Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 08/1806/262. The contractual start date was in December 2009. The final report began editorial review in June 2013 and was accepted for publication in February 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Sheaff et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 NHS commissioning practice and health system governance
Background
Few questions are more important to the NHS than how its commissioners exercise governance over local health economies. Commissioners pay for health care on behalf of patients who cannot do so themselves and on the state’s behalf; in the absence of public ownership and direct managerial control by the state, they also exercise governance over the service providers. This study aims to examine the means, contexts and effects of commissioning practice that was current in 2010–12, that is the activities of assessing health needs, selecting and contracting providers to meet them, monitoring the outcomes and then repeating the cycle. 1,2 We focus on the ways in which health-care commissioners can influence health-care providers within a quasi-market health system.
NHS commissioning: the policy context
Policy initiatives related to commissioning since 1991 have set the basis for current NHS commissioning policy and the system introduced in April 2013. Since 1991, three distinct main commissioning structures have evolved:
-
Population-based commissioning. A single body commissions health services for the entire resident population within its geographical boundaries. This structure includes public health activity, for evaluating population health-care needs and initiating preventative activities. In England, District Health Authorities began commissioning services for populations of 200,000–500,000 people in 1991.
-
General practice-based commissioning. General practices, or another gatekeeper and budget holder, individually or collectively commission services, the general practitioners (GPs) acting as proxies or advocates for their registered patients when making referral decisions. These commissioners tend to serve perhaps 5000–100,000 patients. GP fundholding was the best-known English variant.
-
Client-based commissioning. Patients themselves choose a health provider, which a commissioning organisation then pays on their behalf. Consequently the provider has to be paid per episode of care; in most health systems, through a diagnosis-related group (DRG)-based tariff system. Another variant is to give patients a voucher or budget to pay for care. Client-based commissioning is still an emergent structure in England, represented by the Patient Choice policy, personal health budgets and the ‘payment by results’ (PbR) system (see section Phase 5: 2006–10 – client-based commissioning).
Clinical Commissioning Groups (CCGs), introduced in April 2013, are essentially a variant of population-based commissioning, but also resemble general practice-based commissioning in that GPs play a pivotal role in their governance. One can distinguish six phases of the evolution of NHS commissioning in England.
Phase 1: unitary system (before 1991) and the impetus behind the 1991 reforms
Until the late 1980s, contiguous health authorities (HAs) planned and managed NHS hospital and community health services for a geographically defined population. Services could be organised across the district and integrated, since just one body managed them. Transaction costs were low because decisions were enacted through line management. However, HAs were subject to provider capture, becoming beholden to clinicians (especially doctors) both for technical reasons (to help inform their decision-making) and in consequence of the 1947 settlement between the state and the medical profession, through which the NHS was established. 3 There was also an efficiency trap: ‘good’ providers who attracted more patients incurred greater costs and their service ‘quality’ (especially waiting times) deteriorated.
The NHS financial ‘crisis’ of the late 1980s prompted the Conservative government to announce a widespread review. Though financial in origin, the crisis was to be solved by organisational restructuring. The Working for Patients White Paper4 heralded the end of the unitary system. Enthoven, whose work5 anticipated it, had proposed contracts with individual consultants, but the White Paper was less radical and proposed a market-style relationship between commissioners (‘purchasers’, i.e. HAs) and service providers, albeit with a heavy dose of management intervention and regulation. At varying speeds, NHS providers became self-governing trusts. A late addition to the proposals was GP fundholding, seen as a way of introducing competition between purchasers. Hence the NHS quasi-market was born in April 1991.
Phase 2: 1991–7 – the ‘plurality of purchasing’
Although allegedly incompatible,6 population-based commissioning and GP fundholding coexisted for several years.
Although HAs had sufficient financial clout to engender improvements in provision, they were not so responsive to local needs. Some HAs sought to introduce locality purchasing initiatives, not only to be responsive to local need but also to stem the flow of GPs electing to become fundholders. 7 GP fundholders had relatively little financial power (given the size of their budget compared with a provider’s), but were more agile in securing improvements in certain services for particular groups of patients. The analogy between HA ‘supertankers’ and GP fundholder ‘speedboats’ was apt.
Much concern about GP fundholding centred on fears of ‘cream skimming’ (GPs might avoid ‘unhealthy’ patients in case they cost the GP’s budget more), a two-tier service (some patients might enjoy ‘better’ access to services), higher transaction costs (of negotiating and monitoring contracts) and possible adverse effects on the doctor–patient relationship. In the event there were few cases of cream skimming and few patients were aware whether their GP was a fundholder or not,8 although transaction costs were approximately twice those of HAs. Over time, GP fundholding schemes became smaller and their remit expanded, which complicated the evaluation of them. 9 Some GP fundholders also sought to leverage their financial power by combining in networks (‘multi-funds’), which evolved into more formal total purchasing pilots (TPPs),10 the nearest equivalent commissioning organisation so far to CCGs. Each served about 300,000 people, similar to an HA. By 1997, the variants of GP fundholding covered 53% of the English population,11 equivalent to 10% of the hospital and community health services budget. 12
At this stage client-based commissioning barely existed. Although patients were given some encouragement to move between practices, few did. 8,13 Policy talk about ‘choice for patients’ was thus largely rhetoric.
Phase 3: 1997–2001 – the fall and rise of the practice commissioner
Labour’s 1997 election manifesto declared that it would replace GP fundholding with more collaborative commissioning,11 in language that symbolised a shift away from explicitly market-style relations towards a system of service ‘delivery agreements’ of longer duration than existing contracts. Whereas GP fundholders had real budgets, the replacement system would give general practices ‘indicative’ budgets. Crucially, all GPs in an area would belong to a primary care group (PCG). The 481 English PCG boards were mandated to include nurse and local authority representatives,14 but GPs were in the majority, albeit ‘not very effective’15 in wielding influence. Although the ‘ghost of GP fundholding’ lived on,15 the tension between general practice-based commissioning and population-based commissioning was resolved in favour of the latter, attenuated with strong GP input.
Primary care groups evolved into primary care trusts (PCTs), taking on the former HA role to
become the lead NHS organisation in assessing need, planning and securing all health services and improving health. They will forge new partnerships with local communities and lead the NHS contribution to joint work with local government and other partners. 16
Health authorities were abolished, while NHS performance management regimes and the authority of the Secretary of State were significantly reinforced. 17
Phase 4: 2001–6 – shifting the balance of power?
In 2005, practice-based commissioning (PBC) was introduced to give GPs greater influence over commissioning. PCTs gave general practices ‘virtual’ budgets for health services for their practice patients, but retained the ‘real’ money;18 a system similar to the TPPs. Since PBC budgets were not held at practice level but collectively, PBC represented another variant of the population commissioner model, with stronger GP input than hitherto. PBC practices tended to collaborate to share expertise and resources, designed care pathways jointly19 and encouraged GP engagement with commissioning. However, on balance:
Progress to date has been slow in all sites: very few PBC-led initiatives have been established and there seems to have been little impact in terms of better services for patients or more efficient use of resources. 18
See also Coleman et al. (p. viii). 20
By 2012, ‘David Colin-Thomé, the health department’s lead doctor in primary care, declared it [PBC] to be a “corpse”. A corpse which he judged was “not for resuscitation” ’. 15
Phase 5: 2006–10 – client-based commissioning
In 2006, PCTs were amalgamated, reducing their number from 303 to 152. The number of Strategic Health Authorities (SHAs) was reduced to eight, in ‘what looked remarkably like the reinvention of the regional offices that had been abolished earlier’ (pp. 241–2). 21 Ministers were starting to consider PCTs underpowered in controlling healthcare providers and began considering ‘demand side’ (p. 11)22 reforms. World-class commissioning (WCC) was an attempt to upgrade PCTs’ managerial performance of their commissioning role, and to strengthen PCT commissioning by developing, and evaluating PCT performance against, a set of 10 competencies (www.hsj.co.uk/resource-centre/world-class-commissioning-nhs-sets-out-to-lead-the-world/211288.article) – a development that also illustrated population-based commissioners’ ongoing search for legitimacy. Under the Commissioning for Quality and Innovation (CQUIN) scheme, up to 2.5% of the value of provider contracts was linked to compliance with quality standards; the selection of quality standards changed from year to year, and within limits could be varied at regional level.
Client-based commissioning thus emerged. Hitherto, NHS providers (except GPs) had been paid through block or cost-and-volume contracts. The PbR policy introduced a prospective payment system of paying providers a tariff for each episode of care. These ‘Healthcare Resource Group’ (HRG) tariffs were a variant of the DRG system originally developed in New York. PbR was intended to encourage providers to reduce their costs (to below tariff level) and increase patient throughput (hence reducing waiting times for treatment). Concurrently, the ‘Patient Choice’ policy obliged GPs to offer patients a choice of provider for planned secondary care,23 and the chosen provider was guaranteed the corresponding tariff payment. Following similar schemes for social care,24 a pilot scheme to develop and evaluate personal health budgets was launched. In 2009, a policy that NHS organisations would be ‘preferred providers’ was announced. Nevertheless, the policy of promoting provider competition (including competition between NHS providers) continued during and after 2009.
Phase 6: coalition government
Originally billed as ‘GP commissioning groups’, CCGs are membership organisations of all the GPs serving a geographically defined resident population. Although the nature of this membership role is still emerging, it means that individual practices will not hold commissioning budgets; only the CCG will do so collectively. Thus CCGs represent yet another variant of population-based commissioning, but with still stronger GP input. This time, GPs are ‘required to assume the driving seat of commissioning’ (p. 12). 15 CCGs will also have greater leverage over individual general practices’ performance than did earlier commissioners. CCGs were intended to become responsible for 80% of NHS spending (their 2014 share is almost certainly lower) compared with the initial 30% budget responsibility for GP fundholding in 1991. It remains to be seen whether CCGs will become more like large-scale GP fundholders or more like PCTs.
The Any Willing (later, Qualified) Provider policy widened the range of providers from which patients or GPs could choose, with the aim of adding private providers. The Transforming Community Services (TCS) policy (2011) transferred community health services from PCT ownership and management into separate organisations, most often NHS trusts. The monitor’s role became one of fostering ‘level playing field’ competition between public and private providers. Private firms were permitted to participate in NHS commissioning, through selling data analysis services that model patient demand (as two US health maintenance organisations (HMOs) have done), helping commissioners manage programme budgets, or selling more general commissioning support to NHS commissioners. Further commissioning support work could, according to some, be tendered for private-sector provision.
So, at the time of writing (June 2013), the NHS mainly uses two commissioning structures: a population-based (but GP-controlled) structure and a client-based structure [PbR plus Any Qualified Provider (AQP)]. Traces of general practice-based commissioning are more rhetoric than reality.
Continuities
Certain structural continuities have persisted since 1991. Competing governance structures coexist. 25 Health policy rhetoric about competition has often been accompanied by a strong undercurrent of control and market management, such as brokering individual organisations’ losses at the end of the financial year. 26 Concomitantly, the level of competition has waxed and waned. Throughout the past 20 years, commissioners have preferred to spend their budget on local providers – ‘localism’. 27 While commissioning structures have varied over time, whether NHS funding was expanding or being retrenched, commissioners have retained a rationing role and a function in ensuring equitable allocation of NHS spending.
There has been constant tension regarding the scale of population at which commissioning should take place. 28 The range goes from personal budgets (n = 1) to CCGs and, for rare or specialised treatments, millions. The Secretary of State did not prescribe how many CCGs there should be, but the number authorised (n = 211) is smaller than the original number of PCTs (n = 303), larger than the last generation of PCTs (n = 152) and similar to the number of HAs in 1992 (n = 192). General practice, specialised services and health visiting are commissioned at national level by NHS England.
There has also been a clear shift away from letting general practices decide if they want to commission other services. GP fundholders were volunteers. All practices had to be members of their local PCT, and now CCG. The GPs managing CCGs will have to take responsibility for, and intervene to influence, any apparently poorly performing GPs or general practices in their territory. They will hold individual practices to account for the practice’s commissioning expenditure. In some areas general practices are already being performance managed on this responsibility. General practice itself has been gradually drawn into the orbit of NHS management, partly but not only through successive changes to GP contracts, especially the new general medical services (NGMS) contract introduced in 2004. 29
Contracting methods have also become more sophisticated, block contracts being gradually replaced by cost and volume contracts (sometimes with caps and/or cost-per-case variations at the margin). Starting with a small range of planned acute treatments, PbR tariffs now cover most planned acute care and are being extended into mental and community health services.
Overview
Although the commissioning–provision split is generally accepted, the precise roles that either side plays are not. Given the alleged ‘failures’ of commissioning (and commissioners) over the past 20 years,30 it might appear that the balance of power within the NHS remains weighted towards the providers, in primary31 and secondary care. Equally, commissioners have not always been willing to exercise their powers fully, often ‘colluding’ with providers in support of local services. 27 Their limited data and expertise also put NHS commissioning organisations at a further disadvantage compared with providers. Managerial careers in commissioning, for example, might be short compared with those in NHS trusts. Mean salaries for commissioner chief executives were about £10,000 less than their acute-sector counterparts. 32 Throughout there has been an ongoing tension between the need for a publicly funded service to be answerable to Parliament and the neo-liberal desire for markets and competition, which policy-makers think deliver locally responsive services.
Attributing impacts to commissioning and commissioning practice is a complex and contested activity. Because evaluation was not built into the early periods of commissioning, the evidence for improved outcomes is equivocal. Two reviews8,13 point to some positive outcomes, although other commentators33 are less convinced. This brings us to the question of what existing research shows about the mechanisms by which commissioning works and their effects.
Chapter 2 The research context: commissioning as governance
Governments introducing quasi-markets in health care still wish to avoid uncontrolled ‘market forces’ damaging such politically salient services. An apparent solution is to construct governance structures34 that retain a degree of state control, hence exercise power, over the increasingly independent health-care providers. Someone must also be ‘payer’ on behalf of patients who cannot pay providers directly. Commissioning serves both purposes.
‘Commissioning’ is a very English concept. Elsewhere, diverse organisations fulfil these roles to varying extents: social health insurers [social health insurers (SHIs), e.g. Krankenkassen (Germany), Siekenfonds (the Netherlands)], state bodies [e.g. Medicare (USA)], corporate insurers, charities or mutuals [e.g. Group Health (USA)]. To develop an initial theory of how commissioning works, we therefore drew on research about this range of organisations (and for brevity call them all ‘commissioners’).
International comparisons of health systems35–37 report that commissioners use diverse and multiple means of exercising governance over providers. Many quasi-market health systems hybridise contractual with hierarchical38,39 and networked governance structures. To explain and analyse such complexes therefore required a theoretical framework which accommodated, and related, these diverse governance mechanisms, one capable of combining and integrating more specific theories (e.g. of contract) within a wider, more complex framework. Consequently, and because governance is an exercise of power, we selected the theory of (the multiple) ‘technologies of power’40–42 as an overarching analytic framework. Within it, we applied (a) more specific analytic framework(s) for each of the main media of power (enumerated below), choosing a framework relevant to, and used in, preceding research into commissioning, but with two exclusions. When incompatible alternative theories were available (e.g. negotiated-order versus institutionalist explanations of organisational value-systems), we selected the one most consistent with the overall framework and complementary to the other elements in it. We also excluded essentially normative frameworks, such as neo-classical theories of perfect competition43 or normative managerial accounts of governance. The resulting framework supplements the markets–hierarchy–networks trichotomy of governance structures44 with a more nuanced, specific account of the media of power through which, in different combinations, commissioners might exercise governance over providers.
Many commissioners are also, even mainly, agents of employers, subscribers (consumers),45 shareholders and other interests besides the state. In some health systems, commissioners compete, which in Germany and the Netherlands has led to market concentration on the commissioner side of the market. 46,47 Commissioner competition may accentuate adverse selection, requiring a risk-equalisation system to make risk selection unprofitable. 46 Even competing commissioners often negotiate collectively with providers, attempting to wield power through a de facto monopsony35 (one buyer confronting many sellers), which in a health system with flexible prices would help reduce those prices. 48
Media of power
The ‘therapeutic state’ (p. 254)40 co-opts and adapts the ‘technologies of power’ that it believes will reinforce its control over the population, promote and implement policies (e.g. regarding population health, reproduction, the control of deviancy) and discipline the medical profession accordingly. Foucault argued41 that control within and between organisations occurs through a dispositif: a structured complex of diverse, coexisting technologies of power42 including professional disciplines, surveillance, task sequencing, task distribution, coercion and panoptical control. 49,50 Commissioners generally try to exercise governance over health-care providers by combining several methods in parallel. 51 We call each such method a ‘medium of power’, because each embodies a collection of ‘technologies of power’. 52 These complexes of technologies of power are historical ‘positivities’ that can be identified only empirically, case by concrete case. 53 International overviews35–37 suggest that health-care commissioners generally use one or more of six media of power: managerial performance of commissioning; negotiated order; discursive control; resource dependency and financial incentives; provider competition; juridical control.
Managerial performance of commissioning
Strong management systems are necessary to ensure provider compliance. 54 Some English GPs see commissioning as a substantial ‘job’, others as a supplementary task. They often lack time and skill (e.g. in data analysis) to participate intensively in commissioning; PCTs also lacked the necessary resources. 55 Delegating those tasks to other staff may be cheaper, but can also send an adverse message about the relative importance of these tasks and problems. 56 Although GP fundholding may have fragmented strategic planning,13 their small size and organisational independence enabled fundholding practices to make small local service changes more easily than PCTs. 57
As noted, the managerial performance of commissioning is often regarded as a cycle involving evaluating the health needs of the population that the commissioner serves and then specifying the corresponding services, which requires epidemiological and public health expertise. Few recent studies examine how needs assessment relates to commissioning, although cf. Pickin and St. Leger58 and Milne. 59
A second step is procurement. There are again few studies of NHS procedures for recruiting and selecting providers, letting the contract and negotiating its terms and conditions. At times these procedures have been erratic. PCTs have been known to change their requirements for procuring alternative provider medical services less than 24 hours before the competitors were due to present bids. 60 Furthermore, the choice of provider inherently has a value-laden ‘political’ aspect. 61 Outside the health sector, Cousins and Lawson62 among others describe how corporations normally manage procurement through a supply portfolio approach, relationship management and performance measurement. Socialisation mechanisms, incorporating relational aspects such as supplier conferences and on-site visits, help establish effective communication and information sharing. These in turn support the integration of suppliers and providers into product development. Managerial attention becomes focused on specific aspects of procurement and product development, such as innovation and communication, through performance management processes. Competitive procurement for military equipment produced substantial savings even when the provider did not change,63 for instance. One difficulty, though, is co-ordinating different providers in parallel, especially under conditions of organisational instability. 64,65
Thirdly, commissioners have to audit and monitor provider performance and compliance with commissioners’ aims, and prevent provider ‘opportunism’. 66,67 Transparency of provider activities and costs assists commissioners in these activities,35,68 as does professional expertise in the services concerned. 54 PCT scrutiny of out-of-hours services was least rigorous when the PCT itself supplied them69 and most rigorous when social enterprises did. Bevan and Hood,70 Bevan71 and Gray72 describe how performance targets encouraged upcoding or ‘gaming’ of data returns by both NHS hospitals and general practices, although other studies39,73,74 report the opposite. Bevan71 attributed the weakness of PCT monitoring and control of providers partly to the removal of a regional level mediating between PCTs and the Department of Health (DH),75 and recommended introducing more uncertainty into how NHS provider managers are assessed in order to impede gaming. English GPs valued monitoring data only when they had selected information that would be meaningful and useful to them. 56 ‘Hard’ (measurable) outcomes make it easier for commissioners to monitor providers’ activity,76 even independently of the provider. 77 US local government commissioners self-report more active monitoring than providers perceive. 76 Where only soft outcomes apply, US practice is often to monitor multiple stakeholders’ satisfaction levels with providers. 76 Providers who perceive that their commissioner lacks monitoring expertise, and those who are highly resource dependent on one commissioner, are likely to try to negotiate monitoring methods with their commissioner. 77 US studies also report that commissioning managers often lack the skill and understanding to obtain monitoring data and interpret it in non-simplistic ways. 78–80 To address this point, the NHS introduced the WCC assurance framework, requiring PCTs to evaluate their competencies in procurement and ‘managing the local health system’, among others.
A second-order managerial task is to minimise the transaction costs of the above activities. Divergence between commissioner and provider goals, and hence the cost of monitoring services, is likely to be greater when publicly owned commissioners face corporate rather than ‘third-sector’ providers. 81 Transaction cost theories imply that contractual negotiations demand more resources for infrequently commissioned services that display asset specificity, uncertainty and immeasurability. 82–84 Thus the negotiation of, say, residential care contracts is simpler, cheaper and better adapted to quasi-market institutions than is the negotiation of contracts for mental health services. 85 In services with hard-to-measure outcomes, negotiative monitoring becomes necessary, with raised transaction costs;65 which may partly explain why US non-profit providers are over three times more likely to negotiate outcome monitoring than are for-profit providers. 77 Increased contracting out (of US social care) may come at the price of reducing commissioners’ own capacity ‘to be a smart buyer of contracted goods and services’,86(p. 296),87 although a study of US municipal contracts suggested that including contract management activities in the services bought can offset this problem. 54 However, some US commissioners doubt the probity of contracting out service-monitoring work. 76 In some US states, Medicare has subcontracted health-care commissioning entirely to managed care ‘plans’ (insurers) but how far this arrangement improves health outcomes to compensate for the additional managerial complexity is not well understood.
Economies of scale in commissioning management may be exhausted at quite small population sizes (< 200,000), although the threshold varies by care group (e.g. > 1,000,000 for organ transplants). 88 Qualitative studies83,89 suggest that moving from block to tariff payments (see subsection Resource dependency and financial incentives) raised NHS transaction costs. Longer-term contracts spread the initial transaction costs over a longer period, and flexible, relational working saves the cost of contract revisions. 83 Negotiating with an ‘umbrella group’ for numerous, similar small providers (e.g. general practices) also makes contract negotiation simpler and cheaper. 83 In theory, cheaper or more effective service provision might outweigh higher commissioning transaction costs, although an early New Zealand study cast doubt on this claim. 83 Greaves et al. 90 found no empirical basis for defining an optimal PCT size.
Negotiated order
Commissioners can also influence providers by agreeing with them a division of labour, rights of non-interference91–93 and arbitration procedures should disputes occur,35 establishing an explicit or tacit ‘negotiated order’. 91(p. 147),84,94 Although it might include contract negotiations as a special case, a negotiated order is wider than that. The parties exchange mainly non-monetary benefits: promises of action (or restraint), help in kind, authorisations, material resources, public support and so on. The negotiation may be multilateral and is highly ‘relational’,95,96 reflecting social capital already accumulated, local organisational cultures, micro-politics and personal antagonisms or affinities. The character of a negotiated order is determined by the selection of participants and by agenda control,97–99 that is what is not discussed and how the issues that are discussed are framed. The weaker a commissioner’s bargaining position, the more prudent it may be for them to negotiate about one variable (e.g. price or quality or volume), not several,100 letting other ‘sleeping dogs lie’ (p. 1). 101 English NHS structures at all levels reflect a negotiated order with the medical profession. 3 Bate et al. 102 describe ‘backroom commissioning’ in six PCTs where the chief executives of the largest local NHS organisations struck local deals about resource allocation. With few commissioners and providers, community health services also support negotiative rather than contractual relationships. 27,103 In contrast, commissioner–provider relationships in English social care, with its numerous small providers, ‘barely go beyond the mere business of contracting’ (p. 560). 104
Negotiated order is often criticised for allowing provider ‘capture’ of commissioning because of information asymmetry, because details of providers’ working practices and cost become negotiable only insofar as they are transparent and intelligible to the commissioner;105 professional loyalties and career paths transcend the commissioner–provider split; and commissioners assume that providers always behave in ‘knightly’, not ‘knavish’, ways (p. 67). 106 Such conditions may inhibit commissioners from radically changing existing patterns of provision. 107 Strong relationships between providers and government can also undermine commissioners:
contracting out presumes that the . . . contractor’s job is to act as agent of the government’s policy. The relationship is fractured, however, if contractors create independent political ties with policymakers and thus outflank their administrative overseers. In such cases contractors are less agents than partners, helping to shape the very design of the program, free from any significant oversight, and beneficiary of state and local governments’ dependence on their performance (p. 176). 107
As instances of negotiated order, in the early 2000s PCTs negotiated away financial control in return for providers realising other targets, rapidly increasing PCT deficits. 71 A New Zealand study found that non-governmental organisations were discouraged from participating in commissioning activities that they thought existing providers had already captured. 108
Nevertheless, some health policies encourage primary care doctors to ‘capture’ commissioning. Fundholding and TPPs appeared on balance to reduce elective referral and admission rates, emergency-related occupied bed-days (TPPs only), waiting times for non-emergency treatment109–111 and growth in prescribing costs. They appeared to improve the coordination of primary, intermediate and community support services, financial risk management (TPPs only) and clinicians’ engagement in commissioning. 112,113 However, they also reduced patient satisfaction (fundholding only) and equity of access, increased management and transaction costs and had little impact on how hospital care was delivered. Fundholding furthermore gave commissioning GPs an incentive to refer conservatively,111 despite GPs being insensitive to provider prices. 114
Discursive control
Where the parties trust each other, a stewardship model of governance115,116 applies and the negotiated order rests on discursive control. For persuading providers, commissioners can apply two main types of discursive ‘orders’. 117
Emic discourse is intelligible and morally persuasive to those who inhabit a particular culture, though not necessarily to others. It invokes what are regarded as legitimate normative claims on others’ behaviour, such as the demands of ‘policy’, ‘public opinion’, wider social ideologies (religion, economics, ethics, etc.) and professional ‘discipline’. 52 Thus, strong professional norms of treatment standards prevented Danish hospital ownership making much difference to the clinical quality of orthopaedic care;118 for England, see Waring and Bishop. 119 In the English NHS, managerial targets and their role as agents of central policy120 appear to have the strongest emic influence on NHS trusts, although less upon GPs. 31 A study of three English PCTs found that they regarded central government authority as more influential on providers than contractual mechanisms. 57 Similarly, ‘targets and terror’ were the main influence on providers’ waiting times. 71 Most variants of New Public Management ideas and practices are ‘aimed at “normalising” public sector employment on private sector models’ (p. 1). 121 As a special case of emic discourse, ‘soft coercion’ is the technique of threatening that, if one’s demands are not satisfied, a third party – for instance, a government – will impose a worse solution. 122 Thus, ambulatory care cost control occurred in Germany because SHIs could allude to government threats to control ambulatory doctors’ professional autonomy, which the doctors valued above marginal income gains. 46
Etic discourse (evidential, technical or scientific knowledge) nowadays means, above all, evidence-based medicine (EBM) and epidemiology, whose persuasive power lies in its objectivity and putatively scientific basis, which clinicians regard as authoritative. For commissioning purposes, EBM has the advantage of making increasingly explicit what health impacts and outcomes commissioners can expect from each service they commission, or expect to lose when rationing health care, facilitating commissioners’ monitoring of services provided. By tending to standardise descriptions of treatments and their outcomes – ‘commodification’123 – EBM facilitates the comparison of providers, hence provider competition. In practice, though, evidence is often used as post facto justification of decisions made for other reasons:102 ‘policy-based evidence’. The choice of performance measure itself reflects managers’ and other parties’ interests. 124 Its availability also varies by care group.
Discursive control can also be applied where trust is weak, but then negotiators rely more on other mechanisms to align provider and commissioner interests artificially. 125
Resource dependency and financial incentives
By threatening to reduce or remove resources, a commissioner can exercise power over providers who depend on the commissioner for their resources. 77,126,127 How much power depends upon whether the provider depends heavily or only slightly upon the commissioner for resources;128 on the unit of payment (whether the provider is paid, say, for each episode of care or by large block contracts);35,108 on whether the commissioner pays the provider directly or through an intermediary; on whether the payment is made before or after treatment occurs;1,35 and on whether or not the commissioner’s threat to withdraw resources is credible (the ‘credibility’ of an incentive).
There is strong evidence that using fee for service (FFS) units of payment raises treatment volume and costs: ‘Consequently, not to introduce unregulated fee-for-service reimbursement is one of the few unequivocal lessons of health care financing’ (p. 1580). 46
Block payments enable commissioners to cash-limit the cost of health services, as do spot contracts24 and payments to individual professionals for working a specified period of time. 129 Theoretically, block contracts create an incentive to undertreat, but there is only slight evidence130 that this actually occurs in the NHS. Capitation (subscription) payments for a defined population theoretically have a similar effect per patient, but are also incentives to recruit patients. Flat fees prevent monopoly providers using price discrimination and price fixing. 46 Incentives also motivate data collection regarding the activities and outcomes being incentivised. 89,131
Tariff (e.g. DRG-like) payments incentivise providers to treat more patients. In England, HRG payments to hospitals appeared to reduce average length of stay (ALoS) and increase throughput and the proportion of day cases, with little effect on three quality indicators (changes in in-hospital mortality, 30-day post-surgical mortality and emergency readmission after treatment for hip fracture), and exerted downward pressure on costs. 132,133 In Taiwan, switching from FFS- to DRG-based payments reduced length of stay and intensity of treatment for coronary artery bypass graft and angioplasty patients. 134 Tariff payments may remove incentives for hospitals to transfer services to community care. 135
Pay-for-performance incentives are typically used to incentivise specified care processes,136 on the assumption that if they are evidence based the desired health outcomes will follow. The NHS general practice Quality and Outcomes Framework (QOF) produced high compliance with the stipulated care processes, and little evidence of providers ‘gaming’ the data. 137 Nevertheless, two recent systematic reviews suggest that, overall, evidence about the effects of such payments is ambivalent, especially regarding the integration and continuity of care. 129,138 The effects of incentive payments for service quality may wear off after a few years, both in (US) hospitals139 and in general practice. 140 Financial penalties for high levels of hospital-acquired infection had little effect,141 although incentive payments did improve asthma and diabetes management in a large care network. 142 Penalties were only one mechanism among several for reducing late discharges from NHS hospitals. 143 A systematic review of incentives for individual professionals129 found that payment for working for a specified period was generally less effective, and payment for providing care for a patient or specific population or pre-specified activity or care quality more effective, at influencing care processes, referrals, admissions and prescribing, but not compliance with guidelines. Another systematic review140 found that financial incentives had a small positive effect on the quality of general practice.
Retrospective reimbursement of patients’ treatment costs (e.g. by tariff payment) usually leaves commissioners somewhat passive unless probity problems arise (e.g. overclaiming). Commissioners can influence provider selection only indirectly by framing (‘nudging’) patients’ or gatekeepers’ choices,144 for instance through promotional or ‘educational’ activities. Cost reimbursement appears to be a suitable payment for simple services whose outcomes and production processes are clearly definable, while fixed-cost payments (which can be prospective) are suitable for complex services that have multidimensional, unstable and uncertain goals. 145
The effect of incentives also depends on their credibility. Danish and Swedish hospitals that knew they would be financially supported for other reasons (e.g. rurality) were less dependent on, hence less sensitive to, DRG-like payments than private hospitals. 118,146 NHS hospital managers also initially doubted the stability of the HRG tariffs, hence their value for long-term planning. 132
Prospective payments give commissioners scope to construct incentives and, if they can, to choose how to allocate work between providers, to plan the provision and cost of health care for their population. Strict monitoring of performance targets, coupled with direct incentives to managers, has functioned partly as an alternative to competition as a mechanism for controlling NHS providers. 147 It has also been argued that financial incentives can displace non-financial incentives to provide high-quality care. 148
Provider competition
A credible threat of losing income to another provider accentuates a provider’s resource dependency on the commissioner. 96,149 Yet the mere presence of alternative providers does not necessarily suffice to increase bargaining power; US self-pay patients are charged up to 2.5 times as much as insurers and Medicare are per patient. 150 Rather, commissioner power is maximised by creating a monopsony. 151 During 1997–2002 the fragmentation of English HAs into PCTs, and numerous hospital mergers,152 increased market concentration on the provider side. 153 A common NHS scenario is a large commissioner (HA, PCT, CCG) facing one main provider (e.g. a hospital, mental health trust) with insufficient ‘numbers’ for competition to occur. 147 In, say, Italy, commissioners can take a ‘make-or-buy’ decision66 to operate their own services, which is likely also to make them more proficient in other aspects of commissioning154 and more micro-economically ‘efficient’ for low-contestability, low-measurability services. 66 GP fundholders,11 and later PBC commissioners, as often used their commissioning budgets to ‘make’ new services and care pathways as to ‘buy’ secondary care. Commissioners can also encourage untried providers to tender. The creation of preferred provider organisations offered US insurers a way to control health-care costs without eliminating patient choice. 155 Providers at the margin of financial or technical viability become more susceptible to competitive pressures; cf. Hinings et al. 156 Technical complexity creates asset specificity, reducing providers’ capacity to find alternative commissioners. 157
Commissioners may also be able to set the criteria by which to select providers: at its crudest, price versus non-price (‘quality’) competition. Fixed tariffs are usually thought to force providers to compete only on service quality, but variable tariffs give commissioners greater power to safeguard competition itself and to influence providers in other ways. 158
English147 and US159 studies in the 1990s found an inverse relationship between competition and quality of care but, when prices were fixed, competition improved hospital care quality. Mortality from acute myocardial infarction (AMI) fell in NHS hospitals exposed to greater competition. 160 A review of 68,000 discharges from 160 hospitals during 2003–7161 found, that where competition was more ‘feasible’, AMI mortality rates decreased faster, lengths of stay were shorter and treatment cost the same as elsewhere. Increasing the number of an NHS hospital’s competitors by three was associated with improved hospital management practices estimated to cause a 6% reduction in AMI mortality. 162 The effects of hospital competition on quality, however, appeared different inside and outside London. 163 Even after 2006, patients were more likely to ‘choose’ hospitals that their GP had referred patients to previously. 152 Patient choice effected a small reduction in waiting times. 164 UK studies mostly define health-care ‘markets’ in terms of the distance between patients’ general practices and hospital, an approach that they say ‘accurately reflects the choice sets open to NHS users’ (p. F238). 160 However, what matters for understanding how commissioners (hitherto PCTs, predominantly) harness competition for controlling providers is the choice set open to them. Studies from that angle are rare.
Providers of different ownership in the UK also appear to concentrate on different aspects of service design as their distinct competitive advantage. Corporate independent-sector treatment centres (ISTCs) brought new models of care into the NHS rather than clinical innovation. 165 Personal budgets for social care gave people who employed personal assistants directly (not via a care agency) greater control, continuity and quality of life. 166 Competition between care homes seems to keep prices in check but has little effect on quality. 167 Third-sector providers often have difficulty dealing with NHS commissioners’ procurement systems. 168,169
Findings from the USA are also equivocal, and have to be applied to the very different NHS context with caution. On balance they suggest that provider competition raises hospital quality, particularly for high-risk AMI patients;170–172 but the opposite has also been reported. 173 Some studies have found that competition improved outcomes for HMO-funded hospital patients but worsened them for Medicare-funded patients. 174 Competition had no quality effects for insured patients although it worsened outcomes for the uninsured. 175 Incentive payments for quality improvement had greater effects in less competitive markets. 139 Lower Medicare payments were associated with higher mortality, especially in more competitive markets. 171 Although increased market concentration and hospital volume have contributed to declining mortality with some high-risk cancer operations, declines in mortality with other procedures are largely attributable to other factors. 176 US data from 1990–97 suggested that hospital efficiency increased as one moved away from a very competitive market [Herfindahl–Hirschman Index (HHI) < 0.25], but began to decrease again at HHI > 0.7. Furthermore, HMO market share had a stronger association than HHI with hospital efficiency. 177 Non-profit providers may also be less opportunistic and self-interested,87 which may explain why they were less responsive than for-profits to financial incentives. 178 However, under competitive pressure, non-profit providers began to mimic corporate pricing strategies and merger tactics to increase their market power. 179 Provider competition in the USA reduced the costs of services to institutional180 but not individual payers. Competition made no difference to how closely social service providers in Florida complied with contracts. 181
Juridical control
Commissioners can also use juridical processes to influence providers. In some health systems (e.g. Germany, Russia) commissioners have the right to audit or inspect providers (e.g. to see medical records) to verify if treatments were necessary and/or correctly billed. Commissioners everywhere can seek enforcement of contracts, laws and regulations through the courts or regulators, although, in the ‘new public contracting’, contracts between commissioners and publicly owned providers are enforced – sometimes only weakly or one-sidedly – through hierarchical governance structures rather than the legal system. 38 If they have such discretion, commissioners can simplify contract formulation by supplementing a standard base contract,182 with optional additional clauses per provider, speciality or care group. 83 Complete, presentiated contracts (i.e. contracts which anticipate all main contingencies and specify what will be done should each event occur) are hard to formulate for ‘complex services’ (p. 1). 145 Writing them increases transaction costs. 39 Nevertheless, managed care (with contracts stipulating such practices as making primary and preventative services available to patients and controlling secondary care utilisation) reduced US preventable admissions of over-65-year-olds compared with fee-for-service reimbursement, especially for sicker patients. 183 Long-term contracts reduce transaction costs but also provider contestability, and remove a disincentive for providers to engage in staff development and training. 83 In England, zonal contracts for social care provision create, in effect, local monopolies of provision. 24 NHS hospital contracts generally had greater flexibility at the margin, the more the provider’s spare capacity. 184,185 Yet, however tightly a commissioner tries to specify contract terms, there are always practical limits to the completeness and presentation of contracts;84,186 in practice, a negotiated order (see above) is required to complement them. 39,187 Stable contracts become increasingly relational and may engender stable networks,188 eventually even the replacement of a market or quasi-market with an integrated hierarchy. 82
Although these six media of power are distinct, they interact. Negotiation demands certain managerial skills (performance). A negotiated order rests on agreement about norms and a shared discourse. These norms may include juridical principles besides beliefs about evidence basing, what the law requires, and wider social ideologies. If a competing provider is available, a commissioner’s negotiating position may become stronger. However, whether it has competitors or not, each provider depends on its commissioners for resources, so a commissioner can exploit that resource dependency even when negotiating with a monopoly provider, and even in non-market health systems. To understand how commissioners might exercise governance over providers, it is therefore necessary to understand in a more concrete way how the media of power combine and interact, reinforce or negate each other depending on circumstances.
Modes of commissioning
As noted, commissioners try to exercise governance over providers through particular combinations of media of power. We call each such combination a ‘mode of commissioning’. Globally, many different modes of commissioning are found. The above research findings suggest, in sum, that differences in modes of commissioning help explain:35
-
patterns of provider development, the spread or absence of specific kinds of provider or services; corporatisation and concentration of capital
-
health systems’ capacity for cost control
-
the development and use of evidence-based medicine
-
patterns of managerial development of commissioning and medical involvement therein.
Different types of commissioning organisation are likely to develop different modes of commissioning, whose effects partly depend on how providers react. 24 Except in the extreme case of ‘gridlocked’ governance,189 each mode of commissioning leaves providers some room for manoeuvre. Each medium of power might therefore be expected to have different effects even on similar providers (e.g. university hospitals) according to the institutional context. One might expect different modes of commissioning to develop for, say, diverse care groups. This brings us to our research questions.
Chapter 3 Aims and research questions
Contingency theory83,190 predicts that observed commissioning practice is likely to evolve by trial and error towards the mode(s) of commissioning best adapted to the commissioners’ roles, environment and the specific characteristics of different care groups and services. Furthermore, one mode of commissioning may contain elements of use to another, and the different modes of power interact (whether synergistically or the opposite).
The research aimed to assist this learning by examining existing commissioning practices and their contexts and effects on providers, that is to:
-
examine which commissioning practices emerge and are adapted to different organisational and care-group contexts, including other health systems
-
contribute thereby to governance theory, institutional economics, organisational sociology and organisational theory.
Comparing NHS commissioning with that in other health systems would help illuminate which commissioning practices – those which recur across health systems – are adapted to the structure of quasi-markets per se, and which reflect only the circumstances of the NHS during 2010–12. However, we used the English NHS of 2010–12 as the main context within which to address these aims. Our research questions (RQs) therefore were:
-
How do English health policy-makers and NHS commissioners understand the policy aims of commissioning, and how can governance over providers be exercised through commissioning?
-
How has the reconfiguration of commissioning structures occurred in practice and what shapes this reconfiguration?
-
How far does their commissioning practice allow commissioners to exercise governance over their local NHS health economies?
-
How much room for manoeuvre do NHS commissioners have?
-
What are the consequences, and how do commissioners try to manage them, when commissioning is distributed across different organisations and when it shifts to being client based?
-
How do provider managers respond to commissioning activity?
-
-
How do commissioning practices differ in different types of commissioning organisation and for specific care groups, taking the following care groups as contrasting tracers: unscheduled inpatient care for older people; mental health; public health; and planned orthopaedic care? On which aspects of service provision do different commissioning organisations tend to focus?
-
What factors, including the local health system context, appear to influence commissioning practice and the relationships between commissioners and providers?
We took RQ3 to ask what media of power commissioners use, how and with what limitations. By ‘client-based commissioning’ we mean specifying and paying for services on the basis of each episode of care for each individual patient (tariff payments, personal health budgets). We defined ‘distributed commissioning’ as the joint commissioning of a health-care provider or pathway by several commissioners collaboratively, and ‘room to manoeuvre’ as ‘scope for exercising the media of power over providers’.
Chapter 4 Methods
Research design
Our research design was a multiple mixed-methods191 realistic evaluation. 192 Its components were:
-
Content and discourse analysis of policy documents and interviews with policy-makers and managers to elicit their programme theories of NHS commissioning, answering RQ1 by identifying their understanding of:
-
the intended policy and service outcomes of NHS commissioning
-
the mechanisms that would produce these outcomes.
-
-
A cross-sectional analysis of publicly available managerial data about local health economies (commissioners, providers, socioeconomic context), testing for any associations between commissioners’ characteristics and the policy outcomes identified in the programme theory of NHS commissioning. In agreement with the Health Services and Delivery Research (HSDR) programme, this analysis was regarded as an initial exploration of the value and uses of reanalysing published managerial data to characterise and evaluate the impacts of NHS commissioning. The unit of analysis (‘local health economy’) would for practical purposes be the PCT, considering what data would probably be available. This method contributed to answering RQ3 and RQ5.
-
A systematic comparison of case studies of commissioning in five English case study sites, with induction of common patterns, and exploration and explanation of contrasts. Within each site these case studies were longitudinal, tracing the formation of commissioning structures and practices in recent years. The framework structuring the comparison was the analysis of the media of commissioner power outlined in Chapter 2. This method contributed to answering RQ2, RQ3 and RQ4.
-
A systematic comparison, using the same framework, of patterns across the English case studies with case studies in Germany and Italy. This method contributed to answering RQ3, RQ4 and RQ5.
-
Action learning sets of commissioners from the English, German and Italian case study sites. This contributed to answering RQ1, RQ2 and RQ3.
-
Framework analyses to synthesise the above findings, contributing to answering all of RQ2, RQ3, RQ4 and RQ5 and to testing the programme theory’s underlying assumptions.
These methods fitted together as follows. The discourse and Leximancer analysis revealed the empirical and causal assumptions (programme theory) on which current commissioning policy rests, especially about how commissioners can influence the providers of NHS services (RQ1). Case studies of the development of local commissioning then explored how far the assumed commissioning organisations and systems were present to begin with (RQ2). The case studies were also used to explore which commissioning mechanisms commissioners were using, how they did so (RQ3), if they used different mechanisms for different care groups (RQ4), how providers responded and what contexts appeared to influence providers’ reactions to commissioning (RQ5). Within the data availability constraints, the cross-sectional analysis of managerial data served the same purposes. Action learning was another way to explore, in ‘real time’, what mechanisms commissioners were using. We used the international comparisons to explore and differentiate which commissioning contexts, mechanisms (above all, media of power) and outcomes appear common to quasi-markets more widely, and which are peculiar to English NHS commissioning. Each method contributed some parts of an overall, perforce incomplete, jigsaw of the complex relationships between commissioning organisations, contexts, mechanisms and outcomes. Table 1 gives an overview.
| Research question | Method | Data sources | Analysis |
|---|---|---|---|
| 1. Programme theory | Discourse analysis | Interviews; documents | Leximancer analysis; cognitive frame analysis |
| 2. Development of commissioning | Cross-sectional comparison of longitudinal narratives | Fieldwork (interviews, document collection); published managerial data | Pattern induction from systematic cross-sectional comparison of longitudinal case studies |
| 3. Commissioning practice and governance | Comparative case studies; cross-sectional analysis of published managerial data | Fieldwork (interviews, document collection); published managerial data | Framework analysis comparing uses and limitations of media of power across health economies; inductively classifying commissioning practices; testing associations between commissioning practice and service outcomes |
| 4. Modes of commissioning for different care groups | Framework analysis comparing commissioning practices between tracer groups | ||
| 5. Commissioning practice and commissioner–provider relationships | Framework analysis; empirical testing of programme theory | Results of analyses for RQ1, RQ2, RQ3 | Compare these relationships and their contexts across countries, with programme theory and with initial theoretical frameworks |
Because all the above were undertaken during 2010–12, the cross-sectional study data are for 2008–9 (the latest available in 2010–12). Comparison with published managerial data, where available, helped indicate the likely generalisability of our findings. We also compared our own findings with relevant empirical findings emerging from research studies in the Health Reform Evaluation Programme, HSDR, National Institute for Health and Care Excellence (NICE) and the DH Health Policy Programmes.
We involved patient representatives [through PenPIG, the Patient Involvement Group of the SW Peninsula Collaboration for Leadership in Applied Health Research and Care (CLAHRC)], consulting them before research started about the research questions and overall research design (as expressed in the lay summary) and afterwards about our conclusions (expressed in an executive summary). We involved key commissioning stakeholders – clinicians and managers – through the action learning set described below, and will involve them again in the post-project dissemination activities.
Discourse analysis
Design
The discourse analysis of commissioning policy was carried out to identify the programme theory of NHS commissioning that would apply to CCGs. We analysed key policy documents’, policy-makers’ and managers’ accounts of these matters; cf. Millar et al. 22 We focused on actually occurring texts and utterances rather than their ‘genre’ or ‘conclusion rules’ (p. 278),193 but did regard the texts as a systematic set of ideas, values and problematics. 194
Sampling
Documents
Our sampling strategy was purposive, selecting what policy-makers emphasised as seminal policy statements, hence widely distributed to NHS managers between the general election and the start of legislation (July 2010 to September 2011). The two main documentary samples were:
-
Equity and Excellence: Liberating the NHS195 and its official support documents; this was the most widely distributed policy document concerning NHS commissioning (43,351 downloads in 2012; followed by the NHS Operating Framework at 32,869)
-
the 2012 Act196 and its explanatory ‘factsheets’, including one on service quality subsequently withdrawn from the DH website.
These (see Appendix 1) were downloaded from DH, NICE, Healthcare Commission and National Patient Safety Agency websites.
Oral material
We assembled transcripts of interviews with policy-makers and top-level NHS managers. Returns from interviewing diminished after about 20 interviews but we interviewed 23, whose roles Table 2 summarises. The transcripts (with speeches mentioned below) were inputs for the cognitive frame analysis (see Chapter 5, section Cognitive frame analysis) which supplemented the Leximancer analysis.
| Role | n |
|---|---|
| Current and former parliamentarians | 4 |
| DH policy directors | 5 |
| Directors of national and regional NHS organisations | 5 |
| National local authority organisation representative | 1 |
| Directors of national voluntary organisations | 2 |
| Heads of national medical organisations | 2 |
| Senior official of think-tank | 1 |
| Former NHS Director | 1 |
| Other | 2 |
Many informants were so senior that fuller details would compromise their anonymity. However, their careers and status gave good reason to believe that they would know the rationales for NHS commissioning policy, having been involved in formulating it. The interviews were audio-recorded and transcribed. Interviewees were offered the chance to see and correct their transcript.
Besides the above interviews, we also analysed transcripts of (existing) speeches by national politicians and the NHS Chief Executive about the aims, mechanisms and implementation of the new commissioning system. These included speeches to the House of Commons, Royal College of General Practitioners, British Medical Association, NHS Confederation and The King’s Fund, selected to cover both supportive and unsupportive audiences. We also included evidence to the Commons Health Select Committee from civil servants and NHS managers. Evidence given by independent experts was not included, as they would not necessarily be among the policy authors. For the same reason we did not include evidence, or other speeches and writings, from opponents of the policy.
Leximancer and cognitive frame analyses
To expose the programme theory underlying commissioning policy for the English NHS required exposing what context–mechanism–outcome (CMO) relationships the sample texts stated or implied. Appendix 2 describes Leximancer analysis more fully, but in brief it is an automated form of quantitative content analysis which outputs lists of associated terms (‘concepts’), counts and measures of their co-occurrence, and indexes their original textual occurrences.
Although Leximancer analysis located which CMO relationships the texts most often mentioned, the original documentary formulations were mostly too broad, ambiguous or brief to specify clearly how these mechanisms would work. We therefore conducted a cognitive frame analysis of data from our interviews with parliamentarians and top-level health managers, making a logic analysis197 to elaborate and supplement the policy texts’ accounts of CMO relationships. In doing so, again seeking to relate our informants’ accounts and explanations (frames) to the categories (CMO, media of power) required for a realistic evaluation. Mostly the informants’ accounts were consistent, but where they differed (in emphasis rather than contradicting each other) we took the more prevalent interpretation as more likely to guide commissioning practice. Appendix 2 further describes the cognitive frame analysis. We collated the descriptions of CMO relationships found by these methods and paraphrased them as statements in the form required for empirically testing CMO assumptions, namely ‘Doing X in circumstances M will cause agent A to do Y’, or a logical equivalent.
Cross-sectional analysis of published managerial data
Insofar as data were available, the cross-sectional analysis of published routinely collected managerial data was designed to:
-
provide a sampling frame for the English case studies
-
describe the profile (mix) of commissioning organisation(s)’ practices and resources in the English NHS, allowing categorisation of local health economies in terms of these variables
-
test for associations between health economies’ organisational characteristics (profiles), commissioning practices and published indicators of service outcomes.
The second and third of these also contributed to answering RQ3 and RQ5.
Indicators and measures
Three groups of measures were selected by the following methods and criteria (Appendix 3 explains more fully):
-
Independent variables [(Governance Variable) in the model below] were selected from the published data sets as measures or prima facie proxies for the media of power described in Chapter 2. Suitable data were mostly available only for 2008–9, and only for two media of power (provider competition, managerial performance).
-
Control variables were selected on the basis of existing research into the factors that influence the need and demand for health services. Ideally one would control for all likely confounders that are not under PCT control: population age, sex, ethnicity, income and education profiles and case mix (primary diagnosis, comorbidities, severity of illness). 198,199 Published data allowed only limited controlling for these factors (for instance, PCT income is allocated by criteria intended to reflect – so, in this context, standardise for – population health needs and local service input costs). It would have been desirable to have a control variable that enabled us to control directly for differences in hospital case mix, but in the absence, at the time of the study, of a suitable published variable, deprivation appeared to be the nearest proxy among the control variables available.
-
Dependent variable selection started from lists of the generic health service and health policy outcome indicators200,201 that the Organisation for Economic Co-operation and Development (OECD) and World Health Organization (WHO) use for international comparisons of health systems, and Greaves et al. ’s list,90 which, so far as we were aware, was then the only published study similar to this one.
Table 3 lists the independent variables, controls and dependent variables that we used. Appendix 3 explains more fully how and why they were selected.
| Category | Variable | Mean | Standard deviation |
|---|---|---|---|
| Commissioning governance (independent variables) | |||
| Generic provider competition | HHI | 0.511 | 0.200 |
| Client-based commissioning | Proportion of ‘Choose and Book’ patients | 0.539 | 0.178 |
| Personal health budget pilot (Y/N) (dummy) | N/A | N/A | |
| Practice-based commissioning: % GP participation | 94.766 | 17.494 | |
| Population based competitive commissioning | % of budget spent on local authority and voluntary providers | 5.036 | 5.479 |
| % of budget spent on independent-sector health care | 3.447 | 3.798 | |
| Number of provider contracts | 6.020 | 2.470 | |
| Proportion of PCT budget spent on main provider | 0.572 | 0.318 | |
| PCT management | WCC score | 109 | 21 |
| Controls | Number of PCT mergers | 1.513 | 1.884 |
| PCT income per capita | 1.393 | 0.505 | |
| PCT weighted population | 337,689.4 | 170,141.5 | |
| Indices of deprivation, average score | 23.722 | 8.376 | |
| Service outcomes (dependent variables) | |||
| Quality of care and primary–secondary care co-ordination | Amenable mortality annual rate, all causes, under-75-year-olds, directly standardised | 0.961 | 0.213 |
| Unplanned hospitalisation rate for ambulatory care sensitive chronic conditions, adults, directly age and sex standardised, as % of 2007–8 | 112.516 | 33.176 | |
| Emergency admissions for primary care preventable acute conditions, indirectly standardised, % change since 2007–8 | –3.482 | 13.365 | |
| Emergency admissions for primary care preventable chronic conditions, indirectly standardised, % change since 2007–8 | –6.201 | 15.828 | |
| Emergency readmissions within 28 days of discharge from hospital, adults over 16, indirectly standardised for age, method of admission, spell, diagnosis (ICD-10) and procedure (OPCS version 4), % change since 2007–8 | –3.690 | 6.052 | |
| Ratio of observed to expected emergency admissions for conditions not usually requiring hospital admission, indirectly standardised | 90.502 | 26.213 | |
| Access to care | Mean time waited for admission | 47.461 | 9.218 |
| % change 2007/8 to 2008/9 in proportion of trauma and orthopaedics patients waiting less than 18 weeks from referral to planned treatment | 0.103 | 0.455 | |
| % change 2007/8 to 2008/9 in proportion of all admitted patients waiting less than 18 weeks from referral to planned treatment | 0.579 | 3.348 | |
| % change 2007/8 to 2008/9 in proportion of all non-admitted patients waiting less than 18 weeks from referral to planned treatment | 0.820 | 1.084 | |
| Proportion of patients waiting more than 4 weeks for a first outpatient appointment following GP referral | 0.010 | 0.057 | |
| Monthly mean waiting list, IP and day cases, proportionate to weighted population | 0.011 | 0.004 | |
| Cost control | PCT surplus (deficit marked with –) as proportion of income | –0.273 | 0.501 |
| Hospital activity | Ratio of day cases to admissions | 0.365 | 0.045 |
| Average (mean) length of stay | 5.742 | 0.801 | |
| Finished consultant episodes proportionate to weighted population | 0.325 | 0.117 | |
Although the range of publicly available data at PCT level about the media of power increased during 2010–12, lack of suitable data still limited the scope of the cross-sectional analysis. Only qualitative data can describe discursive control, negotiated order and the contents of contracts. Ad hoc financial incentives to providers also evade managerial data sets. When available at all, quantitative data about patient complaints, prosecutions or disciplinary proceedings against providers record only exceptional events. We could identify which PCTs had personal budget pilot schemes, but NHS managerial data contained little further information about them. Consequently our cross-sectional analysis concentrated on managerial performance and provider competition.
The mean and SD for each measure were calculated from data sets noted in Appendix 3. The independent and control variables shown in Table 3 all had variance inflation factor (VIF) scores between 1.164 and 2.273. In general the different quality indicators for hospital services were not highly correlated,163 but among our selection there were five exceptions (see Appendix 4). Note that PCT budgets did not include the majority of general medical practice (funded from DH budgets).
Data collection
Deprivation data were downloaded from www.gov.uk/government/publications/english-indices-of-deprivation-2010. WCC scores were published in the Health Services Journal. 202 Data from which to estimate hospitals’ ‘market’ shares were obtained from the 2011–12 PCT recurrent revenue allocations exposition book. 203 Otherwise, data were downloaded from the NHS Information Centre website (www.hscic.gov.uk/searchcatalogue). We assembled a database in which the rows were PCTs and the columns contained the above measures and data about PCT characteristics (e.g. extent of practice-based commissioning, presence of personal health budgets, number of recent PCT mergers). Data were for the financial year 2008–9 except for referral to treatment time and WCC data scores, which were reported by calendar year; we used 2009. According to their accompanying documentation the deprivation data were ‘mainly’ for 2008, but reported for 2011 administrative boundaries. We trimmed percentages back to 100% when higher figures (e.g. for data completeness, percentage of GPs involved in practice-based commissioning) were obviously wrong.
Analysis
To measure the relationships between the media of commissioner power (‘governance variables’), dependent variables (policy outcomes) and the main potentially confounding variables, and the relative contributions of each explanatory variable, we used stepwise multiple linear regression with backwards elimination, that is removing all non-significant and/or trivial independent variables until only those that satisfied our declared criteria remained. Our basic model was:
We used four variants of this model, changing the independent [GovernanceVariable] variable to reflect different media of power, including the different quasi-market architectures that coexist in the NHS. The variants of independent variable were therefore:
-
a measure of managerial competence (WCC scores)
-
a generic measure of competition (HHI)
-
four measures indicating the extent of competitive tendering commissioning
-
three measures indicating the extent of individualised commissioning.
For each variant of the independent variables, we repeated the regression with different dependent [Service Outcome] variables, explained below. In all cases PCT Deprivation Index, per capita PCT income and PCT weighted population were included as controls. (It was a policy aim that PCT income should reflect the PCT’s weighted population size, but this was not achieved during PCTs’ existence.) The unit of analysis was the PCT, the main NHS commissioner for the pre-CCG period that the data described, approximately 2 years before the case study fieldwork began. The implications of this time difference are discussed below.
We declared negligible correlation to be one where the estimated standardised beta (β) coefficient was in the range 0.001 > β > –0.001 or adjusted R2 < 0.01. Significant correlation was declared where p ≤ 0.05. Statistical calculations were performed with R (version 3.1.1, The R Foundation for Statistical Computing, Vienna, Austria). In analysing the data we have erred towards conservatism, that is towards statistically underprocessing rather than overprocessing the data. The method of analysis is described more fully in Appendix 2.
Systematic comparison of case studies
Design
Using the frameworks described below, we systematically compared case studies of English local health economies. Because health-care processes (types of interventions, models of care, etc.) are likely to influence commissioning practice, we selected four care groups as ‘tracers’ likely to reveal contrasting commissioning practices:
-
unplanned admissions of people with chronic conditions
-
mental health
-
public health: prevention of diabetes and coronary heart disease through both clinical activity (e.g. statin prescribing) and intersectoral action (e.g. to influence diet and exercise)
-
scheduled orthopaedic surgery.
For differentiating these care groups we took one tracer group in one local health economy as the unit of analysis (‘case’)204 and, otherwise, the whole study site. (By ‘tracer group’ we meant that one group of patients is used to trace a sequence of events which will also happen to other care groups. The tracer group was taken as an instance of a wider, qualitatively similar pattern.) At the start of fieldwork (2010) a ‘local health economy’ corresponded to a PCT and in our study sites this situation did not change as CCGs developed. 205
Sampling
Because we wished to study commissioning as a means of governance under conditions of organisational diversity, we used our PCT database (see Chapter 3, section Data collection) as the sampling frame for a maximum-variety sample of four health economies. Our sampling strategy was to select study sites for early progress towards GP-led commissioning; maximum organisational variety of commissioner; contrasting proportions of budget spent on their main acute hospital (hence prima facie different levels of provider competition); inclusion of at least one site with fragmented commissioning, indicated by a percentage of in-territory spending well below the 57% median for 2008–9, that is so low as to be likely to involve collaboration with other commissioners; and the presence of personal health budget pilot schemes.
We approached 11 potential study sites. One failed to reply. Another initially agreed but then withdrew for reasons unconnected with the study. From the remainder we selected sites with:
-
a newly clustered PCT (‘Shire’) now commissioning three acute hospitals
-
the hitherto commonest NHS arrangement of one (unclustered) PCT commissioning one dominant acute hospital (‘Milltown’)
-
a PCT that was devolving commissioning to a GP-owned social enterprise (community interest company) (‘Porttown’)
-
a PCT where a Darzi polysystem of federated general practices also participated in commissioning (‘Metroland’).
This sample also gave us variety in the amount of commissioner spending on independent-sector providers, ranging from 0.75% (Shire) to 14.5% (Porttown; England mean 3.47%, 2009–10 figures). In addition, we selected a site in which two GP consortia were receiving support from a US corporation in commissioning services for people with chronic health problems (in ‘Livewell’ PCT), which, focusing on just one tracer group, was a mini case study. Table 4 and Appendix 5 describe the resulting sample.
| Pseudonym | Commissioning structure(s) | Local spend on main provider (%) | Personal health budget pilot? | Office for National Statistics classification |
|---|---|---|---|---|
| Main study sites | ||||
| Metroland | Commercial PHC provider (two alternative provider medical services sites + five satellite practices), later added commissioning support role. Polysystem: network of general practices with employed managerial and non-medical PHC clinicians; also providing borough-wide services for specialised forms of PHC | 55 | No | London suburb/large urban |
| Porttown | Social enterprise (CIC). All practices were members. SE employed former PCT commissioning and service improvement team. Seconded staff member from pharmaceutical firm. Externally provided patient surveys | 93 | Yes | Regional city/other urban |
| Milltown | GP consortium taking over (relict) PCT commissioning infrastructure and staff. Based on PBC consortium. All practices are members | 68 | No | Regional city/large urban |
| Shire | Before 2010, general practices organised into six locality commissioning groups. CCG developed on federated model but retaining locality groups, to which relict PCT staff dispersed. No private-sector involvement in commissioning support | 36 | Yes | Rural |
| Mini study site | ||||
| Livewell | US HMO involvement, focus on people with chronic health problems, including older people with recurrent unplanned hospital admissions | 75 | No | Large urban |
In each site we assembled a sample of key informants through discussions with the lead commissioning managers or GPs, who identified the lead commissioning managers for the tracer groups, lead clinicians and managers in secondary care providers (including those for the tracer groups), local authority leads for adult social care and patient or carer representatives. It was noticeable that this snowballing method did not identify PCT Chairs or Non-Executive Directors as key informants, despite their governance roles. However, one of the researchers was a PCT chair (not in a study site). This process yielded a sample of 104 English informants across the categories summarised in Table 5.
| Category | Porttown | Shire | Metroland | Milltown | Livewell |
|---|---|---|---|---|---|
| PCT managers and advisers | 5 (+ 1) | 6 (+ 1) | 9 (+ 1) | 2 (+ 1) | 3 (+ 1) |
| GP commissioners | 5 (+ 1) | 3 (+ 1) | 2 (+ 1) | 3 (+ 1) | 4 (+ 1) |
| Provider managers | 6 | 7 | 5 | 1 | 1 |
| Provider clinicians | 3 | 7 | 5 | 0 | 2 |
| Local authority (including joint appointments) | 6 | 2 | 6 | 2 | N/A |
| Voluntary organisations | 1 | 1 | 1 | 0 | N/A |
| Patient representatives | 1 | 1 | 1 | 0 | N/A |
| Total | 27 (+ 2) | 28 (+ 2) | 29 (+ 2) | 10 (+ 2) | 10 (+ 2) |
Additionally, action learning set participants (shown as ‘+ 1’ in Table 5) from each site made a total of 114.
Data collection
Data were collected from informant interviews and documents. Semistructured interviews used variants of the schedule in Appendix 6. All interviews were digitally recorded and transcribed by professional transcribers, and interviewees were offered the chance to correct their transcript. Our collection of managerial documents was guided by our interviewees, since they were best placed to say which documents were locally seminal. We also collected professional press reportage. As data analysis proceeded, we supplemented these data sources with ad hoc e-mail and telephone enquiries when data triangulation revealed gaps or ambiguities, or if we had reason to believe that circumstances had changed at a particular site.
The concept of power implies a counterfactual account of what providers would otherwise do206 if commissioners were less powerful (and vice versa), which we obtained empirically from informants’ accounts of commissioners’ attempts to change provider practice, of providers’ response(s) and of what happened when providers proposed changes that the commissioners contested.
Coding and analysis
From the theoretical framework described in Chapter 2, we constructed a coding frame (Appendix 7) by which to code case study interview transcripts. To ensure reliability, the researchers cross-checked each other’s coding of an initial maximum-variety sample of transcripts and wrote coding criteria where their initial coding had differed. The coded transcripts were entered into NVivo (version 10, QSR International, Warrington, UK), and nodes created for each of the main concepts in the analytical framework and to identify the study site, professional role, organisation(s) and tracer group(s). As data entry proceeded, we created additional nodes for concepts suggested by the data but which the original coding frame could not accommodate. We thus made both a framework and an inductive (‘ground-up’) analysis of the interview data. NVivo reports for different combinations of nodes were produced, reproducing the source pieces of transcript text. We reduced these data by writing a ‘pithy sentence’ summarising what each report segment said about commissioning for that site and/or care group. We then collated all the pithy sentences (across sites) concerning a research question or part thereof.
We examined how the reconfiguration of commissioning structures occurred in practice and what shaped it by constructing a narrative of those events in each study site during the study period. The action learning sets gave an opportunity for a deeper interpretation of these findings, to correct and update them. Within and across sites, all these materials were then synthesised by the methods reported below.
International comparisons
Design
To discover what other factors, including health system context, influence commissioning practice, we compared our English study sites with two national case studies of European quasi-market health systems. Similarities between commissioning practice in the three countries would suggest which features and consequences of commissioning practice appear to be intrinsic to commissioning in quasi-markets. Differences would suggest features, consequences and problems which were specific to one type of quasi-market, or to such contexts as the political culture of that country. Additionally, examination of well-developed commissioning practice elsewhere might yield findings (e.g. proof-of-concept findings) of practical value for commissioning practice in England. For comparability and to draw these explanatory and practical lessons, we used the same analytical and data-collection methods as for the English case studies.
Sampling
We selected Italy as a Mediterranean health system207 similar to, indeed partly modelled on, the English NHS, and for contrast Germany, a paradigm Bismarckian system of commissioning health services through SHIs, where multiple commissioners commission public and private providers, paying them by DRG-like tariffs. As German and Italian study sites, we chose respectively:
-
one of the largest German SHIs, with 7.2 million members, over 100 years’ experience and a reputation for technically sophisticated commissioning methods
-
the Lombardy and Emilia Romagna health regions, whose health-care commissioning practices have parallels to those in England.
Data collection
German data were collected at national, commissioner and provider levels by mixed methods from the following sources:
-
interviews and discussions with key informants: these were representatives of the three main federal associations of health organisations and the Federal Joint Committee [Gemeinsame Bundesausschuss (GB-A)]; 11 staff, covering a range of functions, at the SHI; and managers from five hospitals (university, third sector and publicly owned) in one of the largest provincial industrial cities
-
grey material including official regulations and guidance, Sozialgesetzbuch V above all
-
participation in three national events involving German SHIs
-
ad hoc enquiries from individual experts
-
published research found by hand-searching journals.
Interviews carried out in 2011–12 were recorded and transcribed. Two of the researchers analysed material in German.
In Italy data were collected at regional, ASL (azienda sanitaria locale, local health authority) and provider level by mixed methods from the following sources:
-
Interviews and discussions with 23 key informants in Lombardy. These included two managing directors (one for secondary and one for primary care) in each of seven ASLs; and seven other managing directors who between them represented each ownership category of provider – public firms (aziende ospedaliere, AOs, the equivalent of NHS trusts), non-profit, for profit, public–private partnership, national research centre – and each of the following levels of provider – acute care, general practice, domiciliary care and residential care. These interviewees were geographically dispersed across the regions. We also interviewed two regional managing directors, one from the health Directorate-General (DG) and one from the family DG (responsible social and health-care activities and organisations).
-
Key documents, above all decrees.
-
Participation in two regional events for heads of primary care (one in Emilia Romagna, one in Lombardy).
-
Ad hoc enquiries from individual experts.
-
Published research found by hand-searching journals.
Material in Italian was translated and initially analysed by one of the researchers and a senior Italian National Health Service (INHS) manager, both native Italian speakers with postgraduate training at English universities.
Analysis
As far as possible, transcripts and texts were directly analysed in the original language to avoid misleading translations (e.g. of the term ‘commissioning’, which has no exact German or Italian equivalent). Data from the German and Italian case studies were assembled into the same framework as used to synthesise data from the NHS case studies, reported below.
Action learning
The action learning set (see Appendix 8) aimed to:
-
refine our research questions and tools in collaboration with commissioning managers and clinicians, test the face validity of emerging preliminary findings with them and consider dissemination strategies
-
bring together an international cohort of interested clinicians, managers and researchers to explore the potential for learning from commissioning experiences in England, Germany and Italy
-
offer busy managers and clinicians a forum for learning and development reflecting their own personal and organisational agendas rather than one imposed by commissioning ‘experts’, as a catalyst for participants to work on their own challenging commissioning problems, capitalising on the knowledge and experience within the set.
Items 2 and 3 would also help generate recommendations for commissioning practice.
One clinician and one manager from each of the five study sites participated in action learning sets between November 2011 and March 2013. At the outset the participants established their own:
-
ground rules (e.g. about confidentiality) for conducting the learning set
-
check-in rules
-
update frequency
-
reporting process, including rules of confidentiality
-
check-out rules, including arrangements for subsequent sets.
Three of the researchers were facilitators. At each meeting we also presented emerging research findings to the participants and provided expert input in specific areas (e.g. supply chain management, findings from other research studies on commissioning). One learning set was combined with a mini-conference in which the learning set members exchanged updates and practical ideas about commissioning with informants from the German and Italian study sites. The learning set members agreed conclusions at each meeting, and from the action learning set overall. The anonymised summary findings were included in the evidence synthesis.
Synthesis
By these methods we assembled and analysed the data summarised in Table 6.
| Method | Interviews | Other material |
|---|---|---|
| Discourse analysis | 23 | 34 policy documents, 7 speeches, 147 grey documents |
| Cross-sectional analysis | N/A | 44 published data sets, 1 dissertation |
| Case studies | 110 | 57 documents, 22 contracts, 111 press reports |
| Learning set | 10 | 5 meetings, mini-conference |
| Germany | 20 | 39 documents, 3 national events |
| Italy | 24 | 14 documents, 2 national events |
| Secondary data | N/A | 412 published papers, 87 research reports |
As noted, the cross-sectional method used pre-CCG data for a period of 2 years before the case study fieldwork.
Data were synthesised by framework analysis. Conceptually this was equivalent to constructing, for each research question, a data grid in which each row contained data relevant to some aspect of that research question and each column represented a site; and then populating the cells with the relevant data from the case study ‘pithy sentences’, cross-sectional analysis, action learning set, international comparisons and other published studies. Collating data this way provided an immediate means of triangulation, revealing gaps, ambiguities or apparent contradictions in the data, prompting supplementary data collection. By noting common or divergent patterns across cells, we ‘read off’ answers to our research questions and discovered where new categories or concepts were required to accommodate unforeseen empirical findings. 208 We also compared our own findings against those from other studies. The same method was used for cross-country comparison except that the virtual columns now represented countries.
A second framework analysis recollated these data under the standard CMO categories of realistic evaluation, which allowed us to evaluate the empirical validity of the programme theory assumption.
Ethics and research governance
South West Research Ethics Committee approval (reference 09/H0206/50) was subject to informant anonymity and to obtaining management permission from each research site, which we did for all the NHS sites. University of Plymouth ethical approval was obtained for non-NHS sites. Obtaining study site access was laborious and slow (many months) because of a combination of site staff overload (see Chapter 6, section Overload), cumbrous procedures for obtaining the permissions, and administrative delays. The growing importance of evidence-based policy-making contrasted with the difficulty of accessing the necessary evidence. No such difficulty arose in Germany or Italy.
Findings
Our findings are presented by research question, indicating as necessary what their evidential basis is.
Chapter 5 How English health policy-makers and NHS commissioners understand NHS commissioning policy
To ask how English health policy-makers and NHS commissioners understood the policy aims of commissioning, and how governance over providers can be exercised through commissioning (RQ1), is to ask what the programme theory of NHS commissioning policy was during 2010–12. Policies state, or assume, that, if policy-makers and managers do what the policy prescribes, then in the prescribed circumstances (which the policy might also attempt to create) a pre-defined set of policy outcomes will result. These assumptions, indeed predictions, are the programme theory underlying the policy. Our discourse analysis was intended to expose what the fundamental documents, key informants and the 2012 Act196 said or implied are the most salient:
-
CMO relationships that NHS commissioning in England involves
-
mechanisms by which NHS commissioners exercise governance (power) over providers.
Specifically, we aimed to reveal what these salient patterns say or imply that the media of power by which English NHS commissioners exercise governance over their service providers will be.
Quantitative (Leximancer) content analysis
The Leximancer analysis aimed to list, and quantify the salience of, the assumptions about the structures, mechanisms and outcomes of NHS commissioning stated in our samples of documentary and oral material. Note that in Leximancer analysis the term ‘concept’ denotes only the repeated co-occurrences of terms in the texts analysed. ‘Themes’ are repeated co-occurrences of concepts. Tables 17, 18 and 19 in Appendix 1 show in descending order of frequency what concepts concerning contexts, mechanisms and outcomes were found when the three text samples were combined. For each of the seven outcome-concepts, Table 20 in Appendix 1 shows how frequently each mechanism-concept co-occurred. Appendix 1 also shows the frequencies of occurrence of concepts relating to the outcomes, mechanisms and contexts for each of the three samples of policy text separately.
The mere presence of these associations did not, however, reveal what specific context–mechanism–outcome relationships the policy texts were assuming. The concepts found by Leximancer analysis were too broad for that. We therefore extracted from the source texts each passage in which these associations occurred. Having removed substantively duplicate passages, we made a précis of each that remained, using a formulation suitable for empirical testing; that is, ‘Doing X under conditions C will cause agent A to do Y’ or a logical equivalent. Sometimes these passages described CMO relationships explicitly but more often they were elliptical, calling on the reader’s background knowledge to supply the implicit missing elements. Then we supplied the apparently missing assumptions, which are italicised to distinguish them from the original explicit texts. Appendix 9 shows what we added, and that the additions were few (5% of the programme theory word count).
The analysed materials contained many assertions about what organisations were needed, their duties and defects in existing commissioning systems. They only briefly described how CCGs, the main NHS commissioning mechanism, would work. Apart from mentioning ‘effective dialogue’ with hospitals, almost all that Equity and Excellence: Liberating the NHS says on that point is that clinical commissioning
will bring together responsibility for clinical decisions and for the financial consequences of these decisions . . . reinforce the crucial role that GPs already play in committing NHS resources . . . increase efficiency, by enabling GPs to strip out activities that do not have appreciable benefits (p. 27). 195
Little detail appeared, either, about the mechanisms of patient involvement in care decisions; about how public health measures, research and evidence basing will improve patient outcomes; about how joint working between NHS commissioning groups and local government, patient involvement, research and evidence basing will help contain NHS costs; or about what makes a provider ‘qualified’. Much of the 2012 Act itself was uninformative on these points (naturally focusing on defining terms, public bodies’ powers of appointment, remuneration, accounting arrangements and amendments to previous law),196 but the official Factsheets published to explain it209–228 did describe examples of effective commissioning. The speeches and, much more, Select Committee material229–236 explained more fully some of the mechanisms and mechanism–outcome relationships left unexplained in the written material. In summary, the policy documents and public debates comprised mostly descriptions of contemporary practice and normative assertions about the new organisations’ roles and duties, but offered only a few, mostly meagre, accounts of the mechanisms or the reasoning behind them, some of which may be post hoc rationalisations. 22
Cognitive frame analysis
To reach a more complete, coherent account of the programme theory, it was necessary to impute more explicitly the missing assumptions that policy documents had left the reader to supply. We used our data from interviews with policy-makers and senior implementers to fill these gaps, especially about what Leximancer analysis had shown to be the most salient CMO relationships in the policy texts: competition (patient choice, contestability), financial incentives and negotiations between commissioners and providers.
There was also the question of how other NHS governance structures would interact with commissioning, and how the different commissioning structures would interact.
Commissioning isn’t the route by which improvement is . . . necessarily . . . driven in the system . . . [But by] peer pressure within providers, professional competition, information data and . . . public pressure around that choice, the extent to which punters will be moving, there will be regulatory pressure at the bottom end as well.
Senior manager 1
Another senior civil servant agreed, adding that accountability and audit arrangements would be stronger than under GP fundholding. Transparent, accessible information would enable patients to compare commissioners and choose their hospital. Regulation would guarantee minimum standards and safety of care.
What the [2012 Health] Bill is trying to do is to try and find a, kind of, pragmatic way through the middle that combines the best aspects of all of those different things. I think if you only have integration that can’t be the way forward and if you only have competition, and no integration, then that can be problematic too in certain circumstances. So I think it’s trying to somehow try and steer the middle ground.
Senior manager 2
The new commissioning mechanisms were intended partly to strengthen commissioners’ control over NHS costs:
[C]ommissioners are . . . most of the time . . . merely acting as literally the payers at the end of the day, on stuff that they don’t really have much control over. . . . And the reason why they’re writing the cheques is that there are a bunch of other people in the system, GPs . . . actually incurring the expenditure.
Senior manager 2
Yet commissioners’ role would be narrow:
[T]he only way a provider is accountable to a CCG is via the contract. There isn’t another thing.
Senior manager 3
Hence:
[T]hat doesn’t really get them [CCGs] into the arena of managing providers within a local health system, it’s completely different from that.
Senior manager 4
Policy-makers suggested that population-based, general practice-based and client-based commissioning were compatible and coherent because they were all designed to commission services on the patient’s behalf:
So the main function of commissioning is to be an effective agent on behalf of the people for whom they are purchasing care in ensuring that people get access to the right level of care or sufficient quality in the system in way that actually doesn’t exceed the amount of money that is available.
Senior manager 1
General practitioners will commission as patients’ proxies, because patients will be able to select GPs for, among other things, referral opportunities:
If people in one geographical area can see in comparison to another nearby geographical area that their GPs are delivering a poorer-quality service with less good outcomes, less access to pharmaceutical products, slower referral times, da, da, da, etc. etc. they’re going to want to say ‘Well why? I’m going to move my personal register to another GP practice’.
[. . .] You seem to be envisaging a situation where if the patient moves their registration then presumably some fragment of the GP’s commissioning budget eventually goes?
Yes, the money for the patient, yes.
As for media of commissioner power, Parliamentarian 2 suggested that, within commissioning consortia, managers would perform much of the commissioning work while GPs undertook the overall governance. For both
a starting point [is], I think in terms of them being clear about your commissioning strategy, and particularly priorities for investment and disinvestment, making sure they are coherent, they tie back to need, they’re affordable, but also that you engage with providers at an early stage.
Senior manager 5
He added that commissioners’ negotiations with hospitals were intended to ‘rebalance, empower commissioners’ in negotiating with providers. GPs could not only negotiate with hospital consultants more critically and in greater depth than lay managers could, but thereby involve consultants in managerial decision-making:
So the aim is to actually increase clinician engagement across the pitch but using GP commissioners as the way in.
Senior manager 3
The negotiations would concern technical efficiency (care pathway design) and service cost, and stimulate consultants to raise the quality of, even reconfigure, secondary care. The concomitant risk was that GPs and consultants might collaborate to stymie provider competition. In a second set of negotiations a CCG’s central co-ordinating body would review its own member practices’ quality of care and ‘work with’ individual practices to improve it:
[S]howing clinical leadership to improve services at scale and pace . . . [so that] the whole primary care body start behaving along the lines of the redesigned services.
Senior manager 6
Peer pressure within CCGs would induce GPs to refer as CCGs want. GPs would also have the interest and capability to integrate more fully the now-fragmented general practice, community health, social care and outpatient services.
Transparency was the main discursive mechanism (as we have called it) putting pressure on providers to improve service quality. Commissioners and patients would be able to
monitor performance using a range of mechanisms . . . There’ll be the hard information they receive, the comparative information they’ve got to look at performance compared with other areas. There’ll be the soft intelligence they get through their own patients, through the public and other parties, HealthWatch, CQC [the Care Quality Commission], the Commissioning Board and so on.
Senior manager 4
Commissioners’ asymmetry of information with secondary providers would be less for GPs (as clinicians) than for non-medical managers. Furthermore:
There is of course a political dimension to this, because any politician, any MP who doesn’t stand up for his or her local hospital won’t be the MP for very long. And that’s why it [commissioning] needs to be clinically led rather than politically led, and also politicians need to say when a clinician says ‘well I think we need to do X, Y and Z’, rather than saying ‘oh no, oh no, how terrible’, say ‘well actually that’s right, I agree with that because it’s going to improve patient outcomes and survival rates, experience etc. etc.’
Parliamentarian 1
Tariff payments would give providers financial incentives and the means to self-finance their own investment and/or disinvestment strategies. Also:
[C]ommissioners will have some say over [tariffs] locally, up to a point, and then the national commissioning board have a key role in structuring the tariff.
Senior manager 1
Tariffs would also make providers face the financial consequences of what they did. Commissioners would be able to
say ‘I’m withdrawing my contract from you in six months if it [your performance] hasn’t improved’ and then you actually do it. . . . And then if you could work it out and you had a failure regime where the service didn’t close but the organisation collapsed and moved to another place [sc. new management], you could see driving improvement being accelerated.
Senior manager 6
They would not have to solve providers’ debt and solvency problems, which would help deal with problematic providers and hospital overcapacity (e.g. in London). Also the new financial incentives would raise service quality:
shifting the least good or the lower mean towards the mean or a bit beyond the mean.
Senior manager 1
Only a limited range of standards would be incentivised across the NHS at any one time. The tariff system might also be revised to include ‘year-of-care’ payments for chronic ill-health, because existing tariffs incentivised providers to increase activity.
Competition was intended to raise service quality, reflecting a general policy assumption that markets ‘deliver efficiency and innovation, and improve the quality of services’ (www.oft.gov.uk/shared_oft/economic_research/oft887.pdf), and increase provider diversity:
so that it’s not a monopolistic capture, you can have more than one provider and you can have some dynamism and change and some sense of challenge.
Senior manager 1
New provider entry was a means of introducing new models of care. (Two different informants both cited Diabetes UK providing primary care management of diabetes as an example.) Similarly, the AQP policy would mean that:
for those procedures where you’re able to specify . . . anybody who can meet the requirement can provide the service . . . I suspect it’s more around pathway diversification so seeing the more traditional forms of pathway delivery being changed.
Senior manager 4
Finally, provider competition would facilitate patient choice of provider, a policy goal in itself. Both interviewees and policy documents mentioned that staff-owned providers (social enterprises etc.) might be commissioned, but their formulations suggested only weak interest. Provider competition was national policy, not discretionary, although local commissioners could decide which services to place under the AQP mechanism rather than competitive tendering.
Informants mentioned juridical controls mainly as mechanisms preventing commissioners (and providers) from acting anticompetitively. The European procurement requirements were, senior manager informants said, very general and high level. The UK government (through the 2012 Act196) would in practice decide what specific procurement requirements NHS commissioners faced and not go far beyond those already applying to PCTs. Professional regulations would prevent competition or patient choice having any adverse effects on quality of care:
[A]ny provider organisation, whether it’s a hospital or a community service or a general practice, they know that at the end of the day their duty is to provide the right care for the individual patient and as an individual clinician they could be in breach of professional regulatory standards or as an organisation they could be in breach of contract if they ever did something that . . . was the wrong decision for that patient.
Senior manager 7
Contracts were seen largely as a framework for specifying services. However:
If GPs and hospital doctors don’t agree or are at war or at least can’t see a way ahead, then actually the contract will not solve any of the issues by and large that they’re throwing up.
Senior manager 8
Disagreements or problems about service redesign, cost or quality would normally be resolved negotiatively.
Policy-makers’ and top managers’ programme theory
Combining the explicit and the imputed material, Figure 1 represents the overall structure of the programme theory of NHS commissioning policy during 2010–12. It combines what have been called ‘clinical’, ‘managerial’ and ‘political’ discourses. 237 Arrows represent the main mechanism–outcome relationships that the policies assumed. Figure 1 represents high-level mechanisms rather than all the intermediate processes nested within them, such as GPs’ and patients’ everyday care choices. Each concrete mechanism noted in Figure 1 may combine several media of power. ‘Providers’ include community health, mental health and non-GP services besides hospitals.
FIGURE 1.
The underlying programme theory: NHS commissioning policy 2010–12. LA, local authority; NCB, National Children’s Bureau; OI, outcome indicator; PH, public health; PHR, primary health care.
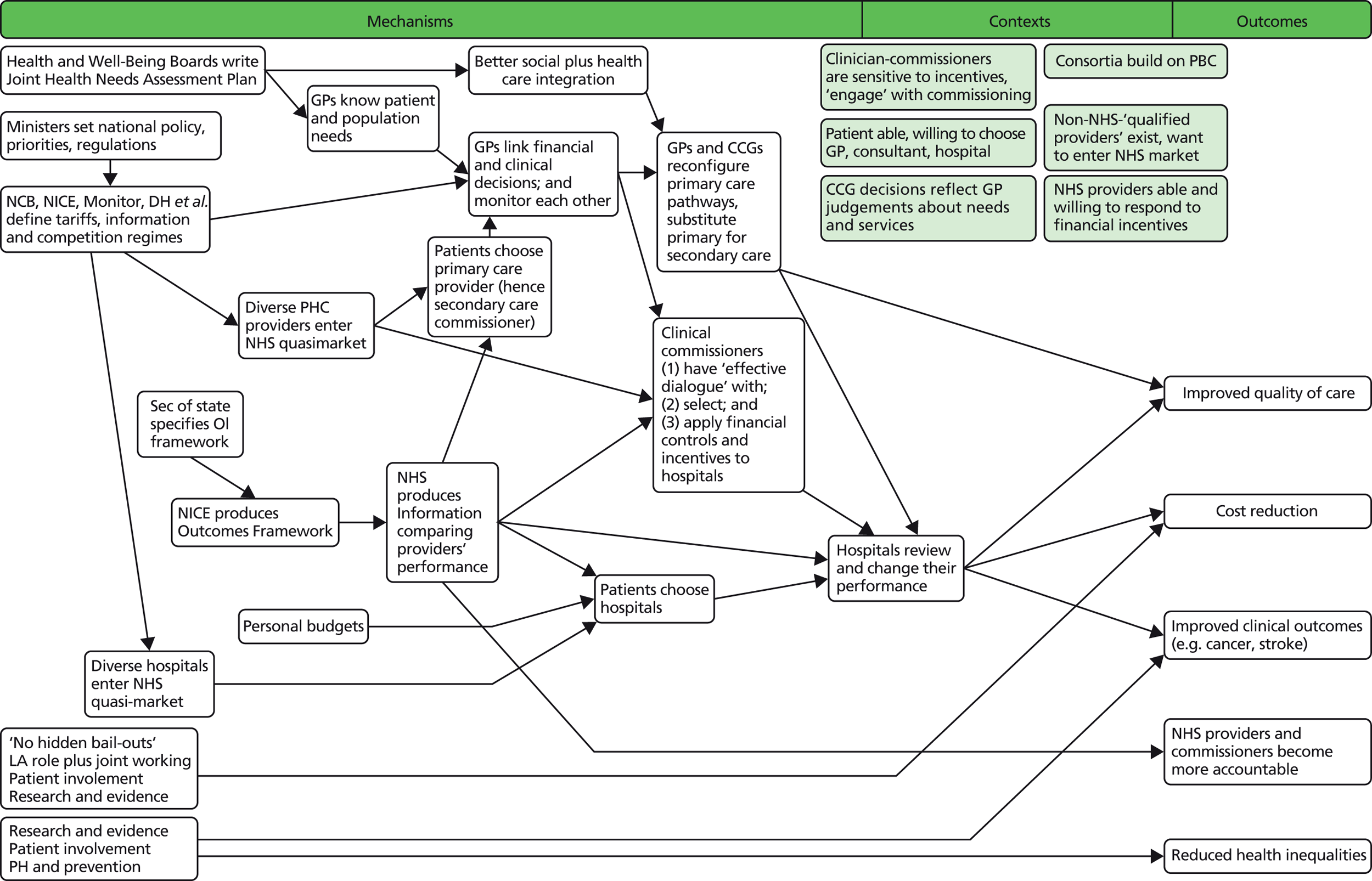
Each arrow in Figure 1 denotes a testable proposition or complex of them. Formulated as CMO propositions, the main programme theory assumptions of NHS commissioning policy were:
PT1: Central government’s decisions and actions lead NHS Commissioning Board, NICE, etc, to set regulations and guidelines that reflect ministers’ priorities.
PT2: Through joint commissioning with local government, commissioners will understand care group and population health needs.
PT3: NHS England’s management and GPs’ knowledge of patient needs together allow and stimulate GP commissioners to link clinical and financial decisions.
PT4: General practitioners’ commissioning role will lead CCGs to review primary care quality.
PT5: General practitioners’ commissioning role and joint commissioning with local government will lead to stronger integration of primary health and social care services (before and after hospital episodes).
PT6: General practitioners’ commissioning decisions, reviews of primary care quality and stronger partnership working with social care will bring about reconfiguration of primary care pathways, removing ineffective activities.
PT7: The reshaping of primary care pathways and the development of new information technology (IT) (online consultations etc.) together result in primary replacing secondary care to some extent.
PT8: General practitioners’ commissioning decisions, the outcomes framework, the presence of alternative providers and patients’ choice of providers (in particular of GPs) together stimulate and enable GPs to exercise greater influence over other providers.
PT9: Increased GP influence over other providers and the substitution of primary for secondary care together improve clinical outcomes.
PT10: Increased GP influence over other providers, GPs’ focus on quality and the substitution of primary for secondary care together improve quality of care.
PT11: Increased GP influence over other providers and the substitution of primary for secondary care together reduce costs of care.
PT12: Ministerial decisions lead NICE to produce the specific outcomes framework.
PT13: The outcomes framework and IT developments result in patients, commissioners and providers themselves having information by which to compare providers’ performance, and in patients and commissioners selecting (and deselecting) providers.
PT14: The outcomes framework, information for patients, provider plurality and (later) personal budgets lead patients and commissioners to choose between (and deselect) providers.
PT15: Commissioners and patients choosing between health-care providers causes the latter to improve clinical outcomes together.
PT16: Commissioners and patients choosing between health-care providers causes the latter to improve quality of care.
PT17: Patients choosing between health-care providers causes the latter to reduce the cost of care.
PT18: Research and evidence production causes health-care providers to improve clinical outcomes.
PT19: Patient involvement in care decisions causes health-care providers to improve clinical outcomes.
PT20: Public health activity causes health-care providers to improve clinical outcomes.
PT21: Refusing ‘bail-outs’ causes health-care providers to reduce costs.
PT22: General practitioner and local government joint commissioning causes health-care providers to reduce costs.
PT23: Patient involvement in care decisions causes health-care providers to reduce costs.
PT24: Research and evidence cause health-care providers to reduce costs.
PT25: The availability of information by which to compare providers’ – and by implication commissioners’ – performance increases NHS organisations’ accountability to the public.
These relationships are moderated by the presence or character of GP engagement with commissioning, local experience of practice-based commissioning, patients’ willingness to choose their hospital and on that basis their GP if necessary, the availability of ‘qualified’ competing providers, and existing providers’ capacity and scope to respond to financial incentives and competitive pressures.
The above propositions, and Figure 1, omit many details, nuances and complications, outlining only the gross overall architecture of the exposed programme theory. As with previous policies,22 the policy aims were broad and difficult to pin down. Nevertheless, the above propositions are amenable to empirical testing in light of NHS commissioning practice, to which we now turn.
Chapter 6 Reconfiguring commissioning structures
Next we consider RQ2: how English NHS commissioning structures were reconfigured during 2010–12, and what factors shaped that reconfiguration. By ‘commissioning structures’ we mean PCTs, the emergent CCGs and local authorities taken together. CCGs ‘went live’ 2 months before the end of the study period. We report who participated, how they were ‘engaged’ and how during 2010–12 CCGs converged from different local origins on a common pattern. These findings are drawn mainly from the English case studies and press reportage.
Reconfiguration as recycling
In all our study sites CCGs evolved from existing organisational structures for GP involvement, but which ones existed, were used and reconfigured varied between sites. In Porttown the starting point was a social enterprise (community interest company), which originated as the practice-based commissioning coordinating body, concentrating on referral management and owned by the city’s GPs. After the 2010 election the PCT transferred the Professional Executive Committee’s (PEC) commissioning functions to it. As its role extended, the social enterprise was ‘rolled up’ into the CCG. Paradoxically, the 2012 Health Act was an impediment. 196 To work around its requirement that the CCG be a statutory body, the PCT created an interim ‘Clinical Commissioning Executive’ to work after the fashion of a holding company. In Milltown those parts of the PCT in which GPs were active (the PEC, various micro-commissioning groups) evolved into the CCG by ‘scaling up’ already-established arrangements. In neither site had the PCT been clustered with another. Metroland split the PCT cluster (and other cross-London groupings) back into four, creating one CCG for each borough in the cluster’s territory. It populated its CCG from an existing polyclinic (or ‘polysystem’):
[S]o they’ve actually basically kept that poly, the sort of, there were, sort of, four, five, if you like groupings within the PCT and they’ve basically kept that within the CCGs.
General practitioner, Metroland
General practitioners involved in the Metroland polysystem became CCG enthusiasts, but others were generally unfamiliar with commissioning. Consequently the new CCG was constructed almost from scratch, initially with six GPs and designated PCT staff to assist them. Shire formed its CCG by clustering two PCTs. One had developed autonomous locality structures that undertook practice-based commissioning. Clinical commissioning programmes were long established there, with PCT, GP, other primary care and local authority representatives meeting acute and mental health trust medical directors every month. This PCT became the platform for CCG formation, absorbing the existing cardiac, stroke and diabetes networks. The other PCT had little practice-based commissioning and had to start recruiting GPs into commissioning work with the other PCT almost from scratch.
The transition to CCGs blurred the division of commissioning labour between PCT, cluster and shadow CCGs, which retarded commissioning work in all four sites. Metroland informants were also uncertain whether the CCG should be shaping or implementing GPs’ wishes. Those in Shire were uncertain whether the CCG should focus on primary or secondary care.
Incremental engagement
Another common pattern across sites was difficulty in recruiting GPs to ‘engage’ with commissioning. PCT informants in Metroland, Shire and (more guardedly) Porttown emphasised how fast this was happening, but some GPs presented a more nuanced view.
Availability
Reconfiguration of the commissioning organisations was hampered by a shortage of GP participants, even where GPs already participated in commissioning. Partly this was a matter of GP availability. Few GPs wanted to participate actively in commissioning because of lack of interest, work overload, multiple commitments or the cost and quality of locum cover. Many GPs simply attached more importance to direct patient care. Most Milltown GPs were unfamiliar with commissioning and not confident about doing it. Few GPs responded to consultations about service changes in Porttown or Milltown. Metroland PCT set up clinical forums with two local acute hospitals. At first few GPs or consultants attended, although later they began initiating discussions with (other) commissioners and seeking their advice. Shire and Porttown GPs were mostly content to leave commissioning to the former PEC members and social enterprise respectively.
Capability
Many GPs still lacked knowledge about commissioning and confidence in their commissioning skills:
Some GPs don’t understand the risk in taking out 30% of inpatient services from a Trust.
Commissioner manager, Metroland
Metroland GPs were still at the stage of familiarising themselves with such policies as Quality, Innovation, Productivity and Prevention (QIPP), so the PCT began education work with them. Some Milltown GPs were confident about the clinical aspects of commissioning but not the other aspects, with which they were less familiar. To address this problem and the lack of GP availability, the study sites used different commissioning support organisations and to different extents. Porttown subcontracted its social enterprise to provide commissioning support and sought advice from its NHS regional procurement organisation. Both Milltown and Metroland relied on cross-PCT commissioning support organisations. Metroland also used management consultancies for a few discrete tasks (see Chapter 7). Shire provided each of the clinical commissioning project group with PCT commissioning and finance manager support, but made little use of commissioning support organisations, apart from some ad hoc external evaluations of proposed or actual service reconfigurations.
Distrust
To assume, as parliamentarians did, that GPs would commission differently from non-medical managers implies possible disagreements between the two. The GPs were most interested in community provision of mental health services, while PCT managers prioritised cost-saving bed closures. These differences tended to reduce GPs’ appetite for helping develop service specifications. Shire PCT managers sided with local hospitals in rejecting GP proposals for direct GP referral to MRI scanning for young people with knee pain (to reduce outpatient referrals) and replacing regular hospital biopsies with GP monitoring of patients screened negative for prostate cancer. Some GPs concluded:
there’s a sort of pretence of [GP] involvement but it doesn’t make any difference.
General practitioner chair of clinical commissioning programme, Shire
It took persistent GP pressure to induce Porttown PCT to support vascular disease checking (a national mandate). The lead GP thought that the PCT had given a pilot project for vascular disease checking, and the evaluation of that project, insufficient practical support, which
makes you pretty impotent when you’re trying to improve your commissioning.
General practitioner cardiology lead
Other GPs became disengaged when they felt that their ideas for better ways of working did not get commissioned because Porttown PCT lacked authority with (other) providers. In Milltown, though, there was little evidence of distrust between GPs and commissioning managers. The PCT had encouraged GP involvement. Its long-established commissioning strategy groups included commissioning managers, GPs and other providers, between whom relationships were friendly.
These disagreements spilled over into the GP body itself. Some GPs felt that their PEC colleagues had ‘gone native’, becoming too compliant with hospital and PCT priorities in Shire. Two or three Porttown GPs were antagonistic towards the social enterprise from which the CCG was built, although most were passive. Having regarded the PCT as a failure, they tarred the social enterprise with the same brush. Some Metroland GPs saw the reconfiguration of commissioning as their chance to get rid of the PCTs, others as an opportunity to recruit PCT commissioning and contract staff. Milltown PCT found it necessary – and hard – to sustain a consistent message about commissioning objectives and how to achieve them (e.g. by closing a walk-in centre).
Study-site PCTs followed a strategy of gradually increasing the above bodies’ commissioning activity and remit, building up trust and reconfiguring commissioning structures incrementally as opportunities arose, so that preponderance gradually shifted from managers to GPs. Methods included:
-
Widening the decisions and issues delegated to shadow CCGs to include such issues as linking commissioning plans to heath outcomes, priority setting, contract management, integrated care, management of long-term conditions in Metroland; referral management, implementation of QIPP priorities in Shire; and contract monitoring with hospital consultants in Porttown. Milltown PCT built on practice-based commissioning groups that involved a mix of stakeholders in reviewing commissioning for specific care groups.
-
Involving GPs throughout the commissioning cycle, for instance in Metroland having a GP chair commissioning meetings on mental health services; or in Porttown scrutinising the business cases for new projects or services.
Our [commissioning] team used to carry laminated copies of the commissioning cycle and every time a GP said ‘Let’s do this’ . . . we’d pull it out of the bag and go ‘right, where on the cycle is that question you are asking?’
Commissioning manager, Milltown
-
Inviting ‘ordinary’ GPs (not previously involved in commissioning) to lead commissioning groups for specific clinical areas, such as clinical pathways, long-term care, apparent hospital ‘over-activity’ (e.g. for myringotomy at Porttown), mental health services, coronary heart disease (CHD) and diabetes prevention, musculoskeletal services, trauma and public health. Milltown introduced formal processes for selecting GPs for some roles rather than relying on ‘usual suspects’ or unskilled volunteers.
-
Inviting GP ‘enthusiasts’ with particular clinical interests to attend meetings to give their opinions (Shire, Porttown).
-
Involving GPs in referral triage, in Porttown by reporting their work and its cost implications through quarterly meetings with a GP committee; and in Metroland by reviewing audit data and observations of local practice.
-
Clinical pathway and service redesign (with PCT staff and hospital consultants), although in Metroland this activity was more fruitful at one hospital than another with ‘less maturity’. Milltown ended up with 42 project groups for these purposes. Clinical commissioning projects served a similar purpose in Shire. Porttown GP leads contributed to redesigning health services for homeless people.
-
Prioritising commissioning work on care groups or problems that interested GPs: specific diseases, such as diabetes (Shire); high-spending services, such as mental health, general medicine (Shire, Metroland, Porttown); and high-volume patient groups (Metroland, Porttown).
-
Primary care trust managers and borough directors collaborating with GP practice managers over budget setting (Metroland); or, in Milltown, identifying clinical and non-clinical commissioning leads in each general practice.
Wider collaboration
A parallel task was to reconfigure joint commissioning with local government and GP negotiations with hospital, mental health and community health services trusts.
Consultants
The fora described above sought expert advice from secondary care clinicians, usually consultants. In Metroland and Shire these meetings became, among other things, a venue for consultants to make presentations about clinical matters (e.g. prescribing for patients with long-term health problems in Metroland). Consultant participation was comparatively straightforward in Milltown, where the lead GP commissioner had strong personal relationships with some consultants and mediated the relationship between them and other GPs; hesitant in Shire, where the consultants were conscious of being both clinical experts and (potentially) organisational or speciality representatives; and patchy in Metroland, where the separate clinical fora for each hospital developed at different rates because at one hospital it was hard to involve the consultants. Corporate providers never participated.
Local government
Joint commissioning with local government also tended to evolve from existing arrangements. A preliminary step was cross-over membership between NHS and council bodies, adding a CCG member or two to the Health and Well-Being Board (Shire, Metroland) and a social services director to the CCG Board (Porttown, Shire, Metroland). The Metroland Director of Social Services attended the meetings of NHS chief executives hosted by the PCT. Porttown and Milltown Directors of Public Health were already joint Local authority (LA) and NHS appointments, as were some of the more junior commissioning managers in Milltown. Existing joint commissioning and public health activities were also broadened and elaborated, making public health an increasingly joint NHS–local authority activity. Porttown PCT was already involved in an existing health theme group and local strategic partnership addressing health inequalities, which developed into the Health and Well-Being Board, using its health inequalities strategy as a basis for joint commissioning plans and activity. Metroland borough council had a long-established Health and Social Care Liaison group, which in 2002 had agreed a concordat with the NHS and established an intermediate care partnership that mostly obviated the need for Section 75 arrangements (although there still were some for mental health services). The Health and Well-Being Board was a successor to this activity. Shire’s long-established joint commissioning board gained a wider remit, but public health work continued more separately.
Overload
These developments occurred despite the disruptive side effects of NHS restructuring on staff turnover (although the disruption was least in Metroland). Three successive changes of Shire commissioning structures meant that:
They [commissioners] never develop that expertise that you can start having a sensible dialogue.
Medical director, Shire
It caused
loss of organisational memory.
General practitioner, Metroland
Staff turnover and increased work demands forced those remaining to prioritise tasks. Metroland and Porttown PCT rotated their attention around care groups so that some service specifications were reviewed in depth with ‘just programme managing essentially’ (manager, Porttown) for the rest. Shire ‘rationalised’ 22 Clinical Commissioning Programmes into 7, aligning each with a national programme budget heading, but also making agendas and meetings (20–40 people) too large for easy decision-making, and mostly irrelevant to the hospitals. This made clinicians see the groups as mostly for information gathering. Other tasks were simply delayed, for instance out-posting hospital diabetic nurses to general practices (to reduce outpatient attendances; Shire) or finalising plans for social work assessments in winter of older people with long-term conditions (Metroland). Commissioners also engaged external commissioning support: management consultants (e.g. to review the viability of rehabilitation beds; Metroland), the London Health Programme (Metroland), the Procurement Supplies Agency (Porttown), the SHA (Shire, Milltown) and independent experts (Shire). Livewell bought substantial support from a US HMO to develop a unified view, across the commissioners, GPs and other primary care providers, about what services should be commissioned, monitored and reviewed. 238 Overload was less evident in Milltown, perhaps because so many GPs contributed to commissioning there. It became more severe the year before CCGs went live, with less work being done on commissioning initiatives, revising service specifications (Metroland) and setting public health priorities (Porttown).
Convergent reconfiguration
Despite their different origins, the study CCGs converged on a common structure, partly stipulated by legislation and central guidance: clinical senates; subgroups for specific care groups, clinical specialities or service problems; and the shadow CCG that from April 2013 would manage the first two. Commissioners created their organisational structures partly in order to involve clinicians (e.g. the 42 project groups in Milltown).
Recycling existing organisations implied recycling the existing local GP leaderships, as others have also found. 239 The Shire GPs dominating service redesign work and chairing clinical commissioning programmes tended to be former PEC members, GPs with a special interest (GPSIs) or, as in Porttown and Milltown, former practice-based commissioning activists. The former PCT chair in Metroland reappeared as assistant director of the CCG. As noted above, Milltown PCT took steps to moderate, but not reverse, this tendency. These continuities of GP leadership, of subgroups doing much of the commissioning, and of non-GP managers doing the commissioning work that GPs would not, seemed to presage more an evolution of commissioning practice than the upheaval, even ‘revolution’, that many commentators and policy-makers predicted before April 2013.
Chapter 7 NHS commissioning practice and governance over health economies
Research question 3 concerned how far NHS commissioning practice in 2010–12 allowed commissioners to exercise governance over their local NHS health economies. Using all the study methods except the international comparisons and Leximancer analysis, this chapter reports how NHS commissioners exercised governance unilaterally over providers. Later chapters consider the rest of RQ3: what room for manoeuvre NHS commissioners had; the consequences of distributed and client-based commissioning; and how providers responded to commissioning activity. By ‘commissioners’ we mean the combination of residual PCT and emergent CCG organisations.
Case study informants’ accounts of current NHS commissioning practice in 2010–12 mainly concerned negotiated order, managerial performance and discursive control, and (less so) provider competition (Table 7).
| Medium | Number of references | Percentage of references |
|---|---|---|
| Managerial performance | 920 | 29 |
| Negotiated order | 845 | 27 |
| Discursive control | 607 | 19 |
| Financial incentives | 252 | 8 |
| Provider competition | 340 | 11 |
| Juridical governance | 180 | 6 |
Since informant responses covered all six media of power, we report how the study site commissioners used each one, and how the media interacted.
Management performance
Separating commissioner and provider forced commissioners to be more deliberate, focused and explicit (documented) in specifying what services they wanted from Porttown and Milltown community health services. Existing providers still won the tender, but had to specify services and costs more precisely.
Service specifications were becoming evidence based, as others have found. 102,240 In all four sites, public health professionals contributed local data on which to base service specifications. Shire PCT did so least, but (like Porttown) did use the Map of Medicine (http://mapofmedicine.com) to redesign care pathways and specify referral criteria. Porttown and Metroland also re-used Hospital Episode Statistics data. Their public health staff contributed to service specifications and pathway design. When evidence was absent or ambivalent, medical consensus or majority opinion was followed – again reported elsewhere102 – and commissioners made more subjective judgements (‘intelligence’) based on financial information, their own perceptions of local services, and staff and patient feedback (e.g. complaints).
Providers, indeed the main provider, played a large part in formulating service specifications. Commissioners in all sites spoke of provider proposals for service provision, which ranged from consultants advising about the evidence base for service specifications (Porttown) to consultants telling commissioners what service changes were feasible (Metroland). Provider input compensated for the commissioners’ lack of clinical and technical knowledge, as provider informants often commented. Nevertheless, mental health commissioners sometimes argued that:
I think that I can commission better because I was involved in providing the service.
Mental health commissioner, Metroland
Clearer service specifications helped in introducing referral-screening criteria aimed at reducing hospital activity by diverting suitable patients to primary or community care, at least for extra-contractual referrals (Metroland). Where referral criteria were lacking, peer review was used, often with consultant (Porttown, Metroland, Shire), and in Shire also physiotherapist, input.
Commissioners in our study sites often felt that they lacked the procurement skills required for dealing with competing providers. They were aware, however, of the transaction costs of procurement work, which they saw as a somewhat futile waste of money and time when only one bidder was available. Informants at Shire contrasted the local authority’s ‘scrupulous’ application of tendering rules with the small number of providers. Our study sites followed official procurement procedures and regulations most carefully for large contracts and when there were two or more bidders, but, if market testing identified only one potential provider and they could keep within EU law, they would avoid tendering.
Commissioners mainly used nationally mandated measures such as target compliance, patient-reported outcome measures (PROMs)241 and DH ‘vital signs’ for monitoring providers. During our fieldwork the latest NHS Operating Framework242 measured recorded quality, resources and reform. Two (of eight) of the headline and nine (of 27) supporting quality measures concerned health outcomes; the rest measured work processes. (No resource or reforms targets concerned health outcomes.) The NHS Outcomes Framework had not yet appeared. 243 Porttown PCT benchmarked its providers against regional comparators, as did Shire. All sites used contract reports that included Monitor’s reporting requirements, QIPP data and exception reports for non-compliance with contract or quality standards. Metroland required local providers to give ‘narrative’ explanations of outliers, exceptions and untoward incidents. Metroland, Shire and Porttown encouraged provider staff to report service quality problems. Porttown commissioned a local firm to undertake patient surveys, but dealt directly with any patient who wrote comments (rather than just scores) on the survey form. Livewell collected data via its telephone helpline.
Although commissioners relied on their providers to supply and interpret monitoring data, providers sometimes withheld information, such as ‘commercially sensitive’ financial data, on the grounds that they had to make a surplus (Metroland). Non-disclosure could have adverse consequences for both sides. Porttown hospital trust masked its financial problems as long as it could until the PCT and hospital found themselves having to make savings exceeding £30M. Tariff payments made provider finances, patient flows and case mix more transparent than did block contracting. Similarly, because there were QOF payments for diabetes and epilepsy treatments, Shire PCT knew how many of those patients were treated, but knew the number of Parkinson’s disease treatments only because it employed a specialist nurse. At Metroland especially, our informants thought that involving GPs made service monitoring more incisive, especially regarding clinical outcomes and cost-effectiveness.
The action learning participants suggested that an important aspect of management performance (especially service specification and contracting) was to promote integration of the disparate primary, secondary and social care pathways that an individual patient followed, although, in practice, commissioning was rarely carried out in this way. Often, discussions between commissioners and providers about how to identify patients with long-term conditions who might be diverted to community care (to reduce costs) reached an impasse. This was an obstacle to reducing inpatient activity.
Looking at all English PCTs cross-sectionally, we had data on 16 service outcomes (see Chapter 4, section Indicators and measures). Only one, PCT surplus/deficit, correlated with PCTs’ summary WCC scores (see Table 23, Appendix 4), and then weakly and in the opposite direction from predicted; larger PCT deficits (or smaller surpluses) were associated with higher WCC scores. However, PCT surplus also correlated negatively (r = –0.319, p < 0.001) with monthly mean waiting list size (combined inpatient and day cases) per 100,000 population: the shorter the waiting list proportionate to population, the smaller the PCT’s financial surplus (or the larger its deficit). The more numerous correlations between the controls and the service outcomes were, with two exceptions, also verging on negligible. One might have expected WCC scores to reflect among other things the implementation of contemporary managerial objectives. 55 If so, our finding casts doubt on the validity of the WCC self-scoring system (which was subsequently discontinued).
During the study period the Francis Report244 exposed a culture of vague monitoring criteria and unrealistically optimistic findings. Francis reported that commissioners (and providers) often responded to prima facie adverse monitoring reports by reinterpreting the findings rather than acting on them. (Stafford was not one of our study sites.)
Negotiated order
Contract negotiations were conducted mostly by chief executive dealing with chief executive, and other non-medical managers dealing with their counterparts (e.g. PCT finance manager with trust finance manager etc.). Senior clinicians sometimes participated, but not uniformly, especially not in negotiations about cost savings. In Metroland mental health trust, even the medical directors were not always involved in such negotiations. Negotiations about the unscheduled care contracts in Porttown involved the PCT and acute trust finance directors, with marginal input from other PCT commissioning staff, let alone anyone else:
It’s just a contractual numbers negotiation.
Commissioning manager, Porttown
Shire was similar. There clinicians’ proposals (e.g. for diabetes pathways) would not necessarily enter contract negotiations. One Metroland consultant believed that ‘difficult’ consultants were kept out of contract negotiations (no one else either corroborated or denied this). One way to bridge the two negotiated orders was by judiciously selecting consultants – and GPs – to involve. Porttown hospital trust involved selected consultants in order to demonstrate to them (and, through them, other consultants) that the trust had obtained the best deal it could. Action learning participants reported instances when a consultant spent much time negotiating the introduction of new services and reconfiguring care pathways with one commissioning manager, only for the agreement to be reversed elsewhere in the PCT. The consultant then felt she had wasted her time and spent less time working with the commissioner.
National policy priorities (targets, budgets) largely set the commissioners’ agenda, as another study102 also found.
Commissioners need to demonstrate that they exercise control. They are only interested in national diktats and money.
Consultant, Metroland
However, the national policy focus did give providers and commissioners common interests, especially concerning hospital referral criteria, substitution of primary for secondary care, compliance with QIPP targets, emergency department (ED) utilisation and hospital outcomes, although Porttown community health service (CHS) managers argued that their commissioners paid too much attention to minutiae (e.g. heart failure nurses’ referral habits). Indeed, our hospital informants described the main commissioning focus as being costs, although in Metroland waiting times were no less central. Action learning set members used the term ‘class hegemony’ to describe the close networks among small numbers of nationally prominent NHS managers, networks which local managers would use when trying to influence the other party in commissioning negotiations.
Financial negotiations were often separate from ‘real-side’ negotiations. In Shire, Metroland and Milltown, a financial agreement (and, in Milltown, also local authority budgets) framed subsequent ‘real-side’ negotiations about service priorities, population needs and service specifications. In Porttown, for instance, the clinical and service specification of a new eating disorder service was adjusted to meet the budget, not vice versa. The main exception was that, when the London Health Programmes awarded contracts for ‘hyper-acute’ trauma and stroke centres, specifications for quick access and clinical quality determined the cost. As others report,102 both financial and ‘real-side’ negotiations were framed by historical patterns:
[W]e commission most things on a historic basis unless there’s a good reason to start arguing and we need to change things . . . you’re basically arguing around the margins with the provider about what changes. But . . . where there are significant risks around delivery . . . you’re likely to take more of [a] care pathway approach to such as A&E [accident and emergency], such as maternity.
General practitioner, Metroland
Commissioners’ proposals for cost containment and service re-profiling were bound to be contentious. Providers who disliked commissioners’ proposals disputed the justifications for them. Shire PCT and one hospital argued inconclusively for years about why ED attendances were increasing. ED consultants blamed the lack of GP availability; the PCT cited its own data and surveys suggesting the opposite.
A second negotiated order involved GPs and consultants (and other secondary care clinicians), who often liked to deal directly with each other, blurring the commissioner–provider distinction (especially in the small-scale Livewell project) and bypassing the aforementioned managerial negotiations. Clinicians’ attitudes towards non-medical commissioners ranged from:
We don’t just want to be a manager with a clinician’s hat on
General practitioner, Porttown
to:
I do my level best not to deal with commissioners.
Consultant, Metroland
Livewell GPs disliked even the word ‘commissioning’. 238 Doctor-to-doctor negotiations could have constructive results for a commissioner. Porttown consultants endorsed changes to ear, nose and throat services as a consequence of dealing directly with the GP organisation, while the GPs questioned and reportedly limited the orthopaedic consultants’ income-maximising activities. The obverse of this medical collegiality was, at times, scepticism about the value of non-medical inputs to commissioning and about managers trying to control things in which they were not competent. There were also limits to medical collegiality:
[O]ne of the hardest things I’ve found is convincing my GP colleagues that the hospital doesn’t have a hidden agenda, it’s not out there to ruin general practice.
General practitioner, Milltown
Porttown and Milltown informants described mediating debates between GPs and consultants. Disagreements about what work should transfer to non-hospital settings soured relationships between Shire GPs and consultants.
In terms of quantity of work and participants, the most important negotiated order was what GPs called ‘micro-commissioning’: interdisciplinary, interorganisational redesign of care pathways, most often (and protractedly) for complex, non-commodified activities such as rehabilitation, chronic obstructive pulmonary disease (COPD), unscheduled care and mental health care. However, care pathways for less organisationally complex care – for example orthopaedic surgery – were also sometimes micro-commissioned. Micro-commissioning typically involved several providers, NHS and local authority commissioners, patient representatives and ‘third-party’ experts such as a lead psychiatrist, public health consultant (Metroland) or immunologist (Porttown), but could also be small scale (e.g. at Livewell). From the pathway design followed decisions about providers’ functions, service access criteria, resource needs – including decommissioning decisions in Milltown – and in Livewell an overall redesign of primary care provision. From these decisions followed service specifications and monitoring arrangements, raw material from which contracts were prepared. Micro-commissioning gave the participating clinicians and providers a head start in bidding for the ensuing contract.
Building up trust with providers took years. It required compromises and trade-offs (as others report39), and partly depended on the personalities and interests involved. After Milltown PCT decommissioned its community matron service, it collaborated with (other) providers to redeploy the community matrons, which the commissioner saw as investing in future goodwill. Metroland PCT agreed that its hospitals could cut beds (hence costs) provided their activity was not reduced, and paid for some (not all) of the above-contract activity that the acute hospital had undertaken. To resolve a potential dispute about upcoding, a private hospital invited Metroland PCT to send a coder to agree the disputed codes jointly with its own coders. Shire PCT claimed to avoid disputes by mutually recognising divergent interests and reaching compromises. As others report,39 regional NHS bodies (SHAs, during most of 2010–12) would sometimes intervene in contract negotiations to exercise hierarchical control over both sides, including dispute resolution. Shared beliefs in a commonality of NHS interests and in NHS-wide interorganisational collaboration, persisting from earlier NHS structures and rules, also helped mitigate tensions and disputes, indeed facilitated micro-commissioning.
In all four sites, patient and carer representatives (e.g. from Diabetes UK) were involved in micro-commissioning and, in Shire, decisions about service closures. Patient voices were not necessarily unanimous. Some patient groups in Shire opposed acute bed closures, while others preferred replacing acute beds with care closer to home. User representatives for Milltown mental health services shifted over years from an adversarial to a more supportive stance. Porttown patients whom the PCT consulted were interested in wheelchair supply but not vascular risk assessment or ISTC orthopaedic services. For mental health, one challenge was to engage with users at the more disabled end of the spectrum, for instance those with chronic schizophrenia. Neither did patient representatives merely respond to NHS initiatives. Porttown patients participating in a regional heart/stroke network (as opposed to the PCT patient consultations) presented their own proposals for a CHD self-help service. Porttown council had learnt that user involvement worked best when users participated in the early stages of service design and specification.
Over time, negotiations usually became more relational as trust and goodwill accumulated, the participants recognising that they would need each other’s help in future. In Milltown and Porttown, GP–consultant relationships rested on the precept ‘If you have got a problem, ring me’, forestalling the use of other media of power. This social capital was reported in Milltown as helping to repair the harm that tariff payments did to commissioner–provider relationships. Metroland also built on the relationships formed in operating its ‘polyclinic’. Because they influenced what media of power a manager was usually inclined to use, certain personal attributes, skills and management style were important for commissioners, as others have also found. 245 One such skill was motivational interviewing (e.g. inviting providers to state their view of the evidence base to frame negotiations in terms that the provider accepts). Another was to blame a third party (e.g. national policy, the behaviour of another local organisation), not the other negotiator, for the dispute. Patience and emotional resilience were two more. 238 A corporate hospital manager explained:
I’m from a sales background so you learn never to burn a good relationship because it costs you down the line.
Private hospital manager, Metroland
Nevertheless, some relationships had already been burned by personality clashes (Milltown), argumentative, competitive and antagonistic negotiating styles (Shire) or bullying:
I’ve been in meetings that were so bad that if you’d filmed them you’d be in front of a court.
General practitioner, Porttown
Indeed, action learning participants suggested that our analytic schema should include bullying as a method which negotiators used.
Discursive control
Etic discourse framed much of the micro-commissioning negotiation mentioned above and was a main currency of provider monitoring. Thus Shire PCT stated that services without an evidence base would be decommissioned. Commissioners in our study sites mainly used nationally promulgated materials when persuading providers to accept commissioners’ proposals, most often NICE guidelines, the Recovery Model, QIPP targets, the Map of Medicine, National Service Frameworks (especially for mental health, older people and CHD) and the Improving Access to Psychological Therapies (IAPT) programme. Before negotiation or monitoring meetings with providers, commissioners would also supply data on local problems to frame the discussion, for example case-load and case mix spreadsheets (Porttown) or studies showing that a walk-in centre raised ED admissions (Milltown).
At times etic persuasion resolved disagreements between commissioner and provider (e.g. about remodelling eating disorder services in Porttown), but not always. Etic arguments could cut both ways, as they did against commissioner proposals for GP triage in EDs (Metroland) or when the Shire mental health provider simply dismissed national guidance about home treatment as ‘out of date’. ‘Evidence’ was sometimes used to justify rather than ground decisions.
Then debate fell back on emic discourse. Commissioners sometimes cited patient consultation (but seldom patient choice) to legitimise their claims on providers. Porttown PCT asked its providers to show evidence of patient – and staff – consultation about proposed service changes. Occasionally, wider ethical imperatives were invoked. The Porttown pathway group for non-psychotic mental health problems succeeded in remodelling services because everyone recognised the fatal consequences when these services fail. ED consultants in Shire argued that, although they could not control which patients presented at the ED, they could not clinically or morally justify sending patients elsewhere either. The argument that proposed service changes would have no bad consequences for patients was often persuasive to provider clinicians. One influential emic argument reflected the relationality mentioned above, expressing a culture of joint responsibility for the local NHS: ‘the [Milltown] way’. Porttown GPs’ leaders said that their GPs had more appetite for collaboration and integrating their work than for competition.
Financial incentives
There was little disagreement that tariff payments incentivised providers to increase the number of patient episodes, which had
driven a wedge between us over the last few years.
Commissioning manager, Milltown
Commissioners asserted that treatment thresholds had fallen and upcoding had appeared. The volume of providers’ activity became the focus of contract negotiations rather than service specifications. However, rising marginal costs of care limited the expansion. The main Porttown hospital had to open wards and theatres at weekends, at costs above the tariff payments. Shire hospitals wanted to discontinue costly out-posted clinics in community hospitals. Tariff payments constrained micro-commissioning by placing a ceiling on the cost of any new care pathway in Metroland.
Unless commissioners responded as reported below, the combination of tariff system, AQP and patient choice rules weakened their power to control provider case load and case mix, hence overall costs, and the sources of service provision. When Metroland PCT and its main hospital agreed a reduced volume of elective activity, the hospital still deliberately delivered more services than agreed, presenting the PCT with a fait accompli and corresponding bill. Shire PCT found its obligation to pay for hospital ‘overperformance’ an obstacle to transferring funds into long-term care. Porttown commissioner and provider informants agreed that tariffs incentivised hospitals not to transfer services to primary care.
Under tightening financial constraints, commissioners in the study sites responded by bundling their tariff payments to providers into blocks (see also Petsoulas et al. 39), the ‘cap-and-collar’ or ‘managed PBR’ system. If provider activity fell below a certain ‘floor’ or (more likely) exceeded a certain ‘ceiling’ (in Metroland, 5% above the expected volume), tariff payments for the marginal activity were reduced by an agreed amount, eventually falling to zero in Porttown. One Shire hospital, though, so far exceeded its expected volume that the PCT exercised its option to pay it on a ‘non-contractual activity’ basis, that is to pay a monthly sum that was retrospectively adjusted for deviations from the level of activity that the PCT had forecast. There were exceptions; Porttown PCT changed its de facto block contract with the ISTC to tariff payments. Nevertheless, the predominant response was bundling in order to dampen what, according to commissioners, were perverse incentive effects.
Block payments were still used for community health and most mental health services. They sometimes prevented providers from being incentivised, even reimbursed, for work. Metroland mental health trust was not commissioned to treat, say, schizophrenics, nor the Shire trust people for autism, but both trusts were still expected to treat them under a block contract, so that the providers either cross-subsidised the work or sought voluntary-sector provision and/or finance. When Porttown GPs began performing minor operations, the local hospital, not the GPs, was still paid under the hospital’s block contract. Not that block contracts inherently denied commissioners scope to incentivise their providers. A block contract between a Metroland provider and PCT shared the costs of referrals above a specified level in return for the provider increasing its bed capacity. Shire PCT used a block contract to offer its community and mental health service a secure income in return for the providers taking an increased case load. Milltown PCT built into its ED block contract an incentive to send suitable patients to an ambulatory care centre, where the average case cost was £70, not £2000. In theory, CQUIN could also be used as a supplementary incentive mechanism, but the targets and payments were in practice decided nationally and regionally. Within the national NGMS contract, Porttown and Shire used QOF payments to incentivise general practices to implement vascular disease checking. Although in practice the study site commissioners did little to measure the volume of work of block contract holders, well-designed block contracts could accommodate strong monitoring arrangements. One in Shire stipulated the quarterly provision of monitoring information, which was used to review and improve performance, with the commissioner having the option of contract termination.
Commissioners also used block payments to hypothecate funding for nationally prioritised services (e.g. early intervention, Metroland). Conversely, block funding made it easy for Metroland to divert £5M from its mental health provider to meet hospital overspend resulting from tariff incentives, although such transfers also occurred in pre-tariff days. When commissioner budgets were tight, the use of block payments compelled providers to negotiate adjustments with the commissioner; but by the same token Milltown PCT found that this tended to lock the commissioner into using existing providers.
Independent-sector treatment centres were initially paid irrespective of what volume of cases they treated246 and so the Metroland ISTC seemed to feel no incentive to engage with GPs and, we were told, ‘cherry-picked’ patients (PCT commissioning manager, Metroland). That corporate provider, at least, seemed to respond to block payments differently from NHS providers, who were more willing to waive their contractual claims on commissioners.
Like others,71,247 we found that our study site commissioners shrank from financially destabilising the main local providers on whom they depended for fulfilling their commissioning duties. Shire PCT did not exercise its option of non-payment when local providers did not comply with their contract. Neither would Shire or Metroland PCTs reduce total tariff payments to reflect a large reduction in admissions. A Milltown commissioning manager argued that it would be short-sighted to disrupt long-standing, usually productive relationships with a provider for the sake of a one-off financial gain. For voluntary and corporate providers, losing an NHS contract was undesirable but not fatal (Shire, Metroland).
The shift towards lower, ‘best-practice’ tariff prices began only at the end of the study period, as did the introduction of mental health tariffs and (in some places but not our study sites) experimental ‘year-of-care’ (in effect, capitation) payments. In our two study sites where they had been trialled, personal health budgets had so far had little perceptible effect:
I don’t know anything about them.
Commissioner, Metroland
Shire PCT was still ‘investigating the use’ of personal health budgets for brain injury patients (PCT commissioning manager, Metroland).
Provider competition
Provider competition was the medium of power about which the most cross-sectional data were available. Preliminary examination (see Table 21, Appendix 4) showed that spending on independent-sector providers correlated negatively with spending on local authority and voluntary-sector providers, consistent with the interpretation that some PCTs used local authority and voluntary-sector provision, and others used independent-sector provision, in response to hospital overload; and that these two options were to some extent alternatives.
Given our data, the theoretical maximum numbers of correlations, with the sign as predicted, that might be found between measures of competition and of policy outcomes were:
-
provider competition, generically: 1 measure (HHI) × 16 service outcomes = 16 possible correlations
-
population-based competitive bidding: 4 measures × 16 service outcomes = 64 possible correlations.
Ignoring negligibly small ones, 3 of the 16 possible predicted correlations between HHI and the selected service outcomes were found (see Table 24, Appendix 7). HHI correlated as predicted with:
-
amenable mortality rate, all causes, under-75-year-olds, directly standardised
-
monthly mean waiting list, in-patient and day cases, proportionate to weighted population (but this correlation was weak)
-
finished consultant episodes (FCEs) proportionate to weighted population.
Twelve of the other 13 predicted correlations between HHI and the policy-relevant service outcomes were not found. The remaining correlation, between HHI and percentage change in the proportion of all non-admitted patients waiting less than 18 weeks for planned treatment, was in the opposite direction from predicted. The following service outcomes were more strongly associated with a control variable, the PCT Deprivation Index, than with HHI:
-
change in emergency admission for primary care preventable chronic conditions
-
change in emergency admission for primary care preventable acute conditions
-
ratio of observed to expected emergency admissions for conditions not usually requiring hospital admission
-
mean time waited
-
ratio of day cases to admissions
-
average length of stay.
Primary care trust income per capita was more strongly associated with PCT budgetary surplus or deficit than was HHI.
Conceivably, though, gross patterns of association between a generic measure of competition (HHI) and the service outcomes might mask more nuanced associations. We therefore repeated the analysis, replacing HHI in turn with each of the four variables indicating the extent of possible provider competition under population-based commissioning. Of 64 possible correlations, we found four, all with the opposite sign from what the programme theory assumed (see Table 25, Appendix 4). Since the other possible associations were either negligible or absent, it appears that, under population-based commissioning, less concentrated provision of secondary care was not associated with ‘better’ performance on the service outcomes that we considered. Again, control variables (especially deprivation) were more often associated with the service outcomes than were those reflecting the extent of provider competition.
This evidence therefore seems mostly against the assumption that provider competition has helped PCTs realise the service outcomes studied. Advocates of competition might reply that these findings occur because NHS organisations are half-hearted about competition, or because a single provider dominates most local NHS health economies. We therefore repeated the analyses for PCTs with the lowest supply-side market concentration only. For PCTs with the lowest quartile of HHI scores, two more correlations with the predicted sign emerged but the previously found correlation between HHI and FCEs proportionate to weighted population disappeared. Thus 4 of the 16 theoretically possible correlations were as predicted (see Table 27, Appendix 4). The findings suggested that less concentrated hospital provision may be associated with ‘improved’ (reduced) unplanned admissions for conditions sensitive to primary and to ambulatory care; but to complicate matters these patterns probably reflect primary care activity besides hospital competition. We also examined whether the correlation between HHI and waiting lists might reflect PCTs’ use of independent-sector hospitals. For the quartile of PCTs with lowest HHI scores, the correlations between the same service outcome measures and PCT spending on independent-sector providers had the opposite sign from that predicted by the programme theory for mean time waited, for average number of patients waiting more than 4 weeks for a first outpatient appointment (proportionate to weighted population) and for inpatient and day-case waiting list (proportionate to population; see Table 28, Appendix 4). These findings appear to suggest, if anything, that PCTs facing the greatest waiting-list challenges responded by buying independent-sector services. However, PCT spending on independent-sector providers did correlate (with the predicted sign) with the improvement compared with the previous year in:
-
percentages of unplanned hospitalisation for chronic ambulatory care sensitive conditions
-
primary care preventable acute conditions
-
emergency readmissions within 28 days of discharge from hospital
-
admitted patients waiting less than 18 weeks from referral to treatment
-
non-admitted patients.
The findings are also consistent with the hypothesis that PCTs that faced the greatest waiting-list challenges were also those where recently discharged patients and those with primary care preventable conditions were less likely to be admitted to hospital via ED. The contrast between these findings and those regarding HHI reflects the non-correlation between HHI and spending on independent-sector providers (r = –0.0508, p = 0.534). Thus 5 of the 16 possible predicted correlations between spending on independent-sector providers and the service outcome measures were found. Again, the service outcomes studied correlated more often with the controls than with the measures of competition or the use of independent providers.
While the above analyses included the four most obvious possible confounders of the above relationships between provider competition and service outcomes, further research may reveal others. These controversial subjects sometimes provoke objections248 that the researchers selected outcomes likely to produce findings supporting their policy preferences. We minimised that risk by analysing multiple outcomes, and some of the outcome measures we used were sensitive to competition; but since our analysis was limited to published data it remains conceivable that yet further outcomes would be more sensitive to competition. Analyses of the relationships between competition and quality are sensitive to the way market size and London factors are entered into the analysis. 163 The present analysis may corroborate that finding: it defines market size as PCT size and did not adjust for London factors. More important, things may have changed since 2009. For one thing, the policy (in 2009) of regarding NHS trusts as preferred providers was supplanted in 2010 by the Any Willing/Qualified Provider policy. Further research to test whether or not that is so will be required when later data are published.
Our case studies did find some evidence of commissioners using provider contestability as a means of control. Porttown PCT opened negotiations with private nursing companies in case the community health services trust proved unwilling to meet the PCT’s service specification, and decommissioned its wheelchair provider. Metroland commissioners used similar threats to reduce the cost of care packages by 20%. Shire PCT found itself new providers for talking therapies, diagnostics and primary care ophthalmology services. However, Milltown used only the alternative secondary care providers (i.e. the ISTC) imposed on them by higher-level NHS management. Like others,249 we found that provider competition occurred mostly for specific care groups and among small community health service providers, although not, in our study sites, only at their geographical margins.
Existing providers were often the only credible bidder. PCTs had usually (including all our study sites) transferred their community health services en bloc either to the existing, near-monopoly mental health or hospital trust, or to a single dedicated NHS trust or a single social enterprise (Porttown, Surrey). The selection criteria in the London Health Programme’s ‘competition’ for hyper-acute stroke centre contracts included having certain numbers of suitably qualified consultants already available. Pharmacy provision of vascular risk checks was ruled out a priori in Porttown. In Shire the criteria for provider selection included provider experience and relationship with the local health community. Sometimes the third sector also contained only one credible bidder: for Shire memory services, the Alzheimer’s Society.
Metroland and Shire allocated emergency work in certain specialities to one hospital and elective work to another. Whether or not a cartel was intended, there were also volume, hence quality and safety, arguments for concentrating these clinical activities. Shire hospitals, we were told, also had informal agreements about not ‘poaching’ each other’s orthopaedic work. London had 10 mental health trusts but they did not compete. In Milltown, services designated as ‘pilot projects’ were exempt from competitive tendering.
We found two contrasting approaches to competition between NHS trusts and ISTCs. It was more common to make ISTCs subcontractors of an NHS acute trust (Shire, Metroland, Milltown), with Metroland PCT initially requiring two of its NHS hospitals to refer a percentage of patients onwards to a selected ISTC. Porttown, however, set up head-to-head competition between its NHS trust and an ISTC and, as a demonstration of intent to the local hospital trust, used its ISTC contract to the full. Other studies show that some165 but not all246 other PCTs also did this. The prospect of losing income to competitors made NHS trusts negotiate more constructively with their commissioners about service changes, for instance in audiology (Shire), ophthalmology and orthopaedics (Porttown).
Consultants’ conflict of interest over private work, reported nearly 20 years ago,250 was still evident. The Porttown ISTC employed its own consultants. Its manager claimed that, insofar as NHS consultants could, through their links with the referral management scheme, influence what choices GPs offered patients, they encouraged referrals to the other local private hospital, where they practised privately. The manager of the large private hospital in Metroland had
an agreement with the [NHS] trust that if they have a consultant who deliberately seems to be keeping their clinic to a minimum so that it will default to the private sector the trust will ring me so that the consultant doesn’t benefit from this behaviour.
Corporate hospital manager, Metroland
She ‘wanted to nip that problem in the bud’ in order to build a strong relationship with the PCT and not endanger her firm’s reputation for probity. Nevertheless, it was not in her hospital’s commercial interest to help the NHS reduce waiting times to the same as those for private hospitals, because that would be a disincentive for patients to buy health insurance and use private hospitals. Consultants using her hospital had the same incentive and would switch patients to other private hospitals if hers appeared to give NHS patients the same access as private patients. Tariff payments were lower than the premium prices once paid to private hospitals, which risked having to pay any costs above tariff level. Some Metroland GPs formed surgical provider groups, sometimes with consultants as members, and were commissioned by the PCT; a US study suggests that such hospitals stimulate demand for complex procedures. 251 Shire PCT found it harder to ensure uniform pathways across independent-sector providers than across NHS acute trusts. NHS trust clinicians were also under managerial pressure to meet NHS waiting-time targets; corporate providers were not. Private mental health services were mainly provided by the third sector, including a service user group (Metroland) and in Milltown a social enterprise involving leading commissioning GPs.
Attributing impacts to provider competition is not straightforward. After the ISTC opened, ALoS for orthopaedic patients in Porttown fell from eight days to four, the combined effect of competition and extra capacity. After hyper-acute stroke services were established in London, stroke mortality fell by 50% but in this case ‘provider substitution’ meant replacing existing treatments with evidence-based alternatives, not provider competition.
As case studies we selected PCTs both with and without multiple hospitals. Like others147,160 we initially equated multiple providers with ‘possible’ provider competition. Our case study findings undermine that assumption. Citing patient reluctance to travel152,252 and difficulty in influencing GP behaviour, the two case study commissioners (Metroland, Milltown) in large conurbations with many other hospitals nearby did not regard hospital competition as feasible or desirable, Milltown describing itself as ‘landlocked’. Metroland commissioners argued that patients prefer going to their local hospital or mental health service. Shire had three hospitals plus a teaching hospital just over its boundary, but still made the case-load allocations reported above. ‘Possible’ competition was not actual competition. Only Porttown stimulated head-to-head hospital competition, but having no other NHS hospital within or near its boundaries, competition there was between the NHS trust, a small private hospital and the ISTC. Even so, Porttown commissioners felt that they had limited competitive leverage over their local foundation trust:
Commissioning is about a power struggle between clout of PCTs and a hospital that will never close.
General practitioner, Porttown
Juridical controls
The standard DH contracts were used everywhere, but they accommodated local variation and their mandatory contents varied by care group. However, they specified only service volumes, not service design, case mix, clinical pathways or (until late in the study period) feedback of monitoring information. Mostly the same contract framework and terms were used for all providers, except that independent providers were always paid the normal HRG tariff (Shire). Additional local performance requirements reflected any local operating framework, health needs assessment (e.g. in Shire) and local agreements about care pathway changes (Metroland). DH control over contract formulation relaxed towards the end of the study period, putting PCTs in a stronger negotiating position by giving them more negotiating latitude about, say, how the 18-week waiting target would be met (Porttown). Some local authority contracts (e.g. in Shire) were for as long as 25 years, making them difficult to terminate early. At the opposite extreme, Porttown awarded annual contracts, creating uncertainty for providers. Community and mental health service contracts were less complete than hospital contracts. Provider non-compliance was initially dealt with by informal discussion. For instance, when a private diagnostics company in Porttown ignored written notice that it had breached its contractual obligation to obtain PCT approval before directly marketing its services to GPs, the next stage was to involve the PCT board, placing the matter in the public domain with possible adverse media coverage for the provider.
More complete contracts made service provision less flexible. Providers became reluctant to do work (e.g. diagnostic tests in Metroland, laparoscopic hernia repairs in Shire) off contract. CHS providers in Porttown complained that the PCT criticised them for not delivering activities that were not stated in the contract. Commissioners were reluctant to pay for off-contract treatments (even when a consultant had already offered to treat the patient), including novel procedures for which no tariff existed (both in Shire).
Informants readily cited local authority standing orders, EU regulations and DH Cooperation and Competition Panel requirements for competitive tendering. Many believed that the DH contestability framework generally permitted PCT collaboration with one provider.
Care Quality Commission (CQC) investigations could also trigger service reconfigurations independently of local commissioners. A CQC enquiry closed one ED and transferred maternity services to another hospital, irrespective of Metroland PCT’s hospital contracts. Adverse CQC reports compelled Porttown PCT to decommission an inpatient learning disability service. Similarly, Monitor imposed its own requirements on providers irrespective of their contracts with commissioners. In response to a financial crisis, Monitor replaced the entire management team in a Shire hospital, which the PCT took as opportunity to make a fresh start in working with its replacement.
In summary, the reconfiguration of commissioning structures (see Chapter 6) was resulting in the negotiated order between commissioners and providers evolving gradually from a predominantly manager-to-manager regime to one with a greater medical admixture. The discourse used in these negotiations correspondingly became somewhat more medicalised. Medical involvement appeared if anything to reduce the weight that commissioners gave to provider competition. The financial incentive regime changed little, being anyway partly beyond commissioners’ control, and juridical control over providers remained marginal.
Chapter 8 Commissioners’ room for manoeuvre
Policy statements about NHS commissioning, and the underlying programme theory, assumed that commissioners would have room for manoeuvre to adapt their commissioning activity, hence service provision, to local circumstances and health-care needs, and to local GPs’ and patients’ preferences. A subdivision of RQ3 was therefore to ask how wide this room was during 2010–12. Drawing on our case studies and secondary sources, we found that commissioners had limited room for manoeuvre both ‘vertically’ (freedom from central control) and ‘horizontally’ (latitude to innovate, experiment and take risks). 253
Certain limits on commissioners’ room for manoeuvre were practically irremovable for commissioners. Paradoxically, as commissioners in Milltown pointed out, evidence-based medicine was one. During the study period, evidence-based guidance and service specifications were becoming more numerous, comprehensive and specific. However, in return for this constraint, commissioners gained increased transparency of providers’ practice and of the quality, safety and outcomes of the commissioned services. 29,123
Like many researchers,27,160,252,254,255 our study site commissioners assumed that patients would not travel to ‘non-local’ providers. Consequently, and because of the physical concentration of hospital services over many years, most PCTs relied on one hospital for about two-thirds of their secondary care. In our case study sites, secondary mental health and community health services provision were similarly concentrated. Metroland and Milltown commissioners knew that the pattern of their unplanned ED admissions also reflected patients’ proximity to (or distance from) a hospital. These conditions limited a priori the scope for provider competition. As commissioners saw it, they also made it imperative not to destabilise these main providers. Two areas in which provider competition was nevertheless feasible were for low- to medium-complexity planned secondary care (competition between NHS trusts and private hospitals) and for certain types of community care and mental health services, for which small private- and third-sector providers sometimes competed.
Other constraints were theoretically more tractable, but not for commissioners. National policy and guidance rather narrowly defined commissioners’ latitude about what services to commission. As others report,256 mental health commissioning was described as:
driven by national ‘must dos’ so you didn’t need to think about it or interpret it.
Mental health commissioner, Metroland
This has most recently referred to national dementia strategy. National policy and guidance also stated how commissioners should select providers and which providers to consider. Shire hospitals tried to turn this requirement on its head, challenging a decision to tender community dermatology and endoscopy services because they were outside the national mandate for tendering. The tariff system had competition-inhibiting implications for private hospitals. One in Metroland – part of a national chain – found that tariff payments decreased its capacity to offer alternatives to NHS provision because the company knew that its overhead costs were higher than in NHS hospitals. The CQUIN and QOF payment systems allowed commissioners a certain discretion in setting provider incentives, but in practice higher NHS management largely decided what behaviours or targets would be rewarded or penalised. SHAs also directed both commissioners and providers. So far as Metroland was concerned, their main interest seemed to be in securing Foundation Trust (FT) status for the NHS trusts; in Porttown, reducing the main hospital’s deficit. Porttown and Milltown commissioners said they faced inconsistent demands from the SHA, PCT cluster and DH. Shire commissioner managers perceived their chief executive as feeling accountable above all to elected representatives and the DH for the use of public funds, which sometimes justified making decisions that other local organisations might not like. Milltown PCT had experienced public opposition to some of its decisions, but did not change them. However, the medical director of one Shire hospital argued that the other side of this coin was that PCTs shrank from making decisions, for fear of public opinion and of the local MP getting involved.
National cost-control imperatives exacerbated conflicts of interest between commissioners and NHS trusts, which protracted negotiations and micro-commissioning discussions, and constrained the extent to which service provision could be reconfigured or depart from historical funding patterns. Some GPs were uninterested in participating in commissioning and, a greater constraint on commissioning, were not amenable to changing their referral habits, referral screening notwithstanding. The staff turnover and overload reported above also limited commissioners’ room for manoeuvre. In theory there was no obstacle – except the cap on commissioning management costs – to commissioners engaging external expert help in writing service specifications and monitoring providers, but they seldom did.
Nevertheless, our case study data and commissioning practice in the case study sites together suggested that the above conditions left commissioners with room for manoeuvre in:
-
prioritising which care groups to concentrate on
-
allocating any additional money that did become available
-
what commissioning support to use
-
which GPs, consultants and others to involve in commissioning negotiations
-
how to redesign or respecify services through micro-commissioning
-
collecting local evidence about services and their effects
-
bundling tariff payments
-
using the elements of QIPP, QOF and other payments that were at their discretion
-
how they filled out the national contract framework
-
how far beyond the legal requirements they took competitive procurement
-
how far they used contestability or discretionary payments to incentivise providers
-
ways of collaborating with local government and/or GPs on admission-reduction projects.
In sum, commissioners’ vertical room for manoeuvre remained narrow. Their horizontal room for manoeuvre was becoming narrower in some ways (having to accommodate local government and GP requirements) but wider in others (possibility of new providers, development of micro-commissioning).
Chapter 9 Distributed commissioning
During 2010–12 there were three main types of distributed commissioning:
-
for about 15% of contracts,128 one PCT (later, CCG) ‘lead’ commissioner commissioning a provider on behalf of all commissioners whose residents the provider treated
-
joint NHS and local authority commissioning of the same provider(s)
-
‘client-based’ commission, effected through the tariff system and personal budget pilot schemes.
Our findings on these points come from the case studies and (to a lesser extent) the cross-sectional analysis.
The lead commissioner approach
In our study sites the nearest PCT or the one sending most patients to the jointly commissioned provider acted as lead commissioner (Shire, Porttown). This happened:
-
For very small care groups (e.g. certain ophthalmological treatments in Metroland, assisted conception in Shire).
-
In dealing with large teaching hospitals in conurbations. Thus Metroland was an associate commissioner for one of the largest London teaching hospitals (‘it’s a Goliath . . . we are small’) and lead commissioner for a smaller one.
-
For larger but evenly dispersed care groups. Thus Porttown PCT was lead commissioner for orthopaedic work for its ISTC on behalf also of three neighbouring PCTs. Before 2010, London PCTs with the same local acute or mental health provider also commissioned them jointly.
Lead commissioning required the associate commissioners to trust the lead commissioner to uphold their interests. Thus, commissioners sending just a few patients to a third-sector provider did not bother attending monitoring meetings because they trusted Porttown as lead commissioner to uphold their interests. Metroland subscribed to a distributed commissioning arrangement in which the lead role rotated between PCTs. PbR also promoted financial transparency, hence trust, between collaborating commissioners. Porttown and fellow commissioners began sharing information about service redesign. Metroland and its three cocommissioning PCTs produced a common commissioning strategy that led in turn to more standardised models of care (e.g. similar home treatment teams for people with dementia), standardised contracts and cost savings (e.g. through sharing older people’s home treatment teams across two PCTs). Shire resolved its disagreement with a neighbouring PCT about access criteria to assisted conception services.
However, commissioning was sometimes only partly standardised and pooled. Even in Metroland, each partner-commissioner also had separate meetings with the mental and community health service trusts about clinical change, information, finance and performance management. Initially each PCT negotiated service volume and costs independently of the other PCTs. Indeed, the mental health trust asked each PCT to keep the details secret lest other PCTs demand the same. After PCTs were clustered, they became more open with each other about such matters.
When different commissioners’ financial or service requirements were too diverse, lead commissioner arrangements broke down. Metroland PCT discovered that a lead commissioner without financial problems was likely to be more financially generous to providers than its less wealthy associate commissioners wanted. Metroland PCT eventually withdrew from jointly commissioning a cardiac service because it felt it could not influence, and hence could not gain much from, lead commissioner arrangements. Shire PCT disengaged from a lead commissioning arrangement that did not give it sufficient clarity about its financial commitment and risks. Discrepant fees for different PCTs’ patients led Porttown PCT to disaggregate the commissioning of the small but sole available provider of eating disorder services. Other disputes between lead and associate commissioners arose because, reflecting their populations’ different needs, they wanted different methods for approving changes to services and decisions about individual patients’ care pathways. Shire PCT withdrew from a dispersed commissioning arrangement because the lead commissioner had unilaterally decided not to stipulate distinct contract terms for Shire patients.
Detaching from a lead commissioning group at times enabled a commissioner to negotiate better terms. When Metroland began commissioning a large teaching hospital directly, it had to pay more attention to and take a stronger role in negotiating with it, obtaining more favourable terms for managing the financial risks of referrals of severely ill patients. Similarly, by negotiating independently, Shire made more flexible contracts with its providers.
While commissioning power was concentrated by having a single lead commissioner for a specialty or condition, the consequences of the lead commissioner model of distributed commissioning still depended on how convergent the different commissioners’ interests were. When they differed substantially, commissioners responded by reverting to separate commissioning. Otherwise, they responded with more standardised service specifications and contracts, gaining countervailing power in dealing with large, even merged, providers.
Joint local authority–NHS commissioning
In our study sites, joint NHS and local authority commissioning was ‘joined at the top’ (p. 21):257 more collaborative at higher (strategic, planning, governance) levels than at the operational level of dealing with service providers.
NHS and local authority commissioning strategies were often coordinated through reciprocal membership of each other’s working committees. Metroland had borough-wide commissioning groups with local authority members, primary care representatives and one patient representative. There was also a Health and Social Care Liaison group, but its only governance function was to manage Section 75 agreements, so the NHS bodies regarded it as a consultative mechanism. Porttown PCT included a local authority representative in its QIPP monitoring meetings. A psychiatrist from the mental health trust and the CCG’s mental health lead GP contributed to local authority commissioning of mental health services. Local authorities and NHS commissioners consulted quite widely about their joint commissioning objectives. Metroland public health leads made a ‘concordat’ and a Joint Strategic Needs Assessment, focusing on reducing health inequalities, which became the basis of a joint commissioning plan. In Shire a joint commissioning board agreed on collaborative work programmes, including hospital discharge management and preventing orthopaedics admissions, although that did not lead to any concrete commissioning decisions. Shire Health Scrutiny Committee still interpreted its role as approving significant variations in NHS services, so one of the Shire hospitals appealed against the commissioners’ proposals for competitively tendering community dermatology and endoscopy services. A local strategic partnership in Porttown aimed its public health priorities at the most deprived areas with poor health outcomes and at leisure, weight management and smoking cessation. The partners intended this work to inform joint commissioning plans. In practice, though, it had little influence on services to reduce childhood obesity or the licensing of fast food and alcohol outlets, although they did jointly commission stroke services.
At a strategic level, commissioning was more often a joint activity for community and mental health than other services. Metroland, Porttown and Shire were already jointly commissioning mental health services (since 1999 in Shire). Metroland and Shire both used Section 256 funds to help finance local authority re-ablement services and in Metroland falls prevention, re-ablement, home support, crisis intervention and home treatment services. The NHS and local authority jointly revised the corresponding care pathways and cofunded health crisis-intervention teams in Metroland, learning difficulties services and voluntary organisations’ memory adviser services in Shire. Shire social care, community hospitals, rehabilitation services and interface (GPSI) services were jointly commissioned, as was the mental health ‘floating’ support service in Porttown. Shire council also contributed to implementing clinical commissioning programmes for stroke, CHD and diabetes.
Being implemented through separate line-management structures, the operational work of provider negotiations, procurement and monitoring were more distinct, reflecting the differences between NHS and local authority regulatory and accountability regimes, financial and planning cycles, and whether local politicians were directly involved. NHS commissioners had larger budgets (for instance £25M vs. £2M for mental health in Shire), but local authorities had more experience of provider competition, commissioning private providers and involving service users in assessing tenders. The nearer to operational level one came, the greater these differences, hence the difficulty co-ordinating the different commissioners and through them the providers. PCT commissioning in Shire was organised by localities, which were coterminous with those of the local authority, but the intermediate care teams commissioned by either organisation were still resourced differently. Ill-defined boundaries between health and social care for, say, re-ablement (NHS) and rehabilitation (local authority) were reported to create commissioning overlaps and duplication. Thinking that trying to pool budgets would cause long delays in commissioning or changing services, local government and NHS commissioners in Shire chose instead to move towards colocation and then full integration of services. They were jointly developing specifications for integrated services, but had not yet commissioned any when our fieldwork finished. Although Porttown council and PCT agreed about mental health service development, their agreement was not translated into combined (mental health) service delivery teams or shared IT systems. In Metroland, both health and social care commissioners saw their role as keeping people out of hospital, but a lot of the real decision-making occurred at senior level in health and social care commissioners separately, ‘so that’s where things start to come apart’. Measuring health and other service outcomes was a new activity for many local authority staff, who discovered that many relevant outcomes (e.g. quality of life) are complex and hard to measure. Metroland borough therefore used falls outcome measures developed by the NHS commissioning support organisation, and some developed for the DH national outcomes framework, collecting its own data (e.g. on older people’s experiences of care homes) to populate them.
To mitigate these differences, NHS and local authority managers at both commissioner and provider levels set up informal, network-like working arrangements. Metroland managers set up an intermediate care partnership without seeking formal Section 75 status for it. Shire PCT and local authority informally agreed not to divert their budgets to other uses without consulting each other.
Nevertheless, points of friction between local authority and NHS managers remained, impeding joint commissioning.
-
Differences in priorities reflected the different accountabilities of NHS managers and local government managers, and, still more, councillors:Local authority manager, Metroland
[T]he big difference is in culture between the NHS and its way of working and local council and its way of working . . . the members of the council are elected members and . . . the NHS is a very different way of working. And, I think there’s going to be, you know, lots of work, as we go forwards, around that culture because it’s just the culture changes will need to happen.
Metroland council found shifting from health-care scrutiny to commissioning partnership a big cultural change. Porttown informants reported deep-rooted differences between elected councillors’, PCT managers’ and CCG members’ priorities, so that joint commissioning requirements could not be agreed, nor joint action taken. TCS and QIPP had made NHS–local authority relationships more ‘spiky’ (GP, Porttown). Different local authority and NHS managerial cultures were also reported in Shire. There especially, the local authority was service provider as well as commissioner, which our NHS informants saw as a conflict of interest.
-
Reconfiguration of NHS commissioners meant that they were no longer coterminous with local authorities. Metroland and Milltown CCGs were coterminous with a borough, but the central support organisation (for commissioners) for Metroland covered eight boroughs, which our informants feared might be hard to reconcile with the council’s wish to focus on local needs and services. When the shadow Shire CCG replaced locality-based PECs, it was coterminous with the county council instead of with several second-tier local authorities. Porttown PCT became part of a CCG locality coterminous with several councils, not just the city council.
-
One party to an agreement unilaterally changed commissioning arrangements and/or services. In Porttown the council established a single point of entry to mental health services, onto which the PCT could not easily map its service-commissioning methods. Metroland borough unilaterally cut £250,000 from mental health contract funding, leaving the PCT to pay for services that the PCT considered should be local authority funded. The PCT’s quick response to news of proposed local authority budget changes pre-empted similar unilateral reductions in Shire.
-
Clinicians were sceptical about whether or not local authorities would commission better services than themselves. For this reason, Porttown GPs were reluctant to publish a tender for mental health services, believing it would precipitate a city council ‘takeover’. The mental health trust was equally sceptical, but still thought it had a better working relationship with the council than with the CCG. In Shire the PCT, local authorities and clinicians had wide-ranging disagreements about strategy, priorities, service specifications and commissioning intentions for mental health services.
-
There were divergent interests and priorities for secondary care, for instance over priorities for disinvesting from inpatient services in Porttown.
The transferred public health activities and staff were the least connected. In Metroland, the role of the public health department was described as primarily strategic, delegating the implementation of its plans to others (disappointing the local authority’s initial hopes that public health staff transferred to it would have implementation experience or expertise), in contrast to Porttown, where the city council delegated the commissioning of drug services to its new public health department. In Shire, a still more silo-like relationship persisted, with public health apparently operating almost (but not completely) in isolation. During our fieldwork Health and Well-Being Boards were still being set up and did not ‘go live’ until late in the study period.
Distributed commissioning involved a negotiated order between commissioners, supplementing the other negotiated orders reported in Chapters 6 and 8. In theory, collaborating commissioners disposed of stronger financial incentives and greater ability to exploit provider competition, but they did not make obviously greater use of either than non-collaborating commissioners did. In joint local authority–NHS commissioning, differences in the discourses that the two kinds of commissioner used in dealing with providers were also apparent. Juridical controls remained marginal.
Client-based commissioning
We defined ‘client-based commissioning’ as specifying and paying for services on the basis of each episode of care for each individual patient (tariff payments, personal health budgets). Chapter 7 reports our main findings about tariff payments in England during 2010–12. As an initial exploration of whether or not service outcomes were associated with provider competition under client-based commissioning rather than population-based commissioning, we repeated the cross-sectional analysis, testing for associations between our 16 available policy outcome data sets and the three indicators showing the extent of provider competition in terms of client-based commissioning. Of the 48 predicted possible correlations only 1 was found (see Table 26, Appendix 4). The presence of a personal budget pilot scheme was associated with an increase in patients being treated within the 18-week target, but the association was weak. Otherwise the associations had the wrong sign, or were negligible or absent. Once again, the control variables were more often, and in this case also more strongly, associated with the service outcomes studied.
Chapter 10 Providers’ responses
Our case studies suggested that, in ascending order of difficulty that they posed for commissioners, providers’ responses to commissioners’ proposals during 2010–12 ranged from negotiated agreement, through inability to respond, to unwillingness, even resistance.
Negotiated agreement
NHS trusts’ responses to commissioners’ demands were never exclusively protectionist. They sometimes made alternative proposals for achieving results that the commissioners also wanted or, at least, were compatible with the commissioner’s priorities. Shire and Metroland hospitals were content to divert patients away provided the necessary alternative community and (social) care was available. Discussions at Metroland solved the problem of how to treat mental health patients who turned up at the ED in the absence of a 24/7 mental health service. Clearly specified, ‘micro-commissioned’ care pathways and common clinical interests were often enough to make providers respond constructively to commissioners’ proposals, especially if additional payment was also available.
Providers’ ability to respond
Even when provider managers agreed with a commissioner about what should be done, they might still be unable to implement their side of the bargain, for instance if consultants were unenthusiastic. In practice, pathway changes and bed reductions could not be made without clinician involvement. Shire hospital informants in particular explained that the hospitals’ ‘corporate’ view was that of the senior managers and consultants who dealt with the PCT, not necessarily that of other hospital staff. Repetitive discussions in Porttown care pathway groups led PCT representatives to doubt if the commissioners’ proposals were ‘getting back to’ hospital consultants (commissioning manager, Porttown). Consultants’ traditional autonomy from management worked against such involvement. In one Shire hospital especially, the consultants had customarily had a free rein to the extent of agreeing activity changes with the PCT without senior management approval. Milltown consultants took legal advice about who was responsible for the safety of patients triaged away from the ED, until their medical director persuaded them that this was a non-problem. In Porttown community services, consultants, psychologists and psychotherapists were reported to be very powerful, and managerial leadership weak, to the extent of its chief executive asking the PCT’s negotiator:
how he could bring about transformation in his organisation, which didn’t inspire hope in me I have to say.
Commissioning manager, Porttown
In a Metroland hospital, distrust between hospital managers and consultants had reached the point where a consultant believed:
Just about the time I started here, or just before, they shut the consultant common room because they were concerned that the consultants were using it to meet and plan the downfall of the executive, literally, at least that’s the story . . . you know, the agendas of consultants are not always the same as those of an executive board.
Surgeon, Metroland
Consultants were consulted about commissioning activity and ‘what we are required to deliver’ (hospital manager, Metroland), but not about curtailing or cutting services.
We found no evidence that NHS trust managers responded to other trusts, commissioners or private providers predominantly by developing competitive strategies, even when (as in Porttown and Shire) they knew that national policy favoured competition and there were ISTCs nearby. Rather, as indicated above, they tended towards more collusive, negotiative strategies (often with tacit commissioner endorsement) to circumvent competition.
Providers’ willingness to respond
A minor though common irritant to providers was commissioners’ demands for detailed information, which providers thought was clinically uninformative, ill chosen or not used once provided. When these requests became vexatious, one of the Shire hospitals merely ignored them. Provider-side informants sometimes interpreted the ideology of a ‘purchaser–provider split’ as endorsing their separation and independence from commissioners. Metroland trusts, we were told, had historically been quite inwardly focused and saw little need to engage with commissioner requirements. Personality clashes [such as the ‘massively adversarial’ relationship between commissioner and hospital chief executives in Porttown (GP, Porttown)] were another exacerbation.
When providers disagreed with commissioner suggestions for restructuring service provision, one response was to make incompatible counterproposals, as has been found elsewhere. 258 A Shire hospital proposed discarding services that it did not want to provide (surgery in community hospitals), protecting existing services (e.g. endoscopy) against provision by alternative providers (GPs in this case) and expanding other services. Especially when commissioner budgets were tight, some commissioner demands were simply not in the provider’s interest:
We call them efficiencies and to some extent they are but they are also service cuts, there’s no two ways about that, and it’s then you go from collaboration to confrontation.
Commissioning manager, Metroland
Shire commissioners were aware that they faced strong providers whose interests lay in maximising income and whose culture was that they, not commissioners, should determine service provision. Even after the medical director and consultants in one Shire hospital had agreed to reduce their high rates of cardiology intervention, hospital managers stopped them because of the financial implications. In Metroland, private care providers sought higher profit levels than the local authority was prepared to fund. Despite engaging in micro-commissioning, some providers (e.g. in Porttown) complained of being unable to influence commissioners. Indeed, the action research participants reported initial resistance by the providers to closer working between community and secondary care services.
When conflicts of interests became palpable, providers might, first, try to force the commissioners’ hand. As reported above, Metroland hospital reneged on its agreement to reduce its case load by 20%, knowing that PbR and AQP rules obliged commissioners to meet the costs anyway. This hospital also made unilateral changes to services (e.g. rapid-access nurse-led pain clinics, arrhythmia clinics) and then expected the commissioner’s post facto endorsement and funding. The main Porttown hospital unilaterally reconfigured stroke services to seek better integration with other providers. The smallest of three Shire hospitals threatened to withdraw its ED service, forcing the PCT to negotiate with another hospital to transfer the service there. Another hospital unilaterally informed the PCT that it would cease doing spinal treatments (it was the sole provider), forcing the PCT to retender the work. A third established a foot surgery department that increased its activity, even though another Shire hospital offered cheaper bio-mechanical alternatives. When Shire PCT could not afford to pay for additional patients to receive non-surgical treatment for prostate cancer, the provider obtained charitable funding and continued the service that way. Such tactics did not always succeed, however. A Metroland consultant raised money to build a cardiac catheter laboratory, but the commissioners refused to meet the running costs.
Arbitration between commissioners and providers rarely took place through any juridical process, although Milltown had agreed formal procedures for negotiating and resolving disputes. More often hospitals in Shire, Porttown and Metroland attempted to go over commissioners’ heads by asking the SHA to overturn agreements with the commissioner. The SHA could impose its preferred solution because it could sack both the provider and the commissioner chief executives if they did not implement it. Similar patterns are reported elsewhere. 39 At times SHA interventions weakened the commissioner’s bargaining position, for instance by imposing on the commissioner – but not providers – a deadline for agreeing contracts.
[Porttown] hospital has always won partly because the SHA undermined the PCT by covertly subsidising [the hospital]’s poor financial problem.
General practitioner, Porttown
However, another SHA refused to do that for the main Metroland hospital.
The commonest response on either side, though, was inertia: the often-reported phenomenon of seemingly endless, unproductive negotiations, even when much joint effort had been put into developing service plans, for example when it was proposed to cut services or change CQUIN payments (Metroland). As an extreme case, the only tangible outcomes of 10 years’ negotiation about ED services in Shire were a patient leaflet explaining the different purposes of EDs and GPs, and training care home staff not to telephone 999 but to use other providers. Especially if there were funding implications (e.g. when setting up an urgent care centre in Metroland), a negotiated agreement often had to be referred back to higher managers on either side, who might not endorse it. NHS providers were not necessarily enthusiastic about acting as autonomous public firms. 253 Corporate providers also had their moments of inertia (e.g. when Metroland PCT tried to renegotiate better terms and when Porttown tried to improve private hospital compliance with the 18-week wait target). Their culture of separation from NHS commissioners naturally ran deeper than in NHS trusts.
In a situation of mutual dependence, a commissioner with only one provider to hand might alternatively capitulate. Thus, Metroland PCT was forced to renegotiate its unrealisable admissions plans partway through the financial year. In the face of consultant opposition, Shire PCT turned down the GP initiatives mentioned above, which, a GP told us, was typical of the PCT’s tendency to placate and prioritise secondary care interests. Falling short of capitulation, Milltown commissioners developed a practice of trying to understand, rather than simply blame, providers whose actions or decisions caused problems for the commissioner. Indeed, a powerful, financially secure hospital trust could come to see its main commissioner as barely relevant to its own plans for strategic and service development.
Making providers more helpful
Providers’ responsiveness to commissioners thus reflected the presence or absence, and depth, of any conflicts of interests between the two. Providers often responded passively, but commissioners could sometimes rouse them into helpfulness by threatening loss of resources (possibly to a competitor) or a third party’s intervention. Porttown PCT had difficulty persuading a local hospital to provide wet age-related macular degeneration treatment as an outpatient service until it threatened to commission an independent provider. The same PCT discovered that, when the mental health trust felt that it might be about to lose resources or services, it became more willing to listen to the commissioner. In Milltown too, the threat of withdrawing the mental health trust’s psychology and rehabilitation service contracts triggered more constructive negotiations and micro-commissioning. More subtly, the Milltown commissioner hinted that, if the community health service specification were ‘refreshed’ in the ways the commissioner wanted, there would be no need to retender the service. In Shire audiology and mental health services, the threat of losing services (hence income) to other providers made the existing providers’ negotiators become more helpful. The availability of a competing provider was one way to make the threat of losing funds credible, but not the only way (see Chapter 7, section Provider competition). The absence of any existing vested interest also gave the commissioner a free hand, for instance when remodelling eating disorders and other non-psychotic mental health-care pathways in Porttown.
Soft coercion took the form of claiming that the SHA would intervene – to everyone’s detriment – if no agreement were reached: a credible threat, as explained above. Shire and Porttown PCTs both argued that the SHA would reduce budgets if QIPP targets were not reached. National financial targets were used as an argument to persuade the Porttown hospital to change its activities. In Milltown the lead GP commissioner represented herself as a ‘buffer’ between GPs and city-level commissioners, representing her own ideas as a lesser evil than what the city-level commissioners might otherwise do.
Our informants did not dwell upon the potential conflict of interest between GPs as commissioners and GPs as providers, although national media and the professional press raised this issue at intervals. Our GP informants who did mention it (e.g. in Metroland) perceived it in terms not of conflict of interest, but of opportunities for general practice entrepreneurship in developing primary care and substituting for secondary care, with little sense of any possible juridical or political implications.
Chapter 11 Commissioning for specific care groups
Services for many care groups were commissioned together in the rather generic ways described above. RQ4, concerning commissioning for specific care groups, turned out (our case studies suggested) to have only a limited empirical application. During 2010–12 only mental health had specialised commissioners and commissioning, in our study sites as elsewhere. Public health was commissioned with a very light touch, if that.
Planned orthopaedics
For many of the more common orthopaedic procedures, measures and outcome indicators were relatively well defined and standardised, as were diagnostic criteria, care pathways, treatment methods and expected outcomes (although not, we were told, for every treatment, e.g. shoulder surgery). Our informants reported using PROMs data (mandatory), the National Hip Fracture Database (except Metroland), ALoS data (NHS Information Centre secondary uses service) and some generic measures applicable to orthopaedics (e.g. the Patient Environment Appraisal Tool) to compare providers’ activity, spending and performance and, in Shire, to assess the risks of reducing orthopaedic surgery provision in order to identify contract priorities. Metroland PCT also monitored hospital infection rates, but reportedly did not react to them. Shire PCT collected GPs’ reports of patients’ reactions to orthopaedic care, including patients who subsequently regretted having had ineffective surgery, with a view to introducing physiotherapy-based advisory services for patients contemplating orthopaedic surgery. For orthopaedics:
[Y]ou can absolutely quantify every stage of that, know what it’s going to be and for 96.4% of the time that will be exactly what happens and then the rest of it there’ll be a few complications.
Commissioning manager, Porttown
Because planned orthopaedic treatments were mostly rather ‘commodified’ it was relatively easy to establish criteria for appropriate referrals and to screen GP referrals accordingly, as Shire, Metroland and Porttown did, in effect making a single point of entry to planned orthopaedic services. Commodification also facilitated the substitution of one provider for another. Indeed, a corporate hospital in Metroland was for a time the PCT’s second largest orthopaedics provider. The predictable costs of much orthopaedic surgery, its high volume and a sufficiently generous tariff meant that:
elective orthopaedics is a money spinner.
Hospital manager, Shire
This applied both for NHS trusts’ ISTCs and for other for-profit providers over a long period. 250 Porttown fully used its orthopaedics contract with its ISTC to give the commissioner (and only incidentally GPs or patients) a choice of provider. Similarly, Shire PCT commissioned three corporate hospitals to do (mainly) joint replacement so that it could stop paying local NHS trusts extra each spring and summer to catch up with the orthopaedic work they had cancelled during the winter. In Metroland, though, both the private hospital and the ISTC were the subcontractors of local NHS trusts, not of the PCT or CCG (see Chapter 7, section Provider competition). However, corporate providers tended to treat only the less complex patients [American Society of Anesthetists classification 1 (ASA 1) to the stable end of ASA 3 comorbidity groups] in Porttown and Metroland. While some Shire NHS trust managers would also have preferred to concentrate on these patients, the consultants favoured a broader, more complex and varied case load.
Commissioners did renegotiate care pathway redesign for orthopaedics, but micro-commissioning had neither the centrality – compared with competition and financial incentives – nor the depth of work found with two other care groups (mental health and recurrent unplanned admissions). Commissioners thus controlled providers of ‘commodified’ planned orthopaedic surgery mainly by a combination of discursive control (evidence-based medicine) and provider competition.
Recurrent unplanned admissions
Commissioners’ efforts to reduce unplanned hospital admissions were impeded by a lack of knowledge of the categories and causes of these admissions. Shire and Porttown commissioners felt unable to predict even the direction of change, let alone number, of unplanned admissions in the coming year. Hospital informants in both sites stated that the underfunding of community services hindered them from discharging unscheduled patients, but PCT funds were mostly committed to hospital services. Shire GPs also perceived community services to be insufficient and so for safety referred older people who fell to an ED. In general, hospital services were commissioned per speciality or group of specialities; no one had dedicated overall commissioning responsibility for people prone to recurrent unplanned admissions.
Competition was of slight use to commissioners for influencing how providers managed this care group. If they required orthopaedic surgery, Metroland patients with long-term conditions and comorbidities were for safety unlikely to be referred to private providers, who merely took the less complex cases. The need to co-ordinate care pathways across multiple organisations was also, our informants thought, hard to reconcile with provider competition. Micro-commissioning was required. Thus the local authority and the mental health trust collaboratively commissioned re-ablement services (Porttown, Metroland, Shire), the Stroke Association to provide postdischarge care, home treatment for end-of-life care (Porttown), case management, carer’s services, intermediate care beds (Metroland) and GP triage of patients entering EDs (Shire, Porttown). In doing so, Shire reduced the number of re-ablement service providers from around 100 to 10. It also supplemented the contract of one local NHS hospital to pay for clearing the discharge backlog. However, both commissioner (in Metroland) and hospital informants (in Shire) claimed that they had difficulty dedicating sufficient time to the laborious tasks of redesigning care pathways for patients at risk of frequent unplanned readmission, especially if case management was envisaged (Shire). Each side recognised the value of such work and each argued that someone else should do it. In Livewell that someone else was a US HMO, engaged by the PCT (under pressure from general practices), which with those general practices comprehensively redesigned services for this care group, building in risk assessment and telephone support services. 238 Learning set members, however, emphasised that these integrative activities were not as routine as they ought to be, because of such impasses as the hospital asking the PCT to identify which patients to divert to community care, and to which services, but the PCT being unable to do so. Metroland PCT did not set targets for hospital discharge or providing services to prevent readmissions. Shire clinicians felt that the psychologists, CPNs and social workers were not much involved with the commissioners’ attempts to reduce unplanned admissions, so those attempts had little effect on working practice.
Prevention of coronary heart disease and diabetes
Coronary heart disease and diabetes prevention concerned two main types of activity and therefore provider. One was activity aimed at changing individuals’ consumption and behaviour patterns, addressing at-risk populations not in their capacity as patients (which most of them were not) but in terms of ‘lifestyle’, as consumers or residents. The other was clinical prevention, addressing at-risk individuals in their capacity as patients, whether undergoing routine health checks (e.g. under the national health checks programme), being treated for CHD and/or diabetes, or being treated for some other condition, and as necessary either treating the patient in general practice or referring the patient on to ‘lifestyle’ (e.g. smoking cessation) or other clinical services.
The commissioning of service providers was an activity ill adapted for stimulating primary prevention259 through ‘New Public Health’ methods – changing lifestyles and consumption patterns or regulating the production, promotion and sale of food etc. 260 – for CHD and diabetes as for many other preventable conditions.
[W]hen you do a needs assessment, this happens especially [with inter-]sector and other partners, they automatically think that you are going to commission a service and sometimes it’s not always about commissioning a service as such because if you’re looking at population health, you know, it might not be it.
Public health doctor, Metroland
One public health informant asserted that commissioning for ‘lifestyle prevention’ is simply not possible, whether through the Local Enhanced Services scheme or in any other way. Commissioners did not discuss long-term prevention much.
Because preventative services would not deliver immediate savings (e.g. within 3 years) they were not a high priority for commissioners, who thought that more pressing tasks such as tackling unplanned admissions had to be handled before moving ‘upstream’ to commission preventative activities. For lack of resources, few ‘lifestyle service’ providers were commissioned, although mechanisms such as the local enhanced services (LESs) provided ways to incentivise providers who did so. Indeed, the Porttown commissioner chief executive rejected public health proposals for the primary prevention of diabetes. Accordingly, public health staff there concentrated on trying to persuade the city council to be stricter in licensing fast food and alcohol retailers, and on carrying out health impact assessments for the council. Shire’s stroke and diabetes networks did succeed in commissioning exercise groups at sports centres, but the financial crisis led the PCT to withdraw finance for a diabetes-prevention pilot. These conditions might partly explain the reports that public health worked somewhat separately, a phenomenon reported beyond our study sites. 261
Secondary prevention, and prevention through clinical activity, was commissioned much as any other primary care clinical intervention, for instance through QOF incentives and LES incentive payments, as others have also reported. 259 Through its GP-owned social enterprise, Porttown PCT provided GPs with access to electrocardiograph machines and a toolkit to assist in vascular risk assessment, although the vascular checks petered out when the pilot project ceased. It also commissioned a small-scale project through which CHS nurses ran CHD and diabetes-prevention clinics in a deprived part of the city. Shire’s public health department set up a hub where GPs could send patients with mild diabetes or CHD for prescribed exercise or weight-loss services. A clinical commissioning project piloted the introduction of an intermediate diabetic care nurse and audited the clinical outcomes. The commissioners agreed to monitor hospitals on (among other measures) diabetics’ blood pressure and body mass index.
Mental health
Mental health service commissioners in our study all faced one near-monopoly NHS mental health trust absorbing above 60% (in Milltown, Metroland and Shire, 80%) of the mental health budgets alongside numerous niche providers, often local authority funded. (Metroland had at least 50, besides contracts for specialist tertiary services.) These small providers included voluntary and charitable providers, churches, counsellors and patient self-help groups, private care homes and domiciliary care. GPs and social services also provided substantial inputs (e.g. older people’s and learning difficulty care homes, day centres, domiciliary re-ablement).
Four media of commissioner power were noticeably weak in mental health care. One was discursive control. Mental health commissioners had only a small evidence base on which to draw. A few well-defined outcome indicators were available (e.g. return to activities of daily life), but our informants generally averred that outcomes were opaque and hard to measure, as well as difficult to relate to national policy, and monitoring data were usually incomplete. As for emic discourse, there were cultural differences between local authority and NHS models of the nature of mental health care and its intended outcomes, reflecting the different professional training and cultures of social workers and clinicians. Porttown, Metroland and Shire informants contrasted the recovery model (on the NHS side) that promotes patients’ active involvement in their treatment and tailoring services to the episodic nature of long-term mental problems versus a social model (on the social work side) offering indefinite low-key support (e.g. housing and employment) to maintain client independence. The medical director of psychiatry in Metroland complained that the social work ethos had gained ascendency, which ‘infuriates’ health workers and ‘disenfranchises’ clinicians. Second, the financial incentives were predominantly mainly block (on the health side) and per diem payments (for some local authority-funded services). The small-scale contracts stipulated patient volume, but seldom costings or performance measures. Against that, it was possible to discuss patient-level events in detail with small providers, which led to problem identification and solving. Monitoring of the large provider relied more on ‘generalisation and anecdote’ (commissioner, Porttown).
Mental health commissioners in all case study sites foresaw difficulties in using tariffs for mental health services, but also that tariffs would provide greater openness and clarity about provider activity and costs. The only scope for competition was among the small non-statutory providers, although Shire had opened negotiations with Mind and Rethink. Even among the smaller providers, though, Metroland PCT had never decommissioned an entire provider except for when a few temporary fixed-term contracts expired. PCTs’ limited tendering capacity and their aim to integrate health and social care were further disincentives to promoting competition.
Mental health care often required the assembly of co-ordinated care pathways across multiple providers, hence micro-commissioning and emic discursive control over providers. Micro-commissioning networks were relatively stable. Users’ voice was often more evident in these networks than in the commissioning of acute care, but users’ input did not necessarily translate into influence over budgets, the commissioners or the main provider. Mental health service commissioners in our study sites were more likely than their acute commissioner counterparts to include (besides managers) former service providers with social work, nursing or mental health provider backgrounds (Shire, Porttown, Metroland). Action learning participants, especially a GP commissioner, argued that too many psychiatrists spent their time medicating patients who do not get better. Consequently patients with drug and alcohol problems did not get access to psychological therapies.
The IAPT programme was an important exception to these patterns. IAPT contracts stipulated outcomes and limited access to services to a fixed number of contacts (20 in Porttown), giving a fixed end-point at which to evaluate treatment outcome. 262 Mental health commissioners in Shire and Porttown perceived in IAPT an evidence-based, outcome-oriented approach to commissioning services that might be adapted for dementia and personality disorder services too. Milltown commissioners also commented that it was
unprecedented . . . quite a sophisticated minimum data set.
Mental health commissioner, Milltown
The IAPT was thus a prototype for extending commodified commissioning further into mental health.
Technical contrasts
Table 8 summarises the empirical contrasts in NHS commissioning practice between these care groups.
| Medium of commissioner power | Care group | |||
|---|---|---|---|---|
| Medium of commissioner power | Mental health | Planned orthopaedic surgery | CHD/diabetes prevention | Older people, recurrent unplanned admissions |
| Management performance | Service specification and monitoring limited and problematic. IAPT a prototype alternative approach | Standardised outcome measures and care processes stipulated | Commissioning largely irrelevant to intersectoral primary prevention. Otherwise, as for primary care generally | Utilisation patterns poorly understood, making contract specification difficult |
| Negotiated order | Micro-commissioning of care pathways in depth, multiple providers and commissioners | Slight: focus on post-discharge care | ‘Horizontal’ negotiation with local government and other interest groups. Some interdisciplinary projects | Micro-commissioning, often at individual patient level (case management) |
| Discursive control | Weak: little evidence (except IAPT) and different NHS and social work models of care | Etic: evidence-based practice and outcome measures | Etic: evidence-based practice and outcome measures | Emic: emphasis on shared targets and cost-control imperatives |
| Financial incentives | Mainly block payments (cost control) but tariffs being introduced | Per-case payments, harnessing provider profit motive | As for primary care generally, but vulnerable to budget cuts | Block contracts with ad hoc supplements |
| Provider competition | Sometimes when dealing with small, third-sector niche providers; otherwise marginal | Applied for high-volume, low- and medium-complexity case loads | Marginal | Marginal |
| Juridical control | Marginal | Marginal | Marginal | Marginal |
These contrasts reflect technical differences across five dimensions between services for these care groups:
-
how far the commissioning of service providers is relevant at all (cf. primary prevention)
-
extent of the available evidence base
-
whether the episode of care and its outcomes are discrete and well defined
-
case mix homogeneity, hence, with (2) and (3), ‘commodification’
-
complexity of provision (number of providers simultaneously involved with one patient), hence the number of commissioners.
Provider responses to commissioners (cf. Chapter 10) also varied by care group. GPs responded to commissioners trying to strengthen clinical preventative services insofar as the services could be financed through LES, and above all the QOF, payment systems, but were otherwise not responsive. Few attempts were made to commission providers of intersectoral health promotion activity, so we had little opportunity to observe how they reacted. Providers of planned orthopaedic surgery responded more as the programme theory of NHS commissioning assumed, readily expanding case-loads when commissioners demanded, often competing with each other. In contrast, mental health providers tended to respond with renewed, or adapted, and collaborative micro-commissioning activity.
Chapter 12 Commissioning practice and health system context
Research question 4 asked what factors, including the local health system context, appear to influence commissioning practice and the relationships between commissioners and providers. Comparisons between NHS commissioning and its counterparts in other health systems indicate which commissioning practices and problems recur across health systems, hence may stem from the structure of quasi-markets per se, and which stem from the particular English NHS context in 2010–12. Insofar as they face similar problems to those of NHS commissioners, other health systems’ solutions or workarounds offer possible practical ‘lessons’, in the sense of empirical proofs of concept, for NHS commissioning practice. Descriptions of the German and Italian health systems are available elsewhere. 263,264 Below, we briefly note the mode of commissioning in each, and then, for each medium of power, possible lessons for NHS commissioning.
Germany
In Germany, the main health-care commissioners were SHIs (‘sick-funds’, Krankenkassen) and Land (provincial) governments. Eighty-seven per cent of the population were SHI members (2012), the remainder privately insured or self-payers. A separate SHI system finances long-term care. 265,266 Hospital ownership is diverse (public hospitals had 49% of beds in 2008, corporate hospitals 15% and charitable hospitals 36%). Acute care is paid for through DRG tariffs. In future, mental health care will be too. Land governments planned the allocation of hospital beds and largely financed the corresponding infrastructure. Patients can self-refer to any ‘ambulatory’ doctor, that is a generalist family doctor or non-hospital specialist. Ambulatory doctors were commissioned by dividing a cash-limited budget according to the points that each doctor earned, with different numbers of points for different medical acts. Reforms in 2004 required SHIs to promote a gatekeeping role for GPs to reduce direct access to specialist services, but in 2007 a survey (O’Shea L. The German Health System. London: Nuffield Trust [unpublished briefing paper]; 2010) showed that 44% of Germans saw two or more specialists in the last year (UK 19%). Cost control is a long-standing national policy. Table 9 summarises the mode of commissioning in the German system.
| Medium of power | Form under case mix commissioning |
|---|---|
| Managerial performance | Case mix modelling + audit + subscriber marketing |
| Negotiated order | Rhineland model (consensus and multistakeholder model) + episode based |
| Discursive control | Emic: solidarity + juridical rights |
| Etic (evidential): case mix data | |
| Financial incentives | Fixed tariffs |
| Provider competition | None that commissioners can harness: referral ‘framing’ at most |
| Juridical | Comprehensive regulation + administrative law |
Managerial performance, negotiated order and juridical controls were the dominant media of power. 267
Management of commissioning
German commissioning practice shows how powerful and sophisticated the monitoring aspect of managerial performance can become. Data were collected in real time. SHIs audited, confirmed and made payments continuously, collecting from hospital bills and medical records data about what activity was being paid for. Such data enabled one SHI, reputedly the most developed in this respect, to make routinely such analyses as volumes of hip-replacement revisions per provider, evaluations of disease-management programme costs and outcomes for diabetes, and analyses of case mix distributions and trends for any geographical level, any provider(s) and any DRG. Each SHI knew its own data for hospital case mix and compared them with the publicly available national figures, interrogating apparent inconsistencies between the two. The Medizinische Dienst der Krankenkassen (MDK), run jointly by the SHIs, routinely reviewed patient case notes in order to verify if the coding and therefore payment were appropriate given the clinical facts, but did not review the effectiveness of care.
Hospital activity was nevertheless far from transparent to German SHIs or patients. 265 German hospital managers told us that when negotiating with commissioners they aggregated data and income data into large blocks:
Why did you decide that?
To make in all one negotiation about the DRGs and one for nursing care for children. And it’s less transparent to the SHIs. . . . We have an orthopaedic department in [hospital 1] and one at [hospital 2], and the SHIs could see from our data, our Excel tables, we have done this here but more there . . . if we handle matters at a large scale we don’t have to discuss these things with the SHI.
Hospital staff also tended to dislike the Medical Review Board and its members.
Lessons for NHS commissioners concern the availability and analysis of performance activity data. DRG adoption alone is insufficient. NHS commissioners’ performance management, cost control and planning roles might be strengthened by having rights of access to provider data but German practice also suggested that gaining the modelling and monitoring benefits of a tariff system requires data warehouses and specialised staff, centralised at the level of some millions of patients, and an extensive IT infrastructure. These specialised functions may be more effectively and cheaply undertaken at regional or subregional level (e.g. by commissioning support units) than at CCG level. However, greater transparency and the resulting commissioner interventions appear, on German evidence, at times to strain relationships between commissioners and providers.
Negotiated order: the Rhineland model
The German health system contains nested negotiated orders at national, Land and provider levels. Annual negotiations involving all main national interest groups (federal associations of SHIs, doctors and dentists, hospitals and patient organisations), co-ordinated by the Gemeinsame Bundesausschuss and with the state as arbiter, agree the broad framework of health service planning and guidelines for quality of care. This ‘Rhine’ or ‘Ordoliberal’ approach was deeply rooted in German political culture. 268 Although binding, these decisions were consensual. Consequently, doctors and SHIs could block changes. For instance, the Association of Ambulatory Physicians vetoed other doctors doing out-of-hospital surgical procedures. Similar negotiations establish a Land bed plan based on predicted needs for hospital services, make regional adjustments to DRG payments, and agree the points tariffs by which ambulatory care doctors are paid.
At provider level, the main currency of commissioning negotiations between SHIs and German hospitals was the number and case mix of episodes and, for ambulatory care doctors, medical acts. To launch the annual contract negotiations, German SHIs sent each hospital spreadsheets of DRG targets. The proposed case mix implied an overall number of DRG points, hence an implied budget. It was possible to reduce, even remove, groups of cases by reallocation within the total number of points, but the system did not so readily allow an overall reduction in case load, case mix or budget. National SHI federations, SHI national offices and local health-manager networks advised and updated SHI negotiators about the commissioning climate and local issues, but the hospitals had better data about their own case mix and internal costs than the SHIs did. The Land plan framed the ensuing commissioner–provider negotiations by defining each hospital’s bed numbers, overall case load, case mix and, in effect, ceiling for SHI-funded activity. Negotiations focused on the hospital’s DRG points allocation, its case mix and the nationally defined growth margin rather than clinical quality. Payment for new treatments not yet in the DRG system and for discretionary services were also negotiated. Assuming that some degree of planning of the overall profile of health-care provision is desirable, the German DRG system instantiated a concrete, detailed way of modelling and managing hospital activity, case mix and revenue costs, although it might be argued that deciding DRG volumes within the constraints of a Land bed plan puts the infrastructural cart before the epidemiological horse of health-care needs.
For NHS commissioning, German experience seems to confirm that a consequence of making DRGs the commissioning currency is to focus commissioners’ negotiations on service volume, case mix and cost rather than on service quality, which commissioners therefore need to manage through another mechanism. Giving hospitals the right to reimbursement for whatever patients they could attract tied the German commissioners’ hands when negotiating with providers. SHIs strengthened their hand by negotiating jointly with providers, and negotiating with each provider separately.
Discursive control
German informants mentioned emic discourses used in commissioning management and negotiations. They tended to refer to the different parties’ rights and obligations under the nationally negotiated agreements and regulations. These arguments cut both ways. When SHIs claimed to represent patients’ interests, the hospitals replied that they – and SHIs – were equally obliged to ensure that patients could get the services that they (patients) chose. Apart from having to work within the Land bed plan, considerations of public accountability did not appear to figure much. Neither did EBM, and still less in primary than secondary care. 269 Provided they stuck to treatments authorised under the Land plan, law and regulations, German hospitals’ treatment methods were beyond SHI scrutiny. The place of EBM was more at national level. When the GB-A decided which new therapies, devices, pharmaceuticals or models of care to include in the DRG tariff, it used above all evidence about effectiveness from the Institut für Qualität und Wirtschaftlichkeit in Gesundheitswesen.
An implication for NHS commissioners appears to be that a shared framework of norms is what makes discursive control possible. The norms do not necessarily have to be technical ones. Neither does the norm of ‘complying with health policy’ have to be defined any single way (e.g. compliance with a negotiated settlement vs. compliance with the latest government pronouncement). What matters is that commissioners and providers share the same norms.
Incentives
Diagnosis-related group-based payments gave hospitals a financial incentive to increase activity,270 whereas the SHIs wished to avoid patient numbers, hence costs, spiralling out of control. Only a few treatments (e.g. short-term nursing care at home) required SHI consent to pay. Otherwise, the DRG tariff system left German commissioners little discretion for using financial incentives to renegotiate provider behaviour locally. As a workaround, SHIs negotiated with hospitals a ‘corridor’ (Flur) for the main groups of DRGs, agreeing an expected level of activity for each, what rebates the SHI would receive should the volume or case mix fall below that range and the payment for justified additional work above it. Since 1998, German SHIs have offered selective contracts, restricting subscribers’ choice of providers in return for lower subscriptions, but many patients assumed that only providers with difficulty attracting patients accepted such contracts.
Neither did the tariff system directly reward providers for improving the clinical quality of care (as opposed to attracting more patients). SHIs had discretion to pay providers for new and off-tariff treatments, but otherwise were obliged to pay for all acute hospital treatment irrespective of quality. Complex and long-term care presented different problems. For chronic care, the SHIs paid a per diem Pflegekost (care cost) and will from 2013 have the option to do the same for some psychiatric services, instead of making cost-plus payments as hitherto. Some experimental integrated care projects constructed interorganisational care pathways linking primary and secondary providers for certain patient groups, but these required specially negotiated contracts because DRGs were available not for network-based care provision, but only for paying single providers. For ambulatory care, the points tariff also had to be modified to accommodate disease-management programmes, that is preventative case management and continuous care for certain chronic conditions (e.g. diabetes, COPD). Some 14,000 such schemes existed but only about 5.5% of people were enrolled in them. Integrated care and disease-management programmes represented only 1% of health-care spending. The benefits appeared to be improved care, at least for diabetics,269 rather than cost savings.
These problems and workarounds have parallels in England. German SHIs independently invented what NHS commissioners call ‘cap-and-collar’ agreements, and independently discovered that the construction of cross-organisational (‘integrated’) care pathways requires substantial modifications to tariff payment systems. A hidden limitation of a tariff system is the requirement for a separate, parallel system for undertaking the commissioning function of managing clinical quality in care providers, raising transaction costs in consequence. It is possible to define DRGs in terms of clinical procedures but this negates a theoretical advantage of DRGs: that providers are paid per episode of care (ideally, by outcome), remaining free to introduce innovative clinical procedures.
Provider competition
Except for selective and integrated care contracts, German commissioners could not choose their providers. Only the Land government could select or deselect hospitals as providers, by including them in the bed plan or not. For ambulatory care doctors and dentists, not even this mechanism was available. The German equivalent of an AQP policy prevented commissioners from using selection (competition) of providers as a means of controlling them, despite – indeed, because of – patient choice of provider.
Hospital capacity was 5.66 acute beds per 1000 population (2010), reflecting German health care’s greater orientation towards secondary rather than primary medical care and community health services, and ‘a hospital on every hill’. In the west, Germany also had a tradition of religious foundations providing hospital care, especially small local hospitals. Corporate providers were also entering the hospital market. That appeared, on German experience, to promote market concentration and centralisation on the provider side, with firms such as Aesculapias developing a strong national organisation to counter those of the SHIs. [Competition between SHIs also produced concentration on the commissioner side of the quasi-market (TK data, 2010), as in the Netherlands. 271] Nevertheless, public- and third-sector hospitals were no less – perhaps more – efficient than private ones. 272,273 Attempts to control the health system by regulation and tariffs pushed provider competition into the marginal ‘windows’274 not foreclosed by regulation, tariff or policy fiat. When competing providers are entitled to payment once patients have chosen them, commissioners’ control over provider costs is weakened from a budgetary cash-limited system into one that, at most, contains care costs within ‘corridors’.
If NHS commissioners are to harness provider competition as a medium of governance, German SHIs’ experience suggests that commissioners need scope to deselect providers, for instance from providing services for specific care groups. Long-term provider competition may become self-weakening as providers merge or fail in the face of competition, which suggests that commissioners would need to be continually searching for possible new providers and (insofar as they can influence such events) default towards taking a critical view of proposed provider mergers. Comparing German and UK experience suggested that the possibility of provider redundancy, hence excess provider capacity, may be required to sharpen provider competition. That would appear to confront commissioners with having to decide whether to control costs through provider competition or by reducing the numbers of providers.
Juridical controls
German commissioning relied on nationally standardised regulations, contracts and legal entitlements, clearly specified decision-making processes and participants in them, and allocations of decision-making powers among particular institutions. The range and number of services offered, and remuneration rates, were stipulated at national level for all SHIs. 263 German SHIs’ obligations to patients were legally prescribed. In disputed cases a first step was to seek an independent opinion from MDK about the medical necessity of the treatment in question, followed by appeal to the Schiedstelle (administrative court) and then to the civil courts, but even Schiedstelle cases were infrequent (maybe one or two a year for the largest hospitals) and expensive (€7000 or more per case). The hospitals won perhaps 80% of these cases. A lesson for NHS commissioners was that, even in the juridically oriented German system, judicial remedies were for commissioners and providers alike costly, unpredictable instruments of last resort, used only exceptionally. Most important, regulations intended to maximise provider diversity and competition for patients removed provider competition as a medium of commissioner power. 267
Italy
Lombardy health policy context
Like its English counterpart, the Lombardy region of the INHS had a quasi-market structure, a mixture of public, third-sector and corporate secondary-care providers, between which commissioners were legally required to ensure fair competition. Public hospitals were semi-autonomous ‘private firms’ (AOs). All organisations wishing to provide publicly funded health care had to pass a four-stage accreditation process, whose last stage was the award of a contract. Local HAs (ASLs) commissioned services for populations of similar size to those of English PCTs, although unlike English CCGs they controlled only 2% of the budget for ambulatory and diagnostic care. The regional authority, a branch of the regional government, commissioned both social care and the rest of health care. It had considerable discretion over what kind of quasi-market structures to establish. It could, for instance, vary the national DRG tariffs and take ‘make-or-buy’ decisions. All region authorities directly managed some hospitals, although Lombardy retained only one (Table 10).
| Model | % | Regions |
|---|---|---|
| Integrated | > 66 | Veneto, Aosta Valley, Trentino Alto Adige, Abruzzi, Molise and Sardinia |
| Mixed, quasi-integrated | 40 < n < 66 | Liguria, Umbria, Marche, Basilicata, Calabria, Piedmont, Emilia Romagna, Tuscany and Puglia |
| Mixed, quasi-separated | 20 < n < 40 | Friuli, Lazio, Campania and Sicily |
| Separated model | < 1 | Lombardy |
Of the media of commissioner power over providers, discursive (ideological) control predominated, followed by negotiated order and the managerial (above all, regional) performance of commissioning. Incentives and provider competition were less important, juridical controls least of all (Table 11).
| Medium of power | Form under surrogate planning (Lombardy) |
|---|---|
| Managerial performance | Programme planning + patient-level care management programmes (pilots only) |
| Negotiated order | Local managerial problem-solving networks |
| Discursive control | Doctrine of subsidiarity + evidence-based protocols |
| Financial incentives | Tariff + per diem + ad hoc payments |
| Provider competition | Limited scope for commissioners to harness + referral ‘framing’ at the margins |
| Juridical | Dual legal and managerial contracts |
Elements of population-based commissioning coexisted with client-based commissioning (DRG tariffs), but the former, undertaken mainly at regional level, predominated. More like the UK than Germany, a range of community health services and intermediate care providers existed.
Managerial performance
Commissioners planned their local health economy. Every January the regional authority set overall inpatient case mix and numbers for each ASL, and the range, level and volume of non-tariff payments (FNTs; see below). Each ASL then made a territorial plan and negotiated contracts with its accredited ‘preferred providers’, chosen on a value-for-money basis. The ASL agreed admission levels with each provider and the contract duration. Providers had two kinds of contract. One, with juridical status, was awarded as the last stage of the accreditation process. It stated the main rules and quality standards with which the provider must comply. An annual operational contract fixed the provider’s budget and activity level for that year, but had no legal status. Both contracts were managed at ASL level, although the regional DGs oversaw the whole process, allocated resources and actually licensed the providers. Comparing the roles of local commissioners (ASL in Lombardy, PCT or CCG in England) and regional organisations made the Lombardy INHS appear more centralised than the English NHS; but it was the reverse at national level. 277 Compared with the English NHS, the strength of this highly vertical system was its control over providers and its homogeneous way of gathering information and data, which has been described (p. 209)276 as a ‘quasi-administered’ system.
Nevertheless we found at regional level a considerable fragmentation of management, a ‘silo’ approach coupled with a lack of information sharing and of transparency in decision-making. In Lombardy, health services commissioning remained divided from that of social services, at both regional and ASL levels. Indeed, the so-called integrated care for frail people with health and social care needs was commissioned by the family DG, even though the regional health fund financed these services. Within each ASL, the social care department (attività socio sanitarie integrate) and its director were responsible to the ASL general director for the key strategic policies, but still maintained a good deal of autonomy, networking with different institutional stakeholders such as the municipalities, social services, schools and other local actors. Other local (ASL) commissioning staff had limited discretion but when they tried to exercise it they were often admonished by the regional DGs. Primary care was an exception due to the social capital on which it called and its different territorial characteristics, which let commissioners collaborate more actively with providers.
Providers’ contracts stipulated external audits of services and peer reviews of service quality. (Each Emilia Romagna hospital also had an advisory committee, which included patient representatives and often conducted user surveys.) Commissioners appeared to consider monitoring by means of administrative data management too laborious and inefficacious as a means of quality control in Lombardy, although inspection of medical records was used in Emilia Romagna. However, monitoring data were not necessarily converted into information through which commissioners could exercise governance over providers:
of course we have all the data and whenever we do something we perfectly know who will be influenced by that intervention and the expected results. . . . We conduct a lot of survey and data analysis, . . . surveys and tables for the national accounting court . . . but no documents and scientific studies have been made. . . . Research of course could be done. But there is also a point of the political willingness and interest in doing that: to open the data and information as well as a clear interest in confronting with other realities.
Director-General, regional government
Health technology assessments and evidence-based protocols were applied, but not systematically and very little by commissioners at ASL level.
For English NHS commissioners, one lesson appears to be that interdisciplinary rather than uniprofessional organisational structures are more conducive to an integrated approach to service commissioning. More striking, though, is the proof of concept of the feasibility of regionally managed commissioning by organisations with the latitude to select providers and set contract duration. To overcome the information asymmetry between providers and commissioners, and to make the health system more transparent to the public, required the political will on the part of the commissioners and the higher-level bodies which oversee them.
Negotiated order
Unlike their NHS equivalents, most senior commissioning managers in Lombardy (and Emilia Romagna) had occupied the same role for 10 years or more. Long-term stability, investment in training commissioners and long-standing relationships with providers gave commissioners a deep knowledge of the regional health system, its development and commissioning mechanisms. These relationships and the trust which had accumulated were an important medium of commissioner influence over providers, especially the AOs but also private providers. Commissioners’ relationships with providers have been described as more like a ‘compact’ than a ‘contract’ (p. 3). 278 In both Lombardy and Emilia Romagna, disagreements between commissioners and providers were usually resolved negotiatively and, in Lombardy, tended to concern quite focused activities and services. It was a way in which clinicians participated in commissioning. (In Emilia Romagna, few people other than clinicians participated.) Most commissioning negotiations were about adjusting recent historical patterns of provision. Nevertheless, there was also an informal vertical hierarchy in decision-making about commissioning, with the regional DGs and directors-general for health and for social care services at its apex. The other important interest group (in both regions) was the GPs’ trade union, which negotiated GPs’ contracts at both national and regional levels.
For NHS commissioners, the Lombardy and Emilia Romagna cases suggest that frequent changes in commissioning personnel may be counterproductive for commissioners’ exercise of ‘relational’ governance over providers. The Italian examples also indicate the practicality of giving clinicians (medical managers) a substantial role on either side in commissioning negotiations.
Discursive control
This negotiated order partly rested, too, on shared ideologies. Because programme planning, resource allocation and therefore commissioning were mainly driven by political decisions, they had an ideological substrate and a disciplinary force over the professionals and managers involved. A regional school for public managers, and training programmes for health-care managers and professionals, helped foster common disciplinary and ideological norms across the regional health system. A key, distinctive shared belief was the idea of subsidiarity, expressed by many theories (e.g. the New Public Management, the so-called Third Way, the new public governance). 279 In Lombardy it shaped a unique view of government, focused not on the division of powers among different layers of government (‘vertical subsidiarity’) but on ‘horizontal’ subsidiarity, conceived as a sort of division of labour between the public sector and civil society. It reinforced the ‘knightly’ public service ethos, (p. 195)280 which interviewees expressed more strongly than provider or professional interests. In Emilia Romagna, in contrast, the Alma-Ata declaration281 was a chief reference point. These (emic) principles appeared more pervasive and influential than evidence-based (etic) discourse.
As with Germany, a lesson for NHS commissioners appears to be that what makes governance by discursive means possible is not so much how the norms are formulated – whether as policy or technical norms – but the fact that commissioners and providers share the same norms.
Financial incentives
Lombardy commissioners’ only lever of control through DRG tariffs was by negotiating a production ceiling in the providers’ contracts. For ambulatory and diagnostic services, a provider was guaranteed 95% of the previous year’s expenditure and case load. For activity from 97% to 103%, the tariff was cut by 30%; from 103% to 106%, it was cut by 60%; and above that the tariff was zero. This arrangement incentivised providers to achieve the 106% level, to grow the next year’s starting budget level. As cost-control pressures increased, ‘ceiling budgets’ were introduced into provider contracts, enforced by tariff caps should service use exceed the planned budget. Neither would the regional authority reimburse providers for treatments not included in its annual plan. In these ways the Lombardy commissioners contained costs by (in effect) constructing a hybrid of cost-and-volume (below the 106% level) and block contracts (above 106%).
In response to other limitations in the tariff system, commissioners kept some services outside it, financing them as ‘functions with no tariff’ (funzioni non tariffate, FNTs). This was partly because tariffs could not be introduced for all services at once. Outpatient, diagnostic and some highly specialised clinical services were still paid for through cost-plus fees for service. Rehabilitation, residential services, domiciliary services and long-term care were still paid for per diem. For other services (A&E, dialysis, foetal and neonatal pathology), commissioners considered payment by DRG undesirable because they believed it would restrict access. Neither was it practicable to finance teaching and research through tariffs. FNTs had also been used to support private and non-profit hospitals that could not access other public funds for their activities, and indeed public hospitals that had exceeded their budgets. However, as cost pressures increased, extra-budgetary payments were gradually reduced. Other exceptions to the tariff system included integrated care management; ASLs would assess each patient’s needs, decide the necessary treatment plan and give the patient a payment voucher to cover the cost. From 2012 the regional DGs paid a variable premium (adjustment) of ± 2% of the budget to providers according to the provider’s performance against certain quality standards. The local ASLs also allocated 2% of each provider’s previous year’s income for activities of its choice.
Lombardy commissioners also adopted programmes to ‘nudge’ patient choice to reduce cross-boundary patient flows, especially for highly specialised services (e.g. neurosurgery), because the Lombardy commissioners would have to pay the regions receiving these patients. (Cross-boundary flow was also an issue in Emilia Romagna.) For example, Mantova ASL, on the border of the Emilia Romagna and Veneto regions, introduced training schemes to encourage GPs to meet their patients’ diagnostic and specialised ambulatory care needs within the region, and created an incentive for hospitals to hire specialists to treat such patients.
In the fact that commissioners in Lombardy independently invented something similar, NHS commissioners may find some endorsement of their own ‘cap-and-collar’ modifications to the HRG system. The experience of commissioning in Lombardy suggests further modifications: retention of pre-DRG payment systems and the application of non-DRG payments to stimulate provider compliance with clinical quality standards, the development of interorganisational care pathways, and provision of specialist treatments within the region.
Provider competition
Until the banking crisis, the system of paying providers for up to 106% of last year’s case load was largely used to foster provider competition. One consequence was that the proportion of small providers fell, partly through mergers. Private providers’ market share increased, partly because of public–private partnership schemes which involved contracting out the operational management, and temporarily the property, of nine AO hospitals, and a network of specialised services and departments, especially for diagnostics and rehabilitation. Private providers concentrated mainly on long-term care, less clinically risky and more lucrative than acute care,276 although provider competition impeded the construction of stroke networks. 282 Since 2002, competition has decreased. Because new provider entry had saturated the supply of hospital beds, both regionally and nationally, a regional decree closed the publicly funded health system to new providers. Fixed tariffs limited the scope for price competition, production ceilings the scope for competition on quality. Consequently the competitive incentives for hospitals, and after 2007 also for diagnostic and laboratory services, to improve services weakened. However, patients’ choice of provider could still slightly change a provider’s share of the INHS quasi-market, and still played a role in rewarding provider quality and the providers’ reputation. Domiciliary care provision was more competitive, but, since the reform of assistenza domiciliare integrata (integrated home care) services was still in a pilot phase, it remains to be seen if that situation will continue. In general, though, provider competition was sacrificed and tariffs ‘bundled’ in the interests of cost control, and to a lesser extent planning. 283,284 This experience and the consequent trade-off decisions appear relevant to NHS commissioning too.
Juridical controls
Through regional law, regulations and decrees, juridical control was pervasive, extending to defining the roles of different types of manager,285 the annually planned workloads and the overall lines of health system development. A major challenge for the Lombardy regional health system was the permanent conflict of competencies and roles between the regional health general directorates and the ASLs, which in practice had only a limited role in actively programming, purchasing and controlling the health services allotted to them. There was no regulatory authority for competition comparable with the UK Office of Fair Trading. Nevertheless, tight financial and juridical regulation left commissioners and providers little margin for autonomy and discretion on either side, defined a clear division of labour between them, and created a joint commitment to avoiding conflicts. Conflicts between providers and commissioners were usually settled informally, either by direct negotiation, or, if still unresolved, by the regional DG, but without any mediation. Doctors in management roles in some providers maintained direct relationships with regional DGs, going over the heads of their ASL. Exceptionally, disputes were taken to the ordinary courts, but the costs were high and procedures time-consuming and, from the commissioners’ standpoint, of little consequence because any remedy or sanction imposed on the provider was usually administrative. The courts seldom withdrew a provider’s accreditation. At most, decrees supplied part of the normative framework through which commissioners might exercise discursive influence over providers.
Although comprehensive juridical powers were available to commissioners, they were used sparingly, commissioners being costly, unpredictable instruments of last resort. The same lesson for NHS commissioners emerges as from the German case.
Factors influencing commissioning practice
Comparing the case studies of Germany and Italy with those in England, certain patterns recur, suggesting that these patterns reflect not local peculiarities of commissioning practice but common characteristics of the different media of governance across the three health systems and, on the basis of that evidence, corresponding lessons for NHS commissioning.
To overcome the information asymmetry between providers and commissioners requires both suitable resources (as the German case suggests) and (as the Lombardy case suggests) political will on the part of the commissioners and of the higher-level bodies to which commissioners are accountable. In all cases the negotiated order between commissioners and providers was coloured at local level by the micro-political relationships between organisations and among individuals, and by the history of past commissioning practice. Negotiations between commissioners and providers required a common discourse. Evidence about clinical practices and models (etic discourse) was one such discourse, although the extent of its use, which organisations most used it, and how, varied considerably across the three health systems. The content of shared emic discourses also varied considerably, reflecting the wider political cultures in which the three health systems were embedded: obedience to ‘policy’ dominated emic discourse in the English NHS; a solidaristic consensus on health policy and regulations generated by the ‘Rhineland’-style political institutions in Germany; and an ideology of subsidiarity in Lombardy. What the three situations had in common, though, was that the shared discourse enabled commissioners to appeal during negotiations to normative assumptions that the providers shared and that moderated the expression and pursuit of the particular interests of an organisation or profession.
In all three countries, DRG tariff payments gave providers strong incentives to gain income by expanding their activity. Whether or not they expanded competitively, at other providers’ expense, seemed to be a secondary question (especially in England and Italy; less so in Germany). This incentive, however, conflicted with cost-control pressures, already present in England and Italy, and emerging in Germany. Commissioners in all three systems – and Poland286 and the USA287 – reacted similarly by bundling tariff payments to weaken tariffs’ expansionary incentive effects on providers and to place an eventual cash limit on commissioner spending. Insofar as tariff payment systems are equated (simplistically, to be sure) with ‘competition’, commissioning practice in all three countries has involved sacrificing ‘competition’ to cost control. 276 In all three systems, a ‘pure’ tariff system tended to weaken commissioners’ control over providers, especially (but not only) by weakening commissioners’ power to select providers. Commissioners in all three health systems also supplemented tariff payments with separate incentives for maintaining clinical quality standards. To promote the ‘integration’ of care for complex and/or chronic conditions across multiple providers, commissioners in all three systems tried to introduce some form of micro-commissioning, although there was less scope for it in Germany and Italy than in England. In all three countries, public- and third-sector providers participated in micro-commissioning but corporate providers hardly at all in England (with the important exception of the US HMO in Livewell).
All three systems had organisationally diverse health-care providers. Irrespective of different modes of commissioning, state-owned tertiary providers tended to concentrate on complex and hard-to-treat (e.g. multiple) conditions. The third sector also provided especially for hard-to-treat conditions, but mostly in community settings (primary and social care). Corporate providers specialised in profitable care, typically high-volume non-urgent acute care, but also some more complex, high-cost acute care (e.g. heart surgery in Germany; complex diagnostics in Italy). However, because for-profit providers preferred lucrative, unproblematic services, they were less likely than public or third-sector providers to be providing services exposed to the causes of conflict noted above, despite their in-built motivation to expand their profits, hence market share, and despite their objectives differing most from commissioners’ objectives.
Commissioning practice always combined different media of commissioner power over providers. That reflects a certain hybridisation of the three systems studied, where Bismarckian elements (above all, tariff systems) coexisted with more Beveridge-like elements (attempts to maintain public accountability and implement regional or national health policy). Managerial performance and negotiated order were important everywhere, but thereafter the relative importance of ideology, financial incentives and competition varied. An elaborated negotiated order was an important, and for commissioners a helpful, part of commissioning practice, but it was not always easily reconciled with provider competition. Similarly, the transparency of providers’ activities and costs helped commissioners exercise control, but was not always reconcilable with provider profit seeking and competition. The dominant mode of commissioning reflected certain quasi-market structures: who owned the commissioners; what kinds of provider (in terms of ownership) were present; the rules for provider entry and exit; and how much discretion the legal and regulatory framework gave commissioners.
Chapter 13 Conclusions
Summary empirical findings
Next we summarise our empirical findings, answering each research question in turn and stating the evidential basis of our answer. Briefly, three parallel strategies to governance coexisted in commissioning practice: a strategy based on trust and relationality; a more incisive, less trustful strategy (willingness to challenge, even replace, providers); and making ad hoc workarounds and modifications to quasi-market structures. After stating what limitations and qualifications apply to the findings, we draw some more enduring, general conclusions.
How do English health policy-makers and NHS commissioners understand the policy aims of commissioning, and how can governance over providers be exercised through commissioning?
Policy-makers’ and managers’ accounts, and the discourse analysis of policy documents (Chapter 5), suggested that the explicit aims in pursuit of which commissioners exercise governance over providers were generally agreed, few and broad. They were to:
-
raise the quality of both primary and secondary care
-
integrate primary health and social care services more fully, especially before and after hospital episodes
-
remove ineffective activities
-
replace secondary with primary care, insofar as is feasible
-
enable patient choice of providers
-
improve clinical outcomes
-
reduce costs of care
-
make GPs (as providers) responsible for the financial consequences of their referral and other treatment decisions (what is called responsibilisation288)
-
increase NHS organisations’ accountability to the public.
Policy-makers assumed that commissioners would exercise governance over providers mainly through the media of managerial performance (rewriting service specifications and service contracts; exploiting new IT to monitor providers’ performance); selecting (or deselecting) providers; discursive control (research and evidence dissemination, disciplinary control over primary care); negotiated orders between NHS commissioners, local and service providers; and financial incentives and competition among and between GPs, other primary care providers and hospitals.
Although they agreed on the broad principles, different informants foresaw a different balance between practice-level and whole-CCG-scale commissioning. They placed different weights on patient choice, including choice of GP (emphasised by parliamentarians) and the AQP policy. National policy-makers, especially parliamentarians, emphasised making GPs financially responsible for their own referral and other treatment decisions. NHS informants paid this, and provider bail-outs, less attention. Some NHS commissioners gave themselves wide interpretive latitude, especially about provider competition and the division of commissioning labour between GPs, NHS managers and local authorities.
From mainly interview-based data at four sites and cross-sectional data analysis, our emerging findings suggested the levels of support or challenge shown in Table 12 for the prior policy assumptions about commissioning. Appendix 10 explains the right-hand column entries more fully.
| Programme theory assumption | Evidence |
|---|---|
| PT1: Central government’s decisions and actions lead NHS Commissioning Board, NICE, etc. to set regulations and guidelines which reflect ministers’ priorities | Beyond remit of this study |
| PT2: Through joint commissioning with local government, commissioners will understand care group and population health needs | Some public health input into service specifications, though limited, but this input was especially in Shire |
| PT3: NHS England’s management and GPs’ knowledge of patient needs together allow and stimulate GP commissioners to link clinical and financial decisions | Existing commissioners tend to deal separately with financial and clinical aspects of services |
| PT4: General practitioners’ commissioning role will lead CCGs to review primary care quality | Weak corroboration |
| PT5: General practitioners’ commissioning role and joint commissioning with local government will lead to stronger integration of primary health and social care services (before and after hospital episodes) | Weak corroboration |
| PT6: General practitioners’ commissioning decisions, reviews of primary care quality and stronger partnership working with social care will bring about reconfiguration of primary care pathways, removing ineffective activities | Micro-commissioning focused more on care pathway redesign than removing ineffective activity |
| PT7: The reshaping of primary care pathways and the development of new IT (online consultations etc.) together result in primary replacing secondary care to some extent | Being attempted through micro-commissioning but IT is marginal. The main reported obstacles are lack of services and of GP clinical skills |
| PT8: General practitioners’ commissioning decisions, the outcomes framework, the presence of alternative providers and patients’ choice of providers (in particular of GPs) together stimulate and enable GPs to exercise greater influence over other providers | GP influence exercised more through a negotiated order than competitive (choice) mechanism. Threat of loss of resources (e.g. to alternative providers) did make providers negotiate more constructively |
| PT9: Increased GP influence over other providers and the substitution of primary for secondary care together improve clinical outcomes | Too early to say yet |
| PT10: Increased GP influence over other providers, GPs’ focus on quality and the substitution of primary for secondary care together improve quality of care | Too early to say yet |
| PT11: Increased GP influence over other providers and the substitution of primary for secondary care together reduce costs of care | Commissioners were containing care costs, but by creating DRG/HRG ‘bundles’ and negotiation rather than substitution |
| PT12: Ministerial decisions lead NICE to produce the specific outcomes framework | Corroborated |
| PT13: The outcomes framework and IT developments result in patients, commissioners and providers themselves having information by which to compare providers’ performance, and in patients and commissioners selecting (and deselecting) providers | Comparison occurred, but commissioners seldom deselected providers. Little evidence yet that patients’ choice much influenced provider performance or sustainability |
| PT14: The outcomes framework, information for patients, provider plurality and (later) personal budgets lead patients and commissioners to choose between (and deselect) providers | As above |
| PT15: Commissioners and patients choosing between health-care providers causes the latter to improve clinical outcomes | As above |
| PT16: Commissioners and patients choosing between health-care providers causes the latter to improve quality of care | As above |
| PT17: Patients choosing between health-care providers causes the latter to reduce the cost of care | Not patient choice but commissioners’ de facto reintroduction of cash-limited block contracts and referral screening were the cost-reduction mechanisms |
| PT18: Research and evidence production causes health-care providers to improve clinical outcomes | Too soon to say. Evidence production continues, but the mechanism for its impact on providers may be as much through NICE, CLAHRCs and professional networks as through commissioning |
| PT19: Patient involvement in care decisions causes health-care providers to improve clinical outcomes | Beyond remit of this study |
| PT20: Public health activity causes health-care providers to improve clinical outcomes | No commissioning linkages between public health activity and provider clinical activities found (except public health input into contract specifications). Commissioning system partly irrelevant to primary prevention |
| PT21: Refusing ‘bail-outs’ causes health-care providers to reduce costs | This event not observed |
| PT22: General practitioner and local government joint commissioning causes health-care providers to reduce costs | Micro-commissioning led to service reconfigurations, cost implications not known |
| PT23: Patient involvement in care decisions causes health-care providers to reduce costs | Beyond remit of this study |
| PT24: Research and evidence cause health-care providers to reduce costs | Beyond remit of this project |
| PT25: The availability of information by which to compare providers’ – and by implication commissioners’ – performance increases NHS organisations’ accountability to the public | Appeared more true of providers (about whose activities more information is available) than commissioners |
Since CCG commissioning was still being established during this study (2010–12), NHS commissioning practice may yet converge more closely upon the programme theory underlying NHS commissioning policy. That said, insofar as the programme theory rests on invalid assumptions, it will be hard to implement and not necessarily have the intended results. The assumptions least consistent with the available evidence are those likely to have the most challenging practical implications for commissioning practice, considered below (section Emerging and adaptive commissioning: practical implications).
In our four case studies we found evidence that the financial and the ‘real’ side (service volume, quality, case mix and outcome) were often decoupled in hospital contract negotiations. Senior managers tended to conduct financial negotiations with little medical participation, under pressure to meet financial targets stemming from national policy, in advance of discussions of care group or population needs. It remains to be seen if matters change as CCGs become more established, but during 2010–12 we found little evidence in our four case studies to support the assumption that management by NHS England and GPs’ knowledge of patient needs will together stimulate GP commissioners to link clinical and financial decisions. Regarding provider competition, a minority of their service outcomes (including some proxy clinical outcomes) improved where multiple hospitals coexisted, although more did not. Our case study commissioners (and other providers) did indeed compare providers against national and regional benchmarks for clinical outcomes and quality, but seldom deselected providers for that (or any other) reason. Our interview evidence suggested that provider competition appeared not to be a strong explanation of those patterns. Insofar as patient choice affected provider performance or sustainability, it was through the medium of tariff payments. Insofar as the overall costs of care are concerned, the evidence from all three countries suggests that this form of patient choice raises, not reduces, the cost of health care. Qualitative evidence from the three countries also suggested that patient choice based on tariff payments undermines commissioners’ capacity to choose providers, whether to improve clinical outcomes or for any other reason. In the four English case study sites, commissioners influenced providers (including fellow GPs) more through a negotiated order and discussions about evidence than through competitive mechanisms, including patient choice. A threat to remove resources (e.g. to alternative providers) made providers more inclined to negotiate constructively with commissioners, but providers were not always willing and/or able to respond to GP (or other) commissioners’ demands.
We consider the practical implications in section Emerging and adaptive commissioning: practical implications below.
How did the reconfiguration of commissioning structures occur in practice and what shapes this reconfiguration?
The four case studies suggested that the factors most shaping CCG formation were GPs’ willingness to participate and the availability of those GPs who were willing. Staff turnover due to restructuring exacerbated overload among commissioners. Where GPs had previously participated in commissioning, CCGs were formed by recycling former PCT and PEC structures and memberships. Elsewhere, individual GP enthusiasts were more relied upon: in our London site, from the polysystem especially. The balance between ‘usual suspect’ and ‘new enthusiast’ GPs in the emerging CCG leaderships depended on which of these two tendencies predominated, and on the quality of earlier relationships between the former PCT or PEC and other GPs. Continuity in GP leadership tended to promote continuity in commissioning activities and priorities. Other GPs were drawn into commissioning incrementally as opportunities arose. The more slowly GP participation grew, the more work and influence remained with non-GP commissioning staff, who were more likely than GPs to favour forming a large CCG; make cost saving a commissioning priority; and not necessarily focus attention on the care groups that most concerned GPs. The more often PCTs had been restructured, the weaker the relationality between commissioners and doctors (both GPs and consultants). The extent and tenor of commissioning discussions between GPs and consultants depended on how far consultants were willing to participate constructively, which varied according to accidents of personality and local NHS history. The more diverse the organisations that were combined (or, for dispersed commissioning, that collaborated), the harder it was for coherent priorities and activities to emerge, the slower they did so and the harder the organisation of commissioning was to reconfigure. Analogous factors applied to the development of joint commissioning with local authorities. In the short term these factors seemed to promote continuity rather than radical breaks in commissioning activities and priorities. Paradoxically, stable commissioning organisation structures (both staffing and learnt commissioning practices) and stable relationships between commissioners and other local organisations made it easier and quicker, in our four case study sites, to establish CCGs and the negotiated order through which CCGs would operate.
How far does current (2010–12) commissioning practice allow commissioners to exercise governance over their local NHS health economies?
Commissioners across our four English case study sites employed all six media of power identified in Chapter 2 (section Media of power). Appendix 11 shows how the different kinds of commissioner that we studied used and combined different media of power.
Management performance: NHS commissioners in our case study sites were in a weak position vis-à-vis providers insofar as they lacked technical expertise for specifying services and interpreting monitoring information, and depended on providers to supply it. In contrast, the German SHI we studied could analyse and model extensive collections of tariff data in depth. Italian ASLs were in an intermediate position.
Negotiated order: Our case study NHS commissioners exercised governance through a negotiated order based partly on contract negotiations, but also heavily dependent on micro-commissioning. Negotiations were often protracted and inconclusive when commissioner and provider interests differed. Then especially, commissioning was often a laborious, uncertain process. By dealing directly with each other, GPs and consultants could sometimes solve practical problems of care co-ordination.
Discursive control: Commissioning agendas were dominated by national policy, evidence-based guidance and a shared culture of loyalty to the local NHS. This pattern emerged both from the local case studies and the policy-maker interviews.
Incentives: Commissioners could influence NHS trusts, our four case studies suggested, by proposing to add or remove resources, competition having an effect largely by making the threat of removal more credible. The cross-country comparison (and published studies) suggested that, despite strengthening service monitoring, tariff payment systems weakened commissioners’ ability to control the volume or costs of care. Commissioners in England, Germany and Italy alike responded by bundling tariff payments.
Competition: Mostly our study site commissioners neither promoted nor greatly exploited provider competition. They were unwilling to destabilise local NHS trusts, whether they depended on one large provider or (e.g. in Shire) several. The same phenomenon was reported in Italy. Across England, our cross-sectional analysis never found above a third of the expected associations between measures of competition and the relevant policy outcomes, and those found were often weaker than the association with contextual variables. Compared with Germany (but less so with Italy), there was little unused hospital capacity.
Juridical controls: Juridical controls were used only exceptionally in all three countries studied. In all three, more complete contracts made it easier both for providers not to provide, and for commissioners not to pay for, off-contract work.
Nevertheless some media of power were always more frequently reported than others. The commissioners we studied in all three countries influenced providers mainly through managerial performance (transparency of provider activity data was important), sustaining a negotiated order (in particular micro-commissioning, where feasible) whose disciplinary basis was evidence basing and shared emic assumptions (although the content of these assumptions varied considerably between countries) and adjusting incentives. Competition gave commissioners power only insofar as they could select providers, and had at most a mixed impact on the service outcomes studied. Juridical controls were marginal to day-to-day commissioning practice in all three countries.
This pattern appeared to reflect three main factors. First, commissioners faced trade-offs between the different media for exercising governance: relationality (and micro-commissioning) versus competition; complete contracts versus flexible service provision; relationality versus juridical controls; and tariff incentives versus commissioners selecting providers. Commissioners’ governance over providers was not necessarily maximised by establishing as many media of power as possible, because some media obstructed others. Second, our four case studies suggested that, insofar as GPs gained influence on commissioning, the shift from PCTs to CCGs meant that commissioning practice relied less upon competition and more upon a negotiated order between GPs and consultants, in which medical discourse became more prominent. There was a greater propensity for micro-commissioning. These changes concerned the ‘real side’ of commissioning practice rather than finance. Third, negotiative and discursive control require trust, the absence of substantial background conflicts of interest between commissioner and provider. Otherwise, the alternative media of power have to be mobilised more fully. Of these, the most potent was for commissioners to use providers’ resource dependency upon the commissioner as a means of influencing the provider: a specific form of financial incentive. The selection of media of power partly reflected factors in the commissioners’ environment (what kinds of provider there were, how they reacted to commissioners’ activity, the structure of the quasi-market itself, regulatory and policy constraints on commissioners) and partly the commissioning organisations’ own activity (who controlled it, what they decided, what adaptive commissioning practices they developed).
How much room for manoeuvre do NHS commissioners have?
The answer to this research question specifies more concretely how the commissioners’ environment and the structure of the internal market limited commissioners’ powers of governance over service providers. In our four English case study sites the commissioners’ environment and the structure of the NHS quasi-market meant that NHS commissioning practice during 2010–12 did not always enable commissioners to exercise governance over providers in respect of:
-
providers unilaterally closing or altering services
-
provider case load (volume), case mix and willingness to treat patients off-tariff
-
ensuring that providers internally implement service changes agreed with commissioners
-
promoting GP and consultant engagement in commissioning activity
-
promoting user involvement in service changes of little interest to them
-
achieving transparency of provider activity and costs
-
monitoring the service and health outcomes of most services
-
stimulating ‘lifestyle change’ activity to address causes of ill health outside the health system
-
user influence on service design, which is feasible only for services that users are interested in changing.
However, the same factors meant that NHS commissioners in the four case study sites could exercise governance over:
-
referral rates, through GP involvement in referral screening and reviewing providers’ clinical activity
-
care pathways, through direct GP–consultant negotiations (which commissioners can only initiate, not control)
-
service specifications, by:
-
micro-commissioning or
-
defining clear outcome indicators and measures for well-defined episodes of care (e.g. IAPT-style contracts); however, the scope for commodifying technically complex, mental health and long-term care involving multiple conditions and/or multiple care providers is limited
-
-
service co-ordination at individual patient or small care group level, through promoting direct GP–consultant contacts for problem solving
-
service models, by appeal to evidence supplemented as necessary with guarantees that changes will have no adverse consequences for patients
-
costs, through block contracts (with safeguards for obtaining sufficient monitoring data) and bundling tariff payments, with below-tariff marginal adjustments to payments
-
service profile, by using block contracts to guarantee certain services financially
-
target compliance, partly through monitoring and, where feasible, provider competition.
In these matters the commissioners could develop adaptive commissioning practices, in the light of how providers responded (see subsection How do provider managers respond to commissioning activity? below).
Our four case studies also suggested that certain limits on NHS commissioners’ manoeuvrability were practically irremovable within any credible scenario for the near future: the content of evidence-based guidance; patients’ mobility between providers; the physical infrastructure of large hospitals; national policy; the tariff system; and medical scepticism or disengagement. Nevertheless, the commissioners we studied did have room for manoeuvre concerning:
-
which care groups to prioritise for commissioning attention and for developing new models of care
-
how to allocate any additional income or savings that did become available
-
what commissioning support to use
-
which GPs, consultants and others to involve in negotiations
-
how to redesign or respecify services through micro-commissioning
-
collecting local evidence about services
-
bundling tariff payments
-
using the discretionary elements of QIPP, QOF and other payments
-
latitude within the DH national contract framework
-
how far beyond the legal requirements they took competitive procurement.
Here too commissioners had scope for decision-making and developing adaptive commissioning practices.
What are the consequences, and how do commissioners try to manage them, when commissioning is distributed across different organisations and when it shifts to being client based?
In our four case study sites, the consequences of the lead commissioner model of distributed commissioning depended on how convergent the different commissioners’ interests were. When they differed substantially, commissioners managed the situation by reverting to separate commissioning arrangements. Otherwise, the main consequence (managerial response) was a move towards more standardised service specifications and contracts, and an increased capacity to countervail the power of large, even merged, providers. In Germany, distributed commissioning took the form of several SHIs negotiating jointly with each provider, although without a ‘lead commissioner’ arrangement. That situation also presupposed that patients subscribed to different SHIs will receive essentially similar care, conforming to national quality standards, Deutsche DRG specifications, and any other requirements that the SHIs could jointly negotiate. In Lombardy, commissioning roles were distributed vertically between regional and local governments, with the result that many commissioning decisions were centralised to regional level.
Because of the different accountabilities, governance structures and working practices in the NHS and local government, joint commissioning in England was ‘joined at the top’ (p. 21)257 rather than at the levels of more concrete commissioning, service design and monitoring, especially in public health. Managers tried to manage these circumstances by setting up ad hoc, informal cross-organisational network arrangements to co-ordinate services. These networking arrangements only partly relied on commissioning mechanisms. They were also found in Italy and Germany.
Combining findings from England, Germany and Italy suggests which consequences of per-patient, tariff-based commissioning may be intrinsic to that form of client-based commissioning. These three tariff systems weakened commissioners’ control over provider activity, case mix and costs but better monitoring information enabled commissioners to devise more sophisticated monitoring and modelling systems. Nevertheless, providers’ activity and cost data were still not sufficiently transparent for commissioners’ purposes. They still left a certain amount of privacy for provider management practices about which commissioners might have wished to have known when negotiating. [Research in this field is currently (2014) in progress.]
Commissioning managers’ main responses to these circumstances were to:
-
retrieve control over costs (and case mix) by bundling tariff payments into blocks with discounts and/or variable payments at the margin
-
devise new forms of capitation payment and block contracts at the margins of, and as agreed exemptions to, the tariff system in England, Italy and Germany
-
supplement tariff payments with additional incentive payment schemes to reward higher-quality services, better outcomes and/or continuity of care. Such were QIPP and QOF payments in England; case management, the Istituti di Ricovero e Cura a Carattere Scientifico (IRCCS) and voucher schemes in Italy; and disease-management programmes in Germany.
In these ways commissioners adapted to, indeed worked around, some of the environmental constraints of commissioning imposed by quasi-market structures, national policy and regulations.
Personal health budgets were still being piloted (and separately evaluated) in England during the study period. They had not yet had much reported impact on NHS commissioning or services in our four main study sites, or the mini-case study site. Our cross-sectional analysis found only 1 of 48 possible correlations between the three measures of the extent of individualised commissioning and the 16 service outcomes studied. The presence of a personal budget pilot scheme was associated with an increase in patients being treated within the 18-week target, but the association was weak. Otherwise, the associations had the wrong sign, or were negligible or absent. Personal health budgets were not yet an important influence on commissioners’ governance over providers.
How do provider managers respond to commissioning activity?
English NHS providers’ responsiveness to the commissioners in our four case study sites reflected the presence or absence, and depth, of any conflicts of interests between the two. On perceiving such a conflict, providers most often responded passively. Negotiations, including micro-commissioning, became protracted and inconclusive. Providers often proposed what services should be commissioned, sometimes as counterproposals to the commissioners’ ideas but also for reasons of their own. They sometimes altered services unilaterally, independently of commissioners’ demands. Providers’ willingness and ability to respond to commissioners’ demands were also conditioned by their internal management, especially consultants’ attitudes to commissioners’ proposals. The internal management of German and Italian hospitals did not appear to involve such sometimes troublesome relationships with their consultant equivalents.
The English commissioners that we studied, however, could sometimes rouse providers into helpfulness by threatening a loss of resources (possibly to a competitor) or an unfavourable intervention from a third party, above all higher-level NHS management. Such powers were not available to German SHIs, but in Italy the ASLs, and still more regional governments, could use discretionary payments for this purpose, although the threat of removing tariff-funded work from providers was not credible.
Provider diversification appeared to generate a similar division of labour in all three health systems. State-owned tertiary providers increasingly concentrated on high-complexity and hard-to-treat (e.g. multiple) conditions. The third sector also provided especially for hard-to-treat conditions. German and Italian corporate providers specialised in profitable care, typically high-volume, non-urgent acute care, but also some more complex, expensive acute care (e.g. heart surgery and diagnostics respectively).
Providers’ responses stimulated commissioners to adapt their selection and use of media of power. Many of these adaptive responses were more sophisticated forms of existing managerial practices (e.g. better data collection and interpretation, greater medical participation in negotiations) but some (e.g. appeal to regional NHS management) used non-market structures.
Commissioning for different care groups
The distinctive patterns of commissioning for our four tracer groups were:
-
Mental health: Evidence-based service specification and monitoring were limited and problematic, although IAPT prototyped an alternative approach. In all three countries studied, micro-commissioning of care pathways often occurred, in our four English case study sites involving multiple providers and commissioners. NHS and social work professionals often had conflicting emic discourses. Mainly block payments were used, although tariffs were being introduced. Many providers were small, specialised third-sector organisations, but commissioners made little use of provider competition.
-
Planned orthopaedic surgery: Outcome measures and care processes were often standardised, based on relatively well-developed evidence-based practice and outcome measures, which facilitated the use of provider competition. There was little micro-commissioning and what there was focused on post-discharge care. Payments were by tariff, which providers found lucrative.
-
Coronary heart disease/diabetes prevention: The commissioning of services was largely irrelevant to the primary prevention of these diseases through intersectoral activities (promoting lifestyle and consumption changes, etc.). To the extent that clinical prevention was possible, it was commissioned much as for primary care generally; that is, by harnessing QOF or LES payments and commissioning community health services projects. For these projects, evidence-based practice and outcome measures were relatively well developed, but as experimental projects they were vulnerable to budget cuts. Commissioners made little use of provider competition.
-
Older people with recurrent unplanned admissions: The causes of these referral patterns were poorly understood, making contract specification difficult. Commissioning relied heavily on micro-commissioning, even case management. As persuasive devices in negotiating with providers, commissioners emphasised the targets and cost-control imperatives that they and the providers shared. Commissioners made little use of provider competition.
Across the three health systems studied, these differences in commissioning practices between care groups appeared to reflect:
-
the extent to which the commissioning of service providers was relevant at all (cf. primary prevention)
-
the extent of the available evidence base
-
case mix homogeneity
-
how well defined the duration and outcomes of episodes of care were
-
the number of providers and commissioners likely to be involved simultaneously with each patient.
Together these factors reflected technical characteristics of the service concerned, not (as we had expected when writing the research protocol) at the level of detailed clinical (or, for intersectoral health promotion, anti-marketing) techniques, but at the level of complexity of the model of care required for each care group. That is, complexity in terms of the variety and range of inputs required and the uncertainties of outcome. The more strongly services showed these characteristics, especially characteristics (2) to (4), the more susceptible they were to ‘commodification’, that is designing, paying for and monitoring services on the basis of standardised, discrete packages of care.
Aspects of service provision on which different commissioning organisations tended to focus
Looking across the three health systems, each variant of each medium of power helped commissioners to influence some, and impeded influencing other, aspects of providers’ services. (Classic tariff systems prevent commissioners from selecting providers; a negotiated order involving clinicians facilitates care pathway design; and so on.) The commissioning organisations that we studied concentrated on managing the aspects of service provision shown in Table 13. The row headings are service characteristics that the programme theory of NHS commissioning, our case study informants (in all three countries) and published managerial data all emphasised.
| Service characteristic | PCT | CCG | LA | SHI | ASL |
|---|---|---|---|---|---|
| Predominant objectives | Implement national policies | Primary–secondary care co-ordination | Elected councillors’ priorities | Remain solvent, recruit subscribers | Implement regional government policy |
| Referrals | Referral volumes, referral criteria, unplanned referrals | Referral criteria, clinical management problems | Redefining eligibility criteria (social care) | Referral volumes, case mix | Cross-boundary patient flows, case load (volume) |
| Finance | Overall costs, prevention of ‘over-activity’ | Overall costs, per diem costs | Overall costs, prevention of ‘overactivity’, risk pooling | Overall costs, prevention of ‘over-activity’ | |
| Care groups | Care groups of interest to secondary providers | Large care groups for whom GPs are responsible | Groups whose care LA funds | Large care groups | Large care groups |
| Provider development | Implement national initiatives, stabilise main providers | Substitute primary for secondary care | Sustain sufficient affordable providers | Within Land plan (hospitals), selective contracts | Develop existing providers through pilot schemes |
| Care-pathway development | Reducing hospital admissions, multiprovider pathways, co-ordinating health and social care | Co-ordinating health and social care | Coordinating health and social care | Disease management, mental health-care networks | Reduce cross-boundary flows, integrate primary and social care |
| Service quality | Care pathway redesign, national guidance and targets | Care pathway redesign, evidence-based practice | Conformity to registration standards | Conformity to national quality standards | Presence of peer-review-based audit systems |
| Provider selection | Main local providers | Main local providers | In-authority providers | Not permitted | Existing providers only |
During a transitional period, the contrasts between PCT and CCG represented ends of a continuum rather than categorical differences. Table 13 shows what the commissioners tried to control. How far they succeeded partly depended on the providers’ responses (see subsection How do provider managers respond to commissioning activity? above) and the local health system context. These differences lead naturally to the following research question.
What factors, including the local health system context, appear to influence commissioning practice and the relationships between commissioners and providers?
Taking the English, German and Italian case studies with the cross-sectional data from England, the commissioning practices and modes of commissioning that we studied appeared to reflect three main groups of factors:
-
the commissioners’ environment, in particular:
-
whom the commissioners were accountable to, and for achieving what ends
-
local histories and existing relationships among commissioners, providers and local government, and between GPs and hospital doctors
-
providers’ resource dependencies on the commissioners
-
socioeconomic characteristics of the population served
-
-
two sets of technical factors:
-
the service technologies (at model of care level) for each care group
-
the inherited physical infrastructure of services: whether they had more or less capacity than commissioners needed, the specialities available, their location, and the availability of alternatives
-
-
commissioners’ own selection of the media of power noted above, and how commissioners developed their commissioning practices, learning from how providers responded.
Relationships between commissioners and providers both influenced commissioning practice and were recreated by it. Through the feedback mechanism of provider responses to commissioning, adaptive commissioning practices emerged from the commissioners. The absence or presence of conflicts of interests between commissioners and providers, attenuated or exacerbated by the local micro-political history of relationships between the organisations and among the individuals involved in commissioning, influenced which media of power commissioners needed to use in their commissioning practice. In England, deprivation, PCT mergers and PCT income (per capita of population) appeared no less, and in many cases more, strongly associated with service use289 and the outcomes we studied than did HHI (a putative measure of competition), independent-sector provision or client-based commissioning.
Relationships between commissioners and providers were defined by the relative importance and operation of, or the absence of, each medium of power discussed in Chapter 2. Each specific combination of these media, and the corresponding commissioning practices, constituted a specific mode of commissioning. Abstracting general patterns from our comparisons of commissioning practice across study sites, countries and tracer groups, three main modes of commissioning were most evident. Concentrating on the commissioner–provider interface, Table 14 contrasts them.
| Medium of power | Case mix commissioning | Surrogate planning | Micro-commissioning |
|---|---|---|---|
| Managerial performance | Case mix modelling + audit + subscriber marketing | Service planning for geographical population | Clinical experience + knowledge of evidence bases |
| Negotiated order | Consensus: multiple commissioners – one provider | Principal–agent | Multiple stakeholder providers, commissioners, patients (and optionally others) |
| Discursive control | Solidarity + juridical rights + case mix data | Policy compliance + EBM + local political culture | EBM + local knowledge + culture of supporting local health system |
| Financial incentives | Tariffs (bundled) | Block payments + ad hoc pay for performance + tariffs (bundled) | Continuity of provider contract |
| Provider competition | None: referral ‘framing’ at most | Provider competition or bilateral monopoly | None: coproduction of care pathways and service specifications instead |
| Juridical | Comprehensive regulation + administrative law | Unwritten constitution + common law | No direct application |
Thus the population-based commissioning structures in England and across the Italian regions sustained a mode of commissioning that we have called ‘surrogate planning’. Client-based commissioning sustained a case mix mode of commissioning, more developed in Germany but having a secondary role in England and Italy too. Micro-commissioning focused more upon service quality; the case mix and surrogate planning modes of commissioning focused more upon finance and performance. To the more limited extent that we could study general practice-based commissioning structures, they especially sustained the micro-commissioning mode. (What we have called general practice-based commissioning is, more precisely, the commissioning structure in which the patient’s primary-care gatekeeper commissions the other health services to which the patient is referred.) The concept of a ‘mode of commissioning’ makes explicit the mechanisms (media of power) by which commissioners attempt to control providers, the requisite contexts (environment) and how the mechanisms interact. Surrogate planning is one specific, concrete instance of a mode of commissioning. Case mix commissioning and micro-commissioning are two more. Each commissioning organisation that we studied combined elements of several modes of commissioning, but one predominated, so that in practice the health systems we studied had hybrid commissioning structures. Under case mix commissioning, managerial performance, negotiated order and juridical controls appeared the dominant media of power. In surrogate planning, a different kind of negotiated order, provider competition and financial incentives and penalties dominated. Micro-commissioning relied on the negotiative use of discursive controls. Other media of power were marginal or absent. Even where the same medium (e.g. negotiated order) was used in different health systems, it took a different form in each, depending on what other media of power coexisted and of course on the national political culture.
Empirical patterns
Our empirical findings – whose limitations we reiterate in the next section – suggest that commissioners depended on three complementary (not alternative) parallel strategies for exercising governance over health-care providers. A strategy of trust, developed through stable working relationships between the individuals representing either side, rested upon a negotiated order and shared normative assumptions. In the CCGs we studied, those relationships were increasingly negotiated between GPs and hospital consultants, and framed in predominantly medical terms. Financial and clinical discussions were kept largely separate. A more distrustful, incisive strategy harnessed the provider’s resource dependency and the commissioner’s capacity (where it existed) to reduce or increase the provider’s income. Both strategies required transparent data about provider activity; commissioners needed to be not only able to access provider data, but also able to analyse the data and willing to confront whatever provider performance issues were exposed. Provider competition and juridical controls had a more ancillary role. Provider competition was one way to make commissioners’ threats to withdraw resources credible. (Another, in Italy, was to allow commissioners a ‘make or buy’ option for procuring services.) In themselves juridical and regulatory controls were a clumsy medium of power, but also a source of shared normative assumptions (e.g. about commissioners’ rights and duties).
The first two strategies took quasi-market structures as given. A third strategy was to modify or work around those structures. If the providers co-operated, a commissioner could in effect modify the separation of competing providers by encouraging them to collaborate, whether by forming care networks or by making one provider the subcontractor of another, ‘lead’, provider. The same can be done among separate, potentially competing commissioners. Commissioners could also modify the incentive structures by adjusting the unit of payment to providers, for instance by bundling tariff payments. These workarounds modified quasi-market structures in the interests, as commissioners saw it, of governance over health-care providers, especially when commissioners had to pursue such aims as cost control, which would have been harder without these market modifications.
These patterns point towards a contingency theory of health-care commissioning (see section Commissioning contingencies). Before outlining it, though, we report the qualifications that attend our empirical findings.
Limitations and qualifications
Specific caveats about the above findings are already stated in the methods and findings chapters. Here we add only more general limitations and qualifications to our conclusions. Beginning with theoretical limitations, other theories, such as sociolegal theory and institutional economics, might also be applied to and tested against our data. It may also still be early to expect a commissioning system undergoing reorganisation during the study period to realise commissioning outcomes first formulated in policy documents during 2010–12, although as Chapter 1 indicates these policies have substantial continuities with longer-established policies.
We did not take our cognitive frame analysis of the programme theory of NHS commissioning as far as a full discourse-historical analysis, or examine how the programme theory is embedded in wider genres and ideologies.
Our findings have, we repeat, a limited empirical basis: a systematic comparison of commissioners in three countries, a specific selection of England-wide data sets, a policy and discourse analysis, and four (for some issues, five) interview-centred case studies in England. We focused on health services, mainly secondary care at that, excluding intersectoral public health, research, training, capital allocation and, above all, long-term care, which in England, Germany and Italy is mostly financed separately. At the time of this study CCGs were still developing. Many details and practicalities of their eventual work remained unknown. The same applied to psychiatric commissioning in Germany. Our cross-sectional analysis was limited to published data, which made only two media of power susceptible to quantitative analysis and left it an open question if other measures of policy outcomes might show greater effects of competition, and if a longitudinal study would. We analysed the WCC competencies only in the aggregate, not how far each competence was separately associated with the health policy outcomes that we studied.
The cross-sectional analysis of managerial data used pre-CCG data for a period 2 years before the case study fieldwork, raising the question of what implications the differences in period for the cross-sectional and the case study data have for the present findings. Obviously no such implications arise from the free-standing conclusions of the cross-sectional study. On balance our findings suggest that commissioning practice in 2010–11 was not so different from 2008–9 that the cross-sectional and the case study data report substantially different commissioning regimes and therefore cannot be combined. Managerial staff turnover was high in our four case study sites but we found little evidence that commissioning practice changed substantially because of that. Indeed services there were reviewed and recommissioned less frequently. There was considerable continuity of GP involvement during 2008–11. If anything, GPs were in those sites less inclined than managers to use competition as a means of influencing providers, but, against that, the government became more inclined to after 2010. Formally, PCTs, not CCGs, were responsible for commissioning throughout. Nevertheless, the ideal solution to this time difference would be to extend both analyses into the period after 2010, yielding a longitudinal study, should the data become available.
Our mixed methods contributed unequally to the findings. The core research was case study findings at four English sites, with some in-depth work on exemplar tracer conditions and some comparative international case studies. Case studies are inherently open to recall and response bias, but triangulation between informants and other data sources reduced the risk. Comparing a variety of commissioners had the methodological advantage of enabling us to contrast varied organisational structures, but at the price of having to rely on the qualitative generalisation of our findings, a step to be taken cautiously. Our case studies covered four of the (then) 152 English PCTs, plus a fifth (Livewell) in part. Fewer case study data, in particular from providers, were available from one site (Milltown) than the other three. In Milltown the three main negotiative orders (GPs with commissioners; commissioner with hospitals; micro-commissioning) were long established and, despite other hospitals being available near its borders, the commissioners made little use of provider competition. If anything, the lower representation of Milltown might have led us to understate the importance of negotiated order versus provider competition as a medium of power. Another empirical limitation is that we did not observe formal commissioning meetings. However, this is less of a limitation than might appear. We found that formal commissioning meetings were not the only venue for commissioning work. Information and ‘intelligence’ sharing, not to mention ‘backroom’ dealing (p. 253),102 mostly occurred elsewhere. In one-to-one interviews, informants were freer to speak candidly and critically than in meetings. Discourses, ideologies and evidence are the same in meetings as elsewhere. In two sites, some of the pivotal meetings were so heated that it is doubtful outsider observers would have been admitted, and if they had been their presence would probably have had Hawthorne effects289 on how the meetings were conducted. From the case studies we have abstracted qualitative generalisations, which will apply more widely only to the extent that the commissioning methods we reported have counterparts elsewhere. However, because NHS commissioning is quite centrally controlled, pursues largely nationally defined objectives and has essentially similar organisational structures across England, our findings may be generalisable with caution. Table 15 shows that for the variables most relevant to commissioning practice and its service outcomes, our study sites (2010–12 data) covered most of the range of variation for England while avoiding outliers, except perhaps for PCT surplus/deficit, where our sites fell within a narrow range (small surpluses).
| Variable | Study site range | England range | England mean |
|---|---|---|---|
| Listed GP patients | 239,641–399,807 | 93,218–1,298,398 | 357,307 |
| % budget spent on largest provider | 36–93 | 24–97 | 66 |
| Independent-sector spending (%) | 0.75–14.5 | 0.01–17.3 | 3.47 |
| HHI | 0.21–0.67 | 0.14–0.93 | 0.51 |
| Average deprivation score | 14.62–36.97 | 8.81–45.0 | 23.64 |
| PCT surplus/deficit (% of allocation) | 0.02–1.7 | –5.23–5.11 | 0.46 |
| PCT income per capita | £799.97–£1947.67 | £343.34–£4907.28 | £1392.33 |
Most but not all of our study sites used private-sector commissioning support, also matching the England-wide pattern. 290
Nevertheless, comparisons with the rest of England, and of the UK, might yield different findings. At cross-country level, we compared just two other countries, although again selecting countries whose health systems have parallels elsewhere. Our selection of study sites meant that this study reported three main generic modes of commissioning, but others exist, including:
-
general practice-based commissioning, under which a general practice, or other primary-care gatekeeper, holds the budget for their use of those services
-
commissioning of health care for occupational groups
-
corporate health insurers’ commissioning of health services
-
commissioning of intersectoral health promotion (smoking-control campaigns, etc.).
Commissioning contingencies: environment, technology and ‘fit’
Empirical findings about CCGs and PCTs have a transient local interest, but taken with the cross-country comparisons they can make a more enduring contribution to explanations of which modes of commissioning and which commissioning practices emerge in different settings, and therefore how governance occurs through commissioning. Our empirical findings suggest a contingency account of how governance is exercised through different modes of commissioning. This study contributes to the study of governance by suggesting outlines of such a theory of commissioning, something which barely exists yet. Pending fuller discussion elsewhere, we note two main sets of external constraints on the modes of commissioning that a commissioning organisation can use: environmental constraints and technical constraints.
The media of power available to commissioners depended on the policy, legal and economic settings and the quasi-market structures within which commissioners worked i.e. the commissioners’ organisational environment. Combining our English (see Chapter 7), German and Italian evidence (see Chapter 12), we distinguished three generic modes of commissioning. Instances of all three were found in each health system, but one tended to predominate. Each mode of commissioning involved a specific configuration of media of power. Certain media of power, in specific forms, were available to commissioners while others were weak or absent (see Tables 9, 11, 13, 14 and 31). In the case of England, our four case studies and the cross-sectional analysis together suggested that only in quite specific circumstances did each medium of power appear to help commissioners exercise governance over providers. Governments’ willingness to face the electoral consequences of confronting providers (see Chapter 5, section Policy-makers’ and top managers’ programme theory) constrained commissioners’ negotiating position; German SHIs were constrained by providers’ legal rights to payment; and so on.
A second set of constraints arose from the technical character of health care for different care groups. Our evidence, mainly from five English case studies (including Livewell) and Germany, suggested distinct patterns of commissioning for different care groups. For each care group, commissioners had selected and developed configurations of the media of power which they considered to be adapted and practically relevant for maintaining commissioners’ governance over the corresponding health services. The technological character of different health services (e.g. for different care groups) had influenced the selection and impact of different media of power – not, as we had expected when writing the study protocol, technology at the level of differences in clinical or therapeutic practice, but at two other levels. One level was that of the characteristics of the model of care typical of that care group. Relevant characteristics were the extent of the available evidence base, case mix homogeneity, whether or not care outcomes were well defined, whether patients usually required a discrete episode of treatment or longer-term care involving multiple providers simultaneously, and whether or not health services or health promotion campaigns were relevant. The other level was that of the providers: minimum size compared with the scale of population health-care needs, which determines whether many providers were required, giving scope for provider competition, or just one; specialities; and geographical dispersal.
Contingency theory291 assumes that an organisation’s structures and managerial practices adapt to ‘fit’ its productive technologies and environment. Typically this adaptation occurs by trial and error. Observation of what adaptations develop, and under which circumstances, suggests which modes of healthcare commissioning appear adapted to which contexts and care groups.
We compared the media of power relevant to commissioning services for each tracer group (see Table 8) with those available to commissioners under each of the three modes of commissioning we studied (see Table 14). The comparison (Table 16) suggests that each mode of commissioning is a better ‘fit’ for some care groups than others. Some modes of commissioning make it easy, and others make it harder, for commissioners to exercise governance over the providers of services which use a particular kind of care ‘technology’. In Table 16, ‘Origin’ means the type of quasi-market setting292 which each mode of commissioning characteristically originated from and was adapted to. ‘Favoured providers’ indicates which type of provider organisations have tended to predominate and which, therefore, commissioners focus upon in that environment. ‘Care networks’ typically consist of public providers, small firms and third-sector organisations, who collectively provide and co-ordinate care for a group of patients. 293 Under ‘technology’, the ‘care groups’ row shows the care groups for whom the fit is closest between the technically relevant configuration of media of power and the mode of commissioning.
| Broad contingency | Specific contingency | Case mix commissioning | Surrogate planning | Micro-commissioning |
|---|---|---|---|---|
| Health system environment | Origin | Compulsory private insurance; social insurance | Managed/planned competition | Primary doctor-based purchasing |
| Provider selection by commissioner | None | Managed systematically | Assembled ad hoc | |
| Favoured providers | Corporate; ‘public firms’; professional partnerships | Public; third sector | Care networks | |
| Care ‘technology’ | Type of episode | Discrete | Almost all | Prolonged and/or recurrent health problems, including those prone to exacerbations or crises |
| Care groups with closest fit | Planned acute care, low to medium complexity (e.g. planned orthopaedic surgery; episodic mild mental health problems; clinical prevention) | Large groups with predictable, understood utilisation patterns (e.g. planned orthopaedic surgery); target populations for intersectoral prevention (e.g. smokers) | Chronic conditions, including degenerative conditions; multiple health problems (e.g. older people having repeated unplanned hospital admissions; chronic and/or complex mental health problems) | |
| Care ‘technology’ | Acute treatment of discrete, independent episodes of ill-health; clinical prevention | Acute care, long-term care, intersectoral prevention | Co-ordinated multiprovider treatment of multiple, recurrent or chronic health problems | |
| Supplementary governance structures | Juridical, planning hierarchy | Hidden hierarchy, networks with other commissioners and small providers | Network | |
Episodic and chronic health problems are of course ends of a continuum. Developments in clinical and therapeutic technologies shift care groups along it, when for instance previously chronic conditions become more effectively treatable. The surrogate planning mode of commissioning appears applicable across most of this continuum for several reasons. Service planning at population level does not require the detailed patient-level service specifications or classifications that case mix commissioning and micro-commissioning do. Population-level norms of provision can be used instead, including norms based on epidemiological and other evidence that explains service utilisation patterns. The surrogate planning mode of commissioning can also accommodate flexible incentives (e.g. DRGs, target-based payments) at the margins of block contracts (though if the marginal incentives became predominant it collapses into case mix commissioning). Of the three modes of commissioning we examined in detail, only surrogate planning could readily accommodate the ‘technology’ of intersectoral health promotion campaigns outside the health sector (e.g. to promote exercise).
Emerging and adaptive commissioning: practical implications
A contingency theory of commissioning identifies factors, some beyond commissioners’ control, which constrain commissioners’ governance over providers. Yet any empirically credible theory must also accommodate our evidence (see Chapter 8) that commissioners nevertheless normally have some room for manoeuvre.
Commissioning practice was made to ‘fit’ the health system environment and/or health care technologies in various ways. Most obviously, commissioners selected or developed a mode of commissioning to fit the care group, their own aims and the health system context. Conversely, governments sometimes mandated a mode of commissioning in order to accommodate certain types of provider and/or care technology. However, care technologies, the demographic and epidemiological patterns which necessitate them, and the science which produces them are not very amenable to manipulation by policy-makers. Our findings suggest that, when there is no close ‘fit’ between organisational environment, care technology and their own aims, commissioners respond with one or more of the following:
-
Workarounds within an existing mode of commissioning. For instance, they tried to modify, amalgamate or invent DRGs for commissioning care for patients with multiple, complex long-term health-care needs.
-
Combining or hybridising several modes of commissioning (e.g. tariff payments with micro-commissioning in CCGs).
-
Supplementing commissioning with non-market governance structures (‘supplementary governance structures’ in Table 16). Thus, difficult contract negotiations in two of our English study sites became occasions when regional NHS bodies exercised hierarchical power (‘hidden hierarchy’). Commissioners in England, Germany and Italy tried to set up care networks to co-ordinate (‘integrate’) care across separate providers. Indeed, under micro-commissioning, contract-based commissioning was an adjunct to care networks rather than vice versa.
-
Neglecting certain care technologies (e.g. before 1990 many east European health systems had few means of commissioning community health services).
The emerging commissioning practices that we have reported were adaptive practical responses to the constraints facing commissioners. CCGs are also likely to have to develop adaptive responses insofar as commissioning policy rests on empirically questionable assumptions (see first section of Chapter 13). These emergent adaptations and their counterparts in Germany and Italy suggest some practical implications.
Our cross-sectional and English case study evidence suggested that provider competition had limited usefulness for governance. It was associated with commissioners achieving a minority, but only a minority, of the policy outcomes we studied, and it remained unclear what primary care providers had also contributed to these outcomes. Sometimes differently owned providers reacted differently to the same commissioning initiatives (see Chapter 7, section Provider competition). An obvious practical implication is that commissioner managers sensitise themselves to the differences in organisational goals, cultures and working practices between public, corporate and third-sector providers. For the ‘integration’ (co-ordination) of multiple providers, provider competition was of little practical relevance. As German SHIs had also concluded, micro-commissioning was also required, which depended on involving the relevant providers and then building long-term working relationships with and among them. Insofar as more diverse providers tended to have more divergent interests, it appeared a lesser evil to recognise the divergent interests rather than try to argue them away. As Williamson’s theory82 implies, these circumstances of asset specificity (of clinical skills), frequent contracts and complex, variegated products (uncertain outcomes) tended to impel commissioners and providers away from market-like relationships towards relationships more like those within a single organisation, although contracting mediated and masked them in quasi-markets.
In any case, when provider competition did occur (e.g. in Germany) providers’ resource dependency was what motivated it. Commissioners could harness that resource dependency directly, even when negotiating with a monopoly provider (see Chapter 10, section Making providers more helpful). Commissioners’ likelihood of success in doing so depended, though, on both sides believing that the commissioner could reduce the resources it allocated to non-compliant providers. However, the very fact that commissioners were exercising governance, that is acting as agents of the government’s, undermined this belief insofar as governments avoided publicly accepting responsibility for such acts (see Chapter 5, section Policy-makers’ and top managers’ programme theory) or when corporate providers were guaranteed NHS contracts. 246 In either event, commissioners ‘go naked into the conference chamber’294 to negotiate with providers.
It is often noted (see Chapter 2, section Negotiated order) that contractual relationships between commissioners and providers require a negotiated order – ‘relationality’ – alongside formal tendering, contract awarding and monitoring. We add that this is not only to compensate for contracts’ incompleteness. Neither is it a complete alternative to the more incisive commissioning strategies mentioned in the section Empirical patterns above. A negotiated order involving influential professionals on the provider side, evidence from our four English case studies (see Chapter 10) suggested, helps to promote understanding, hence willing implementation, of the commissioners’ aims in parts of the provider organisation which are not involved in formal contract or budget negotiations. Post-2010 NHS structures and rules also instituted broader, more systematic collaboration between consultants and GPs, placing GPs (as commissioners) on a more equal footing with consultants. This development, that of micro-commissioning and the strengthening of joint commissioning, attenuated the tripartite structural division which has inconvenienced interorganisational collaboration for the NHS since 1948. All these developments have the practical implication of commissioners adopting a long-term approach to maintaining trust between the parties involved, a task which involves both personal negotiating styles and the stability not just of the organisations but of the personnel involved.
We found in our four English case studies that a stable negotiated order between the ‘lead’ GPs involved in commissioning and the other GPs could be accumulated piecemeal by commissioners taking a flexible opportunistic approach to recruiting interested GPs when new policy initiatives or local project ideas arose. This necessarily happened gradually. Some GPs perceived that hospital interests had ‘captured’ local commissioners. Many GPs and consultants also wanted to avoid being made responsible for linking clinical and financial decisions, equated by some with rationing and commissioner scrutiny of clinical practice. An emergent solution was for commissioners to involve, if not ‘difficult’ GPs and consultants, then at least the stratum of (respectively) lead GPs and medical directors, in financial negotiations, for their support for commissioning decisions might be more persuasive to other doctors than non-medical managers’ opinions.
Besides the use of evidence basing, commissioner governance over providers through a negotiated order required a shared emic discourse. That the discourse is shared was almost as important as its particular content, provided that it legitimised commissioner governance over providers’ activity. Our English and German case studies suggested that norms which overemphasise providers’ independence were counterproductive for governance purposes. Insofar as commissioners can influence providers’ organisational cultures, the practical implications are obvious.
We found two emergent adaptations to client-based commissioning, more extensive in Germany than England or Italy. Our evidence suggested that unmodified tariff payment systems were likely to be counterproductive for the purpose of containing service costs. Tariffs were too marktkonform (market-conforming), that is too similar to prices in conventional markets, which tend to incentivise the open-ended expansion of production and allow only weak governance. 295 Commissioners in all three countries adapted the tariff system by defining ‘bundles’ of tariff payments and using non-tariff rates of payment at the margin, to incentivise a more controlled and focused development of case loads and case mix, and to protect providers that reduced case loads from penalty. Intelligently designed cost-and-volume contracts can be used similarly (Chapter 7, section Financial incentives). Non-tariff payments are anyway required for commissioning intersectoral health promotion. A second adaptation was for commissioners to try to influence providers indirectly by influencing patients’ choices through marketing methods (e.g. health advice services) or ‘nudges’ such as discounts for SHI subscribers, or by influencing GPs’ referral decisions. CCGs in our four study sites and Livewell (and elsewhere, judging by professional press reports) were increasingly attempting to manage GP referrals during 2010–12.
Monitoring information gathered in one commissioning cycle helps inform commissioners in planning the next. The new NHS structures and rules made hospital activity more transparent to commissioners and made commissioners’ plans for service development more explicit, specific and concrete. These are textbook precepts of good planning and project management. NHS commissioners nevertheless often depended on providers to collect and interpret monitoring data. A practical implication, especially observed in Germany, was for commissioners to develop provider activity databases whose data did not depend so heavily on the providers who were being monitored. This was a strength of DRG-based systems. If cost-and-volume contracts are used, the commissioners’ problem was then to obtain similar levels of transparency and information. An obvious practical implication would be to collate, preferably automatically, activity data that ought to be collected anyway at patient level for clinical management reasons, for instance referral data per provider by International Classification of Diseases code. Anonymised data usually suffice. German evidence suggests that it was effort well spent for commissioners to develop the specialised epidemiological and statistical skills for analysing the data. Yet our evidence, from both England and Italy, also confirmed the practical value of supplementing IT-based monitoring with qualitative knowledge of providers’ interests, problems and plans, through a negotiated order with providers. A striking example was the corporate hospital reporting consultant ‘misbehaviour’ (Chapter 7, section Provider competition). The acquisition of skills, links and relationships required stable staffing on both sides, an area in which clinicians’ knowledge and networks especially contributed to commissioning.
In summary, commissioning practice in our four case study sites worked in certain respects differently from what NHS commissioning policy assumed. Financial and ‘real-side’ contract negotiations were partly decoupled, with less clinician involvement on the financial side. Commissioners influenced providers (including fellow GPs) more through a negotiated order and discussions about evidence than through competitive mechanisms (including patient choice). Commissioners routinely compared providers against national and regional benchmarks, but seldom deselected providers for that (or any other) reason. Where multiple hospitals coexisted, analysis of cross-England data suggested that a minority of their service outcomes (including some proxy clinical outcomes) improved, but more did not. Different combinations of the media of power – distinct modes of commissioning – appeared to be required for exercising governance over the providers of services for different care groups, and for different organisational types and sizes of provider. Depending on these circumstances, governance through commissioning appeared to require giving different weights to three parallel strategies for exercising governance over health-care providers: one based on trust and relationality; a more sceptical, challenging strategy; and ad hoc workarounds when quasi-market structures seemed ill-adapted to commissioners’ purposes. A key managerial skill in the commissioners we studied appeared to be that of combining these elements judiciously. In any event, commissioners depended upon the transparency of provider activity data and the ability to analyse it. When commissioners and providers repeatedly have to work around quasi-market structures (e.g. by bundling tariffs, micro-commissioning), wider questions arise about how the health system should be structured.
Further research
Current English health policy assumes that private providers, social enterprises and NHS-owned providers respond differently from NHS commissioners in terms of ‘efficiency’, cost, propensity to innovate and willingness to compete. These differences are assumed to reflect the differences in provider ownership. We found some evidence consistent with this assumption and so, redactions notwithstanding, did the Competition Commission’s 2013 report. 296 It is important for the quality, development, integration and economical provision of NHS-funded care for NHS commissioners to understand what these differences in provider responses are; under what conditions and for which care groups these obtain; and if or how commissioners might deal with these consequences or indeed exploit them. Our evidence also showed the importance of micro-commissioning for certain care groups, raising the question of how to sustain effective micro-commissioning as providers increasingly compete and diversify. As noted, a limitation of the present study was that CCG commissioning had not yet ‘gone live’, making it too early to judge what effects CCG commissioning might have on the substitution of primary for secondary care, and upon cost control.
Our evidence, and its limitations, suggest the following needs, in descending order of importance, for further research to increase knowledge and understanding of:
-
if differently owned providers (corporate, third sector, public, professional partnership, etc.) respond differently from health-care commissioners and, if so, what specific implications for commissioning practice follow
-
the impact of commissioning practices on health system integration when care pathways have to be constructed across multiple providers that must tender competitively for work, perhaps against each other
-
the emergent system-wide effects accumulating, over a period of say 3–5 years, from the separate, competitive commissioning of an assemblage of providers of unequal size and diverse ownership
-
the negotiating practices used within contract negotiations, provider monitoring and problem-solving negotiations, not only in formal meetings but also in the informal micro-politics of deal making, tacit trade-offs and the sharing (or concealment) of activity data, cost data and ‘intelligence’ (qualitative, informal knowledge) between providers and commissioners. This is particularly relevant to monopsony–monopoly negotiations (i.e. a commissioner with its dominant provider).
Additionally:
-
What variants of ways of bundling tariff payments can be found and
-
how do they compare as means of cost control?
-
to what extent do they retain the monitoring-information advantages of classic tariff systems?
-
-
Data availability limited our reanalysis of managerial data to a cross-sectional study design. There remains a need for a longitudinal analysis, as data become available. Our evidence about the difficulty of interpreting such findings suggests that such a study ought to include qualitative research into the organisational mechanisms producing any important patterns found in the quantitative longitudinal study.
-
What commissioning practices and other conditions help CCGs and local government to focus and collaborate – despite our evidence of the difficulties – on managing certain strategically important activities (avoidable admission prevention; making planned care more efficient; primary prevention through intersectoral activity)?
-
Once CCGs have stabilised and matured, what continuities and discontinuities from PCT commissioning practice will they show?
-
What specific managerial skills, and other personal attributes, commissioning managers might require; for instance, which of the WCC competencies remain relevant to NHS commissioning.
Acknowledgements
We gratefully acknowledge the assistance given by our interviewees, who by the terms of our ethical approval must remain anonymous. Those in England contributed despite unusually heavy workload demands. We are also grateful for the assistance of Alessandro Colombo (Éupolis Lombardia), Paul Cousins (Manchester Business School), Andrea Donatini (Emilia Romagna Regional Health Authority), Randall Krackauer (Aetna), Martin Richter (Universität Hohenheim), Judith Smith (Nuffield Trust), Frank Verheyen and Caroline Wagner (both Wissenschaftliches Institut der TK für Nutzen und Effizienz im Gesundheitswesen).
Contributions of authors
Rod Sheaff (Professor, Health Services Research) designed the research, conducted the discourse and cross-sectional analyses, contributed to fieldwork in England, Germany and Italy, synthesised the results and prepared them for publication.
Nigel Charles (Research Associate, Health Services Research) undertook the project management and contributed to the English fieldwork, facilitating the action learning set, discourse analysis, English and German fieldwork, case study analysis and preparing the results for publication.
Ann Mahon (Senior Lecturer, Health Policy and Management) led the action learning set and contributed to research design, discourse analysis, English fieldwork, case study analysis and preparing the results for publication.
Naomi Chambers (Professor, Healthcare Management) contributed to the research design, facilitating the action learning set, discourse analysis, English and German fieldwork, case study analysis and preparing the results for publication.
Verdiana Morando (Research Fellow, Health Services Research) undertook the Lombardy fieldwork, analysed the Italian data, and contributed to the action learning set and preparing the results for publication.
Mark Exworthy (Professor, Health Policy and Management) contributed to the research design, discourse analysis, cross-sectional analysis, English fieldwork, case study analysis and preparing the results for publication.
Richard Byng (Professor, Primary Care Mental Health) contributed to the research design, discourse analysis, cross-sectional analysis, case study analysis and preparing the results for publication.
Russell Mannion (Professor, Health Systems) contributed to the research design, discourse analysis and preparing the results for publication.
Sue Llewellyn (Professor, Accountability and Management Control) contributed to the research design, discourse analysis, Italian fieldwork, case study analysis and preparing the results for publication.
Publications
Chambers N, Sheaff R, Mahon A, Byng R, Mannion R, Charles N, et al. The practice of commissioning healthcare from a private provider: learning from an in-depth case study. BMC Health Serv Res 2013;13(Suppl. 1):S4. doi:10.1186/1472-6963-13-S1-S4.
Sheaff R, Chambers N, Charles N, Exworthy M, Mahon A, Byng R, et al. How managed a market? Modes of commissioning in England and Germany. BMC Health Serv Res 2013;13(Suppl. 1):S8. doi:10.1186/1472-6963-13-S1-S8.
Sheaff R. Plural provision of primary medical care in England, 2002–2012. J Health Serv Res Policy 2013;18(Suppl. 2):20–8.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Sheaff R, Peel V. Best Practice in Health Care Commissioning. Harlow: Longman; 1993.
- Øvretveit J. Purchasing for Health: A Multidisciplinary Introduction to the Theory and Practice of Health Purchasing. Buckingham: Open University Press; 1995.
- Klein R. The New Politics of Health. Harlow: Longman; 1995.
- Working for Patients. London: HMSO; 1989.
- Enthoven A. Managed competition of alternative delivery systems. J Health Polit Policy Law 1988;13:305-21. http://dx.doi.org/10.1215/03616878-13-2-305.
- Mays N, Dixon J. The Plurality of Purchasing. London: The King’s Fund; 1996.
- Exworthy M. A review of recent structural changes to District Health Authorities as purchasing organisations. Environ Plann C: Gov Policy 1993;11:279-89. http://dx.doi.org/10.1068/c110279.
- Robinson R, Le Grand J. Evaluating the NHS Reform. London: The King’s Fund; 1994.
- Peckham S, Exworthy M. Primary Care in the UK: Policy, Organization and Management. Basingstoke: Palgrave; 2003.
- Mays N, Goodwin N, Bevan G, Wyke S. What is total purchasing?. BMJ 1997;315:652-5. http://dx.doi.org/10.1136/bmj.315.7109.652.
- Wainwright D, Calnan M, Exworthy M, Peckham S, Powell M, Hann A. Shaping Health Policy: Case Study Methods and Analysis. Bristol: Policy Press; 2011.
- Dixon J, Le Grand J, Mays N, Mulligan JA. Learning from the NHS Internal Market. London: The King’s Fund; 1998.
- Goodwin N, Le Grand J, Mays N, Mulligan JA. Learning from the NHS Internal Market A Review of the Evidence. London: The King’s Fund; 1998.
- Callaghan G, Exworthy M, Hudson B, Powell M. Prospects for collaboration in primary care: relationships between social services and the new PCGs. J Inter-Prof Care 2000;14:19-26. http://dx.doi.org/10.1080/713678538.
- Timmins N. Never Again? The Story of the Health and Social Care Act 2012. A Study in Coalition Government and Decision Making. London: The King’s Fund; 2012.
- Department of Health . Shifting the Balance of Power: The Next Steps n.d. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/Browsable/DH_4099025 (accessed 7 September 2007).
- Exworthy M, Greener I, Mckee L, Ferlie E, Hyde P. Organising and Re-organising: Power and Change in Health-care Organisations. London: Palgrave Macmillan; 2008.
- Curry N, Goodwin N, Naylor C, Robertson R. Practice Based Commissioning. Reinvigorate, Replace or Abandon?. London: The King’s Fund; 2008.
- Putting Commissioning into Practice: Implementing Practice Based Commissioning through Good Financial Management. London: Audit Commission; 2007.
- Coleman A, Checkland K, Harrison S, Dowswell G. Practice-based Commissioning: Theory, Implementation and Outcome. Manchester: National Primary Care Research and Development Centre; 2009.
- Klein R. The New Politics of the NHS. Oxford: Radcliffe Medical; 2006.
- Millar R, Powell M, Dixon A. What was the programme theory of New Labour’s Health System Reforms?. J Health Serv Res Policy 2012;17:7-15. http://dx.doi.org/10.1258/jhsrp.2011.010189.
- Fotaki M, Roland M, Boyd A, McDonald R, Sheaff R, Smith L. What benefits will choice bring to patients? Literature review and assessment of implications. J Health Serv Res Policy 2008;13:178-84. http://dx.doi.org/10.1258/jhsrp.2008.007163.
- Baxter K, Wilberforce M, Glendinning C. Personal budgets and the workforce implications for social care providers: expectations and early experiences. Soc Policy Soc 2011;10:55-6. http://dx.doi.org/10.1017/S1474746410000382.
- Exworthy M, Powell M, Mohan J. The NHS: quasi-market, quasi-hierarchy and quasi-network?. Public Money Manag 1999;19:15-22. http://dx.doi.org/10.1111/1467-9302.00184.
- Klein R. The troubled transformation of Britain’s National Health Service. N Engl J Med 2006;355:409-15. http://dx.doi.org/10.1056/NEJMhpr062747.
- Exworthy M. Localism in the NHS quasi-market. Environ Plann: Gov Policy 1998;16:449-62. http://dx.doi.org/10.1068/c160449.
- Exworthy M, Moon G. The shape of things to come. Health Serv J 1998;108:20-2.
- Sheaff R. Medicine and management in English primary care: a shifting balance of power?. J Soc Policy 2009;38:627-47. http://dx.doi.org/10.1017/S0047279409990183.
- Commissioning: Fourth Report of Session 2009–10. London: HMSO; 2010.
- Gridley K, Spiers G, Aspinal F, Bernard S, Atkin K, Parker G. Can general practitioner commissioning deliver equity and excellence? Evidence from two studies of service improvement in the English NHS. J Health Serv Res Policy 2012;17:87-93. http://dx.doi.org/10.1258/jhsrp.2011.010176.
- Gould M. PCT chiefs’ pay hike fails to close gap. Health Serv J 2004;112:6-7.
- Hunter D. The Health Debate. Bristol: Policy Press; 2008.
- Rhodes R. Understanding Governance. Buckingham: Open University Press; 1997.
- Glaser W. Paying the Hospital: The Organization, Dynamics, and Effects of Differing Financial Arrangements. San Francisco, CA: Jossey-Bass; 1987.
- Alber J, Bernadi-Schenkluhn B. Westeuropäische Gesundheitsysteme im Vergleich: Bundesrepublik Deutschland, Schweiz, Frankreich, Italien, Großbritannien. Frankfurt: Campus; 1992.
- Roemer M. National Health Systems of the World. Oxford: Oxford University Press; 1993.
- Vincent-Jones P. The new public contracting: public versus private ordering?. Indiana J Glob Leg Stud 2007;14:259-78. http://dx.doi.org/10.2979/GLS.2007.14.2.259.
- Petsoulas C, Allen P, Hughes D, Vincent-Jones P, Roberts J. The use of standard contracts in the English National Health Service: a case study analysis. Soc Sci Med 2011;73:185-92. http://dx.doi.org/10.1016/j.socscimed.2011.05.021.
- Foucault M. Madness and Civilization. London: Tavistock; 1967.
- Foucault M. Discipline and Punish: The Birth of the Prison. London: Allen Lane; 1977.
- Lemke T. ‘The birth of bio-politics’: Michel Foucault’s lecture at the Collège de France on neo-liberal governmentality. Econ Soc 2001;30:190-207. http://dx.doi.org/10.1080/03085140120042271.
- Keen S. Debunking Economics: The Naked Emperor of the Social Sciences. London: Zed Books; 2001.
- Thomson G, Frances J, Levacic R, Mitchell J. Markets, Hierarchies and Networks: The Coordination of Social Life. London: Sage; 1991.
- Van de Ven WPMM. Market-oriented health care reforms: trends and future options. Soc Sci Med 1996;43:655-66. http://dx.doi.org/10.1016/0277-9536(96)00111-6.
- Bärnighausen T, Sauerborn R. One hundred and eighteen years of the German health insurance system: are there any lessons for middle- and low-income countries?. Soc Sci Med 2002;54:1559-87. http://dx.doi.org/10.1016/S0277-9536(01)00137-X.
- Okma KGH, Marmor TR, Oberlander J. Managed competition for Medicare? Sobering lessons from the Netherlands. N Engl J Med 2011;365:287-9. http://dx.doi.org/10.1056/NEJMp1106090.
- Moriya AS, Vogt WB, Gaynor M. Hospital prices and market structure in the hospital and insurance industries. Health Econ Policy Law 2010;5:459-79. http://dx.doi.org/10.1017/S1744133110000083.
- Foucault M. The Archaeology of Knowledge. London: Routledge; 2002.
- Jessop B, Bröckling U, Krasmann S, Lemke T. Governmentality Current Issues and Future Challenges. London: Routledge; 2010.
- Broer T, Nieboer AP, Bal R. Governing mental health care: how power is exerted in and through a quality improvement collaborative. Public Adm 2012;90:800-15. http://dx.doi.org/10.1111/j.1467-9299.2011.01967.x.
- Foucault M. Power/Knowledge. New York, NY: Pantheon; 1980.
- Foucault M. The Birth of the Clinic: An Archaeology of Medical Perception. London: Tavistock; 1973.
- Brown T, Potoski M. Contracting for management: assessing management capacity under alternative service delivery arrangements. J Policy Anal Manag 2006;25:323-46. http://dx.doi.org/10.1002/pam.20175.
- McCafferty S, Williams I, Hunter D, Robinson S, Donaldson C, Bate A. Implementing world class commissioning competencies. J Health Serv Res Policy 2012;17:40-8. http://dx.doi.org/10.1258/jhsrp.2011.011104.
- Checkland K, Coleman A, Harrison S, Hiroeh U. ‘We can’t get anything done because . . .’: making sense of ‘barriers’ to Practice-based Commissioning. J Health Serv Res Policy 2009;14:20-6. http://dx.doi.org/10.1258/jhsrp.2008.008043.
- Abbott S, Procter S, Iacovou N. Clinicians, market players or bureaucrats? Changing expectations of the general practitioner role in the English and Welsh NHS, 1991–2005. J Health Organ Manag 2008;22:433-45. http://dx.doi.org/10.1108/14777260810898679.
- Pickin C, St. Leger S. Assessing Health Need Using the Life Cycle Framework. Buckingham: Open University Press; 1993.
- Milne R. Evidence-based purchasing. Evid Based Med 1996;1:101-2.
- Sheaff R. Plural provision of primary medical care in England, 2002–2012. J Health Serv Res Policy 2013;18:20-8. http://dx.doi.org/10.1177/1355819613489544.
- Macq J, Martiny P, Villalobos LB, Solis A, Miranda J, Mendez HC, et al. Public purchasers contracting external primary care providers in Central America for better responsiveness, efficiency of health care and public governance: issues and challenges. Health Policy 2008;87:377-88. http://dx.doi.org/10.1016/j.healthpol.2008.01.007.
- Cousins P, Lawson P. The effect of socialization mechanisms and performance measures on supplier integration in new product development. Br J Manag 2007;18:311-26. http://dx.doi.org/10.1111/j.1467-8551.2007.00514.x.
- Hartley K. Public purchasing. Public Money Manag 1991;11:45-9. http://dx.doi.org/10.1080/09540969109387641.
- Klijn E-H. Governing networks in the hollow state: contracting out, process management or a combination of the two?. Public Manag Rev 2002;4:149-65. http://dx.doi.org/10.1080/14616670210130516.
- Johnston JM, Romzek BS. Social welfare contracts as networks: the impact of network stability on management and performance. Adm Soc 2008;40:115-46. http://dx.doi.org/10.1177/0095399707312826.
- Preker AS, Harding A, Travis P. ‘Make or buy’ decisions in the production of health care goods and services: new insights from institutional economics and organizational theory. Bull World Health Organ 2000;78:779-90.
- Button M, Leys C. Healthcare Fraud in the New NHS Market: A Threat to Patient Care. London: Centre of Health and the Public Interest; 2013.
- Lindstedt C, Naurin D. Transparency is not enough: making transparency effective in reducing corruption. Int Polit Sci Rev 2010;31:301-22. http://dx.doi.org/10.1177/0192512110377602.
- Colin-Thomé D, Field S. General Practice Out-of-Hours Services Project to Consider and Assess Current Arrangements. London: Care Quality Commission; 2010.
- Bevan G, Hood C. What’s measured is what matters: targets and gaming in the English public health care system. Public Adm 2006;84:517-38. http://dx.doi.org/10.1111/j.1467-9299.2006.00600.x.
- Bevan G. Setting targets for health care performance: lessons from a case study of the English NHS. Nat Inst Econ Rev 2006;197:67-79.
- Gray K, Bailey MF. Non-price competition in NHS secondary care contracting: empirical results. J Health Organ Manag 2008;22:480-95. http://dx.doi.org/10.1108/14777260810898705.
- Rogers R. ‘HRG drift’ and payment by results. BMJ 2005;330. http://dx.doi.org/10.1136/bmj.330.7491.563.
- Campbell S, Reeves D, Kontopantelis E, Sibbald B, Roland M. Effects of pay for performance on the quality of primary care in England. N Engl J Med 2009;361:368-78. http://dx.doi.org/10.1056/NEJMsa0807651.
- Bevan G. Have targets done more harm than good in the English NHS? No. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.a3129.
- Amirkhanyan AA. Monitoring across sectors: examining the effect of nonprofit and for-profit contractor ownership on performance monitoring in state and local contracts. Public Adm Rev 2010;70:742-55. http://dx.doi.org/10.1111/j.1540-6210.2010.02202.x.
- Amirkhanyan AA. Collaborative performance measurement: examining and explaining the prevalence of collaboration in state and local government contracts. J Public Adm Res Theory 2009;19:523-54. http://dx.doi.org/10.1093/jopart/mun022.
- Heinrich CJ. Do government bureaucrats make effective use of performance management information?. J Public Adm Res Theory 1999;9:363-94. http://dx.doi.org/10.1093/oxfordjournals.jpart.a024415.
- Moynihan DP. Why and how do state governments adopt and implement ‘managing for results’ reforms?. J Public Adm Res Theory 2005;15:219-43. http://dx.doi.org/10.1093/jopart/mui012.
- Lambright K. Getting what you ask for: barriers to proper use of service monitoring tools. Am Rev Public Adm 2008;38:362-79. http://dx.doi.org/10.1177/0275074007309150.
- Van Slyke DM. Agents or stewards: using theory to understand the government–nonprofit social service contracting relationship. J Public Adm Res Theory 2007;17:157-87. http://dx.doi.org/10.1093/jopart/mul012.
- Williamson O. Markets and Hierarchies. New York, NY: Free Press; 1975.
- Ashton T. Contracting for health services in New Zealand: a transaction cost analysis. Soc Sci Med 1998;46:357-67. http://dx.doi.org/10.1016/S0277-9536(97)00164-0.
- Macneil IR. Contracts: adjustment of long-term relations under classical, neo-classical and relational contract law. Northwestern Uni Law Rev 1978;72:854-905.
- Felstead A, Ashton D. Tracing the link: organisational structures and skill demands. Hum Res Manag J 2000;10:5-21. http://dx.doi.org/10.1111/j.1748-8583.2000.tb00023.x.
- Van Slyke DM. The mythology of privatization in contracting for social services. Public Adm Rev 2003;63:296-315. http://dx.doi.org/10.1111/1540-6210.00291.
- Feiock RC, Jang HS. Nonprofits as local government service contractors. Public Adm Rev 2009;69:668-80. http://dx.doi.org/10.1111/j.1540-6210.2009.02016.x.
- Bojke C, Gravelle H, Wilkin D. Is bigger better for primary care groups and trusts?. BMJ 2001;322:599-602. http://dx.doi.org/10.1136/bmj.322.7286.599.
- Marini G, Street A. A transaction costs analysis of changing contractual relations in the English NHS. Health Policy 2007;83:17-26. http://dx.doi.org/10.1016/j.healthpol.2006.11.007.
- Greaves F, Millett C, Pape UJ, Soljak M, Majeed A. Association between primary care organisation population size and quality of commissioning in England: an observational study. Br J Gen Pract 2012;62:e46-54. http://dx.doi.org/10.3399/bjgp12X616364.
- Strauss A, Schatzman L, Ehrlich D, Bucher R, Sabshin M, Friedson E. The Hospital in Modern Society. New York, NY: Free Press; 1963.
- Abbott A. The System of Professions: An Essay on the Division of Expert Labor. Chicago, IL: Chicago University Press; 1988.
- Griffiths L. Accomplishing team: teamwork and categorisation in two community mental health teams. Sociol Rev 2008;45:59-78. http://dx.doi.org/10.1111/1467-954X.00054.
- Allen P. Contracts in the National Health Service internal market. Mod Law Rev 1995;58:321-42. http://dx.doi.org/10.1111/j.1468-2230.1995.tb02013.x.
- Granovetter M. Economic action and social structure: the problem of embeddedness. Am J Sociol 1983;41:481-510.
- Mintzberg H. Power in and around Organizations. Englewood Cliffs, NJ: Prentice Hall; 1983.
- Bachrach P, Baratz MS. Power and Poverty: Theory and Practice. London: Oxford University Press; 1970.
- Lukes S. Power. London: Macmillan; 1974.
- Therborn G. The Ideology of Power and the Power of Ideology. London: Verso; 1980.
- Siciliani L, Stanciol A. Bargaining and the Provision of Health Services. York: University of York; 2008.
- Klein R. Policy making in the National Health Service. Polit Stud 1974;22:1-14. http://dx.doi.org/10.1111/j.1467-9248.1974.tb01469.x.
- Bate A, Donaldson C, Murtagh MJ. Managing to manage healthcare resources in the English NHS? What can health economics teach? What can health economics learn?. Health Policy 2007;84:249-61. http://dx.doi.org/10.1016/j.healthpol.2007.04.001.
- Flynn R, Pickard S, Williams G. Contracts and the quasi-market in community health services. J Soc Policy 1995;24:529-50. http://dx.doi.org/10.1017/S0047279400025423.
- Bode I. Co-governance within networks and the non-profit–for-profit divide. Public Manag Rev 2006;8:551-66. http://dx.doi.org/10.1080/14719030601022932.
- Porter A, Mays N, Shaw S, Rosen R, Smith J. Commissioning healthcare for people with long term conditions: the persistence of relational contracting in England’s NHS quasi-market. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-S1-S2.
- Bevan G. Impact of devolution of health care in the UK: provider challenge in England and provider capture in Wales, Scotland and Northern Ireland?. J Health Serv Res Policy 2010;15:67-8. http://dx.doi.org/10.1258/jhsrp.2010.009174.
- Kettl D. Sharing Power: Public Governance and Private Markets. Washington, DC: Brookings Institution; 1993.
- Abel S, Gibson D, Ehau T, Leach D. Implementing the Primary Health Care Strategy: a Maori health provider perspective. Soc Policy J New Zealand 2005;25:70-87.
- Dowling B. Effect of fundholding on waiting times: database study. BMJ 1997;315:290-2. http://dx.doi.org/10.1136/bmj.315.7103.290.
- Dusheiko M, Gravelle H, Jacobs R. The effect of practice budgets on patient waiting times: allowing for selection bias. Health Econ 2004;13:941-58. http://dx.doi.org/10.1002/hec.937.
- Dusheiko M, Gravelle H, Jacobs R, Smith P. The effect of financial incentives on gatekeeping doctors: evidence from a natural experiment. J Health Econ 2006;25:449-78. http://dx.doi.org/10.1016/j.jhealeco.2005.08.001.
- Mannion R. The evolution of general practitioner purchasing in the English NHS: continuity, change and future challenges. Int J Health Serv 2008;38:717-30. http://dx.doi.org/10.2190/HS.38.4.h.
- Greener I, Mannion R. Will practice-based commissioning in the English NHS resolve the problems experienced by GP fundholding?. Public Money Manag 2008;28:231-8. http://dx.doi.org/10.1111/j.1467-9302.2008.00649.x.
- Spoor C, Munro J. Do budget-holding physicians respond to price? The case of fundholding in the UK. Health Serv Manag Res 2003;16:261-7. http://dx.doi.org/10.1258/095148403322488955.
- Berle A, Means G. The Modern Corporation and Private Property. New York, NY: Macmillan; 1932.
- Davis JH, Schoorman FD, Donaldson L. Toward a stewardship theory of management. Acad Manage Rev 1997;22:20-47.
- Fairclough N. Discourse analysis in organization studies: the case for critical realism. Organ Stud 2005;26:915-39. http://dx.doi.org/10.1177/0170840605054610.
- Andersen LB, Jakobsen M. Does ownership matter for the provision of professionalized services? Hip operations at publicly and privately owned clinics in Denmark. Public Adm 2011;89:956-74. http://dx.doi.org/10.1111/j.1467-9299.2010.01881.x.
- Waring J, Bishop S. Going private: clinicians’ experience of working in UK independent sector treatment centres. Health Policy 2012;104:172-8. http://dx.doi.org/10.1016/j.healthpol.2011.07.006.
- Hoque K, Davis S, Humphreys M. Freedom to do what you are told: senior management team autonomy in an NHS acute trust. Public Adm 2004;82:355-75. http://dx.doi.org/10.1111/j.0033-3298.2004.00398.x.
- Pollitt C, van Thiel S, Homburg V. New Public Management in Europe. Manag Online Rev 2007:1-7.
- Courpasson D. Le changement est un outil politique. Rev Fr Gestion 1998;120:6-16.
- Harrison S. Co-optation, commodification and the medical model: governing UK medicine since 1991. Public Adm 2009;87:184-97. http://dx.doi.org/10.1111/j.1467-9299.2009.01752.x.
- Nicholson-Crotty J. Politics, policy, and the motivations for advocacy in nonprofit reproductive health and family planning providers. Nonprofit Volunt Sect Q 2007;36:5-21. http://dx.doi.org/10.1177/0899764006291778.
- Dias JJ, Maynard-Moody S. For-profit welfare: contracts, conflicts, and the performance paradox. J Public Adm Res Theory 2007;17:189-211. http://dx.doi.org/10.1093/jopart/mul002.
- Rhodes RAW. Beyond Westminster and Whitehall. London: Allen & Unwin; 1988.
- Gains F. ‘Hardware, software or network connection?’ Theorizing crisis in the UK Next Steps Agencies?. Public Adm 2004;82:547-66. http://dx.doi.org/10.1111/j.0033-3298.2004.00406.x.
- Fichera E, Gravelle H, Pezzino M, Sutton M. Specification of Financial Incentives for Quality in Health Care Contracts. Manchester: University of Manchester; 2012.
- Flodgren G, Eccles MP, Shepperd S, Scott A, Parmelli E, Beyer FR. An Overview of Reviews Evaluating the Effectiveness of Financial Incentives in Changing Healthcare Professional Behaviours and Patient Outcomes n.d. http://summaries.cochrane.org/CD009255/how-good-are-financial-incentives-in-changing-health-care (accessed 31 December 2012).
- Chalkley M, Tilley C. The existence and nature of physician agency: evidence of stinting from the British National Health Service. J Econ Manag Strat 2005;14:647-64. http://dx.doi.org/10.1111/j.1530-9134.2005.00077.x.
- Maisey S, Steel N, Marsh R, Gillam S, Fleetcroft R, Howe A. Effects of payment for performance in primary care: qualitative interview study. J Health Serv Res Policy 2008;13:133-9. http://dx.doi.org/10.1258/jhsrp.2008.007118.
- Farrar S, Yi D, Sutton M, Chalkley M, Sussex J, Scott A. Has payment by results affected the way that English hospitals provide care? Difference-in-differences analysis. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b3047.
- Is the Treatment Working? Progress with the NHS System Reform Programme. London: Audit Commission; 2008.
- Cheng S-H, Chen C-C, Tsai S-L. The impacts of DRG-based payments on health care provider behaviors under a universal coverage system: a population-based study. Health Policy 2012;107:202-8. http://dx.doi.org/10.1016/j.healthpol.2012.03.021.
- Smith J, Curry N, Mays N, Dixon J. Where Next for Commissioning in the English NHS?. London: Nuffield Trust; 2010.
- Rosenthal MB, Landon BE, Normand S-LT, Frank RG, Epstein AM. Pay for performance in commercial HMOs. N Engl J Med 2006;355:1895-902. http://dx.doi.org/10.1056/NEJMsa063682.
- Doran T, Fullwood C, Gravelle H, Reeves D, Kontopantelis E, Hiroeh U, et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med 2006;355:375-84. http://dx.doi.org/10.1056/NEJMsa055505.
- Herck PV, Smedt DD, Annemans L, Remmen R, Rosenthal MB, Sermeus W. Systematic review: effects, design choices, and context of pay-for-performance in health care. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-247.
- Werner RM, Kolstad JT, Stuart EA, Polsky D. The effect of pay-for-performance in hospitals: lessons for quality improvement. Health Aff 2011;30:690-8. http://dx.doi.org/10.1377/hlthaff.2010.1277.
- Gillam SJ, Siriwardena AN, Steel N. Pay-for-performance in the united kingdom: impact of the quality and outcomes framework – a systematic review. Ann Fam Med 2012;10:461-8. http://dx.doi.org/10.1370/afm.1377.
- Lee G, Kleinman K, Soumerai SB, Tse A, Cole D, Fridkin S, et al. Effect of nonpayment for preventable infections in U.S. hospitals. N Engl J Med 2012;367:1428-37. http://dx.doi.org/10.1056/NEJMsa1202419.
- Levin-Scherz J, DeVita N, Timbie J. Impact of pay-for-performance contracts and network registry on diabetes and asthma HEDIS® measures in an integrated delivery network. Med Care Res Rev 2006;63:14S-28S. http://dx.doi.org/10.1177/1077558705284057.
- Manzano-Santaella A. Disentangling the impact of multiple innovations to reduce delayed hospital discharges. J Health Serv Res Policy 2010;15:41-6. http://dx.doi.org/10.1258/jhsrp.2009.009049.
- Thaler R, Sunstein C. Nudge: Improving Decisions about Health, Wealth, and Happiness. New Haven, CT: Yale University Press; 2008.
- Brown T, Potoski M, Van Slyke D. Complex Contracting: Lessons from the Department of Homeland Security’s Secure Border Initiative n.d.
- Jakobsen MLF. The effects of new public management: activity-based reimbursement and efficiency in the Scandinavian hospital sectors. Scand Polit Stud 2010;33:113-34. http://dx.doi.org/10.1111/j.1467-9477.2009.00241.x.
- Propper C, Burgess S, Gossage D. Competition and quality: evidence from the NHS internal market 1991–9. Econ J 2008;118:138-70. http://dx.doi.org/10.1111/j.1468-0297.2007.02107.x.
- Marshall M, Smith P. Rewarding results: using financial incentives to improve quality. Qual Saf Health Care 2003;12:397-8. http://dx.doi.org/10.1136/qhc.12.6.397.
- Baumol WJ. Contestable markets: an uprising in the theory of industry structure. Am Econ Rev 1982;72:1-15.
- Anderson GF. From ‘soak the rich’ to ‘soak the poor’: recent trends in hospital pricing. Health Aff 2007;26:780-9. http://dx.doi.org/10.1377/hlthaff.26.3.780.
- Light D. From managed competition to managed cooperation: theory and lessons from the British experience. Milbank Q 1997;75:297-341. http://dx.doi.org/10.1111/1468-0009.00058.
- Beckert W, Christensen M, Collyer K. Choice of NHS-funded hospital services in England. Econ J 2012;122:400-17. http://dx.doi.org/10.1111/j.1468-0297.2012.02496.x.
- Dusheiko M, Goddard M, Gravelle H, Jacobs R. Explaining trends in concentration of healthcare commissioning in the English NHS. Health Econ 2008;17:907-26. http://dx.doi.org/10.1002/hec.1301.
- Milward HB, Provan K. Governing the hollow state. J Public Adm Res Theory 2000;10:359-79. http://dx.doi.org/10.1093/oxfordjournals.jpart.a024273.
- Fennell ML, Alexander JA. Perspectives on organizational change in the US medical care sector. Ann Rev Sociol 1993;19:89-112. http://dx.doi.org/10.1146/annurev.so.19.080193.000513.
- Hinings CR, Hickson DJ, Pennings JM, Schneck RE. Structural conditions of intraorganizational power. Adm Sci Q 1974;19:22-44. http://dx.doi.org/10.2307/2391786.
- Williamson OE. Comparative economic organization: the analysis of discrete structural alternatives. Adm Sci Q 1991;36:269-96. http://dx.doi.org/10.2307/2393356.
- Appleby J, Harrison T, Hawkins L, Dixon A. Payment by Results: How Can Payment Systems Help to Deliver Better Care?. London: The King’s Fund; 2012.
- Dranove D, White WD. Recent theory and evidence on competition in hospital markets. J Econ Manag Strat 1994;3:169-20. http://dx.doi.org/10.1111/j.1430-9134.1994.00169.x.
- Cooper Z, Gibbons S, Jones S, McGuire A. Does hospital competition save lives? Evidence from the English NHS patient choice reforms. Econ J 2011;121:F228-F260. http://dx.doi.org/10.1111/j.1468-0297.2011.02449.x.
- Gaynor M, Moreno-Serra R, Propper C. Death by Market Power: Reform, Competition and Patient Outcomes in the National Health Service n.d. www.nber.org/papers/w16164 (accessed 24 January 2013).
- Bloom N, Propper C, Seiler S, Van Reenen J. The Impact of Competition on Management Quality: Evidence from Public Hospitals. London: Centre for Economic Performance, London School of Economics and Political Science; 2010.
- Gravelle H, Santos R, Siciliani L, Goudie R. Hospital Quality Competition under Fixed Prices. York: University of York; 2012.
- Siciliani L, Martin S. An empirical analysis of the impact of choice on waiting times. Health Econ 2007;16:763-79. http://dx.doi.org/10.1002/hec.1205.
- Turner S, Allen P, Bartlett W, Pérotin V. Innovation and the English National Health Service: a qualitative study of the independent sector treatment centre programme. Soc Sci Med 2011;73:522-9. http://dx.doi.org/10.1016/j.socscimed.2011.06.014.
- Glendinning C, Halliwell S, Jacobs S, Rummery K, Tyrer J. New kinds of care, new kinds of relationships: how purchasing services affects relationships in giving and receiving personal assistance. Health Soc Care Comm 2000;8:201-11. http://dx.doi.org/10.1046/j.1365-2524.2000.00242.x.
- Forder J, Allan S. Competition in the Care Homes Market. London: Office of Health Economics; 2011.
- Allen P, Turner S, Bartlett W, Perotin V, Matchaya G, Zamora B. Provider diversity in the English NHS: a study of recent developments in four local health economies. J Health Serv Res Policy 2012;17:23-30. http://dx.doi.org/10.1258/jhsrp.2011.011015.
- Sheaff R, Child S, Schofield J, Pickard S, Mannion R. Understanding Professional Partnerships and Non-hierarchical Organisations. London: National Institute of Heath Research Service Delivery and Organisation Programme; 2012.
- Kessler DP, Geppert JJ. The effects of competition on variation in the quality and cost of medical care. J Econ Manag Strat 2005;14:575-89. http://dx.doi.org/10.1111/j.1530-9134.2005.00074.x.
- Shen Y-C. The effect of financial pressure on the quality of care in hospitals. J Health Econ 2003;22:243-69. http://dx.doi.org/10.1016/S0167-6296(02)00124-8.
- Gaynor M, Moreno-Serra R, Propper C. Can competition improve outcomes in UK health care? Lessons from the past two decades. J Health Serv Res Policy 2012;17:49-54. http://dx.doi.org/10.1258/jhsrp.2011.011019.
- Mukamel D, Zwanziger J, Tomaszewski K. Penetration, competition, and risk-adjusted hospital mortality. Health Serv Res 2001;36:1019-35.
- Gowrisankaran G, Town RJ. Competition, payers, and hospital quality. Health Serv Res 2003;38:1403-22. http://dx.doi.org/10.1111/j.1475-6773.2003.00185.x.
- Volpp KGM, Williams SV, Waldfogel J, Silber JH, Schwartz JS, Pauly MV. Market reform in new jersey and the effect on mortality from acute myocardial infarction. Health Serv Res 2003;38:515-33. http://dx.doi.org/10.1111/1475-6773.00131.
- Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med 2011;364:2128-37. http://dx.doi.org/10.1056/NEJMsa1010705.
- Sari N, Blank J, Valdmanis V. Evaluating Hospital Policy and Performance: Contributions from Hospital Policy and Productivity Research. Oxford: Elsevier; 2008.
- Horwitz J. Why We Need the Independent Sector: The Behavior, Law, &Amp; Ethics of Not-for-Profit Hospitals 2004. http://law.bepress.com/umichlwps-olin/art3 (accessed 15 March 2013).
- Melnick G, Keeler E, Zwanziger J. Market power and hospital pricing: are nonprofits different?. Health Aff 1999;18:167-73. http://dx.doi.org/10.1377/hlthaff.18.3.167.
- Smith P. Achieving Better Value for Money in Health Care. Paris: Organisation for Economic Co-operation and Development; 2009.
- Lamothe M, Lamothe S. Competing for what? Linking competition to performance in social service contracting. Am Rev Public Adm 2010;40:326-50. http://dx.doi.org/10.1177/0275074009337621.
- Lavoie J, Boulton A, Dwyer J. Analysing contractual environments: lessons from indigenous health in Canada, Australia and New Zealand. Public Adm 2010;88:665-79. http://dx.doi.org/10.1111/j.1467-9299.2009.01784.x.
- Basu J, Mobley L. Do HMOs reduce preventable hospitalizations for Medicare beneficiaries?. Med Care Res Rev 2007;64:544-67. http://dx.doi.org/10.1177/1077558707301955.
- Csaba I, Fenn P. Contractual choice in the managed health care market: an empirical analysis. J Health Econ 1997;16:579-88. http://dx.doi.org/10.1016/S0167-6296(96)00533-4.
- Chalkley M, McVicar D. Choice of contracts in the British National Health Service: an empirical study. J Health Econ 2008;27:1115-67. http://dx.doi.org/10.1016/j.jhealeco.2008.05.005.
- Hughes D, Dingwall R. Sir Henry Maine, Joseph Stalin and the reform of the NHS. J Soc Welf Law 1990;5:296-309. http://dx.doi.org/10.1080/09649069008412540.
- Vincent-Jones P. The New Public Contracting: Regulation, Responsiveness, Relationality. Oxford: Oxford University Press; 2006.
- Bolton MK, Malmrose R, Ouchi WG. The organization of innovation in the United States and Japan: neoclassical and relational contracting. J Manag Stud 1994;31:653-79. http://dx.doi.org/10.1111/j.1467-6486.1994.tb00633.x.
- Sheaff R. Governance in gridlock in the Russian health system; the case of Sverdlovsk oblast. Soc Sci Med 2005;60:2359-69. http://dx.doi.org/10.1016/j.socscimed.2004.10.008.
- Morgan G. Images of Organization. Thousand Oaks, CA: Sage; 2007.
- Byng R, Norman I, Redfern S. Using realistic evaluation to evaluate a practice-level intervention to improve primary healthcare for patients with long-term mental illness. Evaluation 2005;11:69-93. http://dx.doi.org/10.1177/1356389005053198.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- Kwon W, Clarke I, Wodak R. Organizational decision-making, discourse, and power: integrating across contexts and scales. Discourse Comm 2009;3:273-302. http://dx.doi.org/10.1177/1750481309337208.
- Hodge B, Coronado G. Mexico Inc.? Discourse analysis and the triumph of managerialism. Organization 2006;13:529-47. http://dx.doi.org/10.1177/1350508406065104.
- Equity and Excellence: Liberating the NHS. London: Department of Health; 2010.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Rey L, Brouselle A, Dedobbeleer N. Logic analysis: testing program theory to better evaluate complex interventions. Can J Prog Eval 2012;26:61-89.
- Devereaux PJ, Heels-Ansdell D, Lacchetti C, Haines T, Burns KEA, Cook DJ, et al. Payments for care at private for-profit and private not-for-profit hospitals: a systematic review and meta-analysis. CMAJ 2004;170:1817-24. http://dx.doi.org/10.1503/cmaj.1040722.
- McBride D, Hardoon S, Walters K, Gilmour S, Raine R. Explaining variation in referral from primary to secondary care: cohort study. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c6267.
- Smith P, Papanicolas I. Health System Performance Comparison: An Agenda for Policy, Information and Research. 2012. www.euro.who.int/en/what-we-do/data-and-evidence/health-evidence-network-hen/publications/2012/health-system-performance-comparison-an-agenda-for-policy,-information-and-research-2012 (accessed 22 January 2013).
- Organisation for Economic Co-operation and Development . Health at a Glance 2011: OECD Indicators n.d. http://dx.doi.org/10.1787/health_glance-2011-en (accessed 23 January 2013).
- World class commissioning league table . Health Service Journal n.d. www.hsj.co.uk/topics/world-class-commissioning-scores-2010/world-class-commissioning-league-table/5018174.article?blocktitle=News&contentID=3619 (accessed 3 February 2015).
- 2011–12 PCT Recurrent Revenue Allocations Exposition Book. London: Department of Health; 2012.
- Yin RK. Enhancing the quality of case studies in health services research. Health Serv Res 1999;34:1209-24.
- Exworthy M, Frosini F, Jones L, Peckam S, Powell M, Greener I, et al. Decentralisation and Performance: Autonomy and Incentives in Local Health Economies. Southampton: National Coordinating Centre for the Service Delivery and Organisation; 2010.
- Ailon G. What B would otherwise do: a critique of conceptualizations of “power” in organizational theory. Organization 2006;13:771-800. http://dx.doi.org/10.1177/1350508406068504.
- Petmesidou M, Guillén AM. ‘Southern-style’ national health services? Recent reforms and trends in Spain and Greece. Soc Policy Adm 2008;42:106-24. http://dx.doi.org/10.1111/j.1467-9515.2008.00598.x.
- Bitektine A. Prospective case study design: qualitative method for deductive theory testing. Organ Res Methods 2008;11:160-80. http://dx.doi.org/10.1177/1094428106292900.
- Factsheet A1: The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet A2: The Case for Change – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet A3: Overview of Health and Care Structures – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet A4: Scrutiny and Improvements – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet B1: Clinically-led Commissioning – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet B2: Provider Regulation to Support Innovative and Efficient Services – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet B3: Greater Voice for Patients – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet B4: New Focus for Public Health – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet B5: Greater Accountability Locally and Nationally – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet B6: Modernising Health and Care Public Bodies – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet B7: Support Workers and Voluntary Registration – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet C1: Improving Quality of Care – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet C2: Reducing Health Inequalities – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet C3: Improving Integration of Services – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet C4: Choice and Competition – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet C5: The Overarching Role (NHS) of the Secretary of State – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet C6: Reconfiguring Services – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet C7: Establishing New National Bodies – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet C8: Embedding Research as a Core Function of the Health Service – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Factsheet C9: Education and Training – The Health and Social Care Act 2012. London: Department of Health; 2012.
- Dorrell S. How NHS and Commissioning Need to Change to Meet Challenges Ahead 2012.
- Lansley A. GP Commissioning and the Future of the NHS 2010.
- Lansley A. A Shared Ambition to Improve Outcomes 2010.
- Lansley A. Shifting Power to the Frontline 2010.
- Howe G. GP Commissioning: Making It Happen 2010.
- Nicholson D. Sir David Nicholson’s Speech to the NHS Confederation 2010.
- Public Accounts Committee . Thirty-Third Report. National Health Service Landscape Review, HC708, 2010–11 n.d. http://www.publications.parliament.uk/pa/cm201012/cmselect/cmpubacc/764/76402.htm.
- Thirteenth Report of Session 2010–12, 17 January 2012. London: HMSO; 2012.
- Rayner M, Scarborough P, Allender S. Values underlying the National Service Framework for coronary heart disease in England: a discourse analysis. J Health Serv Res Policy 2006;11:67-73. http://dx.doi.org/10.1258/135581906776318956.
- Chambers N, Sheaff R, Mahon A, Byng R, Mannion R, Charles N, et al. The practice of commissioning healthcare from a private provider: learning from an in-depth case study. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-S1-S4.
- Sampson F, O’Cathain A, Strong M, Pickin M, Esmonde L. Commissioning processes in primary care trusts: a repeated cross-sectional survey of health care commissioners in England. J Health Serv Res Policy 2012;17:31-9. http://dx.doi.org/10.1258/jhsrp.2011.010191.
- Coronini-Cronberg S, Lee H, Darzi A, Smith P. Evaluation of clinical threshold policies for cataract surgery among English commissioners. J Health Serv Res Policy 2012;17:241-7. http://dx.doi.org/10.1258/jhsrp.2012.012023.
- Black N. Patient reported outcome measures could help transform healthcare. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f167.
- The Operating Framework for the NHS in England 2011/12. London: Department of Health; 2010.
- The NHS Outcomes Framework 2011/12. London: Department of Health; 2010.
- Independent Enquiry into the Care Provided by Mid Staffordshire NHS Foundation Trust 2005–2009. London: HMSO; 2010.
- Checkland K, Snow S, McDermott I, Harrison S, Coleman A. ‘Animateurs’ and animation: what makes a good commissioning manager?. J Health Serv Res Policy 2012;17:11-7. http://dx.doi.org/10.1258/jhsrp.2011.011010.
- Player S, Leys C. Confuse and Conceal: The NHS and Independent Sector Treatment Centres. Monmouth: Merlin; 2008.
- Dixon A, Appleby J, Robertson R, Burge P, Devlin N, Albert HCT. Patient Choice: How Patients Choose and How Providers Respond 2010. www.kingsfund.org.uk/publications/patient-choice (accessed 24 January 2013).
- Pollock A, Macfarlane A, Kirkwood G, Majeed FA, Greener I, Morelli C, et al. No evidence that patient choice in the NHS saves lives. Lancet 2011;378:2057-60. http://dx.doi.org/10.1016/S0140-6736(11)61553-5.
- Frosini F, Dixon A, Robertson R. J Health Serv Res Policy 2012;17:16-22. http://dx.doi.org/10.1258/jhsrp.2011.010194.
- Yates J. Private Eye, Heart and Hip: Surgical Consultants, the National Health Service and Private Medicine. Edinburgh: Churchill Livingstone; 1995.
- Mitchell J. Med Care Res Rev 2007;64:395-41. http://dx.doi.org/10.1177/1077558707301953.
- Hanning M, Åhs A, Winblad U, Lundström M. Impact of increased patient choice of providers in Sweden: cataract surgery. J Health Serv Res Policy 2012;17:101-5. http://dx.doi.org/10.1258/jhsrp.2011.011070.
- Exworthy M, Frosini F, Jones L. Are NHS foundation trusts able and willing to exercise autonomy? ‘You can take a horse to water . . .’. J Health Serv Res Policy 2011;16:232-7. http://dx.doi.org/10.1258/jhsrp.2011.010077.
- Propper C, Damiani M, Leckie G, Dixon J. Impact of patients’ socioeconomic status on the distance travelled for hospital admission in the English National Health Service. J Health Serv Res Policy 2007;12:153-9. http://dx.doi.org/10.1258/135581907781543049.
- Exworthy M, Peckham S. Access, choice and travel: implications for health policy. Soc Policy Adm 2006;40:267-87. http://dx.doi.org/10.1111/j.1467-9515.2006.00489.x.
- Exworthy M, Berney L, Powell M. How great expectations in Westminster may be dashed locally: the local implementation of national policy on health inequalities. Policy Polit 2002;30:79-96. http://dx.doi.org/10.1332/0305573022501584.
- Henderson C, Sheaff R, Dickinson A, Beech R, Wistow G, Windle K, et al. Unplanned Admissions of Older People: Exploring the Issues. London: National Institute of Health Research Service and Delivery Organisation; 2011.
- Checkland K, Harrison S. The impact of the Quality and Outcomes Framework on practice organisation and service delivery: summary of evidence from two qualitative studies. Qual Prim Care 2010;18:139-46.
- Marks L, Cave S, Hunter D, Mason J, Peckham S, Wallace A. Governance for health and wellbeing in the English NHS. J Health Serv Res Policy 2011;16:14-21. http://dx.doi.org/10.1258/jhsrp.2010.010082.
- Health for All by the Year 2000. Geneva: World Health Organization; 1985.
- Hunter D, Perkins N. J Health Serv Res Policy 2012;17:45-52. http://dx.doi.org/10.1258/jhsrp.2012.011127.
- Byng R, Newbold L, Qureshi A, Weyer Brown C, Bannon J, Pooler J, et al. The South West Improving Access to Psychological Therapies (IAPT) Evaluation Study. Plymouth: Peninsula Medical School; 2011.
- Busse R, Riesberg A. Health Care Systems in Transition, Germany 2004. Copenhagen: World Health Organization and European Observatory on Health Systems and Policies; 2004.
- Lo Scalzo A, Donatini A, Orzella L, Cichetti A, Profili S, Maresso A. Italy, Health System Review. Copenhagen: World Health Organization; 2009.
- Glendinning C. Improving equity and sustainability in UK funding for long-term care: lessons from Germany. Soc Policy Soc 2007;6:411-22. http://dx.doi.org/10.1017/S1474746407003727.
- Theobald H. Home-based care provision within the German welfare mix. Health Soc Care Comm 2012;20:274-82. http://dx.doi.org/10.1111/j.1365-2524.2012.01057.x.
- Sheaff R, Chambers N, Charles N, Exworthy M, Mahon A, Byng R, et al. How managed a market? Modes of commissioning in England and Germany. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-S1-S8.
- Hyman R. Britain and the European Social Model: Capitalism against Capitalism?. London: London School of Economics, Institute for Employment Studies; 2008.
- Redaelli M, Meuser S, Stock S. Ambulatory care trends in Germany: a road toward more integration of care?. J Ambul Care Manage 2012;35:182-91. http://dx.doi.org/10.1097/JAC.0b013e31823f0114.
- Vogl M. Improving patient-level costing in the English and the German ‘DRG’ system. Health Policy 2013;109:290-30. http://dx.doi.org/10.1016/j.healthpol.2012.09.008.
- Okma KG. Recent Changes in Dutch Health Insurance: Individual Mandate or Social Insurance. Washington, DC: National Academy of Social Insurance; 2009.
- Helmig B, Lapsley I. On the efficiency of public, welfare and private hospitals in Germany over time: a sectoral data envelopment analysis study. Health Serv Manag Res 2001;14:263-74. http://dx.doi.org/10.1258/0951484011912762.
- Tiemann O, Schreyögg J, Busse R. Hospital ownership and efficiency: a review of studies with particular focus on Germany. Health Policy 2012;104:163-71. http://dx.doi.org/10.1016/j.healthpol.2011.11.010.
- Exworthy M, Powell M. Big windows and little windows: implementation in the ‘congested state’. Public Adm 2004;82:263-81. http://dx.doi.org/10.1111/j.0033-3298.2004.00394.x.
- Boni S, Mapelli V, De Stefano A, Compagnoni V, Gambino A, Ceccarelli A. I sistemi di governance dei Servizi Sanitari Regionali. Formez Quaderno 2007;57:1-314.
- Brenna E. Quasi-market and cost-containment in Beveridge systems: the Lombardy model of Italy. Health Policy 2011;103:209-18. http://dx.doi.org/10.1016/j.healthpol.2011.10.003.
- Lega F, Sargiacomo M, Ianni L. The rise of governmentality in the Italian National Health System: physiology or pathology of a decentralized and (ongoing) federalist system?. Health Serv Manag Res 2010;23:172-80. http://dx.doi.org/10.1258/hsmr.2010.010006.
- Powell M. The ‘Horizontal’ Dimension: Decentralisation, Partnership, and Governance of Welfare 2007. www.irer.it/eventi/governancerelazionigiugno2007/Powell.pdf (accessed 8 June 2013).
- Colombo A. The ‘Lombardy model’: subsidiarity-informed regional governance. Soc Policy Adm 2008;42:177-96. http://dx.doi.org/10.1111/j.1467-9515.2008.00602.x.
- Bartlett W, Le Grand J. Quasi-markets and Social Policy. London: Palgrave Macmillan; 1993.
- Declaration of Alma-Ata. Geneva: World Health Organization; 1978.
- Farinella D, Saitta P, Signorino G. The regionalization of the public health system and new governance models for healthcare: the stroke network case in Italy. World Med Health Policy 2011;3:1-23. http://dx.doi.org/10.2202/1948-4682.1139.
- Baker C, Beglinger JE, Bowles K, Brandt C, Brennan KM, Engelbaugh S, et al. Building a vision for the future: strategic planning in a shared governance nursing organization. Semin Nurs Manage 2000;8:98-106.
- Neri S. La Regolazione dei Sistemi Sanitari in Italia e in Gran Bretagna: Concorrenza, Cooperazione, Programmazione. Milan: Franco Angeli; 2006.
- Mattei P. The enterprise formula, new public management and the Italian health care system: remedy or contagion?. Public Adm 2006;84:1007-27. http://dx.doi.org/10.1111/j.1467-9299.2006.00624.x.
- Kowalska K. Managed care and a process of integration in health care sector: a case study from Poland. Health Policy 2007;84:308-20. http://dx.doi.org/10.1016/j.healthpol.2007.04.009.
- Cutler D, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med 2012;366:1075-7. http://dx.doi.org/10.1056/NEJMp1113361.
- Delbridge R. Surviving JIT: control and resistance in a Japanese transplant. J Manag Stud 1995;32:803-17. http://dx.doi.org/10.1111/j.1467-6486.1995.tb00153.x.
- Roethlisberger FJ, Dickson WJ. Management and the Worker. Cambridge, MA: Harvard University Press; 1939.
- Naylor C, Goodwin N. The use of external consultants by NHS commissioners in England: what lessons can be drawn for GP commissioning?. J Health Serv Res Policy 2011;16:153-60. http://dx.doi.org/10.1258/jhsrp.2010.010081.
- Donaldson L. The Contingency Theory of Organizations. London: Sage; 2001.
- Sheaff R. What kind of healthcare ‘internal market’? A cross-Europe view of the options. Int J Health Plann Manage 1994;9:5-24. http://dx.doi.org/10.1002/hpm.4740090103.
- Southon G, Perkins R, Galler D. Networks: a key to the future of health services. Aust Health Rev 2005;29:317-26. http://dx.doi.org/10.1071/AH050317.
- Bevan A, Dorey P. The Labour Governments 1964–1970. London: Routledge; 2006.
- Williamson O. The Economic Institutions of Capitalism. New York, NY: Free Press; 1985.
- Private Healthcare Market Investigation. London: Competition Commission; 2013.
- GUIDANCE: Assignment for Transition. London: Department of Health; 2011.
- GUIDANCE: Retention and Exist Terms (RETs) for Business Critical Staff. London: Department of Health; 2011.
- The English Indices of Deprivation 2010. London: Department for Communities and Local Government; 2011.
- Public Health England . Health Profiles n.d. www.apho.org.uk/default.aspx?QN=P_HEALTH_PROFILES (accessed 4 December 2014).
- Middleton K. Equity and Excellence: Liberating the NHS for Allied Health Professionals. London: Department of Health; 2010.
- Analytical Strategy for the White Paper and Associated Documents. London: Department of Health; n.d.
- Commissioning for Patients: A Consultation on Proposals. London: Department of Health; 2010.
- Initial Equality Impact Assessment (EqIA) July 2010. London: Department of Health; n.d.
- Nicholson D. Letter to NHS Bodies and Local Authorities, 13 July 2010. London: Department of Health; 2010.
- Local Democratic Legitimacy in Health. London: Department of Health; 2010.
- Regulating Healthcare Providers: A Consultation on Proposals. London: Department of Health; 2010.
- Report of the Arm’s-Length Body Review. London: Department of Health; 2010.
- Additional Annex to Sir David Nicholson’s Letter on ‘Equity and Excellence: Liberating the NHS’: Managing the Transition and the 2011/12 Operating Framework. London: Department of Health; n.d.
- Nicholson D. Letter to NHS Bodies and Local Authorities, 17 February 2011. London: Department of Health; 2010.
- Transparency in Outcomes: A Framework for the NHS. A Consultation on Proposals. London: Department of Health; 2010.
- An Information Revolution Consultation. London: Department of Health; 2010.
- The World Health Report 2000. Health Systems: Improving Performance. Geneva: World Health Organization; 2000.
- Argyris C. On Organisational Learning. Oxford: Blackwell; 1992.
Appendix 1 Inputs to the Leximancer analysis
Published and grey documents analysed (excluding transcripts)
Equity and Excellence 2010. 195
Liberating the NHS – Allied Health Professionals. 301
Liberating the NHS – Analytical Framework. 302
Liberating the NHS – Commissioning for Patients consultation paper. 303
Liberating the NHS – Equality Impact. 304
Liberating the NHS – letter from Sir David Nicolson. 305
Liberating the NHS – Local Democratic Legitimacy in Health Consultation Paper. 306
Liberating the NHS – Regulating Healthcare Providers Consultation Paper. 307
Liberating the NHS – Report of the Arm’s Length Bodies. 308
Liberating the NHS – Transition – Nicholson annex. 309
Liberating the NHS – Transition – Nicholson letter. 310
Liberating the NHS – Transparency in Outcomes: A Framework for the NHS Consultation Paper. 311
Liberating the NHS – An Information Revolution Consultation. 312
Health and Social Care Act 2012. 196
A1. Factsheet – Overview – 24 April 2012. 209
A2. Factsheet – Case for Change – 24 April 2012. 210
A3. Factsheet – Overview of Health and Care Structures – 24 April 2012. 211
A4. Factsheet – Scrutiny and Improvements – 30 May 2012. 212
B1. Factsheet – Clinically Led Commissioning – 24 April 2012. 213
B2. Factsheet – Provider Regulation to Support Innovative and Efficient Services – 24 April 2012. 214
B3. Factsheet – Greater Voice for Patients – 30 May 2012. 215
B4. Factsheet – New Focus for Public Health – 25 April 2012. 216
B5. Factsheet – Greater Accountabilty Locally and Nationally – 25 April 2012. 217
B6. Factsheet – Streamlined Arm’s Length Bodies – 25 April 2012. 218
B7. Factsheet – On Support Worker Regulation – 27 February 2012. 219
C1. Factsheet – Improving Quality of Care [undated]. 220
C2. Factsheet – Tackling Inequalities in Healthcare – 27 April 2012. 221
C3. Factsheet – Promoting Better Integration of Health and Care Services – 27 April 2012. 222
C4. Factsheet – Choice and Competition – 27 April 2012. 223
C5. The Role of the SofS – 30 May 2012. 224
C6. Factsheet – Reconfiguration of Services – 27 April 2012. 225
C7. Establishing New National Bodies – 27 April 2012. 226
C8. Research – 27 April 2012. 227
C9. Education and Training – 27 April 2012. 228
House of Commons Health Committee. 2010. Commissioning. Fourth Report of Session 2009–10. London: HMSO. 30
Leximancer data tables, documentary and oral material samples combined
| Concept | Count |
|---|---|
| Social | 1589 |
| Clinical | 1499 |
| Local | 1436 |
| Public | 810 |
| National | 392 |
| Risk | 174 |
| Concept | Count |
|---|---|
| Commissioner(s)/commissioning | 2292 |
| Provider(s)/provision | 2073 |
| Services | 1844 |
| Care | 1605 |
| NHS | 1562 |
| Patients | 1470 |
| Foundation/trust(s) | 1214 |
| Person/people | 1090 |
| GP(s) | 1072 |
| Secretary (of State) | 887 |
| Consortia | 886 |
| Monitor | 756 |
| Service | 669 |
| Board | 667 |
| System | 658 |
| Information | 625 |
| Act | 514 |
| PCT(s) | 504 |
| (Local) authority | 447 |
| Bodies | 425 |
| Organisations | 399 |
| Government | 382 |
| Health care | 341 |
| National Health Service Act | 330 |
| Management | 275 |
| Money | 273 |
| Staff | 255 |
| Evidence | 192 |
| Treatment | 187 |
| Hospital | 160 |
| Concept | Count |
|---|---|
| Health | 3190 |
| Quality | 839 |
| Outcomes | 512 |
| Needs | 352 |
| Available | 286 |
| Better | 273 |
| Important | 272 |
| Mechanism concepts | Outcome concepts | ||||||
|---|---|---|---|---|---|---|---|
| Health | Quality | Outcomes | Needs | Available | Better | Important | |
| Service(s) | 1627 | 332 | 149 | 149 | 96 | 82 | 63 |
| Care/health care | 1367 | 374 | 263 | 125 | 82 | 115 | 58 |
| Provider(s)/provision | 666 | 244 | 101 | 83 | 59 | 37 | 42 |
| Commissioner(s)/commissioning | 649 | 261 | 175 | 137 | 67 | 58 | 78 |
| NHS | 539 | 216 | 176 | 75 | 50 | 69 | 52 |
| Patient(s) | 441 | 323 | 234 | 153 | 54 | 103 | 54 |
| National Health Service Act | 413 | 20 | 5 | 13 | 37 | 3 | 2 |
| Foundation trust | 347 | 45 | 6 | 23 | 28 | 14 | 18 |
| Person/people | 316 | 75 | 43 | 39 | 38 | 23 | 24 |
| Consortia | 241 | 108 | 88 | 58 | 26 | 21 | 36 |
| GP(s) | 268 | 118 | 94 | 74 | 24 | 30 | 39 |
| Secretary (of State) | 265 | 37 | 31 | 9 | 17 | 6 | 4 |
| Authority (local) | 249 | 13 | 5 | 25 | 2 | 7 | 11 |
| Information | 216 | 66 | 39 | 23 | 48 | 21 | 12 |
| Monitor | 211 | 40 | 4 | 12 | 13 | 4 | 9 |
| Bodies | 184 | 27 | 4 | 15 | 4 | 9 | 9 |
| System | 183 | 112 | 56 | 31 | 15 | 34 | 40 |
| Board (NHS commissioning) | 148 | 41 | 25 | 4 | 14 | 1 | 7 |
| Organisations | 122 | 46 | 19 | 22 | 13 | 16 | 14 |
| Government | 118 | 29 | 33 | 20 | 10 | 12 | 23 |
| PCT(s) | 88 | 39 | 8 | 21 | 12 | 23 | 29 |
| Treatment | 73 | 25 | 16 | 6 | 6 | 6 | 3 |
| Staff | 72 | 17 | 15 | 15 | 12 | 10 | 8 |
| Management | 51 | 53 | 16 | 7 | 10 | 14 | 11 |
| Evidence | 42 | 21 | 22 | 12 | 15 | 6 | 5 |
| Money | 40 | 53 | 18 | 14 | 10 | 25 | 19 |
| Hospital | 40 | 14 | 10 | 6 | 4 | 10 | 1 |
Equity and Excellence: Liberating the NHS and branded supporting documents
In descending order of frequency, the concepts identified concerning contexts were:
-
social
-
local
-
public
-
consultation
-
government
-
transition
-
conditions.
In descending order of frequency, the concepts identified concerning mechanisms were:
-
NHS
-
services
-
patient(s)
-
commissioning
-
consortia
-
GP
-
providers
-
system
-
NHS commissioning board
-
indicators
-
information
-
people
-
organisations
-
health-care
-
provide
-
choice
-
arm’s-length
-
framework
-
White Paper
-
Monitor
-
staff
-
service
-
primary
-
trusts
-
Department (of Health)
-
regulation
-
statutory
-
provider
-
review
-
treatment.
In descending order of frequency, the concepts identified concerning outcomes were:
-
health
-
care
-
well-being
-
quality
-
outcomes
-
improvement
-
available
-
costs
-
appropriate.
In descending order of frequency, the top five mechanisms co-occurring with each context-concept were:
-
social: services, patient(s), NHS, patients, commissioning
-
local: services, patient(s), commissioning, NHS, GP
-
public: patient(s), services, NHS, commissioning, consortia
-
government: NHS, patient(s), services, providers, system
-
transition: system, NHS, commissioning, consortia, GP
-
consultation: patient(s), DH, NHS, indicators, information
-
conditions: people, services, patient(s), providers, indicators.
In descending order of frequency, the top five contexts co-occurring with each outcome were:
-
health: local, public, government, conditions, consultation
-
care: local, public, conditions, government, transition
-
well-being: local, public, government, transition, consultation
-
quality: local, public, government, transition, conditions
-
outcomes: social, public, local, conditions, government
-
improvement: social, local, public, consultation, government
-
available: social, public, consultation, conditions, local
-
costs: social, public, government, consultation + local (joint fourth)
-
appropriate: social, local + public (joint second), government, transition + consultation + conditions (joint fifth).
These patterns are rather consistent. ‘Local’ and ‘public’ co-occurred over 100 times with the first three outcome-concepts; the other contexts co-occurred with them no more than 38 times. With smaller numbers, the same pattern recurred for the other outcome-concepts.
In descending order of frequency, the mechanisms most frequently co-occurring with each outcome were:
-
health: services, NHS, patients, commissioning, consortia
-
care: services, NHS, patients, commissioning, consortia
-
well-being: services, commissioning, NHS, patients, consortia
-
quality: NHS, patient(s), services, commissioning, consortia
-
outcomes: patient(s), NHS, services, commissioning, consortia
-
improvement: patient(s), services, NHS, commissioning, consortia
-
appropriate: NHS, patient(s), system, arm’s-length
-
costs: NHS, services, arm’s-length, organisations, information + system (joint fifth)
-
available: patient(s), NHS, health care, information, indicators.
Again the repetitive pattern is striking, as is the appearance of ‘indicators’ and ‘information’ in relation only to service availability and cost.
Oral material
Concepts concerning contexts were:
-
Local.
-
Clinical.
-
Public.
Concepts concerning mechanisms were:
-
Commiss*.
-
People.
-
Patients.
-
Service(s).
-
System.
-
NHS.
-
Provider(s).
-
Money.
-
Patient.
-
GP(s).
-
Hospital.
-
Primary.
-
PCT.
-
Management.
-
Organisations.
-
Sir David Nicholson.
-
Policy.
-
Competition.
Concepts concerning outcomes were:
-
Care.
-
Quality.
-
Health.
-
Better/best/improve.
In descending order of frequency, the top five mechanisms co-occurring with the three context concepts were now:
-
Local: commiss*, service(s), provider(s), PCT, people.
-
Clinical: commiss*, service(s), people, GP(s), system.
-
Public: service(s), patients, NHS, commiss* + provider(s) (jointly).
The three contexts co-occurred with the four outcomes in the following descending order:
-
Care: local, clinical, public.
-
Quality: local, public, clinical.
-
Health: local, public, clinical.
-
Better/best/improve: local, clinical, public.
In descending order of frequency, the top five mechanisms co-occurring with each of the four outcome-concepts were:
-
Care: primary, service(s), commiss*, people, provider(s).
-
Quality: service(s), commiss*, patients, provider(s), NHS + system (jointly).
-
Health: service(s), commiss*, people, provider(s), system.
-
Better/best/improve: service(s), commiss*, patients, NHS, provider(s).
Appendix 2 Supplementary information on methods
This appendix supplements the corresponding sections in Chapter 4, Methods, of the main body of the report.
Leximancer analysis
Leximancer software, which automates quantified content analysis, proceeds unless otherwise reconfigured as follows.
-
The software divides the study text into two-sentence blocks.
-
It eliminates stop-words (proper names, ‘and’, ‘the’, interviewer name and other terms that are known a priori to be uninformative).
-
Frequent words and frequently associated words are selected as ‘seed words’ (‘concepts’).
-
The software codes the two-sentence blocks according to what concepts are present.
-
It counts the occurrences of codes.
-
The most frequently associated concepts are defined as themes (which can be traced back to their textual sources).
-
By default, Leximancer surfaces the main concepts inductively. The researcher can also rerun Leximancer further times, selecting those inductively found concepts that are relevant to her research questions for grouping into themes. In the present case, we selected the concepts and themes relevant to the power mechanisms discussed in Chapter 2.
The term ‘concept’ has in Leximancer analysis a narrower than usual meaning, denoting ‘co-occurring words’ (as opposed to the more usual use, in research, of a theoretically informed essential definition).
The study ‘text’ can be a combination of documents (including transcripts, laws), spreadsheets, audio and video material. We therefore ran three analyses:
-
Equity and Excellence: Liberating the NHS195 and the official support documents branded as explaining and elaborating it, except for the Assignment for Transition and human resources management documents,297,298 which were irrelevant to a CMO analysis
-
oral material: speeches and interviews
-
the 2012 Act196 with the official explanatory ‘factsheets’, including one on service quality. 209–228
First, we used Leximancer’s default setting to find inductively what themes (and component concepts) were present in the sample. We coded the concepts found as relating to the context, mechanism or outcome of NHS commissioning policy or as ‘stop-words’ (e.g. ‘change’, ‘future’, ‘things’, ‘and’, ‘the’, etc.) for being uninformative, ambiguous (e.g. ‘substitute’), trivial or irrelevant. Approbations, however vague (e.g. ‘best’, ‘improve’), were also coded as outcomes, that is policy or service outcomes. We collapsed duplicate concepts (e.g. ‘patient’ + ‘patients’, ‘GP’ + ‘GPs’, ‘better’ + ‘best’ + ‘improve’). We assumed that the conjunction of concepts or themes denoting a mechanism and/or a context and/or an outcome denoted an existing or proposed CMO relationship. A count of these conjunctions showed which CMO relationships received most coverage in the texts. Because some of these conjunctions (textual proximities) may reflect nothing more than drafting accidents, this method may bias towards overestimating the number of CMO relationships stated in the texts, but if any such overcounting is more or less evenly distributed across the texts, as we have assumed, it will not bias the relative frequencies of the different CMO assertions. From the blocks of texts where Leximancer had found these conjunctions, we extracted any descriptions of CMO relationships and classified the mechanisms according to which media of power they used.
Cognitive frame analysis
Although the quantitative (Leximancer) analysis located which CMO relationships the texts most often mentioned, they were too broad, ambiguous or brief in saying how these mechanisms worked or would work. We therefore made a cognitive frame analysis of data from our interviews with parliamentarians and top-level health managers to elaborate and supplement the accounts of CMO relationships found in the policy texts. In doing so, we again sought to relate the accounts and explanations (frames) that our informants used to the categories (CMO; media of power) required for the present study. Mostly the informants’ accounts were consistent, but where they differed (in emphasis rather than contradicting each other) we took the more often expressed view as the one more likely to guide commissioning in practice.
When policies are controversial, a simple précis of policy documents and transcripts is likely to oversimplify the programme theory by omitting relevant aims, mechanisms and implicit background assumptions. It might also overemphasise spurious rationalisations and the polemics. A more sophisticated discourse analysis is required. We adopted a ‘rhetorical’ variant. 293 This is ‘critical’ in the sense of not necessarily taking all managerial and political rhetoric at face value or as entirely coherent, valid and normatively persuasive. We therefore dispute the suggestion that such critiques are impossible;294 its realist character is just what gives realistic evaluation its critical facet, because a programme theory can be evaluated empirically. Therefore, to the extent that they rely on these empirical assumptions, so can the policies that through the medium of political discourse express a programme theory. Nevertheless, taking policy statements at face value is a necessary starting point and our default assumption until we find reasons to suspend it.
We took the following signs as calling into question if policy documents should be taken only at face value:
-
silences or obviously ambiguous policy positions about important mechanisms or outcomes
-
statements contradicting the balance of evidence available when the policy was formulated
-
apparent contradictions among policy statements that (all supporting the policy) ought to be consistent.
Then a realistic evaluator has to infer and impute the missing assumptions in order to reconstitute the programme theory as completely and explicitly as possible and (to avoid evaluating a ‘straw man’ theory later on) in the most credible form consistent with the explicitly stated elements. We did so by inviting policy-makers themselves to elaborate the missing material at interview.
We collated the descriptions of CMO relationships found by these methods and paraphrased them as statements of the form ‘Doing X in circumstances M will cause agent A to do Y’ (or a logically equivalent statement, e.g. ‘If A does X, B will do Y’), the form required for empirically testing CMO assumptions. In this way we identified the CMO relationships by which policy-makers and top managers assumed NHS commissioning would achieve its intended service outcomes.
Cross-sectional analysis of published managerial data
Before making the regression analyses, we checked for multicolinearity by measuring VIF among the potential independent and control variables in the regression analyses, retaining only variables whose VIF was below the conservative threshold of VIF = 2.5 (hence also the conventional threshold VIF = 5.0).
All analyses were at PCT level. To show effects of, say, provider competition, it is necessary (but not sufficient) to find non-trivial correlations, with coefficients of the correct sign, between the commissioner characteristics and the service outcome variables. Since there are a number of such variables, there would be multiple potential correlations for each commissioner characteristic for which we had data. The higher the proportion of such correlations found having the sign that the relevant element of programme theory predicts, and the stronger those correlations, the stronger would be the evidence supporting the assumption that provider competition has an impact on the policy-relevant service outcomes. Such findings would support the inference that, if PCTs could stimulate (continuing the example) provider competition, the PCTs would thereby help to realise those outcomes. Conversely, the absence of any such correlation, or the presence of correlations with the opposite sign from what the programme theories outlined above assume, would be prima facie evidence against those assumptions.
In the event (see Chapter 7, subsection Provider competition) we found few of the correlations that the programme theory assumed, in particular regarding competition. We therefore tested the robustness and sensitivity of our findings by rerunning the analyses for only the PCTs with the highest levels of competition, that is those in the top quartile for:
-
spend on independent (i.e. for-profit) sector
-
spend on local government sector and voluntary sector combined (not separated in the published data)
-
Herfindahl index.
The top quartile was selected because it contained 38 sites; a smaller selection would allow test results only of dubious validity.
Evidence synthesis
Across the case studies, data were synthesised by framework analysis. Conceptually this was equivalent to constructing, for each research question, a data grid in which each row contained data about a specific aspect of that research question, and each column represented a site, and then populating the cells with the relevant data from the case study collections of ‘pithy sentences’, findings from the cross-sectional analysis, action learning set findings, international comparisons and other published studies. We noted what common or divergent patterns there were across cells and then ‘read off’ the patterns as answers to our research questions. This method also revealed where it was necessary to add new categories or concepts to accommodate unforeseen empirical findings. By combining primary and secondary sources, we were able to compare (indeed check) our own findings against those from other studies.
As necessary, we derived the (equivalent to) row headings for each such systematic comparison from the analytical framework in Chapter 2, the programme theory assumptions found by discourse analysis (see Chapter 5) and by deduction from the research question itself. In this way we nuanced the framework analysis for each research question. Analysing the reconfiguration of commissioning structures (RQ2) required a comparison of longitudinal accounts of the formation and development of commissioning structures in each study site during the study period. Once these histories had been elicited, they too could be systematically compared in the above way. Regarding RQ3(a), the ways in which commissioners changed their commissioning practice in an attempt to influence their providers demonstrated that the commissioners had at least that much freedom of manoeuvre in practice. The limits to this freedom were found by discovering what practical, resource and policy restrictions there were on their freedom to exercise the media of power listed in Chapter 2 over their providers. We identified these limits from our case study materials, policy and regulatory statements. To examine some of the effects of client-based commissioning [RQ3(b)], we relied more on the cross-sectional than the case study data. Analysing the similarities and differences in commissioning practice for different care groups provided the basis for testing some of the theories discussed in Chapter 2 (RQ4). 204
Appendix 3 Measures used in cross-sectional analysis
To select measures we started from internationally recognised generic health service and health policy outcomes indicators that the OECD201 and WHO200 have used for international comparisons of health systems, and Greaves et al. ’s list,90 which so far as we were aware was at the time the only published study similar to this one.
The OECD indicator groupings are:
Quality of care:
-
Care for chronic conditions: avoidable admissions: respiratory diseases; uncontrolled diabetes.
-
Care for acute exacerbation of chronic conditions: in-hospital mortality following acute myocardial infarction, stroke.
-
Patient safety: obstetric trauma; procedural or postoperative complications.
-
Care for mental disorders: unplanned hospital re-admissions for mental disorders.
-
Cancer care: screening, survival and mortality for cervical cancer and breast cancer; survival and mortality for colorectal cancer.
-
Care for communicable diseases: childhood vaccination programmes; influenza vaccination for older people.
Access to care:
-
Unmet health care needs.
-
Coverage for health care.
-
Burden of out-of-pocket health expenditure.
-
Geographic distribution of doctors.
-
Inequalities in doctor consultations.
-
Inequalities in dentist consultations.
-
Inequalities in cancer screening.
-
Waiting times.
Health expenditure and financing [no sub-national indicators].
Long-term care
-
Life expectancy and healthy life expectancy at age 65 years.
-
Self-reported health and disability at age 65 years.
-
Prevalence and economic burden of dementia.
-
Recipients of long-term care.
-
Informal carers.
-
Long-term care workers.
-
Long-term care beds in institutions and hospitals.
-
Long-term care expenditure.
The corresponding WHO indicator groups, from the World Health Report 2000,313 are:
-
Health: level (DALY, disability-adjusted life-year), distribution.
-
Attainment of goals: responsiveness (level, distribution), fairness in financial contribution, health expenditure per capita in international dollars.
-
Population estimates: dependency, life expectancy at birth, probability of dying.
-
Deaths by cause, age, sex, mortality stratum.
-
Burden of diseases: DALY, equality of child survival.
-
Responsiveness: index of responsiveness.
-
Fairness of financial contribution.
-
Health expenditure:
-
total health expenditure as percentage of GDP
-
public, private, out-of-pocket, tax-funded, social security, other
-
public expenditure on health as percentage of total public expenditure
-
per capita health expenditure (total, out-of-pocket, total in international dollars, public in international dollars, out-of-pocket in international dollars).
-
-
Overall health attainment.
The measures Greaves used were:90
-
clinical effectiveness
-
controlled blood pressure in hypertension
-
controlled blood glucose levels in diabetes
-
emergency admissions: acute conditions
-
emergency admissions: chronic conditions
-
premature mortality from all circulatory diseases
-
mortality from causes amenable to health care
-
non-elective readmission rate
-
emergency admissions: acute conditions usually managed in primary care
-
1-year survival index for all cancers
-
breast screening coverage
-
cervical screening coverage
-
uptake of influenza vaccinations by over-65s
-
smoking quitters
-
measles, mumps and rubella vaccination
-
satisfaction with care received [at GP]
-
GP recommendation [whether patient would recommend her GP]
-
staff noticed [patient’s] views
-
agreed with staff about managing problem
-
enough support [in managing long-term condition]
-
tonsillectomy rate
-
did not attend rate
-
excess bed-days per non-elective admission
-
length of stay for fractured neck of femur
-
low-cost statin prescribing
-
see doctor quickly
-
book appointment ahead
-
satisfaction with opening hours
-
2-week cancer wait
-
18-week wait 2008
-
WCC financial governance score
-
Health Care Commission annual health check [score]
-
efficiency and effectiveness
-
work collaboratively with community
-
engagement with clinicians
-
work with providers.
Of all the above indicators, those reporting whole-system characteristics were irrelevant for present purposes, as were indicators related to non-hospital services, that is primary and community care. From what remained, we selected relevant measures, which were:
-
known or could reasonably be assumed to be amenable to health-care provider activity; hence, indirectly amenable to commissioner intervention insofar as it influences provider activity
-
reported at PCT level (found by checking NHS Information Centre website), which requirement ruled out WHO Health Report 2000 indicators, which are all at national level, and many NHS indicators (e.g. electronic patient-reported outcome measures, meticillin-resistant Staphylococcus aureus control, patient complaints), which were published only at provider level; no data were available for community health services
-
reported for the same period as the independent variables (2008–9)
-
relevant to main NHS policy priorities during the last decade
-
closest to the OECD and/or WHO indicator definitions, where there was a choice of indicator.
Because the co-ordination of primary and secondary care was one of the PCTs’ roles as commissioners, we did include indicators/measures of that.
Appendix 4 Cross-sectional data analysis findings tables
| Independent variable | Independent or control variable | r | p |
|---|---|---|---|
| X.4 Choose and book % | X.10 Herfindahl index | 0.258 | 0.001 |
| X.7 Spend on local authority and voluntary sector | X.8 Independent sector spend | –0.639 | < 0.001 |
| X.10 Herfindahl index | X.12 Spend on main provider | 0.305 | < 0.001 |
| X.13 PCT mergers [C] | –0.249 | 0.002 | |
| X.16 PCT weighted population [C] | –0.291 | < 0.001 | |
| X.12 Spend on main provider | X.15 PCT income % [C] | –0.179 | 0.027 |
| Dependent variable | Dependent variable | r | p |
|---|---|---|---|
| X.19 Amenable mortality all causes under 75 yo annual directly standardised | X.27 Emergency admissions not usually requiring hospital admission observed/expected indirectly standardised | 0.269 | < 0.001 |
| X.33 Mean time waited | 0.308 | < 0.001 | |
| X.34 Median time waited | 0.339 | < 0.001 | |
| X.37 Non-admitted patients referral to treatment Dec 2008–Dec 2009 all patients < 18 weeks, % change | 0.184 | 0.02 | |
| X.39 Monthly mean waiting list, IP & day case, per weighted population | 0.249 | 0.002 | |
| X.20 Emergency re-admissions, above 16 yo, indirectly standardised | X.21 Emergency admissions phc-preventable-chronic conditions indirectly standardised | 0.199 | 0.012 |
| X.22 Emergency admissions phc-preventable-acute conditions indirectly standardised | 0.218 | 0.006 | |
| X.23 Emergency admissions for PHC-preventable chronic conditions, per cent improvement from 2007/08 to 2008/09 | 0.344 | 0.002 | |
| X.25 Emergency re-admissions within 28 days of discharge from hospital, adults > 16 yo, indirectly age, method of admission of discharge spell, diagnosis (ICD-10 chapter/selected sub-chapters within medical specialities) and procedure (OPCS 4 chapter/selected sub-chapters within surgical specialities) standardised % | 0.768 | < 0.001 | |
| X.33 Mean time waited | 0.171 | 0.02 | |
| X.21 Emergency admissions phc-preventable-chronic conditions indirectly standardised | X.22 Emergency admissions phc-preventable-acute conditions indirectly standardised | 0.238 | 0.002 |
| X.33 Mean time waited | 0.28 | 0.006 | |
| X.34 Median time waited | 0.164 | 0.039 | |
| X.38 Average number of patients waiting more than 4 weeks for a 1st out-patient appointment following a GP referral/PER 2008–09 weighted population | 0.23 | 0.004 | |
| X.39 Monthly mean waiting list, IP & day case, per weighted population | 0.226 | 0.004 | |
| X.22 Emergency admissions phc-preventable-acute conditions indirectly standardised | X.23 Emergency admissions for PHC-preventable chronic conditions, per cent improvement from 2007/08 to 2008/09 | 0.2 | 0.01 |
| X.25 Emergency re-admissions within 28 days of discharge from hospital, adults > 16 yo, indirectly age, method of admission of discharge spell, diagnosis (ICD-10 chapter/selected sub-chapters within medical specialties) and procedure (OPCS 4 chapter/selected sub-chapters within surgical specialities) standardised % | 0.196 | < 0.001 | |
| X.27 Emergency admissions not usually requiring hospital admission observed/expected indirectly standardised | 0.23 | 0.004 | |
| X.33 Mean time waited | 0.28 | < 0.001 | |
| X.34 Median time waited | 0.286 | < 0.001 | |
| X.38 Average number of patients waiting more than 4 weeks for a 1st outpatient appointment following a GP referral/PER 2008–09 weighted population | 0.206 | 0.009 | |
| X.23 Emergency admissions for PHC-preventable chronic conditions, per cent improvement from 2007/08 to 2008/09 | X.25 Emergency re-admissions within 28 days of discharge from hospital, adults > 16 yo, indirectly age, method of admission of discharge spell, diagnosis (ICD-10 chapter/selected sub-chapters within medical specialities) and procedure (OPCS 4 chapter/selected sub-chapters within surgical specialities) standardised % | 0.298 | < 0.001 |
| X.38 Average number of patients waiting more than 4 weeks for a 1st outpatient appointment following a GP referral/PER 2008–09 weighted population | 0.206 | 0.009 | |
| X.25 Emergency re-admissions within 28 days of discharge from hospital, adults > 16 yo, indirectly age, method of admission of discharge spell, diagnosis (ICD-10 chapter/selected sub-chapters within medical specialties) and procedure (OPCS 4 chapter/selected sub-chapters within surgical specialities) standardised % | X.33 Mean time waited | 0.221 | 0.005 |
| X.34 Median time waited | 0.207 | 0.009 | |
| X.37 Non-admitted patients referral to treatment Dec 2008–Dec 2009 all patients < 18 weeks, % change | 0.217 | 0.006 | |
| X.38 Average number of patients waiting more than 4 weeks for a 1st outpatient appointment following a GP referral/PER 2008–09 weighted population | 0.17 | 0.036 | |
| X.27 Emergency admissions not usually requiring hospital admission observed/expected indirectly standardised | X.33 Mean time waited | 0.195 | 0.014 |
| X.34 Median time waited | 0.269 | < 0.001 | |
| X.39 Monthly mean waiting list, IP & day case, per weighted population | 0.234 | 0.003 | |
| X.33 Mean time waited | X.36 Admitted patients referral to treatment Dec 2008–Dec 2009 all patients < 18 weeks, % change | 0.32 | < 0.001 |
| X.37 Non-admitted patients referral to treatment Dec 2008–Dec 2009 all patients < 18 weeks, % change | 0.33 | < 0.001 | |
| X.39 Monthly mean waiting list, IP & day case, per weighted population | 0.32 | < 0.001 | |
| X.34 Median time waited | X.36 Admitted patients referral to treatment Dec 2008–Dec 2009 all patients < 18 weeks, % change | 0.265 | < 0.001 |
| X.37 Non-admitted patients referral to treatment Dec 2008–Dec 2009 all patients < 18 weeks, % change | 0.202 | 0.018 | |
| X.39 Monthly mean waiting list, IP & day case, per weighted population | 0.414 | < 0.001 | |
| X.36 Admitted patients referral to treatment December 2008–December 2009 all patients < 18 weeks, % change | X.37 Non-admitted patients referral to treatment Dec 2008–Dec 2009 all patients < 18 weeks, % change | 0.295 | < 0.001 |
| X.38 Average number of patients waiting more than 4 weeks for a 1st outpatient appointment following a GP referral/PER 2008–09 weighted population | 0.174 | 0.028 |
| Policy variable | Adjusted r2 | WCC and/or control variable(s) | Estimated standardised coefficient β | p | PT predictsa |
|---|---|---|---|---|---|
| X.19 Amenable mortality | 0.529 | X.17 Deprivation index [C] | 0.017 | < 0.001 | N.A. |
| X.21 Emergency admissions phc-preventable-chronic conditions indirectly standardised, % improvement from 2007/8 to 2008/9 | 0.374 | X.17 Deprivation index [C] | 2.44 | < 0.001 | N.A. |
| X.22 Emergency admissions phc-preventable-acute conditions % improvement 2007/8 to 2008/9 | 0.023 | X.14 PCT Mergers [C] | –0.012 | 0.035 | N.A. |
| X.23 Emergency admissions for PHC-preventable chronic conditions, per cent improvement from 2007/8 to 2008/09 | 0.02 | X.17 Deprivation index [C] | 0.003 | 0.04 | N.A. |
| X.27 Emergency admissions not usually requiring hospital admission observed/expected | 0.1 | X.17 Deprivation index [C] | 1.027 | < 0.001 | N.A. |
| X.37 Non-admitted patients referral to treatment December 2008–December 2009 all patients < 18 weeks, % change 2007/8 to 2008/9 | 0.11 | X.14 PCT Mergers [C] | –0.002 | 0.011 | N.A. |
| X.39 Monthly mean waiting list, IP and day case, per weighted population | 0.36 | X.14 PCT Mergers [C] | 0.001 | < 0.001 | N.A. |
| X.15 PCT income % | –0.002 | < 0.001 | N.A. | ||
| X.49 PCT surplus/deficit | 0.33 | X.13 WCC scores | –0.005 | 0.021 | +ve |
| X.15 PCT income % | 0.545 | < 0.001 | N.A. | ||
| X.53 Ratio of day cases to admissions | 0.125 | X.17 Deprivation index [C] | –0.002 | < 0.001 | N.A. |
| X.55 FCE/weighted population | 0.31 | X.14 PCT Mergers [C] | 0.035 | < 0.001 | N.A. |
| X.15 PCT income % [C] | –0.048 | 0.004 | N.A. |
| Policy variable | Adjusted r2 | Competition and control variable(s) | Estimated standardised coefficient β | p | Predicted signa |
|---|---|---|---|---|---|
| X.18 Amenable mortality | 0.549 | X.10 HHI | 0.154 | 0.008 | +ve |
| X.17 Deprivation index [C] | 0.016 | < 0.001 | N.A. | ||
| X.21 Emergency admissions phc-preventable-chronic conditions, improvement 2007/8 to 2008/09 | 0.374 | X.17 Deprivation index [C] | 2.44 | < 0.001 | N.A. |
| X.22 Emergency admissions phc-preventable-acute conditions % improvement 2007/8 to 2008/9 | 0.081 | X.10 HHI | –0.158 | 0.05 | –ve |
| X.14 PCT mergers [C] | –0.012 | 0.41 | N.A. | ||
| X.17 Deprivation index [C] | 0.306 | 0.027 | N.A. | ||
| X.23 Emergency admissions for PHC-preventable chronic conditions, per cent improvement from 2007/8 to 2008/9 | 0.022 | X.17 Deprivation index [C] | 0.003 | 0.04 | N.A. |
| X.27 Emergency admissions not usually requiring hospital admission observed/expected | 0.101 | X.17 Deprivation index [C] | 1.027 | < 0.001 | N.A. |
| X.33 Mean time waited | 0.028 | X.17 Deprivation index [C] | 0.16 | 0.023 | N.A. |
| X.37 Non-admitted patients referral to treatment < 18 weeks, % change 2007/8 to 2008/9 | 0.135 | X.10 HHI | –0.01 | 0.024 | +ve |
| X.14 PCT mergers [C] | –0.002 | 0.01 | N.A. | ||
| X.39 Monthly mean waiting list, IP and day case, per weighted population | 0.394 | X.10 HHI | 0.005 | 0.002 | +ve |
| X.15 PCT income % [C] | –0.003 | < 0.001 | N.A. | ||
| X.49 PCT surplus/deficit | 0.283 | X.15 PCT income % [C] | 0.533 | < 0.001 | N.A. |
| X.53 Ratio of day cases to admissions (non-standardised) | 0.125 | X.17 Deprivation index [C] | 0.002 | < 0.001 | N.A. |
| X.54 Mean ALoS non-standardised | 0.023 | X.17 Deprivation index [C] | 0.017 | 0.035 | N.A. |
| X.55 Ratio: FCEs/weighted population | 0.33 | X.10 HHI | –0.1 | 0.017 | –ve |
| X.14 PCT mergers [C] | –0.03 | < 0.001 | N.A. | ||
| X.15 PCT income % [C] | –0.04 | 0.008 | N.A |
| Policy variable | Adjusted r2 | Competition variable(s) | Estimated standardised coefficient β | p | PT predictsa |
|---|---|---|---|---|---|
| X.19 Amenable mortality | 0.53 | X.17 Deprivation index [C] | 0.173 | < 0.001 | N.A. |
| X.21 Emergency admissions phc-preventable-chronic conditions indirectly standardised, % improvement from 2007/08 to 2008/09 | 0.374 | X.17 Deprivation index [C] | 2.4351 | < 0.001 | N.A. |
| X.22 Emergency admissions phc-preventable-acute conditions % improvement 2007/08 to 2008/09 | 0.063 | X.11 Number of provider contracts | 0.012 | 0.008 | –ve |
| X.14 PCT mergers [C] | –0.015 | 0.01 | N.A. | ||
| X.23 Emergency admissions for PHC-preventable chronic conditions, per cent improvement from 2007/08 to 2008/09 | 0.062 | X.11 Number of provider contracts | 0.015 | 0.007 | –ve |
| X.17 Deprivation index [C] | 0.004 | 0.005 | N.A. | ||
| X.25 Emergency readmissions within 28 days of discharge from hospital, adults > 16 yo, % improvement from 2007/08 to 2008/09 | 0.027 | X.17 Deprivation index [C] | 0.001 | 0.023 | N.A. |
| X.27 Emergency admissions not usually requiring hospital admission observed/expected | 0.101 | X.17 Deprivation index [C] | 1.027 | < 0.001 | N.A. |
| X.33 Mean time waited | 0.028 | X.17 Deprivation index [C] | –0.16 | 0.023 | N.A. |
| X.39 Monthly mean waiting list, IP & day case, per weighted population | 0.374 | X.14 PCT mergers [C] | 0.001 | < 0.001 | N.A. |
| X.15 PCT income % [C] | –0.002 | 0.001 | N.A. | ||
| X.49 PCT surplus | 0.329 | X.7 Spend on LA & voluntary sector | –2.94 | 0.002 | +ve |
| X.8 Independent sector spend | –2.77 | 0.008 | +ve | ||
| X.15 PCT income % [C] | 0.519 | < 0.001 | N.A. | ||
| X.53 Ratio of day cases to admissions (non-standardised) | 0.173 | X.11 Number of provider contracts | –0.004 | 0.005 | +ve |
| X.12 Spend on main provider | –0.024 | 0.03 | +ve | ||
| X.17 Deprivation index [C] | –0.002 | < 0.001 | N.A. | ||
| X.54 Mean ALoS non-standardised | 0.023 | X.17 Deprivation index [C] | –0.02 | 0.035 | N.A. |
| X.55 (FCE/Weighted population) | 0.27 | X.14 PCT mergers [C] | 0.04 | < 0.001 | N.A. |
| Policy variable | Adjusted r2 | Competition variable(s) | Estimated standardised coefficient β | p | PT predictsa |
|---|---|---|---|---|---|
| X.19 Amenable mortality | 0.529 | X.17 Deprivation index [C] | 0.017 | < 0.001 | N.A. |
| X.21 Emergency admissions phc-preventable-chronic conditions indirectly standardised, % improvement from 2007/08 to 2008/09 | 0.374 | X.17 Deprivation index [C] | 2.44 | < 0.001 | N.A. |
| X.22 Emergency admissions phc-preventable-acute conditions % improvement 2007/08 to 2008/09 | 0.023 | X.14 PCT mergers [C] | –0.012 | 0.035 | N.A. |
| X.23 Emergency admissions for PHC-preventable chronic conditions, per cent improvement from 2007/08 to 2008/09 | 0.022 | X.17 Deprivation index [C] | 0.003 | 0.039 | N.A. |
| X.25 Emergency re-admissions within 28 days of discharge from hospital, adults > 16 yo, improvement from 2007/08 to 2008/09 | 0.027 | X.6 PBC projects GP participation | –0.029 | 0.023 | +ve |
| X.27 Emergency admissions not usually requiring hospital admission observed/expected | 0.101 | X.17 Deprivation index [C] | 1.027 | < 0.001 | N.A. |
| X.33 Mean time waited | 0.024 | X.6 PBC projects GP participation | 4.31 | 0.03 | –ve |
| X.37 Non-admitted patients referral to treatment < 18 weeks, % change 2007/08 to 2008/09 | 0.147 | X.5 Personal health budget pilot | 0.006 | 0.001 | +ve |
| X.15 PCT income % [C] | 0.005 | 0.008 | N.A. | ||
| X.39 Monthly mean waiting list, IP & day case, per weighted population | 0.356 | X.15 PCT income % [C] | –0.002 | < 0.001 | N.A. |
| X.49 PCT surplus/deficit | 0.283 | X.15 PCT income % [C] | 0.533 | < 0.001 | N.A. |
| X.53 Ratio of day cases to admissions (non-standardised) | 0.125 | X.17 Deprivation index [C] | –0.002 | < 0.001 | N.A. |
| X.54 Mean ALoS non-standardised | 0.023 | X.17 Deprivation index [C] | –0.017 | 0.035 | N.A. |
| X.55 (FCE/weighted population) | 0.309 | X.14 PCT mergers [C] | 0.04 | < 0.001 | N.A. |
| X.15 PCT income % [C] | –0.05 | 0.004 | N.A. |
| Policy variable | Adjusted r2 | Competition variable(s) | Estimated standardised coefficient β | p | PT predictsa |
|---|---|---|---|---|---|
| X.19 Amenable mortality | 0.76 | X.10 HHI | 0.308 | < 0.001 | +ve |
| X.14 PCT mergers [C] | 1.96 | < 0.001 | N.A. | ||
| X.16 PCT weighted population [C] | –0.138 | 0.023 | N.A. | ||
| X.17 Deprivation index [C] | 0.498 | < 0.001 | N.A. | ||
| X.21 Unplanned hospitalisation for chronic ambulatory care sensitive conditions (adults) directly age-sex standardised, % improvement since 2007/08) | 0.77 | X.10 HHI | 0.61 | < 0.001 | –ve |
| X.14 PCT mergers [C] | 4.71 | < 0.001 | N.A. | ||
| X.15 PCT income % [C] | 0.161 | 0.027 | N.A. | ||
| X.16 PCT weighted population [C] | –0.3 | < 0.001 | N.A. | ||
| X.17 Deprivation index [C] | –0.16 | 0.006 | N.A. | ||
| X.22 Emergency admissions phc-preventable-acute conditions % improvement 2007/08 to 2008/09 | 0.73 | X.10 HHI | 0.319 | < 0.001 | –ve |
| X.14 PCT mergers [C] | 1.6 | < 0.001 | N.A. | ||
| X.15 PCT income % [C] | 0.204 | 0.003 | N.A. | ||
| X.16 PCT weighted population [C] | 0.249 | < 0.001 | N.A. | ||
| X.23 Emergency admissions for PHC-preventable chronic conditions, per cent improvement from 2007/08 to 2008/09 | 0.69 | X.10 HHI | 0.389 | < 0.001 | –ve |
| X.14 PCT mergers [C] | 0.969 | 0.011 | N.A. | ||
| X.15 PCT income % [C] | 0.215 | < 0.001 | N.A. | ||
| X.16 PCT weighted population [C] | 0.237 | 0.005 | N.A. | ||
| X.25 Emergency re-admissions within 28 days of discharge from hospital, adults > 16 yo, % improvement from 2007/08 to 2008/09 | 0.68 | X.10 HHI | 0.196 | 0.002 | –ve |
| X.14 PCT mergers [C] | 0.815 | 0.042 | N.A. | ||
| X.15 PCT income % [C] | 0.5 | < 0.001 | N.A. | ||
| X.16 PCT weighted population [C] | 0.211 | 0.002 | N.A. | ||
| X.27 Emergency admissions not usually requiring hospital admission observed/expected | 0.645 | X.14 PCT mergers [C] | 2.08 | < 0.001 | N.A. |
| X.15 PCT income % [C] | 0.4 | < 0.001 | N.A. | ||
| X.16 PCT weighted population [C] | 0.283 | < 0.001 | N.A. | ||
| X.33 Mean time waited | 0.697 | X.10 HHI | 0.187 | < 0.001 | +ve |
| X.14 PCT mergers [C] | 1.52 | < 0.001 | N.A. | ||
| X.17 Deprivation index [C] | 0.086 | 0.003 | N.A. | ||
| X.35 Referral to treatment 2008/09 trauma & orthopaedics % change Dec 2008–Dec 2009 | 0.798 | X.10 HHI | 0.37 | < 0.001 | –ve |
| X.14 PCT mergers [C] | 2.42 | < 0.001 | N.A. | ||
| X.15 PCT income % [C] | 0.28 | < 0.001 | N.A. | ||
| X.36 Admitted patients referral to treatment Dec 2008–Dec 2009 % change 2007/08 to 2008/09 | 0.666 | X.10 HHI | 0.13 | 0.027 | –ve |
| X.15 PCT income % [C] | 0.257 | 0.001 | N.A. | ||
| X.16 PCT weighted population [C] | 0.222 | < 0.001 | N.A. | ||
| X.17 Deprivation index [C] | 0.222 | < 0.001 | N.A. | ||
| X.37 Non-admitted patients referral to treatment < 18 weeks, % change 2007/08 to 2008/09 | 0.716 | X.15 PCT income % [C] | 0.267 | < 0.001 | N.A. |
| X.16 PCT weighted population [C] | 0.086 | < 0.001 | N.A. | ||
| X.17 Deprivation index [C] | 0.138 | < 0.001 | N.A. | ||
| X.38 Average number of patients waiting more than 4 weeks for a 1st outpatient appointment following a GP referral/PER 2008/09 weighted population | 0.74 | X.10 HHI | 0.53 | < 0.001 | +ve |
| X.14 PCT mergers [C] | 2.26 | < 0.001 | N.A. | ||
| X.16 PCT weighted population [C] | –0.29 | < 0.001 | N.A. | ||
| X.17 Deprivation index [C] | 0.4 | < 0.001 | N.A. | ||
| X.39 Monthly mean waiting list, IP & day case, per weighted population | 0.665 | X.10 HHI | 0.23 | < 0.001 | +ve |
| X.14 PCT mergers [C] | 4.65 | < 0.001 | N.A. | ||
| X.49 PCT surplus | 0.652 | X.10 HHI | 0.1 | 0.006 | –ve |
| X.14 PCT mergers [C] | 2.01 | < 0.001 | N.A. | ||
| X.17 Deprivation index [C] | 0.18 | < 0.001 | N.A. | ||
| X.55 FCE/weighted population | 0.36 | X.15 PCT income % [C] | –0.012 | < 0.001 | N.A. |
| X.16 PCT weighted population [C] | –0.006 | < 0.009 | N.A. |
| Policy variable | Adjusted r2 | Competition variable(s) | Estimated standardised coefficient β | p | PT predictsa |
|---|---|---|---|---|---|
| X.19 Amenable mortality | 0.73 | X.14 PCT mergers [C] | 1.66 | < 0.001 | N.A. |
| X.15 PCT income % [C] | 0.144 | 0.047 | N.A. | ||
| X.17 Deprivation index [C] | 0.571 | < 0.001 | N.A. | ||
| X.21 Unplanned hospitalisation for chronic ambulatory care sensitive conditions (adults) directly age–sex standardised, % improvement since 2007/08 | 0.7 | X.8 % spent on independent sector healthcare | 0.298 | < 0.001 | +ve |
| X.14 PCT mergers [C] | 2.75 | < 0.001 | N.A. | ||
| X.15 PCT income % [C] | 0.306 | < 0.001 | N.A. | ||
| X.22 Emergency admissions phc-preventable-acute conditions % improvement 2007/08 to 2008/09 | 0.746 | X.8 % spent on independent-sector healthcare | 0.375 | < 0.001 | +ve |
| X.15 PCT income % [C] | 0.293 | < 0.001 | N.A. | ||
| X.16 PCT weighted population [C] | 0.371 | < 0.001 | N.A. | ||
| X.23 Emergency admissions for PHC-preventable chronic conditions, per cent improvement from 2007/08 to 2008/09 | 0.672 | X.15 PCT income % [C] | 0.479 | < 0.001 | N.A. |
| X.16 PCT weighted population [C] | 0.494 | < 0.001 | N.A. | ||
| X.25 Emergency readmissions within 28 days of discharge from hospital, adults > 16 yo, % improvement from 2007/08 to 2008/09 | 0.689 | X.8 % spent on independent-sector healthcare | 0.22 | 0.003 | +ve |
| X.15 PCT income % [C] | 0.56 | < 0.001 | N.A. | ||
| X.17 Deprivation index [C] | 0.27 | < 0.001 | N.A. | ||
| X.27 Emergency admissions not usually requiring hospital admission observed/expected | 0.74 | X.8 % spent on independent-sector healthcare | 0.583 | < 0.001 | –ve |
| X.15 PCT income % [C] | 0.425 | < 0.001 | N.A. | ||
| X.16 PCT weighted population [C] | 0.312 | < 0.001 | N.A. | ||
| X.17 Deprivation index [C] | –0.267 | < 0.001 | N.A. | ||
| X.33 Mean time waited | 0.68 | X.8 % spent on independent-sector healthcare | 0.15 | < 0.001 | –ve |
| X.14 PCT mergers [C] | 0.69 | 0.006 | N.A. | ||
| X.16 PCT weighted population [C] | 0.109 | 0.002 | N.A. | ||
| X.17 Deprivation index [C] | 0.122 | < 0.001 | N.A. | ||
| X.35 Referral to treatment 2008–09 trauma & orthopaedics % change Dec 2008–Dec 2009 | 0.635 | X.14 PCT mergers [C] | 1.9 | < 0.001 | +ve |
| X.15 PCT income % [C] | 0.521 | < 0.001 | N.A. | ||
| X.16 PCT weighted population [C] | 0.212 | 0.002 | N.A. | ||
| X.36 Admitted patients referral to treatment Dec 2008–Dec 2009 all patients < 18 weeks, % change 2007/08 to 2008/09 | 0.69 | X.8 % spent on independent-sector healthcare | 0.316 | 0.01 | +ve |
| X.14 PCT mergers [C] | –1.46 | < 0.001 | N.A. | ||
| X.15 PCT income % [C] | 0.292 | < 0.001 | N.A. | ||
| X.16 PCT weighted population [C] | 0.303 | < 0.001 | N.A. | ||
| X.17 Deprivation index [C] | 0.156 | 0.013 | N.A. | ||
| X.37 Non-admitted patients referral to treatment < 18 weeks, % change 2007/08 to 2008/09 | 0.74 | X.8 % spent on independent-sector healthcare | 0.146 | < 0.001 | +ve |
| X.14 PCT mergers [C] | –0.853 | < 0.001 | N.A. | ||
| X.15 PCT income % [C] | 0.26 | < 0.001 | N.A. | ||
| X.16 PCT weighted population [C] | 0.126 | < 0.001 | N.A. | ||
| X.17 Deprivation index [C] | 0.084 | 0.007 | N.A. | ||
| X.38 Average number of patients waiting more than 4 weeks for a 1st outpatient appointment following a GP referral/PER 2008/09 weighted population | 0.68 | X.8 % spent on independent-sector healthcare | 0.299 | < 0.001 | –ve |
| X.15 PCT income % [C] | 0.259 | 0.002 | N.A. | ||
| X.17 Deprivation index [C] | 0.427 | < 0.001 | N.A. | ||
| X.39 Monthly mean waiting list, IP & day case, per weighted population | 0.74 | X.8 % spent on independent-sector healthcare | 0.57 | < 0.001 | –ve |
| X.14 PCT mergers [C] | 2.578 | < 0.001 | N.A. | ||
| X.49 PCT surplus | 0.72 | X.8 % spent on independent-sector healthcare | 0.45 | < 0.001 | –ve |
| X.17 Deprivation index [C] | 0.135 | < 0.001 | N.A. | ||
| X.55 FCE/weighted population | 0.36 | X.15 PCT income % [C] | –0.012 | < 0.001 | N.A. |
| X.16 PCT weighted population [C] | –0.006 | 0.009 | N.A. |
Appendix 5 Case study site vignettes
Metroland
Metroland is a borough in the London NHS region with a population of about 270,000. It had been served by a PCT whose boundaries corresponded to those of the borough. Before fieldwork started, the PCT had clustered with three neighbouring PCTs, each of which was part of the same conurbation. During fieldwork this cluster had merged with a similarly sized neighbouring cluster.
The population served by the former PCT is in the second quartile of measures of deprivation. The main Public Health England average measures of health in Metroland are mixed compared with the English average. Life expectancy and healthy eating are higher than the English average, but smoking-related deaths and levels of children in poverty are higher than average. Premature mortality caused by CHD is the same as the English average.
There are about 50 GP practices in the borough. The former PCT largely dealt with two acute providers. During the course of fieldwork, one of these providers merged with two other acute providers in other parts of the conurbation. Given the PCT’s proximity to many other acute providers in the city, it also dealt with some of these. About 55% of its allocation was spent on one of the main acute providers and around 33% was spent on two others. Acute services were also offered by two private providers. The original four clustered PCTs shared services with one NHS community and mental health service provider. Some mental health services were also provided by the voluntary sector. The local authority boundaries corresponded to those of the original PCT, which also commissioned adult social and mental health-care services, some jointly with the clustered PCTs.
Subsequent to the clustering of the PCTs, demerging has in effect taken place with the creation of a CCG whose boundaries correspond to that of the original PCT.
Porttown
Porttown is a city with a population of about 260,000. The population served by the former PCT is in the top quartile of measures of deprivation, as measured by income and employment scores. 299 The city has above average poor health for most of the main measures published by Public Health England. For example, life expectancy in the city is lower than the English average and it also ranks below the average for measures of healthy eating and above the average for smoking and premature mortality caused by CHD. The proportion of children living in poverty is about the same as the English average. 300 The Network of Public Health Observatories produces health profiles for each local authority in the UK. These use Office for National Statistics data from the Index of Multiple Deprivation for 2010 for each Lower Super Output Area to describe the sociodemographic characteristics of these authorities (www.apho.org.uk/default.aspx?QN=P_HEALTH_PROFILES).
There are around 40 GP practices in the city. Secondary acute care is provided by one large district general hospital (DGH) and two private hospitals. The DGH accounted for over 90% of the PCT’s spend on its main acute provider. At the time of fieldwork, the PCT retained its public health provider arm, but the commissioning function was in the process of being transferred to the local authority. There is one main NHS provider of community and mental health services, including inpatient provision. There are also out-of-area inpatient services commissioned from the private sector. Mental health services are also provided by a small number of voluntary-sector organisations, some commissioned jointly with the local authority. The PCT boundary was coterminous with the city local authority. The local authority is a commissioner of adult social and mental health-care services.
As with all our study sites, the clinical commissioning group was in the process of being established during the course of fieldwork and in April 2013 it assumed commissioning responsibilities from the former PCT and that of a neighbouring one. The resulting CCG boundaries covered the city and most of the county in which the PCT was located, including another large city. The CCG is divided into three localities. One of these localities covered the former PCT’s catchment area, but also extended into the surrounding rural hinterland to serve a population of about 350,000.
Shire
Shire is a predominantly rural county with a population of about 400,000. Two former PCTs served this population, and had clustered before fieldwork. One covered a largely rural population and the other the main urban centre of the county, consisting of two neighbouring large towns with a combined population of over 300,000. The population served by the former PCTs was in the third quartile of measures of deprivation. The county population has generally better health than the English average. Life expectancy and healthy eating are above the average for England. It also has lower than average rates of smoking, premature mortality caused by CHD and children living in poverty.
There are over 100 GP practices in the county, with nearly half of these in the two main urban centres. There are three DGHs in the county, two of which were in the process of merging during fieldwork. The preclustered PCT that served the urban centre spent around 40% of its allocation on one of the main acute providers and around 90% on all three of the providers in the county. The PCT that had covered the mainly rural areas of the county spent around 36% and 70% respectively on these acute providers. Acute services were also offered by four private providers. There was one provider of community and mental health NHS services in the county, with some provision by the voluntary sector, some of which was jointly commissioned with local authorities. We were unable to gain access to the public health service provider. There were three local authority commissioners of adult social care and mental health-care services. The rural PCT boundaries broadly corresponded to those of the county local authority, and the urban PCT boundaries broadly corresponded to those of the local authorities for the two neighbouring towns.
The clinical commissioning group that was being formed during fieldwork now spans the boundaries of the clustered PCTs; that is, it covers the entirety of the rural and urban areas of the county. The PCT that had covered the mainly rural areas of the county had created a locality structure. This has been retained and adapted to cover the CCG, which is subdivided into 13 localities, each with their own commissioning responsibilities.
Milltown
Milltown has a population of 229,000 and is a city that is part of a large conurbation.
The population within the boundaries of the former PCT is in the top quartile of measures for deprivation. The health of the population is worse than the English average on nearly all of Public Health England’s main measures. Life expectancy in the city is lower than the English average and the proportion of children living in poverty is above the average. It has especially higher than average rates of adult smoking, smoking-related deaths and premature mortality caused by CHD and cancer.
There are just over 50 GP practices in Milltown. Most services are commissioned from two main providers: the acute provider and the mental health provider. About 68% of the PCT’s allocation was spent on the main acute provider and 19% on two others in neighbouring cities. Other services are commissioned from a range of voluntary, community and private-sector providers. Public health commissioning has been transferred to the local authority, which is coterminous with the former PCT patch.
The CCG had been working in shadow form for some time in advance of its legal status. It has assumed the commissioning responsibilities previously held by the Milltown PCT.
Livewell
Livewell was selected as a stand-alone single in-depth case study of a public–private partnership because of government policy to encourage private-sector involvement in commissioning. In this context it involves partnering with a private-sector organisation, as a cocommissioner and provider, to aid whole-system redesign in primary care and to support the commissioning of services for people with long-term conditions at risk of unplanned hospital admissions.
Livewell is an area of the West Midlands characterised by high levels of deprivation, communities with a high proportion of people from diverse minority ethnic backgrounds, poor levels of general health and high levels of chronic disease prevalence. In common with other areas, the health economy is challenged by high and increasing levels of ED attendances and urgent care admissions. Thirty-two different first languages are spoken in the community.
Across the five practices in the Livewell programme, 32% of urgently admitted patients stay in hospital for less than 24 hours; 60% of ED attendances result in patients being discharged, of whom 40% go home without treatment; and there is a large degree of variation in urgent admissions, ED attendances and outpatient referrals between the five practices. In one of the practices, where a more in-depth analysis has been undertaken, 54% of spend has been estimated to be on urgent care, in contrast with inpatient elective (16%), day cases (20%) and maternity (10%).
Driven by the doctors, there was also a series of events held with staff to shape the programme strategy and redesign. Patient participation groups were actively involved on an ongoing basis in design and in offering detailed feedback. Users and care-givers took up structured opportunities for engagement.
Phase 1 of the programme started in 2008 and covered one practice, of 9500 patients. Programme management support was secured from a private-sector health-care commissioning support provider, which also delivered the telephone care-management service. Phase 2 of the initiative, which was conceived in 2010 and sponsored by the local PCT as a fund-to-save initiative (approximately £500,000), comprised five practices covering 50,000 patients and was supported by the same private-sector firm. Redesign of care included an initiative to run group consultations, a think-tank and a telephone care-management service. It is this last, in phase 2 of the project, that is the principal focus of this case study.
Appendix 6 Specimen interview schedule
Appendix 7 Coding frame for case study interview transcripts
| Media of power coding frame v7 | ||||
|---|---|---|---|---|
| All columns Providers can be primary, secondary and public health carers and can be located in the NHS, local authorities, the voluntary sector and private-sector organisations, GPs. Where organisations (e.g. general practices) have both a commissioning and a providing role, we treat those roles separately. |
||||
| Column B sub-codes (B1–B5, in ascending strength of commissioner’s role): B1: Provider force majeure B2: Provider initiated proposal(s) B3: Commissioner deliberately left this issue alone (Klein’s ‘sleeping dogs’ decision) B4: Commissioner initiated proposal(s) B5: Commissioner force majeure |
||||
| Column C sub-codes (annotate descriptions onto transcript) Circumstances which: C1. Limit use of a medium power (e.g. no alternative provider locally, commissioning driven by historical spending patterns) C2. Potentiate the medium (e.g. Secretary of State is local MP) C3. Make the medium of power work unexpectedly (e.g. competition raises not reduces costs) C4. Have other mediating/moderating effects |
||||
| Medium of power | A | B | ||
| Negotiated order (relationality) NB Only negotiations between commissioner and provider, not other negotiations |
M1 | Explicit or tacit mutually agreed arrangements between commissioners and providers about their involvement in and responsibilities for commissioning concerning: | ||
| information sharing | 1 | |||
| division of labour | 2 | |||
| collaboration/participation | 3 | |||
| other | 4 | |||
| Provider competition/contestability | M2 | Commissioners’ attempts to manage competition between providers by deciding (insofar as they are permitted to): | ||
| Criteria for selecting providers | ||||
| package of care | 1a | |||
| price | 1b | |||
| quality | 1c | |||
| Range of providers: | ||||
| inviting new bidders | 2a | |||
| helping establish new providers | 2b | |||
| providing services themselves (the ‘make or buy’ decision) | 2c | |||
| refusing to use particular provider(s) | 2d | |||
| Monopsonisation (number of commissioning-side organisations) | 3 | |||
| Other | 4 | |||
| Financial incentives | M3 | The range of financial incentives to motivate providers: | ||
| unit of payment | 1 | |||
| time of payment | 2 | |||
| conditions for payment | 3 | |||
| bonuses/penalties | 4 | |||
| exemptions from payment | 5 | |||
| other | 6 | |||
| Ideological and disciplinary control (evidence-based medicine, professional ethos, political ideologies) | M4 | Technical or scientific knowledge (evidence-based practice, aetiology, epidemiology, models of care . . .); evaluation and pilot results Occupational ethos, norms of conduct towards peers, superiors, clients and others Wider social ideologies (New Public Management, religion, economics, political belief systems etc.) Appeal to/use of higher managerial or political authority, e.g. top NHS managers’ wishes, ‘target’, ‘policy’, CQC, SHA, DH, Secretary of State, etc Other |
1 2 3 4 5 |
|
| Juridical governance (contracts, law, regulation) | M5 | The extent to which and the means by which commissioners are involved in: | ||
| the specification of contract terms | 1 | |||
| use or threat of coercive enforcement of contracts or legal rights | 2 | |||
| the use of arbitration through the SHA or other third party | 3 | |||
| other | 4 | |||
| Managerial performance of commissioning (managerial performance repertoires) | M6 | Managerial resources for commissioning work: | ||
| Which individuals and occupations (patients, professions, organisations, researchers, mgt. consultants etc.) actively participate and their means of participation | 1 | |||
| Which external bodies (e.g. referral screening bodies, commissioning support, consultancies etc.) support commissioning and how | 2 | |||
| Knowledge of provider’s performance and internal management | 3 | |||
| Transaction costs – economies of scale and scope | 4 | |||
| Understanding of commissioning (principles, rationales, methods) and skills | 5 | |||
| Delegation of commissioning work | 6 | |||
| Other | 7 | |||
| Other | M7 | |||
Appendix 8 Action learning
Action learning set findings are presented following the three aims stated in the methods section:
-
sharing preliminary findings and enhancing the research process (aims 1 and 2)
-
sharing commissioning experiences: international perspectives (aim 3)
-
findings relating to the action learning set process: opportunities for personal and organisational learning and development (aim 4).
Sharing preliminary findings and enhancing the research process
When the first action learning set met (2010), analysis of the first phase of case study site interviews was largely complete. From the analysis we constructed scenarios (Table 30) instantiating answers to the question ‘How does power manifest itself in commissioner–provider relationships?’ and presented them to the learning set. The ensuing facilitated discussion endorsed the face and content validity of the scenarios as instances of uses of the media of power. The scenarios served participants as a framework with which to explore notions of power and how they are enacted in commissioning practice. Participants found scenarios from sites other than their own both familiar and comforting, in that they recognised they were experiencing comparable instances of different media of power.
| Scenario | Characteristics |
|---|---|
| Effective commissioning (service specification, contracts) | Effective commissioning should be about integrating the disparate primary, secondary and social care pathways that an individual patient is on. In practice, commissioning is rarely carried out in this way.Commissioning manager |
| Redirecting resources (service specifications, emic [ideological] control) | Too many psychiatrists are employed medicating patients who do not get better. Consequently, those with drug and alcohol problems do not get access to psychological therapies.GP commissioner |
| Reducing inpatient care (financial incentives, service specification) | The Foundation Trust is asked to reduce costs by reducing in-patient care for those with long-term conditions (LTC) and divert patients to community care. The FT asks the PCT to identify which patients should be diverted in this way and whether appropriate community services exist. But they are unable to identify the patients or the community services. There is an impasse over the means of reducing inpatient activity.FT manager |
| Clinician disengagement (negotiated order) | A consultant spends a great deal of time discussing and agreeing with the lead commissioner the introduction of new services and reconfiguring care pathways. But the agreement is reversed elsewhere in the PCT. The consultant feels he has wasted his time and reduces the time he spends working with the PCT.Secondary care clinician |
| Skill sets (managerial performance/personal power) | There is initial resistance by the providers to closer working between community and secondary care services. The commissioner draws on his previous clinical training to use behaviour and change management methods (such as motivational interviewing skills) to deal with the resistance.Commissioning manager |
Further data analysis had taken place by action learning set 4, to which we fed back the emerging findings. The fifth meeting made a critique of a Nuffield Trust research report on commissioning. The learning set:
-
endorsed the face and content validity of our research findings so far
-
suggested adding ‘class hegemony’ and bullying into the media-of-power schema
-
considered that the research provided a common framework for learning set members to explore their experiences, an opportunity for a more sophisticated discussion of experiences, problems and possible ways forward in the workplace.
Sharing commissioning experiences: international perspectives and those from other sectors
At the ‘mini-conference’, contributors from Techniker Krankenkasse (Germany) and Emilia Romagna health region (Italy) described their own commissioning practice and its impact on health care, offering ‘expert outsider’ insights into the focus, processes and expected effects of their commissioning efforts. We presented more of our research findings and there was a facilitated discussion about the applicability to health-care commissioning of supply-chain management models derived from manufacturing procurement.
The learning set concluded that health-care systems can learn from exploring commissioning and procurement practices in countries with different approaches to funding, structuring and delivering care. Health-care systems can also apply – with adaptations – private-sector procurement processes to state-funded and insurance-based health-care systems. The Cousins Supply Wheel62 depicts the different pressures related to effective supply-chain management (organisational structure, portfolio of relationships, cost–benefit analysis, skills and competencies and performance measures) in other economic sectors. The learning set members found it relevant to NHS providers and commissioners because, with adaptations, it could be used to aid in the development of a ‘contingency’ version of the commissioning repertoire, expressly adapted to different commissioning circumstances. This adapted version includes engagement with users (patients, public and populations), explicit concern about the quality of provision, and management–external factors such as political ‘interference’ and the media.
Personal and organisational learning and development
The action learning helped to resolve real health management problems in health-care commissioning, and through learning at a distance from work and its day-to-day pressures helped to support commissioning staff as they ‘ride the storm’. It involved reframing their management issues or problems, which opened up potential solutions not previously considered – an instance of ‘double-loop’ learning. 314 Box 1 summarises the local contexts and pressures in which the set members were operating.
-
Knitting contracting, strategic commissioning/service redesign and quality and safety together in the right way.
-
Need to align interests in primary, secondary and social care.
-
Short-termism in projects.
-
Newness of clinically led commissioning.
-
Structural transition in general.
-
Workload and quality variability in primary care.
We took care to distinguish the research from the action learning process. The action learning facilitator’s role was to facilitate learning, not to act as expert. Participants were encouraged to bring their own problems and identify actions to enact in the workplace. On behalf of the others, one participant summarised some of the issues they faced in their work and addressed in the learning set meetings (expressed in general terms to protect confidentiality; Box 2).
-
Importance of alignment of interests and transparency in commissioning.
-
Clear aims in contracting, underpinned by sound legal framework.
-
Weaknesses of the quasi-market system.
-
Lack of transparency and poor accreditation/monitoring of performance.
-
Achievements not rewarded and contracts awarded by historical rather than current performance.
-
Lack of information for patients and public to make truly informed choices.
-
Need to balance competing/conflicting interests of organisations/different patient groups.
-
Need to manage conflicting stated aims of the government: competition versus cooperation.
-
Different modes of commissioning: contractual versus negotiated.
-
Different levels of co-operation and trust between providers and commissioners.
-
Improved quality and reduced cost where integrated care has worked.
Action learning involves key interpersonal skills. The learning set supported the development of interpersonal and intrapersonal processes through encouraging and modelling active listening, careful questioning and commitment to action. Although it was self-selected, the group functioned well with high levels of engagement, trust, constructive challenge and questioning. After the final action learning set, a member who is a commissioning manager wrote a reflective piece commenting:
It has been interesting to start to apply theory to our commissioning pursuits more. Our issues are common/universal . . . It was really interesting to get an understanding of [large urban area] initiatives, where scale can be a real help . . . On the whole I think it has consolidated my view about the options open to us within commissioning, levers and incentives, service redesign versus contract and performance. I still think we need to know more about the different contractual models open to us . . . I have been struck by our continued recognition that the determinants of health are many but we are constrained in a system that is mainly health focused or works in silos for the most part. This is very much resonant with how we wish to develop an approach in [site] around using community assets and mixing health and social care interventions together.
Commissioning manager, action learning set
Also:
Reflecting on the [Livewell] partnership with a private organisation, the blurring of commissioning/providing was great and I know some people do question the split and other areas in the world have not gone in this direction. It is significantly easier to develop a pathway yourself if you have received the funding to do so and there is much untapped potential in primary care. This doesn’t translate into a strategy for how all primary care may change the way they are operating though, but does give a couple of examples of how things could be done differently.
Commissioning manager, action learning set
Appendix 9 Précis of programme theory assumptions from Leximancer analysis
Policy texts associate commissioner managerial capacity with the three main mechanisms and with corresponding service outcomes (italicisation indicates assumption imputed by researchers):
-
Specifying service needs:
-
By understanding care group and population health needs of a local population, good communication and engagement with the public, patients and health and social care professionals, commissioners will design service specifications as the basis for contracts with providers.
-
External commissioning support functions will assist the above, and hence will improve the quality of service that CCGs can buy.
-
Commissioners will form groupings of commissioning at different scales for different care groups. For rare diseases, specialised lead commissioners will propose ‘more effective ways of working’ that improve outcomes without more cost.
-
-
Procurement is equated with complying with regulations intended to maintain fair competition; see below.
-
Monitoring: by using measurement (case mix-adjusted NHS Outcomes Framework targets; systems that track expenditure and reconcile activity and expenditure) and the transparency of commissioned providers and general practices, health outcomes commissioners will:
-
improve those health outcomes
-
stimulate the CCG ‘to work with individual practices to address any “concerns” that a practice is causing ineffective or wasteful use of NHS resources’ (p. 29)303
-
help prevent such failures as at Mid Staffordshire NHS Foundation Trust
-
make commissioners more accountable to ‘patients and the public’ for the health outcomes and quality of care that consortia achieve by proxy of their commissioned providers and member practices (p. 3)195
-
benchmark what improvements there have been in service and quality, and pay providers accordingly
-
feed back into the management of procurement and contracting, in a circular annual process.
-
Two main negotiated orders, and their consequences, are described. Only the first is a medium for direct commissioner power over providers.
-
Commissioner–provider. GPs’ involvement in commissioning, that is giving GPs a financial incentive and tighter financial control to design care packages will:
-
result in pathway redesign, removing ineffective activities, and hence may
-
improve clinical outcomes
-
tighten financial control
-
increase service efficiency
-
give general practices more influence over other providers
-
make commissioning organisations focus on hence influence provider quality
-
make GPs take responsibility for the practical (including financial) consequences of their individual patient spending decisions, and hence align macro population and micro patient-level commissioning
-
get the engagement of the people (fellow GPs) on the demand side (for hospital care)
-
involve general practices in partnership working with social care
-
enable GPs to create and lead change (type of change unspecified).
-
-
NHS–local government. By commissioning jointly (e.g. by using pooled budgets, by lead commissioning arrangements and by involving health and social care professionals from all sectors in designing care pathways or care packages), CCGs and local government will:
-
obtain services for older people or children and families that are ‘joined up’ or integrated
-
obtain higher-quality services in terms of patient experience;
-
make more efficient use of NHS resources
-
drive up the quality of general practice
-
give commissioning plans a local (i.e. local authority) perspective.
-
Etic discursive mechanisms for commissioner control over providers are:
-
national commissioning frameworks that help frame the local negotiations
-
research showing new ways of preventing, diagnosing and treating disease, which will increase NHS quality and productivity and support growth in the economy
-
publishing risk-adjusted NHS Outcomes Framework data, which will lead providers to change their working practices as an emic response to etic evidence.
If statements about providers’ obligations are more than exhortations, they imply emic discursive controls over providers. The implied psychological mechanisms are that feelings of obligation among, ultimately, provider managers and clinicians will make them actively fulfil the obligations. Four associations of concepts involving such obligations were:
-
The government guarantees that real-terms health spending will increase in every year of this Parliament, which oblige ‘the NHS’ to cut waste and transform productivity.
-
In return for becoming more empowered, professionals and providers are obliged to be more accountable for the results they achieve.
-
Endorsement by elected members of local authorities gives democratic legitimacy to commissioning plans.
-
General practitioner involvement will make commissioning decisions reflect the needs and wishes of patients and the public; hence they will be a legitimate guide to provider action.
-
In return for their commissioning powers, GPs will be obliged to be responsible and critically compare referrals with others GPs.
Two groups of mechanisms based on financial incentives to providers were found. Commissioners will have some say over local financial incentives on providers and these incentives will increase efficiency in the system, by means of:
-
Incentive mechanisms based on per-patient payments to providers:
-
Per-patient payments will make people opt for that provider.
-
Personal health budgets will lead providers to improve outcomes, transform NHS culture, put patients in control and integrate care across health and social services.
-
Per-patient payments will enable patients to choose which hospital or GP they want to go to.
-
Hospitals will make savings (for them to spend) if they can do a procedure more efficiently than tariff.
-
-
Other financial incentives to providers:
-
Pathway and other new tariffs for community services will stimulate providers to reduce avoidable readmissions and to establish more joined-up working between hospitals and social care following patient discharge from hospital.
-
Payments linked to quality measures in national clinical audits will stimulate providers to improve service quality. Specifically, QOF incentives will stimulate general practices to make continuous improvements in quality of care.
-
Payment for performance will make pharmacies provide high-quality and efficient services, as well as better value in the use of medicines.
-
An incentive structure based partly on balance of need, NICE guidance, etc. will stimulate providers to achieve a limited number of outcomes set by the Secretary of State and commissioning board.
-
Concepts of provider competition (besides ‘competition’, the terms ‘ social market’, ‘patient choice’ and ‘contestable’ provision) were associated with the following effects and mechanisms:
-
Unsatisfactory services will be terminated. In the event of provider underperformance, a local authority should intervene and ultimately retender the contract where that is in the best interests of its local population.
-
Good providers will thrive and poor providers fail. That is, providers will:
-
improve clinical outcomes, adding years to life and life to years
-
increase quality
-
reduce costs, especially on less efficient care
-
innovate
-
increase productivity
-
have a stronger focus on satisfying patient choice
-
read (on the internet) what patients expect and offer it
-
increase efficiency of service provision
-
simplify access, reducing waiting times
-
incur redundancy costs for unsuccessful providers
-
come forward to respond to what commissioners want.
By reshaping markets, commissioners will develop providers to better meet the needs of the population.
-
-
When GP commissioners decide to attain given outcomes, they will decide either to provide the necessary services themselves or to ask secondary providers to change the services accordingly.
Regulation that makes competition occur is directed at commissioners’ behaviour; it is not intended as a mechanism for commissioner control over providers. Juridical concepts concerning regulation, inspection and contracts were associated with certain concepts of their effects:
-
Regulation will remedy problems – including lack of commissioner control over providers – arising from the absence of competition. Then, joint licensing of providers by Monitor and CQC, including imposing special licensing conditions on providers, will:
-
increase (provider) efficiency in the system
-
maintain essential levels of safety and quality
-
ensure continuity of essential services
-
ensure services are financially sustainable
-
maintain a balance of innovation versus standardisation
-
assess clinicians against protocols, which will reduce clinicians’ discretion not to comply with high-quality protocols.
-
-
New forms of contract will:
-
improve the quality of and access to NHS dentistry, especially for schoolchildren
-
improve community pharmacy services’ quality, efficiency and value in the use of medicines
-
give CCGs more influence over providers than PCTs had.
-
-
Inspectorates will have the following effects:
-
The CQC will take enforcement action against health or social care providers not meeting essential levels of safety and quality.
-
Local HealthWatch will investigate and recommend remedies for poor services.
-
Appendix 10 Evidential status of programme theory assumptions
Comparing our evidence with the 24 main assumptions that, according to our analysis in Chapter 5, underlie current commissioning policy for the English NHS, we found that four (PT4, PT5, PT12, PT22) were consistent with our findings. Whether or not another seven (PT1, PT9, PT10, PT18, PT19, PT21, PT24) also were valid remained unknown because the antecedent event (e.g. refusing provider bail-outs) either had not occurred yet or was beyond our remit (e.g. patient participation in care decisions). Another four (PT3, PT17, PT20, PT23) appeared inconsistent with our evidence. Our findings give the remaining ten assumptions (PT2, PT6, PT7, PT8, PT11, PT13, PT14, PT15, PT16, PT25) qualified support because parts of them were corroborated, parts not. The following evidence called programme theory assumptions PT2, PT3, PT6, PT7, PT8, PT11, PT13, PT14, PT15, PT16, PT17, PT20, PT23 and PT25 into question.
PT2: Through joint commissioning with local government, commissioners will understand care group and population health needs of their local population at a macro level.
The above evidence indicated some public health input into the identification of population and care-group health needs, albeit unevenly. Public health input sometimes did find its way into service specifications, but often did not, for two reasons: lack of short-term cost savings made commissioners give preventative interventions low priority; and the intersectoral health-promotion activities (e.g. for smoking control, changing food-consumption patterns) that have the biggest health impacts are effected more by campaigning, economic regulation and legislation than by service commissioning.
PT3: NHS England’s management and GPs’ knowledge of patient needs together allow and stimulate GP commissioners to link clinical and financial decisions.
Our evidence suggests a decoupling, in contract negotiations, of financial from ‘real-side’ discussions, with a tendency under current commissioning practice for senior managers to conduct financial negotiations with little participation by GPs or consultants. The financial discussions were motivated by pressures to meet financial targets set in consequence of national policy, in advance of discussions of care group or population needs. It remains an open question whether that position will change as CCGs become more established.
PT6: GP commissioning decisions reviews of primary care quality and stronger partnership working with social care will bring about a reconfiguration of primary care pathways, removing ineffective activities.
We found evidence suggesting that micro-commissioning (reviews of primary care quality and stronger partnership working with social care) was indeed focused on reconfiguring care pathways, often in primary care. The evidence also suggested that participants were seeking positive benefits (more effective care, better care coordination, demonstrating the value of existing services) rather than activities to stop, although the removal of ineffective activities was occasionally a by-product.
PT7: The reshaping of primary care pathways and the development of new IT (on-line consultations etc.) together result in primary replacing secondary care to some extent.
When a reallocation of income and/or desirable work was implied, GPs and hospitals had competing interests in obtaining (or retaining) the work, which impeded proposals to substitute primary for secondary care. The evidence also suggests that, so far, information technology did not play much of a role in such discussions.
PT8: GPs’ commissioning decisions, the outcomes framework, the presence of alternative providers and patients’ choice of providers (in particular of GPs) together stimulate and enable GPs to exercise greater influence over other providers.
The foregoing evidence indicates that commissioners influenced providers (including fellow GPs) more through a negotiated order and discussions about evidence than through competitive (including patient choice) mechanisms. A threat to remove resources (e.g. to alternative providers) made providers more inclined to negotiate constructively with commissioners, but providers were not always willing and/or able to respond to GP (or other) commissioners’ demands.
PT11: Increased GP influence over other providers and the substitution of primary for secondary care together reduce costs of care.
As noted, we found evidence of certain limitations of GP influence over other providers, and of competitive pressures impeding the substitution of primary for secondary care. There was no evidence that substantial reductions in the cost of care had so far been achieved by these means, but at so early a stage it would be premature to draw firm conclusions on that point.
PT13: The outcomes framework and IT developments result in patients, commissioners and providers themselves having information by which to compare providers’ performance and to allow patients and commissioners to select (and de-select) providers.
And
PT14: The outcomes framework, information for patients, provider plurality and (later) personal budgets lead patients and commissioners to choose between (and deselect) providers.
The evidence confirms that commissioners (and indeed other providers) compared providers against national and regional benchmarks, but that commissioners seldom deselected providers for that (or any other) reason. Insofar as patient choice affected provider performance or sustainability, it was through the medium of tariff payments, which evidence from all three countries showed to increase providers’ activity and commissioners’ costs. IT played little role.
PT15: Commissioners and patients choosing between health-care providers causes the latter to improve clinical outcomes.
And
PT16: Commissioners and patients choosing between health-care providers causes the latter to improve the quality of care.
Evidence from the three countries suggested that, insofar as patient choice involves the tariff system, it reduces or removes commissioners’ capacity to choose providers, whether to improve clinical outcomes or for any other reason. Where multiple hospitals co-existed, a minority of their service outcomes (including some proxy clinical outcomes) improved, although more did not. Our evidence suggests that provider competition appeared not to be a strong explanation of those patterns.
PT17: Patients choosing between health-care providers cause the latter to reduce the cost of care.
Insofar as patient choice involves tariff payments, and insofar as the overall costs of care are concerned, the evidence from all three countries suggests the opposite.
PT20: Public health activity causes health-care providers to improve clinical outcomes.
Our evidence suggests that public health input (such as it is; see Chapter 6, subsection Local government) into contract specifications and provider monitoring is what links public health activity and providers’ clinical activities. The evidence suggests that at present this links is tenuous, however. The commissioning of health-care providers is partly irrelevant to primary prevention.
PT25: The availability of information by which to compare providers’ – and by implication commissioners’ – performance increases NHS organisations’ accountability to the public.
As noted, the evidence suggests that commissioners do compare providers against national and regional data, some of which are publicly available. To that extent, providers became more accountable to commissioners. Existing commissioners were held managerially accountable to central government by the use of similar information (targets, financial out-turns, etc.), but it is still too early to know whether ‘live’ CCGs will be held accountable through similar mechanisms.
In summary, commissioners influenced providers through managerial performance (transparency of provider activity was important), sustaining a negotiated order (in particular micro-commissioning) whose disciplinary basis was evidence basing and shared emic assumptions (although the content of these assumptions varied considerably between countries) and adjusting incentives. Competition gave commissioners power only insofar as they could select providers, and had at most a mixed impact on the service outcomes studied. Juridical controls were marginal to day-to-day commissioning practice.
Appendix 11 Commissioning organisations and media of power
| Medium of power | PCT | CCG | LA | SHI | ASL |
|---|---|---|---|---|---|
| Management performance | Formal service specifications; monitoring mostly through tariff and target data | Developed competitive procurement system | Case mix and cost monitoring; service redesign only at margins | Case mix and cost monitoring | |
| Negotiated order | Intense relationality with main provider(s); micro-commissioning | Contractual character | Collectively at national, Land and provider levels | Intense relationality with main providers | |
| Discourse | Policy + EBM + culture of local collaboration | EBM + shared collegial norms | Normative; council policy | Case mix modelling; solidarity; regulation | Evidence-based protocols + ideology of subsidiarity |
| Financial incentives for providers | Bundled tariffs + target based + ad hoc | Stability of income | Bundled tariffs + cost-plus (some psychiatry) | Bundled tariffs + ad hoc | |
| Provider competition | Limited, some token competition | GPs uninterested in provider competition | For generic services; and where PCTs could influence LA use of central funds | Not available | Closed to all but existing providers |
| Juridical control | Exceptional | ||||
List of abbreviations
- A&E
- accident and emergency
- ALoS
- average length of stay
- AMI
- acute myocardial infarction
- AO
- azienda ospedaliera (hospital public firm, Italy)
- AQP
- Any Qualified Provider
- ASA
- American Society of Anesthetists [classification of patient’s physical status]
- ASL
- azienda sanitaria locale (local health authority, Italy)
- CCG
- Clinical Commissioning Group
- CHD
- coronary heart disease
- CHS
- community health service
- CLAHRC
- Collaboration for Leadership in Applied Health Research and Care
- CMO
- context–mechanism–outcome
- COPD
- chronic obstructive pulmonary disease
- CQC
- Care Quality Commission
- CQUIN
- Commissioning for Quality and Innovation
- DALY
- disability-adjusted life-year
- DG
- Directorate-General
- DH
- Department of Health (England)
- DRG
- diagnosis-related group
- EBM
- evidence-based medicine
- ED
- emergency department
- FCE
- finished consultant episode
- FFS
- fee for service
- FNT
- funzione non tariffata (variable- or off-tariff activity, Italy)
- FT
- Foundation Trust
- GB-A
- Gemeinsame Bundesausschuss (federal negotiating body, Germany)
- GP
- general practitioner
- GPSI
- general practitioner with a special interest
- HA
- health authority
- HHI
- Herfindahl–Hirschman Index
- HMO
- health maintenance organisation
- HRG
- Healthcare Resource Group
- IAPT
- Improving Access to Psychological Therapies
- ICD-10
- International Classification of Diseases, Tenth Edition
- INHS
- Italian National Health Service
- IRCCS
- Istituti di Ricovero e Cura a Carattere Scientifico (hospitals recognised as research centres and receiving additional public funding for that role)
- ISTC
- independent-sector treatment centre (corporately owned but also designated as ‘treatment centre’ or ‘NHS treatment centre’)
- IT
- information technology
- LES
- local enhanced service
- MDK
- Medizinische Dienst der Krankenkassen (medical service for SHIs, Germany)
- NGMS
- new general medical services (contract)
- NICE
- National Institute for Health and Care Excellence
- OECD
- Organisation for Economic Co-operation and Development
- PBC
- practice-based commissioning
- PbR
- payment by results
- PCG
- primary care group
- PCT
- primary care trust
- PEC
- Professional Executive Committee
- PROM
- patient-reported outcome measure
- QIPP
- Quality, Innovation, Productivity and Prevention
- QOF
- Quality and Outcomes Framework
- RQ
- research question
- SHA
- Strategic Health Authority
- SHI
- social health insurance/insurer
- TCS
- Transforming Community Services
- TPP
- total purchasing pilot
- VIF
- variance inflation factor
- WCC
- world-class commissioning
- WHO
- World Health Organization