Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 10/2002/52. The contractual start date was in April 2012. The final report began editorial review in January 2014 and was accepted for publication in June 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by White et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Hospitals feature significantly in the lives of many children who come to harm at the hands of their parents or carers, and diagnostic and other errors are not uncommon. These have proved resistant to standard policy responses, and reviews into decision-making in high-profile cases tend to reassert familiar imperatives – particularly that professionals should ‘share information’ in order to identify and protect children at risk. Despite radical reforms to safeguarding processes and systems over the last 10 years, errors and failures persist in detection and intervention when children at risk present in secondary care. There is no ‘gold standard’ for the diagnosis of child abuse. Harmful incidents to a child are rarely independently witnessed and, unless there is perpetrator confession, reliance is placed on substantiation of reasonable suspicion at case conferences or in the civil courts (that the occurrence of abuse was more likely than not). The consequences of an incorrect diagnosis of child maltreatment in either direction can be catastrophic. A false-negative diagnosis of a ‘sentinel’ or ‘harbinger’ injury, such as facial bruising or oral injury, in a non-independently mobile infant may precede severe and sometimes fatal abuse. 1 A false-positive diagnosis of inflicted injury in a child presenting with, say, a scald could have serious consequences, including needless separation of the child from his or her family. 2
The last decade has seen the rise of the patient safety paradigm in health, with three major reviews taking place in England in 2013 – the Francis, Keogh and Berwick reports – arising from the events at North Staffordshire NHS Foundation Trust. 3–5 These emphasise, variously, social and organisational processes, including the importance of communication, feedback loops, confidential reporting and organisational learning. However, these are rarely modelled in detail to take account of the social and cultural dynamics of child health settings and children’s safeguarding. This remains a relatively neglected area, despite being associated with high risks, including child deaths. For example, while tools exist for detecting risk [it has been estimated that 91.7% of emergency departments (EDs) have some form of written protocol6], little is known of their effectiveness in influencing clinical behaviour, and follow-up of child protection outcomes is typically absent. 7,8 To date, mainstream patient safety research has tended to emphasise safety within clinical specialities, departments or units, such as operating theatres or EDs, with less attention paid to multiagency systems, the wider organisation and beyond. In children’s health care, the complexity of human factors is somewhat broader than in many other clinical domains, not least because the decision-making network is dispersed and the potential risks to children are outside rather than inside the hospital walls. Thus, the interface between hospital-based services for children and local authority children’s social care (CSC) is crucial. Very recently, there has been increased attention to this domain, which is beginning to draw attention to the importance of human and interactional factors,9 with increased emphasis placed on clinical governance through the use of best evidence, audit and, more recently, supervision and peer review. 10
Alongside developments in patient safety, the child protection system has also been subject to a number of major reviews, with the most recent11 making recommendations about the need to move away from a compliance culture, to support professional judgement and to develop learning cultures in CSC organisations. These chime with the recommendations of the Francis,3 Keogh4 and Berwick5 reports, potentially providing an opportunity for a system redesign that takes into account the specific challenges of safeguarding children at risk. This study examines the interstices between hospitals and CSC. It looks in detail at the factors affecting decision-making and knowledge sharing in secondary health-care settings to argue for a more sophisticated engagement with the complex factors at play. It draws substantially on the patient safety paradigm and associated concepts relating to organisational culture and change.
Specifically, the study is focused on supporting and evaluating clinician-led service design in an acute trust in the north-west of England, where the relative neglect of safeguarding in patient safety initiatives had prompted senior clinicians, with strong support from the executive board, to rethink their processes and practices. A suite of initiatives and artefacts has been designed to combine both bottom-up initiatives and top-down governance,12 which has been shown to be effective in promoting cultural change. Their intended outcome is to create a positive safety culture, characterised by openness, justice and learning, where learning from error is regarded as the norm. 13 The various initiatives are described in detail in Chapter 6 of this report, but are summarised below (Table 1).
| Module | Cultural emphasis | Components |
|---|---|---|
| Governance | Promoting board-to-ward communication and feedback | Walkround |
| Electronic reporting | Promoting a reporting culture | Electronic information sharing form based on patient safety principles |
| Quality control (co-mentoring) | ||
| Special circumstances form for maternity cases | ||
| Storytelling | Safeguarding awareness and the sharing of professional knowledge | Case discussions based on systemic incident analysis |
| Digital stories |
Research aims and objectives
This project follows a ‘whole systems’ approach aimed at addressing these deficits in the knowledge base, and is also oriented to action and to creating a culture of safe practice with children at risk, using a user-centred design methodology. It is designed to address the following primary question:
‘Can a safeguarding culture be designed within the hospital environment that will provide the conditions for the detection of children at risk of abuse and support protective actions before discharge, including collaboration with external agencies?’
More specifically, the objectives comprise:
-
the development of a sociologically rich understanding of why diagnostic failures and communication breakdowns occur
-
the design of a suite of integrated interventions for promoting a positive safety culture, following a user-centred approach
-
the evaluation of the effectiveness of this package, including its generalisability across sites.
The project addresses cultural and organisational issues, uses applied methodologies within a multidisciplinary team, makes better use of existing research knowledge through system redesign, and is centrally concerned with knowledge transfer within and between organisations, seeking to provide measurement of quality improvement.
In addition to contributing to the design of innovations in the primary site, the project has been concerned with the adoption of the safeguarding system in new sites. Understanding the transfer of technologies between contexts is crucial if benefits are to be accrued across the NHS. In a review of research on the diffusion of service innovations, Greenhalgh et al. 14 concluded with a call for research to address the following key question:
By what processes are particular innovations in health service delivery and organization implemented and sustained (or not) in particular contexts and settings, and can these processes be enhanced? This question would benefit from in-depth mixed-methodology studies aimed at building up a rich picture of process and impact. 14
The present study aimed directly to address this gap, following the requisite disciplined, eclectic approach. In a recent comprehensive review of technology adoption in health care, the provision of ‘firm evidence of clinical efficacy and cost-effectiveness’ was identified as a primary determinant of successful adoption. 15
Structure of the report
Chapter 2 reviews a diverse range of literature on safeguarding and on organisational systems and cultures. Chapter 3 outlines the methods and natural history of the project. Chapter 4 primarily addresses the first objective of the study – the development of a sociologically rich understanding of why diagnostic failures and communication breakdowns occur – using data from the study to illustrate the everyday complexities of knowledge making and sharing in relation to safeguarding concerns in the hospital context. Chapter 5 builds on this to explore the perspective at the receiving end of information in CSC. Chapter 6 addresses objectives 2 and 3 and details the artefacts in use in site 1 and their evaluation, and also includes a description and formative evaluation of systems in use in site 2. Chapter 7 concludes the study, with particular reflection on the potentialities and challenges of innovation and technology transfer in complex public service bureaucracies. It attends to the principal research question of whether or not a safeguarding culture can be designed that will provide the conditions for the more accurate detection of children at risk of abuse and support protective actions before and after discharge.
Chapter 2 ’Wicked issues’ in safeguarding children
This chapter reviews a range of extant literatures which underpin the study. It begins with an examination of what is known about child protection practice and the complexities of the reasoning processes involved. Attempts to reform policy are critically reviewed. It is argued that the ‘process paradigm’, which sees organisations as technical networks of business processes and has been dominant in the public services [as a central feature of the new public management (NPM)] for at least two decades, is not optimal for children’s safeguarding. 16,17 The chapter then reviews the literature on safety cultures, pivotal to understanding the innovations in our primary site, and concludes with a brief review of some of the seminal work on technology adoption, given our interest in transferring these innovations to other settings.
Policy context
[C]hild protection raises complex moral and political issues which have no one right technical solution. Practitioners are asked to solve problems every day that philosophers have argued about for the last two thousand years . . . Moral evaluations can and must be made if children’s lives and well-being are to be secured. What matters is that we should not disguise this and pretend it is all a matter of finding better checklists or new models of psychopathology – technical fixes when the proper decision is a decision about what constitutes a good society.
p. 24418
Written 30 years ago, this closing paragraph of a detailed ethnography of child protection underscores the ethical imperatives and dilemmas at the core of clinical practice in this area. This counsel has not been heeded, and ‘the child protection system’ has arguably been subject to a series of technical fixes. Thus, the key moral debates have not taken place and service design has tended to be based on a series of misreadings of the realities of the work. This study is focused directly on the pressing matter of ‘design’ and has entailed a detailed examination of everyday safeguarding practices in secondary health settings where problems of detection and action to protect children at risk have proved recalcitrant, despite the fact that statutory frameworks and policy/practice guidelines are well established and that there are ongoing attempts to refine and improve them.
The Children Act 198919 introduced the concept of significant harm as the threshold for justifying compulsory intervention in family life in the best interests of children or unborn babies. 19 Much professional activity in relation to safeguarding children is oriented to deciding whether or not the presenting circumstances constitute ‘reasonable’ cause for referral to CSC for a section 47 investigation. Section 47 of the Act places a duty on local authorities to make enquiries, or cause enquiries to be made, where there is reasonable suspicion that a child is suffering, or is likely to suffer, significant harm. When this threshold for intervention is deemed to be reached, the duty to seek parental consent for information sharing is dispensed with. In many cases, particularly those presenting in secondary health settings, knowledge about the family or child is either too ambiguous or too incomplete to warrant a section 47 referral, even though professionals may have serious concerns about children’s well-being. In these circumstances, they may make a referral under Section 17.1(a) of the 1989 Act19 which gives local authorities a duty to ‘safeguard and promote the welfare of children within their area who are in need’. In relation to both of these categories, local authorities will, in turn, make decisions about whether or not the criteria are met. Thus, a case may be referred to children’s services, but may still fail to make it over the threshold of the ‘front door’. This makes this interface particularly thorny and elevates the importance of professional ‘information practices’, namely the way professionals handle and present information in particular ways to serve particular purposes.
The importance of ‘sharing information’ is underscored in statutory guidance. In 1988, the then Department of Health and Social Security began attending to the need to ensure multiagency working in child protection, producing the first version of Working Together, which provided detailed prescriptions for competent interagency working. 20 These measures were intended to protect children from ‘inter-agency dangerousness’ (p. 13), by ensuring that significant details were passed between agencies. Working Together has been through a number of iterations since, and in its penultimate form in 2010 the document had grown to 393 pages in length as the government tried to pre-empt every communicative eventuality. This has recently been stripped back to 97 pages following attempts to cut the bureaucratic burden in child protection practice,21 but it remains the primary guidance for multiagency working in child safeguarding. The new Working Together to Safeguard Children has the explicit aim of shifting the focus away from processes and onto the needs of the child. 22 However, most of the responsibilities and procedures in this 2013 document remain the same as the 2010 guidance. These are underpinned by a key principle, that ‘safeguarding is everyone’s responsibility’, but this is a deceptively complex imperative in everyday practice, particularly when services are under pressure.
Brandon et al. 23 estimate that, currently, the total number of violent and maltreatment-related deaths of children (0–17 years) in England is around 85 per year. In 50–55 of these cases, death was directly attributable to violence, abuse or neglect, with a further 30–35 in which maltreatment was a factor but not the primary cause. Despite policy changes, the numbers of child deaths has remained relatively constant and, in contrast with their political significance, comparatively low. 24 The most recent data suggest that fewer such deaths are occurring in children already known to the child protection system and in infancy, although this remains the period of highest risk. 23,24 Nevertheless, accurately detecting children at risk without encroaching on the privacy of family life has proved a very vexing problem with a turbulent recent history. Moreover, while secondary health-care settings should provide opportunities to prevent children returning to unsafe situations, or to alert other agencies to potential dangers, there is strong evidence that clinicians under-report child protection concerns9,25,26 and that triggers for reasonable suspicion are highly variable, particularly in relation to older children. 27,28 In one of very few studies examining the interface between hospital services and CSC, Lupton et al. 29 found that clinicians in EDs believed that other agencies and professionals had unrealistic expectations of their role in child protection work. Clinicians’ thresholds for reasonable suspicion are variable and highly subjective. In a ‘judgement analysis’ of the decision-making of a hospital-based child protection team in respect of referral to Social Services,30 involving 915 cases over a 7-year period, it was found that 81.7% of reported cases were substantiated through systematic decision processes that reflected current knowledge. However, single-parent families in financial difficulties were more likely to be reported, a finding that echoes other studies. 31 The authors were unable to determine whether this reflected a true association between low-income, single-parent families and child maltreatment, or a prior bias or stereotypical view of such families.
Under-reporting of suspected child abuse cases tend to reflect clinicians’ personal experience, beliefs and attitudes. 32 Factors associated with under-reporting include prior knowledge of the family,33 lack of confidence in the child protection system and its perceived adverse consequences for the child and family,33,34 and previous negative experiences of the child protection system and the courts. 33–35
Clinicians’ interpretation of ‘reasonable suspicion’ is also highly subjective,36 although a central diagnostic tenet, of an injury being suspicious when the history is inconsistent or implausible, is generally adhered to. 32 Using case vignettes abstracted from real clinical situations, Lindberg et al. 37 showed that experienced paediatricians agreed substantially at either pole of an ordinal scale, from definitely not inflicted (e.g. disinterested witness to a road traffic injury, mimic of bruise such as a birth mark) to definitely inflicted (e.g. unexplained multiple fractures, patterned bruising) injury, but showed considerable variability in agreement with ‘intermediate’ case scenarios (e.g. bruising in a setting of possible ‘easy bruising’). This accords with clinical experience, where diagnostic uncertainty that accompanies such ‘grey’ cases can lead to circumspection and indecision. 38
Despite the emerging evidence base, there are signs of physical injury that remain equivocal and situations where the likelihood of physical abuse is difficult to determine. For example, the characteristics of bruising suggestive of physical abuse are, to some extent, seen in children with an underlying blood coagulation or connective tissue disorder. Both physical abuse and bleeding disorders may coexist and the diagnoses are not mutually exclusive. 39
A suspicious injury may remain the only concern when a child protection investigation has been concluded and known risk factors have been eliminated as far as possible. In these situations, the investigating team will turn to the paediatrician to adjudicate, as the balance lies with the medical evidence alone. This is a very difficult and uncomfortable position for the professional. Could this be a non-intentional, ‘one-off’ injury that, for some reason, was not witnessed; or is the nature of the injury, whether abusive or otherwise, being concealed out of fear of repercussions; or will this be regarded as a ‘harbinger’ if the child represents with a more serious injury?
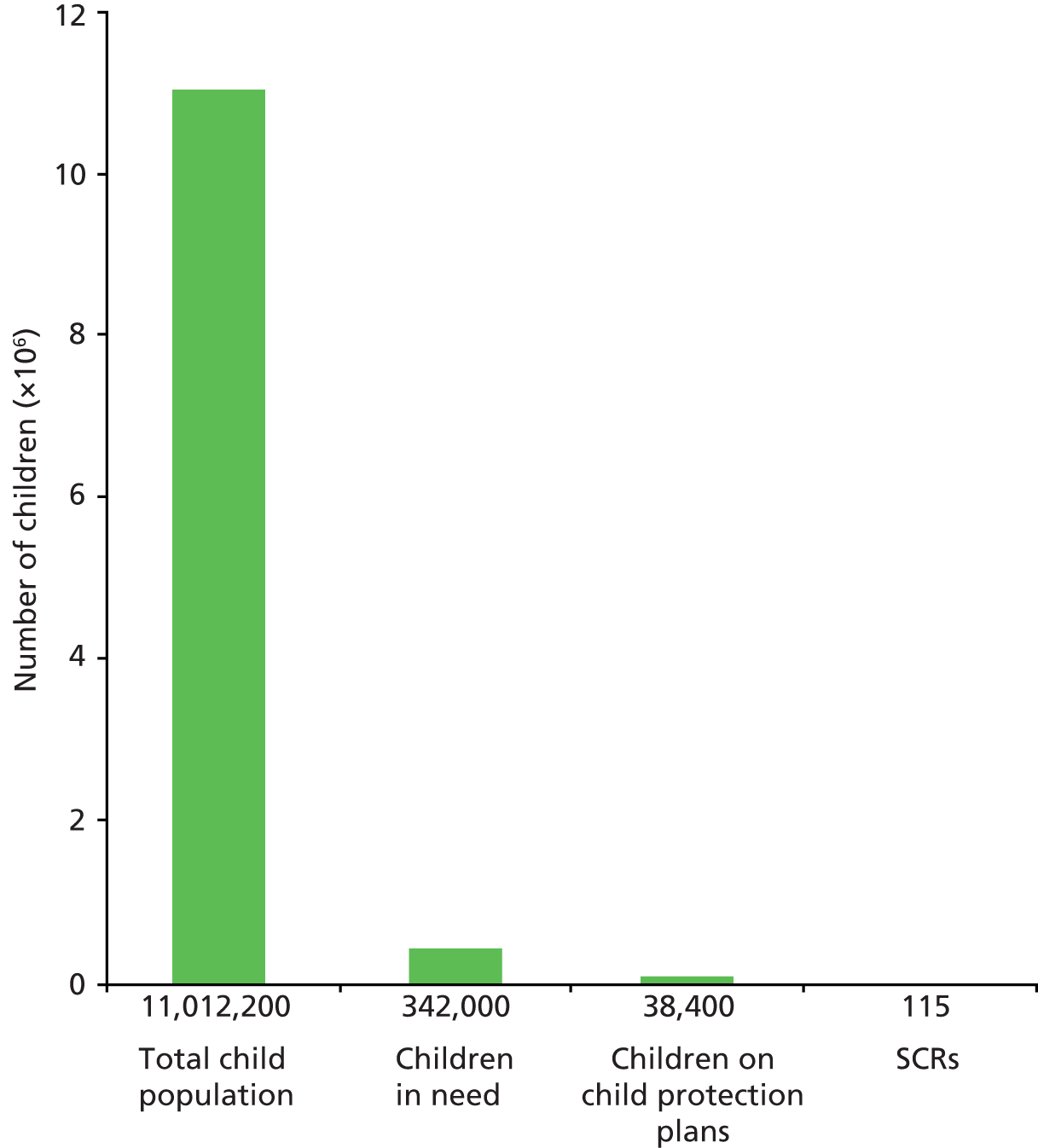
In their review of serious case reviews (SCRs), Brandon et al. 23 note that one-third of the 40 children they studied had a history of missed health appointments; six had been admitted to hospital, one child nine times; and 18 had at least one attendance at an ED. Serious harm is only the tip of the iceberg: the number of other errors is unknown, but will be substantially greater than SCRs suggest. Moreover, the number of children experiencing serious harm clearly hugely outweighs the number of fatalities. This is illustrated in Figure 1, using data from Brandon et al. 23
High-profile stories and media outrage about children who have been neglected or fatally abused at the hands of their parents or carers have driven policy since the death of Maria Colwell in 1973. 40 With the inquiry reports into the deaths of Jasmine Beckford,41 Tyra Henry42 and Kimberley Carlile,43 the late 1980s saw the translation of the notion of danger into one of ‘risk’. As Mary Douglas44 notes, the beginnings of the notion of ‘scientific’ risk assessment had implications for professional and organisational accountability:
The charge of causing risk is a stick to beat authority, to make lazy bureaucrats sit up, to exact restitution for victims. For those purposes danger would once have been the right word, but plain danger does not have the aura of science or afford the pretension of a possible precise calculation.
p. 24
Dingwall et al. ’s18 study of the child protection practices in two social services departments appeared to support the view that the State was reluctant to intervene in family life. The authors referred to the ‘rule of optimism’, by which they meant the pervasive liberal democratic belief that children are usually best cared for within their (birth) families. This idea was (mis)appropriated by the Beckford Inquiry and was taken to mean that it was social workers who were overly optimistic and easily duped by dangerous parents. After the inquiry, Dingwall45 underscored the more general societal meaning of the original statement through the use of the first person plural:
the child protection system contains an inherent bias against intervention anyway. If we wish to change that, then we must confront the social costs . . . that some children will die to preserve the freedom of others.
p. 503
This perspective was more recently reiterated in the family courts:
Society must be willing to tolerate . . . diverse standards of parenting . . . [and] children will inevitably have both very different experiences of parenting and very unequal consequences flowing from it . . . These are the consequences of our fallible humanity and it is not the provenance of the State to spare children all the consequences of defective parenting.
J Hedley, cited in the matter of B (A Child)46
This central moral tension remains between the rights of the many to freedom from scrutiny and intrusive intervention into the intimate spaces of family life, and those of the relatively few who come to serious harm at the hands of their carers. This is rarely, if ever, addressed in policy and procedure, but it renders the accurate detection of children at risk a really ‘wicked issue’ for the human actors involved. The precautionary principle is constantly in a discursive and moral dance with proportionality. Many more children die in road accidents, for example, than at the hands of their significant others. 47 Each violent and retrospectively tragically preventable death has its own effect on this fickle pendulum, potentially shifting the point of balance. The high-profile cases of Victoria Climbié48 and Peter Connelly have had their impacts on policy, which are discussed below. The more recent cases of Keanu Williams and Daniel Pelka in autumn 2013 have provoked further political and media scrutiny of systems and practices, again and understandably with a focus on the prevention of false negatives (i.e. avoiding missed cases) and an assumption that more referrals to CSC will keep children safe. It is easy for these tragic events to drive precipitous policy initiatives which tend to move towards the precautionary pole.
The post-Climbié reforms: strong but wrong solutions?
Victoria Climbié died in London in 2000 as a result of longstanding cruelty at the hands of her great aunt, Marie-Therese Kouao, and Kouao’s partner, Carl John Manning. 48 This triggered a highly influential inquiry into professional and institutional failure, which proved a pivotal catalyst in New Labour’s modernisation agenda for children’s services. Resulting legislative changes, first outlined in the Every Child Matters Green Paper,49 include the establishment of local children’s safeguarding boards, with the responsibility for safeguarding children in local authority areas, conducting reviews on all child deaths, and increased regulation and audit of child protection responses. The government put in place a series of measures intended to enhance information sharing and early intervention, drawing heavily upon information and communication technologies (ICTs) to support their ambitions. 50 These included the establishment of a children’s database (known as ContactPoint), which was intended to hold basic information on all children in an area, with an option for practitioners to record their involvement with a child/young person and, as an early warning, place a ‘flag of concern’ on a child’s records. This has subsequently been scrapped, but there are currently plans to develop a national database by 2015 to record every child who visits hospital accident and emergency (A&E) departments or has out-of-hours general practitioner (GP) consultations. It is proposed that medical staff will be able to see if the children they treat are subject to a child protection plan, meaning that they have already been identified as being at risk. Thus, the search for technical solutions to mediate and augment human communication continues, and these matters are discussed further in later chapters of this report.
The post-Climbié reforms also included aspirations for a ‘common assessment’ process. The common assessment framework (CAF) has been developed as the standard tool for all professionals working with children and families, which can be used for both assessment and referral purposes. 51,52 The aspiration was that a ‘common language’ may develop to improve information sharing and communication between professionals. The inspectorate Ofsted currently uses the numbers of CAFs completed by agencies as a proxy measure for early help, with the apparent assumption that more is better. 53 This places pressure on hospital services to use this rather than other forms of assessment, as we discuss in Chapter 6.
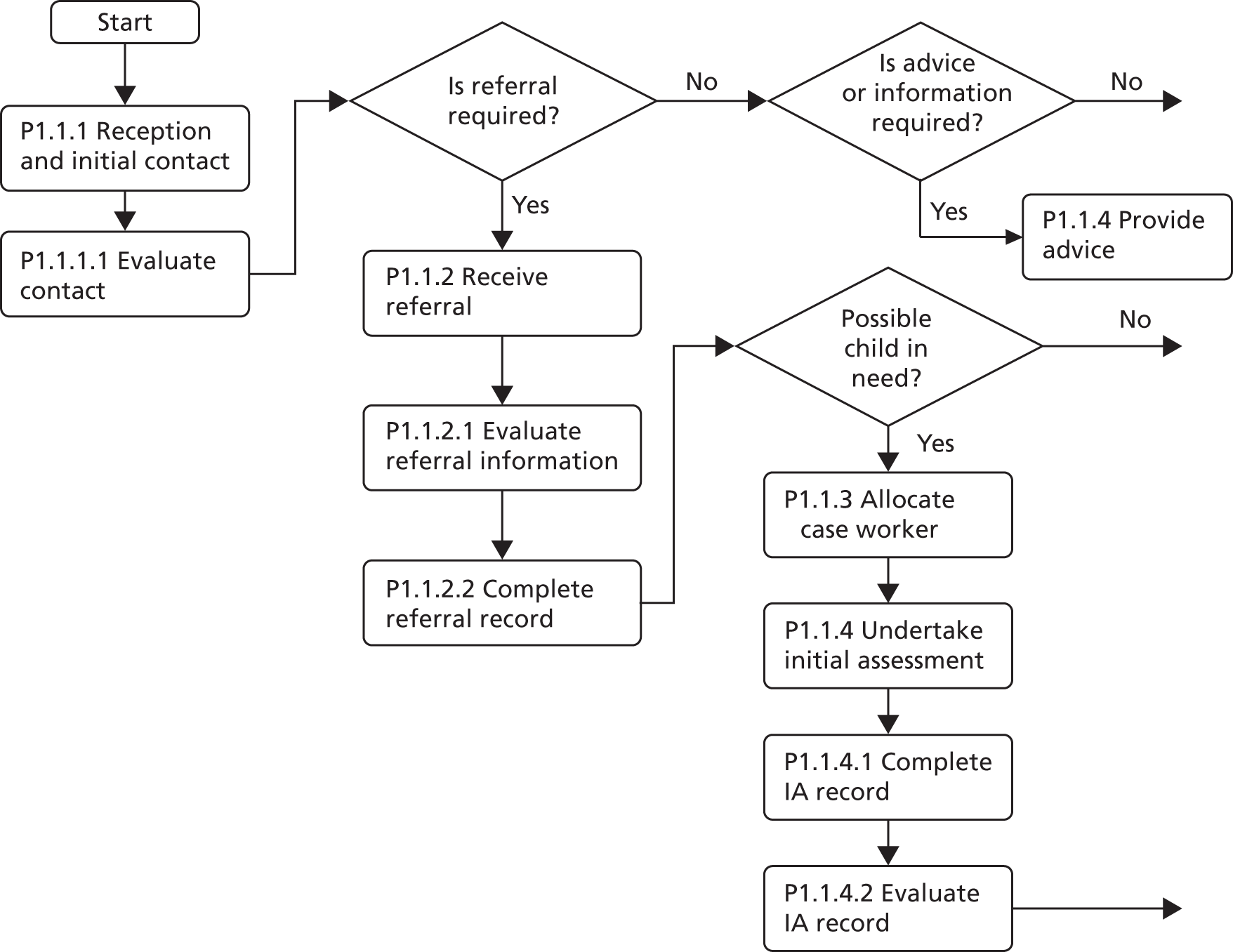
The developments in England post Climbié have led to a highly centralised ‘command and control’ approach to regulating the activities of professionals in the area of child protection. New Labour’s approach to public administration provided a medium for NPM to flourish. 54 The defining contours of NPM were that strong top-down management is the key to quality and performance; that workers are apt to be self-interested and inefficient; that the standardisation of processes and explicit targets drive quality; and that these are ensured by rigorous micromanagement using performance indicators. 55 In the context of human services, and particularly child protection, NPM has been centrally concerned with managing institutional risk,56 and has been accused of creating a climate of ‘targets and terror’. 57 It is in this context that the then New Labour government put in place a series of reforms drawing heavily on concepts of ‘business process management’ (BPM), electronically enacted through the Integrated Children’s System (ICS). 58,59 The ICS attempts to re-engineer and micromanage practice through the imposition of a detailed, workflow model of the case management process and other processes, as Figure 2 demonstrates.
FIGURE 2.
The diagram is adapted from the Children’s Social Care Services Core Information Requirements Process Model. 60 It shows only the initial stages of a much more comprehensive flow chart covering an A3 sheet; the open arrows on the right indicate that the flow continues after these initial steps have been performed. The labelling of the process steps (P.1.1.1, etc.) reflects the hierarchical notational system in the original process model to designate successive steps. IA, initial assessment.
Many of Laming’s48 broad diagnostics of the failures contributing to Victoria’s death are accurate. However, the relative neglect of human, interactional and social factors in the report means that the policy responses, particularly the emphasis on standardised processes and ‘information sharing’ initiatives, have been based on a set of contestable assumptions. 16,61 The most notable of these is that catastrophic child deaths are substantially the result of professionals failing to record or share information. Such failures clearly are not trivial, indeed they are crucial, but they are not necessarily causal. For example, they are ubiquitous features of many cases which do not end catastrophically, as Wastell17 notes:
[T]o be sure that this evidence is decisive, we need to know how often it was present in other cases but did not lead to calamity . . . Unless it can be shown . . . that assessments, information gathering and multi-agency collaboration were conspicuously worse in the serious cases, how can it possibly be claimed that these were critical causal features?
p. 168
For the causal factors in the death of Victoria, it is necessary to look elsewhere. A re-examination of some of the evidence submitted to the Climbié inquiry48 will illustrate this point. In July 1999, Dr Schwartz, consultant paediatrician at Central Middlesex hospital, examined lesions on Victoria’s body. Her clinical opinion was that the marks were self-inflicted due to intense itching from a scabies infection. This opinion differed from a previously expressed and documented diagnosis by a locum registrar, who produced detailed body maps of Victoria’s injuries and was of the view that there was a strong possibility that she had been physically abused. While Dr Schwartz testified to the inquiry that she had made it clear to social services that she could not exclude physical abuse, the production of a medical explanation for some of the injuries proved a highly consequential red herring.
The contact with social services to inform them of the ‘change’ of diagnosis was made by Dr Dempster, a junior doctor unfamiliar with social services and the child protection system. Dr Dempster followed up several unsatisfactory conversations with social workers with the following letter:
Thank you for dealing with the social issues of [Victoria]. She was admitted to the ward last night with concerns re: possible NAI [non-accidental injuries]. She has however been assessed by the consultant Dr Schwartz and it has been decided that her scratch marks are all due to scabies. Thus it is no longer a child protection issue.
There are however several issues that need to be sorted out urgently: 1) [Victoria] and her mother are homeless. They moved out of their B & B accommodation 3 days ago. 2) [Victoria] does not attend school. [Victoria] and her mother recently arrived from France and do not have social network in this country. Thank you for your help.
Laming, p. 25148 (The Victoria Climbié Inquiry, Crown Copyright 2003)
The letter’s communicative intent was to prompt a visit to the hospital by a social worker, but was read by social services as a recategorisation of the case, triggering a quite different organisational response. Brent children’s services had two initial assessment teams: referrals were considered first by the duty team, and, if the referral appeared to relate to ‘a child in need’, the case would remain with them for initial assessment. If, on the other hand, there were child protection concerns, it would be transferred to the child protection team for urgent action. Under the Children Act 198919 and the associated guidance, the category of ‘child in need’ was introduced to signal the importance of offering support to families with a range of needs such as housing. Thus, within the assumptive world of Brent Social Services, the crucial line of Dempster’s letter becomes, ‘Thus it is no longer a child protection issue’ and not the documented ‘urgent’ social matters. The case, therefore, entered a bottleneck in an overstretched duty team, who were dealing with backlog of 200–300 cases per week. While these circumstances are clear, such formal organisational systems and the dysfunctions they produce escaped scrutiny in the enquiry process; indeed, subsequent reforms have prescribed more of them, with time scales imposed on decision-making and assessment, regardless of case complexity. 62 Thus, the interface between other agencies, including hospitals, and CSC became dogged by a preoccupation with ‘thresholds’ and their ‘consistency’, ascribing a technical rationality to what is in fact a complex sense-making process with the potential to distract attention from human factors in the decision process. 63
Thresholds are dynamic. They bend in response to the balance between demand and resources, and are affected by a range of human, social and organisational factors. For example, analysis of the child protection system at a national level has demonstrated that as referral rates increase, the number of ‘non-urgent’ cases allocated falls,62 reflecting rational adaptation and prioritisation at the local level. In such a system, an immobile baby presenting at the ED with an unexplained skull fracture will always make it over the threshold regardless of competing demands, but most children and families referred from health settings to social work services are not like that. A family struggling to cope is also going to struggle to get through the front door of many local authority CSC departments, and they are going to struggle harder on some days than others. Yet a great deal of organisational time is spent crafting ‘thresholds’, and waste in the form of ‘failure demand’ enters the system as cases are batted back and forth, and universal services try to second-guess responses. 64
It is clear that complexities arise from the need to pass what might be speculative and ambiguous information across service boundaries. Communications within a system are embedded in a range of interpretive dichotomies: signal/non-signal; information/noise and pattern/randomness. 65 One reader/hearer may find information where another detects only noise. For the receivers of the referrals, for example, the categories ‘non-accidental injury’ or ‘child protection case’ are the signals they are seeking in the ‘noise’ of the genuine deliberations of doctors, as the latter try to make sense of equivocal cases.
Interactional factors in child health: sharing knowledge
There are two principal literatures which pertain to the complexities of sense-making and knowledge sharing in children’s safeguarding at the agency interface. First, there are problems in translation, interpersonal trust and technological systems where the individuals involved, including sometimes the child, are separated from each other in time and space. Second, there are intrinsic complexities in all clinical and professional decision-making, which are amplified in safeguarding because the presenting ‘symptoms’ are often ambiguous and contestable, and judgements about parenting often require moral evaluations.
Beginning with the first set of factors, research shows that knowledge sharing and learning is influenced by multiple interpersonal, social and organisational factors, including the inhibitory impact of distinct knowledge domains, social hierarchy and low trust. 66 Knowledge sharing throughout child health and social care is, therefore, both ‘slippery’ (difficult to codify) and ‘sticky’ (difficult to share across boundaries), not readily responsive to simplistic exhortations to ‘share information’. 67,68 Mainstream patient safety research has tended to focus within clinical specialities, departments or units, such as operating theatres or EDs, with less attention paid to the interconnections between these areas and the wider organisation and beyond. 69
The identification of children at risk and the sharing of knowledge and decision-making across time and space may properly be conceived as a complex system, whereby interdependencies and couplings between professionals and agencies can be the source of both safety and risk, depending on how they are co-ordinated. The promotion of multiagency working in social work with children and families is promoted as a way to prevent children ‘slipping through the net’ of services, and of ensuring that professionals have the ‘full picture’. 70 Yet research from social psychology71,72 on helping behaviours, and from the USA73–75 on interagency collaboration, has found that where there are increased numbers of people involved, the individual sense of responsibility for a case can, contra to the policy aspiration, be radically reduced. The literature repeatedly emphasises that good communication has the potential to reduce this complexity and support co-ordination, but, thinking back to the example from the case of Victoria Climbié, what does communication mean and how does one know when it has taken place?
Knowledge sharing is more than the transmission of information. It denotes the exchange and use of diverse knowledge, and often more tacit ‘know-how’, between different groups to engender shared understanding and collaborative learning. 76 Knowledge is often elaborated along two lines. For many systems and improvement strategies, such as knowledge management, knowledge is conceived as an explicit, abstract and tangible resource that can be accessed, codified and exchanged (e.g. in formal policies or incident reports). In other words, it is a substantive thing to be shared with others in the form of documents or evidence. This contrasts with the idea that knowledge or know-how is often tacit, experiential, taken for granted and inextricably situated in practice. 77 In this sense, knowledge is difficult to share and it is typically acquired and developed through participation in ‘communities of practice’78 rather than management information systems. In short, knowledge is not a ‘thing’ that a community ‘has’, but rather it is what they ‘do’ and ‘make’, and who they ‘are’. 78 This distinction is important because efforts to understand and, indeed, promote knowledge sharing and collaboration should focus not only on the formal assemblages of knowledge, but also on the more informal and unarticulated manifestations of know-how. Knowledge sharing is, therefore, more than the communication of information, referring also to how the meanings, ‘know-how’ and practices of one group or organisation can be shared and integrated into the practices of another. 79 Recognising these differences, knowledge sharing requires different strategies and practices. So, the sharing of explicit knowledge (e.g. evidence, guidelines or data records) is often related to how it is described, presented and articulated; the extent to which different actors are aware of its availability and utility and can access it; and the ease with which it can be used. In contrast, the sharing of tacit knowledge is often based on more informal, day-to-day interactions around common problems, the creation of opportunities to enable social intercourse and creative problem-solving.
More than this, however, knowledge sharing and collaborative learning involves transforming the form of knowledge. For example, Nonaka80 suggests organisational learning involves the ‘externalisation’ of tacit know-how, so that it can be used by others, but also the ‘internalisation’ of explicit knowledge, so that it can be integrated into daily practices. As such, activities are often needed to translate and transform knowledge between different communities. Returning to our previous example, if a non-mobile infant presents at an ED with a skull fracture, which the parents say has been caused by the infant turning over in his or her cot, there is little externalisation or translation of tacit knowledge required: it is self-evidently implausible, and both the police and CSC will have no difficulty understanding it as such. In this case, the technological systems, whether these be telephones, faxes or information technology (IT) systems, will usually be sufficient to ‘pass’ the information. Any system failure would be readily evident, probably technological in nature, and easily remedied.
However, if the mother of a 5-year-old child on a paediatric ward is seen by the parent of another patient to be shouting at the child ‘inappropriately’, and nursing staff also have a ‘bad feeling’ about the way the parent and child interact, the process of translation is much harder. If the nursing shift changes and the new staff do not directly encounter the parent in contact with the child, further problems ensue. The sense-making is constrained by the local organisational temporal practices which disrupt relationships and reduce or eliminate proximity. This has consequences for the embodied knowledge of the interaction between parent and child, the subsequent production of an externalised ‘rationalisation’ of the observation, and, crucially, a waning of the moral imperative to act. 81 One can now easily see the complexities of knowledge sharing in safeguarding. As Bauman82 notes:
The only space where the moral act can be performed is the social space of ‘being with’, continually buffeted by the criss-crossing pressures of cognitive, aesthetic, and moral spacings. In this space, the possibility to act on the promptings of moral responsibility must be salvaged, or recovered, or made anew.
p. 183
Research points to a range of factors that facilitate or inhibit knowledge sharing. 76,79,83,84 These include the characteristics of both ‘donor’ and ‘recipient actors’, such as their motivations, accessibility, strategies, levels of trust, shared values, hierarchies and absorptive capacity. 85,86 For example, in the commercial world, competitive pressures can inhibit inter-organisational knowledge sharing where it threatens competitive advantage. 76 As discussed, CSC is under systemic pressure to reduce demand on its services and, accordingly, has developed locally ‘rational’, rationing and gatekeeping practices. The structural configuration of relationships between agencies can also channel knowledge flows through ‘central actors’ rather than between peripheral actors,87 or indeed through actors who ought to be peripheral, such as call centre operators, at the expense of a proper dialogue between clinicians and social workers, for example. 88 Similarly, power hierarchies and cultural difference between actors can impact knowledge sharing, especially where powerful actors maintain control of knowledge to advance their own interests. 84,89 For professional work, these issues are exacerbated where expert knowledge is closely linked to sociolegal jurisdictions within the division of labour. 90 CSC is the lead agency for child protection investigations under section 47 of the Children Act 198919 and, as noted above, has a number of systemic pressures which incentivise ‘screening out’ ambiguous referrals by recategorising them as ‘below the threshold’ for intervention.
Making knowledge: the problematics of sense-making
As explained above, there are vexing problems in ensuring effective knowledge sharing in relation to children at risk. However, there are also complex problems in knowledge making for individuals and groups of professionals and clinicians. For example, often children present with a complaint for which there may be biological, neurological, genetic and/or psychosocial explanations. In accomplishing diagnosis, the boundary between biological and psychosocial aetiology is especially problematic. 91 For example, are frequent hospital admissions the result of an intrinsic metabolic disorder, a consequence of emotional maladjustment, because of poor nutrition or inadequate parenting, or do all factors apply?
To find possible clues to diagnostic certainty and avoidance of error in child protection, it is useful to examine the process of decision-making. Munro92 describes two major forms of reasoning as the basis of decision-making practice: intuitive and analytic. Intuition is a cognitive process that ‘somehow produces an answer without the use of a conscious, logical process’. Analytical reasoning is the opposite, ‘a step-by-step, conscious, logical process’ (p. 2). This is akin to the decision-making framework described by Almond93 and Dowie and Elstein,94 which portrays intuition as a subconscious and experiential process, based around ‘common sense’, ‘gut feeling’ and ‘cue and pattern recognition’, in contrast to the analytic or rational model, which is based on logical and systematic methods of gathering information. Both Munro92 and Almond93 argue persuasively that these models exist on a continuum, the process of decision-making often involving decisions within decisions, all of which require careful deliberation and reflection, both at a rational and an intuitive level. Over-reliance on intuition may, in some circumstances, lead to a persistent, negative bias towards, say, low-income, single-parent families in reporting child abuse concerns. On the other hand, evidence-based checklists may be a valuable aid to decision-making, but cannot provide a satisfactory replacement for intuitive judgement.
Furthermore, children frequently injure themselves and the injuries may be medically trivial,95 creating a potential bias towards the default assumption of accidental injury. Children are usually accompanied by parents whom clinicians may find difficult to confront, and their moral evaluations of the parents can also be decisive, especially when the child cannot communicate directly. 25,91,96,97 These difficulties are exacerbated by other human factors. Human beings have particular cognitive biases. We tend to reach conclusions quickly and develop a ‘psychological commitment’ to our first formulation. 94 This is confounded by a tendency to seek out evidence that confirms a hypothesis rather than to search for ‘disconfirming’ evidence, known as ‘confirmation bias’. 98
The case of Peter Connelly (Baby P) illustrates some of these complexities. Peter was observed to be injured very frequently, with a variety of bruises and bumps which became increasingly serious over time. However, Tracey Connelly, Peter’s mother, alleged that he would frequently injure himself and had behavioural disturbances such as head banging, which were also observed by the social worker. A strong (but wrong) hypothesis thus took hold that Peter had a behavioural disorder. In his last few months of life, Peter’s weight was falling dramatically. His father had also raised significant concerns, and told agencies that Tracey Connelly had a new boyfriend. Many agencies were involved with Peter, but the different professionals seemed to be failing to notice or to respond to the deterioration in Peter’s health and development, and to act appropriately in relation to his injuries. Tracey Connelly had been apparently co-operative with services, frequently presenting Peter at the doctor’s surgery, for example, to seek help with what she said was his difficult behaviour.
The intuitive judgements that the professionals had made about Tracey Connelly’s character, and their cognitive commitment to the ‘behavioural disturbance’ hypothesis, led them to pay insufficient attention to clear signs that Peter was being abused. These pressures are challenging to counteract, resisting interventions such as training. 25 Moreover, attempts to increase the reporting of concerns carry their own unintended consequences: the generation of false positives, overloading child protection services, together with buck-passing and discrimination against vulnerable communities. 99 For example, there are concerns that the use of screening instruments and protocols in health services, to assist in the identification of cases where children could be at risk, may not increase accuracy but may instead lead to a rise in the rate of false positives, putting more pressure on strained child protection25,100–103 resources, which could in turn generate more rather than less risk. There are also potentially direct adverse effects on children; for example, a full skeletal survey to screen for unseen injuries can be very distressing, especially for preverbal infants.
Further complicating the picture, as co-operative social animals, humans are equipped with abilities for making intuitive judgements about each other, often of a moral nature. For a long time, at least as far back as Plato, emotions were seen as distinct from our capacity to reason. Emotions were things to be tamed, allowing reasoning to take place uncontaminated. There is now clear evidence that a good deal of ‘rational’ decision-making relies on our capacities as human beings to make sense of the world using our emotions. 104–106 Gut feelings are not impeccable guides to judgement, but neither are they silly and ‘irrational’. They are not inferior to reason. They rely on the capacities of our evolved, social brain, and enable us to act quickly, often with a high degree of accuracy in many different situations. 107 However, intuitive judgments are vulnerable to error, and so critical debate with others is vital in order that professionals learn to recognise and interrogate such biases, choosing whether or not they need to correct them for this particular case, in these individual circumstances. Human beings’ judgements about each other normally stay in the realm of what we think of as common sense. 108 A ‘gut feeling’ can make an individual particularly resistant to change or challenge,109 especially if that gut feeling is masked by a ‘technical’ vocabulary using, for example, psychological theory of one sort or another. A ‘cold’ mother can thus become redescribed as a ‘mother who has failed to bond with her child’, obscuring the fact that the underlying judgement was made on intuitive grounds, not through systematic scientific observation and critical self-questioning.
The presence of other human actors in the right atmosphere of circumspection, challenge and debate may properly work to ‘trouble’ the intuitive reading of a case, but it will not do so unless the organisational cultures encourage this kind of critical questioning. Without such a culture, professionals all too frequently remain in an unquestioning, comfortable, collective settlement about the reality of a family’s circumstances. This may often prove to be right, but is sometimes strong but wrong. This means that the cultures in organisations, and the dominant ideas in a profession at a particular point in time, will affect the rational/emotional/intuitive responses of individual clinicians and teams. It has recently been argued that more attention must be paid to human factors and the interactional complexities of decision-making regarding children at risk of harm. 61 Within CSC, there are promising signs of growing interest in and potential government support for more systemic solutions, focused on human factors, human-centred design, systemic understandings and more complex conceptualisations of culture and governance. 21,110–112
Protecting children: fatal flaws in the process paradigm
In this section, we develop further our analysis of the failure of systems such as the ICS (see The post Climbié reforms: strong but wrong solutions?) which contribute to the mounting evidence that top-down, bureaucratic approaches to safeguarding children, which privilege process over practice, are not the solution; indeed, they can make matters worse, for instance by restricting knowledge sharing between professionals. 59,62,113–115 We argue that such approaches are based on a process paradigm, the assumption that the key to enhancing reliable performance is to standardise the process and enforce compliance to that standard. This paradigm is problematic not only in health and social case, but in the commercial world, too, from which it derives. This is attested by the high rate of failure of BPM initiatives, estimated to be as high as 80%116 The ‘critical success factors’ for BPM initiatives have been well investigated,116 and the degree to which processes can be validly standardised is the decisive factor. Technologies for process management will thus only be effective for standard, routine processes and it is vital to distinguish between these and non-routine counterparts;17 put simply, the message is ‘do not standardise processes which are not standard’. Lillrank and Liukko117 capture this distinction in their ‘quality broom’ metaphor. Using the metaphor of a sweeping brush, they suggest that quality systems work for routine processes requiring compliance with procedure and protocol (the handle end of the broom), whereas flexible, interpretive processes are required for decisions which are non-routine and taken in conditions of uncertainty (the flexible ‘swishing’ end of the broom). For the latter, a quality culture is required. Treating the processes at the interpretive end as though they were processes at the ‘handle end’ will erode the quality culture, trapping professionals in rigid processes.
Lillrank and Liukko117 argue that non-routine processes differ from standard routines ‘in that input is vague and not readily classified into categories . . . Therefore the assessment of an input is an interpretation which must be derived through the search for new information, iterative reasoning, and trial-and-error’ (ibid. p. 42). While standard processes can be managed directly through procedural or technological means, non-routine processes, on the other hand, are often controlled more effectively through indirect means such as professional beliefs and values, personal responsibility; through culture, in other words. 118 Or, as Weick119 put it:
Either culture or standard operating procedures can impose order . . . but only culture also adds in latitude for interpretation, improvisation, and unique action.
Much of the professional task in children’s safeguarding lies at the ‘brush’ end of the quality broom, which explains why rigid process standardisation at the interagency interface is, fundamentally, the wrong approach. The argument encapsulated in the quality broom metaphor is not simplistically for or against standardisation, but for recognition of the diversity within a system and for the deployment of standardisation only in the correct context.
Managers need to decide what should be strictly regulated and what should be left to empowered individuals and groups . . . A great deal of trouble follows, if processes are interpreted as being different from what on closer examination they really are.
Lillrank and Liukko117
The fundamental need to distinguish routine and non-routine processes also appears in the work of the sociotechnical theorist, Calvin Pava. 120,121 In contrast to routine processes, where work follows a linear, sequential ‘conversion process’, non-routine work (the work done by skilled professionals and managers) addresses unstructured or semistructured problems; it is driven by ‘plausible but imprecise information inputs, varying degrees of detail, extended or unfixed time horizons’, and is characterised by fairly broad discretion (p. 48). 120 Non-routine work is characterised by the management of many activities at the same time; non-linear flow (‘a disjointed zigzag process’ of problem-solving on uncertain, shifting terrain); and vocational separatism (professionals are educated experts with a high degree of autonomy). Pava sees non-routine work as consisting of multiple, overlapping deliberations carried on by flexible and fluid networks of individuals (discretionary coalitions). Deliberations are defined as ‘reflective and communicative behaviours’ concerning equivocal, problematic topics. One example of this in social work is the assessment of a child and family’s circumstances and discussion with other professionals, while in medicine an example is differential diagnosis.
Enhancing non-routine work involves the technical analysis of deliberations, looking in particular for important ‘information gaps’. As a sociotechnical theorist, Pava is equally concerned with the social analysis of deliberations, the ‘role network’ identifying who interacts with who, attempting to understand the ‘characteristic values’ for each party and whether they align, converge or conflict. The key to improving performance is to optimise the joint design of the technical subsystem (the deliberations) and the social subsystem (the role networks). Pava suggests, as example interventions, human resource measures to support the formation of effective coalitions (e.g. team-based pay schemes) and technical innovations to support deliberations (e.g. computer conferencing). In relation to safeguarding children, organisational systems are not optimally designed from a sociotechnical perspective, with the social system often neglected. For example, team relationships may be fractured by efficiency-based interventions such as hot-desking and the use of call centres in local authorities.
Safety cultures
The concept of organisational culture is ubiquitous in the discourses of health-care reform and patient safety. 122 Cultures speak themselves through articulations of ‘the way we do things around here’. Especially where work is non-routine and interpretive, they are likely to have profound effects on case formulations and so forth. Culture is known to be a key factor in, for example, the successful adoption of clinical guidelines. 123 The concept has a long history but came strongly to the fore in the 1980s, promoted by management gurus such as Tom Peters. Culture is a promiscuous, protean concept, amorphously defined and difficult to measure,122,124 but always to hand as convenient slogan, explanation, manipulandum, mediating variable, outcome, and so on. In a survey,124 90% of health managers routinely used ‘culture’ to describe the way things happen in the organisation and 99% agreed that understanding culture was important for effective management (53% strongly agreed), yet almost all managers agreed that local cultures can provide significant obstacles to improvements in health-care quality. 124
Schein’s125 conceptualisation of culture as shared basic assumptions, articulated in values which govern how the organisation behaves and visibly manifests itself, has been seminal. Hofstede’s126 framework is also popular, characterising culture in terms of several key dimensions: power distance, uncertainty avoidance, individualism, masculinity and long-term orientation. 126 The competing values framework (CVF) is also widely used in the management literature. The CVF defines culture in terms of two axes: flexibility versus control, and internal versus external orientation. The intersection of these two axes generates four distinctive cultures: clan, adhocracy, hierarchic and market. The CVF has been used, for instance, to study the mediating effect of culture on the success of organisational change initiatives. For instance, Shih and Huang127 found that the process improvement programmes, based on the rigorous management of work processes, tended to fare better in organisations with a hierarchical culture.
A further popular framework is that of Martin128 who argues organisations are not homogenous cultural entities, but comprise different subcultures. In health care, for example, nursing could be characterised as having a stricter disciplinary code than other professional groups. 129 The current study concerns interagency work, and the multiple cultural contexts of different professional groups can be expected to affect the tractability of professional behaviours. Martin identifies three broad categories of subculture: enhancing subcultures (characterised by strong support for the centre), countercultures (characterised by scepticism and dissent) and orthogonal subcultures (defined by occupational group or demographic features). Such subcultural features can modulate change efforts. Ravishankar et al. ,130 for instance, show how the enhancing subculture of one business unit led to the smooth adoption of a centralised IT initiative, whereas a countercultural business unit largely rejected it.
In this work, we are concerned with a very specific aspect of organisational culture, its ‘safety culture’, defined in general by Vincent131 as follows:
[T]he safety culture of an organization is the product of the individual and group values, attitudes, competencies and patterns of behavior that determine the commitment to, and the style and proficiency of, an organization’s health and safety programmes.
p. 273
A positive safety culture is characterised by communication based on mutual trust, shared perceptions of the importance of safety and confidence in the efficacy of safety mechanisms. Vincent131 writes of the importance of an ‘open and fair’ culture, in contrast to the normal organisational tendency to blame people for errors which, by producing defensive strategies, works against safety in the long term by inhibiting the reporting of important safety concerns and incidents:
Punishing people for honest error is not simply unfair and pointless; it is dangerous . . . suppress[ing] the very information you need to create and maintain a place of safety.
p. 277
In a similar vein, Dekker13 has written extensively of ‘Just Cultures’ which simultaneously address the twin, and potentially conflicting, imperatives for accountability and organisational learning. Dekker13 distinguishes two forms of accountability: backward looking (looking for culprits to blame and shame) and forward looking, a form of accountability which ‘brings forward information about needed improvements to people or groups that can do something about it’ (p. 135).
An important strand in the literature on safety culture deals with the characteristics of ‘high-reliability organisations’ (HROs), such as nuclear power plants, aircraft carriers and air traffic control. Some authors believe that health care has much to learn from the culture and practices of such organisations; Vincent131 explicitly likens the typical day in an ED to the situation aboard an aircraft carrier. In both cases, a complex, dynamic situation must be managed: planes must be landed, often in bad weather on a heaving deck; patients must be treated, each different, always under time pressure, sometimes with the threat of violence. In both situations, there is the same overarching imperative: ‘try not to kill anyone’. Dealing with constantly shifting contingencies requires rapid decision-making, co-ordination and mutual adjustment by those involved in the action. This requires a relaxation of hierarchy (of rank and authority), an emphasis on local autonomy and a flexible attitude to procedures. Vincent sees the HRO as a more appealing model for health care than manufacturing, the source of conventional ideas about safety, because production line processes seem to have so little in common ‘with the hands-on, hugely variable and adaptive nature of much work in healthcare’ (p. 278). Vincent cautions, though, that this can be overplayed, as much of health care, such as pharmacy distribution, is routine and predictable.
The distinctive cultural characteristics of HROs are articulated by Weick et al. 132 using the concept of mindfulness. HROs are contrasted with conventional organisations: whereas the dominant concern in the latter is efficiency and success, for the HRO the priority is reliability. Reliability may be defined as ‘the lack of unwanted, unanticipated, and unexplainable variance in performance’ (p. 51). 133 The traditional approach seeks to achieve reliability through the development of highly standardised routines, but this focus on repeatability is problematic: ‘it fails to deal with the reality that reliable systems must perform the same ways even though their working conditions fluctuate and are not always known in advance . . . the idea that routines are the source of reliability . . . makes it more difficult to understand the mechanism of reliable performance under trying conditions’ (p. 35). 132
This brings us back to the ‘quality broom’ metaphor, and the need to distinguish between routine and non-routine processes, also echoed in the work of Pava. What is distinctive of the HRO is not process stability but cognitive stability, i.e. stability in the processes that make sense of the variability; reliability is not the outcome of ‘organisational invariance’, but results from the continuous management of fluctuations. The law of requisite variety is, therefore, at the heart of reliable performance. Crudely speaking, this law stipulates that the ‘variety’ of a ‘control system’ must equal or exceed the variety of that which is being regulated (variety is defined as the number of possible ‘states’ a system can be in). 17 For an organisation to survive in a particular environment, it must be attuned to the variety of its surroundings. If the environment becomes more complex, the organisation must adapt itself in order to manage this variety and to preserve its viability. Two adaptive mechanisms are available:17 variety attenuation describes the process of reducing the variety of the relationship between the organisation and its environment (e.g. a CSC agency restricting its services to only those children at very high levels of risk); variety amplification describes the reverse, for example a hospital sets up a new diabetic clinic, thereby increasing its variety from the perspective of the local population.
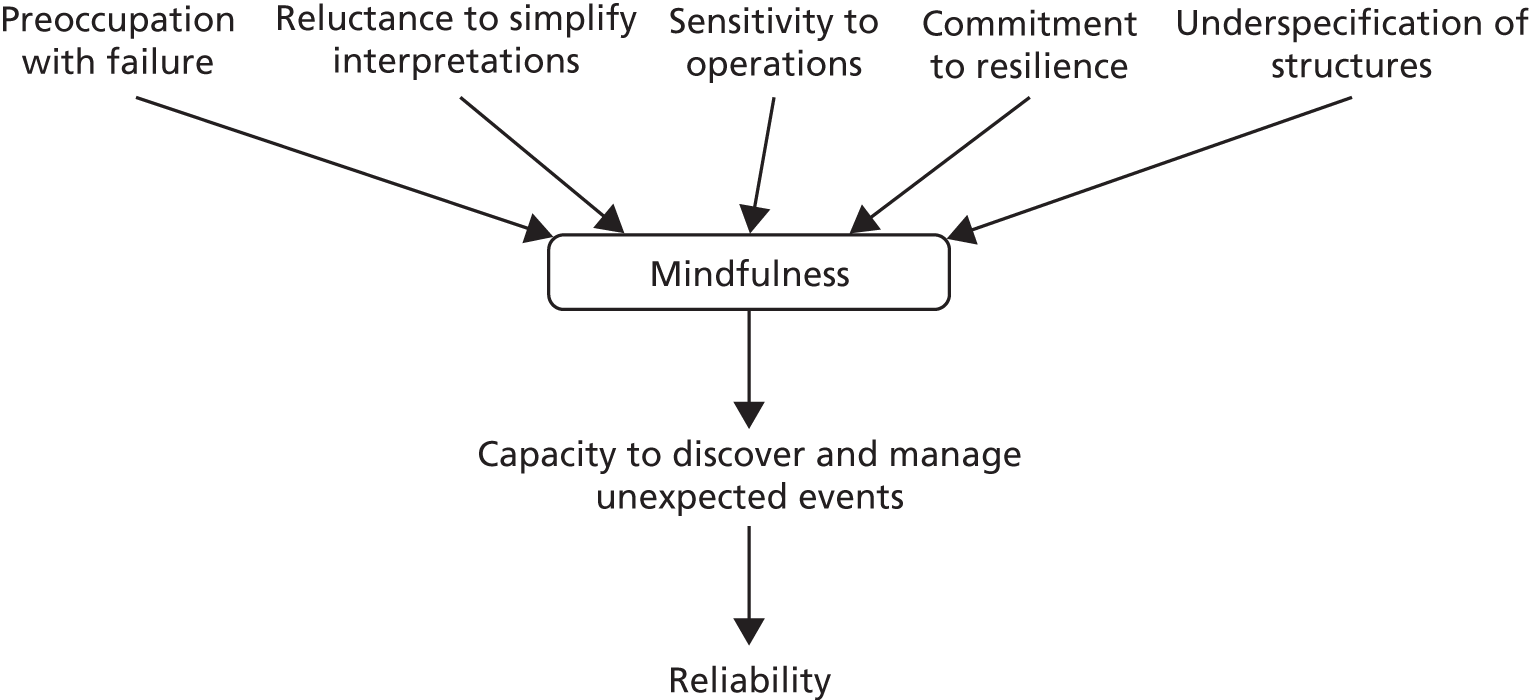
For Weick et al.,132 the ability to anticipate, detect and adapt to unexpected events is key. When new or unexpected events occur, practitioners need ‘to revise their understanding of the situation, their evidence collection and evaluation tactics, or their response strategy’ (p. 35). Continuous awareness of variations, adaptive cognition and flexible action produces orderly, reliable behaviour. Weick and Sutcliffe134 designate this state of cognition ‘mindful infrastructure for high reliability’. It has several key determinants, as depicted in Figure 3.
Weick and Sutcliffe134 define mindfulness as:
The combination of ongoing scrutiny of existing expectations, continuous refinement and differentiation of expectations based on newer experience, willingness and capability to invent new expectations that make sense of unprecedented events, a more nuanced appreciation of context and ways to deal with it, and identification of new dimensions in content that improve foresight and current functioning.
p. 42
The five determinants are briefly explicated as follows. Preoccupation with failure is what gives HROs their distinctive character; because failures are rare events, not only is constant vigilance needed, but there must also be a readiness to seek out more data and broaden the variety of failures given attention. Effective HROs thus encourage the reporting of errors, including near misses. Simplification is an intrinsic property of organisation, enabling complexity to be made cognitively tractable and action to be taken. However, it is potentially dangerous, as it ‘limits the precautions people take and the number of undesired consequence they envisage. Simplification increases the likelihood of surprise’ (p. 41). 134 Sensitivity to operations essentially means having an ‘integrated big picture of operations in the moment’ (p. 43),134 a concept similar to ‘situation awareness’, which has been extensively studied in the human factors literature. Whereas anticipation refers to the prediction of dangers in advance, resilience refers to ‘the capacity to cope with unanticipated changes after they have become manifest, learning to bounce back’ (p. 46). 134 Finally, underspecification of structures refers to the need to create flexibility, building in requisite variety and avoiding procedures that are followed mechanically. These factors are crucial and will be returned to in later chapters of this report.
Technology adoption
The practical centrepiece of the present work is the development of a package of tools aimed at fostering a safeguarding culture. The tools will be developed primarily at one site, and an important aim was to test their general validity by evaluating their adoption by other participating partners. The adoption of innovations is an enterprise fraught with risk, and has been the subject of scholarly research for several decades. Initiatives involving IT, such as those featured here, are notoriously risky: all too many IT projects miscarry, with failure rates as high as 80% reported at one time or another. 17 When information systems involve more than one organisation, the risk of failure is inevitably higher. Research has sought to tease out the ‘critical success factors’, which predispose projects to achieve the desired benefits, and a strong consensus has emerged. Failed projects typically represent management failures of flawed decision-making and lack of engagement; technology per se is seldom to blame. Many in senior positions see technology as a ‘magic bullet’. Markus and Benjamin135 argue that such ‘blind faith’ in technology is the predominant mind-set among managers and executives. There is general agreement that users must be engaged in the development of systems, and that strong commitment at the top of the organisation is also required. It is vital that managers engage with technology, seeing it as an instrument for redesigning their organisation; passively implementing technology developed elsewhere is a recipe for failure. We will return to the need for such a ‘design attitude’ in the chapter on the design and evaluation of the safeguarding package.
The literature on technology innovation and adoption is voluminous and a review is beyond the scope of this work. The seminal work is that of Everett Rogers. Rogers136 portrays the innovation process as a linear sequence of stages, beginning with the initial idea and its development into an adoptable entity, be it product, artefact or service. Whether or not the innovation is adopted is held to depend on a number of critical factors, grouped into three areas: the intrinsic attributes of the innovation itself (e.g. its ‘relative advantage’, complexity and compatibility with existing practices), the effectiveness of marketing and communication on the part of change agents, and the degree of ‘felt need’, resources and capacity for change within the adopter. Rogers’ original work has spawned a vast profusion of derivative models, such as the technology adoption model, which with its various embellishments dominates the research in the field of information systems on technology adoption and diffusion. 137 Alternative theorisations have begun to spring up, such as those based on actor-network theory (for a recent discussion of applications in health care, see Cresswell et al. 138) but models based on Rogers’ continue to hold sway. 137
A pertinent limitation of Rogers’ model is its focus on adoption decisions made by individuals rather than organisations. As Van de Ven139 argues, the process of organisational innovation and adoption is considerably more complex, with multiple potential initiatives unfolding in parallel, all competing for priority in a politically contested milieu. Van de Ven proposes an extension of Rogers’ model to address organisational innovation and its management: the model depicts the organisational innovation process as made up of multiple, non-linear activities and events progressing through time. These can be inventive, developmental or adoption activities, or reflect evolving features of the organisation context (such as changes in norms or reward systems). At any time, the flow of activity can be perturbed by ‘process events’ (shocks, setbacks, learning events, gestating events), which can influence the trajectory of particular innovations.
Conclusion
Patient safety is an international priority140 and the subject of a high-profile NHS initiative, Patient Safety First141 (PSF). There has been a reconceptualisation of clinical risk focusing on latent ‘error provoking conditions’ which create ‘accident opportunities’. 142 It has become increasingly recognised that most harm to patients is not deliberate, negligent or the result of serious incompetence. Instead, harm more usually arises as an emergent outcome of a complex system where typically competent professionals and managers interact in inadequate organisational configurations (inter alia Mannion et al. 122). There has been a gradual recognition within the wider health policy arena that safeguarding (both adults and children) is inextricably linked with quality, governance, safety and dignity. 143 Although these developments have begun to address the safety of children presenting in hospitals, very little reference to safeguarding is made in the Operating Framework for the NHS in England 2011–12,144 and PSF focuses exclusively on ‘in hospital’ threats, not the extra-mural risks to which the children are usually exposed. This reflects general concern that protecting the welfare of children is insufficiently embedded within the thinking and practices of acute NHS trusts. 145
Much research on patient safety to date has also focused on a single clinical environment or organisational setting. 146 There has been a relative neglect of threats to patient safety arising across settings, or where the decision-making depends on a dispersed network. This is often the case in secondary settings where retrenchment of local government services has led to the loss of many hospital-based social work teams. 147 Safeguarding children is interactionally, emotionally and cognitively complex. Signs and symptoms are often ambiguous. It often falls into the interstices between organisations and governance systems, with a consequent lack of clarity about responsibility compounded by endemic problems in communication and knowledge sharing across space, time, and organisational and professional boundaries. 148 As a high-risk, high-blame activity, it is also buffeted by media scandals and political buck-passing,149 which create further barriers to co-operation. Only a thorough understanding of human, social and organisational challenges will afford effective solutions. Chapters 4–6 present data from the study to illustrate, explore and evaluate attempts to provide such remedies.
Chapter 3 Research design and methods
Design science
The proposed investigation follows a design science approach. In contrast to conventional social science (which aims to describe, explain or predict social phenomena150), the aim of design science is to develop a corpus of practically oriented knowledge regarding the design, implementation and use of a general class of artefact, technology or service innovation. 17 In the field of information systems, design science enjoys a well-established tradition with a lineage reaching back over several decades. 151 It also has its votaries in management research. Van Aken152 distinguishes two modes of management research. Mode 1 corresponds to conventional explanatory science. In contrast, the aim of mode 2 research (i.e. design science) is the production of field-tested and grounded ‘technological rules’, i.e. chunks of ‘general knowledge linking an intervention or artefact with an expected outcome in a certain field of application’ (p. 22). 152 Importantly, such rules should be used not as instructions but as design exemplars, to be invoked because of their relevance to resolving a problem. Practitioners then ‘have to translate this general rule to their specific problem by designing a specific variant of it’ (p. 27). 152 The question must always be ‘why does this intervention in this context produce this outcome?’ The rationale of mode 2 research is, thus, to furnish a body of knowledge informing design, which must be applied critically and sensitively to important features of the local context. 17
Design is a core feature of the patient safety paradigm and has been shown to be integral to its success. 12 Design science intrinsically involves the construction and evaluation of an exemplar of the innovation in question, reflexively learning from this real-world action. This is the broad approach to be adopted in this study. A mixed-methods153,154 research design will be followed to evaluate the impact of a package of initiatives (including an electronic reporting tool) designed by clinicians within our primary hospital site, aimed at promoting a safety culture. In the spirit of design science, we will seek to understand if, and in what aspects, this intervention has been effective and the key causal and contextual factors bearing on this outcome. The primary interest will be the impact of the intervention on improved communication and knowledge sharing, particularly with external agencies. For this reason, much of the research has been devoted to understanding generic issues regarding the exchange of knowledge and information between hospitals and community bodies, in particular local authority CSC departments.
Qualitative methods (interviewing and ethnographic observation) have been the main research tools, supplemented by quantitative data where available, to evaluate the impact of the intervention on the volume and quality of communications. Although the study is predominantly qualitative in nature, the use of quantitative data plays an important part, not least in triangulating the interview data in the evaluation of the impact of the ‘package’, and in the usage by staff of various key elements, such as the reporting tool. We recognise that our quantitative analysis is limited; this is because we had no access to raw data (except for a short staff survey) and were reliant on statistics published in internal reports (e.g. average rates of referral to CSC). Nonetheless, the use of such numerical data reflects a different epistemological orientation from purely qualitative research, and hence our approach is best described as mixed methods.
Interrogating organisational culture
There are established tools for assessing cultural change in health care. However, many instruments reflect the same intraorganisational biases of the patient safety literature and the majority explore predefined sets of dimensions which do not fit with the proposed study. 124 The design orientation of the research and the novelty of the clinical problem require a more emergent and open methodological approach. The proper evaluation of a design intervention relies on a rigorous understanding of the realities of everyday practice. Thus, we have drawn substantially on methods associated with interpretive sociology to examine the linguistic and other practices which produce and reproduce ‘cultures’ in our studied organisations.
Professionals are involved in acts of meaning-making, which are often collaborative and are bound by available repertoires of interpretation. Meaning-making is accomplished through language and takes place in particular social and organisational contexts. In order to get their job done, professionals must package their opinions for consumption by others. They must be able to justify, account for and ‘perform’ their judgements. This may be for the patient who has come to their service, or for colleagues, or in some other arena of accountability or judgement-making, such as inspection or a clinical audit. They must also ‘work-up’ a written account of aspects of their thinking for case files, reports and records. Moreover, patients/clients come to services with their own stories to tell. So, the processes of clinical judgement are intrinsically ‘storied’. Professionals ‘take the history’, then retell it in a form consistent with their specialist knowledge. However, professional narratives contain more than specialist knowledge. They attribute cause and effect, and often construct blameworthiness and creditworthiness. Professional stories, even humorous anecdotes, are often moral tales. It is through this interpretive lens that we have analysed the interview data and field notes of observations.
It is easy for the notion of ‘storytelling’ to be misunderstood. We are not suggesting that the patient’s body, or the family’s problems, or the child’s injury, do not exist outside the story. Rather, ‘troubles’ are given particular meanings, which may, for example, construct them as the proper business of the professional, or, alternatively, as the proper business of another. So, narratives attribute cause and effect in particular ways.
In sum, the development of a ‘just culture’ and associated changes in the organisational milieu should be visible in human actions and reportable in professional talk – as evidenced in everyday conversation and in interviews. Anthropological methods have been shown to be a particularly sensitive methodology for assessing cultural change in patient safety studies. 155,156 These were deployed and also triangulated using semistructured interviews and analysis of key metrics such as the number of cases reported or referrals made and so forth. For internal validity, all interviews were fully transcribed. At least two members of the research team were involved in generating coding frames for themes from qualitative data, comparing independent coding of a subset of data to identify and address coding differences and ensure consistency.
Research sites
Three hospital trusts were partners in the study. The first, Pennine Acute Hospitals Trust (PAHT), employs 8820 full-time equivalent (FTE) staff and operates from four sites: Fairfield General Hospital, Bury; North Manchester General Hospital; The Royal Oldham Hospital; and Rochdale Infirmary. PAHT serves the communities of North Manchester, Bury, Rochdale and Oldham, along with the surrounding towns and villages. This area is collectively known as the north-east sector of Greater Manchester and has a population of around 800,000. The second site is one of the largest foundation trusts in the country, with over 11,000 employees providing general and specialist hospital and community care for the people of a large conurbation. Site 2 was chosen for its prima facie similarity to site 1, with a view to exploring technology transfer. As a consequence of the delays in piloting the materials in site 2, data drawn from this site have been primarily used to triangulate and assess the generalisability of those from site 1 in relation to objective 1 of this study, ‘the development of a sociologically rich understanding of why diagnostic failures and communication breakdowns occur’. Site 2 has enabled comparison and theoretical generalisation between cases about the common human, interactional and organisational factors involved in safeguarding children. It has also provided further exemplars of clinician-led innovation which have been formatively evaluated.
The third hospital site was a tertiary specialist centre chosen to provide a strongly contrasting environment in which to evaluate the adoption and use of the tools developed in site 1. Delays in approving the research at that site meant that no fieldwork was performed at site 3; for this reason, it is not identified or discussed further.
As described in Chapter 5, eight local authorities fell into the immediate catchment areas of sites 1 and 2, and fieldwork was carried out in four of these authorities.
Natural history of the project
The project was originally designed to follow a linear trajectory from baseline data and artefact redesign to evaluation, followed by technology transfer and formative evaluation in new sites. The process has been less predictable and more iterative for a variety of reasons:
-
There were significant delays to the project start. Ethical approval was granted 3 months after the project start date, but final research and development (R&D) approval at our primary hospital site was not granted until 6 months after the original project start date. R&D approval at the second hospital site was granted shortly after the site-specific approval process was instigated and fieldwork could begin. As noted, the third hospital site did not complete approvals until the final day of the project and had to be excluded from the study.
-
The design process is not linear. Rather, practices evolve and are embraced and resisted in a number of unpredictable ways. A simple ‘before-and-after’ approach did not lend itself to this. Instead, multiple methods (as noted) were used to examine cultural stasis and change.
-
Technology transfer proved much more challenging than anticipated. Sites 2 and 3 expressed a wish to adopt the information sharing forms from site 1 in April 2012 with a view to piloting their use with two local authorities. At project end, the necessary IT was not in place. Thus, for pragmatic reasons, this site has been used as a comparator with formative assessment of the efficacy of tools specific to that site. Agreement from the neighbouring local authorities to pilot the forms has been in place for some time. Collaboration between the clinicians across the sites continues, with an intention to implement the artefacts as soon as the necessary technology is in place.
Research methods and data collection
An in-depth case study was carried out in site 1. As this is design- and action-oriented research, the primary site was not chosen, or sampled, in the conventional sense; rather, developments were under way at PAHT and required piloting, further design and evaluation. As is common with action research157 and its derivatives, one of the investigators (SS) was also a participant. This ‘complete membership role’158 produces challenges to traditional notions of ‘insider’ and ‘outsider’. However, Strathern159 casts doubt on the distinction between the familiar and unfamiliar, saying that such a criterion would involve ‘impossible measurements of degrees of familiarity’ (p. 16). What is important for Strathern159 is whether or not the researcher and researched share the conceptual frameworks which inform ethnography, thus:
[W]hether anthropologists are at home qua anthropologists, is not to be decided by whether they call themselves Malay, belong to the Travellers or have been born in Essex; it is decided by the relationship between their techniques of organizing knowledge and how people organize knowledge about themselves.
p. 18159
So, from this perspective, validity and reliability do not depend on the ethnographer being an alien, or outsider, in the setting. Indeed, one advantage of turning the ethnographic gaze on the familiar is precisely that it holds the possibility of defamiliarisation of certain routines and practices. In this regard, the academic research team has acted as a ‘critical friend’ in relation to the participant observations undertaken by SS, contributing to the iterative process of design and redesign.
Mixed qualitative methods alongside quantitative analysis of key system metrics were used to bring the design of the various instruments in PAHT to completion. Methods have been designed to ensure the ‘trustworthiness’ of the research in the sense of providing both rigour (process) and relevance (end product). 160 Credibility161 was ensured by triangulation of methods, ongoing and iterative conversations with ‘members’ as part of the design process and piloting, and the independent analysis of transcripts by at least two members of the research team. In addition, credibility is built up through a prolonged engagement in the field and persistent observation and triangulation of data.
The mixed-methods research design has involved the following data collection methods.
Qualitative interviews
Semistructured qualitative interviews were used to understand how safeguarding activity and interprofessional and interagency working were organised and experienced by key clinicians and managers. Interviews were especially important for identifying diagnostic complexities, patterns of knowledge sharing and participants’ knowledge domains, cultures and organisational context. The interviews were designed to be conducted in a semistructured, conversational style, giving participants the opportunity to explore emergent issues. All interviews were guided by, but in practice not limited to, topic guides developed to reflect the study objectives. An example is shown in Appendix 2. Key topic areas were developed within the project team and shared with representatives from the patient and public involvement (PPI) group (see Appendix 15). A key input from the PPI process was the importance of attending to the importance of avoiding an increase in false positives in the safeguarding process.
Interview questions were structured to generate participant narratives. These stories were not read necessarily as ‘truths’ but rather as analytical windows into how participants make sense of and give meaning to ‘child protection’ in the context of their other activities and to make visible aspects of knowledge and culture. Participants were invited, in writing, to participate in the study, which included providing a participant information sheet and an opportunity to contact the project team for further information or to arrange an interview (see Appendix 2). Other participants were recruited during ethnographic observations; for example, where an individual was observed as having an important role in a team meeting, they would be asked to participate in the study and provided with an information sheet and similar contact details. Formal interviews were digitally recorded with the consent of participants and all were transcribed verbatim for the purpose of subsequent data analysis. A total of 60 interviews, most lasting between 1 and 2 hours, were conducted, and the majority were audio recorded. These were supplemented by interviews arising from ethnographic observations which were recorded in detailed field notes.
Fifty-six different individuals were interviewed. A small number of staff were interviewed twice (the heads of safeguarding at the two research sites, and one named nurse) and two community physicians were interviewed together. In total, 58 distinct interviews were carried out. A detailed breakdown by staff group is shown in Table 2.
| Professional role | Number interviewed | ID codes |
|---|---|---|
| Consultant paediatricians | 6 | CP1 to CP6 |
| Named nurse | 4 | NN1 to NN4 |
| Senior executives (e.g. director of nursing, chief executive) | 4 | SE1 to SE4 |
| LA team managers | 8 | TM1 to TM8 |
| Designated nurses | 2 | DN1, DN2 |
| Designated doctor | 1 | DD1 |
| Head of safeguarding | 2 | HS1, HS2 |
| Emergency medicine consultants | 2 | EM1, EM2 |
| Midwives (mostly community, some with specialties, e.g. mental health) | 11 | MW1 to MW11 |
| Nurses (staff nurses, charge nurses, senior nurse mentors) | 10 | N1 to N10 |
| Miscellaneous administrative staff | 2 | AD1, AD2 |
| Community paediatricians | 2 | CMP1, CMP2 |
| Health visitor | 2 | HV1, HV2 |
Focus groups
Two focus groups with nurses based in different settings took place in the primary site, which explored similarities and differences in staff members’ understandings of the safeguarding process.
Observations
Alongside interviews, ethnographic observations of key activities provided a further main source of data. Observations were undertaken in the primary site of:
-
Co-mentoring activities.
-
Walkrounds.
-
Audit meetings.
-
Daily analysis of cases by the named nurse.
-
Design workshops. The academic research team undertook these as non-participant observers with the clinical researchers as participant observers.
To deepen our understanding of the roles and contributions of key individuals, further shadowing observations were also undertaken with key individuals, such as the named nurse for safeguarding and the co-mentors. Handwritten field notes including rich description and separate interpretations were taken, which were later typed up electronically as corresponding text and interpretation. Observations were also undertaken of the sense-making and ‘information practices’ at the receiving end of information sharing in community health settings and CSC.
Analysis of case notes, documents, policies and routine data
During data collection, various audit, strategy and policy documents were collected from both the primary and the second research site. These included formal policies and pathways for referral, patient leaflets and guides, and pictures of posters, fact sheets and other information. The research team also analysed routinely collected performance data relating to safeguarding at each site, including the numbers of referrals to CSC and the quality of information shared. Detailed analysis of decision-making and systemic incidents analysis was undertaken with a sample of four anonymised medical files, selected for their typicality.
Case tracking
In the primary site, a sample of cases which were referred to CSC were tracked. In the second site, referrals were routinely tracked and the research team had access to those data.
Design workshops
Meetings of the whole project team took place approximately every 6 months. These reviewed progress and also functioned as design workshops where innovations were shared and discussed. This created a collaborative clinical network, which continues and has proved very fruitful. There is evidence that this kind of peer support has considerable potential for development nationally.
Quantitative data
To supplement the qualitative data, a range of relevant quantitative metrics were gathered where such data were available and relevant. These data will be introduced and described at various points in the report, primarily in Chapter 6 where they form an important ingredient in evaluating the impact of the ‘design package’. Examples of such metrics include the number of referrals from the hospital to local CSC organisations. A bespoke staff survey of attitudes to safeguarding in PAHT was also carried out.
Data management
All data were managed in accordance with NHS and university research governance frameworks. All interview transcripts were anonymised with pseudonyms, and all identifiable information such as contact details were securely filed. Handwritten ethnographic notes did not include identifiable names and were archived within 48 hours into locked cabinets.
Data analysis
In analysing the interview and focus group data, our approach was as follows. Data were, typically, read by two members of the research team; they were independently coded on the first reading and then codes were compared. We were first concerned with examining the data for themes that related directly to our research questions, for example clinicians’ experience of using the artefacts. Second, an inductive approach was used to locate themes within the data that were not directly and explicitly related to the questions, but which nevertheless were salient within the corpus, or within particular occupational or organisational contexts. Here, we were concerned with understanding the interactional and social contexts in which this work takes place, and the accounts in interviews were seen both as testimony about events that had taken place and as a source of cultural meaning-making and cultural reproduction. In this, we draw on an established tradition in interpretive sociology described by Brewer162 thus:
[F]ragments of recorded talk . . . fieldnotes, and reports of observed actions can reliably represent a social world . . . small scale, micro events in everyday life have at least common features with the broader social world . . .
p. 236
Transcripts were read multiple times by SW and DW and also by CH and EW. Emergent themes were discussed between all of the authors to check for internal validity, accuracy of interpretation, particularly of domain-specific knowledge of particular professionals, and to locate themes for further analysis. Having practising clinicians as part of the research team also allowed for routine ‘member validation’ to check the accuracy of our interpretations of clinical information in particular.
Once themes were identified, these were examined in more detail through further readings of the transcripts, followed by manual coding of the material and its organisation into subthemes. During this process, the transcripts as a whole were continually referred back to, as a means of ensuring that the data and analysis remained grounded and inductive. This analytic process involved the authors in a reciprocal relationship between data themes, the whole corpus, and the empirical and conceptual literatures we had reviewed. As a brief illustration, Table 3 shows two of the primary themes from the initial analysis of the interviews with hospital staff: paediatricians, nurses, senior managers and midwives. For each theme, sample indicative quotations are listed, indexed by keywords. The third column gives the interview identifier used to locate the quotation in the relevant transcript. Given the nature of the two themes illustrated, the majority of comments were sourced from paediatricians or emergency medicine consultants.
| Primary theme (first iteration) | Key words or phrase | Interview reference |
|---|---|---|
| Diagnostic ambiguity/difficulty | Ambiguity/subjectivity | CP4 |
| Intrinsic unpredictability | CP4 | |
| Parental deception | CMP1 | |
| Difficulty of confronting parents | CMP1 | |
| Broken clavicle | CMP1 | |
| Difficulty talking to parents | EM1 | |
| Lots of grey areas | EM1 | |
| Thresholds problematic | EM1 | |
| Grey cases but need all or nothing | EM2 | |
| Munchausen example | EM2 | |
| Not exact science | CP2 | |
| Very emotional stuff | CP2 | |
| Relations with social care | Not invited to case conferences | CP1 |
| Lack of feedback on cases | CP1 | |
| Contrast with colocation | CP1 | |
| Change of social worker | CP1 | |
| No feedback | CP6 | |
| Incomplete information | CP6 | |
| Playing system | CP6 | |
| Delays in response | CP4 | |
| Spider’s web | EM1 | |
| Black hole | EM1 | |
| Windscreen metaphor | EM2 | |
| Limited info in A&E | EM2 | |
| If you can get a sensible social worker | EM2 | |
| No feedback | EM2 | |
| HYPe up referrals | EM2 | |
| One-way street | CP2 |
Service users/public involvement
The area of children’s safeguarding is sensitive; most victims are too young to participate in any meaningful or ethical way and parents often feel shame or anger about the incidents in question. However, the system generates a considerable number of false positives and those who have been falsely accused can be keen to ensure that the system is made more sensitive to these eventualities and to help others who may share the same experiences. The project team established an advisory group comprising parents who had experience of being falsely accused of harming their children and a young mother who experienced the system as a teenaged mother in difficult home circumstances. The advisory group contributed to a design workshop towards the end of the project. This group was recruited through the complaints process at our primary site and through contacts at the Family Rights Group, a charity in England and Wales that advises parents and other family members whose children are involved with, or require, CSC services because of welfare needs or concerns. Two members of the advisory group provided digital stories of their experiences, which are described in Chapter 6. In addition to these project advisory roles, patient representatives have been involved in the production of further digital stories of their experiences to be used in training and education within our primary site. These will be made available to our other site and form part of the transition package detailed in Chapter 6. A full account of the process of patient involvement in the digital stories is provided in Appendix 15.
The research has the full and formal written support of all local safeguarding children boards (LSCBs) in both regions. Support from the LSCBs gave the team access to a wide range of key publics involved in children’s safeguarding and thoroughly mandated the work within all relevant agencies.
Chapter 4 Jigsaw practices and spiders’ webs: pragmatics and problematics of knowledge in safeguarding
This chapter provides an analysis of qualitative and quantitative data across both sites exploring the complexities of knowledge making and knowledge sharing in child protection. It provides a context through which the description and evaluation of the various artefacts designed to enhance safe practice can be interpreted. Though the data do show subtle and important differences in the system responses in each trust, the different sites have not been identified here. This has been an ethical decision as this is a highly sensitive area in which professional error or indecision can have serious consequences for individual managers and clinicians. Systemic differences are articulated elsewhere in this report, but here the focus is on the enduring, intrinsic complexities of the work. It is these human factors that the artefacts described in Chapter 6 have been designed to ameliorate, and a thorough understanding of the nature of the work is a necessary backdrop to the design-oriented aspects of the study.
High-profile cases: blaming and shaming
I think virtually all of the social workers who’ve been caught with one of these cases have been sacked haven’t they . . . I wouldn’t want to be a social worker if you paid me – I don’t know how much you’d have to pay me to – but you know – an awful job – not an awful job but an awful support.
Consultant paediatrician (CP4)
This medical consultant summarises the national climate in children’s safeguarding services. The anticipation of a relatively low-probability but high-consequence catastrophe is always present. It is, thus, important first to underscore the high-blame environment in which intellectually and emotionally challenging decisions and activities take place. This study was foreshadowed by the reports of the deaths of Peter Connelly in 2008 and Khyra Ishaq in 2010, and the conclusion of the criminal case relating to child sexual exploitation in Rochdale and Oldham in 2012, as well as the scandal about Jimmy Savile’s activities in NHS hospitals. In autumn 2013, as the study was concluding, the deaths of Daniel Pelka, Hamza Khan and Keanu Williams reached the headlines. The sites for this study have been directly affected by some of these deaths, with far-reaching effects on organisational culture and professional consciousness, as this community paediatrician describes:
A week or two ago, that the Pelka case came out, a little boy came to clinic who had had a child protection medical done a few months ago and he’d picked up a murmur or something and been put to our clinic. And his mum was a . . . East European of some sort. And although he was not undersized, he looked the most miserable, withdrawn kid you could ever wish to meet and although the medical was inconclusive – bruising was due to being hit by a sibling or something – but – and so – and it’s interesting ‘cause I made a mental note: I’ve got to do something . . . God, that’s really pricked my conscience, hasn’t it?
Community paediatrician (CMP1)
The fear of ‘missing’ a case which ends in a catastrophic death is expressed at all levels in the organisation, as a member of the executive team in one of our sites recounts:
It was on my birthday, when a psychotic woman in [city] murdered her children. I spent the day up there with the GP who’d been desperately calling for help from the police . . . you never know when that day is going to come, do you? And it was dreadful . . . But from a process of how we report up, I’m not concerned about it. But, as I say, I wouldn’t say there wouldn’t be pockets of things that are going to just come out and just, you think, ‘Oh, God’.
Senior executive (SE1)
Attempts to learn from previous deaths also have unintended system effects which consume professional time, as a member of the executive team in one of our sites explains:
And so for me safeguarding children is not something that keeps me awake at night from our organisational point of view, however it is a significant issue in [city] . . . So the issue for us is around the capacity to respond to the amount of business there is out there in relation to safeguarding children. So at any one time we can have a number of serious case reviews that are ongoing far more than I’ve ever come across anywhere else I’ve ever worked. It’s a lot of resource. And of course that resource takes people away from the front line.
Senior executive (SE4)
In both of these cases, from different sites, the respondents’ confidence in their own organisational systems is affirmed; this is unsurprising as it is part of their professional role to ensure this, but the realities and repercussions of terrible events in places outside their control is juxtaposed with this sense of order. These effects are felt every day, in encounters with parents and children:
Things are flaky in safeguarding because it’s not an exact science. It’s just putting things together. Very emotive, very disturbing and distressing for clinicians involved so I think to some extent it’s underestimated what we go through as paediatricians. We’ve got to always have child abuse in the back of our mind when the child comes in and now with what’s gone on in [the north-west] with the sexual abuse . . . – we feel that we are put on a map and with magnifying glasses everybody is looking. That’s how the police and social services feel . . . There are lots of things about child protection which are difficult. Nothing about child protection which is easy and straightforward. Nothing. Absolutely nothing.
Consultant paediatrician (CP4)
The impact of inspection and regulation and the current measures and proxies for performance, themselves affected by scandal, also have effects at board level and throughout the organisation:
So we have to take people away from the doing in order to feed the beast and it can be very frustrating sometimes . . . you know we had to feed the beast again about Savile and we might have to tweak some, you know strengthen some stuff about volunteers. And what is interesting, at today’s safeguarding committee we looked at some of the changes around CRB [Criminal Records Bureau, now known as Disclosure and Barring Service or DBS] processes and how actually we’ll get less information about positive CRBs. At the same time we have got them asking us about you know make sure that you’re safe around Savile issues. It’s just strange.
Senior executive (SE4)
This level of real and perceived scrutiny would affect practice even in routine domains, but the ambiguity and interactional complexity involved in the detection of children at risk of harm means that its effects are intense.
The slipperiness of knowledge making in child health contexts
Safeguarding might be everyone’s business, and vigilance may be vital and culturally valued, but the majority of presenting cases in acute settings are not safeguarding matters. Furthermore, children frequently injure themselves accidentally. Judgement in most cases is based on clinical experience (‘pattern recognition’, where the clinician relies on their knowledge of the particular domain, and of other similar cases they have encountered), and/or on the results of diagnostic tests for particular hypotheses. In relation to children, of course, it also often relies on the clinician hearing a recognisable and morally adequate history from the carer. A suggestion of moral inadequacy on the part of the parents (e.g. that they are trivialising or exaggerating symptoms, or are failing to care for the child) has the potential to raise suspicion, requiring a different range of responses. 91 However, this requires rhetorical and evidential work, and an audience that recognises these factors as clinically relevant. Storytelling in these cases is oriented to characterisations of significant adults, which normalise the presentation, or to descriptions of problematic behaviours or sentinel events, such as injuries or incidents of domestic abuse.
Particular complexities arise when children or young people have been assigned to a clear and unambiguous medical category, but their problems are thought to be exacerbated by either parenting or relationship problems (e.g. children with unstable diabetes whose parents are suspected of mismanaging their diet). These cases involve particularly complex work, as the presence of an ‘intrinsic’ disorder requires that any psychosocial component be argued into existence in the absence of clear evidence. Narratives about these cases have the flavour of detective stories with anomalous physical findings, such as failure to gain weight, set alongside characterisations of carers. These cases often involve practical detective work, rigorous questioning of ‘witnesses’, cross-checking of parental accounts and an almost forensic attention to detail.
Cases may begin as straightforwardly ‘medical’ and evolve gradually to different formulations through formal and informal case-talk between professionals. For example, if a child has cerebral palsy and has difficulty swallowing and chewing, it becomes expectable that his/her weight gain may be slow. This then exists as an available explanation for poor weight gain and, in absence of dramatic weight loss, clinicians need not necessarily investigate further. Further investigation must, therefore, be triggered by something salient, and this is a highly contestable and often practically onerous process relying substantially on moral judgement and techniques of persuasion. Moreover, many candidate safeguarding cases result from clinical contact with adults rather than with children themselves. This may occur in maternity services as a result of concerns about a woman’s drug use, or her exposure to intimate partner violence, or as a result of adults’ presenting at the ED.
Serious physical injury accompanied by an implausible parental explanation is tragic for the child but it is organisationally and clinically easy to manage. Far more common are cases in which the significant players in the family and professional network are dispersed through time and space. The following extract from an interview with an experienced consultant in paediatric emergency medicine illustrates the range of judgement calls and interactional activities required to raise concerns in the ‘swampy lowlands’ of practice.
The problem arises nowadays on actually trying to get [CSC] to accept the referral . . . There was a child recently who attended with her mother. The mother was coming with a very vague condition and was with an older child who was an adult . . . And there was something very concerning but not really clear about the interaction between the mother and the child and they were also from out of area, so one of the nurses raised a concern, said I’m not really sure why they’re here and I started asking the mum why the child wasn’t at school. And you know she couldn’t really answer that and there was a lot of vague questions being answered.
Consultant, emergency medicine (EM2)
Here, the concern is triggered not by the presenting problem, which was ‘very vague’, but by the parent’s inability to answer questions about the child’s school attendance. The account continues:
So this nurse took it upon herself to ring up social services here and said well they've moved to the area recently but the child is not in school and the interaction is not very good and I wondered whether I could refer this child. Maybe you have any further information? And the social worker point blank refused and said ‘Well what do you want me to do? This is out of area and I can’t really do anything’. And meanwhile the 21-year-old sister of this child who was very sensible had rung her own social worker to say that they’ve been in this hospital out of area. And this social worker from [area] then rang back to our nurse and said actually what’s happening is this woman is due to appear in court in 2 days’ time to have the care of her children taken away from her because she’s a known Munchausen’s patient and actually want to place the children in care and so she’s done a runner to your hospital to fake another illness to get away from this court case. So it’s . . . a sensible concern that we wouldn’t have been able to raise if that nurse had not been so persistent. You know if it had been someone junior or with a bit less stamina that would have been dismissed.
Consultant, emergency medicine (EM2)
It is clear that there are many different ways in which this case could have been handled. The child’s ‘vague condition’ could have been treated as a trivial case of parental overanxiety. The nurse might have dismissed her concerns about the interaction, or not have noted these in the first place. The absence of information can be a reason not to take further action as well as a reason to refer; one can conclude that one has ‘the full picture’, or can search further for the ‘missing pieces’ of the jigsaw. All of this is negotiated and argued into being in the encounter itself and ‘backstage’ in talk between clinicians in specific, and often very challenging, clinical contexts.
In the following extract, a community paediatrician discusses concerns about the living conditions of a child with developmental delay:
I saw a child in CDC [Child Development Centre] for the first time last Friday. A bit unkempt, quite greasy hair, some developmental delay . . . I think Mum’s got some learning difficulties, two older children with autism, another child with learning difficulties and I said, ‘How many . . .?’ And then she said, ‘There’s 12 of us that live in the house’. And I said, ‘How many bedrooms?’ ‘Three bedrooms.’ Good attachment, but I’ve written now to the health visitor to say, ‘Can you make sure this family’s getting the right support? Can you check out that the house . . .?’ So it was sort of not true child protection, but . . .
Community paediatrician (CMP1)
The evaluation of the case as being ‘not child protection’ was then gently challenged by a colleague who was also participating in the interview:
Or it’s interesting, there’s the rule of optimism, which is when you say ‘good attachment’, because actually people put on a show when they come out the house, don’t they? And she could be an absolute monster at home.
Community paediatrician (CMP4)
The mandate to ’know’ what does not ‘show’ thus presents the spectre of future harm and professional culpability in a number of presenting cases, where the medical issues are relatively trivial, or are in themselves well monitored and managed. As noted above, this is particularly thorny territory where a child has a diagnosed medical condition, as this nurse based in the ED articulates:
Like, we had an example the other day, on Friday we had a little lad come through and basically he was having an asthma attack but it, kind of, come to light that he’d been at his dad’s for a week and his mum had forgotten to give his inhalers. Now, I don’t believe an adult nurse would necessarily [check with CSC] because he’s come in for an asthma attack, they see the issue of he’s got an asthma attack, whereas from seeing kids all the time, you’d know that if your child had an extensive condition, like an allergy to nuts, you’d always have the Epipen and he did not even have his Epipen, so we looked into it and he was actually known to social services on a plan and dad had like changed his last name in the meantime and he was with dad and they were expecting a baby with somebody else and, in the end, paeds didn’t send him home.
ED nurse (NN4)
Here, the presenting ‘surface’ version of the case and the hidden ‘depth’ and realities are juxtaposed. The propensity to ‘look deeper’, or to ‘seek more information’ or ‘missing pieces’, is not evenly distributed among clinicians. Indeed, the differences in the perspectives of individual clinicians, their credulity, or their sceptical orientation to parental accounts form part of routine organisational storytelling by clinicians about each other. These performative aspects of ‘telling the case’ are as important as the hands-on, diagnostic work in ‘slippery’ cases.
Precaution versus proportion: why safeguarding is a wicked (moral) issue
So how many of these children who you say we missed were actually harmed when they left the hospital?
Paediatrician (field notes, audit meeting)
Two contrasting moral positions can support case formulations about risk, which may be described as ‘proportion’ versus ‘precaution’. That is, the clinician may invoke the precautionary principle – better safe than sorry – or they may instead, like the paediatrician above, assert the necessity for clinical pragmatism and proportionality. These coexist as potential mandates for a diverse range of possible decisions and disposals in individual cases where the presentation is open to interpretation. It is because these two contrasting positions are always available that practice tends to be relatively resistant to control with protocols and guidelines, even where these are clear and unequivocal. For example, our first site has a mandatory process of referral to a paediatric specialist registrar or consultant for children under the age of 1 year presenting with head injuries, burns, bleeding, bruising or fractures, and children who cannot walk independently who have a fracture. Figure 4 shows the protocol displayed prominently in the EDs.
FIGURE 4.
Referral protocol, ED (site 1).
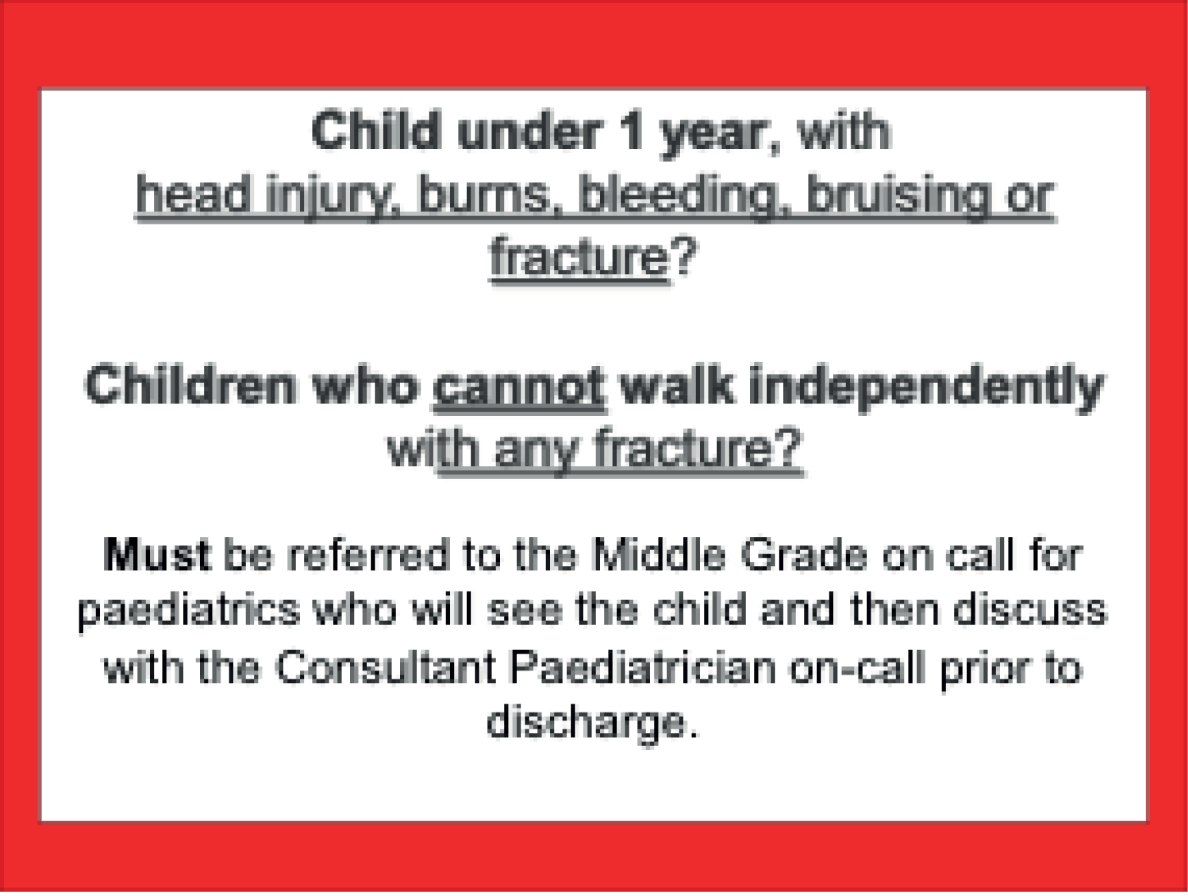
A similar mandate is in place at our second site and national guidelines have recently been produced. 163,164 All cases meeting the criteria must be the subject of a discussion between the doctor/emergency nurse practitioner and the on-call paediatric middle grade, or consultant, at the most appropriate hospital base. This protocol is accompanied by the following flow chart (Figure 5) relating to all children, which has been well received and is considered helpful. The chart guides the process of decision-making aiming to increase the accuracy of detection of non-accidental injuries and other risks.
FIGURE 5.
Detailed flow chart, site 1.
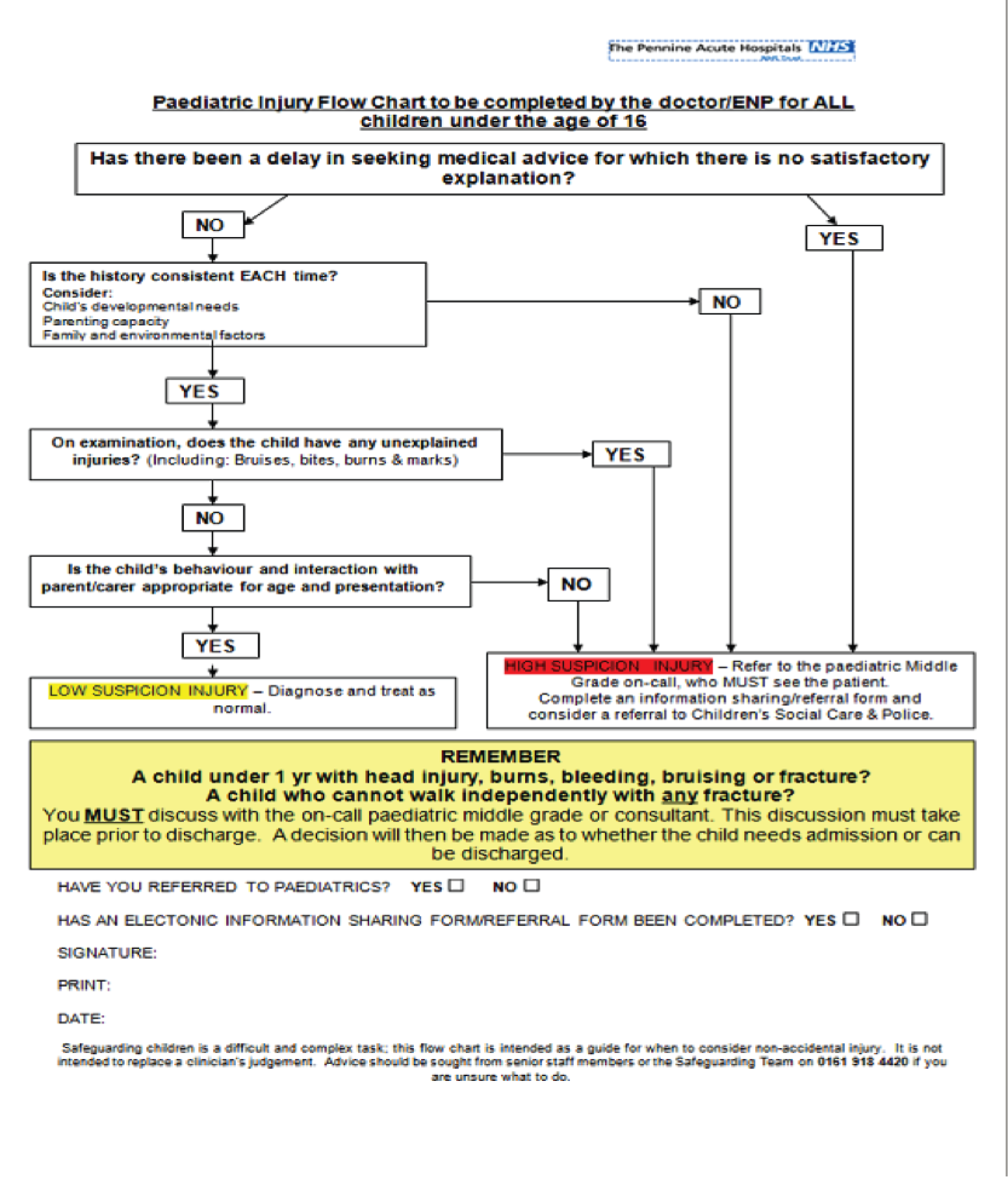
While the flow chart reaffirms the non-negotiable, mandatory nature of referral to paediatrics for under 1-year-old children and fractures in immobile children, it also uses the concept of a ‘low-suspicion injury’, a category into which most children presenting in EDs can be placed, and thus one that is always available in ambiguous cases, even those involving fractures.
This is described below by a consultant in emergency medicine:
I got contacted by one of the paediatricians the other day and it was all about a fractured clavicle. And the history was dah, dah, dah, and the examination was dah, dah, dah and I think we – after all we had a mobile child. And we sort of thought, well, fractured clavicles, you know, you fall over– it’s going to happen and you may not notice it at the time, particularly, but then, apart from the child’s not moving its arm and the mum sought help for that, and then the callus appears. So she’d behaved very appropriately; we decided that it probably was not NAI [non-accidental injury] and that we would just communicate with the health economy and check with the social services that they didn’t have anything bad and leave it at that.
Consultant, emergency medicine (EM2)
An audit examining compliance with the protocol in one of our sites found only 45% adherence to guidelines for children under 1 year of age (n = 39). There is some evidence that novice, and perhaps less than adequately trained, locum staff might be part of the problem. Among the non-referrals, 9 out of 19 (47%) were seen by locums, but this cannot entirely explain or contextualise the clinical decision-making. The majority of non-referred children presented with minor head injuries. The debate at the paediatric audit meeting about the appropriate institutional response to these cases is illustrative of the complexities of decision-making about medically trivial injuries in small children, where ‘surface’ presentation can be easily treated, and where detailed questioning of parents, who are behaving ‘appropriately’, is interactionally and emotionally very difficult and possibly consequential, in terms of either potential complaints or parents becoming wary of presenting with their children in the future. The existence of an absolute, unequivocal and unambiguous referral protocol apparently does not neutralise these factors.
We need to have some balanced thinking because for your benefit and my benefit and the child’s benefit I’d rather take away their discretion, rather than have a Baby Peter on the front doorstep.
Senior nurse (field notes, paediatric audit meeting)
In the above extract, the case for ‘precaution’ is set out. This position typically invokes national, or local, high profile cases: that ‘we don’t want one of those on our doorstep’, and hence the curtailment of discretion, is an important aspect of this position on ensuring safe decision-making and management of institutional risk. However, this position was quickly rebutted by a senior consultant, who invoked the principle of clinical proportionality:
So, should you apply this across the whole population, should every baby that is born have blood sugar checked, bilirubin checked, are safeguarding issues more important? I think we have to prioritise what is important.
Paediatrician (field notes, paediatric audit meeting)
While mandatory referral to paediatrics has a clear impact on paediatric workload, these arguments are a good deal more complex than that.
I get complaints every day from junior doctors and locums. A toddler who is just starting to walk and bangs his head on a table, parents rush to hospital, immediate referral to paediatric registrar for review, 20 patients waiting I mean things need to be prioritised, people have to do their job, you can’t put a blanket rule. I think what’s come across is that cases should be discussed and if the paediatric registrar on one case a day in [hospital] is referred it’s taking 2 hours of the paediatric registrar’s time. We have to be sensible.
Paediatrician (field notes, paediatric audit meeting)
The arguments for ‘proportion’ are typically accompanied by an invocation of the importance of discretion and personal responsibility for ‘thinking’ in all staff, including the junior staff in the ED.
The important thing is the thinking process, if you’re not thinking, these aren’t the only cases you will miss, there are lot more cases. What is important is education and induction of frontline staff to recognise what is normal and what is not, when people don’t do their job right that’s when things go wrong, you can’t have paediatricians holding onto everything.
Paediatrician (field notes, paediatric audit meeting)
In this position, safeguarding is normalised as just like any other decision where the junior staff should refer to their senior, rather than directly to a specialist.
Junior doctors should go to their senior to get advice before referring to another. As a registrar I would have never referred to another specialty without speaking to my senior. That would make the system more robust. Children need to be referred, we must safeguard children, but there has to be some system in place in their own department. A&E staff always refer to us to check the story from paediatric experience. I always ask if the middle grade has seen it, but again they want us to check the story. It’s important to take a very thorough history and examine, and examining is everybody’s job not just the paediatrician. A&E need to be taught to do it better.
Paediatrician (field notes, paediatric audit meeting)
Arguments are also articulated about the nature of expertise, with consultant paediatricians sometimes feeling that they are being treated as experts in domains outside their subject specific knowledge:
My view is most people run away from child protection. It’s always the paediatrician’s problem. Pass the buck to paediatrician, that’s how it is. When it comes to fractures it’s a big nuisance area. We do not see accidental fractures. And orthopaedic doctors see accidental fractures every single day. And then for me as a paediatrician I shouldn’t be saying what is the force needed, when I don’t see 99 children with accidental fractures and orthopaedic guys are the ones who can say yes that’s the force, yes it fits in. Most of the time they will not give a definite opinion and it’s, I guess radiologists do give opinion but they don’t have the history. So the only person who can match both is really the orthopaedic guys. But they don’t want to get involved.
Consultant paediatrician (CP3)
The contending positions, ‘precaution’ versus ‘proportion’, are important for at least two reasons. First, they provide a warrant for failing to follow a mandatory process, morally and emotionally; second, they make an unassailable pragmatic case that if doctors other than paediatricians never have to appraise the story then they will never learn. This illustrates a core problem with designing safeguarding policy: since the inquiry into the death of Victoria Climbié,48 child protection has been deemed to be ‘everybody’s business’.
However, in practice, this is often not the case. This underscores just how difficult the design of protocol and processes are in this area, and gives some indication of why the problems seem to be recurrent and recalcitrant.
It is also important to note that there are potential negative consequences of raising the possibility of non-accidental injury, as this consultant in emergency medicine articulates an organisational effect:
So fractures – lots of children come in with fractures . . . You know you’ve got a child who has had an unwitnessed fall in a garden but they’re ambulant and they’re running around in the garden like a nut case, they scream – you know they [parent] haven’t actually seen that they have fallen off the slide or whatever they have done. You know compared to the other children – yeah, so the potentially inflicted injuries – those sorts of things . . . So there’s lots of triggers of safeguarding from A&E, which is probably better to do it that way rather than the other way round. But once they've been triggered it’s quite difficult to rescind those and [safeguarding leads] have to get involved on some of those occasions and say ‘no, this is just a straightforward fracture’.
Consultant paediatrician (CP4)
However, there are also potentially profound and devastating effects on parents. Thus, the clinicians must be simultaneously oriented to detecting parental deception and avoiding false accusations or excessive risk aversion.
We had a parent who said to us the other day . . . the child had had fallen over in the garden and it had not been witnessed . . . her mum actually said to me ‘if I wanted to I could have lied and told you that she’d fallen over and bashed herself couldn’t I and you’d have been none the wiser that I wasn’t telling the truth and I’d have gone home’ but because she said ‘I didn’t see it’ the child had to stay in for days and days and days and in fact it was nothing . . . I can think of lots of times when my children have – you know they are big and ambulatory now they could potentially do it but you know – so my son had fallen over at nursery and cut his head open on a corner . . . you know and no one had witnessed it. If I’d have brought them straight into A&E after they got back from nursery . . . but you could imagine some people would trigger that and he’s now had two of those, he then cut himself – he’s just bloody accident-prone.
Consultant paediatrician (CP4)
Effects on parents and child of child protection processes can be profound, as this paediatrician articulates:
I noticed this big bruise behind the ear. I wanted to believe it could be an accident. Mum did not know . . . I went back and explained the whole process to the parents, grandma, father, mother, everyone was perfectly co-operative given the difficult circumstances and this was a poorly child as well which made life more difficult for me . . . By the time the social worker came, it was too late to investigate the nursery and so on so the decision was made by the social care to take a PPO [Police Protection Order] . . . It felt over the top but I wasn’t sure of what the legal situation was because it’s not my area so I just went along with the social worker and poor parents were distraught obviously, mother was completely shaking.
Consultant paediatrician (CP3)
Further problems arise in conducting what is, in effect, an investigative interview about childcare, in cases where an adult patient presents without his or her child in the ED demanding skill, experience and seasoned intuition:
So these would be victims of domestic violence, adults with significant mental health problems, not straightforward managed depression but you know people who are clearly in crisis at the moment, people with substance abuse problems, so alcohol and drug problems who’ve got children and that sort of thing . . . And some of our nurses are fantastic at it, you know while they’re doing their medical assessment of the patient they’ll be just having a bit of a chat with them you know ‘Where do you live? I see you live there. Have you got any children? How old are they then? Where do they go to school?’ and because they’ve recognised right from the outset you know this is a woman with bruising to her face or whatever who’s very upset, they have recognised that this might be domestic violence, they will be gathering that information even before the issue of domestic violence is raised as a possibility with the woman. And that’s the difference between an experienced practitioner and somebody who’s new to the role really.
Consultant, emergency medicine (EM2)
Thus far, this chapter has outlined the wider social context of safeguarding which assumes the possibility of actuarial certainty creating a climate of blame and shame. It has also articulated the wicked complexities of making sense of cases, and the moral courage needed both to act and not to act when what you need to ‘know’ does not ‘show’. This is vexing enough within the borders of one complex organisation, but the plot thickens when new players are introduced at the agency margins.
Knowledge sharing in children’s safeguarding: jigsaw practices
[T]here is something of a mismatch between the jigsaw, as articulated in conceptual abstract accounts, and jigsaw practices on the ground. As an abstract metaphor, the jigsaw does not reflect the complexities of building a ‘full’ picture in practice.
Thompson, p. 18770
Thus far, this chapter has described the problematics of professional sense making and diagnosis in child safeguarding contexts. In these domains, further complexities arise from the need to pass unclear, speculative and ambiguous information across service boundaries. The ‘jigsaw’ may be incomplete, and the professional concerned may, or may not, know that some of the pieces are missing. The construction of a ‘full’ picture is inevitably contingent upon actions and talk within settings, and may or may not be subject to ongoing revision. The search for a common language for child welfare has been a veritable holy grail of policy, but in the context of stretched services, where information is often interpreted strategically, it has been elusive, and that should not be a surprise. In the extract below, a paediatrician explains the mismatch in the repertoires of health and CSC, where the latter are seeking certainty in diagnosis about suspected abuse in order definitively to categorise the case as a section 17 or 47 of the Children Act 198919 and hence manage their workflow. Section 17 referrals can be strategically deferred, whereas with an explicit section 47 case, action must be immediate.
We're saying ‘I’m not sure therefore an accident cannot be excluded’ and this is sort of such a difficult term for social care . . . For us it means actually there’s still a possibility, but they’re saying ‘no it’s not a suspected NAI [non-accidental injury]’ that’s what they miss . . . whereas for us it means it’s still possible. So they have different ways to understand our terms, medical terms . . . I mean ‘suspected’, for us, it means different things medically than for social care and I learnt that – yeah that the language is so different.
Consultant paediatrician (CP6), emphasis added
Children’s social care services face unprecedented levels of demand,9 a problem exacerbated by the fact that they are key to other organisations managing their own (institutional) risk. Contact with children or parents, especially in EDs, is fleeting, so there is almost always an information ‘deficit’. This can potentially trigger referrals to CSC on a precautionary basis, as is articulated by this ED consultant who likens the process to diagnostic screening procedures used in biomedicine:
Yeah you have to slightly over-refer in order to be safe . . . So from a social services point of view a lot of these look like an inappropriate referral and some of them are. But you need to accept a certain percentage of inappropriate referrals in order to get the really bad ones. If I ordered 100 CT [computerised tomography] head scans a year and they were all abnormal I would be negligent, I would be a bad doctor, because I need to have about 300 and 200 of those need to be normal in order to get the right threshold.
Consultant, emergency medicine (EM2)
The jigsaw is most frequently used as a metaphor. The pressure to share fragments of a story can be particularly acute in EDs, where contact with patients is fleeting and frequently fraught:
To my mind any pieces of the jigsaw that exist should be sitting in a folder in social care, whether it’s electronic or paper or whatever but there needs to be one place for all the bits of the jigsaw to go otherwise the whole notion of safeguarding doesn’t work. You know if we have got one bit, the GP’s got one bit, the captain of the football team has got one bit, and they’re not in the same place and they never get to the same place, then you cannot recognise that pattern of concern that might be developing . . . And if we’ve got that concern we have to give it to social care partly because someone’s got to co-ordinate it haven’t they? And often, you know the referrals person will say ‘Well can you not liaise that out to this person or that person’ . . . We can’t co-ordinate that from an A&E department. You know that’s just an unrealistic expectation. And social care have, as far as I understand it, the statutory duty to do that.
Consultant, emergency medicine (EM2)
So, if we stay with the jigsaw metaphor, to the recipient a fragment often makes little sense. They are trying to work out the meaning of pieces of jigsaw without having access to the picture on the front of the box. Little wonder, then, that CSC attempt to gatekeep and limit information flow into their organisation, particularly where this is fragmented and difficult to use. However, their health colleagues have equally good organisational reasons for wanting to gatecrash. The boundary difficulties are, thus, complicated by potentially very different interpretive schemata and local exigencies.
It is unsurprising that referral to CSC is one important aspect of managing institutional risk in hospitals at the highest management levels. In the following extract, a member of the executive team in one of our sites explains the recurring tension between precaution and proportion:
Now, I mean, [Head of Safeguarding] has been putting herself about a fair bit and I think – you know – almost to the point of any concern about any patient, ‘Oh, it could be a safeguarding issue’. And I say, ‘Look, hold on; we can’t have everything being a safeguarding issue’. But, she’s a very powerful advocate for that and there is no doubt that, when you actually look at it in the cold light of day – you know – say, well what’s the harm in making the referral? Well none, really, ‘cause someone will look at it in a degree of depth and will establish your suspicions are unfounded. It would be a dreadful occasion, I think, if every single referral was automatically judged to be correct because then you probably aren’t sending enough. You need to have a number where the investigation says no, no; we don’t need to be doing this. You were mistaken. And all I’d say to that is, ‘Fine. I’m reassured’.
Senior executive (SE2)
The identification of safety with high rates of referral shows itself in the following comments from a member of the executive team in another of our sites regarding the occurrence of a dip in referrals, which had clearly been a cause for concern:
In relation to the awareness we have seen, apart from a blip recently, a real improvement in the number of referrals of our staff and I think that’s because staff are now more aware. The training’s kicked in. The awareness has kicked in . . . So we have seen a huge increase in numbers, both for adults and children.
Senior executive (SE4)
Metrics monitored by the trust corroborated this increase, with 620 children having been referred because of safeguarding concerns during the relevant quarter, compared with the average of 449 over the previous year (most referrals reflected emotional concerns and neglect, and the increase had been in these categories rather than physical and sexual abuse). Indeed, the development of a referring culture from a health perspective can be seen as a big step forward when there have been significant and enduring problems in keeping safeguarding concerns at the forefront of busy clinicians’ minds.
It wasn’t so long ago either that they weren’t letting people know. Then they were getting lambasted well you should have done a referral. See this is the culture a little bit in an acute trust. They’re patting themselves on the back still that they have managed to do the referral, because it was not so long ago they didn’t even think, because they don’t tend to think in an acute trust about anybody outside the walls of the hospital.
Head of Safeguarding (HS2)
The systemic effects on CSC are noted by safeguarding professionals in health settings. They are aware of the capacity for fragments of cases histories passed over the agency boundary to create larger haystacks in which the needles are more difficult to find, but they have competing imperatives to ensure vigilance and a referring culture in their clinicians. They are caught in a double bind.
We see quite a consistent pattern in terms of the numbers of referrals that we do as an organisation to local authority around safeguarding concerns. We’ve seen a rise since we started looking at it over the course of this year I think the average is about 450 safeguarding referrals each quarter. But we had one quarter where everything sort of dipped a bit and the kind of feedback that we got from staff at the front line was that they were getting quite a difficult time from the local authority at that point . . . It coincided with a time when in [the local authority] there is very much an approach that they want to reduce the number of referrals going through the front door, that feel they get a lot of referrals that are not child protection. And it’s obviously you know, it’s the argument makes it harder to see what the real child protection is if you don’t get, so it’s that push back really.
Head of Safeguarding (HS2)
While these referral practices makes perfect sense within the hypothetico-deductive logic of biomedicine and the high-blame, high-risk context of institutional accountability in health, the systemic effect on CSC is very significant, as it generates what, for them, is ‘noise’ in a service under pressure. This effect is discussed in detail in the next chapter. It is likely to matter fundamentally whether the referring professional sees themselves, or are systemically situated, as actively spinning a relational knowledge web about a child, as a metaphorical spider, or as the current keeper of just one piece of a jigsaw to be collated and made sense of elsewhere by someone else. The spider metaphor is invoked below and implies a different, more active, relationship with the data gathered:
So there’s conversations to be had with the mother. I would say there’d need to be a conversation with the school which is where this concern has been, you know has originated from and what’s the basis of it, what is the pattern of behaviour you know what have they noticed. You might want to have a chat with the GP. You might want to talk to the school nurse, you know any other agencies who might be involved with the child. So it kind of sends out, it’s like a spider’s web really, you know you start off at the centre but then each pathway you go down gives you different links to other things which need to be pursued.
Consultant, emergency medicine (EM2)
Raising the barrier with technology: call centres and gatekeeping
It has been noted that high demand and referring culture are likely to generate gatekeeping behaviours in CSC. References to difficulties in contacting the services are ubiquitous in the accounts of health staff in both sites and are frequently exacerbated by the configuration of the local authority ‘front door’. The social care agencies, to which our two sites relate, are variously configured, with two using a ‘call centre/information officer’ system and others using various versions of a social work duty desk. The perspectives of CSC are covered in more detail in the next chapter.
I think the perception within medics often is that the social care is so understaffed that they are so stretched that they are often trying to push referrals away if they can – that’s the perception – maybe true or not true – and then putting sort of obstacles in the way so you have to go through the contact centre first and then if you’re trying to get a social worker directly they’re not available, they are out or there’s no one there – that particular person who deals with that case is not in and no one else takes it over. Once you get a mobile phone then it’s easy to contact them.
Consultant paediatrician (CP6)
All of our respondents from health mentioned the importance of having a conversation and speaking directly to the social worker, where ambiguities and nuance can be discussed, with many expressing a wish to have a hospital-based team or worker and referring positively to previous experience of such systems in providing ‘a sounding board’ and opportunity for face-to-face discussion. This is borne out in other research,9 but many referral portals preclude this. The spatial and temporal distance from the other professional is invoked by all respondents as an impediment to the effective communication of ‘intent’ and ‘nuance’, as is described by this consultant in emergency medicine:
It is a complicated business . . . There isn’t a pathway for the key professional at one end to talk to the key professional at the other end. There are too many steps in between and that leads to a dilution of information and omission of information you know, whereas if you were having the conversation directly with the practitioner who’s going to take responsibility for the management of the case thereafter that’s the opportunity for clarifying isn’t it and making that risk assessment but the process doesn’t enable that.
Consultant, emergency medicine (EM1)
The complexity of the referral portal is explained at length here by a senior safeguarding professional:
So that particular local authority has got a call centre at the front of all of its services for children. So the sorts of problems that are reported by staff is that they get cut off, or it just takes a very long time for calls to be put through. This is a service called [XX] and they answer the phone for all of children’s services. So where you want to go with the child protection referrals is just one of the areas they could direct you to. And the idea is I suppose if they ask the right screening questions they can put the calls in the right way . . . So that’s your first obstacle is getting through that [XX]. [Social care] will acknowledge that [XX] is a problem, because it’s a problem to them as well . . . So their social workers are in court and they need to get hold of somebody and they’re ringing they can’t get past it themselves.
Head of Safeguarding (HS2)
‘Having a conversation’ is constructed as a means of removing ambiguity in communicative intent:
Referral doesn’t mean a, I’m handing all this over to you and I’m abdicating all responsibility, it just means the highlighting of a concern. And we know that not all of these concerns result in a section 47. We know that. We know that some of them don’t even result in anything other than a home visit. All we want to do is be taken seriously and you know to get some feedback. That’s all we want.
Consultant, emergency medicine (EM1)
Frequent changes of shift in hospitals and of social worker in CSC disrupt this communicative flow:
I find the way the caseloads change and contacting them very, very difficult, but you have long conversations with one social worker before they become a child protection [case] or, you know, when they’re a child in need and then all of a sudden you have another social worker who then deals with it because it’s now a child protection issue rather than a child in need. And I feel that you have to start again every time and I find that very tricky.
Consultant paediatrician (CP1)
There are ubiquitous complaints about the lack of feedback about referrals from CSC in both sites, with the metaphor ‘black hole’ often deployed, though certain local authorities appear to be more strongly associated with this phenomenon. It is likely that this escalates as a result of the referral system itself, in a positive feedback process. CSC gatekeep and their health colleagues try to gatecrash to manage their own risk in a high-blame environment. Both practices are rational but potentially systemically unsafe, with health staff treating ‘making the referral’ as the end, not the means:
It’s like making a referral into a black hole. That’s what it feels like from our end. The staff meet with resistance to the referral being accepted at all, you know and they’re sometimes told ‘You don’t need to refer this. We don’t need this as a referral’ which you know, well what happens then with the information? . . . So it does feel a bit like well, I’ve made a referral, I’ve done my job, I hope the right things happen for this child now. That’s a bit how it feels.
Consultant, emergency medicine (EM2)
While there is a degree of frustration expressed by health-based staff about this phenomenon, there is also a good deal of sympathy, and the reasons for the difficulties are widely known:
I think there are some very good social workers and they are doing fantastic work and they, you know if you have one of them dealing with it then you are very reassured. And because I’ve been being very senior I very often have this discussion and say ‘I’m referring you this. I’m sending you the form but I’d be quite happy if this can be followed up the next day because I don’t think this child is in immediate danger’ and they will then come up with the appropriate response . . . you get a really fantastic response. But overall I would say that the relationship is a bit strained really because we have been identified as one of the major referral sources for them . . . there’s a reluctance to accept another referral.
Consultant, emergency medicine (EM2)
Given that the lack of routine feedback from CSC was a feature of the Victoria Climbié48 enquiry, it is surprising that this has not be tackled more directly nationally. This senior safeguarding professional reflects on the issues:
So we all say, ‘Yes, we want it’, and they [CSC] always say, ‘Yes, you should have it’, and we never move on from that. ‘Cause it’s like it’s a ‘it would be nice’ instead of an ‘it’s absolutely necessary’. Well, there’s a statutory responsibility to do it and they still don’t do it . . . I’ll tell you why it doesn’t happen is because it never features in a serious case review that this child died because somebody didn’t feedback from the outcome of a referral.
Head of Safeguarding (HS2)
However, there is evidence that this feedback can be ‘designed in’.
It’d be nice if it was done. Does it make a difference to the child if it’s done? Feeding back to people who’ve made a referral is kind of down there on our list of things to do. Even though it’s long been a requirement that they do it. It should be easy. There is one authority who’s doing it. There is one authority that established a formal way of providing feedback in a really clear and useful way. Our named nurse is very impressed with it.
Head of Safeguarding (HS2)
This kind of feedback loop has formed part of system innovations elsewhere in England. 9
The problematics of consent
Information sharing in both directions between CSC and health is further affected by the problematics of consent. In the following extract, a paediatric nurse recounts an incident where CSC did not share information about the offending history of a young person admitted to the ward:
And I’ve also had a 12-year-old child, we had the police – all the social services were aware, he’s in care anyway, I had a policeman ring me 4 hours into the shift to say ‘get that child away from any other children, he’s had violent tendencies towards other children before, he’s set things on fire. Think along the lines of [Robert] Venables’ . . . That was a policeman confidentially ringing being very, very concerned because of this child and as he said it, I looked into the dining room and he was sat next to someone hugging this little boy, like playing, and the parents were there and I felt sick inside thinking, because social services did not tell us any details, ‘no, no, it’s confidentiality for that child’.
Nurse, paediatric focus group
Practical reasoning, institutional procedures and ‘myths’ about consent have a significant impact on decisions to share or not to share information. The threshold for sharing information about a child or family without consent is that there is cause to believe that the child is suffering or likely to suffer significant harm, i.e. that a section 47 investigation may be indicated. However, before the information is shared, it is frequently not possible to make the case for sharing it; this is a thorny problem.
Yeah because if it doesn’t meet the threshold for them to be a referral they can’t share the information with us, which I just think is very unsafe. We know you’re making a referral but it’s probably not going to meet our threshold for child protection so why would we share information with you? It’s that whole, you know, it’s behaviour that doesn’t help us working together isn’t it? You’re worried but you probably don’t need to be.
Head of Safeguarding (HS2)
The need to obtain parental consent to share information is also an interactional factor in health settings. The next chapter describes a case where this was a factor and examines its effects on the system. This issue, as with the others discussed in this chapter, carries a degree of moral hazard: share too little information and interpret confidentiality tightly and children at risk will be missed; do the opposite and create false positives and mistrust among parents in seeking health advice and treatment.
Plugging the information gaps: a case example
It is clear from the discussion so far that there are multiple nodes where communication and detection of risk can fail, even if the clinician is being conscientious in their work – latent conditions for error lurk ubiquitously. 142 Both of our sites had systems in place to plug these potential gaps, particularly in EDs. This involves some form of screening of attendances against risk criteria. A common response to this need is to have a liaison service undertake the screening retrospectively and refer on to either community health services or CSC in cases where the clinicians have failed to spot a risk factor. It has been noted that much effort is directed within acute settings at the identification of harm or potential harm, and within practice is directed at the management of the presenting problem and any further escalation of risk to a child. Within our second case study site, the ‘paediatric liaison role’ played an important part in identifying children and families who needed support to be safe, but who were not deemed to be ‘at immediate risk’ of deliberate harm. The aim of the team is threefold: first, to ensure the provision of relevant and high-quality follow-up care for children attending A&E; second, to facilitate communication effectively across acute and community health settings; and finally, to reduce inappropriate ED attendance by working with community-based teams to encourage and educate families about GPs, health visitors and school nurses.
The paediatric liaison service (PLS) reviews all ED attendances of children aged 0 to 16 years against a set of criteria of ‘protected characteristics’, for example if the child is looked after or if the child has a fracture and is under 2 years old. The liaison officers read the whole form. They ensure that the demographic data are completed, check for the context of the child’s visit and read to see if the child would qualify for further follow-up – regardless of whether or not this has been stated by the attending professional on the ward. The information is deciphered, updated where necessary and uploaded to a community database from which an administrative team contact the relevant health visiting or school nurse team. One in 10 of all referrals lead to a ‘notification’ to a community health team and the liaison officers take the responsibility to suggest further action and to advise the community teams of any background information.
The Head of Safeguarding gave an example of the poor quality of paperwork, and how the pressures on staff in EDs can be responsible for this. The case in question involved a mother who had presented at the ED in the early hours of the morning after taking an overdose. All of the basic details regarding names and addresses had been completed, but the referral simply stated that she had presented at the ED with an overdose:
And we went back to the member of staff and said ‘what did she take, how much did she take, what kind of treatment did she need? Where were her children when she took it? What provision was in place for them to be cared for?’ . . . and we got all that information pulled together fairly quickly and the staff members had that one to one, but what she did say, which is a fair point I suppose, is that on that night in question she had been dealing with that woman who was then stable. She’d done a referral quickly, but was then pulled in to resuss to be with a patient who was really, really unstable. And she just described the difficulties of the environment that is the emergency department.
Head of Safeguarding (HS2)
The PLS is often described as performing a ‘screening’ role because the presumption is that the professional completing the original A&E paperwork would know when the child meets the vulnerability for community health notification. This upfront evidencing is important, as liaison staff do not have the advantage of being with the child and family through the A&E journey. However, the information on the form is often scant, making a decision to notify community health services more difficult:
Somewhere you’ll see someone and they’ll say to you, ‘Oh, did you see that record about such-and-such?’ . . . They’ll go, ‘Oh, I was really concerned about mum’s interaction with the child’. Nothing written in there, so just they might have ticked that as being liaison health visitor input . . . but we are not – no crystal ball; we don’t know what the issue is.
Health visitor (HV1)
In the words of one liaison officer, their account is ‘third hand’. There is a discrepancy in some cases between what the idealised nature of the review is – seeing if the notification box has been ticked, doing demographic investigative work if necessary and notifying the relevant health visitor or school nurse team – and the reality.
What you will see is that, yes, there’s a comment [on the paperwork] about ‘has that clinician who’s having the face-to-face contact with the family – have they thought about the vulnerability criteria?’ which they have got access to, and ‘have they seen whether or not this attendance meets that vulnerability criteria?’ Nine times out of 10 they all tick no, and yet, you know, we’ve already done a notification for this child.
Health visitor (HV1)
In these instances the team spots the detail within the paperwork and ‘we would do the notification’. When asked how often clinicians missed children who met the criteria, the liaison officer replied, ‘Oh, yes, all the time. Yeah’ (AD2). In spite of this, there is no automatic feedback loop to the ED, meaning that under ordinary circumstances, the professional who saw a child would be unaware that a notification to community health had been sent. In some cases where there were real concerns about the safety of a child, the paperwork was so incomplete that the health visitor liaison (HVL) had returned it to the consultant on duty for immediate further action. However, it was only in more worrying cases that the HVL team would go onto the ward to ask for clarification or to push for further action and potentially a referral to social care. In the main, from the point of view of the busy ED, community health remains somewhat out of view.
In addition to clinicians not utilising the vulnerability checklist in instances where the diagnosis is relatively clear, some cases involve a much greater degree of interpretation and subjectivity. One such area is the presentation of adults in A&E who give rise to parenting capacity concerns.
We will also review adult records when the adult has attended with an issue that will impact on their parenting capacity. So we’re talking about domestic abuse, mental health problems, alcohol and drug use and there’s a clear pathway that these notification – these attendances need to be identified by the clinician, they need to ask about responsibility for children and they need to make interagency referrals. And then the completed record needs to be made available for our team. And, again, that’s very spasmodic, isn’t it, how effective that is?
Health visitor (HV1)
In performing this scrutiny and reviewing role, a degree of interpretive work is being undertaken. However, this is muddied when pieces of the jigsaw are missing, where clinicians did not evidence answers about parental responsibility or relationships with CSC in the paperwork. There is more than surface-level screening taking place; there is judgement-based practice, informed by tacit knowledge and previous experience, by a moral orientation to protect both community staff and children and by the institutional guidelines within which they operate. The guidelines act as cultural artefact: inscribed within them are the concerns of the local trusts about the vulnerability levels of disparate groups, registering a hierarchy of risk. In creating notifications for children, the team are managing these risk categories on behalf of the broader local health system, using discretion, experience and interpretive frames to protect and support children and families. Moreover, they go beyond a screening role, a sort of double-check on clinical decision-making, by actively challenging senior medics where necessary. They perform a safety-net role by spotting families in need who might have been overlooked by those on the wards.
In order to co-ordinate follow-up support and to communicate actions across professional boundaries, the PLS had to translate as well as interpret. Through tacit knowledge and experience they have a collected wisdom that enables them not only to pass on information but to do so in a mode and manner that means it is more likely to be acted on. They are selling the notification. In the case of health visitors, the liaison officer said,
‘Cause, you see, health visitors, they don’t need a lot of medical terminology. They just need – you know, there’s no need for that. It just muddies the water for them. They just need to know when they came, why they came and what happened.
Health visitor (HV1)
In the case of child protection medical assessments, the team were cautious about writing too much information in their notification:
When we are doing child protection medicals, we keep it very, very brief. We put the minimum of information. We put the fact they came, that it was undertaken and a contact number for further details.
Health visitor (HV1)
The reason given for this expediency was a concern not to prejudice any further work while any potential investigation was in its infancy. The team also felt that if the issue progressed, then the relevant professionals would be informed by social care in any case. It was not their role to pass on all information to all parties; rather, they translated what they felt to be relevant for those working with the family in the community.
It’s a work in progress as well, you see. I mean, what we see here is the very start of the investigation. So there is no definite diagnosis or, you know, further plan. It’s just the medical’s – the examination’s been undertaken and they’ve – and now it’s in the hands of children’s services or the police and they’re the people that have – you know, and they will only divulge as they feel fit.
Health visitor (HV1)
In speaking of data protection, one of the officers said:
You know, it’s showing information for the benefit of the child, but it’s on a need-to-know basis. And, actually, health visiting teams don’t need to know an awful lot of the stuff that – and if they do, that will be disclosed by social care.
Health visitor (HV1)
So, the purpose of PLS goes well beyond screening. Their activity can curtail or embellish the understanding of associated professionals about family life as they decide how much or how little information to share across agencies and on what terms. By performing the role of a communication hub, the small team have built up detailed knowledge of the social, geographic and institutional topography operating across the area.
The set-up of the PLS reflects the need to manage immediacy within the cacophony of the ED. Certainly, the PLS service takes pressure off the referring agent by focusing the latter’s attention firmly in the direction of social care towards the institutional ‘hot potatoes’ of categories ‘section 17’ and ‘section 47’. The liaison helps to manage a fraught environment on behalf of these acute sites by pre-empting and organising community follow-up. The team will pick up, from a directive in the A&E notes or from their own discretion, those cases that they think could benefit from community health-care involvement. The liaison officers perform safety by challenging medical personnel to think more broadly about risk and harm, and to encourage them to use the protected characteristics as a guide.
We have a link consultant and periodically we will e-mail – and we’ve had times of being very assertive where we have actually collected names – not to pinpoint but we’d have actually sent e-mails to those particular practitioners with the vulnerability criteria and just said, you know, ‘burns are a safety issue’ – those sorts of things. But we’re a bit slack on that because we’re a bit short on the ground and so other things take priority because, you know, it’s about – as long as the child is safe and if we’ve flagged it up.
Health visitor (HV1)
This is not to say that low-level concerns are overlooked or missed. Many respondents had the intuitive sense that all was not well; many described in their notes the appearance of an unkempt child or the dislocated behaviour of a mother. However, several ED nurses commented on their frustration that if they had low-level concerns, for example about feeding or hygiene, they had nowhere to record or refer these concerns. One staff nurse stated:
Sometimes it’s not even that they need a safeguarding referral. It’s just access to the help. There’s no other way of us as nurses on the front line to get people help other than to make referrals.
ED nurse (N5)
They felt that for any action beyond the hallways of the ED to be taken, they had to refer it to CSC. These nurses felt ill-equipped to signpost families because they were not sure what was available locally, be it a Sure Start children’s centre or a local housing office: ‘we would not even know where to get it from or how to’.
In terms of knowledge of community health, two ED nurses seemed uncertain about how to contact health visitors or access school nurses and recognised that this had strategic implications:
I think that’s probably the biggest gap in the service is that probably quite a few people that we safeguard don’t need the safeguarding and it’s the same vulnerable adults. You don’t need safeguarding, they just need help put in place, but there’s no way of doing that.
ED nurse (N5)
Or, as one nurse pithily said, ‘there needs to be something in between all or nothing’.
One paediatric nurse based in ED, who describes herself as ‘passionate about safeguarding’, was aware of the PLS. She said that it offered ‘back-up’ to A&E staff, ensuring that ‘every child has got that [paperwork] so, in theory, it should not get missed’. In being aware of the protected characteristics and in the ways in which information can be passed to health visitors, the paediatric nurse took a more nuanced approach to information sharing:
So if you had a child that had an accidental ingestion of Calpol, that’s safeguarding, because a bottle can do damage. But if it’s the fact that they’ve eaten the end of a candlestick, to me, that’s health visitor, because although they say well they might not have adequate supervision at home, there might be neglect. Well when I’ve had my Godchildren, I’ve sat them in front of a telly while I go and made myself a drink, and it only takes a split second for them to do something. That’s not necessarily the parents not doing their job. If all those things go to safeguarding, then kids are going to get missed.
ED nurse (N4)
In having the liaison officers scan all ED child attendances, the likelihood of children falling through the cracks of provision between acute and community settings is likely to be reduced. However, this reliance on a small number of revolving staff, who in their own words only access ‘third hand’ (AD2) accounts, might be inadvertently contributing to a referral culture that, in the words of one consultant, leads to ‘an all-or-nothing response . . . There isn’t really anything else in between . . . We either refer them or we don’t’ (EM2). By outsourcing responsibility to check for characteristics that trigger community health input, acute staff focus their referring and support behaviours towards social care. This mirrors the sentiment of the two ED nurses who instinctively felt that a social care referral was unnecessary but also felt that without such an action they would struggle to get any additional support for a family. The liaison officers recognised how they might be inadvertently contributing to a culture that is not imbued with community health considerations:
I think there’s underuse of this [protected characteristics] in as far as I – and I guess a lot of that’s to do with the fact that they know that every record will be reviewed in any case, so whether they tick yes or no . . .
Health visitor (HV1)
These two adult staff nurses had only recently found out that adding a red sticker to a patient’s file and leaving it with the ward reception meant that the health visitor would take a closer look at the file. The nurses interviewed said of this informal approach, ‘it’s not a service that is massively known. You only know about that because you did that safeguarding level 3 or whatever it was’ (EW3). The other nurse added, ‘If we don’t use that service we will lose it. And I think it’s just being wasted really . . . that’s something that I’d say 90% of staff don’t know about’ (EW3). This informal approach stands in contrast to the process for referring to CSC, which is painstakingly recorded in multiple textual and digital forms. Rather, the relationship between acute and community health is more permeable and fluid, yet from the descriptions given by nurses it is also more hazy and uncertain. The informal nature of this practice does not mean the nature of the interpersonal communication across professional boundaries is necessarily improved:
With a red dot, yeah you put the red dot on there, what’s going to say reception is going to put that in the pile for health visitor? You don’t get to speak to anyone about it. And that doesn’t really sit well with me.
ED nurse (N5)
In the pressurised environment of ED, establishing the significance of the red dot on a file is unlikely to take priority and does not necessarily foster additional meaningful conversation between the A&E nurse and the health visitor.
The PLS is a useful and successful workaround; it helps to get the job of recognising need and managing safety done without adding additional pressures to a stretched cohort of ED staff. While the PLS team are competent and confident, they are not clinicians working in ED. The service in acting as a citywide portal is stretched. The team often do not have access to a computer, and so have to hand-write and fax details to their administrative team. Whether or not IT would help, though, has been questioned:
Now obviously some of these things can be sent more easily electronically and would not have bits of paper flying around . . . there just is no easy way of doing it. So I mean the individual teams are not always easy to identify, particularly school nursing team . . . and also they swap round and change quite a lot and so it is not perfect.
Head of Safeguarding (HS2)
It can be seen that attempts to ‘plug the gaps’ are themselves interpretive and complex. In our other site, the PLS has been almost entirely phased out based on the view of the safeguarding team that building the screening and quality assurance process into the ‘day job’ of some members of the permanent ED staff is likely to improve organisational learning and communication between ED and community health services. Despite these aspirations, embedding learning has not proved to be a straightforward issue. This co-mentoring initiative is described and evaluated in Chapter 6.
Conclusion
This chapter has described the everyday problematics of knowledge making and knowledge sharing and the climate of real and anticipated blame in secondary health-care settings. Paraphrasing Pava,120,121 we can see that there are multiple concurrent processes at play; people are doing many things at the same time; problem-solving takes place on uncertain, shifting terrain with high levels of vocational separatism and relative professional autonomy, qualities which render simple mandates to follow this or that procedure or process somewhat impotent. In Pava’s120,121 terms, this kind of domain requires the development of reflective and communicative behaviours concerning equivocal, problematic topics to ensure safety. It is in this context that organisational redesign and cultural change are so pressing. That clinicians manage at all to evaluate, judiciously make decisions, communicate sensitively with parents and with clarity with other professionals in these circumstances is noteworthy. In this environment, retrospectively obvious errors will always be a feature, but organisations can support safer practice and identify their own ‘blaming and shaming’ practices, which are acutely felt by staff even at a very senior level, as this consultant articulates:
I think we need – people need more support. There needs to be more resources put into the system, particularly social services. There also needs to be a non-litigious environment and that does occur here so things go wrong ‘what have you done wrong?’, you know particularly the nurses, the nurses get slaughtered. There isn’t any – I mean doctors it’s a bit different – if anyone else would have done the same and as long you’ve not gone and . . . done something really stupid you know . . . You learn from it and that’s important. You weren’t negligent, you weren’t lazy, you weren’t dismissive.
Consultant paediatrician (CP1)
It is to the design of such a just culture that the innovations in Chapter 6 are oriented.
Chapter 5 Is it child protection? Practical reasoning at the local authority front door
The previous chapter outlined the complexities of knowledge making and knowledge sharing from the perspectives of practitioners and clinicians working in secondary health settings. It highlighted the ambiguities in presenting conditions and the difficulty of coding the information so that it is understandable to someone in another agency with different priorities and pressures. The local authorities to which the two trusts relate have been affected by recent high-profile cases. For these reasons, this report throughout has also obscured the identities of individual local authorities where possible and has instead drawn out common systemic factors which are present to a greater or lesser degree across sites. It has been noted that information does not easily cross professional and organisational domains. 165,166 Traditional information theory167 assumed that information could simply be transmitted, as long as it was precise and not disturbed by noise. More recently, it has been recognised that information has to be translated between different sites and, in the process, is transformed. As Winthereik and Vikkelsø168 note:
The basic process of communication is, therefore, one of transformation: the message is sent, but undergoes successive translations as it links with transmitters and receivers and finally with the recipient. This inherent transformation of the message is simultaneously a risk and a source of invention; successful communication, thus, necessarily involves the risk of failure . . . Moreover, an entity changes character as it enters into relations with different other entities (a message inscribed in a letter is not identical with the same message being given over the phone).
p. 47
A distinction can be made between information and knowledge. Rasmussen169 considers that ‘information is the storing, retrieval and processing (objectivation) of knowledge’: knowledge is individual, whereas information is social. Kanfer et al. 170 distinguish between mobile and embedded knowledge:
Knowledge [is] considered ‘mobile’ when it can be codified in a linguistic . . . way and easily transferred or translated from one person or group to another. Knowledge is ‘embedded’ in a social system when it is bound up with a set of communications, practices, and tools that make linguistic codifications difficult.
p. 319
Aas,171 in a study of sentencing in youth justice, also suggests that some knowledge travels and other knowledge does not. Informal knowledge, such as ‘he is a good lad’, may be viewed with suspicion because of its lack of explicitness, transparency and scientific basis, travelling less well than ‘he scored low on a risk assessment instrument’. For the health professional to make a successful referral, they need to communicate their local and personal assessment of children and families into a form of information which the worker in a local authority or other agency can understand and interpret in a sympathetic way without losing the nuanced character of their assessment.
The concept of the ‘boundary object’172 has been developed to identify objects which move across organisational boundaries but are able to be interpreted by different audiences: ‘Boundary objects are both plastic enough to adapt to local needs and constraints of the several parties employing them, yet robust enough to maintain a common identity across sites’ (p. 508). 172 However, Saario et al. 173 conclude that a report on a child transferred between health and social care colleagues is likely to become a boundary object only if it is read, discussed in multiagency meetings and comes to be the definitive description of the child. If successful, it directs the actions of all professionals in the network. They conclude that most do not achieve such a status, and need to be augmented by other actions – e-mails, telephone calls, meetings, and so on. The frequent references to pieces of the jigsaw in the previous chapter underscore that there is a significant risk that data exchanged between health and social care fail to achieve this state, remaining weak, ambiguous and malleable to disposals not intended by the referrer.
The ‘front door’ of children’s social care
Children’s social care organisations have complex systems for processing the information they receive from professionals and the public. As with all ‘people processing organisations’,174 they manage the referral of information, carry out assessments and make decisions about further interventions. How this information is organised and managed affects the whole way in which the service operates and has been the subject of constant reorganisation. As described in Chapter 2, it has also been (and still is) the subject of a performance management regime and a range of indicators which attempt to audit the effectiveness of the system, so the activity at each stage is closely monitored. For example, there are tight timescales for each part of the process and information is recorded in complex forms. 59 How this information about children and families is recorded becomes the basis of future scrutiny and reassessments of families.
As noted, there are two main jurisdictions under which CSC operates, commonly known as child protection and children in need, sometimes referred to as section 47 and section 17 (of the Children Act 1989),19 respectively. Although this categorisation does affect the handling of cases, there are roughly four stages: receive initial information, collect additional information and make an assessment, make a decision and decide on longer-term intervention.
-
Receive information, referred to as the ‘contact’ stage: CSC receives contact from an outside agency or member of the public. At this stage they may decide that the case is inappropriate, signpost the caller elsewhere and take no further action. To make such a decision, they may make some inquiries of the child welfare network (the school, the health visitor, etc.). They may even visit the family.
-
Referral/initial assessment: at this stage, CSC accepts that the referral is relevant for their intervention. If there is an injury to the child or a serious concern, emergency action may take place to ensure that the child is safe. The child might be kept in hospital or moved to a foster home. If the concern is less serious, the child may remain at home but a child protection inquiry would be carried out. Such a decision would involve discussions with the police and other professionals (a strategy discussion). If the case is not considered as ‘child protection’ but as ‘child in need’, an initial assessment will be carried out. Such an assessment has a prescribed format and should involve a visit to the family home and a meeting with the child. Completion of the assessment is expected in 2 weeks (or 7 working days in some local authorities). At this stage, the case might be closed.
-
Detailed assessment: if the initial concerns are substantiated, a more detailed assessment is carried out. For a child protection case, a child protection investigation is carried out and a report is provided for an initial child protection meeting, within 3 weeks of the strategy meeting. For ‘child in need’, a core assessment is expected to take around 2 months. For both assessments, there should be a series of meetings with the family. Evidence will be gathered from other agencies and family members and a detailed report produced. At the initial child protection conference the case can be closed, or a child in need plan or a child protection plan established. Similarly, a ‘child in need’ meeting at the end of the core assessment will have similar options. Some local authorities have developed a single assessment process.
-
Longer-term work: if after the core assessment/child protection conference it is decided that the family need further intervention and support, they are likely to receive a service as a part of a child protection plan or a ‘child in need’ plan. Care proceedings may also be commenced.
This rather complex process of ‘duty and assessment’ involves receiving information, carrying out assessments and making decisions. It is central to the organisation of CSC and determines how the services are organised and how information is received and processed. In most local authorities, the process is divided up in some way, with social workers from different teams carrying out particular elements and tasks.
The NHS trusts within this study interface to a total of eight local authorities within their immediate catchment areas, although sometimes cases can present from much further afield. The research team conducted interviews and observed and discussed information-handling practices in four of these authorities with highest numbers of referrals from the trusts. These will be referred to as LA1, LA2, LA3 and LA4. Within these local authorities, there were major differences in the ways in which the duty and assessment system was organised.
In two large city authorities, the initial contact with CSC was via a centralised call centre, which was part of the general local authority ‘customer contact’ system. A referrer telephones, faxes or posts their initial concerns to a centre which deals with all contact information (stage 1 above). The initial telephone call might be with a ‘customer services officer’ who will take the basic information and pass it on to a member of a social work team based at the call centre. They will consider if the information is relevant for CSC intervention and make initial checks. The social workers in the call centre will not visit the family home or attend a strategy meeting. If the case is considered child protection, the details are immediately sent to the relevant team, and child protection inquiries started by the (duty) social worker in that team. If it is considered to be a ‘child in need’ case, the referral is accepted and a recommendation is sent to the relevant team that they should carry out an initial assessment.
Differences also exist once a team has taken over the referral: they may continue to work with the family until the case is closed or the child is on a care order. That is, there is no split between assessment and longer-term work. However, in other local authorities, transfers after the initial stage may take place. This structure, based on ‘functional specifications’ of the social work task, is increasingly typical of larger local authorities. In the past, large local authorities were often split into districts, which were considered large enough to have their own duty and assessment systems working alongside longer-term social work teams. However, with the increased auditing of referral and assessment systems, centralised systems have been developed, with the aim of developing consistent responses in initial decision-making. 88
The proliferation of call centres brings obvious problems in its wake. In such systems, the social worker in the centralised team has little local knowledge of services or professionals, giving little room for discussions at the initial stage. There is an assumption that the information at this stage speaks for itself and a structured process of information gathering and assessment can begin. It also means that the duty/assessment process is split into two. On day 1, the social worker at the call centre is likely to speak to the referring professional and others in the welfare network to decide whether or not to accept the referral. A second social worker from another team may then complete the assessment but without having had conversations with the other professionals, illustrating concerns about the ‘dilution of information’, raised in the previous chapter, as it passes from the one person to another in the various workflows of the local authorities.
In contrast, in other local authorities, cases typically transfer between teams only after the initial child protection or ‘child in need’ conference, or care proceedings, i.e. after stage 3 above. These tend to be smaller unitary or metropolitan local authorities which do not have to relate to a large number of external agencies. In these structures, the initial contact typically comes to the duty and assessment team which decides if it should become a referral and whether a child protection or ‘child in need’ intervention is appropriate. Social workers in these teams carry out the required assessment, and the case is passed on the appropriate long-term team. The advantage of this structure is that there can be more detailed discussions at the initial stage, including home visits to decide if any form of assessment is necessary and the possibility of more informal discussions with referrers.
Some local authorities, although none in our sample, have a multiagency safeguarding hub (MASH) team, who operate a joint assessment process to decide the appropriate service to assess the child’s needs and identify an intervention. It is not appropriate for this study to address the complexities of multiagency teams as none featured in our sites but discussion can be found in studies by Moran et al. 175 and Forst and Robinson. 176 The MASH team operate before a CSC intervention and are able to manage assessments and interventions of a wide range of concerns, not just CSC referrals.
In summary, the varying scenarios we have outlined in this section mean it is likely that a referrer will receive a contrasting experience of the duty and assessment systems, depending on how the local authority organises their services. This will affect the ‘storytelling’ of both parties, referrer and recipient, about the quality and quantity of referrals from health settings. These stories can be expected to exert a material effect on patterns of referral behaviour and influence information exchange, processing, analysis and decision-making.
Information flows and their assessment
All of the social work team managers in the four local authorities investigated reported categorising the information they receive in two main ways: intermediate risks (triggering child protection inquiries), and concerns about the child development and welfare (more likely to lead to a ‘child in need’ response). Such categories are formal responses to treating information under particular legal frameworks, or bureaucratic workflows, but also initiate particular types of actions and processes. A child protection investigation is clearly different from a ‘child in need’ assessment. Therefore, making the correct decision at the outset is critical, although it is important to note that cases can move between categorisations, and hence processes, as new information, for instance, emerges.
Children’s social care team managers are concerned to know if there are immediate risks to children. This could involve injuries, bruises and marks as well as reported observations of hitting, punching or other inappropriate punishments. Evaluating the details and accuracy of such evidence is, of course, central to the investigation as it could contribute to any police case for prosecution. It may also be necessary to know if the child should be in a safe place, either kept in hospital or moved into foster care.
There’s something not quite right . . . a child’s turned up with an injury and the account doesn’t fit or there’s a delay in medical attention or actually it’s looking like it’s a non-accidental injury.
Team manager (LA1)
Social work managers often rely heavily on the evidence provided by hospital staff for both initial decisions and during the development of an assessment.
If a doctor’s saying it’s a non-accidental injury or it doesn’t fit we would immediately start section 47, we wouldn’t say to a doctor ‘well can you send us the information’, we would get on with it [. . .] so if you can’t get the information from source A you go to source B, ‘how’s the child on the ward, are the parents there, are they being attentive, are they nipping out for fags’, all that sort of stuff, so invariably we’re able to get a conversation going and make a start really.
Team manager (LA1)
Well, I mean, they’re the doctors. You know what I mean? I’m not going to debate the nature of a fracture with them. [Laughing] Either – they need to come off the fence and make a decision.
Team manager (LA4)
In the clearest cases, this will be evidence of injuries to the child or direct observation by staff of incidents in hospital. A CSC manager described a detailed referral from a hospital which reported the case of a child who appeared in A&E with a large bruise. The doctor’s report of his examination was clear enough for the social workers to visit the home to determine whether or not it was accidental:
They said this huge big fireguard had fallen on this child. That might be the case but it would have to do in certain ways . . . what we did do when we got the police together, got on our chargers and went up to the house and indeed, there is this huge, big ugly contraption, so it was consistent.
Team manager (LA2)
Often, reports from hospital staff were unclear regarding whether or not an injury was non-accidental:
Unless it’s slam dunk clear cut, there’s a fair amount of fence sitting . . . Some paediatricians are more able or willing than others to nail their colours to the mast.
Team manager (LA2)
The previous chapter discussed this issue from the point of view of the paediatricians, who often cannot unequivocally exclude accidental injury in many cases. On occasions, the paediatric opinion might appear to shift; for example, one paediatrician was clear at the strategy meeting that an injury was non-accidental, but was less clear in the subsequent report, which made it difficult to present a case in court. Making categorical statements about the likelihood of an injury being inflicted is consequential for paediatricians, and of course for families, but the absence of such categorisations (is it a section 17 or a section 47?) is institutionally problematic. However, as the hospital-based staff understand the pressures on CSC, so CSC also show reciprocal knowledge of the problems of diagnostic ambiguity.
I think they’re naturally guarded because if it ends up in court and although the care proceedings process wasn’t supposed to be adversarial, it is, and if one consultant paediatrician says ‘that’s a spiral fractural’, they’ll find somebody else who’s able to say ‘well actually, you know, he’s got rickets’ or something . . . And understandably, some things are ambiguous and I don’t mind a degree of ambiguity but obviously, if they’re not able to say it’s an NAI [non-accidental injury], then we need more than suspicion to go before a court for an emergency order.
Team manager (LA2)
Examples were provided of instances where mistakes were made through health professionals identifying marks incorrectly, which can produce tensions when precautionary referrals are made as a result. One example was in relation to a Mongolian blue spot, a type of birthmark common among darker-skinned races, such as Asian, East Indian and African people:
It’s not like a bruise that can be a bit yellow here, a bit purple there. But we’ve had two last week of health visitors saying ‘think it’s Mongolian blue spot but I’m not sure’, so we have to do a section 47 because they have sent a Cause for Concern . . . we have to then consult the paediatrician at the hospital to check that and then they have a right go at me saying ‘why are you sending children for Mongolian blue spot–’ and I’m saying ‘I’m not a doctor, even if I know straightaway it’s Mongolian blue spot . . . ‘. We have no choice. That breaks down relationships with consultant paediatricians because they’re on the phone to me saying ‘what are you doing’.
Team manager (LA1)
Sometimes the hospital and the CSC had differing views of a case, with clinical evidence and social evidence not matching up. A baby of 2 months of age in LA4 was found to have bruising which was assessed as unlikely to be accidental. The family were devastated and could not explain how it happened, but co-operated with the investigation. There was no corroborating social evidence: no criminal activity or previous contact with children’s services. A system of constant observation of the family was put in place with the help of family members, both at the hospital and once the baby was allowed to leave with his or her grandparents. It was concluded that perhaps the explanation was the way the new mother had been holding the baby. The hospital here remained ‘worried’ but agreed not to continue with a section 47 investigation, which would have been based solely on the medical concern. Conversely, the social evidence can, on occasion, be misleading. One example was provided from the same local authority where medical evidence was initially seen as not sufficient. A 9-month-old baby was repeatedly brought into hospital for vomiting which increasingly became the subject of suspicion by the hospital staff. As there was no other evidence, the family were ‘given the benefit of the doubt’. However, eventually it was found that the mother had, in fact, fabricated the condition and a section 47 investigation was instigated.
In another local authority (LA3), an example was provided of not just poor communication but also differences regarding the responsibility to share information and hence decision-making. Briefly, there were complaints by other parents in the children’s ward that a parent had hit his or her child on the ward, and he or she was also seen consuming the child’s food. The incident was not observed by the ward staff. The doctor examined the child and could find no marks, and so did not contact CSC or complete an information sharing form. The child was discharged home. Subsequently, an information sharing form was completed by a nurse but sent to the wrong local authority. The CSC team manager received the form 4 days after the child’s discharge. They contacted the hospital for more information but the referrer was on leave. The CSC team manager wanted to call an immediate strategy meeting, which is the normal institutional response to a section 47 referral, but there was little evidence from the hospital and, in particular, there was no record of the witnesses on the ward for the police to interview. Consequently, child protection inquiries could not take place and a social worker visited the home to carry out an initial assessment. The key factor here is that the hospital appeared to have initially made the decision that the incident did not constitute a concern and that it was appropriate to discharge the child without contacting CSC or the police. On subsequent review of the case, a different view, of the need to share information, was given. However, by this late stage the inquiries by the CSC and police had been seriously compromised and could not take place:
I think it could also be people’s different interpretation of a concern really. Because what we have had is two doctors reviewing the child and not find any evidence. The nurse subsequently could have spoken to the safeguarding nurse about it and who has interpreted it slightly differently.
Team manager (LA3)
In summary, where information about risks to children is clear and evidence can be provided, information can be appropriately shared and co-ordinated responses developed between hospitals, CSC and the police. In these circumstances, unambiguous evidence provided by the health professionals is central to subsequent action. However, such evidence is often not so clear and making decisions is less straightforward. In some instances, there are different interpretations as to what constitutes risks to children. These findings reflect previous research,68 but what is interesting here is that differences of opinion and interpretation can continue to take place even in a hospital setting in which sharing concerns both is encouraged and can be carried out by all staff through different communication trajectories. System design can improve situated sense-making, but it cannot eradicate the intrinsic slipperiness of the knowledge about the families and children seen, often very fleetingly, in hospital sites, nor can it neutralise the emotional and moral nature of the decision to probe in order to ‘know’ what does not actually ‘show’. As will be discussed in due course, however, systems and cultures can support reasoned professional debate and discussion about these recalcitrant problems heightening mindfulness and reflexivity.
Concerns about child development and welfare
Hospital staff are also likely to observe less acute concerns regarding children’s health and development and their families’ welfare. These tend to relate to observations of parenting, child–parent interaction or neglect while the children are in hospital, or attendances at hospital associated with their parents’ domestic violence, depression, or drug and alcohol abuse. Platt177 notes referrals of ‘child concern’: ‘there was a general level of concern but not specific harm to the child’ (p. 11). He notes the need for the social worker to be able to develop a ‘broader understanding of the context, especially regarding parental accountability’. However, such information is not always clear, and what might be seen as a concern can be open to different interpretations by different staff.
What do you mean by ‘home conditions’ and then it’s about one person’s perception, isn’t it. So what we tend to do is ring school or nursery or the health visitor and say ‘have you been in lately, have you got any concerns’, sometimes health come back and say ‘it’s always been a bit untidy but we’re not over concerned about it’, so then we’d say ‘well will you monitor it and come back to us’. Then if we’ve got say a 2-and-a-half-year-old, health visitor’s stopped going in a long time ago, we’d have to go out, and actually it’s a little bit cluttered, not enough for us to be involved and that would have helped to have had that on the form.
Team manager (LA1)
A CSC team manager described contrasting interpretations of concern of parental neglect between the A&E department and the children’s ward:
They’re young parents. There is a young newborn baby that was admitted to hospital with bronchiolitis, admitted through accident and emergency but the parent hadn’t brought any milk and any nappies and that was raising concern. The child was transferred to a neighbouring hospital [who] contacted us and basically was asking around discharge of the child as safe and well . . . but given the concerns from [the first hospital] they wanted some advice . . . [Their] view was that the care of the child on the ward had been good and also in an emergency situation a parent doesn’t always think to take nappies and a bottle to hospital. So I think you’ve got a contrast there in terms of escalation of concern.
Team manager (LA3)
There were particular concerns about referrals from the ambulance service:
. . . certainly the ones that you get from the ambulance who go ‘OK, well, you know, she was a bit angry and the house is a bit scruffy’ and you’re kind of left. Obviously, you know, they’ve got a particular job to do but . . .
Team manager (LA2)
The big improvement is, the biggie for me would be the ambulance crew about putting some more meat on the bones. The actual hospital isn’t bad and if it’s not on, we can check it out with [safeguarding] team.
Team manager (LA1)
The big advantage of referrals from the hospitals is that if information is not clear, the children’s safeguarding team in the hospital is able to make contact with the referring hospital professional; they provided ‘quality control at their end’ (LA2). These experiences of referrals from ambulances remind us that CSC receive referrals from multiple agencies, most notably the police reporting incidents of domestic abuse. Thus, information sharing forms from the hospitals enter a competitive space where demand for a service or response always outstrips organisational capacity.
Having a conversation
Chapter 4 noted the importance of ‘relationships’ and ‘conversations’, and this was stressed by both CSC and the hospital-based staff, but organisational structures often disrupt both of these. For health professionals who are well known to the CSC duty and assessment team, it is possible to ‘have a conversation’ (LA2) so that there can be an exchange of information before a formal referral is made.
Some health professionals are not quite sure and we don’t mind that, we promote that, ‘if you’re not sure, ring us’, and they’ll just say ‘can I run this by you, what do you think’ and then we might say ‘it’s not really for us’ . . . If you can have that two-way conversation then it’s loads better. We are very clear, you speak to a qualified worker straightaway, let’s get the concerns down, not three or four times telling your story and you’re fed up or it’s been filtered down.
Team manager (LA1)
Where there is a social work team in the hospital, there are also opportunities for early conversations, with the formal referral then following the prescribed procedures (LA4).
That happens – we have those discussions. I have my discussions with the safeguarding nurses here, the lead safeguarding nurses. The same with [other hospitals] – they would give me a ring and say ‘we’ve got this, what do you think?’ and I’ll say ‘it doesn’t sound right to me . . . we’ll pick up on that’.
Team manager (LA4)
However, such a conversation relies on familiarity between the CSC team managers and referrers from the hospital, which is less likely to happen in large local authorities where referrals are via call centres and can be disrupted by reorganisations in both health and social care, as this designated nurse describes:
What worries me is, for me, that children from [local hospital], when they need inpatients, now have to go [hospital] or [hospital], that is not obviously a choice of [the trust], that’s a consequence of Making it Better (national initiative). What worries me is that they won’t have the relationships with social care in [local area] if a child’s in [the other hospitals]. I’m confident that they can fill the form in, I’m confident that they can do the referral, but I’m less confident that they have those personal relationships, which so much depends on actually, you know, the ward sister picks the phone up and she’s been the ward sister in [local hospital] for donkey’s, she picks the phone up and she has credibility because they know her. And you lose that I think because the services are no longer local.
Designated nurse (DN1)
The problematics of consent
Throughout these exchanges of information between CSC and health professionals, families were often unaware of what was happening. Professionals involved in completing a referral are expected to inform parents and carers that they have concerns and that they will be sending information to CSC. This requires skilful handling and is likely to make staff hesitate, especially if concerns are unclear. Where risks are unambiguous and require medical examination, processes are explicit. If, however, staff are referring concerns after the contact with the hospital has finished, such consent to share is unlikely to have taken place. This can cause problems for the visiting social worker, although often families are understanding:
But that’s what we do, you know, we’re very clear in saying, and we’re open and honest, we work in an open and honest way, we’ll say ‘we know the ambulance crew came out the other day and they raised a few concerns’ and then 9 times out of 10 families say ‘come in’, it’s not a concern and 9 times out of 10, they just need signposting or they need some advice and then there is the odd occasion where you think, goodness me these children shouldn’t be here and it needs quite a lot of work to get this right.
Team manager (LA1)
At the same time, checks by the social workers involving contacting the school or health visitor to help decide whether or not to accept as a referral and start an initial assessment should also take place with the families’ consent.
It’s best to have consent to check with schools and we usually get parental permission, can we check the school, can we check with health, but if we haven’t got that consent because we haven’t been out, then we need to have some informed information before we go out and on child protection, sometimes we have to do that without consent, because we have to look at protecting children.
Team manager (LA1)
To share or not to share? Signal and noise
The previous chapter noted that referral to CSC is one major way in which hospitals self-consciously manage risk to the child and also their own institutional accountability. It is a continual tension when designing systems to encourage referral without creating a ‘referring culture’ of ‘gatecrashing’ the local authorities’ attempts to ‘gatekeep’. Messages are intrinsically contradictory. CSC expected hospitals to provide them with information on risks and concerns about children in order for them to make inquiries and assessments; however, CSC also expected hospital staff to make a judgement about what is an appropriate case to refer and to make clear the reasons for the concerns.
We have to be able to expect hospitals to use some judgement. I don’t think they should be sending everything wanting children’s services to make a judgement about it. Not everything is a safeguarding issue. Children do have accidents. It’s about the circumstances of that, if they’ve been climbing out of a window a storey up then there are potential issues with that. It’s about making judgements and balancing, you know, putting things into a context.
Team manager (LA3)
There was a concern that, on occasion, sending a referral to CSC was seen as offloading a personal worry rather than a considered, professional act:
I’ve done my bit, you know, I passed it over to you, and we still get a lot of that, not necessarily much from [this hospital] but medical professionals, health professionals and indeed education professionals, certain times of the year, you know, I give it to you so I’ve done my bit, I can sleep easy now.
Team manager (LA2)
At the same time, CSC generally express a preference to have information rather than not, particularly if there have been previous concerns:
Yes, yeah absolutely . . . I’d rather that information was sent forward and then we can consider that in some respects, because it does inform. You know we wouldn’t know if a child who we’re currently working with has been admitted to hospital, that is a piece of information that is missing.
Team manager (LA3)
We would never say ‘this isn’t for us’ or ‘this is a waste of time’, never because even if it is, you might think well why would you send this . . . it’s still a piece in the jigsaw for us, so we would still record that information, you never know what else we might have or what may come in, or it might be linked to a sibling or another family member and it’s a piece to a jigsaw for us, so we’re not bothered what we get.
Team manager (LA1)
Well I think all the information’s useful, isn’t it?
Team manager (LA2)
It could be that this is seen as a confusing message, especially for staff new to referral systems – do not send us all your concerns but we do like to have information even if it is not serious enough for us to act on. Where demand is high, the systemic effects can be profound. The following case study describes in more detail day-to-day practice in one children’s services setting where there is a particularly high referral rate.
Gatekeeping and gatecrashing: initial decision-making in a high-demand environment
Local authority 4 is a large urban local authority. All contacts and referrals from other agencies or the public are managed by a central contact centre, as described above, with a central social work team (which we refer to with the pseudonym ‘first contact team’ or FCT) assessing the referral. For cases where assessment by a social worker is not warranted, the FCT might recommend that a health visitor or school nurse carry out a CAF. This is an assessment of the needs of the child and family where the worker considers whether or not their service can offer appropriate help, or if an intervention from a different service is needed. The FCT can also point the referrer towards the other family support services provided by the local authority and voluntary organisations; its mission statement talks of ‘providing reassurance, advice, signposting and guidance and support’. However, given its size, this is not possible on the basis of informal contacts. More often, health professionals can have informal conversations with the hospital social work team, particularly via the safeguarding nurses. The FCT also deals with all general inquires; for example, professionals trying to find out if a family is known to CSC. Consequently, there are a large number of contacts managed by the team, around 200–300 per day.
The FCT is located in a large local authority building near the centre of the city. It is an open-plan office with most staff ‘hot-desking’, but this team has a designated area. There are eight social workers and managers in the team, with four staff managing the work in the ‘inbox’ at any one time. Most referrals from hospitals come either as a secure e-mail or, more often, by fax. For a fax, the referral has be converted into a portable document format (PDF) file to be saved on the CSC system, and as the contents of the PDF file cannot be copied and pasted, the details of the referral have to be retyped into the CSC system. Hospital staff use a short referral form, which asks for basic information about the child, family and referrer. It is much less detailed than the CAF, where the emphasis is on the child’s needs and the provision of evidence. Instead, this form asks about the ‘cause of concern’, which first appeared in the information referral and tracking initiative in 2004, predating the development of the CAF. The distinction between ‘concern’ and ‘need’ has been criticised as a basis for information sharing, as the former is seen as the professionals’ reaction to the circumstances rather than a professional’s assessment of the child’s needs. 178 There is no direct question regarding why a social work assessment is required.
When examining the inbox, the FCT social worker cannot see who has sent the form until it has been opened. They open the referral form and assess the content. Sometimes they are hand written and hard to read. Furthermore, the referrer might have had little contact with the child and family, so the form is often inappropriately completed and has significant details missing. The following extracts are samples of referrals from health settings received by this team on the morning of our observations and are taken from the field notes of the researcher based on conversations with the team manager and the interview transcript.
A midwife from a hospital refers a case of a mother who arrives at hospital unbooked, having received no antenatal care and without baby clothes or nappies. She is concerned whether this is an appropriate environment for the baby to return to home. She has only known the patient for 3 hours. The family speak little English. The FCT manager searches social services records but with little information to identify the family, she has no way of tracing previous concerns.
Referral 1
The main task is to decide whether or not the concerns expressed by the referrer constitute an appropriate referral to CSC. The FCT worker is able to access his or her own records to see if there has been a previous referral or work completed by CSC. However, he or she is unable to contact other professionals without consent from the parents. In this case, therefore, there is not enough information or enough of a concern for the FCT to begin initial inquiries.
Sometimes the decision-making is straightforward, particularly when the medical evidence of an injury to the child is unequivocal. The team immediately pass on the concern for a strategy discussion. Similarly, if the social care need is clear, a decision to complete a child in need assessment is made.
So [the mother] is saying, ‘I’m 5 months pregnant. My two previous children were removed from my care. I’m worried you’re going to take this one. My circumstances are changed. The baby of the father is different. I’m single, I’m at college, things are going fine. I’m rebuilding my life. I want to keep my baby’. So we say, ‘OK, that’s beautiful’. It’s fairly straightforward. We’re going to do something here. We’re going to assess this with an open mind.
Referral 2 (from a health visitor)
Often, however, the FCT worker does not accept that the referrer’s concerns clearly demonstrate that the needs of the child meet the criteria for a social worker assessment. The evidence of the child’s and the family’s needs is clear, but the FCT does not consider that a CSC intervention is appropriate. A particular example is children and young people who attempt suicide.
The example in there was [a child who’s] a bit low, he’s depressed, obviously something’s not right for him. His parents are really supportive. He keeps walking along the train tracks. So then he tries to harm himself. So what he needs is some therapeutic intervention. What he doesn’t need is a statutory social worker, ‘cause they actually don’t do therapeutic work.
Referral 3
Often, the evidence at the early stages of referral is contested, with different views about what is considered appropriate for CSC intervention.
This is a referral from a primary health-care practice about mother’s ability to parent her child. It states that the mother is known to social services, is pregnant, and is suffering from depression. The referral states: ‘I have limited knowledge. I’ve only seen mother and daughter once. Parent mum engaged relatively well during consultation and mum seems attentive to daughter’s needs’. The health professional has however made the referral without the mother’s knowledge and only decided to do so after subsequent discussion with colleagues. The FCT manager is frustrated by the lack of detail and consent. A search of the CSC record reveals that the previous contact was an information sharing request from the police with no concerns about the child’s needs. The FCT manager decides that she will take no further action and reports this decision back to the health-care professional. She is particularly critical of the lack of detail in the referral which might identify appropriate concerns, for example was there something about the mother’s interaction with the child.
Referral 4
There are a number of dilemmas here. First, the FCT manager considers that the concerns should constitute a threat to the child for them to take the case further. There is some exasperation that the referral is unclear. CSC is a statutory service, which must observe the requirements of the 1989 Children Act19 before becoming involved. Second, a health professional who has had only short-term involvement with a family has had little opportunity to carry out initial exploratory work with the mother, and has not sought her consent to make a referral to the CSC, even though this is an expectation of the policy. If the concerns are not about an immediate risk to a child (thereby constituting section 47 inquiries), the CSC is not able to contact other agencies to ask for any appropriate information they might have on the child without the parents’ consent. The FCT manager sees this as a serious matter.
She hasn’t got any consent for this, so we have to bear that in mind, ‘cause we’re not going to breach the mother’s human rights to actually be told that people are concerned about her and make an approach to social care. It’s a basic requirement.
Team manager (FCT)
This now displays a more general problem: who takes responsibility for assessing a child’s needs and identifying an intervention for those situations which are not seen as appropriate for CSC? There are a wide range of potential interventions available in terms of early help, but it is not clear whose responsibility it is to identify and mobilise such services. This is a particular problem for hospital staff who might have brief or short-term contact with children. As noted in the previous chapter, they are less likely to be able to carry out the work needed to gather sufficient evidence about a child’s needs to inform an appropriate intervention, although this is an expectation of LCSB policy. This pressure on CSC to take responsibility for assessing a wide range of concerns, which are not seen as requiring a social work intervention, can create tensions.
Instead of just reacting and referring it, actually, have you done any work with the family? . . . That’s a real pressure for me and it’s always the same hospitals that are creating that pressure. Although [the new LCSB policy] has come in, they actually don’t agree with it. You can tell they don’t, ‘cause they have that approach. So there’s a real conflict developed there where I’m trying to manage that because it’s very important we work well with our partners. I do want them to refer some things to us, but I need them to understand that – and you’ll find that tension.
Team manager (FCT)
Concerns displayed in a referral do not necessarily speak for themselves; moving information between different professionals and agencies requires a translation process, as highlighted in this chapter’s introduction. One option for the hospital professional is to pass on the concerns to primary health professionals, the health visitor, school nurse or midwife, who can have ongoing contact with the child. In this capacity, they could carry out a CAF and develop a lead professional/’team around the child’ process. However, this interface is not always straightforward and lines of accountability are blurred.
A referral was received from a hospital regarding a mother who had attended A&E following an assault and was abusive to the staff. The FCT contacted the health visitor and found that the family were well known. The FCT considered that some work was needed to find out more about the child’s needs and considered that the most appropriate action was the completion of a CAF by the health visitor. However the health visitor did not consider that the child was in need and therefore did not want to do a CAF.
Referral 5
Examples of information and opinion moving back and forth between the hospital and the FCT were provided. Just as information does not speak for itself, so it keeps changing. It needs to be talked up to have the required impact. As discussed in Chapter 4, information flows within and between agencies, and professionals in child welfare are often seen as ‘building a picture’, adding together pieces of information like a ‘jigsaw’. It was noted that this is complex process: the pieces of jigsaw need to be assessed, and finding the full picture is not clear. For the FCT in discussions with health referrers, the negotiation process can also mean that the ‘pieces of the jigsaw’ change shape. As the referral is passed back to the referrer for more information or the referrer puts pressure on the FCT to reconsider their decision, new information is added or old information is reformulated. This phenomenon may be exacerbated by the clearly ‘informational’ and ‘categorical’ role of this team, which does not assess or intervene itself. It does not have to anticipate an encounter with a family or think about what the worker might need to say or do. It is oriented to screening contacts in or, more usually, out of a highly pressured CSC service.
Conclusion
There’s a lot of conflict at the front door.
Team manager
Health and social care professionals are committed to promoting the safety and well-being of children and families. They are also committed to interagency working through sharing information and collaborative interventions. Much effort is exerted in establishing structures and protocols to this end. However, there are a wide range of factors which get in the way. There are different professional perspectives and working practices, organisational structures, and high levels of anxiety and pressure. We have seen how information is changed as it crosses organisational boundaries and, especially where there is a reliance on ICTs, the nature of information exchange has been changed. Lash179 notes the difference between narrative and information:
Unlike narrative, information compresses beginning, middle and end into a present immediacy of a ‘now-here’. Unlike discourse information does not need legitimating arguments, does not take the form of propositional utterance, but works an immediate communicational violence.
p. x
Aas171 notes how the database ‘stacks’ bits of information without providing any commentary on their relative importance and comparability. The order is created by the user. In our data, the CSC gather together a wide range of information from various professionals and have to create a ‘meta-narrative’, but one which fits their own organisational imperatives and actions. While the network of welfare professionals may eventually meet and debate these differences to produce joint action, the majority of cases do not progress that far. There are often misunderstandings of the relative roles and responsibilities of each agency, despite many attempts at joint policies, procedures and protocols. However, there was a striking difference between different local authorities: some CSC see all information on children as relevant (‘we would never say “this is not for us” ’), in contrast to the view that CSC should receive only information which requires ‘a statutory agency, interfering in this family’s life’. The existence of these two potential orientations suggests a need for dialogue and explicit articulation of these standpoints in multiagency training and in discussions within LSCBs. Evidence from innovations within our sites strongly and unsurprisingly suggests that multiagency practice forums, feedback on referrals through a live quality assurance process and multiagency audits in the spirit of organisational learning and within ‘just cultures’ are productive. 9
Chapter 6 The safeguarding package: design and evaluation
The clinical context: Pennine Acute Hospitals Trust
The PAHT provides general and specialist hospital treatment to a population of 800,000 in North East Greater Manchester. The trust is in a process of reconfiguration under the ‘Making it Better’ national initiative,180 focusing on inpatient services for women and children. Despite the existence of clear guidelines, clinical practice regarding child protection varies across the trust sites. In response to this, the PSF approach has being redesigned by the Pennine Acute Safeguarding Children Group and applied to promoting and safeguarding the welfare of children. The aim has been to develop a package of safeguarding artefacts. The project has been led by a senior clinical manager, the Head of Safeguarding, and the design philosophy combines ‘bottom up energy with top down support’, which has been shown to be effective in promoting cultural change (p. 11). 12 The intended outcome is to create a positive safety culture, characterised by openness, justice and learning, where learning from error is regarded as the norm. 13,142
General principles: clinician-led design
The design of the Pennine package has followed a clinician-led approach, with the Head of Safeguarding taking the lead. The general approach followed the broad principles of the SPRINT design methodology, developed by one of the investigators (see Appendix 1 for an overview of SPRINT). As a senior manager, the project exemplifies the importance of managers seeing ‘system design’ as their primary task. This is consistent with current thinking about the managerial role and the importance of managers adopting a ‘design attitude’. Wastell17 argues that managers should see their primary task as ‘systems design’, with the term system denoting ‘the work system’, defined as ‘a system in which human participants and machines perform work using information, technology, and other resources to produce specific products and/or services’ (p. 10). The ‘design attitude’ enjoins a different relationship with technology. Design-minded managers concern themselves not simply with the implementation of technological innovations spawned elsewhere, but with the potential of technology to configure the workplace optimally for service performance and delivery.
The importance of the design attitude at all levels in the management of social care in the times ahead is underscored in the final report of the Munro181 review. Quoting at length from Chapter 7:
Managers have to satisfy the needs of both today and tomorrow. They provide day-to-day management of child protection services. But they also exercise leadership to challenge and bring about change and improvement focused on securing a better future . . . Leadership is much more than the authority of key figureheads. Leadership should be valued and encouraged at all levels . . . It is essential that local leaders fundamentally consider if their service is configured optimally to meet the needs of children and families. Changes will inevitably need to be made and it should be kept continually under review
pp. 106–7 (The Munro Review of Child Protection: Final Report, Crown Copyright 2001, licensed under the Open Government Licence v3.0)
Munro’s final report extols the virtues of good design and cites several examples of what can be achieved when the shackles are loosed of the ‘electronic iron cage’, giving mangers the freedom to develop ‘work systems’ based on local conditions and methods of work, systems which emphasise professional autonomy within a flexible framework of recording and time scales.
To illustrate clinician-led design in action, we use the example of the special circumstances form (SCF) used by community midwives to indicate any concerns they have about expectant mothers. Many of the artefacts in the Pennine package had been substantially designed before the present investigation got under way as a result of delays in approval processes. The SCF was a late addition to the package; it is an electronic version of a yellow paper form then in use, and will be designated eSCF. The design aims for the eSCF were to improve the quality of recording by incorporating principles associated with earlier innovations in information sharing detailed below, and to improve the sharing across organisational boundaries. Typically in the past, the form had been deposited in the patients’ notes but had gone no further afield. A further intention was to raise the threshold for generating forms, as there was a widespread concern that too many were being produced. A ‘drop in the number of forms going forward’ was thus an explicit objective (Pennine Board Report, April 2013, unpublished).
The later phases of the design of the eSCF took place during the research, as well as its implementation. The design of the form was led by the Head of Safeguarding, working very closely with users. So-called ‘table-top’ design meetings were an integral part of the process. At these meetings, a prototype version of the form would be shown to users, and feedback gained from them; other issues regarding the use of the form would also be discussed. Implementation of the form was planned for spring 2013, and a table-top meeting had been convened to demonstrate the final version of the form itself, and the instruction manual. The meeting is described in detail in Appendix 6.
The meeting was held to discuss the following key issues. One important advantage of an online system would be to simplify the logistics of the forms being incorporated into the patients’ hospital notes. For the paper form, this would require the midwife to take the form to the relevant hospital, filing it by hand in the notes. Having an online form would render this journey unnecessary as the hospital staff could do the filing; however, there were concerns that this would not be done reliably enough, given the competing pressures on hospital staff. The second purpose of the meeting was to review and revise the criteria that triggered the production of these forms; a traffic-light system had been proposed, with three levels of severity: red, amber and green (RAG). If the level of concern is judged to be relatively low (green), this should lead to the completion not of a form but just of an entry in the notes.
As noted, a full account of the context for the meeting and a sketch of the meeting itself (reconstructed as closely as possible from field notes) is presented in Appendix 6. Here, we extract some key quotes and provide the gist of the discussion. The following quote, from contemporaneous interviews, shows how indiscriminate the use of the forms had become:
At one time when we started off . . . if someone had a yellow form in their notes it was a big you know, big deal . . . But now it’s almost become a bit of a sort of standing joke in midwifery that ‘Oh what, she hasn’t got a yellow form?’
Specialist midwife (MW6)
I think we’re getting into the realm of erring on side of caution all the time and we are doing them all the time for everybody and that’s my real issue.
Community midwife, team leader (MW6)
A lot of the people who . . . are doing it with good intention . . . But in that process we have lost our capacity to actually see what’s in front of us a little bit. It just feels like the triumph of protocol over common sense.
Specialist midwife (MW6), emphasis added
The meeting itself lasted approximately 2 hours, and involved extensive discussions about the mechanisms for lodging the eSCF in the patients’ notes, leaving two realistic options to be explored further: the midwife continuing to do the job, or it being delegated to the ward-clerk because it was judged that hospital midwives were too busy. The discussion of RAG was also focused and constructive, leading to satisfactory outcomes in terms of defining thresholds, in particular identifying cases of low levels of concern which presently would trigger a form, but in the future should not. Other noteworthy points include the stifling effect of information governance on innovation in the form of a stricture, deemed ‘nonsensical’ by the participants at the meeting, on the sharing of midwifery records with other clinical staff directly involved with the patient’s care. Another point was a mundane but very valuable property of the paper form, namely its yellow colour. This meant that the form would stand out, wherever it was placed in the notes. The printed version of the online form would necessarily be white, which meant careful manual insertion in the notes was even more important to ensure that the form was clearly visible on the top of the file, in the hope that it would remain there, ready for the woman’s admission.
Overview of the Pennine package
The Pennine safeguarding package consists of three modules, each composed of one or more components, addressing different elements of safety culture (Table 4). The various components will now be briefly described.
| Module | Cultural emphasis | Components |
|---|---|---|
| Governance | Promoting board-to-ward communication and feedback | Walkround |
| Electronic reporting | Promoting a reporting culture | SBAR information sharing form |
| Quality control (co-mentoring) | ||
| SCF | ||
| Storytelling | Safeguarding awareness and the sharing of professional knowledge | Case discussions |
| Digital stories |
Walkrounds
To promote an open culture when discussing safety issues and incidents, PSF advocates the use of ‘walkrounds’ by senior staff. This has been adapted by PAHT directly to address safeguarding issues, with the aim of achieving a ‘board-to-ward’, ‘ward-to-board’ governance loop. 118,182
The original walkround protocol consisted of a list of 24 questions. Each quarter, the results of the walkrounds carried out during that period is analysed. Appendix 3 shows the original list of questions, plus a summary of the results for the second quarter of 2012. For each issue identified, the safeguarding team carry out an analysis which is briefly summarised in a third column of the form (not shown), and any relevant actions are indicated. For example, for the protocol question, ‘Can you describe what you would do if you had evidence to suggest a colleague was involved in abusing patients?’, the analysis commented as follows: ‘one person said that they did not know what they would do which is concerning’, and the following action was identified ‘Action: reiterate the need to raise concerns about colleagues in the level 3 safeguarding training’. The quarterly report reviews progress on all actions arising from the previous report.
As a critical element in board-to-ward communication and feedback, the protocol for the walkrounds is kept under regular review to ensure its ongoing relevance to current safeguarding priorities. For example, in 2013, in the wake of the Rochdale and Oldham cases, there was particular concern in the trust about the level of confidence of staff in relation to child sexual exploitation, and the walkround protocol had been adapted to reflect this. This facilitated a detailed discussion at the trust board in the last quarter of the year, which completed the ward-to-board, board-to-ward feedback.
Electronic reporting
The effectiveness of staff in recognising and reporting potential safeguarding risks accurately and promptly to relevant professionals from other organisations, disciplines and agencies is crucial in ensuring effective safeguarding. PAHT had traditionally used a paper system for sharing information across professional and organisational boundaries, known generally as a ‘Cause for Concern’ (CFC) form. However, the effectiveness with which the form was used was a matter of concern, in particular, the thoroughness in recording key information and the lack of clarity regarding the action which was being sought from the recipient by the sender. With the twin aims of expediting communication and improving the quality of referrals, a web-based reporting tool had been designed, largely in advance of the start of the present research, though some refinements were carried out over the early months of our work. This is based on a bespoke adaptation of the NHS ‘Situation, Background, Assessment and Recommendation’ (SBAR) patient safety tool, which provides a memorable mechanism for framing conversations, enabling clarification of what information needs to be communicated and fostering a culture of patient safety. The tool consists of standardised prompt questions within four sections, to ensure that staff are sharing concise and focused information in an accessible narrative form (Box 1).
I am . . .
I am calling about . . . child’s name/family names/adult’s name.
The reason I am calling is . . . child was brought to department today at . . ., etc.
I have assessed the child . . . what investigations have taken place.
B: BACKGROUNDThe child’s demeanour is . . .
The child is accompanied by . . .
Their demeanour is . . .
The social circumstances known to me are . . .
The child’s parents are . . .
The child’s siblings are . . .
Other people in the household are . . .
A: ASSESSMENTChild’s developmental needs: the injury/reason for admission, the cause of complaint/mechanism of the injury, how the history fits the presentation.
Parenting capacity: explanation given to parents, parents’ reaction, parent–child interaction, parents’ comprehension of situation.
Family and environmental factors: safety of home environment, security of environment, issues regarding others sharing home environment.
My concern is: child is/may be at risk or likely to be at risk of significant harm, child is in need, parent(s) require support, advice, help . . .
R: RECOMMENDATIONThis requires further investigation under section 47 of the Children Act 1989. 19
This requires immediate intervention while child is in the department.
The child will be discharged and requires follow-up in the community.
This is for information-sharing purposes only – no action is requested.
The adapted form is designed to promote referrals that clearly express what is expected of the recipient and the level of concern. It is designed to help the sender make explicit what they have observed or heard, and its context, and also to clarify their communicative intent in the form of a recommendation.
The information sharing/safeguarding children referral form, as the full form is known, is described in detail in Appendix 4, which presents the user manual. As a convenient shorthand, we will often refer to the full form simply as the ‘SBAR’. Figure 6 shows a simple completed example of the SBAR section of the form, and a redacted example of the full form is shown in Appendix 5. As described above, an electronic version of the SCF has also been developed, based on the design of the SBAR (for a redacted example, see Appendix 7).
FIGURE 6.
Example of SBAR section of the electronic reporting tool. GCS, Glasgow Coma Scale.

In order to monitor the quality and improve the standards of referral, a quality control system is vital. PSF’s co-mentoring methodology had been adapted to provide this. Co-mentoring has been implemented in EDs; led by specialist band 7 practitioners, it focuses on practice with a view to providing feedback to build trust, raise awareness, and enhance the timely sharing of information. 183 Auditing of records, as the PSF recommends, is part of this, providing feedback when standards are not met.
Storytelling: learning, mindfulness and knowledge sharing
As Weick119 has argued, storytelling is an important device for fostering safety in organisations where reliability, i.e. the avoidance of failure, is the paramount concern. In such circumstance, opportunities for learning through trial and error are limited, and substitutes must be sought in the form of imagination, stories, thought experiments, simulations, etc.
Two storytelling devices feature in the Pennine package: case discussions and digital stories.
Case discussions
A whole-systems approach to the analysis of ‘safeguarding incidents’ (serious failures, near misses and less consequential instances of ‘something going wrong’) is integral to the PSF philosophy,12 focusing on latent conditions142 alongside procedural failure. When safeguarding failures occur in the trust, be they diagnostic errors or breakdowns in communication with other professionals and agencies, these failures are analysed, and practitioners and managers are prompted to consider how lessons learned from incidents can best be shared with peers. The results of these deliberations are brought to regular case discussion workshops involving all professional groups, where the aim is to raise awareness and stimulate learning across the trust. The more salient of these cases are written up for formal dissemination.
The framework developed by Pennine for the sharing of ‘Lessons Learned’ is shown in Appendix 12. It emphasises the work of Reason142 on the promotion of ‘learning cultures’ in the NHS, quoting extensively from the report of National Advisory Group on the Safety of Patients in England. 184 The report poses NHS leaders a challenge to ‘create and support the capability for learning, and therefore change, at scale, within the NHS’ (p. 5),184 warning about focusing on the wrong priorities, such as meeting targets and financial priorities. The report goes on: ‘Rules, standards, regulations and enforcement have a place in the pursuit of quality but they pale in potential compared to the power of pervasive and constant learning’ (p. 6) (A Promise to Learn – A Commitment to Act: Improving the Safety of Patients in England,184 Crown Copyright, 2013).
A completed case pro forma is presented in Appendix 12 for a child in whom non-accidental injuries had been missed (child C). Two further cases are presented in Appendix 10, Baby H: suspected fabricated or induced illness (FII), and Appendix 11, ‘Child M: a study of neglect. The ‘Lessons Learned’ bulletin for child C is shown in Appendix 12. The bulletin was published in March 2013 and distributed throughout the trust as part of the mainstream PSF process. Stories and synopses of significant incidents are also routinely presented at meetings including the trust board.
Digital stories
Digital stories are short videos. They are used as tools to disseminate best clinical practice and to illustrate the root causes of critical incidents. Some of the stories are based on case discussions, others prompted by patient complaints, and they are aimed at improving professional communication and helping parents to understand clinical procedures. At the time of writing, two digital stories had been produced and two were in preparation: the scripts of the two completed stories (Natalie’s story and Jake’s story) are compiled in Appendix 14.
The mechanisms for producing digital stories are noteworthy, requiring considerable professional engagement including a fresh approach to handling complaints from patients and families. At PAHT, all complaints that are in any way related to safeguarding concerns are shared with the Head of Safeguarding, who addresses the concerns in the response to the complainant and contribute to meetings. The use of case studies in training is not new. However, the people about whom they are concerned rarely, if ever, know they are used; the studies rely on a trainer’s interpretation of events and do not represent the voice of the parent or the child. The ‘parent story’ initiative began by taking forward concerns that arose from complaints, and presents the voice of the parent directly. It is captured in a way that cannot be altered and has been approved by the parent him- or herself. The use of complaints, even where not upheld, has been successful in impacting on system design in education and training for health professionals. The added benefit is the sense that the complainants’ voices are heard and continue to be heard long after the bureaucratic processes around the complaint are completed.
The two ‘patient stories’ which have been produced during this project have been invited from parents who have made a complaint where the child protection process has been followed correctly, and therefore, their complaint has not been upheld, but who also wished to meet to express their concerns about communication during the process. On both occasions it was acknowledged that professionals had something to learn about how they communicate with parents while complying with child protection policy; the Head of Safeguarding invited the parents – verbally at the meeting, then later in writing – to meet with her so that their ‘story’ could be captured and used in training. More details of PPI in the production of digital stories may be found in Appendix 14.
Evaluation of the Pennine package
The following sections report the evaluation (using a pragmatic mixed-methods approach, combining interview, observational and numerical data) of the various modules of the Pennine safeguarding package, as follows:
-
walkrounds
-
electronic reporting
-
storytelling.
Walkrounds
Walkrounds were, until recently, mainly performed by the staff of the safeguarding team (typically either the Head of Safeguarding or the named nurse) once per site every quarter. Now, the named doctors are taking a more substantial role, as discussed below. Walkrounds are based on the model of the pilot who walks round the plane before it sets off and checks that all systems are in working order. The walkround protocol consists of a set of questions which can be adapted to reflect changing concerns, aimed generally at checking awareness of key safeguarding issues and procedures and at gauging the effectiveness of training:
We’re the safeguarding hub, we will be the people who walk around and see if what we think is working and happening – people know how to access us, people know how to access training, that some of what we’re teaching and training is going in, that we are making some sort of difference to people’s understanding.
Head of Safeguarding (HS1)
Every quarter, the results are consolidated and a thematic analysis performed, and any actions arising from this are noted, planned and implementation subsequently monitored. The following quote gives an example from the adult safeguarding side:
I’d done an audit on the Mental Capacity Act by looking through records at compliance. That audit told us that, yeah, largely, we were compliant. But when we were doing the walkrounds and said to people, ‘How confident are you about that?’, they didn’t seem to know, and there was a lack of confidence. So we’ve developed on a Mental Capacity Act Implementation Group. We would hope to see a better understanding of the Act as a result of that. So you can see how it’s fed through.
Head of Safeguarding (HS1)
Although the original protocol has remained stable for the first couple of years, it has recently been reworked (see Walkrounds) to reflect changing concerns and priorities, including the increasing concern with child sexual exploitation. This illustrates that the national context and media interest can directly affect safeguarding priorities:
The trust board said, ‘How confident are we that people on the ground have a clue about child sexual exploitation?’ So we’ve integrated that kind of question into the walkround. I’m not sure how it’s worded, because it depends on what the – how the conversation’s done. But it would be something like: ‘You’ve heard about all the child sexual exploitation things that’s going on in Rochdale. How confident are you that you’d know what to do?’ It gives us a flavour of how effective our training is; whether the messages that we are trying to get home are getting there.
Head of Safeguarding (HS1)
It is vital that the walkrounds do not degenerate into a box-ticking exercise, a bureaucratic end rather than a means to cultural understanding and change. The questions are ‘meant to be delivered not as a questionnaire but as a guided conversation’. Maintaining this has not always been easy. HS1 describes the behaviours of some of the staff as follows:
I think that if you spoke to [other staff] about the walkrounds, they would be less positive than I am . . . it’s maybe because it’s just another thing for them to have to do. When they reformed the tool they made it so there was tick-box answers and I looked at it and I said, ‘No, no, no, no. We can’t have tick boxes. We need free-flowing conversation and narrative. It’s an aide-mémoire for things you want to cover. That’s all it is’. But it’s work in progress, but we’re still getting good stuff out of it.
Head of Safeguarding (HS1)
Disciplinary boundaries had initially constrained the implementation of walkrounds, with named nurses initially targeting only nurses, and doctors demonstrating more limited engagement. These trends had recently begun to change, and the walkround system was manifestly becoming more embedded in the organisation:
What we found originally was we would automatically target nurses ‘cause we’re nurses – you know . . . the named nurses would go to nurses. But part of the whole developing of the culture stuff has been bringing our main doctors into this system now, and they target doctors. They do walkrounds, as well. So, actually, we’re doing far more than one per site per quarter . . . bringing them on board to take that culture through was never done before. They were just, ‘yes, we’ve got named doctors and they do a bit of training’, and that was it. That has made a massive difference.
Head of Safeguarding (HS1)
Electronic reporting (Situation, Background, Assessment and Recommendation): the trust perspective
As previously noted, we will adopt the shorthand SBAR to refer to the information sharing/safeguarding children referral form, as the full form is known. SBAR was implemented in the second quarter of 2012, and Table 5 shows the number of referrals per quarter since its inception, and the proportion of those which were section 17 or section 47 referrals (Children Act 1989)19 to CSC. It will be noted that the number of SBARs dipped in the first 6 months of 2013, although there is no obvious explanation for this, and the level has since been restored. It is probably the case that seasonal factors were at play over the winter months, but more data will be required to confirm the replicability of this trend.
| Quarterly period | Total SBARs | s17/s47 referrals | Referrals, % |
|---|---|---|---|
| 2012 Q2 | 1015 | 116 | 11.5 |
| 2012 Q3 | 1094 | 98 | 9 |
| 2012 Q4 | 904 | 86 | 9.5 |
| 2013 Q1 | 842 | 126 | 15 |
| 2013 Q2 | 1008 | 125 | 12.4 |
The Head of Safeguarding was interviewed in July 2013 regarding the success of SBAR. She commented favourably on the use of SBAR, although the need to fax referrals to CSC was a continuing concern:
It’s embedded. People use it, they like it . . . nobody’s filling in the pink things by hand any more. It’s not like we have had to prise them out of their sticky mitts, you know, and say, ‘No, we’re not using those any more!’ It’s like, ‘Thank God for that.’ When you press ‘submit’, it goes to where it needs to go to.
Head of Safeguarding (HS1)
Her view of the improvements is corroborated by this consultant paediatrician:
It’s very efficient. You can complete one in less than 5 minutes and you only have to fax it once and that’s to the local authority . . . and it’s automatically e-mailed to the safeguarding team who then distribute it out to primary care. The prompts that they’ve got down the side really help them to decide what to write in each box. And I think that has really helped. Admittedly sometimes you can have information overload but I don’t think we have information overload, I think the right amount of information is shared about appropriate cases. So that’s really helped.
Consultant paediatrician (CP5)
In order to explore satisfaction with the form, and a number of other issues concerned with children’s safeguarding, including staff confidence and satisfaction with training, a staff survey was carried out at the end of the research (November 2013). The pro forma for the survey is shown in Appendix 13. It was conducted electronically using the ‘Survey Monkey’ package (www.surveymonkey.com). The link to the survey was sent to all staff, as there was no means of selecting the target group, but the covering e-mail indicated that only those involved in children’s safeguarding should complete the form. Three hundred and two responses were received. It is difficult to estimate the response rate given the circumstances of the survey, but of the total complement of clinical staff of 3706 (doctors, n = 765; nurses, n = 2523; midwives, n = 418), the Safeguarding Unit estimate that approximately 60% would have seen the survey as relevant to them, and be working during the period that the survey was carried out. This gives a nominal response rate of approximately 14%.
Question 1 asked respondents to identify their professional group, and question 3 directly addressed satisfaction with the SBAR (results are reported below). Questions 2 and 4 addressed training and confidence (results reported in section 6.7). The remaining questions were included to gain qualitative feedback for the Safeguarding Unit on support, anxieties and improvement ideas, and are not reported in this document. On the subject of SBAR, 188 staff members expressed an opinion, and results confirmed that liking for the form was widespread (Table 6). Overall, 74 used the form and considered it well designed, and a further 108 thought it well designed although they did not use it personally, giving a total of 91.5% who considered the form a useful artefact. Nurses tended to be the main users of the form. Only 16 described the form as ‘not useful’; notably, this group largely comprised hospital midwives who generally have less experience of using computers as part of their routine work (this difference was statistically significant: χ2 = 36.5, degrees of freedom = 1; p < 0.0001).
| Staff category | Not useful | Well designed and I use it myself | Do not use it but well designed |
|---|---|---|---|
| Consultant/midgrade doctors (ED and inpatient) | 3 | 9 | 14 |
| Junior doctors (ED, inpatient and locums) | 0 | 5 | 14 |
| Midwives – hospital | 8 | 4 | 0 |
| Midwives – community | 2 | 9 | 1 |
| Nurses (ED, inpatient and outpatient) | 2 | 27 | 25 |
| Other (allied/blank) | 1 | 20 | 54 |
In the view of HS1, the quality of SBAR completions was also improving and is subject to live quality assurances processes, through co-mentoring and review by the safeguarding team (see Quality control of referrals):
The referrals that we get, we’ll look at all of them – we’ll look at all the information sharing and all the referrals and they, on the whole, are appropriate . . . it’s so easy and quick for them. So I think, anecdotally, that the quality of them is improving. It started off well and then it slipped off, but then I think it’s coming back up again now . . . the poor-quality ones, they’ve not really bothered about what goes into situation, background, assessment . . . but at least their recommendation is clear.
Head of Safeguarding (HS1)
An example of the effectiveness of SBAR is provided by one of the cases subjected to systemic incident analysis (see Child M in Appendix 11). HS1 comments on the case as follows in the context of information sharing:
Child M was an example of the effectiveness of our information sharing forms. Child M was in hospital, the nursing staff were concerned that there were elements of neglect. They did an information sharing form for the school health practitioner . . . the named nurse in the community read it and rang me back and said, ‘We’ve seen your concerns; we’ve got really high concerns about this case’ . . . I had a chat with the ward staff, spoke to this particular doctor and I said ‘So why is this child failing to thrive?’ He says, ‘Cause she’s not been fed’. I said, ‘I’m upgrading it, then, to a section 47 referral’. It shot up because our form went to where it went to, and when she got the information and compared it with the information she’d got – you know, it’s all about joining the dots.
Head of Safeguarding (HS1)
The SBAR-based form was shortlisted for the National Patient Safety Awards in 2013 and was highly commended in the Data and Information category.
Quality control of referrals
As noted above, the co-mentoring system in the ED had been instituted with the aim of improving record-keeping in general, and the quality of SBAR referrals in particular. Typically, each morning one of the mentors works their way through a list of cases from the previous 24 hours. All cases of children under the age of 2 years who attended the ED are inspected on the hospital’s electronic patient record system. Several of these sessions were observed; one such session is reconstructed from field notes in Appendix 9. Of the 18 cases reviewed in that session, there were no safeguarding concerns in 10 cases. Medical notes were satisfactory in the majority, and exemplary in some cases (n = 6). Significant deficiencies were noted in three sets of notes regarding social and/or medical histories. In the eight cases exhibiting safeguarding concerns, five had been appropriately handled, but in three cases, SBARs should have been completed because of multiple attendances.
The mentors report the results of their work to the Safeguarding Unit, and the results of their auditing are summarised in Table 7 regarding the quality of case recording since the inception of co-mentoring in April 2012, when SBAR was first introduced. The table shows that missing social histories in the clinical notes is the worst problem, but that quality has generally improved apart from a dip in early part of 2013. Thirty-two per cent of records were judged as good at the start of the scheme; the most recent audit showed this had improved to 52%. Following an initial rise in the number of SBARs, the average of cases leading to a referral has flattened out to around 10%.
| Period | Total | % good record | % missing social history | % missing medical and/or birth history | % illegible | % SBAR completed |
|---|---|---|---|---|---|---|
| April 2012 to May 2012 | 991 | 32 | 49 | 33 | 1 | 2 |
| August 2012 to October 2012 | 540 | 37 | 43 | 33 | < 1 | 12 |
| December 2013 to January 2013 | 444 | 46 | 45 | 29 | 3 | 7 |
| February 2013 to March 2013 | 300 | 34 | 56 | 43 | 1 | 7 |
| July 2013 to August 2013 | 242 | 52 | 32 | 14 | < 1 | 10 |
Other aspects of the co-mentoring scheme had, however, not been as effective as had been hoped. As noted in Chapter 4, the trust has a policy that all children under 1 year with head injury, burns, bleeding or bruising should be referred to paediatrics. However, this protocol was not being followed consistently and it had been hoped that the co-mentoring would remedy this. The trust covers several hospitals, and the system had been implemented in only one of them, to gain a controlled understanding of its impact. The results had been disappointing, but it was felt that locums were to blame:
We expected in [the hospital implementing co-mentoring] there to be a better result, because of the co-mentoring, but there isn’t. But then we found out that the majority of cases where the referrals are not being made are because the locums haven’t made them. [The hospital] was as bad as everybody else, I thought co-mentoring would nail it. But you can’t nail it with the locums because they can’t learn. ‘Cause they’re in and then they’re gone – you know. So it – we’ll see if this has made a difference for the locums.
Head of Safeguarding (HS1)
The ‘problem with locums’ theme is echoed by the following consultant paediatrician, based in A&E:
[T]he co-mentoring project was intended to find the person who hadn’t done it right, talk to them about it but then get the person to rectify it themselves so that next time they had experience of doing it but also knew what to do. With these locum staff the nursing staff can’t do that at all. They have no way of contacting these locum staff other than via their agency . . . It would take them so long to actually track this doctor down that it would be pointless. So I think what they’re doing in that particular case is they are filling in the gap themselves, dealing with whatever didn’t go right, but that doesn’t mean that there’s been any education for the person who didn’t do it right in the first place so that person will continue to make that same mistake all the time.
Consultant paediatrician (CP6)
Moreover, it is not just locums who are difficult to track down; there are also practical difficulties caused by the temporal and bureaucratic ordering of the hospital including shift patterns. 185,186
The co-mentoring scheme uses permanent clinical staff to check the system for missed cases and to have conversations with the relevant clinicians afterwards to embed learning. It is explicitly designed to ameliorate some of the potential problems with using ‘semidetached’ systems, such as the HVL service discussed in Chapter 4. However, in the busy context of A&E this proves a challenge.
It is difficult though because you know, if they’re on day shifts and the doctor who didn’t do something that he was supposed to do is on night shifts they won’t see that doctor on the day shift for 3 weeks potentially because the doctor will be on a week of nights, have a week off and then maybe on a late shift when they’re on earlies. So it may be actually that they can’t give that kind of feedback to the doctor in real time.
Consultant paediatrician (CP6)
The difficulty of tracking down staff and working with them to improve their case recording and referrals also emerged during our fieldwork observations (see Appendix 9), leading mentors to complete referrals themselves. In addition to the disjuncture created by shift patterns, there are interactional challenges. It can be very difficult to question another clinician’s decision-making and record keeping, even when this is an explicit part of one’s role. This is clearly also affected by professional hierarchy and trust. Making challenge a taken-for-granted aspect of everyday work has required a shift in culture:
But I think that in the majority now realise that what is being done is being done for the benefit of the child and that it is not meant as a direct criticism of their clinical care although in reality it is some form of criticism of their care. But it’s intended to be helpful to try and stop them getting in hot water in the future. And I think that’s the way that we need to phrase it and that’s probably what the nursing staff are doing well because nobody’s come to me to complain to say ‘I can’t believe they’re still looking at our notes’.
Consultant paediatrician (CP5)
Situation, Background, Assessment and Recommendation information sharing form: at the receiving end
It is a noteworthy development that the SBAR-based form has been accepted as a multiagency referral by all the local authorities to which PAHT relates. Referrals were audited by the safeguarding team at Pennine for a sample of cases (section 17 and 47 referrals) to CSC for a 1-month period in mid-2013. The aim was to establish the outcome of the referral and the actions it generated distally at the five CSC locations involved. A total of 27 referrals were made that month, the majority coming from the ED (n = 16). The sample size is small, but, disquietingly, one-third of referrals were not received at two of the local authority destinations, and in a further five cases only the telephone referral and not the written referral had been received. For one local authority, this meant that the majority of referrals were more or less defective (five out of nine). One Head of Safeguarding comments on the missing referrals in that local authority, believing their IT system to be culpable:
Now, the thing about [local authority] is – the ICS is so complicated, they can’t find child protection plans, referrals – they can’t find stuff on their own system. So when we’re ringing up and saying, ‘Have you got it?’, and they’re saying, ‘No’. If you said, ‘Go and have a look somewhere else on the system. You might. . .’ And then, a couple of occasions, they’ve said, ‘Oh, wait a minute. I’ve gone into a different screen and found it’. It’s scary. They can’t find it on their own system.
Head of Safeguarding (HS1)
Six of the 27 referrals were followed up in detail by telephone. Results showed that in all cases, CSC felt that the referrals were appropriate, as illustrated by two examples: (1) the referral concerned a domestic incident and the local authority had allocated the case to a social worker for initial assessment; and (2) following the referral in respect of unexplained bruising and neglect, concerns were such that the child had been discharged into foster care.
The redesigned form has been positively received in community health settings where its communicative clarity and structure is valued:
Historically, the doctors would scribble notes on bits of paper . . . actually social care require a reasonable amount of information, don’t they, they can’t do it off scribbly bits of paper . . . From a designated nurse point of view . . . it is actually a good system. I think it’s useful, I do, I do, I think it’s useful and I think it works and I think it’s easy for staff and it gives some consistency, doesn’t it.
Designated nurse, commissioning (DN1)
Observational studies in these community teams confirmed that the SBAR was generally welcomed. Appendix 8, for instance, details the results of a morning’s observation in one of the teams with the designated nurse, responsible for commissioning (DN2). A total of 286 referrals had been received in the 5 months from May to September 2012 from PAHT. Although sometimes there could be confusion about why a referral had been sent to the community team, the benefits of the system were generally appreciated, although very few required an active response:
The system is definitely useful – we do need the information . . . and the referrals have been getting better recently . . . the ones that would lead to something proactive being done are less than 10% – this could be a phone call, home visit or inviting them to come to clinic.
Designated nurse, commissioning (DN2)
For all referrals, a NHS CFC form has to be completed, and it is noteworthy how much ‘information processing work’ is required to complete this form (see Appendix 8), which is simply stapled to the front of the original referral before filing.
Children’s social care managers in our interviews also tended to welcome the new form. Referring to the traditional handwritten referral, one commented:
In essence, it was just some paediatrician’s handwritten notes, you know, like, ‘therefore’ symbols and triangles and all that sort of stuff which, you know, you can decipher if you have been around long enough! So, yeah, so we get the [SBAR], if it’s coming from them to us, we’d open it up, look at it and obviously you start forming hypotheses or thinking what you’ve got to do next.
Team manager (LA2)
There was some particular concern, though, that in some cases the SBAR provided general comments but there was insufficient information to act.
I’m content with those, I suppose the only thing I would say is some of them lack analysis and reason as to why they are concerned. You know, there needs to be a bit more because of this, because of this, they go ‘I am concerned’ rather than, you know –
Team manager (LA1)
I would say is it’s about the analysis of why you’re referring, being clear about what the issues are, ‘the house is a bit scruffy’, ‘I’m a bit worried about the interaction’, what is the evidence, so what evidence have you got to suggest that there is a cause for concern, rather than I’ve got a cause for concern.
Team manager (LA2)
The CSC managers provided examples of SBARs triggering a ‘child in need’ assessment because of the concerns based on the observations of hospital staff. When asked for examples, the CSC team manager replied:
Well loads, absolute loads. I think we only had one on Monday where a mum had turned up at A&E and I think she had a bad shoulder and talked about domestic violence at home, it was an Asian mum, never spoke to anybody before about it, being knocked about by her partner . . . We go out and see mum at school and it’s very evident there’s a real problem in that house. If that person at A&E hadn’t let us know that, that could have gone undetected for a long time . . . we wouldn’t be doing the work with that mum to make her safe and consequently the child.
Team manager (LA1)
The electronic special circumstances form
The eSCF had gone live in April 2013, as planned. All had not been easy but the system was now in place. Lack of computer experience was a factor in this, according to HS1.
It’s taken a lot of education to get community midwives, particularly. It’s not as much part of their culture to complete electronic anything in the community, as it is in a site hospital. Anyway, it’s getting there and we’ll get less and less complaints. When it first came out, they moaned like hell, but they’re getting there now and they’re coming through.
Head of Safeguarding (HS1)
An important aim of the eSCF, it will be recalled, was to reduce the number of referrals. The total number in 2012–13 prior to the implementation of eSCF was 1808, i.e. 452 per quarter. In the first quarter of 2012, directly after implementation, the figure was roughly the same, at 425, but in the second quarter there was a very conspicuous rise to 622. This, at least, is a positive indication that the system is being well used.
Following on from the design meeting, it is interesting to see what was ultimately decided regarding the placement of the forms in the patients’ notes. HS1 reported that ‘they decided that of the two options, they preferred to do it physically. To come to the hospital and to make sure – to do it themselves’. Regarding the RAG system, although the aim had been to reduce referrals, a ‘safety first’ attitude had inhibited this, as the following quote from a community midwife attests:
We do, we err on the safety caution side with amber because if we’ve had ladies that have said there is not an issue with domestic violence but there’s been one in the past we put it into an amber because our group sort of feel that there could potentially be an issue and it’s sort of ensuring that each time we’re seeing them we’re asking the question have we got an issue? So in a sense we do have probably more ambers than green.
Community midwife, team leader (MW8)
The Head of Safeguarding reflected:
The RAG rating hasn’t happened as I wanted it to happen. We wanted it to be if you RAG it as green, don’t do it at all. That was what it was supposed to be, if you have RAGed it as green, you don’t do a special circumstance, you just record it in the notes routinely. But they can’t let go of that . . . It’s like a security blanket. So, that’s OK. At least they’re RAG rating them as green. So the next step in the evolution will be, now you don’t do one for green.
Head of Safeguarding (HS1)
Storytelling: case discussions and digital stories
It will be recalled that the primary aim of the case discussions was to foster a ‘learning culture’. There had been initial problems in accomplishing this, as the following reflections of the Head of Safeguarding attest:
This is about that learning culture. How do we learn from incidents? How do we reflect on them? One of the vehicles for that was the case discussion meetings, which were in place when we started this project. And it started off very successfully, once every 6 weeks, and then gradually people stopped coming . . . We invited people to submit a case . . . We’d have a big meeting room, and doctors like pictures so they’d usually do a presentation which involved looking at photographs, and we’d have a meeting after. And we had a few of those that were really successful, really valuable . . . but then gradually people started to drift off and I don’t really know why.
The first people to drift off were nurses, really quickly. Bang! They were gone. They saw it as a doctors’ forum, I think. Yeah, I had to drag the nurses into the conversation. The doctors would dominate it if you let them, but then the cases that were brought were brought by doctors. The nurses did not offer any. And then, gradually, doctors stopped coming and we’d just have two or three . . . Some paediatricians didn’t like it because we invited junior doctors and they were consultants and they wanted – they didn’t like washing their dirty linen in public, in front of their juniors.
Head of Safeguarding (HS1)
After this faltering start, the named doctors in two of the hospital sites played a key role in reinvigorating the scheme. Clear targets in terms of training and running case discussions have been pivotal, and the two doctors support each other:
Well, we’ve got set objectives based around the role of the named doctor, so we’re looking at how much training they do, how many subgroups they go to, how many meetings they go to . . . just get them doing tasks, really. But they’re already making a big impact. A massive impact. [Dr X] basically does Oldham and Rochdale, and [Dr Y] does Bury and North, here. And they each have a case discussion meeting at each site. And they both go to each. And they’ve taken off completely now. They don’t call it case discussion meetings. They’ve renamed it peer review meetings because that’s medical meeting terminology . . . There’s something about this – about the – jumping onto the culture that exists instead of imposing your own, and that is that doctors prefer to have things led by doctors.
And it’s making a difference to practice, so I can give you two examples where a paediatrician has taken a case that they’ve been unsure about, they’ve got photographs of a bruised ear, for example, and as a result of the peer – they call it peer review. We’ve had at least two occasions where doctors have taken cases to peer review; the peer review have said, ‘We think that is a bruise. That is an inflicted injury. That isn’t accidental’. And on the basis of that and the reflection that’s taken place, the doctor has changed her report to Children’s Social Care. Which can only be a good thing.
Head of Safeguarding (HS1)
Here, an important point is made about using available and familiar vocabularies to introduce new and unfamiliar practices. We return to this point in the conclusion. There was, however, still progress to be made:
We’ve also had a case where the doctor’s refused to change his opinion. He will not change his opinion, even everybody says, ‘You’re wrong’. He says, ‘I’m not changing my opinion. I was there. I saw the child. You didn’t’. We shouldn’t be relying completely on medical opinion, anyway. Those days should be gone since Cleveland, for sure. But a huge amount of weight is still placed on medical opinion. Especially when he’s saying, ‘It’s accidental’, when everybody else is saying, ‘You can’t do that accidentally.’ But, the culture is changing. The culture is you are supported. You can reflect on your practice. You can change your mind. This is not an exact science. It’s OK to say, ‘I’m not sure. I will go and speak to colleagues and then get somewhere else out of it’.
Head of Safeguarding (HS1)
Nonetheless, the Head of Safeguarding’s conclusion was upbeat; the culture change had been enormous despite the faltering beginnings and the need to develop the same culture among the nurses.
So, you know, in terms of a systematic analysis, or a systemic – we’ve changed the system. For me, that is massive and was completely absent. Completely absent. And that has been a big, big cultural change. So in terms of a learning culture, that has . . . developed massively. We’ve got lots to do, though, ‘cause we need to make that happen for nurses.
Head of Safeguarding (HS1)
At the time of writing, two digital stories have been produced in the form of 10-minute video presentations: Aiden’s story and Natalie’s story. The script of Natalie’s story can be found Appendix 14: it describes the experiences of a teenaged mother, the victim of difficult home circumstances, who was treated unsympathetically by hospital staff in contrast to other professionals (the school teenage pregnancy service). Aiden’s story relates the distressing experience of parents suspected of injuring their child, who had a traumatic full skeletal survey as part of the investigation. As a result the parents assisted in the design of a parents’ guide to skeletal surveys. Two further stories are in preparation, including Jake’s story, discussed below in the interview with HS1 (the draft script is presented in Appendix 14). The fourth, Jilani’s story, represents an instance of severe neglect, detected as a result of effective communication between the hospital and community health. The digital story was produced to illustrate the effectiveness of the information sharing forms. The Head of Safeguarding comments on the value of stories which have such favourable outcomes, in contrast to cases which highlight failure and calamity.
We don’t hear enough of what good looks like. We don’t hear enough of ‘this is what works well’. You can’t always learn from mistakes. You have to learn from – that there’s a positive outcome. And the brilliant outcome for this is that this child is doing really, really well. You can see a change in front of your eyes, which you can with neglect, very often. And the doctor who’s seeing her said it’s the most wonderful thing to see, this skinny, underweight, anaemic creature is now this beautiful, thriving child who is in school for the first time in God knows how long.
Head of Safeguarding (HS1)
Despite some initial reluctance, the doctor concerned had agreed to turn the experience into a digital story and found the experience very rewarding: ‘he made the comment about what a positive experience that was, sharing that learning – what he had learned from it’. From the perspective of the Head of Safeguarding, case discussions and digital stories have promoted the growth of a learning culture:
And this – the difference is, is that Aiden, they thought he had a fracture, but when they looked at it again, it was a vitamin D deficiency anomaly, so there wasn’t anything. In this case, this child had a very suspicious bruise on his ear that is very typical of a pinch. And unexplained. All the referrals went through and everything and they are a lovely family and Mum is absolutely – she says, ‘This has absolutely ripped us apart because we feel like we are being accused’. Well, what seems to have – nobody seems to have said, ‘We’re not accusing you. Someone has hurt your child. We’re not saying it’s you’.
Head of Safeguarding (HS1)
At this point in the interview, the Head of Safeguarding (HS1) referred to Jake’s story mentioned above (see also Appendix 14). The story describes the experiences of Jake’s parents after they found a bruise on his ear after returning from nursery. The draft script takes up the story:
We rang the out-of-hours GP service and were told to take him to the local hospital. We went straight to the ward and understood we were bringing Jake to hospital for some tests to check there was no infection on his ear. We were seen by a paediatrician who spent about 10 minutes looking at Jake, hardly said anything, then went away. Next thing we knew was a social worker was there wanting to speak to us. That’s when it felt that our lives were being blown apart.
Jake’s story (draft script)
The way the case had been handled by CSC is the focus of the story. This had caused enormous distress to the parents, and a letter of complaint had been written about the way they had been treated. The digital story tells the story from the point of view of the aggrieved parents. Although a response had been provided to the letter, the parents were not happy with that, and a meeting was arranged with the Head of Safeguarding (HS1). At the meeting the parents spoke of how the stresses of the initial confrontation with social services had distracted them from thinking carefully about the likely real cause of the child’s injury. The mother observed that it had become apparent to her that the injury had probably happened at nursery. The Head of Safeguarding continued in the interview:
[A]nd if they’d managed to step away from feeling like they were accused for a minute, then they might have been able to see that, but nobody had said to them anything that helped them to get to that other place. And also, when social work came round, she said they said, ‘First of all, we might have to take all three of your children into care’. They’d been mulling it over, when they started thinking about it, her friend had a child with a bruised ear and the friend – who went to the same nursery, and the friend just said, ‘I just thought he must have banged it on the radiator’.
Head of Safeguarding (HS1)
Shortly after the original incident, Jake exhibited another injury:
[W]hen they picked him up from nursery, he had a big, red patch on his face and they said he’d banged his face . . . they’d said to nursery, ‘Did you put the fact that he’d banged his face in your accident book?’ And they said, ‘No, because we thought it was eczema’. And so she [the mother] said, ‘You didn’t think it was eczema. You told me he’d banged his face’. So then all the doubts come – she pulled him out of nursery straight away after that. But it was only after complaining and talking to us that they thought, ‘Hang on a minute. Nobody’s got to the bottom of this’.
Head of Safeguarding (HS1)
The Head of Safeguarding commented on the lessons to be learned, highlighted in the digital story, told from the parents’ perspective:
[W]e give parents the real strong impression that ‘the only people we’re looking at in all this is you. It’s either you or nobody else’. And we need to learn to do that differently.
Head of Safeguarding (HS1)
Above all, the parents highlighted how terrifying the whole experience had been:
‘Put yourself in our shoes. How would you want to feel? You know, you’d want to know what’s happening next.’ She described this horrible feeling of being in their house for 2 weeks, dreading a telephone call and dreading people coming round, ‘cause they had no idea what was going to happen. Tell us it straight. Tell us what’s going to happen very clearly. Don’t leave us in the dark.
Head of Safeguarding (HS1)
The trust do have a leaflet which explains what can be expected after a referral to CSC, but this had not been given to the parents:
I gave that to them and said, ‘If you’d been given that, would it have made a difference?’ And they said at the meeting, ‘No, it’s very legal. It’s very formal and it’s not very parent-friendly’. So they’re going to rewrite a leaflet with me. A parent-written, ‘this is what will happen to you’, kind of thing. So that’s positive, isn’t it?
Head of Safeguarding (HS1)
Digital stories have enabled safeguarding training in the trust to be delivered more efficiently and effectively. They are used concisely to illustrate safeguarding in action and its effects and to stimulate debate. Digital stories also help to carry the patient experience to the trust board, where they are presented and discussed.
Technology transfer and adoption of the package
One aim of the study was the transfer of the Pennine package to our two other sites. Because of various delays, internally at the sites and in the research approval process, this has not occurred, despite considerable enthusiasm for elements of the package, the SBAR in particular. Another aim of the research was to examine innovations in those other sites to see how these could enhance the package. The Head of Safeguarding at site 2 looked forward to an electronic referring system based on SBAR which it was hoped would both improve the quality of the referrals and stimulate a more analytical engagement with the presenting case. Quality of referrals had been identified as an issue in recent inspections:
Well we definitely wanted it and you know there was a lot of enthusiasm obviously from me, from our team. There’s no problem with any of the local authority partners . . . The staff themselves want a form that makes it easier for them to do the right thing, put the right information in. So we got very quick sign up to say this is something we’d embrace, we would trial and we would pilot. Can’t remember when we had that but it was over a year ago.
Head of Safeguarding (HS2)
Despite this enthusiasm, progress had been slow:
The director of IT is great and he is, broadly speaking, very supportive of everything we want to do in safeguarding, but I am one of a big number of people wanting changes to systems [and] they’re implementing huge new electronic patient records system. And I suppose it’s the way big organisations work. I made quite a lot of noise, we pushed quite hard, then you get treated a little bit like well stop being a diva because actually we’ve got all these other pressing priorities.
Head of Safeguarding (HS2)
Current plans are to start implementation in 2014, beginning in paediatrics and paediatric ED, before moving on to the ED. Specific innovations have been planned in relation to electronic transfer of referrals through a secure portal removing the need for insecure faxing which in due course could be adopted in PAHT and elsewhere in the NHS. Getting the electronic portal right has been a significant cause of delay but may well prove to be a considerable improvement on other means of transmission:
So in the future we’re keen to move away from faxing and we are. When we launch the SBAR referral that will be electronically sent with just clicking a submit button will take it automatically through without having to select which social care office it goes to it will just be submitted electronically via a secure e-mail . . . it’s linked to the patient record. So when you go in to the patient records screen there’s kind of a long list of things down the left-hand side. One of them will be safeguarding referral. So it will be visible on everybody’s form, everybody’s record, but obviously you’ll only use it in certain instances. So it will be there on the child and it will automatically populate the child’s details.
Head of Safeguarding (HS2)
Future plans include the potential use of SBAR to replace the CAF; this is also an aspiration at PAHT, but has proved difficult to bring to fruition. The number of CAFs completed is routinely used by inspectorates as a proxy for the amount of early help offered to families. There is perpetual pressure in both of our sites for more CAFs to be completed, particularly in maternity. The CAF has been subject to considerable criticism regarding its design, which tends to make it difficult to tell a family’s story. 113,187,188 Data from PAHT suggest that midwives are using the redesigned SCF and that the information within this describes the needs for early help and that the services are provided appropriately. It seems a sensible aspiration for both sites to seek to make the case for this form to be treated as the equivalent of a CAF, but this aim is likely to be thwarted by concurrent developments within several north-west authorities to develop their own electronic CAFs, which will all differ from each other. The system pressure created as a result may be anticipated to be significant, requiring midwives in particular to complete a range of forms depending on the local authority.
So once we get this prototype going, the next target then will be maternity, because there are big issues with the quality of the information there. That the problem is that what they want the midwives to do is a CAF while they are waiting to refer in, because they won’t have any referrals before 18 weeks . . . So what they’re keen is more of an assessment to be done by the midwife beforehand. So we just need to make that right with them that they would accept a better SBAR – because the CAF is just not intuitive is it?
Head of Safeguarding (HS2)
Resistance, in the form of weariness brought on by incessant change, is nonetheless anticipated, even though the change is for the better:
So it might be that there is a better assessment tool out there anyway that’s going to come on that we can get them to, but of course the fatigue that you then have in organisations who’ve been trying to drive the CAF, you know, to then say to people well actually now we want to do something different, because people do go just oh what another change?
Head of Safeguarding (HS2)
Despite Munro’s arguments for freeing up services to design better systems,11,181 including CAFs, pressure from inspectorates remains a significant source of stasis and a barrier to innovation in this regard.
Service design in site 2
Despite problems in implementing the SBAR information sharing forms, it has been possible to learn from the systems developments in place in our second site. As with our first site, considerable use is made of peer support and review, which is universally welcomed by staff.
The alerts/flagging system
This site has in place a noteworthy ‘flagging system’ to identify children known to be ‘at risk’. Safeguarding policy at this site is to place an alert on the electronic health records of all children for whom safeguarding concerns have been identified. The alert is placed as a result of one of two triggers: the child has been identified in the hospital as requiring referral to CSC, or the child is already subject to a child protection plan. A consultant in emergency medicine describes the system:
We have an electronic patient record for all patients in the trust and so what comes up is a little symbol on the electronic patient record and it comes through, it interfaces through to our computer system that we use in the A&E Department. So we get a symbol that comes up on the main white board screen which looks at all the patients in the department so you can identify that there’s an alert on that particular child . . . what we agreed was that we would just put an alert on saying a safeguarding referral was made on this child on such and such a date and then the person could go in, look at the notes for that data and see what the nature of the referral was, what the concerns were.
Consultant, emergency medicine (EM1)
The medical records on the hospital systems are thus ‘flagged’ when a child is referred to CSC and if they are known to be on a child protection plan. Very brief information is placed behind that flag, indicating which department carried out the referral and the category of concern (physical abuse, neglect, sexual abuse, emotional abuse or concerns about parental capability).
The system is generally positively evaluated by staff, who nevertheless sound a note of caution about its capacity to skew clinical judgement, as this consultant describes:
I think that they are a double-edged sword and I think you know part of what we have to do is to educate our staff about how to interpret the presence of an alert on the child . . . So it should be a trigger for a more careful approach if you like, not that we’re not careful in the first place but just to make you, you know question yourself, is there anything else I’m missing here . . . It’s clearly important that we train staff that the absence of an alert does not mean that this isn’t a safeguarding issue and equally that they understand that what the alert says is that we made a safeguarding referral, not that there was any section 47 or any necessarily significant outcome from it . . . So I think they’re useful as long as your staff are trained to know how to interpret them and you know not to be either falsely reassured or falsely suspicious as a consequence of them.
Consultant, emergency medicine (EM1)
In our first site, there is contrasting scepticism about the value of a flagging system, as this designated nurse relates:
I think every child that comes through the door should be treated on a level playing field and if you’ve got a concern, you’ve got a concern, and having child protection plan isn’t really part of that, you should deal with it on the way it’s presenting to you.
Designated nurse commissioning (DN1)
This debate is important in the context of national plans to develop a system of flagging and alerts in the NHS. Pilots are expected to be in place by 2015. The experience in our second site is that the alerts can be helpful, but must be augmented with training. Staff are aware of the capacity for flags to generate both false positives and false negatives, and the impact of this on novices is likely to be greater. A recent review9 on partnership working between paediatric and child protection services makes a similar point:
Data on any existing involvement with social care can most usefully be used to ‘step up’, but not to ‘step down’ the level of concern . . . it should not lead to trust staff reducing concern or paying less attention to clinical signs of maltreatment when a child is not known to social care.
p. 1
It goes without saying that the accuracy and updating of any database system is crucial. A national database would create problems with consent. That is, it is problematic to flag a child as ‘at risk’ without informing the parents, unless that child has reached the threshold for child protection interventions; as the numbers of children on a plan are in constant flux, significant resource could be expended in keeping the system up to date. Learning from the experiences of local services that have designed alerts systems would seem an essential part of any national design work.
Routine tracking of referrals
When the safeguarding office staff in our second site send a referral, the relevant local authority social care office is telephoned to check that they have received it. This was developed because referrals appeared to go missing, even though fax receipts for them had been received. This follow-up is a significant and time-consuming task which is not routinely undertaken in our first site but generates important feedback on the system.
Well we try to track every referral. The last quarter there were about 20% of referrals where we just didn’t get a response. Tracking the outcomes of referrals is easy on the inpatient children, but the vast majority of our referrals are on, are from the emergency department. Some of those children will be admitted, some not. The vast majority not or it could be an adult that’s presented that’s caused concern of a child protection nature. So they are more tricky. Now the office work with the different local authorities and they were ringing and they were asked not to ring, because obviously that ties up the phone line. Now they do it in writing. So they’ll track them down in writing . . . it’s not very popular, but what we have just sort of said is well we can’t have all these referrals that have been my our staff and not know what’s happening with them. We need to have some sort of record. They just say they’ve not received them.
Head of Safeguarding (HS2)
Data recently provided by the safeguarding unit at our second site showed for the most recent quarter, around 36% of referrals received a social work-led response (initial assessment or section 47/case conference), 22% were deemed to require no further action, and the outcome was unknown in 35% of referrals despite rigorous attempts to obtain this information from social care. The frustration this caused is shown graphically in the following vignette involving the named doctor (ND).
ND had a really bad experience and he did a letter . . . basically you know, he’d spent all day trying to sort out a problem and he’d been batted from pillar to post and he said if I can’t get through he said I am really persistent, which he is, I’ve got a lot of knowledge about the system, I’m quite important, I’m like a named doctor in an organisation, if they can’t listen to me when I’m jumping up and down saying I’m concerned about a child, he said what chance has anybody got?
Head of Safeguarding (HS2)
The routine follow-up of referrals could usefully inform debate within the local system, for example through the LSCBs. It highlights different practices between local authority systems, as we found in our primary site when this activity was undertaken as part of the research.
Concluding points
Cultural change requires real ‘board-to-ward’ engagement. The role of charismatic and dedicated clinical and safeguarding leads appears to be vital. The data from both sites strongly suggest that one key important factor is the direct and day-to-day involvement of the Head of Safeguarding in individual cases, including talking to and meeting with the families and children and being available for open discussion of ambiguities and uncertainties.
So when I first started here we didn’t have a Head of Safeguarding for the trust. And although we had a safeguarding team they were very hands-off from what I remember . . . So there’s been a real change. The setting up of that safeguarding team has really helped promote safeguarding throughout the trust. It’s the actual clinical interest that the team have so that in terms of you know the named nurse for safeguarding children will actually come and see families on the ward and will come and you know actually see patients and families if you want her to. The Head of Safeguarding will come and see families or will come and see patients and will come to the department and will talk about individual cases, not just the high-level strategy stuff and not just pure educational or training stuff. There’s actual real clinical engagement from the team and that’s really how I think it should be.
Consultant paediatrician (CP5)
Training can also play an important part in achieving cultural change, as indicated in the data from the staff survey in PAHT (see Appendix 13). From a total of 301 responses, 146 found the training ‘very useful’ (48.5%), and 140 described it as ‘useful’ (46.5%), i.e. there was a positive response in 95% of cases. Only five said that they had not received any training, while just seven reported a negative opinion (2%). This training appears to lead to a feeling of confidence, with 103 reporting that they were ‘very confident’ regarding their handling of safeguarding concerns, and 174 ‘fairly confident’. Only 6% expressed themselves as ‘unsure what to do’. These statistical results are corroborated by a consultant paediatrician:
The second thing that has really changed is the training programme that I mentioned earlier, that we did have some teaching in the past but the team have really taken on board a kind of work stream to standardise and co-ordinate the training that occurs throughout the whole organisation so that we can be sure what people have had at each level, and by each level there I mean you know we can be sure what the very junior doctors have had and what the very senior doctors have had and that there’s some kind of standardisation between the delivery.
Consultant paediatrician (CP5)
Clinicians, in turn, need support from the trust boards. Similarly, in both sites, the named and designated nurses and doctors provide vital peer support and skills in negotiation with other agencies where cases are contested. However, in both sites, innovation was constrained by exogenous factors such as national initiatives, inspectorates, bureaucratic requirements and the need for adaptations to IT, a point which will be taken up in the next and final chapter.
Chapter 7 Discussion and conclusions
This chapter concludes by drawing together the main findings of the research and outlining what appear to be the primary conditions for successful innovation, for creating ‘just cultures’ and for safer practice. There has been recent work exploring the interface between CSC and hospital sites,9 which underscores the importance of pre-referral discussion, training, audit, the creation of practice forums to reflect upon and debate cases, high-quality information sharing, and so forth. This study substantially replicates those findings, reinforcing in particular the need for more conversations regarding live cases, and for reflective discussions in order to improve mutual understanding and promote organisational learning.
Over the course of the study, we have investigated everyday practices in both research sites in considerable depth. There is convincing evidence of cultural change in PAHT. Case discussions, peer-review meetings, and the openness to being challenged and to changing opinions and processes are evidenced in the interviews and in the everyday practices observed by the team. Moreover, the impact of collaboration between the clinicians across the two hospital sites has been significant and has produced blueprints for further service innovations. For example, the two heads of safeguarding have designed a ‘shaken baby’ app, to help parents to cope with crying babies. Clinicians have described conceptual and emotional benefits of ‘safe’ conversations with others in similar roles in different organisations. This study suggests that creating a system of peer support along these lines could enhance safe practice and produce a ‘design studio’ for the fruitful discussion of future service innovations based on shared learning. The clinicians involved in our study contrast this opportunity with the current form of peer support and review in the NHS, which one describes as ‘not supportive, not done by peers, and feels like another inspection’.
However, our study also supports the view that decisions in relation to safeguarding children are complex and vulnerable. Knowledge sharing, especially between health and social care agencies, can either mitigate or exacerbate this complexity. The evidence-base for the clinical identification of children at risk has been considerably enhanced over recent years, with the publication of systematic reviews of physical injuries, sexual abuse, and emotional abuse and neglect. Validated screening checklists and operational definitions for ‘reasonable suspicion’ of child maltreatment,189 based on Bayesian calculations of conditional probabilities that a given configuration of injuries or symptoms may indicate abuse, are beginning to be developed. However, as this report has repeatedly noted, many children and adults presenting at hospitals do not carry these diagnostic markers. Indeed, most cases are clouded in ambiguity and uncertainty, and hence in personal and organisational risk. Enhancing safe practice in such a precarious world is a challenge.
Candidate success factors in enhancing safe practice
If safeguarding children is to become mainstream patient safety business, high-level organisational strategy matters. In PAHT there has been a steady integration of learning from SCRs, and other child protection-related processes with ‘patient safety’-related incidents. There has been a growing recognition that the same systemic issues impact on safeguarding as well as on the conventional medical domain. Significantly from a cultural perspective, safeguarding is now seen as part of the generic quality framework of the trust and is, for example, incorporated into the ‘lessons learned’ bulletin, which is circulated, posted on the intranet and presented to the patient safety committee.
Using the language of patient safety appears to have been pivotal. Cultures speak themselves, as we noted in Chapter 2, Safety cultures, and making use of a familiar vocabulary and artefacts such as the ‘SBAR’ to redescribe safeguarding as a safety issue, and thus as something fundamental to the functions of an acute hospital, has been part of the success. In the words of the Head of Safeguarding, ‘You’ve got to change how you speak. You’ve just got to change your language’. In so doing, the taken-for-granted beliefs, images, intuition, mental models and technical skills in use through the patient safety paradigm, which are thus part of the interpretive repertoire of clinical staff and managers, have been mobilised to support change and innovation in relation to safeguarding children. Engagement from the executive team and the board has been crucial. A dedication to data gathering and analysis, and the appointment of a Head of Safeguarding who relates directly to the medical director in the hierarchy, have been seen as critical success factors, as this senior executive explains:
The fact that we clearly did make a quite bold statement of, ‘No, no, we’re appointing a Head of Safeguarding; we don’t think the safeguarding nurses on their own are sufficient.’ And the safeguarding nurses are part of the divisional directorate clinical structure; the Head of Safeguarding isn’t. The Head of Safeguarding is apart from the divisional structure where you’re basically asking people to examine their own practice and, sure enough, 9 times out of 10, they’ll say they’ve done it perfectly well. So I think it’s the having the senior, objective opinion which is important.
Senior executive (SE2)
Literature on governance and leadership affirms the importance of using local data to inform decision-making. This can sometimes slip from the priority list in conditions of external scrutiny, central target setting and blame. 190 At PAHT, the gathering of local data to support service design has been prioritised, as outlined below:
I mean I think, to an extent, if you’re relying on external regulation to drive improvements, then . . . if all your aspiration is to discharge your regulatory requirements, then, hey, forget it. You’ve got to have something which is aspiration . . . So, if someone says, ‘Look, there’s a regulatory requirement to do x, y and z’, you’d say, ‘Yeah, but we should be doing that anyway. What we want to know is what’s a, b and c on top of that.’ . . . ’Cause the regulation will probably come out of something that happened 10 years ago and is eventually catching up. If we come across things in day-to-day practice, that should become part of our aims for the future.
Senior executive (SE2)
Nevertheless, the preoccupation with measurable indicators, such as numbers of CAFs completed, by inspectorates and policy-makers, remains a challenge, as (paraphrasing Einstein) many of things that count in enhancing safer practice cannot be counted. The Head of Safeguarding notes ‘you can’t understand the value of things like protecting children from abuse in counting numbers. I’m not sure that that is completely understood’. This reinforces the generic concerns raised in Chapter 2 about the adverse impact of performance management regimes. 57
The experience in PAHT suggests that persistence, resilience and vigilance from the safeguarding leadership and executive teams are crucial. The importance of user-centred design, piloting, incrementalism, and a thorough empirical engagement with everyday practices and emerging patterns of use seem essential, as the Head of Safeguarding notes:
I think priorities are to get underneath this co-mentoring stuff in more detail, really. Yeah, what is really going on there. And to see what the results of this re-audit is going to be and really get underneath that – what is going on here? We have 3 years of these audits, nothing’s changing. And I think I might try focus groups for that. ‘You tell me, instead of me trying to guess at what will make a difference.’ And to carry on. To keep the impetus. To keep the drive.
Head of Safeguarding (HS1)
We have argued that there is evidence of cultural change at PAHT, but practices are dynamic, the walls of the organisation are porous, staff change roles or leave, and adverse incidents receive publicity, often generating precipitous policy shifts. The precaution versus proportion pendulum continues to swing, and there are enduring challenges in creating cultures to support safe practice to which we now turn.
Wicked issues reconsidered
Making the case in safeguarding: interaction, emotion and relationship
All of our respondents mentioned the importance of relationships and conversations. Children’s safeguarding is saturated by the language and techniques of risk. From actuarial risk assessment schedules to centrally designed and mandated templates for assessment in CSC, the presence of a risk apparatus that bears the stamp of instrumental rationality is widespread. While arguably shaped and constrained by this standardising apparatus, practitioners continue to defy its totalising potential. In this study, as in our previous work, we see professional autonomy continuing to hold its ground. 191 The danger of technical procedures functioning as defences for containing anxiety192 and substituting for professional judgement is ever-present, and once such a defensive culture has set in it can be difficult to dislodge, as one experienced midwife pithily observed:
Once that culture’s developed it’s really hard to unpick it because a lot of the people who were doing it are doing it with good intention and they maybe are genuinely fearful that they don’t want to overlook something. But in that process we’ve lost our capacity to actually see what’s in front of us a little bit. It’s a recent thing I think. I would say it’s probably in the last 4 or 5 years that I’ve noticed there’s a definite shift away from, sometimes it just feels like the triumph of protocol over common sense.
Specialist midwife (MW6)
Abstract bureaucratic rules often attempt to erase variability in human performance, but such variety is essential for effective operation. This is the ineluctable principle of requisite variety (see Safety cultures), fundamental to the systems view of organisations. Only humans can amplify the variety necessarily lacking from a rule in order to deal with unique contingencies. The interactive quality of clinical practice renders it an essentially social, interpretive enterprise, in which both the logics and strategies of diagnosis and intervention are fundamentally dependent upon the particulars of individual cases. The assessment of safety or risk results from the contextual detail of the case; ‘risk trade-offs’ are calculated and made in each and every situation, having as much to do with dialogue and the quality of relationships as with this or that next procedure. Practitioners shift between a range of risk management strategies and resources. The logics of risk management strategies are emergent and contingent; they arise in relation to particular cases as reflexive, individualised and tailored responses. Risk assessment practices are embedded in social relations – team culture, patient–clinician relationships – which create unique contingencies. A multiplicity of rationalities are invoked that are not just to do with instrumental concerns, but evoke human virtues of compassion, empathy and a sense of responsibility for others.
Top-down approaches to risk management can be difficult to work around and can inhibit effective and skilled professional practices. Professionals must negotiate the contingencies of each and every case. The curtailment of the reflexive, dialogical spaces necessary to undertake this work thus paradoxically increases the likelihood of error. Face-to-face relationships make safe teams.
[S]imply installing a team structure in an organization does not automatically result in effective teamwork. Effective team performance requires team members’ willingness to cooperate for a shared goal . . . Moreover, effective teamwork depends on effective within-team communication and adequate organizational resources and support. In short, teamwork requires team members to develop a shared awareness of one another’s roles and abilities. Without this awareness, serious but avoidable adverse outcomes may result from a series of seemingly trivial errors that effective teamwork would have prevented.
Baker et al. , p. 10193
Storytelling works in producing learning and mindfulness,132 but ‘teams’ can easily be disrupted by professional hierarchies, bureaucratic processes and structural changes. These findings replicate those of other studies of partnership working and knowledge sharing, and are important for service redesign beyond children’s safeguarding. 194 Moreover, dialogic spaces can be inadvertently designed out by frequent endogenous and exogenous structural and organisational turbulence. These can create barriers to developing cultures that support safer practice. National initiatives intended to improve services, such as ‘Making it Better’, have contributed to the closure of a local hospital, causing anxiety about the threat to the relationships between children, CSC and the hospital staff, for example as we saw in the quotation from the designated nurse (see Chapter 5, Having a conversation).
Design and the management of change in a complex environment
All really important innovations normally start from tiny minorities of people who do use their creative freedom. Yet, it seems, large-scale organisation is here to stay. The fundamental task is to achieve smallness within a large organisation . . . In any organisation, there must be a certain clarity and orderliness. Yet, orderliness is static and lifeless; so there must also be plenty of elbow-room for breaking through the established order, to do the thing never anticipated by the guardians of orderliness. Therefore any organisation has to strive continuously for the orderliness of order and the disorderliness of creative freedom.
Schumacher, pp. 203–4195
Safeguarding takes place in a complex system, and even relatively minor changes within any part of that system can impact on the rest of the system in unpredictable ways. Local interventions to increase safety can paradoxically produce the opposite effect from a systemic point of view, and it is important that managers understand patterns of causality in complex environments, and are alert for potentially dangerous positive feedback loops. Increasing thresholds, for instance, can easily operate to increase rather than decrease demand, in the form of ‘failure demand’ not ‘value demand’, which undermines the organisation’s ability to provide services. 196 The key to improving service quality is to find ways of reducing the former.
Reflecting this complexity, it is even more important that managers adopt a ‘design attitude’. Designers naturally embrace systems thinking, and seek to mitigate unintended consequences through careful experimentation. The conventional model of change in the management literature is characterised by Kawalek197 as top-down, linear and planned, with Kotter’s198 eight-step ‘road map’ being the best known of such classical linear models. However, such orthodoxy has been challenged. Weick199 argues that it is founded on a false analogy with architectural design, ‘that a design is a blueprint constructed at a single point in time, that designs produce order through intention, and that design produces planned change’ (p. 348). Weick199 also argues that organisational design is a quite different process from architectural design: it is dynamic and continuous, partly pre-planned and top-down, but also emergent, spontaneous and organic, more like a recipe than a blueprint. Weick199 suggests a different metaphor, that of improvisational theatre, whose essence is ‘making do’ the creation of order in the moment, in the act of performance: ‘resourcefulness is more crucial than resources – [using] whatever resources and repertoire one has to perform whatever task one faces’ (p. 346). Weick199 argues that bricolage is the quintessence of leadership: ‘the main function of any leader is to draw organisation out of the raw materials of life . . . fixing things on the spot through a creative vision of what is available and what might be done’ (pp. 352–3).
It is this view of change which emerges from this research. In Chapter 2, Technology adoption, we argued that the process of innovation in organisations is complex, with multiple potential initiatives unfolding in parallel, all competing for priority in a politically contested milieu. We depicted the innovation process as made up of multiple, non-linear activities and events progressing through time: these can be concerned with the initial invention itself, its promotion and ‘selling’, or its adoption and implementation. At any time, the flow of activity can be perturbed by ‘process events’, shocks, setbacks and policy changes, which can influence the trajectory of particular innovations and projects. Designing with a blueprint is not feasible when faced with such organisational realities; a ‘design attitude’, embracing pragmatism, experimentation and incrementalism, is essential. This includes the need to embrace proven design methods such as prototyping and the use of ethnographic methods to gain a rich understanding of the complex realities of even mundane practices. 17 The design attitude recognises the complexity of design work in organisations, and the ever-present risk of unintended consequences.
Just as designing requires improvisation and dexterity, the same is true for practising design science in real organisations, as we did here. In this work, we have attempted to respond to Greenhalgh et al. ’s14 call to explore why particular innovations in health care are successful or not, using the mixed methods ‘aimed at building up a rich picture of process and impact’ (p. 620). The research process is at the mercy of the same fluctuating contingencies, meaning that our research plan had to be continually adjusted, with the team forced to trim and tack. In some areas we did more than intended, although not always by the original means, but in others areas our efforts were met with frustration, most notably in the ‘technology transfer’ of the SBAR tool to the second site. Technology adoption by organisations, as we anticipated, is a more complex process than the adoption by individuals. Despite these vicissitudes, the design science approach had afforded not only important theoretical insights but also practical knowledge of how other organisations could deploy these tools, and the difficulties they are likely to encounter. This is the quintessence of design science.
Technology as a fickle friend
The assumption that electronic systems facilitate better ‘information sharing’ merits more critical examination. Poorly designed, or precipitously imposed technologies can act as a barrier to human communication and sense-making. As we saw in the redesign of the SCF for maternity cases in Chapter 6 (see also Appendix 7), in moving to an electronic form the visual cue of the yellow form could have been lost. Recognising the potentially negative ergonomic effect of a new system is an important part of careful system redesign. Newer is not necessarily better, and electronic is not necessarily better either. Electronic systems work well for particular kinds of knowledge. If knowledge is explicit, and expressible, it can be moved around using IT and conveyed in documents, e-mail and databases, as well as through meetings and briefings. However, much of the knowledge in the detection of a child or family at risk is tacit and difficult to codify. It is experiential, active, alive and expressible through direct interaction. 80 When technological developments disrupt this, for example through using a call centre to filter all communication and discouraging staff from talking about cases unless they have received a referral in particular format, or which has already been entered onto the system, then the translation of tacit understandings and ‘gut feelings’ into explicit and communicable knowledge is rendered extremely problematic.
Furthermore, our data suggest that technology may act as either a support or a barrier to change and innovation and also to the adoption of new working practices. Incompatible systems are a recurrent problem at a number of interfaces in both of our sites. This lack of digital unity and the slim promise of any integration soon, means that much of the initial work undertaken by clinicians takes place in a limbo-space between electronic and handwritten, e-mail and fax, telephone call and letter. As one clinician describes, ‘we are partially and embryonically electronic’ (Health Visitor 1, HV1). The array of different systems performing slightly different functions highlights the way in which system design shapes the form and effectiveness of communication across professional boundaries.
Study limitations
It is important to acknowledge the limitations of this study. The first limitation relates to the generalisability of the findings beyond the selected case study sites. We can be reasonably confident about the generic features of professional practice in health and social care, described in Chapters 4 and 5. These chapters take forward but are corroborative of other studies and the extant literature. However, we have not been able to test the transferability of the artefacts from PAHT as we intended, and this formed a significant part of our rationale for having additional sites. We have found the onerous and lengthy process involved in securing access to NHS sites limiting, and a longer-term, more episodic project plan would, on reflection, have worked better, allowing us to follow the process through without incurring additional costs to the National Institute for Health Research (NIHR). This is a challenging model, however, in relation to contracting researchers’ time.
A second limitation relates to the follow-up of cases. It was a requirement of ethical review that only clinician researchers could follow cases through to social care where this involved access to patient identifiable data. This is time-consuming work and was limited by the capacity of busy clinicians. It has thus limited this important aspect of the study. The follow-up of cases which has taken place suggests this is an important fault line in the system and suggests the need for further research in this area and grappling with its complexities in terms of ethics and patient consent where the patient/client is a child. The tension between precaution and proportion has played out in the approval processes of the project itself and has excluded entirely one proposed site from the study. This site was a tertiary children’s hospital and could have yielded helpful contrasts to our other two large acute trusts.
The third limitation relates to the challenge of recruiting participants for interview from certain groups. While we have a good cross-section of professions, selection has by necessity been partly pragmatic, dependent on responses to e-mails and so forth. This was further exacerbated by the loss of our researcher after only a few months and the significant loss of research time as a consequence. Our intention had been to interview staff at least twice as the package was developed. While several principal informants were interviewed a number of times, this was not routine for all informants. This was due primarily to the non-linearity of the design process – there was no simple ‘before’ and ‘after’ in PAHT, and the delays in implementation in site 2 meant that such comparison was also impossible. The saturation of the data suggests that this has not significantly affected the validity of the study – there is a remarkable similarity in accounts from all professional groups across both sites – but it has limited the confidence with which we can makes claims about the evaluation of specific artefacts and their transferability.
Future research
If you want truly to understand something, try to change it.
Kurt Lewin
Health care is an arena of flux and innovation as improvements in quality and efficiency are constantly sought. Despite this, an authoritative review by Greenhalgh et al. 14 has drawn attention to the paucity of in-depth studies of the implementation of service innovations, if they were sustained in particular contexts and settings, and how such processes could be enhanced. This study provides an example of the genre of such work and from our findings we would recommend the following research directions, listed in priority order, addressing the specific area of child protection as well as service improvement more generally.
-
Technology is often portrayed as a mechanism conducive to innovation. However, here we have seen how it can equally well obstruct beneficial change. A paper form can be implemented over a weekend, but electronic forms can take months and years, as we have described. This study suggests that forces of stasis in the NHS are considerable, including those arising from the research and information governance systems. A study which systematically analysed factors that enhance or limit organisational change would help to inform the design of the accountability and governance structures and processes. It is important that such forces for change and stasis are better understood through further research, using similar mixed methods to those employed here.
-
The need to assess technology transfer and local conditions for its success or failure is an important priority. The potential of transferring some of the artefacts developed here, for instance digital stories, into allied organisations, including CSC, would be valuable both to advance the patient safety agenda and to afford an opportunity to study processes of organisational change more generally. Participatory action research methods combined with multimethod ethnography, including analysis of key metrics about referral pathways and decision-making, would be the requisite methodological approach.
-
There are a number of current developments at a policy level which pertain to this research. Government is currently developing the Child Protection Information Sharing project, which is intended to improve information flow within the NHS, particularly between hospitals and CSC. This will create a database of children on a child protection plan and those who are ‘looked after’ (on a care order, or accommodated with parental consent in foster or residential care) by the local authority. This study shows the interpretive and interactional complexities of clinical decision-making and the problems which occur in distinguishing signal from noise. As new information sharing initiatives are implemented, a complex multimethod approach to their evaluation is vital. For example, how will clinicians interpret the information that a child is, or is not, on a plan? The two sites in this study had polar opposite views on whether such data would help or hinder clinical judgement. This remains a pressing empirical question.
-
This study suggests that the configuration of the local authority ‘front door’ may be an important factor in knowledge sharing between health care and CSC. Future work could usefully focus specifically on a comparative analysis of a number of different local authority models, for example a site using a contact or call centre, a site using a MASH and a site using a duty social work system. Again, the methodological approach would need to be similar to that deployed in this study, analysing the human sense-making and the impact of technologies broadly defined to include telephones and faxes, and tracking cases through the system.
In summary, the findings from this study suggest the importance of user-centred design, piloting, incrementalism and a thorough empirical engagement with everyday practices and emerging patterns during implementation. They confirm the value of the design science paradigm, and the need for a flexible, mixed-methods approach in this context. This report may usefully inform the commissioning of future liaison and safeguarding posts within the evolving health economy as we enter a period of considerable change. The findings from this study suggest that this may be particularly challenging, and that future research could usefully track local authority decision-making about resource allocation and commissioning, and its effects on such fragile processes.
Acknowledgements
The financial support of the NIHR Health Services and Delivery Research (HS&DR) is acknowledged: project code 10/2002/52.
Pennine Acute Hospitals Trust provided their consent and access over the course of the project. We are most grateful to clinicians, managers and patient representatives for their engagement with this project.
Heart of England Foundation Trust are also thanked for their consent, support and access to staff.
Maria Kilcoyne, Heart of England Foundation Trust, provided valuable guidance and advice throughout the project.
Dr Michael Plunkett, Heart of England Foundation Trust, provided valuable guidance and advice throughout the project.
Kerry Allen, University of Birmingham, carried out first-stage qualitative fieldwork and analysis.
This report presents independent research commissioned by the NIHR. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR Evaluation, Trials and Studies Coordinating Centre (NETSCC), the HS&DR programme or the Department of Health. The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, Medical Research Council, Central Commissioning Facility, NETSCC, the HS&DR programme or the Department of Health.
Contributions of authors
Professor Susan White, University of Birmingham, led the project, was the main author of the final report and participated in qualitative fieldwork.
Professor David Wastell, University of Nottingham, codesigned research, was the second author of the main report, led the design strand of work, was responsible for collation and analysis of quantitative data and participated in qualitative fieldwork and analysis.
Dr Suzanne Smith, PAHT codesigned research, was lead clinician researcher and facilitated fieldwork access.
Dr Christopher Hall, University of Durham, codesigned research, carried out qualitative fieldwork and analysis and contributed to the final report.
Emilie Whitaker, University of Birmingham, carried out qualitative fieldwork and analysis and contributed to the final report.
Dr Geoff Debelle, Birmingham Children’s Hospital and University of Birmingham, codesigned research, contributed to the final report and provided valuable guidance and advice.
Professor Russell Mannion, University of Birmingham, contributed to the original design and the final report and provided valuable guidance and advice.
Professor Justin Waring, University of Nottingham, contributed to the original design and the final report and provided valuable guidance and advice.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Sheets L, Leach M, Koszewski I, Lessmeier A. Sentinel injuries in infants evaluated for child physical abuse. Pediatrics 2013;131:701-7. http://dx.doi.org/10.1542/peds.2012-2780.
- Komulainen S, Haines L. Understanding Parent’s Information Needs and Experience where Professional Concerns Regarding Non-Accidental Injury were not Substantiated. London: Royal College of Paediatrics and Child Health; 2009.
- Francis R. The Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Keogh B. Review Into The Quality of Care and Treatment Provided by 14 Hospital Trusts in England: Overview Report. London: NHS; 2013.
- Berwick D. Berwick Review Into Patient Safety. London: Department of Health; 2013.
- Sidebotham P, Biu T, Goldsworthy L. Child protection procedures in emergency departments. Emerg Med J 2007;24:831-5. http://dx.doi.org/10.1136/emj.2007.051011.
- Carter YH, Bannon MJ, Limbert C, Docherty A, Barlow J. Improving child protection: a review of training and procedural interventions. Arch Dis Child 2006;91:740-3. http://dx.doi.org/10.1136/adc.2005.092007.
- Louwers C. Screen for child abuse at emergency departments: a systematic review. Arch Dis Child 2010;95:214-18. http://dx.doi.org/10.1136/adc.2008.151654.
- Lewis J. Partnership Working in Child Protection: Improving Liaison Between Acute Paediatric and Child Protection Services. London: Social Care Institute for Excellence; 2013.
- Thomas A, Mott A. Child protection peer review for paediatricians. Child Abuse Rev 2013;22:60-6. http://dx.doi.org/10.1002/car.2201.
- Munro E. The Munro Review of Child Protection. Progress Report: Moving Towards a Child Centred System. London: The Stationery Office; 2012.
- Patient Safety First. London: National Patient Safety Agency; 2011.
- Dekker S. Just Culture Balancing Safety and Accountability. Farnham: Ashgate Publishing Company; 2007.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovation in service organisations. Milbank Q 2004;82:581-629. http://dx.doi.org/10.1111/j.0887-378X.2004.00325.x.
- Organisational and Behavioural Barriers to Medical Technology Adoption. York: NHS Institute for Innovation and Improvement; 2009.
- Featherstone B, White S, Wastell D. Featherstone, B. Ireland’s opportunity to learn from England’s difficulties? Auditing uncertainty in child protection. Ir J Soc Work 2012;12:49-62.
- Wastell DG. Managers as Designers in the Public Services: Beyond Techno-Magic. Axminster: Triarchy Press; 2011.
- Dingwall R, Eekelaar J, Murray T. The Protection of Children: State Intervention and Family Life. Oxford: Blackwell; 1983.
- Children Act 1989. London: The Stationery Office; 1989.
- Working Together: A Guide to Inter-agency Co-operation for the Protection of Children. London: DHSS; 1988.
- Munro E. The Munro Review of Child Protection: Interim Report – A Child’s Journey. Manchester: Department for Education; 2011.
- Working Together to Safeguard Children. London: Department for Education; 2013.
- Brandon M, Sidebotham P, Bailey S, Belderson P, Hawley C, Ellis C, et al. New Learning from Serious Case Reviews: A Two Year Report for 2009–2011. Manchester: Department for Education; 2012.
- Sidebotham P, Atkins B, Hutton J. Changes in rates of violent child deaths in England and Wales between 1974 and 2008: an analysis of national mortality data. Arch Dis Child 2012;97:193-9. http://dx.doi.org/10.1136/adc.2010.207647.
- Gilbert R, Kemp A, Thoburn J. Recognising and responding to child maltreatment. Lancet 2009;373:167-80. http://dx.doi.org/10.1016/S0140-6736(08)61707-9.
- Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE. Performance of screening tests for child physical abuse in accident and emergency departments. Health Technol Assess 2008;12. http://dx.doi.org/10.3310/hta12330.
- Daniel B, Taylor J, Scott J. Noticing and Helping the Neglected Child: Literature Review. London: Department for Children, Schools and Families; 2009.
- Rees G, Stein M, Hicks L, Gorin S. Adolescent Neglect: Research, Policy and Practice. London: Jessica Kingsley Publishers; 2011.
- Lupton C, North N, Khan P. Working Together or Pulling Apart? The National Health Service and Child Protection Networks. Bristol: The Policy Press; 2000.
- Benbenishty R, Davidson-Arad B, Chen W, Glasser S. The decision of hospital-based child protection teams to report to community child protection services. Br J Soc Work 2011;41:1232-50. http://dx.doi.org/10.1093/bjsw/bcq133.
- Ute T, Leventhal J, Yazdgerdi S, Perrin J. Concerns about child maltreatment in hospitalized children. Child Abuse Negl 1997;21:187-98. http://dx.doi.org/10.1016/S0145-2134(96)00144-5.
- Flaherty E, Sege R, Griffin T, LL P. From suspicion of physical child abuse to reporting: primary care clinician decision-making. Pediatrics 2008;122:611-19. http://dx.doi.org/10.1542/peds.2007-2311.
- Jones R, Flaherty E, Binns H, Price L. Child abuse: report of the Child Abuse Reporting Experience Study Research Group. Pediatrics 2008;122:259-66. http://dx.doi.org/10.1542/peds.2007-2312.
- Van Haeringen A, Dadds M, Armstrong K. The child abuse lottery – will the doctor suspect and report?. Child Abuse Negl 1998;30:159-69. http://dx.doi.org/10.1016/S0145-2134(97)00172-5.
- Theodore A, Runyan R. A survey of pediatricians’ attitudes and experiences with court in cases of child maltreatment. Child Abuse Negl 2006;30:1353-63. http://dx.doi.org/10.1016/j.chiabu.2006.05.010.
- Levi B, Dellasega C, Boehmer S. What is reasonable suspicion of child abuse?. J Public Child Welfare 2012;6:56-589. http://dx.doi.org/10.1080/15548732.2012.683374.
- Lindberg D, Lindsell C, Shapiro RA. Variability in expert assessments of physical child abuse likelihood. Pediatrics 2008;121:e945-53. http://dx.doi.org/10.1542/peds.2007-2485.
- Debelle G. Interpreting signs of physical maltreatment: ‘grey case’ and what is ‘reasonably possible’. Paediatr Child Health 2012;22:470-5. http://dx.doi.org/10.1016/j.paed.2012.08.001.
- O’Hare A, Eden O. Bleeding disorders and non-accidental injury. Arch Dis Child 1984;59:860-4. http://dx.doi.org/10.1136/adc.59.9.860.
- Field-Fisher T. Report of the Committee of Inquiry into the Care and Supervision Provided by Local Authorities and Other Agencies in Relation to Maria Colwell and the Co-ordination Between Them. London: The Stationery Office; 1974.
- A Child in Trust: Report of the Panel of Inquiry Investigating the Circumstances Surrounding the Death of Jasmine Beckford. London: London Borough of Brent; 1985.
- Whose Child? The Report of the Panel Appointed to Inquire into the Death of Tyra Henry. London: London Borough of Lambeth; 1987.
- A Child in Mind: Protection of Children in a Responsible Society: Report of the Commission of Inquiry into the Circumstances Surrounding the Death of Kimberley Carlisle. London: London Borough of Greenwich; 1987.
- Douglas M. Risk and Blame: Essays in Cultural Theory. London: Routledge; 1994.
- Dingwall R. The Jasmine Beckford affair. Mod Law Rev 1986;49:489-507. http://dx.doi.org/10.1111/j.1468-2230.1986.tb01700.x.
- Family Law Week . In the Matter of B (A Child) [2013] 2013.
- Kearney J. Perceptions of non-accidental child deaths as preventable events: the impact of probability heuristics and biases on child protection work. Health Risk Soc 2013;15:51-66. http://dx.doi.org/10.1080/13698575.2012.749451.
- Laming H. The Victoria Climbié Inquiry: Report of an Inquiry by Lord Laming. Norwich: Department for Health and Home Office; 2003.
- Every Child Matters. London: Chief Secretary to the Treasury; 2003.
- Hudson J. Digitising the structure of government: the UK’s information age government agenda. Policy Polit 2002;30:515-31. http://dx.doi.org/10.1332/030557302760590431.
- Common Assessment Framework for Children and Young People: Managers’ Guide. London: Department for Education and Skills; 2006.
- Common Assessment Framework for Children and Young People: Practitioners’ Guide. London: Department for Education and Skills; 2006.
- Framework and Evaluation Schedule for the Inspections of Services for Children in Need of Help and Protection, Children Looked After and Care Leavers. Manchester: Ofsted; 2014.
- Dillow C. The End of Politics: New Labour and the Folly of Managerialism. Petersfield: Harriman House; 2007.
- Chard A, Ayre P, Ayre P, Preston-Shoot M. Children’s Services at the Cross-Roads. Lyme Regis: Russell House; 2010.
- Munro E. Managing societal and institutional risk in child protection. Risk Anal 2009;29:1015-23. http://dx.doi.org/10.1111/j.1539-6924.2009.01204.x.
- Bevan G, Hood C. What gets measured is what matters: targets and gaming in the English public health care system. Public Adm 2006;84:517-38. http://dx.doi.org/10.1111/j.1467-9299.2006.00600.x.
- Shaw I, Bell M, Sinclair I, Sloper P, Mitchell W, Dyson P, et al. An exemplary scheme? An evaluation of the integrated children’s system. Br J Soc Work 2009;39:613-26. http://dx.doi.org/10.1093/bjsw/bcp040.
- White S, Wastell D, Broadhurst K, Hall C. When policy o’erleaps itself: the tragic tale of the Integrated Children’s System. Crit Soc Policy 2010;30:405-29. http://dx.doi.org/10.1177/0261018310367675.
- Process Flow Diagram: P1.1 Core Case Management Operations V4.0. London: DCSF; 2008.
- White S, Broadhurst K, Grover C, Jamieson J. Critical Perspectives on Safeguarding Children. Oxford: John Wiley & Sons; 2009.
- Broadhurst K, Wastell D, White S, Hall C. Performing ‘initial assessment’: identifying the latent conditions for error at the front-door of local authority children’s services. Br J Soc Work 2010;40:352-70. http://dx.doi.org/10.1093/bjsw/bcn162.
- Platt D, Turney D. Making threshold decisions in child protection: a conceptual analysis. Br J Soc Work 2014;44:1472-90. http://dx.doi.org/10.1093/bjsw/bct007.
- Masson J, Dickens J. Partnership by Law? The Pre-Proceedings Process for Families on the Edge of Care Proceedings. Bristol: University of Bristol; 2013.
- Serres M. Parasite. Minneapolis, MN: University of Minnesota Press; 2007.
- Cross R, Borgatti SP, Huysman M, Wulf V. Social Capital and Information Technology. Cambridge, MA: MIT; 2004.
- Swan J, Scarbrough H. Knowledge management: concepts and controversies. J Manag Stud 2001;38:913-21. http://dx.doi.org/10.1111/1467-6486.00265.
- Reder P, Duncan S. Understanding communication in child protection networks. Child Abuse Rev 2003;12:82-100. http://dx.doi.org/10.1002/car.787.
- Waring J, Rowley E, Dingwall R, Palmer C, Murcott T. A narrative review of the UK Patient Safety Research Portfolio. J Health Serv Res Policy n.d.;15:26-32. http://dx.doi.org/10.1258/jhsrp.2009.009042.
- Thompson K. Multi-agency information practices in children’s services: the metaphorical ‘jigsaw’ and professionals quest for a ‘full’ picture. Child Fam Soc Work 2012;18:189-97. http://dx.doi.org/10.1111/j.1365-2206.2011.00821.x.
- Latanè B, Darley J. The Unresponsive Bystander: Why Doesn’t He Help?. New York, NY: Meredith Corporation; 1970.
- Kogut T, Beyth-Marom R. Who helps more? How self-other discrepancies influence decisions in helping situations. Judgm Decis Mak 2008;3:595-606.
- Bickman L, Summerfelt WT, Noser K. Comparative outcomes of emotionally disturbed children and adolescents in a system of services and usual care. Psychiatr Serv 1997;48:1543-8.
- Bickman L, Summerfelt WT, Noser K. Long-term effects of a system of care on children and adolescents. J Behav Health Serv Res 1999;26:185-202. http://dx.doi.org/10.1007/BF02287490.
- Glisson C, Hemmelgarn A. The effects of organizational climate and interorganizational coordination on the quality and outcomes of children’s service systems. Child Abuse Negl 1998;22:401-21. http://dx.doi.org/10.1016/S0145-2134(98)00005-2.
- Easterby-Smith M, Lyles M, Easterby-Smith M, Lyles M. Handbook of Organizational Learning and Knowledge Management. Oxford: Blackwell; 2003.
- Blackler F. Knowledge, knowledge work and organizations: an overview and interpretation. Organ Stud 1995;16:1021-46. http://dx.doi.org/10.1177/017084069501600605.
- Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge: Cambridge University Press; 1991.
- Cabrera A, Cabrera EF. Knowledge-sharing dilemmas. Organ Stud 2002;23:687-710. http://dx.doi.org/10.1177/0170840602235001.
- Nonaka I. A dynamic theory of organizational knowledge creation. Organ Sci 1994;5:14-37. http://dx.doi.org/10.1287/orsc.5.1.14.
- Malone R. Distal nursing. Soc Sci Med 2003;56:2317-26. http://dx.doi.org/10.1016/S0277-9536(02)00230-7.
- Bauman Z, Bauman Z. Postmodern Ethics. Oxford: Blackwell; 1993.
- Argote L, McEvily B, Reagans R. Managing knowledge in organizations: an integrative framework and review of emerging themes. Manage Sci 2003;49:571-82. http://dx.doi.org/10.1287/mnsc.49.4.571.14424.
- McDermott R, O’Dell C. Overcoming cultural barriers to sharing knowledge. J Knowl Manag 2001;5:76-85. http://dx.doi.org/10.1108/13673270110384428.
- Cohen W, Levinthal D. Absorptive capacity: a new perspective on learning and innovation. Adm Sci Q 1990;35:128-52. http://dx.doi.org/10.2307/2393553.
- Van Wijk R, Jansen JJ, Lyles MA. Inter- and intra-organizational knowledge transfer: a meta-analytic review and assessment of its antecedents and consequences. J Manag Stud 2008;45:830-53. http://dx.doi.org/10.1111/j.1467-6486.2008.00771.x.
- Owen-Smith J, Powell WW. Knowledge networks as channels and conduits: the effects of spillovers in the Boston biotechnology community. Organ Sci 2004;15:5-21. http://dx.doi.org/10.1287/orsc.1030.0054.
- Coleman N, Harris J. Calling social work. Br J Soc Work 2008;38:580-99. http://dx.doi.org/10.1093/bjsw/bcl371.
- Addicott R, McGivern G, Ferlie E. Networks, organizational learning and knowledge management. Public Money Manage 2006;6:87-94. http://dx.doi.org/10.1111/j.1467-9302.2006.00506.x.
- Abbot A. The System of Professions. Chicago, IL: University of Chicago Press; 1988.
- White S. Accomplishing the case in paediatrics and child health: medicine and morality in interprofessional talk. Sociol Health Illn 2002;24:409-35. http://dx.doi.org/10.1111/1467-9566.00302.
- Munro E. Common errors of reasoning in child protection work. Child Abuse Negl 1999;23:745-58. http://dx.doi.org/10.1016/S0145-2134(99)00053-8.
- Almond P. Approaches to decision-making and child protection issues. Community Pract 2001;74:97-100.
- Dowie J, Elstein A. Professional Judgement: A Reader in Clinical Decision Making. Cambridge: Cambridge University Press; 1988.
- Trocmé N, MacMillan H, Fallon B, De Marco R. Nature and severity of physical harm caused by child abuse and neglect: results from the Canadian Incidence Study. CMAJ 2003;169:911-15.
- Strong P. The Ceremonial Order of the Clinic. London: Routledge and Kegan Paul; 1979.
- Silverman D. Communication and Medical Practice. London: Sage; 1987.
- Wolf FM, Gruppen LD, Billi JE. Differential diagnosis and competing hypotheses heuristic: a practical approach to judgement under uncertainty and Bayesian probability. JAMA 1985;253:2858-62. http://dx.doi.org/10.1001/jama.1985.03350430070028.
- Melton G. Mandated reporting: a policy without reason. Child Abuse Negl 2005;25:9-18. http://dx.doi.org/10.1016/j.chiabu.2004.05.005.
- Barlow J, Fisher J, Jones D. Systematic Review of Models of Analysing Significant Harm. London: Department for Education; 2012.
- Carter Y, Bannon M, Limbert C, Docherty A, Barlow J. Improving child protection: a systematic review of training and procedural interventions. Arch Dis Child 2006;91:740-3. http://dx.doi.org/10.1136/adc.2005.092007.
- Peters R, Barlow J. Systematic review of instruments designed to predict child maltreatment during the antenatal and postnatal periods. Child Abuse Rev 2005;12:416-39. http://dx.doi.org/10.1002/car.821.
- Woodman J, Lecky F, Hodes D, Pitt M, Taylor B, Gilbert R. Screening injured children for physical abuse or neglect in emergency departments: a systematic review. Child Care Health Dev 2007;36:153-64. http://dx.doi.org/10.1111/j.1365-2214.2009.01025.x.
- Damasio AR. Descartes’ Error: Emotion, Reason and the Human Brain. New York, NY: Avon Books; 1994.
- Haidt J. The emotional dog and its rational tail: a social intuitionist approach to moral judgement. Psychol Rev 2001;108:814-34. http://dx.doi.org/10.1037/0033-295X.108.4.814.
- Printz J. The Emotional Construction of Morals. Oxford: Oxford University Press; 2007.
- Gigerenzer G. Reckoning with Risk. London: The Penguin Press; 2002.
- Green J. Epistemology, evidence and experience: evidence based health care in the work of Accident Alliances. Sociol Health Illn 2000;22:453-76. http://dx.doi.org/10.1111/1467-9566.00214.
- Payne J, Bettman J, Koehler D, Harvey N. Blackwell Handbook of Judgment and Decision Making. Oxford: Blackwell Publishing; 2007.
- Fish S, Munro E, Bairstow S. Learning Together to Safeguard Children: Developing a Multi-Agency Systems Approach for Case Reviews. London: SCIE; 2008.
- Wastell D, White S, Broadhurst K, Hall C, Peckover S, Pithouse A. Children’s services in the iron cage of performance management. Int J Soc Welfare 2010;19:310-20. http://dx.doi.org/10.1111/j.1468-2397.2009.00716.x.
- Munro E. A systems approach to investigating child abuse deaths. Br J Soc Work 2005;35:531-46. http://dx.doi.org/10.1093/bjsw/bch194.
- Hall C, Parton N, Peckover S, White S. Child-centric ICTs and the fragmentation of child welfare practice in England. J Soc Policy 2010;39:393-41. http://dx.doi.org/10.1017/S0047279410000012.
- Broadhurst K, White S, Wastell D. Risk, instrumentalism and the humane project in social work – identifying the informal logics of risk management in children’s statutory services. Br J Soc Work 2010;40:1046-64. http://dx.doi.org/10.1093/bjsw/bcq011.
- Peckover S, Hall C, White S. From policy to practice: the implementation and negotiation of technologies in everyday child welfare. Child Soc 2008;23:136-48. http://dx.doi.org/10.1111/j.1099-0860.2008.00143.x.
- Trkman P. The critical success factors of business process management. Int J Inf Manage 2010;30:125-34. http://dx.doi.org/10.1016/j.ijinfomgt.2009.07.003.
- Lillrank P, Liukko M. Standard, routine and non-routine processes in health care. Int J Health Care Qual Assur 2004;17:39-46. http://dx.doi.org/10.1108/09526860410515927.
- Mannion R, Konteh F, Davies H. Assessing organisational culture for quality and safety improvement: a national survey of tools and tool use. Qual Saf Health Care 2009;18:153-6. http://dx.doi.org/10.1136/qshc.2007.024075.
- Weick K. Organizational culture as a source of high reliability. Calif Manage Rev 1987;29:112-27. http://dx.doi.org/10.2307/41165243.
- Pava C. Managing New Office Technology. New York, NY: Free Press; 1983.
- Pava C. Redesigning sociotechnical systems design: concepts and methods for the 1990s. J Appl Behav Sci 1986;22:201-21. http://dx.doi.org/10.1177/002188638602200303.
- Mannion R, Davies H, Harrison S. Changing Management Cultures and Organisational Performance in the NHS. London: SDO; 2010.
- Dodek P, Cahill NE, Heyland DK. The relationship between organizational culture and implementation of clinical practice guidelines: a narrative review. J Parenter Enteral Nutr 2010;34:669-74. http://dx.doi.org/10.1177/0148607110361905.
- Mannion R, Davies H. Measuring and Assessing Organisational Culture in the NHS. London: NCCSDO; 2008.
- Schein E. Organizational Culture and Leadership: A Dynamic View. San Francisco, CA: Jossey-Bass; 1992.
- Hofstede G. Culture’s Consequences: Comparing Values, Behaviors, Institutions, and Organizations Across Nations. Thousand Oaks, CA: Sage Publications; 2001.
- Shih C, Huang S. Exploring the relationship between organizational culture and software process improvement deployment. Inf Manage 2010;47:271-82. http://dx.doi.org/10.1016/j.im.2010.06.001.
- Martin J. Cultures in Organizations: Three Perspectives. New York, NY: Oxford University Press; 1992.
- The Code: Standards of Conduct, Performance and Ethics for Nurses and Midwives. London: Nursing and Midwifery Council; 2008.
- Ravishankar M, Pan S, Leidner D. Examining the strategic alignment and implementation success of a KMS: a subculture-based multilevel analysis. Inf Syst Res 2011;22:39-5. http://dx.doi.org/10.1287/isre.1080.0214.
- Vincent C. Patient Safety. Chichester: Wiley-Blackwell; 2010.
- Weick K, Sutcliffe K, Obstfeld D, Boin A. Crisis Management. Los Angeles, CA: Sage; 2008.
- Hollnagel E. Human Reliability Analysis: Context and Control. London: Academic Press; 1993.
- Weick K, Sutcliffe K. Managing the Unexpected: Assuring High Performance in an Age of Complexity. San Francisco, CA: Jossey Bass; 2001.
- Markus LM, Benjamin R. The magic bullet theory in IT-enabled transformation. Sloan Manage Rev 1997;38:55-68.
- Rogers E. Diffusion of Innovations. New York, NY: Macmillan; 1983.
- Wastell D, McMaster T. Organisational dynamics of technology-based innovation: diversifying the research agenda. J Inf Technol 2008;23:63-70. http://dx.doi.org/10.1057/palgrave.jit.2000133.
- Cresswell K, Worth A, Sheikh A. Actor-network theory and its role in understanding the implementation of information technology developments in healthcare. BMC Med Inf Decis Mak 2010;10:1-13. http://dx.doi.org/10.1186/1472-6947-10-67.
- Van de Ven A, Huber G, Glick W. Organizational Change and Design. Oxford: Oxford University Press; 1993.
- World Alliance for Patient Safety. Geneva: WHO; 2004.
- Carthey J, Clarke J. Patient Safety First: The ‘How to Guide’ for Implementing Human Factors in Healthcare. London: Patient Safety First; 2009.
- Reason J. Human error: models and management. BMJ 2000;320:768-70. http://dx.doi.org/10.1136/bmj.320.7237.768.
- Transparency in Outcomes: A Framework for Adult Social Care. London: DH; 2011.
- Nicholson D. The Operating Framework for the NHS in England 2011/12. London: Department of Health; 2011.
- Kennedy I. Getting it Right for Children and Young People: Overcoming Cultural Barriers in the NHS so as to Meet their Needs. London: Department of Heath; 2010.
- Waring J. Getting to the ‘roots’ of patient safety. Int J Qual Health Care 2007;19:257-8. http://dx.doi.org/10.1093/intqhc/mzm035.
- Rushton A, Beaumont K. Social work in healthcare settings: turning full circle?. Clin Child Psychol Psychiatry 2002;7:295-302.
- Currie G, Waring J, Finn R. The limits of knowledge management for public sector modernisation: the case of patient safety and quality. Public Adm 2008;86:363-85. http://dx.doi.org/10.1111/j.1467-9299.2007.00705.x.
- Vaughan D. The dark side of organizations: mistake, misconduct, disaster. Ann Rev Sociol 1999;25:271-305. http://dx.doi.org/10.1146/annurev.soc.25.1.271.
- Hevner A, March S, Park J, Ram S. Design science in information systems research. MIS Q 2004;28:75-105.
- Wastell D, Sauer J, Schmeink C. Time for a ‘design turn’ in IS innovation research? A practice report from the home front. Inf Technol People 2009;22:325-50. http://dx.doi.org/10.1108/09593840911002441.
- van Aken JE. Management research as a design science: articulating the research products of mode 2 knowledge production in management. Br J Manag 2005;16:19-36.
- Mingers K. Combining IS research methods: towards a pluralist methodology. Inf Syst Res 2001;12:240-59. http://dx.doi.org/10.1287/isre.12.3.240.9709.
- Creswell J, Plano Clark VL. Designing and Conducting Mixed Methods Research. London: Sage; 2010.
- Waring J, McDonald R, Harrison S. Safety and complexity: the inter-departmental threats to patient safety in the operating department. J Health Organ Manag 2006;20:227-42. http://dx.doi.org/10.1108/14777260610662753.
- Waring J, Harrison S, McDonald R. A culture of safety or coping: ritualistic behaviours in the operating department. J Health Serv Res Policy 2007;12:3-9. http://dx.doi.org/10.1258/135581907780318347.
- Stringer E, Genat W. Action Research in Health. Upper Saddle River, NJ: Merrill Prentice Hall; 2004.
- Adler P, Adler P, Lee RM, Renzetti CM. Researching Sensitive Topics. London: Sage; 1993.
- Strathern M, Jackson A. Anthropology at Home. London: Tavistock; 1987.
- Seale C. The Quality of Qualitative Research. London: Sage; 1999.
- Lincoln Y, Guba E. Naturalistic Enquiry. Beverley Hills, CA: Sage; 1985.
- Brewer J. The ethnographic critique of ethnography. Sociology 1994;28:231-44. http://dx.doi.org/10.1177/0038038594028001014.
- Child Protection Companion: Second Edition. London: Royal College of Paediatrics and Child Health; 2013.
- When to Suspect Child Maltreatment. London: NICE; 2013.
- Kripanlani S, LeFevre F, Phillips C, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA 2007;297:831-41. http://dx.doi.org/10.1001/jama.297.8.831.
- Avison D, Young T. Time to rethink health care and ICT. Commun ACM 2007;50:69-74. http://dx.doi.org/10.1145/1247001.1247008.
- Shannon C. A mathematical theory of communication. Bell Syst Tech J 1948;27:379-423. http://dx.doi.org/10.1002/j.1538-7305.1948.tb01338.x.
- Winthereik B, Vikkelsø S. ICT and integrated care: some dilemma of standardising inter-organisational communication. Comput Support Coop Work 2005;14:43-67. http://dx.doi.org/10.1007/s10606-004-6442-9.
- Rasmussen T. Social Theory and Communication Technology. Aldershot: Ashgate; 2000.
- Kanfer A, Haythornthwaite C, Bowker G, Bruce B, Burbules N, Porac J, et al. Modelling distributed knowledge processes in next generation multi-disciplinary alliances. Inf Syst Front 2000;2:317-31. http://dx.doi.org/10.1023/A:1026520728644.
- Aas K. Sentencing in the Age of Information: From Faust to Macintosh. London: Glasshouse Press; 2005.
- Star S, Griesemer J. Institutional ecology, ‘translations’ and boundary objects: amateurs and professionals in Berkley’s Museum of Vertebrate Zoology. Soc Stud Sci 1989;19:387-420. http://dx.doi.org/10.1177/030631289019003001.
- Saario S, Hall C, Peckover S. Inter-professional electronic documents and child health: a study of persisting non-electronic communication in the use of electronic documents. Soc Sci Med 2012;75:2207-14. http://dx.doi.org/10.1016/j.socscimed.2012.08.019.
- Prottas J. People Processing – The Street-Level Bureaucrat in Public Service Bureaucracies. Lexington: Lexington Books; 1979.
- Moran P, Jacobs C, Bunn A, Bifulco A. Multi-agency working: implications for an early-intervention social work team. Child Fam Soc Work 2007;12:143-51. http://dx.doi.org/10.1111/j.1365-2206.2006.00452.x.
- Frost N, Robinson M. Joining up children’s services: safeguarding children in multi-disciplinary teams. Child Abuse Rev 2007;16:184-99. http://dx.doi.org/10.1002/car.967.
- Platt D. Threshold decisions: how social workers prioritize referrals of child concern. Child Abuse Negl 2006;15:4-18. http://dx.doi.org/10.1002/car.929.
- Cleaver H, Barnes J, Bliss D, Cleaver D. Developing Information Sharing and Assessment Systems. Research Report RR597. London: Department for Education and Skills; 2004.
- Lash S. Critique of Information. London: Sage; 2002.
- Making it Better. Assuring High-Quality Care in the NHS. 2013.
- Munro E. The Munro Review of Child Protection: Final Report – A Child-Centred System. London: Stationery Office; 2011.
- Mannion R, Davies H, Marshall M. Cultures for Performance in Health Care. Buckingham: Open University Press; 2005.
- Calnan M, Rowe R. Trust Matters in Health Care. Maidenhead: Open University Press; 2008.
- A Promise to Learn – A Commitment to Act: Improving the Safety of Patients in England. London: National Advisory Group on the Safety of Patients in England; 2013.
- Zerubavel E. Hidden Rhythms: Schedules and Calendars in Social Life. Chicago, IL: Chicago University Press; 1981.
- Zerubavel E. Patterns of Time in Hospital Life. Chicago, IL: University of Chicago Press; 1979.
- Pithouse A, Hall C, Peckover S, White S. A tale of two CAFs: the impact of the electronic common assessment framework. Br J Soc Work 2009;39:599-612. http://dx.doi.org/10.1093/bjsw/bcp020.
- White S, Hall C, Peckover S. The descriptive tyranny of the common assessment framework: technologies of categorization and professional practice in child welfare. Br J Soc Work 2009;39:1197-217. http://dx.doi.org/10.1093/bjsw/bcn053.
- Levi B, Dellasega C, Boehmer S. What is reasonable suspicion of child abuse?. J Public Child Welfare 2012;6:569-89. http://dx.doi.org/10.1080/15548732.2012.683374.
- Miller R, Mannion R, Freeman T, Davies H. Hospital board oversight of quality and patient safety: a narrative review and synthesis of recent empirical research. Milbank Q 2013;91:738-70. http://dx.doi.org/10.1111/1468-0009.12032.
- Wastell D, White S, Broadhurst K. Children’s services in the iron cage of performance management: street-level bureaucracy and the spectre of Švejkism. Int J Soc Welfare 2010;19:310-20.
- Wastell D. The fetish of technique: methodology as a social defense. Inf Syst J 1996;6:25-40. http://dx.doi.org/10.1111/j.1365-2575.1996.tb00003.x.
- Baker D, Gustafson S, Beaubien J, Salas E, Barach P. Medical Teamwork and Patient Safety: The Evidence-Based Relation. Rockville, MD: Agency for Healthcare Research and Quality; 2005.
- Waring J, Marshall F, Bishop S, Sahota O, Walker M, Currie G, et al. An ethnographic study of knowledge sharing across the boundaries between care processes, services and organisations: the contributions to ‘safe’ hospital discharge. Health Serv Deliv Res 2014;2. http://dx.doi.org/10.3310/hsdr02290.
- Schumacher E. Small is Beautiful: A Study of Economics as if People Mattered. London: Vintage; 1993.
- Seddon J. Systems Thinking in the Public Sector. Axminster: Triarchy Press; 2008.
- Kawalek P. The bubble strategy: case study of dynamic, defensible processes in Salford. Int J Public Sect Manage 2007;20:178-91. http://dx.doi.org/10.1108/09513550710740599.
- Kotter J. Leading change: why transformation efforts fail. Harv Bus Rev 1995;74:59-67.
- Weick K, Huber G, Glick W. Organizational Change and Redesign. New York, NY: Oxford University Press; 1995.
- Brandon M, Bailey S, Belderson P, Gardner R, Sidebotham P, Dodsworth J, et al. Understanding Serious Case Reviews and their Impact: A Biennial Analysis of Serious Case Reviews, 2005–07. Norwich: University of East Anglia; 2009.
- Lick DW. A new perspective on organisational learning: creating learning teams. Eval Prog Plan 2006;29:88-96. http://dx.doi.org/10.1016/j.evalprogplan.2005.08.004.
- Argyris C. On Organisational Learning. Malden, MA: Wiley-Blackwell; 1999.
- Munro E. The Munro Review of Child Protection: Part 1 – A Systems Analysis. London: Department for Education; 2010.
Appendix 1 Overview of SPRINT
The SPRINT methodology comprises a generic toolbox of techniques and ‘best practices’ for design. Here, we briefly set out its main principles as these are universal; specific technical details may be found on the SPRINT website (managingbydesign.net) and in Wastell. 17 SPRINT is in the public domain and there are no copyright or commercial interests.
SPRINT comprises three main phases, each defined in terms of a set of aims, and there is a set of tasks within each phase. Phase 1 (investigate process context) is essentially one of analysis. It is the most important phase, and comprises a range of investigative tasks aimed at gaining a thorough ‘diagnostic understanding’ of areas where improvement is sought, including the use of process mapping and ethnographical methods. The general aims are to understand the service context of the project by considering all relevant perspectives, to analyse the effectiveness and efficiency of current processes in this broader context, and to generate ideas for improvements. Phase 2 involves the development of one or more design proposals, setting out ideas for service innovation, backed up by business cases involving clearly specified and measurable outcomes. Phase 3 focuses on implementation, the management of change and evaluation as the basis for continuous improvement.

A number of important principles underpinning SPRINT are as follows:
-
Innovation. SPRINT encourages the search for innovative solutions: although SPRINT emphasises the need to be innovative with technology, it may well be that only a process redesign, a new therapeutic technique or reorganisation of staff is required.
-
Incremental implementation: while design is the exercise of creative imagination, SPRINT acknowledges that implementation is the art of the possible. While it is important to encourage radical ideas, in practice the pragmatics of implementation may oblige a step-by-step approach.
-
Breadth of vision and multiple perspectives: SPRINT recognises that a range of different points of view are relevant to a design project and must be triangulated to develop a full understanding. The importance is stressed of seeking out and examining all stakeholder perspectives.
-
Depth of understanding: the need to develop a rigorous understanding of the realities of everyday practice is a sine qua non, and ethnographic methods are unequivocally recommended. One of the primary reasons for the failure of IT systems is that they are designed on a fictitious view of working practices, gleaned from the procedure manual or indeed from managers who are out of touch with what their staff actually do.
-
User-centred design: a participative approach is indispensable.
-
Evaluation and benefits management: SPRINT stresses the need to set measurable objectives at the outset of projects and to measure achievements against these goals.
-
Evidence-based practice: design should always be informed by the best evidence. As well as gathering detailed local intelligence, SPRINT encourages its users to look externally, at published academic research and at other organisations facing similar issues (benchmarking).
Appendix 2 Interview materials
This appendix contains a sample interview schedule, the consent form and the participant information sheet.
Sample semistructured interview schedule (hospital staff)
Opening:
-
Thank participant for agreeing to be interviewed.
-
Remind about reasons for interview/study: ‘You are being invited to take part in the study because you are involved in the care of patients, the design of systems or receipt of referrals. We want to understand what you see as the factors that support or hinder communication between different professionals, families and children, and how you see this as affecting diagnosis and outcome. These views will help us identify whether the initiatives currently being piloted are working’.
-
Remind about anonymity.
-
Emphasise that interviewee does not have to answer questions they would rather not.
Questions:
-
When were you last concerned that a child in your care might be at risk of abuse? What happened?
-
What helps you to safeguard and promote the health and wellbeing of your patients as much as possible?
-
What do you understand about sharing information to different agencies about safeguarding?
-
Do you think there‘s anything that could improve communication pathways regarding safeguarding between colleagues and professionals from other agencies?
-
What do you think of the ‘walkrounds’ as a way helping communication?
-
What is your opinion of the online referral/information sharing system for safeguarding children?
-
What is the range of support and advice available to you around child protection and how might it be improved?
-
How do you learn about things that have gone wrong in child protection cases and how practice might be improved?
-
What are the ‘pebbles in your shoes’ that get in the way of you safeguarding and promoting the welfare of your patients?
Consent form
Participant information sheet
We would like to invite you to take part in our research study. Before you decide whether you would like to take part we would like you to understand why the research is being done and what it would involve for you. One of our team will go through the information sheet with you and answer any questions you have. Please feel free to talk to others about the study if you wish and do not hesitate to ask us if there is anything that is not clear.
What is the purpose of the study?
Hospitals feature significantly in the lives of many children who are neglected or non-accidentally harmed, but errors in professional decision-making can sometimes occur. In children’s health care, the range of factors affecting such judgements is broader than in many other settings and the network of people involved is dispersed. The interface between hospital-based services for children and local authority children’s social care is particularly important and requires innovative service design. This research will extend and evaluate clinician-led initiatives designed to improve accurate diagnosis, assessment and referral of children who have been harmed, or who are at risk of harm. The aim of the study is to identify interventions and practices that support improved communication between care processes, services and organisations so as to promote safe practice and at the same time reduce the numbers of false positives which cause unnecessary distress to families.
Why have I been invited?
You are being invited to take part in the study because you are involved in the care of patients, the design of systems or receipt of referrals. We want to understand what you see as the factors that support or hinder communication between different professionals, families and children, and how you see this as affecting diagnosis and outcome. We are inviting a range of key professionals involved in the assessment and diagnosis of children presenting in secondary health settings or receiving referrals from them to take part. Together these views will help us identify whether the initiatives currently being piloted are working and help us to redesign and innovate further where necessary. We aim to ensure that our recommendation will be relevant to people, like yourself, who are involved in the organisation and delivery of care in this complex area.
Do I have to take part?
No, it is up to you to decide whether or not to take part. If you do decide to take part you will be given this information sheet to keep and be asked to sign a consent form. If you decide to take part you are still free to withdraw at any time and without giving a reason.
What will happen to me if I take part?
We will ask you to take part in a one-to-one interview with a member of the research team. The interview will ask about your work role to understand how you are involved in the assessment and treatment of children and families, and it will ask you to describe how the current processes are operating in your workplace. The interview will also seek your views about the factors that support or hinder communication and how you see this as accurate assessment of children at risk. We will also ask you for your recommendations to improve current systems and processes.
The interview will last up to one hour, and will be undertaken in a private location of your choosing, such as a departmental office. With your consent, the interview will be recorded to ensure we accurately keep a record of your views, but all personal information will be kept confidential and your anonymity will be maintained.
What will happen to the information I give?
Subject to your written consent interviews will be transcribed by a member of the research team or a confidential transcription service used by the University of Birmingham. After transcription the recordings will be destroyed and the transcripts will be stored on a secure password protected computer. Nobody outside of the research team will have access to the transcripts, but selected and anonymous quotations may be used in the research report or subsequent publications.
What are the possible benefits of taking part?
We cannot promise the study will help you or your service but the information we get from this study will help us identify what is working well and will inform further system design to improve communication and ultimately improve the safety of children attending the hospital.
What if there is a problem?
If you have a concern about any aspect of this study, you should ask to speak to the researchers who will do their best to answer your questions. The Study Lead, Professor Susan White, is also available to answer your concerns and can be contacted by telephone or e-mail. If you remain unhappy you may contact Dr Brendan Laverty, Assistant Director (Contracts and Governance), by telephone or by e-mail.
What if we find something wrong?
We want you to be able to share your views on the safety of the systems and to identify areas where you think errors may occur. However, it is important that if we find something wrong which places patients at risk or in the delivery of patient care, including malpractice or poor performance that we bring this to light and share this information with the team responsible for the patient’s care, as well as local service leaders so that they can act accordingly. Should such an incidence occur it will be referred to Dr Suzanne Smith, Head of Safeguarding, for her to deal with the matter in accordance with Trust processes and procedures. However should it be considered necessary to disclose any information as outlined above we will always inform you of our actions before hand.
Will my taking part in the study be kept confidential?
All information which is collected about you during the course of the research will be kept strictly confidential, stored in a secure and locked office, and on a password protected computer system. Any information about you which leaves the hospital will have your name and work address removed (anonymised) and a unique code will be used so that you cannot be recognised from it. The procedures for handling, processing, storage and destruction of the data meet the requirements of the Data Protection Act 1998.
Your personal data will be kept for up to 1 year after the end of the study so that we are able to contact you about the findings of the study (unless you advise us that you do not wish to be contacted). All research data will be kept securely for 5 years. After this time your data will be disposed of securely. During this time all precautions will be taken by all those involved to maintain your confidentiality and only members of the research team will have access to your personal data.
Authorised representatives of the sponsor or NHS host organisation may have limited access to your personal data in order to monitor or audit our conduct of this research. These representatives are subject to the same duty of confidentiality as the research team.
What will happen if I do not want to carry on with the study?
Your participation is voluntary and you are free to withdraw at any time, without giving any reason, and without your legal rights being affected. If you withdraw then the information collected so far cannot be erased and this information may still be used.
Should you experience distress as a consequence of your participation in the study the researcher will in the first instance offer any clarification you may require. You will also be able to access a confidential counselling service that is accessible to all Pennine Acute Hospital NHS Trust (PAHNT) employees. The counsellors are situated on various sites around the Trust within the Mediscreen Occupational Health Departments at Rochdale Infirmary, Fairfield General Hospital, Royal Oldham Hospital and North Manchester General Hospital. The service comprises a team of dedicated, trained, professional counsellors who work within the guidelines of the British Association of Counselling and Psychotherapy. The service is confidential, flexible and tailored to each individual’s needs. Counselling is a confidential professional service for personal and work related issues.
Who is organising and funding the research?
This research is being organised by the University of Birmingham and is being funded by National Institute for Health Research’s Health Services Research Programme.
Who has reviewed the study?
This study has been reviewed by the NRES Committee North West – Greater Manchester South, which is an independent group of people.
Appendix 3 Example walkround quarterly report
A total of 10 audits were undertaken within the period in question. The following table has been extracted from the quarterly report. It enumerates each question asked in the walkround and summarises the response.
| Question | Response |
|---|---|
| When were you last concerned that a patient in your care might be at risk of abuse? | Three said that they were concerned about a patient within the last month. Six said that they had concerns within the last 2 weeks. One could not recall an event |
| What happened? | Reponses included:
|
| Can you describe what you think defines abuse? | Physical (n = 8), sexual (n = 3), neglect (n = 2), financial (n = 2), emotional (n = 6), verbal (n = 1), anything not in the patient’s best interests (n = 1) |
| Can you describe what would you do if you suspected a patient was being abused? | Raise a safeguarding alert (including adult, child and midwifery forms) (n = 7) Discuss with colleagues including their manager and the safeguarding team (n = 10) Speak with the patient (n = 3) |
| Can you say what training is available around safeguarding? | Classroom safeguarding training (n = 8) E-learning (n = 6) Peer supervision (n = 1) Not aware of any safeguarding training (n = 1) |
| Were you able to safeguard and promote the health and well-being of your patients this week as much as possible? | Yes (n = 8) Mostly (n = 1) No (n = 1) |
| Who do you think is responsible for safeguarding patients’ welfare? | Everybody (n = 10). All agreed that it was everyone’s responsibility and some elaborated to mention which agencies played key roles |
| Can you describe what other agencies are involved in safeguarding apart from in the hospital? | Social care (n = 8), police (n = 7), charities (n = 2), teachers (n = 1), GPs (n = 6), DNs (n = 2), school nurses (n = 2), health visitors (n = 4), midwives (n = 2), security (n = 1) |
| How would you feel if you had to make a referral to the local authority SC about a patient today? | Would not have a problem (n = 5) Fearful (n = 1) It is my job but I would find it upsetting (n = 1) It is my job but I would find it stressful (n = 3) |
| What would you expect to happen after you made a referral? | Feedback (n = 6) Someone will intervene – strategy meeting, come to the ward, etc. (n = 8) |
| What would you do if another health professional disagreed with you about a safeguarding concern? | Five would discuss with the safeguarding team or their manager, four stated that they would still do the referral, one would challenge colleague’s opinion |
| Can you describe what you would do if you had evidence to suggest a colleague was involved in abusing patients? | Involve management (n = 7), discuss with the safeguarding team (n = 4), complete an incident (n = 1), follow whistleblowing policy (n = 1), don’t know (n = 1) |
| Can you describe how you would respond to a child or adult who disclosed abuse? | Discuss with manager/safeguarding team (n = 6), document (n = 4), reassure the patient and tell them what to expect (n = 8), get consent to share information (n = 1), I would feel upset (n = 1), listen (n = 1), be sympathetic (n = 1) |
| What do you know about sharing information to different agencies about safeguarding? | Only share relevant information (n = 4), do not give notes out but we can discuss face to face (n = 1), get consent (n = 2), needs to be in line with Data Protection Act (n = 3) |
| Do you think that there’s anything that could improve communication pathways regarding safeguarding between colleagues and professionals from other agencies? | Suggestions included: No improvements can be made (n = 2) Feedback on referrals and queries (n = 3) More staff (n = 2) Electronic patient notes on a shared system so that all agencies can see when a patient presents, etc. (n = 3) |
| Do you always record your concerns? | Yes (n = 10) |
| Do you know where to seek support and advice? | Yes (n = 10) |
| Have you ever discussed your concerns with patients/relatives? | No (n = 2), yes (n = 8), I have had no reason to do so (n = 1) |
| What do you think the trust could do to make sure we protect patients from abuse? | Answers included: More education and training (n = 4) More staff on the shop floor (n = 1) Better record keeping (n = 1) Patient satisfaction survey (n = 1) |
| What are the pebbles in your shoes that get in the way of you safeguarding and promoting the welfare of patients? | Answers included: Staff shortages (n = 2) Patients who move wards constantly lack continuity of care (n = 1) Too busy (n = 1) Lack of interagency working from CSC (n = 1) CAF paperwork is too bulky (n = 1) Parents who conceal information or are aggressive can be intimidating (n = 2) |
| Can you describe how you would identify early signs of risky behaviours? | Alcoholics (n = 4), drug users (n = 4), unprotected sex (n = 1), repeated admissions (n = 1), aggression (n = 2), fear (n = 1), non-compliant with treatment (n = 2), inconsistent history (n = 1) |
| What do you understand as acceptable in terms of restraint? | It is used to protect the patient or others from harm (n = 5) |
| What do you think that the trust can do to make sure patients’ dignity, rights and best interests are met? | Answers included: Training/discussions re safeguarding (n = 2), treat everyone as an individual (n = 1), nothing (n = 1), patient surveys (n = 2) |
Appendix 4 Electronic Cause for Concern referral form (user guide)
This appendix presents a synopsis of the user manual for the electronic CFC/Safeguarding Children Referral form. The purpose of the form is to allow practitioners from all areas to highlight concerns to relevant community health professionals. In addition, the form serves as a referral form to alert CSC (where a child is at risk of significant harm) or where a child is identified as ‘in need’ (Children Act 1989). 19 This booklet aims to help practitioners to work their way through the new form.
1. Access the form
To access and use the electronic Cause for Concern/Safeguarding Children Referral form follow the instructions below:
-
Access the Trust intranet and go into the interactive menu.
-
Select the online form icon at the top of the page.
-
Select the Cause for Concern/Safeguarding Children Referral form icon.
2. Patient details
Complete patient’s hospital and/or NHS number and the patient’s date of birth (mandatory field) and click ‘get patient details’. Once the details have been received the screen will self-populate with all of the necessary details such as GP and NHS number and should look like the screen below:
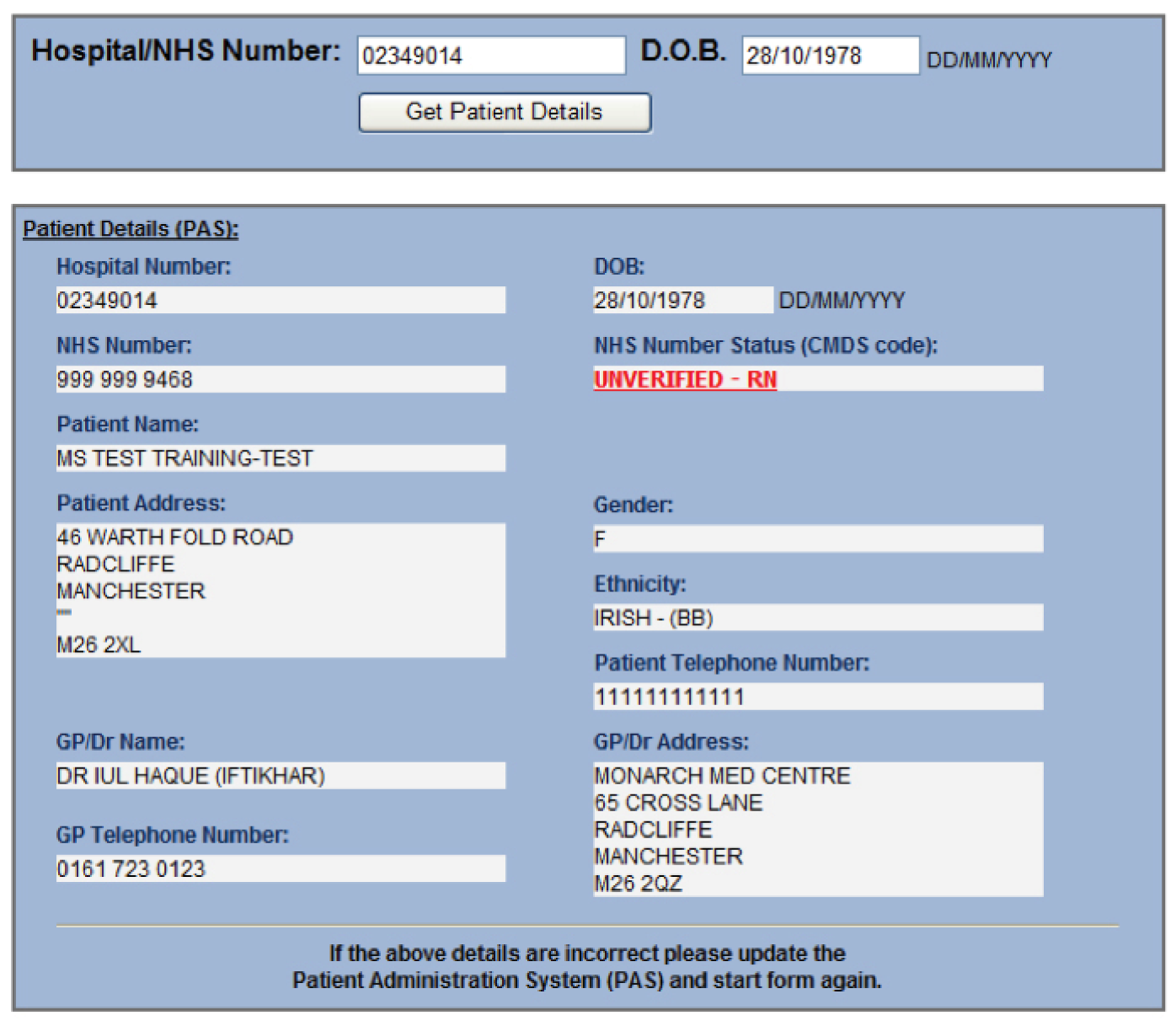
3. Referrer’s details
This box is important, as it will provide professionals from other agencies with details on how to contact you if they need to discuss the referral you have made.
4. Referral type
It is crucial that you identify the CORRECT referral type. Guidance as to the meaning of the options is given below.
Information sharing: This category is to be used when we wish to share a concern such as safety in the home with the community professionals involved in the child’s life. This information is then sent to either the school nurse or the health visitor. This is not a referral to children’s social care.
Child in need – section 17:
A child is in need if:
-
He is unlikely to achieve and maintain, or to have to opportunity of achieving or maintaining, a reasonable standard of health or development without the provision of services by the local authority.
-
Health or development it to be significantly impaired or further impaired without the provision of such services.
-
He is disabled.
Child protection – section 47:
Where there is reasonable cause to suspect that a child is suffering or is likely to suffer significant harm. This can include harm or likelihood of harm, which is attributable to a lack of adequate parental care or control.
5. Primary carers
-
Identify the person that the child lives with and who provides most of the care for that child – it may not necessarily be a parent.
-
It is mandatory to provide details on parental responsibility. If you are unsure about what this is, click the highlighted box and guidance will point you in the right direction.
-
Complete details of family composition/significant others. It is important to question if the child has any siblings and who else lives in the household.
6. SBAR: Situation/Background/Assessment/Recommendation
-
Complete SBAR boxes in as much detail as possible using the prompts in the right-hand boxes. These prompts can be copy and pasted into the information boxes to provide the beginning of your sentence which may help save time if necessary.
-
Use of the SBAR tool will produce a referral which is clear and accurate.
-
Respond to the question about whether or not the child is aware of the information sharing/referral and select from the drop-down box yes, no or N/A.
-
Respond to the question about whether or not the parent/carer is aware about the information sharing/referral.
-
If the answer to this question is ‘no’ then a box will pop onto the screen asking for details why they have not been informed.
-
If the answer is ‘no’ and you are making a child in need s17 referral, a pop up box will remind you that consent is required for this referral type.
-
Complete the free-text box requesting details of the parent/carers view of the referral (this is a mandatory field). You can include details of the parent’s reaction when they were informed.
-
Complete the question about whether or not a CAF/Common Assessment Framework has been completed for the child/young person. The CAF is a nationally standardised process designed to help practitioners get a complete picture of a child’s additional needs at an early stage. If you answer yes to this question then the form will ask for the agency name and lead professional.
-
Complete the final field prompting any further information which you may wish to be included; this may be information which will help the referral process or can be used to include extra information about siblings, etc.
-
Submit the form.
-
If the referral type is ‘information sharing’ the form will automatically be submitted to the Trust Safeguarding Team who will ensure it is securely delivered to the appropriate Named Nurse Team in the community.
-
If the referral type is ‘child protection s47’ or child in need s17’ once you have clicked ‘submit form’ you must print the form and fax it to the relevant local authority where the child resides. This must be done after you have telephoned through your referral. A list of phone and fax numbers will appear on the screen once you have clicked send.
When you have submitted the form the Trust Safeguarding Team will ensure it is securely delivered to the appropriate Named Nurse Team in the community.
Appendix 5 Information sharing/safeguarding children referral form
Appendix 6 Design in action: a case study
The sharing of information in midwifery is achieved with use of a form called the Special Circumstances Form (SCF). The transfer of this paper form and sharing it across organisational boundaries has at times been problematic. The form has now been developed as an online facility. The rate of information sharing from the forms has remained stable as it has always been well used. The criteria for using the form has changed to raise the threshold when it would be used so we expect to see a drop in numbers of forms going forward.
Pennine Board Report, April 2013
Context: the triumph of protocol over common sense
Hospital-based and community midwives are critical players in the identification of women who may be at risk during pregnancy from, for example, substance, or domestic abuse and also are often the first professionals to identify potential danger to an as yet unborn infant. The midwives differ from many other professionals in the system in that their relationship with the women with whom they work extends over time and their knowledge of the women’s personal and social circumstances can be considerable. This contrasts with ‘brief hospital encounters’, though there can be a downside, as one senior practitioner astutely observed:
[S]ometimes if you work in areas of high social deprivation and you’re in and out of houses all the time where standards may be, for example physical cleanliness levels or interaction with children are very poor. It can start to feel a bit normal to you. You can normalise because you’re not seeing the wider picture. I don’t think that happens straight away but it does happen if you’re working in those areas for prolonged periods. You sort of, it’s almost like your thresholds for acceptability reduce down a little bit too much.
Specialist midwife (MW6)
Knowing women over extended periods, midwives are in touch with changing circumstances over the course of the pregnancy, potentially altering the nature of the midwife’s relationship with the woman. Self-evidently, newborn infants are also at particularly high risk of harm if their basic care needs are not met, or if they are injured accidently or non-accidentally. Thus, midwives are likely to encounter a considerable number of ‘special circumstances’, knowledge of which they may wish to share with other agencies, including CSC. The complexities are exacerbated by the fact that CSC do not usually accept referrals relating to unborn infants until 18–20 weeks of gestation.
The SCF for Pennine was the subject of a design project initiated during the course of the research. There were two key aims: first, to replace the paper forms with an online system, and second, to review and revise the criteria which triggered the production of these forms. An important advantage of an online system would be to simplify the logistics whereby the forms were incorporated into the patients’ hospital notes. It is clearly critical that this information is available to hospital staff when the woman is admitted for delivery, and, to ensure that they stand out in the notes, the forms are printed on yellow paper. However, the forms are completed by midwives in the community, and to ensure that they are lodged in the notes the midwife must physically transport them to the relevant hospital, filing them by hand in order to alert attending staff when the woman presents in labour. This is evidently time-consuming, and by obviating the need for such a journey, the online system should bring real benefits, as the following interview extracts with two community midwives attest:
We do a special circumstance form for ladies’ case notes. It’s a yellow form that gets entered into the notes. It’s going to be going online soon which is going to be a bonus for us because the problem we have now at [location] is the lady’s case notes are kept here until she’s 28 weeks then they get sent to Oldham. So if we have got to update these forms we have to drive to [location], park up, walk a million miles to just write in the notes. So it’s going to be online so the updates can be done online which will be much, much better.
Community midwife (MW5)
We’re going online with the system and I think being online if we have to update somebody’s notes we have got to where the case notes are held so it’s often difficult trying to actually get to, you know, so I think once it’s online that will be better, things will be updated live rather than a few days later when you get the opportunity to do it.
Community midwife (MW7)
A more fundamental problem with the ‘yellow forms’ is the progressive lowering of thresholds since the form was first introduced; originally, these were produced only for serious cases, but now they have become the norm:
[A]t one time when we started off the system of the yellow form we used to call it, if someone had a yellow form in their notes it was a big you know, big deal – ‘She’s got a yellow form. She’s got a yellow form’ and a report was always handed over – ‘She’s got a yellow form’ and the circumstances. But now it’s almost become a bit of a sort of standing joke in midwifery that ‘Oh what, she hasn’t got a yellow form?’.
Specialist midwife (MW6)
‘Cos years ago those yellow forms – we have had them quite a long time but they were only done for serious cases. But it’s as these lists come up, you must do them for this, this, this and this, that’s when it becomes, it’s not a big deal any more . . . It’s not like an alert – ooh you know, just check that out. So if they could change that, that would be better because you could have the yellow for the serious ones, the ones that really need concern but then a different colour for the ones that are a history of, just watch out kind of thing.
Community midwife (MW5)
The senior midwives we interviewed, mainly team leaders, provided numerous examples of situations where special circumstances were produced needlessly:
But the trouble with these yellow forms are the form is done for anybody with a history of depression for example. So say I was 16, my mother died, I was going through my GCSEs [General Certificate of Secondary Education] and I was depressed, I would have a form done. I’m now 30 years old, pregnant and in a happy marriage. It’s not relevant any more. Yes the history’s there but there was a reason for it. And I’ve now passed through that. I’m happy. There’s no problem. Yet she gets a form.
Community midwife (MW5)
So is the fact that someone’s had postnatal depression 2 years ago, is that going to change – but she presents as well today – is that going to change the way that you manage her care? . . . So therefore I would not generate a special circs [circumstances] form ‘cos it’s a paper exercise and it’s not actually doing anything to improve that patient journey. . .
Specialist midwife (MW6)
I mean my issue is with special circs [circumstances] is that we do a special circ for everything. And I think we have got to be realistic that not everything needs to be documented. There are things that don’t need to be documented. Depression that they had 20 years ago doesn’t really need to be documented if it was treated, dealt with and there’s been no reoccurrence.
Community midwife (MW8)
Defensive practice was driving the reduction in thresholds and broadening of categories, in the view of senior professionals:
But this fear that it’s not a case of ‘I know somebody who that happened to and they happened to in court’, it’s just like just to be on the safe side, so it just becomes a paper trail . . . a lot of special circs forms are generated for that reason and that’s what we need to clarify in the trust I think.
Specialist midwife (MW6)
MW6, a specialist in mental health, saw this symptomatic of a more general cultural shift:
And I think there’s a growing culture amongst health professionals generally of being afraid of not referring, of overlooking and there’s a growing culture of referral for purposes of covering one’s own back as opposed to a referral because you believe that it’s in the best interests of the patient that you’re looking after . . . And what that does for the women that I look after is just cause unnecessary anxiety and is a fruitless process a lot of the time.
Specialist midwife (MW6)
The categories and criteria for which a SCF is deemed appropriate have thus become too broad. SCFs can cover a wide range of issues with no sensitivity to current assessment of risk. Too many are being completed and this is creating a problem in differentiating between levels of risk and danger.
I think we’re getting into the realm of erring on side of caution all the time and we’re doing them all the time for everybody and that’s my real issue. I get 20, 30 referrals a week which when you have to go through that . . . by the time I’ve gone through all them the time I’ve spent and I’ve reduced it down so much the amounts that really are not necessary, we spend more time doing that bit rather than looking at the ones that really are an issue and they’re the ones that can easily be missed.
Community midwife (MW8)
It gets bigger and it grows. It’s just like practices sort of mushroom really in hospitals very quickly and before no time at all something has become routine-ised that was not routine-ised. The referrals are up so there’s two ways of looking at it. People say we are getting so much better at detecting where there’s child protection issues now ‘cos we generate all these special circumstances forms. We’re getting much more vigilant about safeguarding . . . I think some of us think are we just generating a load of forms that we don’t need.
Specialist midwife (MW6)
Once that culture’s developed it’s really hard to unpick it because a lot of the people who were doing it are doing it with good intention and they maybe are genuinely fearful that they don’t want to overlook something. But in that process we have lost our capacity to actually see what’s in front of us a little bit. It’s a recent thing I think. I would say it’s probably in the last 4 or 5 years that I’ve noticed there’s a definite shift away from, sometimes it just feels like the triumph of protocol over common sense.
Specialist midwife (MW6)
The table-top meeting
The design of the online system was progressed over 2012, with the aim of launching the system in the spring of 2013. The team attended a key ‘table-top’ design meeting in November 2012 which directly addressed the issues noted above. Attendees at the meeting included the Head of Safeguarding (HS), the named nurse for safeguarding (NN), the Head of midwifery (HM), a senior hospital midwife (SM) and two community midwives (CM1, CM2). The first part of the meeting considered the logistics of filing the electronic forms, more specifically the thorny issue of ‘updates’. The second half turned attention to the question of thresholds, with the aim of reducing the number of filings; this was a key trust objective, as the epigraph to this chapter attests.
The ’updating issue’ relates to the fact that SCFs are not one-off referrals. If the mother condition changes on subsequent midwife visits after the original filing, an ‘update’ must be filed. Although there had been general support for online submission in earlier meetings, the situation was not straightforward, as the need still existed for the electronic documents to be printed off and put securely in the notes. This caused obvious complications, potentially undermining the benefits of the online systems. The Head of Safeguarding described the two options for handling the updates in particular:
We’ve two options really. Option A, when the form is electronically updated the midwife prints them off and trots off to wherever the notes are in order to file them in the notes, or B, it’s up to the hospital midwives to check the file on every maternity service admission and print off the updates and file them in the notes.
To focus discussion, the Head of Safeguarding presented the following case scenario:
The community midwife sees a mother every week . . . the concerns relate to domestic violence. The initial special circumstances form is a low-level concern relating to partner’s controlling behaviour but the updates show rising levels of concern. What do you feel about that?
A brief discussion ensued summarised by the following salient points:
I realise that she’s working in [X] and still has to make the journey but I would still go with A, that the person updating it should do it.
I was just thinking that, with B, a labour ward midwife, she’s got a lot to do before she goes on the system to check everything, so it would be hard for her.
So you don’t want option B?
No . . .
No, we all agree with that.
No, that would not be secure, it would not be robust enough.
The only thing they could do would be to ring the ward clerk, and get them to print off the update and put it in the notes.
And would that be acceptable?
Yeah . . .
The Head of Safeguarding then presented a variation on the original scenario:
Let’s look at another scenario I dreamed up because women might not always come into maternity services when they are pregnant. It’s the same patient with a broken wrist after an accident that needs surgery, so she’s admitted to an orthopaedic ward. Admissions note the initial spec circ form [special circumstances form], and no questions are asked because it’s very low level. That’s the danger of relying on the hospital midwives to print off . . . you don’t see the creeping levels of concern. If they saw the updater, they might think of contacting children’s social care. What we don’t want to do is to introduce extra risk into a system and currently you would have all the updates in the patient notes – they open the notes and they can see the rising levels of concern.
In the ensuing discussion, the idea of an electronic alert on the patient administration system (PAS) was raised, which would draw attention to the submission of the updates. This took the conversation in an interesting direction:
The thing is, you could have an alert on PAS, it ticks the box to a certain extent but it’s still not as good as what they get now which is they open the notes and it’s there. And they won’t be able to access it because special circs forms can only be accessed by midwives, and they’d have to ring a midwife to print it off and put it in the notes.
But what’s the point of a spec circs form if other professionals can’t see it?
What are we saying that only midwives can look at special circs forms, why don’t we make them available to everybody? You could have your alert and if they want to have a look they could look. What did we make it that only midwives could look at it?
Because Information Governance were not happy about having so much confidential information on a shared drive, but we got passed that by saying only midwifery staff will have it.
But that’s nonsense. All the people who would have access to it have access to the patient’s notes . . . it’s only professionals. It’s dangerous to be honest with you. The shared drive, it’s not as if the public can see it and who would want to go and look at the midwifery notes anyway! I’ll have a word with Information Governance and override that . . . and then we could go for a failsafe couldn’t we. We’d have an alert on PAS just in case they’re not printed off and put in the notes. . .
The discussion concluded as follows:
At the last meeting, we had a lot of midwives saying get the hospital midwives to do it, but we have identified that is is probably building risk into the system. We’ve got a strong view that it’s safer for community midwives to do it themselves or we’ve got the option of ward clerks doing it. Could we agree that? I prefer the ward clerk one . . .
We’d have to make sure that the community midwife was always responsible for the filing, either they do it themselves or ensure that the ward clerk does.
To be absolutely clear, we ditch option B. We’ll include those two options then. Midwives will get that question then, that they have completed it . . . that is my input and I have made sure that it’s gone in the notes.
The second half of the meeting addressed the design of a traffic light system to attempt to standardise criteria for triggering SCFs. Again, the Head of Safeguarding led the discussion:
Does anyone think that the thresholds are right . . . this is a good time to look at this because we’re launching a new system. We’ve got so many flags on the system that it’s the cases with no flags that jump out. So if we want to change it. We need to define the criteria . . . we can do that now, it’s the best time.
Scenarios such as historic depression, raised in our contextual interviews with the senior midwives, featured in the ensuing discussion, the feeling being that such cases should not generate special circs forms, in and of themselves. SM offered the following hypothetical example of domestic violence:
Can I get your thoughts on a woman with previous DV [domestic violence]? The protocol says that we should get in touch and find out about the current partner.
That‘s not right, not if there are no new concerns. If she’s covered in bruises, that’s different.
The reason is because it shows they’re generally more vulnerable to any sort of abuse, that’s what we were told.
But that should be because she’s been specifically identified as a specially vulnerable person, not just because she’s had DV in the past. Lots of women would be mortified to think that . . . it has to be because she’s been identified as a specially vulnerable person. And you’d know why that was, for instance because she’s got learning disabilities. You need to use your professional judgement, not lists of criteria.
The debate continued, and is paraphrased below:
If she had previous depression and a teenage pregnancy, is that green or amber?
The thing is this is not the only piece of information; it’s in the notes that she’s had another baby and will include somewhere that she had postnatal depression. The purpose of special circumstances is not to give a potted history of everything that’s happened before; it’s to draw attention to something that’s extremely relevant to this pregnancy.
What would partner substance misuse come under? We get quite a few Asian women whose partners misuse, but they never do . . . would it be a green so we were aware of it?
It could be, but what is the impact . . . if it’s a big impact then it would be amber. . .
That’s the danger of lists . . .
As soon as you give lists, you close down professional judgement. What matters is whether in your judgement some extra intervention is needed. If you decide it’s something that you need to keep your eye on, just you, then it’s low level. If you need to keep your eye on it and maybe tell someone else, then it’s an orange . . . and if you think it needs a multiagency response potentially then higher. It’s defining your professional judgement not giving lists.
But there’s an anxiety when it comes to things like serious case reviews, that’s where the lists provide reassurance so it’s important how we word it . . .
We will need to provide some examples, but they should be examples not lists.
Yeah, that’s good way of approaching it.
And you can always make it an amber if you’re feeling nervous about it . . . and we can always review things down the line.
Appendix 7 Special circumstances referral form (redacted)
Appendix 8 A morning in community services
This appendix describes one of the team’s visits to community services. It provides a synopsis of the field notes taken by the researcher. The visit lasted approximately two-and-a-half hours. Most of the time was spent with the designed nurse, DN2.
Field notes: visit to community services
DN2 led me [the researcher] through a typical morning, reviewing referrals, which had come in the previous day and overnight. Three staff work in the office: DN2, a specialist nurse for safeguarding children (SN) and an administrative support officer (AD1). DN2 logs into her NHS e-mail; there is a generic safeguarding stream which goes to all in the office, with separate substreams from the police, the ambulance service and PAHT. Normally, SN scans all the referrals, flagging them as green (AD1 can handle) or red (SN needs to look at these herself).
We looked at the first couple of cases.
The first was a ‘section 17 referral’. The presenting incident at A&E was a mother with a drug overdose. While there were obvious Child Protection (CP) concerns, there were no details of the children on the referral: in cases like this ‘It can take half a day to track the children down’, she commented. DN2 queried the absence of a CAF. More importantly, because this was section 17, it should have gone to Children’s Services: ‘this happens all the time . . . we’re constantly sending things back, but nothing happens’.
We looked at the next referral, ‘information sharing’, with Health Visitor. DN2 observed that ‘this what should happen . . . But it’s often a bit cryptic what comes through, for example – child had bump to the head while playing – home safety check please. But health visitors don’t do this any more! There a lack of understanding at the hospital of what Universal Services can do’. Although there was nothing in the referral to suggest safeguarding concerns, ‘we have to do something, we have to pass it to the health visitor . . . this causes so much work’.
For all referrals, a ‘NHS Cause for Concern’ form has to be completed. This specifies the source of the concern (PATH, NHS Direct, etc.) and the action to be taken by the relevant ‘Health Practitioner’: there are four options (several may apply):
-
add to the chronology of significant events
-
file in health records
-
for information only
-
consider contacting family (home visit).
‘We look in the records, and if there are no other indications, then the referral and the completed CFC will just be filed in the folder for that health visiting or school nurse team.’ This is what happened to the referral in question. All details on the referral are also checked by SN on the child health system (e.g. GP details, addresses, etc.) who finally prints off the referrals, stapling the CFC to the front before sending it to the appropriate area team.
We then discussed the referrals in relation to the organisation of community services in the area. There were approximately 40 health visitors and 30 school nurses in the workforce, and the conurbation was divided into four areas. Some statistics are kept as part of a Governance Report, which DN1 showed me. A total of 286 CFCs had been raised in the 5 months from May to September 2012 as a result of referrals from PAHT: ‘the ones that would lead to something proactive being done are less than 10% – this could be a phone call, home visit or inviting them to come to clinic’. We worked out that this corresponded to approximately two referrals per day, i.e. less than one would require a ‘proactive response’ per week. The volume from the hospital was completed dwarfed by the blizzard of domestic violence referrals from the police: in July, 243 police referrals had been received compared with 72 from PAHT.
Again, DN2 mentioned the inappropriate section 17s: ‘the hospital has the duty to make the referral to Children’s Social Care, not to us’. She went on to give a further example of a 13-year-old child with multiple A&E attendances as the victim of assault – ‘we kept sending it back but we eventually had to refer it to CSC’.
We then discussed benefits, problems and improvements. The following points were made:
-
‘The safeguarding team [at the hospital] need a better understanding of what we can do – we’d be happy to go in and help them understand better our work – It would be useful for safeguarding staff and co-mentors to spend time shadowing health visitors.’
-
‘Too many referrals are to cover people’s backs.’
-
‘The systems is definitely useful – we do need the information . . . and the referrals have been getting better recently.’
-
‘The A&E ones are the problem – not getting parental consent.’ BT showed me an example of a case where a mother had been shouting aggressively at the child. The form indicated that the parents had not been informed of the referral because the nurse ‘did not want to cause tension between staff and parents’. ‘But this just puts the health visitor in a very difficult position – you can’t just turn up and say I believe you kicked off at the hospital.’
Appendix 9 Co-mentoring: a typical day in accident and emergency
This section provides a summary of one of the team’s visits to the A&E department in order to observe the co-mentoring process in action. The researcher sat alongside the mentor as she worked her way through the list of cases that had been flagged the previous day. The co-mentoring protocol requires that all relevant cases are reviewed by the mentors. This typically takes around 2 hours, but took a little longer that morning as the mentor gave a brief commentary on each of the cases. A short interview was conducted after the observational session had concluded.
On the morning in question, there were 18 cases in the list. A summary is provided in the following table, reconstructed from the researcher’s field notes. Note that the abbreviation CM identifies the mentor.
Case 1. Child had spot on hand. There had been four previous attendances and the child had left without being seen. A SBAR should have been sent. Details on PAS checked: who brought the child, next of kin (same address?), GP details. CM completes a SBAR.
Case 2. Minor head injury (cut) to toddler. No obvious concern but family had left without being seen. SBAR had been sent.
Case 3. Child with diarrhoea and vomiting, seen by doctor. No safeguarding concerns, but CM finds it hard to decipher the record – medical details only – no social history. CM notes that the doctor is a regular locum and she has spoken to him already, but he takes no notice. CM comments that ‘this is the main problem . . . Junior doctors are much more responsive especially if they have been in paeds’. Middle grade doctors are ‘receptive but slip after a while and need a prod’.
Case 4. Same locum. CM notes again no family history, no birth history.
Case 5. 22-month-old girl, with vomiting. Good set of notes, no concerns.
Case 6. First attendance, child fell off swing and limping. No problems with documentation, and no safeguarding concerns.
Case 7. Child suffering ‘febrile convulsions’. CM notes that this is not uncommon in under-5-year-olds, but there were five previous attendances. A SBAR should have been done, but not so. CM completes SBAR to be sent to the Health Visitor for ‘information sharing’ and follow-up.
Case 8. Child had ingested disinfectant. A SBAR was mandatory, and had been completed with the child referred to the KOALA unit.
Case 9. Another ingestion. A SBAR had been done and the child referred to paeds.
Case 10. The child had stood on a hair straightener, and burned foot. There had been five previous referrals. A SBAR should have been done, but not so. CM completed SBAR for the Health Visitor for ‘information sharing’ and follow-up. She notes that ‘Heath Visitors are getting lots more referrals now’.
Case 11. Baby with vomiting. CM noted recording was reasonable but ‘hard to read’. No safeguarding concerns.
Case 12. Toddler with nappy rash. No concerns except junior doctor’s handwriting.
Case 13. A child with rash, possible chickenpox. CM comments admiringly on excellent recording by the nurse practitioner. No safeguarding concerns.
Case 14. No concerns. Child had been referred to out-of-hours GP.
Case 15. Child with rash, possible chickenpox. Again, good recording by nurse practitioner noted. There had been five previous attendances. A SBAR should have been done, but not so. CM completed SBAR, for the Health Visitor for ‘information sharing’ and follow-up, noting that ‘it helps to educate the Heath Visitors’.
Case 16. Child crying when normally doesn’t. Again, excellent recording by nurse practitioner noted. Parents reassured and advised to follow up with GP. All well.
Case 17. Child with cold experiencing difficulty breathing. Doctor has seen child and referred to paeds: ‘Another decent set of notes’.
Case 18. Child with temperature, query tonsillitis. No birth history, family history and social history. Otherwise no concerns.
KOALA, Kid's Observation and Assessment Liaison Area.
CM was interviewed for 30 minutes or so, after the session. The following key points were made:
-
Because cases are reviewed on the following day, or later, the member of staff responsible for the SBAR is not readily accessible, so the mentors typically complete any SBARs which should have been completed.
-
CM felt that the system was ‘definitely beneficial – we pick up lots of omissions and the quality of the documentation is much better’.
-
‘Locums are the main problem, but not sure what we can do.’
-
Multiple attendances are the main cause of omitted SBARs.
-
Histories are also inconsistently recorded.
CM went on to make several suggestions for improvement:
-
Multiple visits should be much more clearly flagged on the PAS: ‘many people don’t think this is important’. There is just a small icon in the top left hand corner of the screen.
-
The SBAR form is satisfactory, but its completion is intrinsically time-consuming.
-
Make less use of locums.
-
The results of the mentoring process should be fed back into the induction of new rotations of doctors.
-
There are many reasons why the SBAR is not completed, for example the nurse is too busy, and leaves for later; the nurse leaves it for the doctor, but the patient is then discharged without a SBAR and the doctor does not inform the nurse that it has not been done.
Appendix 10 Case study (Baby H)
Case study: suspected fabricated or induced illness July 2013 – Baby H
Baby H was a 12-month-old baby girl who first came to the attention of paediatricians on 7 December 2012. Parents had called an ambulance at 02.25 that morning. Dad was with the baby when he heard her crying. He went to her at about 2 a.m. and noted she was making sounds as if her upper respiratory tract was blocked. He called the ambulance. A paramedic witnessed Baby H as vacant and not fully alert. In A&E, doctors felt that the ‘floppy episode’ was due to an upper respiratory tract infection with mucous blocking the upper airway. Baby H was admitted for observation and discharged later the same day.
On 25 January 2013 at 04.19 hours the hospital received a standby call for resuscitation. Baby H’s mother was woken up by Baby H crying. Mum found Baby H grunting, looking pale and breathing slowly. She called an ambulance. On examination at hospital, Baby’s oxygen levels were low and Baby H was upset. After oxygen was administered Baby recovered well. She was discharged on 27 January.
On 15 March 2013 the hospital received another standby call at 04.49 hours. Baby H had had chickenpox for several days. Mum got up to get a drink and found Baby to be gasping for breath. When the rapid response vehicle arrived Baby H was grey, unresponsive and making very little respiratory effort. She did not respond to oxygen therapy and was making a moaning cry on the way to hospital. On examination at hospital, doctors queried sepsis as the cause of her collapse. Baby was given antibiotics directly into her bone (interosseous). She was admitted to high-dependency unit (HDU) and was discharged on 19 March 2013.
On 3 April 2013 at 04.32 hours, the hospital received another standby call for resuscitation. Mum found Baby H gasping for breath. On examination in hospital Baby H appeared pale, floppy, vacant and gazing. After 20 minutes in resuscitation, Baby H was witnessed to have another episode where she became pale and unresponsive. Baby was admitted to the children’s unit.
Baby H was still in hospital on 12 April 2013. At 04.00 hours, Mum, who was resident, alerted staff to the fact that Baby H was struggling to breathe and was unresponsive. She was resuscitated, transferred to HDU and quickly recovered as before.
Paediatricians were starting to question what was happening at this point. They began to consider other differential diagnoses. FII was part of this consideration. The trust safeguarding team were contacted on 10 April 2013 by one of their most senior consultant paediatricians who was also designated doctor in one of the Clinical Commissioning Group areas within the trust footprint. He reported to the Head of Safeguarding that he was concerned and that, in the light of numerous normal tests, ‘we could really now be dealing with FII’. Further investigations were ordered and arrangements made for Baby H to be nursed in an open bay on the ward on her return from HDU rather than go back to the single room she had come from.
It was agreed that Baby H would not be discharged. The Head of Safeguarding recommended a professionals meeting to include CSC to ensure that everyone had the opportunity to discuss health and social issues with the family and assess the level of professional concern and necessity for action. Nursing staff were asked to pay particular attention to parent–child interaction on the ward.
Investigations/observations
During her stay in hospital, Baby H had a battery of investigations including bloods, toxicology, computerised tomography (CT) scan, skeletal survey, ophthalmology, electroencephalogram (EEG) and magnetic resonance imaging (MRI) scan. All were normal.
Baby H’s parents were described as quite passive in nature and noted not to ask a lot of questions regarding their baby’s care. Mum sometimes seemed quite flat. She had told staff she had recently had the unpleasant task of agreeing to end active treatment for her brother who was on life support; this was on the same day that Baby H was first brought to hospital. It was noted that Mum was resident with Baby H and Dad and siblings visited appropriately.
Liaison
The family included 10 children all living in the same house. No concerns existed with regard to the family from the point of view of the health visitor. No historical concerns were documented with child health. The family were not known to the named nurse for child protection in the community or to CSC. Checks were made with neighbouring hospitals and there were no concerns expressed from these quarters. The GP was contacted and expressed no concerns about the family.
In keeping with national and local guidance on FII, the safeguarding team agreed to liaise with a senior social worker and invite them to a professionals meeting to discuss the emerging issues from the case. The team manager for the local area office was contacted and this was put to her. She asked that a referral be made through the contact centre in the usual way. However, the safeguarding team felt that the threshold for a referral had not been met and wanted a conversation to gauge opinion before going straight to referral.
The Head of Safeguarding at CSC was contacted and she agreed initially that at this stage a formal referral was not necessary. The meeting invite, due for the 26 April, was again extended to the social work team manager. On the 25 April, an e-mail exchange took place between the Head of Safeguarding at PAHT and CSC.
The Head of Safeguarding at CSC stated that:
When we spoke a week ago you informed me that additional tests were to be done to rule out any other possibility for the baby’s difficulties . . . In holding the meeting arranged for tomorrow I presume these tests have now been done and have shown no organic cause for the six occasions on which she has had to be resuscitated? If that is the case then there are clearly significant concerns for her safety and protection and this is emphasised by the collapse she experienced whilst in hospital and led to her being moved from the privacy of a cubicle to a public ward. I understand that mother has been present throughout the child’s stay in hospital and was there at the time of her last collapse in the cubicle. I can see no other course of action that would not require the involvement of children’s social care at this stage and I presume you are of the same mind given your request for their attendance at tomorrow’s meeting . . . social work assessments are needed at the very least and action to safeguard the child cannot be ruled out. I must advise you to make a referral via the contact centre as a matter of urgency. It can be made clear that the child is currently safe . . . This will ensure that the referral is well managed and is not escalated unnecessarily.
The reply from the Head of Safeguarding at PAHT was intended to reassure CSC that, if it was felt the child was at risk or likely to be at risk of significant harm, then a referral would be forthcoming. However, she added:
. . . that is not where we are at the moment. Some tests remain outstanding and it is certainly not clear that the child’s condition is being induced. The point of the professionals meeting is to gather together our information with that of other professionals to help us identify the nature of the risk and what next steps should be to manage it. We have prepared a chronology which throws a slightly different light on things as there has been some professional witness to some of the incidents of collapse. We need to consider this in context of medical examination findings. It would be useful to have social work team manager with us during these deliberations . . . This is an extremely uncertain and delicate case which, if handled badly, could impact on the long term outcomes for the child. As soon as we have some consensus re: balance of probability then we will make a referral (or not).
A telephone discussion followed whereby it was pointed out that a referral was necessary to enter the case onto ‘the system’, thus explaining the activity of the social worker in attending the professionals meeting. The Head of Safeguarding at PAHT again resisted the request to make a referral because in doing so there would be a documented concern of significant harm which was not a true reflection of the professional opinion at the time. It was suggested that a referral be made just to get it on the system, but that health professionals could be assured nothing would be done until agreement was reached that this met the threshold for intervention. There was no agreement about this course of action.
Further conversations highlighted the concern in CSC that the hospital was allowing unsupervised contact between mother and baby and that presented a risk given the uncertain circumstances.
On 26 April, the professionals meeting took place and the social work team manager attended. Information was shared and a plan put in place that included:
-
Health Vision will visit the property to ascertain sleeping arrangements
-
doctor will complete outstanding tests such as MRI and sleep study
-
Baby H to remain in hospital until tests completed and plan of action devised by professionals, nursed in an open bay
-
to contact CSC and the police if mother tries to leave with Baby
-
CSC to complete background checks on siblings and parents.
Diagnosis
In early May, Baby H was transferred to a specialist hospital for sleep studies. On 15 May 2013, the consultant paediatrician at PAHT verbally confirmed with the Head of Safeguarding that the results from the extensive sleep studies, taken over 5 days, showed that Baby H was suffering from complex partial epilepsy. It was agreed that FII was no longer a feature of the case. The Head of Safeguarding at CSC was informed that no child protection referral would be forthcoming.
Baby H was transferred back to PAHT and work began with the parents to prepare Baby for discharge. Specialist training and equipment was to be ordered and in place prior to discharge. On 4 June 2013, Baby H experienced another episode from which she did not recover. Her heart stopped, she could not be resuscitated and she died. Concern about the cause of death and Baby H’s condition continued post mortem. However, a vast series of tests showed nothing to suggest that her death was as a result of FII.
Systemic analysis
Reporting culture: systems and technology
Systems and technology influenced interagency discussion and co-operation. The opportunity to have a conversation with a social worker was governed by the need to enter the activity on ‘the system’, the initiation of which could only be achieved by a referral. This is despite the fact that the health professionals were not ready to make a referral. This was doubted by CSC who suggested we had reached that threshold and that was why we had moved baby and mother out of a single room into a four-cot bay. Reassurances were given by the Head of Safeguarding at CSC that if a referral was made and the system triggered, there would be no intervention and emphasised the point of the referral would be to open the gateway into the service. This was challenged by the hospital who felt that a referral under the Children Act 198919 would signal a level of concern, that the child was at risk of significant harm, that did not exist at that point, although it was constantly part of differential diagnosis considerations.
Informed culture: dealing with uncertainty
The Safeguarding Unit made reference to the fact that the hospital was leaving mother unsupervised with her baby and this concerned them. Significance was placed on moving mother and baby into a more open bay area. While it was acknowledged this was to facilitate observation, the hospital emphasised that it was not an indication that a decision had been reached about significant harm. This level of uncertainty proved very challenging to CSC who went on to indicate that the hospital should make a referral so that CSC could control the level of contact mother had with her baby. The risks that this posed in terms of identifying whether or not FFI was taking place was apparently not considered. The lack of evidence to support an application to court to secure the necessary authority to limit mother’s contact was also not considered. The need to apply a procedure as a means of securing a level of certainty and assurance that ‘something was being done’ seemed to override the facts of the case including the fact that the clinical staff would not support the recommended action.
The lack of diagnosis was less alarming to clinicians than to CSC who quickly assimilated that the cause was non-organic even though this had not been established or mentioned by medical staff. The need to ascribe the ‘non-organic’ status of the child’s condition was a key concern to CSC and the link between lack of diagnosis and concerns for safety and protection were automatically made with a level of certainty that was not apparent in the discourse of hospital staff who were more prepared to tolerate a level of uncertainty than CSC. This tolerance was probably underpinned by their constant and ongoing experience and interaction with the mother and her baby.
I presume these tests have now been done and have shown no organic cause for the six occasions on which she has had to be resuscitated? If that is the case then there are clearly significant concerns for her safety and protection and this is emphasised by the collapse she experienced whilst in hospital and led to her being moved from the privacy of a cubicle to a public ward.
The fear of consequences of not intervening and not applying procedures in this case seemed to be founded on a rapid hypothetico-deductive reasoning normally confined to the realms of case reductionism prominent in the field of medical science. The family were not known to CSC and no concerns had been expressed by any professionals in relation to the family. Indeed, contact with professionals was limited to essential contacts, probably due to the fact that there were nine other children in the household. The level of concern around significant harm from social care seemed to be based purely on the lack of diagnosis, observations about mother’s demeanour and the uncertainty of hospital staff and their decision to move mother and baby to a more visible area. Without any further information this lead to a false positive identification. When the certainty of a diagnosis was reached, all concerns disappeared.
Conclusion
The need for a professional conversation with colleagues from other agencies is an essential feature of working together. The need to have ‘a case’ inputted onto ‘a system’ in order for that conversation to occur will hinder vital professional interaction and is highlighted by Munro. 11 The practice of having ‘a discussion’ is included in Working Together to Safeguard Children:22
All professionals share appropriate information in a timely way and can discuss any concerns about an individual child with colleagues and local authority children’s social care.
p. 7 (Working Together to Safeguard Children, Crown Copyright 2013, licensed under the Open Government Licence v3.0)
The need to balance evidence as part of the process of balancing risk is also highlighted:
No system can fully eliminate risk. Understanding risk involves judgement and balance. To manage risks, social workers and other professionals should make decisions with the best interests of the child in mind, informed by the evidence available and underpinned by knowledge of child development.
p. 22 (Working Together to Safeguard Children, Crown Copyright 2013, licensed under the Open Government Licence v3.0)
The lack of tolerance of uncertainty coupled with the need to govern conversation through the presence and input on a system is prevalent in this case and could potentially have resulted in an inappropriate intervention removing a mother from her child prior to her death.
Plan
-
Case reviewed at peer review/case discussion meeting.
-
Multiagency review/reflective practice session agreed, to be facilitated by LSCB Independent Chair.
Appendix 11 Case study (Child M)
Case study neglect: Child M
On 24 April, Child M presented to A&E at PAHT, brought in by ambulance at 01:07 hours with a history of being found on the bathroom floor by mum and with being unresponsive. There was also a history suggestive of possible fits and vomit found in the toilet. On arrival to A&E her temperature was very low (34.4 °C) and she was drowsy and not fully responsive. Both her feet were red and a chronic ulcer was found on her left ankle. She also had skin spots on her right shoulder suggestive of sore skin or pressure ulcer. Child M’s blood test showed low sodium levels (salt level) in her blood and she was treated with intravenous (i.v.) antibiotics and given i.v. fluids. There was no high-dependency bed at the local hospital so she was transferred to another PAHT site in the early hours for ongoing care. She was initially thought to have meningitis or encephalitis-like illness but a lumbar puncture later ruled it out. She had a CT brain scan which showed non-specific dilatation of ventricles (fluid-filled cavities inside the brain) but MRI scan was normal. She gradually improved and by the next day she was fully conscious and started eating orally. Subsequent blood tests showed that she had gross nutritional deficiencies.
An information sharing form was raised and the SBAR included the following information:
Situation: child brought to department as standby reduced GCS? Fit, concern for child’s health as underweight for age; also due to ulcerated L ankle which had for 3 months.
Background: child attend as less responsive, brought with mum, stated had diarrhoea for few days, also extremely red feet up to ankles, parent states seen GP but had the ankle and feet problem for 3 months.
Assessment: low temperature? Fits, rash, mum states she likes to pick scab; that’s why not healed on ankle but is an extensive wound and general poor hygiene, mum stated dirty due to dogs.
Recommendation: admitted for continuing management, feel maybe parents need some support and education help with child.
GCS, Glasgow Coma Scale.
The information sharing form was sent by nursing staff on the ward for the attention of the school health practitioner on the day of admission. The form was forwarded to the named nurse in the community by the hospital safeguarding team.
The following Wednesday (5 working days later) the named nurse contacted the hospital safeguarding team to say that the school health practitioner had serious concerns about the child particularly with respect to neglect. Information shared was that Child M appeared hungry at school in the past and was observed to go looking for food. The school health practitioner had made a referral to CSC in the recent past. The hospital nurses noted that Child M did not have enough clothes provided and appeared quite sad and withdrawn, seeking attention from the nurses intermittently.
On the basis of their conversation, the hospital Head of Safeguarding upgraded the ‘information sharing’ status of the form to ‘child protection referral s47’. The referral was rung through to CSC, the referral faxed and confirmation received that the case had been allocated to a social worker the same day.
History from mother
When asked, Child M’s mother told the doctor at the hospital that Child M had had diarrhoea for a few days prior to admission but was not unwell with it. She said that she was found in the bathroom on 24 April 2013 and had vomited in the toilet. The mother had taken Child M down the stairs and given her a drink; Child M then had a generalised shake of her limbs which appeared like a fit, lasting about 5 minutes, and stopped on its own. After that Child M’s mother called the ambulance. She said that she had noted Child M’s swollen feet in the last 6 months had attended the GP surgery regarding this. Child M’s mother explained that the ulcer on her left ankle was secondary to a graze which Child M had picked. She also mentioned that Child M was a very fussy eater, like herself. She said that things had improved since she (the mother) had a new partner. Child M was reported to have always had a good appetite but was always small and mother did not think there was anything wrong. Child M’s mother reported that Child M had been home schooled being taught by stepdad since December 2012 as the family planned to moved to the south of the country and she was missing a lot of school in between when they were going to the south to look for property. On further questioning, while taking a more detailed background history about moving schools twice, mother explained that Child M was previously referred to Social Services due to concerns regarding neglect and not being fed. The first time it occurred was 4 years ago and prompted a school move. The same thing occurred at the next school over 1 year ago.
At this point Child M was also attending school, having wet herself on the way to school and reporting that mother was not changing and cleaning her appropriately. Mother mentioned that both times she was taken to the same Social Worker and both times it was proven ‘that Child M was lying as one who wants to be at the centre of attention’.
Previous medical history and background
Child M was born by normal delivery weighing 6 pounds 4 ounces. She was brought to hospital once for possible irritable hip but otherwise remained healthy. Her development was normal and there was no concern about her hearing or vision. She was up to date with her immunisations and not currently on any regular medication. There was no concern about her sleep and she did not have any tendency to self-harm. She last attended school in December 2012. Mum described her as bossy at times at school and there was some concern in the past regarding bullying both as perpetrator and/or victim of bullying.
Family history and composition
Child M lives with her mother and stepdad. There were two other boys aged 10 months old and 2 years old both to mother and stepdad. There were two other children of stepdad from a previous relationship; a son aged 14 years and a daughter aged 12 years. The 14-year-old son lived in the same household as Child M but the daughter usually lived with her mum and stayed with her dad on Tuesdays and Thursdays. There were no significant health problems in the family apart from the 14-year-old who suffered from behavioural problems and issues around soiling.
A medical was completed and the consultant paediatrician recorded the following:
Child M has presented with a seizure which was most likely secondary to low sodium (salt level.) This has now corrected but we have the following concerns:
-
She is significantly underweight and short for her age.
-
She has shown a very good appetite and at one point we had to control her oral intake as she was showing signs of refeeding syndrome (a condition where chronically malnourished children – if allowed to feed – can develop life-threatening salt depletions.) Child M showed a drop of phosphate and magnesium after starting feeding and a dietitian had to be involved.
-
She has some significant nutritional deficiencies for which a medical cause has not been found so far. She has also shown good weight-gain while an inpatient.
-
There have been previous concerns regarding neglect and lack of food.
-
The family has also moved schools and now she is getting home schooling. This could have been triggered by professionals raising concerns about neglect.
He concluded that he was concerned the Child M’s poor nutritional status was secondary to gross neglect and pointed to the significant weight gain recorded during her stay in hospital. On 7 May 2013, a strategy meeting was held on the children’s ward. An Emergency Protection Order had been made in respect of Child M but not the siblings. Foster carers were identified and planned a visit that day. No unsupervised contact was allowed between parents and Child M, including telephone contact. The social worker described the outcome of her visit to the family home where it was identified that there was no sign of Child M having lived there. She had no bedroom and would sleep on the landing or in the bath. She was kept away from the kitchen by means of keeping the dogs in there in the knowledge that Child M was scared of them.
Child M was discharged later that week.
Follow-up
On the 15 July, Child M was reviewed in outpatients clinic by the consultant who treated her in hospital. He documented that her body mass index was now above average, she was at school and seemed much happier. The consultant confirmed that the turnaround in Child M’s condition was not due to any special treatment other than placing her in a different environment and providing her initially with vitamin supplements. He concluded: ‘I am convinced that she had reached that state due to gross neglect on the part of her previous carers and not due to any malabsorption or any other medical reason’.
Systemic analysis
Establishing the context
The enhanced reporting culture within PAHT and the use of the online information sharing tool had an important impact on this case. The SBAR reflects a level of concern that does not meet the threshold of a referral to CSC. Although not a particularly good example of how SBAR can be completed, it provided a clear indication to the named nurse who read it that the level of concern in the hospital was at a different level to the school health practitioner, prompting the telephone call to the trust safeguarding team.
During the following 5 days, concern in the hospital was growing. The fact that the concern was both validated and heightened from another source, the school health practitioner, added to the overall context in which assessments then occurred. This resulted in a clarity of reporting from the consultant that helped ensure the application for an Emergency Protection Order was successful. The combination of information and sharing of levels of concern in a timely manner avoided the ‘start again syndrome’ so often associated with failures to recognise and respond to cases of neglect. 23
Learning culture
The system of peer review incorporating reflective practice and providing opportunities for clinical supervision within an educative and supportive context is central to developing a learning culture. A series of peer review/case discussion meetings are becoming more established within PAHT, led by the safeguarding team and attended mainly by paediatricians.
This case was taken to peer review meeting to highlight the positive lessons learned. Individual feedback was given to the practitioners who were involved in the case and their response is a reminder of the point made by Munro11 that most of us work in our chosen professions in health and social work because we want to do the right thing and make people’s lives better. The e-mail reply from the consultant stated:
Thanks for the lovely email. I indeed felt vey good yesterday seeing her in my clinic happy, thriving and altogether a different girl than when I first met her in the ward. I will love to present her case in any meetings, just let me know in good time. Well done to you and all involved.
Opportunities to recognise what ‘good looks like’ are as important as recognising mistakes. The case has been commissioned by the LSCB as a SCR.
Reporting culture
Following the trust safeguarding team’s upgrading of the information sharing form to a referral form, the telephone call and the faxing of the referral as per normal procedures, conversations between the trust Head of Safeguarding and the named social worker revealed that the social worker was unaware of the referral from the trust, even though this was the basis of the rapid allocation of the case on the same day as the referral. The social worker repeatedly informed the Head of Safeguarding that the only referral they had on the system was that from the school health practitioner several weeks previously. This supports findings from the audit into section 47 referral cases where some teams could not find the paperwork that followed the telephone referral and of which the trust safeguarding team had a copy. As a result the trust’s safeguarding support manager now rings the relevant local authority contact centre on receipt of every section 47 referral to check that they have received the paperwork. In some cases, they have not and it is sent again. In other cases, the paperwork, which is scanned into the electronic system, is found on a different screen. Further work is required to explore practice of electronically filing faxed referral forms.
Appendix 12 ‘Lessons Learned’ framework
This appendix describes the ‘Lessons Learned’ framework developed by PAHT. These are three sections: (1) the first is a verbatim transcription of the Framework itself as published in the trust; (2) the second provides an example of a completed pro forma; and (3) the third shows the ‘Lessons Learned’ bulletin produced by this case and distributed throughout the trust.
Developing a safeguarding learning culture: aligning safeguarding, quality and patient safety
The key driver in the modern NHS is the achievement of quality rooted in patient-centred care and underpinned by clinical effectiveness, patient safety and patient experience. This has been most recently reinforced by Sir Bruce Keogh, National Medical Director for the NHS in England, in his review of the quality of care and treatment provided by 14 hospital trusts in England,4 and by a report by the National Advisory Group on the Safety of Patients in England: ‘A Promise to Learn – A Commitment to Act: Improving the Safety of Patients in England’. 184
The emphasis on the learning culture described by Reason142 is especially prevalent in the latter with calls for the NHS to embrace an ethic of continual learning ‘top to bottom and end to end’ (p. 5). 184 The authors pose NHS leaders a challenge to ‘create and support the capability for learning, and therefore change, at scale, within the NHS’ (p. 5). 184 The group warn about focusing on the wrong priorities, such as meeting targets and financial priorities, and thereby missing the point. They state (p. 6):184
Rules, standards, regulations and enforcement have a place in the pursuit of quality but they pale in potential compared to the power of pervasive and constant learning.
National Advisory Group on the Safety of Patients in England. A Promise to Learn – A Commitment to Act: Improving the Safety of Patients in England, Crown Copyright, 2013
The words ‘child protection’ or ‘safeguarding’, or even ‘abuse’, do not appear in either of these reports but it is not a challenging step to recognise that protection from harm includes protection from abuse and neglect (the word ‘neglect’ does appear on numerous occasions). At the same time, it would not be challenging to sideline child protection into a specialist ‘silo’ that is not concerned with achieving quality of care for patients in the NHS.
The governance structure within PAHT includes safeguarding within the Clinical Governance and Quality and patient safety structure. Learning lessons from child protection SCRs was seen as something different to learning lessons from clinical incidents and serious untoward incidents. However, the new draft quality strategy makes explicit reference to safeguarding and the Trust Quality Assurance Framework includes a ‘Lessons Learned’ element that includes lessons from child protection investigations and SCRs. This has resulted in a wider sharing of lessons learned beyond the boundaries of paediatrics.
The first SCRs that was shared as part of the new PAHT ‘Lessons Learned’ framework was that of Child C, a 5-month-old who attended the hospital as an emergency case, suffering from two skull fractures and bruising to the side of the face.
‘Lessons learned’ pro forma: example case
| Incident/complaint/claim/other? | SCR – commissioned by Oldham LSCB |
| What and how did it happen? Root cause – what happened? Consider the care and service delivery problems Provide an overview |
At the age of 5 months Child C was admitted to hospital in an emergency. Medical examination and investigations revealed that Child C has sustained two skull fractures, along with bruising to the side of the face. Child C’s mother and father who lived together could offer no satisfactory explanation as to how the injuries were caused. As a consequence Child C’s sibling (Child B) was examined and was found to have current and older injuries. Sibling 1 the eldest child was not found to have any injuries The family had been known to children’s social care since approximately 22 months prior to Child C’s injuries and 10 months earlier it was reported that Child B had bruising and scratches that required further investigation. Child B had a medical with a consultant paediatrician who found and confirmed that the possibility of non-accidental injury could not be ruled out, however, it was also stated that the injuries could be consistent with an explanation that an older sibling (Sibling 1) had caused them. This explanation became the accepted position and the focus was on supervision of the children and work was undertaken by children’s social care and the health visitor to help the family One month later Child B was observed to have bruising to the face, a different consultant paediatrician also revealed bruising to the child’s back. The medical concluded that the injuries could be accidental as Child B was an active and inquisitive toddler, and again supervision was the focus The case was closed to children’s social care following a period of assessment and work with the family two month prior to the birth of Child C (seven months prior to Child C’s injuries). At the age of 5 months old, Child C presented to the hospital with serious non-accidental injuries. The injuries sustained by Child C caused agencies to reconsider the response to the injuries observed to Child B and the decision was to undertake a SCR |
| Why did it happen and what was its impact on the patient, staff and trust? | The report clearly concludes that an opportunity to protect Child B was missed during the two medical interventions. The report notes that in June and July 2011 Child B was seen by different paediatricians and that, whilst both followed the trust guidelines, the practice fell below expected standards because a rule of optimism was followed and explanations by the children’s mother and father were accepted without challenge. There is a need for change to organisational culture rather than simply an individual deficit |
| What can we learn? | The report makes a number of important findings, and makes recommendations to address the issues where suboptimum practice is identified as follows: A need to provide a standardised medical report that is widely shared with relevant child protection agencies The need for medical reports to use phrases and language that provides clarity of intent The need to ensure then when undertaking a medical examination under safeguarding procedures, the context of any such previous medical reports are highlighted and considered That paediatrician’s undertaking medicals under safeguarding procedures need to maintain a degree of what Lord Laming referred to as ‘healthy scepticism’ and ‘respectful uncertainty’ That a second opinion culture is promoted in cases which proves difficult to reach judgement |
| What action is needed to reduce recurrence? | The recommendations for action are as follows: To introduce a trust medical report template To develop quality control of section 47 medical reports To formalise peer support Ensure case notes are available for each section 47 medical examination to ensure information is available from previous medicals |
| What were the key themes that were highlighted? | Information sharing Standardisation of phrases and language that provides clarity of intent Access to notes when undertaking a child protection medical Maintaining a healthy degree of scepticism when dealing with child protection Peer support |
| Who needs to be informed? | Women and children’s division |
| Areas for action requiring a cross divisional approach? | No |
| Please share these lessons learned with the right staff at the right time in the right format ‘To provide the very best care for each patient on every occasion’ |
|
The ‘Lessons Learned’ bulletin for the preceding case
Appendix 13 Pro forma of staff survey
Appendix 14 Two digital stories
This appendix contains the scripts for two of the digital stories that have been developed: Natalie’s story and Jake’s story. The latter was still in production at the time of writing.
Script of Natalie’s story
I wasn’t what you’d call a ‘good’ pupil at school. My mum and dad drank loads on a daily basis and I was out drinking every night too. A year before I became pregnant I was self-harming in order to cope with the arguments at home and having to look after my brother who is 2 years younger than me.
I was 15 and got pregnant and was still out drinking. I didn’t understand what it all meant – I was 15! I did have a social worker who did her best to help but to be honest I wasn’t very honest about my situation and refused to tell any professional who my son’s dad was as if I had I knew there would be a lot of questions asked about the age difference and was worried that I wouldn’t be able to keep my baby.
Now I know more about social work and what could have happened, I probably would have benefited from having a pre-birth assessment just so I was better prepared to deal with the demands of becoming a parent (I don’t think I would have struggled half as much!)
Initially no one expected anything of me. I didn’t have to go to school and I had to motivate myself to set up meetings with the teachers at the school to tell them that I wanted to stay in education while I was pregnant. This was hard because I had never had a good relationship with them and knew that they would think I wouldn’t succeed because of my behaviour and my attitude towards members of staff. When I did, though, I was given a huge amount of support from school. The head of the behaviour unit really encouraged me and made every effort to ensure that I could complete my coursework and GCSEs despite being pregnant.
Before Connor was born I made arrangements for his arrival, I decorated my room a couple of weeks before and had everything ready for him. There was no dad on the scene and that’s how I wanted it. No one ever asked me about Connor’s dad again. The professionals involved did not really quiz me in any great depth and as much as I was glad about this at the time I know I was trapped in an emotionally abusive relationship which could have potentially affected my ability to be a good mum.
It didn’t hit me till I was being wheeled out of theatre after having a Caesarean and I was holding my baby boy – that things started to change. I just remember kissing his head and being overwhelmed by this feeling I didn’t really understand at the time.
I’ve had to be strong though – some people didn’t make it easy for me. On the postnatal ward I wasn’t shown how to bath or feed my baby. I had no idea that I would lose so much blood and found myself having to clean it up from the toilet floor because I didn’t want to be a nuisance. I already had the feeling the midwives did not like me. They would coo over other people’s babies and their attitude towards me was different. I felt judged as a single teenage mother. I was asked if I wanted to breastfeed. I explained that I didn’t think I could because I had to go back to school. They could have sat with me and helped me work out how I could establish breastfeeding and continue it and still go to school but they didn’t. They had no interest in me or the fact I wanted to go back to school and finish my exams. I felt they frowned upon me – even for cuddling Connor too much!
I learned nothing from the midwives in the hospital. I couldn’t wait to get out of hospital but when I did I thought – ‘heck, what now?’. I remember ringing the teenage pregnancy midwife, Janine, after 3 days of being at home. I had met her antenatally but didn’t particularly like her or engage with her because to be honest I just thought she was a busy body. Three days after I’d had Connor I rang her, though, crying to her that Connor would not stop crying. She was there in minutes. She took him off me and was reassuring me all the time that I was doing OK, I was doing a good job. She went through how I should wash and sterilise the bottles and basically taught me the things I think I should have already been shown in hospital.
When he was about 7 weeks old, Connor was really poorly and had to be admitted to hospital for an operation to counter the pyloric stenosis he was suffering with. I became aware there were parents with babies that were suffering much worst conditions and I would listen to them crying and worrying about them. I suddenly realised how much I wanted Connor to be OK – how much I loved him and more importantly how to be his mum.
He recovered fully after his operation. I went back to school and took Connor with me. It wasn’t easy – I was bullied and ridiculed by the people I used to drink and smoke weed with. I managed to avoid them by using a different entrance. I can honestly say that if I hadn’t had ‘Learning Base’ and hadn’t had the help of the learning mentors, I would never have gone back.
From where I am now I can look back and see so many opportunities for professionals. An opportunity taken was when Janine dropped everything to see me when Connor wouldn’t stop crying. She talked me down over the phone and helped me calm down. Other professionals though assumed that I was living with my parents and was therefore well supported but that was not the case for me. Had I not made the effort and asked for support I would have stayed at home and become more and more socially isolated.
I needed to get course work finished for my exams. The art teacher was amazing and sat with Connor while I worked. The learning support team were brilliant. Before I went onto college I went to Connexions to see the teenage pregnancy adviser. They told me about my entitlements and what my dad needed to claim until I was 18. My parents were big drinkers so I didn’t get to see much of the money. Connexions helped me apply for benefits and apply for college. They told me I was entitled to a ‘Care to Learn’ nursery place and helped me find a nursery. They also put me in touch with a tenancy support worker so I could find my own place.
What kept me motivated was the fact that I didn’t want Connor to grow up like I did through a really dysfunctional childhood. Mum was worse than Dad for the drinking and I decided I just didn’t want to be in it any more. I got a house before my 17th birthday. I was classed as estranged from my parents so got my own benefits of about £45/week and £60 tax credits and child benefit. Connexions helped me learn about practical budgeting and helped me fill out EMA and travel expenses forms when I started college in September.
All the ‘good’ that I experienced throughout that 2-year period helped get me to college. It gave me reassurance that having a baby doesn’t mean life stops. At college I met a really good friend who helped decorate my house. I had and still have a good social life! I’m also still in touch with Learning Base staff, Connexions workers and family support worker.
What about my mum and dad? Before I moved out I had an honest chat with Dad and told him I needed his help. He could have ignored me but he responded. He got up at the same time as me and took Connor to nursery. I am really close to my dad now. My relationship with my mum is still a bit delicate. She has referred to me as an irresponsible parent in the past when she caught me dancing around the kitchen with Connor. I couldn’t believe she was telling me how to parent after the childhood she had given me!
As for Connor – he has turned everyone’s lives around. He is my little angel. Both mum and dad no longer drink and both are in employment. Connor spends loads of time with them on the weekends. I love it when people say ‘Is this your little boy, he’s so polite, so well mannered’ and he is. He has a wonderful sense of humour. He’s a really good artist and an actor. He’s got an amazing personality and brilliant sense of humour. Although gets a little too cheeky sometimes!
I live in my own home with Connor and I have just finished my social work degree. Looking back, it could have been so different. I know I was on the path of self-destruction and can honestly say that if I had not have had my son I would probably be dead.
He really has turned my life around and I know that without him I wouldn’t have had the passion or determination to make a good future for us.
Yeah, being a teenage parent is hard and without support things can go wrong. But with the right support in place and professionals along the way who genuinely want it to work, it could be the best possible outcome. I know it is for me!
Script of Jake’s story: ‘Tell us straight’
Jake is a happy 2-year-old boy who lives at home with us and his two older siblings of 8 years and 5 years. One Friday, we picked him up from nursery and were told that he’d banged himself and had a red mark on his cheek. Jake didn’t seem particularly bothered and didn’t mention it at home so we thought nothing more about it. Jake tells us everything. He is a chatterbox and tells us everything that he’s seen and done and anything that has happened to him. He told us he’d tumbled off a bike at nursery and we took it that was where he had banged his face.
That weekend, we were bathing Jake. He has a lot of blond curly hair which covers his ears. In the bath, his hair was wet and we clearly saw a dark bruise on the top of his ear, behind it and inside the top of it. We also noticed a dot lower down inside his ear which we thought was as a result of his banging it when he had the accident with the bike at nursery. We checked on the internet about ear bruising and noticed that it can be a sign of infection and a developing problem. We rang the out-of-hours GP service and were told to take him to the local hospital.
We went straight to the ward and understood we were bringing Jake to hospital for some tests to check there was no infection on his ear. We were seen by a paediatrician who spent about 10 minutes looking at Jake, hardly said anything, then went away. Next thing we knew was a social worker was there wanting to speak to us. That’s when it felt that our lives were being blown apart. The social worker told us the doctor thought the injury to be suspicious and looked like it had been inflicted, not that it had been caused accidentally as we had assumed. We couldn’t believe what we were hearing. We felt accused – mortified. How could anyone think we could hurt our children? They are our lives. Our world revolves around them. Surely children bruise their ears all the time? We had so many questions but no one seemed willing to spend time to answer them for us.
The social worker visited us at home and actually said that the worse case scenario was that our three beautiful children would be taken into care. We were devastated and terrified at the same time. We knew we had not hurt Jake. The social worker said she could see we were a nice family and this would just be a formality and she would have to check with the GP to see if he had any concerns about us. The GP rang us and told us the social worker had been in touch. He told them it was ridiculous that anyone could suggest that we had hurt our son.
The social worker said she would be back in touch and keep us informed. We did not hear anything. For two long weeks we did not dare to go out in case someone called. We just wanted this nightmare to end. Every time the phone rang we wondered if it would be someone telling us they were going to take our children into care. Eventually, we rang and asked what was happening. The social worker was on holiday! She was supposed to have sent us a form and claimed she had pushed it through the letterbox but we had been waiting every day for some form of communication and knew for a fact nothing had been pushed through our letterbox. We were in the dark and hadn’t got a clue about what was going on.
Eventually we were told the case was closed – but we still had lots of questions. We wrote to the hospital and met the consultant paediatrician who had advised on Jake’s injury. Our questions were answered, explanations were given and we began to realise that Jake couldn’t have hurt his ear by banging it on the handlebar of the bike. We were shown information that helped us understand that although we knew we had not hurt him, perhaps someone else had. We have had to push for this information though, it hasn’t been offered to us. Everyone seems to have done their bit of form filling and box ticking and social workers have seemed happy to accept we haven’t hurt our son, but have they made enquiries about the times he was at nursery and not with us? It seems all the focus was on us – we must have caused the injury. When everyone had ticked their boxes and decided it wasn’t us, why didn’t they look elsewhere – the injury still happened?
At the time when we were at the hospital with Jake we would have welcomed the opportunity to ask questions and have them answered but it felt like no one wanted to talk to us. We were accused. If someone had said something like ‘no one is being accused but we think someone has hurt your child’, it would have helped us understand what was going to happen next and we wouldn’t have felt so scared. Perhaps the doctor was trying not to upset or offend us – but the truth is we would prefer to be told straight about what they think has happened and be told straight about what is going to happen. There’s no point in trying to fluff it up. It doesn’t help. It makes things worse. We should not be left not knowing what is going on.
We know why child protection procedures are in place and now accept why they were followed when Jake turned up with the bruising on his ear. We understand that now but we didn’t at the time and no one tried to tell us. It might not be easy for hospital staff to know what to say when they have to make a referral to children’s social care so this story is intended to help professionals to do the right thing and do things right:
-
Put yourself in our shoes. How would you feel if your child came home with a bruise that you wanted to seek advice about and then you find yourself feeling accused of causing it? Think; it might be someone else who has caused this. Perhaps you could say ‘someone has hurt your child’.
-
Tell us straight – don’t try and fluff it up. It doesn’t help. We need to know you think this injury is inflicted and that it needs to be investigated. Don’t leave us not knowing. How would you feel being left in the dark for weeks and weeks? Please, tell us straight.
-
Tell us what is going to happen. Don’t leave us guessing. You might need to say it a few times but please, let us know – what is the procedure you are following and what can we expect to happen next.
We don’t want another child abuse tragedy any more than you do. We know why you have to follow procedures. Help us to understand, give us time to ask questions and please, just tell us straight.
As for Jake, we took him out of the nursery. We could not be confident he had not been hurt there and no one was going to find out for us. What if he was hurt there? What if other children will be hurt by someone who is still there? Makes you think, doesn’t it?
Appendix 15 Patient and public involvement in digital stories
At PAHT, all complaints that are in any way related to safeguarding concerns are shared with the Head of Safeguarding, who addresses the concerns in the response to the complainant and contributes to meetings. These complaints furnish potentially valuable patient stories, providing a powerful mechanism for enhancing PPI.
Two recent ‘patient stories’ have been invited from parents who have made a complaint where the child protection process has been followed correctly, and therefore their complaint has not been upheld, but who also wished to meet to express their concerns about communication during the process. On both occasions it was acknowledged that professionals had something to learn about how they communicate with parents while complying with child protection policy, and the Head of Safeguarding invited the parents verbally at the meeting, then later in writing, to meet with her so that their ‘story’ could be captured and used in training.
Both sets of parents consented to the Head of Safeguarding contacting them to make arrangements to see them in their own homes and discuss the key learning points they wanted to get across. The different sets of parents took different routes from this point on. It was emphasised to both sets of parents that there was no expectation being placed upon them and revisiting the events that led to the complaint might prove unpleasant for them and they might wish to withdraw their consent at any point.
Deborah, who worked with the trust to produce ‘Aiden’s story’, met with the Head of Safeguarding at her home to discuss the general format of the digital story and agree the use of pictures, music, text and voiceover. Paula went through the story again with the Head of Safeguarding and emphasised the key points she wanted to make within the confines of a story that would last between 2 and 6 minutes. Deborah wrote the ‘script’ and agreed some small edit points with the Head of Safeguarding. The script was passed to the trust e-learning team along with some digital photos of Aiden to include in the story. These were edited together with library pictures and music. Deborah then came to the trust premises to record a voice over. She wanted this to be clearly attributed to her and to be about her son and the credits show this. Deborah signed ‘release’ forms to provide written consent to the use of the story in training. The trust newsletter did a piece on the launch of the DVD and issued a press release. Deborah commented on several occasions that the process was ‘therapeutic’ for her. She was extremely happy with the results.
The DVD is now used regularly in face-to-face child protection training and has been shown to the trust board.
The second set of parents had a different experience. As part of the complaint process they moved from a position where they felt unfairly accused of abuse to a position where they acknowledged that their child had sustained an inflicted injury but with no idea as to who had inflicted it. Their attentions turned to their nursery provider and that was still being played out when the Head of Safeguarding visited their home, with their consent, to begin the ‘story’ process.
The initial meeting with the parents went very well and the parents explained that they wanted them and their children to remain completely anonymous, which did not present a problem. It was clear, however, that there was still a lot of emotion surrounding the incident that led to the complaint. Both parents wanted the Head of Safeguarding to write their story and this was done using the words in their complaint letter, the words minuted at the complaint meeting and the words used in their home. The key messages and the language to describe them were agreed in the home and the Head of Safeguarding prepared a short piece for their approval. At each stage of contact with both parents, the Head of Safeguarding invited the parents to step out of the process. On receipt of the written story the parents e-mailed back to say that the process was proving too painful for them and they wanted to put it behind them. They stated that they felt confident that the Head of Safeguarding understood their perspective and would use their words as agreed to express the key messages they wanted to get across. They gave full consent to continue to develop a digital story but without their further input and without naming them or their children. They took some comfort from the fact that the work would continue and would be used to educate health professionals.
The third digital story did not arise via a complaint but included an opportunistic encounter with a teenage pregnancy midwife and one of her previous patients, whom she discussed with the Head of Safeguarding in supervision. The story of a determined young woman achieving career and academic success against all the odds and flouting all stereotypes was felt to be a powerful story that would have a high impact in training and education. The teenage pregnancy midwife contacted her ex-patient and asked if she wanted to engage in the ‘parent story’ process.
Natalie was extremely cautious to start with and agreed to provide her contact details to the Head of Safeguarding to discuss the process and to seek some assurances. Natalie was on the point of qualifying as a social worker and wanted full assurance that her story would not include any detail that identified her or her son. This was given and she met with the Head of Safeguarding on trust premises at Natalie’s request. Natalie preferred to tell her story while the Head of Safeguarding wrote, rather than produce it herself as Deborah had done. It was longer than the previous digital story but contained more than a single incident. After their meeting the Head of Safeguarding prepared a written ‘script’ and sent it to Natalie. Natalie returned it with some amendments and reordered the content. She was very uncertain about leaving in a reference to her ex-partner and the fact that he was emotionally abusive. It was agreed she would leave it in as it could always be edited out if necessary.
The completed script went to the e-learning team who recorded a voiceover using their own staff as Natalie did not want to risk being recognised by her voice. There were no pictures of her or her child and the story was made up largely of animated shapes. An early draft of the digital story was sent to Natalie. It was not finished and the whole story was not told. She was pleased with the progress made but still uncertain about the reference to her ex-partner. Shortly after this, the Head of Safeguarding sent her the completed story with the reference to the ex-partner still included. When she saw the whole thing Natalie was completely satisfied that it should remain and remarked on how powerful the story was and how moving for her in a positive way. How she had triumphed over so much adversity filled her with a sense of pride when she saw it captured on DVD – even though it was her story and she knew it. The final edit was completed and a launch for its use in training planned. As reference is made to other agencies, the relevance of this story goes beyond health professionals but extends to other agencies. The plan is to share the DVD with all four LSCBs within the PAHT footprint, with Natalie’s consent and knowledge.
The use of case studies in training is not a new thing. However, the people about whom they are concerned rarely, if ever, know they are used; they rely on a trainer’s interpretation of events and do not represent the voice of the parent or the child. The ‘parent story’ initiative that began from taking forward concerns that arose from complaints presents the voice of the parent directly and is captured in a way that cannot be altered and that has been approved by the parent themselves. The use of complaints, even where not upheld, has been successfully utilised to impact on system design around education and training for health professionals. The added benefit is the sense that the complainants experience that their voices are truly heard and continue to be heard long after the bureaucratic processes around the complaint are completed.
Appendix 16 Revised synopsis of study protocol
Improving practice in safeguarding at the interface between hospital services and children’s social care: a mixed-methods case study
Research question and research objectives
Can a safeguarding culture be designed within the hospital environment that will provide the conditions for the detection of children at risk of abuse and support protective actions before discharge, including collaboration with external agencies? Specific objectives include:
-
the development of a sociologically rich understanding of why diagnostic failures and communication breakdowns occur
-
the design of a suite of integrated interventions for promoting a positive safety culture, following a user-centred approach
-
the evaluation of the effectiveness of this package, including its generalisability across sites.
Background
Policy context: safeguarding and patient safety
Secondary health care should provide opportunities to prevent children returning to unsafe situations, or to alert other agencies to potential dangers, but there is strong evidence that clinicians under-report child protection concerns26 and that thresholds for reasonable suspicion are highly variable. In one of very few studies examining the interface between hospital services and children’s social care, Lupton et al. 30 found that clinicians in EDs believed that other agencies and professionals had unrealistic expectations of their role in child protection work. Workload pressures, ambiguous physical signs and the lack of wider information on the child and the family were seen to limit the role they staff could play in identification. In their review of serious case reviews (SCRs), Brandon et al. 200 note that a third of the 40 children they studied had a history of missed health appointments; six had been admitted to hospital, one child nine times, and 18 had at least one attendance at ED. Serious harm is only the tip of the iceberg: the number of other errors is unknown but will be substantially greater than SCRs suggest.
The persistence of failure to recognise children at risk and intervene appropriately in hospital settings is all the more disquieting given the plethora of reform initiatives rolled out since the death of Victoria Climbié,48 including the establishment of local children’s safeguarding boards and increased regulation and audit of child protection responses. Improving information sharing between agencies is emphasised in these reforms, resulting in a variety of complex forms and processes, often embedded in IT systems. Although expounded with strong claims that they would prevent future tragedies, the death of Peter Connelly (Baby P) showed many of the same system failures, especially at the interface with secondary health care. Given mounting evidence that top-down, bureaucratic approaches to safeguarding children have had paradoxical consequences, including restricting knowledge sharing between professionals,59,62,113–115 it has been argued that more attention must be paid to human factors and the interactional complexities of decision-making regarding children at risk of harm. 61 Within children’s social care, there are promising signs of growing interest in, and potential government support for, more systemic solutions, focused on human factors and human-centred design. 21,110,112,191
Within the NHS, systems approaches have a longer history and initiatives based on these principles have seen significant advances over the last decade. Patient safety is an international priority140 and the subject of a high-profile NHS initiative, Patient Safety First (PSF). There has been a reconceptualisation of clinical risk focusing on latent ‘error provoking conditions’ which create ‘accident opportunities’. 142 It has become increasingly recognised that most harm to patients is not deliberate, negligent or the result of serious incompetence. Instead, harm more usually arises as an emergent outcome of a complex system where typically competent professionals and managers interact in inadequate organisational configurations. 122 There has been a gradual recognition within the wider health policy arena that safeguarding (both adults and children) is inextricably linked with quality, governance, safety and dignity. 143 Although these developments have begun to address the safety of children presenting in hospitals, only scant reference to safeguarding is made in the Operating Framework for the NHS in England 2011/12144 and PSF focuses exclusively on ‘in hospital’ threats, not the extramural risks to which the children are usually exposed. This reflects general concern that protecting the welfare of children is insufficiently embedded within the thinking and practices of acute NHS trusts. 145 Much research on patient safety to date has also focused on a single clinical environment, or organisational setting. 69,146 There has been a relative neglect of threats to patient safety arising across settings, or where the decision-making depends on a dispersed network. This is often the case in secondary settings where retrenchment of local government services has led to the loss of many hospital-based social work teams. 147 Safeguarding children often falls into the interstices between organisations and governance systems, with a consequent lack of clarity about responsibility compounded by endemic problems in communication and knowledge sharing across space, time, organisational and professional boundaries. 148 As a high-risk, high-blame activity it is also buffeted by media scandals and political buck-passing149 which create further barriers to co-operation.
Human and interactional factors in child health: sense-making and knowledge sharing
In child health settings, clinical sense-making can be particularly complex. For example, often children present with a complaint for which there may be biological, neurological, genetic and/or psychosocial explanations. In accomplishing diagnosis, the boundary between biological and psychosocial aetiology is especially problematic. 91 For example, are frequent hospital admissions the result of an intrinsic metabolic disorder, a consequence of emotional maladjustment, poor nutrition, inadequate parenting, or do all factors apply? Furthermore, children frequently injure themselves and the injuries may be medically trivial,95 creating a potential bias towards the default assumption of accidental injury. Children are usually accompanied by parents whom clinicians may find difficult to confront and their moral evaluations of the parents can be decisive especially when the child cannot communicate directly. 26,91,96,97 Add in the intrinsic biases of human information processing (the tendencies to reach conclusions quickly, to develop a ‘psychological commitment’ to an anchor hypothesis and seek only confirmatory evidence:94,98 we have a powerful force-field for case formulations to be strong but wrong. These pressures are challenging to counteract, resisting interventions like training. 25 Moreover, attempts to increase the reporting of concerns carry their own unintended consequences: the generation of false positives, overloading child protection services, buck-passing and discrimination against vulnerable communities. 99 There are potentially direct adverse effects on children, for example a full skeletal survey to screen for unseen injuries can be very distressing, especially for preverbal infants. In a safeguarding context, further complexities arise from the need to pass what might be unclear, speculative and ambiguous information across service boundaries. Research shows that knowledge sharing and learning is influenced by multiple interpersonal, social and organisational factors, including the inhibitory impact of distinct knowledge domains, social hierarchy and low trust (e.g. Cross and Borgatti66). Knowledge sharing throughout child health and social care is thus both ‘slippery’ (difficult to codify) and ‘sticky’ (difficult to share across boundaries), not readily responsive to simplistic exhortations to ‘share information’. 67,68
Only a thorough understanding of human, social and organisational challenges will afford effective solutions. For example, one of the applicants has synthesised theories within organisational studies, medical sociology and public policy to develop an inclusive and pragmatic conceptual heuristic of the range of possible factors that shape knowledge sharing. This has the potential to generate lessons to improve learning and patient safety in hospital discharge, which have applicability to similar trans- and extramural risks associated with safeguarding children. 148 The heuristic embraces the domains of knowledge, culture and organisation, helping explain the challenges and potential solutions to knowledge sharing across complex occupational or organisational boundaries. Knowledge addresses what safety issues are under consideration; culture refers to how different groups act and interact within different communities and professions; and organisation is implicated in terms of the location and medium of the exchange, including the possibility of overlapping and ambiguous processes, regulatory regimes and technologies through which clinical practice takes place. This framework enables assessment of the impact of different reporting systems when children are perceived to be at risk, and the barriers to learning from adverse events (like diagnostic errors) to guide service improvement which can be used to design a safeguarding culture. It will be utilised in this study as indicated below.
Summary of need
Health need: children’s safeguarding has been a neglected area of patient safety despite being associated with high risks, including death. While isolated tools exist for detecting risk (Sidebotham et al. 6 estimate that 91.7% of EDs have some form of written protocol), little is known of their effectiveness in influencing clinical behaviour and follow-up of child protection outcomes is typically absent. 7,8 Here we will follow a ‘whole systems’ approach aimed at creating a culture of safe practice with children at risk, using a user-centred design methodology; this will be rigorously evaluated. While focused on secondary care, there will be primary health benefits in terms of prevention of harm and provision of timely intervention. We will identify lessons for other general and specialist child health settings and local authority children’s services to enhance the effectiveness of technology transfer.
Express need: the study aligns with the HSR aims – to understand and improve patient safety, patient experience and effectiveness of care. We offer a novel approach to a neglected safety problem featuring user-centred design, evaluation and technology transfer drawing upon the expertise of a multidisciplinary research team.
Sustained interest and intent: despite radical reforms to safeguarding processes and systems over the last 10 years, errors and failures persist in detection and intervention when children at risk present at secondary care, suggesting that there has been insufficient attention to human and interactional factors. This is a matter of priority importance for the NHS.
Organisational focus consistent with HSR mission: the research contributes directly to the strategic priorities of the HSR programme. It addresses cultural and organisational issues, uses applied methodologies within a multidisciplinary team, makes better use of existing research knowledge through system redesign, and is centrally concerned with knowledge transfer within and between organisations, seeking to provide measurement of quality improvement
Generation of new knowledge and prospects of change: there is a growing evidence of the social and organisational processes involved in children’s safeguarding, including the importance of communication, feedback loops, confidential reporting and organisational learning, but these are rarely modelled to take account of the social and cultural dynamics of child health settings. Moreover, existing research rarely addresses directly the issue of patient safety in relation to trans- and extra-mural risks.
Building on existing work: the study builds on previous work to understand, and develop interventions to enhance, safe practice across care processes and organisations. The team has extensive experience of related research (see references).
The clinical context: Pennine Acute Trust and clinician-led system design
The Pennine Acute Hospitals NHS Trust (PAHT) provides general and specialist hospital treatment to a population of 800,000 in NE Greater Manchester. It provides emergency services, diagnostics, medicine, surgery, specialist (HIV/AIDS) and women and children’s services, employing 8820 FTE staff. The Trust is in a process of reconfiguration under the ‘Making it Better’ national initiative, focusing on inpatient services for women and children. Despite the existence of clear guidelines, clinical practice regarding child protection varies across the Trust sites and even within specific services. For example, there is an explicit and unambiguous requirement that children under one year of age presenting at EDs with bruises, bleeding or fractures should be referred to the paediatrician on call, yet there are routine breaches of this protocol. In response to such failures, the Patient Safety First approach is being redesigned by the Pennine Acute Safeguarding Children Group and applied to promoting and safeguarding the welfare of children. The developments ‘combine bottom up energy with top down support’ (p. 11)12 which has been shown to be effective in promoting cultural change. The intended outcome is to create a positive safety culture, characterised by openness, justice and learning, where learning from error is regarded as the norm. 13,142 Various specific initiatives are under way.
-
Walkrounds. To promote an open culture when discussing safety issues and incidents PSF advocates the use of ‘walkrounds’ by senior staff. This has been adapted by PAHT directly to address safeguarding issues, and is currently being piloted, before implementation across each area within children’s services and EDs. Targets will be set in order to measure effectiveness. Notes taken during walkrounds will be regularly collated and analysed feeding the findings to the Trust Board via the Clinical Governance and Quality Committee and also to practitioners through the Pennine Acute Safeguarding Children Group to achieve a ‘board to ward’ and ‘ward to board’ governance loop. 118,122,182
-
Systemic incident analysis. A whole systems approach to the analysis of ‘safeguarding incidents’ (serious failures, near misses and less consequential instances of ‘something going wrong’) is being developed, focusing on latent conditions alongside procedural failure. Diagnostic errors and failures to communicate effectively with other professionals and agencies will be emphasised, and practitioners and managers prompted to consider how lessons learned from incidents can best be shared with peers. Congruent with a learning culture, a more robust system of peer review and clinical supervision (incorporating reflexive practice) is being developed. Application of the systems approach will be embedded within the preparation and dissemination of SCRs, with progress on actions fed back through a variety of methods (newsletter, training).
-
Electronic reporting. The effectiveness of staff in recognising and reporting potential safeguarding risks accurately and promptly to relevant professionals from other organisations, disciplines and agencies is crucial. PAHT have a paper system for sharing information across professional and organisational boundaries known generally as a ‘cause for concern’ form. However, the degree to which professionals consider it necessary to raise concerns differs across the organisation and across different clinical areas. A web-based tool is being designed (based on an adaptation of PSF’s SBAR tool) to promote referrals that clearly express what is expected of the recipient and the level of concern.
-
Digital stories and service user engagement. The use of PPI in child protection is challenging, but parents who have submitted official complaints about their experience of child protection procedures within the Trust are being approached. Videos (‘digital stories’) are being produced. These are presented by the parent, and are aimed at improving professional communication and helping parents to understand clinical procedures. Early experiments have shown considerable promise. Digital stories are also planned both to disseminate best clinical practice and to illustrate the root causes of critical incidents.
-
Co-mentoring and auditing. PSF advocates the use of risk assessment tools, and an adaptation of this is being developed within PAHT. A co-mentoring system is proposed201 which provides feedback to staff on cases where a different intervention might have benefited the child, thus embedding ‘double loop learning’. 202 This directly supports the aim of the ‘Munro Review of Child Protection’ which seeks ‘a less prescriptive working environment with more room for professional judgement’ (p. 1.11). 203 Co-mentoring will be piloted in ED, led by specialist Band 7 practitioners. It will focus on practice with a view to providing feedback to build trust, raise awareness, and enhance timely sharing of information. 183 Auditing of records, as the PSF recommends, will be part of this, providing feedback when standards are not met.
The following table shows how these initiatives map into the heuristic framework set out above as their primary (✗✗) and secondary (✗) focus as partial solutions:
| Intervention | Knowledge | Culture | Organisation |
|---|---|---|---|
| Walkrounds | ✗✗ | ✗ | |
| Systemic incident analysis | ✗✗ | ✗ | |
| Electronic reporting | ✗ | ✗✗ | |
| Digital stories and service user engagement | ✗✗ | ✗ | |
| Co-mentoring and auditing | ✗✗ | ✗ |
Research design and methods
The investigation follows a design science approach, involving a mix of quantitative and qualitative methods. In contrast to conventional social science (which aims to describe, explain or predict social phenomena) the aim of design science is to develop a corpus of practically-oriented knowledge regarding the design, implementation and use of a general class of artefact, technology, or service innovation. 17 Design is a core feature of PSF and has been shown to be integral to its success. 12 Design science intrinsically involves the construction and evaluation of an exemplar of the innovation in question, reflexively learning from this real-world action. Given its practical orientation, design science is characterised by robust eclecticism in terms of theory and method. Reflecting this, a range of research methods are used, following a broad user-centred approach, which is vital in health and social care. Ethnographic analysis, for instance, is indispensable in order to understand professional practice. On the theoretical side, several relevant perspectives are applied, with a particular focus on organisational culture.
The concept of organisational culture is ubiquitous in the discourses of health care reform and patient safety. It is known to be a key factor in the successful adoption of clinical guidelines, for example. 123 Yet culture is a contestable concept and has been rigorously interrogated. 124 There are established tools for assessing cultural change in health care. However many instruments reflect the same intra-organisational biases of the patient safety literature generally and the majority explore predefined sets of dimensions which do not fit with the proposed study. 124 The ongoing design orientation of the research and the novelty of the clinical problem required a more emergent and open methodological approach, introduced above and described in practical terms below. That is, the development of a ‘just culture’ and associated changes in the organisational milieu should be visible in human actions and reportable in professional talk – as evidenced in everyday conversation and in interviews. Anthropological methods, have been shown to be a particularly sensitive methodology for assessing cultural change in patient safety studies. 155,156 These are deployed and also triangulated using semistructured interviews and analysis of key metrics such as the number of cases reported, the numbers of complaints received and so forth. For internal validity,161 all interviews are fully transcribed with least two members of the research team involved in generating coding frames for themes from qualitative data, comparing independent coding of a subset of data to identify and address coding differences and ensure consistency.
Work package 1: research planning and preparation
WP1 is directed towards preparing and planning the study securing ethical and other approvals conducting a synthesis of existing literatures and assembling the PPI group.
Work package 2: completion of design phase 1
Use of mixed qualitative methods, for example interviews with clinicians, non-participant observation of everyday practice and the prototypes in-use and (re)design workshops, to bring the design of the various instruments in Pennine to completion. A broad user-centred approach is adopted, now widely embraced as a highly effective approach to service design, within the public sector in particular. 17 The following table summarises each intervention, the research methods needed to complete the design and the primary outputs.
| Intervention | Status | Research methods | Primary output |
|---|---|---|---|
| Walkrounds | Prototype being piloted | Observation Interviews with executive directors | Revised walkround protocol and good practice guidelines |
| Systemic incident analysis | Prototype system being designed | Retrospective file research Interviews with senior practitioners involved in the cases above |
Revised protocol/methods and training materials Case studies |
| Electronic reporting | Paper systems: including referral forms, SBAR Web-based prototype |
Observation of practice and interviews with users (mainly nurses) in ED, paediatric wards, antenatal Interview referral team managers, one in each of the four local authorities User-centred design workshop |
Structured electronic reporting tool for internal and external referrals |
| Digital stories and service user engagement | One story had been produced at the start of the study | Development of three further stories collaboratively with clinicians and families was undertaken | Portfolio of digital stories |
| Co-mentoring and auditing | Pilot system being designed for ED | Observation of training of co-mentors in pilot study User-centred design workshop |
Protocol and training materials Case studies |
Work package 3: evaluation phase
This involves a systematic internal and external evaluation focused on the quality of decision-making regarding safeguarding. This included interviews with clinicians and managers, audits of cases and critical incident analysis building on the work in place in Pennine to assess reporting and decision-making.
| Intervention | Evaluation |
|---|---|
| Walkrounds | Observation in two separate months and interviews with sample of key staff in walkround sites (wards sisters, junior doctors) Analysis of metrics (no. of walkrounds and actions) to examine trends over the period of the study |
| Systemic incident analysis | Ongoing audit of new incidents Interviews with clinicians and managers identified as having played a key role in sample) of the above |
| Electronic reporting | Observation of current practice and interviews with key internal users in the various sites of use: ED, maternity, and paediatric inpatients Tracking and auditing of referrals to local authorities Online survey of all clinical staff at PAHT |
| Digital stories and service user engagement | Interviews with safeguarding staff |
| Co-mentoring and auditing | Observation of current practice and use of routinely collected audit data Interview with mentors and a sample of ‘novices’ |
Work package 4: technology transfer/generalisability
In addition to the innovations in PAHT, we are concerned with the adoption of the safeguarding system in new sites. Understanding the transfer of technologies between contexts is crucial if benefits are to be accrued across the NHS. In a review of research on the diffusion of service innovations, Greenhalgh et al. 14 concluded with a call for research to address the following key question:
By what processes are particular innovations in health service delivery and organisation implemented and sustained . . . and can these processes be enhanced? This question, probably the most serious gap in the literature we uncovered, would benefit from in-depth mixed-methodology studies aimed at building up a rich picture of process and impact.
p. 620
The present study aims to addresses this gap. However, it proved impossible to implement the suite of initiatives designed in PAHT to other identified sites due to problems in adapting IT systems in one site and failure on the part of the other site to process R&D approval until the final day of the project. An additional site was thus used as a comparator to explore the generalisability of the findings on sense-making, professional reasoning and interagency communication from the primary site.
Glossary
- Designated doctor/nurse
- Based in primary care trusts, these individuals take a professional and strategic lead on all aspects of the health service contribution to safeguarding children.
- Named doctor/nurse
- Based in acute trusts, these individuals provide advice and expertise and promote good practice within the organisation.
List of abbreviations
- A&E
- accident and emergency
- BPM
- business process management
- CAF
- common assessment framework
- CFC
- Cause for Concern
- CSC
- children’s social care
- CT
- computerised tomography
- CVF
- competing values framework
- ED
- emergency department
- eSCF
- electronic special circumstances form
- FCT
- first contact team
- FII
- fabricated or induced illness
- FTE
- full-time equivalent
- GP
- general practitioner
- HDU
- high-dependency unit
- HRO
- high-reliability organisation
- HSDR
- Health Services and Delivery Research
- HVL
- health visitor liaison
- ICS
- integrated children’s system
- ICT
- information and communication technology
- IT
- information technology
- i.v.
- intravenous
- LSCB
- local safeguarding children board
- MASH
- multiagency safeguarding hub
- MRI
- magnetic resonance imaging
- NETSCC
- NIHR Evaluation, Trials and Studies Coordinating Centre
- NIHR
- National Institute for Health Research
- NPM
- new public management
- PAHT
- Pennine Acute Hospitals Trust
- PAS
- patient administration system
- portable document format
- PLS
- paediatric liaison service
- PPI
- patient and public involvement
- PSF
- Patient Safety First
- R&D
- research and development
- RAG
- red, amber and green
- SBAR
- Situation, Background, Assessment and Recommendation
- SCF
- special circumstances form
- SCR
- serious case review