calculated. As can be seen in Table 9, there were good ICCs (> 0.6) for total score, emotional, conduct and pro-social behaviour. This indicates good test–retest reliability.
| SDQ scale | ICC (n) |
|---|---|
| Total difficulties | 0.713 (71) |
| Emotional symptoms | 0.622 (72) |
| Conduct problems | 0.707 (71) |
| Hyperactivity/inattention | 0.569 (71) |
| Peer problems | 0.450 (72) |
| Pro-social behaviour | 0.604 (73) |
| Impact score | 0.566 (68) |
Table 10 shows the mean differences between the two scores.
| SDQ subscale | Mean | SD | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Total difficulties | 0.394 | 4.2 | –0.605 | 1.393 |
| Emotional symptoms | –0.028 | 2.0 | –0.501 | 0.445 |
| Conduct problems | 0.000 | 1.4 | –0.325 | 0.325 |
| Hyperactivity/inattention | 0.056 | 1.6 | –0.312 | 0.425 |
| Peer problems | 0.347 | 1.8 | –0.069 | 0.763 |
| Pro-social behaviour | 0.123 | 1.8 | –0.301 | 0.547 |
| Impact score | 0.118 | 2.5 | –0.478 | 0.713 |
Factor analysis and internal consistency
Table 11 shows the internal consistency (using Cronbach’s alpha) for the sub-scales and total score. Overall, this was ‘good’ for the total score and emotional scores. It could be considered ‘acceptable’ for the impact score. It was less good for the other subscales.
| SDQ scale | Cronbach’s alpha |
|---|---|
| Total difficulties | 0.735 |
| Emotional symptoms | 0.707 |
| Conduct problems | 0.480 |
| Hyperactivity/inattention | 0.232 |
| Peer problems | 0.208 |
| Pro-social behaviour | 0.420 |
| Impact score | 0.662 |
Table 12 shows the findings for the Varimax rotated factor analysis. The five-factor solution explained 48% of the variance. All five factors had eigenvalues > 1. The factor structure was examined by identifying the factor loadings, taking the highest factor loading where there were similarities between factors. The following shows the factor loadings for each factor, along with the amount of variance for each factor (all > 0.4).
| SDQ scale | Components (47.5%) | ||||
|---|---|---|---|---|---|
| 1 (16.1%) | 2 (9.1%) | 3 (8.1%) | 4 (7.3%) | 5 (6.9%) | |
| Emotional symptoms | |||||
| I get a lot of headaches, stomach-aches or sickness | 0.57 | 0.027 | 0.145 | −0.164 | 0.259 |
| I worry a lot | 0.748 | −0.087 | 0.059 | −0.065 | 0.22 |
| I am often unhappy, down-hearted or tearful | 0.673 | −0.182 | −0.258 | −0.243 | 0.069 |
| I am nervous in new situations. I easily lose confidence | 0.54 | −0.082 | −0.071 | −0.037 | −0.043 |
| I have many fears, I am easily scared | 0.438 | 0.141 | 0.068 | 0.475 | 0.065 |
| Conduct problems | |||||
| I get very angry and often lose my temper | 0.581 | 0.045 | −0.037 | 0.068 | 0.353 |
| I usually do as I am told | 0.036 | 0.03 | 0.653 | −0.074 | −0.049 |
| I fight a lot. I can make other people do what I want | 0.408 | 0.171 | 0.098 | 0.09 | −0.191 |
| I am often accused of lying or cheating | 0.637 | 0.021 | 0.133 | 0.115 | −0.076 |
| I take things that are not mine from home, school or elsewhere | 0.378 | −0.15 | −0.253 | −0.197 | −0.239 |
| Hyperactivity/inattention | |||||
| I am restless, I cannot stay still for long | 0.198 | −0.115 | −0.033 | 0.307 | 0.643 |
| I am constantly fidgeting or squirming | 0.084 | 0.327 | −0.466 | 0.026 | 0.324 |
| I am easily distracted, I find it difficult to concentrate | 0.546 | 0.178 | 0.436 | 0.162 | 0.109 |
| I think before I do things | 0.078 | −0.559 | −0.047 | −0.055 | −0.004 |
| I finish the work I’m doing. My attention is good | 0.14 | −0.463 | 0.543 | 0.092 | 0.017 |
| Peer problems | |||||
| I am usually on my own. I generally play alone or keep to myself | 0.532 | −0.119 | −0.507 | 0.057 | −0.092 |
| I have one good friend or more | −0.059 | −0.078 | −0.178 | 0.803 | 0.004 |
| Other people my age generally like me | 0.116 | −0.476 | 0.465 | 0.263 | 0.137 |
| Other children or young people pick on me or bully me | 0.675 | 0.133 | 0.006 | 0.081 | −0.17 |
| I get on better with adults than with people my own age | 0.142 | 0.327 | −0.005 | −0.287 | −0.347 |
| Pro-social behaviours | |||||
| I try to be nice to other people. I care about their feelings | −0.054 | 0.139 | 0.001 | −0.174 | 0.704 |
| I usually share with others (food, games, pens etc.) | 0.015 | 0.052 | −0.107 | −0.623 | −0.009 |
| I am helpful if someone is hurt, upset or feeling ill | 0.124 | 0.621 | 0.013 | −0.074 | 0.256 |
| I am kind to younger children | 0.153 | 0.532 | 0.249 | −0.255 | −0.314 |
| I often volunteer to help others (parents, teachers, children) | −0.026 | 0.632 | −0.335 | 0.078 | −0.025 |
The scores did not map exactly to the subscales as seen in validation papers from other languages and cultures. Emotional and conduct questions loaded within one factor. The hyperactivity and pro-social scales included three of the five questions. Peer problem questions were identified by only one question (I have one good friend or more). The fifth factor was loaded on the question ‘I am restless, I cannot stay still for long’.
Validation of parent version of the British Sign Language Strengths and Difficulties Questionnaire
The validation of the deaf parent SDQ is based on 191 respondents.
Parent British Sign Language Strengths and Difficulties Questionnaire scores
Table 13 shows the mean scores for the total and subscale score.
| SDQ subscale | Mean | SD | n |
|---|---|---|---|
| Total difficulties | 13.2 | 6.7 | 189 |
| Emotional symptoms | 3.3 | 2.6 | 191 |
| Conduct problems | 2.8 | 2.0 | 190 |
| Hyperactivity/inattention | 4.0 | 2.2 | 189 |
| Peer problems | 3.1 | 2.1 | 190 |
| Pro-social behaviour | 7.5 | 1.8 | 191 |
| Impact score | 1.2 | 2.0 | 187 |
Classification of parent British Sign Language Strengths and Difficulties Questionnaire scores using existing coding frame
Table 14 shows a breakdown of the SDQ scores using the existing SDQ coding frame to categorise young people as normal, borderline or abnormal based on parent scores. On the total score 28% were classified as abnormal, 18% borderline and 55% as normal.
| SDQ subscale | Normal (%) | Borderline (%) | Abnormal (%) | Total |
|---|---|---|---|---|
| Total difficulties | 103 (55) | 33 (18) | 53 (28) | 189 |
| Emotional symptoms | 107 (56) | 28 (15) | 56 (29) | 191 |
| Conduct problems | 95 (50) | 27 (14) | 68 (36) | 190 |
| Hyperactivity/inattention | 140 (74) | 21 (11) | 28 (15) | 189 |
| Peer problems | 82 (43) | 46 (24) | 62 (33) | 190 |
| Pro-social behaviour | 165 (86) | 11 (6) | 15 (8) | 191 |
Concurrent validity
Table 15 shows the parent SDQ score and subscale scores by gold standard clinical assessment.
| Question | Response and significance | Total difficulties | Emotional symptoms | Conduct problems | Hyperactivity/inattention | Peer problems | Pro-social behaviour | Impact score |
|---|---|---|---|---|---|---|---|---|
| Does the child have an affective/mood disorder? | p-value | 0.286 | 0.199 | 0.24 | 0.463 | 0.592 | 0.765 | 0.336 |
| No | 12.7 (6.5) 146 | 3.1 (2.6) 147 | 2.6 (1.9) 146 | 3.9 (2.1) 146 | 3 (2.1) 147 | 7.7 (1.6) 147 | 1.2 (1.9) 147 | |
| Borderline | 12.8 (5.7) 4 | 4 (1.2) 4 | 2.5 (2.1) 4 | 3 (1.4) 4 | 3.3 (2.9) 4 | 8.3 (2.1) 4 | 2 (1.8) 4 | |
| Yes | 17.4 (9.6) 5 | 5 (3.2) 6 | 4 (2.8) 6 | 4.8 (3.1) 5 | 4 (2.2) 5 | 7.7 (1.6) 6 | 2.2 (3) 6 | |
| Does the child have an anxiety disorder? | p-value | 0.004 | < 0.001 | 0.271 | 0.753 | 0.009 | 0.069 | 0.007 |
| No | 12.1 (6) 126 | 2.9 (2.5) 128 | 2.6 (1.9) 127 | 3.9 (2.2) 126 | 2.8 (2) 127 | 7.8 (1.5) 128 | 1 (1.8) 128 | |
| Borderline | 15.4 (7.7) 24 | 4.5 (2.6) 24 | 3.2 (2.2) 24 | 3.9 (1.8) 24 | 3.8 (2.6) 24 | 7.4 (2) 24 | 1.8 (1.9) 24 | |
| Yes | 20.8 (9.5) 4 | 7 (3.2) 4 | 3.5 (1.7) 4 | 4.8 (3.3) 4 | 5.5 (3) 4 | 6 (0.8) 4 | 3.8 (3.2) 4 | |
| Does the child have a hyperkinetic disorder (or ADHD)? | p-value | < 0.001 | 0.051 | < 0.001 | 0.031 | 0.002 | 0.123 | < 0.001 |
| No | 12.4 (6.1) 143 | 3.1 (2.6) 145 | 2.6 (1.9) 144 | 3.9 (2.1) 143 | 2.9 (2) 144 | 7.7 (1.6) 145 | 1.1 (1.8) 145 | |
| Borderline | 20.5 (8.1) 6 | 5.2 (3) 6 | 4.3 (2.2) 6 | 5.2 (1.3) 6 | 5.8 (2.7) 6 | 6.3 (2) 6 | 2.7 (2.2) 6 | |
| Yes | 23.3 (5.8) 3 | 5.7 (2.3) 3 | 6.3 (1.5) 3 | 6.7 (4.2) 3 | 4.7 (1.5) 3 | 7.7 (0.6) 3 | 6.3 (1.5) 3 | |
| Does the child have a conduct/oppositional defiant disorder? | p-value | < 0.001 | 0.344 | < 0.001 | < 0.001 | 0.001 | 0.011 | < 0.001 |
| No | 11.6 (5.9) 120 | 3.1 (2.4) 122 | 2.2 (1.8) 121 | 3.6 (2) 120 | 2.7 (1.9) 121 | 7.8 (1.6) 122 | 0.9 (1.8) 122 | |
| Borderline | 17.7 (6.7) 31 | 3.8 (3.3) 31 | 4.2 (1.5) 31 | 5.5 (2.1) 31 | 4.2 (2.6) 31 | 7.1 (1.5) 31 | 2.3 (2) 31 | |
| Yes | 20 (1.4) 2 | 4 (1.4) 2 | 6.5 (2.1) 2 | 4 (0) 2 | 5.5 (2.1) 2 | 5.5 (0.7) 2 | 4 (1.4) 2 | |
| Does the child have any attachment difficulties or an attachment disorder? BOTH | p-value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | 0.093 | < 0.001 |
| No | 11.5 (5.7) 130 | 3 (2.3) 132 | 2.3 (1.8) 131 | 3.5 (2) 130 | 2.7 (1.9) 131 | 7.7 (1.6) 132 | 1 (1.9) 132 | |
| Borderline | 17.1 (4) 15 | 2.5 (2.9) 15 | 4.1 (1) 15 | 6.7 (0.7) 15 | 3.8 (2.2) 15 | 7.5 (1.1) 15 | 2.3 (1.3) 15 | |
| Yes | 26 (3.4) 8 | 8.3 (0.9) 8 | 5.8 (1.2) 8 | 5.1 (2.5) 8 | 6.9 (1.1) 8 | 6.5 (1.6) 8 | 3.6 (2.1) 8 | |
| Does the child have an adjustment disorder? BOTH | p-value | 0.001 | < 0.001 | 0.008 | 0.331 | 0.089 | 0.033 | 0.003 |
| No | 12.4 (6.2) 146 | 3 (2.5) 147 | 2.6 (1.9) 147 | 3.9 (2.2) 146 | 3 (2) 146 | 7.7 (1.5) 147 | 1.1 (1.9) 147 | |
| Borderline | 20.7 (7.8) 7 | 6.9 (2) 8 | 4.6 (1.8) 7 | 4.7 (1.5) 7 | 4.3 (3.2) 8 | 6.5 (2.5) 8 | 3.1 (2) 8 | |
| Yes | 0 (0) 0 | 0 (0) 0 | 0 (0) 0 | 0 (0) 0 | 0 (0) 0 | 0 (0) 0 | 0 (0) 0 | |
| Does the child have any uncommon disorders? BOTH | p-value | 0.022 | 0.081 | 0.121 | 0.206 | 0.04 | 0.468 | 0.376 |
| No | 12.8 (6.3) 150 | 3.2 (2.6) 152 | 2.7 (2) 151 | 3.9 (2.1) 150 | 3 (2.1) 151 | 7.7 (1.6) 152 | 1.2 (1.9) 152 | |
| Borderline | 2.5 (0.7) 2 | 0 (0) 2 | 0.5 (0.7) 2 | 2 (0) 2 | 0 (0) 2 | 8.5 (0.7) 2 | 0 (0) 2 | |
| Yes | 0 (0) 0 | 0 (0) 0 | 0 (0) 0 | 0 (0) 0 | 0 (0) 0 | 0 (0) 0 | 0 (0) 0 | |
| Does the child have an autism spectrum disorder? BOTH | p-value | 0.982 | 0.449 | 0.589 | 0.285 | 0.958 | 0.826 | 0.359 |
| No | 12.9 (6.6) 151 | 3.3 (2.6) 153 | 2.7 (2) 152 | 3.9 (2.1) 151 | 3.1 (2.2) 152 | 7.7 (1.6) 153 | 1.2 (1.9) 153 | |
| Borderline | 12 (0) 1 | 1 (0) 1 | 1 (0) 1 | 7 (0) 1 | 3 (0) 1 | 8 (0) 1 | 0 (0) 1 | |
| Yes | 13.5 (9.2) 2 | 1.5 (2.1) 2 | 3.5 (3.5) 2 | 5 (4.2) 2 | 3.5 (0.7) 2 | 7 (0) 2 | 3 (4.2) 2 |
The total score is significantly associated with anxiety disorders, ADHD, conduct disorders, attachment and adjustment disorders.
Test–retest reliability
Table 16 shows the descriptive summary of the retest scores.
| SDQ subscale | Mean (SD) n |
|---|---|
| Total difficulties | 12 (6.6) 143 |
| Emotional symptoms | 3.2 (2.6) 146 |
| Conduct problems | 2.3 (1.9) 146 |
| Hyperactivity/inattention | 3.7 (2.2) 144 |
| Peer problems | 2.9 (2) 146 |
| Pro-social behaviour | 7.4 (1.9) 147 |
| Impact score | 1 (1.8) 144 |
Table 17 shows the ICCs. As can be seen in the table, there was a good correlation for the total and subscales. This indicates good test–retest reliability as defined by a correlation coefficient of at least over 0.6 for each group.
| SDQ scale | ICCs (n) |
|---|---|
| Total difficulties | 0.746 (143) |
| Emotional symptoms | 0.769 (146) |
| Conduct problems | 0.676 (146) |
| Hyperactivity/inattention | 0.656 (144) |
| Peer problems | 0.650 (146) |
| Pro-social behaviour | 0.598 (147) |
| Impact score | 0.657 (144) |
Table 18 shows the mean difference between the test and retest scores.
| SDQ subscale | Mean | SD | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Total difficulties | 0.909 | 4.653 | 0.140 | 1.678 |
| Emotional symptoms | 0.110 | 1.808 | −0.186 | 0.405 |
| Conduct problems | 0.486 | 1.594 | 0.226 | 0.747 |
| Hyperactivity/inattention | 0.243 | 1.795 | −0.053 | 0.539 |
| Peer problems | 0.089 | 1.665 | −0.183 | 0.361 |
| Pro-social behaviour | 0.259 | 1.631 | −0.007 | 0.524 |
| Impact score | 0.153 | 1.539 | −0.101 | 0.406 |
Factor analysis and internal consistency
Table 19 shows the Cronbach’s alpha for the subscales and total score for the parent version of the SDQ. The Cronbach’s alpha was good for the total score, emotional and impact score. It was less good for the other subscales.
| SDQ subscale | Cronbach’s alpha |
|---|---|
| Total difficulties | 0.842 |
| Emotional symptoms | 0.701 |
| Conduct problems | 0.529 |
| Hyperactivity/inattention | 0.585 |
| Peer problems | 0.580 |
| Pro-social behaviour | 0.424 |
| Impact score | 0.723 |
Table 20 shows the findings for the Varimax rotated factor analysis. The five-factor solution explained 50% of the variance. All five factors had eigenvalues > 1. The factor structure was examined by identifying the factor loadings, with the highest factor loading taken where there were similarities between factors. Table 20 shows the factor loadings for each factor, along with the amount of variance for each factor. The scores did not map exactly to the subscales as seen in other validation papers. Emotional questions loaded mainly within one factor, but the same factor also included peer problem questions. Conduct was spread across factors. The hyperactivity scale splits between two factors. The pro-social scales included three of the five questions. The fifth factor included two questions: ‘Generally obedient, usually does what adults request’ and ‘Considerate of other people’s feelings.’
| SDQ subscale | Components (50%) | ||||
|---|---|---|---|---|---|
| 1 (17.3%) | 2 (2.4%) | 3 (2.1%) | 4 (2.1%) | 5 (1.6%) | |
| Emotional symptoms | |||||
| Often complains of headaches, stomach-aches or sickness | 0.662 | −0.077 | 0.002 | 0.119 | −0.014 |
| Many worries, often seems worried | 0.708 | 0.134 | 0.068 | 0.085 | 0.039 |
| Often unhappy, down-hearted or tearful | 0.773 | 0.129 | −0.095 | 0.118 | −0.052 |
| Nervous or clingy in new situations, easily loses confidence | 0.190 | 0.707 | −0.118 | 0.013 | 0.067 |
| Many fears, easily scared | 0.679 | 0.217 | 0.022 | −0.090 | 0.150 |
| Conduct problems | |||||
| Often has temper tantrums or hot tempers | 0.574 | 0.158 | 0.366 | 0.191 | −0.088 |
| Generally obedient, usually does what adults request | 0.241 | −0.017 | 0.247 | −0.011 | −0.617 |
| Often fights with other children or bullies them | 0.559 | 0.339 | 0.145 | 0.284 | 0.034 |
| Often lies or cheats | 0.203 | −0.047 | 0.346 | 0.500 | −0.146 |
| Steals from home, school or elsewhere | 0.313 | 0.425 | 0.256 | −0.015 | 0.143 |
| Hyperactivity/inattention | |||||
| Restless, overactive, cannot stay still for long | 0.122 | 0.055 | 0.098 | 0.846 | 0.066 |
| Constantly fidgeting or squirming | 0.136 | 0.039 | −0.202 | 0.774 | 0.044 |
| Easily distracted, concentration wanders | 0.283 | 0.070 | 0.512 | 0.306 | 0.150 |
| Thinks things out before acting | −0.074 | 0.003 | 0.173 | 0.034 | −0.593 |
| Sees tasks through to the end, good attention span | 0.043 | −0.041 | 0.767 | −0.180 | −0.033 |
| Peer problems | |||||
| Rather solitary, tends to play alone | 0.464 | 0.304 | 0.245 | 0.329 | 0.057 |
| Has at least one good friend | 0.547 | 0.108 | 0.155 | 0.230 | −0.074 |
| Generally liked by other children | 0.072 | 0.425 | 0.416 | 0.121 | −0.123 |
| Picked on or bullied by other children | 0.674 | 0.178 | 0.197 | 0.158 | −0.223 |
| Gets on better with adults than with other children | 0.448 | −0.068 | −0.187 | −0.159 | 0.239 |
| Pro-social behaviour | |||||
| Considerate of other people’s feelings | 0.126 | −0.050 | 0.270 | 0.114 | 0.638 |
| Shares readily with other children (treats, toys, pencils etc.) | 0.048 | −0.179 | −0.588 | −0.085 | 0.234 |
| Helpful if someone is hurt, upset or feeling ill | −0.352 | −0.563 | 0.088 | −0.010 | 0.250 |
| Kind to younger children | 0.054 | −0.639 | −0.141 | −0.030 | −0.144 |
| Often volunteers to help others (parents, teachers, other children) | −0.124 | −0.605 | −0.104 | −0.028 | 0.274 |
Validation of teacher version
There was a total of 77 deaf teaching staff. Of these, 27 were deaf teachers of the deaf and 50 were deaf teaching assistants.
Teacher Strengths and Difficulties Questionnaire scores
Table 21 shows the mean scores for the total score and the subscales.
| SDQ subscale | Mean | SD | Valid n |
|---|---|---|---|
| Total difficulties | 12.8 | 6.1 | 74 |
| Emotional symptoms | 3.2 | 2.3 | 74 |
| Conduct problems | 2.4 | 2.3 | 74 |
| Hyperactivity/inattention | 4.2 | 2.5 | 74 |
| Peer problems | 3.0 | 1.9 | 74 |
| Pro-social behaviour | 6.6 | 2.3 | 74 |
| Impact score | 1.1 | 1.6 | 73 |
One of the teachers and two of the teaching assistants did not fully complete questionnaires.
Classification of teacher report scores using existing coding frame
Table 22 shows a breakdown of the SDQ scores using the existing SDQ coding frame to categorise young people as normal, borderline or abnormal based on teacher scores. On the total score 31% were classified as abnormal, 23% borderline and 46% as normal.
| SDQ subscale | Normal (%) | Borderline (%) | Abnormal (%) | Total |
|---|---|---|---|---|
| Total difficulties | 34 (46) | 17 (23) | 23 (31) | 74 |
| Emotional symptoms | 45 (61) | 11 (15) | 18 (24) | 76 |
| Conduct problems | 43 (58) | 9 (12) | 22 (30) | 74 |
| Hyperactivity/inattention | 55 (74) | 3 (4) | 16 (22) | 74 |
| Peer problems | 50 (68) | 8 (11) | 16 (22) | 74 |
| Pro-social behaviour | 53 (72) | 8 (11) | 13 (18) | 74 |
Concurrent validity
Table 23 shows the deaf teacher SDQ scores and subscale scores by gold standard clinical assessment.
| Question | Response and significance | Total difficulties | Emotional symptoms | Conduct problems | Hyperactivity/inattention | Peer problems | Pro-social behaviour | Impact score |
|---|---|---|---|---|---|---|---|---|
| Does the child have an affective/mood disorder? | p-value | 0.496 | 0.661 | 0.553 | 0.741 | 0.636 | 0.915 | 0.513 |
| No | 12.3 (6.2) 47 | 3.1 (2.4) 47 | 2.5 (2.4) 47 | 3.9 (2.7) 47 | 2.9 (1.8) 47 | 6.8 (2.1) 47 | 1.1 (1.7) 46 | |
| Borderline | 8.0 (0) 1 | 2.0 (0) 1 | 1.0 (0) 1 | 3.0 (0) 1 | 2.0 (0) 1 | 7.0 (0) 1 | 0.0 (0) 1 | |
| Yes | n/a | n/a | n/a | n/a | n/a | n/a | n/a | |
| Does the child have an anxiety disorder? | p-value | 0.16 | 0.049 | 0.609 | 0.29 | 0.173 | 0.044 | 0.589 |
| No | 11.7 (6.1) 41 | 2.8 (2.3) 41 | 2.5 (2.5) 41 | 3.7 (2.7) 41 | 2.7 (1.7) 41 | 7.0 (2.0) 41 | 1.1 (1.7) 40 | |
| Borderline | 15.3 (6.4) 7 | 4.7 (2.7) 7 | 2.0 (2.1) 7 | 4.9 (1.7) 7 | 3.7 (2.1) 7 | 5.3 (2.2) 7 | 1.4 (1.5) 7 | |
| Yes | n/a | n/a | n/a | n/a | n/a | n/a | n/a | |
| Does the child have a hyperkinetic disorder (or ADHD)? | p-value | 0.021 | 0.037 | 0.117 | 0.544 | 0.046 | 0.003 | 0.281 |
| No | 12.3 (5.9) 44 | 3.0 (2.3) 44 | 2.5 (2.4) 44 | 4.0 (2.7) 44 | 2.8 (1.7) 44 | 6.7 (2) 44 | 1.1 (1.7) 43 | |
| Borderline | 6.7 (1.5) 3 | 2.3 (1.2) 3 | 0.0 (0) 3 | 2.3 (1.2) 3 | 2.0 (1) 3 | 9.7 (0.6) 3 | 0.0 (0) 3 | |
| Yes | 26.0 (0) 1 | 9.0 (0) 1 | 5.0 (0) 1 | 5.0 (0) 1 | 7.0 (0) 1 | 2.0 (0) 1 | 3.0 (0) 1 | |
| Does the child have a conduct/oppositional defiant disorder? | p-value | 0.047 | 0.786 | 0.018 | 0.009 | 0.575 | < 0.001 | 0.222 |
| No | 11.1 (5.5) 24 | 3.0 (2.3) 24 | 1.5 (1.9) 24 | 4 (2.9) 24 | 2.6 (1.9) 24 | 7.6 (1.6) 24 | 0.9 (1.6) 23 | |
| Borderline | 12.4 (6.5) 21 | 3.0 (2.3) 21 | 3.1 (2.7) 21 | 3.2 (1.7) 21 | 3.0 1.5) 21 | 6.5 (2) 21 | 1.1 (1.8) 21 | |
| Yes | 20.3 (5.1) 3 | 4.0 (4.6) 3 | 4.7 (0.6) 3 | 8 (2.6) 3 | 3.7 (3.1) 3 | 2.3 (0.6) 3 | 2.7 (0.6) 3 | |
| Does the child have any attachment difficulties or an attachment disorder? BOTH | p-value | 0.001 | 0.001 | < 0.001 | 0.197 | 0.08 | 0.338 | < 0.001 |
| No | 11.5 (5.9) 30 | 2.8 (2.2) 30 | 1.7 (1.9) 30 | 4.4 (2.8) 30 | 2.5 (1.6) 30 | 7.1 (2.5) 30 | 0.8 (1.3) 29 | |
| Borderline | 10.5 (4.9) 12 | 1.9 (1.2) 12 | 3.2 (2.1) 12 | 2.8 (2) 12 | 2.6 (1.4) 12 | 6.1 (1.4) 12 | 0.8 (1.9) 12 | |
| Yes | 24.0 (1.7) 3 | 7.0 (1) 3 | 8 (1) 3 | 4.3 (0.6) 3 | 4.7 (0.6) 3 | 7.7 (0.6) 3 | 4.7 (0.6) 3 | |
| Does the child have an adjustment disorder? BOTH | p-value | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| No | 12.2 (6.2) 48 | 3.1 (2.4) 48 | 2.4 (2.4) 48 | 3.9 (2.6) 48 | 2.9 (1.8) 48 | 6.8 (2.1) 48 | 1.1 (1.7) 47 | |
| Borderline | n/a | n/a | n/a | n/a | n/a | n/a | n/a | |
| Yes | n/a | n/a | n/a | n/a | n/a | n/a | n/a | |
| Does the child have any uncommon disorders? BOTH | p-value | 0.399 | 0.661 | 0.857 | 0.274 | 0.636 | 0.126 | 0.513 |
| No | 12.3 (6.2) 47 | 3.1 (2.4) 47 | 2.4 (2.4) 47 | 3.9 (2.6) 47 | 2.9 (1.8) 47 | 6.7 (2.1) 47 | 1.1 (1.7) 46 | |
| Borderline | n/a | n/a | n/a | n/a | n/a | n/a | n/a | |
| Yes | 7 (0) 1 | 2 (0) 1 | 2 (0) 1 | 1 (0) 1 | 2 (0) 1 | 10 (0) 1 | 0 (0) 1 | |
| Does the child have an autism spectrum disorder? BOTH | p-value | 0.061 | 0.018 | 0.457 | 0.128 | 0.063 | 0.011 | 0.457 |
| No | 11.8 (5.9) 46 | 3.0 (2.3) 46 | 2.3 (2.4) 46 | 3.7 (2.6) 46 | 2.8 (1.7) 46 | 7.0 (2) 46 | 1.0 (1.7) 45 | |
| Borderline | 26.0 (0) 1 | 9.0 (0) 1 | 5.0 (0) 1 | 5.0 (0) 1 | 7.0 (0) 1 | 2.0 (0) 1 | 3.0 (0) 1 | |
| Yes | 16.0 (0) 1 | 0.0 (0) 1 | 4.0 (0) 1 | 9.0 (0) 1 | 3.0 (0) 1 | 3.0 (0) 1 | 2.0 (0) 1 |
Test–retest reliability
Table 24 shows the descriptive summary of the retest scores.
| SDQ subscale | Mean | SD | n |
|---|---|---|---|
| Total difficulties | 10.9 | 6.2 | 46 |
| Emotional symptoms | 2.4 | 2.2 | 46 |
| Conduct problems | 2.1 | 2.2 | 46 |
| Hyperactivity/inattention | 3.7 | 2.6 | 46 |
| Peer problems | 2.7 | 1.6 | 46 |
| Pro-social behaviour | 6.4 | 2.5 | 46 |
| Impact score | 0.9 | 1.3 | 46 |
To compare the two scores, the ICCs were calculated. As can be seen in Table 25, there were good ICCs (> 0.6) for the total score and subscales. This indicates good test–retest validity.
| SDQ scale | ICC (n) |
|---|---|
| Total difficulties | 0.830 (46) |
| Emotional symptoms | 0.759 (46) |
| Conduct problems | 0.743 (46) |
| Hyperactivity/inattention | 0.714 (46) |
| Peer problems | 0.664 (46) |
| Pro-social behaviour | 0.831 (46) |
| Impact score | 0.767 (46) |
Table 26 shows the mean differences in scores between teacher BSL SDQ test and retest.
| SDQ subscale | Mean | SD | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Total difficulties | 1.717 | 3.594 | 0.650 | 2.785 |
| Emotional symptoms | 0.543 | 1.516 | 0.093 | 0.994 |
| Conduct problems | 0.500 | 1.735 | −0.015 | 1.015 |
| Hyperactivity/inattention | 0.478 | 1.941 | 0.098 | 1.055 |
| Peer problems | 0.196 | 1.327 | −0.198 | 0.590 |
| Pro-social behaviour | 0.478 | 1.441 | 0.050 | 0.906 |
| Impact score | 0.239 | 1.099 | −0.087 | 0.566 |
Factor analysis and internal consistency
Table 27 shows the Cronbach’s alpha for the subscales and total score for the teacher version of the SDQ. The Cronbach’s alpha was good for the total score and subscales. It was least good for peer problems.
| SDQ scale | Cronbach’s alpha |
|---|---|
| Total difficulties | 0.738 |
| Emotional symptoms | 0.690 |
| Conduct problems | 0.607 |
| Hyperactivity/inattention | 0.697 |
| Peer problems | 0.515 |
| Pro-social behaviour | 0.664 |
| Impact score | 0.781 |
Table 28 shows the findings for the Varimax rotated factor analysis. The five-factor solution explained 54.9% of the variance. All five factors had eigenvalues > 1. The factor structure was examined by identifying the factor loadings, with the highest factor loading taken where there were similarities between factors. The following shows the factor loadings for each factor, along with the amount of variance for each factor (all > 0.4).The scores did map closely to the subscales as seen in other validation papers. Emotional questions loaded mainly within one factor, but also included peer problem questions (this was seen in the parent validation). Conduct scales included three of the five questions. The hyperactivity scales included all the five questions. The pro-social scales included four of the five questions.
| SDQ subscale | Components (54.9%) | ||||
|---|---|---|---|---|---|
| 1 (13.7%) | 2 (12.5%) | 3 (10.8%) | 4 (9.9%) | 5 (7.1%) | |
| Emotional symptoms | |||||
| Often complains of headaches, stomach-aches or sickness | 0.181 | −0.122 | −0.449 | 0.357 | 0.273 |
| Many worries, often seems worried | 0.174 | 0.670 | 0.207 | 0.341 | −0.012 |
| Often unhappy, down-hearted or tearful | −0.015 | 0.460 | 0.157 | 0.707 | −0.109 |
| Nervous or clingy in new situations, easily loses confidence | −0.068 | 0.744 | 0.008 | −0.179 | −0.063 |
| Many fears, easily scared | −0.144 | 0.609 | 0.030 | 0.292 | −0.222 |
| Conduct problems | |||||
| Often has temper tantrums or hot tempers | −0.262 | 0.087 | 0.037 | 0.687 | 0.001 |
| Generally obedient, usually does what adults request | −0.519 | 0.000 | 0.145 | 0.317 | 0.350 |
| Often fights with other children or bullies them | −0.365 | −0.161 | 0.059 | 0.554 | 0.363 |
| Often lies or cheats | −0.069 | 0.043 | 0.118 | 0.118 | 0.693 |
| Steals from home, school or elsewhere | −0.010 | 0.114 | −0.042 | 0.354 | −0.022 |
| Hyperactivity/inattention | |||||
| Restless, overactive, cannot stay still for long | −0.001 | −0.179 | 0.588 | 0.509 | −0.222 |
| Constantly fidgeting or squirming | 0.041 | −0.150 | 0.702 | 0.161 | −0.011 |
| Easily distracted, concentration wanders | −0.063 | 0.118 | 0.754 | 0.162 | 0.378 |
| Thinks things out before acting | −0.041 | 0.056 | 0.634 | −0.062 | 0.017 |
| Sees tasks through to the end, good attention span | −0.378 | 0.315 | 0.542 | −0.128 | 0.409 |
| Peer problems | |||||
| Rather solitary, tends to play alone | −0.211 | 0.678 | −0.314 | 0.171 | 0.123 |
| Has at least one good friend | −0.257 | 0.565 | 0.073 | −0.025 | 0.024 |
| Generally liked by other children | −0.617 | 0.260 | 0.129 | 0.178 | −0.233 |
| Picked on or bullied by other children | 0.175 | 0.629 | −0.094 | 0.269 | 0.394 |
| Gets on better with adults than with other children | 0.360 | 0.016 | −0.357 | 0.259 | 0.024 |
| Pro-social behaviour | |||||
| Considerate of other people’s feelings | 0.111 | 0.052 | 0.058 | 0.185 | −0.467 |
| Shares readily with other children (treats, toys, pencils etc.) | 0.714 | −0.177 | 0.075 | −0.111 | 0.307 |
| Helpful if someone is hurt, upset or feeling ill | 0.701 | −0.168 | −0.139 | 0.067 | −0.292 |
| Kind to younger children | 0.673 | −0.059 | −0.055 | −0.027 | −0.240 |
| Often volunteers to help others (parents, teachers, other children) | 0.773 | 0.097 | 0.055 | −0.123 | −0.119 |
Comparison of deaf teachers and deaf teaching assistants
Table 29 shows the mean scores for the deaf teacher BSL SDQ comparing deaf teachers and deaf teaching assistants. There are no statistically significant differences between deaf teachers and deaf teaching assistants.
| SDQ subscale | Deaf teacher | Deaf teaching assistant |
|---|---|---|
| Total difficulties | 11.9 (6) 26 | 13.3 (6.2) 48 |
| Emotional symptoms | 3.2 (2.2) 26 | 3.2 (2.3) 48 |
| Conduct problems | 2 (2.2) 26 | 2.6 (2.3) 48 |
| Hyperactivity/inattention | 3.8 (2.7) 26 | 4.4 (2.4) 48 |
| Peer problems | 2.9 (2.2) 26 | 3 (1.8) 48 |
| Pro-social behaviour | 7 (2.4) 26 | 6.4 (2.2) 48 |
| Impact score | 1.2 (1.7) 25 | 1 (1.5) 48 |
Inter-rater agreement
Inter-rater agreement for the deaf child self-report Strengths and Difficulties Questionnaire
Inter-rater agreement of the deaf child Strengths and Difficulties Questionnaire and their parents
Table 30 shows the scores for the subscales and total scale where there are paired data between the deaf young person’s self-report SDQ and their parent’s completed questionnaire.
| SDQ subscale | Rater | Mean | n | SD | Test statistic (degrees of freedom), p-value |
|---|---|---|---|---|---|
| Total difficulties | Child | 14.03 | 104 | 5.623 | 1.121 (103), p = 0.265 |
| Parent | 14.99 | 104 | 8.248 | ||
| Emotional symptoms | Child | 3.62 | 110 | 2.682 | 0.029 (109), p = 0.977 |
| Parent | 3.63 | 110 | 2.749 | ||
| Conduct problems | Child | 3.08 | 106 | 1.928 | 0.266 (105), p = 0.791 |
| Parent | 3.16 | 106 | 2.641 | ||
| Hyperactivity/inattention | Child | 4.06 | 104 | 1.800 | 2.366 (103), p = 0.020 |
| Parent | 4.73 | 104 | 2.612 | ||
| Peer problems | Child | 3.46 | 106 | 1.593 | 0.398 (105), p = 0.692 |
| Parent | 3.57 | 106 | 2.567 | ||
| Pro-social behaviour | Child | 7.15 | 110 | 1.736 | 0.350 (109), p = 0.727 |
| Parent | 7.25 | 110 | 2.480 | ||
| Impact score | Child | 2.00 | 97 | 2.500 | 0.472 (96), p = 0.638 |
| Parent | 1.85 | 97 | 2.468 |
The only subscale that showed a significant difference was the hyperactivity score (p = 0.020), where the mean difference was 0.673 (2.901), with parents scoring their children significantly higher.
Table 31 shows the correlation between the paired scores. Overall, the correlations were fairly weak.
| SDQ subscale | n | Correlation | p-value |
|---|---|---|---|
| Total difficulties | 104 | 0.250 | 0.011 |
| Emotional symptoms | 110 | 0.264 | 0.005 |
| Conduct problems | 106 | 0.211 | 0.030 |
| Hyperactivity/inattention | 104 | 0.175 | 0.076 |
| Peer problems | 106 | 0.234 | 0.016 |
| Pro-social behaviour | 110 | 0.202 | 0.034 |
| Impact score | 98 | 0.249 | 0.013 |
Inter-rater agreement of the deaf child Strengths and Difficulties Questionnaire and their teachers
Table 32 shows the scores for the subscales and total scale where there are paired data with the teacher completed questionnaire. In all the scales, the teacher scored the child lower than the self-reported SDQ scores. There were significant differences for the emotional, conduct, peer, impact and total scales (p < 0.01).
| SDQ subscale | Rater | Mean | n | SD | Test statistic (degrees of freedom), p-value |
|---|---|---|---|---|---|
| Total difficulties | Child | 14.44 | 90 | 5.561 | 3.979 (89), p < 0.001 |
| Teacher | 11.16 | 90 | 7.679 | ||
| Emotional symptoms | Child | 3.87 | 94 | 2.637 | 3.293 (93), p = 0.001 |
| Teacher | 2.79 | 94 | 2.739 | ||
| Conduct problems | Child | 3.03 | 91 | 1.900 | 4.091 (90), p < 0.001 |
| Teacher | 1.89 | 91 | 2.218 | ||
| Hyperactivity/inattention | Child | 4.08 | 91 | 1.809 | 0.475 (90), p = 0.636 |
| Teacher | 3.92 | 91 | 3.081 | ||
| Peer problems | Child | 3.72 | 90 | 1.690 | 3.898 (89), p < 0.001 |
| Teacher | 2.71 | 90 | 2.245 | ||
| Pro-social behaviour | Child | 7.19 | 94 | 1.821 | 0.752 (93), p = 0.454 |
| Teacher | 6.98 | 94 | 2.342 | ||
| Impact score | Child | 2.09 | 85 | 2.443 | 3.500 (84), p = 0.001 |
| Teacher | 1.06 | 85 | 1.530 |
Table 33 shows the correlation between the paired scores. Overall, the correlations were fairly weak.
| SDQ subscale | n | Correlation | p-value |
|---|---|---|---|
| Total difficulties | 90 | 0.333 | 0.001 |
| Emotional symptoms | 94 | 0.294 | 0.004 |
| Conduct problems | 91 | 0.170 | 0.108 |
| Hyperactivity/inattention | 91 | 0.290 | 0.005 |
| Peer problems | 90 | 0.242 | 0.021 |
| Pro-social behaviour | 94 | 0.150 | 0.150 |
| Impact score | 85 | 0.116 | 0.289 |
Inter-rater agreement for the deaf parent Strengths and Difficulties Questionnaire
Inter-rater agreement of the deaf parent Strengths and Difficulties Questionnaire and child Strengths and Difficulties Questionnaire
Table 34 shows the scores for the subscales and total scale where there are paired data with the parent-completed questionnaire. In all the scales, the parent scored the child higher than the self-reported SDQ scores. There were significant differences for the emotional, conduct, peer and total scales (p < 0.01).
| SDQ subscale | Rater | Mean | n | SD | Test statistic (degrees of freedom), p-value |
|---|---|---|---|---|---|
| Total difficulties | Parent | 14.13 | 83 | 6.998 | 4.159 (82), p < 0.001 |
| Child | 11.37 | 83 | 5.298 | ||
| Emotional symptoms | Parent | 4.18 | 89 | 2.618 | 2.926 (88), p = 0.004 |
| Child | 3.35 | 89 | 2.603 | ||
| Conduct problems | Parent | 2.99 | 84 | 2.114 | 3.581 (83), p = 0.001 |
| Child | 2.24 | 84 | 1.502 | ||
| Hyperactivity/inattention | Parent | 3.96 | 83 | 2.260 | 1.235 (82), p = 0.220 |
| Child | 3.61 | 83 | 1.866 | ||
| Peer problems | Parent | 3.30 | 84 | 2.264 | 4.129 (83), p < 0.001 |
| Child | 2.40 | 84 | 1.908 | ||
| Pro-social behaviour | Parent | 7.39 | 89 | 1.663 | 1.906 (88), p = 0.060 |
| Child | 7.87 | 89 | 1.707 | ||
| Impact score | Parent | 1.62 | 81 | 2.278 | 2.663 (80), p = 0.009 |
| Child | 0.90 | 81 | 1.772 |
Table 35 shows the correlation between the paired scores. Overall, the correlations were moderate for the total score and for emotional, conduct and peer subscales.
| SDQ subscale | n | Correlation | p-value |
|---|---|---|---|
| Total difficulties | 83 | 0.546 | < 0.001 |
| Emotional symptoms | 89 | 0.473 | < 0.001 |
| Conduct problems | 84 | 0.479 | < 0.001 |
| Hyperactivity/inattention | 83 | 0.231 | 0.036 |
| Peer problems | 84 | 0.560 | < 0.001 |
| Pro-social behaviour | 89 | 0.039 | 0.717 |
| Impact score | 81 | 0.306 | 0.005 |
Table 36 shows the agreement between the deaf parent and child (kappa = 0.214). Overall, of the 42 parents who scored their child as normal, 39 of the children scored normal on the self-report. Where parents scored the child as abnormal (32 children), only seven of these children scored abnormal on the self-report.
| Self report SDQ total difficulties | Deaf parent total difficulties | Total | ||
|---|---|---|---|---|
| Normal | Borderline | Abnormal | ||
| Normal | 39 | 8 | 19 | 66 |
| Borderline | 3 | 1 | 6 | 10 |
| Abnormal | 0 | 0 | 7 | 7 |
| Total | 42 | 9 | 32 | 83 |
Inter-rater agreement of the deaf parent Strengths and Difficulties Questionnaire and child’s teacher Strengths and Difficulties Questionnaire
Table 37 shows the scores for the subscales and total scale where there are paired data with the deaf parent and teacher-completed questionnaire. In all the scales, the parent scored the child higher than the teacher SDQ scores. There were significant differences for all subscales except the pro-social subscale.
| SDQ subscale | Rater | Mean | n | SD | Test statistic (degrees of freedom), p-value |
|---|---|---|---|---|---|
| Total difficulties | Parent | 14.04 | 123 | 6.575 | 8.346 (122), p < 0.001 |
| Teacher | 8.37 | 123 | 7.422 | ||
| Emotional symptoms | Parent | 3.42 | 124 | 2.570 | 6.362 (123), p < 0.001 |
| Teacher | 1.85 | 124 | 2.354 | ||
| Conduct problems | Parent | 3.06 | 124 | 2.116 | 7.607 (123), p < 0.001 |
| Teacher | 1.52 | 124 | 2.162 | ||
| Hyperactivity/inattention | Parent | 4.31 | 124 | 2.176 | 3.849 (123), p < 0.001 |
| Teacher | 3.22 | 124 | 2.839 | ||
| Peer problems | Parent | 3.37 | 123 | 2.299 | 7.436 (122), p < 0.001 |
| Teacher | 1.80 | 123 | 1.990 | ||
| Pro-social behaviour | Parent | 7.49 | 124 | 1.755 | 1.388 (123), p = 0.168 |
| Teacher | 7.16 | 124 | 2.304 | ||
| Impact score | Parent | 1.29 | 120 | 1.880 | 3.297 (119), p = 0.001 |
| Teacher | .69 | 120 | 1.511 |
Table 38 shows the correlation between the paired scores between the deaf parent and teacher. Overall, the correlations were moderate for the total score and for emotional, conduct and peer subscales. They were weak for hyperactivity/inattention and impact.
| SDQ subscale | n | Correlation | Significance |
|---|---|---|---|
| Total difficulties | 123 | 0.426 | < 0.001 |
| Emotional symptoms | 124 | 0.384 | < 0.001 |
| Conduct problems | 124 | 0.450 | < 0.001 |
| Hyperactivity/inattention | 124 | 0.233 | 0.009 |
| Peer problems | 123 | 0.412 | < 0.001 |
| Pro-social behaviour | 124 | 0.167 | 0.063 |
| Impact score | 120 | 0.325 | < 0.001 |
Table 39 shows the agreement between the deaf parent and teacher (kappa = 0.203). Overall, of the 55 children (deaf or hearing) scored by their deaf parents as normal, 47 were scored as normal by the teachers. Of the 39 children scored as abnormal by their deaf parents, only 12 were scored by the teacher as abnormal.
| Teacher total difficulties coded | Deaf parent total difficulties | Total | ||
|---|---|---|---|---|
| Normal | Borderline | Abnormal | ||
| Normal | 47 | 20 | 20 | 87 |
| Borderline | 5 | 5 | 7 | 17 |
| Abnormal | 3 | 4 | 12 | 19 |
| Total | 55 | 29 | 39 | 123 |
Inter-rater agreement for the deaf teacher Strengths and Difficulties Questionnaire
Inter-rater agreement of the deaf teacher Strengths and Difficulties Questionnaire and the child Strengths and Difficulties Questionnaire
Table 40 shows a summary of scores for deaf teacher and child.
| SDQ subscale | Rater | Mean | n | SD | Test statistic (degrees of freedom), p-value |
|---|---|---|---|---|---|
| Total difficulties | Child | 13.59 | 41 | 4.582 | 0.448 (40), p = 0.657 |
| Teacher | 13.10 | 41 | 6.160 | ||
| Emotional symptoms | Child | 3.55 | 44 | 2.416 | 0.267 (43), p = 0.791 |
| Teacher | 3.43 | 44 | 2.500 | ||
| Conduct problems | Child | 2.93 | 41 | 1.506 | 1.768 (40), p = 0.085 |
| Teacher | 2.22 | 41 | 2.092 | ||
| Hyperactivity/inattention | Child | 3.80 | 41 | 1.990 | 1.768 (40), p = 0.172 |
| Teacher | 4.49 | 41 | 2.951 | ||
| Peer problems | Child | 3.71 | 41 | 1.601 | 1.313 (40), p = 0.197 |
| Teacher | 3.22 | 41 | 2.162 | ||
| Pro-social behaviour | Child | 7.23 | 44 | 1.179 | 1.589 (43), p = 0.119 |
| Teacher | 6.68 | 44 | 2.239 | ||
| Impact score | Child | 2.10 | 39 | 2.393 | 2.260 (38), p = 0.030 |
| Teacher | 1.21 | 39 | 1.559 |
Table 41 shows the correlation between deaf teacher and child scores.
| SDQ subscale | n | Correlation | p-value |
|---|---|---|---|
| Total difficulties | 41 | 0.183 | 0.252 |
| Emotional symptoms | 44 | 0.341 | 0.023 |
| Conduct problems | 41 | 0.013 | 0.935 |
| Hyperactivity/inattention | 41 | 0.238 | 0.134 |
| Peer problems | 41 | 0.228 | 0.151 |
| Pro-social behaviour | 44 | 0.231 | 0.132 |
| Impact score | 39 | 0.269 | 0.097 |
Inter-rater agreement of the deaf teacher Strengths and Difficulties Questionnaire and the parent Strengths and Difficulties Questionnaire
Table 42 shows a summary of scores for each pair between deaf teacher and parent. In each case, the deaf teacher scored lower than the parent.
| SDQ subscale | Rater | Mean | n | SD | Test statistic (degrees of freedom), p-value |
|---|---|---|---|---|---|
| Total difficulties | Parent | 15.69 | 64 | 6.414 | 4.151 (59), p < 0.001 |
| Teacher | 12.45 | 64 | 6.218 | ||
| Emotional symptoms | Parent | 3.02 | 64 | 2.554 | 0.054 (63), p = 0.957 |
| Teacher | 3.00 | 64 | 2.175 | ||
| Conduct problems | Parent | 3.61 | 64 | 2.113 | 4.016 (63), p < 0.001 |
| Teacher | 2.53 | 64 | 2.309 | ||
| Hyperactivity/inattention | Parent | 5.72 | 64 | 2.340 | 4.129 (63), p < 0.001 |
| Teacher | 4.17 | 64 | 2.440 | ||
| Peer problems | Parent | 3.34 | 64 | 2.227 | 1.915 (63), p = 0.060 |
| Teacher | 2.75 | 64 | 1.808 | ||
| Pro-social behaviour | Parent | 7.16 | 64 | 1.962 | 1.510 (63), p = 0.136 |
| Teacher | 6.66 | 64 | 2.379 | ||
| Impact score | Parent | 1.93 | 60 | 1.912 | 3.351 (59), p = 0.001 |
| Teacher | 1.03 | 60 | 1.626 |
Table 43 shows the correlation between the deaf teacher and parent scores.
| SDQ subscale | n | Correlation | p-value |
|---|---|---|---|
| Total difficulties | 64 | 0.513 | 0.000 |
| Emotional symptoms | 64 | 0.531 | < 0.001 |
| Conduct problems | 64 | 0.531 | < 0.001 |
| Hyperactivity/inattention | 64 | 0.214 | 0.089 |
| Peer problems | 64 | 0.258 | 0.039 |
| Pro-social behaviour | 64 | 0.267 | 0.033 |
| Impact score | 60 | 0.317 | 0.014 |
Multi-informant Strengths and Difficulties Questionnaire algorithm
Table 44 shows the overall prediction of child psychiatric diagnoses from the symptom and impact scores derived from the existing SDQ multi-informant algorithm (see Appendix 1).
The following table shows the findings for the 144 deaf children. Overall, 37% were rated as having a probable psychiatric disorder. This was much lower in the community (26%) than in the NDCAMHS group (81%).
| Category of disorder | Rating | Total, n (%) | Community, n (%) | NDCAMHS (clinical case), n (%) |
|---|---|---|---|---|
| Prediction of a hyperactivity/inattention disorder | Unlikely | 105 (73) | 92 (79) | 13 (48) |
| Possible | 31 (22) | 20 (17) | 11 (41) | |
| Probable | 8 (6) | 4 (3) | 3 (11) | |
| Prediction of a conduct disorder | Unlikely | 73 (51) | 67 (58) | 5 (19) |
| Possible | 31 (22) | 29 (25) | 2 (7) | |
| Probable | 40 (28) | 20 (17) | 20 (74) | |
| Prediction of an emotional disorder | Unlikely | 98 (68) | 89 (77) | 9 (33) |
| Possible | 24 (17) | 15 (13) | 8 (30) | |
| Probable | 22 (15) | 12 (10) | 10 (37) | |
| Prediction of any psychiatric disorder | Unlikely | 51 (35) | 50 (43) | 1 (4) |
| Possible | 40 (28) | 36 (31) | 4 (15) | |
| Probable | 53 (37) | 30 (26) | 22 (81) |
Sensitivity and specificity of British Sign Language Strengths and Difficulties Questionnaire versus clinical assessment
The probable/possible diagnosis of a psychiatric disorder derived from the SDQ was compared with the eight questions relating to having a disorder from the clinical interview or clinical note review (using either borderline/probable or no clinical diagnosis). For the eight questions, where a borderline or yes was recorded for any of the questions, the patient was coded as having a clinical diagnosis of a psychiatric disorder. Table 45 shows the data. The sensitivity of the SDQ was 81% (71–90%) and the specificity was 42% (29–52%).
| Prediction of any psychiatric disorder (SDQ) | Clinical diagnosis | ||
|---|---|---|---|
| No | Borderline/yes | Total | |
| Unlikely | 15 | 8 | 23 |
| Possible/probable | 21 | 35 | 56 |
| Total | 36 | 43 | 79 |
Where the multi-informant SDQ coded unlikely/possible or probable as a threshold against a probably clinical diagnosis for caseness, then the sensitivity of the SDQ was 76% (58–89%) and the specificity was 73% (64–78%) (see Table 46).
| Prediction of any psychiatric disorder (SDQ) | Clinical diagnosis | ||
|---|---|---|---|
| No/borderline | Yes | Total | |
| Unlikely/possible | 39 | 6 | 45 |
| Probable | 15 | 19 | 34 |
| Total | 54 | 25 | 79 |
Rasch model
Confirmatory factor analysis
Data from 650 baseline assessments based upon 306 children were included in the analysis. Looking separately at the SDQ as completed by parents, teachers and children, and allowing for local dependency within domains (correlated errors), the data failed to satisfy the strictest interpretation of a CFA on all occasions, either as a five-factor structure, or as a second-order factor structure after omitting the pro-social scale (Table 47, analyses 1–12).
| Analysis | Description | Group | Chi-square | Degrees of freedom | p-value | CFI | TLI | RMSEA |
|---|---|---|---|---|---|---|---|---|
| 1 | SDQ-5 factor | Parents | 642.1 | 265 | < 0.001 | 0.832 | 0.810 | 0.071 |
| 2 | SDQ-5 factor | Teachers | 475.5 | 265 | < 0.001 | 0.939 | 0.930 | 0.062 |
| 3 | SDQ-5 factor | Child | 539.9 | 265 | < 0.001 | 0.718 | 0.680 | 0.071 |
| 4 | SDQ-20 first- to second-order factor | Parents | 445.9 | 166 | < 0.001 | 0.856 | 0.835 | 0.077 |
| 5 | SDQ-20 first- to second-order factor | Teachers | 347.7 | 166 | < 0.001 | 0.932 | 0.922 | 0.072 |
| 6 | SDQ-20 first- to second-order factor | Child | 337.6 | 166 | < 0.001 | 0.814 | 0.788 | 0.071 |
| 7 | SDQ-5 factora | Parents | 593.8 | 261 | < 0.001 | 0.852 | 0.830 | 0.067 |
| 8 | SDQ-5 factora | Teachers | 433.1 | 263 | < 0.001 | 0.950 | 0.943 | 0.055 |
| 9 | SDQ-5 factora | Child | 530.5 | 264 | < 0.001 | 0.726 | 0.689 | 0.071 |
| 10 | SDQ-20 first- to second-order factora | Parents | 371.9 | 161 | < 0.001 | 0.892 | 0.872 | 0.068 |
| 11 | SDQ-20 first- to second-order factora | Teachers | 324.0 | 165 | < 0.001 | 0.940 | 0.931 | 0.068 |
| 12 | SDQ-20 first- to second-order factora | Child | 320.6 | 165 | < 0.001 | 0.832 | 0.836 | 0.068 |
| Ideal values | > 0.05 | > 0.95 | > 0.95 | < 0.06 |
Exploratory factor analysis
An EFA found that, while a five-factor solution satisfied an RMSEA value of < 0.06, the pattern of factors varied between parents, teachers and children, and that only the pro-social and emotional domains, as originally specified, emerged as valid domains for parents and teachers, and for parents and children, respectively. The peer domain failed to emerge in its original format within any group.
Relaxing the criteria of RMSEA to < 0.1 in the EFA, in order to identify a potential set of unidimensional items that can be considered by the Rasch analysis, found a two-factor solution which showed the pro-social set of items loading on one factor, and all other items on the second factor (RMSEA 0.092). This gives some credence to the possibility of a total score from the remaining four domains.
The data were then fitted to the Rasch measurement model. Initially (Table 48, analysis 1) the data for the total SDQ (20 items) showed considerable misfit to model expectations. Furthermore, there was a breach of the unidimensionality and local independence assumptions. Upon examination (of the residual correlations) it was evident that locally dependent items clustered within the four domains. Consequently, the data were resolved as four testlets, and then showed good unidimensionality but still some misfit to the model expectations (see Table 48, analysis 2). The value A is a proportion of the common (non-error) variance. The bifactor solution showed that 89% of the non-error variance was common when summating the four domains into a total score; thus, 11% of the variance had to be discarded to obtain the unidimensional latent estimate.
| No. | Description | Group | Chi-square | Degrees of freedom | p | Residual item | Residual person | Person Separation Index reliability | % tests > 5% | 95% CI | A | n | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||||||||||
| 1 | SDQ-20 | All | 701.84 | 180 | < 0.001 | 0.304 | 2.36 | −0.155 | 1.18 | 0.80 | 14.3 | 12.8 to 15.8 | – | 912 |
| 2 | SDQ-20–4 domain | All | 80.07 | 36 | < 0.001 | 0.228 | 1.75 | −0.358 | 1.01 | 0.72 | 3.1 | 1.7 to 4.5 | 0.89 | 912 |
| 3 | SDQ20–4 domain split | All | 92.73 | 72 | 0.051 | −0.102 | 1.22 | −0.404 | 1.00 | 0.71 | –b | – | – | – |
| 4 | SDQ20–4 domain | Baseline | 55.22 | 36 | 0.021 | −0.101 | 1.80 | −0.402 | 1.05 | 0.70 | 3.3 | 1.6 to 5.0 | 0.87 | 668 |
| 5 | SDQ20–4 domain | Parent baseline | 36.24 | 36 | 0.457 | −0.111 | 1.32 | −0.394 | 1.04 | 0.68 | 3.4 | 0.8 to 6.0 | – | 280 |
| 6 | SDQ20–4 domain | Teacher baseline | 14.87 | 12 | 0.248 | −0.239 | 0.42 | −0.398 | 1.20 | 0.58 | 2.7 | 0.5 to 5.8 | – | 193 |
| 7 | SDQ20–4 domain | Child baseline | 19.98 | 12 | 0.067 | 0.294 | 1.05 | −0.319 | 0.99 | 0.66 | 3.7 | 0.5 to 6.6 | – | 195 |
| 8 | Pro-social | Child | 17.32 | 10 | 0.068 | 0.160 | 1.03 | −0.311 | 1.47 | 0.23 | – | – | – | 165 |
| Ideal values | > 0.05 a | < 1.4 | < 1.4 | > 0.70 | < 5.0 | LCI < 5.0 | ||||||||
The potential source of misfit was investigated further. Given the way in which response options are interpreted within this BSL framework, for example by judging facial expression, which may represent a continuous expression of emotional intensity, the consistency of the scoring of each item may have potential to create disordering of response thresholds, where the increase in the score of any particular item may not be reflected by an increase in the underlying trait of difficulties. This inconsistency is known as threshold disordering and may contribute to misfit. This was not the case for the SDQ, where, out of the 20 items which form the total score, only two items failed to make the transition from one category to the next in a way which reflected the increase in the underlying trait of difficulty, and this disordering was only marginal and not statistically significant. This confirms that the interpretation of magnitude of any particular item is working as expected, where an increase in score on the item reflects an increase in the underlying trait of difficulties.
Differential item functioning was observed for several domains. For example, there was significant DIF by gender on the emotional domain (Figure 4). Thus, at any level of difficulties, females were more likely to score higher on the emotion domain than were males. Likewise, teachers were likely to rate children lower than others on the conduct domain. There was also significant DIF by time on the peer domain. All the sources of DIF were subsequently accounted for by splitting domains such that, for example, two emotional domains were created, one for each gender. This resolved misfit to the model (see Table 48, analysis 3). A comparison of those who completed the SDQ with and without BSL (parent, teacher and self-report) showed that DIF by BSL was largely absent. Only for the self-completed SDQ for the peer domain did a difference occur. Those using BSL reported a higher score on this domain.
FIGURE 4.
Differential item functioning for emotional symptoms by gender.
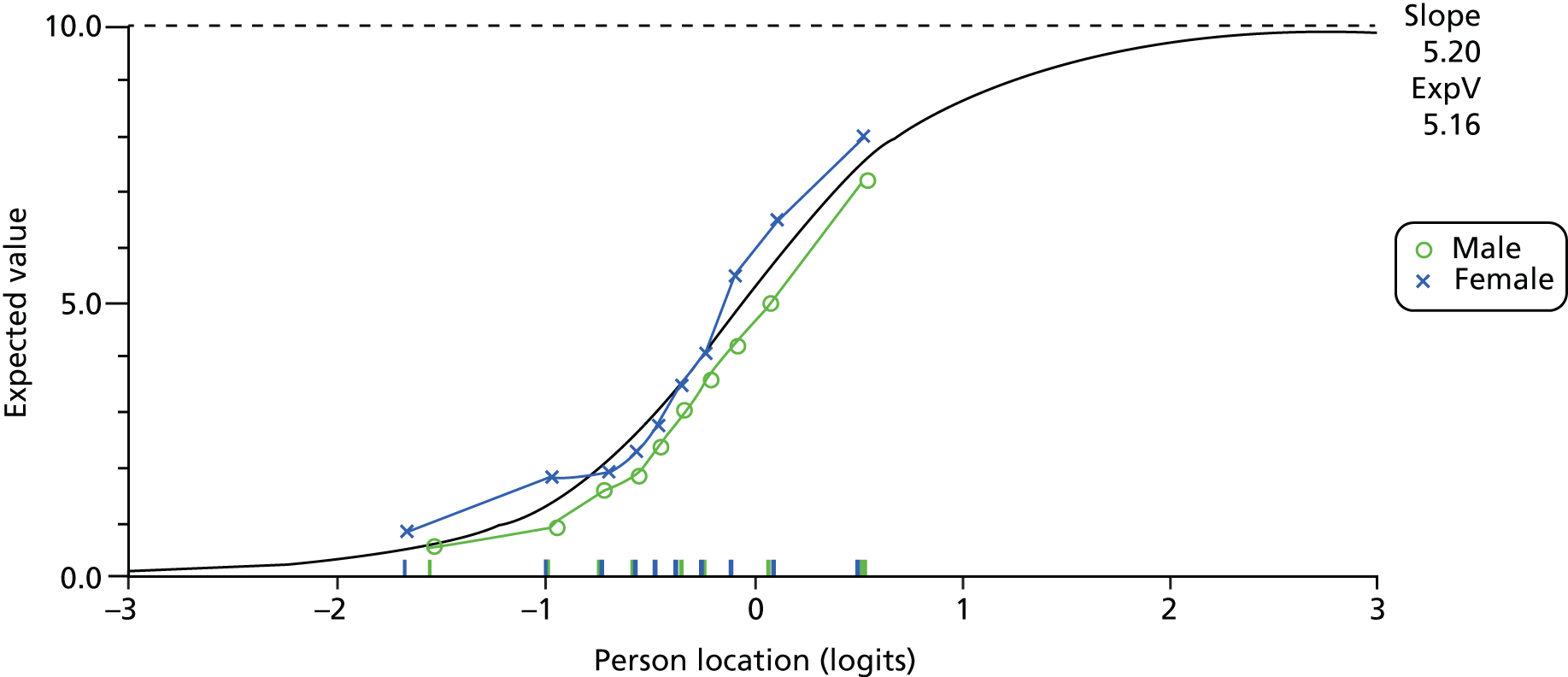
Figure 5 shows the person–item distribution for the total sample. The total sample was then disaggregated into various groups to obtain a more in-depth understanding of how the scale worked, and where some of the problems may be found. All such analyses were undertaken with the testlet (four domains) approach. The baseline data, and each of the responder groups at baseline, showed good fit to model expectations (see Table 48, analyses 4–7). However, in each case, reliability was below that acceptable for group use. DIF was found by gender (of child) for both parental and self-report and there was some DIF by location for parental report.
FIGURE 5.
Person–item distribution of total sample (n = 971).
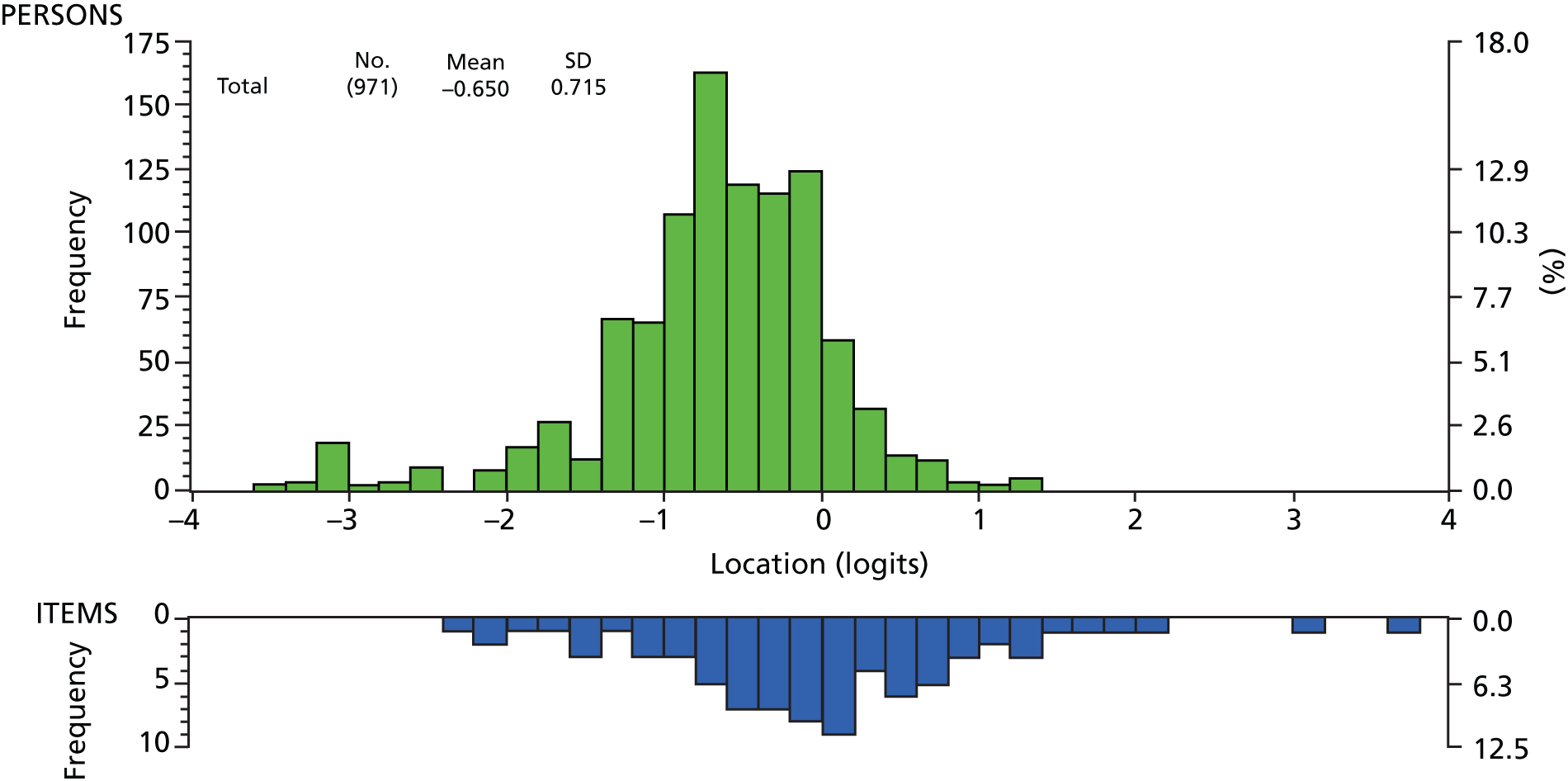
For completeness, the items within the pro-social subscale were examined. Only the self-report satisfied Rasch model expectations but the reliability was extremely low, and thus the scale was of little use.
Discussion of validation
Recruitment was good, with 144 deaf young people who were deaf BSL users, 191 deaf parents who were BSL users and 77 deaf teachers and teaching assistants who were BSL users. An additional 55 hearing young people aged 11–16 years, 74 hearing parents and 127 hearing teachers were recruited as part of the validation process. Recruitment proved to be difficult in the early stages of the study for various reasons, including that many people did not respond to packs they had been sent, that some professionals were too busy or found it difficult to pass on packs to potential participants and that some participants found there to be too much information (required by research governance regulations) to digest or to see ‘the wood from the trees’ (as one participant put it). We found that mainstream schools were less likely to want to be involved: of those approached, 28% of secondary schools with hearing-impaired units and 16% of primary schools with hearing-impaired units became involved, in contrast to deaf-specific schools (91% becoming involved). We also found that several deaf participants had concerns about confidentiality and some parents were also concerned that screening their child for ‘mental health’ problems might have negative consequences by labelling them. After workshop discussions and PPI advice we adapted our recruitment strategy to include more face-to-face meetings, improved information leaflets and more focus on providing reassurance about issues important to potential participants, such as confidentiality. We considered and implemented a range of other ways of improving accessibility, for example by arranging for Deaf and hearing research assistants to make trips to schools to give presentations and meet teachers and parents for information meetings. This greatly improved our ability to recruit participants into the study.
Of the young people who were recruited, 91% described themselves as having severe to profound deafness (80% profound). This is not surprising given that these groups are more likely to learn BSL. Of the 11- to 16-year-old young people, 15% had no form of hearing aids or cochlear implants. This is a choice that some deaf young people make. A total of 75% had some BSL in their families (38% of this was fluent), so many young people are using BSL despite the fact that it is not regularly used at home. Many of these young people were in schools where they had strong peer relationships with other deaf young people who were BSL users. Approximately one-third of young people used cochlear implants. We had a multiethnic group, because of our intention not to exclude families from ethnic minority backgrounds. Some 66% of deaf young people described no learning disabilities or learning difficulties, so this was a mixed sample of recruits.
Using the existing SDQ coding frame, 18% of young people scored themselves as having an ‘abnormal’ score (39% abnormal or borderline); 28% of parents scored their child as abnormal (46% abnormal or borderline); and 31% of teachers scored children and young people as abnormal (54% abnormal or borderline).
The study found that the self-report BSL SDQ shows statistically significant differences between the clinical and community samples for total score, emotional subscale, hyperactivity/inattention subscale and conduct subscale, but not for the peer problems and pro-social behaviour subscales. This means that the translated questionnaire can discriminate between the community and the clinical sample for all but the peer problems subscale (the pro-social subscale being a ‘strength’ subscale). After adjusting for gender, there is still a significant difference (p = 0.015). The areas where the questionnaire does not discriminate may be related to the Deaf experience. Deaf young people have peer relationship issues not because of mental disorder, but due to language and communication barriers with peers. Also, social and emotional developmental delay is common in deaf children and some deaf children have higher rates of selective peer groups, and this could impact on the peer problems and pro-social scores.
The self-report BSL SDQ was shown to be valid against the gold standard clinical interview, and therefore would be able to be used as a screening tool to identify clinical cases, particularly when considering the total difficulties score.
There was a statistically significant difference between genders on the total score and emotional subscale across the whole group and when we analysed by community and clinical groups. This is likely to reflect the increased prevalence of emotional difficulties in girls of this age group, which will be reflected in the total score.
Factor analysis
The original authors report a five-factor structure113 and some other studies use CFA to support this. 187 In a sample of 1686 parent-rated translated SDQs in Germany188 from a mixed community and clinical sample, principal components analysis extracts five factors accounting for 53.9% of the variance. Our study had similar findings, with a five-factor model accounting for 55% of the variance for the teacher version, 50% for the parent version and 48% for the self-report version. Some studies have suggested some modifications189 to the five-factor structure. 190 A Hebrew version finds five factors but in both the parent and the self-report version the peer problems factor disappears, with the five items going into four different factors on each and the hyperactivity and inattention factor splitting into two. 191 Five factors are also found in the Russian version but with low enough factor loadings for the authors to suggest that inadequate psychometric characteristics make it ‘unsatisfactory’ for use in Russian adolescents. 192 This is a problem not only for translated versions. A large US cohort found a three-factor structure was a better fit for the self-report version of the English SDQ,192 and that factor loadings and subscale reliabilities were low for the five-subscale version. A group considering the US self-report SDQ suggested a three-factor solution based on pro-social behaviours, internalising problems and externalising problems,193 and some similarities to this model were found in a large Finnish study of 1458 13- to 17-year-olds where, for boys, symptoms of conduct problems, emotional problems and hyperactivity/inattention are ‘fused’ on factor analysis. 194 An Italian study with 1394 children aged 8–10 years also found that this three-factor model fitted best. 195 As an example, this three-factor model yields Cronbach’s alpha coefficients for internal consistency of 0.67 (0.63–0.69) for pro-social behaviours, 0.63 (0.60–0.66) for externalisation problems and 0.54 (0.49–0.57) for internalisation problems for the overall sample. Goodman and colleagues196 reporting on an epidemiological study of 5- to 16-year-old children in the UK suggested that a three-factor model may be useful in low-risk samples. A study comparing the self-report version in five European countries (Italy, Sweden, Cyprus, Germany and the UK) found that a three-factor model (with internalising, externalising and pro-social subscales) fitted better in Cyprus, with five factors fitting better in Germany, but fit indices for both models were ‘poor’ for the UK, Sweden and Italy. 197 They suggested that removing the inversely expressed items improved the goodness of fit. The internal consistency and validity of the SDQ total difficulties score were good for most countries, and this accords with our findings.
Our factor analysis suggests that a good use of the BSL SDQ is as a screening tool to identify young people with mental health problems with sensitivity and specificity both above 70% when using the upper threshold on the multi-informant algorithm. Looking at concurrent validity, the BSL SDQ versions were able to identify attachment and conduct disorders in all three versions, ADHD in parent and teacher versions and anxiety disorders in child and parent versions.
In summary, the psychometrics for the BSL version of the SDQ are not dissimilar to other translated versions.
There are several reasons why differences in factor structure from the original version may exist. It has been proposed that the reverse items in the SDQ may be confusing for some and that the psychometrics improve when they are removed. 197 We should always consider the possibility that a translation from the written form of an oral/written language to a visual language carries with it complexities that make accurate translation of meaning more difficult, as we have discussed at length in Chapter 2, Stage 1. However, our findings are not very different from other written to written translation studies reported and the variance of factor solutions are very similar (as described in Factor analysis above).
Deaf cultural norms are significantly different from spoken English. 148 This means that there may be different expectations from deaf adults regarding the behaviour of children and young people, with respect to what is ‘normal’. Examples of this were seen within the clinical validation interviews, where parents reported on emotional symptoms that levels of social confidence/worries depended very much on the environment, and they found the question difficult to answer. They reported that the child could present very differently in a Deaf environment from a hearing one. The same might be true for some of the conduct subscale items. It is our clinical experience that a lot of behavioural presentations are in fact due to underlying communication difficulties for a deaf child in a hearing environment, rather than a primary behaviour disorder.
Other studies show strong associations between different factors, for example between parent-rated conduct and hyperactivity/inattention191,198 and between conduct and emotional scores191 in Hebrew-speaking children. Another example of this was a study in Norway that found that, across ethnic groups, the correlation coefficients between the hyperactivity/inattention factor and the conduct problems factor were high (range 0.76–0.92), suggesting that they did not reliably represent distinct constructs in adolescents. 199 In our findings, the fact that emotion and conduct items load together in both the self-report and parent BSL SDQs suggests a complex relationship between emotional problems/anxiety and behaviours associated with frustration such as temper tantrums. The finding that theory of mind is delayed in many deaf children82 may be related, as empathy delays can be associated with emotional, social and behavioural problems. Put another way, empathy problems may lead to internalising problems in some children and externalising problems in others. This could be explored in further research.
Rasch factor analysis
Using the Rasch analysis, the CFA failed to support the five-factor structure of the SDQ, as well as the four-domain-based total score. An initial EFA failed to derive any meaningful structure that was consistent across the parent–teacher–child response structures. Various reports on the SDQ based upon this approach have been published with different degrees of support for the original structure, sometimes arguing for a three- or two-domain structure. 192,194,197,200,201 Furthermore, there are suggestions that the scale lacks cultural invariance, working differently in different countries, even where the language is the same. 193 The finding in the current study that the structure varies by parent–teacher–child completion has also been reported elsewhere. 189 The various issues arising from analysis of the scale have led some to argue that the SDQ total score should be used in preference to the various subscale scores. 199 Consequently, the findings in the current study are not atypical and may not be a function of the novel approach of delivering the scale through BSL.
Some of the reasons for that lack of stability may have emerged in the Rasch analysis. Other than substantive breaches of the local independence assumption, dealt with by creating testlets, item bias emerged in the DIF tests. Thus, the emotional domain needed to be split for gender, and also there were some differences in the way in which teachers assessed their pupils, and also between the baseline and follow-up study in the test–retest component. All these biases can be accommodated within the Rasch measurement framework through the item split technique, and thus unbiased latent estimates can be obtained which provide valid ways to compare, for example, gender or test–retest. Nevertheless, outside this framework these biases may contribute to the lack of stability of the scale. Furthermore, the use of small subscales with cut-points where gender bias is present may lead to misinference about diagnostic allocation, where, for example, girls are more likely to achieve an above cut-point score on the emotional domain than boys, at the same level of overall difficulties. The absence of DIF for completion by BSL confirms the success of the adaptation procedure and the comparability of the BSL version with the original. Only the self-completed version for the peer domain showed a significant (higher) difference in response at any level of the trait.
Another concern is the level of reliability reported in this study, and in others. 113,202 Where clinical cut-points are used, which can be viewed as high stakes, reliability should be in excess of 0.9. 203 These levels are never achieved for this scale, and some reports have subscales well below that required even for group comparisons.
Given fit to the Rasch model, then, the raw score of the SDQ-20 (total score) is a sufficient statistic to estimate magnitude of difficulties. It is valid for each group (parents, teachers and self-completion) independently and when pooled together after adjustment for item bias (e.g. the conduct domain by teacher). Consequently, the differences in estimates of difficulties between the different assessors can be evaluated without the risk of bias caused by the DIF (in this case domain functioning). Thus, all assessments can be placed on the same unbiased metric.
The low reliability may be a function of the sample having similar levels of difficulties. Figure 2 shows that the majority of assessments allocate subjects into a range of just one logit (between –1 and 0 logits). This typically reduces reliability, as the scale cannot separate out this large group over this narrow range. This is commonly seen in other samples (e.g. undergraduate examinations) where all the respondents are clustered together over a very narrow range of marks. Thus, it is possible that the reliability may be depressed because of this concentration of location.
As BSL is accessible only through someone’s production, as it has no written form, prosodic features such as speed and intensity of articulation and facial expression are necessarily present. In written language, such features are not present (except as, for example, punctuation marks or writing style), and so a written questionnaire can present as more neutral, as it has no inherent ‘tone of voice’. Using the Rasch analysis we were able to explore if there was any disordering of response thresholds, where the increase in the score of any particular item may not be reflected by the increase in the underlying trait of difficulties. This inconsistency is known as threshold disordering. This was not the case for the SDQ, where, out of the 20 items which form the total score, only two items failed to make the transition from one category to the next in a way which reflected the increase in the underlying trait of difficulty, and this was not significant. This suggests that respondents were able to see questions as distinct and an increase in score on the item reflected an increase in the underlying trait of difficulties.
Subscales and internal consistency
Several studies report specific subscales being below acceptable limits in the specific psychometrics (Cronbach’s alpha coefficients). 202,204 It is common in studies from different countries for items to load on to different subscales from the ones intended from the original. For example, in the Spanish teacher version205 two of the hyperactivity/inattention items load better onto the conduct subscale and two of the items for the peer problems scale load better onto the conduct problems subscale. Similar problems are found with the parents subscale. In the Italian version195 Cronbach’s alpha coefficients (internal consistency/reliability) improve when certain poorly performing items are removed. Such studies discuss possible problems with translation, subtle meaning or cultural interpretation of behaviour. Five items show factor loadings less than 0.35 and three of these items are from the peer subscale. Other studies from other languages and cultures find similar problems with loading of items. 188,206,207
The original reports of the English SDQ described Cronbach’s alpha scores of 0.73 for the total difficulty scale. 113 This study had total difficulty Cronbach’s alphas of 0.735 for the self-report version, 0.842 for the parent version and 0.738 for the teacher version, which are not dissimilar. The mean and range from a review of 26 studies208 in various languages for parents showed 0.67 (0.54–0.84) for pro-social behaviour, 0.76 (0.58–0.85) for hyperactivity/inattention, 0.66 (0.46–0.76) for emotional problems, 0.58 (0.46–0.76) for conduct problems, 0.53 (0.30–0.76) for peer problems and 0.80 (0.69–0.87) for total difficulties. For teachers, weighted mean internal consistency and ranges are 0.82 (0.79–0.86) for pro-social behaviours, 0.83 (0.66–0.89) for hyperactivity/inattention, 0.73 (0.63–0.80) for emotional problems, 0.70 (0.63–0.84) for conduct problems, 0.63 (0.35–0.77) for peer problems and 0.82 (0.62–0.85) for total difficulties. In a more recent study of five European countries,197 self-report Cronbach’s alphas for some subscales for conduct disorders were 0.45 for German 12- to 17-year-olds but 0.12 in Cyprus and 0.02 in Sweden. Similarly the peer problems subscale showed coefficients of 0.54 in Germany and 0.5 in Italy, but 0.15 in Cyprus. In the Spanish version for teachers, the subscale Cronbach’s alphas range from 0.64 to 0.85 and in the parent version from 0.58 to 0.77. 205 In other translated versions, the internal consistency Cronbach’s alpha coefficient is very low,206 ranging between 0.30 and 0.83. For subscales, only parent and teacher hyperactivity/inattention and teacher pro-social subscales had Cronbach’s alpha greater than 0.7 in this study. Again, this is not dissimilar from other studies. In the Israeli version only the total difficulties scale and the hyperactivity/inattention subscale for parent and adolescent had Cronbach’s alpha scores of 0.7 or above. 191 The Russian self-report version finds Cronbach’s alpha of 0.7 or above in only the emotional subscale. 192 The remaining subscales have scores ranging from 0.44 to 0.60. The Swedish version finds scores between 0.51 and 0.76, with the latter the highest score for the total score. 209 Other studies also show low reliability. 194,198,210 One study suggests that one of the problems is that none of the subscales are truly unidimensional. 190 Di Riso and colleagues195 suggest that instruments should be striving for very high Cronbach’s alphas of 0.90 or above. Few studies achieve this and our Cronbach’s alpha scores are broadly in the ranges of other translation studies.
Cultural differences in SDQ research
In the current study the mean female self-report scores were higher for all subscales and the total score than those for UK children. 162 For example, the UK mean total score for 11- to 16-year-olds is 10 and our study found 15.5 in the community sample. The male scores were similar between Deaf and UK mean scores, except that both males and females had higher peer problem scores than the UK young people. It is not uncommon to find differences between cultures such as studies reporting differences between UK children and Arab,211 Norwegian212 or Russian192 children. The Norwegian study suggested under-reporting of SDQ emotional symptoms by Norwegian adults (compared with British adults) in those children with emotional disorders. Parents of deaf children appear to report higher rates of problems than their teacher or self-report equivalents.
Compared with British hearing children,1 Dutch,204 Norwegian212 and Hebrew children191 have lower mean scores on emotional subscales, while the Russian teacher version reports higher means for emotional problems than the UK sample. 213 Deaf girls in particular seem to have higher rates of emotional problems in both our community and clinical samples. Any cultural differences could be related to differences in actual morbidity, attributions, levels of tolerance, expectation/fear of being judged in differing societies or other factors. This has yet to be more comprehensively researched.
One study that explored an ethnic minority (Pakistani) in its country (Norway) found that, while questionnaire items showed loadings above 0.4 on all the subscales, six items were below 0.30 in the Pakistani group199 when using the same Norwegian version. There was no apparent difference between first- and second-generation ethnic minority responses, suggesting the language was not solely responsible for problems with the subscales. This is a clue that cultural factors are relevant.
Some authors suggest real cultural differences in behaviours, or language differences or response style differences. 199 There may also be some kind of measurement artefact214 related, for example, to social desirability and openness about symptoms or questions. Translation issues discussed in Chapter 2 have also been highlighted by others, including the non-equivalence of translated items. 214
Other authors have made reference to subtle differences in meaning or severity when words or phrases are translated in different languages in different cultures. 191,214 Response styles may also vary across cultures. 197
Gender
In this study we found that girls in both community and clinical samples scored higher on the total difficulties scale when scored by teachers or parents. This is similar to Finnish,194 Hebrew191 and Dutch202 studies showing higher informant total scores for girls, although the French214 and Chinese206 translations had higher scores for boys. The Italian study of 8- to 10-year-olds shows girls and boys roughly equivalent for total difficulties but girls higher for emotional problems and on the pro-social subscale195 and this study also found that girls had higher scores on the emotional problems and pro-social subscales. Most studies score boys higher for hyperactivity/inattention and girls higher for pro-social behaviour, but our sample showed no statistically significant difference between genders. As discussed above, these findings suggest that deaf girls struggle more than boys with emotional problems in both the community and clinical samples.
Test–retest reliability
In this study the test–retest reliability ICC is 0.830 for the total difficulties scores, and for the subscale scores ranges between 0.664 and 0.831. Interestingly the best ICC, of 0.831, is for the pro-social subscale. This may reflect the fact that deaf teaching staff know their students better and can observe pro-social activity on a regular basis. Broadly speaking, test–retest results are equivalent to those in the original and other versions of the SDQ.
The original study reporting the UK version of the SDQ reported test–retest reliability of 0.62. 113 The lowest mean from six studies of informants for 4- to 10-year-old children208 is 0.65 for parent-rated pro-social behaviour, with means of 0.66 for the emotional, conduct and peer problems scales. Teacher test–retest correlations are better, with the means for different subscales between 0.72–0.85. Some studies have shown low test–retest reliability, with for example a range of 0.40–0.79 in the Chinese study. 206 It found ICCs between 0.45 and 0.71 for the self-report version, between 0.60 and 0.77 for the parent version and between 0.65 and 0.88 for the teacher version. This accords with other studies in that teacher versions have better test–retest reliability than other versions and that the self-report pro-social subscale has the lowest retest scores of the self-report subscales.
Inter-rater reliability (cross-informant correlations)
In general, Goodman113 reports good cross-informant correlations compared with other instruments. However, this study found that subscale agreement between parents and teachers ranged from 0.214 to 0.531, with 0.513 for the total score and 0.317 for the impact score. The weighted mean correlations between subscales for parent and teacher versions in a review of eight studies of 4- to 12-year-olds ranged from 0.26 to 0.47. 208 Other studies looking at inter-rater reliability correlations also found similar ranges, such as 0.23–0.49 reported for subscales of the Chinese version of the SDQ. 206
This study found similar paired sample correlations between 0.175 (hyperactivity subscale) and 0.264 (emotional subscale) for the deaf child and parent comparisons and between 0.150 (pro-social behaviour) and 0.294 (emotional subscale) for the deaf child and teacher comparisons. Deaf parent comparisons with self-report versions range from 0.039 (pro-social subscale) to 0.560 (peer subscale) and with teacher versions range from 0.167 (pro-social subscale) and 0.450 (conduct subscale). Our study found 0.039–0.560 for deaf parent subscale comparisons with self-report and 0.130–0.341 for deaf teacher comparisons with self-report. All of these are very similar, suggesting that our inter-rater agreement statistics are very similar to those of a range of other cross-cultural translations of the SDQ. The pro-social subscale had poor inter-rater reliability. This is not dissimilar to other studies but could also point to a lack of awareness of parents and teachers about the experiences of deaf young people.
For the SDQ self-report version, the only subscale that showed significant difference from the parent SDQ was the hyperactivity subscale. Where parents scored significantly higher, this may be because of differences in awareness, attitudes, expectations or fund of knowledge issues, or it may be because there are cultural differences in behaviour. Young people may regard their behaviour as less problematic or more acceptable and not have wider groups of peers to compare against. This hypothesis may be strengthened by the finding that, for the deaf parent SDQ, there were significant differences from the young person self-report SDQ on emotional, conduct and peer subscales, with parents scoring higher on those subscales. They also scored higher than the teachers in all subscales other than pro-social scale.
The parents consistently scored higher than the teachers.
This raises some interesting questions about how deaf parents perceive their children (both deaf and hearing offspring), and also how deaf young people are perceived. It may be a cultural phenomenon, or linked to fund of knowledge deficits, or related to relative social isolation, or changes in expectations, awareness or attitudes. We are unable to be certain, but this is an interesting area for future research.
Validity and discriminative power in identifying a clinical sample
There were significant differences between the clinical and community samples for total score and for the emotional and conduct subscales.
The standard multi-informant SDQ algorithm for generating a final score for caseness found that 81% of the clinical samples were identified and 26% of the community samples were identified. When using this algorithm against the gold standard clinical assessment we found good sensitivity (81%) and low specificity (42%) when using ‘probable’ or ‘possible’ caseness as a threshold, and good sensitivity (76%) and good specificity (73%) when using only ‘probable’ caseness as a threshold. Both of these have better sensitivities than the original UK studies but lower specificities. This means higher numbers of false positives if this tool is used as a screening instrument.
As discussed through the report, our hypothesis about this would be relating it to the clinical deaf population. It is our clinical experience, for example, that deaf young people referred for a behaviour problem often have underlying emotional, developmental or communication disorders.
The SDQ has been translated into over 60 languages. There are therefore numerous papers describing validation. Some examples include research from Germany,188 Israel,191 Russia192 and the Islamic Republic of Iran. 215 Many of these do not use gold standards to validate the child versions but may use other questionnaire-based instruments such as the Child Behaviour Checklist. 188 Some studies explore cross-informant agreement between different versions of the SDQ, for example comparing the child version with parent or teacher versions. 188,215 Some use semistructured clinical interviews such as the Development and Well-Being Assessment (DAWBA) inventory,191 while some, like our study, have used clinical interviews. 215
We chose to use clinical assessment to make it ecologically valid but also because there are no other gold standards available for validation in deaf children, meaning we had limited options.
Chapter 4 General discussion
This complex and important research project has shown that we have established the levels of validity of all versions of the BSL SDQ. This is broadly equivalent to other translated versions. We therefore now have a BSL questionnaire which can be used for mental health screening and also establishing outcomes within specialist CAMHS.
The original authors of the SDQ describe sensitivity of 94.6% and specificity of 63.3%. 113 However, the original study uses the DAWBA, which is derived from and dependent on the SDQ. Other studies have since explored this further. In the other studies, only moderate correlations are found for the parent (r = 0.38) and teacher (r = 0.46) versions of the SDQ and the clinician-rated Health of the Nation Outcome Scales216 for Children and Adolescents. 217 Correlations of 0.43 for ADHD, 0.30 for conduct disorder and 0.26 for emotional disorders are found between independent clinician diagnoses and diagnoses generated by SDQ algorithm. 218 The original authors also point out that identification for eating disorders and certain types of anxiety disorder (specific phobia, agoraphobia, panic disorder and separation anxiety) has a sensitivity below 50%. 114 Using a ROC analysis,219 the German version of the SDQ found that the resulting area under the curve value of 0.829 on the total difficulties score shows good discrimination between clinical and community samples. 188
Our study, as with other cultural groups as disparate as Arab,211 UK196 and Norwegian,199 found the strongest findings in relation to total difficulties score. As with other studies,191,220,221 this study has found that the SDQ shows higher mean scores in children and young people in a clinical sample with psychiatric disorders than a community sample.
Limitations and study challenges
General limitations of the study included the length of time it took to translate the SDQ into BSL. This was because the process was more complex when translating from a written language to a visual one (see Chapter 2). This led to significant time pressures as the study unfolded.
We also found that the system of national portfolio research recruitment across the country did not lend itself well to a study with deaf people. For example, most clinical studies officers in the comprehensive local research network system have limited or no training in working with deaf people. This created additional time and resource pressures, and was resolved only by our team travelling long distances and sometimes staying in hotels overnight to facilitate recruitment.
Some challenges are discussed below under subheadings.
Recruitment within the Deaf community
The process of recruitment was difficult for a variety of reasons. In the UK, the Deaf community is a close-knit group. The most recent prevalence rates for BSL users in England estimates that there are approximately 125,000 deaf adults who use BSL as their main form of communication. 222 The 2012 Consortium for Research into Deaf Education survey51 suggests that only 5–8% of deaf young people are BSL users; the others rely on spoken English or multimodal forms of communication, such as SSE. SSE is not in itself a language and, although the translators who developed the BSL SDQ were keen to be inclusive, the team were conscious that they were developing a signed language version of the SDQ, available in full BSL. Around 90% of deaf young people are born to hearing families, and therefore struggle to acquire language at the same rate as their hearing peers, because the necessary conditions for language acquisition are less likely to be met.
There were concerns from some members of the Deaf community about confidentiality, which in some cases seemed to be a barrier to participation. Although reassurances were given, some families struggled with the concept and clearly felt uncomfortable with who knew what about their child, particularly in regard to the necessity for a clinical interview; several families expressed concerns about this and questioned the need for it. There was a suspicion among many, in particular deaf parents, that the clinicians were looking for problems with their child. In these circumstances, it was highly beneficial that several of the research assistants were deaf themselves, and able to allay fears about the purpose and nature of the clinical interviews and the security of the study data.
Recruitment of clinical cases
It was expected that the clinical CAMHS teams would be able to recruit approximately half of the young people for the study. In reality this proved not to be the case. We needed regular prompts and encouragement to remind clinicians to consider the study. There was anxiety about the inclusion criteria and also that involvement might cause additional stress. It is also true that the clinicians were very busy and finding time to prioritise research was not easy.
Recruitment of deaf teachers
Only a limited number of qualified teachers in the country are deaf. We were able to recruit 27 deaf teachers and 50 teaching assistants (nine of these were described as BSL instructors and one was described as a child care officer, but all of them were involved in communication and teaching assistant support within the classroom).
The number of deaf teachers in England is relatively small, because of the large challenges that deaf people have in obtaining the necessary qualifications and the gradual reduction over the last 15 years in deaf schools across the country, with an inclusion policy that sees many deaf children placed in mainstream education. In these circumstances, schools often recruit deaf teaching assistants in order to facilitate communication and learning. Many of these deaf teaching assistants work closely with deaf children, and are very well placed to fill out the BSL SDQs in relation to the children they teach. We therefore thought that it was important to recruit them into our study to explore if reliability was as good for teaching assistants as it was for teachers in this group; we found that it was.
Using online delivery
It was found that the online system was particularly useful for retesting participants. In these cases, respondents were already familiar with the research process and had experienced answering the questionnaire once on a previous occasion. However, for participants new to the research it was less beneficial, as researchers found that almost all participants involved in the study appreciated the opportunity to ask questions face to face, and discuss their involvement in the research.
There were additional drawbacks in that it was not possible to enter data offline and upload them at a later date when internet connection had been established, meaning that all participants had to have access to internet connections to make use of this system. While in large cities this was not a problem, during recruitment in the south-west and other rural areas of the country where internet access is poor it did cause problems. These stemmed from not being able to establish internet connection at all, or it not being at fast enough speeds to stream SDQ BSL video questions smoothly enough to be understood.
Equally, because the videos were hosted on the Manchester video library service (VLS), occasions when this site was closed for maintenance caused disruption to the streaming of the videos within the questionnaires. For example, at one point the VLS was completely updated over several weeks, meaning that every video had to be re-embedded within the questionnaires, as the coding had changed. As the research team was not based within the University of Manchester, the team was unaware of this for a significant period of time.
There were considerable limitations within setting up and securing the SelectSurvey database, in that there was a lack of close technical support available to the team, and it is a complex system to use and manage, with several different components. Funding was not sought for a part-time study technician, or technical support costs; this team would recommend that future studies include such funding in setting up similar projects. While it is clearly a useful piece of software that can bring many benefits to the recruitment phase of such a study, great care must be taken in the design and maintenance of such a study, and teams must plan effective ways of setting up and managing the challenges associated with using online systems in their research.
The online system was, for some participants, difficult to use without researcher contact. Participants are required to enter some basic information about themselves and their enrolment in the research (e.g. date of birth, participant number). Although these instructions are available in both BSL and English, following the research procedures has been much easier when supervised by a researcher who can help explain the process in a responsive way. This is particularly true for the younger participants in the research, who may have significant lack of access to a ‘fund of knowledge’. Thus, many of the benefits that one may expect such a system to reap became limitations. While in some senses the system was able to save considerable time and travel costs, the quality of information was poorer and participants were less easily engaged to stay involved with all the individual steps of the research process. This may have been partly a result of design and presentation, and has yielded useful information for future studies.
Non-responders and potential sample bias
While some previous, clinic-based, studies were able to obtain very high rates of parent report alongside child/young person self-report,188 other studies found high levels of non-response, particularly with the parent version. 204 This Dutch study also found (when analysing the teacher and self-report questionnaires) that the children of parents who did not return a SDQ had significantly more conduct, hyperactivity/inattention and peer problems.
We found that schools were particularly keen to become involved if they were deaf residential schools. By contrast, mainstream schools with deaf children had much lower take-up rates. This may have created a bias, but it is not possible to know the direction of this bias without further study.
Mental health problems are thought to occur in about 10% of 5- to 16-year-olds1 in the UK. Our study cannot claim to examine prevalence in a population because it is not a population sample. Our sample has come mainly from two groups. The first is from a clinical group of young people being seen by NDCAMHS (a highly specialised nationally commissioned service), and the second is from the community. Those recruited from the community have come largely through approaches to primary and secondary schools that include deaf children, but also through our network of contacts in the Deaf community and through teachers of the Deaf who see most children with deafness of 40 dB and above. There are therefore likely to be selection biases. The clinical group includes mainly children and young people who have been unable to access generic CAMHS, or who have been referred to us because of our expertise in seeing children and families whose first language is BSL. In the community setting there are likely to be a number of selection biases, and some of these have been identified in earlier sections. Biases can operate in both directions. For example, this may include culturally Deaf families avoiding the study because of perceived stigma and worried parents seeking out participation in the hope of eliciting support for their child.
Mean scores of total difficulties are reported across five different countries by Essau and colleagues. 197 Adolescents in the UK and Germany report significantly higher problems than in Sweden, Cyprus and Italy, and there are various statistically significant differences in the subscales across countries. High means (equivalent to those in Germany and the UK in this study) have previously been found in China223 and Holland. 202 These studies, alongside studies of different ethnic groups in the same country, for example Israel224 and Norway,199 suggest that it is not safe to use similar thresholds for total or subscales across different ethnic groups.
Gold standards
Even when the recruitment figures are met, there have still been issues in terms of how to validate the BSL SDQs, as there are no other validated mental health instruments (either questionnaires or semistructured interviews) designed specifically for this population. The current gold standard is a full clinical interview with a semistructured questionnaire, administered by a clinician with specialist knowledge of both Deaf culture and mental health, with a qualified interpreter used to working in child mental health services. All clinicians who administered clinical interviews as part of this study had at least BSL level 3, but used interpreters at all times. However, this has meant much greater resources have needed to be introduced to the project, as the recruitment centres cover large geographical areas, and the clinicians must be accompanied by qualified BSL/English interpreters in order to conduct the level of assessment required. The whole interview was interpreted from English to BSL (clinician to family) and then interpreted back from BSL to English (family to clinician). As the research was carried out nationwide, there were problems establishing consistency in interpreters being used; for instance, it would not be cost-effective having an interpreter based in Newcastle travelling down to London for the interview. There has been nationwide training for interpreters working with NDCAMHS, and interpreters who had received this training were used whenever possible. All clinicians had at least 5 years’ experience of working with deaf children in child mental health services, and some had considerably more. There are no deaf BSL-using clinicians working within the NDCAMHS teams who were available to undertake these interviews.
Language and linguistic challenges
One issue that is likely to be influential in the interpretation of the data concerns the highly heterogeneous nature of the language used by the deaf children who participated. This is partly related to the influence of the age of acquisition of a signed language, and also the lack of early childhood experiences of visual language. There will also be issues with the relative knowledge of certain aspects of language, such as social and emotional language. Thought was given to the practicalities of assessing the children’s language level using standardised tools. However, given the extreme shortage of experienced language therapists who have experience and knowledge of sign language, this was not possible. It is also not likely to be possible in practice, for example in population screening. The researchers noted the highly heterogeneous life histories of the children who participated. They differed not only in age of acquisition of a sign language, but also in the extent to which they could be considered bilingual. This is not simply an issue about language competence; some aspects of language (emotions, attitudes, etc.) may be more readily expressed in one language than another, depending on the child’s experiences. We had no way of controlling for this, but it remains an important issue for future research. Some mechanism for controlling language experiences and competencies would yield richer data.
Ethical issues
Ethical issues were discussed on a regular basis, particularly in regard to the identification of some young people who had emotional or behavioural difficulties but were not currently receiving support. Where this became apparent for families within the context of the research, we were able to reassure them and direct them to appropriate services, and we had many sources of feedback to suggest that this was valued and that outcomes for children were improved as a result. This was known to have happened on four separate occasions as part of the validation interview process. For three families it led to a referral to the NDCAMHS team in their locality, and, for one family, directing to another appropriate voluntary sector service. The clinical members of the research team facilitated this. One family was referred to children’s social services for family support after the clinical interview validation visit. This was done after discussion with the family because of the pressures it was under.
There was some confusion on the part of one deaf parent about what the research involved, and she did express some frustration to the clinical interviewer. She was recruited after a talk at a Deaf club, and said that afterwards she was worried that others at the Deaf club might have thought that her child had a mental health problem. We reviewed the process of that recruitment and were satisfied that it had been done sensitively, and this parent was reassured about the nature of the research and that she was not approached because anyone had concerns about her child’s mental health.
In our experience, a number of young people and families from the community sample found it a very useful process to take part in the project. A number of hearing parents, who had no particular clinical concerns about their children, nevertheless enjoyed a discussion with an experienced NDCAMHS clinician about the general developmental aspects and experiences of deaf young people.
Working with deaf people and the deaf community
Historically, the Deaf community has been an oppressed group, and hearing researchers conducting research ‘on’ deaf people, compounded with a stigma of ‘mental health’ in this instance, has often meant it has been difficult to persuade participants that this research is simply checking the validity of a signed language translation. This had an impact upon how the entire research process was framed when approaching individuals to take part in the study, in that we wished to ensure fully informed consent without arousing concern in people. In order to make sure that this was addressed, the team largely focused on face-to-face appointments before consent had been obtained, where participants could ask as many questions as they wanted and develop a better concept of the overall project aims. Qualitative feedback from participants has supported this as a strategy, in that people report feeling that when we have visited them on more than one occasion they have a better understanding of the process and what they need to do.
Another important cultural issue is that many deaf people, when they are growing up, may have been teased or taunted because of their use of language, the sound of their voice, or their inability to hear. Many of these taunts involve stigmatising phrases using words such as ‘mental’. For those deaf adults (parents and teachers or adolescents) who are being asked to fill in a questionnaire in BSL, there are therefore issues that resonate with them, when the term ‘mental health screening questionnaire’ is used. This presented challenges for our research team in terms of developing an understanding with the Deaf community about the importance of the research. This required considerable engagement with the Deaf community to explain the importance of improving the emotional and psychological well-being of young people by identifying their difficulties accurately and early. While many in the Deaf community understood this, there were also many others who remained highly suspicious. The team was committed to upholding the principles of informed consent to take part in research, and several discussions within the team were held to think about issues with the type of language and wording used in explaining the aims and components of the study to prospective participants. For example, rather than referring to ‘clinical interviews’, these were presented as ‘informal discussions with people that work at the Deaf Children, Young People and Family Service, like a psychologist or a psychiatrist’.
Deaf researchers
One advantage of our research team was the presence of five Deaf researchers (three research assistants, one collaborator and one clinical studies officer) who were an integrated part of the team. They could communicate one to one with deaf children and young people as well as deaf teachers and parents, and this meant direct communication was possible without the need for an interpreter. Both deaf and hearing researchers supported each other and brought a range of skills into the team. Deaf researchers also made high-quality links with the Deaf community and had great credibility in environments such as Deaf youth clubs, where they were seen as positive role models. Similarly, many hearing families valued contact with hearing and Deaf researchers who often visited in pairs. The management of the study was highly collaborative.
There were some important issues around confidentiality. Some Deaf communities are small, and Deaf members of the research team often knew deaf families who were participating. We took special care to be clear about confidentiality with participants and to have high standards of information governance.
A positive outcome to one visit was noted, as one of the children involved in the research was visibly affected by the exposure to a Deaf professional being respected among hearing professionals.
Working with interpreters
British Sign Language interpretation was also vital in the management of the research project. While the main research centre was in York, Deaf research assistants in other areas of the country working independently from the clinical NDCAMHS staff were given regular supervision. BSL interpreters facilitated a number of telephone calls, face-to-face supervisions and steering groups throughout the entirety of the study, aiming to ensure good communication among all members of the research team.
There were, however, certain barriers when working within different NHS trusts, which sometimes made communication difficult for all researchers, as the use of video-conferencing facilities such as Skype and FaceTime is not allowed between some NHS trusts. This meant that communication was often confined to e-mail, or telephone calls only when BSL interpreters were available. This raises some important learning points for future studies, in thinking about how such teams should be organised. It was felt at times that it would have been considerably more beneficial if everyone had shared a base and travelled across the country as needed. This facilitates much better communication in a mixed hearing/deaf environment, but also presents a greater burden of travel times and costs.
Sociocultural issues
Most of the young people who filled in the self-report questionnaire were profoundly deaf (79.9%). This is as expected, as children with mild to moderate deafness often attend mainstream schools and choose oral communication over BSL. We did, however, have some moderately and severely deaf young people who regarded themselves as fluent in BSL. Some of these young people were in deaf families, had close associations with other deaf young people who used BSL fluently, or were in schools where BSL was used regularly.
Deafness presents in many different ways and it is not possible to define all deaf people as one group. 225 The Deaf community is important to many deaf people, especially the 5–10% born to a deaf parent or parents. Deaf parents can be strong positive role models, which benefits their children. 226 Deaf culture refers to a sense of belonging and shared values that communities experience, where sign language is central. 227 Deaf is spelt with a capital D by some to signify cultural identity, and is not necessarily related to level of hearing loss. Many deaf people are sensitised to power imbalances between deaf and hearing people. Many dislike terms such as ‘hearing impairment’, ‘hearing disability’ or even ‘hearing problems’, seeing these terms as pejorative. It has been suggested that mental health difficulties in deaf people are not due to being deaf per se, but are largely to do with living in an environment that is not deaf aware or deaf friendly. 15
Deaf parents usually bring children up within the Deaf culture. Deaf children in hearing families face a range of experiences, ranging from a bicultural/bilingual upbringing to those who avoid Deaf culture and choose spoken language as the main mode of communication that they pursue for their child. 228 This may change when the child becomes older and makes choices of their own.
Summary of linguistic issues
The translation phase of this research shows that there were difficulties in selecting particular signs, and modifying the register of the signing in order to maximise participants’ understanding of the concept of the questionnaire. 121 However, this has also had a negative impact upon the ease with which we have recruited participants. When visiting schools or families and giving examples from our newly translated questionnaires, we found that because of some of the regional variation in sign selection, or the extent to which a deaf young person might use a mixture of signed and oral communication methods, some questions are not clear to them. From a research perspective, it is imperative that we know if the instruments are reliable and valid, yet this has proven quite distressing for some young people still developing their ‘Deaf identity’ and realising that they are not perhaps fluent enough to understand the whole questionnaire.
Patient and public involvement
Patient and public involvement was a central part of our research. Given the cultural and linguistic issues described above, and also given specific differences in the rates of mental health problems in deaf children, with a range of different causative associations and pathways, it was very important that we brought a keen understanding of service users and representatives of deaf children and young people (such as the NDCS) into the research team. For this reason, the NDCS and a service user parent of two deaf children were on the steering committee for our research. We made good use of focus groups, of both deaf young people and deaf adults, in commenting on drafts of the self-report, parent and teacher versions of the SDQ produced by the translation and back-translation teams. We also took advice from linguists and a variety of deaf professionals working within child mental health services. Advice from Deaf researchers, including those employed by us, and also by the SORD team at Manchester University, was sought and given. Deaf parents have also been involved in the lay summary of this report, and the NDCS will be involved in its dissemination, subject to approval by the National Institute for Health Research (NIHR).
Focus groups
As part of the PPI, participants from the focus groups were given opportunities to comment on the processes and materials.
Steering groups
Co-applicants from voluntary organisations such as the NDCS and BATOD were regularly invited to steering groups, both in the development phase and throughout the running of the study. They were able to provide several important contributions, particularly with respect to the recruitment phase of the study. The NDCS in particular gave valuable support in accessing their groups, providing information about the feasibility of recruitment in terms of areas where there were particularly strong BSL groups, and the idea of giving a small reimbursement to participants for taking part. All these ideas were eventually taken forward and integrated into the study protocol in time for the recruitment phase of the research.
Deaf service advisors
The NDCAMHS employs several Deaf service consultants, whose job it is to provide support to the clinical teams in making sure that the service is accessible, and that clinical and strategic developments are considered from a Deaf perspective. These professionals were able to provide regional and national support to the research assistants, particularly with regards to recruiting community sample participants. As well-connected members of the Deaf community, they were able to facilitate access to the Deaf community as well as a multitude of deaf professional contacts, who in turn were able to promote the study throughout England. This proved extremely valuable in terms of recruitment, as people were much more willing to engage when approached through a previously known contact. The value of having strong professional networks should not be underestimated when conducting research within tight-knit communities such as the Deaf community.
Feedback from participants
Through the reflective notes of the research assistants working on the project, we were able to gather direct feedback from participants about particular elements of the questionnaire. All participants were given the opportunity, following completion of the questionnaire, to offer feedback on the process to the researcher. This feedback was captured by the researcher. Researchers were also trained to observe particular cues where participants may not have understood questions throughout the questionnaire. This was discussed with the participants after completion of their involvement in the research, to ascertain what they had understood by the questions. This information was routinely entered into the study database.
Feedback from deaf parents
Many parents reported problems with question number 1. They were unclear whether the placement meant that the child’s or other people’s views needed to be considered. Another question was about being ‘unhappy’. The presentation of the sign in this was reported to be ambiguous, and so parents were unsure whether it referred to being happy or unhappy. However, other parents thought that it was a good presentation of the information, and one parent reported that it had made her think twice about her child, who was already known to CAMHS. Deaf parents reported that they sometimes felt questions were difficult to answer, as their answers would be different depending on whether their child was in a hearing or Deaf environment. Deaf parents also commented that they appreciated the presentation in BSL, but they would have greatly appreciated more examples.
Feedback from deaf teachers
There was a mixed response in terms of feedback from the teachers. Some reported that the SDQ in BSL was very clear and understandable. Some stated that the structure was not clear; for example, in the first question it was unclear whether the child was to think of others or it was asking what others thought about the child. Others reported that they would have liked more pronounced lip patterns, as, when a verb and adverb were created in one sign, for example to ‘WALK-QUICKLY’, it was ambiguous exactly what adverb the verb was conveying.
One researcher noted a general response to their arrival within a mainstream context as being that of surprise from the young people that a professional visiting the school would be a deaf person. This was noteworthy to the researcher, as they in turn were surprised to find this response in 2013. It appeared to be a negative response to encounter, but alternatively it was encouraging for the researcher to see that their presence did offer the opportunity for the young people to observe for themselves a potential role model in a deaf person who was a professional, and to gain a sense that this was indeed possible.
Feedback from deaf young people
Many deaf young people reported problems with questions 2 and 10. They stated that they were unsure what the person was referring to, and it would have been helpful to have more lip pattern to help identify this. For example, a BSL mouth pattern was used in a question about stealing, but some of the young people were unsure if this then meant taking and if so taking what, leading to confusion in some young people. In addition, they stated that they would have liked to see more examples being used to help create the concept in a way they clearly understood. A number reported that they felt it was difficult to connect with the presenter because of the style of presenting in BSL that they had adopted. Some mentioned that they found the regional variation a problem. Others, however, stated that they felt the presentation was clearly understandable. In summary, the feedback was very mixed, with many finding the BSL version straightforward to understand.
Recommendations for future research
Priority 1
Use the SDQ BSL version alongside other validated versions of the SDQ to scope the mental health needs of deaf children in England.
This study has shown that the BSL SDQ is an adequate screening instrument for deaf children and young people, particularly as an overall screening instrument for mental health problems.
The translation and validation of the SDQ in BSL enables comparative research to take place with deaf children who are BSL users. A research priority would be to carry out a national study of deaf children to scope the mental health needs of deaf children and to compare different subpopulations. This will help us better understand the prevalence of mental health problems and the needs of deaf children in different settings or backgrounds, and plan services to meet those needs.
Priority 2
There is a need to develop better instruments for deaf children from basic principles (i.e. not translated versions). These need to be designed specifically for deaf children and be culturally and linguistically appropriate.
Anxiety disorders, behaviour problems230 and low self-esteem231 have been proposed as more common in deaf children, and the development of new instruments for deaf young people, through research, would enable us to explore this further. A priority therefore is to develop further instruments specifically for deaf children for particular disorders. These could focus around depression, quality of life and anxiety. It would allow better monitoring of interventions for this group.
Priority 3
We need to understand better why it is that deaf children have higher rates of mental health problems and to develop early interventions that prevent children who are deaf having mental health problems.
Further research should take place to understand the high rates of mental health problems evident in deaf young people found in this and other research. We need to urgently research why this increase continues against a backdrop of changes in education policy, newborn screening and technological advances (e.g. cochlear implantation). Qualitative research with deaf children, teachers of the deaf and parents will help us understand the experiences of deaf children and the impact of a range of factors on their mental health.
A large follow-up cohort of deaf children would be helpful. This would be methodologically robust with rich information across a range of ages and domains. This could include detailed epidemiological information and birth-related data as well as social, family, communicative and educational information. This would help us better understand associations with mental health problems. From this it would be possible to develop early intervention research including clinical trials (e.g. parenting interventions) and policy-based research (e.g. educational interventions) that seeks to improve child mental health outcomes for deaf children.
Conclusions
We have learnt a great deal, alongside colleagues from other institutions interested in furthering our understanding of the Deaf experience, from the translation of a screening tool for mental health problems in children and young people into BSL. These methodologies can be used in future work in this field.
We have established the levels of validity of a BSL translation of the most commonly used mental health questionnaire for children and young people in deaf young people, deaf parents and deaf teachers. This validation has shown that it is robust enough to be used as a screening instrument for mental health problems in deaf children and young people, or by deaf parents or teachers responding on behalf of a child. This is an important first step in better understanding the needs of deaf children and young people in the UK, and will hopefully lead to further research on their mental health and well-being.
Acknowledgements
We are particularly grateful to all of our research participants who gave up their time to support this study. There are several key contacts within schools, voluntary organisations and our other National Deaf Children Young People and Family Services without whom this research would not have been possible. We would also like to thank all the translators and interpreters for their advice and support throughout this study, and the valuable contributions to the design and conduct of this study made by the project steering committee.
Thanks for excellent administration support from Catherine Arthurson and research governance committee support from Caroline Mozley, Damon Foster, Sinead Audsley and Alison Thompson. Thanks to Jules Bersford-Dent, Dani Varley, Jenny Sweetman and David Marshall for support with proofreading.
This report presents independent research commissioned by the NIHR (project number 09/2000/43). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the HS&DR Programme, the NIHR, the NHS or the Department of Health.
Contributions of authors
*Dr Sophie Roberts (Consultant Child and Adolescent Psychiatrist, Mental Health and Deafness) cowrote the grant application, coled the research, and made a substantial contribution to the design, fieldwork and data interpretation.
*Professor Barry Wright (Consultant Child and Adolescent Psychiatrist, Mental Health and Deafness) wrote the protocol and cowrote the grant application, coled the research and made substantial contribution to the design, fieldwork and data interpretation.
*Ms Kate Moore (Research Trial Coordinator, Mental Health and Deafness) established the study at inception and made substantial contributions to the day-to-day management of the research between 20 June 2011 and 31 July 2013.
*Ms Josie Smith (Clinical Studies Officer, Mental Health and Deafness) led the recruitment aspects of the study. She was Research Trial Coordinator between 1 August 2013 and 10 April 2014.
*Dr Victoria Allgar (Statistician) carried out all statistical analysis (except Rasch analysis) and contributed to the report.
*Professor Alan Tennant (Statistician) carried out Rasch analysis and wrote relevant sections of the report.
*Ms Caroline Doherty (PPI) attended steering group meetings and made contributions to the protocol and report.
*Ms Ellen Hughes (Research Assistant) made contributions to fieldwork in the North and South West, and contributed substantially to the report.
*Ms Danielle Collingridge Moore (Research Fellow) was involved in supporting the early development and set-up of the study, and contributed to Chapter 2.
*Dr Richard Ogden (Linguist) contributed to linguistic aspects of translation work and relevant sections of the report.
*Ms Helen Phillips (Research Assistant) made substantial contributions to the fieldwork in the Midlands and contributed elements to the report.
*Ms Lilli Beese (Research Assistant) made substantial contributions to the fieldwork in London and the South East and contributed elements to the report.
*Dr Katherine Rogers (Research Fellow) supported online SDQ, managed Manchester University data housing and contributed to Chapter 2 of the report.
Collaborators
*Ms Kosar Qaddus (Research Assistant) made substantial contributions to the fieldwork in Somerset.
*Ms Isobel Barlow (Research Assistant) made contributions to the fieldwork in the North and South West.
*Ms Naomi Hooke (Research Assistant) was involved in supporting the early development work of the research.
Dr Sophie Bennett (Research Assistant) was involved in preparing the grant application and protocol.
Ms Emma Burton (Research Assistant) assisted with the recruitment in London.
Ms Justine Durno (Research Assistant) assisted with the recruitment in London.
Ms Lisa Hackney (Clinical Studies Officer) made contributions to the fieldwork in the North and South West.
*Ms Di Baines (Clinical Studies Officer) assisted with recruitment.
Ms Jules Beresford Dent (Clinical Studies Officer) proofread a final version of the report.
Dr Maria Gascon-Ramos (Principal Investigator for Somerset Partnership NHS Foundation Trust) carried out clinical interviews.
*Dr Rob Walker (Principal Investigator for Dudley and Walsall Mental Health Trust) carried out clinical interviews.
*Dr Andrew Holwell (Principal Investigator for South West London and St George’s Mental Health NHS Trust) carried out clinical interviews.
*Professor Bryony Beresford (Co-applicant) attended steering group meetings.
*Ms Mary Dawson (PPI) attended steering group meetings.
*Ms Rachael Hayes (NDCAMHS, North) advised about deaf experience.
*Dr Charlotte Glenister (Somerset Partnership NHS Foundation Trust) attended early steering groups.
Dr Victoria Fernández García de las Heras (NDCAMHS, London) carried out clinical interviews.
*Dr Sarah Kent (NDCAMHS, Midlands) carried out clinical interviews.
Dr Hannah George (NDCAMHS, North) carried out clinical interviews.
Dr Nicoletta Gentili (NDCAMHS, Midlands) carried out clinical interviews.
Dr Sarah Woodhead (NDCAMHS, North) carried out clinical interviews.
Ms Hayley Ford (NDCAMHS) carried out clinical interviews.
*Ms Hilary Sutherland (Deaf Advisor, NDCAMHS, Taunton) gave deaf experience advice and supported the Research Assistant in Taunton.
Ms Michelle Crellin (Parent Representative) advised on the protocol and study documentation.
Mr Steve Powell (Chief Executive, SignHealth) gave consultation to the steering group and supported recruitment.
With particular thanks to Professor Robert Goodman, original author of the SDQ, who consulted with us on the process of translation and authorised the final translated version.
*Steering group members.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Meltzer H, Gatward R, Goodman R, Ford T. Mental health for children and adolescents in Great Britain. Int Rev Psychiatry 2003;15:185-7. http://dx.doi.org/10.1080/0954026021000046155.
- Hindley P, Hill P, McGuigan S, Kitson N. Psychiatric disorder in deaf and hearing impaired children and young people: a prevalence study. J Child Psychol Psychiatry 1994;35:917-34. http://dx.doi.org/10.1111/j.1469-7610.1994.tb02302.x.
- Meadow K, Trybus R. Behavioral and Emotional Problems of Deaf Children: An Overview. Hearing and Hearing Impairment. New York, NY: Grune and Stratton; 1979.
- Mejstad L, Heiling K, Svedin C. Mental health and self image among deaf and hard of hearing children: Project MUSE. Am Ann Deaf 2009;153:504-15. http://dx.doi.org/10.1353/aad.0.0069.
- Van Eldik T, Treffers P, Veerman J, Verhulst F. Mental health problems of deaf Dutch children as indicated by parent’s responses to the Child Behaviour Checklist. Am Ann Deaf 2004;148:390-5. http://dx.doi.org/10.1353/aad.2004.0002.
- Vostanis P, Hayes M, Du Feu M. Behavioural and emotional problems in hearing impaired children: a preliminary study of teacher and parent ratings. Eur J Spec Needs Educ 1997;12:239-46. http://dx.doi.org/10.1080/0885625970120306.
- Van Gent T, Goedhart A, Hindley P, Treffers P. Prevalence and correlates of psychopathology in a sample of deaf adolescents. J Child Psychol Psychiatry 2007;48:950-8. http://dx.doi.org/10.1111/j.1469-7610.2007.01775.x.
- Hindley P. Psychiatric aspects of hearing impairments. J Child Psychol Psychiatry 1997;38:101-17. http://dx.doi.org/10.1111/j.1469-7610.1997.tb01507.x.
- Landsberger S, Diaz D. Inpatient psychiatric treatment of deaf adults: demographic and diagnostic comparisons with hearing inpatients. Psychiatr Serv 2010;61:196-9. http://dx.doi.org/10.1176/appi.ps.61.2.196.
- Van Eldik T. Behavior problems with deaf Dutch boys. Am Ann Deaf 1994;139:394-9. http://dx.doi.org/10.1353/aad.2012.0280.
- Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. http://dx.doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Freeman R, Malkin S, Hastings J. Psychosocial problems of deaf children and their families: a comparative summary. Am Ann Deaf 1975;120:275-304.
- Cornes A, Rohan M, Napier J, Rey J. Reading the signs: impact of signed versus written questionnaires on the prevalence of psychopathology among deaf adolescents. Aust N Z J Psychiatry 2006;40:665-73.
- Beaton D, Bombardier C, Guillemin F, Ferraz M. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000;15:3186-91. http://dx.doi.org/10.1097/00007632-200012150-00014.
- Polat F. Factors affecting psychosocial adjustment of deaf students. J Deaf Stud Deaf Educ 2003:325-39. http://dx.doi.org/10.1093/deafed/eng018.
- Hindley P. Mental health problems in deaf children. Curr Paediatr 2005;15:114-19. http://dx.doi.org/10.1016/j.cupe.2004.12.008.
- Stevenson J, Richman N. Behaviour, language and development in three year old children. J Autism Child Schizophr 1978;8:299-313. http://dx.doi.org/10.1007/BF01539633.
- Hindley P, Kroll L. Theoretical and epidemiological aspects of attention deficit and overactivity in deaf children. J Deaf Stud Deaf Educ 1998;3:64-72. http://dx.doi.org/10.1093/oxfordjournals.deafed.a014341.
- Sinkkonen J, Weisel A. Issues Unresolved: New Perspectives on Language and Deaf Education. Washington, DC: Gallaudet University Press; 1998.
- Brown A, Cohen P, Greenwald S, Susser E. Nonaffective psychosis after prenatal exposure to rubella. Am J Psychiatry 2000;157:438-43. http://dx.doi.org/10.1176/appi.ajp.157.3.438.
- Chalmers D, Stewart I, Silva P, Mulvena A. Otitis Media with Effusion in Children: The Dunedin Study. London: Mac Keith Press; 1989.
- Chess S, Fernandez P. Impulsivity in rubella deaf children: a longitudinal study. Am Ann Deaf 1980;125:505-9. http://dx.doi.org/10.1353/aad.2012.1329.
- Pless I, Power C, Peckham C. Long-term psychosocial sequelae of chronic physical disorders in childhood. Pediatrics 1993;91:1131-6.
- Sculerati N. Analysis of a cohort of children with sensory hearing loss using the SCALE systematic nomenclature. Laryngoscope 2000;110:787-98. http://dx.doi.org/10.1097/00005537-200005000-00009.
- Das V. Aetiology of bilateral sensorineural hearing impairment in children: a 10 year study. Arch Dis Child 1996;74:8-12. http://dx.doi.org/10.1136/adc.74.1.8.
- Sculerati N. Analysis of a cohort of children with sensory hearing loss using the SCALE systematic nomenclature. Laryngoscope 2000;110:787-98. http://dx.doi.org/10.1097/00005537-200005000-00009.
- Das V. Aetiology of bilateral sensorineural hearing impairment in children: a 10 year study. Arch Dis Child 1996;74:8-12. http://dx.doi.org/10.1136/adc.74.1.8.
- Bess F, Dodd-Murphy J, Parker R. Children with minimal sensorineural hearing loss: prevalence, educational performance and functional status. Ear Hear 1998;19:339-54. http://dx.doi.org/10.1097/00003446-199810000-00001.
- Bernstein V, Denno L. Repetitive behaviors in CHARGE syndrome: differential diagnosis and treatment options. Am J Med Genet A 2005;133A:232-9. http://dx.doi.org/10.1002/ajmg.a.30542.
- Tamayo M, Maldonado C, Plaza S, Alvira G, Ge T, Zambrano M. Neuroradiology and clinical aspects of Usher syndrome. Clin Genet 1996;50:126-32. http://dx.doi.org/10.1111/j.1399-0004.1996.tb02366.x.
- Souriau J, Gimenes M, Blouin C, Benbrik I, Benbrik E, Churakowskyi A. CHARGE syndrome: developmental and behavioural data. Am J Med Genet 2005;133A:278-81. http://dx.doi.org/10.1002/ajmg.a.30549.
- Wachtel L, Hartshorne T, Dailor A. Psychiatric diagnoses and psychotropic medications in CHARGE syndrome: a pediatric survey. J Dev Phys Disabil 2007;19:471-83. http://dx.doi.org/10.1007/s10882-007-9064-6.
- Stefanis N, Thewissen V, Bakoula C, van Os J, Myin-Germeys I. Hearing impairment and psychosis: a replication in a cohort of young adults. Schizophr Res 2003;85:266-72. http://dx.doi.org/10.1016/j.schres.2006.03.036.
- Waldeck T, Wyszynski B, Medalia A. The relationship between Usher syndrome and psychosis with Capgras syndrome. Psychiatry Interpers Biol Processes 2001;64:248-55. http://dx.doi.org/10.1521/psyc.64.3.248.18467.
- Mangotich M, Misiaszek J. Atypical psychosis in Usher syndrome. Psychosomatics 1983;24:674-75. http://dx.doi.org/10.1016/S0033-3182(83)73178-6.
- Kitson N, Thacker A, Hinkley P, Kitson T. Mental Health and Deafness. London: Whurr; 2000.
- Zwiebel A. More on the effects of early manual communication on the cognitive development of deaf children. Am Ann Deaf 1987;134:16-22. http://dx.doi.org/10.1353/aad.2012.0828.
- Vernon M. Fifty years of research on the intelligence of deaf and hard of hearing children: a review of literature and discussion of implications. J Deaf Stud Deaf Educ 2005;10:225-31. http://dx.doi.org/10.1093/deafed/eni024.
- Schildroth A. Congenital cytomegaolovirus and deafness. Am J Audiol 1994;3:27-38. http://dx.doi.org/10.1044/1059-0889.0302.27.
- Tellier A, Cormier-Daire V, Abadie V, Amiel J, Sigaudy S, Bonnet D, et al. CHARGE syndrome: report of 47 cases and review. Am J Med Gen 1998;76:402-9. http://dx.doi.org/10.1002/(SICI)1096-8628(19980413)76:5<402::AID-AJMG7>3.0.CO;2-O.
- Emerson E, Einfeld S, Stancliffe R. The mental health of young children with intellectual disabilities or borderline intellectual functioning. Soc Psychiatry Psychiatr Epidemiol 2010;45:579-87. http://dx.doi.org/10.1007/s00127-009-0100-y.
- Fortnum H, Stacey P, Summerfield A. An exploration of demographic bias in a questionnaire survey of hearing-impaired children: implications for comparisons of children with and without cochlear implants. Int J Pediatr Otorhinolaryngol 2006;70:2043-54. http://dx.doi.org/10.1016/j.ijporl.2006.07.014.
- Morton C, Nance W. Newborn hearing screening: a silent revolution. N Engl J Med 2006;354:2151-64. http://dx.doi.org/10.1056/NEJMra050700.
- Hintermair M. Parent resources, parental stress, and socioemotional development of deaf and hard of hearing children. J Deaf Stud Deaf Educ 2006;11:493-51. http://dx.doi.org/10.1093/deafed/enl005.
- Moeller M, Schick B. Relations between maternal input and theory of mind understanding in deaf children. Child Dev 2006;7:751-66. http://dx.doi.org/10.1111/j.1467-8624.2006.00901.x.
- Meadow-Orlans K, Mertens D, Sass-Lehrer M. Parents’ Early Experiences with Deaf and Hard of Hearing Children. Washington, DC: Gallaudet University Press; 2003.
- MacTurk R, Meadow-Orlans K, Koester L, Spencer P. Social support, motivation, language and interaction: a longitudinal study of mothers and deaf infants. Am Ann Deaf 1993;138:19-25. http://dx.doi.org/10.1353/aad.2012.0575.
- Calderon R, Greenberg M, Kusche C, Martin D. Advances in Cognition, Education and Deafness. Washington, DC: Gallaudet University Press; 2000.
- Rutter M. A children’s behaviour questionnaire for completion by teachers: preliminary findings. J Child Psychol Psychiatry 1967;8:1-11. http://dx.doi.org/10.1111/j.1469-7610.1967.tb02175.x.
- Wake M, Hughes E, Poulakis Z, Collins C, Rickards F. Outcomes of children with mild–profound hearing loss of 7 and 8 years: a population study. Ear Hear 2004;25:1-8. http://dx.doi.org/10.1097/01.AUD.0000111262.12219.2F.
- CRIDE Report on 2012 Survey on Educational Provision for Deaf Children in England. London: Consortium of Research in Deaf Education (CRIDE); 2012.
- Powers S. Influences of student and family factors on academic outcomes of mainstream secondary school deaf students. J Deaf Stud Deaf Educ 2003;8:57-78. http://dx.doi.org/10.1093/deafed/8.1.57.
- Stinson M, Antia S. Considerations in educating deaf and hard-of-hearing students in inclusive settings. J Deaf Stud Deaf Educ 1999;4:163-75. http://dx.doi.org/10.1093/deafed/4.3.163.
- Power S, Hyde M. The characteristics and extent of participation of deaf and hard of hearing students in regular classes in Australian schools. J Deaf Stud Deaf Educ 2002;7:302-11. http://dx.doi.org/10.1093/deafed/7.4.302.
- Crocker S, Edwards L, Austen S, Crocker S. Deafness in Mind. Working Psychologically with Deaf People across the Lifespan. London: Whurr; 2004.
- Gregory S, Bishop J, Sheldon L. Deaf Young People and Their Families: Developing Understanding. Cambridge: Cambridge University Press; 1995.
- Power S. An analysis of deaf pupils’ examination results in ordinary schools in 1996. Deafness Educ Int 1998;22:30-6.
- Huttunen K, Sorri M. Long-term outcome of early childhood hearing impairments in northern Finland. Scand Audiol 2001;30:106-8. http://dx.doi.org/10.1080/010503901300007236.
- Strong M. Language Learning and Deafness. Cambridge: Cambridge University Press; 2007.
- Schick B, de Villers P, de Villers J, Hoffmeister R. Language and theory of mind: a study of deaf children. Child Dev 2007;78:376-96. http://dx.doi.org/10.1111/j.1467-8624.2007.01004.x.
- Moores D, Anderson K, Ayers K, Krantz K, Lafferty M, Locke M. Issues and trends in American Annals of the Deaf publications 2001–2007. Am Ann Deaf 2008;153:99-120. http://dx.doi.org/10.1353/aad.0.0020.
- Wauters L, Van Bon W, Tellings A. Reading comprehension of Dutch deaf children. Reading Writing 2006;19:49-76. http://dx.doi.org/10.1007/s11145-004-5894-0.
- Yoshinaga-Itano C, Sedley A, Coulter D, Mehl A. Language of early and later identified children with hearing loss. Pediatrics 1998;102:1161-71. http://dx.doi.org/10.1542/peds.102.5.1161.
- Kyle F, Harris M. Concurrent correlates and predictors of reading and spelling achievement in deaf and hearing school children. J Deaf Stud Deaf Educ 2006;11:273-88. http://dx.doi.org/10.1093/deafed/enj037.
- Gibbs S. The skills in reading shown by young children with permanent and moderate hearing impairment. Educ Res 2004;46:17-24. http://dx.doi.org/10.1080/0013188042000178791.
- Patel V, Flisher A, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet 2007;369:1302-13. http://dx.doi.org/10.1016/S0140-6736(07)60368-7.
- Baron-Cohen S, Leslie A, Frith U. Does the autistic child have a ‘theory of mind’?. Cognition 1985;21:37-46. http://dx.doi.org/10.1016/0010-0277(85)90022-8.
- Russell P, Hosie C, Gray C, Scott C, Hunter N. The development of theory of mind in deaf children. J Child Psychol Psychiatry 1998;39:903-10. http://dx.doi.org/10.1017/S0021963098002844.
- Courtin C. The impact of sign language on the cognitive development of deaf children: the case of theories of mind. J Deaf Studies Deaf Educ 2000;5:266-76. http://dx.doi.org/10.1093/deafed/5.3.266.
- Peterson C, Siegal M. Insights into a theory of mind from deafness and autism. Mind Lang 2000;15:123-45. http://dx.doi.org/10.1111/1468-0017.00126.
- Peterson C. Drawing insight from pictures: the development of concepts of false belief in children with deafness, normal hearing and autism. Child Dev 2002;73:1442-59. http://dx.doi.org/10.1111/1467-8624.00482.
- Peterson C, Siegal M. Deafness and theory of mind. J Child Psychol Psychiatry 1995;36:458-74. http://dx.doi.org/10.1111/j.1469-7610.1995.tb01303.x.
- Courtin C, Melot A. Metacognitive development of deaf children: lessons from the appearance–reality and false belief tasks. Dev Sci 2005;8:16-25. http://dx.doi.org/10.1111/j.1467-7687.2005.00389.x.
- Steeds L, Rowe K, Dowker A. Deaf children’s understanding of beliefs and desires?. J Deaf Stud Deaf Educ 1997;2:185-95. http://dx.doi.org/10.1093/oxfordjournals.deafed.a014324.
- Figueras-Costa B, Harris P. Theory of mind development in deaf children. J Deaf Stud Deaf Educ 2001;6:92-102. http://dx.doi.org/10.1093/deafed/6.2.92.
- Lundy J. Age and language skills of deaf children in relation to theory of mind development. J Deaf Stud Deaf Educ 2002;7:41-56. http://dx.doi.org/10.1093/deafed/7.1.41.
- Woolfe T, Want S, Siegal M. Signposts to development: theory of mind in deaf children. Child Dev 2002;73:768-78. http://dx.doi.org/10.1111/1467-8624.00437.
- Terwogt M, Rieffe C. Deaf children’s use of beliefs and desires in negotiation. J Deaf Stud Deaf Educ 2004;9:27-38. http://dx.doi.org/10.1093/deafed/enh013.
- Peterson C. Theory of mind development in oral deaf children with cochlear implants of conventional hearing aids. J Child Psychol Psychiatry 2004;45:1096-10. http://dx.doi.org/10.1111/j.1469-7610.2004.t01-1-00302.x.
- Remmel E, Peters K. Association for Psychological Science 18th Annual Convention. New York, NY: Marriott Marquis; 2004.
- Rhys-Jones S, Ellis H. Theory of mind deaf and hearing children’s comprehension of picture stories and judgments of social situations. J Deaf Stud Deaf Educ 2000;5:248-65. http://dx.doi.org/10.1093/deafed/5.3.248.
- Wright B, Oakes P. Does socio-emotional developmental delay masquerade as autism in some deaf children?. Int J Ment Health Deafness 2012;2:45-51.
- Kvam M. Sexual abuse of deaf children: a retrospective analysis of the prevalence and characteristics of childhood sexual abuse among deaf adults in Norway. Child Abuse Negl 2004;28:241-51. http://dx.doi.org/10.1016/j.chiabu.2003.09.017.
- Titus J, Schiller J, Guthmann D. Characteristics of youths with hearing loss admitted to substance misuse treatment. J Deaf Stud Deaf Educ 2008;13:336-50. http://dx.doi.org/10.1093/deafed/enm068.
- Mullen P, Martin J, Anderson J, Romans S, Herbison G. Childhood sexual abuse and mental health in adult life. Br J Psychiatry 1993;163:721-32. http://dx.doi.org/10.1192/bjp.163.6.721.
- Kluwin T, Stinson T, Colarossi G. Social processes and outcomes of in-school contact between deaf and hearing peers. J Deaf Stud Deaf Educ 2002;7:200-13. http://dx.doi.org/10.1093/deafed/7.3.200.
- Hindley P, Hindley P, Kitson N. Mental Health and Deafness. London: Whurr; 2000.
- Landgraf J, Abetz L, Ware J. Child Health Questionnaire (CHQ): A User’s Manual. Boston, MA: Health Institute, New England Medical Center; 1996.
- Arnold P, Atkins J. The social and emotional adjustment of hearing impaired children integrated in primary schools. Educ Res 1991;33:223-8. http://dx.doi.org/10.1080/0013188910330307.
- Nunes T, Pretzlik U, Olsson J. Deaf children’s social relationships in mainstream schools. Deafness Educ Int 2001;3:123-36. http://dx.doi.org/10.1179/146431501790560972.
- Davis J, Elfenbein J, Schum R, Bentler R. Effects of mild and moderate hearing impairments on language, educational and psychosocial behaviour of children. J Speech Hearing Disord 1986;51:53-62. http://dx.doi.org/10.1044/jshd.5101.53.
- Punch R, Hyde M. The social participation and career decision making of hard of hearing adolescents in regular classes. Deafness Educ Int 2005;7:122-38. http://dx.doi.org/10.1179/146431505790560365.
- Fellinger J, Holzinger D, Sattel H, Laucht M. Mental health and quality of life in deaf pupils. Eur Child Adolesc Psychiatry 2008;17:414-23. http://dx.doi.org/10.1007/s00787-008-0683-y.
- Center for Disease Control and Prevention . Prevalence of Autism 2007. www.cdc.gov/ncbddd/autism/data.html (accessed 7 August 2009).
- Regional and National Summary Report of Data from the 2007–2008 Annual Survey of Deaf and Hard of Hearing Children and Youth. Washington, DC: GRI, Gallaudet University; 2008.
- Roper L, Arnold P, Monteiro B. Co-occurrence of autism and deafness. Autism 2003;7:245-53. http://dx.doi.org/10.1177/13623613030073002.
- Mandell D, Novak M, Zubritsky C. Factors associated with age of diagnosis among children with autism spectrum disorders. Pediatrics 2005;116:1480-6. http://dx.doi.org/10.1542/peds.2005-0185.
- Martin D, Bat-Chava Y. Negotiating deaf hearing relationships: coping strategies of deaf boys and girls in mainstream schools. Child Care Health Dev 2003;29:511-21. http://dx.doi.org/10.1046/j.1365-2214.2003.00371.x.
- National Institute for Health and Care Excellence . Cochlear Implants for Children and Adults With Severe to Profound Deafness 2009.
- Dammeyer J. Psychosocial development in a Danish population of children with cochlear implants and deaf and hard-of-hearing children. J Deaf Stud Deaf Educ 2010;15:50-8. http://dx.doi.org/10.1093/deafed/enp024.
- Wheeler A, Archbold S, Gregory S, Skipp A. Cochlear implants: the young people’s perspective. J Deaf Stud Deaf Educ 2007;12:303-16. http://dx.doi.org/10.1093/deafed/enm018.
- du Feu M, Fergusson K. Sensory impairment and mental health. Adv Psychiatr Treat 2003;9:95-103. http://dx.doi.org/10.1192/apt.9.2.95.
- Kvam M, Loeb M, Tambs K. Mental health in deaf adults: symptoms of anxiety and depression among hearing and deaf individuals. J Deaf Stud Deaf Educ 2007;12:1-7. http://dx.doi.org/10.1093/deafed/enl015.
- Mitchell T, Broham L. The psychological treatment needs of deaf mental health patients in high secure settings: a review of literature. Int J Forensic Ment Health 2011;10:92-106. http://dx.doi.org/10.1080/14999013.2011.577135.
- Austen S, Graham J, Baguley D. Ballantynes’ Deafness. Chichester: Wiley-Blackwell; 2009.
- Sass-Lehrer M. Programs in Services for Deaf and Hard of Hearing Children and Their Families: The Young Deaf or Hard of Hearing Child. Baltimore, MD: Paul H. Brookes Publishing; 2003.
- Yoshinaga-Itano C. From screening to early identification and intervention: discovering predictors to successful outcomes for children with significant hearing loss. J Deaf Stud Deaf Educ 2003;8:11-30. http://dx.doi.org/10.1093/deafed/8.1.11.
- Moeller M. Early intervention and language development in children who are deaf and heard of hearing. Pediatrics 2000;106. http://dx.doi.org/10.1542/peds.106.3.e43.
- Watkin P, McCann D, Law C, Mullee M, Petrou S, Stevenson J. Language ability in children with permanent hearing impairment: the influence of early management and family participation. Pediatrics 2007;120:e694-e701. http://dx.doi.org/10.1542/peds.2006-2116.
- Calderon R, Naidu S. Further support for the benefits of early identification and intervention for children with hearing loss. Volta Rev 2000;100:53-84.
- Watkins S, Taylor D, Mikalich E. SKI-HI Curriculum: Family Centered Programming for Infants and Young Children with Hearing Loss. Logon, UT: Utah State University; 2004.
- Goodman R, Meltzer H, Bailey V. The Strengths and Difficulties Questionnaire: a pilot study on the validity of the self-report version. Eur Child Adolesc Psychiatry 1998;7:125-30. http://dx.doi.org/10.1007/s007870050057.
- Goodman R. Psychometric properties of the Strengths and Difficulties Questionnaire. J Am Acad Child Adolesc Psychiatry 2001;40:1337-45. http://dx.doi.org/10.1097/00004583-200111000-00015.
- Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br J Psychiatry 2000;177:534-9. http://dx.doi.org/10.1192/bjp.177.6.534.
- Mathai J, Anderson P, Bourne A. Use of the Strengths and Difficulties Questionnaire as an outcome measure in a child and adolescent mental health service. Australas Psychiatry 2003;11:334-7. http://dx.doi.org/10.1046/j.1440-1665.2003.00544.x.
- Callaghan J, Young B, Pace F, Vostanis P. Evaluation of a new mental health service for looked after children. Clin Child Psychol Psychiatry 2004;9:130-48. http://dx.doi.org/10.1177/1359104504039177.
- Ford T, Tingay K, Wolpert M. CORC’s survey of routine outcome monitoring and national CAMHS dataset developments: a response to Johnston and Gower. Child Adolesc Ment Health 2002;11:50-2. http://dx.doi.org/10.1111/j.1475-3588.2005.00390.x.
- Health and Social Care Information Centre . Child and Adolescent Mental Health Services Data Set 2014. www.hscic.gov.uk/CAMHS (accessed 21 October 2014).
- National Health Service . Children &Amp; Young People’s IAPT 2014. www.cypiapt.org/children-and-young-peoples-project.php?accesscheck=%2Findex.php (accessed 21 October 2014).
- Beresford B, Clarke S, Greco V. Referrers’ use and views of specialist mental health services for deaf children and young people in England. J Ment Health 2010;19:193-201. http://dx.doi.org/10.3109/09638230902968159.
- Moore K, Moore D, Wright B, Ogden R, Rogers K. Overcoming the challenges of translating mental health instruments into sign languages. Int J Ment Health and Deafness 2013;1:20-9.
- Rogers K, Young A, Lovell K, Campbell M, Scott P, Kendal S. The British Sign Language versions of the Patient Health Questionnaire, the Generalized Anxiety Disorder 7-Item Scale, and the Work and Social Adjustment Scale. J Deaf Stud Deaf Educ 2013;18:110-22. http://dx.doi.org/10.1093/deafed/ens040.
- Brauer B. Adequacy of translation of the MMPI into American Sign Language for use with deaf individuals: linguistic equivalency issues. Rehabil Psychol 1993;38:247-60. http://dx.doi.org/10.1037/h0080302.
- Rogers K. An Investigation into the Relationship between the Perceived Strengths and Difficulties of Deaf Young People and their Self-Esteem. Manchester: University of Manchester; 2008.
- Cornes A, Brown P. Mental health of deaf adolescents: an investigation using an Auslan version of the Strengths and Difficulties Questionnaire. Deafness Educ Int 2012;14:161-75. http://dx.doi.org/10.1179/1557069X12Y.0000000009.
- Crowe T. Cross-cultural instrument translation: assessment, translation, and statistical applications. Am Ann Deaf 2005;150:67-72. http://dx.doi.org/10.1353/aad.2005.0020.
- Vernon M, Miller K. Interpreting in mental health settings: issues and concerns. Am Ann Deaf 2001;146:429-34. http://dx.doi.org/10.1353/aad.2012.0200.
- Rogers K, Young A, Lovell K, Evans C. The challenges of translating the Clinical Outcomes in Routine Evaluation – Outcome Measure (CORE-OM) into British Sign Language. J Deaf Stud Deaf Educ 2013;18:110-22. http://dx.doi.org/10.1093/deafed/ens040.
- Montoya L, Egnatovitch R, Eckhardt E, Goldstein M. Translation challenges and strategies: the ASL translation of a computer-based, psychiatric diagnostic interview. Sign Lang Stud 2004;4:314-44. http://dx.doi.org/10.1353/sls.2004.0019.
- Lipton D, Goldstein M, Fahnbulleh F, Gertz E. The interactive video-questionnaire: a new technology for interviewing deaf persons. Am Ann Deaf 1996;141:370-8. http://dx.doi.org/10.1353/aad.2012.0228.
- Steinberg A, Lipton D, Eckhardt E, Goldstein M, Sullivan V. The diagnostic interview schedule for deaf patients on interactive video: a preliminary investigation. Am J Psychiatry 1998;155:1603-4.
- Every Child Matters. London: The Stationery Office; 2003.
- Department of Health . Department of Health 2014. www.gov.uk/government/organisations/department-of-health (accessed 21 October 2014).
- UK Council on Deafness . Annual Report 2004 n.d. www.deafcouncil.org.uk/docs/repo4.doc (accessed 6 September 2012).
- Sutherland H, Young A. Research with deaf children and not on them: a study of method and process. Child Soc 2013;28:366-79.
- Greco V, Beresford B, Sutherland H. Deaf children and young people’s experiences of using specialist mental health services. Child Soc 2009;23:455-69. http://dx.doi.org/10.1111/j.1099-0860.2008.00176.x.
- CAMHS Outcome Research Consortium . CORC 2014. www.corc.uk.net (accessed 21 October 2014).
- Beresford B, Greco V, Clarke S, Sutherland H. An Evaluation of Specialist Mental Health Services for Deaf Children and Young People. York: Social Policy Research Unit, University of York; 2008.
- Schembri A, Cormier K, Johnston T, McKee D, McKee R, Woll B. Sociolinguistic Variation in British, Australian and New Zealand Sign Languages. Cambridge: Cambridge University Press; 2010.
- Schembri A, Johnston T, Bayley R, Cameron R, Lucas C. Oxford Handbook of Sociolinguistics. Oxford: Oxford University Press; 2013.
- Quinn G. Schoolization: an account of the origins of regional variation in British Sign Language. Sign Lang Stud 2010;10:476-501. http://dx.doi.org/10.1353/sls.0.0056.
- Sutton-Spence R, Woll B. The Linguistics of British Sign Language: An Introduction. Cambridge: Cambridge University Press; 1998.
- Mellman L. Countertransference in court interpreters. J Am Acad Psychiatry Law 1995;23:467-71.
- Brennan M, Brien D, Brennan M, Brien D. Dictionary of British Sign Language/English. London: Faber and Faber; 1992.
- Liddell S. Grammar, Gesture and Meaning in American Sign Language. Cambridge: Cambridge University Press; 2003.
- Lane H, Philip F. The Deaf Experience: Classics in Language and Education. Washington, DC: Gallaudet University Press; 2006.
- Ladd P. Understanding Deaf Culture: In Search of Deafhood. Clevedon: Multilingual Matters; 2003.
- Ladd P, Lane H. Deaf ethnicity, deafhood and their relationship. Sign Lang Stud 2013;13:565-79. http://dx.doi.org/10.1353/sls.2013.0012.
- Grosjean F. Bilingualism, biculturalism, and deafness. Int J Bilingual Educ Bilingualism 2010;13:133-45. http://dx.doi.org/10.1080/13670050903474051.
- Plaza-Pust C, Morales-Lopez E. Sign Bilingualism Language Development, Interaction, and Maintenance in Sign Language Contact Situations. Studies in Bilingualism. Amsterdam: John Benjamins Publishing Company; 2008.
- Mason K, Rowley K, Marshall C, Atkinson J, Herman R, Woll B. Identifying specific language impairment in deaf children acquiring British Sign Language: implications for theory and practice. Br J Dev Psychol 2010;28:33-49. http://dx.doi.org/10.1348/026151009X484190.
- Norbury C, Bishop D, Briscoe J. Production of verb morphology: a comparison of SLI and moderate hearing impairment. J Speech Lang Hear Res 2001;44:165-78. http://dx.doi.org/10.1044/1092-4388(2001/015).
- Douglas S, Craig C. Collaborative and iterative translation: an alternative approach to back translation. J Int Mark 2007;15:30-43. http://dx.doi.org/10.1509/jimk.15.1.030.
- Wang W, Lee H, Fetzer S. Challenges and strategies of instrument translation. West J Nurs Res 2006;28:310-21. http://dx.doi.org/10.1177/0193945905284712.
- Acquadro C, Conway K, Hareendran A, Aaronson N. Literature review of methods to translate health-related quality of life questionnaires for use in multinational clinical trials. Value Health 2008;11:509-21. http://dx.doi.org/10.1111/j.1524-4733.2007.00292.x.
- Cha E, Kim K, Erlen J. Translation of scales in cross-cultural research: issues and techniques. J Adv Nurs 2007;58:386-95. http://dx.doi.org/10.1111/j.1365-2648.2007.04242.x.
- Peña E. Lost in translation: methodological considerations in cross-cultural research. Child Dev 2007;78:1255-64. http://dx.doi.org/10.1111/j.1467-8624.2007.01064.x.
- Lee C, Li D, Arai S, Puntillo K. Ensuring cross-cultural equivalence in translation of research consents and clinical documents: a systematic process for translating English to Chinese. J Transcult Nurs 2009;20:77-82. http://dx.doi.org/10.1177/1043659608325852.
- Jones E, Boyle J. Working with translators and interpreters in research: lessons learned. J Transcult Nurs 2011;22:109-15. http://dx.doi.org/10.1177/1043659610395767.
- Graybill P, Aggas J, Dean R, Demers S, Finigan E, Pollard R. A community-participatory approach to adapting survey items for deaf individuals and American Sign Language. Field Methods 2010;22:429-48. http://dx.doi.org/10.1177/1525822X10379201.
- Engleghard GJ. Invariant Measurement: Using Rasch Models in the Social, Behavioural and Health Sciences. New York, NY: Routledge; 2013.
- n.d. www.sdqinfo.com/bb1.html (accessed 26 October 2014).
- International Classification of Diseases. Geneva: World Health Organization; 2010.
- International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use n.d. www.ich.org (accessed 26 October 2014).
- Perneger T. What’s wrong with Bonferroni adjustments. BMJ 1998;316:1236-8. http://dx.doi.org/10.1136/bmj.316.7139.1236.
- Cronbach L. Coefficient alpha and the internal structure of tests. Psychometrika 1951;16:297-333. http://dx.doi.org/10.1007/BF02310555.
- George D, Mallery P. SPSS for Windows Step by Step: A Simple Guide and Reference 11.0 Update. Boston, MA: Allyn and Bacon; 2003.
- Fleiss J. The Design and Analysis of Clinical Experiments. New York, NY: John Wiley & Sons; 1986.
- Milfont T, Fischer R. Testing measurement invariance across groups: application in cross-cultural research. Int J Psychological Res 2010;3:111-21.
- Rasch G. Probabilistic Models for Some Intelligence and Attainment Tests. Chicago, IL: University of Chicago Press; 1960.
- Tennant A, McKenna S, Hagell P. Application of Rasch analysis in the development and application of quality of life instruments. Value Health 2004;7:22-6. http://dx.doi.org/10.1111/j.1524-4733.2004.7s106.x.
- Luce R, Tukey J. Simultaneous conjoint measurement: a new type of fundamental measurement. J Math Psychol 1964;1:1-27. http://dx.doi.org/10.1016/0022-2496(64)90015-X.
- Van Newby A, Conner G, Bunderson C. The Rasch model and additive conjoint measurement. J Appl Meas 2009;10:348-54.
- Andrich D. Rating scales and Rasch measurement. Expert Rev Pharmacoeconom Outcome Res 2011;11:571-85. http://dx.doi.org/10.1586/erp.11.59.
- Wind S, Engelhard G. How invariant and accurate are domain ratings in writing assessment?. Assessing Writing 2013;18:278-99. http://dx.doi.org/10.1016/j.asw.2013.09.002.
- Fischer GH, Molenaar IW. Rasch Models: Foundations, Recent Developments, and Applications. New York, NY: Springer; 1995.
- Teresi J, Kleinman M, Ocepek-Welikson K. Modern psychometric methods for detection of differential item functioning: application to cognitive assessment measures. Stat Med 2000;19:1651-83. http://dx.doi.org/10.1002/(SICI)1097-0258(20000615/30)19:11/12<1651::AID-SIM453>3.0.CO;2-H.
- Arnold SF. Sufficiency and invariance. Stat Probability Lett 1985;3:275-9. http://dx.doi.org/10.1016/0167-7152(85)90044-6.
- Masters G. A Rasch model for partial credit scoring. Psychometrika 1982;47:149-74. http://dx.doi.org/10.1007/BF02296272.
- Linacre J. Sample size and item calibration stability. Rasch Meas Trans 1994;7:328-31.
- Smith E. Detecting and evaluation the impact of multidimensionality using item fit statistics and principal component analysis of residuals. J Appl Meas 2002;3:205-31.
- Marais I, Andrich D. Formalizing dimension and response violations of local independence in the unidimensional Rasch model. J Appl Meas 2008;9:200-15.
- Wainer H, Kiely G. Item clusters and computer adaptive testing: a case for testlets. J Educ Meas 1987;24:185-202. http://dx.doi.org/10.1111/j.1745-3984.1987.tb00274.x.
- Reise S, Morizot J, Hays R. The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Qual Life Res 2007;16:19-31. http://dx.doi.org/10.1007/s11136-007-9183-7.
- Andrich D. Cronbach’s Alpha in the Presence of Subscales n.d.
- Tennant A, Conaghan P. The Rasch measurement model in rheumatology: what is it and why use it? When should it be applied, and what should one look for in a Rasch paper?. Arthritis Rheum 2007;57:1358-62. http://dx.doi.org/10.1002/art.23108.
- Sanne B, Torsheim T, Heiervang E, Stormark K. The Strengths and Difficulties Questionnaire in the Bergen child study: a conceptually and methodologically motivated structural analysis. Psychol Assess 2009;21:352-64. http://dx.doi.org/10.1037/a0016317.
- Becker A, Woerner W, Hasselhorn M, Banaschewski T, Rothenberger A. Validation of the parent and teacher SDQ in a clinical sample. Eur Child Adolesc Psychiatry 2004;13:11-6. http://dx.doi.org/10.1007/s00787-004-2003-5.
- Van Roy B, Veenstra M, Clench-Aas J. Construct validity of the five-factor Strengths and Difficulties Questionnaire (SDQ) in pre-, early, and late adolescence. J Child Psychol Psychiatry 2008;49:1304-12. http://dx.doi.org/10.1111/j.1469-7610.2008.01942.x.
- Mellor D, Stokes M. The factor structure of the Strength and Difficulties Questionnaire. Eur J Psychol Assess 2007;23:105-12. http://dx.doi.org/10.1027/1015-5759.23.2.105.
- Mansbach-Kleinfeld I, Apter A, Farbstein I, Levine S, Ponizovsky A. A population-based psychometric validation study of the Strengths and Difficulties Questionnaire – Hebrew version. Child Neurodev Psychiatry 2010;1:1-12.
- Ruchkin V, Koposov R, Schwab-Stone M. The Strength and Difficulties Questionnaire: scale validation with Russian adolescents. J Clin Psychol 2007;63:861-69. http://dx.doi.org/10.1002/jclp.20401.
- Dickey W, Blumberg S. Revisiting the factor structure of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry 2004;43:1159-67. http://dx.doi.org/10.1097/01.chi.0000132808.36708.a9.
- Koskelainen M, Sourander A, Vauras M. Self-reported strengths and difficulties in a community sample of Finnish adolescents. Eur Child Adolesc Psychiatry 2001;10:180-5. http://dx.doi.org/10.1007/s007870170024.
- Di Riso D, Salcuni S, Chessa D, Raudino A, Lis A, Altoe G. The Strengths and Difficulties Questionnaire (SDQ): early evidence of its reliability and validity in a community sample of Italian children. Pers Individual Diff 2010;49:570-5. http://dx.doi.org/10.1016/j.paid.2010.05.005.
- Goodman A, Lamping D, Ploubidis G. When to use broader internalizing and externalizing subscales instead of the hypothesized subscales on the Strengths and Difficulties Questionnaire (SDQ): data from British parents, teachers and children. J Abnorm Child Psychol 2010;38:1179-91. http://dx.doi.org/10.1007/s10802-010-9434-x.
- Essau C, Olaya B, Anastassiou-Hadjicharalambous X, Pauli G, Gilvarry C, Brayet D., et al. Psychometric properties of the Strength and Difficulties Questionnaire from five European countries. Int J Methods Psychiatr Res 2012;21:232-45. http://dx.doi.org/10.1002/mpr.1364.
- Ronning J, Handegaard B, Sourander A, Morch W. The Strengths and Difficulties Self-Report Questionnaire as a screening instrument in Norwegian community samples. Eur Child Adolesc Psychiatry 2004;13:73-82. http://dx.doi.org/10.1007/s00787-004-0356-4.
- Richter J, Sagatun Å, Heyerdahl S, Oppedal B, Røysamb E. The Strengths and Difficulties Questionnaire (SDQ) – self-report: an analysis of its structure in a multiethnic urban adolescent sample. J Child Psychol Psychiatry 2011;52:1002-11. http://dx.doi.org/10.1111/j.1469-7610.2011.02372.x.
- Niclasen J, Teasdale T, Andersen A, Skovgaard A, Elberling H, Obel C. Psychometric properties of the Danish Strength and Difficulties Questionnaire: the SDQ assessed for more than 70,000 raters in four different cohorts. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0032025.
- Curvis W, Mcnulty S, Qualter P. The validation of the self-report Strengths and Difficulties Questionnaire for use by 6- to 10-year-old children in the UK. Br J Clin Psychol 2014;53:131-7. http://dx.doi.org/10.1111/bjc.12025.
- Muris P, Meesters C, Eijkelenboom A, Vincken M. The self-report version of the Strengths and Difficulties Questionnaire: its psychometric properties in 8- to 13-year-old non-clinical children. Br J Clin Psychol 2004;43:437-48. http://dx.doi.org/10.1348/0144665042388982.
- Bland J, Altman D. Multiple significance tests: the Bonferroni method. Br Med J 1995;310. http://dx.doi.org/10.1136/bmj.310.6973.170.
- van Widenfelt B, Goedhart A, Treffers P, Goodman R. Dutch version of the Strengths and Difficulties Questionnaire (SDQ). Eur Child Adolescent Psychiatry 2003;12:281-9. http://dx.doi.org/10.1007/s00787-003-0341-3.
- Rodriguez-Hernandez P, Betancort M, Ramirez-Santana G, Garcia R, Sanz-Alvarez EJ, De las Cuevas-Castresana C. Psychometric properties of the parent and teacher versions of the Strength and Difficulties Questionnaire (SDQ) in a Spanish sample. Int J Clin Health Psychol 2012;12:265-79.
- Du Y, Kou J, Coghill D. The validity, reliability and normative scores of the parent, teacher and self report forms of the Strengths and Difficulties Questionnaire in China. Child Adolesc Psychiatry Ment Health 2008;2. http://dx.doi.org/10.1186/1753-2000-2-8.
- Obel C, Heiervang E, Rodriguez A, Heyerdahl S, Smedje H, Sourander A. The Strengths and Difficulties Questionnaire in the Nordic countries. Eur Child Adolesc Psychiatry 2004;13:32-9. http://dx.doi.org/10.1007/s00787-004-2006-2.
- Stone L, Otten R, Engels R, Vermulst A, Janssens J. Psychometric properties of the parent and teacher versions of the Strengths and Difficulties Questionnaire for 4–12 year olds: a review. Clin Child Fam Psychol Rev 2010;13:254-74. http://dx.doi.org/10.1007/s10567-010-0071-2.
- Smedje H, Broman J, Hetta J, von Knorring A. Psychometric properties of a Swedish version of the Strengths and Difficulties Questionnaire. Eur J Child Adolesc Psychiatry 1999;8:63-70. http://dx.doi.org/10.1007/s007870050086.
- Giannakopoulos G, Tzavara C, Dimitrakaki C, Kolaitis G, Rotsika V, Tounas Y. The factor structure of the Strengths and Difficulties Questionnaire (SDQ) in Greek adolescents. Ann Gen Psychiatry 2009;8:1-7. http://dx.doi.org/10.1186/1744-859X-8-20.
- Thabet A, Stretch D, Vostanis P. Child mental health problems in Arab children: application of the Strengths and Difficulties Questionnaire. Int J Soc Psychiatry 2000;46:266-80. http://dx.doi.org/10.1177/002076400004600404.
- Heiervang E, Goodman A, Goodman R. Nordic advantage in child mental health: separating health differences from reporting style in a cross-cultural comparison of psychopathology. J Child Psychol Psychiatry 2008;49:678-85. http://dx.doi.org/10.1111/j.1469-7610.2008.01882.x.
- Safronova M, Slobodskaya H, Goodman R, Savina N. Psychological health of schoolchildren and socioeconomic status of a family. Siberian Psychol Mag 2003;18:78-85.
- Shojaei T, Wazana A, Pitrou I, Kovess V. The Strengths and Difficulties Questionnaire: validation study in French school-aged children and cross-cultural comparisons. Soc Psychiatry Psychiatr Epidemiol 2009;44:740-7. http://dx.doi.org/10.1007/s00127-008-0489-8.
- Ghanizadeh A, Izadpanah A, Abdollahi G. Scale validation of the Strengths and Difficulties Questionnaire in Iranian children. Iranian J Psychiatry 2007;2:65-71.
- Gowers S, Harrington R, Whitton A, Lelliott P, Beevor A, Wing J. Brief scale for measuring the outcomes of emotional and behavioural disorders in children: Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA). Br J Psychiatry 1999;174:413-16. http://dx.doi.org/10.1192/bjp.174.5.413.
- Mathai J, Anderson P, Bourne A. Austr N Z J Psychiatry 2004;38:639-43. http://dx.doi.org/10.1080/j.1440-1614.2004.01428.x.
- Mathai J, Anderson P, Bourne A. Comparing psychiatric diagnoses generated by the Strengths and Difficulties Questionnaire with diagnoses made by clinicians (SDQ) as a screening measure prior to admission to a child and adolescent mental health service (CAMHS). Adv Ment Health 2004;1:235-46. http://dx.doi.org/10.5172/jamh.1.3.235.
- Fawcett T. An introduction to ROC analysis. Pattern Recognit Lett 2006;27:861-74. http://dx.doi.org/10.1016/j.patrec.2005.10.010.
- Goodman A, Goodman R. Strengths and Difficulties Questionnaire as a dimensional measure of child mental health. J Am Acad Child Adolesc Psychiatry 2009;48:400-3. http://dx.doi.org/10.1097/CHI.0b013e3181985068.
- Marzocchi G, Capron C, Di Pietro M, Duran Tauleria E, Duyme M, Frigerio A. The use of the Strengths and Difficulties Questionnaire (SDQ) in Southern European countries. Eur Child Adolesc Psychiatry 2004;13:1140-6. http://dx.doi.org/10.1007/s00787-004-2007-1.
- IPSOS Mori . IPSOS Mori GP Survey 2010. www.gp-patient.co.uk/results (accessed 31 March 2011).
- Yao S, Chang C, Zhu X, Jing X, McWhinnie C, Abela R. Measuring adolescent psychopathology: psychometric properties of the self-report Strengths and Difficulties Questionnaire in a sample of Chinese adolescents. J Adolesc Health 2009;45:55-62. http://dx.doi.org/10.1016/j.jadohealth.2008.11.006.
- Farbstein I, Mansback-Kleinfeld I, Levinson D, Goodman R, Levav I, Vograft I. Prevalence and correlates of mental disorders in Israeli adolescents: results from a national mental health survey. J Child Psychol Psychiatry 2010;51:630-9. http://dx.doi.org/10.1111/j.1469-7610.2009.02188.x.
- Munoz-Baell I, Ruiz M. Empowering the deaf: let the deaf be deaf. J Epidemiol Community Health 2000;54:40-4. http://dx.doi.org/10.1136/jech.54.1.40.
- Woolfe T, Smith P. The self-esteem and cohesion to family members of deaf children in relation to the hearing status of their parents and siblings. Deafness Educ Int 2001;3:80-96. http://dx.doi.org/10.1179/146431501790561043.
- Meadow-Orlans K, Erting C. Deaf People in Society: Mental Health and Deafness. London: Whurr; 2000.
- Communicating with Your Deaf Child. London: NDCS; 2011.
- Heiervang E, Goodman R. Advantages and limitations of web based surveys: evidence from a child mental health survey. Soc Psychiatry Epidemiol 2011;46:69-76. http://dx.doi.org/10.1007/s00127-009-0171-9.
- Roberts C, Hindley P. The assessment and treatment of deaf children with psychiatric disorders. J Child Psychol Psychiatry 1999;40:151-67. http://dx.doi.org/10.1111/1469-7610.00430.
- Hindley P, Kitson N, Graham J, Martin M. Ballantyne’s Deafness. London: Whurr Children; 2001.
Appendix 1 Strengths and Difficulties Questionnaires multi-informant algorithm
Strengths and Difficulties Questionnaire: predictive algorithm in SPSS
The predictive algorithm is based on up to 12 input variables:
phyper = SDQ hyperactivity score from parent SDQ
thyper = SDQ hyperactivity score from teacher SDQ
shyper = SDQ hyperactivity score from self-report SDQ
pconduct = SDQ conduct problems score from parent SDQ
tconduct = SDQ conduct problems score from teacher SDQ
sconduct = SDQ conduct problems score from self-report SDQ
pemotion = SDQ emotional symptoms score from parent SDQ
temotion = SDQ emotional symptoms score from teacher SDQ
semotion = SDQ emotional symptoms score from self-report SDQ
pimpact = SDQ impact score from parent SDQ
timpact = SDQ impact score from teacher SDQ
simpact = SDQ impact score from self-report SDQ
The algorithm generates four output variables:
sdqed = prediction of an emotional disorder
(0 = unlikely, 1 = possible, 2 = probable)
sdqcd = prediction of a conduct disorder
(0 = unlikely, 1 = possible, 2 = probable)
sdqhk = prediction of a hyperactivity disorder
(0 = unlikely, 1 = possible, 2 = probable)
anydiag = prediction of any psychiatric disorder
(0 = unlikely, 1 = possible, 2 = probable)
set format = f8.0.
computevarmis = 0.
recode varmis (0=sysmis).
execute.
if (phyperge 0 and pimpactge 0) phk=0.
if (phyperge 6 and pimpactge 1) phk=1.
if (phyperge 7 and pimpactge 2) phk=2.
if (phyperge 9 and pimpactge 1) phk=2.
execute.
if (shyperge 0 and simpactge 0) shk=0.
if (shyperge 6 and simpactge 1) shk=1.
if (shyperge 7 and simpactge 2) shk=2.
execute.
if (thyperge 0 and timpactge 0) thk=0.
if (thyperge 6 and timpactge 1) thk=1.
if (thyperge 7 and timpactge 2) thk=2.
execute.
compute pshk=phk.
execute.
if (sysmis(phk)) pshk=shk.
execute.
if (phkge 0 or shkge 0 or thkge 0) sdqhk=0.
if (pshk=2 or thk=2) sdqhk=1.
if (pshk=1 and thk=1) sdqhk=1.
if (pshk=1 and sysmis(thk)) sdqhk=1.
if (sysmis(pshk) and thk=1) sdqhk=1.
if (pshk=2 and thk=1) sdqhk=2.
if (pshk=2 and thk=2) sdqhk=2.
execute.
if (pconductge 0 or tconductge 0 or sconductge 0) sdqcd=0.
if (pconductge 4 or tconductge 3 or sconductge 5) sdqcd=1.
if (pconductge 5 and pimpactge 2) sdqcd=2.
if (tconductge 4 and timpactge 2) sdqcd=2.
if (sconductge 6 and simpactge 2) sdqcd=2.
if (sysmis(pimpact) and sysmis(timpact) and sysmis(simpact)) sdqcd = varmis.
execute.
if (pemotionge 0 or temotionge 0 or semotionge 0) sdqed=0.
if (pemotionge 5 and pimpactge 1) sdqed=1.
if (temotionge 5 and timpactge 1) sdqed=1.
if (semotionge 6 and simpactge 1) sdqed=1.
execute.
compute pem= 0.
if (pemotionge 6 and pimpactge 2) pem=1.
execute.
compute tem= 0.
if (temotionge 6 and timpactge 2) tem=1.
execute.
compute sem= 0.
if (semotionge 7 and simpactge 2) sem=1.
execute.
compute allem= pem + tem + sem.
if (allemge 1) sdqed=2.
if (allem=1 and sdqcd=2) sdqed=1.
if (allem=1 and sdqhk=2) sdqed=1.
if (sysmis(pimpact) and sysmis(timpact) and sysmis(simpact)) sdqed = varmis.
execute.
if (sysmis(sdqed) and sysmis(sdqcd) and sysmis(sdqhk)) anydiag = varmis.
if (sdqedge 0 or sdqcdge 0 or sdqhkge 0) anydiag=0.
if (sdqedge 1 or sdqcdge 1 or sdqhkge 1) anydiag=1.
if (sdqedge 2 or sdqcdge 2 or sdqhkge 2) anydiag=2.
execute.
delete variables varmis phk shk thk pshk pem tem sem allem.
List of abbreviations
- ADHD
- attention deficit hyperactivity disorder
- ANOVA
- analysis of variance
- ASD
- autism spectrum disorder
- BATOD
- British Association of Teachers of the Deaf
- BSL
- British Sign Language
- CAMHS
- Child and Adolescent Mental Health Services
- CFA
- confirmatory factor analysis
- CFI
- comparative fit index
- CHARGE syndrome
- C coloboma of the eye, central nervous system anomaliesH heart defectsA atresia of the choanaeR retardation of growth and/or developmentG genital and/or urinary defects (hypogonadism)E ear anomalies and/or deafness
- CORC
- CAMHS Outcome Research Consortium
- DAWBA
- Development and Well-Being Assessment
- DIF
- differential item functioning
- EFA
- exploratory factor analysis
- HI
- hearing impaired/impairment
- ICC
- interclass correlation coefficient
- IQ
- intelligence quotient
- IRT
- item response theory
- NDCAMHS
- National Deaf Child and Adolescent Mental Health Service
- NDCS
- National Deaf Children’s Society
- NIHR
- National Institute for Health Research
- OCD
- obsessive–compulsive disorder
- PPI
- patient and public involvement
- RMSEA
- root-mean-square error of approximation
- SD
- standard deviation
- SDQ
- Strengths and Difficulties Questionnaire
- SORD
- Social Research with Deaf People
- SSE
- Sign Supported English
- TLI
- Tucker–Lewis index (non-normed fit index)
- ToD
- teacher of the deaf
- VLS
- video library service