Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 09/1002/09. The contractual start date was in February 2011. The final report began editorial review in April 2014 and was accepted for publication in October 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
During part of the duration of this project, Jonathan Klein received a grant from Southampton Clinical Commissioning Group for another project, which did not constitute any conflict of interest.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Wye et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Changes to health-care commissioning during the lifetime of the study
Recent history suggests that there will always be some mix of public sector, clinician and commercial involvement in NHS health-care commissioning, even if the balance shifts under successive governments. This research spanned 6 turbulent years within the NHS, during which that balance changed considerably.
This study was conceived in 2008, at the time the then Labour government emphasised improving the competencies of commissioners through World Class Commissioning (WCC). 1 At this time, NHS commissioning was mainly led by managers in about 150 organisations known as ‘primary care trusts’ (PCTs). The main vehicle to draw on clinical expertise was known as ‘practice-based commissioning’ (PBC), which was established in 2005, and later promoted under the WCC initiative. PBC, however, struggled to engage clinicians. 2 Meanwhile, commercial providers were gaining greater ground with the advent of the Framework for procuring External Services for Commissioners (FESC), launched in November 2007. FESC was an initiative whereby 14 commercial providers went through an authorisation process and were approved to aid PCTs in commissioning health-care services.
When this study was designed and submitted at the outline stage in August 2009, NHS health-care commissioners were defined as ‘PCT managers’, clinical input to commissioning was relatively minimal or variable across the country and the outlook for commercial companies was promising.
This changed substantially after funding for the study was awarded in June 2010. After the 2010 election, the Conservative–Liberal Democrat coalition government brought in a major NHS reorganisation with the stated aim of transferring commissioning power from managers to clinicians, specifically general practitioners (GPs). With Liberating the NHS,3 PCTs were to be abolished by April 2013 and their commissioning responsibilities allocated to over 200 Clinical Commissioning Groups (CCGs) and NHS England. Public Health, which for many PCTs had been an important conduit of research evidence, moved to local authorities. The analytical function of PCTs was hived off into independent commissioning support units (CSUs) expected to be self-sufficient by 2016. A major impact of the Health and Social Care Act of 20124 was to externalise much of what had been previously internal to local commissioning organisations (e.g. analytics, Public Health).
Unsurprisingly with this degree of flux, identifying the ‘commissioners’ became increasingly difficult during fieldwork, as PCTs moved into PCT clusters, shedding staff through reconfigurations, CCGs emerged out of General Practice Commissioning Groups and PCTs, and CCGs negotiated the transition of commissioning responsibilities. PCTs no longer contracted commercial companies for commissioning support, as PCTs were soon to be defunct, and neither did CCGs, as CCGs often did not hold budgets because they were in shadow form. The term ‘external provider’ became synonymous with ‘commercial provider’, although the implications of Liberating the NHS3 meant that the health-care market was increasingly open to not-for-profit organisations such as social enterprises and the voluntary sector.
When fieldwork began in early 2011, a commissioner could be defined as either a PCT manager or a GP commissioner and clinical input was increasing, but contracts with external providers such as commercial companies and not-for-profits were limited. Protests led by groups such as 38 degrees (www.38degrees.org.uk) and Keep our NHS Public (www.keepournhspublic.com) were common, because of fears that Liberating the NHS3 would privatise the running of the NHS. Moreover, the proposed changes had limited support from doctors, without whom they would flounder. 5 In the summer of 2011 in light of the controversy, the coalition government instituted a ‘pause’ for further consultation, which added confusion and delay to the commissioning reforms and our project. Over the 2 years of data collection since, the situation has settled and it is possible to delineate commissioners and those who provide commissioning support and advice. This culminated with authorisation of CCGs in April 2013.
At the time of writing (early 2014), about 60% of the commissioning budget and contingent responsibilities lay with CCGs, which had substantial clinical leadership. Commercial companies were steadily increasing their business, with the aid of the ‘Lead Provider Framework’ which included assured suppliers of health and social care support services. 6 These suppliers were winning contracts from CCGs and, in some cases, forming partnerships with CSUs, many of which employed former PCT staff. In addition, a host of external providers taking multiple organisational forms had sprung up. 7,8
Research questions and objectives
Throughout the span of the study, our chief interest was exploring knowledge exchange processes between those responsible for NHS health-care commissioning with others internal and external to their organisations, even as those classified as ‘internal’ and ‘external’ were continually changing. We used the term ‘knowledge exchange’ (rather than ‘knowledge transfer’ or ‘research implementation’) as information, research evidence, expertise, skills and innovations such as research-based software are all forms or applications of ‘knowledge’, and ‘exchange’ best describes how knowledge is transformed through the interaction of two or more parties. We wanted to know what knowledge was needed, where it was obtained and how it was transformed and fed into NHS commissioners’ decision-making. Although we had a particular interest in research-based evidence, for the purposes of this study all sources of knowledge were included.
The reorganisation of commissioning following the 2012 Health and Social Care Act4 impacted on our exploration of the research questions. The upheavals were a major part of the context in which the participants in our research were operating, and the impact of the Act was a running theme throughout our data. However, that process of change was a unique event that we were not funded to evaluate. Although this inevitably remained an important part of the context, we eventually took the view that it should not form a major part of our analysis.
The focus of enquiry on knowledge exchange remained constant, although the research questions and aims were regularly updated because of the changing NHS landscape. By adopting a qualitative approach using ethnographic techniques, the study was flexible enough to adapt. Moreover, it complemented other research commissioned by the National Institute for Health Research (NIHR) Services Delivery and Organisation research programme such as the use of evidence in health-care management decisions,9 health-care managers’ use of and access to management research,10 management practice among middle managers and GPs11 and the commissioning of long-term conditions. 12 Those studies have given a valuable picture of how PCT managers and GPs drew on research evidence and other sources to inform their commissioning decisions. This study builds on that literature by providing early insight into CCGs and the growing band of external purveyors of knowledge and information including commercial providers, not-for-profit agencies, CSUs and Public Health.
The study was structured around four research questions. They were:
-
How do health-care commissioners access research evidence and other sources of knowledge to aid their commissioning decisions?
-
What is the nature and role of agencies that provide commissioning expertise from the public (e.g. Public Health), private (e.g. commercial providers) and other sectors (e.g. not-for-profit)?
-
What are the processes by which health-care commissioners transform information provided by other agencies into useable knowledge that is embedded in commissioning decisions?
-
What are the benefits and disadvantages?
In answering these questions, this study had the following objectives:
-
to describe models of commissioning expertise, including private (e.g. commercial providers) and public sector (e.g. clinical consortia, specialist commissioning)
-
to elucidate how diverse health-care commissioners and other providers of commissioning expertise access, assimilate, integrate and utilise managerial and clinical research
-
to establish how existing professionals with expertise in commissioning from the public (e.g. Public Health practitioners) and private sector (e.g. management consultants) transform and market their managerial and clinical knowledge
-
to examine how knowledge is exchanged between commercial agencies and public sector bodies and how that knowledge is embedded and applied in the commissioning process
-
to explore the perceived benefits and disadvantages of these exchanges
-
to identify actionable messages and disseminate them to commissioners, policy-makers and external providers using effective knowledge exchange strategies.
Structure of this report
The next chapter of this report covers the methods used in the study, including information on the case sites. Chapter 3 is the first results chapter and discusses the nature of commissioning. Chapter 4 covers models of commissioning to provide greater understanding of what commissioners do, before going on to describe the contributions of others such as commercial providers to commissioning processes. Chapter 5 focuses on the knowledge acquisition and Chapter 6 discusses knowledge transformation. Chapter 7 covers the role and function of external providers. Chapter 8 offers in-depth accounts of three contractual relationships. Chapter 9 reports the benefits and disadvantages of these processes and Chapter 10 details the key findings and implications of this study.
Box 1 summarises the key points of this chapter.
-
The aim of this research is to study knowledge exchange between those responsible for commissioning NHS services and external agencies.
-
Since this project was conceived in 2008, the NHS landscape has changed remarkably as a result of the organisational changes set out in Liberating the NHS. 3 Consequently, several functions that were formerly considered ‘internal’ in PCT structures (e.g. analytics or Public Health) now have ‘external’ status.
Chapter 2 Methods
Research design
The aim of this research was to study knowledge exchange between NHS commissioners and internal and external agencies. We chose a case study design as case studies are useful in answering exploratory questions, especially when the investigator has little control over events and when the focus is a contemporary phenomenon with real-life context. 13 Within the cases, we collected data through a variety of ethnographic techniques such as semistructured interviews, observations and documentary analysis. We provide more details about data collection and analysis later in this chapter, but first, we discuss recruitment. Because of the complexities, a major portion of this chapter is dedicated to explaining how, who and why we recruited participants as we did. This detail has been provided also because the scientific advisor from our funders, NIHR Health Service and Delivery Research, asked for a full description to give guidance to those wishing to study commercial providers in the future, as this has rarely been accomplished before in this context.
The phenomenon in this research was knowledge exchange, but identifying case boundaries proved challenging. Reassuringly, Ragin and Becker argue that it is counterproductive to have strong preconceptions of the case boundaries as this hampers conceptual development. Instead, researchers need to continually ask themselves ‘What is the case?’, to reconfigure what is inside (and outside) case boundaries and reclarify the phenomenon under study. 14 This was certainly our experience.
Initially, our intention was to construct cases around contracts of 6 months’ duration or more with significant knowledge exchange between commercial providers and their NHS clients. These criteria were selected to exclude one-off consultancy activities such as contract negotiation or pathway development, where knowledge exchange was presumed to be minimal. Our assumption was that each contract would clearly engage a set of external providers and their NHS clients and data collection would involve gathering sets of accounts from both.
Ethical permission was obtained from South West Research Ethics Committee 2 on 25 November 2010 (10/H0206/52). Local research governance approvals were obtained from all 11 PCTs where the study external providers were working. Service support costs were agreed to cover the study costs of participants, but no one asked for financial reimbursement for taking part.
Recruitment of external providers
To recruit commercial providers, our starting point was that the study lead (LW) had a long-standing relationship with the chief executive of one commercial provider. Relying on these types of prior contacts to recruit study participants is an accepted feature of ethnographic15 and case-study research. 13 The chief executive first informally sounded out the key leads from other commercial providers verbally and then by e-mail, furnishing an information sheet about the study, which was then supplied by the research team. Where a commercial provider showed interest, contact details were supplied to LW, who followed up with a telephone call and further written information. Only two commercial providers were approached and both agreed (see Recruitment and data collection via the first commercial provider and Recruitment and data collection via the second commercial provider for further details). We attempted to recruit a third commercial provider without this introduction and received no response.
Through our work with Swallow, we encountered a not-for-profit agency that offered a software tool marketed and supported by Swallow. Given that our fieldwork with Swallow and Heron suggested that antipathies towards the for-profit sector might hamper knowledge exchange, we recruited this not-for-profit (Jackdaw – pseudonym) to learn more about how such organisations fared (see Recruitment and data collection via not-for-profit agency for further details).
Four CCGs located in areas where Swallow and/or Heron had worked were also recruited (see Recruitment of Clinical Commissioning Groups for a fuller explanation). Through fieldwork with these CCGs, we encountered many other external providers offering support to commissioners including freelance analysts and former NHS commissioners, for-profit organisations with particular subject and methods expertise and not-for-profit agencies lobbying for particular patient groups. Furthermore, as discussed in Chapter 1, several units that started out as ‘internal’ moved to external provider status such as Public Health. Wherever possible, we interviewed these providers to augment our understanding of the type, range and usefulness of external provider input to commissioner decision-making.
Recruitment and data collection via the first commercial provider
Data collection started with Swallow, a medium-sized UK-based commercial company that worked exclusively with public sector clients in health, education and government. Offering a suite of software tools for invoice validation, auditing best place of care, risk prediction and predictive modelling, Swallow consultants often had NHS or public service backgrounds in analytics or commissioning.
When fieldwork began in early 2011, Swallow was engaged in two contracts that met our criteria, but one was nearly finished; we therefore chose the second, which was just beginning the second of 4 years. Worth over £20M with 40–50 Swallow staff involved, this contract was one of the largest ever negotiated between commercial providers and NHS commissioners. With the contract covering an entire region, the aim was to deploy the suite of software tools to the analytics units of local commissioning organisations, train NHS analysts in using the tools and supply ‘wrap around’ support from consultants with commissioning expertise to help commissioners translate output from the tools into commissioning decisions. Importantly, the contract dictated that although Swallow staff could operate the tools and recommend actions to ‘realise benefits’ (estimated at £200M), the NHS staff were tasked with putting those recommendations into effect. Swallow received payment only once both parties agreed that the ‘deliverables’ had been met.
With respect to our study, this contract afforded multiple avenues of enquiry (and potential cases), as several commissioning organisations were involved. Interviewing began with the Swallow director and programme manager for the contract. Through snowball sampling, we interviewed a further 13 Swallow staff including analysts and those with commissioning expertise, making a total of 15 Swallow interviews. We also observed one internal and one mixed Swallow/NHS meeting and one informal and three formal training events led by Swallow staff for NHS participants. Moreover, Swallow was particularly generous in sharing documentation such as training materials, progress reports, PowerPoint (Microsoft Corporation, Redmond, WA, USA) presentations and software guides.
By the end of the summer of 2011, saturation was reached with Swallow professionals, as little new information was emerging, but further data collection with their NHS clients was necessary. Wherever possible, we approached NHS staff observed and named in interviews by Swallow staff; however, few NHS staff agreed to be interviewed, partly because of the heightened turbulence resulting from the recent reorganisations and possibly because our independence might have been questioned as our introductions had come via Swallow. We planned to recruit more through future observations, as the changes in the NHS settled. However, our potential pool of NHS clients suddenly dried up as Swallow was bought out by a much bigger company (Tern), which abruptly discontinued involvement in the study in September 2011, preventing the identification of potential new candidates. In total, we interviewed 10 NHS staff in direct contact with Swallow before losing access.
This left us with murky case boundaries. The data did not fall neatly into matched Swallow–NHS accounts within specific geographical areas around a clear contract, partly because of the paucity of NHS data but also because Swallow consultants worked across several PCTs, making data concentration more difficult. An exception was the use of a Swallow tool for auditing best place of care.
Developed in North America, this tool consisted of care standards informed by research-based evidence and expert opinion. Clinical auditors applied the standards in real time, inputting data from patient notes to determine if current inpatients were in the best place of care. A previous audit using this tool at a local hospital had not been very successful. Swallow staff had exclusively conducted the first audit and their results were challenged by the acute providers. Nine months later, a second audit was initiated, which coincided with our fieldwork. This second audit was led jointly by the PCT and acute and community providers with Swallow support. In this instance, we interviewed the Swallow tool lead, observed a NHS/Swallow planning meeting, interviewed four NHS staff (two commissioners and two senior provider managers) and attended a CCG meeting where the results of the audit were presented. Documentary evidence included meeting minutes, the audit tool template, the software product guide, a draft action plan for the PCT, an audit report and e-mails between LW and commissioners several months after the audit.
This body of evidence gave useful, balanced information about the phenomenon of knowledge exchange between commissioners and commercial providers and so became a separate Swallow ‘case’ known as ‘Swallow tool’. Other Swallow interview, observation and documentary data were amalgamated into this second distinct Swallow case, albeit with only a few NHS accounts dispersed across several geographical areas known as ‘Swallow’. Some NHS participants appear in more than one case study and only three are exclusive to the ‘Swallow’ case. The Swallow data provided valuable information about the methods and mind-set of Swallow consultants. Moreover, two of the commissioning organisations ultimately recruited in the latter half of fieldwork were located in the region of the original Swallow contract.
Recruitment and data collection via the second commercial provider
Shortly after our contact with Swallow was prematurely terminated, data collection started with Heron in the autumn of 2011. Heron was a UK subsidiary of a much larger international company. Heron offered software tools for invoice validation and risk prediction, in addition to an electronic tool that advised GPs on the most clinically effective and cost-effective medications for their patients during consultations.
Heron’s staff of around 130 people with analytical, project management and clinical backgrounds included approximately 10% who were North American. Again, data collection started with senior leaders, specifically the head of Heron UK and a director, and continued with Heron personnel identified through snowball sampling. At the close of fieldwork, saturation with Heron was reached, with 16 interviews with project managers, analysts and clinical staff, one observation of a training session and documentation such as marketing brochures, e-mails and the website.
Findings emerging from Swallow suggested that little knowledge exchange with commissioners occurred in the early to mid-point of contracts. So, with Heron, we wanted contracts that had either finished or were towards their end. Data collection started with Heron during the ‘hunger gap’ between the PCTs disbanding and CCG authorisation in the autumn of 2011 to summer 2012, when few commercial opportunities arose. Our quest to find mature or completed contracts was well timed, because Heron had four contracts with former PCTs that met our criteria. This was rapidly reduced to three, because relationships with NHS clients at a fourth site were somewhat precarious. Although Heron were not averse to including this site in the study, they felt that limited knowledge had been exchanged, compared with the others.
One contract was for Westhide (pseudonym). Starting in 2009, the remit of this 3-year rolling contract was for Heron to directly manage a portfolio of contracts with a group of acute trusts offering specialist care to patients with rare conditions. This provided unique insight into how commercial providers would manage commissioning responsibilities if these functions were outsourced. Unfortunately, although we interviewed four of the eight frontline Heron staff working on this project, only two NHS participants were willing to be interviewed. One was interviewed in 2012 when we were in the field and she suggested three other possible NHS participants, none of whom agreed to be interviewed. In fact, two sent an identically worded e-mail:
Many thanks for your e-mail but I am going to have to decline your request to assist with this research.
Surmising that perhaps the timing of interview invitations was unfavourable, we made a final attempt to find NHS candidates for this potential case in early 2014. Three new NHS names were suggested, of whom one responded to requests for an interview. Although this was better than before, two NHS client interviews were not sufficient to include Westhide as a case site in its own right. Instead, its data formed part of the ‘Heron’ case study (see Chapter 4, Commercial provider commissioning model).
Heron also put forward a second contract with Deanshire. We contacted the NHS project manager lead for Deanshire on several occasions by e-mail and got no response. Heron also contacted this lead on our behalf without success. Eventually, we bypassed this individual, requested permission to recruit the CCG directly from its board and were given approval. Three NHS participants subsequently interviewed had contact with Heron.
In contrast, recruiting from the third Heron contract was relatively smooth. The ‘Penborough’ contract initially ran for 2 years and was renewed for a third. It had three aims: (1) to increase the competency of commissioners for WCC assurance; (2) to develop a community engagement model to feed into commissioning decisions; and (3) to support the integration of health and social care in commissioning. With a few reminders and some prodding, three NHS participants with direct contact with Heron were interviewed.
Once again our data did not neatly fall into paired Heron–NHS accounts around a clear contract, except for Penborough. So, we separated out the Penborough data into their own case (see Penborough, below) and amalgamated the 16 Heron interviews, one observation, documentation and five NHS participant interviews into a case called ‘Heron’.
Recruitment and data collection via not-for-profit agency
As previously mentioned, having collected data from two commercial providers, we were interested in learning more about the not-for-profit sector. Our point of contact with Jackdaw was a Swallow NHS participant, who took part in Jackdaw training. This training came about when the Swallow contract was renegotiated (for a second time), following the takeover of Swallow by Tern in the summer of 2011. The NHS negotiators stipulated greater contact between the original developers of Swallow’s tools (i.e. Jackdaw and several other companies) and the wider NHS clients.
Jackdaw was a very small not-for-profit provider, which had developed and refined a risk prediction tool through research carried out over 30 years, and continued its strong links with academic institutions. At the time of data collection, the UK branch of Jackdaw consisted of one full-time consultant who reported to a managing director in Europe, both of whom were interviewed. Through didactic, online webinars, the knowledge exchanged in this particular case study was between Jackdaw staff (nationally and internationally) as tool experts and seven NHS clients of diverse backgrounds (analytics, commissioning) from different commissioning organisations to help the NHS clients become ‘superusers’. We invited all seven NHS participants to interview and three accepted. We also ‘observed’ a virtual webinar session. Data were collected from May 2012 to January 2013.
We would have liked to have recruited further not-for-profit organisations, but the only other potentially suitable candidate did not respond to requests for interview. Thus, our conclusions about the role of not-for-profit agencies are somewhat tempered.
Recruitment of Clinical Commissioning Groups
By May 2012, when data collection with Swallow and Heron was complete, concerns were rising about the lack of NHS participation in the study. Moreover, preliminary findings suggested that capturing impact on commissioning decisions was difficult, as it was largely analysts who benefited (or not) from the use of the software tools. This meant that answering our research questions about how commissioners (i.e. decision-makers) accessed, transformed and used external knowledge was impeded. We had shied away from more direct recruitment of CCGs as commissioners’ attention was understandably absorbed by changes in the NHS. However, in the summer of 2012, we decided to proactively target the CCGs where Swallow and Heron had been most active, inviting staff from these CCGs into the study regardless of their previous level of contact with Swallow and Heron. Two CCGs were recruited from Swallow’s geographical patch (Norchester and Carnford) and two from where Heron had previous contracts (Penborough and Deanshire).
Norchester
To recruit Norchester, LW opportunistically met an influential Norchester GP at a conference. This academic GP agreed to an interview and then liaised with the chief operating officer of the CCG on our behalf to recruit the CCG.
Norchester CCG was a highly research-aware organisation, largely because of the involvement of this GP academic. Although Norchester was in an affluent area in England, the CCG was facing considerable financial challenges with targeted savings of over £20M by 2014. Nationally known for its pioneering initiatives, the CCG’s primary, somewhat high-risk, strategy for reducing unsustainable spending was to modify about 40% of their contracts by (1) rewarding providers on the basis of achieving outcomes such as fewer deaths in hospital rather than activity (e.g. number of procedures) and (2) commissioning a lead provider who then subcontracted other providers. Information and knowledge to support this work came from local CSU analysts employing Swallow’s risk prediction tool and several commercial and not-for-profit agencies with expertise in Public Health, contracting, business case development and condition expertise.
Norchester was split into localities of different sizes; the largest locality covered a population of 150,000. The CCG was in considerable flux during the first period of fieldwork (summer 2011), which had stabilised by the second period of fieldwork (December 2012 to May 2013), shortly before authorisation. Public Health and CSU colleagues (formerly known as the ‘Decision Support Unit’) were colocated in the same building, although some Public Health professionals also worked in local authority premises. Participants for Norchester were selected on the basis of involvement with Swallow and its tools and role in organisation (e.g. senior leaders). Again, snowball sampling was the principal method of identifying appropriate candidates. Data collection is itemised in Table 1.
| Data type | Data source |
|---|---|
| Observations and associated documents (two observations, total duration 5 hours 50 minutes, 28 documents) | CCG shadow governing body meetings December 2012 (held in public, 10 meeting papers) and January 2013 (not held in public, 18 meeting papers) |
| Interviews (11 interviews, total transcribed duration 8 hours 4 minutes) | Four members of the CCG shadow governing body: a CCG accountable officer (GP), two locality leads (both GPs), and a practice manager |
| Four analyst/information staff: a PCT lead analyst, a chief information lead, a PCT/CSU analyst and a freelance analyst | |
| CCG R&D lead (GP), ex-PCT chairperson (GP), CCG associate director of strategy and governance | |
| Additional documents (11 documents, seven websites) | CEO’s report November 2013, commissioning report Phase 1 March 2013, report of workshop event January 2013, three board papers November 2013 Questions to the board September and December 2013, statements on procedures of limited clinical value from 2009, 2012 and 2013 (accessed from Norchester website 6 December 2013) |
| Websites of three organisations working with the CCG |
Carnford
We were directed to Carnford via a Swallow NHS participant. Carnford covered a 210,000+ population with generally low deprivation in England, and was one of several CCGs operating in the same county. They were under serious financial pressure, having received one of the lowest allocations in England, and felt that ‘operating at the edge of bankruptcy’ had been normalised in their area. There was a lot of interest in data and tools as a route to finding solutions to their problems, and those offering knowledge based on research evidence were enthusiastically received. Public Health and the local CSU were both working closely with the CCG to find ways to provide the knowledge and support they wanted, but the CCG had also engaged an external provider with an accountancy background (Bullfinch: pseudonym) to work on a number of specific projects.
Our first interview was with a GP who was using the Swallow risk prediction tool for end-of-life care. This GP was a member of the Unscheduled Care Board (UCB) that reported to the ‘Clinical Cabinet’, which was described as the CCG’s ‘engine room’ where clinical priorities were identified and work streams were monitored. Perhaps because our entry point was via the UCB, data for this CCG were more operational than strategic. Participants for Carnford were selected on the basis of role in the organisation (e.g. senior leaders, purveyors of research or data) and involvement with Swallow and its tools. Observation at meetings and snowball sampling were the principal methods of identifying appropriate candidates. Data collection ran from May 2012 to May 2013 and is itemised in Table 2.
| Data type | Data source |
|---|---|
| Observations and associated documents (five observations, total duration 13 hours, 12 documents) | November 2012 (five meeting papers), January 2013 (minutes only) and February 2013 (four meeting papers) meetings of UCB |
| March 2013 meeting of Clinical Cabinet (agenda only) | |
| May clinical reference group meeting (agenda only) | |
| Interviews (11 interviews, total transcribed duration 6 hours 55 minutes) | Five members of the Clinical Cabinet: CCG accountable officer/Clinical Cabinet chairperson, unscheduled care lead (also chairperson of UCB), research/education/innovation lead, IT lead and Public Health representative |
| Three other members of UCB: lead on integrated care teams, integrated services programme manager (contractor), and Public Health consultant | |
| CSU information analyst working with UCB, CSU director of performance and development, and a freelance analyst who was involved in evaluating risk stratification tools for the local PCTs | |
| Additional documents (five documents, one website) | Briefing paper from Public Health on unplanned hospital admissions, two issues of the local ‘Clinical Bulletin’, and two ‘pathway tool project’ documents |
| CCG website |
Penborough
Penborough CCG had contracted Heron for 3 years. This CCG covered a population of about 160,000 and was in the most deprived quintile of local authority areas in England. NHS commissioners in Penborough had a history of working in close partnership with the local authority to achieve an integrated commissioning strategy for health and social care. With the Health and Social Care Act 2012,4 this partnership was maintained and many key staff from the former commissioning structure were retained. Working collaboratively with providers, the local authority, the community and other CCGs was an ethically driven approach, but was also seen as the most efficient and effective way of commissioning. They were idealistic, positive and regarded themselves as an effective commissioning organisation. They also had the confidence to openly admit in CCG board meetings and interviews where improvements could be made.
As stated previously, our entry point to this CCG was two Heron consultants. In keeping with a CCG that prioritised patient involvement and integration with social care, this case had the broadest range of participants. These were selected to include senior leaders, and those involved with Heron and its tools, but also to reflect the organisation’s focus on including knowledge from clinical, managerial and community perspectives. Observation at meetings and snowball sampling were the principal methods of identifying appropriate candidates. Data collection took place from February 2012 to May 2013 and is itemised in Table 3.
| Data type | Data source |
|---|---|
| Observation and associated documents (five observations, total duration 12.5 hours, 54 documents) | Three sequential bimonthly public meetings of the CCG governing board, covering January to May 2013. Documents: 14 to 16 papers available in advance of each meeting |
| One bimonthly CCG governing board workshop (April 2013). Documents: agenda and copies of two presentations | |
| One monthly meeting of the council formed of representatives from each practice in the CCG (May 2013). Documents: agenda and copies of four presentations | |
| Interviews (12 interviews, total transcribed duration 7.5 hours) | Seven members of the CCG governing board: chairperson, vice chairperson (who is also chairperson of the Council of Members), finance director/deputy chief executive, Public Health director (who is also lead for well-being and prevention), sustainable services director, adult social care advisor and GP representative (who is also clinical lead for the unscheduled care) |
| Four other CCG members: deputy chief finance officer, innovation and research lead, service manager lead for unscheduled care and community representative for unscheduled care | |
| Two staff from private provider Heron Ltd who had worked with the organisation before the transition to CCG structure (joint interview) | |
| Additional documents (seven documents, two websites) | Set of six documents and one web-based tool relating to business case/service proposal development processes |
| Memorandum of Understanding with Public Health | |
| CCG website |
Deanshire
Coterminous with its local authority, Deanshire was a county-wide CCG serving a largely rural population of approximately half a million. The practices making up the CCG were organised into localities, each of which nominated a representative to sit on the Clinical Operations Group, the ‘engine room’ of the CCG. Deanshire had a somewhat conservative ethos in ensuring that the CCG ticked the right boxes and was seen to be above board, possibly to maintain its reputation as a leading commissioning organisation, but there were also several examples of innovative, inspiring projects focusing on improving patient care carried out by committed staff.
Like Penborough, Deanshire had formerly contracted Heron but our entry point to this CCG was through the director of commissioning development, who suggested that we focus our enquiry on two commissioning initiatives: the reablement project and the acute stroke project. Work on the reablement project began in 2010 and rollout of the redesigned reablement service across the county was ongoing at the time of data collection. The acute stroke project was at a much earlier stage and grew out of broader work around stroke, which had been instigated by the CCG in response to poor outcomes in Deanshire.
Heron’s presence in the data collected from the CCG was minimal, largely because the contract had stopped several years prior to fieldwork, but other commercial providers of commissioning expertise were visible. These included a commercial company that had worked on the reablement project and a project management contractor who was working on the acute stroke project. Participants for Deanshire were selected basis of role in the organisation (e.g. senior leaders) or in one of the two projects which had been selected as foci. Observation at meetings and snowball sampling were the principal methods of identifying appropriate candidates. Data collection took place from January to April 2013 and is itemised in Table 4.
| Data type | Data source |
|---|---|
| Observations and associated documents (four observations, total duration 9 hours 45 minutes, 43 documents) | December 2012 CCG governing body public meeting. Documents: agenda and 10 meeting papers |
| February and May 2013 Clinical Operations Group meetings (March/April meetings closed to non-CCG members). Documents: agenda and eight meeting papers (February), plus agenda and 17 meeting papers | |
| Acute stroke project meeting in February 2013. Documents: agenda and four meeting papers | |
| Interviews (14 interviews, total transcribed duration 9 hours 44 minutes) | Seven members of the CCG: governing body chairperson, clinical operations group vice chairperson, director of clinical commissioning development, director of strategy and patient engagement, head of pathway development, head of federation development and a commissioning manager |
| One member of local authority staff, who had worked with the NHS commissioners on the reablement project, and one Public Health consultant | |
| Five commercial providers of commissioning expertise: two staff each from two large companies which had worked in the area, and one project manager who worked as a contractor on the acute stroke project | |
| Additional documents (one document, one website) | ‘Prioritisation principles’ document for planning |
| CCG website |
Summary of cases and data collection methods
At the completion of fieldwork, eight cases were identified from the data and we had a spread of data with NHS and external provider accounts. In total, we collected interview data from 92 participants [47 NHS clients, 36 external provider consultants and nine other participants (e.g. freelance consultants, lay representative and so on)] and conducted 25 observations.
Interview participants were sent information sheets electronically before interviews and written (or recorded) consent was obtained. The initial topic guide was devised by the research team and covered type of information wanted, sources of information, and how that information was accessed and fed into decision-making. The topic guide was regularly revised as new questions emerged and others appeared to have been answered. Interviews were face to face or by telephone, depending on the preference of the participant and practicalities. Lasting 20–60 minutes, all interviews were recorded and transcribed.
Prior permission to observe activities was obtained by researchers before attending events. Chairpersons and training leads mentioned the research and researcher’s presence at the start of events, sometimes with the researcher absent from the room. Observation notes were taken, with the help of an aide memoire based on the research questions. Notes taken during observation included details of who was present, room layout, verbal exchanges, participant reactions and researcher reflections. Observation notes were typed up as soon as possible after the data were collected. All interview and observation participants were given pseudonyms.
A range of documentary data were collected to supplement, confirm and challenge emerging findings from interview and observation data. These included meeting minutes, reports, websites, marketing material, press releases and e-mails. These data fed into the second phase of data analysis (Table 5).
| Case | NHS | Total NHS | External provider | Total external | Total NHS plus external | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GP commissioner | Commissioner | Analyst | Other NHS | Commercial/not-for-profit | Freelance | Public Health | Local authority | Lay | ||||
| Swallow | 1 | 2 | 15 | 25a | ||||||||
| Swallow tool | 2 | 2 | 1 | 5 | ||||||||
| Heron | 2 | 1 | 16 | 17 | ||||||||
| Jackdaw | 2 | 1 | 2 | 5 | ||||||||
| Norchester CCG | 5 | 3 | 2 | 1 | 11 | |||||||
| Carnford CCG | 5 | 2 | 2 | 2 | 11 | |||||||
| Penborough CCG | 2 | 5 + 1 | 2 | 2b | 1 | 1 | 12b | |||||
| Deanshire CCG | 2 | 5 | 2 + 2b | 1 | 1 | 14b | ||||||
| Total | 15 | 17 | 9 | 6 | 47 | 36 | 4 | 3 | 1 | 1 | 47 | 92 |
Data analysis
Several theoretical influences were present in our thinking while we were analysing the data, including ideas from the knowledge management literature.
Brown and Duguid’s notion16 of the ‘social life of information’ was useful. They argue, for example, that innovative knowledge ‘flows in social rather than digital networks’, and see successful innovation as dependent on ‘the bringing together of abstract information and situated knowledge’. They emphasise the importance of local knowledge and the role of social networks in grounding knowledge in practical contexts. They stress that informal exchanges such as stories are key to the way that knowledge moves through organisations. 17 Consequently, the notion of ‘communities of practice’ was also key to our analysis, as an important way in which people share knowledge and also connect informally and formally across boundaries, such as departments, disciplines and organisations, to share expertise and learning and to develop knowledge-in-practice. 18,19 Gabbay and le May’s work on collective mindlines provides a further dimension to the role of collective sense-making in primary care decision-making. 20,21 These ideas are concordant with Weick’s analyses of collective ‘organisational sense-making’, where context and understanding are mutually enacted. 22
Nonaka’s model of knowledge creation,23 which describes how knowledge is created and assimilated, also seemed relevant. This suggests a sequence of conversions of knowledge between tacit and explicit that enable people in organisations to share (mostly practical) knowledge. This author originally described a continuing cycle of socialisation (learning how things are actually done day to day in that organisation), externalisation (exposing implicit and tacit knowledge, e.g. through story-telling and mutual observation), combination (of that explicit knowledge with other sources of knowledge often in guidance documents, manuals or intranets) and internalisation (by individuals working in that environment). However, subsequent critiques have suggested that this so-called ‘SECI cycle’ misunderstands the nature of tacit knowledge and that a more nuanced view is required. Cook and Brown, for example, argue that organisations come to know by ‘bridging epistemologies’ in a process of productive enquiry termed a ‘generative dance’. 24 Nonetheless, the underlying SECI elements still seemed germane to the way commissioners might treat knowledge.
Analysis was guided by constant comparison methods, whereby data were compared across categories, continually refined and fed back into further data collection (and analysis) cycles, as is usual with high-quality qualitative studies. 25 Preliminary analysis started in June 2011, a few months after data collection began. The research team had regular face-to-face meetings every 6 months and teleconferences in between (about every 6–8 weeks). In preparation, individual team members were sent two to three pieces of data (e.g. two interviews and an observation) and asked to read through these documents, identify emerging themes and key learning points, reflect on the research questions and suggest any possible new questions for the topic guide. Covering all eight cases, eight batches of data were analysed and discussed successively.
The next phase of analysis began in May 2013, when fieldwork came to a close. The research associate (EB) developed a coding framework, in collaboration with LW and AC, based on the research questions. Using NVivo software (QSR International, Warrington, UK), she systematically coded cases independently. In addition, EB and LW developed 20–50-page case summaries for each case. Drawing on all interview, observation and documentary data for each case, these summaries included a ‘thumbnail sketch’, key findings, details of data collection and useful quotes. Each summary was structured into:
-
models of commissioning
-
external providers
-
knowledge/information accessed
-
knowledge transformation processes
-
benefits/disadvantages.
From October 2013, every member of the research team read the summaries independently and wrote up their reflections. Drawing on the research questions, each researcher conducted a cross-case analysis, identifying key themes common to the cases as well as discrepant data. In January 2014, we held a day-long meeting to discuss and agree themes. As in past team meetings, discrepant data were debated, with data confirming/negating particular positions presented, until agreement among the group was reached. In fact, disagreements tended to be more about nuances rather than clear differences in perspectives.
A final stage of analysis took place while writing up the report. Data were compiled and compared separately for each of the five domains (e.g. models of commissioning, external providers) from the data summaries, analyses from previous team meetings and sometimes the sound files from digitally recorded steering meetings. Draft chapters were produced, distributed to the team for comment and revised.
One key question was whether or not to undertake, as part of this report, a substantial analysis of the impact of the 2012 Health and Social Care Act4 on the world we were studying, or whether or not to allow it be included just as a part of our findings on knowledge exchange. The arguments in favour of the former were that we had considerable (if serendipitous) data about the NHS participants’ experience of the changes, that these underlay the relationships that underpinned the knowledge exchange, and that this unique context needed to be explicated in full. The counterarguments were that we had not designed our data gathering to answer questions about that context. Our job was to understand knowledge exchange between the various agencies involved, whose changing roles would inevitably emerge as we presented the findings. What mattered for our study was that commissioners were always operating in difficult organisational and political circumstances, and so we should focus not on the features of a unique event, but those that were likely to be common to a wide range of circumstances. There was also, it must be said, an underlying set of political tensions to our debating this point: the desire to provide evidence that exposed the disruption to commissioning versus the professional necessity of maintaining the political neutrality of a research report about knowledge exchange. Our final decision was that although the results and discussion chapters refer to the vicissitudes created by the 2012 Health and Social Care Act4 as it pertains to knowledge transfer, we would not explicitly present data on the impact of this Act on the NHS.
Challenges
There were several challenges in working with commercial and not-for-profit providers. The first concerned research governance. External provider consultants moved around NHS organisations quickly and freely, but as researchers we could not. For example, initially the second audit using the Swallow tool was planned for the week after the stakeholders’ meeting. This audit was to take place in two settings: an acute and a community trust. To understand more about informal ways of exchanging knowledge, the research team were keen to observe the audits in practice. However, obtaining the necessary permissions from these two NHS settings took several weeks. In this instance, the date of the audit was fortunately postponed and local permissions came through for the acute trust in time. Other opportunities were missed, though, because local governance processes were not quick enough.
Research governance issues also affected the study methodology. In the original protocol, we had planned to shadow five commercial consultants over several time periods to observe where they obtained their knowledge and how this was fed into client decision-making; but, in addition to difficulties with research governance processes, which meant that the research team was unlikely to have permission to enter the same premises as the external consultants, a further complication was that few consultants were willing to be observed. They were highly (and understandably) sensitive to the impression an accompanying researcher might make on their clients. Several also voiced concern about patient confidentiality, fears that were not assuaged on presentation of documents evidencing local research and development permissions. Moreover, external consultants were highly autonomous and readily refused requests to take part in shadowing, despite their line manager’s encouragement. So, we abandoned the idea of shadowing and instead carried out observations of meetings and training events, which helped to identify study participants.
Another challenge centred around anonymisation and confidentiality. Given the commercial sensitivities of the data, transcripts, summaries and observation notes were password protected. It is always problematic to write an account of this sort while holding to one’s assurance to participants that the data will be kept anonymous and unattributable. In drafting this report, the demands of providing enough information for ‘rich description’ were weighed against the possibilities of unmasking. This was challenging in an arena where commercial providers knew their competitors well. In addition, the commissioning organisations were also quite distinct. Thus, in presenting quotes, participants’ professional backgrounds are cited and a distinction is made between NHS and external providers, but employing organisations are not identified. In order to not single out the one not-for-profit provider, this company and its two commercial competitors have all been identified as ‘commercial provider’. We have done our very best to maintain anonymity by giving the sites fictional names and using false names for specific individuals, but, inevitably, some readers will still be able to identify the sites. We hope that participants will accept that anyone who recognises a site will probably already be close enough to them to be well aware of most of the matters raised, and that no harm will result.
Dissemination
As this was a study about exchanging knowledge, dissemination of findings to target audiences such as commissioners and external providers was an essential part of the original bid. Accordingly, we put forward the idea of setting up a reference group of interested commissioners and external providers from the case sites who would act as a dissemination group, helping us to find key messages for wider dissemination throughout the lifetime of the study. This plan was modified, because early attempts to feed back to commercial providers as ‘critical friends’, with a view to having them subsequently join such a dissemination reference group, created significant consternation.
For example, in March 2011, a few months after fieldwork began with the first case (Swallow), we were asked to furnish Swallow with our observation notes of a Swallow team meeting. These were raw data, noting who sat where and who talked to whom, and appeared fairly innocuous. However, subsequently, a Swallow team member got in touch to say:
I have to say I wasn’t aware you’d be feeding back in this way. I’d certainly value an opportunity to discuss your interpretation of my performance given what has been written.
E-mail, 21 March 2011
We subsequently learnt that several members of the team were under consideration for promotion and felt that our account of their behaviour (e.g. X looking at computer) did not reflect well on them. For a short time, the continuing participation of Swallow hung in the balance. Ultimately, a key senior leader decided that the notes were not prejudicial and they should continue with the study. Unsurprisingly, those who had objected refused all further invitations to take part in the study.
Moreover, we were becoming increasingly aware of the commercial sensitivities of our research. Although regular feedback to research participants through reference groups was our original intention, we did not want to endanger the study. Consequently, we left dissemination to towards the end, although an independent academic met with us mid-study to identify any emerging findings.
Significant dissemination opportunities arose about 9 months before the study ended. A NHS manager was seconded from a commissioning organisation and attached to the project to develop and carry out knowledge mobilisation. Modelled on the defunct Service Delivery and Organisation Management Fellow scheme and paid for by local Research Capacity Funding, this NHS manager became invaluable as the study drew to a close. She helped to interpret the commissioning data (e.g. reports, business cases), clarified anomalies in the data and identified local commissioners who would be willing to develop a knowledge mobilisation strategy. The outputs of this work are presented in Chapter 10 and Appendix 1.
Reflexivity and the research team
The use of external providers in NHS commissioning is highly sensitive and controversial. We were aware of the potential research team members to unwittingly view the data through preconceived prejudices. To address this, three measures were adopted.
The first was the composition of the research team. This included two commissioners (one clinical and one non-clinical) and academics with policy, management, Public Health and methodological backgrounds. The research team also had a mixture of views including sceptics and those who were more neutral about the contributions of commercial providers, including one who had previously worked for a commercial provider. Thus, throughout the duration of the project, team members challenged each other’s views.
The second was the introduction of explicit reflexive activities when fieldwork began (January 2011) and at our final analysis steering meeting (January 2014). The key question asked of all team members was:
What are your preconceptions, assumptions, prejudices and views about: a) the use of external providers in the NHS, b) the implications of the White Paper [Liberating the NHS], especially shifting commissioning to GP consortia?
Team members provided either written or verbal accounts, which were recorded and transcribed. Interestingly, these individual accounts charted a similar trajectory with regard to the use of external providers. The more sceptical members of the team initially had an ‘antipathy’ towards commercial providers that ‘softened’ through data collection with Swallow consultants, as this agency was ‘populated with people who shared the ideology/aims of the NHS [and] genuinely wanted to make a difference to patient care’. However, once the senior management team at Swallow was replaced and former Swallow interviewees found jobs elsewhere, original ‘fears/prejudices were (utterly) confirmed’. These were not shifted much with further collection of Heron data. Meanwhile, those with more neutral views remained relatively constant. However, overall team members did develop a more nuanced perception of the advantages and disadvantages of commercial providers. With regard to the implications of Liberating the NHS,3 the team was unanimous in having serious concerns about the abilities of GPs to take on their new commissioning roles.
Another measure to encourage reflexivity was that the final steering group meeting was chaired by an external academic with a background in knowledge exchange. Apart from summarising key findings and helping us to clarify our thoughts, an important task of this chairperson was to ensure that suppositions and hypotheses were backed with data. However, interestingly, the research team reached consensus with rapid accord.
The impact of these activities was that as we were aware of each other’s (and our own) preconceptions, we became quite adept at ensuring that contributions were challenged, especially during analysis. Often, the contributor themselves would flag up that a particular insight might be due to a preconception or attitude. It meant that the team frequently questioned each other and explored assumptions.
Box 2 summarises the key points of this chapter.
-
Using a case study design, although the phenomenon under study remained constant, identifying the case and its boundaries was challenging. Eventually, eight cases of knowledge exchange between NHS commissioners and other agencies emerged. Four were case studies that had external providers as the unit of analysis and four had a commissioning organisation as the unit of analysis.
-
Data collection included 92 interviews of NHS and external provider staff, 25 observations of meetings and training events and documents such as meeting minutes, websites and marketing brochures.
-
Challenges included variable willingness for potential interviewees to participate, slow research governance processes that stopped researchers from shadowing external consultants, safeguarding of commercially sensitive data and maintaining participant anonymity.
-
Our initial intention to disseminate findings as the study progressed was reversed early on because of sensitivities around data sharing. Instead, a NHS commissioner was seconded into the team towards the end of the project to set up a group of commissioners to identify actionable messages. Similarly, she also worked closely with a former commercial provider consultant to develop actionable messages for this audience.
-
Given the controversial nature of this project, the research team considered it appropriate to generate and share their observations about their own preconceptions and changing views at key points in the study trajectory.
Chapter 3 Processes of commissioning
Introduction
Before presenting findings about how commissioners access, transform and apply knowledge from different sources, greater awareness is needed of what health-care commissioners actually do. It is also important to contextualise this study by elucidating how commissioning was understood at the time of fieldwork.
This chapter presents background information from other literature (e.g. Department of Health and other studies) and findings from our own data. The background section begins with a brief history of commissioning and contracts. This is followed by a discussion of theoretical models of commissioning and a description of ‘real-life’ commissioning from other studies. The chapter concludes with findings from our study on the various pressures that commissioners needed to satisfy when making commissioning decisions.
A brief history of commissioning and contracts
Commissioning in England and Wales has had many incarnations. Before 1991, the commissioning of health care was carried out by local authorities. With the 1990 NHS and Community Care Act,26 the Conservative government created ‘purchasers’ and ‘providers’, whereby purchasing was carried out by health authorities and family health service authorities, the latter focusing on general practices. Primary care groups were established in 1999, bringing together health authorities and family health service authorities. Primary care groups, however, were short lived, and by 2002 they had amalgamated into the larger organisational form of PCTs. PCTs were allocated about 80% of the NHS budget, incorporating Public Health and community health services. They were also responsible for the broad clinical governance of general practices and some types of contracts with general practices, although GPs were still personally responsible under law and professional regulations for their clinical practice. 11 In April 2013, as part of the Health and Social Care Act 2012,4 PCTs were abolished and their functions distributed among local authorities, CSUs, NHS England and CCGs.
Clinical Commissioning Groups became the latest attempt to involve clinicians in commissioning. The first was in the 1990s, when the Conservative government brought in GP fundholding. Fundholding general practices negotiated their own contracts with hospitals, made decisions about which providers and services they would use and often deployed surpluses to develop innovative new services. GP fundholding was abolished by the Labour government in 1998 in response to accusations that it had been creating a two-tier NHS. 27
‘Total purchasing pilots’ were another variation of general practice commissioning that also operated in the 1990s. 28 Results from an evaluation suggested that the level of achievement varied widely between pilots and included reductions in the length of stay and emergency admissions. However, total purchasing pilots were also associated with higher direct management costs per head and needed heavy financial investment in their organisational development. In 2005, PBC was introduced. This gave general practices the power to spend NHS allocations locally, but the engagement of GPs was patchy,2 perhaps partly because no real funding followed the decision-making.
As commissioning organisations have evolved with more (or less) clinical input, so have the nature of provider contracts. Initially, most contracts were ‘block’, whereby an amount was agreed for a predetermined set and number of activities. The disadvantage of block contracts was that those providers that performed more than the anticipated number of activities did not get paid for this extra work. In 2003–4, Healthcare Resource Groups (HRGs) were established, and so instead of paying an average price for an activity, activities were split into different clinical categories that were aligned on a cost basis. However, more detail was still needed and so ‘payment by results’ was brought in, whereby each patient event had a HRG converted into a price for individual item billing. A limitation of payment by results was that often activities outside acute hospitals had no set price, such as those carried out in community services. Moreover, the emphasis continued to be on activity rather than quality of care or outcomes.
More recently, interest has grown in ‘outcomes-based commissioning’, whereby payment is contingent on meeting an agreed set of outcomes. Sometimes more than one provider is necessary to deliver these outcomes and a lead provider will subcontract relevant services from other providers. The advantage of this approach is that services are purchased on the basis of needs but, thus far, outcomes-based commissioning has proved difficult to implement, with substantial resistance from powerful acute hospitals. 29 Another contractual innovation originating from social care is ‘micro commissioning’, whereby clients/patients have personal budgets and agree a care package in collaboration with social workers/GPs. Outcomes-based commissioning and micro commissioning are still relatively rare within the health-care sector, although we encountered both during this study. Generally, we found that commissioning organisations tended to use a combination of block and activity-based contracts when negotiating with providers.
What do commissioners do?
Definitions of commissioning
A literature review by the University of London found many definitions of ‘commissioning’, which varied across public sectors. 30 In asking for definitions of commissioning from our study participants, a NHS commissioning director said that ‘ideal’ commissioning was the ‘right balance’ between ‘strategic focus on needs assessment and service strategy delivered through contracting’ utilising Public Health and analysts to understand needs, commissioning staff with service specific knowledge to ‘build up a picture of what the whole system needs to look like’ and contracting staff ‘with technical skills to make sure that we use the contracts to deliver that’ (Paula, NHS senior commissioning manager).
Other answers included ‘everything but provision’ (Donald, CCG chairperson) but others argued that provision was also a form of commissioning, as every time a GP issued a prescription or made a referral it had commissioning implications (Jen, commercial consultant). A long-term conditions study also concluded that the ‘strict separation’ of commissioning and provision was notional. 31 The definition of commissioning has even inspired several YouTube™ videos (search www.youtube.com under ‘what is commissioning?’).
Commissioning frameworks
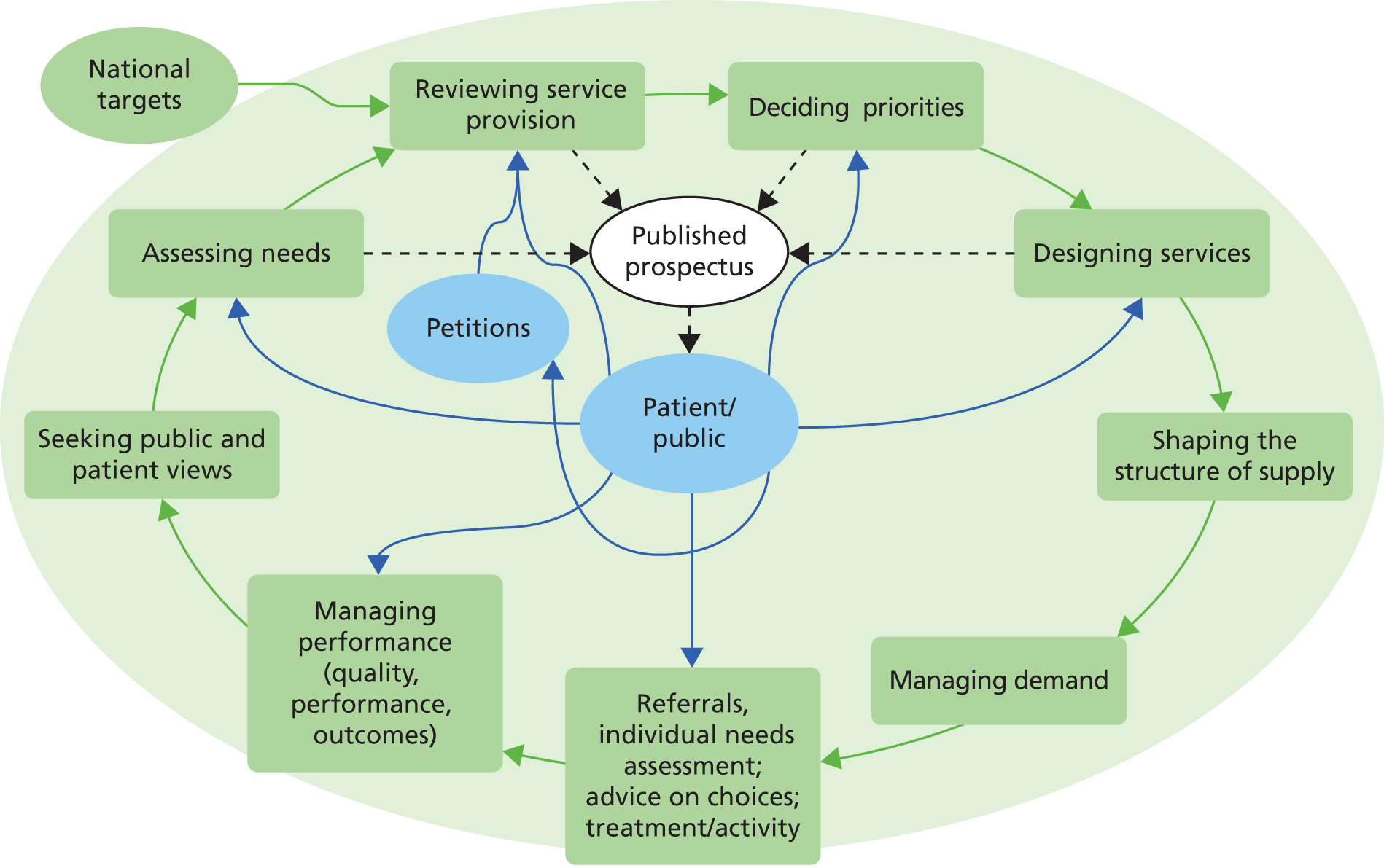
An early, simple conceptual framework of purchasing (the forerunner of commissioning) was suggested by Øvretveit and colleagues using the plan-do-study-act model. 32 Several years later, the Department of Health developed a much more complex model to include functions such as assessing needs, designing services, managing demand and managing performance (Figure 1).
FIGURE 1.
Commissioning framework. Source: Health Reform in England: Update and Commissioning Framework. 33 Copyright Yorkshire and the Humber Public Health Observatory.
The Institute of Public Care split commissioning activities into commissioning and procurement. They expanded and refined the framework to include other common commissioning activities such as gap analysis, business case appraisal, service evaluation, development of service specifications, contract management, performance management and resource allocation Figure 2. Clearly, over the past 20 years, the role of commissioners has evolved substantially.
FIGURE 2.
Institute of Public Care model of commissioning. Reproduced with permission from Developing Intelligent Commissioning Yorkshire and the Humber Joint Improvement Project. Commissioning Model: IPC Joint Model for Public Care. URL: www.yhsccommissioning.org.uk/index.php?pageNo=594. 34

The literature
In comparing these frameworks with ‘real-life’ commissioning, recent studies found that the work of commissioners is complex, disjointed, mutable and fast paced. Moreover, high-quality, effective commissioning is difficult to achieve, not least because the link between commissioning processes and outcomes is tenuous.
In their study of health-care middle managers in four PCTs,11 Checkland and colleagues concluded:
The generic managerial work undertaken by PCT middle managers was messy, fragmented and largely accomplished in meetings . . . [There was] evidence of confusion and overlap between the various commissioning teams and groups. Managers struggle with this and appear to compensate by dividing up their personal responsibilities into ‘pieces of work’.
p. 11
The aim of an action research study led by Smith and colleagues was to learn more about the ‘nitty gritty’ of commissioning long-term conditions in three PCTs. 12 Based on their findings, plus previous work, they suggested that there were two cycles of commissioning. The first was the annual contractual cycle, which was labelled as ‘transactional’. The second cycle was ‘interpersonal’, built on trust, common values, and established and new networks. They identified nine activities of effective commissioning (e.g. getting the balance right between interpersonal and transactional aspects, strong focus on monitoring and using information to inform review). The researchers also detailed seven key themes:
-
The ‘commissioning cycle’ is a misnomer as developmental commissioning running over many years ran in parallel with annual contractual aspects of commissioning.
-
An ‘extraordinary’ level of effort went into commissioning, and this often seemed ‘disproportionate’ to the anticipated or actual outcomes.
-
Many different individuals carried out commissioning tasks including managers and clinicians from providers, GPs, voluntary sector representatives and PCT commissioners. Clinicians’ role was primarily as champions for change.
-
Money was at times peripheral, with the majority of spending remaining in block contracts.
-
Changes brought about through commissioning were incremental. Success was more likely with ‘bite-sized’ completion of tasks within a wider plan.
-
External drivers such as national guidance played a powerful role.
-
Commissioners within this study worked within a context of uncertainty, as fieldwork took place while PCTs were winding up and CCGs emerged.
In our study, participants also mentioned the fast-paced nature of commissioning, whereby those providing support had to be highly flexible to changing needs.
You have to go in with a blank sheet of paper and almost listen to their requirements from the ground up again and see has the landscape changed? Commissioning requirements are a moving feast. Does your tool still – is it still relevant?
Randall, freelance analyst
Our study participants highlighted several processes, skills and viewpoints necessary for commissioning not previously mentioned. With their strategic overview, commissioners took ‘a whole systems approach to the way we develop services and pathways’ (Jane, NHS commissioning manager), because providers may be overly focused on ‘their services, their staff, their accountability’ (Abbie, NHS commissioning manager). Furthermore, leadership and persuasion skills were crucial to link providers together and manage tensions that competing agendas invariably generated. Commissioners, however, did not just have to influence providers. Successful commissioners also continually worked with and competed against their commissioning colleagues. For example, in one CCG we observed a commissioner present a business case for a lymphoedema service to the CCG board. The board had to consider the merits of funding this business case compared with several others recently submitted by other local commissioners; the lymphoedema business case was in direct competition with other proposals.
Having outlined the processes that commissioners engage in and provided a flavour of the shifting, challenging nature of their role, the rest of this chapter focuses on results from our study. The next section covers the reasons that prompted commissioners to look for information and the various pressures they needed to satisfy.
Commissioning decision-making
Observations of CCG meetings, reinforced and explored through interview and documentary evidence such as CCG meeting minutes, suggested that the push for commissioners to seek information arose either because they were told to take a course of action or because they wanted to take a course of action and they needed to find out how best to proceed. In both situations, which occurred commonly across the sites, relevant information was necessary to justify the decision and to persuade others to approve and/or follow the suggested course. Decision-making was assisted through repeated cycles of finding information, persuading others, justifying proposals, finding more/different information, persuading others, etc.
The impetus when commissioners were ‘told’ might be a top-down edict from the Department of Health or Strategic Health Authority; for example, the implementation of NHS 111 and ‘telehealth’ were major national initiatives during fieldwork. One CCG found that generating their own data from the first few patients using telehealth (specifically looking at hospital utilisation) was helpful in beginning to persuade some sceptical colleagues and to start developing an ‘evidence base’ to justify the decision. Commissioners might not have agreed with the directive or believed in its merit for their local population but, regardless, such activities became a ‘must do’ which led to the search for viable supporting information.
Alternatively, commissioners sometimes looked for information when no predetermined course existed. Sometimes, local information prompted changes. For example, in response to service user feedback one commissioning organisation needed information to develop a reablement project for those with long-term conditions. To help to decide a course of action, persuade others and justify their decisions, commissioners drew substantially on several sources including mapped patient pathways, shadowing key clinicians and meetings between service users and senior commissioners. These senior commissioners needed to be convinced of the priority of the problem and merit of the proposed solution to allocate funding and give senior-level support.
In either situation (being told to or wanting to make changes), commissioners searched for and pulled in information, when information was needed. Commissioners required information to build a cohesive, convincing case. In comparing GP decision-making with GP commissioner decision-making, one participant said that as a GP the decision was between the GP and the patient, but as a commissioner the decisions ‘have to stand up to extremely close, possibly legal scrutiny and have to be owned by the organisation’ (Angus, GP commissioner). As they came from publicly accountable organisations, commissioning decisions had to be resilient to challenges from many possible directions.
For example, challenges might come from clinicians and health-care provider organisations that needed to make changes themselves in order for the initiative to be a success. We encountered multiple examples of this, including commissioners in two case site CCGs who were rolling out risk assessment tools to general practice staff, with variable success.
Service users and the public sometimes needed to be persuaded. In one CCG, engaging the public was a way to smooth the introduction of potentially unpalatable service alterations.
You’re talking about moving one thing to another site: people see that as closure. It’s a political football . . . This engagement of lay members is to get them to kind of carry the message and hold you to account before – rather than at the end stage going, ‘Well we didn’t feel like we were involved in this,’ you carry them through.
Vidur, GP commissioner
Given the political nature of the NHS, the press sometimes posed challenges. Commissioning organisations wanted to avoid negative media attention. In observations of the boards of two CCGs, managing media coverage was an issue. In one, a GP commissioner’s remarks had been misconstrued, leading the local newspaper to headline that the board planned to close some hospital wards. In the other, the board discussed managing a local protest by the political group ‘38 Degrees’, which objected to the opening of the NHS to commercial companies. A GP commissioner from a third CCG predicted that some of their future decisions about using commercial providers would probably result in headlines.
You could see tabloid press headlines, ‘Money from NHS spent by non-NHS manager doing consultancy work’.
Anthony, GP commissioner
Commissioners also needed to build a persuasive case to convince those with a policy or performance management role, such as the Department of Health and Strategic Health Authorities (and now NHS England area teams). National or regional directives could take the form of goal setting such as the NHS Outcomes Framework or specific targets such as ‘95% of patients attending accident and emergency departments should be seen within 4 hours’. In addition, there was general commissioning guidance such as the development of commissioning strategic plans and the Everyone Counts: Planning for Patients 2013/201435 from the national NHS Commissioning Board. Commissioning organisations followed national and regional directives with varying degrees of enthusiasm and compliance. For example, one CCG went through the process of tendering services for the ‘any qualified provider’ requirements, although they were perfectly happy with their current provider.
Again it was an example of centralisation of things coming down from above. They said that we had to put out two or three services to any qualified provider. So the cluster decided what we should do. And one of them was ultrasound, non-obstetric ultrasound, which we have an absolutely excellent service provided by the hospital, even routine ones are done within a week, brilliant service. So why do we do it? So there’s all this process and people – they ended up with a list of seven providers. But, you know, it was a complete waste of time and money.
David, CCG chairperson
Sometimes commissioners were keen to follow national mandates, as these aligned with local agendas. For example, one CCG capitalised on national policy leanings on commissioning lead providers to subcontract to other providers. Several board documents mentioned that local activities had had substantial ‘interest from Number 10’ (i.e. the Prime Minister’s office) (board meeting papers). Another CCG exhibited resistance to several national directives and consequently experienced pressure to comply.
I just see how the world works and the pressure that organisations are put under if they don’t conform. You know, these words like, ‘You are at risk. Your organisation is at risk. You are at personal risk for this.’ And that’s not a nice thing to be (sic) on your shoulders.
Because things are different here?
Yeah, or because we don’t agree with national diktat. We don’t think this works and we want to do this.
Yeah, so you’re identified as risky?
Yeah and then you get lots of phone calls, and the chief exec gets phone calls, and he has to speak to you going, ‘Oh I’m getting a lot of flak about this. Can you not just smile sweetly and say you’ll engage?’
Vidur, GP commissioner
Although commissioners were less likely to need to justify their decisions to this audience, ‘evidence purveyors’ were another source of pressure. ‘Evidence purveyors’ were those that generated or located data or knowledge that might inform decision-making, such as Public Health, CSUs, Strategic Clinical Networks, Academic Health Science Networks (AHSNs), Collaborations for Leadership in Applied Health Research and Care (CLAHRCs), commercial and not-for-profit providers working in collaboration with the CCGs and academic researchers. The ‘evidence’ they provided might be unsolicited or be couched in such a way as to be experienced as a pressure, for example the championing of the recommendations from the annual Joint Strategic Needs Assessments (JSNAs) carried out by Public Health. There was considerable variability in terms of the level of impact made by these external agencies across the commissioning case sites. Although their role is discussed in-depth in a later chapter, commissioners in one CCG in particular were, apparently, highly influenced by Public Health.
I think two areas where we’ve made a big difference is around diabetes, in terms of using a combination of the evidence from local data and from national audit, in conjunction with the evidence of what worked, to actually persuade CCGs that – to look at the way that they are commissioning diabetes services, and the model, and to think about that . . . and around the evidence for diabetes education. The other area would be in evidence for cardiac and pulmonary rehab and in the familial hypercholesterolemia where we did a bit of work and actually have used the evidence of effectiveness of screening . . . to actually get all the CCGs to agree to commission a service which we didn’t have before.
Sandra, Public Health consultant
In addition to managing these external forces, commissioners also had to convince their internal colleagues within their particular organisational culture. Sometimes, a particular ethos permeated an organisation, which meant that certain decisions were more acceptable than others. In one CCG, the optimistic, ‘can-do’ culture influenced decision-making. The term ‘cynical’ emerged in several interviews as a pejorative term applied to those who raised queries about the feasibility of certain plans.
From the provider stuff, I think I’ve got the experience to know what is possible and what probably isn’t, and probably being a realist . . . what the cynics call realism, and it’s supposed to be cynical, I’m accused of that sometimes. I think it’s just being realistic.
David, CCG chairperson
In summary, commissioners had to influence and collaborate with many external and internal interested parties to build a cohesive case for taking a particular course of action. This included clinicians and other health-care providers, service users, the public, the press, national and regional policy and performance managers, evidence purveyors and internal colleagues (Figure 3).
FIGURE 3.
Pressures on commissioners.
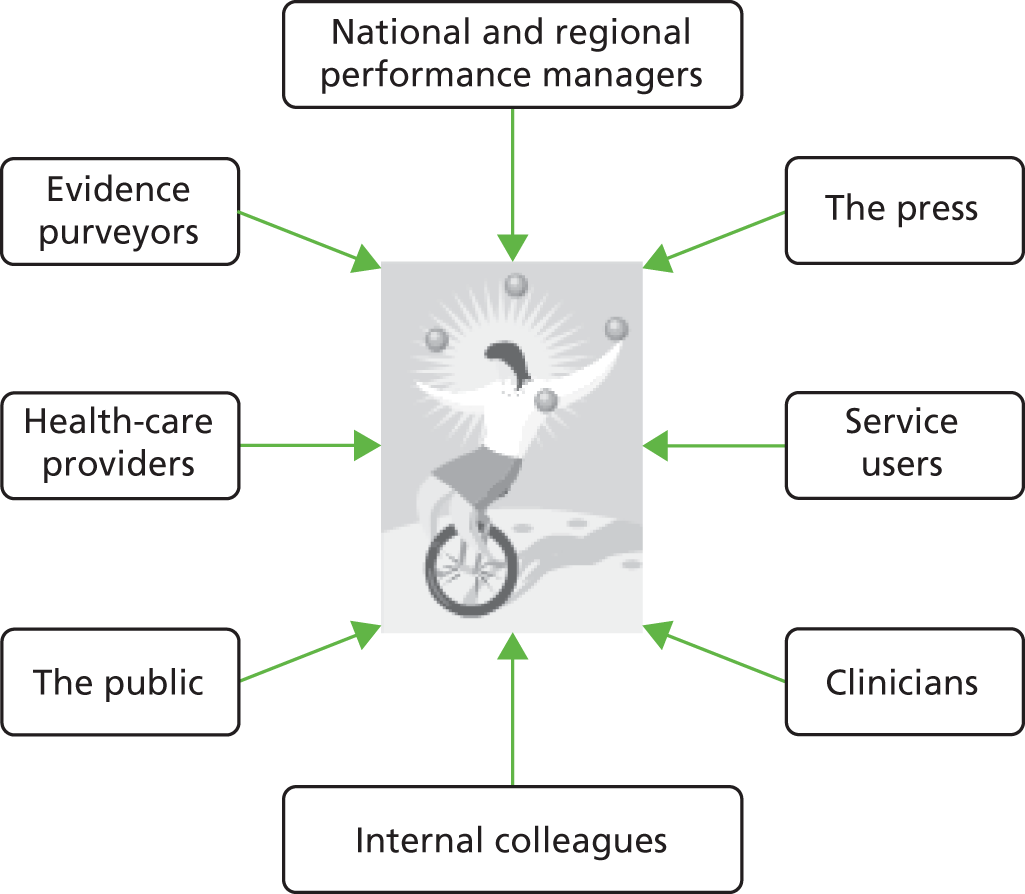
Not all forces came into play in every decision-making process and there was also variability in the strength of each, as a proposal traversed through different stages. Invariably, however, in the centre of this web of these pressurising forces, the commissioners juggled competing agendas, priorities, power relationships, demands and their own inclinations – to make the ‘best’ decision circumstances allowed. Just as there is an ‘art of medicine’, this was the ‘art of commissioning’. Thus, to a large extent, commissioning was a matter of pulling together the appropriate knowledge and information that would satisfice (a portmanteau word of satisfy and suffice introduced by Simon in 195636) competing agendas, and manoeuvring the implications of that knowledge through a complex system (Figure 4). Box 3 summarises the key points of this chapter.
FIGURE 4.
Commissioning as satisficing: (1) the naive view and (2) the view suggested by our data.
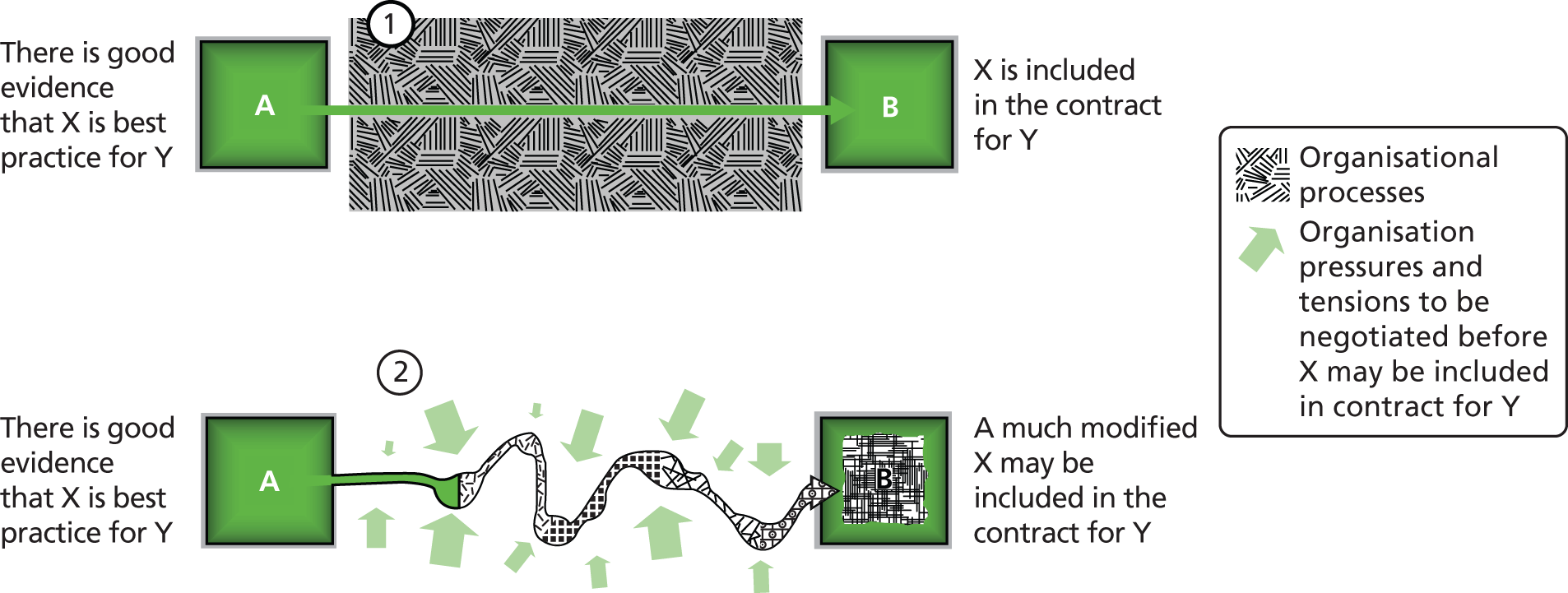
-
Health-care commissioning is messy, fragmented and fast paced.
-
Commissioning activities include needs assessment, service design, performance management, business case development, development of service specifications, service evaluation, contract management and resource allocation.
-
Commissioners sought information to build a cohesive, convincing case to inform or persuade others take a course of action.
-
Commissioner juggled competing agendas, priorities, power relationships, demands and their own inclinations – to make the ‘best’ decision circumstances allowed. This was the ‘art of commissioning’.
-
Commissioning largely consisted of drawing together the appropriate knowledge and information that would ‘satisfice’ these competing agendas and manoeuvring that knowledge through a complex system.
Chapter 4 Models of commissioning
Introduction
Having discussed the nature of commissioning in general, we now set out the specific models of commissioning identified in this study. The term ‘model’ is used in respect of broad functional types and not, for instance, conceptual frameworks or programme theories. The three models of commissioning were clinical commissioning, integrated health and social care commissioning, and commercial provider commissioning. Although versions of the first two models have existed for the past two decades, the third model of commercial provider commissioning is new within the English NHS context.
We make no claim that these are the only three models, but they are the ones that emerged from interview and observation data, and were categories imposed by the researchers, not the participants themselves. Moreover, the models were not mutually exclusive. For example, all of the CCG sites exhibited variants of the clinical commissioning model; the integrated health and social care model was dominant in one commissioning organisation with pockets evident in two others; the commercial provider model was the rarest, as we only found one example where commercial providers had taken over commissioning activities wholesale.
A key point to make is that in drawing together the entire data set, commonalities across the CCG case sites are perhaps overplayed. In fact, the CCG case sites were highly heterogeneous in their configurations and in how they operated. Every CCG case site had its own unique blend of commissioning models to help find its way in balancing and managing competing demands. Moreover, each commissioning model emphasised a particular type of knowledge. The principal argument of this chapter is that different models of commissioning necessarily demand different types of knowledge.
Clinical commissioning
National policy
Although various policy changes have aimed to involve clinicians in commissioning, the 2012 Health and Social Care Act4 brought about a seismic change by establishing over 200 CCGs to replace PCTs across England. Clinical in this case means GPs, as the majority of CCGs were led by GPs,37 although each CCG had a secondary care consultant on its CCG board and a nurse lead for quality. In April 2013, GPs became responsible for 60% of the NHS budget, principally to commission acute and community services. There was substantial variety in how CCGs were configured. For example, some CCGs were a small ‘fleet of foot commissioning body buying in what it needs’ (Simon, CCG chairperson) and some had their own in-house finance and analytical departments.
Although all general practices were legally obliged to belong to a CCG, CCGs were membership organisations, where interested clinicians could opt in (or out). 38 As one chairperson said:
Being part of a CCG and being involved in the CCG are two separate things.
Malcolm, CCG chairperson
The hope was that as local general practices participated in decision-making, they would abide by those decisions, change their behaviours and ‘play by the rules’ (Tom, CCG chairperson). As one CCG chairperson mentioned in an account of dealing with unengaged GPs, ‘you keep looking at the CCG as this third party over there when actually the CCG is you’ (Malcolm, CCG chairperson). However, during fieldwork, several participants worried that general practices would withdraw, unless the ‘central command and control’ style of the NHS was eased to permit more local autonomy.
What we have tried to do is generally take on board the expectations of this redesign, which was to put clinicians at the heart of it, and so we have embedded clinicians throughout the organisation at pretty much most levels, to lead and drive the commissioning. And, as I said, it’s a challenge for us, because whatever is being said, there is still a top-down command and control, a tight grip wanted from the centre at the NHS management line, to ensure and assure that we are going to deliver 20 billion pounds savings. And I absolutely understand that. Versus the expression ‘going to let 1000 flowers bloom’ to allow the GPs to expand and be creative. And I think management at the local level has got that difficult relationship to manage. Because it won’t take much to pee the GPs off and make them walk away from this.
Sarah, NHS commissioning manager
The contribution of clinical commissioners
This section refers mainly to the contribution of GP in their role as commissioners rather than as providers of care. According to one participant, the same GP ‘noisy lights’ still held commissioning roles, as had previously been the case (Patricia, commercial consultant). However, other long-serving commissioning managers from more than one study CCG case site noted that CCGs were more clinically driven than previous commissioning organisations. One commissioner with over 25 years’ experience commented that at board level the clinical commissioning had wrought ‘much more conversation and thinking about . . . clinical knowledge’ (Carla, NHS commissioning manager). One GP clinical lead believed that clinical commissioning meant that raw data were interpreted with a ‘clinical eye’, which would reduce instances of drawing misleading conclusions that might lead to unfair resource allocations to general practices (Patrick, GP commissioner).
We regularly observed clinical input to commissioning decisions in observations of CCG meetings. For example, in one CCG the group were looking at an unscheduled care dashboard to attempt to identify patient groups that could be diverted from hospital. Two GPs had prolonged discussion about cellulitis, applying their clinical knowledge to interpret information from the dashboard.
[Anthony continues getting Teresa to open different bits on the dashboard. He says there are lots of areas which appear to be ‘low hanging fruit’, and mentions cellulitis. He says ten people a month were being admitted with that, and asks why they weren’t being cared for in the community [he says something about what treatment would be], and also says something about the mindset around admissions.]
Be a bit careful about whether it is actually cellulitis they are being admitted for – often it is because there has been a social care breakdown.
But they still should not be an acute admission – in that case they should be admitted to a nursing home.
It is still not as simple as putting in a venflon. Anthony says that this kind of data still gives them a way to look at things which need sorting. He says DVTs are another example.
Meeting observation
Several participants, including GP commissioners, commented that an advantage of involving GPs in commissioning was that GPs were ‘closer’ to patients, which made decisions more ‘real’. GPs also had useful local knowledge of how the health-care system worked. Although during fieldwork the specific contribution of GPs was still being worked out, several participants mentioned that GPs were well suited to developing services and designing patient pathways. We observed many examples of clinical commissioners involved in service redesign and provision, such as establishing a GP role in hospital emergency departments. In addition to service development, GP commissioners were identified by participants as having an important role in challenging their hospital consultant colleagues.
It’s so predictable . . . you always go through the same process that they [hospital] are particularly hard done by, they have cut everything to the bone, and there’s all these vital initiatives that [the local health-care economy] must have, and we’re so far behind everywhere else, and GPs are wonderful, they only refer things that absolutely need doing, and we never see anybody for a follow up, and all this stuff, you know, this comes out. And finding places, clinical areas where you can begin to change behaviour is hugely difficult. So what I think we have to do, as GPs, is to try and anticipate and understand those areas. So this is what I regard as almost the only bit that GP commissioners add value, is that we hopefully can see through the guff that our clinical colleagues in specialties will put up and begin to challenge some of that. But of course that’s quite difficult. They are the experts and so on.
Angus, former PCT chairperson and GP
To change GP behaviour, this participant said that GPs liked information that suggested they were ‘in the middle’ of the pack and that if they were not, their behaviour could be shifted, but only if the data were trustworthy (Angus, former PCT chairperson and GP). Another agreed saying ‘If there’s a really good arguments, if you can see the graphs, see the numbers people will almost change overnight because they generally want to do the right thing’ (Patrick, GP commissioner). One chairperson from another CCG recounted that ‘one of the powerful phrases’ he had heard from a GP was ‘show me the data and I’ll sort myself out’.
So a lot of the time people just don’t know that the way they’re behaving clinically is at variance with their colleagues. They may not know that they ask for 50% more ultrasound scans than anybody else. And if you point that out to them, then they can actually say, ‘Oh OK, right, every time I write ultrasound scan perhaps I should go and talk to a colleague and say would you have done that, should I be doing something differently?’ So it’s not necessarily being done in a judgemental way; it’s being done in a sort of actually just to inform you and see if you can solve the problem yourself.
Tom, CCG chairperson
Another CCG chairperson recounted two examples of behavioural change due to peer review. Once was when data suggested that his own behaviour with X-ray referrals meant that his practice was the second highest user of X-ray services in the CCG, and the other instance was with a GP colleague.
We’ve got a GP who has been known about by the PCT for years, who spends exactly twice as much on drugs as anyone else in our group. [PCT chief executive] would go round and plead with him. He’d be very polite, give him tea, coffee, biscuits, anything he liked, but what really mattered [was] controlling his prescribing expenditure. Since he’s had peer review, and charts up on the wall showing where he is with his peers, he’s accepted mentorship from one of our GP leads, you know, and he’s starting to make some progress. In other words, he’d flick a V sign at the, you know, the managers, but he doesn’t do that to his peers.
Martin, CCG chairperson
Challenges
During fieldwork from 2011 to 2013, several challenges were noted facing the introduction of CCGs. GPs carried out their commissioning duties in addition to their ‘day job’ as GPs. In working two jobs, interview participants had widespread concerns that GPs had insufficient time for commissioning. Moreover, several voiced fears that if pushed to choose, GPs would keep their clinical jobs because their commissioning activities were extraneous. At least one GP commissioner voiced the attitude of many in stating that he was still mainly a ‘jobbing GP’ (Anthony, GP commissioner).
Several participants noted that GPs needed to shift from their ‘provider’ stance to a wider population perspective, mindful of the wider system. Without this wider system view and an understanding of the impact of their decision-making, GP commissioners could inadvertently make the situation worse. For example, one participant was concerned that GPs might not have sufficient understanding of the financial implications of service changes. He gave a complicated account of how if some hospital services were moved into the community or private sector, the hospital would still have the same overheads and this would be passed on to commissioners’ bills. Commissioners would then become trapped because the costs at the hospital would stay the same (or increase) and they would also be paying for a similar service elsewhere, in effect paying twice. He believed that the only way to actually save any money was to take entire services out of the hospital and commission them elsewhere, such as the British Pregnancy Advisory Service (Joel, commercial analyst). This was quite a sophisticated argument, possibly unknown to many GP commissioners (or, indeed, NHS commissioning managers).
Another commissioning manager gave a different example of how inexperienced GP commissioners could accidentally create more problems.
I think – engineering analogy coming again – it’s really easy to try and fix something at one part of the system and make it worse somewhere else. So you can focus around a particular issue, let’s imagine you look at a rapid response community service, and you employ a team of nurses to respond to medical crises that would normally have ended up in A&E [accident and emergency], and it looks like you’re doing a really good job. You’re recording the fact that you’re avoiding all of these admissions, but what you’re not recording is what happens to those people in 30 days, 90 days, whether they’re going back in twice as many times. So that’s just an arbitrary example of how easy it is within all of this to try and focus on something and fix something, but actually make it worse somewhere else.
Alan, commissioning manager
Given these concerns, fears were commonly voiced from NHS commissioning managers, commercial providers, Public Health professionals and the GPs themselves that GPs lacked the necessary skills.
I mean where do we get the expertise? . . . You know, are GPs born managers? . . . I now find at the end of my career that slightly perversely I’m having to sort of learn new skills to supposedly support the care of my patients.
Roger, GP commissioner
An experienced commissioning manager identified those skills as understanding legal duties and responsibilities such as budgets, managing contracts and poorly performing providers and identifying and interpreting information, especially around costs and cost utilisation (Paula, NHS senior commissioning manager). Although some GPs had previously been involved in commissioning, it was a major leap from project-based PBC to strategically managing million-pound budgets across whole health economies in CCGs. For some, amassing this expertise within 2 years was daunting. In fact, when asked what he would do when the PCT dissolved, one CCG chairperson responded candidly, ‘Cry’ (Martin, CCG chairperson). However, these data were collected from 2011 to early 2013, when CCGs were still in the authorisation phase; their confidence may have grown as they moved from shadowing PCTs to full responsibility.
Having worked internationally, analysts from one commercial provider expressed several other concerns about the implications of the policy of clinical commissioning on data collection and interpretation. One pointed out that with the slimming down of commissioning, those left had to be more multiskilled. An American analyst commented that by shifting financial responsibility to providers, which was also a trend in the USA, ‘there should be a pretty heavy incentive for these groups to have analytics so they can manage their populations’ (Sergio, commercial analyst). Another analyst agreed noting that GP commissioners were not going to understand cost and utilisation modelling and so there was a ‘kind of commissioning support service that will be probably more essential now than even it was before’ (Brenda, commercial analyst). Tim thought that the advent of CCGs meant lots of smaller contracts with smaller data sets, which were more difficult to manage. This would increase the amount of analyst time needed to reconcile those data sets (Tim, commercial analyst).
Integrated health and social care commissioning model
Definitions and challenges
The second model identified from our data was integrated health and social care commissioning. Often known as joint commissioning, this has been a policy feature since the split between Health and Local Authorities in 1991. Some policy initiatives focused on pooling health and social care budgets, initially with the Health Act Flexibilities in 1999 and later in 2006. 39 Most recently in the 2013 Spending Review, the government committed £3.8B to the ‘Better Care Fund’ by ‘top slicing’ a proportion of funding allocated to CCGs into pooled funds for health and social care. 40 This was not new money.
In general, the NHS has been responsible for health care, while local authorities deliver social care, for example help with bathing and dressing for the frail elderly living at home. However, clarifying needs as health or social care can be challenging, with some care recipients experiencing duplication while others fall through the gaps. A major reason for disagreement is that health and social care have separate budgets, and so the classification of a particular need as ‘health’ or ‘social’ care has financial implications.
One participant, with a specific remit to develop joint commissioning, commented that health and social care were not ‘easy bedfellows’, partly because their approaches to commissioning came from ‘medical research’ and ‘social science’ mind-sets, respectively. He noted that despite ‘desperate’ attempts to integrate health and social care, ‘it’s very, very hard because . . . it’s two silos with a lot of aggro’, which was mirrored from government level to the local system (Percy, former PCT chief executive officer and Department of Health senior manager, now freelance consultant). Moreover, a recent study found that despite widespread perceptions of the benefits for patients, there was limited evidence that joint commissioning improved outcomes,41 although a former King’s Fund fellow argued that such evidence was difficult to generate, partly because other initiatives might also have had an impact on outcomes. 42
Examples from the Clinical Commissioning Group case sites
The level of involvement of local authorities into NHS commissioning strategically varied across CCG case sites. In one, a Social Services representative sat on one of the key CCG decision-making forums but did not make any comments in any observed meetings. In two others, Social Services representatives attended and made several contributions. The fourth was striving to be a fully integrated organisation and not only included local authority representatives (who appeared to be highly influential in observations of meetings), but also articulate elected councillors. At operational level within the CCG case sites, integration of health and social care took forms such as integrated health and social care teams, jointly funded collaborative projects and overarching programmes.
In one commissioning case site, the integrated services programme was repeatedly discussed at meetings of the UCB. This programme sought integration of different health sectors (i.e. acute and community) as well as health and social care. It emphasised operational changes, such as improving information sharing so that social care needs could be identified and addressed within health assessments. An integrated care team made up of a GP, a community matron, a community nurses and an adult services social worker aimed to offer ‘joined up care’ to those with long-term conditions (press briefing). Another prominent initiative integrated a walk-in centre and a GP out-of-hours service with the emergency department so that all urgent care was located in one place. A joint discharge scheme had been set up and the first few patients had been through this successfully. The UCB were considering joint care packages to prevent the delay of discharge from hospitals because of questions about the appropriateness of health or social care.
With regards to impact, at one UCB meeting a ‘taking stock’ discussion noted positive culture change, for example with providers from hospitals and community sharing information, but joint commissioning was not yet a reality. Instead, in an interview, the freelance consultant leading this work commented that the intermediate aim was to develop joint service specifications, which he coined as ‘complementary commissioning’, before pooled budgets were achievable. Participants were generally enthusiastic about this programme, but more progress was needed.
In a second commissioning organisation where we found evidence of integrated health and social care commissioning, 11 organisations from across voluntary, health and social care sectors worked together to support individuals ‘to get back on their feet following treatment in an acute or community hospital’ (briefing paper, January 2012). The impetus for this initiative was feedback from patients that their needs were not being met. With help from a commercial agency using a methodology focused on patient experience, the project team mapped current services and detailed five patient pathways. They also carried out service user consultations, stakeholder engagement and shadowing exercises. The shadowing included professionals from different organisations observing each other at work and teams of professionals from both social and health care (including senior managers) visiting service users. This was particularly insightful in clarifying service user needs.
So we took a group of professionals, occupational therapists, physiotherapists, social worker, care worker . . . So they went into somebody’s home . . . they learnt [that] having a professional doing something led to a greater quality of interaction. So you can sit down with a cup of tea and say, ‘I’m here to listen to you. Tell me about yourself,’ but they got a lot more in terms of understanding what was going on with that person from working with them around helping them to walk or helping them to do something, that was consistent. It just was a more natural conversation. They’d bump into the MBE medal on the wall and have a conversation around that, and there were things that helped them [professionals] to understand what mattered to them [service users].
Daniel, commercial consultant
From these activities, the team reported to the CCG board:
Assessment and treatment was undertaken in silos – the results of this validated the observations from our initial shadowing work that service users felt passed from service to service without being fully understood or [having] the things that mattered to them addressed in a meaningful way. The consequences of this for the system are a huge amount of unnecessary cost, duplication, waste, inefficiency and low morale with services responding to a significant amount of failure demand, seeing the same service users again and again.
Briefing paper
The intervention designed was an integrated service consisting of NHS staff (occupational therapist, physiotherapist) and social services professionals (occupational therapist, social worker, care worker supervisor). This was piloted at a GP surgery and then spread across the locality with five further integrated teams. The integrated teams were ‘not constrained by organisational barriers and systems’ and were encouraged to develop innovative approaches to problems (briefing paper).
An evaluation of the service was carried out by the local Public Health director comparing a cohort of service users with non-service users (control group), with the intended outcomes of reduction in hospital admissions and social care packages. The results were a small reduction in the hospital admissions between the 12 months before and 3 months after the intervention for the service users (no mention of comparison with control group). The cost of social care packages, however, went up for both the service user and control groups, although it was significantly less for service users (briefing paper). Using a researchers’ lens, the conclusions would be that the effect of the intervention was weak, as there was no reduction in hospital admissions between the intervention and control group and the costs of social care packages increased. (NB: we did not have access to the original report.) Interestingly, these findings were reported differently at the CCG governing board meeting.
The principal outcomes of the study indicated: a significant difference between the patient groups in the number of hospital re-admissions and a significant reduction in social care costs.
Meeting minutes
Based on the data we have, in being transmitted to the board the impact of the intervention became substantially overstated. These minutes also mention that the occupational therapists had reported a ‘re-discovery of their skills’ and GP feedback was positive (meeting minutes). The project was recommissioned at £250,000 annually on a recurring basis. Interview participants had widespread enthusiasm for this project, citing how it had improved morale.
For another commissioning organisation, integration of health and social care commissioning occurred strategically and operationally and permeated every aspect of their approach. It appeared to have unanimous support, although dissent on this front might be difficult in an organisation so committed. Health and social care had pooled their entire budgets several years ago, partly in a ‘defensive’ move to stop the local PCT from being amalgamated with neighbouring PCTs in early reforms. They made infrastructure changes, such as moving Public Health and children’s services to the local authority and shifting adult social care services into health. The aim was to create an ‘integrated system as opposed to an integrated single organisation’, although one participant noted that this was difficult when issues of ‘self-preservation’ arose (Alan, NHS commissioning manager). Decisions were taken with ‘a no detriment advantage [in] that everything we do is about no detriment to the other party’ (George, Social Services manager). This meant that in making commissioning decisions, the board, including the highly vocal locally elected councillors, deliberated on the effect of actions both on key health outcomes such as hospital admissions and on social care indicators such as residential care placements.
A CCG director described the social care voice as ‘very strong’ (Carol, NHS commissioning manager) and interview and observation data suggested that those from the local authority were highly influential. Moreover, lay members and patients played a major role. The CCG chairperson was a lay representative, with a GP as vice-chairperson. Small, three-person teams, consisting of a clinical lead, a service manager and a lay person, led each of their seven work streams (e.g. unscheduled care, disabilities, older people). The CCG had set up a community forum whose members worked in various capacities across the CCG. Furthermore, ideas for service changes were put to a ‘Dragon’s Den’ panel of service managers, clinicians and lay people.
The impetus for such high levels of community involvement appeared partly as a result of ethical values, but also because of a desire for informed community debate on the most difficult issues facing the commissioning organisation. Community knowledge was important in challenging clinical knowledge and priorities and engagement also sought to achieve acceptance of difficult decisions and public behaviour change. However, such openness to public involvement also brought difficulties; for example, a CCG board member had accidentally caused an outcry from remarks made in a radio programme and we observed a member of the public heatedly challenge the CCG board in a public meeting. (NB: the CCG members addressed this individual by his first name and invited him to talk with the deputy director further, and so presumably he was well known.)
Commercial provider commissioning model
Outsourced contract
For the third model we have coined the term ‘commercial provider commissioning’, which applies only to instances where the commissioning is done exclusively by the external provider. Although in this study commercial providers mainly had a role in advising and supporting clients through the deployment of tools and commissioning expertise, we found one example of ‘commercial provider commissioning’, where commissioning had been completely outsourced to external providers. The commercial provider had taken over all aspects of the commissioning process, including contracting and performance management. (NB: the use of the term ‘commercial provider’ in this context does not refer in any way to commercial providers of actual health-care services such as private hospitals).
This started in 2009. The commercial provider team managed the contracts of a group of large, powerful acute providers, which were ‘very expensive and quite difficult to control’ (Joel, commercial consultant). The remaining NHS staff managed another set of contracts with acute providers in a different geographical area. The commercial provider team consisted of a programme manager, nurses, administrators and ‘lots of analysts’. Although the NHS and commercial provider teams were colocated on the same site, there was a clear split in their remits and significant hostility from the NHS team, which may be a reason why only one operational NHS team member was willing to participate in this study.
Definition of commissioning by commercial providers
While participants from advisory commercial providers defined commissioning in a variety of ways, often comparable with NHS study participants, the definition offered from the company with the outsourcing contract was consistently in terms of managing supply, demand and consumer engagement. Managing supply was defined as getting the right providers, contracts and management processes, which one participant thought was ‘simple’ (Larry, commercial consultant). Managing demand was ensuring that providers deliver the right health care, which another said was critical to ensure that ‘people are only passing deeper into the system at the appropriate point’ (Jemma, commercial consultant). Managing the health-care consumer was about interacting with patients and the public to navigate their way through the system.
The importance of data
Crucial to the commissioning ethos of this commercial provider was to ‘use data to drive decision making’ (Kristen and Thomas, commercial consultants). They largely saw the ‘problem’ as a NHS driven by politics and people rather than by data. Several participants talked about the provision of data to ‘move you beyond that purely political/anecdotal approach’ (Jemma, commercial consultant). Another said ‘we have always said data are the lifeblood of any organisation’ (Dennis, commercial consultant). They wanted to ‘integrate the system’ by linking medical records, through better analysis of data to understand ‘what’s driving your costs’ and by engaging patients to change their behaviour. Moreover, the aim of their interventions was to develop or find a ‘single source of the truth’ (i.e. reliable, consistent data). This phrase emerged repeatedly in interview and observation data.
Analysts for this outsourced service undertook ‘forensic investigation of the data’, mainly finding errors in coding leading to overcharging (Joel, commercial analyst). However, when the commercial provider team started the contract, there was ‘pretty much no data’ and so the hospital providers ‘kind of managed themselves with little contract management’ (Harlow, commercial analyst). Only 2 of the 17 hospitals supplied hospital (Secondary Uses Service) data, which:
. . . gives you granularity that finally you can start unpicking exactly what’s going on for the patient, you can start looking at pathways and so on . . . [otherwise you are paying] for something that you don’t even know what it is.
Dennis, commercial consultant
The approach the commercial provider took with hospital providers was to say:
‘If you don’t supply us with this data, we can’t validate our patient activity, therefore we are not going to pay for it.’ So slight – at times, very antagonistic approach. And I remember we sent out these letters and we were lambasted and lambasted by the PCTs, lambasted by the providers.
Dennis, commercial consultant
In an attempt to reduce the hostility between the commercial provider, acute providers and PCTs, a NHS commissioner was seconded for 1 year to the commercial provider mid-contract. During fieldwork, several participants noted that relationships had since significantly improved. This ‘firm but principled’ stance of ‘no data, no payment’ (Dennis, commercial consultant) suggests that the commercial provider was willing to sacrifice comfortable relationships for the provision of good-quality, useable data. This is not to say that all commercial companies would prioritise data and relationships similarly.
Accountability and performance management
In addition to prioritising measurement and data capture, another characteristic of commercial provider commissioning was the emphasis on accountability and performance management. For this contract, the commercial provider placed nurses into hospitals to verify patient notes against invoices, as often commissioners have limited ways of checking the accuracy of claims. Feedback from the hospitals was that clinicians were essential in this role to make clinical judgements. A commercial provider thought that embedding the nurses in the hospital teams was ‘invaluable’ in identifying anomalies because ‘every single patient going into that trust is being reviewed by our nurse on site’ (Dennis commercial consultant). For example, if there was any bed blocking, the nurses would ‘pick up the phone’ to contract leads and investigate further. The nurses also regularly reported back performance management issues to the PCTs. Another participant was less positive about the embedded nurses, seeing it as a lost opportunity, as, apart from ‘one or two significant issues’ of quality and safety, the nurse did not capitalise on driving up quality or challenging clinical behaviours. Measuring the impact of the nurses was also difficult, and this initiative was stopped.
Knowledge needs
Within each of the models, different types of knowledge were privileged (Table 6). Local clinical knowledge from GPs was prioritised in the clinical commissioning model, service user knowledge was key in the integrated health and social care model and analysts’ knowledge of capturing and interpreting data was crucial in the commercial provider model. This is explained further in the following sections.
| Model | Clinical commissioning | Integrated health and social care | Commercial provider |
|---|---|---|---|
| Knowledge privileged | GP | Service user | Analyst |
| Knowledge provided by privileged source |
|
|
|
| Knowledge wanted but unavailable |
|
|
|
| Type of activities |
|
|
|
| Advantages/disadvantages | ‘Real’ decisions made closer to patients Lack of commissioning knowledge |
Make unpopular decisions more palatable? Commissioning decisions more open to public criticism |
Financial savings Over-reliance without skills transfer |
Knowledge needs for clinical commissioning
Within clinical commissioning, local GP knowledge of the health economy and service provision was important. As key gatekeepers, they were assumed to provide an understanding of how best to deliver care to patients. However, GP commissioners were cautious about relying on their local knowledge alone. In our observations of commissioning meetings, clinical commissioners repeatedly called for evidence to inform which services to commission anew and which services to recommission. This did not have to be research based, but clinical commissioners were clearly uncomfortable making decisions in a vacuum. Clinical commissioners were also wanted robust evaluation ‘to say “yes” and it is delivering what we expected – or it isn’t’ (Clara, NHS commissioning manager). For example, one CCG chairperson mentioned that they had about eight different initiatives to address problems around delayed transfer of care, but no mechanism to find out if any were ‘contributing well or contributing badly to that final outcome’ (Simon, CCG chairperson).
In terms of information, NHS commissioning managers and commercial providers commented that clinical commissioners needed information faster than PCTs, as GPs were used to ‘real-time’ data with general practice information technology (IT) systems. In one commissioning study site, extensive work was undertaken to update a pathway tool with locally informed pathways, which, the lead was pleased to report in a board meeting, appeared increasingly used during consultations. In another commissioning organisation, several participants talked about wanting the ‘holy grail of a very simple, understandable dashboard for the general financial picture that is useable and understandable to GPs’ (Craig, GP commissioner). Ideally, they wanted this tool to track real-time activity and financial flows to find out how money was spent.
We observed anxieties around discrepant data in several commissioning meetings and this concern also surfaced regularly in interview data. For example, one CCG chairperson said that disagreements about data were a ‘fundamental flaw of our system’ (Simon, CCG chairperson). Another GP commissioner was keen to get consistent data because of the situation of ‘oh God, we went to this meeting with one set of figures, now I see another set that tell a completely different story’ (Angus, GP commissioner). One GP clinical lead commented:
I think GPs have a very limited tolerance for being given information in data, and as soon as you present, you have two different sets of data, they typically devalue both of them and believe neither of them.
Craig, GP commissioner
This issue was of high priority to clinical commissioners, as they were well aware that without consistent data, behavioural change among their colleagues was unlikely. However, several participants also mentioned that the lack of consistent data or repeated requests for further information was sometimes an excuse for clinical commissioners to delay or avoid taking difficult decisions.
I sometimes get quite frustrated at people’s constant requests for more and more and more local data, and more and more and more analysis, when really it’s quite clear what we need to do, and actually more data is not going to change the actions that you need to take . . . actually, you know, it’s almost like that’s just a mechanism for not taking [laughs] any action.
Sandra, Public Health consultant and GP
Knowledge needs for integrated health and social care commissioning
The knowledge privileged in health and social care commissioning in two of the three examples was largely that of service users. In the integrated project, service users were the reference point in understanding what worked (and what did not) and their perspectives were gathered in various ways (pathways, consultations, shadowing). Similarly, mechanisms for incorporating service user views and their expertise were instituted in the third commissioning organisation including service users as strategic leads, elected councillors as board members, and a community forum. In comparison, the data for one CCG suggested service user involvement were minimal.
Do you see any patients around here today? No. So I think it is a bit about getting patients involved, both in advising, helping with decision making and then communicating decisions to the public. I think to have laypeople communicating messages would be very powerful alongside clinicians or board members or politicians or whatever. And at the moment we have very little of that.
Anthony, GP commissioner
External expertise also contributed to integrated health and social care commissioning initiatives. For example, a large international accountancy consultancy helped with the urgent care initiative and was rated highly by the CCG chairperson. Elsewhere, a commercial consultancy was brought in to use their systems methodology to map and understand ‘customer’ demand. (NB: in briefing papers, terminology such as ‘failure demand’ appear regularly, suggesting that at least some commissioners had become highly adept in its use.) Several participants were positive about the contribution of this consultancy. In another example, Public Health led on the evaluation of an initiative. Finally, in one commissioning case site, a commercial provider supplied expertise to set up a ‘Community Forum’ and small group structures, which was also appreciated.
Knowledge needs for commercial provider commissioning
Given the emphasis on good-quality data, unsurprisingly analysts’ expertise was highly valued in the commercial provider commissioning model. This was crucial to feed into and inform decision-making. Pulling together data from disparate sources and increasing its quality had been a major task. Keeping on top of the contract also required excellent analytical skills. A NHS client said that the key to this contract was that the commercial provider did ‘the basics really well’, which resulted in savings estimated at over £1M in the first year.
Initially within the contract, a clear knowledge translation strategy had been costed in by the commercial provider so that a NHS team could pick up the skills of the commercial provider, but this was eliminated early on by the NHS client to reduce contract costs. Therefore, scant ‘legacy planning’ was in place and the costs of the contract were likely to increase again, once the commercial provider left. However, there was little evidence that the commercial provider would leave, as the initial contract for 3 years was renewed for 2 more, and then after a further tending exercise the commercial provider was awarded another 3-year contract with an extended 2-year option. By 2019, the commercial provider may have run this outsourced commissioning service for 10 years with no mechanisms in place to transfer skills into the NHS/CSU. This further deskilled local NHS/CSU analysts and commissioners and effectively made the NHS clients completely reliant on commercial provider support.
Box 4 summarises the key points in this chapter.
-
Three models of commissioning were identified from our data: clinical commissioning, integrated health and social care commissioning and commercial provider commissioning. However, even within any particular model, there was considerable variance in practices, procedures and underlying attitudes and values.
-
Every CCG had its own unique blend of these commissioning models.
-
Different types of knowledge were privileged in the different models. Local clinical knowledge from GPs was prioritised in the clinical commissioning model, service user knowledge was key in the integrated health and social care model and analysts’ knowledge of capturing and interpreting data was crucial in the commercial provider model.
-
With their clinical knowledge of patient needs and local knowledge of the health economy, GP commissioners had an important role in generating ideas for improved services and pathways. They also were called on to challenge hospital consultants and their GP peers.
-
The knowledge that clinical commissioners wanted was evidence of which services to commission and ways to determine if their initiatives made a difference. Calls for reliable, trustworthy data were frequent, as without these, there was limited impact in changing clinical behaviour.
-
Examples of integrated health and social care commissioning included overarching programmes of work, integrated health and social care teams and specific projects. One CCG merged its health and adult social care budgets to create an ‘integrated system’, whereby the implications of decisions were considered on both health and social care outcomes, the social care voice was ‘very strong’ at all levels of the organisation and service users had major roles in decision-making and leading initiatives.
-
A commercial provider won an outsourced contract to take over commissioning responsibilities for a NHS team. In this model, high-quality data to ‘drive decision making’ was emphasised along with accountability and tight performance management of providers (no data, no payment). In addition, nurses were embedded in acute hospitals to audit patient notes. Good relationships between commercial providers, commissioners and health-care providers were secondary to good-quality data. Without mechanisms to transfer commercial provider skills into the NHS, the NHS clients have become completely reliant on the commercial provider, as the contract is now expected to run for at least 10 years.
-
Clinical commissioners wanted ‘real-time’ data on activity mapped against financial flows; NHS health-care commissioners in general wanted service evaluations to find out if their initiatives had made a difference.
Chapter 5 Knowledge acquisition
Introduction
This chapter addresses the research question:
How do health-care commissioners access research evidence and other sources of knowledge to aid their commissioning decisions?
For clarity, ‘commissioner’ is defined as any individual employed by a CCG (or PCT, which pre-dated CCGs) who makes decisions affecting health-care delivery or provision. Although we recognise that external providers from CSUs and Public Health may be involved in work that impacts on health care and experience the same or similar knowledge transformation processes, in this chapter ‘commissioner’ refers to PCT/CCG commissioners, regardless of clinical or managerial background.
Chapter 4 provided data on knowledge needs and sources for the different models of commissioning. This chapter describes knowledge acquisition and the following chapter presents findings on knowledge transformation. However, the distinction between knowledge acquisition and transformation is blurred, as transformation occurs from the moment knowledge is acquired. Nevertheless, for the purposes of reporting, the findings have been artificially separated into two chapters.
To recap, the data informing the next three chapters comes from eight case studies. The four case studies of CCGs were:
-
Carnford CCG – struggling financially, highly collaborative with its providers and reliant on the use of tools and the data produced from those tools to influence commissioning decisions.
-
Deanshire CCG – relatively confident as a commissioning organisation, focused on governance, carrying out some innovative projects in partnership with commercial providers.
-
Norchester CCG – financially challenged, emphasis on (ideally academic research) evidence-based policy-making, piloting new ways of commissioning contracts, with substantial aid from commercial and not-for-profit providers.
-
Penborough CCG – creating an integrated network of health and social care provision, with a heavy emphasis on public involvement throughout, historically extensive use of commercial, not-for-profit and freelance providers.
In addition, we draw on data from the four case studies of commercial and not-for-profit providers working in contractual relationships with NHS clients. These were:
-
Heron – a multinational commercial company with a suite of tools and mixed UK/non-UK staff, offering analytics and project management.
-
Jackdaw – small, international, not-for-profit offering one tool.
-
Swallow – a national commercial company with a suite of tools staffed largely by ex-NHS personnel offering analytical and commissioning expertise.
-
Swallow Tool – an exemplar of Swallow and NHS clients (PCT, acute and community providers) working together to audit best place of patient care using an electronic tool.
We start with sources and types of knowledge identified by participants, along with details of the ways in which knowledge was acquired. The chapter concludes with a discussion of the relatively modest role of research evidence in commissioning.
Sources and types of knowledge
Classification of sources
In building a cohesive case for action, practising the art of commissioning and manoeuvring their proposals through the system, commissioners sought knowledge and information from many sources to determine, clarify, substantiate and defend their position. An overview of those sources commonly named by commissioners and observed in commissioning meetings is detailed in Tables 7–10, categorised as ‘people’, ‘organisations’, ‘tools’ and ‘research based’. These tables have been constructed by a commissioner working with our research team using the categories commonly understood by commissioners, and are not exhaustive, as other sources and types of knowledge undoubtedly exist and these sources offer other types of knowledge not named by participants. As this is not a quantitative survey, we make no claims to the representativeness of this classification, nor do we attribute weightings to the particular factors. However, Clarke and colleagues conducted a survey on sources of evidence used by commissioners,43 which offers additional useful information.
| Clinicians | Commissioning managers | Analysts | Patients and the public | Freelance consultants |
|---|---|---|---|---|
| Local relationships and history | Local relationships and history | Local relationships and history | Local experience of services and personnel | Local relationships and history (if former staff) |
| How services operate | ‘Whole-picture view’ | Hospital and primary care data | How services operate | Project-based experience |
| Possible improvements | Finance and budgets | Software tool operation | How they might be better served | Specific skills (e.g. analysis) |
| Primary care data | Performance | Data and their interpretation | Products | |
| Condition-specific expertise | Legal responsibilities | Local benchmarking and modelling | Experience and knowledge of the conditions | |
| Some knowledge of academic research | Contracting and procurement | |||
| Experiential knowledge (e.g. which services are not managing referrals well) | Experiential knowledge (e.g. how to steer commissioning decisions through the system) | Experiential knowledge (e.g. what data to trust and not to trust) | Experiential knowledge (e.g. how to put pressure on the system) | Experiential knowledge (e.g. ways to present information for local commissioners) |
| Department of Health | NICE | NHS Improving Quality | Public Health | CSU | ‘Think tanks’ (e.g. The King’s Fund) | Royal Colleges | Local health-care providers | Other CCGs/CSUs and health-care providers | Commercial and not-for-profit providers |
|---|---|---|---|---|---|---|---|---|---|
| Best practice guidance | Clinical guidelines | Best practice guidance | JSNA | Local relationships and history | Best practice guidance | Best practice (e.g about safety) | Local relationship and history | Best practice guidance | Clinical/project management |
| National Outcome Frameworks | Case studies | Rapid research evidence appraisal | Contracting and procurement | Organisational development | Activity data | Literature reviews | Sophisticated data interrogation skills | ||
| Commissioning guidance | Improvement tools | Service evaluation | Human resources | Research reports | Performance data | Patient pathways | Best practice guidance national and international | ||
| Publications | |||||||||
| Organisational development | New development in clinical field | Commissioning experience | |||||||
| Liaison with commercial providers | Horizon scanning | ||||||||
| Horizon scanning |
| Electronic software tools | National benchmarking | National and local dashboards | Business system/quality improvement techniques, (e.g. LEAN) | Locally developed models (e.g. commissioning intelligence) |
|---|---|---|---|---|
| Scenario generating tool | Comparison with other CCGs/CSUs/health-care providers | Comparison with other CCGs/CSUs/health-care providers | Project management | |
| Pathway tool | What’s not working | What’s not working | ||
| Invoice management | Activity and referral data (local) | |||
| Risk prediction | ||||
| Prescription alternatives | ||||
| Bespoke dashboards |
| Journals and bulletins | Search engines | Universities | Cochrane | CLAHRC, AHSN and PCRN | Electronic newsletters |
|---|---|---|---|---|---|
| BMJ | MEDLINE | Local university | Systematic reviews | Future sources of research | Local clinical briefings |
| British Journal of General Practice (BJGP) | Google Scholar™ | York (mentioned twice in different CCGs) | Public Health observatories | ||
| Drugs and Therapeutics | The King’s Fund | ||||
| MHRA Drug Alerts | NHS Improving Quality | ||||
| Health Service Journal (HSJ) |
Which sources are commissioners more likely to trust?
Among national sources, commissioners appeared to trust certain organisations more, namely the National Institute for Health and Care Excellence (NICE), The King’s Fund and NHS Improving Quality (formerly NHS Institute for Innovation and Improvement). Participants viewed NICE as providing rigorous, but not always easily applicable, information. NHS Improving Quality and The King’s Fund were useful sources of best practice guidance and new ways of commissioning. In contrast, several participants, especially GP commissioners, seemed sceptical about the rigor of the information from the Department of Health.
Local information often trumped generalised research-based knowledge or information from other localities. For example, ‘telehealth’ was a national ‘must do’, but clinicians were wary about its local applicability. In one CCG, a local Public Health consultant compiled a briefing about the academic research evidence behind ‘telehealth’. This briefing appeared to reconfirm, and perhaps even strengthen, the CCG’s stance that ‘telehealth’ was not a useful intervention. One month later, a health-care provider implementing ‘telehealth’ presented data on the first eight patients presenting at their local service and noted the reduction in hospital admissions. His conclusion was ‘the data is showing that it’s really starting to make a benefit’. Although the committee considering ‘telehealth’ did not completely reverse their earlier position, they became more positive.
We’re not entirely sure but it seems to have some evidence that something happening.
Can you tell us the key areas where it’s starting to show benefit? COPD [chronic obstructive pulmonary disease] isn’t.
Heart failure.
It’s soft measures such as empowerment.
Telemedicine helping people to feel they can take control but it’s hard to measure.
Marvellous!
So watch this space.
Meeting observation
Although many factors might have contributed to the group’s more welcoming response to ‘telehealth’, the presentation of positive local data appeared persuasive enough to start to reverse previously held opinions substantiated by research evidence.
Mechanisms for acquiring knowledge
Verbal
The mechanisms whereby commissioners acquired knowledge included conversations, stories and documentation.
Verbal exchange was particularly well suited to the fast-paced, rapidly changing environment in which commissioners worked. Conversations were an important way of getting information quickly through chance encounters, formal meetings and informal gatherings. The contingent nature of these exchanges, however, meant that if a different combination of individuals had happened to meet, different knowledge would have been acquired and perhaps a different set of decisions would have been made.
. . . popping in to see various GPs on my way somewhere else because they had 5 minutes to spare and wanted to chat. But we’ve come up with these ideas, and it’s just been because we’ve sat there and had the time to chat.
Randall, freelance analyst
Knowledge was also acquired through stories. Sometimes stories were told to substantiate a viewpoint, and sometimes stories about patients and services were recounted to appeal to ‘common sense’ and/or make an emotional impact.
So the example that we used, and that really hit the team, was a chap who was having problems with dexterity in his hands – has anybody related this story to you already?
No, no, not this one.
. . . And the clothing side, he was struggling to do his buttons and to do the collars of his shirt. They spent some time with him and, you know, the house was clean, he was a very proud person. And the old approach would either be to put in a package of care around help to dress himself, or making him wear some sort of T-shirt or something. Actually we were able to take his own formal shirts, and behind the buttons put in some Velcro, so that he could wear his own shirts and have that sense of self-esteem, and not have somebody coming in every day which, you know, the learning from the team was people lose their independence the more they have people doing for them. So those types of simple things, but you can imagine, in a normal system, if you said, ‘Well I need to put some Velcro in,’ you know, they’d be hunting for the Velcro budget, we don’t have one, put in a ‘package of care’ around clothing!
Daniel, commercial consultant
Stories could be powerful in influencing commissioning decision-making. For example, a commissioning manager said that stories were important to persist with proposals through the lengthy, repeated decision-making cycles.
And I have often thought in the past you need the story of the change. Because ideally from the time you’ve gone through health scrutiny committee, the CCG, other local groups, other stakeholder groups and especially if you get to a procurement exercise where actually you might draw services to a close and you know people may be TUPE’d [Transfer of Undertakings] or made redundant and there’s some heavy duty consequences for people, you need a compelling story. And often that is much more powerful than data that you want to throw at people, and so having the clinical stories is really important and the patient’s story is really, really key.
Harry, NHS commissioning manager
But not everyone was in favour of stories. A Public Health consultant noted that GP commissioners tended to be ‘overly swayed by these hugely dramatic stories that clinicians would come in with based on individual patient anecdotes’ (Mary, Public Health consultant).
Documentation
Although substantial knowledge acquisition occurred through informal conversation, more formal verbal exchanges such as meetings were recorded, to leave a paper trail documenting discussions for accountability purposes. Commissioners had substantial access to other documentation, much of which was unsolicited. Documentation was often sent electronically. Documentation included performance, activity, financial and referral data from a range of health-care providers, directives and guidelines from the Department of Health and regional bodies, meeting papers, business cases, reports, patient satisfaction surveys, guidelines and pathways. Often key points were summarised on a side of A4 or an executive summary, possibly because the volume of reading was unmanageable. For example, governing board members had usually at least a dozen documents of several pages each to read before monthly meetings. Presumably to make this task easier, many documents had standardised cover sheet with information such as title, purpose of the paper and action required. In some cases, executive summaries of one page or shorter directly followed these cover sheets.
Despite this ‘overabundance’ of information, which meant that CCGs were ‘absolutely swimming in data’, a CCG chairperson said they had ‘a staggering lack of . . . intelligent data’ (Simon, CCG chairperson). One way of finding missing but desired information was through the internet. GP commissioners and commissioning managers recounted how they used Google™ or Google Scholar to find the relevant information to contribute to discussions with colleagues, inform thinking about service provision and substantiate the decisions already made.
I go onto Google Scholar or Google, and it’s not very difficult to type in key words like ‘CCG’ or ‘PBC’ or ‘PCT budget allocation evidence’, and Google is phenomenal, and Google Scholar will obviously just give you the articles, and you can usually get there on a single page, obviously go a little bit further, read some of the subreferences, etc., extract the key data and some of the graphs, put it onto a PowerPoint, and either present it at a board meeting or in one-to-one discussion with colleagues.
Patrick, GP commissioner
The process mentioned above of reading the subreferences, extracting the key data, entering findings onto a PowerPoint presentation and presenting the data to colleagues clearly illustrates the simultaneous processes of knowledge acquisition and transformation, as sifting, selecting, rejecting, synthesising and incorporating takes place to reshape the original knowledge (see Chapter 6, Ways knowledge is treated).
Useful but overlooked sources
Although where and how commissioners acquired information was important, the obvious sources that were overlooked were also interesting. For example, several participants from one commercial provider pointed out the vast number of good-quality data that commissioners did not use, including Public Health data sets. Another former commissioning manager recounted how she had been unaware of the wealth of information available to her from internal sources when she had worked within the NHS, and so had not known what to ask for.
. . . when they [commercial providers] came in and said, ‘Who is driving your costs?’ at which point I was like, ‘What do you mean? I don’t understand that question’. I’ve got this demographic. I’ve got this population, deprived population here and here. I’ve got this overall growth in population, and this wodge of money at that hospital, and that wodge of money at this hospital. That was my data points. And they came in and said, ‘Well who is driving your costs?’ and came back with a pile of paper this high saying, ‘All these people have been in hospital more than three times in the last 12 months, they’re driving your costs’. I didn’t know I had that data, I didn’t know to ask for it, and now I know.
And where did they get that data from?
From my own IMT [information management technology] department!
Kirsten, commercial consultant
Research evidence
This section discusses the limited impact that research made on commissioning, usually appearing digested in other forms such as NICE guidance, locally developed briefings and embedded within software tools. However, we did identify a couple of examples of explicit use of research in one site in the form of evidence reviews drafted by local Public Health consultants. Elsewhere, another CCG was attempting to become a more robust ‘evidence based commissioner’.
Implicit use of research evidence
For commissioners, the word ‘evidence’ often meant any source of information other than personal experience and anecdotes. When asked about the use of evidence in commissioning decisions, participants often mentioned best practice guidance, hospital and primary care data and Department of Health documentation.
Academic research made a fleeting appearance and was usually embedded within other forms. Most participants did not talk about research evidence unprompted and research evidence was only formally presented at two of observed board meetings (of the same CCG). Instead, participants at another commissioning organisation talked about how research was implicit ‘in the system’ (Alan, NHS commissioning manager), although there was no formal mechanism or any obvious attempt to check if it was being appropriately and systematically adduced. Instead, clinicians and commissioners were ‘expected to keep on top’ of their area (Alan, NHS commissioning manager) sometimes by having their ‘ear to the ground’ with national and local networks (Vidur, GP commissioner). The expectation was that clinical commissioners would bring a research perspective with up-to-date, research-based assessments. In an observation of one CCG meeting, this higher level of understanding of research was visible when a GP commissioner explained ‘funnel plots’ to his colleagues, although we do not know if GP commissioners as a profession were this knowledgeable.
Difficulties with using academic research
When asked about academic research, participants mainly talked about the difficulties in accessing and using research. These included ‘academically very robust’ interventions not working in clinical practice (Jane, NHS commissioning manager), the difficulties in finding applicable, relevant research or tools, the challenge in drawing conclusions from literature reviews when there were substantial variations in the intervention, lack of commissioner time and skills to do comprehensive reviews, difficulties in interpreting the ‘spin’ within abstracts (Mary, Public Health consultant) and the length of time for locally commissioned research to produce meaningful outputs.
One Public Health consultant discussed the difficulties in making research digestible for consumption by commissioners.
So there is an issue around the evidence, and often it’s very sort of generalised, the conclusions can be quite vague, so it’s quite difficult to turn that into kind of an operational plan. Then you need to pull the evidence together, and there’s always the risk that you’ve missed out a really critical recent study which contradicts everything else. Then you’ve got to find a receptive audience, and often it will come across as being quite kind of ivory tower, and is this really of direct relevance to what we’re trying to do?
Rick, Public Health consultant
Explicit use of research (or research-like) evidence
However, research-based information was sometimes evident. Two commissioners (from different CCGs) mentioned conducting literature reviews for specific projects, or contracting commercial providers to review the literature for them. Many participants mentioned NICE guidelines. Although NICE guidance was described as ‘hard edged’ with stronger links to academic research (Karen, Public Health consultant), it was not mandatory to apply, and locally implementation was sometimes problematic if local services did not exist to support the guidelines. Another GP commissioner made the point that NICE guidance was ‘absolutely crucial’ to decision-making but ‘we know we would go bust if we implemented all of them’. So, they picked the ‘best ones’, defined as the most ‘do-able’ (Patrick, GP commissioner).
Local service evaluations were mentioned by participants from three CCGs, when they were asked about research. These included a controlled cohort study of the reablement project, a cohort study mapping the service usage of 50 patients at a local hospital and a controlled cohort study on the impact of case management on hospital usage. The controlled cohort study was led by a local academic GP and was mentioned by several participants, as the findings of this study had a clear impact on commissioning decisions because the CCG decided not to expand the case management service; the evaluation had found that little difference between the case and control groups. However, the nature of the contract was such that the CCG could not recoup the costs of the service, although they did decide not to increase their investment.
Public Health was cited in response to queries about accessing research evidence, for example the Public Health consultant who drafted a briefing on ‘telehealth’ for one subcommittee, but carrying out a robust evidence review was time-consuming. Nonetheless, the subcommittee appeared enthusiastic about this these evidence appraisals.
Teresa comments that this presentation is very, very helpful. People are interested in more reviews of research evidence around unscheduled care, to help with things like education and self-management . . .
Value of this is that if we think of new initiatives we want you to be critical . . .
. . . Can we give things to you (Public Health consultant) to check out?
That is the sort of input we want, and have not had in past.
Meeting notes
Yet despite this enthusiasm, the subcommittee members appeared at a loss in applying the information, especially as much of the research evidence was about ineffective interventions. For example, in observing a meeting where an evidence review on interventions to prevent unplanned hospital admissions was presented, the committee scanned through the interventions, a short discussion ensued on the benefits and disadvantages of one intervention with inconclusive evidence (‘telemedicine’) and the document was then put to one side. We do not know if the document fed into their future thinking, but its use seemed cursory. This group did not appear to consider the disinvestment opportunities highlighted by these reviews. The Public Health consultant who prepared these reviews was aware that the group struggled to apply the information usefully.
Another issue I think, so for instance Sarah Purdy’s work [on unscheduled care], an awful lot of it was like, ‘Well there is no evidence that this works and there’s no evidence that that works.’ And that, it’s really interesting, but then you think, well if we are trying to get people who have these really kind of strict targets, real pressure to reduce costs, and to just come in every month saying ‘We’ve looked at this and it doesn’t work,’ then that’s quite a difficult position to be in.
Rick, Public Health consultant
Evidence-based commissioning
Although in three CCGs research evidence was not particularly drawn on, the ethos of one CCG was explicitly grounded in evidence-based policy-making. This was visible throughout the organisation. In meetings, participants, including lay representatives, often asked ‘where’s the evidence?’ and in interviews participants from this CCG regularly talked about how the application or lack of research evidence affected decision-making.
I’ve had conversations [with colleagues] about, ‘Well, you know, we shouldn’t be putting that down to say it will make savings because there’s no evidence that it will,’ versus me saying, ‘But actually we’ve still got a statutory responsibility to deliver a balanced plan, and if I take those savings out they need to come from somewhere else.’
Carla, NHS commissioning manager
One GP commissioner from the same CCG noted that the repeated refrain for evidence for which they are ‘always duty bound’ can stop decision-making by commissioners.
. . . [they become] frozen because you can’t make pragmatic decisions. Because it’s like America is out there but they will not set sail until they know it’s there . . . So with interventions like ‘telehealth’, ‘they’ll say ‘well we are not doing that.’
Patrick, GP commissioner
Briefings
A formal mechanism for improving the evidence-based practice of GPs was clinical briefings drafted and sent out by a GP commissioner from one study CCG. Initially, these clinical briefings just went to one practice, but then the CCG disseminated the briefings across the patch. The briefings evolved from focusing on clinical evidence to including updates from local services, such as feedback from local hospitals on problematic referrals. Again, in the act of acquiring information for the briefings, the GP commissioner was already transforming knowledge as some information was discarded and other information was selected, reshaped and synthesised to reflect local circumstances.
Within the commercial providers, regular briefings were drafted and disseminated. The information from these briefings was sometimes passed on to the NHS clients via e-mail. One commercial consultant had a self-appointed task of pulling together regular briefings with research from ‘think tanks’, NHS Improving Quality, Public Health observatories and ‘leaders of thinking’. He also included information from Deloitte on health-care innovation (North American), McKinsey, the Mayo Clinic and Dartmouth Atlas to ‘bring in stuff that might be a bit different from what you normally see on the Department of Health websites’ (John, commercial provider). Once John left the company, however, no one appeared to take up this role – another example of the way in which knowledge acquisition was dependent on the happenstance of who was present. Conversely, in the other commercial company, this role was formalised, as a designated consultant sent out weekly bulletins. If this staff member was unavailable, another was appointed to this task. The consensus from commercial provider staff at both companies was that these briefings had helped them become more evidence based.
Commercial providers and academic research
Many software tools marketed by commercial providers were predicated on academic research. For example, one tool arose from decades of academic research initiated by clinical teams. Development of the tool was ongoing and one external provider encouraged researchers around the world to carry out independent studies using the tool. Results were published on its website ‘to impart knowledge of how it’s been applied in different areas’ and establish ‘rigour’ (Stan, commercial analyst). Consultants from the company regularly attended academic conferences where they gave presentations on the tool and made ‘opportune’ contacts (Katie, commercial consultant). Engaging academics was important to the success of rolling out the tool.
And how important do you think universities are in terms of expansion?
Extremely. Absolutely, that’s the key, and that’s what differentiates us from [competitors] that we are research oriented, and that’s what the [tool] is based on.
Katie, commercial consultant
In summary, commissioners defined evidence in many ways, but not usually in terms of academic research. Academic research was occasionally explicitly sought, but usually it had been digested, transformed and embedded into forms such as NICE guidance, software tools, the clinical knowledge of GP commissioners and local briefings, presentations and conversations. Importantly, commissioners did not usually check or confirm the standing of rigorous evidence in such sources, but took it on trust. When commissioners had more direct access to research evidence, they had reservations about and difficulties in applying it to local circumstances. Ironically, a negative consequence of evidence-based commissioning was that without robust evidence commissioners became stalled in their decision-making. The general interest in using research evidence was encouraging, but difficulties in finding applicable, user-friendly research and its inconsistency in providing useful, accessible conclusions meant that the impact of academic research evidence on commissioning decisions was limited.
Box 5 summarises the key points of the chapter.
-
Sources of information for commissioners included people such as clinicians, commissioning managers, analysts, patients and the public, commercial and not-for-profit providers and freelance consultants; organisations included local public health departments, CSUs, health-care providers, Department of Health, NICE and think tanks such as The King’s Fund and the Nuffield Trust. Tool-based information came from software tools from commercial providers, national benchmarking and local dashboards.
-
Local data often trumped national or research-based information.
-
In acquiring information, conversations and stories were important, as oral methods were fast and flexible which suited the changing world of commissioning. Unsolicited documentation was ubiquitous and often sent electronically. Commissioners used internet search engines such as Google and Google Scholar to find required information.
-
Once acquired, indeed in the very act of its acquisition, information went through many cycles to be rejected, filtered, embellished and/or modified before further dissemination.
-
Commissioners often did not use information sources available such as Public Health data sets and CSU data.
-
Academic research was occasionally sought, but usually was already digested, transformed and embedded into NICE guidance, software tools, GP clinical knowledge, presentations, conversations and local briefings. Its provenance and appropriateness was taken on trust and not checked. Disinvestment opportunities highlighted by research reviews did not trigger debates or influence commissioners’ thinking.
-
The general interest in using research evidence was encouraging, but difficulties in finding applicable, user-friendly research and its inconsistency in providing useful, accessible conclusions meant that the impact of academic research evidence on commissioning decisions was limited.
Chapter 6 Knowledge transformation
Introduction
This chapter addresses the research question:
What are the processes by which health-care commissioners transform information provided by other agencies into useable knowledge that is embedded in commissioning decisions?
Having discussed knowledge acquisition, this chapter discusses knowledge transformation, although as stated previously the phenomena of knowledge acquisition and transformation are inextricably linked. Because this is a study of knowledge transformation between commissioners and external providers, we will provide examples involving commercial, not-for-profit and freelance providers, public health departments and CSUs.
Knowledge transformation necessarily involves the acquisition and modification of information. In analysing our data, we identified five conduits through which knowledge was acquired and transformed. We use the term ‘conduit’ deliberately to emphasise the sense that knowledge flowed through these channels between two or more parties whose exchanges involved both receiving and transmitting information, sometimes simultaneously, and to evoke the transformational flow of that we observed. The conduits were, of course, inevitably intertwined and interlinked, but are treated separately here for the sake of clarity.
-
Interpersonal relationships, whereby commissioners sought information held by others with whom they had ongoing relationships.
-
People placement, whereby commissioners accessed information embodied by external provider consultants with particular skills, experiences, backgrounds and expertise, who were placed among them.
-
Governance, whereby commissioners were expected in their role as publicly accountable, statutory organisations to act on information from elsewhere (e.g. Department of Health, NHS England teams) or set up internal structures and processes.
-
Copy, adapt and paste, whereby commissioners accessed information from elsewhere which might be locally applicable.
-
Product deployment, whereby commissioners accessed information held in electronic or non-electronic tools and methods produced by the external contractors and deployed by or for the clients.
These five conduits were not the only ones commissioners and external providers employed, but they were most commonly found across case sites to a larger or lesser extent. To increase the potential usefulness and application of the knowledge passing through these conduits, commissioners continually carried out two processes: contextualisation and engagement. Contextualisation involved taking knowledge and filtering and focusing it through a local lens. Engagement entailed promulgating and refining the knowledge further by involving, informing, enthusing and/or motivating the right people.
These conduits were employed at various times during the decision-making trajectory, from the moment that a commissioner asked, ‘What do I need to know and from what/whom will I get the information I need?’. Through these conduits, commissioners collaborated with many colleagues internal and external to identify gaps in their current knowledge, attempt to fill those gaps, assess the usefulness of the information received, apply what was useful and modify/discard what was not, identify new information gaps, attempt to fill those gaps, assess usefulness and so on. These iterative, repeated cycles were continually layered and multifaceted, making the tracking of any particular information/knowledge (such as research evidence) and its trajectory difficult to trace.
This chapter describes the five knowledge transformation conduits, the processes that commissioners used to maximise the use of knowledge and the ways knowledge was treated.
Interpersonal relationships
Interpersonal relationships came into play when commissioners sought information held by others with whom they had ongoing relationships. For example, one commissioning organisation contacted consultants from a local not-for-profit organisation to ask for possible external organisations with specialised skills to inform a contracting initiative. Because professionals from the two organisations had worked together before, the commissioners knew that the not-for-profit agency was well placed to advise them. Of all the conduits, interpersonal relationships appeared the most influential and were implicitly nested into people placement and product deployment.
Interpersonal relationships were visible at different times and played out in key relationships. Some key relationships were positive and some less so, which led to varying levels of impact. For example, one commercial provider allocated consultants with experience in commissioning to help staff from commissioning organisations to interpret data from software tools. A few commissioning consultants were ‘very, very good individuals within [commercial provider] who added a huge amount of value in terms of helping people with their commissioning problems’ (Alfred, NHS client). Others appeared less useful to commissioners and made less progress.
In one commissioning organisation, interpersonal relationships were closely linked to colocation and the face-to-face, informal contacts that colocation permits. In interview, a GP commissioner noted the number of desks he sat away from the Director of Finance (two) and the Director of Public Health (eight) in their open-plan office, and credited this proximity with the high level of collaboration. A freelance analyst working with this CCG was also aware of the importance of informal, face-to-face encounters with local GPs.
If you’ve got trust and if you’ve got experts in both domains really closely engaged, literally, and by that I mean literally sat at the same computer fiddling around with stuff on the screen, bouncing ideas off each other, that for me was where all these light bulb moments came.
Randall, freelance analyst
One Public Health consultant talked about how through building relationships, Public Health had transformed commissioners’ understanding of the commissioning cycle, highlighting the importance of needs assessment. This was particularly important given how thinly stretched the Public Health team was across five CCGs.
I suppose what we’ve done a lot over the last two years has been around really relationship building. Because one of the problems with having five CCGs and a sort of relatively lean Public Health team is actually, you know, physically being able to be a presence which, I mean I know that just being somewhere is not the same as imparting but if you’re never there and they can’t see you, that is a problem . . . I think we’ve been very successful there with the CCGs actually supporting them to understand the commissioning cycle, and that it starts with a needs assessment.
Sandra, Public Health consultant
With commercial providers, interpersonal relationships sometimes appeared to depend on a perception of shared ‘public sector values’ such as partnership, knowledge freely exchanged and the primacy of patient benefit (Alfred, NHS client). We observed several instances where commercial consultants attempted to capitalise on their NHS credentials and knowledge to build relationships.
. . . to get credibility if they’ve not seen your CV [curriculum vitae] beforehand, is that I’ve worked in the NHS, so I’m clinically intelligent in that sense, and I’ve been in their shoes most of the time, so I’ve often been in the wards with people that I’m working alongside and I try to understand what their issues are. But I can also work with them as a person, so who they are and what issues they are facing. And I mean I know that’s very effective, because I get an awful lot of disclosure very early on in terms of what the real issues are for people.
Jessie, commercial consultant
In summary, interpersonal relationships manifested themselves in different ways, but often appeared dependent on informal, face-to-face encounters and demonstrating shared values through claims of belonging to the ‘NHS family’.
People placement
Another conduit, closely linked to the above, was people placement, whereby the necessary skills, expertise, background and experiences were embodied in the professionals themselves. Ideally, these individuals were embedded within a client organisation. An example of people placement was when a commercial company located two nurses at acute hospitals to check invoices against patient notes. Commonly, the intention behind people placement was to inject knowledge into the health-care system and to foster interpersonal relationships.
Several types of external providers employed the conduit of people placement. For example, a CSU provided regular senior manager input at senior management team meetings and an analyst embedded within the CCG.
Well, we have a very good contact at the CSU, Mike. He comes to our senior management team meetings now once a fortnight. And what we’ve managed to do with his help and support really is get his team to see themselves as welcome within our building . . . And so we need to build up some of the personal relationships which always make these things easier. And we need some of the ease of communication which comes from somebody being on the next desk rather than at the end of the telephone or e-mail.
Tom, CCG chairperson
Although it was relatively rare, some commercial companies managed to embed consultants into NHS organisations, but only if commissioning organisations were receptive.
It was very much a place of work as well, so we stayed up there during the week, so it wasn’t a transient thing either we absolutely became part of their organisation. And we were invited to everything that was to do with that organisation, weren’t we? Whatever happened we were – one of us was involved in something that was going on in there. And so because we were there, and we were very visible, and we were in the same building as the four commissioning group leads, directors, we were very available, weren’t we? (Yeah) And we had lots of drop in questions, so they regularly came to us with questions that weren’t necessarily related to the piece of work that we were doing with them at the time. So they would come for advice and help, wouldn’t they?
And I think because we had built that relationship, we were then seen as an organisation coming in that they didn’t feel threatened by.
Patricia and Helen, commercial consultants
Former public sector organisations such as CSUs employed the people placement conduit with perfunctory matching of skill sets to client needs. With commercial providers, the process of people placement appeared more sophisticated, as the matching of consultant and NHS client was fundamental to success. Good matching considered discipline (e.g. analyst to analyst), previous experience in the care sector (e.g. mental health) and skills and expertise (e.g. knowledge of contracting). One commercial provider, either accidentally or intentionally, also allocated consultants whose personality type filled gaps on the management team (e.g. ‘completer/finishers’ vs. ideas initiators). Some clients wanted international experts rather than ‘recycled NHS managers’ (Kristen, senior commercial consultant), but other clients preferred working with those with NHS background. Softer skills were also necessary.
The front man, Tim, was very good, he knew his stuff, he could hold his own with the GPs, he worked well with the colleagues, didn’t wind anybody up and we had a very productive year out of that working relationship.
Kurt, NHS analyst
Commercial consultants were allocated to projects on the basis of client needs, which were often unclear and highly changeable. Commercial consultants could suddenly be reallocated, leaving NHS clients somewhat bereft.
There’s a piece of work that the PCT want to do which is more about looking at different kinds of contracting options for the future. And we’ve got an expert in that, and it seems absolutely daft me spending ages reading up and scratching my head and only being able to give them part of the solution, when actually John can do it all. And he’s really wanted to get his teeth into something like that. So I’ve explained to them [the clients], ‘This is our expert. I will be moving back. John is going to be doing this piece of work’. But, they’re not happy – I think they’re not happy about me stepping back, but they know that they’ll get what they need and at the end of the day, that’s what they’re paying for.
Jessie, commercial consultant
Although the conduit of people placement relied on the knowledge embodied within individuals, those individuals often chose to relocate. For example, about 20% of study participants at one commercial provider left before fieldwork stopped 6 months later. Many went on to work for rival commercial companies, taking their expertise with them. We also encountered NHS participants who straddled the NHS/commercial provider divide by working concurrently for both. During the data collection phase, no one voiced concern about this intermingling and exchange between the NHS and commercial companies. Subsequently, however, a programme broadcast on BBC Radio 4 questioned the impact of secondments of NHS staff into large commercial providers and vice versa. 44
Governance
Another conduit through which knowledge was obtained and transformed was governance, which we use here in the very broad sense of the structures and processes which shape ‘the way we do business’. Governance is a similar conduit to the others in that knowledge is exchanged and transformed between two or more parties, sometimes from national/regional bodies such as the Care Quality Commission or NHS England and sometimes between different local committees. Knowledge to inform governance came from sources such as national ‘must dos’ and guidance, local financial data and patient-level data. Unlike the other conduits whereby the commissioner actively sought information, with this conduit the commissioner was often the (unwilling) recipient. The governance conduit was visible in processes and structures adopted by CCGs and the way decisions were made. For example, with clinical commissioning medical input was now much more likely to inform decision-making.
In the old days decisions made by the PCT would be made according to what the Department of Health required, the Strategic Health Authority required, the managers thought was appropriate and then we’d also consult with the clinicians . . . and that’s how it would go through. Now it starts with a clinician, the whole innovation, the whole idea. The clinicians drive it through and they bring it to the governing body and say, ‘This is what we want to happen – is it feasible to make it happen?’ The governing body then, as the name suggests, looks at the governance of it, and that’s the right way. That’s a big shift in where the responsibility, where the accountability, where the innovation and the service provision comes from.
Malcolm, CCG chairperson
Because probity and accountability were so important to CCGs, proposals went through several decision-making cycles before ultimate approval. This often frustrated commercial providers and freelance consultants, who complained of slow NHS decision-making, such as Brian:
Think about the decision route. From the project board to the Operations Group – the papers are already out for the March Operations Group meeting.
Why does the Operations Group need to make the decision?
It needs to be the whole community, can get it into the March agenda. [Len is Operations Group chairperson.] [Kevin asks about terms of reference and whether they have delegated decision-making powers.]
Can’t possibly expect every decision to go to them? This isn’t a major decision.
This is our top priority.
The more you push it up the governance ladder the harder it is to make a decision.
The expectation was that we were coming back with a recommendation.
So we will inform them and explain why. Not the same as asking ‘do you agree’?
We are asking for an endorsing decision from them.
Meeting notes
Interestingly, Brian, the freelance consultant above, was a former PCT chief executive, so he was presumably well accustomed to the exigencies of public sector accountability. But a recent study suggests that these structures have become even more prolific with the advent of the Health and Social Care Act 20124 and CCGs. 45 Because proposals were repeatedly discussed in decision-making cycles across several decision-making groups, it was often hard to determine what and when decisions were taken, who was involved or what information had contributed. Nonetheless, as public money was involved, proposals were necessarily subjected to substantial scrutiny.
Besides decision-making processes and structures, the governance conduit was evident in other aspects, including setting strategy, finance, risk and information management. The conduit of governance was most visible in our observations of CCG board and subcommittee meetings. For example, we observed a freelance consultant presenting her report on the Francis Inquiry to a CCG governing body, which considered the implications of the report operationally and strategically. This report necessitated a response from every CCG as a national mandate. The consultant, who was an ex-NHS colleague, took the 290 recommendations of the Francis report, synthesised them into a few categories and benchmarked local performance against these categories. CCG board members found this report ‘really helpful’, especially as the consultant’s assessment was that the commissioning organisation was ‘not starting from zero’ (Hannah, commissioning manager). This then influenced their subsequent decisions on developing a strategy for quality assurance.
The governance conduit was visible in policies around data sharing, which often had a major impact on limiting or preventing knowledge transformation. The desire to use patient-level data to link across data sets was increasing, as commissioners from several of the study CCGs developed patient pathways to inform their commissioning decisions. But this coincided with greater stringency around data protection.
For example, one commissioning organisation wanted to link up their dashboard with hospital data to the risk prediction tool at patient level to learn more about where in their pathways patients stopped using NHS services. Information governance stipulations were that linkage of patient-level data could occur only if there was direct patient benefit to the patients involved. But in the case of the dashboard, direct patient benefit could not be demonstrated, so this linkage was not permitted. Distinguishing between data linkage for ‘direct patient benefit’ versus ‘commissioning’ was not straightforward.
Think that would be great and if the hospital could tell us what happened to them. Can we share that data between hospital and community (i.e. trace a patient journey through)?
[Yvonne says no but Sally says yes.]
Because patient’s been discharged we couldn’t argue that it’s for the benefit of that patient. But you could anonymise. But you couldn’t then link without an identifier to community provider data.
Couldn’t someone call the patient and ask if they could use their data?
If we want to use data for performance we can take to (something).
As long as anonymised that’s fine.
Meeting notes
Moreover, although a participant said that GPs were less enthusiastic about using patient data for ‘planning’ purposes rather than direct patient outcomes (Sanjay, GP commissioner), when GP commissioners realised the restrictions around use of patient-level data for commissioning, there was considerable outrage.
You can’t beat actually following case notes.
That was shot down due to information governance.
Rubbish!! [He is really indignant].
If it is a clinician to clinician discussion you’ll be fine.
In that case I’ve breached information governance lots of times.
There is a distinction if you are looking at the data for a cost saving versus a care issue. General group response is that ‘it is all patient care’.
Meeting notes
In another commissioning organisation, data sharing with commercial providers was an important concern. To populate software tools, commercial providers needed access to patient data sets from different health-care sectors. For the risk prediction tool, all the data for the local general practices and hospitals were held in a data warehouse by a third-party commercial company. This same company also held national NHS data, and so NHS data governance requirements were all met. Nonetheless, several GPs voiced concerns about releasing their data without patient permission, as they were alarmed about data handling.
I know a lot about it, because I’m extremely sceptical because I did not like the idea of [commercial provider] having all of our data. People completely do not understand the data flows and the IT implications of what they were suggesting. So it takes primary care data, merges it with secondary care data, then what people didn’t really realise is that there is a third data set which had no information governance surrounding it whatsoever, apart from [commercial provider] could use it for whatever they wanted and sell it to the highest bidder.
Really?
Well I’m exaggerating slightly.
Patrick, GP commissioner
One practice manager said that he and his colleagues had similar concerns about the association of the risk prediction tool with a commercial company, as practice managers were beginning to see themselves as ‘guardians of the patients’ data’ (Adrian, practice manager). Once the contract with the commercial provider ended, however, the CCG was ‘desperate’ to share patient-level data and roll out the tool, but it was tied up in information governance (Patrick, GP commissioner).
Not all CCGs were concerned about data sharing with commercial providers. An analyst at the same CCG as above noted that data sharing was hampered because influential GPs were ‘at the cautious end of the spectrum in terms of data sharing’ (Charles, NHS analyst). He commented that GPs in a neighbouring county had 100% uptake of the risk stratification tool, because there was not the same level of concern and the other county also had ‘people at very senior level who were driving the value of the risk prediction tool’ both clinicians and managers. Another reason Charles thought practices were reluctant to sign up was that the sign-up documentation was lengthy and technical.
In summary, the governance conduit was mainly visible through decision-making and information governance. With decision-making, because proposals were considered by many different committees, the knowledge was constantly reshaped. Information governance could halt knowledge transformation by forbidding linkage of patient data sets and because of alarm around commercial providers having access to patient data.
Copy, adapt and paste
Another conduit was ‘copy, adapt and paste’, whereby innovations, ideas, tools, pathways, guidance, service redesign and so forth were taken from one context and adapted to a different programme, project, organisation, health-care economy or sector. One commercial consultant, who was a former public sector employee, commented that there was an ‘almost pathological desire’ to ‘copy and paste’ in the NHS (Felicity, commercial consultant). One GP commissioner noted that commissioners were good at ‘foraging around to find something roughly right’, but then had difficulties in testing the robustness of the borrowed concept (Ciara, GP commissioner). To make the imported knowledge work, commissioners and clinicians had to contextualise and adapt the concept locally.
We found many examples of copy, adapt and paste across the case site CCGs. For example, one CCG adopted ‘copy, adapt and paste’ with a commercial pathway tool. Based on NICE guidelines and tailored to reflect local pathways, this electronic pathway tool was intended to sit on GPs’ desktops to provide evidence-based pathways accessible during consultations. This had been adapted in a neighbouring county, to great acclaim. A CCG borrowed and paid for their neighbour’s modified pathway tool and adapted it further to meet their requirements by adding information about local services.
‘Copy, adapt and paste’ was encouraged by copious documentation on best practice, disseminated from the Department of Health, The King’s Fund, NHS Improving Quality and other organisations. One commissioning organisation was constantly ‘horizon scanning’ to look out for pioneering initiatives to appropriate ‘because there are loads out there’ (Carol, NHS commissioning manager). Sometimes, they contracted external commercial providers to ‘bring in research from other areas that says over here they are doing this and how that might be adapted or adopted here’ (Hilda, lay representative). But often they conducted those searches themselves.
Research in this modern world is very quick, you know, it’s really very, very easy to find out who’s doing what. So if you look at A&E and put in GPs in there, you know, I know there’s been national research done, I know there’s The King’s Fund stuff, but in 10 minutes I could go online and find out which other hospitals are publishing information about trying it. So it’s relatively easy to pick a subject matter and say what’s going on out there.
Alan, NHS commissioning manager
In summary, ‘copy, adapt and paste’ was so ubiquitous in the case sites that it was sometimes hard to trace back to the original source of the innovation. Few ideas or ‘innovations’ seemed genuinely original. Moreover, each time an innovation was appropriated into a new context, its content was further modified.
Product deployment
Another related conduit of knowledge was product deployment. Product deployment consisted of the production and dissemination of information via tools, often combined with training in their use that was produced by the external contractors. In one commissioning organisation, the tool was a system-wide business method. Developed from managerial research into organisational behaviour from the 1980s, the aim was to move organisations from a ‘command and control’ ethos to focusing on customer needs. The commercial provider contributed the method and the client brought local knowledge. Although the idea of seeing the organisation from the service user perspective is not new, the combination of the knowledge of the consultants (who were often ex-clients of the method) with an overarching method that prioritised ‘principles’ over ‘rules’ (e.g. downgrading box ticking to meet governance requirements) seemed to change the way that service redesign was viewed.
And I think what I’ve learned, which actually, in some ways, when I say it out loud seems so simplistic, is that actually, if we do the right thing for our patients, then it actually is cheaper, quicker, more efficient, more effective.
Jane, NHS commissioning manager
But a non-electronic tool was unusual. In this study, product deployment usually involved software tools developed by commercial providers for invoice validation, scenario modelling and risk prediction. Risk prediction tools were most common. These tools aggregated hospital and primary care data to work out the current and predicted costs of patients based on their conditions. This information was usually used to identify patients at high risk of hospital admissions for interventions such as case management by community matrons, although one CCG was piloting use of the tool for resource allocation to general practices.
Training NHS staff in operating the tools was part of product deployment. One tool provider set up virtual online webinars, whereby NHS clients were taught advanced operational skills by international experts in the risk prediction tool (see Chapter 8, External provider 1). Another risk prediction provider organised face-to-face multidisciplinary sessions, either in GP practice premises or at the headquarters of the commercial company. Participants at these training sessions tended to be practice managers, community nurses, pharmacy leads, commissioning managers and GP clinical leads. The format of the training sessions was interactive PowerPoint presentations followed by a demonstration of the tool populated with local data.
A critical moment in the sessions was the identification of local high-risk service users, as this was a test of the tool’s accuracy and usability. If ‘the usual suspects’ (i.e. known patients) (Ginny, external consultant) were identified and no new information was provided, NHS clients might conclude that the tool offered no added value. But if too many patients unknown to the clinical team were identified, the conclusion could be that the tool was inaccurate. In comparing data output from the tool with their clinical and practice-based knowledge, clinicians formed judgments about the usefulness of the tool.
Two commercial providers used a strategy of training NHS/CSU trainers who in turn trained other NHS/CSU staff. The NHS/CSU trainers came from different backgrounds, including primary care commissioning and information. They taught general practice staff and community matrons and others how to use the tools through group presentations and ‘sitting by Nelly’ methods. However, several NHS trainers noted that those trained to use the tools quickly forgot those skills, as neither the CCG nor other general practice staff requested any output. The skills were not drawn on frequently enough to embed the knowledge (see Chapter 8, External provider 1).
NHS/CSU analysts were key to the implementation of these software tools, as analysts tended to have day-to-day operational responsibility. But the capacity of analysts available within the NHS was low, especially during fieldwork when PCTs were losing staff in the turmoil following the 2012 Health and Social Care Act. 4 Instead, commercial providers trained anyone who showed up from the commissioning organisation to training sessions, which might include those who were uncomfortable with anything more complicated than spreadsheets.
But in one commissioning agency, the NHS analysts were an equal match for the sophisticated expertise of commercial providers. In working closely with the commercial providers to run and test a scenario-generating tool, the NHS analysts identified several ways that the tool could be improved and made these adaptations themselves within the software. These suggestions were then incorporated into the next version of the tool by the commercial provider and rolled out to other clients. Some commercial provider consultants, mainly those with lead responsibility for a particular tool, actively sought these opportunities to enhance tool performance. This was an example of genuine knowledge exchange whereby both commercial provider and NHS client benefited.
Knowledge transformation processes
In adapting and applying knowledge accessed through these conduits, two processes were regularly employed: contextualisation and engagement.
Contextualisation
Contextualisation involved taking information from elsewhere and applying a local lens or filter. Commissioners had an essential role in contextualising the knowledge to local circumstances, but sometimes external providers had to undertake contextualisation as well so that the knowledge was fit for commissioners. When appropriating information from elsewhere, one commissioning manager commented that someone ‘always says our system is not like that’ (Clara, NHS commissioning manager), and so the knowledge needed to be contextualised to overcome this hurdle. One commissioning manager said that contextualisation was the ‘crux’ of commissioning.
I think that’s the crux of our job. It’s really interesting, because you read what you read, and you find out what you can, but then it has to be applied locally. And all localities are different, you know. If you look at [our CCG], for instance, we’ve only X population in our entire area. Geographically it’s relatively small and urban compared to say our neighbours in [county name]. So that alone says something about how you start to think about things. And a lot of activity, research, JSNAs, a lot of Public Health driven sort of surveys about where your deprivation is – all that information is available. And so you have to then balance best practice against what’s reality locally, what you’re doing already good and bad locally.
Alan, commissioning manager
The inherent transferability between the original context where the information was generated and the local situation was important and participants varied in views on how close that matching had to be.
If evidence or trials show that it works elsewhere then we have to believe that it can work here too.
Agree but we can’t assume that it will all work here because the data elsewhere may say 200 but it won’t be 200 here. Need to look at all of the pieces not just one part.
Meeting notes
Contextualisation repeatedly appeared in product deployment. The type of knowledge and information built into software tools was often based on academic research evidence or expert consensus that was not UK based. Often, tools needed ‘Anglicisation’. This contextualisation was crucial, as without high NHS applicability clients tended to dismiss the tool. Some contextualisation was undertaken by external provider staff, but, to make some tools useful, NHS analysts provided further contextualisation for the local health-care economy.
Moreover, NHS clients had to know what to do with the data and needed help applying data outputs to commissioning decisions. Ideally, commissioners had access to an ‘interpreter’ who was known and trusted to assist with this type of contextualisation. For example, in one CCG, a CSU analyst attended meetings where she had a regular slot to present a dashboard and work through the implications of the data with committee members. In another CCG, a GP commissioner talked about his concern that, without a trusted interpreter, commercial providers might take advantage of GP commissioners.
But, you know, what do you do with that data? We know that it must be saying something to us, the fact that a little old lady has had three falls, the ambulances have been round a few times, that probably is telling us something about her, that she’s not very stable. But it doesn’t tell us that she’s somebody that necessarily needs to be assessed by the team. And when our team resources are really very, very stretched, we’re in a bit of a dilemma. We’ve now got a waiting list for people to be assessed, and half of them, I suspect, will be assessed and it will be decided that they hadn’t really got a big problem at all. So somebody coming in and saying, ‘Oh yeah, we recognise all of that, we can do something with that,’ sounds superficially very appealing. Now some of it may be complete bullshit and they may just be angling to get into the markets and that’s what worries me.
Roger, GP commissioner
Contextualisation was integral to the ‘copy, adapt and paste’ conduit and manifested in interpersonal relationships and people placement, where through relationships and by combining knowledge and expertise, knowledge could be transformed into a more useable, applicable form. Training on the tools alone did not appear to be sufficient in helping commissioners to maximise their use of the tools. The outputs had to be interpreted and contextualised by those who understood the tools, so that local commissioners could digest and apply the information. Otherwise, NHS clients did not know what to do with the data. Contextualisation was less evident in governance processes, although translating national and regional mandates required some contextualisation.
Engagement
Another knowledge transformation process was engagement. Engagement was about taking transformed knowledge and exposing and refining it further by involving the ‘right people’. The right people might have important information or perspectives, be positioned to instigate behavioural change (or show reason why that could or should not happen) and/or could tap into local or national networks to make the initiative a success. Again, commissioners were crucially placed to undertake local engagement, but external providers also actively used engagement strategies.
Local commissioner-led engagement was evident with service redesign initiatives, whereby commissioners drew on the experience of those ‘round the table’ (Abbie, NHS commissioning manager). Moreover, engagement of clinicians into commissioning initiatives was discussed across all case sites. For example, in one CCG meeting the group talked about progress on engaging ophthalmologists in developing a community service. Engaging GP practices was also a common topic.
And one other positive thing I think is that in previous times it’s been incredibly difficult to actually engage general practice in some of the quality improvement work because, understandably, you know, independent contractors, getting GPs to come to meetings and do things if you can’t fund them and things is quite difficult, and now obviously that is a role [for GP commissioners].
Sandra, Public Health consultant
With appropriate governance, engagement was visible to ensure that the right people were involved in decision-making. This signalled that the relevant organisations had been consulted and took responsibility. Being perceived as engaging appropriately was a high priority with one CCG, where very large meetings with many different organisational representatives were held, although input from some was minimal (i.e. Public Health, Social Services). In another, the process of engagement led to a different (and smaller) mix of elected councillors and a lay representative as chairperson.
In one contract, engagement by the external provider was clearly implicated in the vicissitudes of the contract’s success. The commercial provider first deployed a team of analysts with little commissioning expertise or NHS knowledge and minimal focus on relationship building and engaging local commissioners. The NHS client complained. The commercial provider then allocated a cohort of new management consultants, many with a background in the NHS, with a remit of ‘commissioner engagement’ to help to interpret and use the data. Some successfully developed interpersonal relationships. The NHS clients were happier. However about a year later, changes within the commercial provider meant that the emphasis shifted and engagement moved more to the background. Moreover, the commercial provider blocked NHS clients from having any direct contact with subcontractors of the tools because of concerns that the NHS clients would drop the main contractor in favour of the subcontractors. This stifled knowledge exchange. The contract was renegotiated; the termination date was brought forward by several months and the NHS clients directly contracted further training from a subcontracted company. Changing levels of commissioner engagement had an impact on the success of this contract.
In summary, engagement helped to spread, and further transformed, knowledge. Engagement was particularly necessary with product deployment, as ample data from this study suggested that without engaging the right people such as influential GPs and practice managers, as well as commissioners, the roll-out and use of software tools was frustrated. Interpersonal relationships enhanced product deployment and appeared to facilitate greater understanding (and possibly use) of the tool outputs generated. Engagement was highly visible within governance.
Model of knowledge conduits and transformation processes
Figure 5 represents the findings of this chapter visually, setting out the relationships between the different knowledge conduits and commissioners’ knowledge transformation processes. In Chapter 8, details from vignettes will be added to the template below to provide examples.
FIGURE 5.
Template of conduits and transformation process. CAP, copy, adapt and paste; G, governance; IR, interpersonal ralationships; PD, product deployment; PP, people placement.
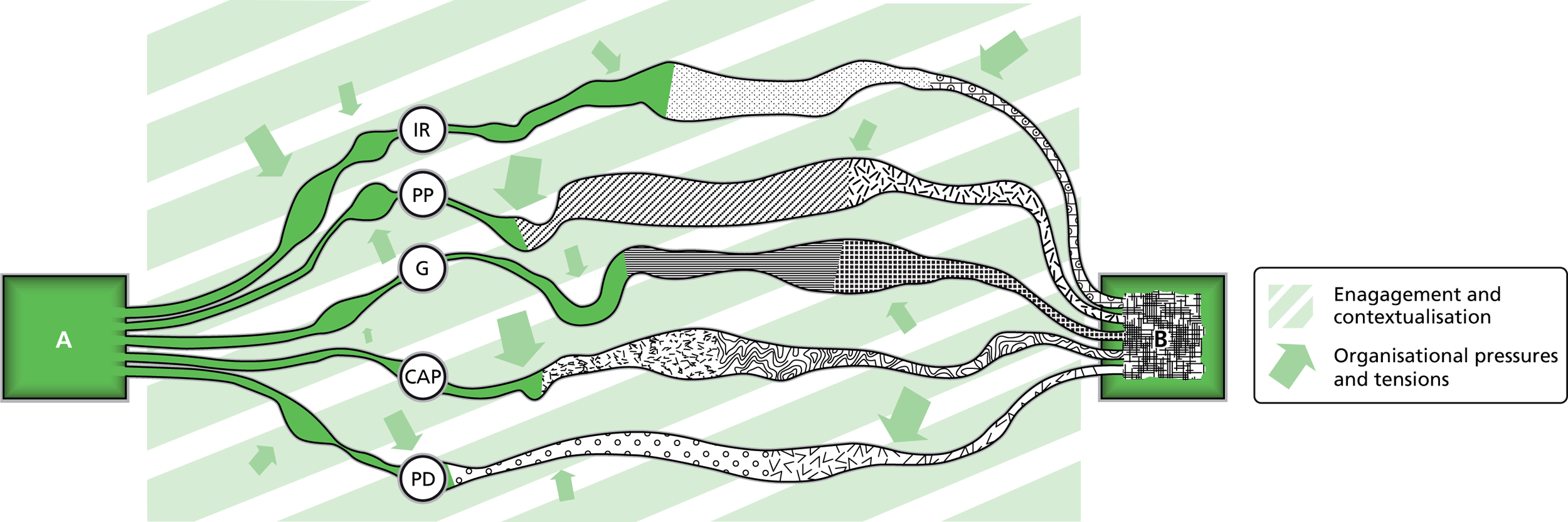
Ways knowledge is treated
As stated previously, we found that knowledge acquisition and transformation were interwoven, with little to differentiate knowledge acquisition from knowledge transformation, as every transfer from one source to another entailed someone’s knowledge acquisition, during which it was at least to some extent altered. In contextualising and engaging, commissioners employed many ways of treating that knowledge. These actions are set out in Figure 6 and are not presented in any quantifiable way. They emerged from taking multiple accounts in the data in turn and analysing how the information had been treated. Through this continual, repeated sifting and milling, useful information was retained and passed on, while less helpful knowledge was discarded. The ways that commissioners treated knowledge were similar to the ways that multisectoral policy-making groups and clinical communities of practice treat knowledge in developing their ‘mindlines’. 20,21,46,47
FIGURE 6.
Ways of treating knowledge.

Box 6 summarises the key points of the chapter.
-
The conduits through which knowledge was transferred were:
-
interpersonal relationships, whereby commissioners sought information held by others with whom they had ongoing relationships
-
people placement, whereby external staff were embodied with particular skills, experiences, backgrounds and expertise and were ideally embedded within the clients’ organisation
-
governance, whereby commissioners received and applied knowledge as publicly accountable officials
-
copy, adapt and paste, whereby commissioners accessed information from initiatives elsewhere and applied locally
-
product deployment, whereby commissioners accessed information held in electronic or non-electronic tools and methods.
-
-
Within these conduits, knowledge was not merely transferred but transformed.
-
Many of the activities of knowledge transfer, exchange and transformation were motivated by the ‘juggling’ art of commissioning discussed in Chapter 3, which entailed the need to manoeuvre information through the system in an optimal manner that, by ‘satisficing’ competing pressures, altered the knowledge itself.
-
Commissioners employed contextualisation and engagement to localise the knowledge and spread it to the right people. In undertaking these processes, knowledge was treated in many ways, such as reshaping, discarding and telling.
-
Face-to-face encounters were important in facilitating interpersonal relationships. People placement and product deployment implicitly relied on activating the interpersonal relationship conduit, which led to greater success in contractual relationships. Without this comingling of conduits, commissioners struggled to interpret data outputs without an interpreter on hand.
-
Information, innovations and ideas were so modified that sometimes the original provenance was difficult to ascertain.
-
Information governance hampered the flow of knowledge by limiting access to patient-level data for pathway mapping and linkage of data sets. Some general practice staff had concerns about data sharing with commercial providers.
-
Of all the conduits, interpersonal relationships appeared most crucial in influencing commissioning decisions.
Chapter 7 The role and nature of external providers
Introduction
This chapter answers the research question:
What is the nature and role of agencies that provide commissioning expertise from the public (e.g. Public Health), private (e.g. commercial providers) and other sectors (e.g. not-for-profit)?
Having discussed knowledge acquisition and transformation in commissioning, we now focus on external providers. As mentioned previously, we use the term ‘external provider’ for several different types of organisations. These include former public-sector bodies such as Public Health and the information function of PCTs that have now predominantly moved into CSUs. This term also includes commercial and not-for-profit companies, freelance consultants and voluntary agencies, although no data were collected from the voluntary sector.
The chapter starts with a classification and description of the types of external providers encountered during fieldwork. An exploration of CSUs and Public Health follows. We then present information on why commissioners use for-profit and not-for-profit consultants and what these consultants offer. The final section covers the views of participants on for-profit and not-for-profit providers.
Who are the external providers?
Classification
During the two-and-a-half years of fieldwork from 2011 to mid-2013, our four case study CCG commissioners worked with many different external providers. We have listed these below, categorised as public, commercial, not-for-profit and voluntary sector, along with the work these organisations (or individuals) were engaged in, where known. Some functions were carried out by multiple organisations; for example, evidence reviews were conducted by commercial companies and public health departments. This list is not exhaustive, as occasionally participants mentioned that external providers had been contracted, but the provider was not named and no further details were available.
The breadth of external providers and their level of involvement suggest that there was substantial external provider presence in NHS commissioning during the fieldwork period, some of which pre-dated the 2012 Act. 4 Table 11 gives an overview of the range and type of external providers working across the four CCGs.
| Provider | Contribution |
|---|---|
| Public sector foundation | |
| Public Health | JSNA and identification of local priorities, well-being and prevention, rapid evidence reviews, health impact assessments, service evaluation, evidence interpretation, horizon scanning |
| CSUs | Transactional (e.g. payment of invoices, contract monitoring, budgeting), performance management, data analysis, bespoke analytical tools, service evaluation, HR, media support, organisational development |
| Primary Care Research Network | No current role but suggestion of contribution to setting up and delivering local research projects |
| Leadership Academy | Learning and development for CCGs |
| Commercial | |
| Bazian | Literature review |
| BDO Consulting | Service review, horizon scanning, capacity filling, data analysis |
| Beacon | Mental health specialists, developing pathway approach to severe mental health |
| Boston Consulting | No information about contribution |
| Capita | Software tool deployment |
| Cobic | Programme management, specialise in developing outcomes-based commissioning |
| CSL | No information about contribution |
| Ernst & Young | No information about contribution |
| KPMG | No information about contribution |
| PricewaterhouseCoopers | Organisational development |
| Swan Partners | Modelling and future spend |
| United Healthcare | Software tool development, commissioning support |
| Vanguard | Development of pathways |
| Freelance consultants (pseudonyms) | |
| Brian | Project manager for condition specific project. Ex-public sector |
| Harold | Analyst developing tool. Ex-NHS |
| Percy | Project manager for portfolio of work. Ex-NHS |
| Randall | Analyst developing tool. Ex-NHS |
| Tina | Responding to Francis report and undertaking project on improving quality. Ex-NHS |
| Not-for-profit | |
| ACG International | Software tool development |
| The King’s Fund | Organisational development |
| Solutions for Public Health | Programme management, event management |
Commissioning support units
Having provided an overview of the different types of external providers, we will discuss each one in turn, except for the voluntary sector, for which we have few data.
Commissioning support units officially came into existence in April 2013, a month before the bulk of the fieldwork stopped. At the time of writing this report (spring 2014), the future of CSUs seems uncertain, as there is substantial debate about reorganising CSUs, merging them and/or creating partnerships between CSUs and commercial organisations. Uncertainty was a feature also during fieldwork, but this was mainly focused around the role of CSUs and ways that CSUs and CCGs could work together. Sometimes this relationship was challenging, partly because CCG clients often were not clear about the problem, the intended outcome, ways to monitor progress or the unintended consequences of their interventions. The CSU–CCG relationship could also be hampered by CCGs making a ‘deluge of requests’ for data, many of which were quite similar. This led to ‘muck spreading’ rather than a strategic approach.
A variety of different staff in CCGs ask a very large number of questions of our informatics function, some of which are different questions, or slightly different questions, so that they’re not asking in a joined-up way, if you see what I mean. But equally our staff, sort of under that deluge of requests, run the risk of just sort of getting stuck in front of their screen trying to find answers to those requests . . . it’s rather at the moment as if between us we’re driving a muck spreader, and we’re spreading masses of information all over the place. Whereas actually what we’ve got to do is target the fertiliser where the plant is.
Mike, CSU analyst
Commissioning support units and study Clinical Commissioning Groups
The four case CCGs contracted three different CSUs. The CCGs had quite distinct relationships from their CSU.
One CCG had a large internal team to avoid dependence on the CSU, which they felt was too removed. A participant intimated that the ‘best’ former PCT staff had been cherry picked by the CCG and those without posts then went to the CSU. This CCG bought financial services and ‘transactional’ activities such as payment of invoices, but the CCG still carried out internal finance reporting such as budget reports and contract monitoring. Another participant was clear that he would prefer CSUs not undertake service design, as local knowledge was needed. The general sense from this CCG was that the CSU was an external organisation.
Commissioning Support Unit staff embedded within this CCG included a pharmacy advisor, human resources support and a small team for extra contractual activity. A participant said that embedding CSU staff within the CCG was key, as GPs liked to work with those they knew. Without embedding CSU staff, the likelihood was that the CCG would create internal support services duplicating those offered by the CSU.
GPs tend to work on a one-to-one relationship, and better the devil they know sort of example. So to work with an anonymous organisation, they will find a challenge. And I can see Clinical Commissioning Groups up and down the country wanting to recreate lots of commissioning support services within their own environment, because they’ll be wanting to build relationships with people they know.
Sarah, NHS commissioning manager
In another CCG, the CSU and CCG worked more closely together. This particular CCG was keen on using data and tools to inform commissioning. The CSU carried out routine data analyses, but they also built bespoke tools and supported software tools from commercial and not-for-profit providers. The CSU ‘offer’ included media support, responses to Freedom of Information requests, public and practice engagement, human resources and organisational development, recruitment, workforce planning support, risk management, information governance, IT support to the CCG and general practices, horizon scanning and financial activities such as managing staff payments. The CSU also offered a scheme to fill ad hoc capacity gaps in the CCG.
The CCG had a close relationship with a senior CSU manager and a CSU analyst; the latter ‘had been around for donkey’s years’ and took the role of ‘principal analyst’ (Connie, CSU analyst). She was highly regarded and well embedded within the commissioning organisation with her own desk. Because of this long-standing relationship, this analyst believed that she was not seen as a threat when requesting commissioning plans or making suggestions. Her role was to liaise with the CCG and the team back at the CSU offices that did ‘a lot of the actual [number] crunching’ (Connie, CSU analyst). CCG staff could also use her as an access point to find relevant expertise within the CSU. Another important role was interpretation, as this analyst helped CCG commissioners to understand outputs from the CSU.
Some of the reports can be quite monstrous. And, you know, they were bravely wading through it all, which was frustrating for them, and it wasn’t fair on them, because there should have been someone there to assist them.
Connie, CSU analyst
In observations, the reliance of the CCG on this principal analyst was notable. During one meeting of a subcommittee, she was not able to attend and the members had no access to the dashboard tracking unscheduled admissions. This caused significant consternation and some negativity.
[Morris asked if it was possible to have an update on the gaps in the dashboard.]
We have no dashboard.
The difficulty is that the information service hasn’t been able to complete the work we wanted them to do because they were doing the QIPP [Quality, Improvement, Productivity and Prevention] information plan and HRGs, so staff were pulled off our stuff. We are not happy about this and are trying to get it resolved.
We felt we were getting real traction in November.
Difficult times at the moment, changes in the system are having an impact but we are where we are . . .
Very frustrating.
Don’t give up hope. Connie will be back on it.
Presumably we are paying. If she is not available then they have to get someone else.
Meeting notes
Commissioning support units and commercial providers
Having looked at the relationship between CSUs and the study CCGs, we now discuss general findings about the interactions between CSUs and commercial providers.
Commissioning Support Units had complicated relationships with commercial providers, working sometimes in collaboration and sometimes in competition. For example, one CSU manager commented that in her experience CSUs and commercial providers best worked together in partnership whereby CSU staff offered local knowledge to sense check and interpret the data.
[Commercial provider] have come in and developed the data warehouse to take the SUS [Secondary Uses Service] data. But the data warehouse has only become useful because our data managers have got involved in looking at that and interpreting the data for them to say, ‘Right well you’ve got um – um you’ve matched this particular data item wrong,’ or, ‘You’ve got to filter for this,’ or, ‘You need to be aware of that,’ and then quality checking the information, so that they’ve actually set up the data warehouse to process the information correctly.
Joan, CSU manager
Another CSU manager planned to offer a mediation service, whereby CCGs could go to CSUs to identify commercial and not-for-profit providers for other work. But there were signs in some CCG–CSU relationships that CCGs might turn to commercial providers out of dissatisfaction with CSU performance.
I think that’s bizarre. At the end of the day, if we’re having this sort of contract arrangement, then if we’re saying to an organisation, ‘We’re paying you X number of pounds to provide us with the data,’ they can’t come back and say, ‘Well we can’t do it because we’re too busy doing something else,’ having agreed to undertake that body of work. They’re essentially in breach of contract . . . I think what’s probably going to happen is I think they’re going to shoot themselves in the foot potentially. Because I think people will go outside of the CSU when they’re allowed to.
Anthony, GP commissioner
Competition between CSUs and commercial providers became increasingly common over the study as they bid for the same business. One commissioning manager recounted an experience when a CSU did not bid for a contract because among the competition was a commercial company with whom the CSU had previously worked. His interpretation was that the CSU knew that they would struggle to win the contract, because the analytical service of the commercial provider was superior.
In April 2014, we conducted our final interview. This was 1 year after CSUs had been launched and 18–24 months after our initial data collection. Although the viewpoint of this particular commissioning manager might be uncommon, he mentioned that in tendering exercises the quality of bids from the CSUs had been disappointing.
And I suppose there is a sort of basic commercial lesson to be learnt out of this in that if the CSUs are moving as they are towards a place where they need to go out and win business, they need to raise their game substantially both in terms of their customer orientation, just the whole sort of attitude, but also in terms of the amount of careful, competent work that they need to put into preparing bidding documentation, because some of it was just woefully inadequate really.
Jacob, NHS commissioning manager
In summary, the relationships between CCG and CSUs varied from distant to quite close, with some CSUs offering a broad spectrum of services. In general, CCGs trusted that the CSUs had the interests of CCGs at heart, but in practice there were concerns that the CSUs struggled to manage the demands of multiple commissioning clients and produce useful output. Embedding CSU staff within CSUs was common. The relationship between CSUs and commercial providers could be collaborative or competitive and there were some concerns that CSUs were not competitive enough and/or not adept at bidding for contracts.
Public Health
Like CSUs, Public Health was a former PCT in-house function separated from commissioning with the 2012 Health and Social Care Act. 4 Public Health maintained its public sector status, so commissioning colleagues tended to trust the motivations of their Public Health colleagues. But Public Health had moved into local authorities. One consultant, who was a former NHS analyst, was concerned that this would marginalise Public Health still further, as historically the links between local government and NHS organisations had been tenuous.
All CCGs in this study accessed Public Health for information on JSNA to determine the priorities for their population. But, beyond that, clinical commissioners had differing perceptions on the usefulness of Public Health.
In one CCG, Public Health had a clear role in accessing, synthesising and interpreting research evidence, as a Public Health consultant had carried out evidence reviews for a subcommittee. His motivation was to find ways that Public Health could engage with and influence CCGs. In addition to evidence reviews, this local public health department had undertaken ‘deep dive’ needs assessments, pathway redesign, individual funding request evidence reviews, strategy development, input into Quality, Improvement, Productivity and Prevention (QIPP) plans and had helped to ‘interpret things like the Vitamin D guideline from the CMO [Chief Medical Officer] letter’ (Sandra, Public Health consultant). They also contributed to a service specification on cardiac rehabilitation. Moreover, they brokered relationships between a local charity promoting an exercise referral scheme with the relevant GP commissioning lead.
Within this CCG, one GP commissioner was enthusiastic about Public Health involvement in commissioning with their ‘massive amount of expertise’ and valuable local memory (Ralph, GP commissioner). Another GP commissioner was less clear about the contribution that Public Health could make, noting that Public Health kept asking the CCG what was needed, but as a new organisation the CCG neither could clarify their needs nor understood what Public Health could offer. However, although the relationship between this CCG and Public Health was still under construction, substantial goodwill clearly existed between the two.
In another CCG, the relationship appeared less promising. Two GP commissioners commented that they did not have a clear vision of how Public Health fit, although the post of Director of Public Health was a joint appointment between the CCG and the local authority to help collaboration. They thought that the Director of Public Health overemphasised well-being, inequality, deprivation and prevention. In observations, the Director of Public Health presented data in a way that appeared to confuse GP commissioners. Nonetheless, the Director of Public Health was a widely visible, vocal member of the CCG governing body. In this particular CCG, the ability of Public Health to influence the CCG appeared to rest quite heavily with one individual.
In summary, during fieldwork the role of Public Health was still under discussion. Commissioners tended to trust the intentions of their Public Health colleagues, but views on the usefulness of output varied. Several participants commented that Public Health overemphasised the well-being and deprivation agenda at the expense of producing service evaluations and evidence reviews that would be of more use to commissioners.
Commercial and not-for-profit providers
Reasons for working for commercial and not-for-profit providers
The rest of the chapter covers commercial and not-for-profit providers. First, we will present reasons that NHS professionals moved to commercial and not-for-profit providers and then discuss cultural differences between the NHS and commercial sectors, reasons for contracting commercial external providers and attitudes towards the use of commercial and not-for-profit providers.
In interviews, we found that many consultants from for-profit and not-for-profit providers had ex-public sector or NHS backgrounds. Ex-public sector professionals said that they joined for-profit and not-for-profit companies for several reasons. Two former information managers believed in the product of a not-for-profit and wanted to promote it more widely. Another ex-information manager moved to commercial consultancy because he became ‘fed up with the NHS’. He thought he would have more influence outside than in (Rhett, commercial analyst). After over 15 years in the NHS, Jessie also felt that she could make more of a difference from the outside. Inside the NHS, she often felt ‘constrained’, whereas now ‘there’s more opportunity and I’ve found that I’ve been able to be more effective in driving change and changing people’s behaviours and attitudes than I was when I was an [NHS] employee’ (Jessie, commercial consultant).
For analysts, the differences between employment in the NHS and commercial sector were particularly stark. The main reasons for departure from the NHS were career progression and job satisfaction. An analyst said that in the PCT he felt like ‘a small piece in a larger clockwork’, whereas with the commercial provider he had ‘free rein’ to make decisions which made him feel ‘more important’ (Ranulph, commercial analyst). After 12 years in the NHS, Doug left because of lack of progress in IT project management. He was interested in independent contracting or interim management but needed more private sector experience. Only one participant raised the issue of pay, claiming that salaries in the NHS and commercial sector were commensurate, although this is difficult to believe given the tendency for NHS analysts to be graded at bands 5 or 6 (currently £21,478–34,530 annually).
Joel appreciated that commercial analysts were allocated work on the basis of their skills and the ‘whole emphasis is a lot less about hierarchy’ (Joel, ex-NHS commercial analyst). In the NHS, the quantity and quality of analysts was substandard, as ‘one of the frustrations with the NHS is that they don’t reward excellence and knowledge’ (Joel, commercial analyst). Because analytical staff had limited prospects, good analysts tended to leave or went into management, which meant that they were not benefiting the ‘coal face’. This is a familiar management problem.
A NHS commissioning manager who had worked with both NHS and commercial analysts thought that the NHS analysts were ‘a fairly dejected bunch who are not very loved or cared for’. This was reflected in the quality of their work.
I think the NHS, they don’t have the same motivation to trawl through the detail that [commercial provider] have. My experience of information staff in the NHS is they’re kind of a fairly dejected bunch who are not very loved or cared for. And I think that sort of is reflected in the quality of the work they produce. They sort of churn out the monthly monitoring reports or a standard monthly interpretation of ‘We’re over-performing in cardiac, we’re under-performing in urology,’ and that’s about it. And the [commercial provider] analysts seem much more interested in understanding what the data is telling them, so moving on from just analysing data to the sort of information intelligence insight end of the spectrum.
Paula, NHS commissioning manager
Several former NHS analysts now working for commercial companies agreed that NHS work was dull and the focus was not on interpretation, whereas commercial analysts were more knowledgeable about data application.
I was in a meeting this morning with um – I won’t name the PCT, but it was a PCT. I spoke to two analysts and the programme manager, and the programme manager knew what they were doing, the analysts were contractors who were just brought in and knew the nuts and bolts of it, but didn’t have any knowledge, and were just there to churn out the information. And I think the difference is that our analysts actually know a bit more than just churning out the data, because they can apply more knowledge around the business and the NHS.
Howard, commercial analyst
Cultural differences between the NHS and commercial providers
Working harder and faster
Several people used the word ‘liberating’ to describe their experience of working for commercial providers, as their ideas were given substantial internal support, which was less common in the NHS. A difference that Jen noted was that commercial provider staff worked harder and faster and ‘no’ was not an option. ‘If a customer asks for it then work it out’ (Jen, commercial consultant). Tim said that moving to the commercial provider was a ‘massive shock’ because the NHS was ‘very relaxed; there weren’t many demands put upon you,’ whereas in a private company there were. Patricia and Janine also thought that commercial companies worked faster, whereas in the NHS there was substantial discussion before any action, arguably to meet the governance rules for a publicly accountable agency.
Moreover, commercial consultants said that many NHS projects were not followed through. But work streams contracted with commercial providers also failed to materialise. For example, one PCT asked a commercial provider to facilitate workshops with GPs on their information needs, as part of the transition to CCGs. The commercial provider then developed a survey of GPs with the aim of assessing GP knowledge about commissioning. This survey was never administered. In another example, a major consultancy worked with one PCT to develop a Public Health forecasting model, but the analyst kept finding ‘glitches’ and informed the management consultancy. Eventually the project was dropped, as both the management consultancy and the health-care clients lost interest.
Working to the brief
Jen noted that results were more important than process for commercial providers. Jemma and Howard made similar comments, while Vicky said that commercial providers thought about commissioning in terms of ‘what are the key problems we’ve got to solve? . . . What are we actually looking to achieve?’ (Vicky, commercial analyst). Perhaps because of the iterative nature of commissioning, NHS clients often struggled to conceptualise work in these terms, so the brief was unclear and the value for money difficult to assess.
So I – I think that there is a – it’s ambiguous about the value for money that people of [commercial provider] give, to be quite honest with you . . . I mean to be fair to them; they’re not given a clear brief.
Percy, freelance consultant
Unclear briefs not only resulted from lack of precision around problems and outcomes, but also raised potentially unrealistic expectations of what commercial providers could offer.
I think my view, and especially going through that process of that change, was the NHS [client] did not know what they wanted. And I think sometimes they think, if they have the private industry come in, we’ll give them all the answers. But you can’t give them the answers without knowing the question.
Patricia, commercial consultant
The lack of clarity about problems and outcomes that affected the quality of briefs repeatedly arose in one contract. Within the commercial company itself, the consultants could not agree the level of detail needed in a brief before it was signed off by both parties. Some consultants wanted very clear remits and milestones while others were prepared to be more flexible. When the senior management team at this company changed, the previously more easygoing, adaptable approach of some consultants was replaced by a strict edict to only ‘work to the brief’. Any activity not detailed in full would require extra payment. One client said that it was ‘much more obvious that they’ve allocated 3.25 hours to do a task and then they are out of there’.
Previously, as clients we’d say, ‘We’d like this room painted red’. And [commercial provider] would respond, ‘Fine, red, what colour red? Okay we’ve got it’. And now under new management they say, ‘We’ll buy 3 litres of red gloss paint and we’ll paint this wall X and it will take Y amount of time’.
Susie, NHS client
Eventually the commercial provider’s insistence on only working to the brief was a contributory factor to the premature cessation of the contract.
Finding ‘ethical’, non-profit-driven commercial companies
Possibly to assuage misgivings about moving from the public to private sector, many ex-NHS consultants unsurprisingly stressed the ‘ethical’ nature of their commercial provider, stating that the principal intention of these companies was to improve the NHS, not generate profits for shareholders.
Doug said that he chose to work for his external provider because it was ‘not totally corporate’ and ‘there was a real sense that we are here to improve the NHS not to make money out of it’ (Doug, commercial analyst). Jemma had worked in a pharmaceutical company, the NHS and a commercial provider. She felt uncomfortable ‘ethically’ in the pharmaceutical company and happier in the NHS, and thought the commercial provider was a ‘really nice balance between that ethical and commercial approach’. She explained that although the commercial company was ‘fuelled by commercial drivers at the end of the day which influences the way we work and the decisions we make’, there was a ‘genuine interest in producing outcomes for the benefit of people other than our own organisation’ (Jemma, commercial consultant). She was ‘shocked’ when she moved into the NHS because of the way in which ‘people detached themselves as individuals from the NHS as a system’ and the need to ‘feed the beast’, which was ‘demotivating’ (Jemma, commercial consultant).
Tim had worked in the NHS as an analyst and subsequently with a commercial provider for 6 years. Working for the NHS was ‘rewarding because I was doing something for the NHS and therefore kind of for people in general’. In moving to the commercial provider, he felt he retained that sense of doing ‘something which I felt was actually going to have benefit’ (Tim, commercial analyst). Tim finished his interview by saying that his company was not out to ‘take over the NHS’ but to help patients, albeit in a different way.
At the end of the day, it’s about helping patients. I think the good thing about [commercial provider] is that I think pretty much everybody in this place has that same mentality. And a lot of people come out of the NHS, a lot of people are ex-nurses and such like, and still have that same kind of mentality, that they do just want to help patients, but just in a different way.
Tim, commercial analyst
In summary, often consultants with for-profit or not-for-profit companies had ex-NHS or public sector backgrounds. Reasons for leaving the NHS included lack of promotion prospects, frustration with the NHS system and belief in greater influence from outside. Although consultants worked harder in the commercial sector than the NHS, employment by commercial companies was ‘liberating’ and appeared to give greater job satisfaction, perhaps because of fewer regulations. A major difference between the NHS and commercial sector was ‘working to the brief’, which meant that consultants had to be adaptable enough to meet clients’ changing needs without taking on too much extra, unpaid work. The general sense of many accounts was that working for the NHS was a bit of a backwater and talented ex-NHS staff convinced themselves that they could still contribute to the NHS, and possibly make an even bigger impact, through working for commercial companies, although our data on benefits do not support this to any great degree (see Chapter 9).
Why were external providers contracted?
To justify their expense, commercial consultants had to provide evidence that their contribution added value over and above what was already accessible. NHS clients contracted commercial and not-for-profit providers for many reasons. A commercial consultant identified the following:
-
to help develop commissioners and commissioning skills
-
as a stopgap when short of staff
-
to help meet specific ‘deliverables’
-
to turn around less mature, struggling commissioning organisations
-
to have someone from outside identify what is not realistically going to work
-
to add value to what is already planned.
A NHS commissioning manager said the advantages of external providers were their independence and credibility. For example, an external consultancy was brought in to carry out a service review in a controversial area, independent of the acute providers and commissioners.
Elsewhere, a NHS commissioner mentioned that a commercial provider brought ‘a fresh pair of eyes’ (Lynn, NHS commissioning manager). Sometimes this ‘fresh’ perspective was solicited to help commissioning organisations find previously unidentified savings, although this did not always materialise, often ‘because it was just telling us what we already knew’ (Paula, NHS commissioning manager). Sometimes, the ‘fresh’ perspective was also wildly inaccurate; for example, a commercial provider overestimated potential savings from decommissioning ‘procedures of limited clinical value’ by comparing the PCT with the rest of the country without taking into account local circumstances. In another example, analysts and commissioners attempted to replicate the work of the commercial provider to identify savings, but the calculations of the local analyses did not correspond to those of the external provider.
Once the teams looked into the data further – well there’s two things, (a) it was quite difficult to look into the data further because we didn’t have the level of detail that supported the high level figures; [(b)] when we did our own analysis looking into it further, we couldn’t find the same opportunities.
Joan, CSU analyst
One commercial consultant talked about how external providers gave the ‘bigger picture’. For some CCGs, this bigger picture was international and commercial and the providers were contracted specifically for access to this expertise. This was especially important for CCGs that wanted to move ‘further and faster’ (Sarah, NHS commissioning manager). Others opted for UK-based companies because they wanted those who ‘spoke fluent NHS’ rather than ‘fluent expert’ (Susie, senior NHS analyst). For example, we observed how a UK-based consultant regularly drew on her knowledge of how commissioning organisations elsewhere in the UK faced similar problems, but we were unable to collect any NHS client views to assess the helpfulness of these narratives.
One commercial consultant thought that commercial providers had access to other sources of information ‘that allow them to join the dots in a different way’ by convening a ‘bigger, richer group of people together who have got more brain power and experience than they would be able to deploy in a PCT’ (Rhett, commercial analyst). Another analyst shared that view, having just moved from the NHS. He said that the commercial company created ‘more of a product than an information team on its own’, through collaborations of commercial, NHS and academic partners. They had ‘academics coming and scrutinising the work’ which increased rigour and led to ‘sell[ing] a product that bears up’ (Ranulph, commercial analyst). Nonetheless, when this particular contract came to an end, the NHS clients opted to retain and pay for half of the products on offer.
Sometimes commercial providers were contracted for their project management expertise. In one contract, a company developed complicated benefits realisation maps to identify and track benefits. These detailed:
-
‘enablers’ (such as software tools)
-
actions to change (e.g. ‘implement engagement strategy for GPs and providers’)
-
outcomes (e.g. ‘full GP engagement is achieved’)
-
benefits (e.g. reduced referrals)
-
objectives (e.g. ‘By the end of 2011 we will have implemented a system of strategies and processes which will result in a reduction in spend of XXX by 2012’).
In this contract, the enablers were within the control of the commercial company, but the actions leading to outcomes, benefits and achievement of objectives were not. Nonetheless, this commercial company did not receive payment until both parties agreed that the benefits had been ‘realised’. The actions for change on which the success of the contract hinged were actually enormous projects in their own right, dependent on commissioning clients to initiate and carry out. Moreover, these documents implied a linear model of change, where one action neatly led on to and triggered the next, whereas the literature is clear that NHS change management is much messier, multidirectional and complicated. 48–50 Unsurprisingly, a NHS client said that it was difficult to see what value these benefit realisation maps had added. Moreover, in summing up the overall impact of this contract, one consultant concluded that little progress had been made in the first 18 months.
I think that we’ve provided the enablers in many instances, whether that enabler is a piece of analytical work or a tool or even people, whatever it is, but there are no actions being taken, and therefore no outcomes being achieved, and very little benefits.
Paddy, commercial consultant
Gap filling (i.e. replacing missing staff) was another reason for contracting external providers, although both NHS clients and commercial consultants had concerns about using commercial staff in this way because assessing added value from gap filling was difficult. Gap filling was especially common in 2012 when many PCT staff left; for example, one commissioning organisation lost one-third of its staff. But rather than just making up numbers, sometimes external providers were contracted to fill skills gaps for specific projects. For some CCGs, attracting staff with the right skills was a perennial problem because their organisations were small. In one particular CCG, which was geographically isolated in a deprived part of the country, a partial solution was a cadre of trusted, known, ex-NHS freelance consultants.
In summary, external providers were brought in for their knowledge, skills and extra manpower. The knowledge of the ‘bigger picture’ could be national or international, based on different ways of manipulating data or being an outsider. But sometimes commercial and not-for-profit consultants were just filling temporarily vacated posts. Assessing the added value that commercial providers contributed over and above what was already available was important in assessing their usefulness. This task, already a difficult one for the clients, was even harder when consultants were principally gap fillers.
What do external providers do?
Consultants carried out a variety of different tasks, projects and roles in case study CCGs. For example, one commercial company collected data for a national review on hospital mortality rates and carried out a horizon-scanning exercise to identify interventions in primary and secondary care that reduced hospital demand. They also supported the CCG’s work on planning for future demand. Furthermore, this CCG worked with a freelance ex-NHS colleague on their quality agenda. They also sought help from not-for-profit companies with specialist expertise. In this CCG, drawing on the expertise and support of external providers was fairly common.
In another CCG, two freelance consultants were highly visible. One was a former PCT chief executive who was semiretired and carried out some consultancy work around integration across care sectors. The other was a retired former NHS analyst who was supporting the CCG with software tool development. In addition, two major management consultancies had helped draft commissioning strategies as part of the authorisation process. A third commercial company had significant input into a project aimed to consolidate urgent care services in one location. This commercial consultancy carried out numerous tasks such as identifying reasons for urgent care use and modelling workflows.
We’re trying to redesign the emergency department and integrate the walk-in centre which was closing and we’re trying to integrate some of that function, along with the GP out of hours, and put all of that into one place with the emergency department, so that you’ve got one place to go to for all emergency care. And then the patients are streamed either to a GP or primary care nurse or to the emergency department, depending on who is the most appropriate person to be dealing with their condition. Now what Bullfinch Partnership were able to do for us was, firstly they said, ‘Well these are the fifty commonest reasons that people come to the emergency department. And can you say which direction those people should go, i.e. primary care or emergency department? And if it’s a mixture, then roughly what percentages?’ And then they went away and got the data for the emergency department, from the walk-in centre and the out of hours, and they were able to model for us what the likely need would be for clinicians at various times of the day. So quite technical, needs a bit of number crunching, needs a bit of input from us as well, but they went away and did that work and we were able to see that actually in the daytime we would only need one GP staffing that particular part. Out of hours would be different. But, you know, it answered that question for us.
Tom, CCG chairperson
In another PCT, a commercial company assisted with data analysis and helped build a bespoke tool.
We were looking at dashboards, we looked at things like [commercial provider A] and I think it was [commercial provider B] or whatever it is . . . And this is information to tell us what’s going on in the system, you know, what’s happening to emergency admissions, are they going up or down? And PBC practices have a budget, so are practices on budget or below budget or overspending or underspending etc.? And so [commercial company C] helped us look at the other people’s (). We also looked at some of the other stuff and we came to a general conclusion, which [commercial company C] are happy to back, that none of them actually did the business, including their own. So we actually then said, ‘Right, we’re going to build our own.’ So we built our own dashboard. [Commercial company] gave us advice but mainly it was – it wasn’t trying to lead us anywhere. That dashboard we have now sold into other areas, so that’s being used in [county X] and it was shortlisted in the Y Awards.
Kurt, NHS analyst
In another CCG, multiple companies were engaged specifically for work around a contracting initiative. A local not-for-profit agency provided co-ordination, programme management and some event management, especially in the first phase of the initiative. They also supplied clinical leads. A NHS commissioning client said that working with this not-for-profit was like ‘working with another PCT’ (Clara, NHS commissioning manager). This not-for-profit organisation also sourced three other companies to work on the contracting initiative. We know little about the first. The second was a condition-specific consultancy contracted to challenge local acute clinicians and provide data to compare the local CCG against international benchmarks. This was a relatively new, clinically led organisation that ‘based a lot of evidence of practical experience and outcomes from the US’ (Clara, NHS commissioning manager). Another organisation was commissioned for their expertise in modelling current and future spend for the new contracts. In addition to these three, a fourth commercial company was involved in developing new ways of contracting. Their role was principally one of programme management, helping the CCG to identify its goals and processes of achieving them, deploying commercial consultants to support the process and providing links and introductions to other useful companies. The multiplicity of tasks and functions and finding the right external providers to deliver them shows the complexity involved in contracting commercial providers.
In summary, external providers undertook a wide variety of tasks including project management, gap analysis, forecast modelling, event management, pathway development, software tool development, analytics and stakeholder engagement. The matching of the external provider to the task relied less on the organisational form (i.e. commercial, not-for-profit, freelance) and more on the skills, experience and expertise on offer.
Views on external providers
Without hard measures of impact, opinions on the usefulness of external providers varied. The experience of one CCG chairperson was that overall commercial providers were not ‘leagues above the PCT . . . [because the] private sector is very variable and I’m not absolutely convinced that they’re necessarily better than the PCT’ (Martin, CCG chairperson).
Another participant said that the primary benefit of one contract was that PCTs were more likely to collaborate with each other. For example, use of the software tools meant that issues around GP practices’ reluctance to share patient data with commissioning organisations had been tackled.
I don’t think in terms of the actual expertise or capabilities that [commercial provider] brought fundamentally a lot of anything new or different. But maybe it was the effort that we all put into getting it up and running and collaborating and working together on things like information governance protocol that helped to accelerate some of the development.
Andrew, CSU analyst
Another client with a different provider thought the real strength of the commercial provider was its analytical team and approach to data. He thought they did ‘a bloody good job’.
And the great strength I think of the service that [commercial provider] provided is that they had a strong analytical component in the team and were very data-savvy essentially and drove a lot of their forecasting on the basis of a good, forensic analysis of what the data was telling them, which is also the way that they’d managed to squeeze savings out of providers by challenging inconsistencies in the provision of reporting from the providers that indicated that there were flaws in the data that was being reported, so the misattribution of activity in the contract. So they did a bloody good job in my opinion.
Jacob, NHS commissioning manager
However, this might be a minority view, as only one other NHS client working on this contract with this commercial provider agreed to be interviewed. Although not as effusive, she also thought that the commercial provider had made a useful contribution.
Trust and usability (i.e. ease and acceptability of use) were important factors in contributing to opinions on the usefulness of the contributions of freelance, not-for-profit and commercial providers. Commercial providers were often viewed with substantial suspicion, but they themselves believed that if the quality of their work was high this negativity could be overcome. In some cases, we found this to be true, as a couple of commercial providers produced output of considerable value, such as savings on acute hospital contracts and improved national ranking of the commissioning organisation. But often client feedback was mixed or lukewarm, with observations that the output was not quite right. In contrast, generally the output of freelance consultants was highly valued, usually because these now independent consultants often had the advantage of previous employment by the client. For example, we observed a former nurse colleague now working as a freelance consultant praised repeatedly at a CCG board meeting for her concise presentation style and the quality of her reports, which members found easy to digest. In another CCG, several participants were positive about the abilities of a freelance analyst, whom one described as ‘brilliant’, who once had worked in a local GP practice (Adrian, practice manager). In both cases, the freelance consultants were able to contextualise their work with remarkable accuracy, because of extensive familiarity through their previous employment with the client.
With regard to trust, client views on commercial providers were influenced by beliefs about the level of threat such companies posed for destabilising the NHS and the perception of what external providers could offer.
There’s a risk to the fundamental structure of the NHS and it’s a slippery slope to privatisation. If you look at the CSU, then it has the contract management of the Acute Trusts, and the primary care sector [NB: Informant incorrect as NHS England contracts primary care sector]. That’s a lot of clout. Now if hypothetically that purchasing power for NHS services was outsourced to a private sector provider then you are basically making some fundamental changes to the structure of the NHS. Now that’s my kind of knee-jerk reaction response. However if you look at the NHS as a brand it’s a very complicated brand and there’s lots of public private sector enterprise that make the NHS function, you know. And there are examples of private sector organisations that have been far more efficient than our historic NHS counterparts. And so it’s very possible for private sector companies to provide services for the NHS in accordance with NHS values. So I am less concerned about the involvement of the private sector, as a concept than some others might be.
Harry, NHS commissioning manager
A GP clinical lead had no objection in principle to using commercial providers, although he was deeply committed to the NHS.
But in all honesty, if they [the commissioning organisation] are not cutting the mustard, well why not go to KPMG or something and get them to do a body of work for us? And spend the public money getting a private organisation to do a body of work for a public organisation? I personally would not have a fundamental ideological aversion to that, although I am firmly, deeply ideologically committed to the NHS and do not want to do things which destabilise it, but recognise actually we need to look at it very differently and spend our monies differently.
Anthony, GP commissioner
One GP localities lead was similarly pragmatic. He had ‘no problem’ with paying for commercial tools ‘as long as the cost of it is commensurate with the potential benefit that we can get’ (Craig, GP commissioner). Another GP commissioner seemed resigned to the influx of commercial provider support within commissioning, because GPs did not have the skills themselves. Other GP commissioners were more negative. One said that he did not trust any of the big ‘consultancies that come in and fiddle about . . . give you some data and then disappear’. He went on to explain that the information had to arrive on his desk consistently from a trusted information provider with whom he had a long-term relationship (Angus, GP commissioner). He also said that he did not believe that the information provided by commercial providers was any better.
Now I don’t think that for pure knowledge or information they’re any better at what they do. They’re glossier and they talk the talk, but I don’t think there’s any intrinsic reason why they should be cleverer than an internal service.
Angus, GP commissioner
Another GP commissioner was ‘wary’ of the commercial provider ‘agenda to make money without having some of the other aims that non-private providers might have’ such as ‘providing health care to the local community in the best way possible’. She was more comfortable about not-for-profit agencies and thought that ‘having a little bit of alternative provision can be helpful for commissioners so that they can actually get the main deliverer to deliver what they want’ (Ciara, GP commissioner).
A senior CSU manager, who eventually went to work for a not-for-profit, thought that the organisational form was not as important as ensuring similarity in values.
[We] have met with [commercial provider] on a kind of fortnightly basis and we’ve developed, I think, a very healthy relationship with them. And my view as to why that is, is that [commercial provider]’s value set lies much more with our value set. And they’re a small company, I think they’ve only got less than 30 employees; all of them are ex-NHS staff.
Alfred, CSU analyst
In contrast, some participants were concerned with the ‘predatory’ behaviour of commercial companies. For example, one GP commissioner, who was leading on the implementation of a software tool by one company, was contacted by a rival company claiming that their tool was superior. Given that software tools were not his area of expertise, this GP commissioner was perplexed about how to proceed. This ‘predatory’ behaviour also concerned a CSU manager.
And what [commercial provider] has been doing, it seems, is sort of trying to pick off each CCG. And potentially there is a real commercial risk to the NHS there, because you’ve now got eight people who could be told, ‘Well I’m sorry, that’s just what you’ve got to pay’. They’ve not got any commercial skills.
Mike, CSU manager
Although we have limited data, concerns about the use of private providers were raised by two members of the public as part of the public questions in a CCG board meeting. The CCG response was that private providers have been part of the system for years and GP practices could be considered independent contractors (meeting minutes). The point about GP practices was also made by a lay representative on another CCG board.
GPs sometimes are put as, ‘Well you know, they have this great big heart, and they’re just going to do everything for everyone’ . . . sometimes perpetuated by GPs themselves, you know, ‘We’re only here to save lives’. And the large salary and contract that comes with it of course but, so, but they are primarily businesses. They want to function by delivering good-quality health care to their patient group and they win contracts for doing that and they get paid well for doing that, as is rightly the case. So like any business, that’s how they operate.
Malcolm, lay representative
In summary, commercial consultants knew some clients might view them as threats but believed that this could be overcome through good performance. This was less problematic for freelance consultants, who were often former colleagues of their clients, as the perception of threat or a conflict of values was less. Not-for-profit agencies and commercial companies that convincingly demonstrated NHS ‘values’ were more likely to be trusted. Nonetheless, clinical commissioners’ views on commercial providers were ambivalent. Some GP commissioners were happy to contract commercial providers if the benefits were worthwhile; others recognised that the lack of GP commissioning skills warranted greater use of commercial providers and others were inherently distrustful and believed that the offer of commercial providers was no better than that of NHS (or ex-NHS) staff. For this last group, not-for-profit organisations were more acceptable.
Box 7 summarises the key points of the chapter.
-
Trust plus usability influenced views on the usefulness of external output. Freelance consultants generally had a NHS background and were viewed as less threatening than commercial providers. Their output was well contextualised to their client, as often freelance providers were former employees and so had useful local knowledge. In contrast, although commercial consultants often had ex-NHS or public sector backgrounds, they were sometimes viewed as threats, the usefulness of their output was variable and they lacked local knowledge. Not-for-profit providers encountered less hostility than commercial companies.
-
The breadth of external providers and their level of involvement suggest that there was substantial external provider presence in NHS commissioning during the fieldwork period, which included 18 months prior to the passing of the 2012 Health and Social Care Act. 4
-
The relationships between CCG and CSUs varied from distant to quite close, and views about CSU contributions ranged from inadequate to highly valuable. CSUs and commercial companies’ relationships could be collaborative and/or competitive.
-
The move to local authorities increased the marginalisation of Public Health in commissioning. Some participants thought that Public Health overstressed the inequalities agenda at the expense of input such as service evaluations and evidence reviews. However, although the evidence reviews produced by one Public Health consultant were appreciated, they did not seem to inform the thinking of commissioners in one case site.
-
NHS analysts were particularly drawn to working for commercial companies, as NHS work was often mundane with scant opportunity to interpret, as opposed to merely produce, data. NHS analysts felt isolated and unable to effect much change on commissioning.
-
CCGs contracted external providers for their knowledge, skills and expertise in many areas including project management, forecast modelling, event management, pathway development, software tool development, analytics and stakeholder engagement. Commercial providers sometimes brought a specialist ‘big picture’ view and sometimes were just filling gaps in the staffing.
-
The matching of the external provider to the task relied less on the organisational form (e.g. commercial, freelance, not-for-profit) and more on the skills, experience and expertise on offer.
Chapter 8 Accounts of NHS and external provider contracts
Introduction
This aim of this chapter is to provide in-depth accounts to illustrate the points made in previous chapters. These vignettes offer a wealth of material that is difficult to present out of context, given the multilayered, multifaceted nature of knowledge exchange. Each vignette was built around a contractual relationship between NHS clients and commercial or not-for-profit providers. Some of the vignettes describe an entire contract, while others illustrate just one component. To maximise anonymity, the providers will be known as ‘external provider 1’, ‘external provider 2′ and ‘external provider 3’; no distinction is made between for-profit and not-for-profit providers and quotes are not attributed. A summary of key points follows each vignette.
External provider 1
Background
External provider 1 was a small international company that marketed a software tool developed and refined from decades of academic research. Academics carried out studies with the tool in different countries, tested its viability, amended the algorithms and presented findings at conferences, which helped to contextualise the tool, provided credibility and reached new markets.
It’s often that the academicians (sic) through publications, through presentations and conferences and so on that proves the [tool’s] viability within a particular country or setting and demonstrate its value. And then the government gets – you know – it gets their attention. But it has already the acknowledgement and the credits that come from having been already vetted out in an academic setting.
External provider 1’s business model was based on keeping their company small and relying on other larger locally based companies with licences to provide software, training and the ‘wrap arounds’ (or ‘front end’) which were software/user interfaces. The advantage of working through suppliers was that these larger companies could ‘exploit the system’ by ‘react[ing] much more strongly to a market or emerging market’ and were big enough for initiatives such as FESC and the Lead Provider Framework. As an international company, external provider 1 also valued the local knowledge these larger suppliers had and received ‘added value’ such as the ‘report generator, additional analytical tools or consulting that they [the suppliers] offer the user’.
A disadvantage of working through local suppliers was that the licensed suppliers were selective about the level and type of knowledge that filtered through to end users, as the aspects of the product that local suppliers highlighted varied. For example, external provider 1 noticed that one supplier was ‘much more interested in the delivery of information, how it looks and feels and so on’ because they were an informatics company, while another prioritised the ‘managerial aspects’ because it was a ‘classic management consultancy’. This meant that the management consultancy ‘struggled with not being able to understand the subtleties in the technology and how sometimes a particular report in terms of the way it looks is actually important to whether it gets adopted or utilised in any way’.
Knowledge exchanged
This vignette begins with a NHS team acting on behalf of a consortia of commissioning organisations contracting a licensed supplier of external provider 1’s tool. The terms of that particular contract were that no direct contact was allowed between external provider 1 and NHS staff; all contact had to be filtered through the licensed supplier. (The latter was concerned that, with unmediated contact, the clients might decide to contract external provider 1 directly and sidestep the local supplier.) Consequently, NHS end users were unable to develop more advanced skills, as they were working with a supplier with less understanding of the tool than the clients would have liked. However, the contract with the licensed supplier was eventually renegotiated by the NHS contracting team, lifting the clause of no contact. External provider 1 was then contracted directly.
To facilitate knowledge exchange, external provider 1 arranged for experts in designing the software tool to teach selected NHS end users more advanced skills. Known as ‘superusers’, the NHS participants worked across several different PCTs, were chosen by their local PCT and had a variety of backgrounds including analysts, commissioning managers and project managers. The contract between external provider 1 and the NHS was for several modules of advanced training in the tool. The experts were located in North and South America and were chosen because they had developed particular aspects of the tool. At a pre-arranged time, the superusers would log on to a webinar. The expert could not be seen but his/her voice would talk users through a series of slides. Simultaneously, superusers could write notes to each other or the expert or ask questions by raising their virtual hand. Sometimes there was a long enough time lag until the expert noticed the question that the webinar could already be on a completely different topic. At the end of the set of modules, the superusers sat an exam and received a qualification.
The training was technical and oriented to the US health-care system, although a consultant from external provider 1 told us that each module was revised prior to the webinars to contextualise for the particular country. To help contextualise and embed the knowledge further, they used several mechanisms, for example:
-
Two knowledge brokers were present at every session: a consultant from external provider 1 and an information manager who worked for the NHS team that set up the contract and who knew the superusers well.
-
Superusers were given homework. Homework questions for module 2 included ‘describe the risk factors that are included’ as well as an opportunity to identify ‘take home messages’ and further questions. To improve their understanding, superusers were allocated time to compare their homework when they met at other forums.
-
The superusers were sent the slides a few days before along with some background reading to prepare for online sessions.
-
One participant organised a full-day revision session, when the course was nearly completed.
-
External provider 1 supplied manuals to users about the system with every variable described, but other manuals could also be downloaded.
Knowledge transformation
The tool necessitated GP practice-level data and generated output on patients that were at higher risk of using health services. One superuser’s role was to embed the software tools into GP practices and encourage GP practice staff to use them. In transforming her learning about the software tool to GP practices, she selected aspects of the webinar learning that were germane to practice managers and administration staff and dejargonised the language.
There are a number of reports within the tool, so I focus on two reports that they need. The first one is the case management report, which has their entire practice population within it. And then you apply a series of filters to only have those patients that you want to look at. And that’s taking a very broad approach. And then there’s also an approach where you can concentrate on specific disease conditions. So I concentrate on those two reports mainly. And then I go into the report and I go through column by column so they understand what each column means. And I put it into terminology that they can understand. And then, while I’m there, we actually run a report, we put it into Excel, I go through the filters so I’m showing them how to do it, and actually often I get them to do it. So I get them to do the picking rather than me, so that when I leave they’ve actually got a list of patients. And I think, at the point I leave, they do understand. I think the problem comes because they don’t access it often enough, so by the time they need to go back into it they’ve forgotten. So what I’ve done is produce a PowerPoint presentation with step by step instructions so they can refer to that.
We obtained a copy of this PowerPoint presentation and each slide is a screen shot of a menu on the tool with a red circle around the option to generate case management reports for the Quality and Outcomes Framework. Although this superuser said that general practices did not want to learn how to operate the tool as they had little time, tool operation was the focus of her teaching. Instead, general practices wanted the superuser to analyse the data and send practices the results, and then practices could ‘get on with it’. But information governance stipulations meant that neither the PCT nor this superuser had permission to access to the relevant practice data.
Another superuser who was trained in advanced skills had an analytics background. A major initial challenge was that he had no access to the tool, so it was like ‘trying to be a car salesman and sell a car by describing it to people. We were on a hiding to nothing’. A further complication was that a tool with the same function from a different provider had been operational for over 5 years locally and this was ‘not always flavour of the month’ with GPs sceptical about case management. To remove the association with case management and market the tool more successfully, this superuser showed differences in standardised mortality rates and type of disease by practice to identify novel ways of allocating resources to general practices. This strategy was apparently successful, as after one presentation one locality increased its take up from three to all 10 practices. In training general practice staff, he tended to ‘dive straight into using the tool’ with a case report and explain terms and concepts as he went along.
As a primary care commissioner, another superuser said that the tool was used in several ways. The first was to identify a case list for the community matrons, which longer term could feed into an ‘overhaul’ of the community matron contract and a change in referral criteria. Second, she said that ‘a lot of’ commissioners ask her to run the tool to see if there is ‘anything interesting’ about a particular cohort of patients. For example, to reach elderly individuals who needed some care but were not housebound or known to health-care providers, the CCG had set up drop-in clinics in church halls and sheltered accommodation staffed by community matrons, pharmacists and voluntary sector staff (e.g. Age Concern). To ‘populate those clinics’, the superuser devised an algorithm and ran it in the tool, for example over age 60 years, several comorbidities, ‘a couple of hospital counts’. This list of patients identified was further refined when passed on to the GP practices who then decided if the tool had identified the right people. This ‘did actually throw up people they [general practices] might not have thought about’. The feedback the superuser and her team got from the practices about using the tool in this way was ‘quite, quite promising’.
Challenges
One challenge was that some general practices were not motivated to use the tool. A superuser reported that, once general practice staff were taught, those skills were forgotten, as the tool was infrequently used. Another superuser noted that, because practices were not asked to identify patients as a part of any programme or initiative, the tool was not used routinely. That particular version of the tool also did not allow for stripping out of certain patients (e.g. pregnant women, those with transplants), which meant lists of patients were produced that the practices could not manage. Moreover, trend data did not exist to track patients over time, thereby determining whether or not the tool and consequent interventions made a difference. For these reasons, practices sometimes did not ‘see the point’ in investing their time in the tool.
Another challenge was around data accuracy. For example, one superuser recounted how raw data were extracted from primary care, linked with secondary care data, cleaned and ‘put through the grouper’ (the algorithm). But the result wasn’t ‘right’. The superuser and her team identified that the problem was not with the tool, but with the ‘wrap arounds’ from the other suppliers. Consequently, the CCG had considerable concerns about using the tool and had not launched the ‘charm offensive’ with the general practices. Moreover, the superuser and her colleagues had to learn about technical aspects of the tool which they ‘shouldn’t need to know but we’re feeling we do need to know because we can’t ask the right questions’. However, overall, this superuser was positive about the benefits of this tool; she just thought that the package with multiple suppliers was too complicated. As these data were collected in 2012 and several versions of the tool will have been rolled out since then, these problems may now be corrected.
Views on the training
Satisfaction with the training depended on expectations. One superuser with a commissioning background identified her objectives from the training as:
Technical expertise about how the data is extracted, how it’s cleaned, the algorithm that’s supplied and the outputs that the [tool] gives and in addition to that they [external provider 1] will be in the best position to understand how best to use it.
She said the training left her ‘better informed’ but ‘more confused’, because of its technical detail. When probed about ‘how best to use it’, this superuser said that there were lots of ways to ‘cut the data’ and at the moment a ‘generic approach’ was employed, but she wanted someone from external provider 1 to work with her and a commissioner for long-term conditions ‘to actually think about the best way to get maximum results’, perhaps by developing a strategy focusing in-depth on one condition such as chronic obstructive pulmonary disease or diabetes. She wanted the tool contextualised to her immediate concerns, which was difficult without a tool expert on hand. She also wanted an opportunity to blend her local knowledge with expert knowledge to identify where the tool could make a difference. The absence of a strategy for using the tool with general practices meant that the superuser did not have much clarity about the direction she should be taking with practices and, in turn, practices were less receptive to ‘getting on board’. Her learning from the training did not address this.
Another superuser found external provider 1’s training interesting, not least because she learnt what the tool could do without the ‘front end’ (i.e. ‘wrap arounds’) provided by other suppliers. This superuser thought that the original training by the local supplier did a ‘good job in trying to get across the things we needed to know at the time’ and it was ‘a very useful introduction to what actually is quite complicated’. Through actual use of the tool over time, this superuser found that the implications of some of the training were not appreciated until she was working with live data. She thought that ‘the training is obviously very necessary, but also there’s a period of time of actually using data and reflecting back on things that’s also very important’.
Benefits and disadvantages
At the time of fieldwork in 2012, the benefits of the software tool appeared to be more theoretical than actual, perhaps because superusers had just been trained. A member of the NHS team that procured the tool said he ‘absolutely’ believed that the tool could be useful for commissioners, but thus far making a difference was ‘more the exception than the rule’. Other mechanisms were needed to capitalise on the tool, such as good-quality community matrons, ‘integrated’ working relationships between community matrons and GPs and regular patient review to ensure that the information generated was useful. This participant identified many difficulties, including the inherent challenges in changing the status quo, the complicated environment, the range of stakeholders across multiple organisations who did not necessarily buy into the change objectives, and the short-term focus on ‘today’s problem today’ leading to managing the ‘minutiae’, which militated against longer term strategic thinking, induced a lack of relevant skills among managers in interpreting information, and limited leadership at senior management level to champion the tool.
Another superuser thought that a potentially powerful way of using the tool for practices would be in ‘case-mix adjustment’. Currently, practices were judged against an overall average (i.e. average number of hospital admissions by practice). Using data from 10 practices in one locality, he identified the practice that had the greatest opportunity to lower admissions, which would not have been selected through usual methods. This example was also brought up by a local GP clinical lead, who felt that this application was potentially very powerful. He was also relatively positive about the tool because it had addressed some long-standing problems about resource allocation to GP practices that the clinical lead had been aware of since fundholding days.
As both of these examples suggest, in general, participants identified how the tool might influence commissioning, rather than examples of actual impact.
Box 8 summarises the key points from the first vignette.
This vignette illustrates how knowledge transforms through multiple processes. In one example, a superuser applied her recently acquired knowledge from the webinar training to devise an algorithm to identify elderly patients for a multidisciplinary intervention (product deployment). But before contacting these people, this list was again transformed by general practice staff who weeded out those who were not suitable (interpersonal). The processes of engagement (with general practices) and contextualisation (of the algorithm and the original list) were also evident.
In another example, a superuser copied the steps to generating a case management report into a PowerPoint presentation with screen shots and red highlights (copy, adapt and paste) and then trained general practice staff through ‘sitting with Nelly’ sessions where she passed on her knowledge (people placement). General practice staff did not want to learn how to manipulate the data themselves, but data protection rules meant that only they could have access to practice data to transform it into useful knowledge (governance). The superuser contextualised the webinar knowledge to focus on areas of key interest to general practices and through face-to-face visits engaged practice staff to use very limited aspects of the tool (interpersonal knowledge transformation).
Other key points from this vignette include:
-
External provider 1 worked through academic channels. They encouraged independent assessment of the tool, posted published papers on their website and attended academic conferences to make contacts. Academics not only were knowledge producers but they also (unwittingly) marketed knowledge to extend external provider 1’s reach.
-
The tool was bought by a NHS team on behalf of several commissioning organisations and then allocated to NHS staff who had no input into the selection of the tool nor any clear information need that the tool was meeting. Consequently, NHS users were left to puzzle out not only how to use the tool but what problems it could address. One superuser found that this lack of clarity impacted on her ability to engage GP practices.
-
Although the NHS clients recognised the high calibre of expert knowledge, there was agreement that the training included excessive technical detail. Some said it was too focused on the American health-care model and not on how the tool could best be used in English commissioning contexts.
-
Because it was so small, external provider 1 worked through much local commercial companies to market its tool, which led to complicated arrangements which impacted on data quality and created concerns about competition hampering knowledge exchange.
-
During fieldwork (May to August 2012), difficulties cited with the tool included its overly American lexicon and conceptualisation of health-care systems, its lack of filtering mechanisms and its discrepancies between raw and processed data. These may have by now been resolved with successive versions of the tool, but were sufficient to lead to the postponement of rolling out the tool to GP practices in one commissioning organisation.
-
Transformation of knowledge to GP practices was through the NHS ‘superusers’ acting as intermediaries. They offered training but, because there was no impetus on GP practices to subsequently use the tool to produce information, the skills and knowledge transferred could be lost.
-
Apart from identifying patients from case management, which arguably was for clinical rather than commissioning purposes, actual use of the tool to inform commissioning was relatively limited during fieldwork (2012). Exceptions were that the tool had been used innovatively to identify prospective users of an outreach clinic for the elderly and the ‘case mix adjustment’ aspect of the tool to identify GP practices with the most potential to reduce hospital admissions.
-
Nonetheless, an analyst superuser and a GP clinical lead were enthusiastic about the tool, and another superuser with a commissioning background thought it was ‘quite promising’. A third superuser was less convinced.
Figure 7 explicates visually a few of the transformative processes in this vignette. Chronologically, this starts at the bottom with product deployment.
FIGURE 7.
Transformation processes in vignette 1. CAP, copy, adapt and paste; G, governance; IR, interpersonal relationships; PD, product deployment; PP, people placement.
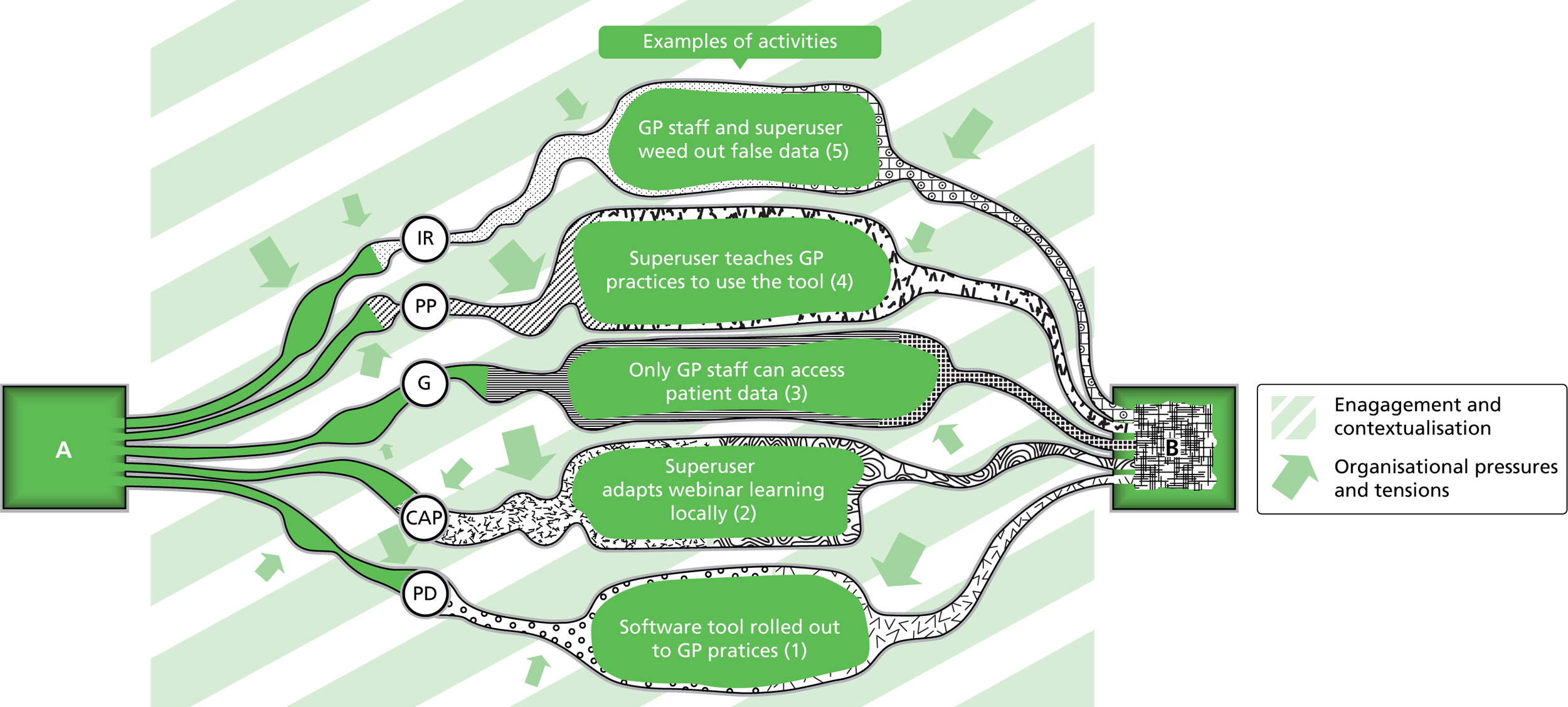
Table 12 illustrates how the differing agendas and pressures of the key parties affected their knowledge exchange activities.
| External provider 1 (tool developer) | Local supplier (tool supplier) | Superusers | Commissioners | GP practices |
|---|---|---|---|---|
| Aims | ||||
|
|
|
|
|
| Activities to meet aims (or not) | ||||
|
|
|
|
|
Figure 8 illustrates how the tool, the knowledge embedded in it and the information derived were transformed by the key players in the knowledge exchange conduits. The ways that these key actors ‘framed’ that knowledge are indicated by the changing shape of the knowledge that each set of actors had about the tool, for example the shift from the tool being framed at its inception as evidence-based knowledge with deep and wide academic credentials to a deliberately simplified and, therefore, useful piece of saleable software.
FIGURE 8.
The transformation of knowledge in vignette 1. CAP, copy, adapt and paste; IR, interpersonal relationships; PD, product deployment.
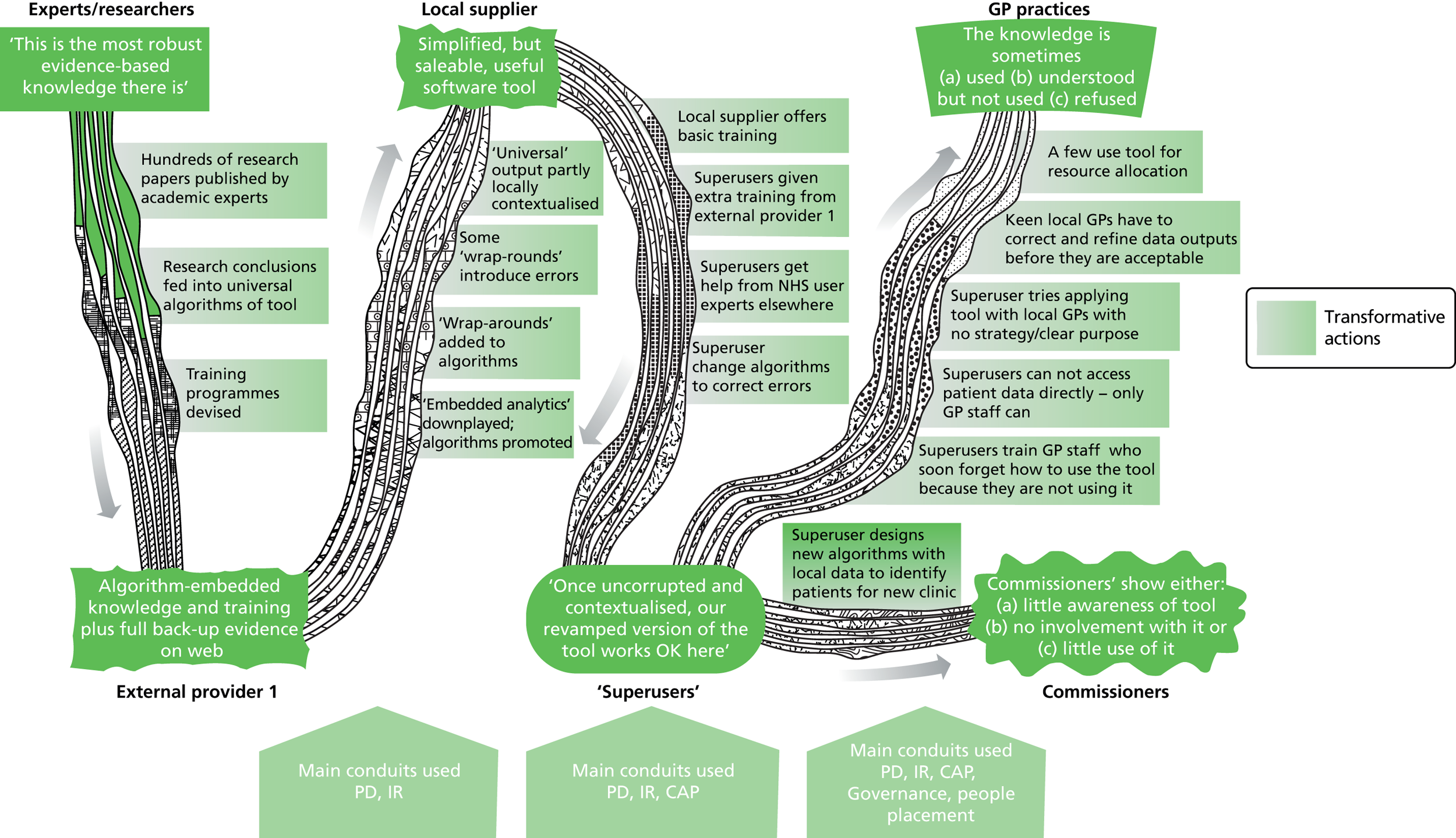
External provider 2
The software tool
External provider 2 was a large UK-based company that supported several software tools, some developed in-house and some developed elsewhere. Consequently, they had a large team of analysts. The tool in this vignette was developed by another commercial company. It used ‘evidence based protocols’ to assess whether or not a patient or cohort of patients were in the best place of care for their particular needs; for example, those in hospital might be better placed in community settings. According to the product guide, the ‘evidenced based protocols’ that informed the tool were ‘developed and maintained by a Global Clinical Panel of over 800 independent experts including UK based clinicians’. These guidelines were ‘compared with the clinical evidence within Map of Medicine and NICE guidelines and found to be 97% compliant’ (product guide). No further information was available about where or how these guidelines were generated. However, there were references to academic research within the tool.
Although local commissioners had not specifically requested or sought this tool, it was available for regional use. The local hospital had higher than average emergency hospital admissions and the decision was made to conduct audits using this software tool to determine if patients were misplaced in acute settings. Essentially, the audit consisted of clinically qualified staff (i.e. ‘reviewer’) entering patient data by working through a number of screens checking boxes. The reviewer would enter supplementary notes to explain reasons for his or her decisions. The tool then reported whether or not the patient ‘qualified’ by meeting the criteria for care in that particular setting. As the audits took place in ‘real time’, care providers would be available to answer any queries of the reviewers arising from patient notes.
The first audit
A first audit of the local hospital using the software tool was carried out solely by staff from external provider 2 in the autumn of 2010. One NHS client said that ‘the first audit was a disaster really’. He identified several problems, the first being the lack of detail. For example, the tool gave the proportion of those who could have been given care elsewhere without any details about why or where.
It gave us no details. So when we got that we felt that that was unhelpful because a percentage figure didn’t give us any idea of what was required, who those patients were, were there any themes in that? And what facilities were required? So if it was say falls, you know, what’s required? What would we have to put in? Because they assumed that there was a physician who would go and visit the patients at home, and constant nursing support at home, which wasn’t available.
Once the notes were reviewed, they found that ‘whoever applied it, applied it without any common sense at all’, giving them ‘ridiculous’ results. This was thought to be a problem not with the tool, but with its application. Hospital clinicians retested the patients who had been ‘non-qualifying’ and found that nearly all qualified. Examples of those initially classified as ‘non-qualifying’ included a pregnant woman who was ‘essentially killing her baby’, which led to a statutory legal admission, and a man with repeated chest pains who needed a coronary angiogram which could not be administered at home; the tool said that he was suitable for home care. These anomalies were not because the tool was North American (although several participants commented about the challenges in applying a North American tool) but because ‘it was just a complete misunderstanding or very, very poor assessment’. We do not know who within external provider 2 carried out the assessments.
The hospital wanted the PCT board to consider the revised results, but the PCT commissioners were reluctant.
They had just fed back and signed off the protocol . . . One of the PCTs said that they didn’t really care whether it was accurate or not, it gave them the message they wanted . . . they actually refused to look at it.
Eventually, the PCT and external provider 2 were persuaded to examine the revised data and they agreed that the quality of the audit was poor.
And they said ‘Look if you really want us to see your data, if it would help for us to go through your data, we’ll set up a meeting’. And I said, ‘Look, it’s not my data, it’s your data. It’s not going to help me in any way at all. I’ve read it, I understand it. It’s just that you’re planning all around this, and you haven’t looked at the data yourself, and consistently won’t look at it’. So they at that point said, ‘All right we will look at it. And we’ll bring it there with external provider 2’. And I brought the notes and we went through it. And at that point the PCT were completely shocked. So external provider 2 said they just didn’t understand why it had been so poor. And the PCT, I could see they were quite shocked, because I think they at that point felt that I just didn’t like the result of it and was arguing on the edges or the extremes, but in truth it was really, really very poorly done.
The second audit
The experiences of the first audit obviously had a major impact on the planning of the second. Commissioners leading on the second audit did lots of ‘one to one talking, listening to their concerns’ to get the right people back on board. The argument used was that the second audit was using internal people with local knowledge of organisations that external provider 2 did not have. Moreover, the second audit would have joint PCT–care provider ownership with adequate clinical leadership. In addition, the settings expanded to include acute, community and social service premises, including the medical admissions unit, community hospital wards and social service wards. The population under study was all those aged over 70 years currently located in those settings during the 7 days of the audit. The knowledge wanted from the review was:
Are patients being admitted appropriately?
For the patients who are in beds who could go home today?
For the patients who are in beds who could receive a different level of care from another provider?
Meeting minutes
There were some concerns about whether or not the software tool would provide all the necessary information needed, especially around capacity. A bespoke questionnaire was to be administered in tandem with the tool when auditing. Additional information collected by the questionnaire would include:
Is there an existing care package?
Did the patient have a ‘telecare’ service available?
Does the patient live alone?
Meeting minutes
Staff from the hospital meant to develop this further, but a participant subsequently said this questionnaire was never devised. It was not entirely clear if an explicit decision was taken or if the questionnaire dropped off the agenda. Regardless, these data were not collected.
For the health-care staff to undertake the audit themselves, training was necessary. The tool developer (not external provider 2) carried out the training. The training was intended for 5 days, but local reviewers could not be released for that amount of time, so the training was cut down to 2 days. Reviewers included two managers with nursing backgrounds, a consultant community nurse, an acute hospital nurse, a discharge liaison officer without a clinical background and a social worker. Only two reviewers were in current clinical practice. Seven reviewers were trained but five carried out the audit. As part of the training, the reviewers developed a glossary to translate American nomenclature into terms suitable for this particular health-care economy. While entering the data into the tool, consultants from external provider 2 were on hand within the setting to answer any questions. At the end of every day, the reviewers met a senior hospital consultant to discuss any cases found to be ‘disqualifying’ and analytics staff (not clear if PCT or commercial based) then generated data reports.
Knowledge transformation
Two key streams of knowledge were exchanged in this vignette. The first was about the tool and was between external provider 2 (including their tool developers) and local stakeholders and reviewers. The medium was formal meetings with PowerPoint presentations and didactic, face-to-face training of local reviewers both delivered by commercial consultants. But one reviewer said that the real learning came from using the tool because of misconceptions of how the tool operated.
Because we didn’t have an understanding of how the tool actually worked, when we set up that workshop. We were very much posing the questions of: what should be included in the audit, what shouldn’t be, what types of questions should we be asking in the audit? Thinking that an audit would be questioner-based, that you would present – you know, if you’ve got these clinical notes in front of you, you’d also have a list of questions at the side of you and you would answer those questions, if that makes sense. Where the audit tool itself isn’t like that at all. So I think we had a misconception of what the tool looked like.
This comment is slightly confusing, however, as several workshop participants had been involved in the first audit and so, presumably, were familiar with the tool. Nonetheless, the second audit generated ideas among commissioners, community and hospital providers about how to use the tool next time around. One was to follow patients through their journey from day one of admission to test suitability daily to inform length of stay and another was as a 24-hour ‘snapshot’ of A&E.
The conceptual model of the tool was especially useful to hospital staff. They replicated the approach (without the tool) in ‘several audits of little areas’.
I think the whole question of looking at admissions and what was required, and what services could be put around it, is one that is so obvious that actually we weren’t thinking about it. So although the audit didn’t achieve that, or the first one didn’t do it, and the methodology seemed so obvious, the questions seemed so obvious, we weren’t doing it, so I think it was quite useful for the initial concept, because it is a simple concept . . . and I think they’ve [commercial provider] brought that.
This conceptual shift had generated substantial enthusiasm, but neither the hospital nor commissioners said that they would use the tool itself again. Moreover, the hospital would not work with external provider 2 again.
A second stream of knowledge centred on outputs from the tool and how those outputs informed commissioners’ decision-making, as a NHS participant said that a key problem was acting on the findings. Despite numerous requests, we never obtained the final report from either the first or the second audit. However, we did collect a PowerPoint presentation for an audit using the software tool at a neighbouring hospital a year earlier. This provided an account of the tool outputs.
This report presented separate findings into acute admissions and long stay with ‘headline’ information for each. This information was then broken down further for each category, into ward, ward type, specialty, patient age and admission day. Additional information on patient characteristics (e.g. lives alone) and admission source (e.g. GP) was given for long stay. Alternative levels of care were identified for all three categories (e.g. acute admissions, long stay). Results from qualitative interviews with clinical and managerial staff were then presented in terms of ‘opportunities identified’. The report gave separate recommendations for commissioners and providers, for example ‘Review sub-acute provider admission criteria and admission protocols in consultation with acute provider. Implement monitoring arrangements to ensure that these are adhered to and remain based on level of care need’. The report finished with ‘next steps’ (report).
Although we did not obtain a copy of the final report for the audits under study, a participant said that 28% of patients could have been cared for elsewhere in the first audit, while the second audit found that 24% of patients were in a suboptimal care setting. Although the difference between the two audits was minimal, the results of the second audit were widely accepted, whereas the first audit was highly contested and led to the disengagement of the hospital. Consequently, the first audit did not generate much knowledge transfer. A participant in both audits said that the second was more successful than the first because of local involvement across providers and the commissioning organisations. This created ‘a much better understanding of what was actually happening in hospitals’ across the health economy, which was ‘invaluable’. Local engagement led to local ownership.
In the findings presented to the PCT board, recommendations included conducting an audit with the 50- to 60-year-old age group, given that fewer over-70s were in hospital and community settings than anticipated. This also meant that commissioners needed to look elsewhere in the system to reduce hospital demand. However, it is unclear whether or not these recommendations were taken on board, as a subsequent e-mail in late 2011 said that ‘the results have not been used in any commissioning decisions’. The timing of the publication of the report coincided with the height of the turbulence from the 2012 Act and the departure of the PCT champion to a new job, so possibly other factors contributed to its limited impact on commissioning.
Benefits and disadvantages
A participant said that the local stakeholders could have conducted the audit without the software tool, but it would have been ‘very qualitative’ and the same quality of data would not have been produced.
Generally, local stakeholders found the second audit ‘very useful’, but not because the tool gave much insight into unplanned hospital admissions, nor did it provide information to feed into planning for future care. This was partly because the questionnaire to collect these data was not developed but also because of ‘gaps’ in the information provided by the reviewers, including the lack of recording of NHS number. Without current clinical backgrounds and possibly because of the abbreviated training, some reviewers ‘struggled’ and the quality of data was poorer than anticipated.
Nonetheless, the audits had an entirely unexpected outcome, in that relationships between the hospital, community providers and commissioners improved, particularly through the fieldwork phase of the second audit when local reviewers, commercial consultants and hospital staff met daily to consider the doubtful cases. Several participants stressed how important this improvement in relationships was, as previously the hospital had not worked well with the commissioners or the community providers, ostensibly for over 20 years. A participant said that ‘it made us start talking about data rather than prejudiced opinions’, which meant that formerly fractious conversations were now based around ‘evidence’.
I’d say [I had a] very negative experience from working with this tool and the way it was applied. But ultimately it might have been the trigger to really make some very big changes in the health economy, in terms of making us realise we have to work better together. And that probably was more valuable than the tool ever could be. So paradoxically [the commercial company] helped. And I think they helped because it was the beginning of saying, ‘We’re going to talk about evidence rather than about opinions’.
In sum, the application of the tool mended historically fragmented relationships, built trust within the local health economy and helped the hospital to consider other ways of grappling with a longstanding problem. But the commercial provider played a minor role, mainly in offering a forum for the stakeholders to work together and providing knowledge about the tool.
Box 9 summarises the key points from the second vignette.
In this vignette, engagement was a central issue. For example, before running the second audit the right people had to be re-engaged, following the ‘disastrous’ impact of the first. Governance also played a major role with the first audit, as the PCT commissioners were unwilling to consider revised results because their decisions and plans had already been made.
The knowledge transformation processes of interpersonal relationships, product deployment and people placement were particularly visible during the auditing process. Reviewers came from many different backgrounds (acute, community, social services and commissioning). They pooled and shared their clinical, service and organisational-based knowledge through daily, face-to-face debriefings (interpersonal relationships) and with the help of the software tool (product deployment) created new understandings. People placement was also evident, whereby the reviewers took knowledge out of the audit settings back to inform their organisational bases. This was particularly useful with the acute hospital, as little previously was known. In this way, difficult relationships between different sectors of the local health-care economy were improved. After the audit, the most noticeable knowledge transformation process was ‘copy, adapt and paste’, whereby the hospital staff took the underlying concept of the tool and applied this approach in audits in other areas of the hospital.
Other key points from this vignette include:
-
The tool tended to be ‘one size fits all’, which was not fit for purpose. Contextualisation was necessary first for the UK (e.g. lexicon and sectors) but also for the particular health economy (i.e. to match which services are locally available). The tool was too crude to change practice, but it was a starting point.
-
To use a tool successfully, it was necessary to understand it. Moreover, a software tool such as this required actual use to comprehend its full potential. Having expert advice on tool use was also necessary. Ideally, tool analysis needed to be complemented with the collection of other data.
-
Assessing what was appropriate for individual patient care was subtle, and the danger of any rigid framework was that it lost that subtlety and threw up apparent negative findings that were debatable.
-
The particular value of the tool and intervention by the external provider was as a trigger for reflection on health-care processes and policy at a far deeper level than previously. A disturbing possibility is that it was the poor quality of the initial audit, and the subsequent wrangles, that proved to be the key catalytic feature.
Figure 9 below illustrates a few of the transformative processes in this vignette. Chronologically, this starts with number (1). Table 13 details the motives behind these transformations further. Figure 10 summarises a few of the crucial transformations that the key actors in this vignette undertook to reshape the tool, its embedded knowledge and the information derived from it. It also illustrates the way they framed the status of that knowledge as a result of their contextual demands and constraints, and their worldviews.
FIGURE 9.
Transformative process in vignette 2.
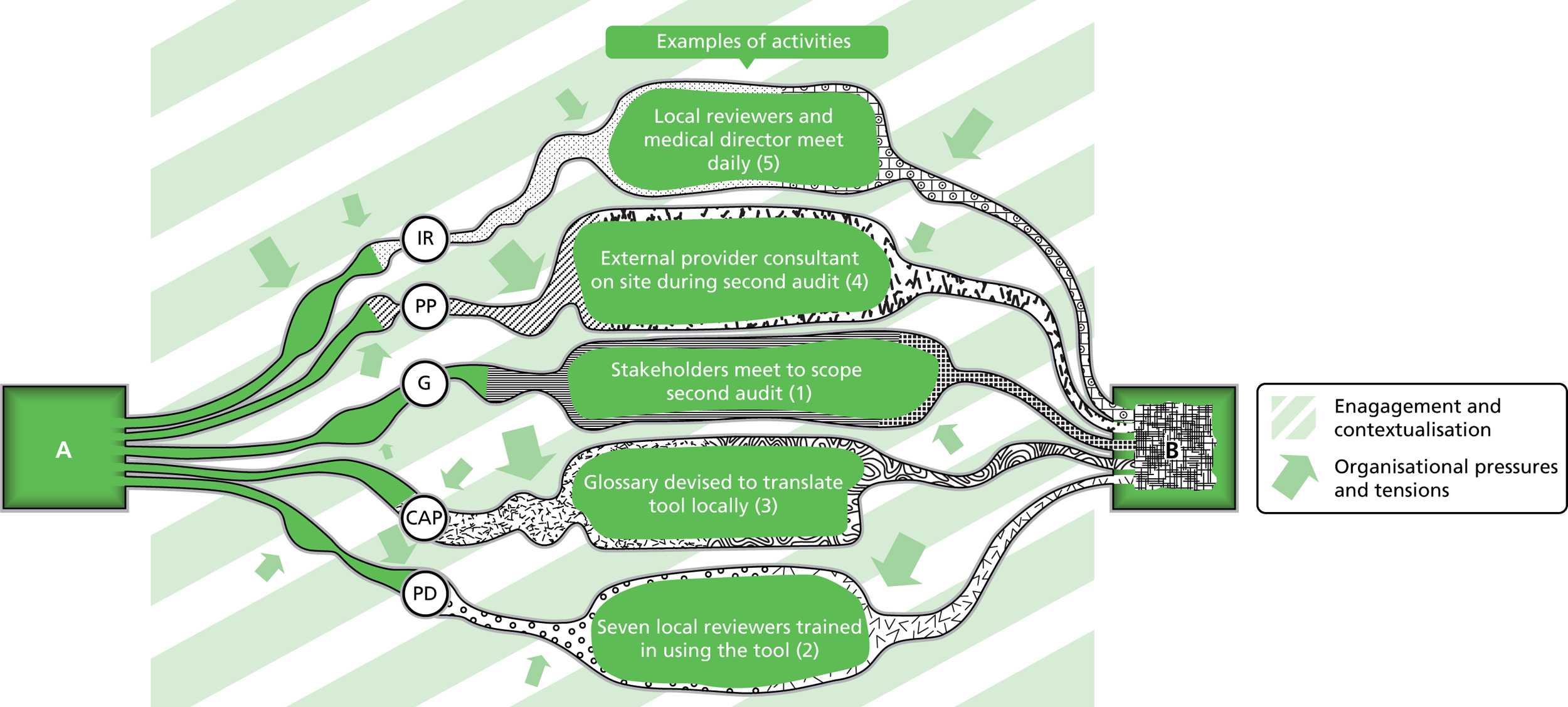
FIGURE 10.
The transformation of knowledge in vignette 2. EP2, external provider 2; CAP, copy, adapt and paste; G, governance; IR, interpersonal relationships; PD, product deployment; PP, people placement.
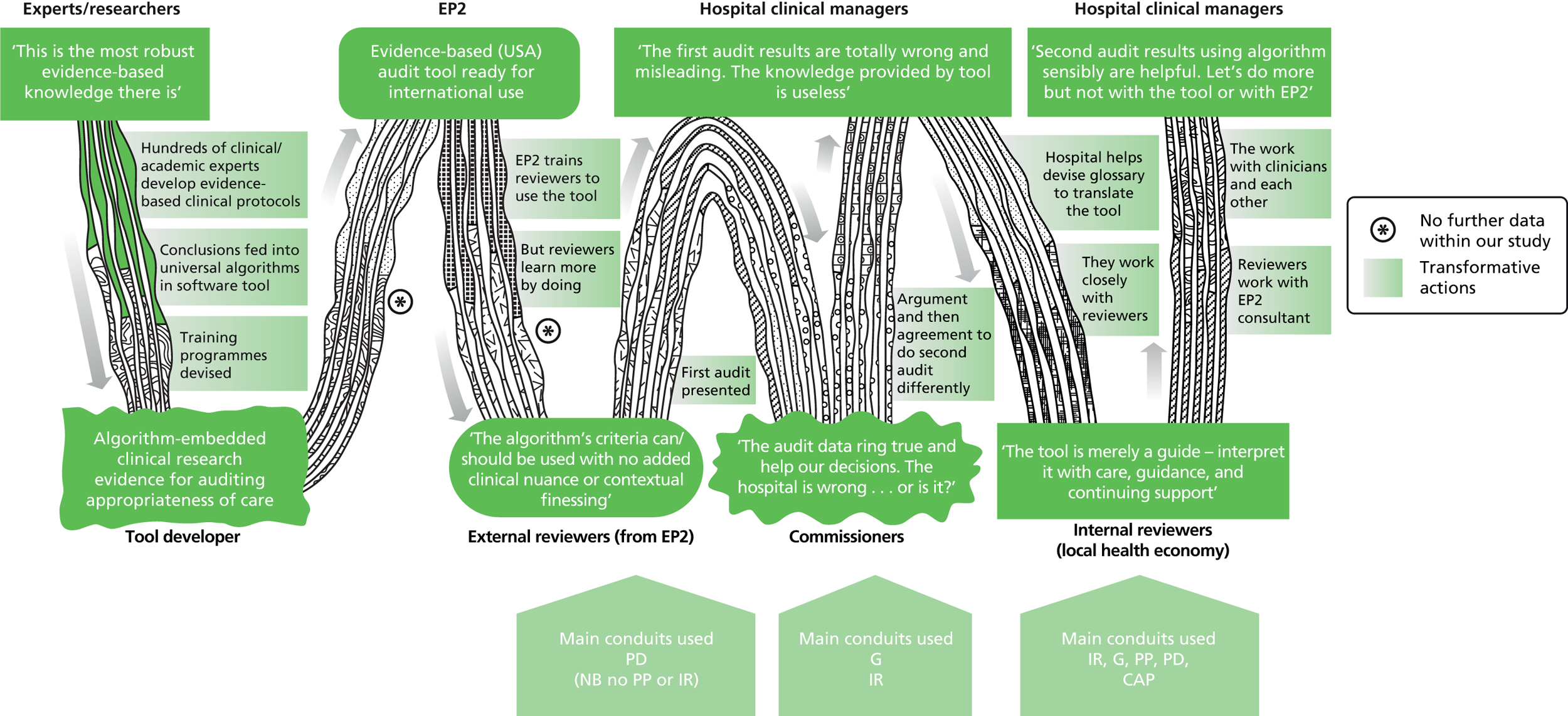
| External provider 2 (tool supplier) | Reviewers | Acute hospital trust clinical managers | PCT commissioners |
|---|---|---|---|
| Aims | |||
|
|
|
|
| Activities to meet aims (or not) | |||
|
For provider 2 reviewers (first audit):
|
|
|
External provider 3
Background
External provider 3 was a UK subsidiary of a North American health-care corporation with an international portfolio. Although in the UK external provider 3 employed over 100 staff, they had access to several thousand North American employees, who acted as international experts, developed software tools and sometimes filled UK staff shortages.
In 2008, external provider 3 won a 2-year contract to carry out several specific pieces of work for a PCT. During the first year of the contract these were renegotiated and four main work streams emerged: (i) support for WCC; (ii) complex case management, including the introduction of a software tool; (iii) development of a ‘savings cabinet’; and (iv) consultancy/coaching work with newly appointed directors within the local commissioning structures. This vignette focuses on work streams (i) and (ii). Various extensions meant that the contract eventually lasted 3 years.
External provider 3 had five to six whole-time equivalent staff working on the contract, but this involved eight main individuals. As well as a programme manager and a clinical lead, there were two North Americans who spent a substantial amount of time on site, an associate programme manager, one or two people for ‘actuarial-type work’ and an analyst. Some of these staff were ‘coming and going’, but a feature of the work seemed to be the continual presence on site over a long period of time of the clinical lead and the associate programme manager.
Knowledge wanted
The commissioners in this vignette worked within a strong local culture of collaboration, innovation, public engagement/accountability and transparency. They were very open to working with external agencies to support their commissioning activities, and did so regularly because sometimes they were unable to attract candidates with the necessary experience. Being able to recognise where external support would be helpful was an area where the NHS clients felt skilled. During fieldwork, several NHS staff spoke about the importance of building up a network of external organisations and individuals who had the right knowledge and skills. The expense, however, was mentioned as an important constraint on accessing external support.
At the time of tendering for this contract, which pre-dated the 2012 Act by several years, the commissioners were ‘trying to go from good to great as a commissioner’. To achieve this, they wanted to look outside the NHS as ‘we wanted to set our aspirations greater than just what was available nationally and look at some of the good practice internationally.’ Contracting a company with a North American base was, therefore, particularly appealing. Consultants from external provider 3 described the commissioners at this particular NHS site according to Belbin’s team roles. 51
So they were the plants and shapers, but they weren’t the completer finishers. I would say that that was evident when we were working with them, that they had a huge amount of ideas. Lots of shaping, lots of meetings, huge meeting culture, and then the actual discipline of completing it and measuring was not there.
The external provider 3 consultants assigned to the contract saw themselves as ‘completer finisher’ personalities which complemented the missing skills within the PCT. Both external provider and NHS staff spoke about the degree of focus on performance management as one of the key differences between their organisations. Another commissioner summarised the knowledge and skills which he thought external provider 3 had brought to the NHS client organisation as good, real-time analysis, programme management, engagement and coaching.
World Class Commissioning work stream
External provider 3 described a ‘gap analysis’ based on the success criteria for WCC as ‘hard going’ for both sides, but also ‘the key’. Through the gap analysis, the external providers sought to help the commissioners understand the assurance process. The consultants went through each commissioning competency and challenged the commissioners to ‘demonstrate that you actually do that. Give me the tangible evidence’. The gap analysis also facilitated communication within the NHS client organisation, leading to the discovery of duplicated work.
A ‘massive programme of work’ was then undertaken to prepare for the next WCC assurance day. An early task was to work with commissioners to identify who should be part of the WCC process ‘not just having the same people that put their hands up, but actually who does need to be involved’. This included identifying the stakeholders external to the commissioning organisation: ‘if you don’t start engaging with them as of day one, when they do get contacted they are going to give a very different message to what you think they will’. The external providers said that the commissioners recognised that project management was not one of their strengths, and so training was provided: ‘a lot of the stuff that we did was around developing staff to take on projects’. They also provided information about tools which could be used for particular tasks, and further training around these.
The commercial consultants mainly drew on best practice examples nationally and internationally, identified from existing and new contacts to inform this work. Some of this knowledge came from colleagues working at other NHS sites who had already gone through the WCC process. The external consultants on site brought in experts from external provider 3 to the NHS client site, including North American staff who provided some training. But they also made contacts based on publicly available information and facilitated exchange of knowledge between NHS organisations.
Case-management work stream
A NHS commissioning manager described the second work stream as ‘a project directly to support adult social care and community nursing to think about what we needed to make that work here’. First, a software tool was used to identified the ‘riskiest population’ in each of the localities, and then the external providers ‘sat down with the community matrons’ to compare the lists of patients produced by the tool with current patient lists (presumably based on clinical judgement). They found little overlap. External provider staff said that this had ‘really started [NHS clients] to ask questions’. Agreeing how to proceed had been a long process, necessitating going ‘back quite a few steps’ to discuss the basic principles of case management and the definition of a ‘complex’ patient. External provider staff felt that NHS staff sometimes did not have thinking space or ‘someone next to you challenging’ your assumptions. The software tool, and the external provider staff supporting it, had provided this challenge. This led to changes in the implementation of case management.
As part of this work stream, the clinical lead from external provider 3 was involved in project meetings with the leaders of the NHS clinical teams and she also ran sessions directly with nurses and social care workers. This consultant said that within the existing case-management programme ‘there was nothing to say whether what they were doing was actually adding value anywhere in the system’. So, as evidence to evaluate the impact of the existing case-management programme was not being generated, this was something else offered by external provider 3.
In addition, the personal qualities of the external provider lead were appreciated. A NHS client said that the external provider clinical lead was ‘a skilled programme manager’ and had clinical knowledge and experience as a nurse, a combination missing from their own organisation at that time. Actually having carried out case management elsewhere, and speaking from that experience of changes, the various benefits and pitfalls, was key to the external provider’s value. The NHS commissioning lead was also a clinician and this similarity in backgrounds meant that the external provider clinical lead had ‘very ably’ supported him to get other clinicians on board.
Challenges
The main challenges, which were raised by both sides, were those of defining what work was needed and ensuring the work remained relevant and useful in a constantly changing commissioning environment. A NHS commissioning manager felt that several factors had affected the relevance and usefulness of work done by various external providers for her organisation. She felt that either partner could be ‘at fault’, with the brief sometimes not having been that good, but also ‘what is brought is not quite as relevant as it could have been’. The political climate had changed after work was commissioned, meaning that it was no longer as acceptable. The contract was sufficiently flexible for changes to be made when needed, although this did take a good deal of time and energy. The long timescale of the contract facilitated this, as did the mutual goodwill to engage.
Views on the work
The NHS commissioners expressed positive views about the quality of the work conducted by external provider 3. The clinical lead assigned to the project was rated particularly highly, and was seen to have good credibility based on her ‘sound knowledge’. A commissioning manager said that the external provider had ‘much better horizon scanning, because they were looking internationally’, while another manager emphasised how the external provider had been skilled at interrogating data, identifying areas which needed work, and coming up with ‘good tools which we could use’. Another commissioner described external provider 3 as having ‘both the tools and the understanding of those tools’. The manager who had been closely involved in the case management work was very satisfied.
What we’re buying is a polished product for something that we want to do anyway. But of course you then come into the aspect of how they support us to get going, and that’s a standard supplier/provider thing, and we’re very happy with that, I think they do a very good job. If I didn’t, they wouldn’t get any more business.
A GP commissioner was less sure about whether or not the contract had been a good use of resources:
They did some work here but for what we paid them I’m not sure. It was somewhat difficult to understand exactly what they achieved in the end. So I think if you’re going to do that you’ve got to be very clear about getting value for money because it can be very expensive . . . you know, well it’s the cynical idea, isn’t it? You get management consultants in to tell you what you know already. They just go round, you know, finding, you know, and producing, probably hopefully producing solutions that you may not have seen, but probably you have seen, but not been really able to put into effect.
The quality of the work was not the only factor affecting how useful it ended up being, and this senior manager’s view that some streams were very useful and others less so was a fair reflection of our data overall.
There were some really good pieces of work where we were looking at things such as risk stratification and programmes of work going forward, and those worked quite well . . . I think both of us [external provider and clients] probably felt, at the end of the day, that we’d got some really good things out of it but perhaps not as much as we had hoped.
Benefits and disadvantages
The external provider staff assigned to the contract felt that it had gone particularly well, saying that their organisation was really proud of this project. They described knowledge transfer as having been a pillar which stood alongside all of the work streams, and that this was important to their professional integrity. The benefits perceived by the NHS clients included those linked to specific projects but also more general skills and approaches which they felt they had acquired through the work.
And they have supported us in making us better at doing the evidence. Because external provider 3 will never do anything without having some data analysis, they’d have almost a hypothesis to do something and then they’d test that out . . . So I think they have made us more organised in that way.
A commissioning manager referred to a ‘commissioning toolkit’ of ‘those types of technical things that we would need to support us going forward, which we’ve used’. She felt that the external providers had led by example but had also set up the systems and processes that ‘then enabled us to see and learn how to do that type of process’.
The WCC work stream had been very effective in moving the NHS client up the national rankings, but it was not clear what the impact was on their actual commissioning at the time. A minority of NHS clients were uncertain about the ongoing value of the work a few years down the line and in a very different commissioning landscape.
The case-management work stream had challenged how community services were being targeted, and had engaged clinical, social care and management staff in negotiating agreed definitions of targets and objectives for case management. A system for measuring outcomes was also introduced. However the ultimate outcome of the work was beyond the control of both external provider 3 and the commissioners, as it required the service providers to deliver the benefits. Restructuring of community services owing to national level initiatives was seen by a commissioning manager as having limited the impact. This was ‘absolutely nothing to do with the expertise we brought in’.
Yeah I suppose, hmm, [long pause] I mean to some extent, you know, to some extent we’ve gone as far as we can at the moment on that particular case-management initiative. And I would point to it and say that was a result of their involvement.
Nevertheless, this work was described by another commissioner as having been ‘the biggest gain’ on the contract. He commented that the external providers were ‘very good’ at working with professional groups and felt that an opportunity was missed in not bringing the external providers together with clinicians earlier. Another commissioning manager also felt that the clinician engagement had worked well, and that it was where some of the legacy lay, as it was ‘real for people, and it’s not just feeling as if it’s a theoretical exercise, so people can see that there has been a change that are using the systems’.
The WCC work stream is depicted in Figure 11. Although the numbers indicate possible chronological order, this was not entirely clear from the data. Moreover, because the WCC aspect of this vignette is derived mainly from the experiential knowledge of external consultants, using data to develop tables and models tracking the transformation processes of that knowledge was difficult. So, no table or figure equivalent to those in External provider 1 and External provider 2 accompany this vignette.
FIGURE 11.
Transformative proccesses in vignette 3.
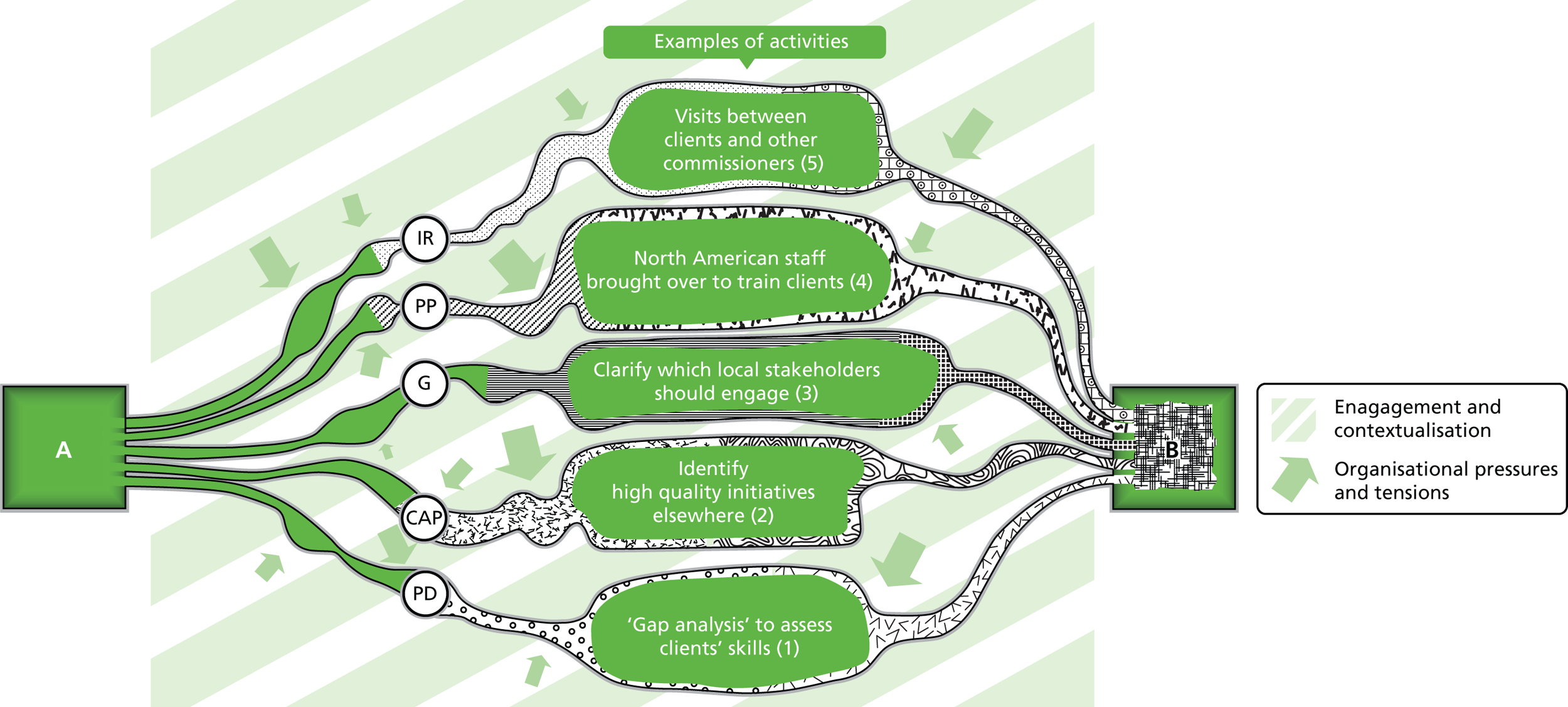
Box 10 summarises the key points of the third vignette and Box 11 summarises the key points in the chapter.
Several knowledge conduits were employed in this vignette. As this was an organisation comfortable with the idea of ‘buying in’ knowledge and skills as and when required, knowledge was acquired from the people brought in (people placement). The commissioners had a strong interest in exploring international best practice (copy, adapt and paste), but they did this via the presence of those external provider 3 staff within their organisation. External provider 3 staff drew on knowledge from their colleagues working elsewhere in the UK as well as from North America to find good examples of best practice (interpersonal relationships). They also searched the internet and made contact with other NHS organisations to find initiatives which had worked well elsewhere which could be adapted for this NHS client (copy, adapt and paste). The application of the tool triggered a renegotiation of the client’s approach to case management, and the use of gap analysis had been crucial in identifying the tasks for the WCC work (product deployment).
The local culture within the NHS client resulted in governance processes which prioritised collaboration, innovation, transparency and engagement, and this may have been behind the strong relationship which developed with the external provider. External provider 3 staff commented on how this relationship had gone beyond what was usually developed with most NHS clients, where external providers were sometimes perceived as a threat. The embedding of external providers and the duration of the contract had also facilitated this relationship. This relationship and level of access allowed added more value, and trumped some negative associations of their private-provider identity encountered elsewhere.
Contextualisation was also very visible within this vignette. The external providers’ engagement with professional groups was seen as central to the progress which had been made with case management. Both the software tool and the case management methodology which external provider 3 had brought to their NHS client had originated in North America and had been contextualised, first, for the UK context, and then another level of contextualisation was added at the level of the local client site.
-
Knowledge transformation processes were multilayered, multifaceted and nested within each vignette in various ways.
-
These vignettes demonstrate that external providers may offer ‘solutions looking for problems’ rather than developing solutions in response to real problems experienced on the ground.
-
Examples of knowledge obtained via interpersonal relationships included professionals from commissioning, hospital, community and social services pooling their knowledge in daily face-to-face encounters when auditing and external providers contacting colleagues for best practice advice.
-
Product deployment included the training and use of software tools and gap analysis to inform competency development work.
-
Governance was less evident, and sometimes stopped knowledge transformation from occurring, for example when a PCT did not consider revised results from an audit after board decisions were made or when national imperatives superseded local decisions.
-
Examples of copy, adapt and paste included modifying software training tool materials for general practices, adopting the conceptual approach of a software tool (without using the tool itself) and applying (modified) successful WCC initiatives from elsewhere.
-
Examples of people placement included embedding external provider staff in a commissioning organisation and assigning a project manager to teach general practice staff use of a software tool in another.
-
Contextualisation in these vignettes largely occurred around adapting North American software tools to local English health economies through glossaries and the interpretation efforts of external providers.
-
Engagement was visible throughout the vignettes; for example, when commissioners worked to re-engage health-care providers after an unsuccessful first audit, general practice staff were introduced to software tools and professional groups were enthused to achieve ‘World Class Commissioning’.
-
The result of the knowledge exchanges and transformative processes, shaped by the key actors’ contextual drivers, constraints and worldviews, was to produce not only actual changes in the knowledge base but also a range of different ways of framing the external providers’ tools that were being used and the information the tools generated.
-
Highly skilled external consultants working in welcoming organisations that added value beyond what was available locally and deliberately drew on multiple knowledge transformation conduits appeared more successful.
Chapter 9 Benefits and disadvantages
Introduction
Having discussed knowledge acquisition and transformation and the role of external providers, we now address the research question:
What are the benefits and disadvantages?
When originally conceiving this question, we were particularly interested in how knowledge exchange between commercial providers and NHS clients influenced commissioning decisions. However, our analyses suggested that answering this question was much more complicated than just looking at impact on commissioning. In assessing benefits and disadvantages, the implicit questions to be considered are: benefits of what and for whom?
In thinking through ‘of what’, our main focus of interest was external provider–NHS contractual relationships, particularly commercial and not-for-profit providers. The ‘what’ also included their products such as software tools, new information (often from the tools) and use of knowledge conduits such as people placement. In terms of ‘for whom’, the principal client audiences identified were commissioners and analysts. But each of these audiences was heterogeneous, with a multitude of clients with different expectations. For example, senior commissioners might be interested in strategic gains and improvements in their organisation’s prestige, while the focus of junior commissioners might be more operational, such as support in developing patient pathways. Similarly, those involved in the production and marketing of information included CSU senior managers interested in better leverage in the health-care market, middle managers who wanted to enhance day-to-day relationships with their clients and those at the coalface who churned out the data looking to do so more quickly and easily. In addition, a secondary group of NHS clients was the health-care providers who were affected by data collection and interpretation.
A further potential beneficiary audience was the commercial and not-for-profit providers, who wanted to exploit the potential of their software tools and attract other clients with their growing knowledge base. Because these external providers were also made up of professionals with heterogeneous disciplines, occasionally one professional group (say analysts) would conclude that a particular contract had been successful, citing post-contractual NHS-commercial analyst collaborations, while staff with other perspectives involved in the same contract stated that the contract was not particularly successful, because senior management relationships had soured between clients and the external provider.
Thus assessing benefit depended on what was under consideration and who was making the judgement as well as what had been produced. Furthermore, clients weighed up useful output against expense.
Don’t ask me about value for money on those things because, you know, from the private sector, and in the public sector, external consortia of that type is very, very, very expensive. And there tends not to be a formal measure of how much you got for that.
David, CCG chairperson
In Chapter 8, we presented accounts of the perspective of NHS clients along with details on the nature and benefits of the collaboration. Data to inform this chapter come from the three vignettes in Chapter 8 along with several other contracts between NHS clients and external providers. All were with commercial and not-for-profit agencies except the final two. These included:
-
training NHS commissioners and analysts to become ‘superusers’ of a software tool (see Chapter 8, External provider 1)
-
the training and use of an electronic auditing tool to determine best place of care (see Chapter 8, External provider 2)
-
developing the commissioning competencies and performance of a commissioning organisation (see Chapter 8, External provider 3)
-
supporting the reintegration of those with long-term conditions into the community
-
training and deployment of a suite of software tools
-
an outsourced commissioning unit
-
supporting a new contracting initiative
-
developing and using a dashboard for unplanned hospital admissions (CSU)
-
project to improve condition-specific outcomes for an acute condition (freelance consultant).
For several contractual relationships (a, b, c, d, e and h), we have sufficient data from the external provider and NHS clients to draw conclusions. For (f) we were unable to recruit sufficient NHS clients, and for (g) and (i) we were prevented from collecting sufficient accounts from external providers. Nonetheless, we have ample data to inform this chapter.
We begin with a discussion about the unhelpful factors that hindered knowledge exchange in the NHS generally, before focusing specifically on knowledge exchange with external providers. We then set out the challenges in assessing the impact of contracts between the NHS and commercial/not-for-profit sector, followed by a set of useful criteria to judge that impact. The chapter ends with findings on what did and did not work well.
Gap between analysts and commissioners
Several participants mentioned that the schism between health-care analysts and commissioners was particularly unhelpful in fostering knowledge exchange. Initially, commissioners and analysts were colocated within PCTs and were then generally separated out into two organisations with the 2012 Health and Social Care Act4 (CCGs and CSUs). But even before the Act, these two communities did not work well together, as other studies have shown. 52 A former NHS analyst thought that separating analytics from commissioning was ‘absolutely’ wrong for the fast-paced, highly changeable environment of commissioning.
So this sort of siloed approach where one set of people come up with the requirements and they give the requirements to this other set of people who go away, beaver away and then deliver it, I just don’t think that works. I think that’s absolutely set up to fail.
Randall, freelance analyst
This gap affected not only analysts and managers in commissioning organisations, but also those working within acute hospital trusts. A former head of IT for a hospital recounted how he bridged the manager/analyst gap by instituting a policy of asking analysts to follow up managers’ requests by initiating personal contact to find out more about what information was wanted and how it would be used, because historically analysts had not furnished the right information. Similarly, the former head of information for a commissioning organisation set up an exchange between PCT and acute hospital analysts so that they could learn more about each other’s environments and use of information. These are both examples of people placement.
Within commercial provider organisations, we found that the gap between analysts and commissioners (or project leads) was much less evident, even though many commercial participants had ex-NHS backgrounds. Possibly this was because commercial companies deliberately cross-fertilised individuals with different backgrounds. For example, a commercial company said that their ‘standard team’ consisted of a project manager, a clinical lead and an analyst. As a result, analysts were highly knowledgeable about commissioning and how best to produce useful data and managers and clinical leads knew how to use data to inform change. This level of interdisciplinary working was noticeably absent from the NHS sites.
Another long-standing contribution to the schism between analysts and managers was that the trigger for data production was the ‘wrong way round’. Data tended to be generated and then a use for this data was sought, instead of managers first defining a problem and then analysts generating the information for a solution.
It always starts with the data, stick it in a big warehouse, then they think, ‘Well what should we do with this?’ and then we start pushing out, coming out with reports and saying, ‘Do you like these reports?’ Rather than starting from the other side, which is the commissioner has this burning urge to answer this particular question that is relevant to making an actual decision. So OK, so we need to answer this question: how are we going to go about answering it?
Randall, freelance analyst
Difficulties in measuring the impact of contracts
Commissioner/analyst silos
The gap between analysts and commissioners also created difficulties in measuring the impact of contracts between the NHS and external providers. A major product of commercial/not-for-profit providers in this study was the generation of good-quality data using sophisticated tools. But within the NHS generally, data were not used to generate change. Therefore, this affected the assessment of the impact of these contracts. Moreover, because interventions were software-tool based, NHS/CSU analysts were more likely to benefit from contracts with commercial and not-for-profit providers through more powerful, easier ways of generating data. But benefits such as easier data generation often were not noticed by commissioners, as commissioners had little knowledge of the work of the analysts. The schism between these two professional groups meant that an appreciation and understanding of the impact of these contracts might not have percolated through the system. However, sometimes commissioners did notice. In one contract, NHS commissioning clients clearly identified how detailed analysis of data from invoice validation software had led to million-pound savings.
Dependency on other factors outside control
A further difficulty in measuring the impact of contracts was that often the change indicated was outside the influence of the external provider (and sometimes the commissioner).
For example, the purpose of many software tools was to identify populations for care interventions. Assessment of impact depended not only on the quality of the software tool, but also on the care intervention. If there was no care intervention, a poor-quality care intervention, or one that affected few people, then the benefits of the tool were blunted. Moreover, the benefits often were not realised for a long time, which frustrated short-term assessments of the impact.
The question that I get asked most often . . . is, ‘Well where’s the evidence that having [software tool] makes a difference?’ And er it’s an incredibly difficult question to answer because – and my stock response is, ‘Well actually having a system that combines data, runs it through an algorithm and provides you with a set of information on its own isn’t going to make any difference. But if you’ve got good-quality community matrons, if you’ve got GP practices that have an integrated care team, where GPs and community matrons and possibly social workers meet together on a regular basis and review patients from the [software tool] list, and you’ve then got a willingness to change the care pathway for those patients, then you will see a change, and you will see an improvement’.
And is that happening anywhere?
Um yeah there’s er – I think it’s probably more an exception than the rule.
Alfred, NHS analyst
Sometimes NHS clients accepted that the impact of the tools was dependent on the behaviour of others and these did not negatively influence their view of the commercial provider. Elsewhere, commissioners were less sanguine.
And they spent £5,000,000 on it and they were busy, I went down to the meetings down in [X] on a regular basis, and every time, every meeting I went to they were saying, ‘Oh well, yeah, it’s all rolled out across [County A] and [County B] you know, I can’t understand why you don’t use it.’ I said, ‘Well what have they achieved?’ They said, ‘Well they’re finding – they’re finding out lots of things.’ I said, ‘Yeah but what have they actually achieved?’ and nobody could tell me a single thing that had happened as a result of it.
Patrick, GP commissioner
Changing priorities
Another challenge in measuring benefits was the changeable nature of commissioning. Both commercial providers mentioned contracts that initially had substantial knowledge exchange mechanisms and that were subsequently dropped from the contract when more pressing needs arose.
And one of the biggest challenges for us around the skills transfer is the recognition of what our clients need to do to be ready to take it. So going back to the [software] tool we are using, the process has been designed whereby we would do the first round of audit in the setting. The next round 6 months later, we would coach and mentor the PCT staff to do that in a community setting, so they learn how to use the tool with a member of our team sat next to them. And they would be trained in how to get the outputs from it. What happened in practice was the PCT said, ‘We don’t have the staff to be able to do that so what we’d like to do is pay you extra to do the audit for us again’. So I’ve written and said, ‘Okay, we could do that, but you’re not going to get the transfer of knowledge and skills’. So we have to be really, really careful. Our whole ethos is that they get this knowledge and skills so they get the benefits but if a client chooses not to do what they need to do, we have to be very, very explicit. Because if we get to the end of this and they say, ‘Well you haven’t told us how to do this; it all gets very, very muddly’.
Lana, commercial consultant
In some situations, the commercial providers genuinely wanted to maximise knowledge exchange, but the NHS clients were not very interested. In others, the commercial providers did not appear to value knowledge exchange. One contract became particularly difficult because the NHS clients believed that the commercial providers deliberately avoided transferring knowledge to keep the clients dependent.
Isolating desired consequences
Another difficulty in assessing the benefit of contracts with external providers arose from the complexity of the NHS and the wider health and social care system. Benefits from one intervention might easily create unintended, negative consequences elsewhere. Moreover, isolating the benefits of one particular intervention was difficult if multiple changes were taking place within the health economy concurrently.
Sometimes you might have a very successful project, but it will be swamped by something else. For instance, we had a pathology lab project, and I believe it was quite successful on the elements that they were targeting, but the overall pathology results showed a huge increase because there had been a new policy put in around dementia testing, which involved eight different pathology tests.
Connie, CSU analyst
Benefits slow to materialise, subtle and difficult to measure
Benefits were often slow to be realised. For example, an experienced senior commissioner was brought in about 18 months into a 3-year contract to give notice of its termination as the NHS clients thought it was not working well. This manager thought that the difficulties were because the contract was underfunded and forecasting of overspend ‘tended to bounce around quite a bit from one month to the other’ (Jacob, commissioning manager). He convinced the NHS clients to continue with the contract, arguing that 18 months was too early to reap the benefits. The volatility calmed down over the next few months, as the commercial provider had predicted. In the following year, the full budget was allocated, the savings target was delivered in full and the ‘overall contract envelope came in pretty much on the button which is quite an achievement really I think for [commercial company] given the amount of change and sort of chaos frankly that was going on in the system at the time’ (Jacob, NHS commissioning manager).
Although the success of this commercial provider was recognised, a few commercial consultants and a Public Health consultant mentioned that sometimes the benefits from their contributions might be overlooked. This could be because as knowledge was transformed, tracing it back to the source was challenging, but also because often benefits were subtle, such as changes in attitudes, relationships or dynamics. For example, a commercial consultant recounted how the use of a software tool had improved local relationships:
I mean I think that we have added value to the organisation, and added skills and expertise. I’m trying to think, if you went in there, would they say, ‘Oh, you know, this is what we did before and this is what we did now’. I think they would see some changes in terms of just working around some of the day-to-day commissioning issues. I don’t think what we have affected is some of this – well I think we have affected the dynamic relationship with the provider actually. I think we’ve certainly added some expertise and some clinical expertise in terms of the work around [software tool]. So an area where they thought they had a problem but there had never been the evidence to have that kind of discussion with the clinicians. Yeah so I think they might say that – you know, or they didn’t have the analytics or the – so I think they would probably say that some of their – they are now almost better equipped to make those decisions or to have the discussions.
Betty, commercial consultant
Interestingly in this case, the perspectives of NHS clients who used this commercial provider concurred with regard to the development of better relationships with acute providers and production of evidence informed discussions, although they categorically stated that the commercial provider had not brought clinical expertise (see Chapter 8, External provider 2). Neither have they elected to buy the tool again.
Moreover, even when changes could be identified and agreed, quantifiable measurement was open to extensive negotiation. For example, in calculating the savings accrued by deploying a software tool, a participant said that nurses who were embedded into acute hospitals to check invoices had looked into 150 cases and ‘made real patient impact’. A monetary figure was put against this in terms of the savings realised from earlier discharges and reductions in pre-operative lengths of stay. But this figure was not convincing enough; the nurses were pulled from the hospitals and moved back into the internal audit team because it was ‘very hard to quantify those savings’ (Dennis, commercial consultant).
In summary, there were many reasons that made demonstrating the benefits of contracting external providers challenging. These included:
-
the split between analysts and commissioners which left commissioners uninformed about the value of external provider input
-
the dependence of benefit generation on other professional groups within the system who were outside the influence of the external provider
-
changing commissioning agendas, which led to the prioritisation of different benefits
-
the complexity of the NHS, which meant that benefits in one area could lead to disadvantages elsewhere
-
the usual challenges in outcome measurement, such as difficulties in attributing causality, or in distinguishing and quantifying the impact of earlier or more subtle inputs.
Generally, perceptions of change depended on the agenda and position of the informant. Commercial consultants and the NHS clients responsible for their contracting understandably claimed greater evidence of added value to justify the expense, while those with more negative views of external providers or decision-makers who did not see directly the contribution of the external providers were more likely to downplay or overlook external provider contributions.
Indicators of a useful contractual relationship
Given the challenges and complexities in identifying and measuring benefits, NHS clients and external providers developed other ways of judging success.
One was that the products were still in use. An analyst described one contract as a ‘really positive experience on both sides’ as the clients were ‘still using my stuff’ such as databases, which the commercial company had sold for a (notional) penny (Joel, commercial analyst). But not all products were maintained. A ‘prioritisation framework’ for one CCG was discontinued, because it was too prescriptive and the scoring mechanism did not capture difficult judgements. Instead, the NHS clients brought in a set of prioritisation guidelines based around ‘must dos’ and benefits for patients.
Another sign of a useful contractual relationship was that the company was recontracted because ‘if you use a service that works well you tend to use it again’ (Tom, CCG chairperson). Several participants from two different contracts with a particular commercial provider mentioned further work and contract extensions as evidence of success. Further work and contract extensions were likely to come about only if the contractual targets and the brief were met to the satisfaction of the client. In one contract, this was clearly not the case, as the contract was docked by 25% because of client dissatisfaction with performance.
Another way of judging success was that the commercial company used the NHS clients as references. One NHS client, who worked with multiple commercial companies, noted that one tended to refer prospective clients to them while another did not. Moreover, no mention of this contract existed on the commercial provider’s website.
We’re less of an important client than we were, almost. That’s what it feels like . . . It’s not a flagship for [commercial provider A] as it had been . . . And I don’t think that they would immediately recommend us as a reference to another client. In contrast [commercial provider B] . . . are referring people to us . . . and I’ve had phone calls and e-mails from [CCG A] and [CCG B] in terms of people making enquiries about what we’re using [software tool] for and how does it work and what is [commercial provider B] like as a supplier . . . I don’t think [commercial provider A] thinks that we would probably speak very highly of them.
Alfred, NHS client
In summary, the indicators of a useful contract were:
-
Output from the contract was still in use.
-
The external provider was recontracted by the client.
-
The client provided positive references for the external provider for future clients.
What does not work well
Aggressive, strategic marketing
Several factors could negatively affect the contractual relationship. As mentioned in Chapter 7, several participants had concerns about the profit-making agendas of commercial companies. For example, a Public Health consultant talked about attending a conference where commissioners were ‘pressurised’ to purchase their products. Another participant was suspicious about the claims about software tools, because he thought that these might stem more from a desire for profit rather than usefulness.
And I think there is huge value in going to the States and looking at those tools and saying, ‘Well which one of these works in the UK?’ Not, as the management consultants are doing at the moment, looking at them and saying, ‘Which one can we make (the biggest) profit margin on in the UK?’ And I suspect (why) [software tool 1] have been touted fairly heavily by [commercial provider A] is because [software tool 1] come with a much lower price tag than [software tool 2] which, you know, are owned by [commercial provider B] and – and [commercial provider B] don’t give things away.
Harold, freelance consultant
Limited desire for external provider support
A major factor influencing success was the desire for external provider support. Being told what to do was endemic in the NHS, and NHS professionals were used to having to try to find some merit in hierarchically imposed interventions, programmes and tools that were unsolicited or appeared not to meet their needs. In one contract, after a tendering process that took nearly a year, the client needs had changed and so the ‘solution’ no longer addressed a clear ‘problem’. Moreover, it was never clear whether or not frontline, operational analysts, on whom the success of the venture depended, had been consulted or engaged. One freelance consultant with a view from the sidelines, said that he thought that this particular contract was ‘appalling and shambolic’ on both sides. For example, he claimed that NHS staff ‘intentionally sabotaged projects’ (although details were not provided), because of ‘anti-private sector sentiment’. Meanwhile, there were competence issues with the commercial provider who could not deliver or ‘get the requirements quite right’ because they had a ‘less than helpful customer’. In his view it was unsurprising that the success of this contract had been ‘patchy’ (Randall, freelance consultant).
Participants discussing other contracts noted the difference between those clients who were ‘forced’ to work with external providers because they were poorly performing and those who were more ‘open to knowledge’ (Joel, commercial analyst). Hostility from NHS staff stopped knowledge transfer in several contracts, as this process was possible only if both sides were receptive.
Potentially I think what’s been challenging across the project generally is a little bit of hostility initially from the NHS staff definitely, all blame on their side I would say. But that, I think, has created quite a difficult relationship, and I think that is impeding what could otherwise be really good knowledge transfer.
Paula, NHS commissioning manager
Lack of clarity around the brief
If a contractual relationship had not been desired or sought, or even when it had, a related difficulty was lack of clarity about how to maximise the contribution of the external provider. A commercial consultant thought that the NHS clients were not getting the best out of one contract because PCTs did not know what they wanted.
I’m probably being unfair, but from the PCT perspective, I don’t think they’ve actually sat down and thought, ‘How can we really get the best value for money from this particular contract in terms of sharing knowledge?’
Georgia, commercial consultant
A CCG chairperson also felt that the reason this contract had not turned out as intended was because ‘there was not enough intelligence in the commissioning of that set up in the first place. In other words, the commissioners didn’t really know what they wanted’. This meant that the private providers were not clear on what they were supposed to deliver ‘and there was not then the engagement between the intelligent commissioner and the intelligent provider to actually deliver a product that was really useful’ (Simon, CCG chairperson).
A NHS commissioning manager from another CCG thought that commissioners overfocused on the ‘holy grail’ among tools at the expense of thinking through what information tools might provide to create change.
Actually these things are tools and they’re not perfect. They’re giving you a clue and pointers, but at the end of the day you have to interpret them and apply [laughs] a bit of common sense, and actually take some action. And I suppose that’s all it is. I think people spent such a lot of time talking about tools and not enough time in actually thinking about systems and what we needed to do.
Sandra, Public Health consultant
This lack of clarity about the purpose of external provider support was a common refrain across the case sites. Partly this stemmed from minimal knowledge about what external providers could offer, but the rapidly changing needs of NHS clients also exacerbated this difficulty. To redress this confusion, help clarify the brief and generate enough work to justify the costs of the contract, one external provider held meetings with senior commissioners and analysts attached to the contract across several organisations. The aim was to identify three clear projects for each organisation, develop an action plan and track progress. This resulted in several impressive, colour-coded documents with progress quantified in percentages for each project. Moreover, the office walls of the commercial provider were covered in different coloured Post-it® notes with information about progress and the occasional headline, for example ‘All project deliverables for April achieved!’ However, 3 months later when enquiring about these action plans, we were told that they were out of date and no longer in use.
Sometimes another contributing factor was that the NHS client who first contracted the external provider was no longer available, leaving a gap in terms of understanding the purpose and vision behind the contract. This was especially true in contracts that relied heavily on one manager to develop the tender.
One of the critical things that happened, in fact it was their start day was – I became seriously ill and I was taken out of the system for 6 months. So having done all the work up, all the negotiation . . . So there was a steep learning curve, having built that relationship with me, and working with me and understanding what I wanted, and I went off on the day that they arrived, and other people had to try and pick that up. But I would say, regardless of that, I’m not saying that there wouldn’t have been difficulties even if I had been there.
Sarah, NHS commissioning manager
Without a vision about the purpose of the brief, clients often struggled to know how best to interpret and apply the output, so little happened. Sometimes the presentation was a ‘glossy’ document that was not amenable to application, perhaps because of limited resources dedicated to implementation.
But I think a lot of these large consultancy firms come in, they go through the data which is corrupt and needs uncorrupting, and then they give you a load of information. But when you try and put it in, it doesn’t do anything. So I mean [commercial provider] so they’re very good at coming and giving you a false sense of security as to what you’re doing . . . But they’re also not given the time to actually make the change, you know. So they’ll keep coming in to give you a diagnosis, but it tells you what you already know. But they’re not really given the opportunity to implement . . . there’s lots of money been spent on that sort of information, but it doesn’t get transferred to the organisation.
Percy, freelance consultant
Output of limited value
NHS clients also tended to not value the contributions of external providers if external provider output was not very helpful. In addition to the many examples reported earlier, analysts from one CCG compared the positive predictive values of several different risk predictions tools using local data. They found the results were ‘pretty disappointing’, as in general these tools identified only one ‘true’ positive for about ‘five to six’ false positives (meaning that for every five to six patients that the tool suggested needed interventions, only one genuinely did). They went on to calculate the costs and found that given the number of false positives, any intervention, to be cost neutral, would have to save around £700 a year per patient, which was not feasible. This contributed to their lack of engagement with the tool. Reportedly, those who undertook this work said the results were fed back to the external providers who ‘didn’t want to know’, although there could be many reasons for this, including concerns about the robustness of the analysis.
In summary, unhelpful factors included:
-
aggressive marketing by commercial providers
-
limited interest in external provider support from NHS clients
-
lack of clarity and vision around the contract’s purpose
-
limited impact, for example owing to restricted resources, an unclear brief or departure of the client who originally let the contract
-
limited emphasis on implementation in favour of strategy
-
outputs of limited value
-
lack of early involvement of those expected to use the external services
-
changing commissioning environment and priorities.
What works well
Understanding clients and the market
Having discussed challenges, we now focus on factors that facilitated contractual relationships between the NHS and external providers.
In comparing and contrasting various providers, one participant said that some commercial providers ‘really got it’, meaning that client needs and the health-care market were understood.
We worked with [commercial provider A] and it’s a struggle, if you know what I mean. And the reason I’m thinking it’s a struggle is I’m thinking that these guys just don’t know health care . . . They’re trying to be management consultants, they’re trying to fit – you know, they’re trying to support CSUs as if we just ought to be generic businesses: we’re not generic businesses, we’re health businesses and you need to understand health care. My challenge is the support we need needs to make us the best in giving commissioning support. We need to be able to articulate the question, you know, we think commissioning support in the future will be all about X or Y or Z or what does transformation mean, what does outcomes based commissioning mean? And actually when you speak to this particular advisory, they can’t really answer those questions.
Kurt, NHS analyst
He went on to say that external providers who met clients’ needs and had insight into the ‘market’ were more likely to produce something useable and thought provoking. This participant, as well as others, seemed to suggest that when contracting external providers, NHS clients were looking for something that went over and above what was generally available.
Given the rapidly changing nature of commissioning, external providers who regularly revisited objectives, adjusted to the changing environment and contextualised their support appropriately were better placed to meet or exceed expectations.
That was one of the things I really found was that, you know, it seemed to be that every 3 months there was a different tune in town, you know, there was a completely different emphasis on what needed to be figured out or worked on now and so it’s quite easy for something to be the flavour of the month at one time and then for it to be almost accepted as standard or potentially not to be relevant any more.
Randall, freelance analyst
Helping clients to do the work themselves
Other participants mentioned that helping clients to do the work themselves, rather than doing the work for them, was beneficial. Of course, clients needed to co-operate for this to occur. For example, one participant mentioned a previous experience working with commercial providers on market analysis whereby the management consultants ‘upskilled’ the NHS staff through the use of tools ‘and we had to do it ourselves’. She thought that this work was ‘really excellent’ (Paula, NHS commissioning manager). A commercial provider echoed that embedding knowledge transfer through upskilling enhanced the value of their work.
You asked about what else do we bring to the table. I think it is that piece of our knowledge transfer. It’s that we do like to be an organisation that it’s not that we go in there, we deliver and we walk away, but we go in there, we deliver, we show them how to do it and then we walk away. And that was very much a focus at [CCG].
Yeah that’s a really good point actually.
Even though we had four work streams eventually, there was this pillar next to all those four work streams that we had to be able to, as an organisation internally demonstrate knowledge transfer.
And we know they’ve continued to do the work that we started there. And in fact we’re going back to do some more work with them. I’m going back to do some training with them at the beginning of March. So we do know that they are continuing on that work . . . And that’s really – and I think, personally for us two, we were really keen on that when we were coming towards the end of the contract, that we’d left everything that we could possibly leave with them.
Patricia and Helen, commercial consultants
There was an interesting paradox in this account, in that the commercial providers wanted to avoid dependency but simultaneously mentioned being recontracted for further work as evidence of success.
Developing non–threatening relationships
Not all successful contracts appeared to depend on developing longer term relationships, but some did. Non-threatening relationships were particularly helpful.
I think sometimes we don’t have the – I don’t wanna call it a luxury – but sometimes you don’t have the time to build that relationship. We were able to build, as a team, not just myself and Helen, but as a wider team we were able to build a relationship with the people that we were working with and others, so it gave us a greater understanding of being able to identify what would help them and what wouldn’t, and then to challenge that when needed . . . And I think because we had built that relationship, we were then seen as an organisation coming in that they didn’t feel threatened by.
Patricia and Helen, commercial consultants
However, not all longer term contracts resulted in better relationships. Another commercial provider with a 3-year contract kept switching embedded consultants, depending on the changing needs of clients’. This interrupted developing relationships and left some clients ‘not happy’ (Jessie, commercial consultant).
An ideal contractual relationship?
One particular commercial company stood out in that their NHS clients were uniformly very pleased. A NHS commissioner said that the partnership with the commercial company worked well and was different from other external providers because they went at the slower pace of the NHS and did not say ‘you’ve got it all wrong’.
I think what made the difference was the specific individuals understood that we couldn’t change the whole of the NHS overnight because some of their observations about how health and social care work . . . [showed that] this is a big, enormous beast. It’s a bit like the cruise liner; you can’t turn it on a coin very quickly. And I think sometimes the management consultants, people coming externally from private organisations feel very frustrated and tied by what we’re trying to work within, and our ability to make big change quickly . . . So, I think what made it work with [commercial company] was that they were willing to go at our pace, and understand that there was some parameters we couldn’t change rather than coming in saying, ‘oh, you’ve got it all wrong’.
Jane, NHS commissioning manager
In contrast, an ex-NHS freelance consultant working with the same CCG was struggling, perhaps because he was given to challenging the client.
One of the things that I’m trying to do within the organisation, which has got nothing to do with this project, is I’ve said to Abbie and to Kevin who is the MD [managing director], ‘Your method of delivering projects isn’t working’. You know, ‘You just don’t have a project – a change of culture in the organisation, and you need to think about that, and this is how you can do it’.
Brian, freelance consultant
Not only was the approach of the successful commercial company less confrontational, but they also motivated senior leaders to shadow clinical teams to have ‘normative’ experiences with patients themselves to learn the reasons for change. Patient stories were also effective in communicating difficulties with the current system back to the organisation, as the lesson of these stories was that the organisation was delivering poor experiences and outcomes in exchange for highly expensive interventions from health and social care. In addition, the success of the commercial company was contingent on local commissioners doing the work themselves and not ‘being done to’.
Yeah I think the key point here is often with external organisations there is an expectation that they will come and do it to you . . . our approach is very much that we have expertise around the design and management of work but we have no understanding of your particular area, and it is your responsibility to improve your system, but hopefully we can help with that. But it’s about you doing it to yourself.
Daniel, commercial consultant
The example of this commercial provider seems to suggest that the key ingredients for success were going at the pace of the organisation, taking a piecemeal approach, involving senior leaders ideally through arranging encounters between senior leadership, clinical teams and patients, using patient stories to illustrate the case for change and ensuring that the client organisation does the work. Elsewhere, we found that commercial providers drew on some of these principles but not all.
In summary, the key feature of successful contractual relationships between NHS clients and external providers were:
-
the providers’ ability to understand and respond to the clients’ needs and market
-
flexibility as circumstances change
-
facilitating activities so that clients do the work themselves and gain skills
-
non-threatening, non-confrontational approach of the external provider
-
working to the time frames/constraints of the clients in a piecemeal approach.
Box 12 summarises the key points in the chapter.
-
External providers who understood the health-care system and could add value to existing contributions were more appreciated, as were those who incorporated knowledge transfer so that clients were not dependent long term.
-
Good relationships between the external provider and client also facilitated better knowledge exchange. Knowledge exchange was possible only if both sides were receptive.
-
The long-standing NHS schism between analytics and commissioning was particularly relevant in impeding knowledge exchange. External providers in this study tended to deploy software tools for better data generation. So, in assessing impact, commissioners often could not identify benefits because it was not they themselves but their analysts who were the primary audience.
-
Benefits were often theoretical about what software tools could do, rather than actual benefits in terms of the production of useful information that fed into commissioning decisions and led to changes.
-
Because capturing benefits was problematic, other indicators were used to make judgements such as contract extensions, new contracts with former clients, products still in use and the client supplying good references.
-
A primary reason for unsuccessful contracts was that clients did not want to work with external providers. Contractual relationships were sometimes ‘forced’ because of concerns around NHS performance or in response to Department of Health directives. Other times, frontline operational staff did not identify the same need for assistance as their colleagues who had contracted the external provider.
-
Another inhibiting factor was lack of clarity around the brief, often because the client was not entirely clear about the problem, the nature of the proposed solution or the desired outcome. The rapidly changing nature of the commissioning environment meant that it was difficult but important to keep the brief relevant. Successful external providers continually readdressed objectives, recognising the heterogeneity of needs within the client organisation.
Chapter 10 Discussion and conclusion
Introduction
The purpose of this chapter is to summarise key points from the results, relate our findings to the literature, consider the implications and present actionable messages. This chapter also covers suggestions for future research and starts with strengths and weaknesses.
Strengths and weaknesses
This research is one of the first in-depth studies of commissioning following the 2012 Health and Social Care Act. 4 We have depicted the new landscape and captured the roles of different players in this latest version of the NHS. In the transitional period between PCT and CCG that this study largely describes (although two contracts pre-dated 2010), relationships between NHS commissioners and external providers might have been operating in such disadvantageous circumstances that the report findings could err on the side of pessimism about the workability and value of the external support to commissioners. However, in one contract that we tracked from 2010 to 2013, although the turbulence created by the 2012 Act was not helpful, the difficulties experienced appeared more attributable to the use of the conduits (or lack of it) than other contextual factors.
Commercial and not-for-profit providers permitted substantial access, although more perspectives from NHS clients, especially operational analysts and commissioners, would have been welcomed. These views were difficult to obtain, partly because the turbulence of the 2012 Act meant that many NHS professionals were preoccupied with the danger of losing their jobs. Entering the field via the commercial provider may have affected NHS recruitment, as we might have been overly associated with the commercial sector. We would have liked to have studied more ‘negative’ cases from one commercial provider, who steered us away from less successful contracts. Nonetheless, ample data were collected, both positive and negative, to create several coherent case studies of knowledge exchange, which we believe offer genuine insight and provide conclusions based on carefully collected and analysed data.
In using a case study design, we generated accounts with rich, detailed transferable learning. Drawing on multiple data sources (interviews, observations and documentation) and comparing across data sources was a particular strength. Case studies offer the opportunity for what Stake53 calls ‘naturalistic generalisation’, whereby ‘readers recognise in case study details and find descriptions that resonate with their own experiences . . . [and then] transfer of knowledge from a study sample to another population’. 53 A similar notion is ‘the shock of recognition’ suggested by Meyer54 in her account of action research methodology. The researcher’s account sparks a process of identifying with the data and comparing and contrasting (perhaps rejecting or denying) with the reader’s own experience of, and insights into, similar situations so that they can make valid inferences that illuminate their understanding. This type of generalisation seems apt for a study of knowledge exchange in commissioning, given that commissioners appear particularly proficient in recognising how evidence and experience from elsewhere apply to their own context.
As for ‘user involvement in the study’, we considered at the outset the potential contribution of patient and public involvement in the research, but as few have understanding of commissioning, we instead framed ‘involvement’ in terms of maximising commissioner input regularly throughout the study. This included having two commissioners as co-applicants, who attended team meetings and played active roles in the analysis (see Tables 7–10), asking two commissioners to take the lead for identifying ‘actionable messages’ and organising a workshop with several different commissioners from health and social care organisations to improve our understanding of commissioning and help to develop the actionable messages. Accessing and orchestrating this exceptional level of involvement of a ‘target audience’ throughout the lifetime of the study was a key part of our approach.
Summary of key findings
Our fieldwork produced a large amount of information about the disruptions and difficulties as well as the new opportunities that the 2012 Health and Social Care Act4 created for the knowledge exchange we were studying, but after much internal debate we had decided not to present that information beyond allowing it to remain as a constant leitmotiv through our findings. Otherwise, this might be seen to be transgressing important academic and political requirements for research reports. It is perhaps worth noting that this decision was itself a poignant echo of the way that commissioners too had to transform their data into products that would be accepted, taken seriously and used. Knowledge production and knowledge transformations in any field are rarely free of such tensions and all knowledge exchanges and their products – including not just commissioning briefs but research reports such as this – are inevitably a compromise shaped by the pragmatic political and professional requirements of their context.
In this study of knowledge exchange between external providers and health-care commissioners, we found that commissioners wanted information to try to build a cohesive, persuasive case to determine a course of action. Knowledge acquisition and transformation were tightly interwoven, as knowledge was continually reshaped, adjusted and repackaged. Flexible, fast media such as conversations and stories, rather than written documentation, were especially suited to knowledge exchange with commissioners. The commissioning landscape was ever-changing, sifting and reprioritising, and commissioners needed knowledge providers who could keep up.
In seeking knowledge from external providers, health-care commissioners tapped into potentially helpful sources of information from five conduits (often in combination):
-
interpersonal relationships
-
embedded or allocated intermediaries (people placement)
-
directives, organisational structures and processes (governance)
-
best practice or innovations from elsewhere (‘copy, adapt and paste’)
-
software tools or non-electronic methods and training (product deployment).
Commissioners, often in partnership with others, would contextualise knowledge obtained through these conduits to apply it to local circumstances while trying to engage the ‘right people’ to refine the knowledge and ensure wider awareness. Thus, knowledge accessed through these conduits was transformed through the contextualisation and engagement processes into locally applicable information. This often happened in the very act of acquiring the knowledge.
Implicit in people placement was the intention of forming interpersonal relationships through which key stakeholders could be engaged and opportunities for contextualisation identified. Unsurprisingly, commercial and not-for-profit providers tended to favour people placement and interpersonal relationships along with product deployment. Freelance consultants relied on interpersonal and people placement, although we found one example of product deployment by an ex-NHS analyst. CSUs behaved similarly to commercial and not-for-profit providers by utilising interpersonal relationships, people placement and product deployment extensively to contextualise and engage, with some evidence of ‘copy, adapt and paste’. Public Health was an interesting anomaly, as in influencing commissioners they heavily depended on interpersonal relationships and inclusion in governance structures such as membership of key boards. They appeared to have no recourse to product deployment and little opportunity to draw on people placement, as Public Health staff were already stretched. Moreover, their contributions were not quite aligned with the requirements of commissioners, some of whom claimed that Public Health overstated the health promotion and deprivation agenda at the expense of potentially more useful service evaluations and evidence reviews. However, one public health department was experimenting with ‘copy, adapt and paste’ by searching for research evidence for rapid reviews requested by commissioners.
There were several examples of commercial and not-for-profit providers depending almost exclusively on product deployment. This was not successful for several reasons. First, focusing only on product deployment favoured analysts who understood and appreciated the tools. But this was less helpful for commissioners and other key stakeholders such as general practice staff and community nurses, who were generally less proficient in database manipulation and preferred other ways of knowledge acquisition. By privileging product deployment and, consequently, analysts, external providers were missing (and even annoying) target audiences of decision-making commissioners. Second, the gap between analysts and those commissioners meant that the knowledge generated by analysts was unlikely to flow through to the right commissioners. Third, because in many cases the tools were allocated ‘top down’ rather than purposefully selected by the actual intended users, there was no clear commissioning ‘problem’ identified for data output to supply a ‘solution’. In fact, sometimes the outputs created a problem by identifying more patients who needed care for whom services were already lacking. Finally, commissioners often did not understand the output from the tool and struggled to contextualise it, not least because the tools frequently came from North America. Consequently, the data were not used or applied, which meant that commissioners’ assessments of external provider contribution were lukewarm.
These failings might be rectified though the incorporation of people placement and the development of interpersonal relationships. With embedded staff, or dedicated staff at the very least, commissioners had support in contextualising the data outputs. This was highly visible in one contract that started with complete reliance on product deployment, with little success. The external provider then embedded commissioning experts to help form relationships and interpret the data. This appeared to have some success, until the contract changed again. In a different contract that was heavily based on data output production, a commercial project manager commented that local clients relied on meetings with him before reading and applying data outputs, even though the contract (and presumably the meetings) had been running for 3 years. In contrast, a NHS project manager who had received advanced skills training on a software tool nevertheless wanted interdisciplinary meetings comprising her, a tool expert and a commissioning lead to suggest where data outputs could inform strategy. Without this, she struggled to apply the outputs from the tool meaningfully or to engage GP practices. External providers that did not draw on people placement and interpersonal relationships, in addition to product deployment, blunted their impact.
Contractual relationships between external providers and health-care commissioners were improved when external consultants mimicked the knowledge acquisition and transformation processes of commissioners themselves. Two highly regarded commercial consultants were embedded for about 3 years in a commissioning organisation (people placement) where they developed many longer term interpersonal relationships. Part of their work involved rolling out a software tool (product deployment), but they also accessed knowledge through ‘copy, paste and adapt’ by horizon scanning for examples of best practice and identifying highly rated commissioners elsewhere for their clients to visit. In addition, these consultants continually contextualised information received from various sources and engaged professional audiences such as primary care clinicians. This contract was deemed a success in helping the organisation meet its goals and was extended (see Chapter 8, External provider 3). Elsewhere, a CSU analyst was embedded within a commissioning organisation (people placement) where she already had many long-standing relationships (interpersonal relationships). Her job was to develop a dashboard (product deployment), and contextualise the outputs from this tool in formal and informal meetings that engaged the potential users. This dashboard and the analysts’ input were considered a great success, although the commissioners had some reservations about the CSU more generally. In both these cases, these external providers, who had excellent interpersonal skills, went further than utilising known commissioner conduits; they ‘went native’ by closely approximating commissioner behaviour. However, they still provided a welcome channel to and from the outside, bringing in expertise and additional support when needed.
Not all successful contracts depended on consultants ‘going native’. In another partnership, the external providers allocated consultants (people placement) to teach a business-system approach (product deployment) that relied on ‘principles’ rather than ‘rules’ and prioritised the experience of the ‘customer’ (i.e. the patient). The engagement aspect was particularly notable, as senior commissioning and provider managers, in another form of people placement, shadowed frontline clinical staff, observed care needs first hand and talked to patients, which led to powerful ‘normative’ experiences making a persuasive case for change. External consultants were not embedded, but were available to support and guide, while commissioners and other stakeholders were responsible for contextualising and hence learnt how to use the method themselves. In reflecting on the elements of success, NHS clients mentioned external consultants’ acceptance of the slow pace of change in the NHS and their non-threatening approach whereby external consultants did not criticise. Commissioners highly rated this contractual relationship because they learnt a valuable skill which they could apply elsewhere and they saw that the work made a difference to patient care.
In these successful contracts, key ingredients were that the external consultants, through placement and relationships, had an excellent understanding of clients’ needs by becoming embedded in the client’s world and produced highly valued output that the clients would not have generated on their own. These external consultants continually went back to clarify the brief to ensure that output was relevant to the ever-changing commissioning context. Of course, many external providers would relish the opportunities afforded by this level of access, but clients needed to trust the motivations of external providers and/or be persuaded by the usefulness of their output. This was difficult if the products were mainly aimed at analysts rather than commissioners. Moreover, sometimes external providers just did not deliver what the clients expected to even their minimal levels of satisfaction, much less produce something of value beyond expectations.
Theoretical underpinnings
In understanding our results, several theoretical frameworks proved appropriate, as they have grappled with, and provided enlightening accounts of, similar phenomena in other contexts that are germane to this study. We make no claim that these are the only potentially useful frameworks [e.g. we do not refer here to Nonaka’s widely cited ‘SECI spiral’ (see Chapter 2, Data analysis), which ultimately seemed less relevant to our findings than the models discussed below]. Nor do we assert that the frameworks we adduce below are anything approaching a comprehensive attempt to link our findings with all the relevant literature. Such an exercise would be massively beyond the scope of this work, even as regards the core topic of knowledge exchange, let alone wider matters such as organisational decision-making, the private–public sector interface, innovation theory, improvement theory, the impact of central policy on local services, change management, absorptive capacity of organisations and management styles, to name just a few of the possible candidates raised by our findings. We therefore limit ourselves here to explicating the theoretical frameworks that most informed our thinking because they were the most relevant and illuminating as regards our main research questions.
The social psychologist Karl Weick, in his highly influential studies of organisations, has characterised sensemaking – which is usually a retrospective justification of a decision rather than a proactive deliberation – as a process of enactment followed by selection and then retention of some new information that the actor needs to understand in context. 22 By ‘enactment’, he means that people recreate in their own minds (perhaps collectively) the situation to which the new information pertains, and at the same time ‘bracket’ some (not all) of the raw new information for further inspection. What gets picked up in this way (and what gets ignored to a greater or lesser degree) depends on both the mental models that people already possess and on the environment or situation in which or for which they are processing the information. Enactment is an active process; people do not just passively receive data, they question and explore in ways guided by their mental models and their environment (which to some extent they are also enacting through the very process of sensemaking, e.g. by using the new information to help to recreate, consolidate or alter their situation). ‘Selection’ is about choosing meaning for the new information, which can be interpreted in all sorts of ways; but people tend to select interpretations (often guided by past interpretations) that best fit both the new information and the circumstances they are enacting. ‘Retention’ is about holding on to the most successful interpretations of the new information in that context. The result of these processes is that people retrospectively recast the new information so that it can fit their (partly newly enacted) circumstances – hence the term ‘retrospective sensemaking’. Within an organisation, these interpretations become shared mental models that, among other things, guide future enactment and selection, shaping not only how future decisions are made and justified but also the organisational context in which they are made.
Many of our findings were phenomena that seem to correspond to the enactment and selection phases of Weick’s model. We regularly observed how participants compared, tested and queried new information, sometimes using a clinical lens (GP commissioners), sometimes using a managerial one (commissioning managers) and sometimes using a technical one (analysts). In doing so they were ‘enacting’ the data and the circumstances they interpreted as being relevant to it, for example what the audit results in vignette 2 meant and how they were or were not valid in their hospital. Selection was also evident as our participants interpreted the data and gave it meaning. For example, in understanding data on unscheduled hospital admissions, several GP commissioners discussed clinical reasons that patients with cellulitis might be admitted and alternative care provided for these patients that had a quite different meaning and implications from the analysts’ and the managers’ interpretations.
The partly shared mental model that an organisation (e.g. a CCG or subgroups within it, such as analysts or GPs or boards) successfully develops, consciously or otherwise, will be one that fits both their local context and their way of doing business (what one is supposed to do and how). Thus, each organisation worked out its own unique set of shared mental models (including acceptable ways of doing things), for example with one commissioning organisation focusing on integrated health and social care and another emphasising the importance of good governance, but with subgroups or communities whose shared view might vary from each other’s and the espoused mental models. Moreover, any such set of mental models depended on a continuing process of negotiation between the key actors within the organisation(s) that might or might not result in a consensus. (Compare, for example, the rifts that developed after the first audit in vignette 3 with the all the key parties’ acceptance of shared view after the second audit.) At an individual and a collective level, we observed participants drawing on what Gabbay and le May have called their ‘mindlines’. 20,21 Mindlines are described as internalised, collectively reinforced and often tacit guidelines about handling complex situations. They are informed by training, experience, interactions, reading, local circumstances and a host of other sources, including the collective views of colleagues on how things should be done (‘collective mindlines’). 21 Originally described as the means by which clinicians adduce, combine and use different kinds of evidence when deciding how to manage patients, they are also applicable to other complex but routine decision-making situations. Among commissioners, their mindlines allowed them to weave their way through an uncertain maze of often contradictory tensions, constraints and demands, and arrive at politically and organisationally satisfactory solutions. This recalls Gabbay and Le May’s analogy in which new knowledge in a health-care system is like a soft and malleable ball, which not only changes direction every time it is hit, sometimes unpredictably, but also morphs each time it is hit or transferred from one actor (one component of the system) to another. 21 The image in Figure 4 conveys a similar idea.
The notion of mindlines was evident also in the way that participants accessed, transformed and applied knowledge. For example, GP commissioners would refer to patient stories, articles that they had read and conversations with colleagues when interpreting data and making decisions about potential interventions to judiciously build the case for the action they were proposing. Mindlines, which are often shared through such informal means, help to explain why the same information was processed and understood in different ways, as it was combined with different information by different individuals in different professional and organisational groups. For example, the potential of risk profiling to allocate general practice budgets on the basis of multimorbidity was exciting to analysts because this was a new way to use a tool, but some GPs reacted with weariness, as previous risk prediction tools had not been very helpful. Both analysts and GPs were using the given knowledge about risk profiling (and/or the tool) to solve different sets of problems and were drawing on their own (but different) mindlines based around past experience, adeptness at software usage and understanding of local priorities.
Mindlines and sensemaking activities take place within ‘communities of practice’ and other knowledge-based groups. Communities of practice consist of groups of people with a common purpose or passion who ‘1) connect pockets of expertise, 2) diagnose and address recurring problems, 3) analyse knowledge related sources of uneven performance, 4) link and coordinate unconnected activities and initiatives addressing similar knowledge domain’. 19 Communities of practice, which are ubiquitous in health service organisations,55 can foster the creation of new knowledge and ways of doing things, and in the course of sharing knowledge also develop a shared understanding and sense of identity. While much of the activity that these groups undertake will be in the form of discussing knowledge, some also work with tools, and the group learns from its experience with the tools. This relates to another distinction we have observed, namely that between knowledge-sharing and knowledge-nurturing communities. 56
Examples of communities of practice included groups of analysts within and across organisations, the community of decision-making commissioning managerial staff and some communities of GP commissioners. Such groups were an important part of what Brown and Duguid17 have called the ‘social life’ of knowledge, a concept relevant to our findings not only because it deals with the influence of social networks on the processing of knowledge, but also because it touches on innovation theory – how such knowledge does or does not lead to new ways of doing things in an organisation. The commissioning knowledge that was being exchanged (or not) within and between the communities of practice clearly had its ‘social life’. Ideas were shared, stories exchanged, knowledge modified and reshaped or even rejected as the participants learnt from and reinforced the mindlines within their own communities. But as is often the case with such communities, the knowledge also tended not to cross over between some communities (e.g. GPs to analysts; commissioners to commercial providers), which obstructed its flow. This may be why people placement and product deployment played such an important role as knowledge conduits; they helped to cross the barriers between the different (and differing) communities. This problem resonates with the now widespread acceptance that practitioners should be involved in knowledge creation and, vice versa, that researchers need to engage practitioners early in their research if they want their results to be implemented – the argument for coproduction,57 or what van de Ven calls ‘engaged scholarship’. 58 Not only knowledge creation, but also knowledge acquisition and transformation may be similarly improved by closer working between the two camps of, say analysts (external or internal) and commissioners.
As far as the tools are concerned, it was not so much the tools themselves as the underlying models they implied that were the key aspect being transmitted and transformed through product deployment. The tools, or the underlying models, may become boundary objects,59 enabling understanding, communication and sharing between different groups (such as NHS/CSU analysts and tool providers but not – unfortunately – between the communities of commissioners and analysts). Where NHS clients felt that a tool was not working, this might indicate a breakdown in sensemaking, as the framework of meaning on which the tool was based did not fit well with the commissioning organisation’s framework of meaning. This could lead to either the dismissal of the tool (which we observed with general practices around risk stratification tools) or to some kind of synthesis into a new framework of meaning (such as the scenario generating tool that was modified by NHS analysts). The data resulting from the tools could also of themselves be boundary objects that allowed better dialogue and joint decisions. This happened for example in vignette 2, after the second set of mutually acceptable audit data had become a means to achieving a useful dialogue between groups that had hitherto been at loggerheads.
Choo’s four-way classification of decision-making was also useful. 60 His two-by-two table (low/high uncertainty about goals vs. low/high procedural uncertainty) suggests four ideal types of modes – ‘rational’ decision-making (high certainty on both axes), ‘process’ decisions (high certainty on procedure, low on goal), ‘political’ decisions (low procedure, high goal) and anarchy (both low) – helped to make sense of the data, as did his suggestion that an organisation’s decision style can be a hybrid of these modes, which alters over time. With some commissioning and external provider organisations the process mode seemed to dominate: goals were clear, but the alternatives to reach them were not, and the organisation was working through a process of searching for (or creating) and evaluating alternatives. Choo suggests that as the organisation becomes more familiar with the alternatives open to it, the process becomes more routinised and moves towards the rational mode. Many of our data suggested that commissioning organisations operated in the anarchic mode (high uncertainty for both the goals and the procedures, which was exacerbated by the reorganisation of commissioning that was underlying the activities). Problems met solutions fairly randomly and there was also perhaps something of the political mode, where much effort went into setting out cases for alternative goals (low goal uncertainty due to ‘must do’ targets but high procedural uncertainty about how best to achieve them). Arguably, some external provider organisations such as Heron were in the rational mode while most commissioning organisations aspired to be, where everything was routine, so that they would have the luxury of straying into the political mode every now and then to question what they were doing. This was especially evident in one commissioning organisation where we were asked to inform the chief accountable officer if we found any software tool to manage all of commissioning activity in real time linked to financial data with the robustness of prescribing analysis and cost prescribing data. In effect, the organisation wanted the ‘holy grail’ of commissioning with this magical, non-existent tool. But most commissioning organisations were probably operating in the process mode, or even the anarchic mode (which might, or might not, be regarded as dysfunctional under the highly uncertain circumstances in which they were operating).
Choo’s anarchic mode is also related the much earlier ‘garbage can’ model of decision-making,61 which was originally proposed as an empirically based counterpoint to the predominance of over-rational and theoretical notions of managerial behaviour. It suggests that organisational decisions are often made in a kind of organised anarchy in which managers, their goals, the problems, their causes, the effects and the alternative solutions are all poorly defined, as are the processes by which the managers, who may themselves be in a state of flux, have to make decisions, often hurriedly, under pressure and in the face of competing and irreconcilable interests. This complex of circumstances, so frequently described for managerial or policy decisions in other sectors, is redolent of the situation sometimes described by the commissioners in our case studies. It may help to explain the kind of (sometimes serendipitous) satisficing that we suggested characterised the knowledge utilisation and transformation entailed by many commissioning decisions (see Chapter 3, Figures 3 and 4).
Recent literature on commissioning
Our study was commissioned in a call with several other studies that explored knowledge exchange with health-care commissioners. In addition, a call a year earlier focused on how health-care managers used evidence. Many of those studies are now published.
Swan and colleagues explored the use of evidence by health-care commissioners in PCTs. 9 They found that evidence and decisions were coproduced and identified several ‘inter-dependencies’ that mediated evidence. ‘Process interdependencies’ included role, project, management, governance, expertise and relational. Furthermore, another set of interdependencies were categorised under ‘task’. Their key findings were that information does not speak for itself and that experts were needed to translate evidence. There is overlap between Swan’s ‘process interdependencies’ and our knowledge conduits, and in both studies the importance of translation and contextualisation was highlighted. Swan and colleagues concluded that, in transferring knowledge to commissioners, case studies might be a more effective medium and make information more usable.
Checkland and colleagues’ work on the role of middle managers in PCTs collected data on clinical and commissioning managers. They found that commissioning was ‘messy’ and ‘fragmented’. 62 They identified the role of the ‘animateur’ defined as someone who managed disparate groups of professionals over which the commissioner had little control to engage in a particular course of action,63 which appears similar to our concept of engagement. Checkland and colleagues also found that middle managers managed information in several directions: up, down, internally and externally. This concurs with our research.
Smith and colleagues12 studied commissioning for long-term conditions, finding that commissioners balanced two commissioning ‘cycles’. One was relational and the other was transactional. They identified skilled managers and accurate and timely data as the keys to helping and hindering effective commissioning. They also developed indicators of effective commissioning.
Dopson and colleagues10 explored health-care managers’ use of management research in six ‘knowledge economies’, including a commissioning organisation. They found that managers were most oriented to their own experiential knowledge and that of others within their community of practice. ‘Knowledge leaders’ tried out, tested, transposed and contextualised evidence from elsewhere10 and, in close accord with our own findings, the researchers noted the social processes of evidence acquisition and transformation.
Our study and the ones named above draw out similar points in terms of the importance of relationships, the social processes of knowledge acquisition and transformation, the multiple ways and directions in which managers accessed and spread knowledge and the fundamental ‘coproduction’ of both evidence and decision-making.
Outsourcing in the NHS
This study and others9,12,62 have stressed the importance of interpersonal relationships for commissioners to acquire, transform and apply useful information. But these relationships are harder to create and sustain across organisational boundaries. With the 2012 Health and Social Care Act, many more organisational boundaries were created with the transfer of public health departments into local authorities and new organisations such as CSUs. Numerous commercial and not-for-profit providers with competitive mindsets also entered the market offering data management and information services. This curtailed exchange of knowledge, as providers were reluctant to share knowledge and information with rivals.
Effectively with this panoply of information providers, not only did the 2012 Health and Social Care Act create more conducive conditions for competition, but it also introduced outsourcing to health-care commissioning. Outsourcing is common in the private sector. The conventional wisdom is that ‘organisations should choose to outsource carefully selected, non-core activities that can be accomplished quicker, cheaper and better’ elsewhere. 64 This raises questions about the role of information in commissioning, predominantly delivered by CSUs and other external agencies. Our findings confirmed that the provision of information is not, and cannot be considered, an activity that is ‘non-core’ to commissioning. Our study casts doubt on the expectation that the expertise of those supplying locally usable information could be regarded as a commodity independent of the work of commissioning, either now or in the foreseeable future. On the contrary, the acquisition and transformation of knowledge remained central to the decision-making required of the commissioners that we interviewed and observed. We did not obtain information on the financial costs of outsourcing, that is external organisations, whether CSUs, commercial or not-for-profit agencies, were ‘quicker, cheaper and better’ than in-house facilities. However, any such cost–benefit calculation should take account of the additional opportunity costs of the time and effort that was needed for the information exchange to be maintained effectively across the new organisational boundaries, not to mention the costs of the failure of that transformation to occur satisfactorily, as well as the benefits of the external agencies’ contributions, which as we showed in Chapters 7 and 9 were difficult to quantify.
External providers were often brought in without much thought to fostering knowledge exchange or longer term benefits. Our case studies revealed that NHS commissioners could become reliant on outside organisations, whether from commercial or not-for-profit organisations, to satisfy the information needs that were fundamental to their decision-making. The result of this trajectory could be that commissioners face the risk of long-term dependency on external providers, particularly if no explicit knowledge transfer mechanisms exist and/or can be made to work effectively. We found some evidence that this was occurring already. In one contract between a CCG and a CSU, the reallocation of the embedded CSU analyst to other work, besides that of developing a dashboard for an unscheduled care subcommittee, meant that the subcommittee became severely stalled over the weeks that the analyst was missing. Moreover, despite the analyst’s regular attendance at the meetings, the subcommittee members appeared unable to interpret data from the dashboard without her input. In another contract, the commissioning function was completely outsourced to a commercial provider who installed information systems, utilised their own commercial analysts to undertake ‘forensic analytics’ and delivered substantial savings by ‘doing the basics really well’. After renewing the contract for 5 years, the NHS clients had become used to a really well-performing team. After a further tendering exercise the contract was extended for another 3 years with an additional 2-year option. The benefits of this possibly 10-year contract could be that the NHS clients will have received a high-quality service (hopefully), but the disadvantages could be that, should this contract be discontinued, no one else has been trained to deliver the same service. Nor are the NHS clients able to capitalise on the commercial provider’s expertise in replicating this success elsewhere. Although in the first few years of the contract, NHS analysts worked alongside the commercial team, and so could have been given these skills, this component of the contract was too expensive and the NHS client declined. With the latest contract, knowledge exchange mechanisms were difficult to incorporate, as it was not clear to whom commercial analysts would transfer their skills. Their former NHS colleagues were now housed in rival organisations – CSUs.
Thus, outsourcing seems to have made the transfer of valuable knowledge and skills from commercial and other external providers to NHS clients even more difficult than it was. Ironically, although the 2012 Health and Social Care Act eased the way for greater commercial, not-for-profit and other external provider involvement in the NHS, the same Act may have established substantial barriers to NHS clients actually learning from these external providers to benefit the NHS.
Alternatively, instead of commercial and not-for-profit providers taking over functions of NHS commissioners through outsourcing, they could genuinely add value to help strengthen and improve the NHS by skilling up NHS professionals. Particularly useful knowledge transfer would be around ‘forensic’ approaches to data analysis, novel ways of interpreting data, teaching commissioners how to interpret data and helping NHS/CSU analysts gain greater understanding of how data can inform commissioning. Commercial providers also have useful knowledge in project management, in terms of clarifying the ‘problem’ first before producing data to identify the ‘solution’. Drawing on people placement, external providers could embed external consultants with the right combination of experience, skills and personality types to complement those missing in NHS client organisations, so that when the contract finishes, the organisation is better equipped than before. Knowledge transfer should be a core component in contracts between NHS clients and external providers, where the NHS clients have the capacity to take on board new skills.
Actionable messages
To identify actionable messages from our study, we carried out two processes with some of the main potential target audiences. The first was that two team members, both with commissioning backgrounds who had worked in various organisations including PCTs, CCGs, CSUs and commercial consultancies, read through the eight case summaries and identified actionable messages for each one (see Appendix 1). The second was an event where a group of commissioners, information managers and a few of the team academics listened to the ‘stories’ presented in Chapter 8. The group then commented on how these stories matched their own experiences and contributed further key actionable messages for commissioners and information specialists. In combining across these two sets, the following messages were the common ones that emerged.
Commissioning managers
-
Before purchasing a tool or external support, a clear problem of importance to commissioners and/or analysts needs to be identified with a shared understanding of how the tool or external support can resolve the problem and contribute to the solution.
-
Those drawing up contracts with external providers need to fully engage from the start the staff who will be the recipients of the external expertise or expected to utilise it, ensuring that all parties understand and agree about the nature the problems being addressed and the proposed approach to their solution. Contracts with external agencies coproduced by all of the actively interested parties may have a greater chance of successful results.
-
Commissioners may need to take note of, and make better use of, the knowledge conduits and transformation processes that we have elicited (i.e. interpersonal, people placement, governance, ‘copy, adapt and paste’ and product placement).
-
Careful thought is needed when embedding individuals, considering not only skill set, experience and knowledge but also personality type. Commissioners need to be clear about what type of individuals are missing or poorly represented from their organisation.
-
With many service change and transformation projects as much focus needs to be given to implementation as to the process and deployment of the tool itself. Commissioning organisations need to acknowledge this in their plans with their knowledge exchange partners (e.g. external providers, hospital managers, clinicians, etc.) and make decisions with this in mind.
-
Commissioning organisations need to build in knowledge transfer as a key requirement to contracts with external providers, which may help to retain and develop in-house skills. This is a vital step for commissioners using external providers to take full advantage of the potential for knowledge exchange and training on offer.
Commissioning support units
-
Commissioning support units or equivalent public organisations with a mandate for ‘business intelligence’ need to develop and maintain cultures that value staff – focusing on individuals, teams and organisations in terms of drive, performance and contribution, to foster healthy conduits for knowledge exchange.
-
External providers, and particularly CSUs, need to help their commissioner clients define the scope and detail of the support they require. Having loose service-level agreements based on individuals and long-term support to programmes is unlikely to deliver the outcomes needed or sustainability for commissioners.
-
The role of commissioning analysts may need to be reconfigured to ensure that their training and activities includes interpreting and contextualising data outputs. This may help to make NHS analytics a more credible profession with their commissioner colleagues. There is also a need to upskill commissioners so that they know how to use their analysts better. Better structures and processes to encourage interpersonal interactions between the two ‘camps’, including widespread use of people placement, may be a useful way to help achieve better mutual understanding, if not actual ‘coproduction’ or ‘engaged scholarship’ in the knowledge transformations that result.
-
Commissioning support units should understand that most valuable knowledge transfer occurs via good personal relationships, and set up their structures and processes in such a way as to ensure that their staff can develop such relationships with their local clients.
-
It may also be useful to prioritise knowledge management and knowledge exchange within organisational development work, ensuring that attention is paid to this when reorganisations are planned and rolled out.
External providers
These findings are relevant for all types of external providers we encountered within the study, be they freelance, not-for-profit, commercial or CSUs.
-
Ideally, knowledge transfer drawing on the five conduits should be a core offer from external providers.
-
It would be helpful to provide interpretation of data and practical (not merely technical) assistance with tools to drive change. We found that transferring operational or technical knowledge of a tool alone is often not enough.
-
When working in the NHS, external providers might be more successful if they adapted their expectations to fit clients’ reality and negotiated mutually acceptable understandings and time frames about the use of the techniques and knowledge they are purveying. Pressing the contractor’s own values and time scales onto the client rarely yielded the desired result.
-
It would be useful if external provider staff, including CSUs, regularly asked clients to define (and redefine) the problem and intended outcome and were amenable to adapting and adjusting the project timetable accordingly.
-
Where possible, external providers could helpfully ensure that the work was carried out by or jointly with clients, so the clients took ownership, and skills were more likely to be transferred. Although this may appear to undercut the future for the external provider’s services, it is also likely to increase the chances of the outputs being trusted and useful, which may actually increase the prospects of repeat business.
-
Costing in the resources needed for genuine knowledge exchange and implementation of change might mean more contracts were successful, for example by acknowledging and allowing the time needed to build local relationships.
-
The commissioning organisations in our case studies preferred the following from external providers, who may consider making them a core part of their work with the NHS:
-
long-term contracts/relationships
-
continuity of workforce/relationships
-
flexible and adaptable capacity
-
experienced staff
-
clinical knowledge/subject matter experts with good interpersonal skills rather than just technical or project management skills
-
contextual understanding.
-
Implications for future research
Future research evolving from this study has already been commissioned. The study lead obtained a NIHR Knowledge Mobilisation fellowship with the aim of increasing collaborations between NHS commissioners and primary care academics. This will run from June 2014 to June 2017. Specifically, she will develop communities of practice consisting of patients, clinicians, researchers and commissioners to evaluate health-care services, drawing on researchers’ methodological knowledge. This work will be heavily informed by the learning from this study. Furthermore, we have identified several areas where further research would be helpful.
Replication
There would be some merit in repeating this work, given that it was carried out at a time of particular turmoil in the NHS, to see the extent to which those organisational exigencies affected some of the findings.
Knowledge exchange
-
To what extent do clinicians and managers from primary, secondary and community care draw on the conduits and transformation processes identified in our study? What is their impact and how is that affected by different circumstances?
-
Are these knowledge exchange conduits amenable to deliberate and productive manipulation and, if so, to what extent do such interventions improve the process and outcomes of knowledge exchange?
Commissioning
-
Can and should NHS and commercial health-care providers be commissioned in the same way?
-
What are the ‘core skills’ required for the commissioning of the health service and where should they reside?
Public Health
-
What are the characteristics of public health departments that successfully meet commissioners’ needs?
Commissioning support units
-
How do the role, training and skills of health-care analysts need to change to make working in CSUs an attractive option?
-
How can CSUs and commercial/not-for-profit providers work together to maximise knowledge exchange?
Commercial, not-for-profit and freelance providers
-
What are measurable outcomes of utilisation of commercial and not-for-profit agencies and how do they compare?
-
Given that this study focused mainly on commercial providers who offered software tools, what is the contribution of commercial providers that primarily provide management consultancy?
-
How successful is the ‘Lead Provider Framework’ in identifying and securing effective collaborations?
Conclusion
Commissioners had to influence and collaborate with many external and internal parties to build a cohesive case for taking any particular commissioning decision. Amid a web of competing agendas, priorities and power relationships, as well as their own professional, organisational and political norms, commissioners had to make the ‘best’ decision that the often conflicting pressures, constraints and tensions allowed. The ‘art’ or ‘craft’ of commissioning was, in essence, pulling together the appropriate knowledge and information, including the tools for producing it to satisfy competing agendas, and manoeuvre it through a complex system. That process inevitably meant that knowledge was continually being altered to meet those multifaceted requirements.
We identified three models of commissioning in our particular case studies: clinical, integrated health and social care, and commercial provider commissioning. Different types of knowledge were privileged in the different models. Local clinical knowledge from GPs was prioritised in the clinical commissioning model, service user knowledge was key in the integrated health and social care model, and analysts’ knowledge of capturing and interpreting data was crucial in the commercial provider model. All commissioning organisations displayed various blends of these models.
Commissioners were highly pragmatic in their use of knowledge. Research evidence usually appeared in a digested format such as NICE guidelines and often required further contextualisation, such as locally devised clinical briefings or reviews, before being considered. Commissioners did not appear to consider the ways that negative research evidence that could inform disinvestment opportunities.
We identified five main conduits that commissioners used to access and transform knowledge. They were:
-
interpersonal relationships
-
people placement (embedded staff)
-
governance (e.g. national directives, local procedures)
-
copy, adapt and paste (best practice from elsewhere)
-
product deployment (software tools).
Within those conduits, media such as conversations and stories fitted particularly well with the fast-changing, flexible world of commissioning, and often ‘trumped’ hard data that could be questioned or sidelined on account of their low perceived usability. Local data often were more persuasive than national or research-based information.
As knowledge was exchanged through these conduits, it was iteratively refocused, reshaped or rejected, largely through two transformative processes:
-
contextualisation (amending it to suit local circumstances), and
-
engagement (involving the key players for whom the knowledge would have an impact).
This was true both in the act of obtaining the knowledge, and subsequently when it was being actively reshaped and repackaged as moved between and within organisations and key personnel. These processes were redolent of some of the notions that underpinned our analysis, especially collective organisational sensemaking, ‘the social life of knowledge’, the development of collective mindlines, and the role of communities of practice.
External providers that maximised their use of these conduits and transformation processes were more successful. Interpersonal relationships were especially important to help contextualise the knowledge for local application and engage the ‘right people’ to refine the knowledge further. External providers that mainly targeted NHS/CSU analysts (e.g. through product deployment alone) were less likely to influence commissioners, because of the long-standing schism between analysts and commissioners. Some commercial providers bridged this gap by creating interdisciplinary teams of analysts, project managers and clinicians. But elsewhere, because of this split, the sporadic use of the knowledge conduits and the variable production of output over and above what was already available, many contracts within our case studies were perceived by our research participants as being only partly successful. Success was, however, difficult to define or assess, let alone quantify. Trust and usability influenced client views on usefulness of external provider contributions.
An impact of the 2012 Health and Social Care Act was to further distance information producers (i.e. health-care analysts) from information users (i.e. commissioners) by creating organisational boundaries that were barriers to knowledge exchange. Consequently, commissioning organisations often did not capitalise on contractual relationships with external providers by learning new skills. If the NHS is to benefit from the expertise that external providers have to offer, then wherever possible, knowledge exchange and development of skills within commissioning teams should be components in every contract.
Acknowledgements
Thanks to all the participants who gave us their accounts, despite considerable time pressures, and often allowed observation of their meetings and training events. We are especially grateful to the three external provider organisations and four CCGs that took part. In addition, thanks to the following people:
Rachel Anthwal, NHS Fellow at University of Bristol and Programme Manager at South West CSU, for leading on the development and writing-up of actionable messages and commenting on draft reports.
Claire Barry, independent art director, for patiently turning John Gabbay and Andrée le May’s sketches for Figures 4, 5 and 7–11 into the finished illustrations.
Maya Bimson, formerly of NHS Bristol and United Health Care, for supporting the project since its inception, offering health-care commissioning insight and developing actionable messages for external providers.
Gene Feder, Professor, University of Bristol, for support as and when needed and for reading the final version of the report.
William House, former GP and practice-based commissioner, for supporting the project in its early stages and providing GP commissioning insight.
Andrée le May for attending a mid-project meeting as a ‘critical friend’, chairing a cross-case analysis session, contributing to the figures and commenting on drafts.
Tim Wye, Bristol City Council Social Services, for social care insights.
Other commissioners and analysts who participated at various points of the project to provide frontline input and helped to develop actionable messages for commissioners and CSUs included:
Michael Bainbridge, Somerset CCG.
Jude Carey, NHS Fellow at the University of Bristol and Bristol CCG.
Neil Riley, South West CSU.
Adwoa Webber, Bristol CCG.
Contributions of authors
Lesley Wye (Research Fellow, School of Social and Community Medicine, University of Bristol) was principal investigator, conceived the study and was responsible for its overall direction. She contributed to research design, carried out primary data collection for two sites and contributed to data collection for the others, analysed data within cases and across cases, drafted the final report and contributed to actionable message development.
Emer Brangan (Research Associate, School of Social and Community Medicine, University of Bristol) contributed to primary data collection in six case sites, analysed data within sites and across cases, commented on all drafts of the drafts, wrote vignette 3 and contributed to actionable message development.
Ailsa Cameron (Senior Lecturer, School of Policy Studies, University of Bristol) contributed to research design, data analysis and cross-case analysis, and commented on some drafts of the report.
John Gabbay (Emeritus Professor, Wessex Institute for Health Research and Development, University of Southampton) contributed to research design, data analysis, cross-case analysis, actionable message development and developing the diagrams, co-drafted sections of Chapter 10 and commented in detail on all drafts of the report.
Jonathan Klein (Senior Lecturer, Southampton Management School, University of Southampton) contributed to research design, data analysis, cross-case analysis and actionable message development, and commented on all drafts of the report.
Catherine Pope (Professor, Faculty of Health Sciences, University of Southampton) contributed to research design, data analysis and cross-case analysis, and commented on some drafts of the report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- World Class Commissioning. London: Department of Health; 2007.
- Lewis R, Curry N, Dixon M. Practice Based Commissioning: From Good Idea to Effective Practice. London: The King’s Fund; 2007.
- Liberating the NHS. London: Department of Health; 2010.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Doctors Told To Deal Bill A Death Blow. London: British Medical Association; n.d.
- Lead Provider Framework. Redditch: NHS England; 2014.
- Mapping The Market Commissioning Support Services. London: Gateway Reference; 2013.
- Mapping The Market II Commissioning Support Services. London: Cagora; 2014.
- Swan J, Clarke A, Nicolini D, Powell J, Scarbrough H, Roginski C, et al. Evidence In Management Decisions: Advancing Knowledge Utilisation in Healthcare Management. Warwick: University of Warwick; 2012.
- Dopson S, Bennett C, Fitzgerald L, Ferlie E, Fischer M, Ledger J, et al. Health Care Managers Access and Use of Management Research. Final Report 2012.
- Checkland K, Snow S, McDermott I, Harrison S, Coleman A. Management Practice in Primary Care Organisations: The Roles and Behaviours of Middle Managers And GPs: Final Report 2011.
- Smith J, Shaw S, Porter A, Rosen R, Blunt I, Davies A, et al. Commissioning High Quality Care For People With Long Term Conditions: An Action Research Study 2013.
- Yin R. Case Study Research. London: Sage; 2002.
- Ragin C, Becker H. What is a Case?. New York, NY: Cambridge University Press; 1992.
- Hammersley M, Atkinson P. Ethnography: Principles and Practice. London: Routledge; 1995.
- Brown J, Duguid P. Local knowledge: innovation in the networked age. Manag Learn 2002;33:427-37. http://dx.doi.org/10.1177/1350507602334002.
- Brown J, Duguid P. The Social Life of Information. Boston, MA: Harvard Business School Press; 2000.
- Wenger E. Communities of Practice: Leaning, Meaning and Identity. New York, NY: Cambridge University Press; 1998.
- Wenger E, McDermott R, Snyder W. Cultivating Communities of Practice. Boston, MA: Harvard Business School Press; 2002.
- Gabbay J, le May A. Evidence based guidelines or collectively constructed ’mindlines?’ Ethnographic study of knowledge management in primary care. BMJ 2004;329:1013-18. http://dx.doi.org/10.1136/bmj.329.7473.1013.
- Gabbay J, le May A. Practice-Based Evidence for Healthcare. Oxford: Routledge; 2011.
- Weick K. Sensemaking in Organisations. London: Sage; 1995.
- Nonaka I. A dynamic theory of organizational knowledge creation. Organ Sci 1994;5:14-37. http://dx.doi.org/10.1287/orsc.5.1.14.
- Cook S, Brown J. Bridging epistemologies: the generative dance between organisational knowledge and organisational knowing. Organ Sci 1999;10:381-400. http://dx.doi.org/10.1287/orsc.10.4.381.
- Patton M. Qualitative Research and Evaluation Methods. London: Sage; 2002.
- NHS and Community Care Act 1990. London: The Stationery Office; 1990.
- Kay A. The abolition of the GP fundholding scheme: a lesson in evidence-based policy making. Br J Gen Pract 2002;52:141-4.
- Goodwin N, Mays N, McLeod H, Malbon G, Raftery J. Evaluation of total purchasing pilots in England and Scotland and implications for primary care groups in England: personal interviews and analysis of routine data. BMJ 1998;317:256-9. http://dx.doi.org/10.1136/bmj.317.7153.256.
- Williams D. Exclusive: trusts force delay in outcomes based commissioning plan. Health Serv J 2013.
- Newman M, Bangpan M, Kalra N, Mays N, Kwan I, Roberts T. Commissioning in Health, Education and Social Care Models, Research Bibliography and In-Depth Review of Joint Commissioning between Health and Social Care Agencies. London: EPPI Centre Institute of Education, University of London; 2012.
- Porter A, Mays N, Shaw S, Rosen R, Smith J. Commissioning healthcare for people with long term conditions: the persistence of relational contracting in England’s NHS quasi-market. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-S1-S2.
- Øvretveit J. Purchasing for Health: A Multi-Disciplinary Introduction to the Theory and Practice of Commissioning. Buckingham: Open University Press; 1995.
- Department of Health . Health Reform in England: Update and Commissioning Framework 2006. www.yhpho.org.uk/default.aspx?RID=10297 (accessed 10 March 2014).
- Commissioning Model: IPC Joint Model for Public Care. n.d.
- NHS England . Everyone Counts: Planning for Patients 2013 14 n.d. www.england.nhs.uk/everyonecounts/ (accessed 12 February 2015).
- Simon HA. Rational choice and the structure of the environment. Psychol Review 1956;63:129-38. http://dx.doi.org/10.1037/h0042769.
- Checkland K, Coleman A, Segar J, McDermott I, Miller R, Wallace A, et al. Exploring the Early Workings of Emerging Clinical Commissioning Groups: Final Report. London: PRUCOMM, London School of Hygiene and Tropical Medicine; 2012.
- Naylor C, Curry N, Holder H, Ross S, Marshall L, Tait E. Clinical Commissioning Groups: Supporting Improvement in General Practice?. London: The King’s Fund and Nuffield Trust; 2013.
- NHS Act 2006 Partnership Arrangements. London: Department of Health; 2006.
- Jordan J. The Impact of the Better Care Fund on CCGs Explained. London: Health Service Journal; 2014.
- Dickinson H, Glasby J, Nicholds A, Sullivan H. Making sense of joint commissioning: three discourses of prevention, empowerment and efficiency. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-S1-S6.
- Thiel V. Where is the Evidence for Promoting Integrated Care?. London: Health Service Journal; 2014.
- Clarke A, Taylor-Phillips S, Swan J, Gkeredakis E, Mills P, Powell J, et al. Evidence-based commissioning in the English NHS: who uses which sources of evidence? A survey 2010/2011. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2013-002714.
- Cox S. The Accountant Kings 2014. www.bbc.co.uk/programmes/b03wpjjq (accessed 10 April 2014).
- Checkland K, Allen P, Coleman A, Segar J, McDermott I, Harrison S, et al. Accountable to whom, for what? An exploration of the early development of Clinical Commissioning Groups in the English NHS. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2013-003769.
- Gabbay J, le May A, Jefferson H, Webb D, Lovelock R, Powell J, et al. A case study of knowledge management in multiagency consumer-informed ‘communities of practice’: implications for evidence-based policy development in health and social services. Health 2003;7:283-310.
- Hopthrow T, Feder G, Michie S. The role of group decision making processes in the creation of clinical guidelines. Int Rev Psychiatry 2011;23:358-64. http://dx.doi.org/10.3109/09540261.2011.606539.
- Wye L, McClenahan J. Getting Better With Evidence. London: The King’s Fund; 2001.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. http://dx.doi.org/10.1111/j.0887-378X.2004.00325.x.
- Crilly T, Jashapara A, Trenholm S, Peckham A, Currie G, Ferlie E. Knowledge Mobilisation in Healthcare Organisations: Synthesising Evidence and Theory Using Perspectives of Organisational Form, Resource Based View of the Firm and Critical Theory 2013.
- Belbin RM. Management Teams: Why They Succeed or Fail. Oxford: Butterworth-Heinemann; 2010.
- Brailsford S, Bolt T, Bucci G, Chaussalet T, Connell N, Harper P, et al. Overcoming the barriers: a qualitative study of simulation adoption in primary care trusts in the NHS. J Operational Res Soc 2013;64:157-68. http://dx.doi.org/10.1057/jors.2011.130.
- Stake R. The Art of Case Study Research. London: Sage; 1995.
- Meyer J. Evaluating action research. Age Ageing 2000;29:8-10. http://dx.doi.org/10.1093/oxfordjournals.ageing.a008104.
- le May A. Communities of Practice in Health and Social Care. Oxford: Blackwell; 2009.
- Klein J, Connell N, Meyer E. Knowledge characteristics of communities of practice. Knowledge Manag Res Pract 2005;3:106-14. http://dx.doi.org/10.1057/palgrave.kmrp.8500055.
- Nutley S, Walter I, Davies H. Using Evidence: How Research Can Inform Public Services. Bristol: The Policy Press; 2007.
- van de Ven A, Johnson P. Acad Manag Rev 2006;31:802-21. http://dx.doi.org/10.5465/AMR.2006.22527385.
- Star S, Griesemer J. Institutional ecology, ‘translations’, and boundary objects: amateurs and professionals in Berkeley’s Museum of Vertebrate Zoology, 1907–1939. Soc Stud Sci 1989;19:387-420. http://dx.doi.org/10.1177/030631289019003001.
- Choo CW. The Knowing Organization: How Organizations Use Information to Construct Meaning, Create Knowledge, and Make Decisions. New York, NY: Oxford University Press; 2006.
- Cohen M, March J, Olsen J. A garbage can model of organizational choice. Admin Sci Q 1972;17:1-25. http://dx.doi.org/10.2307/2392088.
- Checkland K, Harrison S, Snow S, Coleman A, McDermott I. Understanding the work done by NHS commissioning managers: an exploration of the microprocesses underlying day-to-day sensemaking in UK primary care organisations. J Health Organ Manag 2013;27:149-70. http://dx.doi.org/10.1108/14777261311321752.
- Checkland K, Snow S, McDermott I, Harrison S, Coleman A. ‘Animateurs’ and animation: what makes a good commissioning manager?. J Health Serv Res Policy 2012;17:11-7. http://dx.doi.org/10.1258/jhsrp.2011.011010.
- Ward J, Peppard J. Strategic Planning for Information Systems. Hoboken, NJ: Wiley; 2002.
Appendix 1 Actionable messages
External provider analysis
| Key findings | Actionable messages |
|---|---|
| The approach by Swallow shows limited understanding of the local context, drivers and needs of the PCTs/CCGs. This may have been in part to do with a regional group acting as the intermediary, but not completely | Before bidding for work, try to understand context, needs and drivers within the client organisations as much as possible from different levels. Trusting in the perspective of those who contract you alone may not be sufficient. Better contextual understanding will assist in:
|
| The processes and systems within Swallow did not seem strategic, as any member of the PCT was able to initiate a project. This policy may have come about because Swallow had so little buy-in from the commissioning organisations that they were willing to take on any work, regardless of relevance, to build relationships and show value. But this lack of strategic focus made it difficult to show how the projects undertaken contributed to the delivery of the contract | With longer term contracts on which payment is dependent on delivery, systems and processes primary focus needs to be on contract delivery for the client and the external provider. External providers could consider discussing how to manage tangential work during the procurement process to manage client expectations |
| Swallow believed their tools to be superior to any in use within the PCTs, but from information provided did not evidence how. They therefore encountered resistance from PCT staff to use the new tools | Understand clients’ use of tools and their ongoing needs, and provide tools that meet these. This could be pragmatic use of the tool, as well as the strategic use of the tool. Again, obtaining information from all levels of client organisations, including operational analysts, is key |
| Commissioning engagement leads were often moved around between different PCTS. Yet one of the key findings is that these leads stressed that building relationships and trust were integral to success in engaging clients | Providing consistency for clients and staff where relationships are good might need to be prioritised over other considerations, possibly even consultant skill sets |
| Scenario generating tool was being marketed to assist commissioners in understanding the impact of commissioning decisions on the system. However, the tool included only acute sector data. This, therefore, is not able to assist commissioners to understand the impact on the whole health system for which they are responsible | A generic tool should be marketed for what it can deliver and not over sold. Loss of credibility is a risk if this happens |
| Best place of care tool is a North American tool that Swallow has not adapted for the UK market. This highlights, again, the one-size-fits-all mentality | As tool providers there is a need to adapt tools from abroad to ensure that they reflect the systems in which they will be used. Not only do these need to be adapted nationally for the UK market, but also locally for each health-care economy where they are used |
| Knowledge transformation processes to NHS clients outlined how Swallow focussed on GP practices. This shows a lack of understanding of the complexities and enormities of local health systems, as well as lack of strategic thought. If the organisation had focussed on PCT staff as a train the trainer model, PCT staff could have then been used to transfer the knowledge to GP practices, in which they had established relationships | If transferring knowledge to ensure independence after you have left is a driver, then a clear strategy on how this can most easily and sustainably be achieved is essential |
| Slow decision-making cycles in the NHS is noted as problematic to delivery, and, therefore, payment to the external provider. As Swallow had numerous ex-NHS staff why was this not known and planned for? | When working in the NHS build processes, systems and expectations that fit with the decision-making cycles of the NHS. This appears to be key to successful contracts |
| Key findings | Actionable messages |
|---|---|
| There was no translation into commissioning impact. There is no point in having a tool without knowing how it will be used effectively | Do not just provide a tool and training. Make sure you work with clients to maximise its use effectively. Presumably, Swallow have learning from others areas that could be drawn on |
| The phase I audit used Swallow staff solely. Was this the provider’s advice/experience on what works best? Involvement of the PCT/CCG is not clear in the planning of the audit | Tool providers need to bring expertise in tool deployment, but ultimately work collaboratively with clients to ensure the tool deployment and use is agreed by all parties |
| When conducting the second audit the evidence notes that reviewers without a clinical background, as well as all auditors being new to the tool, had a process of familiarisation throughout the audit period | To ensure that the mistakes of the first audit were not repeated, the provider could have provided a person with a strong clinical background to ensure the consistent use of the tool |
| Key findings | Actionable messages |
|---|---|
| The tool was allocated to commissioners who had no input into which tool was selected or a priori information need that the tool was meeting. Consequently, NHS users were left to puzzle out not only how to use the tool but what problems the tool could address | CCGs need to understand the problem that needs solving and their key requirements for a solution. Do not jump to buying the tool without understanding its potential or the impact of its use in practice. Ask for examples of how it has been used elsewhere and contact several previous users – not just champions suggested by the consultancy. This investment of time may save substantial money later |
| The content and delivery of the training did not suit all clients | External providers need to consider clients’ needs for learning, rather than providing recycled training used for other clients. The training should include how the tool can be used in health-care transformation, preferably in a similar context |
| Technical training was not sufficient for clients to understand how best to use the tool | External providers should work collaboratively with clients to devise strategies for using the tool, help interpret the data and demonstrate how the interpreted data can be used |
| Jackdaw worked through other suppliers to market their tools | Tool developers need to be aware that working through other suppliers may impede skills transfer, which in turn will reflect poorly on the reputation of your tool |
| Jackdaw noted that ‘there are “implementation studies” which use “action research” to get the tool into practice, which are less likely to be published because concerns around breaching confidentiality of the site or patients’ | External provider should be able to provide solid examples of the implementation of the tool and its effectiveness, even if these are not published in peer-reviewed press. CCGs should request this |
| Key findings | Actionable messages |
|---|---|
| All those interviews came across as confident; from the data provided this could be perceived by clients as arrogant and patronising. There was a consistent underestimation of the skills, abilities and knowledge of NHS commissioners and analysts | External providers as organisations and individuals within them need to constantly be sensitive to how their confidence and clear preconceptions and opinions of NHS staff could come across negatively to clients. The external provider will need to avoid being tarnished with being predatory and overly controlling/influencing of CCG clients |
| Kristen talks of her experience of being a commissioner in the NHS and Heron working with her. She noted the power of her Heron colleague asking pertinent questions such as ‘why do they do it like that?’ | External providers are not asking anything remarkable. CCGs need to question whether or not they listen more to external providers than to their own staff. Who should be asking the same questions? |
| Heron note that they offer using ‘data to drive decision making’. This is very different from the other cases looked at as the other examples have focused on use of tools, rather than the data/intelligence gleaned from them to influence/drive decisions | Using ‘data to drive decision-making’ is a unique selling point for the external provider in comparison with other commercial providers whose main focus was the selling of products/tools. Other external providers could consider this line of approach, using the tools as the key to extracting the intelligence/data |
| Heron have a model for project delivery in teams, the contrast being made that NHS staff work in silos | CCGs and CSUs need to make matrix working a reality and break down departmental boundaries that can hinder project delivery |
| Heron employees talked about their organisation having ‘value’ and ‘drive’. This is predominant in the culture of this organisation. Contrasting the NHS, which certainly is value based, it lacks a systematic culture on drive | CCGs and CSU need to foster a culture for their organisations where values and drive for individuals, teams and the organisation as a whole is developed and prized |
| Performance management of staff was clear within Heron. The NHS could learn a lot from this, where success and failure is often attributed to an individual, rather simplistically and dangerously | CCGs could learn from external providers in terms of performance management of staff, where the focus is on affirmation and acknowledgement of contribution, not on success or failure of an individual |
| ‘What clients want are people to help them understand the data’ | External providers need to understand CCG clients often want not only the data, but assistance in how to use it |
| ‘You can’t give them the answers without knowing the question’. This has strong echoes of Carnford | External providers can help CCGs to understand their local context through asking the right questions and eliciting the answer |
| Dennis notes knowledge transfer was an element of the Westhide contract with Heron; however, it was removed owing to cost pressures | Knowledge transfer could be argued to be the most important aspect of the Westhide contract. For external providers this may be advantageous as it creates reliance. For CCGs it shows a lack of strategic thinking on skills needs and gaps in the future |
| Knowledge transfer is mentioned as a factor to help success, as NHS staff learn new skills but also understand the local context | External providers need to consider knowledge transfer as an offer to CCGs; this would be attractive. CSUs need to consider how they market as they have knowledge to transfer, but also know the local context |
| Key findings | Actionable messages |
|---|---|
| The decision support unit/CSU is viewed by many senior leaders as providing the ‘mundane stuff’ – analytics/intelligence | CSUs need to be able to communicate the breadth of skills contained within their staff, selling the extent of their capabilities rather than transactional processes. If they do not there is a real risk to CCGs not seeing the added value they bring, and pull staff in house/or CSU staff leave as not being used to their full potential |
| Randall (freelance analyst) was highly regarded for ‘providing timely, useful information . . . a real understanding of GP needs . . . and the flexibility respond to commissioners’ iterative, evolving demands.’ This should be the standard rather than the exception | External providers, including CSUs, should understand the CCG environment, being adaptable and responsive, as well as understand their needs will be a key to success |
| The size of the CSU working with Norchester discussed by many outlining the differing views on advantages and disadvantages Advantages:
Disadvantages:
|
The size of a CSU could provide opportunities for economies of scale and spread of ideas; however, being able to offer skills transfer as part of the offer to CCGs will be attractive to CCG leaders who are keen to ensure that skills are retained within their organisation |
| A CSU staff member noted that other external providers were ‘quite removed from day to day business and worked to specifications’. This could be viewed as an advantage as external providers can concentrate on the project/work they have been defined, and not pulled in different directions, as is the risk with CSUs | CSUs need to take advantage of local knowledge/networks but still need rigour of an external provider to define work packages with clients, to ensure delivery |
| Angus reflected that ‘some individuals are particularly good at understanding what you need and delivering it’ | Clients find it hard to hire for projects and not for people. External providers therefore need to understand this and use methods to communicate the benefits of a team-based approach to delivery |
Angus noted that to trust the information provided by external providers he required two things:
|
When going through procurement and after winning the contract, external providers need to have a strategy around how their contribution aligns with the clients’ goals and aims and how they plan to develop a long-term relationship |
| This case study noted caution in relation to primary care data sharing, and reflects the debate/view held nationally in primary care. Adrian noted that ‘practice managers are beginning to see themselves as “guardians of patients’ data”‘ | External providers need to understand and consider this carefully when bidding for work. The assumption is often data will be shared, whereas this is most often not the case. Contingency plans should be developed during procurement to address the situation if the external provider cannot get access to the data |
| Throughout the case study there is wariness from a number of CCG staff and local GPs in the use of the commercial external providers. However, it is interesting to note that a number of organisations are emerging using the NHS logo and brand but are in fact non for-profit/profitable organisations. The concerning aspect of this is that they are not being transparent in the fact that they are non-NHS organisations | CCGs need to have robust systems and processes to decide which organisations to work with to ensure the appropriate use of public funding. A lot could be learned from systems used by medicines management teams in working with the pharmaceutical industry |
| Simon noted that ‘the private providers weren’t clear on what they were supposed to deliver and there was not then the engagement between the intelligent commissioner and the intelligent provider to actually deliver a product that was really useful’ | External providers and particularly CSUs need to help CCGs define the scope and detail of the support they require. Having loose service-level agreements based on individuals and long-term support to programmes, will not deliver the outcomes needed, or sustainability for CSUs |
| Simon commented that tool ‘was probably just what we need’ but that there is not clarity about ‘what I can do differently because I know this’ | External providers must understand that selling a tool is not enough; clients (meaning all stakeholders, not just senior leaders who have contracted you) need to understand the benefits offered by the tool and how it will be implemented and its impact evidenced |
| Key findings | Actionable messages |
|---|---|
| A key finding was the suspicion and belief in the predatory behaviour of external providers | External providers are usually aware of this common mind-set within the NHS. Could you sell the benefits, but also be honest about the current limitations with clients? |
| Roger, the GP lead for integrated care teams, reflected the commonly held view emerging from many case studies that CCGs and clinical leads want the answer to problems they face, as he states ‘nobody seems to be able to say that this or isn’t the right way of doing it’ | External providers need to robustly evaluate implementation in order to build the body of evidence |
| Roger expresses a view that CCGs have a desire to have skills, knowledge and capacity to do the majority of work in house, as he states ‘so we could do it all locally. But when you look at the enormity of the task, you just wonder whether – or I just wonder whether the resources are there’ | External providers could explore knowledge transfers as a credible part of their offer to clients. Consideration needs to be given about the sustainability of this as a model, particularly for CSUs who are currently more geographically constrained |
| Mike’s view that CSUs could act as gatekeepers/contractor for CCGs working with commercial providers, despite his insistence that it was a role to ‘protect CCG from the commercial provider.’ It could conversely be seen as creating dependency on the CSU, by the CCG | Despite CSU currently being part of the NHS, they are arm’s length and are external providers. Consideration needs to be given to how they therefore interact with CCGs and other external providers alike, so as not to alienate potential clients/partners |
| The emerging theme of collaboration came up with Tom saying ‘come and work at our desks. Come and meet the team and feel part of the team. Though you are working at arm’s length and for a different employer, what you do is absolutely integral to what we’re doing’ | CSUs and other external providers need to consider the benefits of short- and/or long-term colocation, ideally having staff embedded within the CCG |
| The tools being derived originally from America was raised once again in this case study. However, as the tool was to predict the accuracy for insurance companies, this is still relevant for the NHS, as a publicly funded organisation. However, the CCGs view is that this discredits it | External providers need to consider how they market the tool and its origins. The fact that the tool would work in the NHS to keep costs down could be sold as a benefit |
| Discussion on focus of tools thresholds of 1% and 25%, 5% still small numbers at the top of the pyramid. One Public Health consultant wanted to look at lower down the pyramid for preventative interventions. He acknowledged that this was unlikely as CCGs were ‘trying to fire fight’ | External provider risk prediction/stratification tool providers should assess and advise CCGs on short-term/longer term goals/interventions and which will have the biggest impact |
| Harold had done statistical analysis on the risk prediction tool’s predictive value and found it to be low. When he approached, regional group and Jackdaw, both were resistant to acknowledge the analysis or do further analysis | CCGs need to ensure they have the appropriate skills to assess the effectiveness of the tool they use preferably independent analysis of the algorithm behind the tool (if available) |
| One freelance consultant acknowledged that a lot of business within the CCGs and former PCTs was generated because of the NHS inability to share knowledge – ‘knowledge management in the NHS is very poor. And particularly with all the changes so with the PCT disappearing there’s no work stream about, you know knowledge management being transferred’ | CCGs and CSUs could add value and save duplication of effort by working effectively across NHS organisational boundaries to share knowledge. As well as establish effective knowledge management systems for the organisation |
| Key finding | Actionable message |
|---|---|
| Sarah states that ‘you can have all the technical skills you like, if you haven’t got relationship management skill in terms of managing the system, the technical skills won’t get you anywhere’ | CCGs, CSUs and external providers can all benefit from understanding that good tools, good data and crucially good translation/communication are key to success. Not mutually exclusive, but a combination of these |
| ‘The role of these agents was the credibility and “independence” they brought to the process’ | CSUs need to consider and be aware of how they are viewed by CCGs. Will they be seen as independent and credible or more of the same NHS? How they market and evidence this may be key to success |
| Consultants noted that NHS staff had lots of ideas but they didn’t have ‘the actual discipline of completing it and measuring it was not there.’ Could this explain the NHS brain drain to external providers? | CCGs and CSUs need to develop performance cultures where staffs are valued for their contribution, performance and drive |
| ‘Hilda expected the CSU to have data analysis and health economics skills and experience’ | CSUs should consider how they can improve their offer for these services |
| Penborough had retained a large internal team, so had reduced reliance on the CSU. Alan went on to note that for service redesign it was important to retain local input, and he did not seem to see this as something the CSU could provide | CSUs need to consider how they market themselves to maximise their client base. Key messages may be for some local CCGs ‘local and responsive’ |
| Penborough CCG set expectations that knowledge would be transferred as part of the hand over process. This is the first example seen of a CCG proactively stating and expecting this | CCGs need to build in knowledge transfer as a key requirement to contracts with external providers |
| Vidur talks about presentation from PWC costing lots with lots of flow charts, but that ‘I don’t think it’s a good use of my time, or my learning style’ (Vidur) | External providers need to understand the multiple ways to present findings to CCGs/clinicians. What would work well and why, as well as what did not work well? |
| Key finding | Actionable message |
|---|---|
| From reviewing the people interviewed working for consultancies with a NHS background. Why is there a NHS brain drain to external providers? | CCGs should consider proactive recruitment and retention policies which value individuals’ contribution, drive and performance (see Penborough above) |
| ‘What made it work was external provider were willing to go at our pace and understand that there were some parameters we couldn’t change, and worked at our pace with us, rather than coming in and saying, oh you’ve got it all wrong’ | External providers/CSU should note this clearly effective approach of working with CCGs, at the pace and style they have |
| External provider used patient stories to communicate effectively. This seemed to work well, with only one person noted as saying it was ‘anecdote’ | CCGs, CSUs and external providers should consider the use of stories as an effective technique, backing up messages with data could be a powerful combination |
| Outlines a situation when Brian (freelance consultant) articulated the problem, but Kevin (CCG accountable officer) found a solution | External providers need to not just define problems, but find realistic solutions. Be realistic with yourselves and clients in terms of what is possible to change as well as the timeframe to do this |
| Brian (freelance consultant) is noted as needing ‘some guidance’ | CCGs/CSUs need to look for and test for technical and interpersonal skills for internal and external recruitment processes |
| ‘If we actually did the right things for patients first, then we find we get those outcomes as a secondary consequence’ | Focusing on quality patient improvements rather than money-saving efficiency schemes will be attractive to clinically-led CCGs |
| External provider notes that they are ‘principles drive versus rules driven’. This is very clever marketing, as they are one of the few case studies to show a clearly defined methodology | Having a few clear and simple messages that are marketed well can be a highly effective strategy for external providers |
Glossary
- Analytics
- A term used to refer to quantifiable data such as activity and performance data produced by health-care analysts.
- Collaboration for Leadership in Applied Health Research and Care
- A collaboration between universities and their NHS partner organisations.
- Commercial provider
- An organisation that supplies health care or services to make a profit. Also known as ‘for profit’ and ‘private’.
- Dashboard
- A succinct data set that identifies performance against commissioning key performance indicators. Normally comes with a red, amber, green rating.
- Joint Strategic Needs Assessment (JSNA)
- A priority-setting exercise carried out by public health departments.
- NHS provider
- An organisation that provides health-care services to the NHS, for example a hospital.
- Not-for-profit
- An organisation that supplies health-care or services without the aim of making a profit. Examples include social enterprises.
- Primary care provider
- An organisation that offers primary care services such as general practices.
- Quality, Improvement, Productivity and Prevention (QIPP)
- A Department of Health-led initiative to transform NHS services to make £20B of efficiency savings.
- Secondary care provider
- Another term for hospital.
- Unscheduled Care Board
- Subcommittees of commissioning organisations that focus on hospital issues.
- World Class Commissioning
- An assurance programme instituted by the Labour government in 2008, designed to improve commissioning practice in primary care trusts, which were the primary local commissioning organisations from 2001 to 2013.
List of abbreviations
- A&E
- accident and emergency
- AHSN
- Academic Health Science Network
- CCG
- Clinical Commissioning Group
- CLAHRC
- Collaboration for Leadership in Applied Health Research and Care
- CSU
- commissioning support unit
- FESC
- Framework for procuring External Support for Commissioners
- GP
- general practitioner
- HRG
- Healthcare Resource Group
- IT
- information technology
- JSNA
- Joint Strategic Needs Assessment
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PBC
- practice-based commissioning
- PCT
- primary care trust
- QIPP
- Quality, Improvement, Productivity and Prevention
- SECI
- socialisation, externalisation, combination, internalisation
- UCB
- Unscheduled Care Board
- WCC
- World Class Commissioning