Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 10/1011/67. The contractual start date was in October 2011. The final report began editorial review in October 2013 and was accepted for publication in February 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Disclaimer
this report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Lea et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
A lack of ‘joined-up’ working between the health and social care sector and the criminal justice system (CJS) has been reflected in a number of tragic events, resulting in serious case reviews and subsequent inquiries. 1–5
The aim of the Interface Project was to examine and explore current practice relating to the management of individuals with enduring moderate to severe mental health needs (EMHN), specifically at those points where they interface with the NHS and CJS, and to ascertain how such practice can be enhanced. Three stages of work were conducted, each guided by a set of research questions.
Stage 1
-
1. How are the practice implications of current national policy relating to the management of individuals with EMHN being interpreted at local level?
-
2. How has Cornwall articulated national policy into practice benchmarks where the NHS and police are required to work together?
Stage 2
-
3. What are the organising principles that precipitate a joint working decision, by either the NHS or the police?
-
4. What is the decision-making process and who is involved in it?
-
5. Is the decision-making process consonant with local practice guidelines and national policy implications?
-
6. What is the impact of these decisions on the service user?
-
7. What is the impact of these decisions on the NHS and police organisations?
-
8. What are the economic costs associated with current and potentially enhanced practice?
Stage 3
-
9. What are the barriers and facilitators to the multiagency management of individuals with EMHN?
-
10. What are the implications of the research for national policy and practice?
The research project became known as the Interface Project in the early stages of the work in order to contextualise the work and provide the research with an identity. The terms ‘research project’ and ‘Interface Project’ are therefore used interchangeably throughout the report.
Chapter 2 Background
The national context
Throughout the last 20 years, and especially the latter part of the last decade, there has been an escalating debate about how individuals with EMHN might best be managed within and between the NHS and CJS. It is widely recognised by mental health practitioners, the police and the courts that these individuals repeatedly come to the attention of the CJS, with their journey into and out of the CJS being conceptualised as a ‘revolving door’. 6 The Department of Health (DH) has been proactive in commissioning a considerable amount of research in an effort to understand how this cycle might be broken. In 1992, Dr John Reed, in the first of a series of reports, reviewed ‘health and social services for mentally disordered offenders and others requiring similar services’. 7 Among the many recommendations made, Reed stressed that a flexible, multiagency, partnership approach was essential to bring about change.
It is unfortunate, but telling, that 21 years on, Reed’s primary recommendation has been only partially heeded. Indeed, the term ‘silo working’8 has been used to describe the paucity of interaction and engagement between services. Lord Bradley’s inquiry into how people with ‘mental health problems or learning disabilities’ fare within the CJS conceded that since Reed, little had changed except the ‘political and social context’. 6 Baroness Corston’s equally wide-ranging review of ‘women with particular vulnerabilities in the CJS’ identified similar shortcomings to Bradley, but suggests too that where women are concerned, a radically different and holistic approach is required. 9 Rutherford explored the extent to which interagency working or ‘convergence’ has developed, the obstacles that still exist to a wider take up, and the limits that (may) need to be applied to the convergence process to retain professional and ethical boundaries. 8
Her Majesty’s Inspectorate of Constabulary (HMIC) has encouraged the police to embrace the operational and financial benefits to be had from partnership working in all areas of policing;10 Flanagan, in his comprehensive review of policing, arrived at the same conclusions. 11 Perhaps with one eye to the extensive post-Bradley implementation process, the National Policing Improvement Agency in conjunction with the DH produced detailed guidance on how the police should respond to people with ‘mental ill-health and learning disabilities’. They, like others, identify that police officers have little or no formal training in diagnosing or dealing with mental ill-health. 12
Although mental ill-health is not indicative of any latent propensity to criminality or dangerousness, stereotypically, those who live with it are invariably perceived to be predisposed or inclined to both. On the street, where the police are both the first and last resort in dealing with individuals deemed to be experiencing mental ill-health, the ‘successful resolution’ of an incident – the bridge jumper, for example – depends on the unique contextual details of the event in question. These, in turn, will determine the legal powers available to the officer and the sort of action he or she may take. The process of rationalising and interpreting these contextual and legal elements is, of course, informed by the ideological imperatives (the received wisdom) of the police organisational milieu; this may well be quite different to the occupational imperatives of the mental health professional, the social worker, ambulance staff, or general medical practitioners. Moreover, the police imperative may very well conflict or compete with the occupational imperatives of others and the long-term prognosis of the individual concerned. For those whose levels of ‘dangerousness’, criminality and psychiatric diagnosis are such that they are not subject to any formal interagency process such as Multi-Agency Public Protection Arrangements (MAPPA) or Safeguarding Children or Vulnerable Adult protocols and procedures, this is especially so. As many practitioners within the CJS and the statutory and voluntary mental health services have long been aware, these ‘gaps’ in the system are what ensure that many individuals with mental ill-health are destined to make unnecessary and inappropriate forays into the CJS. For a large number of people, this experience is as damaging as it is avoidable.
The need for research
The research literature calls for increased cross-sectoral case- or data-linkage studies to examine service users’ interaction with services to enhance service user outcomes (e.g. Ferrante13). Furthermore, such methods are useful in enabling researchers to identify service user outcomes for populations such as those targeted in this study, which are often considered marginalised or hard to reach. 14 Triangulating data contained in routinely collected data sources with primary data enables not only a holistic picture of the service user experience to be obtained, but also connections between and utilisation of findings to be understood. For example, there has been a recent call for longitudinal studies that include the analysis of administrative or secondary data in combination with validation through primary data collection to provide comprehensive understanding of interactions between services. 15 The Interface Project responded to these suggestions through the qualitative analysis of predominantly secondary data together with a small amount of primary data to enable a ‘thick description’16 of service user journeys and inter- and intra-agency decision-making to be obtained, examined and understood. This broad application of qualitative methodologies fulfils recommendations for the wider use of qualitative methodologies in mental health research to enable the exploration of research areas that are not conducive to the application of purely quantitative methods. 17 The current study also seeks to address three research priorities identified through a consultation exercise:
-
researching care pathways and transitions between services (in this case within and between the CJS and mental health services)
-
research to improve the quality of mental health care in the CJS (through understanding the interactions between CJS staff and service users and mental health professionals)
-
enabling meaningful involvement of service users in the planning and delivery of services (through involvement and consultation of service users on and with the project team and via consultation with service users regarding project findings, and developing implications for research through focus groups). 17
A great deal of the existing research identifies or acknowledges the ‘gaps’ that exist in the interface between CJS and NHS mental health service provision, and the sort of individuals who regularly find themselves falling into those interagency voids. The practicalities of implementing a ‘national intention’ are complex, and necessarily subject to a local interpretation: for example, for a variety of contextual reasons what works well in cosmopolitan inner city London may be less likely to succeed if transplanted to the more isolated districts of rural Cornwall. This project sought to illuminate the nature of these gaps both nationally (through a practice-focused review of existing documentation) and locally (through a detailed study of Cornwall’s attempt to translate EMHN policy into practice guidelines for NHS/CJS interface working), in order that interagency decision-making, communication and service delivery are improved.
It is essential that rigorous academic research is conducted in order to understand the disparate processes and outcomes in relation to individuals with EMHN across the country, in order to address the inevitable inconsistency and lack of coherence between policy and practice. Furthermore, as the current situation demonstrates, a lack of dialogue within the same organisation and between organisations ensures that individuals ‘known’ to all or some of them are frequently not dealt with in a truly integrated or genuinely informed way. If the ‘silo mentality’ stifles interagency dialogue and inhibits practitioners and managers from exploring every option when dealing with those individuals who are known to a number of organisations, it also exaggerates the distinct and seemingly competing occupational aims and cultures of those involved. Thus, an important aim of the research was not only to find ways to promote greater interagency dialogue, but also to explore how practitioners from different organisations might develop genuine partnerships in dealing with individuals who are known to a range of organisations. A ‘case-linkage’ methodology offered a useful and exciting means of finding ways to include a range of relevant practitioners and professionals into the health-care process and improving continuity of care and access.
Reflecting local need
Against the above background, the research arose out of a small pilot project, set up to scope the need associated with individuals having EMHN and care plans who are also known to the police. The project was set up as a partnership between the local policing area in East Cornwall and the Cornwall Partnership NHS Foundation Trust (CFT) funded by the NHS. This pilot identified the scale of the need and resulted in a partnership bid to the National Institute for Health Research (NIHR) to conduct the Interface Project.
Cornwall’s partnership working with individuals who may encounter health and social services and the CJS has pockets of exemplary practice. These include co-ordinated activities around the use of Section 136 of the Mental Health Act (MHA),18,19 the operation of drug treatment requirements as part of Community Rehabilitation and Punishment Orders, the enactment of the MAPPA and maintaining performance with regard to prison transfer targets for mentally disordered offenders. Multiagency collaboration is underpinned by a local forum, the Peninsula Criminal Justice Agencies Group (formerly the Mentally Disordered Offenders Group), where major stakeholders (Crown Prosecution Service, probation, primary care trusts, local authorities, police and provider trusts) are represented. Inevitably, where specific services or activities are underpinned by statutory requirements, clarity and delivery are enhanced. Local experience is that where the legal and statutory basis of provision is unclear and risk is possible but uncertain, then co-ordination of activities relies on the interpretation of service mandates by authoritative individuals who may have competing agendas (e.g. risk management vs. capacity management).
Research into practice
It is widely acknowledged that the translation or implementation of research findings into practice must occur more frequently and widely. Indeed, implementation in mental health practice has been described as ‘embryonic’. 20 Within the Interface Project, therefore, an iterative process of ‘translational forecasting’ enabled potential opportunities for the translation of research findings into practice to be explored and optimised as they become available in real time.
Within the research framework, specific models and strategies for facilitating the implementation of findings were reviewed. The literature recognises that innovation adoption fails to achieve long-term implementation due to deficiencies in the implementation strategy rather than due to those in the innovation itself (e.g. Klein and Sorra21). Therefore, the concept of a translational continuum was of particular relevance, involving an explicit focus on translating research findings into practice from the outset of the research to ensure adoption, early and enduring implementation of recommendations and actions based on the research findings. 20,22
Chapter 3 Methodology
Overview
A three-stage methodology was used to achieve the aims and objectives outlined in Chapter 1 (two using secondary data and one gathering a small amount of primary data). Stage 1 involved a review of documentation pertaining to the translation of national policy into regional/local practice guidance in the area of EMHN. Stage 2 represented the main body of work and was a case-linkage study involving NHS case records and police case records for individuals with multiple mental health episodes, deemed of moderate risk, and known to the police. Stage 3 explored the barriers and facilitators to the effective multiagency management of this vulnerable group in the light of evidence from the review exercise against the findings from the case-linkage study. The three stages are presented in this report as distinct sections containing methods and findings for each stage. Quotations are provided in the findings of stages 2 and 3 to illustrate the themes emerging from the analysis; it should be noted that the use of offensive language in quotations has been retained to remain true to the original voice of the participants.
Conceptual framework and design
The project was informed by a conceptual and methodological framework developed by the project team to successfully evaluate a range of multiagency services and initiatives through the rigorous application of mixed methods. 23 This framework was responsive to identified need,24 adopting Burke’s25 principles of participatory evaluation. Burke (1998, pp. 44–5)25 posits seven principles of participatory evaluation:
(1) The evaluation must involve and be useful to the program’s end users; (2) the evaluation must be context-specific, rooted in the concerns, interests and problems of the program’s end users; (3) the evaluation methodology respects and uses the knowledge and experience of the key stakeholders. (4) the evaluation is not and cannot be disinterested; (5) the evaluation favors collective methods of knowledge generation; (6) the evaluation (facilitator) shares power with the stakeholders; (7) the participatory evaluator continuously and critically examines his or her own attitudes, ideas and behavior.
These principles were operationalised in the Interface Project through the engagement of stakeholders at all stages of the research/evaluation process to ensure the meaningful utilisation of project findings26 and enhance multiagency working and service user outcomes. The framework was further informed by the tenets of community psychology, which espouse collaborative working with traditionally marginalised groups and understanding people within their social contexts. 27
Implementation science in action
The current research constituted a single-site study in Cornwall. The research team adopted a two-pronged approach to the dissemination and implementation of the research findings:
-
thorough and considered implementation of the findings in the county of Cornwall across police, NHS and third sector organisations
-
dissemination of the research findings nationally to both academic and practice communities through a consultative process focused on the translation of the findings into different local contexts.
Implementation in Cornwall: the praxis-oriented dialogue model
A social constructionist epistemology and central tenets of community psychology form the basis for what the authors’ term the praxis-oriented dialogue (PoD) model of implementation. Social constructionism is a theory of knowledge which is broadly concerned with the ways in which reality is actively constructed, rather than pre-existing. 28 Psychological and social phenomena, in particular, are constructed or coconstructed with others and there is an emphasis on the role of language and discourse as the medium through which meaning and understanding are created. As presented above, community psychology advocates explicitly focussing on the experience of those individuals traditionally marginalised by society within a democratised research process.
This model was explicitly defined within the Interface Project, building on the methodology that Lea and Callaghan had been using in their work for many years. It articulates implementation as integral to the research process, considered from research conception and embedded in research design, rather than simply constituting a ‘research phase’. The PoD model reflects a set of principles that inform the process of research, to maximise engagement, ownership and translation into practice. Thus, the PoD model set the context for the way in which qualitative and quantitative data would be collected and analysed as part of a mixed-methods approach to research design. The PoD model is particularly appropriate for health-care research relating to interagency and joint service development, delivery and innovation. A set of three core and three operational principles define the model representing its epistemological basis and methodological foundation.
Knowledge is socially constructed
The discipline of the sociology of scientific knowledge reminds us that all knowledge is socially constructed, and recognises the existence of powerful ‘ideological commonplaces’ relating to the tacit ‘how to’ knowledge associated with socialisation into different professions, disciplines and their respective cultures. Understanding the intersubjective, intertextual and fundamentally dialogic nature of social life and being mindful that all language is dynamic, relational and engaged in the redescription of the world is fundamental to the effective and successful implementation of research findings. Understanding that knowledge is socially constructed enables researchers to acknowledge that as research findings are translated into practice contexts they will be redefined and reinterpreted in that context; a new set of meanings may be created. Furthermore, in mental health service delivery, benefits can be derived from researchers, practitioners and service users working together to coconstruct the meaning of the research. Specially, the ‘over to you’ approach that characterises much dissemination activity can create a barrier between research and practice and risks the impact of research being ‘lost in translation’.
Research is explicitly committed to critiquing the status quo and building a more just society
The notion of ‘research as praxis’29 is fundamental to the PoD model. Praxis involves putting ideas or theories into action or practice through a reflective process, which aims to achieve change. The elements at the core of research as praxis are that those being researched are involved in the research through a ‘democratized process of inquiry characterized by negotiation, reciprocity, empowerment’, acknowledgement that research cannot ever be neutral30 and that research thus framed is ‘explicitly committed to critiquing the status quo and building a more just society’;29 that is, it aims to transform. Indeed, at the core of much health and social care research is a concern to provide an evidence base for practice to transform services such that they offer enhanced user care. As researchers, practitioners and service users, we are committed to using the rigours of research to enable positive social change and ensure ‘sustainable co-creation processes that model, seed, and support progressive change agendas’. 31
Practice-informed research is as important as research-informed practice
Evidence-based, or research-informed, practice is central to best practice. However, the authors argue that the notion of ‘practice-informed research’ is equally important in health-care research generally and particularly in relation to research into mental health care service delivery. Thus, research arises from challenges in the current practice context, and is developed and designed in relation to that context. For example, the benefits of ‘bottom-up, clinician-conceived and directed clinical intervention research, coupled with collaboration from research experts’32 have been noted. This approach increases the likelihood that research is relevant, appropriate and significant to practice and, therefore, that the potential for effective and sustained implementation will be realised. Research-informed practice and practice-informed research lead to both improved practice and improved research in the challenging context of mental health care service delivery.
‘Implementation’ should be thoroughly embedded within the research
Building on the first three principles, the PoD model asserts that researchers should contemplate implementation from the outset of a research project, and that this approach should inform both the governance and process of the research. Although many funding bodies require dissemination and implementation strategies to be included in research proposals, research suggests that these are often insufficient to effect successful translation of findings to practice. Research-driven change is complex and invariably impacts on individual practitioners and support staff at various levels of the target organisation, as well as potentially affecting ways of working between individuals, sections, departments and other agencies. In order for implementation to be effective, Eccles et al. 33 noted the importance of having a health-care workforce that can sustain implementation in the clinical setting as a matter of routine. Including practitioners as members of the research team assists in privileging the importance of implementation right from the start and in being mindful of the context within which research findings will need to be applied. Furthermore, permitting the dialogic and intertextual nature of social life into the research team allows for the development of a sensitive, appropriate and realistic implementation strategy. Operationally, thoroughly embedding implementation within the Interface Project will enable timely identification of barriers and facilitators to implementation, key gatekeepers and champions, relevant practice meetings and events to attend. This allows projects to map out a ‘timeline of engagement’, informing the implementation strategy over the lifetime of the project.
Key stakeholders need to be engaged in a meaningful, authentic way
In a context of increasing ‘transdisciplinarity’,34 considerable benefit can be derived from establishing a multidisciplinary research team, including academics from different disciplines as well as practitioners and service users, and from key stakeholders’ meaningful and authentic engagement in the research. Although the attendant diversity of views can be challenging, the consequent reciprocal understanding enables appropriate contextualisation of the research and lays the foundations for effective implementation while building joint accountability, responsibility, investment and ownership. This aligns with Baker et al. ,35 who regard translation as a ‘new, broader, collaborative approach that brings clinicians, researchers, patients, and managers together to improve care’.
Stakeholder engagement and the associated successful implementation of research can be facilitated further through the integration of researchers within health-care organisations as Eccles et al. 33 noted: ‘Implementation research and implementation researchers need to be embedded within the NHS’. The benefits of this approach include enabling key elements of the research to progress (e.g. data collection, case-linkage); increased engagement of individuals and organisation with the research; increased collaborative working; increased shared investment in the successful outcome of the research; enhanced understanding and appreciation of roles (both research and practice); and increased rapport and trust leading to joint problem-solving in the face of gate-keeping. Taken together, these benefits positively influence the likelihood of the successful implementation of research findings in the service context.
The relationship between researchers and practitioners is respectful and appreciative
Shotter has argued that ‘too often’ researchers act as ‘external observers of others’ conduct’ (unpublished paper cited in Lather31). This leads to a divide between ‘researcher’ and ‘researched’ (whether health-care provider or user) and fuels the translation gaps identified by Cooksey. 36 Therefore, the PoD model asserts that although the nature of stakeholders’ engagement may vary, both researcher and researched should be involved together in the research process. Furthermore, such relationships must be characterised by genuine mutual respect and appreciation, the valuing of all contributions, and equality. Achieving such relations involves overcoming the sometimes competing cultures that define different professions, and the mistrust that can exist between researchers and practitioners that is sometimes fuelled by perceptions that researchers are making ‘diagnostic pronouncements’31 about current service delivery. However, it is through effective, constructive relationships that translation can best be achieved.
National consultation and dissemination: moving beyond Cornwall
Although this study involved a single site, given the rationale for the research and the ongoing challenges of managing this vulnerable, marginalised and under-researched population, it was decided to explore the applicability of the research findings beyond Cornwall. A national consultation and dissemination strategy was developed early on in the project to address this. Four sectors were identified and targeted, as illustrated in Figure 1, mirroring the key stakeholder groups engaged in the research and responsible for the management and research of individuals with EMHN. These were the police, the NHS, third-sector organisations and the academic community. Within each of these sectors, key individuals and/or organisations as relevant were directly targeted with a view to sharing the research findings and consulting on their implications for differing contexts. This process (illustrated in Figure 2), was greatly facilitated by the academic–practice collaboration described above and informed by the PoD model, as the team had knowledge of and access to a wide variety of influential individuals nationally through academic and practice contacts and networks.
FIGURE 1.
Key national sectors for consultation on and dissemination of findings.
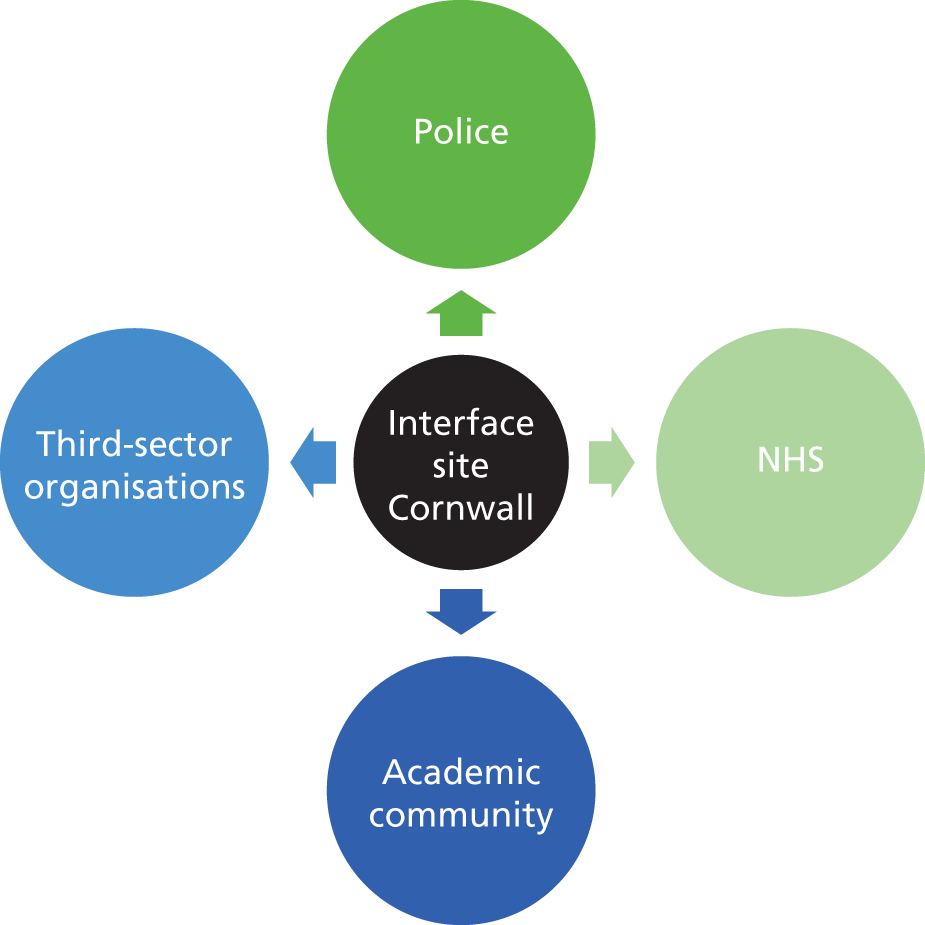
FIGURE 2.
Dissemination strategy beyond Cornwall.

A central focus of this strategy was a targeted Interface National Stakeholder Consultation event, held at the Institute of Psychiatry, King’s College London, on 10 September 2013.
Research capacity building
The research team were committed to ensuring that research capacity was developed within the partner organisations. Although elements of the PoD model support the activity of research capacity building, this was seen as an element of the project that required explicit action to ensure that the research had both positive and lasting impact in practice organisations. In order to ensure that this was being achieved, the team used the components of Cooke’s framework for analysing research capacity building to ensure a holistic approach. 37 Each of these components are presented below, detailing how they were fulfilled by the Interface Project.
Skills and confidence building: developing appropriate skills and confidence through training and creating opportunities to apply skills
Due to the participatory approach of the PoD model, members of the research team from practice organisations received research training and development from the proposal stage of the research. Academics ensured that practice-based members of the team were able to develop according to their interests and the needs of the research. The success of this approach is reflected in the development by practice staff of a bid for research funding to investigate the efficacy and utility of a custody service innovation. The approach also contributed to a police research team member successfully applying for a Winston Churchill Fellowship to examine the implementation of Mental Health Courts and Crisis Intervention Teams in Chicago and Baltimore, USA. Furthermore, through the embedding of the Interface research manager in the CFT Centre for Mental Health and Justice, staff and trainees were able to access expertise and advice as appropriate when embarking on evaluations and audits to monitor aspects of work of the team and scope for further funding.
Close to practice: to enable implementation/utility
As described, the research manager and research assistant were integrated into CFT and Devon & Cornwall Police (DCP), each receiving honorary contracts in order to undergo relevant training to facilitate access to systems and sites. Part-time (approximately 2 days a week) situation of the research manager in the CFT Centre enabled the formation of links to facilitate:
-
development of the detailed process of case extraction and linkage according to protocols and guidance within each organisation
-
implementation of findings of current research
-
potential opportunities for research/evaluation support
-
potential opportunities for collaboration beyond the current project
-
potential opportunities for staff development
-
potential opportunities for service delivery research/evaluation as a follow on/beyond the current project.
Linkages and collaborations
Although three members of the original project team had worked together previously on a variety of criminal justice-related projects, Interface Project funding enabled the development of a team that not only strengthened the partnership with DCP but also extended to the CFT (including mental health and social care), primary care (through the health for homeless service that were instrumental in the service user consultation) and third-sector agencies. This not only enhanced the implementation of the findings of the Interface Project as described above, but developed both academic–practice relationships and collaborations between practice organisations. Examples of how such collaborations have impacted on practice as a result of this project include:
-
provision of support for the development of a business case for the innovative custody liaison and diversion service
-
provision of advice with regard to the development of the street triage service delivery model for Section 136 detentions and associated evaluation
-
a successful collaborative proposal developed to support pump prime of evaluation of service delivery model from the Institute of Health and Community, Plymouth University, Plymouth
-
development of CFT risk assessment training.
Appropriate dissemination: to maximise impact
Dissemination was undertaken from the earliest available opportunity in order to embed the research in the practice organisations. Presentations were made at a CFT Research Continuing Professional Development event to raise awareness among CFT staff, at an event held on World Mental Health Day in order to disseminate information to service users, and at a police joint health commissioning day to ensure that members of DCP were aware of the research. Meetings also took place with Mental Health Team (MHT) leads in order to disseminate project aims and objectives and plan implementation from the outset. Additionally, following completion of the clinical audit, meetings and consultations were held between inpatient and community service line leads to disseminate clinical audit findings and support the development of recommendations and actions. The research manager was also a member of the CFT Research and Innovation Committee.
Continuity and sustainability: maintenance and continuity of newly acquired skills and structures to undertake research
Through the participatory approaches highlighted above, practice members of the team were able to gain experience in a range of research skills including writing funding proposals; applications to the National Research Ethics Service (NRES) and the National Information Governance Board (NIGB); research design; data collection; data analysis and service user consultation. As such, team members gained confidence to enable them to disseminate these newly acquired skills within their organisations. Furthermore, and importantly, the embedding of researchers and conduct of the project directly in and with practice engendered the development of a research culture within these organisations with consideration of the value of research and evaluation to support practice and in the design and development of service.
Infrastructures: structures and processes set up to enable smooth and effective running of research projects
The methodology employed to conduct the case-linkage study necessarily relied on access to systems, including mental health records and police intelligence systems. The researchers worked with the practice organisations to develop information-sharing protocols to support the work of the project. This was facilitated through the inclusion of the force data protection officer and the CFT information governance manager on the Project Steering Group to monitor the requirements of the project in the light of the agreements in place. These structures and processes, set up early in the project, were invaluable in the application to the Ethics and Confidentiality Committee of the NIGB for Section 251 support. Owing to both the established collaborative relationships and the clear protocols already in place, a successful application was made that received Secretary of State approval to access records for the purpose of the research. Additionally, these structures and processes enabled the development of further interagency work that required cross-system access and analysis such as the current CFT audit of the new custody liaison and diversion service.
Finally, the formal buyout and associated subcontracts between the practice organisations and lead academic institution enabled planned, effective and sustainable management of protected time for practitioner members of the research team. This also enabled an explicit link to be made between practitioner–researchers’ current roles and their role in the research team, which further underlined research as a core activity for these individuals and more generally in their teams.
Project management
As per the protocol, the project was managed by a collaborative team of academics, practitioners and service user researchers, experienced in working in multisite, multidisciplinary initiatives. The project was headed by Professor Lea (Institute of Psychiatry, King’s College London) who has considerable experience in leading this type of academic and community work, including having occupied key roles in the Local Strategic Partnership of Plymouth with responsibility for co-ordinating and delivering outputs and outcomes. Regular monitoring and reporting was undertaken in order to ensure project progress and success. Figure 3 presents the project management structure and associated communication and dissemination channels.
FIGURE 3.
Project management structure.
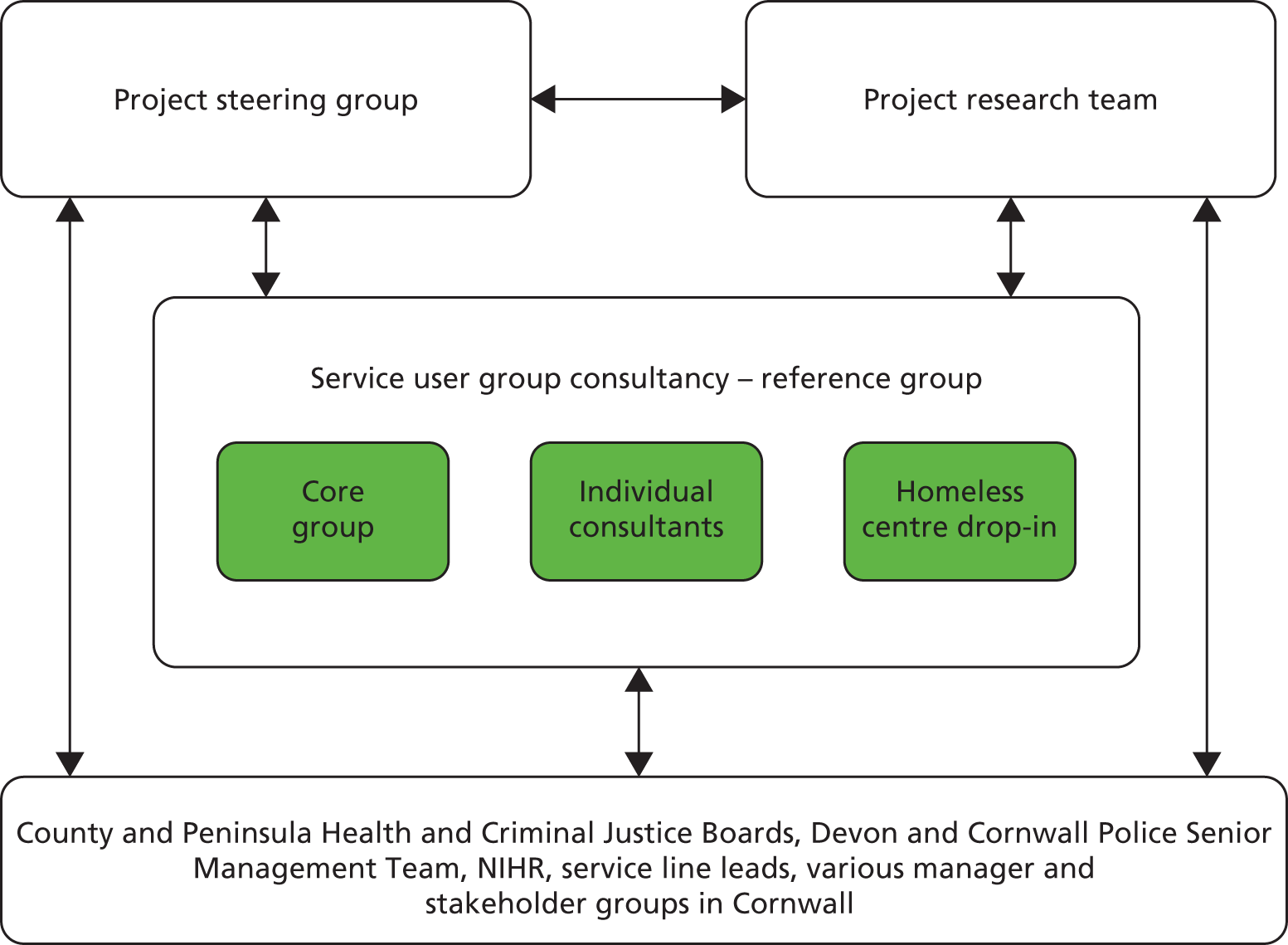
Three distinct groups conducted, monitored and consulted on the research, these being the research team, the steering group, and the service user reference group respectively. The research manager and research assistant were present at all steering group, research team and patient and public involvement (PPI) sessions, providing continuity and a single point of reference across the groups. A service user consultant, employed by the trust, sat on both the steering group and reference group, liaising and communicating between the two. Wider collaboration and consultation with service users is described in detail in the methods and discussion sections of this report. Practice members of the research team took on additional dissemination roles, promoting the project at regional and local meetings, which they attended as part of their formal roles. The research manager represented the project specifically at the Local Health and Criminal Justice Boards, Section 136 meetings and in communicating findings to trust service line leads and force staff as appropriate. The interactions between the different elements of project management within the project are illustrated in Figure 3.
Steering group
The project reported to a steering group comprising team members, stakeholders from the NHS, police, third sector and service users – representing the main organisations with an interest in the research. The terms of reference of the group included responsibility for monitoring the delivery of milestones to time and on budget, ensuring the appropriateness of the communication and dissemination strategy associated with the project and receiving interim and final reports. Membership of the steering group extended during the course of the research to include individuals within statutory and third-sector organisations with key strategic and practice-based roles in both the management of individuals with EMHN and/or information governance in the practice organisations in which the research was based. The steering group was chaired by an independent chair, Professor Rod Sheaff, who has experience as a principal investigator on NIHR-funded projects. Meetings were held quarterly throughout the project until the last meeting on 20 September 2013.
Research team
The full project research team met bimonthly [in person or via telephone conferencing/voice over internet protocols (in this case Skype™; Skype Ltd, Rives de Clausen, Luxembourg)]. The meetings were held in the south west in various locations hosted by each of the participating organisations. Each meeting was chaired by Professor Lea or Dr Callaghan (research manager) in person and included the regular evaluation of project performance, both financial and non-financial, ensuring that any necessary corrective actions were undertaken in a timely manner. The research team meetings were important in ensuring that the research was being conducted rigorously and answering the research questions defined in the protocol. Furthermore, practice-based research team members were able to highlight changes in policy and practice that could affect the conduct of the research and/or the context in which implications from the research would be drawn. The membership of the research team changed from the original fund holders, specifically in relation to the police fundholders and health economics academics, with all changes to the team approved by the Health Services and Delivery Research (HS&DR) programme.
The roles of the members of the research team were as follows: Dr Callaghan (Research Manager, Plymouth University) was responsible for day-to-day operational project management and liaison with NHS and police colleagues; Susan Eick (Research Assistant, Plymouth University) supported the work of the Research Manager and day-to-day operation of the project; John Morgan (fund holder, CFT) facilitated the conduct of the project and implementation strategy within the Trust; Chief Inspector Mark Bolt (fund holder, DCP) facilitated the conduct of the research within the force; Dr Diana Rose (fund holder, Institute of Psychiatry) guided the development of the PPI strategy for the project; Dr Anita Patel (fund holder, Institute of Psychiatry) led the health economics component of the Interface Project until she went on maternity leave, specifically she was responsible for overseeing the development of the methodology and data collection; and Professor Graham Thornicroft (fund holder, Institute of Psychiatry) provided specialist advice and guidance on elements of the project.
In summary, a framework of robust governance structures ensured effective delivery of outputs and outcomes including project management, financial tracking, risk management and performance management. These structures also provided a forum for robust discussion and appraisal of the research and the associated implementation and dissemination activity.
Changes to the original protocol
A number of necessary changes were made to the original project protocol as described in the original application. Where required, changes were submitted to and approved by the NRES and substantial changes to the project were approved by the HS&DR programme (refer to Appendix 1 for full details of changes). Most significant were the changes to the identification of cases for the case-linkage study following support from the NIHR and Section 251 approval from the NIGB, and changes to the recruitment strategy for the stakeholder consultation. A 3-month funded extension to the project was also permitted to allow the application to the NIGB and an amendment to the original NRES application to take place.
Ethical approval for the study was sought from the South West Research Ethics Committee of the NHS NRES, the Institute of Psychiatry, King’s College London (as the sponsor) and the Faculty of Health, Education and Society Human Ethics Subcommittee of Plymouth University (responsible for the delivery of the research). Approval was also obtained from the Royal Cornwall Hospitals Trust Research and Development Department as the research site. The research team sought appropriate approval for all amendments. The research was also adopted by the NIHR Mental Health Research Network (MHRN) and was supported by the team based in CFT.
Inclusion of a clinical audit
Originally, as described in the project proposal, the researchers anticipated that the participant pool for the case-linkage study (stage 2) would be drawn from a clinical audit that would be undertaken by CFT as part of their Skillshare initiative. However, Skillshare was disbanded due to funding issues and the audit was not conducted as planned. This therefore necessitated the CFT to conduct the audit as part of the Interface Project with the support of the researchers so that case-linked individuals could still be identified to form the participant pool for the research.
Application for support in terms of Section 251 of the NHS Act (2006)
An application was made to the Ethics and Confidentiality Committee of the NIGB for their support in terms of Section 251 of the NHS Act (2006),38 by setting aside the common law duty of confidentiality. The application process is described in the following section.
Team changes
As the project progressed, the roles of team members evolved, particularly in the case of two of the police representatives on the original bid who retired during the project. As they were no longer representative of the police, they were transferred from the research team to the steering group (Police Constable Dr Nick Lynn and Detective Superintendent Iain Grafton OBE). Changing team members allowed the project to retain the two retired police representatives’ expertise and advice while allowing a new team member from the force to join the research team (Chief Inspector Mark Bolt). In addition, the lead for the health economics component of the study, Dr Anita Patel, had to suspend involvement on the project at the point where health economic data collation for analysis was started. Ms Margaret Heslin conducted the health economic component under the supervision of Dr Barbara Barrett.
Recruitment process
After the protocol was amended to take into consideration the change to the recruitment process supported by Section 251 support from the NIGB, a decision was taken to seek support from the local MHRN to gain consent from potential service user participants in stage 3 of the project. As a project on the MHRN Portfolio, the MHRN local team were able to liaise with care teams to locate potential service users and distribute recruitment packs on behalf of the researchers.
Stakeholder consultation
Changes were made to aspects of the data collection in stage 3. For the stakeholder focus groups, it was envisaged that a nominal group technique would be used. Once the framework analysis progressed in stage 2, it was realised that not all decisions applied to each of the stakeholder groups, making it difficult to use the technique with the same questions across all the groups. Therefore, the findings related to service decision-making were presented to the stakeholders and groups selected the decisions most relevant to them for further discussion. Questions were developed to prompt discussion of experiences in relation to presented findings, specific to the police, mental health services and service users. The national stakeholder element of stage 3 was originally envisaged as involving telephone focus groups. However, this was replaced with a face-to-face consultation event to increase participation, group synergy and rapport. The event reflected the PoD implementation model used in the project and event feedback suggested that it was very well received (see Chapter 6, National consultation findings).
The original proposal, original protocol and final protocol approved by the NIHR are provided in Appendix 1 for further reference.
Application to the National Information Governance Board
In the early stages of the clinical audit conducted in stage 1 it became clear that the recruitment process through care teams that had originally been envisaged would not fulfil the sample requirements for the case-linkage study (stage 2). Findings revealed that approximately 35% of the potential participants for this research were not on the current caseload of a secondary MHT at any one time. Consequently, this proportion of the potential participant pool for the case-linkage study could neither be screened according to the agreed inclusion and exclusion criteria, nor invited to provide their informed consent to participate in the research. This group of identified cases arguably included the most vulnerable of individuals who were at the centre of this research and who Lord Bradley argued to be most at need. 6 Not only do they continually enter and leave the CJS through a revolving door but further, as the audit revealed, this pattern is mirrored in their use of mental health services. In order to include this group, it was deemed necessary (by the research team, steering group and service user consultants) to apply to the Ethics and Confidentiality Committee of the NIGB for Section 251 support of the NHS Act (2006). 38 This permission sets aside the common law duty of confidentiality to enable access to mental health records without consent.
Application to the NIGB was a rigorous process involving all four partner agencies in the rewriting of the study protocol, development of a secure data extraction and pseudonymisation process, and the implementation of data transfer risk assessments and system security policies to enable the lawful and secure extraction and transfer of data for the purpose of the research. The research received Secretary of State approval for Section 251 support on 12 October 2012 and it was noted by the NIGB that the research was of ‘huge public benefit’.
Patient and public involvement: the Interface Service User Consultative Group
Introduction
Patient and public involvement has been an integral and informative part of the project from the outset. PPI through direct consultation and collaboration on elements of the study methods has occurred from the early stages of the research through to the findings in this report.
Summary of patient and public involvement
Integrally, the project has been supported and directed by Dr Diana Rose, Co-Director of the organisation Service Users in Research Enterprise (SURE). Dr Rose was an original fund holder and as such, has had input on the study methods and the development of PPI consultation throughout the project. Dr Rose is a member of the research team and the project steering group; the latter also included a further member, Kate Atkinson, who is employed by CFT as a service user consultant. Additionally, some members of the research team have had life experience of being users and/or carers in receipt of the services explored in the research. Direct PPI in the project management provided expert knowledge to develop a ‘reference group’, an independent group of service users who could be consulted on the project as it progressed.
The aim of having a strong PPI component in the project was to provide meaningful advice for the project from service users’ perspectives, ensuring the research findings were relevant to service users, and to improve implementation and translation of the findings. Adhering to the collaborative nature of the research, all stakeholders, including professionals and service users, needed to be involved in directing the research and interpreting the findings.
Through discussions with Dr Rose, it was decided that a reference group, representative of service users who had experience of mental health services and the police, should be created. No such reference group within the target population existed in Cornwall.
Method of consultation
The following describes the process used to set up the reference group.
Initially, recruitment was to be attempted through information packs distributed via care teams in Cornwall. In a similar vein to the original methods for the case-linkage study, care teams were asked to identify people they believed would be willing to take part and whose involvement would not impinge on their care. Unfortunately, only one person volunteered through this process (and did not actually take part once consultation began). To improve the chances of recruitment, all groups in Cornwall in contact with mental health service users were approached and provided with recruitment leaflets to distribute to their clients. Additionally, a précis of the project was provided to display in open access areas and on organisation websites. The choice of dissemination contacts and the recruitment leaflet were guided by Miss Atkinson.
Once this process was initiated, interest in the project snowballed, with professionals and service users getting in contact to ask for leaflets to distribute. Over 300 leaflets were distributed throughout Cornwall. From this recruitment, a core reference group of 12 individuals was formed. The consultants met as a group on a bimonthly basis and individually with members of the research team depending on their mental health needs (one individual consistently met the researchers on a singular basis and two interchanged between group and one-to-one meetings). Six group meetings (with an average of nine attendees) were held in a public building in central Cornwall and five individual meetings were held (on university property or in the locale of a third-sector organisation) over the lifetime of the project. Two researchers attended each meeting and facilitated the group. Consultants were given £20 and paid travel expenses for each meeting they attended. Copies of claim forms and group meeting minutes/individual meeting notes were circulated to service user consultants after each meeting.
Once the group commenced, it was realised that although the group members had experience of both services as service users or carers, they did not represent the majority target group represented in the research. The initial group was 75% female, > 35 years old and had limited recent experience with the police. Results from the audit in stage 1 illustrated that the consultation needed to target young males in repeat contact with the police for suspected substantive offences in hard to reach populations. To address this, the research team liaised with ‘Health for Homeless’ to set up drop-in sessions in a homelessness centre in Cornwall. To approach the homeless population was a suggestion made by the main consultative group. This resulted in consultation with three young males and one female with recent contact with the services.
When devising a format for the reference group, discussions were held with administrators of existing service user groups and Plymouth University’s Human Resources and Finance departments. Literature and guidance from organisations such as the MHRN and SURE were reviewed. Advice was sought from the facilitator of an existing service user consultative group for a social work programme at Plymouth University. The following key aspects of administering a reference group were adopted:
-
terms of reference and ground rules
-
fully minuted group meetings
-
summarised individual meetings
-
clear accounting, with claim forms copied to consultants
-
secure and confidential storage of contact details.
Contributions of the group to the research
As well as the PPI support received from Dr Rose and Miss Atkinson described above, the reference group has contributed to the following aspects of the project, resulting in formal changes to research methods and the interpretation of findings. Changes to the research design were formalised in the information sheets, consent forms and other relevant documents; in turn, these changes led to amendments to the research ethics application and changes to the research protocol. The input of the reference group has helped to frame the findings. The challenges and impacts of the group are discussed in Chapter 7 of this report.
-
NIGB application The group was consulted on the appropriateness of applying to the NIGB for permission to access data without consent. The group agreed with this approach and emphasised the importance of gaining accurate data to help improve services over the concern about accessing data without permission.
-
Information sheets and consent form The documents developed by the research team early in the project were reviewed by the group. Following their suggestions, changes were made to the layout; the principal change was a bulleted summary on the first page, highlighting the main points from the information sheet. From reviewing the consent form, the group decided that potential research participants should be offered the option of taking part in an interview and focus group, rather than one or the other.
-
Research participant recruitment method The group provided advice on recruitment methods for the stakeholder consultation in stage 3, including the concept of drop-in sessions at homeless centres (which was used as a method of recruitment for the service user consultation and for recruiting participants for stage 3).
-
Logistics of service user consultations and research participation The group provided guidance relating to suitable times to start and finish consultations and research interviews/focus groups with mental health service users, for example:
-
hold meetings in the afternoon to allow people to travel and time for medication to take effect, but finish in time for people to leave before it gets dark
-
hold meetings in neutral locations acceptable to users of police and mental health services
-
pick suitable days of the week to ensure support services were available post consultation (not on a Friday so people were not in crisis over a weekend)
-
suitable length of time for consultation meetings, research interviews and focus groups with an emphasis on the ability to take breaks during participation.
-
-
Dissemination The group suggested outputs for the research that would be meaningful for service users, including dissemination to third-sector organisations such as Mind, the Revolving Doors Agency and Age UK. Representatives of these organisations were invited to the national stakeholder event.
-
Discussion of findings At each stage of the research, results were presented to the reference group as they became available. This allowed the group to discuss the findings and compare them with their own experiences. Throughout the consultation, the group has made suggestions as to how services could be improved, in addition to their advice on the research itself.
-
Review of implications for research and final report At the end of the project, a final meeting was held with the group in the form of a workshop to present the findings and ask for feedback on the main implications of the research. Further consultation was sought from the group on the following topics, which arose from the process of setting up the group and from feedback given by group members.
-
UK Border Agency requirements Due to new requirements from the UK Border Agency, universities have to ask for proof of identity before making payments to anyone employed in any activity, even if this is to pay expenses to volunteers. The consultants were asked for their feedback on this requirement and how it might affect their participation in research and service consultations as it seemed to pose some challenges. This consultation was written up in a short report and disseminated internally to the Human Resources and Finance departments at Plymouth University.
-
Disclosure barring service checks A recurring theme was the impact of police records on future employment prospects. Due to this, a police force data protection officer was asked to provide a summary of information that could be given to service users on request during the project relating to disclosure barring service checks. The group reviewed the information in terms of applicability and ease of understanding.
Chapter 4 Stage 1: policy into practice review and clinical audit
Introduction to stage 1
A short practice-focused review was undertaken to illuminate how national policy has been interpreted and translated at the regional/local level. This involved two elements: a review of relevant regional/local documents nationally; and an audit to identify and analyse local need within offender populations at the stages of the CJS identified in the Bradley report (Custody and Neighbourhood Policing6). This work extended the pilot review that formed the impetus for this research and complements existing policy-focused reviews and a local trust-based audit.
Policy review
Policy review method
A review was conducted of national and local policy, guidelines, supporting documents and related reports. The search process was internet based, searching government departmental sites, third-sector organisation sites, and using the search engine Google (Google Inc., Menlo Park, CA, USA). Search terms for regional/local documentation included formal descriptors (e.g. mental health issues, suicidal, Section 136). Information on national recommendations was collated into single documents to understand the policy landscape post the Bradley report. 6
Pertinent documents were analysed using thematic analysis to identify core features and themes associated with the developing practice guidelines or benchmarks with which to assess practice quality and standards. Standards on which to assess the audit findings were developed from this review. The recommendations pulled from the review were used to frame and compare the findings from the case-linkage component of the research in stage 2.
Policy into practice review
The practice-focused review illuminated how national policy relating to individuals with EMHN has been interpreted and translated at the regional (south west) and local (Cornwall county) levels to inform practice. The main aim of the review was to answer the first two project research questions:
-
How are the practice implications of current national policy relating to the management of individuals with EMHN being interpreted at local level?
-
How has Cornwall articulated national policy into practice benchmarks where the NHS and police are required to work together?
Commissioned national recommendations for practice
Much of the national focus for the management of EMHN stems from Lord Bradley’s review. 6 Building on the key recommendations of the 2009 review, the DH responded with New Horizons: A Shared Vision for Mental Health,39 providing a broad overview of actions that could be taken to improve the lives of individuals with mental health issues. Actions generated from the report included specific suggestions for improving the journeys of service users through the CJS pre and post prosecution. These actions were further defined in Improving Health, Supporting Justice: The National Delivery Plan of the Health and Criminal Justice Programme Board,40 which reiterated Bradley’s recommendations,6 devising objectives to meet the recommendations nationally. Key deliverables were suggested for each of the main services involved in the care of individuals as they progressed through the CJS. There were six overall strands from the plan:40
-
The need for a systematic and joint NHS/CJS approach to offender health.
-
Needs assessments to help inform commissioning decisions about mental health services for offenders, both in the community and for those in prison or in secure mental health services.
-
A systematic approach to supporting people with mental health problems at police stations and at courts, through liaison and diversion services: provision of high-quality assessments; diversion of people to health and social care services as appropriate; support of decisions about the range of sentencing options by the courts.
-
Continued investment in mental health awareness training for frontline CJS staff.
-
Embedding the care programme approach (CPA) throughout the CJS.
-
Working to reduce the transfer times from prison to mental health bed for individuals under Section 47/48 of the MHA. 19
In line with the Interface Project’s research questions, the specific recommendations of the Bradley report6 pertaining to types of police contact that are particularly relevant for this research have been explored. Service users with EMHN may interact with the police in one of three ways: detention under Section 136 of the MHA;18,19 detention in custody for a substantive offence; or police contact not resulting in detention but pertaining to welfare issues, low level offending, antisocial behaviour (ASB), etc.
The Bradley report6 remained the key source of recommendations throughout the research window (18 April 2011 to 8 June 2012). However, in 2013 two major reports were published. 41,42 They both propose new recommendations, although the reports also call for some of Bradley’s original recommendations to be actioned 14 years on. The latest recommendations are important in providing a context for how the findings of this research are relevant to current and future practice. These new recommendations form part of the framework for the implications for research provided at the end of this report. The specific recommendations relating to detention under Section 136 are provided in Boxes 1 and 2.
All partner organisations involved in the use of Section 136 of the Mental Health Act 2007 should work together to develop an agreed protocol on its use.
Discussions should immediately commence to identify suitable local mental health facilities as the Place of Safety, ensuring that the police station is no longer used for this purpose.
The Codes of Practice should be amended to bring detention times for those detained in police custody under section 136 in line with the PACE [Police and Criminal Evidence Act 198443], allowing a maximum of 24 hours in police custody (out of the maximum of 72 hours for which they can be detained overall). The period of detention should be subject to regular, independent reviews by both police and health officials to ensure that:
action is taken to transfer the detained person to a health-based Place of Safety as soon as is practicable; or
An assessment is carried out as soon as possible at the police station, where any transfer to a health-based Place of Safety may cause unnecessary delay.
Any assessments which are needed, once the 24 hours in police custody has elapsed, should be undertaken in a hospital.
Clinical Commissioning Groups and local social services should assure themselves that they have commissioned sufficient capacity to meet the demand for assessment under section 136, and that multiagency working is effective.
Commissioners and providers of social services and health services should ensure that they identify periods of demand for the reception and assessment of persons detained under section 136 and that they effectively manage resources to meet this demand.
Police custody officers should ensure that a full explanation is recorded in the custody record as to why a person detained under section 136 has not been accepted into a health-based Place of Safety.
The Mental Health Act 1983 should be amended to remove a police station as a Place of Safety for those detained under section 136, except on an exceptional basis (namely, where a person’s behaviour would pose an unmanageably high risk to other patients, staff or users of a health-care setting).
The recommendations relating to custodial detention for individuals who are suspected of committing a substantive offence are provided in Boxes 3 and 4.
Information on an individual’s mental health or learning disability needs should be obtained prior to an Anti-Social Behaviour Order or Penalty Notice for Disorder being issued or for the pre-sentence report if these penalties are breached.
All police custody suites should have access to liaison and diversion services. These services would include improved screening and identification of individuals with mental health problems or learning disabilities, providing information to police and prosecutors to facilitate the earliest possible diversion of offenders with mental disorders from the CJS, and signposting to local health and social care services as appropriate.
Liaison and diversion services should also provide information and advice services to all relevant staff including solicitors and appropriate adults.
The MPS [Metropolitan Police Service] and its NHS partners should immediately implement the Bradley Report recommendation so that all police custody suites should have access to liaison and diversion services.
Additionally, a group of recommendations from the reports relate to all forms of detention in a custody centre, therefore are relevant to both Section 136 and custody detentions in a police custody centre. These recommendations are provided in Boxes 5 and 6.
A review of the role of Appropriate Adults in police stations should be undertaken and should aim to improve the consistency, availability and expertise of this role.
Appropriate Adults should receive training to ensure the most effective support for individuals with mental health problems or learning disabilities.
The NHS and the police should explore the feasibility of transferring commissioning and budgetary responsibility for health-care services in police custody suites to the NHS at the earliest opportunity.
Mental health nurses with experience related to offenders must be available to all custody suites as required. The MPS should conduct a 360 degree review every six months to ensure that they are accessing the proper advice from psychiatric nurses in the delivery of health care in custody suites.
Practices and policies in custody suites must acknowledge the needs of people at risk on grounds of their mental health issues as part of pre-release risk assessment and take appropriate steps, to refer them to other services and to ensure their safe handover to relatives, carers or professionals.
The MPS [Metropolitan Police] should adopt the Newcastle health screening tool or one that meets the same level of effectiveness for risk assessment in all custody suites.
The main recommendations from the earlier Bradley report6 and the two recent reports41,42 concern Section 136 and custody, and are related to the detention and management of individuals in both these processes. However, Bradley also suggested preventative measures that could be taken to reduce offending, including two measures of particular relevance to the non-detention contact group identified within this research:
1. Local Safer Neighbourhood Teams should play a key role in identifying and supporting people in the community with mental health problems or learning disabilities who may be involved in low-level offending or anti-social behaviour by establishing local contacts and partnerships and developing referral pathways.
2. Community support officers and police officers should link with local mental health services to develop joint training packages for mental health awareness and learning disability issues.
Reproduced with permission from the DH6
Although the above recommendations are important for practice relating to individuals with EMHN in the CJS, the main underpinning factors for practice arise from legislation defined in Acts of Parliament and the related Codes of Practice pertaining to those Acts. The main acts are discussed in the following section. These acts, in part, inform the recommendations made by Bradley and others.
UK legislation
Framing all government guidelines and reports are the legal requirements of Acts of Parliament relating to mental health and the CJS. Legislatively, the main Acts of Parliament that inform practice relating to individuals with EMHN and their interactions with the CJS are:
-
the Mental Capacity Act 2005 (MCA)44
-
the Police and Criminal Evidence Act 1984 (PACE)45
-
the Criminal Justice Act 2003 (CJA)46
-
the Data Protection Act 1998 (DPA). 47
For each of these acts, a code of practice has been developed which guides national interpretation of the acts to inform practice.
Mental Health Act 1983 c.20, revised 2007 c.12
The code of practice for the MHA48 notes that the guidance is not mandatory. Principally, the purpose of the MHA code of practice is:
Decisions under the Act must be taken with a view to minimising the undesirable effects of mental disorder, by maximising the safety and wellbeing (mental and physical) of patients, promoting their recovery and protecting other people from harm. 48
In reviewing the MHA code of practice, the most relevant sections to management of individuals with EMHN in the CJS were from the section on ‘Guidance on Section 136: mentally disordered people found in public places’ (pp. 74–86). 48 This section of the code of practice defines that to be sectioned the individual needs to be in a public place and in immediate need of care or control. Removal to a place of safety (which could be a purpose built Section 136 suite, custody, the individual’s home or other care settings) may take place if a police officer believes it is necessary in the interests of that person, or for the protection of others. A person can be taken to a place of safety to enable the person to be examined by a doctor and interviewed by an approved mental health professional (AMHP), so that care and treatment can be arranged:
It is not a substitute for an application for detention under the Act, even if it is thought that the person will need to be detained in hospital only for a short time. It is also not intended to substitute for or affect the use of other police powers. 48
The maximum allowable period of detention is 72 hours (consecutive detentions are unlawful).
The MHA code of practice highlights the importance of jointly agreed local policies to govern the use of Sections 135 and 136. Section 135 is a magistrates order applied for by an AMHP for a person who is refusing to allow mental health professionals into their residence for the purposes of a Mental Health Act assessment (MHAA). Police officers are provided with the right to enter the property and to take the person to a place of safety.
Local Social Services Authorities, hospitals, NHS commissioners, police forces and ambulance services should ensure that they have a clear and jointly agreed policy for use of the powers under sections 135 and 136, as well as the operation of agreed places of safety within their localities. 48
When considering service users who come into contact with police and the health service for incidents other than sections 135 or 136, there is guidance in the code of practice relating to police powers for conveying patients between hospitals and returning patients who abscond (p. 93)48 and for dealing with patients who are absent without leave (AWOL) (pp. 174–7). 48
Mental Capacity Act 2005 c.9
The MCA came into force in 2007, providing a legal basis for providing care and treatment for adults lacking mental capacity to give consent. 49,50 The MCA is primarily aimed at health professionals and the code of practice indicates that decisions about mental capacity should be taken by a health professional. The code of practice does provide guidance that:
All reasonable steps which are in the person’s best interests should be taken to prolong their life
Paragraph 5.31 (p. 79)50
Sometimes people who lack capacity to consent will require emergency medical treatment to save their life or prevent them from serious harm. In these situations, what steps are ‘reasonable’ will differ to those in non-urgent cases. In emergencies, it will almost always be in the person’s best interest to give urgent treatment without delay.
Paragraph 6.35 (pp. 104–5)50
Police do not have the power to detain under the MCA, but may be in a position to act in the best interests of a person where an officer perceives that an individual does not have mental capacity. The MCA was not used in any of the incidents discussed in this report.
Police and Criminal Evidence Act 1984 c.60
Police guidance comes directly from the PACE43 and other relevant criminal acts. Relevant sections for custodial detention of individuals with mental ill health are in Code C: code of practice for the detention, treatment and questioning of persons by police officers. Within Code C, particularly the following referenced pages, there are guides for police officers dealing with people defined as a ‘mentally disordered or otherwise mentally vulnerable person’. 45 Of particular relevance to the findings in this research and to individuals with EMHN are the general descriptions of custody management (pp. 2–5), assigning an appropriate adult (AA) (pp. 9–10, 16), and the conditions of detention and the care and treatment of detainees (pp. 23–29). 43 Guidance for dealing with detainees is further provided in sections relating to cautions, interviews, detention extensions and charging in Code C of PACE.
Criminal Justice Act 2003 c.44
The CJA defines the powers and duties of the police in relation to dealing with offenders. 46 Criminal offences are defined within this Act. Common law ‘offences’, such as breach of the peace (BoP), are not deemed a criminal offence and therefore not covered by this Act. Other common public order offences such as affray are defined under the Public Order Act 1986,51 and therefore individuals with EMHN committing these types of offences will be subject to the Public Order Act. The only provision of the CJA directly pertaining to individuals with mental health concentrates on mental health treatment requirements; however, this relates to court rather than police powers.
Data Protection Act 1998 c.29
The DPA came into force in 2000. 47 It is designed to protect individual rights and introduce transparency about data usage and data handling. Schedule 1 of the Act defines the eight principles of data protection, where data should be:
-
processed fairly and lawfully
-
processed for limited purposes
-
adequate, relevant and not excessive
-
accurate and up to date
-
not kept longer than necessary
-
processed in accordance with the data subject’s rights
-
secure
-
not transferred to countries outside European Economic Area without adequate protection.
Data sharing is an important part of interagency working. The DPA ensures that personal data remains confidential but does make provision for disclosures of confidential information. Section 29 relates to allowable disclosure between the police and health services if the disclosure is for the purpose of preventing or detecting crime including the apprehension or prosecution of offenders. 47
The above national recommendations and relevant legislation provided the framework within which the practice investigated in the Interface Project was situated and in terms of which it was analysed. The following section outlines relevant practice-based protocols, which reflect local interpretation of national legislation and recommendations.
Regional and local interpretation and practice
In order to understand the local context within which service user journeys were undertaken, regional and local policy documents and practice-based protocols were reviewed and members of the NHS and police in Cornwall were informally consulted about the translation of national policy and the law into practice. Regionally, across Devon and Cornwall, ‘Section 136 Mental Health Act 1983 Operational Protocol for Devon, Cornwall and the Isles of Scilly’52 has been developed, deriving from the MHA and code of practice. The interagency development of this regional protocol meets the recommendation of the MHA code of practice for joint working and was developed by the collaboration referred to as the Peninsula Criminal Justice Agencies group. In conjunction with this, a further regional protocol was developed for Section 135 detentions ‘Section 135 (1) (2) Mental Health Act 1983 Operational Protocol for Devon, Cornwall and the Isles of Scilly’. 53
Additionally, CFT has produced a local operational policy specifically relating to their Section 136 suite at place of safety. 54 Provision of a designated place of safety for the detention of individuals under Section 136 means that Cornwall has followed the guidance of the MHA to provide a facility for such detentions. As the designated place of safety for Section 136 detentions in Cornwall, the Section 136 suite should be considered before detaining an individual in custody. There are exceptions to this, as described in the protocol:
Reproduced with permission from CFT54
The above documents are the only formalised documentation specific to Section 136 and the custody of individuals with EMHN. However, there is a formal process for recording police contact with vulnerable adults with or without mental health issues, even if the police contact does not result in detention. DCP have developed a system known as the Neighbourhood Harm Reduction Register (NHRR). The NHRR was developed in response to the murder of Steven Hoskin, a vulnerable adult living in Cornwall who had multiple contacts with the NHS and the police prior to his death in 2006. 55 The NHRR covers:
all residential addresses where there are three or more visits from the police over a three-month period. Three calls in three months are seen as the trigger level. The Harm Reduction spreadsheet is designed to identify these addresses on a quarterly basis56
A serious case review into Steven’s murder resulted in a set of multiagency and single-agency recommendations and actions. 55 The following tables highlight the recommendations from the review aimed specifically at CFT (Box 7) and DCP (Box 8), the two organisations from which data were sourced for this research.
Where a threshold for risk is crossed, non-engagement and non-attendance should not be a barrier to internal multidisciplinary discussion and wider multiagency liaison and consultation. High risk cases amongst referrals should be highlighted for multidisciplinary discussion at the weekly team meeting and with outside agencies where appropriate and legal.
To improve co-ordination of the referral pathway to mental health services for homeless people, especially where there are frequent changes of address, even if discussion takes place with relevant agencies without face to face contact with the client/patient. This can only take place if a risk assessment indicates that confidentiality and consent issues can be over-ridden in the interest of public protection.
Training for adult protection, particularly the identification of vulnerable adults at risk runs alongside training for child protection and safeguarding children for all staff within Cornwall Partnership Trust. Multiagency training may be of additional benefit and should be targeted at key professionals.
A more co-ordinated approach to individuals presenting with personality disorders and requesting treatment should be agreed between Cornwall and Isles of Scilly Primary Care Trust and Cornwall Partnership Trust. This should then be explicitly commissioned using as its basis the National Institute for Mental Health in England paper: ‘personality disorder: no longer a diagnosis of exclusion’.
Following arrest for an offence or detention under section 136 of the Mental Health Act, (at about 7-14 days) where there has been a mental health outcome, there should be a follow up review between police and psychiatrist (responsible clinician under the 2007 Act) to assess whether the outcome has achieved the correct goals of treatment or criminal responsibility and to re-assess risk management.
Adult Protection training is reviewed in line with this Serious Case Review, specifically aimed at the issues of identification and awareness of a vulnerable adult and procedures to instigate once the identification has been made. This will require rolling out to all operational staff with immediate effect.
That a list is forwarded to Police of all persons within the Adult Protection process and that these named persons are all created as Nominal Records on the police computer and have an Adult Protection Flag placed on the nominal. That any person who has an Adult Protection Flag has a warning marker (SIG warning) put in place on the address where they reside. Any person coming into contact with police staff for any reason who has an Adult Protection marker against them or SIG [street index gazetter] warning on their address should have circumstances passed to either Adult Social Care or the Department of Children, Young People and Families (possible use of 121a form) and Neighbourhood Teams.
Any police staff coming into contact with a person deemed to be vulnerable/in the Adult Protection process, and there is obvious concern regarding their welfare, or that of any other persons they have direct contact with, should take advice from the Adult Protection Officer. That these incidents are monitored and prioritised by the Adult Protection Officers working within Basic Command Unit ensuring compliance with policy and concerns are shared and highlighted to Social Services i.e. either Adult Social Care or the Department of Children, Young People and Families.
That where an individual is identified as posing a threat to the community, consideration should be given to progress the individual within the MAPPA system. Thereby ensuring a multiagency review of the risk and action as deemed appropriate and managed by an appropriate agency’
In addition to the NHRR, CFT have created mental health liaison forums for subMAPPA information exchange and have appointed a psychiatric nurse dedicated to the problems of homeless people. 55 Steps taken to meet the recommendations from the Steven Hoskin serious case review and the national recommendations will be discussed within the context of the findings from stage 2 of this research.
In summary, the review of relevant national recommendations, legislation and regional and local protocols framed the exploration of service user journeys in the audit, case-linkage study and stakeholder consultation stages of this research. The translation of policy into practice can be subject to interpretation, and as such, can lead to differences in service user management and care. Research questions 1 and 2 are answered further under each relevant section in the results and discussion sections of this final report, thereby contributing to an understanding of the challenges associated with delivering consistent, excellent, multiagency management and care of individuals with EMHN.
Clinical audit
Introduction
The audit sought to address the following aim: to identify and calculate the number of EMHN individuals who are currently accessing mental health services of the trust who interfaced with the CJS in the second quarter of 2011 (weeks 16–30).
Clinical audit methods
Criminal justice system-derived case identification
Initial case identification was made from the NHRR and the National Strategy for Police Information Systems (NSPIS) Custody System in the second quarter of 2011 (18 April–30 July 2011). Each identification process is detailed below:
Neighbourhood Harm Reduction Register
The 12 NHRRs for Cornwall were used to identify potential audit cases. Entries on the registers are based around addresses to which the police have been called at least three times in 3 months. Data entered for each address varies both within and between registers. Figure 4 provides an overview of the identification process.
-
Where a principal person (PP; the main person at the address that calls relate to) was identified on the register, the individual was automatically entered onto the case list (see Figure 4, box 1).
-
The PP was then located on the Operational Information System (OIS) and all associated persons’ (APs; individuals associated with the PP) entries examined. Where an AP of the PP was (1) involved in an incident within the time frame or (2) associated with the address in the NHRR, they were included in the case list (see Figure 4, box 2).
-
The address of all PPs was entered into a View Street Index (VSI) search on OIS. All APs of the address who were (1) involved in an incident in the time frame and (2) associated with the address subjected to the VSI search were included in the case list.
-
Where only an address was identified on the register (see Figure 4, box 3), the address was entered into a VSI search on OIS. All APs of the address who were (1) involved in an incident in the time frame and (2) associated with the address subjected to the VSI search were included in the case list (see Figure 4, box 4).
FIGURE 4.
Case identification methodology using the NHRR and Operational Information System.
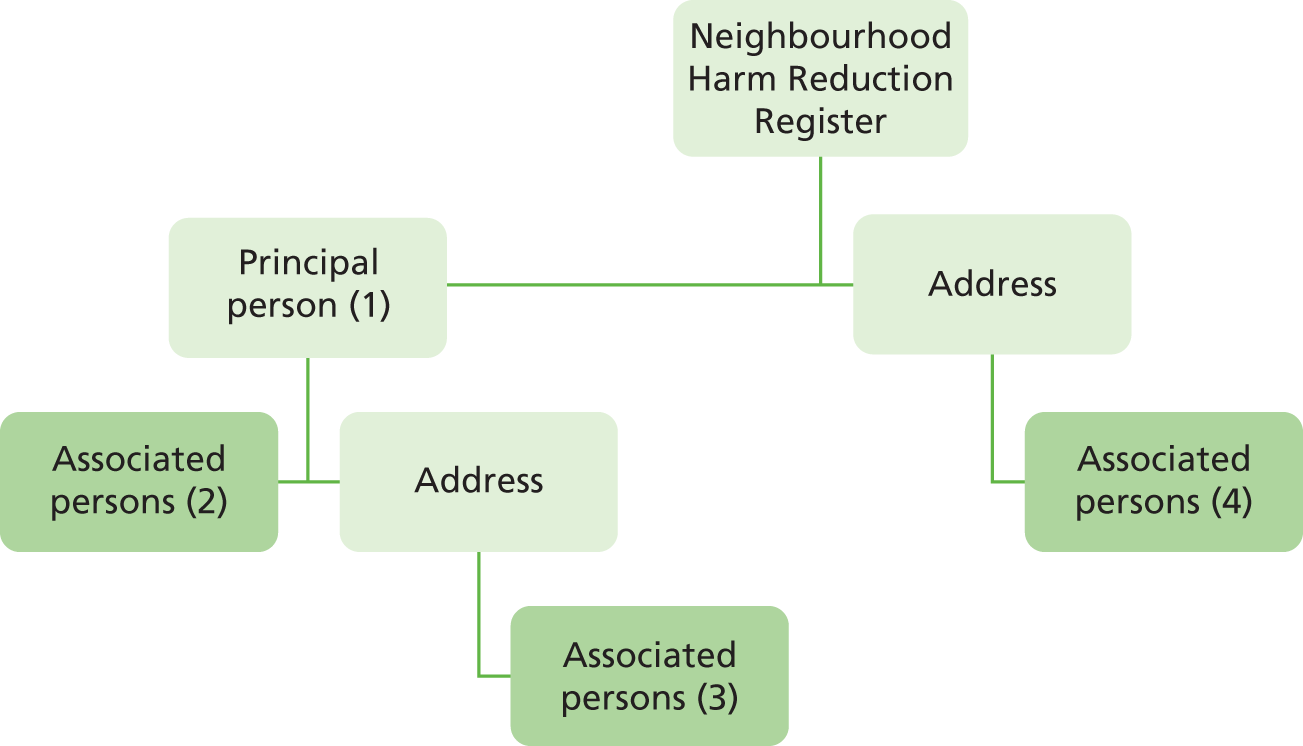
National Strategy for Police Information Systems Custody System
The procedure used to identify individuals from the Custody System and each of the custody centres in Cornwall to be case-linked was as follows:
-
‘Custody Record’ was selected as the chosen data source to be searched.
-
Each custody centre in Cornwall was searched for records that related to custody entries in weeks 16–30 of 2011 inclusive.
-
Each search provided a list of custody records. Data of individuals aged > 18 years (i.e. date of birth prior to 18 April 1993) within the period of the audit were collected.
The name and date of birth of each identified individual were recorded and stored on a secure spreadsheet on a DCP secure server.
Cornwall Partnership NHS Foundation Trust-derived case identification and data collection
Due to CJS record keeping practices during the audit period, in order to identify Section 136 detentions that were taken directly to the place of safety, it was necessary to request a performance management report of the audit period. Cases were included in the sample if:
-
they were detained under Section 136 by the police and transported directly to the place of safety, and
-
had a record of this detention on CJS systems (in order that records could be case-linked).
Clinical audit findings
Full sample
Criminal justice system-derived cases
Figure 5 illustrates the process by which linked cases were identified. A total of 2717 individuals were recorded on police custody records and the police NHRR as having interacted with the police in the second quarter of 2011. Of these, 529 had a record on the RiO system. There were nine deaths and one imprisonment between initial recorded police contact and case-linkage, resulting in 519 (19.1%) linked cases (i.e. individuals who also had a record on RiO). Of these, 321 (61.8%) were identified solely through custody records, 120 (23.1%) were identified through the NHRR and 78 (15.0%) were identified through both custody records and the NHRR (Table 1).
FIGURE 5.
Flow chart of case identification process (CJS-derived cases).

| Case identification findings | Custody records only | NHRR only | Individual has contact recorded in both custody and NHRR |
|---|---|---|---|
| Total sample of police contacts in audit period (> 18 years old) | 2021 | 536 | 160 |
| Number of linked mental health cases | 321 | 120 | 78 |
| Percentage of linked mental health cases | 16 | 22 | 49 |
| Percentage of linked cases for sample | 19 | ||
NHS-derived cases
Thirty-four individuals were recorded as being detained under Section 136 at the place of safety. Of these, 30 had a corresponding record on DCP CJS databases and were aged > 18 years. Seven of the cases had been identified previously through the CJS-derived sample selection, two of which were recorded on OIS as attending the custody centre first, and were therefore removed from the sample. There were three deaths in the group before the audit commenced and one incident was recorded as an inappropriate use of Section 136. Of the remaining 24 cases, 15 (62.5%) had records for Section 136 place of safety detentions only; one (4.2%) had a custody record; five (20.8%) had additional NHRR or OIS logs; and three (12.5%) had records across all systems.
Type of criminal justice system contact
Type of CJS contact was examined for each of the 538 cases recorded. The majority (83.6%, n = 450) had one type of interaction with the police during the audit period, with 16.4% (n = 88) recorded as having two or more different types of interaction with the police during this window. Table 2 shows the proportion of type of contact recorded across the CJS systems for the sample.
| Type of CJS contact | Number of individuals | % |
|---|---|---|
| Section 136 | 45 | 8.4 |
| Custody (crime) | 285 | 53.0 |
| NHRR | 120 | 22.3 |
| Section 136 and custody (crime) | 6 | 1.1 |
| Section 136 and NHRR | 8 | 1.5 |
| Custody (crime) and NHRR | 67 | 12.5 |
| Section 136, custody (crime) and NHRR | 7 | 1.3 |
The most frequent single form of contact was custody (crime), followed by NHRR and Section 136. In terms of cases with multiple contact types in the audit period, the majority were recorded as interacting with the police through arrest for a substantive offence as well as incidents recorded on the NHRR (n = 67, 76.1%). Thirteen (19.7%) of the individuals detained by the police under Section 136 were also recorded as being detained in custody for an offence within this time frame. Similarly, 15 (22.7%) of those detained under Section 136 were recorded as being involved in an incident linked to the NHRR.
In order to ensure that the audit findings were implemented in the trust, an implementation strategy was developed. Participatory methods were employed to develop recommendations and actions based on the findings in collaboration with service managers. The strategy and associated recommendations and actions are presented in Appendix 6.
Chapter 5 Stage 2: case-linkage study
Introduction
Stage 2 comprised two elements: first, analysis of secondary case-linked data from cases identified by the audit presented above; and second, a health economic component designed to track costs incurred in client journeys and compare these with alternative models of enhanced practice.
Case-linkage study method
Sampling method
This stage of the case-linkage study concerned the identification and examination of 80 of the 538 cases that had been in receipt of NHS services and had contact with the police in the second quarter of 2011, identified by the clinical audit in stage 1. All 538 cases identified in the audit were subjected to a case selection process. A random selection of 80 cases from the audit was made using a stratified sampling framework. The framework focused on cases with two or more referrals to mental health services in Cornwall. Examination of these specific cases identified two broad referral groups comprising 277 cases:
-
long-term referral group – cases with EMHN illustrated by open ongoing referral not discharged at the time of first police contact in the audit period (n = 159)
-
short-term referral group – cases with EMHN illustrated by multiple referrals pre/post/at time of first police contact in the audit period (n = 118).
The sampling framework was designed to reflect the full range of service user experiences with both mental health and police services in Cornwall (those with both short- and long-term referrals with varying degrees and type of police contact). The sample was further stratified based on the type of CJS contact (in the 3-month audit period) into the following groups:
-
custodial detention for a substantive offence (identified through NSPIS custody records)
-
detention under Section 136 of the MHA
-
incidents entered on the NHRR
-
cases with two or more of the above contact types.
Based on the above categorisation, proportionate sampling was used to determine a representative sample from the 277 cases. The proportions were based on the proportional representation of each police contact type within the short- and long-term referral groups identified above (Table 3). The frequency of police contact type under each referral group was calculated and the proportionate number of cases in each group to constitute the required sample of 80 cases was identified. All 277 cases were assigned a number and a random number table was used to assign the appropriate number and type of cases to each group.
| Police contact type | Long-term referral group | Short-term referral group |
|---|---|---|
| Section 136 | 6 | 4 |
| Custody (crime) | 18 | 15 |
| NHRR | 13 | 8 |
| Complex | 9 | 7 |
| Total | 46 | 34 |
Data collection
Data were collected from police and mental health records for each of the 80 individuals for 12 months from the index police contact in the second quarter of 2011. The relevant documents identified for inclusion in the analysis from each system are detailed in Appendix 3.
Pseudonymisation process and data security
The confidentiality of person identifiable data was assured through a rigorous data access and pseudonymisation method, developed and agreed by the research team and partner agencies. Approval was granted by the NIGB for one researcher (the research manager) to access personal identifiable data from the RiO mental health system. The research assistant accessed data from the police systems under the data processing agreement with DCP. Reversible pseudonymisation (to enable back linking to the personal identifier in case of dissent) was utilised to both facilitate accurate case-linkage and enable depersonalisation of data. Cases were assigned a novel randomly generated PseudoID, which acted as an alias within the newly created pseudonymised, depersonalised data sets (quantitative worksheets) and data corpuses (qualitative data). PseudoIDs therefore enabled a link between such data and the personal identifiable data. A data flow diagram of the pseudonymisation process is included in Appendix 4.
All data collected were depersonalised and stored according to the pseudonymisation process. All personal data were stored on the practice organisations’ secure servers. All depersonalised data were transferred to secure university servers using encrypted hard drives and a force issue IronKey® (Imation Corporation, Oakdale, MN, USA) according to the regulations of the organisation. Prior to data transfer, a pseudonymisation and depersonalisation check was made by the trust information governance lead and the force data protection officer.
Case-linkage data analysis
A combination of quantitative and qualitative analyses were used.
Quantitative analysis: core demographic information of all 80 selected cases identified were collated and analysed descriptively. Data were captured using Microsoft Excel 2010 (Microsoft Corporation, Redmond, WA, USA) and imported into Statistical Packages for the Social Sciences version 19 (SPSS; SPSS Inc., Chicago, IL, USA) for analysis. Categories used to defined variables collaged for the case-linkage data are provided in Appendix 2.
Qualitative analysis: framework analysis was employed in order to organise and analysis the data. Framework analysis enables the systematic management and analysis of qualitative data, allowing in-depth exploration of the data while maintaining a transparent audit trail. 57 This form of analysis is being used increasingly in health-care research as its analytic rigour enhances the validity of findings. While sharing similarities with thematic analysis, framework analysis involves a series of interconnected stages that enable the researcher to explore the data until a coherent account emerges. 58
A full pilot was conducted on two individual cases. Documents were created from the various data fields (see Appendix 3) by copying and pasting into word processing files. These files were depersonalised and pseudonymised before being uploaded into NVivo 2010 version 9 (QSR International, Warrington, UK). All records over a defined 12-month period were accessed. NVivo was used to organise and structure the analysis ensuring the centralising of data from the variety of sources and the systematic analysis of the data corpus. Data were coded independently by two researchers and analysed using framework analysis. 58 Qualitative data from the databases were analysed within a framework using the following process:
-
data management
-
immersed in data through data collection and depersonalisation process
-
data familiarisation: read and coded case-linked files
-
developed skeleton framework
-
-
descriptive accounts
-
individual coding within framework
-
summarising and synthesising the range of data: refining initial themes and categories
-
-
explanatory accounts
-
developing patterns within concepts/themes
-
-
interpretation/finding meaning.
Specific frameworks evolved from the data for each area of police contact. These are described in more detail in the findings for stage 2.
The following sections seek to address the research question, ‘How are the practice implications of national policy relating to the management of individuals with EMHN being interpreted at a local level? To illustrate this, pertinent policy is highlighted throughout the findings in relation to case analyses.
Case-linkage study: Section 136 findings
Introduction
The aim of this element of the project was to explore the journeys of individuals within the case-linkage sample who experienced a detention under Section 136 of the MHA.
Sample characteristics
Of the 80 cases selected for the case-linkage study, 23 were detained under Section 136 within the research window (i.e. the year following the index police contact in the 3-month period in which cases were originally identified). Of these, the majority (n = 17, 78.3%) were detained under Section 136 once, with four individuals being detained twice, one three times and one individual being detained four times over the course of the year following initial identification. Therefore, the following analysis relates to 23 individuals who account for 32 Section 136 detentions.
Ten individuals were male and 13 female. Of the 14 records available, 13 cases were recorded as single and one as married or having a civil partner. The average age of the group at the point of their first detention in the research window was 35.7 years (range 18.8–73.3 years). Twenty individuals were recorded as living in privately rented/owned accommodation, one in a hostel/assisted living, one in another care setting (e.g. residential care) and one individual was recorded as residing in a hospital setting at the time of data collection. All 20 records of ethnicity were white British (one individual refused to disclose their ethnicity and two were not recorded). Nineteen of the 23 individuals examined were recorded as unemployed at the time of data collection. One individual was a student, one retired and two were unrecorded.
Police contact
Contact in the research window
For 10 of the 23 individuals, this was their index police contact in the research window (i.e. first police contact in the second quarter of 2011). Eleven individuals detained under Section 136 had also been arrested for a substantive offence in the research window, with seven being arrested once during this period and the remaining four individuals being arrested two, three, four and six times respectively.
For five individuals, their Section 136 detention was the first time they had been in custodial detention.
Eight of the 23 cases were recorded in the NHRR within the research window, indicating that there were calls to their address at least three times in a 3-month period within this time frame.
Police warning flags
The frequency of cases with Police National Computer (PNC) warning flags is presented in Figure 6. Eighteen individuals had PNC warnings on their criminal intelligence system (CIS) records, 10 of whom had two or more flags.
FIGURE 6.
Frequency of PNC warnings (n = 18 individuals).
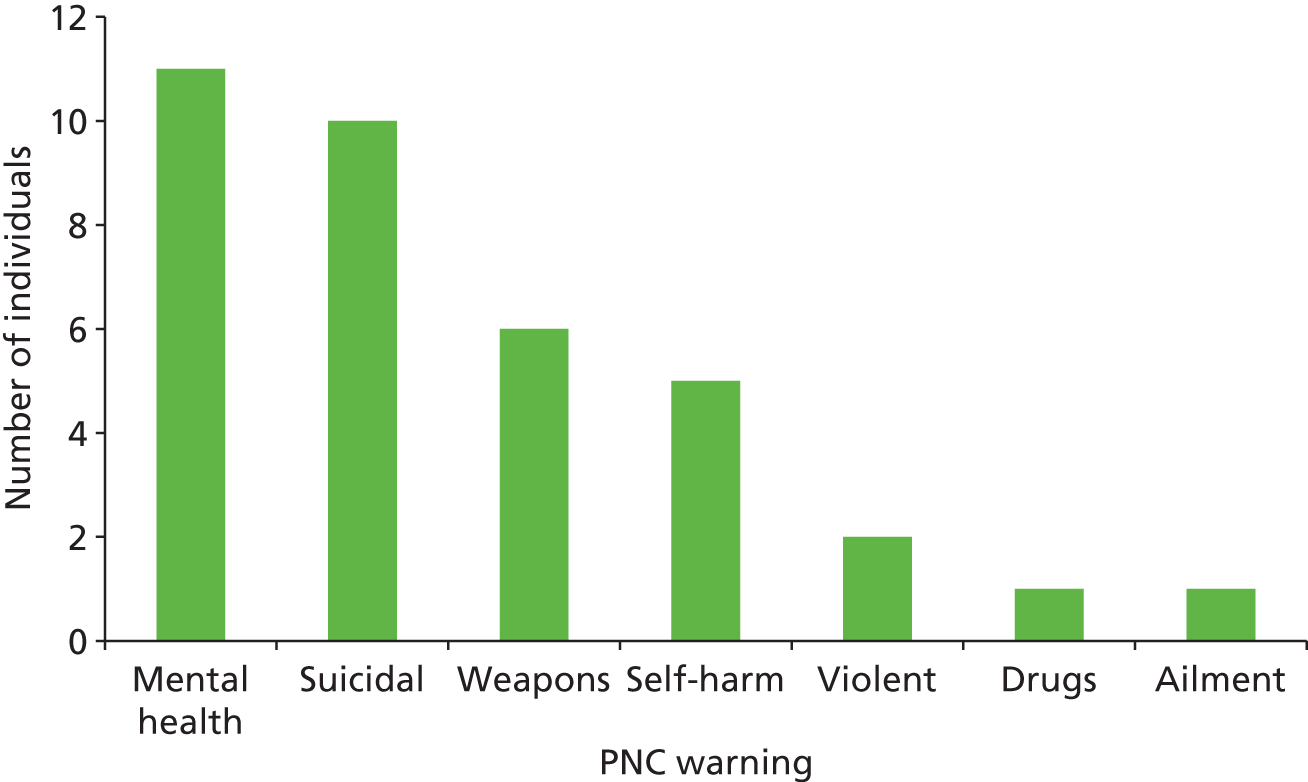
Eight of the 23 individuals included in the sample had a local warning flag on their record (Table 4). Seven had a single warning and one had both a location ban and a special need warning. Seven of the eight individuals with local warning flags also had PNC warnings. The one individual who had a local warning only was flagged for the Multi-Agency Risk Assessment Conference (MARAC).
| Local warning | Number of individuals |
|---|---|
| Vulnerable adult | 4 |
| Location ban | 2 |
| MARAC | 1 |
| Special need | 2 |
Mental health contact
For 20 of the 32 contacts, the individual was on the caseload of a care team at the time of detention. Eight contacts were on the caseload of one care team (six general secondary mental health services and two acute health problem management teams). Seven contacts were related to individuals on the caseload of a general secondary MHT and a further care team including acute mental health problem management (n = 2); offender-specific services (n = 3); specialist services (n = 1); and learning disability (LD) services (n = 1). Finally, five contacts were on the caseload of two general secondary MHTs with one of these, in addition, being on the caseload of the early intervention team (EIT) at the time of detention.
Formal police recording of mental health history
Recording of mental health using the PNC warning flag system was explored. After any incident where mental health issues are a precipitating factor for police contact, the reporting officer has the option of adding a PNC warning flag for mental health, suicidal or self-harm to the PNC system, providing a warning of mental health issues for future contact with the individual. Eleven individuals had a mental health warning flag attached to their police record, four of which comprised their sole recorded warning for use by the police. Seven individuals had two or more warnings additional to mental health. Three individuals had one additional warning (two suicide and one weapons); one individual had two additional warnings (suicide and weapons); and three individuals had additional warnings of suicide and self-harm with two of these having third warnings of weapons and violence attached to their records. All but one of these cases had a warning indicative of mental health issues in addition to the mental health warning.
Table 5 presents the warnings attributed to the remaining seven individuals (out of the 18 individuals with a PNC flag) who did not have a mental health flag. Although they did not have a mental health flag, five had warnings of behaviour that could be attributed to mental health needs (i.e. self-harm and suicide). It is unknown whether attaching suicide and self-harm warnings without a mental health flag is deliberate or due to individual differences between recording officers in the interpretation of the need for a warning flag or the understanding of mental illness and related behaviours.
| Case | Warning 1 | Warning 2 | Warning 3 |
|---|---|---|---|
| 1 | Drugs | ||
| 2 | Weapons | ||
| 3 | Suicide | ||
| 4 | Suicide | ||
| 5 | Suicide | Self-harm | |
| 6 | Suicide | Weapons | |
| 7 | Suicide | Self-harm | Weapons |
Section 136 decision framework
Four main decision-making points were identified through a review of policy documentation, consultation with practice partners (both police and mental health) and service users. It was intended to identify critical decision points at which there was a decision regarding the management of the individual and/or the possibility of diversion from police and/or mental health services. The four decision points were:
-
initial decision to detain under Section 136
-
location of detention
-
request and conduct MHAA
-
outcome of MHAA.
Framing the findings around decision-making processes enabled the findings to be explored in the context of the research questions relating to stage 2 of the research and provided evidence for answering the questions in Chapter 7 of this report. The research questions guiding the case-linkage study were as follows:
-
What are the organising principles that precipitate a joint working decision, by either the NHS or the police?
-
What is the decision-making process and who is involved in it?
-
Is the decision-making process consonant with local practice guidelines and national policy implications?
-
What is the impact of these decisions on the service user?
-
What is the impact of these decisions on the NHS, and police organisations?
It would be expected that decision 1 (initial decision to detain under Section 136) would be primarily taken by the police with possible input from services who may have called the police or who the police may contact (e.g. in the case of a missing person), and decision 4 (outcome of MHAA) would be within the remit of mental health practitioners (Section 12 doctor and AMPH) with information provided by other MHTs/services as appropriate. Decisions 2 and 3, however, would be expected to involve a higher level of interagency collaboration in order to reach an outcome or achieve diversion from Section 136.
Two researchers familiarised themselves with the data with regard to the above decisions in order to devise a framework within which each decision could be understood and within which data could be organised that would enable each case to be represented within each of the above decisions. The researchers were aware that although using secondary mental health and police records as the data corpus, these could be divided/viewed in two formats, i.e.:
-
data used by professionals to inform their decision-making at the time of the incident and for the duration of the detention process (i.e. historical data)
-
data compiled to log each incident and associated detention – this can be instantaneous and retrospective.
Two broad themes were identified through this process, each comprising two and three subthemes respectively. Table 6 presents the framework within which data were organised and coded under each of the above definitions.
| Framework theme | Framework subtheme | Definition |
|---|---|---|
| Informational | Individual factors | Factors directly related to the individual (e.g. behaviour, history). Any information that could not be ascertained without being witnessed or background information provided about the individual |
| Context | Situational factors, including presenting environment; social environment of the individual; perceptions/interpretations of others; how the individual interacts with the environment | |
| Operational/procedural | Information sharing | Use of information within/across systems; information gathered, recorded and shared at the current event; recording of shared information |
| Risk management | Assessment of and response to risk based on information provided (i.e. under informational theme and information subthemes above) | |
| Care management | Management of the individual in terms of both process (following policy/guidelines) and care (best interests of the individual). Can also involve the care of others associated either with the presenting situation or the individual themselves. Care management either moves the individual forward through the process to the next decision point or facilitates diversion from Section 136 |
In order to capture and represent a holistic account of the service user journey through the Section 136 detention process, it was necessary to ensure that all data gathered pertaining to each detention was utilised and accounted for within the analysis. As mentioned above, although some data were not direct contemporaneous accounts of the pivotal decision point, it is possible that the circumstances surrounding these points and information used prior to the decision being reached would drive the conclusion of each decision. Therefore, it was essential that data to be used to examine each decision point were standardised across all cases. Table 7 provides a summary of the data used to examine each of the decision points.
| Decision | Data |
|---|---|
| Decision 1: decision to detain under Section 136 | All information used to make the decision All procedures carried out to fulfil decision |
| Decision 2: location of detention | All information used to make the decision regarding location of detention All procedures conducted to make decision regarding location of detention and conduct detention in that location |
| Decision 3: conduct of MHAA | All information and procedures post detention and pre MHAA All information and procedures regarding discharge where MHAA does not occur All information used to make the decision to conduct MHAA All procedures conducted to make decision to conduct MHAA |
| Decision 4: outcome of MHAA | All information and procedures post MHAA All information used to make the decision to discharge/refer/section under the MHA All procedures conducted to make decision to discharge/refer/section under the MHA Outcome of MHAA |
The following sections present the analysis of each of the above decision points based on the above framework.
Decision 1: decision to detain under Section 136 of the Mental Health Act (1983/2007)
The first decision to be addressed by this analysis is the decision by a police officer to detain an individual under Section 136 of the MHA. The decision is influenced by a number of factors, discussed under the following headings:
-
Source of contact
-
Level of response
-
Location of initial decision
-
Police communication with mental health services.
Source of contact
Of the 32 contacts, 29 were initially directed towards the police through police call handlers or presentation at a police station. Calls were made either by a family member/partner or carer (n = 9, 28.1%), ambulance personnel or ambulance control (n = 7, 21.9%), the individual calling the police themselves in order to highlight their situation (n = 7, 21.9%), or a member of the public expressing concern or by a care team (n = 2, 6.3%). One service user initiated their detention by presenting themselves at a police station. Three further contacts were instigated through direct contact with the police (not through a call handler): one individual was found wandering in traffic, one was brought directly to the attention of police via a reporting person (RP) during patrol, and one individual was detained following being returned home by the police after another incident and the individual subsequently threatening to injure themselves with a knife.
Level of response
Operational Information System logs were examined to determine the level at which the police were required to respond to each incident. Thirteen incidents incurred an immediate response (response within 20 minutes of receipt of call), 14 incidents a prompt response (response within 1 hour of receipt of call) and three incidents a routine response (response within 48 hours of receipt of call). Two detentions had no recording of response: one did not have a police record of the detention and one individual presented themselves at a police station.
Operational Information System logs also provided attendance classifications, thereby offering a rationale for the initial incident response (the two aforementioned detentions without OIS logs are not included here). The highest proportion of attendances were for reasons of public safety relating to concern for or collapse of the individual themselves (n = 21). In the remaining cases, classifications included ASB (n = 4), a missing person (n = 2), suspicious circumstances (n = 1), a domestic incident (n = 1) and violence (n = 1) – linked to risk of violence from others.
Location of initial detention
Figure 7 presents the location of apprehensions and where the decision to detain under Section 136 was made. It can be seen that although all detentions were conducted in a public place, seven were conducted in areas that could be considered of heightened potential risk (i.e. railway station, track, bridge and beach), thereby supporting the rationale for detention in terms of risk to self (see below).
FIGURE 7.
Location of initial Section 136 detention. Numbers represent the number of detentions conducted in each location.
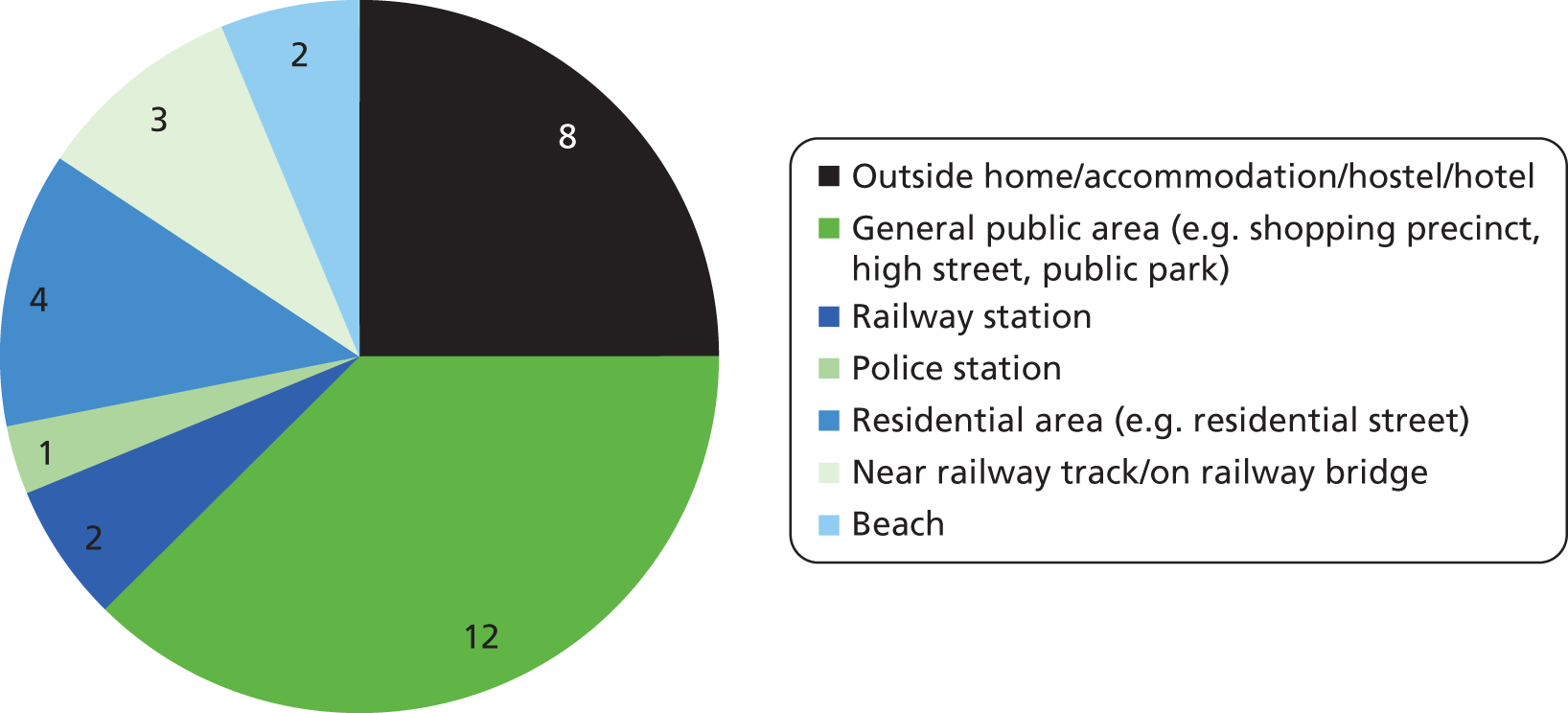
Police communication with mental health services
Examination was made of the OIS logs and mental health progress notes of each case to determine if police made contact with mental health services prior to making the decision to detain under Section 136, thereby either confirming the need for detention or providing the possibility of diversion. In the case of 21 (66%) detentions there was no contact between the police and mental health services prior to detention (i.e. between initial call regarding the individual and decision to detain under Section 136).
For the remaining 11 cases, there was a record of contact between services on OIS logs. Communication of such communication in progress notes was not routinely recorded. The researchers examined the direction of contact (i.e. if the police or mental health services instigated the contact), the degree of success in terms of making contact and the impact of successful contact on the decision to detain. Five cases had a record of successful contact between services, and an additional record of an impact of this contact on the decision to detain under Section 136. In two of these five successful contacts, the mental health and social care services recommended and supported police detention under Section 136 (one contact was instigated by the individual’s MHT). In one of the five cases, contact was made by the individual’s pastoral care team providing the police with sufficient historical information about the individual to support their decision that detention under Section 136 was both required and appropriate. For the fourth case, a discussion between services regarding the individual’s safety precipitated the decision to detain under Section 136. Finally, discussion about the situation of one service user between a social worker from the MHT and police led to the responsibility for that service user to remain with the police, which led directly to Section 136 detention:
Probably be voluntary attendance to [psychiatric hospital] as saying if she doesn’t see a psychiatrist she will kill herself . . . Trying to call numbers to see if they would accept
OIS log
t/c [telephone call] from police and ambulance crew who have been called to [service user]’s cousins address. [service user] was in the house when she became agitated, carried out some DSH [deliberate self-harm] on herself and threatened to hurt other people. Police were called and are trying to decide whether to charge her or whether she needs mental health assessment. I advised that this was a police decision but it does appear [service user] may be attempting to get herself admitted to hospital. The emergency services will carry on with their assessment of the situation.
Progress notes
In the remaining six cases (two of which were out of area), communication between services did not directly impact on the decision to detain under Section 136. However, in the case of one service user, communication between services had the potential to divert from detention. Despite this, due to the level of risk perceived by the attending officers, the individual was detained upon leaving their property:
Female was detained as the on paramedics arrival female said she was going to hang herself and listening to voices in her head telling her to kill herself. We have explained to [psychiatric hospital] she had to be in a place of safety.
Progress notes
Telephone call with emergency care practitioner who has been in attendance at SU’s [service user’s] home address. He informed me that he had treated and closed her wounds. However was expressing concern that the police were still in attendance and planning on waiting for SU to step outside her property and detain her on a Section 136. The emergency care practitioner informed me that SU had been speaking to him throughout, good eye contact and showed some humour. He reports that he had spoken with my colleague from [location] and understood that her presentation has remained unchanged. Informed the care practitioner of her review with the consultant prior to discharge. I repeated to him what the police are proposing. He informed me that the police are going to wait for her outside to have a cigarette and pick her up on a Section 136. Discussed how this course of action is bad practice and should not happen.
OIS log
Framework analysis of decision to detain
Framework analysis was undertaken of all the depersonalised documentation related to the decision to detain under Section 136. Themes are supplemented by descriptive analysis of cases in order to contextualise the themes and relate their proportionate applicability. Four themes emerged from the analysis of decision 1:
-
risk to self
-
risk to others
-
known to services
-
outcome considerations attempted diversion from Section 136.
Theme 1: risk to self
In order to assess contemporaneous decision-making by the police it was necessary to ensure that the researcher used information that was both available to police and recorded as a result of the incident (indicating information available directly from the presenting situation being witnessed and dealt with by police officers). As such, data were restricted to OIS logs with information supplemented by information provided by police to MHTs and recorded in the mental health progress notes. All 32 contacts were perceived as being a risk to themselves by the attending police officers. Figure 8 presents the categorised factors that precipitate a decision to detain under Section 136 due to risk to self.
FIGURE 8.
Categorisation of risk to self for Section 136 detentions (n = 32).
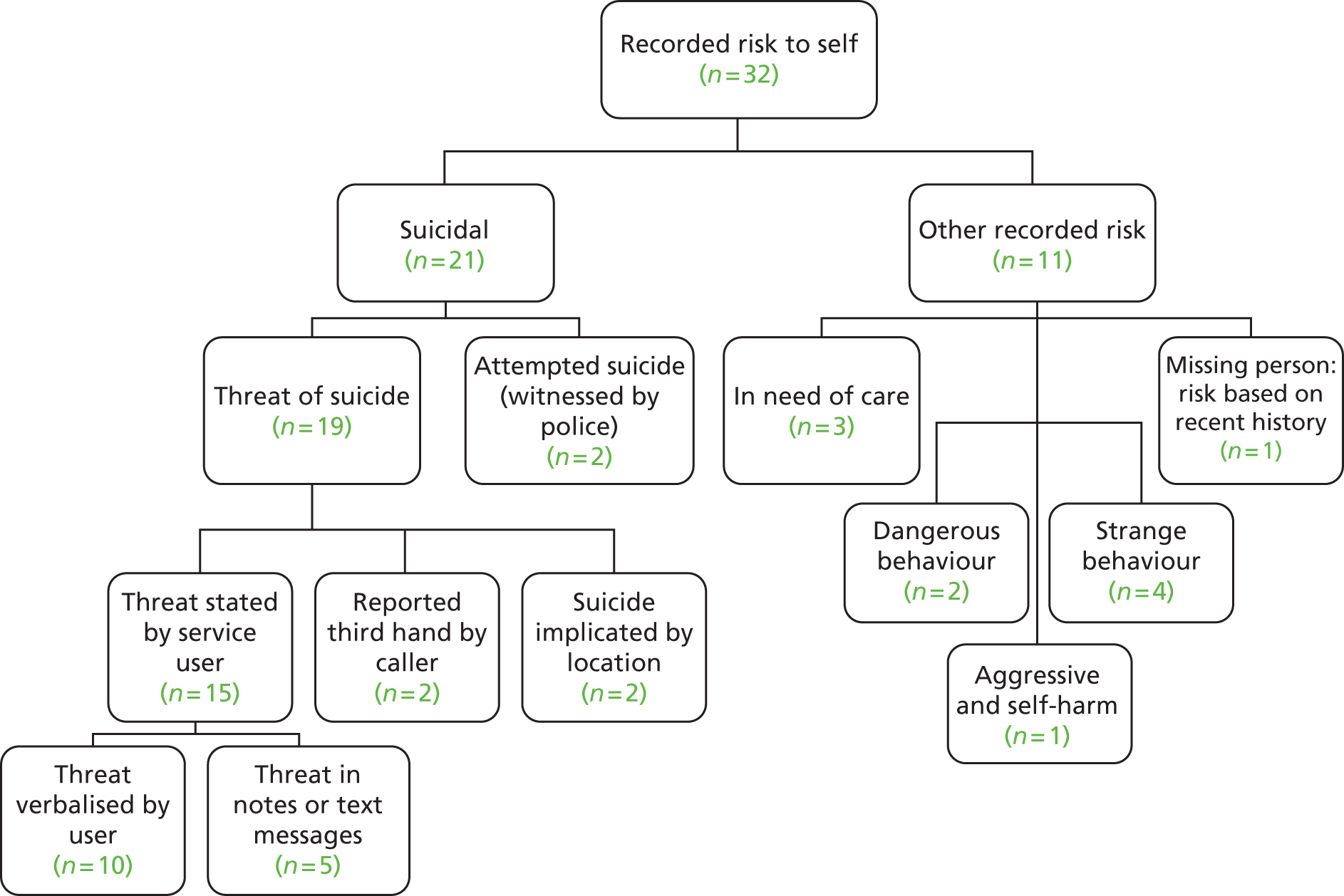
Two cases were witnessed as attempting suicide at the scene: one individual had thrown themselves from a window and one individual had attempted hanging. Three individuals were witnessed to be engaging in deliberate self-harm (DSH) at the time of detention: two by cutting (one with razor blades) and one by hitting herself in the face. Eight individuals were classed as missing persons during the initial logs relating to their detentions. It was only for these latter missing person cases that officers were able to collect historical information that facilitated a more detailed assessment of risk, including history of self-harm or mental health conditions (e.g. depression, anxiety) and recent overdose.
Information with regard to risk to self was categorised into the following:
-
immediate threat/danger to self
-
threat of suicide
-
DSH
-
behaviour perceived as indicative of mental illness.
In four instances, officers perceived immediate risk to self. Three of these were due to the behaviour of the individual (attempting suicide) and two to location. Three were also viewed as a risk to others (two at the time of apprehension, one while in custody). In all four cases, the police were required to intervene at the point of the individual taking an action which put them at risk. For example:
refers to report of concern welfare. DP [detained person] barricaded in room attempting to self harm. Ambulance attended. Unable to treat due to demeanour. Police attended and DP attempted to throw herself out of window headfirst. Taken outside to ambulance. Behaviour deteriorated. Sect 136
OIS log
girl tried to hang herself
OIS log
Threat of suicide was verbally stated by the individual and relayed to the call operator or response officers in 10 incidents recorded in OIS logs. These ranged from a general statement of suicidal intent to more specific information with regard to the method of suicide considered by the individual. For example:
concern for welfare [service user], 30yrs. was on phone to RP [reporting person] feeling suicidal.
OIS log
DP [detained person] has attended police station . . . DP [detained person] stated that he intending committing suicide by taking an overdose
Custody front sheet
concern for welfare – female on the line saying she can’t take it anymore . . . caller is walking at some speed – she is stating that she needs to end it she is asking me to stay on the phone as she is scared.
OIS log
In five of the 19 cases where threat of suicide was recorded, the individual left notes to be found in the event of their death or sent text messages intimating that they were suicidal:
RP [reporting person] has received 4 texts – ‘can’t do this anymore’ ‘ending it’ ‘just wanted to say goodbye, hope you get better’.
OIS log
she is very depressed and has a long history of suicide attempts. she has sent a message to a friend of hers today saying she doesn’t see the point of carrying on.
OIS log
Two of the 19 individuals were apprehended on or near a railway line, which police officers assessed as indicating imminent potential risk to the individual. For example:
RP [reporting person] states female is now standing in the middle of the tracks
OIS log
female saying she is going to kill herself saying she is going to the bridge – caller just shouting at me . . . with female on the bridge
OIS log
In the remaining two cases, threat of suicide was reported by the caller.
girlfriend saying she is feeling suicidal . . . circumstances log [number] refers. police called by male stating his girlfriend was threatening to commit suicide, d/p [detained person] located clearly distressed & stating she was hearing voices telling her to hurt herself, d/p has history of self harming & detained for her own safety.
OIS log
Recording of self-harm in police logs illustrated that officers relied on historical and observational information to determine if this was or might be an issue in their assessment of risk. The researchers examined information on both historical and current self-harming behaviour available to officers when making the decision to detain under Section 136. Information on historical self-harm was recorded in 10 logs, including PNC warnings (n = 5) and recent self-harming behaviour (n = 5), including carrying of implements used to self-harm and recorded observations of self-harm. For example:
**high risk** based on current state of mind and recent attempts to self harm/suicide
OIS log
Imminent risk: razor blades in handbag – self harmed last night when missing.
OIS log
Other than the two attempted suicides presented above, directly observed DSH was recorded in the OIS records of five detentions with the individual either engaging in the behaviour in front of the police or having visible injuries attributable to DSH, for example:
23 yr old female self harmed – hitting herself in face – wants to knife herself and other people – [service user] – schitzophrenic female back of AMB [ambulance] – has harmed herself not threatened anyone whilst been here
OIS log
female safely off the track – cuts to her arms AMB [ambulance] to check her over
OIS log
Although not necessarily linked to suicide threat, self-harming behaviour or historical risk of self-harm contributed to the responding officer’s decision to detain for the purpose of care and control.
Figure 8 shows nine individuals were recorded as not presenting with suicidal ideation or behaviour but displayed behaviour that police associated as reflecting mental health needs. Four individuals were perceived as displaying ‘strange’ behaviour and were under the influence of alcohol or drugs on detention. Although these individuals were not explicitly threatening or attempting suicide, or posing a risk to others, their behaviour (and in the example below, location) indicated a level of potential risk that precipitated detention under Section 136:
DP [detained person] found on beach heavily intoxicated in possession of paracetamol, behaving very irrationally, rambling uncontrollably, history of MH [mental health] issues, fear she will harm herself if not detained
OIS log
Police perceived three of the individuals to be in need of care due to their behaviour and/or presenting situation. The following example is of an individual presenting with no imminent risk to himself or others, but acting in such a manner as to require immediate care that, due to presence of the police at the scene, precipitated a detention under Section 136:
male not properly dressed and appears confused – caller tried to speak with him but male could not talk very well. male also appears to have soiled himself
OIS log
Finally, two individuals were viewed as exhibiting dangerous behaviour, one at the scene of the incident (walking in among moving traffic) and one attempting to exit a moving vehicle. In both of these cases, the risk to self translated to risk to others, presented below.
Theme 2: risk to others
Thirteen Section 136 detentions involved individuals who were perceived by attending police officers as being a risk to others at the time of apprehension. This was characterised either by threat or actual violence to specific single and multiple individuals including professionals such as:
-
The attending ambulance crew (n = 3, one individual also threat to mother, see below).
-
OIS log
OIS: f/AMB [call from ambulance crew] – called to a 20 yrs old male self harming – threatening further violence – autistic patient who also has ADHD [attention deficit and hyperactivity disorder]
-
OIS log
girl tried to hang herself – now being violent (call made by crew)
-
-
Police (n = 2).
-
OIS log
the DP [detained person] was completely uncooperative and had been violent towards officers so was taken to cell and searched by PC [police constable]
-
-
Health workers (n = 1, one individual also threat to partner, see below).
-
OIS log
could hear disorder in background CPN [community psychiatric nurse] is female and male driver, patient in back of car. they are transporting him to [mental health hospital 3] taking him to [custody suite] att because of behaviour – 2 CPNs with him are arranging MHT to attend [custody suite] within next 1–2 hours to do assessment
-
Non-professionals deemed at risk were:
-
The individual’s partner due to violence (n = 2, one individual also threat to health worker, see above).
-
OIS log
RP [reporting person] states his friend and him are at the sig being threatened with violence by this female as she has had too much to drink and they want her removed, RP [reporting person] also sounded in drink.
-
-
The individual’s mother (n = 1, one individual also threat to ambulance worker, see above).
-
OIS log
further call from AMB [ambulance] to say male getting aggressive now he has just assaulted his mother
-
-
The individual’s child due to the child being present during the incident (n = 1, also threat to public, see below).
-
OIS log
caller on matched log is happy to keep an eye on her as she appears very distressed – caller more concerns for the child.
-
Public safety was perceived as being an issue due to the individual wandering in traffic (n = 1); threatening behaviour to the public (n = 1, also threat to child, see above); intimidating behaviour in a shop (n = 1); attempting to break into surrounding properties (n = 1); and threatening to stab others (n = 1). Finally, one individual was perceived as a risk to others due to his fear that he would harm his family following self-presentation at a police station. A further detention involved an individual who was deemed a risk to others once in custody by the police.
Tasers were authorised to potentially manage three incidents, although they were not used. Rationales for authorisation included aggression by the individual, violence by the individual toward their partner and the individual threatening to stab others.
Theme 3: known to services
Whether or not the individual was known to the police was information used in making the decision to detain under Section 136. The 32 OIS logs associated with each incident, were examined to determine if this was the case. One incident did not have an associated police record (the contact and detention was recorded only in mental health records).
Eighteen individuals were recorded as known to the police through PNC warnings. Of these, eight individuals had a PNC warning for mental health and of the seven who had a PNC marker other than for mental health, five had a warning for behaviour associated with mental health issues (i.e. suicide or self-harm).
Examination was made of OIS logs to determine the knowledge of the individual by the responding officers and/or call operators, and showed this was the case in eight incidents. Seven of the incidents in which police officers and/or call handlers had previous knowledge of the individual were related to two service users with multiple Section 136 detentions in the research window: one with four recorded detentions and one with three recorded detentions. For the individual who had four Section 136 detentions, call handlers provided the response officers with information on his mental health and forensic history. For the individual with three Section 136 detentions, examination of OIS logs indicate an escalation in knowledge, from the call handler being aware of the individual being left at home by an ambulance crew immediately prior to the incident (first detention) to the call handler being aware of the individual’s behaviour (second detention), to both the call handler and response officers recording previous knowledge of the individual’s behaviour (third detention):
local officers well aware of female
OIS log
Additionally, and also presented above, individuals were currently on the caseload of, and therefore known to, mental health services in the case of 20 Section 136 detentions. Contact was made between police and mental health services prior to 11 of the detentions examined here in relation to the decision to detain under Section 136. The following examples show how knowledge of the individual by mental health services coupled with this communication between services can both support the decision to detain under Section 136 and provide information to help the police with their enquiry when an individual is missing:
I spoke to the police officer who said he was reluctant to take [service user] back to [residence] as he would leave immediately they left and they did not have the resources to keep returning him to [residence]. in view of his vulnerability i suggested that they consider a Section 136 to maintain his safety and dignity.
OIS log
[Officer] spoken to [service user]s CPN [community psychiatric nurse], a [CPN], she has not heard anything from [service user] over last couple of days, she says she has a support worker in [support worker], she starts work at 1600 and shall also try to contact [service user] then . . . log numbers passed to both, however they can only suggest we look at cemetery which has already been checked. please advise btp [British Transport Police], in case travels into Devon, no destinations known ATT [at the time].
OIS log
Theme 4: outcome considerations – attempted diversion from Section 136
Although the factors discussed above impacted on the initial decision to detain under Section 136 for the majority of detentions, in some cases, services suggested potential alternatives to Section 136. In one case, the police attempted to involve the home treatment team (HTT) in order to avoid the individual being detained, but due to the unavailability of the HTT until the following day, and on assessing the potential risk to that individual, they were detained under Section 136. However, diversionary measures that offer the support required to keep individuals (and in some cases, others) safe cannot always be identified. For example, in the case of one individual’s detention, he was not perceived as being a risk to himself or others, and the police attempted to find an alternative to his management. However, social services advised that he be detained at a place of safety because, despite the individual’s residential home being happy to reaccept him, they would not be able to maintain his safety as they were unable to lock the doors.
contacted by staff member at [residence] as SU [service user] was causing a disturbance in [home town] the police were with him. SU was confused and disoriented and had been incontinent of urine. I spoke to the police officer who said he was reluctant to take SU back to [residence] as he would leave immediately they left and they did not have the resources to keep returning him to [residence]. In view of his vulnerability I suggested that they consider a Section 136 to maintain his safety and dignity.
Progress notes
Records also showed examples of further attempts at diversion prior to police involvement. In one case, the individual recognised the service user had mental health issues and had called the out of hours MHT. However, on not receiving a reply and having continuing concern for the individual, it was deemed necessary to call the police. Furthermore, in the case of a Section 136 detention that occurred out of the force area, the individual themselves attempted to divert the Section 136 by communicating with the relative who called local police to report them missing. Initially, Section 136 was thought to not be applicable as the individual was found in their hotel room. However, once the individual was taken informally to an out of county police station, they were then detained under Section 136:
contacted [other Force] and they have the female at [out of county] police station and the have been updated on the last and the female is currently in the process of section 136.
OIS log
Decision 2: location of detention
The second decision to be addressed here is that of the location of the detention of the individual under Section 136. Figure 9 presents the location of detention and associated transfer of the 32 detentions under examination. Of these, 19 were detained solely in a police custody suite and nine (two out of county) solely in the NHS place of safety. Two of the 19 detentions that occurred solely in the custody suite were initially taken to the place of safety but not admitted due to rationales associated with resource and alcohol intake (addressed in more detail below). Three further contacts spent a proportion of their detention within the police custody environment being transferred from there to the place of safety (n = 1) and general hospital (n = 2). Finally, one individual was originally to be detained in custody but was transferred en route to an acute psychiatric ward following information regarding his current Section under the MHA.
FIGURE 9.
Location of Section 136 detentions.
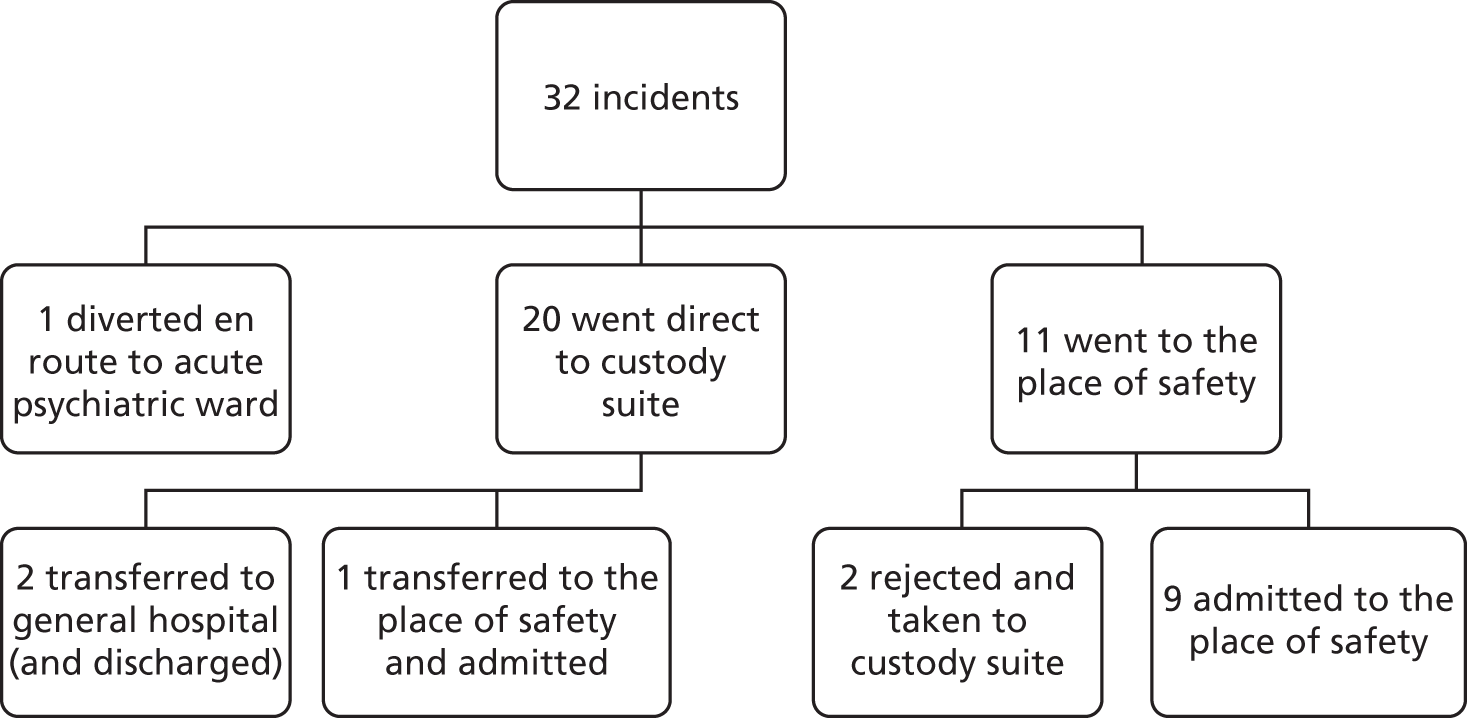
Time detained in both custody and the place of safety was examined. Of the 19 detentions that occurred solely in custody, the mean duration of detention was 14 hours 17 minutes (range 3 hours 24 minutes–36 hours 36 minutes). Only two of the nine detentions that took place exclusively in the place of safety had a recorded time of detention (4 hours 28 minutes and 4 hours 40 minutes respectively). Overall, the mean duration of detentions for which records were available was 12 hours 45 minutes (range 3 hours 24 minutes–36 hours 36 minutes). All of the detentions in custody were within the 72-hour maximum allowable time in detention for Section 136 in accordance with the MHA.
Both agencies’ information systems were examined to determine which made the decision as to the location of the detention, and the rationale for that decision. The local Section 136 protocol identifies that if an individual is under the influence of drugs or alcohol or is violent, this is an exception to the recommendation that Section 136 detentions should be located in the place of safety. 52 Examination of OIS logs and progress notes provided the rationales for 21 of the 22 custody detentions. Table 8 presents the decision-making agency and associated rationale for each of the 22 cases. In line with the findings of the recent HMIC (2013) report,41 the main rationales for location centred on those highlighted in the local protocol, i.e. alcohol consumption, violence and resource. In general, police made the majority of decisions with regard to rationales concerning alcohol consumption or violence. The majority of MHT rationales concerned resource or lack thereof.
| Agency making decision | Rationale | Number of contacts |
|---|---|---|
| Police | Alcohol only | 5 |
| Alcohol and violence | 5 | |
| Violence only | 2 | |
| MHT | Alcohol | 1 |
| Resource | 6 | |
| Violence | 1 | |
| Police and MHT | Violence | 1 |
| Unknown | Unknown | 1 |
Framework analysis of location decision
The themes below provide the rationales that supported the decisions to detain in the main locations, i.e. custody and the place of safety:
-
alcohol and drug consumption
-
risk of violence
-
resource.
Theme 1: alcohol and drug consumption
Alcohol consumption was a precipitating factor in the decision to locate 11 detentions in custody. The police officers’ decisions to locate 12 detentions in custody due to alcohol consumption and violence show adherence to the local Section 136 protocol. For the three detentions that were initially located in custody but were later transferred to either general hospital or the place of safety, the police made the initial location decision due to alcohol and did not involve the place of safety as they were clearly following protocol. In the case of one of the two detentions that were initially taken to the place of safety but not admitted, alcohol consumption was given as the rationale for non-admittance. However, the officers’ records show that although officers were following protocol in that they did not assess these individuals as intoxicated, the place of safety staff took a different interpretation of the protocol, which prevented location of the service user at the place of safety. This illustrates the importance of interpretation of protocol with regard to alcohol consumption.
Theme 2: risk of violence
As shown, presentation of violent/aggressive behaviour together with known alcohol consumption was the rationale for five police decisions to detain in custody. Violence was the sole rationale for the police decision to detain in custody in two cases. Police and mental health services came to a joint decision to detain one individual in custody as it was determined that he was too aggressive to be detained at the place of safety. Violence was only used by mental health services as the rationale for one custody detention. The decision to detain an individual considered to be violent is in line with local protocol,52 which states that in cases where the individual is assessed as violent or there is concern regarding the potential for violence, the individual should not be detained in the place of safety.
From police records, only one of the nine exclusively place of safety detentions presented as violent at the time of apprehension.
male kicking off with AMB [ambulance] they state he needs an immediate section
OIS log
This individual was en route to custody when the MHT received information that he was already under Section 3 of the MHA and therefore diverted to their service. An examination of the available mental health risk assessments was conducted that revealed seven contacts had a risk assessment within the 9 months prior to the date of their detention, of which two had a record in their mental health notes of historical violence to staff (one also had a known history of violence to family that was specifically recorded). Other indications of violence contained in risk assessments included hostage taking, weapons and warnings to staff only to visit the individual in pairs [this individual had been risk assessed specifically for violence using the Historical Clinical Risk Management-20 (HCR-20)]. Therefore, for those cases that were detained in the place of safety, historical violence indicators in mental health risk assessments did not preclude them from entry to the place of safety.
Theme 3: resource
Table 8 shows that six individuals were unable to be detained at the place of safety due to issues regarding resource in terms of capacity (n = 3) or technical issues including, broken alarms, locking systems and lighting (n = 3). Officers were informed of these issues during calls made to the Section 136 suite to check availability. None were recorded as being either under the influence of alcohol or violent/aggressive and so met the protocol requirements for entry to the place of safety. Although the suite itself has the capacity to detain two individuals unless one detainee is aged <16 years, capacity is also determined by perceived risk from detainees, available staffing levels and the individual needs of the detainees (Mr Andrew Fox, Head of Social Work, CFT, 2013, personal communication). The following example illustrates capacity issues at the place of safety:
call from [custody suite] to advise that [service user] had been picked up by the police in the town and had been taken on a section 136 to the station. [service user] states she is hearing voices and wants to commit suicide.advised police that we were struggling to find beds as this was the 3rd section 136 at [place name] tonight. tel[ephone] call to [professional],on call manager for the west.advised her of the current situation and the lack of bed space.
Progress notes
Lack of capacity is an acceptable exception to locate a detention in the place of safety noted in the Section 136 protocol. 52 Technical issues are not specifically highlighted in the protocol as a legitimate exception. However, as the safety of service users and staff is fundamental to the protocol, this was regarded as an unavoidable exception. An example of such a technical issue is illustrated below:
female detained Section 136 – [Place of safety] unable to take her…why won’t [Place of safety] take her? . . . no panic alarms working so can’t accept anyone
OIS log
The location of detention itself can impact on resources available in custody to manage the individual once detained. The following examples, although not impacting on the decision as to the location of detention itself, illustrate issues of resource that are affected by the decision to locate a detention in custody. The failure of the place of safety to accept an individual has implications for the police in terms of their resources. Specifically, if the service user is female, a female detention officer must be available to appropriately manage the individual, as shown in the following extracts.
now at [MHL1] – cannot take anyone due to fault with their alarm unit now on the way to you – do you have female do [detention officer] working pse [please]
OIS log
Cust Sgt [custody sergeant] asking for another 1 poss [possible] another female to assist will need to be strip searched
OIS log
The following OIS log details the impact on not only the custody centre but the level of police response available for the geographic area. This followed the decision by the place of safety not to admit the service user due to their consumption of a glass of wine, thereby raising a debate in the interpretation of the protocol as shown in the following log extract:
for inspector [name] to review please the consequence of this on a busy night was that [custody suite] went migrate red due to the needs of this individual which had severe impact on local response cover due to the volume of logs and prisoners pending review by Insp [inspector] [name] – thanks
i will e-mail ins [inspector] [name] about this and ask him to review acquaint himself with this state of affairs and raise it yet again with [Place of safety]. log can be closed.
OIS log
female coming back initially to prevent bop [breach of the peace] . . . will need 2 female officers to search her
OIS log
Decision 3: to conduct a Mental Health Act assessment
During detention under Section 136, there is a set process for managing the individual in custody or the place of safety. All individuals detained at the place of safety are formally assessed under the MHA. In the research site, prior to July 2013, an informal mental health assessment [often recommended by the health-care professional (HCP)] was conducted in order to ascertain if a request needed to be made for a MHAA (as of July 2013, MHAAs are mandatory for all Section 136 detentions). It is accepted that a MHAA should be conducted following request by the forensic medical examiner (FME) (PACE code of practice C). In the case of twenty-two contacts, individuals spent some or all of their detention in police custody suites (one being transferred to the place of safety and two to hospital). At the outset of detention under Section 136 in custody, detention officers undertake a standard risk assessment (which forms part of the custody record on NSPIS). The FME’s decision is based on this risk assessment, the circumstances of the original detention, information gathered during the individual’s time in custody, and how the person presents during the FME’s examination.
The risk assessment consists of standard questions, including self-reported mental health history, self-harm, recent alcohol use and medical history. The self-harm question is twofold, with opportunity for the custody officer to enter their own observation of self-harm. Of the 19 who remained in custody for the duration of their Section 136 detention, 17 self-reported as having currently or historically self-harmed. All 19 of those detained in custody for the duration of their Section 136 detention were recorded by the police as having currently or historically self-harmed.
Mental Health Act assessments were conducted in 25 of the 32 detentions. Figure 10 presents the number of MHAAs conducted and the rationales for those cases in which a formal assessment was not conducted. In the seven cases where a MHAA was not conducted, detention logs and medical forms were examined to ascertain the rationales for this.
FIGURE 10.
Mental Health Act assessment outcomes.
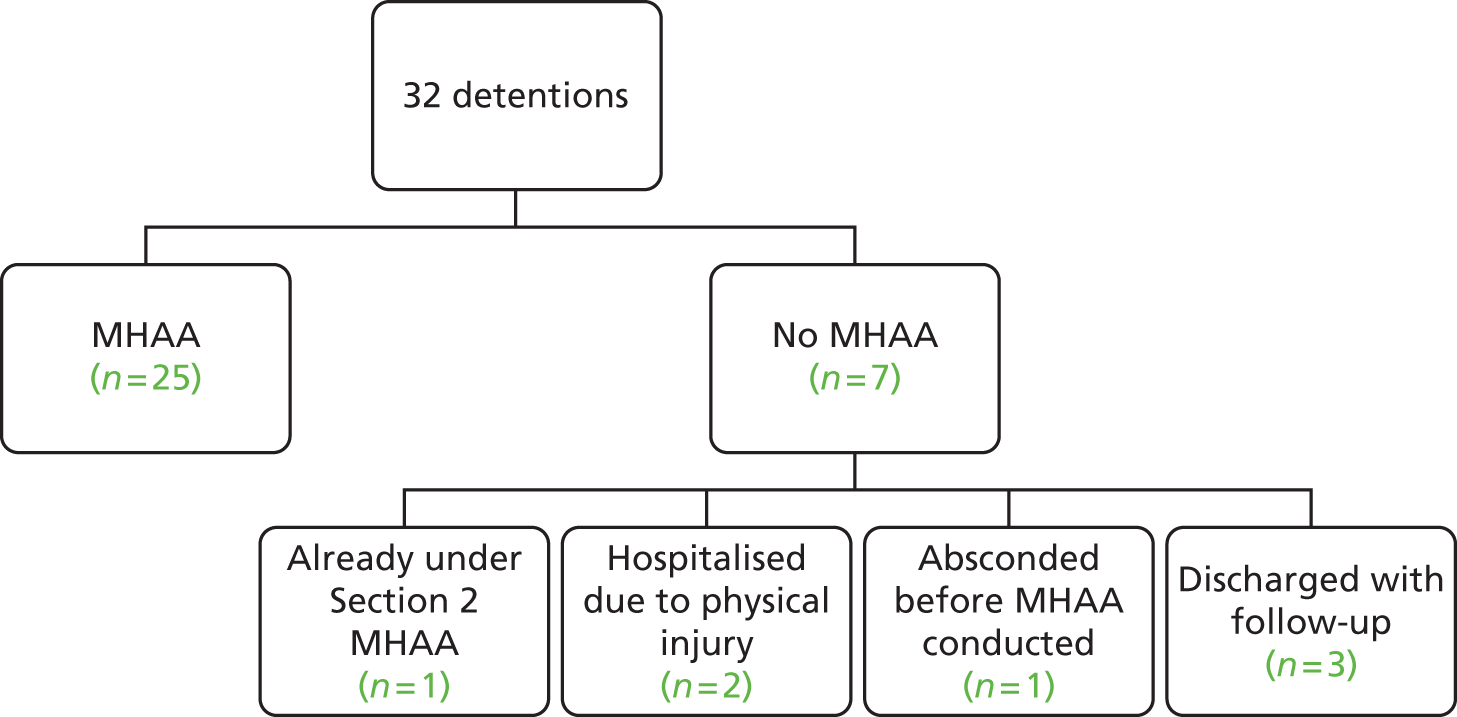
Of those not assessed, one was found to be under Section 2 of the MHA at the time of detention and subsequently transferred en route to psychiatric hospital, so a Section 136 MHAA was not necessary. Two individuals were discharged from general hospital following treatment for physical injury; therefore, they would have been assessed at the hospital, possibly by adult psychiatric liaison (APL) or the HTT and discharged, for example:
Re the call from [HTT CONTACT] – before the decision is made to release this DP [detained person] – I need the FME to speak with the hospital staff/[HTT CONTACT] to resolve whether she is to be released straight from hospital . . . Spoke with FME – agreed that the d/p [detained person] would return to custody for Dr to assess – contacted the AMHP [HTT CONTACT] who advised that the officers had left the hospital with the DP – enqs [enquiries] made to try and ascertain where they have taken the DP
OIS log
Three cases were discharged due to, or with the understanding that, some form of follow-up would occur. Two of these cases were based in custody for their detention; after assessment by the FME, one was recorded as not having suicidal ideation and had future care appointments in place, and the second was discharged home after discussion with the MHT, resulting in agreement that a follow-up appointment would be provided. The third contact with follow-up care in place had been detained in the place of safety and, after an informal assessment, was discharged home with a referral to the HTT and agreed follow-up from the Community Mental Health Team (CMHT) within 7 days. This was against current protocol but based on the presenting behaviour of the individual and her willingness to engage with services offered. For example:
A 20 year old student with a history of self harming behaviours and low mood, [service user] lacks appropriate alternative coping strategies and is impulsive in her behaviours. [service user] described wanting to change and willing to except help from services. At this time it is not felt that [service user] is displaying mental illness to the nature and degree warranting a Mental Health Act assessment with a view to hospital admission. She remains an ongoing risk of self harm but has agreed to all support offered and a management plan for today, which will be reviewed by HTT later today.
Progress notes
The final contact out of the seven not formally assessed under the MHA following Section 136 detention absconded before the MHAA could take place and was discharged home on being located by the police.
Framework analysis of decision to conduct a Mental Health Act assessment
Twenty-five Section 136 detentions resulted in a MHAA, of which 18 were conducted in police custody. The following themes emerged as instrumental in the FME’s decision to request, and for the MHT to carry out, a formal MHAA in custody:
-
the impact of alcohol
-
mental health history
-
presenting situation
-
resource.
Data supporting this decision-making were identified either in the detention log or medical form (by the FME) or the mental health progress notes entered retrospectively by the MHT.
Theme 1: the impact of alcohol
While someone is detained in police custody, the initial decision to request a MHAA lies with the FME who then requests this from the MHT. In some cases, particularly where the individual was not under the influence of alcohol, the detention under Section 136 was sufficient to prompt the FME to request a MHAA. In these instances, the request was viewed as a routine continuation of the management of the individual through the Section 136 detention process:
will benefit from a MHAA . . . Medical advice DP [detained person] will require a MHAA, assessment requested. Spoken to HTT WEST [NAME] which will pass the information to AMHP and will arrange a MHAA to take place, will call back with an eta [expected time of arrival]
Custody medical form
Intoxication at the time of detention, however, often prevented the decision to request a MHAA as a straightforward follow-on from detention. Twelve individuals were recorded as being under the influence of alcohol when they were detained under Section 136. It was not always clear if their behaviour at the incident that precipitated detention was due to the effects of alcohol or a potential mental health need. In these cases, the FMEs were recorded as conducting an informal mental health assessment when the individual was no longer intoxicated in order to determine the need for a formal MHAA without the potentially confounding effects of alcohol:
Will require MH [mental health] assessment by FME in morning when sober. Medical advice. Referred for formal MHAA.
Custody medical form
Once she had sobered she was assessed by the FME and at that time continued to have suicidal ideation, therefore a MHAA was requested.
Progress notes
Theme 2: mental health history
Mental health history was used by the FMEs to provide support for their rationale to request a MHAA. This information was often provided by the service user in the initial risk assessment and/or the assessment conducted by the FME. Self-report of mental health conditions, diagnoses and previous contact with mental health services aided the FME in building up a picture of the extent of need and previous mental health service input. The persistence of this need also provided impetus for the MHAA request. In the following example, the individual reported both the duration of mental health needs and specific diagnoses which, together with the presenting situation and detention, provided support for the need for a formal assessment under the MHA:
Long h/o [history of] mental health problems. Reports PTSD [post-traumatic stress disorder], depression and OCD [obsessive compulsive disorder]
Custody medical form
Communication between the FME and the MHT facilitated knowledge exchange with regard to mental health history and the presenting situation. In the following case, the FME’s contact with the individual’s MHT provided historical information about the individual’s behaviour in relation to her presentation in custody (non-compliance with medication). Due to the potential for increased risk associated with this behaviour, this provided the main driver for requesting a MHAA in custody:
MHAA requested with AMHP [NAME], she said the morning team which starts @0900hrs will call custody with an ETA [expected time of arrival] for the assessment. DP [detained person] will benefit from further assessment as has become noncompliant with her medication for 1 week and does not need her medication anymore. Discussed with AMHP, DP’s has become non-complaint with medication in the past and then DP becomes unwell. DP has High Risk Behaviour tendencies when upset, which is a possibility due to her recent situation at home and with her personal life. This warrants a MHA assessment at custody and not in the community.
Detention log
In a further example, discussion of the individual’s current behaviour in the context of their mental health history revealed a pattern of potentially escalating behaviour that warranted further attention by services through a MHAA:
P/c [phone call] from Dr[FME], FME at 2.20am. He was asking for advice about [service user]. He had redressed her arms. She had many cuts on both arms and had ‘written’ ‘help me’ on one. She had been picking at her wounds. [FME] reported that she was sober, alert and wanting to go home. He asked if he should release her. I explained a little about her background and that her behaviour recently was becoming increasingly risky. I was not prepared to advise alone. I suggested I would seek views of the duty consultant and call him back.
Progress notes
P/C [phone call] to Dr[name], duty consultant. After hearing of [service user]’s history and recent events he and I concluded that [service user] should be assessed fully.
Progress notes
Theme 3: presenting situation
On receiving a request from the HCP for an initial assessment of mental health needs, the FME conducted an assessment of those individuals detained in custody. In general, records showed that an assessment of the presenting situation included evaluation of both mental state and personal care as well as any change in presentation during detention.
Mental state was assessed through self-report during discussion with the individual, direct observation during assessment and detention logs, and reports of officers who had been conducting regular checks on the individual throughout the detention. Records showed that assessment focused on what was perceived to be paranoid or delusional behaviour. The following extracts from the custody medical form of individuals being assessed by the FME show examples of paranoid and delusional beliefs that were seen to precipitate the need for a MHAA:
Today seems paranoid – believed police were trying to kill her and her child.
Custody medical form
DP [detained person] stated she does want to be alone, she stated she hears voices and would like kill herself.
Custody log
Other detention related issues? – ‘Yes. states she hears voices all the time’
Medical form
Assessment of personal care included the individual’s ability both to self-care and engage with services, including the potential to engage with services in the community should the individual be discharged without being formally assessed, as well as compliance with medication. The following extract from a custody medical form shows how an individual’s overt non-compliance with medication can have a direct impact on the FME’s perception of the need for a MHAA:
DP [detained person] is noncompliant with her medication and is refusing to start taking them again. DP stated she is on various medication but feels better now and does not want them. DP called the police tonight and stated she does not want to live anymore. DP has changed her statement and stated to me that she does not remember. MHAA requested for the morning (DP is well known to the CMHT) due to 1. DP Noncompliant with medication. 2. High risk behaviour when upset. 3. DP calling police and going missing tonight and stated she is afraid she will harm herself. 4. DP stated she does not remember saying or doing anything tonight and that everyone is lying that she called the police.
Custody medical form
Perceptions of individuals’ ability to self-care involved an assessment of risk of self-neglect. An individual’s inability to engage in appropriate self-care was evidenced by historical knowledge (either from self-report or discussion with the MHT), circumstances of the detention and/or direct observation of current presentation. The following example from a custody medical form relates to an individual for whom a MHAA was requested due to both mental state and concerns for self-neglect due to the circumstances in which they presented at the time of detention and continued to present in custody:
Seen re Section 136 assessment. Brought in very confused & self neglected after call from concerned MOP [member of public] – out on road, shuffling, very self neglected, covered in own faeces, confused ++, refused to return to own address, brought in on Section 136 as concerns for personal safety . . . Unable to assess MH [mental health] fully but no SI [suicidal ideation] expressed, denies ideas DSH. D/W [detainee with] AMHP [NAME] who is here for another DP [detained person], agrees.
Custody medical form
The above discussion showed that change in presentation when an individual has been under the influence of alcohol can determine the decision to request a MHAA. In the same way, change in presenting situation with regard to mental state and behaviour can also impact on this decision. In the following example, the change in the individual’s behaviour, coupled with the assertion by the FME that he would not engage with services in the community if released, drove the decision to contact the AMHP to request formal assessment:
advised DP [detained person] that I will go to speak with the MH [mental health] team and get back to him in regards to if he will be assessed in custody or not. I spoke with OOH [out of hours] MH team AMHP [NAME], I advised her that he appears well to be sent to home address with no MHAA in the custody, she agreed. I went to talk to DP that he will be going home and he became upset and stated that he wants to be released now and became aggressive and punched and kick the cell door. He stated he will make his own way back to [home town] from [police station]. DP became unpredictable and irrational and refused to give his address. The Custody srgt [sergeant] assisted me when I went to see DP and concluded that he will not release DP with this presentation of unpredictability and irrationality. I have spoken with AMHP [NAME] and requested her for full assessment on the new presentation and that he will not keep his appointments in the community and that he will require further assessment (which he missed) which can be arranged at the custody under the MHA and that he will benefit from a period of further assessment at the hospital due to his unpredictability, vulnerability and non compliance with medication and him not attending his assessment set out in the community.
Medical form
Theme 4: resource
The availability of resource emerged as relevant to the decision to request a MHAA, in terms of staffing and in timing of the MHAA. First, both the required levels of staffing (including Section 12 doctors and an AMHP) and the co-ordination recommended by the MHA (which recommends that all practitioners conduct the assessment simultaneously) carry resource implications. It could be argued that this is further exacerbated in a large rural site due to geography and associated logistics. The following extracts from a police detention log and mental health progress notes, respectively, highlight these resource issues in making the decision to request a MHAA:
have called home treatment team and spoken to AMHP [name] she stated they can not get any Dr’s at this time as there are two more 136 at [place name]. she stated it will probably be some time this afternoon before anyone will be available. she will contact when arranged.
Detention log
It was now almost 3am and I was unlikely to find a s12 [Section 12 of the Mental Health Act 1983;18200719] doctor who would respond as they would be working in the morning.
Progress notes
Resource as a precipitating factor in the decision to not request a MHAA can have a negative outcome for the individual, particularly in terms of timing of the MHAA. As shown, individuals can be detained under Section 136 for up to 72 hours. However, this duration of detention, particularly in custody, is not considered to be in the best interests of the individual. Where timing of either the FME assessment or the MHAA could potentially prolong detention, efforts were made by police to provide solutions to expedite the process of requesting and securing a formal MHAA for detained individuals. The following entry in a detention log illustrates one officer’s attempt to reduce the time required to wait for an assessment of need for MHAA by the FME:
Considered transferring DP [detained person] to [place name] to assist in speeding up the FME assessment, but it is likely DP will need to be dealt with by her own team and this will not happen until the morning, therefore no benefit to a transfer.
Detention log
Decision 4: outcome of Mental Health Act assessment
Of the 25 contacts that were formally assessed under the MHA, five were detained following MHAA (four detained under Section 2, one under Section 3), and one was informally admitted to inpatient psychiatric care. Nineteen contacts were not detained in hospital for further assessment or treatment.
Of those detained in hospital after their MHAA, only one was not on the caseload of a care team at the time of detention. Four of the five individuals on caseload were under the care of a CMHT with additional care provided by APL (referred 1 day prior to detention; detained Section 2); day resources team and EIT (detained Section 2); day resource team (Section 2); and forensics (informally admitted) respectively. The individual who was detained under Section 3 was on the caseload of the HTT 1 day prior to detention.
Framework analysis of decision on outcome of Mental Health Act assessment
Formal recording of the MHAA and related progress note entries were examined to determine the precipitating factors in the decision to detain under the MHA. The framework employed to analyse the data utilised information and operational/procedural categories to understand the decision-making process among the professionals conducting MHAAs. Four themes emerged from the data that revealed these factors: imminent risk; existing formal management arrangements; informal social care/management support arrangements; and behaviour. Each of these is considered below in relation to those who were subsequently detained under the MHA and informally admitted following MHAA.
Theme 1: imminent risk
The imminent risk associated with managing the care of an individual in the community was a major consideration in the decision to detain under the Mental Heath Act following formal assessment. As was the case when considering risk in the initial decision to detain under Section 136, risk was assessed according to risk to self (the individual) and risk to others, both of which are presented below.
As previously discussed, all detentions under Section 136 in this sample were perceived as being a risk to self by the attending officers. Further assessment of risk to self was undertaken within the MHAA to determine if the individual remained at risk. For example, it was noted above that risk to self at detention could be due to the location of the individual on apprehension (e.g. on a railway bridge). Although location was not a factor during assessment, the MHT would need to assess if the individual was likely to return to the risk location on discharge. Furthermore, for those individuals threatening suicide, the potential and imminency of this risk was reassessed. The following example is an extract from the mental health progress notes of an individual whose continued elevated potential risk to self was a factor in the decision of the MHT to detain under Section 2:
At the moment she is in a low period and has constant thoughts of wanting to end her life. Decision made to detain given significant risks to self (recent significant paracetamol overdose and being found on train tracks last night).
Progress notes
As presented above in relation to the FME’s decision to request a MHAA, intoxication was a factor that changed the perception of risk to self. In the following examples, individuals who were considered a suicide risk at detention did not express the intent to commit suicide when no longer under the influence of alcohol and therefore were no longer considered a risk. They were therefore able to receive appropriate care in the community without the need for detention:
acute suicidality under the influence of alcohol and social adversity, with underlying depression. suicidality now resolved in sobriety and ready to return home with appropriate support.
Progress notes
[service user] had recovered from her drinking yesterday and denied any further thoughts of suicide.
Progress notes
Consideration of risk to others contributed to almost half of police decisions to detain under Section 136. As with risk to self, risk to others was reassessed in the MHAA to assess the potential for continued risk and to determine the imminence of this risk and thereby the need for detention:
Discussed case with Dr. [name] Duty Con Psyh. [consultant psychiatrist] and Dr. [name] S.12 agreed she had a degree of capacity, but she may pose a risk to her child without back up care and support for her and [daughter], also with no medication to manage her mental health overnight would place her and child at risk. [service user] was placed under Section 2 of the M.H. act 83-07.
Progress notes
Furthermore, analysis showed that in some cases, a combination of risk to self and risk to others was explicitly stated as supporting the rationale for formal admission. In the example below, imminent risk to self and others coupled with lack of appropriate informal support to manage the individual’s behaviour was a factor in the decision to detain.
[service user] was admitted under the M.H. Act due to risk she pose to herself and other (son). She would be managed at home overnight if medication was available with the support of her ex-partner, but given that they are no safeguard her risk was too high to remain at home.
Progress notes
Conversely, the decision not to detain in the example below was based in part on the lack of risk posed by the individual either to himself or others:
no evidence of risk to self or others due to mental illness
Progress notes
Theme 2: formal management
Although all but one of the individuals detained following MHAA were on caseload at the time of detention, effective management due to being both known to services and under current care was not guaranteed following detention. Therefore, the MHAA included assessment of level of engagement with services and compliance with medication from historical records, the report of third parties and self-reports. Engagement and compliance were varied across cases and recorded as factors in the decision for formal admission. The following example is of an individual who was not detained, partly due to his expressed commitment to engage with short-term intensive support from the HTT:
He said he was happy to accept support from HTT in the short term and agreed to daily visits, he also agreed to use the telephone service if he was feeling suicidal, saying that he had found talking with us useful today. He said he did not want to go to hospital, but rather get on with his life. Given the guarantees we did not feel he was detainable; he also was very distressed about been locked in a cell, therefore forcing him to be in hospital would have proved counter theraputic.
Progress notes
In contrast, the following extract is from the notes of an individual who was detained under Section 2 following both multiple Section 136 detentions in the research window and observation of lack of engagement with services:
She has been supported by the HTT over the past couple of days but today has refused to engage.
Progress notes
Lack of engagement with services in the following example was coupled with lack of compliance in taking medication. In this case, both factors contributed to the decision to detain the individual under the MHA as it could not be guaranteed that community services could deliver the care and management required.
Had earlier refused to see the CMHT as he was convinced that he was going to die complained of chest pain. Has been refusing to take his meds consistently in the community.
Progress notes
Similarly, decision to detain in the example below was precipitated by both lack of service engagement and non-compliance with medication. The individual was offered informal admission to ensure compliance with medication that had affected his sleeping pattern. However, on indicating he would not engage with the voluntary service offered, detention under Section 2 of the MHA was viewed as the only course of action available to ensure he received the care and management required.
He has not been compliant with meds recently and has had very little sleep. Was offered an informal admission which he initially appeared to accept. However when I returned to the cell to go over this again with him and ascertain whether he had understood this he refused and given the concerns of assessors was detained under s2 [Section 2 of the Mental Health Act 1983;18 200719] MHA
Progress notes
Theme 3: informal management
The availability of informal support and management from family, friends and other carers was a further important factor in the decision to detain following MHAA. Every MHAA includes consultation with family or carers where applicable and appropriate, and evaluation of whether or not family and/or carers are willing to and capable of providing the required support. The availability of this type of support, or lack thereof, can impact on the decision to detain, as illustrated in the following two examples:
Has good supportive relationship with grandparents, a poor one with his mother, and says he has never seen his father
Progress notes
little support from family: [service user]’s nearest relative is her son [son]. He is currently away on holiday in [overseas] with his friend. [service user] have since spoke to him via his friend phone letting him know what her current situation is. In view of this and [service user] not able to remember contact details of her son’s friend I was unable to have a discussion with her NR [nearest relative].
Progress notes
It was also important to review regularly the ability of family member/carers to maintain support for their relatives suffering from mental health conditions. This ability may change as a result of the individual becoming more challenging or the personal circumstances of the family member/carer. The following example involves an individual who was detained under Section 136 twice in the research window; the extract relates to his first detention. An entry in the mental health progress notes shows how the individual’s mother, who cares for him, is finding managing his condition increasingly challenging and describes the support that she herself requires in order to effectively care for her son. On the second detention, due in part to the potential risk to his mother which prevented her from being able to manage him at home, the individual was detained under Section 2 of the MHA.
Mum agreed that [service user] could go there this evening but is finding it increasingly difficult to know how to manage [service user]. Mum has done lots of research on BPD [bipolar disorder] but is unclear how best to respond when [service user] in crises. She has not had a carers assessment and she agreed that she would find this useful. Mum has had her own counselling at the GP [general practitioner] and is due to cease this shortly, she would be interested in any support groups for carers. Mum said that part of the problem has been [service user]’s refusal for information to be disclosed to mum, agreed I would discuss this with her and ask that a carers assessment and support be officered to [service user]’s mum.
Mental health progress notes
Theme 4: behaviour
Behaviour that precipitated the decision to detain following MHAA, similar to that which drove the decision to request a MHAA by the FME, often centred around behaviour considered to indicate underlying delusional beliefs. In term of the MHAA, this behaviour was either directly observed by the professionals undertaking the assessment or was described by the individual themselves. For example:
Assessed by Dr[medical 1] and Dr[name] S12s [Section 12 of the Mental Health Act 1983;18 200719] and [name] AMHP. Presented as confused, thoughts being blocked and felt the cell was being bugged. Felt that his flat would have been ransacked whilst in custody and believed that this had been transmitted to him. He also felt that his computer will be being used and his phone but could not explain by who or why. Paused for long periods between answering questions and often appeared to lose concentration.
Progress notes
Additionally, consideration of mental state contributed to the decision-making process when individuals were unable to look beyond the present, with a bleak or limited outlook toward the future. The following extract from the formal recording of the MHAA in the mental health notes of an individual detained under Section 2 of the MHA showed that this feeling of hopelessness toward the future contributed to the assessment of risk and, therefore, to the need for detention:
[service user] very emotional at times, concerns that she had no sense of hope and could see no way forward. Given level of risk and recent high risk behaviour decision to detain for assessment.
Progress notes
Certain types of behaviour in the custody centre and during assessment also elevated the potential risk to self to such an extent as to warrant detention. The following extract from the formal record of the MHAA presents the rationale for the need to detain for further assessment under the MHA as in part attributable to this. Furthermore, in this case, health professionals took into account that the level of informal management in place was unable to meet the needs of the individual given the presenting behaviour:
Patient presented as mono-syllabic and totally uncooperative. Following interview whilst professionals were discussing options patient locked herself in the toilet and stuffed toilet paper in her mouth. Presented in a teenage tantrum manner. It was felt that admission was perhaps not clinically the right way to go but given her behaviours whilst in the suite and the fact that her father was unable to cope and unable to maintain her safety and she would consequently have nowhere to go there was no other option than to admit to hospital. As she would not go as an informal patient she was detained under S2 [Section 2 of the Mental Health Act, 1983;18 200719].
MH1
Lack of insight on the part of the individual was also taken into consideration in the decision to detain following assessment. Perceived lack of insight included denial of mental health condition or diagnosis and irrationality:
GP [general practitioner] diagnosed bipolar disorder but patient refuses to belief this is the case
Progress notes
[service user] was not clear about exactly why she had gone to the railways station. She said she was in the station toilets when the police detained her. She said she was not planning to throw herself in front of a train and pointed out that, at the railway station, the train would be travelling at low speeds or even stopped and then it would be difficult to throw oneself in front of the train there.
Progress notes
In comparison, the behaviour of individuals who were not detained was perceived quite differently by the MHT. As might be anticipated, these individuals displayed an absence of the behaviours that were viewed as being indicative of a mental health condition requiring assessment and potential treatment. Furthermore, they displayed insight:
No evidence of thought disorder, no delusions, no abnormal perceptions. Has insight and has accepted support.
Mental health core assessment
Evidence of good personal interaction, appropriate engagement with the questions in the assessment and the individual’s positive demeanour were associated with decisions not to detain following assessment:
[service user] presented as bright and friendly. He had good eye contact and did not present as depressed or anxious.
MH1
[service user] had stopped taking her prescribed medication. This may have contributed to her presentation of underlining irritability and elevation in mood. There were no obvious signs of [service user] being troubled by intrusive thoughts. She maintained good eye contact and although some of her answers were a little evasive in the main she did answer coherently. Reasonable eye contact and rapport.
Progress notes
As was the case with the FME decision to request a MHAA, the MHT also assessed any changes in behaviour during the assessment, including those that could be indicative of alcohol withdrawal rather than mental illness requiring detention under the MHA. Other changes in behaviour were also noted that enabled the team to differentiate between behaviour that indicated a condition requiring detention or that which could be treated in the community. In the following example, elevated mood of the individual on seeing her family indicated that the flattened affect with which she initially presented was not pervasive:
Appeared tearful at times, initially flat but becoming more spontaneous and smiled when her mother and boyfriend arrived.
Progress notes
Follow-up in the community following Mental Health Act assessment
Nineteen of the 25 individuals formally assessed under the MHA were not detained. Progress notes and the formal recording of the MHAA were examined to determine if there was any follow-up care or management of these individuals; this ranged from no plan by mental health services to enhancement of care plans. Five individuals were not provided with any follow-up, with three of these advised to contact their general practitioner (GP) (one was provided with a letter to support this). Four individuals were advised to continue with the support of their current care teams (including HTT and CMHT). For one of these individuals the MHT liaised with the current care team to ensure that the existing package of care was continuing. One further individual who was not on the caseload of mental health services, but was being supported by domestic violence (DV) services run by the police, was advised to remain engaged with these services following detention. Eight individuals were offered enhanced care following MHAA. Of those, five were not on the caseload of a MHT at the time of detention: of which three were referred to either a CMHT or HTT, one was referred to an alcohol specialist nurse and one was put in touch with CPN support. Of the three that were on the caseload of general secondary mental health services, two were to be followed up by their current care teams and one was to be provided with support with her current housing needs.
Post-detention actions by the police
Actions taken by the police to follow-up an individual at the point of disposal and afterwards were explored by looking at the final outcomes on detention logs and whether information about an incident had been entered into new or existing non-crime vulnerable adult records. In some cases, the police provided referrals and support in addition to that provided by the MHT listed above. This included transport home and between hospitals (n = 5), advice and directions as to how to return home (n = 1), advice regarding housing (n = 2), and making direct contact with services on behalf of the individual (n = 1). Finally, two individuals were offered referrals to external service, these being drug and alcohol services and a women’s rape and sexual abuse centre.
Recording of non-crime vulnerable MHA records by police would have been required for nine of the incidents as they occurred in October 2011 or later, from when a record of a Section 136 incident was required, including the outcome from the mental health services. However, in three cases, a record was not created.
In the four cases predating October 2011, entries were made in the pre-existing non-crime vulnerable adult records (n = 3) and information was recorded retrospectively in a record linked to a later event (n = 1).
Summary
There is a clear policy and local protocol that aims to support decision-making throughout the Section 136 decision-making process. However, the findings above show understanding and interpretation of protocol, as well as limitations regarding availability and utility of resource, impact on the successful interagency management of individuals through the detention process. Although police had knowledge of the mental health needs of the majority of individuals, there was minimal recording of information exchange, which could have the potential to enhance management at the time of detention. Furthermore, it is clear that in the sample under examination here, a minority (28%) of individuals formally assessed under the MHA were detained under the Act following assessment. However, almost half of those not detained were offered a form of enhanced care or management, for which a MHAA was not necessary but expedited access to this care. The findings suggest, therefore, that services should be in place to facilitate the timely access to care and support for individuals in crisis who are not detainable under the Act, thereby avoiding the trauma of detention under Section 136 and MHAA.
Case-linkage study: custody findings
Introduction
The aim of this element of the project was to explore the journeys of individuals within the case-linkage sample who experienced a custodial detention due to suspicion of an offence.
Sample characteristics
Fifty-two of the 80 service users who were included in the case-linkage study were arrested for a substantive offence in the year following their index police contact. They were examined for this research, accounting for 126 offences (mean = 2.4 offences, range 1–10 offences). Seventeen (32.7%) were female and 35 (67.3%) were male with a mean age of 33.6 years (range 18–67 years). Thirty individuals were recorded as single, seven were married or had a civil partner, one individual was divorced or in a civil partnership that had been dissolved, one was widowed or a surviving civil partner and 13 did not have a record of their marital status. Forty-five (86.5%) individuals lived on their own or in privately rented accommodation, five (9.6%) lived in a hostel or assisted living, one lived long term in a hospital setting and one lived care of an address (no further information was available). Fifty (96.2%) individuals were recorded as white British; in one case, the client refused to record their ethnicity and the remaining individual did not have a record. The majority were unemployed (n = 45, 86.5%); two were employed in elementary occupations (cleaner and waitress); one was in a professional occupation; one in an associate professional and technical occupation; one a process, plant and machine operative; one self-employed; and the remaining individual was retired.
Police contact
Arrests in the research window
Figure 11 provides the reason for each of the 126 arrests of the 52 individuals examined. It can be seen that the largest group is that regarding offences against people, followed by breach of warrants/orders and prison recalls [which accounted for 29 arrests (23.0%)] and public order offences [accounting for 26 arrests (20.6%)].
FIGURE 11.
Reason for arrest in the research window (n = 126). Numbers represent the number of arrests in each category.
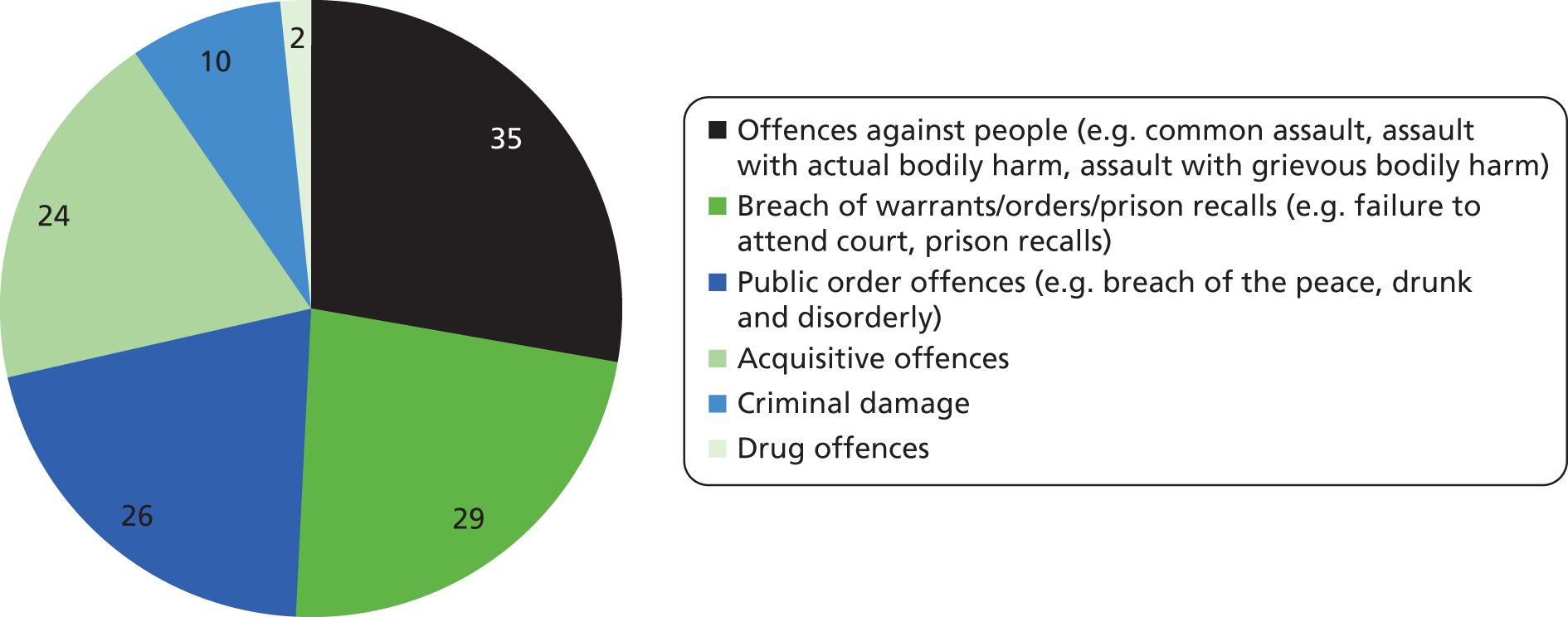
Contact in research window
Ten individuals who were arrested for a substantive offence in the research window were also detained under Section 136 of the MHA. Of these, five were recorded as both being detained under Section 136 and on the NHRR. Twelve individuals included in the custody analysis were also recorded on the NHRR.
Police warning flags
Examination was made of the CIS to determine the warning flags attached to individuals’ records that could influence decision-making at the time of detention. A full explanation of the PNC and local warning categories is given in Appendix 2. The frequency of cases with PNC warnings is presented in Figure 12. Thirty-three individuals had PNC warnings on their CIS records and 19 did not.
FIGURE 12.
Frequency of PNC warnings (n = 33 individuals).
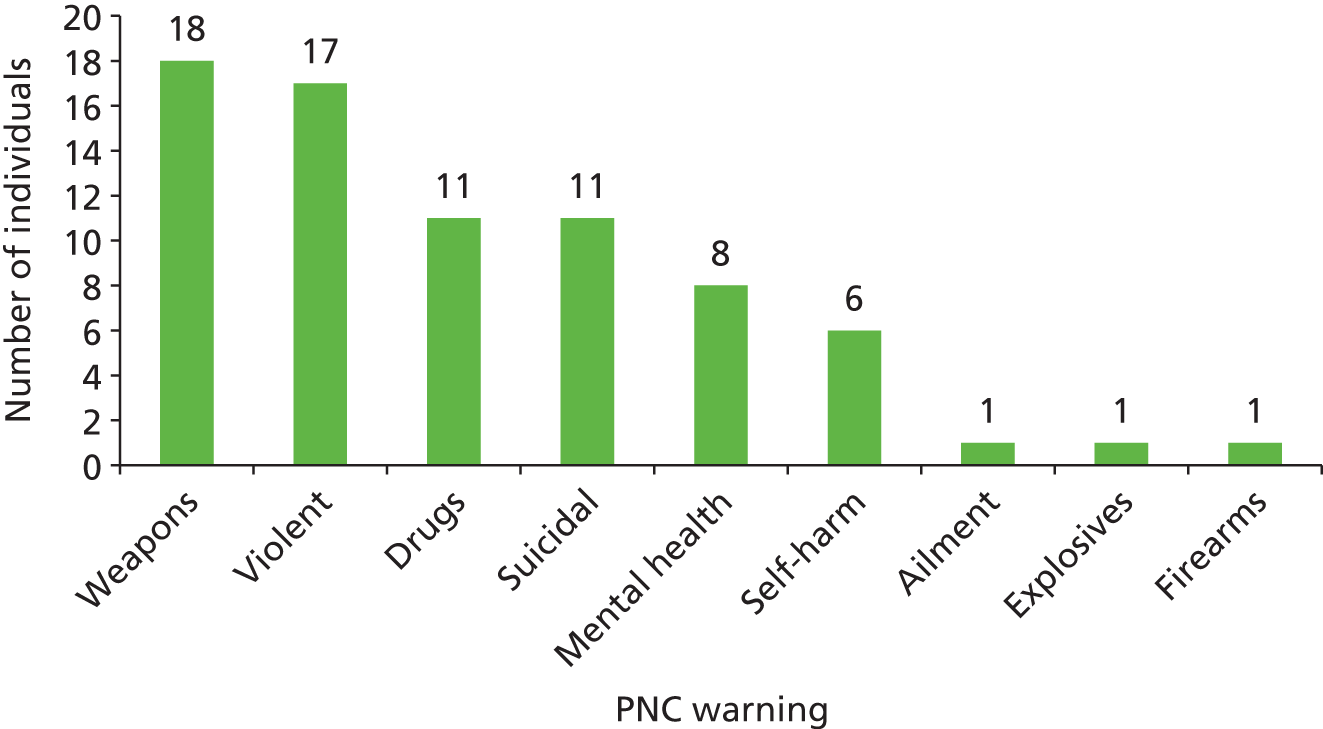
Three individuals were recorded in the research window as having their first custody detention for a substantive arrest (as recorded on custody risk assessments in NSPIS). Of these, one had a subsequent detention in the research window and the remaining two had a record on the NHRR. Seven individuals did not have a complete risk assessment on entering custody and so it was not known if they had previous detentions.
Twenty of the 52 individuals included in the sample had a local warning flag on their record, 10 with one local warning, and 10 with up to three local warnings on their record (Figure 13).
FIGURE 13.
Number of individuals with local warnings (n = 20). a, Penalty notices for disorders; b, individual has been involved in (though not necessarily convicted of) an offence of a sexual nature; c, alcohol referral scheme; d, the individual has entered into an ASB contract with the police; e, individuals who have alternate identities or other names they use.
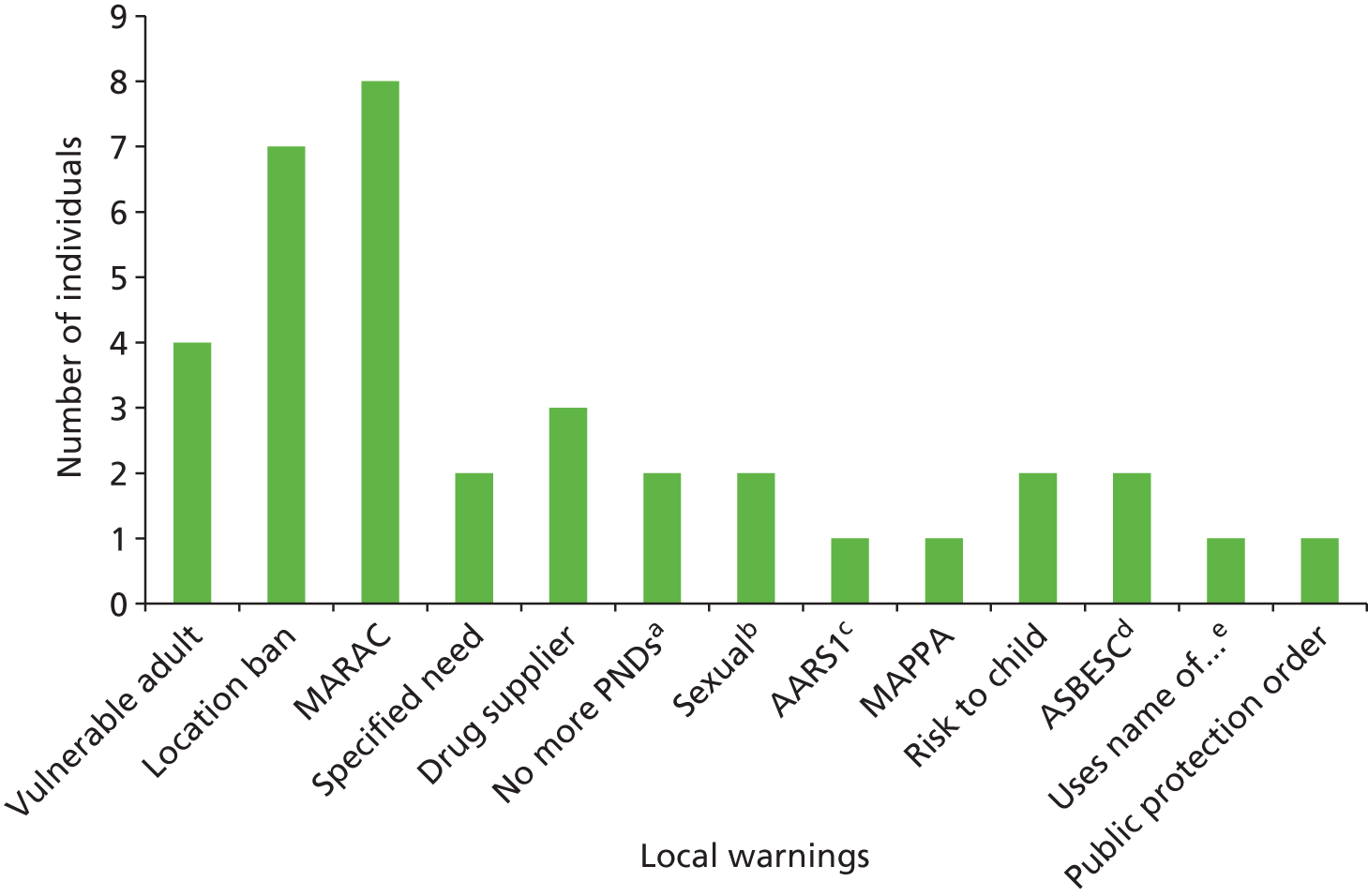
Further examination was made of the records of those individuals with a PNC mental health warning. As presented (see Figure 12), eight individuals had a PNC warning for mental health; for two of these individuals, this was the sole warning on their record. Table 9 presents the further attributed warnings for the remaining six individuals with a mental health marker. It can be seen that with the exception of case one below, all cases also have a suicide and/or self-harm warning within their record.
| Case | Warning 1 | Warning 2 | Warning 3 |
|---|---|---|---|
| 1 | Weapons | ||
| 2 | Weapons | Suicidal | |
| 3 | Ailment | Self-harm | |
| 4 | Suicidal | Violent | Weapons |
| 5 | Violent | Weapons | Self-harm |
| 6 | Suicidal | Violent | Weapons |
Table 10 presents the warnings attributed to the remaining 25 individuals who did not have a mental health marker. Of these, 11 had warnings on their records, which could be perceived as indicative of mental health issues (i.e. suicidal or self-harm). Seven of these individuals had a PNC warning for suicide, three for self-harm and one individual had warnings for both suicide and self-harm.
| Number of cases | Warning 1 | Warning 2 | Warning 3 | Warning 4 |
|---|---|---|---|---|
| 2 | Suicidal | |||
| 2 | Self-harm | |||
| 1 | Violent | |||
| 2 | Drugs | |||
| 2 | Weapons | |||
| 1 | Suicidal | Self-harm | ||
| 1 | Suicidal | Weapons | ||
| 1 | Suicidal | Violent | ||
| 2 | Suicidal | Violent | Weapons | |
| 1 | Suicidal | Violent | Drugs | |
| 1 | Self-harm | Violent | Weapons | Drugs |
| 1 | Violent | Weapons | ||
| 4 | Violent | Weapons | Drugs | |
| 1 | Violent | Firearms | Explosives | |
| 3 | Weapons | Drugs |
Mental health contact
Individuals’ contact with mental health services at the time of arrest was examined by identifying first if they were on the caseload of a MHT, and second which team or teams were currently caring for them. This information is useful in determining if being on the caseload of a MHT is a precipitating factor in the decision to instigate information exchange while in custody.
At the time of arrest, 55 of the 126 (43.7%) contacts were related to an individual who was on the caseload of a MHT or MHTs. Forty-six contacts were related to individuals who were on the caseload of a single MHT at the time of arrest; this comprised 38 on the caseload of secondary mental health services, one under a team within the acute mental health problem management category, four in general LD services and three in offender specific services. Nine contacts were related to an individual on the caseload of general secondary mental health services and one additional team: electroconvulsive therapy (n = 1); offender-specific services (n = 3); acute mental health problem management teams (n = 2); specialist teams (n = 2) and EITs (n = 1). Furthermore, of those cases related to an individual on the caseload of general secondary mental health services, seven were on the caseload of two teams and two contacts were on the caseload of three teams within this category.
Custody decision framework
Akin to the Section 136 framework, four main decision points were identified through review of policy, consultation with both professionals and service users and familiarisation with the data. The data familiarisation process was undertaken within the framework of informational themes (including individual factors and context of the call) and informal operational/procedural themes (including information sharing, risk management and care management). Through this process, the decisions taken by and between services to manage and care for these individuals emerged iteratively from the data. A number of subdecisions within each of the four main decision points were also identified:
-
decision to detain and conduct of arrest
-
– decision to instigate information exchange
-
– decision to detain
-
– decision to use restraints
-
– decision to authorise tasers/deployed armed response officers
-
-
detention management decisions
-
– decision to instigate information exchange
-
– decision to request an AA
-
– decision to extend the PACE clock
-
-
decision to conduct a MHAA
-
decision regarding the outcome of the MHAA and custody disposal.
Decision 1: decision to detain and conduct of arrest
Operational Information System logs were examined to identify the origin of the caller/alert to the incident to which response officers were called and culminated in an arrest. Figure 14 presents the proportion of offences that were alerted by identified categories of caller.
FIGURE 14.
Distribution of type of caller (n = 126).
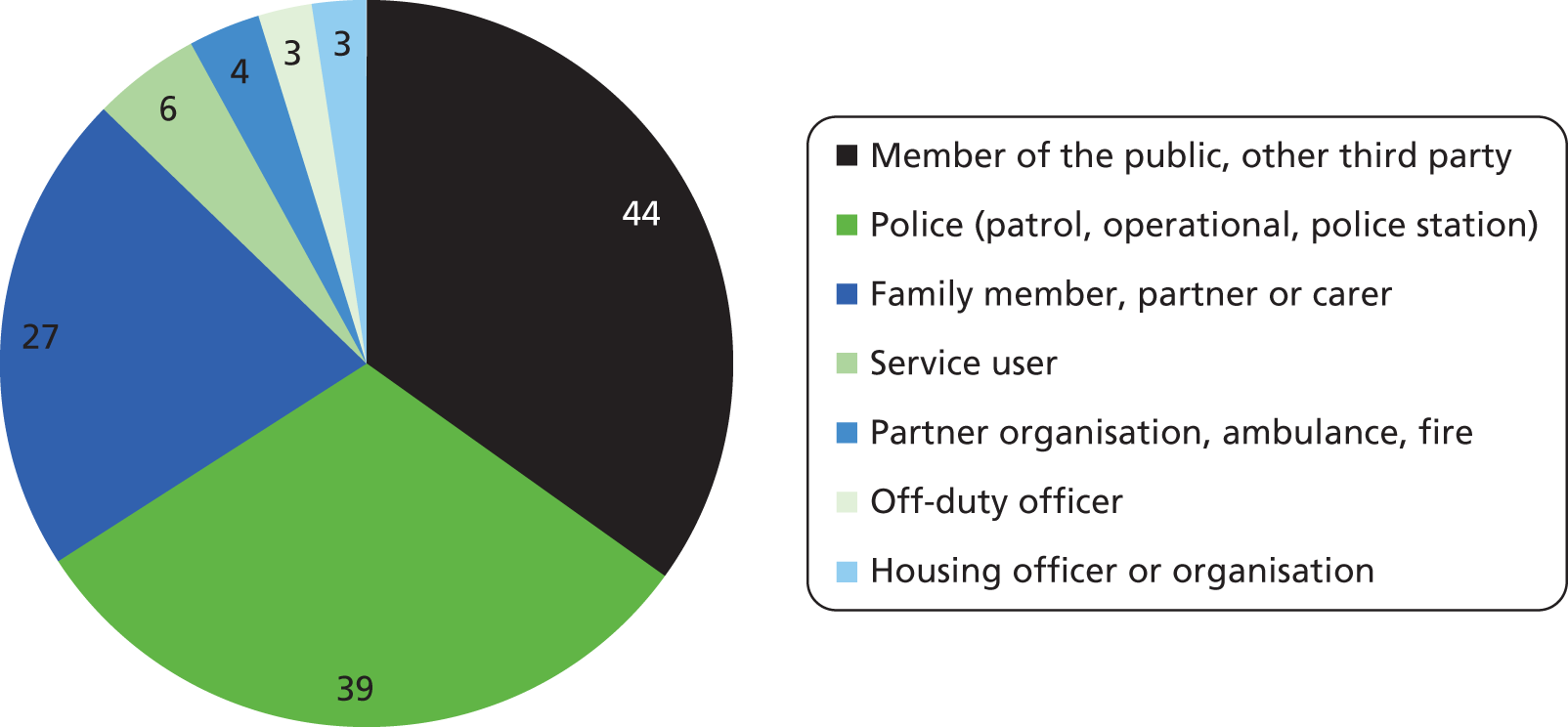
Response officers were requested to attend 81 of the 126 (64.3%) incidents via the police control room (therefore having an OIS log). Level of response to the call was recorded in all 81 detentions. Of those recorded, 49 (60.5%) were assigned immediate response (within 20 minutes of receipt of call), 27 a prompt response (within 1 hour of receipt of call) and five a routine response (within 48 hours of receipt of call). Response level was compared for the reason for arrest (cited in custody front sheets from NSPIS) (Table 11). The majority of immediate responses were linked to offences against people and public order offences (which relates to potential risk to others). Those cases where the level of response was not recorded relate to incidents which were attended but the call was not taken by the control room, therefore representing responses made directly by officers to follow-up an offence, breaches and where the officers were on patrol and witnessed an incident.
| Type of offence | OIS log not available | Routine | Prompt | Immediate |
|---|---|---|---|---|
| Offences against people | 6 | 0 | 10 | 19 |
| Public order offences | 6 | 0 | 7 | 13 |
| Theft offences | 12 | 1 | 4 | 7 |
| Breach of warrants/orders/prison recalls | 16 | 4 | 4 | 5 |
| Criminal damage | 3 | 0 | 2 | 5 |
| Sexual offences | 0 | 0 | 0 | 0 |
| Drug offences | 2 | 0 | 0 | 0 |
Framework analysis of decision to detain and conduct of arrest
Framework analysis was undertaken of all the depersonalised documentation related to custody detention. Three themes emerged from the analysis of decision 1:
-
decision to instigate information exchange
-
decision to use restraints in the conduct of arrest
-
decision to authorise tasers.
Theme 1: decision to instigate information exchange
As discussed, although police may have knowledge of mental health issues of individuals, this knowledge is often limited to PNC warnings, their own past experience of the individual and information conveyed by operators. It is useful to examine the rationales for information exchange between services in order to understand the nature and degree of success of communication and the impact that this has on the care/management of the individual and their disposal. Contact was made with MHTs associated with individuals prior to five arrests. For example, the following notes were recorded on OIS logs pertaining to contact made with the individual’s CPN:
just taken the call from [CPN: manager of CMHT] she has been speaking to SU [service user] and can clearly hear the sound of hissing gas in the background of the call.
OIS log
Although the information exchange in this case did not directly aid the decision to detain, it did open up the lines of communication between services and supported the joint management of the individual through his detention and subsequently.
Furthermore, in one case, contact from the housing provider of the individual to the police and to mental health services provided information that both alerted the police to the offence and provided information required by mental health services to aid their decision to conduct a MHAA:
[service user] did not attend clinic today. Informed by [housing professional] at 4.30pm that they have had to alert the police because he is armed with a machete as well as a firearm (air rifle/pistol). Endorsed their decision to call the police. Informed that I would alert HTT and duty consultant but that the police needed to be informed that a psychiatric assessment needed to be conducted under safe circumstances. HTT alerted. Discussed with duty consultant and background details given.
Progress notes
Information exchange also provided police with reassurance as to the management of the individual. For example, in the case below, direct contact with the support worker provided information as to the mental state of the individual to be detained and the level of need in terms of mental health input required on detention:
[NAME] who is support worker says she isn’t coming round, she is quite happy that [service user] and [service user friend] remain there are on their own and capable to look after themselves. She considered it attention seeking as [service user] is new to the house and has taken the attention away from [service user friend]. Support worker’s number has been given to [service user] who says she is happy to speak to them at any point during the night but won’t be attending
OIS log
The decision to instigate information exchange between services at the point of despatch of officers to the scene was guided by prior knowledge of mental health issues associated with the person concerned. This knowledge stemmed from either the experience of the police officers themselves and/or the operators relaying information to officers from their own direct experience of co-ordinating previous incidents and/or from their examination of associated police records. Examination of the records in relation to these precipitating factors is provided below.
Operational Information System records were examined to determine the degree of police knowledge of the individual on apprehension/arrest. Thirteen individuals were known to the response officers dispatched to the incident. Longstanding knowledge of the individual was indicated in six logs ranging from understanding their behaviour (and potential impact on contact): ‘male known to u can be a bit of a handful’; ‘please be mindful of male’; ‘walks as though he is drunk’ to acknowledgement of their knowledge of the individual: ‘units aware of male’; ‘have dealt with this female before’, ‘male is subject to a tag at this time’. Response officer awareness of mental health issues was recorded in two cases reflecting prior knowledge and recent experience of police contact with the individual: ‘female was 136 in [area] other day she mentioned about killing herself‘; ‘officers were called to this address only yesterday which resulted in arrest of [service user wife] there is a longstanding history of mental health and domestic violence issues between [service user and service user wife]’. Finally, knowledge of the individual also originated from very recent contact with the individual in five cases: ‘taken in earlier for BoP’, ‘earlier attendance at address’, ‘third time we have dealt with her today’, ‘aware of the male attended last night also’, ‘identified from earlier incident’.
Operators relayed information gleaned from either their own knowledge of the individual/incident (due to recent incidents in which they had a co-ordinating role), information collected from examination of OIS logs or information provided by the RP, in some cases in real time. One hundred and three of the detentions examined here had an OIS log related to the incident immediately prior to and at the time of detention. In one example, the operators examined the non-crime vulnerable adult record on CIS, which had a direct impact on the officers’ decision to detain the individual. In the case of two examples, operators were able to provide information regarding mental health issues or history (e.g. recent Section 136 detention, history of suicide attempts and past methods thereof) to aid officers in making decisions regarding either detention itself and/or management of the individual. Other examples of information provision by operators included information regarding circumstances of recent incidents (n = 2), incidents specific to DV (n = 2), whether the individual was currently under warrant or wanted for other offences (n = 2), current reported whereabouts of the individual (n = 1), whereabouts of other APs involved in the crime (n = 1), conversation with the individual (n = 1) and finally, one report of the breadth of information/logs available regarding the individual under investigation.
Theme 2: decision to use restraints in the conduct of arrest
The Independent Commission on Mental Health and Policing’s recent (2013)42 report highlighted the disproportionate use of restraint with regard to the cases examined. Due to the secondary data on which the case-linkage study relies, factors covered in the report such as length of time in restraints could not be examined in this research. However, recorded rationales for restraint were identified and coded through examination of the OIS logs. Restraints in the form of handcuffs were used in 46% of arrests (n = 58). Thirty seven (63.8%) of these involved an individual recorded as being under the influence of alcohol/drugs, which could be a contributory factor in the decision to use restraints due to the potential for unpredictable behaviour. There is no regulation for officers to record a rationale for their decision to use restraints during detention. However, specific rationales were available for 11 of the 58 (19%) detentions in which restraints were used and fell within three themes. Each theme is noted below with example quotations from OIS logs:
i. Use of restraints for the individual’s own safety (n = 5).
lady in cuffs for her own safety
female did try to out a ligature around neck – string from clothing (in van)
No injuries or threats made to officers at scene. Captor deployed to stop subject injuring herself.
male is banging his head on the van and thrashing around.
male is banging his head against the cage
ii. Use of restraints to maintain the safety of others (n = 4).
male says if I take the handcuffs off him he is going to smash my face in and everyone around him.
DP [detained person] asked to wait outside for officers but refused myself and PS [police sergeant] attempted to escort DP outside he became violently aggressive and was take to the floor where he proceeded to spit in my face – arrested placed in cuffs and escorted to cell.
would advise Taser. Units to effect arrest as male can be unpredictable and known to use drugs. [incident where restraint was used and Taser also authorised]
Female wasn’t pleased to see us now under arrest for breach of the peace and was quite violent on arrest.
The rationale provided for the use of restraints for one individual was due to both safety of the individual herself and others: ‘has tried to strangle herself in the back of a van with a sock’; ‘DP [detained person] in handcuffs as attacked police at the scene of arrest’.
iii. Use of restraints to aid the conduct of the detention (n = 1).
Finally, one rationale was based on the need to conduct the arrest, as the service user was uncooperative:
[service user] is in the house refusing to come out so have to put the door in.
Although the records examined show that restraints were used in almost half of the arrests examined here, due to the lack of rationales for the majority of these cases and the lack of measure of effectiveness in meeting the identified rationales, it is not possible to conclude as to whether or not the use of restraints in this sample was disproportionate.
Theme 3: decision to authorise tasers
The Metropolitan Police Service survey ‘Mental Health and the Police’, cited in the Independent commission on Mental Health and Policing’s report,42 reported that 34% of taser deployments were linked to individuals or incidents related to mental health. The Commission further reported that in the cases that they examined, officers were unable to comment on the efficacy of taser deployment in the management of detention. In the current research, tasers were authorised but not deployed during the conduct of five arrests and armed response officers were deployed to a single further incident. In order to understand the precipitating factors for the decision to deploy, OIS was examined to determine the rationale for authorisation. For all incidents, including that to which firearms officers were deployed, the rationale was based on the potential or actual possession of a weapon by the individual. With regard to the taser authorised incidents, potential or actual possession of knives were the basis of the rationale in the case of three incidents:
knife mentioned
threatened mother with knife
knife – male had a knife in his back pocket and showed them the knife but did not take it out of his pocket they only saw the handle – black, about a 3 inch blade – poss. a veg knife.
In addition, a general threat of possession/use of weapons was the rationale for the remaining two incidents:
male is stood on the top of his car and has dented his roof. RP told him to get off and he said no! he’s possibly in possession of a weapon also but caller can’t see what it is.
male armed himself with an iron bar, mother will not let us in.
The clear rationale for deployment of firearms officers to the scene of the final incident was potential possession of a crossbow:
**note PNC marker – possible possession Crossbow** asks if [housing organisation name] have any restrictions of holding these items in his room . . . having these items in his room is not an offence as such . . . to clarify last their policy is that ‘he cannot have weapons on the property’
As noted, although tasers and armed response were authorised for the above incidents, none were deployed and the decisions not to deploy was not available for scrutiny in the secondary data analysed for this research, as these were not recorded.
Decision 2: detention management decisions
Lord Bradley’s report6 recommended access to liaison and diversion services for individuals with mental health needs; this was echoed recently by the Independent Commission on Police and Mental Health report. 42 The latter report further recommended access to mental health nurses in all custody suites. At the time the data used for the purpose of the current research was recorded, there was no custody liaison and diversion service or specialist mental health nurse provision in the research site. Therefore, access to mental health services was via referral by the HCP, usually a general nurse in the custody centre and/or the force medical examiner. A custody liaison and diversion service was implemented in the research site in the month following the end of the research window and is included as a model of enhanced care in the health economics section of the report (see Health economics component).
Framework analysis of decisions concerning detention management
Three themes emerged relating to detention management decisions:
-
decision to instigate information exchange between services
-
decision to request an AA
-
decision to authorise PACE clock extensions.
Theme 1: decision to instigate information exchange between services
Records were examined to determine both the level of mental health service involvement and communication with MHTs during detention. As highlighted above, examination of current caseload at the time of arrest was made in order to identify if current access to mental health services was a precipitating factor in the decision to instigate information exchange. Fifty-five related to an individual on caseload at the time of detention (Figure 15). For 25 (45%) of these detentions, there was communication between police and MHTs during detention (Table 12). Regarding the 71 detentions related to an individual not on caseload at the time of detention, there were only eight (11%) records of communication between police and MHTs. Therefore, there was a higher proportion of information exchange between services for those cases on caseload at the time of arrest than for those not on caseload, suggesting caseload status as a precipitating factor underpinning this decision. Although not clear from the records available, such communication may be facilitated by the service user or family/friends present at the incident, informing the police of the caseload status of the individual. Mental health progress notes, custody medical forms, and detention logs were examined to determine the origin of initial contact, the rationale for contact, and any information exchange due to the call.
FIGURE 15.
Degree of communication between police and MHT depending on caseload status of individual.
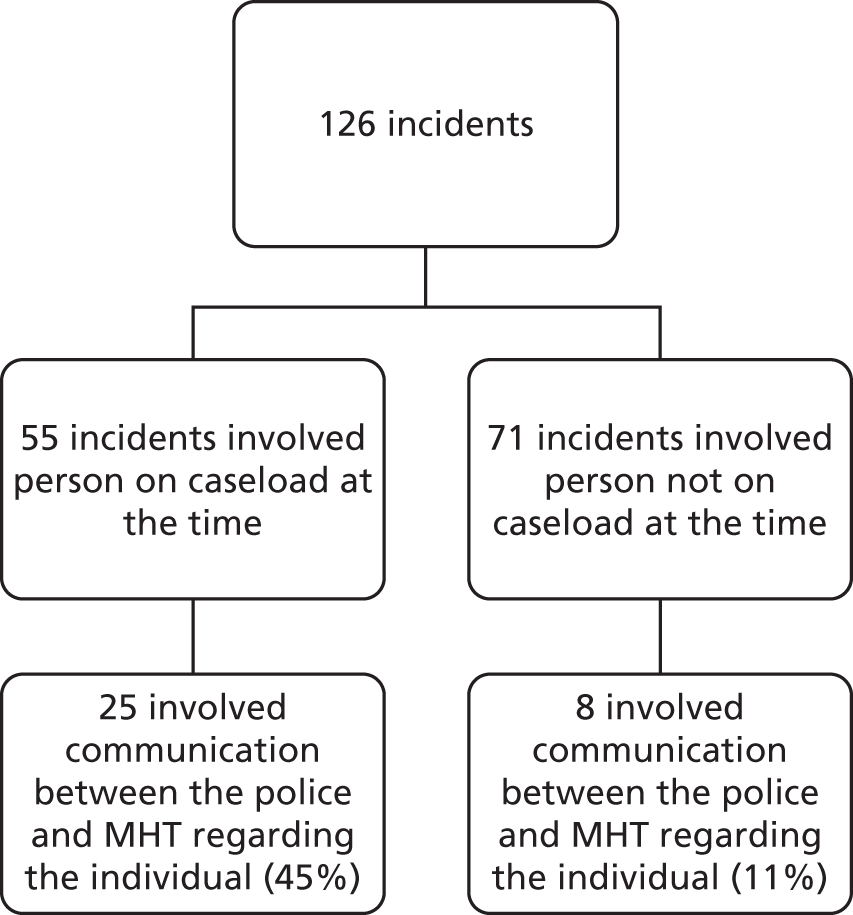
| Profession instigating information exchange | Number of individuals |
|---|---|
| Police | 10 |
| FME | 6 |
| HCP | 4 |
| FME and police | 2 |
| MHT | 1 |
| AA | 2 |
Ten of the 25 (40%) recorded communications for those contacts on caseload were directly between police officers and the MHT. Four of these contacts involved provision of information regarding the arrest of the individual. Five included requests for an AA, including highlighting the need for an AA for court and two included a request for MHAA. In one instance, the detained individual requested that his CPN be made aware of the detention. In terms of the care and management of the individual, one contact involved a request for a CPN to provide support for the individual, one consisted of a request for information as to the nature of the current support received by the individual and one requested information as to the possible support that could be provided by the individual’s supported housing on their release. In two cases, information exchange between police and mental health services culminated in a recorded joint decision. In one of these cases, a joint decision regarding support in custody was made between services because of this communication due to the individual having a general anaesthetic for electroconvulsive therapy in the last 24 hours. In the second case, the information was to inform the FME’s assessment which would be fed back to the MHT with a plan of management for the individual.
Six (24%) of the 25 contacts on caseload where there was communication with mental health services during detention were directly between the FME and mental health services. Two of these were recorded solely as direct requests to conduct a MHAA. In the third case, a joint decision was made between the FME and MHT not to conduct a MHAA and in a fourth, an assessment other than a formal MHAA was requested by the FME, which resulted in the individual being referred to a CMHT. The final two examples were requests by the FME, first for information regarding if the individual was fit to release and second, to request that the individual’s care co-ordinator contact the custody centre following the individual’s return from accident and emergency (A&E).
Four of the 25 contacts on caseload where there was communication between services during detention were between the HCP and MHTs. In all four of these cases, records showed provision of information concerning the details of arrest with one individual explicitly requesting that the MHT were made aware of the detention through the HCP. These communications also involved requests for information to facilitate management of the individual in custody. This included requesting (and questioning) the level of support currently being received by the individual, requesting additional support for the individual while in custody, requesting general information about the individual and asking for corroboration of information provided by the individual with regard to previous section and future mental health service appointments.
In two cases both the police and FME contacted mental health services, both of which involved requests for MHAAs, provision of information regarding the detention and in one case, the raising of police concerns about releasing the detained individual due to threats made to harm others.
In one case, the MHT had called the police prior to detention to report the service user as a missing person, which had facilitated continued communication through to ensuring support in court from a court liaison nurse. Finally, in two cases there was recorded communication between the AA and the mental health services. In one instance, this communication also involved the HCP and related to an enquiry regarding the individual’s medication following release from custody. Communication facilitated arrangements to be made to ensure that the prescription required contained the correct information to meet the needs of the service user. In the other example of AA–MHT communication, the AA’s communication with a social worker led to a referral for the individual to social care services.
Six of the eight communications relating to contacts that were not on caseload at the time of arrest were directly between police officers and mental health services (Table 13). Of these, five were solely to request an AA. The remaining two examples were communications between the MHT and HCP and the FME and police respectively. Rationales for communication included the provision of information regarding the arrest, information requested as to the mental health condition of the individual and alerting the MHTs that requests for MHAAs may be required.
| Profession instigating information exchange | Number of individuals |
|---|---|
| Police | 6 |
| HCP | 1 |
| Police and FME | 1 |
Theme 2: decision to request an appropriate adult
The decision to request an AA for an individual in custody lies with the custody sergeant. According to PACE, ‘When the custody officer has any doubt about the mental state or capacity of a detainee, that detainee should be treated as mentally vulnerable and an AA called’. Forty-two requests for an AA were recorded in the detention log and/or the custody medical form, of which 30 had an explicit rationale recorded for the request. Table 14 shows the proportion of rationales provided under each category. Mental health was either the sole or a contributory precipitating factor in the rationale for requesting an AA in 19 cases, with a specific diagnosis of a mental health condition being a factor forming the next largest group (n = 11, with three cases also explicitly recording a statement of concern regarding mental health). Diagnoses included schizophrenia, bipolar disorder, borderline personality disorder and psychosis. Rationales identified as implicit within the records by the researchers concerning mental health were recorded due to one detention involving a MHAA where attending mental health practitioners acted as AAs and the other detention involving an FME assessment for a MHAA during the course of the detention.
| Rationale | Number of contacts |
|---|---|
| Mental health sole rationale (stated) | 9 |
| Mental health (implicit) | 2 |
| Diagnosis | 11 (3 with statement regarding general mental health) |
| Past AA attendance | 3 (2 with mental health stated) |
| Named mental health professional and mental health stated | 3 |
| Mental capacity | 2 (same individual, two different dates) |
Detention logs, custody medical forms and mental health progress notes were examined to determine the rationale for requesting an AA. Eighty-six (68.9%) cases did not have AA support during detention. Thirty-one (24.6%) detentions had a record of attendance of an AA, and the remaining 11 (7.1%) had no record of AA attendance although attendance had been requested. This did not necessarily highlight that an AA had not attended, but may have reflected lack of explicit recording of attendance. Of the 31 requests that culminated in AA attendance, 19 were made by the HCP and the remaining 12 were made by the detention officers alone.
Theme 3: decision to authorise Police and Criminal Evidence Act 1984 clock extensions
The ‘PACE clock’ refers to the 24 hours in which police are able to detain and charge individuals following arrest. The PACE43 requires that a detained person (DP) has the validity for detention regularly reviewed. An individual can be released or charged at any time while detained. On arrest, a person should be taken directly to a police station and custody of that individual should be handed over to an officer of at least the rank of sergeant (constable only in exceptional circumstances). The role of the receiving officer, referred to as the custody officer is to determine that the arrest was lawful and that there is sufficient evidence to charge that person for the offence for which they have been arrested. If there is insufficient evidence to charge, the custody officer may authorise the detention of that person in order to secure and obtain evidence or to obtain evidence by questioning. As soon as there is sufficient evidence to charge, the person must be charged and released either with or without bail.
Reviews are made at regular interviews throughout the detention process. The role of the reviewing officer is to ensure there are sufficient grounds for further detention and that the investigation into the offence is taking place expeditiously. The time of the first detention is known as the ‘relevant time’. Approximately 6 hours after the relevant time, an officer of at least the rank of inspector must review the reasons for detention and, if appropriate, authorise further detention for the same reasons as above. Following this, 9 hours after the first review (or 15 hours after the relevant time, whichever is the sooner), a further review must be conducted by an inspector or above and, if required, further detention can be authorised.
After 24 hours following the arrest, the DP must either be charged and released with or without bail or released from custody unless a superintendent authorises detention for up to a further 12 hours. This authorisation can only take place following the second inspector’s review. A superintendent’s extension is rare and usually only considered for a serious offence. Following this, and only in extreme cases, a further extension of detention can be obtained from a magistrate’s court for up to a total of 72 hours.
Examining detentions within this sample, the mean time spent in custody was 9.2 hours (range = 0.25–27.00 hours). According to PACE, detentions in custody should not exceed 24 hours without charge. Therefore, the rationales to extend the time in custody over the 24 hours, and the total time held, in the case of four detentions were examined here (Table 15). One of these detentions (27 hours in custody) was a failure to answer police bail, which is not subject to PACE and, therefore, is not included in the findings below (see Table 15). Mental health needs and the provision and arrangement of assessment supported the rationales associated with two of the remaining three PACE clock extensions. Although it is ultimately a police decision to review and extend the clock in accordance with PACE, this can be due to delays that are not under the control of the police, as was the situation in the final case examined. The following extract records the rationale for an extension due to a delay in the arrival of the team to conduct a MHAA:
the grounds are DP has been in custody on sus [suspected] criminal damage and has been awaiting mental Health assessment before he can be spoken to with regard to allegations. This is just commencing and as such, he will not have had the allegation put to him within the 24 hour period. Requests made for review of his detentions and a further 4 hours to allow for interview and any further enquiries to take place I authorise further detention of SU [service user] without charge until 20:00
Detention log
| Case | Hours in custody | Reason for arrest | Rationale for extension | Disposal |
|---|---|---|---|---|
| 1 | 26.0 | Offences against people | Reasonable grounds to believe that it is necessary in order to obtain a charging decision | Charged and detained for court |
| 2 | 25.5 | Criminal damage | Custody staff advise concerns for mental health – doctor at location to assess; reasonable grounds to obtain charging decision, preserve evidence, secure evidence | NFA |
| 3 | 26.0 | Public order offence | MHAA being arranged. Necessary to detain for individual’s own protection | Charged and detained for court |
Decision 3: decision to request a Mental Health Act assessment
The decision to request a MHAA in custody lies with the FME. Seven (5.6%) detentions involved a MHAA in custody. All MHAAs were recorded by both agencies (i.e. in the Police detention logs/medical forms and mental health MHAA forms/progress notes). All of these records were examined to determine the decision-making process for each MHAA request/decision to conduct an assessment. As presented above, following data familiarisation, the coding framework applied in the Section 136 analysis was found to be relevant to these data. Three themes emerged from the data related to the request for MHAAs following custody arrest that also emerged from the Section 136 analysis, these being detention circumstance, presenting situation, and resource/availability. An additional theme that did not emerge from the Section 136 analysis was identified in the custody analysis, this being the provision of a specific rationale for requesting a MHAA.
Framework analysis of decision to request a Mental Health Act assessment
Three themes emerged concerning the decision to request a MHAA:
-
detention circumstance
-
presenting situation
-
resource/availability.
Theme 1: detention circumstance
Analysis of the circumstance of the detention showed that assessment of risk to self and others was an important factor in the decision to conduct a MHAA and mirrors the precipitating factors that underpinned the decision to detain the individual. Risk to others was a factor in the rationales for all seven MHAAs. In one case, the need for a MHAA due to threatening behaviour constituted the main rationale for the initial detention.
Informed by [housing professional] at 4:30 pm that they have had to alert the police because he is armed with a machete as well as a firearm (air rifle/pistol) Endorsed their decision to call the police.Informed that I would alert HTT and duty consultant but that the police needed to be informed that a psychiatric assessment needed to be conducted under safe circumstances. If patient not admitted or not taken into custody I will attempt an urgent assessment next week to evaluate risk to others in light of today’s information
Progress notes
P/c [phone call] from [service user]s mum prior to midnight, she had called the police earlier today and they had agreed to take her to a women’s refuge for her safety . . . she was then made aware that they had attended her home and removed [service user] for common assault, he had pushed her across the landing earlier . . .
Progress notes
Risk to self was evident in the rationales for four of the seven requests for MHAAs. All of these cases involved DSH at the time or immediately prior to detention. In the examples below, the need for a MHAA again links back to the original rationale for the detention:
PC [police constable] from police to [professional]. they have detained her on a SCT 136 [section 136; there was a misunderstanding about the detention which was for a Breach of the Peace] after been called by her mother, she absconded when they arrived and was found cutting herself; taken back to mother’s where she resumed cutting herself and had to be handcuffed, paramedics attended to the cuts. [Professional] liaised with the ward who felt she was not appropriate to be supported in 136 suite, so will be taken to custody.
Progress notes
DP has attended hospital in early hours for attention to cut to left wrist/arm (not assessed as DP refused) also for MHA. DP became too aggressive & was bought to custody.
Custody medical form
Theme 2: presenting situation
The presenting situation in custody also supported the rationale to request a MHAA. Regular checks are made on detained individuals, which include monitoring of behaviour to ensure that assessments by the HCP and FME are made as appropriate. Behaviour recorded by the attending officer, detention officer, reviewing officer or HCP influenced the decision to conduct a MHAA and the outcome of that assessment. A range of behaviour recorded in the detention logs, custody medical forms and mental health progress notes emerged as underpinning the rationale to request a MHAA.
Lack of co-operation with officers or medical staff was noted in two of the seven cases in which a MHAA was requested. In the following example, information conveyed by the HCP to the MHT detailed the difficulty in appropriately assessing the individual due to uncooperative behaviour:
[name] said that he was now settled and been sleeping since 23.00, he said [service user] had been uncooperative, refusing to speak to custody nurse, [name] had yet to see him being currently at [place name].
Progress notes
Perceptions of behaviour apparently indicative of mental health issues also contributed to the rationale for MHAA requests. Assessment of this behaviour following direct observation was evident in the rationales for five of the seven MHAAs and included behaviours perceived as reflecting paranoia and auditory hallucinations:
Some paranoid ideas and bizarre statements expressed in patient known to drugs team who has been described by them as psychotic and who has been referred to CMHT
Progress notes
P/C [phone call] from dr. [name] at [custody]. [service user] presenting much the same as 2 weeks ago but with superficial cuts to arms. States she is hearing voices.
Progress notes
He is presenting as paranoid, suspicious
Progress notes
DP is presenting with paranoia, odd behaviour, agitation, pressure of speech.
Custody medical form
Monitoring of detained individuals enabled any change or continuation in behaviour to be assessed and recorded. Three of the individuals for whom a MHAA was requested and conducted presented with suicidal ideation on detention. The persistence of this ideation was an influential precipitating factor in the request for a MHAA, particularly where this persisted when the individual was no longer under the influence of alcohol:
FME continued to request MHAA due to suicidal ideas.
Custody medical form
He is now not under the influence of alcohol. [service user] is now stating that he intends to swim out to sea and drown himself once released.
Custody medical form
Further persistent behaviour that contributed to the rationale to conduct a MHAA included that which indicated a risk to others. In the following example, the continuation of threatening behaviour toward others was recorded in the custody medical form:
DP seen in cell as volatile & making threats to harm others. DP is visibly agitated & angry, no evidence to suggest alcohol intake & drug use denied. Vital signs normal.
Custody medical form
Finally, the individual’s presenting situation could have a direct impact on the resource allocation and timing of the MHAA. The data show that the delay in despatching the MHT to conduct a MHAA could be due to acting in the individual’s best interests and the conduct of an appropriate and accurate formal assessment of the individual’s mental health under the Act. For example, if the individual had consumed alcohol, a MHAA could not be conducted until they were no longer under the influence and were able to be appropriately assessed:
Discussed with AMHP [NAME]. Advises I speak to duty consultant Dr [NAME] who is here to see another DP currently. Is FTD [fit to detain] in interim. They will arrange review tomorrow by own team when sober.
Custody medical form
Theme 3: resource/availability
Resourcing issues represented another factor that influenced the decision to request a MHAA. For five of the seven MHAA requests, resource issues were recorded as causing a delay in the conduct of the MHAA. As presented above for two cases, this resulted in their detention being extended beyond the 24-hour PACE clock. Generally, resource issues were related to staffing. In the example below, the mental health staff had already conducted a MHAA assessment and there was no capacity to conduct another MHAA until the following morning:
Informed Custody Sgt [sergeant] that MHA assessment will be arranged for morning of 11/7/11 as AMHP has just returned from MHA assessment (5 am) and it will not be able to set up MHA assessment until day shift comes on duty at 8 am. Custody Sgt ok with this but said that [service user]’s Mother had been informed that MHA assessment would take place at 10 pm last night by the mental health team and would be upset that this did not happen. I said [service user]’s Mother will be informed when MHA assessment takes place.
Progress notes
In a further case, resource issues drove a request by the MHT for a review of the current situation by the FME to ascertain whether or not a MHAA was still required. The request was refused by the police, however, as not conducting a MHAA following the original request by the FME would go against policy (PACE code of practice C: Fit to detain, fit to interview).
T/C [telephone call] from [L33] asking expected time for the MHAA. Informed them that no time had yet been set but once a time had been arranged they would be informed. Also asked if their FME had seen [service user] again but was told this would not happen now because the request for a MHAA has been requested and accepted
Progress notes
The availability of specialist staff members able to best assess and manage the individual was also seen to guide the dispatch of MHTs to conduct formal assessments under the MHA. In the following example, a team could have been sent out to assess the individual and not doing so would have an inevitable impact on police resource in the custody suite due to the consequent retention of the individual in custody. However, as the individual was resting, it was considered in his best interests to delay the assessment until his care team were available the next day, as they would be best placed to assess and deliver care:
PNs [name] was concerned that duty consultant be contacted re: any instructions Dr [Medical 1] may have left but felt that the assessment could take place in the morning as [service user] now settled. I agreed to call duty consultant (Dr [name]) who on hearing information agreed that as [service user] was settled and sleeping that the assessment would be preferable for the morning by his own team.
Progress notes
Decision 4: decision regarding the outcome of a Mental Health Act assessment and custody disposal
The outcome following the MHAA was either to be detained under the MHA or not detained. Two of the seven individuals who were formally assessed were detained under Section 2 of the Act, and five were not detained. There were no voluntary admissions. All of the individuals who were not detained following formal assessment were offered some form of enhanced care/management following MHAA. Individuals were offered a variety of enhanced care according to their presentation and their existing care arrangements (where applicable). Table 16 provides details as to the type of enhanced management offered to individuals who were not detained following formal assessment.
| Case | Enhanced care/management |
|---|---|
| 1 | Offered referral to CMHT but refused |
| 2 | Daily support from HTT: double-handed visits. Change in medication |
| 3 (assessment 1) | Referral to CMHT; manager of CMHT to be provided with details of outcome of MHAA. Follow-up to CMHT of potential rehabilitation placement |
| 3 (assessment 2) | Referred to supported accommodation; service user to contact CMHT and support worker |
| 4 | Joint management meeting set up between clinical team and police. Consideration to be given to treatment of condition in a specialised setting |
Framework analysis of decision to detain under Mental Health Act
The framework used to understand decision to detain under the MHA with regard to outcomes of MHAAs following Section 136 detentions was applied to the decision to detain on formal assessment under the Act in custody following arrest. MH1 forms used to record details and outcome of MHAAs were examined to determine the precipitating factors in the decision to detain following MHAA. For two cases, progress notes detailing the MHAA were examined due to, first, one case detailing minimal information regarding the current MHAA in the MH1 and second, an MH1 not being available in the health-care notes.
The mental health code of practice criteria for applications for detention under Section 2 state that in order to make an application, the following must be met:
Analysis focused on identifying the precipitating factors that enabled an assessment against the MHA criteria above. Four themes emerged from the data that brought understanding in terms of the rationale for detention, which reflect the themes that emerged from the analysis of decision to detain under the Act following Section 136 detentions:
-
imminent risk
-
existing formal management arrangements
-
existing informal social care/management arrangements
-
behaviour.
Theme 1: imminent risk
Mental health professionals conducting the MHAA evaluated the potential imminent risk of the individual both to themselves and to others in making the decision to detain under the MHA. Each of these forms of risk is presented below with reference to how they informed the decision to detain.
Perception of risk to self by the assessing MHT was recorded in all cases that were formally assessed under the MHA. In the two cases that involved detention under the MHA, the first was regarded as a risk to self through self-neglect and the second due to not being able to leave the house because of his mental state. However, as detailed below, both of these cases were further concurrently assessed as an imminent risk to others, which combined with risk to self, drove the decision to detain. In the cases of those individuals who were assessed but not detained, risk to self-behaviours recorded in the mental health notes included both historical and current, observable DSH or suicide, for example:
[service user] was at her mother’s home and was self-harming superficially to her arms. She ran off so mother informed the police. She was returned by the police but continued to self-harm. She became very difficult and was detained for breach of the peace and taken to [custody centre]. They did not pursue the B of P [breach of the peace] but requested a MHA assessment
MH1
Solely historical risk, however, was not considered sufficient for risk to self to be a precipitating factor in the decision to detain. For example, although one individual had a historical recording of suicide and DSH risk, this was not considered relevant to the current presenting situation. Therefore, in this case, the lack of current risk to self was directly attributable to the decision not to detain:
There appeared, to all those involved in this assessment this afternoon, to be no evidence at this time of [service user] having overt plans of either suicide or deliberate self-harm, and no evidence of him requiring hospital admission at this stage.
MH1
As noted above, perception of risk to others was recorded in the mental health notes of both cases in which individuals were detained under Section 2 following MHAA. Both individuals had presented with behaviour that put others at risk and further, was likely to pose a risk in the immediate future, in comparison with those who were not detained as an outcome of MHAA whose risk to others was not assessed as requiring immediate detention to mitigate risk.
Detained case one: According to [professional] manager at [service provider] fellow residents have complained about [service user] stealing from the kitchen and harassing a female resident by hiding her things. It has also come to light that [service user] has weapons in his room including a homemade crossbow, a machete, an air gun, and an axe. He is also stockpiling bits of bicycle in his flat. He is said to be firing his air gun out of the window. [service user] had locked himself in his room and police had to break in.
MH1
Detained case two: MHA undertaken at [custody centre] [service user] assaulted his mother the previous evening she thought he was going to push her down the stairs she grabbed onto a door frame a friend who was in the property heard the commotion and came to help. [service user mother] sought [housing agency] apparently the police were going to transport her but she missed them at pickup point police went to house and [service user] was arrested. [service user mother] has been spending much of her time out of the property through fear [service user mother] reports that he had been responding to the internet part of his beliefs is that the lady who lives next door is part of the stalking, she is expecting a baby so there were concerns for her safety
MH1
The individual related to the second case was formally assessed under the MHA in custody following arrest on a previous occasion in the research window to that in which he was detained. On that occasion, risk to self was recorded predominantly as threats but without the level of seriousness or imminence necessitating further detention:
T/C [telephone call] from Dr. [name] at [custody centre] raising concerns about [service user]. he was arrested last night under the influence of alcohol for common assault, after going to a bar, and when asked to leave hitting the doorman
Progress notes
However, at the second arrest related MHAA in the research window, risk to others had become both imminent and serious, thereby raising the need for intervention by the MHT under the Act.
She also said he believed his stalker’s sister lived next door to her. He shouts about her sometimes, and has said he is going round, but has never got up from his seat when saying this; she has told him she will phone 999 if he goes to, which she says she would.
Progress notes
Theme 2: existing formal management arrangements
Assessment was made of individuals’ current access to and engagement with services during the MHAA. The two cases that culminated in detention under Section 2 of the Act, although known to services, either did not have formal management in place at the time of detention or were not engaging with services in a way that facilitated the support that they required. Detention was therefore in part determined by the current or historical level of engagement with community services, which could necessitate admission to ensure engagement and therefore effective assessment and treatment. For example, detained case one:
[service user]’s family, professionals, his housemates and managers of [supported housing] have all expressed concern over the past few weeks. He has not been seen by CMHT over this period though attempts have been made.
MH1
Detained case two:
His mother Mrs. [service user mother] informed Dr. [name] that AMHP [name] contacted her on the 11th April with regards to an MHA planned for the 13th April. Mrs. did not hear any more and the MHA did not happen. He was discharged from EIT in January 2011. He moved back to his mother’s from [place name] and has not left the house for about four months because of his paranoid beliefs . . . He said he would be happy to try a different anti-psychotic and engage with HTT. We stressed that we could not guarantee no side effects with anything, but pointed out the risks of becoming increasingly psychotic, and stressed if he was concerned about medication to discuss it with workers so changes could be made without risking relapse
MH1
In the case of the five contacts who were not detained following formal assessment and who were not currently on the caseload of a care team, as presented above, enhanced care/management was offered in the form of referrals to CMHTs following release from custody. However, in these cases, as in the following example, the MHT assessed the individual’s potential for successful engagement:
[service user] is a 35 year old man, whom had recently been discharged from CMHT, and has had various previous contacts with psychiatric services. [service user]’s diagnosis has been unclear, but he has reportedly suffers from a psychotic or paranoid illness, and has suffered from anxiety and severe depression for some years. However, over the preceding few months [service user] had reportedly been improving in his mental health and, although remaining low in mood, appearing to reach a relatively stable point and not wishing to have further active contact with the CMHT at this time. He was therefore discharged on 12/4/11 . . . However, their remained the need for [service user] to be re-referred to Psychiatric Services, primarily for a review of psychiatric medications, as well as a review of the need for him to receive at least short-term support from the CMHT whilst his social situation remains a current active stressor within his life. Dr to complete a referral to CMHT services for immediate review. [service user] is happy with this plan, and reports he would be willing to see a consultant further. [service user] reports that he has plans to go into detox and rehab at ‘[rehab]’, has reportedly been referred and is awaiting placement. This will need confirmation by the CMHT when contact is re-instigated. A call was made by myself to ‘[rehab]’ at approx. 6pm to investigate [service user]’s referral, and a message left for day-time
MH1
Theme 3: existing informal care/management arrangements
Assessment was made of the degree of informal care and management available to the individual on release from custody. Providers of support could include family and friends able to support the individual with, for example, social care needs, their behaviour because of their condition and engagement with services. Existence of informal support/management reduced the need for consideration of formal admission. For example, in the case of the second detained case above, who had a previous custody MHAA in the research window, his mother’s willingness to support her son with enhanced HTT input prevented a formal admission at this point. However, with increased risk to others (including his mother) 2 months later at the second custody MHAA, this informal management was not possible and in part drove the decision to detain under Section 2 of the MHA. First MHAA:
She felt that home treatment was the best way forward, and was happy to have him home with support. She said she felt he wanted support, but people have not come out to help him, and he has not been able to leave the house to go to see others. She would like for him to look at supportive living in the future, but is concerned he wishes to leave Cornwall and he will not cope. HTT number given, she has agreed to phone 999 if she feels threatened.
MH1
Second MHAA:
He has had limited food and water. It was decided to detain for a further period of assessment and because of the uncertainty of his behaviour was transferred to [Acute Psychiatric Ward]
MH1
Theme 4: behaviour
Assessment necessarily included the individual’s presenting behaviour at the time of assessment. In terms of the two cases who were detained under the MHA, both presented with behaviour perceived to be delusional, with corroborating information from both third-party report and direct observation. Detained case one:
He has been described as ‘floridly psychotic’ and seems to have delusional ideas about seeing scorpions. This has come from his family and was the case a few days ago. Present at the interview were Drs [name] and [name]. Both S12 [Section 12] and [professional] AMHP. [service user] was prepared to say very little other than the female resident had been bothering him for 25 years. This was clearly odd, as he had only known this person for a short time. He refused to say anything else went to the toilet and then returned to his cell. He was brittle resentful and there were also signs of self-neglect.
MH1
Detained case two:
When we interviewed him he admitted to us he was hearing voices and that he was being watched plotted against on the internet and Facebook [Facebook Inc., MenloPark, CA, USA] he couldn’t explain why or how anyone would want to do this
MH1
Furthermore, following assessment of mental capacity, in the case of detained case one, there were also concerns with regard to capacity that contributed to the decision to detain. Detained case one:
There is some doubt about his insight and capacity to make rational decisions.
MH1
Although it was recorded for detained case one that there was ‘no reason to doubt capacity’, the record also showed that there was some difficulty in adequately assessing the individual that could impact on capacity assessment, and therefore on the potential for risk to the individual that could influence the decision to detain.
The outcome of the assessment of behaviour was markedly different with regard to the five cases not detained under the Act following formal assessment. In some cases, the assessing clinicians/practitioners did not agree with the individual’s self-report of presenting symptoms:
[service user] suggesting she has psychotic symptoms but professionals do not feel this was the case. PD [personality disorder] diagnosis accurate . . . Has capacity for actions
MH1
In other cases, the presenting mental state did not influence capacity or require immediate acute care as would be provided by formal admission. Example one:
Concern emerged upon his return to the Police station and his presenting low mood and suicidal ideation. Dr [name] [service user] presented as slightly withdrawn initially, but was soon able and willing to engage in lengthy conversation regarding his arrest, his past and his current situation. Throughout the interview [service user] appeared to be somewhat anxious, and regretful of the incidents that had led to his arrest and consequent assessment, although not distressed or overtly depressed in mood. He maintained good insight into his previous suicidal ideation and suicide attempts and was able to identify his apparent progress in terms of his long-term recovery, and the progress he had made over the previous year. Having said this, he appeared to be realistic about his continuing struggle with his mental health, his alcohol addiction, and his housing situation. Equally, no evidence today of psychosis, although overt reports of struggling with his paranoid thoughts when in particularly stressful situations or when drinking heavily. No medical recommendations were made.
MH1
Example two:
No evidence of mental disorder warranting admission formal or informal. No evidence of hopelessness or plans. No evidence of significant mood disorder or psychosis. Had full capacity to understand the assessment and the outcome, as well as being fully able to engage in conversation about his future and make active plans in an attempt to resolve his difficult social situation.
MH1
Care/management of detained individuals post-Mental Health Act assessment/detention
Post detention actions taken by the police
For those cases who were not detained, any actions taken by the police post MHAA were also explored to determine if support/management by the police affected outcome for the individual. In two cases, the custody officers were concerned about access to accommodation once the individual was released from custody. Subsequently, police provided support via communication with family or housing to ensure that accommodation was available:
spoke with [service user]s mother who stated will arrange for her keys and other belongings to be dropped at station within 30 mins or so
Detention log
DP cannot return to accommodation in [AREA] due to 2 breaches re leaving accommodation overnight and Social services are not assisting for accommodation at this stage. AMHP has stated that he will have to arrange his own accommodation and that he has told her that he will stay with a friend and is aware he must remove property by 21.00 tonight. DP has money and is able to get train back to [AREA].
Detention log
In a further two cases that were not detained following MHAA, transport was arranged for the individual, with one individual taken home by patrol officers and one prepared for transportation to court by the officers managing his detention.
Action taken. Full details of the d/p’s [detain person’s] self-harm issues given to Reliance officers [NAME] and [NAME] – d/p was clothed in track suit bottoms, paper knickers, t shirt and flip flops – d/p handed to reliance for court with fully completed PER and medication
Detention log
In another two cases not detained following MHAA, the police provided individuals with additional support in the form of information regarding other agencies and services additional to that provided by the MHT:
she did not wish to be referred to any support agencies – provided with a Samaritans leaflet and also MH [mental health] literature.
Detention log
MHA team carried out assessment and decided to release him. They have contacted New Connexions for him to stay there tonight. Given Partnership Agency information and Samaritans card.
Detention log
In the final case regarding an individual who was formally assessed but not subsequently detained under the Act, the detention officers took extra steps to try to support the individual by attempting to influence the MHT’s decision to detain under the MHA following their persistent assessment of risk with regard to the presenting situation. The example below provides the rationale as to why the decision was taken not to detain under the MHA following assessment:
Discussions with Sergeant [name] ([custody centre]), [professional] and [psychology 1]. Sergeant [name] concerned about releasing [service user] in the face of the threats she has made to harm others and herself. He asked if I would reconsider admission. I informed sergeant [name] that I appreciated and shared his concern but did not believe that admission was appropriate and I would organise a meeting between the police and ourselves as soon as practical to work out strategies for jointly addressing the risks she presented [professional] shares my view that Hospitalization would have been inappropriate given that she was fundamentally threatening criminal behaviour.
Progress notes
Custody disposal outcomes
Police recorded disposals for all cases arrested in the sample were examined. Figure 16 presents the disposal categories for all custody detentions. The largest disposal category concerned there being no further action (NFA) by the police (n = 38, 30.2%) following detention. Therefore, although individuals would have a custody record and a record on CIS, the case regarding the original offence would not be taken any further by the CJS, often due to lack of evidence and therefore the potential strength of the case at court.
FIGURE 16.
Disposal categories for all custody detentions (n = 126). Numbers represent the number of detentions in each disposal category.
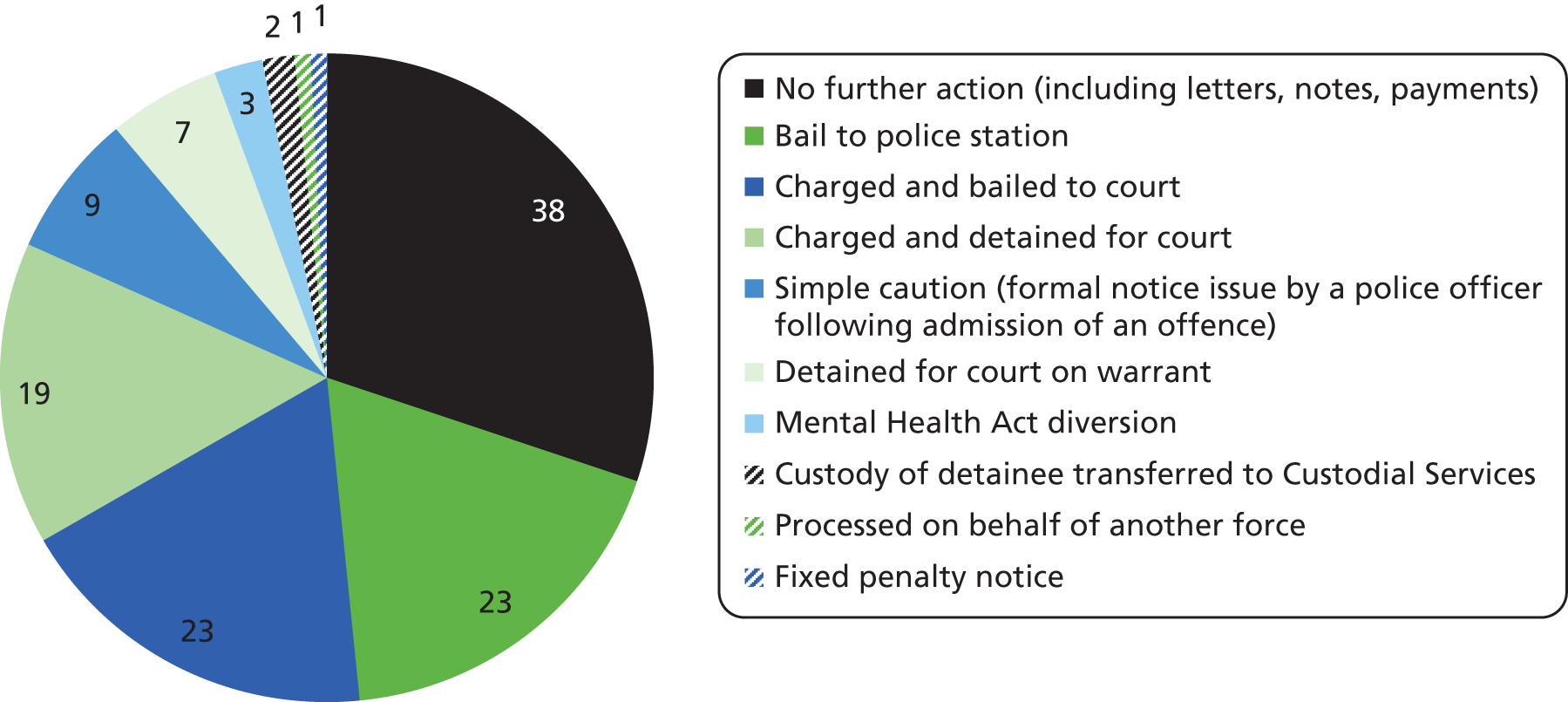
The data were examined to explore the disposal category for each offence type (Table 17). It can be seen that the majority of offences categorised under public order received NFA and, furthermore, NFAs following public order offences were the highest group within this disposal category. Additionally, a high proportion of cases in which individuals were arrested for offences against people were also NFA. MHA diversion was recorded for three contacts: one public order offence (detained Section 2 MHA); one contact due to an offence against people (detained Section 2 MHA) and one breach of bail or an order (individual not detained under the MHA). The highest number of police detentions following arrest was for arrests related to breaches of bail and orders.
| Type of offence | Charged and detained for court | NFA | Simple caution | Bail to police station | Detained for court on warrant | Custody of detainee transferred to custodial services | Charged and bailed to court | MHA diversion | Processed on behalf of another force | Fixed penalty notice | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Offences against people | 2 | 15 | 4 | 10 | 0 | 0 | 3 | 1 | 0 | 0 | 35 |
| Public order offences | 1 | 14 | 4 | 3 | 0 | 0 | 2 | 1 | 0 | 1 | 26 |
| Theft offences | 3 | 4 | 1 | 7 | 0 | 0 | 9 | 0 | 0 | 0 | 24 |
| Breaches | 11 | 2 | 0 | 2 | 7 | 2 | 3 | 1 | 1 | 0 | 29 |
| Criminal damage | 1 | 3 | 0 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 10 |
| Drug offences | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Total | 19 | 38 | 9 | 23 | 7 | 2 | 23 | 3 | 1 | 1 | 126 |
Summary
This section of the report has presented the research findings in relation to the journeys of 52 individuals through mental health and police services specifically in relation to custody detentions. There were relatively few instances of police knowledge of the mental health needs of these individuals as indicated by markers on the police systems, with alternative markers such as self-harm and suicide not explicitly linked to potential mental health issues. Although recorded information exchange between services prior to or at the time of detention was low, where such communication was recorded, this proved useful to both services in their management of these individuals. Furthermore, the findings regarding detention management suggest that communication between police and mental health services during detention is more likely if the individual is on the current caseload of a secondary MHT. Although almost half of the detentions involved the use of restraint, there was limited recording of rationales. However, of those available rationales, all but one were clear in their application to mitigate against risk of harm either for the individual or others. The findings showed an AA attended a quarter of the detentions under examination here, with the most common determining factor in attendance being a clearly defined diagnosis of mental health condition. These findings are discussed in relation to relevant policy and protocol in the discussion section of the report.
Case-linkage study: non-detention contact findings
Introduction
Fifteen individuals from the case-linkage sample had neither a Section 136 detention nor a custody arrest for the 12 months following their index police contact in the second quarter of 2011. It was considered vital to include these individuals’ experiences in the case-linkage analysis for the following reasons:
-
Post-Bradley reports and recommendations support the need for diversion for individuals with mental health issues who interface with the CJS. It is useful, therefore, to examine the journeys of mental health service users who come into contact with the police but who did not escalate to Section 136 detentions or custody arrests within the research window.
-
Although the Section 136 and custody findings reported herein are looked at as specific contact types, most of those individuals also had non-detention contact with the police; therefore, the types of non-detention contacts described below reflect the journeys of those individuals as well.
-
In general, research focuses on police contacts that culminate in a detention. By identifying the decisions that are made in managing those individuals who are not detained, it can arguably be possible to develop research to further examine how decisions can be made to avoid criminal justice crises and ensure individuals are effectively managed to achieve enhanced mental health outcomes.
Sample characteristics
Of the 80 cases selected for the case-linkage study, 15 individuals were in contact with the police but had no detentions within the research window (i.e. the year following the index police contact in the 3-month period in which cases were originally identified). These 15 individuals were associated with 418 police contacts. The number of police contacts per individual ranged from 1 to 296 (average 28 contacts per person). Two hundred and seventy-eight (66.5%) contacts were not attended by police officers.
Eight of the 15 individuals were female, and seven were male. Of the 10 records available for marital status, seven cases were recorded as single and three as married or having a civil partner. The average age of the group at the point of their first contact in the research window was 41.5 years (range 21.2–85.0 years). Twelve of the individuals were recorded as living in privately rented/owned accommodation, two in hostels/assisted living and one in another care setting (e.g. residential care) at the time of data collection. All of the cases were white British apart from one white Irish. Six of the 15 individuals were recorded as unemployed at the time of data collection, one worked in an elementary occupation, two were retired and six were unrecorded.
Police contact
Reason for police contact
The reasons for the 418 contacts were broadly categorised into the groups in Figure 17, providing an overview of whether or not the call was related to concerns for welfare, linked to a criminal activity, logging of incidents, etc. For 327 incidents, the call was related to the welfare of the individual. For the one individual with the highest call volume (296 contacts in total), the calls related to misplaced calls, trying to contact family members and carers, loneliness, etc., associated with the individual’s dementia. The other 31 contacts in this group were linked to the individuals’ behaviour during the call or concerns of a third party. The next highest proportion of reasons for calls involved 29 incidents related to reporting by the individual or a concerned caller, including reporting further information linked to a previous incident, reporting non-urgent incidents, providing intelligence requested by the police, provision of information by a partner agency, etc. A further 27 contacts related to non-crime domestic incidents between partners and family members. The remaining call types are categorised in Figure 17 and involved small numbers of incidents.
FIGURE 17.
Types of call.
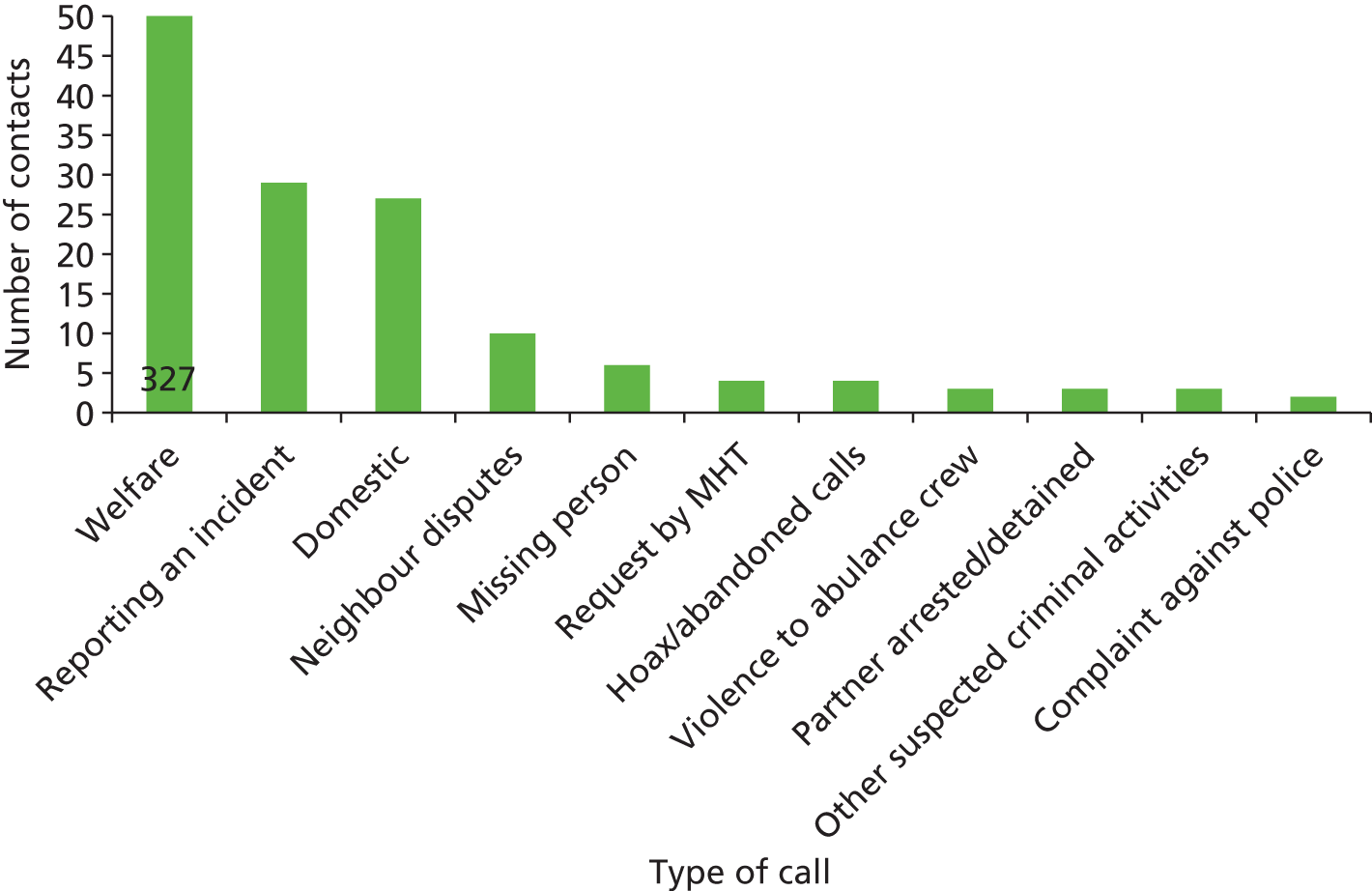
Types of police contact in the research window
None of the 15 individuals were detained by the police during the research window. For 10 of the individuals, their contact with the police had triggered the individual’s address to be recorded on the NHRR (if there were three calls to the police regarding the address in a 3-month period), eight of which were named as a PP (i.e. their name was recorded on the NHRR alongside the address). The five individuals not recorded on the NHRR did not meet the criteria, as four had fewer than two incidents each over the year and one had five incidents but none in the same NHRR quarter.
In the eight cases involving a PP at the address on the NHRR, data were available for warning markers entered by officers to highlight issues relating to that person. These markers are summarised in Figure 18, which indicates that five of the eight individuals recorded on the NHRR had a mental health marker. Therefore, only 33% of the 15 individuals were highlighted on the NHRR as having mental health issues, despite those individuals being case-linked on RiO.
FIGURE 18.
Non-detention contact group individuals with NHRR warning markers (n = 8).
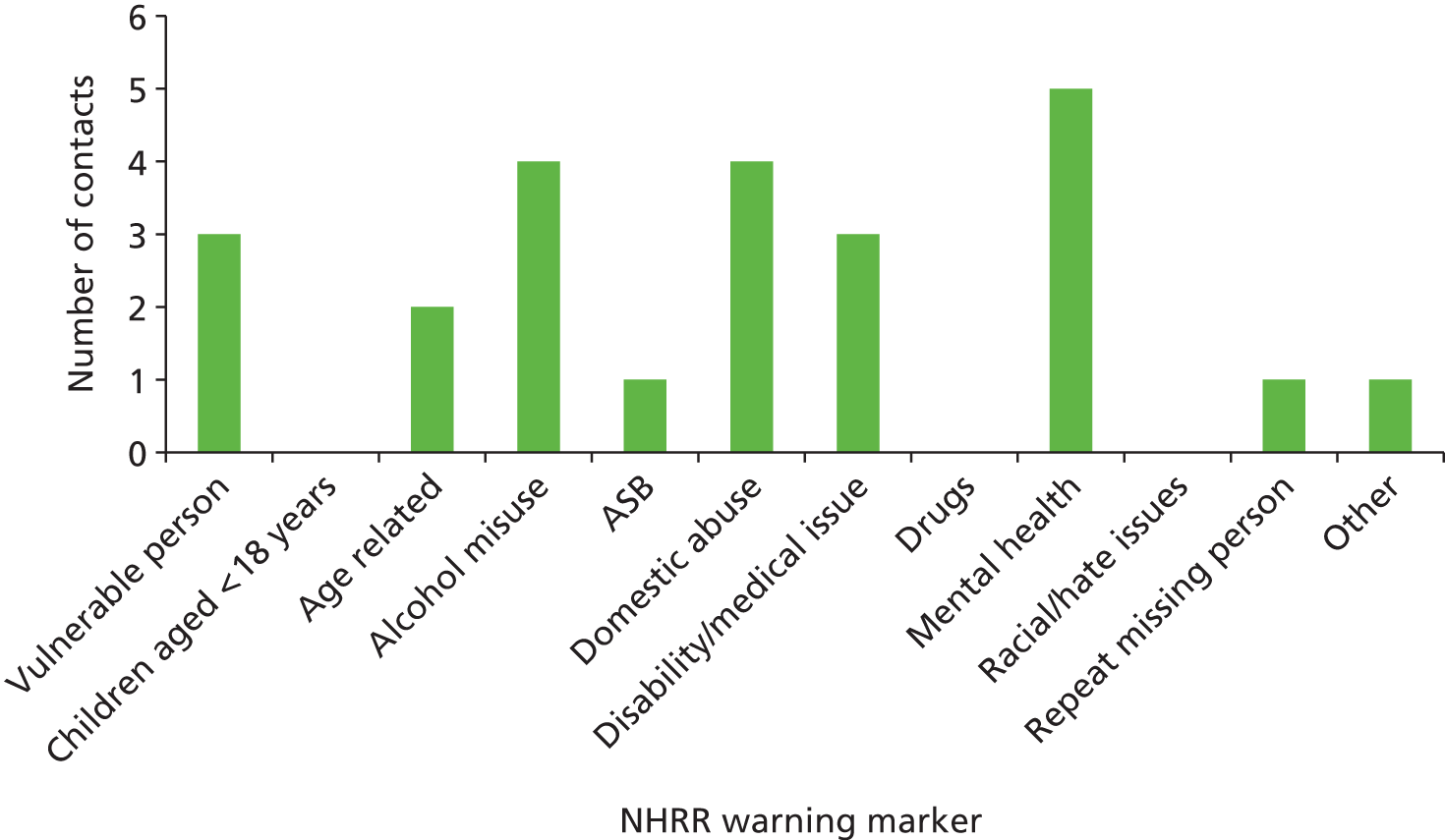
Ten individuals had a non-crime vulnerable adult record linked to their CIS records. These are generally created when a referral to the police is received from another organisation, for example adult social care, and will relate to an incident or concerns raised, usually about the care and management of the individual. It is then allocated to an ‘officer in charge’ who takes responsibility to collate action. The non-crime vulnerable adult records explored in this research contained long-term plans for an individual as well as interagency information exchange. The records seemed to be used in place of problem solving plans (PSPs), which are normally created as part of the solution to a long-term problem, often including individuals whose behaviour is affecting service delivery or the local community (definitions of non-crime vulnerable adult records and PSPs – Chief Inspector Mark Bolt, personal communication).
Table 18 compares NHRR entry with the number of OIS logs associated with that individual, whether or not they had a non-crime record and/or corresponding warning markers and flags. All individuals with more than 10 OIS logs (n = 5) had non-crime vulnerable adult records. Of the 10 individuals who had fewer than 10 OIS logs, only two had a non-crime vulnerable adult record indicating that records were being created for those individuals who were repeatedly in contact with the police.
| Case | Individual on NHRR | Warning marker (NHRR) | Non-crime vulnerable adult | Warning flag (PNC or local) | Number of OIS logs |
|---|---|---|---|---|---|
| 1 | No | N/A | No | No | 2 |
| 2 | Yes | Vulnerable adult, disability, mental health, missing person | Yes | Local: vulnerable adult | 296 |
| 3 | Yes | Alcohol misuse, disability, mental health | Yes | PNC: violent, self-harm, suicidal | 14 |
| 4 | Yes | Vulnerable adult, disability, mental health | Yes | Local: vulnerable adult | 15 |
| 5 | Yes | Vulnerable adult, alcohol misuse, DV, mental health | Yes | Local: risk to child | 30 |
| 6 | Yes | Mental health | Yes | None | 6 |
| 7 | Yes | ASB, DV | No | None | 7 |
| 8 | No | N/A | No | None | 1 |
| 9 | Yes | Alcohol misuse, DV | No | None | 5 |
| 10 | Yes | Not PP | No | No | 6 |
| 11 | No | N/A | Yes | Local: vulnerable adult | 1 |
| 12 | Yes | Alcohol misuse, DV | No | No | 2 |
| 13 | No | N/A | No | PNC: mental health and weapons Local: drug supplier |
5 |
| 14 | Yes | Not PP | Yes | Local: risk to child | 27 |
| 15 | No | N/A | No | Local: drug supplier and risk to child | 1 |
To determine the uniformity of recording of warnings across police systems, the warning markers on the NHRR were noted against available PNC warnings on CIS. Two of the 15 individuals examined here had PNC warning flags (see Table 18). Seven of the 15 individuals included in the sample had a local warning flag on their CIS record. It can be seen from Table 18 that recording of markers on the NHRR and warning flags on the PNC did not always match; for example, a vulnerable adult marker is noted on the NHRR entry for case 11 but there is no similar warning flag on the PNC system. Control operators and response officers do not have access to NHRR, and therefore would not see those warnings when responding to an incident.
Mental health contact
Nine of the 15 individuals were on the caseload of a MHT at the time of their index contact in the research window. Individuals were either on the caseload of one (n = 7) or multiple (n = 2) secondary MHTs. Examining the 418 contacts, in 334 the individual was on the caseload of a single team category, and in 16 the individual was linked to two or more team categories. The remaining 68 contacts were related to individuals not on caseload at the time of police contact. Descriptions of the care team categories are provided in Appendix 2. The majority (n = 324) of contacts related to individuals on the caseload of general secondary mental health services; one case accounted for 296 of these contacts as they were on the caseload of the CMHT for all their contacts. In respect of the remaining 28 contacts where the individual was on the caseload of secondary mental health, for 12 contacts, the individuals were on the caseload of the CMHT, 15 with the complex care team and one with the day resource team. Due to the small sample size (n = 15 individuals), the care team categories relating to the caseload of each individual are provided in Table 19.
| Case | Total number of contacts | Number of contacts on each team |
|---|---|---|
| 1 | 2 | Not on caseload for any contacts |
| 2 | 296 | All 296 on caseload of CMHT (secondary) |
| 3 | 14 | All 14 on caseload of AOS, for seven contacts, also with acute teams |
| 4 | 15 | All 15 on caseload of a complex care team (secondary) |
| 5 | 30 | One on an acute team caseload, 29 not on caseload |
| 6 | 6 | All six on psychological therapies (specialist), for three contacts, also with secondary (all three on CMHT, with one contact also on day resource team) |
| 7 | 7 | Three contacts on CMHT (secondary), for two contacts also with a learning disabilities team. Not on caseload for four contacts |
| 8 | 1 | On AOS caseload |
| 9 | 5 | Not on caseload for any contact |
| 10 | 6 | All six on EIT, for two contacts also with AOS |
| 11 | 1 | On learning disabilities caseload |
| 12 | 2 | Not on caseload for any contact |
| 13 | 5 | Three on CMHT (secondary), for two contacts also on AOS, one on AOS only, one not on caseload |
| 14 | 28 | Three on CMHT (secondary) |
| 15 | 1 | Not on caseload for contact |
Non-detention decision framework
Unlike the Section 136 component and aspects of the custody component of this research, analysis of the decisions that were undertaken in the management of the 15 ‘non-detention’ individuals could not be guided by a specific policy/protocol. Consultation with practice-based members of the research team, however, revealed aspects of best practice and local initiatives (such as the NHRR described above) that support the identification and management of individuals with mental health issues who come into contact with the police. As discussed under the policy review section of this report, Bradley made recommendations relating to supporting individuals who are linked to low level offending or ASB to prevent further offending and detention. 6 Particular to this group of individuals, and Cornwall, are the recommendations that emerged from the Steven Hoskin serious case review. 55 The researchers were cognisant of these recommendations when analysing and interpreting the non-detention data.
As with the previous analyses, the data familiarisation process was undertaken within the framework of informational themes (including individual factors and context of the call) and informal operational/procedural themes (including information sharing, risk management and care management). Through this process, the decisions taken by and between services to manage and care for these individuals emerged iteratively from the data. As a consequence, a sequence of broad decisions and subthemes encompassing the management of an individual not requiring detention emerged as follows.
Decision 1: decision to dispatch response officers
-
Perception of immediacy of need
-
response classification
-
origin of call
-
type of call
-
perception of risk.
-
-
Individual’s history
-
review and interpretation of previous OIS logs
-
operators’ recent experiences of dealing with the individual
-
information provision by police/police staff.
-
Decision 2: decision not to detain/officers’ responses
-
Awareness of mental health.
-
Interagency information exchange.
-
Authorisation of tasers.
-
Diversion from detention.
Decision 3: decision to provide further support/joint management
-
Referral to Neighbourhood Beat Teams (NBTs).
-
Joint management of individual.
-
Police aftercare.
Decision 4: decision to conduct a Mental Health Act assessment
The above decisions capture the contact process from the initial call received by the operator – including how this was dealt with by the operator, and responding officer – through their management once in attendance of an incident and where applicable, ongoing management. The following sections describe the context of each decision in relation to the 418 contacts examined.
Decision 1: decision to dispatch response officers
As with the Section 136 and custody analysis, the first decision in the process involved control room operators’ decisions regarding the necessity to dispatch response officers to an incident. For the 15 non-detention individuals, the decision to dispatch emerged as a major decision because of the number of contacts in this group where the decision was to grade a call as ‘non-attendance’ (n = 278).
Framework analysis of the decision to dispatch response officers
Analysis showed that the decisions to dispatch were based on the following themes:
-
Perception of immediacy of need
-
response classification
-
origin of call
-
type of call
-
perception of risk.
-
-
Individual’s history
-
review and interpretation of previous OIS logs
-
operators’ recent experiences of dealing with the individual
-
information provision by police/police staff.
-
Each of these themes relate to the operators’ decisions to dispatch officers to an incident and are discussed in turn below.
Theme 1: perception of immediacy of need
The grading and classification of an incident by the operator and their decision to dispatch a response officer or not depended on the origin of the call, what the context of the call was (type), and the operator’s perception of risk to the individual and others. As part of the operator’s assessment of a call, they provide a grading of the level of necessary attendance and a classification of the type of call. To provide context for the operators’ decisions to dispatch, the grading and classification of the 418 contacts are discussed first.
Operational Information System logs were examined to determine the response level and classification assigned to each contact by the operator. Of the 418 contacts, 27 were graded as ‘immediate’ (response within 20 minutes of receipt of call), 80 ‘prompt’ (response within 1 hour of receipt of call) and 89 ‘routine’ (response within 48 hours of receipt of call). The remaining logs (n = 222) were graded as ‘non-attendance’. The non-attendance grading does not reflect the actual number of non-attendances (n = 278), as although 56 contacts were initially graded for a response, due to changes during the course of a call, attendance in these cases was deemed to be no longer required. In addition to response level grading, classifications were assigned, thereby providing a categorised rationale for each contact. The classifications are provided in Table 20.
| Classification | Frequency |
|---|---|
| Public safety: concern/collapse/ill/injured/trapped | 171 |
| Administration: information/intelligence | 84 |
| Public safety: domestic incident | 27 |
| Public safety: hoax call to emergency services | 27 |
| ASB: nuisance | 24 |
| Crime related: acquisitive, sexual offence, violence, other crime | 23 |
| Administration: contact record, police generated resource act, complaint against police, emergency incident create, messages | 15 |
| ASB: personal | 14 |
| Public safety: suspicious circumstances/insecure premises/vehicle | 13 |
| Public safety: abandoned call | 14 |
| Public safety: missing person | 6 |
Operational Information System logs were examined to identify the origin of the call (i.e. the person making the call). Table 21 presents the proportion of contacts that were alerted by identified categories of caller. The majority of contacts were made directly by the service user (83%), although when attended incidents were looked at in isolation, the proportion of calls logged by the service users dropped to 55%. Indeed, the calls least likely to result in a decision to attend were made by the individuals themselves (23%).
| Individual or organisation | Number of contacts (n = 418) | % of contacts (n = 418) | Number of attended contacts (n = 140) | % of attended contacts (n = 140) | % of calls resulting in attendance |
|---|---|---|---|---|---|
| Third party | 20 | 4.8 | 15 | 10.7 | 75 |
| Police (patrol, operational, police station) | 1 | 0.2 | 1 | 0.7 | 100 |
| Family member, partner or carer | 26 | 6.2 | 25 | 17.9 | 96 |
| Service user | 347 | 83 | 80 | 57.1 | 23 |
| Partner organisation, ambulance, fire | 10 | 2.4 | 10 | 7.1 | 100 |
| MHT | 6 | 1.4 | 4 | 2.9 | 68 |
| Housing officer or organisation | 1 | 0.2 | 1 | 0.7 | 100 |
| Social services | 3 | 0.7 | 1 | 0.7 | 33 |
| Third sector support organisation | 4 | 1.0 | 3 | 2.1 | 75 |
Type of call received by the operator had an impact on the perception of the immediacy of need. The types of calls were summarised in Figure 17. The following provides examples of those calls.
Most calls related to concerns for welfare. A concern for welfare reported by the service user seemed to be the most likely to end in non-attendance by officers (n = 219), followed by routine (n = 53), then prompt (n = 44). The findings were influenced by one individual whose calls, although welfare related, were considered to be nuisance calls by the services as they congested the police control room system and the switchboard of the mental health service (who were also in receipt of repeat calls). The individual’s repeat calls were associated with their dementia. In response, the police set up a non-attendance plan for the individual which specified that unless there was a perceived immediate threat to self or others, the operator could automatically grade the response as non-attendance. This plan was devised in agreement with social services, the MHT, and the individual’s health-care assistant providers. Examples of logs associated with this individual read:
usually non-attendance – welfare package in place
OIS log
Other examples of calls relating to welfare including concern for an individual due to their mental or physical state included:
caller has mental health problems told me that she is a psychopathic murderer and she thinks there is someone wandering around outside her property asked her parents to phone and ask for police to attend but does not appear that they have
OIS log
concerns for welfare gent [gentleman] is very confused on line saying he is blind and that following his wife leaving him believe this relates to log 649 2808 he has not had his meds for 2 days. Am unable to get gent to understand re contacting doctor and he appears very confused.
OIS log
The next largest group of types of calls related to reporting (i.e. the caller ringing to provide information requested by the police, reporting further incidences linked to a historical event or reporting historical events, etc.). Contacts relating to reporting were only graded as non-attendance in one incident. Fifteen were graded as routine, eight prompt and three immediate. The three immediate responses related to the individual reporting something that would have a potential risk to a third party. The single reporting call that related to a non-attendance was made to relay information not requiring any response:
. . . caller believes that the ambulance man that collected him today dropped a mobile – as when he returned from the hospital he has found it – but does not know how to use it.
OIS log
As mentioned, reporting could also relate to an incident where the operator perceived a risk to the individual or others and therefore made the decision to grade the response as immediate:
loud banging noise like someone kicking the door then sounds of muffled shouting then someone ran down the stairs
OIS log
The next largest group of types of calls was domestic incidents. Due to the obvious risk to self and others, none of these calls were graded as non-attendance. The majority were graded as prompt (n = 13), followed by immediate (n = 7) and routine (n = 6). The following example relates to grading as immediate for a domestic incident:
Elderly male caller, gave the details, said he was frightened then hung up couldn’t hear me ask if he needed an ambulance.
OIS log
The slower response gradings were linked with domestic incidents where the operator knew the level of risk due to historical domestic incidents at the individual’s address.
The remaining types of calls involved small numbers. These included hoax calls (e.g. an individual trying to acquire a lift from the police) and a call where once officers attended the incident, the individual could not remember making the call. These types of calls may highlight welfare issues, even where the police did not attend.
The type of risk posed by the individual to themselves or others as recorded in the OIS logs was categorised by the researchers (Figure 19) in order to identify any patterns in relation to the operators’ perceptions of risk and subsequent dispatch of officers. It can be seen from Figure 20 that the vast majority of non-attended incidents had no discussion of risk in the logs. Where there was an indication of risk either due to the individual’s behaviour, risk from others or third-hand reports of risk, the incident was at least twice as likely to be attended by police officers than not.
FIGURE 19.
Categorisation of level of risk derived from OIS logs for attended contacts (n = 140).
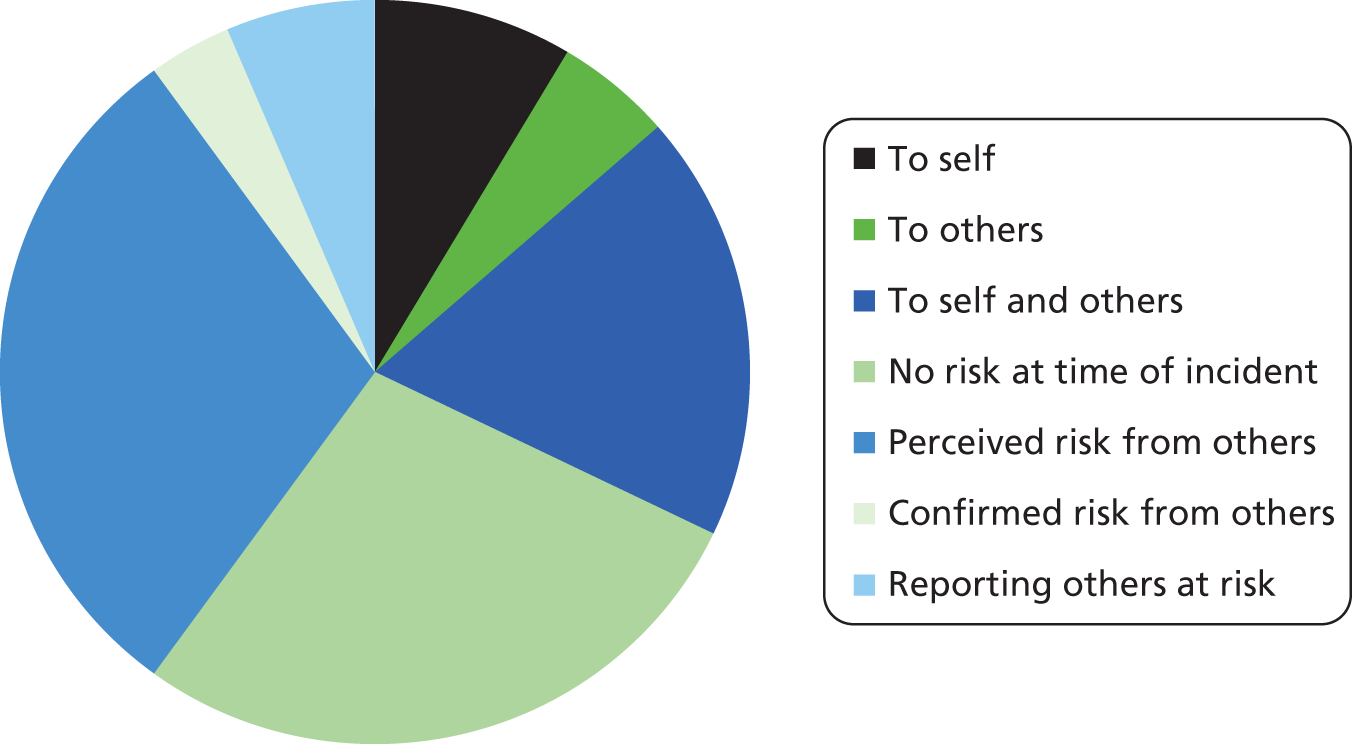
FIGURE 20.
Categorisation of level of risk derived from OIS logs for non-attended contacts (n = 278).
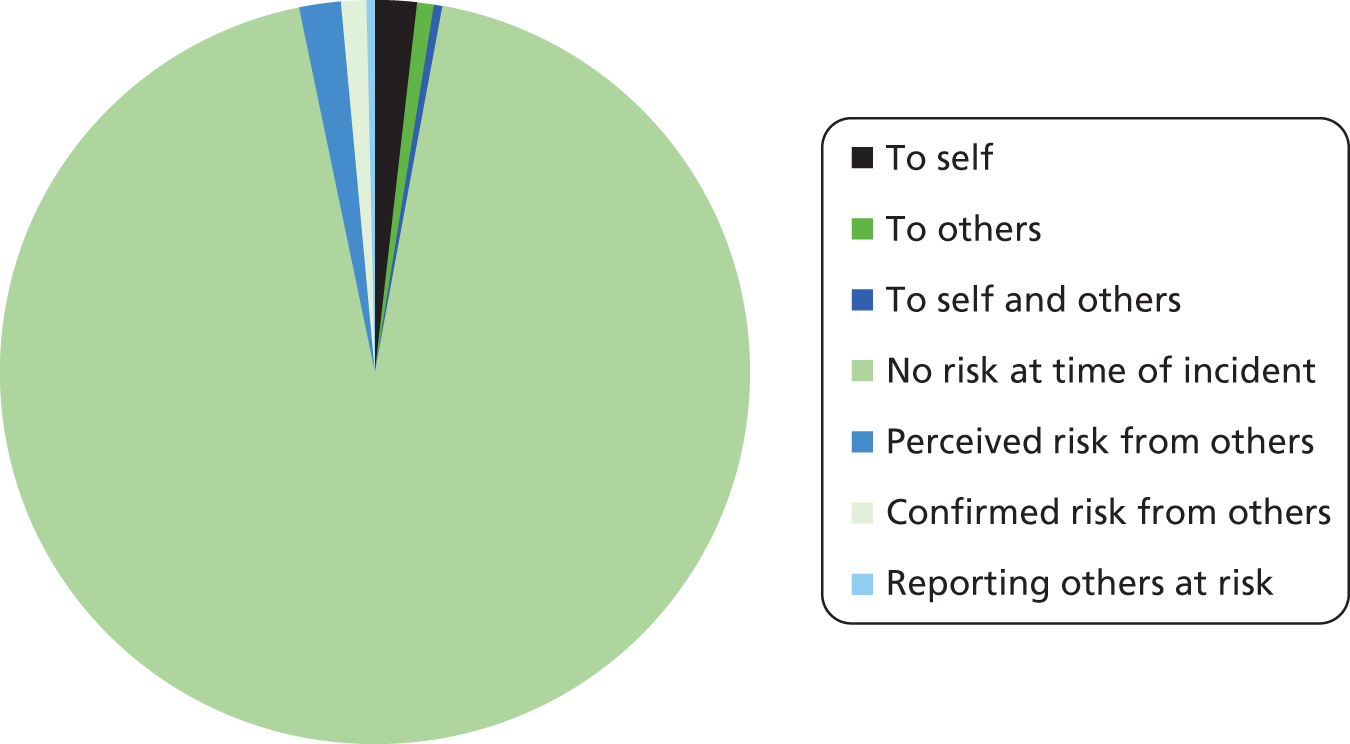
Theme 2: individual’s history
Operators’ decisions to grade and dispatch response officers were also based on historical information about the individual. This could be from recorded experience in logs or personal experience as described under the headings below. Previous knowledge of the individual was mentioned in 365 contacts (87%).
On receipt of a call to the control room, in most cases the operator reviewed previous logs related to that individual (AP search) and/or the address of the incident (VSI function). The researchers examined references made by the operators to previous logs and how they used them to deal with repeat callers, particularly to identify individuals who were known to the police because of nuisance calls. Examples of logs related to previous incidents recorded on OIS logs include:
grading amended due to VSI. There is a need for the relevant agencies to be involved and NBM [neighbourhood beat manager] to be aware.
OIS log
couple is well known to us – is probably domestic
OIS log
Of particular relevance to this research were references to the individual’s mental health status. This informed both decision 1 and how the officers responded to the incident (decision 2). This is discussed further under Decision 2: decision not to detain/officers’ responses.
female is [service user] no first name or dob [date of birth] – does have MH [mental health] issues – female is likely to go mad at officers
OIS log
It was clear from OIS records that some individuals were recognised by operators due to their repeat caller status. This prior knowledge was relayed to response officers on the ground and informed the action taken. Examples of records pertaining to prior knowledge include:
I believe several of my colleagues have also spoken to [service user] on the 999.
OIS log
I have spoken to/been screamed at 4 times today by [service user] on that occasion it was about her electric fire not working
OIS log
The operators would also note if they had previous experience of how to deal with the individual concerned. Lord Adebowale’s report has suggested that information provided by operators to response officers needs to be enhanced. 42 For example, in the case of the following individual, due to the intelligence gathered and interpreted by the operator, it was not necessary to dispatch response officers to attend:
we do not attend logs for [service user] or create them we just update [non-crime vulnerable adult record]
OIS log
On receipt of a call, as well as reviewing logs as presented above and liaising with fellow operators, operators communicate with officers on patrol and NBTs to gain intelligence on appropriate responses in relation to the individual. This can provide information on whether or not the matter called in is already being dealt with and if appropriate management has already been put in place, thereby negating the need for further intervention:
Caller vulnerable adult 999 advice provided from DC [detective constable] [name]. I have already spoken with [service user] regarding this in the presence of his appropriate adult [name]. I gave him advice to phone 999 if anyone attended his H/A [home address] making threats.
OIS log
on going drawn out situation that the local policing team are aware of – will speak to the NBM [neighbourhood beat manager] now and appraise him of the log and those involved – will ask him to speak to the parties in due course – no offences
OIS log
Three OIS logs demonstrated how information provided by the officer directly influenced the operator’s decision to dispatch a response, as demonstrated by the following examples:
unit has had dealings with [service user] before and happy to pop out for a welfare check
OIS log
aware of male and case in question – will attend and assist
OIS log
Decision 2: decision not to detain/officers’ responses
Once response officers had been dispatched to deal with an incident, those attending had to make a decision about how to respond at the incident. As discussed in Decision 1: decision to dispatch response officers, prior knowledge of the individual played a part in how decisions were made to dispatch an officer; the same information helped the responding officers to decide on their response. Provision of information to the officer about the individual and the circumstances were sourced from the operators’ interactions with the caller, warning flags on the PNC and notes about behaviour on previous logs. An important factor, particularly for this research, was police knowledge of individuals’ mental health as discussed in the logs. This knowledge then informed related decisions to contact mental health services. Additionally, in some cases, diversions from possible detention were noted in the logs and the rationales given as to why an officer might have considered detention.
Framework analysis of decision not to detain and response
The response officer’s decisions are discussed under the following themes:
-
awareness of mental health
-
information exchange
-
authorisation of tasers
-
diversion from detention.
Theme 1: awareness of mental health
To understand whether or not officers dealt with the incidents with any knowledge that the individual had mental health issues, the OIS logs were explored to search for any mention of mental health. Awareness of mental health issues was noted in 359 of the 418 logs (86%). Only one individual in the non-detention group had a PNC mental health flag, meaning that little information was gained about mental health from the PNC warning flags. Although the NHRR included mental health and vulnerable adult markers, as described in Table 18, this information would not have been available to the response officers unless they were in contact with NBTs. Therefore, awareness of mental health issues was largely dependent upon the knowledge of the operators (experience and searches) and the officers.
The relationship between being on the caseload of the care team at time of contact and police awareness of mental health in the logs was explored to determine if this had any impact on police awareness of mental health at the time of an incident. Findings indicated that police awareness was recorded in more logs when the person was on the caseload of a MHT. For contacts on caseload at the time of contact (n = 350), awareness of mental health issues was mentioned in 333 (95%) logs. Where the individual was not on caseload (n = 68), awareness of mental health issues was mentioned in 26 (38%) logs.
In some cases, the individual’s history was not the source of raising awareness of mental health, but how the person presented during the call or once officers interacted with the individual. In three cases, the caller’s description of the individual highlighted that they had mental health issues, assisting the attending officer in understanding what they might encounter:
rambling call from male with mental health problems
OIS log
In three further cases, it was the individual’s presentation at the scene of the incident that led to officers’ awareness of mental health issues:
AIO [all in order] here. Female has MH [mental health] issues. Spoken to other residents on same floor but nothing heard by them
OIS log
with lady now – 2 care workers here ATT [attendance/attended] – female has severe MH [mental health] issues and carers state she probably disposed of Tel no.s herself
OIS log
Theme 2: information exchange
Police communication with a MHT was noted in 50 of the 418 logs and nine logs noted communication with social services. For six of the 50 contacts, the MHT initiated the phone call to the police and for three of the nine social service calls, social services initiated the call; therefore, these nine cases do not relate to a decision to instigate information exchange by the police. However, as they pertained to communication and joint working between the services, they were still explored. For two of the nine partner organisation initiated contacts, the call was made to ask for police to escort an individual to a MHAA. The other calls initiated by the partner organisations included three calls to report a missing person and four calls to update police intelligence, including:
-
corroborating that an individual was having a problem with a prowler
-
reporting the recent return of a family member from hospital
-
providing contact details for social services for a repeat caller
-
informing the police that a safeguarding process had been put in place.
The following text relates to one (from the MHT) of the two calls for assistance to escort an individual to a MHAA. Corresponding texts from the RiO progress notes and OIS log relating to the call show how responsibility for dealing with the individual moves between the services during the incident.
Found to be missing from the ward during hourly checks at 11 am. Ward searched, grounds searched and 2 x staff searched [L19] town including Asda. Mobile phone tried, going straight to answer phone. Reported missing to the police and at 12:35. Attempts made to contact [individual mother], next of kin with no success, staff to continue attempts to make contact. Log number. This morning reports of [individual] being a little quieter in mood but no obvious sign of distress. Reported as moderate risk to self, low risk of harm to others.
Progress notes
called [name] ward they are sending someone down with a car – they have no other means of transport -they’ll try and get her in the car and take it from there . . . [service user] handed over to staff will update compact at the station
OIS log
The following texts illustrate the calls made by the MHT or social services to update police intelligence:
R/p [reporting person] wanted to warn us in case we receive any calls from the female who is known for making spurious calls to the police, female may genuinely be reporting sus circs [suspicious circumstances].
OIS log
R/p [reporting person] wishing to inform us that [wife] is likely to be going on leave from hospital tomorrow and returning to address with husband
OIS log
For the remaining 41 of the 50 logs where communication with the MHT was noted, the calls were made by the police during the logged incident. In 19 cases, this related to the aforementioned individual with dementia, where part of the vulnerable adult plan for dealing with the individual required the police to inform the individual’s MHT and social services that contact had been made with the police. For the remaining 12 logs where communication occurred (and was not initiated by the MHT), the reasons were as follows. Most communication related to requests for intervention from the MHT during an incident (two contacts where the individual was the focus of the call and four contacts where the individual’s partner needed care). In the example below, the police called a MHT to obtain care for an individual; however, the MHT required a definitive request from the police. The police officer at the scene discussed how to progress with the attending ambulance crew:
I have spoken to females mental health worker – they will not come out unless we actually [operator] 2022 [time] 22/02 [date] request them ourselves . . . paramedic is going to speak to [mental health hospital] to find out what the best course of action is re this
OIS log
For three of the 12 contacts, communication was simply to inform the MHT of an incident for their records. This exemplifies good practice concerning information sharing and up-to-date record keeping.
no stated incident or reason for the call for intel [intelligence] submission re the male & notification to local MH [mental health] team.
OIS log
The three remaining contacts relate to calls by the police to gain information about an individual’s current care. In one, the police needed to find out when a MHAA was going to be conducted, in the second, they needed information about the care of an individual’s partner, and the third related to confirming that a care package was in place with a long-term care team. An example of the police contacting the MHT for information about current care is provided below:
I have also spoken to [name] of adult social care who has passed Mr through to the long term care team. They are aware of [service user] as they were informed of his wife’s departure some two days ago. Awaiting call back from [name] of the long term care team to see what actions have been put in place.
OIS log
Being on the caseload of a care team did not seem to influence if the MHT or social services were called. For those contacts where the individual was on caseload (n = 350), police contacted the MHT in 43 cases (12%) (social services in eight logs). For those not on caseload at time of contact (n = 68), police contacted the MHT in seven logs (10%) (social services in one log).
Theme 3: authorisation of tasers
Tasers were authorised for two of the incidents but not deployed. Alcohol or drugs were not mentioned in either of those incidents. Violence was highlighted in one of the taser-related OIS logs. In one of the incidents, the individual was deemed to be a risk to themselves and others and, in the other, the service user was perceived to be at risk from others. As with the Section 136 and detention incidents, tasers were deployed when weapons were indicated. For the one contact where tasers were authorised for an individual in the sample, the incident relates to a call from the MHT asking for assistance in taking someone sectioned under Section 3 of the MHA to hospital:
from FIM [force incident manager], I understand social workers have no way of dealing with a male who could potentially cause harm with a knife. He has been asked to give the knife up but refused. The social workers have requested police assistance and raise concerns if not done sooner rather than later as he may go missing potentially with the knife. I will authorise Taser for the protection of officers and staff as this male has a knife and states it is for his protection.
OIS log
Theme 4: diversion from detention
For nine contacts, there was a discussion of potential response options relating to detaining the individual under Section 136 or arresting them for an offence. Discussions about Section 136 detentions were instigated by the MHT as an option for returning an informal patient into their care or to ensure that the individual was dealt with safely if their behaviour deteriorated:
. . . as mentioned previously they believe she is safe with a friend but asks if she is seen out and about during the night in a distressed state pls [please] could officers consider Section 136 – there are no immediate concerns and medical staff plan to do an assessment later today . . .
Progress notes
have phoned RP [reporting person] again to find out what they want us to do with the male when he is located. They initially stated for police to return him as he is a vulnerable adult but explained to him that we have now powers as such as he is an informal patient. they have asked if police could try to encourage him to come back to the ward – police can give [Place of safety] a call to see if they can come and collect him – they have also said that he is posing a risk to others/himself, he can be detained Section 136 and brought back that way
OIS log
During the latter incident, the police indicated that it was their responsibility to make the decision as to whether or not to detain under Section 136 and that a detention could not be directed by the MHT:
. . . units will decide if he is displaying sect 136 or not . . . they will not bring him in on it just because sig [street index gazetteer] suggest it.
OIS log
Similar to the log entry above, the following example involved consideration of how to deal with someone who is not engaging with the MHT and how police involvement can be used to achieve treatment for the individual:
AIO [all in order] here. female has MH [mental health] issues. Spoken to other residents on same floor but nothing heard by them. Night staff due in shortly but female is calm now and ok going back to her room . . . – call from Dr [name] to say they have attended her h/a [home address] (sig) [street index gazetteer] to do assessment on the female but she is not there – as mentioned previously they believe she is safe with a friend but asks if she is seen out and about during the night in a distressed state pls [please] could officers consider s.136 – there are no immediate concerns and medical staff plan to do an assessment later today
OIS log
In six logs, the possibility of arresting the individual for a substantive offence was mooted. In two cases, this was in an attempt to halt the individuals from making nuisance calls to the services.
this will need to be crimed and further updates ref [mental health] MH and capacity of female placed on crime. E-mail sent to officer requested this is crimed in line . . . I am speaking to local PCSO [police community support officer] – female will not have capacity and we will confirm this SS [social services]
OIS log
The following quote relates to the same log and provides a short rationale as to why the incident did not result in criminalisation; the individual was thought not to have the mental capacity to take responsibility for her actions:
this lady is ill, not a criminal
OIS log
In the second contact, related to nuisance calls, threat of arrest was used as a measure to reduce the volume of calls:
. . . nothing wrong with her. She claims swollen AMB [ambulance] needed x-ray. She does not. She said she will continue phoning for police and AMB. She has been told she will be arrested if she does, but she didn’t seem to care so may get more calls from her.
OIS log
For the other four contacts that made reference to the use of arrest, the use of police power was used as a way of encouraging engagement with mental health services or as an alternative if intervention by the MHT was not successful. The following extract reflects a discussion with the service user about the need to use police powers if they continued with non-engagement:
spoke with [MH (mental health) team] who has had no joy re MH assessment. She stated that the only option potential is to deal with [service user] with the crime. And possible assessment then. However she will be writing a letter to [service user] today stating that if there is no cooperation then it will be handed over to police.
Progress notes
This communication is potentially an example of local services meeting the recommendation from the Steven Hoskin serious case review, as ‘where a threshold for risk is crossed, non-engagement and non-attendance should not be a barrier to internal multi-disciplinary discussion and wider multi-agency liaison and consultation’. 55
One log gives an example of where intervention by the MHT and returning an individual to hospital would prevent a BoP, thereby removing the need to detain that person using police powers for the protection of others:
spoken to staff at [name] ward [mental health hospital] they are happy for [wife] to be returned to there as a place of safety-concerned if she remains at the location there will be a BoP
OIS log
Decision 3: decision to provide further support/joint management
Support during and after the incident was provided by the police, partner and third-sector agencies, or informally provided by family and carers. The main route of follow-up management apart from contact with the MHT or social services was to refer the incident to the NBT. Other referrals and follow-up methods included a referral to a DV officer and two referrals to housing officers to secure a property. Additionally, responding officers would:
-
add information to/create non-crime vulnerable adult records
-
ensure a family member/friend/carer was available to support the individual.
Framework analysis of decision to provide support and joint management
The decisions relating to providing follow-up support are discussed under the following headings:
-
referral to NBTs
-
joint management of individual
-
police aftercare.
Theme 1: referral to Neighbourhood Beat Teams
In 103 incidents, the contact was logged with the NBT for further action. Operators ‘actioned’ NBT intervention, which would then result in a follow-up telephone call, visit to the individual or an update of information in the log or non-crime vulnerable adult plan for the individual.
I have spoken with the r/p [reporting person], who states that she has had [service user] calling out to her from a vehicle. The r/p has stated that she does not wish to get [service user] in to trouble and does not want her arrested. The r/p has finally agreed to a mediation between the two parties with local NBT officers present to resolve the situation. I will email the NBM [neighbourhood beat manager] for the area to arrange a suitable time for this to happen.
OIS log
Referrals for NBT contact were mostly for welfare issues (n = 82). The remaining cases involved neighbourhood disputes (n = 8) and reports of alleged ASB and harassment (n = 13).
Theme 2: joint management of individual
The data for the 15 individuals in the non-detention group revealed joint management between the police and NHS as part of the resolution of an incident. As mentioned previously under Theme 2: information exchange, some joint management involved information sharing only, ensuring each agency was kept up to date with the individual’s latest care needs and their interactions with services.
For five contacts there were recorded interactions between the services to jointly manage the individual at the end of or after police contact. In the following example, a DV officer liaised with social services and created a log about an upcoming multiagency meeting. The officer details how their interaction with social services will inform the meeting and may aid joint management of the individual and their partner.
f/DVO [from domestic violence officer] – I have spoken to [name] who is the lead for adults safeguarding – he has arranged a meeting with [service user] doctors and CPN, etc. at [name] surgery at 2.00 pm Monday 16th may, it is hoped that at this meeting the GP’s will be forced into acting on ‘best interest’ with regard to [service user] and [husband] unfortunately as things are at the moment, [husband] makes a complaint, [service user] has no capacity, so is not arrestable, and then [husband] will do work with SS [social services] or doctors to protect himself. DVO will supply a detailed history to try to show the impact that this ongoing problem is causing all agencies.
OIS log
In another case, an officer liaised with a CPN before making a decision to issue a harassment warning. The CPN was able to give officers their opinion of the situation; officers issued the warning, but were aware that the harassment may have been two sided between the individual and a neighbour:
[service user] does have m/h [mental health] issues and is under CPN [name] of [mental health hospital] . . . I have spoken to [CPN] and she is aware of the ongoing issues between [service user] and [AP1; associated person 1]. CPN was under the impression the harassment was the other way round and it was in fact [service user] being harassed by [AP1] . . . harassment warning to be issued to [service user] and then [AP1] updated and intel [intelligence] to be input. But officers to be aware [service user] may make a counter allegation.
OIS log
The issue of intervention, whether by the police or MHT, was discussed in relation to lack of engagement by another individual. This led to a discussion of responsibility for the individual if they continued non-engagement with services:
I have spoken with [service user] who was at home with his mother. He is having delusional thoughts and seeing things. He is safe and well but flatly refuses to engage with the MHT. Unfortunately, mother is not strong willed enough to persuade him to see the MHT and has in the past been obstructive towards their intervention. No offences and no concern for [service user]’s welfare he is just a poorly man who will not seek help. – there is nothing we can do- the MH [mental health] team are the only people that can help him – but he is still refusing their help all resources leave scene/dispatch cancelled etc. Advise MH team no in log – and close plse [please] – OOH [out of hours] MHT have been advised and will pass this onto [EIT contact]
OIS log
The following example illustrates joint discussions about pursuing a criminal matter associated with another individual:
I have spoken with pc [police constable] [name] who was dealing with previous vulnerable adult matters concerning [service user] and [service user 2]. Message from switchboard stating that social worker phoned. I have attempted to contact him but he was not available, message left for him to call back. This matter is a historic report and as a result is not time critical. I suspect that it will be best dealt with by raising a non-crime vulnerable adult and progress matters in conjunction with social services. Have read log and agree that domestic side to be closed and none va [non-crime vulnerable adult] will address the issues alleged with multi agency input this matter is a historic report and as a result is not time critical. I suspect that it will be best dealt with by raising a non-crime vulnerable adult and progress matters in conjunction with social services.
Progress notes
In the final case where joint management was noted, the potential impact of police involvement in the management of an individual was discussed, and how this would impact on their health. This led to discussions with the police about suitable times and methods for approaching the individual to continue their investigation:
Tel call from [individual] this evening. Very tearful and initially it was very difficult to engage in conversation with him he is feeling very confused, scared and frightened and states he is struggling to cope with day to day living. He feels unable to leave his home for fear of his safety. He is also very worried about having to go to [custody suite] police station at 11 am in the morning. He isn’t sure why he is having to go but is convinced he will be going to prison for 5 years. Tried to reassure him but it was very difficult due to his distress. I am sending this to the CMHT as I am unsure what current support, if any, is being offered to [individual]
Theme 3: police aftercare
Examples of pastoral care provided by the police were recorded in some logs, reflecting actions beyond their normal duty of care, highlighting a compassionate and caring response on the part of some officers. Due to the vulnerability of the individual and the lack of available family or care support, in the following example, officers ensured the individual’s basic needs were met:
on leaving [service user] I ensured he was fed and watered by making him a cup of tea and a pot noodle snack.
OIS log
In another example of police aftercare, police took steps to ensure that an individual would be able to get to a police station for questioning and that an AA would be in place:
having read the updates Mr [service user] will need to be seen at a police station for the first response book completion. I have spoken to him and arranged to have him collected at 1000 in the morning as previously arranged the only difference being we will need to go and get him from around the corner. PS [police sergeant; name] has the matter in hand, [AP2; associated person 2] the friend will also be attending and can act as app. adult for the purposes of the booklet completion.
OIS log
Further to the above log, the police raised concerns about the care in place for this individual and highlighted that he may have been overlooked by services, despite potentially suffering domestic abuse. This case reflects good practice in relation to the recommendations of Bradley6 and the Steven Hoskin serious case review55 whereby support should be in place for individuals who may be missed because they are not detained and not associated with crime:
[name] has concerns for [service user]’s welfare, care & support whilst she is being dealt with by other agencies. It appears that [service user] maybe ‘going under the radar’ for care and support by all agencies. [service user] is unaware that [names from housing co.] are reporting this to the police. due to the difficulties this causes any approach the pol [police] make on the back of this call from [name], I have located this log and explained that I will ask units dealing, if they could use this log/call from the AP as a means to get [service user] to reveal the current circs [circumstances] he is living under in being a male victim of dv [domestic violence]?. I have also explained the need to continue their liaison with him and to use this as a means to encourage him to report to the pol and other supported agencies in Cornwall that deal with male d/v. am aware retired Insp. [inspector] [name] dealt with this very issue.
OIS log
Resolving a neighbour dispute constituted a follow up measure for another individual and involved linking with the housing officers to manage the situation:
both of [neighbours] complaints are in the process of being dealt with by pc [police constable] [name] and [name] – housing . . . [service user] is due in for an interview next Tuesday. [service user] discussed her and her sons concerns and increasing anxiety linked to allegations from [address]
OIS log
Decision 4: decision to conduct a Mental Health Act assessment
Five of the 15 individuals received a MHAA during the research window. Three of these were directly related to the police contacts initiated by a MHT or social services for assistance in escorting the individual to hospital for a MHAA, or to return an AWOL individual to receive a MHAA. Thus, the decision to conduct a MHAA did not result from police contact in these three cases, but was the reason for that contact. Of the remaining two cases, one had no police involvement and was assessed under the MHAA after presenting at general hospital and being assessed by an APL team as requiring a MHAA. The final case involved a police contact related to an individual who was telephoning the police, ambulance, and mental health services stating that she was suicidal. All five MHAAs resulted in detention under the MHA (two under Section 3 and three under Section 2).
Framework analysis of decision to conduct a Mental Health Act assessment
The one case that resulted from multiple contacts with the police and partner agencies is explored in more detail below, as it illuminates a case where contact was not instigated by the MHT or social services and shows an effective multiagency response to an individual’s needs. It provides a good example of where risk is effectively transferred between services, and the rationales for taking certain actions are clearly recorded. The initial contact with the police was made by the individual calling and stating that she was suicidal but did not feel supported by the MHT:
RP [reporting person] states that she has been calling [mental health hospital] on [Tel no] to try and speak to her crisis worker ‘[name]’ she states that the staff on the SWB there have been very aggressive with her on the phone – even though she is feeling suicidal she states that she explained to them how she was feeling and apparently the female on the SWB [switchboard] put the phone down on her stating ‘don’t talk about it go and do it’. Caller is even more distressed now and feeling even more suicidal.
The operator liaised with an officer on patrol who indicated that the individual may be attention seeking, an opinion based on prior experience of the caller. Officers were dispatched to the incident. Awareness of the caller’s mental health issues led to a call to a MHT made by the ambulance crew also on the scene of the incident:
paramedic is going to speak to [mental health hospital] to find out what the best course of action is re this . . . paramedics spoken to ooh [out of hours] doctors to make twds [towards] so that they can section her
OIS log
Further to contact made by the ambulance crew, the police called the MHT to find out how long it would take for a doctor to attend the incident. This section in the individual’s progress notes also highlights intra-agency communications amongst the MHTs:
Pls [please] call [mental health hospital] – do they have any idea of ETA [expected time of arrival] for Dr to attend re this? – speaking to [mental health hospital] they advise Dr [name] has called the home treatment team regarding female. I am being put through to him now he is awaiting a call back from MH [mental health] team to attend and meet him there . . . he has spoken to [mental health hospital] switchboard and they will get the MH team to call him urgently.
Progress notes
Through joint information and guidance from the paramedics, MHT and Serco, the police made the decision to leave the individual in the care of friends. Provision of advice that the police could leave the scene was corroborated in the progress notes:
will update paramedics and will leave female in the care of her friends who will call 999 should she need help in the night.
OIS logs
The following day, further communication was made by the MHT to inform police they had attempted to conduct a MHAA at the individual’s home address. Keeping the police informed of the progress of the case is an example of appropriate information sharing between services in action:
pls [please] see update – Dr did attempt assessment at h/a [home address] no immediate concerns and will try again later
OIS logs
The final decisions concerning this individual were captured in her progress notes. Due to the individual’s presenting behaviour, and the fact that informal information provided by her father indicated that she was a substantial risk to herself, she was detained under Section 2 of the MHA.
she [individual] stated she was quite happy to talk with me so I then asked to speak again to the paramedic. I agreed that he and the police could leave and that I would continue to make contact by phone with [individual] overnight and assess the need for any more pro-active face to face assessment or MHA. At this point both the paramedic and police left . . . I spoke again with [individual] who still remained pleasant and talkative but she would not agree to utilise any PRN [pro re nata: when required] medication she may have had, and felt she would not sleep. She spoke again about wishing to see a priest. I asked [individual] about options for the night of how she might stay safe and included within that an offer for hospital admission which she refused. She agreed that she would not go out again tonight and that I could call her back later. I then called her father whose number had been passed to me from switchboard. He expressed his concerns for [individual]’s current situation. He reflected that in his experiences, her reassurances of not having intentions to harm herself or take overdoses are often not adhered to and he ultimately requested for a mental health act assessment to be carried out on [individual] tonight. I therefore discussed the situation with AMHP [social work 2] and on call consultant – dr. [medical 13] who felt that there was now no other option but to take on a MHA assessment tonight. Alongside dr. [name] they have arranged to meet [individual mother] (nearest relative) at [individual]’s home at 00.30 this morning.
Progress notes
Summary
In summary, the ‘non-detention’ group, although representing a small number of individuals, represented a large number of varied contacts with the police that in some cases resulted in effective interagency communication and management of the individual. Unlike the Section 136 and custody analysis, the non-detention analysis was necessarily weighted towards the early decisions made by the operator and response officer as decisions concerning detention were not applicable. The themes emerging from the data were more fluid and not easily defined due to the lack of national and local policy and protocol aimed at this group. Findings indicate that local services have attempted to meet the recommendations made by Bradley, namely to ‘identify and support people in the community with mental health problems or learning disabilities who may be involved in low-level offending or anti-social behaviour by establishing local contacts and partnerships and developing referral pathways’. 6 This was exemplified by the discussions around joint management decisions on care and management, and information sharing to update each other.
Importantly, the 15 service users in this group could represent individuals where diversion is working effectively, as they have not reached detention level contact in the research window. Equally, they could be seen as being on the cusp of detention and therefore need to be carefully monitored to avoid contact with services escalating. The findings from this group show that police contact does not necessarily involve a risk to self and others requiring immediate response, but does highlight where concern for welfare can be managed effectively by both services. Finally, they also revealed the potential pressure that one individual can put on the services through misplaced calls creating implications for what are already stretched resources, and how this pressure can be mitigated through good interagency collaboration.
Although these findings suggest that more work needs to be done in relation to access to and consistent use of PNC and NHRR warnings relating to individuals’ mental health, in light of the recommendations of the Steven Hoskin serious case review,53 they indicate genuine attempts at joint referral pathways in meeting the needs of this particular group of individuals with EMHN.
Health economics component
Background
The aim of the economic component of this study was threefold: to conduct a cost analysis, estimating the total costs of clients moving though the current pathways based on observed criminal justice and health service activity identified through a case-linkage exercise; to use these data to create a decision-analytic model (using a decision tree) to map an approximation of client progress through criminal justice services complete with attached costs and probabilities; and to use this, combined with recommendations from key policy documents, to create a series of alternative models that represent the estimated potential CJS cost impacts of enhancements to current practice on decision-making processes and client journeys. Such scenario modelling can prove very informative for service/policy evaluation and appraisal in the absence of ‘harder’ evidence on cost impacts (see McCrone et al. 59 for an example).
Cost analysis of case sample
Methodology
Perspective
Total costs were calculated from a service provider perspective, including the mental health, social and criminal justice services. The total costs of mental health and social care services were computed for each participant by combining the following costs: inpatient services, client contact (including contacts at community clinics, the client’s home, at hospitals, GP surgeries, public places, custody centres, supported/residential/nursing housing, and contacts by phone), meetings in the absence of client and patient assessments.
Criminal justice services were defined in this study as contacts with the police (i.e. telephone calls to the police, police attendance at incidents, arrest and removal to a place of safety under Section 136). Police attendance was defined as at least one police officer attending an incident. Court proceedings and prison were not able to be included in this study. The total costs of contacts with criminal justice services were computed for each participant by combining the following costs: initial contact costs (cost of contacting the police, police attendance, ambulance attendance at incident), custody costs (length of stay in custody suite, MHAAs, HCP triage, FME, AMHP, hospital attendance) and other costs (transport, follow-up calls by police and escorting). Total costs per participant were computed by combining total mental health, social care costs and criminal justice services costs. Contact with the police was defined as any incident which was logged by OIS.
Due to the novel and complex nature of the study and the population, only major cost drivers were included, therefore providing an estimate of the general order of magnitude of cost impacts linked to criminal justice pathways. Thus, for CJS costs, costs such as police attendance, ambulance attendance, or custody time (see Appendix 5 for full list) were included, but minor contributors to total costs that required more detail than was available in files, such as communication within the CJS or liaison with other agencies, were excluded.
Data were collected using the case-linkage method (see Case-linkage study method). Mental health and social care data were collected from RiO, the electronic patient record system used to support Mental Health and Learning Disabilities services. 60 RiO covers mental health service use only. All data were collected from case records. RiO data fields used for the purpose of data extraction included the client diary of appointments, progress notes which detail non-diarised contact, referral and inpatient records, assessment records and MHAA outcomes. CJS data was collected via OIS and NSPIS custody records. Data were extracted on an incident basis according to actions taken (number and type), duration of incidents and associated actions and resource allocation.
Data collection and subsequent costing was for a 1-year retrospective research window within the period 18 April 2011 to 8 June 2012 depending on the date of the index police contact of each case (data were collected for 12 months following index police contact in the dates set for the clinical audit).
As mentioned above, this novel and complex method of case-linkage required new approaches to data collection in a criminal justice context. Therefore, the application of standard questionnaires or data extraction tools, as commonly used for economic analysis of this type, was not possible. Instead, spreadsheets were created to record service use that allowed for the addition of new services to be added as they became apparent from case records identified through the case-linkage exercise (Tables 22 and 23).
| Health and social care use | ||||
|---|---|---|---|---|
| Person 1 | Day 1 | |||
| Person 1 | Day 2 | |||
| Person 1 | Day 3 | |||
| Person 2 | Day 1 | |||
| Person 2 | Day 2 | |||
| Person 2 | Day 3 | |||
| CJS use | |||||
|---|---|---|---|---|---|
| Person 1 | Incident 1 | ||||
| Person 1 | Incident 2 | ||||
| Person 2 | Incident 1 | ||||
| Person 2 | Incident 2 | ||||
| Person 2 | Incident 3 | ||||
All costs were reported in pounds sterling at 2011/12 prices. Where prices from previous years were used, these were inflated to 2011/12 prices. Unit costs were applied to resource use data to calculate total costs per client. Unit cost estimates, their sources and any assumptions made for their estimation are detailed in Appendix 5. Unit costs were a combination of national and local depending on availability. Discounting was not necessary as all costs related to a 1-year period.
Data were analysed using SPSS for Windows (version 20) and Stata (version 11; StataCorp LP, College Station, TX, USA). Despite the skewed nature of the cost data, the mean and standard deviations (SDs) for cost data are reported as recommended by Barber and thompson. 61 Interquartile range (IQR) and 95% confidence intervals (CIs) of cost data [obtained by non-parametric bootstrap regressions (1000 repetitions)], bias corrected and accelerated are reported as recommended by Efron. 62 Predictors of costs were examined using bootstrap regressions (ordinary least squares) of costs and the following predictors: age, gender, marital status, living situation, ethnicity, employment status, referral status (long term vs. short term) and residence (out of county vs. in county).
Resource use data were collected from electronic records for specific clients. For the CJS data there were occasions where number of police in attendance was recorded but the duration of attendance was missing (34 incidents, 4% of all incidents). In these circumstances, the mean duration for those with a police attendance was imputed for those with a missing value. Within the mental health and social care data, there were several occasions (16 incidents, 15% of clients) where there was information that meetings in the absence of a client had occurred, but the details of the professionals in attendance of those meetings were missing. In these cases, the cost of two nurses was assumed to reflect the level of service contact that would have taken place. In several cases there was information that the client met with a HCP, but there was missing information on the details of the professional (111 incidents, 7% of all incidents). Here, a mean average cost of health-care contacts for observable cases was used as a substitute cost.
Results: cost analysis of case sample
Service use data from the case-linkage study was available for 55 clients (inclusive of those where some data linkage was required).
Resource use
Health care
Of the 55 clients, all had at least one contact with mental health and social care services over the 1-year period. Thirteen (23.6%) had at least one inpatient stay. For these clients, the mean number of days as an inpatient over 1 year was 89.85 (SD 91.50) days. The range was 5–310 days.
Of the 55 clients, 49 (89.1%) clients had at least one client assessment during the 1 year, 52 (94.5%) clients had at least one meeting with a professional and 37 (67.3%) clients had at least one meeting between professionals in the absence of the client.
Criminal justice services
Of the 55 clients, all 55 had at least one contact with criminal justice services over the 1-year period. The number of contacts (separate incidents) with criminal justice services ranged from 1 to 293. The median number of contacts was seven (IQR 3–14). One client was recorded as having 293 contacts (incidents recorded on OIS that did not result in a detention), which was unusually high compared with the other clients included in the sample. The next most frequent number of contacts was 35. For the outlier client, almost 90% of these contacts (261 contacts out of 293) had minimal CJS resource use. This was either a call to police which required NFA, or a call to police that required a follow-up call from the police.
The combined number of contacts with police for the whole sample was 783. Of these, 461 (58.9%) required at least one police officer attendance. One client required a total of 47 police officers in attendance for one incident. This was a fairly unusual client since the next most frequent number of police officers in attendance was 21. Of those incidents that had a police officer in attendance, the median was three officers (IQR 2–5).
Of the 783 contacts, 98 (12.5%) involved some time in custody. Of those, the median time was 8 hours 38 minutes (IQR 4 hours–15 hours 30 minutes). The range was from 15 minutes to 41 hours 30 minutes. Twelve clients (12.2%) had a MHAA.
Costs
Health care
Total mental health and social care costs were non-normally distributed and positively skewed (Figure 21). The mean cost per person over the 1-year period was £10,812.08 (SD £23,714.39; IQR £386.33–6335.31; 95% bootstrapped CI £6054.86 to £19,726.27). The range was £41.70–108,434.80.
FIGURE 21.
Distribution of total mental health and social care costs.
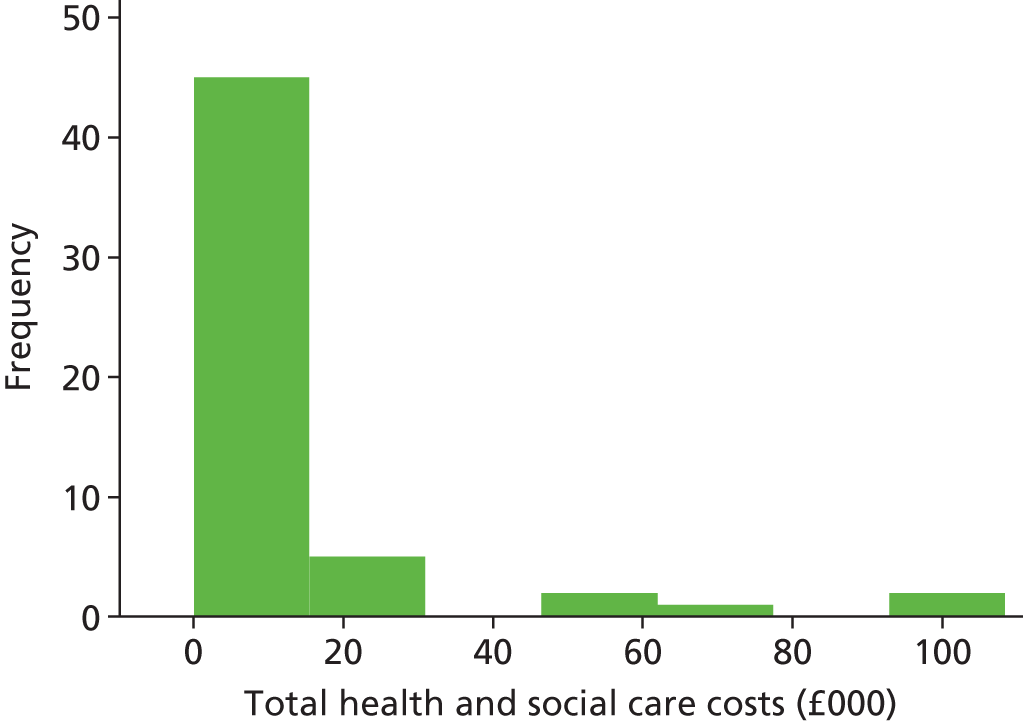
Figure 22 shows the mean proportions of mental health-care costs. It shows that the major cost contributor was inpatient services, which accounted for 76% of the total.
FIGURE 22.
Mean proportions of mental health-care costs.
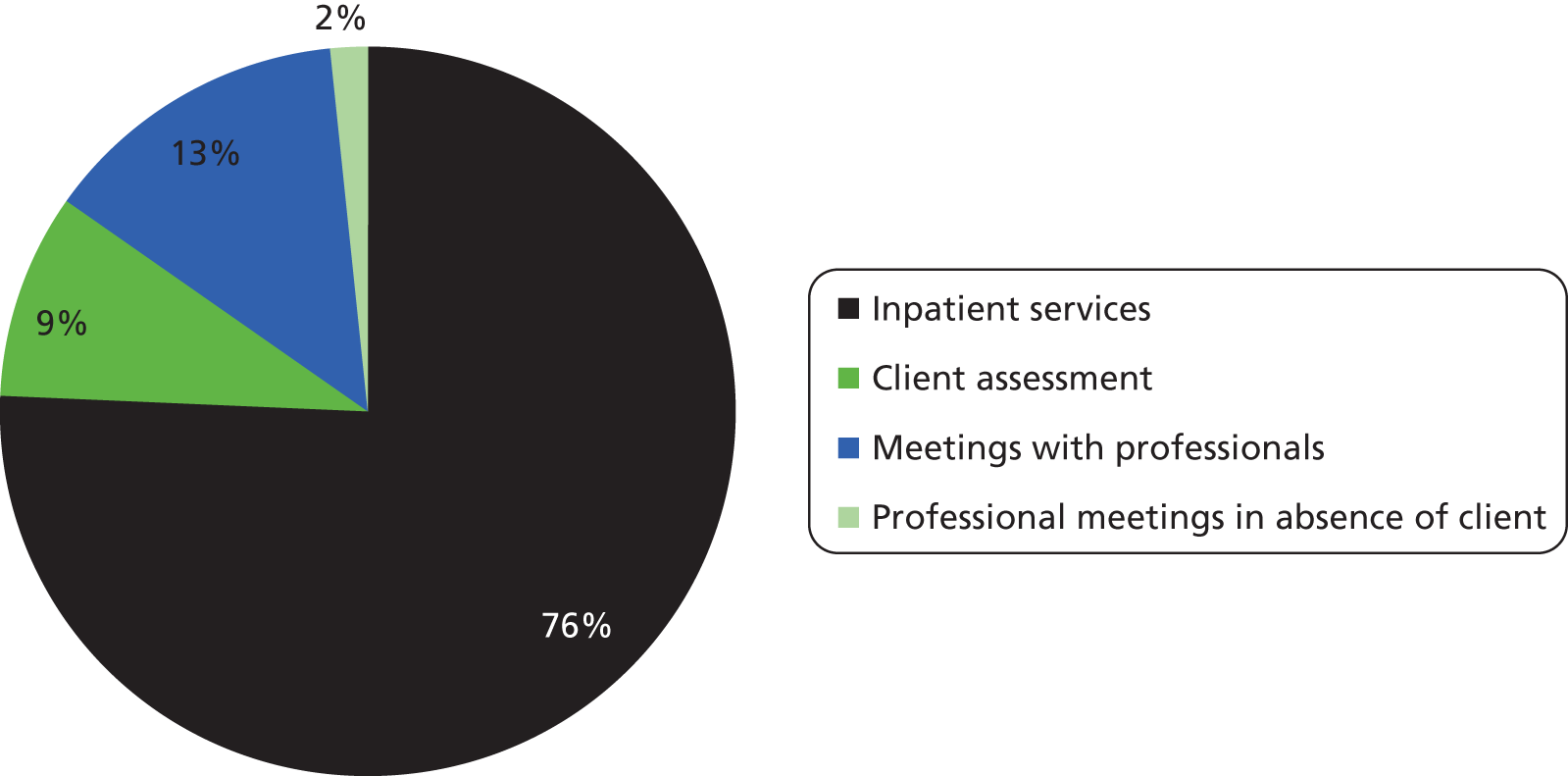
Criminal justice system
Total costs associated with criminal justice service contacts were also non-normally distributed and positively skewed (Figure 23). The mean cost per person over the 1-year period was £4551.88 (SD £4460.90; IQR £1359.99–7019.72; 95% bootstrapped CI £3551.48 to £6058.47). The range was £42.48–23,840.88.
FIGURE 23.
Distribution of total costs associated with criminal justice services.
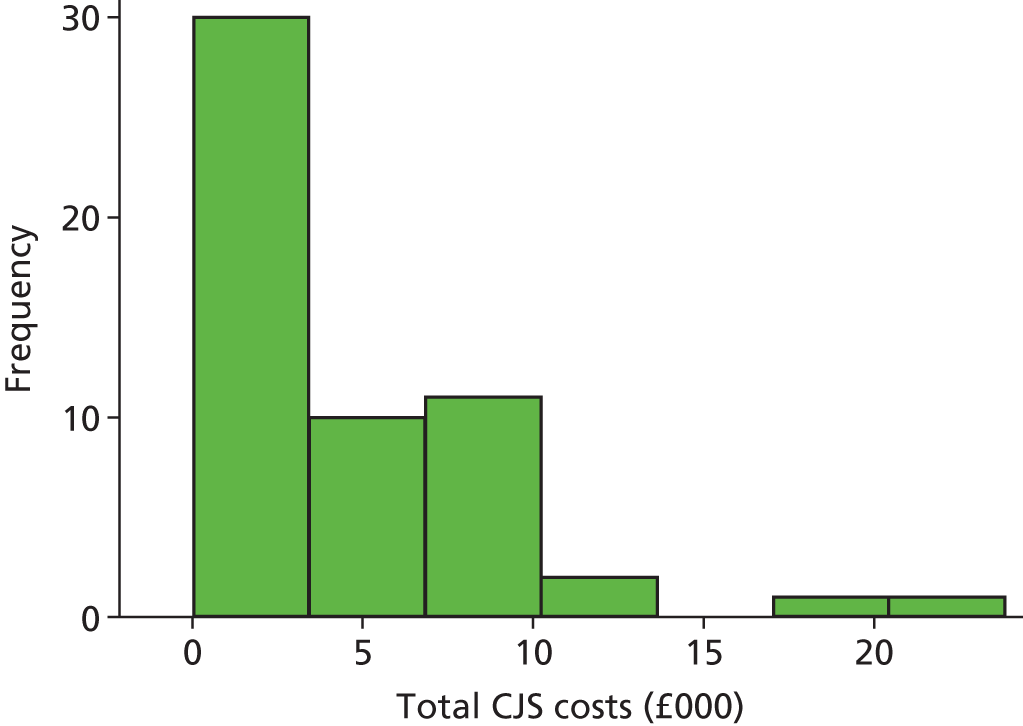
Figure 24 shows the mean proportions of criminal justice service costs, examined by incident rather than by client. It shows that the major cost contributor was police attendance at incidents, accounting for 59% of total costs. This was followed by custody costs.
FIGURE 24.
Mean proportions of CJS costs.
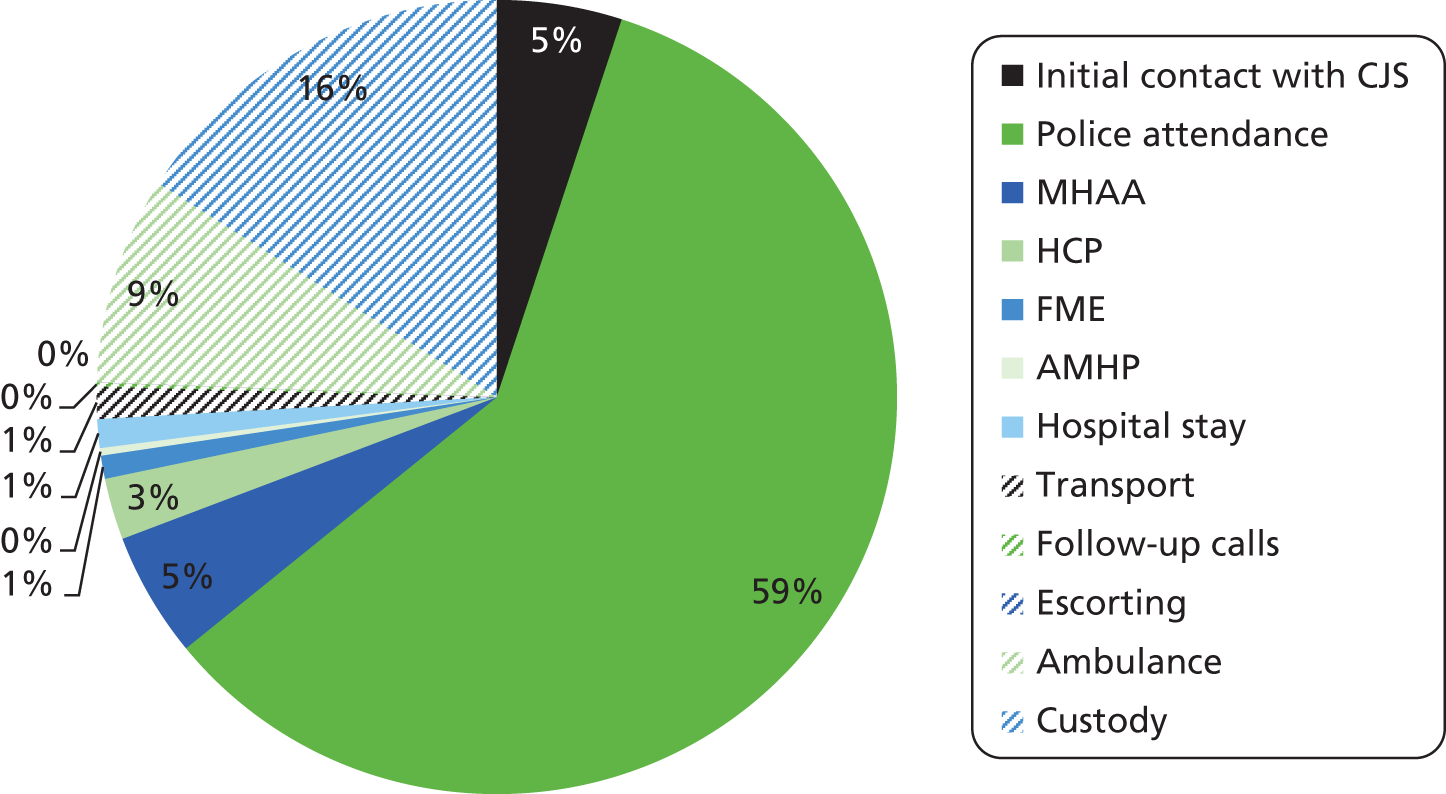
Total costs
Total health and social care costs were non-normally distributed and positively skewed. The mean cost per person over the 1-year period was £15,363.95 (SD £24,007.21; IQR £2647.46–14,961.50; 95% bootstrapped CI £10,688.52 to £24,960.44). The range was £529.30–112,862.70.
Predictors of cost
A univariable analysis of factors associated with cost based on baseline characteristics was undertaken. Table 24 shows that the only variable associated with costs was whether or not the client was a long-term referral, with short-term referral having a higher mean difference in costs £12,849.98 (95% bootstrapped CI £3944.91 to £29,191.59).
| Predictor | Mean difference (£) | Bootstrapped 95% CI (£) (bias corrected and accelerated) |
|---|---|---|
| Age | ||
| Age | 216.55 | –290.18 to 1270.48 |
| Gender | ||
| Male | – | – |
| Female | 708.99 | –10,270.25 to 15,854.59 |
| Marital status | ||
| Single/divorced | – | – |
| Married | 1868.04 | –14,147.99 to 43,911.99 |
| Living situation | ||
| Hostel/assisted living/other | – | – |
| Client home (privately owned/rented) | 2799.10 | –31,558.78 to 15,322.20 |
| Ethnicity | ||
| White British | – | – |
| White other | 2543.56 | 0 to 10,469.58 |
| Employment status | ||
| Unemployed | – | – |
| Other | 2669.42 | –9330.46 to 27,248.79 |
| Referral status | ||
| Substantive referrals | – | – |
| Non-substantive referrals | 12,849.98 | 3944.91 to 29,191.59 |
| Residence | ||
| Out of county | – | – |
| In county | 10,137.70 | 0 to 21,070.38 |
Pathways analysis
Methodology
A decision-analytic model was built based on the current pathways through criminal justice services experienced by people with mental health problems. The model is, by necessity, a simplified representation of services and thus only includes the key components of the pathway. As such, it focuses on the main cost drivers, which are contacts with CJS, police attendance, custody, and assessment; plus the inpatient element of the health and social services pathway. The inclusion of inpatient costs as the only health and social services cost was thought to be valid as inpatient services have previously been found to be the major cost driver in mental health service costs. 59 Additionally, all clients were known to mental health services at the beginning of the study and were therefore likely to be in contact with community care services already. Therefore, any referral to community mental health-care services was treated as a continued cost rather than a new additional cost. The costs used to generate pathway costs, detailed in Appendix 5, are a combination of existing unit costs and activity costs generated through the case-linkage exercise (Tables 25–27).
| Item | Unit | Unit cost (£, 2011/12 prices) | Source | Assumptions |
|---|---|---|---|---|
| Section 136 suite | Per occurrence | 1388 | DH65 | Cost as an acute psychiatric ward for 1 bed-day plus a MHAA |
| MHAA | Per occurrence | 1059 | Curtis64 | Based on the assumption of 3 hours for two Section 12 doctors plus an AMHP |
| HCP triage | Per occurrence | 92 | Curtis64 | Assumed 1 hour; cost at the mid-point of an advanced nurse and FME as it could be either |
| FME | Per occurrence | 132 | Curtis64 | Assumed medical consultant for 1 hour |
| Admission | Per admission | 13,719 | DH65 | Based on the unit cost of £329 per acute psychiatric care bed-day multiplied by the average number of days per admission in this sample = 41.7 days |
| Street triage | Per contact | 53 | Curtis64 | Costed as assertive outreach; per hour of patient contact; assuming 1 hour of contact |
| Link worker | Per contact | 68 | Curtis64 | Assumed mental health nurse; per hour of face-to-face contact; assume 1 hour contact; excluding qualifications |
| Item | Unit | Unit cost (£, 2011/12 prices) | Source | Assumptions |
|---|---|---|---|---|
| Time in custody for those who were on a Section 136 and taken to custody | Per custody occurrence | 497 | Chief Inspector Mark Bolton, DCP, 2013, personal communication | Cost based on the mean number of hours in custody for those who were under a Section 136 and taken to custody: 12.42 hours multiplied by the unit cost per hour in custody of £40 |
| Time in custody for those who were arrested | Per custody occurrence | 384 | Chief Inspector Mark Bolton, DCP, 2013, personal communication | Cost based on the mean number of hours in custody for those who were arrested: 9.60 hours multiplied by the unit cost per hour in custody of £40 |
| Item | Unit | Unit cost (£, 2011/12 prices) | Source | Assumptions |
|---|---|---|---|---|
| Cost of police attendance for those who were on a Section 136 | Per occurrence | 495 | DCP July 2013 | Cost based on the mean number of minutes of total police attendance per incident for those who were detained Section 136: 510.63 minutes multiplied by the unit cost per minute for a police officer of £0.97 |
| Cost of police attendance for those who were arrested | Per occurrence | 457 | DCP July 2013 | Cost based on the mean number of minutes of total police attendance per incident for those who were arrested: 471.55 minutes multiplied by the unit cost per minute for a police officer of £0.97 |
| Cost of police attendance for those who were not arrested or detained Section 136 | Per occurrence | 267 | DCP July 2013 | Cost based on the mean number of minutes of total police attendance per incident for those who were not arrested or detained Section 136 but did have police attend the incident: 275.54 minutes multiplied by the unit cost per minute for a police officer of £0.97 |
Probabilities for the decision tree estimate the proportion of clients who follow specific cost-generating pathways subsequent to key decision points in the system. A model for current care pathways was based on data collected as part of stage 2 (case-linkage). Probabilities were determined by calculating the proportion of clients moving through each arm of the pathway based on all incidents. Although there were only 55 clients in the study, the clients had a total of 783 incidents, from which the probabilities were calculated (see Appendix 5).
Probabilities used in the modelling of enhanced pathways of care were based on assumed deviations from current probabilities observed for the existing standard pathways and were informed by policy recommendations or changes to practice in Cornwall that have been adopted or are currently being advised. One-way deterministic sensitivity analyses were used to assess the sensitivity of conclusions made about the cost of new care pathways to changes in key assumptions made about cost and probabilities.
Results: pathways analysis
The following pathway analyses examine the standard pathway at the time of the study (model 1: options within what could be considered ‘care as usual’) and pathways based on actual or potential practice enhancements (models 2–4). These enhancements were selected due to changes in local practice since data collection (models 3 and 4); imminent changes to local practice (model 2) and recommendations from the Bradley report6 (model 4).
Model 1: standard pathways at time of study
The standard care pathway at the time of the study is shown in Figure 25. The decision-analytic model indicates that a person who enters the pathway had an average cost for that incident of £521.63. For 100 people entering the pathway, the estimated cost was £52,163. This is much lower than the average cost in the costs analysis section above, because the modelling is based on each incident whereas costs reported in the cost analysis were based on the cost per client for a year.
FIGURE 25.
Model 1: standard pathways at time of study. S12, Section 12; S136, Section 136.
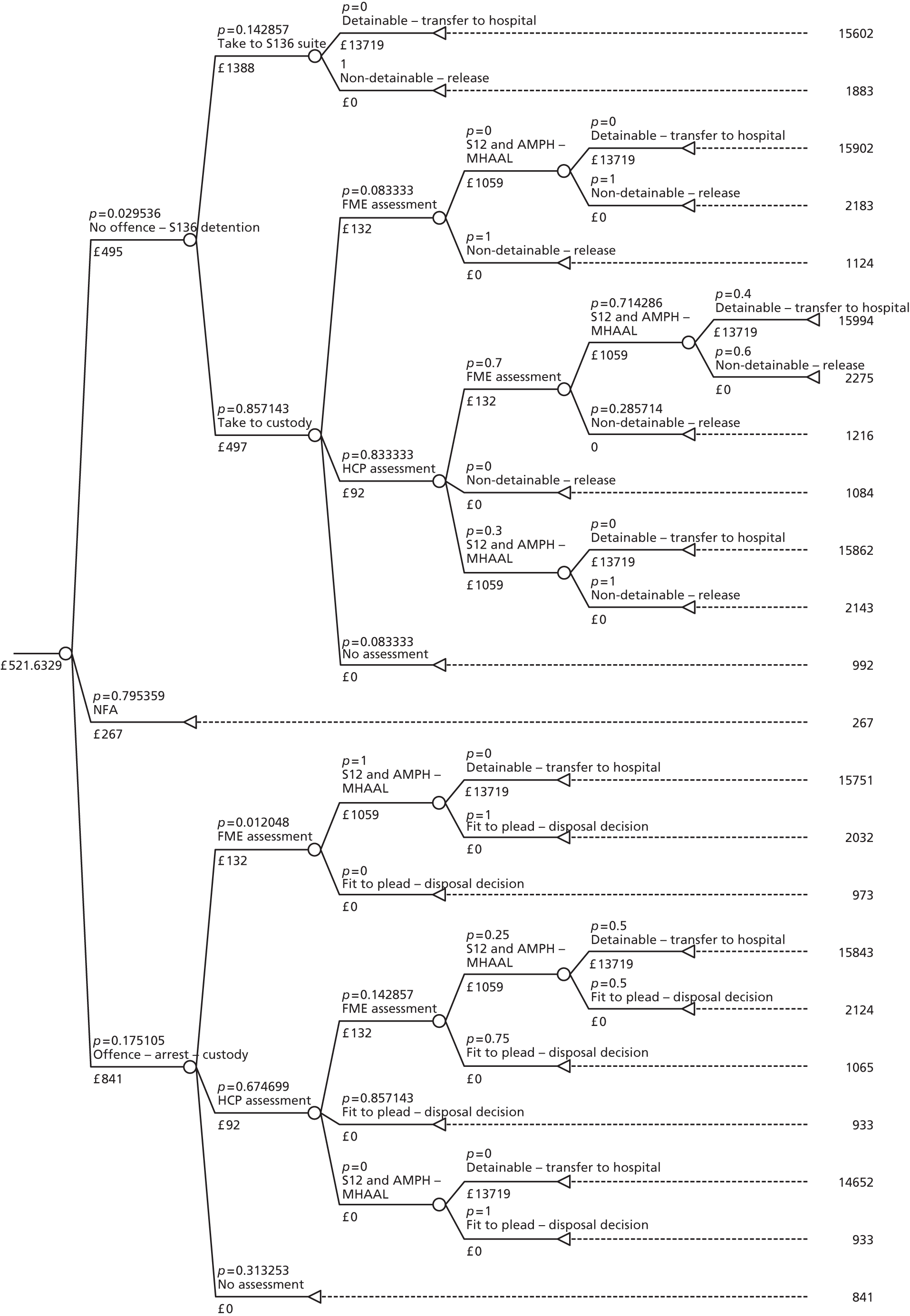
Model 2: standard pathway plus enhancement of street triage
The standard pathway of care plus enhancement of street triage is shown in Figure 26. A recent press release from the government63 described the new concept of street triage, which involves mental health nurses accompanying officers to incidents where there is an indication that someone is in need of mental health support to provide assessment, care and treatment as quickly as possible. Initial pilots show that street triage can help keep people out of custodial settings thus reducing the demands on police time. Based on the modelling, it was estimated that the cost of each police attendance would increase as a consequence of the additional cost of a street triage contact, estimated at £53 per hour of patient contact (costed as assertive outreach, assuming 1 hour of contact64). The model was based on the assumption that the street triage would have no effect on the number of incidents in which the police took NFA or that resulted in the arrest of the client. It was also based on the assumption that the probabilities of going to a Section 136 suite or custody would be halved, and that half of clients entering through that arm of the pathway would avoid being detained Section 136 and be referred to appropriate services via street triage contacts. It is important to note these are assumptions based on an informed judgement as to the likely impacts of street triage and not on any direct evidence as to how this is likely to impact on policing and other criminal justice activity.
FIGURE 26.
Model 2: standard pathways plus enhancement of street triage. a, Probability missing. S12, Section 12; S136, Section 136.
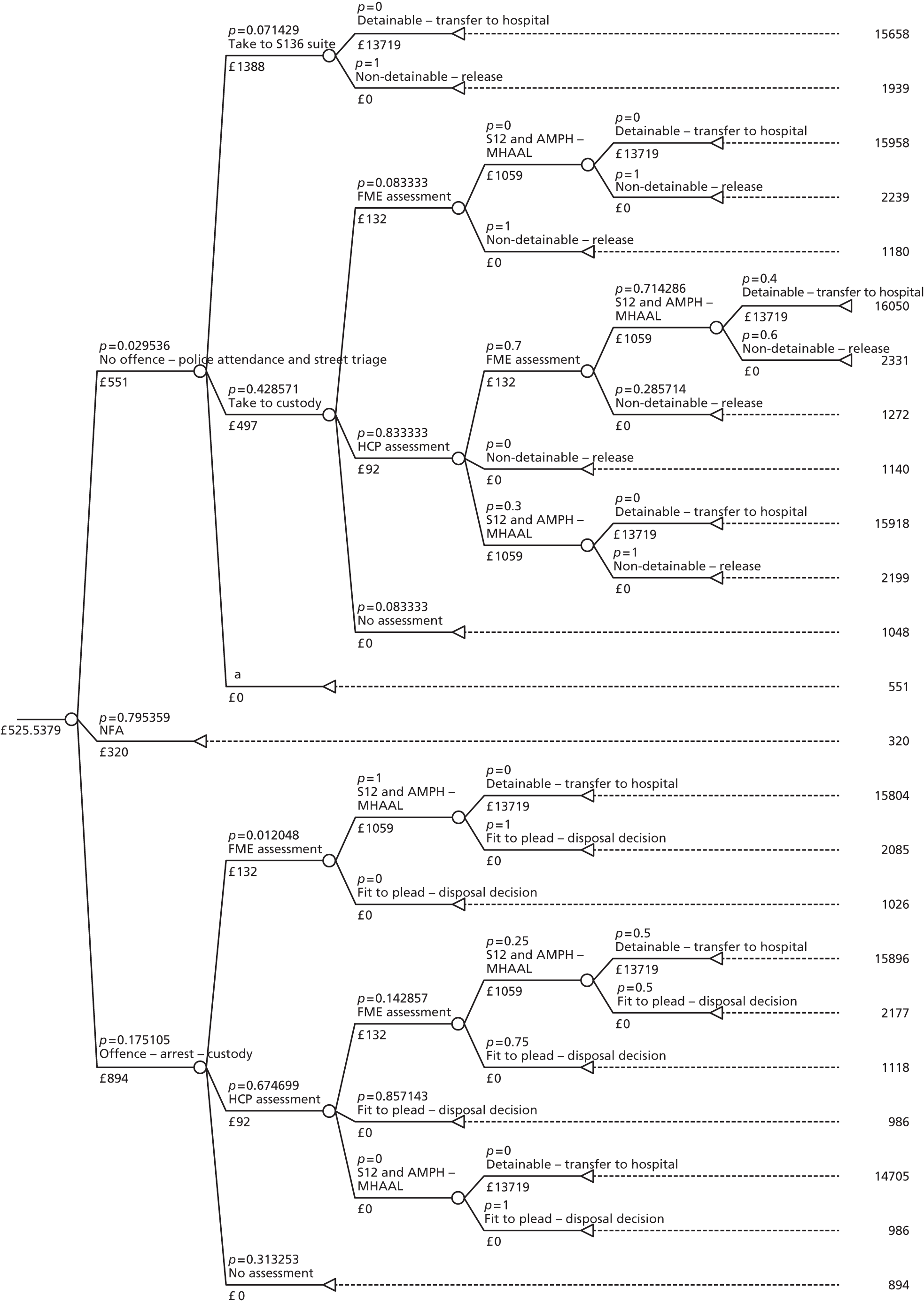
Given the assumed costs and probabilities, the average cost per incident was £525.54 compared with £521.63 in the standard pathway. For 100 people entering the criminal justice pathway, the estimated cost was £52,554 compared with £52,163 in the standard pathway. This represents an increase in costs of less than 1% compared with the original standard pathway. If the probability of a client entering the street triage referral arm was reduced to 0.2, the average cost per incident increased to £555.05. For 100 people entering the pathway, the estimated cost was £55,505. This was an increase of 6% in comparison with the original standard pathway. A further sensitivity analysis was conducted assuming street triage only influenced entry into custody via a Section 136, and not through entry into Section 136 suite. The probability of a client entering the Section 136 suite arm of the pathway was kept at the standard pathway value of 0.14 (to two decimal points), the probability of entering the custody – Section 136 arm of the pathway – was increased to 0.69 (to two decimal points) and the street triage referral arm was reduced to 0.17 (to two decimal points). This is equivalent to street triage reducing those taken to custody on a Section 136 by 20%. Based on these assumptions, the average cost per incident was increased to £556.22. For 100 people entering the pathway, the estimated cost was £55,622, giving an increase of 6% compared with the original standard pathway.
A further sensitivity analysis was conducted based on the finding from the data that of all those who are put on a Section 136, only 25% end in a detention with the other 75% going through the pathway but not ending in a detention. If street triage were to prevent the 75% who do not end in detention from entering the Section 136 arm, the average cost per incident would be £500.95 compared with £521.63 in the standard pathway. For 100 people entering the criminal justice pathway, the estimated cost was £50,095 compared with £52,163 in the standard pathway. This is a reduction of 4% on the original standard pathway.
Although in each of these analyses, street triage is assumed to reduce either the number of cases entering custody on a Section 136, or the number of cases entering custody on a Section 136 plus the number of cases being taken to a Section 136 suite, the reduction in costs that result from this are not great enough to offset the added cost of street triage. However, at this individual resource level, the estimates used in this report suggest that the introduction of street triage will not increase costs dramatically, even if substantive changes are made to key assumptions in the model that drive costs.
As with all decision-analytic models, there are a number of limitations that are discussed below.
Model 3: standard pathway plus enhancement of Mental Health Act assessments for all Section 136 detainees
The standard pathway of care plus enhancement of MHAAs for all Section 136 detainees is shown in Figure 27. The figure shows that the need for FME and health-care practitioner assessment has now disappeared as all Section 136 clients have a full MHAA. The current probability of detention was estimated on the basis of information from the standard pathway on the numbers of clients being detained or not in the entire custody – Section 136 arm (0.17 probability of detainment vs. 0.83 probability of non-detainment). Therefore, the only change in this model compared with the standard model is that the ‘taken to custody’ arm has now been reduced to reflect that all cases receive a MHAA and this leads to detention or not. Given the assumed costs and probabilities associated with MHAA enhancement, the average cost per incident was £526.40 compared with £521.63 in the standard pathway. For 100 people entering the pathway, the estimated cost was £52,640 compared with £52,163 in the standard pathway. This was an increase of less than 1% compared with the original standard pathway.
FIGURE 27.
Model 3: standard pathways plus enhancement of MHAA for all Section 136 detainees. S12, Section 12; S136, Section 136.
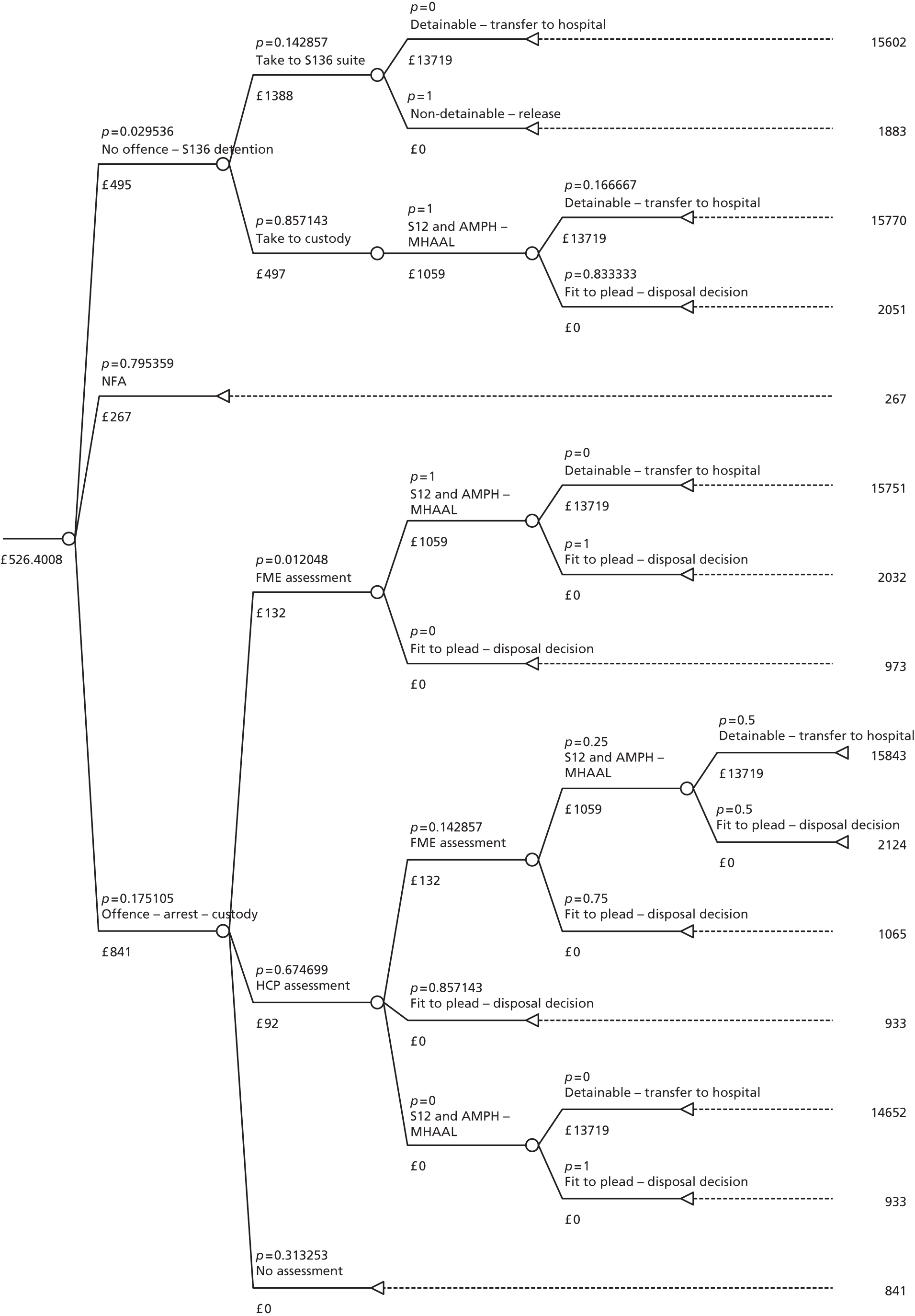
A sensitivity analysis was conducted that assessed how much the costs of this new pathway would change if it were to also include the cost of contact with an FME in all custody cases as well as the cost of a MHAA. This was included as it reflects practice in Cornwall, and resulted in an average cost per incident of £529.74. For 100 people entering the pathway, the estimated cost was £52,974. This was 2% higher than the original standard pathway. A further sensitivity analysis was conducted that included the cost of contact with an FME and a HCP in all custody cases as well as the cost of a MHAA. This resulted in an average cost per incident of £532.07. For 100 people entering the pathway, the estimated cost was £53,207. This was also 2% higher than the original standard pathway.
Similar to street triage, the estimates used suggest that the introduction of MHAAs for all Section 136 detainees would not increase costs dramatically, even after allowing for the inclusion of additional activities as part of this pathway. Limitations are discussed below.
Model 4: standard pathway plus enhancement of link worker at custody outreach level
The standard pathway of care plus the enhancement of a link worker at the custody outreach level is shown in Figure 28. This enhancement is developed from a number of documents, most notably the Bradley report, which states that ‘All police custody suites should have access to liaison and diversion services’. 6 Figure 28 shows that the link worker only covers clients in custody on an arrest as this is what is currently being implemented in Cornwall. The link worker contact has been estimated at £68 per hour of face-to-face contact (costed as a mental health nurse; assuming 1 hour of contact, excluding qualifications64). This cost has been added to the cost of arrest assuming every case will be checked as being known to mental health services and it is assumed to require 1 hour of face-to-face contact with a client and offered contact with the link worker. No changes to probabilities have been made. Therefore, the only change in this model from the standard model is the additional cost of a link worker. The average cost per incident was £533.54 compared with £521.63 in the standard pathway. For 100 people entering the pathway, the estimated cost was £53,354 compared with £52,163 in the standard pathway. This led to an increase of 2% compared with the original standard pathway.
FIGURE 28.
Model 4: standard pathways plus enhancement of link worker at custody level.
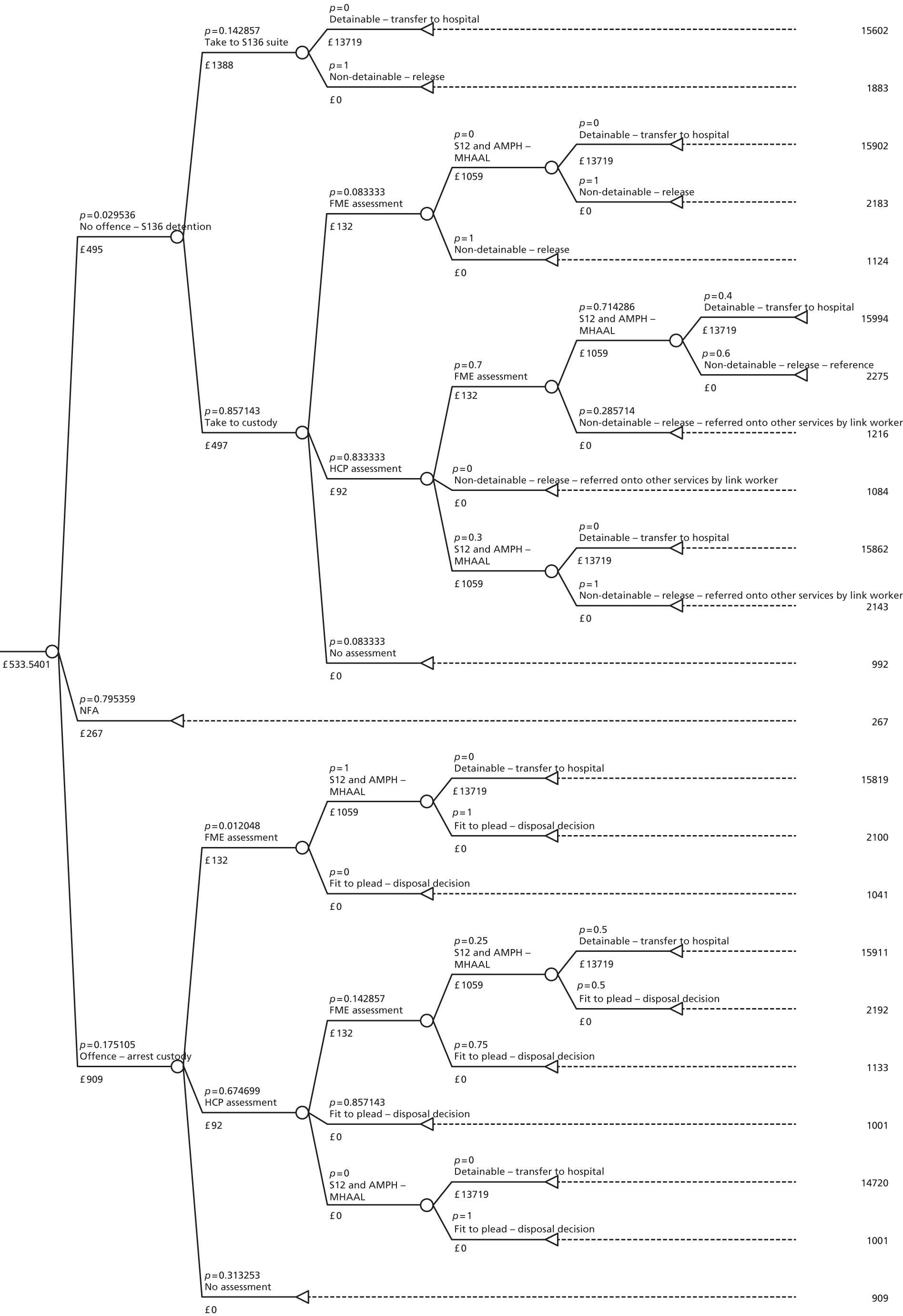
For the sensitivity analysis, assumptions based on the cost of the link worker were changed to assume that contacts with link workers on arrest would amount to 3 hours of face-to-face contact, increasing the link-worker cost to £204. This resulted in an increase in the average cost per incident to £557.35. For 100 people entering the pathway, the estimated cost was £55,735. This was an increase of 6% compared with the original standard pathway.
The enhancement of a link worker at the custody outreach level appears to not increase cost greatly. This finding is robust even when costs are challenged in sensitivity analyses.
This inclusion of a link worker at the custody outreach level has the potential to improve outcomes for clients. A report by James concluded that ‘Intervention at the police station may help prevent more serious offending’. 66 This could also lead to potential cost savings in the long run by reducing the likelihood of re-entering the CJS. However, it is beyond the scope of this report to model these outcomes.
Health economics discussion
Cost analysis of case sample
Findings
The finding that the mean cost per client per year was large (£15,364) was unsurprising, as was the finding that costs varied widely between clients. However, the finding that short-term referral clients had higher costs compared with long-term referrals could be useful. As discussed earlier, short-term referral clients were those who were on the caseload of a care team on a short-term referral at the time of the index police contact in the 3-month audit period. This was compared with long-term referral clients who were on the caseload of a MHT for at least 2 months at the time of the index police contact in the 3-month audit period. The association between higher costs and having less contact with mental health services offers an insight into costs and resource use, suggesting this could be a potential area to target in order to reduce overall costs, including those impacting on the CJS. A more detailed future evaluation of factors driving costs (beyond the scope of this analysis) would add further insight.
The cost analysis also suggested that the major cost contributor to mental health service costs was inpatient services, and the major cost contributor to criminal justice service costs was police attendance at incidents. Again, this new evidence on the major cost drivers gives some insight into the potential benefits to police and the health-care system if enhanced pathways can be devised that effectively manage and improve behavioural outcomes in this client group.
Strengths and limitations
The cost analysis had some limitations. The main limitation revolves around which costs have been included. The health and social care costs that have been estimated only included mental health-care costs and ignored physical health-care costs. Recent literature indicates that there is an association between physical health problems and mental health problems,67 thus the cost of physical health services in this sample could be substantial, assuming that services are responsive to these sorts of needs for people with mental health problems. Physical health-care costs were not examined within this study but are an important area of potential future research. Similarly, the costs of specialised accommodation were not considered. This is a costly resource and could have the potential to dramatically influence the scale of overall costs estimated. Thus, future research should aim to include this within the analyses. Due to available resources, the cost analyses were also only based on 55 cases. Future research in this area using a larger sample would lead to a more precise estimate of costs.
The cost analysis based on the case-linkage data also had some important strengths. This was a novel study, which is just the first step in studying the complex interface between health and social care and criminal justice services. As well as providing information on an under-researched area, it is also useful in informing future directions of research.
Pathways analysis
Findings
Each model suggests minimal effects on individual level costs of each enhancement compared with current practice, even when substantial changes are made to key assumptions used to estimate costs. However, when considering the total volume of clients who could potentially be affected by new service enhancements, the overall resource investment in services required could be significant. For example, with link workers, a whole new team of people may need to be employed if every person who is arrested is to be assessed on arrival at a police station and the extension of this service to cover ‘out of hours’ arrests, arguably when many clients require link worker input, would increase resource requirements further. However, the potential impact of this initial resource investment, given the aim of such custody liaison services to reduce recidivism and enhance diversion to appropriate mental health services, should ultimately reduce as service is implemented and embedded.
It must also be borne in mind that costings and subsequent pathway modelling are specific to the CJS (excluding courts and post-sentencing costs) and local mental health and social care services in Cornwall, and do not necessarily represent what might happen elsewhere, as there is likely to be considerable national variation in how people are managed in the interaction between CJS and wider services.
Strengths and limitations of the decision-analytic models
General limitations of decision-analytic models apply to the models in this study. For example, most of the probabilities in the enhanced models are based on informed assumptions as there was no data or literature to further inform the modelling of enhanced pathways. Although this limits the validity of the models, the models were externally assessed by relevant stakeholders, thereby testing the general credibility and validity. The modelling also does not attempt to make any assessment regarding the longer-term impacts of service enhancements and, therefore, whether or not the costs of service enhancement estimated here are justified in terms of any longer-term benefits that may be delivered through better client outcomes.
Each of the pathway models also had some specific limitations. Model 2 has the limitation of not having taken into account the potential effects of street triage on police attendances that result in arrest or NFA. This is likely to have the effect of increasing the mean cost per incident further as a much larger number of clients would receive this service, but the scale of this increase is unknown. This has not been modelled as it is unclear whether or not the service would even be viable for this group of clients. Model 3 has the limitation that it has not accounted for the knock-on effect of increased time in custody due to increased waiting time for MHAAs, which stakeholders have informed the researchers are likely due to the increased number of clients who require an assessment of this type. It would be expected that this would increase costs, perhaps dramatically, but again the scale of this increase in unknown.
There are a number of strengths of the decision-analytic models. First, the standard pathway model was built on observed activity (albeit for a limited number of individual cases) linked to existing pathways. This formed the basis for the development of the models used to estimate the cost of the enhanced pathways, thus increasing their validity in terms of providing a reasonable baseline against which to assess cost impacts in each case. Second, the researchers avoided an overly complex, and therefore, non-transparent, model and have focused on identifying and estimating key cost drivers linked to the identified service enhancements. Third, much of the probability data in the standard model was based on data collected in the attached case-linkage study. 68 However, this is an observational study and as such is susceptible to bias;69 this could have led to inaccurate probabilities in the standard model and thus inaccurate probabilities in the enhanced models.
Overall implications for future research
As mentioned above, in terms of the cost analysis, it was not possible in the context of this study to include all potential service components. Future research could, for example, examine the costs linked to contact with physical health-care resources and specialised accommodation. Furthermore, cost analyses by themselves are not enough to provide information on whether or not pathway enhancements offer value for money and represent a cost-effective use of resources. 70 This, in combination with a more comprehensive examination of service costs, would require a full and robust evaluation of the impact of pathway developments on client outcomes and a subsequent assessment of the benefits linked to any improvement in outcomes observed.
Chapter 6 Stage 3: stakeholder consultation
Introduction
In the light of the review stage, evidence against the findings of the case-linkage study, service users, NHS and police practitioners and managers were consulted to consider barriers and facilitators to the effective multiagency management of this vulnerable group. The aims of the stakeholder consultation were to:
-
identify the barriers and facilitators to the multiagency management of individuals with EMHN
-
develop implications of the research for national policy and practice.
Additionally, the stakeholder consultation sought to address the research question: how are the practice implications of national policy relating to the management of individuals with EMHN being interpreted at a local level? Local interpretation of national policy is illustrated through both service user and professionals’ lived experience of being in receipt of and delivering practice.
A two-pronged approach was implemented to achieve comprehensive stakeholder consultation: first, a local consultation with mental health and police professionals and joint agency service users in the research site and second, a national event including a range of stakeholders from across the country. Each of these consultations is presented below with reference to the aims detailed above.
Consultation methods
Local stakeholder consultation
Recruitment
Service user and professional stakeholders were consulted with regard to the findings of the case-linkage study to provide their perceptions of the barriers and facilitators to achieving effective interagency joint working/management of individuals with EMHN. Professional participants from both mental health services and the police were recruited through e-mail distribution lists, team and service managers and word of mouth due to the researchers being embedded within the organisations. Concerted efforts were made by the researchers to encourage participation from mental health services, but unfortunately, participation was limited. Fourteen of the 25 (56%) police officers who were invited to participate in the research consented to take part and attended a focus group. Officers including an officer from the British Transport Police (BTP), police community support officers, detention officers and response officers, participated in two focus groups in the east and west of Cornwall. Two of the six (33.3%) AMHPs who were sent a recruitment pack took part in a focused discussion. One of the 26 Section 12 doctors (3.8%) who were invited to take part in the research took part in a semistructured interview. Finally, the nurse from the APL team invited to participate in the study took part in a semistructured single participant interview.
Recruitment for the service user consultation was undertaken using two methods. First, the MHRN approached the care teams of individuals identified through the clinical audit as having contact with the police in the audit period. The care co-ordinators of 57 potential participants who were identified in the audit and currently on the caseload of a care team were approached by the MHRN team to screen them against the following criteria:
-
capacity to consent
-
participation could lead to deterioration in the health of potential participants
-
inclusion could potentially threaten their interactions with the current care team
-
approaching the individual could precipitate harmful behaviours to themselves or others.
The care co-ordinators of 30 of the 57 (52.6%) individuals identified were successfully contacted and the screening process conducted. Care co-ordinators advised against the recruitment of 12 of the 30 (40%) individuals. The remaining 18 (60%) individuals were invited to participate in the research by the MHRN. Three of the 18 invited consented to take part in the research by sending a completed consent form to the research team. However, one individual did not supply contact details and the remaining two individuals returned their consent forms following completion of data collection and analysis.
Second, the research team worked directly with a third-sector homeless agency that had previously been involved with the research regarding the service user consultative group. Eight joint agency service users were recruited to participate in a focus group with the support of this organisation. Six men and two women attended the focus group. Participants had a mean age of 45 years (range 23–61 years). A poster advertising the project was displayed in the common room of the local shelter, together with recruitment packs, in order that potential participants could make a decision as to whether or not they wished to take part. All potential participants who signed up to take part in the research attended the focus group. Staff at the shelter were on hand in order to answer any questions about the study, or to signpost individuals to the researchers if they were not able to respond to queries themselves.
Procedure
All professional and service user focus groups and interviews were preceded by a presentation detailing the findings of the study, including the identified decision-making points. Professional participants were then asked to consider each of the identified decisions that were relevant to their practice in terms of the barriers and facilitators to making these decisions. Following presentation of the main findings, service user participants were asked to reflect on their experience of joint service use and answer the following five questions:
-
What are your experiences of the police when dealing with your mental health needs?
-
What are your experiences of joint care provided by the police and MHT?
-
What do you think could be changed to get the services working together more?
-
Have you had any follow-up contact with the police after police contact?
-
Have you had any follow-up contact with the MHT after police contact?
Focus groups and interviews were digitally recorded and transcribed verbatim. Data were analysed using thematic content analysis. All transcripts were coded independently by two researchers. The researchers met regularly to discuss codes and emerging themes.
For the purpose of clarity, professional and service user findings from the local consultation are presented separately below. Furthermore, due to the small numbers of health professional participants, quotes from this group are not attributed to specific professionals in order to preserve confidentiality.
National stakeholder consultation
The Interface National Stakeholder Event was an integral element of stage 3 of the Interface Project. The event aimed to disseminate the process and findings of the Interface Project to a national audience of practitioners from across mental health services and the police in order to generate discussion about the generalisability of findings and implications for research and practice. Furthermore, it was intended to develop collaborative links in order to scope opportunities for further research.
The event was hosted by the Interface Project research team at the Institute of Psychiatry, King’s College London, and publicised through predominantly targeted invitations to health professionals and the police, as well relevant third-sector organisations. Members of the project steering group suggested potential delegates and national organisations to invite in the first instance (e.g. members of the Police Mental Health National Forum) and a snowball methodology was used thereafter. In order to facilitate small group work as well as larger discussions, a target figure of 42 delegates was set. Despite an effort being made to invite an equal number of police and health professionals, delegate numbers were markedly weighted towards the police, as shown in Table 28. Two consultant service users from the Interface Service User Consultative Group attended and presented their experiences of service delivery and involvement with the research.
| Stakeholder | Number attending event |
|---|---|
| Police | 25 |
| Health professionals | 12 |
| Charity | 3 |
| Home Office | 2 |
| Service users | 2 |
The day was structured to include general discussion as well as specific focus on Section 136, the management of individuals with EMHN in custody, and service user engagement in research and practice.
Stakeholder consultation findings
Local consultation findings
Professional stakeholders
Five core themes emerged across the professional focus groups and interviews. These included:
-
interpretation of protocol
-
resource and availability
-
information sharing
-
risk assessment and responsibility.
Each of these themes will be presented below in terms of barriers and facilitators to achieving successful interagency working and any improvements to practice and policy posited by participants.
Theme 1: interpretation of protocol
The first theme concerned the interpretation of protocol and the impact that this has on practice and joint working activity. Necessarily, this focused on detentions under Section 136 of the MHA as this (as presented in the policy review above) has a local protocol, which interprets national policy within the local context. In terms of Section 136, the police focus groups centred predominantly on the decisions that police need to take in their practice of managing individuals to be detained under Section 136; within the context of the research findings, these being decision one (decision to detain under Section 136) and decision two (location of detention). Police officers frequently discussed the location of an individual’s detention in respect of Section 136 detention. Location decisions were seen to have the greatest impact on police management of individuals with mental health issues and involved greater communication with MHTs. The following subthemes focus on police discussion of the barriers and facilitators to practice surrounding the decision, in terms of the interpretation of the local Section 136 protocol52 regarding alcohol intake and violence. The discussion is centred on police perceptions of this interpretation of the protocol due to the low participation rate from mental health services and there being no participation from place of safety staff in the consultation.
The police highlighted the issue of varying interpretation of the protocol concerning acceptance of a Section 136 detention at the place of safety, and intoxication as a significant barrier to the appropriate interagency management of service users. Staff at the place of safety were perceived to have a different understanding to the police as to what was acceptable in terms of alcohol consumption in order to enable a detention in the place of safety. The local protocol states that an alternative to the place of safety should be sought as the location of the detention ‘where there is suggestion or evidence of alcohol or drug abuse to the point of intoxication rendering that individual unfit to have a MHAA undertaken’. 52 These varying interpretations were viewed by participants as creating a barrier in achieving what officers saw as the best outcome for the individual (i.e. detaining in the place of safety rather than in custody):
We’ve had people through custody that have been refused at place of safety for things like well they’ve had a glass of white wine with their Sunday lunch.
Police
That’s something that’s being addressed, because it’s a case that, er, because it’s sometimes being put forward that it’s a case of whether or not they’ve had a drink, I think the actual protocol states as to whether they’re drunk.
Police
Although, as noted in the case-linkage study above, police in the main make their own assessment of level of intoxication to determine the location of detention for individuals detained under Section 136, officers perceived that their own judgement on acceptable intoxication levels was being called into question by staff at the place of safety. For example, when the staff at the place of safety called for a breathalyser test, this was viewed not only as inaccurate interpretation of protocol, but further, as questioning police expertise. Although this particular request for the specific measure of alcohol consumption was provided in two examples by police officers, there was a general consensus that the police assessment of consumption would not be viewed as reliable by the MHT, with a further perception of a degree of mistrust with regard to their motivation for requesting locating a detention in the place of safety. This perception of inaccuracy of judgement created another barrier in locating a detention in the place of safety:
I was actually asked to breathalyse someone, having 136ed [detained the individual under Section 136 MHA] them, because they were a danger to themselves, they threatened that they were going to hurt themselves, kill themselves, but they got treatment that day. I 136ed because I was concerned they were going to be a risk to themselves and possibly to others. I took them to [Place of Safety]; I was asked to breathalyse them and I argued that point, saying I don’t see the relevance of that
Police
But they indicated to me that was their policy, so I did it, and knowing it was going to be zero because the bloke hadn’t touched a drop, and he needed help, and you know . . .
Police
Well I had a big debate on the day, I wasn’t really very happy about the whole question of alcohol because, as you rightly said, every one of us here knows that we’re supposedly experts in what we consider drunkenness. I thought that was a hurdle that was put in place, because it was almost like they didn’t want to take them for whatever reason.
Police
Police participants believed that that non-acceptance of an individual on the grounds of alcohol consumption when perceived by officers as having been low, was linked to place of safety staff perceptions of risk to themselves and other staff. Police perceived staff at the place of safety to be selectively misinterpreting the protocol according to the effect this may have on the working of the place of safety and the impact on staff:
And if they’re intoxicated then that’s not really a reason to not detain them unless they are so heavily intoxicated that it’s affecting their working. So a glass a wine with your Sunday lunch or what have you, a lady off the [unclear] who had been drinking several gin and tonics and what have you, they did accept because overall it wasn’t raising the risk to themselves.
Police
Differing interpretations of the guidelines regarding alcohol by the agencies managing these individuals were compounded by individual differences in interpretation within agencies as shown in the following quotations:
And I think . . . I don’t know if this is the time to do it or later, but it’s different staff have a different interpretation of the rules. So some staff at place of safety will accept nearly all the time and some will refuse nearly all the time. But if you presented the same person to one they will refuse them, the next one will accept the same person, well that’s the perception I have.
Police
That’s wrong, that’s not their policy, and there are some operatives that interpret the policy over there somewhat more strictly than perhaps is expected.
Police
As with the interpretation of the protocol in relation to alcohol, differences in interpretation were also perceived to exist around violence. The local protocol states: ‘where the person concerned is violent or where the arresting officer is concerned that the person may be violent. The overall consideration must always be the safety of everyone involved’. 52 Specifically, police and place of safety staff interpreted both protocol and presenting situations differently, with place of safety staff viewing an individual as being a risk and police believing them not to be so. Furthermore, officers highlighted that some place of safety staff sometimes interpreted risk to be high when police did not think there was a threat of violence. This again reflected individual interpretation of the protocol:
I’ve taken people to place of safety and I represented them when I didn’t think they would, and I’ve taken them, when one’s asked for fag as he’s got out of the car and I said, ‘No, you can’t do that.’ And he said, ‘Oh, for f***’s sake.’ And so he’s not coming, he’s violent. He’s never been violent in his life and all he’d said is the F word, I won’t repeat it. Anyway they refused him on that ground. So it’s such a wide between who you get and you know.
Police
There was a perception that the staff at the place of safety had their own risk assessment system, partly based on historical records associated with that individual, together with an assessment of the potential risk to staff and the working of the place of safety as presented in terms of alcohol above. It was felt that there was some ambiguity in the protocol as to whether the assessment should be based on the current presenting situation and/or historical assessment of risk. Police participants reported that assessment of risk was often based on historical mental health-based information rather than presenting situation interpreted and communicated by the police officers:
You ring up, it’s a mobile number – the officers on the street have detained someone, rung the suite at [Place of Safety] or have turned up, then they’ll turn around, check the records and that’s when the officers will be directed as to where they believe would be the most appropriate place of detention. Because – this is what I was talking about last week – they didn’t have any violent markers or anything like that on our system. He’s been dealt with on a number of occasions. He’s compliant, all the rest of it. But they did have their own risk assessment, they had a marker for themselves and they based it on that marker as opposed to how he was presenting at that particular time.
Police
We have people turned down from [Place of Safety] who are not under the influence of alcohol, not under the influence of drugs, compliant, but because they have a warning marker on their records from some time back, they will still say ‘no, there’s potential for them to be violent’ and again, it comes back, well that’s unfortunately – I imagine quite common – with some people with mental health illness, because of their frustrations, because of their illness, for whatever reason, there is a chance of some kind of violence to be displayed. But as soon as that’s on their record, it would appear, they go direct to custody.
Police
Officers indicated that issues of capacity and resource at the place of safety had an impact on their interpretation of risk of violence due to the assessment of potential for violence and the ability of staff to effectively manage the individual. Furthermore, police perceived that the systems in place within the place of safety did not sufficiently support the MHT to ensure both effective management and staff safety:
And the thing with place of safety is they don’t shut their doors, they won’t shut the doors on anybody until someone’s been sectioned, whereas in there they’ll put them in a cell and shut the door and say that they’re not allowed to say, ‘Keep the doors open.’ And that’s what concerns me. So there is two sides to it. So they can just attack the staff and there quite often is just one female member of staff there and if you take one male in they know the door’s open and has got access to her. And that’s what makes them twitchy, because they’re not allowed to lock doors.
Police
Police participants who faced challenges in the interpretation of protocol around alcohol consumption were required to resolve the issue on a case-by-case basis. There was a sense of frustration among police participants that, although dealing with each case separately resolved the issues for that individual and issues between staff/agencies at the time, this piecemeal approach did not facilitate consultation or impact on the Section 136 protocol itself and therefore practice more widely. One example in a MHT showed how recognised potential for protocol misinterpretation consolidated into an effort to ensure lasting, widespread change. Varying interpretation of protocol had been causing issues for practice which was overcome with positive and sustained effort through collaborative working and ultimately, change to protocol. In response to a change in the Section 136 protocol, both the MHT and police worked collaboratively to agree on and bring clarity to protocol interpretation with regard to the movement of service users during a Section 136 detention. This enabled the change in protocol to have a positive impact on joint practice and the management of service users:
But basically we work with the police to say well, these are the options and in practically all of the, most of the, well at least two of the options we need the police’s active cooperation in this. In that you’re the one’s going to be transporting the patient around the county and need to continue to be involved until someone says we don’t need you anymore, really. And that, I think that’s improved the situation. I can’t recall how long it’s been officially in place for about six months, but I think it’s been piloted and the agreement was there for quite a bit longer. And to some degree it’s reduced the amount of patients who appear to have been brought here against their will, under arrest for breaching the peace and then de-arrested once they arrived here. Which has been a way the police bring people to emergency departments throughout Britain for years, actually, and is poor practice, but you know, it’s not an easy thing to argue against, really.
HCP
Theme 2: resource availability
Theme one was predominantly based on police focus group data. However, all participants spoke about varying resource issues that impacted on their ability to effectively manage individuals with EMHN and further access to appropriate treatment for these individuals. The following section focuses on these resource issues in terms of (1) impact of resource and, in particular, staffing issues at the place of safety; (2) resource-based treatment options that impact on MHAA outcomes; and (3) logistical challenges and associated impact on both management and outcomes for the individuals concerned. Throughout the data related to resource, professionals described a tension between the need to work within and understand resource restrictions (within their own and other agencies) and provision of management/care in the best interests of the service user.
As presented in the theme above, because one of the major challenges to the police in effectively managing individuals with mental health needs was the ability to detain in the place of safety, resource issues at the place of safety were mainly discussed by this participant group. This predominantly centred on the availability of resource at the place of safety and the impact this has on their ability to locate individuals detained under Section 136 at the place of safety rather than in custody. The local protocol states that an alternative location for detention should be sought: ‘Where [Place of Safety] is in use and has no further capacity available’. 38,52 Aside from recognition of capacity issues stated by the protocol, there was a degree of understanding among police participants that limited resource at the place of safety meant that in some cases, to continue detention, custody was the only option:
You’ve got the 136 suite manned by one person in a suite with a locked door that can’t be locked because they haven’t been sectioned . . . the 136 suite is not sufficiently manned and it’s not fit for purpose.
Police
The impact of resource issues on the ability to manage violence within the place of safety was highlighted in the section regarding violence in theme one above. Officers viewed the protocol as limited in terms of provision of service in the place of safety for individuals presenting with violent behaviour and felt these limitations were driven by issues of resource (i.e. resource driving protocol rather than needs of the individual):
If they had enough staff at [Place of Safety] they could deal with potentially violent patients as well. It’s probably sheer numbers that prevents them from deciding to take them.
And do you think that would reduce the number of detainees?
Yes.
Furthermore, staffing restrictions culminating in understaffing and inadequate security arrangements to deal with this were perceived as impacting on assessment of risk from violence, thereby creating a barrier to accepting individuals into the place of safety.
They’ve got, it’s an absolutely bizarre system where they’ve got key coded entry so if the nurse . . . and I’m saying female because it could be either, presses a panic button I think they have to go through these doors, one opens before the other can open and it takes probably about a minute to get to them because of the internal door system. So there is two sides to every story. They’re nervous about their own security, so that’s why some are more twitchy than others about saying it’s a violent marker, because we’re bringing them under mental health and they leave the doors open.
Police
However, although the police were understanding of the impact of limited resources on the ability of place of safety staff to accept individuals detained under Section 136, this decision consequently impacted on the police in terms of their own resources and created a barrier in their ability to practice effectively. As one officer noted:
But again, I think it’s because the resource that we have is not sufficiently staffed or got sufficient money there to be able to resource it properly. No reflection on the individuals there because they’re a single person with a potentially violent person. I know what my feelings would be if I was in that situation. But that doesn’t help the boys and girls on the street at 2 o’clock in the morning.
Police
The availability of appropriate treatment was necessarily discussed solely by the health professionals who took part in the consultation. Discussions centred on the provision of care for individuals, first in terms of providing formal assessment under the MHA and second, with regard to the decision to detain under the MHA following assessment. In terms of detaining under the MHA, it is essential that the facility is available for assessment/treatment as applicable. One HCP highlighted some of the difficulties in conducting a MHAA in a general hospital, and A&E specifically, and in doing so recognised the subsequent resource implications for the police due to the lack of specialist resource/provision to deal with potentially challenging behaviour. This can therefore have an impact on location of the MHAA and the way in which individuals are managed through the detention process:
So on some occasions it’s assessed that that patient isn’t manageable in the A&E department without the police being there, and so you have to say to the police, well and we cross hairs with the MHAA, you have to say to the police, well, we’ll arrange that here, in which case you’re here for the next hour and a half, two hours because we can’t manage this patient without your presence. Or they go back to custody and we, the Mental Health Act Assessment carries on from there. So there’s that option. Or, as we discussed with Place of Safety, they’re medically clear here and in terms of supervision and care, doesn’t need necessarily the police with them, but would still need 136 suite level of mental health observation and care, which is again a difficult thing to provide in the A&E department.
HCP
A further issue raised by another HCP who participated in the consultation was the availability of treatment following MHAA. This participant perceived a direct impact of resource on decision to detain following formal assessment. As prescribed in the MHA, admission following formal assessment under the MHA can only be recommended if the appropriate, recommended care is available. Where the resource is not available, it is possible that individuals may not be recommended for detention under the MHA even if this would be in their best interests. Therefore, the decision to detain can be driven by resource availability rather than the needs of the individual.
And I think the other thing that it may throw up is, I think, decision-making is sometimes impacted about the availability of the resource because at the moment, Cornwall has got a problem that we don’t have beds to admit people to, but actually it’s a national problem so sometimes you’re on call and there will not be a mental health bed in the whole of the county . . . to admit somebody to. So actually, that definitely affects your decision-making process if you know, I think, the . . . or the decision-making does go up unconsciously if you know there is no way to admit this person.
HCP
Due to resource issues with regard to acute psychiatric bed space both locally and nationally, a decision to detain involves a cost–benefit analysis of detention against removing the individual from local support structures. Therefore, the individual needs of service users need to be taken into account and balanced with resource availability when considering the best mental health outcome for that individual:
Sometimes, you know, when you have to make the decision about detaining somebody, it has to be the sort of last alternative in doing the least amount of harm option. Sometimes you have to decide between, for instance having somebody who’s got a terminally ill wife at home, they’re in their 60s, they’ve never left Cornwall, getting them admitted to Northampton or – the other day I had to – the only bed was in Scotland, you know, are you going to do more harm by taking them away, hundreds of miles to admit them or do you sort of just try and make do in the community and carry on for a bit longer. So, those things really do affect the decision-making process.
HCP
Mental Health Act assessments require the co-ordination of at least one Section 12 doctor and one AMHP to assess the individual. An application for detention following MHAA requires the support of two medical recommendations. According to the MHA, AMHPs have overall responsibility for ensuring the co-ordination of the MHAA. Furthermore, the MHA recommends that, unless there is good reason (not defined within the MHA), that assessment should be undertaken jointly. This presents particular challenges to AMHPs who not only have to deal with issues of staffing but also, in a rural area such as the research site, the physical travel and time issues in organising a joint assessment. The AMHPs who participated in the consultation discussed the resource and logistical issues in relation to organising and conducting a MHAA. As presented in the case-linkage study above, on requesting a MHAA, delays were often experienced due to resource issues in terms of staffing levels (often impacted by the time of day/night of requests) and spikes in levels of need. A change in protocol requiring mandatory MHAAs for all Section 136 detentions precipitated discussion regarding the resource issues in co-ordinating formal assessments. In terms of resource, HCP participants were concerned as to the impact that the inevitable increase in MHAAs will have on service:
Well it’s horrendous [slight laughter from member of the group]. It’s been since the 1st of July and it’s . . . we’re doing loads more MHAAs in custody and I’m hoping at the end of this month we’re going to get the numbers just to see how many more, but obviously that’s going to have an impact, not that that doesn’t have an impact on what you’re looking at . . . those groups of people, but from here on . . .
HCP
Furthermore, participants recognised that this will also impact on police resources and, importantly, the management/welfare of service users, particularly those who are detained in custody:
Yeah, yeah. Massively. And the other thing, the impact that this has . . . well it is starting to and it will if it continues, is that because we’ve got more people are going to be in custody longer. I mean I know we’ve got 72 hours, but I think the policy is something . . . response within six or seven hours, but people are waiting in custody and I know a young lad the weekend before last spent nearly 48 hours in custody because, and again, and if you’re talking overnight, we have one AMHP on duty for the whole of Cornwall for overnight. Now I know we only have one Section 12 doctor, but obviously there’s a limit to what one person can do. So the upshot of it is that people are going to be sitting in custody longer, which is not good.
HCP
Additionally, there was some discussion about the lack of understanding of resource limitations and implications between services. As the following example shows, differing remits of organisations can limit the ability of practitioners to provide what they would regard as an optimal service. However, this needs to be balanced with the reality within which services can be delivered and understood by partner agencies:
I mean the police who do provide an emergency response, and their blue light, they rush out there and then they ring us and they say, ‘This person needs a MHAA now.’ And, like you said, that person could be in [place name] and I’m in . . . I’ve got to get two doctors, it’s going to take a couple of hours depending on where they are and what time they can do and I think the police find that really frustrating, because they’re used to rushing out, blue light, ‘We’re here now’. So when we say, ‘Well, OK. We are going to be two and a half hours.’ ‘Well, we can’t stay here for two and a half hours.’ So it causes clashes because we work on a different . . . I mean it would be great if we had two doctors and an AMHP in a car [group laughter] sitting there, not doing anything . . . we’re going to rush out. I’d love to be able to do that [slight laughter]. But that can be an issue, it can be a problem . . .
HCP
Theme 3: information sharing
Timely, accurate and proportionate information sharing within and between services was viewed across all professional groups as key to effective interagency management of individuals with EMHN. Issues that were discussed in relation to facilitators and barriers to information sharing included the past experience of staff (both in terms of sharing information and of the individual) and knowledge to facilitate appropriate information sharing.
It was clear in the focus group discussions with the police that they perceived accurate and timely information sharing from the outset of an incident as one of the main potential facilitators of management of individuals with EMHN. In discussing decision one (decision to detain) in relation to both Section 136 detentions and arrests for substantive offences, police officers noted the importance of having accurate and contemporaneous information while they are en route to respond to a request for attendance. Discussion related to the time pressures on officers to gather and synthesise information that would enable them to respond to incidents and manage individuals more appropriately. Furthermore, they highlighted limitations to their access to police records (e.g. response officers do not have access to OIS) as a barrier to their work and management of individuals with mental health issues. The experience of both the operator providing information to officers from command and control, coupled with the experience of the response officer themselves, were seen as key in the delivery of timely and effective information exchange:
But again it comes down to personalities and experience. Some coms [communications] operators when they’re on, you know that when they tell you to go, whilst you’re going there they’re going to tell you everything you need to know on the way, and you don’t even have to ask. There’s two or three very good on that but they’ve been there a long time. But it’s a very pressurised job and there is a high turnover of staff. And so we don’t always have people staying around and getting experience. So if you’re as experienced as we are, we have to prompt them to find this information for you, it’s okay. But if you’re not [unclear speech – 1:27:21] doing it then there’s a potential there, but again it’s down to the individuals involved.
Police
Information provision en route to an incident was viewed as enabling response officers to build a picture as to the appropriate response to ensure effective management of the individual. However, if the information provided is inaccurate, this may impact on the officer’s justification of their response when an incident is later reviewed:
Well often you get called to a job, you get given information en route to that job, and it’s only when you arrive you think ‘hang on a minute, I think this information I’ve got isn’t entirely correct, and you have to justify your actions thereafter, that they were detained because A, B and C. So it’s not always as reported.
Police
All professional groups expressed a lack of clarity about the structures and processes in place to facilitate information sharing. Health practitioner participants discussed issues with regard to both appropriateness of information sharing and knowledge in terms of what could be lawfully shared between agencies, as well as channels of communication that would facilitate lawful and appropriate sharing of personal information.
Health-care professional participants discussed the imperative to share information based on their knowledge of the findings of serious case reviews that revealed missed opportunities for intervention due to lack of timely and appropriate sharing of information that could have saved the lives of service users. Participants placed both the safety of the individual and the safety of the professionals managing that individual as the drivers for proportionate sharing of personal information:
It’s a need to know. It’s for safety of the police officers and the safety of others and the person involved. So that’s kind of the premise that I work on and most of the time that’s reciprocated by the police. It’s we’re in this situation, it’s a crisis, what can you tell me about this person? And what’s going to keep me safe, what’s going to keep others safe and . . . ?
HCP
Police focus groups revealed an additional lack of clarity in terms of channels of communication to enable information sharing. There was a degree of confusion about who they could contact to obtain information about an individual in order to make a decision regarding their management, particularly prior to or at the point of detention. Police participants were aware of the telephone number of the place of safety in order to highlight a detention under Section 136, and officers located in the custody suites were able to contact the MHT in order to either request an AA or MHAA. However, despite recognising the utility of contemporaneous information about an individual at the time of an incident, there was limited knowledge as to how this communication could be achieved. As one HCP participant highlighted, this is not because the information is not available or that there is no system to support this information sharing, but that there is limited knowledge of the process of obtaining information held on the mental health system by the police on the ground:
Well, they can do that. I mean, they can phone up the crisis team any time of night, who can give them the information if we’re holding information, and that has always been available. It doesn’t get used . . . After hours, the crisis team are there, they’ve always been there and the police have always been able to make use of that. I don’t think they do at all.
HCP
Confidentiality in terms of information sharing was discussed across all professional groups and, again, was noted as requiring clarity, particularly in terms of criteria for lawful breaches of confidentiality between agencies. As noted above, confidentiality breaches were considered appropriate if this mitigated potential risk to service users and professionals and consequently kept people safe. However, knowledge of what can be shared often impedes information sharing and, therefore, effective management/care:
Again, information governance gets interpreted differently by different people . . . I think we feel much more comfortable about breach of confidentiality, need to know, when actually this is in the patient’s best interest, where other people will be, ‘Can’t tell you anything. Can’t tell you anything. I don’t know. Confidentiality, can’t . . . ‘ and, you know, people have always been at loggerheads about that . . .
HCP
Theme 4: risk assessment and responsibility
Discussion across all participant groups focused on the responsibility that professionals from each agency assume at different periods of the service user journey within and between services. This discussion centred on the assessment of and responsibility for risk for the individual concerned and, additionally, the issues involved in the transfer of risk as the individual moves from being the responsibility of one service to another. In the main, this theme emerged in relation to the police assessment of risk and the response to both this assessment and subsequent transfer of responsibility to mental health services. The following sections present the issues raised by police and mental health professionals in both the assessment of and responsibility for risk of individuals who move between services.
Police participants discussed the assessment of risk at the time of detention. Participants were in agreement with the research findings that risk to self and others were the primary precipitating factors that they considered in making a decision to detain an individual under Section 136. For example:
The biggest issue is those first two on the top left, I think – risk to self and risk to others. That’s the first thing I would think of –
Yeah, definitely –
Everything else is a bolt on, isn’t it, as you go through the process.
They’re the only two that I, to be fair, have really used. If they say they’re going to hurt themselves, or hurt someone else, then what do we do with them on a day to day basis?
Officers felt confident in assessing risk to self and others where there were clear risk indicators such as DSH, threat of or attempt at suicide (risk to self) or violence/aggression/threats (risk to others). This confidence was reduced when individuals presented with behaviour that they viewed as potentially indicative of mental illness but that was not perceived as directly contributing to risk. In the following example, police discuss how, in such ambiguous cases, they use wider contextual factors to assess indirect/potential future risk to self and/or others:
Because I mean, the fact of the matter is, when you’ve got someone like that, if someone is in the square and as far as they’re concerned, they can see pink elephants flying round their head and so on, then they’re not in need of immediate care and control, which obviously is what gives the power to 136. So unless they are really a risk to self or a risk to others, then those two have to be clarified prior to any decision for a 136 . . . I think sometimes with the pink elephant ones, it also depends where they are, because they can become a risk to themselves through others as well, by their behaviour.
Police
Police participants were aware that their assessment of risk was often called into question by mental health services and that they were criticised for apparent inappropriate use of Section 136 when HCPs perceive that alternative action (or no action) could or should be taken to manage the individual concerned without the need for detention. Officers voiced the concern that detention was perceived by mental health services as potentially creating a barrier in the management of individuals who they themselves viewed as being in need of care and control. However, they asserted that given their remit in terms of being the first to respond to an incident, and the imperative to act on the presenting situation in order to fulfil their duty as sworn officers, they needed to make decisions quickly and deal with the immediacy of the situation:
So someone threatening to jump off and hurt themselves/harm themselves and you say, well it’s easy for the doctor to say that because he wasn’t there at the time and I’m sure he would jump off a chair with a noose around.
You’ll have to act on it.
Police
As was the case in terms of resource, above, police participants felt that they were often required to compromise the long-term best interests of the service user due to the responsibility for risk necessitated by their role, and through their being the first to respond to an incident. The assessment of risk by police officers discussed above is bound by their need to deal with the immediacy of the situation presented to them on arrival at an incident. Police participants further voiced the concern that although they were required to make decisions to protect individuals and the public, they did not always feel supported by their organisation to make decisions that were in the best interests of the individual. Officers were aware that detention was not always in the long-term best interests of the individual and may not be the course of action supported by the individual’s MHT. However, due to their role and the perception that they will need to assume the subsequent responsibility in terms of risk for any action they took, the impetus to take diversionary action was generally diminished. Without the support of the organisation, officers were more likely to engage in what they perceived as risk-averse behaviour in making the decision to detain under Section 136, thereby creating a potential barrier to long-term effective management and co-operative interagency working.
Everyone’s afraid to say no in case something does happen and then everybody gets the finger pointed at them.
Police
Furthermore, a component of the risk assessment was based on the police interpretation of the individual’s mental capacity at the time to make a decision about their own safety. Police participants perceived that their interpretation of mental capacity and the need for care and control was at odds with that of mental health service professionals’ interpretation of detentions under Section 136 (i.e. that all those detained under Section 136 should be potentially detainable under Sections 2 or 3 of the MHA or able to be recommended for informal admission).
If someone’s sat on a bridge and you go to them and say, ‘I’m going to jump.’ ‘Why?’ ‘I want to kill myself, [unclear speech – 29:08], my wife’s died, I’ve lost my two children. I can’t see the point of carrying on.’ Are they sane or are they insane? Are they in need of immediate care? . . . Possibly not. Are they making a sound judgement? And lots of doctors have told me that in custody, just because they say they’re going to kill theirself doesn’t mean that they need any . . . got any requirements under the Mental Health Act, you know they’re going to be released from custody. So it’s a brave decision to say, ‘I’m leaving you here, you make your own decision.’ Technically they’re not . . .
We can’t do that though can we? We can’t do that.
Discussion also took place as to how this hurdle to achieving support for officers to engage in decision-making based on the considered best interests of service users could be overcome. As the example below shows, in order for this to be achieved, not only would officers need the support of their organisation but also effective communication with and support from the MHT in order to have up-to-date information about the individual’s needs and contingency plans:
I think that’s the crux. I think if officers that did attend and were prepared to make quite robust, almost brave decisions, because she’s attention seeking, she knows – she does it when she comes into custody, in cells, she knows even then what to do to get the attention. If individual officers knew they had the support of the organisation to be able to turn around and say ‘no, there’s a care plan in place, we’re not going to deal with you’, or even if the organisation said ‘right, we’re not going to send police officers’ – but that’s not going to happen, so police officers are then faced with what they’ve got knowing that if something goes wrong on that odd occasion where she may do something unintentionally – she’s attention seeking but she goes too far – it’s going to be these poor sods gripping a rail in front of [place name] and explaining why they didn’t do what they should do.
Police
Furthermore, as one HCP participant noted, although the information required to support officers to make these decisions is available through the crisis team, it is currently underused. This again highlighted a lack of knowledge about currently available information sharing structures.
What they don’t realise is, yes, you can say, ‘Yes, we know this patient. Yes, they have a care team,’ and actually, you don’t have to give them the information but you can go and look and see that there is a contingency plan. ‘Do you know what, maybe you’d want to ask this person whether they’ve done this, this and this or you could get them to phone us and talk to us’.
HCP
Police participants discussed how the responsibility for the individual’s risk was often passed between services. The local protocol stipulates responsibility for police officers as follows:
To offer every assistance to the hospital staff and the AMHP to ensure the safety and security of the detainee, themselves, all other patients and staff at all times. To remain at the hospital until this detaining report is fully completed and handed to the nurse in charge. AND the nurse has settled the detainee, commenced the assessment process and has decided that police presence is no longer required. 52
In terms of the protocol, AMHPs have responsibility for the transport and care of those individuals detained under the MHA following formal assessment until hand over is complete with the receiving inpatient facility. However, there are periods during the service user journey through Section 136 detentions, for example the time immediately prior to, or at the time of detention, when responsibility is not clearly defined or supported by local protocol. This is further exacerbated in the case of management of individuals with mental health issues who have been arrested for an offence, for whom professionals do not have a locally agreed shared protocol to facilitate management. Police participants described what they experienced as being a relatively common occurrence of MHTs passing on the responsibility of risk for an individual to the police due to the time of the week and resource:
It’s like the four o’clock phone call on a Friday and the MHT is saying that there’s a concern for welfare for someone and they haven’t got anyone to
It’s a common theme.
Just pass it over to the police, yeah.
Only because it’s four o’clock on a Friday.
Police
In the case of the following officer’s experience, differing perceptions of professionals as to their remit is seen as at odds with the understanding of that remit by other agencies and can compromise the management and what is considered to be in the best interests of the individual in crisis:
I would go as far as to say generally negative experiences, yeah. One lady had also had a home visit and smashed her whole flat and then stormed out saying that she was going to jump in front of the nearest lorry that she could find. And her friend who was in the house followed, called us . . . so we actually detained her very promptly and 100 yards down the road detained her at the side of the lorry that she was trying to make efforts to jump under the lorries that was going past. So we put a phone call back through to the MHT who were conducting the home assessment and it was quite clear that they thought it’s no longer their responsibility, can go down to [place of safety], which may have been the right decision for them to make, I’m not saying it wasn’t. However it seemed, looking at the overall care and what’s in the best interest for that lady, that seemed to be the most invasive way of doing it. But generally negative.
Police
Health professional participants were aware of the difficulty for police in terms of their responsibility for risk. Some health professional participants saw this exemplified in their discussion of the rationale for the recent change to mandatory MHAAs for Section 136 detentions. Therefore, by formally assessing all individuals detained under Section 136, it would be possible to provide a rationale as to why they were not admitted and the responsibility not to detain following assessment would not lie with the police:
My feeling is I think there’s an issue about people being discharged from 136s, leaving custody and then something happening to them, but I also wonder whether there is a cost implication, because obviously the police have to pay for the FME and I know there aren’t many FMEs when they’re driving around Devon and Cornwall, so there’s that impact as well. But I think it’s because of the first, because there’s been a lot of . . . so I’m guessing that if someone has a full Mental Health Act Assessment and they’re then discharged and something happens, then you can trace back the reasons why the person was discharged. Does that make sense?
HCP
More widely, risk responsibility was discussed in the context of understanding roles and associated responsibilities. This was exemplified through the following health professional’s comment on the lack of understanding as to who is responsible for aspects of management of service users who come into contact with mental health services and the police. As was highlighted above in the discussion concerning information sharing, rigorous definition of responsibility in terms of interagency communication and alerting with regard to individuals in crisis is seen as an enhancement of practice that would decrease the chance of missing opportunities for intervention and benefit the mental health outcomes of service users.
Because, you know, there’s custody liaison nurses started, but, we’re yet to meet with them, but we’re not clear, I don’t think, of their role or responsibilities regarding these patients yet. How the responsibility for the communication is shared about these patients, I suppose. There’s not many of them, but the patients with problem diagnosis of anti-social personality disorder and serious forensic violence histories, because we see if there’s a particular crisis or a particular increase in substance misuse or something like that that’s going on, or housing, or whatever else problems going on with these patients, then the A&E department will see them. And that’s a danger sign in that if you’re gonna kill yourself or kill somebody else you’ve probably attended an A&E department in the weeks preceding that, or months preceding that. We don’t, I don’t think any of us feel that we get much support from forensic services or MAPPA or anything else when we raise concerns about these patients.
HCP
Summary
In general, professional participants were aware of the barriers that affect their own agency’s management of individuals with EMHN. However, professionals described a lack of understanding of the pressures and limitations by other agencies and the scarce allocation of resources in the provision of care for individuals with mental health needs who present to both services. Furthermore, although there are processes in place to support information sharing, these are not widely known across services, placing a barrier in the way of effective interagency management.
Overall, there are differing interpretations of protocol and policy impact across a range of key areas, including assessment of alcohol consumption and risk of violence in order to access the place of safety, assessment of risk to self and others in relation to precipitating the decision to detain under Section 136, and what constitutes proportionate and lawful information sharing to maintain the safety of service users, staff and the public. A tension emerged from these discussions between what is in the best interests of the service user and the options available to the service with responsibility of the service user at that time. This leads to strain between services as they make efforts to meet the aims of their respective organisations and manage their corporate responsibility to service users within the context of often absent or ill-defined and understood protocols and compounded by resource shortages.
Service user findings
Service user participants had a range of experience in terms of mental health service and police contact. In relation to mental health service contact, participants had experience of secondary, acute and specialist community services as well as inpatient services. Their experience of police contact included arrests for drug, public order offences and offences against people, Section 136 detentions and where officers had concern for their welfare. In discussing the questions presented above, participants identified barriers and facilitators and suggested improvements that could be made to effective management/joint management of individuals with mental health needs across both police and mental health services, elements of which were evident in four main themes that emerged from analysis of the data. The themes were:
-
police understanding of mental health
-
information sharing
-
professional roles and responsibilities
-
understanding the needs of service users.
Each of these themes are presented below with reference to examples from the focus group.
Theme 1: police understanding of mental health
The majority of service user discussion focused on police management of individuals with mental health issues. One of the main barriers perceived by service users to police achieving effective management was their inability first to recognise behaviour as precipitated by mental ill health and second, to understand presenting behaviour as indicative of crisis point. With respect to the latter, one service user described an example of an attempted suicide where they were in contact with the police but no follow-up contact was provided, either by the police or mental health services. Lack of police understanding was perceived as a barrier to the police providing appropriate and effective management of individuals suffering from acute mental health issues. In the following quote, lack of understanding of how someone with bipolar disorder might react to the police was provided by a service user as an example of this barrier:
In the experiences I’ve had, and I’ve seen people who’ve got things like bipolar, or depression, and they get arrested, right, in my experience if someone put their hand on me, Police officer or doesn’t matter who it is, I’d go off on one – because I just react to it, it’s instinct to react, yeah, so they give you a bit of a hard time and all the rest of it, you know, what have you – and then when they realise you’ve got this bipolar, you’ve got this manic depression, after they’ve beaten you up and thrown you around or whatever, I think they need to stop and find out if you have got mental health issues. They need to look at that first before they start all the rough stuff and judging who you are.
Additionally, service users saw a barrier in terms of the perceived lack of understanding by the police of comorbidity of mental health and drug/alcohol issues. This was viewed as a pervasive attitude where service users perceived that the police did not believe that individuals who had issues with drugs did not have mental health issues that required referral/treatment, but, rather they should be managed primarily as under the influence of drugs. Lack of understanding of these issues was viewed as the mismanagement of incidents, potentially resulting in negative impacts on service users and inappropriate application of resource, to the point where it could escalate a situation:
In my experience, I had a paranoid psychosis in the public toilets, and the way the Police dealt with it was – to me, I wasn’t a raving lunatic. I was coming off a long induced drug binge but the way they did it was it was all sealed off and there were negotiators, and there was nobody whatsoever to meet any mental health needs, you know what I’m saying? To me if the GP would have come along and given me an injection and put me to sleep for a day, it would have solved everybody’s problems. Because that’s all I needed to do, basically. You know, I needed rest. But the way they handled it was totally off the wall. Because to me, it would have been more sensible to approach . . . with a steady approach, you know what I’m saying? One on one, or two – if they fear for one’s safety, send two. Because that softly softly approach, to anybody in that frame of mind, is a lot more easier than . . . They’re surrounding you by a lot of people and then they’re all like – Yeah, because I came out of the toilets and they trussed me up like a chicken. Do you know what I’m saying? And to me that was senseless.
Where service users had good experiences of police management when they were experiencing crisis, this was generally due to the individual officer’s knowledge of mental health and mental health services. As such, service user participants suggested training in mental health for police officers and, further, the designation of police officers with a specialism in mental health. By having enhanced training and specialist officers, service users expressed the belief that this would improve understanding of mental health conditions and the individuals concerned:
Yeah, but the Police don’t understand mental health. But I think that in that, there should be Police officers that specialise in mental health, because at least that way they’re doing their Police role and their mental health role. Because at least then – And then there’s that little bit of empathy then. Because then if need be, if they need to be a Police officer they can go and do that, if they really need someone for mental health and there’s someone working, they know then – they understand.
Theme 2: information sharing
One of the major perceived facilitators in the management of individuals with EMHN experienced by service user participants was information sharing between the police and mental health services. Although it was recognised that this should be proportionate and appropriate, service users agreed it was necessary in order to effectively manage joint agency service users and expressed surprise that information was not more frequently and formally shared. Service users perceived that a lack of appropriate information sharing could provide a barrier to effective management.
So would you prefer it if the police could actually see your information?
Absolutely, yeah! They should have easier – easy access to your medical records.
It should just come up on the main part of your . . . what’s wrong with you, you know.
Service users provided examples of instances when joint management was enhanced through information sharing conducted in their best interests. Service users appreciated the police providing the MHT with information in order that they could start to deal with the presenting situation and seek to meet the needs of the service user from the point of police contact:
I mean, what I found is at least they can do a proper handover. Then the mental health people know what they’re walking into, they know what the problem is, they know what the mood is. They’ve got a better idea of what your immediate need is going to be.
The following example is of a service user who felt directly supported by police to access mental health services. This showed how provision of information about the incident by the police to mental health services can enhance the experience of the individual concerned and expedite the service user’s journey to appropriate treatment. For this individual, this prevented retraumatisation by preventing him from having to relive the experience by having to recount the incident.
The other thing I did which helped me a lot was they spoke to them first and explained the more traumatic part of what I’d explained to them, so I wouldn’t have to go through it for a third time that day. Because they had it all written down in their notes . . . Because then by the time the mental health team spoke to me, they knew –everything . . . the worst part of it, what had been going on . . . I suffer from PTSD [post-traumatic stress disorder], so the problem is it’s recurring over and over and over. And I don’t want to go through it again and again, I mean I was killing myself because it was the only way I could make the replays stop.
Although there was agreement within the group that services should share information in order to improve service user care, service users felt that at each step in their management they should be consulted about intended information sharing in order that they are fully informed of the process:
But I think they should tell us as well – I think the Police should say, I’m putting you in touch with this person, don’t just do it because then you’re going to think well hang on, why . . . they’ve done it without telling you.
Service users were clear in their support for and understanding of the need for enhanced information sharing between services in order to improve outcomes for individuals with mental health needs. Participants felt that agencies had restricted access to records from other agencies, and that this created a barrier to appropriate management. In order to change this situation and enhance interagency management and understanding of the mental health needs of individuals, service users felt that accessibility of records to appropriate agencies should be improved. Specifically, services users highlighted the efficacy of strategic information sharing at a point when it would be most useful for the police when making a decision. Early access to information when en route to an incident was perceived by participants as a way to enhance the management of individuals with mental health illness:
If they’ve got something like that and they actually get the name of the person before they go out to the scene, then there is absolutely no reason why they shouldn’t then be saying, right – oh it’s so-and-so, wait a minute, there’s a mental health disorder, we need to send one of these officers.
Furthermore, there was recognition of the need for enhancement to current record keeping techniques in order to ensure that the police have access to records with accurate and up-to-date information to improve the provision for repeat service users. In the following example, service users posited a method of ensuring that records are updated to benefit the police and with the consent of the service user:
This is probably a stupid idea, but you know when you go in a doctor’s office, surgery, and you get a little clipboard, and they give you – put your name and address, and all your bits and your health – I’m thinking, maybe, you could do something like that if you get arrested or whatever, or . . . then they can take it off and look, maybe they could put that on their computer for next time. Or whatever. They’ve got the information they need, but they haven’t got the information they really really need.
Theme 3: professional roles and responsibilities
Service user participants discussed their understanding that mental health and police services had defined roles and remits in order to fulfil the work of their respective organisations. They recognised that in dealing with mental health service users who come to the notice of the police, these roles were sometimes blurred, particularly for police who often found themselves on the front line of dealing with such individuals. This situation whereby professionals were attempting to balance the expectations of their respective service, whilst having to simultaneously fulfil the role of the other service, created a significant perceived barrier in the management of service users:
The police are law and order, they’re not a local charity – you know what I mean. And that 50–50 doesn’t work. The police are law and order, to keep the peace. The mental health team are there for care and attention. So they’ve got a job to do . . .
Furthermore, service users recognised the frustrations of individual professionals who wanted to deliver an optimal service for those with mental health issues created through the limitations placed on services relating to their roles:
They want the right person to help you, rather than them trying to deal with it and they can’t. They just try and put you through to someone else.
Interestingly, service users recognised that although services should be available and responsive to their needs, that there was some onus on them (as service users) to actively engage with services in order that they might be effectively managed and receive the care appropriate to their needs. Therefore, in order to improve interagency management, part of the responsibility was perceived to lie with the service user to recognise that they are in need of help and take steps to accept what is being offered:
Yeah. To me it comes back to the issue of if you want the help that’s there, sometimes you’ve got to make that first step yourself, haven’t you. You’ve got to say, right I’ve hit rock bottom, I don’t want this anymore, right. And anybody that can do that, or try to do it, these people can then work – like [Service User 2] said, there’s a budget they work by, but I’ve never ever known [agency] turn anybody away.
Additionally, in taking responsibility to access care, engaging with services and affecting change in their lives, service users expressed the need for this to be recognised by services, so that attitudes and treatment of the individual by professionals should be adapted as they assumed responsibility for and changed their lives:
Until only about 12 months ago, the only contact I used to get – I used to get hustled in the street all the time by them, but in the last 12 months I’ve got to be honest and say there’s been a complete turnaround, because I suppose they see a change in me. You know, I get the odd one and I’ve had it, who say leopards don’t change their spots as far as I’m concerned, and I said well they do, mate. He said they don’t change their spots, the spots just get bigger until the colour completely changes. But generally I’ve found overall there is a change of attitude towards me, because I suppose they can see a change, you know what I’m saying? Because I’m no longer this, in their eyes, raving lunatic walking around, psychotic or paranoid or whatever, and causing them work as far as they’re concerned, you know.
Rather than more strictly delineating professional roles and responsibilities in order to improve the situation with regard to the barriers presented above, it was clear that service users perceived specialist integrated services as being the optimal method to provide the structure to improve care/management. Service users had some knowledge of and were positive about the recently implemented custody liaison and diversion service in the research site. Furthermore, as the following extract exemplifies, service users could see the value of integrated police and mental health services that were able to facilitate timely access to services and support for service users:
The thing is, how do they define mental health? And we all know it’s a minefield. You know, I think you can get, like I say if you’ve got CPNs or drug workers in the Police station, which is a good thing, but all the multiple agencies need to be working together and to have first-hand experience. And like [service user 1] said, this is the breakdown, it’s law and order against care and attention, and you’re always going to get that . . . you need somebody that can liaise between the two – in the ideal world
Theme 4: understanding the needs of service users
Although the service users felt that some police professionals understood elements of mental health conditions and mental illness, there remained a lack of understanding of service users’ needs and how to ensure those service users were able to access appropriate services. In the first instance, at the very least, there was a call for the police to recognise when individuals were requesting help:
Well, they think you’re psychotic if you ask them for help. They think you’re gone in the head. And I was like, no, I’m not gone in the head, I was like I just need help, and they were like we’re going to section you, and I was like I don’t need sectioning, I just want help.
Not all of the participating service users had received care/management follow-up from the police following contact; however, those that did had found this useful and supportive. Examples included follow-up letters and the offer of support when required and the understanding of when the service user was able to self-manage their needs more and move away from the support of the services:
They sent me letters, to make sure that I was all right . . . Oh yes, and in the end I just like got hold of them to say I’m now living in blah blah blah, I’ve got this help and this support, and if I need your help I’ll contact you, and they were like that’s fine. But they’ve always said that if I need them, they’re there.
Another facilitator linked to management of service user needs was that of ensuring a single point of contact who would be consistent in the provision of support. Support facilitated by the same individual throughout their journey gave service users confidence and facilitated engagement with all services. For example:
Yeah. I mean, he wasn’t in uniform or nothing. But because he just made me feel like he was a normal person. But he come with me once a month whenever I’d see me counsellor, he used to come with me, just to make sure I was ok . . . Because obviously he was the one who’d put me through to the mental health team. And then obviously he followed it all through right until the end.
Furthermore, the following example presents another impact of consistency with respect to changing their attitude to police services and potentially encouraging them to seek help when previously they would not have felt supported to do so:
It’s the same one that’s done, like, from the start to finish, rather than someone else coming in and having to explain to that person, it just gets boring saying the same thing, but it’s the same one that’s stuck throughout the whole . . . It destroys the stereotype for me, you’re left with the feeling that I could approach them if I knew something was going to happen and I was out somewhere, if there was a Policeman around I probably wouldn’t be able to get anywhere near the right response . . . but you feel it wasn’t this horrible thing that if I’m contemplating something to stop the . . . and if there’s one walking down the road you can metaphorically grab them and say that you need their help, look I’m in danger of hurting myself.
An important factor perceived as necessary to improve service user journeys was a diversionary approach to individuals with EMHN so that a contact with the police did not necessarily end in detention, or mental health services could be accessed before an incident escalated to the point where police had to attend. An example of this was to have knowledge of out of hours access to mental health services (for both the service user and police):
It’s better to talk to someone without them going ‘oh yeah we’re going to section you’. I don’t want to be sectioned, I just want to talk to someone. And then it took a few weeks, and then I finally got a phone number that you can call now. You can text them out of – like, quite late at night –
Out of hours.
Yeah, and they’re bloody helpful.
Oh ok. So you could have done with just being given that to begin with.
Yeah, if they’d have given me that in the first place it would have been a completely different story . . .
Summary
Service users, although having experienced a range of barriers in interagency management of incidents in which they were involved with both services, were keen to share potential facilitators and suggest improvements in service that could enhance interagency care. Overall, early joint service intervention and provision of an integrated care package was an important factor in all the themes. An exemplar was provided by one service user who had been in contact with the police at crisis point and from that point on had a quick and supportive journey through the services:
I was arrested by them, they found me in the middle of a suicide attempt, and the way they approached it was only one of them approached me, the other one was about 50 metres away. I later found out that it was one of my friends who’d alerted them to the suicide attempt so they arrived knowing what it was and I was more a danger to myself than anyone else. They sat down, talked to me rather quietly for at least 30 minutes, they weren’t arresting me, but if necessary to protect myself they would, they asked me if I was with a doctor down there, I said no I’m not registered with a doctor. They said, what we’re going to do, we’re going to take you to a GP surgery now, we’re going to get you registered with him, but then before we leave we’re going to make sure that that GP has contacted mental health services, and we’ll wait until someone arrives from there before we leave, but we’ll just be in the surgery, we won’t be in the doctor’s waiting room. I was lucky I got the two most reasonable police officers in Cornwall! . . . I mean it was 4 o’clock in the afternoon of the same morning that I was brought in here [referring to the shelter], sedated by the mental health team, so I could start the process of putting my life back together.
The above example highlights some of the main factors discussed in the group and exemplifies where all aspects came together to create what could be deemed as a gold standard scenario, including joint working, information sharing, diversion from custody, understanding of mental health needs and expedient routes for treatment. Furthermore, the above example highlights intervention by a third-sector organisation, in this case the homeless shelter in which the focus group took place. Third-sector support, particularly in the form of housing, money management, addictions, etc., was viewed as vital by the group.
Well I’ve been here two years and nine months now, and I’m waiting for a, like, to move into a council property. I’ll probably be here for another year. But I can’t slate [the shelter] whatsoever. If it wasn’t for them, I wouldn’t be what I was now. I’d still be an alcoholic, and I’d still be taking drugs.
In summary, the service users wanted to see an improvement in the awareness and knowledge of mental health issues within the police. Although it was viewed that general training of the police force would be beneficial, the service user participants perceived the development of specialist officers as having more far reaching impact. Services could be greatly improved by the sharing of information, with proportionate and necessary sharing of information between the police and mental health teams to expedite and smooth the transition between services.
Fundamentally, having accessed services at a time of crisis, participants could see the challenges service users posed to the two services that attempted to deliver care and manage them effectively – despite the barriers in achieving this. The police were viewed as the service that often needs to deal with the immediacy of situations with potential risks to the individual themselves and/or to others. Although the service users understood that the police needed to deal quickly with incidents, they highlighted the need for officers to consider the needs of service users in managing situations where mental health may be an issue. Although no comment was made in relation to the adherence or otherwise with policy or protocol, recommendations made by service users included integrated liaison services, the need for diversionary services and that of mental health training for police officers reflect the recommendations made in Lord Bradley’s 2009 report. 6
Finally, both professionals and service users focused on two key areas in the management of individuals with EMHN. First, both consultations generated discussion with regard to interagency information sharing. Both groups (i.e. professionals and service users) could see the benefit of accurate and timely information sharing that would benefit interagency working and the professionals involved in delivering service, and have both immediate and long-term benefit to service users as they move between services. Both groups were keen for there to be clear and transparent processes and procedures to support information sharing to be of most benefit to interagency working and service user outcome. Second, both groups raised the tensions and dilemmas with regard to role, remit and responsibility of police and mental health professionals. Both groups recognised that the boundaries in role and remit are often blurred, creating a barrier to the effective interagency management of mental health service users who come into contact with the police. Training, the development of joint protocols with clear delineation of responsibility and a clear shared understanding of roles, and appropriate resourcing of provision or at least awareness of the impact of under-resourcing for service providers and service users, were viewed as potential facilitators to effective interagency management.
Each of the elements presented on the day (Section 136, custody and service user engagement in research and practice) are presented below with reference to engagement methods and emergent themes.
Section 136
Members of the research team (practitioners and academics) presented the main findings of the case-linkage study related to Section 136 detentions. The presentation was used as a springboard that informed a group work session using vignettes based on case examples to stimulate discussion around the relevance of the findings to the attendees, as well as the common and divergent themes across services and geographical areas. Much of the discussion centred on the consequences to police officers of not detaining individuals under Section 136:
-
Most groups discussed the possible disciplining of officers for not detaining under Section 136 someone who subsequently self-harms or commits suicide. It was noted that officers are fearful to not use Section 136, as this can be seen to protect them from future recriminations. Further discussion within this theme centred on the lack of knowledge of alternatives to Section 136 available to police officers that would still provide the level of management required by the individual in order to mitigate against risk.
-
One group noted that training inspectors as well as constables on the use of Section 136 would be beneficial, to ensure a full understanding of the implications and ground-level challenges across the board.
-
Most groups went on to discuss the public perception of the role of police to make any given situation safe. With this in mind, participants expressed understanding of the challenges for officers to walk away from public situations in which individuals are presenting with potentially risky behaviour.
The rapid dissemination of police actions in such situations through the use mobile phone cameras and social media can impact on practice and the way situations such as these are managed.
Custody
Members of the research team (practitioners and academics) presented the case-linkage study findings relating to those cases with an arrest in the research window. As with the Section 136 session, the presentation informed a group work exercise using vignettes based on linked cases to stimulate discussion around the relevance of findings as well as emergent themes across professions and localities. The themes that emerged from these discussions were:
-
Most groups discussed the generalisability of the custody findings and speculated on whether or not a similar pattern of offence and detention management practices found in Cornwall prevailed across the UK. Discussion suggested that different areas may respond to policy guidance differently, although common challenges emerged. It was generally agreed that further research would be valuable in this area.
-
Most groups felt that there was a need for creative solutions to providing individuals with mental health needs in custody with access to suitable AAs.
-
The point was raised across the groups that there is need for service provision for mental health crises or emergencies that parallels that of physical health emergencies. Thus, discussion focused on a process more like A&E in terms of care and management.
Service user involvement
Presentations were given on service user involvement in research and service user involvement in the Interface Project. Furthermore, as noted above, two service user consultants from the Interface Project service user consultative group presented their experience of mental health and police services and their involvement in the research. These presentations were generally well received, as reflected in the event feedback; for example, particular positives included ‘Listening to perspectives of service users and stakeholders was very informative and useful’; ‘Service user perspective’; ‘Mr [service user’s] presentation was very engaging and informative’. Presentations were followed by a general discussion. The main themes of this were:
-
the challenges associated with engaging this population meaningfully and effectively; it was noted that the Interface Project was the only community forensic mental health research project with a service user reference group
-
the benefits of achieving such engagement for research and practice
-
the unique insights afforded by hearing first-hand the experiences of this group
-
meaningful engagement of service users in research was discussed (consultation was seen to have direct transformational benefits for service users by giving them a voice in the research process, impacting on the conduct of the research and enhancing their confidence).
Generic themes
Over the course of the day a set of overarching generic themes emerged. These included:
-
The need to raise the profile of the challenges of mental health and policing Delegates were delighted to have the opportunity to discuss the challenges and share best practice across sectors, but felt that more needed to be done in terms of enabling continued discussion that can influence government policy and practice. Academic research, rooted in collaborative methodology, was seen as key in facilitating this.
-
The need for a common language Delegates argued for the need to ensure that across sectors and organisations, professional and para-professionals (including government ministers and civil servants) are using a common language to avoid confusion, enhance understanding and drive clarity.
-
Information sharing and governance A significant focus of discussion was information governance and information sharing between agencies in order to manage effectively individuals with mental health needs across services. Discussion centred around the functionality and usability of record systems for practitioners on the ground and, in particular, the fragmented systems that prevented coherent management of individuals across geographical areas. For example, it was noted that RiO does not speak to social care systems such as Framework-I, and that these organisation- rather than service user-centred systems perpetuate silo working, maintaining a barrier to effective recording and information sharing. Furthermore, it was suggested that many people are happy for their information to be shared, and many indeed already assume that it is shared between organisations such as the police and mental health services. Consultation with service users was considered important in this regard.
-
Budget management There was a discussion amongst delegates regarding the need for consultation on the commissioning of services and, in particular, the current drive toward the transfer of custody health-care commissioning to the NHS.
-
The opportunity to network and share practice across organisations and the UK The need for opportunities such as the organised day was highlighted repeatedly, noting the value of sharing practice, joint problem solving and the possibility of lobbying for appropriate change. Even colleagues from the same county reported having met up for the first time due to the event and asserted the benefits of this. A number of delegates highlighted this when asked about the most useful aspect of the day: ‘Networking across other regions and accessing info and details of colleagues’; ‘Networking, sharing practice, procedures’; ‘Multiple providers and agencies willing to enter into discussions’.
Chapter 7 Discussion
The Interface Project arose out of the identified need to enhance service provision for individuals with EMHN who have contact with the CJS. Three stages of research were undertaken to answer a set of research questions pertaining to the relevant policy and legislation that frames this area of practice; the decision-making processes that impact the journeys of service users as they revolve between mental health services and CJS, including a health economics study; and the barriers and facilitators to providing an integrated pathway of care across agencies managing people with EMHN. The focus of the research was on the activity at the interface of mental health services and the CJS, and the implications of the single or joint agency decisions made at this interface for service users and providers.
Mental health service users interface with the police in one of three main ways, as shown in our findings: (1) Section 136, (2) detained in custody for a substantive offence, or (3) non-detention police contact. Due to the substantial differences in these three journeys, these findings needed to be considered separately. This analysis revealed a set of common and divergent findings across the three groups and pertaining to the full sample of the case-linkage study.
The common findings across the Section 136, custody and non-detention journeys of service users were:
-
The profile of service users across all three journey groups was similar in respect to ethnicity (94% white British or Irish), employment status (75% unemployed) and marital status (77% single).
-
The importance of information sharing early on in an incident and throughout its progress was evident across groups. Where this occurred, service users experienced more seamless and appropriate management and service providers felt more informed and supported in making decisions about such management.
-
Prior knowledge of, and recorded information about, the individual was beneficial to understanding the contact situation, responding to it and informing decisions as to appropriate management of the situation.
-
Although the assessment of risk was pivotal to a number of decisions affecting the service user journey across journeys and services, perceptions of risk differed between police and mental health professionals due to their different occupational imperatives. Thus, police officers respond to incidents through the principles of command and control while mental health professionals are concerned for the longer-term care and management of the individual.
-
Where the individual was detained, similar themes emerged in relation to the request and conduct of MHAA. These were risk to self and others, formal and informal support arrangements in the community, and presenting behaviour (where there was a MHAA).
-
Issues of resource were prevalent in all detention cases (Section 136 and custody) including availability of acute psychiatric care beds, pressure on place of safety and custody suites, and availability of staff to conduct a MHAA. These issues had direct, negative effects on service user management and on mental health and police services.
-
There was evidence in all three groups of police officers’ care beyond control, whereby they have gone beyond their responsibility to manage risk to ensure that an individual is safe and secure (e.g. has got home after being detained).
A number of key differences were found between the three types of service user journey:
-
The presence of protocol to inform and structure management of the individual was different across the three groups, being most visible in regard to Section 136 and least visible in relation to non-detention cases. Existence of protocol impacts consistency of approach to management, both by the police and mental health services. As less guidance is available, so greater diversity of outcome for service users is apparent and services experience greater challenge in terms of making an appropriate decision in the best interests of the individual.
-
Differences were apparent between groups in relation to the amount of prior information and knowledge there was available in relation to individuals’ mental health history. Thus, a greater number of PNC warning flags (78% vs. 63% vs. 13%, respectively) including mental health warnings on the police systems were associated with the Section 136 sample than either custody detentions or non-detentions. This impacts on the knowledge available regarding the individual at an incident and on the degree of communication between police and mental health services, with greater communication in respect of Section 136 cases.
-
There were differences between the groups in relation to whether or not the individual was on the caseload of a MHT at the time of contact with police. Substantially more police contacts involved an individual on caseload at the time of contact in the Section 136 (63%) group than in the custody (44%) or non-detention group (31%; single case accounting for majority of incidents removed). Furthermore, more information exchange between services was seen where the individual was on caseload.
-
The profile of service users differed in relation to gender; slightly more females were sectioned under Section 136 (57% female and 43% male), more males were detained in custody (33% female and 67% male), and similar numbers of males and females were reported in the non-detention sample as Section 136 (53% female and 47% male). Individuals in the non-detention group were slightly older (mean = 41.5 years; range 21.2–85.0 years) than those in either the Section 136 (mean = 35.7 years; range 18.8–73.3 years) or custody groups (mean = 33.6 years; range 18.0–67.0 years).
-
In terms of making the initial decision to detain or attend an incident, contextual factors such as location were seen to be more influential in the case of Section 136 detentions with regard to risk than in custody/non-detention contacts.
The findings have implications for policy and practice, and inform recommendations for research that are grounded in the experience of service users, mental health and police professionals on the ground and their wider organisations. The discussion of the findings with regard to implications and recommendations is centred on two main issues to have emerged from the research: information governance and moving from interagency working to an integrated service. These issues were key in professional and service user stakeholders’ consideration of the findings of the case-linkage study in the light of current service delivery and experience of service respectively. Figure 29 provides a suggested operational process involving the development of a joint agency steering group to inform and drive recommended actions derived from the research findings. The figure identifies the key co-commissioning stakeholders in the outcomes of those service users whose journeys bring them into contact with health providers and criminal justice agencies. The findings and process of this research underline the importance of bringing a picture of the lived experience of mental health service users to the attention of all agencies responsible for commissioning in order that they can co-operate in maximising the outcomes for these individuals through requirements in service specifications and the application of contracting levers such as the Quality, Innovation, Productivity and Prevention programme. A locally-based joint agency steering group, or offender health partnerships board would constitute a forum in which information about need and vulnerability can be shared, where conflicting priorities could be discussed and resolved and in which the operation of information sharing agreements around the target population could be monitored.
FIGURE 29.
Recommended actions for commissioners.
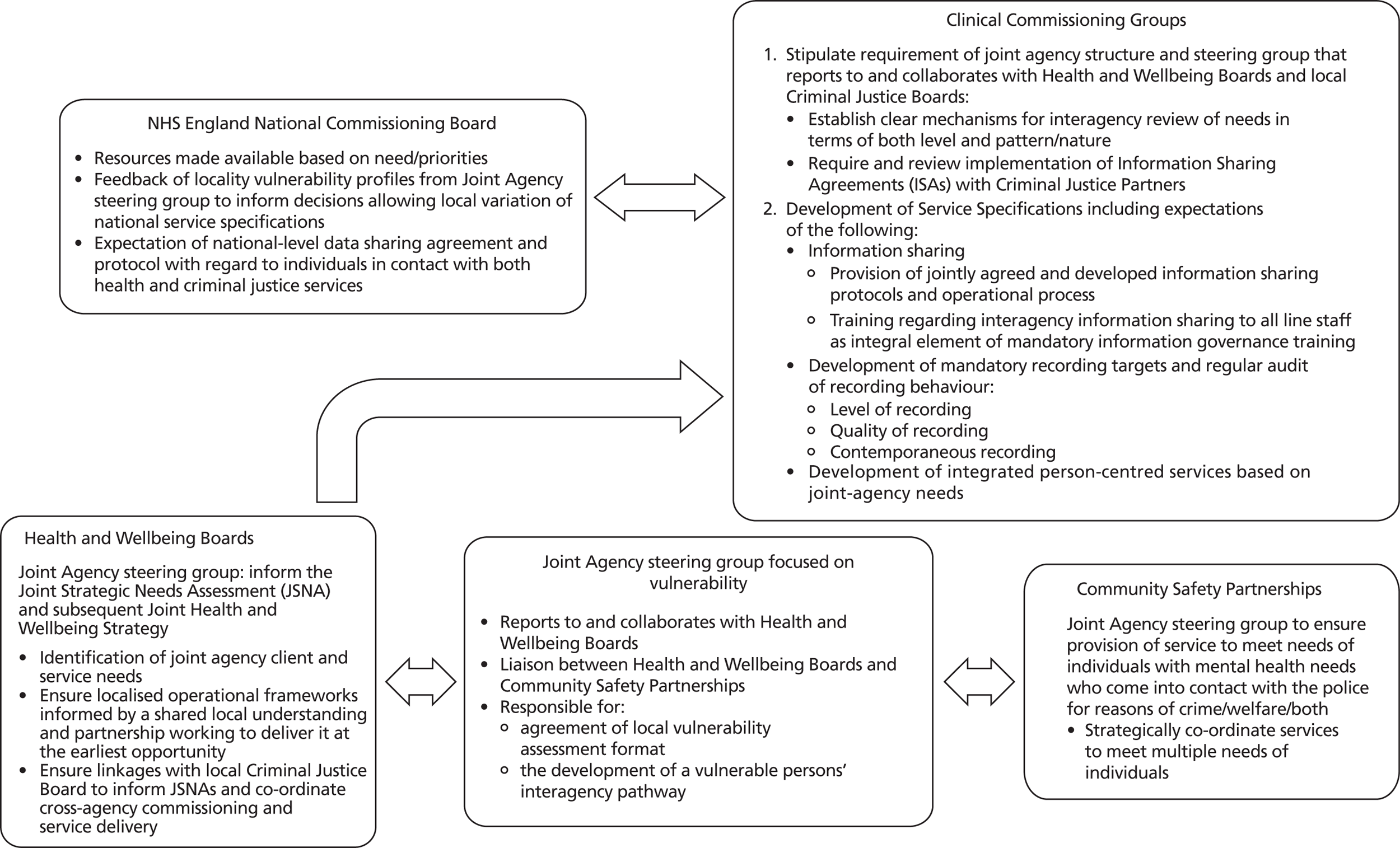
Information governance
The issue of information governance pervaded the Interface Project, in terms of the methodology employed in the research and as a major issue to emerge from the research findings. The case-linkage methodology and reliance on routinely collected case file data necessitated a strong focus on information governance within the research. Use of these data for the purpose of research enabled discussion with practitioners and service users, which highlighted the importance of interagency information governance processes and structures, the need for functional and usable systems to both support and operationalise these processes, and staff provided with the skills, knowledge and support to maximise the utility of systems for the best outcomes for practice and ultimately service users. Information governance for the management of joint service users of the police and mental health services is governed by the DPA47 for both the police and mental health services with additional governance of the NHS Act 200638 in terms of the common law duty of confidentiality and Caldicott principles, which govern the use of patient information in NHS organisations.
The findings of the case-linkage study highlighted instances when information exchange between services took place and were beneficial to the decision-making process, interagency working and enhanced service user outcomes. Service users who took part in the stakeholder consultation supported the view that agencies should communicate about those individuals in their care and provided examples of benefit of such exchange from their own experience. Professional stakeholders, although understanding the benefits of information exchange for their practice and service user outcomes, expressed concern with regard to both assessment of proportionate and appropriate sharing of personal information and lack of awareness of processes to support and mechanisms to facilitate and operationalise this.
There are formalised processes for information exchange between services for the purpose of public protection; for example, MAPPA are bound by legislation (i.e. CJA). However, as has been shown by the current study, the majority of EMHN individuals who come into contact with the police are not managed by such formal processes; rather, information exchange about these individuals is governed by exclusions to the first principle of the DPA (the processing of personal data fairly and lawfully) that permit third-party disclosure in the case of, among others, prevention/detection of crime and the prevention of physical/mental harm to the individual and/or others. Furthermore, and also as shown by the current study, the majority of individuals who come into contact with the police either through Section 136 detentions or custody arrests, if on caseload of secondary mental health services are on the caseload of general secondary mental health services and not offender-specific services who routinely liaise with the police to support service users. Therefore, the majority of joint agency service users are managed by professionals who may not have specialist knowledge to enable them to appropriately and confidently disclose information to other agencies that could effectively enhance management. Although health professionals and police are provided with training, the extensive mandatory training burden on staff and the reliance on e-learning-based principles rather than scenario-based training methods with no supporting joint protocol does not adequately support staff.
Information sharing is also either facilitated or obstructed by systems designed to support the recording and accessing of information. Two main issues were highlighted by this study in this regard; first, the usability and functionality of systems for front-line staff both inputting and retrieving information, and second, the communication between systems or lack thereof. Both the case-linkage study, which itself relied on the recording systems under discussion here, and the stakeholder consultation highlighted how access to timely historical information, for example regarding risk or contingency plans, can aid effective management through accurate information about an individual to support practice and/or to provide accurate information within their own agency or to share with other agencies. However, it is clear that the systems used to support the work of agencies are not designed to support interagency management and therefore perpetuate the silo working that has been implicated in so many of the serious case reviews. National stakeholders called for systems that could ‘talk to each other’, breaking the insular recording and working patterns of agencies in order to centre system requirements on individuals. Service user consultation highlighted the potential willingness of service users to enable agencies to share proportionately information that could have the potential of enhancing practice and, importantly, meeting the needs of service users.
Due to the methodology employed by the current study, accuracy of record keeping emerged as an important issue, not only for interagency management but also for the research process itself. Accurate information that can be retrieved in a timely fashion at the point of need is crucial. The findings have indicated that relay of information by operators to response officers en route to, or at the time of, incidents can enhance officers’ management of EMHN individuals through the provision of information regarding mental health condition and recent police incidents in which they have been involved. Similarly, staff at the place of safety need to be able to assess potential detainees’ risk of violence in order to make a decision with regard to location of detention in the place of safety. The research process itself highlighted the need for minimum standards of recording and systems that support the rapid retrieval of information in order to accurately and efficiently use information available when staff require it on the ground, and to ensure comprehensive and accurate auditing of practice. This was highlighted in particular with regard to the recording of rationales for the use of restraints and the recording of requests for AAs and associated rationales.
Figure 30 highlights the main points for transferable learning and recommended actions for local NHS practice derived from the research findings related to information governance.
FIGURE 30.
Transferable learning for local NHS practice and recommended actions: information governance.
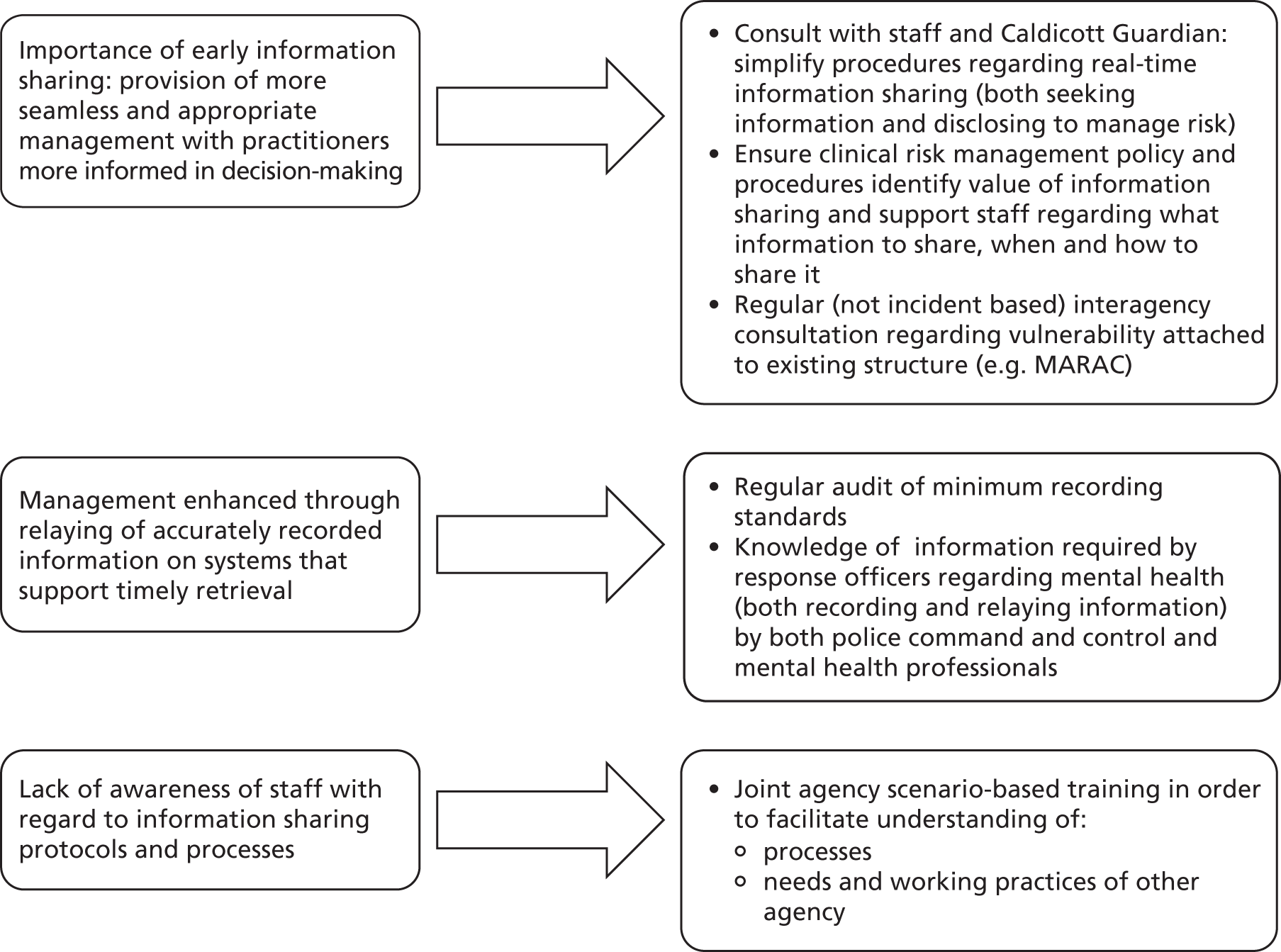
From interagency working to integrated service
This project focused on interagency decision-making in the service journeys of mental health service users who come into contact with the police. The impetus for this research, in part, came from the need to ensure effective interagency working to prevent service users from falling between services, as highlighted by recent serious case reviews. The findings of the main case-linkage study and the stakeholder consultation highlighted the concern of professionals in both their responsibility for the risk of individuals and their respective organisations’ (lack of) support when removing their agency from this responsibility/handing responsibility to the other service. Additionally, the service user consultation called for clearly delineated responsibility in combination with staff knowledge of mental health within an integrated service centred on the needs of service users.
The stakeholder consultation and findings of the main study further raised the issue of differing interpretations of protocols designed to support effective interagency management. Even in the case of Section 136, which has clearly defined policy interpreted at a local level in line with Lord Bradley’s recommendations,6 protocols are variously interpreted leading to disparate modes of management across cases and less than optimal outcomes for service users. Overall, analysis of service user journeys in this project, and the identified opportunities for service users to fall between services as decisions are variously made regarding their management, points towards the need for a move from interagency working to truly integrated services centred on the service user where agencies have an equal responsibility for their management and a shared stake in the service being delivered.
The health economics component of this study modelled the potential economic impacts of two such integrated service enhancements: a custody liaison service providing mental health nurses in the custody environment to assess and refer individuals who have been arrested and (may) require mental health input; and a street triage service providing mental health professional support to police officers at the point of detention for Section 136. The pathways analysis points towards the efficiency of the development of the above integrated service models, which were shown to have a minimal effect on individual level costs compared with current practice. Although the roll out of these services to all of those who qualify could escalate resource allocation, it is argued here that the diversionary role of such services could ultimately reduce the population requiring such services, thus reducing need and potentially cost.
This evidence supports the recent government funding of pilot street triage schemes for potential Section 136 detentions for the following reasons:
-
Street triage models provide an integrated service with joint protocols to jointly manage individuals in crisis, in order to ensure that they receive an appropriate response and service to meet their needs.
-
Enhancement of crisis care that will not only support officers in making the decision to detain under Section 136, but also meet the need highlighted by the national professional stakeholders in terms of an emergency service for mental health needs to mirror that currently provided for physical health needs.
-
Such an integrated service, designed to divert individuals to appropriate care and management at the point of need, would ensure that those who are in need of enhanced management but are not detainable under the MHA for assessment and/or treatment do not need to be subjected to unnecessary detention under Section 136 and formal assessment in order to expedite their access to care.
The evidence further supports the need for joint training of police and mental health professionals in line with the recent joint HMIC, Care Quality Commission (CQC) and Her Majesty’s Prison report recommendations:41,42 joint agency training, including legal powers but with particular regard to protocol in order that a common understanding and interpretation is developed and consolidated in practice. Also, in line with this report, refresher training should be provided, enabling changes in protocol to be updated among the workforce, confirmation of protocol interpretations to be achieved and challenges in operationalisation of protocol to be resolved.
Figure 31 highlights the main points for transferable learning and recommended actions for local NHS practice derived from the research findings related to this theme.
FIGURE 31.
Transferable learning for local NHS practice and recommended actions.
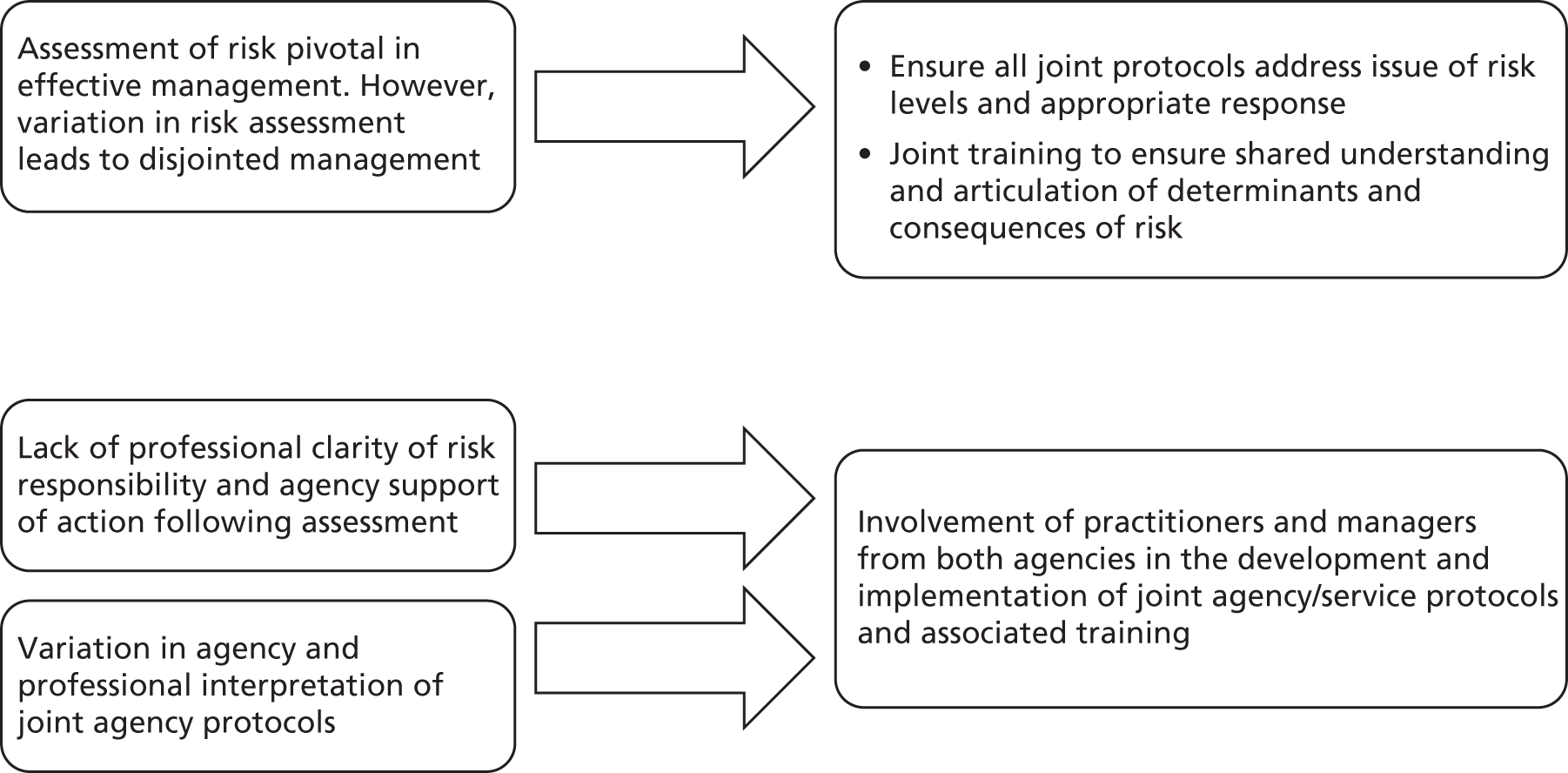
Patient and public involvement: impact, challenges, lessons learnt
Patient and public involvement and the development of the Service User Consultative Group was considered a strength of the Interface Project. However, ensuring meaningful engagement of service users was not without its challenges. As presented in Chapter 3, the recruitment method for the group required revision to secure participation and ensure representation of experience in terms of mental health need and type of police contact. Administrative challenges included ensuring parity in terms of payment for service users’ time and access with regard to location and methods of consultation with the group. The research team resolved these issues through a combination of collaboration with partner and third-sector organisations and flexibility to ensure openness and equity of access throughout the project. Finally, ensuring that consultation was meaningful to the research and to participating service users was central to the research. This was assured by:
-
ensuring the group was heard and meaningful changes made to the research in response to feedback
-
the group was representative of the target population of the research
-
service user consultation was communicated to all elements of the project management structure.
Patient and public involvement has had wide-ranging impacts on the project and the service user consultants themselves. The contributions made by the consultants have been discussed in detail in Chapter 3. In summary, PPI has had a meaningful impact on the study design, recruitment and consultation, and has helped frame the research findings. The consultation process has had a positive impact on the service users involved in the research, who have demonstrated a positive response to their involvement and expressed a strong interest in continuing to consult on research. In particular, the group emphasised the importance of being involved in a meaningful process, seeing evidence of the consultation put into action and the importance of perceiving that they might be able to improve service user experience through their journeys through mental health and police services. Consultants also recognised the positive effect that involvement in the research had on their confidence and personal development.
The service user consultation of the Interface Project was considered to have been both successful and impactful in terms of the conduct and validation of the research. To the authors’ knowledge, this is the first successful community forensic mental health reference group for research in the UK and as such it provides a model for other projects. Lessons learned for future research include consultation with service users from the outset of project conception; collaboration with third-sector agencies in the recruitment of consultants; flexibility in consultation method to suit the needs of service users; maintaining focus on the needs of the research and ensuring parity in terms of service user inclusion and remuneration.
Limitations
The Interface Project suffers three main limitations. First, the data for the project’s main study involved the police and mental health records associated with 80 services users’ journeys over the period of a year. This sample size could be considered low, particularly once the findings were categorised according to types of police contact. However, the data corpus was extremely substantial (e.g. in the case of one individual their data comprised 286 pages of data drawn from police and NHS records, and the full corpus took up one-third of the faculty’s allocated server space). The number of police contacts per individual ranged from 1 to 296, and for each police contact police and mental health data were examined. Nevertheless, the findings of the study need to be interpreted with caution.
Second, the single-site nature of the research further limits the generalisability of the findings. Cornwall is a rural locale with a low, dispersed population and no city-sized conurbation; as such, it is not representative of all other counties in England. However, a single site was appropriate given the substantial complexity of the research area and the need for an associated innovative study design and methodology to meet the research objectives. Thus, this approach has enabled the methodology to be successfully trialled including managing complex, intra and interservice relationships; data sharing and data access; managing a large volume of highly sensitive, linked data; and the engagement of service users meaningfully in the research. Consequently, as noted by participants at the national stakeholder consultation, the Interface Project provides a model for extending the research to other sites nationally. Additionally, the national event demonstrated that the findings resonated with senior managers in the police and NHS from other counties in England, as similar data storage systems are used by the police and mental health services and services are working to common codes of practice through local interpretation.
Third, the recruitment of participants to the study in stages 2 (service users) and 3 (service users, police and mental health professionals) proved challenging. This was resolved in stage 2 through the change to the recruitment methodology and the successful application to NIGB for Section 251 approval, which resulted in a more representative sample through the application of a stratified random sampling approach than would have been achieved through the original consent route. There were two recruitment issues that impacted on stage 3 of the research. First, the recruitment of service users through the local mental health clinical research network was not as successful as anticipated. Owing in part to the need for the network research officers to recruit through care teams and the associated resource implications, recruitment of individuals identified through the clinical audit was not successful. Although three individuals indicated their interest in participating in the research, consent forms were received after data collection had ceased. Fortunately, due to the very successful relationships with third-sector organisations through the service user consultation element of the project, the team recruited the expected number of service users to participate in stage 3. However, mental health professional participation was low (and similarly relatively few mental health professionals attended the national stakeholder event). Low levels of recruitment, despite substantial effort, appear to be a reflection of the roles and responsibilities of mental health professionals who were challenged to make the time to be involved due to work commitments. This limits the findings of stage 3 in terms of mental health professionals’ perspectives. Finally, although police officers reflecting a range of ranks were readily recruited into stage 3, as well as a representative of the BTP and police community support officers, due to the emergence of the importance of communication from command and control from the analysis in the case-linkage study, representation from call operators would have been a valuable addition to the police stakeholder consultation discussions.
Given the importance of the PoD model in framing the research process, it is appropriate to reflect on its success. Certainly, the model has been extremely effective in thoroughly engaging stakeholders in the development, process and early implementation of findings. This is significant, as the discipline of ‘implementation science’ continues to note the challenges of securing the effective uptake of research findings in health-care contexts. However, the model is similar to others rooted in a social constructionist epistemology and informed by a participatory evaluation methodology, both within health care and other disciplines. For example, McWilliam et al. ’s71 ‘participatory social interaction approach’ to knowledge translation has much resonance with our approach. These authors adopt a critical and constructivist approach to knowledge, incorporating a sensitive appreciation of the hierarchical system of power relations within health-care organisations that form the context of implementation, a focus on social interaction through social phenomenology and a participatory approach. It would be worth exploring and comparing the relative merits of these different approaches in the future. Furthermore, as participatory research is characterised by conducting research ‘with’ and not ‘on’ people,72 thereby ensuring that the research is owned by both the participants in the research and the researchers, this type of research is time-consuming. It would be fair to say that delivering this project to time was challenging. Although we would argue that the benefits outweigh this disadvantage, the time taken to engage stakeholders meaningfully and continue to invest in those relationships throughout the research should not be underestimated.
Strengths
This research has a number of strengths. First, to the knowledge of the authors, this is the first time that case-linkage of police and mental health records yielding such a substantial corpus of data has been achieved in the UK. The methodology is both complex (engaging agencies; obtaining ethical approval; gaining access through NIGB) and resource intensive (researcher time for data extraction, depersonalisation, management and analysis). However, the ability to understand the decision-making process from the records of both agencies provides a unique perspective on the drivers for the decisions made as well as the challenges and facilitators to interagency management of joint service users.
Second, as noted above, the sample size in this study could be considered a limitation in terms of the quantitative analysis that could be undertaken. However, the extensive nature of both the police and mental health data yielded for each case provided a rich data corpus that facilitated the in-depth qualitative work examining the nuances of the decision-making process of professionals managing each type of police contact. The detailed examination of 80 cases enabled the researchers to make best use of this rich data in order to uncover the precipitating factors and processes that underpin such decisions. It should be reiterated that the research relied on routinely collected data from each agency and further noted that these data are not in a format conducive to detailed examination for the purpose of research. This means that such detailed qualitative work as undertaken for this project is both painstaking and time intensive. For example, the rationale supporting the use of restraints by a police officer in the course of a detention could be buried in a single line within 25 pages of text from the detention log of a single detention. By focussing in such detail on what may be considered a limited sample, the research has identified a range of factors that influence interagency decision-making that can now be scrutinised across research sites and a wider population of service users.
Third, as presented within the PPI sections in this report, service user involvement has been highly successful in this project, having a significant impact not only on the research itself but also on the service users themselves. To the knowledge of the authors, the service user consultative group developed to support the work of the project is the only reference group formed to consult on research examining joint service provision in a community forensic population. Furthermore, despite the potential challenges in identifying and engaging with this population, the research team both maintained the momentum and membership of the core group, and ensured the authentic representation of those members of the population whose needs often preclude them from having a voice in the process and conduct of research.
Finally, the approach developed by the first two authors and applied in the Interface Project ensured true partnership from the outset through engagement with practitioners and their respective organisations and embedding of researchers within the agencies under examination. Not only did this facilitate the process of the research (exemplified in the partnership working involved for the NIGB application) but imbued a strong sense of ownership of the research on the part of both CFT and the police, making the findings of the research and their implementation of critical importance to both organisations.
Recommendations
The project has given rise to three sets of recommendations relating to future research.
Recommendations based on project findings
-
The Interface Project was a test site for an innovative case-linkage study that included qualitative analysis of interagency decision-making, economic analysis of costs and potential service enhancements. However, the study was conducted in a single predominantly rural site in the south-west of England. Replication of this study is recommended in further sites in England and Wales to examine potential variation in decision-making and costs according to differences in a variety of variables including geographical area, urbanisation, demographic differences, protocol interpretation, resource and service provision. It is further recommended that replication of the research should be made in sites representative of more ethnically diverse populations.
-
The findings showed that a very small proportion of individuals with a custody detention following arrest were formally assessed under the MHA. The research identified the precipitating factors in the decision to request a MHAA and the decision to detain further under the MHA, for those who were formally assessed. It is recommended that further research is undertaken to identify those cases where decisions were made to not assess and detain under the MHA, and the outcomes of those decisions for the individual. The Section 136 and stakeholder consultation findings revealed a discrepancy between how place of safety staff assessed violence risk for admission and how police officers perceived that these assessments were made. Additionally, police officers perceived that mental health staff viewed their assessment of risk at the time of detention under Section 136 as resulting in inappropriate Section 136 detentions. It is recommended, that further research:
-
specifically examines assessment of risk in the light of protocol interpretation
-
includes both primary and secondary data in order to triangulate the precipitating factors informing assessment and driving related decisions.
-
-
It is recommended that future research employs a Realist Evaluation approach. 73 This approach could further enhance the contextual sensitivity of findings through understanding the mechanisms underpinning the practices identified in this research, as well as the conditions required to trigger these mechanisms to produce enhanced management outcomes. The adoption of this approach could increase the generalisability and translation of research findings of benefit to service providers, commissioners and ultimately service users.
Recommendations based on themes and implications
-
Training One of the implications drawn from the findings of the research for practice was for scenario-based interagency training of police and mental health professionals with regard to information sharing and protocol adherence and interpretation. It is recommended that further research should explore the development and utility of such training, and the impact thereof on practice and interagency management.
-
Integrated service Recent developments and government-funded pilots have enabled the implementation of integrated services such as custody liaison and diversion and street triage. It is recommended that research should be undertaken with regard to professional decision-making of such services with a particular focus on risk responsibility and interprofessional communication and information exchange. It is essential that such research is longitudinal in order to ensure that the diversionary impact of such services is explored within service user journeys, and that a health economics aspect is included in order to identify resource implications over time.
Recommendations relating to re-use of the data corpus
As noted, the research has produced an extensive and rich data corpus. The research team acknowledge that due to the success of the NIGB application, they have been in a privileged position to be able to examine the journeys of arguably the most vulnerable service users as they interface with both police and mental health services.
-
It is recommended that future research using these data could take a discursive approach to understanding the way in which risk is negotiated and understood between and within services.
-
A separate study exploring mental health professional and police conceptions of mental health and EMHN service users using a discursive approach would also offer an innovative and important contribution to existing knowledge.
-
Two observations were made by the researchers in their extraction and management of the data corpus. First, that a significant proportion of the cases examined for the purpose of this research were currently or had been victims of sexual violence either as adults or in childhood. Second, a number of the female cases included in the sample were mothers whose children had been removed from their care. Although neither of these issues could be explored within the remit of the current research, discussion between the researchers based on observation of the data indicated that both of these issues had an effect on the mental health, mental health service and police contact of the individuals examined. It is, therefore, recommended that further research focus on the impact of these two issues on police and mental health service user journeys.
Acknowledgements
This project has been dependent on the goodwill and time of numerous people and organisations. We have many people to thank. First, we need to thank our service user consultants for their invaluable time, input, support and inspiration. In connection with the group, we would particularly like to thank Kate Atkinson for her support and advice. Service user involvement in this project was greatly enhanced by recruitment provided by Cornwall Health for Homeless and Coastline Housing, to whom we are very grateful.
We are also indebted to all the members of the steering group for their helpful guidance throughout the project. Professor Rod Sheaff chaired the group and two of our original fund holders, Dr Nick Lynn and Iain Grafton OBE, were also members. We would particularly like to thank Julia Moore, Force Mental Health Liaison, for her help in accessing data and for her advice. We would like to thank Andy Fox (Head of Social Care) for supporting and raising awareness of the project in social care in Cornwall. Thank you also to Barry Marsh, who brought valuable insight to the project, representing Mid-Cornwall Lifestyles.
For their immensely valuable help in preparing the NIGB application, we would like to thank the Force Data Protection Officer as well as the Trust Information Governance Lead and Head of Records Management, Plymouth University and the teams that worked with them to progress the application. Dr Ellen Wilkinson (Medical Director of CFT), who has been supportive of the research and the NIGB application in particular. Finally, thank you to the staff at the Centre for Mental Health and Justice (CFT) and the training team at Crownhill police station for their patience and support provided to the researchers.
A special thank you must be given to James Brown (Institute of Psychiatry, Psychology and Neuroscience, King’s College London) for being so supportive and diligent in his work related to the project, particularly in organising the national stakeholder event.
The host institutions, the Institute of Psychiatry, Psychology and Neuroscience (King’s College London), Plymouth University, CFT and DCP and many members of staff in each organisation have made this project possible; in particular, we want to thank our colleagues in finance, human resources, information and technology information governance in each organisation.
This research could not have been conducted without the generosity of CFT and DCP in working with us in true partnership – we have appreciated this enormously – the project’s success is an achievement that should be shared with all our collaborators and consultants.
This report contains public sector information licensed under the Open Government Licence v2.0. Open Government licence was confirmed to cover the reproduction of quotes from the Bradley Report,6 Steven Hoskin Serious Case Review,55 Acts and Codes of Practice. CFT’s copyright statement confirms permission to reproduce the Longreach House Place of Safety Assessment Suite Operational Policy54 for the purpose of research. Turning Point confirmed permission to reproduce quotes from Lord Adebowale’s report. 42
Contributions of authors
The authors contributed to the following aspects of the project and report:
Susan Lea Original concept, project lead, overall design, data analysis, drafting and report revising.
Lynne Callaghan Original concept, research manager, overall design, health economic component design, case-linkage, health economic and stakeholder data collection, data analysis, drafting and report revising.
Susan Eick Case-linkage, health economic and stakeholder data collection, data analysis, drafting and report revising.
Margaret Heslin Health economics component data analysis, drafting and revising.
John Morgan Original concept, data collection support, practice-based review of interpretation of findings, overall design and data analysis.
Mark Bolt Data collection support and practice-based review of interpretation of findings.
Andrew Healey Health economics component drafting and revising.
Barbara Barrett Health economics component drafting and revising.
Diana Rose PPI design and support and report revising.
Anita Patel Original concept, overall design, health economic component, drafting and revising.
Graham Thornicroft Expertise in UK mental health policy, related research programmes and projects, expertise in implementation science.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
This report contains transcripts of interviews conducted in the course of the research, or similar, and contains language which may offend some readers.
Publications
Presentations
Callaghan L. Enhancing the Multi-Agency Management of Individuals with Enduring Moderate to Severe Mental Health Needs (EMHN): Client Journeys and the NHS/CJS Interface Cornwall Partnership NHS Foundation, Mental Health Team Continuing Professional Development, Pentire Hotel, Newquay, Cornwall, 26 October 2011.
Morgan J, Bolt M, Callaghan L, Marshall D. Cornwall Joint Working. Police Health Care Commissioning Stakeholder Day, China Fleet Country Club, Saltash, Cornwall, 30 May 2012.
Callaghan L, Eick S. Enhancing the Multi-Agency Management of Individuals with Enduring Moderate to Severe Mental Health Needs (EMHN): Client journeys and the NHS/CJS Interface World Mental Health Day Event, Cornwall, 10 October 2012.
Lea SJ, Callaghan L, Morgan J, Grafton I, Bolt M, Thornicroft G, et al. Exploring Inter-Agency Decisions at the Mental Health/Criminal Justice Interface: Preliminary Findings From a Case-Linkage Study, Institute of Psychiatry, King’s College, London, 14 March 2013.
Callaghan L, Eick S, Rose D, Morgan J, Bolt M, Atkinson K, et al. Developing Authentic and Sustained Service User Involvement In Research With Hard to Reach Groups: The Case of the Interface Project. Institute of Health and Community, Community Engagement Conference 2013 Programme, Roland Levinsky Building, University of Plymouth, 20 March 2013.
Poster only
Lea SJ, Callaghan L, Morgan J, Lynn N, Thornicroft G, Grafton I, et al. Enhancing the Multi-Agency Management of Individuals with Enduring Moderate to Severe Mental Health Needs (EMHN): Client Journeys and the NHS/CJS Interface. Faculty of Health, Education and Society Launch, Plymouth University, 14 September 2011.
Lea S. Tracking Interagency Collaboration in Relation to Individuals with Enduring Mental Health Needs: A Case-Linkage Study. NIHR MHRN 2012 National Scientific Meeting, Birmingham, 25–27 April 2012.
Callaghan L, Morgan J, Grafton I, Bolt M, Thornicroft G, Rose D, et al. Examining Service User Journeys Through Mental Health Services and the Criminal Justice System: The Interface Project. Cornwall Research Forum, The Knowledge Spa, Truro, 29 June 2012.
Callaghan L, Morgan J, Grafton I, Bolt M, Thornicroft G, Rose D, et al. Examining Service User Journeys Through Mental Health Services and the Criminal Justice System: The Interface Project. Plymouth Hospitals NHS Trust Conference, Derriford Hospital, Plymouth, 14 September 2012.
Callaghan L, Morgan J, Eick S, Watson D, Furbear T, Grafton I, et al. Using Case-Linkage Methodology with Hard-to-Reach Populations: The Experience of the Interface Project. MHRN National Scientific Meeting 2013, The Grand Connaught Rooms, London, 20 March 2013.
Briefing papers
Lea S, Callaghan L, Grafton I, Bolt M, Morgan J, Thornicroft G, et al. The Interface Project: Enhancing the Multi-Agency Management of Individuals with Enduring Moderate to Severe Mental Health Needs Briefing Paper for the Independent Police Complaints Commission.
Lea S, Callaghan L, Grafton I, Bolt M, Morgan J, Thornicroft G, et al. Briefing Paper for the Revolving Doors Agency. The Interface Project: Enhancing the Multi-Agency Management of Individuals with Enduring Moderate to Severe Mental Health Needs Revolving Doors Agency, Borough High Street, London SE1 1JG.
References
- Birchard M. The Birchard Enquiry. London: The Stationery Office; 2004.
- Magee I. The Review of Criminality Information 2008. http://tna.europarchive.org/20100419081706/http://www.police.homeoffice.gov.uk/publications/operational-policing/review-criminality-information/roci-full-report2835.pdf?view=Binary (accessed 4 October 2011).
- Laming L. The Victoria Climbié Inquiry. London: The Stationery Office; 2003.
- Laming L. The Protection of Children in England: A Progress Report. London: The Stationery Office; 2009.
- Docking M, Grace K, Bucke T. Police Custody as a ‘Place of Safety’: Examining the Use of Section 136 of the Mental Health Act 1983. London: Independent Police Complaints Commission; 2008.
- Bradley K. The Bradley Report: Lord Bradley’s Review of People with Mental Health Problems or Learning Disabilities in the Criminal Justice System. London: Department of Health; 2009.
- Review of Health and Social Services for Mentally Disordered Offenders and Others Requiring Similar Services Report of the Official Working Group for People with Special Needs. London: Department of Health and Home Office; 1992.
- Rutherford M. Blurring the Boundaries: The Convergence of Mental and Criminal Justice Policy: Legislation Systems and Practice. London: Sainsbury Centre for Mental Health; 2010.
- Corston J. The Corston Report: A Review of Women with Particular Vulnerabilities in the Criminal Justice System. London: The Home Office; 2007.
- Her Majesty’s Inspectorate of Constabulary . Getting Together. A Better Deal for the Public Through Joint Working 2009. www.hmic.gov.uk/media/getting-together-a-better-deal-for-the-public-through-joint-working-20090608.pdf (accessed 4 June 2011).
- Flanagan R. The Review of Policing Final Report. London: Home Office; 2008.
- Briefing Note on Recognising Mental Ill Health and Learning Disabilities. Wyboston: National Policing Improvement Agency; 2010.
- Ferrante A. The use of data-linkage methods in criminal justice research: a commentary on progress, problems and future possibilities. Current Issues Crim Just 2008;20.
- Larney S, Burns L. Evaluating health outcomes of criminal justice populations using record linkage: the importance of aliases. Eval Rev. 2011;35:118-28. http://dx.doi.org/10.1177/0193841X11401695.
- Fisher WH, Simon L, Roy-Bujnowski K, Grudzinskas A, Wolff N, Crockett E, et al. Risk of arrest among public mental health services recipients and the general public. Psychiatr Serv. 2011;62. http://dx.doi.org/10.1176/appi.ps.62.1.67.
- Geertz C. Thick Description: Toward an Interpretive Theory of Culture. The Interpretation of Cultures: Selected Essays. New York, NY: Basic Books; 1973.
- Greatley A, Naylor C, Wallcraft J, Samale C. Research Priorities for Service User and Carer-Centred Mental Health Services: Consultation Report. Report for the National Coordinating Centre for NHS Service Delivery and Organisation. London: Research & Development National Coordinating Centre for NHS Service Delivery and Organisation; 2007.
- Mental Health Act 1983 c.20. London: The Stationery Office; 1983.
- Mental Health Act 2007. London: The Stationery Office; 2007.
- Tansella M, Thornicroft G. Implementation science: understanding the translation of evidence into practice. Br J Psychiatry 2009;195:283-5. http://dx.doi.org/10.1192/bjp.bp.109.065565.
- Klein KJ, Sorra JS. The challenge of innovation implementation. Acad Manage Rev 1996;21:1055-80.
- Thornicroft G, Lempp H, Tansella M. The place of implementation science in the translational medicine continuum. Psychol Med 2011;41:2015-21. http://dx.doi.org/10.1017/S0033291711000109.
- Creswell JW. Research Design. Qualitative, Quantitative, and Mixed Methods Approaches. London: Sage; 2009.
- Wadsworth Y. Responsive Evaluation: New Directions for Evaluation, No. 92. San Francisco, CA: Jossey-Bass; 2001.
- Burke B. Evaluating for a change: reflections on participatory methodology. New Dir Eval 1998;80:43-56. http://dx.doi.org/10.1002/ev.1116.
- Papineau D, Kiely MC. Participatory evaluation in a community organization: fostering stakeholder empowerment and utilization. Eval Program Plan 1996;19:79-93. http://dx.doi.org/10.1016/0149-7189(95)00041-0.
- Orford J. Community Psychology: Challenges, Controversies and Emerging Consensus. Chichester: John Wiley & Sons Ltd; 2008.
- Nightingale D, Cromby J. Social Constructionist Psychology: A Critical Analysis of Theory and Practice. Buckingham: Open University Press; 1999.
- Bakhtin M, Emerson C HM, McGee V. Speech Genres and Other Late Essays. Austin, TX: University of Texas Press; 1986.
- Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implementation Sci 2007;2:40-8. http://dx.doi.org/10.1186/1748-5908-2-40.
- Lather P. Research as praxis. Harvard Educ Rev 1986;56:257-77.
- Rogers EM. Diffusion of Innovations. New York, NY: Free Press; 1995.
- Eccles MP, Armstrong D, Baker R, Cleary K, Davies H, Davies S, et al. An implementation research agenda. Implementation Sci 2009;4:18-24. http://dx.doi.org/10.1186/1748-5908-4-18.
- McWilliam C, Kothari A, Ward-Griffin C, Forbes D, Leipert B. South West Community Care Access Centre Home Care Collaboration (SW-CCAC): evolving the theory and praxis of knowledge translation through social interaction: a social phenomenological study. Implementation Sci 2009;4:26-39. http://dx.doi.org/10.1186/1748-5908-4-26.
- Baker R, Roberton N, Rogers S, Davies M, Brunskill N, Khunti K, et al. The National Institute of Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for Leicestershire, Northamptonshire and Rutland (LNR): a programme protocol. Implementation Sci 2009;4:72-6. http://dx.doi.org/10.1186/1748-5908-4-72.
- Cooksey D. A Review of UK Health Research Funding. London: The Stationery Office; 2006.
- Cooke J. A framework to evaluate research capacity building in health care. BMC Fam Pract 2005;6. http://dx.doi.org/10.1186/1471-2296-6-44.
- National Health Service Act (2006) c.41. London: The Stationery Office; 2006.
- New Horizons A Shared Vision for Mental Health. London: DH; 2009.
- Improving Health, Supporting Justice: The National Delivery Plan of the Health and Criminal Justice Programme Board. London: The Stationery Office; 2009.
- A Criminal Use of Police Cells? The Use of Police Custody as a Place of Safety for People with Mental Health Needs’. London: HMIC; 2013.
- Adebowale V. Independent Commission on Mental Health and Policing Report. London: Independent Commission on Mental Health and Policing; 2013.
- Home Office . Police and Criminal Evidence Act 1984 (PACE) and Accompanying Codes of Practice 2010. www.homeoffice.gov.uk/publications/police/operational-policing/pace-codes/ (accessed 25 September 2013).
- Mental Capacity Act 2005. London: The Stationery Office; 2005.
- Police and Criminal Evidence Act 1984 (Pace) Code C Revised Code of Practice for the Detention, Treatment and Questioning of Persons by Police Officers. 2013.
- Criminal Justice Act 2003 c.44. London: The Stationery Office; 2003.
- Data Protection Act 1998 c.29. London: The Stationery Office; 1998.
- Code of Practice. Mental Health Act 1983. Published Pursuant to Section 118 of the Act. London: DH; 2008.
- Implementing the Mental Capacity Act 2005 – Guidance for Police. London: Metropolitan Police; 2013.
- Mental Capacity Act 2005 Code of Practice. London: The Stationery Office; 2007.
- Public Order Act 1986. London: Her Majesty’s Stationery Office; 1986.
- Section 136 Mental Health Act 1983 Operational Protocol For Devon, Cornwall and the Isles of Scilly. Cornwall: The Peninsula Criminal Justice Agencies Group; 2009.
- Section 135 (1) (2) Mental Health Act 1983 Operational Protocol For Devon, Cornwall and the Isles of Scilly. Cornwall: The Peninsula Criminal Justice Agencies Group; 2005.
- Longreach House Place of Safety Assessment Suite – Operational Policy. Cornwall: Cornwall Partnership NHS Foundation Trust; 2009.
- Flynn MC. The Murder of Steven Hoskin: A Serious Case Review. Cornwall: Cornwall Adult Protection Committee; 2007.
- Why a Neighbourhood Harm Reduction Spreadsheet?. Cornwall: Devon & Cornwall Police; 2010.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage Publications; 2003.
- Smith J, Firth J. Qualitative data analysis: the framework approach. Nurse Res 2011;18:52-6. http://dx.doi.org/10.7748/nr2011.01.18.2.52.c8284.
- McCrone P, Dhanasiri S, Patel A, Knapp M, Lawton-Smith S. Paying the Price: The Cost of Mental Health Care in England to 2026. London: The King’s Fund; 2008.
- Southern Health NHS Foundation Trust . RiO Mental Health &Amp; Learning Disabilities 2013. www.southernhealth.nhs.uk/knowledge/rio-mhld/ (accessed 4 September 2013).
- Barber JA, Thompson SG. Analysis and interpretation of cost data in randomised controlled trials: review of published studies. BMJ 1998;317:1195-200. http://dx.doi.org/10.1136/bmj.317.7167.1195.
- Efron B. Better bootstrap confidence intervals. J Am Stat 1987;82:171-85. http://dx.doi.org/10.1080/01621459.1987.10478410.
- Department of Health . Extending the Street Triage Scheme: New Patrols With Nurses and the Police 2013. www.gov.uk/government/news/extending-the-street-triage-scheme-new-patrols-with-nurses-and-the-police (accessed 13 September 2013).
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: University of Kent, Personal Social Services Research Unit; 2012.
- Department of Health . NHS Reference Costs 2010 11 2011. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_131140 (accessed 4 September 2013).
- James D. Police station diversion schemes: role and efficacy in central London. J Forensic Psychiatry 2000;11:532-55. http://dx.doi.org/10.1080/09585180010004801.
- Naylor C, Parsonage M, McDaid D, Knapp M, Fossey M, Galea A. Long-Term Conditions and Mental Health 2012. www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/long-term-conditions-mental-health-cost-comorbidities-naylor-feb12.pdf (accessed 13 September 2013).
- Soto J. Health economic evaluations using decision analytic modeling. Int J Technol Assess Health Care 2002;18:94-111.
- Susser E, Schwartz S, Morabia S, Bromet E. Psychiatric Epidemiology. Oxford: Oxford University Press; 2006.
- Byford S, Torgerson DJ, Raftery J. Cost of illness studies. BMJ 2000;320. http://dx.doi.org/10.1136/bmj.320.7245.1335.
- McWilliam C, Kothari A, Ward-Griffin C, Forbes D, Leipert B. South West Community Care Access Centre Home Care Collaboration (SW-CCAC) . Evolving the theory and praxis of knowledge translation through social interaction: a social phenomenological study. Implementation Sci 2009;4:26-39. http://dx.doi.org/10.1186/1748-5908-4-26.
- Swain J, French S, French S, Sim J. Physiotherapy: A Psychosocial Approach. Oxford: Butterworth-Heinemann; 2004.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- NHS Direct . NHS Direct 2011. www.nhsdirect.nhs.uk/about/~/media/files/boardpapers/november2010/board%20scorecard%20-%20header%20sheet.ashx (accessed 10 June 2011).
Appendix 1 Changes to project
Appendix 1 includes the original research proposal (confidential personal and financial details removed), the original protocol and the final protocol. Table 29 below shows the major amendments to the project and the dates of these changes.
| HS&DR protocol | REC amendment | Reason for amendment |
|---|---|---|
| Upload date: 19 December 2012 | Amendment upload date: 15 October 2012 | Change of case-linkage case identification following Section 251 approval from the NIGB |
| Upload date: 7 May 2013 | Amendment upload date: 4 March 2013 | Change of recruitment strategy for stakeholder consultation |
ORIGINAL RESEARCH PROPOSAL
ORIGINAL PROTOCOL
Enhancing the Multi-Agency Management of Individuals with Enduring Moderate to Severe Mental Health Needs (EMHN): Client Journeys and the NHS/CJS Interface.
1. Aims/Objectives:
The aim of the proposed research is to examine and explore current practice relating to the management of individuals with enduring moderate to severe mental health needs (EMHN), specifically at those points where they interface between the NHS and criminal justice system, and to ascertain how such practice can be enhanced. Three stages of work are planned, each guided by explicit objectives. Stage two represents the major study to be undertaken and therefore the bulk of the work.
a. Stage One
-
1. How are the practice implications of current national policy relating to the management of individuals with EMHN being interpreted at local level?
-
2. How has Cornwall articulated national policy into practice benchmarks where the NHS and Police are required to work together?
b. Stage Two
-
3. What are the organising principles that precipitate a joint-working decision, by either the NHS or the Police?
-
4. What is the decision-making process and who is involved in it?
-
5. Is the decision-making process consonant with local practice guidelines and national policy implications?
-
6. What is the impact of these decisions on the service user?
-
7. What is the impact of these decisions on the NHS, and Police organisations?
-
8. What are the economic costs associated with current and potentially enhanced practice?
c. Stage Three
-
9. What are the barriers and facilitators to the multi-agency management of individuals with EMHN?
-
10. What are the implications of the research for national policy and practice?
2. Background:
Throughout the last twenty years, and more especially the latter part of the last decade, there has been an escalating debate about how individuals with EMHN might best be managed within and between the NHS and criminal justice system (CJS). It is widely recognised by mental health practitioners, the Police, and the courts that these individuals repeatedly come to the attention of the CJS, with their journey into and out of the CJS being conceptualised as a ‘revolving door’ (Bradley, 2009). The Department of Health (DoH) has been proactive in commissioning a considerable amount of research in an effort to understand how this cycle might be broken. In 1992 Dr John Reed, in the first of a series of reports, reviewed ‘health and social services for mentally disordered offenders and others requiring similar services’. Among the many recommendations made, Reed stressed that a flexible, multi-agency, partnership approach was essential to bring about change. It is unfortunate, but telling, that eighteen years on that call has been only partially heeded.
The lack of ‘joined-up’ working between the health and social care sector and the CJS is reflected in a number of tragic events which have resulted in serious case reviews and subsequent inquiries (Bichard 2004; Magee 2008; Laming 2003; Laming 2009; IPCC 2010). Indeed, the term ‘silo working’ (Rutherford 2010: 74) has been used to describe the paucity of interaction and engagement. Lord Bradley’s inquiry (2009) into how people with ‘mental health problems or learning disabilities’ fare within the criminal justice system, concedes that since Reed, little has changed except the ‘political and social context’ (Bradley 2009: 9). Baroness Corston’s (2007) equally wide-ranging review of ‘women with particular vulnerabilities in the criminal justice system’ identifies similar shortcomings to Bradley; but suggests too that where women are concerned, a radically different and holistic approach is required. Most recently, Rutherford (2010) has explored the extent to which inter-agency working or ‘convergence’ has developed, the obstacles that still exist to a wider take up, and the limits that (may) need to be applied to the convergence process to retain professional and ethical boundaries.
Her Majesty’s Inspectorate of Constabulary (HMIC 2005; 2009) has, meanwhile, been applying pressure to the Police to embrace the operational and financial benefits to be had from partnership working in all areas of policing: Flanagan, in his comprehensive review of policing (2008), arrived at the same conclusions. Perhaps with one eye to the extensive post-Bradley implementation process, the National Policing Improvement Agency (NPIA) in conjunction with the DoH (2010) has produced detailed guidance on how the Police should respond to people with ‘mental ill-health and learning disabilities’ (2010); they, like others, identify that police officers have little or no formal training in diagnosing or dealing with mental ill-health. Although mental ill-health is not indicative of any latent propensity to criminality or dangerousness: stereotypically, those who live with it are invariably perceived to be predisposed or inclined to both. On the street, where the Police are both the first and last resort in dealing with individuals deemed to be experiencing mental ill-health, the ‘successful resolution’ of an incident – the bridge jumper for example – depends on the unique contextual details of the event in question. These, in turn, will determine the legal powers available to the officer and the sort of action he or she may take. The process of rationalising and interpreting these contextual and legal elements is, of course, informed by the ideological imperatives (the received wisdom) of the Police organisational milieu; this may well be quite different to the occupational imperatives of the mental health professional, the social worker, ambulance staff, or general medical practitioners. Moreover, the Police imperative may very well conflict or compete with the occupational imperatives of others and the long-term prognosis of the individual concerned. For those whose levels of ‘dangerousness’, criminality, and psychiatric diagnosis are such that they are not subject to any formal inter-agency process such as Multi Agency Public Protection Arrangements (MAPPA) or Safeguarding Children or Vulnerable Adult protocols and procedures, this is especially so. As many practitioners within the CJS and the statutory and voluntary mental health services have long been aware, these ‘gaps’ in the system are what ensure that many individuals with mental ill-health are destined to make unnecessary and inappropriate forays into the CJS: for a large number of people, this is an experience that is as damaging as it is avoidable.
The research literature calls for increased cross-sectoral case or data linkage studies to examine service users’ interaction with services to enhance service user outcomes (e.g. Ferrante, 2009). Further, such methods are useful in enabling researchers to identify service user outcomes for populations such as those targeted in this study which are often considered marginalised or hard to reach (Larney & Burns, 2011). Triangulating data contained in routinely collected data sources with primary data enables not only a holistic picture of the service user experience to be obtained but also connections between and utilisation of findings to be understood. For example, Fisher et al (2011) call for longitudinal studies that include the analysis of administrative or secondary data in combination with validation through primary data collection to provide comprehensive understanding of interactions between services. The qualitative analysis of predominantly secondary data together with a small amount of primary data collection and analysis will enable a ‘thick description’ (Geertz, 1973) of service user journeys and inter- and intra-agency decision-making to be obtained, examined and understood. This broad application of qualitative methodologies fulfils Greatley et al’s (2007) recommendation of the wider use of qualitative methodologies in mental health research to enable the exploration of research areas that are not conducive to the application of purely quantitative methods. The current study also seeks to address three of Greatley et al.’s research priorities identified through their consultation exercise, these being, first, researching care pathways and transitions between services (in this case within and between the CJS and Mental Health Services); research to improve the quality of mental health care in the CJS (through understanding the interactions between CJS staff and service users and Mental Health Professionals) and third, enabling meaningful involvement of service users in the planning and delivery of services (through involvement and consultation of service users on and with the project team and via consultation with service users regarding project findings and developing recommendations through focus groups).
3. Need:
Against the above background, the proposed research arises out of a small pilot project, set up to scope the need associated with individuals having EMHN and care plans who are also known to the Police. The project was set up as a partnership between the Local Policing Area (LPA) in East Cornwall and the Cornwall Partnership Foundation NHS Trust, and is funded by the NHS. This pilot has identified the scale of the need and resulted in this partnership bid to the Service Delivery and Organisation programme.
The research will utilise predominantly existing data and an element of primary data with the overall aim of enhancing practice in relation to decision making and the organisation and delivery of health care for individuals with EMHN who interface with the Criminal Justice System (CJS). A great deal of the existing research identifies or acknowledges the ‘gaps’ that exist in the interface between CJS and NHS Mental Health service provision, and the sort of individuals who regularly find themselves falling into those inter-agency voids. The practicalities of implementing a ‘national intention’ are complex, and necessarily subject to a local interpretation: for example, for a variety of contextual reasons what works well in cosmopolitan inner city London may be less likely to succeed if transplanted to the more isolated districts of rural Cornwall. This project will therefore seek to illuminate the nature of these gaps both nationally (through a practice-focused review of existing documentation) and locally (through a detailed study of Cornwall’s attempt to translate EMHN policy into practice guidelines for NHS/CJS interface working) in order that inter-agency decision making, communication and service delivery are improved.
It is essential that rigorous academic research is conducted in order to understand the disparate processes and outcomes being achieved across the country in order to address the inevitable incoherence between policy and practice nationally. Furthermore as the current situation demonstrates, a lack of dialogue within the same organisation and between practitioners between organisations ensures that individuals ‘known’ to all or some of them are frequently not dealt with in a truly integrated or genuinely informed way. If the ‘silo mentality’ stifles inter-agency dialogue and inhibits practitioners and managers from exploring every option when dealing with those individuals who are known to a number of organisations, it also exaggerates the distinct and seemingly competing occupational aims and cultures of those involved. Thus an important aim of the proposed research is not only to find ways to promote greater inter-agency dialogue; but also to explore how practitioners from different organisations might develop genuine partnerships in dealing with individuals who are known to a range of organisations: a ‘case-linkage’ methodology offers a useful and exciting means of finding ways to include a range of relevant practitioners and professionals into the health care process and improving continuity of care and access.
Cornwall’s partnership working with individuals who may come into contact with Health, Social Care and Criminal Justice Services has pockets of exemplary practice, including coordinated activities around the use of section 136 of the Mental Health Act, the operation of Drug Treatment requirements as part of Community Rehabilitation and Punishment Orders, the enactment of the Multi-Agency Public Protection Arrangements and maintaining performance with regard to Prison Transfer targets for mentally disordered offenders.
Multi-agency collaboration is underpinned by a local forum, the Local Criminal Justice Agencies Group (formerly the Mentally Disordered Offenders Group), which relates to a peninsular-wide group where major stakeholders (CPS, Probation, Primary Care Trusts, Local Authorities, Police and Provider Trusts) are represented. Inevitably, where specific services or activities are underpinned by statutory requirements, clarity and delivery are enhanced. Local experience is that where the legal and statutory basis of provision is unclear and risk is possible but uncertain, then coordination of activities relies on the interpretation of service mandates by authoritative individuals who may have competing agendas (e.g. risk management vs. capacity management).
4. Methods:
Conceptual Framework and Design:
The project will be informed by a conceptual and methodological framework developed by the project team to successfully evaluate a range of multi-agency services and initiatives through the rigorous application of mixed methods (Creswell, 2009). This framework is responsive to identified need (Wadsworth, 2001), adopting Burke’s (1998) principles of participatory evaluation through the engagement of stakeholders at all stages of the research/evaluation process to ensure the meaningful utilisation of project findings (Papineau & Kiely, 1996) in order to enhance multi-agency working and service user outcomes. The framework is further informed by the tenets of community psychology which espouse collaborative working with traditionally marginalised groups and understanding people within their social contexts (Orford, 2008).
A three-stage methodology will be used to achieve the aims and objectives outlined above (two using secondary data and one gathering a small amount of primary data). Stage one involves a review of documentation pertaining to the translation of national policy into regional/local practice guidance in the area of EMHN. Stage two represents the main body of work and is a case-linkage study involving NHS case records and Police case records for individuals with multiple mental health episodes, deemed of moderate risk, and known to the Police. Stage three explores the barriers and facilitators to the effective multi-agency management of this vulnerable group in the light of evidence from the review exercise against the findings from the case-linkage study.
Stage 1 Policy into practice review and custody and outreach planning audit:
A short practice-focused review will be undertaken to illuminate how national policy has been interpreted and translated at the regional/local level. This involves two elements: a review of relevant regional/local documents nationally, and an audit to identify and analyse local need within offender populations at the stages of the Criminal Justice System identified in the Bradley Report (Custody and Neighbourhood Policing). This work extends the pilot review that formed the impetus for this research, complements existing policy focused reviews and a local Trust based audit.
-
Review: Search terms for regional/local documentation would include formal descriptors (e.g. mental health issues, suicidal, Section 136) to capture organisational ‘flags’, and more colloquial terms (e.g. bizarre, strange, mad, CPN and Psychiatrist) that police officers might use when submitting narrative text as part of intelligence submissions or in making updates to crime investigation screens. Documents from both elements will be analysed using thematic content analysis to identify core features and themes associated with the developing practice guidelines or benchmarks with which to assess practice quality and standards. Standards on which to assess the audit findings will be developed from this review.
-
Audit: Cases to be identified from the following Police databases for the second quarter of 2011 (weeks 16–30):
-
National Strategy for Police Information Systems Custody Systems (3 Custody Centres in Cornwall).
-
Neighbourhood Harm Registers (12 current registers in Cornwall).
-
Identified nominals will be case-linked with the BT-RIO System (NHS records system used by the Forensic Mental Health Team in Cornwall Partnership NHS Foundation Trust) to identify and calculate the number of individuals with enduring moderate to severe mental health needs (EMHN) who are currently accessing Mental Health Services of the Trust and who interface with the CJS. The planning and implementation of these audits will be conducted with service user involvement.
Stage 2 Case linkage study:
A case-linkage study will be undertaken linking NHS case files and Police intelligence files for individuals with multiple mental health episodes, deemed of moderate risk and known to the Police identified by the audit above. The focus of the research will be Cornwall Partnership Foundation NHS Trust. In each case, the client journey through the NHS and CJS will be explored with a specific focus on patient needs, organisational decision-making, multi-agency partnership working and decision outcomes for both client and organisations through the qualitative analysis of case files and associated documentation. Specifically, this would include examining the frequency of opportunity for engagement between the NHS and CJS to enhance outcomes for the client, the number of opportunities that led to active engagement, evidence of disclosure between the organisations, and evidence of direct joint working in the development of client care plans. Principles governing decision making through client journeys will be examined in the context of local practice guidelines and national policy implications.
Given resource scarcity within all of the public agencies involved in managing individuals with EMHN, it is important to consider the economic implications of current and alternative models of working. To better inform decisions about joint working we will undertake a costing study within this phase of work which estimates and compares costs associated with (a) current practice and (b) potential enhancements to current practice (based on local and national guidelines and policy).
This study comprises two elements, first, analysis of secondary case-linked data from cases identified by the audit presented above and second, a health economic component to track costs incurred in client journeys and compare these with alternative models.
The cases identified by the audit presented above will be used as the first stage of the identification of cases for the main case-linkage study secondary data analysis for which approval will be sought from the relevant NHS Research Ethics Committee, Trust Research and Development office and ethics committees within the Higher Education partners.
a. Secondary data analysis:
This stage of the case-linkage study concerns the identification and examination of cases identified by the custody and outreach planning audit described above that have been in receipt of NHS services and accessed the CJS.
-
All potential cases for inclusion in the research identified by the audit are to be subjected to a two-pronged screening process to ensure individuals’ protection from harm, first using both NHS and Police-derived exclusion criteria and second through consultation with relevant care teams. NHS exclusion criteria include: a. Police involvement was considered on the basis of disruptive behaviour but ultimately never sought by the clinical team; b. that to approach the person at the time of the study would lead to mental health deterioration; c. that to approach the person for inclusion in the study would threaten their ability to work with the current care team; d. that to approach the person for inclusion would precipitate behaviours liable to cause harm to themselves or others. Police exclusion criteria include: a. subject of an ongoing investigation as a suspect due to the potential for operational compromise; b. subject of an ongoing investigation as a victim/witness due to the potential to breach the Criminal Procedure and Investigations Act (1996); c. where Police intelligence suggests that contacting the individual would increase risk of harm to the person or to others. As a further safeguard, the clinical psychologist deployed to the study would liaise with the current or most recent care team and/or GP as appropriate to aid the decision to approach the person for inclusion.
-
Cases identified through the above screening process will be invited to participate in the study by allowing the research team access to their records on both the BT RIO and CIS systems for the purposes of the study [to be conducted in accordance with the British Psychological Society Code of Ethics and Conduct, August 2009]. Potential participants will be sent a study information sheet and consent form in order that they can provide their informed consent to allow access to their records.
-
Receipt of informed consent from invited individuals will confirm the final sample of cases to be included in the study.
-
The applicants have conducted a feasibility study to identify appropriate records to be included in the data corpus which enable the capture of a holistic view of participant journeys through, within and between the CJS and Mental Health Services. Each of these records can be saved electronically and/or printed in hard copy for the purposes of analysis. The relevant documents identified for inclusion in the analysis are detailed below.
-
Identified CJS records/databases: Data to be generated from CJS records are located within separate databases.
-
Criminal Intelligence system (CIS). Individual records comprise a number of screens. The front screen for each case contains basic demographic information, flags and warnings as appropriate. The ‘back screens’ for each case provide detail and a rich picture of participants’ interactions with the CJS and other services as reported by Police staff. These data can be printed in hard copy and stored securely on University of Plymouth and King’s College London property for analysis.
-
Operational Information System (OIS). This system contains the initial detailed logs created by police officers following a reported incident. The log is generated from the information that the police call handler obtains from the caller, it is graded and a response is generated. Due to the level of detail required to be entered into the OIS, inclusion of these data to the data corpus enables the researchers to examine the decision making processes of the police in their interactions with participants and other professionals both within the CJS and inter-agency. These detailed logs can be printed and stored in order to be analysed as in 5.a above. The OIS represents up to the first 72 hours of any case, after which the case is entered onto the CIS described above.
-
National Strategy for Police Information Systems (NSPIS) Custody System. This system provides current and archived data relating to individuals who have been through the three custody suites in Cornwall. A proportion of participants may be taken to the custody suite in Plymouth despite being resident in Cornwall dependent on the location of initial interaction with the Police. The front screen pertaining to each individual provides a table with basic demographics and rationale for custody (e.g. Section 136 and/or alleged offence). The detention log in the back screens of this system provides a timetable of procedures and context to a range of decision-making processes including authorisation for searches, checks on individuals and calls and logs of requests for examination and advice from medical practitioners with responses. A diary also contains pertinent dates such as those required to answer bail. All data contained within these records can be printed and scanned for the purpose of analysis.
-
Police National Computer (PNC). Although the three systems used above are routinely used throughout Police Constabularies across the country, the PNC is the only national database. As such, on identifying participants, it is possible to check the PNC to gather data on potential police interaction outside the Devon and Cornwall Police Force. Data is comparable to that generated from CIS to which the PNC is linked.
-
-
Identified NHS records/databases: Cornwall Partnership Foundation NHS Trust (CPFT) initiated use of the BTRIO system in August 2010 for all service users with severe and enduring mental health needs. RIO is an electronic health record which captures referral processing, details of assessments and ongoing care. CPFT uses RIO to record all interactions with service users, all care plans and all risk assessments. The feasibility study identified a range of folders within the system that would enable the researchers to gain a holistic picture of participants’ access to and interactions with Mental Health Services. Further, it was clear that the level of detail of the combined documents would enable the researchers to answer the research questions. The following list details the folders that have been identified to be included in the data corpus. All documents can be converted into encrypted Microsoft Word or Pdf documents to be stored securely for analysis.
-
Core assessment:
-
– Overview: participants’ physical and psychological health, treatment and care management.
-
– Ongoing: Mental Health/Children’s legislation: contains Mental Health and Forensic details.
-
-
Client referral/screening: referral into and out of Mental Health services, brief referral details.
-
Client related data views:
-
– Progress note overview: all documented interactions with the service user from August 2nd 2010, print options allow for review over a user specified time period if required.
-
– Risk overview: risk assessment details covering risks to and from the service user.
-
– Diary view: All face to face interactions between participants and professionals and between professionals regarding participants.
-
– Clinical Documentation list: a list of documents stored electronically, including those received by the Trust and those sent.
-
-
-
Analysis: A combination of quantitative and qualitative analyses will be used.
-
Quantitative analysis: Core demographic information of all cases identified via the audit that fulfil the screening criteria detailed above will be collated (estimated 800–1000 cases). Descriptive analyses will be conducted to gain a picture of the sample. Data would be captured through the use of Microsoft Excel and imported into Statistical Packages for the Social Sciences (SPSS) for analysis. It is estimated that approximately 10% of individuals will provide informed consent (i.e. 80–100 cases) to their records being used in the case linkage study. Therefore, statistical analyses will be undertaken to compare the core demographics of full and subsamples to assess the representativeness of the final sample obtained.
-
Qualitative analysis: A full pilot will be conducted on two consenting cases. Documents will be anonymised and either converted or scanned into electronic text documents and uploaded into NVivo. All records over a defined 12 month period will be accessed. The data corpus will be necessarily complex and rich. Using NVivo to organise and structure the analysis will ensure the centralising of data from the variety of sources presented above and systematic conduct and record of the analysis of this large data corpus. Data will be coded independently by two researchers and analysed using thematic content analysis (Smith, 1992). Functionalities to check for reliability of coding provided by NVivo such as Coding Comparison Queries will be conducted. Any differences will be resolved through discussion of the key themes and the interpretations placed on them.
-
-
Member validation will be sought through service user involvement at relevant stages throughout the analysis.
b. Health economics component:
The Health economics component of the study will examine data gathered from the in-depth study of the sub-sample of cases examined for the case linkage study (stage 2b above). The methods for this aspect of the study will be as follows:
-
For the selected sample, we will utilise CJS data (from NSPIS, CIS, PNC and OIS) and case-linked NHS data (from the BT RIO database) to sequentially map actual individual-level client journeys and processes of decision-making, accounting for all individuals and agencies involved, for the 12 month retrospective time period in which cases will be examined.
-
Based on the finding of the case-linkage study (stage 2b above), we will then generate a series of alternative pathway scenarios which represent the assumed potential impacts of key enhancements to current practice on decision-making processes and client journeys at a broad level (e.g. a sub-MAPPA process).
-
The core impacts of these alternative scenarios will then be translated into pragmatic and specifically defined hypothesised impacts on the way the CJS and NHS manage cases; such impacts will be applied to the sample individual-level data in turn (and in combination if appropriate). Depending on the nature of the potential impacts, each will affect variable proportions of the sample data, depending on relevance to actual journeys. The individual-level data will thus represent actual client journeys and a series of alternative journeys based on the hypothesised effects of enhanced practice on the individual. Such scenario modelling can prove very informative for service/policy evaluation in the absence of ‘harder’ evidence (see McCrone et al. (2008) for an example).
-
The researchers will then apply unit costs to individual-level resource use associated with actual and alternative journeys to calculate a series of total resources costs for each individual. This will allow the statistical comparison of total mean costs associated with actual pathways and alternative scenarios and the identification of any potential additional costs (or savings), and changes in the balance of costs between different sectors (e.g. NHS vs. police), associated with moving from current to enhanced practice.
Stage 3 Stakeholder consultation:
Service users, NHS and Police practitioners and managers will be consulted to consider in the light of evidence of the review stage against the findings of the case-linkage study, barriers and facilitators to the effective multi-agency management of this vulnerable group.
-
Service users who indicate that they would be interested in taking part in a focus group on consenting to the access of records for the case-linkage study would again be subjected to the two-pronged screening process detailed above to ensure protection of harm due to the time period between initial expression of interest and this stage of the project.
-
Service users in the final screened sample would be sent a study information sheet and consent form to invite them to participate in this stage of the study. The research assistant will then contact potential participants via their preferred mode of communication and arrange a convenient time and date for the focus group. Two focus groups will be conducted with each stakeholder group comprising 6–8 participants in each group (n = 36–48).
-
NHS and Police practitioners and managers who took part in the Skills Share initiative would be invited to take part in this stage of the study and sent a study information sheet and consent form. On receipt of completed consent forms the research assistant will contact potential participants to arrange a convenient time and date for a focus group. Focus groups will be uniprofessional in order to allow practitioners and managers to speak freely regarding inter-agency relationships and associated benefits and barriers.
-
Focus groups will be structured by the application of aspects of the Nominal Group Technique (NGT). Participants will be introduced to aims and objectives of the project as a whole, given a short presentation of the findings of the previous two stages of the study and asked if they have any questions.
-
Following this introduction, participants will be asked to consider questions related to the aims of this stage of the study in the light of the findings, i.e. concerning the barriers and facilitators to achieving effective multi-agency working for EMHN individuals.
-
Following presentation of these questions, participants will be requested to complete the five stages of the NGT (Lloyd-Jones, Fowell & Bligh, 1999). These include the (i) ‘silent phase’ (participants are asked to individually write down or consider their answers to the questions posed), (ii) ‘item generation or round robin phase’ (participants break into two smaller groups and write a comprehensive list of items collated from those written individually with the aid of the facilitators if required), (iii) ‘item clarification’ (discussion to determine the meaning of items), (iv) ‘voting phase’ (participants will be asked to rank order emerging barriers and facilitators in terms of their relevance or importance to their lived experience and/or professional practice) and (v) ‘reassembly of the group’ (participants will reform as the original group to discuss the issues raised in the break-out groups).
-
As well as collection of written data generated in the groups, both the break-out groups and final group discussions will be digitally recorded with the participants’ permission and transcribed verbatim.
-
Appropriate descriptive and inferential statistics will be used to analyse the ranked responses generated from the first four stages of the NGT.
5. Plan of Investigation and Timetable:
| Dates | Activity | Key Milestones |
|---|---|---|
| Pre-funding/post-approval period (June–September 2011) | ||
| July |
|
|
| August |
|
|
| September |
|
|
| October 2011–March 2012: Practice-focused review and custody and outreach audit | ||
| October–November |
|
|
| December–January |
|
|
| February–March |
|
|
| April 2012–January 2013: Case-linkage study | ||
| April |
|
|
| May–June |
|
|
| July |
|
|
| August–November |
|
|
| December 2012–January 2013 |
|
|
| February–June 2013: Focus group study and stakeholder validation | ||
| February |
|
|
| March–April |
|
|
| May–June |
|
|
6. Project Management:
The project involves a collaborative team of academics and practitioners, experienced in working in multi-site, multi-disciplinary initiatives. The project is led by Professor Lea (Institute of Psychiatry, KCL) who has considerable experience in leading this type of work, including having occupied key roles in the Local Strategic Partnership of Plymouth with responsibility for coordinating and delivering outputs and outcomes.
Regular monitoring and reporting is an important tool in controlling projects and an essential part of good project management practice. The project will report to a Project Steering Group comprising team members, stakeholders from the NHS and Police, and service users. The group will be chaired by an independent chair, who will be selected in consultation with the NIHR MHRN. Meetings will be held quarterly. The terms of reference will include responsibility for monitoring the delivery of milestones to time and on budget; responsibility for ensuring the appropriateness of the communication and dissemination strategy associated with project; and receiving interim and final reports.
The full Project Team will meet bi-monthly. These meetings will be held in the South West and always attended by Professor Lea in person. The other three London-based colleagues will attend meetings as appropriate virtually, using Skype, or in person when possible. These meetings will include the regular evaluation of project performance, both financial and non-financial, and ensuring that any necessary corrective actions are undertaken in a timely manner.
In the South West, Dr Callaghan, Research Manager, will be responsible for day-to-day, operational project management and liaison with NHS and Police colleagues. A framework of robust, strictly applied systems will ensure effective delivery of outputs and outcomes. These include: project management, financial tracking, risk management, and performance management. Relationships between the NHS team member, the Police team members and Dr Callaghan and Professor Lea are well established and this bid has resulted out of their previous joint working.
The team is used to maintaining regular, effective communication and contact via range of methods including face-to-face, Skype, and mobile technology.
7. Service Users/Public Involvement:
The team has been informed by guidance on best practice in engaging service users in research (i.e. INVOLVE guidance on involving marginalised/vulnerable people in research; advice from the Service User Research Enterprise at King’s). Two consultant service users have been involved in the project since the outline proposal stage. Consequently, service users will participate actively to the research in a number of ways:
-
Dr Diana Rose, co-director of SURE (the Service User Research Enterprise) is a member of the project team.
-
The two consultant service users currently engaged in the project (through the NHS Forensic Mental Health team), and referred to above, will be members of the Project’s Steering Group. This role was decided upon in dialogue with the service users themselves who felt that this level of engagement was appropriate to their needs.
-
A service user reference, or LEAP, group will be established to provide autonomous, independent advice on all aspects of the research process. Reference group members will be engaged through relevant NHS and Police service user fora. All service users involved in the project will contribute to the dissemination of the work, in accordance with their needs, including report writing, seminars, presentations and workshops. Service users will also contribute actively to the development of practice principles and regional targets.
8. References
- Bichard A. The Bichard Inquiry Report. London: The Stationery Office; 2004.
- Bradley K. The Bradley Report: Lord Bradley’s review of people with mental health problems or learning disabilities in the criminal justice system. London: Department of Health; 2009.
- Burke B. New Directions for Evaluation. 1998.
- Corston J. The Corston Report: a review of women with particular vulnerabilities in the Criminal Justice System. London: Home Office; 2007.
- Cornwall people profile. Cornwall: Community Intelligence, Cornwall Council; 2010.
- Cornwall Council . Deprivation 2010. URL: http://www.cornwall.gov.uk/default.aspx?page=22134 (accessed 10 May 2011).
- Creswell J.W. Research Design. Qualitative, quantitative, and mixed methods approaches. London: Sage; 2009.
- Ferrante A. The use of data-linkage methods in criminal justice research: a commentary on progress, problems and future possibilities. Current Issues in Criminal Justice 2009;20:378-92.
- Fisher W., Simon L., Roy-Bujinowski K., Grudzinskas A., Wolff N., Crockett E., et al. Risk of arrest among public mental health services recipients and the general public. Psychiatric Services 2011;62:67-72.
- Flanagan R. The Review of Policing Final Report. London: Home Office; 2008.
- Geertz Clifford. The Interpretation of Cultures: Selected Essays. New York: Basic Books; 1973.
- Greatley A., Naylor C., Wallcraft J., Samale C. Research Priorities for Service User and Carer-Centred Mental Health Services: Consultation Report 2007.
- Her Majesty’s Inspectorate of Constabulary . Getting Together. A Better Deal for the Public through Joint Working 2009. URL: www.hmic.gov.uk/SiteCollectionDocuments/. /THM_20090609.pdf (accessed 30 August 2010).
- Her Majesty’s Inspectorate of Constabulary . Closing the Gap. A Review of the ‘fitness for purpose’ of the Current Structure of Policing in England and Wales 2005. URL: http://www.wlga.gov.uk/download.php?id=852&l=1 (accessed 30 August 2010).
- Independent Police Complaints Commission . Investigation into Essex Police Contact With Maria Stubbings Prior to Her Murder in December 2008 2010. URL: www.ipcc.gov.uk/maria_stubbings_commissioner_s_report.pdf (accessed 01 September 2010).
- Larney S., Burns L. Evaluating health outcomes of criminal justice populations using record linkage: the importance of aliases. Evaluation Review 2011;35:118-2.
- Lord Laming. The Victoria Climbié Inquiry. London: The Stationery Office; 2003.
- Lord Laming. The Protection of Children in England: A Progress Report. London: The Stationery Office; 2009.
- Lloyd-Jones G., Fowell S., Bligh J.G. The use of the nominal group technique as an evaluative tool in medical undergraduate education. Medical Education 1999;33:8-13.
- McCrone P, Dhanasiri S, Patel A, Knapp M, Lawton-Smith S. Paying the Price: The Cost of Mental Health Care in England to 2026 n.d.
- Magee I. The Review of Criminality Information 2008. URL: http://tna.europarchive.org/20100419081706/http://www.police.homeoffice.gov.uk/publications/operational-policing/review-criminality-information/roci-full-report2835.pdf?view=Binary (accessed 30 August 2010).
- National Policy Improvement Agency and the Department of Health . Guidance on Responding to People With Mental Ill Health or Learning Disabilities 2010. URL: www.npia.police.uk/en/docs/Mental_ill_Health.pdf (accessed 30 August 2010).
- Orford J. Community Psychology: Challenges, controversies and emerging consensus. Chichester: John Wiley & Sons Ltd.; 2008.
- Papineau D., Kiely M.C. Participatory evaluation in a community organization: Fostering Stakeholder empowerment and utilization. Evaluation and Program Planning 1996;19:79-93.
- Review of Health and Social Services for Mentally Disordered Offenders and Others Requiring Similar Services Report of the Official Working Group for People with Special Needs. London: Department of Health and Home Office; 1992.
- Rutherford M. Blurring the Boundaries: The convergence of mental and criminal justice policy, legislation, systems and practice. Sainsbury Centre for Mental Health; 2010.
- Smith C.P. Motivation and personality: Handbook of thematic content analysis. New York: Cambridge University Press; 1992.
- Wadsworth Y. Responsive Evaluation: New Directions for Evaluation, No.92. San Fransisco: Jossey-Bass; 2001.
LATEST PROTOCOL
Enhancing the Multi-Agency Management of Individuals with Enduring Moderate to Severe Mental Health Needs (EMHN): Client Journeys and the NHS/CJS Interface.
3. Aims/Objectives
The aim of the proposed research is to examine and explore current practice relating to the management of individuals with enduring moderate to severe mental health needs (EMHN), specifically at those points where they interface between the NHS and criminal justice system, and to ascertain how such practice can be enhanced. Three stages of work are planned, each guided by explicit objectives. Stage two represents the major study to be undertaken and therefore the bulk of the work.
a. Stage one
-
1. How are the practice implications of current national policy relating to the management of individuals with EMHN being interpreted at local level?
-
2. How has Cornwall articulated national policy into practice benchmarks where the NHS and Police are required to work together?
b. Stage two
-
3. What are the organising principles that precipitate a joint-working decision, by either the NHS or the Police?
-
4. What is the decision-making process and who is involved in it?
-
5. Is the decision-making process consonant with local practice guidelines and national policy implications?
-
6. What is the impact of these decisions on the service user?
-
7. What is the impact of these decisions on the NHS, and Police organisations?
-
8. What are the economic costs associated with current and potentially enhanced practice?
c. Stage three
-
9. What are the barriers and facilitators to the multi-agency management of individuals with EMHN?
-
10. What are the implications of the research for national policy and practice?
4. Background:
Throughout the last twenty years, and more especially the latter part of the last decade, there has been an escalating debate about how individuals with EMHN might best be managed within and between the NHS and criminal justice system (CJS). It is widely recognised by mental health practitioners, the Police, and the courts that these individuals repeatedly come to the attention of the CJS, with their journey into and out of the CJS being conceptualised as a ‘revolving door’ (6). The Department of Health (DoH) has been proactive in commissioning a considerable amount of research in an effort to understand how this cycle might be broken. In 1992 Dr John Reed, in the first of a series of reports, reviewed ‘health and social services for mentally disordered offenders and others requiring similar services’ (7). Among the many recommendations made, Reed stressed that a flexible, multi-agency, partnership approach was essential to bring about change. It is unfortunate, but telling, that eighteen years on that call has been only partially heeded.
The lack of ‘joined-up’ working between the health and social care sector and the CJS is reflected in a number of tragic events, which have resulted in serious case reviews and subsequent inquiries (1–5). Indeed, the term ‘silo working’ (Rutherford 2010: 74) (8) has been used to describe the paucity of interaction and engagement. Lord Bradley’s inquiry (2009) into how people with ‘mental health problems or learning disabilities’ fare within the criminal justice system, concedes that since Reed, little has changed except the ‘political and social context’ (6). Baroness Corston’s (2007) equally wide-ranging review of ‘women with particular vulnerabilities in the criminal justice system’ identifies similar shortcomings to Bradley; but suggests too that where women are concerned, a radically different and holistic approach is required (9). Most recently, Rutherford (2010) has explored the extent to which inter-agency working or ‘convergence’ has developed, the obstacles that still exist to a wider take up, and the limits that (may) need to be applied to the convergence process to retain professional and ethical boundaries (8).
Her Majesty’s Inspectorate of Constabulary (10) has, meanwhile, been applying pressure to the Police to embrace the operational and financial benefits to be had from partnership working in all areas of policing: Flanagan, in his comprehensive review of policing, arrived at the same conclusions (11). Perhaps with one eye to the extensive post-Bradley implementation process, the National Policing Improvement Agency (NPIA) in conjunction with the DoH (2010) has produced detailed guidance on how the Police should respond to people with ‘mental ill-health and learning disabilities’(12); they, like others, identify that police officers have little or no formal training in diagnosing or dealing with mental ill-health. Although mental ill-health is not indicative of any latent propensity to criminality or dangerousness: stereotypically, those who live with it are invariably perceived to be predisposed or inclined to both. On the street, where the Police are both the first and last resort in dealing with individuals deemed to be experiencing mental ill-health, the ‘successful resolution’ of an incident – the bridge jumper for example – depends upon the unique contextual details of the event in question. These, in turn, will determine the legal powers available to the officer and the sort of action he or she may take. The process of rationalising and interpreting these contextual and legal elements is, of course, informed by the ideological imperatives (the received wisdom) of the Police organisational milieu; this may well be quite different to the occupational imperatives of the mental health professional, the social worker, ambulance staff, or general medical practitioners. Moreover, the Police imperative may very well conflict or compete with the occupational imperatives of others and the long-term prognosis of the individual concerned. For those whose levels of ‘dangerousness’, criminality, and psychiatric diagnosis are such that they are not subject to any formal inter-agency process such as Multi Agency Public Protection Arrangements (MAPPA) or Safeguarding Children or Vulnerable Adult protocols and procedures, this is especially so. As many practitioners within the CJS and the statutory and voluntary mental health services have long been aware, these ‘gaps’ in the system are what ensure that many individuals with mental ill-health are destined to make unnecessary and inappropriate forays into the CJS: for a large number of people, this is an experience that is as damaging as it is avoidable.
The research literature calls for increased cross-sectoral case or data linkage studies to examine service users’ interaction with services to enhance service user outcomes e.g. (13). Further, such methods are useful in enabling researchers to identify service user outcomes for populations such as those targeted in this study, which are often considered marginalised or hard to reach (14). Triangulating data contained in routinely collected data sources with primary data enables not only a holistic picture of the service user experience to be obtained but also connections between and utilisation of findings to be understood. The qualitative analysis of predominantly secondary data together with a small amount of primary data collection and analysis will enable a ‘thick description’ (16) of service user journeys and inter- and intra-agency decision-making to be obtained, examined and understood. This broad application of qualitative methodologies fulfils Greatley et al’s (2007) recommendation of the wider use of qualitative methodologies in mental health research to enable the exploration of research areas that are not conducive to the application of purely quantitative methods (17). The current study also seeks to address three of Greatley et al.’s research priorities identified through their consultation exercise, these being, first, researching care pathways and transitions between services (in this case within and between the CJS and Mental Health Services); research to improve the quality of mental health care in the CJS (through understanding the interactions between CJS staff and service users and Mental Health Professionals) and third, enabling meaningful involvement of service users in the planning and delivery of services (through involvement and consultation of service users on and with the project team and via consultation with service users regarding project findings and developing recommendations through focus groups) (17).
3. Need:
Against the above background, the proposed research arises out of a small pilot project, set up to scope the need associated with individuals having EMHN and care plans who are also known to the Police. The project was set up as a partnership between the Local Policing Area (LPA) in East Cornwall and the Cornwall Partnership NHS Foundation Trust (CFT), and is funded by the NHS. This pilot has identified the scale of the need and resulted in this partnership bid to the SDO.
The research will utilise predominantly existing data and an element of primary data with the overall aim of enhancing practice in relation to decision making and the organisation and delivery of health care for individuals with EMHN who interface with the Criminal Justice System (CJS). A great deal of the existing research identifies or acknowledges the ‘gaps’ that exist in the interface between CJS and NHS Mental Health service provision, and the sort of individuals who regularly find themselves falling into those inter-agency voids. The practicalities of implementing a ‘national intention’ are complex, and necessarily subject to a local interpretation: for example, for a variety of contextual reasons what works well in cosmopolitan inner city London may be less likely to succeed if transplanted to the more isolated districts of rural Cornwall. This project will therefore seek to illuminate the nature of these gaps both nationally (through a practice-focused review of existing documentation) and locally (through a detailed study of Cornwall’s attempt to translate EMHN policy into practice guidelines for NHS/CJS interface working) in order that inter-agency decision making, communication and service delivery are improved.
Cornwall’s partnership working with individuals who may come into contact with Health, Social Care and Criminal Justice Services has pockets of exemplary practice, including coordinated activities around the use of Section 136 of the Mental Health Act, the operation of Drug Treatment requirements as part of Community Rehabilitation and Punishment Orders, the enactment of the Multi-Agency Public Protection Arrangements and maintaining performance with regard to Prison Transfer targets for mentally disordered offenders.
Multi-agency collaboration is underpinned by a local forum, the Local Criminal Justice Agencies Group (formerly the Mentally Disordered Offenders Group), which relates to a peninsular-wide group where major stakeholders (CPS, Probation, Primary Care Trusts, Local Authorities, Police and Provider Trusts) are represented. Inevitably, where specific services or activities are underpinned by statutory requirements, clarity and delivery are enhanced. Local experience is that where the legal and statutory basis of provision is unclear and risk is possible but uncertain, then coordination of activities relies on the interpretation of service mandates by authoritative individuals who may have competing agendas (e.g. risk management vs. capacity management).
It is essential that rigorous academic research is conducted in order to understand the disparate processes and outcomes being achieved across the country in order to address the inevitable incoherence between policy and practice nationally. Furthermore, as the current situation demonstrates, a lack of dialogue within the same organisation and between practitioners between organisations ensures that individuals ‘known’ to all or some of them are frequently not dealt with in a truly integrated or genuinely informed way. This potentially stifles inter-agency dialogue and inhibits practitioners and managers from exploring every option when dealing with those individuals who are known to a number of organisations, it also exaggerates the distinct and seemingly competing occupational aims and cultures of those involved. Thus an important aim of the proposed research is not only to find ways to promote greater inter-agency dialogue; but also to explore how practitioners from different organisations might develop genuine partnerships in dealing with individuals who are known to range of organisations: a ‘case-linkage’ methodology offers a useful and exciting means of finding ways to include a range of relevant practitioners and professionals into the health care process and improving continuity of care and access.
Moreover, it is vital that steps are taken to facilitate the adoption and implementation of recommendations developed from the research findings. Focus on implementation in mental health practice has been described as, ‘embryonic,’ (18). An iterative process of ‘translational forecasting’ will enable potential opportunities for the translation of research findings into practice being explored and optimised as they become available in real time. The research methodology is sensitive to understanding barriers and facilitators to implementing potential research findings, and these are studied and addressed explicitly as part of the Interface Project. Developing a method to forecast implementation will be achieved through a number of steps:
-
The multidisciplinary research team’s identification of key personnel and processes where change can be instigated and negotiated in their respective organisations.
-
The case-linkage study, which includes mapping key decision-making pathways and processes within and between organisations.
-
The detailed and comprehensive engagement of members of the research team with all stakeholder groups throughout the research process, thereby facilitating communication and dissemination of research findings and implementation opportunities.
Within the research framework, specific models and strategies for facilitating the implementation of findings have been reviewed. The literature recognises that innovation adoption fails to achieve long-term implementation due to deficiencies in the implementation strategy rather than due to those in the innovation itself e.g. (19). Therefore, the concept of a translational continuum is of particular relevance, involving an explicit focus upon translating research findings into practice from the outset of the research to ensure adoption, early and enduring implementation of recommendations and actions based on the research findings (18, 20).
Through identification of key individuals, groups and processes within and across agencies from the work of the research team throughout the life time of the project, the iterative process described above will enable real-time testing of the potential for and operationalisation of implementation as findings emerge. The research manager (Dr Lynne Callaghan – LC) will, through the development of her collaborative work within each agency, identify key individuals, groups/committees and commissioners who make key strategic, corporate decisions that would, in principle, support innovation adoption and implementation with whom to explore potential for implementation.
4. Methods:
Conceptual Framework and Design: The project is informed by a conceptual and methodological framework developed by the project team to successfully evaluate a range of multi-agency services and initiatives through the rigorous application of mixed methods (21). This framework is responsive to identified need (22), adopting principles of participatory evaluation through the engagement of stakeholders at all stages of the research/evaluation process to ensure the meaningful utilisation of project findings in order to enhance multi-agency working and service user outcomes (23, 24). The framework is further informed by the tenets of community psychology, which espouse collaborative working with traditionally marginalised groups and understanding people within their social contexts (25).
A three-stage methodology will be used to achieve the aims and objectives outlined above (two using secondary data and one gathering a small amount of primary data). Stage one involved a review of documentation pertaining to the translation of national policy into regional/local practice guidance in the area of EMHN. Stage two represents the main body of work and is a case-linkage study involving NHS case records and Police case records for individuals with multiple mental health episodes, deemed of moderate risk, and known to the Police. Stage three explores the barriers and facilitators to the effective multi-agency management of this vulnerable group in the light of evidence from the review exercise against the findings from the case-linkage study.
Stage one Policy into practice review and custody and outreach planning audit:
A short practice-focused review was undertaken to illuminate how national policy has been interpreted and translated at the regional/local level. This involved two elements: a review of relevant regional/local documents nationally, and an audit to identify and analyse local need within offender populations at the stages of the Criminal Justice System identified in the Bradley Report (Custody and Neighbourhood Policing). This work extended the pilot review that formed the impetus for this research, complements existing policy focused reviews and a local Trust based audit.
-
Review: Search terms for regional/local documentation included formal descriptors (e.g. mental health issues, suicidal, Section 136) to capture organizational ‘flags’, and more colloquial terms (e.g. bizarre, strange, mad, CPN and Psychiatrist) that police officers might use when submitting narrative text as part of intelligence submissions or in making updates to crime investigation screens. Documents from both elements were analysed using thematic content analysis to identify core features and themes associated with the developing practice guidelines or benchmarks with which to assess practice quality and standards. Standards on which to assess the audit findings were developed from this review.
-
Audit: Cases were identified from the following Police databases for the second quarter of 2011 (weeks 16–30):
-
National Strategy for Police Information Systems Custody Systems (All Custody Centres in Cornwall)
-
Neighbourhood Harm Reduction Registers (12 current registers in Cornwall)
-
Identified nominals were case-linked with the BT-RiO System (NHS records system used by the Forensic Mental Health Team in CFT) to identify and calculate the number of individuals with enduring moderate to severe mental health needs (EMHN) who are currently accessing Mental Health Services of the Trust and who interface with the CJS. The planning and implementation of these audits were conducted with service user involvement.
Stage two Case-linkage study:
A case-linkage study will be undertaken linking NHS case files and Police intelligence files for individuals with multiple mental health episodes, deemed of moderate risk and known to the Police identified by the audit above. The focus of the research will be CFT. In each case, the client journey through the NHS and CJS will be explored with a specific focus on patient needs, organisational decision-making, multi-agency partnership working and decision outcomes for both client and organisations through the qualitative analysis of case files and associated documentation. Specifically, this would include examining the frequency of opportunity for engagement between the NHS and CJS to enhance outcomes for the client, the number of opportunities that led to active engagement, evidence of disclosure between the organisations, and evidence of direct joint working in the development of client care plans. Principles governing decision making through client journeys will be examined in the context of local practice guidelines and national policy implications.
Given resource scarcity within all of the public agencies involved in managing individuals with EMHN, it is important to consider the economic implications of current and alternative models of working. To better inform decisions about joint working we will undertake a costing study within this phase of work, which estimates and compares costs associated with (a) current practice and (b) potential enhancements to current practice (based on local and national guidelines and policy).
This study comprises two elements, first, analysis of secondary case-linked data from cases identified by the audit presented above and second, a health economic component to track costs incurred in client journeys and compare these with alternative models.
The cases identified by the audit presented above will be used as the first stage of the identification of cases for the main case-linkage study secondary data analysis for which approval will be sought from the relevant NHS Research Ethics Committee, Trust Research and Development office and ethics committees within the Higher Education partners.
In the original study methods, access to patient identifiable data was to be limited to individuals who had provided full informed consent for such access. The participant pool for case-linkage was derived from the registered clinical audit described under Stage one. Findings from the audit revealed that approximately 35% of the pool were not on current caseload, and therefore did not have a current care team. As potential participants were to be accessed through their care teams to enable screening (to ensure that it would be safe and appropriate to approach them for consent), this meant that potential participants had to be in contact with a care team. Consequently, as 35% of these individuals did not have a current care team, this proportion of the potential participant pool could neither be screened using agreed inclusion and exclusion criteria, nor invited to provide their informed consent to participate in the research as originally proposed. Further interrogation of the audit data revealed that the 35% of people without current care included individuals who Lord Bradley (2009) argued to be most at need. Applying the originally intended recruitment procedures as operationalising the common law duty of confidentiality would mean that this group of cases could not be included in the research, their needs remaining both unresearched and unmet.
An application was made to the Ethics and Confidentiality Committee of the National Information Governance Board (NIGB) for their support in terms of Section 251 of the NHS Act (2006), by setting aside the common law duty of confidentiality. A three-month funded extension to the project was approved by the NIHR HS&DR (project funder) to allow the application to the NIGB and an amendment to the original National Research Ethics Service application to take place.
a. Secondary data analysis:
This stage of the case-linkage study concerns the identification and examination of cases identified by the custody and outreach planning audit described above that have been in receipt of NHS services and accessed the CJS.
All potential cases for inclusion in the research identified by the audit are to be subjected to a case selection process. A random selection of 100 cases from the audit will be made using a stratified sampling framework. The framework will be based on reflecting case characteristics, concentrating on cases with 2 or more referrals to mental health services in Cornwall. The framework will reflect the full range of service user experiences with both mental health and police services in Cornwall. Stratification categories will be based (1) type of CJS contact (NSPIS; NHRR; Section 136 detentions; multiple: complex); (2) frequency of CJS contact; (3) referral status at time of police contact (current ongoing referral; current ongoing referral and referral specific to police contact; only referral specific to police contact; no current referral).
The relevant documents identified for inclusion in the analysis are detailed in Appendix 3 of this report.
The confidentiality of person identifiable data will be assured through the following pseudonymisation and data access method, which has been developed and agreed by the research team, CFT and DCP. The research manager (LC) and research assistant (Susan Eick – SE) will access case records of 80–100 cases identified by application of the sampling frame on both the RiO mental health and CJS systems. Reversible pseudonymisation (to enable back-linking to the personal identifier in case of dissent) will be utilised to both facilitate accurate case-linkage and enable depersonalisation of data. Cases will be assigned a novel randomly generated PseudoID, which will act as an alias within the newly created pseudonymised, depersonalised data sets (quantitative spreadsheets) and data corpuses (qualitative data). Such PseudoIDs will therefore enable a link between such data and the personal identifiable data. A data flow diagram of the pseudonymisation process is supplied with this application. Each entry below corresponds to an element on this data flow and labelled accordingly. Although this application pertains specifically to the accessing of health records, the parallel process for accessing CJS data is included in the data flow and the description below.
1. Creation of a Master Index:
-
Personal identifiers (name and date of birth) of the cases identified by the registered audit will be randomly assigned a PseudoID. These linked data will be held in a single Excel worksheet on a secure drive on the Trust N3 server. 100 cases identified by the stratified sampling frame will be marked within this master index as those required for examination for the case-linkage study.
-
Access CFT Master Index: LC, John Morgan (JM), SE, Trust Information Governance (IG) Lead
-
-
A copy of the Master Index will be held in a single Excel worksheet on a secure drive on the DCP server. 100 cases identified by the stratified sampling frame will be marked within this master index as those required for examination for the case-linkage study. Access CJS Master Index: LC, SE, Force Data Protection Officer.
2. Data access:
-
Data will be accessed on the RiO mental health records system for each case. Records will be accessed in the CFT Forensic Mental Health Team Offices. The worksheet containing the personal identifiable data and PseudoID will be accessed from a CFT laptop in a docking station connected to the CFT network allowing access to the dedicated server drive. The RiO record of each case to be examined for the research will be accessed from the same laptop.
-
Access: LC, JM, SE, Trust IG Lead
-
-
Data will be accessed from the CJS systems for each case. Records will be accessed from a docked networked laptop or networked PC in Crownhill Police station, Plymouth. The worksheet containing the personal identifiable data and PseudoID will be accessed from a DCP laptop in a docking station/PC connected to the DCP network allowing access to the researcher’s police server drive. The CJS record of each case to be examined for the research will be accessed from the same laptop.
-
Access: LC, SE, Force Data Protection Officer
-
3. Data collation and storage:
-
RiO data required to answer the research questions will be collated and stored under PseudoID in Microsoft Excel and Word files on the dedicated server drive.
-
Access: LC, JM, SE, Trust IG Lead
-
-
CJS data required to answer the research questions will be collated and stored under PseudoID on Microsoft Excel and Word files on the Police server drive.
-
Access: LC, SE, Force Data Protection Officer
-
3. Data depersonalisation and storage:
-
RiO-derived collated data will be depersonalised. Depersonalisation will include removing any identifying features from the data including names, addresses and distinguishing features of cases. All data will be depersonalised including that of service users, all third parties and organisations. All data will be stored on the dedicated server drive as above.
-
Access: LC, JM, SE, Trust IG Lead
-
-
CJS-derived collated data will be depersonalised. Depersonalisation will include removing any identifying features from the data including names, addresses and distinguishing features of cases. All data will be depersonalised including that of service users, all third parties and organisations. All data will be stored on the Police server drive as above.
-
Access: LC, SE, Force Data Protection Officer
-
4. Pseudonymisation and depersonalisation check:
-
The Trust IG Lead will work with the Research Manager (LC) to ensure that data are appropriately pseudonymised and depersonalised.
-
The Force Data Protection Officer will work with the Research Manager (LC) to ensure that data are appropriately pseudonymised and depersonalised.
5. Data transfer and storage:
-
Pseudonymised and depersonalised RiO-derived data will be stored and transferred on a Trust issue encrypted hard drive.
-
Pseudonymised and depersonalised CJS-derived data will be stored and transferred on a Police issue IronKey.
-
Access: Whole research team (LC, JM, SE, Susan Lea (SL), Graham Thornicroft (GT), Anita Patel (AP), Barbara Barrett (BB), Diana Rose (DR), Iain Grafton (IG), Mark Bolt (MB), and Margaret Heslin (MH).
-
6. Data linkage and storage:
-
Pseudonymised, depersonalised RiO and CJS-derived data linked via PseudoID and stored on dedicated server drives and encrypted hard drives at Plymouth University and King’s College for analysis. Hard copies of pseudonymised depersonalised data will be stored in locked filing cabinets on University premises (Plymouth and King’s College). Data will be exported to Statistical Packages for the Social Sciences (quantitative data derived from Excel spreadsheets created above and NVivo (qualitative data derived from Word documents created above) as appropriate.
-
Access: Whole research team (LC, JM, SE, SL, GT, AP, BB, MH, DR, IG, MB).
-
7. Securing of Master index:
-
On completion of project, the Master index at both sites will be limited to contain only RiO number (CFT data) and Nominal code (CJS data) and PseudoID. The electronic file and all data contained on the server drives of each organisation will be deleted. A hard copy of the resulting limited Master Index will be created and stored under each organisation’s Records, retention, and Destruction Schedule.
-
Access CFT Master Index: Trust IG Lead.
-
Access CJS Master Index: Force Data Protection Officer.
-
Additional points:
-
Only those research team members with substantive or honorary contracts with CFT (LC, JM & SE) and who are Trust Information Governance trained will have access to the personal identifiable data and case records (in RiO and CJS systems) in order to collate and depersonalise data. Only the aforementioned research team members will have access to the Master Index and PseudoID for each case and be able to link to this alias in order to access therefore the personal identifiable data. All those with access to personal identifiable information for the purposes of research (LC, SE and JM) are fully aware of their responsibilities in terms of data processing, the Data Protection Act (1998) and the Caldicott Principles.
-
No hard copies of personal identifiable data will be made. Hard copies of depersonalised data under PseudoID 2 will be made for the purpose of analysis and stored in locked filing cabinets in King’s College London and Plymouth University.
-
The CFT IG Lead will audit the researchers’ access to records on RiO for the purpose of patient safety and to comply with information governance requirements. The DCP Data Protection Officer will audit researcher access to CJS systems
Analysis: A combination of quantitative and qualitative analyses will be used
-
Quantitative analysis: Core demographic information of all 100 selected cases identified via the audit will be collated. Descriptive analyses will be conducted to gain a picture of the sample. Data would be captured using Microsoft Excel and imported into Statistical Packages for the Social Sciences (SPSS) for analysis. Statistical analyses will be undertaken to compare the core demographics of full and subsamples to assess the representativeness of the final sample obtained.
-
Qualitative analysis: A full pilot will be conducted on two individual cases. Documents will be anonymised and either converted or scanned into electronic text documents and uploaded into NVivo. All records over a defined 12 month period will be accessed. The data corpus will be necessarily complex and rich. Using NVivo to organise and structure the analysis will ensure the centralising of data from the variety of sources presented above and systematic conduct and record of the analysis of this large data corpus. Data will be coded independently by two researchers. Functionalities to check for reliability of coding provided by NVivo such as Coding Comparison Queries will be conducted. Any differences will be resolved through discussion of the key themes and the interpretations placed on them.
Member validation will be sought through service user involvement at relevant stages throughout the analysis.
b. Health economics component
The Health economics component of the study will examine data gathered from the in-depth study of the sub-sample of cases examined for the Case-linkage study (Stage two above). The methods for this aspect of the study will be as follows:
-
For the selected sample, we will utilise CJS data (from NSPIS, CIS, NHRR, PNC and OIS) and case-linked NHS data (from the BT RiO database) to sequentially map actual individual-level client journeys and processes of decision-making, accounting for all individuals and agencies involved, for the 12 month retrospective time period in which cases will be examined.
-
Based on the finding of the case-linkage study (Stage two a above), we will then generate a series of alternative pathway scenarios which represent the assumed potential impacts of key enhancements to current practice on decision-making processes and client journeys at a broad level (for example, a sub-MAPPA process).
-
The core impacts of these alternative scenarios will then be translated into pragmatic and specifically defined hypothesised impacts on the way the CJS and NHS manage cases; such impacts will be applied to the sample individual-level data in turn (and in combination if appropriate). Depending on the nature of the potential impacts, each will affect variable proportions of the sample data, depending on relevance to actual journeys. The individual-level data will thus represent actual client journeys and a series of alternative journeys based on the hypothesised effects of enhanced practice on the individual. Such scenario modelling can prove very informative for service/policy evaluation in the absence of ‘harder’ evidence (see (51) for an example).
-
The researchers will then apply unit costs to individual-level resource use associated with actual and alternative journeys to calculate a series of total resources costs for each individual. This will allow the statistical comparison of total mean costs associated with actual pathways and alternative scenarios and the identification of any potential additional costs (or savings), and changes in the balance of costs between different sectors (e.g. NHS vs. police), associated with moving from current to enhanced practice.
Stage three Stakeholder consultation:
Service users, NHS and Police practitioners and managers will be consulted to consider in the light of evidence of the review stage against the findings of the case-linkage study, barriers and facilitators to the effective multi-agency management of this vulnerable group.
-
Service users: One hundred randomly selected cases identified by the audit will be entered into a screening process, carried out by relevant current care teams. All current prisoners will be excluded from the potential participation pool for the stakeholder consultation. Current care teams will be asked to identify and exclude potential participants from the pool identified by the audit where:
-
identified individuals do not have the capacity to consent
-
participation could lead to deterioration in the health of potential participants
-
inclusion could potentially threaten their interactions with the current care team
-
approaching the individual could precipitate harmful behaviours to themselves or others.
-
-
CJS records will be checked to ensure that no current prisoners are contacted to take part in the research.
-
In addition to the above recruitment process, participants will be recruited through third sector homelessness agencies to ensure full demographic representation (homeless; young men; offenders) of service user stakeholders. Recruitment will be via individual staff members, and recruitment posters and leaflets left at drop-in centres. Participants will be self-selecting and therefore will not go through the screening process described above. However, the researchers will work with agencies to ensure that it is appropriate to approach individuals for inclusion in the research. Potential participants will be sent a recruitment pack (prepared by the researchers) including an invitatory letter, study information sheet, consent form and freepost envelope. Care teams will seek informed consent from participants identified in the participant pool on behalf of the researchers as they have legitimate access to their records for the purpose of treatment and therefore does not breach the common law duty of confidentiality. Recruitment will also be aided by the Cornwall based team of the Mental Health Research Network who will both liaise with care teams and approach potential participants.
-
Participants will be asked to provide their informed consent by return of a completed consent form in the freepost envelope, via email or via text message directly to the researchers. Care teams will be informed of all participants consenting to take part in the research. Participants will be resent recruitment packs if potential participants have not indicated their consent within two weeks of receipt of the original pack. If after two weeks, the potential participant has not responded they will not be contacted again.
-
Following receipt of completed consent forms, the research assistant (SE) will contact potential participants via their preferred mode of communication and arrange a convenient time and date for the focus group or interview. Service users will be given the choice of taking part in a single participant interview, in order to avoid excluding those who do not feel comfortable in participating in a group discussion.
-
Practitioners will be recruited via the Mental Health Team Leads (NHS) and the Force Mental Health Liaison Officers (CJS) via email. Potential participants will be sent a study information sheet and consent form.
-
On receipt of completed consent forms, the research assistant (SE) will contact potential participants to arrange a convenient time and date for a focus group. Focus groups will be uniprofessional in order to allow practitioners and managers to speak freely regarding inter-agency relationships and associated benefits and barriers.
-
Focus groups will be structured by the application of aspects of the Nominal Group Technique (NGT). Participants will be introduced to aims and objectives of the project as a whole, given a short presentation of the findings of the previous two stages of the study and asked if they have any questions. Following this introduction, participants will be asked to consider questions related to the aims of this stage of the study in the light of the findings, i.e. concerning the barriers and facilitators to achieving effective multi-agency working for EMHN individuals. Following presentation of these questions, participants will be requested to complete the five stages of the NGT (Lloyd-Jones, Fowell & Bligh, 1999). These include the (i) ‘silent phase’ (participants are asked to individually write down or consider their answers to the questions posed), (ii) ‘item generation or round robin phase’ (participants break into two smaller groups and write a comprehensive list of items collated from those written individually with the aid of the facilitators if required), (iii) ‘item clarification’ (discussion to determine the meaning of items), (iv) ‘voting phase’ (participants will be asked to rank order emerging barriers and facilitators in terms of their relevance or importance to their lived experience and/or professional practice) and (v) ‘reassembly of the group’ (participants will reform as the original group to discuss the issues raised in the break-out groups). As well as collection of written data generated in the groups, both the break-out groups and final group discussions will be digitally recorded with the participants’ permission and transcribed verbatim. Appropriate descriptive and inferential statistics will be used to analyse the ranked responses generated from the first four stages of the NGT.
-
Two focus groups will be conducted with each stakeholder group comprising 6–8 participants in each group (n = 36–48).
-
5. Plan of Investigation and Timetable:
| Dates | Activity | Key Milestones |
|---|---|---|
| Pre-funding/post-approval period (June–September 2011) | ||
| July |
|
|
| August |
|
|
| September |
|
|
| October 2011–March 2012: Practice-focused review and custody and outreach audit | ||
| October–November |
|
|
| December–January |
|
|
| February–March |
|
|
| April 2012–January 2013: Case-linkage study | ||
| May |
|
|
| June |
|
|
| August |
|
|
| August |
|
|
| August |
|
|
| September |
|
|
| October–November |
|
|
| October–February 2013 |
|
|
| March–April 2013 |
|
|
| May–September 2013: Focus group study and stakeholder validation | ||
| March–May |
|
|
| May–June |
|
|
| June–September |
|
|
6. Project Management:
The project involves a collaborative team of academics and practitioners, experienced in working in multi-site, multi-disciplinary initiatives. The project is led by Professor Lea (Institute of Psychiatry, KCL) who has considerable experience in leading this type of work, including having occupied key roles in the Local Strategic Partnership of Plymouth with responsibility for coordinating and delivering outputs and outcomes.
Regular monitoring and reporting is an important tool in controlling projects and an essential part of good project management practice. The project will report to a Project Steering Group comprising team members, stakeholders from the NHS and Police, and service users. The group will be chaired by an independent chair, who will be selected in consultation with the NIHR MHRN. Meetings will be held quarterly. The terms of reference will include responsibility for monitoring the delivery of milestones to time and on budget; responsibility for ensuring the appropriateness of the communication and dissemination strategy associated with project; and receiving interim and final reports.
The full Project Team will meet bi-monthly. These meetings will be held in the South West and always attended by Professor Lea or LC, the Research Manager in person. The other three London-based colleagues will attend meetings as appropriate virtually, using Skype, or in person when possible. These meetings will include the regular evaluation of project performance, both financial and non-financial, and ensuring that any necessary corrective actions are undertaken in a timely manner.
In the South West, LC will be responsible for day-to-day, operational project management and liaison with NHS and Police colleagues. A framework of robust, strictly applied systems will ensure effective delivery of outputs and outcomes. These include: project management, financial tracking, risk management, and performance management. Relationships between the NHS team member, the Police team members and LC and Professor Lea are well established and this bid has resulted out of their previous joint working.
The team is used to maintaining regular, effective communication and contact via range of methods including face to face, Skype, and mobile technology.
7. Service Users/Public Involvement:
The team has been informed by guidance on best practice in engaging service users in research (i.e. INVOLVE guidance on involving marginalised/vulnerable people in research; advice from the Service User Research Enterprise at King’s). Two consultant service users have been involved in the project since the outline proposal stage. Consequently, service users will participate actively to the research in a number of ways:
-
Dr Diana Rose, co-director of SURE (the Service User Research Enterprise) is a member of the project team. Two of the two consultant service users currently engaged in the project (through the NHS Forensic Mental Health team), and referred to above, one is a member of the Project’s Steering Group. This role was decided upon in dialogue with the service users themselves who felt that this level of engagement was appropriate to their needs.
-
A Service User Consultative Group (SUCG) will be established to provide autonomous, independent advice on all aspects of the research process. Consultants were recruited via mail shots to Cornwall based public and third sector services. Interested individuals will meet approximately quarterly at a neutral location to advise on the project. The group will be run by the Research Manager and the Service User Consultant, who will provide a link for the SUCG to the project Steering Group.
All service users involved in the project will contribute to the dissemination of the work, in accordance with their needs, including report writing, seminars, presentations and workshops. Service users will also contribute actively to the development of practice principles and regional targets.
Appendix 2 Data categories
Care team categories
| Team category | Team | Description |
|---|---|---|
| General secondary mental health service assessment, support, treatment and management Moderate intensity services |
CMHT | Broad range of cases and services spanning mental illness and personality disorder at various stages of recovery |
| Veterans service | Assessment and signposting or treatment of mental health difficulties arising from armed service | |
| Rehabilitation outreach | Specifically for service users graduating from inpatient recovery units | |
| Housing support/day resources | Service users requiring enabling with daily structure and accommodation | |
| Specialist epilepsy service | Assessment and treatment of epilepsy. Liaison with family and carers with regard to management of condition | |
| Memory clinics | Assessment and diagnosis of dementia by memory assessment practitioners | |
| Acute mental health problem management Very high intensity services |
HTT | Individualised, intensive support for individuals experiencing acute mental or emotional health problems. Approved mental health practitioners from HTTs conduct MHAAs in custody and place of safety |
| APL | Assessment of individuals who attend the A&E department and who have mental health problems or have deliberately harmed themselves | |
| Acute psychiatric inpatient services | Acute psychiatric inpatient services for individuals admitted voluntarily or under the MHA following MHAA | |
| General LD services Moderate intensity services |
Adult learning disabilities | Assessment, enablement, support risk management |
| Specialist input teams: working alongside CMHT or functional (AOS/EIT) services | Personality disorder | Assessment, consultation and focused treatment of people with personality disorders |
| Psychological therapies | Assessment, formulation, consultation and treatment for mental health problems presenting in secondary care services | |
| Eating disorders services | Community-based psychosocial assessment. Formulation, consultancy and treatment for individuals with a clinical diagnosis of an eating disorder | |
| Offender specific services | Forensic services | Assessment, formulation, consultation, treatment and management of mentally disordered offenders who have committed serious offences |
| Court liaison service | Assessment, liaison and brief intervention arising from appearance at court | |
| Functional teams: constituted with a clear remit to focus services on priority needs groups | EIT | Provision of prompt assessment and treatment of psychosis in its first presentation to mental health services, up to age 35 years |
| Assertive outreach team | Provision of intensive support to individuals with complex and long-term mental health conditions to stabilise symptoms, prevent relapse and encourage engagement with services | |
| ECT | Provision of ECT |
Marital status
-
Not recorded.
-
Single.
-
Married/civil partner.
-
Divorced/person whose civil partnership has been dissolved.
-
Widowed/surviving civil partner.
Accommodation
-
No fixed abode.
-
Client home (privately owned/rented).
-
Hospital setting.
-
Other care setting.
-
Client/carer/family home.
-
Hostel/assisted living.
-
Bail hostel.
-
Care of.
-
Not known.
-
Guesthouse.
-
Workplace/shop.
-
Campsite.
Ethnicity
Ethnicity was collated using the 16 + 1 self-defined classification system from the National Census [Department of Health. National Standards for Ethnic Group and Related Matters. URL: http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/publicationsandstatistics/publications/publicationspolicyandguidance/browseable/dh_5319155 (accessed 28 November 2014)]:
-
0. Not recorded.
-
1. White British.
-
2. White Irish.
-
3. Any other white background.
-
4. White and black Caribbean.
-
5. White and black African.
-
6. White and black Asian.
-
7. Any other mixed background.
-
8. Asian-Indian.
-
9. Asian-Pakistani.
-
10. Asian-Banglideshi.
-
11. Any other Asian background.
-
12. Caribbean.
-
13. African.
-
14. Any other black background.
-
15. Chinese.
-
16. Any other ethnic group.
-
17. Client refused.
-
18. Client unable to chose.
-
19. Not known/unable to request.
Occupation
The Office for National Statistics occupational classification system was used to categorise occupations of cases with additional categories (10 onwards) added for clarity [Office for National Statistics. SOC2010 Volume 1 Structure and Descriptions of Unit Groups. 2010. URL: www.ons.gov.uk/ons/guide-method/classifications/current-standard-classification/soc2010/soc2010-volume-1-structure-and-descriptions-of-unit-groups/index.html#5 (accessed 28 November 2014)]:
-
Managers, directors and senior officials.
-
Professional occupations.
-
Associate professional and technical occupations.
-
Administrative and secretarial occupations.
-
Skilled trades occupations.
-
Caring, leisure and other service occupations.
-
Sales and customer service occupations.
-
Process, plant and machine operatives.
-
Elementary occupations.
-
Employed.
-
Unemployed.
-
At home mum/housewife.
-
Student.
-
Unknown.
-
Retired.
-
Self-employed (not classified).
Local warning flag warnings (from the criminal intelligence system)
-
AARS1 (alcohol referral scheme).
-
ASBESC (the nominal has entered into an ASB contract with the police).
-
ASBO (antisocial behaviour order).
-
Complete.
-
Conceals (hides weapons on person).
-
DASSP (domestic abuse serious or serial perpetrator).
-
DNA required.
-
Drug supplier.
-
FIB Interest (Force Intelligence Bureau).
-
FIU Interest (Financial Investigation Unit).
-
Location ban.
-
MAPPA.
-
MARAC.
-
MoPI (management of police information).
-
Name used by . . . (nominal uses other names or has done in the past or that others use the name: either way).
-
No more PNDS (penalty notice for disorder).
-
PPO (public protection order).
-
Pub watch (pub watch scheme where person is known to local licensees).
-
Risk to child.
-
Sex Off Reg (on sex offenders register).
-
Sex SOPO (sexual offences prevention order).
-
Sexual [nominal has been involved in (though not necessarily convicted of) an offence of a sexual nature].
-
SMRS1 (substance misuse referral scheme).
-
Spec need (specified need).
-
UNHMP (convicted sex offender who is currently in HM Prison Service).
-
Uses name of . . . (nominals who have alternate identities or other names which they use).
-
Vulnerable adult.
Police National Computer warning flags
-
Ailment (DP has ailments and/or disabilities).
-
Alleges (allegations made against police or support staff that are unfounded).
-
Alleges sexual assault.
-
Conceals (carries concealed weapons).
-
Contagious (DP is a carrier of a disease, which is contagious and may be a hazard to others).
-
Drugs (arrest for possession, manufacture/production or possession with intent to supply any illegal drug).
-
Escaper (DP may attempt to escape custody).
-
Explosives (circumstances involving the unlawful possession or criminal use of explosives in any circumstances).
-
Firearms (circumstances involving the criminal possession or use of a firearm).
-
Mental health (DP is the sufferer of a mental condition or disorder).
-
Offends Vulne (offences against vulnerable adults).
-
Self-harm (DP has previously self-harmed).
-
Suicidal (has attempted or is likely to attempt suicide).
-
Violent (DP may resort to violent behaviour).
-
Weapons (DP may use or carry weapons).
Appendix 3 Data collection fields
Criminal justice system data
Identified CJS records/databases.
The data generated from CJS records were located within separate databases.
-
CIS. Individual records comprise a number of screens. The front screen for each case contains basic demographic information, flags and warnings as appropriate. The ‘back screens’ for each case provide detail and a rich picture of participants’ interactions with the CJS and other services as reported by police staff. The following fields will be accessed:
-
Subfield 1: nominal menu.
-
Subfield 1: nominal index update main screen.
-
Reason: demographics, PNC warnings and rationale, local warnings and rationale
-
-
Subfield 2: nominal index update secondary screens.
-
Reason: details of offence/incidents. Free text: report and rationales of arresting.
-
-
-
OIS. This system contains the initial detailed logs created by operators and officers following a reported incident. The log is generated from the information that the police call handler obtains from the caller, it is graded and a response is generated. Owing to the level of detail required to be entered into the OIS, inclusion of these data to the data corpus enables the researchers to examine the decision-making processes of the police in their interactions with participants and other professionals within both the CJS and interagency. The OIS represents up to the first 72 hours of any case, after which the case is entered onto the CIS described above. The following fields will be accessed:
-
Subfield 1: AP’s view.
-
Reason: confirming identification (linkage), PNC warning flags (e.g. suicidal, etc.).
-
-
Subfield 2: associated incidents/persons.
-
Reason: collate number of incidents in research window, rationale for call, real-time log, identification of RPs (including HCPs).
-
-
-
NSPIS custody system. This system provides current and archived data relating to individuals who have been through the three custody suites in Cornwall. A proportion of participants may be taken to the custody suite in Plymouth despite being resident in Cornwall dependent on the location of initial interaction with the police. The front screen pertaining to each individual provides a table with basic demographics and rationale for custody (e.g. Section 136 and/or alleged offence). The detention log in the back screens of this system provides a timetable of procedures and context to a range of decision-making processes including authorisation for searches, checks on individuals and calls and logs of requests for examination and advice from medical practitioners with responses . . . The following fields will be accessed:
-
Subfield 1: custody record.
-
Reason: PNC source documents.
-
-
Subfield 2: custody record front sheet.
-
Reason: initial reason for arrest, place of arrest/custody, circumstances of arrest, demeanour on arrival (substance use, mental state), prior offender.
-
-
Subfield 2: detention log.
-
Reason: real-time log of custody attendance, medical assessments, interactions with health/medical practitioners, Section 136, disposal.
-
-
Subfield 2: risk assessment.
-
Reason: mental health issues, risk to self/others.
-
-
Subfield 1: custody record.
-
Reason: detention management.
-
-
Subfield 2: national medical form.
-
Reason: HCP assessment of state (physical and mental health), examination and observation completed, medication, risk of self-harm, plan of treatment/referral, plan of observation/rousing, log of HCP movement times.
-
-
-
NHRR. This is a spreadsheet-based system. Information is collated for addresses in the 12 policing areas of Cornwall based on repeat calls to addresses (three or more calls to the police in 3-monthly periods). The following fields will be accessed:
-
Subfield 1: location.
-
Reason: neighbourhood.
-
-
Subfield 1: history of attendance.
-
Reason: number of attendances to address.
-
-
Subfield 1: risk identified.
-
Reason: risk tendency score, PSP.
-
-
Subfield 1: underlying issues.
-
Reason: vulnerable person, children aged < 18 years, age-related alcohol misuse, ASB, domestic abuse, disability/medical, drugs, mental health, racial/hate, repeat missing person/truancy, other.
-
-
Subfield 1: free text.
-
Reason: opinion of reporting officer/main rationale for calls giving rise to inclusion to NHRR, rationale behind/expansion on underlying issues, background to incidents.
-
-
-
PNC. Although the three systems used above are routinely used throughout police constabularies across the country, the PNC is the only national database. If the researchers find an incident(s) in OIS or CIS relevant to the research within the 12-month period, an application was made to view that data to the relevant data processing officer from the relevant force.
Health data
Identified NHS records/databases: CFT initiated use of the BT RiO system in August 2010 for all service users with severe and EMHN. RiO is an electronic health record, which captures referral processing, details of assessments and ongoing care. CFT uses RiO to record all interactions with service users, all care plans and all risk assessments. The feasibility study identified a range of folders within the system that would enable the researchers to gain a holistic picture of participants’ access to and interactions with mental health services. Furthermore, it was clear that the level of detail of the combined documents would enable the researchers to answer the research questions. The following list details the folders that have been identified to be included in the data corpus.
Core assessment
-
Subfield: core assessment.
-
Form: presenting situation and referral outcome decision.
-
Reason: professional decision-making: provides rationale for referral based on presenting situation of service user.
-
-
Form: social history/care management form.
-
Reason: professional decision-making: level of vulnerability and management in the 12-month research window.
-
-
Form: mental health legislation/protection of vulnerable adults.
-
Reason: professional decision-making: critical interagency information in the 12-month research window.
-
-
Form: forensic and probation history.
-
Reason: professional decision-making: history in the 12-month research window and comparison with CJS recording.
-
-
Form: substance and alcohol use.
-
Reason: professional decision-making: recording of problematic substance and alcohol use can be recorded here or provide indication of escalation to problematic use within the 12-month research window. Impacts on CJS involvement.
-
-
Form: problematic substance and alcohol use.
-
Reason: professional decision-making: as above.
-
-
Form: mental state examination.
-
Reason: professional decision-making and health economics: provide evidence of assessment taking place and joint decision-making.
-
-
Form: client and carers understanding of assessment.
-
Reason: professional decision-making: provides details of client role in decision making.
-
-
Form: formulation/summary.
-
Reason: professional decision-making and health economics: provides summary of core assessment of service user.
-
-
-
Subfield: core assessment overview – point in time.
-
Reason: professional decision-making and health economics: provides overview if presenting situation and associated issues within the 12-month research window.
-
Risk information
-
Subfield: HCR-20.
-
Reason: professional decision-making and health economics: DH violence risk assessment tool, evidence of an assessment being carried out within the study window, factors leading to this decision and impact on professional decision-making.
-
-
Subfield: risk assessment.
-
Reason: professional decision-making and health economics: evidence of assessments carried out in the 12-month research window with information including risk of harm to self, harm to others, accidents, other risk behaviours, factors affecting risk, summary of assessment.
-
-
Subfield 2: view risk incidents history.
-
Reason: professional decision-making: evidence of incidents recorded in the progress notes assessed by professionals as involving risk.
-
-
Subfield: safeguarding children – adult form 1.
-
Reason: professional decision-making and health economics: evidence of concern for welfare of children.
-
-
Subfield: safeguarding children – adult client form 2.
-
Reason: professional decision-making and health economics: evidence of child/children specifically at risk: check if form completed (not for content).
-
-
Subfield: risk incidents/risk history.
-
Reason: professional decision-making: evidence of incidents recorded in the progress notes assessed by professionals as involving risk.
-
Role as carer information
-
Subfield: carer assessment overview.
-
Reason: professional decision-making and health economics: evidence of carer involved in care of service user, evidence of assessment of needs of carer in the 12-month research window.
-
-
Subfield: carer care plan review.
-
Reason: professional decision-making and health economics: evidence of review of carer needs in the 12-month research window.
-
Specialist assessments
-
Subfield: observation/seclusion.
-
Form: access to fresh air, observation, seclusion.
-
Reason: health economics: assessments carried out during any inpatient admission in the 12-month research window.
-
-
Outcome measures
-
Subfield: clustering assessment.
-
Reason: professional decision-making and health economics: Health of the Nation Outcome Scale outcome measure.
-
-
Subfield: clustering allocation.
-
Reason: professional decision-making and health economics: allocation to superclass and cluster outcome measures.
-
-
Subfield: experience of service.
-
Reason: professional decision-making: service user perspective of journey.
-
-
Subfield: Health of the Nation Outcome Scales (older adults; HoNOS65+).
-
Reason: professional decision-making and health economics: outcome measure for specific client group (older adults).
-
-
Subfield: Health of the Nation Outcome Scales (acquired brain injury; HoNOS-ABI).
-
Reason: professional decision-making and health economics: outcome measure reflecting specific client need.
-
-
Subfield: Health of the Nation Outcome Scales (learning disabilities; HoNOS-LD).
-
Reason: professional decision-making and health economics: outcome measure reflecting specific client need.
-
-
Subfield: Health of the Nation Outcome Scales (secure care; HoNOS Secure).
-
Reason: professional decision-making and health economics: outcome measure for service users discharged from inpatient care by tribunal in the 12-month research window.
-
Care planning, care programme approach and reviews
-
Subfield: care planning – clients.
-
Reason: professional decision-making and health economics: evidence of care planning in the 12-month research window.
-
-
Subfield: care plan contacts.
-
Reason: professional decision-making and health economics: provision of information to client in the 12-month research window: journey quality.
-
-
Subfield: care plan distribution.
-
Reason: professional decision-making: other services provided with care plan.
-
-
Subfield: crisis, relapse and contingency plan.
-
Reason: professional decision-making and health economics: rationale for interagency involvement.
-
-
Subfield: CPA management.
-
Reason: professional decision-making and health economics: number of CPA episodes in the 12-month research window.
-
-
Subfield: CPA review.
-
Reason: professional decision-making and health economics: detail of reviews conducted in the 12-month research window.
-
-
Subfield: pre-discharge planning.
-
Reason: professional decision-making: liaison with other services prior to discharge and cross check with progress notes.
-
-
Subfield: MAPPA review.
-
Reason: professional decision-making and health economics: evidence of review conducted in the 12-month research window.
-
-
Subfield: Section 117 review management.
-
Reason: professional decision-making and health economics: evidence of review conducted in the 12-month research window: after care (inpatient admission) plan relevant to condition for which detained. Evidence of service user right to be offered such a plan.
-
Medicines management and electroconvulsive therapy
-
Subfield: clinical management plan.
-
Reason: health economics: evidence of plan being completed in the 12-month research window.
-
-
Subfield: electroconvulsive therapy treatment.
-
Reason: health economics: evidence of treatment provision in the 12-month research window.
-
Progress notes
-
Reason: professional decision-making and health economics: progress notes of all health and social care professionals in contact with service user in the 12-month research window.
Diagnosis
-
Reason: professional decision-making and health economics: diagnoses made in the 12-month research window.
Clinical documentation
-
Subfield: document list view form: list of letters/related documents.
-
Reason: professional decision-making and health economics: letters/documents between professionals related to service user care in the 12-month research window.
-
Client-related data views
-
Subfield: care plan overview – point in time.
-
Reason: professional decision-making: direct access to care plan in action on specified dates within the 12-month research window.
-
-
Subfield: client diary view.
-
Reason: professional decision-making and health economics: all appointments in the 12-month research window (including those cancelled); referrals and associated rationales.
-
-
Subfield: HCR-20 overview.
-
Reason: professional decision-making and health economics: summary of HCR-20 H Factors for assessments made in the 12-month research window.
-
-
Subfield: inpatient care plan.
-
Reason: professional decision-making and health economics: problems and interventions during inpatient admissions in the 12-month research window.
-
-
Subfield: inpatient care plan – point in time.
-
Reason: professional decision-making and health economics: problems and interventions during inpatient admissions in the 12-month research window. Access on specific dates.
-
-
Subfield: progress note view.
-
Reason: professional decision-making and health economics: access to progress notes on specified dates.
-
-
Subfield: risk overview – point in time.
-
Reason: professional decision-making and health economics: summary of risk assessment in action at specified point in time.
-
-
Subfield: safeguarding children – adult client.
-
Reason: professional decision-making and health economics: evidence of child/children specifically at risk: check if form completed (not for content). Access to assessments on specified dates.
-
-
Subfield: safeguarding children – adult client – overview.
-
Reason: professional decision-making and health economics: summary of evidence of child/children specifically at risk: check if form completed (not for content). Access on specified dates.
-
-
Subfield: RiO significant events.
-
Reason: professional decision-making and health economics: incidents of significance flagged within the progress notes.
-
Mental Health Act
-
Subfield: Mental Health 1 assessments.
-
Reason: professional decision-making and health economics: assessments completed in the 12-month research window.
-
-
Subfield: client sections – history.
-
Reason professional decision-making and health economics: history of sections in the 12-month research window.
-
-
Subfield: Section 132 rights.
-
Reason: professional decision-making and health economics: record of rights explained in research window; level of service user understanding.
-
Archived forms
-
Form: safeguarding children summary, current interventions including medication, referral outcome decision.
-
Reason: professional decision-making and health economics: forms related to assessments conducted and decisions made within RiO data fields in the 12-month research window and evidenced in archived forms.
-
Appendix 4 Pseudonymisation process

Appendix 5 Health economics component: unit costs
Criminal justice system unit costs
| Item | Unit | Unit cost (£, 2011/12 prices) | Source | Assumptions |
|---|---|---|---|---|
| Initial contact section | ||||
| Contact with police | Per contact | 16 | NHS Direct74 | Based on cost of NHS direct phone call |
| Police attendance | Per minute | 0.97 | DCP July 2013 | Assume a police constable; £56.58 per hour full economic cost ignoring special rates (i.e. public holiday rates); cost per minute based on actual police attendance time |
| Ambulance called | Per occurrence | 230 | CFT July 2013 | Total cost of each of the paramedic services divided by the total number of contacts |
| Custody section | ||||
| Length of stay in custody suite | Per hour | 40 | DCP July 2013 | Cost based on individual contact time: based on average cost per detainee of £328 per custody occurrence and the average stay of 8.5 hours |
| MHAA | Per occurrence | 1059 | DH65 | Based on the assumption of 3 hours for two Section 12 doctors plus an AMHP |
| HCP/triage | Per occurrence | 92 | DH65 | Assumed 1 hour; cost at the mid-point of an advanced nurse and FME as it could be either |
| FME | Per occurrence | 132 | DH65 | Assumed medical consultant for 1 hour |
| AMHP | Per occurrence | 54 | DH65 | Assumed social worker for 1 hour |
| Hospital attendance | Per occurrence | 586 | CFT July 2013 | Based on non-elective inpatient (short stay) – cost per stay |
| Other section | ||||
| Transport | Per occurrence | 117 | DCP July 2013 | Assume two police constables for 1 hour. |
| Follow-up calls by police | Per occurrence | 4.87 | DCP July 2013 | Assume one police constable for 5 minutes |
| Escorting | Per occurrence | 117 | DCP July 2013 | Assume two police constables for 1 hour |
Mental health and social care unit costs
| Item | Unit | Unit cost (£, 2011/12 prices) | Source | Assumptions |
|---|---|---|---|---|
| Mental health inpatient | ||||
| Acute psychiatric | Per bed-day | 329 | DH65 | – |
| PICU | Per bed-day | 647 | DH65 | – |
| Dementia ward | Per bed-day | 340 | DH65 | – |
| Rehabilitation ward | Per bed-day | 289 | DH65 | – |
| Low secure ward | Per bed-day | 441 | DH65 | – |
| Client diary | ||||
| Community clinic | ||||
| Medical | Per occurrence | 125 | DH65 | Mental health consultant services; community setting; follow-up attendance face to face; adult other services |
| Nursing | Per occurrence | 34 | Curtis64 | Assume mental health nurse; per hour of face-to-face contact; assume 30-minute appointment; excluding qualifications |
| Social work | Per occurrence | 78 | Curtis64 | Social worker adult services; per hour of face-to-face contact; assume 30-minute appointment; excluding qualifications |
| Psychology | Per occurrence | 136 | Curtis64 | Per hour of client contact; assume 1-hour appointment; excluding qualifications |
| Non-clinical | Per occurrence | 14 | Curtis64 | Assume social work assistant; per hour; assume 30-minute appointment |
| AMHP | Per occurrence | 78 | Curtis64 | Assume social worker; cost as above |
| Police | Per occurrence | 58 | DCP July 2012 | Assume two police constables for 30 minutes; full economic cost for a constable ignoring special rates, i.e. public holiday rate |
| GP | Per occurrence | 36 | Curtis64 | Per patient contact lasting 11.7 minutes; excluding qualifications; including direct care staff costs |
| Therapy | Per occurrence | 30 | Curtis64 | Assume occupational therapist; assume 1 hour; excluding qualifications |
| Senior practitioner HTT | Per occurrence | 188 | DH65 | Mental health specialist teams – adult – crisis resolution HTTs; face to face |
| Inpatient | ||||
| Medical | Per occurrence | 0 | – | Assumed this would be included in the cost of inpatient bed-day |
| Nursing | Per occurrence | 0 | – | Assumed this would be included in the cost of inpatient bed-day |
| Social work | Per occurrence | 113 | Curtis64 | Cost as home visit – assuming there is a similar cost with the inclusion of travel time |
| Psychology | Per occurrence | 197 | Curtis64 | Cost as home visit – assuming there is a similar cost with the inclusion of travel time |
| Non-clinical | Per occurrence | 20 | Curtis64 | Cost as home visit – assuming there is a similar cost with the inclusion of travel time |
| AMHP | Per occurrence | 113 | Curtis64 | Cost as home visit – assuming there is a similar cost with the inclusion of travel time |
| Police | Per occurrence | 58 | DCP July 2012 | Cost as home visit – assuming there is a similar cost with the inclusion of travel time |
| GP | Per occurrence | 92 | Curtis64 | Cost as home visit – assuming there is a similar cost with the inclusion of travel time |
| Therapy | Per occurrence | 43.5 | Curtis64 | Cost as home visit – assuming there is a similar cost with the inclusion of travel time |
| Senior practitioner HTT | Per occurrence | 188 | DH65 | Cost as normal HTT – assume HTTs always work in the community so keep at fixed cost |
| Client home | ||||
| Medical | Per occurrence | 181 | DH65 | Mental health consultant services; community setting; follow-up attendance; face to face; adult other services; combined with community nurse home visit ratio (1.45) |
| Nursing | Per occurrence | 49 | Curtis64 | Assume mental health nurse; per hour of face-to-face contact; assume 30-minute appointment; excluding qualifications; combined with community nurse home visit ratio (1.45) |
| Social work | Per occurrence | 113 | Curtis64 | Social worker adult services; per hour of face-to-face contact; assume 30-minute appointment; excluding qualifications; combined with community nurse home visit ratio (1.45) |
| Psychology | Per occurrence | 197 | Curtis64 | Per hour of client contact; assume 1-hour appointment; excluding qualifications; combined with community nurse home visit ratio (1.45) |
| Non-clinical | Per occurrence | 20 | Curtis64 | Assume social work assistant; per hour; assume 30-minute appointment; combined with community nurse home visit ratio (1.45) |
| AMHP | Per occurrence | 113 | Curtis64 | Cost as social worker above |
| Police | Per occurrence | 58 | DCP July 2012 | Assume two police constables for 30 minutes; full economic cost for a constable ignoring special rates, i.e. public holiday rate |
| GP | Per occurrence | 92 | Curtis64 | Per patient out of surgery visit lasting 23.4 minutes; excluding qualifications; including direct care staff costs |
| Therapy | Per occurrence | 44 | Curtis64 | Assume occupational therapy; excluding qualifications; assume 1-hour appointment; combined with community nurse home visit ratio (1.45) |
| Senior practitioner HTT | Per occurrence | 188 | DH65 | Cost as normal HTT; assume HTTs always work in the community so keep at fixed cost |
| General hospital | ||||
| Medical | Per occurrence | 171 | DH65 | Mental health consultant services; outpatient setting; follow-up attendance face to face; adult other services |
| Nursing | Per occurrence | 34 | Curtis64 | Cost as community contact |
| Social work | Per occurrence | 78 | Curtis64 | Cost as community contact |
| Psychology | Per occurrence | 136 | Curtis64 | Cost as community contact |
| Non-clinical | Per occurrence | 14 | Curtis64 | Cost as community contact |
| AMHP | Per occurrence | 78 | Curtis64 | Cost as community contact |
| Police | Per occurrence | 58 | DCP July 2012 | Cost as community contact |
| GP | Per occurrence | 92 | Curtis64 | Cost as home visit; assuming that there is a similar cost with the inclusion of travel time |
| Therapy | Per occurrence | 30 | Curtis64 | Cost as community contact |
| Senior practitioner HTT | Per occurrence | 188 | DH65 | Cost as normal HTT; assume HTTs always work in the community so keep at fixed cost |
| GP surgery | ||||
| Medical | Per occurrence | 36 | Curtis64 | Cost as GP below |
| Nursing | Per occurrence | 34 | Curtis64 | Assume mental health nurse; per hour of face-to-face contact; assume 30-minute appointment; excluding qualifications |
| Social work | Per occurrence | 78 | Curtis64 | Cost as community contact |
| Psychology | Per occurrence | 136 | Curtis64 | Cost as community contact |
| Non-clinical | Per occurrence | 14 | Curtis64 | Cost as community contact |
| AMHP | Per occurrence | 78 | Curtis64 | Cost as community contact |
| Police | Per occurrence | 58 | DCP July 2012 | Assume two police constables; assume 30-minute event |
| GP | Per occurrence | 36 | Curtis64 | Assume per patient contact lasting 11.7 minutes; excluding qualifications; including direct care staff costs |
| Therapy | Per occurrence | 30 | Curtis64 | Cost as community contact |
| Senior practitioner HTT | Per occurrence | 188 | DH65 | Cost as normal HTT; assume HTTs always work in the community so keep at fixed cost |
| Supported housing/residential/nursing home/homeless hostel/probation service/custody centre/magistrate service/day resource centre/public place | ||||
| Medical | Per occurrence | 181 | DH65 | Cost as home visit; assuming there is a similar cost with the inclusion of travel time |
| Nursing | Per occurrence | 49 | Curtis64 | Cost as home visit; assuming there is a similar cost with the inclusion of travel time |
| Social work | Per occurrence | 113 | Curtis64 | Cost as home visit; assuming there is a similar cost with the inclusion of travel time |
| Psychology | Per occurrence | 197 | Curtis64 | Cost as home visit; assuming there is a similar cost with the inclusion of travel time |
| Non-clinical | Per occurrence | 20 | Curtis64 | Cost as home visit; assuming there is a similar cost with the inclusion of travel time |
| AMHP | Per occurrence | 113 | Curtis64 | Cost as home visit; assuming there is a similar cost with the inclusion of travel time |
| Police | Per occurrence | 58 | DCP July 2012 | Cost as home visit; assuming there is a similar cost with the inclusion of travel time |
| GP | Per occurrence | 92 | Curtis64 | Cost as home visit; assuming there is a similar cost with the inclusion of travel time |
| Therapy | Per occurrence | 44 | Curtis64 | Cost as home visit; assuming there is a similar cost with the inclusion of travel time |
| Senior practitioner HTT | Per occurrence | 188 | DH65 | Cost as normal HTT; assume HTTs always work in the community so keep at fixed cost |
| Phone call | ||||
| Medical | Per occurrence | 25 | DH65 | Mental health consultant services; community setting; follow-up attendance non-face to face; adult other services |
| Nursing | Per occurrence | 6.7 | DH65 | Assume same proportion of community costs as a psychiatrist face to face vs. non-face to face (20%) |
| Social work | Per occurrence | 16 | DH65 | Assume same proportion of community costs as a psychiatrist face to face vs. non-face to face (20%) |
| Psychology | Per occurrence | 27 | DH65 | Assume same proportion of community costs as a psychiatrist face to face vs. non-face to face (20%) |
| Non-clinical | Per occurrence | 2.8 | DH65 | Assume same proportion of community costs as a psychiatrist face to face vs. non-face to face (20%) |
| AMHP | Per occurrence | 16 | DH65 | Assume same proportion of community costs as a psychiatrist face to face vs. non-face to face (20%) |
| Police | Per occurrence | 4.9 | DCP July 2012 | Assume same proportion of community costs as a psychiatrist face to face vs. non-face to face (20%) |
| GP | Per occurrence | 22 | Curtis64 | Assume same proportion of community costs as a psychiatrist face to face vs. non-face to face (20%) |
| Therapy | Per occurrence | 6 | Curtis64 | Assume same proportion of community costs as a psychiatrist face to face vs. non-face to face (20%) |
| Senior practitioner HTT | Per occurrence | 38 | DH65 | Assume same proportion of community costs as a psychiatrist face to face vs. non-face to face (20%) |
| Assessments | ||||
| Social inclusion | Per assessment | 7 | Curtis64 | Assume family support worker (band 4), 15 minutes; per hour; assume not face to face with client |
| Referral screening | Per assessment | 67 | Curtis64 | Assume mental health nurse (band 5), 1 hour; per hour; excluding qualifications; assume face to face with client |
| Police screening request | Per assessment | 126 | Curtis64 | Assume community nurse (band 6), 3 hours; per hour; excluding qualifications; assume not face to face with client |
| Court diversion | Per assessment | 42 | Curtis64 | Assume community nurse (band 6), 1 hour; per hour; excluding qualifications; assume not face to face with client |
| Information sharing | Per assessment | 35 | Curtis64 | Assume mental health nurse (band 5), 1 hour; per hour; excluding qualifications; assume not face to face with client |
| Presenting situation and referral outcome decision | Per assessment | 141 | Curtis64 | Assume mental health nurse (band 5), 3 hours; per hour of patient-related work; excluding qualifications; assume some face-to-face contact |
| Risk assessment | Per assessment | 70 | Curtis64 | Assume mental health nurse (band 5), 2 hours; per hour; excluding qualifications; assume not face to face with client |
| HCR-20 | Per assessment | 210 | Curtis64 | Assume community nurse (band 6), 5 hours; per hour; excluding qualifications; assume not face to face with client |
| Safeguarding children | Per assessment | 70 | Curtis64 | Assume mental health nurse (band 5), 2 hours; per hour; excluding qualifications; assume not face to face with client |
| Carer care plan review | Per assessment | 53 | Curtis64 | Assume mental health nurse (band 5), 1.5 hours; per hour; excluding qualifications; assume not face to face with client |
| Clustering assessment and allocation | Per assessment | 35 | Curtis64 | Assume mental health nurse (band 5), 1 hour; per hour; excluding qualification; assume not face to face with client |
| Care plan entry | Per assessment | 12 | Curtis64 | Assume mental health nurse (band 5), 20 minutes; per hour; excluding qualifications; assume not face to face with client |
| Crisis relapse and contingency plan | Per assessment | 34 | Curtis64 | Assume mental health nurse (band 5), 30 minutes; per hour; excluding qualifications; assume face-to-face contact |
| MAPPA review | Per assessment | 78 | Curtis64 | Assume advanced nurse (band 7), 1.5 hours; per hour; excluding qualifications; assume not face to face with client |
| Mental Health 1 assessment | Per assessment | 1059 | Curtis64 | Assume social worker adult services, consultant psychiatrist and registrar. Social worker adult services, 3 hours; per hour of patient-related work; excluding qualifications. Consultant psychiatrist, 3 hours; per hour of patient-related work; excluding qualifications. Registrar, 3 hours; per hour for 48-hour week; excluding qualifications |
| Meetings in absence of client (the cost of meetings in the absence of the client was calculated using cost per profession with times for each meeting applied) | ||||
| Medical | Per hour | 124 | Curtis64 | Assume consultant psychiatrist; per contract hour; excluding qualifications |
| Nursing | Per hour | 35 | Curtis64 | Assume mental health nurse; per hour; excluding qualifications |
| Social work | Per hour | 39 | Curtis64 | Social worker adult services; per hour; excluding qualifications |
| Psychology | Per hour | 60 | Curtis64 | Clinical psychologist; per hour; excluding qualifications |
| Non-clinical | Per hour | 28 | Curtis64 | Assume social work assistant; per hour |
| AMHP | Per hour | 39 | Curtis64 | Assume social worker adult services; per hour; excluding qualifications |
| Police | Per hour | 58 | DCP July 2012 | Assume one police constable; per hour of full economic cost; ignoring special rates, i.e. public holiday rate |
| GP | Per hour | 118 | Curtis64 | GP; per hour of general medical services activity; excluding qualifications; including direct care staff costs |
| Therapy | Per hour | 30 | Curtis64 | Assume occupational therapist; per hour; excluding qualifications |
| Senior practitioner HTT | Per hour | 39 | Curtis64 | Assume social worker adult services; per hour; excluding qualifications |
| Health visitor | Per hour | 43 | Curtis64 | Health visitor; per hour; excluding qualifications |
| Residence manager | Per hour | 37 | Curtis64 | Assume care home manager; per hour |
| Housing officer | Per hour | 39 | Curtis64 | Assume social worker adult services; per hour; excluding qualifications |
| Ward manager | Per hour | 52 | Curtis64 | Assume nurse team manager; per hour; excluding qualifications |
| MHA manager | Per hour | 52 | Curtis64 | Assume nurse team manager; per hour; excluding qualifications |
| Probation officer | Per hour | 39 | Curtis64 | Assume social worker adult services; per hour; excluding qualifications |
| Homeless key worker | Per hour | 39 | Curtis64 | Assume social worker adult services; per hour; excluding qualifications |
| Meeting | Source | Assumed time | ||
| Interagency co-ordination meeting | DCP July 2012 | 90 minutes | ||
| Tactical intervention meeting | DCP July 2012 | 30 minutes | ||
| Risk management meeting | DCP July 2012 | 90 minutes | ||
| MARAC | DCP July 2012 | 90 minutes | ||
| CPA | DCP July 2012 | 60 minutes | ||
| Management meetings | DCP July 2012 | 60 minutes | ||
Probabilities entered into the decision-analytic modelling
| Event point | Probabilities (to two decimal points) | Source of information |
|---|---|---|
| Following police attendance: | Data collected in Interface Project; only for those with a police attendance | |
| Section 136 detention | 0.03 | |
| Arrest | 0.18 | |
| NFA | 0.80 | |
| Section 136 detention | ||
| Following Section 136 detention: | Data collected in Interface Project; only for those with a police attendance | |
| Take to Section 136 suite | 0.14 | |
| Take to custody | 0.86 | |
| Following MHAA following being taken to Section 136 suite: | Data collected in Interface Project; only for those with a police attendance | |
| Detained – transfer to hospital | 0.00 | |
| Not detainable – release | 1.00 | |
| Following being taken to custody: | Data collected in Interface Project; only for those with a police attendance | |
| FME assessment | 0.08 | |
| HCP assessment | 0.83 | |
| No assessment | 0.08 | |
| Following FME assessment: | Data collected in Interface Project; only for those with a police attendance | |
| MHAA | 0.00 | |
| Not detainable – release | 1.00 | |
| Following HCP assessment: | Data collected in Interface Project; only for those with a police attendance | |
| FME assessment | 0.70 | |
| MHAA | 0.30 | |
| Not detainable – release | 0.00 | |
| Following FME assessment after HCP assessment: | Data collected in Interface Project; only for those with a police attendance | |
| MHAA | 0.71 | |
| Not detainable – release | 0.29 | |
| Following MHAA after FME assessment following HCP assessment: | Data collected in Interface Project; only for those with a police attendance | |
| Detained – transfer to hospital | 0.40 | |
| Not detainable – release | 0.60 | |
| Arrest | ||
| Following arrest: | Data collected in Interface Project; only for those with a police attendance | |
| FME assessment | 0.01 | |
| HCP assessment | 0.67 | |
| No assessment | 0.31 | |
| Following FME assessment: | Data collected in Interface Project; only for those with a police attendance | |
| MHAA | 1.00 | |
| Not detainable – release | 0.00 | |
| Following HCP assessment: | Data collected in Interface Project; only for those with a police attendance | |
| FME assessment | 0.14 | |
| MHAA | 0.86 | |
| Not detainable – release | 0.00 | |
| Following FME assessment after HCP assessment: | Data collected in Interface Project; only for those with a police attendance | |
| MHAA | 0.25 | |
| Not detainable – release | 0.75 | |
| Following MHAA after FME assessment following HCP assessment: | Data collected in Interface Project; only for those with a police attendance | |
| Detained – transfer to hospital | 0.50 | |
| Not detainable – release | 0.50 | |
Appendix 6 Implementation strategy following clinical audit
The following pages summarise the recommendations and action plan following the clinical audit as agreed with the trust. The implementation process diagram shows the stages of development of this plan and the participatory nature of the process.
Summary of recommendations
Three themes emerged from the review of the audit findings, these being raising awareness, recording and RiO functionality.
| Theme | Recommendations |
|---|---|
| 1. Raising awareness |
|
| 2. Recording behaviour |
|
| 3. RiO functionality |
|
Action plan
The action plan below was prepared in consultation with service line leads and other key stakeholders in order to ensure maximisation and sustainability of impact of the findings and recommendations of the audit.
-
To organise an interagency meeting to discuss recording behaviour in relation to Section 136. (Responsibility: LC to arrange a meeting with key representatives from mental health, social work and police services.)
-
To feed findings and recommendations regarding awareness and recording concerning risk assessment recording fidelity to the Trust Risk Policy Development Group. (Responsibility: JM.)
-
To ensure recommendations regarding awareness and recording with regard to care planning are incorporated into CPA policy and training. (Responsibility: JM to ensure CPA policy reviewer is briefed of recommendations.)
-
To feed recommendations regarding RiO functionality to care process design groups in hospital, complex care and community business lines to ascertain need and drive the processing of appropriate RiO change request forms. (Responsibility: LC and JM with the collaboration of above business lines.)
-
Continue to host the Interface Project and learn from the emerging data in the following areas:
-
– linked cases where police contact was not recorded on RiO
-
– decision-making and communication on high risk/high need patients
-
– inviting LC to attend Cornwall’s Offender Health Partnership board. (Responsibility: JM through Interface Project research meetings.)
-
Implementation process

Glossary
- Appropriate adult
- A relative, guardian, person responsible for care or social worker (person who is not a police officer) who must be present if a young person or vulnerable adult is to be searched or questioned in police custody (Great Britain. Police and Criminal Evidence Act 1984 Code C. London: Her Majesty’s Stationery Office; 1984).
- Approved mental health professional
- A person approved by local authorities to implement elements of the Mental Health Act [see amended Mental Health Act 2007 (Great Britain. Mental Health Act 2007. London: The Stationery Office; 2007)].
- Associated person
- A person associated with a police incident and named on the log for that incident.
- Care programme approach
- A UK system of delivering community services to those with mental illness.
- Care Quality Commission
- Non-departmental public body of the government established to regulate and inspect health and social care services in England.
- Community psychiatric nurse
- Psychiatric nurse based in a community rather than hospital setting.
- Criminal intelligence system
- Police record system containing criminal and non-crime records.
- Criminal Justice Liaison and Diversion team
- A team with the task of diverting offenders with mental health needs away from the criminal justice system into the care of health and social services.
- Criminal justice system
- System of law enforcement directly involved in apprehending, prosecuting, defending, sentencing and imprisoning those who are suspected of, or have been charged with, criminal offences.
- Criminal Records Bureau
- See Disclosure and Barring Service.
- Detained person
- Person held in police custody.
- Disclosure and Barring Service
- Organisation responsible for processing criminal record checks.
- Fit to detain
- Medically fit to remain in police custody.
- Fit to interview
- Medically fit to take part in a police interview.
- Forensic medical examiner
- Forensic medical examiners (formerly known as police surgeons) are usually general practitioners, who are self-employed, independent and individually appointed to provide their services to relevant police forces.
- Long-term referral (group)
- Case who had been on the caseload of a Mental Health Team for at least 2 months at the time of the index police contact in the audit period.
- Multi-Agency Public Protection Arrangements
- Interagency group tasked with the management of registered sex offenders, violent and other types of sexual offenders, and offenders who pose a serious risk of harm to the public.
- Multi-Agency Risk Assessment Conference
- Interagency group brought together to deal with domestic abuse.
- Neighbourhood Harm Reduction Register
- Register of addresses where there have been three or more incidents in one quarter of the year. Contains information of the principal person at that address.
- Operational Information System
- This system contains the initial detailed logs created by the police during and following a reported incident.
- Police National Computer
- Computer system used across the UK by law enforcement organisations.
- Principal person
- Main individual linked to police incidents at an address registered on the Neighbourhood Harm Reduction Register.
- Short-term referral (group)
- Case who was on the caseload of a Mental Health Team for less than 2 months at the time of the index police contact in the audit period.
- Single point of contact
- An officer advising and assisting on all aspects of an investigation relating to communication of data and with communication service providers.
- View Street Index
- Search function on the Operational Information System for identifying previous incidents or individuals through addresses.
List of abbreviations
- A&E
- accident and emergency
- AA
- appropriate adult
- AMHP
- approved mental health professional
- AP
- associated person
- APL
- adult psychiatric liaison
- ASB
- antisocial behaviour
- AWOL
- absent without leave
- BoP
- breach of the peace
- BTP
- British Transport Police
- CFT
- Cornwall Partnership NHS Foundation Trust
- CI
- confidence interval
- CIS
- criminal intelligence system
- CJA
- Criminal Justice Act 2003
- CJS
- criminal justice system
- CMHT
- Community Mental Health Team
- CPA
- care programme approach
- CPN
- community psychiatric nurse
- DCP
- Devon & Cornwall Police
- DH
- Department of Health
- DP
- detained person
- DPA
- Data Protection Act 1998
- DSH
- deliberate self-harm
- DV
- domestic violence
- EIT
- early intervention team
- EMHN
- enduring moderate to severe mental health needs
- FME
- forensic medical examiner
- GP
- general practitioner
- HCP
- health-care professional
- HCR-20
- Historical Clinical Risk Management-20
- HMIC
- Her Majesty’s Inspectorate of Constabulary
- HS&DR
- Health Services and Delivery Research
- HTT
- home treatment team
- IQR
- interquartile range
- LD
- learning disability
- MAPPA
- Multi-Agency Public Protection Arrangements
- MARAC
- Multi-Agency Risk Assessment Conference
- MCA
- Mental Capacity Act 2005
- MHA
- Mental Health Act
- MHAA
- Mental Health Act assessment
- MHRN
- Mental Health Research Network
- MHT
- Mental Health Team
- NBT
- Neighbourhood Beat Team
- NFA
- no further action
- NHRR
- Neighbourhood Harm Reduction Register
- NIGB
- National Information Governance Board
- NIHR
- National Institute for Health Research
- NRES
- National Research Ethics Service
- NSPIS
- National Strategy for Police Information Systems
- OIS
- Operational Information System
- PACE
- Police and Criminal Evidence Act 1984
- PNC
- Police National Computer
- PoD
- praxis-oriented dialogue
- PP
- principal person
- PPI
- patient and public involvement
- PSP
- problem solving plan
- RP
- reporting person
- SD
- standard deviation
- SURE
- Service Users in Research Enterprise
- VSI
- View Street Index