Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 10/1013/42. The contractual start date was in January 2012. The final report began editorial review in March 2014 and was accepted for publication in September 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Sally Brearley acted as the Chair of the Prime Minister’s Nursing and Care Quality Forum from January 2011 to December 2013.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Maben et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction and background
Introduction
This report describes the second phase of a study investigating the impact of a move to all single room accommodation in a new hospital. It draws upon data from phase 1 of the study, which was funded by the Engineering and Physical Sciences Research Council (EPSRC) through the Health and Care Infrastructure Research and Innovation Centre (HaCIRIC) at Imperial College London. In phase 1 we carried out in-depth research on care delivery, working practices and staff and patient experiences in the old hospital buildings (Pembury Hospital and Kent and Sussex Hospital) during the period in the run-up to the move to the new Tunbridge Wells Hospital, giving us baseline, ‘before’, practices and experiences in four cases (postnatal ward, acute assessment unit, acute general surgery ward and older people’s ward). We also undertook interviews with 20 key stakeholders including the architects, builders and senior nursing staff and executives in the trust. This phase 1 work was completed in August 2011. 1
The study reported here (phase 2) was undertaken at Maidstone and Tunbridge Wells NHS Trust’s new 512-bed hospital in Pembury, Kent – the Tunbridge Wells Hospital – and two hospitals which acted as controls (steady state and new build) between 2012 and 2013. We have (with the trust’s permission) deliberately chosen not to try to anonymise the 100% single room new build hospital at Tunbridge Wells, as it would be very difficult to do so and by not doing so we have been able to use photographs and plans, which greatly add to the data. Tunbridge Wells Hospital was completed in December 2010, with women’s and children’s services moving into the building in January 2011 and the remaining clinical services following in September 2011. It is the first district general hospital in England with single rooms throughout the inpatient accommodation. Data collection for this phase of the study was undertaken 12–15 months after the move to avoid teething problems and to try to capture working practices and experiences once they had had a chance to bed down.
Together, phases 1 and 2 deliver a project that answers significant questions for health care generally and the NHS in particular: how does the move to all single room hospital accommodation impact upon care delivery and working practices, staff experience, patient experience, costs and safety?
Background
Historically, the principles of hospital design have been based on Florence Nightingale’s 19th-century observations about the advantages of natural light, ventilation and cleanliness. 2 Long open wards of about 30 beds became the standard inpatient accommodation in hospitals globally. 3 Over the years, clinical practice and opinions about health care have changed and the suitability of open wards in modern hospitals has been called into question. 4 In the 1950s, new build hospitals experimented with ‘racetrack’ wards, where beds are arranged round the periphery with a corridor or ‘track’ surrounding the offices and other ancillary areas. 5 More recently, hospital design has used multibedded bays, which usually contain four to six beds. 6 Meanwhile, private health-care facilities have mainly single rooms. At the present time, internationally, the case is being made for more single room accommodation in new hospital designs, and some researchers argue for the abolition of all shared accommodation. 7 This is largely based on the belief that patients prefer single rooms and benefit from improved patient outcomes compared with hospital wards. 8 Hospital designs based on higher proportions of single room accommodation are likely to impact on patients’ health outcomes, staff and organisations but the nature and extent of the impact is as yet unclear. 9
Research on single room accommodation is a relatively new area within hospital design. 10 Evidence-based hospital design aims to improve outcomes for specific design characteristics or interventions,11 including room occupancy, ventilation systems, the acoustic environment, views of nature/landscapes,12–14 lighting, ergonomic design, and floor layouts and work settings. 2,15,16 More is now known about the impact of hospital design on patient safety,17 patient and staff satisfaction, a patient’s stress experience and organisation performance metrics. 18 For example, good design can reduce injury from falls, infections and medical errors; it can minimise environmental stressors19,20 and enhance pain control. 21 However, design decisions about hospital accommodation are not only based on scientific evidence such as patient outcomes; they also involve value-based judgements such as patient preferences for care, operational judgements about demand or changing clinical needs and priorities, and economic considerations. 8 An area of developing research is flexibility of hospital design to accommodate future changes in service delivery based on medical requirements (e.g. acuity-adaptable rooms) and patient preferences (e.g. private or semiprivate). 22 Advances have also been made using participatory ergonomics to involve staff in designing work spaces5 and to involve patients in hospital design. 11,23 Evidence from the USA11 and from UK childbirth environments suggests that the involvement of patients in ward and hospital design can improve health-care outcomes. 24,25
UK context
The proportion of single rooms in UK NHS hospitals is on the rise. 2 In UK hospitals, the percentage of single rooms as a proportion of total available beds increased from 22.6% in 2002–3 to 32.7% in 2009–10. Since 2001, Department of Health guidance has been that ‘the proportion of single rooms in new hospital developments should aim to be 50% and must be higher than the facilities they are replacing’. 3 Thus, increasingly, new hospital design includes greater proportions of single room accommodation and, in some cases, all single rooms. 26
The argument for single rooms in NHS hospitals is gaining prominence in the context of increasing public and political expectations about the quality of health care in general. 27 Political aspirations for more single room hospital accommodation are, in part, a response to a perceived public desire for such accommodation, and to provide greater privacy and dignity in NHS hospitals. 28 Single rooms can address a patient’s dislike of mixed-sex accommodation and difficulties of accommodating patients according to gender, by eliminating mixed-sex wards or bays. 29 Problems with mixed-sex bathrooms can remain, unless the rooms are en suite – a move that is relatively easy with new builds, but may be harder if existing facilities are being converted. 28 Single rooms mean that patients are unlikely to need to be moved because a bay needs to ‘change sex’ or because they need to be isolated;30 this potentially reduces stress for patients and risk of infection spread. 31 In the UK independent sector, the use of single room accommodation is far more common than in the NHS and it has been suggested this contributes to its lower rate of health-care-associated infections (HCAIs). 32 HCAI (also referred to in the medical literature as nosocomial infection) has become more common as medical care has grown more complex, causing significant morbidity, mortality and cost internationally. 33 Reduced HCAI is an important potential outcome of single room hospital design and we examine the issues in several sections of this report. In the next section we summarise existing evidence on infection rates and single room hospital design. Part of the argument in favour of single rooms is that they can also be used to accommodate diverse functions, such as patient recovery after surgery or other procedures and providing in situ medical treatment – for example wound dressing and physiotherapy – as well as offering flexible accommodation for many different types of patient, such as maternity, mental health and paediatric, together with the equipment required for each specialty. 8
At the time of research commissioning, there were no NHS hospitals and few general wards in the UK with all single room accommodation, and the opportunities for evaluation were limited. Bevan ward at Hillingdon Hospital is one of the few test wards in the UK supported by the Department of Health and the National Patient Safety Agency (NPSA). Evaluation of Bevan ward based on patient and staff perspectives shows a range of perceived positive outcomes for staff and patients (including patient privacy and comfort, prevention of infection, reduction in medication errors, ease of toileting and bathing). However, Bevan ward is the only ward with 100% single rooms in an otherwise unchanged estate, so it provides limited evidence for whole hospital redesign, where multifunction rooms for nurse breaks, staff bases and communal social spaces for patients and visitors would be needed. 34
At the present time, there is little good-quality evidence from UK hospitals about the likely impact of single room accommodation on patients, staff or health-care organisations. Such evidence is much needed to inform decisions about single rooms and the extent to which they may be associated with inflated capital outlays and capital costs, augmented staffing levels, reduced patient safety and greater staff walking distances. 35 Economic considerations are also important when NHS managers have to make efficiency savings to meet rising health-care costs36 yet maintain the quality of, and access to, health care. Most available evidence (discussed in the next section) derives from studies in the USA and Scandinavia, and, while some evidence may be transferable, not all is likely to directly translate to the UK because of different financial, cultural and organisational systems. Gaps in the evidence are discussed in the next section.
Current state of the evidence
In this part of the report we draw together evidence from the health-care literature to examine what is known about the impact of single room accommodation and to identify gaps in the evidence. We explore impact in terms of the range of potential advantages and disadvantages for patients and staff and potential economic outcomes. These are summarised in Boxes 1–3 and discussed below.
-
Potential advantages for patients include increased privacy, dignity and less disruption from other patients. Improved control over their environment could mean greater comfort, enhanced sleep, enhanced contact with families, better communication with staff and increased patient satisfaction.
-
Potential outcome advantages include fewer medication errors, reduced infection rates and faster patient recovery rates.
-
Potential disadvantages include less surveillance by staff; increased failure to rescue and increased rates of slips, trips and falls; reduced social interaction and greater patient isolation.
-
Perceived advantages for staff include potential for more personalised patient contact and potentially fewer interruptions.
-
Perceived disadvantages include increase in staff travel distances (less time for direct care); potential need for an increase in staffing levels as a result of more single rooms and/or adjustments to staff skill mix; increase in staff stress, staff working in isolation and increased risks to personal safety.
-
Perceived economic advantages include potential for cost savings associated with reduced length of stay, reduced infection rates and fewer medication errors.
-
Perceived economic disadvantages include increased land and building costs, increased maintenance costs and increased staffing costs.
For patients, a potential advantage of single room accommodation could be increased privacy, dignity and comfort. 11,37,38 However, the evidence does not clearly point to a preference for single rooms among patients and little is known about patient preferences across different age and cultural groups. 39 One UK survey (IPSOS Mori) found that around 35% of the public preferred single rooms, while around 40% preferred small (single-sex) bays. 28 However, this was a survey of the perceived (and future) needs and desires of the general public, not of hospital patients, who, when sick, may express different preferences. It is important to note that for many patients the privacy associated with single rooms may not be as important as other aspects of the hospital environment, such as a sense of safety, security or connection. A recent Scandinavian study showed that positive aspects of multibedded accommodation included a patient culture of taking care of one another and enjoying the company of other patients, which gave a sense of security to both patients and nurses. However, these advantages were slight and could easily become disadvantages if roommates were very ill or confused. 40 There is some evidence that single rooms are associated with greater patient satisfaction: a Welsh hospital with 100% single rooms reported 95% satisfaction. 41 Results from the York Health Economics Consortium evaluation of the pilot ward of 100% single rooms at Hillingdon Hospital suggest that patients in single rooms were more satisfied than those in multibedded rooms [yet infection rates did not decrease and length of stay (LOS) was unaltered]. 29
In other studies, patients rated privacy and personal space as important but they also said that when ill they wanted nurses to be closer. 12,13,42 There is also evidence of more speech privacy and higher patient-reported satisfaction with doctor and nurse communication in single room patient accommodation. 11 A study of patient–physician communication in the Netherlands suggested that patients find it easier to raise questions with staff during ward rounds in single rooms than in multibedded rooms and feel that staff are more empathetic towards them. 43
There is potential for improved outcomes for patient safety with single rooms. Single rooms could mean fewer medical errors because of less interruption and distraction,29 and room design that incorporates dedicated space for patient supplies and medication can help to reduce medication errors. 20 In 2007, the NPSA undertook a study including a review of empirical evidence, an analysis of National Reporting and Learning Systems (NRLS) data and interviews with clinicians and staff with experience of current conditions, who would be directly affected by the use of single rooms. 38 These authors concluded that if there is good design (layout which includes observation points and large glazed windows and doors) the evidence does not suggest that single rooms reduce staff-to-patient observation or increase accidents or ‘near miss’ events.
The evidence of associations between single rooms and HCAI, including evidence of causal effects on infection rates is complex. Relevant research is dispersed across clinical, service management and design literatures8,11,44 and extends to include themes of infection control effectiveness, transmission routes, the impact of movement patterns between health-care institutes, the development of antimicrobial resistance and strain competitiveness or cocolonisation. 45 Specific studies relate to different types of impact or measures of infection, clinical settings, population groups, different types of infection site (e.g. respiratory, urine, wound, blood) and organisms, including Escherichia coli (Migula 1895) Castellani and Chalmers 1919, methicillin-resistant Staphylococcus aureus Rosenbach 1884 (MRSA), Clostridium difficile (Hall and O’Toole 1935) Prévot 1938 (C. diff. ) and Pseudomonas Migula 1984. 33 It is known that HCAIs are spread by numerous paths including surfaces (especially hands), air, water, intravenous routes, oral routes and surgery. 8,9 Some authors suggest that single rooms improve infection control because of better physical design46,47 that enables patient isolation at admission, decontamination after discharge and maintaining clean air. 11 Mechanisms for the reduction of infections through single rooms could include reduction of person-to-person contacts and limiting the spread of infection by person–surface–person contacts. 48 However, the relationships are complex, and multiple organisational and management factors, such as clinical leadership and staffing, are also known to have a significant impact on infection control in hospitals. 49 Staff infection control knowledge50 and risk perceptions of HCAI within different clinical environments may also influence HCAI rates. 51 Models of nursing may also be an important factor; for example, the ‘cohorting’ of patients, by grouping together infectious patients and nursing them within an area of a hospital ward to reduce spread of infection, can be more easily achieved with single rooms. However, to be effective, staff cohorting is also essential (having a cohort of staff who work only with ‘infected’ patients),52 and this may be as hard to achieve in single room accommodation as in other designs. The high degree of heterogeneity of studies, together with inter-related causal factors described above, makes it difficult to draw clear conclusions about causal effects of single rooms on HCAI rate. Two rigorous systematic reviews have been conducted to summarise the evidence on the association of single room accommodation and HCAI. Dettenkofer et al. 53 included 17 historic and prospective cohort studies between 1975 and 2001 in their systematic review (details of these findings can be found in Appendix 1). The majority of studies were conducted in intensive care units (ICUs; n = 9), followed by surgical wards (n = 4), isolation units (n = 2) and general hospitals (n = 2). Three out of nine studies in ICUs reported a reduction of infections, while no reduction was found for postoperative wound infections in the four studies of surgical wards. A subsequent review by Whitehead et al. 54 identified two additional studies between 2001 and 2006. The two studies, in neonatal55 and paediatric intensive care settings,56 showed a reduction of the mean number of infections in isolation or single rooms in comparison with multibedded bays (further detail of these studies is in Appendix 1); reduced HCAI rates may also be related to shorter LOS associated with single rooms. More recent studies all conducted in ICUs57–60 have shown a reduction in several types of infections including MRSA and C. diff. Meta-analysis of infection rate from studies of single rooms is problematic because of different study designs, patient groups, types of infection or organism under consideration, and geographical setting. 53,61 Furthermore, there is evidence that HCAI rates usually show a short-term decline following any move to a new hospital building but that the effect is short-lived. 62 Furthermore, findings from studies of isolation rooms may not be transferable to single room accommodation because of differences in patient confinement, ventilation, barrier nursing or other infection control measures to limit transmission risk. 32,39 While an association of single room accommodation and decreased infection rates is repeatedly shown in intensive care settings including paediatric populations,53,57–61 for all other patient populations evidence of an association of single room accommodation and HCAIs is absent or equivocal. For the purposes of our study and research questions (listed in Chapter 2, Research questions), we consider infection rate as a possible safety outcome associated with single room accommodation, as explained in Chapter 2, Staff travel distances.
There is some evidence that patients in single rooms recover faster than those on wards. 11,37,38 This has been attributed to lower patient stress, but other factors that influence a healing environment, such as being able to see daylight and nature views or infection control practices, may have a more significant impact on patient recovery outcomes. 11
Although some patients may prefer and benefit from single rooms, this is not the case for all patients. Single rooms could mean less surveillance by staff, increased failure to rescue, increased rates of slips, trips and falls,41 and patients experiencing falls unnoticed. 11,37,38,63 Potential disadvantages may also include reduced social interaction64 and greater patient isolation. 11,26,38 For some patient groups, such as people with a stroke65 or mental health problems,66 the isolating effects of single rooms could impede the therapeutic process and overall experience of care. Research on routine isolation of infected patients in hospitals31 provides strong evidence about the negative impact of isolation. In a systematic review of 16 studies, the majority showed that isolation had a negative impact on patients’ mental well-being and behaviour, including depression, anxiety and anger, and that some health-care workers spent less time with patients in isolation,67 which may have implications for patients in single rooms per se. An interview study of people with cancer in Denmark68 found that refuge from fellow patients was hard to achieve in multibedded rooms and the fact that personal conversations might be overheard by fellow patients caused patients to withhold important information from health-care professionals. Despite the challenges, 18 of the 20 patients (10 male and 10 female) preferred the companionship associated with multibedded rooms.
Young people in hospital may prefer the company and security of sharing accommodation with people their own age. 69 Other patient groups may value different aspects of hospital environments; for example, new mothers may want a family-centred environment which can support bonding with their baby and developmental care;70,71 stroke patients benefit from environments that support physical activity;65 and patients who are receiving long-term critical care may benefit most from an environment that enables them to maintain the personal activities of daily living. 72 Patients near the end of life and their families may want an environment that provides a sense of emotional or physical proximity to loved ones. 73 These aspects of the hospital environment may be more important than single rooms in influencing patient satisfaction74 and health-care quality. 75
Aspects of hospital and ward design have the potential to impact on all health-care staff; however, there is little UK research evidence about staff perceptions or experiences of delivering care to patients in single room accommodation or the impact on morale, motivation and staff engagement. A report by the York Health Economics Consortium described advantages of single room accommodation for staff. This included the potential for more personalised patient contact and fewer interruptions to care delivery. 29 However, as these outcomes are so closely linked to staffing and other variables it is difficult to control for these factors or to say what the impact on patient outcomes at ward level might be.
Possible disadvantages of single rooms could include increased distances for staff to walk. However, the evidence relating to ward layout and nurses’ observation,2 walking distances76 and workload4 is complex, making it difficult to draw conclusions about implications for staff, patient care or outcomes. Several authors have suggested the potential need for an increase in staffing levels as a result of more single rooms and/or adjustments to staff skill mix. 26,37,38 The NPSA study refuted the suggestion that single-patient rooms require increased levels of staff to prevent patient alienation. 38 However, no patients were directly involved in the study, suggesting this statement is based on the evidence from other countries. A US study using comparative design to investigate how clinicians perceive, evaluate and adjust to a new hospital environment found the single-patient room model increased the workload of many clinicians and their stress had increased after 15 months. 77 The study showed that employees with 3 or more years of service had significantly higher stress than others, suggesting that staff with established work patterns may find it more difficult to adjust to new hospital designs. Staff stress could be greater if they feel less able to monitor patients, have less time for direct care or are less visible to patients. 30 Staff working in single room hospitals may spend more time working in isolation, which could have negative implications for team working, innovation78 and staff well-being,79 but there is little UK evidence to support these suggestions. Staff working in isolation may experience greater risks to personal safety from violence, aggression or physical assault,80 and factors which are known to trigger anger and aggressive behaviour (e.g. emotional anxiety, patient stress, lack of hydration/nutrition) could be harder to detect and respond to if patients are in single rooms. 81
A study by the Commission for Architecture and the Built Environment16 found links between hospital design and nurse recruitment, retention and productivity. Overall, however, there is not yet sufficient evidence available in the UK to be able to draw valid and reliable conclusions in terms of the impact on nursing workforce requirements, or indeed requirements of other staff groups.
The economic advantages and disadvantages of single rooms have also been debated in the literature. As part of the present research study we undertook a focused literature review of the economic impact of single rooms (see Appendix 1). The review explored evidence on building costs, staff costs and outcomes as reported in the research literature. Overall, the review found little comparable evidence about the construction and operating costs associated with single room accommodation. The majority of studies are not based in the UK and, even within the UK, construction costs are likely to vary with geographic setting and hospital design. In general, a single room (and en suite bathroom) requires more space and this may need extra land, depending on the site and building design. 82–84 Acuity-adaptable rooms can cost even more because of the need for more space and equipment, but some cost savings may be made because of a reduced need for patient transfers. 85 Maintenance costs per square metre are likely to be the same, but the greater space requirement for ward areas means that overall maintenance costs may be higher. It is not possible to say whether or not single rooms increase staffing costs because of the scarcity of evidence for impact on staffing levels or skill mix. 6 Although many claims have been made about the cost savings associated with single room accommodation – including reduced LOS, infection rates and fewer medication errors61,86 – there is very little evidence from well-designed research studies to support these claims.
Summary
Internationally, health systems and individual hospitals are keen to explore higher proportions of single room accommodation in new builds, but little is known about the impact of this type of accommodation on patients, staff and organisations.
In the UK, NHS providers are encouraged by Department of Health guidance to provide higher proportions of single room accommodation (the aim is 50%) in any new hospital builds. As yet, there are few wards or hospitals in the UK with all single room accommodation and the opportunities for evaluation have been few.
Evidence-based health-care design is a growing area of research. To date, little empirical work on single rooms has been undertaken in the UK, with most research emanating from the USA and Scandinavia. The available evidence is equivocal, suggesting a range of potential benefits for patients and staff but also a range of potential disadvantages.
Potential advantages of single room accommodation include increased patient privacy, greater dignity and less disruption from other patients. If patients have improved control over their environment this could mean greater comfort, enhanced sleep, enhanced contact with families, better communication with staff and increased patient satisfaction. Improved outcomes could include fewer medication errors, reduced infection rates and faster patient recovery rates. Staff could experience more personalised patient contact and fewer interruptions.
Potential disadvantages of single room accommodation include less surveillance by staff; increased failure to rescue and increased rates of slips, trips and falls; reduced social interaction and greater patient isolation; increase in staff travel distances (less time for direct care); potential need for an increase in staffing levels as a result of more single rooms and/or adjustments to staff skill mix; increase in staff stress; staff working in isolation; and increased risks to personal safety.
The impact of single room accommodation on staff-to-patient observation, staffing levels, adjustments to staff skill mix and staff travel distances is unclear.
However, important issues that require further research include concerns about potential additional workload,4 stress79 and risks to staff;30,77,80,81,85 less patient surveillance;11,37,38 and patients feeling isolated or alienated. 38,68,69
There is limited evidence about the costs and economic outcomes of higher proportions of single room accommodation. 82–84 In the UK there is insufficient strong evidence to be able to draw valid and reliable conclusions about single rooms or models of hospital design based on this type of accommodation. The international health-care literature shows that decisions around ward design are complex and trade-offs are likely to be necessary between evidence-based designs, patient and staff preferences, changes in clinical needs/demand and economic considerations.
Further research and evaluation of UK hospitals is needed to build evidence to inform and improve ward and hospital designs at ward and hospital level and nationally, including:
-
examining impact on patient outcomes at hospital level including implications for having sufficient beds and safe hospital occupancy87,88
-
addressing how to ensure privacy when it is needed and also facilitate communication and social interactions to make a period of hospitalisation more manageable for patients68 and more satisfactory for staff
-
exploring issues of managing risk/safe care practices associated with single rooms, for example staff ability to deliver direct patient care while also monitoring other patients on the ward and making judgements about priorities of caregiving. 12,13,42
These emergent issues reinforce the need for research to examine single rooms not only as physical spaces but as personal, social and cultural spaces of caregiving.
Chapter 2 Methods
Introduction
This report is based on data collected during the second phase of a two-phase longitudinal mixed-methods study. Phase 1 data are reported fully in a separate report,1 although they are used throughout the report as a basis for comparison and to orientate readers to key phase 1 findings. The case study methods and data collected in this study (phase 2) replicate as far as possible the case study methods and data collected in phase 1 (Table 1).
| Aims: to identify the impact of the move to 100% single room accommodation on: | Research question(s) | Methods |
|---|---|---|
| Care delivery and working practices | How are work patterns disrupted and reconstituted, including through trial-and-error use of new approaches (and to what extent are these successful/unsuccessful)? | Case study data:
|
| Staff experience | How are staff perceptions and experiences of the move to single rooms shaped by formal organisational and change management processes? What are the advantages and disadvantages of a move to all single rooms for staff? Does the move to all single rooms affect staff experience and well-being, and their ability to deliver effective and high-quality care? |
Case study data:
|
| Patient experience | What are the advantages and disadvantages for patients of a move to all single rooms? How does the move to all single rooms affect patient experience and well-being? Does it affect diverse patient groups differently? |
Case study data:
|
| Safety outcomes (including falls and infection rates) | What are the influence and costs of a move to a new hospital with 100% single rooms compared with the nearest equivalent design with standard proportions of single rooms? What impact do different percentages of inpatient single rooms have on patient safety outcomes (including falls and infection rates) compared with standard accommodation? |
Quasi-experiment secondary data:
|
| Costs | How does the move to all single rooms affect costs, including nurse staffing, patient services and costs associated with adverse patient events? How do different percentages of in-patient single rooms (50–100%) influence costs? What is the influence of a move to a new hospital (compared with no move) on costs? |
Cost analysis secondary data:
|
Research approach
The research includes a pre/post mixed-methods evaluation in a single hospital within which there are three distinct but related workstreams:
-
a before-and-after mixed-methods case study design (with four nested cases) within a single hospital
-
a quasi-experimental before-and-after study using two control hospitals (one steady state and one move to new build with fewer than 100% single rooms)
-
an analysis of comparative costs associated with single rooms.
This chapter provides an overview of the research approach and questions. It also presents the methods used and provides details of the study design, sampling, data collection and analysis.
In our original project proposal we included applying a realist evaluation framework1 to explore the effect of single rooms in different circumstances and on different stakeholder groups. This proposal was reconsidered during the project for a variety of reasons. First, and most importantly, realist evaluation is an approach developed for evaluating large-scale complex social change programmes. While bringing a new hospital into operation has some similarities with implementing a programme, important differences became apparent to the project team that made a realist framework problematic to apply. 89–91 Second, during the course of the project, unresolved methodological issues relating to how to define context–mechanism–outcome configurations that form the basis for realist analysis became the focus of critiques of the approach. 92,93 In view of these, the research team decided that there were few advantages in adopting a realist framework over and above using conventional methods, such as case study and quasi-experimental design. However, our approach has been broadly informed by ‘realist’ perspectives, particularly in terms of identifying stakeholder intentions; utilising their knowledge of ‘how things work’ on the ground; and defining and testing ideas about ‘what works’ in different contexts. Thus, our aim was still to understand what worked and for whom, in what circumstances, and how.
Research ethics and patient and public involvement
The study was approved by Maidstone and Tunbridge Wells NHS Trust Research and Development department as a service evaluation project in July 2009 and access renewed for phase 2 in December 2012 (reference 09/07/049A). Ethical approval was obtained from King’s College London Psychiatry, Nursing and Midwifery Research Ethics Subcommittee (approval granted January 2010 and for phase 2 in January 2012, reference PNM/09/10-30).
Patients and the public were involved throughout this study, as detailed in Appendix 2.
Research questions
The research seeks to identify the impact of the move to 100% single room accommodation on five key areas:
-
care delivery and working practices
-
staff experience
-
patient experience
-
safety outcomes
-
costs.
The overall aim of the project is to explore the implications for the clinical workforce and patients of a move from ‘traditional’ facilities – comprising primarily open-plan ‘Nightingale-style’ wards – to a newly built facility in which all accommodation is in single rooms.
Table 1 provides details of the specific research aims, the research questions that align with these and the principal methods that were used to gather data to answer them.
Before-and-after mixed-methods case study
A before-and-after mixed-methods case study design was used to explore the impact of the move to all single room hospital accommodation on care delivery, working practices and staff and patient experience. Phase 1 data provide a ‘baseline’ understanding of care delivery, working practices and staff and patient experience in four case study wards (see Appendix 3 and phase 1 report). 1
The following sections describe the main components of data collection for the pre-/post-move evaluation: interviews with key stakeholders to explore the organisational context in which the move took place and the ‘nested’ ward case studies. The latter had five components: observation of practice; measurement of staff travel distances; a staff questionnaire survey; interviews with staff; and interviews with patients. A separate section describes how the data were analysed.
Four case study adult inpatient wards were purposively selected to encompass a range of different clinical areas and patient groups. Wards selected were acute assessment, surgical, medical (older people) and maternity (see Chapter 4 for full descriptions of each case study ward, including their physical layout and staffing). Case study data collection was undertaken between September 2012 and June 2013. Staff and patients invited to take part received an information sheet about the research study (see Appendix 4).
Organisational context: key stakeholder interviews
Data on organisational context were collected through a series of key stakeholder interviews (n = 41) which were undertaken between August 2009 and July 2010 for phase 1 (n = 20) (see Appendix 5 for phase 1 sample and interview guide) and between August 2012 and May 2013 for phase 2 (n = 21). In addition to these interviews in phase 2, a mini focus group was undertaken with Allied Health Professionals (AHPs). Trust staff interviewed were sampled purposively and through snowball sampling (Table 2).
| Senior trust staff | Medical staff and AHPs | Case study ward managers and ward clerk |
|---|---|---|
| Interim director of nursing Head of nursing for emergency services Head of nursing for surgery Head of midwifery/head of women’s, children’s and sexual health services/coclinical director for maternity services Deputy director of infection prevention and control Assistant director estates and facilities Therapy manager Senior matron safeguarding vulnerable adults |
Consultant respiratory physician Medical director (and consultant in anaesthetics and intensive care) Senior physiotherapist (n = 2) (orthopaedic and medical rehabilitation) Senior occupational therapist (n = 2) (acute and orthopaedic) Dietitian Speech and language therapist Mini-focus group with five participants (all different from the above): one dietitian, two occupational therapists and two physiotherapists |
Ward manager – surgery (interview also involved junior sister/practice development nurse) Ward manager – acute elderly care Ward manager – AAU Ward manager – postnatal and transitional care unit Ward clerk/administrator (AAU) |
Key stakeholders were provided with the staff research interview information sheet (see Appendix 4), which lasted 30–60 minutes. The topic guide prompted exploration of the early challenges and experiences across the trust and issues of implementation relating to transition to all single room ward accommodation (see Appendix 6).
Observation of practice
Procedure
The aim of the observation of practice was to understand how and where staff spent their time and determine if the proportion of time they spent on each activity changed following the move. Staff members were approached by either the ward manager or the researcher prior to the shift to assess willingness to be shadowed, and the researcher explained the research and that participation was voluntary, prior to obtaining consent. All observation was carried out by the same member of the research team in order to ensure consistency in data collection across the four case study wards and across study phases. Observation involved shadowing individual nursing and midwifery staff members (both registered and assistant staff) for between 4 and 8 hours and recording their activity using a structured time and motion data collection tool. Observation was undertaken during the day only (between 07.00 and 20.00) and should, therefore, be regarded as indicative rather than representative.
The data collection tool was developed by the research team using HanDBase (version 4, DDH Software, Inc., Wellington, FL, USA) software, and drew on a similar tool used in health-care research designed and developed by Westbrook and Ampt94 (WOMBAT – Work Observation Method by Activity Timing). Time-stamped data were collected using a HanDBase custom form interface on a hand-held computer [personal digital assistant (PDA)]. The form contained a series of categories, each with a popup list of options or subcategories. Additional detail was collected in relation to two activity categories (direct care and face-to-face professional communication), which were predicted to change most in the all single room ward, and via a ‘Twitter’ box allowing the recording of additional short verbatim notes relating to working practices and effectiveness. Activity categories are detailed in Box 4.
-
Direct care.
-
Documentation.
-
Escort/transfer patient.
-
Indirect care.
-
Medication tasks (including medication administration).
-
Personal/social.
-
Professional communication.
-
Ward-related (including cleaning, bed-making, stocking utility room, and linen trolleys).
See Appendix 7 for a full list of the HanDBase form categories and tables of definitions.
Participants
A mix of nurses, midwives and health-care assistants (HCAs) (to be shadowed) were sampled in order to understand differences between these groups. A total of 19 members of staff were observed before the move and 24 after the move to the new build. No members of staff were observed both times, so the design was purely a between-sites comparison. Numbers of staff observed and hours of observation per ward are shown in Table 3.
| Staff group | Phase | Hours observation (number of staff shown in brackets) | Total | |||
|---|---|---|---|---|---|---|
| Acute assessment | Medical (older people) | Surgical | Maternity | |||
| Nurses/midwives | Pre | 23 (3) | 13.5 (2) | 19.25 (3) | 14.75 (3) | 70.5 (11) |
| Nurses/midwives | Post | 27.4 (5) | 23.2 (4) | 23.2 (4) | 22 (4) | 95.8 (17) |
| HCAs | Pre | 6 (1) | 15.25 (2) | 12.5 (2) | 14.5 (3) | 48.25 (8) |
| HCAs | Post | 5.6 (1) | 8.5 (2) | 10.5 (2) | 11.2 (2) | 35.8 (7) |
| Total | 62 (10) | 60.45 (10) | 65.45 (11) | 62.45 (12) | 250.35 (43) | |
Staff travel distances
Procedure
Staff travel distance data were collected by pedometer. The researcher had 10 pedometers that could be used at any one time. The pedometer model was the ‘OMRON Walking Style II’ (OMRON Healthcare UK Ltd, Milton Keynes, UK), chosen because it has high accuracy. The mechanism works whether it is in a pocket or attached and does not count false steps such as bending or jumping. The devices recorded the number of steps taken, but not distance. The pedometers were attached to the participant’s belt or placed in a pocket. These were distributed and collected by the researcher before and after the shadowing sessions. The quality of the pedometer was commented on by participating staff, who displayed high motivation to wear the device.
Participants
During the time when observation data were being collected, all staff members on duty were invited to wear pedometers to record the number of steps taken. This usually involved the same cluster of rooms in which the researcher was observing but could involve staff on other clusters. Travel distance data were collected from 109 staff: 53 staff (49%) before the move and 56 (51%) after the move. A small number of staff (n = 5, 4%) were observed at both times: one registered nurse (RN) and four HCAs. A number of staff contributed more than one observation session: 85 provided one session, 18 provided two sessions, 5 provided three sessions and 1 provided four sessions. A total of 140 data collection sessions occurred. There were 73 sessions (52%) collected prior to the new build and 67 sessions (48%) after the new build. The average number of sessions per member of staff was 1.38 and 1.20, respectively. Table 4 shows the number of hours of data collection and the number of participants.
| Staff group | Phase | Hours pedometer data (number of staff shown in brackets) | Total | |||
|---|---|---|---|---|---|---|
| Acute assessment | Medical (older people) | Surgical | Maternity | |||
| Nurses/midwives | Pre | 111 (11) | 54 (5) | 74 (8) | 40 (5) | 279 (29) |
| Post | 58 (9) | 27 (7) | 59 (8) | 33 (6) | 177 (30) | |
| HCAs | Pre | 30 (1) | 118 (11) | 49 (6) | 39 (6) | 236 (24) |
| Post | 24 (5) | 62 (12) | 54 (7) | 11 (2) | 151 (26) | |
| Total | Pre | 141 (12) | 172 (16) | 123 (14) | 79 (11) | 515 (53) |
| Post | 82 (14) | 89 (19) | 113 (15) | 44 (8) | 328 (56) | |
| Grand total | All | 223 (26) | 261 (35) | 236 (29) | 123 (19) | 843 (109) |
Staff survey
Survey design
The survey was developed by the research team to probe perceptions of many aspects of the ward environment, and questions were generated by reviewing the literature including previous studies of ward design and the tools they used. 95–97 It included a new 152-item questionnaire designed specifically for this study, and a validated teamwork and safety climate survey98 (see Appendix 8). After generating a pool of potential items, a group of health services researchers reviewed and iteratively revised the items to ensure that there was no overlap or repetition, that the wording was consistent and non-biased, and that all theoretically relevant topics were included. The draft survey was then pilot tested by a group of 20 nurses attending postgraduate training, who provided feedback on timing, wording, clarity and layout. Changes were incorporated into the final version. The survey included categorical questions, using Likert scales and yes/no answers, and open-ended questions designed to capture more nuanced data about staff experiences. The sections in the survey were:
-
perceptions of current ward layout, environment, facilities and information and communications technology (ICT) in relation to patient facilities, staff facilities, effect on teamwork, care delivery, safety and privacy
-
perceptions of the move to 100% single room wards
-
teamwork and safety climate
-
preference in relation to the proportion of beds in single rooms versus bays
-
job satisfaction
-
well-being and stress
-
demographic details.
A small number of questions were rephrased for coherence following the move (see Appendix 9).
The survey included an adapted version of the 22-item version of the Teamwork and Safety Climate Survey. 98 This is a validated survey consisting of two scales to measure perceptions of teamwork and three to measure safety climate. The final adapted teamwork and safety climate scale within the survey consisted of 24 items with Likert-type scales ranging from 1 (strongly disagree) to 5 (strongly agree) (see Appendix 8).
Procedure
A copy of the survey was addressed to each ward staff member and placed in a box (in either the ward manager’s office or the staff break room) for collection by staff when they were next on duty. Staff were informed about the survey by ward managers (on several occasions) and the researcher during observation sessions. Posters publicising the study and reminder posters (after 2 weeks) were also put up on the wards to encourage responses. A prize draw incentive was offered to staff completing the survey (£75 Marks & Spencer gift card for each ward). Completed surveys were returned directly to the research team using a Freepost reply envelope.
Participants
The total survey population was 176 before the move and 204 after the move. The overall response rate was 31% before the move and 27% after it. Fifty-five participants completed the pre-move survey and the same number completed the post-move survey. Nineteen participants took part in both the before and after surveys. The survey respondents were predominantly female; one male completed the pre-move survey and three males completed the post-move survey. The survey respondents were RNs/midwives and HCAs/care support workers. The number of staff participating from each case study ward before and after the move is shown in Table 5, and the respondents who were RNs or registered midwives (RMs) and HCAs are shown in Table 6.
| Phase | Ward | Total | |||
|---|---|---|---|---|---|
| Maternity | Surgery | Older people care | Acute assessment | ||
| Pre | 17 | 15 | 11 | 12 | 55 |
| Post | 26 | 14 | 11 | 4 | 55 |
| Total | 43 | 29 | 22 | 16 | 110 |
| Phase | HCAs | Registered nurses/midwives | Total |
|---|---|---|---|
| Pre | 16 | 39 | 55 |
| Post | 16 | 39 | 55 |
| Total | 32 | 78 | 110 |
Staff interviews
Procedure
Staff were recruited through the ward managers and by the researcher while conducting observation on the wards. Staff were reminded that participation was voluntary. Of 24 staff interviewed, 10 had also been shadowed by the researcher. Interviews were conducted on the wards in a private room or quiet area and lasted 30–60 minutes. The staff interview topic guide (see Appendix 10) covered the following areas:
-
staff experience – working differently/new ways of working
-
ward layout including layout of single rooms and en suites
-
staff communication and teamwork
-
perceptions of patient experience.
Half of the total interviews additionally involved reflexive photography. 99 Reflexive photography – a type of photo-elicitation technique where research participants take photographs – formed the main focus of ‘reflective’ discussion during the subsequent interview. The approach allows the research participant to talk about the significance and meaning of photographs which represent their perspective on the topic in question. Reflexive photography was used in this research to both generate a visual record of the work environments and also encourage research participants to critically analyse the ward layout, environment and facilities. It was used to prompt deeper consideration of positive and negative aspects of the work environment, and encourage participants to ‘view’ the environment in a new way or light, reassessing those aspects that are taken for granted. 100
Staff taking part in reflexive photography interviews were provided with a 27-exposure single-use disposable camera and a sheet of information and guidelines about reflexive photography (see Appendix 11). Staff were asked to take a minimum of five photographs of aspects of the ward environment. The researcher collected the cameras from the wards and returned at a later date with the photographs, which were discussed during one-to-one photo-elicitation interviews. Staff participating in reflexive photography interviews took between 5 and 27 photographs (phase 1, median 9, total 128; phase 2, median 7, total 114).
Participants
In-depth interviews were conducted with nursing staff (registered and assistant staff) in phases 1 and 2 (a total of 48 interviews). In each phase, six interviews were carried out on each case study ward (Table 7).
| Staff group | Phase | Staff interviews (photo elicitation in brackets) | Total | |||
|---|---|---|---|---|---|---|
| Acute assessment | Medical (older people) | Surgical | Maternity | |||
| Nurses/midwives | Pre | 5 (3) | 2 (2) | 4 (2) | 5 (3) | 16 (10) |
| Post | 5 (3) | 3 (1) | 6 (3) | 5 (2) | 19 (9) | |
| HCAs | Pre | 1 (0) | 4 (1) | 2 (1) | 1 (0) | 8 (2) |
| Post | 1 (0) | 2 (1) | 1 (1) | 1 (1) | 5 (3) | |
| Total | Pre | 6 (3) | 6 (3) | 6 (3) | 6 (3) | 24 (12) |
| Post | 6 (3) | 5 (2) | 7 (4) | 6 (3) | 24 (12) | |
| Grand total | All | 12 (6) | 11 (5) | 13 (7) | 12 (6) | 48 (24) |
Patient interviews
Procedure
Patients were recruited in two ways. For three wards (acute assessment, surgical and maternity), the trust sent a letter to recently discharged patients on behalf of the research team. Patients could then choose to opt in by returning a reply slip directly to the research team. Patients were interviewed between 2 and 4 weeks following discharge from hospital. The majority of interviews were conducted in respondents’ own homes (n = 24). Three interviews were conducted by telephone and one at another health-care facility at the request of participants. Interviews lasted 60–75 minutes (telephone interviews lasted up to 30 minutes) and patients received a £25 cash payment for giving up their time to participate.
An alternative method was used to recruit four of the patients on the medical (older people) ward because of the importance of identifying patients who were cognitively able to give informed consent, and concerns about the potential burden placed on frail older patients in participating in an interview following discharge. The ward manager, in consultation with staff, recommended patients that the researcher could approach to provide information about the research. The researcher introduced herself to these patients, provided them with a copy of the patient information sheet and returned to discuss willingness to participate 48 hours later. Patients were reassured that participation was voluntary. Patients were interviewed in their single room, were cognitively well and were able to participate fully in interviews, which were tape recorded and transcribed verbatim.
Interviews were conducted using a topic guide (see Appendix 12) which focused on patient experiences of the physical environment and their overall experience of care, including:
-
feeling comfortable
-
feeling safe
-
interaction with staff
-
interaction with visitors.
Participants
A total of 32 in-depth patient interviews were conducted in both phases 1 and 2 (with between 4 and 12 patients per case study area) (see Appendix 13 for pre-move sample). Table 8 provides a breakdown of key characteristics of patients interviewed, including LOS, age, parity (maternity patients) and gender.
| Key demographics | Ward | Total | |||
|---|---|---|---|---|---|
| Medical assessment unit | Older people | Emergency surgery | Postnatal | ||
| LOS (range) | 24 hours to 7 days | 6 days to 5 weeks | 24 hours to 9 days | 48 hours to 7 days | – |
| Mean age | 62 years (range 44–74 years) | 82 years (range 70–95 years) | 66 years (range 45–84 years) | 35 years (range 26–49 years) | – |
| Paritya | |||||
| Primiparous | N/A | N/A | N/A | 5 | – |
| Multiparous | 3 | ||||
| Female | 4 | 4 | 3 | 8 | 19 |
| Male | 4 | 4 | 5 | N/A | 13 |
| Total (interviews per ward) | 8 b | 8 | 8 | 8 | 32 |
Data analysis
Time and motion personal digital assistant observation, pedometer and survey data analysis
Time and motion PDA observation data were exported from the handheld computers to Microsoft Excel 2007 (Microsoft Corporation, Redmond, WA, USA) for analysis. Pedometer data were entered into Excel for analysis and staff survey data were entered and analysed in SPSS (Statistical Product and Service Solutions version 22, IBM Corporation, Armonk, NY, USA) (see Chapter 5 for full details of analysis integrated with results reporting).
Interviews with key stakeholders, staff and patients
Qualitative in-depth interviews with key stakeholders, staff and patients were digitally recorded and transcribed verbatim. Qualitative data were analysed using a framework approach, a method which involves the systematic analysis of verbatim interview data within a thematic matrix. 101 The key topics and issues emerging from the interviews were identified through familiarisation with interview transcripts as well as reference to the original objectives of the case study research, the topic guides and phase 1 data. However, new themes and issues were also allowed to emerge inductively from data. A series of thematic charts was developed and data from each transcript were summarised under each theme (see Appendix 14 for an example). This facilitated detailed exploration of the charted data, in order to map and understand the range of views and experiences in different themes as well as allowing comparison across cases and groups of cases. Recurring and significant core concepts or dimensions of experience themes were identified through an exploration of associations between the themes, and among cases in the coding matrix. This helped to develop an understanding of the range of experience of the study participants.
Data synthesis occurred as part of the analytical process, and connections were made between qualitative and quantitative data sources in order to identify core themes and connections. We aimed to balance the emic versus etic position following Greenhalgh et al. ’s work90 and have drawn upon the work of Happ et al. 102 to undertake a concurrent mixed analysis for complementarity and completeness.
Quasi-experimental before-and-after study
Design
To isolate any effect of single room accommodation on safety outcomes, a quasi-experimental approach (as a before-and-after study with non-equivalent controls) was taken. 103
Selection of comparator sites
The new Tunbridge Wells Hospital is a 100% single room facility. Main characteristics required of potential comparator sites were (1) no change but planning to move in the future (indicating wards that were nearing the end of their expected useful life, to ensure comparability with the ‘intervention’ site) and (2) moving to a new building with mixed accommodation with 50% single rooms (as a control for changes associated with a move to a new facility but not 100% single rooms). After several potential NHS trusts were contacted, one hospital in the South West region (no move, planned move in 2014) and one hospital in London (new building, mixed accommodation, move in 2011) agreed to participate in the study (Table 9).
| Characteristic | Acute assessment | Older people | Surgical | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Tunbridge Wells | Mixed accommodation | Steady state | Tunbridge Wells | Mixed accommodation | Steady state | Tunbridge Wells | Mixed accommodation | Steady state | |
| n | 17,457 | 4948 | 24,747 | 1600 | 1779 | 1580 | 4938 | 1821 | 8388 |
| Age | 57.5 | 52.8 | 64.8 | 84.4 | 80.5 | 82.9 | 60.7 | 55.0 | 50.2 |
| LOS | 1.3 | 1.1 | 1.5 | 27.4 | 12.9 | 13.8 | 7.2 | 8.1 | 1.9 |
| Charlson comorbidity index (%) | 8.2 | 4.3 | 9.5 | 11.8 | 4.9 | 16.5 | 10.6 | 9.4 | 4.1 |
Analytical approach
Theoretically, the comparison of trusts by trends of infections or safety events could be conducted at the individual, ward or hospital level. However, safety incidents such as falls, as well as hospital-acquired infections, are usually recorded in dedicated reporting systems, which contain information only about the harmed patients, thereby excluding information about the overall population of the ward or the trust. These data are often used for performance measurement and are available on the ward and/or trust level as volume-standardised rates (e.g. falls per 1000 bed-days). While individual-level data would allow risk adjustment and therefore reduce selection bias in the comparison of trusts or wards, individual-level data are rarely available in routine data. A different way of addressing selection bias is based on risk stratification, which groups in strata patients with similar characteristics. Analysing at the ward level by comparing wards of the same type (e.g. medical ward) partially achieves this goal, since most wards have specific populations where patients share similar characteristics. Therefore, safety incidents and hospital-acquired infection rates are analysed on the ward level. In addition, we use administrative data containing information on age, LOS, primary diagnosis based on the International Classification of Diseases, Tenth Edition (ICD-10),104 Healthcare Resource Group (HRG) codes, and diagnoses used in the Charlson comorbidity index,105 to match wards with similar characteristics between trusts and to identify changes in the population over time.
Assessing trends before and after the move, or identifying differences between trusts, and associating these trends with a single room effect requires four conditions to be met: (1) the outcomes of interest (safety events, hospital-acquired infections) change after the move to the ‘intervention’ (single room) site, while (2) the core characteristics of the patient population remain the same over time and (3) the core characteristics of the patient populations of the compared wards at the different trusts are broadly similar. Finally, (4) any identified effect is strongest at the single room site (Tunbridge Wells Hospital), weaker at the new building with mixed accommodation site and not present at the steady state control site. Based on these considerations, we first considered the data from Tunbridge Wells Hospital. When trends of a single room effect supported by statistical process control charts (SPCs) were apparent, we considered the comparator sites to assess if the pattern of results was consistent with a single room effect.
Statistical process control charts
Given the nature of the available data as monthly rates, and to analyse changes in safety events and hospital-acquired infection outcomes before and after the move, the analysis was conducted as an interrupted time-series analysis augmented by SPCs. SPCs plot the outcome of interest over time on a chart which contains a centre line (representing the mean) and upper and lower confidence limits, which are defined as three standard deviations below or above the centre line. SPCs allow differentiating between common cause variation, which refers to random error, and special-cause variation, which arises from actual changes in the level of the variable of interest. 106 Several rules identify special-cause variations, of which two are of particular interest to identify changes to safety events after the move: (1) one data point outside the confidence limits and (2) eight or more data points above the centre line. 106 This approach was taken because of the nature of the available data (generally monthly reports of rates over relatively short time periods). A regression-based analysis would be more appropriate if it were possible to risk adjust for differences in patient characteristics. However, this was not possible given the available data. Another alternative would have been to pool all data before and all data after the move and test for differences. However, this would have not allowed us to identify the patterns we have found. We therefore believe that this was the most appropriate approach to the data that we were able to collect.
For all outcomes, u-charts with Cornish–Fisher (CF) expansion were used, which are appropriate to handle varying sample sizes and count data with a Poisson distribution. 107 All charts were plotted with the Improved Quality Control Charts (IQCC; version 0.5; http://cran.r-project.org/web/packages/IQCC) package in R (version 3.1.1, The R Foundation for Statistical Computing, Vienna, Austria).
Matching
To identify similar wards across sites, individual-level data for age (mean), LOS (mean) and the percentage of diagnosis included in the Charlson comorbidity index were aggregated at ward level and inspected for matching with existing case study wards. Wards that most closely matched the aggregated measures and were of the same ward type (e.g. surgery) as the case study wards were selected for inclusion in the study (see Table 9). The wards at the new build mixed accommodation control site consisted before the move of eight-bedded, three-bedded and single rooms. With the move, the proportion of single rooms increased from 14% to 38% for the three included wards. The steady state control site had less than 10% single rooms.
Data management
Trusts were asked to provide data for a 3-year period from January 2010 to December 2012. Outcome data (safety events and hospital-acquired infections) were requested for the four case study wards (acute assessment, older people, surgery and maternity) at the old Pembury Hospital and their succeeding wards at the new Tunbridge Wells Hospital. These outcomes are all regarded as being sensitive to the quality and quantity of nursing care provided, with some (falls, infections) reflecting specific challenges or hypothesised advantages attributed to single rooms. 108 The same was requested from four wards of the same type at each of the control sites. Because of the low incidence – pressure ulcers, falls, MRSA and C. diff. – maternity wards were excluded from further analyses.
Routine data are captured in various ways. Table 10 summarises the sources and definitions of the different outcome and risk stratification variables. Data were received from several departments within each trust, including finance, human resources, infection control and nursing management. While definitions of ‘incidents’ recorded in this routine quality data are generally standardised (e.g. using recognised grading systems for pressure ulcers), the approaches to gathering data may not be. There is a risk of under-reporting. However, as the key aim was not to compare trusts but to scrutinise (differences in) changes within trusts, these data remain potentially useful, if limited.
| Variable | Source | Definition |
|---|---|---|
| Outcome | ||
| Falls | Incident reports | (Falls per month per ward/bed-days) × 1000 |
| Pressure ulcer | Incident reports | (Pressure ulcers per month per ward/bed-days) × 1000 |
| Medication error | Incident reports | (Medication errors per month per ward/bed-days) × 1000 |
| MRSA | Infection control | (MRSA cases per month per ward/bed-days) × 1000 |
| C. diff. | Infection control | (C. diff. cases per month per ward/bed-days) × 1000 |
| Matching/risk stratification | ||
| Age | Administrative | Mean |
| LOS | Administrative | Mean |
| Primary ICD-10 | Administrative | 10 most frequent four-digit ICD-10 codes |
| HRG | Administrative | Five most frequent HRG subgroups |
| Charlson index | Administrative | Percentage of diagnoses included in the Charlson index |
| Bed-days | Administrative | Sum of LOS per month per ward |
| Staffing | ||
| WTE all nursing staff | Finance | Total nursing hours per patient-day |
| WTE RNs | Finance | Total registered nursing hours per patient-day |
| WTE temporary staff | Finance | Temporary nursing hours per patient-day |
Data availability
Because of the diverse range of sources, analysis on the ward level and changes in the data infrastructure, not all data were available for all wards throughout the investigation period from January 2010 to December 2012 (Table 11).
| Area | Variable | Tunbridge Wells | Mixed accommodation | Steady state | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Acute assessment | Surgery | Older people | Acute assessment | Surgery | Older people | Acute assessment | Surgery | Older people | ||
| Staffing | Total nursing hours per patient-day | 36 | 36 | 36 | N/A | 36 | 36 | 36 | 36 | 36 |
| Total registered nursing hours per patient-day | 36 | 36 | 36 | N/A | 36 | 36 | 36 | 36 | 36 | |
| Temporary nursing hours per patient-day | 36 | 36 | 36 | N/A | 36 | 36 | N/A | N/A | N/A | |
| Case mix | Age | 36 | 36 | 36 | 32 | 32 | 32 | 36 | 36 | 36 |
| LOS | 36 | 36 | 36 | 32 | 32 | 32 | 36 | 36 | 36 | |
| Volume | 36 | 36 | 36 | 32 | 32 | 32 | 36 | 36 | 36 | |
| HRG | 36 | 36 | 36 | 32 | 32 | 32 | N/A | N/A | N/A | |
| ICD-10 | 36 | 36 | 36 | 32 | 32 | 32 | 36 | 36 | 36 | |
| Outcomes | Falls | 36 | 36 | 36 | 26 | 26 | 26 | 36 | 36 | 36 |
| Pressure ulcer | 36 | 36 | 36 | 27 | 33 | 33 | 36 | 36 | 36 | |
| Medication error | 36 | 36 | 36 | 26 | 26 | 26 | N/A | N/A | N/A | |
| C. diff. | 36 | 36 | 36 | 36 | 36 | 36 | 36 | 36 | 36 | |
| MRSA | 36 | 36 | 36 | 36 | 36 | 36 | 36 | 36 | 36 | |
Missing data handling
For the mixed accommodation new build site, only 32 months of administrative data were available, which would have reduced the observation period that could be matched to outcome data. To impute the missing aggregate bed-days we calculated the mean and standard deviation of the previous 5 months (all post-move phase) and used these values assuming a normal distribution to randomly generate and impute four aggregate values. For missing outcome and staffing data, listwise deletion was used, which subsequently reduced the number of available time points.
Cost analysis
Design
Available data are described above (see Tables 10 and 11). Where possible, we aimed to gather differences in terms of unit of resources and outcomes before and after the move to single room design. Where it was feasible and relevant, changes in resource consumption and outcomes were investigated using real costs (e.g. cleaning and staff costs).
Data collection from expert opinion
A range of experts from the architecture, construction and facilities management industries were consulted, along with experts from hospital management and operations. The aim of these interviews was to seek views on the relative impact of different hospital designs on costs and resource use. These experts also provided opinion on the emerging research findings. Use of expert opinion is a relatively informal technique, but can be useful in clarifying the issues relevant to a particular topic and its evaluation, especially where the available research evidence or data are poor. Individual experts can be consulted, but groups of experts together are generally preferred to draw on a wide range of experience. 109
We drew up a list of experts from personal contacts and used a snowball sampling strategy to add to this list, and to include those connected with hospital construction (Table 12). Experts were contacted directly through e-mails or telephone, and meetings were arranged in person. An interview schedule with the main discussion topics was prepared in advance, together with a list of questions to be addressed (see Appendix 15). Nine experts were gathered in a group setting in order to stimulate and allow different perspectives or opinions to be discussed. One-to-one telephone interviews were arranged with three other experts.
| Institution/role | Skills/expertise |
|---|---|
| Director of Gateway Reviews and Estate Facility Management for NHS | Construction management, PFI |
| Commercial Leader of Laing O’Rourke Construction Ltd | Construction management, PFI |
| Bid Manager at Laing O’Rourke | Architectural design, health care |
| BIM Specialist at Skanska | Architectural design, health care |
| Managing Director at Steffian Bradley Architects | Architectural design, health care |
| Director at Steffian Bradley Architects | Architectural design, health care |
| Strategic advisor at comparator site (new build) | Strategic estate advice |
| General Manager – Facilities at Maidstone and Tunbridge Wells NHS Trust | Facility management, hospital management |
| General Manager at Maidstone and Tunbridge Wells NHS Trust | Facility management, hospital management |
| Associate Director of Nursing at Maidstone and Tunbridge Wells NHS Trust | Nursing management, staff management |
| Head of Domestic Services at comparator site (steady state) | Facility management |
| Head of Financial Management at Maidstone and Tunbridge Wells NHS Trust | Management finance, costing, health care |
Analytical approach
Construction and facilities management costs
Construction and operating/maintenance costs were assessed using a combination of data from the literature (see Chapter 2 and Appendix 1); the outline business case for the new hospital; stakeholder views; the health-care premises cost guides; and Estates Return Information Collection (ERIC) data over a sample of hospitals. Net present value of construction costs and life-cycle operating costs were assessed using a 3.5% discount rate over the first 30 years and a 3% discount rate for the next 30 years, making a total of 60 years.
An estimate of the difference in cleaning costs over 1 year was calculated using administrative data and assuming three different scenarios: 100% single rooms, 50% single rooms and 100% multi-bedded rooms. Costs were assessed assuming each hospital would host the same number of patients but in three different room designs.
Cost of nurse staffing before and after the move to single rooms
The cost impact of changes in nursing whole-time equivalent (WTE) before and after the move using the actual monthly WTE in each case study ward was assessed. The monthly WTE of each staff category (bank nurses, agency nurses, trained and untrained nurses) was costed using the monthly salary in each salary band. This was drawn from Royal College of Nursing (RCN)110 data on pay rates for bands 1–9 for each year from 2009 to 2012110 and data on unit cost of health and social care111 to estimate the unit cost for WTE.
The average monthly WTE has been multiplied for the corresponding monthly pay rate in each month. The 2010–11 pay rate was used for monthly WTE before the move and the 2011–12 pay rate for the monthly WTE after the move. Pay rate differs according to staff band; therefore, we applied the salary corresponding to each band using the average of all pay scales in each band.
Extra nursing time, workload and patient contact time
We used monthly data from January 2010 to August 2011 for the period before the move and data from September 2011 to December 2012 for the period after the move.
We used the time (in seconds) of the activities nurses spent in contact with patients (e.g. direct care, indirect care or medication activities at the bedside) using the inclusion and exclusion criteria (Tables 13–16). Data were carefully analysed to exclude any direct care where the patient was not present (e.g. with relatives or while the patient was away) and included any indirect care, ward-related activity or medication activities where the patient was present with the nurse (e.g. helping the patient in the toilet, taking temperature in the ward, escorting the patient to another ward). The time in seconds before and after the move spent in contact with patients was compared with the total time of a 12-hour shift (in seconds) to calculate the proportion of patient contact activities over all the nurses’ activities during a shift.
| Activity | Location | Comment on activity for inclusion (I) or exclusion (E) | Time (seconds) | |
|---|---|---|---|---|
| Before | After | |||
| Direct care | At bedside | All activities of direct care at bedside are in contact with patient (I) | 33,150 | 37,404 |
| No value | If there is no location we assume it is direct care with the patient (mainly all these activities are with the patient, e.g. ‘check male patient ok as walking down ward’) (I) | 782 | 0 | |
| Nursing team | Nurse is clearly with a relative and not with patient (e.g. ‘relative asking re social services’) (E) | (69) | (119) | |
| On ward | Unless it is clearly stated otherwise, nurses are in contact with the patient (e.g. ‘assisting patient walking’, ‘walking with patient to loo’) (I) | 1662 | 2368 | |
| Activities with relatives where the patient is clearly not there (e.g. ‘speak with relative’, ‘bed 20 buzzing’) (E) | 0 | (284) | ||
| Toilet | All activities of direct care in the toilet are in contact with patient (I) | 705 | 612 | |
| Documentation | At bedside | All activities of documentation at bedside are in contact with patient, unless explicitly stated that the patient is away (e.g. ‘care plan re what eaten’) (I) | 2224 | 1031 |
| All other locations (office, nurse station) | Documentation activities away from the bed are not in contact with patient, unless clearly stated (E) | (5475) | (10,243) | |
| Indirect care | At bedside | Mainly cleaning (but the patient not there) (E) | (98) | (804) |
| Patient’s toilet | Cleaning while the patient is not there (e.g. ‘cleaning commode while patient is not there’) (E) | 0 | (172) | |
| Mainly cleaning but without the patient (e.g. ‘cleaning commode while patient is chatting with carer’) | (260) | 0 | ||
| All other locations | These activities are not in contact with patient (E) | (7705) | (10,020) | |
| Medication | At bedside | Distribution of medication and help patients taking medication (I) | 7321 | 2366 |
| All other locations | Mainly medication preparation, not in presence of patients (E) | (6541) | (7365) | |
| Ward related | At bedside | Doing menu for food (in presence of patient) (I) | 851 | 259 |
| All other locations | Patient is not present (E) | (11,910) | (11,291) | |
| All other activities | In all locations | Patient is not present (E) | (24,487) | (39,213) |
| Total seconds of patient contact | 46,695 | 44,040 | ||
| Activity | Location | Comment on activity for inclusion (I) or exclusion (E) | Time (seconds) | |
|---|---|---|---|---|
| Before | After | |||
| Direct care | Bedside | All activities of direct care at bedside are in contact with patient (I) | 27,258 | 39,365 |
| No value | If there is no location we assume it is direct care with the patient (mainly all these activities are with the patient, e.g. ‘take patient to treatment’) (I) | 361 | 0 | |
| Nursing team | Nurse is clearly with a relative and not with patient (e.g. ‘relative asking re patient’) (E) | (539) | 0 | |
| Off ward | Escorting patient (e.g. ‘escorting patient to smoke’) (I) | 1111 | 0 | |
| On ward | Unless it is clearly stated otherwise, nurses are in contact with the patient (e.g. ‘assisting patient walking’) (I) | 246 | 250 | |
| Speaking with relative (patient is clearly away) (E) | (154) | (505) | ||
| Toilet | All activities of direct care in the toilet are in contact with patient (I) | 33 | 0 | |
| Reception | Nurse is clearly with a relative and not with patient (e.g. ‘relative asking’) (E) | 0 | (365) | |
| Shared patient area | With patient (I) | 0 | 57 | |
| Documentation | At bedside | All activities of documentation at bedside are in contact with patient, unless explicitly stated that the patient is away (e.g. ‘care plan re what eaten’) (I) | 1511 | 1584 |
| All other locations | Documentation activities away from the bed are not in contact with patient, unless clearly stated (E) | (9990) | (8887) | |
| Indirect care | At bedside | Treating patient with infection (e.g. ‘C. diff. + patient’) (I) | 0 | 118 |
| Mainly cleaning (but the patient not there) (e.g. ‘patient outside for cigarette’) (E) | (320) | (150) | ||
| All other locations | These activities are not in contact with patient (E) | (8684) | (13,818) | |
| Patient to ASU (patient is present) (I) | 32 | 0 | ||
| Medication | At bedside | Distribution of medication and help patients taking medication (I) | 0 | 5869 |
| All other locations (office, nurse station) | Mainly medication preparation, not in presence of patients (E) | –4239 | –9517 | |
| Other | At bedside | Doing menu for food (in presence of patient) (I) | 24 | 0 |
| Other locations | Patient is not present (E) | –31,037 | –31,166 | |
| Ward related | At bedside | Doing menu for food (in presence of patient) (I) | 1360 | 811 |
| All other locations | Patient is not present (E) | –13,436 | –6691 | |
| Escort | At bedside | Preparing patients for transfer (I) | 152 | 0 |
| Off ward | Mainly not with patients unless patient has oxygen (E) | –818 | 0 | |
| Patient is present (I) | 2271 | 0 | ||
| Total seconds of patient contact | 34,359 | 48,054 | ||
| Activity | Location | Comment on activity for inclusion (I) or exclusion (E) | Time (seconds) | |
|---|---|---|---|---|
| Before | After | |||
| Direct care | At bedside | All activities of direct care at bedside are in contact with patient (I) | 16,878 | 33,138 |
| No value | If there is no location we assume it is direct care with the patient (mainly all these activities are with the patient, e.g. ‘helping patient’) (I) | 6630 | 0 | |
| Nursing team | Nurse is clearly with patient (e.g. ‘patient asking re discharge’) (I) | 0 | 491 | |
| Office space | Nurse is clearly with a relative and not with patient (e.g. ‘sorting parking with dad’) (E) | (176) | 0 | |
| On ward | Unless it is clearly stated otherwise, nurses are in contact with the patient (e.g. ‘assisting patient walking’) (I) | 0 | 1091 | |
| Parking (E) | (52) | 0 | ||
| Shared patient area | With patient (I) | 1546 | 356 | |
| Corridor | Nurse is with patient (e.g. ‘taking temperature’) (I) | 266 | 0 | |
| All other locations | With patient (I) | 0 | 41 | |
| Documentation | At bedside | All activities of documentation at bedside are in contact with patient, unless explicitly stated that the patient is away (e.g. ‘care plan re what eaten’) (I) | 0 | 274 |
| All other locations | Documentation activities away from the bed are not in contact with patient, unless clearly stated (E) | (20,881) | (26,506) | |
| Indirect care | At bedside | These activities are not in contact with patient (e.g. while patient away) (E) | (1067) | (56) |
| No value | These activities are not in contact with patient (e.g. while patient away) (E) | (1755) | 0 | |
| Activity in presence of patient (e.g. catheter) (I) | 175 | 0 | ||
| Ward support | Mainly kitchen, no patients (E) | (4323) | (8982) | |
| Medication | At bedside | Distribution of medication and help patients taking medication (I) | 80 | 391 |
| All other locations | Mainly medication preparation, not in presence of patients (E) | (2201) | (4697) | |
| Ward related | At bedside | Not completed; not clear if patient is present (E) | (326) | (581) |
| Other locations | Not completed; not clear if patient is present (E) | (18,059) | (11,647) | |
| Escort | Off ward | Mainly not with patients unless patient has oxygen (E) | (1458) | (2397) |
| Total seconds of patient contact | 25,575 | 35,782 | ||
| Activity | Location | Comment on activity for inclusion (I) or exclusion (E) | Time (seconds) | |
|---|---|---|---|---|
| Before | After | |||
| Direct care | At bedside | All activities of direct care at bedside are in contact with patient (I) | 34,642 | 36,111 |
| No value | If there is no location we assume it is direct care with the patient (mainly all these activities are with the patient, e.g. ‘helping patient’) (I) | 1642 | 0 | |
| Nursing team | Nurse is clearly with patient (e.g. ‘escorting patient’) (I) | 260 | 0 | |
| On ward | Unless it is clearly stated otherwise, nurses are in contact with the patient (e.g. ‘assisting patient walking’) (I) | 1028 | 416 | |
| Ward support | Patient is present (I) | 32 | 0 | |
| Shared patient area | With patient (I) | 0 | 597 | |
| Toilet | All activities of direct care in the toilet are in contact with patient (I) | 1138 | 0 | |
| Documentation | At bedside | All activities of documentation at bedside are in contact with patient, unless explicitly stated that the patient is away (e.g. ‘care plan re what eaten’) (I) | 1055 | 0 |
| At bedside | Patient not in bed (E) | (28) | 0 | |
| All other locations | Documentation activities away from the bed are not in contact with patient, unless clearly stated (E) | (6442) | (10,025) | |
| Indirect care | At bedside | These activities are not in contact with patient (e.g. while patient away) (E) | (1271) | (55) |
| Ward support and other | Mainly kitchen, no patients (E) | (8763) | (9965) | |
| Medication | At bedside | Distribution of medication and help patients taking medication (I) | 4116 | 6063 |
| All other locations | Mainly medication preparation, not in presence of patients (E) | (3693) | (9590) | |
| Other | At bedside | With patient doctor doing exams (I) | 1284 | 0 |
| Not with patient (E) | (2235) | (1042) | ||
| Other locations | Not with patient (E) | (36,013) | (36,497) | |
| Ward related | At bedside | Not completed; not clear if patient is present (E) | (1162) | (378) |
| Other locations | Nurse is not with patient (E) | (11,054) | (11,425) | |
| Escort | At bedside | Board for patient to be transferred/care treatment | 551 | 302 |
| Off ward | Not with patient | (320) | 223 | |
| Total seconds of patient contact | 45,748 | 43,712 | ||
We used the actual monthly WTE nurse data in each case study ward to control for the number of nurses working during the period of time used in the analysis. The WTE time has been transformed into monthly hours assuming a nurse works 37.5 hours/week. We used the monthly patient bed-days on the case study wards to control for the total number of patient-days in the same time frame. The proportion of contact time was applied to the total nurse hours per patient-day (NHPPD) to provide an estimate of the patient contact time per patient-day (Tables 13–16).
Summary
The research includes a pre/post mixed-methods evaluation in a single hospital within which there are three distinct but related workstreams:
-
a before-and-after mixed-methods case study design (with four nested cases) within a single hospital
-
a quasi-experimental before-and-after study using two control hospitals (steady state and move to new build with less than 100% single rooms)
-
an analysis of costs associated with single rooms.
The research seeks to identify the impact of the move to 100% single room accommodation on five key areas:
-
care delivery and working practices
-
staff experience
-
patient experience
-
safety outcomes
-
costs.
The research has been undertaken within a case study framework, seeking to provide a holistic understanding of the 100% single room design, and, specifically, what works in what circumstances.
Data collection has involved the following:
-
key stakeholder interviews with trust staff and Private Finance Initiative (PFI) consortium members
-
attendance at trust ‘single room working group’ meetings
-
case study research on four wards [acute assessment, medical (older people), surgical and maternity] including a staff survey, observation of staff, pedometer data, staff interviews (including photographs) and patient interviews
-
routine data including bed occupancy, staffing, payroll, LOS, build costs, infection rates, falls, pressure ulcers and administrative patient data.
Chapter 3 Developing the single room hospital and organisational support for single room working
Introduction
This chapter aims to provide sufficient context on the evolution and development of the new hospital and its 100% single room design to enable an understanding of the subsequent findings. It also seeks to detail the formal organisational and change management processes to allow us to answer the research question: How are staff perceptions and experiences of the move to single rooms shaped by formal organisational and change management processes? It draws on data gathered in phase 1 from interviews with key stakeholders during 2008–9 and in phase 2 during 2012–13 (see Chapter 2 for details). These include stakeholders who had key roles in planning and managing the new hospital development, and ward managers. Some of those interviewed for the evaluation had taken up their posts after the design of the building was signed off, and became involved with the development when the build was under way or at the stage of developing operational policies. Indeed, interviewees highlighted the long time scale and complexity of the process, which included designing a new hospital; a PFI build; reconfiguring services in the trust and local health economy; operationalising single room wards; and moving services, staff and patients to the new hospital.
Evolution of the new Tunbridge Wells Hospital at Pembury
Maidstone and Tunbridge Wells NHS Trust is a large acute hospital trust providing general hospital services to 500,000 people living in the south of west Kent and parts of the north of East Sussex. It also provides cancer services for the whole of Kent and for Hastings and Rother. Until September 2011, the trust operated from three hospital sites (Maidstone Hospital, Kent and Sussex Hospital in Tunbridge Wells, and Pembury Hospital).
The new Tunbridge Wells Hospital, built on the old Pembury Hospital site, has been fully open since late September 2011 and replaces Kent and Sussex Hospital and Pembury Hospital. It was built under the PFI scheme, whereby a hospital is designed and built by private companies which are repaid by the NHS trust over a period of 25–40 years. Following service reconfiguration, the new hospital has become the trust’s centre for trauma surgery, orthopaedics, and women’s and children’s care, including consultant-led maternity services.
To set the build in context and to understand potential facilitators and barriers to operationalising the 100% single room design, Table 17 provides a timeline of the new hospital development and details key dates in the history of the PFI procurement and build. This chapter explores important factors which have influenced the change process, including key drivers for the 100% single room design of the hospital; the design of the wards and single rooms itself; the affordability review and changes in the scope of the PFI scheme; the change in leadership and impact on the change process; and the role of the single room working group.
| Date | Event |
|---|---|
| 2000 | Merger of Mid-Kent Healthcare NHS Trust and Kent and Sussex Weald NHS Hospitals Trust to form Maidstone and Tunbridge Wells NHS Trust |
| February 2001 | Government approves initial business case for new hospital |
| December 2003 | Planning permission for new hospital upheld following judicial review |
| 2004 | Development of output specifications and approval of outline business case. Trust advertises for PFI partner |
| January 2005 | Issue of PITN to shortlisted bidders (n = 3). PITN includes (DH Estates) requirement that 50% of patient accommodation be provided in single rooms. Involvement of NPSA as advisors to trust |
| May 2005 | Submission of responses to PITN by bidders. Visit by director of nursing and estates director to US facility (new St Joseph’s Hospital, West Bend, WI) with NPSA. St Joseph’s was designed with input from health care and systems engineering to develop a set of design recommendations to guide the design of a new hospital facility focused on patient safety |
| July 2005 | Shortlisting of two bidders and issue of FITN. FITN reflects learning from visit to St Joseph’s and asks bidders to present how their proposed designs are designed for patient safety. FITN includes requirement for 100% single room design |
| October–December 2005 | First outbreak of bacterial infection C. diff. at Maidstone and Tunbridge Wells NHS Trust; Healthcare Commission investigation found that the trust failed to identify the outbreak at the time |
| April 2006 | Submission of responses to FITN by bidders |
| April–September 2006 | Second C. diff. outbreak; Healthcare Commission investigation found that the trust was slow to respond to second outbreak (e.g. isolation ward not established until August) |
| June–October 2006 | Affordability review of PFI health projects led by Richard Glenn on behalf of DH and HM Treasury. Scope of project shrinks, requiring bids to be revised |
| May–December 2007 | Submission of Appointment Business Case for external review by DH, HM Treasury and SHA |
| October 2007 | Healthcare Commission report published highlighting 90 patient deaths between April 2004 and September 2006 in which hospital-acquired C. diff. was a definite or probable cause of death. During the same period a further 255 patients had died having contracted C. diff. Publication of the report prompts resignations of CEO, chairman and director of nursing. New CEO appointed, along with an interim director of nursing |
| November 2007 | Health Secretary announces preferred PFI bidder, a consortium led by Equion, a division of infrastructure developer John Laing. Partners include Laing O’Rourke (contractor responsible for design and build), Anshen + Allen (architect), HCP Social Infrastructure (UK) Ltd (project management and clinical leadership) and Interserve (hard facilities management, i.e. repair and maintenance) |
| March 2008 | Financial close and construction commences of all single room 513-bed district general hospital. PFI agreement is over 30 years with capital build cost of £237M |
| August 2008 | New permanent director of nursing takes up post |
| June–July 2009 | Single room ‘mock up’ opens on site for clinical staff to review, create ‘snagging’ list and explore feasibility of any desired design tweaks |
| August 2009 | First site visit by National Nursing Research Unit research team. Visit is hosted by director of nursing and includes tour of new hospital building site, attendance at trust KPI meeting, and presentation of research project to trust staff including ward managers following KPI meeting |
| August–September 2009 | Review of trust’s preparedness to bring new hospital into operational use. Revision of governance structure to involve operational staff |
| September 2009 | Draft decant (move and migration) strategy produced by construction consultancy company, Cyril Sweett Limited |
| November 2009 | Establishment of single room working group (chaired by director of nursing) |
| February 2010 | Public anxiety over service reconfiguration plans relating to removal of consultant-led maternity services from Maidstone site to new hospital’s centre of expertise leads to referral of decision by Kent County Council to Secretary of State for Health |
| April 2010 | Communications consultancy Freshwater commissioned to conduct an audit and provide audit report and strategy for communicating service change. Audit finds that staff perceive a lack of communication, rumours and misinformation are an issue, and that there is patchy understanding of trust’s strategic direction. Key issue is lack of clinical ‘champions’ to articulate service changes messages. Widespread concerns around single rooms identified |
| May/June 2010 | Visit to new St Olav’s Hospital, Trondheim, Norway, by senior nursing team |
| November 2010 | Handover to trust of new building for women’s and children’s services |
| December 2010 | Ruling by Health Secretary that consultant-led maternity services at Maidstone can close in September 2011 as planned, and services be centralised at new hospital |
| January 2011 | Closure of old Pembury Hospital and move of services into new hospital |
| May 2011 | Handover to trust of rest of building (wards, accident and emergency) |
| September 2011 | Closure of Kent and Sussex Hospital and move of services into new hospital |
Drivers for 100% single room design
The planning of new inpatient accommodation is guided by Health Building Note 4 (HBN 04). In 1997, HBN 04 recommended that in new hospital projects a minimum of 50% of in-patient beds should be in single rooms. The rationale underlying this recommendation includes rising patient expectations (including in relation to privacy and dignity), movement towards greater patient choice and the prevention of HCAIs. The preliminary invitation to negotiate (PITN), issued by the trust in January 2005, incorporated this guidance for 50% of in-patient accommodation to be provided in single rooms.
A key driver for the 100% single room design of the new Tunbridge Wells Hospital was the involvement of the NPSA in the PFI procurement process. The NPSA championed designing for patient safety, and promoted an all single room design as an important patient safety solution, particularly in relation to infection control, but also as a means of reducing patient falls, stress (caused by noise and sleep deprivation) and LOS. Single rooms were also seen as means of improving staff-to-patient communication, patient confidentiality and privacy, family support and patient satisfaction. The NPSA’s view was based on the same evidence base reported in Chapter 1, and acknowledged potential negative effects of single rooms including a requirement for increased nursing resource, reduced staff-to-patient observation and social isolation of patients, as well as increased building costs (see Chapter 1). Through the NPSA’s involvement, both the trust and PFI consortia were actively encouraged to consider the option of 100% single rooms in the new hospital. This shaped the procurement process, and by final invitation to negotiate (FITN) the specification for the new hospital included the requirement for 100% single rooms. Overall, this design decision would add 1% to the capital build cost, which was considered acceptable.
Thus, in a relatively short period of time (from PITN in Jan 2005 to FITN in July 2005), the 100% single room design was fixed. Members of the winning PFI consortium and the trust acknowledged that the design was driven by the involvement of the NPSA and the competitive nature of PFI procurement (see Appendix 16 for a summary of the business case).
It was also critical that the trust board approved the decision. The then chief executive was described as a powerful ‘champion’ of the 100% single room design (quotation not attributed for confidentiality). The motivation for the trust was related primarily to building a patient-centred and safe environment, but also – as perceived by the PFI consortium and members of the trust’s new hospital development team – to the associated kudos or notoriety for being the first district general hospital in England to have all single rooms.
We were informally I suppose pushing the 100% single rooms through PITN. The FITN came out and had 100% single rooms in it. So we were probably quite closely aligned with the trust. And I think the people in the trust could see the benefits of it [. . .] all the things that should flow from 100% single rooms with infection control, slips and trips, and all the rest of it. But maybe there’s an ego factor as well, I believe.
Phase 1 key stakeholder interview (KSI) 20, PFI consortium contractor
[There was] kudos about being the first . . . full-blown NHS general hospital . . . to have all of its inpatient accommodation in single rooms, both elective and emergency.
Phase 1 KSI1, trust clinical planner
Ward and room design for the new hospital
The design of the inpatient wards and the individual single rooms was both a response to the construction site itself (a difficult sloping site, but with views across woodland listed as an area of outstanding natural beauty) and an attempt to alleviate concerns regarding staffing levels required to nurse patients in single rooms (see Appendix 16). Wards were designed to enhance the therapeutic environment by maximising direct sunlight and views across the countryside in patient rooms (Figure 1). This led to a ‘perimeter’ design, with patient rooms wrapped around the outside of ward ‘fingers’, with inboard en suite facilities (i.e. located internally, on the corridor side of the room) and ward support facilities down the centre (Figure 2). The ‘perimeter’ design restricts visibility from the corridor. A number of features were incorporated into the design to alleviate this, including a vision panel in the door with a direct line of sight to the patient bed head (Figure 3), decentralised staff bases and distributed touch-down bases. The ward layout was designed to minimise walking distances for nurses, and communication was to be facilitated by technology such as Vocera (wireless hands-free voice communication system, Vocera, San Jose, CA, USA).
FIGURE 1.
New hospital during construction: old Pembury Hospital in the foreground.

FIGURE 2.
Floor plan showing ‘perimeter’ design of new hospital with single rooms wrapped round the outside of each ward ‘finger’ and ward support facilities down the centre. Reproduced with kind permission from Stantec.

FIGURE 3.
Internal view of single room 1 illustrating position of bed head in relation to en suite facilities and door (with vision panel) to corridor.

Another ‘safety’ feature was the standardisation of patient room layout (Figure 4). The room has the en suite facilities on the bed head wall with a handrail to facilitate safe access for patients mobilising independently (see Figure 3). A clinical hand wash basin is located close to the entrance of the room, opposite the en suite facilities, to support hand hygiene prior to patient contact (see Figures 3 and 5). The specification for the design of the single room was influenced by a visit to a facility in the USA by the trust director of nursing and estates director with the NPSA during the procurement process (see Table 17 and Change in leadership and impact on the change process).
FIGURE 4.
Single room plan showing en suite facilities jutting into corridor. Reproduced with kind permission from Stantec.
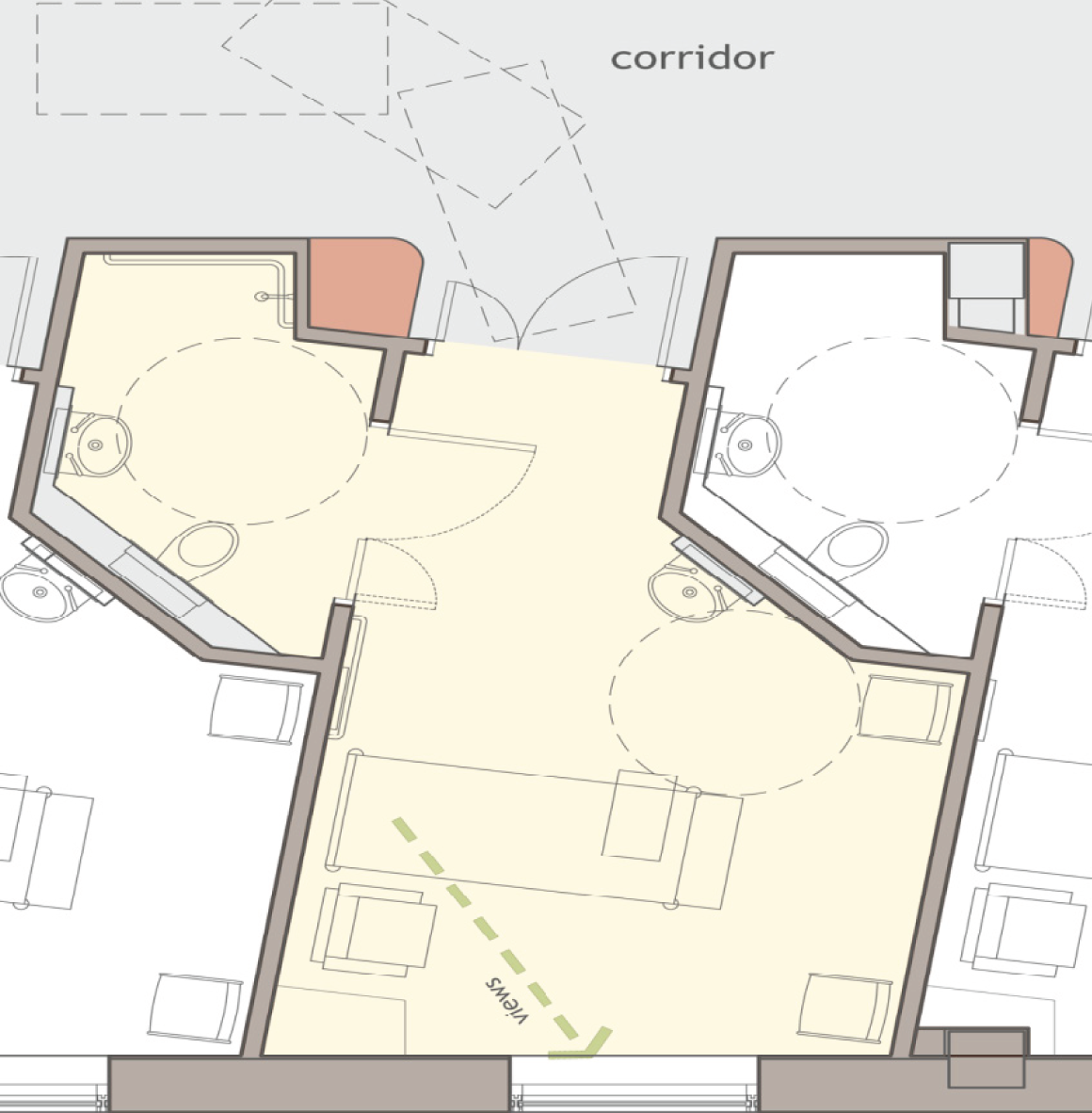
FIGURE 5.
Internal view of single room 1 illustrating position of clinical hand wash basin and full height glazing to maximise views and natural light.

Affordability review and scope of the Private Finance Initiative scheme
The scope of the overall PFI scheme was reduced in 2006 following the affordability review of PFI schemes undertaken by the Private Finance Unit of the Department of Health on behalf of the Treasury. At this point, public spaces were reduced in size (e.g. the entrance to the hospital and the restaurant). While the review did not lead to any changes to the wards in terms of number of beds and size of patient rooms, there were other key changes which had implications for the operationalisation of the wards. For example, ‘soft’ facilities management services, including ICT, ward housekeepers and ward stewards (providing a 24-hour infrastructure and administrative role) were to be provided in house rather than through the PFI project company.
The PFI went from being a ‘chocolate chip’ to a ‘vanilla’ PFI, that’s what we call it. We were providing all the soft services at one stage . . . in terms of the ward support . . . we were working on sort of a housekeeper type model that the person that came and did the cleaning was the same person that brought people their food, and they would build up a relationship with the patient. They weren’t going to be providing any nursing care, but they would be another person that was providing support to patients and could potentially take some of the pressure off the nursing staff.
Phase 1 KSI20, PFI consortium contractor
Change in leadership and impact on the change process
During the PFI procurement and build process, the trust was subject to an investigation by the Healthcare Commission into deaths related to outbreaks of the bacterial infection C. diff. (see timeline in Table 17). Following the well-publicised Healthcare Commission investigation into infection control failures at the trust, there was a change in leadership, with most members of the small team involved in the PFI procurement process and key design decisions for the new hospital leaving the trust in autumn 2007.
For the incoming chief executive and interim nursing director, the Healthcare Commission findings set out clear priorities relating to improving staffing levels and implementing robust infection control protocols. The outcome of the investigation also led to a complex set of tensions with implications for the new hospital build. Discontinuity in project leadership within the trust was a particular issue; there was a lack of ownership of and buy-in to the 100% single room design, and lack of confidence in the design decision, among members of the new senior team. The context for change in relation to the new hospital and single room working had shifted from a ‘receptive’ to a ‘non-receptive’ context. 112
The incoming chief executive was concerned about whether or not the 100% single room design was appropriate for an acute hospital and explored with the new hospital development team if there was an option to change the design to a 50/50 split between bayed areas and single rooms.
Any change at this stage in the procurement process had prohibitive financial implications; the narrow template of the wards, with single rooms designed around the perimeter, meant incorporating four-bed bays would be impossible within the proposed design. Furthermore, following the Healthcare Commission report there was a political imperative to ensure that Tunbridge Wells had a new hospital, and the chief executive was under pressure to sign up to the new hospital within the PFI procurement timetable (financial close was reached in March 2008 and construction started).
It became very clear there was a window of opportunity for a new hospital. If that window of opportunity – which was actually quite narrow – was missed in any way, there wouldn’t be a new hospital in Pembury [. . .] So in a sense a [100%] single room [design] became a bit of a side issue because the issue became, ‘Do you want a new hospital or not in Tunbridge Wells?’ and that was easier to justify. Albeit it was done both by ourselves and the SHA [Strategic Health Authority] very much with our eyes open in terms of some of the problems that still needed to be resolved, not least the finances, not least the actual operational policy and how these single rooms would operate. So it wasn’t an ideal situation.
Phase 1 KSI7, trust chief executive
While the trust necessarily focused on resolving the day-to-day operational shortcomings of the organisation, transformation work relating to the new hospital and single room working was delayed. The disjuncture caused by the change in leadership and loss of knowledge of those who were closely involved in the build meant that engagement with bringing the new hospital into operational use was not high on the agenda of senior staff at the trust. The PFI consortium project manager was concerned about the impact this lack of engagement might have on operationalising the single room wards and getting staff to think about work differently.
I started to worry that . . . we would build something that would become a white elephant, because none of the transformation work would happen . . . I was really worried that the new team [. . .] weren’t part of the journey, they didn’t necessarily agree with the destination anyway, and I don’t know if they did or they didn’t because we didn’t have that level of engagement . . . I was really, really worried that the trust would not then engage with the clinical teams and get them to think about how they change their practice, and how they work on a dispersed nursing basis, and that they do their workforce planning and all the rest of it.
Phase 1 KSI19, PFI consortium project manager
Throughout the construction of the new hospital there was little joint working between the new hospital development team and clinical stakeholders. Communication was not helped by a lack of staff continuity. Key information necessary for defining how the wards would operate in practice was shared with clinical stakeholders via the research team, rather than via any formal or informal channels of communication within the trust or between the trust and the PFI consortium. A research interview in June 2010 with the architect revealed that the general adult wards had been designed with the intention that a decentralised nursing team would relate to each ‘cluster’ of 10 patient rooms; the director of nursing appeared unaware of that feature.
Clinical staff involvement in the design process
A review of the trust’s preparedness to bring the new hospital into operational use was undertaken in August–September 2009. The review assessed the governance structures in place and identified an absence of operational staff involvement in processes and preparation for taking over the new hospital. The governance structure was revised to involve operational staff in the management and progression of the redevelopment programme, working group deliverables were set and meeting structures were realigned. User groups that had been involved at the FITN stage – particularly in relation to the layout of the single rooms – were reconvened as ‘move’ and ‘migration’ working groups, led by divisional project managers seconded to the role from within the trust. The focus of the working groups was mainly the decant strategy, including the movement of equipment and safe move of patients.
A communications strategy audit commissioned by the trust in the first quarter of 2010 identified widespread concern about single room working and a lack of clinical ‘champions’ to communicate service change messages. The report recommended a comprehensive programme of staff communication, including updates for clinical staff on recommended best practice for nursing patients in single rooms. Most stakeholders interviewed thought that more involvement of clinical staff in the early stages of the design process would have been beneficial. Plans of the new hospital were available but staff interviewed said they had difficulty interpreting architectural drawings. From plans alone they had not been able to visualise aspects of the wards and rooms, or appreciate the length of the wards. With hindsight, some respondents suggested that elevations of the internal features of the ward would have been helpful, particularly the view from the nurses’ bases, which might have allowed design issues affecting clinical practice (such as windows in the doors and the position of the bed in the room) to have been identified earlier and ameliorated. Others felt that being able to experience the proposed design, in the form of a physical mock-up of a single room and a ward, would have allowed them to assess if it enabled safe and efficient clinical practice.
The divisional project managers arranged site visits for their user groups, although it was only when the new hospital was being built that a single room mock-up was made available for staff to review; access was limited to small groups and at restricted times. The mock-up revealed issues with the layout of the room and its fixtures and fittings, but it was too late to make any significant changes without prohibitive cost implications:
the mock-up of the room was fantastic, we went in and then we discovered where we’d put the toilet roll holder wasn’t very conducive, you were swinging round like this, and there wasn’t enough room. [. . .] we sat on the loo, we did all of that, but it was too late, the hospital was already designed, the plumbing was already in.
Phase 2 KSI24, senior nurse manager
This senior nurse felt strongly that clinical processes should determine ward and room design and clinical staff should have been more involved before the plans were signed off. Asked for advice for others designing single room wards, interviewees agreed that early mock-up of the single room was vital and as many staff as possible should experience and assess the proposed design:
really it would have been so easy for us to [. . .] measure the size of the room, map it out on the floor, stick a bed in there, even if it’s an old bed, a chair, a table, whatever we wanted in there and mock up the layout, spray on the ground even, what the bathroom was going to look like. But say, ‘How do we want it to work?’ rather than, ‘This is the design, do you like it?’ [. . .] And if you can, do a group [of rooms] rather than just the one. So, if you’re going to have a mixture of side rooms and bays, then make sure that works for you. [. . .] And get as many staff from a ward area to walk through that mock-up area [. . .] to see, ‘Will this work for me?’
KSI24, senior nurse manager
Some stakeholders also questioned the uniformity of single room design in the new hospital and the lack of flexibility to accommodate particular types of patient or specialised practice, which potentially could have been built into the design.
I think nurses are very innovative about making things work and we can make silk purses out of sows’ ears, and quite often we do. [. . .] I think that one of the frustrations is there’s only so much flexibility in a single room [with this design]. So if you can build flexibility into your design that’s where people can be innovative and it keeps it dynamic as well. And you can keep your patients safer.
KSI24, senior nurse manager
Developing operational policies and procedures
Lack of planning for operationalising single room wards was identified following the change in leadership at the trust. However, substantial transformation work did not begin until a single room working group, chaired by the director of nursing services, was established in November 2009, less than 2 years before the new hospital opened. Trust executives and the working group realised that the hospital design was based on the assumption that ICT and other technology would support staff – ‘we planned our hospital imagining the I[C]T was going to be there for us’ (KSI24) – but ‘good ideas’ had not been translated into concrete plans, at least not in time for the opening of the new hospital. Attention became concentrated on resolving ‘the practical issues’ of staffing, equipping and running single room wards.
A number of visits by senior managers and clinicians were made to see other hospitals with single room wards and these provided important opportunities for transferring learning. The visit by members of the senior nursing team to St Olav’s Hospital in Trondheim, Norway, in May–June 2010 was perceived as pivotal in informing decisions about operationalising the wards, although with hindsight some members of the group felt that an earlier visit would have been even more valuable. The terms of reference for the visit included informing the development of operational policy and procedures, workforce planning and ICT solutions to support patient care. Lessons learnt were fed back to working groups, and senior nursing staff were able to communicate positive messages relating to single room working and patient experience.
Senior nurse managers saw the Trondheim visit as important in helping them with nurse workforce planning, in particular in thinking about nursing wards in clusters, rather than as a whole ward. Looking back at their decisions on staffing levels, senior staff judged that they were broadly correct and most wards had ‘done okay’ (quote not attributed for confidentiality). However, one manager recalled that ‘the work we did around sorting out staffing levels was actually quite painful [. . .] I can’t tell you how many scenarios I worked up’ and felt ‘pressurised not to put in an expensive skill mix’ (KSI23). It had been difficult to assess the staffing required in certain specialist areas, some of which had run into difficulties after the move because the volume of work was higher than had been expected. Reflecting on the experience of determining nursing establishments for the new wards, a senior nurse manager concluded that single rooms were ‘a red herring’ when working out staffing levels and that focusing on staff–patient ratios was more helpful:
If you look at the current thinking where one [nurse] to five [patients] is considered good, one to seven is pushing you into a little bit of a risky zone, one to eight, one to nine is really where you don’t want to be, it’s exactly the same with single rooms. So the wards here that worked well right from the start, in their cluster of 10 [rooms] have two RNs and a health-care support worker, they never ran into problems.
KSI21, senior nurse
Despite this favourable assessment, the same manager also referred to problems experienced at the new hospital, when general wards had to bring in ‘specials’ – additional nursing staff – to care for patients with dementia who were at risk of falling. The need for extra staff was explained as part of adapting to the new environment, while nurses were ‘fine tuning processes of delivery of care and how you organise your workload during the course of a shift’ (KSI21). In support of this explanation, it was said that the use and costs of employing temporary staff had subsequently decreased. However, by the end of the first year, increases in nursing establishment and ‘tweaks’ to skill mix had been agreed for a number of wards (see Chapters 4 and 9).
Although the visit to Trondheim in June 2010 was positive, there was limited time relative to the move dates (January and September 2011) to develop a comprehensive transition strategy for single room working, and progress tended to be piecemeal. Some important operational details were clarified at a late stage and decisions to purchase equipment were delayed, which had implications for how staff perceived and experienced the move in terms of nursing practice on the single room wards. Examples include:
-
Equipment unavailable: the design of the en suite toilet required a customised sanitary chair for patients unable to use the toilet independently. The decision to purchase sanitary chairs was not made until early September 2011 and this equipment was not available when services moved to the new hospital later that month.
-
Unforeseen equipment requirements: a requirement was identified for ‘patient status at a glance’ information to be displayed at the entrance to each patient room (for example to indicate infection control pathway information or nutrition status) but there was no means to do this. The solution – magnetic strips on the door – was not put in place until after the move. The wards also lacked a central, whole ward ‘patient status at a glance’ board and there was no suitable space for one, so a board for each cluster of 10 rooms was provided.
-
New working practices not implemented and insufficient equipment: despite widespread concern among staff about the risks of patients falling in single rooms, attention focused on militating against it only after the move, when it became apparent that the number of falls had increased. The side room protocol that was in use at the old hospital had not been revised and intentional ‘rounding’ (regular nursing rounds) had not been formalised as part of the operating procedure for single room wards. The need to carry out fall assessments and identify patients at risk had to be reinforced after the move, and only later were wards provided with antislip socks and pressure alarm mats, sometimes in insufficient quantities.
-
Reorganising nursing teams: a policy or standard operating procedure for a ‘nurse/midwife in charge’ on the single room wards [based on the role as operated at Hillingdon Hospital’s single room pilot ward, shared with trust staff via the National Nursing Research Unit (NNRU) research team] was not drafted until July 2011, leaving little time for dissemination to ward staff and any briefing about and trial of new ways of working. After the move it was found that wards had interpreted this role differently and required clarification about its supervisory nature and responsibilities, and the requirement for the nurse in charge to be easily contactable, by carrying a wireless telephone with a dedicated telephone number.
Although visits to other hospitals were an important way of learning about single room working and helped the development of operational policies, some senior managers felt that there had been missed opportunities for learning from the move of women’s and children’s services in January 2011, 9 months before the relocation of the general wards and services. A senior nurse commented ‘I don’t think there was enough open feedback about what had gone well and not gone well with the women and children’s move’ (KSI23).
Preparing clinical staff for single room working
Staff engagement and communication prioritised move and migration issues rather than considering clinical practice in the new environment. There was general agreement among key stakeholders and clinical staff interviewed after the move that staff had been anxious about moving into the new hospital, but there were different opinions about whether or not more could have been done to prepare for working on single room wards. Some senior nurse managers thought that securing strong ward leadership had been a crucial factor in successful transition to the new hospital. Ward manager appointments were made well ahead of the move and having ‘the right leaders in place’ was seen as an important resource for managing organisational anxiety (this and other quotes not attributed for confidentiality). ‘Everybody was nervous [. . .] But I think with the right leaders in place it was positive’ (KSI23).
As outlined above, site visits were arranged for staff before the new hospital was complete but clinical staff said that they did not find these brief visits particularly useful because the hospital was empty and had no signage, and there was little to help them envisage what working on the wards would be like:
it was difficult for it to be more than a walk round. And people [. . .] still couldn’t quite envisage how it was going to be when they were actually on site. So I think everybody did feel quite disorientated.
KSI31, ward manager
The visits were also primarily about the layout of the single room, and staff were not challenged to think about work practices beyond it, for example working on a ward with 30 single rooms/clusters of 10 rooms in small teams. Ward managers reported almost exclusively focusing on moving equipment, setting up the wards and transferring patients safely, and ‘hadn’t prepared in any way’ for working differently. Three of the four ward managers interviewed suggested that it would have been neither possible nor desirable to prepare staff in advance for the ‘unknown quantity’ of single room working.
I don’t think any of us had any concept of how it was going to work. I think we actually had to just walk in there and start. I think that was the only way we could have done it. I think you could have prepared yourself to death and I don’t think it would have particularly helped. [. . .] I mean we didn’t even know how our teams were going to work to start with. All we wanted to do really was to get our patients over safely and then we just thought we’ll work from there on, and we just did, didn’t we?
KSI33, ward manager
The fourth ward manager held a different view and felt that more preparation would have helped staff adapt to the new environment faster and more easily:
[I]t would have been nicer to have more time for staff familiarisation and things like doing skills drills [. . .] where you really think about what to do if something happens in this room. Where do we go? What do we do? How do we call people? Where is the equipment stored? That sort of thing. That’s really difficult to do in an area which you have very limited access to. And until we were virtually moving in we didn’t have the equipment, so it was very difficult to do those dummy runs if you haven’t got a clinical room full of the equipment . . .
KSI31, ward manager
A medical consultant also thought that clinical staff should have been encouraged to think about working in the new environment and how it might affect their routines:
Yes, we had plans on the walls, everyone could see them [. . .] we hadn’t really figured out what they meant. [. . .] I don’t think we paid attention to what we would all be doing. So I suppose by simulating our working day, or saying I’ll come in here, I’ll do that, people could have got into their head what they were going to have to do.
KSI28, medical consultant
Some clinical staff had been part of discussions about working in the new hospital, but these focused largely on ICT to assist staff in the delivery of care. Expectations had been raised about the extent of technological support that would be available to staff – for example, systems enabling patients to be monitored at a central point and handheld electronic devices for recalling and recording patient information – and some staff were both surprised and disappointed to discover when they arrived on the wards that this ‘selling point’ of the new hospital had not been realised. Moreover, they found that ICT and telephone communication systems did not function well initially and staff received little help or training in using equipment with which they were unfamiliar, such as wireless telephones:
[W]e were under the impression I[C]T was going to be all singing all dancing, and it wasn’t really. We could have done almost with someone from I[C]T on the ward each day helping us. [. . .] That was the biggest thing that let us down, I feel, was I[C]T.
KSI33, ward manager
The focus on ICT during development of the new hospital was reported to have distracted nurses from addressing more important issues, such as coping with the increased throughput of patients and effective bed management in the single room environment.
We spent 2 years talking about those things and that was a complete waste of conversation and our time [. . .] You’ve got a patient who is very dependent coming in, but the only room that’s empty is the one that’s furthest away [from the nursing station]. [. . .] We may have been thinking more about that before we came over if we hadn’t been so distracted by all of this I[C]T promise that has never [happened].
KSI30, ward manager
Post-move support for single room working
The priority given to the move and migration strategy (which all staff felt went very well), rather than to considering how staff would work in the new hospital, left staff ill-prepared for the challenges they encountered when they started working on single room wards. The chief executive was quoted in the local press saying:
Although we didn’t aim to do this, our staff were conditioned to thinking that the move itself was the end, they did an awful lot of work and tirelessly worked towards the closing down of the K&S [Kent and Sussex Hospital] and the move to the new hospital, and psychologically they felt that was it, but in actual fact it was only the start of the journey. I don’t think we’d anticipated that dip just after we moved quite as well as we could have done.
Chief executive115
Staff recollections of the first days in the new hospital convey the sense of anxiety, the sheer hard work and the extent of the change required, primarily because of single rooms, often compounded by other issues such as ward layout, nurse staffing, size of the hospital and case mix:
[I]t’s actually been really hard work [. . .] adjusting the way we work [. . .] You had to change the way that you nursed. You had to change the way that you thought, the way that you looked at things, and then you lost all that familiarity [. . .] the majority of staff in that first 3 or 4 months, if they’d been offered positions anywhere else [. . .] they’d have just walked away from it all.
KSI30, ward manager
Staff did not criticise management for the lack of preparation and generally minimised problems they encountered, for example with telephones and ICT, referring to them as ‘teething problems’ and ‘bedding in’. However, many staff spoke about the length of time it took to get used to the new environment; in most cases this was at least 6 months and it was only at interview over 1 year after the move that they described feeling more settled and able to make improvements.
A senior nurse thought that project teams that had helped with the move had been disbanded too early: ‘some of them might have run out of steam slightly before the move. I think they should have continued for 3 months to help with the bedding-in’ (KSI23). She also suggested that a formal review of lessons learnt by managers after 3 months in the new hospital would have been useful: ‘We did have a post-move clinical reference group, but it was terribly flat’ (KSI23). Ward managers and other senior nurses established regular meetings (such as the ward support group), which were a useful forum for discussing and resolving difficulties encountered in delivering services and sharing examples of effective practice:
[W]e used to have a meeting [. . .] every Friday, for an hour [. . .] for about the first 9 months, where we would tweak things. So, somebody was having problems with getting meals, it would be discussed at that meeting, and catering would be there, and we’d say, ‘What are we doing?’ [. . .] so we were trying to get immediate responses.
KSI24, nurse manager
In this group ward managers presented their difficulties, such as ineffective working or unsafe practice, and these narratives highlighted problems and triggered a search for solutions. While ward managers supported their staff to adapt to working on the single room wards, there was little evidence of other help provided for ward nurses, AHPs or doctors, and there was no forum for staff to share and learn from each other. Aspects of ward design and their perceived consequences that created particular problems for nurses included lack of visibility of patients and other staff, a perceived rise in falls, and the system of secure ward entry and exit. This last was not a nursing responsibility, yet nurses found that they were expected to deal with it, because there was no one else to do so.
Support for single room working had three key elements:
-
development of new processes and ways of working
-
implementation of tools to optimise single room working
-
reinforcement or reapplication of existing protocols and procedures.
See Chapter 6 for a discussion of these in more detail. However, it is important to emphasise here that new processes and ways of working were developed only after the move, in ways that were ad hoc and typically by using trial and error. Essential protocols and processes, for example the hourly rounds protocol and standard operating procedure for a ‘nurse/midwife in charge’, were not developed until after the initial phase of the move, when staff also had to implement a plethora of other new protocols and procedures.
I think our poor staff were a bit bombarded with, number one, trying to understand a new site, and getting to grips with a new way of working, especially if they were on a Nightingale ward, very, very different for them, plus, I don’t know, half a dozen at least, if not more, new policies that were implemented at that time as well. [. . .] I did really feel for them, and I think they were a bit punch drunk, I think, with everything new and everything different [. . .] But they’ve embraced it and moved with it.
KSI27, senior nurse
Other issues were that ICT was not fully functional; equipment such as customised sanitary chairs and patient status at a glance boards was not available initially; and staff were not familiar with tools they needed to use, for example wireless telephones. Finally, because of the nature of single room working there was a need to reinforce procedures and protocols, such as fall assessments and infection control procedures. Basic infection control principles were revisited to counter the myth that patients in single rooms were protected from hospital-acquired infections, and to prevent staff becoming complacent:
I think people [. . .] have a belief that because patients are in single rooms, there is no risk of infection. And that is a mind-set that we’re busily trying to change.
KSI27, senior nurse
Just to remind staff not to be complacent. Don’t think just because they’re in single room that there isn’t a risk of infection, that infections can still travel from room to room, [. . .] because there isn’t that visual reminder that you have to do anything different with them, because every patient’s in the same situation. So, reminding them about signage, keeping doors closed . . . keeping those messages alive.
KSI27, senior nurse
There were some distinct differences in practice between wards in the new hospital and those at Kent and Sussex Hospital. In the latter almost every patient in a single room had an infection and there were visual reminders for these patients with a trolley and signage near the patient’s bed. This was not the case in the new hospital. Every single room had gloves, aprons, etc., at the doorway and so it was not immediately obvious to staff that they had to care for some patients (with infection) differently; the visual cues were not there.
Chapter summary
As a result of the main focus being on the move itself and getting patients safely transferred, new processes and ways of working were developed only after the move, in ways that were ad hoc and typically by using trial and error. Nurses on the wards encountered a variety of challenges that had not been foreseen before the move because operational procedures had been incompletely specified or staff had not been prepared for new ways of working, for example new ways of working to ensure patients’ safety and care quality; new ways of working as a team; locating and communicating with colleagues; and ensuring good patient experience. All of these key aspects are explored in much more detail in the following chapters.
Chapter 4 The case study wards
Introduction
This chapter provides information about the layout and key characteristics of the four case study wards. It begins with an overview of their location and physical environment at the old hospitals. This is followed by descriptions of each ward in the new Tunbridge Wells Hospital, including the physical environment (illustrated with floor plans) and highlights salient continuities and changes in ward organisation and staffing. This chapter provides the context for interpreting the findings from the research reported in subsequent chapters.
Case study wards before the move
Three of the case study wards were located at the Kent and Sussex Hospital in Tunbridge Wells, which opened in 1934 as a purpose-built facility. It featured south-facing traditional Nightingale wards (with rows of beds on either side) and three-quarter-height glazing, designed to maximise fresh air and sunlight to support patient recovery. During the Second World War, six wartime emergency huts were added to the hospital footprint. Two of these were demolished in the 1980s, when a new accident and emergency (A&E) wing was added to the hospital. The acute assessment ward (redesignated medical assessment unit in the new hospital) was located in this wing and was the most modern of the case study wards. The older people’s ward was in one of the four remaining wartime emergency huts. The surgical ward was a light and airy, high-ceilinged Nightingale ward in the original 1930s buildings.
The fourth ward (maternity) was located on the old hospital site at Pembury. The original building was a workhouse that opened in 1836, was extended during the 19th century, and became a county hospital in 1938. The maternity ward was on the first floor of the Victorian buildings (built c. 1890) with the delivery suite some distance away on the ground floor in ‘temporary’ flat-roofed accommodation opened in 1969. A special care baby unit was also located on the ground floor.
Diagrams of the four case study wards before the move are provided in Appendix 17. The following photographs (Figures 6–10) illustrate some features of the wards.
FIGURE 6.
Front of Kent and Sussex Hospital.

FIGURE 7.
Accident and emergency wing, Kent and Sussex Hospital.

FIGURE 8.
South-facing Nightingale wards with curved fire escapes at Kent and Sussex Hospital (surgical ward shown at level 3).

FIGURE 9.
View of four wartime emergency huts at Kent and Sussex Hospital.

FIGURE 10.
Maternity ward at old Pembury Hospital (showing postnatal section on the first floor).

Case study wards in the new hospital
Acute admissions unit
The acute admissions unit (AAU) admitted patients from A&E for further assessment, diagnosis and treatment, prior to discharge or transfer to a specialist ward. Patients were intended to stay in the unit for a maximum of 48 hours, which was extended if beds on other wards were not immediately available. The AAU admitted 350–400 patients per month, including many who were acutely ill or in an unstable condition.
The AAU was adjacent to the A&E department and had 30 single patient rooms around the perimeter of the ward, with ward support facilities down the centre, as shown in the ward diagrams (see Appendix 18). Compared with the old hospital’s acute assessment ward, which had 16 beds in a compact layout of three bays, the AAU was a much larger and longer ward, designed to be nursed as two sides (14 beds and 16 beds). Through trial and error, nursing staff found it better to work as three teams each responsible for clusters of 10 rooms, although this configuration did not fit so well with features of the ward layout (staff bases, call bell system, location of facilities) (see Chapter 6, Maintaining teamwork and communication). Ward-based medical staff used a room in the central area of the ward, occupying space that on other wards was used for storage; no additional storage was provided on the AAU. There was no day room for patients. The staff break room was located off the ward and shared with A&E, as it had been at the old hospital. Nursing staff considered it too far away and instead used a small interview room on the ward, which also housed a desk and work station and had no window or kitchen facilities. Table 18 shows the staffing allocation for the AAU after the move. The nurse staffing ratio decreased slightly (from 1 : 4 to 1 : 4.2) and the HCA staffing ratio increased (from 1 : 16 to 1 : 10) (Table 19).
| Ward | Number of beds | Early | Late | Night | |||
|---|---|---|---|---|---|---|---|
| RNs | HCAs | RNs | HCAs | RNs | HCAs | ||
| AAU | 30 | 7a | 3 | 7a | 3 | 5b,c | 2 |
| Older peopled | 30 | 6a | 4 | 4a | 4e | 4c | 2 |
| Surgical | 30 | 7a | 3 | 4a | 3 | 4c | 2 |
| Postnatal | 31 | 4 | 4 | 4 | 2 | 4 | 2 |
| Time | Beds | RNs (ratio of RNs to beds) | HCAs (ratio of HCAs to beds) |
|---|---|---|---|
| Pre move | 16 | 4 (1 : 4) | 1 (1 : 16) |
| Post move | 30 | 7 (1 : 4.2) | 3 (1 : 10) |
On the AAU the ward manager and some of the nursing staff had transferred from the previous ward, which had a high turnover of staff and recruitment problems. A cadre of newly qualified nurses was recruited before the move and a further cohort from Portugal joined after the move. The ward continued to have difficulties retaining staff; consequently, the workforce included a high proportion of inexperienced nurses, and bank and agency staff were used to fill vacancies.
The AAU had a medical team based on the ward, and dedicated physiotherapists and occupational therapists (OTs). The ward clerks staffed a desk near the ward entrance from 09.00 to 22.30 daily – the longest of all the case study wards – consistent with patterns of 24-hour activity and visitor access on this busy ward.
Older people’s ward
This case study ward was one of two older people’s wards in the new hospital and admitted patients with a variety of medical conditions, diagnoses and disabilities, including dementia and impairments of mobility, eyesight, hearing and speech. The ward had 30 beds (28 before the move), including 10 orthogeriatric beds (typically patients with fractured neck of femur). Patient LOS varied greatly: some patients were discharged within a few days, but those with more complex needs tended to stay much longer if there were delays in finding an appropriate placement. After the move to the new hospital, patient stay decreased but not as much as expected; staff attributed the smallness of the decrease to the ward’s changing case mix (see Chapter 8). Nurses said they were caring for higher-dependency patients, with increasingly complex conditions and comorbidities, including physical disabilities and cognitive impairment, and there were more patients requiring intensive rehabilitation. As on the old ward, staff found it challenging to care for patients who were confused, demanding or aggressive, but their greatest concern on the new ward was the risk of patients falling.
The older people’s ward was located on level 2 of the new hospital and had 30 single rooms (see Appendix 18, Figure 44). Nursing staff were deployed in three teams, each relating to a cluster of 10 rooms. It had a similar layout to most of the general wards, with three nursing stations, centralised ward support facilities and a small patient day room, which could accommodate a maximum of six patients. Despite its limitations, the day room was used regularly to hold a ‘lunch club’ for five or six patients, and staff had plans to create another communal area for patients. The reception desk was covered by the ward clerk from 08.00 to 15.00. There was a staff break room on the ward.
The staffing allocation for the older people’s ward after the move is shown in Table 18 above. After the move the nurse staffing ratio increased substantially (from 1 : 9.5 to 1 : 5) and the HCA staffing ratio decreased (from 1 : 5.6 to 1 : 7.5) (Table 20).
| Time | Beds | RNs (ratio of RNs to beds) | HCAs (ratio of HCAs to beds) |
|---|---|---|---|
| Pre move | 28 | 3 (1 : 9.3) | 5 (1 : 5.6) |
| Post move | 30 | 6 (1 : 5) | 4 (1 : 7.5) |
An extra member of staff had recently joined the weekday day shift to co-ordinate discharge planning. The ward reported a fairly stable nursing workforce with a core of experienced nurses and HCAs, although, in the first year, periods of short-term sickness absence and unfilled vacancies led to increased use of bank nurses and agency staff.
The ward nursing team was formed when the new hospital opened and comprised staff from six wards at the old hospital. The new ward manager was newly appointed and it was her first substantive ward management post. The team reportedly ‘gelled’ quickly and, despite the ward manager being seconded to another hospital in the trust for 3 months of the first year, staff interviewed said that they worked together well and there was a good atmosphere on the ward. The ward manager provided leadership in ‘caring thoughtfully’ for patients with dementia, which she acknowledged as a ‘real passion’. Two medical consultants and their teams were based on the ward and there were twice-weekly multidisciplinary team (MDT) meetings, including nursing staff, physiotherapists, OTs and the care managers who had aligned themselves to the ward.
Surgical ward
This case study ward admitted acutely ill patients for emergency or unscheduled surgery, providing pre- and postoperative care (or conservative management) and rehabilitation, and specialising in upper gastrointestinal and colorectal surgery. Before the move, the ward accommodated elective and emergency surgical patients, and beds were often used for patients from other specialties. The number of beds reduced from 35 to 30, and in the new hospital included four beds designated for patients with C. diff. infections. Average patient LOS was just over 7 days before the move and increased slightly after the move. Nurses said that they now had older and more dependent patients, which could make nursing ‘heavy going’.
The surgical ward had an almost identical footprint and layout to the acute older people’s ward (see Appendix 18, Figure 45); nursing staff were deployed in three teams each relating to a cluster of 10 rooms. The small room assigned for a patient day room (as on the older people’s ward) was not used for this purpose; staff could take relatives there if a patient died, for example, and patients’ relatives occasionally slept there. The reception desk was covered by the ward clerk from 08.00 to 15.00. There was a staff break room on the ward.
The staffing allocation for the surgical ward after the move is shown in Table 18. After the move, the nurse staffing ratio increased (from 1 : 5.8 to 1 : 4.3) and the HCA staffing ratio decreased (from 1 : 7 to 1 : 10) (Table 21).
| Time | Beds | RNs (ratio of RNs to beds) | HCAs (ratio of HCAs to beds) |
|---|---|---|---|
| Pre move | 35 | 6 (1 : 5.8) | 5 (1 : 7) |
| Post move | 30 | 7 (1 : 4.3) | 3 (1 : 10) |
Staff turnover was said to be relatively low and there was a core group of experienced and competent staff. About one-third of the nursing staff were from the Philippines, where some had experienced nursing patients in single rooms.
The ward manager, who had been in post for more than 10 years, the nursing team and the ward clerk all transferred together from the old hospital, preserving continuity of leadership, ward identity and an ethos of strong teamwork and high standards of care. Medical cover for the ward was provided alternately by two surgical teams (upper gastrointestinal and colorectal) and the team in charge changed every 3 or 4 days. The ward clerk played a key role helping the clinical team to work effectively, particularly managing telephone communication.
Postnatal ward
Maternity services from two trust hospitals were centralised in a wing of the new hospital dedicated to women’s and children’s services: the unit from old Pembury Hospital moved into the building in January 2011 followed later that year by services from Maidstone (see Chapter 3). The antenatal ward, delivery suite and neonatal unit were on one floor; on the level above was postnatal and transitional care (for babies requiring additional treatment or observation). Although midwives perceived they were busier than before, managers pointed out that the total number of births had not changed and it was likely that staff perceptions were influenced by the size of the new unit. The postnatal ward had 31 beds, almost double the number on the previous ward at Pembury Hospital (n = 16). Patient LOS ranged from 24 hours after uncomplicated deliveries to 2 weeks for babies or for women needing extra care.
This part of the hospital had a different ward footprint, with a shorter ward ‘finger’ and a large curved area at the end of the building (see Appendix 18, Figure 46). The ward was originally planned to be dedicated to postnatal care, but a section was redesignated as gynaecology beds that were nursed and managed separately. This divided the postnatal ward into two distinct zones, with 16 beds on the ‘finger’ and 15 on the curve, nicknamed ‘the west wing’. Each zone had two midwife bases, with staff at each covering seven or eight rooms. Ward support facilities had been reallocated between postnatal and gynaecology, leaving ‘the west wing’ with inadequate support, which staff found inefficient and inconvenient. The patient lounge was described by midwives as ‘not appealing’, ‘underused’ and not big enough to accommodate women with their babies. Initially, ward clerks were at the reception desk for a few hours a day, but subsequently staffing was extended to cover peak evening visiting time. The staff break room was located just outside the ward.
The staffing allocation for the postnatal ward after the move is shown in Table 18. After the move, the midwife staffing ratio increased slightly (from 1 : 8 to 1 : 7.75), as did the HCA staffing ratio (from 1 : 10.6 to 1 : 7.75) (Table 22).
| Time | Beds | RMs (ratio of RMs to beds) | HCAs (ratio of HCAs to beds) |
|---|---|---|---|
| Pre move | 16 | 2 (1 : 8) | 1.5 (1 : 10.6) |
| Post move | 31 | 4 (1 : 7.75) | 4 (1 : 7.75) |
Midwives and support workers rotated on a 6-monthly basis between the antenatal unit, delivery suite and postnatal ward, although a few staff worked permanently on the postnatal ward. The workforce included a high proportion of long-service midwives and HCAs. The ward manager post was created when the two maternity units merged, and included responsibilities in the wider maternity department that sometimes took the ward manager away from the ward. Unlike the other case study wards, there was no shift co-ordinator role on the postnatal ward, although designating a ‘midwife in charge’ on each shift was under consideration. There were no formal ward rounds: paediatricians had a room on the ward and doctors usually discussed a patient only with the midwife responsible.
Summary
Each of the four case study wards had a different set of circumstances to deal with in terms of staffing, leadership, comparative ward size, and layout and deployment of staff, ward support and wider MDT interactions. Some wards had day rooms and staff rest rooms that were well used, while others adapted and made do with rooms which were not purpose built. What they all had in common was a move from multibedded facilities, where work patterns and teamwork were embedded, to the challenges of working in wards with 100% single rooms. Each ward had its own set of challenges to manage. The advantages and disadvantages for staff and patients are explored in depth in the following chapters (see Chapters 5–7).
Chapter 5 Case study quantitative data findings
Introduction
This chapter provides the results of the analysis of quantitative data from three different sources:
-
Staff activity: task time distribution. Observations of staff activities were undertaken in each study ward to understand the types of tasks undertaken by staff and the proportion of time spent on each. Staff were shadowed by a researcher who logged their activities.
-
Staff travel distances. These were collected by staff wearing pedometers. These data were collected before and after the shadowing sessions.
-
Staff experience surveys. Staff surveys on each ward were conducted before and after the move to the new hospital and these data provide a comparison of perceptions of the ward environment in the old and new wards.
The survey probed perceptions of many aspects of the ward environment before and after the move. As discussed in Chapter 3, the trust, the designers and stakeholders held various expectations about the benefits of the 100% single room design. We examined whether or not these expectations (or hypotheses about the effect of the move) were fulfilled. Specifically, the new hospital was designed to increase patient comfort, prevent infections, reduce numbers of patient falls, reduce patient stress, increase patient-centred care and increase the time spent by nurses on direct care (see Appendix 16). Concerns were raised about the possible reduction in staff observing and monitoring patients, increased travel distances and patient isolation.
This chapter primarily addresses the following two research questions:
-
What are the advantages and disadvantages of a move to all single rooms for staff?
-
Does the move to all single rooms affect staff experience and well-being and their ability to deliver effective and high-quality care?
Staff activity: task time distribution results
Preliminary analysis showed that five activity categories accounted for 78% of observation data before the move and 83% of observation data after the move. This meant that numbers in the remaining categories were too low for analysis, so all subsequent analyses were confined to these five categories: direct care, indirect care, professional communication, medication tasks and ward-related activities. Proportion of time was derived by calculating the duration of each event from its start and end time, and then aggregating duration by activity for each observation session. The number of events for each activity was also counted (Table 23).
| Time | Number | Minimum | Maximum | Suma | Mean | SD |
|---|---|---|---|---|---|---|
| Pre move | 19 | 106 | 242 | 3372 | 177 | 40 |
| Post move | 24 | 80 | 211 | 3679 | 153 | 33 |
Proportion of time spent in each type of activity was analysed using a general linear model with proportion of time as the dependent variable. The first model consisted of a single independent variable for before and after the new build and was used to ascertain the effect of the move to a new build, prior to adjusting for other variables. To this model were added ward (maternity, surgical, older people, AAU), staff group (midwife, RN, HCA) and day of the week. This second model was used to ascertain the effect of the move to the new build having adjusted for these variables.
Events were defined as a switch of activity (either to a new activity or to continue a previously interrupted activity) and were captured by a new entry in the PDA. The number of events (new or continuation of a previous activity) per hour was modelled in the same way except that a generalised linear model with a Poisson distribution and shift length in hours specified as offset (equivalent to modelling the hourly rate) was fitted to the data. An unadjusted analysis (before and after the new build only) and adjusted analysis (before and after the new build, ward, staff group and day of week) were performed.
Analysis of medication tasks was confined to RNs only. The fact that RMs work only on the postnatal ward means that it would not be possible to interpret whether any obtained results were due to the effect of the professional group or the ward. Therefore, staff group (i.e. midwives) was dropped from this model. On average the number of events (either new or continuations of previous activities) observed per session was higher before the move than after (177 vs. 153).
However, the move to the new build did not result in a significant change to the proportion of time spent on different activities (Table 24). Although there was an increase in the proportion of direct care, indirect care, professional communication and medication tasks and a decrease in ward-related activities such as cleaning, bed making and stocking the utility room in adjusted analyses, none of these changes was statistically significant (see Table 24).
| Activity | Pre move | Post move | Mean difference | 95% confidence interval | Significance | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | L95% | U95% | Mean | L95% | U95% | ||||
| Direct care | |||||||||
| Unadjusted | 29.7 | 23.7 | 35.7 | 33.0 | 27.5 | 38.5 | –3.3 | –11.2 to 4.6 | 0.400 |
| Adjusted | 33.5 | 27.4 | 39.5 | 37.9 | 31.5 | 44.3 | –4.5 | –11.7 to 2.8 | 0.219 |
| Indirect care | |||||||||
| Unadjusted | 7.9 | 5.8 | 10.0 | 9.4 | 7.9 | 10.9 | –1.5 | –3.9 to 0.9 | 0.222 |
| Adjusted | 6.8 | 4.5 | 9.0 | 8.5 | 6.1 | 10.9 | –1.7 | –4.4 to 1.0 | 0.204 |
| Professional communication | |||||||||
| Unadjusted | 15.2 | 11.2 | 19.3 | 17.8 | 15.1 | 20.4 | –2.5 | –7.0 to 2.0 | 0.268 |
| Adjusted | 15.3 | 11.9 | 18.8 | 16.0 | 12.3 | 19.6 | –0.7 | –4.8 to 3.5 | 0.748 |
| Medication tasksa | |||||||||
| Unadjusted | 10.8 | 4.2 | 17.5 | 13.3 | 8.5 | 18.1 | –2.4 | –10.0 to 5.1 | 0.513 |
| Adjusted | 11.8 | 6.0 | 17.6 | 12.4 | 7.2 | 17.5 | –0.6 | –8.7 to 7.5 | 0.880 |
| Ward-related activity | |||||||||
| Unadjusted | 13.9 | 8.2 | 19.7 | 9.2 | 5.4 | 13.0 | 4.7 | –1.8 to 11.2 | 0.148 |
| Adjusted | 10.8 | 6.1 | 15.5 | 9.4 | 4.4 | 14.4 | 1.4 | –4.3 to 7.0 | 0.622 |
Table 25 shows results for the analysis of the number of events per hour. The adjusted number of recorded events per hour decreased significantly for direct care (p = 0.039) and professional communication (p = 0.002), and increased significantly for medication tasks. A decrease in the number of events per hour for an activity, and no change in the proportion of time spent on that activity, suggests that there were fewer interruptions during these tasks and work was, therefore, less fragmented. This interpretation is supported by qualitative data showing that nurses could focus on direct care and communication tasks more easily in the single room environment. Staff had difficulty locating each other and also felt reluctant to interrupt a colleague providing direct care in a single room, and there were more frequent structured opportunities for professional communication within the small nursing teams.
| Activity | Pre move | Post move | Risk ratio | ||||
|---|---|---|---|---|---|---|---|
| Rate | 95% confidence interval | Rate | 95% confidence interval | eβ | 95% confidence interval | Significance | |
| Direct care | |||||||
| Unadjusted | 7.75 | 7.26 to 8.26 | 6.80 | 6.36 to 7.26 | 1.14 | 1.04 to 1.25 | 0.005 |
| Adjusted | 7.95 | 7.32 to 8.65 | 7.12 | 6.48 to 7.81 | 1.12 | 1.01 to 1.24 | 0.039 |
| Indirect care | |||||||
| Unadjusted | 3.58 | 3.26 to 3.94 | 4.13 | 3.80 to 4.49 | 0.87 | 0.76 to 0.98 | 0.028 |
| Adjusted | 3.19 | 2.78 to 3.66 | 3.63 | 3.15 to 4.19 | 0.88 | 0.76 to 1.02 | 0.082 |
| Professional communication | |||||||
| Unadjusted | 6.78 | 6.33 to 7.27 | 6.37 | 5.95 to 6.82 | 1.07 | 0.97 to 1.17 | 0.201 |
| Adjusted | 6.89 | 6.31 to 7.53 | 5.80 | 5.24 to 6.42 | 1.19 | 1.06 to 1.33 | 0.002 |
| Medication tasksa | |||||||
| Unadjusted | 2.66 | 2.30 to 3.07 | 4.48 | 4.08 to 4.93 | 0.59 | 0.50 to 0.70 | < 0.001 |
| Adjusted | 2.62 | 2.26 to 3.05 | 3.62 | 3.19 to 4.11 | 0.72 | 0.59 to 0.88 | 0.001 |
| Ward-related activity | |||||||
| Unadjusted | 3.15 | 2.85 to 3.49 | 2.77 | 2.50 to 3.07 | 1.14 | 0.98 to 1.31 | 0.080 |
| Adjusted | 2.30 | 1.99 to 2.66 | 2.49 | 2.12 to 2.91 | 0.92 | 0.77 to 1.11 | 0.401 |
The number of events per hour increased significantly for medication tasks (p = 0.001), showing increased fragmentation for this task. Again, this interpretation is supported by the qualitative data showing that when staff entered a patient room to administer medication they were likely to engage in other direct care activities; thus medication administration was not carried out in a single medication round, but integrated into patient care activities generally.
We also assessed the changes in patients’ contact time per patient-day to check if nurses spent more time with the patient instead of doing other activities. The analysis draws on day shift observation data (based on 118.5 hours of staff shadowing before the move and 254.5 hours after the move). The proportion of contact time was applied to the total NHPPD to provide an estimate of the patients’ contact time per patient-day (see Table 26).
| Measure | Older people’s ward | AAU | Maternity ward | Surgical ward | ||||
|---|---|---|---|---|---|---|---|---|
| Before | After | Before | After | Before | After | Before | After | |
| Total observed patient contact (seconds) | 46,695 | 44,040 | 34,359 | 48,054 | 25,575 | 35,782 | 45,748 | 43,489 |
| Total observed time (seconds) | 103,412 | 123,379 | 104,034 | 119,153 | 105,895 | 119,762 | 116,729 | 122,689 |
| Proportion contact time over total (% over total) | 0.45154 | 0.35695 | 0.33027 | 0.40330 | 0.24151 | 0.29878 | 0.39192 | 0.35447 |
| Hours of patients contact over 12 hours (B) | 05:25 | 04:17 | 03:57 | 04:50 | 02:53 | 03:35 | 04:42 | 04:15 |
| Difference (before and after) of contact (minutes) every 12 hours | –68 | 53 | 41 | –27 | ||||
| Average monthly WTE | 32.38 | 44.13 | 27.48 | 47.77 | 86.91 | 144.86 | 42.22 | 41.29 |
| Average monthly nurse hours | 5262 | 7172 | 4465 | 7762 | 14,123 | 23,540 | 6861 | 6709 |
| Average monthly patient-days | 1296 | 1120 | 486 | 791 | 1471 | 1914 | 1011 | 961 |
| Average NHPPD | 4.1 | 6.4 | 9.2 | 9.8 | 9.6 | 12.3 | 6.8 | 7.0 |
| Proportion of patient contact over total activities × NHPPD | 1.8 | 2.3 | 3.0 | 4.0 | 2.3 | 3.7 | 2.7 | 2.5 |
| Difference of patient contact per patient-day (hours) | 0.45 | 0.93 | 1.4 | –0.2 | ||||
| Difference of patient contact per patient-day (minutes) | 27 | 56 | 81 | –11 | ||||
| % difference | 25 | 30 | 58 | –7 | ||||
After the move, the contact time per patient-days increased in all units, apart from surgery, where there was a decrease in direct care and an increase in indirect care activities, for example medication activities and professional communication, and essential ward/patient care activities.
These changes are the result of a combination of two factors: a change in the proportion of care (i.e. an increase/decrease in the time spent with the patient) and a change in NHPPD (i.e. an increase/decrease in the number of nurses working full-time during a day).
Staff travel distances results
Statistical analysis
The data were analysed using a repeated measures general linear mixed model (GLMM) with steps per hour as the dependent variable and pre/post new build, ward (maternity, surgical, older people, AAU), observation session (repeated measure), staff group (midwife, RN, HCA) and day of the week as independent variables. The first GLMM analysis investigated the main effects of ward, pre/post move, staff group and day of the week. The second GLMM analysis investigated the interactions between pre/post move and ward, and between pre/post move and staff group. Because midwives were employed only on the maternity ward, there was potential confounding between the effects of ward and staff type. Initial analyses confirmed that removing maternity from the analyses improved the fit of the models. The first sensitivity analysis added a variable to the model that indicated whether or not a member of staff contributed to both the pre- and post-build samples. Only five staff contributed to both. The effect on the overall results was minor. A second sensitivity analysis fitted a model to first observation session data only, but allowed data to repeat across individual staff before and after the build. We report the results below, including where sensitivity analyses identified differences.
The data set contains information on 140 sessions collected on 53 staff (49%) prior to and 56 staff (51%) after the new build. A number of staff contributed more than one observation session: 85 provided one session, 18 provided two sessions, five provided three sessions and one provided four sessions. There were 73 sessions (52%) collected prior to the new build and 67 sessions (48%) after the new build. The average numbers of sessions per member of staff were 1.38 and 1.20, respectively. A small number of staff (n = 5, 4%) were observed at both times (one RN and four HCAs). Table 27 shows descriptive data for ward and staff group.
| Group | Before new build | After new build | ||||||
|---|---|---|---|---|---|---|---|---|
| Number of observation sessions | Mean | Range | SD | Number of observation sessions | Mean | Range | SD | |
| Ward | ||||||||
| Maternity | 14 | 630 | 380–1007 | 194 | 8 | 687 | 463–1008 | 211 |
| Surgical | 17 | 653 | 354–996 | 152 | 22 | 793 | 419–1274 | 247 |
| Older people | 23 | 664 | 361–965 | 158 | 21 | 845 | 553–1229 | 193 |
| AAU | 19 | 773 | 479–1007 | 181 | 16 | 880 | 469–1311 | 254 |
| Staff group | ||||||||
| Midwife | 7 | 475 | 380–640 | 94 | 6 | 583 | 463–683 | 99 |
| RN | 32 | 639 | 354–1007 | 178 | 29 | 827 | 419–1311 | 240 |
| HCA | 34 | 768 | 470–1007 | 131 | 32 | 853 | 469–1274 | 220 |
| Total | 73 | 683 | 354–1007 | 175 | 67 | 817 | 419–1311 | 231 |
The unadjusted means (see Table 27) show an increase in the number of steps per hour for all wards and staff groups. Staff working on the older people’s ward (from 664 to 845) and RNs (from 639 to 827) have seen the biggest increases.
Table 28 shows results for the main effects of ward, pre/post move, staff group and day of the week. The number of steps per hour increased significantly from a mean of 715 before the move to a mean of 839 [F(1,83) = 10.36; p = 0.002] after the move. HCAs took significantly more steps per hour than nurses [F(1,83) = 8.01; p = 0.006]. There were also significant differences between days of the week [F(4,21) = 3.40; p = 0.027]. There was no significant difference between wards in the distances travelled (Table 29).
| Source | Numerator df | Denominator df | F | Significance |
|---|---|---|---|---|
| Ward | 2 | 89.251 | 2.375 | 0.099 |
| Pre/post | 1 | 83.369 | 10.361 | 0.002 |
| Staff group | 1 | 82.744 | 8.009 | 0.006 |
| Day of week | 4 | 21.304 | 3.403 | 0.027 |
| Main effect | Mean | 95% confidence interval | Standard error | df |
|---|---|---|---|---|
| Ward | ||||
| Surgical | 746.224 | 677.846 to 814.601 | 34.374 | 82.310 |
| Older people | 742.913 | 679.206 to 806.620 | 32.060 | 88.556 |
| AAU | 843.230 | 768.182 to 918.278 | 37.766 | 88.363 |
| Phase | ||||
| Pre | 715.663 | 659.846 to 771.481 | 28.032 | 77.056 |
| Post | 839.248 | 786.866 to 891.630 | 26.355 | 87.117 |
| Staff group | ||||
| RN | 719.222 | 666.644 to 771.800 | 26.442 | 84.478 |
| HCA | 835.689 | 776.300 to 895.079 | 29.848 | 80.953 |
| Day of the week | ||||
| Monday | 741.312 | 655.436 to 827.187 | 42.848 | 54.843 |
| Tuesday | 777.115 | 692.873 to 861.358 | 42.300 | 76.367 |
| Wednesday | 755.842 | 690.048 to 821.635 | 32.229 | 30.291 |
| Thursday | 717.955 | 645.887 to 790.022 | 35.438 | 33.377 |
| Friday | 895.054 | 813.920 to 976.189 | 39.796 | 31.297 |
Table 30 shows results for the interactions between pre/post move and ward, and between pre/post move and staff group. Neither of the two interactions was statistically significant.
| Source | Numerator df | Denominator df | F | Significance |
|---|---|---|---|---|
| Ward | 2 | 84.165 | 3.084 | 0.051 |
| Pre/post | 1 | 79.605 | 8.064 | 0.006 |
| Staff group | 1 | 78.399 | 9.402 | 0.003 |
| Day of week | 4 | 16.204 | 2.673 | 0.070 |
| Ward × pre/post | 2 | 82.450 | 0.641 | 0.529 |
| Staff group × pre/post | 1 | 76.482 | 3.481 | 0.066 |
The estimated marginal means (Table 31) showed that there was an increase from pre to post build across all wards. Although the size of this increase did not differ significantly between wards, the increases in the surgical and older people’s wards were larger than for the AAU. RNs experienced a larger increase (from 624 to 811) in the number of steps per hour (from 3.74 to 4.86 miles) than HCAs (from 828 to 862 steps; from 4.96 to 5.17 miles).
| Interaction effects | Ward | Mean | 95% confidence interval | Standard error | df |
|---|---|---|---|---|---|
| Pre | Surgical | 689.468 | 589.662 to 789.274 | 50.188 | 83.952 |
| Older people | 654.297 | 560.517 to 748.077 | 47.077 | 75.094 | |
| AAU | 834.224 | 717.999 to 950.449 | 58.270 | 69.703 | |
| Post | Surgical | 808.083 | 716.470 to 899.697 | 45.991 | 75.279 |
| Older people | 820.963 | 733.337 to 908.589 | 44.103 | 89.452 | |
| AAU | 880.431 | 780.455 to 980.408 | 50.311 | 88.382 | |
| Pre | RN | 623.967 | 549.679 to 698.255 | 37.304 | 76.621 |
| HCA | 828.026 | 735.557 to 920.495 | 46.318 | 66.286 | |
| Post | RN | 811.322 | 737.286 to 885.358 | 37.230 | 83.973 |
| HCA | 861.663 | 784.430 to 938.896 | 38.825 | 82.223 |
The estimated marginal means from the second sensitivity analysis suggested a decrease in the number of steps per hour for the AAU from 901 to 836 and for HCAs from 876 to 855, rather than an increase as shown in Table 31. The change in means for the remaining two wards and for RNs, from pre to post build, were in the same direction, and of the same order of magnitude (see Table 31).
Staff experience survey
Results
Because of staff leave, shift patterns and staff turnover during the course of the study, it was not possible to use a completely within-subjects design, in which the pre- and post-move surveys were completed by the same people. Despite this, 19 participants did complete surveys at both times, which meant a mixed within- and between-subjects design. One potential problem with this is that the subgroup who completed both surveys could have been sensitised to the research questions and, therefore, could have been more likely to report differences after the move than those who completed only one survey; that would bias our results. We addressed this by treating the design as a between-subjects design and checking for bias by comparing the results of our analyses for the whole group with separate within-subjects analyses on the subgroup who completed both surveys. The results were identical except for a small difference: perceptions of the effect of the accommodation on the delivery of care approached significance (0.099) in the within-subjects analysis whereas for the whole group this effect was significant (0.011). This can be attributed to lack of power in the subsample of 19. On this basis we proceeded with the analysis by treating the ‘before’ and ‘after’ samples as independent groups.
There were 152 items in the staff survey. Our approach to analysis was multifaceted. First, we explored the potential for grouping questions into subscales that would summarise a topic area. We thematically analysed the questions to determine those that were likely to be measuring attitudes to related aspects of the ward design, and then tested these subscales using statistical reliability analysis. Where reliability was not adequate we revised the items in the subscales until we had identified coherent subscales. These were then analysed using independent sample t-tests to determine if post-move responses were significantly different from the pre-move scores for each subscale. Similar analyses were undertaken for the teamwork and safety climate scales. Qualitative open-ended questions were analysed thematically using a content analytic approach. The well-being and stress items were compared before and after the move using the Pearson chi-squared test and Fisher’s exact test when expected frequencies were less than 5.
One of the aims of the study was to investigate if there were differences between the case study wards in their perceptions of the positives and negatives of the new single room accommodation. However, the relatively small number of staff in each of the case study wards meant that it was not possible to explore this question statistically. We therefore used correspondence analysis and perceptual mapping to examine the interaction between ward attributes and case study wards. Correspondence analysis is an exploratory mapping tool that allows visualisation of relationships in the data that would be difficult to identify if presented in a table. 114 It is related to other techniques such as factor analysis and multidimensional scaling. It does not rely on significance testing and is best viewed as an exploratory technique that provides insights into the similarities and differences between two variables. 115 Correspondence analysis does not address questions of whether or not there were differences in ratings between the attributes (e.g. whether or not privacy for patients was rated more highly than staff teamwork). Instead, it focuses on the differences between case study wards and the interaction between ratings and wards. It allows an examination of to what extent which wards are associated with particular ratings. In this way it allows us to qualitatively explore the quantitative data.
Ward environment survey subscales
Ten reliable subscales were formed. Table 32 shows the subscales and example items from each.
| Subscale | Description | Example question |
|---|---|---|
| Efficiency of the physical environment | Factors affecting work efficiency | Supplies/equipment always available |
| Care delivery | Factors affecting how care is delivered | Space at patients’ bedsides is sufficient for staff to provide care with ease |
| Staff amenity | Whether or not the ward is pleasant, agreeable and comfortable for staff | Staff rest area aids relaxation/recuperation |
| Patient amenity | Whether or not the ward is pleasant, agreeable and comfortable for patients | Adequate space for patients to move about the ward |
| Infection control | Factors facilitating infection control | The ward design/layout is helpful for isolating patients with infections |
| Privacy/confidentiality | Whether or not it is possible to maintain patient privacy and confidentiality in different situations | Maintaining patient confidentiality |
| Teamwork | Factors affecting how work is co-ordinated between team members | Ability of staff to spontaneously discuss issues of care |
| Patient safety | Factors affecting the safety of patients | Safety and security of patients |
| Staff safety | Factors affecting the safety of staff | Safety and security of staff |
| Family/visitors | Factors facilitating the involvement of family and visitors | Participation of family members in patient care |
Appendix 19 contains a complete list of all items used for each subscale.
Table 33 summarises the statistical analysis of the subscales showing means, Cronbach’s alpha and the number of items for each subscale before and after the move. According to accepted criteria,115 alpha above 0.60 is acceptable for exploratory analyses, above 0.70 is acceptable for confirmatory purposes and above 0.80 is good for confirmatory purposes. Obtained coefficients were generally good, ranging mostly between 0.67 and 0.92. The lowest alpha, of 0.53, was obtained for the family/visitors subscale after the move, suggesting that this subscale is not internally consistent. However, the pre-move alpha was good (0.70), so it was decided to retain this subscale for exploratory purposes.
| Subscale | Phase | Mean score | Cronbach’s alpha | Number of items | ||||
|---|---|---|---|---|---|---|---|---|
| Acute assessment | Medical (older people) | Surgical | Maternity | All | ||||
| Efficiency of physical environment | Pre | 2.86 | 3.36 | 2.53 | 2.65 | 2.80 | 0.77 | 10 |
| Post | 2.87 | 3.50 | 3.64 | 2.99 | 2.99 | 0.82 | 10 | |
| Care delivery | Pre | 3.29 | 3.65 | 3.30 | 2.76 | 3.20 | 0.72 | 6 |
| Post | 2.21 | 3.05 | 3.37 | 2.64 | 2.88 | 0.72 | 6 | |
| Staff amenity | Pre | 3.63 | 3.06 | 2.43 | 2.88 | 2.95 | 0.73 | 8 |
| Post | 2.53 | 3.23 | 3.48 | 3.14 | 2.99 | 0.80 | 8 | |
| Patient amenity | Pre | 2.73 | 3.26 | 2.81 | 2.62 | 2.82 | 0.83 | 14 |
| Post | 3.09 | 3.30 | 3.75 | 3.36 | 3.43 | 0.79 | 14 | |
| Infection control | Pre | 2.58 | 3.81 | 2.33 | 2.53 | 2.75 | 0.71 | 2 |
| Post | 4.25 | 3.82 | 4.57 | 4.27 | 4.25 | 0.67 | 2 | |
| Privacy/confidentiality | Pre | 2.38 | 3.48 | 2.35 | 2.22 | 2.54 | 0.92 | 4 |
| Post | 4.13 | 4.23 | 4.54 | 4.25 | 4.31 | 0.72 | 4 | |
| Teamwork | Pre | 3.48 | 4.09 | 3.73 | 3.09 | 3.55 | 0.90 | 11 |
| Post | 2.43 | 3.27 | 3.20 | 2.79 | 2.97 | 0.92 | 11 | |
| Patient safety | Pre | 2.97 | 3.82 | 3.32 | 2.96 | 3.23 | 0.73 | 5 |
| Post | 2.75 | 3.13 | 3.37 | 3.46 | 3.32 | 0.63 | 5 | |
| Staff safety | Pre | 3.11 | 3.65 | 3.28 | 2.87 | 3.19 | 0.80 | 5 |
| Post | 2.75 | 3.20 | 3.13 | 3.13 | 3.10 | 0.71 | 5 | |
| Family/visitors | Pre | 2.92 | 3.06 | 2.71 | 2.44 | 2.75 | 0.70 | 3 |
| Post | 3.25 | 3.67 | 4.21 | 3.92 | 3.89 | 0.53 | 3 | |
Table 34 shows the results of independent sample t-tests comparing subscale scores before and after the move. Staff perceived significant improvements in the efficiency of the physical environment, the patient amenity, the effect of the environment on infection control, patient privacy, and family and visitors. The largest increases were found for perceptions of infection control and patient privacy. Perceptions of the effect of the ward environment on teamwork and care delivery were significantly more negative after the move. There were no significant differences in staff perceptions of staff facilities, patient safety and staff safety.
| Subscale | Phase | Mean | SD | t | p-value |
|---|---|---|---|---|---|
| Efficiency of physical environment | Pre | 2.81 | 0.67 | –3.346 | 0.001a |
| Post | 3.24 | 0.70 | |||
| Care delivery | Pre | 3.20 | 0.66 | 2.59 | 0.011a |
| Post | 2.88 | 0.67 | |||
| Staff amenity | Pre | 2.95 | 0.67 | -0.373 | 0.710 |
| Post | 2.99 | 0.73 | |||
| Patient amenity | Pre | 2.82 | 0.64 | –5.52 | < 0.001a |
| Post | 3.43 | 0.50 | |||
| Infection control | Pre | 2.75 | 1.11 | –8.39 | < 0.001a |
| Post | 4.25 | 0.73 | |||
| Privacy | Pre | 2.54 | 1.15 | –10.14 | < 0.001a |
| Post | 4.31 | 0.59 | |||
| Teamwork | Pre | 3.55 | 0.64 | 4.34 | < 0.001a |
| Post | 2.96 | 0.77 | |||
| Patient safety | Pre | 3.23 | 0.69 | –7.32 | 0.466 |
| Post | 3.32 | 0.67 | |||
| Staff safety | Pre | 3.19 | 0.68 | 0.67 | 0.502 |
| Post | 3.10 | 0.75 | |||
| Family/visitors | Pre | 2.74 | 0.77 | –8.60 | < 0.001a |
| Post | 3.90 | 0.63 |
Although all subscales showed moderate to very good reliability, changes were not uniform for all items in every subscale; there were some exceptions to the overall trend. Overall ratings for the subscale ‘efficiency of physical environment’ increased, but ratings for the item ‘ward design/layout minimises walking distances for staff’ decreased. These perceptions were confirmed by our findings from the analysis of travel distances showing that staff took significantly more steps after than before the move. Some aspects of the design increased the amenity of the ward for staff but others did not. For example, staff toilet facilities, locker facilities and space at staff bases were rated more highly but ratings for social interaction and natural light decreased. These positive and negative aspects meant there was no significant difference in staff amenity before and after the move. The new ward was rated as much more positive for patients but there were reduced scores for three items after the move: social contact between patients, ability of patients to see staff and way finding. All aspects of teamwork and training were rated less positively, except for the item ‘discussing patient care with colleagues’, which increased. This finding is supported by our analysis of observation data showing that professional communication activities were less fragmented.
Although there were no significant differences in the effect of the ward layout on perceptions of patient safety, examination of the items showed that ratings for two items increased (‘minimising risk to patients of physical/verbal abuse from other patients/visitors’ and ‘minimising the risk of medication errors’) while ratings for two items decreased (‘responding to patient calls for assistance’ and ‘minimising the risk of falls/injury to patients’). This suggests that, although staff thought some risks to safety were reduced, they perceived an increased risk of falls and delays in responding to calls for assistance. Staff perceptions of a rise in risk of falls are detailed in Chapter 6. Staff also reported being unable to hear calls for assistance when in a single room with a patient.
There were five items that did not fit into any of the subscales. These items were analysed singly using Fisher’s exact test and the results are shown in Table 35. There was a significant relationship between the move and ratings for the number and location of hand basins, ease of keeping patient areas clean and quiet, and the overall comfort of patients, which all increased after the move. There was no relationship between the move and judgements of whether or not the location of the dirty utility room (where bedpans are stored and disposed of) reduces cross-contamination.
| Item | Fisher’s exact test | Exact p-value |
|---|---|---|
| Number and location of clinical hand wash basins supports good hand hygiene | 19.46 | < 0.001a |
| Location/layout of dirty utility reduces risk of spillages/cross-contamination | 3.91 | 0.43 |
| Overall comfort of patients | 28.82 | < 0.001a |
| Easy to keep patient care area quiet | 60.98 | < 0.001a |
| Easy to keep patient care areas clean | 19.59 | < 0.001a |
The distribution of responses for the four significant items showed that significantly more staff rated these aspects of single room accommodation as more positive after the move than before (Tables 36–39).
| Number and location of CHWBs supports good hand hygiene | Before or after move | Total | |
|---|---|---|---|
| Before | After | ||
| Strongly disagree | 2 | 1 | 3 |
| Disagree | 14 | 6 | 20 |
| Neither agree nor disagree | 7 | 4 | 11 |
| Agree | 29 | 23 | 52 |
| Strongly agree | 3 | 21 | 24 |
| Total | 55 | 55 | 110 |
| Overall comfort of patients | Before or after move | Total | |
|---|---|---|---|
| Before | After | ||
| Very unhelpful | 4 | 1 | 5 |
| Unhelpful | 16 | 1 | 17 |
| Neither helpful nor unhelpful | 15 | 7 | 22 |
| Helpful | 13 | 31 | 44 |
| Very helpful | 7 | 14 | 21 |
| Total | 55 | 54 | 109 |
| Easy to keep patient care areas quiet | Before or after move | Total | |
|---|---|---|---|
| Before | After | ||
| Strongly disagree | 20 | 3 | 23 |
| Disagree | 25 | 6 | 31 |
| Neither agree nor disagree | 3 | 7 | 10 |
| Agree | 3 | 34 | 37 |
| Strongly agree | 0 | 5 | 5 |
| Total | 51 | 55 | 106 |
| Easy to keep patient care areas clean | Before or after move | Total | |
|---|---|---|---|
| Before | After | ||
| Strongly disagree | 3 | 3 | 6 |
| Disagree | 14 | 1 | 15 |
| Neither agree nor disagree | 12 | 9 | 21 |
| Agree | 19 | 32 | 51 |
| Strongly agree | 3 | 10 | 13 |
| Total | 51 | 55 | 106 |
Expectations before the move and reality after the move
Before the move, staff were asked to rate on a five-point scale whether they thought single rooms would be better or worse for different aspects of clinical work (e.g. minimising the risk of patient falls, maintaining patient confidentiality, knowing when other staff might need help). After the move they again rated whether single rooms were better or worse for clinical work, thus providing a measure of whether or not their expectations about single rooms were met in reality. The questions were a subset of 23 questions from the first part of the survey and were analysed using Fisher’s exact test.
Results (Table 40) showed that staff perceptions of whether or not single rooms were better than multibedded wards changed after the move for five items. Staff perceptions of whether or not single rooms were better for responding to calls for assistance, knowing when other staff might need help and minimising walking distances were rated as worse or much worse by significantly more staff after than before the move. Staff rated single rooms as positive for patient sleep and rest and for interactions between patients and visitors after the move.
| Item | Fisher’s exact test | p-value |
|---|---|---|
| Minimising falls/injury to patients | 1.12 | 0.923 |
| Minimising need to move patients within the ward | 5.96 | 0.192 |
| Keeping patient areas clean | 5.68 | 0.217 |
| Communication between nursing staff and patients | 7.12 | 0.191 |
| Participation of family member in care | 4.24 | 0.370 |
| Responding to patient calls for assistance | 10.14 | 0.029a |
| Preventing/controlling hospital-acquired infections | 6.18 | 0.066 |
| Patient sleep and rest | 6.49 | 0.049a |
| Ease of taking patients to toilet/bathroom | 5.44 | 0.138 |
| Ability of staff to deliver high-quality care to all patients | 6.52 | 0.231 |
| Maintaining patient confidentiality | 3.86 | 0.235 |
| Minimising risk to staff of physical/verbal abuse | 8.09 | 0.082 |
| Knowing when other staff might need a helping hand | 10.75 | 0.010a |
| Ability of patients to see staff | 5.19 | 0.117 |
| Patient privacy | 3.84 | 0.121 |
| Patient interaction with visitors | 8.94 | 0.051a |
| Minimising staff walking distances | 13.36 | 0.006a |
| Minimising risk to patient of verbal/physical abuse | 7.39 | 0.113 |
| Social contact between patients | 3.57 | 0.487 |
| Overall comfort of patients | 3.88 | 0.400 |
| Minimising risk of medication errors | 6.39 | 0.112 |
| Staff spending time with patients | 8.30 | 0.068 |
| Monitoring patients | 4.07 | 0.234 |
Tables 41–45 show the distribution of significant responses.
| 100% single rooms, Responding to patient calls for assistance | Before or after move | Total | |
|---|---|---|---|
| Before | After | ||
| Much worse | 3 | 16 | 19 |
| Worse | 18 | 18 | 36 |
| No different | 20 | 15 | 35 |
| Better | 5 | 4 | 9 |
| Much better | 2 | 1 | 3 |
| Total | 48 | 54 | 102 |
| 100% single rooms, Patient sleep and rest | Before or after move | Total | |
|---|---|---|---|
| Before | After | ||
| Much worse | 0 | 0 | 0 |
| Worse | 0 | 1 | 1 |
| No different | 1 | 3 | 4 |
| Better | 15 | 24 | 39 |
| Much better | 39 | 26 | 65 |
| Total | 55 | 54 | 109 |
| 100% single rooms, Knowing when other staff might need a helping hand | Before or after move | Total | |
|---|---|---|---|
| Before | After | ||
| Much worse | 18 | 37 | 55 |
| Worse | 24 | 12 | 36 |
| No different | 5 | 4 | 9 |
| Better | 3 | 2 | 5 |
| Much better | 0 | 0 | 0 |
| Total | 50 | 55 | 105 |
| 100% single rooms, Patient interaction with visitors | Before or after move | Total | |
|---|---|---|---|
| Before | After | ||
| Much worse | 3 | 1 | 4 |
| Worse | 3 | 3 | 6 |
| No different | 14 | 5 | 19 |
| Better | 15 | 26 | 41 |
| Much better | 13 | 19 | 32 |
| Total | 48 | 54 | 102 |
| 100% single rooms, Minimising staff walking distances | Before or after move | Total | |
|---|---|---|---|
| Before | After | ||
| Much worse | 13 | 30 | 43 |
| Worse | 14 | 15 | 29 |
| No different | 13 | 4 | 17 |
| Better | 7 | 4 | 11 |
| Much better | 0 | 2 | 2 |
| Total | 47 | 55 | 102 |
Teamwork and safety climate survey
To take into account our changes to the survey, we combined the four items about the quality of communication with doctors, nurses, nursing assistants and AHPs with the items in the information handover subscale to form a new subscale of seven items. Although this is different from the scales reported by Hutchinson et al. ,98 reliability analysis confirmed the original factor structure of the survey. There were two teamwork subscales and three safety climate subscales with good to high reliability (Table 46). See Appendix 20 for a list of the items contained in each subscale.
| Subscale | Phase | Mean score | Cronbach’s alpha | Number of items | ||||
|---|---|---|---|---|---|---|---|---|
| Acute assessment | Medical (older people) | Surgical | Maternity | All | ||||
| Teamwork | ||||||||
| Input into decisions | Pre | 4.17 | 3.85 | 4.06 | 3.50 | 3.86 | 0.77 | 6 |
| Post | 3.46 | 3.88 | 3.83 | 3.47 | 3.65 | 0.87 | 6 | |
| Information handover and communication | Pre | 4.17 | 4.04 | 4.07 | 3.62 | 3.95 | 0.71 | 7 |
| Post | 3.25 | 3.72 | 3.79 | 3.49 | 3.59 | 0.80 | 7 | |
| Safety climate | ||||||||
| Attitudes to safety within own team | Pre | 3.87 | 4.02 | 4.27 | 3.53 | 3.90 | 0.79 | 5 |
| Post | 3.65 | 3.82 | 4.04 | 3.46 | 3.69 | 0.83 | 5 | |
| Overall confidence in safety of organisation | Pre | 3.36 | 3.09 | 3.16 | 2.92 | 3.11 | 0.76 | 3 |
| Post | 2.50 | 3.09 | 3.21 | 2.89 | 2.99 | 0.73 | 3 | |
| Perceptions of management’s attitudes to safety | Pre | 3.44 | 3.18 | 3.71 | 3.04 | 3.34 | 0.83 | 3 |
| Post | 2.25 | 3.27 | 3.33 | 3.16 | 3.16 | 0.78 | 3 | |
Mean scores for all subscales decreased following the move. Independent sample t-tests showed that ratings for information handover and communication decreased significantly following the move [t = 3.23, degrees of freedom (df) = 108, p = 0.002], indicating that information exchange and sharing within teams was perceived to be worse after the move. There were no other significant differences.
Correspondence analysis
Correspondence analysis transforms cross-tabulated data into a biplot showing distances between variables. In this study, case study ward was a column variable and mean questionnaire subscale score was a row variable (see Table 33). As appropriate when analysing mean scores, Euclidean distance was used and standardisation by removing row means was used. 114,116 This means that differences between the subscale means were not represented in the perceptual map, as we were not interested in whether or not, for example, infection control was rated more highly than privacy. Differences between wards, contained in the columns, were of interest and are represented in the perceptual map. Separate analyses were conducted for before and after the move and for the ward attributes and teamwork/safety climate survey.
Figure 11 shows perceptual maps of the association between ward attributes and wards before and after the move. The pre-move map shows that the points on the map were dispersed, indicating that the ratings were not strongly associated with particular wards. There was one exception in that ratings for the efficiency of the physical environment, privacy and infection control were higher for the older people’s ward than for the other wards. The post-move map shows that the highest ratings for the efficiency of the physical environment, the delivery of care, the staff facilities and teamwork were obtained in the older people’s and surgical wards, indicated by proximity on the map. Ratings for patient amenity, infection control, privacy and family/visitors were highest for the surgical ward. High ratings for patient safety were obtained in maternity and the surgical ward. Ratings for staff safety were similar in the older people’s, surgical and maternity wards. The acute assessment ward was not associated with any particular ward attributes, as was the case before the move.
FIGURE 11.
Perceptual maps of (a) pre- and (b) post-move ward attributes by ward.
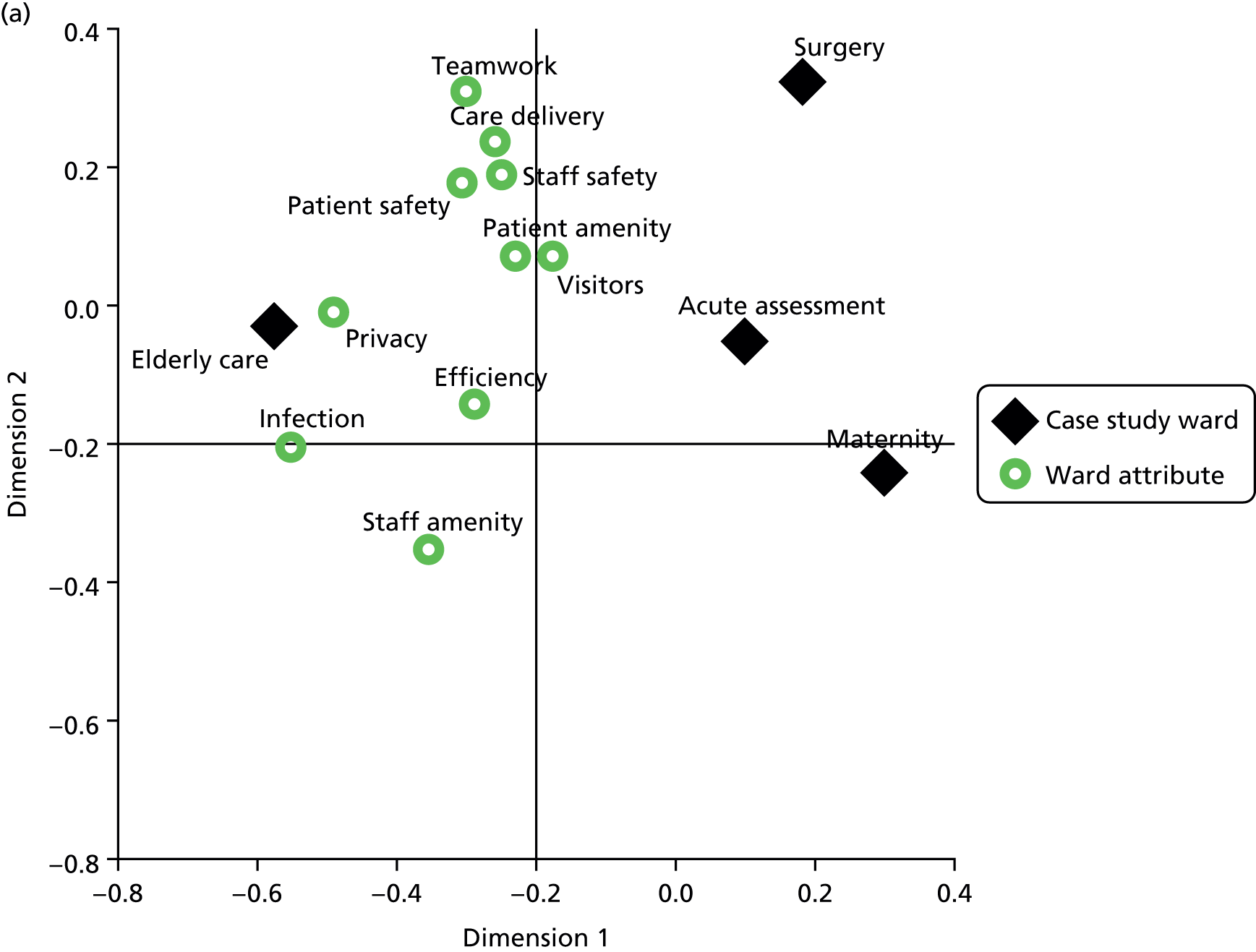
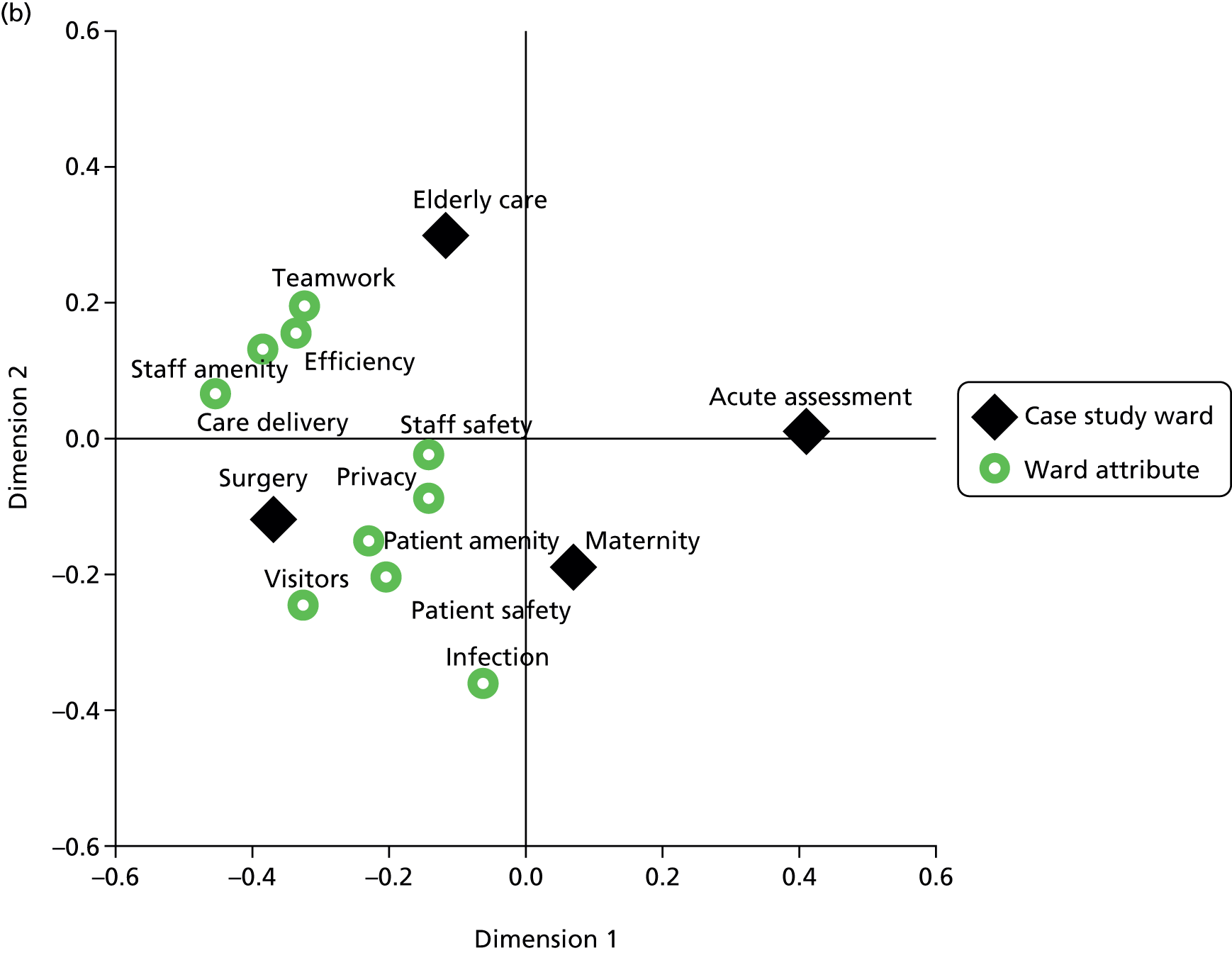
Figure 12 shows perceptual maps before and after the move of the association between teamwork/safety climate ratings and wards. The teamwork/safety climate survey consisted of two teamwork subscales – team input into decisions, and information handover and communication – and three safety climate subscales – attitudes to safety within own team, overall confidence in safety of organisation and perceptions of management attitudes to safety. The pre-move map shows that ratings of input into decisions, information and handover, and overall confidence in safety of the organisation were highest for the acute assessment ward. Ratings of safety attitudes within the team and management attitudes to safety were highest for the surgical ward. After the move, the surgical ward had the highest ratings for safety attitudes within the team, overall attitudes to safety and management; ratings for team input into decisions and information handover and communication were highest for the older people’s ward. Ratings for all safety climate subscales decreased in the acute assessment ward, which is indicated on the perceptual map by its location in a quadrant by itself. Maternity scores did not show a consistent pattern.
FIGURE 12.
Perceptual map of (a) pre- and (b) post-move ratings of teamwork/safety climate by ward. Att., attitude; mgt., management.
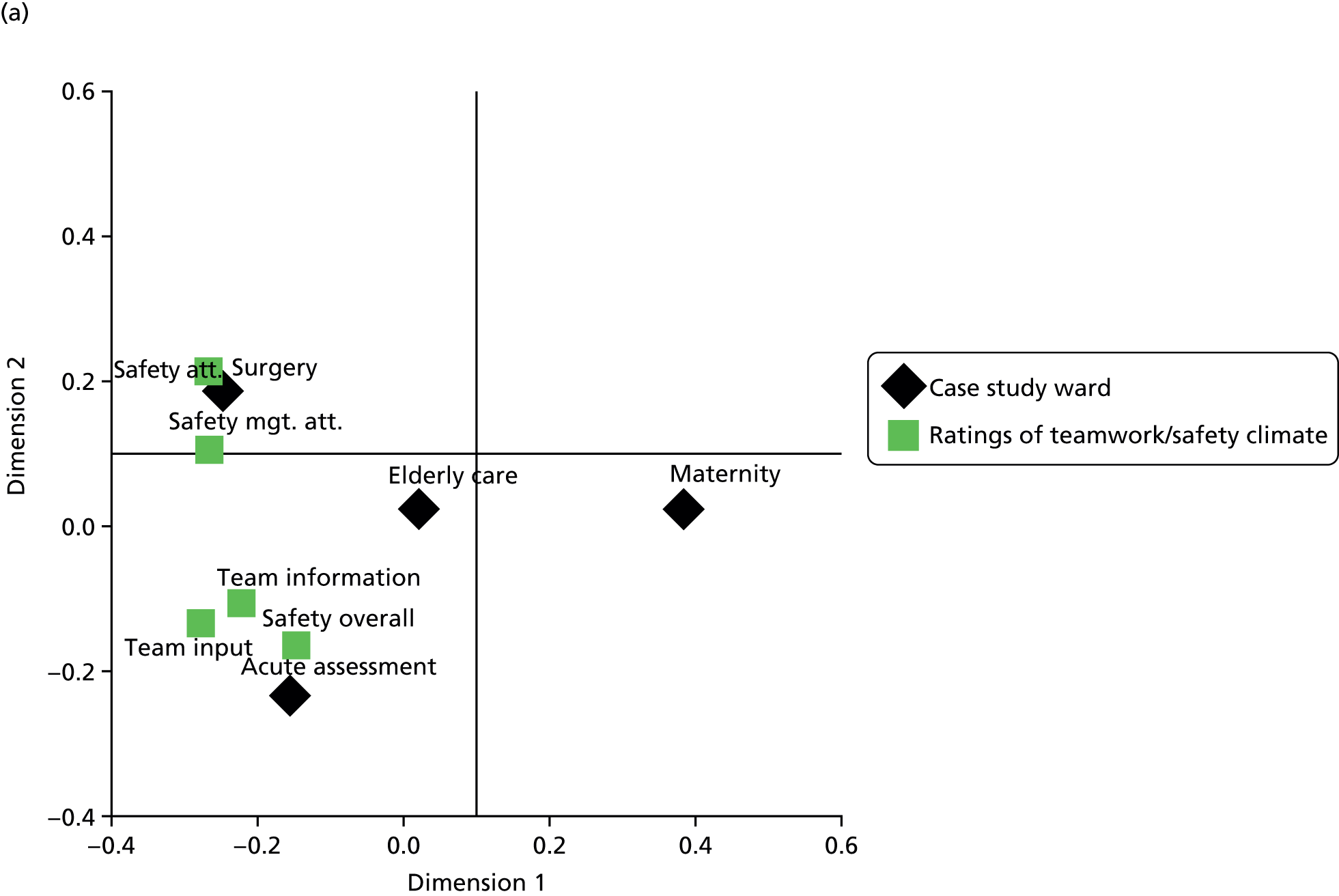
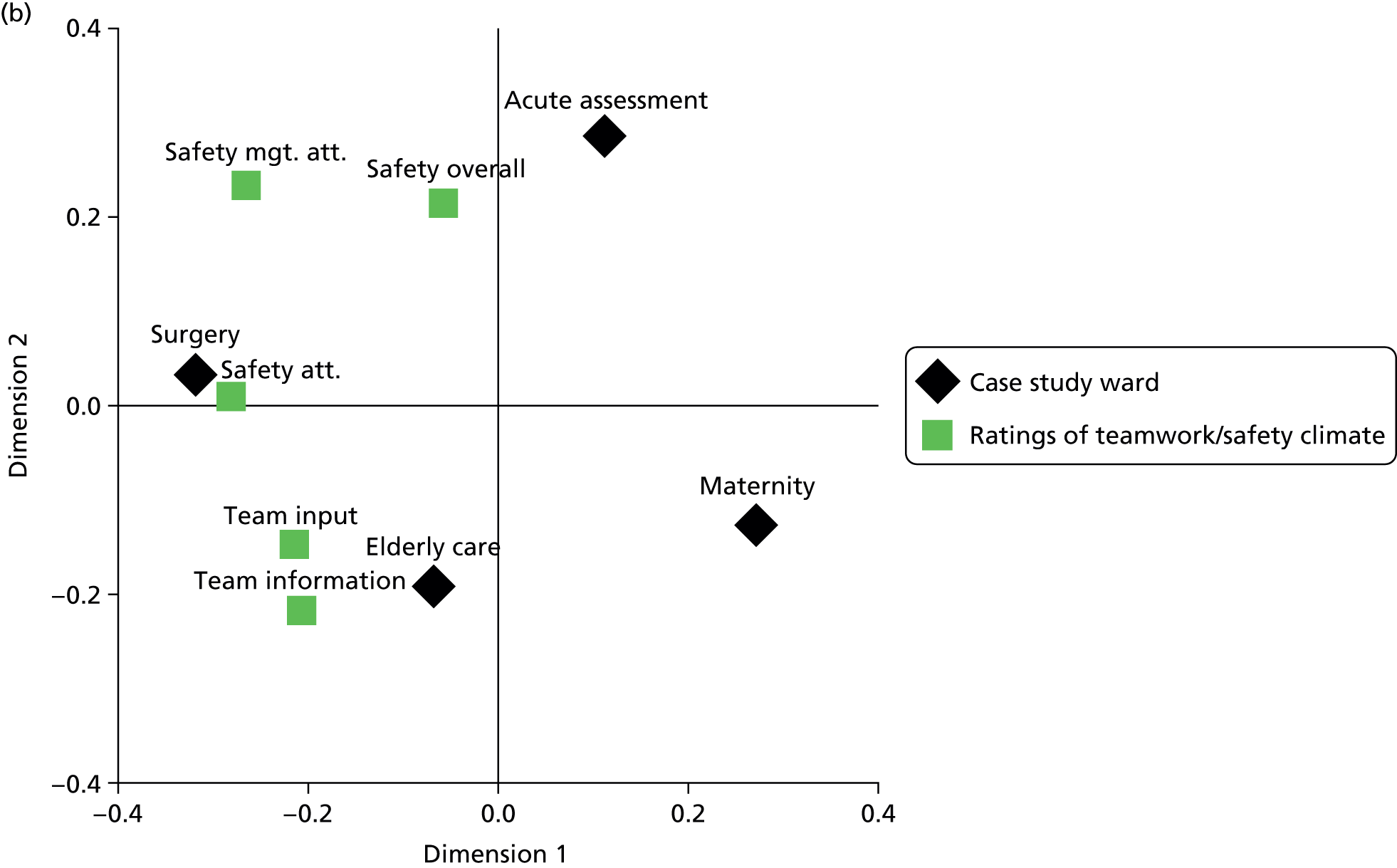
These maps reveal some differences between wards in perceptions of the ward environment and show that perceptions were different before and after the move.
Staff ward preferences
Nursing staff were asked to indicate whether they would prefer single rooms, multibedded accommodation or a combination. There was a range of views (Figure 13). In each phase, fewer than 18% of staff indicated a preference for 100% single rooms. The most common preference in each phase was a combination of 50% of beds in single rooms and 50% in bays (see Figure 13). In the pre-move survey, more staff reported a preference for more beds in bays (n = 20) than in the post-move phase (n = 12).
FIGURE 13.
Nurse preferences for single room or multibedded accommodation.
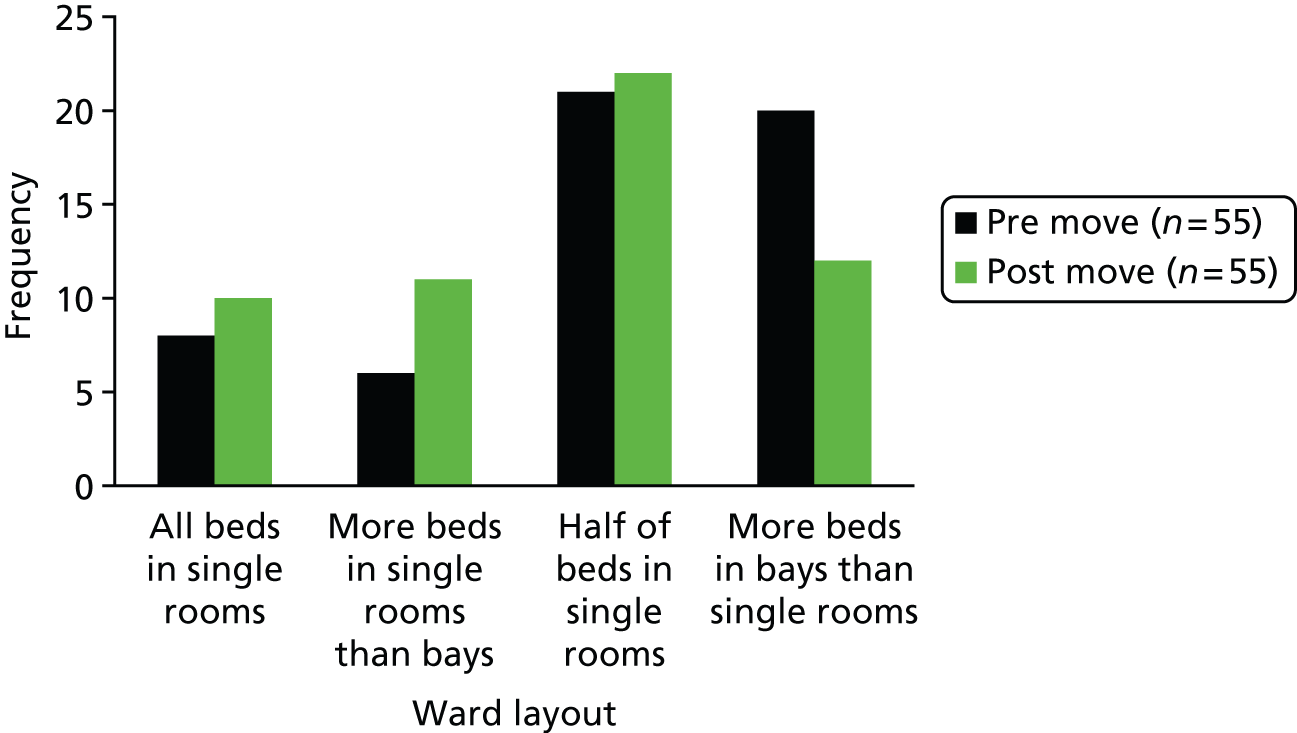
Staff stress and well-being
There were five categorical questions about staff well-being that investigated whether or not they had experienced injuries and harassment in the previous 12 months (Table 47). There were three items about job stress that asked participants to rate their stress on a five-point Likert scale (Table 48). Results showed no differences in staff well-being and stress before and after the move.
| Item | χ2a | df | p-valueb |
|---|---|---|---|
| During the last 12 months have you been injured or felt unwell as a result of moving and handling? | 0.842 | 1 | 0.359 |
| During the last 12 months have you been injured or felt unwell as a result of needlestick and sharps injuries? | 0.000 | 1 | 1.00 |
| During the last 12 months have you been injured or felt unwell as a result of slips, trips and falls? | 0.000 | 1 | 1.00 |
| In the last 12 months have you personally experienced physical violence, harassment, bullying or abuse from patients or partners/relatives/visitors? | 1.545 | 1 | 0.214 |
| In the last 12 months have you personally experienced physical violence, harassment, bullying or abuse from colleagues? | 0.000 | 1 | 1.00 |
| Item | χ2 | df | Exact p-valuea |
|---|---|---|---|
| I often feel under a lot of pressure at work | 3.32 | 3 | 0.359 |
| I worry a lot about my work outside working hours | 0.60 | 4 | 0.985 |
| My job is very stressful | 1.820 | 4 | 0.863 |
Staff were asked 10 questions about their satisfaction with their own performance of various tasks during their last shift, and one question about their overall job satisfaction. Results (Table 49) showed no significant effect for any of the job satisfaction items.
| Item | χ2 | df | p-value |
|---|---|---|---|
| Satisfaction with performance of physical care | 1.29 | 4 | 0.871 |
| Satisfaction with performance of emotional care | 3.61 | 4 | 0.467 |
| Satisfaction with performance of monitoring/recording observations | 5.80 | 4 | 0.213 |
| Satisfaction with performance of pain management | 4.03 | 3 | 0.282 |
| Satisfaction with performance of activities of daily living | 5.43 | 4 | 0.268 |
| Satisfaction with performance of educating/teaching patients/family | 1.82 | 4 | 0.839 |
| Satisfaction with performance of medication administration | 4.00 | 4 | 0.364 |
| Satisfaction with performance of preparing patients for discharge | 1.66 | 4 | 0.799 |
| Satisfaction with performance of care planning/co-ordination | 1.58 | 4 | 0.812 |
| Satisfaction with performance of documenting care | 2.83 | 4 | 0.620 |
| Satisfaction overall with job | 5.07 | 4 | 0.303 |
Qualitative survey data
Four open-ended questions were used to gain qualitative data about staff attitudes. The questions were:
-
What two things do you think would most improve the current ward environment for staff?
-
What two things do you think would most improve the current ward environment for patients?
-
Before move:
-
What two things are you most looking forward to in relation to the move to 100% single rooms in the new hospital?
-
What two things are you most concerned about in relation to the move to 100% single rooms in the new hospital?
-
-
After move:
-
What two things do you like the most about single room wards in the new hospital?
-
What two things do you dislike most about single room wards in the new hospital?
-
In the following sections we present the results of the thematic analysis with frequency data (almost equal numbers of staff responded before and after the move, n = 55 and n = 54 respectively) and examples from participants’ written responses where appropriate. Table 50 shows that staff identified a number of things that would improve the ward accommodation for patients. The need for more space, improved patient facilities, privacy, and rest and sleep were largely met, since there were fewer people identifying these as needs after the move. However, the need for improved patient–staff ratios and a day room to provide patient social interaction were still reported after the move.
| Improvement needed | Phase | Mean | Total | |||
|---|---|---|---|---|---|---|
| Acute assessment | Medical (older people) | Surgical | Maternity | |||
| More space around patient beds | Pre | 2 | 4 | 7 | 8 | 21 |
| Post | – | – | – | – | – | |
| Improved staff–patient ratio/more quality time with staff | Pre | 2 | 5 | 3 | 1 | 11 |
| Post | 1 | – | 4 | 5 | 10 | |
| Improved heating/lighting/ventilation | Pre | 1 | – | 3 | 1 | 5 |
| Post | – | – | 1 | 1 | 2 | |
| Improved patient toilet/bathroom facilities | Pre | 1 | 1 | 2 | 5 | 9 |
| Post | – | 1 | 2 | – | 3 | |
| Improved patient privacy | Pre | 5 | 1 | 2 | 7 | 15 |
| Post | – | – | – | 1 | 1 | |
| Improved rest and sleep | Pre | 1 | 1 | 3 | 2 | 7 |
| Post | – | – | – | – | – | |
| Day room/TV/social interaction | Pre | 6 | 5 | 4 | 1 | 16 |
| Post | 5 | 7 | 15 | 30 | 57 | |
The need that staff perceived before the move for space around patient beds and staffing levels had decreased after the move (Table 51). However, ventilation/heating/lighting, access to equipment and supplies and facilities for staff, including staff bases, were identified as needing improvement after move. In addition there was a need for improvements in monitoring patients, keeping track of colleagues, reducing isolation and reducing walking distances. These have all been identified by other parts of our results (see Chapter 6).
| Improvement needed | Improvement needed | Mean | Total | |||
|---|---|---|---|---|---|---|
| Acute assessment | Medical (older people) | Surgical | Maternity | |||
| More space around patient beds | Pre | 3 | 6 | 5 | 8 | 22 |
| Post | – | – | – | 3 | 3 | |
| Improved staff–patient ratio/more quality time with staff | Pre | 4 | 6 | 2 | 2 | 14 |
| Post | – | 2 | 1 | 1 | 4 | |
| Access to equipment and supplies | Pre | 4 | 4 | 2 | 5 | 15 |
| Post | – | 1 | 14 | 16 | 31 | |
| Improved facilities for staff | Pre | 1 | – | 2 | 4 | 7 |
| Post | 3 | 1 | 6 | 3 | 13 | |
| Improved staff bases | Pre | 3 | – | 2 | 5 | 10 |
| Post | – | – | 2 | 6 | 8 | |
| Improved heating/lighting/ventilation | Pre | 2 | 1 | 1 | 1 | 5 |
| Post | – | 2 | 2 | 2 | 6 | |
| Monitoring patients | Pre | – | – | – | – | – |
| Post | – | 1 | 2 | 5 | 8 | |
| Improved ability to find staff | Pre | – | – | – | – | – |
| Post | – | 1 | 2 | 3 | 6 | |
| Reduced staff isolation/increased safety | Pre | – | – | – | – | – |
| Post | – | 1 | 1 | – | 2 | |
| Reduced walking distances | Pre | – | – | – | – | – |
| Post | 1 | 1 | 1 | – | 3 | |
Staff were asked about the features of the ward they were most looking forward to in the pre-move phase, and most liked in the post-move phase (Table 52). Results showed that staff most liked the increased patient privacy, patient sleep and rest, increased space, working in a modern environment and improved patient bathroom facilities.
| Most looking forward to/most liked | Examples | Phase | Maternity | Surgery | Older people | Acute assessment | Total |
|---|---|---|---|---|---|---|---|
| Improved patient privacy |
|
Pre | 9 | 4 | 5 | 2 | 20 |
| Post | 24 | 9 | 9 | 3 | 45 | ||
| Improved patient sleep and rest |
|
Pre | 4 | 4 | 3 | 1 | 12 |
| Post | 11 | 1 | – | 1 | 13 | ||
| More space around beds |
|
Pre | 2 | 7 | 3 | – | 12 |
| Post | 1 | 5 | 2 | 1 | 9 | ||
| Working in a modern environment |
|
Pre | 7 | 3 | 2 | 5 | 17 |
| Post | – | – | – | – | – | ||
| Improved patient toilet/bathroom |
|
Pre | 2 | 3 | 3 | 1 | 9 |
| Post | 3 | 2 | 1 | 1 | 7 | ||
| Infection control |
|
Pre | – | 1 | 1 | 2 | 4 |
| Post | 3 | 1 | 2 | 1 | 7 | ||
| Improved quality of care |
|
Pre | 1 | 1 | – | 1 | 3 |
| Post | 1 | 4 | 1 | – | 6 | ||
| Overall patient comfort |
|
Pre | 1 | – | 1 | 3 | 5 |
| Post | 3 | 1 | 1 | – | 5 | ||
| Decreased need to move patients |
|
Pre | – | 2 | – | – | 2 |
| Post | – | – | – | – | – | ||
| Better for relatives |
|
Pre | 1 | – | 1 | – | 2 |
| Post | 1 | 1 | 1 | 1 | 4 | ||
| Easier environment to work in |
|
Pre | 1 | 1 | – | 3 | 5 |
| Post | 1 | 2 | – | – | 3 | ||
| Other |
|
Pre | 1 | 1 | 1 | 3 | 6 |
| Post | 1 | – | – | – | 1 |
Table 53 shows that staff were most concerned about being able to monitor patients, patient isolation and the risk of falls. Being unable to find staff and increased walking distances also emerged as features staff disliked about single rooms.
| Most concerned about/most dislike | Examples | Phase | Maternity | Surgery | Older people | Acute assessment | Total |
|---|---|---|---|---|---|---|---|
| Observing/monitoring patients |
|
Pre | 12 | 8 | – | 8 | 28 |
| Post | – | 8 | 5 | 3 | 16 | ||
| Patient isolation |
|
Pre | 5 | 6 | 7 | 4 | 22 |
| Post | – | 2 | 2 | 1 | 5 | ||
| Patient safety/falls increase/not seeing falls |
|
Pre | 2 | 8 | 9 | 3 | 22 |
| Post | – | 3 | 5 | 1 | 9 | ||
| Staffing levels |
|
Pre | 5 | 2 | – | – | 7 |
| Post | – | 1 | – | – | 1 | ||
| Finding staff/equipment/keys |
|
Pre | – | – | 1 | – | 1 |
| Post | – | 3 | – | – | 3 | ||
| Increased workload/distances |
|
Pre | 1 | – | – | 1 | 2 |
| Post | – | – | 2 | 1 | 3 | ||
| Teamwork |
|
Pre | 4 | – | – | 1 | 5 |
| Post | – | – | – | – | – | ||
| Staff safety |
|
Pre | 1 | 2 | 1 | 1 | 5 |
| Post | – | 1 | – | – | 1 | ||
| Patients can’t see that staff are busy |
|
Pre | – | – | – | – | – |
| Post | 4 | 2 | – | – | 6 | ||
| Changed patient expectations/viewed as a hotel |
|
Pre | – | – | – | 1 | 1 |
| Post | – | 3 | – | – | 3 | ||
| Other |
|
Pre | 3 | 2 | 1 | 1 | 7 |
| Post | – | 2 | 4 | 1 | 7 |
Summary
-
Most staff would prefer a mix of single rooms and multibedded rooms on wards.
-
Staff activity events observed per session were higher after the move and direct care and professional communication events per hour decreased significantly, suggesting fewer interruptions and less fragmented care.
-
A significant increase in medication tasks among recorded events suggests medication administration was integrated into patient care activities and was not undertaken as a medication ‘round’.
-
Travel distances increased for all staff, with highest increases for staff in the older people’s ward and surgical wards and for RNs/RMs.
-
Staff perceived that the new accommodation was better for:
-
efficiency in carrying out tasks
-
patient amenity, including comfort, space, sleep, light and ventilation
-
infection control
-
patient privacy
-
patient interaction with family/visitors and their involvement in care.
-
-
In open comments, staff most liked the increased patient privacy, working in a modern environment, improved patient sleep and rest, and space around the bedside.
-
Staff perceived that the new accommodation was worse for:
-
delivery of care, including factors such as spending time with patients, communication with patients, monitoring patients and remaining close to patients, responding to calls for assistance, minimising the risks to staff, minimising walking distances and staff spending time with patients
-
teamwork, including being able to locate staff, obtain assistance from colleagues, informal learning, keeping team members updated, discussing care with colleagues and knowing when other staff might need help.
-
-
In addition, in open comments staff were most concerned about patient isolation, the risk of falls and staff isolation.
-
There were no perceived differences in staff amenity and patient and staff safety.
-
Ratings for information handover and communication decreased significantly following the move. This suggests that information exchange and sharing within teams – and between professions – was perceived to be worse after the move.
-
Different wards valued different aspects of the ward environment.
-
Ratings for staff toilet facilities, locker facilities and space at staff bases were rated more highly but ratings for social interaction and natural light decreased.
-
No differences were found in staff job satisfaction, well-being or stress before and after the move.
-
The need for improved patient–staff ratios and a day room to provide patient social interaction was still reported after the move.
Chapter 6 Staff experiences of the advantages and challenges of single rooms: adaptations to work patterns
Introduction
This chapter explores staff experiences of working on single room wards. It is based primarily on analysis of in-depth interviews with nursing and midwifery staff working on the four case study wards, undertaken approximately 1 year after the new hospital opened. Some of those interviewed took photographs of the aspects of the new environment they found positive and negative (see Chapter 2); a selection of these images is used to illustrate our findings. The analysis also draws on data from interviews with AHPs, medical staff and nurse managers, together with researcher observations on the wards.
Before the move, staff working on open-plan wards valued the visual and aural proximity they had with patients and colleagues, which offered three key benefits: (1) enhanced surveillance and monitoring of multiple patients, (2) increased opportunities for teamwork and communication and (3) facilitation of social contact between patients. However, proximity between patients on open-plan wards was also perceived by staff to have negative consequences in terms of ensuring privacy, dignity and confidentiality for patients and in increased risks of infection. Staff also identified deficiencies in the layout and facilities of the open-plan wards which created obstacles to delivering effective and efficient care (see Appendix 3 and Maben et al. 1).
This chapter primarily addresses the following research questions:
-
What are the advantages and disadvantages for staff of a move to all single rooms?
-
How are work patterns disrupted and reconstituted, including through trial-and-error use of new approaches (and to what extent are these successful/unsuccessful)?
We begin with a summary of perceptions of the positive and negative aspects of single room wards before the move to the new hospital, based on in-depth interviews with nursing and midwifery staff and a questionnaire survey. 1 Nursing staff foresaw four main advantages of single room wards and four main disadvantages. These provide the structure for exploring staff experiences after the move. In the post-move interviews, staff described an additional challenge associated with single rooms – managing time and prioritising workloads – which had not been previously expected. Some aspects of single room wards presented challenges for staff that required adaptation or changes to the work patterns that had been established on open-plan wards. Where staff identified challenges we also explore how they responded to alter their ways of working.
Pre-move findings: staff perceptions of single room wards
Most nurses and midwives who were interviewed or responded to the questionnaire had already taken part in an induction programme (including a tour of the new hospital) so they were able to anticipate the likely advantages and challenges of working in a hospital with all single room patient accommodation. Perhaps not surprisingly, the expected advantages were the converse of the perceived inadequacies of the old hospital wards, and the challenges mirrored aspects of working on open-plan wards that they found beneficial. Diverging from this pattern was the concern expressed by nurses about having sufficient staff to provide safe and high-quality care: this was perceived to be a challenge at the old hospital and was expected to continue after the move. Before the move, nursing staff expected that single rooms would have four main advantages and four main challenges (Table 54).
| Advantages | Challenges |
|---|---|
| Privacy, dignity and confidentiality; more personalised patient care Staff expected single rooms with en suite toilets and showers to improve patient experience, most notably by offering increased privacy, dignity and confidentiality. They thought patients would be less disturbed by ward activity or other patients and get better sleep and rest. Although staff valued the visual and aural contact with patients on open-plan wards, they recognised that discussion of personal or intimate issues was constrained, so they looked forward to developing closer relationships with patients and providing more personalised care |
Reduced visibility of patients: difficulties monitoring and safeguarding patients Nurses and midwives were concerned that single rooms would make it more difficult and time-consuming for them to monitor patients and maintain patient safety. In particular, they worried that patients would be at increased risk of falling because staff might not see or hear patients attempting to move unaided or be able to respond quickly enough to prevent a fall |
| Improved room design; improved care delivery Nurses expected that increased space and improved facilities in patients’ rooms with well-designed and well-equipped single rooms and en suite facilities would create a better working environment, enabling staff to deliver care effectively |
Social isolation of patients Staff members were concerned that some patients might miss social contact with other patients and feel isolated and lonely |
| Improved ward design; increased efficiency The design and layout of wards in the new hospital, with centralised support (e.g. treatment room, utility, kitchen), sufficient storage, more bases for staff and provision of staff facilities, were expected to provide a better working environment for nurses and midwives and improve efficiency |
Maintaining teamwork and communication Staff expected that they would spend more time working alone and have fewer opportunities to be with their colleagues. They felt it was possible that they too could become isolated and lonely |
| Reduced risk of infection Staff expected single rooms with en suite facilities and well-designed wards to facilitate improved infection control |
Staffing levels to support safe and effective care Staff questioned if staff–patient ratios in the new hospital would be sufficient to support safe and effective nursing and midwifery practice on single room wards |
Post-move findings: staff experiences of expected advantages
This section explores how staff actually experienced working in the new hospital during the first year. The four advantages expected by staff before the move structure the findings. We consider the extent to which expectations were met (or not) and highlight any unanticipated effects.
Privacy, dignity and confidentiality; more personalised patient care
Staff compared single rooms favourably with open-plan wards in terms of providing privacy, dignity and confidentiality for patients. Patients had their ‘own space’, including an en suite bathroom and toilet, where personal care could take place away from other patients. A staff nurse on the surgical ward (S16) said that she would ‘hate to go back to nursing patients behind curtains’ because, ‘dealing with gastric surgery, it can be embarrassing when patients don’t make it to the toilet in time [. . .] now they have the dignity and privacy of being in their own room.’
Single rooms were also seen as advantageous as they allowed patients to sleep, rest and recuperate without disturbance. They could also better accommodate visitors. Privacy was particularly valued for patients who were seriously or terminally ill and for their families. This had been difficult to provide on open-plan acute wards. Staff also felt that single rooms helped facilitate discussion with patients and families together.
I think from a privacy and dignity point of view, when patients are dying, or when relatives are in there, or in extremis, when you don’t really want the next patient to be making a noise, then [single rooms are] fantastic. [. . .] I used to feel very embarrassed when people would be at the nursing station or having a joke about something and somebody’s dying 3 yards away, and the relatives are round the bed. I found that very uncomfortable.
KSI28, consultant
[At the old hospital] you’d have to find a room outside the ward to bring the family to, to have a discussion with them, whereas here, you might be able to speak a bit more openly and privately with the family and with the patient present. Almost have a mini-MDT with the family and the patient in their room.
AHP40, dietitian
Patients also said they liked the confidentiality afforded by the single room, and the privacy and flexibility it gave for visitors (patient interview data – see Chapter 7).
In the survey, staff gave higher ratings to single room wards for patient amenities, especially patient privacy; patient comfort, space, sleep, light and ventilation; also patient interaction with family/visitors and their involvement in care (see Chapter 5).
At interview, nurses and AHPs said that single rooms enabled them to ‘focus on the patient’ and respond with appropriate emotional engagement. One HCA described how moving between rooms allowed her to adjust her manner to suit each patient’s circumstances. The privacy afforded by single rooms meant communication with patients could be more open. Staff also reported less likelihood of interruption and distraction. ‘You’re able to give your patient the attention and care because you’re with them; you haven’t got someone else shouting from the other side of the room for you’ (M01). Observation on the wards suggested that staff were more likely to respect patients’ privacy – perhaps because rooms were perceived as the patient’s personal space. This was reinforced by staff knocking on the door before entering ‘so that the patient feels they’ve got some control over their environment’ (S16).
[At the old hospital] I could be doing a personal task, giving someone’s bottom a wash, and a doctor would put their head through the curtains, even though you had ‘Do Not Disturb’ [. . .] And the poor patient would be mortified. Whereas now, we shut the door, we close the screens, yes sometimes you see them peek, but the moment they see nurse, pinny, back to them, they’re away and they don’t come in. So they respect the privacy a bit more as well. So that is better.
S11, staff nurse, surgical ward
Observation of staff activity suggested that after the move they experienced fewer interruptions when providing care (see Chapter 5, Staff activity: task time distribution results).
Staff associated spending uninterrupted time with individual patients with providing effective and personalised care. However, nurses and midwives also explained that the potential of the single rooms for developing better relationships with their patients was not always fully realised, because they felt unable to give sufficient time and attention to each patient. The tensions staff experienced around apportioning time between patients and prioritising their workload was an important theme in the interviews. While this is an issue recognised by nursing staff in many settings, for staff interviewed in this study the all single room environment accentuated the tensions, which they linked to not being able to see and interact with a number of patients at the same time. Staff had not foreseen that the move would make this aspect of practice more challenging (see An unforeseen challenge: time management and prioritising workloads below).
Improved room design; improved care delivery
Staff thought that single rooms provided an improved working environment for delivering patient care and described the rooms as modern, clean, spacious and safe. The en suite facilities were considered to be one of the most positive aspects, allowing nursing staff to more easily assist patients with personal care. Nurses particularly valued being able to give patients showers, and sensed that this was appreciated. A staff nurse took a photograph of the en suite shower (Figure 14) to illustrate that showering patients was now ‘so much easier’ and ‘much more civilised and pleasurable’ (S16). This view was also expressed by other nurses.
FIGURE 14.
The en suite shower. Taken by S16, staff nurse, surgical ward.

[The single rooms] are really accessible and for patients that want to hold on to things while they’re walking, they’ve got bars around the side, from the bed to the bathroom, they’ve got the bars alongside of the toilet and the bars on the wall to hold onto, bars by the shower, so I think that’s really good. The floors are non-slip as well, so I stand patients up quite confidently in there, without worrying that they’re going to slip because they’ve got that special dappling. And again, they just look cleaner, they look tidier. The bathrooms are really spacious as well, and it’s just the freedom that it gives patients.
S14, HCA, surgical ward
In the survey, staff perceived significant improvements in the efficiency of the physical environment on single room wards in terms of carrying out tasks (see Chapter 5).
Although staff generally thought single rooms were a ‘huge advantage’ when delivering patient care, they also identified less positive aspects of the particular room design. Five main issues were identified from our analysis of staff interviews and participant-produced photography, which were also observed by the researcher when shadowing staff:
-
room layout: getting beds into/out of patient rooms
-
en suite bathroom layout
-
windows in patient rooms
-
location of the nurse call cancel button
-
patient televisions.
It should be emphasised that these were issues specific to the Tunbridge Wells Hospital design rather than generic problems of single rooms per se. However, for staff they created obstacles to safe and efficient working or diversions from direct patient care, which they found frustrating (presented in Table 55 and illustrated by Figures 15–17). Some issues also had an impact on quality of care and patient experience. Most of the problems had not been picked up in the mock-up of the single room during the design process and became apparent only once the new hospital was operational.
| Patient room design issue | Staff comments |
|---|---|
| Room layout getting beds into/out of rooms Patient chair positioned between bed and en suite bathroom to facilitate mobilisation to the toilet (not as envisaged in plans) creates difficulties when moving trolleys/beds because of angle of the entrance and position of the clinical hand wash basin. AHPs found room layout awkward when using equipment (see Figure 15). In the original design the location of the patient chair was expected to be on the opposite side of the bed, but this would have located patients further away from the entrance to the en suite facilities |
|
| En suite bathroom layout Criticisms of the en suite design included lack of space to manoeuvre wheelchair/walking frame; location of the toilet paper dispenser (behind the toilet, which required patient on toilet to twist around and reach up, which was difficult for some without assistance); and long support rails either side of the toilet that got in the way. These problems were worse in several rooms on each ward: one of these is shown in Figure 16 |
|
| Windows inpatient rooms The full-height glazing with a view outside was seen as a positive feature of the patient room. However, the window itself had no retainer to hold it open and adjust the amount of ventilation. Nurses found this frustrating and were often observed propping objects against the window in attempts to give a patient optimal fresh air |
|
| Location of the nurse call cancel button The nurse call cancel button was located behind the patient’s bed in a position that was difficult for some nurses to reach (see Figure 17) |
|
| Patient televisions Every patient room was equipped with a wall-mounted television (funded by the League of Friends). Patients and visitors had difficulty getting the televisions to work and remote controls frequently went missing. Staff were irritated by having to attend to problems with televisions because it took them away from clinical work |
|
FIGURE 15.
Patient chair next to en suite door, impeding bed moves. Taken by S15, staff nurse, surgical ward.

FIGURE 16.
Layout of en suite where position of sink limits access to toilet. Taken by OP24, HCA, older people’s ward.

FIGURE 17.
Location of nurse call cancel button behind patient bed. Taken by S15, staff nurse, surgical ward.

Improved ward design; increased efficiency
Staff made many positive comments about the ward environment in the new hospital. They found it clean, spacious, modern and quiet and calm, and compared it favourably with the ‘hustle and bustle’ of open-plan wards. Staff felt proud of the new hospital and privileged and professional working in it.
It’s light; it looks clean, whereas although I think [the old hospital] was clean, it never looked clean because it was such an old building. [. . .] It just looks more professional. I feel better about my job, I feel like a professional working in a professional environment.
S11, staff nurse, surgical ward
One aspect of the new wards noted by staff was their length in comparison with the open wards they had worked on previously, which meant they had to walk increased distances. This was particularly apparent to nurses on the AAU, which in the old hospital was a compact shape with half the number of beds.
I spend hours walking round and round and round in figures of eight [. . .] It’s good for my figure but it hurts my feet. It’s just the sheer size in comparison to the old [ward] that was tiny.
M05, junior sister, AAU
After the move to the new hospital, staff walked increased distances. The greatest increases took place on the older people’s and surgical wards (see Chapter 5, Staff travel distances results).
Nursing and midwifery staff identified features of the new ward design that facilitated working efficiently and effectively, but the benefits were sometimes offset by challenges that hindered and frustrated them. We highlight here five aspects of ward design, discussed in interviews and observed by the researcher while on the wards, which staff experienced as having both benefits and challenges:
-
ward support facilities
-
ward entry system
-
nurse call system
-
staff break rooms
-
natural light in staff work areas.
These aspects (presented in Table 56 and illustrated by Figures 18–20) were not consistent across all four case study wards, because of variations in ward design and operational issues, nor were they equally salient for all staff working on a ward.
| Aspect of ward design | Benefits identified by staff | Challenges identified by staff |
|---|---|---|
| Ward support facilities Centralised ward support facilities (e.g. clean and dirty utility, drug preparation room, kitchen) located down the middle of the ward with doors to the corridor either side (see ward layout plans in Appendix 18) were intended to provide adequate storage space and minimise walking distances |
A ‘big improvement’ especially in terms of storage and organisation, e.g.:
|
Some aspects considered inadequate or poorly designed, e.g. cupboards in the clean utility room were difficult to access because drug trolleys were stored in the room; the controlled drug cupboard was badly located and too small; and drawers were difficult to pull in and out. On some wards location of store rooms increased distances staff had to walk:
|
| Ward entry system Staff (ward clerks or receptionists when on duty, nurses at other times) operated the secure ward entry system to allow patients and visitors to enter and exit. Some wards had a second set of security doors with no entry buzzer |
Nurses on the older people’s ward felt that the double security doors kept their patients safe:
|
Operating the entry system was frustrating for nurses because it interrupted clinical work:
|
| Nurse call system Patient call bells switch on a light outside the room; monitor screens at the nurses’ stations indicate room number and distinguish call bells pressed in the room or bathroom |
|
The light outside one room on each ward was difficult to see. The monitors at the decentralised nurse bases had a smaller, simplified display, which staff found more difficult to read:
|
| Staff break rooms Ideally, staff wanted a dedicated break room located on the ward, which enabled them to take breaks even if the ward was busy, knowing their colleagues could call them back if necessary |
The surgical ward and the older people’s ward had break rooms on the ward with a window, fridge, sink and microwave (see Figure 19):
|
The AAU and the postnatal ward had break rooms off the ward shared with other departments, which some staff did not use. AAU staff took breaks in a small interview room on the ward:
|
| Natural light in staff work areas Ward design maximised natural light in patient rooms, but daylight came into other ward areas only at the end of the double corridor and in the reception area |
Staff on the surgical ward said they preferred parts of the ward with natural light and particularly commented on the views from the windows in the reception area:
|
Blinds in patient rooms were often closed while nurses were delivering care, so they could be working for extended periods in artificial light:
|
FIGURE 18.
The clinical room on the surgical ward. Taken by S16, staff nurse, surgical ward.

FIGURE 19.
The staff break room on the surgical ward. Taken by S14, HCA, surgical ward.

FIGURE 20.
Interview room on AAU used as a staff break room.

Staff who identified problems associated with ward support facilities (e.g. location and adequacy of storage space, utilities, kitchens), ward entry arrangements and the nurse call system, also felt their ability to work efficiently was affected, particularly by increasing the distances they had to walk.
In the staff survey, overall ratings for the item ‘efficiency of physical environment’ improved, but ratings for the item ‘ward design/layout minimises walking distances for staff’ worsened. Analysis of travel distances showed that staff took significantly more steps after than before the move (see Chapter 5).
Staff well-being was affected by inadequate break rooms and lack of natural light on the wards. In general, however, staff perceived the advantages of the new working environment as outweighing the disadvantages.
The staff survey showed that some aspects of the design had improved staff amenities, e.g. toilet facilities, locker facilities and space at staff bases, but that others worsened, e.g. social interaction and natural light (see Chapter 5).
Reduced risk of infection
Staff expected that single rooms would reduce infection risk. Certainly the new wards were perceived by staff to support good hygiene practices, with no-touch clinical hand wash basins in every patient room, and personal protective equipment, alcohol hand gel and antibacterial wipes available from wall-mounted dispensers outside every room. This provided a visual reminder for staff entering a patient room to comply with infection control procedures (Figure 21).
FIGURE 21.
Protective equipment, alcohol hand gel and antibacterial wipes outside the patient room. Taken by OP25, junior sister, older people’s ward.
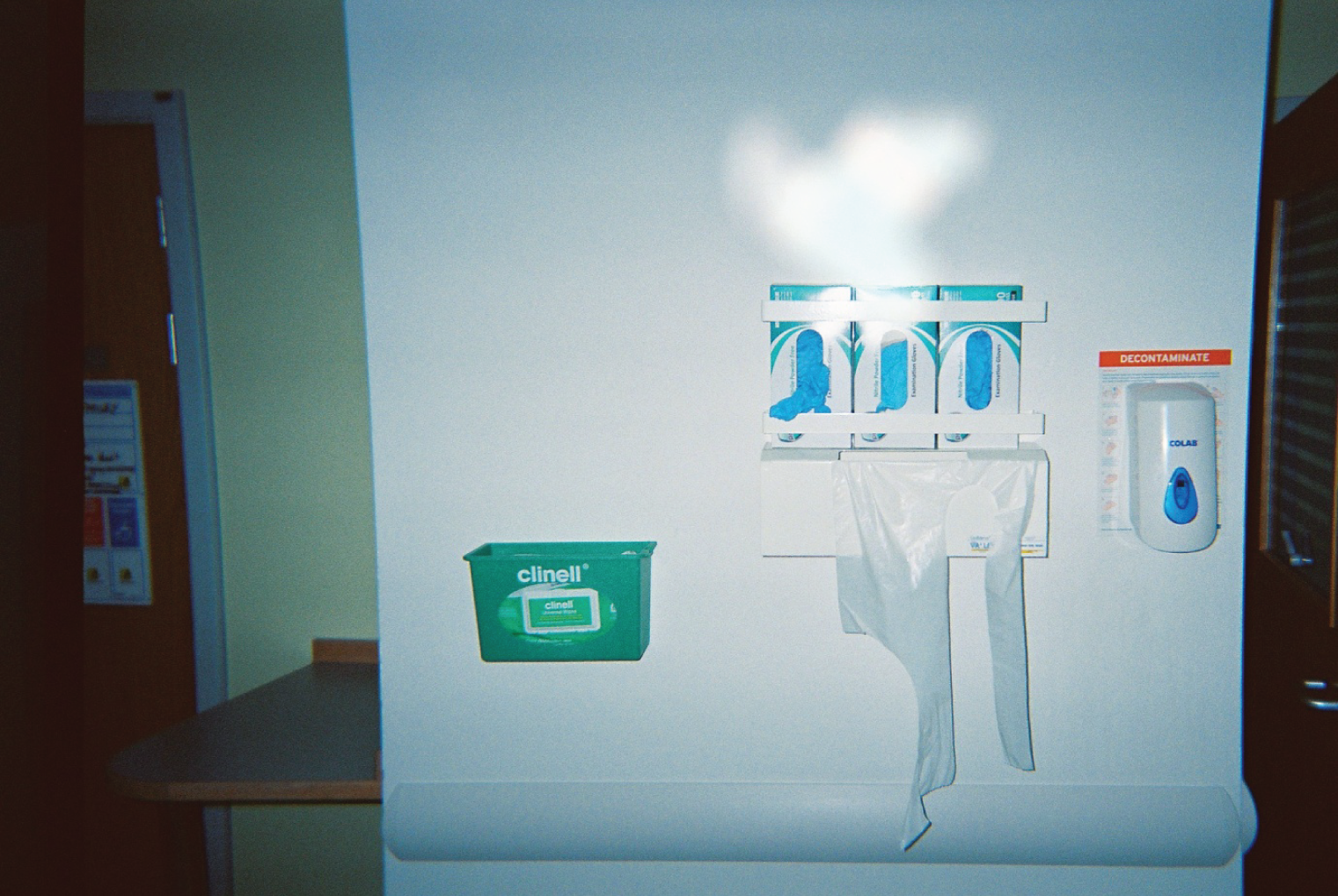
I’ve taken a picture of the gloves on the wall, just outside the general patients’ room, the gloves, alcohol dispenser, aprons, and the wipes [. . .] they’re very clean, clear, easy to refill and they really benefit from being where they are, which is perfect, the fact that they’re outside every single patient’s room, there’s no question about it.
OP25, junior sister, older people’s ward
Because you’ve got individual basins, you’re not sharing a sink. You’re able to wash your hands very quickly after having patient contact, rather than having to walk around looking for a basin to use. [. . .] So you just feel that you’re able to carry out infection control procedures more effectively.
S16, staff nurse, surgical ward
However, staff attitudes to infection control had to be challenged to avoid complacency associated with the belief that single rooms solved all infection control issues (see Chapter 3). On open wards, staff could see which patients had infections (e.g. trolley with gloves and wipes by the bed and signage). After the move, a warning system was introduced: magnetic signs on room doors to indicate specific procedures that staff should follow.
In the survey staff rated the ward environment better for infection control (see Chapter 5).
Summary: were the expected advantages of single room wards confirmed?
In general, staff found that single rooms brought the advantages they expected, but the benefits were not always fully realised because of unforeseen issues in the new environment. Staff found that single rooms improved privacy, dignity and confidentiality for patients, allowing them to rest and recuperate without disturbance, and were better for visitors. Single rooms facilitated communication with patients, as staff could spend time caring for individual patients without interruption. However, contrary to expectations, single rooms did not necessarily enable staff to deliver more personalised care, because they felt unable to give sufficient time and attention to each patient. The challenges experienced around dividing time between patients and prioritising workload had not been foreseen by staff (see An unforeseen challenge: time management and prioritising workloads, below).
The design of patient rooms and wards in the new hospital largely met staff expectations for an improved working environment, and supported staff working more effectively. However, various aspects of the design of rooms and wards at Tunbridge Wells Hospital presented obstacles to safe and efficient working (room and bathroom layout) and increased the distances they had to walk (location and adequacy of storage space, utilities). Staff also felt that they were diverted from patient care by the ward entry and nurse call system, and that their own well-being was affected by inadequate break rooms and lack of natural light. However, in general the design benefits were felt to outweigh these issues. Staff liked the new hospital (clean, spacious, modern, quiet and calm) and it gave them a real sense of professionalism. They also perceived single rooms as reducing the risk of infection. Managers feared this would lead to complacency about infection control, so they reasserted infection control policy and developed a visual warning system to prompt staff to take specific measures before entering a patient’s room.
Post-move staff experiences of expected disadvantages
This section explores the four disadvantages of single room wards which staff had foreseen before the move (see Table 54). We consider the extent to which expectations were met (or not) and highlight any unforeseen aspects of the move. Each disadvantage is followed by a section outlining how work patterns were adapted to meet these challenges.
Reduced visibility of patients: difficulties monitoring and safeguarding patients
The biggest challenge experienced by staff working on the single room wards was surveillance and monitoring of patients. In interviews carried out before the move, nurses and midwives represented the open-plan ward as a panoptic space that enabled them to observe and control what went on within it. They could see and hear patients easily, acknowledge requests for help and prioritise their responses. In contrast, they found that the possibilities for such panoptic surveillance were severely curtailed by the design of the single room wards.
When we were on an open ward I could walk on the ward and I could view everybody. And when you knew your patient you could see [if they didn’t look well]. Whereas now I can walk up and down the rooms, but as soon as I’m in a room I’m away from everybody. [. . .] That time has gone where you could just stand and have a quick chat with a patient while you were still keeping an eye on everybody else.
S11, staff nurse, surgical ward
[Some clusters of rooms] they’re just corridors, if you’re in the first room, you can’t hear the last room. So if there’s a machine buzzing, say you’re in 11 and there’s a machine buzzing in 21, until you physically get down the corridor a bit more you can’t hear it.
S15, staff nurse, surgical ward
Staff described how visibility of patients from the ward corridor was limited to the patient room they were directly outside, and then only if the door or vision panel in it was open (Figure 22). Although the bed head was visible from the doorway, the line of sight into the rest of the room was interrupted by the wall of the adjacent room’s en suite bathroom. Each en suite bathroom also protruded into the ward corridor (‘inboard’ single room design) obscuring the view of patient room doors for staff looking down the corridor (Figure 23).
FIGURE 22.
Door to a patient room, showing Vistamatic vision panel. Taken by OP24, HCA, older people’s ward.

FIGURE 23.
Single corridor with rooms opposite each other. Taken by S16, staff nurse, surgical ward.

Sixty-two per cent of respondents in the staff survey felt that responding to patient calls was worse in single rooms than in multibedded wards (see Chapter 5).
All staff interviewed perceived that lack of visibility of patients in the single room wards had contributed to an increase in falls in the new hospital. Experienced nursing staff thought that it had been easier to prevent falls in multibedded accommodation because they could ‘keep an eye’ on patients and were more aware of warning signals, such as patients becoming agitated or attempting to get up from their chair or bed. Nurses also described how on open-plan wards they would be alerted by other patients calling them when they saw a patient at risk of falls begin to move, which enabled staff to respond in time to ensure the patient was safe. In contrast, ‘You’re not able to predict things as easily when people are behind closed doors’ (S16).
Last week, we had about three people [. . .] climbing out of beds and falling [. . .] And I know on an open ward [patients] can still climb out of bed but at least as you’re walking up and down the ward you could physically see them [. . .] now the only time we know somebody has fallen out is when we hear the clump and they’re on the floor.
S15, staff nurse, surgical ward
Nursing staff on the acute wards expressed anxiety, concern and distress about falls, which a ward manager confirmed were ‘a big fear’ in the new hospital; confused patients and those with dementia were particularly difficult to safeguard from falling. It was generally felt that the new environment placed additional demands on nurses in terms of monitoring patients.
The next section explores how staff adapted their working patterns in response to the challenge of reduced visibility of patients and the perceived increased risk of falls.
Adapting work patterns to monitor and safeguard patients
On multibedded wards, nurses and midwives had been able to monitor a number of patients simultaneously, but patients in single rooms could only be observed individually, which meant that nurses had to change some established ward routines:
You have to adjust your nursing practice just to make sure that everybody is seen and you keep an eye on them the whole time. With the bays you’d go in to see one patient but then subconsciously you’re eyeballing everybody else, making sure everybody else is okay. Whereas here you have to physically go into each and everybody’s rooms, or stop and have a look at them.
M03, staff nurse, AAU
Staff described opening doors to improve their view of patients from the ward corridor. If doors were closed, nurses liked the blinds in the door vision panel (Vistamatic, Hainault, Essex, UK) to remain open, although it was designed to give patients control.
Room check procedures
The side room protocol from the old hospital was to be implemented on the new wards and updated to include hourly checks on patients to ensure they were safe and their nursing care needs were met. Ward managers and staff found that with the upheaval of the move it took time to establish systematic monitoring, but room checks soon became successfully embedded in both ward routines and individual nurses’ practice.
On the AAU, staff also expected AHPs and medical staff to alert them to potential problems. This approach was endorsed by nurse managers, who wanted all ward staff to take responsibility for ensuring patients’ comfort and care.
I walk around with my head permanently fixed to the side that all the rooms are on, just checking [. . .] I’ve just adapted. I now look into every single room every time I walk past and I make the effort to go into the rooms. [. . .] It becomes part of the routine rather than anything else. [. . .] And the physios do the same; they point things out to us. The pharmacist does the same thing. We all keep a lookout and tell each other if we’re worried about someone, which we did before, but before you could see [patients], you can’t now.
M05, junior sister, AAU
Most wards aimed for hourly checks (3-hourly on the postnatal ward) and nurses were required to document patient checks. Staff compliance with documentation proved more difficult to achieve and ward managers described having to ‘reinforce’ this systematic recording. A recurrent theme in the interviews was the amount of ‘paperwork’ staff had to complete. Some nurses were resistant to change that involved more form filling, especially if it duplicated other documentation and took time away from delivering patient care.
There seemed to be variation in room-checking procedures between the four case study wards, which suggested that wards may have been adapting room checks to address local issues. Some AAU nurses found a new lengthier form demanding to complete: ‘We don’t always fill them in because there’s so many boxes to tick’ (M04). However, if documentation was not completed, this could generate additional, and possibly unnecessary, checks.
Nurse managers were aware that the quality of room checks could be variable and that there could be a ‘danger of moving towards a tick box mentality’ (KS21). They thought that well-organised and efficient ward routines, with task-focused care scheduled at regular intervals throughout the day, would ensure that ward staff interacted with patients at least every hour. Patient-focused care could then be integrated into these routines, eliminating the need for separate checking. However, some ward nurses perceived carrying out room checks as additional work, which increased the pressures on them and the difficulties they experienced in prioritising their workload (see An unforeseen challenge: time management and prioritising workloads).
Seriously ill or highly dependent patients who required frequent monitoring would often have a dedicated nurse stationed in their room or directly outside (a nurse ‘special’). On an open ward, a nurse responsible for observing one vulnerable patient would usually monitor other patients. On a single room ward this was not possible, which put extra pressure on the team working in that ‘cluster’ of rooms, although agency or bank nurses could be brought in as ‘specials’.
Safeguarding patients from falls
Following the move to the new hospital and an increase in the incidence of falls, ‘specials’ were widely used to safeguard patients, particularly those who were confused or had dementia and were at risk of falling, but this was a costly and unsustainable approach. A variety of other measures were introduced to reduce falls: falls assessments on admission, falls training for staff and increased frequency of room checks. Low-profile beds, antislip socks, coloured wrist bands, signage on room doors, and bed and chair pressure mat alarms were also used. Nurses on the older people’s ward and AAU spoke favourably about pressure mat alarms and the older people’s ward manager said they ‘helped us cut down on the use of specials’.
The three general wards had tried to replicate an approach to safeguarding patients commonly used on open wards: moving a patient at risk of falls closer to the nurses’ station, to facilitate monitoring and rapid intervention if they attempted to mobilise. There were different views about the effectiveness of this approach. On the surgical ward, bed moves were rare and thought to be of limited value for increased surveillance because nurses no longer spent much time at their station. On the AAU, patients were moved to rooms nearer to the nurses’ station, where staff could respond quickly to alarms. However, the ward manager also drew attention to the disruption caused by bed moves, including additional cleaning, which was costly (see Chapter 9).
On the older people’s ward, where the majority of patients were said to be at risk of falls, the highest-risk patients were grouped together in a cluster of 10 rooms that was allocated a higher level of staffing. Here, patient rooms were on either side of the corridor and nurses therefore felt that they could see and hear patients better than elsewhere on the ward. Initially, ‘the zone’ – as the cohort area was known – was full and one nurse was allocated to constantly check the patients and respond to pressure-mat alarms. As the number of high-risk patients fluctuated, the ward manager adjusted staffing levels in the nursing team accordingly, and successfully decreased use of specials on the ward.
It seems to work at the moment, as soon as we get new confused, disorientated patients who are at risk, we try and put them on antislip socks, alarm mat and, as soon as there’s a discharge in the zone, then we’ll swap them over and try and control the situation, increase staffing, drop staffing – we just take it moment by moment.
OP25, junior sister, older people’s ward
In addition, some patients in the zone, especially those with cognitive impairments, were brought out of their rooms to sit in the corridor, which facilitated monitoring and rapid responses to pressure mat alarms, while allowing staff to continue with routine tasks and delivering care. It also provided patients with some stimulation and opportunities for social interaction with each other and with ward staff. However, this arrangement was considered far from ideal; in the words of a senior nurse, it was ‘a perverse situation’, not least because it demonstrated that staff had to work around ward design to safeguard patients. For staff, it raised questions about the suitability of single rooms for older, cognitively impaired patients:
[in the zone] at the moment, we’ve got most of the high-risk falls [patients] sitting outside in the corridor. So, if they’re going to sit them out in the corridor, then why are you having single rooms?
OP24, HCA, older people’s ward
Creating the zone and using multiple measures to safeguard patients from falls was thought to have succeeded: ‘it does take more work; more organisation, but it’s for the good of the patients and it helps safeguard. It does work so far’ (OP25). The older people’s ward, with leadership from the ward manager, had developed a concerted response to the challenge of falls. Staff had adapted their work patterns to safeguard patients and there was a sense of shared learning and commitment to working together to improve care quality and safety. Nurses recognised that they would never completely eradicate falls, but felt they were doing ‘the best we can’ to protect patients.
In contrast, staff on the AAU expressed less confidence in their ability to safeguard patients. Some nurses found the number of falls on the ward distressing and difficult to reconcile with their duty to care for patients. A sense of responsibility for not preventing falls was associated with feelings of personal failure and low morale. Other nurses described becoming fatalistic about falls: ‘some people are destined to fall whatever you do’ (M05).
Social isolation of patients
Before the move to the new hospital, nursing staff were concerned that single room wards would reduce opportunities for interaction between patients and could result in some patients feeling isolated. Staff interviewed after the move felt their experiences confirmed that social isolation was a disadvantage of single room wards, describing how lack of social contact with other patients could influence not only patients’ satisfaction with their hospital stay, but also their emotional well-being and recovery. Social isolation of patients in the new hospital was compounded by ward design with limited day rooms (surgical, older people’s and postnatal wards) or none at all (AAU). Staff thought that the rooms were too small, inconvenient for patients to access, uncomfortable and unattractive (Figure 24). They felt that provision of social or communal space for patients should have been given much higher priority.
FIGURE 24.
Day room on surgical ward, with narrow access and limited visibility. Taken by S16, staff nurse, surgical ward.

Staff accounts tended to associate isolation with particular groups of patients, notably older, less independent patients, including those who were confused or cognitively impaired, and whose stay in hospital lasted more than a few days. Nurses expressed concern about these patients and felt they benefited least from single room wards. Although staff valued the contribution of volunteers, who talked or read to patients on the general wards, there was consensus that voluntary help alone could not resolve the problem. Without the company of other patients, older patients were described as becoming lonely, withdrawn, unhappy, discouraged and less motivated to engage with the therapeutic efforts of staff.
I just do sometimes feel sorry for the older patients that are in for weeks [and] don’t necessarily have a lot of contact with other people. And I guess mood has a massive impact on everything in hospital, on your recovery, on your eating, on how likely you are to get up and work with the physio that day. And sometimes if you’ve other patients motivating you, or even just speaking to you, it just picks up your mood, it can help.
AHP40, dietitian
At interview, patients said they rarely interacted with other patients in the new hospital. For some, this led to a sense of isolation and they wanted the opportunity to socialise with other patients (see Chapter 7).
Staff also recognised that patients of all ages could be disadvantaged by not mixing with others; hearing their experiences was thought to help individuals assess their own progress and could be reassuring, motivating and encouraging:
for postnatal ladies it’s important that they can see what’s going on around them and it’s not all about them and their baby [. . .] they don’t understand that every baby feeds all the time and cries and everything. They can’t see what is normal and I think they think, ‘My baby is going to feed and go to sleep for 6 hours’. But if they see the other women struggling as well it sort of normalises it for them.
PN36, midwife, postnatal ward
Socially isolated patients were seen as likely to make more demands on staff, for example pressing call bells frequently or talking a lot to keep nurses in the room with them. For some staff this created tensions because they wanted to alleviate patients’ loneliness but felt that they had no time to talk.
It tends to be older patients who have no company at home [. . .] especially if they’re being barrier nursed and the door needs to be closed, they find it very isolating, and I’ve had quite a few older people get quite upset. And then the impact it has on us because they’re lonely, they’ll be pressing their bell all the time for nothing other than just wanting someone to be there with them, [but] you just don’t have that time [. . .] Yeah, and if they don’t see you for a little while, patients often think you must not be doing anything.
M01, HCA, AAU
The fact that some patients might think staff were not busy or working hard (as indicated by the quote above), was something most nurses and midwives alluded to in the interviews and clearly found challenging. They felt that this misperception increased demands on staff and denigrated their professionalism. For staff, a significant negative aspect of single room wards was that patients were unable to see them working, and therefore could not judge whether or not it was appropriate to seek attention. Having no cues about ward activity that could help them modify their demands, patients in single rooms became what some nurses’ narratives described as ‘demanding’, ‘difficult’ or ‘more selfish’ in single rooms. There was also a general view that the style and quality of the single room accommodation influenced some patients to behave as though they were in a hotel rather than a hospital and to treat staff accordingly.
Adapting work patterns to reduce patient isolation
Use of day rooms
Staff on all the case study wards would have liked more social interaction among patients; however, without expensive structural alterations, the design and layout of the wards offered limited possibilities for recreating the communal aspects of open plan wards. Only the older people’s ward had established regular use of the day room, using it to hold a ‘lunch club’ for five or six patients, the maximum number it could accommodate. Staff had to adjust their routines to get patients into the room before lunch was served, but they endorsed the value of the lunch club, particularly for patients with dementia. There were plans to create another, more homely, communal space in the ward reception area.
Encouraging patients to leave their rooms
Other wards put more emphasis on encouraging mobile patients to come out of their rooms for therapeutic reasons and to facilitate social interaction. Staff had been surprised to find that independent patients rarely ventured outside their rooms. Admission procedures included ‘orientation to the room’ for the patient, but staff on the surgical ward found they needed to take a more proactive approach, giving patients ‘permission’ to leave their room and encouraging them to walk around.
Midwives on the postnatal ward were particularly concerned about women ‘isolating themselves’ in their rooms. ‘Orientation’ for postnatal patients included an explanation of ward facilities, and a booklet. Information about the ward was also provided during antenatal care. However, midwives felt that these approaches would succeed in overcoming isolation only if more spacious and attractive communal areas were provided and women had a reason to use them, for example to eat their meals. Some midwives were pessimistic about recreating the communal aspects of postnatal care that had facilitated peer support among women on the old wards, and also regretted no longer offering demonstrations and teaching for groups of patients.
The single room postnatal ward had enabled changes in policy regarding visitors. Fathers were now allowed to stay overnight in rooms with their partners, although no beds or bedding were provided for them. This development divided staff opinion. One point of view, often vigorously expressed, was that fathers ‘got in the way’ and made midwives’ jobs more difficult. The alternative perspective was that fathers supported their partners, which reduced demands on staff, and they should be encouraged to stay. There were clearly unresolved tensions for midwives around adapting to having fathers on the ward, which influenced patient experience (see Chapter 7).
Maintaining teamwork and communication
Nursing staff anticipated that they would spend more time working alone on single room wards, and were concerned about maintaining contact and communication with colleagues, which they considered essential to delivering effective nursing care. Open-plan wards enabled nurses to see, hear and interact with each other, which facilitated co-ordinating patient care and providing each other with assistance; this indicated good teamwork that was universally valued. After the move, staff felt that this quality of teamwork had been difficult to recreate. Nurses described seeing less of their colleagues, being unaware of what was happening in other parts of the ward, and sometimes feeling isolated. One of the main difficulties described by staff was finding colleagues to obtain assistance and information. This was a cause of much frustration, especially for HCAs.
It can be a bit difficult sometimes, if you’re really stuck and, you know, I’ve been hanging out of rooms calling for a nurse sometimes, but if somebody’s in another room, you can’t see them. [. . .] [If] you really need a nurse, or you really need somebody to come and help you, then you have to go through all the rooms to try and find them [. . .] So if you do need assistance [. . .] we often just press the call buzzers ourselves.
S14, HCA, surgical ward
Well, I suppose sometimes, on a really busy day, you can feel a bit isolated [. . .] I know you shouldn’t, but at times it does make you put your own health at risk. I’ve done that with my own back, you just think, ‘Oh I can’t find anyone, [the patient] desperately needs the toilet, I’m going to help them’.
OP23, HCA, older people’s ward
The staff survey found that ratings of teamwork were lower after the move, including being able to locate staff and obtain assistance from colleagues, informal learning, keeping team members updated and discussing care with colleagues (see Chapter 5).
Allied Health Professionals and medical staff said that after the move it took them more time to find nursing staff and speak to them about patients. Nurses generally were perceived to be busy and therefore less interruptible or available. Nursing staff also thought that single room wards had disrupted interaction with colleagues from other professions. Nurses said that they might not notice a doctor or AHP going into a patient’s room, and unless the professional made an effort to find them, or the patient told them, they would have no immediate information about the encounter.
The teamwork subscale in the staff survey showed that ratings of information handover and communication between professions were significantly lower after the move (see Chapter 5).
The size and design of general wards required nursing staff to work in small, decentralised teams, caring for patients in a cluster of 8 to 10 rooms, and based at a nearby nursing station. One member of each team was responsible for carrying a wireless telephone, so that they were contactable by the shift co-ordinator or supervisor, and the receptionist could forward calls relating to patients in that cluster directly to the team. A shift co-ordinator or supervisor was responsible for overseeing the ward as a whole, which was thought to help the ward team function efficiently.
Nurses were generally positive about working in decentralised teams and felt that good communication and co-operation were important in helping staff deliver effective patient care. However, there was also a widespread perception that decentralised working had reduced opportunities for interaction among the wider ward nursing team. Many nurses and midwives said that they had now less professional and social contact with colleagues; they felt that this not only was a personal loss, but also detracted from the sense of community in the hospital:
there’s a feeling that it’s almost like three separate wards, in a way. You’re very much self-contained within your own team. Whereas before, I think there was far more interaction between nurses.
S16, staff nurse, surgical ward
Some nurses spoke positively about the nursing team on their ward but others felt that the mutual support they had experienced on multibedded wards could not always be relied on in the new hospital. A staff nurse spoke candidly about her experience of, and attitude to, reciprocity among nurses:
to be honest I’ve got enough on my plate with my 10 beds. Unless somebody needs me, [when] they can come and get me, I’m too busy. It sounds awful, but they’ve got their 10, I’ve got my 10. I think it’s a bit like that. [. . .] You get the right group of people on shift and we do try and muck in and help each other out. If one end is particularly quiet they will go and help out the end that is busy. But some people will just think, ‘Thank God, I’ve got a quiet day today,’ and make the most of it.
S11, staff nurse, surgical ward
Some experienced nurses also indicated that single room wards impacted on the ability to support, train and develop staff. They explained that it was more difficult to supervise juniors: ‘that is a direct result of the environment really, because you can’t eyeball nurses enough to know that they’re drowning and they need help’ (M06). There were also fewer opportunities for informal learning than on multibedded wards.
You overhear someone working behind a curtain and you pick up and you think, ‘That was a really nice thing they did for that patient. Maybe I’ll try that’. I think that’s definitely missing, picking up on things from each other that way, because [. . .] it’s not as easy to hear how they interact with people.
M05, junior sister, AAU
Adapting work patterns to improve communication and teamwork
Establishing decentralised teams
Two of the case study wards (older people and surgery) had deployed staff as envisaged during the development of the new hospital with decentralised nursing teams related to clusters of 10 rooms; a configuration that was supported by the ward design. The ward layout on the AAU was different: it had been designed to be nursed as two ‘sides’ of 14 and 16 rooms. Although nominally divided into two teams, staff initially replicated how they had worked previously, with each qualified nurse taking individual responsibility for five to seven patients. The ward manager described how this approach did not transfer successfully:
The staff found that very, very difficult [. . .] they weren’t supporting each other and felt that they were working very much in isolation, [they] weren’t taking breaks on time and were generally becoming more and more stressed and burnt out. We sat down at a team meeting and said, ‘How else do you think we can do it?’
AAU ward manager
The nurses decided that they wanted to try the system used on other wards, with teams relating to clusters of 10 rooms, even though the layout of the AAU did not support this arrangement.
We went from two teams to three teams. Same staffing levels [but now] two qualified and one CSW [care support worker] [work together as a team] to 10 patients. [. . .] It was as if the smaller team were able to talk to each other, recognise, support each other in decisions; tell each other what was going on. [. . .] Suddenly it all clicked and it all made much more sense. [. . .] It was from that point they started to manage things that little bit better. There was less stress on the ward. It was as though they’d taken ownership of it.
AAU ward manager
Staff felt that nursing in small teams made working on the single room ward easier, particularly by enabling them to share the workload and cover each other for breaks.
We’ve sucked it, we’ve seen, we’ve changed it, we’ve sucked it again [. . .] we’ve changed the way staffing is allocated seven times and this does seem to be the best way that it works, with the least amount of stress. [. . .] So, although [a team has] got 10 patients, and we expect them to know their 10 patients, you’ve got someone to cover you. [. . .] So now our staff are getting breaks, whereas before we went through about a 6-month period where people weren’t having anything to eat or drink for twelve and a half hours.
M06, junior sister, AAU
Team nursing was seen as ‘quite a culture change’ for nurses used to working individually. They had to learn to ‘let go’ and ‘rely on each other’ when working together, which could be ‘quite stressful still because they’ve got to trust the other person’ (M05). Other nurses alluded to the high level of trust required for teams to function effectively in the single room environment, where staff rarely worked within sight of each other.
Staff working in decentralised teams had also developed new approaches to planning the delivery of care. As there was less likelihood of impromptu face-to-face interaction on single room wards, nurses found they needed to be more systematic about ‘catch ups’ to share information about patients and plan their work. Most staff thought that this had improved communication among staff working in a small team.
Maintaining situation awareness (the supervisor role)
Decentralised nursing teams were said to work well, but staff felt that the ward team as a whole now lacked coherence. Nurses handed over in each area separately, and midwives handed over midwife to midwife. The surgical ward had retained a central handover for all staff every morning, which the ward manager felt was important for communication, maintaining ward identity and counteracting the ‘segregation’ created by decentralised working. Nurses liked this arrangement, but found that during the shift they lost touch with developments outside their ‘cluster’:
in the morning, we all sit and have a handover together, so that’s quite nice, and then you split off. [. . .] You meet together when you’re mixing your drugs and [at patients’] lunchtime, but that’s about it. So you don’t really know what the other teams are going through – if they’re really busy – unless they ask you for help. That can be quite hard.
S12, staff nurse surgical ward
On the general wards the shift co-ordinator or supervisor (often the ward manager) was the only nurse with a brief to maintain an overview of activity on the ward as a whole. For some nurses this was a new role and even experienced nurses considered it more demanding than being nurse-in-charge on an open-plan ward. For the junior sister quoted below it had been ‘quite a learning curve’.
[When I’m] in charge, having 30 patients in your head rather than 16 is a bit more of a challenge, also just the geography of the place, it’s huge, and getting used to having a mobile phone on you the whole time [. . .] because people can’t see you, they have to phone you. It’s a different environment, it’s been quite a learning curve. [. . .] I have to learn how to stop one person in each of the three teams, at least twice a day, and go, ‘Right, run through your patients with me, tell me what’s happening, give me some feedback,’ on a more official, structured basis than when we were a smaller [ward] team, because it was easier to pick it up as you overheard them talk to one another.
M02, junior sister, AAU
Communication tools on the ward
Staff clearly had a preference for face-to-face interaction and saw other means of communication, such as wireless telephones and whiteboards, as less satisfactory. Wireless telephones were provided for nurses, but a number of these had gone missing soon after the hospital opened, so they were typically held by the shift co-ordinator and one member of each nursing team. Most nurses and midwives said that they found them intrusive when caring for patients, although a few nurses liked the flexibility they offered.
If I’m honest I try to avoid carrying the phone, because I find it really intrusive if I’m busy looking after somebody in a room [. . .] I’d rather come out of the room on my terms, and go and answer the phone, than feeling [. . .] I’m busy trying to help this baby feed or I’m doing a tube feed or whatever, and I’ll have to answer my phone [. . .] It’s not appropriate and it’s heavy in your pocket actually, so I’m not a great fan.
PN32, midwife, postnatal ward
[T]he phone system is really good. You carry your own phone. You can make a call while you’re in somebody’s room if you need to. You don’t have to go out to a desk to access the telephone. You can give patients’ families your direct number. So from the communication side of things, that’s been a big plus I think. [. . .] If you’re doing a dressing or doing something like toileting a patient, then you don’t answer it, it just goes to missed calls and you can retrieve it when you’re free. So yeah, I love that side of things.
S16, staff nurse, surgical ward
Nurses seemed to have had little training to help them use the telephones effectively. Telecommunications could have helped locate staff on the ward, but this was rarely suggested.
Whiteboards in patient rooms and ‘patient status at a glance’ boards were ways of sharing information about patient care that did not require personal contact. Staff were accustomed to using patient status boards at the old hospital (although in the new build these had not been installed when the hospital opened) but the white boards in patient rooms were an innovation that had to be integrated into work patterns. Some nurses found them particularly useful: ‘a good communication tool. Anything that means I get less interrupted I like’ (M05). Some staff, including AHPs, questioned if all ward staff read and acted on the information they displayed and others suggested they were not kept up to date or fully utilised, particularly for communicating with patients and their families.
Staffing levels to support safe and effective care
Before the move to the new hospital, nurses and midwives expressed concerns about staffing levels, and this was a recurrent theme in post-move staff interviews. Nurses felt that more staff were required in the new hospital to aid patient surveillance and overcome the challenges identified above. After the move, staff reported that they were ‘busier’, which they attributed to both service reconfiguration and the single room wards. Nurses in the new hospital described themselves as under greater pressure than they had been when working on open-plan wards, using terms such as ‘constantly running’ or ‘pulled’; they felt they had insufficient time for patient care:
if everything is going smoothly the nursing levels are fine [. . .] Mornings aren’t too bad [. . .] But this afternoon [. . .] it’s just one trained, one care assistant. I’ve had a patient from ITU [intensive therapy unit] that needs constant monitoring, I had a patient dying and the relatives needed quality time with me and their loved one, and then I had a patient that suddenly became septic, and a patient that was on a blood transfusion, all at the same time. And with one trained member of staff and one care assistant it wasn’t safe at all.
S11, staff nurse, surgical ward
Some ward managers said that increased staffing levels were necessary. However, other managers thought that at least some of the pressures experienced by nurses were not connected with the size of the workforce; rather they were due to staff not prioritising their workloads or managing their time effectively. Staff also identified this as an unforeseen challenge of working on single room wards (see section An unforeseen challenge: time management and prioritising workloads).
Summary: were the expected challenges of single room wards confirmed?
All of the challenges foreseen by staff arose in practice and required accommodation and adaptations to working patterns. Some challenges became more significant than expected because they were compounded by other factors in the new environment. The most important challenge for staff was surveillance and monitoring of patients because the design of the single room wards limited the visibility of patients even more than expected. Staff on the general wards had introduced a variety of measures to facilitate monitoring and prevent falls. Staff considered social isolation a real disadvantage for patients and staff on single room wards. Some groups of patients, notably those who were older, confused or cognitively impaired, were perceived to be most affected, becoming lonely and more likely to make demands that staff saw as inappropriate or excessive. Staff had limited scope to increase interaction among patients, because day room facilities on the wards were inadequate or non-existent. As staff had expected, maintaining teamwork and communication on single room wards presented a variety of challenges. Staff adapted successfully to working in decentralised nursing teams, although finding the optimal configuration required trial and error on one ward. Decentralised working disrupted the coherence of the ward team as a whole and some nurses noticed less trust and reciprocity among staff. Experienced nurses found it harder to supervise staff and there were fewer opportunities for informal learning. Face-to-face communication was more difficult to accomplish, but alternative methods that could have saved staff time, such as telecommunications and whiteboards, were not well established.
Staff expressed concerns that staffing levels on the new wards were insufficient to support safe and effective care, but some pressures may have been due to difficulties managing time and prioritising their workload, the final and unforeseen challenge identified by staff.
An unforeseen challenge: time management and prioritising workloads
Staff felt that single rooms ensured privacy, which improved their interaction with patients and potentially enabled them to deliver more personalised patient care. However, they described tensions in terms of managing their time and dividing their attention between all the patients they were caring for on a shift. Apportioning time equally or fairly to patients was not such a problem on open-plan wards where staff were visible to patients and could interact with them collectively as well as individually. Staff faced a dilemma: they could offer patients in single rooms a better quality of individual care, but they were also required to explicitly divide their time among them and therefore could not always give everyone the time they would have liked to. This resulted in nurses feeling ‘bad’, ‘frustrated’ and unable to ‘give [their] best’:
Nursing in rooms is completely different to a bay [. . .] you feel that you can’t give every single patient equal attention I suppose, whereas I could before. I could stand in the middle. I could chat to all of them as a whole, they could all interact with each other, whereas now it’s very much one on one or two with one and you almost feel guilty not being able to spend as much time with them as you could.
M05, junior sister, AAU
Varying acuity levels meant that staff had to concentrate on patients with the greatest need for care and would possibly see patients needing only routine observation no more than twice during a shift; qualified staff found that situation unsatisfactory.
The other afternoon I just felt I was being pulled; I managed, but I was being pulled. And I kept thinking, ‘I know I need to go and see this patient because I’ve not personally seen this patient for quite a while,’ but I had some quite demanding relatives and one of my patients was becoming unwell, they were just on the edge, so I had to keep a close eye on them as well. I just think sometimes I want everything to slow down a bit so that I can give what I want to give: give my best.
OP21, junior sister, older people’s ward
Another source of anxiety for staff was that while in a patient’s room they could not see or hear other patients who might need them, which sometimes prevented them from giving that patient their full attention: ‘you’re very aware that you’re talking to somebody but at the same time listening out for anything else going on, the emergency buzzer even or the other call buzzer systems’ (PN31). Staff also recognised the ‘danger’ of clinical interactions in single rooms becoming prolonged. Staff described being ‘stuck’ in a room or finding it ‘difficult to get away’ and sometimes feeling that patients were ‘keeping’ them.
Staff recognised that single rooms facilitated delivering personalised patient care, yet most found themselves struggling to achieve this goal. Nurses described the strain of managing demands on their time and highlighted the impact this could have on developing relationships with patients. Some staff suggested that, as a result, care in the new hospital was becoming more task orientated than on the old wards, and a ward manager felt this was diminishing nurses’ job satisfaction.
You don’t develop a relationship [with the patient] any more because you’re very aware that if you’re in a room for any length of time there’s nobody in the main corridor [. . .] patients in the other rooms are alone. You can’t share your time with four people in the same go, and that makes things very, very difficult. [. . .] All you hear is the pumps bleeping and things like that, and you just feel more task orientated. [. . .] You’re just going in to do the task and go away. I don’t think [staff] are enjoying it quite as much.
KSI30, ward manager
One-third of staff thought that the move would make no difference to time spent with patients, 13% thought it would increase and 41% felt it would decrease. After the move, only 18% felt there was no difference, with 55% suggesting time with patients had reduced and 24% that it had increased (see Chapter 5).
Interviews with patients found that not all of them experienced a sense of connection with staff and, for those individuals, care felt task-driven and functional (see Chapter 7).
Adapting work patterns to improve time management and prioritise workload
To address the tensions of managing time and prioritising workloads, nurses and midwives took a more systematic approach to delivering care, with greater emphasis on assessment and planning rather than working in a reactive and fragmented way.
Forethought, awareness and planning
With greater distances to walk on the single room wards, staff found it beneficial to think ahead and ensure they gathered everything they needed before going into a patient’s room. A junior sister described how managing team workload required more ‘awareness’ than on multibedded wards, and staff needed to explicitly divide up tasks.
You need to be a lot more aware of your time management and how long you spend in each room [and] patient priority, who’s your unwellest and who you need to spend more time with. I think in bay nursing you’re not quite so aware of that because you’re eyeballing them constantly [. . .] That’s part of learning to deal with team nursing [. . .] you’re going to start in room 1, and the [auxiliary] need to start in room 10, and we’ll meet in the middle. But that still means the people in rooms 5 and 6 don’t get seen for an hour.
M06, junior sister, AAU
Another nurse described how she integrated doing observations and drug rounds, which took more time but allowed her to make a full assessment of each patient and prioritise their care:
In the morning when I’m doing the drug rounds [. . .] I always make sure [. . .] that the boards are all updated [. . .] that their obs [observations] are okay. I’ve then got to give the medication. So I do spend a bit of time with each of my patients, [. . .] I always prefer to do the obs with the medication in the morning because I just check everything, eyeball each patient and make sure they’re okay [. . .] and that means that when I’ve finished I can plan the rest of my day. If someone’s a little bit poorly I can go back and check on them [. . .] instead of getting caught up with all the washes. [. . .] If you do all your washes first then start eyeballing each of your patients some of them could be in serious problems.
M03, staff nurse, AAU
Prioritising care and sharing workload
A nurse on the older people’s ward described how a team would respond to a patient becoming more acutely ill by ‘escalating’ care: allocating one member of the team to concentrate exclusively on caring for that patient.
A staff member can say, ‘actually, I need to concentrate on this patient only’, so the two other staff on that zone [HCAs] assume I’m not going to be available because I’m concentrating on this priority. [. . .] The staff nurse takes a step to the side and says, ‘I’m not assisting with any of the daily activities, I’m going to concentrate on this. Come and get me if you need anything urgently’. The supervisor or the ward manager obviously is aware that is happening and they can also support the team members as well. That seems to work.
OP25, junior sister, older people’s ward
Supervisors or shift co-ordinators were felt to play an important role in helping staff manage their workload, by prompting or endorsing decisions to escalate care. In addition, they could step in to help at busy times, often with tasks that would otherwise take nurses away from delivering direct patient care. This was also thought to be a valuable aspect of the newly established discharge co-ordinator post on the older people’s ward.
Summary
Advantages and challenges of single room working
Staff working on single room wards experienced the advantages they had expected before the move, although the expected benefits were not always fully realised because of issues and challenges in the new environment. Staff found that:
-
Single rooms improved privacy, dignity and confidentiality for patients, allowing them to rest and recuperate without disturbance, and were better for visitors. Single rooms were perceived to facilitate communication with patients and reduce interruptions. However, staff found single rooms did not always enable more personalised patient care, because they felt unable to give sufficient time and attention to each patient.
-
The design of patient rooms and wards met many staff expectations for an improved working environment and supported them to deliver efficient and effective care. However, staff also identified various design elements specific to Tunbridge Wells Hospital that presented obstacles to safe and efficient working, increased the distances they had to walk, diverted them from patient care and affected their well-being.
-
Staff liked the new hospital (clean, spacious, modern, quiet and calm), which gave them a sense of professionalism.
-
Staff believed that the new wards supported good hygiene practices and reduced the risk of infection. However, to avoid complacency, managers reinforced infection control policy and developed a visual warning system to prompt staff to take specific measures before entering a patient’s room.
Staff working on single room wards experienced the four main challenges they had anticipated before the move, which in some cases represented more significant disadvantages than expected. Staff found that:
-
The design of the wards limited visibility of patients even more than they had anticipated. Their greatest challenge was monitoring and safeguarding patients, especially those at risk of falls, which increased pressure on staff.
-
Social isolation was a real disadvantage for patients and staff on single room wards. Patients, who were older, confused or cognitively impaired, were perceived as most affected, becoming lonely and more likely to make demands on staff that were considered inappropriate or excessive. Staff wanted to increase interaction among patients but had limited options because of the lack of communal space on the wards.
-
The quality of ward teamwork enjoyed in the old hospital had been difficult to recreate on the new wards. Staff adapted to decentralised nursing teams, but experienced less interaction with colleagues and disruption to the ward team as a whole, resulting in diminished trust and reciprocity among staff; difficulties supervising staff; and fewer opportunities for informal learning. Face-to-face communication was harder to accomplish, but aids that would have saved staff time (telephones and whiteboards) were not well established.
-
Concerns were expressed that staffing levels on the new wards were not always sufficient to support safe and effective care.
Staff also highlighted an unanticipated challenge of time management and work prioritisation in single rooms. They had to divide their time between patients individually and could not give the time and care they wanted, resulting in frustration and dissatisfaction. Some nurses suggested that care had become more task orientated.
Disruption and reconstitution of work patterns
-
Staff developed new ways of working and new processes of care. Successful examples included monitoring patients; decentralised nursing teams; supervisory roles for situation awareness; regular room checks; and falls interventions.
-
Trial and error was a feature of innovations, with staff teams trying, for example, different ways of preventing falls and different configurations of decentralised teams.
-
Locating colleagues to obtain information and assistance was one of the main difficulties described by staff, and was, on the whole, unresolved by new ways of working.
-
New ways of working that were considered successful had some disadvantages; for example, room checks supported surveillance and helped reduce patient isolation, but increased paperwork and risked a ‘tick box’ approach to care. In addition, sitting patients at a high risk of falls in the corridor might have prevented falls, but it was considered ‘perverse’ in an all single room hospital.
-
Tools to optimise single room working were largely underutilised; they were most extensively adopted for falls prevention and less well embedded in terms of enhancing team and patient/staff communication.
-
Staff recognised that they required different strategies for time management and prioritisation on single room wards, to enable them to divide their time between patients and feel satisfied that they were giving all patients sufficient personalised care. Building good teamwork may help, but nurses found patients’ expectations and inability to assess the extent of demands on staff complicated finding satisfactory approaches.
Chapter 7 Patient experience of the single room ward environment
Introduction
This chapter explores the experiences of patients on single room wards. It presents findings from a thematic and cross-case analysis of 32 in-depth interviews conducted with patients who had recently stayed, or were currently staying, on the four case study wards at the Tunbridge Wells Hospital. Information about how the analysis was conducted and characteristics of the sample can be found in Chapter 2.
This chapter addresses the following research questions:
-
What are the advantages and disadvantages for patients of a move to all single rooms?
-
How does the move to all single rooms affect patient experience and well-being?
-
Does it affect diverse patient groups differently?
It begins with a summary of findings from interviews with patients in multibedded accommodation at the old hospitals, which are presented in full in the phase 1 evaluation report. 1 This is followed by an exploration of patient experiences of single rooms in the new hospital. Four key themes or dimensions emerged from analysis of patient interviews, which specify different facets of patients’ overall experience of staying in single rooms. These dimensions – labelled ‘comfort’, ‘control’, ‘connection’ and ‘isolation’ – are defined and then each is explored in turn, using quotes from patients to illustrate their experiences. Finally, we consider patients’ preferences for single room or shared accommodation in hospital.
Pre-move findings: patient experience of shared accommodation
Analysis of interviews with patients on the old multibedded rooms revealed that the physical environment influenced three key dimensions of patient experience – security, community and physical comfort – which contributed to patients’ overall assessment of their stay in hospital.
-
Security: positive perceptions of security were related to staff proximity; ability to witness staff caring for other patients and observe staff competence; and social interaction with staff. Feelings of insecurity were associated with ‘rushed’ care and staff who did not have time to get to know patients. The ward layout and perceived pressure on staff contributed to patients on the postnatal ward feeling especially insecure.
-
Community: multibedded rooms allowed patients to engage actively or passively in the patient community. Many patients enjoyed the company and camaraderie on the ward and derived emotional comfort from social interaction. However, the condition or behaviour of other patients could change the community dynamic on the ward; for example, cognitively well patients on the older people’s ward felt more isolated if they were with predominantly cognitively impaired patients.
-
Physical comfort: patients’ experiences of physical comfort were influenced by many aspects of the ward environment. Discomfort was associated with shared toilet facilities; lack of space around the bed; and inability to control lighting, temperature and noise.
In the pre-move data, patients’ experiences of shared accommodation shaped their views on single rooms in the new hospital. Maternity patients expressed a preference for single rooms, which they expected would provide more security, privacy and physical comfort than an open ward. Other patient groups were ambivalent about single rooms, identifying potential benefits (sleep, rest and en suite facilities) and disadvantages (loss of proximity to staff, loneliness and isolation).
Post-move findings: patient experience of single room accommodation
Key dimensions of post-move patient experience
Analysis of interviews with patients carried out after the move to the new hospital revealed that their experiences of single rooms had four key dimensions: comfort, control, connection and isolation.
-
Comfort: the dimension of comfort was common to patient experience before and after the move. Patients in single rooms identified aspects of the environment that contributed to their comfort, particularly the en suite facilities, in contrast to patients on the old wards, who experienced significant levels of discomfort. The design of the room helped reduce patients’ anxiety, promote rest and sleep, and support physical comfort.
-
Control: patients interviewed after the move talked much more about aspects of experience that related to being in control while staying in hospital. The privacy of the single room meant patients felt that they retained their independence and freedom; they were able to do what they liked, when they liked and in their own time. They perceived the room as their own space and compared it with being at home. It was important to patients that they were not being observed by others, so they did not feel self-conscious; the room allowed them to be ‘backstage’ and removed any anxiety associated with impression management. 117
-
Connection: this dimension relates to the quality of interaction with staff experienced by patients in single rooms. Patients felt connected when they had good communication and relationships with staff; they did not feel alone. In contrast, patients who perceived staff as ‘too busy to talk’ and care as task oriented felt a sense of disconnection. They were disinclined to initiate conversation with staff and found time passing slowly.
-
Isolation: patients who felt little connection with staff were likely to report feeling isolated in single rooms. Isolation was also associated with unmet expectations of interaction with other patients on the ward; some patients who missed company felt confined in their rooms.
Comfort
An important difference between pre-move and post-move patient experience was in perceptions of comfort. Patients on the old wards identified aspects of ward design and facilities as increasing their discomfort. In contrast, patients in the new wards were universal in their praise for the comfort afforded by the single room environment. The language patients used to describe the environment often included frequent comparisons with a ‘hotel’, with patients favourably comparing the standard of accommodation and level of comfort with that experienced in a hotel room.
You had a shower, toilet, and washing facilities. Got your own TV, which when you’re in hospital you want something to do, which is a bonus [. . .] I would rate it really as probably on a par with a three-star hotel [. . .] That’s how good it was.
P11, male surgical patient, age 70 years
I went into the room, a beautiful room, lovely condition, lovely toilet and bathroom, I’ve got to say. To stay there is like a five-star hotel. It’s lovely.
P15, female surgical patient, age 65 years
Patients noted the quality of the lighting, ventilation and views from the bed and these were important factors in the overall levels of comfort experienced. There was also a sense in which patients experienced these aspects of the environment as healing or aids to their recovery.
The lighting was fantastic, because obviously, there are different settings. So I could turn the main lights off and you had some lights you could control behind your bed [. . .] You could turn the up light or the down light on, so the lighting was fantastic.
P1, male AAU patient, age 44 years
The temperature was fine and there was a long window, floor to ceiling, which I could open easily. [. . .] That was nice, very nice. [. . .] by the Sunday I could get out of bed and just go and open my window, which was lovely.
P2, female AAU patient, age 74 years
To be able to look out and see the trees and the sunlight, and the sky when it turns a different colour [. . .] it’s lovely to look at [. . .] just being able to look up, where trees are, and look up at the sky and the sunlight [. . .] It makes a difference, [. . .] you just feel happier [. . .] in spite of everything.
P21, female patient, older people’s ward, age 85 years
Patients with recent experience of shared hospital accommodation acknowledged that the single rooms gave them peace and quiet, compared with the noise of an open or bay ward environment. They described disturbed nights and feeling exhausted and in need of sleep following their discharge from an open ward. In contrast, single rooms meant patients were able to sleep well at night, and rest during the day. Postnatal patients also experienced reduced anxiety about their own baby crying and better sleep in comparison with postnatal patients interviewed in the pre-move study.
I know you can’t say, ‘I don’t want to be in that ward’, but if you have someone in there that has got dementia, it’s very frustrating because they don’t settle [. . .] Your whole time that you stay in there is a constant being awake, listening [. . .] whereas when you’re in a room and you’re on your own, you haven’t got anybody. You couldn’t hear a sound in that room, not a sound.
P15, female surgical patient, age 65 years
The single room is, I think, the most perfect solution they came up with because [. . .] sometimes babies are crying constantly, [. . .] but I had that peace and at least if baby was asleep, I could also go to sleep because there wasn’t anyone next to me with a baby crying or anything.
P26, postnatal patient, age 26 years
All patients interviewed found having an en suite toilet and shower particularly beneficial. The proximity of the en suite facilities meant that patients could easily mobilise to the toilet or shower, either independently or with assistance. For older, frail patients, this meant being able to enjoy a shower and a hair wash, and was a great source of comfort.
This business of having a nice wet room is marvellous. They wheel you in, strip you off, hose you down, rub soap all over you, hose you down again, dry you, and whip you back into bed again. It’s quick and easy for them. I mean, when you think of that and a blanket bath – what a performance that is – they [en suite facilities] really are [marvellous].
P12, male surgical patient, age 84 years
I’ve been in there [en suite]. Mind you, they have to help to get me in there. But what surprised me so was that I had a shower, yes. And at the same time as having the shower, they’ve washed my hair, yes. And that was wonderful! [laughs].
P21, female patient, older people’s ward, age 85 years
Staff considered en suite facilities an important advantage of single rooms because they made it easier to assist patients with personal care. Nurses particularly valued being able to give patients showers, and sensed that this was appreciated (see Chapter 6, Improved room design; improved care delivery).
For many patients, the privacy of the en suite toilet was important; they did not have to feel embarrassed about using the toilet or not getting to the toilet in time.
The first few days I couldn’t go to the toilet normally [. . .] With my problem [diverticulitis], having my own toilet was brilliant.
P11, male surgical patient, age 70 years
I only just made it into my bathroom in time [. . .] I would have been so embarrassed, if I’d had to go out of my [room] and across the corridor and feel sick, and wet myself, I would just die of embarrassment [. . .] but there it was absolutely fine.
P16, female surgical patient, age 45 years
The en suite bathroom also meant patients could be as comfortable as they would be at home, being able to keep their toiletries in the bathroom, take their time and, for postnatal ward patients, leave the door open so that they could hear their baby.
If I think back to when I’d had surgery [at Maidstone], it’s a communal toilet, so you’re kind of in and out as quick as you can. And the fact that it was more difficult to wash and stuff in a communal bathroom, rather than if you’ve got your own private one, and you can spread out and just feel much nicer, much more like you’re at home or wherever. So, I think that made a big difference.
P7, female AAU patient, age 44 years
Being a new mum you didn’t really want to leave your baby at all, so I’d leave the door of the en suite open and I could still hear [baby] [. . .] it was just convenient that when you’ve got a newborn, sometimes it just feels like you haven’t got a minute to yourself, so just to quickly be able to pop to the loo. And especially to keep changing pads and things like that, so you need all of those essentials nearby.
P30, postnatal patient, age 29 years
Control
The second dimension of experience identified from the post-move interviews was ‘control’. Control rarely featured in patients’ accounts of staying on open wards. In single rooms, control was closely associated with privacy and freedom; not being observed by others; and retaining independence and agency. The level of physical comfort discussed above supported patients’ sense of control. Female patients also talked about being able to ‘think’ what they liked, and valued not having to worry about what other patients might be thinking about them. Patients compared the single room with being at home, in their own space, with similar control and privacy.
Being in a room on my own where I didn’t have to talk to people if I didn’t want to, I could watch the telly, I’d got my iPad, I’d got stuff that I could amuse myself with [. . .] And the fact that I’d got privacy, and things like being able to go to sleep when I wanted, and wake up when I wanted, was really beneficial [. . .] not being disturbed by other people. So, I was quite happy to be in my own room, and I think I would have been really unhappy to be on a ward.
P7, female AAU patient, age 44 years
I love it in here, because you can do what you like, think what you like, and [. . .] go to sleep, and look at magazines.
P21, female patient, older people’s ward, age 85 years
You’ve got your own TV [. . .] when I was alone in here, when [baby] was sleeping I would catch up a little bit on things that are happening in the world, what I would do at home anyway [. . .] even if [baby] cries I can take my time to get out of the bed and take her. There’s no hurry, ‘Oh, my god, she’s crying. Maybe she’ll wake up the baby next to me’. It was a home from home.
P26, postnatal patient, age 26 years
Patients also reported that having their own space and privacy meant they felt relaxed.
When you’ve got your room it’s just nicer, it makes you feel more relaxed [. . .] you’ve still got your little bit of independence [. . .] your space rather than just a curtain between you and the next bed.
P16, female surgical patient, age 45 years
It just gives you time to properly relax, and you haven’t got other people shouting across the ward, and other people perhaps who are very ill and making a lot of noise. You don’t get to hear all that. It’s just nice because you can relax in your own time. You’re given that privacy, and that’s what I like.
P14, female surgical patient, age 72 years
Staff interviews and observation on the wards suggested that staff perceived the room as a patient’s ‘own space’ and they understood it was important for patients to have control over their environment. Staff respected patients’ privacy by knocking on doors before entering rooms (see Chapter 6, Privacy, dignity and confidentiality; more personalised patient care).
In the pre-move interviews, anxiety and vulnerability due to lack of privacy were most evident in the experiences of postnatal ward patients. In the post-move interviews, all patients talked about the enhanced confidentiality offered by the single room, but postnatal patients were especially grateful for the privacy afforded by the single room. In one case, a mother was able to ‘speak frankly’ with staff about her baby’s medical condition [talipes (clubfoot)] and appreciated being able to concentrate only on her baby without having to see babies with normal feet. For another mother, the privacy of the room was helpful in her feeling comfortable asking about what to expect following her caesarean section (c-section).
With having medical check-ups on [baby] having my own room meant I could speak frankly. You didn’t feel that somebody was going, ‘Oh?’ And his feet were really bad, [. . .] we knew about it from 21 weeks, but seeing his little feet all pushed in, it was quite a thing to get your head around and deal with, and it was nice not to be looking at some other baby whose legs were fine.
P32, postnatal patient, age 32 years
You can ask them anything [. . .] I had a c-section and I would ask them about the pains, the bleeding, the catheters, how everything worked. Because it’s private, I felt comfortable and they could even show me and [. . .] actually demonstrate it for me.
P26, postnatal patient, age 26 years
Finally, another key factor in patients’ experience of control was the privacy and flexibility of the single room environment for having visitors. Patients described being able to talk to their visitors freely and in confidence and liked the longer visiting hours and relaxed attitude of ward staff towards the length of visits. For parents, the single room was especially valued for ensuring a relaxed visit, for both patient and child(ren). Patients did not have to worry about their visitors disturbing other patients.
I’ve done quite a lot of visiting in hospitals, in wards, and I do think visiting in here is very much easier, in single rooms. [There’s] more space. And there’s more confidentiality, you feel not everyone’s hearing your business [. . .] it is nice really [visitors] can come whenever they like, in a single room, and that’s a very big bonus.
P17, female patient, older people’s ward, age 80 years
It was lovely because you had the privacy. So my daughter, she climbed onto the bed with me and had a cuddle, she felt more relaxed to be able to do that, whereas in the other hospital I could tell that she was self-conscious because there were a lot of people watching [. . .] [children] can talk, joke, laugh and be more relaxed in themselves, which was good for me, being the patient, because you get more out of the visit. They [wife, daughter and son] tended to stay longer as well [. . .] I think they extended their visits because you don’t feel like you’re in people’s way so much.
P1, male AAU patient, age 44 years
Staff interviewed thought that single rooms were better for visitors, affording privacy and confidentiality, which they saw as particularly important for seriously ill patients and their families. Staff surveyed rated single rooms as better or much better for patient interactions with visitors (see Chapter 5). Staff also valued single rooms for discussion with patients and families together (see Chapter 6, Privacy, dignity and confidentiality; more personalised patient care).
Although the single room was viewed as beneficial for visitors, postnatal patients felt that they had little control in relation to fathers staying overnight following the birth of their child(ren), a new policy enabled by single rooms. There was a lack of information about what fathers could expect, except that they would need to bring their own bed (e.g. camp bed or airbed) and bedding. One patient and her partner were able to plan in advance, but this was as a result of a visit that had been arranged because of the patient’s disability. The patient was extremely positive about midwives’ support and the environment enabling her independence, and was grateful her partner could stay. Other postnatal patients experienced a lack of control and increase in anxiety because of the lack of facilities and encouragement for fathers to stay overnight.
For him to come and stay would mean bringing a blow-up mattress [. . .] If there was a bed there, or even if there was a couch that he could lie down on, then he definitely would have stayed [. . .] It was really hard for both of us, him having to leave . . . especially his [baby’s] first night, second night [. . .] I was very emotional, I was exhausted, yes, and it’s your baby, you just want to be there. So it was really tough having to say goodbye and him going home.
P32, postnatal patient, age 32 years
It is a really important time in a family, when you have a baby, and it would have been nice for [partner] to spend the baby’s first night there, with her [. . .] If he knew that he was going to be able to get some comfortable sleep, he would have stayed. [It] would have made me less anxious, if he could have been there.
P25, postnatal patient, age 40 years
Fathers staying overnight on the postnatal ward had divided staff opinion. Some midwives interviewed felt that fathers should be given more encouragement to stay, but others felt that they made midwives’ jobs more difficult (see Chapter 6, Social isolation of patients).
Connection
The main interaction or connection patients had with other people, apart from their visitors, was with staff, including nursing and/or midwifery staff, AHPs, medical staff, domestic staff and catering staff. There was also interaction with volunteers, for example volunteer readers on the older people’s ward and breast feeding peer supporters on the postnatal ward. Unlike in the pre-move wards, patients had limited, if any, interaction with other patients.
In contrast to the wholly positive experiences of comfort and control in single rooms described above, there was a dichotomy in patients’ experiences of connection. Patients reported similar frequencies of visits to their room by the various staff groups listed above, and they described nursing staff conducting regular intentional ward rounds (usually stating that nursing staff came hourly to ask them if they needed or wanted anything). However, the quality of interaction with staff was experienced differently.
For one group of patients, the single room was perceived as ‘a busy place’, where there was ‘always some activity’, where you were rarely ‘on your own’, and ‘weren’t isolated’. Staff were ‘always in and out’, ‘always checking on you’ and ‘always asking’ if they needed anything. This activity and communication with different staff led to a sense of connection for these patients. As one patient described it, they ‘weren’t isolated’.
If you’re in hospital, you’re ill, you’re not there for a holiday, and if you’re ill you need a lot of treatment, you have your blood pressure taken three times a day, your temperature and all that, they have to draw blood samples to send for analysis. So you are being constantly attended by nurses because of your condition. Also people are coming in and taking orders for meals and meals are coming in, so actually, a [single room] is a very busy place, you’re not on your own, hardly ever.
P12, male surgical patient, age 84 years
They came in quite often, because obviously you had the cleaner come in, and then I had several blood tests so somebody else came in [. . .] They were taking your pulse maybe three times a day, and then there was the meal times and the coffee times. So there was always some activity [. . .] you weren’t isolated.
P4, female AAU patient, age 74 years
Some patients thought that the single room enabled staff to give them undivided attention and supported one-to-one care. Other patients thought that staff had been trained in interpersonal skills, which improved the quality of interaction.
Nothing was too much trouble. I didn’t feel like I was sharing somebody with everybody else, I felt like she was my midwife [. . .] there was real one-to-one care and attention being provided for me, and I think that’s part of what you get with having a room on your own, because you’re not conscious of other people being around, the midwives aren’t conscious and distracted by what’s going on elsewhere.
P25, postnatal patient, age 40 years
They stood still and listened. They didn’t try to get away quick. You know how if somebody has got to go and do something else so they’re backing away. They didn’t do that [. . .] When they came in you wouldn’t have thought that they’d been rushing about with somebody else and then come panting up to you. That didn’t happen. I think they must be trained in that way, that they can shut off from one and go to the next one. It’s wonderful what they do. [. . .] I was perfectly happy in there, really I was.
P14, female surgical patient, age 72 years
In contrast, the other group of patients, although reporting a similar frequency of interactions with staff, perceived these interactions as largely task driven or functional rather than relational, and as a consequence said they found the single room ‘very quiet [. . .] you never saw anybody’ (P9), and that staff were ‘very distant’ and ‘busy’, and ‘did not have time to chat’. This led to patients feeling disconnected and disinclined to ask questions or ‘delay’ staff; consequently some needs might be unmet. It also meant that patients felt the day went very slowly.
They didn’t really have time to chat. [. . .] They just came in and did what they had to do, the temperatures and blood pressures, and things like the obs, as they call them. And that was it [. . .] You get more time [in a multibedded bay], not to chat to the staff, but to ask them questions, because they’re in a bay more than they are in a single room. They would only come to your room just to see if you’re okay, every so often or if you called them.
P10, male surgical patient, age 71 years
They’re [nursing staff] mostly quite friendly [. . .] but of course, they’ve all got their own jobs to do and they can’t stay and talk or anything [. . .] it is a long old time from 7 in the morning until 7 at night.
P24, female patient, older people’s ward, age 78 years
The dichotomy of experience in relation to a sense of connection with staff suggests that there may be variability between wards and among different staff members in the quality of intentional rounding. Some patients experienced lack of continuity in the staff caring for them, which interfered with establishing a sense of connection. Team nursing and intentional rounding integrated with task-based care may result in several different members of staff delivering care to a patient during a shift. The patient quoted below links discontinuous, task-focused care with missed opportunities to increase his comfort.
One nurse takes your blood pressure and another takes your blood sugar [. . .] and the way they do it, they’ve got all the records, it’s time to do insulin, they come in, ‘Hello, Mr X, you need your insulin injection’. They do it and walk straight out. So, there is no chance to say anything that has just cropped up, like, ‘Could you open the window? Could you close the window? Could you turn the light off?’[. . .] and those ordinary things you don’t need to make a great fuss about, but you can ask for in passing [on an open ward].
P23, male patient, older people’s ward, age 80 years
Senior nursing staff recognised that there was variability in intentional rounding (see Chapter 6, Reduced visibility of patients: difficulties monitoring and safeguarding patients) and that staff needed to be encouraged to enter the room and stand close to the patient, rather than simply ‘popping their head round the door to see if patients are okay’. This would encourage patients to ask questions or make requests. The quality of intentional rounding is also heavily dependent on staffing levels, and, where wards are short-staffed or staffed by agency staff, the quality of intentional rounding may suffer. Patients frequently mentioned how busy staff seemed to be, and this is perhaps surprising given the lack of visibility for patients of the ward beyond their own single room. However, it was clear from patients’ accounts that staff were monitoring patients regularly, carrying out hourly room checks, which helped patients in single rooms – like patients on open wards, who could see nurses going about their work – to feel safe and secure, even if they did not always experience a sense of connection with the staff who checked on them.
There were other simple, yet important to patients, measures that encouraged connection between staff and patients. One such measure was putting nursing staff names on patient whiteboards in the room, so that patients knew who was caring for them that shift. Patients reported variation in this practice, and highlighted how important it was for them as a means of building rapport in the single room environment.
The highlights are they [. . .] introduced their self to you. You know, ‘Hello, Mr _____ , I’m so-and-so’, and they used to put on the board, Sister in Charge, blah, blah, blah, and you knew exactly who you were dealing with.
P11, male surgical patient, age 70 years
I think the first couple of days, they came in and they wrote on the board who was in charge and so on. That happened for a couple of days, and then it didn’t happen afterwards [. . .] It was quite nice to have a name, because if you’re not seeing people going up and down, there’s no kind of other rapport with anybody, so it’s quite nice to know who’s who.
P7, female AAU patient, age 44 years
Staff interviewed felt that single rooms could facilitate relationships with their patients and the delivery of personalised care, yet most found themselves struggling to achieve this goal because they felt unable to give sufficient time and attention to each patient (see Chapter 6, section An unforeseen challenge: time management and prioritising workloads).
In the survey, staff rated delivery of care (including factors such as spending time with patients, communication with patients, monitoring patients and remaining close to patients) worse in single rooms than on the old wards (see Chapter 5).
Isolation
For some patients, lack of interaction with other patients was a striking feature of their stay in hospital, and led to strong feelings of isolation in some cases.
It would have been nice to have been able to see other people, or maybe just to chat with other mothers [. . .] If you’re in an open ward, you just see people coming and going [. . .] you can chat to people across the ward [. . .] you can see other people going through what you’re going through [. . .] I just wanted to get home [. . .]because there isn’t anyone to chat to and I just felt a little bit isolated being in the room on my own.
P31, postnatal patient, age 36 years
Once you’re on the mend and you can get up out of bed that’s when it seems to be very lonely in a way, and isolated, I suppose [. . .] and the days and the nights seemed very, very long [. . .] If you’re alone in a room you tend to think about your illness more than if you’re chatting to somebody about the weather or your car, or something like that. That’s how I felt.
P10, male surgical patient, age 73 years
I don’t like it here [. . .] It’s boring sitting indoors all day either watching [TV] or reading [the paper] and looking at four walls. You can talk to [other patients on an open ward/bay]. Who are you going to talk to here? There’s nobody to talk to. The staff, you do talk to them sometimes but they’re busy, they’ve got their work to do.
P19, male patient, older people’s ward, age 86 years
Staff considered lack of social contact among patients a real disadvantage of single room wards. They felt that it could influence patients’ satisfaction with their hospital stay and their emotional well-being and recovery (see Chapter 6, section Social isolation of patients). Staff associated loneliness particularly with older, less independent or confused patients, but patient interviews indicate this experience was more widespread.
The isolation and lack of interaction experienced by some patients led to them feeling confined or constrained in their single room, and patients described a lack of information from staff about day room facilities or other communal areas that they could access (although patients in the AAU had no day room).
It did get a little bit lonely [. . .] you don’t really get to talk to many people, other patients. [. . .] I wanted to go for a walk just to get out of the room and maybe have a chat with someone. You do start to feel a little bit stir crazy stuck in a room [. . .] I don’t know if there was a common area, no one ever said. No one basically told me the rules, that you’ve got to stay in your room or if you want you can go and get a cup of coffee and sit in this room and watch a bit of TV with other people. So I guess if anything could be improved it could be telling patients what they can and can’t do. You know, is it okay to leave the ward? [. . .] I kind of felt like I had to stay in my room.
P1, male AAU patient, age 44 years
I did feel that perhaps I’d get shouted at if I walked past the nurses’ station [. . .] I did feel constrained to stay and not explore too much; they could help that by saying, ‘Well, no, if you walk up that corridor, there’s a communal room there’. And so you would feel that you can walk there.
P8, male AAU patient, age 69 years
Staff on some wards reported taking a more proactive approach to encouraging mobile patients to leave their rooms and walk around for therapeutic reasons and to facilitate social interaction (see Chapter 6, Social isolation of patients).
Staff considered the limited day room facilities a disadvantage of the new hospital. The AAU did not have a day room, and the older people’s ward was the only other case study ward which made structured use of its day room, running a lunch club for patients (see Chapter 6). Some patients particularly wanted opportunities to interact with other patients, and made suggestions for how this could be encouraged by staff.
They do have a lunch club which operates on lots of days of the week, but it depends on the nurses being able to take the time to take you down there and be with you [. . .] I go down there most days [. . .] I like talking to the other patients and finding out why they’re there [. . .] When it’s cancelled and I have to sit in here it’s terrible.
P24, female patient, older people’s ward, age 78 years
I think maybe that [patient interaction] could have been encouraged [. . .] maybe the midwives could say, ‘Right let’s all come and have a cup of tea together,’ or something like that. I don’t know if that would be a way forward to socialise a bit more, and just to share your stories maybe, a bit like mother and toddler groups that I’m trying to get to now.
P30, postnatal patient, age 29 years
Summary of advantages and disadvantages
The advantages and disadvantages of single room accommodation identified by patients are summarised in Table 57, which also shows how particular advantages and disadvantages relate to the four dimensions of patient experience discussed above. Patients felt safe and secure because staff carried out regular monitoring. Patients experienced high levels of comfort and control in single rooms, which enhanced their well-being. Some patients felt a sense of connection with staff, which improved their experience; others felt a sense of disconnection, which detracted from their experience, and intensified feelings of isolation resulting from the absence of a community of patients. For some patients the inability to interact with other patients negatively influenced their overall experience of staying on an all single room ward.
| Advantages and disadvantages of single rooms identified by patients | Positive and negative influences on experience and well-being identified by patients |
|---|---|
| Regular monitoring by staff Irregular monitoring and lack of continuity of staff |
Patients feel safe and secure Patients feel less safe and secure and less connected |
| High-quality accommodation, with en suite facilities Easy to maintain personal hygiene; patients particularly valued ability to shower and wash hair Privacy preserves dignity, especially in relation to bodily functions Space for personal effects Lighting, ventilation, window and view Soundproofing, no noise or disturbance |
HIGH LEVEL OF COMFORT Cleanliness associated with positive feelings, pleasure Reduced embarrassment and anxiety Feels like home Improved mood Better sleep; well rested No anxiety about disturbing other patients |
| Having ‘own space’ with personal effects allows independence and choice TV in room; can adjust light, temperature and ventilation Privacy: unobserved by other patients Confidentiality of interaction with staff Facilitates visiting: fewer constraints on visits in terms of timing, duration and number of visitors. Quality of interaction with visitors improved. No concerns about disturbing other patients |
HIGH LEVEL OF CONTROL Self-determination, sense of freedom Feels like home, happier No anxiety associated with impression management: can ‘be myself’, more relaxed, no embarrassment Promotes information seeking and engagement with staff Reduced isolation Patient and visitors more relaxed Increased emotional support |
| Postnatal patients wanted partners to stay overnight but found obstacles to achieving this |
REDUCED LEVEL OF CONTROL
Increased anxiety and isolation Reduced practical and emotional support |
| Good quality of interaction with staff: staff perceived as giving full attention, listening, interested in the patient as a person Poor quality of interaction with staff: care perceived as episodic and task driven, staff as ‘busy’ |
HIGH LEVEL OF CONNECTION Patient feels at the centre of activity Patient able to ask for information and help Emotional support SENSE OF DISCONNECTION Patient feels alone, marginal Patient reluctant to ask questions or make requests, hence needs unmet Feeling of time passing slowly |
|
No community of patients; few opportunities for social interaction; unable to see what others are doing; no chance to share experiences
No guidance on appropriate behaviour on the ward; no information about communal facilities; unsure about whether or not can leave room |
ISOLATION Loneliness, boredom, unhappiness Unable to normalise experiences No social or emotional support from other patients Feel restricted and confined Physical activity reduced Anxiety about breaking ‘rules’ |
Patient preferences for single room versus multibedded accommodation
Patients were asked at interviews about their preferences for single room or shared accommodation and on the basis of their responses were categorised into three groups: those stating a preference for single rooms; those stating a preference for multibedded accommodation; and those who were ambivalent. Patients with a preference for single rooms were the largest group (21 of 32, roughly two-thirds of those interviewed). All four case study wards were represented in this group, with five patients each from the AAU, the older people’s ward and the surgical ward, and six patients from the postnatal ward. These patients felt the advantages of the single room in terms of comfort and control outweighed any disadvantages in relation to connection with staff and isolation, and having en suite facilities and a television was particularly important to them.
This, I would think, wins out over the ward. Because of the advantages, I mean you’ve got your own wash hand basin, you’ve got your own toilet, you’ve got your own television. No, really it would win out.
P18, male patient, older people’s ward, age 70 years
Seven patients stated a preference for multibedded accommodation; the main reason given was interaction with other patients. These patients were from three of the four case study wards, with two patients each from the AAU and the older people’s ward, and three patients from the surgical ward. Six of the seven patients were male and one was female. There was variation in their LOS and age (LOS range 1–9 nights, age range 47–86 years).
Postnatal patients largely expressed a preference for single room accommodation, consistent with the phase 1 findings that all postnatal patients said they would prefer a single room. However, two of these postnatal patients were also represented in the group of four patients who were ambivalent. For these patients the benefits of the single room in terms of comfort and control outweighed the disadvantage of feeling isolated, but isolation and loneliness were significant downsides to their experience of the single room. Patients holding this ambivalent position were from three of the case wards: two postnatal patients (both first-time mothers), a male AAU patient (age 44 years) and a female patient on the older people’s ward (age 78 years). These patients wanted more opportunities to go out of their rooms and meet other patients.
Does all single room accommodation affect diverse patient groups differently?
Single rooms were a clear preference for many patients (and most postnatal patients) but a significant minority, including patients of varying ages and patient groups, wanted greater choice, in terms of either having the option of shared accommodation or being able to interact with other patients in communal spaces of the hospital. Approximately one in three patients interviewed (11 of 32) experienced lack of interaction with other patients as a main disadvantage of the single room. More male patients (6 of 13) expressed a preference for multibedded accommodation to counteract this experience of isolation, but female patients also wanted opportunities to interact with other patients.
It was very mixed for me. The concept I think is great and it’s great that people have that choice but I think going to the future, it should be a choice, not ‘Yes, you’re going to have a room by yourself’.
P8, male AAU patient, age 69 years
It is important to reiterate here that these preference findings are based on qualitative data from four case study wards and are not necessarily generalisable to other settings or groups of patients. It is also important to note that in the older people’s ward we were not able to interview patients who were very sick or who had dementia or delirium, and our sample primarily comprised older people in the designated orthopaedic beds. Trauma patients, paediatric patients and patients with dementia may have different preferences and particular experiences of the single room environment that are not adequately represented by the four core concepts discussed above.
While staff associated loneliness particularly with older, less independent or confused patients, patient interviews indicate this experience was more widespread and experiences more varied. Maternity patients expressed a preference for single rooms, which they expected would provide more security, privacy and physical comfort than an open ward. Patients across all groups identified the potential benefits (sleep, rest and en suite facilities) and the disadvantages (loss of proximity to staff, loneliness and isolation).
Summary
-
There were four core dimensions of patient experience of the single room environment. These were comfort, control, connection and isolation.
-
Patients experienced high levels of comfort in the single rooms, particularly in relation to the en suite toilet facilities, lighting, ventilation, having a view from a window and noise levels. The single room was frequently compared favourably with a hotel or home environment.
-
Patients also experienced a high degree of control in the single room. The privacy of the single room meant patients could do as they pleased at any time, without worrying about other patients. Consequently, they reported feeling relaxed. Patients also enjoyed the confidentiality afforded by the single room, and the privacy and flexibility it gave for visitors.
-
Postnatal patients experienced lack of control in relation to fathers staying overnight on the ward, due to inadequate provision of information and facilities, and some midwives’ ambivalence about this policy.
-
Patients reported similar frequencies of visits to their single room by various staff, and all patients described nursing staff conducting regular intentional ward rounds. However, there was a dichotomy in patient experiences of connection with staff, with one group of patients experiencing a sense of connection, while a second group of patients did not. For this second group, care was experienced as largely task driven and functional.
-
The experience of disconnection might be explained by variability in intentional rounding by nursing and midwifery staff. Patients also valued other measures that supported connection, such as writing staff names on patient whiteboards.
-
Interaction with other patients was largely absent from patient experiences in the new hospital. For some patients this led to a sense of isolation. Patients wanted to have the opportunity to socialise with other patients to counter this isolation.
-
Approximately two in three of the 32 patients interviewed expressed a clear preference for single room accommodation in hospital. The benefits of the single room in terms of comfort and control outweighed any disadvantages for these patients.
-
Approximately one in three of the 32 patients struggled with an absence of interaction with other patients and a consequent sense of isolation. Seven patients stated a preference for multibedded accommodation because of this, including six male patients, half of the men interviewed. Four patients wanted better day-room provision or structured activities for patients to facilitate interaction.
Chapter 8 Single rooms and patient safety: before-and-after study with non-equivalent controls
Background
The hospital environment in general and single room accommodation in particular are potentially important factors influencing the quality of the care provided and patient outcomes (see Chapter 1). Two areas that have received much attention for the effect of single rooms on health-care quality are infection rates and adverse events.
The mechanism considered for the reduction of infections through single rooms is the reduction of person-to-person contacts as well as limiting the spread of infection by person–surface–person contacts. 48 Two rigorous systematic reviews have been conducted to summarise the evidence on the association of single room accommodation and HCAIs. Dettenkofer et al. 53 included 17 historic and prospective cohort studies between 1975 and 2001 in their systematic review. The majority of studies were conducted in ICUs (n = 9), followed by surgical wards (n = 4), isolation units (n = 2) and general hospitals (n = 2). Three out of nine studies in ICUs reported a reduction of infections while no reduction was found for postoperative wound infections in the four studies of surgical wards. No reduction in infections was documented for isolation wards, although increasing the number of beds per room led to an increased number of infections in acute medical wards. A second review by Whitehead et al. 61 identified two additional studies between 2001 and 2006. Those studied were assessed as having a lower risk of bias. The two studies, in neonatal and paediatric intensive care settings, showed a reduction of the mean number of infections in isolation or single rooms in comparison with multibedded bays. More recent studies all conducted in ICUs57–60 have shown a reduction in several types of infections including MRSA and C. diff. In summary, an association of single room accommodation and decreased infection rates was repeatedly shown in intensive care settings including paediatric populations; however, for all other patient populations evidence of an association of single room accommodation and nosocomial infections is absent or equivocal.
In addition to HCAIs, several adverse events such as falls or medication errors have been highlighted as being potentially affected by single room design. 48,118 However, the evidence is scant. In their systematic review, van de Glind et al. 86 could only identify opinion articles, which reported a decreased rate of medication errors due to improved patient registration and reduced mix-up of patients through single rooms. Anecdotal evidence suggests a potential increased risk of falls through single rooms, because nurses have less opportunity to see patients and keep them under surveillance and therefore a reduced opportunity to detect imminent fall situations. While it is recognised that a number of environmental factors are associated with fall rates,32 an association of falls and single rooms in particular has not yet been investigated.
Therefore, we undertook a comparative quasi-experimental study that aimed to identify how moving to single room accommodation influences hospital-acquired infection and adverse events compared with remaining in multibedded accommodation or moving to mixed accommodation. Specifically, we analysed the changes in outcomes in wards moving from existing traditional wards within the trust to the new all single room hospital and compared it with outcomes in matched wards in two control hospitals: one which moved to a new build with mixed accommodation and one which acted as a ‘steady state’ control with traditional wards and no move during the study period. We set out to examine the plausibility of the hypotheses that any changes are specifically associated with the move to all single rooms as opposed to the provision of modernised accommodation or secular trends (e.g. staffing changes due to financial pressures or changes in the patient population).
Results
Special-cause variation at Tunbridge Wells Hospital
Overall, 15 36-month periods of outcome data were available from Tunbridge Wells Hospital. Falls, pressure ulcers, medication error, C. diff. and MRSA rates were available for all three wards (acute assessment, older people and surgical).
Five of the eleven time series revealed special-cause variation that could be associated with moving to the new Tunbridge Wells Hospital: increased fall, pressure ulcer and C. diff. rates in the older people’s ward and temporary increases in falls and medication errors in the acute assessment unit (Figures 25–28).
FIGURE 25.
Older people’s ward at Tunbridge Wells: u-chart with CF expansion – (a) falls, (b) pressure ulcers and (c) C. difficile. CL, centre line; LCL, lower control limit; StdDev, standard deviation; UCL, upper control limit.

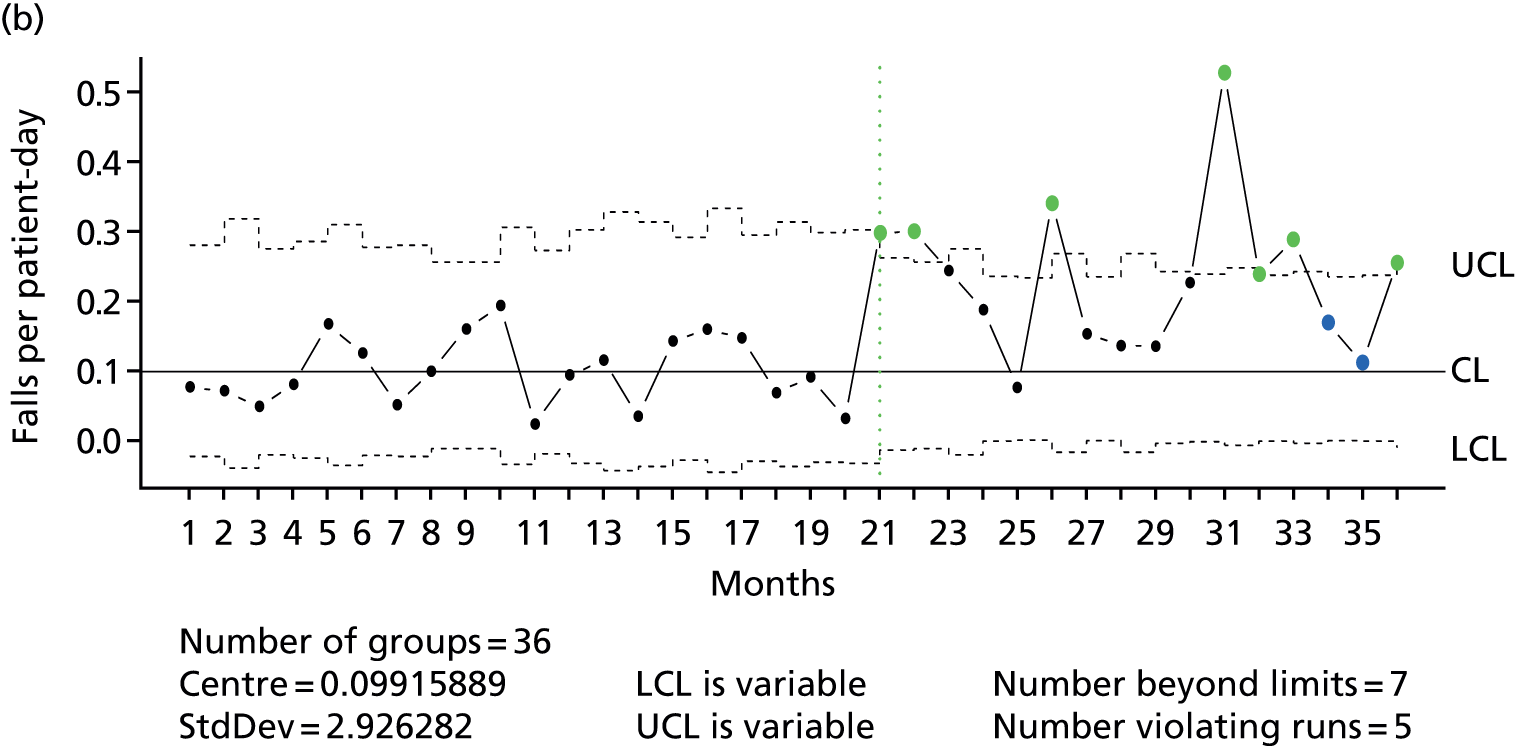
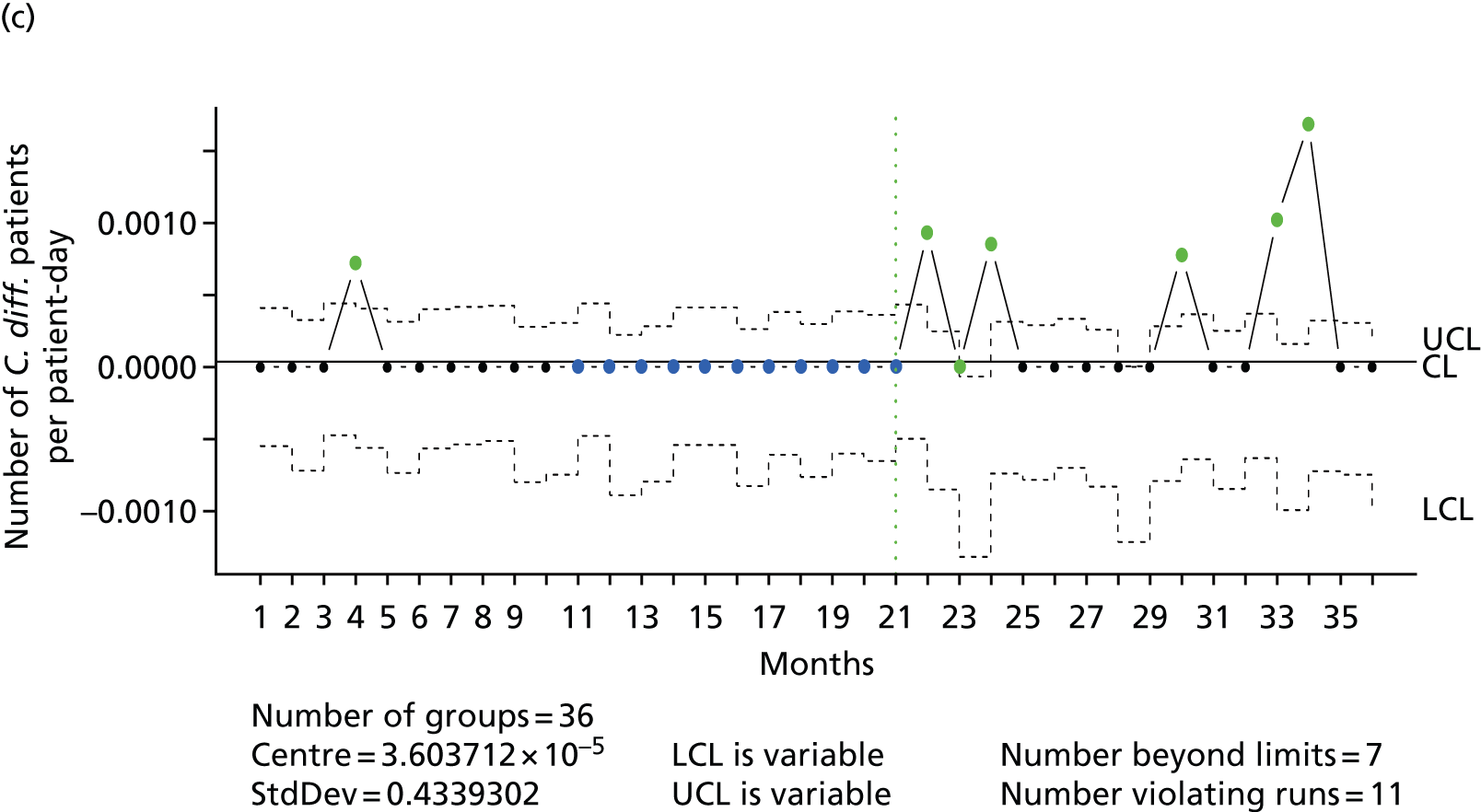
FIGURE 26.
Older people’s ward at Tunbridge Wells: case mix – (a) LOS and (b) HRG codes.
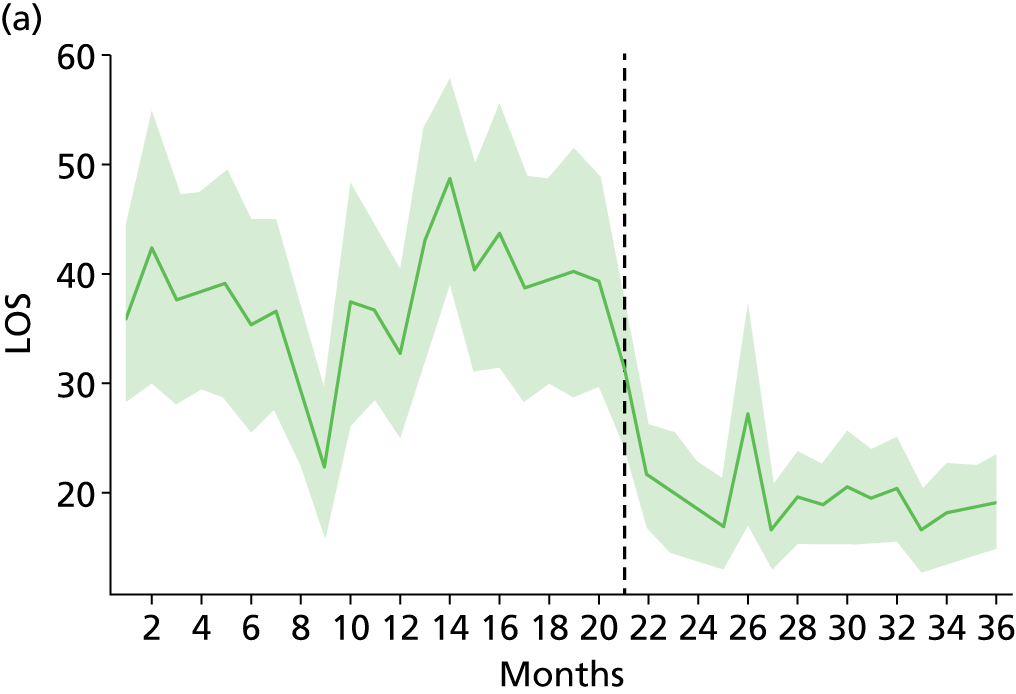

FIGURE 27.
Acute assessment unit at Tunbridge Wells Hospital: u-chart with CF expansion – (a) falls and (b) medication errors. CL, centre line; LCL, lower control limit; StdDev, standard deviation; UCL, upper control limit.
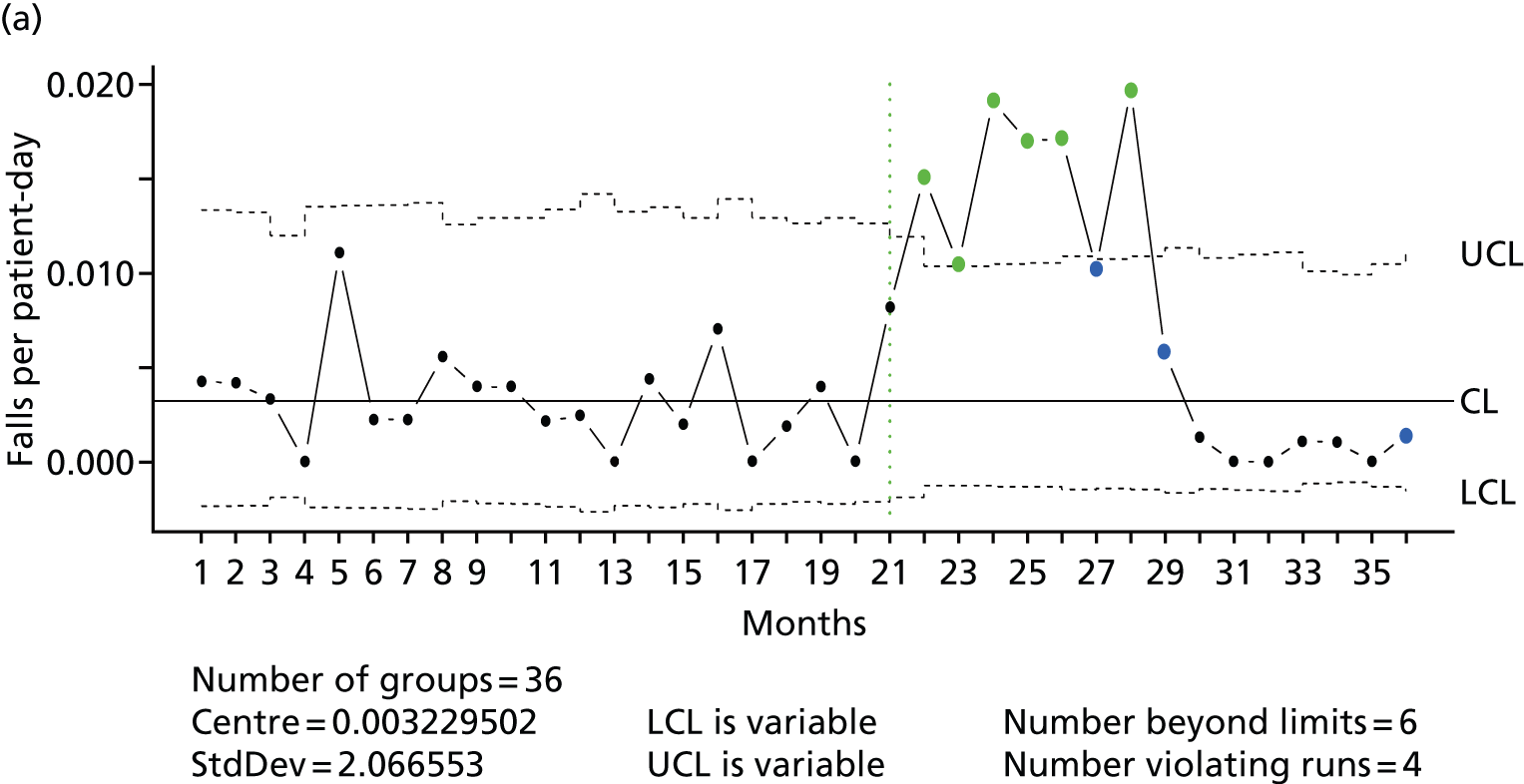
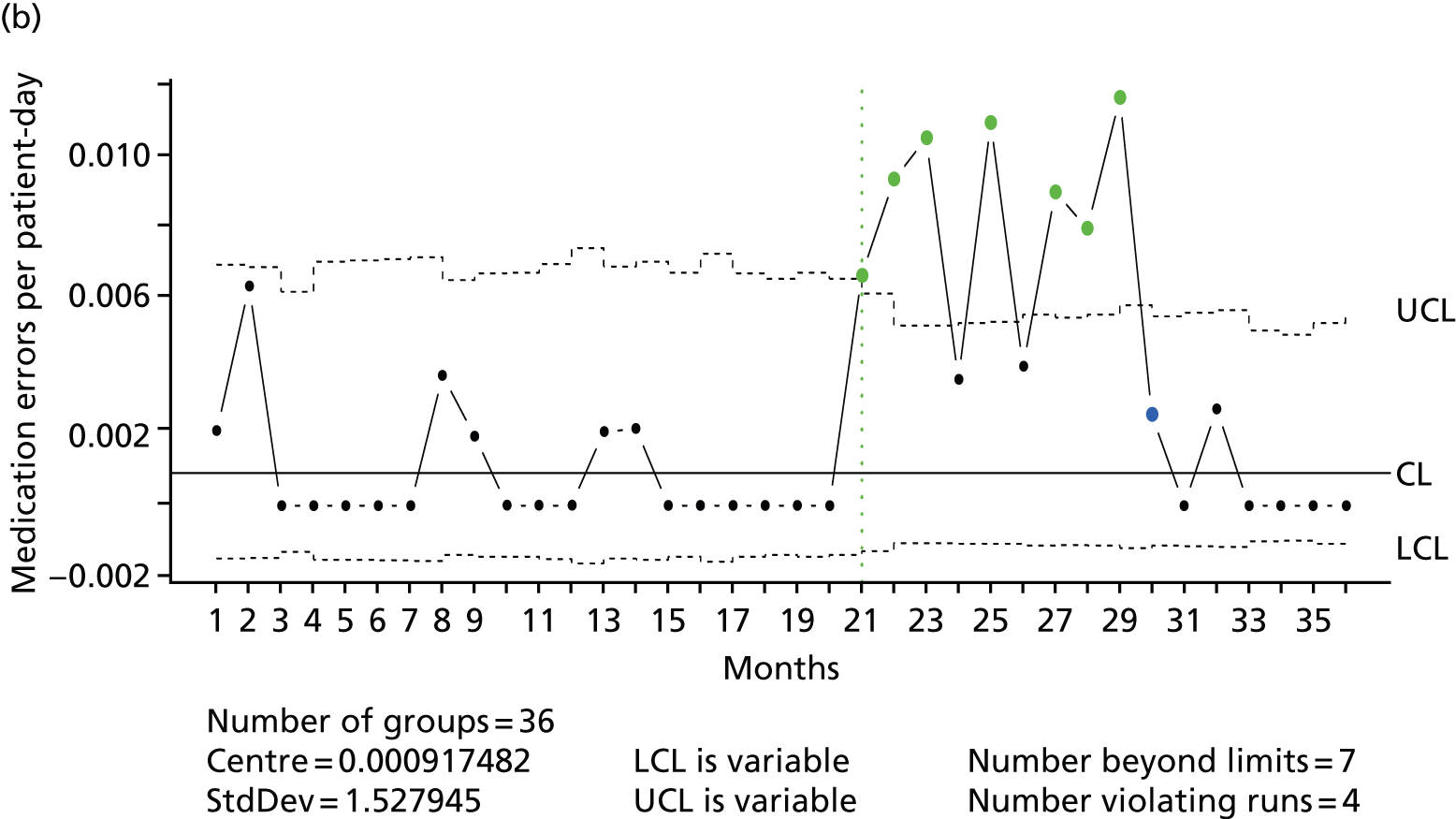
FIGURE 28.
Acute assessment unit at Tunbridge Wells Hospital: case mix – (a) LOS and (b) HRG codes.

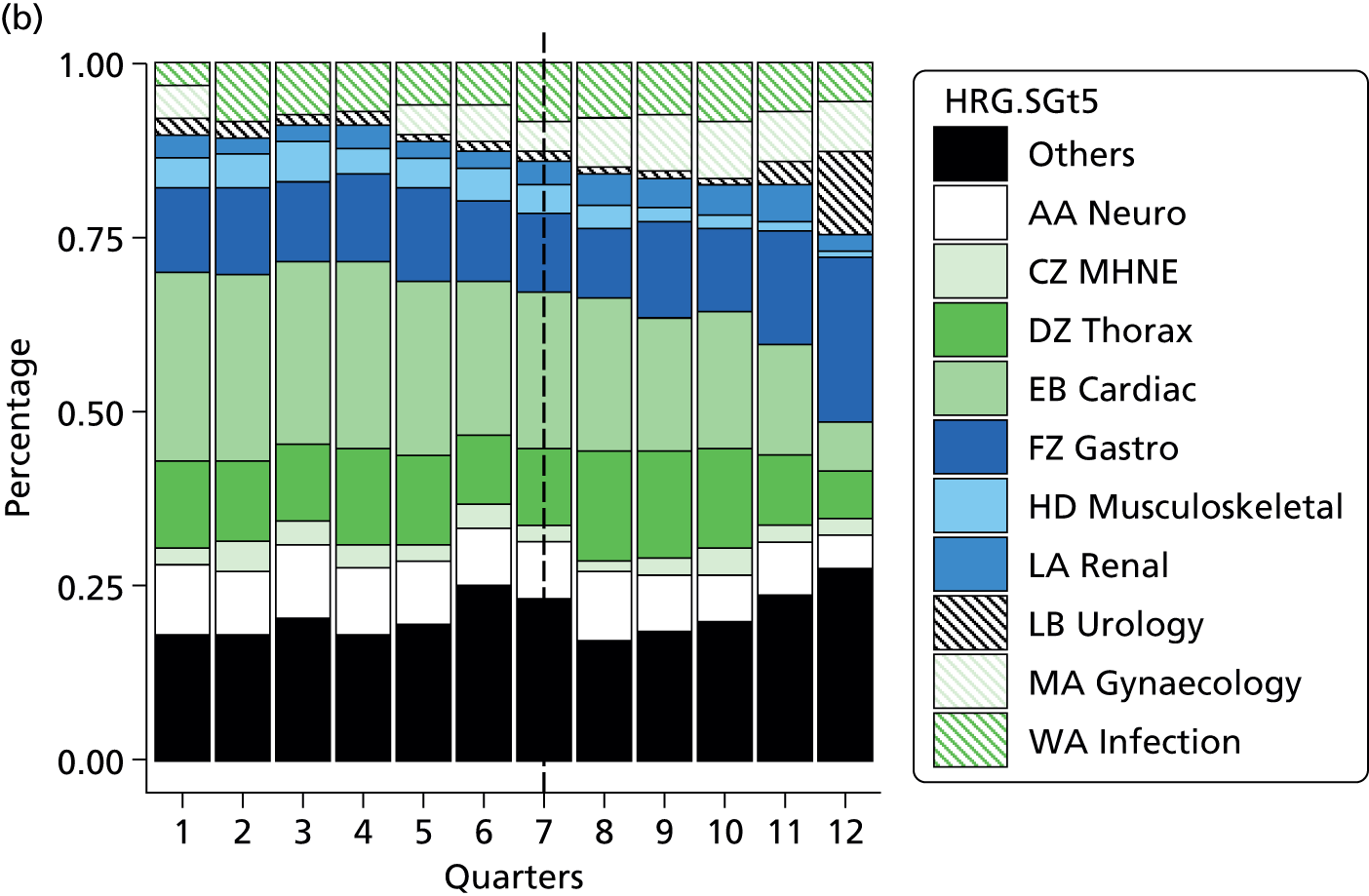
Figures 25 and 26 show a pronounced increase in fall, pressure ulcer and C. diff. rates at the older people’s ward at Tunbridge Wells Hospital that occurred after the move to single rooms. Two criteria for special-cause variation are met: overall 17 measurement points above the upper control limits (indicated in blue) and more than seven consecutive points above the centre line (indicated in green). However, the case mix of this ward changed substantially in the same time period: the LOS decreased from 37 to 20 days and the proportion of orthopaedic trauma patients (orthopaedics/trauma HRG subgroup) increased from 4.6% to 24.8%, which, therefore, does not allow us to attribute the changes in falls and pressure ulcers rates to single room accommodation (for additional case-mix data see Appendix 21).
In the acute assessment unit, falls and medication errors at Tunbridge Wells Hospital were increased but returned after 7–9 months to the same levels as before the move (see Figures 27 and 28). In the same time period, LOS increased from 1.2 to 1.4 days and some changes in case mix (e.g. a reduction of the cardiac HRG subgroup by 7%) could be observed. Because the change in adverse events is not sustained, it is unlikely that the change in case mix is the sole cause (for additional case-mix data see Appendix 21). Therefore, this change might be attributed to the move to single rooms.
Special-cause variation at new build with mixed accommodation comparator site
Although data from the case study wards at Tunbridge Wells Hospital did not show a clear consistent single room effect, the new build with mixed accommodation comparator site provides another opportunity to explore single rooms (Figures 29–32). In particular, the temporary increase in falls and medication errors on the AAU is a possible (temporary) single room effect, but might simply be associated with general disruption associated with a move to a new environment. Overall, 15 24- to 36-month time series across all wards and outcomes were available from the new build mixed accommodation control site. Whereas in the AAU at Tunbridge Wells Hospital we saw a temporary increase of medication errors and falls following the move, no such special-cause variation could be identified in any ward in the new build mixed accommodation comparator site (see Figures 31 and 32). Although there were special-cause variation events visible, these were either single time points below or above the control limits or violating runs (seven consecutive runs below/above the centre line) not synchronous to the move. These were therefore discarded as potentially attributable to a move or to an increase in the proportion of single rooms.
FIGURE 29.
Older people’s ward at new-build mixed accommodation control site: u-chart with CF expansion – (a) falls and (b) pressure ulcers. CL, centre line; LCL, lower control limit; StdDev, standard deviation; UCL, upper control limit.
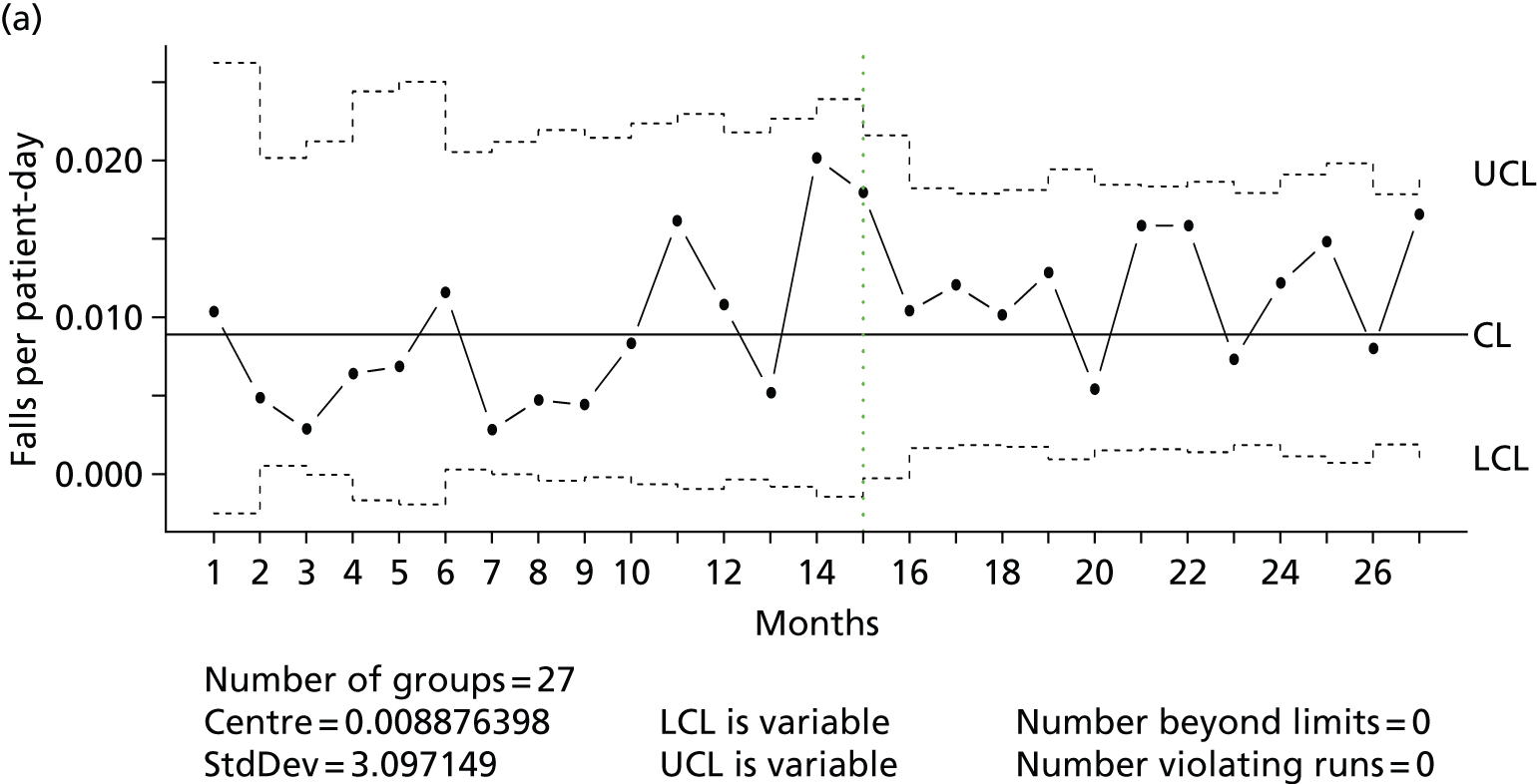
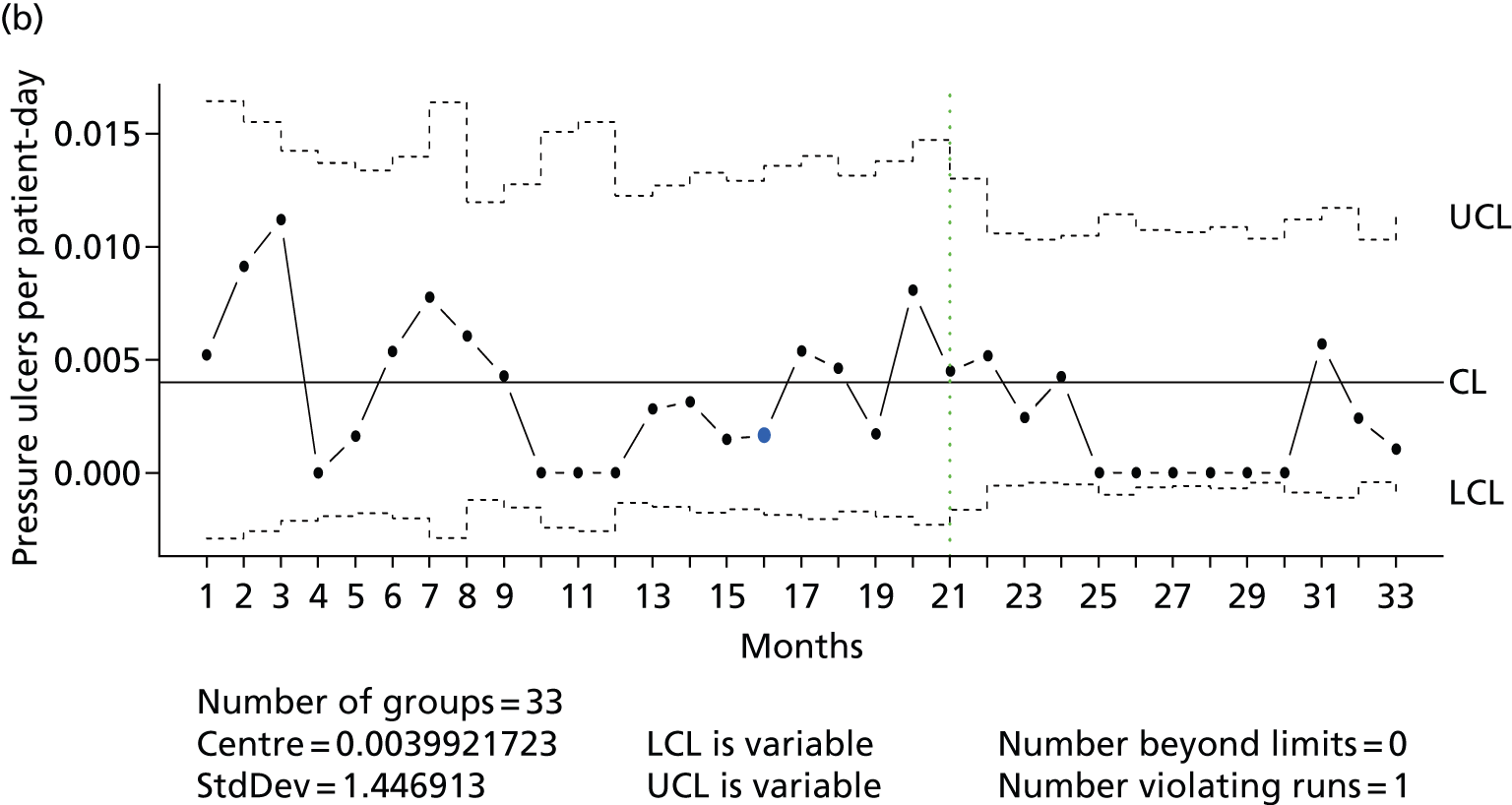
FIGURE 30.
Older people’s ward at new-build mixed accommodation control site: case-mix – (a) LOS and (b) HRG codes.
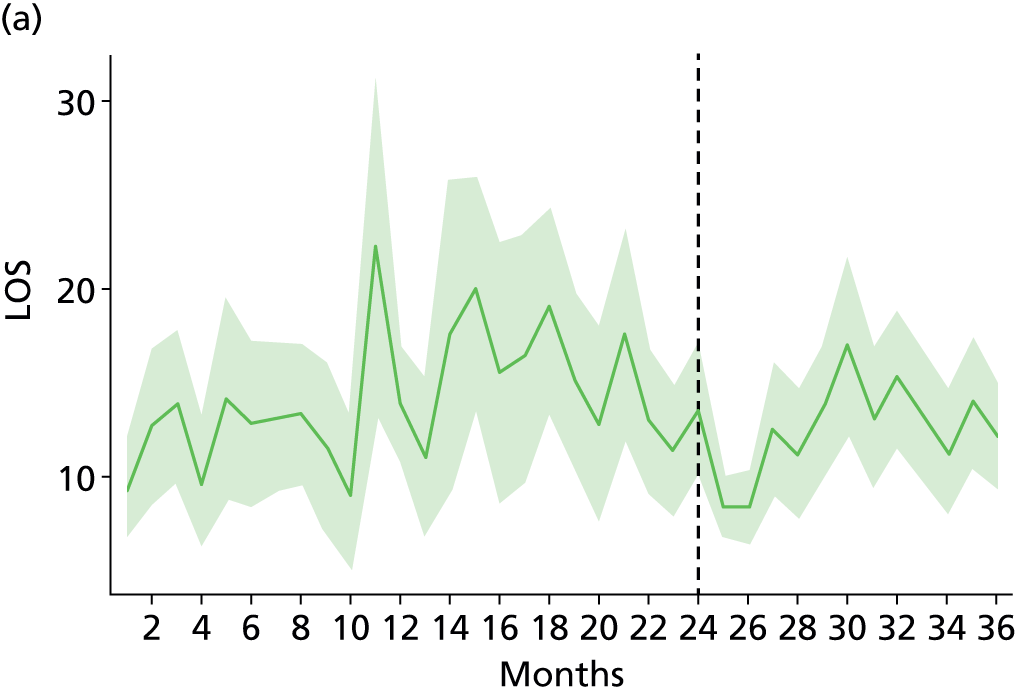
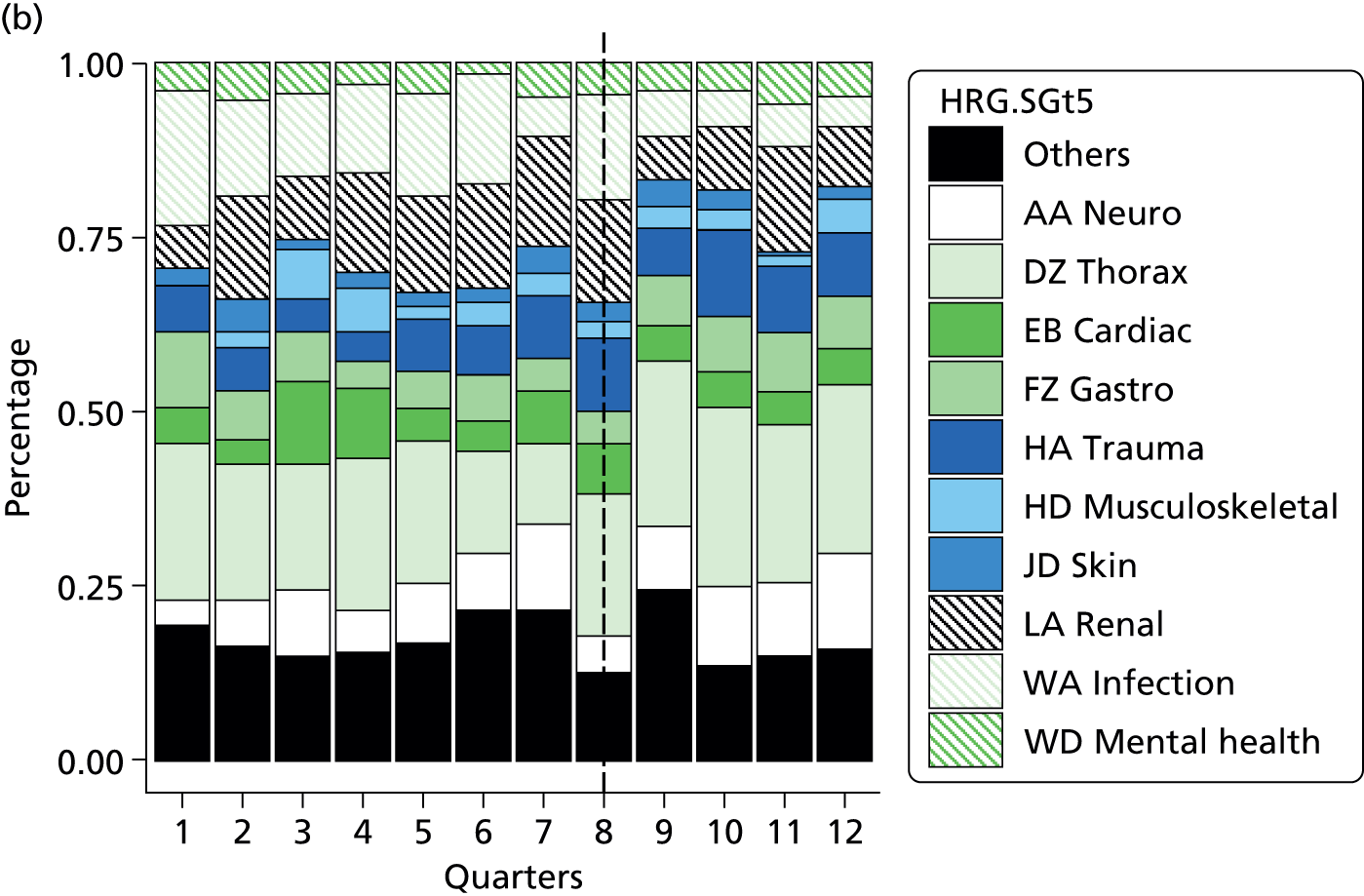
FIGURE 31.
Acute assessment unit at new-build mixed accommodation control site: u-chart with CF expansion – (a) falls and (b) medication errors. CL, centre line; LCL, lower control limit; StdDev, standard deviation; UCL, upper control limit.

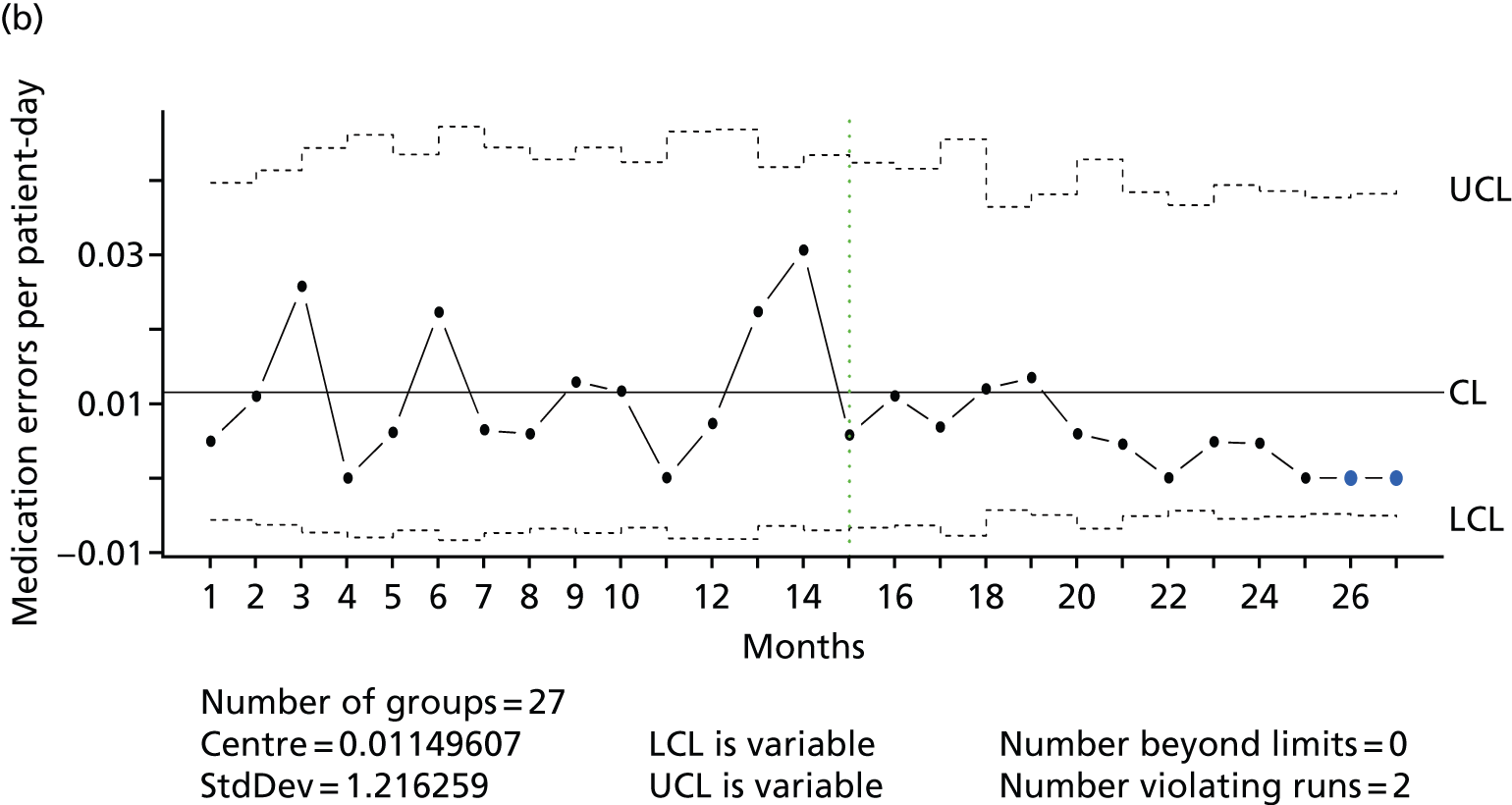
FIGURE 32.
Acute assessment unit at new-build mixed accommodation control site: case-mix – (a) LOS and (b) HRG codes. MHNE, mouth, head, neck and ears.
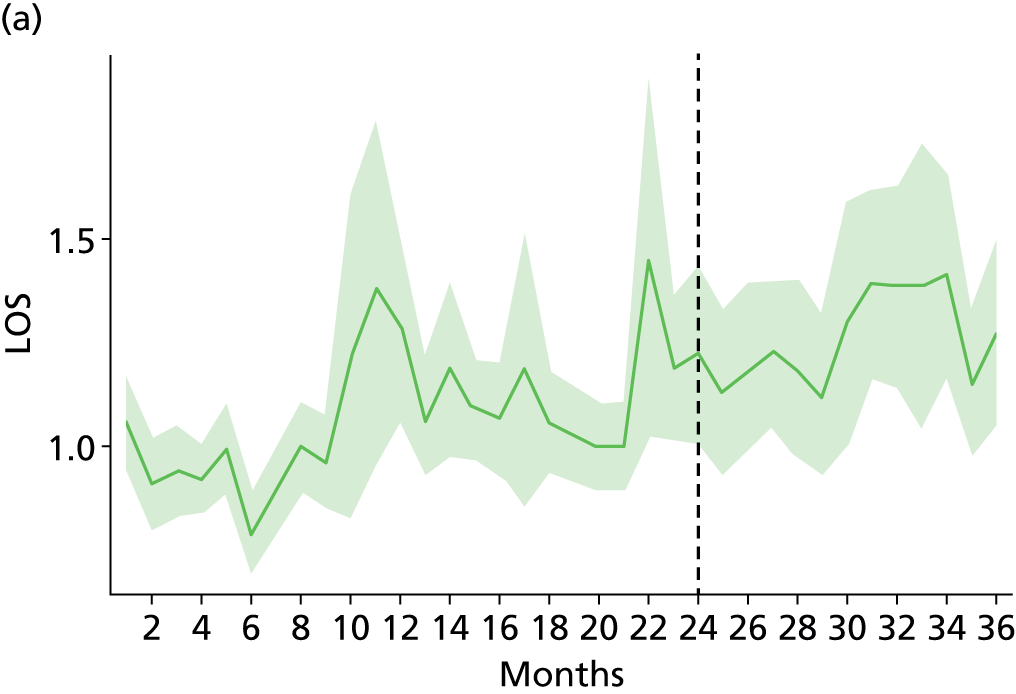

Special-cause variation at steady state comparator site
Overall, 12 36-month time series across the three wards for fall, pressure ulcer, MRSA and C. diff. rates were available from the steady state control site. Various special-cause variations were present at the older people’s ward (Figures 33 and 34) and the AAU at the steady state control site (Figures 35 and 36). For example, the fall rate on the older people’s ward declined while the pressure ulcer rate at the AAU increased, indicating in both cases that the patient population changed to some extent; however, other factors might have played a role too.
FIGURE 33.
Older people’s ward at steady state control site: u-chart with CF expansion – (a) falls and (b) pressure ulcers. CL, centre line; LCL, lower control limit; StdDev, standard deviation; UCL, upper control limit.
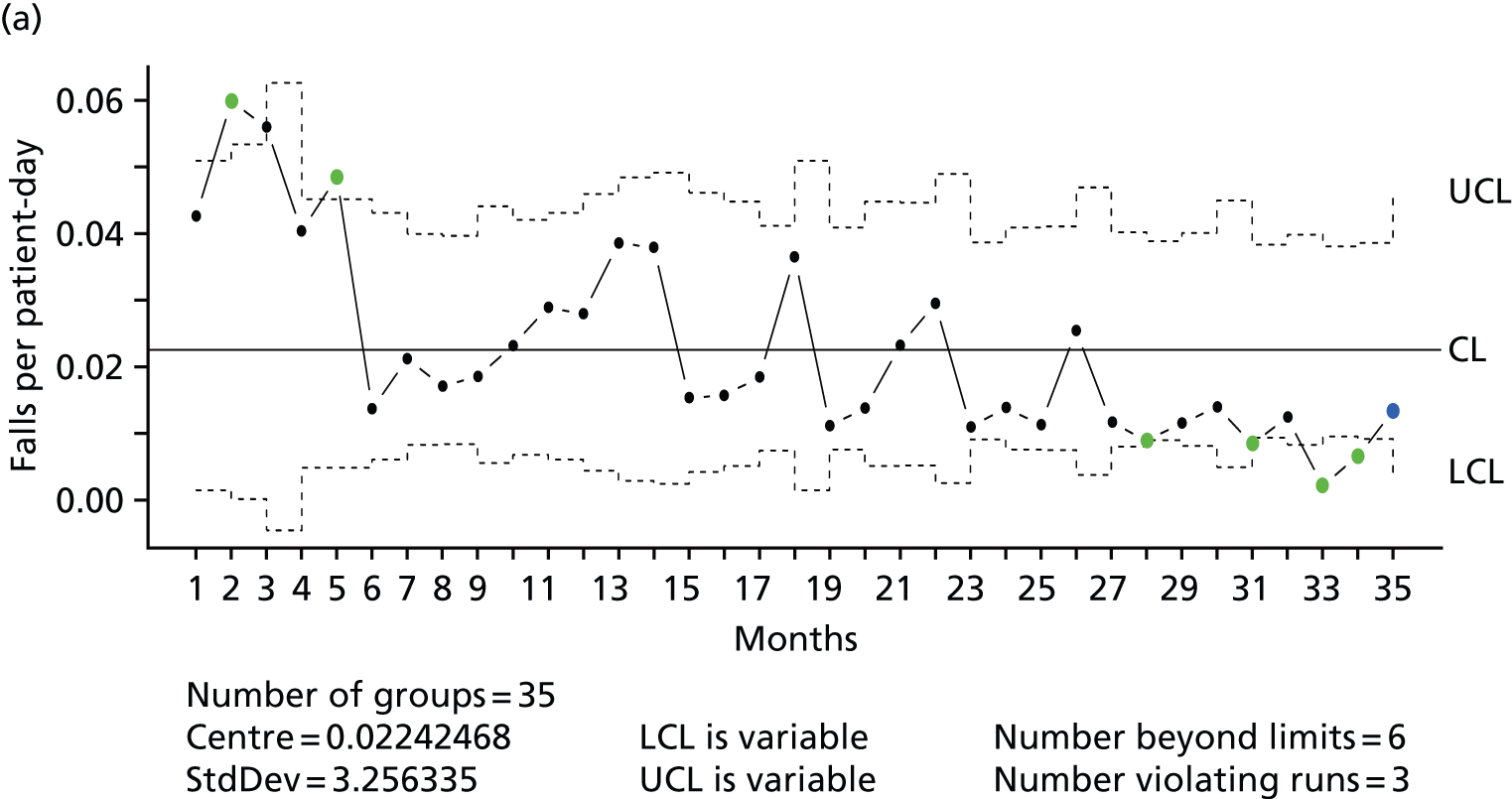
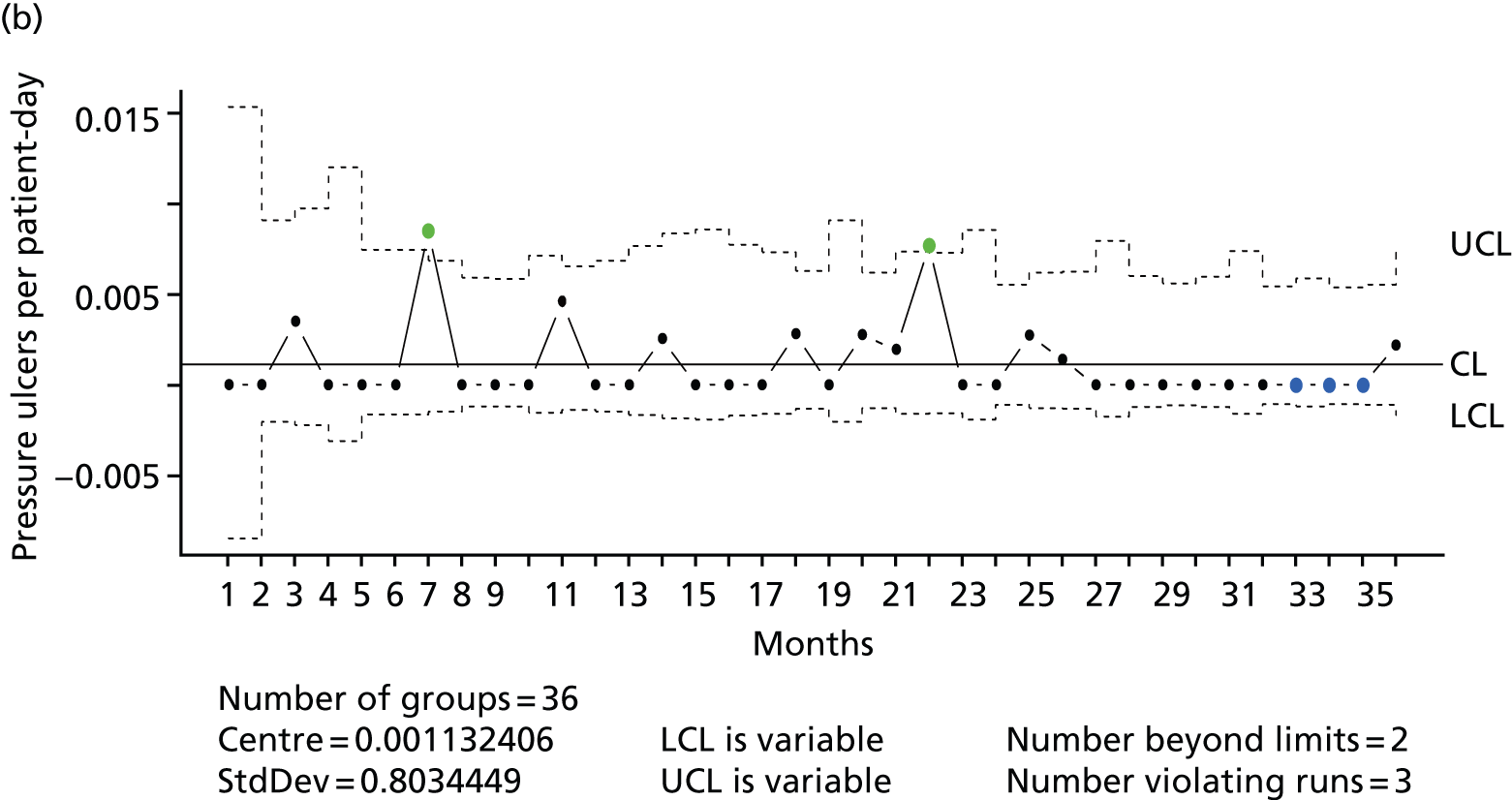
FIGURE 34.
Older people’s ward at steady state control site: case mix – (a) LOS and (b) ICD-10 codes. HS, health services.
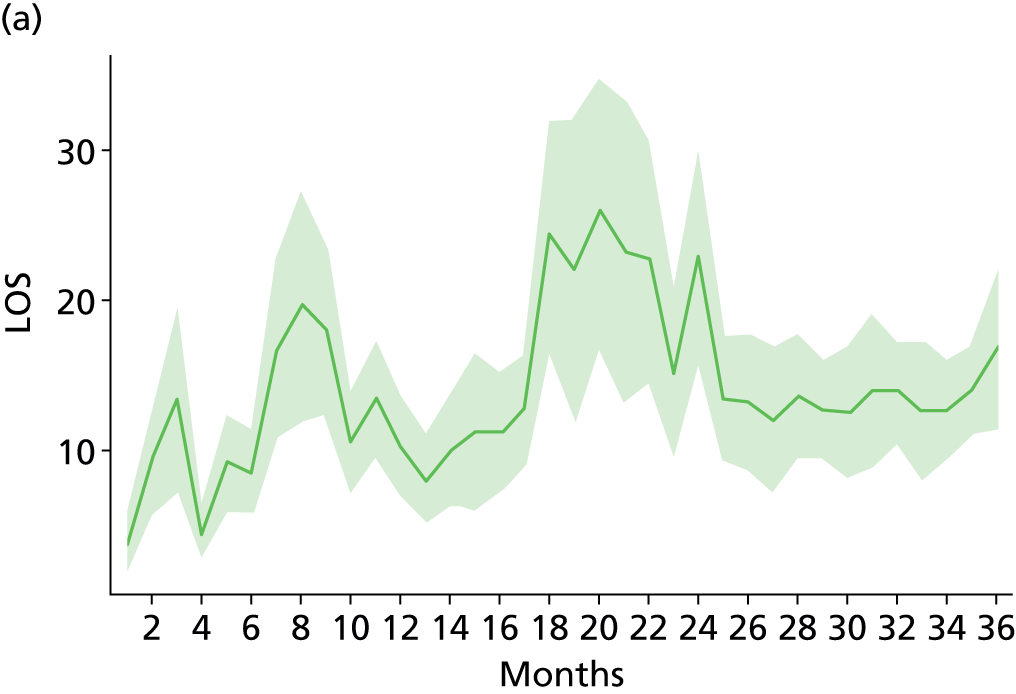

FIGURE 35.
Acute assessment unit at steady state control site: u-chart with CF expansion – (a) falls and (b) medication errors. CL, centre line; LCL, lower control limit; StdDev, standard deviation; UCL, upper control limit.

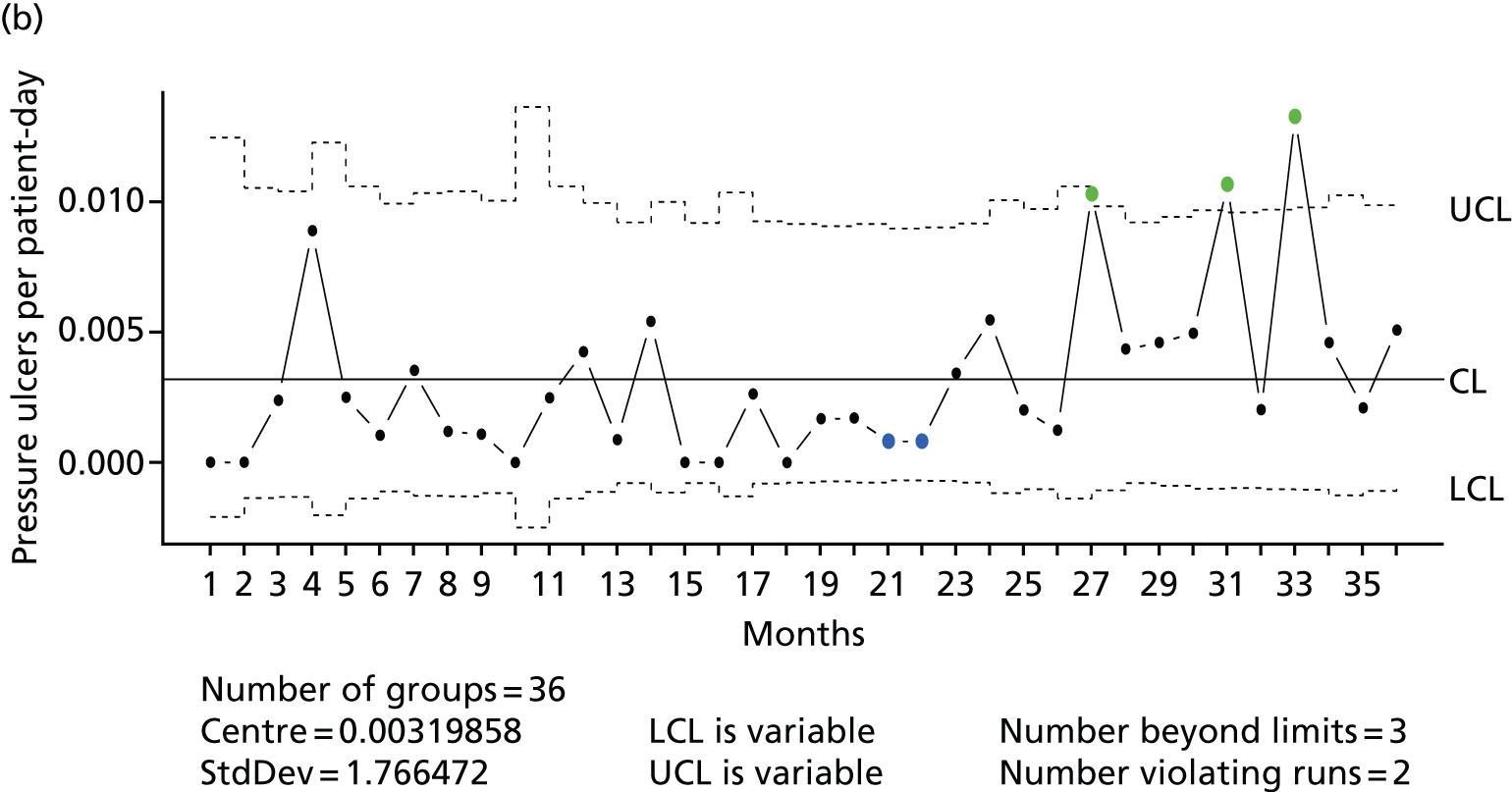
FIGURE 36.
Acute assessment unit at steady state control site: case mix – (a) LOS and (b) ICD-10 codes. HS, health services.
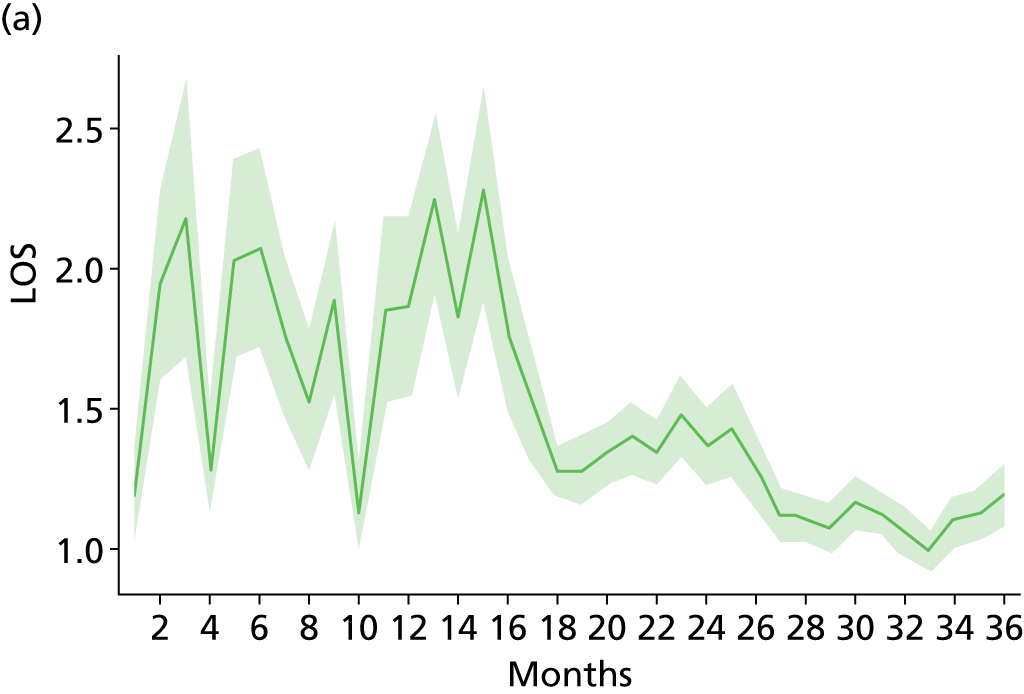
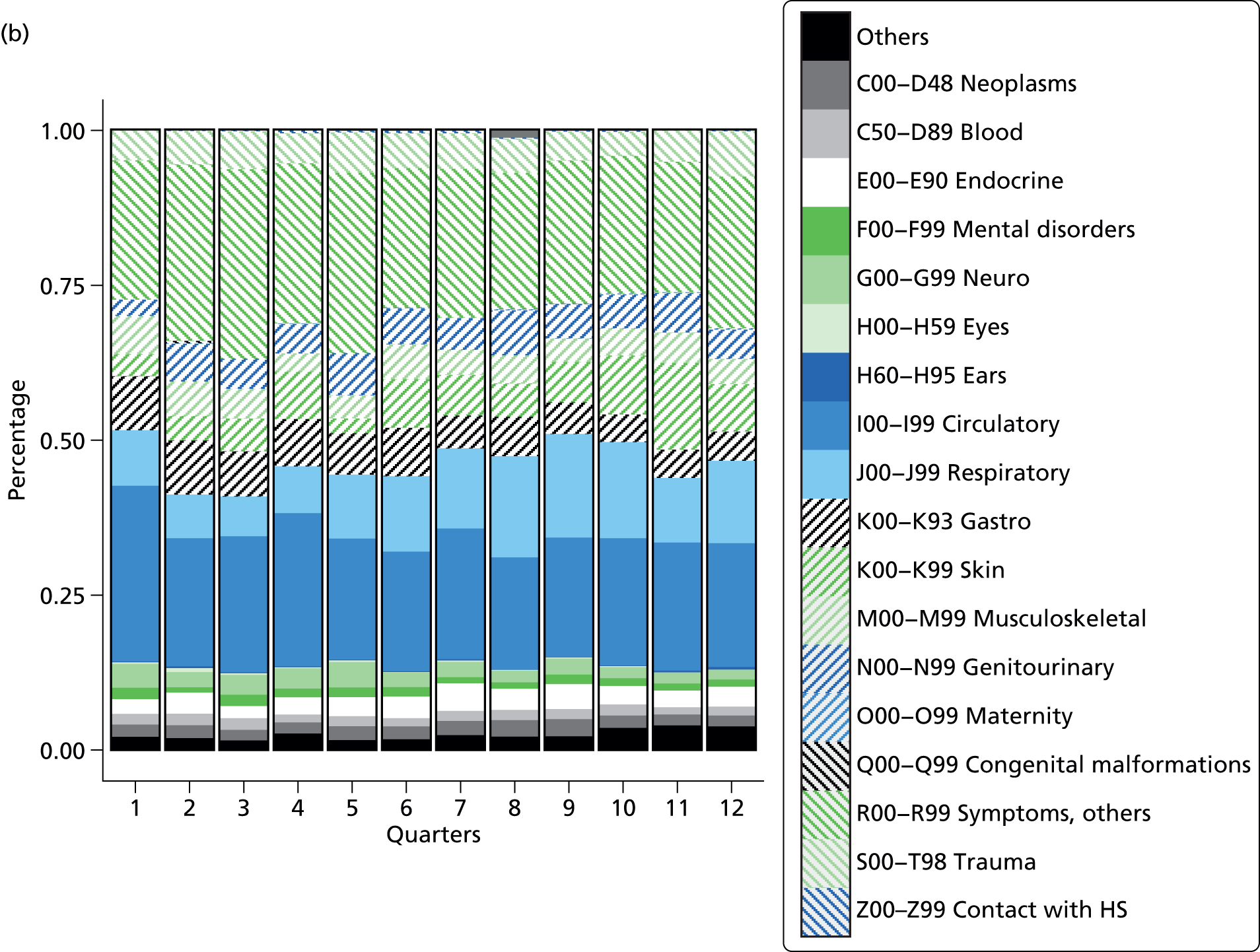
Trust-level fall trend
Staff at Tunbridge Wells Hospital reported increased fall rates after the move. Triggered by this and the evidence from the older people’s ward and AAU, we also analysed the overall fall rate for the entire trust, including data from the old Kent and Sussex Hospital before the move, Tunbridge Wells after the move and the old hospital in Maidstone.
From April 2011 to September 2013, falls in the trust increased from 4.74 to 7.84 falls per 1000 bed-days, which represents an increase of 65% (Figure 37). To assess changes in the underlying risk of the trust population, we took the percentage of patients with an increased fall risk as simple measure of fall risk. We defined patients with an increased risk as patients (1) having one of the Charlson comorbidity diagnoses or (2) having a diagnosis that specifically indicates a high risk of falls or (3) over the age of 70 years (see Appendix 22 for more details). In the time period from April 2011 to December 2012 (which is the overlap of the planned study period and the trust-level data that were available) the fall risk increased in close proportion to the fall rate (see Figure 37). The correlation between the fall risk and the fall rate is strongly positively associated (r = 0.68). Thus, although there has been a clear sustained increase in the rate of falls, it is not possible to attribute this clearly to single rooms per se given the overall increase of patients at risk of falls.
FIGURE 37.
Standardised fall rate and percentage of patients with increased fall risk. Lines are based on LOcal regrESSions (LOESS). Black dashed line represents the time of the move. Grey shading represents the 95% CI area.
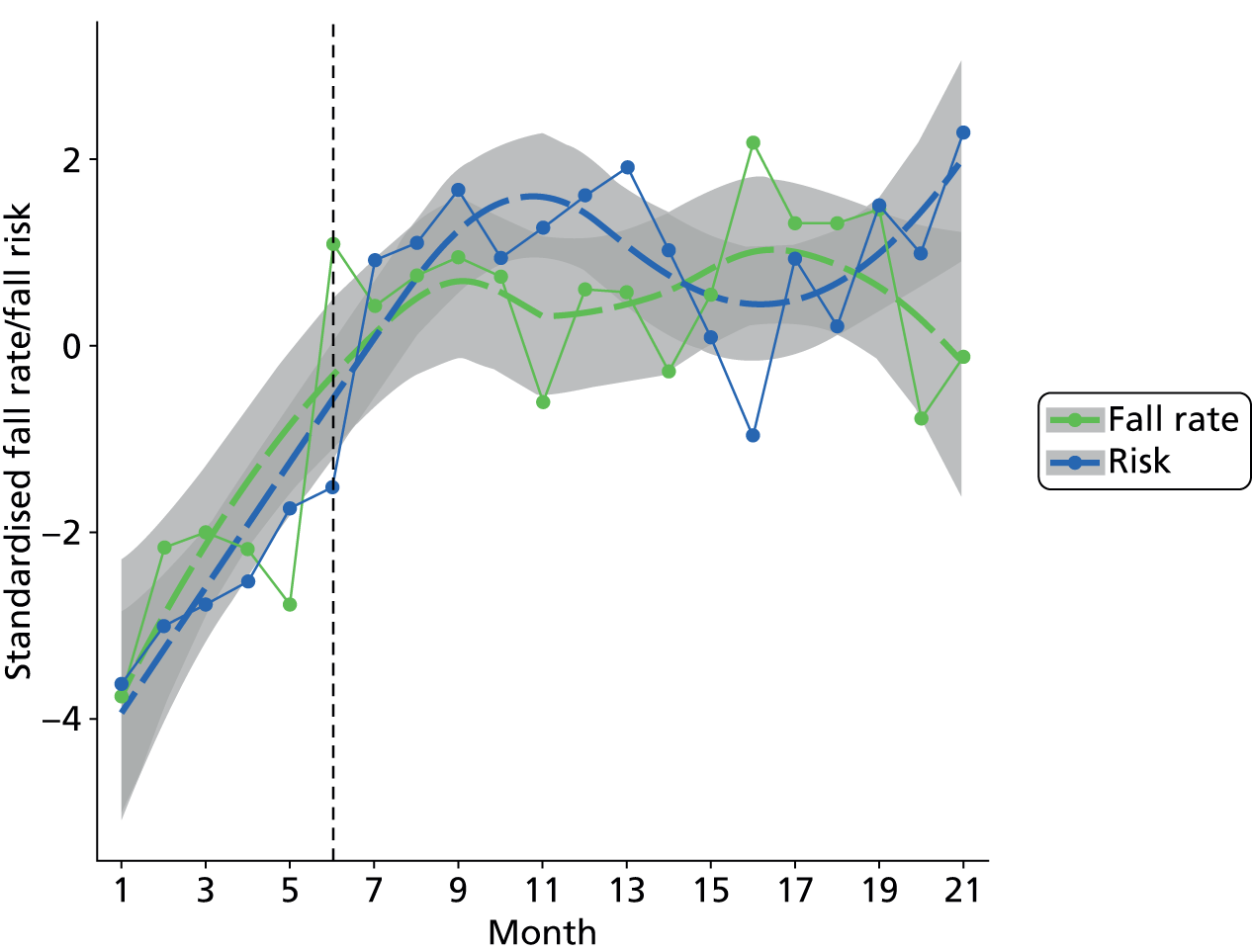
National infection trends
Infection rates are the safety outcomes which have gained the most attention in empirical research on the effect of single rooms. This study has 18 time series of infection rates (MRSA and C. diff. for each study ward). Although 18 time series were available, nine of these referred to MRSA, which had a very low incidence at all sites. For example, there was only one documented MRSA case at Tunbridge Wells Hospital on the three wards over 36 months. Although the incidence of C. diff. was higher, in comparison with MRSA it was still low. Two (AAU at Tunbridge Wells Hospital and the surgical ward at the steady state control site) of the nine time series had fewer than five cases, which did not allow any further scrutiny. Of the remaining seven time series, six showed a reduction in C. diff. rates (one at Tunbridge Wells Hospital, three at the mixed accommodation site and two at the steady state control site). Only one did show an increase (older people’s ward at the single room site; see Figures 25 and 26). Given the low incident rates at all sites, the research team decided to investigate how the national trends for MRSA and C. diff. have developed in the investigation period from 2010 to 2012.
The mandatory reporting for Public Health England includes MRSA bacteraemia and C. diff. and data are published regularly. Figure 38 shows the mean standardised quarterly MRSA rate. MRSA infections decreased from 279 cases in the first quarter of 2010 to 92 in the fourth quarter of 2012. This trend is also visible for Tunbridge Wells Hospital. Trust-level data for C. diff. are not publicly reported, but the overall national trend is similar: the trust-apportioned number of infections decreased from 3489 (Q1, 2010) to 1525 (Q4, 2012), which represents a reduction of 56% in the 3-year period.
FIGURE 38.
Quarterly standardised MRSA counts for NHS England (National) and Maidstone and Tunbridge Wells (M/TW). Lines are based on LOcal regrESSions (LOESS). Black dashed line represents the time of the move. Grey shading represents the 95% CI area.

Summary
Assuming a dose–response relationship, a single room effect would be more pronounced at the 100% single room site at Tunbridge Wells Hospital and to a lesser extent at the mixed accommodation site. The planned comparator analysis included 30 time series (three wards and five outcomes at the single room site and the mixed accommodation site) where the effect of single rooms could have been observed. Ultimately, five time series showed a special-cause variation following the move. Three time series showing an increase of falls, pressure ulcers and C. diff. infections at the older people’s ward at Tunbridge Wells Hospital (see Figures 25 and 26) could be related to a change in case mix rather than moving to single rooms and were not confirmed at the mixed accommodation site. The only time series with special-cause variation synchronous with the move without substantial case mix changes was at the AAU at Tunbridge Wells Hospital, with increases of falls and medication errors (see Figures 27 and 28). Although this could indicate an effect of single room accommodation, the increase was only temporary, and fall and medication error rates decreased to previous levels 6–9 months after the move. This peak was not confirmed at the new build mixed accommodation site. The temporary nature of this increase and the lack of confirmation at the mixed accommodation control site support an alternative explanation, which would describe this increase of safety events as move related, but probably more related to disruptions to the work flow than to single rooms. This disruption seems most likely to be associated with a move to a new environment and the need to adjust work patterns following the move. Some of the disruptions and need for adaptation may be associated with the environment (single rooms); however, increases were temporary and no similar pattern was observed in the control wards which also experienced a move and an increase in single beds, which suggests that it is not inevitable and/or that increased risk is not intrinsically associated with single rooms. It may be avoidable and it certainly seems that, given time, adaptations can be made to reduce it. Although this conclusion must be interpreted in the light of an overall increase in falls at the trust level, the strong correlation between changes in this rate and change in patient-level risk factors associated with service reconfigurations makes it hard to conclude that single room accommodation is the cause.
Conclusions
The results fit into the wider literature, which showed a link between single bed accommodation and reduced infection rates in intensive care populations, but not in general medical or surgical populations. Although this is one of the few studies investigating single room accommodation and safety events, we could not find a consistent pattern for any of the safety events. For all special-cause variations that coincided with the move to single rooms, we found plausible alternative explanations (e.g. case mix) or disruption through the reorganisation of the services after the move.
Chapter 9 Cost impact of a single room hospital design
Introduction
In this chapter we explore the cost impact of a single room hospital design using the available data from the comparator study. As well as collecting available data on costs and activity, we consulted a range of experts from the construction and facilities management sectors, and hospital operation and management, to seek views on the relative impact of different hospital designs on costs and resource use. These experts participated in a group and one-to-one telephone interviews and provided opinion on the emerging research findings (see Chapter 2 and Appendices 1 and 15 for more details).
We focus especially on costs in relation to construction and facilities management, operational costs such as cleaning and catering, and nurse staffing costs. For construction and facilities management costs we consider how different percentages of single rooms (50% and 100%) influence costs. Please note that all costs are as close to accurate as possible, but some are estimates. Uncertainty was dealt with in the model through sensitivity testing using the range of reported figures. We also consider the impact of all single room accommodation on costs associated with falls, LOS and infection control. However, it was not possible to perform a full analysis of the costs of changes to falls, medication errors and hospital-acquired infections (see Chapter 8) because of insufficient data on these events. As will be shown, it was also generally impossible to attribute observed differences to a ‘single room effect’.
Building and maintenance costs
There is very limited research, little consensus and consequently a degree of uncertainty over the comparative construction cost of all single room hospitals versus hospitals with a mix of multibedded wards and single rooms (see Chapter 8). One estimate, based on a hypothetical scheme in an NHS trust, suggested an additional space cost per bed per day of 5.14% for an all single room hospital compared with one with 50% single rooms82 (see Appendix 1). However, our expert interviewees felt that this extra cost would probably be rather less than 5% compared with construction costs across the entire facility. The reason for the hypothesised extra cost is that a design based on all single rooms requires more floor area in the nursing areas than a multibedded room design, and therefore additional construction costs. Other hospital floor areas (theatres, imaging, diagnostics, outpatients/consulting rooms and support utilities) would broadly be the same as for any other recent build, as would the corridors and non-core ancillaries such as car parking.
Refurbishment and maintenance costs are partly influenced by the rate of patient turnover and rate of bed occupancy. There is huge variability in refurbishment/renewal cycles, ranging from redecoration every 3–5 years to renewal of furniture every 8–10 years, flooring every 15–20 years and lighting every 25–30 years. There is not thought to be a significant difference in maintenance costs per square metre or per bed space between single and multiple occupancy designs. However, it would be reasonable to assume that any additional floor area needed for a single room design requires greater total annual running costs such as energy, and periodic refurbishment and renewal capital costs.
Construction and facilities management costs at Tunbridge Wells Hospital
Over the life cycle of a hospital, there is typically a 1 : 1 : 20 ratio of capital expenditure to estates-related operational expenditure to medical costs in discounted cash flow terms; that is, if it costs £100M to build a hospital, it will cost about the same in discounted total maintenance costs through its lifespan, but 20 times that in costs relating to the provision of medical care. 119–123 This means that any overall (small) increase in initial capital expenditure or annual estates-related operational expenditure would be negligible compared with the total life-cycle running costs of a hospital.
To get a feel for the significance of the identifiable incremental costs of the 100% single room design of Tunbridge Wells Hospital, we modelled the cash flows over the full assessed project life of 60 years (using a 3% discount rate), of which around half falls within the scheme’s PFI contract. This review was based largely on data in the original outline business case for the new hospital. While the absolute figures date back to 2004, they nevertheless provide an order of magnitude estimate for the impact, given that the ratios between the various parameters will not have changed significantly since then. This analysis shows 1 : 1 : 12 ratios of capital expenditure (including major life-cycle work) to estates-related operating costs (building running costs, equipment upgrades) to medical costs.
In net worth terms (i.e. discounted cash flow, net present value at 3%), were the capital expenditure and operating cost to have been decreased by building a conventional 50% single room facility and assuming (conservatively) 5% and 10% reductions, the full life-cycle costs of the site would have reduced by only 0.7% and 1.4% of the original respectively.
However, given that, in the case of Tunbridge Wells Hospital, the construction company contends that the higher proportion of single rooms did not lead to any increased floor area, we can assume that capital expenditure and estates-related operational expenditure (i.e. ‘hard facilities management’) are scarcely higher, if at all, than in a 50% single room hospital.
Cleaning and ‘hotel’ costs
Housekeeping costs vary from hospital to hospital according to space, utility costs, staff capacity and staff cost. The literature suggests cleaning costs are higher in single room hospitals because of increased numbers of bathrooms, doors and pieces of furniture, and greater floor area. 61 This was confirmed by our expert interviews and the Tunbridge Wells Hospital administrative data. However, the relationship between cleaning costs and design can be hard to interpret. A single room might be much easier to clean because the space is wider and there are fewer obstacles than in multibedded rooms, but any time savings are offset by the additional time required to clean the larger number of bathrooms. In a multibedded room design there are fewer bathrooms but larger common areas to clean.
Generally, our experts felt that the time required for cleaning a single room design hospital was longer. This was confirmed by the general manager of facilities at Maidstone and Tunbridge Wells NHS Trust, who suggested that for general cleaning it takes around 10 minutes to clean a bed space in a multibedded design and around 25 minutes for a single room.
According to administrative data from Maidstone and Tunbridge Wells NHS Trust (2012–13), in a 100% single room hospital the domestic cleaning labour cost per room per day is £7.88 for a standard clean, including single bathrooms and associated areas. In a multibedded design, the domestic cleaning labour cost per bed area per day is £5.44, including the allocated costs for bathrooms and common areas.
In the model below we assume the same area in square metres to build three different models of hospital: one with 100% single rooms; one with 50% single room design and 50% multibedded rooms; and one with multibedded accommodation only. There is a standard number of rooms that could be created for a given floor area depending on the room type and mix, with differences in the total areas among the three designs due to differences in the corridor space required (Table 58). Assuming that each ward has 28 patients:
-
in a 100% single room hospital: 28 single rooms with one assisted bathroom per room
-
in a 50% single room hospital: 14 single rooms (12 semiambulant en suite and two disabled en suite), three rooms with four beds with three disabled en suite bathroom and three with water closet (WC), one room with two beds with a semiambulant en suite and one assisted bathroom
-
in a 100% multibedded room hospital: seven rooms with four beds, seven disabled en-suite disabled bathrooms, seven WC and one assisted bathroom.
| Room type | 100% singles | 50% single/50% multibedded | 100% multibedded | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Number of rooms | Area per room (m2) | Total area (m2) | Number of rooms | Area per room (m2) | Total area (m2) | Number of rooms | Area per room (m2) | Total area (m2) | |
| Single room | 28 | 19 | 532 | 14 | 19 | 266 | |||
| Semiambulant en suite | 26 | 4.5 | 117 | 12 | 4.5 | 54 | |||
| Disabled en suite | 2 | 6.5 | 13 | 2 | 6.5 | 13 | |||
| Four-bed bay | 3 | 64 | 192 | 7 | 64 | 448 | |||
| Disabled en suite | 3 | 6.5 | 19.5 | 7 | 6.5 | 45.5 | |||
| WC-only en suite | 3 | 2.5 | 7.5 | 7 | 2.5 | 17.5 | |||
| Two-bed bay | 1 | 36 | 36 | ||||||
| Semiambulant en suite | 1 | 4.5 | 4.5 | ||||||
| Assisted bathroom | 1 | 15 | 15 | 1 | 15 | 15 | 1 | 15 | 15 |
| Total area (m2) | 677 | 607.5 | 526 | ||||||
Applying the cleaning cost to each type of room we can see the relative difference in costs of each configuration (Table 59). The total cost of cleaning a ward in a 100% single room hospital would be £228.52, compared with £149.40 in a 50% single room hospital and £160.20 in a hospital with 100% multibedded rooms. Assuming that, as in Tunbridge Wells Hospital, there are 500 bed spaces, the cost per patient per day ranges from £5.34 to £8.16. The total annual costs for cleaning a 500-bed all single room hospital are 53% higher than for a 50 : 50 mixed accommodation hospital. While this is clearly a considerably higher annual cost for a trust, spread over the lifetime of a hospital in relation to medical costs, which may be 20 times higher, this would be marginal.
| Room type | 100% singles | 50% single/50% multibedded | 100% multibedded | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Number of rooms | Unit cost (£) | Total cost (£) | Number of rooms | Unit cost (£) | Total cost (£) | Number of rooms | Unit cost (£) | Total cost (£) | |
| Single room | 28 | 7.88 | 220.64 | 14 | 7.88 | 110.32 | |||
| Semiambulant en suite | 26 | 12 | |||||||
| Disabled en suite | 2 | 2 | |||||||
| Four-bed bay | 3 | 5.44 | 20.32 | 7 | 7.88 | 152.32 | |||
| Disabled en suite | 3 | 7 | |||||||
| WC-only en suite | 3 | 7 | |||||||
| Two-bed bay | 1 | 5.44 | 10.88 | ||||||
| Semiambulant en suite | 1 | ||||||||
| Assisted bathroom | 1 | 7.88 | 7.88 | 1 | 7.88 | 7.88 | 1 | 7.88 | 7.88 |
| Total cost per ward | 228.52 | 149.40 | 160.20 | ||||||
| Cost per patient | 8.16 | 5.34 | 5.72 | ||||||
| Daily cleaning cost per 500 patients | 4080.71 | 2667.86 | 2860.71 | ||||||
| Annual cost | 1,489,200 | 973,769 | 1,044,159 | ||||||
Impact on distribution of meals to patients
Moving from multiple to single room design has implications for the way patient meals and refreshments are administered. Multibedded wards allow more patients to be served at the same time, whereas distribution of meals to rooms in the single room model potentially requires more time for distribution because of layout.
Administrative data from Tunbridge Wells Hospital show a 49% increase in the cost of preparing and serving meals after the move to the new hospital. However, according to interviewees this was largely due to a change from a central kitchen to a ward-based kitchen model, a decision taken at the planning stage and not directly related to the single room design. It is, therefore, not possible to draw any firm conclusions on the impact of single room design on catering costs in Tunbridge Wells Hospital.
Impact on staffing costs
Planned investment in nursing staff
Before the move, in November 2010, an investment of an additional £1,669,000 per year in additional nursing staff was planned (Table 60). This comprised three main components:
-
an additional number of WTE nurses, midwives and support staff required across the wards, to cope with the additional surveillance required by the single room design
-
an increase in price of WTE
-
an increment in the number of beds in a number of wards.
| Area | Previous hospital | Proposed new hospital | Difference | Previous WTE/bed | Proposed new hospital WTE/bed | Total change in WTE/bed | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beds | WTE | Cost per year (£000) | Beds | WTE | Cost per year (£000) | Beds | WTE | Cost per year (£000) | ||||
| General wards | 528 | 693.52 | 20,957 | 505 | 679.19 | 20,624 | –23 | –14.33 | –333 | 1.31 | 1.34 | 0.03 |
| Maternity | 60 | 204.73 | 8632 | 71 | 225.83 | 9381 | 11 | 21.1 | 749 | 3.41 | 3.18 | –0.23 |
| AAU Pembury | 16 | 27.81 | 902 | 30 | 48.59 | 1537 | 14 | 20.78 | 635 | 1.74 | 1.62 | –0.12 |
| A&E | 0 | 48.95 | 1796 | 0 | 56.34 | 2034 | 0 | 7.39 | 238 | |||
| Acute stroke unit | 9 | 17.54 | 580 | 8 | 21.23 | 726 | –1 | 3.69 | 146 | 1.95 | 2.65 | 0.70 |
| Arrivals and discharge | 0 | 2.58 | 79 | 0 | 3.28 | 76 | 0 | 0.7 | –3 | |||
| Coronary care unit | 6 | 15.29 | 583 | 6 | 17.14 | 603 | 0 | 1.85 | 20 | 2.55 | 2.86 | 0.31 |
| Neuro rehab ward (Kent and Sussex Hospital) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| ITU | 7 | 42.72 | 1712 | 6 | 44.86 | 1792 | –1 | 2.14 | 80 | 6.10 | 7.48 | 1.38 |
| Outpatients | 0 | 28.25 | 942 | 0 | 33.31 | 1006 | 0 | 5.06 | 64 | |||
| Other areas | 52 | 330.03 | 11,688 | 49 | 330.03 | 11,688 | –3 | 0 | 0 | 6.35 | 6.74 | 0.39 |
| Paediatrics | 75 | 120.65 | 4467 | 69 | 114.39 | 4406 | –6 | –6.26 | –61 | 1.61 | 1.66 | 0.05 |
| Gynaecology | 32 | 50.85 | 1570 | 28 | 53.31 | 1636 | –4 | 2.46 | 66 | 1.59 | 1.90 | 0.31 |
| Endoscopy | 6 | 19.83 | 550 | 12 | 20.74 | 587 | 6 | 0.91 | 37 | 3.31 | 1.73 | –1.58 |
| Pre assessment | 0 | 4.61 | 144 | 0 | 6.35 | 173 | 0 | 1.74 | 29 | |||
| Theatres | 0 | 186.57 | 6276 | 0 | 193.37 | 6279 | 0 | 6.8 | 3 | |||
| Total | 791 | 1793.93 | 60,878 | 784 | 1847.96 | 62,548 | –7 | 54.03 | 1670 | 2.27 | 2.36 | 0.09 |
The additional resources were to be allocated across the hospital according to the specific needs of wards in terms of patients’ age, acuity and severity of their illness, ward design and staff requirements. In the ITU, for example, the number of nurses per bed is generally higher than in other units because patients need extra surveillance124 and so the planned investment in staff was higher. Table 60 reflects staffing at the time of opening; there were further investments in staffing in the subsequent 3–6 months, notably in A&E and the AAU.
Overall, under the planned investment at Tunbridge Wells Hospital there was a 0.9% decrease in beds, a 3% increase in WTE staff and a 2.7% increase in total costs. There was, therefore, a slight increase in the number of WTE staff per bed. Assessing how much of the planned investment was the result of a ‘single room effect’ is, however, not possible. In some areas (maternity, paediatrics, gynaecology and endoscopy) the changes were part of an overall review of nursing levels and the general restructuring of patient pathways made possible by local reconfiguration following the construction of the new hospital. In addition, part of the planned investment (£1,143,000) is attributable to a combination of an increase in the number of nurses (extra 54 WTE staff) and an annual adjustment of nursing pay during this period. 110 It is difficult to say how much of this sum is due to pay adjustment, as it differs across nursing bands. There was also a change in the number of beds in some wards. In the AAU, for example, the number of beds increased by 14, with a total increase of 20.78 WTE comprising 9.88 WTE trained nurses and 3.45 WTE assistant support staff; the maternity ward grew by 11 beds and 21.10 WTE (see Table 60).
The cost of staff (no split between RN and HCA was available) per patient bed after the move increased in general wards by £1150 per bed per year (3% more). In the acute stroke unit, however, there was a very large increase in staff cost per bed (£26,340 or 41% more), while in the ITU the cost per bed increased by £54,071 (22%). This was because of the increased planned investment in comparatively high-cost staff in these units and the small number of beds. The ACU and the ITU are the units with the most severe and life-threatening illnesses and injuries that require constant close monitoring and support from nurses. In general in these units the ratio of nurses to beds is 1 : 1 or 1 : 2 (in other wards this can be 1 : 6 or more).
In the AAU, the planned cost of staff per bed decreased by £5148 per bed per year (9% less). This is because of an increment in the denominator – the number of beds – from 16 to 30 and, although there was a planned investment in more staff, this investment did not bring the AAU up to the same level of staff per bed as it had had before the move (Table 61).
| AAU | Total before | Total after | Difference |
|---|---|---|---|
| A&C/senior manager bank total | 0.00 | 0.12 | 0.12 |
| A&C/senior manager substantive total | 0.22 | 1.60 | 1.37 |
| A&C/senior manager staff total | 0.22 | 1.72 | 1.49 |
| Nurse agency total | 1.54 | 4.71 | 3.17 |
| Nurse bank total | 2.80 | 5.05 | 2.25 |
| Nurses substantive – registered total | 16.68 | 26.57 | 9.88 |
| Nurses substantive – assistant total | 6.61 | 10.07 | 3.45 |
| Nursing total | 27.64 | 46.39 | 18.75 |
| Ward total | 27.86 | 48.11 | 20.25 |
| Number of beds | 16 | 30 | |
| Registered nurses WTE/bed | 1.04 | 0.89 | |
| Assistant nurses WTE/bed | 0.41 | 0.34 | |
| Other staff WTE/bed | 0.29 | 0.38 | |
| Total ward staff WTE/bed | 1.74 | 1.60 |
Actual nursing whole-time equivalent cost before and after the move to single rooms
Planned staffing may not reflect the actual staffing deployed. Administrative data on staffing levels show that there was a change in the number of WTE nurses after the move to single room design. Comparing the data in the 19 months before the move with data for 19 months after the move, up to March 2013 (most recent data available), there was an overall increase in WTE nurses and also a change in the skill mix of staff (Tables 61–63). We assessed the WTE staffing for the 19 months before September 2011 (date of the move) and the 19 months after the move (until March 2013). An average monthly number of WTE staff has been assessed before and after the move. A number of WTE staff per bed has been calculated by dividing the average monthly WTE by the number of beds in the ward before and after the move.
| Older people’s ward | Total before | Total after | Difference |
|---|---|---|---|
| A&C/senior manager substantive total | 1.47 | 1.01 | –0.46 |
| A&C/senior manager bank total | 0 | 0 | 0 |
| A&C/senior manager total | 1.47 | 1.01 | –0.46 |
| Nurse agency total | 0.12 | 1.35 | 1.24 |
| Nurse bank total | 3.62 | 6.42 | 2.80 |
| Nurses substantive – registered total | 2.901 | 20.75 | 7.85 |
| Nurses substantive – assistant total | 14.47 | 14.67 | 0.21 |
| Nurse total | 31.10 | 43.20 | 12.09 |
| Agency total | 0.00 | 0.00 | 0.00 |
| Ward total | 32.57 | 44.21 | 11.64 |
| Number of beds | 28 | 30 | |
| Registered nurses WTE/bed | 0.46 | 0.69 | |
| Assistant nurses WTE/bed | 0.52 | 0.49 | |
| Other staff WTE/bed | 0.65 | 0.29 | |
| Total ward staff WTE/bed | 1.16 | 1.47 |
| Surgical ward | Total before | Total after | Difference |
|---|---|---|---|
| A&C/senior manager bank total | 0.05 | 0.13 | 0.08 |
| A&C/senior manager substantive total | 1 | 1 | 0 |
| A&C/senior manager staff total | 1.05 | 1.13 | 0.08 |
| Nurse agency total | 0.09 | 0.38 | 0.29 |
| Nurse bank total | 4.27 | 4.51 | 0.24 |
| Nurses substantive – registered total | 24.01 | 23.46 | –0.55 |
| Nurses substantive – assistant total | 13.02 | 12.03 | –0.99 |
| Nursing total | 41.39 | 40.38 | –1.01 |
| Ward total | 42.44 | 41.51 | –0.93 |
| Number of beds | 35 | 30 | |
| Registered nurses WTE/bed | 0.69 | 0.78 | |
| Assistant nurses WTE/bed | 0.37 | 0.40 | |
| Other staff WTE/bed | 0.15 | 0.20 | |
| Total ward staff WTE/bed | 1.21 | 1.38 |
In the AAU there was a 73% increase in WTE (from 27.86 to 48.11 WTE), resulting from the recruitment of additional trained nurses and agency nurses (see Table 61). However, the AAU increased from a 16-bedded unit to a 30-bedded unit; thus, if we compare the WTE per bed before and after the move, the ratio decreased from 1.74 to 1.60, that is there were fewer members of staff per bed (see Table 61). This trend perhaps underlies findings from our interview data which suggest that staff felt extremely pressurised in this ward. Temporary bank and agency staffing was used to cover shortfall due to (1) short notice absence, (2) increased acuity and (3) vacancies.
In the older people’s ward there was a total increment of 142% in WTE (from 32.57 to 44.21), with a significant use of agency nurses and untrained nurses (see Table 62). However, the number of beds increased by only two, with the result that the number of WTE staff per bed grew from 1.16 to 1.47 of all staff (see Table 61). A senior nurse manager confirms that some of this increase also reflects the change in case mix. The ward cares for patients on the fractured neck of femur (broken hip) pathway, for 48 hours after operation; the older people’s ward in the old accommodation (before the move) did not routinely do this.
It was not possible to extract the postnatal ward figures from the data because of the way maternity services operate, with staff moving frequently to ensure one midwife to every mother in established labour. The senior nurse for midwifery confirmed there was no WTE increase for the new postnatal ward, as all the staffing increase was to staff the new birth unit.
The only ward registering a decrease in WTE was the surgical ward, with a 2% reduction in WTE (see Table 63). Because the number of beds also decreased, the WTE-per-bed ratio slightly increased from 1.21 to 1.38.
Cost of nurse whole-time equivalent changes before and after the move to single rooms
See Chapter 2 for details of the approach to assessing the cost impact of changes in nursing WTE before and after the move.
The average monthly WTE pay rate before and after the move was assessed in each case study ward, except maternity. It was not possible to undertake this calculation for maternity, as we have only all staffing figures including community midwifery and it was not possible to calculate accurate bed numbers. The difference in monthly nursing cost, and cost per bed, before and after the move is summarised (Tables 64–66). The results show that there was an increase in the cost of nursing/midwifery staff in the AAU and older people’s case study wards but not the surgery unit.
-
In the AAU there was a total average monthly increase of £42,301 after the move, with a decrease of £225.90 per bed (see Table 64).
-
In the older people’s ward the average monthly cost increased by £22,315, partly because of an increase in RNs. The monthly staff cost per bed increased by £604 (see Table 65).
-
The surgery unit is the only unit that registered a decrease in the average monthly cost of staff (£12,213). As the number of beds decreased from 35 to 30 the average cost per bed increased, but only by £66 (see Table 66).
| AAU | Before (2010–11) | After (2011–12) |
|---|---|---|
| A&C/senior manager bank (band 8) | £11 | £414 |
| A&C/senior manager substantive (band 8) | £1245 | £5632 |
| A&C/senior manager staff total | £1255 | £6047 |
| Nurse agency total (band 5) | £4418 | £8785 |
| Nurse bank total (band 5) | £4839 | £9071 |
| Nurses substantive – registered | ||
| Band 5 | £30,924 | £49,297 |
| Band 6 | £3489 | £9457 |
| Band 7 | £2933 | £2933 |
| Nurses substantive – registered total | £37,345 | £61,687 |
| Nurses substantive – assistant | ||
| Band 2 | £8012 | £6491 |
| Band 3 | £221 | £6309 |
| Nurses substantive – assistant total | £8233 | £12,800 |
| Nursing total | £56,089 | £98,390 |
| Difference in monthly WTE pay | £42,301 | |
| % difference | 75% | |
| Number of beds | 16 | 30 |
| Average monthly cost per bed | £3505.56 | £3279.67 |
| Older people’s ward | Before (2011–12) | After (2011–12) |
|---|---|---|
| A&C/senior manager substantive (band 8) | £4932 | £3755 |
| A&C/senior manager substantive total | £4932 | £3755 |
| Nurse agency total (band 5) | £136 | £2505 |
| STT agency (band 5) | £3 | N/A |
| Nurse bank total (band 5) | £7050 | £12,275 |
| Nurses substantive – registered | ||
| Band 5 | £20,750 | £36,258 |
| Band 6 | £3797 | £4172 |
| Band 7 | £2933 | £2933 |
| Nurses substantive – registered total | £27,479 | £43,362 |
| Nurses substantive – assistant | ||
| Band 2 | £17,515 | £15,350 |
| Band 3 | £1516 | £3700 |
| Nurses substantive – assistant total | £19,032 | £19,050 |
| Nursing total | £58,632 | £80,947 |
| Difference in monthly WTE pay | £22,315 | |
| % difference | 38% | |
| Number of beds | 28 | 30 |
| Average monthly cost per bed | £2094.00 | £2698.25 |
| Surgical ward | Before (2011–12) | After (2011–12) |
|---|---|---|
| A&C/senior manager bank total (band 8) | £202 | £394 |
| A&C/senior manager substantive (band 8) | £5197 | £3556 |
| A&C/senior manager staff total | £5400 | £3950 |
| Nurse agency total (band 5) | £89 | £687 |
| Nurse bank total (band 5) | £8358 | £8693 |
| Nurses substantive – registered | ||
| Band 5 | £41,172 | £41,475 |
| Band 6 | £16,058 | £4685 |
| Band 7 | £6734 | £2933 |
| Band 6 | £1349 | N/A |
| Nurses substantive – registered total | £69,148 | £58,472 |
| Nurses substantive – assistant | ||
| Band 2 | £15,371 | £14,641 |
| Band 3 | £982 | £689 |
| Nurses substantive – assistant total | £16,353 | £15,331 |
| Nursing total | £99,347 | £87,133 |
| Difference in monthly WTE pay | –£12,213 | |
| % difference | –12% | |
| Number of beds | 35 | 30 |
| Average monthly cost per bed | £2838.48 | £2904.45 |
Staff walking time
Analysis of staff activity and walking time data (see Chapter 5) shows that after the move to single rooms the time spent on direct and indirect care changed in all wards and nurses and midwives in all wards walked more than before the move.
Staffing costs are not affected by the time spent walking; rather, they are affected by the total numbers of hours worked. However, there is an opportunity cost associated with time spent walking: this time is not available for other activities such as spending time with patients or administrative activities. Spending more time walking longer distances might also affect staff performance as nurses suffer from greater fatigue; thus efficiency or effectiveness might be reduced.
The costs associated with falls
Almost 209,000 falls were reported in hospitals in England in 1 year to October 2012. 125 Of those, 61,000 (in round numbers) involved harm to patients: 55,000 involved a low degree of harm, 5000 moderate harm and 898 severe injuries, such as hip fractures and head injuries. In 2007 the Patient Safety Observatory estimated that falls cost the NHS £15M per year, equivalent to a cost of £92,000 a year for a 800-bed acute hospital trust. 126 On average, a fall cost the NHS £73.33. 126
Some falls result in litigation. During 2005, the NHS Litigation Authority (NHSLA) received notification of 102 claims of clinical negligence relating to patients falling in hospital settings. 128 These claims cost over £3M in compensation. However, it is difficult to estimate the cost of a single claim after a fall (unitary claim).
In Tunbridge Wells Hospital, there was an initial increase in falls in all the wards after the move to single room design (data for the maternity unit are not available), followed by a decrease (see Chapter 8).
Table 67 shows the difference in falls rate [monthly falls per patient (FPP) in each unit] before and after the move. Assuming the average number of patients remains constant we calculated the potential cost impact of the change over 1 year in each unit (the maternity unit was not included). If these differences were due to the single room design, an increase in falls as in the AAU or older people’s ward would increase associated costs by £7571 in a year, but this would be partially offset by a reduction in falls in the surgery unit. However, although there was certainly a perception among staff that the loss of visibility as a result of single rooms meant that falls increased and were harder to prevent (see Chapter 6), there is no clear evidence that the observed changes in the rate of falls – and associated costs – are related to the move to a single room design.
| Administrative data | AAU | Older people’s ward | Surgical ward |
|---|---|---|---|
| Average FPP/per month before the move | 0.00381 | 0.09916 | 0.01189 |
| Average FPP/per month after the move | 0.01194 | 0.23039 | 0.00368 |
| Difference in average FPP before and after | 0.00814 | 0.13123 | –0.00821 |
| % difference before and after | 214% | 132% | –69% |
| Average patients in 1 year | 1400 | 700 | 6792 |
| Difference in number of falls over 1 year | 11 | 92 | –56 |
| Unitary cost | £73.33 | £73.33 | £73.33 |
| Total difference in cost per year | £835.12 | £6736.07 | –£4088.02 |
Changes in length of stay
After the move to single room design there was a change in the LOS and number of bed-days in some wards (see Chapter 8). In the AAU the average LOS increased, while in the older people’s ward it decreased. The AAU did not initially have an ambulatory model, but following closer management patients were moved promptly to inpatient wards after a 48-hour LOS. Following the move, the older people’s ward had 10 orthopaedic rehab beds, so these patients move through the system faster than patients with complex needs; this is largely a result of pathway and case mix changes, and changes in the local health-care economy. In the surgery unit there was no immediate change after the move but after 6 months there was a substantial increase in LOS, followed by a sudden decrease, which can in part be explained by changes in patient pathways: initially, in the new hospital, surgical patients were outlying in other specialties; following a review of pathways (moved overnight electives, etc.) medical outliers took up surgical beds.
We explored the possibility of investigating the cost impact of the change in LOS using the LOS trim-point (the number of days after which the tariff no longer covers the inpatient stay and an additional daily cost is required for each extra day) for each patient and multiplying the difference in days for the daily tariff. By analysing the number of days exceeding the trim-point and applying the extra daily tariff beyond the trim-point it is theoretically possible to assess the cost of extra LOS. However, there were insufficient control variables in the available data to check for this, and it would not be possible to ascribe the extra cost or saving to the hospital design itself.
The costs associated with hospital-acquired infections
The majority of studies show a reduction in hospital-acquired infection rates for single rooms, but there are also a few showing no differences or even higher infection rates in single rooms. It is generally very difficult to control for confounding factors when investigating the impact of building design on the transmission of infection. It may be that in some cases infections decrease because of better ventilation system, hand washing and other precautionary measures rather that isolation.
Data on hospital-acquired infection rates at Tunbridge Wells Hospital show very low rates of C. diff. in the case study wards both before and after the move (see Chapter 8).
Table 68 shows the average monthly differences in C. diff. infection rates (number of infections per patient per month) before and after the move. The older people’s ward registered an increase in the number of C. diff. cases after the move, while the AAU and surgery unit registered a decrease (see Chapter 8).
| Administrative data | AAU | Older people’s ward | Surgical ward |
|---|---|---|---|
| AIPM before the move | 0.00010 | 0.001351 | 0.002828 |
| AIPM after the move | 0.00008 | 0.006217 | 0.001366 |
| Difference in AIPM before and after | –0.00003 | 0.00487 | –0.001462 |
| % difference in AIPM before and after | –27% | 360% | –52% |
| Average patients per unit in 1 year | 1400 | 700 | 6792 |
| Difference in number of infections in a year | 0 | 3 | –10 |
| Unit cost to treat C. diff. infections | £6738.00 | £6738.00 | £6738.00 |
| Total incremental cost per year | –£258.74 | £22,949.44 | –£66,887.38 |
Assuming the average number of patients remains constant, we calculated the cost impact of the change over 1 year in each unit. There are no UK estimates of the cost of C. diff. infections per patient. We therefore used a recent US study which estimated that C. diff. treatment and LOS costs amount to £6738 (95% confidence interval £5444 to £8105). 127
Using these figures per patient implies that the increase of infections in the older people’s ward would have increased the costs for additional treatments by £22,949 per year, but this would have been offset by a reduction of infections in the surgical ward and AAU saving £66,887 per year. However, as in the case of falls, we cannot directly ascribe these changes to the move towards a single room hospital design.
Chapter summary
We found that construction costs at Tunbridge Wells Hospital are reported to be no higher as a result of its all single room design, because no additional ward space was required. Any increase in maintenance and refurbishment costs over the lifetime of the hospital would be outweighed many times by the total life-cycle costs associated with medical care.
It was hard to identify any clear cost effect associated with single rooms, apart from increased cleaning costs. However, these would represent a very small share of total lifetime operating costs of the hospital, although clearly in any given year they represent a potential additional burden on trust budgets.
While there may have been some impact on operational costs arising from increased numbers of staff, this is partially due to the change in number of beds, the cost of staff time and change in the skills mix of staff. While there may have been some possible loss of staff efficiency due to challenges in surveillance and additional walking, it is not possible to say what impact this has on clinical outcomes.
There is no clear evidence of a cost impact of single rooms in terms of falls, LOS and hospital-acquired infections.
Chapter 10 Conclusions: were the expected benefits of and concerns about the 100% single room design realised?
Introduction
We have brought together our findings in a cross-case analysis, which considers how the four case study wards fared in the move to the new hospital, bringing together key findings from previous chapters. The focus is particularly on the context and characteristics of the wards; initiatives taken by staff to adapt to the new environment; and outcomes for patients and staff (see Appendix 23).
In this chapter we examine the extent to which our results demonstrate the anticipated benefits of 100% single room design, drawing on the findings from five key evaluation data sets, relating to:
-
staff experience
-
patient experience
-
costs
-
safety outcomes
-
care delivery and working practices.
The trust, designers and stakeholders held various expectations about the benefits of the 100% single room design (see Appendix 16). Specifically, the new hospital was designed to:
-
increase patient comfort, reduce patient stress and enhance healing
-
improve patient-centred care and increase the time spent by nurses on direct care
-
prevent infections
-
reduce patient falls.
Potential problems were recognised as:
-
reduced observation and monitoring of patients and increased travel distances for staff
-
patient isolation
-
possible increase in nurse staffing required.
Although attempts were made to overcome these issues in the design and planning stages, our findings suggest there were still negative consequences for patients and staff. We also discuss the impact of the move on teamwork and staff working practices, and highlight the implications of our findings for future hospital design and for clinical practice on single room wards. Finally, we assess the extent to which 100% single bedroom design ‘works’ and offer recommendations for future research.
Increase patient comfort, reduce stress and enhance healing
Patient comfort was undoubtedly enhanced by single rooms, which were acceptable to patients, indeed warmly welcomed by many, who found the benefits outweighed any disadvantages. This study is the first to find that the majority of patients (two-thirds of those interviewed: 21 out of a total of 32) preferred single rooms to multibedded wards. Patients liked the high-quality accommodation, the comfort of en suite facilities, natural views, temperature, lighting and noise levels and the confidentiality, control, privacy and flexibility afforded by the single room. Staff also emphasised the benefits for patients. This supports the literature which highlights increased privacy, dignity and comfort. 11,37,38 Short-stay and postnatal patients liked single rooms the most, and postnatal patients were relieved not to have their baby’s crying disturbing others, which they reported as much less stressful for them. Patients also liked the space and privacy to be with their friends and relatives and the opportunities that some visitors were allowed (fathers; relatives of older people and dying patients) to stay overnight with the patient. Again, this has the potential to enhance healing and reduce patient anxiety and stress, which some patients alluded to. Patients valued reduced noise levels, and the ability to close the door and sleep well, undisturbed by other patients or staff. They also noted the large windows with views of the wooded valley as restful and enjoyable. The rooms and setting were ‘luxurious’ by most standards, which may be part of their appeal and may be unique to this particular build.
Patients were less likely to be moved than in the old multibedded wards (to comply with single-sex accommodation), also potentially reducing stress. 31 Previously, there was little evidence about the preferences of patients from different age and cultural groups. Our findings suggest that, while staff felt that single rooms were less suitable for older people, older patients themselves did not concur, with patients across a wide age range preferring single rooms. Patients appeared to weigh up the pros and cons and, while some highlighted drawbacks, most thought the en suite bathroom and other elements of comfort (e.g. enhanced sleep quality) outweighed the disadvantages. However, we took a purposive sample, which included mainly people of white British origin, and we were not able to interview patients who were very unwell or had cognitive impairments, so generalisability of the findings should be treated with caution.
Design implications
-
The en suite bathroom is an important element of single room design significantly enhancing privacy and dignity for patients.
-
Provision of pull-down beds or sofas in bedrooms that convert to beds for relatives of sick and dying patients and new mothers would improve patient experience and enable relatives to support patients.
-
The view from the single room window enhances well-being and patient experience, as does patient control over temperature and lighting.
Improve patient-centred care and increase the time spent by nurses on direct care
Staff reported being able to spend more time with some patients and sometimes to offer care that was more personalised and individualised. However, this was not always possible and more time did not always mean more personalised care. Once in the single room, nurses were less likely to be interrupted by others, and our structured observation study shows that nurses in the AAU and midwives on the postnatal ward spent more time at the bedside after the move. However, nurses reported struggling to divide their attention between all the patients they were caring for (in contrast to open bedded bays in the old setting) and found time management and prioritisation of workloads challenging in the new environment. More opportunities to prepare for working on all single room wards might have revealed this issue earlier and allowed staff to develop strategies for managing their time and resources. Nurses had to work differently to ensure that all patients were seen regularly, requiring teamwork with support staff and implementation of regular hourly intentional rounds (or 3-hourly on the postnatal ward). Patients generally knew that they were being regularly observed and monitored, although some felt isolated and experienced care as task-focused (see sections Reduce patient falls and reduce observing and monitoring of patients and Patient isolation). This finding suggests that how intentional rounding is carried out has important implications for patient experience: rounds should include meaningful contact with patients rather than only task-focused care.
The literature suggests that ill patients wanted nurses to be closer. 12,13,42 Some patients in our study reported a high level of connection with staff, with staff perceived to be giving them full attention, listening and interested in the patient as a person, while others felt a sense of disconnection. A study of cancer patients in Denmark68 found that refuge from fellow patients was hard to achieve in multibedded rooms and the fact that personal conversations might be overheard by fellow patients caused important information to be withheld from health-care professionals. Patients and staff in our study noted the increased speech privacy afforded by single rooms, which they felt allowed patients to raise difficult issues and better patient–staff relationships to develop, supporting previous research. 11,43
Implications for practice
Our findings suggest it would be beneficial for managers planning a similar move to:
-
encourage staff to prepare and rehearse for working in single rooms well ahead of moving
-
provide support and training for staff regarding time management and dividing attention between patients in single rooms
-
promote intentional rounding that includes meaningful contact with patients, not just task-orientated care.
Infection prevention
Because of the fall in infection rates nationally and low incidence at our study site and comparator hospitals, it is difficult to conclude from our data that it is the ‘single room’ factor that prevents infection. Our interview with the infection control team member warned against staff complacency and that single rooms were not the ‘be all and end all’ in terms of infection prevention, and staff should be reminded about good practice. This supports Dowdeswell et al. ,8 who suggest that good infection control practices, such as access to hand washing facilities and hand hygiene, are more important factors in reducing HCAI rates than single rooms per se (cf. Wojgani et al. 128), although compliance may be facilitated by careful design and location in a single room, along with toilets that are not shared between patients. Certainly the evidence here cannot be interpreted as providing generalisable evidence that single rooms play no part in the control of infection. Staff in this study perceived single rooms to be an important element in preventing infection, and felt nursing patients in single rooms facilitated infection control practice, including providing good access to hand washing facilities and facilities to isolate patients. In our study, the infection control team reported that, during a norovirus outbreak, the spread at Tunbridge Wells Hospital was more limited than at Maidstone Hospital (with open bay wards).
Implication for practice
-
Infection control policies require continued vigilance and reinforcement; enhanced signage and training to remind staff of infection control good practice may help to avoid staff complacency.
Reduce patient falls and reduce observing and monitoring of patients
Before Tunbridge Wells Hospital opened there was an expectation that falls would decrease, yet the evidence suggests single rooms could mean less surveillance by staff and increased rates of slips, trips and falls41,129 and falls that are unnoticed by staff or other patients. 37,38,63 To minimise falls, the rooms had non-slip flooring and inboard bathrooms with bathroom doors on the bed head wall with hand rails (to prevent falls risk by patients walking across an open floor to get to the bathroom). However, staff reported that the flooring was ‘very hard’ and the inboard bathrooms (which protrude into the corridor, reducing visibility) meant that staff sight lines were limited to one patient (and then only if the door or blinds were open). With good design (layout which includes observation points and large glazed windows and doors) there is no evidence to suggest that single patient rooms reduce staff-to-patient observation. 38 However, at Tunbridge Wells Hospital the inboard bathrooms coupled with reduced glazing (the bi-fold door was glazed in the original design; this was changed during the build) resulted in significantly reduced visibility for staff, especially compared with the open wards they had worked on previously. One of the most important themes in staff interviews was concern about reduced visibility and surveillance of patients. Staff also noted that on open wards other patients and visitors would alert staff to patients getting out of bed or at risk of falling, a warning system that was not available on single room wards. Staff found the loss of panoptic surveillance one of the most important disadvantages of the new wards and perceived falls had increased. The comparator study shows that, following the move, falls increased on general wards; but they increased throughout the trust. At Tunbridge Wells Hospital only the AAU had a falls increase not accounted for by case-mix changes and therefore related to the move. This increase was temporary and fall rates decreased to previous levels 6–9 months after the move, so we cannot attribute the increase in falls to the single room design. One suggestion for the reduction is that the interventions staff introduced eventually (optimal deployment of staff; one-to-one ‘specialing’ of patients; patient cohorting; alarm mats; etc.) helped reduce falls. The comprehensive fall reduction plan detailed in the business plan for the new hospital was not evident on the wards and staff did not mention this at interview. Our findings suggest that a focus on the move and migration left staff unprepared for working in an unfamiliar and challenging new environment, so that some of the new approaches to monitoring and safeguarding patients were initially absent and then took time to bed in.
Design implications
-
It is vital to maximise visibility on single room wards, in particular into rooms (by extensive glazing) and along corridors (by creating uninterrupted views).
-
Technological solutions to assist monitoring and surveillance of high-risk patients may be required.
Implications for practice
-
A comprehensive single room working policy and falls strategy, which has been tried and tested before the move, is required.
-
Established work patterns are disrupted by moving to a new environment, and reconstituting them in ways appropriate to the new setting may require trial and error. Adaptation could be facilitated by encouraging staff to anticipate working on single room wards and giving them opportunities to trial their plans.
Increased travel distances for staff
Our findings suggest this concern was well founded. Staff walking distances increased, particularly for staff on the surgical and elderly wards and for RNs (who walked an extra mile per shift after the move), confirming Trant’s35 findings. There are design solutions which can help reduce excessive walking and allow higher global visibility. 130,132 At Tunbridge Wells Hospital, the restricted line of sight into the room and the ward layout, with most rooms adjacent to each other along a corridor ‘finger’, may have exacerbated increased walking by nursing staff. Staff also spoke of the whole hospital being ‘large’ with long corridors and walking distances between wards and other departments, for example pharmacy and theatres. Another explanation could be the implementation of hourly intentional rounding and the need to go in and out of each patient’s room for monitoring and surveillance purposes rather than simply walking down an open ward once and seeing 10–12 patients on one journey. Increased walking can have opportunity costs and may also affect staff performance. Nurses reported the walking ‘exhausting’ and ‘hard on the feet’, potentially causing nurses to suffer from greater fatigue; thus, efficiency or effectiveness might be reduced.
Design implication
-
Minimise staff walking distances as far as possible with central facilities, short corridors and double-loaded corridors (rooms on either side).
Patient isolation
The main disadvantage of single rooms for approximately one-third of patients was a sense of isolation, and patients missed the opportunities for interaction with other patients that they expected on a hospital ward, confirming previous findings. 11,26,38 For some patient groups, for example stroke patients65 and mental health patients,66 the isolating effect of single rooms could impede the therapeutic process and overall experience of care. In our study, patients and staff noted the potential for loneliness, boredom and the loss of a chance to share and normalise their experiences (midwives highlighted the importance of this for new mothers), as well as the lack of opportunities for distraction and social interaction offered by multibedded wards. Staff on the older people’s ward had tried to ameliorate these disadvantages, setting up a lunch club for patients in the day room, and they were planning to refurbish an area between the wards as a communal space for activities or for relatives to sit with patients. On other wards day rooms were rarely used, or had been designated for other purposes, and staff deplored the lack of space for patients, although the loss of day rooms in acute hospitals appears to be a wider trend. Patients needed guidance on the location of any communal facilities; they also felt unsure whether or not they were allowed to leave their room and staff reported reluctance of some to do so. Staff on the maternity ward had developed a ‘welcome to the ward’ booklet which gave women information about shared spaces and how to meet others on the ward. However, all staff thought that their initiatives to facilitate interaction among patients were unlikely to succeed without the provision of more attractive and welcoming spaces for patients and visitors.
Design implication
-
Maximise communal spaces for patient and visitor use and make the space usable, welcoming and appealing to patients.
Implication for practice
-
Patients need to be orientated to the whole ward, not just the single room, and benefit from opportunities to socialise with other patients where this is appropriate.
Possible increase in nurse staffing required
The literature suggests there may be a need for an increase in staffing levels and/or adjustments to staff skill-mix as a result of increased single room occupancy. 26,37,38 Our study has provided detailed evidence of the nurse staffing before and after the move to the new hospital and shows that for all of our case study wards (except the AAU) the WTE nursing staff per bed increased after the move. Nursing costs per bed have increased accordingly. In our case study ward that was the exception to this trend – the AAU – staff reported feeling under increased pressure and compromised because they were not able to give patients the quality of care they wished to provide. Some nurses said that they were thinking of leaving and morale on the ward was evidently low. Our findings suggest that this was related to insufficient nurse staffing levels, but we are unable to attribute causality.
Implication for practice
-
Nurse staffing and skill mix is likely to require review and augmentation.
Staff working practices and teamwork
Nurses’ accounts detail a sense of anxiety, frustration, hard work and the need to work very differently in the new hospital primarily because of single rooms. The nature of tasks undertaken by nursing staff did not change, but they had to adapt their working practices and our findings suggest many felt ill-prepared for the new ways of working required on single room wards. There were few clinical champions for single room working and divided opinions about whether or not preparation would have helped: some staff felt the only way to learn was on the job, while others felt more could have been done beforehand. Many new ways of working were trialled and were eventually successful; for example team cluster organisation on the AAU, or patient cohorting and lunch clubs on the older people’s ward.
Nurses encountered a variety of challenges they were unprepared for because issues had not been foreseen or operational procedures had been incompletely specified, for example, to ensure patient safety and care quality; new ways of working as a team; locating and communicating with colleagues. Staff reported feeling isolated from each other and the wider nursing team, and found that they had to make special efforts to keep up to date with each other and the patients in their cluster. Challenges they identified included obtaining assistance from colleagues, informal learning, keeping team members updated and discussing care with colleagues. Doctors and AHPs found locating nursing staff difficult, which made communication difficult. At the time data were collected (over 1 year after the move) there was little indication that these issues were improving following a period of ‘bedding down’. The reduced visibility of staff appears to be a difficult challenge to overcome. Thus, our findings suggest that a move to all single rooms may have significant implications for the nature of teamwork and informal learning (i.e. observing how colleagues handle situations and role modelling) in the longer term.
Implications for practice
-
Clinical champion posts could be beneficial: to work with staff before the move to prepare for different ways of working and after the move to resolve problems.
-
Single room wards can impede communication and teamwork; managers and staff need to find ways to maintain teamwork and facilitate informal learning, for example work with organisational development teams and improve use of communication aids.
Do single rooms ‘work’?
Overall, ‘it depends’ on whose perspective and over what time scale. They certainly ‘work’ for some patients, but staff put in a lot of effort and used their initiative in an attempt to make them work for all patients.
Two-thirds of patients in our small sample expressed a preference for single rooms following the move and spoke of the three Hs – hotel, home and hospital – to convey the feeling that single rooms allowed them to experience the comfort and control of home or a hotel in a hospital environment. However, the majority of staff still expressed a preference for retaining some multibedded patient accommodation (see Figure 6), but after experiencing single room working they were more favourable towards this design than before the move. In preparing for any such move, attention needs to be given to possible increases in risk associated with disruptions caused by a move and the need to adapt work patterns. Detailed planning is required and staff need to be given opportunities to anticipate and plan for changed work patterns.
Evidence from this study in relation to patient safety, clinical outcomes and cost is mixed. A policy of routine provision of single room accommodation for general wards cannot be justified solely on the grounds of controlling infection, because infection rates had decreased nationally prior to the move to the new hospital. Although there may be a role for single rooms, the costs of increased single room provision need to be compared with the likely costs of other strategies for infection control. Reduced medication errors have been claimed as a possible benefit of single rooms, with consequent cost savings. We found no support for this rationale in our study. It has been suggested that single rooms may affect falls rates. Although in this study falls increased after the move, single rooms are unlikely to be the cause; indeed moving itself, with the associated system disruptions, may be a more likely explanation for our findings. In terms of cost, additional construction costs for 100% single over 50% single rooms are insignificant over the lifetime of a typical hospital, as are additional cleaning costs. However, cost needs to be measured against longer-term and wider benefits. We found no clear evidence for infection control or medication error benefits, and the falls evidence is ambiguous, but potential benefits in terms of reduced lengths of stay and improved outcomes remain a possibility. The main driver for choosing single or multibedded accommodation is likely to come down to the relative costs and other considerations, such as patient preference and experiences. The 100% single room hospital design is extreme and participants in this study (including patients) expressed a desire for flexibility, with a mix of single rooms and multibedded patient accommodation.
Overall implications for policy and planning
This study is one of very few to have examined in depth the experiences of patients and staff in single room hospital accommodation and therefore it provides valuable evidence to guide policy, planning and hospital design. The study attempted to answer the question: what are the advantages and disadvantages of single rooms for different groups of staff and patients and for different quality outcomes? Alongside this question it is important to understand that a move to all single rooms in a new hospital involves major changes to all aspects of clinical work and therefore the impact of the layout of the rooms cannot be entirely separated from the way that staff and managers manage their work in single rooms. The success or failure of the design is not the only important question. How well working practices can be matched to the design to produce good outcomes is just as important. Based on the results of the study we highlight the following overall implications:
-
Based on our data, there appear to be no strong economic or safety reasons for choosing 100% single rooms and strong arguments for including a mix of single rooms and multibedded accommodation. Although many patients and some staff preferred single rooms because of the comfort, privacy and opportunity for personalised care they offered, this was not the case universally; indeed, most staff did not prefer single rooms, while most patients did. However, some patients would have preferred multibedded accommodation because of the opportunity for social interaction and the proximity to staff; the latter is particularly important for critically ill patients, those with dementia and those at risk of falling, in terms of safe and effective care. There therefore seem good reasons from the perspective of patient care and efficiency of working to choose a mix of single rooms and multibedded accommodation. In other new hospital builds it is, therefore, important to give careful consideration to the mix of accommodation types.
-
The process of planning a new hospital is vital to its success and involves the co-ordination of a large number of stakeholders. It is vital that sufficient time and effort be invested in ensuring that there is optimum co-ordination between the designers, builders and the staff who will work in the new hospital. In particular, there needs to be early discussion of the impact on clinical work of design decisions, and the need for adaptation of work processes to fit the new building and how to prepare for this. It is important that this process include a wide range of clinical representatives and managers who are supported to engage in this vital planning work as early as possible, but at least 1–2 years before the move (see implications for practice 3, 6, 8 and 9 below).
-
In any move to all single rooms or a large proportion of single rooms, maximisation of design features and technology to ensure that the design is successful and that standards of care are not reduced is key. The provision of day rooms to enable patient social interaction is important to overcome patient isolation. Staff will spend considerably more time working alone in rooms with patients and therefore there is the potential for negative impacts on communication between team members, on the availability of team members to back each other up and on the ability of team members to plan and co-ordinate their work. Communication technology (and support and training to ensure its optimum use) can be a vital part of overcoming these problems and therefore important to retain in the full specification (see implication for design 7 and implication for practice 7 below). Active monitoring and management of changes in work practices during and after the move will be required. Policies for infection control and preventing falls will need to be reconsidered and revised to ensure that they are suitable for the new environment, and constant monitoring of these and similar indicators will be needed to ensure fast detection of any problems. A process for reporting and resolving unforeseen problems caused by the design and resources for rectifying these is required (see implications for practice 1–3, below).
-
Finally, a move to a new building with a significantly different layout requires advance preparation and practice to enable staff to devise and become familiar with new working practices. Detailed preparation needs to occur well in advance of the move and involve all staff. This should include site visits; simulated practice, including team working, in a mocked-up single room and whole-ward (with multiple single rooms) environment; and discussion of potential problems and solutions. Simulated practice could also be helpful for identifying problems and testing solutions prior to the final design being accepted (see implications for practice 3, 4, 7, 8 and 9, below).
Summary of design and practice implications
Implications for design
-
The en suite bathroom is an important element of single room design significantly enhancing privacy and dignity for patients.
-
Provision of pull-down beds or sofas in bedrooms that convert to beds for relatives of sick and dying patients and new mothers would improve patient experience and enable relatives to support patients.
-
The view from the single room window enhances well-being and patient experience, as does patient control over temperature and lighting.
-
It is vital to maximise visibility on single room wards, in particular into rooms (by extensive glazing) and along corridors (by creating uninterrupted views).
-
Technological solutions to assist monitoring and surveillance of high-risk patients may be required.
-
Minimise staff walking distances as far as possible with central facilities, short corridors and double-loaded corridors (rooms on either side).
-
Maximise communal spaces for patient and visitor use and make the space usable, welcoming and appealing to patients.
Implications for practice of 100% or large proportion of single rooms
-
Encourage staff to prepare and rehearse for working in single rooms well in advance of moving.
-
Provide support and training for staff regarding time management and dividing attention between patients in single rooms.
-
Promote intentional rounding that includes meaningful contact with patients, not just task-orientated care.
-
Infection control policies require continued vigilance and reinforcement; enhanced signage and training to remind staff of infection control good practice may help to avoid staff complacency.
-
A comprehensive single room working policy and falls strategy, which has been tried and tested before the move, is required.
-
Established work patterns are disrupted by moving to a new environment, and reconstituting them in ways appropriate to the new setting may require trial and error. Adaptation could be facilitated by encouraging staff to anticipate working on single room wards and giving them opportunities to trial their plans.
-
Patients need to be orientated to the whole ward, not just the single room, and benefit from opportunities to socialise with other patients where this is appropriate.
-
Nurse staffing and skill mix is likely to require review and augmentation.
-
Clinical champion posts could be beneficial: to work with staff before the move to prepare for different ways of working and after the move to resolve problems.
-
Single room wards can impede communication and teamwork; managers and staff need to find ways to maintain teamwork and facilitate informal learning, for example work with organisational development teams and improve use of communication aids.
It would beneficial for managers planning a similar move to:
-
encourage staff to prepare and rehearse for working in single rooms well ahead of moving including attention to team working issues
-
provide support and training for staff regarding time management and dividing attention between patients in single rooms
-
promote intentional rounding that includes meaningful contact with patients, not just task-orientated care
-
actively monitor and manage changes in work practices and any changes in patient experience indicators during and after the move.
Recommendations for future research
We recommend that future research should:
-
explore design solutions to improve patient surveillance, facilitate team working and reduce walking distances for staff
-
investigate patient experience and preferences more extensively, with a larger patient sample, and in hospital builds with different proportions of single rooms and varying ward designs
-
investigate carer’s experience so that the most vulnerable/frail patient experiences – including the experiences of those with a disability or with dementia – can be taken into consideration
-
explore the longer-term impact of single room working on the nature of staff teamwork and informal learning
-
assess the longer-term impact of single rooms on quality of care and clinical outcomes, including LOS, falls, medication errors, infection control, and surveillance and monitoring of patients
-
take case-mix changes, and therefore risk adjustment strategies, into account.
Acknowledgements
Our thanks go to all the patients and staff who participated in this research, through completing a survey, and/or being interviewed or observed as part of our fieldwork, or securing and preparing safety and outcomes data for us. We are also grateful to the NHS trust senior managers and other interviewees from the building and architecture world for giving us their time to talk about the early planning and design stages of the project. Grateful thanks to Flo Panel-Coates, John Kennedy and Avey Bhatia, directors of nursing, and Sarah Fielder, Lead Nurse of the Infection Prevention Team at Maidstone and Tunbridge Wells Trust, for their support for the project. We would also like to thank the staff of the two comparator sites for their support of the study. Steve Wright from the European Centre for Health Assets and Architecture (ECHAA) provided invaluable help on the capital cost data. Thank you also to Stephanie Waller, project administrator; Sarah Jane Besser, research associate, who supported the survey data analysis; Elizabeth Morrow, who supported literature reviewing; and the EPSRC HaCIRIC, which provided funding for phase 1 of the study, allowing us the ‘before’ data with which to compare our findings.
Finally, we are grateful to the following members of the Advisory Group for their advice on the study design and support along the way:
-
Ileana Alexandratos, Stantec Architects
-
Martin Allinson, Laing O’Rourke
-
Marie Batey, Hillingdon Hospital
-
Jennifer Bostock, lay member
-
Sally Brearley, lay member and visiting Senior Research Fellow in Patient and Public Involvement
-
Siobhan Callanan, Maidstone and Tunbridge Wells NHS Trust
-
Christine Chapman, lay member
-
Jackie Churchward-Cardiff, HCP Social Infrastructure (UK) Ltd
-
John de Pury, NHS Confederation
-
Robert Gregory, NHS South East Coast
-
Gavin Hailes, Laing O’Rourke
-
Jane Hendy, Surrey University
-
Keith Hurst, independent analyst
-
Liz Jones, Department of Health
-
Marjorie Kingston, North Bristol NHS Trust
-
Michael Phiri, University of Sheffield
-
Francesca Simoni, Stantec Architects
-
Sally Smith, Maidstone and Tunbridge Wells NHS Trust
-
Danielle Tucker, Imperial College London
-
Jonathan Wilson, Stantec Architects
-
other representatives of Maidstone and Tunbridge Wells NHS Trust.
Contributions of authors
Jill Maben (Director, National Nursing Research Unit), principal investigator, led the overall study design, managed the research associate and led and undertook data collection, analysis and final report writing.
Peter Griffiths (Professor of Health Services Research) contributed to overall study design, led the comparator study design and analysis, contributed to report writing and gave final approval of the manuscript.
Clarissa Penfold (Research Associate) contributed to overall study design, led and conducted data collection and analysis of case study qualitative data, contributed to report writing and gave final approval of the manuscript.
Michael Simon (Faculty Research Fellow) conducted data collection and analysis of comparator study, drafted that section of this report and gave final approval of the manuscript.
Elena Pizzo (Research Associate) worked with James Barlow on the design, analysis and write-up of the costing study, conducted data collection and analysis of cost data and gave final approval of the manuscript.
Janet Anderson (Senior Lecturer) contributed to overall study design, led the case study quantitative analysis and report write-up and gave final approval of the manuscript.
Glenn Robert (Professor of Healthcare Quality and Innovation) contributed to overall study design and report write-up and gave final approval of the manuscript.
Jane Hughes (Independent Researcher) undertook additional data analysis of case study qualitative data, contributed to report write-up and gave final approval of the manuscript.
Trevor Murrells (Statistician/Research Data Manager) contributed to overall study design, quantitative analysis and report write-up and gave final approval of the manuscript.
Sally Brearley (Visiting Senior Research Fellow in Patient and Public Involvement) contributed to overall study design and report write-up and gave final approval of the manuscript.
James Barlow (Chair in Technology and Innovation Management – Healthcare) contributed to overall study design, worked with Elena Pizzo on the cost study design, analysis and write-up, contributed to report writing and gave final approval of the manuscript.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Maben J, Penfold P, Glenn R, Griffiths P. Evaluating a Major Innovation in Hospital Design: Workforce Implications and Impact on Patient and Staff Experiences of All Single Room Hospital Accommodation 2012. www.kcl.ac.uk/nursing/research/nnru/publications/Reports/Single-Room-Hospital-Accomodation---HaCIRIC-Phase-1-Report---June-2012.pdf (accessed 9 January 2015).
- Hurst K. UK ward design: patient dependency, nursing workload, staffing and quality – an observational study. Int J Nurs Stud 2008;45:370-81. http://dx.doi.org/10.1016/j.ijnurstu.2006.09.007.
- Hutton J. NHS Hospitals. House of Commons Hansard 2004.
- Lawson B, Phiri M, Wells-Thorpe J. The Architectural Healthcare Environment and its Effects on Patient Health Outcomes: A Report on an NHS Estates Funded Research Project. London: The Stationery Office; 2003.
- Hignett S, Duffy V. Advances in Human Aspects of Healthcare. Boca Raton, FL: CRC Press; 2012.
- Hurst K. Do single rooms require more staff than other wards?. Nurs Stand 2009;24.
- Pennington H, Isles C. Should hospitals provide all patients with single rooms?. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f5695.
- Dowdeswell B, Erskine J, Heasman M. Hospital Ward Configuration Determinants Influencing Single Room Provision. NHS Estates England: European Health Property Network; 2004.
- Codinhoto R, Tzortzopoulos P, Kagioglou M. Effects of the Built Environment into Health Outcomes: Challenges in Building the Evidence Base 2008. www.haciric.org/library (accessed 9 January 2015).
- Sternberg E. Healing Spaces: The Science of Place and Well-being. Cambridge, MA: Belknap Press of Harvard University Press; 2009.
- Ulrich RS, Zimring C, Zhu X, DuBose J, Seo H-B, Choi Y-S, et al. A review of the research literature on evidence-based healthcare design. HERD 2008;1:61-125.
- Lawson B, Phiri M. Hospital design: room for improvement. Health Serv J 2000;110:24-7.
- Pattison HM, Roberston CE. The effect of ward design on the well-being of post-operative patients. J Adv Nurs 1996;23:820-6. http://dx.doi.org/10.1111/j.1365-2648.1996.tb00056.x.
- Ulrich RS. Visual landscapes and psychological well-being. Landscape Res 1979;4:17-23. http://dx.doi.org/10.1080/01426397908705892.
- Couper RTL, Hendy K, Lloyd N, Gray N, Williams S, Bates DJ. Traffic and noise in children’s wards. Med J Aus 1994;160:338-41.
- The Role of Hospital Design in the Recruitment, Retention and Performance of NHS Nurses in England. London: Commission for Architecture and the Built Environment (CABE); 2004.
- Reiling J, Hughes RG, Murphy MR, Hughes RG. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality (US); 2008.
- Ferguson T. Creating healing environments with evidence-based design. Occup Health Saf 2010;79:14-6.
- Joseph A, Ulrich R. Sound Control for Improved Outcomes in Healthcare Settings. Concord, CA: Center for Health Design; 2007.
- Joseph A. The Role of the Physical and Social Environment in Promoting Health, Safety, and Effectiveness in the Healthcare Workplace. Concord, CA: Center for Health Design; 2006.
- Malenbaum S, Keefe F, Williams A, Ulrich R, Somers T. Pain in its environmental context: implications for designing environments to enhance pain control. Pain 2008;134:241-4. http://dx.doi.org/10.1016/j.pain.2007.12.002.
- Arnolds I, Nickel S. Multi-period layout planning for hospital wards. Socio-Econ Plan Sci 2013;47:220-37. http://dx.doi.org/10.1016/j.seps.2013.02.001.
- Bate P, Mendel P, Robert G. Organising for Quality: The Improvement Journeys of Leading Hospitals in Europe and the United States. Oxford: Radcliffe Publishing; 2008.
- Are Women Getting the Birth Environment They Need?. London: National Childbirth Trust; 2005.
- Newburn M, Singh D. Creating a Better Birth Environment: An Audit Toolkit. London: National Childbirth Trust; 2003.
- Snow T. Planning the future of ward design. Nurs Stand 2008;23:12-3.
- Privacy and Dignity: A Report by the Chief Nursing Officer into Mixed Sex Accommodation in Hospitals. London: Department of Health; 2007.
- Public Perceptions of Privacy and Dignity. London: Department of Health; 2007.
- Lowson K, Kelly J, Bending M, Whitehead S, Wright D, Lowson P, et al. Cost-effectiveness of Hospital Design: Options to Improve Patient Safety and Wellbeing – Final Report. York: Health Economics Consortium; 2011.
- Moore A. NHS Single Rooms: Preferences and Privacy 2009. www.hsj.co.uk/resource-centre/nhs-single-rooms-preferences-and-privacy/1982526.article (accessed 9 February 2015).
- Loveday HP, Wilson JA, Pratt RJ, Golsorkhi M, Tingle A, Bak A, et al. National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2014;86:S1-S70. http://dx.doi.org/10.1016/S0195-6701(13)60012-2.
- Ulrich RS, Zimring C, Zhu X, DuBose J, Seo HB, Choi YS, et al. A review of the research literature on evidence-based healthcare design. HERD 2008;1:61-125.
- Sydnor ER, Perl TM. Hospital epidemiology and infection control in acute-care settings. Clin Microbiol Rev 2011;24:141-73. http://dx.doi.org/10.1128/CMR.00027-10.
- Tobari ET. The Influence of Design on Staffing Performance. Paper Presented at ‘Bevan Ward: Generating New Knowledge?’ 2008.
- Trant K. Ward design must not be restricted to single rooms. Nurs Times 2010;106.
- Progress in Making NHS Efficiency Savings, 2011–2012. London: Department of Health; 2013.
- Mooney H. Single rooms: a blueprint for better care?. Nurs Times 2008;104:14-6.
- Young P, Yarandipour R. Examining the case for single rooms. Health Estate 2007;61:85-6.
- Chaudhury H, Mahmood A, Valente M. Advantages and disadvantages of single- versus multiple-occupancy rooms in acute care environments: a review and analysis of the literature. Environ Behav 2005;37:760-86. http://dx.doi.org/10.1177/0013916504272658.
- Persson E, Määttä S. To provide care and be cared for in a multiple-bed hospital room. Scand J Caring Sci 2012;26:663-70. http://dx.doi.org/10.1111/j.1471-6712.2012.00976.x.
- Okeke J, Daniel J, Naseem A, Ramakrishna S, Singh I. Impact of all single rooms with ensuite facility in an acute care hospital in Wales (UK). Age Ageing 2013;42:iii1-11.
- Hutton A. Issues in clinical nursing: consumer perspectives in adolescent ward design. J Clin Nurs Inq 2005;14:537-45. http://dx.doi.org/10.1111/j.1365-2702.2004.01106.x.
- van de Glind I, van Dulmen S, Goossensen A. Physician–patient communication in single-bedded versus four-bedded hospital rooms. Patient Educ Couns 2008;73:215-19. http://dx.doi.org/10.1016/j.pec.2008.07.004.
- Roode S, Goossensen A. Do patients in hospitals benefit from single rooms? A literature review. Health Policy 2007;84:153-61. http://dx.doi.org/10.1016/j.healthpol.2007.06.002.
- van Kleef E, Robotham JV, Jit M, Deeny SD, Edmunds WJ. Modelling the transmission of healthcare associated infections: a systematic review. BMC Infect Dis 2013;13. http://dx.doi.org/10.1186/1471-2334-13-294.
- Gaudart J, Cloutman-Green E, Guillas S, D’Arcy N, Hartley J, Gant V, et al. Healthcare environments and spatial variability of healthcare associated infection risk: cross-sectional surveys. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0076249.
- Stockley JM, Constantine CE, Orr KE. Association of Medical Microbiologists’ New Hospital Developments Project Group . Building new hospitals: a UK infection control perspective. J Hosp Infect 2006;62:285-99. http://dx.doi.org/10.1016/j.jhin.2005.03.015.
- Zimring C, Joseph A, Choudhary R. The Role of the Physical Environment in the Hospital of the 21st Century: A Once-in-a-Lifetime Opportunity 2004.
- Griffiths P, Renz A, Hughes J, Rafferty AM. Impact of organisation and management factors on infection control in hospitals: a scoping review. J Hosp Infect 2009;73:1-14. http://dx.doi.org/10.1016/j.jhin.2009.05.003.
- Santiano N, Caldwell J, Ryan E, Smuts A, Schmidt HM. Knowledge and understanding of patients and health care workers about multi-resistant organisms. Healthcare Infect 2014;19:45-52. http://dx.doi.org/10.1071/HI13027.
- Morrow E, Griffiths P, Rao GG, Flaxman D. ‘Somebody else’s problem?’ Staff perceptions of the sources and control of methicillin-resistant Staphylococcus aureus. Am J Infect Control 2011;39:284-91. http://dx.doi.org/10.1016/j.ajic.2010.06.018.
- National Nursing Research Unit . Does ‘Cohort Nursing’ Help Control Healthcare Acquired Infection? 2007. www.kcl.ac.uk/nursing/research/nnru/policy/Policy-Plus-Issues-by-Theme/hownursingcareisdelivered/PolicyIssue4.pdf (accessed 9 February 2015).
- Dettenkofer M, Seegers S, Antes G, Motschall E, Schumacher M, Daschner F. Does the architecture of hospital facilities influence nosocomial infection rates? A systematic review. Infect Control Hosp Epidemiol 2004;25:21-5. http://dx.doi.org/10.1086/502286.
- Whitehead S, Bending M, Lowson K, Saxby R, Duffy S. Cost-effectiveness of Hospital Design: Options to Improve Patient Safety and Wellbeing. York: Health Economics Consortium (YHEC); 2011.
- Rosenblum S. Single Family Room Care: Before and After Data 2005.
- Ben-Abraham R, Keller N, Szold O, Vardi A, Weinberg M, Barzilay Z, et al. Do isolation rooms reduce the rate of nosocomial infections in the pediatric intensive care unit?. J Crit Care 2002;17:176-80. http://dx.doi.org/10.1053/jcrc.2002.35809.
- Bracco D, Dubois M-J, Bouali R, Eggimann P. Single rooms may help to prevent nosocomial bloodstream infection and cross-transmission of methicillin-resistant Staphylococcus aureus in intensive care units. Intensive Care Med 2007;33:836-40. http://dx.doi.org/10.1007/s00134-007-0559-5.
- Cheng V, Tai J, Chan W, Lau E, Chan J, To K, et al. Sequential introduction of single room isolation and hand hygiene campaign in the control of methicillin-resistant Staphylococcus aureus in intensive care unit. BMC Infect Dis 2010;10. http://dx.doi.org/10.1186/1471-2334-10-263.
- Bonizzoli M, Bigazzi E, Peduto C, Tucci V, Zagli G, Pecile P, et al. Microbiological survey following the conversion from a bay-room to single-room intensive care unit design. J Hosp Infect 2011;77:84-6.
- Teltsch DY, Hanley J, Loo V, Goldberg P, Gursahaney A, Buckeridge DL. Infection acquisition following intensive care unit room privatization. Arch Intern Med 2011;171:32-8. http://dx.doi.org/10.1001/archinternmed.2010.469.
- Whitehead S, Bending M, Lowson K, Saxby R, Duffy S. Cost-Effectiveness of Hospital Design: Options to Improve Patient Safety and Wellbeing. Systematic Literature Review of Single Rooms. York: Health Economics Consortium; 2010.
- Davis GS, Sevdalis N, Drumright LN. Spatial and temporal analyses to investigate infectious disease transmission within healthcare settings. J Hosp Infect 2014;86:227-43. http://dx.doi.org/10.1016/j.jhin.2014.01.010.
- Singh I, Okeke J. Risk of inpatient falls is increased with single rooms. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f6344.
- Bernhardt J, Cumming T. The elephant in the single room debate: keeping patients active. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f6333.
- Bernhardt J, Dewey H, Thrift A, Donnan G. Inactive and alone: physical activity within the first 14 days of acute stroke unit care. Stroke 2004;35:1005-9. http://dx.doi.org/10.1161/01.STR.0000120727.40792.40.
- Levitt G. Infection control for MRSA in a psychiatric hospital. Gen Hosp Psychiatry 2014;36:422-4. http://dx.doi.org/10.1016/j.genhosppsych.2014.02.005.
- Abad C, Fearday A, Safdar N. Adverse effects of isolation in hospitalised patients: a systematic review. J Hosp Infect 2010;76:97-102. http://dx.doi.org/10.1016/j.jhin.2010.04.027.
- Larsen L, Larsen B, Birkelund R. A companionship between strangers: the hospital environment as a challenge in patient–patient interaction in oncology wards. J Adv Nurs 2013;70:395-404. http://dx.doi.org/10.1111/jan.12204.
- Morgan H. Single and shared accommodation for young patients in hospital: Helen Morgan considers the importance of designing hospital units that ensure patient safety and security without limiting the opportunity for socialisation. Paediatr Care 2010;22:20-4. http://dx.doi.org/10.7748/paed2010.10.22.8.20.c7997.
- White R. Designing environments for developmental care. Clin Perinatol 2011;38:745-9. http://dx.doi.org/10.1016/j.clp.2011.08.012.
- Cone S, Short S, Gutcher G. From ‘baby barn’ to the ‘single family room designed NICU’: a report of staff perceptions one year post occupancy. Newborn Infant Nurs Rev 2010;10:97-103. http://dx.doi.org/10.1053/j.nainr.2010.03.002.
- Mammen J, Laude C, Costello B. Relational sustainability: environments for long-term critical care patients. Crit Care Nurs Q 2014;37:53-66. http://dx.doi.org/10.1097/CNQ.0000000000000005.
- Brereton L, Gardiner C, Gott M, Ingleton C, Barnes S, Carroll C. The hospital environment for end of life care of older adults and their families: an integrative review. J Adv Nurs 2011;68:981-93. http://dx.doi.org/10.1111/j.1365-2648.2011.05900.x.
- Gill L, White L. A critical review of patient satisfaction. Leaders Health Serv 2009;22:8-19.
- Naidu A. Factors affecting patient satisfaction and healthcare quality. Int J Health Care Qual Assur 2009;22:366-81. http://dx.doi.org/10.1108/09526860910964834.
- Hendrich A, Chow M. Maximising the Impact of Nursing Care Quality: A Closer Look at the Hospital Work Environment and the Nurses Impact on Care Quality. Martinez, CA: The Center for Health Design; 2008.
- Maguire D, Burger K, O’Donnell P, Parnell L. Clinician perceptions of a changing hospital environment. Health Environ Res Des J 2013;6:69-7.
- Fay D, Borrill C, Amir Z, Haward R, West MA. Getting the most out of multidisciplinary teams: a multi-sample study of team innovation in health care. J Occup Organ Psychol 2006;79:553-67. http://dx.doi.org/10.1348/096317905X72128.
- Borrill C, West M, Shapiro D, Rees A. Team working and effectiveness in health care. Br J Healthcare Manag 2000;6:364-71. http://dx.doi.org/10.12968/bjhc.2000.6.8.19300.
- Ferns T. Violence, aggression and physical assault in healthcare settings. Nurs Stand 2006;21:42-6. http://dx.doi.org/10.7748/ns2006.12.21.13.42.c6389.
- Hollinworth H, Clark C, Harland R, Johnson L, Partington G. Understanding the arousal of anger: a patient-centred approach. Nurs Stand 2005;19:41-7. http://dx.doi.org/10.7748/ns2005.05.19.37.41.c3875.
- Ward Layouts with Single Rooms and Space for Flexibility. London: The Stationery Office; 2005.
- Harrison S. Single rooms boost morale. Nurs Stand 2005;19.
- Adamson D. The Use of Single Patient Rooms Vs. Multiple Occupancy Rooms in Acute Care Environments: Comparative First Cost Analysis of Single and Multiple Occupancy Patient Rooms 2003.
- Sadler BL, Berry LL, Guenther R, Hamilton DK, Hessle FA, Merritt C, et al. Fable hospital 2.0: the business case for building better health care facilities. Hastings Cent Rep 2011;41:13-2.
- van de Glind I, de Roode S, Goossensen A. Do patients in hospitals benefit from single rooms? A literature review. Health Policy 2007;84:153-61. http://dx.doi.org/10.1016/j.healthpol.2007.06.002.
- Jones R. Factors determining the need for single room accommodation in hospital. Br J Healthcare Manag 2011;17:316-17. http://dx.doi.org/10.12968/bjhc.2011.17.7.316.
- Jones R. Hospital bed occupancy demystified and why hospitals of different size and complexity must operate at different average occupancy. Br J Healthcare Manag 2011;17:242-8. http://dx.doi.org/10.12968/bjhc.2011.17.6.242.
- Redfern S, Christian S, Norman I. Evaluating change in health care practice: lessons from three studies. J Eval Clin Pract 2003;9:239-49. http://dx.doi.org/10.1046/j.1365-2753.2003.00387.x.
- Greenhalgh T, Humphrey C, Hughes J, MacFarlane F, Butler C, Pawson R. How do you modernise a health service? A realist evaluation of whole-scale transformation in London. Milbank Q 2009;87:391-416. http://dx.doi.org/10.1111/j.1468-0009.2009.00562.x.
- Rycroft-Malone J, Fontenla M, Bick D, Seers K. A realistic evaluation: the case of protocol-based care. I. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-38.
- Marchal B, van Belle S, van Olmen J, Hoerée T, Kegels G. Is realist evaluation keeping its promise? A review of published empirical studies in the field of health systems research. Evaluation 2012;18:192-21. http://dx.doi.org/10.1177/1356389012442444.
- Øvretveit J. How Does Context Affect Quality Improvement? Perspectives on Context: A Selection of Essays Considering the Role of Context in Successful Quality Improvement. London: Health Foundation; 2014.
- Westbrook J, Ampt A. Design, application and testing of the Work Observation Method by Activity Timing (WOMBAT) to measure clinicians’ patterns of work and communication. Int J Med Inform 2009;78:S25-S33. http://dx.doi.org/10.1016/j.ijmedinf.2008.09.003.
- Chaudhury H, Mahmood A, Valente M. Nurses’ perception of single-occupancy versus multioccupancy rooms in acute care environments: an exploratory comparative assessment. Appl Nurs Res 2006;19:118-25. http://dx.doi.org/10.1016/j.apnr.2005.06.002.
- West P, McDonagh S, Burke M, Trueman P. Evaluation of Hillingdon Hospital Single Rooms Pilot Site – Part 1: Final Literature Review and Final Report. London: Department of Health; 2010.
- France DJ, Throop P, Walczyk B, Allen L, Parekh AD, Parsons A, et al. Does patient-centered design guarantee patient safety? Using human factors engineering to find a balance between provider and patient needs. J Patient Saf 2005;1:145-53. http://dx.doi.org/10.1097/01.jps.0000191550.92042.36.
- Hutchinson A, Cooper KL, Dean JE, McIntosh A, Patterson M, Stride CB, et al. Use of a safety climate questionnaire in UK health care: factor structure, reliability and usability. Qual Saf Health Care 2006;15:347-53. http://dx.doi.org/10.1136/qshc.2005.016584.
- Hurworth R. The use of photo-interviewing: three examples from health evaluation and research. Eval J Australas 2005;4:52-6.
- Banks M. Visual Methods in Social Research. London: Sage; 2001.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analysing Qualitative Data. London: Routledge; 1994.
- Happ MB, Dabbs AD, Tate J, Hricik A, Erlen J. Exemplars of mixed methods data combination and analysis. Nurs Res 2006;55:S43-9. http://dx.doi.org/10.1097/00006199-200603001-00008.
- Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-experimental Designs for Generalized Causal Inference. Boston: Houghton Mifflin; 2001.
- ICD-10: International Statistical Classification of Diseases and Related Health Problems. Geneva: World Health Organization; 2004.
- Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130-9. http://dx.doi.org/10.1097/01.mlr.0000182534.19832.83.
- Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care 2003;12:458-64. http://dx.doi.org/10.1136/qhc.12.6.458.
- Ryan TP. Statistical Methods for Quality Improvement. Hoboken, NJ: Wiley; 2011.
- Griffiths P, Jones S, Maben J, Murrells T. State of the Art Metrics for Nursing: A Rapid Appraisal. London: National Nursing Research Unit, King’s College: London; 2008.
- Yousuf MI. Using experts’ opinions through Delphi technique. Pract Assess Res Eval 2007;12:1-8.
- Royal College of Nursing . Pay Rates 2011 2012 n.d. www.rcn.org.uk/support/pay_and_conditions/pay_rates_20112012 (accessed 3 December 2014).
- Curtis L. Unit Costs of Health and Social Care 2012 2012. www.pssru.ac.uk/project-pages/unit-costs/2012/ (accessed 3 December 2014).
- Pettigrew AM, Ferlie E, McKee L. Shaping Strategic Change: Making Change in Large Organizations – The Case of the National Health Service. London: Sage; 1992.
- Sussex Courier . Trust Boss Grilled on Birth Pains of Hospital 2012. www.courier.co.uk/Trust-boss-grilled-birth-pains-hospital/story-15255966-detail/story.html (accessed 9 February 2015).
- Ivy J. Higher education institution image: a correspondence analysis approach. Int J Educ Manag 2001;15:276-82. http://dx.doi.org/10.1108/09513540110401484.
- Garson D. Validity and Reliability. Asheboro, NC: Statistical Associates Publishing; 2013.
- Correspondence Analysis and Multidimensional Scaling Using PASW Categories. Chicago, IL: SPSS Inc; 2009.
- Goffman E. The Presentation of Self in Everyday Life. New York, NY: Doubleday; 1956.
- Huisman ERCM, Morales E, van Hoof J, Kort HSM. Healing environment: a review of the impact of physical environmental factors on users. Building Environ 2012;58:70-8. http://dx.doi.org/10.1016/j.buildenv.2012.06.016.
- Australian Government Productivity Commission . Public and Private Hospitals 2009.
- Whole Life Costing. London: Constructing Excellence; 2004.
- Hospital Financing in Seven Countries. Washington, DC: Office of Technology Assessment, U.S. Government Printing Office; 1995.
- Redeveloping the Royal Liverpool University Hospital. Liverpool: The Royal Liverpool & Broadgreen University Hospitals NHS Trust; 2009.
- Hood R, Husband D, Yu F. Recurrent Expenditure Requirements of Capital Projects Estimation for Budget Purposes. Washington, DC: The World Bank; 2002.
- Galley J, O’Riordan B. Guidance for Nurse Staffing in Critical Care. London: Royal College of Nursing; 2003.
- National Institute for Health and Care Excellence . Older Patients at High Risk of Hospital Falls 2013. www.nice.org.uk/newsroom/news/OlderPatientsHighRiskHospitalFalls.jsp (accessed 3 December 2014).
- Slips, Trips and Falls in Hospital. London: National Patient Safety Agency; 2007.
- Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med 2013;173:2039-46. http://dx.doi.org/10.1001/jamainternmed.2013.9763.
- Wojgani H, Kehsa C, Cloutman-Green E, Gray C, Gant V, Klein N. Hospital door handle design and their contamination with bacteria: a real life observational study. Are we pulling against closed doors?. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0040171.
- Ugboma I, Drahota AK, Higgins B, Severs M. Effect of bedroom size on falls in hospital: does one size fit all?. J Am Geriatr Soc 2011;59:153-4. http://dx.doi.org/10.1111/j.1532-5415.2011.03466.x.
- Shepley MM, Davies K. Nursing unit configuration and its relationship to noise and nurse walking behavior: an AIDS/HIV unit case study. AIA Acad J 2003;6:12-4.
- Hendrich A, Chow MP, Bafna S, Choudhary R, Yeonsook Heo Y, Skierczynski A. Unit-related factors that affect nursing time with patients: spatial analysis of the time and motion study. Health Environ Res Des J 2009;2:5-20.
- Ulrich R, Zimring C, Xiaobo Q, Anjali J, Choudhary R. Role of the Physical Environment in the Hospital of the 21st Century. Concord, CA: The Centre for Health Design; 2004.
- Thompson JD, Goldin G, Thompson JD, Goldin G. The Hospital: A Social and Architectural History. London: Yale University Press; 1975.
- Chaudhury H, Mahmood A, Valente M. The Use of Single Patient Rooms vs. Multiple Occupancy Rooms in Acute Care Environment: A Review and Analysis of the Literature. Vancouver, BC: Simon Fraser University; 2003.
- Delon GL, Smalley HE. Applications of the Nursing Unit Methodology 1970.
- Batchelor GJ, Esmond TH. Maintaining high quality patient care while controlling costs. Healthcare Financ Manag 1989;43:21-2.
- Yafchak R. A longitudinal study of economies of scale in the hospital industry. J Health Care Finance 2000;27:67-89.
- Smet M. Cost characteristics of hospitals. Soc Sci Med 2002;55:895-906. http://dx.doi.org/10.1016/S0277-9536(01)00237-4.
- Boardman AE, Forbes D. A benefit–cost analysis of private and semi-private hospital rooms. J Benefit–Cost Anal 2011;2:1-27.
- Preliminary Comparative Cost Study: One Bedroom versus Two-Bed Room Cost Comparison. Vancouver, BC: BTY Group; 2003.
- Harris DS, Shepley MM, White RD, Kolberg KJS, Harrell JW. The impact of single family room design on patients and caregivers: executive summary. Perinatology 2006;26:S38-48. http://dx.doi.org/10.1038/sj.jp.7211583.
- Bobrow M, Thomas J, Rea K. Building Type Basics for Healthcare Facilities. New York, NY: John Wiley & Sons; 2000.
- Paatela M. Modern Trends in Hospital Design in Finland 2000. http://www.paatela-arch.fi/main.html (accessed February 2014).
- Ulrich RS. Creating a Healing Environment With Evidence-Based Design 2003.
- Williams MA, Marbury SO. Innovations in Healthcare Design: Selected Presentations from the First Five Symposia on Healthcare Design. New York, NY: John Wiley & Sons; 1995.
- Hurst K. Do single rooms require more staff than other wards?. Nurs Stand 2009;24.
- Barlow G, Sachdev N, Nathwani D. The use of adult isolation facilities in a UK infectious diseases unit. J Hosp Infect 2002;50:127-32. http://dx.doi.org/10.1053/jhin.2001.1138.
- Silini E, Locasciulli A, Santoleri L, Gargantini L, Pinzello G, Montillo M, et al. Hepatitis C virus infection in a hematology ward: evidence for nosocomial transmission and impact on hematologic disease outcome. Haematologica 2002;87:1200-8.
- Montecalvo MA, Jarvis WR, Uman J, Shay DK, Petrullo C, Horowitz HW, et al. Costs and savings associated with infection control measures that reduced transmission of vancomycin-resistant enterococci in an endemic setting. Infect Control Hosp Epidemiol 2001;22:437-42. http://dx.doi.org/10.1086/501931.
- McManus AT, Mason AD, McManus WF, Pruitt BA. A decade of reduced gram-negative infections and mortality associated with improved isolation of burned patients. Arch Surg 1994;129:1306-9. http://dx.doi.org/10.1001/archsurg.1994.01420360096013.
- Heddema ER, van Benthem BHB. Decline in incidence of Clostridium difficile infection after relocation to a new hospital building with single rooms. J Hosp Infect 2011;79:93-4. http://dx.doi.org/10.1016/j.jhin.2011.03.028.
- Bettin K, Kolb S, Clabots C, Gerding D. Frequency of introduction and acquisition of Clostridium-Difficile (Cd) by patients in private versus multibed rooms. Clin Res 1990;38.
- Thompson JT, Meredith JW, Molnar JA. The effect of burn nursing units on burn wound infections. J Burn Care Rehabil 2002;23:281-6. http://dx.doi.org/10.1097/00004630-200207000-00011.
- Cepeda JA, Whitehouse T, Cooper B, Hails J, Jones K, Kwaku F, et al. Isolation of patients in single rooms or cohorts to reduce spread of MRSA in intensive-care units: prospective two-centre study. Lancet 2005;365:295-304. http://dx.doi.org/10.1016/S0140-6736(05)17783-6.
- Duffin C. Private rooms in hospital ‘would hasten recovery’. Nurs Stand 2002;16.
- Gallant D, Lanning K. Streamlining patient care processes through flexible room and equipment design. Crit Care Nurs Q 2001;24:59-76. http://dx.doi.org/10.1097/00002727-200111000-00006.
- Williams B, Rago K, Gamberg P. Impact of discontinuing isolation after heart transplantation. J Transplant Coordination 1995;5:31-4.
- Hendrich A, Nyhuis A, Kippenbrock T, Soja ME. Hospital falls: development of a predictive model for clinical practice. Appl Nurs Res 1995;8:129-39. http://dx.doi.org/10.1016/S0897-1897(95)80592-3.
- Flaherty JH, Tariq SH, Raghavan S, Bakshi S, Moinuddin A, Morley JE. A model for managing delirious older inpatients. J Am Geriatr Soc 2003;51:1031-5. http://dx.doi.org/10.1046/j.1365-2389.2003.51320.x.
- The Patient Room of the Future. Batesville, IN: Hill Rom Publications; 2002.
- Evaluation of Single Room Ward at Hillingdon Hospital: Literature Review. York: University of York; 2010.
- Maki DG, Alvarado CJ, Hassemen CA, Zilz MA. Relation of the inaminate environment to endemic nosocomial infection. N Engl J Med 1982;307:1562-6. http://dx.doi.org/10.1056/NEJM198212163072507.
- Shepley MM. Predesign and postoccupancy analysis of staff behavior in a neonatal intensive care unit. Child Health Care 2002;31:237-53. http://dx.doi.org/10.1207/S15326888CHC3103_5.
- Hilton BA . Res Nurs Health 1985;8:283-91.
- Velarde N, Gunsalus KC, Piano F. Diverse roles of actin in C. elegans early embryogenesis. BMC Dev Biol 2007;7. http://dx.doi.org/10.1186/1471-213X-7-142.
- Phiri M. Does the Physical Environment Affect Staff and Patient Health Outcomes: A Review of Studies and Articles 1965–2005. London: The Stationery Office; 2006.
- Brand CA, Sundararajan V. A 10-year cohort study of the burden and risk of in-hospital falls and fractures using routinely collected hospital data. Qual Saf Health Care 2010;19. http://dx.doi.org/10.1136/qshc.2009.038273.
Appendix 1 Health economics literature review
Introduction
We carried out a scoping review of existing research on the economic impact of a single bedroom design in terms of building costs, staff costs and outcomes, to summarise the evidence between December 2012 and April 2013. We also undertook interviews to collect expert opinions where the evidence from the literature was not available or not clear.
The literature indicates that evidence on the effect of a single room hospital is ambiguous. It is not possible to say with certainty whether or not the single room design has an impact on infection rates, LOS, patient satisfaction and other outcomes and costs. The main studies have been conducted in the USA and the results are difficult to generalise, so there is a lack of evidence in UK settings.
A systematic literature review of single room hospitals was conducted by Whitehead et al. ,61 to investigate whether or not hospital design contributes to improving patients’ outcomes and influences their recovery, and to understand the impact of room design on infection rates, LOS, adverse events, medication errors, patient satisfaction and costs. The results show that excluding medication errors, which tend to decrease in single rooms compared with multioccupancy rooms, there is no unique effect of single rooms on all other outcomes and costs. Another literature review86 concluded that single rooms have a moderate effect on patients’ satisfaction with care, noise, quality of sleep, privacy and dignity, but the impact on hospital infection rates is not clear and there is no evidence on LOS or safety. A literature search conducted by Ulrich and Zimring132 found a relatively small number of robust articles (out of approximately 600 articles reviewed) that related building design to patient safety.
Research question
The main research question was: how does the design of the hospital (specifically a single room environment) impact on costs and outcomes for the hospital and patients? This review sought to identify the effectiveness evidence, economic evidence and cost of different design options. This evidence was then used to provide data for an assessment of changes in capital and operational costs associated with an all single room hospital and one with 50% single rooms compared with a ward-based design.
Selection of studies
The following databases were searched: MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Health Management Information Consortium (HMIC), Cochrane Database of Systematic Reviews (CDSR), PsycINFO, the American Economic Association’s electronic bibliography (EconLIT) and Sociological Abstract. Searches were initially taken to identify studies concerned with the impact of single rooms in general terms, using as main research criteria ‘single rooms’ and ‘building design’. Studies were selected if directly related to ‘single rooms’ or ‘room design’, including one or more of the outcomes ‘infection rates’, ‘length of stay’, ‘adverse events’, ‘medication errors’, ‘patient satisfaction’ and ‘cost data’.
This review was undertaken at the beginning of the study and the time frame 1980–2012 was chosen for the search, as earlier studies were difficult to access and less relevant as conditions and expectations have changed. Of more than 200 papers, 38 papers were included in the review.
Highlights from the literature review
Some significant claims are made for the benefits of single rooms in these studies, but many are small scale and not robustly designed. Moreover, the results are specific to particular institutions studied or settings, such as US hospitals, and may be difficult to generalise. Early studies include those of Thomas and Goldin in 1975133 (cited by Chaudhury et al. 134) and Delon and Smalley. 135 Thomas and Goldin argued that multiple-occupancy rooms were the most efficient in economic terms, as patients can be placed along one corridor to be supervised, reducing nurse travelling time. According to Delon and Smalley,135 nursing costs associated with time spent walking increase proportionally as the number of patients in rooms decreases, and are higher in single room hospitals.
Construction costs
The review revealed that there are very few papers that address the relationship between hospital’s construction cost or operating costs and room occupancy. Most articles on hospital expenditure dealt with overall capital or operating cost and methods of cost reduction in hospital construction. 136–138
Despite a high variability in terms of space and hospital design building, there are standards for the minimum space required per single bedroom. In general, a private room requires more space than a single bed in a semiprivate room (around 40.51 m2 vs. 26.66 m2) according to a Canadian study. 139 To obtain extra space the hospital needs more land or to extend itself in a higher number of floors. In both cases there is a higher overall development cost that will depend on whether or not the new hospital is being built on land already owned by the hospital and, if not, on the local land market.
Construction costs will also vary according to local market and site conditions. Harrison83 found that the cost of building a hospital with single rooms is on average 6% higher than a traditional one. However, while total hospital construction costs include many elements such as the exterior shell, interior, functional equipment, mechanical, electrical and plumbing costs, different studies incorporate different costs, making comparison hard. Costs will vary according to room attributes such as size of windows, type of floor material, walls and ceilings.
The general assumption has been that the cost per square metre of a single room is higher than a multiple occupancy ward, especially if it includes a private bathroom. Adamson84 found that costs of construction per patient are 48% higher for single rooms (US$182,400 compared with $122,550 per patient). Other research from the same period also found higher costs for single rooms. 140,141 In the UK, the cost per bed in one planned hospital was about 14% higher for an all single room hospital than for one with 50% single rooms (£66,333 per bed for 100% single rooms and £58,324 for 50% single rooms). 82 However, it is not clear what the basis of the cost is and what is included or not.
Maintenance costs
Hospital rooms are subject to minor refurbishing and maintenance, such as new fixtures, flooring, wall coverings and furniture every 10 years. According to our expert interviews, these costs are generally 10% of construction costs. The literature does not mention any difference in maintenance costs between a multiple occupancy and a single room hospital, as this partly depends on the speed of patients’ turnover in a hospital.
Operating costs
Operating costs account for over 70% of the hospital overall costs and are usually the same as capital cost within the first 3 years after construction. 142,143 Hardly any research addresses how patient room design affects hospital expenditure in terms of costs. According to some authors operating costs are reduced in single rooms compared with multioccupancy rooms because of a reduction in labour costs and patient transfers within the hospital, as well as higher bed occupancy rates. These authors argue that, even with higher costs of construction, furniture, maintenance, housekeeping, energy and nursing, single rooms can match the per diem cost of multibedded rooms because of the higher occupancy rate. 142,144 They also argue there are operating cost reductions due to lower patient transfer costs.
Housekeeping costs vary from hospital to hospital according to space, utilities costs, staff capacity and staff cost. There is very little in the research literature on cleaning costs in single room hospitals versus multiple occupancy wards. In a study conducted by the University of York in 2010, cleaning costs were expected to rise by as much as 75% in single rooms because of the increase in floor area, the larger number of bathrooms to be cleaned, more doors and windows, and more furniture in the rooms. 61
Staffing costs
There is little evidence on the impact of single rooms on staffing costs. One study reports that nursing care costs in single rooms are almost double those in shared rooms (US$8430 for patients in single rooms and $4265 for multibedded rooms). 145 However, in another study, moving from multiple occupancy to single rooms was reported to increase ward staffing by only 2–4%61 and the results may reflect the approach to allocation of staff rather than nursing needs. In general, single rooms may require more staff than other wards146 and, because of longer distances travelled, beds in single rooms require around 20 minutes more nursing time per day. 139
Infection control
One of the main methods recommended for infection control in hospital is isolation. Barlow et al. 147 found that, in a multibedded bay, 7.5% of patients had infections in acute and medical wards in the UK. Isolation is possible through confinement of the patient in a single room with suitable ventilation systems. 134,144 Single rooms are recommended for patients suffering from staphylococcal pneumonia, skin lesions or MRSA, as they carry organisms that can lead to environmental contamination. Isolation is also recommended as a preventative measure for hepatitis C148 and vancomycin-resistant enterococci. 149
Over half of the studies included in this review reported data on infection rates for different room designs. Some report a significant decrease of infection rates in single rooms compared with multiple occupancy rooms. A 20% reduction in costs associated with infection was reported by Sadler et al. 85 In a case– control study of 78 patients in open space and 115 in single rooms in Israel meeting almost all National Institute for Health and Care Excellence (NICE) methodology criteria, the mean number of infections per child was 1.87 in isolation rooms compared with 3.62 in multiple bedrooms. 56 In a study based on expert opinions, meeting some of the NICE criteria, Harrison83 found an 11% decrease in hospital-acquired infection when a US hospital moved to a new single room building. A reduction in hospital-acquired infection, from 17.7% to 5.9%, was also registered in a small neonatal ICU moving from an open design to single rooms,56 although this study could not be assessed for quality. Similar results were found in a large retrospective cohort study of 2519 burns patients, which reported that the incidence of gram-negative bacteraemia was 31.2% in open wards and 12% in single rooms. 150 A decline in incidence of C. diff. infection after relocation to a new hospital building with single rooms was reported by Heddema and van Benthem. 151 A reduction of nosocomial bloodstream infection and cross-transmission of MRSA was reported in single room designs for ICUs. 57
A few studies report an increase of infections in single rooms. In a limited case–control study of patients admitted to a surgical ward, the acquisition of C. diff. was 9.9% for patients in single rooms, compared with 1.9% in four-bed rooms. 152 A retrospective study, fulfilling some NICE criteria,153 shows that the rate of infections for burns patients increased from 10.8% to 47.1% during the renovation of a hospital from multiple to single rooms, and was still significantly higher after the renovation (23.8%). It is not clear, however, why this might be the case and whether single rooms were directly causal or some other disruptions to work patterns may have been the cause. Finally, Cepeda et al. 154 show that moving MRSA-positive patients into single rooms or bays does not reduce cross-infection. Moreover, because transfer and isolation of critically ill patients in single rooms carries potential risks, they argue that the findings suggest that re-evaluation of isolation policies is required in ICUs where MRSA is endemic.
Length of stay
Studies have demonstrated that using single rooms has the potential to reduce length of patients stay in hospital,144 possibly thanks to the effect of better consultations and treatment, better sleep and fewer adverse events on patient recovery. 155 Some of this work has claimed very large falls in LOS. In a non-empirical study, Gallant and Lanning156 claim that patients remaining in one single acuity-adaptable room throughout their stay tended to recover faster, with patient stay in a hospital in California reduced from 9.5 to 5.4 days in five diagnostic diagnosis-related groups. Ben-Abraham et al. 56 found the LOS to be lower for patients in isolation rooms in a paediatric ICU: an average of 11 days for patients in single rooms compared with 25 days for those in six-bed units.
Other studies have made more modest claims. For example, Sadler et al. 85 suggested that design features appeared to contribute to a 10% reduction in LOS. A lower difference was registered in patients in neonatal intensive care unit (NICU) single rooms with a LOS of 36.2 days instead of 38.3 in open NICU. 56 Thompson et al. ,153 in a good-quality retrospective study, found the LOS of burns patients was similar for the periods before, during and after the renovation of the burns isolation units to single room accommodation. A retrospective study meeting almost all quality criteria found heart transplant patients had longer stays if treated in a single room (9.5 days) than in ward-based accommodation (6.1 days). 157 Similar findings were reported for surgical ward patients (9.6 vs. 7.6 days),155 although the methodology was less robust in this study.
Patient falls
Falls often occur when patients are alone and attempting to go to the bathroom,158 but patient characteristics are also a critical influence on the occurrence of falls, so the evidence is hard to interpret. Older, frail or delirious patients and males, generally with a longer LOS, are more likely to experience adverse events. 134 For these reasons, it has been suggested that multioccupancy rooms with increased surveillance may be more appropriate than single rooms for those patients who require constant supervision and who are more likely to fall in hospital. 134 A study on delirious elderly patients (who are highly susceptible to falling) shows that patients have fewer falls in multioccupancy rooms than in a single room. 159
There are also important factors that can reduce the risk of falls, including greater monitoring by staff members or family members. 158 Private room designs that support the presence of family members are said to reduce the incidence of patient falls,144 as well as environmental factors such as supports, reduced clutter and trip hazards that might be better managed in single rooms. Sadler et al. 85 suggest that design features may help to reduce falls by one-third, but it is not clear how much is attributable to single room design.
Adverse events and medication errors
One study reports that 40% of nursing staff stated that the likelihood of medication errors was high or very high in multibedded rooms, compared with 10% for single rooms. 134 Research conducted by NHS Estates in 2005 shows that medication errors fell by 67% after a coronary ICU was moved from two-bedded to single rooms. 82
Transfer costs
Studies suggest that there are more patient transfers from multioccupancy rooms than from single rooms. 160 Patient transfers within the hospital from one ward to another can result from many factors, including the need for privacy, disruptive patients and infection control issues. 139 The transfer time from a critical care room to a patient room is approximately 7 person-hours, so the provision of a single acuity-adaptable care room reducing the need to move a patient may lead to a reduction in costs. 142,156 In a US study conducted in a new hospital with 348 single rooms, there was a reduction of US$500,000 per year in transfer costs compared with the old multiple occupancy hospital. 144
Conclusions
The literature review indicated that evidence on the impact of single rooms is mixed. There are many claims for the benefits, but it is not possible to say with certainty that single rooms have a positive impact on factors such as infection rates and LOS. Many studies are small scale, contextually specific or poorly designed, so it is not possible to establish whether the effects claimed are attributable to room design or other factors are at play. Moreover, as they refer to other settings (mainly in the USA), it is difficult to translate the findings directly to the UK context.
We also interviewed a number of expert informants involved in the design, procurement and construction of new hospital facilities in the UK to seek up-to-date opinions on the differences in construction, maintenance and operating costs. Their conclusions are summarised in Table 69.
| Cost item | Single room | Multiple occupancy room | References |
|---|---|---|---|
| Land costs | (=) not a big difference between SB and MB | (=) not a big difference between SB and MB | (–) Expert opinion, 2012: there might be a land saving because old buildings were generally built in more than one block, whereas now they tend to build in a compact building with more floors. (+) Expert opinion, 2012: costs increase if foundations need to be heavier |
| Exterior building cost | (=) not a big difference | (=) not a big difference | (=) Expert opinion, 2012: there is little difference in the exterior building costs of hospitals with single rooms or multibedded rooms |
| Interior building costs | (+) more walls; (+) more doors; (+) if the building develops on more floors there might be an increasing cost, but the difference is not relevant; (–) some treatment rooms may not be necessary if the patient can be treated in bedroom | (–) less space required | (+, =) Expert opinion: interior building costs may be more expensive in terms of walls and doors. If the building has more floors there might be a difference in costs, but this is marginal and can be disregarded. Some treatment rooms may no longer be necessary if the treatments can be done in the room In terms of construction costs to build new rooms, there might be an increase in costs due to the number of walls, windows, pipes, connections and pieces of equipment |
| Construction costs for corridors | (+) more space required | (–) less space required | (+, =) Expert opinion: construction costs for corridors may be the same, although more space might be required in a hospital with single rooms |
| Construction costs to build new rooms | (+) higher costs to build walls, windows, equipment, pipes, connections | (–) lower costs and more shared items | (+) Adamson:84 cost for construction US$182,400 per patient for single rooms and $122,550 per patient for mixed rooms. (+) NHS estates:82 cost per bed for 100% single rooms was £66,333, and £58,324 for 50% single rooms. (+) Harrison:83 cost for building a hospital with single rooms is 6% higher than a traditional building, but can be recovered after 1 year |
| Construction costs to replace single bedrooms/mixed | (+) higher for single bedrooms | (–) lower | (+) BTY group:140 cost to replace single rooms with two-bed rooms US$153,000 per patient for single rooms; $134,000 for two-bedded rooms |
| Functional equipment | (+) equipment is required in each room | (–) some shared equipment | (+) Expert opinion: functional equipment and monitoring equipment cost may vary according to the hospital design |
| Monitoring equipment | (+) equipment is required in each room; ( = ) may vary according to building choices | (–) some shared | (+, =) Expert opinion |
| Acuity-adaptable rooms | (+) requires more space and more service | (–) | (+) Sadler et al.:85 inclusion of monitoring equipment within patient’s room increases investment in hospital infrastructure but reduces patients transfer; US$4500 per room |
| Windows | (+) more windows required; (+) larger windows are generally preferred because patients can see the ground and the sky outside (this can affect their health); beds need to be positioned in the right way | (–) one window every two or four beds; difficult to see outside if not close to window | (+) Sadler et al.:85 natural light and nature views are instrumental to patient’s recovery, US$750 per room to increase window size. (+) Expert opinion: larger windows are generally preferred because patients can see the ground and the sky outside (this can affect their health); beds need to be positioned in the right way. (–) Decreased cost of ventilation Window costs may rise because more windows are required; larger windows are preferred because patients can see the ground and the sky outside, with a positive impact on their well-being. In single rooms each patient can easily decide to open the window without affecting other patients, so the air quality is generally better and requires less mechanical ventilation. There is a standard regulation for ventilation and in single rooms mechanical ventilation is required even if there is a window. In bathrooms more mechanical ventilation is required |
| Bathrooms | (+) one bathroom for each room (the bathroom is the same in MB and SB but the number of bathrooms per patient is different) | (–) one bathroom shared every three or four patients | (+) Sadler et al.:85 increased costs for bathrooms with double door access US$12,800 per room. (+) Expert opinion: there is an increase in building costs for bathroom as the number of bathrooms per patient is higher. (+) Expert opinion: there is an increase in maintenance costs because the bathrooms need to be cleaned and water flow checked regularly The costs for bathrooms increase in a single room design, especially if each room has a private bathroom. The bathroom design is generally the same, but there is a higher overall cost due to the increased number of rooms and additional plumbing, pipes, connections and maintenance costs. In single rooms there is a higher need for hand basins and hand-rub dispensers in each room |
| Hoists; ceiling-mounted patient lift | (=) if each bed has one hoist there is not much difference between SB and MB; (+) if they are ceiling mounted there is an increase in costs, but not very high (around £1200 net cost per room) | (–) they are generally mobile and shared | (=, +) Expert opinion: the cost for hoists and ceiling-mounted lifts depends on the hospital design. If there are ceiling-mounted lifts in each room the cost will be around £1200 per room. (+) Sadler et al.:85 US$2,805,800 |
| Enhanced indoor air quality cost | (+) maybe requires more air conduct.; (=) there is a standard regulation for ventilation and SB needs to have mechanical ventilation even if there is a window; (+) more bathroom ventilation required; (–) less mechanical ventilation in use | (=) there is a minimum requirement of ventilation; (+) in MB there is more need of mechanical ventilation | (=, +, –) Expert opinion: (+) maybe requires more air conduct.; ( = ) there is a standard regulation for ventilation and SB needs to have mechanical ventilation even if there is a window; (+) more bathroom ventilation required; (–) less mechanical ventilation in use. (+) Sadler et al.:85 US$10,400 per unit |
| Decentralised nurse stations | (+) more stations (one main + two sub); should be positioned to allow the nurse to view the patient from a distance | (–) fewer stations | (=) Expert opinion: cost of nurse stations is not significantly greater. Generally with single room designs there is a main nurse station with two substations, which are positioned in a way that allows checking patients from a distance; should allow nurse to view patients’ head from a distance. (+) Sadler et al.:85 increased costs for decentralised substations for nurses US$1000 per station |
| Hand hygiene/washing basins | (+) one in each room | (–) shared | (+) Expert opinion: one in each room, included in bathroom costs; Sadler et al.:85 US$750/sink; $25 hand dispenser; $235,875 hand-washing sinks in 300 patient rooms, automated alcohol-based hand-rub dispenser at each bedside |
| Medication area task lighting | (=) if each room has its own light | (=) | (=) Expert opinion: medication area task lighting should not change as in each room there is light and it very much depends on the bed design |
| Noise-reducing costs | (=) regulations for noise reduction are the same for SB and MB; (–) noise should be reduced by more walls and more doors | (+) can be more expensive to try reducing noise in MB | (=) Expert opinion: regulations for noise reduction are the same for SB and MB; (–) noise should be reduced by more walls and more doors; in terms of noise reduction there are the same standard regulations for single and multibedded rooms, so there should not be a difference in costs. In single rooms the noise should be reduced by the presence of doors and walls |
| Electrical costs | (=) generally the same, as there are standard regulations; (+) increased to bring electricity in more bathrooms | (=) | (=) Expert opinion: generally the same, as there are standard regulations; (+) increased to bring electricity in more bathrooms |
| Light control | (=) if lights are bed embedded there is no much difference | (–) shared big lights; (–) more consumption in one MB room there is only one patient (or not fully utilised room) | (=) Expert opinion: if lights are bed embedded there is not much difference; there are standards regarding lighting and heating for both single and multibedded rooms. In single rooms there might be a higher cost to bring light in a higher number of bathrooms, but there is a more efficient use of heating as empty rooms do not need energy |
| Energy demand | (=) not a big difference; (–) it is possible to switch off heating in empty rooms; (+) more expensive to heat SB than MB | (+) not fully utilised rooms can have a waste of energy | Expert opinion: (+) more expensive to heat SB than MB |
| Plumbing costs | (+) more bathrooms to be connected | (–) same pipes serve more patients | Expert opinion: (+) more bathrooms to be connected |
| Water demand | (+) more water required for maintenance of bathroom pipes | (–) shared bathrooms, less water demand | Expert opinion: (+) more water required for maintenance of bathroom pipes |
| TV | (=) if one for each patient, or (+) if there was a shared TV; (+) increased cost for lost/stolen remote controls | (–) more distraction from other patients | Expert opinion: (+) there is likely to be a TV screen in each single room and this can lead to increasing maintenance costs, and occasional loss of remote controls |
| Cleaning costs | (+) larger areas and more rooms and bathrooms to clean | (–) shared areas | Expert opinion: (+) the housekeeping manager of Maidstone Hospital was interviewed to gather information regarding the costs associated with maintenance and cleaning. The interview highlighted that cleaning costs are generally higher in single rooms than in multibedded rooms. The domestic cleaning labour cost per room per day is £7.88 for a standard clean and includes single bathrooms and associated areas. The domestic cleaning labour cost per bed area per day is £5.44 per room and incorporate the allocated costs for bathrooms and associated areas. York study161 |
| Housekeeping and operating costs (based on wards area) | (=) not a big difference in meal administration (sometimes the person bringing the food may also do other services, e.g. cleaning; not clear how this can impact) | (–) shorter distance walked | Expert opinion: the housekeeping manager of Maidstone Hospital was interviewed to gather information regarding the costs associated with housekeeping and the same applies for cleaning |
| Staff health-care provision | (+) longer distance travelled by nurse and doctors | (–) shorter distance travelled by nurse and doctors | (+) Williams et al.:145 higher nursing care costs for patients in single rooms ($8340) than in multibedded rooms (US$4265) for heart transplant |
| Maintenance costs (new fixture, flooring, wall coverings and furniture every 10 years) | (=) not a big difference between SB and MB; (+) in SB there is the need to keep things working even if the bed is empty or the patient is immobilised (toilet flush, shower) to avoid water stagnation or damage; (+) need to check the temperature of water in each bathroom | (–) less maintenance required | Expert opinion |
Summary
Construction costs and operating costs
Construction costs vary with the geographical setting and the design of the hospital. In general a single room requires more space (and a private bathroom) and this may need extra land or space, possibly at a higher cost.
Maintenance costs are the same and vary according to patient occupancy and throughput; the presence of a bathroom for each room may increase the maintenance and cleaning costs. Housekeeping costs may vary according to the space and the staff capacity, but they are expected to rise.
Ward staffing
Number of nursing staff may or may not rise, but the time for travelling and surveillance may increase, with an increase in costs.
Length of stay
Length of stay may decrease because patients appear to recover faster in single rooms. This may be because of better sleep, lower risk of adverse events and infections, and higher privacy leading to better management of patients. However, LOS might also increase because patients feel more comfortable and less inclined to press for discharge, or because of an increase in adverse events and falls.
Infection rates
The majority of the studies show a reduction in infection rates for single rooms,55,56,83,134,150,153 but there is also a study showing no differences162 and at least one study with higher infection rates in single rooms. 152 It is generally very difficult to control for confounding factors and it may be that in some cases infections decrease because of better ventilation systems, hand washing and other precautionary measures rather than isolation.
Falls
Falls are related to LOS and patient recovery time. Falls are generally expected to rise because of the reduced level of observation, from staff and other patients. Falls risk might be reduced by greater monitoring by family members, when present in single rooms.
Medication errors and costs
As medication errors and infection rates may fall in single room hospitals, associated costs may decrease too.
| Outcomes | Single room | Multiple occupancy room | Reference |
|---|---|---|---|
| Patient falls | (+) increases if patients are not sufficiently monitored; (–) in a single room the bathroom is inside and closer, so the probability of falling is decreased; (–) decreases if there is monitoring equipment in each room and if there are acuity-adaptable rooms, larger bathrooms, lifts; (+) may increase if the bathroom is closer because the patient is more confident and attempt to go to the toilet alone | (+) increased if bathrooms are not close to bed; (+) increased because patients need to move from bed to medication room; (–) other patients in the room can help and reduce the fall risk | (–) Expert opinion; Sadler et al.:85 falls are reduced in single rooms; Shepley;163 Ulrich and Zimring132 |
| Patient transfers | (–) reduced transfer to medication rooms, as medications can be done in room; (–) fewer transfers due to bad relationships with roommates | (+) more frequent | (–) Bobrow and Thomas:142 substantial reduction in transfer costs following a move from multibedded to single room hospital. An extra US$500,000 spent on patient transfers in the old hospital because of infection control issues or problems with other patients in shared rooms |
| Diagnostic and treatment service delay | (–) reduced delays if in each room there is monitoring equipment; (=) the same as MB | (+) more frequent | (–) Sadler et al.:85 reduced if the monitoring equipment is in the room |
| Adverse drug event/medication errors | (–) less frequent | (+) more frequent in wards where there are more patients all together | (–) Chaudhury et al.:95,134 probability of medication errors is generally higher in double occupancy rooms than in single rooms. (–) NHS estates:82 medication errors decrease by from 90% to 67% moving to a single room |
| Acquired infections | (–) less frequent as patients are more isolated | (+) more frequent in wards where there are more patients all together, especially in certain wards | (–) Barlow et al.:147 in open-bay bed, 7.5% of patients had infections. (–) Ben-Abraham et al.:56 lower infection rates in child in isolation rooms than in open six-bed space. (–) Harrison:83 reduction in hospital-acquired infection by 11% moving to single rooms. (–) Rosenblum:56 reduction in hospital-acquired infections moving from an open design to single rooms. (–) McManus:150 single bed isolation associated with reduction in infection in comparison with open ward. (–) Chaudhury et al.:134 lower infection rates in single rooms. (=) Maki et al.:162 insignificant difference in nosocomial infections. (+) Thompson:153 higher infection rates of 47.1% in single rooms compared with 10.8–20.8% in multibedded rooms; (+) Bettin et al.:152 higher C. diff. acquisition (9.9%) in single rooms than in multibedded rooms (5.8% in two-bed rooms and 1.9% in four-bed rooms) |
| Length of stay | (–) room design should help patient to recover early | (+) longer LOS | (–) Ben-Abraham et al.:56 lower LOS for patients in single rooms in paediatric ICU (11 days in single room, 25 days in six-bed room). (–) Rosenblum:56 shorter LOS in NICU single rooms (36.2 days) than in open NICU (38.3 days). (=) Thompson et al.:153 no significant difference in LOS between single and multibedded rooms. (+) Williams:157 higher LOS for transplanted patients in single room (9.5 days) than in shared rooms (6.1 days). (+) Bettin et al.:152 higher LOS for surgical ward patients in single bedrooms (12.2 days) than in two-bed rooms (9.6 days) or four-bed rooms (7.6 days)86 |
| Nursing turnover | (–) reduced nurse turnover (depends on design) | (+) | (–) Sadler et al.85 |
| Nurse injuries | (–) reduced in single room for the presence of more space | (+) | (–) Sadler et al.:85 reduced nurse injuries in single room because of more space |
| Energy demand | (=) not very different from MB; (+) need to heat more rooms | (–) less energy demand per patient | (+) Sadler et al.:85 expert opinion |
| Noise level | (–) reduced in general by the new building regulations (ceilings, floors); (–) single rooms have more walls, more doors, so much quieter place | Multiple occupancy rooms are associated with lack of privacy, higher noise level and sleep disturbance144,145 | (–) Sadler et al.:85 reduced noise level |
| Sleep quality | (+) sleep quality is improved in SB | (–) sleep is generally poor and there are distractions from other patients | (+) Expert opinion. Chaudhury et al.:95 patient’s comfort is higher in single room. Velarde et al.165 |
| Social interaction | (–) patients get bored easily; (–) for children’s wards, SB are not advised, (–) more isolation | (+) better for children; (+) more options to talk with other patients, visitors, (+) less isolation | (–) Phiri 2006166 |
| Safety | (–) older patients feel more vulnerable if alone | (+) presence of other patients may give more support | (–) Chaudhury et al.;39 expert opinion |
| Dignity and privacy | (+) more dignity and privacy | (–) reduced by the presence of other patients, visitors | (+) Velarde 2007165 |
| Clinical awareness | (+) more confidence; being in a single room the patient feels more free to explain problems to clinicians; this translates to a better diagnosis and a quick recovery | (–) patients less confident to talk about their own problems in presence of other patients; they neglect to report problems, leading to late diagnosis and slower recovery | (+) Expert opinion |
Appendix 2 Patient and public involvement in the study
In our project proposal we said that we would ‘engage user groups with interests in the built and healing environments of care and regional and national patient organisations and public engagement networks’. This we did. We recruited three patient and public advisors to the project advisory group during 2012–13 and had members attending in September 2012, March 2013 and September 2013. They were also available to comment outside our advisory group meetings and did so occasionally. Ms Sally Brearley, our public contributor co-applicant, has been an active member of the research team throughout our study and has helped recruit public contributors as patients or members of the public who have advised us during the study. Our public contributors as patients or members of the public on the study are as follows:
-
Ms Marlene Moura (until July 2012)
-
Ms Christine Chapman
-
Ms Jennifer Bostock (from July 2013)
-
Ms Sally Brearley (co-applicant and co-author).
These advisors commented upon and advised on wording in patient information literature, on study design and on issues of patient recruitment, and we actively involved representatives in data interpretation, writing and commenting on drafts of the report. We made changes to the reporting of our patient interview data and added and amended our conclusions and implications sections based on feedback. Sally Brearley is a co-author of the report.
We are now engaging with our public contributors in terms of our dissemination plans, in which we plan to include patients, public and user/networks, colleagues and centres to promote and publicise the findings and to help us produce lay summaries of research. Public contributors and patient and user groups will be invited to our project report dissemination event (following peer review).
Appendix 3 Phase 1 key findings
Pre-move findings: staff perceptions of multibedded wards
Benefits
Staff working on the largely open-plan wards in the old hospital particularly valued the visual and aural proximity they had to patients and colleagues, which they thought offered three key benefits:
-
Enhanced surveillance and monitoring of multiple patients: nurses felt that they could quickly and easily ‘keep an eye’ on patients; rapidly identify changes in a patient’s condition or risks to patient safety and intervene appropriately; promptly acknowledge patients’ requests for assistance; and prioritise responding to requests.
-
Increased opportunity for teamwork and communication: nurses valued being able to see colleagues at work and interact with them easily, particularly to offer or request help with tasks. It was easy to maintain situation awareness, which contributed to the smooth running of the ward; and staff felt part of a ‘whole ward’ team responsible for all patients.
-
Facilitation of social contact between patients: proximity between beds on open wards facilitated social contact between patients, which nurses felt had benefits for staff, especially on busy wards where they had little time for sustained interaction with individuals, and for patients, in terms of morale, supporting recovery and relieving boredom.
Deficiencies
However, proximity between patients on open-plan wards were also perceived by staff to have negative consequences in terms of:
-
ensuring privacy, dignity and confidentiality for patients
-
increased risks of infection.
Staff also identified deficiencies in the layout and facilities of the open-plan wards in old hospital buildings, which were seen as creating obstacles to delivering effective and efficient care, including:
-
lack of space, particularly around patient beds, and difficulties accessing limited patient toilet and bathroom facilities, which impeded nurses delivering direct care to patients
-
difficulty accessing equipment and supplies, because of dispersed support areas on the ward; insufficient or cluttered storage space; and limited availability of equipment
-
inadequate bases for nursing staff, which were frequently shared with other professionals, and provided insufficient work space and restricted access to computers and telephones
-
poor provision of facilities for staff, including insufficient and/or inconveniently located break rooms, kitchens and toilets.
Nurse–patient ratios on the wards were also a cause for concern among staff.
Pre-move findings: patient perceptions of multibedded wards
-
The physical environment of the case study wards influenced three key dimensions of patient experience. These were security, community and physical comfort.
-
Patients’ perceptions of security were influenced by the open ward environment. Positive perceptions of security were related to staff proximity and the ability to observe staff competence, witness the care of others and engage in social interaction with staff.
-
For some patients, the hectic nature of the ward environment contributed to feelings of insecurity as patients felt that care was ‘rushed’ and staff did not have time to ‘comfort’ or ‘get to know’ patients.
-
The physical layout and perceived temporal pressure on staff on the maternity ward led to patients feeling especially insecure.
-
Multibedded rooms enabled patients to passively or actively engage in a patient community. Proximity of other patients helped ‘pass the time’, and many patients enjoyed the camaraderie of shared accommodation. Interaction with other patients could be an important source of emotional comfort, giving patients a sense of purpose.
-
The therapeutic aspects of a community of patients could be negated by the condition or behaviour of other patients. Confused or disruptive patients could change the community dynamic on the ward. For cognitively well patients on the medical (older people’s) ward, the prevalence of dementia and confusion among other patients led to heightened feelings of isolation.
-
Sharing accommodation with other patients was particularly troublesome for maternity patients. Patients on the maternity ward experienced an acute lack of privacy, which led to considerable emotional discomfort and anxiety.
-
Open ward accommodation had multiple implications for patients’ experiences of physical comfort. Availability of food and drink, location and size of shared toilet facilities, space around the bed, and lighting, temperature and noise were potential sources of discomfort which could be alleviated or exacerbated by the physical environment.
-
Patients’ views on single rooms were influenced by their experiences of shared accommodation. Maternity patients expressed a clear preference for single room accommodation as a means of improving maternity patient experience. This preference was related to the lack of security, privacy and physical comfort experienced in the open ward environment.
-
Other patient groups held an ambivalent position in relation to single room accommodation. While sleep and rest and en suite facilities were regarded as definite benefits, patients were concerned about the loss of proximity to staff and about loneliness and isolation.
Appendix 4 Staff and patient project information sheets
Appendix 5 Pre-move stakeholder interview sample and interview guide
| Senior trust staff | Trust New Hospital Development Team | PFI consortium |
|---|---|---|
| Chief executive Medical director Director of nursing Deputy chief operating officer Head of service reconfiguration Director of service improvement Head of equality and governance Non-executive director (patient experience) |
Estates development director Redevelopment programme director Clinical planner Non-clinical planner Programme manager Divisional project managers (planned; emergency; support; women’s and children’s) |
Project manager/clinical lead Builder Architect |


Impact of hospital ward design on staff and patient experiences
Research objectives for stakeholder interviews:
Note on use of this topic guide:
We wish to encourage participants to discuss their views and experiences in an open way without excluding issues that may be of importance to individual participants and the study as a whole. Therefore, unlike a survey questionnaire or semi-structured interview, the questioning will be responsive to respondents’ own experiences, attitudes and circumstances.
The following guide does not contain pre-set questions but rather lists the key themes and sub-themes to be explored with each participant. This allows the interviewer to formulate questions which are responsive to each individual participant. The topic guide does not include follow-up questions like ‘why’, ‘when’, ‘how’, etc. as it is assumed that participants’ contributions will be fully explored throughout in order to understand how and why views, behaviours and experiences have arisen. While all topics will be covered with each participant, the order in which issues are addressed and the amount of time spent on different themes will vary between participants.
Introduction
-
Introduce self, NNRU.
-
Introduce research (funding, research design, outputs).
-
Explain: confidentiality, tape recording, length of interview, nature of discussion (specific topics to address, but conversational in style, in your own words, no right or wrong answers), reporting and data storage/archiving.
-
Any questions.
-
Obtain written consent.
The ‘story’
-
Tell me when you first heard about the project . . .
-
When did you become involved?
-
What happened next . . .
-
-
Tell me the story of this project – what were the key events/turning points/decisions and key individuals?
‘Actors’
-
Whose bright idea was this build? What was the starting point? How much of a priority was all single rooms in new build?
-
CAST LIST – who was involved from the beginning?
-
Who made the decisions?
-
Who were the champions and activists for this [in M&TW (Maidstone and Tunbridge Wells NHS Trust)?]
-
Driven clinically or estates and facilities?
-
Were there any major disagreements (regarding single rooms)?
-
What evidence base was used?
-
Local community reactions/actors?
-
Externally – SHA role? DH role/support?
-
-
Where did you go to find out ‘how to do this’? (especially re single rooms)
-
NHS estates info?
-
PEBBLE involvement?
-
-
Have there been major shifts since the new ‘top team’ came in? What are these?
-
Who on the Exec board is responsible for the new build? Is someone on Exec board responsible for single rooms?
-
To what extent have the service re-design team [OD (organisational development)] been involved?
-
What thought has been given to patient experience improvement?
-
Which (ten) people do you think it is important for us to speak to get a good overview of the organisational context and decision making re single rooms?
Single rooms
-
How much of a priority are single rooms in new build?
-
How much consideration has been given to the advantages and/or disadvantages for staff of the move to all single rooms?
-
How was the room layout and design agreed (outboard bathrooms)?
-
How much consideration has been given to the advantages and/or disadvantages for patients of the move to all single rooms?
-
-
How committed is the leadership to notion of single rooms? How do you think others in the organisation view single rooms?
-
Is there a sense of shared purpose re single rooms?
-
-
Tell me about decision making processes in the course of the design and development:
-
e.g. Were any nurses/Drs/patients involved? How?
-
-
To what extent have (senior) managers in the trust begun to engage with the issue of organisational and change management processes related to the move to all single rooms?
-
Did they meet with architects? How were decisions made – e.g. re 2 metres of track for hoists as opposed to 3
-
-
How do you think single rooms will improve the working environment for staff and patients?
-
Are you part of any wider networks/organisations implementing single rooms? How are you in touch with them?
-
What would success look like to you re single rooms? Would others agree with you?
Process/outcomes
-
What do you consider to be the key issues that you would like to pass on/communicate to the research team about the new build in relation to this project and the move to all single room accommodation?
-
Hindsight is a wonderful thing – what have you learnt (your top tips) in relation to this project – what would you pass on to other trusts going through a similar process?
-
Anything else you would like to add?
Appendix 6 Stakeholder interview guide

Evaluating a major innovation in hospital design: workforce implications and impact on patient and staff experiences of all single room hospital accommodation
Research objectives for stakeholder interviews:
Aim of key stakeholder interviews is to further understand early challenges and experiences across the Trust, context, embedding, and issues of implementation relating to transition to all single room ward accommodation, and to identify the impact of the move to 100% single room accommodation on:
Care delivery and working practices:
-
To what extent are work patterns disrupted and reconstituted, including through trial and error of new approaches?
Staff experience:
-
How are staff perceptions and experiences of the move to single rooms shaped by formal organisational and change management processes?
-
Are there advantages and disadvantages for staff of a move to all single room accommodation?
-
Does the move to all single room accommodation affect staff experience and wellbeing and their ability to deliver effective and high quality care?
Patient experience:
-
Are there advantages and disadvantages for patients of a move to all single room accommodation?
-
Does the move to all single room accommodation affect patient experience and wellbeing?
-
Does it affect diverse patient groups differently?
Note on use of this topic guide:
We wish to encourage participants to discuss their views and experiences in an open way without excluding issues that may be of importance to individual participants and the study as a whole. Therefore, unlike a survey questionnaire or semi-structured interview, the questioning will be responsive to respondents’ own experiences, attitudes and circumstances.
The following guide does not contain pre-set questions but rather lists the key themes and sub-themes to be explored with each participant. This allows the interviewer to formulate questions which are responsive to each individual participant. The topic guide does not include follow-up questions like ‘why’, ‘when’, ‘how’, etc. as it is assumed that participants’ contributions will be fully explored throughout in order to understand how and why views, behaviours and experiences have arisen. While all topics will be covered with each participant, the order in which issues are addressed and the amount of time spent on different themes will vary between participants.
Introduction
-
Introduce self, NNRU.
-
Introduce research (funding, research design, outputs).
-
Explain: confidentiality, tape recording, length of interview, nature of discussion (specific topics to address, but conversational in style, in your own words, no right or wrong answers), reporting and data storage/archiving.
-
Any questions.
-
Obtain written consent.
What’s it been like?
-
[Coming up to] 12/18 months since the move – explore what first year/18 months in the new hospital has been like
-
Explore respondent’s feelings about the new hospital
-
What’s good about the new hospital
-
Anything not so good
-
-
Reflections on any initial ‘teething’ problems
-
What were these, how resolved/plans to resolve
-
Respondent’s own hopes/concerns about the move to single rooms (if they had any) – were these realised
-
-
[For ward-based staff] Whether respondent, in their role, has had to work differently (compared to working in K&S/Pembury)
-
How and with what effects/impact
-
Staff experience
-
Feedback from staff team about working on the new ward
-
Explore whether/how staff team members have had to work differently (compared to working in Kent &Sussex/Pembury)
-
Probe in relation to pre-move concerns:
-
Monitoring patients
-
Patient isolation
-
Falls increase/not seeing falls
-
Staff isolation/safety
-
-
-
Explore effectiveness of new operational policies/new ways of working
-
Explore implementation and operation of:
-
Ward-based medical & AHP teams
-
Nurse-in-charge/shift coordinator policy
-
Changes to domestic and catering service delivery
-
Falls risk assessment
-
Single room protocol and intentional rounding (if implemented)
-
Patient status at a glance information
-
Operation of ward reception
-
Open visiting
-
-
-
Explore how well the physical design of the ward and single rooms works for delivery high quality care
-
Prompt in relation to:
-
Centralised ward support facilities
-
Decentralised staff bases & clusters/cohorts of single rooms
-
Layout of single room (vision panel, space around bed, location of CHWB, location and accessibility of en suite, use of sani chairs/commodes/hoists)
-
Patient privacy & dignity during intimate procedures/toileting
-
Nurse call system (including integrated nurse call)
-
Staff–patient relations
-
Temperature, noise, lighting
-
Security and any access/egress issues
-
Staff rest/relaxation (facilities for staff)
-
Any other issues (e.g. location of ICT, pneumatic tube system, vertical and horizontal links to other related departments)
-
-
-
Staff communication and team working
-
Explore in relation to:
-
Awareness of general running issues
-
Doubling up
-
Informal learning
-
Effectiveness and use/uptake of wireless phones
-
Patient status at a glance information
-
-
Patient experience
-
Feedback from patients
-
Explore what works and what doesn’t work so well for patients
-
Explore in relation to:
-
Patients feeling safe and secure (e.g. staff–patient relations, competence and proximity of staff, witnessed care of others, social context, privacy and dignity)
-
Patient community (e.g. passive and active experiences)
-
Physical comfort (e.g. availability of food and drink, en suite location and layout, space, TV, lighting, temperature and noise)
-
-
Organisational context
-
Explore respondent’s perceptions about how well prepared staff were for working in all single room wards
-
Discuss what worked well in preparing for transition (e.g. processes that have supported staff in being flexible and adaptable in the new ward environments)
-
Discuss what didn’t work so well
-
-
Explore respondent’s perceptions about how committed staff were to all single room wards at time of the move
-
Explore reasons and impact
-
Explore any change over time
-
Final observations
-
If had to do it again, is there anything respondent would do differently
-
Explore in relation to:
-
– Design (including 100% single rooms)
-
– Pre-move preparation
-
– Work processes/operational policies (design and implementation)
-
-
-
Any advice for other trusts undertaking similar projects
-
Anything respondent would change to:
-
Improve staff experience
-
Improve patient experience
-
-
Anything respondent misses about the ward at Kent & Sussex/Pembury
Appendix 7 List of personal digital assistant categories and definitions
| Main category | Popup list (select one) |
|---|---|
| TASK STATUS | New [task/patient] Continuation [of previous task/of care for patient] Return [to an earlier task] Pause session End session |
| ACTIVITY | Direct care [enter subcategory in DC TYPE] Documentation Escort/transfer patient Indirect care Medication tasks [including medication administration] Personal/social Professional communication [enter subcategory in PC TYPE] Ward-related Other |
| DC TYPE [Direct care subcategories] | Admission/discharge Assessment/monitoring Assistance with activities of daily living Care/treatment/intervention Cleaning/bed making [patient present] Communication with patient Education/teaching Mobilising patient Other |
| PC TYPE [Professional communication subcategories] | Administrative Being taught Discussing patient care Providing advice Providing assistance Seeking advice Seeking assistance Shift report Other handover Review/update patient status board Teaching (informal) Other |
| LOCATION | At bedside Off ward Office space On ward [any patient care area, but not at patient bedside] Staff area [change, toilet, break room] Staff base [ward office, interview room] Ward support area [clean/dirty utility, supply/store room, kitchen/pantry, medication storage/preparation area] |
| WITH 1 | Allied Health Professional Assistant/support worker Doctor Domestic services Maintenance/ICT/equipment Midwife Nurse Nurse practitioner Patient/relative Play leader/nursery nurse Porter Practice Development Nurse Student Volunteer Ward clerk/receptionist Ward manager/coordinator Other |
| WITH 2 | Popup list as for With 1 |
| WITH 3 | Select number of additional people involved in activity/interaction |
| MODE/DEVICE | CoW [Computer-on-Wheels] Face to face Laptop/tablet Mobile/smart phone Non-verbal Pager PC Telephone Wireless telephone Other |
| ‘TWITTER’ | Manually enter details of any observed problems relating to the layout, environment, facilities, technology (including ICT) and equipment. Include details relating to interruptions, frustrations or difficulties staff member had with completing task/activity |
| DATE | Date record entered (recorded automatically) |
| TIME | Time record entered (recorded automatically) |
| Subcategory | Definition |
|---|---|
| Direct care | Tasks directly involved with patient care including specialist/technical care, assistance with activities of daily living, direct communication with patient and/or relatives |
| Documentation | Documentation (excluding medication documentation), paper or electronic (including updating patient status at a glance information) |
| Escort/transfer patient | Escorting or accompanying patient to another ward/department, transfer patient to a different room (e.g. for diagnostic procedure/treatment) |
| Indirect care | All tasks indirectly related to patient care of a specific patient, not covered elsewhere (e.g. in documentation, professional communication) including reviewing results, planning care |
| Medication tasks | All tasks associated with medication, including preparation, administration, documentation, checking, etc. |
| Personal/social | Meal breaks, toilet breaks, breaks, etc.; all non-work-related communication, category includes complaining and expressing frustration about work |
| Professional communication | All communication (except medication task-related communication) between health professionals; see Table 4 for subcategory definitions |
| Ward-related activities | Any ward-related activity including bed management, staff rotas, non-patient-related clerical/administrative work, keeping stores stocked/delivering supplies, making beds, preparing/checking equipment, attending meetings, cleaning, serving meals/drinks |
| Other | Any other activity |
| Subcategory | Definition |
|---|---|
| Admission/discharge | Any activity relating to admission or discharge which directly involves the patient |
| Assessment/monitoring | Visual observation, vital signs |
| Assistance with activities of daily living | Bathing, feeding, toileting, shaving |
| Care/treatment/intervention | E.g. wound care and dressing, procedures and treatment, intravenous site change, urinary catheter infection |
| Cleaning/bed making | Cleaning patient care area, changing bed linen (performed by the staff member for a patient under their care, e.g. following incontinence/vomiting) |
| Communication with patient | General communication (talking with/listening to), reassuring patients/relatives, helping confused patients, responding to non-medical queries |
| Education/teaching | Providing specific education about patient’s condition and management |
| Mobilising patient | Assisting patient in mobilising (e.g. postop) |
| Other | Any other direct care activity |
| Subcategory | Definition |
|---|---|
| Administrative | Any communication related to running of the ward in general (e.g. staffing, bed allocation, staff co-ordination, staff meeting, scheduling) |
| Being taught (informal) | Being taught new skills or information (informal) |
| Discussing patient care | Discussing patient status or care plan, validation (verifying accuracy or appropriateness of a decision, procedure, care plan, strategy, approach) |
| Providing advice | Providing advice or guidance relating to a skill or clinical knowledge (telling ‘how to’) |
| Providing assistance | Providing assistance with equipment, procedures, data entry, locating people or items |
| Seeking advice | Seeking advice or guidance relating to a skill or clinical knowledge (asking ‘how to’) |
| Seeking assistance | Seeking assistance with equipment, procedures, data entry, locating people or items |
| Shift report/other handover | Excluding main shift report |
| Teaching (informal) | Teaching new skills or information (informal) |
| Other | Any other professional communication |
Appendix 8 Staff survey (medical assessment unit version)
Appendix 9 Changes made to staff survey in new hospital
The pre-move and post-move questionnaires were similar except that a small number of questions were rephrased for coherence following the move. For example, before the move participants were asked about which two aspects of the new hospital they were most looking forward to and which two aspects they were most concerned about. In the post-move phase the questions were reworded to ask what two aspects staff most liked about single room accommodation and what aspects they most disliked.
The survey included an adapted version of the 22-item version of the Teamwork and Safety Climate Survey. 98 This is a validated survey consisting of two subscales to measure perceptions of teamwork and three to measure safety climate. The teamwork subscales are input into decisions, collaboration with other staff and information handover. The safety climate subscales are attitudes to safety within own team, overall confidence in the safety of the organisation and perceptions of management’s attitudes to safety. We adapted the wording of some items to make it clear that the question was asking about the ward environment rather than the whole hospital (e.g. ‘Briefings are common on this ward’ compared with the original item, ‘Briefings are common where I work’). In the original scale there was a question in each teamwork subscale about the quality of collaboration: one about collaboration with senior doctors and one about collaboration with nurses. Because we were interested in the quality of communication in the team as a whole, we reworded these items to that effect and added two similar items asking about quality of communication with nursing assistants and AHPs. The final adapted teamwork and safety climate scale within the survey consisted of 24 items with Likert-type scales ranging from 1, strongly disagree, to 5, strongly agree.
Appendix 10 Staff interview topic guide

Evaluating a major innovation in hospital design: workforce implications and impact on patient and staff experiences of all single room hospital accommodation
Research objectives for staff interviews:
-
Does the move to all single room accommodation affect staff experience and wellbeing?
-
How does the physical environment impact on the experience of staff providing care to patients and how does this influence staff ability and capacity to deliver high quality care?
-
Does it affect staff working practices and are these changed?
-
Does it affect ability of staff to deliver high quality patient care?
-
Are there advantages for staff of a move to all single room accommodation?
-
Are there disadvantages for staff of a move to all single room accommodation?
Note on use of this topic guide:
We wish to encourage participants to discuss their views and experiences in an open way without excluding issues that may be of importance to individual participants and the study as a whole. Therefore, unlike a survey questionnaire or semi-structured interview, the questioning will be responsive to respondents’ own experiences, attitudes and circumstances.
The following guide does not contain pre-set questions but rather lists the key themes and sub-themes to be explored with each participant. This allows the interviewer to formulate questions which are responsive to each individual participant. The topic guide does not include follow-up questions like ‘why’, ‘when’, ‘how’, etc. as it is assumed that participants’ contributions will be fully explored throughout in order to understand how and why views, behaviours and experiences have arisen. While all topics will be covered with each participant, the order in which issues are addressed and the amount of time spent on different themes will vary between participants.
Introduction
-
Introduce self, NNRU
-
Introduce research (funding, research design, outputs)
-
Explain: confidentiality, tape recording, length of interview, nature of discussion (specific topics to address, but conversational in style, in your own words, no right or wrong answers), reporting and data storage/archiving
-
Any questions
-
Obtain written consent
Background
Aim: to gather background contextual information which may have a bearing on experiences and can be followed up and explored during interview
-
Personal circumstances (grade of staff; where work; how long worked in Trust etc. – check whether worked at Kent & Sussex or old Pembury hospital before move)
-
Previous experience as member of staff elsewhere
Recent experience as member of staff in clinical service at Maidstone and Tunbridge Wells NHS Trust
Aim: to capture spontaneous reflections on recent experience and what aspects were important to participant
-
What has it been like working in new ward area?
-
Overall impression of/feelings towards new ward and new hospital
-
Experience (best and worst aspects of experience including reflections on any ‘teething’ problems)
Staff experience: overall experience
Aim: to encourage participant to reflect spontaneously on the physical environment in relation to staff experience
-
Positive aspects of physical environment (layout, environment, facilities)
-
Negative aspects of physical environment (layout, environment, facilities)
-
Affects different staff groups differently?
Staff experience: working differently/new ways of working
Aim: to explore working in new environment in more detail
-
Explore whether/how staff team members have had to work differently (compared to working in Kent & Sussex/Pembury)
-
Probe in relation to pre-move concerns:
-
Monitoring patients
-
Patient isolation
-
Falls increase/not seeing falls
-
Staff isolation/safety
-
-
Explore effectiveness of new operational policies/new ways of working
-
Explore implementation and operation of:
-
Ward-based medical & AHP teams
-
Nurse-in-charge/shift coordinator policy
-
Changes to domestic and catering service delivery
-
Falls risk assessment
-
Single room protocol and intentional rounding (if implemented)
-
Patient status at a glance information
-
Operation of ward reception
-
Open visiting
-
Ward layout including layout of single rooms and en suites
-
-
Explore how well the physical design of the ward and single rooms works for delivery high quality care
-
Prompt in relation to:
-
Centralised ward support facilities (and walking distances)
-
Decentralised staff bases & clusters/cohorts of single rooms
-
Layout of single room (vision panel, space around bed, location of CHWB, location and accessibility of en suite, use of sani chairs/commodes/hoists)
-
Patient privacy & dignity during intimate procedures/toileting
-
Nurse call system (including not having integrated nurse call)
-
Staff–patient relations
-
Temperature, noise, lighting
-
Security and any access/egress issues
-
Staff rest/relaxation (facilities for staff)
-
Any other issues (e.g. location of ICT, pneumatic tube system, vertical and horizontal links to other related departments)
-
-
Staff communication and teamwork
-
Staff communication and team working
-
Explore in relation to:
-
Awareness of general running issues
-
Doubling up
-
Informal learning
-
Effectiveness and use/uptake of wireless phones
-
Patient status at a glance information
-
Staff safety & well-being (if not discussed above)
-
Patient experience
Aim: to understand staff perceptions’ of the patient experience relating to aspects of the physical environment
-
Feedback from patients
-
Explore what works and what doesn’t work so well for patients
-
Explore in relation to:
-
Relational aspects of care
-
Patients feeling safe and secure (e.g. staff–patient relations, competence and proximity of staff, witnessed care of others, social context, privacy and dignity)
-
Socialisation including visitors and patient community (e.g. passive and active experiences)
-
Physical comfort (e.g. availability of food and drink, en suite location and layout, space, TV, lighting, temperature and noise)
-
Final observations/suggestions for improvements
Aim: to obtain staff suggestions for what would improve the physical environment and close interview on a positive note
-
If had to do it again, is there anything respondent would do differently/or, if new in Trust, any changes respondent would make
-
Explore in relation to:
-
Design (including 100% single rooms)
-
Pre-move preparation
-
Work processes/operational policies (design and implementation)
-
-
Anything respondent would change to:
-
Improve staff experience
-
Improve patient experience
Anything respondent misses about the ward at Kent & Sussex/Pembury
Anything else would like to add.
Appendix 11 Reflexive photography information

Impact of hospital ward design on staff and patient experiences
King’s College London Psychiatry, Nursing and Midwifery Research Ethics Subcommittee ref no. PNM/09/10-30
Information and guidelines for taking part in reflexive photography
What is the purpose of reflexive photography?
Reflexive photography is a data collection method in which research participants take photographs and then discuss and reflect on these images during an interview with a member of the research team. We are keen to capture visual records of the ward before and after the move to the new Tunbridge Wells Hospital at Pembury, and would like this visual record to be created by you, so that we can understand the physical environment of the ward as you see it.
What will taking part involve?
We will provide you with a single use disposable camera to take photographs of your ward. We would like you to take at least five photographs. You should always use the flash when taking photographs.
You are free to take photographs of any aspect of the work environment that you think is important.
For example, you might want to photograph aspects of the physical environment (e.g. ward design, layout, environment, facilities, technology and equipment) that you consider to be helpful or unhelpful. You might include photographs of what you consider the best and worst areas of the ward, or a particular area or piece of equipment that helps or hinders your work.
You may take photographs of any area of the ward, including non-patient and staff areas. Please remember not to put yourself or others at risk when taking photographs.
You should avoid including identifiable people in your photographs (e.g. staff, patients or visitors). If you want to include people in any of your photographs, you should do so in such a way that they cannot be identified (e.g. we should not be able to see their face in the photograph).
We will collect the camera back from you after two weeks and get the photographs developed.
We will arrange an interview with you. This will take place with a member of the research team who will share your photographs with you and ask you talk about what they show and your reasons for taking them. With your permission the interview will be audio recorded, so we have an accurate record of what you tell us (the recording will be deleted after transcription). The photographs and interview data will then be analysed by the research team.
Will the photographs and interview data be confidential?
Your interview and photographs will be anonymised. This means you will be assigned a ‘participant identification code’ so no-one outside the research team will be able identify you as having taken the photographs, or through anything you tell us in the interview. If you do accidentally include identifiable people in any of your photographs these will be shredded following the interview.
We will ask you to sign a consent and image release form prior to taking part. This means that you are giving your permission for the research team to keep the photographs you take and use them alongside data from the interview for analysis and the purposes of dissemination of research findings (e.g. in a report of the research). Anonymised photographs selected for inclusion in research reports will be submitted to Maidstone & Tunbridge Wells NHS Trust, and only used with Trust permission.
If you have any queries, please do not hesitate to contact Clarissa Penfold, Lead Researcher,
Appendix 12 Patient interview topic guide
Impact of hospital ward design on staff and patient experiences
Research objectives for patient interviews:
-
Does the move to all single room accommodation affect patient and carer experience and wellbeing?
-
Does it affect diverse patient groups (e.g. pregnant women, the elderly) differently?
-
Are there advantages for patients of a move to all single room accommodation?
-
Are there disadvantages for patients of a move to all single room accommodation?
Note on use of this topic guide:
We wish to encourage participants to discuss their views and experiences in an open way without excluding issues that may be of importance to individual participants and the study as a whole. Therefore, unlike a survey questionnaire or semi-structured interview, the questioning will be responsive to respondents’ own experiences, attitudes and circumstances.
The following guide does not contain pre-set questions but rather lists the key themes and sub-themes to be explored with each participant. This allows the interviewer to formulate questions which are responsive to each individual participant. The topic guide does not include follow-up questions like ‘why’, ‘when’, ‘how’, etc. as it is assumed that participants’ contributions will be fully explored throughout in order to understand how and why views, behaviours and experiences have arisen. While all topics will be covered with each participant, the order in which issues are addressed and the amount of time spent on different themes will vary between participants.
Introduction
-
Introduce self, NNRU
-
Introduce research (funding, research design, outputs)
-
Explain: confidentiality, tape recording, length of interview, nature of discussion (specific topics to address, but conversational in style, in your own words, no right or wrong answers), reporting and data storage/archiving
-
Any questions
-
Obtain (written) consent
Background
Aim: to gather background contextual information which may have a bearing on experiences and can be followed up and explored during interview
-
Personal circumstances (main daytime activity, who live with)
-
Previous experience as hospital in-patient
Recent experience as patient in clinical service at Maidstone and Tunbridge Wells NHS Trust
Aim: to capture spontaneous reflections on recent experience and what aspects were important to participant
-
Length of stay
-
Overall impression of ward and hospital
-
Experience (best and worst aspects of experience)
-
Satisfaction (how satisfied overall with care and treatment received)
Experience of being admitted to ward
Aim: to understand ‘touch point’ and significance for overall experience
-
First impressions of ward environment (welcoming/unwelcoming, homely/clinical, friendly/frightening)
-
Staff
-
Ward (and layout of ward)
-
Other patients
-
Orientation to ward and facilities
Feeling comfortable
Aim: to understand aspects of the physical environment which influenced perceptions of comfort
-
Impressions of ward environment over time
-
General impact of environment on experience of feeling comfortable
-
Bed and other furniture (e.g. chair, bedside cabinet)
-
Facilities (toilets, showers/baths, day room)
-
Ward layout (accessibility, noise, privacy etc.)
-
Décor
-
Entertainment/communication (television, radio, telephone)
-
During the day (noise, lighting, ventilation, temperature)
-
Views from bed, views from windows
-
At night (noise, temperature, lighting, quality of sleep)
-
Other patients
-
Any times/experiences when felt particularly uncomfortable
-
Any times/experiences when felt particularly comfortable
Feeling safe
Aim: to understand aspects of the physical environment which influenced perceptions of safety
-
General impact of environment on experience of feeling safe
-
Security of belongings
-
Nurse call system/calling for assistance (ease or difficulty during day and night)
-
Moving around the ward (any concerns re falls and injury)
-
Visibility of staff
-
Privacy, dignity, confidentiality
-
Cleanliness and hygiene on the ward (including experience of staff hand washing)
-
Any times/experiences when felt particularly unsafe
-
Any times/experiences when felt particularly safe
Interaction with staff
Aim: to understand role of physical environment in patients’ interactions with staff
-
General atmosphere on ward (friendly, unfriendly)
-
Staff behaviour and how interacted with patients (who, for what reason, how often)
-
Relationships with staff (explore for different staff groups: domestics; assistant/support workers; midwives/nurses; doctors)
-
Positive experiences
-
Negative experiences
-
Ways in which physical environment made interactions easier/more difficult (privacy, dignity, confidentiality)
Interaction with visitors
Aim: to explore how the physical environment made visiting enjoyable/less enjoyable
-
Visiting times and visitors
-
Facilities for visitors (chairs, refreshments etc.)
-
Staff interaction with visitors
Suggestions for improvements
Aim: to obtain patients’ suggestions for what would improve the physical environment and close interview on a positive note
-
Ward layout
-
Other aspects of physical environment (noise, lighting, heating, ventilation)
-
Facilities (toilets and bathrooms, day rooms, entertainment and telephones etc.)
-
Visibility of staff
-
Visitors
-
Looking back now is there anything in particular that would have made your experience better/easier?
-
How do you think we can improve patient experiences within these services?
-
What matters most to you as a patient?
-
Explore views on new hospital (100% single rooms) – what would be their choice if had to go into hospital again?
-
Anything else would like to add
End interview and make respondent payment
Appendix 13 Pre-move patient interview sample
| Key characteristics | Case study ward | Total | |||
|---|---|---|---|---|---|
| Acute assessment | Medical (older people) | Surgical | Maternity | ||
| LOS (range) | 24–48 hours | 2–6 weeks | 24 hours–14 days | 24 hours–5 days | – |
| Mean age (years) | 57 (range 42–73) | 87 (range 83–94) | 58 (range 19–77) | Not collected | |
| Paritya | |||||
| Primiparous | – | – | – | 5 | |
| Multiparous | 5 | ||||
| Female | 3 | 2 | 6 | 10 | 21 |
| Male | 2 | 2 | 7 | – | 11 |
| Total (interviews per ward) | 5 | 4 | 13 | 10 | 32 |
Appendix 14 Example of interview framework analysis
| Respondent ID | Summary | Quotations |
|---|---|---|
| MAU01 | R had experience 5 years ago of 5 days on a mixed ward while undergoing cruciate ligament reconstruction. R felt there was a lack of privacy on open ward – which was ‘much improved’ at TWH – but clarified that it was as much about other patient’s privacy and dignity as his own. Had been looking forward to transfer to neurological ward as was getting a bit lonely on MAU, but found the reality to be a disappointment – was exhausted by lack of sleep on the neuro ward, and didn’t find other patients that friendly – although he did start chatting towards end of 2-day stay – so could be a function of LOS at both hospitals, i.e. need long enough LOS to get lonely in SR and again to interact with other if on shared accommodation. However, despite loneliness R would choose a SR again:
|
|
| MAU02 |
|
|
| MAU03 |
|
|
| MAU06 | Describes experience of 4-bedded bay at St Thomas’ – and although can have patients who talk too much – a SR can be ‘ever so lonely’ at times. See new TWH as great improvement on old Nightingale wards of K&S – but feels 4-bed bays work well. [THIS R HAD NO CHILDREN – LIVED A LONELY LIFE TRAPPED IN HIS HOUSE DUE TO HIS HEALTH CONDITION AND OBESITY – HOSPITAL WOULD BE AN OPPORTUNITY FOR MORE SOCIAL EXISTENCE BUT NOT IN SR ENVIRONMENT]
|
|
| MAU07 | R preferred privacy of SR, and comfort – having control over lighting was improved in SR compared to bay at Maidstone where she had surgery earlier in treatment for breast cancer. Had shared bay with a woman who had been moaning and quite negative and R didn’t feel that was what she needed – especially at time when R might have been feeling vulnerable. R liked SRs for privacy aspect, and ability to be more mobile in room compared to in a bed space on shared bay. Liked ability to do as she pleased
|
|
| MAU08 |
|
|
Appendix 15 Expert interview schedules for construction costs and ward services data collection
Interview schedule for construction costs data collection
Title of interview: The cost of construction and cost drivers in a single room design hospital compared to a multi-room hospital
Date and time:
Location:
Subject interviewed:
Introduction time: 5–10 minutes
Welcome – thank you
Introductions: introduce myself, my background and my role in the project
Project description – explain rational and aim of the study
The economic evaluation, explain aims
Explain aim of the meeting and interview: which information and data I’m trying to capture
Explanation of data protection, no right or wrong
Introductions of interviewed: role and time spent in the position
Main interview time: 60 minutes
-
Construction costs
-
What are the main drivers in construction costs of a hospital?
-
We have a list of costs and we will go through it to check your opinions regarding main differences between a single and multi-bedded room hospital.
-
-
Land cost
-
Is there a difference in land cost comparing a SB [single bedded] and MB [multibedded] hospital?
-
What are the costs?
-
-
Exterior building costs
-
Is there a difference in exterior building costs comparing a SB and MB hospital?
-
Can you give an estimate?
-
-
Interior building costs
-
Is there a difference in interior building costs comparing a SB and MB hospital?
-
What about walls, doors, corridors, floors?
-
Is there a standard regulation in building materials, spaces?
-
Can you give an estimate of differences in costs?
-
Other comments
-
-
Construction costs for corridors
-
Is there a difference in corridors comparing a SB and MB hospital?
-
Does this have an impact in terms of costs?
-
Can you give an estimate?
-
-
Construction costs to build new rooms
-
Is there a difference in building single rooms instead of multiple rooms?
-
What about walls, windows, pipes, connections?
-
Is there a big difference in terms of costs?
-
Can you give an estimate?
-
-
Construction costs to rebuild single rooms from an old hospital
-
Is it an option to build a hospital from a previous construction?
-
Is it less expensive?
-
Can you give an estimate?
-
-
Functional and monitoring equipment
-
Is there a difference in functional equipment between single rooms and multiple rooms?
-
What about walls, windows, pipes, connections?
-
Is there a big difference in terms of costs?
-
Can you give an estimate?
-
-
Acuity-adaptable room
-
Is there a difference in acuity-adaptable rooms in SB and MB hospitals?
-
Is there a big difference in terms of costs?
-
Can you give an estimate?
-
-
Windows
-
Is there a difference in number of windows in SB and MB hospitals?
-
Is there a big difference in terms of costs?
-
Can you give an estimate?
-
-
Electrical costs
-
What are the main differences in terms of electrical costs?
-
More connections?
-
-
Energy costs
-
What are the main differences in terms of energy consumption in a SB and MB hospital?
-
Any estimate of the costs?
-
-
Plumbing costs
-
What are the main differences in terms of plumbing costs in a SB and MB hospital?
-
-
Lighting costs
-
What are the main differences in terms of lighting tools in a SB and MB hospital?
-
Is it possible to control for lighting in a SB when it’s empty? (Saving)
-
-
Heating costs
-
What are the main differences in terms of heating costs in a SB and MB hospital?
-
Is it possible to control heating and lighting in a SB when it’s empty? (Saving)
-
-
Water demand and costs
-
What are the main differences in terms of water demand and costs in a SB and MB hospital?
-
-
Rooms
-
Differences in spaces and room configuration: can you describe what is the difference between SB and MB?
-
Is there any standard regulation in terms of space, materials?
-
-
Bathrooms
-
Differences in spaces and bathrooms configuration: can you describe what is the difference between SB and MB? (the bathroom is en suite)
-
Is there any standard regulation in terms of space, materials?
-
What is the difference in costs?
-
-
Enhanced air
-
In the literature we have noticed that single room hospitals have enhanced air. What is your opinion?
-
What about windows?
-
-
Noise reduction costs
-
What about noise reduction? In SB noise should be reduced because of walls and doors. Are there any other noise reduction systems?
-
What is the cost?
-
-
Basins and hand washing
-
Number of hand washing. Is there a standard?
-
What is the cost?
-
-
Nurse stations
-
How many nurse stations?
-
What is the cost for nurse stations?
-
-
Monitoring equipment
-
What can you tell me about monitoring equipment?
-
Any changes? Differences in costs?
-
-
Technology
-
Any difference in technology in SB design?
-
What are the costs?
-
-
Hoists
-
What about hoists in rooms?
-
Any differences in costs?
-
-
Medication rooms
-
In SB can patients get medication in their room, so there is no need for medication rooms?
-
Any changes in costs?
-
-
Maintenance costs
-
What are the main maintenances for a SB? (flooring, new fixtures, wall painting)
-
When is maintenance request? Every 5–10 years? of what?
-
Do you think maintenance costs are higher in a single room design?
-
An estimate?
-
How much maintenance costs impact on overall cost of construction?
-
-
Main impressions regarding single room design compared to the multiple room design: can you please say what are the main impressions regarding a single room design hospital?
-
Other issues and comments
Final questions and conclusions time: 5–10 minutes
Tour of the hospital time: 10–20 minutes
Thanks and goodbye time: 2 minutes
Interview schedule for housekeeping data collection
Title of interview:
Date and time:
Location:
Subject interviewed:
Introduction time: 5–10 minutes
Welcome – thank you
Introductions: introduce myself, my background and my role in the project
Project description – explain rational and aim of the study
The economic evaluation, explain aims
Explain aim of the meeting and interview: which information and data I’m trying to capture
Explanation of data protection, no right or wrong
Introductions of interviewed: role and time spent in the position
Main interview time: 60 minutes
-
Cleaning in general
-
Differences in spaces and room configuration: can you describe what is changed? Number of rooms, number of beds, number of bathrooms, shape of the ward.
-
New materials used.
-
What are in general the main issues/problems with cleaning?
-
How long does it take to clean a ward?
-
How would you compare cleaning a single room ward to a multiple room ward?
-
Other comments.
-
-
Cleaning rooms
-
Differences in spaces and room configuration: can you describe what is changed? Number of rooms before and after.
-
What are in general the main issues/problems with cleaning room?
-
How long does it take to clean a room?
-
What about cleaning of windows?
-
How many times do you clean it?
-
When the patient is admitted – during stay and when discharged.
-
Are there any ‘dead times’?
-
Other comments.
-
-
Cleaning bathrooms
-
Differences in spaces and bathroom configuration: can you describe what is changed? Every room has a bathroom
-
What are in general the main issues/problems with cleaning bathroom?
-
How long does it take to clean a bathroom?
-
How many times do you clean it?
-
When the patient is admitted – during stay and when discharged
-
Other comments
-
-
Cleaning wards (kitchen, common areas etc.)
-
Differences in spaces and ward configuration: apart from rooms and bathrooms is there a difference in cleaning corridors, common areas, and kitchen?
-
What are in general the main issues/problems with cleaning ward now?
-
How long does it take to clean?
-
How many times do you clean it?
-
-
Cost of cleaning
-
How much does it cost to clean a single room (including bathroom and common areas) compared to a multiple room (including bathroom and common areas)?
-
Estimates?
-
How can I get cost data on this? Contact person
-
-
TV and TV remote issue
-
I’ve been told that there is a problem with TV and remotes in rooms. Can you tell me what has happened?
-
Which do you think is the main reason for lost remotes?
-
What are the implications?
-
Any estimate of the costs?
-
Contact reference?
-
-
Basins and hand washing
-
Number of hand washing. Changes and issue with cleaning?
-
-
Nurse stations
-
How many nurse stations?
-
Any issue or problem with nurse stations?
-
-
Monitoring equipment
-
What can you tell me about monitoring equipment?
-
Any changes?
-
-
Technology
-
Which technology has been introduced with the move? Wireless phone?
-
-
Hoists
-
What about hoists in rooms? Any change before and after the move?
-
-
Medications
-
What is changed in terms of time for medications?
-
Is it better in a single room?
-
Are patients treated in their room or transferred to a medication room in the ward?
-
Are you aware of any medication errors before and after the move?
-
Who is the contact person to ask?
-
-
Therapy and drug administration
-
What is changed in terms of time for drug administration?
-
Is it better in a single room?
-
Are you aware of any errors in drug administration before and after the move?
-
Who is the contact person to ask?
-
-
Infection control
-
There is evidence in the literature that single room hospitals have a lower rate of hospital acquired infection. Are you aware of this?
-
Do you know of any change in infection rates after the move?
-
Who is the contact person to ask?
-
-
Patients falls
-
There is evidence in the literature that single room hospitals might have an impact in the rate of patients’ falls during stay. Are you aware of this?
-
Do you know of any change in falls after the move?
-
What do you think is the main reason for a decrease/increase of falls in a ward?
-
Who is the contact person to ask?
-
-
Patients transfer
-
There is evidence in the literature that single room hospitals might have an impact in the number of patient transferrals. For example because of issues with roommates. Are you aware of this?
-
Do you know of any change in transfers after the move?
-
Who is the contact person to ask?
-
-
Maintenance costs
-
What is changed in terms of maintenance of rooms? For example water flushing in bathrooms
-
Do you think maintenance costs are higher in a single room design?
-
Who is the contact person to ask?
-
-
Staff. Let’s talk about staff now. We are going to assess the impact in terms of staff time and workload of a single room design.
-
Are you aware of changes in staff? Staff workload?
-
Do they need to walk more? Distances?
-
Who is the contact person to ask?
-
-
Staff turnover
-
Are you aware of changes in staff turnover after the move?
-
Who is the contact person to ask?
-
-
Staff injuries
-
Are you aware of any staff injured after the move? Do you think this is related to the single room design?
-
Who is the contact person to ask?
-
-
Main impressions regarding single room design compared to the multiple room design: can you please say what are the main impressions regarding a single room design hospital?
-
Other issues and comments
Final questions and conclusions time: 5–10 minutes
Tour of the hospital time: 10–20 minutes
Thanks and goodbye time: 2 minutes
Appendix 16 Business case
Key points from Pembury appointment business case and final invitation to negotiate
Patient safety key driver behind design – 3 key aspects to be met by design
-
control of infection
-
patient privacy
-
supporting effective communication (working practices and facilities designed to support multi-media tri-partheid [staff, patients, carers] communications).
Appointment business case (ABC) and FITN outline that nursing staff will be required to work very differently/organise work differently, as follows.
Increase in amount of purposeful nursing time (from 30–40% to 50–60%) achieved through:
-
Distributed nursing stations (without seats) that enhance nurse/patient and patient/nurse visibility and availability.
-
Near-patient data entry engendering closer proximity of nurses and patients.
-
Patient safety benefits of single rooms (lower falls, nosocomial infections, medication incidents, medical devices errors).
-
Ward based staffing supported by supernumerary Band 7 role to facilitate a more efficient site practitioner service (ward stewards to provide an infrastructure and administrative role within the wards on a 24/7 basis).
Reduction in ward walking distances (despite increased floor areas of the wards) achieved through:
-
Design (Nursing Team Stations ‘proximity prioritised’ to patient bed areas to reduce distances travelled by staff).
-
Ward housekeeper role – undertaking duties previously carried out by RNs.
-
Changes to day-to-day organisation of nursing on the wards (management model where care is co-ordinated closer to the patients).
-
Walking to access supplies minimised by design.
Involvement of visitor and carers in care without creating undue demands on staff and other patients.
-
ABC notes that demands are placed on nurses from carers who are present in greater numbers for more of the time, and that this creates additional physical and emotional labour for nursing staff leading to greater turnover in the initial phases.
Use of technological aids (e.g. Vocera) to improve timeliness and effectiveness of communication between staff and staff and staff and patients.
Standard Inpatient Wards designed to allow maximum flexibility in cohorting patients or care teams in response to the dependency of patients/infection control needs/specialities.
-
Graduated care concept on each ward (so Enhanced/Acute care at front end of inpatient units).
Nurse staffing in 100% single rooms:
-
ABC suggests evidence does not support the need to increase nursing numbers to effective provide care but does indicate a higher turnover of staff in the initial phases of 100% single room development, as result of additional physical and emotional labour for nursing staff from carers present in greater numbers for more of the time.
-
MTW benchmarks consistently at the lower end of National Standards (see Audit Commission study 2005 and National Audit Office study 2006.
-
100% single rooms and a greater acuity of patient, creates need to review nursing numbers and skill mix.
-
greater focus will be placed on how nurses work within a given resource, to increase the amount of proposed direct patient care as a proportion of the working day.
-
the Trust will be piloting new ways of working prior to the commissioning of the new hospital (e.g.) working from distributed nursing stations.
-
Introduction of Information Technology based tools to assist the Nurse in day to day duties will help to ensure that the patient receives the best care possible. (e.g.) near patient data entry, Vocera communication technology.
-
FITN outlines key environmental features and their benefits
Wards must have natural light, beds take priority over staff and have natural light and a view from bed and sitting in a chair.
Bedrooms and bathrooms need to be sized to provide optimum physical and psychological patient care from staff and lay carers and self-care by patients.
Patient control of personal ambient environmental temperature and lighting.
Bedside entertainment to include PC, e-mail, telephone and television.
Physical facilities and infrastructure to support negotiation of balance between communality [socialisation] and individuality [privacy] according to circumstances of patients and to allow safe, timely and effective care.
All beds should be visible from a staff point to enhance staff-patient and patient staff visibility – sightlines to be prioritised along with distributed staff bases.
CHWB to ensure hand hygiene before every patient contact.
Ward security – remote visualisation of visitors at the entrance possible from workstations through visual display and intercom (voice and video intercom).
En-suites will be close to the bed area in order to minimise the potential for patient falls, as per emerging evidence.
Appendix 17 Pre-move case study ward layouts
This appendix presents ward layouts at Kent and Sussex Hospital and Pembury Hospital prior to the move to Tunbridge Wells Hospital.
FIGURE 39.
Acute assessment ward layout. Reproduced with kind permission from Stantec and Laing O’Rourke (colours added by the report authors).
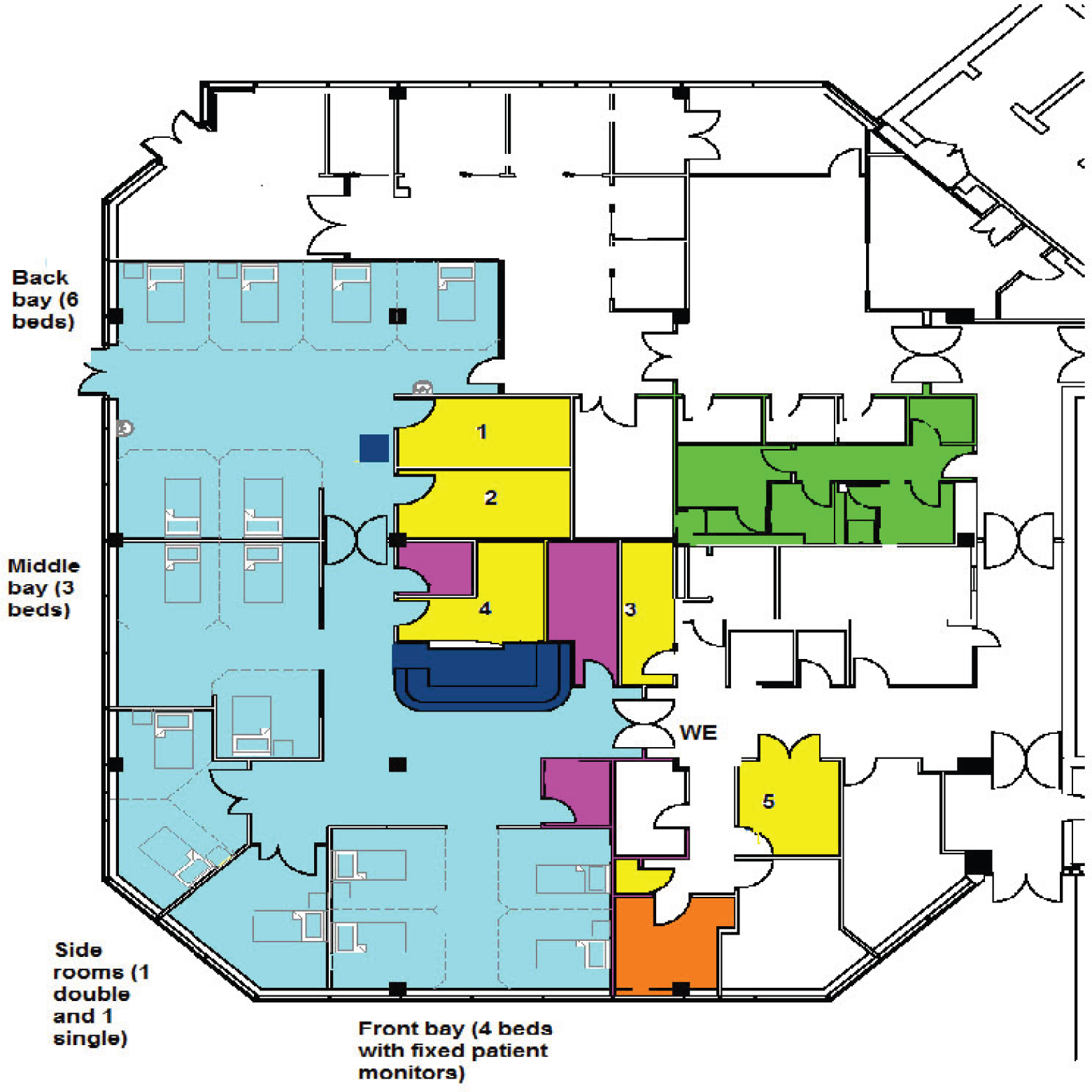
FIGURE 40.
Medical (older people’s) ward layout. Reproduced with kind permission from Stantec and Laing O’Rourke (colours added by the report authors).
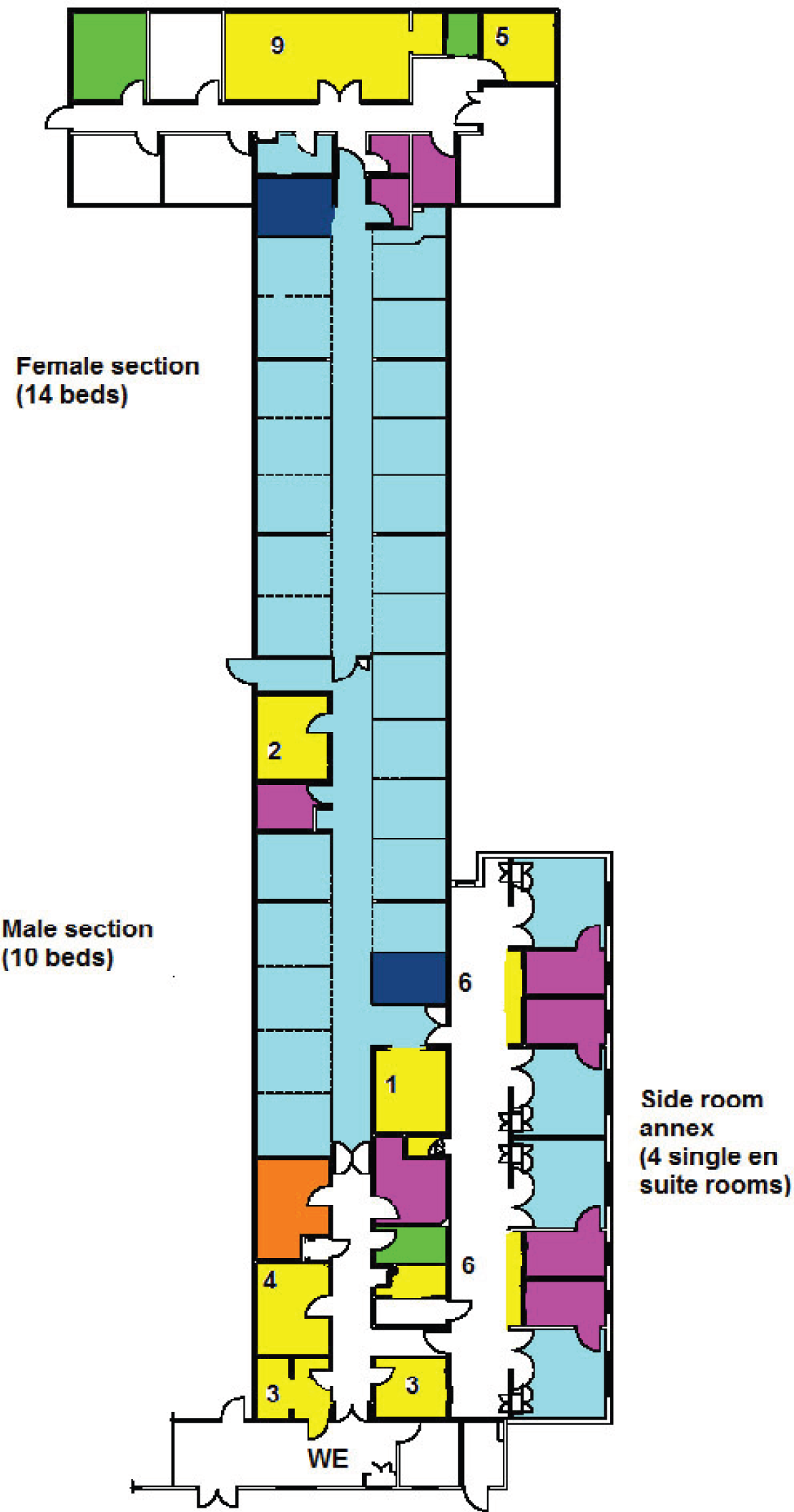
FIGURE 41.
Surgical ward layout. Reproduced with kind permission from Stantec and Laing O’Rourke (colours added by the report authors).
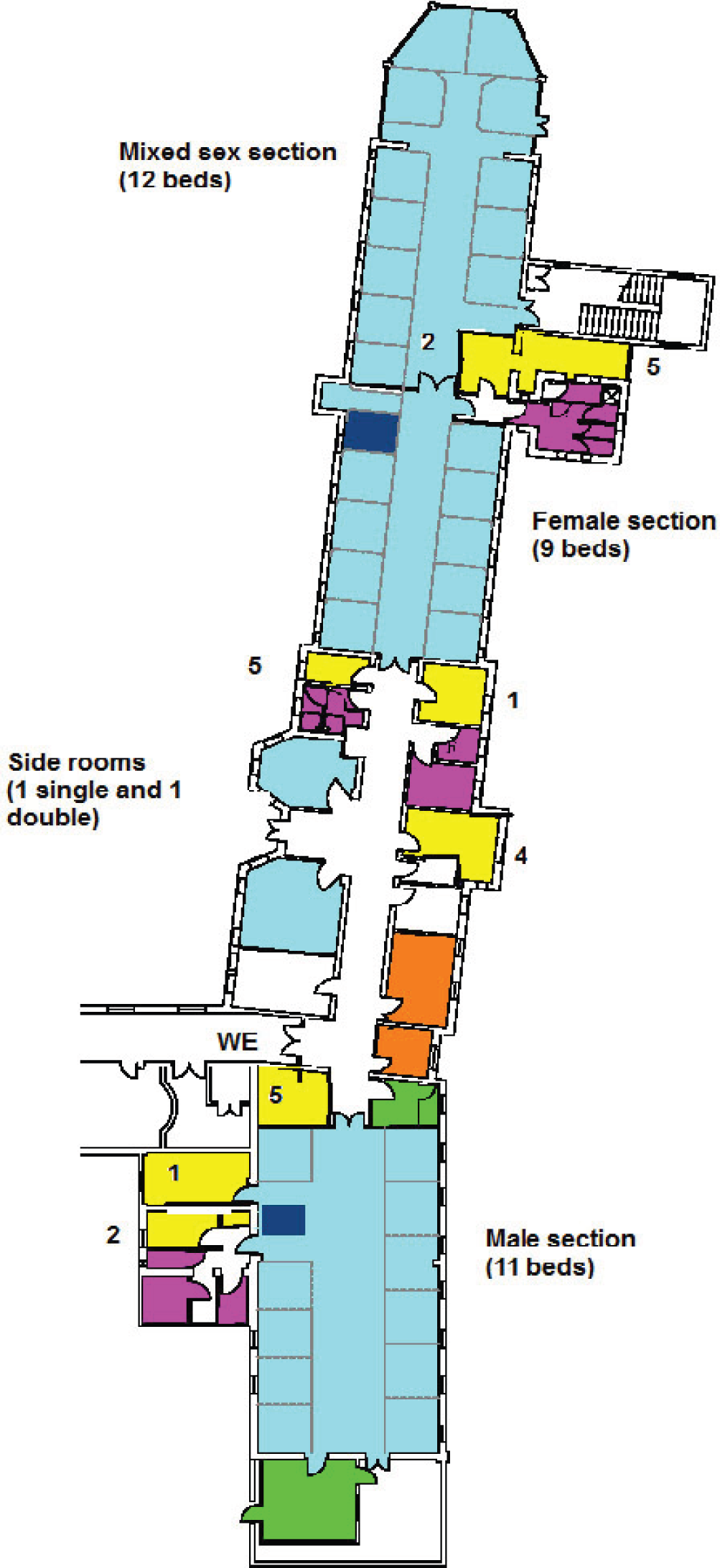
FIGURE 42.
Maternity ward layout. Reproduced with kind permission from Stantec and Laing O’Rourke (colours added by the report authors).
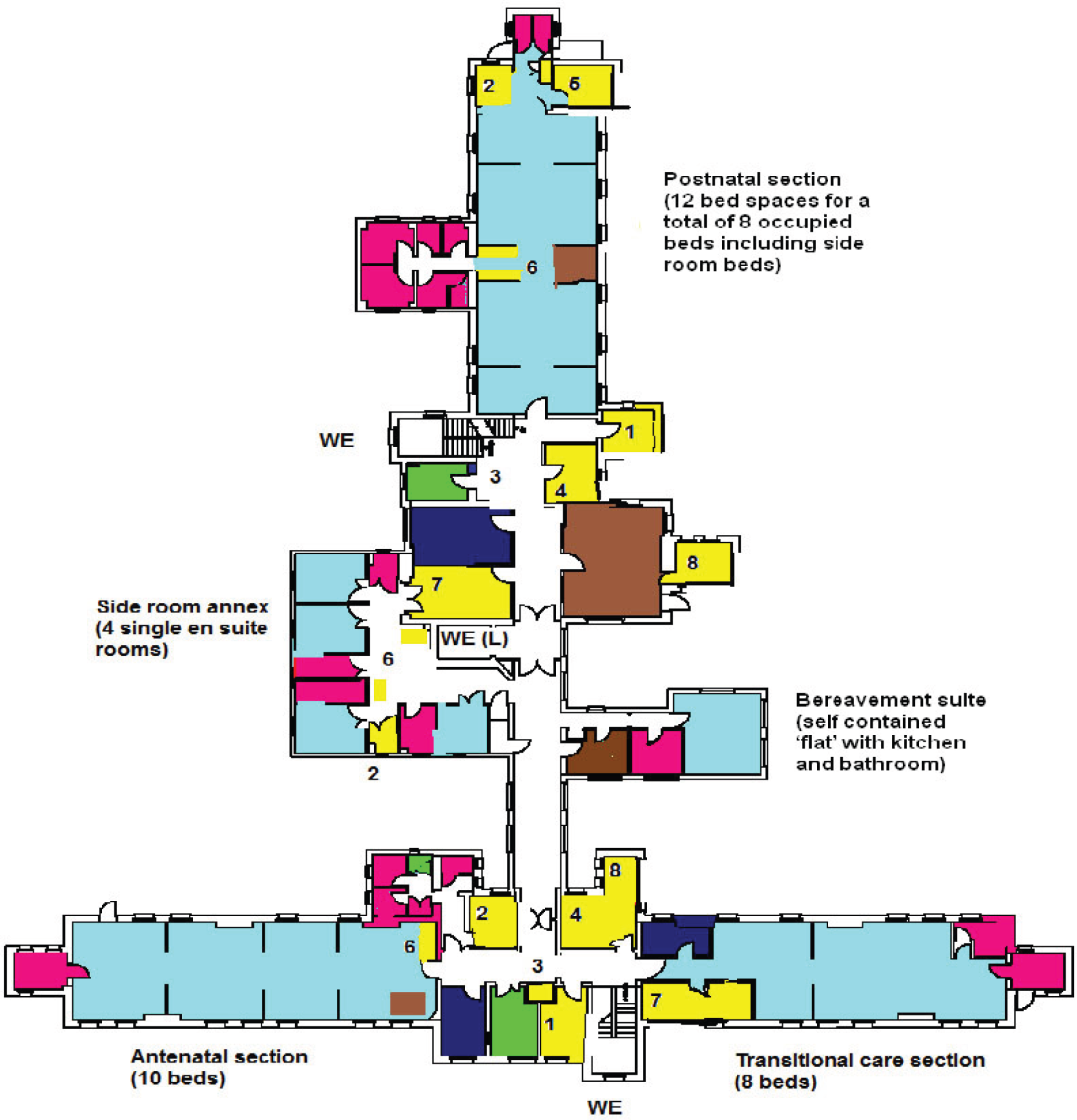
Appendix 18 Ward diagrams in Tunbridge Wells Hospital
This appendix presents case study unit/ward layout diagrams at the new Tunbridge Wells Hospital.
The layouts relate to the main body of the unit/ward and exclude the waiting areas and other facilities outside the unit/ward entrances.
FIGURE 43.
Acute assessment unit layout. Reproduced with kind permission from Stantec and Laing O’Rourke (colours added by the report authors).

FIGURE 44.
Older people’s ward layout. Reproduced with kind permission from Stantec and Laing O’Rourke (colours added by the report authors).
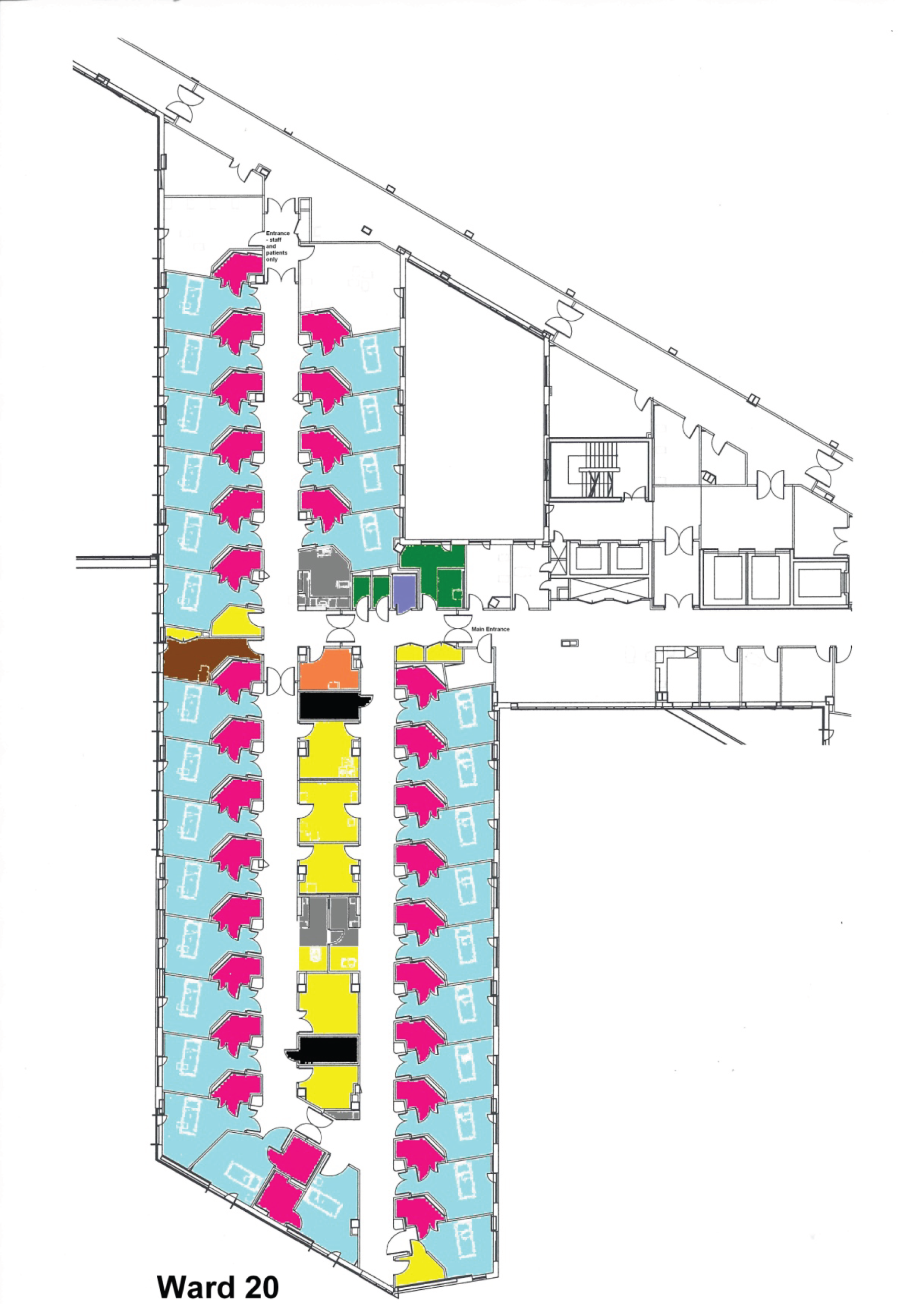
FIGURE 45.
Surgical ward layout. Reproduced with kind permission from Stantec and Laing O’Rourke (colours added by the report authors).
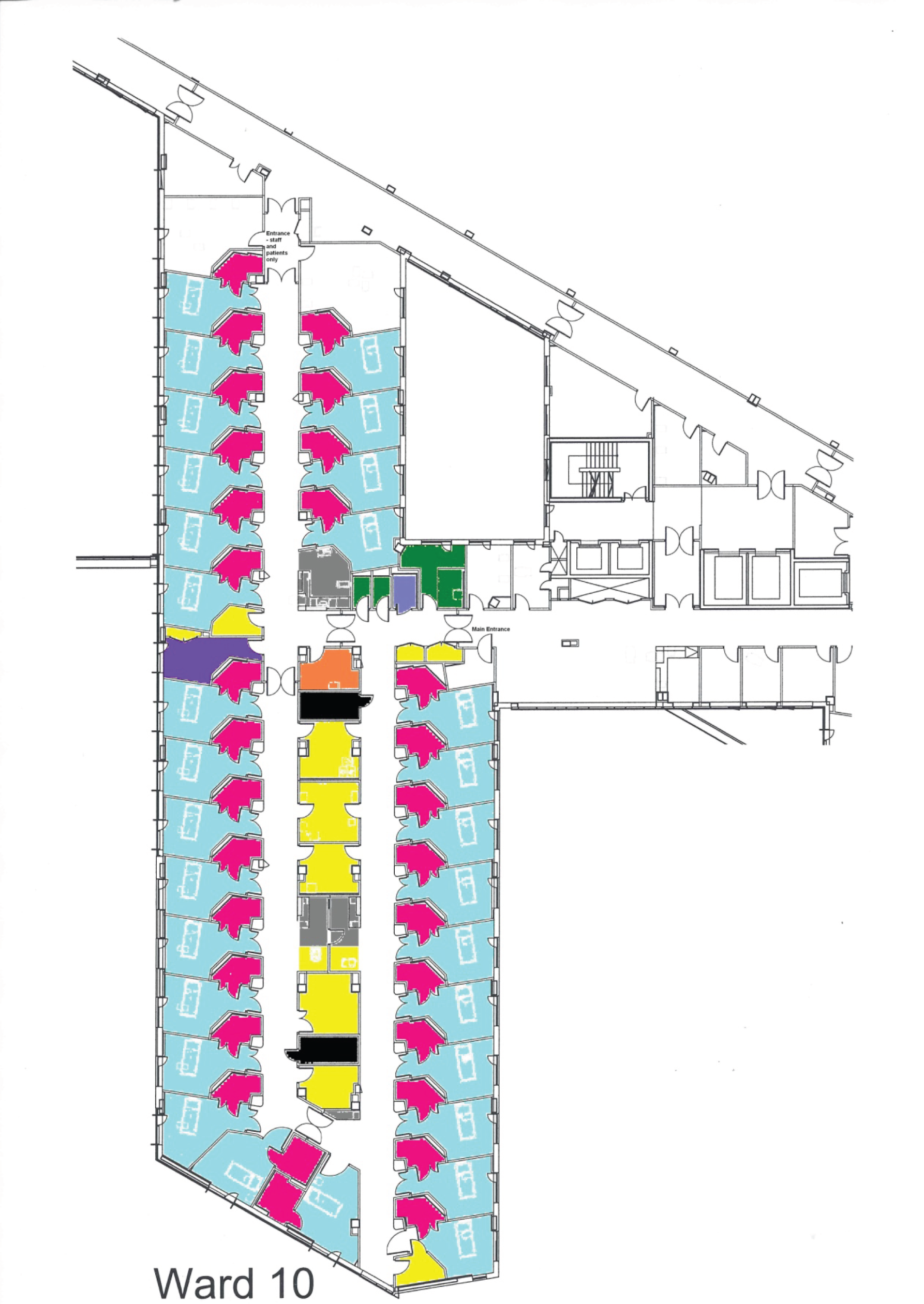
FIGURE 46.
Postnatal and transitional care ward layout. Reproduced with kind permission from Stantec and Laing O’Rourke (colours added by the report authors).

Appendix 19 Ward environment subscale items
Efficiency of physical environment
-
Supplies/equipment always available.
-
Lighting levels easy to adjust.
-
Storage space adequate.
-
Ward design/layout minimises walking distances for staff.
-
Easy to adjust temperature.
-
Medication storage/preparation area adequate.
-
Supplies/equipment easily accessible.
-
Ward design/layout minimises need to move patients within the ward.
-
Availability of computers/ICT adequate.
-
Easy to chart/document care close to patient.
Staff amenity
-
Staff toilet facilities adequate.
-
Easy for new staff to find way about.
-
Staff have regular access to designated rest area.
-
Staff changing/lockers adequate.
-
Adequate space at staff bases.
-
Staff rest area aids relaxation/recuperation.
-
Adequate natural light for staff.
-
Social interaction among ward staff.
Patient amenity
-
Patient toilets good size and access.
-
Patients able to see staff from bed.
-
Most patients have window view of natural setting from bed.
-
Easy for patients/visitors to find way within ward.
-
Easy for patients to get to toilet/bathroom (alone or assisted).
-
Ventilation adequate.
-
Adequate natural light for patients.
-
Sufficient patient toilets and bathrooms.
-
Adequate space for patients to move about the ward.
-
Adequate storage for patients’ clothes/belongings.
-
Facilities provided for patients/visitors adequate.
-
Patient sleep and rest.
-
Social contact between patients.
-
Easy to keep patient care areas quiet.
Privacy/confidentiality
-
Privacy for patients during examination.
-
Maintaining patient confidentiality.
-
Privacy for patients during bathing/toileting.
-
Privacy for patients when giving medical history or being advised.
Teamwork and training
-
Obtaining assistance.
-
Monitoring new/junior team members.
-
Communication between nursing staff and doctors.
-
Knowing when other staff might need a helping hand.
-
Informal learning.
-
Obtaining advice from colleagues.
-
Finding a staff member.
-
Being aware of general running issues on the ward.
-
Ability of staff to spontaneously discuss issues of care.
-
Ability of staff to keep each other updated re general running issues.
-
Discussing patient care with colleagues.
Patient safety
-
Safety and security of patients.
-
Minimising risk to patients of physical/verbal abuse from other patients/visitors.
-
Responding to patient calls for assistance.
-
Minimising risk of falls/injury to patients.
-
Minimising the risk of medication errors.
Staff safety
-
Minimising risk to staff of moving and handling injuries.
-
Minimising risk to staff of slips, trips and falls.
-
Minimising risk to staff of physical/verbal abuse from patients/visitors.
-
Safety and security of staff.
-
Minimising risk to staff of sharps injuries.
Care delivery
-
Ability of staff to deliver high-quality care for all patients.
-
Staff spending time with patients.
-
Communication between nursing staff and patients.
-
Ward layout makes it easy to monitor patients.
-
Location of staff bases enables staff to remain close to patients.
-
Space at bedside sufficient for staff providing care.
Family/visitors
-
Participation of family members in patient care.
-
Patient interaction with visitors.
-
Adequate space for family/visitors at bedside.
-
Easy for patients/visitors to find way within ward.
Infection control
-
Ward design/layout helpful for isolating patients with infections.
-
Number and location of CHWBs supports good hand hygiene.
-
Preventing and controlling hospital-acquired infections.
Appendix 20 Teamwork and safety climate items
Input into decisions
-
Staff input is well received on this ward.
-
Decision-making on this ward uses input from relevant staff.
-
Disagreements on this ward are resolved appropriately (i.e. not who is right, but what is best for the patient).
-
It is easy for staff on this ward to ask questions when they do not understand.
Information handover and communication
-
I know the first and last name of all the staff I worked with during my last shift.
-
Important issues are well communicated at shift changes.
-
Briefings are common on this ward.
-
Satisfaction with quality of communication with doctors.
-
Satisfaction with quality of communication with registered nursing staff.
-
Satisfaction with quality of communication with nursing assistant/support staff.
-
Satisfaction with quality of communication with Allied Health Professionals.
Attitudes to safety within own team
-
I am encouraged by my colleagues to report any patient safety concerns I may have.
-
The culture on this ward makes it easy to learn from the errors of others.
-
I receive appropriate feedback about my performance.
-
Medical errors are handled appropriately on this ward.
-
I know the proper channels to which I should direct questions regarding patient safety.
Overall confidence in safety of the organisation
-
The levels of staffing on this ward are sufficient to handle the number of patients.
-
I would feel safe being treated as a patient on this ward.
-
Trust management does not knowingly compromise the safety of patients.
Management attitudes to safety
-
This organisation is doing more for patient safety now than it did one year ago.
-
Leadership is driving us to be a safety-centred organisation.
-
My suggestions about safety would be acted upon if I expressed them to management.
Appendix 21 Additional case-mix data for Tunbridge Wells
FIGURE 47.
Patient characteristics: acute assessment unit, Maidstone and Tunbridge Wells Hospital. (a) Charlson index diagnoses; (b) nurse staffing; (c) age; and (d) LOS. Dashed line marks time of move; green shading indicates 95% confidence intervals from non-parametric bootstrap. RNHPPD, RN hours per patient-day; tmpHPPD, temporary staff hours per patient-day; TNHPPD, total nursing hours per patient-day.

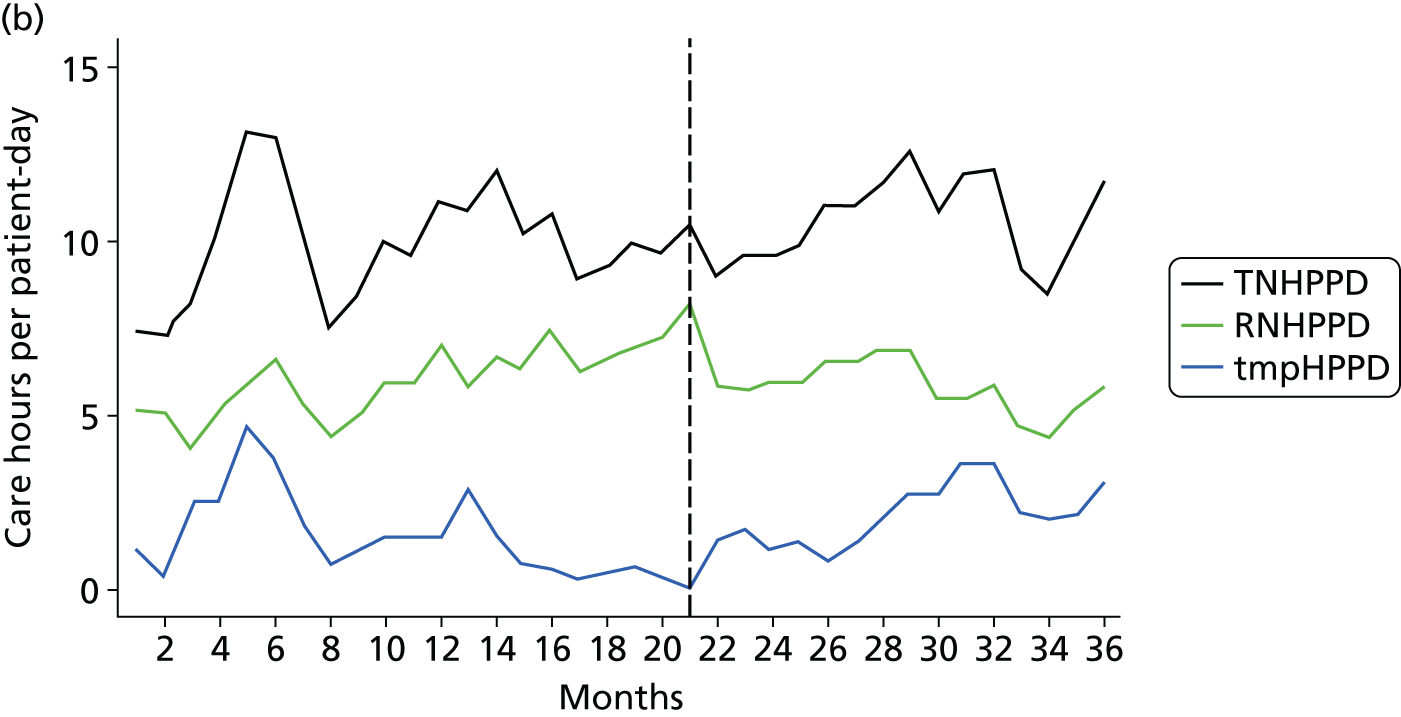

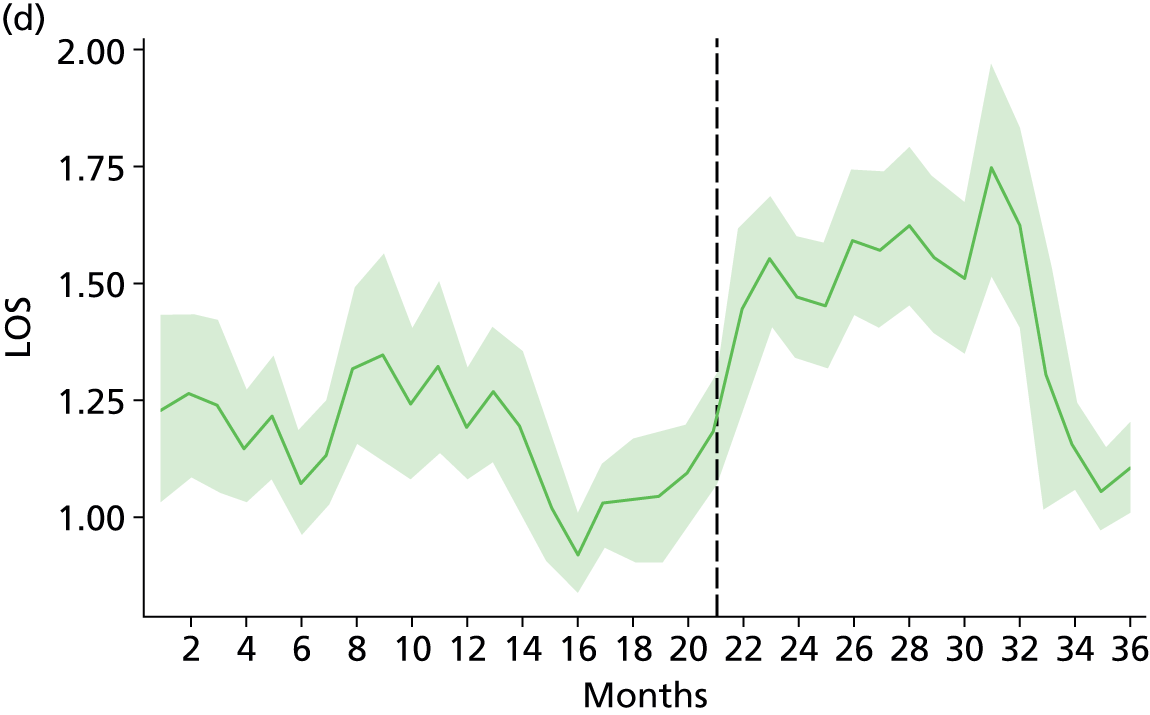
FIGURE 48.
Patient characteristics: older people’s care ward, Maidstone and Tunbridge Wells Hospital. (a) Charlson index diagnoses; (b) nurse staffing; (c) age; and (d) LOS. Dashed line marks time of move; green shading indicates 95% confidence intervals from non-parametric bootstrap. RNHPPD, RN hours per patient-day; tmpHPPD, temporary staff hours per patient-day; TNHPPD, total nursing hours per patient-day.
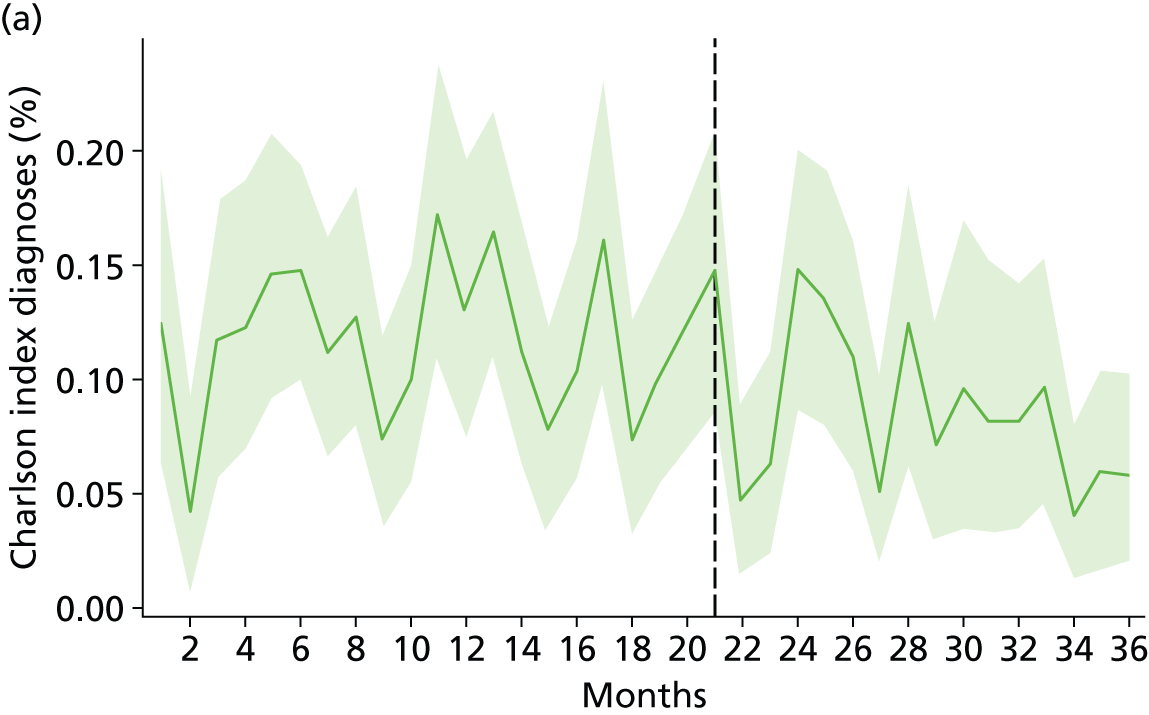
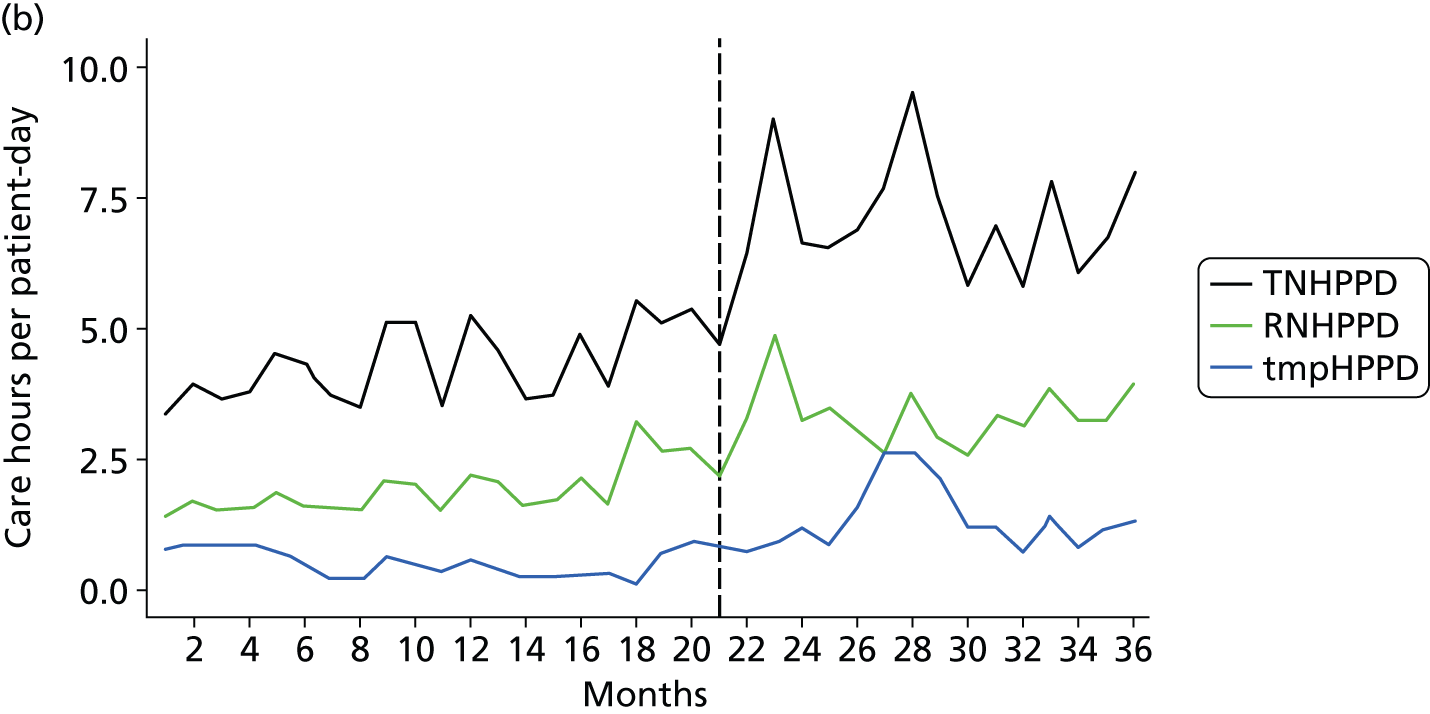
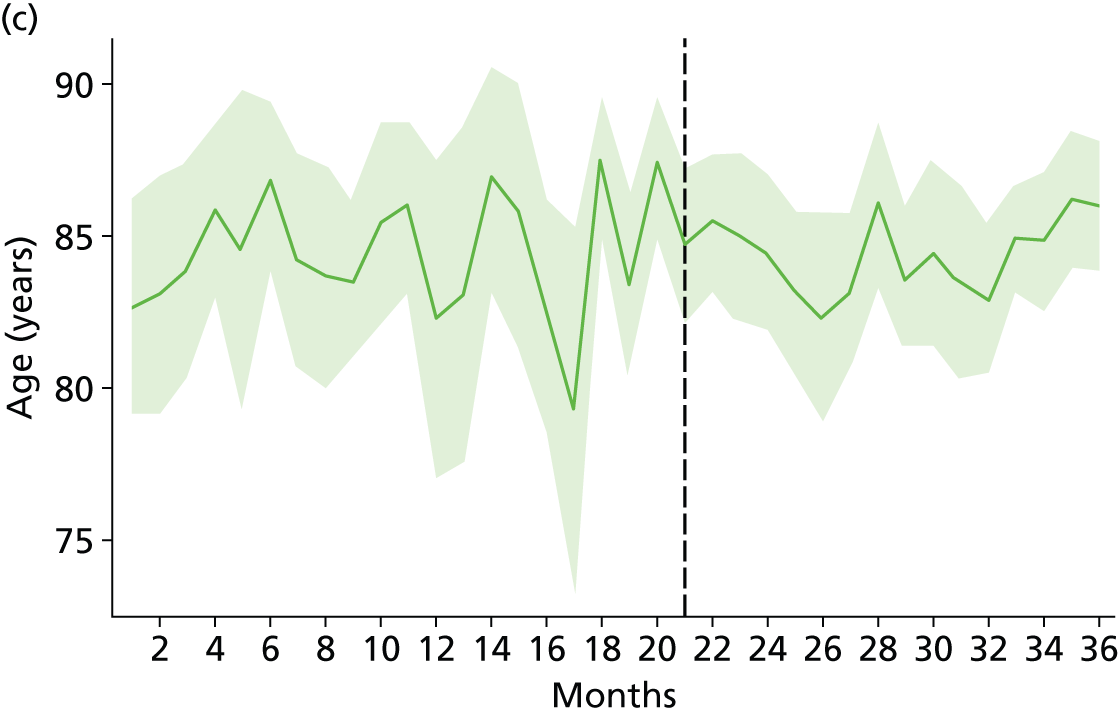
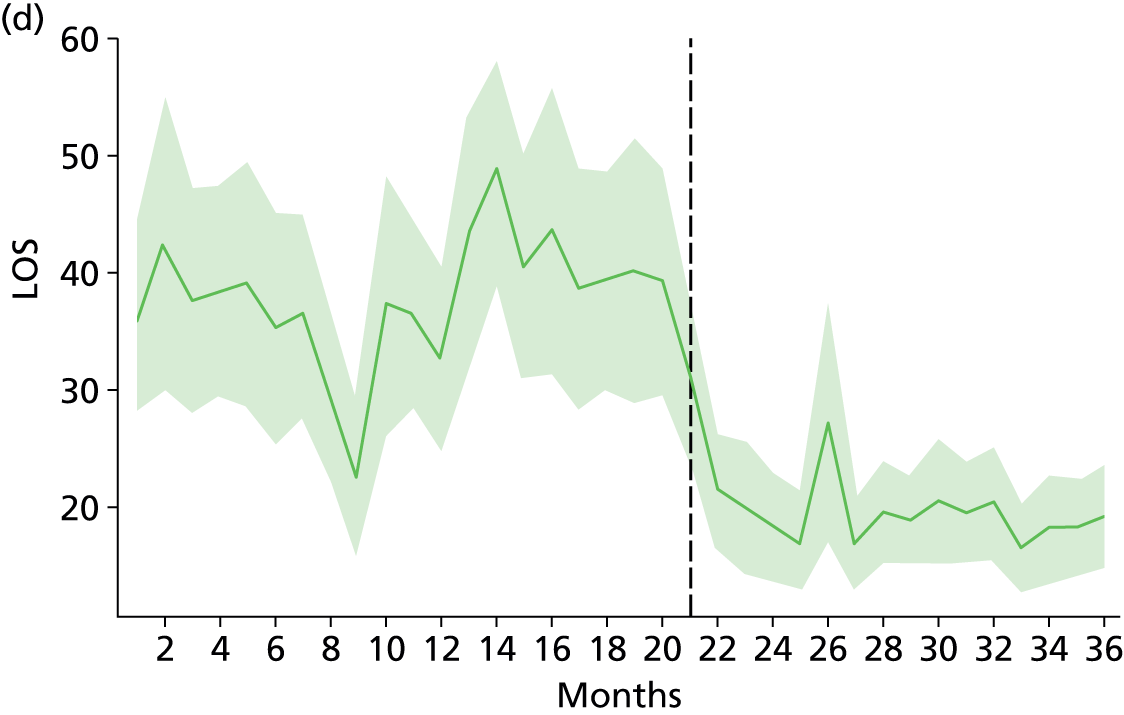
FIGURE 49.
Patient characteristics: surgical ward, Maidstone and Tunbridge Wells Hospital. (a) Charlson index diagnoses; (b) nurse staffing; (c) age; and (d) LOS. Dashed line marks time of move; green shading indicates 95% confidence intervals from non-parametric bootstrap. RNHPPD, RN hours per patient-day; tmpHPPD, temporary staff hours per patient-day; TNHPPD, total nursing hours per patient-day.
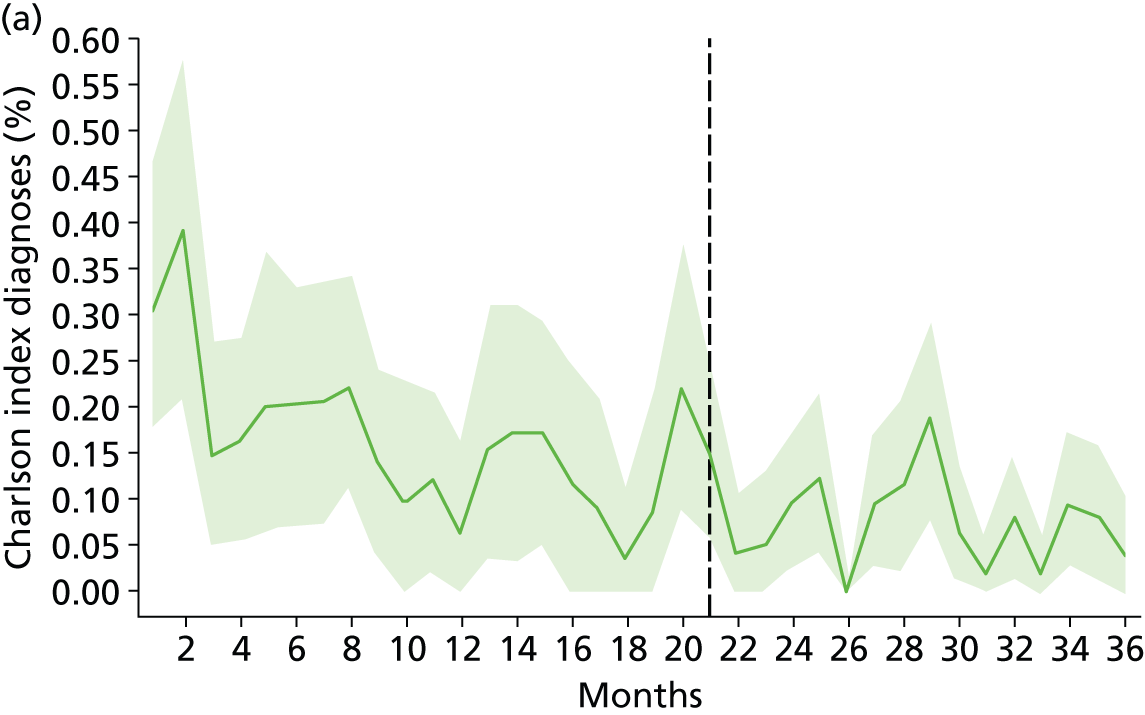
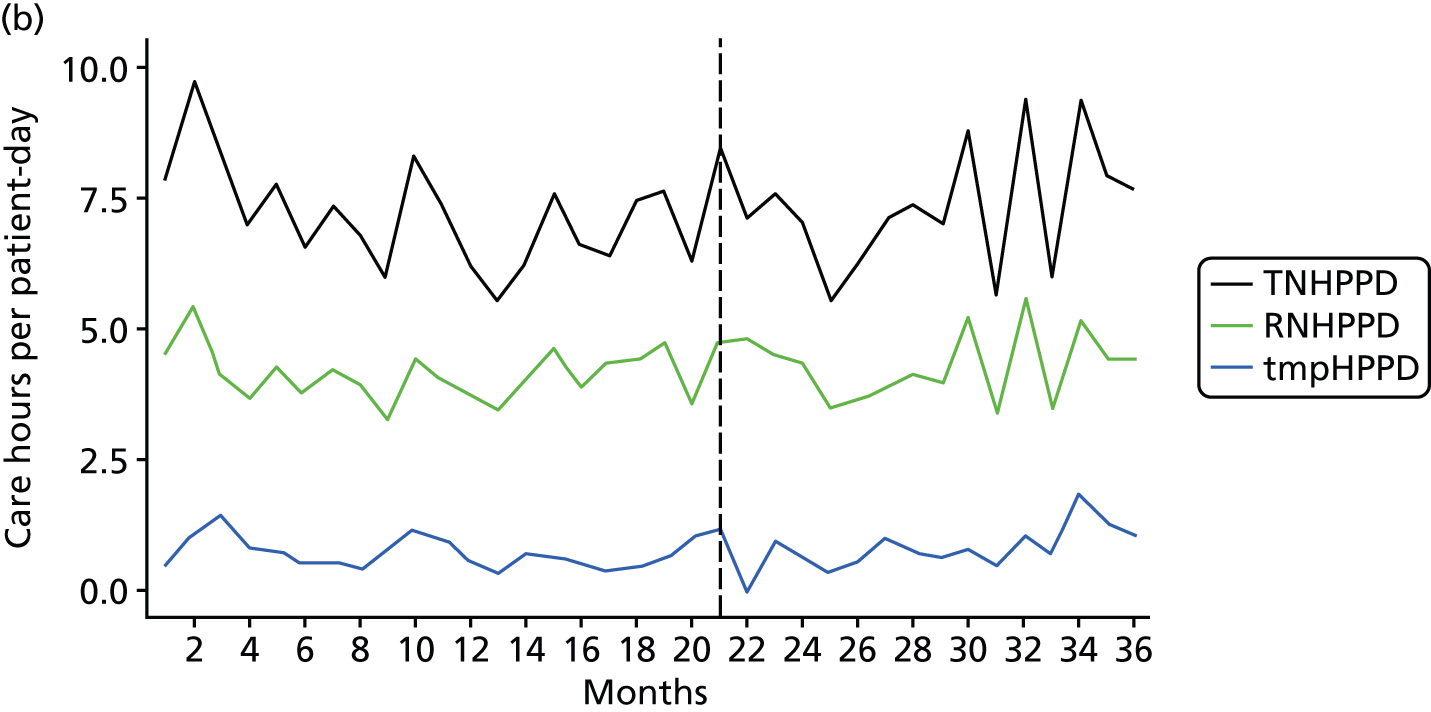
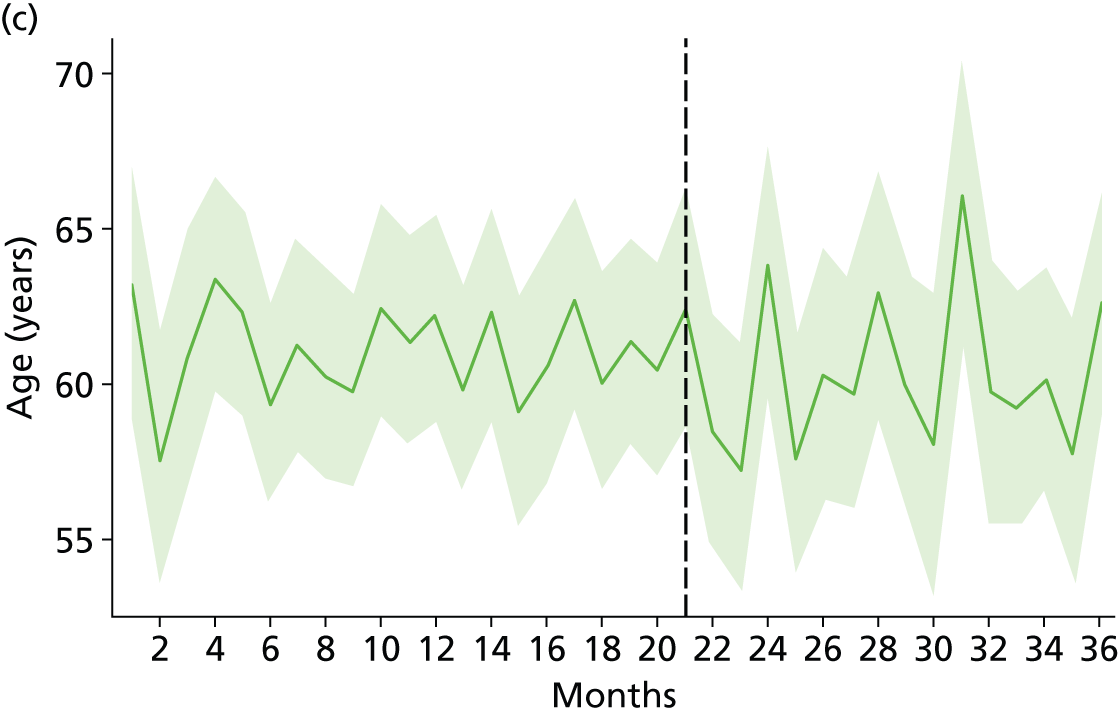
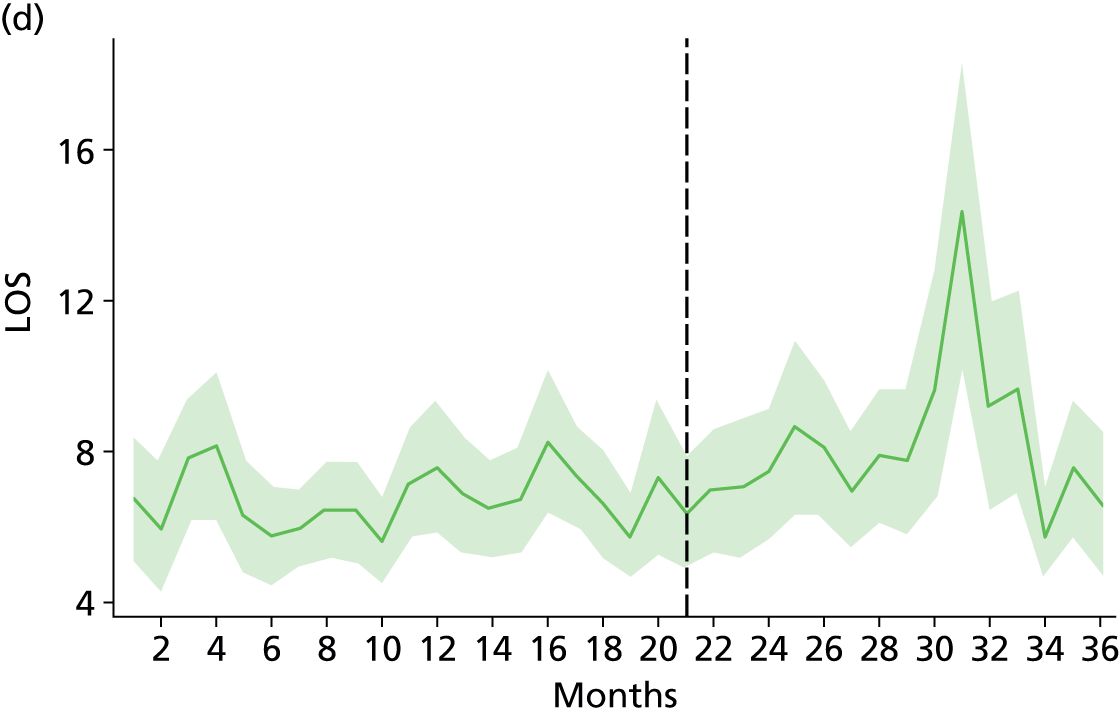
Appendix 22 Definition of fall risk by International Classification of Diseases codes
Based on Brand et al. 167 and using coding from Quan et al. ,105 we modelled fall risk as the proportion of patients having at least one of the following primary diagnosis or being 70 years or older.
| Charlson comorbidities from Quan et al., 2005105 | ICD-10 code |
|---|---|
| Myocardial infarction | I21.x, I22.x, I25.2 |
| Congestive heart failure | I09.9, I11.0, I13.0, I13.2, I25.5, I42.0, I42.5–I42.9, I43.x, I50.x, P29.0 |
| Cerebrovascular disease | G45.x, G46.x, H34.0, I60.x–I69.x, F00.x–F03.x, F05.1, G30.x, G31.1 |
| Dementia | F00.x–F03.x, F05.1, G30.x, G31.1 |
| Mild liver disease | B18.x, K70.0–K70.3, K70.9, K71.3–K71.5, K71.7, K73.x, K74.x, K76.0, K76.2–K76.4, K76.8, K76.9, Z94.4 |
| Diabetes with chronic complication | E10.2–E10.5, E10.7, E11.2–E11.5, E11.7, E12.2–E12.5, E12.7, E13.2–E13.5, E13.7, E14.2–E14.5, E14.7 |
| Hemiplegia or paraplegia | G04.1, G11.4, G80.1, G80.2, G81.x, G82.x, G83.0–G83.4, G83.9 |
| Renal disease | I12.0, I13.1, N03.2–N03.7, N05.2–N05.7, N18.x, N19.x, N25.0, Z49.0–Z49.2, Z94.0, Z99.2 |
| Any malignancy, including lymphoma and leukaemia, except malignant neoplasm of skin | C00.x–C26.x, C30.x–C34.x, C37.x–C41.x, C43.x, C45.x–C58.x, C60.x–C76.x, C81.x–C85.x, C88.x, C90.x–C97.x |
| Metastatic solid tumour | C77.x–C80.x |
| AIDS/HIV | B20.x–B22.x, B24.x |
| Fall risk diagnosis from Brand et al., 2010167 | ICD-10 code |
|---|---|
| Ataxia | G110, G111, G112, G113, G114, G118, G119, R270, R278 |
| Deafness | H90.x, H910, H911, H912, H913, H918, H919, Q780 |
| Delirium | F050, F051, F058, F059, F104, F106, F114, F124, F134, F144, F154, F164, F174, F184, F194, F430 |
| Osteoporosis | M80, M81, M82 |
| Parkinson’s disease | G20 |
| Vision impairment | H53, H54 |
Appendix 23 Cross-case analysis of the four case study wards
Here, we consider how the four case study wards fared in the move to the new hospital. Findings are brought together to explore similarities and differences between the wards and possible reasons for the findings. The focus is particularly on the context and characteristics of the wards; initiatives taken by staff to adapt to the new environment; and outcomes for patients and staff.
Context and characteristics
All the wards relocated to single room accommodation in the new hospital, but they varied substantially in the nature and extent of other changes they had to cope with. ‘Ward’ is also a proxy for patient groups with particular characteristics and needs; distinct groups of staff with a variety of assets and priorities; and a particular place in the organisation. Key stakeholders and staff identified a range of contextual factors and characteristics which they felt compounded or buffered the challenges inherent in moving to the new hospital. Our summary of the nature and scale of these changes and challenges is displayed visually below (Table 77). A challenge in the physical environment of the wards identified by the research team has also been added, namely whether the design supported decentralised nursing teams relating to clusters of 10 rooms or was different from this ‘standard’ plan for general wards. Two wards (older people’s and surgery) conformed to the standard plan and two (AAU and postnatal) deviated from it. The AAU had a unique layout that staff found difficult to adapt to; the postnatal ward layout supported midwives’ established practice, but its design integrity was compromised by a section being assigned to another specialty.
| Context and characteristics | Ward | |||
|---|---|---|---|---|
| AAU | Older people | Surgical | Postnatal | |
| New ward design and layout ‘non-standard’ | +++ | – | – | ++ |
| Increase in number of beds | +++ | – | – | +++ |
| Change in patient characteristics | ++ | + | ++ | – |
| Proportion of high-risk dependent patients needing frequent monitori ng | ++ | +++ | ++ | + |
| Nursing team discontinuity | ++ | +++ | + | ++ |
| Leadership discontinuity | – | +++ | – | ++ |
| Post-move decrease in nurse staffing level | +++ | – | – | – |
| Staff turnover/lack of experience/use of agency staff | +++ | ++ | + | + |
| Policy changes affecting ward environment | ++ | – | – | ++ |
Other challenges at ward level included an increased number of beds on the ward (for the AAU and the postnatal ward, the number doubled); patient characteristics; discontinuities in the staff team; and staffing issues such as turnover and mix of experience. Finally, two wards were affected by system or policy changes that signalled both opportunities and challenges. Service reconfiguration gave the AAU a more prominent role in the new acute hospital, where maintaining the flow of emergency admissions through the system was paramount, putting additional pressures on staff in the unit. The merger of maternity services, which increased the size of the postnatal ward, was also associated with discontinuities in staffing and leadership and the introduction of new policies and procedures, including allowing fathers to stay overnight. These contextual changes determined the extent and type of change staff had to cope with and influenced the character and culture of the wards. The AAU appears to have faced the most challenges, with changes in size of the ward, increased acuity of patients and a decreased level of staffing coupled with a legacy of staffing difficulties that remained unresolved. The older people’s ward faced challenges of monitoring dependent and confused patients in single rooms, with a newly formed team and leadership. The surgical ward appears to have the most favourable context for the move, with fewest concurrent changes.
The issues identified here as ‘contextual’ can be seen as dynamic and inter-related, changing over time and having the potential to interact with each other in unpredictable ways to create new opportunities or constraints. For example, discontinuities in leadership or staff are not inherently negative; they can bring new blood, skills and ideas to a ward. Some issues may amplify disadvantage; for example a decrease in staffing level for a ward with pre-existing staffing difficulties may exacerbate recruitment and retention problems, which in turn almost certainly affect the development of nursing teams. Contextualising the case study wards also allows us to consider the interplay between context and the processes adopted and adapted by staff after the move to the new hospital.
The process of adapting to the single room environment
The all single room wards in the new hospital had important benefits for patients and staff, but they also posed particular challenges for nurses, who had to use their ingenuity to adapt their work patterns and processes to deliver safe and effective care, as discussed in Chapter 6. All the wards responded to the challenges of establishing decentralised nursing teams, monitoring patients, managing the risk of falls, and reducing patient isolation by selecting from a repertoire of conventional methods and, in some cases, developing novel approaches tailored to the particular requirements of patients, staff and ward. A summary of where the wards focused their efforts is provided in Table 78. The differences between wards are due to the salience of the various challenges and how wards used the resources available to them. The priority for the AAU was initially finding a configuration of decentralised nursing teams that enabled staff to work effectively in the ‘non-standard’ ward layout, a protracted process that was described by staff as disruptive and stressful (see Chapter 6). The older people’s ward took a concerted ‘belt and braces’ approach to its biggest challenge, preventing falls, employing all available methods. The surgical ward focused on supporting the ward team, with its established leadership and team work, to deliver good care overall rather than prioritising one particular challenge of single room working. For the postnatal ward, isolation of patients was seen as the most significant challenge, and multiple methods were used to try to increase interaction among patients. None of the wards focused on time management and prioritisation of care, highlighted by nursing staff as a significant issue in the new environment, and largely left to individuals to resolve. Further exploration of this aspect of nursing practice to identify strategies that would help nurses and nursing teams allocate and manage resources (their time, skills and knowledge) appropriately in the single room environment could help to improve patient experience and staff job satisfaction.
| Adaptive approach | Ward | |||
|---|---|---|---|---|
| AAU | Older people | Surgical | Postnatal | |
| Developing decentralised teams/deployment of staff | +++ | ++ | + | + |
| Emphasis on monitoring patients, room checks | ++ | +++ | ++ | + |
| Falls prevention initiatives, e.g. equipment, bed moves, cohorting to manage risk | ++ | +++ | ++ | – |
| Leadership and vision to guide staff initiatives | + | +++ | +++ | + |
| Emphasis on teamwork and communication/mutual support/supervisor role | ++ | + | +++ | + |
| Changing ward environment to recreate panoptic/communal spaces | – | +++ | – | ++ |
| Changing patient expectations and behaviour | + | + | ++ | +++ |
| Staff time management and prioritisation | + | + | + | + |
Achievements and outcomes
The wards adapted to the new hospital environment at different rates but all were functioning satisfactorily a year after the move. The patient outcomes measured in the study and the achievements identified by staff on the wards are linked with summaries of the contextual issues and staff initiatives to adapt work patterns (discussed earlier in this appendix) in Table 79. This cross-case comparison of patterns of context, processes and outcomes enables possible explanations for similarities or differences in outcome to be explored.
| Context | Processes | Outcomes |
|---|---|---|
| AAU Non-standard ward layout Very busy ward, 24-hour emergency admissions, short LOS Double number of beds Decrease in staffing level Continuity of leadership; high turnover and imbalance in staff experience; use of agency staff Reconfigured local service increases external pressures on ward |
Developing small teams to suit ward layout protracted process of trial and error by staff Room checks emphasised and elaborated but evidence of staff non-compliance Initiatives to prevent falls not consistent or coherent |
Staff report transition difficulties: take more than 6 months to settle in Post-move increased rates of falls and medication errors for 6 months+ then return to lower level Poor staff experience, low morale, fatalism about falls ‘It’s all about discharge’ |
| OLDER PEOPLE’S WARD Standard ward layout supports nursing 10-room clusters High proportion of patients confused and at risk of falls, long LOS Slight increase in number of beds Increase in staffing level Discontinuity in leadership and nursing team Periodic use of agency staff |
Consistent and comprehensive initiative to prevent falls, using tools, procedures and notably cohorting high-risk patients Manipulating the ward environment to manage risk and recreate panoptic/communal spaces. Seeking resources to create more communal space Leadership and vision of ‘thoughtful dementia care’ strongly supported by staff |
Nursing team reportedly coheres quickly Post-move higher rates of falls and pressure ulcers sustained, but consistent with changed ward case mix Staff confident they are doing ‘the best we can’; good morale; ideas, plans for change to improve patient experience |
| SURGICAL WARD Standard ward layout supports nursing 10-room clusters Change from elective to emergency surgery, increase in LOS Slight reduction in number of beds Increase in staffing level Continuity of leadership; stable and experienced nursing team |
Strong leadership with emphasis on communication and mutual support, pivotal role of shift co-ordinator, reinforcing procedures such as room checks Attempts to change patient expectations and behaviour, particularly leaving room to mobilise |
Ward nursing team reportedly adapts fairly rapidly Post-move no significant change in patient outcomes Confidence in standard of care delivered, good staff morale, but ward teamwork and trust thought to have declined |
| POSTNATAL WARD Original ward layout compromised Double number of beds Slight increase in staffing level Experienced staff; low turnover; rotation every 6 months New leadership Policy change allowing fathers to stay overnight |
Ward layout supports established pattern of midwife caring for seven or eight patients Modifications to communal spaces Attempts to alter patient expectations and behaviour to increase interaction Variable staff support for fathers policy |
Staff adapt to ward layout but highlight inefficiencies Patient experience mixed: privacy valued but isolation a problem for some Staff concern about unit being ‘impersonal’ and perceived change in midwife role in postnatal care |
Patient outcomes
In terms of patient outcomes, coinciding with the move there were significant increases in the rates of falls and medication errors on the AAU and significant increases in the rate of falls and pressure ulcers on the older people’s ward. On the older people’s ward the rates remained high and are consistent with the changed case mix of the ward (see Chapter 8). On the AAU the rates fell back to pre-move levels after 6–9 months, suggesting that they were associated with adaptation to the new environment. Interestingly, the timing of the return of outcome measures to pre-move levels coincides with staff reports of settling into the new pattern of decentralised working when, to quote the ward manager, ‘suddenly it all clicked’ and staff ‘started to manage things that little bit better’ (see Chapter 6). However, in a complex environment, attributing an outcome to be a single factor is probably too simplistic. For example, the fall rate may also have been influenced by hospital-wide initiatives (provision of equipment, reinforcement of policies and procedures). Other interventions that we have not considered may be implicated. However, it is intriguing that the AAU’s rate of falls and of medication errors stabilised at around the same time, a pattern not found on the other case study wards. This example flags up the importance of the ward layout supporting a configuration of nursing teams that staff can make workable in practice. It also seems likely that pre-existing staffing difficulties on the AAU and the post-move reduced investment in staffing (not experienced by any other case study ward) may have played a part in the difficulties of adapting to the new environment.
Staff experience and well-being
When interviews with staff were carried out, the rate of falls on the AAU had returned to the pre-move level and the rate on the older people’s ward was consistently higher. However, AAU staff were less confident about their ability to prevent falls than staff on the older people’s ward and this was reflected in staff morale. No adaptive effect was detected in outcome measures for the older people’s ward, despite its newly formed ward team. However, what distinguished this ward was the ward manager’s leadership in caring for people with dementia and the ‘belt and braces’ approach to safeguarding patients at risk of falls. Staff were emotionally engaged with the concerted effort to prevent falls, which may have been more effective in bringing them together as a team than an initiative to build teams per se.
Longstanding leadership and an established team were important assets that the surgical ward brought to the new environment and used to good effect. This ward had no significant post-move increase in rates of adverse outcomes. The ward manager introduced various initiatives to support good communication and maintain whole ward teamwork. Staff morale remained high but nurses found that decentralised teams had a divisive effect that was difficult to overcome. Difficulties of finding acceptable alternatives to preferred face-to-face communication with colleagues and the erosion of teamwork and trust, despite efforts to sustain them, are important negative findings in relation to single room wards that merit further investigation, since they have longer-term implications for the development of nursing teams.
Leadership and co-ordination
Nurse managers considered that selecting the right ward sisters to provide leadership was important for securing successful transition to single room working in the new hospital. Our findings provide some support for that view, but the AAU experience suggests that that effective leadership, like any other factor in isolation, is necessary but not sufficient to enable rapid adaptation to the single room environment. The shift co-ordinator role was also an important innovation on the older people’s and surgical wards (the AAU had this role previously) that appears to have been vitally important for maintaining situation awareness across the whole ward. Some less experienced staff interviewed found the demands of this role challenging, which raises questions about preparing staff to take on this and similar co-ordinating and supportive roles.
Patient experience
The surgical ward and the postnatal ward made efforts to encourage mobile patients to leave their rooms to exercise and interact with other patients. Both wards were limited by the inadequate and unattractive social spaces provided for patients and it was not clear how successful their efforts were. Since isolation was one of the main disadvantages of single rooms identified by patients and staff, and staff felt considerable discomfort because they had no time to talk to patients who were simply lonely, it seems important for both patient and staff to find effective ways of enabling social interaction among patients that do not make too many additional demands on staff.
The postnatal ward was different from the general acute wards in many respects. Although midwifery staff considered a high proportion of single rooms an appropriate design for a postnatal ward, not least because patients wanted them, they experienced challenges in delivering care that required adaptations at least as significant as those on the acute wards. Midwives particularly noted the ‘isolating’ effect of single rooms on postnatal women; this had consequences for their practice, restricting them to mainly individual interaction, with few opportunities to work informally with groups of women, as they had done on multibedded wards. The change in policy allowing fathers to stay overnight also altered the ward social environment in ways that some midwives were finding difficult to adapt to. The study suggests that single room working combined with other significant policy changes intended to make care more ‘patient centred’ created tensions for professionals that raised questions about their role and the nature of the service they were providing.
Summary
Bringing together the evaluation findings for the four case study wards we found that:
-
The AAU had to cope with multiple contextual challenges and experienced difficulties adapting to single room working, which were reflected in outcomes, with rates of falls and medication errors initially increasing and then falling back to pre-move levels. Staff morale on the ward was low.
-
The older people’s ward, despite a disrupted nursing team and a patient group that was particularly challenging to care for in the single room environment, found ways of adapting rapidly and managed to keep falls at a rate consistent with the ward case mix. A comprehensive and coherent approach to preventing falls was in place and staff morale was good.
-
The surgical ward had fewer contextual challenges to cope with and continuity of nursing team and leadership were assets that may have helped rapid adaptation to the new environment, with minimal impact on outcomes. Staff were confident and morale was good.
-
The postnatal ward had some significant contextual challenges, including fathers staying overnight, which had implications for midwifery practice. Staff had adapted to the new environment, but for some tensions remained, and raised questions about midwives’ role and the nature of the service they were providing.
Glossary
- Charlson index diagnosis
- Diagnosis included in the Charlson comorbidity index.
- Cornish–Fisher expansion
- A mathematical expression used to approximate the quantiles of a random variable based only on its first few cumulants.
- Cronbach’s alpha
- A measure of internal consistency of scale items.
- HanDBase software
- Relational database manager for iPhone and iPod touch and other handheld computing devices, personal digital assistants, smartphones and desktops.
- Healthcare Resource Group
- Grouping of diagnoses and procedures used for costing purposes by the NHS.
- Healthcare Resource Group subgroup
- Also known as chapter: one of the 22 major categories used to classify HRG codes.
- Length of stay trim-point
- Number of days after which the tariff no longer covers the inpatient stay and an additional daily cost is required for each day.
- Listwise
- A method for handling missing data. In this method, an entire record is excluded from analysis if any single value is missing.
- LOESS
- A form of locally weighted polynomial regression.
- Pearson chi-squared test
- A test of the independence of two categorical variables.
- Poisson distribution
- A discrete probability distribution used for count data such as falls.
- Rounding
- A method of approximating a number to its nearest place value.
- Specials
- One-to-one nursing which closely supervises a patient at risk of falls, wandering, etc.
- U-chart
- An attribute control chart that monitors count data over time for varying sample sizes.
- Vismatic
- Door vision panel.
List of abbreviations
- A&E
- accident and emergency
- AAU
- acute admissions unit
- AHP
- Allied Health Professional
- CF
- Cornish–Fisher
- c-section
- caesarean section
- df
- degrees of freedom
- EPSRC
- Engineering and Physical Sciences Research Council
- FITN
- final invitation to negotiate
- FPP
- falls per patient
- GLMM
- general linear mixed model
- HaCIRIC
- Health and Care Infrastructure Research and Innovation Centre
- HBN
- Health Building Note
- HCA
- health-care assistant
- HCAI
- health-care-associated infection
- HRG
- Healthcare Resource Group
- ICD-10
- International Classification of Diseases, Tenth Edition
- ICT
- information and communications technology
- ICU
- intensive care unit
- ITU
- intensive therapy unit
- KSI
- key stakeholder interview
- LOS
- length of stay
- MDT
- multidisciplinary team
- MRSA
- methicillin-resistant Staphylococcus aureus
- NHPPD
- nurse-hour per patient-day
- NNRU
- National Nursing Research Unit
- NPSA
- National Patient Safety Agency
- OT
- occupational therapist
- PDA
- personal digital assistant
- PFI
- Private Finance Initiative
- PITN
- preliminary invitation to negotiate
- RCN
- Royal College of Nursing
- RM
- registered midwife
- RN
- registered nurse
- SPC
- statistical process control chart
- WC
- water closet (toilet)
- WTE
- whole-time equivalent