Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 10/1008/12. The contractual start date was in September 2011. The final report began editorial review in October 2012 and was accepted for publication in September 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
The University of Warwick received funding from National Institute for Health Research (NIHR) in order to support this work; this money was paid to the institution and not to any of the authors, other than to cover relevant travel expenses. Professor Aileen Clarke is a member of the NIHR Journals Library Editorial Board for which money is paid to the institution.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Fisher et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
The clinical role of the ambulance service has changed dramatically over the last few decades. The 1980s saw the widespread introduction of paramedics and the possibility of delivering life-saving interventions, the 1990s saw more sophisticated equipment and the development of national clinical guidelines, with treatments expanding to cover many diseases in addition to immediately life-threatening conditions, and, in the 2000s, work progressed on ambulance services undertaking definitive care, discharging patients either after telephone advice alone or after face-to-face contact. Over this time, more specialist roles have developed, requiring advanced skills for specific individuals. This has all been accompanied by a continuing increase in the number of 999 calls and individual incidents. All these factors increase the potential risks of adverse events (AEs) in ambulance care as more complex treatments and procedures are undertaken.
The costs of AEs in the health-care setting are considerable at both the personal and institutional levels. Most information on, and research in, patient safety is based on hospital data, with some in primary care, but little is known about patient safety in ambulance services in which the environment, the personnel and the conditions seen can mean that AEs may differ. A retrospective review of medical records in two UK hospitals estimated that 1 in 10 patients experiences an AE,1 with 50% of such events potentially having been preventable had lessons been learnt from previous incidents. 2 Despite the increasing body of evidence informing on the occurrence of AEs within hospitals, corresponding data informing on patient safety when using ambulance services are lacking.
The publication of two seminal reports To Err is Human: Building a Safer Health System3 and An Organisation with a Memory4 more than 10 years ago highlighted an urgent need to systematically study and understand the extent and nature of harm that patients are exposed to in health-care settings. These reports led to the initiation of studies to quantify the incidence of harm, predominantly in hospital-based care and qualitative research to identify the failure mechanisms that result in patient harm. The research showed that underlying attitudes and assumptions concerning safety within health-care settings are a serious obstacle to implementing sustainable improvements. The ability to quantify the safety culture (i.e. safety-related attitudes, staff values and beliefs) of an organisation, and then go on to develop a systems-oriented safety culture, became a major aim. The growing focus on safety interventions has led to the publication of an increasing body of literature that describes interventions and attempts to quantify patient benefit. There is obviously a risk when introducing these interventions into ambulance services without first making a diagnosis of the safety issues.
Patient safety has moved up the agenda for the hospital setting; however, there is little documented evidence as to how ambulance services identify issues or assess the impact of AEs. As < 50% of ambulance services and none of the associated professional bodies signed up to the Patient Safety First campaign,2 safety could be construed to be a lower priority for NHS ambulance services than for hospital services in the NHS. Before the start of this project, a preliminary review of the published literature concerning patient safety in ambulance services showed that the evidence base for patient safety in ambulance services lags behind those for other health-care sectors; furthermore, there is no systematic evidence review to direct policy, service delivery and future research.
An additional preliminary review of websites relating to patient safety identified few resources for ambulance services and no specific consideration of the applicability of generic interventions to this setting. National Patient Safety Agency (NPSA) data identified a wide variation in AE reporting between ambulance services and showed that fewer incidents were reported than by other health-care sectors. Potential reasons for this remain unclear, but it is generally accepted that low AE rates are usually owing to poor reporting rather than because incidents are not occurring. A recent PhD thesis5 suggested that prioritisation of work to improve clinical quality in line with national performance targets may take attention away from patient safety; alternatively, the safety culture in ambulance services may not be conducive to disclosure of AEs. There is clearly a need for further work to explore how ambulance services respond to patient safety issues and to understand how to optimise their engagement with safety initiatives.
There is a growing focus on patient safety across all health-care sectors and, although litigation in ambulance services is infrequent,6 rates are increasing. There is, therefore, an urgent need for robust evidence synthesis to characterise the evidence base associated with AE reporting in NHS ambulance services. This scoping review will help to highlight gaps in understanding and to direct future research and, as such, this project represents a starting point for prioritising and improving ambulance service safety processes in order to make patient care safer.
Chapter 2 Research questions and objectives
The aim of this scoping review was to identify and synthesise the available evidence relating to patient safety when using ambulance services and to identify gaps in the evidence base concerning UK ambulance services and their international equivalents. It should be noted that this review will highlight research concerning patient safety when using ambulance services and identify which questions and topics remain unanswered. Therefore, specific clinical, process or organisational questions, such as the safety of endotracheal intubation in the pre-hospital environment, cannot be definitively answered by this review, as they will need to be the subject of specifically designed reviews. It should also be noted that the search strategy (see Table 1) was designed to find studies concerning patient safety in ambulance services; therefore, not all studies on a particular topic will be found, only those that specifically explore patient safety or use the term ‘safety’ or its variants in the paper are identified.
Three research questions were defined for the project:
-
What is the national and international evidence base for patient safety in ambulance services?
-
What are the significant gaps in the evidence base for which research might add value, through either addressing new questions or replicating international research in the NHS setting?
-
What are the priorities for future policy and research?
The objectives were:
-
To undertake a scoping systematic literature review and seek opinion and advice from ambulance experts to identify the current body of evidence related to patient safety, and identify gaps in the evidence base in UK ambulance services and their international equivalents.
-
To review and analyse documents/reports/data to determine patient safety processes in English ambulance services.
-
To synthesise the evidence to identify significant gaps in the evidence base and recommend research that might add value, through addressing new research questions, replicating inadequately powered studies or replicating international research in the NHS setting.
-
To undertake a prioritisation exercise with key stakeholders in ambulance service patient safety to consider the findings of the evidence synthesis, in order to gain consensus for future policy and research.
-
To disseminate the findings of this scoping exercise, evidence synthesis and prioritisation exercise on patient safety in ambulance services and relevant related emergency services, setting out the recommendations for best use of the available evidence to direct policy and practice, highlighting gaps in the evidence base and indicating prioritised future research needs.
Chapter 3 Scoping systematic literature review
Introduction
Patients contacting the emergency services proceed through a number of processes from initial contact, telephone-based assessment and prioritisation, on-scene assessment, management and discharge or transfer to further care. At all these points, ambulance clinicians and staff process information and make decisions concerning their responses. In the vast majority of cases, these will be in the patient’s best interest; however, in some cases, things go wrong, and decisions at an individual, process or organisational level can lead to an AE. 6,7
A rapid evidence synthesis exploring patient safety in ambulance services was conducted in 2010. It demonstrated a paucity of evidence with no overall systematic review being available (see Appendix 1, or www.warwick.ac.uk/ambulancesafety8). As a starting point to this project, a full scoping systematic literature review was required to comprehensively identify the available evidence on patient safety including evidence not available in electronic databases. The aim of this scoping review was to identify and describe research related to patient safety within ambulance services and identify where questions and topics remain unanswered. It was not designed to answer specific clinical, process or organisational questions such as ‘what is the safety and effectiveness of paramedic endotracheal intubation?’ Such questions would require a subject-specific systematic review. This scoping systematic review has identified citations that specifically explore patient safety or use the term ‘safety’ or its variants.
Aims and clinical questions
The aim of the scoping systematic review was to identify and map the available evidence relating to patient safety when using ambulance services and to identify gaps in the evidence base in UK ambulance services and their international equivalents.
Specific research questions were defined as:
-
What is the national and international evidence base for patient safety when using ambulance services?
-
Where are the gaps in the evidence base regarding patient safety when using ambulance services?
Methods
Study design
A scoping systematic review of the literature was undertaken following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, when appropriate (see Appendices 1 and 2). 9
No restrictions were placed on study design and both prospective and retrospective data were included; no language restrictions were applied.
Literature reports were included in the scoping systematic review if they considered any patient (child or adult) receiving health care from ambulance services or transferred to further care by ambulance services. Reports were eligible if they considered any setting (pre-hospital, primary or secondary care) in which patients received health care, in part or in full, from ambulance services.
Primary outcomes considered in the analysis of patient safety reporting comprised avoidable harm, risk of harm, morbidity and mortality arising from medical error, AEs, litigation cases or other patient safety incidents.
Search strategy for eligible studies
The search strategy used for this scoping systematic review is detailed in Table 1. It was developed in MEDLINE and searches of other databases were adapted from this template.
| # | Searches |
|---|---|
| 1 | Safety |
| 2 | Exp Safety/ |
| 3 | Safety management |
| 4 | Exp Safety management/ |
| 5 | Safety indicator$ |
| 6 | Patient safety |
| 7 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 |
| 8 | Pre-hospital OR pre hospital OR pre-hospital |
| 9 | Ambulance$ |
| 10 | Transportation of patient$ |
| 11 | Emergency medical service$OR EMS |
| 12 | Paramedic$ |
| 13 | Emergency care assistant$ |
| 14 | Emergency medical technician$ |
| 15 | Advanced practitioner$ |
| 16 | Community first responder$ |
| 17 | Exp Transportation of Patients/ |
| 18 | Exp Ambulances/ |
| 19 | Exp Emergency Medical Technicians/ |
| 20 | Exp Allied Health Personnel/ |
| 21 | Exp Emergency Medical Services/ |
| 22 | 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21 |
| 23 | 7 AND 22 |
| 24 | Limit 18 to yr=“1980-current” |
In discussion with the steering group, further medical subject headings (MeSH) and key terms relevant to patient safety and the ambulance services were collated. Using different combinations, 27 search strategies were developed and tested against a set of key papers related to patient safety. The search strategy selected achieved high sensitivity and moderate specificity and performed better than a validated search filter. 10
Data sources
Databases were searched from 1 January 1980 to 12 October 2011 and included MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science, Science Direct, Emerald, Education Resources Information Center (ERIC), Applied Social Sciences Index and Abstracts (ASSIA), Social Services Abstracts, Sociological Abstracts, International Bibliography of the Social Sciences (IBSS), PsycINFO, PsycARTICLES, Health Management Information Consortium, NHS Evidence, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, NHS Economic Evaluation Database and Health Technology Assessment, the FADE Library, Current Awareness Service for Health (CASH), OpenDOAR (Directory of Open Access Repositories) and Open System for Information on Grey Literature in Europe (OpenSIGLE). Zetoc (The British Library’s Electronic Table of Contents) was used for the main journals in the field/conference proceedings. Reference lists from key papers and citations identified as being potentially relevant were also searched.
A Google search of websites was conducted using the advanced search option, which initially considered the first 20 pages of results. In addition, the NHS Confederation website was searched.
It is argued that searching electronic databases alone will find only approximately half of the relevant literature on pre-hospital topics;11 therefore, experts were consulted to ensure that any new data were included in the scoping systematic review process.
Screening
The titles and abstracts of all retrieved citations were screened by six reviewers for their relevance to the topic of patient safety when using ambulance services. Disagreements concerning relevance were resolved by discussion with an additional reviewer who had not been involved in the initial screening. The full text was retrieved for all citations considered potentially relevant.
Literature selection
Literature selection criteria were kept broad, in line with the aims and intentions of a scoping review. The decision to use broad criteria was based on discussion with experts in emergency medicine and patient safety; input from the project advisory group (see Acknowledgements) was also sought.
Inclusion criteria
Citations were included in the scoping systematic review if they contained original data concerning any patient for whom ambulance services had been contacted and the outcome was avoidable harm/risk of harm by acts of omission or commission.
Exclusion criteria
Citations were excluded if they:
-
were off topic, for example road traffic collisions
-
considered the wrong setting
-
considered the wrong population, for example related to the safety of staff rather than patients
-
did not provide research methods, for example overviews, opinion, letters, comments, etc.
-
contained research that was reported elsewhere
-
had a study that was in progress or planned, but with no preliminary findings reported
-
were not specific to ambulance services-general care/guidance
-
did not have an available English abstract
-
had research that had been superseded
-
reported from a disaster or military context
-
were a retracted paper.
The full table of excluded studies can be found in Appendix 4 or at www.warwick.ac.uk/ambulancesafety and the reason for exclusion with the number excluded in each category can be found in Appendix 5.
Data extraction
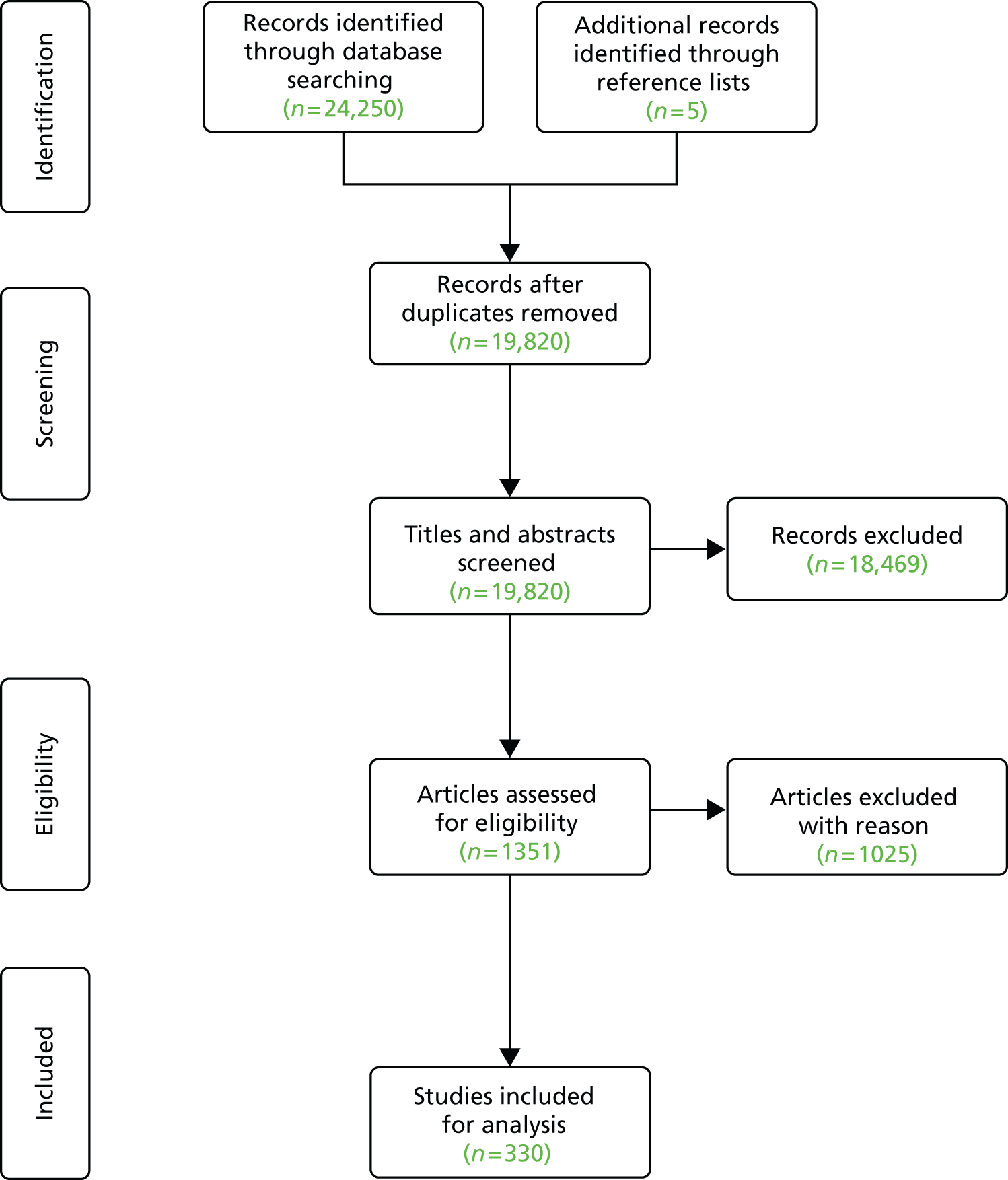
The search identified 24,255 studies, of which 330 were identified as relevant and included in the review (Figure 1). Although the search identified a large number of citations that addressed the topic under consideration, many gave opinions and comments on patient safety and were excluded as they did not contain assessable data. The majority of the studies were observational, including cohort studies, case–control studies, case reports and surveys. Some studies reported randomised controlled trials (RCTs) and there were some systematic reviews.
FIGURE 1.
Study identification (PRISMA) revised.
Information on study design, year and country of publication, environment, participants, interventions and outcomes was extracted using the predefined data extraction form.
Planned analysis
This scoping systematic review will identify citations that specifically explore patient safety or use the term ‘safety’ or its variants. As a scoping systematic review, it is not possible to answer specific clinical, process or organisational questions such as ‘what is the safety and effectiveness of paramedic endotracheal intubation?’, as such questions would require a subject-specific systematic review; therefore, it is not appropriate to combine data for a meta-analysis and a narrative analysis will be presented.
The data were mapped against the patient safety frameworks listed below, in a card-sorting task with the steering group. The frameworks are designed to account for factors contributing to patient safety incidents. Each framework focuses on different aspects of patient safety, as they explore different perspectives, including systems approaches and incident types:
-
Agency for Healthcare Research and Quality (AHRQ) conceptual framework
-
London Protocol
-
National Reporting and Learning Service framework
-
Patient Safety First Safety Domains
-
Yorkshire Contributory Factors framework.
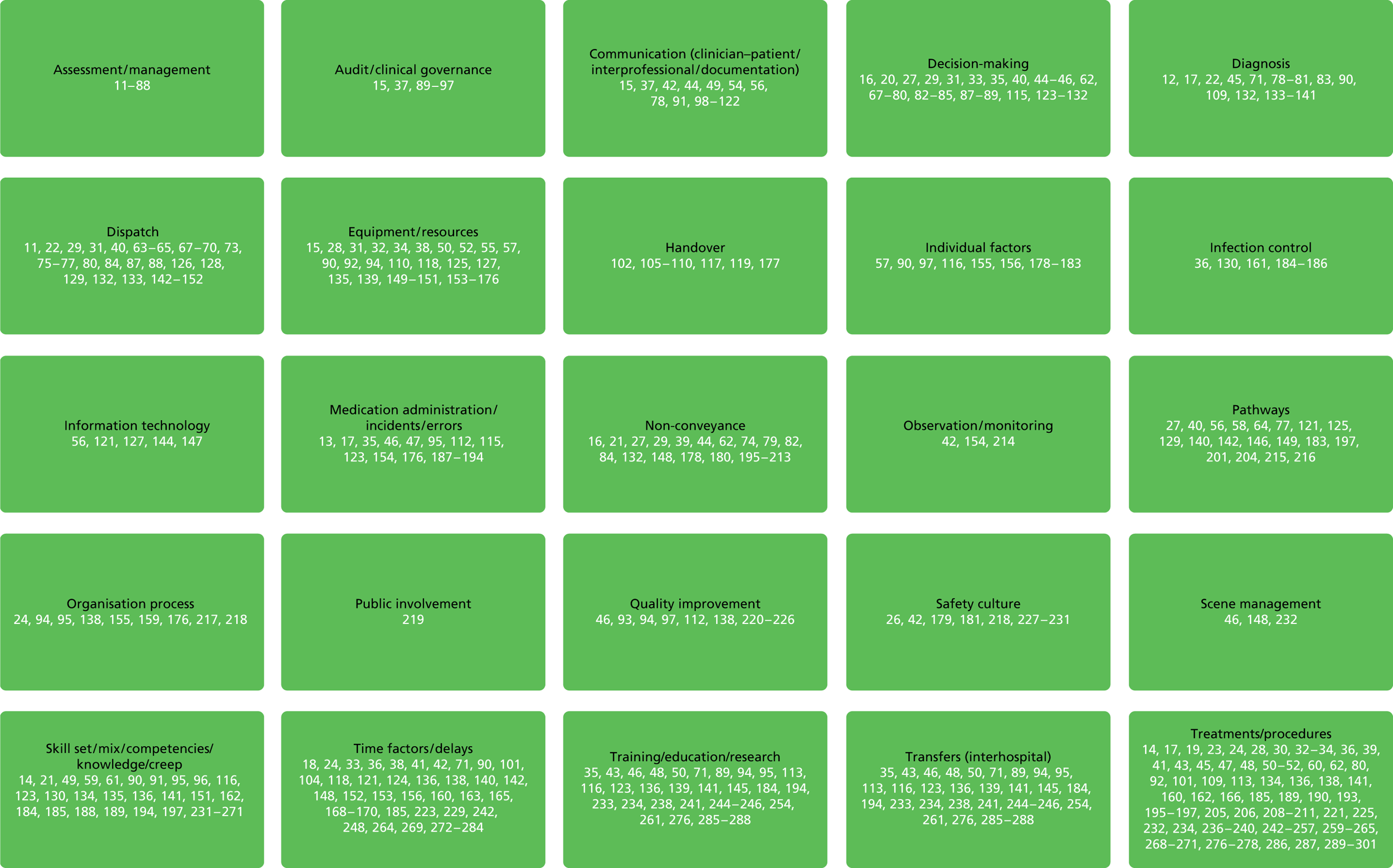
The mapping exercise demonstrated that no one single framework could adequately account for the breadth of evidence retrieved from the scoping systematic review. Therefore, the card-sorting exercise was repeated to develop a new framework that could account for the data, and the resulting topic grid comprised 25 topic areas (Figure 2).
FIGURE 2.
Literature topic areas.
Results
A total of 330 studies met the inclusion criteria. The majority of the studies were from the USA (53%, 175/330), and studies undertaken in the UK accounted for 18% (60/330) of the papers found.
The remaining studies were from Australia, Austria, Belgium, Canada, Crete, Denmark, France, Germany, Greece, Hong Kong, Ireland, Israel, Italy, Japan, the Netherlands, New Zealand, Norway, Portugal, Singapore, Slovenia, Spain, Sweden, Switzerland and Turkey. Studies undertaken in the UK accounted for 18% (58/316) of the papers found. There were 11 systematic reviews/meta-analyses and 13 RCTs. The remainder of the studies were non-RCTs, observational studies, consensus statements and case reports, and two studies were undertaken in two locations. 253,302
The diversity of topics, the poor descriptions of methods and the range of outcome measures meant that it was not possible to combine data from studies in this scoping review. Equally, no standardised quality scoring system was possible. Study type is included in the summary tables as this gives an indication of one aspect of the quality of the evidence. The narrative text below also describes limitations and other aspects of quality of key papers.
Terminology
The literature used a wide range of variable terminologies. As this report considers patient safety from an international perspective, descriptions of personnel, processes and organisations, etc. will vary.
Evidence
The issue of patient safety is a cross-cutting theme relevant to all areas of ambulance service activity, including systems and processes, and clinical and non-clinical staff. This review found research across a broad range of topics and the data have been categorised and tabulated as follows (see Tables 2–8). Studies that examined the transfer of patients (n = 69); assessment and management including diagnosis, treatment, medication, skills and training (n = 135); non-conveyance including telephone advice, treat and discharge on scene and alternative pathways (n = 40); safety culture (n = 20); dispatch (n = 27); equipment (n = 11); and communication (n = 20).
In tabulating the data broadly it should be noted that some cases might be relevant in one or more tables. Therefore, in line with the remit of this scoping review, and to provide as much information to readers on the research undertaken and uncertainties found, a research grid comprising 25 topic areas was developed (see Figure 2). Studies were assigned to categories by their primary and secondary themes. For example, studies looking at patient handover between ambulance clinicians and emergency staff would be listed under handover and under communication.
The evidence tables contain the following study characteristics: citation, design, intervention, duration of the intervention, sample size, inclusion criteria, setting, outcomes, follow-up when applicable, and study findings. The tables are organised in terms of study design:
-
evidence syntheses (meta-analysis, systematic review)
-
experimental designs (RCT, non-RCT)
-
observation studies (before-and-after study/interrupted time series, case–control study, cohort study)
-
other (survey, consensus, case study).
Transfers
A large body of evidence was identified on the topic of transfers (Table 2); 71 papers were found that explored a number of topics, including the efficacy and appropriateness of helicopter transfer, and others compared direct transfer to trauma centres and stabilisation with subsequent transfer for serious life-threatening conditions, generally demonstrating benefit of direct admission to a major trauma centre. The results of these studies gave conflicting results regarding the benefits and cost–benefits of helicopters and most have methodological issues that may bias results. A systematic review by Taylor et al. ,183 looking at the clinical effectiveness and cost-effectiveness of helicopter emergency medical services (EMS), found that helicopter transfer was generally more expensive than ground transport. However, given the variation in study designs, it was not possible to determine either the clinical effectiveness or the cost–benefit of these services and they recommended that an important factor in the determination of clinical and cost–benefit would be determined by local system factors.
| Author(s), year, study design, country | Population, patient number | Intervention/process or topic | Results | Headline |
|---|---|---|---|---|
| Goodloe et al. 2012,175 retrospective observational study, USA | Transported patients, n = 129,110; stretcher incidents, n = 23 | Transfer/stretcher events | No injuries occurred during the study period. Four EMS providers sustained minor injuries | Only a few personnel injuries occurred and no patient injury was reported. Safety for personnel and patients could be enhanced by educational initiatives |
| Thomas et al. 2011,221 systematic review, UK | N/A | Transfer/guidelines for critically ill adults | 17 recommendation categories with subcategories for patient and staff safety during critical care transfers | Increased safety |
| White et al. 2011,150 prospective cohort study, USA | Injured patients ≥ 16 years, n = 557 | Transfer/air medical transport utilisation | Overall mortality was 2%; 48% (266/557) had one of four outcomes: in-hospital mortality, emergent surgery, blood transfusion, intensive care unit admittance. Factors associated with mortality were age (> 44 years) and GCS score; few pre-hospital criteria were associated with clinically important outcomes | Guidelines are needed to avoid over-triage of air medical transport |
| Garwe et al. 2011,215 retrospective cohort study, USA | Critical injured patients, N = 1998: direct transfer, n = 1398; secondary transfer, n = 600 | Transfer/direct to a major level 1 trauma centre | Threefold increase in mortality at 2 weeks for patients undergoing secondary transfer (hazard ratio 2.7, 95% CI 1.31 to 5.6) | Critically injured patients should be transferred directly to a level 1 trauma centre. Those needing stabilisation at non-tertiary facilities should be treated without delay |
| Cooney et al. 2011,273 prospective observational study, USA | Adults and children arriving at ED, n = 483 | Time/ambulance off-load delay | Ambulance off-load delay ranged from 0 to 157 minutes. A high National Emergency Department Overcrowding Score may predict delays | Ambulance off-load delay is a significant risk to patient safety |
| Dhindsa et al. 2011,278 retrospective observational study, USA | Patients with acute myocardial infarction, n = 17 | Transfer/door-to-balloon time | Group one: 13/17 patients were transported by ground EMS and 1/17 was a walk-in patient; group two: 3/17 patients were transported by helicopter. Door-to-balloon times: group one, 53.5 minutes (range 34–84 minutes); and group two, 18 minutes (range 10–64 minutes) | Transport by helicopter has the potential to reduce door-to-balloon time for patients with myocardial infarction |
| Wigman et al. 2011,145 survey, the Netherlands | European helicopter EMS, n = 55 | Transfer/air medical transport utilisation | 50 services used criteria based on injury mechanism including fall from height, lengthy extrication and significant injury | Lack of uniformity in criteria for helicopter emergency medical service activation |
| Dalawari et al. 2011,100 retrospective review, USA | Patients ≥ 65 years transferred to ED from a nursing home. N = 80 patients: n = 40 with transfer form and n = 40 with no transfer form | Transfer/forms | 16 information points were considered essential; 71% of information was documented with the form compared with 28% without (p ≤ 0.001) | Patient transfer form enhances provision of key information |
| Yeh et al. 2011,275 retrospective review, USA | Calls with dispatcher-identified stroke symptoms, n = 2800 | Time/responding with lights and sirens | 98.3% used red lights and sirens; achieved faster response time of 1 minute 52 seconds (95% CI 1 minute 21 seconds to 2 minutes 22 seconds) | Clinical significance unknown |
| American College of Emergency Physicians 2011,303 consensus, USA | Patients not requiring advanced life support level care or evaluation at an ED, n = N/A | Transfer/direct to alternative care | Key elements: EMS physician medical director oversight of development, implementation, continuous improvement of policy and procedure quality, and research of alternative transportation or destination decisions; educational programmes; compliance with dispatch criteria, and patient preferences | EMS systems that choose to implement such options, either during dispatch or following on-scene evaluation by field personnel, should develop a formal programme |
| Gustafsson et al. 2010,116 observational study, Sweden | Interview of nurse specialists, n = 30 | Transfer/interhospital | Worries and concerns by nurse specialist involve being unable to influence transport situations; used acquired knowledge and experience as well as colleagues to resolve situations | Specialist training and team approach to transferring critically ill patients |
| Houston and Pearson 2010,135 questionnaire, UK | Medical/clinical directors, n = 13 | Transfer/ambulance provision for children < 15 years of age | 77% response rate. Minimum response was ambulance technician crewed with an emergency care assistant; six out of nine trusts employ emergency care assistants; 85% had no budget for paediatric care training; and 31% responded that it is possible/highly likely that someone with no specific paediatric training could be the first responder | It is important that adequate training is provided – new pre-hospital guidelines provide extended guidance for this patient group |
| Marques-Baptista 2010,281 retrospective review, USA | Transports, n = 112 | Time/responding with lights and sirens | Time difference of transport with vs. without lights and sirens was –2.62 minutes (95% CI –2.60 to –2.63 minutes). 4.5% (5/112) of patients received time-critical hospital interventions. No patient received time-critical interventions within the time saved by using lights and sirens | Lights and sirens may save time |
| Taylor et al. 2010,183 retrospective review, Australia | N/A | Transfer/air medical transport utilisation | Cost and effectiveness of HEMS varied considerably between studies. A number of studies found HEMS to be cost-effective | A general assessment was not possible and further studies necessary in addressing economic and clinical evidence related to HEMS |
| Greenwood and Heninger 2010,103 case report, USA | n = 1 | Transfer/interhospital | Patient transferred to wrong destination. Driver failed to hear new destination | Individual communication failure |
| Singh et al. 2009,304 retrospective cohort study, USA | Patients > 18 years, n = 19,228 | Transfer/air medical | 5.1% of patients had critical events: haemodynamic deterioration (3.2%, n = 613), major resuscitative procedure (2.1%, n = 413) and death (0.1%, n = 12). First-attempt intubation 64.5% for oral and 75.0% for nasal intubations. Unintentional extubation in five cases | Critical events were mostly associated with pre-transport complications |
| Knapp et al. 2009,31 prospective observational study, USA | Adults with minor medical conditions, n = 93 (11 patients refused to participate) | Transfer/via taxi to further care | 10% (9/93) were admitted, no AEs resulting from transfer method | Use of taxis raised concern owing to potential underestimation of condition severity |
| Ursic et al. 2009,305 observational study, Australia | N = 1952; n = 962 pre- and n = 990 post-service operating | Pathways/direct admission to a trauma service | Significant reduction (p = 0.024) in death rate for severely injured patients (injury severity score of > 15). No difference in overall mortality or morbidity | Reduction in death rate for severely injured patients |
| McGrath et al. 2009,152 retrospective review, USA | Patients with STEMI, n = 32 | Time/reducing time to reperfusion | Correlation between patient stabilisation and total episode time | Areas to consider to reduce times are communication between referring agency and HEMS and stabilising patients for transfer |
| Meisel et al. 2009,172 retrospective review, USA | Patients arriving by ambulance, n = 14,505 | Transfer/utilisation of ambulances and insurance type | In the low acuity group, ambulance transfer was associated with private health insurance | Insurance type is associated with transfer to further care for general and low-acuity patients |
| Goldhill et al. 2009,220 consensus guideline, UK | N/A | Transfer/interfacility | Recommendations for transfers include assessment of necessity to transport, involvement of senior staff, standardisation of communication, competency of transfer staff, regular audit and review of transfer service | Transfer can be safely accomplished even in extremely ill patients |
| Frendl et al. 2009,71,284 consensus statement, USA | N/A | Time/reducing time to reperfusion | Pre-hospital 12-lead ECG can reduce time to reperfusion | A whole-system approach is required to improve service delivery |
| Moga and Harstall 2008,124 systematic review, Canada | Interfacility transport of patients for trauma, injury and medical reasons, n = N/A | Transfer/air medical transport utilisation and safety | Patients transported by helicopter showed a benefit in terms of survival, time to reach a health-care facility, time to definitive care and outcomes of treatment compared with ground transport | Overall, patients transported by helicopter showed survival benefit |
| Shah et al. 2008,131 RCT, UK | Surveys, n = 138 | Transport to PED | Only transport by EMS was found to be acceptable. PED more acceptable than primary care doctor, urgent care centre or no transport and physician appointment in 24 hours | EMS only mode of transport acceptable for parents of paediatric emergencies |
| Poitras et al. 2008,121 case–control study with historical comparison, Canada | STEMI patients transferred for PCI, N = 43: n = 21 from ED and n = 22 direct transport following ECG transmission | Time/ECG transmission to reduce time to reperfusion | The time to primary PCI was 111 minutes and reduced to 57 minutes after the introduction of ECG transmission and direct transfer. 100% of patients met door-to-balloon standard following ECG transmission and direct transfer compared with 28% before the initiative | ECG transmission and direct transfer can reduce the delay in receiving definitive treatment |
| Gratton et al. 2008,148 observational study, USA | 911 calls, N = 63,042: n = 5865 staged calls, n = 57,177 non-staged calls | Time/response times and staging ambulances at dangerous scenes | The response time was significantly longer when ambulances were staged (11.13 minutes compared with 5.55 minutes; p < 0.001) | Staging ambulances increases response times, which may affect patient outcomes especially in time-critical cases |
| Yeung et al. 2008,258 questionnaire survey, Hong Kong | Emergency nurses, n = 51 | Transfer/interfacility transport by registered nurses | Participants with more clinical experience demonstrated significantly better test scores. A total of 59% (30/51) encountered an AE en route | Emergency nurses in Hong Kong have good knowledge of interfacility transport |
| Seymour et al. 2008,192 retrospective review, USA | Patients receiving mechanical ventilation, n = 191 | Transfer/interfacility | No major AE occurred during flight | Major AEs are rare during interfacility rotary-wing transfer of critical ill, mechanically ventilated patients |
| Mariani et al. 2008,306 review, Italy | Transfers, n = 644 | Transfer/interhospital from spoke to hub hospitals | Low number of incidents which were associated with pre-existing instabilities | Transfers from spoke to hub can be done easily safely, with a low incidence of adverse events, which are related to pre-existing signs of instability |
| Hoot et al. 2007,307 observational study, USA | Observations, n = 7948 | Transfer/predicting ED crowding and ambulance diversion | ED was on ambulance diversion 30% of the time | There is a paucity of evidence regarding ambulance diversion |
| Khaleghi et al. 2007,168 observational study, USA | Hospitals, n = 5 | Time/bypass | The number of hours on bypass were pre-trial 112.2, during the trial 0.3, and post-trial 47 | Minor effect on the number of patients in EDs |
| Belway et al. 2006,235 systematic review, Canada | Critically ill adults or children n = N/A | Transfer/specialist transport personnel | Six studies found and one demonstrated improved outcome | Little evidence that having specialist transport personnel improved outcome |
| Pham et al. 2006,160 systematic review, N/A | N/A | Transfer/ambulance diversion | Ambulance diversion is frequent and occurrence is increasing. Ambulance diversion is more likely on Monday mid-afternoon and early evening, during influenza infection periods and when the hospital is at capacity | There is a paucity of evidence concerning ambulance diversion |
| Vilke et al. 2006,170 before-and-after study, USA | N/A | Transfer/voluntary diversion guidelines | 3-year follow-up with comparison of 12-month period 2001–2 with 2004–5: ambulance journeys increased by 10,657 runs; bypass hours decreased by 32,328 hours; patients with hospital requests that were bypassed decreased by 13,721 | A community-wide approach to reduce ambulance diversion is sustainable |
| Thomas et al. 2006,182 questionnaire, USA | Flight nurses, n = 10 | Transfer/cognitive performance of staff | Cognitive function does not differ between 12- and 18-hour shift as long as adequate daily sleep is maintained | Further research required |
| MacDonald et al. 2006,301 literature review, Canada | Intubated and mechanically ventilated adult patients, n = 245 | Transfer/AE and important prognostic factors associated with interfacility transport of intubated and mechanically ventilated adult patients | Most common indication for transport was a need for investigations and/or specialist care. Insufficient data exist to draw firm conclusions regarding the mortality, morbidity or risk factors associated with the interfacility transport of intubated and mechanically ventilated adult patients | Further study is required to define the risks and benefits of interfacility transfer in this patient population |
| Flabouris et al. 2006,15 review, Australia | Doctors and paramedics using air and road transport, four organisations contributed reports, n = 125, documenting 272 incidents | Transfer/retrieval incident register | 91% of incidents were considered preventable. 59% of incidents led to harm including one death | A quality improvement tool |
| Lerner 2006,72 literature review, USA | N/A | Transfer/American College of Surgeons field triage guidelines | There is insufficient evidence to support the overall American College of Surgeons field triage criteria. However, the physiological and anatomical steps had the best evidence to support them | More evidence required for American College of Surgeons field triage criteria |
| van ‘t Hof et al. 2005,140 randomised controlled study, the Netherlands | Patients > 80 years with chest pain for > 30 minutes with signs of ST elevation; N = 467: direct transfer, n = 209; referral via non-PCI centre, n = 258 | Transfer/direct transfer to PCI compared with transfer via non-PCI centre. On-TIME study | Significantly faster time to treatment of 177 minutes compared with 208 minutes (p < 0.01); significantly higher initial patency rate, 44% compared with 35% (p < 0.045); significantly better reperfusion (myocardial blush grade 3), 59% compared with 47% (p < 0.02) | Direct transfer to PCI centre was associated with a shorter time to treatment and improved angiographic and clinical outcome |
| Al Darrab et al. 2005,165 before-and-after study, Canada | N/A | Transfer/ambulance bypass guidelines | Pre-intervention monthly ambulance transports, 1454 (95% CI 1333 to 1575); post-intervention, 1643 (95% CI 1552 to 1735); combined monthly bypass hours decreased from 189.5 hours (95% CI 134.9 hours to 244.1 hours) to 5 hours (95% CI 3.1 hours to 6.9 hours) | Guidelines were effective at reducing ambulance bypass hours |
| Vilke et al. 2004,118 observational study, USA | Patients transported in an advanced life support ambulance, n = 235,766 | Transfer/ambulance diversion guidelines | There was a significant decrease in ambulance diversion during the study period from 1320 pre-trial to 322 during the trial | Community approach reduced ambulance diversion and increased likelihood of transfer to the requested hospital |
| Larson et al. 2004,149 retrospective review, USA | Trauma patients < 19 years, direct transfer, n = 379 intermediate stabilisation, n = 842 | Transfer/direct transfer to trauma centre compared with transfer after intermediate facility stabilisation | Mortality was significantly lower for patients with major trauma transferred after stabilisation (5.5% compared with 8.7%; p < 0.05) | Stabilisation prior to transfer may improve survival |
| Redd and Bair 2003,52 retrospective review, USA | N/A | Transfer/diversion policy | Pre-diversion compared with diversion period: 428% increase in ED closure hours; 32% reduction in ambulance runs | Diversions have implications for training and patient care |
| Schull et al. 2003,308 retrospective review, Canada | Patients with chest pain, N = 3609: n = 1547 low overcrowding, n = 2062 high overcrowding in ED | Transfer/ambulance diversion and pre-hospital delay | Transport interval significantly increased by 28%, 13.4 minutes vs. 17.2 minutes (p < 0.001) | ED overcrowding is associated with pre-hospital delay |
| Lee et al. 2002,174 observational study, Singapore | Transfers from nursing homes, n = 201 | Transfer/utilisation of ambulances | 35% by public ambulances, 36% by private ambulances, 27% by nursing home ambulance and 1.5% by relative | Inappropriate utilisation of public ambulances |
| Steele 2002,169 prospective review, USA | Episodes of ambulance diversion, n = 1845 | Transfer/ambulance diversion | For 744 days during the 881-day study period (29 months), at least one of three EDs was on diversion and for 440 days, all three were on diversion. Average time on ambulance diversion was 6.8 hours per day | Ambulance diversion occurs regularly and reflects high ED demand |
| Ruger et al. 2002,173 retrospective review, USA | Patients arriving at ED in 1 year, n = 58,277 | Transfer/utilisation of ambulances | 72% of patients categorised as resuscitation/emergency were EMS transported and 31% provided own transport. 0.2% of EMS transports were for patients with sore throat | Inappropriate utilisation of ambulances is a patient safety issue |
| Anonymous 2002,153 case report, USA | Infant (10 months) with febrile seizure, n = 1 | Time/delay | Ambulance lost en route, delay resulted in brain damage | Training issue |
| Ho and Lindquist 2001,283 prospective observational study, USA | Ambulance service runs, n = 67 | Transfer/lights and sirens | On average, 3.63 minutes were saved when lights and sirens were used | Lights and sirens may save time |
| Caulkins 2001,178 retrospective review, USA | Paramedics on 8-, 12- and 16-hour shifts, n = 600; patients, n = 2806 | Transfer/staff attitude | There was no significant difference between the last hour and the rest of the shift | No effect of admittance patterns and end of shift |
| Gatsoulis et al. 2000,243 retrospective review, Greece | Pre-hospital deaths, n = 46 | Transfer/preventable pre-hospital trauma deaths | 21 deaths were registered at the scene, 19 occurred during transportation, three in casualty, two in theatre, and one in the computerised tomography scanner. 21 deaths could not have been prevented, 20 could possibly have been prevented and five could definitely have been prevented. 41% (19/46) were due to head injury and 59% (27/46) to other causes; of these, 52% (24/46) were due to haemorrhagic shock, when pre-hospital care was delayed. Six deaths at the scene resulted from head injuries, four from heart and lung rupture and one from carotid rupture; 22 of the non-instantaneous deaths were due to haemorrhagic shock and three to head injury. The average time from the scene to hospital was 60 minutes (range 20–160 minutes). Pre-hospital providers did not have advanced skills | A two-track strategy is needed to reduce the occurrence of preventable death, based on pre-hospital care and prevention |
| Braithwaite 2000,309 review, UK | N/A | Transfer/neonatal | Incubators amplify low-frequency sounds, with sound levels in a potentially hazardous range; noise and vibration can be reduced; siren and light effectiveness is poor but increases noise. Securing incubators requires ‘improvisation’; incubators are too heavy for fittings and can be torn free in an accident | Traditional ambulance design does not consider the neonatal transport needs |
| Heightman 2000,218 case study, USA | N/A | Transfer/to the ambulance | During transfer to the ambulance the patient became combative | Advised by manager to let go of stretchers, etc., if the patient was combative even if subsequently injured |
| Selevan et al. 1999,310 observational study using matched pairs, USA | Patients hospitalised for chest pain or related complaints, N = 6596: transferred, n = 3298; direct admission, n = 3298 | Transfer/diversion | No significant difference in in-hospital death rate. Significant difference in length of stay, intensive care length of stay and care in another facility for some centres | Benefit for some conditions |
| Brown et al. 1999,272 observational study, USA (related 2000)311 | Ambulance responses with lights and sirens, n = 32 | Time/responding with lights and sirens | Significantly faster response times for journeys with lights and sirens | Clinically relevant in a few cases |
| Kost and Arruda 1999,73 retrospective chart analysis, USA | Children transported by ambulance, n = N/A | Transfer/utilisation of ambulances in patients presenting to a PED, regarding both medical necessity and insurance status (aged 2 weeks to 19 years) | Medicaid patients are significantly more likely to use ambulance transportation. They also account for 60% of the unnecessary transports | Inappropriate use of ambulance transportation is common in this paediatric population |
| Eckstein et al. 1999,171 retrospective review, USA | Air ambulance-transported patients ≤ 18 years, n = 260 | Transfer/air medical transport utilisation | 175 reports available: 18% (32/175) of patients were admitted to intensive care; 4% (7/175) were taken to an operating room; 33% (57/175) were discharged home from the ED. Injury Severity Score (n = 146): 84% (122/146) of patients scored 0–15; 14% (21/146) scored 16–30; 2% (3/146) scored > 30 | Paediatric patients are overtriaged for air ambulance transport |
| Ruckoldt et al. 1998,214 randomised prospective study, Germany | Patients requiring ventilation for secondary interhospital transfer, n = 24 | Transfer/additional monitoring with pulse oximetry and capnometry | Complications during transport: 71.4% (30/42) pre-hospital; 63.3% (19/30) during transport with additional monitoring. Additional monitoring identified: hypoventilation, 33% (3/9); partial tube displacement, 22% (2/9); tube disconnection, 11% (1/9 detected immediately). Without additional monitoring: tube displacement was detected at destination, 22% (2/9); complications were detected during transport, 11% (1/9) | Additional monitoring allowed early and reliable detection of potentially life-threatening events during transport of ventilated patients |
| Ho and Casey 1998,279 prospective observational study, USA | Ambulance runs, n = 64 | Time/responding with lights and sirens | Time saved using lights and sirens was, on average, 3.02 minutes | Lights and sirens may save time |
| Snooks et al. 1996,216 mixed methods: retrospective analysis of cases combined and literature analyses, UK | Patients transported by air or ground, n = N/A | Transfer/air medical transport utilisation, cost and benefits | There were no improvements in response times and the time on scene was longer for helicopter-attended patients. Survival of trauma or cardiac patients was not improved, nor was an improvement in the general health status or aspects of daily living in helicopter-attended patients | Results suggest that HEMSs are costly, health benefits are small and there exist only limited circumstances to improve it in England and Wales |
| Van Wijngaarden et al. 1996,151 retrospective review, Canada | Trauma patients, n = 97 | Transfer/air medical transport utilisation | The majority of transfers warranted air ambulance and only 5% were overtriaged | There may be concerns that the undertriage rate is too high |
| Hunt et al. 1995,280 observational study, USA | Transports using lights and sirens, n = 50; simulated transports using no lights and siren, n = 50 | Time/responding with lights and sirens | Transports with lights and sirens were on average 43.5 seconds faster than transports without | Lights and sirens may save time |
| Lavis et al. 1995,18 case study, UK | Patient in clinical trial with blunt trauma, n = 1 | Transfer/pre-hospital triage | Patient initially transferred to GP unit with a Revised Trauma Score of 11/12; transferred to district general hospital 128 minutes post accident in cardiac arrest. Laparotomy 25 minutes after arrival; patient died during surgery owing to torn portal vein | Need for care pathways to be developed by ambulance service for appropriate transfer |
| Barry and Raiston 1994,154 observational study, UK | Children admitted to intensive care unit after transfer, n = 56 | Transfer/interhospital by land ambulance | Most transfers were complicated by AEs. No deaths during transfer | AEs may occur in critical care transfer |
| Sagawa et al. 1994,53 observational study, Japan | Cardiac patients transferred for non-invasive examination, n = 10; healthy volunteer, n = 1 | Transfer/stress during transfer | Increased stress on outward journey | Stress during transfers may adversely affect a patient’s condition |
| Madar and Milligan 1994,157 case study/audit, UK | Infants requiring transfer in incubators | Transfer/neonatal safety and security | Road traffic collision led to the incubator being torn from its mountings and the infant thrown out. Audit led to more secure mountings | No evaluation of the initiative |
| Stohler et al. 1991,37 retrospective audit, USA | Patients transported to further care, n = 327 | Transfer/air medical transport utilisation | 90.8% (297/327) of transfers were justified. Action plans were developed to reduce the occurrence of non-justified air transfer | Resulted in a decrease in the number of non-justified air transfers |
| Low et al. 1988,312 review, USA | Obstetric patients, n = 357 | Transfer to further care by air ambulance | Air transfers were significantly longer (p < 0.05). One in-flight delivery | Safe to transfer obstetric patients using HEMS |
| Bleiler 1982,159 case study, USA | Patient with cardiovascular disease, n = 1 | Transfer to home state | Patient died during transfer | Air taxis must provide basic medical care and have an attendant in addition to the pilot |
Some studies have explored the clinical effectiveness of transmitting the patient’s data during transfer to identify the destination for optimal treatment. Although one study evaluated the effect of transmitting video data,56 most considered the effect of transmitting an electrocardiogram (ECG) on reducing the delay in receiving definitive treatment and its effect on patient outcome. These studies strongly suggested that ECG transmission could reduce time to reperfusion by alerting cardiac centres or facilitate redirection of the ambulance to a cardiac centre. However, these were mostly carried out before paramedics were trained to read ECGs and may now have been superseded. Larger studies of telemedicine have also cast doubt on the clinical advantages of such technologies, although the benefits of pre-alerting may reduce time to treatment. The increasing availability of wireless technology and more bandwidth promises new ways for ambulance staff to both send patient data and receive information that can help in their management. 313
A number of the studies considered the equipment and staff required for safe transfer of adults and children to health-care facilities. This research has highlighted the importance of training team members for safe patient transfer. This has been incorporated into best practice guidance and so is believed to be normal practice. Consideration of the safety of transporting infants and children314 has been the subject of little research; those reports that are available stress the importance of securing incubators and children, although there are few data concerning this type of incident.
A number of studies addressed the effects of ambulance diversion. Studies have shown that this is a regular occurrence, although less so in the UK than in other countries, and reflects emergency departments (EDs) overcrowding especially at times known to be busy (Monday afternoons, during the winter or flu outbreaks and when the hospital is at, or nearly at, capacity). Use of guidelines has been shown to reduce ambulance diversion at such times. Although ambulance diversion is associated with increased length of time to definitive care, Pham et al. 160 suggests there is a paucity of evidence on other outcomes. Some studies have also looked at delays in admitting patients on arrival at the ED;273,308 Cooney et al. 273 suggest that off-load delay is a significant risk to patient safety.
One study148 reported on ambulance staging during a major incident, while other emergency services made the scene safe. Although staging significantly increased response time, it is difficult to see how it could be eliminated.
There is some research considering the potential benefits of using sirens and lights on reducing transfer time, while addressing the risk of ambulance staff being distracted by the noise. There is some research on the use of noise-attenuating headwear.
Assessment and management, including diagnosis, treatment, medication, skills and training
Since the introduction of resuscitation procedures in the 1970s, the development of paramedics as autonomous practitioners, and medical input such as that from the British Association for Immediate Care, the skill set of pre-hospital practitioners and the treatments provided has increased. Outcomes for patients have improved for conditions such as cardiac arrest, myocardial infarction and stroke. The largest volume of literature, with 139 papers identified, considers assessment and treatment, especially those directed towards cardiac conditions (Table 3). Guidelines with the supporting evidence for the safety and efficacy of pre-hospital resuscitation have been developed by the International Liaison Committee on Resuscitation and readers are directed to www.ilcor.org or www.resus.org.uk.
| Author(s), year, study design, country | Population, patient number | Intervention/process or topic | Results | Headline |
|---|---|---|---|---|
| McDermott et al. 2012,193 RCT, Ireland | Advanced paramedic trainees, n = 18 | Medication/intranasal medication vs. intravenous medication by advanced paramedic trainees | Study demonstrated that, among advanced paramedic trainees, the IN route of medication administration is significantly faster, better accepted and perceived to be safer than using the i.v. route | Study underlines that IN medication administration could be considered more frequently when administering emergency medications in a pre-hospital setting |
| Putzer et al. 2013,315 randomised, crossover study, Austria | Advanced life support certified paramedics, n = 25 | Treatment/comparing mechanical chest compression device (LUCAS™; Physio-Control Inc., Lund, Sweden) and manual chest compressions in a simulated CPR scenario during helicopter rescue | LUCAS performed correctly more often than in tthe manual group | Further clinical trials are warranted to confirm the potential benefits offered by LUCAS CPR in helicopter rescue |
| National Prescribing Centre 2012,95 scoping exercise (focus groups and interviews), UK | Front-line practitioners, controlled drug accountable officers; senior advisors from national agencies, n = N/A | Medication/management of controlled drugs | Nine recommendations. Operational personnel may not have a good understanding of legislation relating to management of controlled drugs. Gaps in legislation can lead to potential problems | Controlled drug accountable officers must ensure that robust standard operating procedures are in place in line with legislation and work with regulators, local intelligence networks and police |
| Breckwoldt et al. 2012,236 prospective observational study, Germany | Proficient (physicians ≥ 5 years’ experience), n = 10; experts (anaesthetists ≥ 5 years’ experience), n = 9 | Treatment/endotracheal intubation | ETI experience differed between groups, expert status was associated with fewer incidents of ‘difficult ETI’ and a higher proportion of ETI decisions | The study describes expert behaviour on an empirical basis; ‘expert’ emergency physicians were more likely to choose endotracheal intubation than ‘proficient performers’ and made more use of technical and pharmacological facilitation |
| Kahveci et al. 2012,86 observational study, Turkey | Patients, n = 731 | Assessment/triage decisions by paramedics and emergency residents | Agreement between the triage decisions made by paramedics and by emergency residents was 47% (3L triage scale) and 45% (5L triage scale) | Triaging is commonly performed by nurses in the American emergency system and triage by paramedics is not common |
| Leblanc et al. 2012,300 simulated study, Canada | Advanced care paramedics, n = 22 | Skills/paramedics’ ability to care for patients during stressful events | More errors of commission in the patient care documentation following high-stress scenarios | Results highlight the importance of developing systems and training interventions aimed at supporting and preparing emergency workers who face acute stressors as part of their everyday work |
| Eastwood et al. 2013,288 survey, Australia | Paramedic students, n = 176 | Medication/drug calculation | 52% response rate. Nearly 24% of questions were answered incorrectly, with just over 36.6% not attempted at all. There were 48.5% conceptual errors, 31.1% arithmetical errors and 17.4% computational errors | This study revealed that many undergraduate paramedic students were not capable of performing basic mathematical calculations, even in a non-stressful classroom situation |
| Price et al. 2012,230 survey, Australia | AEs recalled by paramedics, n = 370 | Diagnosis/contributing factors to AEs | Identifying the deterioration was the number one contributing factor to AEs | Patient assessment during transfer is important to identify deterioration |
| Kupas et al. 2012,176 retrospective review, USA | EMS agencies, n = 9 | Medication/carrying and storing medications that have the potential for causing a medication administration error or patient harm | 38 medication safety issues identified: 16 were considered to be high risk, 14 moderate risk and eight low risk for patient harm. All related to medications carried by the EMS. Reviewing medication stored at EMS stations, eight safety issues were identified (five moderate and three low risk) | Understanding medical safety issues may assist EMS agencies in reducing the potential for a medication error and of patient harm |
| Drew et al. 2011,277 RCT, USA | Patients ≥ 30 years old with chest/anginal pain calling 911, N = 794: intervention group ECG transmission to ED and alarm, n = 403; control group usual care, ECG on arrival, n = 391 | Management/ECG monitoring and transmission to reduce treatment times in acute coronary services | Significant decrease of 59 minutes in time to first ECG for the intervention group (p < 0.0001); significant increase of 2 minutes on-scene time for intervention group (p < 0.001). No significant difference in door-to-balloon time or patients with STEMI undergoing reperfusion within 90 minutes | ECG transmission reduces time to treatment |
| Thomas et al. 2011,287 before-and-after study, USA | Transport nurses, n = 12 | Training/complex airway management | Training improved first-attempt intubations significantly from 19% to 36% 1 month after training, but not 1 year after training | Benefit for training, but rapid skill deterioration |
| Weiss et al. 2012,35 before-and-after study, USA | Subjects restrained by EMS personnel, n = 618 | Management/CR, protocol – midazolam (Hypnovel®, Roche) | Pre-CR group: 43% experienced decreased agitation; post-CR group: 49% experienced decreased agitation. Subjects receiving midazolam experienced a significantly greater decrease in agitation score (–17 ± 21 vs. –7 ± 17) [measured on a validated agitation behaviour scale with a parametric (Rasch) adjustment] than those without CR | CR seems safe and effective and could improve the management of severely agitated patients |
| Harris et al. 2011,245 prospective observational study, UK | Intubations, n = 481 | Skills/tracheal intubation | Rates of successful tracheal intubation were first attempt, 87.5%; first and second attempt, 98.8%; third attempt, 99.8% | Intubation attempt success rates were affected by specialty and the length of anaesthetic training |
| Palazzo et al. 2011,259 prospective observational study, USA | Patients undergoing airway management by helicopter EMS, n = 619 | Skills/endotracheal intubation | Intubation success rate of first provider: first attempt, 70.7%; second attempt, 60.3%; third attempt, 40%. Second provider success was not affected by failed attempts by the first provider. Success rate was not associated with bougie use, type of transport (scene or interhospital) or patient age. Provider experience was associated with a higher success rate | Provider experience is associated with first intubation success rate |
| Jensen et al. 2011,46 Delphi study, Canada (related 2010)294 | Advanced care paramedics, n = 17; medical directors, n = 7 | Assessment/clinical decision-making for high-acuity calls | 42 decisions in six categories: airway management, assessment, cardiac management, drug administration, scene management and general treatment. Significant differences between paramedics and medical directors occurred for 12% (5/42) of decisions (p < 0.05) | Consensus was seen for most clinical decisions, with most agreement for assessment |
| Hussmann et al. 2011,36 retrospective review, Germany | Trauma patients: intubated, n = 600; non-intubated, n = 600 | Treatment/pre-hospital intubation | Significant increase in rescue time for intubated patients 82.3 minutes compared with 64.8 minutes (p < 0.001) | Pre-hospital intubation is associated with risk and should be carefully considered except in clear cases of post-traumatic apnoea |
| Chan et al. 2010,112 before-and-after study, Australia | Paramedics, N = 200: n = 100, pre-intervention; n = 100, post-intervention. Patients ≥ 18 years taking four or more medications | Training/importance of patients bringing their medicines to the ED to reduce medication errors | Significant increase (p < 0.001) in patients’ own medicines brought to ED. Resulted in a significant reduction in medication errors post intervention (p < 0.001) | Paramedics bringing patients’ own medicines to hospital can reduce prescribing errors on admission |
| Sulis et al. 2010,161 before-and-after study, USA | Standardised environmental targets, n = 5010 | Infection control/decontamination in critical care transport | Cleaning of targets improved from 12% to 78% (p < 0.00005). Significantly greater increase in equipment cleaning in ground ambulances between each transport vs. air ambulances (98% vs. 67%; p < 0.00005) | Causes of incomplete cleaning: joint cleaning by crew members, ineffective technique, completing patient-related tasks |
| Cushman et al. 2010,238 retrospective cohort study, USA | RSIs, n = 163 | Skills/effect of adding close concurrent and retrospective physician oversight | No significant increase in intubation success rate. Increase in appropriate patient selection | Physician oversight improved patient selection for RSI |
| Wang et al. 2010,267 retrospective review, USA | Pre-hospital clinicians, n = 4846; cardiac arrests, n = 21,753 | Skills/experience and intubation success | High success rate for clinicians with a high level of experience with cardiac arrests 1.48 (95% CI 1.15 to 1.89) and medical non-arrests 1.55 (95% CI 1.08 to 2.22). In trauma non-arrests success rate was not related to experience | Experience improves intubation success for some conditions |
| Matthews et al. 2010,92 audit, UK | Patients with major conditions, n = 443 | Treatment/administration of oxygen in line with British Thoracic Society’s recommendations | 86% of cases were treated in accordance with Joint Royal Colleges Ambulance Liaison Committee guidance in terms of receiving or not receiving oxygen and 73% were treated in full compliance (correct device and flow rate). A total of 8% of cases received oxygen inappropriately and 3% were denied oxygen inappropriately. Only 4 out of 14 cases with acute exacerbation of COPD had oxygen saturation < 88%, but 12 were given oxygen and 10 developed oxygen saturation > 92% | High rate of compliance with oxygen guidelines |
| Batchelder et al. 2009,286 prospective study, UK | Paramedic n = 6 and physicians n = 6 | Training/12-hour training course using simulation; pre-hospital anaesthesia | Mean time from arrival to tracheal tube cuff increased by > 3 minutes; number of safety-critical events fell in later simulations (median 1.0 vs. 3.5). Critical events included failure to both assess the airway and reassess before extending anaesthesia | Limited generalisability |
| Cobas et al. 2009,237 prospective observational study, USA | Adult trauma patients with emergency pre-hospital airway management, n = 203 | Treatment/endotracheal intubation | 203 patients (15%) received pre-hospital airway management: 69% (n = 140) were successfully intubated in the field | Failed endotracheal intubation was not significantly associated with hospital mortality |
| Davis et al. 2009,241 prospective observational study, USA | EMT, n = 22 | Training/self-injectable adrenaline | Baseline knowledge was significantly different from immediate after training and at 3-month follow-up | Poor knowledge of self-injectable adrenaline |
| Olasveengen et al. 2009,260 prospective observational study, Norway | Patients with on-traumatic out-of-hospital cardiac arrest, n = 1128 | Skills/physician-manned vs. paramedic-manned ambulances | Survival after out-of-hospital cardiac arrest was not different for patients treated in a physician-manned ambulance | Skill mix did not influence survival in cardiac arrest |
| Wang et al. 2009,255 prospective observational study, USA | Patients receiving out-of-hospital endotracheal intubation, n = 1954 | Treatment/endotracheal intubation | 1954 patients received endotracheal intubation: 22.7% (n = 444) experienced one or more errors. 73% of patients died, 27% survived to hospital discharge | Endotracheal intubation errors were not associated with early or later death |
| Siriwardena et al. 2009,184 before-and-after study, UK | Paramedics, N = 100: intervention group, n = 50; control group, n = 50 | Treatment/intervention to reduce unnecessary cannulation. Taught to team leaders to cascade | There was a non-significant reduction in inappropriate cannulation rates in the intervention area (95% CI 1.0% to 0.0%) compared with the control area (95% CI 2.5% to 2.6%), and a significant reduction in cannulation rates in the intervention area (95% CI 9.1% to 6.5%) compared with an increase in the control area (95% CI 13.8% to 19.1%). Paramedics in the intervention area were significantly more likely to use correct hand-washing techniques post intervention (95% CI 74.5% vs. 14.9%) | Intervention can lead to improvements in appropriate cannulation |
| Berg et al. 2009,316 observation study, USA | First responder, n = N/A | Training/video laryngoscopy to facilitate intubation in remote training programme | Remote training for intubation is feasible and comparable with face-to-face training | Video laryngoscopy can accelerate introduction of life-saving technologies |
| Cobas et al. 2009,237 observational study, USA | Trauma patients requiring pre-hospital airway assessment and management, n = 230 | Treatment/pre-hospital intubation | 31% (63/203) had failed intubation, 29% (18/63) survived to discharge, 39.6% (25/63) had unrecognised oesophageal intubation. No difference in mortality for those properly intubated and those not | High rate of failed intubation |
| Coleman et al. 2009,49 observational study, UK | Patient case notes, n = 480 | Skills/safety and quality of care by ECPs compared with nurse practitioners, GPs and community paramedics | Significantly higher scores for quality of care, assessment and record keeping for ECPs | Small differences unlikely to be clinically significant |
| Dixon et al. 2009,50 observational study, Ireland | Paramedics with basic life support certification, n = 19 | Training/use of bag valve mask, laryngeal mask airway and laryngeal tube airway | Correct ventilation: 15% with the bag valve mask, 19.2% with the laryngeal mask, and 23.5% with the laryngeal tube. Gastric ventilation: 9.7% with the bag valve mask, 15.8% with the laryngeal mask, 0.31% with the laryngeal tube | The laryngeal tube airway was most effective |
| Woollard et al. 2009,162 observational study, UK | Pre-hospital laryngoscopists, n = 65 | Treatment/use of bougies and malleable stylet in simulated pre-hospital intubations | Intubation success: 57% (37/65) with the malleable stylet; 9–34% (6–22/65) with bougies | Highest intubation success rate was with the malleable stylet |
| Dobson et al. 2009,134 retrospective study, Canada | Patients with heart failure, n = 94 | Diagnosis/heart failure and furosemide administration | Doctors confirmed 60/94 patients as having congestive heart failure. 63.8% agreement with paramedic administration of furosemide; 34/94 diagnosed with pneumonia (41.2%), acute coronary syndrome (23.5%) and COPD (20.6%) | Low rates of agreement for diagnosis |
| Jones et al. 2009,30 questionnaire, UK (related 2011)317 | Chief executives and medical directors of 13 UK ambulance service trusts and two voluntary ambulance service | Management/dressings | 27% of services had wound management policy in place. Methods used for haemostasis: pressure and elevation. Cleansing: sterile saline or water. 100% ambulance service used analgesics [Entonox®, (BOC) morphine, paracetamol or ibuprofen] Dressings: great variation |
No national standard in place for wound management |
| Mirarchi et al. 2009,33 survey, USA | EMTs and paramedics, n = 150 | Assessment/interpretation of living will and its impact on life-saving care | 90% of respondents determined the patient’s code status to be do not resuscitate and 92% defined their understanding of do not resuscitate as comfort care/end-of-life care. In clinical situations, do not resuscitate classification resulted in a lack or delay in life-saving intervention | Incorporating a code status into the living will produced statistically significant increases in the provision of life-saving care |
| Eastwood et al. 2009,194 literature review, Australia | Paramedics, n = N/A | Medication/paramedics’ ability to perform drug calculation | Only three small studies identified. Studies indicate a significant lack of mathematical proficiency among the paramedics sampled | Further studies are needed |
| Boyle 2009,90 retrospective review, Australia | CCRTF reports, n = 6 | Treatment/pre-hospital errors of preventable deaths of road traffic fatalities | The number of preventable deaths increased from 1999 onwards coinciding with introduction of the state trauma system and ALS for paramedics | Multiple factors led to failure: inadequate facilities/personnel, non-adherence to guidelines/standards/management plans, misinterpretation, lack of clinical examination or diagnostic procedure |
| Cooper and Grant 2009,197 review, Australia | N/A | Skills/activity and impact of new and emerging out-of-hospital emergency care roles | ECP and paramedic practitioner have an impact on patient care: average reduction in conveyance rate of 25%, improved interprofessional working, immediacy of treatment and referral and high patient satisfaction | New roles increase non-conveyance rate |
| Frendl et al. 2009,71 retrospective review of records, USA | Patients with suspected stroke/TIA, n = 154 | Training/Cincinnati Pre-hospital Strike Scale for accurate stroke identification | Paramedic training in the Cincinnati Pre-hospital Strike Scale, or its use, had no impact on the accuracy of their identification of patients with stroke/TIA or on-scene time | Limited impact of training |
| Howerton and Watson 2010,248 retrospective review, USA | Intubations, n = 913 | Skills/length of time on duty and intubation success | Increasing success of intubation to the 10th hour on duty followed by a decline | Observation only, further research needed |
| Bernius et al, 2008,187 prospective experimental study, USA | Pre-hospital care providers, N = 523: unaided n = 277, aided n = 246 | Medication/calculate medication doses/endotracheal tube size | 33% incorrect in the unaided vs. 6.6% in the aided group | Large proportion of incorrect calculations with the calculation aid |
| Lobel et al. 2008,318 observational study, USA | Patients requiring airway management, N = 775: pre-etomidate use, n = 255; post-etomidate use, n = 520 | Treatment/etomidate-facilitated intubation | Mixed findings for the effectiveness of etomidate | Further evidence required |
| Warner et al 2008,254 retrospective review, USA | Advance life support calls, n = 20,330 | Treatment/needle thoracostomy | 39 patients (0.2%) had at least one nasopharyngeal tube placed for suspected tension pneumothorax. 22 patients (56.4%) were in circulatory arrest with 12 suffering traumatic arrest and 10 non-traumatic pulseless electrical activity arrest; the remaining 17 were non-arrest cases, 16 with traumatic injury and one with a spontaneous tension pneumothorax. Blunt trauma predominated (48.7%) in both arrest and non-arrest groups | Identified as a safe protocol for the correct placement of nasopharyngeal tubes, including a medical control system allowing for physician input for patients not in arrest |
| Hein et al. 2008,246 prospective audit, Australia | Paramedical staff attempting insertion of a laryngeal mask airway n = 179, patients n = 164 | Treatment/audit of laryngeal mask airway use | 74% insertions were successful, 45% of first attempts were successful, 20% of second attempts were successful and 9% needed three or more attempts | Reported failures were ascribed to patient anatomy (n = 13), technique (n = 9), airway soiling (n = 7), the device (n = 6), trismus (n = 1), high GCS score (n = 1), trauma (n = 1) or unknown reasons (n = 5) |
| Lecky et al. 2008,141 retrospective review, UK | N/A | Treatment/emergency intubation | Results indicate no differences in survival or neurological outcome between paramedic intubation vs. bag–valve–mask ventilation and after hospital intubation by emergency physicians | The efficacy of emergency intubation as currently practised has not been rigorously studied |
| Iqbal et al. 2009,319 before-and-after study, UK | Paramedics, N = 100: intervention group, n = 50; control group, n = 50 | Training/cannulation | A significant reduction in cannulation rates was achieved in the intervention group (9.1% to 6.5%) compared with an increase in cannulation rates in the control group of 13.1% to 19.1% | The intervention can lead to improvements in appropriate cannulation |
| Williams et al. 2007,81 prospective single-blinded observational pilot study, Australia | Students, n = 32 | Skill/assessing undergraduate paramedic student ability to accurately identify the J point and ST segments on ECGs | In most cases, they were able to recognise ST segment elevation; however, definition of the amount of ST segment elevation varied greatly and one-quarter of students did not complete all four J point estimations | Study identified significant variation in students’ interpretation of J point and ST segment in ECG analyses |
| Armstrong et al. 2007,89 prospective observational study, UK | Paramedics and technicians, n = 17; patients, n = 103 | Training/cervical spine clearance | 67% (69/103) patients underwent cervical spine clearance; 87.0% (60/69) were discharged at scene; and 33% (34/103) could not have their cervical spine cleared safely at scene | Cervical spine clearance by trained paramedics on scene may have positive impact on patient care |
| Parwani et al. 2007,251 prospective observational study, USA | Licensed practising paramedics, n = 53; patients undergoing emergency intubation, n = 2853 | Skill/ability to inflate the cuff of an endotracheal tube to a safe pressure | 66% inflated cuff to a pressure greater than the manometer upper limit; 13% were able to identify an overinflated cuff by palpation | Paramedics are poor at inflating endotracheal tube cuffs to a safe pressure and estimating safe pressures |
| Wirtz et al, 2007,257 prospective observational study, USA | Critically ill patients, n = 192 | Skills/intubation in the field or < 10 minutes after admission | 9% (n = 12) of pre-hospital intubations were misplaced; five patients survived to discharge | Misplaced ET tubes affect survival |
| Kerry et al. 2007,113 before-and-after study, UK | COPD patients, n = 100 | Management/impact of lung alert cards | 73/100 patient’s hospital medical notes were available: the incidence of type 2 respiratory failure decreased from 31% to 17%; the need for non-invasive ventilation decreased from 27% to 14%; length of stay decreased by 1 day | Some evidence for the benefits of alert cards in patients with COPD |
| Yaghoubian et al. 2007,320 retrospective review, USA | Trauma patients with truncal injury and hypotension < 90 mmHg, n = 194 | Treatment/adherence to fluid therapy guidelines | 25% (49/194) received < 100 cc of i.v. fluids. Patients receiving > 100 cc had a significantly lower mortality rate than those receiving < 100 cc (21% and 35% respectively; p = 0.04); after adjusting for trauma severity, there were no significant differences in survival related to pre-hospital fluid administration | Fluid therapy guidelines may not be adhered to |
| Vilke et al. 2007,321 survey, USA | Paramedics, n = 32 | Medication/errors | Response rate 83%: 21% of errors occurred during paediatric response calls, with 42% being dose related. Most errors occurred between hours 2 and 7 or 11 and 12 of the shift. 9.1% of paramedics reported making one error in the previous 12 months: 63% were dose related, 33% were protocol errors, 21% were use of the wrong administration route and 4% were use of the wrong medication. Reasons given were failure to check, unfamiliar medication, calculation error, over/under dose | The shift hour may affect AEs |
| Acker et al. 2007,222 consensus, USA | N/A | Management/stroke guidelines | Appropriate processes are needed for dispatch for rapid access to EMS. EMS responders should receive training, protocols and tools that meet ASA/AHA guidelines. Collaboration in the development of EMS training, assessment, treatment and transport protocols. Patients should be transported to the nearest stroke centre | Training and updates for dispatch personnel |
| Wang et al. 2006,256 prospective observational study, USA | Study of rescuers from 42 advanced life support EMS services reporting information on patient encounters | Treatment/endotracheal intubation errors and their associations with patient and EMS system characteristics | Errors were most pronounced for patients < 6 years, non-arrest patients and trauma patients and were less likely for patients receiving neuromuscular blocking agents; error rates were lower for EMS services performing more intubations annually but higher for services with more patient contacts | Endotracheal intubation success with experience |
| Garza et al. 2006,299 retrospective cohort study, USA | Patients with primary cardiac arrest, n = 557 | Treatment/pre-hospital intubation | Overall survival to discharge was 19%: 15% (68/454) of intubated patients survived to discharge and 37% (38/103) of non-intubated patients survived to discharge | Pre-hospital intubation of cardiac arrest patients was associated with higher mortality |
| Isaak 2006,58 retrospective cohort study, USA | Trauma patients, n = 261 | Assessment/GCS score as sole criterion for transport to trauma centre | 40% (104/261) of trauma patients met the need for trauma centre care. Using GCS score of ≤ 14, the sensitivity and specificity for trauma centre transport were 66% and 59%, respectively | GCS score of ≤ 14 in isolation lacks accuracy |
| Michael et al. 2006,47 retrospective cohort study, USA | Patients with isolated extremity injuries, n = 953 | Management/socioeconomic factors and analgesia in pre-hospital care | 29% (279/953) received morphine. Statistically significant effects for males, with benefits in terms of pain severity and time in pre-hospital care. No differences for age, income or ethnicity | Females are less likely to receive pre-hospital analgesia for an isolated extremity injury |
| Derr et al. 2006,225 retrospective review, USA | Patients with acute decompensated heart failure: treated with conventional therapy, n = 63; treated with continuous positive airway pressure, n = 65 | Treatment/continuous positive airway pressure | Continuous positive airway pressure improved oxygen saturation (15.2% vs. 11.9%), decreased respiratory rate (4.7 breaths/minute vs. 1.8 breaths/minute) and decreased mortality rate (13.8% vs. 17.5%) | Continuous positive airway pressure shows improved outcome for acute decompensated heart failure patients in the pre-hospital setting |
| Fakhry et al. 2006,242 review, USA | Trauma patients, n = 1117 | Treatment/RSI | 175/1117 trauma patients had attempted RSI; 169 patients had successful on-scene RSI with 70% of patients intubated at the first attempt, 89% at the second and 96% by the third. Complications included right mainstem intubation: 2.9%, and endotracheal tube being dislodged en route: 1.2% | Attempted RSI was associated with increased on-scene time |
| Shewakramani et al. 2006,322 retrospective review, USA | Burns patients transported by helicopter emergency medical service, n = 100 | Treatment/adequacy of fluid resuscitation following the Parkland formula | 52% (52/100) of patients received inadequate fluid resuscitation (< 50% or > 200%) | Patients received fluid volumes outside of those indicated by the Parkland formula |
| Wang et al. 2006,256 retrospective review, USA | Patients with severe traumatic brain injury; more than or equal to three on abbreviated injury scale, n = 4098 | Treatment/endotracheal intubation either in pre-hospital care or ED | Death rate higher for pre-hospital intubation and worse neurological and functional outcomes | Pre-hospital intubation was associated with higher mortality and worse outcome |
| Svilaas et al. 2005,138 cohort study, the Netherlands | Patients transferred to a catheterisation lab for PCI, n = 207; via protocol, n = 103; usual care, n = 104 | Management/Groningen STEMI protocol | Process mapping and development of the protocol led to a reduction in the distance travelled for the protocol group (43 km compared with 58 km). Faster time from symptom onset to balloon time in the protocol group (203 minutes compared with 251 minutes) | Faster time from symptom onset to balloon time and less travel |
| Febra and Lufinha 2005,298 retrospective cohort study, Portugal | Patients with transcutaneous external cardiac pacing, n = 46; with cardiac arrest, n = 20; with bradycardia, n = 26 | Treatment/transcutaneous external cardiac pacing | Transcutaneous external cardiac pacing resulted in 54% (25/46) haemodynamic stability; 15% (7/46) death; 30% (14/46) sustained shock; overall success rate (defined as hospital admission) was 65% | Transcutaneous external cardiac pacing was associated with better survival rates |
| Bair et al. 2005,265 prospective observational study, USA (related Smith and Bair, 2003323) | Patients with non-tracheal intubation arriving in the ED, n = 1643 | Skills/pre-hospital intubation | 2% (35/1643) patients had unrecognised, non-tracheal intubations; 49% (17/35) were potentially recognisable based on paramedic documentation of clinical findings. More frequent use of end-tidal carbon dioxide level or using multiple confirmation techniques may help to identify non-tracheal intubation | Recommendation for the use of end-tidal carbon dioxide monitoring |
| Price et al. 2005,85 prospective study, USA | Transported patients, n = 411 | Assessment/determining whether or not EMS personnel can use selective diversion and accurately predict which patients will require a critical care bed and which patients are unlikely to require admission to hospital | EMS provider predicted that 59.9% will be discharged, but the actual number was 61.6%. 23.3% will be admitted to a floor bed and 16.8% to a critical care bed, but the actual numbers were 24.1% and 9.95%, respectively | EMS providers appear to be capable of using selective diversion categories |
| Sukumaran et al. 2005,232 prospective observational study, UK | Trauma patients, n = 21,417 | Skills/triage by paramedics and technicians to a resuscitation area | Paramedics attended more severely injured patients, had longer pre-hospital times and patients treated by paramedics were taken more often to intensive care unit, operating theatre or mortuary | Paramedics manage more severely injured patients |
| Firanescu et al. 2005,14 observational study, the Netherlands | Patients requiring thrombolysis, n = 151 | Treatment/the outcome of pre-hospital thrombolysis including time delay, percentage reperfusion, reocclusion, stroke, death, need for PCI and the number of protocol violations | Ambulance paramedic diagnosis was made in 8 ± 6 minutes, with thrombolysis in 13 ± 7 minutes. In 2% of patients the thrombolytic agent was erroneously administered without complication; the median time from onset of symptoms to treatment was 112 ± 77 minutes; 5% of patients died in the first 30 days and 2% suffered intracerebral haemorrhage. Reperfusion was documented in 76% of patients, 18% reoccluded in the following 24 hours; 37% of patients required rescue/facilitated PCI; and after 3 months, 9% of patients had severely impaired left ventricular function | High level of rescue/facilitated PCI |
| Bultman et al. 2005,292 observational study, USA | Adults with shortness of breath, n = 467 | Treatment/CPAP | 47% (218/467) used CPAP and 53% (249/467) did not. Conventional treatment and CPAP offer similarly effective treatment by both medic and patient assessment | Some evidence for the use of CPAP |
| Winslow et al. 2005,28 observational study, USA | Patients with pre-hospital spinal immobilisation, n = 224 | Management/unnecessary pre-hospital spinal immobilisation | Immobilisation was correctly applied in 90% of cases: 68% (202/224) were justified by National Emergency X-Radiography Utilization Study criteria; 32% (72/224) were unnecessarily immobilised | Spinal immobilisation may be overused and exclusion criteria not exploited |
| Cameron et al. 2005,324 retrospective review, Australia | Patients with severe head injury GCS score of < 9, n = 455 | Treatment/intubation with sedation and without drugs and RSI | Patients intubated without drugs or with sedation were at an increased risk of mortality compared with patients receiving RSI | RSI intubation reduced mortality risk |
| Davis et al. 2005,240 retrospective review, USA | Trauma patients, n = 81 | Treatment/thoracostomy | 136 procedures (89 needle thoracostomy and 47 tube thoracostomy). Incidence of complications was low. Aeromedical crew selected patients appropriately to undergo needle thoracostomy or tube thoracostomy | Life-saving procedure with few complications |
| McDermott et al. 2005,136 retrospective audit, Australia | Fatal road traffic collision victims, n = 243 | Management/preventable deaths | 591 inadequacies were identified; 77% (187/243) were pre-hospital errors/inadequacies of which 67% (135/243) [sic] contributed to death | Lessons learnt can reduce errors |
| Rea et al. 2004,190 case–control study, USA | Patients treated by EMTs, n = 66: cases (treated with adrenaline), n = 22; controls, n = 44 | Treatment/adrenaline for treatment of anaphylaxis | Cases were more likely to report a history of anaphylaxis, upper airway symptoms and shortness of breath. Agreement of use/not use of adrenaline between EMT and physician: 86% (57/66) of events | EMTs can discriminate whether or not to use adrenaline |
| Barsuk et al. 2005,234 prospective non-randomised study, Israel | First-year doctors who attended a 2-day advanced trauma life support course in the previous year, n = 72: pre-intervention, n = 36, intervention, n = 36 | Management/enhanced advanced-trauma life support to evaluate pre-hospital trauma management | 56% (20/36) no cricoid pressure assessment; 52% (11/21) successful first attempt; 48% (10/21) poor chest drain management; 73% (11/15) no airway/breathing assessments as per head injury protocol | Incidence of common mistakes was lower in the intervention group. Simulation-based training advocated |
| Jones et al. 2004,247 prospective observational study, USA | Medical patients, n = 160; trauma patients, n = 48 | Skills/intubation | 208 out-of-hospital intubations by paramedics were assessed: 12 (5.8%) endotracheal tubes were incorrectly placed outside the trachea. This comprised 10/160 medical patients (6.3%) and 2/48 trauma patients (4.2%); of the 12 misplaced endotracheal tubes, a verification device was used in 25% of cases | High rates of misplaced ET tubes |
| Newgard et al. 2004,45 prospective observational study, USA | Children evaluated at a crash scene, n = 141; staff from 20 fire stations | Diagnosis/validation of clinical decision rule to identify severely injured children | Sensitivity 100% (95% CI 40% to 100%), specificity 73% (95% CI 65% to 80%) for severe injury; sensitivity 67% (95% CI 22% to 96%), specificity 73% (95% CI 64% to 80%) for specialised trauma care | Identified severely injured children; may prove more reliable than previous rules |
| Barton et al. 2004,262 retrospective observational study, USA | Patients undergoing emergency intubation, n = 2853 | Treatment/RSI | 68% (1944/2853) of intubations were performed using RSI and 32% (909/2853) used other methods. Success rate: RSI 93% (1807/1944); other methods 85% (777/909) | Air medical crews are more confident using RSI than other methods. RSI success rate is high |
| Domeier et al. 2004,263 before-and-after study, USA | Trauma patients with GCS score of 3 to 8 for whom resuscitation was indicated, n = 321 | Training/6-hour didactic and mannequin training for RSI | 85.1% survival for study RSI patients | EMS protocols for paramedic RSI improve intubation and survival |
| Vilke et al. 2004,43 before-and-after study, USA | Patients, N = 5562: pre-intervention, n = 2741; post-intervention, n = 2821 | Training/introduction of a treatment protocol and pain scale. Educational intervention | Patients were 18 times more likely to have a pain assessment performed in the field after the educational intervention (RR 18.11, 95% CI 10.61 to 30.93) | Increased analgesia administration and pain management awareness |
| Kryder et al. 2004,261 retrospective observational study, USA | Patients requiring emergency intubation, n = 386 | Treatment/endotracheal intubation | Intubation was attempted in 11% (42/386) of patients and was successful in 24% (10/42, 95% CI 11% to 37%). Factors associated with failure to attempt intubation were GCS score of ≥ 9 (OR 18.2, CI 6.5 to 29.9), failure to obtain intravenous access (OR 1.8, 95% CI 0.9 to 2.7) performing bag–valve–mask or positive-pressure ventilation (OR 50.4, 95% CI 12.8 to 88.0) | More training might be beneficial to improve out-of-hospital personnel intubation skills |
| Dadkhah et al. 1999,139 observational study, USA | Patients with suspected acute myocardial infarction, n = 247 | Diagnosis/point-of-care testing – Rapid Bedside Cardiac Markers and 12-lead ECG pre-hospital | 11.3% (28/247) of patients with acute myocardial infarction were identified pre-hospital; 3.6% (9/247) were missed, but all had initial non-diagnostic ECGs/Rapid Bedside Cardiac Markers but subsequent positive Rapid Bedside Cardiac Markers | Paramedics can identify patients with acute myocardial infarction using point-of-care testing |
| Barton et al. 2004,60 retrospective review, USA | Patients with oral intubation, n = 2853 | Treatment/laryngoscopic grading system | 2853 patients had a total of 3827 oral intubation attempts; 83% (3171/3827) had laryngoscopy grades recorded. Laryngoscopic grade significantly correlated with overall success and number of intubation attempts | Recording laryngoscopic grade can aid recognition of difficult airways |
| Goebel et al. 2004,17 retrospective review, USA | Patients aged ≥ 14 years treated with adenosine for paroxysmal supraventricular tachycardia, n = 224 | Diagnosis/paramedic rhythm misidentification | Misidentification rates of 9–31% | Inappropriate administration of adenosine in 20% of cases |
| McGlinch and Weller 2004,226 retrospective review, USA | Respiratory or haemodynamic problems and a GCS score of < 8, n = 71 | Treatment/rapid sequence intubation | 38% (27/71) of patients died of these, 8% (6/71) suffered cardiac arrest immediately following RSI. Of the 58 patients meeting the criteria for RSI but who subsequently were not intubated, 28% (15/58) [sic] died | RSI did not appear to improve patient outcomes |
| Martin et al. 2004,23 case report, USA | Patient, n = 1 | Treatment/intracranial insertion of a nasopharyngeal airway in a patient with craniofacial trauma | While intracranial insertion of a nasopharyngeal airway is rare, it is catastrophic. Oropharyngeal airways may be used but definitive securing with an endotracheal tube or, if necessary, a surgical airway is preferred | Intracranial insertion of a nasopharyngeal airway is catastrophic |
| Keeling et al. 2003,41 prospective study, UK | Analysis of data concerning diagnoses made by physicians and paramedics, paramedics’ hypothetical decisions to treat and event timings | Diagnosis/feasibility and safety of pre-hospital thrombolysis | Paramedic diagnosis sensitivity was 71% and specificity was 97% for 660 cases; the median call to potential needle time was 28 minutes and for STEMI the median time saved was 48 minutes. The < 60-minute call to needle time goal was met in 95% of cases and 22% of patients would have received thrombolysis within 60 minutes of symptom onset | Benefits demonstrated in this hypothetical study |
| Bledsoe 2003,25 case report, USA | Adult male trauma patient, n = 1 | Assessment | Incomplete physical examination led to overlooked open sucking wound | Thorough physical examination is essential if initial diagnosis does not match symptoms |
| Alldredge et al. 2001,296 RCT, USA | Patients aged ≥ 18 years, with a pre-hospital diagnosis of status epilepticus, N = 205: lorazepam, n = 66; diazepam, n = 68; placebo, n =71 | Medication/comparison of lorazepam and diazepam | Convulsions ceased in the ED for 59% of patients receiving lorazepam, 43% receiving diazepam and 21.1% receiving the placebo. OR indicated that termination of convulsion is more likely in patients receiving lorazepam than diazepam or placebo | Benzodiazepines are safe and effective when administered pre-hospital by paramedics in the management of status epilepticus. Results confirmed in a meta-analysis by Millikan et al., 2009325 |
| Bahner 2002,233 prospective observational study, USA | Paramedics and nurses, n = 6 | Training/1-day sonography training course: 4 hours on physics, FAST and image quality, 2 hours’ practical training | Scoring of image quality immediately after training was 31.3/40 (n = 72 images), and 5 months after training the average had improved to 29.5/40. Personnel more confident after training | Training improves confidence and skill retention |
| Birk et al. 2002,326 prospective observational study, Denmark | Ambulance technicians, n = 56; patients requiring transfer to further care, n = 5516 | Treatment/unnecessary interventions | Oxygen was administered to 47.7% (2630/5516) of patients, though 71% (1872/2630) had no indicators for administration. ECG was performed on 22.4% of patients (1237/5516), of whom 47.2% (584/1237) showed no symptoms or signs of compromised circulation | Indications for interventions were broad |
| Grmec et al. 2002,55 prospective observational study, Slovenia | Trauma patients ≥ 16 years, n = 286 | Diagnosis/Mainz Emergency Evaluation System and Revised Trauma Score | Outcome prediction was 79.6% with Mainz Emergency Evaluation System and 75.8% with Revised Trauma Score; no statistically significant difference between systems | Mainz Emergency Evaluation System can be used to predict outcome for trauma patients, both in isolation and in combination with other diseases |
| Lord and Parsell 2002,57 prospective observational study, Australia | Patients requiring ambulance transport, n = 262 | Management/visual analogue scale to measure pain | Mean reduction in pain score (20 mm is benchmark for clinically significant reduction) between initial assessment and hospital arrival: 18.2 ± 23.9 mm; 33% (86/262) received no analgesia with the difference in pain score in the non-analgesia group; 3.1 mm (95% CI –2.3 mm to 8.5 mm). Staff attitudes may affect pain management and use of pain scales | Oligoanalgesia is an issue |
| Kelly et al. 2002,83 retrospective sample analysis, Australia | Trauma deaths, n = 222 | Assessment/determining the most effective cut-off of TRISS-derived probability of survival | New cut-off level of TRISS-PS for trauma systems could identify 90% of avoidable deaths with 80% specificity | Further research required |
| Cameron et al. 2002,327 retrospective data review, Australia | N/A | Assessment/predictive model for triage | Physiology data are good predictors of likelihood of death and severe injury requiring intensive care | Further research required |
| Shaban et al. 2002,186 survey, Australia | Paramedics, n = 1258 | Training/infection control | 55% response rate. Knowledge of infection control (waste disposal, staff health, exposure and decontamination) was poor | Need for education about infection control in pre-hospital care |
| Davis et al. 2002,239 review, USA | N/A | Treatment/RSI | Recommendations: close medical direction; training and continuing education; patient monitoring, drug storage and delivery, and confirmation and continuous monitoring of tube placement; use of a standardised protocol; availability of back-up airway devices | Highlighted key points regarding RSI in the US system |
| Lefrancois and Dufour 2002,19 review, Canada | Patients, n = 133 | Treatment/oesophageal tracheal combitube (Combitube™, Kendall-Sheridan Corporation, Argyle, NY, USA) used by an emergency medical/defibrillation technician in cardiorespiratory arrest patients | In 95.4% of patients, the oesophageal tracheal combitube was placed successfully; ventilation was successful in 91.4% of patients. No oesophageal lesions or significant injury to airway structures were seen during autopsy | Immediate complications were not necessarily related to the device |
| Tindall 2002,56 case study, USA | Patient with chest pain, n = 1 | Diagnosis/telepresence | The medical director assessed the patient via video and vital signs data were transmitted from the scene. The medical director directed tests and order medications and monitored response. A diagnosis was made and the patient was transported directly for primary PCI | Diagnosis in the field led to faster treatment |
| Matera 2002,22 case report, USA | EMT, n = 1 | Diagnosis/wrong diagnosis on the basis of the dispatch call | The EMT had problems making a diagnosis because of information given in the dispatch call, as evidence at the event supported differential diagnoses | It is important to consider differential diagnoses based on patient symptoms |
| Hick et al. 2001,328 prospective observational study, USA | Combative patients, n = 53 | Medication/intramuscular droperidol (Xomolix®, ProStrakan) (2.5 mg to 5 mg) for the management of combative patients | Significant differences in agitation score pre- and post-administration; one patient required supplemental oxygen, but no other AEs reported; droperidol was ineffective in one patient | Intramuscular droperidol is safe and effective for use in sedating combative patients |
| Katz and Falk 2001,270 prospective observational study, USA | Patients requiring airway management, n = 108 | Skills/recognition of misplaced endotracheal tube by paramedics | 25% (27/108) had misplaced endotracheal tubes: 33% (9/27) had tubes in the hypopharynx; of these 33% (3/9) died; 67% (18/27) had tubes in the oesophagus; of these, 56% (10/18) died | The incidence of misplaced endotracheal tubes is high |
| Gilbert 2001,276 observational study, Norway | Patients receiving pre-hospital thrombolysis, n = 33 | Training/2-day training course for ambulance staff, community doctors and dispatch nurses | Good compliance with the protocol. 80% of patients receiving thrombolysis had acute myocardial infarction confirmed. Time was saved | Training increases compliance with the protocol |
| Brown and Thomas 2001,268 retrospective review, USA | N = 36: flight nurses, n = 34, paramedics, n = 2 | Treatment/blind nasal tracheal intubation in-hospital (n = 15) or pre-hospital (n = 21) | 48% (10/21) failure rate in pre-hospital compared with 7% (1/15) in-hospital | May indicate less on-scene practice of blind nasal tracheal intubation |
| Mackay et al. 2001,189 retrospective case note review, UK | Patients with GCS score of < 12, head injury, agitated, chest injury with inadequate ventilation, multisystem trauma, N = 359; anaesthetists, n = 10; emergency doctors, n = 9 | Skills/comparing anaesthetists vs. emergency physicians during pre-hospital RSI | Emergency doctors were more likely to classify a patient as a difficult intubation and more likely to intubate patients with GCS score of > 12 and had four failed intubations. Anaesthetists had two failed intubations | ED doctors more likely than anaesthetists to intubate patients with GCS score of > 12 |
| Wang et al. 2001,269 retrospective review, USA | Patients requiring airway management, n = 893 | Skills/patient condition and paramedic performance of endotracheal intubation | 86% (771/893) of endotracheal intubations were successful. Significant difference (p < 0.001) in ETI success rate between cardiac arrests 93% (551/591) and non-cardiac arrests 73% (220/302) | ETI more successful in patients with cardiac arrests |
| Liberman et al. 2000,295 meta-analysis, Canada | N/A | Treatment/advanced life support | 174 articles on pre-hospital advanced and basic life support reviewed; the weighted OR for dying was 2.59 for patients receiving advanced life support compared with basic life support | Literature failed to demonstrate a benefit for on-site advanced life support for trauma patients |
| Morrison et al. 2000,264 meta-analysis, Canada | Acute myocardial infarction patients from six randomised trials, n = 6434 | Treatment/pre-hospital thrombolysis | Significant decrease in all-cause mortality among patients with pre-hospital thrombolysis compared with hospital thrombolysis (OR 0.83, 95% CI 0.70 to 0.98) | Pre-hospital thrombolysis saves lives |
| Gausche et al. 2000,329 quasi-randomised trial, USA | Patients aged < 12 years requiring airway management, n = 830 | Treatment/bag–valve–mask only vs. bag–valve–mask ventilation plus endotracheal intubation | No significant difference in survival for bag–valve–mask (30%; 123/404) vs. ETI (26%; 110/416), nor in rate of achieving good neurological outcome for bag–valve–mask (23%; 92/404) vs. ETI (20%; 85/416) | No benefit for the addition of endotracheal intubation to bag–valve–mask |
| Askitopoulou et al. 2000,38 observational study, Austria | Pre-hospital patients, N = 171; trauma patients, n = 73, non-trauma, n = 98 | Assessment/HECTOR Emergency Scales | Detected vital signs changes more rapidly than the Revised Trauma Score | Improved patient evaluation |
| Meyer et al. 2000,249 prospective observational study, France | Children with severe head trauma [mean age 7.5 years (SD 4.3 years); 14% aged < 2 years], n = 188 | Treatment/emergency tracheal intubation | 78% intubated at scene, 10% at local hospital and 12% in trauma centre. Trainees more frequently reported multiple intubation attempts and difficulties. Pre-hospital incidents occurred in 25% of patients: 19% cough, 2% gastric content inhalation, 3% spasm, 8% vomiting, 12% haemodynamic variations. Hypoxaemia occurred in 14 intubated children (7.5%) and in five non-intubated children (2.6%). Operator experience influenced the number of attempts and type of drug used; immediate incidents were noted in 25% of patients. Drug regimen but not level of consciousness influenced the incidence of immediate incidents | Physician training and adequate medication were the main factors influencing successful intubation |
| Hubble et al. 2000,188 observational study, USA | Paramedics, n = 109 | Medication/calculation – 10-item medication calculation examination | Overall performance on the drug calculation examination was poor. The mean score was 51.4% (SD 27.4). Intravenous flow rate problems and medication bolus problems were calculated correctly in 68.8% of the cases, followed by non-weight-based medication infusions (33.9%), weight-based medication infusions (32.5%) and percentage-based medication infusions (4.5%) | Poor medication calculation skills |
| Snooks et al. 2000,130 observational study, UK | Paramedics undertaking cannulation, n = 183 | Skills/appropriateness of cannulation | 81% (149/183) of cannulations were clinically appropriate; paramedics who cannulated more frequently were significantly more likely to cannulate appropriately (p = 0.05). Kappa of 0.43 for raters | There remains a high level of inappropriate cannulation and the low level of agreement between raters may suggest the level is higher |
| Franklin et al. 2000,54 retrospective review, USA | Patients with a pre-hospital blood pressure recorded, n = 4437 | Diagnosis/hypotension ≤ 90 as an indicator for ED trauma team activation | Hypotension was recorded in 18% (791/4437) of patients. < 50% required surgery, primarily for haemorrhage. The mortality rate for patients with pre-hospital hypotension was 12% | Hypotension may be a useful indicator for trauma team usage |
| Pace and Fuller 2000,250 retrospective review, USA | Adults and children, n = 150 | Training/administration of succinylcholine to facilitate endotracheal intubation | 13% complication rate (19 patients, 95% CI 8% to 18%). 5% serious cardiac complication rate (seven patients, 95% CI 1% to 8%). No cases of unrecognised oesophageal intubation | Succinylcholine appeared to aid intubation in patients not in cardiac arrest but is not without complication risk |
| Sloane et al. 2000,252 retrospective review, USA | Adult trauma patients requiring complex airway management, n = 314 | RSI: in pre-hospital setting vs. in trauma suite | No differences in effectiveness (97.9% pre-hospital, 98.5% in hospital) and no AEs were reported | No difference in successful intubations between the two groups, nor statistical difference in success rates, number of attempts, or immediate intubation events in the procedure |
| Schade et al. 2000,291 case report, USA | Trauma patient, n = 1 | Treatment/intracranial insertion of a nasopharyngeal airway in a patient with craniofacial trauma | An oropharyngeal airway is preferred, but if paramedics are trained in only nasopharyngeal airways then it should be removed as soon as possible | Airway management in patients with craniofacial trauma is more complex |
| Brown and Fowler 1999,285 questionnaire, USA | N = 141: administrators, n = 53; associate of applied science paramedics, n = 25; certified paramedics, n = 63 | Training/evaluation of EMS educational programmes | Both paramedic groups rated preparation time for patient care duties as good or excellent, except during 12-lead ECG interpretation. Certified paramedics gave significantly lower ratings for preparation time for non-patient care duties, which need additional emphasis in education programmes. EMS educational programmes in North Carolina adequately prepare students to work as paramedics | There is added value to associate of applied science paramedic education when compared with the traditional certificate education programme |
| Nicholl et al. 1998,48 quasi-randomised study, UK | Patients with trauma, N = 2045; attended by paramedics, n = 1440, or by technicians, n = 605 | Treatment/comparison of outcomes when treated by EMT with basic life support training and paramedic with advanced life support training | Significantly longer on-scene time (12 minutes; p < 0.01) and a greater number of avoidable deaths occurred with paramedics (p = 0.02). Patients with haemorrhage had a higher risk of death, but survivors had better outcomes | No evidence that pre-hospital events were avoidable |
| Schmidt et al. 1998,253 prospective observational study, Germany and USA | Patients with chest injuries, n = 624 | Treatment/chest tube placement by aeromedical service | 10% (63/624) patients received chest tubes. Four chest tubes needed repositioning in hospital because of malfunctioning or mal-positioning. No infections occurred during hospital stay | Pre-hospital chest tube thoracostomy is safe |
| Bassene et al. 1998,166 observational study , Belgium | Patients with cervical spine lesion requiring airway management, n = 5 | Treatment/fibre optic intubation | Patients were immobilised with cervical collar. In 80% of patients (4/5), intubation was straightforward; in one case intubation was difficult owing to several unsuccessful and traumatising attempts by the first physician on the scene | Fibre optic intubation may reduce hypoxia risk and be useful for difficult intubations |
| Lowe et al. 1998,266 observational study, USA | Patients requiring complex airway management. Flight nurses and paramedics, n = 198 | Skills/RSI protocol | No significant differences in the number of successful RSI pre and post protocol (79% and 84.7%, respectively) | Facial trauma, combativeness, vomiting and nasal bleeding were associated with unsuccessful RSI |
| Qazi et al. 1998,78 observational study, USA | Paediatric blunt trauma patients, n = 192 | Diagnosis/determining the value of paramedic judgement in determining the need for trauma team activation for paediatric blunt trauma patients | EMT judgement alone of the need for TTA for paediatric blunt trauma patients is not sufficiently sensitive to be of clinical use. The paramedic disposition decisions from the scene were always accurate | Further research needed |
| Smith et al. 1998,330 retrospective chart review, USA | Patients coded as CVA or TIA, n = 96 | Diagnosis/accuracy of paramedic diagnoses of CVA or TIA | 49 patients had the diagnosis confirmed. An additional 32 patients were identified to have primary conditions other than CVA/TIA. The positive predictive value was 77% for paramedic identification of acute stroke | Triage and identification CVA/TIA is vital to care and associated with good clinical decision-making |
| Rottman et al. 1997,24 before-and-after study, USA | Patients with altered level of consciousness, non-traumatic chest pain or shortness of breath. N = 2581: before, n = 287; after, n = 2294 | Assessment/online medical control by EMS-certified nurses | Significant but small differences in on-scene time (1 minute; p < 0.03) | Improved on-scene time and appropriateness of therapeutic decisions |
| Linn et al. 1997,20 retrospective study, Israel | Trauma patients assessed using detailed questionnaire, n = 186 | Diagnosis/trauma patients | Blunt trauma diagnoses were missed more often than penetrating injuries; feasible diagnoses were missed in two of four paralysis cases, approximately one-third of crush injuries and one-quarter of fractures | Blunt trauma more difficult to diagnose than penetrating trauma |
| Schaider et al, 1995,137 prospective cross-sectional study, USA | Patients, n = 102 | Diagnosis/chest pain or shortness of breath | For organ system diagnosis, the paramedics had an 82% accuracy (p = 0.05) rating. For specific cardiac and pulmonary diagnosis, paramedics had good concordance with emergency physicians | Overall, paramedics have excellent diagnostic agreement with emergency physician diagnosis by organ system. They retained good agreement on specific cardiac diagnoses and pulmonary diagnosis |
| Nardi et al. 1995,331 prospective review, Italy | Patients with severe TRISS > 15, alive at the scene, required intensive care and ventilation, n = 222 | Treatment/application of advanced-trauma life support | n = 82, EMT transfer to nearest hospital; n = 98, EMT transfer to trauma centre; n = 42, transferred to trauma centre by helicopter emergency medical service with anaesthetist | – |
| Massarutti et al. 2006,332 prospective observational study, Italy | Patients with severe trauma Revised Trauma Score of 9.6 ± 2.7, requiring thoracotomy, n = 55 | Treatment/on-scene simple thoracotomy | On-scene thoracotomy significantly improved oxygen saturation (p < 0.05). Pneumothorax/haemopneumothorax confirmed in 91.5% of cases. No major bleeding reported | On-scene simple thoracotomy safe and effective |
| Wolfberg et al. 1995,217 discussion of consensus, USA | N/A | Medication/implementation of two consensus-based processes to standardise and streamline how new drugs and devices are introduced into pre-hospital practice | Processes for review and classification of devices; for addition of medications to the drug list. Standardised tool ensures that addition of medication is evidence based not led by salesmanship. Ensures accurate, fair and consistent evaluations of devices | Standardised tools ensures accurate evaluations of devices |
| Holliman et al. 1994,142 review of run sheets, USA | ALS runs, n = 2001 | Treatment/using a ‘standing orders’ protocol system | The physician error rate decreased from 2.6% in the previous study; the on-scene time interval did not increase with the standing orders system; there was a decrease in overall error rate in the pre-hospital care system and a slight decrease in the mean on-scene time interval | Paramedic errors occurred at a low frequency with the standing orders system |
| Haynes and Pritting, 1993, 333 observational study, USA | Patients, n = 266 | Training/enhanced training for ambulance clinicians in rural areas | Mean transfer time 41 minutes; transfer appropriate in 94% of cases; ED agreed with diagnosis in 75% of cases | Low rate of agreement with diagnosis |
| York et al, 1993,185 retrospective review, USA | Patients with thoracic trauma, n = 246 | Treatment/thoracostomy (chest tube/needle); comparison of air medical crews vs. physician trauma service | No difference between groups. Air medical crews with the correct training can safely perform the procedure | Training improves thoracostomy success rate |
| Aufderheide et al. 1992,12 prospective study, USA | Pre-hospital stable adult patients with non-traumatic chest pain, n = 439 | Diagnosis/accuracy of base-station, emergency physician, pre-hospital thrombolytic candidate selection | Diagnosis of acute myocardial infarction; 8.7% had pre-hospital diagnostic ECGs and 2.7% were selected by emergency physicians as candidates for thrombolytic therapy. 70% of patients with myocardial infarction had checklist exclusions for thrombolytic therapy. The median time from chest pain onset to paramedic arrival for patients with myocardial infarction was 60 minutes and the estimated average time saved had pre-hospital thrombolytic therapy been available was 101 ± 81 minutes | The predictive value of the paramedic decision to give pre-hospital thrombolysis was 100% |
| Bruns et al. 1992,13 prospective observational study, USA | Patients receiving morphine sulphate in pre-hospital setting, n = 84 | Medication/appropriate administration of Minijet® morphine sulphate (UCB Pharma) to patients assessed for ischaemic chest pain and/or pulmonary oedema | Overall paramedic accuracy of assessment 77% (95% CI 73% to 82%). Appropriateness of therapy 88% (95% CI 85% to 92%). Complication rate 6% (95% CI 2% to 12%) | Low frequency of inappropriate MS administration and complication rate from both erroneous and inappropriate drug administration |
| Sterba 1991,293 prospective randomised study, USA | Volunteers, n = 8 | Treatment/pre-hospital rewarming | Inhalation rewarming and/or peripheral rewarming did not significantly influence rewarming rates | Inhalation rewarming and peripheral rewarming are not recommended for pre-hospital use |
An issue that has accounted for the majority of studies identified by this review is pre-hospital intubation, especially regarding paramedic intubation. Until recently, the procedure was considered the gold standard for pre-hospital care of patients with compromised airways, but debate has led to some ambulance services restricting the use of pre-hospital endotracheal intubation without the administration of drugs and advocating use of supraglottic airway devices as an alternative. The evidence presented in these tables describes a wide range of field observational studies, simulation studies and e-learning. The studies provide mixed evidence as to the effectiveness of intubation except in cases of severe hypoxia. The quality of the literature varied with much evidence reported in conference abstracts that have not been subsequently published in peer-reviewed journals, which may be a consequence of weak design. However, some well-designed studies are now being undertaken which may soon provide a clear answer as to the appropriateness of endotracheal intubation.
Direct transfer for specialist treatment has also been shown to be of benefit for myocardial infarction (and direct transfer to intervention centres), stroke (to hyperacute stroke units) and major trauma (to designated major trauma centres).
For some important topics there is a paucity of research, for example informing on the administration of intravenous fluids during management of trauma. There is also little research on the use of restraint, both chemical restraint provided by the ambulance service and the recognition of patient difficulties during restraint by others (e.g. the police); this is of concern especially in the light of criticisms of ambulance services by coroners in cases where patients have died from asphyxiation following police restraint.
The nature of this review means it has not identified studies of the safety of drug administration specifically in pre-hospital care; much of the consideration as to the safety of treatments in pre-hospital care has been undertaken in broader clinical trials. There is a paucity of high-quality assessments regarding their safety outside these trials when introduced into routine practice. There is also a lack of information regarding the use of complex diagnostics. Most studies address specific conditions, whereas most presentations are symptom based and the diagnosis may not be known until arrival in hospital.
Non-conveyance including telephone advice, treat and discharge on scene and alternative pathways
Table 4 summarises the research that considers interventions designed to reduce the number of patients conveyed to further care, with the aim of reducing costs of either the 999 response or ED attendance, while also reducing patient inconvenience by ensuring they received the right care in the right place. The search identified 39 papers that explored this topic and the evidence describes a range of interventions for children, adults in particular groups (e.g. the elderly or fallen patients) or for specific conditions such as hypoglycaemia, convulsions, poisoning or minor injuries; management of such situations is in some cases directed by a protocol or guideline. The studies detailed by the systematic review often give poor information on the training undertaken to allow ambulance clinicians to make non-conveyance or treat-and-leave decisions, meaning that the handling of such situations may not be consistent and raising concerns that such an intervention may not be implemented safely.
| Author(s), year, study design, country | Population, patient number | Intervention/process or topic | Results | Headline |
|---|---|---|---|---|
| Halter et al. 2011,27 observational study, UK | N = 12: paramedic, n = 1; technicians, n = 11 | Non-conveyance/clinical decision tool for fallen patients | Decision to convey: based on loss of consciousness, pain, injuries, long lie and medical condition. Continuing assessment of medical history, medications, condition, mobility, and social and environmental factors | Decisions based on prior knowledge; most completed the tool retrospectively after decision had been made. Considered an aid to documentation |
| Maggiore 2011,180 case report, USA | 2-year-old girl | Non-conveyance/decision-making | A 2 year old with breathing difficulty died following a decision that transfer was unnecessary | Non-conveyance requires extensive assessment and patient agreement |
| 50-year-old male | Non-conveyance/failure to transport | A man died after reporting severe abdominal pain and waiting 30 hours with 10 calls for EMS, who could not reach the patient’s home owing to snow. Ambulance personnel insisted that the patient walk the short distance to the ambulance; as the patient was unable to walk, the ambulance left the scene | ||
| Fitzpatrick and Duncan 2009,39 systematic review, UK | Patients with hypoglycaemia signs and symptoms, n = N/A | Treat and leave/hypoglycaemia | 2–7% risk of repeat hypoglycaemic events | Safety of treat and leave unknown |
| Brown et al. 2009,29 literature review, N/A | N/A | Non-conveyance/systematic review of the US paramedics’ ability to determine medical necessity of ambulance transport | 214 abstracts evaluated. 61 studies selected for full review. Only a few studies available that met the criteria. Results do not support the practice of paramedics determining whether or not patients require ambulance transport | No evidence to support reliability of decision-making |
| Meisel et al. 2009,125 retrospective cohort study, USA | Patients aged > 18 years transferred to ED, n = 1102 | Non-conveyance/Philadelphia EMS admission rule for guiding admission to an ED (six elements score of 0–14). The score consisted of six weighted elements that generated a total score (0–14): age ≥ 60 years (3 points); chest pain (3 points); shortness of breath (3 points); dizzy, weakness, or syncope (2 points); history of cancer (2 points); and history of diabetes (1 point) | 34% had a score of ≥ 4, of whom 77% were admitted. 29% had a score of ≥ 5, of whom 80% were admitted | Validation of this rule; further studies needed to determine impact and feasibility |
| Al-Sulaiti et al. 2009,207 review of clinical records, UK | Non-conveyed 999 callers, n = 734 | Non-conveyance/decision-making | Non-conveyance of patients is a significant consideration for ambulance service. Early findings indicate that non-conveyance of 999 callers leads to significant utilisation of resources with potential clinical risks | Recontact can lead to significant utilisation of resources |
| Mason et al. 2008,21 cluster randomised controlled study, UK | Patients aged ≥ 60 years of age with minor injury or illness, n = 2025 | Treat and leave/assessment and management of minor conditions by extended-role paramedic practitioners in comparison with ED treatment | 10.9% had an unplanned ED attendance within 7 days, of whom 74% re-presented with a condition related to their index episode. No significant differences were seen between intervention and control groups in terms of re-presentation | Paramedics with extended training are able to treat patients with minor conditions |
| Strote et al. 2008,210 prospective observational study, USA | Patients with stable hypoglycaemia receiving pre-hospital care, n = 203 | Treat and leave/comparison of technician and paramedic treatment of hypoglycaemia cases where the patient was left at home | 54% (110/203) treated by technicians and 46% (93/203) by paramedics. There were no significant differences in outcome or satisfaction for patients treated by technicians or paramedics (p > 0.5) | Safe to leave patients at home following a hypoglycaemic episode when treated by technicians |
| Gray and Walker 2008,79 observational study with historical control, UK | Patients with breathing difficulties aged < 65 years, n = 186 | Non-conveyance/increasing the role of ECPs within the ambulance service | The ECPs showed decreased rates of admission to hospital in both groups at initial contact and at 28 days | A balance between patient safety and avoiding ED attendance and hospital admissions |
| Widiatmoko et al. 2008,334 observational study, N/A | N/A | Non-conveyance/dispatch of district nurse or emergency nurse practitioner with a paramedic to low-priority calls | Reduction in conveyance rate was noted as patients were treated on scene. Service has the potential to be cost-effective | Potential benefits |
| Mason et al. 2007,62 RCT, UK | Older patients with minor acute conditions, N = 3018: intervention, n = 1549; control, n = 1469 | Treat and leave/using trained paramedic practitioners with extended skills | Paramedics with extended skills can provide a clinically effective alternative to standard ambulance transfer and treatment in an ED for elderly patients with acute minor conditions | Positive correlation between paramedic being trained with extended skills and a reduction in hospital admission and patients’ satisfaction |
| Gray and Wardope, 2007,199 prospective observational study, UK | Paramedics and technicians, n = 354 | Non-conveyance/guidelines for no injury, minor limb injury, resolved hypoglycaemia and convulsion | There was 60% compliance with the guidelines with inappropriate non-conveyance due to hypoglycaemia 3% (2/69), epilepsy 4% (1/23), no apparent injury 20% (17/84) and minor limb injury 48% (28/58). 48% of patients not transferred were originally ‘category A’/’delta’ calls. Some patients refused transfer but no data were provided | Poor compliance with guidelines. Poor specificity and sensitivity for existing guidelines |
| Porter et al. 2007,202 focus groups, UK | Pre-hospital clinicians, n = 25 | Non-conveyance/perception of non-conveyance decisions | The approach is to minimise risk and protect selves by taking the patient to the hospital. Ambulance service unsupportive in cases of problems | Non-conveyance is the individual’s decision |
| Kahalé et al. 2006,82 prospective cohort study, Canada | Children aged < 16 years assessed but not transported, n = 345 | Non-conveyance/characteristics, reason and outcomes | 15% (51/345) of non-conveyed children were seen in an ED within 48 hours, of these 8% (4/51) were admitted to hospital. Most non-transported children did not require immediate or urgent medical care. Both parents and paramedics provided input into the non-transport decision | Paramedic documentation for the reasons for non-transport should be improved |
| Haines et al. 2006,200 prospective observational study, USA | Patients aged < 21 years old with a specific condition, n = 704 | Non-conveyance/decision-making | Younger patients were significantly more likely to require admission (p = 0.002). No paediatric intensive care unit admission or deaths | Non-conveyance decision-making was safe and efficient |
| Schmidt et al. 2006,59 retrospective review, USA | EMS runs, n = 1501; patients, n = 1059 | Non-conveyance/factors predicting non-transport and mortality rates in an emergency medical service system with a non-transport policy | Older patients (median age 60 years) were more likely to be transported, whereas race, frequency of call, mutual aid or time of day did not significantly influence probability of transport | Data suggest that EMS-initiated non-transport is influenced only by age and chief complaint and may not result in insignificant mortality |
| Snooks et al. 2006,204 retrospective review, UK | Patients aged ≥ 65 years contacting ambulance service following a fall, N = 534; followed-up, n = 175 | Non-conveyance/attendance following 999 call for a fall | 36% (194/534) were left at home; 86 patients recontacted within 2 weeks of the fall; 2.3% fatality rate | It is not safe to leave patients who fall at home |
| Dale et al. 2004,40 RCT, UK | Category C patients (not requiring an ambulance), n = 330 | Telephone advice/triage and advice by nurse/paramedic using decision support software | In 14.6% of cases, at least one member of the review panel considered the patient to need an ambulance in 14 minutes (35/231) | Decision support software may be safe for managing some category C calls |
| Snooks et al. 2004,132 RCT, UK | Intervention group, n = 257; control group, n = 537 | Treat and leave/develop and evaluate ‘treat and refer’ protocols for trained ambulance crews | ‘Treat and refer’ protocols did not increase the number of patients left at home, but were used by crews and were acceptable to patients | Did increase the job cycle time, some safety issues were identified. Introduction is complex and the content of protocols requires further study |
| Slattery and Heck 2004,44 retrospective cohort study, USA | Patients aged 6 months to 98 years calling 911, for whom a decision was made not to convey them to hospital, n = 732 | Non-conveyance/decision-making and documentation | 18% (131/732) had abnormal vital signs. 24% (172/732) were difficult, if not impossible, to establish decision-making capacity because of being a minor (n = 111), being intoxicated (n = 45) or because of communication barriers (n = 16). 19% (142/732) had advanced care provided (12-lead ECG, intravenous access, parenteral medications) and were subsequently released. Adequate medical history was recorded and physical examination performed in 82% (602/732) and 68% (495/732) of the cases, respectively. Paramedics documented that they had encouraged transport in 35% (258/732) of the cases; 15% (112/732) explained the risks of not being transported; 24% (173/732) enlisted the help of others; 1% (8/732) contacted medical control; 19% (140/732) instructed patients to call 911 back if their condition worsened or if they changed their mind | Processes for non-conveyance require improvement |
| Cain et al. 2003,196 prospective observational study, Canada | Patients aged > 15 years with blood glucose levels < 4 mmol/l, patients: repeat calls, n = 57; total episodes, n = 220 | Treat and leave/hypoglycaemic episode treated and patient left at home | 66% (145/220) of episodes were not transferred. Repeat episodes occurred after a mean of 41 days (± 54 days). No significant difference in incidence of repeat episodes between transported and non-transported patients | Hospital admission is rarely required for hypoglycaemic episodes and recurrences within 48 hours were uncommon. Advice is important for follow-up care |
| Gratton et al. 2003,16 prospective observational study, USA | Transported patients with completed data forms, n = 825 | Non-conveyance/decision-making | Emergency physicians: 30% (248/825) transports were not necessary; paramedics: 29% (236/825) transports were not necessary. Using blinded determination based on the same criteria, paramedics and physicians had agreement on medical necessity of patient transport to ED in 76.2% of cases assessed; 11% (92/825) patients were undertriaged by paramedics | Paramedics cannot reliably predict which patients require transfer to the ED |
| Lerner et al. 2003,208 prospective observational study, USA | Patients with hypoglycaemia signs and symptoms, n = 36 | Treat and leave/hypoglycaemic episode treated by paramedics and patient left at home | 91% (33/36) did not experience a recurrence of the hypoglycaemic episode; 8% (3/36) experienced a recurrence and, of these, one patient was found unresponsive | Paramedics can safely treat a hypoglycaemic episode and leave the patient at home |
| Schaefer et al. 2002,335 RCT, UK | Patients: intervention, n = 1016; matched control, n = 2617 | Non-conveyance/EMTs to reduce ED use of non-urgent patients | Based on physician review and patient interview, the alternate care intervention appeared to be safe and satisfactory | An EMS-based programme may represent one approach to limiting non-urgent ED use |
| Silvestri et al. 2002,203 prospective observational study, USA | Patients contacting 911 who did not require ED transfer, n = 313 | Non-conveyance/decision-making | Paramedic assessment was 81% sensitive (95% CI 72% to 88%) and 34% specific (95% CI 28% to 41%) at predicting requirement for ED care. 32% of cases (27/85) for which paramedics felt transfer was unnecessary met criteria for ED treatment, including 15 (18%) admissions and five (6%) admissions to intensive care | Paramedics cannot reliably predict which patients require transfer to the ED |
| O’Cathain et al. 2002,219 before-and-after study, UK | 911 callers before EMD system, n = 493; after EMD system, n = 466 | Telephone advice/acceptability of an EMD system | The proportion of callers who were satisfied increased from 78% (before) to 86% (after). Two particular problems were identified: some callers were advised to take actions that were subsequently not needed and a small number of callers felt that the ambulance crew did not treat the situation as seriously as they would have liked | Introducing EMD increases the amount of first aid and general advice given to callers and led to an overall increase with the service |
| Hauswald 2002,201 survey, USA | Chart review, n = 183 | Non-conveyance/decision-making | Alternative transport was recommended for 97 patients and 23 needed ambulance transport. Non-ED care was advocated for 71 patients and 32 needed ED care | Paramedics cannot reliably predict which patients require transfer to the ED |
| Anderson et al. 2002,195 retrospective review, Denmark | Patients with hypoglycaemia signs and symptoms, n = 587 with 1148 hypoglycaemic episodes | Treat and leave/hypoglycaemic episode treated by mobile intensive care unit and patient left at home | 84% (964/1148) did not experience hypoglycaemia recurrence in subsequent 72-hour period. Level of care and treatment before arrival of pre-hospital care were predictors of transfer to further care. Poor compliance with leave at home advice was seen in those with recurrence | It is safe to treat a hypoglycaemic episode and leave the patient at home in most instances |
| Smith et al. 2001,84 RCT, UK | Callers phase 1, n = 38; phase 2, n = 133 | Telephone advice/transferring non-urgent 911 calls to a telephone consulting nurse | Transferring calls resulted in fewer basic life support responses and no adverse patient outcome, while maintaining high patient satisfaction | Major implications for communities interested in efficient use of emergency medical service resources |
| Mechem et al. 2001,198 prospective observational study, USA | Patients with signs and symptoms of convulsion, n = 52 | Treat and leave/treatment of convulsion, patient left at home as refused transfer | 94% (49/52) did not experience recurrence in the subsequent 72-hour period. 38% (20/52) contacted their GP; no deaths were reported | Most patients did not experience hypoglycaemia recurrence. Advice should be given on the risk of recurrence |
| Gerlacher et al. 2001,74 cross-sectional study, USA | Paediatric patients, inclusion group, n = 3057; control group, n = 12,302 | Non-conveyance/pre-hospital evaluation of non-transported paediatric patients by a large emergency medical service system | Non-transport was less common in the first 2 years of life and during the hours of midnight to 06.00. Among non-transported patients, personnel of paramedic units had significantly better documentation of contact with OLMC than did personnel of ambulance unites | Non-transport was less common in children under 2 years of age and during early morning hours |
| Schmidt et al. 2000,61 retrospective review, USA | Patients, n = 1300 | Non-conveyance/decision on conveyance by EMTs using protocol with four levels | From 3% to 11% of patients determined on scene not to need an ambulance had a critical event | EMS systems need to determine an acceptable rate of undertriage |
| Burstein et al. 1996,212 prospective observational study, USA | Patients who refused transfer to ED, n = 321 | Non-conveyance/outcomes of patients who refused medical assistance | Follow-up was successfully obtained for 199 out of 321 patients enrolled (62%), of these, 48% (95/199) sought care within 1 week for the same complaint and, of these, 13 were admitted. Six of these 13 had a cardiac or respiratory complaint and one of the 13 died | Focus on reducing refusal of medical assistance for patients with serious complaints |
| Anderson et al. 1998,336 prospective observational study, USA | Patients contacting 911 with signs and symptoms of poisoning, n = 258 | Pathways/diverting 911 calls to a poison centre | Home treatment recommended for 69% (179/258) of patients. Two patients suffered moderate effects, one major effects and one died | Study supports poison centre management of most calls |
| Mechem et al. 1998,211 retrospective review, USA | Patients with hypoglycaemia signs and symptoms, n = 103 | Non-conveyance/treatment of hypoglycaemic episode, with patient left at home on refusal of transfer | 91% (94/103) did not experience recurrence; 9% (9/103) suffered a hypoglycaemia recurrence and recontacted the ambulance service | It is safe to treat a hypoglycaemic episode and leave the patient at home with advice on the risk of recurrence |
| Socransky et al. 1998,206 retrospective review, Canada | Patients aged ≥ 18 years with blood glucose levels < 80 mg/dl, n = 374 (571 hypoglycaemic episodes) | Treat and leave/hypoglycaemic episode comparing those transferred with further care with those refusing transfer | 72% (412/571) refused transfer and 6% of refusers (25/412) suffered recurrence. There was no significant difference in recurrence rates between transferred and non-transferred patients | It is safe to treat a hypoglycaemic episode and leave the patient at home |
| Yaxley et al, 1993,205 retrospective review, UK | Patients with hypoglycaemia signs and symptoms, n = 28 | Treat and leave/treatment of hypoglycaemic episode and the patient left at home | 25 patients avoided hospital admission. No side effects or complications were reported | It is safe to treat a hypoglycaemic episode and leave the patient at home |
| Sprehn et al. 1992,209 retrospective review, Denmark | Patients with severe hypoglycaemia signs and symptoms, n = 180 | Treat and leave/treatment of hypoglycaemic episode in mobile intensive care unit and patient left at home | 69% (125/180) of patients avoided hospital admission; 1% (2/180) experienced secondary hypoglycaemia | Pre-hospital treatment is beneficial |
| Zachariah et al. 1992,213 retrospective review, USA | Non-conveyed patients following ambulance request, n = 158 | Non-conveyance/outcomes of patients | 59% (93/158) were followed up. Of these, 60/93 (64.5%) subsequently sought care from a physician, 15/60 of whom (25%) were later admitted, two to an intensive care unit and two died. In 43 out of 93 (46%) cases, the patient refused transport. Paramedics declined transport or mutually agreed not to transport in 50 out of 93 cases (54%), the latter accounting for 11 of the 15 hospitalisations (73%) | Serious outcomes occurred for some patients not transferred to further care |
The evidence for patient safety in association with non-conveyance or treat-and-leave interventions is mixed. Some studies have shown that patients suffering hypoglycaemic episodes can be safely treated at home, while others report relapses and recontact with the ambulance service. A number of reasons are proposed for this difference: failure to follow the protocol or guidelines, leave-at-home advice is inadequate, and the type of sulphonylureas the patient is taking can affect recurrence.
In addition to specific interventions, details of the outcomes for patients who are denied or refuse treatment are also considered and show mixed results and some safety concerns for those left at home.
The overall evidence on non-conveyance/treat-and-leave shows mixed findings, but does not contain sufficient detail to determine the absolute risks of such interventions or the criteria for ensuring that they are safe and effective.
Safety culture
The Department of Health publication An Organisation with a Memory4 has contributed to a growing interest in the topic of safety culture within the NHS. Research has shown that factors such as an emphasis on production, efficiency and cost, or professional norms for perfectionism among health-care providers, may combine to create a culture contradictory to the requirements of patient safety. 337 The establishment of a ‘no-blame’ culture has become an important aim within the NHS in order to facilitate the reporting of and the learning from incidents. The NPSA seven steps to patient safety include the establishment of a safety culture as first step. 338 It is recognised that major cultural transformations must accompany structural and procedural changes in order to achieve and sustain desired improvements in quality and safety of care. 339
The notion of safety culture was first explored in safety-critical industries following major disasters, most notably the Chernobyl nuclear accident in 1986. 340 A common definition of safety culture in the nuclear industry that is now widely adopted across industries suggests that:
The safety culture of an organisation is the product of individual and group values, attitudes, perceptions, competencies and patterns of behaviour that determine the commitment to, and the style and proficiency of, an organisation’s health and safety management. Organisations with a positive safety culture are characterised by communications founded on mutual trust, by shared perceptions of the importance of safety and by confidence in the efficacy of preventive measures.
Health and Safety Commission341
Safety culture has been described as ‘the way safety is done around here’. 342 What people believe about safety and the importance given to safety within an organisation will strongly influence their decisions, and these beliefs and attitudes are shaped by individual experience and by interacting with and observing peers. 340 In the literature there is a distinction between safety culture and safety climate. Safety climate commonly refers to more readily measurable aspects of safety culture343 and can be regarded as the surface features of the underlying safety culture. 344 Assessment of safety climate is becoming increasingly popular and is conducted using quantitative safety climate questionnaires. A deeper understanding of safety culture requires qualitative methods, as it is concerned with the more enduring underlying culture. 340
In health care, the quantitative assessment of safety climate using questionnaires is an established approach and recommended by bodies such as the Joint Commission. 342 Such assessments can be used to:
-
identify areas for improvement and raise awareness about patient safety
-
evaluate patient safety interventions and track changes over time
-
conduct internal and external benchmarking
-
fulfil directives and regulatory requirements. 337
There are a number of tools for measuring safety culture/safety climate in health care and a review about their validity and reliability is provided in a study by Flin et al. 344 A national survey on the adoption of culture assessment tools within NHS England found that around one-third of NHS organisations are using such tools. 339 In England, the most commonly used tool is the Manchester Patient Safety Framework (MaPSaF),338 reported to be used by 28% of organisations in the survey. MaPSaF is a method for self-reflection about safety culture within a group setting rather than an assessment of climate based on questionnaires. Another tool frequently used is the Safety Attitudes Questionnaire,343 which is reported to be used by 7% of organisations in the survey. In the USA, the Hospital Survey on Patient Safety Culture developed for the AHRQ345 is another prominent questionnaire-based instrument. For both Safety Attitudes Questionnaire and the AHRQ surveys, there is increasing evidence available about the validity and reliability of their dimensions.
The studies reported in the present review examine how the safety culture of the organisation affects patient safety and the likelihood that AEs are reported and acted on (Table 5). Twenty-two studies were identified with mixed results; some studies argued that reporting AEs is uncommon owing to not knowing how to report these, or because of staff being concerned about the consequences, as the research suggests that some organisations have a culture of blame. The wider aspects of safety culture and its impact on minimising risk and reducing harm have not been well studied in ambulance services. However, it is recognised that safety culture and human factors are relatively new research topics in health care. It is important that organisations have a safety culture in which staff feel comfortable reporting incidents, as some studies indicate a high level of incidents and near misses. One study found a low likelihood of disclosing an error to a patient. 228 Studies have also shown that it is unlikely that an AE will be reported to the patient. 42,347
| Authors, year, study design, country | Population, patient number | Intervention/process or topic | Results | Headline |
|---|---|---|---|---|
| MacDonald et al. 2011,346 modified Delphi review, Canada | Experts in EMS and transport medicine, n = 16 | Patient safety/categorisation of AEs and near misses to standardise terminology | Categories were: incident type, patient outcome, patient characteristics, contributing factors and hazards, event detection, organisational outcomes, rectifying action, and interventions to reduce risk | A taxonomy can be used to classify adverse events and near-misses in transport medicine. Further evaluation of the taxonomy is required |
| Patterson et al. 2010,181 observational study, USA | EMTs from 61 organisations, n = 1715 | Safety culture/safety attitudes in EMS | Safety culture scores were higher for air medical teams and organisations with fewer employees. Safety culture scores were lowest for paramedics and for pre-hospital nurses and employees with least experience | No common AE classification available |
| Alvarez-Ortiz 2010,191 case series study, Spain | Patients, n = 5624 | Safety culture/frequency, type and severity of AEs | 2.3% (131/5624) experienced a pre-hospital AE, 40.5% of which were preventable. 44 AEs originated in ambulatory care and 85 in non-ambulatory care; AEs were mainly related to medication | High level of preventable AEs |
| Patterson et al. 2010,302 cross-sectional survey, USA and Canada | Surveys from three EMS agencies, n = 77 | Safety culture/measuring dimensions of workplace safety culture | 78% response rate with a positive perception reported for safety climate, job satisfaction, perception of management; fewer than half of respondents had positive perception of teamwork climate, working conditions and stress recognition | EMS workplace culture varies across agencies |
| Atack and Maher 2010,123 interview, Canada | EMS experts, n = 16 | Safety culture/EMS professional opinion on issues associated with patient safety | Two key issues identified were clinical decision-making (related to expanding role of EMS staff) and the focus and relationship of EMS with health care (move from public safety to health care) | Developing and supporting sound clinical judgement for patient safety |
| Cushman et al, 2010,179 ethnography: event reports/semistructured interviews/focus group, USA | EMS providers managing children, N = 51: event reports, n = 11; semistructured interviews, n = 17; focus groups, n = 23 | Patient safety/perceptions of factors related to AEs | 61 AEs. Five factors were considered to impact on safety culture: uncommon reporting, blaming others, stress, errors of omission and limited training | Under-reporting of AEs and lack of training in children’s EMS |
| Stella et al. 2010,42 pilot study, prospective descriptive study, Australia (related Stella et al. 2008347) | Incidents, n = 454 from 230 cases | Safety culture/pre-hospital critical incident monitoring system | Mean of 2.0 incidents per case. Incident types: communication, n = 101; prolonged time, n = 93; resources, n = 20; equipment, n = 15; resuscitation, n = 41; other treatment problems, n = 41; guideline deviation, n = 19; diagnostic error, n = 9; interference, n = 9; injury, n = 1; and other, n = 42. Management problems included prolonged time at the scene, n = 56, and inadequate documentation, n = 47. System inadequacies included communication with other services, n = 18, and dispatch communication problems, n = 12 | Good evidence for safety reporting systems |
| Turner and Bjarkoy 2011,223 mixed methods (data review, consensus workshop, Delphi survey, pilot studies), UK | N/A | Quality improvement/clinical quality indicators for category B calls | Preliminary findings: 50% of category B calls are within 5/32 dispatch categories, half of the patients have some assessments, only 10% have intervention | Project is ongoing. Preliminary findings available |
| Meisel et al. 2008,348 review, USA | N/A | Safety culture/introduction of a complementary patient safety or pre-hospital care model using injury prevention and control principles | Injury prevention and control principles comprised retrospective chart review, direct observation and self- and peer-reporting. Patient safety surveillance was particularly challenging | Pre-hospital AE surveillance may uncover as yet unidentified weaknesses |
| Fairbanks et al. 2008,227 mixed methods, USA | Interviews, n = 15; focus group participants, n = 23; events, n = 61 | Safety culture/patient safety/focus groups, interviews, event reporting to examine the perceptions of EMS providers regarding near misses and AEs in out-of-hospital care | 44% (27/61) of events were near misses and 56% (34/61) were AEs. Error types included clinical judgement (54%), skill performance (21%), medication events (15%), destination choice (5%) and others (3%). For the 21 cases for which the provider discussed the event: 48% were reported to a physician, 43% to a supervisor and 19% were never reported. None was reported to the patient | High level of AEs |
| Donald and Paterson 2007,91 questionnaire, UK | Pre-hospital staff, n = 45 | Safety culture/incident reporting | 34/45 questionnaires returned. Lack of understanding on how to report critical incidents. Little opportunity to discuss events and vocalise concern | More training on reporting AEs |
| Cooper et al. 2007,271 12-month mixed-methods clinical case study, UK (related study Cooper et al. 2007231) | Observations of ECPs, n = 24; interviews with ECPs and stakeholders, n = 45; audit of patients, n = 611 | Patient safety/collaborative practices and patient care | Collaborative performance of ECPs varies with leadership rating. Communication ability, teamwork and leadership performance were greater for higher grade ECPs. Collaboration influenced by the ECP role, education and training and cultural perspectives. Appointment of ECP clinical leads, training in communication skills, clinical supervision and multiprofessional ECP appointment to improve impact on patient care | Study suggests that collaborative practice of ECPs has an impact on patient care |
| Stephenson 2007,34 mixed methods (interviews, focus groups, surveys), Canada | Volunteers, n = 20 | Safety culture/impact of procedural checklist on medical error |
|
Implement pre-hospital procedural checklist with non-punitive programmes to track and assess medical error |
| Hobgood et al. 2006,228 survey, USA | EMTs, n = 283 | Safety culture/disclosure of medical errors | 55% (157/283) reported having made no medical errors during the previous year, 35% (100/283) reported one or two errors and 9% (26/283) reported more than two errors. 89% (112/126) of those reporting at least one error identified it themselves with < 15% of errors identified by patients, supervisors, nurses, fellow workers or physicians; 6% (7/126) did not report the error. Reporting to the receiving hospital was most common regardless of error type or severity. In hypothetical cases, severe errors were identified 93% of the time, but the ability of providers to identify mild errors significantly varied. Severe errors were more likely to be reported to the supervisor or medical director. The threshold for disclosure of an error to the patient was low | Providers can identify, report and disclose errors hypothetically, but may not apply skills in practice |
| Levick and Swanson 2005,349 prospective observational study, USA | N/A | Safety culture/a real-time driver performance monitoring and feedback device | During 18 months, using 36 vehicles in a metropolitan EMS group, with > 250 drivers and > 1.9 million recorded miles, performance improved from a baseline low of 0.018 miles between penalty counts to a high of 15.8 miles between counts. Seatbelt violations dropped from 13,500 to four | Performance monitoring and feedback can improve skill |
| O’Connor et al. 2002,350 review, USA | N/A | Safety culture/errors occurring during EMS care including types of error, barriers, identification and possible solutions | Barriers to error identification involve inadequate for evaluating errors and a lack of accurate and reliable measurement and analysis methods for errors, and also the culture of blame and litigation prevailing in our society | Managers to identify target areas by process mapping, specifically focusing on areas in which serious AEs may occur |
| Anonymous 2001,26 personnel view, USA | Patient with convulsions, n = 1 | Safety culture/ad hoc safety culture/self-learning | Misdiagnosis of seizure (confusion between seizure and syncope). Medical director asked paramedic to prepare a lecture for continuing education session, which has been classed as most effective punishment | Self-learning improved knowledge in this case – new ways of learning lessons |
| O’Connor and Megargel 1994,351 before-and-after study, USA | Paramedics, n = N/A | Quality improvement/developing a mechanism for conveying quality improvement results to paramedic to improve chart documentation | The use of quality improvement feedback had little effect on psychomotor skills, but had a dramatic effect on chart documentation and behaviour. ETI documentation rate 84% before and 98.8% after quality improvement programme, unjustified trauma scene times decreased from 24.8% to 1.4% | The use of quality improvement feedback is recommended as a means of correcting charting deficiencies or modifying behaviour |
| Spaite et al. 1990,97 audit, USA | Paramedics, n = N/A | Safety culture/data entry compliance | Following introduction of new data collection tool, 25% of data were missing. After 3 months, significant improvement in compliance with only 5% incomplete | Non-completion decreased because data completion became a quality indicator |
| Pons et al. 1985,96 observational study, USA | Paramedics, n = 78 | Safety culture/field instructor programme: orientation and evaluation | 88% (69/78) completed the course, with 12% (9/78) identified as poor and dismissed | Field assessment for new staff |
There is a lack of research that directly measures aspects of safety culture using recognised tools and, compared with research in secondary care, it appears that there is a lack of any tool specifically aimed at assessing safety culture or safety climate in ambulance services. For this reason, most of the reviewed work is either speculating on the impact of culture or extrapolating from poor incident reporting levels.
Dispatch
In February 2012, the ambulance services in England received 701,841 calls relating to 526,918 incidents and 496,678 face-to-face responses. Central to the safe and effective delivery of health care it is important that an appropriate and timely response is provided. In the UK, a number of policies and reports have been issued by the governmental bodies (Taking Healthcare to the Patient;352 Changing Times: Sustaining Long Term Performance Against Call Connect for NHS Ambulance Services;353 and A Vision for Emergency and Urgent Care: The Role of Ambulance Services354), which set standards and provides guidance for call handling in the provision of both clinical advice (hear and treat) and mobile health care (see and treat).
A number of researchers have looked at the development of computer-aided systems with decision-making software that have assisted services in managing the growing number of pathways for the best care of patients. There were 27 studies reporting on patient safety in relation to dispatch that looked at the difficulties in introducing new technology (see Table 6), criteria-based protocols, the overtriage for air ambulances, diverting to alternative care pathways and patient safety issues related to language barriers and its effect on treatment delay. The argument for the need of dispatch systems has now been accepted and the required research is about continuous improvement in the sensitivity and specificity of the systems in detecting serious illness or injury and in detecting patients suitable for telephone advice only. The system failures reported in these studies related to the introduction of computer-aided dispatch systems in ambulance control centres have been largely overcome. The work on safety of the individual protocols for dispatch systems is mostly old and much research relates to specific conditions rather than the entirety of dispatch.
There is little published research on the safety and effectiveness of support systems used in dispatch that looks at true outcomes rather than adherence to the system (Table 6). Much has been superseded by new protocols and support systems. The new dispatch system being adopted across England, NHS Pathways, does not yet have published peer reviewed research to support it, although in an interim evaluation, Turner et al. 64 evaluated outcomes for non-ambulance response calls and concluded that it was as safe as the current system in use by ambulance services in England. Other research is limited on the degree to which language barriers are an issue in delaying treatment. However, given that 2.8% (13,690/496,678) of patients receiving either telephone advice or a face-to-face response contact the ambulance service again within 24 hours following closure of the call or discharge of the patient, it is clear that research exploring the safety of these systems for patients is required. This is in addition to gaining an understanding of the saving in resources that might result.
| Authors, year, study design, country | Population, patient number | Intervention/process or topic | Results | Headline |
|---|---|---|---|---|
| Jones et al. (on behalf of the ESCORTT group), 2012,355 retrospective chart review, UK | Calls to EMS, n = 592 | Dispatch/relationship between reported symptoms and dispatch in cases of stroke | Most frequently reported symptoms were collapse or fall (26%) and stroke (25%). Callers identifying patient with having a stroke were correct in 89% of cases. Calls were dispatched as stroke in 45% of cases. Of the first reported signs, Face Arm Speech Test stroke symptoms were mentioned in < 5% of the cases. However, speech problems were the most commonly reported signs | Callers who contacted EMS for suspected stroke were often correct. Calls categorised as stroke by the emergency medical dispatcher were commonly confirmed as stroke in the hospital |
| Zimmer et al. 2010,109 prospective observational design, Germany | Paramedics, n = 80 | Dispatch/40 video emergency dispatch scenarios | There were > 7 unsafe acts per scenario. The number of unsafe acts per dispatch scenario (mean ± SD) were: advanced life support 6.8 ± 3.9; bronchial asthma 8.1 ± 3.9; pulmonary embolism 4.0 ± 1.6; multiple trauma 9.3 ± 3.2 | Considerable number of unsafe acts and poor communication |
| Deakin et al. 2009,69 retrospective call analysis, UK | Patients having called ambulance service and admitted to hospital, n = 4810 | Dispatch/sensitivity of telephone-based triage software to identify stroke patients | 126/4810 patients were diagnosed as having a stroke. The sensitivity of AMPDS version 11.1 software (Priority Dispatch Corporation, Salt Lake City, UT, USA) was 47.62%, the specificity 98.68%. Fewer than one-quarter received highest priority ambulance response | Classification and dispatch for stroke needs strengthening |
| Buck et al. 2009,65 retrospective review, USA | Transported patients, n = 3474 | Dispatch/diagnostic accuracy of the current national dispatch protocol guiding cases of stroke | Dispatchers assigned a code of potential stroke to 44.8% of patients with a final discharge diagnosis of stroke of TIA | Dispatchers fail to recognise more than 50% of potential stroke calls, using MPDS |
| Clawson et al. 2008,133 retrospective observational study, UK | Calls to EMS, n = 1,137,873 | Dispatch/MPDS predicting cardiac arrest and high-acuity chest pain patients | Chest pain-related priority levels were associated with high-acuity illness | Changes required to the MPDS |
| Ramanujam et al. 2008,75 retrospective observational study, USA | Patient cases identified with dispatch determinant of stroke, n = 882 | Dispatch/assessing the accuracy of stroke identification in EMD with high compliance to MPDS protocol and paramedics using CSS | Of 882 patients with a dispatch determinant of stroke using MPDS stroke protocol, 367 had a final discharge diagnosis of stroke (42%). Of 477 patients with a paramedic assessment of stroke using CSS, 193 had a final discharge diagnosis of stroke (40%) | EMD using MPDS stroke protocol with a high compliance has a higher sensitivity than paramedics using CSS in identifying stroke |
| Turner et al. 2008,64 mixed methods (interviews, discussion and document review), UK | Calls to EMS, n = 80,000 | Dispatch/evaluating the accuracy and safety of NHS Pathways | NHS pathways assign 10% fewer calls to category A when compared with other ambulance services. 10% of calls are assigned to 1-hour delay or category C (no ambulance). Only 3% are assigned to alternative responses. Risk of undertriage is low at only 0.034% | NHS Pathways appears to be at least as safe as the current alternative call assessment and prioritisation system used in England. No judgement made whether or not it is a better service |
| Clawson et al. 2008,67 retrospective review, UK | ‘Unknown problem’ situations, n = 3947 | Dispatch/MPDS protocol to distinguish acuity of patients when little clinical information is known | Statistically significant association between clinical dispatch determinant codes and case outcomes was observed. Dispatch protocol for unknown problems successfully differentiates between low-acuity and non-cardiac arrest patients when patient’s information on standing, sitting, moving or talking can be determined | Additional information is needed for MPDS to categorise ‘unknown problem’ calls |
| Flynn et al. 2006,76 retrospective review, Australia | Ambulance dispatch records for suspected cardiac arrest, n = N/A | Dispatch/sensitivity/specificity of MPDS to detect cardiac arrest | The results indicated that cardiac arrests are correctly identified in 76.7% (95% CI 73.6% to 79.8%) of cases | Despite the positive results, room for improvement exists to maximise chances for survival in out-of-hospital cardiac arrest |
| Feldman et al. 2006,70 retrospective review, Canada | EMS calls, n = 102,582 | Dispatch/relationship between MPDS dispatch priority and out-of-hospital Canadian Triage and Acuity Scale | MPDS exhibits a moderate sensitivity and specificity for detecting high acuity of illness or injury. Cardiac arrest protocol was the best-performing protocol | This performance analysis may be used to identify target protocols for future improvements |
| Hinchey et al. 2007,66 retrospective review, USA | ‘Alpha’-coded transports, n = 2121 | Dispatch/appropriateness of assigning alpha using MPDS | Using standard MPDS protocols, dispatchers accurately identified 99% of patients who did not demonstrate high-acuity illness or injury | Using standard MPDS protocols to accurately identify 99% of patients who do not demonstrate high-acuity illness or injury |
| Reilly 2006,80 mixed methods: survey and retrospective review of medical records, USA | Cardiac-related EMS calls, n = 104 | Dispatch/relationship between dispatches of a cardiac nature in a MPD system and the actual clinical diagnosis | 28.6% of the patients were actually diagnosed with a cardiac-related condition. In this suburban community, the MPD system overtriages emergency medical responses to cardiac emergencies | Overdispatch could result in the only advanced life support (paramedic) unit in the community being unavailable in certain situations |
| Price 2006,229 semistructured interviews, UK | Paramedics, n = 20 | Dispatch/response time targets as quality indicator | Response time targets are not evidence based. Paramedics believe response time targets are inadequate quality indicators, are vulnerable to ‘fiddling’ and dominate ambulance service culture | There is a need for less simplistic quality indicators that recognise that there are many stages between a patient's call for help and safe arrival in hospital |
| Heward et al. 2004,63 before-and-after study, UK | Calls with suspected cardiac arrest, n = N/A | Dispatch/identification of cardiac arrest patients with AMPDS | Implementation of AMPDS gave rise to an excess of 200% in the accurate detection of patients suffering from cardiac arrest by EMDs working in emergency communication centre | Implementation of AMPDS increased accurate identification of patients in cardiac arrest |
| Hayes et al. 2004,126 mixed methods, New Zealand | Command and control dispatchers, n = 14 | Dispatch/complex dispatch | Complex decision strategies were made by command and control dispatchers | Decision-making may be enhanced by redesign of displays |
| Schmidt 2003,146 prospective cohort study, USA | Patients in low-acuity triage, n = 656 | Dispatch/diverting 911 calls to appropriate traditional or alternative routes of care using a decision tree | The decision rule allowed 10% of patients to be triaged to an alternative resource | 911 calls may be safely referred to other agencies |
| Dale et al. 2003,129 retrospective review; pragmatic controlled trial, UK | EMS calls: intervention, n = 635; control, n = 611 | Dispatch/telephone assessment and triage for callers who present with non-serious problems | Findings indicate that the assessment of a category C call identifies patients who are less likely to require ED care. Nurses were more likely than paramedics to assess calls as requiring an alternative response to emergency ambulance dispatch | Could have a significant impact on emergency ambulance dispatch rates |
| Wilson et al. 2002,11 systematic literature review, UK | N/A | Dispatch/priority dispatch of emergency ambulances and clinical outcomes | 19.6% of the papers were related to the prioritisation of emergency ambulances, only 6.1% contained original data. Two papers support the concept that criteria-based dispatch improves outcome. Two papers support criteria-based dispatch in improving ambulance utilisation | There is very little evidence to support the effect of the prioritisation of emergency ambulances on patient outcome |
| Holtermann 2002,128 prospective observational study, USA | Patients making a 911 call, n = 1438 | Dispatch-/criteria-based dispatch guidelines | Dispatchers using the criteria-based dispatch guidelines achieved a predictive value of 99% determining who did not require an advanced life support response (sensitivity 89% and specificity 90%) | Trained dispatchers can use criteria-based dispatch guidelines to identify non-urgent 911 callers |
| Thakore et al. 2002,88 retrospective review, UK | Patients, n = 471 | Dispatch/prioritisation of ambulance dispatch | Result shows that a system of directing the ambulance service to true emergency cases would lead to an increase in the number of such patients to survive as well as reducing the risk to ambulance crews and other road users. Hence, response time could be reduced and resources directed towards the true emergency cases | Introduction of priority-based dispatch system could reduce response time and focus on the seriously ill cases |
| Lerner et al. 2000,274 prospective observational study, USA | Ambulance, fire, police and public safety answering points, n = 25 | Dispatch/ quantification of time difference between the multiagency responders and the atomic clock | Time difference ranged from –551 to 117 seconds (mean difference 61.2 ± 120.3 seconds) in week 1 and from –103 to 79 seconds (mean difference 36.9 ± 33.4 seconds) in week 2; time deviations between week 1 and 2: 0 seconds for one centre, 1–30 seconds for 12 centres, 31–60 for four centres and > 60 seconds for five centres. The time difference might be clinically significant for quality improvement tasks and medical legal reviews for which multiple centres are involved | Discrepancies were not consistent over time, with implications for multiagency responses and time-dependent review |
| Nicholl et al. 1999,143 observational study, UK | EMS calls, n = 1126 | Dispatch/safety of priority dispatch systems | Four cases of undertriage according to ‘expert’ panel (serious head injury, child with meningococcal meningitis, cardiac arrest and unconscious in street after hypoglycaemia). Estimated risk of serious underprioritisation was 1 in 2200 | Low-priority C calls should be responded to as soon as possible rather than immediately |
| Porteous et al. 1999,68 retrospective review of medical records, USA | Medical records of patients treated for stroke or TIA, n = 182 | Dispatch/abilities of dispatchers in recognising the symptoms of stroke | Of the 182 patients, 53% used EMS. Dispatcher coded 31% of their 911 calls as stroke. The word ‘stroke’ was used by 51% of callers; only 41% of ambulances were sent at high priority | EMS dispatch protocols should be more sensible for identifying an actual stroke to ensure a more accurate and timely ambulance dispatch |
| Beynon-Davies 1999,356 case history, UK | N/A | Dispatch/London ambulance service computer-aided dispatch system | System failure led to incorrect allocation of resources, for example multiple vehicles dispatched to the same incident or the nearest vehicle not dispatched | System failures are complex and technical, cognitive and organisational aspects need to be considered. Similar finding by Brooks et al. 2008147 |
| Wastell and Newman 1996,144 observational study, UK | Control room operational staff, n = N/A | Dispatch/psychophysiological evaluation (work demand and stress levels) pre- and post-implementation of the ALERT (MIS Emergency Systems Ltd, Northwich, UK) computerised dispatch system | Computerisation of ambulance control room operations was abandoned in London where management was reported to be weak and industrial relations poor. Manchester showed an improvement in meeting the 8-minute target (55.4% pre-ALERT to 64.4% post-ALERT) in a period when the number of emergency incidents increased from 14,300 to 16,500 per month. Heart rate and systolic blood pressure were recorded as higher when using the paper-based system, statistically significant only for blood pressure (p < 0.05) | Need to consider the effects on staff of new working practices |
| Kothari et al. 1995,77 retrospective pre-hospital records analysis, USA | Pre-hospital records, n = 4413 | Dispatch/to evaluate the frequency/accuracy in diagnosing stroke by pre-hospital care system dispatcher, EMTs and paramedics | EMS dispatcher correctly identified 52% and paramedic correctly identified 72% of cases for which a patient actually suffered a stroke or TIA. Pre-hospital personnel arrived at the scene to examine potential stroke patients in a mean of 3 minutes after an emergency call was received by the dispatcher | Pre-hospital evaluation of potential stroke patients can be accomplished promptly after the EMS system is activated |
| Lammers et al. 1995,87 retrospective pre-hospital and emergency ED chart review, USA | Patients with abdominal pain, n = 788 | Dispatch/rates of undertriage/overtriage of six ambulance dispatch protocols | Of the 788 patients included in the study, 7.8% had conditions defined as emergencies. Four of six protocols overtriaged between 10% and 51% and undertriaged between 4% and 7%. None was more effective than another | Dispatch protocols not validated |
Equipment
There was little evidence on issues of patient safety in relation to equipment with only 11 studies identified (Table 7). There was some descriptive research on AEs related to stretcher incidents, but most such cases related to stretcher collapse, although some reports were of patients being dropped. There was some research on defibrillator use resulting in ignition and causing fires and patient injury; however, this is a known hazard and necessary precautions are thoroughly described in guidelines and advanced life support courses. The use of adhesive pads has also resulted in some research relating to defibrillators being outdated for the UK.
| Authors, year, study design, country | Population, patient number | Intervention/process or topic | Results | Headline |
|---|---|---|---|---|
| Dante et al. 2009,32 observational study, USA | Patients in cardiac arrest, n = 50 | Equipment/on-board monitoring of lateral and axial acceleration during transportation | For 49% of journeys, acceleration was > 93 m/s2. For 60% of journeys, there was significant risk of loss of balance | Balance loss may result in injury or poor-quality CPR |
| Wang et al. 2009,158 retrospective audit, USA | AEs involving ambulance stretchers, n = 671 | Equipment/stretcher incidents | AEs involved collapsed stretcher, n = 360 (54%, 95% CI 50% to 57%); broken, missing, malfunctioning parts, n = 189 (28%, 95% CI 25% to 32%); patient dropped or fell, n = 48 (7%, 95% CI 5% to 9%); and fastening failure, n = 4 (1%, 95% CI 0% to 2%). Over half of incidents involved stretcher collapse | Improved feedback mechanisms for the locking system are needed |
| Høyer et al. 2008167, case study, Denmark | Junior doctors undertaking simulated resuscitation, n = 72 | Equipment/defibrillator design | In 5 of 192 of defibrillation attempts, the monitor was powered off leading to a 24-second delay in defibrillation | Redesign may prevent this problem |
| Saini 2007,127 survey, USA | EMS clinicians and paramedic students, n = 39 | Equipment/electronic decision support tools | Paper-based decision support tools rated low for ease of use | Electronic decision support tools are helpful, but some alerts need to be modified |
| Ferreira and Stanley 2005,357 mixed methods, UK | Ambulance clinicians, n = 8 | Equipment/testing a carry chair with wheels vs. the usual carry chair | During descent and ascent a significantly lower force was needed to carry the patient (p < 0.05) | During ascent, benefits were fewer and the task of carrying patients was physically demanding |
| Eckstein and Chan 2004,163 prospective longitudinal study, USA (related Eckstein and Chan, 2003358) | N/A | Equipment/ambulance availability | 21,240 incidents in which ambulances were out of service owing to ED crowding. Median waiting time was 27 minutes | ED crowding has a great impact on ambulance availability |
| Lindstrom 2004,289 case report, USA | Adult female, n = 1 | Equipment/clothing ignited after defibrillation | Patient was obese and in a Stokes basket. Defibrillator use in the vicinity of oxygen has a fire risk, and there may be problems if the patient is hairy or wet | Electrodes should be applied properly |
| Polk et al. 2004,359 case report, USA | Pregnant women, n = 3 | Equipment/portable ultrasonography device in obstetric care | Portable ultrasonography device was successfully used to revise diagnosis during decision-making of whether or not to transport and further management | A portable ultrasonography device is beneficial in giving additional information to air medical personnel |
| Vourvahakis et al. 2002,164 prospective observational study, Crete | Patients, n = 221 | Equipment/laryngeal mask | Patients: 140 cardiorespiratory, 70 respiratory arrest, nine multiple trauma, and two burn episodes. Following a 12-hour training course, paramedics placed the laryngeal mask at first attempt in 94% (208/221) of cases | The laryngeal mask is a valuable tool in the pre-hospital setting |
| Chollet et al. 1999,155 prospective evaluation, France | Checklists, n = 3276 | Equipment/evaluation of checklists for critical equipment on ambulances | 0.5% (16/3276) of checklists not filled out and 19.5% (639/3276) were incomplete. Tested the efficacy of ambulance equipment checklist. After 1 year, there was 100% compliance in using the checklist, mean completion time reduced from 52 ± 19 minutes to 28 ± 10 minutes after 1 year, with 7.6% of incomplete equipment in the field. 7.6% of equipment abnormalities identified could have had repercussions in the field; compliance with checks was 76% at 1 month, increasing to 100% by 1 year | Compliance can be improved with the correct incentives |
| Dahlgren et al. 1997,360 observational study, USA | N/A | Equipment/performance in helicopters, for example exposure to abnormal temperatures, vibration, shock and electromagnetic fields | Ventilators had problems with the driving gas at subzero temperatures and with vibration. Suctioning proved difficult at lower than –5 °C owing to freezing of mucus. The aircraft motor interfered with equipment motors. Plastic tubes were affected by the cold and very sensitive to vibration and shock | Extreme cold can cause equipment issues and, thus, equipment needs to be protected by storing it in appropriately warm areas of the aircraft |
There is little research on the effects of transported patients and equipment being exposed to abnormal temperatures, vibration, shock and electromagnetic fields. However, there is also growing recognition of the potential safety concerns associated with loss of balance that might result in injury and/or poor-quality treatment en route; it is recognised that the rate and depth of compressions are important for quality cardiopulmonary resuscitation (CPR) and off-balancing forces could affect the quality of such techniques to an unknown extent.
Research has shown that equipment failure can have serious repercussions for patients’ safety and the use of checklists, a process borrowed from the aviation industry, has shown some promise in helping avoid such incidents.
Communication
Communication failures are a recognised threat to patient safety. 361 The British Medical Association’s Safe Handover denotes ‘the transfer of professional responsibility and accountability for some or all aspects of care for a patient, or group of patients, to another person or professional group on a temporary or permanent basis’ (quotation reproduced with permission from the British Medical Association). 362 Handover may occur between members of the same profession, for example during nursing shift change or between individuals belonging to different medical professions or even different organisations, such as the ambulance service handover to the ED. Handover is a frequent and highly critical task in clinical practice as it ensures continuity of care and provides clinicians with an opportunity to share information and plan patient care. 363 Ideally, handover should be thought of as a dialogue that creates shared awareness and provides an opportunity for discussion and recovery as participants bring different perspectives and experiences to this interaction. 364,365
There is now a large body of evidence and a number of systematic reviews that suggest that inadequate handover practices are putting patients at risk. 366–370 Inadequate handover can create gaps in the continuity of care and contribute to AEs. 371 Some of the AEs associated with inadequate handover include increased length of stay,372 treatment delays,364,373 repetition of assessments and confusion regarding care. 374 In time-critical environments such as EDs, the additional burden put on already stretched resources owing to inadequate handover poses a risk not only to the individual patients handed over but also to other patients in need of urgent care. 364
Handover practices show a lot of variability and frequently there are no agreed approaches to provide structure and consistency to the handover process. 107,374,375,376–383 This may lead to handovers of very variable quality and it may make the handover process more difficult, in particular for junior staff who need to adapt to different personal styles of their senior colleagues. Studies also found that there is little formal training in handover provided within the curriculum of medical schools and within the organisations themselves. 377,378,380,384–386 Further barriers to effective handover that have been identified in the literature include multitasking and lack of active listening,107 busy work environment and frequent interruptions,387 content omission388 and inconsistent and incomplete documentation. 381,389
There were 20 studies exploring safety issues in relation to communication between health-care professionals and organisations (Table 8). The majority of these were studies involving handover from ambulance clinicians to ED staff. Research indicates that handovers can be stressful, chaotic, short and may omit transfer of important information. In one study, > 60% of relevant data were not related to ED staff. 108 The data most likely to be conveyed included fluid administration, immobilisation details and drug and oxygen administration, although the rates of reporting of these important facts varied markedly between studies. Some studies reported that staff receiving the patient needed to ask for supplementary information; however, it was also found that receiving staff could be inattentive and lack active listening skills necessitating that information previously conveyed needed to be repeated. It is suggested that three factors influence handover quality: information transfer, shared understanding and the working environment.
| Authors, year, study design, country | Population, patient number | Intervention/process or topic | Results | Headline |
|---|---|---|---|---|
| Siemsen, et al. 2012,122 interview study (semistructured), Denmark | Interviews, n = 47 | Handover/health-care professionals’ attitudes and experiences | We identified eight particular factors having an impact on patient safety in handover: communication, information, organisation, infrastructure, professionalism, responsibility, team awareness and culture | Study revealed that handovers represent complex situations and that the organisation did identify patient handover as a critical safety issue |
| Bergrath et al. 2011,98 prospective observational study, Germany | 29 EMS teams, each consisting of one physician and two paramedics | Documentation/standardised simulated case scenarios (STEMI and multiple trauma) | Use of telemedicine resulted in no significant difference in documentation. STEMI scenario: total of 140 medications given – 22% (31/140) incorrect documentation and 10% (14/140) undocumented; multiple trauma: total of 138 medications given – 22% (31/138) incorrect documentation and 12% (16/138) undocumented. Blood pressure and ECG rhythm were mainly complete and documented correctly; 12-lead ECG diagnosis, onset of symptoms often incorrect or undocumented | Patient care documentation weak even in optimal, stress-free situations. Monitors storing vital data could improve documentation |
| Rehn et al. 2011,390 observational study, Norway | Emergency service personnel, n = 93 | Communication/the use of Optimal Patient Evacuation Norway (OPEN) | Improved interdisciplinary co-operation (p < 0.001) | It is possible to improve patient transportation |
| Dalto et al. 2011,111 retrospective observational study, USA | Quality assurance reports submitted in 2009 for transport of adults, children and neonates, n = 278 | Communication/errors | 64 communication errors were identified in 58 reports (21% of 278). Of the 64 identified communication errors, only 28% (18/64) were classified by the staff as communication errors; 66% (42/64) failure to establish a channel; 33% (21/64) failure of having a shared mental model; and 2% (1/64) level 2 error | Recognition and classification of communication errors need to be improved |
| Waldron and Sixsmith 2011,108 survey, USA | Surveys of ED physicians on cases brought into ED by paramedics. Phase 1 (usual triage), n = 163; phase 2 (research assistant referred handover information), n = 116 | Communication/transfer of information from paramedic to ED physician | Mode of arrival correctly identified by physician in 86% (140/163) of cases in phase 1 and 85% (99/116) in phase 2; identified all procedures performed in 16% (phase 1) vs. 47% (phase 2); identified administration of any oral medication in 83% (phase 1) vs. 91% (phase 2) | Physicians remain unaware of most out-of-hospital procedures and medications given to their ED patients. The addition of a verbal report offers only a modest improvement in overall accuracy |
| Evans et al. 2010,102 prospective study, Australia | Handovers of trauma patients, n = 25 | Handover/information loss between scene and trauma centre | 75% (171/228) of data items handed over by paramedics were documented by trauma team. Trauma team least likely to document treatment provided in pre-hospital setting and signs and symptoms in in-hospital setting. 9% of information was not documented by either paramedics or trauma team, resulting in lost information | High level of information not documented |
| Meisel et al. 2010,105 prospective observational study, USA | Handovers, n = 60; paramedics, 39%, emergency medicine technicians, 61%; hospital staff, 5% | Handover/discordance between record and verbal report | Handover time was 5 seconds to 22 minutes (median 1.79 minutes); 31% had ≥ 1 abnormal vital sign on record, of these, 69% were reported as normal or not reported at all | Discordance was not associated with patient or provider characteristics, or any situational variable |
| Greenwood and Heninger 2010,103 retrospective case report, USA | Trauma patient during interfacility transport, n = 1 | Communication/investigating EMS communication failure | Trauma patient during interfacility transport, n = 1 | Structured forms of communication are critical for limiting failure in high-risk medical settings |
| Manser et al, 2010,110 mixed-methods design (observation and questionnaire), Switzerland | Patient handovers, n = 126 | Handover/development of a rating tool | Three factors influenced handover quality: information transfer (p ≤ 0.001), shared understanding (p ≤ 0.001) and working atmosphere (p ≤ 0.01) | Interdisciplinary dynamics in addition to information transmission affect the quality of handover |
| Deakin et al., 2010,101 review of records, UK | Calls, n = 42 | Communication/telephone CPR for bystander CPR | 45% (19/42) cases were confirmed as cardiac arrest. Bystander CPR rate was 68% (13/19) cases. Telephone CPR instructions increased the number of children who received bystander CPR. Effectiveness limited by delays delivering basic life support | Efficacy of telephone resuscitation scripts unknown |
| Frakes et al. 2009,115 prospective review, N/A | Patients transferred to hospital receiving medication, n = 42 | Documentation/medication documentation and reporting intervention; a prompted second verbal report | A significant increase in documentation accuracy (p < 0.05) was reported; 64% (27/42) of cases had full details of medications administered documented | Problems remain with communication regarding medication |
| Cwinn et al. 2009,99 retrospective review, Canada | Patients transferred from nursing home to ED, n = 384 | Communication/frequency and type of clinically important information gaps | Important information gaps occurred in 86% of cases. Information gaps in reason for transfer, baseline cognitive function, vital signs, advanced directives, medication, activities of daily living, and mobility. Use of standardised transfer was associated with a limited reduction in information gaps | Standardised protocol improves information transfer |
| Owen et al. 2009,107 interviews, Australia | Paramedics and hospital receiving staff, N = 50: paramedics, n = 19; nurses, n = 15; doctors, n = 16 | Handovers/perceived problems | Problems perceived by staff: number of handovers, stressful and chaotic ED, short handover period, lack of training for giving handover and difficulties in receiving staff retaining verbal information. Recommendations were made to ameliorate these deficiencies | Standardised approach needed with multidisciplinary training |
| Grow et al. 2008,104 retrospective observational study, USA | All patients for whom an ambulance was dispatched, n = 629,738 | Communication/treatment delays resulting from language barriers | 2.4% (15,620/629,738) experienced pre-hospital delay with 0.3% (2052/629,738) experiencing treatment delay secondary to language. The most common reasons were weather (45.5%), language barrier (13.1%) and prolonged extrication (6.9%) | Language can be a barrier to care in the pre-hospital setting |
| Jenkin et al. 2007,119 survey, UK | ED staff and ambulance clinicians, n = 80 | Handover/patient handover at ED | ED staff should demonstrate active listening as handover information needed to be repeated | Handovers for critically ill patients should be delivered in two stages, with immediate information given and then followed up after initial treatment |
| Meisel et al. 2006,120 retrospective review, USA | n = 578 patients transferred to the ED | Documentation/transferring pre-hospital trip sheet data to patient notes | In 35% (203/578) of cases, important clinical variables such as low blood glucose, abnormal blood pressure, pulse rate, oximetry, drug allergy or medications administered were not recorded from the trip sheet to the patient’s notes | Some important clinical information was not transferred from the pre-hospital record to the patient’s notes |
| Brady et al. 2004,117 prospective observational study, USA | Patient handovers, N = 296: 27% chest pain; 26% motor vehicle crash; 16% dyspnoea; 15% fall; 11% seizure; 5% stroke; 1% assault | Handovers/from EMS to ED | 296 handovers: 44% (1947/4425) of possible data were transferred; 37% (1649/4425) of transferred information was offered by emergency services; 7% (298/4425) were requested by ED personnel. No significant difference was seen between participant satisfaction and the amount of information transferred (p = 0.85) | Incomplete information given to ED personnel. Physician satisfaction was not related to the number of data relayed |
| Sillesen et al. 2004,391 observational study with historic control group, Denmark | Patients with clinical signs of acute myocardial infarction, N = 107; n = 17 received primary PCI | Communication/ECG transmission to cardiologist | 86% of ECGs were transmitted successfully. No difference in pre-hospital time between groups. Significant difference of 68 minutes for door to intervention for the intervention group (p < 0.05) | Transmission of pre-hospital ECG can reduce time to treatment for patients with STEMI |
| Thakore and Morrison 2001,177 survey, UK | Ambulance clinicians to medical staff, n = 97 | Handover/at ED | Medical staff: handovers were variable between crews and radio reports were not well structured (especially in the context of self-poisoning, paediatric emergencies and chest pain). Medical staff were generally less satisfied with the reporting of vital signs than the history provided. Ambulance crews: medical staff did not pay attention. Ambulance crews were satisfied with handover quality | Need a consistent approach and training |
| Strong and Thompson 2000,114 retrospective review, USA | Reports of trauma patients transferred via helicopter emergency medical service, n = 48 | Documentation/medication documentation and reporting | 1012 decisions in 48 reports, grouped to yield 48 unique decisions, top 10 most frequent decisions were analysed. Adequate documentation was found to support decision-making of top 10 problems (fluids, immobilisation, ventilation, oxygen, safety, monitor, intubation, i.v. access, hot/cold load, neuromuscular blockage) | Documentation supports decision-making, but rationale is not usually documented |
Many studies argued the need for a standardised approach to handovers combined with training in order to improve patient safety and ensure important information concerning the patient’s illness, medical history and treatment received is related to the receiving staff. It has also been suggested that training in this area would be beneficial.
The findings and suggestions for improvement are largely consistent with the general literature on handover (see Communication and Table 8). More recently, the use of the age, time, mechanisms, injury, signs, treatments (ATMIST) protocol has been recommended for use for the handover of trauma patients. As with other standardisation attempts of handover [e.g. the use of situation, background, assessment, recommendation (SBAR)], the aim is to provide structure to the communication process, thereby ensuring greater reliability and potentially also speeding up the handover. ATMIST is an example of a tool developed specifically for a particular context (trauma patients), as opposed to generic tools, such as SBAR. ATMIST can also be used for handover of medical patients (note that ‘M’ changes its meaning to medical complaint and ‘I’ to investigations in this context). There is a need for studies that investigate the impact of the use of tools such as ATMIST. 375
There is a lack of research on the systems aspects of communication, for example the performance-influencing factors that impact on the quality of handover. There is a current research project looking at emergency care handover including the handover from ambulance service to ED,392 which addresses these issues and summarises the existing literature.
Discussion
The scoping systematic review identified a total of 330 studies covering a wide range of topics that explored different aspects of safety in the pre-hospital health-care setting. The majority of the evidence was directed towards assessment, management and treatment. Although there was evidence exploring ambulance dispatch systems at the time of their introduction, there is little evidence to support improvements. The large numbers of papers, the low quality of much of the research and the lack of uniformity of methodologies has made synthesis of the evidence complex. A narrative approach has been utilised because data could not be combined and the resources for a scoping exercise prevented more in-depth analysis.
In line with the remit to map the evidence, a research grid identifying 25 topic areas was developed (see Figure 2). This enabled the evidence to be presented by primary and secondary topics and highlight areas in which research has been undertaken. It should be noted that topic areas are not mutually exclusive and individual publications may be listed under multiple areas.
The key findings of the scoping literature review were:
-
conflicting evidence on the clinical effectiveness of helicopter transfer, but recognised as more expensive
-
transmission of patient data from scene may be useful if it adds to the skills of a paramedic
-
lack of evidence regarding transfer of critically ill children
-
delay in offloading patients at the ED is recognised as a significant risk
-
mixed evidence on endotracheal intubation; further studies are already in progress
-
direct transfer (bypassing local units) shown to be clinically effective for some conditions
-
paucity of evidence on safety of intravenous fluids
-
lack of specific evidence regarding medication safety in pre-hospital care
-
evidence supports non-conveyance of some specific conditions, for example epileptic fits and hypoglycaemia
-
training requirements to support non-conveyance are not well described and, therefore, limit implementation
-
research on non-conveyance is generally poor quality
-
culture is blamed for poor reporting, but a causal link is poorly demonstrated
-
lack of any direct measurement of aspects of safety culture
-
most evidence on dispatch systems is historical from the time of introduction
-
lack of evidence of safety of developments of ambulance dispatch using patient outcome measures
-
research on ambulance handover has shown use of various tools may improve quality
-
lack of research on systems factors influencing quality of handover.
Chapter 4 Document review and analysis
In response to changes in out-of-hours cover and the national pressure to reduce hospital admissions, the scope of ambulance service activity has changed dramatically in both volume and breadth over the last 10 years. The principles of ‘see and treat’ (ambulance staff assessing and completing relevant treatment without onward transport) have evolved so that ambulance services increasingly take responsibility for an entire patient health-care episode. As a result, there is an increasing need for a strong patient safety culture in ambulance services that should include positive leadership and an environment that promotes quality and patient safety.
This chapter seeks to identify the prominence of patient safety activity reported in publicly available documents produced by ambulance services. The first element of the review concentrates on the views of ambulance services and perceptions of patient safety. The second element examines issues identified by agencies such as the NPSA, the NHS Litigation Authority (NHSLA) and coroners’ reports under rule 43.
Annual reports and quality accounts
Introduction
Annual reports
NHS foundation trusts are required by law (NHS Act 2006)393 to produce an annual report. Such reports are laid before parliament each year and then published to the wider community. Reports follow a defined structure394 that specifies a directors’ report including a management commentary, a remuneration report, the disclosures set out in the NHS foundation trust code of governance, a quality report, staff survey, regulatory ratings, other disclosures in the public interest, a statement of the accounting officer’s responsibilities and an annual governance statement.
NHS organisations can highlight information such as:
-
patient care activities
-
descriptions of how an NHS trust uses its foundation trust status to develop services and improve patient care (note that at the time of this research, no ambulance trusts had achieved foundation trust status)
-
performance against key health-care targets
-
procedures for monitoring health-care improvements and progress towards national and local targets
-
information concerning Care Quality Commission (CQC) assessments
-
the response of the NHS foundation trust to recommendations, progress towards targets, key quality improvements, new or revised services, service improvements, improvements in patient/carer information and information on complaint handling.
Quality accounts
Quality accounts are annual reports generated to describe service quality to the public. 395 The primary purpose of quality accounts is to ‘encourage boards and leaders of healthcare organisations to assess quality across all healthcare services they offer. They allow leaders, clinicians, governors and staff to demonstrate their commitment to continuous, evidence-based quality improvement, and to explain their progress to the public.’ [© Crown copyright 2010, Contains public sector information licensed under the Open Government Licence v2.0 (URL: www.nationalarchives.gov.uk/doc/open-government-licence/version/2/)]. 395 The first statutory quality accounts were published in 2011, covering activity for 2009/10.
The content of quality accounts is less stringently regulated than that of annual reports. Although some parts of a quality account are mandatory, most content can be determined locally. Mandatory elements are:
-
review of ambulance services
-
decisions on areas of improvement (at least three priorities) that the service commits to for the next year and is required to report on at the end of that year
-
national and local audits
-
clinical research
-
Commissioning for Quality and Innovation goals
-
a CQC statement
-
data accuracy.
Aim
The aim of this study was to identify, characterise and compare patient safety issues, activities and priorities in English ambulance services by analysing annual reports and quality accounts.
Methods
A document review of ambulance trust annual reports and quality accounts was conducted. Annual reports for the period 2010/11 and quality accounts for the period 2010/11 were retrieved for all English ambulance trusts from their respective websites.
Annual reports
Annual reports were read in their entirety by one researcher. Subsequently, two annual reports were coded using descriptive coding. The researcher applied codes to describe the topic of data items that had a relevance to patient safety using the definition of patient safety and the inclusion criteria predefined for the systematic review. Unrelated data were discarded. The coding for these two annual reports was reviewed by a second researcher during meetings. Disagreements were resolved in discussion. The remaining annual reports were then coded by one researcher independently (these can be viewed in Appendix 6 or at www.warwick.ac.uk/ambulancesafety). Main categories of topic areas were identified in a project meeting through clustering of the codes.
Quality accounts
Quality accounts were read in their entirety by one researcher. Data items that described trust priority areas for 2010/11 relating to aspects of patient safety were coded using descriptive codes. Owing to the structured nature of quality accounts, no review by a second researcher was deemed necessary. Main categories of trust priorities relating to patient safety were identified in a project meeting through clustering of codes.
Results
Annual reports
Annual reports for all English ambulance services (n = 11) were identified and reviewed. All reports followed the prescribed structure in terms of director and finance reporting; they ranged in length from 35 to 173 pages with considerable variation, for example in style and the number of illustrations.
Searching the annual reports for the free-text term ‘patient safety’ produced a range of hits (Figure 3); one service did not mention ‘patient safety’, whereas three ambulance services dedicated a whole chapter to the topic. The absence of the identifying phrase ‘patient safety’ does not necessarily mean that an annual report failed to discuss safety concerns or activities; the ambulance service (service 2) that did not use the phrase provided considerable data concerning improved turnaround times that had been identified as a system issue with a detrimental effect on patient care; the use of control centres providing senior-level clinical advice to address hear and treat/referral demands; and public engagement to collect feedback and patient experiences while promoting an open and fair culture. Furthermore, ambulance service 2 mentioned ‘patient safety’ eight times in its quality account for the same year. As such, the search for the term ‘patient safety’ was not a rigorous identifier of such activities.
FIGURE 3.
Number of times ‘patient safety’ was mentioned in annual reports and quality accounts by 11 English ambulance services.
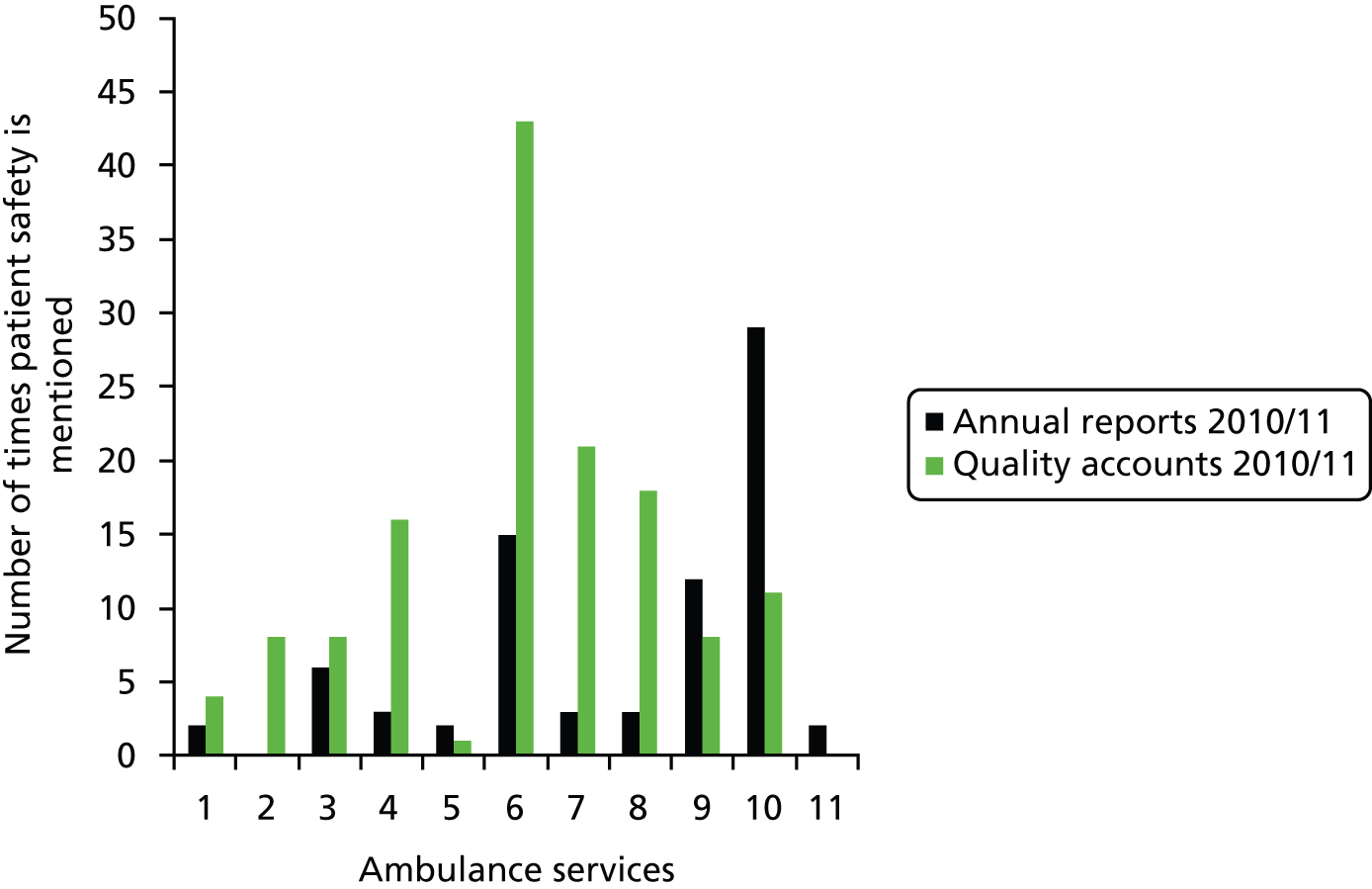
The detailed review of the text of each report identified the following categories of topic areas:
-
reported patient safety issues: cleanliness and infection control, safeguarding, response time targets, other (including patient falls, handover delay, dementia and pain management)
-
improved care: NHS and alternative pathways, patient record forms, see/hear and treat/refer, other (including medicine management, computer-aided dispatch, new equipment and training and skill enhancement)
-
incident reporting and complaints
-
CQC compliance status
-
NHSLA level
-
recognition of new clinical indicators
-
public involvement: patient experience, end-of-life care
-
patient safety activities: campaigns, research, other (patient questionnaires)
-
safety culture including non-punitive reporting systems and being open
-
internal control
-
foundation trust status.
These categories of safety topics included methods of performance measures (numbers 4–6 and 11 above) and issues/activities concerning patient safety (numbers 1–3 and 7–10 above). Topic areas in both types of categories show that annual reports tended to focus on service performance and compliance with national standards.
Quality accounts
The consistent structure used for quality accounts enabled analyses to focus on safety priorities identified by ambulance services for 2010/11. Five of 11 English ambulance services did not group priorities under the areas of patient safety, clinical effectiveness and patient experience while the other six did; only two ambulance services clearly stated whether their 2010/11 priorities had been met.
Review of the areas prioritised by 11 English ambulance services in 2010/11 identified activities grouped under the six categories (Figure 4). Infection prevention and control was prioritised by seven ambulance services; safeguarding was prioritised by four ambulance services; patient safety incidents and culture were prioritised by four ambulance services; use and development of care pathways was prioritised by four ambulance services; the improvement of operational effectiveness was prioritised by five ambulance services; and public involvement and response to public needs was prioritised by four ambulance services.
FIGURE 4.
Categories of trust priorities and number of ambulance services prioritising these categories in 2010/11.

Operational effectiveness and public engagement are usually associated with patient experience rather than patient safety; only two such activities were clearly stated as patient safety priorities.
Activities to promote or prioritise patient safety that were reported by ambulance services in annual reports and quality accounts comprised:
Infection prevention and control
-
review and standardisation of cleaning products
-
training and audit
-
appointment of an infection control nurse specialist/lead for infection prevention and control/hygiene assistants
-
infection prevention and control notice boards
-
job descriptions obliging new staff to comply with infection prevention and control policies and procedures
-
improved availability of hand-washing materials
-
provision of spill kits and sanitary wipes
-
issuing regular letters to staff to remind them of the importance of training
-
roll-out of the ‘cleaner care’ initiative.
Safeguarding
-
partnership work with other trusts
-
job descriptions obliging staff to make safeguarding a priority
-
education and awareness
-
advice and information provision on the staff intranet
-
revision of a referral system
-
communication with relevant agencies across the region
-
increasing the number of safeguarding referrals
-
introduction of a single point of access to which crews refer.
Patient safety incidents and culture
-
improved reporting of patient safety incidents
-
development of patient safety strategy through four work streams
-
education and awareness
-
use of the SBAR technique as a structured communication tool
-
introduction of patient safety visits
-
commissioning of programmes with the NHS institute for innovation and improvement
-
cultural and safety surveys of staff
-
monitoring of medication errors to ensure mitigation before trends develop
-
introduction of a ‘managing medicines’ group
-
employment of ambulance pharmaceutical advisor
-
referral of patient experiences to the board.
Care pathways and clinical decision-making
-
introduction of new care pathways for stroke, heart attack and major trauma
-
facilitating continuous accessibility to stroke thrombolysis
-
public engagement
-
partnerships across different NHS bodies
-
introduction of pre-hospital therapeutic hypothermia
-
reinforcement of the ‘see and treat’ procedure.
Operational effectiveness
-
optimising patient handover by increasing the rate of patient care record submission, posting patient care record submission audit findings on the staff intranet, reintroduction of security wallets and use of an archiving company
-
improving availability of vehicles and equipment for staff
-
new care triage system for NHS pathways
-
identification of frequent callers and supporting nursing homes to prevent unnecessary calls
-
increasing the number of registered paramedics
-
electronically linking the patient care record to the initial emergency call to ensure completeness of health-care records and improved care quality
-
use of electronic patient care records
-
initiation of a learning academy for new call takers and protocol review for existing call handlers.
Public involvement/identifying patient needs
-
partnership with other health-care providers to reduce the number of calls and admissions
-
establishment of systems for entering end-of-life management plans into call centres
-
education of staff in regional hospices
-
development of a clinical dashboard to inform the public about care quality
-
recruitment of an end-of-life project lead
-
development of rapid transfer procedures to enable end-of-life patients to die in a setting of their choice
-
development of the ‘chain of survival’ partnership
-
recruitment of additional community-first responders, staff responders and introduction of public-access defibrillators.
We mapped the themes identified in the literature review to the themes that were identified in the review of ambulance performance documents, Figure 5. There were matches between fifteen (green boxes on Figure 5) domains out of the 25 domains identified during the literature review. Reporting in the ambulance documents universally followed a fairly standard pattern of (1) description of problem, (2) description of proposed/implemented solution and (3) effect of solution. Although there was modest agreement between the topics identified through the literature search, we found no references that the patient safety literature had been consulted in scoping the solutions to the patient safety issues identified.
FIGURE 5.
Mapping domains identified in the literature review and review of ambulance service documents.

Discussion
Exploring the published annual reports and quality accounts of ambulance services provided evidence that issues related to patient safety were frequently reported in these documents. There was a lack of concise or consistent terminology used when describing patient safety issues. This meant that at times it was difficult to clearly identify issues as patient safety as opposed to delivery of clinical care. It was noted that most reporting occurred in relation to reporting performance against external targets such as EMS response time, infection prevention and control, etc. Although this provides some reassurance that performance targets are identifying issues about patient safety, the apparent lack of a systematic approach from a patient safety perspective in most services raises uncertainty about the comprehensiveness or thoroughness by which patient safety issues are addressed. It further suggests that performance measurement drives safety initiatives and that a culture of meeting targets is deeply engrained. For example, infection prevention and control was the area that more than half of ambulance services prioritised in 2010/11. Activities in this area focused on staffing, training and raising staff awareness; however, no reports of infection due to uncleanliness were described to explain why these activities were initiated.
Activities grouped under care pathways included the prioritisation of alternative pathways for stroke and trauma patients in order to reduce hospital admission, reflecting a response to national priorities. Patient safety activities also reflected the uptake of ideas relating to the Patient Safety First campaign, although only five ambulance services signed up. The review did identify examples of best practice and these are highlighted particularly in category 2 above (see Results, Annual reports) and included attempts to improve reporting of patient safety incidents through staff engagement. The SBAR was adopted by one service to improve communication, particularly around handover.
There was a degree of commonality between the categories identified in these reports and the high-level themes identified during the literature review (15 out of 25 matches). We found no evidence that the contemporary literature had been consulted by ambulance services in scoping solutions to the problems identified. However, as reported in Chapter 3, the bulk of the literature focused on assessment, management and treatment, which may explain the lack of drawing on published evidence to scope solutions to patient safety problems.
This review aimed to understand ambulance service perceptions concerning patient safety but is based on what the ambulance services report in official documents, the format and subheadings of which are centrally prescribed. It is therefore possible that patient safety activities may not be fully reflected in the content of these reports. From these reports, the extent to which ambulance services prioritise patient safety cannot be determined and the question remains whether or not the way ambulance services think about safety and the way in which it is reported should be addressed.
Conclusions
There is little consistency regarding the information on attitudes and approaches to patient safety as presented in the official reports produced by ambulance services. The apparent lack of a common language and terminology makes it difficult to determine the extent to which patient safety is being addressed within ambulance services. This hinders the ability to draw conclusions whether or not the safety issues perceived as priorities for ambulance services meet the patient safety needs identified by organisations such as the NPSA, NHSLA and by coroners’ reports.
National Patient Safety Agency patient incident report data
Introduction
In 2000, the Department of Health published four requirements to be met by the NHS to facilitate learning from AEs, comprising:
-
unified mechanisms for AE reporting and analysis
-
a more open culture in which errors or service failures can be reported and discussed
-
mechanisms to ensure that when lessons are identified, the necessary changes are put into practice
-
a wider appreciation of the value of the system approach to preventing, analysing and learning from errors. 1
The NPSA was established in 2001 to identify patient safety issues nationally, collate confidential incident reports and find appropriate solutions to the causal event, and provide feedback to enable organisations to improve patient safety. 2 The resulting patient safety incident report data are published on a 6-monthly basis for every health-care trust. They present statistics on reported patient safety incident types according to NPSA categories, publish a comparison of the statistics for individual organisations and assess reports of incidents and near misses by looking at the frequency of reporting and degree of harm. Trusts receiving the reports are encouraged to act on them to improve patient safety. The first NPSA Patient Safety Incident Report data were published in March 2009. 396
Aim
The aim of this study was to review NPSA incident report data for English ambulance services to consider the occurrence of patient safety incidents and the main incident types.
Methods
Incident report data for English ambulance services were accessed and downloaded from the Organisation Patient Safety Incident Reports on the NPSA website397 for the reporting periods from:
-
April 2010 to September 2010
-
October 2010 to March 2011
-
April 2011 to September 2011.
Data for the individual ambulance services were collated in a single database and displayed comparatively using descriptive statistics and a summary of trends was reported. It was initially hoped that some secondary analysis of data might be possible. Unfortunately, because of the reorganisation of the NPSA, it was not possible to obtain this level of data in the required timescale.
Results
Figure 6 shows AEs reported by the 10 English ambulance services during the 6-month assessment periods from April 2010 to September 2011. Ambulance services are presented in order of decreasing size (resident population served in 2010/11). When considering the data for April to September 2011, there is a trend for ambulance services serving greater numbers of people to report more incidents. For four ambulance services (East of England, West Midlands, London and North East) AE reporting increased from April 2010 to September 2011 and, in contrast, the numbers of AEs reported decreased for the North West, Yorkshire and South Western. In London and the North East the number of events reported increased dramatically by three and eight times, respectively, for April to September 2011 as compared with the previous 6-month period. For the other trust areas the number of AEs reported fluctuated over the assessment period.
FIGURE 6.
Incidents reported to the NPSA by ambulance trusts in 2010–11. a, Ambulance services that joined the Patient Safety First campaign.

The percentage of reported incidents per 999 call is highly variable between ambulance services, with a range from 0.042 to 0.165 (Table 9). It is recognised that the variation in reporting rates has two main influences: a low rate may be caused by a failure to report incidents within the organisation, which may be related to organisational culture; however, a low rate may, more rarely, also be due to few incidents. In most scenarios, it is generally accepted that a high rate of reporting of low-level incidents is a positive sign and indicates a culture open to learning from such reports. Without more detailed analysis, including looking at the ratio of severe to minor incidents reported, no further judgement can be made on the significance of this variation.
| Ambulance trust | Number of incidents reported to NPSA | Number of 999 calls | % incidents per 999 call |
|---|---|---|---|
| East Midlands | 531 | 893,067 | 0.059 |
| East of Englanda | 625 | 1,040,073 | 0.060 |
| Great Western | 166 | 394,251 | 0.042 |
| London | 935 | 1,587,198 | 0.059 |
| North East | 253 | 542,226 | 0.047 |
| North West | 1152 | 1,351,995 | 0.085 |
| South Centrala | 261 | 585,111 | 0.045 |
| South East Coasta | 242 | 871,551 | 0.028 |
| South Westerna | 986 | 596,870 | 0.165 |
| West Midlandsa | 706 | 1,095,653 | 0.064 |
| Yorkshire | 832 | 923,840 | 0.090 |
Delays in reporting AEs to the NPSA are summarised in Figure 7. In the reporting period from April 2011 to September 2011 the mean time to reporting incidents to the NPSA was 36 days.
FIGURE 7.
The time delay in reporting incidents to the NPSA by English ambulance services in 2010–11 (the line indicates the mean reporting delay of 36 days).

Figure 8 shows the proportion of incidents reported by ambulance services in comparison with other care environments and suggests that ambulance services may be less likely to report than other hospital settings. However, it is possible that differences may relate to the sizes of the different care settings and the duration of care (ambulance services care for patients for a very short period of time compared with other NHS organisations).
FIGURE 8.
Proportion of AEs reported to the NPSA by different care settings for a 3-month reporting period between April 2010 and March 2011. This figure is based on dates that incidents were reported to have occurred. Data from National Reporting and Learning System, NHS England, reproduced with permission. URL: www.nrls.npsa.nhs.uk/resources/healthcare-setting/ambulance-service/. Contains public sector information licensed under the Open Government Licence v2.0, www.nationalarchives.gov.uk/doc/open-government-licence/version/2/.
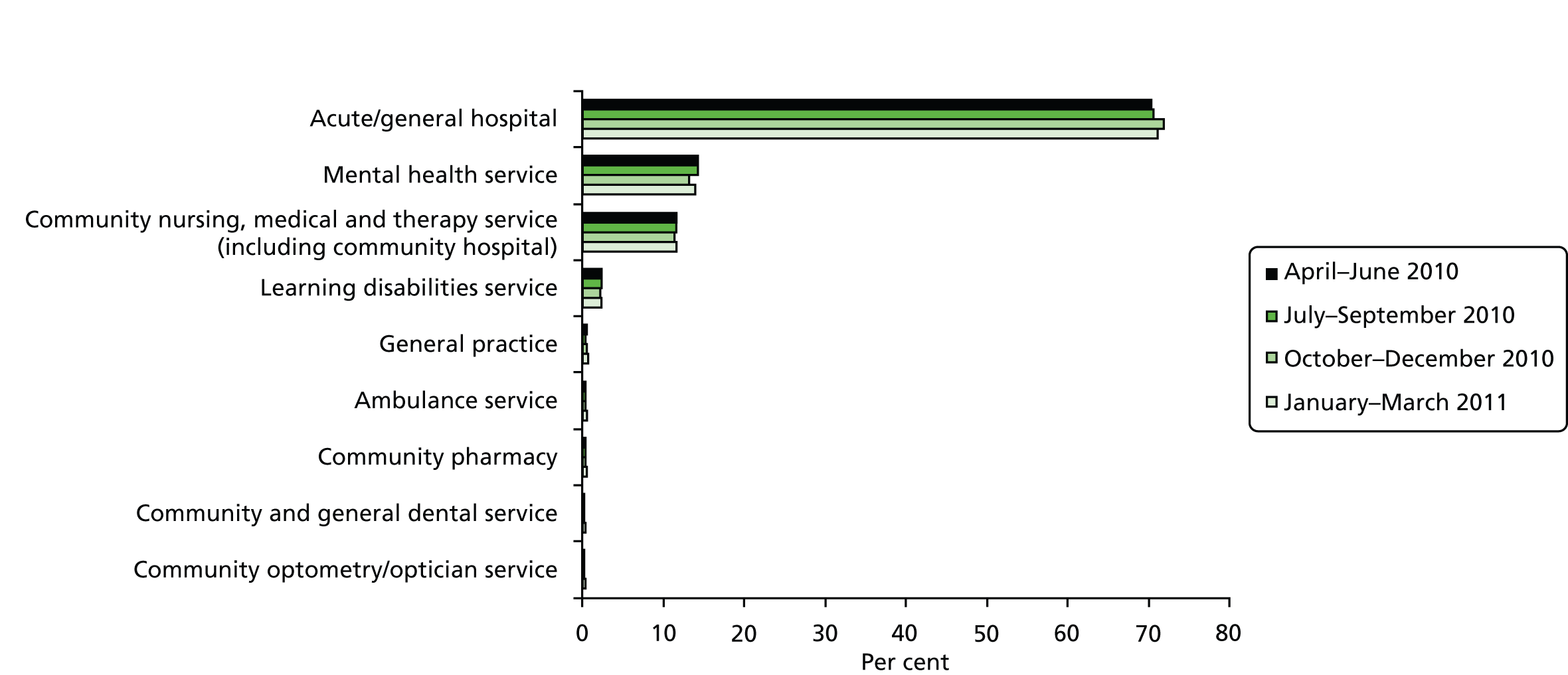
Reporting of AEs to the NPSA by ambulance services classified by incident type is presented in Figure 9; the data suggest that ambulance services most frequently report patient safety issues concerning access, admission, transfer and discharge, and patient accidents (any incident resulting in avoidable harm). Self-harming behaviour and infection control were reported at lower frequencies.
FIGURE 9.
The proportions of incidents reported to the NPSA by ambulance services by incident type (April 2010–March 2011). Contains public sector information licensed under the Open Government Licence v2.0 (URL: www.nationalarchives.gov.uk/doc/open-government-licence/version/2/).
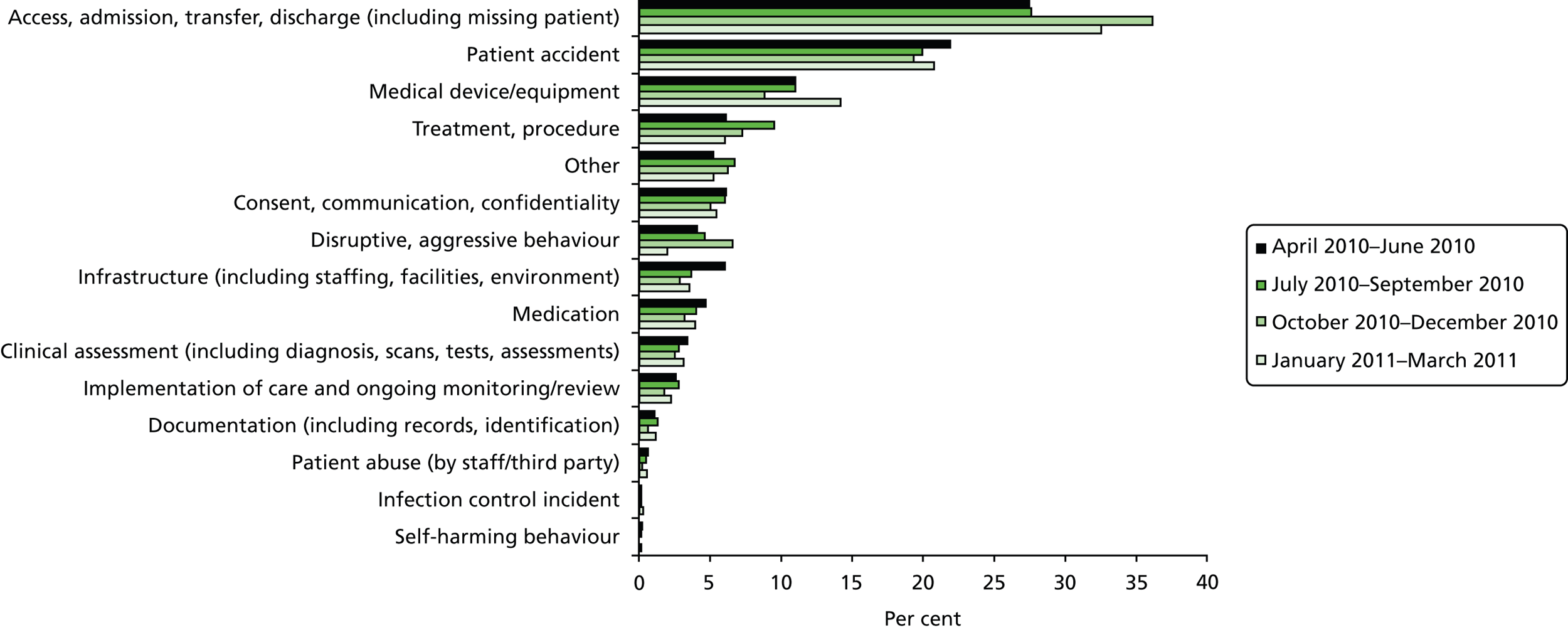
Discussion
The NPSA has developed a system to collate and review confidential patient safety incident reports on a national basis from all care settings. The data are publicly available and a rich source of summary data on AE reporting. This evaluation found that relative to other health-care sectors (e.g. acute hospital trusts, community services and mental health services) ambulance services report small numbers of incidents annually. There is variation in the frequency with which ambulance services reported incidents. This did not seem to be related to the size of ambulance service and may reflect different thresholds for reporting. Consequently, analysis of data reported to the NPSA is likely to miss a number of unreported incidents.
There was consistency over time in the themes that prompted reports. Access, admission, transfer, discharge (including missing patients) were reported most frequently and patient accidents were the next most common incidents; however, the absence of accident reduction activity in the quality accounts and annual reports suggests that ambulance service activity regarding patient safety is not focused on those events that occur most frequently. Therefore, published literature examining incident reports probably also lacks a focus on events that occur with a high degree of frequency.
These categories map to 9 of the 25 topic areas highlighted in the literature review (assessment/management, communication, decision-making, dispatch, equipment, medication, non-conveyance, transfers, and treatment/procedure). This analysis was limited by restricting it to the publicly available material that has been analysed by the NPSA. The reason for this was the abolishment of the NPSA in April 2012, which meant that we were unable to receive the data as we needed them. Overall, the analysis of the National Reporting and Learning System (NRLS) data may help to understand the present safety issues. However, any analysis will be limited because of the classification system of reported incidents, which is designed for secondary care and not ambulance services.
NHS litigation authority data
Introduction
There is an increasing trend towards litigation in health services both nationally6 and internationally. Litigation incurs costs for the NHS health-care budget and finances used would be better spent on patient care. 6 The causes of litigation are varied and include communication errors,103 road traffic collisions,398 negligence, treatment delays,399 and inadequate assessment and/or treatment. It is important to understand the nature of incidents to enable lessons to be learnt by ambulance services.
Aims
The aims of the study were to assess the pattern of litigation claims against ambulance services in England; to consider whether or not the number of cases increases over time; what the causes, outcomes, and costs of litigation are; and what lessons can be learnt.
Methods
This study retrospectively reviewed claims reported to the NHSLA by ambulance service trusts in England over the period 1995/96 to 2010/11. Reports were assessed if they related to the pre-hospital care (including health-care settings allied to pre-hospital care) and litigation arising from emergency and transport services. Incidents could involve adults or children receiving pre-hospital care. As the data set was anonymised, details of the claimant’s age, sex and presenting condition were not provided; sex was sometimes indicated, but was not systematically reported. The anonymised data were collated and analysed using IBM Statistical Product and Service Solutions (SPSS) version 19.0 software (IBM Corporation, Armonk, NY, USA) and the data set comprised 733 cases. One case was input as a negative value and, as the NHSLA was unable to provide an explanation, the case was excluded from analyses.
The main outcome measure assessed was the number of claims that resulted from mistakes and/or poor service and the cost of such claims.
Results
Open compared with closed cases
Of the assessed cases, 20.6% (151/732) were open, 78.6% (575/732) closed and 0.8% (6/732) were classified as ‘incident’ at the time of this study; the definition for incident cases could not be clarified. For all six incident cases, no damages were awarded but all other data points for the claimants were available. Therefore, for the purposes of these analyses, incident cases were treated as open.
Specialties involved
Although the primary specialty involved in the litigation incident was pre-hospital care, 15 other specialties were also involved including accident and emergency (A&E), primary care, mental health services and obstetrics, and dual-specialty involvement accounted for 14.2% of cases (104/732).
Trends in litigation
The number of litigation claims increased over the time period from 1995/6 to 2005/6 and thereafter numbers plateaued. In 1995/6, there were three claims compared with 77 in 2005/6 (Figure 10). Data for 2010/11 were incomplete at the time of this study.
FIGURE 10.
The number of litigation claims per annum from 1995/6 to 2010/11 (n = 733).

Litigation causes
Litigation resulted from a wide variety of causes, and in 8.2% (60/732) of cases was due to multiple factors. The primary cause of incidents is presented in Table 10. Of the 32 categories identified, the most common causes of litigation were lack of assistance (26.1%, 191/732), failed or delayed treatment (18.4%, 135/732), failed or delayed admission to hospital (12.0%, 88/732) and failed or delayed diagnosis (10.8%, 79/732).
| Cause of incident | % (n/all incidents) |
|---|---|
| Lack of assistance/care | 26.1% (191/732) |
| Failed/delayed treatment | 18.4% (135/732) |
| Failed/delayed admission to hospital | 12.0% (88/732) |
| Failed/delayed diagnosis | 10.8% (79/732) |
| Failed/delayed referral to hospital | 6.4% (47/732) |
| Inappropriate treatment | 4.5% (33/732) |
| Failure to recognise a complication | 3.1% (23/732) |
| Failure to supervise | 3.1% (23/732) |
| Inadequate nursing care | 2.6% (19/732) |
| Equipment malfunction | 1.6% (12/732) |
| Operator error | 1.5% (11/732) |
| Lack of facilities/equipment | 1.4% (10/732) |
| Other/unknown/not specified | 2.5% (18/732) |
| Error with agent/dose/route, etc. | 0.8% (6/732) |
| Application of excess force | 0.7% (5/732) |
| Wrong diagnosis | 0.5% (4/732) |
| Assault, etc., by hospital staff | 0.4% (3/732) |
| Failure to act on abnormal test results | 0.4% (3/732) |
| Incorrect injection site | 0.4% (3/732) |
| Slip or trip | 0.4% (3/732) |
| Failure to warn/informed consent | 0.3% (2/732) |
| Fell into/from an object | 0.3% (2/732) |
| Infusion problems | 0.3% (2/732) |
| Medical errors | 0.3% (2/732) |
| Defective tools/equipment | 0.1% (1/732) |
| Inappropriate discharge | 0.1% (1/732) |
| Injuries to others by patient | 0.1% (1/732) |
| Intraoperative problems | 0.1% (1/732) |
| Intubation problems | 0.1% (1/732) |
| Manual handling | 0.1% (1/732) |
| Self-harm | 0.1% (1/732) |
| Failure to carry out observations | 0.1% (1/732) |
The outcome of litigation incidents
A total of 47 outcomes were reported for litigation incidents and 10.1% (74/732) of cases had multiple outcomes. In 25.7% (188/732) of cases, the incident led to death of the patient. Other serious outcomes are described in Table 11. In some cases, the incident outcome had serious and permanent consequences for both the patient and their family in terms of lifestyle and well-being: in 5.5% (40/732) of cases the patient suffered brain damage; other life-limiting conditions included paraplegia (1.5%; 11/732), amputation (1.2%; 9/732), cerebral palsy (1.1%; 8/732), tetraplegia/quadriplegia (1.1%; 8/732), stroke (0.8%; 6/732), partial paralysis (0.3%; 2/732) and incontinence (0.1%; 1/732).
| Outcome of incident | % (n/all incidents) |
|---|---|
| Fatality | 25.7% (188/732) |
| Unnecessary pain | 24.0% (176/732) |
| Fracture | 9.4% (69/732) |
| Brain damage | 5.5% (40/732) |
| Psychiatric/psychological damage | 3.3% (24/732) |
| Poor outcome: fractures, etc. | 3.0% (22/732) |
| Bruising/extravasation | 2.6% (19/732) |
| Spinal damage | 2.6% (19/732) |
| Cardiac arrest | 2.3% (17/732) |
| Additional/unnecessary operation(s) | 1.6% (12/732) |
| Paraplegia | 1.5% (11/732) |
| Amputation (lower) | 1.2% (9/732) |
| Joint damage | 1.2% (9/732) |
| Tissue damage | 1.2% (9/732) |
| Cerebral palsy | 1.1% (8/732) |
| Nerve damage | 1.1% (8/732) |
| Tetraplegia/quadriplegia | 1.1% (8/732) |
| Loss of baby | 0.8% (6/732) |
| Other | 0.8% (6/732) |
| Scarring | 0.8% (6/732) |
| Stroke | 0.8% (6/732) |
| Unknown | 0.7% (5/732) |
| Meningitis | 0.5% (4/732) |
| Other visual problems | 0.5% (4/732) |
| Burn(s) | 0.4% (3/732) |
| Cardiovascular condition | 0.4% (3/732) |
| Dislocation | 0.4% (3/732) |
| Multiple injuries | 0.4% (3/732) |
| Not specified | 0.4% (3/732) |
| Orthopaedic injuries | 0.4% (3/732) |
| Respiratory disorder/failure | 0.4% (3/732) |
| Bladder damage | 0.3% (2/732) |
| Other infection | 0.3% (2/732) |
| Partial paralysis | 0.3% (2/732) |
| Perforation | 0.3% (2/732) |
| Rupture | 0.3% (2/732) |
| Stillborn | 0.3% (2/732) |
| Anaphylactic shock/allergic shock/allergy | 0.1% (1/732) |
| Bowel damage/dysfunction | 0.1% (1/732) |
| Developmental delay | 0.1% (1/732) |
| Facial injuries | 0.1% (1/732) |
| Head injuries | 0.1% (1/732) |
| Incontinence | 0.1% (1/732) |
| Liver damage | 0.1% (1/732) |
| Loss of lung | 0.1% (1/732) |
| Lung disease | 0.1% (1/732) |
| Multiple disabilities | 0.1% (1/732) |
| Oedema | 0.1% (1/732) |
| Reduced life expectancy | 0.1% (1/732) |
| Removal of testicle | 0.1% (1/732) |
| Tendon damage | 0.1% (1/732) |
Location of the incident
Litigation incidents arose at a number of different locations, but most took place in the patient’s home (42.6%; 312/732) or in the ambulance/during transfer to further care (14.8%; 108/732). The remaining locations where the incident occurred are listed in order of frequency: public place, ambulatory care/diagnostic treatment centre, clinical area, A&E, non-clinical area, unknown, call/control centre, support services, general practitioner (GP) surgery, health centre/out-of-hours centre, nursing home, day care services, outpatient department, prison/remand centre, residential care home, dental surgery, or intermediate care setting.
Costs of litigation
For most closed litigation claims (60.2%; 346/575) no damages were paid. The highest amount awarded was £2.8M, with an average cost per settlement of £10,591.57. The highest settlements (≥ £500,000) were for cases of brain damage. Costs were incurred by claimants undertaking litigation and the highest cost reported was £200,000. The average cost for claimants was £4526.88 [standard deviation (SD) £16,296.28]. Costs for defending claims were also reported, with the highest being £122,160.06 and the average cost of defence being £2482.65 (SD £8584.45).
The total cost of claims per year was highest in 2001/2 when settlements reached £3.5M, after which there was a decline with £105,997 paid in damages to 30 claimants in 2009/10 (Table 12). However, the total amount paid in 2001/2 was skewed by one large payment of £2.8M and, if this is excluded from the analyses, there was a gradual reduction in the amount paid out from 2004/5.
| Year | Number of cases | Total cost per year (£) | Mean (£) | SD |
|---|---|---|---|---|
| 1995/6 | 3 | 8000.00 | 2666.67 | 4618.80 |
| 1996/7 | 1 | 0 | N/A | N/A |
| 1997/8 | 6 | 85,000.00 | 14,166.67 | 34,701.10 |
| 1998/9 | 20 | 241,500.00 | 12,075.00 | 33,823.18 |
| 1999/00 | 35 | 28,875.00 | 825.00 | 2213.39 |
| 2000/1 | 41 | 69,795.25 | 1702.32 | 4600.23 |
| 2001/2 | 51 | 3,549,916.66 | 69,606.21 | 3.94 |
| 2002/3 | 54 | 966,648.87 | 17,900.91 | 70,335.40 |
| 2003/4 | 53 | 144,609.00 | 2728.47 | 5207.76 |
| 2004/5 | 60 | 1,162,000.70 | 19,366.68 | 43,847.97 |
| 2005/6 | 70 | 435,938.60 | 6227.69 | 13,352.60 |
| 2006/7 | 62 | 353,858.25 | 5707.39 | 19,665.68 |
| 2007/8 | 37 | 300,622.18 | 8124.92 | 25,280.65 |
| 2008/9 | 45 | 291,549.55 | 6478.8789 | 16,108.54 |
| 2009/10 | 30 | 105,997.00 | 3533.2333 | 6767.04 |
| 2010/11 | 7 | 8719.00 | 1245.57 | 1937.90 |
The gradual reduction in the amount paid to claimants is mirrored by a reduction in the cost of defending these actions since the peak in 2001/2. Details of the 15 most costly litigation claims are presented in Appendix 7.
Discussion
Although the number of litigation claims has plateaued since 2006/7 and the amount of compensation claimants receive has decreased, claims are still made against the ambulance service. The most common reasons for claims include lack of assistance or care, failed or delayed treatment, failed or delayed transfer and failed or delayed diagnosis. The exact cause of litigation incidents was generally unclear and the level of detail provided in the source data set was insufficient for detailed analysis.
Most damages were awarded when the incident resulted in a fatality but the highest levels were awarded when the incident led to brain damage, in recognition of the need for lifetime care. The decrease in the amount of damages paid over time does not appear to be owing to the ambulance service mounting a fierce defence of the action, as the cost of defending cases also fell since the peak in 2001/2.
A number of limitations seriously impact the interpretations that can be drawn from the litigation data presented here. Certain anomalies in the data set could not be explained by the NHSLA, such as the inclusion of minus values for damages and the ‘incident’ category included in the closed and open variable, and no data were provided on patient age, sex, presenting condition or the discipline and level of experience of the ambulance clinician. Incident descriptions were poor, there were no data on the ambulance services involved and it was therefore unclear whether or not some services are subject to more litigation than others. The data from the litigation agency are limited, as not all safety incidents will be reported.
There is also concern regarding the validity of the data provided by the NHSLA. In 2008, Dobbie and Cooke6 published an analysis of litigation claims from 1995 to 2005 and reported 17 cases for which the damages exceeded £1M; however, only one settlement for damages exceeded £1M in our data set for 1995 to 2011. It is difficult to explain this discrepancy, which has not been clarified by the NHSLA. As a result, definitive conclusions cannot be drawn concerning the number of litigations cases brought over time.
The top 10 causes of incidents (see Table 10) resulting in litigation have been mapped against the 25 topic areas and found to encompass eight of these: assessment/management, diagnosis, equipment/resources, individual factors, non-conveyance, observation/monitoring, skill set and treatment/procedures. However, it is recognised that the ability to detect all categories is limited by the coding system used, hence some underlying causes may be omitted.
Conclusions
This analysis provides a snapshot of patient safety incidents over a 15-year period, providing limited data on the nature, cause and costs incurred. Although the data suggest a plateau in the number of litigation claims against the ambulance service and a decrease in the cost of damages paid over recent years, limitations in incident description and data set quality preclude in-depth analysis of the cause. However, given the inadequacies in the data set it is difficult to draw definitive conclusions, one area that ambulance services should examine and aim to reduce is the number of incidences of failed or delayed treatment.
The NHSLA should consider the limitations in the quality of its data and aim to develop a more consistent, detailed and reliable reporting system.
Coroners’ reports
Introduction
Her Majesty’s Coroner is responsible for investigating sudden, unnatural or unexplained deaths as well as sudden deaths in the community and deaths for which the cause is uncertain; therefore, situations when there are concerns about the care received prior to death are referred to the coroner. The coroner (or their officer) will investigate the circumstances surrounding the death and will decide whether or not an inquest is to be held. When an inquest is held, witnesses are called (e.g. clinical staff, pathologist, relatives) to present evidence relevant to the cause of death. If inquest evidence suggests that there might be a risk of future deaths and action is needed to prevent recurrence, the coroner prepares a report under rule 43, which suggests actions to prevent future deaths. These reports can be served to all involved or with an interest in an incident and require a response by the recipients stating whether or not the suggested actions will be taken and, if they are not going to be taken, indicating the reason why.
Aim
The aim was to summarise the issues that caused the coroner to send a report to an ambulance service under rule 43 in order to identify patient safety incidents with ambulance service involvement.
Methods
Summaries of the coroners’ reports were accessed at www.justice.gov.uk/publications/policy/moj/summary-of-reports-and-responses-under-rule-43-of-the-coroners-rules. 400 The summaries of coroners’ reports issued from 2008 to 2011 were screened for ambulance service involvement and relevant documents were then downloaded for review. This period was chosen because 2008 is the time when the letters became publicly available in one location. To obtain letters before this time would have required contacting every coroner and this was not considered feasible.
A thematic analysis was undertaken to identify patient safety issues that triggered coroners’ reports. For consistency, the categories identified for use in the prioritisation exercise (see Chapter 6) were used for classification of the summaries of the coroners’ reports. The summaries were analysed with a view to identifying potential patterns in incident types and the receiving ambulance service.
The decision to issue a rule 43 letter is personal to the coroner when he or she believes that it may prevent a similar future death. The number undertaken by each coroner is highly variable. The information recorded on this database has been abstracted by a non-researcher at the Ministry of Justice and it is, therefore, their opinion of the key issues that are analysed. Although this study adds information about some cases, it cannot be considered a representative sample of coroners’ cases when safety issues were present.
Results
The search identified 25 reports sent to ambulance services between July 2008 and March 2011. Of these, 22 involved nine English ambulance services. Figure 11 illustrates the number of reports sent to each ambulance service, taking into account the number of people served. Given the small number issued, the findings suggest an even spread of coroners’ reports across the majority of English ambulance services.
FIGURE 11.
Number of coroners’ reports received by English ambulance services between July 2008 and March 2011.
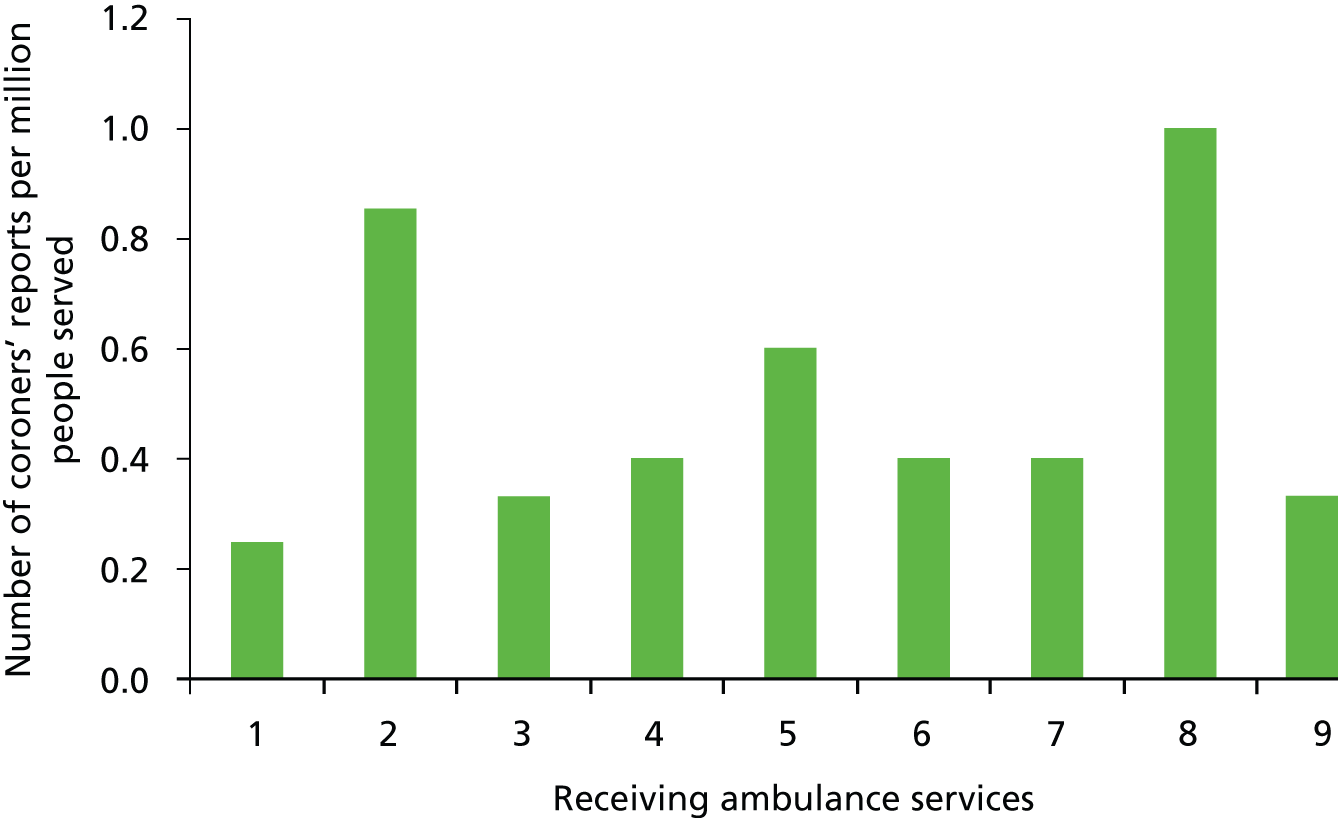
Table 13 details the actions required by rule 43 notices. The patient safety issues that triggered more than half of coroners’ reports related to communication issues and patient assessment skills. Communication was the main focus of seven notices and, of these, four related to communication between the ambulance service and hospitals, two related to internal communication issues and one related to interagency (police) communication. Assessment was relevant to eight notices (four relating to assessment/treatment of specific conditions, three to clinical assessment skills and one to record keeping). Other notices were grouped under the headings of training (one), treatment (four), organisation/culture (three) and equipment (two).
| Category | Rule 43 ruling |
|---|---|
| Communication | Hospital and ambulance service to consider improving communication between health professionals |
| To consider the relationship between the ambulance service and hospital staff and the process of transmitting ambulance records to A&E staff to enable continuity of care | |
| Ambulance service to consider a review of transmission of ambulance records to hospital staff to enable continuity of care | |
| To consider sending notification of road closures by e-mail rather than post, or consider if such information could be integrated with central control/ambulance navigation systems | |
| To consider disseminating guidance to all ambulance trusts about best practice for communications between call centres and ambulance crews | |
| To consider a review of the police airwave system and communication between police and ambulance services when ambulance personnel attend the scene of a violent incident | |
| To consider a review of policy to enable the communication of important patient medical information to the ambulance area responding to the request | |
| Assessment | Ambulance service to include a pain score on their record sheet |
| Ambulance service to consider reminding technicians to conduct their own medical assessments | |
| Ambulance service to consider a review of guidelines for assessment of patients who appear drunk | |
| Ambulance service to consider a review of guidance when an ambulance is called to a police station | |
| To consider provision of ambulances to people advised to contact the emergency services if their condition deteriorates after discharge from hospital following major surgery | |
| To consider incorporating other sources of information at initial diagnosis, particularly the ambulance service’s patient report form; reviewing procedures for assessment of fitness for discharge and reviewing policy on initiating serious untoward incident procedures | |
| To consider issuing guidance to operators to ask callers what drugs the patient has taken (if any) | |
| To consider a review of how information provided to the ambulance service and NHS Direct is assessed and to ensure that a diagnosis of metabolic ketoacidosis is considered when symptoms could indicate this condition | |
| Training | To consider a review of training on excited delirium and risk assessment both at the scene of arrest and the police station; the use of police vehicles to transport prisoners to hospital; guidance on monitoring and observing prisoners; guidance for forensic medical examiners at the police station; guidance on calls to the ambulance service and how they should be handled |
| Treatment | To consider a review of protocols and guidance on prescribing antibiotics in A&E when a patient displays possible symptoms of meningitis; to consider guidance to ambulance staff on keeping possible items of evidence and accurate recording of observations |
| To consider providing adrenaline, amiodarone and atropine to ambulance services in different coloured boxes to avoid confusion | |
| To continue efforts to provide places of safety for people with mental health concerns | |
| To consider allowing patients to use walking aids with which they are familiar, including when travelling by ambulance | |
| Organisation/culture | To consider evidence from the inquest in carrying out the critical incident review |
| Ambulance service to consider a review of its policy on solo responders attending emergencies and crew meal break arrangements | |
| To consider disseminating the action plan arising from their serious untoward incident investigation to all ambulance services throughout England | |
| Equipment | To consider providing equipping ambulance crews with equipment to effect forcible entry and training in its use |
| To consider rigorous servicing of all defibrillator equipment in accordance with service schedules; decommissioning and replacing all defibrillator batteries and improving ambulance staff training in the use of defibrillators |
Discussion
This study of coroners’ rule 43 reports identified 25 notices that were issued over a 3-year period (2008–11). The main reason for serving a rule 43 coroners’ report to ambulance services involved communication issues. Ambulance services often represent the first point of contact for a patient with acute, potentially life-threatening events. Communication plays a key role in ensuring effective dispatch (from the control centre to the scene), liaison with relevant agencies (e.g. police, carers) at the scene and ensuring that information obtained at the first contact is recorded and communicated effectively to hospital staff (in the event the patient is transferred to hospital) or those responsible for follow-up care (e.g. social services, GPs). Successful communication requires a systems approach to ensure that information is passed effectively within and between organisations. The seven rule 43 notices identified by this study provide examples of where communication may have failed and contributed to the death of a patient. Ensuring that ambulance services have effective communication systems in place is an important priority.
The second key theme of the coroners’ reports related to weaknesses in patient assessment and identified areas such as deficiencies in record keeping, and assessment and management of specific clinical conditions. Some, but not all, issues arose in the context of patients assessed on scene and when a decision was made to leave the patient at the scene rather than transfer them to hospital for further assessment and treatment. Such a see-and-treat approach has the potential to be resource effective, but requires careful evaluation to ensure that patient outcomes are improved rather than a delay being experienced in provision of necessary care; ensuring that the see-and-treat approach retains a focus on patient outcome is key to the provision of safe and effective care. The inclusion of recontact rates in national quality indicators represents a useful starting point for this process.
It is recognised that the information from this study may not be representative, as it covers only cases for which a coroner issues a rule 43 notice. The decision to do this is at the personal discretion of each coroner.
The review of rule 43 notices was useful in highlighting examples of lapses in patient care pathways that resulted in death. However, shortcomings in this evidence must be acknowledged: 25 reports is a small number and is an insufficient basis for development of firm conclusions; the reports are associated with individual patient cases and generalisation of the results is not necessarily appropriate; summary reports provide little information that is suitable for analysis or to facilitate identification of underlying safety issues; and, finally, the number of reports received by an ambulance service should not be used to reflect the quality of services offered, as the number of reports also relates to the number of people served and the coroner’s perception of the incident.
All the rulings were mapped to three topic areas of the 25 highlighted in the literature review, namely assessment/management, communication and non-conveyance.
Chapter 5 Staff and user perception in ambulance services
Introduction
Although ambulance services have traditionally responded to targets and requirements placed on them, little is known concerning staff and user perceptions of areas of concern for patient safety. Three approaches were used to inform aspects of staff and user perceptions of ambulance services. The first involved the development of an ambulance service questionnaire, which was distributed to ambulance service medical directors, and focused on potential safety concerns; the second involved a questionnaire based on the London Protocol that was distributed to a patient and public forum of an NHS ambulance service addressing a broad spectrum of ambulance service provision; and the third involved assessing the perceptions of ambulance service staff regarding patient safety by analysing data from the ambulance service safety prioritisation event.
The ambulance service medical directors’ questionnaire
Aims
The aim of this component was to understand how different groups perceived safety issues in ambulance services. The first group to be surveyed was the medical directors of the ambulance services.
Developing the survey measure
Preliminary interviews: in order to identify patient safety issues of potential concern to ambulance services and their users, a series of face-to-face interviews to identify themes were conducted to inform the development of a broader questionnaire. A small sample of ambulance services was approached for permission to interview the medical director, the clinical governance lead and the risk management lead or their equivalent; these individuals were considered key to establishing and maintaining safety culture within the ambulance service.
Three ambulance services agreed to participate as pilot sites and the eight interviews occurred between December 2011 and May 2012. This period was protracted as a result of increased winter pressures within the ambulance service. The interviews were based on three open questions, each with a distinct objective.
Question 1: ‘What in your opinion are the most important issues facing the ambulance service with respect to patient safety?’ The objective of this question was to identify those areas that stakeholders within the ambulance service perceived to be key in maintaining safe and effective services.
Question 2: ‘What sort of documentation exists within the trust around patient safety and can we access it?’ The objective of this question was to determine how ambulance service trusts communicate their patient safety message to operational staff and the level of priority associated with this message.
Question 3: ‘Are you aware of any literature at national or local level that addresses patient safety issues (reports, guidance, etc.)?’ The objective of this question was to identify the literature utilised by the ambulance service to guide policy-making. It also served to ensure that all patient safety documentation of importance to ambulance services was identified by the research team and included in the systematic review.
The interviews were quite open-ended and notes were made by one member of the team, while another team member undertook questioning and exploration of the issues raised. A list of topics mentioned by each interviewee was produced and the lists were compared to identify areas of agreement and overlap; the degree of overlap was high and it was not felt necessary to conduct further exploratory interviews.
Questionnaire
In order to extend coverage and obtain the perceptions of all medical directors of the ambulance service, a questionnaire was constructed based on the open interviews (see Appendix 8 or www.warwick.ac.uk/ambulancesafety). All points mentioned by at least two respondents in the pilot interviews were included resulting in a list of 10 topic areas that were perceived as potentially impacting on patient safety.
The 10 areas were:
-
delay in gaining access to hospital
-
equipment failure/shortage
-
call handling triage/categorisation
-
decision to leave at home
-
medication errors
-
skill mix of available staff
-
increased clinical intervention
-
handover process at hospital
-
resources available to respond
-
allocation of patients at colocated sites (A&E/minor injury units).
The questionnaire was distributed to the medical directors of all English ambulance services (n = 11) and a response was received from seven. Medical directors were asked to rate each item in terms of importance on a scale of 1 to 10, with 10 being most important.
Results
The scores for each participant on the ambulance service questionnaire were collated and analysed using IBM SPSS version 19.0. The mean scores for each item were calculated and are presented in Table 14; a higher score representing a perceived greater safety risk.
| Factor | Mean rating |
|---|---|
| Delay in gaining access to hospital | 8.6 |
| Handover process at A&E | 6.6 |
| Call handling triage/categorisation | 6.0 |
| Decision to leave at home | 5.6 |
| Resources available to respond | 5.3 |
| Equipment failure/shortage | 4.6 |
| Increased clinical intervention | 4.5 |
| Skill mix of staff available | 4.1 |
| Allocation of patients at colocated sites | 4.0 |
| Medication errors | 3.6 |
Although any cut-off from these sets of scores would be arbitrary, it would appear that ‘delay in gaining access to hospital’ at 8.6 is by some margin seen as a key safety issue (see Table 14). If we view overall ratings above five as suggesting importance then the next groups are relatively similar, with perhaps ‘handover process at A&E’ (6.6) and ‘call handling triage/categorisation’ (6.0) as of slightly more concern. Although this was a small sample (n = 7), it does represent the views of over half of the most senior clinical staff in ambulance services.
The areas scoring a mean score greater than five represented four areas of the 25 topics from the literature review, namely dispatch, handover, non-conveyance and time factor/delay.
The patient and public forum questionnaire
Aims
The aim of the study was to establish the opinions and perceptions of potential users of ambulance services as related to patient safety in ambulance services and the factors that have an impact on it. It was felt that useful insights might be gained from non-ambulance staff who had an understanding of how ambulance services function and are organised, and an awareness of some of the challenges faced by ambulance services.
Methods
In order to engage with members of the public and potential ambulance service users who had an understanding of how ambulance services operate, a meeting was arranged with the patient and public forum of a large metropolitan ambulance service. A short presentation relating to the purpose of the meeting and collection of data were provided, following which meeting attendees were asked to complete a questionnaire. Attendees were not obliged to participate and had the option of completing the questionnaire anonymously.
The questionnaire comprised two sections, the first of which contained 49 questions and the respondent was asked to rate, using a 10-point Likert scale, how important they felt each issue was for ambulance services. A score of 1 rated the area as being of little concern with respect to patient safety, whereas a score of 10 rated the area as being of major concern with respect to patient safety. The questions were derived from work initially undertaken by the study team and the expert review group to develop a framework to categorise findings from the systematic literature review (see Chapter 3). This initial work analysed and compared the existing AHRQ conceptual framework, the London Protocol, the National Reporting and Learning Service framework, the Patient Safety First Safety Domains and the Yorkshire Contributory Factors Framework. All items identified from each of the frameworks were collated into a table and then each item was recorded on a card. Duplicate cards were removed. Each of the elements identified on the remaining cards was incorporated into section one of the patient and public forum questionnaire.
The second section asked respondents to identify what they believed to be the five most important factors affecting patient safety in ambulance services (not in order of importance). Additionally, a free-text area was provided for respondents to add any additional information that they felt was important.
Results
Nine attendees of the patient and public forum meeting agreed to participate and completed questionnaires. The scores for each participant on the ambulance service questionnaire were collated and analysed using IBM SPSS version 19.0. The mean scores for each element were calculated and are presented in Table 15; a higher score representing a perceived greater safety risk.
| Dimension | Element | Mean score |
|---|---|---|
| Patient factors | Patient language and communication | 7.8 |
| Personality and social factors | 5.7 | |
| Patient factors, e.g. mobility | 6.8 | |
| Patient condition or illness | 8.3 | |
| Staff factors | Education and training (level of) | 8.2 |
| Clinical knowledge (level of) | 8.7 | |
| Clinical assessment skills (level of) | 8.5 | |
| Critical thinking or clinical decision-making abilities (level of) | 8.3 | |
| Active individual failure | 8.0 | |
| Staff physical and mental health | 7.4 | |
| Staff individual factors, e.g. personality/human factors | 7.0 | |
| Safety knowledge | 8.3 | |
| Team factors | Supervision | 8.0 |
| Leadership and line management | 8.1 | |
| Team structure (congruence, consistency, leadership, etc.) | 7.8 | |
| Team communication | 8.3 | |
| Work environment | Care setting/physical environment/weather | 6.5 |
| Staffing levels and skills mix | 8.4 | |
| Correct skills deployment | 7.9 | |
| Operational efficiency | 7.8 | |
| Shift patterns | 8.7 | |
| Staff workload | 8.4 | |
| Task and technology factors | Communication systems (information technology) | 7.9 |
| Infection prevention and control | 8.6 | |
| Decision-making aids | 7.7 | |
| Availability and use of protocols/guidelines | 8.1 | |
| Design, availability and maintenance of equipment | 8.1 | |
| Availability and accuracy of test results | 7.9 | |
| Vehicles | 8.0 | |
| Organisational and management factors | Policies, standards and goals | 7.0 |
| Safety culture and priorities | 8.3 | |
| Organisational culture | 8.0 | |
| Implementation of care, review, monitoring | 8.0 | |
| Documentation (records and identification) | 7.6 | |
| Financial resources and constraints | 7.2 | |
| Organisational structure | 7.3 | |
| Institutional context factors | Organisational performance (target mentality) | 6.8 |
| NHS executive | 6.6 | |
| Consent, communication, confidentiality | 7.4 | |
| Support from central functions | 7.9 | |
| Links with external organisations | 6.8 | |
| External policy | 7.1 | |
| Economic and regulatory context | 7.2 | |
| Outcomes | Care pathways, including non-transport | 8.0 |
| Access, admission, transfer, discharge | 7.2 | |
| Public involvement and expectation (end of life; destination alternatives) | 7.1 | |
| Safeguarding | 8.1 | |
| Medication errors | 7.9 | |
| Falls | 8.0 |
In section 2, attendees were also invited to identify what they perceived to be the five most important safety concerns (not in any particular order) and a free-text area was provided to allow attendees the freedom to raise any other issues they felt were important considerations that may not have been included within the questionnaire. There was considerable variation in these elements and it was not possible to summarise these data without losing a considerable number of viewpoints; however, it would not be unreasonable to draw the conclusion that the primary areas of concern relating to patient safety in ambulance services, from the perspective of participant feedback in the free-text section, could be broadly categorised as falling within the domains of clinical capability of individual ambulance clinicians and communication skills. Pressures placed on ambulance staff regarding workload were also identified as an area of concern by participants. Responses to section two are included in Appendix 9.
Discussion
There was a high level of consistency in responses to specific questions when comparing services that returned questionnaires. However, the overall ratings showed a degree of discrepancy when comparing services (one service had an average overall rating of 6.9 and another of 4.1). This suggested that different services applied the rating scales differently or they perceived different levels of risk to be associated with the different areas surveyed in the questionnaire. The most obvious area in which there were differences in ratings for different services was ‘call handling triage/categorisation’ (for which scores ranged from two to nine) and ‘decision to leave at home’ (for which scores ranged from two to nine). The observation that the most discrepant scores were associated with three services indicates differential experiences of these safety concerns. The additional ad hoc data given by participants of the prioritisation event were remarkably consistent with the main questionnaire findings.
There is considerable agreement among those involved in delivering ambulance services that operational delivery of services is key, with the highest safety risks cited by ambulance service medical directors being delays in gaining access to hospital and the patient handover process on reaching EDs. These findings indicate a pressing need for interorganisational research and the development of interventions spanning the link between ambulance services and emergency care.
The patient forum exercise provides limited insight into the perceptions of the wider public with respect to what is important in terms of patient safety in ambulance services. Although the number of participants was low, it is apparent that perceptions of the patient and public forum are different from those of the ambulance service medical directors. Members of the patient and public forum had an excellent understanding of the issues facing ambulance services, yet their perceptions of what is important in relation to patient safety were not directly aligned with ambulance service perspectives. Those areas scoring a mean score greater than eight represented nine of the 25 topic areas from the literature review, namely assessment/management, communication, equipment/resources, individual factors, infection control, non-conveyance, safety culture, skill set and training.
Results of the patient and public forum exercise suggest that patients believe factors influencing the initial assessment undertaken by the responding ambulance clinician have the most significant impact on their safety, with operational issues being less important.
Care Quality Commission National Health Service staff survey data
Aim
The aim of this reanalysis of the NHS staff survey data was to analyse data specifically related to staff perceptions of patient safety within the ambulance services in England.
Methods
The postal questionnaire (www.nhsstaffsurveys.com)401 was sent by the Picker Institute on behalf of the Department of Health to 366 NHS organisations in England encompassing 250,000 NHS staff. The questionnaire comprised 167 questions, as detailed in Appendix 10. This study includes secondary analysis of data from the NHS Staff Survey 2011, which was obtained from the UK Data Archive and used with permission. The 2011 NHS Staff Survey was managed by the Picker Institute on behalf of the Department of Health. The survey was originally developed and run by Aston Business School on behalf of the CQC (and predecessor organisations) from 2003 to 2010. From 2013, the Picker Institute manages the survey on behalf of NHS England and copyright for the survey is held with NHS England. Further details about the survey programme are available at www.nhsstaffsurveys.com. 401
All full- and part-time salaried staff who were employed by the NHS on 1 September 2011 were eligible to take part. The sample size per trust was based on workforce size and participants were randomly selected from all staff groups in the trust. The questionnaire process was managed by a company external to the trust in order to maintain confidentiality.
This analysis considered data from participants in paid employment in ambulance services including health-care settings allied to pre-hospital care. This analysis considered data only from the 12 ambulance services in England.
Outcome measures included:
-
Patient safety: reporting errors that affect patients or staff; fairness for staff involved in an error, near miss or incident; being encouraged to report an error, near miss or incident; reports being treated as confidential; trust blame/punishment for in an error, near miss or incident; information given about an error, near miss or incident; lessons learnt; and hand cleansing available.
-
Training and supervision/education: taught courses, supervised on-the-job training, mentoring, shadowing, appraisal, equality and diversity, health and safety, violence and aggression, infection control, handling confidential data, and information provision to patients.
-
Continuing professional development: keeping up to date, personal development plans, computer skills and suggesting improvements to patient care.
-
Culture: involved and consulted on workplace changes, recognition of good work, managerial support, effective top-down communication, patient care as a trust priority, trust manager commitment to patient care, staff informed about important changes, whistle-blowing, raising concerns and managers acting on staff feedback.
-
Organisational demands/processes: work demands/pressures (time, staff, maintaining standards), availability of supplies, vehicles in good repair, safe working environment and quality of care.
Results
Anonymised data were collated by the Picker Institute (on behalf of the Department of Health) and made available on the website in a number of formats. The data provided by ambulance services were downloaded and analysed using IBM SPSS version 19.0. The data set comprised 3823 returns from the London, Great Western, North East, North West, Yorkshire, East Midlands, West Midlands, East of England, South East, South Central and South West ambulance services.
The overall response rate was 45%, with the highest response from the East of England ambulance service, from which 65% of staff approached completed the survey; however, in East Midlands and North West ambulance services, only just over one-third of those approached completed the survey.
Items relating to the perception of respondents considering ‘patient safety’ a priority for their ambulance service are shown in Table 16. The data show that a high proportion of respondents had witnessed an incident (error or near miss) that had affected a patient and 17.5% (670/3823) had reported an error/near miss that had caused harm to a patient. The majority of respondents (69.2%, 2644/3823) perceived that their service encourages incident reporting. Over 25% (977/3823) of respondents perceived that their service blamed or punished staff for incidents (errors and near misses) and 29.7% (1134/3823) stated that staff were not treated fairly following an incident. A total of 22.3% (854/3823) of respondents perceived that their trust takes action to ensure they do not happen again.
| Item | % | n/N | Missinga |
|---|---|---|---|
| Saw error/near miss that affected patients | 21.1 | 806/3823 | 71 |
| Fairness for staff involved in an error | 29.7 | 1134/3823 | 53 |
| Encouraged to report an error/near miss | 69.2 | 2644/3823 | 50 |
| Reported an error/near miss that hurt patient | 17.5 | 670/3823 | 3022 |
| Incident treated as confidential | 41.5 | 1585/3823 | 1 |
| Trust blamed/punished staff for an error/near miss | 25.6 | 977/3823 | 60 |
| Staff informed about an error/near miss | 19.3 | 738/3823 | 60 |
| Lessons learnt from an error/near miss or incident | 22.3 | 854/3823 | 58 |
A wide variety of training was provided by ambulance services (Table 17). The majority of services (69.9%, 2674/3823) provided training in the form of taught courses, with over 40% (1536/3823) providing e-learning. Fewer than 30% reported one-to-one training such as supervised training on the job (28.2%, 1079/3823) or shadowing (14.4%, 550/3823). Almost 70% (2527/3823) of respondents reported receiving an appraisal.
| Item | % | n/N | Missinga | N/A |
|---|---|---|---|---|
| E-learning | 40.2 | 1536/3823 | 32 | – |
| Information provision to patients (within the last 12 months) | 16.8 | 643/3823 | 118 | 744 |
| Handling confidential data (within the last 12 months) | 34.9 | 1334/3823 | 83 | 127 |
| Infection control (within the last 12 months) | 54.3 | 2077/3823 | 77 | 222 |
| Major incident | 29.7 | 1134/3823 | 110 | 149 |
| Violence and aggression | 34.5 | 1318/3823 | 80 | 245 |
| Health and safety (within the last 12 months) | 54.5 | 2085/3823 | 55 | 32 |
| Equality and diversity | 44.0 | 1683/3823 | 78 | – |
| Appraisal | 66.1 | 2527/3823 | 129 | – |
| Shadowing | 14.4 | 550/3823 | 33 | – |
| Supervised on-the-job training | 28.2 | 1079/3823 | 31 | – |
| Taught courses | 69.9 | 2674/3823 | 34 | – |
| Continuing professional development | ||||
| Suggest improvements to patient care | 42.6 | 1629/3823 | 27 | – |
| Computer skills | 10.9 | 416/3823 | 116 | 252 |
| Personal development plan | 48.7 | 1861/3823 | 1493 | – |
Table 18 shows responses for questions related to organisational safety culture. A total of 84.5% (3231/3823) of respondents indicated that they knew the procedures for reporting concerns about negligence or wrongdoing by staff, 57.4% (2193/3823) perceived that their trust provides feedback concerning changes made in response to incidents and < 40% (1414/3823) perceived their service considered patient care a trust priority.
| Item | % | n/N | Missinga |
|---|---|---|---|
| Involved in workplace changes | 23.8 | 909/3823 | 41 |
| Managerial support | 47.6 | 1819/3823 | 17 |
| Effective top-down communication | 34.1 | 1305/3823 | 44 |
| Sections of organisation communicate effectively | 9.2 | 352/3823 | 37 |
| Patient care is a trust priority | 37.0 | 1414/3823 | 54 |
| Trust managers committed to patient care | 29.7 | 1136/3823 | 0 |
| Staff kept informed about important changes | 57.4 | 2193/3823 | 0 |
| Know how to report wrongdoing | 84.5 | 3231/3823 | 52 |
| Raising concerns | 55.4 | 2117/3823 | 1 |
| Mangers act on staff feedback | 14.5 | 553/3823 | 39 |
Table 19 explores the organisational demands placed on staff. Almost 62% (2360/3823) of staff perceived that their service was maintaining standards and 77.7% (2970/3823) were providing quality of care. A total of 34.1% (1304/3823) of participants perceived that their service provided a safe working environment and 18.2% (696/3823) of respondents indicated that vehicles were kept in a good state of repair.
| Item | % | n/N | Missinga | N/A |
|---|---|---|---|---|
| Cannot meet work demands/pressures on time | 35.0 | 1339/3823 | 49 | – |
| Sufficient staff | 29.5 | 1127/3823 | 36 | – |
| Maintaining standards | 61.7 | 2360/3823 | 43 | – |
| Availability of supplies/equipment | 46.2 | 1765/3823 | 41 | – |
| Vehicles in good repair | 18.2 | 696/3823 | 42 | 486 |
| Safe working environment | 34.1 | 1304/3823 | 41 | 524 |
| Quality of care | 77.7 | 2970/3823 | 28 | 499 |
Discussion
This CQC survey showed that a high proportion of respondents had witnessed an incident, although fewer had actually reported it. The exact reasons for non-reporting are unclear, although the majority of respondents perceived that their ambulance service encouraged reporting. Over one-quarter stated that their trust blamed or punished staff involved in incidents and almost one-third perceived that staff are not treated fairly following incidents. It is of concern that respondents perceived that, in the majority of cases, no action is taken to ensure that incidents do not happen again.
Although the majority of respondents perceived that they were delivering quality of care and that standards were maintained, a large proportion of staff felt they could not meet work demands and pressures on their time and almost one-third reported insufficient staff. It is of concern that over one-third of respondents felt that their service was not a safe working environment.
In terms of patient safety culture, the majority of respondents perceived that their trust encourages incident reporting; however, this could be higher if services consider how they could address the perceived lack of confidentiality and the perception that staff involved in an incident are not treated fairly and blamed or punished.
Given the poor response rate and the level of missing data, this survey may under-report incidents. The CQC should work to improve the response rate to this important survey to improve the utility of these data in improving patient safety for ambulance services.
Conclusions
There was considerable agreement among those involved regarding which issues they believe are central to delivering safe ambulance services, with operational delivery of services being key. Patients, on the other hand, perceive technical/knowledge aspects of the patient–clinician interaction to be most important in optimising service safety and effectiveness.
The overall findings from the CQC indicate some areas of concern, especially regarding the number of incidents occurring, the low incident reporting and the perception that lessons are not being learnt. An additional concern is that over one-third of staff reported work demands that they could not meet.
Chapter 6 Prioritisation exercise
Introduction
In order to make valid recommendations for future research directions for UK ambulance services, the data collected and collated from the three work streams, the systematic review (see Chapter 3), the document and database review (see Chapter 4) and ambulance service staff interviews (see Chapter 5), needed to be collated and prioritised. The prioritisation exercise used a modified Delphi method. This technique is particularly useful when there is a wide range of views and opinions. Undertaking it as a conference ensured that all participants were fully aware of the research findings and also allowed for more discussion of areas of differing opinion, while maintaining individual anonymous voting.
Aim
The aim of the prioritisation exercise was to provide an evidence-based ranked list of research priorities for ambulance services in England and Wales.
Methods
A modified three-stage Delphi process was used to prioritise the data generated during this project. The Delphi process is a means of obtaining expert consensus by taking into account all participants’ opinions. Voting is anonymous and participants are less influenced by group pressures that are known to affect decision-making. Therefore, opinions are more likely to be based on the participant’s knowledge and real-world experience than on the official position of the organisation. We ensured participant knowledge by presenting the findings of all components of this research, which was followed by question and answer sessions and group discussions; the discussion groups were pre-allocated by the research team to ensure a spread of ambulance services, professional groups and lay people in each.
An invitation to participate was sent to the medical directors of all UK ambulance services, with each able to send up to four representatives, including lay members. Of the 60 potential attendees, 20 (33%) participated and participants included paramedics, clinical advisors, quality managers, risk and governance managers, lay individuals and medicine and research managers. Two external researchers attended the prioritisation exercise as observers, but were not eligible to vote (because of the potential for bias as their research is in a related field).
Identification of research categories (Delphi step 1)
Research topics were identified from the systematic review, the document and database review, and ambulance service staff interviews. At the meeting of the expert advisory group, research topics were collated and presented on individual cards. The group were asked to review the research topics and consider whether or not there were any other topics they would like to add. A card-sort task402 was then undertaken for which group members were asked whether or not each research topic could be considered under one of five frameworks: the AHRQ conceptual framework, the NRLS, London Protocol,403 Patient Safety First domains and the Yorkshire Contributory Factors Framework. 404 Although the London Protocol was applicable to nearly all data, some topics could not be categorised and, after discussion, it was agreed that nine superordinate categories best accounted for the data.
Prioritisation of superordinate categories (Delphi step 2)
Having heard the presentations on each part of this research project, participants were allowed time for discussion. Participants were asked to vote on how important they felt it was for ambulance services to address each superordinate category in terms of patient safety, using a 10-point Likert scale, where 1 was not important and 10 was extremely important. Electronic voting was used to ensure individual anonymity and the data were analysed immediately, displayed graphically and then discussed.
Prioritisation of subcategories (Delphi step 3)
The highest ranking superordinate categories were divided into subcategories and participants were asked to vote on how important they felt it was for ambulance services to address each in terms of patient safety, using a 10-point Likert scale, where 1 was not important and 10 was extremely important. Electronic voting was used and the data were analysed immediately, displayed graphically and then discussed.
Open questionnaire
After voting, participants were asked to complete an open questionnaire to identify additional research priorities.
Data analysis
Voting was anonymous and undertaken electronically using the Turn Point System. Responses were not weighted and the median score for each superordinate category or subcategory was calculated, ranked and tabulated.
Results
Data from the systematic review, document and database review, the ambulance service medical directors’ interviews and the expert advisory group identified 89 research subcategories. These were collapsed into nine superordinate categories (Table 20). Categories receiving the highest rankings and considered priority research topics for ambulance services comprised patient treatment and clinical procedures, and training and knowledge management; the lowest ranking topics were equipment and information technology support and timeliness of care.
| Rank order | Research topic | Median score |
|---|---|---|
| 7.5 | Patient treatment and clinical procedures | 9 |
| 7.5 | Training and knowledge management | 9 |
| 6.5 | Patient assessment skills | 8 |
| 6.5 | The culture of the organisation | 8 |
| 4.5 | Staff factors | 7 |
| 4.5 | The processes and procedures of the organisation | 7 |
| 3 | Communication issues | 6 |
| 1.5 | Equipment and IT support | 5 |
| 1.5 | Timeliness of care | 5 |
The subcategories of the two highest ranking topics (patient treatment and clinical procedures, and training and knowledge management) were also scored. Table 21 shows that the highest ranking was afforded to decision-making for non-conveyance; recognition of serious illness, undertaking observations and clinical decision-making also received high rankings. The highest ranking subcategories for training and knowledge management were afforded to knowledge transfer and treatment error.
| Rank order | Research topics | Median score |
|---|---|---|
| Patient treatment and clinical procedures | ||
| 4 | Decisions on non-conveyance | 9 |
| 3 | Recognition of serious illness | 8 |
| 3 | Undertaking observations | 8 |
| 3 | Clinical decision-making | 8 |
| 1 | Patient monitoring | 6 |
| Training and knowledge management | ||
| 5 | Knowledge transfer | 9 |
| 4 | Treatment errors | 8 |
| 3.5 | Training implementation | 7 |
| 3.5 | Changing roles | 7 |
| 2 | Safeguarding | 6 |
| 1 | Infection prevention and control issues | 5 |
Participants listed 29 additional research priority areas using the open questionnaire. Only 4 of the 29 were considered new and these were patient/public expectation to be conveyed, public expectation/patient choice, staff selection and referral to other services (Box 1).
Ability to challenge.
Activation times – do they help or hinder?
Appropriateness of activation.
Appropriateness of early warning scores.
Assessment.
Behaviour and attitude.
Clinical integration of services.
Clinical supervision.
Communication at handover to other services, e.g. GP.
Culture.
Delay at hospital.
Education/training.
Effective patient feedback on care.
Feedback on referrals to other services.
Feedback/assurance – how do we know what we are doing is right?
Hear and treat.
Human factors.
Leadership (clinical).
Leaving people at home.
Non-conveyance.
Perceptions of patients and public (expectation to be conveyed).
Public expectation/patient choice.
Public health.
See and treat.
Selection/education of clinical staff.
Selection/education of control staff.
Skill mix – planning for future.
Treatment.
What is appropriate clinical supervision and how to monitor competence.
Discussion
Decision-making for non-conveyance, recognition of serious illness, undertaking observations and clinical decision-making, knowledge transfer, and treatment errors were identified by the expert group as the most important for ambulance services to address to improve patient safety.
It is important to note that, during voting, the differences between the categories being ranked was not great, indicating that all research areas were considered important. This may reflect the paucity of pre-hospital care research compared with other urgent care disciplines, such as emergency and critical care medicine. The emphasis on topics such as non-conveyance and assessment/recognition of serious illness may reflect organisational pressures and the increasing numbers of calls and incidents that the ambulance service is required to manage.
Communication and organisational culture have been common themes in the various components of research. In the prioritisation exercise, these two topics may have been hidden under other titles and may be a component of many of the areas prioritised.
This study does have limitations. Any Delphi-type process is dependent on the audience and the numbers participating were small; however, it was decided that the benefits of a face-to-face meeting (presentation of the research in depth, ability to question the researchers and the opportunity to discuss with other stakeholders) meant the opinion would relate more directly to this research and that this outweighed the disadvantages of sample size. A Delphi process relies on each person giving a view that is independent of others and, although all participants were in the same room, the use of electronic voting should have removed any peer pressure or group bias in voting. The invitation list was deliberately wide and, therefore, the low response rate may be expected but could lead to some bias. Despite the limitations listed above, 86% of participants represented the service under consideration and, therefore, results could be considered to be relevant to that service.
The methodology of voting on the superordinate categories, and the selection of the subcategories from within these, could lead to a single important subcategory from a lower prioritised superordinate category being omitted. The potential for this causing bias was considered less than the risks of fatigue from voting for all subcategories.
Conclusions
This prioritisation exercise clearly indicates the need for high-quality research across many areas of pre-hospital practice to improve patient safety, particularly focusing on clinical skills, alternative pathways enabling discharge of patients by the ambulance service and methods of ensuring effective knowledge transfer.
Chapter 7 Discussion
This scoping exercise has used a multimethods approach, consulting a wide range of patients and professionals, and has highlighted the paucity of good evidence to support patient safety initiatives relating to ambulance services. The existing data sources do not enable ambulance services to study the causation of AEs or to understand the clinical risks. Equally, there is a lack of evidence concerning the effectiveness of specific interventions.
Summary of the main findings
The scoping systematic review identified a wide range of papers, but they were mostly small studies of poor quality with variable outcome measures. We do not believe it would be possible to combine studies using meta-analysis to create more meaningful results.
The literature review highlighted a paucity of high-quality literature: most studies were small and undertaken at single locations. They often did not give sufficient detail for the reader to understand the generalisability or applicability of the findings. Ambulance transfer to some specific specialist centres has been shown to be safe and effective, but the bypassing of local EDs for many conditions has not been conclusively proven as safe. Equally the safety of ‘hear and treat’ has some evidence to support its operational effectiveness, but there are few studies to demonstrate clinical safety. ‘See and treat’ at the scene has less supporting evidence, except for a few pilot trials involving intensive training and specific patient groups. Equipment failure mainly relates to stretcher collapse causing injury or the well-recognised hazards of defibrillators. The search found only one study related to the appointment of staff96 and the issue of competency and appointing new staff was raised as a concern by members of the Delphi panel. The overarching impact of the organisational culture and context in safety in ambulance services has not been studied and is mainly limited to studies detailing an impact on incident reporting.
Official reports from ambulance services were highly variable in their patient safety content; their lack of standardisation makes it difficult to draw conclusions about safety priorities or concerns. However, the reports did describe some common topics including infection control, safeguarding, alternative care pathways and safety culture. It appeared that these may result from national priorities and targets rather than from the analysis of an individual ambulance service of its own safety issues.
The NPSA data for ambulance services were difficult to interpret as they are presented in a framework designed for all providers; for example, falls may include safety issues unique to the ambulance service such as falls from stretchers and carrying patients down stairs. Ambulance services appear to be relatively slow at reporting incidents. Four categories accounted for the majority of cases: access/admission/discharge, patient accidents, devices and equipment, and treatment. These may link to the alternative pathways mentioned in official reports but otherwise appear to address different aspects.
Litigation data were recognised to be of poor quality for the purpose of this scoping exercise, which identified the key causes of litigation incidents as associated with lack of care, failed or delayed treatment, failed or delayed admission, failed or delayed diagnosis, and failed or delayed referral. Once again, this highlights the skills and competencies needed for introduction of alternative pathways, particularly those enabling ambulance services to effect discharge.
Coroners’ reports also reflect a tip of the iceberg, relating only to unexpected deaths and having variable thresholds of usability. A high proportion of the reports highlighted communication or patient assessment skills as the main issue, while others commented on training, treatment, culture and equipment. Once again, the issues around alternative pathways have been highlighted as a major safety concern. It is acknowledged that there are aspects including communication and culture that may not have been explicitly mentioned in other data sources but may be underlying root causes.
Interviews with medical directors and senior staff highlighted 10 main issues of concern: three related directly to alternative care pathways (call handling triage/categorisation, decision to leave at home, allocation of patients at colocated sites), two indirectly to clinical skills (medication errors, increased clinical intervention) and two to handover at the ED (delay in gaining access to hospital, handover process at the hospital) along with equipment failure/shortage, skill mix of available staff and resources available to respond. The handover rated most highly as an area of concern. The patient forum tended to highlight the areas of clinical skills and decision-making, as well as communication.
The CQC staff survey had a low response rate, but some clear trends highlighted issues around the culture inhibiting safe practices and lack of feedback mechanisms. They were also critical of the level of training, which may be particularly important for the new skills required in alternative pathway design.
This scoping exercise clearly illustrates the lack of quality information available regarding ambulance service patient safety in the UK. The findings confirm a consensus of opinion and are supported by evidence, or lack of it, that key areas for future work in patient safety in ambulance services are alternative pathways (including the relevant clinical training), knowledge transfer, communications (including dispatch systems and handover at EDs) and safety culture. In particular, there is a paucity of evidence around human factors and organisational culture. This is now being increasingly recognised as a key area for improvement to minimise risk and reduce harm across a wide range of topic areas. Most improvement appears to take a single intervention approach rather than a systems-thinking approach.
The findings are relevant to commissioners, and non-conveyance and the research in assessment/recognition of serious illness (including the appropriateness of using early warning scores) are areas that should be prioritised. Ambulance services should look further into aspects of communication and culture to further understand how they impact on the quality of the care being offered.
Overarching themes of the combined results
The matrix of 25 topic areas developed in the literature review has been used to illustrate the issues detected by the various components and demonstrate the recurring themes. This is illustrated in Figure 12.
FIGURE 12.
Mapping domains identified by different components of the scoping review. Topics are colour coded by frequency of detection by different components of this scoping review. Dark green, detected by six components; light blue, detected by five components; dark blue, detected by four components; light green, detected by three components; mid green, detected by two components; mid blue, detected by one component. A, annual reports; C, coroners; D, Delphi; L, literature; M, medical directors; N, NHS LA; O, NPSA; P, public engagement.

Four areas were highlighted by five of the eight studies:
-
assessment/management
-
communication
-
equipment/resources
-
non-conveyance.
These are all topics with a large amount of literature to inform initial decision-making, although, as highlighted in the scoping review, the quality is poor. Other topics in order of the number of methods that detected them as an issue are shown in Figure 12.
Throughout this work, two major cross-cutting themes also emerged:
-
The information was not recorded in a consistent manner in various databases, nor in their descriptions in the literature. This lack of definition and consistency of use makes information difficult to interpret and implement change based on the data. Therefore, we recommend that this is addressed in future work.
-
The information from organisations and individuals revealed that there was little systematic use of the literature or databases. This may be cultural, or may be because of the difficulty of obtaining or utilising the information. We hope this report will aid this, but also encourage more evidence-based decision-making in patient safety in ambulance services.
Strengths and limitations of the scoping exercise
This scoping exercise used multiple methods to obtain information of patient safety in ambulance services. By using a wide variety of sources, we have been able to look at the issue from a range of perspectives and have used numerous experts with differing areas of interest to obtain our information. This was a scoping exercise with limited resources and, therefore, we were unable to go into depth in some areas. Quality assessment in the literature was limited and we were not able to undertake secondary analysis of databases.
However, all the methods also have specific limitations:
-
Literature review – there may be some relevant papers that do not include safety-type terms that are not included here. This may be particularly true for specific clinical procedures for which the paper considered a number of care providers and not just ambulance services.
-
Review of annual reports and quality reports – these reports do not have a detailed specification for inclusion and exclusion. The absence of a specific requirement for reporting on patient safety may mean it is a lower priority for the organisation, that it is hidden under another title or simply omitted because there is no direct mandate to report it.
-
NPSA incident reporting data – the limitations of this type of data have been widely studied. Most importantly, high reporting rates can indicate a good reporting culture rather than poor care. 405 There is equally no benchmarking for ambulance services as the nature of their work means they can only be compared with each other (a small sample) and not other NHS providers.
-
NHSLA data – these are not designed to be used to support safety improvement. As such, the reliability of the data for this purpose is poor and can only be used as indicative and not as quantitative data.
-
Interviews and questionnaires to staff – the interviews appeared to reach saturation, but this could reflect the small group of staff who often meet together having a unified view rather than signalling true agreement of views.
-
The CQC staff survey – this achieved a poor response and may be susceptible to completion bias, with those most dissatisfied being more likely to complete the survey.
-
The prioritisation exercise – this attempted to unify the diverse evidence sources but there may have been a selection bias in those who attended. The general seniority of staff may have led to overemphasis on operational issues and less attention to factors such as strategy and culture, for which they may be partly responsible.
By using multiple methods and cross-tabulating the results, the impact of the limitations associated with the specific tools on the overall results of the scoping exercise should be reduced.
Chapter 8 Conclusions
Implications for health care
Important strategic decisions have to be made by ambulance services, but there is no high-quality evidence to inform these decisions or to indicate that current models of care are safe. There are no data on the level of clinical risk in the system, nor how such risks can be mitigated. It appears that patient safety needs to become a more prominent consideration for ambulance services. This study identified many reports of cases for which operational pressures, including targets, were perceived to be more important than patient safety in ambulance services. The culture of the organisation needs to be understood and with consideration being given to the influence this can have on patient safety.
As ambulance services develop, new models of working need to ensure that staff are adequately trained and have means of monitoring clinical risks and intervening if required. Feedback mechanisms are often an important step in this process and the complexity of training staff who work in a mobile workforce and are often isolated from colleagues appears to be a recurring issue in safety reports. Providers and commissioners need a full understanding of the safety implications of introducing new models of care, which is currently undertaken with little supportive evidence; however, this also needs an inherent culture of critical evaluation.
Clinical studies undertaken in secondary care are often applied to ambulance service practice because of lack of specific evidence, although it is often difficult to extrapolate the findings. Therefore, current national guidelines often rely on consensus opinion regarding applicability in the pre-hospital environment. Ambulance services could be helped by a review of national databases to determine whether or not they can respond to the specific needs of this small, but important, group of users.
We recommend that ambulance services review patient safety in the four key areas that consistently appeared as concerns and for which evidence exists, namely:
-
patient assessment and management
-
communications
-
equipment and resources
-
non-conveyance.
Implications for research
Most of the research identified during this study is of poor quality and often relates to small studies in individual ambulance services. This suggests that future research needs to implement larger studies that are adequately powered to demonstrate an effect. Ambulance services are relatively new to clinical research and the absence of quality data that is specific to the pre-hospital care environment may reflect that immaturity. Research support for ambulance services and encouraging increased links with academic institutions may be appropriate. The areas of greatest concern and for which there is a need for major research projects are:
-
understanding the clinical effectiveness and safety of alternative pathways
-
understanding how knowledge transfer is best achieved in ambulance services with their dispersed and mobile workforce
-
understanding how communication in ambulance services can be improved; this covers a range of topic areas including 999 call handling, patient communication and handover to EDs
-
understanding the influence of the organisational culture on patient safety and how this can be continuously improved. The historical background of ambulance services may mean different approaches are required from those in other parts of the NHS.
Pre-hospital care research is required in many areas related to patient safety including basic safety science, looking at how best to measure and analyse safety to give reliable data to enable good monitoring and detection mechanisms.
Dissemination of the findings of the evidence synthesis and prioritisation exercise concerning patient safety when using ambulance services and relevant emergency services will involve presentation of the work described in this report in academic peer-reviewed publications, policy briefings and at methodological- and content-based seminars, conferences and meetings. The website www.warwick.ac.uk/ambulancesafety will provide a project summary, access to this report, newsletters and links to publications; newsletters will be produced and sent for wide distribution, for example to The Joint Royal Colleges Ambulance Committee, Faculty of Pre-hospital Care, Directors of Clinical Care and to the British Paramedic Association/College of Paramedics. In addition, the findings will be reported at national and international conferences.
Acknowledgements
We would like to thank all the participants involved in this research: the ambulance service staff interviewees and participants in the prioritisation workshop and the Delphi exercise. We are particularly grateful to Geoff Aitchison, the patient representative who assisted with the development of the grant application and in the initial planning of the project.
Prioritisation workshop/Delphi panel members
Malcolm Alexander, patient forum, London Ambulance Service NHS Trust; Gethin Bateman, Welsh Ambulance Service NHS Trust; Nick Bell, London Ambulance Service NHS Trust; Nichola Bramhall, East Midlands Ambulance Service NHS Trust; Adele Dean, West Midlands Ambulance Service NHS Trust; Ed England, South Central Ambulance Service NHS Foundation Trust; Tony France, East of England Ambulance Service NHS Trust; Darren Harding, London Ambulance Service NHS Trust; Geraint Harris, North West Ambulance Service NHS Trust; Maxine Johnson, The University of Sheffield; Tim Jones, Welsh Ambulance Service NHS Trust; Paul Kelly, Scottish Ambulance Service Special Health Board; Kevin Mackway-Jones, North West Ambulance Service NHS Trust; Andy McGonnigle, East of England Ambulance Service NHS Trust; Rachel O’Hara, The University of Sheffield; Steve Page, Yorkshire Ambulance Service NHS Trust; Dave Partlow, South Western Ambulance Service NHS Foundation Trust; Tim Pearce, Welsh Ambulance Service NHS Trust; Mary Peters, North West Ambulance Service NHS Trust; Daniel Phillips, East of England Ambulance Service NHS Trust; Richard Whitfield, Welsh Ambulance Service NHS Trust; and David Whitmore, London Ambulance Service NHS Trust.
Advisory group members
We are indebted to the advisory group members for their helpful comments during development of the systematic review protocol, guidance on data sources for document review, input into the interview questions, feedback on categorising research topics and comments on the final report. Their contributions helped us shape the recommendations made in this report.
The advisory group members were: Ann Keogh, Director of Medical Safety, Heart of England NHS Foundation Trust; Kevin Mackway-Jones, Medical Director for North West Ambulance Service NHS Trust; Anthony Marsh, Chairman of the Association of Ambulance Chief Executives; Jacky Swan, Warwick Business School; Nathan Taylor, West Midlands Ambulance Service NHS Trust; and Alison Walker, Medical Director for Yorkshire Ambulance Service NHS Trust.
We would also like to thank Owen Hammett and Oliver Morgan for their help with screening citations and extracting data for the systematic review, Raymond Pang for his help with preparing and screening data for the litigation analysis, and Julie Eastgate for assistance with preparing this report.
Project management
Dr Rose Jarvis (Project Manager, Division of Health Sciences) contributed to the preparation of the grant proposal, undertook overall project management, organised the prioritisation exercise and contributed to the report writing.
Contribution of authors
Dr Joanne D Fisher (Senior Research Fellow, Division of Health Sciences) designed, undertook and wrote up the rapid review of patient safety in the ambulance service in support for the scoping review grant application; contributed to the design of the methodology and was lead writer for the scoping review grant application; contributed to the design of the research protocol, undertaking the systematic and write-up of the report section; analysed the data from the litigation authority data and write-up of the report section; analysed the data from the staff survey and write-up of the report section; and contributed to the write-up of the prioritisation exercise.
Mrs Karoline Freeman (Research Fellow, Division of Health Sciences) contributed to the design of the methodology of the systematic review and ambulance service document review, development of the search strategy, undertaking of the systematic review, write-up of the systematic review report section, review of the annual reports and quality accounts, review of the coroners’ reports and the write-up of the ambulance service documents, coroners’ report summaries and NPSA patient safety incident reports.
Professor Aileen Clarke (Professor of Public Health, Division of Health Sciences) was involved in design and writing of the grant application and research protocol and contributed to the design and undertaking of the systematic review and the prioritisation exercise and to the writing-up of the report.
Professor Peter Spurgeon (Professor of Health Services Management, Division of Health Sciences) designed the interview component of the project and undertook interviews of senior ambulance staff, undertook analysis of interview responses and codesigned the patient/public forum questionnaire, led the analysis of questionnaire responses and participated in the overall design of the project.
Mr Mike Smyth (Senior Research Paramedic, West Midlands Ambulance Service) made contributions to review of papers, codesigned interview questions, undertook interviews of senior ambulance staff, analysed interview responses outlining potential areas for medical director questionnaire, designed patient/public forum questionnaire, visited patient/public group, discussed project, obtained patient/public perspective via questionnaire, analysed questionnaire responses, presented results at consensus conference, and drafted relevant section for final report.
Professor Gavin D Perkins (Professor of Critical Care Medicine, Warwick Clinical Trials Unit) provided input into study design, obtained funding, led the evaluation of ambulance service documents, coroners’ report summaries and NPSA patient safety incident reports and contributed to writing the final report.
Dr Mark-Alexander Sujan (Associate Professor of Patient Safety, Division of Health Sciences) provided input to the study design, assisted with screening publications for the systematic literature review, and contributed to writing the final report.
Professor Matthew W Cooke (Professor of Emergency Medicine, Division of Health Sciences) was the overall lead for the project and the guarantor of the results. He led the proposal development and the design of each of the components. He was the final judge of papers in the literature review and also helped develop the search strategy and exclusion criteria. He was the lead for the prioritisation exercise. He oversaw all the results and writing of the various sections and led the writing of the final conclusions as well as contributing to the whole final report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Vincent C. Adverse events in hospitals. BMJ 2001;322:517-19. http://dx.doi.org/10.1136/bmj.322.7285.517.
- Carruthers I, Philip P. Safety First: A Report for Patients, Clinicians and Healthcare Managers. London: The Central Office of Information; 2006.
- Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Washington, DC: National Academy Press; 1999.
- An Organisation With a Memory: Report of an Expert Group on Learning from Adverse Events in the NHS. London: The Stationery Office; 2000.
- Wankhade P. Performance Management and Cultures in Health Care: Case Study Evidence from the NHS Ambulance Service in the United Kingdom. Liverpool: University of Liverpool; 2009.
- Dobbie AE, Cooke MW. A descriptive review and discussion of litigation claims against ambulance services. Emerg Med J 2008;25:455-8. http://dx.doi.org/10.1136/emj.2007.052324.
- Colwell CB, Pons P, Blanchet JH, Mangino C. Claims against a paramedic ambulance service: a ten-year experience. J Emerg Med 1999;17:999-1002. http://dx.doi.org/10.1016/S0736-4679(99)00131-6.
- Cooke MW. CSI – Patient Safety in Ambulance Services n.d. www.warwick.ac.uk/ambulancesafety (accessed August 2014).
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies that Evaluate Health Care Interventions: Explanation and Elaboration. PLOS Med 2009;6. http://dx.doi.org/10.1371/journal.pmed.1000100.
- Tanon AA, Champagne F, Contandriopoulos AP, Pomey MP, Vadeboncoeur A, Nguyen H. Patient safety and systematic reviews: finding papers indexed in MEDLINE, EMBASE and CINAHL. Qual Saf Health Care 2010;9:452-61. http://dx.doi.org/10.1136/qshc.2008.031401.
- Wilson S, Cooke M, Morrell R, Bridge P, Allan T. A systematic review of the evidence supporting the use of priority dispatch of emergency ambulances. Prehosp Emerg Care 2002;6:42-9. http://dx.doi.org/10.1080/10903120290938760.
- Aufderheide TP, Keelan MH, Hendley GE, Robinson NA, Hastings TE, Lewin RF. Milwaukee prehospital chest pain project – phase I: feasibility and accuracy of prehospital thrombolytic candidate selection. Am J Cardiol 1992;69:991-6. http://dx.doi.org/10.1016/0002-9149(92)90852-P.
- Bruns BM, Dieckmann R, Shagoury C, Dingerson A, Swartzell C. Safety of pre-hospital therapy with morphine sulfate. Am J Emerg Med 1992;10:53-7. http://dx.doi.org/10.1016/0735-6757(92)90127-J.
- Firanescu C, Wilbers R, Meeder JG. Safety and feasibility of prehospital thrombolysis in combination with active rescue PCI strategy for acute ST-elevation myocardial infarction. Neth Heart J 2005;13:300-4.
- Flabouris A, Runciman WB, Levings B. Incidents during out-of-hospital patient transportation. Anaesth Intensive Care 2006;34:228-36.
- Gratton MC, Ellison SR, Hunt J, Ma OJ. Prospective determination of medical necessity for ambulance transport by paramedics. Prehosp Emerg Care 2003;7:466-9. http://dx.doi.org/10.1080/31270300220X.
- Goebel PJ, Daya MR, Gunnels MD. Accuracy of arrhythmia recognition in paramedic treatment of paroxysmal supraventricular tachycardia: a ten-year review. Prehosp Emerg Care 2004;8:166-70.
- Lavis M, McCarthy S, Jenkins NH. The continuing need to formalize pre-hospital triage, highlighted by a case of unusual injury. J Accid Emerg Med 1995;12:206-7. http://dx.doi.org/10.1136/emj.12.3.206.
- Lefrancois DP, Dufour DG. Use of the esophageal tracheal combitube by basic emergency medical technicians. Resuscitation 2002;52:77-83. http://dx.doi.org/10.1016/S0300-9572(01)00441-5.
- Linn S, Knoller N, Giligan CG, Dreifus U. The sky is a limit: errors in prehospital diagnosis by flight physicians. Am J Emerg Med 1997;15:316-20. http://dx.doi.org/10.1016/S0735-6757(97)90025-5.
- Mason S, Knowles E, Freeman J, Snooks H. Safety of paramedics with extended skills. Acad Emerg Med 2008;15:607-12. http://dx.doi.org/10.1111/j.1553-2712.2008.00156.x.
- Matera P. Working under the wrong assumption. JEMS 2002;27.
- Martin JE, Mehta R, Aarabi B, Ecklund JE, Martin AH, Ling GS. Intracranial insertion of a nasopharyngeal airway in a patient with craniofacial trauma. Mil Med 2004;169:496-7.
- Rottman SJ, Schriger DL, Charlop G, Salas JH, Lee S. On-line medical control versus protocol-based prehospital care. Ann Emerg Med 1997;30:62-8. http://dx.doi.org/10.1016/S0196-0644(97)70113-6.
- Bledsoe B. Uncover hidden trauma. JEMS 2003;28.
- Anonymous . Punishment with a point. JEMS 2001;26.
- Halter M, Vernon S, Snooks H, Porter A, Close J, Moore F, et al. Complexity of the decision-making process of ambulance staff for assessment and referral of older people who have fallen: a qualitative study. Emerg Med J 2011;28:44-50. http://dx.doi.org/10.1136/emj.2009.079566.
- Winslow JA, Goodman C, McMahon B. Unnecessary prehospital spinal immobilization. Ann Emerg Med 2005;46. http://dx.doi.org/10.1016/j.annemergmed.2005.06.229.
- Brown LH, Hubble MW, Cone DC, Millin MG, Schwartz B, Patterson PD. Paramedic determinations of medical necessity: a meta-analysis. Prehosp Emerg Care 2009;13:516-27. http://dx.doi.org/10.1080/10903120903144809.
- Jones AP, Allison K, Wright H, Porter K. Use of prehospital dressings in soft tissue trauma: is there any conformity or plan?. Emerg Med J 2009;26:532-4. http://dx.doi.org/10.1136/emj.2008.058255.
- Knapp BJ, Tsuchitani SN, Sheele JM, Prince J, Powers J. Prospective evaluation of an emergency medical services-administered alternative transport protocol. Prehosp Emerg Care 2009;13:432-6. http://dx.doi.org/10.1080/10903120902935256.
- Dante S, Herken U, Hammer T, Kurz M. Description of the acceleration forces affecting balance of pre-hospital providers while delivering cardio-pulmonary resuscitation. Circulation 2009;120.
- Mirarchi FL, Kalantzis S, Hunter D, McCracken E, Kisiel T. TRIAD II: do living wills have an impact on pre-hospital lifesaving care?. J Emerg Med 2009;36:105-15. http://dx.doi.org/10.1016/j.jemermed.2008.10.003.
- Stephenson LS. How Can the Use of Pre-Hospital Procedural Checklists Impact Patient Care in a Traditional Paramedic Culture?. Victoria, BC: Royal Roads University; 2007.
- Weiss S, Peterson K, Cheney P, Froman P, Ernst A, Campbell M. The use of chemical restraints reduces agitation in patients transported by emergency medical services. J Emerg Med 2012;43:820-8. http://dx.doi.org/10.1016/j.jemermed.2011.02.019.
- Hussmann B, Lefering R, Waydhas C, Ruchholtz S, Wafaisade A, Kauther MD, et al. Prehospital intubation of the moderately injured patient: a cause of morbidity? A matched-pairs analysis of 1,200 patients from the DGU Trauma Registry. Crit Care 2011;15. http://dx.doi.org/10.1186/cc10442.
- Stohler SA, Schwartz RJ, Kent Sargent R, Jacobs LM. Quality assurance in the Connecticut helicopter emergency medical service. J Air Med Transp 1991;10:7-11.
- Askitopoulou H, Vourvahakis D, Panagopoulos D, Mamidakis E. HECTOR emergency scale (HES) for the evaluation of prehospital emergencies. Eur J Anaesthesiol 2000;17. http://dx.doi.org/10.1097/00003643-200000002-00568.
- Fitzpatrick D, Duncan EAS. Improving post-hypoglycaemic patient safety in the prehospital environment: a systematic review. Emerg Med J 2009;26:472-8. http://dx.doi.org/10.1136/emj.2008.062240.
- Dale J, Williams S, Foster T, Higgins J, Snooks H, Crouch R. Safety of telephone consultation for ‘non-serious’ emergency ambulance service patients. Qual Saf Health Care 2004;13:363-73. http://dx.doi.org/10.1136/qshc.2003.008003.
- Keeling P, Hughes D, Price L, Shaw S, Barton A. Safety and feasibility of prehospital thrombolysis carried out by paramedics. BMJ 2003;327:27-8. http://dx.doi.org/10.1136/bmj.327.7405.27.
- Stella J, Bartley B, Jennings P. Introduction of a prehospital critical incident monitoring system – final results. Prehosp Disaster Med 2010;25:515-20.
- Vilke GM, Marcotte A, Metz M, Ray L. Pain management in the out-of-hospital setting. Ann Emerg Med 2004;44. http://dx.doi.org/10.1016/j.annemergmed.2004.07.207.
- Slattery DE, Heck J. An opportunity for reform: a comprehensive evaluation of non-transport patterns in an urban emergency medical services setting. Ann Emerg Med 2004;44. http://dx.doi.org/10.1016/j.annemergmed.2004.07.341.
- Newgard CD, Hui S, Griffin A, Lewis RJ. Prospective validation of an out-of-hospital decision rule to identify severely injured children involved in motor vehicle crashes. Ann Emerg Med 2004;44. http://dx.doi.org/10.1016/j.annemergmed.2004.07.210.
- Jensen JL, Croskerry P, Travers AH. Consensus on paramedic clinical decisions during high-acuity emergency calls: results of a Canadian Delphi study. CJEM 2011;13:310-18.
- Michael GE, Sporer KA, Youngblood GM. Socioeconomic and clinical factors associated with prehospital analgesia. Ann Emerg Med 2006;48.
- Nicholl J, Hughes S, Dixon S, Turner J, Yates D. The costs and benefits of paramedic skills in pre-hospital trauma care. Health Technol Assess 1998;2.
- Coleman P, O’Hara R, Mason S, O’Keeffe C. The quality and safety of emergency care practitioner care. Emerg Med J 2009;26. http://dx.doi.org/10.1136/emj.2009.075416g.
- Dixon M, Carmody N, O’Donnell C. The effectiveness of supraglottic airway devices in prehospital basic life support airway management. Emerg Med J 2009;26. http://dx.doi.org/10.1136/emj.2009.075416d.
- Davies A, Mylonas MJ, Ferguson A-L, Hutton A. Case: failure of ambulance crew to treat patient: R (1&2) and M(3) v Welsh Ambulance Service NHS Trust. Clin Risk 2009;15:207-9. http://dx.doi.org/10.1258/cr.2009.090064.
- Redd JM, Bair AE. Implications of ambulance diversion. Ann Emerg Med 2003;42:S1-109.
- Sagawa K, Inooka H, Inooka E. Mental State of Cardiac Patients During Ambulance Transportation n.d.
- Franklin GA, Boaz PW, Spain DA, Lukan JK, Carrillo EH, Richardson JD. Prehospital hypotension as a valid indicator of trauma team activation. J Trauma 2000;8:1034-7. http://dx.doi.org/10.1097/00005373-200006000-00006.
- Grmec S, Schaubach T, Stok E, Ferk J. Comparison of Mainz Emergency Evaluation System (MEES) and Revised Trauma Score (RTS) for prediction of mortality of trauma patients. Prehosp Disaster Med 2002;17.
- Tindall RD. Saving Lives in Real-Time: A Pre-Hospital Telementoring Case n.d.
- Lord B, Parsell B. Use of visual analogue scale for measurement of pain in the prehospital setting. Prehosp Disaster Med 2002;17.
- Isaak S. Is prehospital GCS alone adequate to determine need for a trauma center?. Ann Emerg Med 2006;48.
- Schmidt MJ, Handel D, Lindsell CJ, Collett L, Gallo P, Locasto D. Evaluating an emergency medical services-initiated nontransport system. Prehosp Emerg Care 2006;10:390-3. http://dx.doi.org/10.1080/10903120600725918.
- Barton ED, Swanson ER, Hutton KC. Laryngoscopic visualization grade predicts difficult intubations by air medical crews in the out-of-hospital setting. Ann Emerg Med 2004;44.
- Schmidt T, Atcheson R, Federiuk C, Mann NC, Pinney T, Fuller D, et al. Evaluation of protocols allowing emergency medical technicians to determine need for treatment and transport. Acad Emerg Med 2000;7:663-9. http://dx.doi.org/10.1111/j.1553-2712.2000.tb02041.x.
- Mason S, Knowles E, Colwell B, Dixon S, Wardrope J, Gorringe R. Effectiveness of paramedic practitioners in attending 999 calls from elderly people in the community: cluster randomised controlled trial. BMJ 2007;335. http://dx.doi.org/10.1136/bmj.39343.649097.55.
- Heward A, Damiani M, Hartley-Sharpe C. Does the use of the Advanced Medical Priority Dispatch System affect cardiac arrest detection?. Emerg Med J 2004;21:115-18. http://dx.doi.org/10.1136/emj.2003.006940.
- Turner J, Lattimer V, Snooks H. An Evaluation of the Accuracy and Safety of NHS Pathways. London: Department of Health; 2008.
- Buck BH, Starkman S, Eckstein M, Kidwell CS, Haines J, Huang R. Dispatcher recognition of stroke using the national academy medical priority dispatch system. Stroke 2009;40:2027-30. http://dx.doi.org/10.1161/STROKEAHA.108.545574.
- Hinchey P, Myers B, Zalkin J, Lewis R, Garner D. Low acuity EMS dispatch criteria can reliably identify patients without high-acuity illness or injury. Prehosp Emerg Care 2007;11:42-8. http://dx.doi.org/10.1080/10903120601021366.
- Clawson J, Olola C, Heward A, Patterson B, Scott G. Ability of the medical priority dispatch system protocol to predict the acuity of ‘unknown problem’ dispatch response levels. Prehosp Emerg Care 2008;12:290-6. http://dx.doi.org/10.1080/10903120802100787.
- Porteous GH, Corry MD, Smith WS. Emergency medical services dispatcher identification of stroke and transient ischemic attack. Prehosp Emerg Care 1999;3:211-16. http://dx.doi.org/10.1080/10903129908958939.
- Deakin CD, Alasaad M, King P, Thompson F. Is ambulance telephone triage using advanced medical priority dispatch protocols able to identify patients with acute stroke correctly?. Emerg Med J 2009;26:442-5. http://dx.doi.org/10.1136/emj.2008.059733.
- Feldman MJ, Verbeek PR, Lyons DG, Chad SJ, Craig AM, Schwartz B. Comparison of the medical priority dispatch system to an out-of-hospital patient acuity score. Acad Emerg Med 2006;13:954-60. http://dx.doi.org/10.1111/j.1553-2712.2006.tb00341.x.
- Frendl DM, Strauss DG, Underhill BK, Goldstein LB. Lack of impact of paramedic training and use of the Cincinnati prehospital stroke scale on stroke patient identification and on-scene time. Stroke 2009;40:754-6. http://dx.doi.org/10.1161/STROKEAHA.108.531285.
- Lerner EB. Studies Evaluating Current Field Triage: 1966–2005. Prehosp Emerg Care 2006;10:303-6. http://dx.doi.org/10.1080/10903120600723921.
- Kost S, Arruda J. Appropriateness of ambulance transportation to a suburban pediatric emergency department. Prehosp Emerg Care 1999;3:187-90. http://dx.doi.org/10.1080/10903129908958934.
- Gerlacher GR, Sirbaugh PE, Macias CG. Prehospital evaluation of non-transported pediatric patients by a large emergency medical services system. Pediatr Emerg Care 2001;17:421-4. http://dx.doi.org/10.1097/00006565-200112000-00005.
- Ramanujam P, Guluma KZ, Castillo EM, Chacon M, Jensen MB, Patel E. Accuracy of stroke recognition by emergency medical dispatchers and paramedics – San Diego experience. Prehosp Emerg Care 2008;12:307-13. http://dx.doi.org/10.1080/10903120802099526.
- Flynn J, Archer F, Morgans A. Sensitivity and specificity of the medical priority dispatch system in detecting cardiac arrest emergency calls in Melbourne. Prehosp Disaster Med 2006;21:72-6.
- Kothari R, Barsan W, Brott T, Broderick J, Ashbrock S. Frequency and accuracy of prehospital diagnosis of acute stroke. Stroke 1995;26:937-41. http://dx.doi.org/10.1161/01.STR.26.6.937.
- Qazi K, Kempf JA, Christopher NC, Gerson LW. Paramedic judgment of the need for trauma team activation for pediatric patients. Acad Emerg Med 1998;5:1002-7. http://dx.doi.org/10.1111/j.1553-2712.1998.tb02780.x.
- Gray JT, Walker A. Avoiding admissions from the ambulance service: a review of elderly patients with falls and patients with breathing difficulties seen by emergency care practitioners in South Yorkshire. Emerg Med J 2008;25:168-71. http://dx.doi.org/10.1136/emj.2007.050732.
- Reilly MJ. Accuracy of a priority medical dispatch system in dispatching cardiac emergencies in a suburban community. Prehosp Disaster Med 2006;21:77-1.
- Lord B, Williams B, Boyle M. Paramedic identification of ECG J Point and ST segments: a pilot study. AJP 2007;5. http://ro.ecu.edu.au/jephc/vol5/iss2/5.
- Kahalé J, Osmond MH, Nesbitt L, Stiell IG. What are the characteristics and outcomes of nontransported pediatric patients?. Prehosp Emerg Care 2006;10:28-34. http://dx.doi.org/10.1080/10903120500373322.
- Kelly AM, Nicholl J, Turner J. Determining the most effective level of TRISS-derived probability of survival for use as an audit filter. Emerg Med 2002;14:146-52. http://dx.doi.org/10.1046/j.1442-2026.2002.00309.x.
- Smith W, Culley L, Plorde M, Murray JA, Hearne T, Goldberg P, et al. Emergency medical services telephone referral program: an alternative approach to nonurgent 911 calls. Prehosp Emerg Care 2001;5:174-80. http://dx.doi.org/10.1080/10903120190940092.
- Price TG, Hooker EA, Neubauer J. Prehospital provider prediction of emergency department disposition. Prehosp Emerg Care 2005;9:322-5. http://dx.doi.org/10.1080/10903120590962012.
- Kahveci FO, Demircan A, Keles A, Bildik F, Aygencel SG. Efficacy of triage by paramedics: a real-time comparison study. J Emerg Nurs 2012;38:344-9. http://dx.doi.org/10.1016/j.jen.2011.03.004.
- Lammers RL, Roth BA, Utecht T. Comparison of ambulance dispatch protocols for nontraumatic abdominal pain. Ann Emerg Med 1995;26:579-89. http://dx.doi.org/10.1016/S0196-0644(95)70008-0.
- Thakore S, McGugan EA, Morrison W. Emergency ambulance dispatch: is there a case for triage?. J R Soc Med 2002;95:126-9. http://dx.doi.org/10.1258/jrsm.95.3.126.
- Armstrong BP, Simpson HK, Crouch R, Deakin CD. Prehospital clearance of the cervical spine: does it need to be a pain in the neck?. Emerg Med J 2007;24:501-3. http://dx.doi.org/10.1136/emj.2006.041897.
- Boyle MJ. Comparison overview of prehospital errors involving road traffic fatalities in Victoria, Australia. Prehosp Disaster Med 2009;24:254-61.
- Donald M, Paterson B. Introduction of an electronic debrief and governance tool in prehospital care. Emerg Med J 2007;24:363-6. http://dx.doi.org/10.1136/emj.2006.043539.
- Matthews A, Gavin C, O’Driscoll BR. Audit of pre-hospital oxygen therapy by North West Ambulance Service (NWAS) one year after publication of new JRCALC guidance for oxygen use. Thorax 2010;65. http://dx.doi.org/10.1136/thx.2010.151068.32.
- Achieving Improvements Through Clinical Governance. London: The Stationery Office; 2003.
- Safeguarding Children: A Review of Arrangements in the NHS for Safeguarding Children. London: Care Quality Commission; 2009.
- Safe Management and Use of Controlled Drugs in the Ambulance and Paramedic Services in England. Department of Health; n.d.
- Pons PT, Dinerman N, Rosen P, Dernocoeur K, Coxon K, Marlin R. The field instructor program: quality control of prehospital care, the first step. J Emerg Med 1985;2:421-7. http://dx.doi.org/10.1016/0736-4679(85)90251-3.
- Spaite DW, Hanlon T, Criss EA, Valenzuela TD, Meislin HW, Ross J. Prehospital data entry compliance by paramedics after institution of a comprehensive EMS data collection tool. Ann Emerg Med 1990;19:1270-3. http://dx.doi.org/10.1016/S0196-0644(05)82286-3.
- Bergrath S, Rortgen D, Skorning M, Fischermann H, Beckers SK, Mutscher C. Emergency mission documentation in simulated care: video-based error analysis. Anaesthetist 2011;60:221-9. http://dx.doi.org/10.1007/s00101-010-1790-y.
- Cwinn MA, Forster AJ, Adam Cwinn A, Hebert G, Calder L, Stiell IG. Prevalence of information gaps for seniors transferred from nursing homes to the emergency department. CJEM 2009;11:462-72.
- Dalawari P, Duggan J, Vangimalla V, Paniagua M, Armbrecht ES. Patient transfer forms enhance key information between nursing homes and emergency department. Geriatr Nurs 2011;32:270-5. http://dx.doi.org/10.1016/j.gerinurse.2011.05.001.
- Deakin CD, Evans S, King P. Evaluation of telephone-cardiopulmonary resuscitation advice for paediatric cardiac arrest. Resuscitation 2010;81:853-6. http://dx.doi.org/10.1016/j.resuscitation.2010.02.007.
- Evans SM, Murray A, Patrick I, Fitzgerald M, Smith S, Andrianopoulos N, et al. Assessing clinical handover between paramedics and the trauma team. Injury 2010;41:460-4. http://dx.doi.org/10.1016/j.injury.2009.07.065.
- Greenwood MJ, Heninger JR. Structured communication for patient safety in emergency medical services: a legal case report. Prehosp Emerg Care 2010;14:345-8. http://dx.doi.org/10.3109/10903121003760788.
- Grow RW, Sztajnkrycer MD, Moore BR. Language barriers as a reported cause of prehospital care delay in Minnesota. Prehosp Emerg Care 2008;12:76-9. http://dx.doi.org/10.1080/10903120701709878.
- Meisel ZF, Peacock N, Mechem CC. EMS to ED handoffs: a prospective observational analysis. Ann Emerg Med 2010;56:S87-8. http://dx.doi.org/10.1016/j.annemergmed.2010.06.313.
- Murray S, Crouch R, Pope C, Lattimer V, Thompson F, Deakin C, et al. Improving the quality of ambulance crew hand-overs: a qualitive study of knowledge transfer in emergency care teams. Emerg Med J 2011;28. http://dx.doi.org/10.1136/emj.2010.108605.19.
- Owen C, Hemmings L, Brown T. Lost in translation: maximizing handover effectiveness between paramedics and receiving staff in the emergency department. Emerg Med Australas 2009;21:102-7. http://dx.doi.org/10.1111/j.1742-6723.2009.01168.x.
- Waldron R, Sixsmith D. Emergency physician awareness of out-of-hospital procedures and medications. Ann Emerg Med 2011;58. http://dx.doi.org/10.1016/j.annemergmed.2011.06.397.
- Zimmer M, Wassmer R, Latasch L, Oberndörfer D, Wilken V, Ackermann H, et al. Initiation of risk management: incidence of failures in simulated emergency medical service scenarios. Resuscitation 2010;81:882-6. http://dx.doi.org/10.1016/j.resuscitation.2010.03.009.
- Manser T, Foster S, Gisin S, Jaeckel D, Ummenhofer W. Assessing the quality of patient handoffs at care transitions. Qual Saf Health Care 2010;19:1-5.
- Dalto J, Thomas F, Weir C. Analyzing communication errors in an air medical transport service. Air Med J 2011;30. http://dx.doi.org/10.1016/j.amj.2011.07.007.
- Chan EW, Taylor SE, Marriott J, Barger B. An intervention to encourage ambulance paramedics to bring patients’ own medications to the ED: impact on medications brought in and prescribing errors. Emerg Med Australas 2010;22:151-8. http://dx.doi.org/10.1111/j.1742-6723.2010.01273.x.
- Kerry AL, Lobo C, Milanes S, Curtis J, Maskell NA. Audit reviewing the impact of lung alert cards and ambulance crew education on inappropriate oxygen prescribing in patients with COPD. Thorax 2007;62:A64-149.
- Strong C, Thompson CB. Documentation of decision-making during air transport. Air Med J 2000;19:77-82. http://dx.doi.org/10.1016/S1067-991X(00)90026-9.
- Frakes MA, Robinson KJ, McQuay J. Evaluation of a modified sign-out on emergency department documentation of medications administered by critical care transport teams. Air Med J 2009;28:246-7.
- Gustafsson M, Wennerholm S, Fridlund B. Worries and concerns experienced by nurse specialists during inter-hospital transports of critically ill patients: a critical incident study. Intensive Crit Care Nurs 2010;26:138-45. http://dx.doi.org/10.1016/j.iccn.2010.01.002.
- Brady W, Carr G, Ilton J, Robbins K. Emergency medical services transfer of patient information to emergency department personnel. Ann Emerg Med 2004;44. http://dx.doi.org/10.1016/j.annemergmed.2004.07.212.
- Vilke GM, Castillo EM, Metz MA, Ray LU, Murrin PA, Lev R, et al. Community trial to decrease ambulance diversion hours: the San Diego county patient destination trial. Ann Emerg Med 2004;44:295-303. http://dx.doi.org/10.1016/j.annemergmed.2004.05.002.
- Jenkin A, Abelson-Mitchell N, Cooper S. Patient handover: time for a change?. Accid Emerg Nurs 2007;15:141-7. http://dx.doi.org/10.1016/j.aaen.2007.04.004.
- Meisel ZF, Mechem CC, Shofer FS, Feinberg DM, Pollack CV. Discrepancies between the prehospital and hospital record: what is the value of the trip sheet?. Ann Emerg Med 2006;48. http://dx.doi.org/10.1016/j.annemergmed.2006.07.688.
- Poitras J. Delays to angioplasty for patients with ST-elevation myocardial infarction are reducible by ambulance diversion based on a out-of-hospital electrocardiogram. Ann Emerg Med 2008;52. http://dx.doi.org/10.1016/j.annemergmed.2008.06.187.
- Siemsen IM, Madsen MD, Pedersen LF, Michaelsen L, Pedersen AV, Andersen HB, et al. Factors that impact on the safety of patient handovers: an interview study. Scand J Public Health 2012;40:439-48. http://dx.doi.org/10.1177/1403494812453889.
- Atack L, Maher J. Emergency medical and health providers’ perceptions of key issues in prehospital patient safety. Prehosp Emerg Care 2010;14:95-102. http://dx.doi.org/10.3109/10903120903349887.
- Moga C, Harstall C. Air Ambulance Transportation with Capabilities to Provide Advanced Life Support. Edmonton, Canada: Institute of Health Economics; 2008.
- Meisel ZF, Mathew R, Wydro GC, Crawford Mechem C, Pollack CV, Katzer R. Multicenter validation of the Philadelphia EMS admission rule (PEAR) to predict hospital admission in adult patients using out-of-hospital data. Acad Emerg Med 2009;16:519-25. http://dx.doi.org/10.1111/j.1553-2712.2009.00422.x.
- Hayes J, Moore A, Benwell G, Wong BLW. Ambulance Dispatch Complexity and Dispatcher Decision Strategies: Implications for Interface Design n.d.
- Saini D. Information Needs of Pre-Hospital Care Providers – A Requirements Analysis n.d.
- Holtermann K. Dispatch of 9-1-1 calls – a prospective study of criteria-based dispatch for determining the allocation of EMS resources. Prehosp Disaster Med 2002;17.
- Dale J, Higgins J, Williams S, Foster T, Snooks H, Crouch R. Computer assisted assessment and advice for ‘non-serious’ 999 ambulance service callers: the potential impact on ambulance despatch. Emerg Med J 2003;20:178-83. http://dx.doi.org/10.1136/emj.20.2.178.
- Snooks H, Halter M, Lees-Mlanga S, Koenig KL, Miller K. Appropriateness of intravenous cannulation by paramedics: a London study. Prehosp Emerg Care 2000;4:156-63. http://dx.doi.org/10.1080/10903120090941434.
- Shah MN, Davis CO, Bauer C, Arnold J. Preferences for EMS transport and pediatric emergency department care. Prehosp Emerg Care 2008;12:169-75. http://dx.doi.org/10.1080/10903120801907059.
- Snooks H, Kearsley N, Dale J, Halter M, Redhead J, Cheung W. Towards primary care for non-serious 999 callers: results of a controlled study of ‘Treat and Refer’ protocols for ambulance crews. Qual Saf Health Care 2004;13:435-43. http://dx.doi.org/10.1136/qshc.2003.007658.
- Clawson J, Olola C, Heward A, Patterson B, Scott G. The Medical Priority Dispatch System’s ability to predict cardiac arrest outcomes and high acuity pre-hospital alerts in chest pain patients presenting to 9-9-9. Resuscitation 2008;78:298-306. http://dx.doi.org/10.1016/j.resuscitation.2008.03.229.
- Dobson T, Jensen JL, Karim S, Travers AA. Correlation of paramedic administration of furosemide with emergency physician diagnosis of congestive heart failure. J Emerg Prim Health Care 2009;7.
- Houston R, Pearson GA. Ambulance provision for children: a UK national survey. Emerg Med J 2010;27:631-6. http://dx.doi.org/10.1136/emj.2009.088880.
- McDermott FT, Cooper GJ, Hogan PL, Cordner SM, Tremayne AB. Evaluation of the prehospital management road traffic fatalities in Victoria, Australia. Prehosp Disaster Med 2005;20:219-27. http://dx.doi.org/10.1017/S1049023X00002570.
- Schaider JJ, Riccio JC, Rydman RJ, Pons PT. Paramedic diagnostic accuracy for patients complaining of chest pain or shortness of breath. Prehosp Disaster Med 1995;10:245-50.
- Svilaas T, Dijk WA, Busman JP, Dassen WRM, de Vos R, Zijlstra F. The Groningen Ambulance Study n.d.
- Dadkhah S, French SC, Fisch-Cook C, Cook E, Miller M, Chan S, et al. Now evaluate chest pain with 12-lead electrocardiograms and rapid markers for early recognition of myocardial infarctions in the ambulance (new ERA). Ann Emerg Med 1999;34. http://dx.doi.org/10.1016/S0196-0644(99)80262-5.
- van ‘t Hof AWJ, van de Wetering H, Ernst N, Hollak F, de Pooter F, Suryapranata H. A Quantitative Analysis of the Benefits of Pre-Hospital Infarct Angioplasty Triage on Outcome in Patients Undergoing Primary Angioplasty for Acute Myocardial Infarction n.d.
- Lecky F, Bryden D, Little R, Tong N, Moulton C. Emergency intubation for acutely ill and injured patients. Cochrane Database Syst Rev 2008;2. http://dx.doi.org/10.1002/14651858.CD001429.pub2.
- Holliman CJ, Wuerz RC, Meador SA. Decrease in medical command errors with use of a ‘standing orders’ protocol system. Am J Emerg Med 1994;12:279-83. http://dx.doi.org/10.1016/0735-6757(94)90138-4.
- Nicholl J, Coleman P, Parry G, Turner J, Dixon S. Emergency priority dispatch systems: a new era in the provision of ambulance services in the UK. Prehosp Immediate Care 1999;3:71-5.
- Wastell D, Newman M. Information Systems Development in the Ambulance Service: A Tale of Two Cities n.d.
- Wigman LD, van Lieshout EMM, de Ronde G, Patka P, Schipper IB. Trauma-related dispatch criteria for Helicopter Emergency Medical Services in Europe. Injury 2011;42:525-33. http://dx.doi.org/10.1016/j.injury.2010.03.015.
- Schmidt T, Neely KW, Adams AL, Newgard CD, Wittwer L, Muhr M, et al. Is it possible to safely triage callers to EMS dispatch centers to alternative resources?. Prehosp Emerg Care 2003;7:368-74. http://dx.doi.org/10.1080/10903120390936590.
- Brooks L, Fitzgerald G, Atkinson C. Using Actor Network Theory to Interpret the Introduction of Information Systems Within the London Ambulance Service n.d.
- Gratton M, Garza A, Salomone JA, Shearer J. Ambulance staging for potentially dangerous scenes: another hidden component of response time. Ann Emerg Med 2008;52. http://dx.doi.org/10.1016/j.annemergmed.2008.06.194.
- Larson JT, Dietrich AM, Abdessalam SF, Werman HA. Effective Use of the Air Ambulance for Pediatric Trauma n.d.
- White L, Cudnik M, Werman H. Can prehospital triage criteria predict clinical outcomes for trauma patients transported by air. Air Med J 2011;30. http://dx.doi.org/10.1016/j.amj.2011.07.010.
- Van Wijngaarden M, Kortbeek J, Lafreniere R, Cunningham R. Air Ambulance Trauma Transport: A Quality Review n.d.
- McGrath CP, Rosen GS, Bechtel GA. Improving bedside to departure care in air transport of ST segment elevation myocardial infarction patients: a 2-year retrospective study of performance. Air Med J 2009;29:84-7. http://dx.doi.org/10.1016/j.amj.2009.11.001.
- Anonymous . Ambulance errors lead to $10.2 million settlement. Healthc Risk Manag 2002;24:2-3.
- Barry PW, Ralston C. Adverse events occurring during interhospital transfer of the critically ill. Arch Dis Child 1994;71:8-11. http://dx.doi.org/10.1136/adc.71.1.8.
- Chollet C, Ricard-Hibon A, Marty J. Evaluation of a check list for devices used in prehospital emergency medicine. J Euro Urg 1999;12:139-47.
- Levick N, Swanson J. An optimal solution for enhancing ambulance transport safety: a real-time driver performance monitoring and feedback device. Ann Emerg Med 2005;46:S112-13. http://dx.doi.org/10.1016/j.annemergmed.2005.06.415.
- Madar RJ, Milligan DW. Neonatal transport: safety and security. Arch Dis Child 1994;71:F147-8. http://dx.doi.org/10.1136/fn.71.2.F147-a.
- Wang HE, Weaver MD, Abo BN, Kaliappan R, Fairbanks RJ. Ambulance stretcher adverse events. Qual Saf Health Care 2009;18:213-16. http://dx.doi.org/10.1136/qshc.2007.024562.
- Bleiler E. How safe are air ambulances?. Med Econ 1982;59.
- Pham JC, Patel R, Millin M, Kirsch TD, Chanmugam A. The effects of ambulance diversion: a comprehensive review. Acad Emerg Med 2006;13:1220-7. http://dx.doi.org/10.1111/j.1553-2712.2006.tb01652.x.
- Sulis C, Estanislao R, Wedel S. Completeness of cleaning critical care transport vehicles. Air Med J 2010;29.
- Woollard M, Lighton D, Gregory P, Munro G, Jenkinson E, Hamilton L. Malleable stylet vs re-useable and disposable bougies in a model of difficult intubation: a randomised cross-over trial. Emerg Med J 2009;26. http://dx.doi.org/10.1136/emj.2009.075416l.
- Eckstein M, Chan LS. The effect of emergency department crowding on paramedic ambulance availability. Ann Emerg Med 2004;43:100-5. http://dx.doi.org/10.1016/S0196-0644(03)00747-9.
- Vourvahakis D, Zeaki M, Zervopoulos M, Zigoura A, Pyrros D. Laryngeal mask: experience from prehospital use at EKAB in Heraklion, Crete. Prehosp Disaster Med 2002;17.
- Al Darrab A, Fernandes CM, Worster A, Woolfrey K, Moneta S. A city wide approach to reduce ambulance diversion: the Hamilton model. Ann Emerg Med 2005;46:40-1. http://dx.doi.org/10.1016/j.annemergmed.2005.06.154.
- Bassene PH, d’Hollander A, Faller JP, Kara A, Braun JB. Pre-hospital tracheal intubation assisted by fibroscopy in patients with suspicion of cervical spine lesion: a pilot study. Crit Care 1998;2.
- Høyer C, Christensen E, Eika B. Adverse Design of defibrillators: turning off the machine when trying to shock. Ann Emerg Med 2008;52:512-14. http://dx.doi.org/10.1016/j.annemergmed.2007.11.037.
- Khaleghi M, Loh A, Vroman D, Chan TC, Vilke GM. The effects of minimizing ambulance diversion hours on emergency departments. J Emerg Med 2007;33:155-9. http://dx.doi.org/10.1016/j.jemermed.2007.02.014.
- Steele R. Incidence of ambulance diversion in a small US community. Ann Emerg Med 2002;40.
- Vilke GM, Castillo EM, Stepanski BM, Murrin PA, Upledger-Ray L, Metz MA, et al. San Diego County patient destination trial to decrease ambulance diversion hours: three year follow-up. Ann Emerg Med 2006;48. http://dx.doi.org/10.1016/j.annemergmed.2006.07.760.
- Eckstein M, Jantos T, Kelly N. Air ambulance utilization of pediatric transport in an urban setting. Ann Emerg Med 1999;34. http://dx.doi.org/10.1016/S0196-0644(99)80114-0.
- Meisel ZD, Branas C, Pines JM. Type of insurance is associated with ambulance use for transport to emergency departments in the United States. Ann Emerg Med 2009;54.
- Ruger JP. Ambulance utilization practices: is 911-taxi a myth?. Ann Emerg Med 2002;40.
- Lee SW. The use of ambulance services in the transfer of residents from community step-down facilities to a local emergency department. Ann Emerg Med 2002;40.
- Goodloe JM, Crowder CJ, Arthur AO, Thomas SH. EMS stretcher ‘misadventures’ in a large, urban EMS system: a descriptive analysis of contributing factors and resultant injuries. Emerg Med Int 2012. http://dx.doi.org/10.1155/2012/745706.
- Kupas DF, Shayhorn MA, Green P, Payton TF. Structured inspection of medications carried and stored by emergency medical services agencies identifies practices that may lead to medication errors. Prehosp Emerg Care 2012;16:67-75. http://dx.doi.org/10.3109/10903127.2011.621046.
- Thakore S, Morrison W. A survey of the perceived quality of patient handover by ambulance staff in the resuscitation room. Emerg Med J 2001;18:293-6. http://dx.doi.org/10.1136/emj.18.4.293.
- Caulkins CG. On the scene. Do paramedics make an effort not to transport at the end of their shifts?. Emerg Med Serv 2001;30:83-5.
- Cushman JT, Fairbanks RJ, O’Gara KG, Crittenden CN, Pennington EC, Wilson MA. Ambulance personnel perceptions of near misses and adverse events in pediatric patients. Prehosp Emerg Care 2010;14:477-84. http://dx.doi.org/10.3109/10903127.2010.497901.
- Maggiore WA. Failure to transport: new lawsuits, old trends. EMS Insider 2011;38:2-3.
- Patterson PD, Huang DT, Fairbanks RJ, Simeone S, Weaver M, Wang HE. Variation in emergency medical services workplace safety culture. Prehosp Emerg Car 2010;14:448-60. http://dx.doi.org/10.3109/10903127.2010.497900.
- Thomas F, Hopkins RO, Handrahan DL, Walker J, Carpenter J. Sleep and cognitive performance of flight nurses after 12-hour evening versus 18-hour shifts. Air Med J 2006;25:216-25. http://dx.doi.org/10.1016/j.amj.2006.06.005.
- Taylor CB, Stevenson M, Jan S, Middleton PM, Fitzharris M, Myburgh JA. A systematic review of the costs and benefits of helicopter emergency medical services. Injury 2010;41:10-2. http://dx.doi.org/10.1016/j.injury.2009.09.030.
- Siriwardena AN, Iqbal M, Banerjee S, Spaight A, Stephenson J. An evaluation of an educational intervention to reduce inappropriate cannulation and improve cannulation technique by paramedics. Emerg Med J 2009;26:831-6. http://dx.doi.org/10.1136/emj.2008.071415.
- York D, Dudek L, Larson R, Marshall W, Dries D. A comparison study of chest tube thoracostomy: air medical crew and in-hospital trauma service. Air Med J 1993;12:227-9. http://dx.doi.org/10.1016/S1067-991X(05)80187-7.
- Shaban R, Creedy D, Clark M. Ambulance and anthrax – the challenge of infection control and infectious disease in paramedic emergency care. Prehosp Disaster Med 2002;17:S45-6.
- Bernius M, Thibodeau B, Jones A, Clothier B, Witting M. Prevention of pediatric drug calculation errors by prehospital care providers. Prehosp Emerg Care 2008;12:486-94. http://dx.doi.org/10.1080/10903120802290752.
- Hubble MW, Paschal KR, Sanders TA. Medication calculation skills of practicing paramedics. Prehosp Emerg Care 2000;4:253-60. http://dx.doi.org/10.1080/10903120090941290.
- Mackay CA, Terris J, Coats TJ. Prehospital rapid sequence induction by emergency physicians: it is safe?. Emerg Med J 2001;18:20-4. http://dx.doi.org/10.1136/emj.18.1.20.
- Rea TD, Edwards C, Murray JA, Cloyd DJ, Eisenberg MS. Epinephrine use by emergency medical technicians for presumed anaphylaxis. Prehosp Emerg Care 2004;8:405-10. http://dx.doi.org/10.1016/j.prehos.2004.05.006.
- Alvarez-Ortiz NJ, Aranaz Andrés JM, Gea Velázquez De Castro MT, Miralles Bueno JJ. Pre-hospital adverse events: a way to go. Rev Calid Asist 2010;25:28-33. http://dx.doi.org/10.1016/j.cali.2009.07.009.
- Seymour CW, Kahn JM, Schwab CW, Fuchs BD. Adverse events during rotary-wing transport of mechanically ventilated patients: a retrospective cohort study. Crit Care 2008;12:1-10. http://dx.doi.org/10.1186/cc6909.
- McDermott C, Collins NC. Prehospital medication administration: a randomised study comparing intranasal and intravenous routes. Emerg Med Int 2012;2012:1-5.
- Eastwood KJ, Boyle MJ, Williams B. Paramedics’ ability to perform drug calculations. West J Emerg Med 2009;10:240-3.
- Anderson S, Hogskilde PD, Wetterslev J, Bredgaard M, Møller JT, Dahl JB. Appropriateness of leaving emergency medical service treated hypoglycemic patients at home: a retrospective study. Acta Anaesthesiol Scand 2002;46:464-8. http://dx.doi.org/10.1034/j.1399-6576.2002.460424.x.
- Cain E, Ackroyd-Stolarz S, Alexiadis P, Murray D. Prehospital hypoglycemia: the safety of not transporting treated patients. Prehosp Emerg Care 2003;7:458-65. http://dx.doi.org/10.1080/312703002193.
- Cooper SJR, Grant J. New and emerging roles in out of hospital emergency care: a review of the international literature. Int Emerg Nurs 2009;17:90-8. http://dx.doi.org/10.1016/j.ienj.2008.11.004.
- Mechem CC, Barger J, Shofer FS, Dickinson ET. Short-term outcome of seizure patients who refuse transport after prehospital stabilization. Acad Emerg Med 2001;9:231-6. http://dx.doi.org/10.1111/j.1553-2712.2001.tb01298.x.
- Gray JT, Wardrope J. Introduction of non-transport guidelines into an ambulance service: a retrospective review. Emerg Med J 2007;24:727-9. http://dx.doi.org/10.1136/emj.2007.048850.
- Haines CJ, Lutes RE, Blaser M, Christopher NC. Paramedic initiated non-transport of pediatric patients. Prehosp Emerg Care 2006;10:213-19. http://dx.doi.org/10.1080/10903120500541308.
- Hauswald M. Can paramedics safely decide which patients do not need ambulance transport or emergency department care?. Prehosp Emerg Care 2002;6:383-6. http://dx.doi.org/10.1080/10903120290937978.
- Porter A, Snooks H, Youren A, Gaze S, Whitfield R, Rapport F, et al. ‘Should I stay or should I go?’ Deciding whether to go to hospital after a 999 call. J Health Serv Res Policy 2007;12:S1-32.
- Silvestri S, Rothrock SG, Kennedy D, Ladde J, Bryant M, Pagane J. Can paramedics accurately identify patients who do not require emergency department care?. Prehosp Emerg Care 2002;6:387-90. http://dx.doi.org/10.1080/10903120290937987.
- Snooks HA, Halter M, T Close JC, Cheung WY, Moore F, Roberts SE. Emergency care of older people who fall: a missed opportunity. Qual Saf Health Car 2006;15:390-2. http://dx.doi.org/10.1136/qshc.2006.018697.
- Yaxley L, Aldridge V, Almond J, Greenwood RH, Heyburn PJ, Harradence F, et al. Ambulance personnel can successfully treat severe hypoglycaemia. Practical Diabetes 1993;10:67-8. http://dx.doi.org/10.1002/pdi.1960100210.
- Socransky SJ, Pirrallo RG, Rubin JM. Out-of-hospital treatment of hypoglycemia: refusal of transport and patient outcome. Acad Emerg Med 1998;5:1080-5. http://dx.doi.org/10.1111/j.1553-2712.1998.tb02666.x.
- Al-Sulaiti M, Snooks H, Porter A. Non-conveyance of 999 callers: early findings related subsequent health services callers. Emerg Med J 2009;26. http://dx.doi.org/10.1136/emj.2009.075416h.
- Lerner EB, Billittier A, Lance DR, Janicke DM, Teuscher JA. Can paramedics safely treat and discharge hypoglycemic patients in the field?. Am J Emerg Med 2003;21:115-20. http://dx.doi.org/10.1053/ajem.2003.50014.
- Sprehn M, Pedersen CB, Sorensen MB, Bendtson I. Emergency prehospital treatment of severe hypoglycemia in the Copenhagen Municipality. A retrospective analysis of 180 episodes. Ugeskr Laeger 1992;154:1101-4.
- Strote J, Simons R, Eisenberg M. Emergency medical technician treatment of hypoglycemia without transport. Am J Emerg Med 2008;26:291-5. http://dx.doi.org/10.1016/j.ajem.2007.05.030.
- Mechem CC, Kreshak AA, Barger J, Shofer FS. The short-term outcome of hypoglycemic diabetic patients who refuse ambulance transport after out-of-hospital therapy. Acad Emerg Med 1998;5:768-72. http://dx.doi.org/10.1111/j.1553-2712.1998.tb02502.x.
- Burstein JL, Henry M, C, Alicandro J, Gentile D, Thode HC, Hollander JE. Outcome of patients who refused out-of-hospital medical assistance. Am J Emerg Med 1996;14:23-6. http://dx.doi.org/10.1016/S0735-6757(96)90007-8.
- Zachariah BS, Bryan D, Pepe PE, Griffin M. Follow-up and outcome of patients who decline or are denied transport by EMS. Prehosp Disaster Med 1992;7:359-64.
- Ruckoldt H, Marx G, Leuwer M, Panning B, Piepenbrock S. Pulse oximetry and capnography in intensive care transportation: combined use reduces transportation risks. Anasthesiologie 1998;33:32-6.
- Garwe T, Cowan LD, Neas BR, Sacra JC, Albrecht RM. Directness of transport of major trauma patients to a level 1 trauma center: a propensity-adjusted survival analysis of the impact on short-term mortality. J Trauma Acute Care Surg 2011;70:1118-27. http://dx.doi.org/10.1097/TA.0b013e3181e243b8.
- Snooks HA, Nicholl JP, Brazier JE, Lees-Mlanga S. The costs and benefits of helicopter emergency ambulance services in England and Wales. J Public Health 1996;18:67-7. http://dx.doi.org/10.1093/oxfordjournals.pubmed.a024465.
- Wolfberg DM, Verdile VP, Flinn RD. Incorporating drugs and devices into emergency medical services systems. Prehosp Disaster Med 1995;10:189-94.
- Heightman AJ. Patient security redefined. JEMS 2000;25.
- O’Cathain A, Turner J, Nicholl JP. The acceptability of an emergency medical dispatch system to people who call 999 to request an ambulance. Emerg Med J 2002;19:160-3. http://dx.doi.org/10.1136/emj.19.2.160.
- Goldhill D, Gemmell L, Lutman D, McDevitt S, Parris M, Waldmann C. AAGBI Safety Guideline: Interhospital Transfer. London: The Association of Anaesthetists of Great Britain and Ireland; 2009.
- Thomas AN, Harvey JR, Hurst T. Standards for Capnography Guidelines (2011) 2011. www.ics.ac.uk/education/capnography_guidelines (accessed 6 September 2012).
- Acker JE, Pancioli A, Crocco TJ, Eckstein MK, Jauch EC, Larrabee H, et al. Implementation strategies for emergency medical services within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association expert panel on emergency medical services systems and the stroke council. Stroke 2007;38:3097-115. http://dx.doi.org/10.1161/STROKEAHA.107.186094.
- Turner J, Bjarkoy M. Developing new performance indicators for ambulance service category B calls. Emerg Med J 2011;28. http://dx.doi.org/10.1136/emj.2010.108605.21.
- Lloyd MS, Heeke B, Walter PF, Langberg JJ. Hands-on defibrillation: an analysis of electrical current flow through rescuers in direct contact with patients during biphasic external defibrillation. Circulation 2008;117:2510-14. http://dx.doi.org/10.1161/CIRCULATIONAHA.107.763011.
- Derr C, O’Conner B, Klash A, Galwankar S, MacLeod S. The use of continuous positive airway pressure for the treatment of acute severe pulmonary edema in the prehospital setting. Ann Emerg Med 2006;48. http://dx.doi.org/10.1016/j.annemergmed.2006.07.765.
- McGlinch B, Weller E. Patient outcomes following prehospital rapid sequence intubation for medical emergencies. Crit Care 2004;8. http://dx.doi.org/10.1186/cc2753.
- Fairbanks RJ, Crittenden CN, O’Gara KG, Wilson MA, Pennington EC, Chin NP, et al. Emergency medical services provider perceptions of the nature of adverse events and near-misses in out-of-hospital care: an ethnographic view. Acad Emerg Med 2008;15:633-40. http://dx.doi.org/10.1111/j.1553-2712.2008.00147.x.
- Hobgood C, Bowen JB, Brice JH, Overby B, Tamayo-Sarver JH. Do EMS personnel identify, report, and disclose medical errors?. Prehosp Emerg Care 2006;10:21-7. http://dx.doi.org/10.1080/10903120500366011.
- Price L. Treating the clock and not the patient: ambulance response times and risk. Qual Saf Health Care 2006;15:127-30. http://dx.doi.org/10.1136/qshc.2005.015651.
- Price R, Bendall JC, Patterson JA, Middleton PM. What causes adverse events in prehospital care? A human-factors approach. Emerg Med J 2012;30:583-8. http://dx.doi.org/10.1136/emermed-2011-200971.
- Cooper S, O’Carroll J, Jenkin A, Badger B. Collaborative practices in unscheduled emergency care: role and impact of the emergency care practitioner – quantitative findings. Emerg Med J 2007;24:630-3. http://dx.doi.org/10.1136/emj.2007.048058.
- Sukumaran S, Henry JM, Beard D, Lawrenson R, Gordon MW, O’Donnell JJ, et al. Prehospital trauma management: a national study of paramedic activities. Emerg Med J 2005;22:60-3. http://dx.doi.org/10.1136/emj.2004.016873.
- Bahner DP. Prehospital ultrasonography training: a five-month pilot study. Ann Emerg Med 2002;40.
- Barsuk D, Ziv A, Lin G, Blumenfeld A, Rubin O, Keidan I. Using advanced simulation for recognition and correction of gaps in airway and breathing management skills in prehospital trauma care. Anesth Analg 2005;100:803-9. http://dx.doi.org/10.1213/01.ANE.0000143390.11746.CF.
- Belway D, Henderson W, Keenan SP, Levy AR, Dodek PM. Do specialist transport personnel improve hospital outcome in critically ill patients transferred to higher centers? A systematic review. J Crit Care 2006;21:8-17. http://dx.doi.org/10.1016/j.jcrc.2005.12.008.
- Breckwoldt J, Klemstein S, Brunne B, Schnitzer L, Arntz H-R, Mochmann H-C. Expertise in prehospital endotracheal intubation by emergency medicine physicians – comparing ‘proficient performers’ and ‘experts’. Resuscitation 2012;83:434-9. http://dx.doi.org/10.1016/j.resuscitation.2011.10.011.
- Cobas MA, De la Pena MA, Manning R, Candiotti K, Varon AJ. Prehospital intubations and mortality: a level 1 trauma center perspective. Anesth Analg 2009;109:489-93. http://dx.doi.org/10.1213/ane.0b013e3181aa3063.
- Cushman JT, Hettinger AZ, Farney A, Shah MN. Effect of intensive physician oversight on a prehospital rapid-sequence intubation program. Prehosp Emerg Care 2010 n.d.;14:310-16. http://dx.doi.org/10.3109/10903121003760200.
- Davis BD, Fowler R, Kupas DF, Roppolo LP. Role of rapid sequence induction for intubation in the prehospital setting: helpful or harmful?. Curr Opin Crit Care 2002;8:571-77. http://dx.doi.org/10.1097/00075198-200212000-00015.
- Davis DP, Pettit K, Rom CD, Poste JC, Sise MJ, Hoyt DB, et al. The safety and efficacy of prehospital needle and tube thoracostomy by aeromedical personnel. Prehosp Emerg Care 2005;9:191-7. http://dx.doi.org/10.1080/10903120590924500.
- Davis JE, Churosh N, Borloz M, Howell J. Knowledge of self-injectable epinephrine technique among emergency medical services providers. Ann Emerg Med 2009;1. http://dx.doi.org/10.1016/j.annemergmed.2009.06.139.
- Fakhry SM, Scanlon JM, Robinson L, Askari R, Watenpaugh RL, Fata P, et al. Prehospital rapid sequence intubation for head trauma: conditions for a successful program. J Trauma Injury Inf Crit Care 2006;60:997-1001. http://dx.doi.org/10.1097/01.ta.0000217285.94057.5e.
- Gatsoulis N, Tzafestas N, Damaskinos A. Pre-hospital trauma deaths in a tourist region in Greece. Prehosp Immediate Care 2000;4:117-21.
- Hein C, Owen H, Plummer J. A training program for novice paramedics provides initial laryngeal mask airway insertion skill and improves skill retention at 6 months. Simul Healthc 2010;5:33-9. http://dx.doi.org/10.1097/SIH.0b013e3181b5c3fb.
- Harris T, Lockey D. Success in physician prehospital rapid sequence intubation: what is the effect of base speciality and length of anaesthetic training?. Emerg Med J 2011;28:225-9. http://dx.doi.org/10.1136/emj.2009.088302.
- Hein C, Owen H, Plummer J. A 12-month audit of laryngeal mask airway (LMA) use in a South Australian ambulance service. Resuscitation 2008;79:219-24. http://dx.doi.org/10.1016/j.resuscitation.2008.06.014.
- Jones JH, Murphy MP, Dickson RL, Somerville GG, Brizendine EJ. Emergency physician-verified out-of-hospital intubation: miss rates by paramedics. Acad Emerg Med 2004;11:707-9.
- Howerton D, Watson B. An air medical company’s review of crew duty time and the effects on endotracheal intubation success rates. Air Med J 2010;29.
- Meyer PG, Orliaguet G, Blanot S, Jarreau MM, Charron B, Sauverzac R, et al. Complications of emergency tracheal intubation in severely head-injured children. Paediatr Anaesth 2000;10:253-60. http://dx.doi.org/10.1046/j.1460-9592.2000.00496.x.
- Pace SA, Fuller FP. Out-of-hospital succinylcholine-assisted endotracheal intubation by paramedics. Ann Emerg Med 2000;35:568-72. http://dx.doi.org/10.1016/S0196-0644(00)70029-1.
- Parwani V, Hoffman RJ, Russell A, Bharel C, Preblick C, Hahn IH. Practicing paramedics cannot generate or estimate safe endotracheal tube cuff pressure using standard techniques. Prehosp Emerg Care 2007;11:307-11. http://dx.doi.org/10.1080/10903120701348248.
- Sloane C, Vilke GM, Chan TC, Hayden SR, Hoyt DB, Rosen P. Rapid sequence intubation in the field versus hospital in trauma patients. J Emerg Med 2000;19:259-64. http://dx.doi.org/10.1016/S0736-4679(00)00235-3.
- Schmidt U, Stalp M, Gerich T, Blauth M, Maull KI, Tscherne H. Chest tube decompression of blunt chest injuries by physicians in the field: effectiveness and complications. J Trauma 1998;44:98-101. http://dx.doi.org/10.1097/00005373-199801000-00010.
- Warner KJ, Copass MK, Bulger EM. Paramedic use of needle thoracostomy in the prehospital environment. Prehosp Emerg Care 2008;12:162-8. http://dx.doi.org/10.1080/10903120801907299.
- Wang HE, Cook LJ, Chang CC, Yealy DM, Lave JR. Outcomes after out-of-hospital endotracheal intubation errors. Resuscitation 2009;80:50-5. http://dx.doi.org/10.1016/j.resuscitation.2008.08.016.
- Wang HE, Lave JR, Sirio CA, Yealy DM. Paramedic intubation errors: isolated events or symptoms of larger problems? These emergency treatment errors could be an important indicator of out-of-hospital care quality. Health Aff 2006;25:501-9. http://dx.doi.org/10.1377/hlthaff.25.2.501.
- Wirtz DD, Ortiz C, Newman DH, Zhitomirsky I. Unrecognized misplacement of endotracheal tubes by ground prehospital providers. Prehosp Emerg Care 2007;11:213-18. http://dx.doi.org/10.1080/10903120701205935.
- Yeung KL, Yeung GWY, Chan MWS, Lee SB, Choi KT, Lee LL. Knowledge of inter-facility transport among emergency nurses in Hong Kong: a questionnaire survey. Int Emerg Nurs 2008;16:159-64. http://dx.doi.org/10.1016/j.ienj.2008.05.001.
- Palazzo K, Stuhlmiller D, Funk D, Tilney P, Thomas S. Analysis of HEMS individual endotracheal intubation attempt. Air Med J 2011;30. http://dx.doi.org/10.1016/j.amj.2011.07.006.
- Olasveengen TM, Lund-Kordahl I, Steen PA, Sunde K. Out-of hospital advanced life support with or without a physician: effects on quality of CPR and outcome. Resuscitation 2009;80:1248-52. http://dx.doi.org/10.1016/j.resuscitation.2009.07.018.
- Kryder GD, Jang TB, Tan D. Key factors in out-of-hospital intubation suggested for further training. Ann Emerg Med 2004;44. http://dx.doi.org/10.1016/j.annemergmed.2004.07.331.
- Barton ED, Swanson ER, Hutton KC. Success and failure rates of rapid sequence intubation versus non–rapid sequence intubation by air medical providers in 2,853 patients. Ann Emerg Med 2004;44.
- Domeier RM, Chudnofsky CR, Frederiksen SM, Colone P. The effect of paramedic rapid sequence intubation on outcome in trauma patients. Ann Emerg Med 2004;44. http://dx.doi.org/10.1016/j.annemergmed.2004.07.381.
- Morrison LJ, Verbeek PR, McDonald AC, Sawadsky BV, Cook DJ. Mortality and prehospital thrombolysis for acute myocardial infarction: a meta-analysis. JAMA 2000;283:2686-92. http://dx.doi.org/10.1001/jama.283.20.2686.
- Bair AE, Smith D, Lichty L. Intubation confirmation techniques associated with unrecognized non-tracheal intubations by pre-hospital providers. J Emerg Med 2005;28:403-7. http://dx.doi.org/10.1016/j.jemermed.2004.12.008.
- Lowe L, Sagehorn K, Madsen R. The effect of a rapid sequence induction protocol on intubation success rate in an air medical program. Air Med J 1998;17:101-4. http://dx.doi.org/10.1016/S1067-991X(98)90103-1.
- Wang HE, Balasubramani GK, Cook LJ, Lave JR, Yealy DM. Out-of-hospital endotracheal intubation experience and patient outcomes. Ann Emerg Med 2010;55:527-37. http://dx.doi.org/10.1016/j.annemergmed.2009.12.020.
- Brown J, Thomas F. What happens with failed blind nasal tracheal intubations?. Air Med J 2001;20:13-6. http://dx.doi.org/10.1016/S1067-991X(01)70093-4.
- Wang HE, O’Connor RE, Schnyder ME, Barnes TA, Megargel RE. Patient status and time to intubation in the assessment of prehospital intubation performance. Prehosp Emerg Care 2001;5:10-8. http://dx.doi.org/10.1080/10903120190940254.
- Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med 2001;37:32-7. http://dx.doi.org/10.1067/mem.2001.112098.
- Cooper S, O’Carroll J, Jenkin A, Badger B. Collaborative practices in unscheduled emergency care: role and impact of the emergency care practitioner – qualitative and summative findings. Emerg Med J 2007;24:625-9. http://dx.doi.org/10.1136/emj.2006.043943.
- Brown L. Do warning lights and sirens reduce ambulance response times?. Ann Emerg Med 1999;34. http://dx.doi.org/10.1016/S0196-0644(99)80141-3.
- Cooney DR, Wojcik S, Seth N. 117 Can NEDOCS score be used to predict ambulance offload delay?. Ann Emerg Med 2011;58. http://dx.doi.org/10.1016/j.annemergmed.2011.06.144.
- Lerner EB, Billittier AJ, Adolf JE. Ambulance, fire, and police dispatch times compared with the atomic clock. Prehosp Emerg Care 2000;4:28-30. http://dx.doi.org/10.1080/10903120090941597.
- Yeh C, Bloom E, Ramanujam P. A comparison of time to scene response intervals for acute stroke: Is time saved by red lights and siren response?. Ann Emerg Med 2011;1. http://dx.doi.org/10.1016/j.annemergmed.2011.06.398.
- Gilbert M. Save time, save lives in acute MI: preliminary results from a local community model for early, prehospital thrombolysis in Troms county, Norway. Acta Anaesthesiol Scand Suppl 2001;115.
- Drew BJ, Sommargren CE, Schindler DM, Benedict K, Zegre-Hemsey J, Glancy JP. A simple strategy improves prehospital electrocardiogram utilization and hospital treatment for patients with acute coronary syndrome (from the ST SMART Study). Am J Cardiol 2011;107:347-52. http://dx.doi.org/10.1016/j.amjcard.2010.09.027.
- Dhindsa HS, Lovelady J, Nicholson B, Reid R. Does the use of helicopter EMS reduce door to balloon time for STEMI Patients?. Air Med J 2011;30:255-6. http://dx.doi.org/10.1016/j.amj.2011.07.011.
- Ho J, Casey B. Time saved with use of emergency warning lights and sirens during response to requests for emergency medical aid in an urban environment. Ann Emerg Med 1998;32:585-8. http://dx.doi.org/10.1016/S0196-0644(98)70037-X.
- Hunt RC, Brown LH, Cabinum ES, Whitley TW, Prasad NH, Owens CF, et al. Is ambulance transport time with lights and siren faster than that without?. Ann Emerg Med 1995;25:507-11. http://dx.doi.org/10.1016/S0196-0644(95)70267-9.
- Marques-Baptista A, Ohman-Strickland P, Baldino KT, Prasto M, Merlin MA. Utilization of warning lights and siren based on hospital time-critical interventions. Prehosp Disaster Med 2010;25:335-9.
- O’Brien DJ, Price TG, Adams P. The effectiveness of lights and siren use during ambulance transport by paramedics. Prehosp Emerg Care 1999;3:127-30. http://dx.doi.org/10.1080/10903129908958920.
- Ho J, Lindquist M. Time saved with the use of emergency warning lights and siren while responding to requests for emergency medical aid in a rural environment. Prehosp Emerg Care 2001;5:159-62. http://dx.doi.org/10.1080/10903120190940056.
- Frendl DM, Palmeri ST, Clapp JR, Hampton D, Sejersten M, Young D. Overcoming barriers to developing seamless ST-segment elevation myocardial infarction care systems in the United States: recommendations from a comprehensive prehospital 12-lead electrocardiogram working group. J Electrocardiol 2009;42:426-31. http://dx.doi.org/10.1016/j.jelectrocard.2009.03.011.
- Brown LH, Fowler NH. An evaluation of EMS educational programs in North Carolina. Prehosp Emerg Care 1999;3:157-62. http://dx.doi.org/10.1080/10903129908958925.
- Batchelder AJ, Steel A, Mackenzie R, Hormis AP, Daniels TS, Holding N. Simulation as a tool to improve the safety of pre-hospital anaesthesia – a pilot study. Anaesthesia 2009;64:978-83. http://dx.doi.org/10.1111/j.1365-2044.2009.05990.x.
- Thomas F, Rhoades C, Carpenter J, Holleran R, Handrahan D. Difficult airway simulator intubation success rates using commission on accreditation of medical transport systems training standards. Air Med J 2011;30:208-15. http://dx.doi.org/10.1016/j.amj.2010.12.001.
- Eastwood K, Boyle MJ, Williams B. Mathematical and drug calculation abilities of paramedic students. Emerg Med J 2013;30:241-2. http://dx.doi.org/10.1136/emermed-2011-200929.
- Lindstrom A. Patient’s clothing ignites during defibrillation. JEMS 2004;29:20-1.
- Steinbruner D, Mazur R, Mahoney PF. Intracranial placement of a nasopharyngeal airway in a gun shot victim. Emerg Med J 2007;24. http://dx.doi.org/10.1136/emj.2007.046490.
- Schade K, Borzotta A, Michaels A. Intracranial malposition of nasopharyngeal airway. J Trauma 2000;49:967-8. http://dx.doi.org/10.1097/00005373-200011000-00032.
- Bultman LL, Mahoney B, Fringer R. Effectiveness of prehospital continuous positive airway pressure in treating adult respiratory distress. Ann Emerg Med 2005;46. http://dx.doi.org/10.1016/j.annemergmed.2005.06.416.
- Sterba JA. Efficacy and safety of prehospital rewarming techniques to treat accidental hypothermia. Ann Emerg Med 1991;20:896-901. http://dx.doi.org/10.1016/S0196-0644(05)81434-9.
- Jensen JL, Croskerry C, Travers AH. Consensus on paramedic clinical decisions during high acuity emergency calls: results of a Canadian Delphi study. CJEM 2010;12:229-78.
- Liberman M, Mulder D, Sampalis J. Advanced or basic life support for trauma: meta-analysis and critical review of the literature. J Trauma 2000;49:584-99. http://dx.doi.org/10.1097/00005373-200010000-00003.
- Alldredge BK, Gelb AM, Isaacs SM, Corry MD, Allen F, Ulrich S. A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N Engl J Med 2001;345:631-7. http://dx.doi.org/10.1056/NEJMoa002141.
- Morales JM, Rodriguez MM, Terol J, Torres A, Alvarez JM. Nursing records with standardized nursing language in prehospital emergency care: from utopia to reality. Int J Nurs Terminol Classif 2003;14. http://dx.doi.org/10.1111/j.1744-618X.2003.032_9.x.
- Febra C, Lufinha A. Prehospital transcutaneous cardiac pacing in bradycardia and asystole. Crit Care 2005;9. http://dx.doi.org/10.1186/cc3371.
- Garza AG. Prehospital intubation is associated with increased mortality in primary cardiac arrest patients with ventricular fibrillation. Ann Emerg Med 2006;48. http://dx.doi.org/10.1016/j.annemergmed.2006.07.761.
- LeBlanc VR, Regehr C, Tavares W, Scott AK, MacDonald R, King K. The impact of stress on paramedic performance during simulated critical events. Prehosp Disaster Med 2012;27:369-74. http://dx.doi.org/10.1017/S1049023X12001021.
- MacDonald RD, Adhikari NKJ, Scales DC, Wax RS, Stewart TE, Ferguson ND, et al. Outcomes of interfacility critical care adult patient transport: a systematic review. Can J Anaesth 2006;53:A417-18. http://dx.doi.org/10.1007/BF03022513.
- Patterson PD, Huang DT, Fairbanks RJ, Wang HE. The emergency medical services safety attitudes questionnaire. Am J Med Qual 2010;25:109-15. http://dx.doi.org/10.1177/1062860609352106.
- American College of Emergency Physicians . EMS as an essential public safety service. Policy statement. Ann Emerg Med 2011;57:313-14. http://dx.doi.org/10.1016/j.annemergmed.2010.11.018.
- Singh JM, MacDonald RD, Bronskill SE, Schull MJ. Incidence and predictors of critical events during urgent air-medical transport. Can Med Assoc J 2009;181:579-84. http://dx.doi.org/10.1503/cmaj.080886.
- Ursic C, Curtis K, Zou Y, Black D. Improved trauma patient outcomes after implementation of a dedicated trauma admitting service. Injury 2009;40:99-103. http://dx.doi.org/10.1016/j.injury.2008.06.034.
- Mariani M, Musso P, Dalmasso M. Feasibility and safety of transferring patients with acute coronary syndrome between hospitals. Trends Med 2008;8:49-54.
- Hoot NR, Zhou C, Jones I, Aronsky D. Measuring and forecasting emergency department crowding in real time. Ann Emerg Med 2007;49:747-55. http://dx.doi.org/10.1016/j.annemergmed.2007.01.017.
- Schull MJ, Morrison LJ, Vermeulen M, Redelmeier DA. Emergency department overcrowding and ambulance transport delays for patients with chest pain. CMAJ 2003;168:277-83.
- Braithwaite I. Issues in neonatal transport: improving safety for patients and staff. J Neonatal Nurs 2000;6:65-9.
- Selevan JS, Fields WW, Chen W, Petitti DB, Wolde-Tsadik G. Critical care transport: outcome evaluation after interfacility transfer and hospitalization. Ann Emerg Med 1999;33:33-4. http://dx.doi.org/10.1016/S0196-0644(99)70414-2.
- Brown LH, Whitney CL, Hunt RC, Addario M, Hogue T. Do warning lights and sirens reduce ambulance response times?. Prehosp Emerg Care 2000;4:70-4. http://dx.doi.org/10.1080/10903120090941696.
- Low RB, Martin D, Brown C. Emergency air transport of pregnant patients: the national experience. J Emerg Med 1988;6:41-8. http://dx.doi.org/10.1016/0736-4679(88)90250-8.
- Orthner H. Advanced Communication Infrastructure for Pre-Hospital EMS Care n.d.
- Widner-Kolberg MR. Immobilizing children in care safety seats – why, when, and how. J Emerg Nurs 1991;17:427-8.
- Putzer G, Braun P, Zimmermann A, Pedross F, Strapazzon G, Brugger H, et al. LUCAS compared to manual cardiopulmonary resuscitation is more effective during helicopter rescue – a prospective, randomized, cross-over manikin study. Am J Emerg Med 2013;31:384-9. http://dx.doi.org/10.1016/j.ajem.2012.07.018.
- Berg BW, Beamis EK, Murray WB, Boedeker BH. Remote videolaryngoscopy skills training for prehospital personnel. Stud Health Technol Inform 2009;142:31-3.
- Jones A, Allinson K, Wright H, Porter K. Use of prehospital dressings in soft tissue trauma: is there any conformity or plan?. Emerg Med J 2009;26:532-4.
- Lobel D, Likourezos A, Farahani C, Podolsky S. Successful implementation of an etomidate-facilitated endotracheal intubation protocol in an urban ground transport ambulance system. Ann Emerg Med 2008;52. http://dx.doi.org/10.1016/j.annemergmed.2008.06.191.
- Iqbal M, Banerjee S, Spaight A, Stephenson J, Siriwardena AN. Prehospital intravenous cannulation: reducing the risks and rate from inappropriate venous access by paramedics. Emerg Med J 2009;26. http://dx.doi.org/10.1136/emj.2009.075432a.
- Yaghoubian A, Lewis RJ, Putnam B, De Virgilio C. Reanalysis of Prehospital Intravenous Fluid Administration in Patients With Penetrating Truncal Injury and Field Hypotension n.d.
- Vilke GM, Tornabene SV, Stepanski B, Shipp HE, Ray LU, Metz MA. Paramedic self-reported medication errors. Prehosp Emerg Care 2007;11:80-4. http://dx.doi.org/10.1080/10903120601021358.
- Shewakramani S, Harrison TH, Nardelli B, Thomas SH. Adequacy of fluid resuscitation during transport of burn patients. Ann Emerg Med 2006;48. http://dx.doi.org/10.1016/j.annemergmed.2006.07.690.
- Smith D, Bair AE. Intubation techniques associated with unrecognized nontracheal intubations by out-of-hospital providers. Ann Emerg Med 2003;42:S1-109.
- Cameron PA, Gabbe B, Bernard S, Mulholland S. Does intubation prehospital improve outcomes for head injured patients. Ann Emerg Med 2005;46. http://dx.doi.org/10.1016/j.annemergmed.2005.06.413.
- Millikan D, Rice B, Silbergleit R. Emergency treatment of status epilepticus: current thinking. Emerg Med Clin N Am 2009;27:101-13. http://dx.doi.org/10.1016/j.emc.2008.12.001.
- Birk HO, Henriksen LO. Ambulance-technicians’ indications for prehospital interventions. Prehosp Disaster Med 2002;17.
- Cameron P, Gabbe B, Finch C, McNeil J, Smith K, Wolfe R. Prehospital predictors of major injury. Prehosp Disaster Med 2002;17:S8-9.
- Hick JL, Mahoney BD, Lappe M. Prehospital sedation with intramuscular droperidol: a one-year pilot. Prehosp Emerg Care 2001;5:391-4. http://dx.doi.org/10.1080/10903120190939571.
- Gausche M, Lewis RJ, Stratton SJ, Haynes BE, Gunter CS, Goodrich SM. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. JAMA 2000;283:783-90. http://dx.doi.org/10.1001/jama.283.6.783.
- Smith WS, Isaacs M, Corry MD. Accuracy of paramedic identification of stroke and transient ischemic attack in the field. Prehosp Emerg Care 1998;2:170-5. http://dx.doi.org/10.1080/10903129808958866.
- Nardi G, Massarutti D, Kette F, De Monte A. Pre-hospital care for severe trauma patients: on the field ATLS and helicopter transport are associated with a sharp reduction in mortality. Clin Intensive Care 1995;6.
- Massarutti D, Trillo G, Berlot G, Tomasini A, Bacer B, D’Orlando L. Simple thoracostomy in prehospital trauma management is safe and effective: A 2-year experience by helicopter emergency medical crews. Eur J Emerg Med 2006;13:276-80. http://dx.doi.org/10.1097/00063110-200610000-00006.
- Haynes BE, Pritting J. A rural emergency medical technician with selected advanced skills. Prehosp Emerg Care 1999;3:343-6. http://dx.doi.org/10.1080/10903129908958966.
- Widiatmoko D, Machen I, Dickinson A, Williams J, Kendall S. Developing a new response to non-urgent emergency calls: evaluation of a nurse and paramedic partnership intervention. Prim Health Care Res Dev 2008;9:183-90. http://dx.doi.org/10.1017/S1463423608000765.
- Schaefer RA, Rea TD, Plorde M, Peiguss K, Goldberg P, Murray JA. An emergency medical services program of alternate destination of patient care. Prehosp Emerg Care 2002;6:309-14. http://dx.doi.org/10.1080/10903120290938355.
- Anderson BD, Manoguerra AS, Haynes BE. Diversion of 911 poisoning calls to a poison center. Prehosp Emerg Care 1998;2:176-9. http://dx.doi.org/10.1080/10903129808958867.
- Nieva VF, Sorra J. Safety culture assessment: a tool for improving patient safety in healthcare organizations. Qual Saf Health Care 2003;12:ii17-23. http://dx.doi.org/10.1136/qhc.12.suppl_2.ii17.
- NPSA . Manchester Patient Safety Framework (MaPSaF) – Acute 2006. www.nrls.npsa.nhs.uk/EasySiteWeb/getresource.axd?AssetID=60013&type=full&servicetype=Attachment (accessed 12 January 2011).
- Mannion R, Konteh FH, Davies HTO. Assessing organisational culture for quality and safety improvement: a national survey of tools and tool use. Qual Saf Health Care 2009;18:153-6. http://dx.doi.org/10.1136/qshc.2007.024075.
- Eurocontrol/FAA . Action Plan 15 Safety: Safety Culture in Air Traffic Management – A White Paper n.d. www.eurocontrol.int/safety/gallery/content/public/library/Safety%20Culture/Safety_ATM_WhitePaper_final%20low.pdf (accessed 12 January 2011).
- Organising for Safety: 3rd Report of the ACSNI Study Group on Human Factors. London: HSE Books; 1993.
- Pronovost P, Sexton B. Assessing safety culture: guidelines and recommendations. Qual Saf Health Care 2005;14:231-3. http://dx.doi.org/10.1136/qshc.2005.015180.
- Sexton J, Helmreich R, Neilands T, . The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res 2006;6. http://dx.doi.org/10.1186/1472-6963-6-44.
- Flin R, Burns C, Mearns K, Yule S, Robertson EM. Measuring safety climate in health care. Qual Saf Health Care 2006;15:109-15. http://dx.doi.org/10.1136/qshc.2005.014761.
- Sorra JS, Nieva VF. Hospital Survey on Patient Safety Culture. Rockville, MD: Agency for Healthcare Research and Quality; 2004.
- MacDonald R, Yelle R, Oake-Vecchiato JA, Melis C, Bigham BL. Derivation of a taxonomy to categorize adverse events and near-misses in transport medicine. Air Med J 2011;30:254-5. http://dx.doi.org/10.1016/j.amj.2011.07.008.
- Stella J, Davis A, Jennings P, Bartley B. Introduction of a prehospital critical incident monitoring system – pilot project results. Prehosp Disaster Med 2008;23:154-60.
- Meisel ZF, Hargarten S, Vernick J. Addressing prehospital patient safety using the science of injury prevention and control. Prehosp Emerg Care 2008;12:411-16. http://dx.doi.org/10.1080/10903120802290851.
- Levick NR, Swanson J. An optimal solution for enhancing ambulance safety: implementing a driver performance feedback and monitoring device in ground emergency medical service vehicles. Annu Proc Assoc Adv Automot Med 2005;49:35-50.
- O’Connor RE, Slovis CM, Hunt RC, Pirrallo RG, Sayre MR. Eliminating errors in emergency medical services: Realities and recommendations. Prehosp Emerg Care 2002;6:107-13. http://dx.doi.org/10.1080/10903120290938913.
- O’Connor RE, Megargel RE. The effect of a quality improvement feedback loop on paramedic skills, charting, and behavior. Prehosp Disaster Med 1994;9:35-9.
- Taking Healthcare to the Patient: Transforming NHS Ambulance Services. London: Department of Health; 2005.
- Changing times – Sustaining Long-Term Performance Against ‘Call Connect’ for NHS Ambulance Services. London: Department of Health; 2008.
- A Vision for Emergency and Urgent Care – The Role of Ambulance Services. London: NHS Confederation; 2008.
- Jones SP, Carter B, Ford GA, Gibson JM, Leathley MJ, McAdam JJ, et al. The identification of acute stroke: an analysis of emergency calls. Int J Stroke 2013;8:408-12. http://dx.doi.org/10.1111/j.1747-4949.2011.00749.x.
- Beynon-Davies P. Human error and information systems failure: the case of the London ambulance service computer-aided dispatch system project. Interact Comput 1999;11:699-720. http://dx.doi.org/10.1016/S0953-5438(98)00050-2.
- Ferreira J, Stanley L. Assessment of the Use of Carry Chairs by UK Ambulance Staff n.d.
- Eckstein M, Chan LS. The impact of emergency department crowding on paramedic ambulance availability. Ann Emerg Med 2003;42:S1-109.
- Polk JD, Merlino JI, Kovach BL, Mancuso C, Fallon WF. Fetal evaluation for transport by ultrasound performed by air medical teams: a case series. Air Med J 2004;23:32-4. http://dx.doi.org/10.1016/j.amj.2004.04.005.
- Dahlgren BE, Hogberg R, Nilsson HG. Portable, but suitable: devices in prehospital care might be hazardous to patient or to aviation safety. Prehosp Disaster Med 1997;12:64-7.
- Crossing the Quality Chasm: A New Healthcare System for the 21st Century. Washington, DC: National Academy Press; 2004.
- Safe Handover: Safe Patients. London: BMA; 2004.
- Joint Commission on Accreditation of Healthcare . Focus on five. Strategies to improve hand-off communication: implementing a process to resolve questions. Joint Commission Perspectives on Patient Safety 2005;5.
- Apker J, Mallak LA, Gibson SC. Communicating in the ‘Gray Zone’: perceptions about emergency physician–hospitalist handoffs and patient safety. Acad Emerg Med 2007;14:884-94.
- Jeffcott SA, Ibrahim JE, Cameron PA. Resilience in healthcare and clinical handover. Qual Saf Health Care 2009;18:256-60. http://dx.doi.org/10.1136/qshc.2008.030163.
- Raduma-Tomàs MA, Flin R, Yule S, Williams D. Doctors’ handovers in hospitals: a literature review. BMJ Qual Saf 2011;20:128-33. http://dx.doi.org/10.1136/bmjqs.2009.034389.
- Wong MC, Yee KC, Turner P. Clinical Handover Literature Review. Sydney, NSW: Australian Commission on Safety and Quality in Healthcare; 2008.
- Bost N, Crilly J, Wallis M, Patterson E, Chaboyer W. Clinical handover of patients arriving by ambulance to the emergency department – a literature review. Int Emerg Nurs 2010;18:210-20. http://dx.doi.org/10.1016/j.ienj.2009.11.006.
- Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Qual Saf Health Care 2010;19:493-7. http://dx.doi.org/10.1136/qshc.2009.033480.
- Patterson WS, Wears RL. Patient handoffs: standardised and reliable measurement tools remain elusive. Jt Comm J Qual Patient Saf 2010;36:52-61.
- Cook RI, Render M, Woods DD. Gaps in the continuity of care and progress on patient safety. BMJ 2000;320:791-4. http://dx.doi.org/10.1136/bmj.320.7237.791.
- Horwitz L, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med 2006;166:1173-7. http://dx.doi.org/10.1001/archinte.166.11.1173.
- Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med 2005;80:1094-9. http://dx.doi.org/10.1097/00001888-200512000-00005.
- Ye K, McD Taylor D, Knott JC, Dent A, MacBean CE. Handover in the emergency department: deficiencies and adverse effects. Emerg Med Australas 2007;19:433-41. http://dx.doi.org/10.1111/j.1742-6723.2007.00984.x.
- Talbot R, Bleetman A. Retention of information by emergency department staff at ambulance handover: do standardised approaches work?. Emerg Med J 2007;24:539-42. http://dx.doi.org/10.1136/emj.2006.045906.
- McFetridge B, Gillespie M, Goode D, Melby V. An exploration of the handover process of critically ill patients between nursing staff from the emergency department and the intensive care unit. Nurs Crit Care 2007;12:261-9. http://dx.doi.org/10.1111/j.1478-5153.2007.00244.x.
- Catchpole K, Sellers R, Goldman A, McCulloch P, Hignett S. Patient handovers within the hospital: translating knowledge from motor racing to healthcare. Qual Saf Health Care 2010;19:318-22. http://dx.doi.org/10.1136/qshc.2009.026542.
- Philibert I. Use of strategies from high-reliability organisations to the patient hand-off by resident physicians: practical implications. Qual Saf Health Care 2009;18:261-6. http://dx.doi.org/10.1136/qshc.2008.031609.
- Marshall S, Harrison J, Flanagan B. The teaching of a structured tool improves the clarity and content of interprofessional clinical communication. Qual Saf Health Care 2009;18:137-40. http://dx.doi.org/10.1136/qshc.2007.025247.
- Johnson JK, Arora VM. Improving clinical handovers: creating local solutions for a global problem. Qual Saf Health Care 2009;18:244-5. http://dx.doi.org/10.1136/qshc.2009.032946.
- Bomba D, Prakash R. A description of handover processes in an Australian public hospital. Aust Health Rev 2005;29:68-79. http://dx.doi.org/10.1071/AH050068.
- McCann L, McHardy K, Child S. Passing the buck: clinical handovers at a tertiary hospital. N Z Med J 2007;120.
- Vidyarthi AR, Arora V, Schnipper JL, Wall SD, Wachter RM. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med 2006;1:257-66. http://dx.doi.org/10.1002/jhm.103.
- Arora VM, Johnson JK, Meltzer DO, Humphrey HJ. A theoretical framework and competency-based approach to improving handoffs. Qual Saf Health Care 2008;17:11-4. http://dx.doi.org/10.1136/qshc.2006.018952.
- Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH. What are covering doctors told about their patients? Analysis of sign-out among internal medicine house staff. Qual Saf Health Care 2009;18:248-55. http://dx.doi.org/10.1136/qshc.2008.028654.
- Cleland JA, Ross S, Miller SC, Patey R. ‘There is a chain of Chinese whispers . . .’: empirical data support the call to formally teach handover to prequalification doctors. Qual Saf Health Care 2009;18:267-71. http://dx.doi.org/10.1136/qshc.2008.029983.
- Cheung DS, Kelly JJ, Beach C, Berkeley RP, Bitterman RA, Broida RI, et al. Improving handoffs in the emergency department. Ann Emerg Med 2010;55:171-80. http://dx.doi.org/10.1016/j.annemergmed.2009.07.016.
- Arora V, Johnson J, Lovinger D, Humphrey HJ, Meltzer DO. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care 2005;14:401-7. http://dx.doi.org/10.1136/qshc.2005.015107.
- Arora V, Julia K, Lovinger D, Seiden SC, Meltzer D. Medication discrepancies in resident sign-outs and their potential to harm. J Gen Intern Med 2007;200:1751-5. http://dx.doi.org/10.1007/s11606-007-0415-x.
- Rehn M, Vigerust T, Andersen JE, Krüger AJ, Lossius HM. Major incident patient evacuation: full-scale field exercise feasibility study. Air Med J 2011;30:153-7. http://dx.doi.org/10.1016/j.amj.2011.01.005.
- Sillesen M, Sejersten M, Strange S, Clemmensen P. Telemedical Transmission of Prehospital ECG’s in Patients With Acute Chest Pain n.d.
- Sujan MA, Chessum P, Rudd M, Fitton L, Inada-Kim M, Spurgeon P, et al. Emergency Care Handover (ECHO study) across care boundaries: the need for joint decision making and consideration of psychosocial history. Emerg Med J 2015;32:112-8. http://dx.doi.org/10.1136/emermed-2013-202977.
- National Health Service Act 2006. London: The Stationery Office; 2006.
- Monitor . NHS Foundation Trust Annual Reporting Manual 2011 12 2012. www.monitor-nhsft.gov.uk/sites/default/files/Annual_Reporting_Manual_2011-12%20-%20final_2.pdf (accessed 21 May 2014).
- Department of Health . Quality Accounts Toolkit 2010 11 – Advisory Guidance for Providers of NHS Services Producing Quality Accounts for the Year 2010 11 2010. www.gov.uk/government/uploads/system/uploads/attachment_data/file/216185/dh_122540.pdf (accessed 21 May 2014).
- National Patient Safety Agency . Organisation Patient Safety Incident Reports n.d. www.nrls.npsa.nhs.uk/patient-safety-data/organisation-patient-safety-incident-reports/ (accessed 21 June 2012).
- National Patient Safety Agency . Organisation Patient Safety Incident Reports n.d. www.nrls.npsa.nhs.uk/patient-safety-data/organisation-patient-safety-incident-reports/directory/?q=0%C2%ACambulance%C2%AC (accessed 13 May 2012).
- Wang HE, Fairbanks RJ, Shah MN, Abo BN, Yealy DM. Tort claims and adverse events in emergency medical services. Ann Emerg Med 2008;52:256-62. http://dx.doi.org/10.1016/j.annemergmed.2008.02.011.
- Clark JR. Delay in Treatment. Air Med J 2011;30:117-19. http://dx.doi.org/10.1016/j.amj.2011.03.001.
- Policy paper . Summary of Reports and Responses under Rule 43 of the Coroners Rules n.d. www.justice.gov.uk/publications/policy/moj/summary-of-reports-and-responses-under-rule-43-of-the-coroners-rules (accessed 7 November 2011).
- National Health Service National Staff Survey. 2011. Essex: Data Archive [distributor]; 2013.
- Paul CL. A modified Delphi approach to a new card sorting methodology. Journal of Usability Studies 2008;4:7-30.
- Taylor-Adams S, Vincent C. System Analysis of Clinical Incidents: The London Protocol. Imperial College London, London: Clinical Safety Research Unit; 2012.
- Lawton R, McEachan RRC, Giles SJ, Sirriyeh R, Watt IS, Wright J. Development of an evidence-based framework of factors contributing to patient safety incidents in hospital settings: a systematic review. BMJ Qual Saf 2012. http://dx.doi.org/10.1136/bmjqs-2011-000443.
- Edmondson AC. Learning from mistakes is easier said than done: group and organizational influences on the detection and correction of human error. J Appl Behavl Sci 1996;32:5-28. http://dx.doi.org/10.1177/0021886396321001.
- Stymiest DL. Joining forces. Integrating utility and emergency management for better patient safety. Health Facil Manage 2003;16:26-9.
- Stoop JA. Independent accident investigation: a modern safety tool. J Hazard Mater 2004;111:39-44. http://dx.doi.org/10.1016/j.jhazmat.2004.02.006.
- Danielson NE. EtO Emergency. Think safety before a spill. Mater Manag Health Care 1998;7.
- McNamara R, Yu DK, Kelly JJ. Public perception of safety and metal detectors in an urban emergency department. Am J Emerg Med 1997;15:40-2. http://dx.doi.org/10.1016/S0735-6757(97)90045-0.
- Thompson MR. The three Rs of fire safety, emergency action, and fire prevention planning: promoting safety at the worksite. AAOHN J 2003;51:169-79.
- Hawkins MR. National Flight Nurses Association . NFNA safety survey: a report of data collected in 1988 versus 1998. Air Med J 2000;19:128-33. http://dx.doi.org/10.1016/S1067-991X(00)90002-6.
- Bottle A, Aylin P. Application of AHRQ patient safety indicators to English hospital data. Qual Saf Health Care 2009;18:303-8. http://dx.doi.org/10.1136/qshc.2007.026096.
- Van De Velde M, Kuypers M, Teunkens A, Devroe S. Risk and safety of anesthesia outside the operating room. Minerva Anestesiol 2009;75:345-8.
- Lundstrom T, Pugliese G, Bartley J, Cox J, Guither C. Organizational and environmental factors that affect worker health and safety and patient outcomes. Am J Infect Control 2002;30:93-106. http://dx.doi.org/10.1067/mic.2002.119820.
- Rall M, Dieckmann P. Safety culture and crisis resource management in airway management: general principles to enhance patient safety in critical airway situations. Best Pract Res Clin Anaesthesiol 2005;19:539-57. http://dx.doi.org/10.1016/j.bpa.2005.07.005.
- Vaast P, Puech F. Safety of patient transport for in utero fetal indication. J Gynecol Obstet Biol Reprod (Paris) 2001;30:S25-8.
- Cosby KS, Croskerry P. Profiles in patient safety: authority gradients in medical error. Acad Emerg Med 2004;11:1341-5. http://dx.doi.org/10.1111/j.1553-2712.2004.tb01925.x.
- Anonymous . Strategies to improve patient and healthcare provider safety in patient handling and movement tasks. Rehabil Nurs 2005;30:80-3. http://dx.doi.org/10.1002/j.2048-7940.2005.tb00366.x.
- Flannery RB. Theories of human violence: implications for health care safety. Int J Emerg Ment Health 2004;6:105-10.
- McDaniel L. Is your facility’s emergency response strategy updated?. Biomed Instrum Technol 2005;39:413-5.
- McLaughlin N. First, do no harm. Patient welfare should come first in flight and legislation. Mod Healthc 2008;38.
- Cosby KS, Croskerry P. Patient safety: a curriculum for teaching patient safety in emergency medicine. Acad Emerg Med 2003;10:69-78. http://dx.doi.org/10.1111/j.1553-2712.2003.tb01981.x.
- Valentin J. International Commission on Radiation Protection . Prevention of high-dose-rate brachytherapy accidents. ICRP Publication 97. Ann ICRP 2005;35:1-51.
- Kahn LH. Biodefense research: can secrecy and safety coexist?. Biosecur Bioterror 2004;2:81-5. http://dx.doi.org/10.1089/153871304323146379.
- Balonov M. International Atomic Energy Agency . Exposures from environmental radioactivity: international safety standards. Appl Radiat Isot 2008;66:1546-9. http://dx.doi.org/10.1016/j.apradiso.2007.10.013.
- Burkle FM, Hayden R. The concept of assisted management of large-scale disasters by horizontal organizations. Prehospital Disaster Med 2001;16:128-37.
- Anonymous . Emergency management standards clarified. Jt Comm Perspect 2002;22.
- Jessup R. ERG: an essential first responder resource. Occup Health Saf 2008;77.
- Sudakin DL, Trevathan WR. DEET: a review and update of safety and risk in the general population. J Toxicol Clin Toxicol 2003;41:831-9. http://dx.doi.org/10.1081/CLT-120025348.
- Osimitz TG, Grothaus RH. The present safety assessment of DEET. J Am Mosq Control Assoc 1995;11:274-8.
- Garcia J. A call to action. JEMS 2002;27.
- Benson NH, Hunt RC, Tolson J, Stone CK, Sousa JA, Nimmo MJ. Improved flight following through continuous quality improvement. Air Med J 1994;13:163-5. http://dx.doi.org/10.1016/S1067-991X(05)80107-5.
- MacDonald E. Knowing our limits. Air Med J 2009;28. http://dx.doi.org/10.1016/j.amj.2009.04.014.
- Wiwanitkit V. Transport nurse safety practice: requirement in developing countries. Air Med J 2010;29. http://dx.doi.org/10.1016/j.amj.2009.12.001.
- Shanaberger CJ. Field operations and written policy. What you do not know can hurt you. Greater Houston Transport v Zrubeck. J Emerg Med Serv JEMS 1993;18.
- Zigmond J. Flying in the face of danger. A spate of air ambulance crashes has raised questions about safety, but providers say the service offers overwhelming benefits. Modern Healthcare 2008;38:6-7.
- Slattery DE, Silver A. The hazards of providing care in emergency vehicles: an opportunity for reform. Prehosp Emerg Care 2009;13:388-97. http://dx.doi.org/10.1080/10903120802706104.
- MacDonald E, Heffernan J. Safety above all: an Air Medical Safety Advisory Council update. Air Med J 2002;21:15-6. http://dx.doi.org/10.1016/S1067-991X(02)70049-7.
- Jagim M, Wylie MA. Slam on the brakes. How EMS providers can prevent motor vehicle injuries. J Emerg Med Serv JEMS 1997;22:84-6.
- Waller PF. Challenges in motor vehicle safety. Annu Rev Public Health 2002;23:93-113. http://dx.doi.org/10.1146/annurev.publhealth.23.100901.140522.
- Simsic JM, Masterson K, Kogon BE, Kirshbom PM, Kanter KR. Pre-hospital discharge car safety seat testing in infants following congenital heart surgery. Pediatric Cardiology 2008;29:313-16. http://dx.doi.org/10.1007/s00246-007-9021-2.
- Nordberg M. Improving ambulance safety. Emerg Med Serv 2006;35.
- Batchelor T. A step toward safety. NIOSH study shows improved reach in Winter Park ambulance design. EMS Magazine 2009;38:71-2.
- Erich J. Ambulance safety: what’s new, what’s needed. Emerg Med Serv 2002;31:51-4.
- Levick N. Rig safety 9-1-1: what you need to know about ambulance safety & standards. J Emerg Med Serv JEMS 2008;33:66-7. http://dx.doi.org/10.1016/S0197-2510(08)70380-2.
- Lutz S. Professionals seek improved air ambulance safety record. Mod Healthc 1987;17.
- Amintabish S. Fire safety in health care facilities. J Acad Hosp Adm 1997;9:55-62.
- Barbey JT, Roose SP. SSRI safety in overdose. J Clin Psychiatry 1998;59:42-8.
- Kroesen GA. Risks and safety standards of flying intensive care units. Acta Anaesthesiol Scand Suppl 1996;109:108-9.
- Errando CL, Blasco P. Drug administration errors in departments of anaesthesiology, intensive care recovery, and emergency: improving safety and quality assurance. Rev Esp Anestesiol Reanim 2006;53:397-9.
- Goupil MT. Occupational health and safety emergencies. Dent Clin North Am 1995;39:637-47.
- McCusker J, Roberge D, Vadeboncoeur A, Verdon J. Safety of discharge of seniors from the emergency department to the community. Healthc Q 2009;12:24-32. http://dx.doi.org/10.12927/hcq.2009.20963.
- Sklar DP, Crandall CS, Zola T, Cunningham R. Emergency physician perceptions of patient safety risks. Ann Emerg Med 2010;55:336-40. http://dx.doi.org/10.1016/j.annemergmed.2009.08.020.
- Hohenhaus SM. Leading the revolution: supporting and sustaining a culture of safety in the emergency department. J Emerg Nurs 2009;35:354-5. http://dx.doi.org/10.1016/j.jen.2009.03.008.
- Hicks CM, Bandiera GW, Denny CJ. Building a simulation-based crisis resource management course for emergency medicine, phase 1: Results from an interdisciplinary needs assessment survey. Acad Emerg Med 2008;15:1136-43. http://dx.doi.org/10.1111/j.1553-2712.2008.00185.x.
- Barata IA, Benjamin LS, Mace SE, Herman MI, Goldman RD. Pediatric patient safety in the prehospital/emergency department setting. Pediatr Emerg Care 2007;23:412-18. http://dx.doi.org/10.1097/01.pec.0000278393.32752.9f.
- Brown M. Medication safety issues in the emergency department. Crit Care Nurs Clin North Am 2005;17:65-9. http://dx.doi.org/10.1016/j.ccell.2004.09.009.
- Cadwell SM. Pediatric medication safety in the emergency department. J Emerg Nurs 2008;34:375-7. http://dx.doi.org/10.1016/j.jen.2008.04.014.
- O’Neill KA, Shinn D, Starr KT, Kelley J. Patient misidentification in a pediatric emergency department: patient safety and legal perspectives. Pediatr Emerg Care 2004;20:487-92. http://dx.doi.org/10.1097/01.pec.0000136895.99271.86.
- Ferns T, Cork A, Rew M. Personal safety in the accident and emergency department. Br J Nurs 2005;14:725-30. http://dx.doi.org/10.12968/bjon.2005.14.13.18458.
- Nelstrop L, Chandler-Oatts J, Bingley W, Bleetman T, Corr F, Cronin-Davis J, et al. A systematic review of the safety and effectiveness of restraint and seclusion as interventions for the short-term management of violence in adult psychiatric inpatient settings and emergency departments. Worldviews Evid Based Nurs 2006;3:8-18. http://dx.doi.org/10.1111/j.1741-6787.2006.00041.x.
- Schenkel S. Promoting patient safety and preventing medical error in emergency departments. Acad Emerg Med 2000;7:1204-22. http://dx.doi.org/10.1111/j.1553-2712.2000.tb00466.x.
- Campbell SG, Croskerry P, Bond WF. Profiles in patient safety: A ‘perfect storm’ in the emergency department. Acad Emerg Med 2007;14:743-9.
- Chamberlain JM, Slonim A, Joseph JG. Reducing errors and promoting safety in pediatric emergency care. Ambul Pediatr 2004;4:55-63. http://dx.doi.org/10.1367/1539-4409(2004)004<0055:REAPSI>2.0.CO;2.
- Ciesielski G, Clark N. Safety in the emergency department: it’s about time. Kans Nurse 2007;82:3-6.
- Manno EM. Safety issues and concerns for the neurological patient in the emergency department. Neurocrit Care 2008;9:259-64. http://dx.doi.org/10.1007/s12028-008-9111-x.
- Taylor TB. Threats to the health care safety net. Acad Emerg Med 2001;8:1080-7. http://dx.doi.org/10.1111/j.1553-2712.2001.tb01119.x.
- Ternov S, Akselsson R. System weaknesses as contributing causes of accidents in health care. Int J Qual Health Care 2005;17:5-13. http://dx.doi.org/10.1093/intqhc/mzi006.
- Adams JG, Biros MH. The endangered safety net: establishing a measure of control. Acad Emerg Med 2001;8:1013-15. http://dx.doi.org/10.1111/j.1553-2712.2001.tb01106.x.
- Anonymous . JCAHO’s safety goals – the clock is ticking, will your ED be compliant?. ED Manag 2005;17:73-5.
- Anonymous . ENA study cites barriers to NPSG compliance. ED Manag 2009;21:45-6.
- Cone DC, Davidson SJ. Hazardous materials preparedness in the emergency department. Prehosp Emerg Care 1997;1:85-90. http://dx.doi.org/10.1080/10903129708958794.
- Friedland LR. Universal precautions and safety devices which reduce the risk of occupational exposure to blood-borne pathogens: a review for emergency health care workers. Pediatr Emerg Care 1991;7:356-62. http://dx.doi.org/10.1097/00006565-199112000-00010.
- Anonymous . This year, surveyors to look for patient flow problems: identify bottlenecks now. Hosp Peer Rev 2005;30:1-5.
- Anonymous . Joint Commission’s 2007 National Patient Safety Goals will revamp emergency department nursing practice. Hosp Case Manag 2006;14:142-4.
- Australasian College for Emergency Medicine . Violence in emergency departments. Emerg Med Australas 2004;16. http://dx.doi.org/10.1111/j.1742-6723.2004.00604.x.
- Shaw KN, Ruddy RM, Olsen CS, Lillis KA, Mahajan PV, Dean JM, et al. Pediatric patient safety in emergency departments: unit characteristics and staff perceptions. Pediatrics 2009;124:485-93. http://dx.doi.org/10.1542/peds.2008-2858.
- McKinley A. Health care providers and facilities issue brief: health facilities: year end report – 2004. Issue Brief Health Policy Track Serv n.d.:1-12.
- Casteel C, Peek-Asa C, Nocera M, Smith JB, Blando J, Goldmacher S, et al. Hospital employee assault rates before and after enactment of the California hospital safety and security act. Ann Epidemiol 2009;19:125-33. http://dx.doi.org/10.1016/j.annepidem.2008.10.009.
- Dixon-Woods M. Why is patient safety so hard? A selective review of ethnographic studies. J Health Serv Res Policy 2010;15:11-6. http://dx.doi.org/10.1258/jhsrp.2009.009041.
- Griffin E. Effective systems documentation: essential for safety management. J Healthc Qual 1995;17:26-7. http://dx.doi.org/10.1111/j.1945-1474.1995.tb00776.x.
- Kennedy TJT, Regehr G, Baker GR, Lingard LA. ‘It’s a cultural expectation . . .’ The pressure on medical trainees to work independently in clinical practice. Med Educ 2009;43:645-53. http://dx.doi.org/10.1111/j.1365-2923.2009.03382.x.
- Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M. Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol 2004;99:2051-7. http://dx.doi.org/10.1111/j.1572-0241.2004.40017.x.
- Leonidas T. Balance of power. 5 steps to creating an emergency power master plan. Health Facil Manage 2004;17:20-4.
- Singer SJ, Gaba DM, Falwell A, Lin S, Hayes J, Baker L. Patient safety climate in 92 US hospitals: differences by work area and discipline. Med Care 2009;47:23-31. http://dx.doi.org/10.1097/MLR.0b013e31817e189d.
- Oakley J. Simplifying the management of the environment of care. Radiol Manage 1997;19:33-41.
- Lucas AJ. Improving medication safety in a neonatal intensive care unit. Am J Health-Syst Pharm 2004;61:33-7.
- McCarthy PM, Gaucher KA. Fire in the OR – developing a fire safety plan. AORN J 2004;79:588-97. http://dx.doi.org/10.1016/S0001-2092(06)60910-1.
- Farah RA, Aquino VM, Munoz LL, Sandler ES. Safety and cost-effectiveness of outpatient total body irradiation in pediatric patients undergoing stem cell transplantation. J Pediatr Hematol Oncol 1998;20:319-21. http://dx.doi.org/10.1097/00043426-199807000-00007.
- Maggiore WA, Palmer RB. Exercise restraint. Medical & legal issues you must understand to protect the patient & yourself. JEMS 2002;27:84-8.
- Takada S. Principles of chemotherapy safety procedures. Clin Tech Small Anim Pract 2003;18:73-4. http://dx.doi.org/10.1053/svms.2003.36618.
- Benveniste KA, Hibbert PD, Runciman WB. Violence in health care: the contribution of the Australian Patient Safety Foundation to incident monitoring and analysis. Med J Aust 2005;183:348-51.
- Brasic JR, Fogelman D. Clinician safety. Psychiatr Clin North Am 1999;22:923-40. http://dx.doi.org/10.1016/S0193-953X(05)70134-9.
- Johnston T, Moser R, Moeller K, Moriarty TM. Intraoperative MRI: safety. Neurosurg Clin N Am 2009;20:147-53. http://dx.doi.org/10.1016/j.nec.2009.04.007.
- Mohammed NB, NoorAli R, Anandakumar C, Qureshi RN, Luby S. Management trend and safety of vaginal delivery for term breech fetuses in a tertiary care hospital of Karachi, Pakistan. J Perinat Med 2001;29:250-9. http://dx.doi.org/10.1515/JPM.2001.036.
- Moore EE. Acute care surgery: the safety net hospital model. Surgery 2007;141:297-8. http://dx.doi.org/10.1016/j.surg.2007.01.004.
- Asplin BR. Tying a knot in the unravelling health care safety net. Acad Emerg Med 2001;8:1075-9. http://dx.doi.org/10.1111/j.1553-2712.2001.tb01118.x.
- Bremner JD, Wingard P, Walshe TA. Safety of mirtazapine in overdose. J Clin Psychiatry 1998;59:233-5. http://dx.doi.org/10.4088/JCP.v59n0505.
- Krug SE. The art of communication: strategies to improve efficiency, quality of care and patient safety in the emergency department. Pediatr Radiol 2008;38:S655-9. http://dx.doi.org/10.1007/s00247-008-0893-y.
- Scalise D. Six sigma in action. Case studies in quality put theory into practice. Hosp Health Netw 2003;77:57-62.
- Weller JM, Merry AF, Robinson BJ, Warman GR, Janssen A. The impact of trained assistance on error rates in anaesthesia: a simulation-based randomised controlled trial. Anaesthesia 2009;64:126-30. http://dx.doi.org/10.1111/j.1365-2044.2008.05743.x.
- Goldmann D, Kaushal R. Time to tackle the tough issues in patient safety. Pediatrics 2002;110:823-6. http://dx.doi.org/10.1542/peds.110.4.823.
- Garnerin P, Pellet-Meier B, Chopard P, Perneger T, Bonnabry P. Measuring human-error probabilities in drug preparation: a pilot simulation study. Eur J Clin Pharmacol 2007;63:769-76. http://dx.doi.org/10.1007/s00228-007-0319-z.
- Stahel PF, Fakler JKM, Flierl MA, Moldenhauer K, Mehler PS. Current concepts of patient safety: rapid response system. Unfallchirurg 2010;113:239-46. http://dx.doi.org/10.1007/s00113-009-1734-7.
- Stahel PF, Mehler PS. Medical emergency teams and rapid response triggers – the ongoing quest for the ‘perfect’ patient safety system. Crit Care 2009;13. http://dx.doi.org/10.1186/cc8052.
- Moldenhauer K, Sabel A, Chu ES, Mehler PS. Clinical triggers: an alternative to a rapid response team. Jt Comm J Qual Patient Saf 2009;35:164-74.
- Lamont T, Luettel D, Scarpello J, O’Driscoll BR, Connew S. Improving the safety of oxygen therapy in hospitals: summary of a safety report from the National Patient Safety Agency. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c187.
- Ma P-l, Xi X-m, Lin H-y, Xu Y, Du B, Zhao H-l, et al. Prospective, multi-centre investigation on safety of critical patients in intensive care units. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2007;19:614-18.
- Benjamin DM. Reducing medication errors and increasing patient safety: case studies in clinical pharmacology. J Clin Pharmacol 2003;43:768-83. http://dx.doi.org/10.1177/0091270003254794.
- Marken PA, Pies RW. Emerging treatments for bipolar disorder: safety and adverse effect profiles. Ann Pharmacother 2006;40:276-85. http://dx.doi.org/10.1345/aph.1G112.
- Basch EM, Servoss JC, Tedrow UB. Safety assurances for dietary supplements policy issues and new research paradigms. J Herbal Pharmacother 2005;5:3-15.
- Exadaktylos AK, Haffejee F, Wood D, Erasmus P. South African Red Cross Flying Doctors Service quality and safety in the rural and remote South African environment. Aust J Rural Health 2005;13:106-10. http://dx.doi.org/10.1111/j.1440-1854.2005.00663.x.
- Ciarlet M, Schodel F. Development of a rotavirus vaccine: clinical safety, immunogenicity, and efficacy of the pentavalent rotavirus vaccine, RotaTeq. Vaccine 2009;27:G72-81. http://dx.doi.org/10.1016/j.vaccine.2009.09.107.
- Novoa AM, Perez K, Borrell C. Evidence-based effectiveness of road safety interventions: a literature review. Gac Sanit 2009;23.
- Wan W, Le T, Riskin L, Macario A. Improving safety in the operating room: a systematic literature review of retained surgical sponges. Curr Opin Anaesthesiol 2009;22:207-14. http://dx.doi.org/10.1097/ACO.0b013e328324f82d.
- Velianoff GD. Overcrowding and diversion in the emergency department: the health care safety net unravels. Nurs Clin North Am 2002;37:59-66. http://dx.doi.org/10.1016/S0029-6465(03)00082-3.
- Trzeciak S, Rivers EP. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J 2003;20:402-5. http://dx.doi.org/10.1136/emj.20.5.402.
- Miller K. Pharmacological management of hypertension in paediatric patients. A comprehensive review of the efficacy, safety and dosage guidelines of the available agents. Drugs 1994;48:868-87. http://dx.doi.org/10.2165/00003495-199448060-00004.
- Wozniak EJ, Wisser J, Schwartz M. Venomous adversaries: a reference to snake identification, field safety, and bite-victim first aid for disaster-response personnel deploying into the hurricane-prone regions of North America. Wilderness Environ Med 2006;17:246-66. http://dx.doi.org/10.1580/06-WEME-CO-005R.1.
- Woudenberg F, van der Torn P. Emergency exposure limits: a guide to quality assurance and safety. Qual Assur 1992;1:249-93.
- Woolf AD. Safety evaluation and adverse events monitoring by poison control centers: a framework for herbs & dietary supplements. Clin Toxicol 2006;44:617-22. http://dx.doi.org/10.1080/15563650600795578.
- Welles WL, Wilburn RE, Ehrlich JK, Floridia CM. New York hazardous substances emergency events surveillance: learning from hazardous substances releases to improve safety. J Hazard Mater 2004;115:39-4. http://dx.doi.org/10.1016/j.jhazmat.2004.05.009.
- Van Tilburg C. Backcountry snowboarding: medical and safety aspects. Wilderness Environ Med 1996;7:225-31. http://dx.doi.org/10.1580/1080-6032(1996)007[0225:BSMASA]2.3.CO;2.
- Isbister JP. The risk/benefit equation for therapeutic plasma exchange. Analysis of the rationale for and the safety aspects of therapeutic plasma exchange. Curr Stud Hematol Blood Transfus 1990;57:10-3.
- Jaffe KM. Paediatric trauma rehabilitation: a value-added safety net. J Trauma 2008;64:819-23. http://dx.doi.org/10.1097/TA.0b013e318165f177.
- Kelly DL, Conley RR, Carpenter WT. First-episode schizophrenia: a focus on pharmacological treatment and safety considerations. Drugs 2005;65:1113-38. http://dx.doi.org/10.2165/00003495-200565080-00006.
- Kleiman NS. Primary and secondary safety endpoints from IMPACT II. Integrilin to Minimise Platelet Aggregation and Coronary Thrombosis. Am J Cardiol 1997;80:29B-33B. http://dx.doi.org/10.1016/S0002-9149(97)00574-2.
- Kleindorfer PR, Elliott MR, Wang Y, Lowe RA. Drivers of accident preparedness and safety: evidence from the RMP Rule. J Hazard Mater 2004;115:9-16. http://dx.doi.org/10.1016/j.jhazmat.2004.06.016.
- Kopaladze RA. Methods for the euthanasia of experimental animals – the ethics, esthetics and personnel safety. Usp Fiziol Nauk 2000;31:79-90.
- Lode H. Safety and tolerability of commonly prescribed oral antibiotics for the treatment of respiratory tract infections. Am J Med 2010;123:S26-38. http://dx.doi.org/10.1016/j.amjmed.2010.02.004.
- Ta VM, Frattaroli S, Bergen G, Gielen AC. Evaluated community fire safety interventions in the United States: a review of current literature. J Community Health 2006;31:176-97. http://dx.doi.org/10.1007/s10900-005-9007-z.
- Quail MT, Shannon MW. Pralidoxime safety and toxicity in children. Prehosp Emerg Care 2007;11:36-41. http://dx.doi.org/10.1080/10903120601023289.
- Pellatt GC. The safety and dignity of patients and nurses during patient handling. Br J Nurs 2005;14:1150-6. http://dx.doi.org/10.12968/bjon.2005.14.21.20076.
- Read JS, Newell MK. Efficacy and safety of cesarean delivery for prevention of mother-to-child transmission of HIV-1. Cochrane Database Syst Rev 2005;4.
- Guise J-M, Lowe NK, Connell L. Patient safety in obstetrics: what aviators, firefighters and others can teach us. Nurs Womens Health 2008;12:208-15. http://dx.doi.org/10.1111/j.1751-486X.2008.00325.x.
- Saizonou J, De Brouwere V, Vangeenderhuysen C, Dramaix-Wilmet M, Buekens P, Dujardin B. Audit of the quality of treatment of “near miss” patients in referral maternities in Southern Benin. Sante 2006;16:33-42.
- Dart RC, Green JL, Bogdan GM. The safety profile of sustained release paracetamol during therapeutic use and following overdose. Drug Saf 2005;28:1045-56. http://dx.doi.org/10.2165/00002018-200528110-00005.
- Bratton RL. Advising patients about international travel. What they can do to protect their health and safety. Postgrad Med 1999;106:57-64. http://dx.doi.org/10.3810/pgm.1999.07.605.
- Conwit RA, Hart RG, Moy CS, Marler JR. Data and safety monitoring in clinical research: a National Institute of Neurologic Disorders and Stroke perspective. Ann Emerg Med 2005;45:388-92. http://dx.doi.org/10.1016/j.annemergmed.2004.08.006.
- Jones CT. Annual administrative reviews: safety. Hospitals 1973;47:101-2.
- Joseph AP, Hunyor SN. The Royal North Shore Hospital inquiry: an analysis of the recommendations and the implications for quality and safety in Australian public hospitals. Med J Aust 2008;188:469-72.
- Pringle R. Safety of surgery in elderly. Ann Acad Med Singapore 1991;20:260-4.
- Tiguert R, Rigaud J, Fradet Y. Safety and outcome of early catheter removal after radical retropubic prostatectomy. Urology 2004;63:513-17. http://dx.doi.org/10.1016/j.urology.2003.10.042.
- Nadzam D, Westergaard F. Pediatric safety in the emergency department: identifying risks and preparing to care for child and family. J Nurs Care Qual 2008;23:189-94. http://dx.doi.org/10.1097/01.NCQ.0000324580.82428.70.
- Sorra JS, Dyer N. Multilevel psychometric properties of the AHRQ hospital survey on patient safety culture. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-199.
- Barer AS. Medical aspect of cosmonauts’ safety during emergency landing. Respicere et prospicere. Aviakosm Ekolog Med 2008;42:3-20.
- Timmermann A. Modern airway management – current concepts for more patient safety. Anasthesiol Intensivmed Notfallmed Schmerzther 2009;44:246-55. http://dx.doi.org/10.1055/s-0029-1222432.
- Tice MA. Patient safety: honoring advanced directives. Home Healthc Nurse 2007;25:79-81. http://dx.doi.org/10.1097/00004045-200702000-00005.
- Faddy SC, Garlick SR. A systematic review of the safety of analgesia with 50% nitrous oxide: can lay responders use analgesic gases in the prehospital setting?. Emerg Med J 2005;22:901-8. http://dx.doi.org/10.1136/emj.2004.020891.
- Schwaab B, Katalinic A, Riedel J, Sheikhzadeh A. Pre-hospital diagnosis of myocardial ischaemia by telecardiology: safety and efficacy of a 12-lead electrocardiogram, recorded and transmitted by the patient. J Telemed Telecare 2005;11:41-4. http://dx.doi.org/10.1258/1357633053430412.
- Oemrawsingh PV, Bosker HA, Manger CV, van der LA, Bruschke AV. Safety and efficacy of thrombolysis during ambulance transportation of patients with an acute heart infarct. Ned Tijdschr Geneeskd 1989;133:354-8.
- Barry J. The HoverMatt system for patient transfer: enhancing productivity, efficiency, and safety. J Nurs Adm 2006;36:114-17. http://dx.doi.org/10.1097/00005110-200603000-00003.
- Schneider C, Gomez M, Lee R. Evaluation of ground ambulance, rotor-wing, and fixed-wing aircraft services. Crit Care Clin 1992;8:533-64.
- Wilson P. Fasten their seatbelts: legal restraint of children in car seats and road ambulances. Paediatr Nurs 2007;19:14-8. http://dx.doi.org/10.7748/paed2007.09.19.7.14.c4451.
- Cox K. When angels fly with eagles: safety as a culture. Air Med J 2002;21:17-22. http://dx.doi.org/10.1016/S1067-991X(02)70081-3.
- O’Neil J, Yonkman J, Talty J, Bull MJ. Transporting children with special health care needs: comparing recommendations and practice. Pediatrics 2009;124:596-603. http://dx.doi.org/10.1542/peds.2008-1124.
- Hearns S, Shirley PJ. Retrieval medicine: a review and guide for UK practitioners. Part 2: safety in patient retrieval systems. Emerg Med J 2006;23:943-7. http://dx.doi.org/10.1136/emj.2006.038075.
- Vidacovich B. From idea to innovation: tips for engineering safety, comfort & communications into your next ambulance. JEMS 2008;33:60-6. http://dx.doi.org/10.1016/S0197-2510(08)70160-8.
- Benedek DM, Fullerton C, Ursano RJ. First responders: mental health consequences of natural and human-made disasters for public health and public safety workers. Annu Rev Public Health 2007;28:55-68. http://dx.doi.org/10.1146/annurev.publhealth.28.021406.144037.
- Frakes MA, Kelly JG. A survey of adherence to community-generated safety guidelines in rotor-wing air medical programs. Air Med J 2007;26:100-3. http://dx.doi.org/10.1016/j.amj.2006.06.039.
- Davis J. Medical errors and patient safety. Issue brief. Issue Brief Health Policy Track Serv 2010:1-36.
- Semonin-Holleran R. Ambulance safety: is it an emergency nursing problem?. J Emerg Nurs 2008;34:98-9. http://dx.doi.org/10.1016/j.jen.2008.02.005.
- Limmer D. 10 commandments for EMS survival. JEMS 2000;25:24-30.
- McClincy WD. Manufacturing an EMS response. Emerg Med Serv 1999;28:67-9.
- McLaughlin S. Ready for anything. A look at the Joint Commission’s new emergency management standards. Health Facil Manage 2007;20:39-40.
- Manser T. Teamwork and patient safety in dynamic domains of healthcare: a review of the literature. Acta Anaesthesiol Scand 2009;53:143-51. http://dx.doi.org/10.1111/j.1399-6576.2008.01717.x.
- Rischitelli G, Harris J, McCauley L, Gershon R, Guidotti T. The risk of acquiring hepatitis B or C among public safety workers: a systematic review. Am J Prev Med 2001;20:299-306. http://dx.doi.org/10.1016/S0749-3797(01)00292-6.
- Garrison HG. Feasibility for an EMS workforce safety and health surveillance system. Ann Emerg Med 2007;50:711-14. http://dx.doi.org/10.1016/j.annemergmed.2007.10.010.
Appendix 1 Rapid evidence synthesis
A preliminary search of the evidence on patient safety in the ambulance service
Introduction
The costs of medical errors are considerable at both a personal and an institutional level. 1 It is estimated that 1 in 10 patients in UK hospitals suffers an AE1 yet 50% of such incidents could be avoided if lessons had been learnt from previous incidents. 2
The publication of two seminal reports, To Err is Human: Building a Safer Health System3 and An Organisation with a Memory,4 10 years ago highlighted the fact that there was an urgent need to understand systematically the extent and nature of harm that patients suffer during their contact with health-care services. This gave rise to a surge in research papers in the following years that aimed to quantify the incidence of harm, predominantly in hospital-based care. This was followed by more qualitative studies that tried to understand the mechanisms for failure that give rise to patient harm. Soon it was realised that the underlying attitudes and assumptions about failures and safety within the NHS and health-care in general were a serious obstacle to sustainable improvements in patient safety. The quantification of the safety culture (i.e. the safety-related attitudes, values and beliefs of staff) of an organisation and the development of a systems-oriented safety culture became a second major aim with an increasing number of both quantitative and qualitative papers in the field. We are now at the stage when there is a growing focus on patient safety interventions themselves, with some literature describing interventions qualitatively, but the majority of papers attempting to quantify the benefit to patient outcomes of certain interventions.
The Department of Health introduced the NRLS in 2004. The NRLS, designed to sit alongside local reporting systems, enables NHS staff in England and Wales to anonymously record patient safety incidents and near misses (when patient safety incidents were avoided). These reports are analysed to discover patterns in the data that may suggest measures to improve patient safety and prevent further patients being exposed to the same risk. Reporting across health-care sectors is variable; in 2009 EDs reported more than 600 serious/fatal events compared with only 14 reported by ambulance services in England (NPSA, personal communication); therefore, the extent of harm and risk in the ambulance service remains unknown. The reason for the disparity in reporting is unclear, but suggests failure to report, as there are indications that some systems within the ambulance service may be a threat to patient safety; for example, the lack of consistency in equipment, consumables and vehicle layout (NPSA).
Although some ambulance services are focusing on safety, < 50% of ambulance services and none of their related professional bodies signed up to the Patient Safety First campaign. Given that safety is a national priority, and there is an increase in litigation rates, it is unclear why ambulance services are not prioritising this issue. One reason may be that ambulance services are prioritising meeting targets;2 the culture in the ambulance service may not be conducive to disclosure of AEs. A further reason may be a lack of evidence of the impact of AEs within the ambulance service upon patient safety.
In order to explore the extent and quality of evidence available to ambulance services and to determine whether or not a systematic review and synthesis of the evidence on patient safety in pre-hospital care would be an important step in focusing attention on patient safety and guiding initiatives, a preliminary search of the evidence was undertaken.
Methods
We searched for all study designs and no language restrictions on patient safety in pre-hospital care in the MEDLINE database using the strategy detailed in Table 22. Additional studies were identified from the reference lists and experts on the team.
| # | Searches | Results |
|---|---|---|
| 1 | (pre hospital or pre-hospital or prehospital).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier] | 6642 |
| 2 | ambulance.mp. or exp Ambulances/ | 8018 |
| 3 | emergency.mp. or exp Emergencies/ | 160,983 |
| 4 | emergency medicine.mp. or exp Emergency Medicine/ | 10,926 |
| 5 | paramedic.mp. or exp Allied Health Personnel/ | 37,185 |
| 6 | emergency medical services.mp. or exp Emergency Medical Services/ | 74,593 |
| 7 | emergency medical technicians.mp. or exp Emergency Medical Technicians/ | 4384 |
| 8 | 1 or 2 or 3 or 4 or 5 or 6 or 7 | 206,583 |
| 9 | exp Safety/ed, lj, st, sn, td [Education, Legislation & Jurisprudence, Standards, Statistics & Numerical Data, Trends] | 3270 |
| 10 | 8 and 9 | 201 |
| 11 | limit 10 to humans | 157 |
Results
Studies were selected by one reviewer (JDF) and were included if they reported data on any aspect of patient safety in the ambulance service. Studies focusing on vehicle accidents were excluded.
The search revealed 185 studies of which 24 were identified as relevant and included in the review (Figure 13). Excluded studies and the reasons for exclusion are listed in Table 23.
FIGURE 13.
Evidence selection process for the preliminary search of MEDLINE based on PRISMA.
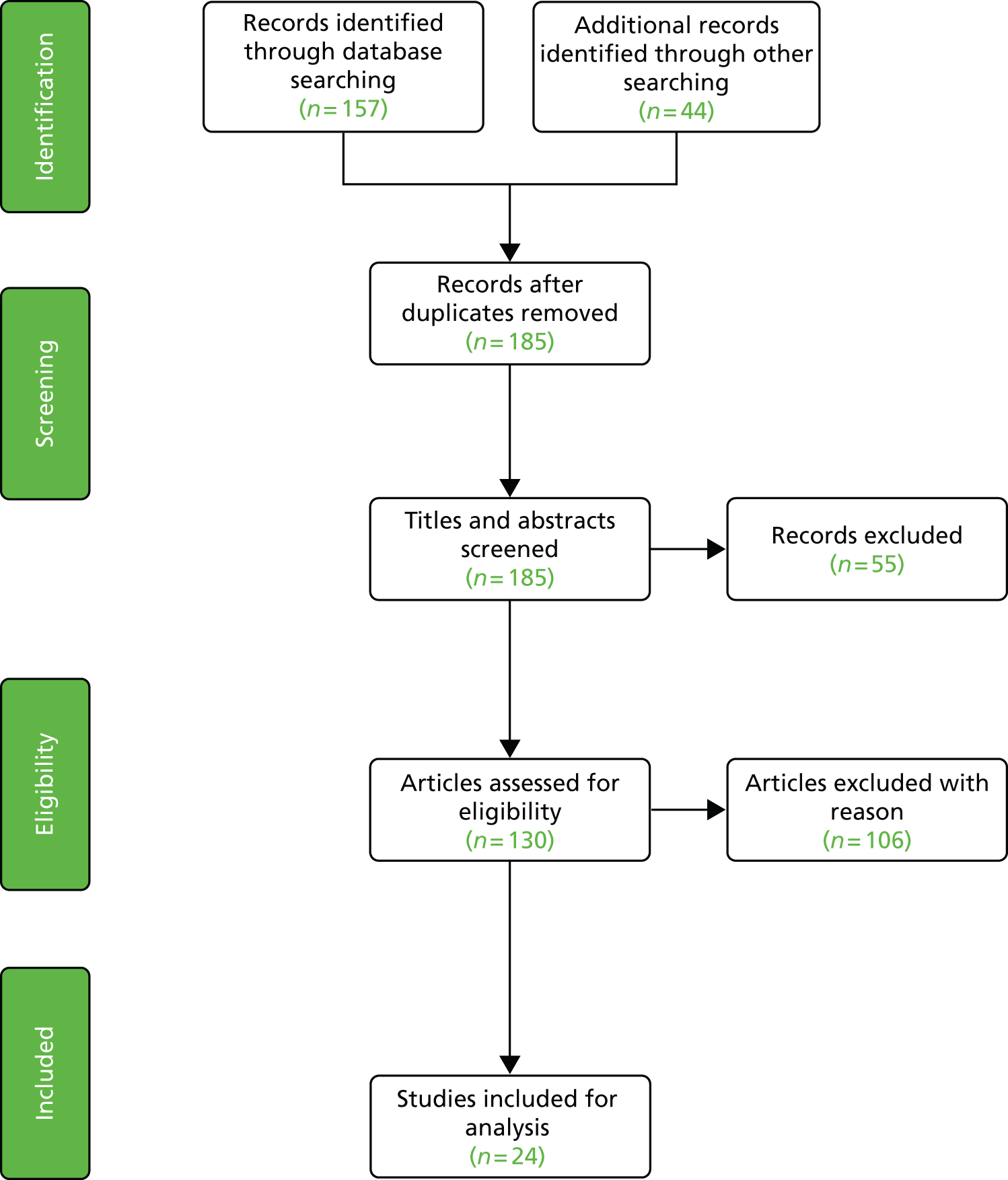
| Study | Topic | Reason |
|---|---|---|
| Stymiest, 2003406 | Major incident | Not relevant |
| Stoop, 2004407 | Interagency major incident planning | Not relevant |
| Danielson, 1998408 | Hazardous waste | Not relevant |
| McNamara, 1997409 | Public and staff safety in ED using metal detectors | In ED |
| Thompson, 2003410 | Fire safety in departments | Not relevant |
| Hawkins and National Flight Nurses Association, 2000411 | Staff air safety of nurses | Not relevant |
| Bottle and Aylin, 2009412 | Application of AHRQ to hospital data | Not relevant |
| Van De Velde et al., 2009413 | Risk and safety of anaesthesia outside the operating room: NORA | Not relevant |
| Lundstrom et al., 2002414 | Safety and culture | Not relevant |
| Rall and Dieckmann, 2005415 | High reliability organisation principles to airway management: routine airway | Not relevant |
| Vaast and Puech, 2001416 | Safety and transportation | Not relevant |
| Cosby and Croskerry, 2004417 | Authority gradients in medicine | Not relevant |
| Anonymous, 2005418 | Handling | Not relevant |
| Flannery, 2004419 | Violence in health-care settings | Not relevant |
| McDaniel, 2005420 | Disaster planning | In secondary care |
| McLaughlin, 2008421 | Safety and air transportation | Not relevant |
| Cosby and Croskerry, 2003422 | Teaching patient safety and in training and certification requirements | Not relevant |
| Valentin and International Commission on Radiation Protection, 2005423 | High-dose-rate brachytherapy | Not relevant |
| Khan, 2004424 | CBRN | Not relevant |
| Balonov and International Atomic Energy Agency, 2008425 | CBRN | Not relevant |
| Cosby and Croskerry, 2004417 | Authority gradient | Not relevant |
| Burkle and Hayden, 2001426 | Co-ordination design | Not relevant |
| Anonymous, 2002427 | Not relevant | |
| Jessup, 2008428 | Not relevant | |
| Sudakin and Trevathan, 2003429 | Safety regarding DEET | Not relevant |
| Osimitz and Grothaus, 1995430 | Safety regarding DEET | Not relevant |
| Garcia, 2002431 | Excluded: transport | |
| Benson et al., 1994432 | Air transport safety | Excluded: transport |
| Benson et al., 1994432 | Flight following in-air medical transport | Excluded: transport |
| MacDonald, 2009433 | Air medical transport | Excluded: transport |
| Wiwanitkit, 2010434 | Transport nurse safety practice: requirement in developing countries | Excluded: transport |
| Shanaberger, 1993435 | Excluded: transport | |
| Zigmond, 2008436 | Transport safety | Excluded: transport |
| Slattery and Silver, 2009437 | Excluded: transport | |
| McLaughlin, 2008421 | Excluded: transport | |
| MacDonald and Heffernan, 2002438 | Excluded: transport | |
| Jagim and Wylie, 1997439 | Excluded: transport | |
| Waller, 2002440 | Safer vehicles, improved traffic records, more effective enforcement, enormously improved EMS | Excluded: transport |
| Simsic et al., 2008441 | Safer vehicles | Excluded: transport |
| Nordberg, 2006442 | Safer vehicles | Excluded: transport |
| Batchelor, 2009443 | Safer vehicles | Excluded: transport |
| Erich, 2002444 | Safer vehicles | Excluded: transport |
| Levick, 2008445 | Safer vehicles | Excluded: transport |
| Lutz, 1987446 | Safer vehicles | Excluded: transport |
| Amintabish, 1997447 | Fire safety in health care | |
| Barbey and Roose, 1998448 | Mortality associated with SSRI overdose | Harm reduction/drugs |
| Kroesen, 1996449 | Air safety crashes | Human error more frequent cause of helicopter accidents than technical failure |
| Errando and Blasco, 2006450 | Medication errors | In critical care |
| Goupil, 1995451 | Harm to patients and staff | In dental office |
| McCusker et al., 2009452 | Discharge from ED | In ED |
| Sklar et al., 2010453 | In ED | |
| Hohenhaus, 2009454 | In ED | |
| Hicks et al., 2008455 | In ED | |
| Barata et al., 2007456 | Medication errors | In ED |
| Brown, 2005457 | Medication errors | In ED |
| Cadwell, 2008458 | Medication errors | In ED |
| O’Neill et al., 2004459 | Medication errors: misidentification | In ED |
| Ferns et al., 2005460 | Staff safety | In ED |
| Nelstrop et al., 2006461 | Restraint and seclusion as interventions | In ED |
| Schenkel, 2000462 | Preventable AE | In ED |
| Campbell et al., 2007463 | Error-producing conditions in ED | In ED |
| Chamberlain et al., 2004464 | Safety in ED | In ED |
| Ciesielski and Clark, 2007465 | Safety in ED-reducing delays and attendances | In ED |
| Manno, 2008466 | Safety of neurological patient | In ED |
| Taylor, 2001467 | Health-care safety net in the USA | In ED |
| Ternov and Akselsson, 2005468 | Study of the causes of accidents leading to death in ED | In ED |
| Adams and Biros, 2001469 | In ED | |
| Anonymous, 2005470 | Medication errors | In ED |
| Anonymous, 2009471 | Medication errors, overcome those barriers | In ED |
| Cone and Davidson, 1997472 | In ED | |
| Friedland, 1991473 | In ED | |
| Anonymous, 2005474 | Overcrowding | In ED |
| Anonymous, 2006475 | In ED | |
| Australasian College for Emergency Medicine, 2004476 | In ED | |
| Shaw et al., 2009477 | In ED | |
| McKinley, 2004478 | In ED | |
| Casteel et al., 2009479 | Staff safety | In ED/mental health |
| Dixon-Woods, 2010480 | Patient safety narrative review of four reports of ethnographic studies | In ED/OR |
| Griffin, 1995481 | Equipment safety | In health care |
| Kennedy et al., 2009482 | Medical trainees and asking for help | In hospital |
| Sebastian et al., 2004483 | Surgery | In hospital |
| Leonidas, 2004484 | In hospital | |
| Singer et al., 2009485 | In hospital | |
| Oakley, 1997486 | In hospital | |
| Lucus, 2004487 | Medication errors | In ICU |
| McCarthy and Gaucher, 2004488 | Fire prevention | In OR |
| Farah et al., 1998489 | Safety of delivering total body irradiation | In outpatient setting |
| Maggiore and Palmer, 2002490 | In pre-hospital care | |
| Takada, 2003491 | Drug errors in chemotherapy | In secondary care |
| Benveniste et al., 2005492 | Staff safety: assault | In secondary care |
| Brasic and Fogelman, 1999493 | Staff safety: assault | In secondary care |
| Johnston et al., 2009494 | Intraoperative MRI: safety | In secondary care |
| Mohammed et al., 2001495 | Obstetrics and breech delivery | In secondary care |
| Moore, 2007496 | Surgery: the safety net hospital model | In secondary care |
| Asplin, 2001497 | Uninsured and underinsured residents in the USA | In secondary care |
| Bremner et al., 1999498 | Overdose and mirtazapine | In secondary care |
| Cheng et al., 2004431 | Coronary artery bypass graft surgery | In secondary care |
| Anonymous, 2005474 | Overcrowding | In ED |
| Krug, 2008499 | In ED | |
| Scalise, 2003500 | Six-sigma | In hospital |
| Weller et al., 2009501 | In hospital | |
| Goldmann and Kaushal 2002502 | Medication errors | In hospital |
| Garnerin et al., 2007503 | Data modelling for drug safety | In hospital |
| Stahel et al., 2010504 | In hospital | |
| Stahel and Mehler, 2009505 | In hospital | |
| Moldenhauer et al., 2009506 | Resuscitation | In hospital |
| Lamont et al., 2010507 | Oxygen safety | In hospital |
| Ma et al., 2007508 | In ICU | |
| Benjamin, 2003509 | Medication errors | |
| Marken and Pies, 2006510 | Safety and tolerability of new drugs | Mental health |
| Basch et al., 2005511 | Use of dietary supplements: adverse effects and interactions lead to increased emergency attendances | No data |
| Exadaktylos et al., 2005512 | Providing flying doctor service | No safety |
| Ciarlet and Schodel, 2009513 | Vaccine development: pentavalent rotavirus vaccine RotaTeq | Not pre-hospital |
| Novoa et al., 2009514 | Road safety interventions in reducing road traffic collisions | Not pre-hospital |
| Wan et al., 2009515 | Operating theatre safety | Not pre-hospital |
| Velianoff, 2002516 | Overcrowding in ED | Not pre-hospital |
| Trzeciak and Rivers, 2003517 | Overcrowding in ED | Not pre-hospital |
| Miller, 1994518 | Hypertension and children | Not relevant |
| Wozniak et al., 2006519 | Snake identification | Not relevant |
| Woudenberg and van der Torn, 1992520 | Chemical exposure limits | Not relevant |
| Woolf, 2006521 | AEs for herbs and dietary supplements | Not relevant |
| Welles et al., 2004522 | Hazardous substance release | Not relevant |
| Van Tilburg, 1996523 | Snowboarding safety | Not relevant |
| Isbister, 1990524 | Therapeutic plasma exchange | Not relevant |
| Jaffe, 2008525 | Effectiveness of paediatric rehabilitation | Not relevant |
| Kahn, 2004424 | Biodefence | Not relevant |
| Kelly et al., 2005526 | Schizophrenia and safety | Not relevant |
| Kleiman, 1997527 | Platelet aggregation and coronary thrombosis | Not relevant |
| Kleindorfer et al., 2004528 | Accident frequency and accident severity at covered facilities | Not relevant |
| Kopaladze, 2000529 | Euthanasia of vertebrate animals | Not relevant |
| Lode, 2010530 | Antimicrobial safety and RTI | Not relevant |
| Ta et al., 2006531 | Fire safety interventions | Not relevant |
| Quail and Shannon, 2007532 | Safety of pralidoxime | Not relevant |
| Pellatt, 2005533 | Handling patients | Nurses |
| Read and Newell, 2005534 | Obstetrics and gynaecology | |
| Guise et al., 2008535 | Obstetrics and gynaecology | |
| Saizonou, 2006536 | Obstetrics and gynaecology | |
| Dart et al., 2005537 | Sustained release paracetamol (acetaminophen) and overdose | Overdose |
| Novoa et al., 2009514 | Prevention of RTCs | Prevention |
| Bratton, 1999538 | Travel advice and primary care | Primary care |
| Conwit et al., 2005539 | Safety and research | Safety and research |
| Jones, 1973540 | Safety reviews in hospitals | Secondary care |
| Joseph and Hunyor, 2008541 | The Royal North Shore Hospital inquiry | Secondary care |
| Pringle, 1991542 | Safety and surgery | Secondary care |
| Tiguert et al., 2004543 | Retropubic catheters and radical prostatectomy | Secondary care |
| Nadzam and Westergaard, 2008544 | Secondary care | |
| Sorra and Dyer, 2010545 | AHRQ and hospital survey on patient safety culture | Secondary care: in hospital |
| Barer, 2008546 | Landings | Space travel |
The review revealed a small number of studies that explored safety in health care that focused on a number of broad topic areas: assessment and treatment,13,39,40,547,548–551 moving and transporting patients,552–558 patient/staff well-being,559 education228,286,560–562 and planning. 563–565 Of the eligible studies, 11 were reviews of the evidence39,547,548,549,552–554,566–568 (Table 24); however, no overall systematic review of the evidence for safety in pre-hospital care was found. Although no formal evaluation of the evidence was undertaken, the quality of the retrieved evidence varied markedly.
| Study and country | Topic | Indicative categories: patient safety, staff safety and well-being |
|---|---|---|
| Fitzpatrick and Duncan, 2009,39 UK | Repeat hypoglycaemic events | Patient safety: extent and nature of harm/intervention(s) to improve patient safety |
| Timmermann, 2009,547 Germany | Airway management training | Patient safety: intervention(s) to improve patient safety |
| Dale et al., 2004,40 UK | Safety of telephone advice for patients requesting an ambulance | Patient safety: intervention(s) to improve patient safety |
| Barry, 2006,552 USA | HoverMatt system: transferring patients | Patient safety: intervention(s) to improve patient safety |
| Manser, 2009,566 Switzerland | Teamwork and patient safety | Patient safety: safety-related culture, attitudes and behaviour |
| Schneider et al., 1992,553 USA | Safety and transportation | Patient safety: intervention(s) to improve patient safety, also including staff safety |
| Tice, 2007,548 USA | Advanced directives as reportable medical errors | Patient safety: extent and nature of harm |
| Wilson, 2007,554 UK | Restraint of children in ambulance and thus safety of all occupants | Patient safety: intervention(s) to improve patient safety |
| Cox, 2002,555 USA | Air safety | Patient safety: intervention(s) to improve patient safety |
| Frakes and Kelly, 2007,560 USA | Adherence to safe practice recommendations | Patient safety: safety-related culture, attitudes and behaviour |
| O’Neil et al., 2009,556 USA | Safe transport of patients | Patient safety: extent and nature of harm/intervention(s) to improve patient safety |
| Davis, 2010,561 USA | Medication errors | Patient safety: extent and nature of harm/intervention(s) to improve patient safety |
| Hobgood et al., 2006,228 USA | Reporting errors: culture | Patient safety: safety-related culture, attitudes and behaviour |
| Hearns and Shirley, 2006,557 UK | Safety in retrieval | Patient safety: intervention(s) to improve patient safety |
| Faddy and Garlick, 2005,549 Australia | Pain relief | Patient safety: intervention(s) to improve patient safety |
| Limmer, 2000,563 USA | Emergency planning | Patient safety: extent and nature of harm/intervention(s) to improve patient safety |
| McClincy, 1999,564 USA | Emergency planning | Patient safety: extent and nature of harm/intervention(s) to improve patient safety |
| McLaughlin, 2007,565 USA | Emergency planning | Patient safety: extent and nature of harm/intervention(s) to improve patient safety |
| Schwaab et al., 2005,550 Germany | Pre-hospital diagnosis of myocardial ischaemia by telecardiology | Patient safety: intervention(s) to improve patient safety |
| Burns et al., 1992,13 USA | The safety of patients receiving morphine sulphate in pre-hospital | Patient safety: intervention(s) to improve patient safety |
| Batchelder et al., 2009,286 UK | Teaching anaesthesia to doctor–paramedic teams using simulation | Patient safety: intervention(s) to improve patient safety |
| Oemrawsingh et al., 1989,551 Netherlands | Thrombolysis during ambulance transfer | Patient safety: extent and nature of harm/intervention(s) to improve patient safety |
| Semonin-Holleran, 2008,562 USA | Orientation of equipment and resources for nurses accompanying patients | Patient safety: extent and nature of harm/intervention(s) to improve patient safety |
| Vidacovich, 2008,558 USA | Engineering and safety, comfort and communications in ambulances | Patient safety: extent and nature of harm/intervention(s) to improve patient safety |
The literature formed two categories, one that explored issues related to patient safety and the other relating to staff safety and well-being. The eligible literature was mapped based on the above framework (Figure 14).
FIGURE 14.
Evidence framework for mapping ambulance service safety literature.

Discussion
The majority of these studies focus on aspects of patient safety, with fewer than one-third exploring safety issues related to staff. Overall, the studies were interventional with few exploring safety-related culture, attitudes and behaviour. There was a paucity of literature reporting methodological approaches to analysing patient and staff safety and well-being in ambulance services. No relevant methodological papers were found; two studies were identified that explored the application of tools designed by the AHRQ for patient safety but these reported data in other health-care sectors. 412,545
Conclusion
Overall, the review found a paucity of literature. It is clear that the evidence base on safety in ambulance services is lagging behind other health-care sectors, with patchy literature on patient safety interventions; thus, the extent of harm and risk is unknown. With no systematic review there is no evidence on which to base policy and direct future research.
Appendix 2 Compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist
| Section/topic | Checklist item | How fulfilled in this report |
|---|---|---|
| Title |
|
Yes – we identify the report as a systematic review (contents page and Chapter 3) |
| Abstract |
|
Yes – the systematic review is summarised in the report abstract |
| Introduction |
|
Yes – the rationale for the systematic review is described (see Chapters 1 and 3) |
|
Yes – an explicit statement of the questions being addressed is given (see Chapter 3, Aims and clinical questions) | |
| Methods |
|
Yes – the protocol is available at: www.warwick.ac.uk/ambulancesafety |
|
Yes – study characteristics including type, participants, intervention, and outcome measures are described (see Chapter 3, Methods) | |
|
Yes – the information sources are described (see Chapter 3, Methods) | |
|
Yes – the search strategy for MEDLINE is presented (see Chapter 3, Methods) and the search strategies for the remaining databases are presented in Appendix 3 | |
|
Yes – the process for selecting studies is given (see Chapter 3, Methods) | |
|
Yes – the following data were extracted into tables by one of four reviewers: citation, design, intervention, duration of the intervention, sample size, inclusion criteria, setting, outcomes, follow-up (if applicable), and study findings | |
|
Yes – the variables for which data were sought are listed (see Chapter 3, Methods) | |
|
N/A – risk of bias of individual studies was not assessed as a narrative synthesis of the data has been performed | |
|
N/A – summary measures have not been reported as a narrative synthesis of the data has been performed | |
|
N/A – data were not combined as a narrative synthesis of the data has been performed | |
|
N/A – risk of bias across studies was not assessed as a narrative synthesis of the data has been performed | |
|
N/A – additional analyses, for example sensitivity or subgroup analyses, metaregression, have not been done as a narrative synthesis of the data has been performed | |
| Results |
|
Yes – the number of studies screened, assessed for eligibility, and included in the systematic review, with reasons for exclusions at each stage, are presented (see Chapter 3, Results and Figure 1) |
|
Yes – characteristics for each study are presented (see Chapter 3, Tables 2–8) | |
|
Yes – risk of bias of individual studies was not assessed as a narrative synthesis of the data has been performed | |
|
Yes – summary data are presented in the evidence tables | |
|
N/A – meta-analysis was not performed | |
|
N/A – risk of bias across studies was not assessed as a narrative synthesis of the data has been performed | |
|
N/A – additional analyses, for example sensitivity or subgroup analyses, metaregression, have not been done as a narrative synthesis of the data has been performed | |
| Discussion |
|
Yes – the main findings and key recommendations are provided for health-care providers, and policy makers (see Abstract and Chapters 7 and 8) |
|
Yes – as this is a scoping review the limitations are discussed in terms of the review process and narrative analysis | |
|
Yes – interpretation of the results in the context of other evidence, and implications and recommendations for future research, is presented (see Chapter 3, Discussion and Chapter 7) | |
| Funding |
|
Yes – explicit reference is made to the source of funding for this scoping review (see Abstract) |
Appendix 3 Search strategies
EMBASE
Searched:1 January 1980 to 12 October 2011.
Search strategy
-
safety management.mp.
-
safety indicator*.mp.
-
patient safety.mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
prehospital.mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
pre-hospital.mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
pre hospital.mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
4 or 5 or 6
-
Ambulance*.mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
transportation of patient*.mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
(Emergency medical service* or EMS).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
paramedic*.mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
exp patient transport/
-
emergency care assistant*.mp.
-
emergency medical technician*.mp.
-
advanced practitioner*.mp.
-
community first responder*.mp.
-
exp emergency health service/
-
exp ambulance/
-
paramedical personnel/ or exp paramedical profession/
-
7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19
-
exp patient safety/
-
safety.mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
21 or 22
-
1 or 2 or 3 or 23
-
20 and 24
-
limit 25 to yr=“1980 –Current”
Cumulative Index to Nursing and Allied Health Literature (CINAHL)
Searched: 1 January 1980 to 12 October 2011.
Search strategy
| # | Query | Limiters/Expanders |
|---|---|---|
| S18 | (S12 or S13 or S14 or S15 or S16) and (S11 and S17) | Limiters - published date from: 19800101-20111012 |
| S17 | S12 or S13 or S14 or S15 or S16 | |
| S16 | TX patient safety | |
| S15 | TX safety indicator* | |
| S14 | TX safety | |
| S13 | “safety management” | |
| S12 | (MH “Patient Safety+”) | |
| S11 | S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 | |
| S10 | TX advanced practitioner* | |
| S9 | TX transportation of patient* | |
| S8 | TX community first responder* | |
| S7 | TX emergency care assistant* | |
| S6 | TX “allied health personnel” OR paramedic* | |
| S5 | TX emergency medical service* OR EMS | |
| S4 | TX ambulance* OR prehospital OR “pre hospital” OR “pre-hospital” | |
| S3 | (MH “Allied Health Personnel”) | |
| S2 | (MH “Emergency Medical Technicians”) OR (MH “Prehospital Care”) | |
| S1 | (MH “Emergency Medical Services+”) OR (MH “Transportation of Patients+”) OR (MH “Ambulances”) |
Web of Science
Searched: 1 January 1980 to 18 October 2011.
Search strategy
| #6 | #5 AND #4 DocType=All document types; Language=All languages; |
| #5 | Topic=(patient safety) OR Topic=(“safety management”) OR Topic=(“safety indicator*”) DocType=All document types; Language=All languages; |
| #4 | #3 OR #2 OR #1 DocType=All document types; Language=All languages; |
| #3 | Topic=(“advanced practitioner*”) OR Topic=(“community first responder*”) OR Topic=(“transportation of patient*”) DocType=All document types; Language=All languages; |
| #2 | Topic=(“allied health personnel”) OR Topic=(paramedic*) OR Topic=(“emergency care assistant” OR “emergency medical technician*”) DocType=All document types; Language=All languages; |
| #1 | Topic=(pre-hospital OR prehospital OR “pre hospital”) OR Topic=(ambulance*) OR Topic=(“emergency medical service*” OR EMS) DocType=All document types; Language=All languages; |
The Cochrane Library
Searched: 1 January 1980 to 2 November 2011.
Search strategy
ID Search
#1 MeSH descriptor: [Ambulances] explode all trees
#2 MeSH descriptor: [Transportation of Patients] explode all trees
#3 MeSH descriptor: [Emergency Medical Technicians] explode all trees
#4 MeSH descriptor: [Emergency Medical Services] explode all trees
#5 prehospital or “pre hospital” or pre-hospital OR ambulance*OR paramedic* OR patient near/3 transportation OR “emergency medical services” or “emergency medical service” or EMS OR “emergency care assistant” or “emergency care assistants"
#6 “emeregncy medical technician” or “ emergency medical technician” OR “advacned pratitioner” or “advanced practitioners” OR “community first responder” or “community first responders"
#7 #1 or #2 or #3 or #4 or #5 or #6
#8 MeSH descriptor: [Safety Management] explode all trees
#9 MeSH descriptor: [Safety] explode all trees
#10 “patient safety” or “safety management” or “safety indicator” or “safety indicators”
#11 #8 or #9 or #10
#12 #7 and #11
Science Direct
Searched: 1 January 1980 to 17 October 2011.
Search strategy
((“transportation of patient*”) OR ((“allied health personnel” or “emergency care assistant*”) OR (“community first responder*”) OR (“emergency medical technician*” or “advanced practitioner”) OR (EMS OR “emergency medical service*” or paramedic*) OR ({pre-hospital} OR “pre hospital” OR prehospital or ambulance*))) AND (“safety management” or “patient safety” OR “safety indicator”)
Education Resources Information Center (ERIC)
Searched: 1 January 1980 to 1 November 2011.
Search strategy
((cabs(safety) or cabs(“safety management”) or cabs(“patient safety”) or cabs(“safety indicator”) or cabs(“safety indicators”)) OR su.EXACT(“Risk Management” or “Safety”)) AND ((cabs(prehospital) or cabs(“pre-hospital”) or cabs(“pre hospital”) or cabs(ambulance*) or cabs(transportation near/3 patient*) or cabs(“emergency medical service”) or cabs(“emergency medical services”) or cabs(EMS) or cabs(paramedic*) or cabs(“emergency care assistant”) or cabs(“emergency care assistants”) or cabs(“emergency medical technician”) or cabs(“emergency medical technicians”) or cabs(“advanced practitioner”) or cabs(“advanced practitioners”) or cabs(“community first responder”) or cabs(“community first responders”)) OR su.EXACT(“Emergency Medical Technicians” or “Allied Health Personnel” or “First Aid”)) AND (su.EXACT “Safety regulations” or su.EXACT “Personal safety” or su.EXACT “Public safety” or su.EXACT “Road safety” or su.EXACT “Safety” or safety or “safety management” or “patient safety” or “safety indicator” or “safety indicators”)
Social Services Abstracts and Sociological Abstracts
Searched: 1 January 1980 to 31 October 2011.
Search strategy
(((prehospital or “pre hospital” or “pre-hospital”) OR (ambulance* or “transportation of patients” or “patient transportation”) OR (“emergency medical services” or “emergency medical service” or EMS or paramedic*) OR (“emergency care assistant” or “emeregncy care assistants” or “emergency medical technician” or “emergency medical technicians”) OR (“advanced practitioner” or “ advanced practitioners” or “community first responder” or “community first responders”)) OR su.EXACT(“Emergency Medical Services” or “Paramedical Personnel”)) AND (su.EXACT(“Safety”) OR (safety or “patient safety”) OR (“safety management” or “safety indicator” or “safety indicators”))
Emerald
Searched: 1 January 1980 to 12 October 2011.
Search strategy
Content = All content, (ambulance* OR pre hospital OR prehospital OR paramedic OR emergency medical service* OR EMS in All fields) AND (patient safety in All fields), between 1980 & 2012
Centre for Reviews and Dissemination, York
Searched: 1 January 1980 to 2 November 2011.
Search strategy
(Exp all trees ambulances/ OR exp all trees transportation of patients/ OR exp all trees emergency medical services/ OR exp all trees emergency medical technicians/ OR prehospital OR pre hospital OR pre-hospital OR ambulance* OR transportation of patient* OR emergency medical service* OR EMS OR paramedic OR emergency care assistant* OR emergency medical technician* OR advanced practitioner* Or community first responder*) AND (exp all trees safety management/ OR safety management OR safety OR patient safety OR safety indicator*)
PsycINFO and PsycARTICLES
Searched: 1 January 1980 to 1 November 2011.
Search strategy
(su.EXACT((“Emergency Management”) OR (“Risk Management”) ) OR su((EXACT(“Safety” ) OR safety)) OR (“patient safety” OR “safety management”)) OR ((“safety indicator” OR “safety indicators”)) AND (((((“pre-hospital” OR “pre hospital” OR prehospital ) OR (ambulance* OR paramedic*)) OR (transportation NEAR/3 patient* OR “emergency medical service” OR “emergency medical services” OR EMS)) OR (“emergency care assistant” OR “emergency care assistants” OR “emergency medical technician” OR “emergency medical technicians”)) OR ((“advanced practitioner” OR “advanced practitioners” OR “community first responder” OR “community first responders”)) OR su.EXACT((“Emergency Services”) ) OR su.EXACT(“CPR” OR “Life Sustaining Treatment” ) OR su.EXACT((“Allied Health Personnel” OR “Fire Fighters” OR “Rescue Workers” ) ))
Applied Social Sciences Index and Abstracts (ASSIA)
Searched: 1 January 1980 to 1 November 2011.
Search strategy
(prehospital OR “pre-hospital” OR “pre hospital” OR ambulance* OR paramedic* OR transportation NEAR/3 patient* OR “Emergency medical service” OR “Emergency medical services” OR EMS OR “Emergency care assistant” OR “Emergency are assistants” OR “Emergency medical technician” OR “Emergency medical technicians” OR “Advanced practitioner” OR “Advanced practitioners” OR “Community first responder” OR “Community first responders” OR su.EXACT “Ambulance services” OR su.EXACT “Emergency services” OR su.EXACT “Fire services” OR su.EXACT “Rescue services” OR su.EXACT “Emergency transport”) AND (su.EXACT “Safety regulations” OR su.EXACT “Personal safety” OR su.EXACT “Public safety” OR su.EXACT “Road safety” OR su.EXACT “Safety” OR safety OR “safety management” OR “patient safety” OR “safety indicator” OR “safety indicators”)
International Bibliography of the Social Sciences (IBSS)
Searched: 1 January 1980 to 31 October 2011.
Search strategy
(safety OR “safety management” OR “patient safety” OR “safety indicator” OR “safety indicators”) AND (prehospital OR “pre hospital” OR “pre-hospital” OR ambulance* OR paramedic* OR transportation NEAR/3 patient* OR “emergency medical service” OR “emergency medical services” OR EMS OR “emergency care assistant” OR “emergency care assistants” OR “emergency medical technician” OR “emergency medical technicians” OR “advanced practitioner” OR “advanced practitioners” OR “community first responder” OR “community first responders”)
Dissertation and theses
Searched: 1 January 1980 to 31 October 2011.
Search strategy
(safety OR “safety management” OR “patient safety” OR “safety indicator” OR “safety indicators”) AND (prehospital OR “pre hospital” OR “pre-hospital” OR ambulance* OR paramedic* OR transportation NEAR/3 patient* OR “emergency medical service” OR “emergency medical services” OR EMS OR “emergency care assistant” OR “emergency care assistants” OR “emergency medical technician” OR “emergency medical technicians” OR “advanced practitioner” OR “advanced practitioners” OR “community first responder” OR “community first responders”)
Subjects included:
nursing OR public health OR health care management OR management OR health education OR public policy OR studies OR mental health OR organizational behavior OR medicine OR communication OR economics OR health care OR transportation planning OR information technology OR pharmacology
NHS Evidence
Searched: 1 January 1980 to 14 November 2011.
Search strategy
(prehospital OR pre-hospital OR ambulance) AND “patient safety”
NHS confederation (1 January 1980 to 15 November 2011)
All of these: ambulance
The exact phrase: patient safety
OpenDOAR (Directory of Open Access Repositories)
Searched: 1 January 1980 to 15 November 2011.
Search strategy
Ambulance AND patient safety
Pre-hospital AND patient safety
Open System for Information on Grey Literature in Europe (OpenSIGLE)
Searched: 1 January 1980 to 15 November 2011.
Search strategy
Ambulance* OR paramedic* OR prehospital OR pre-hospital
Zetoc
Searched: 1 January 1980 to 14 November 2011.
Search strategy
Ambulance
Prehospital
Pre-hospital
The FADE Library
Searched: 1 January 1980 to 23 November 2011.
Search strategy
Search anywhere: (safety OR “patient safety” OR “health and safety”) AND (“ambulance services” OR paramedic OR “emergency medical services” OR transport))
Current Awareness Service for Health (CASH)
Searched: 1 January 1980 to 14 November 2011.
Search strategy
ambulance
Pre-hospital
Prehospital
Paramedic
Searched: 1 January 1980 to 22 November 2011.
Search strategy
The exact phrase: patient safety
Any of these: ambulance OR prehospital OR pre-hospital OR paramedic OR EMS
Appendix 4 Table of excluded studies
| Number | Reason |
|---|---|
| 1 | Off topic, for example road traffic collisions |
| 2 | Considered the wrong setting |
| 3 | Considered the wrong population, for example related to the safety of staff rather than patients |
| 4 | Did not provide research methods: overviews, opinion, letters, comments, etc. |
| 5 | Research was reported elsewhere |
| 6 | Study was in progress or planned with no preliminary findings reported |
| 7 | Not specific to ambulance services – general care/guidance |
| 8 | English abstract was not available |
| 9 | Research had been superseded |
| 10 | Disaster or military context |
| Study reference | Reason |
|---|---|
| Abbadi SM. Pre-hospital emergency care in remote areas in Jordan. Crit Care 2001;5:171 | 4 |
| Abbas HAE, Bassiuni NA, Baddar FM. Perception of front-line healthcare providers toward patient safety: a preliminary study in a university hospital in Egypt. Top Adv Pract Nurs 2008;8:11 | 2 |
| Abercrombie D. Critical patients, critical choices. Emerg Med Serv 1993;22:40–5 | 4 |
| Adams CA. Basic knowledge. Emerg Med Serv 2001;30:17 | 1 |
| Agarwal S, Swanson S, Murphy A, Yaeger K, Sharek P, Halamek LP. Comparing the utility of a standard pediatric resuscitation cart with a pediatric resuscitation cart based on the Broselow tape: a randomized, controlled, crossover trial involving simulated resuscitation scenarios. Pediatrics 2005;116:e326–33 | 2 |
| Alakeson V. Quality, Innovation, Productivity and Prevention (QIPP) and Personal Health Budgets. SCIE Social Care Online. Wythall: In Control; 2010 | 7 |
| Alam HB, Velmahos GC. New trends in resuscitation. Curr Probl Surg 2011;48:531–64 | 4 |
| Alam HB. Advances in resuscitation strategies. Int J Surg 2011;9:5–12 | 3 |
| Alexander-Bratcher KM. Spotlight on the safety net. Mecklenburg Emergency Medical Services Agency. N C Med J 2007;68:286–7 | 4 |
| Allison K, Porter K. Consensus on the pre-hospital approach to burns patient management. Accid Emerg Nurs 2004;12:53–7 | 7 |
| Al-Shaqsi SZK. Response time as a sole performance indicator in EMS: pitfalls and solutions. Open Access Emerg Med 2010;2:1–6 | 4 |
| Alvarez G, Coiera E. Interdisciplinary communication: an uncharted source of medical error? J Crit Care 2006;21:236–42 | 2 |
| Ammar A. Advanced technology does not work by itself. Prehosp Disaster Med 2002;17:S9 | 10 |
| Amnis A. Safe and Effective Service Improvement Using a ‘Lean’ Approach. National Electronic Library for Medicines. London: NICE; 2011 | 4 |
| Anderson PB. A comparative analysis of the emergency medical services and rescue responses to eight airliner crashes in the United States, 1987–1991. Prehosp Disaster Med 1995;10:142–53 | 1 |
| Anderson B. Being in the right place at the right time. Occup Health Saf 2000;69:64–6 | 4 |
| Anderton D. Rationalising the Use of Dipyridamole Suspension. National Electronic Library for Medicines. London: NICE; 2009 | 2 |
| Andrus CH, Villasenor EG, Kettelle JB, Roth R, Sweeney AM, Matolo NM. ‘To err is human’: uniformly reporting medical errors and near misses, a naïve, costly, and misdirected goal. J Am Coll Surg 2003;196:911–18 | 4 |
| Department of Health. How to Use Essence of Care 2010. SCIE Social Care Online. Wythall: In Control; 2010 | 7 |
| Department of Health and Health Protection Agency. Clostridium difficile Infection: How to Deal with the Problem. National Electronic Library for Medicines. London: NICE; 2008 | 7 |
| Department of Health, NHS. Developing the NHS Performance Regime. London: Department of Health; 2008 | 7 |
| Department of Health. Overview and Scrutiny of Health – Guidance. London: Department of Health, 2003 | 7 |
| Department of Health. Raising Standards: Improving Performance in the NHS. London: Department of Health; 2003 | 7 |
| Department of Health. NHS Knowledge and Skills Framework. London: Department of Health; 2004 | 7 |
| Taylor JRA. Improvement partnership for ambulance services: what we do and how we do it. In Rawlins MD, Littlejohns P, editors. Clinical Excellence; Delivering Quality in the NHS 2005. Oxford: Radcliffe Publishing; 2005. pp. 95–8 | 1 |
| Department of Health. High Quality Care for all: NHS Next Stage Review Final Report. London: Department of Health; 2008 | 7 |
| Department of Health. Framing the Contribution of Allied Health Professionals. London: Department of Health; 2008 | 7 |
| Department of Health. Religion or Belief: A Practical Guide for the NHS. National Electronic Library for Medicines. London: NICE; 2009 | 1 |
| Merkur S, McDaid D, Mladovsky P. Chronic Disease Management and Remote Patient Monitoring: European Observatory on Health Systems and Policies. Brussels: European Observatory on Health Systems and Policies, WHO European Centre for Health Policy; 2010 | 7 |
| Department of Health Quality Framework Programme. Quality Accounts Toolkit: Advisory Guidance for Providers of NHS Services Producing Quality Accounts for the Year 2009/2010. London: Department of Health; 2010 | 7 |
| Department of Health, NHS Flu Resilience. Learning the Lessons from the H1N1 Vaccination Campaign for Health Care. London: Department of Health; 2010 | 1 |
| Department of Health. Essence of Care 2010. London: Department of Health; 2010 | 7 |
| Department of Health, NHS Finance, Perfomance and Operations Directorate. The NHS Performance Framework: Implementation Guidance: April 2010. London: Department of Health; 2010 | 7 |
| Department of Health, NHS Medical Directorate. The Framework for Quality Accounts: Response to Consultation. London: Department of Health; 2010 | 7 |
| Department of Health. Using the Commissioning for Quality and Innovation (CQUIN) Payment Framework. London: Department of Health; 2010 | 7 |
| Department of Health, NHS Finance, Performance and Operations Directorate. NHS Performance Framework: Implementation Guidance – April 2011. London: Department of Health; 2011 | 7 |
| Department of Health. Guidance and Competences for the Provision of Services using Practitioners with Special Interests: Urgent and Emergency Care. London: Department of Health; 2009 | 7 |
| NHS Plus, Royal College of Physicians, Faculty of Occupational Medicine. Varicella Zoster Virus – Occupational Aspects of Management. London: Royal College of Physicians and Faculty of Occupational Medicine; 2010 | 1 |
| Anonymous. Paramedic drafts EMS safety bill. EMS Insider 1995;22:3 | 3 |
| Anonymous. New FDA reporting rules take effect this month. EMS Insider 1996;23:1 | 4 |
| Anonymous. COBRA decisions put hospital staff on the spot . . . Consolidated Omnibus Budget Reconciliation Act. J Healthc Risk Manag 1996;18:155 | 2 |
| Anonymous. Medical emergencies aloft: are airlines equipped? University of California, Berkeley, wellness letter 1997;14:2 | 1 |
| Linn R, Werfel P, Brown J. Safety first . . . ‘practice makes permanent’. JEMS 1999;2:14 | 4 |
| Anonymous. Are you ready for JCAHO’s new restraint standards? RN 2000;63:24hf7–8 | 4 |
| Anonymous. Alert: state wants EMS error reports. EMS Insider 2001;28:7 | 4 |
| Anonymous. Patient-safety considerations. EMS Insider 2002;29:3 | 4 |
| Anonymous. Use score card to boost quality. ED Manag 2002;14:114–17 | 2 |
| Anonymous. A positive sentinel event? AI says it’s possible: use root-cause analysis in excellent outcomes, too. Healthcare Benchmarks Qual Improv 2002;1:16–18 | 2 |
| Anonymous. At a glance. OR Manager 2002;18:32 | 1 |
| Anonymous. Thrombolytics safe for ambulance use. Pharm J 2002;269:772 | 4 |
| Anonymous. These tools show cause of close calls, adverse events. J Healthc Risk Manag 2003;25:3–4 | 2 |
| Narinder T. Building safer healthcare systems: a case for error-in-medicine curriculum in medical training. Med J Armed Forces India 2003;59:273 | 2 |
| Rabinovici R, Frankel H, Kaplan L. Trauma evaluation and resuscitation. Curr Probl Surg 2003;40:599–681 | 4 |
| Anonymous. AHP project launched to raise awareness of patient safety. Podiatry Now 2004;7:14 | 4 |
| Anonymous. Do your staff members risk misidentifying patients? ED Nursing 2004;7:93–5 | 2 |
| Anonymous. Ask Sirenhead. Stop the blow hard. JEMS 2004;29:120 | 3 |
| Anonymous. NZNO welcomes coroner’s report recommendations. Kai Tiaki Nurs N Z 2004;10:11 | 2 |
| Braun BI, Darcy L, Divi C, Robertson J, Fishbeck J. Hospital bioterrorism preparedness linkages with the community: improvements over time. Am J Infect Control 2004;32:317–26 | 1 |
| Royal College of Nursing. RCN Review of the Year and Summary Accounts 2003/2004. London: Royal College of Nursing; 2004 | 1 |
| Anonymous. Using medication reconciliation to prevent errors. Jt Comm J Qual Patient Saf 2006;32:230–2 | 2 |
| Anonymous. An obstacle to error reporting remains. Pharm J 2006;276:252 | 2 |
| Anonymous. Prescribing safely. Pharm J 2006;276:554 | 2 |
| News in brief. Emerg Nurse 2007;15:2 | 4 |
| Frew SA. EMTALA compliance could have stopped failure cascade. ED Legal Letter 2007;18:6–8. | 2 |
| Mackersie RC, Dicker RA. Pitfalls in the evaluation and management of the trauma patient. Curr Probl Surg 2007;44:778–833 | 4 |
| Anonymous. Into the wild. Midwifery Matters 2008;117:7–8 | 1 |
| Anonymous. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008;133(Suppl. 6):381S–453S | 2 |
| Anonymous. Bibliography and Other Resource Materials for Advancing Patient And Family-Centered Care. Bethesda, MD: Institute for Family-Centered Care; 2008 | 1 |
| Monitor. Identifying Risk, Taking Action: Monitor’s Approach to Service Performance in NHS Foundation Trusts. London: Monitor; 2008 | 7 |
| Anonymous. Research worth reading. EMS Insider 2009;36:10–11 | 5 |
| Anonymous. MHRA 2009 Liaison Officer Conference: Medicines and Healthcare Products Regulatory Agency. London: Medicines and Healthcare products Regulatory Agency; 2009 | 1 |
| Harvey S, Liddell A, McMahon L. Windmill 2009: NHS Response to the Financial Storm. London: The King’s Fund; 2009 | 1 |
| Anonymous. CLIR launches EMS Voluntary Event Notification Tool. EMS Insider 2010;37:11 | 4 |
| Anonymous. Noticeboard. Emerg Nurse 2010;18:10 | 4 |
| Anonymous. Standards for the Care of Critically Ill Children (4th Edition). Royal College of Anaesthetists. London: The Paediatric Intensive Care Society; 2010 | 2 |
| Anonymous. London Child Protection Procedures: 4th Edition, 2010. London: London Safeguarding Children Board; 2010 | 7 |
| Anonymous. The GAT Handbook 2011–2012. London: Association of Anaesthetists of GB and Ireland; 2011 | 1 |
| Anonymous. 1000 Lives Plus (archived) – Welsh Ambulance Service Trust. Secondary 1000 Lives Plus (archived) – Welsh Ambulance Service Trust 2010. URL: www.wales.nhs.uk/sites3/page.cfm?orgid=781&pid=47103 (accessed 22 April 2013) | 4 |
| Council GM. Treatment and Care Towards the End Of Life: Good Practice in Decision Making. London: General Medical Council; 2010 | 1 |
| Anonymous. 10 steps to establish an EMS risk management program. EMS Insider 2011;38:10 | 4 |
| Anonymous. Psoriasis: Clinical Knowledge Summaries. London: NICE; 2010 | 1 |
| Anonymous. Facing the Future: A Review of Paediatric Services. London: Royal College of Paediatrics and Child Health; 2011 | 2 |
| Anonymous. Deep Vein Thrombosis. Clinical Knowledge Summaries. London: NICE; 2009 | 4 |
| Anonymous. Atrial Fibrillation. Clinical Knowledge Summaries. London: NICE; 2009 | 2 |
| Department of Health. Ambulance Quality Indicators. East Midlands Strategic Health Authority. London: Department of Health; 2011 | 1 |
| Anonymous. Clinical Governance Reading List. London: The King’s Fund; 2009 | 7 |
| Anonymous. Angiox 250mg Powder for Concentrate for Solution for Injection or Infusion – Summary of Product Characteristics. Electronic Medicines Compendium. London: NICE; 2010 | 7 |
| House of Commons Health Committee. Alcohol: First Report of Session 2009–10, Volume 1: Report, Together with Formal Minutes. London: House of Commons Health Committee; 2010 | 7 |
| House of Commons Health Committee. Commissioning: Fourth Report of Session 2009–10. London: House of Commons Health Committee; 2010 | 7 |
| House of Commons Health Committee. The Use of Overseas Doctors in Providing Out-Of-Hours Services. London: House of Commons Health Committee; 2010 | 1 |
| House of Commons Health Committee. Public Health: Twelfth Report of Session. London: House of Commons Health Committee; 2010–12, 2011 | 7 |
| Anonymous. Major Projects Authority Programme Assessment Review of the National Programme for IT. London: Cabinet Office; 2011 | 7 |
| House of Commons Health Committee. Annual Accountability Hearing with Monitor: Tenth Report Of Session 2010–12. London: House of Commons Health Committee; 2011 | 1 |
| National Audit Office. Department of Health – Improving Emergency Care in England. National Audit Office Report (HC 1075, 2003–04). London: National Audit Office; 2004 | 7 |
| Committee HoCPA. The National Programme for IT in the NHS: progress since 2006. London: House of Commons Public Accounts Committee; 2008 | 7 |
| Klein S, McCarthy D. Gundersen Lutheran Health System: Performance Improvement Through Partnership. New York, NY: The Commonwealth Fund; 2009 | 1 |
| House of Commons Health Committee. The Use of Management Consultants by the NHS and the Department of Health: Fifth Report of Session 2008/9. London: House of Commons Health Committee; 2009 | 1 |
| National Audit Office. A Short Guide: The NAO’s Work on the Department of Health. London: National Audit Office; 2010 | 1 |
| Anonymous. Statement of Financial Entitlements (Amendment) Directions 2011. National Electronic Library for Medicines. London: NICE; 2011 | 1 |
| National Audit Office. National Health Service Landscape Review. NAO Report (HC 708 2010–2011). London: National Audit Office; 2011 | 1 |
| The London NHS Confederation. Grand Designs: The New London NHS. London: NHS Confederation; 2003 | 1 |
| Strategic Health Authority PPI Leads Network. Performance Improvement Framework for Patient and Public Involvement in the NHS. London: Department of Health; 2003 | 4 |
| NHS Connecting for Health. Department of Health Issues Guidance on Informatics Planning for 2009/10. National Electronic Library for Medicines. London: NICE; 2008 | 1 |
| NHS. Darlington PCT Prospectus 2009/10. County Durham: Darlington Primary Care Trust; 2008 | 7 |
| Authority LSH. Clinical Workforce Productivity in London’s Health Sector: Final Report – Appendices. London: NHS London; 2008 | 1 |
| NHS Confederation. NHS Confederation Annual Review 2007–2008. London: NHS Confederation; 2008 | 7 |
| NHS London. NHS London Annual Report 2007/2008. London: NHS; 2009 | 7 |
| Department of Health, NHS. Toolkit for High Quality Neonatal Services. London: Department of Health; 2009 | 2 |
| Keasey K, Malby R, Turbitt I, Veronesi I, Neogy I. National Inquiry into Fit for Purpose Governance in the NHS. University of Leeds, Leeds: Centre for Innovation in Health Management; 2009 | 7 |
| Department of Health, Agency HP. Pandemic (H1N1) 2009 Influenza: Summary Infection Control Guidance for Ambulance Services During an Influenza Pandemic. London: Department of Health; 2010 | 7 |
| Centre NI. Statistics on Sickness Absence Rates in NHS April to June 2009. National Electronic Library for Medicines. London: NICE; 2009 | 1 |
| The NHS Confederation and Independent Healthcare Advisory Service. What’s it all for? Removing Unnecessary Bureaucracy in Regulation. London: NHS Confederation; 2009 | 7 |
| NHS. Bedside Guide. London: Royal Free Hampstead NHS Trust; 2009 | 1 |
| Department of Health. NHS 2010–2015: From Good to Great: Preventative, People-Centred, Productive. London: Department of Health; 2009 | 7 |
| NHS Improvement. An Integrated Approach: The Transferability of the Winning Principles – Sharing the Learning. Coventry: NHS Improvement; 2010 | 1 |
| Anonymous. Independent Inquiry into Care Provided by Mid Staffordshire NHS Foundation Trust: January 2005-March 2009: Volume 1. London: Department of Health; 2010 | 1 |
| NHS Lothian. Living and Dying Well in Lothian. Edinburgh: NHS Lothian; 2010 | 7 |
| Edwards N. The Triumph of Hope Over Experience: Lessons from the History of Reorganisation. London: NHS Confederation; 2010 | 7 |
| The NHS European Office. Representing the NHS in Europe – Three Years of Achievement. London: NHS Confederation; 2010 | 7 |
| NHS Institute for Innovation and Improvement, King’s College London. Large Scale Change – NHS Mobilisation. Coventry: NHS Institute for Innovation and Improvement; 2010 | 7 |
| London N. Workforce for London Progress Report: Implementation – Turning Strategy into Action. London: NHS London; 2010 | 7 |
| Molyneux P. Health and Housing: Worlds Apart? Housing Care and Support Solutions to Health Challenges. Association of Public Health Observatories. London: National Housing Federation; 2010 | 7 |
| Programme NNEoLC. Talking Needs Action Training Needs Analysis: The Pilot Sites Report their Findings for End of Life Care Communication Skills. SCIE Social Care Online; 2010. National Health Service. National End of Life Care Program. URL: http://beta.scie-socialcareonline.org.uk/talking-needs-action-training-needs-analysis-the-pilot-sites-report-their-findings-for-end-of-life-care-communication-skills/r/a11G000000181ZZIAY (accessed 26 June 2014) | 7 |
| Department of Health. The NHS Outcomes Framework 2011/12. SCIE Social Care Online. London: Department of Health; 2010 | 7 |
| NHS Institute for Innovation and Improvement. Medical Leadership Competency Framework: Enhancing Engagement in Medical Leadership (3rd Edition). London: NHS Institute for Innovation and Improvement and Academy of Medical Royal Colleges; 2010 | 7 |
| NHS Institute for Innovation and Improvement. Annual Report and Accounts of the NHS Institute for Innovation and Improvement 2009–10. Coventry: NHS Institute for Innovation and Improvement; 2010 | 7 |
| Department of Health. Liberating the NHS: Report on the Arms-Length Bodies Review. London: Department of Health; 2010 | 7 |
| Department of Health. Guidance on the NHS Standard Contract for Acute Hospital Services 2010–11. London: Department of Health, 2010 | 2 |
| Health Mandate. Accounting for Quality: An Analysis of the Impact of Quality Accounts in the NHS. London: Public Health England; 2010 | 7 |
| Davis F. Paediatric Emergency Care. London: NICE; 2010 | 7 |
| Bevington J. Healthy Boards for a Healthy London. London: NHS London; 2011 | 7 |
| Willson A, Seddon J, Brogan A, Jones C, Davies J, Matthias J. 1000 Lives Plus and the NHS Agenda – Lessons from Systems Thinking: All Wales Medicines Strategy Group. NHS Wales; 2011. URL: www.wales.nhs.uk/sites3/Documents/781/Systems (accessed 28 July 2014) | 4 |
| NHS Evidence. Transport Service for Dialysis Patients: To Improve Quality. QIPP – NHS Evidence. London: NICE; 2010 | 1 |
| NHS Institute for Innovation and Improvement. London KsC. Improving Healthcare Quality at Scale and Pace – Lessons from the Productive Ward. Releasing Time To Care Programme – Full Report. Coventry: NHS Institute for Innovation and Improvement; 2010 | 2 |
| NHS Employers. Quality and Outcomes Framework Guidance for GMS Contract 2009/10. London: British Medical Association and NHS Employers; 2009 | 7 |
| Department of Health. Liberating the NHS: Greater Choice and Control: Government Response: Extending Patient Choice of Provider (Any Qualified Provider). London: Department of Health; 2011 | 7 |
| NHS Confederation. NHS Confederation Annual Review 2010–11. London: NHS Confederation; 2011 | 7 |
| Ambulance Service Network. Critical Care Paramedics: Delivering Enhanced Pre-Hospital Trauma and Resuscitation Care: A Cost-Effective Approach. London: NHS Confederation; 2011 | 4 |
| Monitor. NHS Foundation Trusts: Consolidated Accounts 2010/11. London: Monitor; 2009 | 7 |
| NICE. CG109 Transient Loss of Consciousness in Adults and Young People: Ambulance Service Slide Set. London: NICE; 2010 | 4 |
| NHS Scotland. Partnership for Care Scotland’s Health White Paper. Edinburgh: The Scottish Government; 2003 | 1 |
| NHS Quality Improvement Scotland. The Provision of Safe and Effective Primary Medical Services Out of Hours Standards Aug 2004. Healthcare Improvement Scotland. Edinburgh: NHS Quality Improvement Scotland; 2004 | 1 |
| NHS Quality Improvement Scotland. Report of Evidence Based Assessments from SHTG Aug 2008. Healthcare Improvement Scotland. Edinburgh: NHS Quality Improvement Scotland; 2008 | 7 |
| Scottish Government Health Directorates. Delivering Better Health, Better Care through Continuous Improvement: Lessons from the National Programmes. Edinburgh: NHS Scotland; 2008 | 4 |
| NHS Scotland. Wheelchair and Seating Services Modernisation: Action Plan. SCIE Social Care Online. Edinburgh: NHS Scotland; 2009 | 1 |
| The Scottish Government. National Guidance for Child Protection in Scotland: 2010. SCIE Social Care Online. Edinburgh: NHS Scotland; 2010 | 7 |
| WHO. Assessment of Health Security and Crises Management Capacity, Republic of Moldova. WHO Regional Office for Europe. Copenhagen: WHO; 2009 | 1 |
| WHO. Assessment of Health Security and Crises Management Capacity, Armenia. WHO Regional Office for Europe. Copenhagen: WHO; 2009 | 7 |
| WHO. Emergency Medical Services Systems in the European Union. WHO Regional Office for Europe. Copenhagen: WHO; 2010 | 1 |
| Vaillard J, Lai T, Bevan G. Estonia Health System Performance Assessment: 2009 Snapshot. WHO Regional Office for Europe. Copenhagen: WHO; 2010 | 1 |
| Anonymous. Promote safety in air ambulances by taking a stand against drugs. Hosp Employee Health 1989;8:87 | 4 |
| Anonymous. ‘Patient Safety Act’ introduced. Geriatr Nurs 1996;17:199–200 | 4 |
| The Hospital Infection Control Practices Advisory Committee Centers for Disease Control and Prevention Public Health Service USDoH, Human S. Part II. Recommendations for prevention of infections in health care personnel. Am J Infect Control 1998;26:328–54 | 3 |
| Anonymous. Meningitis and meningococcemia. Emerg Nurse Leg Bull 1998;24:2–7 | 7 |
| Anonymous. Missed subdural hematoma: $25 million. Healthc Risk Manag 1999;21:3–4 | 2 |
| Anonymous. Diagnostic failure causes death: $4 million verdict. Healthc Risk Manag 2000;22:3–4 | 2 |
| Hall Y. Misdiagnosis results in death, $1 million verdict. Healthc Risk Manag 2000;22:2–3 | 2 |
| American College of Emergency Physicians Board of Directors. Alternate ambulance transportation and destination. Ann Emerg Med 2008;52:594 | 4 |
| Anonymous. Check your stretcher fasteners. EMS Insider 2001;28:4 | 4 |
| Anonymous. Improper IV leads to amputation. Healthc Risk Manag 2001;23:2–4 | 2 |
| Anonymous. Injury prevention model broadens safety scope: create situations where human error can’t happen. Healthc Risk Manag 2002;24:3–4 | 4 |
| Anonymous. Research update. Poor communication key to clinical errors. Aust Nurs J 2002;10:18 | 3 |
| Medicine PaD. Abstracts of scientific and invited papers for 6th Asia-Pacific Conference on Disaster Medicine, Fukuoka, Japan, 18–22 February 2002. Prehospital Disaster Med 2002;17:S1–35 | 10 |
| Anonymous. Heart attack and triage: $25 million FL settlement. Healthc Risk Manag 2002. URL: www.highbeam.com/doc/1G1-206631117.html (accessed 28 July 2014) | 2 |
| Anonymous. Relatives plan to sue after death of overdose patient who was kept waiting. Nurs Times 2003;99:5 | 2 |
| Anonymous. Medical condition list and appropriate use of air medical transport. Air Med J 2003;22:14–19 | 1 |
| Anonymous. Don’t harm patients with high-alert drugs. ED Nurs 2004;7:88–9 | 2 |
| Anonymous. Policy statement. EMS as an essential public safety service. Ann Emerg Med 2004;43:152 | 4 |
| Anonymous. Ambulance safety becomes a priority. EMS Insider 2004;31:5 | 4 |
| The National Prescribing Centre. Supplementary Prescribing National Prescribing Centre. London: The National Prescribing Centre (now part of NICE Medicines and Prescribing Centre); 2004 | 7 |
| Jones D, Mitchell A. Lean Thinking for the NHS. London: NHS Confederation; 2008 | 7 |
| Anonymous. Designing future ambulance transport for patient safety. J Oper Depart Pract 2006;2:16 | 4 |
| Anonymous. NIH funds pilot program for EMS error reporting system on a national basis. EMS Insider 2006;33:7 | 4 |
| South Western Ambulance Service. What is NHS Pathways? Secondary What is NHS Pathways? Exeter: South Western Ambulance Service; 2011 | 4 |
| Anonymous. Last word. JEMS 2007;32:114 | 4 |
| Anonymous. Top 5 in the news. Jt Comm Perspect Patient Saf 2007;7:2 | 5 |
| Royal College of Obstetricians and Gynaecologists. Standards for Maternity Care. London: Royal College of Obstetricians and Gynaecologists; 2008 | 7 |
| Anonymous. Let’s Talk About Restraint: Rights, Risks and Responsibility. London: Royal College of Nursing; 2008 | 4 |
| Anonymous. Disruptive Innovation – What Does it Mean for the NHS? London: NHS Confederation; 2008 | 4 |
| Anonymous. Engaging Clinicians in a Quality Agenda. Penarth: All Wales Medicines Strategy Group; 2008 | 7 |
| Healthcare Commission. State of Healthcare 2008. London: Healthcare Commission; 2008 | 7 |
| Anonymous. Georgia Situation Report No. 4, 9 September 2008. WHO Regional Office for Europe. Copenhagen: WHO; 2008 | 1 |
| Anonymous. High Court judgement Oakes v Neininger & Ors EWHC 548 (QB) (19 March 2008) 2012. URL: www.casecheck.co.uk/CaseLaw.aspx?EntryID=14543 (accessed 24 September 2012) | 4 |
| European Health Telematics Association. Sustainable Telemedicine: Paradigms for Future-Proof Healthcare. Brussels: European Health Telematics Association; 2008 | 7 |
| Goodrich J, Cornwell J. Seeing the Person in the Patient: The Point of Care Review Paper. London: The King’s Fund; 2008 | 7 |
| Anonymous. Stepping Up: Using Health Standards to Improve Public Health. London: Faculty of Public Health; 2009 | 7 |
| Anonymous. Safeguarding Adults: Report on the Consultation on the Review of ‘No Secrets’. London: Department of Health; 2009 | 7 |
| Anonymous. Last word: the ups & downs of EMS. JEMS 2009;34:82 | 4 |
| Anonymous. Clinical rounds. Medical air transport: cracks in the system lead to adverse events. Nursing 2009;39:23 | 5 |
| Anonymous. Patients’ lives at risk during NHS transfers. Oper Theatre J 2009;223:4 | 4 |
| NHS Confederation. Ambulance Service Network Annual Report 2008–09. London: NHS Confederation; 2009 | 7 |
| Department of Health. The Year 2008/09: Third Annual Report of NHS Chief Executive. National Electronic Library for Medicines. London: NICE; 2009 | 7 |
| KPMG. Learning and Implications from Mid Staffordshire NHS Foundation Trust. London: KPMG; 2009 | 1 |
| Arr-Jones G, Bussey A, Golding M, Wolper S, Mellor L, Fittock A. Patient Group Directions December 2009. Wright J, editor. Liverpool: National Prescribing Centre; 2009 | 4 |
| Health Service Commissioner for England. Listening and Learning: the Ombudsman’s Review of Complaint Handling by the NHS in England 2009–10. London: Health Service Commissioner for England; 2010 | 7 |
| Carayon P, Karsh BT, Cartmill RS. Incorporating Health Information Technology into Workflow Redesign. Rockville, MD: Agency for Healthcare Research and Quality; 2010 | 2 |
| College of Emergency Medicine. Emergency Medicine Consultants – Workforce Recommendations. London: College of Emergency Medicine; 2010 | 7 |
| HM Government. Working Together to Safeguard Children: A Guide to Inter-Agency Working to Safeguard and Promote the Welfare of Children. London: HM Government; 2010 | 7 |
| NHS Confederation. NHS Confederation Annual Review 2009/10. London: NHS Confederation; 2010 | 7 |
| Department of Health. Review of Early Warning Systems in the NHS: Acute and Community Services. London: Department of Health; 2010 | 7 |
| Anonymous. ACEP to promote EMS ‘Culture of Safety’ strategy. EMS Insider 2010;37:5 | 4 |
| Anonymous. Ambulance Services England 2009–10. Leeds: Health and Social Care Information Centre; 2010 | 4 |
| Regulation and Quality Improvement Authority. Report of the RQIA Review of Intrapartum Care. Belfast: Regulation and Quality Improvement Authority; 2010 | 1 |
| NHS Confederation. Improving Quality and Productivity in the NHS whilst Facing the Financial Pressures. London: NHS Confederation; 2010 | 7 |
| Nursing and Midwifery Council. Standards for Medicines Management. London: Nursing and Midwifery Council; 2008 | 3 |
| Gaynor M, Moreno-Serra R, Propper C. Death by Market Power: Reform, Competition and Patient Outcomes in the National Health Service. Cambridge, MA: National Bureau of Economic Research; 2010 | 7 |
| Department of Health. National Quality Board Annual Report 2009/10. London: Department of Health; 2010 | 7 |
| Royal College of Nursing. Standards for Infusion Therapy. London: Royal College of Nursing; 2010 | 3 |
| Royal College of Nursing. Frontline First Interim Report. London: Royal College of Nursing; 2010 | 3 |
| Royal College of Psychiatrists. MARSIPAN: Management of Really Sick Patients with Anorexia Nervosa. London: Royal College of Psychiatrists; 2010 | 1 |
| National Institute for Health Research. Embedding Health Research: National Institute for Health Research Annual Report 2009/10. London: NIHR; 2010 | 1 |
| Anonymous. Professionalism in Healthcare Professionals. London: Health and Care Professions Council; 2011 | 1 |
| Anonymous. Patient safety pulse: your patient safety news. Jt Comm Perspect on Patient Saf 2011;11:2 | 2 |
| Anonymous. Benzodiazepine and Z-Drug Withdrawal. Clinical Knowledge Summaries. London: NICE; 2009 | 1 |
| Department of Health. Informatics Planning 2010/11. London: Department of Health, 2009 | 7 |
| Monitor. Monitor’s Annual Report and Accounts 2010/11. London: Monitor; 2011 | 1 |
| Argent VP. Pre-hospital risks of the reconfiguration of obstetric services. Clin Risk 2010;16:252–5 | 4 |
| Aronson JK. Medication errors. In Aronson JK, editor. Side Effects of Drugs Annual. Amsterdam: Elsevier; 2010. pp. 903–22 | 4 |
| Arthur J. Statistical Process Control for Health Care. Chico, CA: Quality Digest; 2008 | 4 |
| Arvanitoyannis IS. ISO 14000: A Promising New System for Environmental Management or Just Another Illusion? In Arvanitoyannis IS, editor. Waste Management for the Food Industries. Amsterdam: Academic Press, 2008. pp. 39–96 | 1 |
| Asaeda G, Braun J, Prezant D. Keeping patients SAFE New York City providers respond to sexual assault victims. JEMS 2011;36:52–3 | 2 |
| Asakawa Y, Takahashi R, Kagawa J. Falling accidents among metropolitan elderly resulting in emergency ambulance transfer. Nihon Ronen Igakkai Zasshi 2001;38:534–9 | 2 |
| Link H, editor. Interleukin-2-Haltige Ambulance Therapie des Metastasierenden Nierenzellkarzinoms. Ergebnisse und Perspektiven in der Hamatologie und Onkologie. Cologne: Springer; 1995 | 2 |
| Au M, Felt-Lisk S, Anglin G, Clarkwest A. Using Health IT: Eight Quality Improvement Stories. Rockville, MD: Agency for Healthcare Research and Quality; 2010 | 7 |
| Augustine JJ. Unconventional patient positioning. Emerg Med Serv 1998;27:60–61, 63–4 | 4 |
| Augustine JJ. Prehospital rounds. Barrels of bad news. Emerg Med Serv 2005;34:41–2 | 4 |
| Augustine JJ. Heavy subjects: delivery of emergency care to obese patients. JEMS 2007;32:74–6, 78–81, 83–5 | 4 |
| Augustine JJ. ‘How many can you take?’ A medical mass-casualty incident requires consultation and coordination in its response. EMS Mag 2007;36:23, 25–7 | 4 |
| Augustine JJ. Why won’t he wake up? Altered LOC, decreased respirations & pinpoint pupils provide clues to a medication mishap. EMS Mag 2007;36:25, 27 | 2 |
| Augustine JJ. Potty mouth. EMS Mag 2009;38:18, 20 | 1 |
| Augustine JJ. Hold your fire! EMS World 2010;39:24–8 | 1 |
| Backes P. GFR regulations on medical apparatus: what are the consequences for the emergency ambulance service. Notfall Medizin 1986;12:71–7 | 1 |
| Roger NB. Clinical governance. Int Congress Ser 2004;1272:64–71 | 2 |
| Ballard KA. Reply by Karen Ballard to: letter to the editor by Tammy Kane (30 April 2004). Online J Issues Nurs 2004;9:1 | 4 |
| Banks A, Dracup K. Factors associated with prolonged prehospital delay time in African Americans with an acute myocardial infarction. Am J Crit Care 2006;15:149–57 | 1 |
| Barishansky RM. 10 minutes with Deb Funk. Emerg Med Serv 2004;33:28, 31 | 1 |
| Barishansky RM. Vehicle ops. Next generation ambulance puts safety first. Emerg Med Serv 2005;34:30–1 | 1 |
| Barishansky RM, O’Connor KE. Expert advice. Bariatric patients pose weighty challenges. EMS Insider 2007;34:4–5 | 3 |
| Baskett PJF. Nitrous oxide in pre-hospital care. Acta Anaesthesiol Scand 1994;38:775–6 | 1 |
| Batalingaya F. Nutrition survey in Mauritania. Prehosp Disaster Med 2002;17(Suppl. 2):S21 | 1 |
| Batchelor T. A step toward safety. NIOSH study shows improved reach in Winter Park ambulance design. EMS Mag 2009;38:71–2 | 3 |
| Bates KD. Critical decisions. EMS Mag 2009;38:47–50 | 4 |
| Baxter WA. Office improvement . . . ‘The advancing anatomy of an ambulance’. JEMS 1997;22:14 | 4 |
| Becker RC. Hemostatic aspects of cardiovascular medicine. In Kitchens CS, Alving BM, Kessler CM, eds. Consultative Hemostasis and Thrombosis. Philadelphia, PA: W.B. Saunders; 2007. pp. 339–69 | 2 |
| Vemulapalli S. Ambulance safety revisited. Emerg Med Serv 1997;26:14–15 | 1 |
| Beckerman B. Lights and sirens revisited . . . Pitt’s response (August, 1997) to my recent letter to the editor. Emerg Med Serv 1997;26:12–14 | 4 |
| Beckerman B, Smith M. Selective spinal immobilization. Emerg Med Serv 2003;32:12–14 | 4 |
| Beeman L. Basing a clinician’s career on simulation: development of a critical care expert into a clinical simulation expert. In Kyle R, Murray W, eds. Clinical Simulation. Oxford: Academic Press; 2008. pp. 31–51 | 4 |
| Blair B. Teamwork makes magic: air medical transport conference 2001. Air Med J 2001;20:20–21 | 1 |
| Bellazzini MA, Rankin PM, Quisling J, Gangnon R, Kohrs M. Formal testing and utilization of streaming media to improve flight crew safety knowledge. Air Med J 2008;27:84–98 | 1 |
| Bennett P. Environmental governance and private actors: enrolling insurers in international maritime regulation. Polit Geogr 2000;19:875–99 | 1 |
| Berg W, Avery SK. Rainfall variability over the tropical pacific from July 1987 through December 1991 as inferred via monthly estimates from SSM/I. J Appl Meteorol 1994;33:1468–85 | 1 |
| Berger W, Figueira I, Maurat AM, Bucassio EP, Vieira I, Jardim DR, et al. Partial and full PTSD in Brazilian ambulance workers: prevalence and impact on health and on quality of life. J Trauma Stress 2007;20:637–42 | 3 |
| Bergmo TS. Can economic evaluation in telemedicine be trusted? A systematic review of the literature. Cost Eff Resour Alloc 2009;7:18 | 2 |
| Berkow LC. Strategies for airway management. Best Pract Res Clin Anaesthesiol 2004;18:531–48 | 2 |
| Bernstein A. Sanctioning the ambulance chaser. Loyola Los Angel Law Rev 2008;41:1545–84 | 1 |
| Bertocci GE. Special issue on wheelchair transportation safety – introduction. Med Eng Phys 2010;32:229 | 4 |
| Bhanji F, Soar J. Do smartphones help deliver high-quality resuscitation care? Resuscitation 2011;82:1377–8 | 7 |
| Bilukha OO, Brennan M, Woodruff B. Injuries from landmines and unexploded ordnance in Afghanistan. Prehosp Disaster Med 2002;17(Suppl. 2):S36 | 1 |
| Bing-Wen J, Mo-Gin W. Studies on the prophylactic-therapeutic effects of rhubarb on lung injury caused by abdominal infection in rats. Prehosp Disaster Med 2002;17(Suppl. 2):S78–9 | 1 |
| Birlik G, Sezgin OC, Geridonmez SG. 16th International Congress on Sound and Vibration. Sound and Vibration. Krakow: Auburn, AL; 2009 | 3 |
| Biros MH. Research without consent: current status. Ann Emerg Med 2003;42:550–64 | 4 |
| Bitterman RA. Patient Safety Organizations: protecting peer review materials and improving patient safety? ED Legal Letter 2007;18:85–8 | 2 |
| Blacker N. Abstract. Shift hours in the Australian ambulance industry: workforce health and safety, patient, and public safety. J Emerg Prim Health Care 2007;5:1 | 3 |
| Blackledge CG, Jr., Veltri MA, Matlin C, Sparkes W, Lehmann CU. Patient safety in emergency situations: a web-based pediatric arrest medication calculator. J Healthc Qual 2006;28:27–31 | 2 |
| Blanda M, Gallo UE. Emergency airway management. Emerg Med Clin N Am 2003;21:1–26 | 4 |
| Bleetman A. Overview of management of minor head injuries. J Paramedic Pract 2009;1:280–7 | 4 |
| Blevins MR. Old tool new use. Emerg Med Serv 2004;33:16–18 | 4 |
| Bloom MA. Land versus air ambulance: safety issues. J Neonatal Nurs 2002;8:11–14 | 4 |
| Blumen IJ, Coto J, Maddow CL, Casner M, Felty C, Arndt K, et al. A safety review and risk assessment in air medical transport. Air Med J 2002;21:1–63 | 1 |
| Boe J, Dennis JH, O’Driscoll BR. European Respiratory Society Guidelines on the Use of Nebulizers. Lausanne: European Respiratory Society; 2004 | 7 |
| Boersma, E. Improved Electrocardiographic Criteria for Confirmation of Acute Myocardial Infarction with Application in Pre-hospital Thrombolysis. Computers in cardiology. Vienna: IEEE; 1995 | 9 |
| Boivin WS, Boyd SM, Coletta JA, Neunaber LM. Measurement of radiofrequency electromagnetic fields in and around ambulances. Biomed Instrum Technol 1997;31:145–54 | 1 |
| Bolton P, Bass J, Murray L, Lee K, Weiss W, McDonnell SM. Expanding the Scope of Humanitarian Program Evaluation. Annual Humanitarian Health Conference. Amsterdam: World Association for Disaster and Emergency Medicine; 2007 | 1 |
| Boncinelli S, Doni L, Librenti M, Marsili M. Comfort and safety in ambulance transportation. Minerva Anestesiol 1991;57:1561–4 | 8 |
| Boorman S. The Boorman Review: NHS Health and Well-Being Review – Interim Report. London: Department of Health; 2009 | 1 |
| Bounes V, Ducasse JL. Pain in pre-hospital setting. Med Urg 2009;2:387–90 | 7 |
| National Audit Office. NAO Report (HC 101 2007–2008): Caring for Vulnerable Babies: The Reorganisation of Neonatal Services in England. London: National Audit Office; 2007 | 7 |
| National Audit Office. National Audit Office Report (HC 493 2002–03): NHS (England) Summarised Accounts 2001–02. London: National Audit Office; 2003 | 1 |
| Bodker S, Kyng M, Schmidt K, editors. Informing Collaborative Information Visualisation through an Ethnography of Ambulance Control. European Conference on Computer Supported Cooperative Work; 1999 Sep; Copenhagen | 1 |
| Bowler PA. Interhospital transfer for primary percutaneous coronary intervention: a community hospital’s experience. J Emerg Nurs 2006;32:486–90 | 2 |
| Boyd CR, Hungerpiller JC. Patient risk in prehospital transport: air versus ground. Emerg Care Q 1990;5:48–55 | 4 |
| Pybus R. 1996 Safety Management: Strategy and Practice. Oxford: Butterworth-Heinemann; 1996 | 1 |
| Boyle S. Health systems in transition: United Kingdom (England) – Health System Review. Health Syst Transit 2011;13:1–486 | 7 |
| National Audit Office. NAO Report (HC 484-I 2007–08): The National Programme for IT in the NHS: Progress since 2006. London: National Audit Office; 2008 | 7 |
| Bradbeer PVG, Findlay C, Fogarty TC. An ambulance crew rostering system. In Cagnoni S, editor. Real-World Applications of Evolutionary Computing. Lecture Notes in Computer Science (Volume 1803). Edinburgh: Springer; 2000 | 1 |
| Bradley VM. Placing emergency department crowding on the decision agenda. J Emerg Nurs 2005;31:247–58 | 2 |
| Bramstedt KA, Simeon DJ. The challenges of responding to ‘high-tech’ cardiac implant patients in crisis. Prehosp Emerg Care 2002;6:425–32 | 4 |
| Brennan MB, Salama P, Ansari A, Dadgar N. Implementation of an extended age-range mass measles campaign in Afghanistan. Prehosp Disaster Med 2002;17(Suppl. 2):S4–5 | 1 |
| Brindley PG. Medical simulation: no longer ‘why’ but ‘how’. J Crit Care 2009;24:153–4 | 4 |
| Bristow A. Medical helicopter systems: recommended minimum standards for patient management. J R Soc Med 1991;84:242–4 | 4 |
| Brown DG, Skylis TP, Sulisz CA, Friedman C, Richter DK. Sterile water, and saline solution: potential reservoirs of nosocomial infection. Am J Infect Control 1985;13:35–9 | 2 |
| Bruce ML, Sones SS, Peck B. Medication safety. Implications for EMS. Emerg Med Serv 2003;32:97–100 | 4 |
| Bruyninckx R, Van Den Bruel A, Aertgeerts B, Van Casteren V, Buntinx F. Half of the patients with chest pain that are urgently referred are transported in unsafe conditions. Eur J Emerg Med 2008;15:330–3 | 2 |
| Bruzzone LE, Lazzarotto MP, Molfino RM, Zoppi M, International Association of Science and Technology for Development. Parallel robot for ambulance stretcher active suspension: mechanical modelling and simulation. In Hamza MH, editor. Modelling, Identification and Control; Proceedings of the IASTED Conference. Innsbruck, Austria: ACTA; 2002 | 1 |
| Burke K. Tackling health and safety difficulties within the NHS. Personnel Today 2003:11 | 3 |
| Burn J, Lockhart G. All Change Please: Putting the Best New Healthcare Ideas into Practice. London: Policy Exchange; 2008 | 1 |
| Cabridain M-O. Managerial procedures and hospital practices: a case study of the development of a new medical discipline. Soc Sci Med 1985;20:167–72 | 4 |
| Caldicott D. Tactical emergency medical support in Australia. Prehosp Disaster Med 2002;17(Suppl. 2):S19 | 7 |
| Callaham ML. Prophylaxis with zidovudine (AZT) after exposure to human immunodeficiency virus: a brief discussion of the issues for emergency physicians. Ann Emerg Med 1991;20:1351–4 | 3 |
| Callaham ML. Journal performance report for 2010. Ann Emerg Med 2011;58:223–4 | 1 |
| Cameron P, Gabbe B, Finch C, McNeil J, Smith K, Wolfe R. Prehospital predictors of major injury. Prehosp Disaster Med 2002;17(Suppl. 2):S8–9 | 1 |
| Cappato R, Curnis A, Marzollo P, Mascioli G, Bordonali T, Beretti S, et al. Prospective assessment of integrating the existing emergency medical system with automated external defibrillators fully operated by volunteers and laypersons for out-of-hospital cardiac arrest: the Brescia Early Defibrillation Study (BEDS). Eur Heart J 2006;27:553–61 | 3 |
| Car J, Lang B, Colledge A, Ung C, Majeed A. Interventions for enhancing consumers’ online health literacy. Cochrane Database Syst Rev 2011;6:CD007092 | 1 |
| Castillo EM. Collaborative to decrease ambulance diversion: the California Emergency department diversion project. J Emerg Med 2011;40:300–7 | 7 |
| Catlett CL. Where’s that disaster manual?! The training of clinicians on hospital disaster plans. Prehosp Disaster Med 2002;17(Suppl. 2):S27 | 4 |
| Cayten CG, Quervalu I, Agarwal N. Fatality analysis reporting system demonstrates association between trauma system initiatives and decreasing death rates. J Trauma 1999;46:751–6 | 7 |
| Challen K. Early warnings? Please include the ED in your ViEWS. Resuscitation 2011;82:631 | 2 |
| National Patient Safety Agency. Clarification of NPSA Safer Practice Notice on Use of NHS Number as National Identifier for all Patients. National Electronic Library for Medicines. London: NICE; 2009 | 2 |
| Chang KS. Design of disaster decision making system using petri-net. Prehosp Disaster Med 2002;17(Suppl. 2):S68 | 7 |
| Chartrand H, Dick T. You can’t care too much . . . ride along. September issue. EMS Mag 2009;38:12–14 | 4 |
| Cheeseman M, Scott A, Weber K. NHS Direct Referred Enquiries: Is There a Training Need for UKMi? Edinburgh: Proceedings of the 35th UKMi Practice Development Seminar; 2009. 50 (Poster 19). National Electronic Library for Medicines. London: NICE; 2009 | 4 |
| Chen R-J. Early traumal care needs and controversies. Chang Gung Med J 1996;20:163 | 2 |
| Chen MJ. Delayed diagnosis of appendicitis in the elderly. Prehosp Disaster Med 2002;17(Suppl. 2):S72 | 2 |
| Chen WL. Characteristics, problems, and suggestions for evacuation of mass wounded and sick. Prehosp Disaster Med 2002;17(Suppl. 2):S72 | 4 |
| Cheney PR, Fullerton-Gleason L, Gossett L, Weiss SJ, Ernst AA, Sklar DP. Evaluation of restraint use in Emergency Medical Services (EMS) and the correlation with assaults on EMS personnel. Ann Emerg Med 2005;46(Suppl. 3):32 | 3 |
| Cheremisinoff NP, Bendavid-Val A. Green Profits: The Manager's Handbook for ISO 14001 and Pollution Prevention. Burlington: Butterworth-Heinemann, 2001 | 1 |
| Cherry RA, Bradburn E, Nichols PA, Snavely TM, Boehmer SJ, Mauger DT. Outcome assessment of blunt trauma patients who are undertriaged. Surgery 2010;148:239–45 | 2 |
| Chevallet D, Gerbet JY, Roy H, Gouret E. Using self-made software for managing a forward medical post. Prehosp Disaster Med 2002;17(Suppl. 2):S37–8 | 2 |
| Chiarugi F, Trypakis D, Kontogiannis V, Lees PJ, Chronaki CE, Zeaki M, et al. Continuous ECG monitoring in the management of pre-hospital health emergencies. Comput Cardiol 2003;30:205−8 | 9 |
| Chivers S, Gifford P. Manual handling in the health services. Physiotherapy 1999;85:103 | 4 |
| Chotani RA, Spangler JMM. Health indicators for conflict prevention. Prehosp Disaster Med 2002;17(Suppl. 2):S35 | 1 |
| Chung W, Magid D, Maciosek M, Brumbaugh J, Colwell C, Bass R, et al. Emergencies passing by: a national study of ambulance diversion trends. Ann Emerg Med 2002;40(Suppl.):93 | 1 |
| Churchill N, editor. Health Innovations: More for Less in Healthcare. London: The Smith Institute; 2010 | 7 |
| Cimolino U, Holz C. Innovation in the Dusseldorf ambulance service – new ambulances [German]. Notarzt 2001;17:128–31 | 4 |
| Clancy CM. Care transitions: a threat and an opportunity for patient safety. Am J Med Qual 2006;21:415–17 | 2 |
| Clancy CM. Improving the safety and quality of care transitions. Aorn J 2008;88:111–13 | 1 |
| Clark D. Disciple of safety: keepin’ it clean. FireRescue Magazine 2001;19:17 | 4 |
| Clark S, Faunt J, Pradhan M, Adams R, Hill A. Workflow assessment. In Coiera E, Simpson C, editors. HIC 2003 RACGP12CC Handbook of Abstracts: Combined Conferences of the Eleventh National Health Informatics Conference, Health Informatics: Applying Socio-Technical Practices and Principles and Twelfth National RACGP Computer Conference, General Practice: Beyond the Box: Making IT Work for GP’s and Patients. Darlington Harbour, Sydney: Health Informatics Society of Australia (HISA) and Australian College of General Practitioners (RACGP); 2003:79 | 2 |
| Clark P. An Emergency Department Patient's Perception of Safety. PhD thesis. San Antonio, TX: University of Texas Health Science Center; 2010 | 1 |
| Clark JR. Delay in treatment. Air Med J 2011;30:117–19 | 4 |
| Clark JR. Mother’s little helper: the problem of narcotic diversion. Air Med J 2011;30:294–6 | 1 |
| Clemmer TP, Thomas F. Transport of the critically ill. Crit Care Med 2000;28:265–6 | 4 |
| Clough C. Developing Health and Health Care: A Strategy for Shropshire, Telford and Wrekin. Report of a meeting of the National Clinical Advisory Team held at Shrewsbury and Telford Hospital 13 January 2009 | 4 |
| Coeytaux RR, Williams JW, Chung E, Gharacholou SM. ECG-Based Signal Analysis Technologies. Rockville, MD: Agency for Health Research and Quality; 2011 | 2 |
| Coghlan A. A life and death dilemma. New Sci 2006;192:8–9. | 7 |
| Cohen MR. Medication errors – masking the truth? Nursing 2002;32:30 | 2 |
| Cohen MR. Medication errors. Nursing 2008;38:12 | 2 |
| Coleman P, O’Keeffe C, Mason S. Emergency care practitioners: shaping a new type of practitioner from existing NHS clinical roles. Emerg Med J 2009;26:3 | 1 |
| Cone DC. Knowledge translation in the emergency medical services: a research agenda for advancing prehospital care. Acad Emerg Med 2007;14:1052–7 | 4 |
| Connell LJ. Aviation incident reporting: your contribution to EMS safety. Air Med J 1998;4:14–16 | 1 |
| Counselman FL, Flomenbaum NE. Malpractice counsel. Emerg Med 2010;42:22 | 2 |
| Cox DM. Commentary on medication mishaps: avoiding inappropriate use of prehospital meds. Emerg Med Serv 1993;3:12–22, 25–26 [original article Holliman CJ, Wuerz RC, Meador SA. Medical command errors in an urban advanced life support system. Ann Emerg Med 1992;21:347–50] | 5 |
| Craven R. Have ambulance, will travel. Emerg Med Serv 1992;21:47–8 | 4 |
| Crawford I, Mackway-Jones K, Russell D. Specification and selection of Chemical Personal Protective Equipment (CPPE) for Health Service First Responders – the United Kingdom approach. Prehosp Disaster Med 2002;17:S58 | 3 |
| Criss EA. Research review: what current studies mean to EMS. JEMS 2008;33:40 | 1 and 4 |
| Cronin KA. Acute stroke: a descriptive study of mode of arrival, pre-hospital diagnosis, duration of symptoms, and treatment. Ann Emerg Med 2006;48:42 | 2 |
| Independent Reconfiguration Panel. Advice on NHS Service Change in East Kent: Independent Reconfiguration Panel. London: NICE; 2003 | 7 |
| Crossman M. Technical and environmental impact on medication error in paramedic practice: a review of causes, consequences and strategies for prevention. Australas J Paramedicine 2009;7 | 4 |
| Curry N, Ham C. Clinical and Service Integration: The Route to Improved Outcomes. London: The King’s Fund; 2010 | 7 |
| Curry P. Electronic Data Exchange Between Ambulance Services and Provider Units. London: Exchanging Healthcare Information Conference. 1996:93–5 | 9 |
| Curtis LT. Prevention of hospital-acquired infections: review of non-pharmacological interventions. J Hosp Infect 2008;69:204–19 | 2 |
| Cutchis PN, Smith DG, Wenstrand DS, Wiesmann WP. Evolution of a new series of self-contained micromechanical ventilators for prehospital use [4615–29]. In Vo-Dinh T, Grundfest WS, Benaron DA, editors. Biomedical Diagnostic, Guidance and Surgical-Assist Systems. San Jose, CA: SPIE; 2002 | 1 |
| Davidson SJ. Errors in emergency medicine: not quite random ruminations of a curmudgeon. Acad Emerg Med 2000;7:1334 | 4 |
| Evaluating Telecare and Telehealth Interventions: WSDAN Briefing Paper. London: The King’s Fund; 2011 | 7 |
| Davis JE, Churosh N, Borloz M, Howell J. Knowledge of self-injectable epinephrine technique among emergency medical services providers. Ann Emerg Med 2009;54(Suppl.):S36 | 7 |
| De Lorenzo RA. A review of spinal immobilization techniques. J Emerg Med 1996;14:603–13 | 4 |
| Dees L. Perceived Effects of Sleepiness and Sleep Deprivation Among Firefighters and Emergency Medical Services Providers Working a 24/48 Shift Schedule. PhD Thesis. Denton, TX: Texas Woman's University; 2009 | 3 |
| Degnan BA, Murray LJ, Dunling CP, Whittlestone KD, Standley TD, Gupta AK, et al. The effect of additional teaching on medical students’ drug administration skills in a simulated emergency scenario. Anaesthesia 2006;61:1155–60 | 3 |
| Dellborg M. Percutaneous coronary intervention or thrombolytics in ST-elevation infarction. What is the emperor really wearing? Scand Cardiovasc J 2002;36:197–200 | 4 |
| Demmons LL. Chasing ambulance safety. Air Med J 2005;24:112–16 | 1 |
| Dernocoeur K. Soap for safety. Emerg Med Serv 2000;29:28 | 4 |
| Dick T. EMS reruns. Fox in the henhouse: when the accused is a caregiver. Emerg Med Serv 2005;34:40 | 1 |
| Dick T. Tricks of the trade. Three good rules AKA think before you transfer. JEMS 2011;36:30 | 1 |
| Dixon A, Robertson R, Appleby J, Burge P, Devlin N, Magee H. Patient Choice: How Patients Choose and How Providers Respond. London: The King’s Fund; 2010 | 7 |
| Dobbie AE, Cooke MW. A descriptive review and discussion of litigation claims against ambulance services. Emerg Med J 2008;25:455–8 | 4 |
| Dodd RS. Readers write. J Air Med Transp 1991;10:7–8 | 1 |
| Doyle TJ, Vissers RJ. An EMS approach to psychiatric emergencies. Emerg Med Serv 1999;28:87, 90–3 | 4 |
| Drew BJ, Dempsey ED, Joo TH, Sommargren CE, Glancey JP, Benedict K, et al. Pre-hospital synthesized 12-lead ECG ischemia monitoring with trans-telephonic transmission in acute coronary syndromes: pilot study results of the ST SMART trial. J Electrocardiol 2004;37:S214–21 | 6 |
| Drummond KW, Baumann MR, Strout TD. Identifying predictors for accurate diagnosis of acute shortness of breath in prehospital patients treated with albuterol and furosemide. Ann Emerg Med 2005;46(Suppl.):61 | 7 |
| Duckett S. Second wave reform in Alberta. Healthc Manage Forum 2010;23:156–8 | 1 |
| Dunbar CN. Are there holes in the HC safety net? Nurs Spectr NY NJ Ed 2005;17:NJ/NY4–5 | 2 |
| Dykes L, McDowell D, Griffiths E, Taylor R. Angels with wings (and morphine): do RAF winchmen need to be paramedics? Emerg Med J 2009;26:4 | 2 |
| Dyson E, Smith GB. Common faults in resuscitation equipment – guidelines for checking equipment and drugs used in adult cardiopulmonary resuscitation. Resuscitation 2002;55:137–49 | 7 |
| Easter JS. Higher severity of illness in pediatric patients presenting at night and by ambulance. Ann Emerg Med 2008;52(Suppl.):S165 | 1 |
| Eburn M, Bendall JC. The provision of ambulance services in Australia: a legal argument for the national registration of paramedics. J Emerg Prim Health Care 2010;8 | 4 |
| Edwardson O. Major incident command and control: ‘communications: the key to an effective response’. Prehosp Disaster Med 2002;17(Suppl. 2):S37 | 4 |
| Eis D, Geisel U, Sonntag HG. Experiences with an Ambulance for Environmental Medicine at the University of Heidelberg/Germany. Home Care: Umwelt und Gesundheit. Dusseldorf: Gustav Fischer; 1994 | 1 |
| Engum SA, Mitchell MK, Scherer LR, Gomez G, Jacobson L, Solotkin K, et al. Prehospital triage in the injured patient. J Pediatr Surg 2000;35:82–7. | 2 |
| Erich J. Ambulance safety: what’s new, what’s needed. Emerg Med Serv 2002;31:51–4,56,58 passim | 4 |
| Erich J. An instant to decide, a lifetime to regret: the aftermath of ambulance accidents. Emerg Med Serv 2005;34:27, 37–8 | 1 |
| Erich J. Rules of the road. The must-haves of an effective vehicle-safety program. Emerg Med Serv 2007;36:69–73, 75–8 | 4 |
| Erich J. Acceleration forces. What EMS needs to know about balance vs. driving forces in the back. EMS World 2010;39:S14–15 | 5 |
| Estner H, Gunzel C, Wilhelm K, William F, Land eV D. Current benefit from AEDs. Prehosp Disaster Med 2002;17(Suppl. 2):S50–1 | 7 |
| Evans C, Howes D, Pickett W, Dagnone L. Audit filters for improving processes of care and clinical outcomes in trauma systems. Cochrane Database Syst Rev 2009;4:CD007590 | 4 |
| Facey M. ‘Maintaining talk’ among taxi drivers: accomplishing health-protective behaviour in precarious workplaces. Health Place 2010;16:1259–67 | 1 |
| Anonymous. ‘Adverse event’ reporting systems yield benefits: result: system changes that may prevent patient injuries. EMS Insider 2007;34:1–2 | 4 |
| Fallat ME, Overton JW Jr, Emergency Services-Prehospital S, Executive Committee of the American College of Surgeons Committee on T. Air medical transport safety. Bull Am Coll Surg 2007;92:19–23 | 1 |
| Fang J. The Chinese health care regulatory institutions in an era of transition. Soc Sci Med 2008;66:952–62 | 7 |
| Federal Communications Commission. Public safety bureau launched by FCC. Emerg Med Serv 2006;35:28 | 1 |
| Feiner B. Heart sounds: prehospital cardiac care faces unique challenges. Emerg Med Serv 1995;24:16 | 4 |
| Fernandes RM, Bialy LM, Vandermeer B, Tjosvold L, Plint AC, Patel H, et al. Glucocorticoids for acute viral bronchiolitis in infants and young children. Cochrane Database Syst Rev 2013;6:CD004878 | 2 |
| Fertel N, Lederman B. Applying hospital deployment for emergencies in real events. Prehosp Disaster Med 2002;17(Suppl. 2):S74–5 | 4 |
| Firanescu C, Wilbers R, Meeder JG. Safety and feasibility of prehospital thrombolysis in combination with active rescue PCI strategy for acute ST-elevation myocardial infarction. Neth Heart J 2005;13:300–4 | 4 |
| Fitch J. System strategies. Failure is not an option, but success is. EMS Insider 2011;38:4–5 | 4 |
| Fitzgerald M. Successfully reducing medical errors in the ED. Injury 2010;41(Suppl. 1):S37 | 2 |
| Fitzpatrick RW, Pate RG. A Taste of Each Other’s Medicine: National Electronic Library for Medicines. Health Service Journal Resource Centre article. London: NICE; 2008 | 2 |
| Fitzpatrick MA. Improving triage of patients with chest pain. Med J Aust 2003;178:364–5 | 2 |
| (CMACE) CfMaCE. Maternal Obesity in the UK: Findings from a National Project. London: Centre for Maternal and Child Enquiries; 2010 | 1 |
| Fjaer RB. Intervention in measles epidemics. Prehosp Disaster Med 2002;17(Suppl. 2):S5 | 1 |
| Flodgren G, Parmelli E, Doumit G, Gattellari M, O'Brien MA, Grimshaw J, et al. Local opinion leaders: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2011;8:CD000125 | 7 |
| Flomenbaum NE. The challenges of consultations. Emerg Med 2007;39:8 | 2 |
| Flory D. The Quarter: Quarter 1, 2009/10. London: Department of Health; 2009 | 7 |
| Flynn G. Community consultation for emergency exception to informed consent: how much is enough? Ann Emerg Med 2008;51:416–19 | 1 |
| Fonne V, Myhre G. Crew Concepts in the Air Ambulance Service of Norway. Hayward BJ, Lowe AR, editors. Australian Aviation Psychology Symposium. Aldershot: Aviation resource management; 2000 | 4 |
| Foot C, Raleigh V, Ross S, Lyscom T. How do Quality Accounts Measure Up? Findings from the First Year. London: The King’s Fund; 2011 | 7 |
| Foot R, Semple Y, Mulholland P. Medicines Utilisation Data: A Vital Commodity in Today’s NHS. National Electronic Library for Medicines. London: NICE; 2009 | 7 |
| Forry S. Mechanism of injury. Making a vital assessment tool work. JEMS 1992;17:73–6 | 4 |
| Foresman-Capuzzi J. Reply. J Emerg Nurs 2011;37:312–13 | 4 |
| Forsström J. Why certification of medical software would be useful? Int J Med Inf 1997;47:143–51 | 7 |
| Fortin W. Need a TIP? . . . November Publisher’s Page, ‘Repairing the safety nets’. JEMS 1996;21:12–13 | 4 |
| Fourie P. Respiratory sinus arrhythmia feedback for enhanced parasympathetic responses in clients diagnosed with post-traumatic stress disorder and anxiety: a case study. Prehosp Disaster Med 2002;17(Suppl. 2):S75–6 | 1 |
| Frakes MA. Rapid sequence induction medications: an update. J Emerg Nurs 2003;29:533–40 | 2 |
| Frakes MA, High K, Stocking J. Transport nurse safety practices, perceptions, and experiences: the air and surface transport nurses association survey. Air Med J 2009;28:250–5 | 1 |
| Frazer RS. Air medical accidents involving collision with objects. Air Med J 2001;20:13–16 | 1 |
| Frazer E. Ensuring quality patient care and safety for patients requiring air transport. Lippincott’s case management: managing the process of patient care. Lippincotts Case Manag 2006;11:187–9 | 4 |
| Frazer E. A change in culture is required. Air Med J 2008;27:202–3 | 1 |
| French A, Nedza A. Better health care: organizations focus on decreasing EMS clinical errors. EMS Insider 2001;28:6 | 4 |
| Friendship J. Editorial. Aust Emerg Nurs J 2004;7:3–5 | 1 |
| Fromm Jr RE, Varon J. Critical care transport. Crit Care Clin 2000;16:695–705 | 4 |
| NHS Confederation patient safety fact sheets. National Electronic Library for Medicines. London: NICE; 2009 | 4 |
| Furness D, Gough B. From Feast to Famine: Reforming the NHS for an Age of Austerity. London: Social Market Foundation; 2009 | 4 |
| Gabbott D, Smith G, Mitchell S, Colquhoun M, Nolan J, Soar J. Cardiopulmonary resuscitation standards for clinical practice and training in the UK. Accid Emerg Nurs 2005;13:171–9 | 9 |
| Gadon L, Johnstone L, Cooke D. Situational variables and institutional violence: a systematic review of the literature. Clin Psychol Rev 2006;26:515–34 | 2 |
| Gaiser RR. Teaching airway management skills: how and what to learn and teach. Crit Care Clin 2000;16:515–25 | 1 |
| Gaitini LA, Yanovsky B, Somri M, Tome R, Mora PC, Frass M. Prospective randomized comparison of the EasyTube and the esophageal-tracheal Combitube airway devices during general anesthesia with mechanical ventilation. J Clin Anesth 2011;23:475–81 | 2 |
| Gale R. Environmental costs at a Canadian paper mill: a case study of Environmental Management Accounting (EMA). J Clean Prod 2006;14:1237–51 | 1 |
| Gallagher CJ, Akerman RR, Castillo D, Matadial CM, Shekhter I. On the road with the simulator. In Kyle RR Jr, Bosseau Murray W. Clinical Simulation. Oxford: Academic Press; 2008 | 4 |
| Gandy G. Immobilization errors in EMS. Emerg Med Serv 2004;33:93–7 | 4 |
| Gandy WE. What must a claimant prove? EMS World 2011;40:44 | 3 |
| Garcia A. Critical care issues in the early management of severe trauma. Surg Clin North Am 2006;86:1359–87 | 2 |
| Garcia T. Addressing airway issues: how to keep ETI a prehospital skill. JEMS 2011;36:82–3, 85, 87 | 4 |
| Garpenby P. Resource dependency, doctors and the state: quality control in Sweden. Soc Sci Med 1999;49:405–24 | 1 |
| Garrett BM, MacPhee M, Jackson C. Implementing high-fidelity simulation in Canada: reflections on 3 years of practice. Nurse Educ Today 2011;31:671–76 | 7 |
| Gausche M, Seidel JS. Out-of-hospital care of pediatric patients. Pediatr Clin North Am 1999;46:1305–27 | 4 |
| Gausche-Hill M, Lewis RJ, Henderson DP, Haynes BE. Design and implementation of a controlled trial of pediatric endotracheal intubation in the out-of-hospital setting. Ann Emerg Med 2000;36:356–65 | 6 |
| Gausche-Hill M. Integrating children into our emergency care system: achieving the vision. Ann Emerg Med 2006;48:131–4 | 7 |
| Gebbie KM, Merrill J. Identification of emergency preparedness competencies for the healthcare workforce. Prehosp Disaster Med 2002;17(Supp. 2):S65 | 7 |
| Geelen-Baass C, Geelen-Baass B. Abstract. To prescribe or to administer? That is the question. J Emerg Prim Health Care 2007;5:2p | 1 |
| Geidl L, Deckert Z, Zrunek P, Gottardi R, Sterz F, Wieselthaler G, et al. Intuitive use and usability of ventricular assist device peripheral components in simulated emergency conditions. Artif Organs 2011;35:773–80 | 1 |
| Georges J-L, Livarek B, Gibault-Genty G, Aziza JP, Hautecoeur JL, Soleille H. Reduction of radiation delivered to patients undergoing invasive coronary procedures. Effect of a programme for dose reduction based on radiation-protection training. Arch Cardiovasc Dis 2009;102:821–7 | 1 |
| Georges JL, Gibault-Genty G, Charbonnel C, Aziza J-P, Fetoui A, Pessenti-Rossi D, et al. Radiation protection and arterial route in interventional cardiology. Ann Cardiol Angeiol 2009;58:366–72 | 1 |
| Gershon RRM, Qureshi KA, Morse SS, Berrera MA, Cruz CBD. Bioterrorism-related beliefs, attitudes, and behaviors of community-based clinicians. Prehosp Disaster Med 2002;17(Suppl. 2):S48 | 7 |
| Gershon RRM, Vlahov D, Hogan EA, Cruz CBD. Ethical and logistical challenges of conducting research involving world trade center survivors. Prehosp Disaster Med 2002;17:S28 | 1 |
| Geyer N. Ethics and law. Nurs Update 2000;24:15 | 4 |
| Gibson SC, Ham JJ, Apker J, Mallak LA, Johnson NA. Communication, communication, communication: the art of the handoff. Ann Emerg Med 2010;55:181–3 | 2 |
| Gilboy N, Flanagan T. You be the jury: was the standard of care met? J Emerg Nurs 2007;33:579–81 | 2 |
| Gillespie J. Creative procurement for your simulation program. In Kyle RR Jr, Bosseau Murray W. Clinical Simulation. Oxford: Academic Press; 2008 | 1 |
| Gillies MA, Pratt R, Whiteley C, Borg J, Beale RJ, Tibby SM. Therapeutic hypothermia after cardiac arrest: a retrospective comparison of surface and endovascular cooling techniques. Resuscitation 2010;81:1117–22 | 2 |
| Giordano R. Leadership Needs of Medical Directors and Clinical Directors. London: The King’s Fund; 2010 | 7 |
| Glarum J, Birou D, Cetaruk E. Command and Control. Hospital Emergency Response Teams. Boston, MA: Butterworth-Heinemann; 2010:1–17 | 2 |
| Goldhaber SZ. Thrombolysis for pulmonary embolism. Prog Cardiovasc Dis 1991;34:113–34 | 4 |
| Goldmann K, Z. Ferson D. Education and training in airway management. Best Pract Res Clin Anaesthesiol 2005;19:717–32 | 2 |
| González Gómez JM, Chaves Vinagre J, Ocete Hita E, Calvo Macías C. Nuevas metodologías en el entrenamiento de emergencias pediátricas: simulación médica aplicada a pediatría. An Pediatr (Barc) 2008;68:612–20 | 7 |
| Gorvin D. Tennessee EMS task force. Hosp Aviat 1988;7:41–2 | 4 |
| Gould Dinah J, Moralejo D, Drey N, Chudleigh Jane H. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Rev 2010;9:CD005186 | 2 |
| Govindaraju V,Milewski R. Automated Reading and Mining of Pre-Hospital Care Reports. Computer-based Medical Systems. Bethesda, MD: IEEE Computer Society; 2001 | 4 |
| Greb I, Wranze E, Hartmann H, Wulf H, Kill C. Analgesia for extremity trauma by rescue paramedics. Data on safety and effectiveness of prehospital administration of morphine [German]. Notfall Rettungsmed 2011;14:135–42 | 7 |
| Grevstad U, Gregersen P, Rasmussen LS. Intravenous access in the emergency patient. Curr Anaesth Crit Care 2009;20:120–7 | 2 |
| Gropper MA, Matthay MA. Look before you leap: how do intensivists improve care for critically ill patients? Am J Med 2004;116:206–7 | 2 |
| Gryniuk J. The role of the flight paramedic in air medical safety and crew resource management. Air Med J 2003;22:12–14 | 1 |
| Gupta KJ, Nolan JP. Emergency general anaesthesia for hypovolaemic trauma patients. Curr Anaesth Crit Care 1998;9:66–73 | 2 |
| Gurm HS. [Commentary on] Neighborhood income, health insurance, and prehospital delay for myocardial infarction: the Atherosclerosis Risk in Communities study. ACC Cardiosource Rev J 2008;17:27–8 | 7 |
| Guyette FX. Rapid sequence intubation and rapid sequence airway [book review]. Ann Emerg Med 2010;55:232 | 4 |
| Gwinn R. Up-front about errors: EMS system introduces proactive error reporting system. JEMS 2003;28:84–9 | 4 |
| Habler OP, Messmer KFW. 4 artificial oxygen carriers. Best Pract Res Clin Anaesthesiol 1997;11:289–300 | 4 |
| Hafter JL. Expert advice: insights & innovations from top industry professionals. EMS patient-safety recommendations. EMS Insider 2002;29:6 | 4 |
| Hagberg JM. Exercise assessment of arthritic and elderly individuals. Best Pract Res Clin Rheumatol 1994;8:29–52 | 1 |
| Hague E. Question time. Physiother Frontline 2010;16:4–5 | 4 |
| Hains IM, Marks A, Georgiou A. Non-emergency patient transport: what are the quality and safety issues? A systematic review. Int J Qual Health Care 2011;23:68–75 | 1 |
| Hajjar JH, Budd HA, Wachtel Z, Howhannesian A. Ambulatory radical retropubic prostatectomy. Urology 1998;51:443–8 | 1 |
| Hall M. Acute kidney injury. Found Years 2008;4:183–7 | 4 |
| Hall AP, Davies MJ. Diabetic emergencies in acute/critical care. Found Years 2008;4:230–3 | 4 |
| Hallstrom A, Rea TD, Sayre MR, Christenson J, Cobb L, Mosesso VN Jr, et al. The AutoPulse Assisted Prehospital International Resuscitation (ASPIRE) trial investigators respond to inhomogeneity and temporal effects assertions. Am J Emerg Med 2010;28:973–6 | 4 |
| Hankins D. Culture of safety. Air Med J 2011;30:241–2 | 4 |
| Harding M-L. Stretcher cases. Health Serv J 2002;114:32–3 | 4 |
| Hart PD. Complying with the bloodborne pathogen standard: protecting health care workers and patients. AORN 2011;94:393–9 | 4 |
| Heavrin BS, Barrett TW, Schriger DL. The national report card on the state of emergency medicine: answers to the January 2009 Journal club questions. Ann Emerg Med 2009;53:828–34 | 4 |
| Hedlund J, Arnold R, Cerrelli E, Partyka S, Hoxie P, Skinner D. An assessment of the 1982 traffic fatality decrease. Accid Anal Prev 1984;16:247–61 | 1 |
| Heidrich O, Harvey J, Tollin N. Stakeholder analysis for industrial waste management systems. Waste Manag 2009;29:965–73 | 2 |
| Heightman AJ. From the editor. Not all scars are ugly. JEMS 2004;29:12 | 4 |
| Heightman AJ. Last word. Kids cruise safely. JEMS 2005;30:122 | 1 |
| Hemmerling TM. Automated anesthesia. Adv Anesth 2007;25:17–39 | 1 |
| Henderson E. EMT-paramedics in the emergency department setting: a perspective on the value of the EMT-paramedic to patient care outcomes in the emergency department. J Emerg Nurs 2009;35:501–3 | 4 |
| Herm SM, Scott KA, Copley DM. ‘Sim’ sational revelations. Clin Sim Nurs 2007;3:e25–30 | 3 |
| Hertelendy AJ. Prehospital care in rural settings. Prehosp Disaster Med 2002;17:S77 | 4 |
| Hertzum M. Breakdowns in collaborative information seeking: a study of the medication process. Inf Process Manag 2010;46:646–55 | 2 |
| Higgins SL, Herre JM, Epstein AE, Greer GS, Friedman PL, Gleva ML. A comparison of biphasic and monophasic shocks for external defibrillation. Prehosp Emerg Care 2000;4:305–13. [Erratum published in Prehosp Emerg Care 2001;5:78] | 2 |
| Higgins J, Wilson S, Bridge P, Cooke MW. Communication difficulties during 999 ambulance calls: observational study. BMJ 2001;323:781–2 | 1 |
| Hignett S, Griffiths P. Risk factors for moving and handling bariatric patients. Nurs Stand 2009;24:40–8 | 3 |
| Hignett S, Crumpton E, Coleman R. Designing emergency ambulances for the 21st century. Emerg Med J 2009;26:135–40 | 1 |
| National Collaborating Centre for Acute Care. Venous Thromboembolism. London: Royal College of Surgeons; 2008 | 2 |
| Hill JW, Powell P. The national healthcare crisis: is eHealth a key solution? Bus Horizons 2009;52:265–77 | 7 |
| Hilson G, Nayee V. Environmental management system implementation in the mining industry: a key to achieving cleaner production. Int J Miner Process 2002;64:19–41 | 1 |
| Hilson G. Defining ‘cleaner production’ and ‘pollution prevention’ in the mining context. Miner Eng 2003;16:305–21 | 1 |
| Hirabayashi Y, Seo N. Tracheal intubation by non-anesthesia residents using the Pentax-AWS airway scope and Macintosh laryngoscope. J Clin Anesth 2009;21:268–71 | 2 |
| Hobgood CD, John O, Swart G. Emergency medicine resident errors: identification and educational utilization. Acad Emerg Med 2000;7:1317–20 | 3 |
| Hobgood C, Xie J, Weiner B, Hooker J. Error identification, disclosure, and reporting: practice patterns of three emergency medicine provider types. Acad Emerg Med 2004;11:196–9 | 2 |
| Hobgood C, Anantharaman V, Bandiera G, Cameron P, Halpern P, Holliman CJ. International Federation for Emergency Medicine model curriculum for emergency medicine specialists. Afr J Emerg Med 2011;1:85–95 | 3 |
| Hockberger RS, Binder LS, Chisholm CD, Cushman JT, Hayden SR, Sklar DP. The model of the clinical practice of emergency medicine: a 2-year update. Ann Emerg Med 2005;45:659–74 | 2 |
| Hoffman JR, Schriger DL, Votey SR, Luo JS. The empiric use of hypertonic dextrose in patients with altered mental status: a reappraisal. Ann Emerg Med 1992;21:20–4 | 1 |
| Hogan MP, Boone DC. Trauma education and assessment. Injury 2008;39:681–5 | 4 |
| Hohenstein C, Fleischmann T. Patient safety in a high risk area – a Critical Incident Reporting System (CIRS) in the field of prehospital emergency medicine. Notarzt 2007;23:1–6 | 4 |
| Holden RJ, Karsh B-T. The technology acceptance model: its past and its future in health care. J Biomed Inform 2010;43:159–72 | 7 |
| Holleran R. Remembering Michelle North. Air Med J 2005;24:22–4 | 1 |
| Holliman CJ, Field JM, Meador SA, Wuerz RC. Medication mishaps: avoiding inappropriate use of prehospital meds. Emerg Med Serv 1992;21:21–2, 25–6 | 4 |
| Hon C-Y, Gamage B, Bryce EA, LoChang J, Yassi A, Maultsaid D, et al. Personal protective equipment in health care: can online infection control courses transfer knowledge and improve proper selection and use? Am J Infect Control 2008;36:e33–7 | 2 |
| Hood DD, Kneale TD, Hanson ME, Alexander SB. Global applications of the LSTATTM patient care platform. Prehosp Disaster Med 2002;17:S55 | 2 |
| Hopmeier MJ, Carmona R, Noji E. Mundane to critical: the need for transition from individual care to population health maintenance and support. Prehosp Disaster Med 2002;17:S28 | 1 |
| Horton JN, Harmer M. The selection of trainees. Best Pract Res Clin Anaesthesiol 1994;8:575–89 | 3 |
| Hoskins JD, Graham RF, Robinson DR, Lutz CC, Folio LR. Mass casualty tracking with air traffic control methodologies. J Am Coll Surg 2009;208:1001–8 | 1 |
| Houghland JE, Druck J. Effective clinical teaching by residents in emergency medicine. Ann Emerg Med 2010;55:434–9 | 2 |
| Hoyle L. Condition yellow: a hospital-wide approach to ED overcrowding. J Emerg Nurs 2013;39:40–5 | 4 |
| Hu P, Defouw G, Mackenzie C, Handley C, Seebode S, Davies P, et al. What is happening to the patient during pre-hospital trauma care? AMIA Annu Symp Proc 2006:955 | 6 |
| Huda Q, Malik SMMR. High risk areas for public health emergencies: a risk assessment model for conducting vulnerability analysis of hazard prone areas in Bangladesh. Prehosp Disaster Med 2002;17(Suppl. 2):S12–13 | 1 |
| Hüter L, Schwarzkopf K, Rödiger J, Preussler NP, Schreiber T. Students insert the laryngeal tube quicker and more often successful than the esophageal–tracheal combitube in a manikin. Resuscitation 2009;80:930–4 | 3 |
| Hughes JD. Quality products & resources. J Healthc Qual 2002;24:55–6 | 2 |
| Hunt EA, Fiedor-Hamilton M, Eppich WJ. Resuscitation education: narrowing the gap between evidence-based resuscitation guidelines and performance using best educational practices. Pediatr Clin North Am 2008;55:1025–50 | 7 |
| Husband J, Gordon I, Ebdon-Jackson S, Miles K, Cook G, Dubbins P, et al. PET-CT in the UK: British Nuclear Medicine Society. London: Royal College of Radiologists; 2005. | 1 |
| Hutchings A, Durand MA, Grieve R, Harrison D, Rowan K, Green J, et al. Evaluation of the modernisation of adult critical care services in England. BMJ 2009;339:b4353 | 1 |
| Iedema RAM, Jorm C, Braithwaite J, Travaglia J, Lum M. A root cause analysis of clinical error: confronting the disjunction between formal rules and situated clinical activity. Soc Sci Med 2006;63:1201–12 | 2 |
| Iedema RAM, Jorm C, Long D, Braithwaite J, Travaglia J, Westbrook M. Turning the medical gaze in upon itself: root cause analysis and the investigation of clinical error. Soc Sci Med 2006;62:1605–15 | 2 |
| Iremonger C. Guide to Facilitating Clinical Audit Across Different Care Settings. London: Healthcare Quality Improvement Partnership, 2010 | 7 |
| Iserson KV, Lindsey D. Research on critically ill and injured patients: rules, reality, and ethics. J Emerg Med 1995;13:563–7 | 4 |
| Iserson KV. Ethical principles – emergency medicine. Emerg Med Clin N Am 2006;24:513–45 | 4 |
| Itani M, Rosenblatt WH. New airway techniques. Semin Anesth Perioper Med Pain 2003;22:3–10 | 4 |
| Jacob S, Jacoby J, James R, Heller M. Ambulance transport: why ED patients choose as they do. Ann Emerg Med 2006;48(Suppl.):54 | 1 |
| Jacobson S. Avoidable errors in emergency practice. Feeling no pain . . . diagnosis of appendicitis. Emerg Med 2000;32:68, 75 | 4 |
| Jagim M. 1 – La comunicación en el servicio de urgencias. In Lorene N, Ms, Rn, Cen, Laura M. Criddle MRCCCC, editors. Sheehy. Manual de Urgencia de Enfermería (Sexta Edición). Madrid: Elsevier España; 2007. pp. 3–14 | 8 |
| Jakubowski E, Pelaseyed S. Eleventh Futures Forum on the Ethical Governance of Pandemic Influenza Preparedness. WHO Regional Office for Europe. Copenhagen: WHO; 2010 | 1 |
| Jallon R, Imbeau D, de Marcellis-Warin N. A process mapping model for calculating indirect costs of workplace accidents. J Saf Res 2011;42:333–44 | 1 |
| Jarvis NW, Heightman AJ. Who’s to blame? . . . ‘The Trojan Horse of EMS’. JEMS 2001;26:12, 14–15 | 4 |
| Javitt JC, Rebitzer JB, Reisman L. Information technology and medical missteps: evidence from a randomized trial. J Health Econ 2008;27:585–602 | 2 |
| Jensen JL, Croskerry P, Travers AH. Paramedic clinical decision making during high acuity emergency calls: design and methodology of a Delphi study. BMC Emerg 2009;9:17 | 6 |
| Johannigman JA, Branson RD, Edwards MG. Closed loop control of inspired oxygen concentration in trauma patients. J Am Coll Surg 2009;208:763–8 | Retracted |
| Johnson KMS. What is the best transportation for a person without head control? SCI Nurs 1992;9:144 | 4 |
| Jonsson E, Banta HD. Health care technology in Sweden. Health Policy 1994;30:257–94 | 7 |
| Johnson C, Holloway CM. A survey of logic formalisms to support mishap analysis. Reliabil Eng Syst Saf 2003;80:271–91 | 7 |
| Johnson A, Schweitzer D, Ahrens T. Time to throw away your stethoscope?: Capnography: evidence-based patient monitoring technology. J Radiol Nurs 2011;30:25–34 | 2 |
| Jones SE. Prehospital 12-lead ECGs. Ann Emerg Med 1991;20:942–3 | 4 |
| Jones JS, Gengerke J, Kenepp G, Krohmer J. Integration of emergency medical services and special weapons and tactics teams: a decade of experience. Ann Emerg Med 2005;46(Suppl. 3):32 | 1 |
| Jørgensen TH. Towards more sustainable management systems: through life cycle management and integration. J Clean Prod 2008;16:1071–80 | 4 |
| Judge T. AAMS: the price/value equation. Air Med J 2005;24:139–40 | 4 |
| Junglas I, Abraham C, Ives B. Mobile technology at the frontlines of patient care: understanding fit and human drives in utilization decisions and performance. Decis Support Syst 2009;46:634–47 | 7 |
| Kahveci FO, Demircan A, Keles A, Bildik F, Aygencel SG. Efficacy of triage by paramedics: a real-time comparison study. J Emerg Nurs 2012;38:344–9 | 2 |
| Kannampallil TG, Schauer GF, Cohen T, Patel VL. Considering complexity in healthcare systems. J Biomed Inform 2011;44:943–7 | 7 |
| Kantayya VS, Lidvall SJ. Community health centers: disparities in health care in the United States 2010. Dis Mon 2010;56:681–97 | 2 |
| Kaplan K, Mestel P, Feldman DL. Creating a culture of mutual respect. AORN 2010;91:495–510 | 2 |
| Karagiannis G-M, Piatyszek E, Flaus J-M. Industrial emergency planning modeling: a first step toward a robustness analysis tool. J Hazard Mater 2010;181:324–34 | 1 |
| Karapetrovic S, Casadesús M. Implementing environmental with other standardized management systems: scope, sequence, time and integration. J Clean Prod 2009;17:533–40 | 1 |
| Kashuk JL, Halperin P, Caspi G, Colwell C, Moore EE. Bomb explosions in acts of terrorism: evil creativity challenges our trauma systems. J Am Coll Surg 2009;209:134–40 | 4 |
| Kawagoe JY, Graziano KU, Valle Martino MD, Siqueira I, Correa L. Bacterial reduction of alcohol-based liquid and gel products on hands soiled with blood. Am J Infect Control 2011;39:785–7 | 7 |
| Keating RJ, LaRusso NF, Kolars JC. Perceived impact of duty hours limits on the fragmentation of patient care: results from an academic health center. Am J Med 2005;118:788–93 | 4 |
| Keegan L. Reflection on the universal nature of vulnerability. Explore J Sci Healing 2006;2:365–7 | 1 |
| Kelley D. Last word. JEMS 2001;26:98 | 1 |
| Kelly B. Taking community to heart: air medical transport conference. Air Med J 2002;21:20–3 | 1 |
| Keriel-Gascou M, Figon S, Letrilliart L, Chaneliére M, Colin C. Classifications et définitions des événements indésirables associés aux soins primaires: une synthèse de la littérature. Presse Med 2011;40:e499–505 | 7 |
| Kessler C, Chen J, Dill C, Tyndall G, Olszyk MD. State of affairs of emergency medicine in the Veterans Health Administration. Am J Emerg Med 2010;28:947–51 | 2 |
| Khorram Manesh A, Hedelin A, Ortenwall P. Hospital-related incidents: causes and its impact on disaster preparedness and prehospital organisations. Scand J Trauma Resusc Emerg Med 2009;17:26 | 2 |
| Kim JY, Kim CL, Chung CH. Modeling of nuclide release from low-level radioactive paraffin waste: a comparison of simulated and real waste. J Hazard Mater 2002;94:161–78 | 1 |
| Kim HR, Choi G-S, Lee W, Chung KH, Kang MJ, Lee C-W. The research reactor radiation emergency countermeasure system in Korea. Ann Nucl Energy 2010;37:175–9 | 1 |
| King M, Taigman M, Bass B. The top seven EMS problem areas. Emerg Med Serv 2004;33:88 | 4 |
| Kipor GV. Findings of health reporting as criteria of preparedness in emergencies. Prehosp Disaster Med 2002;17(Suppl. 2):S66 | 1 |
| Kirmani JF, Janjua N, Al Kawi A, Ahmed S, Khatri I, Ebrahimi A. Therapeutic advances in interventional neurology. NeuroRX 2005;2:304–23 | 1 |
| Kitchiner R. The role of the personal digital assistant (PDA) in chiropractic practice. Clin Chiropr 2006;9:119–28 | 1 |
| Kivi AL, Hedelin A, Ortenwall P. Regional command and control of the health emergency services in the western part of Sweden. Prehosp Disaster Med 2002;17(Suppl. 2):S36 | 4 |
| Kleinschmidt KC. Elder abuse: a review. Ann Emerg Med 1997;30:463–72 | 2 |
| Knor J. Unconsciousness in Diabetic Patients in Prehospital Emergency Care (PEC). Diabetes a Neuropsychicka Onemocneni; Prednasky 6. Celostatniho Diabetologickeho Sympozia. Brno: Hradec Kralove; 2004 | 4 |
| Koita J, Riggio S, Jagoda A. The mental status examination in emergency practice. Emerg Med Clin N Am 2010;28:439–51 | 2 |
| Kokai Y, Masuda F, Horiike S, Sekine Y. Recent development in open systems for EMS/SCADA. Int J Electr Power Energy Syst 1998;20:111–23 | 1 |
| Koppel A, Kahur K, Habicht T, Saar P, Habicht J, van Ginneken E. Health Systems in Transition. Estonia. Health systems review. European Observatory on Health Systems and Policies. WHO Regional Office for Europe. Copenhagen: WHO; 2010 | 4 |
| Korol IE. The main tasks in offering medical aid to a burned patient in the pre-hospital stage. In Masellis M, Gunn SW, editors. Burns and Fire Disaster: The Management of Burns and Fire Disasters; Perspectives 2000. Boston, MA: Springer; 1995 | 4 |
| Koschel MJ. ‘Rap’ in the streets: a retrospective look at the use of rapacuronium for prehospital rapid sequence induction. Air Med J 2001;20:18–19 | 4 |
| Koskela M. Expert views on environmental impacts and their measurement in the forest industry. J Clean Prod 2011;19:1365–76 | 1 |
| Kourniotis SP, Kiranoudis CT, Markatos NC. A systemic approach to effective chemical emergency management. Safety Science 2001;38:49–61 | 1 |
| Kovacs G, Bullock G, Ackroyd-Stolarz S, Cain E, Petrie DA. A randomized controlled trial on the effect of educational interventions in promoting airway management skill maintenance. Ann Emerg Med 2000;36:301–9 | 3 |
| Anonymous. Prescribing errors. Nurses’ Drug Alert 2002;26:89–90 | 2 |
| Koziol CA, Cuddeford JD, Moos DD. Assessing the force generated with application of cricoid pressure. AORN 2000;72:1018–30 | 7 |
| Krausmann E, Mushtaq F. Learning lessons from tunnel accidents – recommendations in support of the implementation of Article 15 on Reporting of the EU Directive 2004/54/EC. Saf Sci 2010;48:230–7 | 1 |
| Kyle R Jr, Bosseau Murray W. Clinical Simulation. Oxford: Academic Press; 2008. pp. 591–622 | |
| Ramaswami R, Sivarajan KN, Sasaki GH. Optical Networks; A Practical Perspective. 3rd edn. Boston, MA: Morgan Kaufmann; 2010 | 1 |
| Ramaswami R, Sivarajan KN. Optical Networks; A Practical Perspective. 2nd edn. San Francisco, CA: Morgan Kaufmann; 2002 | 1 |
| Kuusniemi KS, Olkkola KT. Opioids in emergency medicine – are we treating pain adequately? Scand J Pain 2011;2:185–6 | 4 |
| Glavin R, Shemanko GA, Hwang JCF, Bencken B, Chow RE, Naik VN. How to fit in while standing out. In Kyle RR Jr, Bosseau Murray W. Clinical Simulation. Oxford: Academic Press; 2008. pp. 69–70 | 4 |
| Kynman G. Thrombolysis: the development of unit guidelines. Intensive Crit Care Nurs 1997;13:30–41 | 7 |
| Labkoff SE, Yasnoff WA. A framework for systematic evaluation of health information infrastructure progress in communities. J Biomedical Inform 2007;40:100–5 | 7 |
| Lagodimos AG, Chountalas PT, Chatzi K. The state of ISO 14001 certification in Greece. J Clean Prod 2007;15:1743–54 | 1 |
| Lamb PJ. Diagnostics studies of growing season rainfall fluctuations in central North America. Pb Reports 1993:283–6 | 1 |
| Lambie L, Mattke S. Selecting Indicators for the Quality of Cardiac Care at the Health Systems Level in OECD Countries. OECD health technical papers no. 14. Paris: OECD; 2004 | 1 |
| Landeweerd JA, Kant I. Working postures and physical load of ambulance nurses. In Ozok AF, Salvendy G, editors. Advances in Applied Ergonomics. Istanbul, Turkey: USA Publishing Corporation; 1996 | 3 |
| Larsson TJ, Betts NJ. The variation of occupational injury cost in Australia; estimates based on a small empirical study. Saf Sci 1996;24:143–55 | 3 |
| Lassalle V, Berton J, Bouhours G, Péres M, Bossard G, Granry JC. Enquête européenne sur la pratique de la simulation médicale pédiatrique. Ann Fr Anesth Reanim 2009;28:628–33 | 7 |
| Letaief M, Hassine M, Bejia I, Ben Romdhane F, Ben Salem K, Soltani MS. Paramedical staff knowledge and practice related to the blood transfusion safety. Transfu Clin Biol 2005;12:25–9 | 2 |
| Laurie DC. Medical waste: science vs. politics. AORN 1992;55:855–63 | 7 |
| Lavery GG, Jamison CA. Airway management in the critically ill adult. In Joseph EP, Phillip Dellinger R, editors. Critical Care Medicine. Philadelphia, PA: Mosby; 2008. pp.17–37 | 4 |
| Leather AJM, Butterfield C, Peachey K, Silverman M, Sheriff RS. International health links movement expands in the United Kingdom. Int Health 2010;2:165–71 | 1 |
| Lee J-W, Oh S-H, Byun E-B, Kima JH, Kima JH, Woonc JH, et al. Inactivation of Enterobacter sakazakii of dehydrated infant formula by gamma-irradiation. Radiat Phys Chem 2007;76:1858–61 | 1 |
| Lee C, Uijtdehaage S, Coates WC. Emergency medicine interest group curriculum: faculty and preclinical student opinions differ in a formal needs assessment. J Emerg Med 2011;40:218–24 | 1 |
| Predicting Ambulance Diversion in an Adult Emergency Department using a Gaussian Process. American Medical Informatics Association; Biomedical and Health Informatics: from Foundations to Applications to Policy. Chicago, IL. Bethesda, MD: American Medical Informatics Association; 2007 | 2 |
| Legido-Quigley H, McKee M, Nolte E, Glinos IA. Assuring the Quality of Health Care in the European Union. A Case for Action. WHO Regional Office for Europe. Copenhagen: WHO; 2010 | 7 |
| Lenehan GP. Head for the hill. J Emerg Nurs 2005;31:335 | 2 |
| Leong MKF, Ponampalam R, Lee FCY, Goh SH. Hazmat Medical Life Support Program, Ministry of Health, Singapore. Prehosp Disaster Med 2002;17:S84 | 7 |
| Leong MT, Ghebrial J, Sturmann K, Hsu CK. The effect of vinegar on colorimetric end-tidal carbon dioxide determination after esophageal intubation. J Emerg Med 2005;28:5–11 | 7 |
| Lepik KJ, Levy AR, Sobolev BG, Purssell RA, DeWitt CR, Erhardt GD. Adverse drug events associated with the antidotes for methanol and ethylene glycol poisoning: a comparison of ethanol and fomepizole. Ann Emerg Med 2009;53:439–450.e10 | 7 |
| Levick N. Establishment and applications of a nationwide pediatric emergency care applied research network. Prehosp Disaster Med 2002;17(Suppl. 2):S11 | 7 |
| Levick N. Rig safety 9-1-1: what you need to know about ambulance safety & standards. JEMS 2008;33:66–7 | 4 |
| Levitan R, Ochroch EA. Airway management and direct laryngoscopy: a review and update. Crit Care Clin 2000;16:373–88 | 7 |
| Levy PD. Development of a model lay-person ambulance service in rural Jamaica. Ann Emerg Med 2006;48:70 | 3 |
| Lewis R. Diabetic emergencies: Part 1. Hypoglycaemia. Accid Emerg Nurs 1999;7:190–6 | 2 |
| Liao T-Y, Hu T-Y. A CORBA-Based GIS-T for Ambulance Assignment. Application-Specific Systems, Architectures and Processors. San Jose, CA: application-specific systems, architectures and processors. IEEE Computer Society; 2002 | 4 |
| Lilford R, Mohammed MA, Spiegelhalter D, Thomson R. Use and misuse of process and outcome data in managing performance of acute medical care: avoiding institutional stigma. Lancet 2004;363:1147–54 | 2 |
| Lin C-C, Chen KF, Shih C-P, Seak C-J, Hsu K-H. The prognostic factors of hypotension after rapid sequence intubation. Am J Emerg Med 2008;26:845–51 | 2 |
| Linder G, Murphy P, Streger MR. You did what? Clinical errors in EMS. Emerg Med Serv 2001;30:69–71 | 4 |
| Linwood R, Day G, FitzGerald G, Oldenburg B. Quality improvement and paramedic care: what does the literature reveal for pre-hospital emergency care in Australia? Int J Health Care Qual Assur 2007;20:405–15 | 4 |
| Lopez-Herce J, Urbano J, Carillo A, Matamoros M. Resuscitation training in developing countries: importance of a stable program of formation of instructors. Resuscitation 2011;82:780–1 | 4 |
| Lorenz V, Rich JM, Schebesta K, Taslakian S, Müllner M, Frass M. Comparison of the EasyTube® and endotracheal tube during general anesthesia in fasted adult patients. J Clin Anesth 2009;21:341–7 | 2 |
| Lott C, Araujo R, Cassar MR, Di Bartolomeo S, Driscoll P, Esposito I. The European Trauma Course (ETC) and the team approach: past, present and future. Resuscitation 2009;80:1192–6 | 7 |
| Lowes T, Sharley P. Oxygen conservation during long distance transport of ventilated patients. Air Med J 2005;24:164–71 | 4 |
| Ludwig S. Pediatric emergency medicine: what lies ahead. Clin Pediatr Emerg Med 2001;2:280–3 | 4 |
| Lufinha A, Ferreira C. Prehospital emergency medicine and non-heartbeating donors: is there a future together? Crit Care 2005;9:P250 | 1 |
| Luppa PB, Müller C, Schlichtiger A, Schlebusch H. Point-of-care testing (POCT): current techniques and future perspectives. Trends Analyt Chem 2011;30:887–98 | 7 |
| Luten R, Broselow J. Rainbow care: the Broselow–Luten system. Implications for pediatric patient safety. Ambul Outreach 1999;Fall:14–16 | 2 |
| Lyden PD, Marler JR. Acute medical therapy. J Stroke Cerebrovasc Dis 1999;8:139–45 | 2 |
| Lyle K, Thompson T, Graham J. Pediatric mass casualty: triage and planning for the prehospital provider. Clin Pediatr Emerg Med 2009;10:173–85 | 4 |
| Mace SE, Mayer TA. Triage. In Jill MB, MD, MBE, FACEP FAAP editor. Pediatric Emergency Medicine. Philadelphia, PA: W.B. Saunders; 2008. pp. 1087–96 | 4 |
| Mackenzie CF, Hu P, Sen A, Dutton R, Seebode S, Floccare D, et al. Automatic pre-hospital vital signs waveform and trend data capture fills quality management, triage and outcome prediction gaps. AMIA Annu Symp Proc 2008;6:318–22 | 6 |
| Mackersie RC. Pitfalls in the evaluation and resuscitation of the trauma patient. Emerg Med Clin N Am 2010;28:1–27 | 4 |
| MacLeod N. Building a culture for safer systems: the experience of ambulance trusts. Prof Nurse 2004;19:457–60 | 4 |
| Madden AP, Barham C. Clinical systems. Anaesth Intensive Care Med 2007;8:518–19 | 2 |
| Magnussen J, Vrangbaek K, Saltman RB. Nordic Health Care Systems. Recent Reforms and Current Policy Challenges. WHO Regional Office for Europe. Copenhagen: WHO; 2010 | 7 |
| Maguire T. Yellow card reporting. Pharm J 2005;275:605 | 2 |
| Mahesh P, Ward B, Bustillo P. 102 Patient safety and quality assurance in HDR application of cancer treatment from the technologists viewpoint. Radiother Oncol 1996;39(Suppl. 1):S26 | 1 |
| Mahowold MW. Diagnostic testing: sleep disorders. Neurol Clin 1996;14:183–200 | 1 |
| Malamed S. Sedation. 5th edn. St. Louis, MO: Mosby; 2009 | 7 |
| Maloney J. Terrorism 101: introduction to terrorism and its medical implications. Prehosp Disaster Med 2002;17(Suppl. 2):S32–3 | 7 |
| Maloney J. Echocardiography in initial assessment of trauma patients. Prehosp Disaster Med 2002;17:S55 | 4 |
| Malmstrom L. Mass-gathering medical care in the Stockholm area – a review. Prehosp Disaster Med 2002;17(Suppl. 2):S41 | 7 |
| Maltezou HC, Wicker S, Borg M, Heininger U, Puro V, Theodoridou M, et al. Vaccination policies for health-care workers in acute health-care facilities in Europe. Vaccine 2011;29:9557–62 | 3 |
| Anonymous. CAS Communication: Medical Patient Weighing Scales: National Electronic Library for Medicines. London: NICE; 2010 | 2 |
| Mandt MJ, Roback MG. Assessment and monitoring of pediatric procedural sedation. Clin Pediatr Emerg Med 2007;8:223–31 | 4 |
| Maniscalco PM, Rubin DL. EMS incident management: the safety sector. Emerg Med Serv 1998;27:59–61 | 4 |
| Manser T. Managing the aftermath of critical incidents: meeting the needs of health-care providers and patients. Best Pract Res Clin Anaesthesiol 2011;25:169–79 | 1 |
| Manson S. Safeguarding Adults: The Role of Health Service Practitioners. London: Department of Health; 2011 | 7 |
| Manwaring JC, Conway GA, Garrett LC. Epidemiology and prevention of helicopter external load accidents. J Saf Res 1998;29:107–21 | 1 |
| Marazza D, Bandini V, Contin A. Ranking environmental aspects in environmental management systems: a new method tested on local authorities. Environ Int 2010;36:168–79 | 1 |
| Marcus GM, Keung E, Scheinman MM. The year in review of clinical cardiac electrophysiology. J Am Coll Cardiol 2009;54:777–87 | 2 |
| Margheri M, Meucci F, Falai M, Comeglio M, Giglioli C, Chechi T. Transferring patients for direct coronary angioplasty: a retrospective analysis of 135 unselected patients with acute myocardial infarction. G Ital Cardiol (Rome) 2001;2:921–6 | 2 |
| Marhavilas PK, Koulouriotis D, Gemeni V. Risk analysis and assessment methodologies in the work sites: on a review, classification and comparative study of the scientific literature of the period 2000–2009. J Loss Prev Process Industries 2011;24:477–523 | 1 |
| Marimon F, Llach J, Bernardo M. Comparative analysis of diffusion of the ISO 14001 standard by sector of activity. J Clean Prod 2011;19:1734–44 | 1 |
| Mak BLM, Chan WWH, Wong K, Zheng C. Comparative studies of standalone environmental reports – European and Asian airlines. Transport Res Part D: Transport Environ 2007;12:45–52 | 1 |
| Markenson D, Krug S. Developing pediatric emergency preparedness performance measures. Clin Pediatr Emerg Med 2009;10:229–39 | 4 |
| Martens PR, Russell JK, Wolcke B, Paschen H, Kuisma M, Gliner BE. Optimal response to cardiac arrest study: defibrillation waveform effects. Resuscitation 2001;49:233–43 | 9 |
| Martin RC, Laxson RR, Wierzbicki JG, Rivard MJ, Fontanesi J. 104 Development of high activity 252Cf sources for neutron brachytherapy. Radiother Oncol 1996;39(Suppl. 1):S26 | 1 |
| Martin PS. National EMS culture of safety update. Air Med J 2011;30:242–3 | 4 |
| Martini DR. Psychiatric emergencies. Clin Pediatr Emerg Med 2004;5:143–5 | 2 |
| Marx JA. Methods of diagnostic peritoneal lavage – better to be safe. Am J Emerg Med 1989;7:452–3 | 1 |
| Mast CR. Walk in someone else’s shoes . . . ‘Caught in the Cross Fire’. JEMS 1998;23:10–12 | 4 |
| Mataria A, Khatib R, Donaldson C, Bossert T, Hunter DJ, Alsayed F, et al. The health-care system: an assessment and reform agenda. Lancet 2009;373:1207–17 | 4 |
| Maxatadze D, Metreveli Z, Chixradze K, Kereselidze T. One-year Georgian experience of nitrous oxide usage in prehospital care and analgesia during transportation. Prehosp Disaster Med 2002;17:S80–1 | 10 |
| Mayfield T. 1996 safety survey. Air Med J 1996;2:29–32 | 3 |
| Mayville ML. Debriefing: the essential step in simulation. Newborn Infant Nurs Rev 2011;11:35–9 | 4 |
| Mazighi M, Derex L, Amarenco P. Prehospital stroke care: potential, pitfalls, and future. Curr Opin Neurol 2010;23:31–5 | 4 |
| McAdams T. Using emerging aircraft technologies to enhance safety and patient care. Air Med J 1998;4:5 | 4 |
| McCabe PJ, Schad S, Hampton A, Holland DE. Knowledge and self-management behaviors of patients with recently detected atrial fibrillation. Heart Lung 2008;37:79–90 | 2 |
| McCarthy D, Mueller K, Wrenn J. Mayo Clinic: Multidisciplinary Teamwork, Physician-Led Governance, and Patient-Centered Culture Drive World-Class Health Care. The Commonwealth Fund; August 2009. URL: www.whynotthebest.org/uploads/download/74 (accessed 28 July 2014) | 1 |
| Healthcare Quality Quest. Report on Published Job Descriptions for Clinical Audit Staff: Healthcare Quality Improvement Partnership. London: Healthcare Quality Improvement Partnership; 2009 | 1 |
| Anonymous. Health System Snapshots: Perspectives from Six Countries. WHO Regional Office for Europe. Copenhagen: WHO; 2008 | 7 |
| McDaniel-Hohenhaus S, Frush KS. 7. Development of an E-learning program for use of the Broselow–Luten pediatric system. J Emerg Nurs 2003;29:417 | 4 |
| MacDonald M. We are a SAFE program because . . . Air Med J 2006;25:238–9 | 3 |
| McDonald KM, Schultz E, Albin L, Pineda N, Lonhart J, Sundaram V. Care Coordination Measures Atlas. Rockville, MD: Agency for Health Research and Quality; 2011 | 7 |
| McDonnell SM, Yassin AS, Brown WG, Perry HN, Thacker SB. Measuring Health Program Effectiveness in the Field: An Assessment Tool. Annual Humanitarian Health Conference. Amsterdam: World Association for Disaster and Emergency Medicine; 2007 | 2 |
| McFee RB, Abdelsayed GG. Clostridium difficile. Dis Mon 2009;55:439–70 | 4 |
| McGovern BA, Garan H, Buskin JN. Treatment of ventricular arrhythmias. Curr Probl Cardiol 1988;13:790–859 | 4 |
| McGuinness B, O’Hare J, Craig D, Bullock R, Malouf R, Passmore P. Statins for the treatment of dementia. Cochrane Database Syst Rev 2010;8:CD007514 | 1 |
| McKee M, Black N. Does the current use of junior doctors in the United Kingdom affect the quality of medical care? Soc Sci Med 1992;34:549–58 | 2 |
| McKenzie P, Mackson E, Morris R. Incorporating TRM into daily operations: the immediate structured debrief. Air Med J 2000;19:117 | 4 |
| McNutt RA, Abrams R, Arons DC, Patient Safety Committee. Patient safety efforts should focus on medical errors. JAMA 2002;287:1997–2001 | 4 |
| Melton K, Pettett G. Transport of the ventilated infant. In Goldsmith J, Karotkin E, eds. Assisted Ventilation of the Neonate. 5th edn. Philadelphia, PA: W.B. Saunders; 2011. pp. 531–41 | 4 |
| Menegazzi JJ, Fuller FP, Pace SA. Succinylcholine-assisted endotracheal intubation by paramedics. Ann Emerg Med 2001;37:360–1 | 5 |
| Messahel FM, Al-Qahtani AS. Transport management of the critically ill. Outcome of study with recommendations. Saudi Med J 2004;25:533–4 | 1 |
| Metcalfe S, Reilly I. Foot and Ankle Injection Techniques. Edinburgh: Churchill Livingstone; 2010 | 4 |
| Metzger JC, Marcozzi DE. Tactical EMS. In Ciottone GR, Anderson PD, Auf Der Heide E, Darling RG, Jacoby I, Noji E, et al., eds. Disaster Medicine. 3rd edn. Philadelphia, PA: Mosby/Elsevier; 2006. pp. 297–301 | 4 |
| Mika L. Mission impossible? Is safety still first within the air medical industry? Air Med J 2000;19:117 | 4 |
| Millard WB. The cost of koi: evidence-based design in emergency medical facilities. Ann Emerg Med 2007;50:267–71 | 2 |
| Miller K. A case manager’s perspective of patient transport. Case Manager 2004;15(Suppl. 2):2–4 | 4 |
| Mireles M, Bledsoe B. Grand delusions . . . ‘missed pericardial tamponade’ call [in Grand Rounds, May 2005 JEMS]. JEMS 2005;30:16–18 | 4 |
| Mirza M, Saini D, Brown TB, Orthner HF, Mazza G, Battles MM. Expert validation of the knowledge base for E-CAD – a pre-hospital dispatch triage decision support system. AMIA Annu Symp Proc 2007;11:1052 | 6 |
| Mitchell A, Pearson L. First trip – safe trip? Infant 2009;5:65–7 | 4 |
| Mlott K. How errors happen . . . medication safety: implications for EMS. Emerg Med Serv 2003;32:97–106 | 4 |
| Montgomery J, Mitty E, Flores S. Resident condition change: should I call 911? Geriatr Nurs 2008;29:15–26 | 2 |
| Moon T, Broome R. Air medical safety program. Top Emerg Med 1994;16:31–7 | 1 |
| Moore PK, Moore EE, Moore FA. Exception from informed consent requirements for emergency research. Surgery 2009;145:630–5 | 1 |
| Morrow D, Rondinelli D. Adopting corporate environmental management systems: motivations and results of ISO 14001 and EMAS Certification. Eur Manag J 2002;20:159–71 | 1 |
| Morse SS, Qureshi K, Gershon RRM, Hogan E. ‘Diseases of bioterrorism’ training program for emergency medical services personnel. Prehosp Disaster Med 2002;17(Suppl. 2):S33 | 4 |
| Mosca DL. The human factors team and accumulative impact of the ‘microtrauma’ of daily practice in emergency personnel. Prehosp Disaster Med 2002;17(Suppl. 2):S54 | 3 |
| Moskop JC, Geiderman JM, Hobgood CD, Larkin GL. Emergency physicians and disclosure of medical errors. Ann Emerg Med 2006;48:523–31 | 2 |
| Moskop JC, Sklar DP, Geiderman JM, Schears RM, Bookman KJ. Emergency department crowding, part 1 – concept, causes, and moral consequences. Ann Emerg Med 2009;53:605–11 | 2 |
| Motoyama EK, Gronert BJ, Fine GF. Induction of anesthesia and maintenance of the airway in infants and children. In Etsuro KM, MD, Davis PJ, MD, editors. Smith’s Anesthesia for Infants and Children. Philadelphia, PA: Mosby, 2006. pp. 319–58 | 2 |
| Mulligan, T. The development of emergency medicine systems in Africa. Afr J Emerg Med 2011;1:5–7 | 4 |
| Murata A, Matsuda S, Mayumi T, Okamoto K, Kuwabara K, Ichimiya Y. Multivariate analysis of factors influencing medical costs of acute pancreatitis hospitalizations based on a national administrative database. Dig Liver Dis 2012;44:143–8 | 1 |
| Murlidhar V, Desa NJ, Roy N. Quality of emergency trauma care in India: an analysis based on TRISS methodology in Mumbai University Hospital. Prehosp Disaster Med 2002;17(Suppl. 2):S81 | 2 |
| Murphy P, Taigman M. Oops! EMS mistakes. JEMS 1998;23:37–8, 40–2 | 4 |
| Murray-Davis B, Marshall M, Gordon F. What do midwives think about interprofessional working and learning? Midwifery 2011;27:376–81 | 2 |
| Muscarella LF. Prevention of disease transmission during flexible laryngoscopy. Am J Infect Control 2007;35:536–44 | 4 |
| Nakano S, Justo RN, Koido Y, Yamamoto Y. Transportation of neonates with congenital heart disease: appropriate respiratory management. Prehosp Disaster Med 2002;17(Suppl. 2):S81–2 | 7 |
| Nakaya J, Kimura M, Hiroi K, Ido K, Yang W, Tanaka H. Genomic Sequence Variation Markup Language (GSVML). Int J Med Inf 2010;79:130–42 | 1 |
| Nelson AL, Collins J, Knibbe H, Cookson K, de Castro AB, Whipple KL. Safer patient handling. Nurs Manage 2007;38:26–32 | 3 |
| Nelwan SP, Kors JA, Meij SH, Boersma H, Simoons ML. Efficacy of a Reduced Lead Set for Pre-Hospital Triage of Thrombolytic Strategies. Conference presentation. Chicago, IL: Computers in Cardiology; 2004 | 9 |
| Newgard C. Validation of probabilistic linkage for matching de-identified ambulance records to a state trauma registry. Ann Emerg Med 2005;46(Suppl.):45 | 1 |
| Newgard C. Agreement of existing and imputed prehospital data in a state trauma registry when compared to ambulance data. Ann Emerg Med 2005;46(Suppl.):62 | 1 |
| Nguyen HB, Daniel-Underwood L, Van Ginkel C, Wong M, Lee D, Lucas AS. An educational course including medical simulation for early goal-directed therapy and the severe sepsis resuscitation bundle: an evaluation for medical student training. Resuscitation 2009;80:674–9 | 3 |
| National Institute for Health and Clinical Excellence. CG102 Bacterial Meningitis and Meningococcal Septicaemia in Children: Audit Support – Clinical and Organisational Criteria. London: NICE; 2010 | 7 |
| Nichols AB, Werfel P. Calculation error. JEMS 2002;27:15 | 4 |
| Niederle T, Standen P. Enhancing standards in rural CBR management. Prehosp Disaster Med 2002;17(Suppl. 2):S14–15 | 2 |
| Nielsen JU. The nurse in prehospital treatment in Holstebro, Ringkoebing County, Denmark. Poster presentation. Acta Anaesth Scand Suppl 1999;114:107 | 4 |
| Nikus K, Lähteenmäki J, Lehto P, Eskola M. The role of continuous monitoring in a 24/7 telecardiology consultation service – a feasibility study. J Electrocardiol 2009;42:473–80 | 1 |
| Nishimoto E. International SOS mass casualty evacuation – Bali 12 October 2002. Prehosp Disaster Med 2002;17(Suppl. 2):S21–2 | 4 |
| Noble D. Global learning, sharing and advancing: a knowledge-based approach. Prehosp Disaster Med 2002;17(Suppl. 2):S33 | 4 |
| Noble D. Rapid vascular access device. Prehosp Disaster Med 2002;17(Suppl. 2):S54 | 4 |
| Noble D. M.I.E.C.O.TM (Minimally Invasive Endo Corporeal Oxygenation): non-pulmonary oxygenation method. Prehosp Disaster Med 2002;17:S82 | 1 |
| Nolan JP, Hazinski MF, Billi JE, Boettiger BW, Bossaert L, de Caen AR. Part 1: Executive summary: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation 2010;81(Suppl 1):e1–25 | 4 |
| Nolan JP, Soar J, Perkins GD. Resuscitation 2010 in review. Resuscitation 2011;82:145–8 | 4 |
| Nolte E, Roland M, Damberg CL, Mattke S, Cacace M, Goshev S. Informing the Development of a Resource Allocation Framework in the German Healthcare System. Technical report. Cambridge: Rand Corporation, Europe; 2011 | 1 |
| Nowak RM, Sen A, Garcia AJ, Wilkie H, Yang JJ, Nowak MR, et al. Noninvasive continuous or intermittent blood pressure and heart rate patient monitoring in the ED. Am J Emerg Med 2011;29:782–9 | 2 |
| Nunez JF. MEDJET International . . . the story. Hosp Aviat 1989;8:19–25 | 4 |
| O’Byrne WT III, Weavind L, Selby J. The science and economics of improving clinical communication. Anesthesiol Clin 2008;26:729–44 | 7 |
| O’Connor RE, Slovis CM, Hunt RC, Pirrallo RG, Sayre MR. Eliminating errors in emergency medical services: realities and recommendations. Prehosp Emerg Care 2002;6:107–13 | 4 |
| O’Driscoll BR, Howard LS, Davison AG. Guideline for Emergency Oxygen Use in Adult Patients. London: British Thoracic Society; 2008 | 7 |
| Ofori G, Gang G, Briffett C. Implementing environmental management systems in construction: lessons from quality systems. Building Environ 2002;37:1397–407 | 1 |
| Ohashi N. New responses and precautions resulting from mass poisonings in Japan. Prehosp Disaster Med 2002;17(Suppl. 2):S88 | 4 |
| Ohta G, Kamada F, Teramura N, Hojo H. 5GHz W-LAN Verification for Public Mobile Applications – Internet Newspaper on Train and Advanced Ambulance Car. Conference Presentation. Consumer Communications and Networking Conference. Las Vegas, NV. Piscataway, NJ: CCNC; 2004. pp. 569–74 | 4 |
| Olia PM, Mollica TV, Vanni E. A report on emergency service by ambulance with doctor on board of the Emergency Department of Prato, Italy. Crit Care 2001;5:P172 | 1 |
| Olola CHO, Narus S, Nebeker J, Poynton M, Hales J, Rowan B. The perception of medical professionals and medical students on the usefulness of an emergency medical card and a continuity of care report in enhancing continuity of care. Int J Med Inf 2011;80:412–20 | 2 |
| Olshaker JS. Managing emergency department overcrowding. Emerg Med Clin N Am 2009;27:593–603 | 4 |
| Oluwadiya KS, Olakulehin AO, Olatoke SA. Pre-hospital care of the injured in south western Nigeria: a hospital based study of four tertiary level hospitals in three states. Annu Proc Assoc Adv Automot Med 2005;49:93–100 | 4 |
| Ong MEH, Ho KK, Tan TP, Koh SK, Almuthar Z, Overton J, et al. Using demand analysis and system status management for predicting ED attendances and rostering. Am J Emerg Med 2009;27:16–22 | 2 |
| Ornato JP, Peberdy MA, Reid RD, Feeser VR, Dhindsa HS. Impact of resuscitation system errors on survival from in-hospital cardiac arrest. Resuscitation 2012;83:63–9 | 2 |
| Osborn HH, Kayen D, Horne H, Bray W. Excess ventilation with oxygen-powered resuscitators. Am J Emerg Med 1984;2:408–13 | 9 |
| Oster NS, Doyle CJ. Critical incident stress and challenges for the emergency workplace. Emerg Med Clin N Am 2000;18:339–53 | 3 |
| Otteni JC, Ancellin J, Cazalaà JB, Clergue F. Pollution et rétropollution du réseau de distribution d’un gaz médical. Ann Fr Anesth Reanim 1994;13:713–25 | 2 |
| Mannan S. Lees’ Loss Prevention in the Process Industries. 3rd edn. Burlington, MA: Butterworth-Heinemann; 2005 | 2 |
| Pagán A, Curty R, Rodriguez MI, Pryor F. Emergency – total power outage in the OR. AORN 2001;74:514–16 | 2 |
| Pandor A, Goodacre S, Harnan S, Holmes M, Pickering A, Fitzgerald P, et al. Diagnostic management strategies for adults and children with minor head injury: a systematic review and an economic evaluation. Health Technol Assess 2011;15:1–202 | 2 |
| Paradis NA, Young G, Lemeshow S, Brewer JE, Halperin HR. Response to ASPIRE investigators. Am J Emerg Med 2010;28:976–8 | 5 |
| Paradis N, Young G, Lemeshow S, Brewers J, Halperin H. Inhomogeneity and temporal effects in AutoPulse Assisted Prehospital International Resuscitation – an exception from consent trial terminated early. Am J Emerg Med 2010;28:391–98 | 6 |
| Parr M. Prehospital airway management for severe brain injury. Resuscitation 2008;76:321–2 | 4 |
| Parsons RL, Miller SA. Analytical considerations for genotoxic and other impurities. In Satinder A, Stephen S, eds. Separation Science and Technology. London: Academic Press; 2011. pp. 171–94 | 1 |
| Patel VL, Yoskowitz NA, Arocha JF, Shortliffe EH. Cognitive and learning sciences in biomedical and health instructional design: a review with lessons for biomedical informatics education. J Biomed Inform 2009;42:176–97 | 2 |
| Patterson PD, Huang DT, Fairbanks RJ, Simeone S, Weaver M, Wang HE. Variation in emergency medical services workplace safety culture. Prehosp Emerg Care 2010;14:448–60 | 3 |
| Patterson M, Rick J, Wood S, Carroll C, Balain S, Booth A. Systematic review of the links between human resource management practices and performance. Health Technol Assess 2010;14:1–334 | 7 |
| Patterson ES, Rogers ML, Tomolo AM, Wears RL, Tsevat J. Comparison of extent of use, information accuracy, and functions for manual and electronic patient status boards. Int J Med Inf 2010;79:817–23 | 2 |
| Patterson PD, Suffoletto BP, Kupas DF, Weaver MD, Hostler D. Sleep quality and fatigue among prehospital providers. Prehosp Emerg Care 2010;14:187–93 | 3 |
| Peach LC, Rankin E. Building a culture of evidence-informed decision making in the community. Healthc Manage Forum 2011;24(Suppl 1):S17–20 | 2 |
| Pearce A, Caldicott DGE, Edwards NA, Eliseo T. Medical awareness and response to incidents at major hazard facilities. Prehosp Disaster Med 2002;17(Suppl. 2):S83 | 2 |
| Peberdy MA, Ottingham LV, Groh WJ, Hedges J, Terndrup TE, Pirrallo RG, et al. Adverse events associated with lay emergency response programs: the public access defibrillation trial experience. Resuscitation 2006;70:59–65 | 3 |
| Pérez ES, Yepez LA, de la Mota IF. Simulation and optimization of the Pre-hospital Care System of the National University of Mexico Using Travelling Salesman Problem Algorithms. Ottawa, Canada: Summer Computer Simulation Conference: Red Hook; 2010 | 1 |
| Perhats C, Valdez AM, St Mars T. Promoting safer medication use among older adults. J Emerg Nurs 2008;34:156–8 | 4 |
| Perina DG, Beeson MS, Char DM, Counselman FL, Keim SM, McGee DL. The 2007 model of the clinical practice of emergency medicine: the 2009 update: 2009 EM model review task force. Ann Emerg Med 2011;57:e1–15 | 7 |
| Perkins GD. Simulation in resuscitation training. Resuscitation 2007;73:202–11 | 7 |
| Phillips DP, Christenfeld N, Glynn LM. Increase in US medication-error deaths between 1983 and 1993. Lancet 1998;351:643–4 | 2 |
| Phillips L, Brown L, Campbell T, Miller J, Proehl J, Youngberg B. Recommendations for the use of intraosseous vascular access for emergent and nonemergent situations in various healthcare settings: a consensus paper. J Emerg Nurs 2010;36:551–6 | 4 |
| Pichon LC, Arredondo EM, Roesch S, Sallis JF, Ayala GX, Elder JP. The relation of acculturation to Latinas’ perceived neighborhood safety and physical activity: a structural equation analysis. Ann Behav Med 2007;34:295–303 | 1 |
| Pierce PF, Evers KG. Global presence: USAF aeromedical evacuation and critical care air transport. Crit Care Nurs Clin North Am 2003;15:221–31 | 1 |
| Plani F, Carson P. The challenges of developing a trauma system for indigenous people. Injury 2008;39:(Suppl 5):S43–53 | 4 |
| Pocock N. Report Suggests Many Trusts Still Not Complying with all NPSA Alerts within Deadline: National Electronic Library for Medicines. London: NICE; 2011 | 7 |
| Pocock N. Update to Safer Spinal (Intrathecal), Epidural and Regional Devices Alert: National Electronic Library for Medicines. London: NICE; 2011 | 2 |
| Polinder S, Segui-Gomez M, Toet H, Belt E, Sethi D, Racioppi F, et al. Systematic review and quality assessment of economic evaluation studies of injury prevention. Accid Anal Prev 2012;45:211–21 | 2 |
| Pollack CV Jr, Diercks DB, Roe MT, Peterson ED. 2004 American College of Cardiology/American Heart Association Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction: implications for emergency department practice. Ann Emerg Med 2005;45:363–76 | 4 |
| Popovic A. Air medical and specialty care ground transportation: a primer for case managers. Case Manager 2004;15(Suppl 2):5–7 | 1 |
| Porter B. From the ground up. Emergency 1985;17:26–9 | 4 |
| Porter A, Button L, Duff K, Evans A, Snooks H, Lowe R, et al. When would you call 999? Perceptions of emergency ambulances’ role in unscheduled health care. Emerg Med J 2009;26:3 | 1 |
| Porter M (foreword). Quality Time: The Value of Consultants’ Supporting Professional Activities to the NHS. London: British Medical Association; 2010 | 7 |
| Post WM, Sramek M, Koster RW, Zocca V. Demo of FreeCall, a system for ambulance dispatching. In Andreassen S, Engelbrecht R, Wyatt J, editors. Artificial Intelligence in Medicine. Amsterdam: IOS Press; 1993. pp. 271–3 | 4 |
| Powell LH, Calvin Jr JE, Mendes de Leon CF, Richardson D, Grady KL, Flynn KJ. The Heart Failure Adherence and Retention Trial (HART): design and rationale. Am Heart J 2008;156:452–60 | 1 |
| Powell MR. Analyzing the power and error of Listeria monocytogenes growth challenge studies. Inter J Food Microbiol 2009;136:10–17 | 1 |
| Pozzi Frazer E. Past, present, and future perspectives of air medical safety. Emerg Care Q 1991;6:16–26 | 4 |
| Pratt RJ, O’Malley B. Supporting evidence-based infection prevention and control practice in the National Health Service in England. The NHS/TVU/Intuition approach. J Hosp Infect 2007;65(Suppl 2):142–7 | 4 |
| Preobrazhensky V. Treatment of children with explosive trauma. Prehosp Disaster Med 2002;17(Suppl. 2):S24 | 2 |
| Pronovost P, Weast B, Schwarz M, Wyskiel RM, Prow D, Milanovich SN. Medication reconciliation: a practical tool to reduce the risk of medication errors. J Crit Care 2003;18:201–5 | 2 |
| Proudfoot S, Moore P, Levine R. Safety in numbers: a survey on ambulance patient compartment safety. JEMS 2007;32:86–8, 90 | 3 |
| Pullen RL Jr. Smooth patient transfers, Part III: Using a hydraulic lift for patient transfer. Nursing 2008;38:54–6 | 2 |
| Pyne SW. Mass-participation event coverage. In Seidenberg P, Beutler A. The Sports Medicine Resource Manual. Philadelphia, PA: W.B. Saunders; 2008. pp. 31–6 | 4 |
| Quattrini V, Swan BA. Evaluating care in ED fast tracks. J Emerg Nurs 2011;37:40–6 | 2 |
| Quinn JV, Mahadevan SV, Eggers G, Ouyang H, Norris R. Effects of implementing a rapid admission policy in the ED. Am J Emerg Med 2007;25:559–63 | 2 |
| Raleigh VS, Foot C. Getting the Measure of Quality: Opportunities and Challenges. London: The King’s Fund; 2010 | 7 |
| Rall M, Stricker E, Reddersen S, Zieger J, Dieckmann P. Mobile ‘In situ’ simulation crisis resource management training. In Kyle R, Bosseau Murray W. Clinical Simulation. Oxford: Academic Press; 2008. pp. 565–81 | 4 |
| Rateau F, Levraut L, Colombel AL, Bernardb J-L, Quarantac JF, Cabarrotd P, et al. Check-list ‘Patient Safety’ in the operating room: one year experience of 40,000 surgical procedures at the university hospital of Nice. Ann Fr Anesth Reanim 2011;30:479–83 | 2 |
| Raveen N. Emergency care in Africa. Afr J Emerg Med 2011;1:51–2 | 4 |
| Rea T, Plorde M, Silvestri S, Rothrock SG, Pagane JR. Diagnosis and triage by EMS professionals (multiple letters). Prehosp Emerg Care 2003;7:295–7 | 5 |
| Ream KA. Journal update. Inside Washington. J Emerg Nurs 2000;26:51A-53 | 4 |
| Rebmann T, Wagner W, Warye K. APIC’s role in emergency management: proceedings of the 2008 APIC Emergency Preparedness Mini-Summit. Am J Infect Control 2009;37:343–8 | 4 |
| Rebmann T. APIC State-of-the-art Report: the role of the infection preventionist in emergency management. Am J Infect Control 2009;37:271–81 | 7 |
| Rebuge Á, Ferreira DR. Business process analysis in healthcare environments: a methodology based on process mining. Inf Syst 2012;37:99–116 | 2 |
| Ren-Da L, Zhang HQ. Treatment of critical multiple traumatic wounds complicated with MOF, Septic OPSI. Prehosp Disaster Med 2002;17:S81 | 4 |
| Reschreiter H, Kapila A. Sedation in adults. Surgery 2006;24:342–5 | 2 |
| Resnic FS, Foody J. Special topics. J Am Coll Cardiol 2006;47(Suppl. 11):D41–4 | 2 |
| Reyes SD, Stillsmoking K, Chadwick- Hopkins D. Implementation and evaluation of a virtual simulator system: teaching intravenous skills. Clin Sim Nurs 2008;4:e43–9 | 3 |
| Rhodes M, Tinkoff G. Trauma outcomes. In Juan AA, MD, FACS, FCCM, Trunkey DD MF, editors. Current Therapy of Trauma and Surgical Critical Care. Philadelphia, PA: Mosby; 2008. pp. 758–62 | 2 |
| Richards M. Extent and Causes of International Variations in Drug Usage: A Report for the Secretary of State for Health. London: Department of Health; 2010 | 7 |
| Ridley S. Secondary transport of the critically ill. Anaesth Intensive Care Med 2004;5:20–3 | 4 |
| Riegel B, Mosesso VN, Birnbaum A, Bosken L, Evans LM, Feeny D. Stress reactions and perceived difficulties of lay responders to a medical emergency. Resuscitation 2006;70:98–106 | 1 |
| Ripanu A, Oprisan M, Nemtisor E, Chiriacescu M, Lazaroiu L, Alexandrescu P, et al. Ambulance services and emergency rooms healthcare information system. Curr Perspect Healthc Comput Part 1–2 1998:443 | 4 |
| Roberts I, Allsop P, Dickinson M, Curry P, Eastwick-Field P, Eyre G. Airway management training using the laryngeal mask airway: a comparison of two different training programmes. Resuscitation 1997;33:211–14 | 3 |
| Roberts KH, Bea RG. When systems fail. Organ Dyn 2001;29:179–91 | 1 |
| Rosen M, West R, eds. Clinical Governance in Pre-Hospital Care. Quality Measures for the Emergency Services. London: Royal Society of Medicine; 2000 | 4 |
| Robinson B. Limited Horizons, Limited Influence: Information Technology Experts and the Crisis of the London Ambulance Service. Technical expertise and public decisions. Princeton, NJ: IEEE; 1996 | 4 |
| Robinson K. ‘To err is human . . .’ patient safety initiatives for EMS. J Emerg Nurs 2002;28:47–8 | 4 |
| Roedig E. Primary and Secondary Air Medical Transport in Ambulance Helicopters. Current aeromedical issues in rotary wing operations: problemes actuels de medecine aeronautiques poses par les operations utilisant des voilures tournantes. San Diego, CA: NATO; 1998 | 4 |
| Rokos IC, French WJ, Mattu A, Nichol G, Farkouh ME, Reiffel J, et al. Appropriate cardiac cath lab activation: optimizing electrocardiogram interpretation and clinical decision-making for acute ST-elevation myocardial infarction. Am Heart J 2010;160:995–e8 | 2 |
| Romero C, Ventura S, Gibaja EL, Hervás C, Romero F. Web-based adaptive training simulator system for cardiac life support. Artif Intell Med 2006;38:67–78 | 2 |
| Rondinelli DA, Vastag G. Global corporate environmental management practices at Alcoa. Corporate Environ Strategy 2000;7:289–97 | 1 |
| Roos LL, Menec V, Currie RJ. Policy analysis in an information-rich environment. Soc Sci Med 2004;58:2231–41 | 4 |
| Rosen KR. The history of medical simulation. J Crit Care 2008;23:157–66 | 4 |
| Ross AK, Eck JB. Office-based anesthesia for children. Anesthesiol Clin 2002;20:195–210 | 2 |
| Rubin M. Get a clue. EMS World 2011;40:57–64 | 4 |
| Ruter A, Gustafsson L, Wikstrom T. Medical management in major incidents. Prehosp Disaster Med 2002;17(Suppl. 2):S36–7 | 4 |
| Russo SG, Eich C, Barwing J, Nickel EA, Braun U, Graf BM, et al. Self-reported changes in attitude and behavior after attending a simulation-aided airway management course. J Clin Anesth 2007;19:517–22 | 2 |
| Rzepnicki TL, Johnson PR. Examining decision errors in child protection: a new application of root cause analysis. Children and youth services review 2005;27:393–407 | 2 |
| Sabatine MS, Antman EM, Widimsky P, Ebrahim IO, Kiss RG, Saaiman A, et al. Otamixaban for the treatment of patients with non-ST-elevation acute coronary syndromes (SEPIA-ACS1 TIMI 42): a randomised, double-blind, active-controlled, phase 2 trial. Lancet 2009;374:787–95 | 2 |
| Sachdeva RC, Jain S. Making the case to improve quality and reduce costs in pediatric health care. Pediatr Clin North Am 2009;56:731–43 | 7 |
| Sachedina N, Donaldson LJ. Paediatric mortality related to pandemic influenza A H1N1 infection in England: an observational population-based study. Lancet; 376:1846–52 | 1 |
| Sahdev P, Lacqua MJ, Singh B, Dogra TD. Road traffic fatalities in Delhi: causes, injury patterns, and incidence of preventable deaths. Accid Anal Prev 1994;26:377–84 | 1 |
| Saiboon IM, Jaafar MJ, Ahmad NS, Ahmad Z, Hamzah FA, Jamal SM. Simulation based education in delivering emergency medicine module. Procedia Soc Behav Sci 2011;18:388–93 | 1 |
| Saini D, Sandhu A, Gori MM, Orthner HF. A study design for comparing electronic patient care report (ePCR) with paper PCR in pre-hospital care. AMIA Annu Symp Proc 2005;2005:1103 | 6 |
| Sakatani K, Ono T, Kobayasi Y, Hikita S, Saito M. Modeling of Patient’s Blood Pressure Variation During Ambulance Transportation [6794–127]. In Minoru S, editor. Mechatronics, MEMS, and Smart Materials, Proceedings of the SPIE, Volume 6794, article id. 67943K, Bellingham, WA: ICMIT; 2007 | 1 |
| Salaripour M, McKernan P, Devlin R. Evaluation of a hospital-wide infection prevention & control certification program: increasing the quality limits for patient safety and staff satisfaction. Am J Infect Control 2006;34:E59–60 | 2 |
| Salem MR, Baraka A. Confirmation of tracheal intubation. In Carin AH, Mda2 – Carin A. Hagberg MD, eds. Benumof’s Airway Management. 2nd edn. Philadelphia, PA: Mosby; 2007. pp. 697–727 | 4 |
| Salem MR. Verification of endotracheal tube position. Anesthesiol Clin 2001;19:813–39 | 7 |
| Saltman RB, Bankauskaite V, Vrangbaeck K. Decentralization in Health Care. Strategies and Outcomes. WHO Regional Office for Europe. Copenhagen: WHO; 2010 | 7 |
| Saltman RD, Busse R, Mossialos E. Regulating Entrepreneurial Behaviour in European Health Care Systems. WHO Regional Office for Europe. Copenhagen: WHO; 2010 | 7 |
| Salvucci A, Jr. Medical abstract reviews. Medication calculation skills. Emerg Med Serv 2000;29:95 | 5 |
| Salvucci A, Jr. Medical abstract reviews. ED diversions and delays in care. Emerg Med Serv 2003;32:41, 120 | 5 |
| Salvucci A, Jr. Medical abstract reviews. Delays in AMI treatment. Emerg Med Serv 2006;35:38–40 | 5 |
| Salvucci A, Jr. Identification and reporting of errors. Emerg Med Serv 2006;35:38 | 5 |
| Saltzherr TP, Wendt KW, Nieboer P, Nijsten MW, Valk JP, Luitse JS. Preventability of trauma deaths in a Dutch Level-1 trauma centre. Injury 2011;42:870–3 | 2 |
| Sampalis J, Boukas S, Tamim H. Comparison of the Pre-Hospital Index (PHI) and the Revised Trauma Score (RTS) in Identifying Patients with Major Trauma. Proceedings of the 40th Annual Conference of the Association for the Advancement of Automotive Medicine, Vancouver, Canada, October, 1996 | 4 |
| Sanderson LM, Collins JW, McGlothlin JD. Robot-related fatality involving a U.S. manufacturing plant employee: Case report and recommendations. J Occup Accid 1986;8:13–23 | 1 |
| Sandhu H, Carpenter C, Freeman K, Nabors SG, Olson A. Clinical decisionmaking: opening the black box of cognitive reasoning. Ann Emerg Med 2006;48:713–19 | 2 |
| Sandhu B, Devadason D. Management of diarrhea. In Wyllie R, Hyams JS. Pediatric Gastrointestinal and Liver Disease. 4th edn. St. Louis, MO: W.B. Saunders; 2011. pp. 1002–11 | 4 |
| Santos G, Mendes F, Barbosa J. Certification and integration of management systems: the experience of Portuguese small and medium enterprises. J Clean Prod 2011;19:1965–74 | 2 |
| Sarr MG. The electronic environment: how has it, how will it, and how should it affect us? J Gastrointest Surg 2001;5:572–82 | 7 |
| Sasson C, Keirns CC, Smith DM, Sayrec MR, Macyd ML, Meurer WJ. Examining the contextual effects of neighborhood on out-of-hospital cardiac arrest and the provision of bystander cardiopulmonary resuscitation. Resuscitation 2011;82:674–9 | 3 |
| Saurman E, Perkins D, Roberts R, Roberts A, Patfield M, Lyle D. Responding to mental health emergencies: implementation of an innovative telehealth service in rural and remote New South Wales, Australia. J Emerg Nurs 2011;37:453–9 | 1 |
| Saxena SK, Pandey AK, Tandon P, Chakravarty R, Reddy AV, Dash A, et al. A novel approach to prepare 90Y–EGMP patches for superficial brachytherapy. Appl Radiat Isot 2009;67:1416–20 | 1 |
| Saxton JW, SherUnger S. Medico-legal aspects and concerns in quality assurance in the United States. Best Pract Res Clin Gastroenterol 2011;25:409–17 | 1 |
| Scarano Jr RM, Bryant B. Federal preemption of state regulation over air ambulances. Air Med J 2009;28:77 | 4 |
| Schafheutle EI, Seston EM, Hassell K. Factors influencing pharmacist performance: a review of the peer-reviewed literature. Health Policy 2011;102:178–92 | 2 |
| Schelper RL. Vascular anatomy. Clin Nutr 2002;21(Suppl. 1):113 | 1 |
| Schexnayder SM, Storm EA, Stroud MH, Moss MM, Ross AS, Fiser RT. Pediatric vascular access and centeses. In Fuhrman BP, Zimmerman JJ. Pediatric Critical Care. St. Louis, MO: Mosby; 2011. pp. 139–63 | 4 |
| Schinco M, Tepas JJ III. Beyond the golden hour: avoiding the pitfalls from resuscitation to critical care. Surg Clin North Am 2002;82:325–32 | 1 |
| Schneider SM, Gardner AF, Weiss LD, Wood JP, Ybarra M, Beck DM, et al. The future of emergency medicine. Ann Emerg Med 2010;56:178–83 | 2 |
| Schneider EC, Hussey PS, Schneyer C. Payment Reform: Analysis of Models and Performance Measurement Implications. Technical report. Cambridge: Rand Corporation, Europe; 2011 | 1 |
| Schnelle DD, Difato L, Guzman R, Jones BE, Gatelya M, Cullen C. Chemical-Biological-Radiological-Nuclear (CBRN) analytical framework based upon the ‘guidelines for emergency response in the utstein style’. Prehosp Disaster Med 2002;17(Suppl. 2):S3 | 10 |
| Ruckoldt H, Marx G, Leuwer M, Panning B, Piepenbrock S. Pulse oximetry and capnography in intensive care transportation: combined use reduces transportation risks. German. Anasthesiol Intensivmed Notfallmed Schmerzther 1998;33:32–6 | 1 |
| Schrover IAJM. Ten years SHE-improvements on a chemical and nuclear research-site – learning drivers. Saf Sci 2008;46:551–63 | 1 |
| Schultz M. Sales representatives in the OR: are they prepared? AORN 1994;59:651–62 | 1 |
| Schwartz JM, Heitmiller ES, Hunt EA, Shaffner DH. Cardiopulmonary resuscitation. In Davis PJ, Cladis FP, Motoyama EK. Smith’s Anesthesia for Infants and Children. Philadelphia, PA: Mosby; 2011. pp. 1200–49 | 7 |
| Schwenk M, Kluge S, Jaroni H. Toxicological aspects of preparedness and aftercare for chemical-incidents. Toxicology 2005;214:232–48 | 7 |
| Segerstrom J. Rescue roundup. Adv Rescue Technol 2005;8:26–32 | 4 |
| Seigel TA, McGillicuddy DC, Barkin AZ, Rosen CL. Morbidity and mortality conference in emergency medicine. J Emerg Med 2010;38:507–11 | 2 |
| Sekimoto M, Imanaka Y, Kobayashi H, Okubo T, Kizu J, Kobuse H. Impact of hospital accreditation on infection control programs in teaching hospitals in Japan. Am J Infect Control 2008;36:212–19 | 2 |
| Semonin-Holleran R. The tapestry of emergency nursing. J Emerg Nurs 2010;36:96 | 1 |
| Semper MM, González de Garibay AS. Historia clínica informatizada: 8 años de experiencia en un servicio médico quirúrgico. Rev 2010;25:173–80 | 2 |
| Sennik D. NHS Medical Device Training Goes Online: National Electronic Library for Medicines. London: NICE; 2009 | 7 |
| Severin PN, Cortez EP, McNeal CA, Kramer JE. Considerations of pediatric simulation. In Kyle R, Bosseau Murray W. Clinical Simulation. Oxford: Academic Press; 2008. pp. 411–21 | 2 |
| Shaban R, Wyatt Smith C, Cumming J. Uncertainty, error and risk in human clinical judgement: introductory theoretical frameworks in paramedic practice. Australas J Paramed 2004;2 | 4 |
| Shabetai R, Sahn DJ. Abstracts of papers to be presented at the 36th Annual Scientific Session of the American College of Cardiology, New Orleans, Louisiana, March 8–12, 1987. J Am Coll Cardiol 1987;9(Suppl. 1):1A-255A | 1 |
| Shah AN, Frush K, Luo X, Wears RL. Effect of an Intervention Standardization System on Pediatric Dosing and Equipment Size Determination. A Crossover Trial Involving Simulated Resuscitation Events: National Electronic Library for Medicines. London: NICE; 2003 | 2 |
| Shalit M, Lewin MR. Medical care of prisoners in the USA. Lancet 2004;364(Suppl. 1):34–5 | 4 |
| Shanaberger CJ. Don’t drop the patient! JEMS 1989;14:68–9 | 4 |
| Sharley P, Griggs B. Secondary aeromedical evacuations post-Bali bombings. Prehosp Disaster Med 2002;17(Suppl. 2):S22 | 1 |
| Sheehy SB. A visitor’s guide to the streets . . . prehospital care . . . a guide for the first-time field observer. J Emerg Nurs 1989;15:517–20 | 1 |
| Penzel T, Salmons S, Neuman MR, eds. Development of Biotelemetry System for Advanced Emergency Care in Ambulance. Marburg, Germany: Biotelemetry; 1997 | 9 |
| Shin JJ, Randolph GW, Rauch SD. Evidence-based medicine in otolaryngology, part 1: the multiple faces of evidence-based medicine. Otolaryngol Head Neck Surg 2010;142:637–46 | 1 |
| Shiring P. Safety A.S.A.P. The ambulance safety awareness program at Baldwin EMS. JEMS 2007;32:54–8 | 4 |
| Sibbald B. Delegating away patient safety. Can Nurse 1997;93:22–6 | 3 |
| Sibbald WJ. Outcomes research and the politics of health care: where have we been and where are we going? J Crit Care 2001;16:133–5 | 2 |
| Sidebotham P, Fox J, Horwath J, Powell C, Perwez S. Preventing Childhood Deaths: A Study of ‘Early Starter’ Child Death Overview Panels in England: SCIE Social Care Online. London: Department for Children, Schools and Families; 2008 | 1 |
| Siff J. Medical malpractice and risk management – part ii of ii. ED Legal Letter 2010;21:133–8 | 2 |
| Simon A, Bernardo M, Karapetrovic S, Casadesús M. Integration of standardized environmental and quality management systems audits. J Clean Prod 2011;19:2057–65 | 1 |
| Simon A, Karapetrovic S, Casadesus M. Evolution of integrated management systems in Spanish firms. J Clean Prod 2012;23:8–19 | 1 |
| Simpson P, Keating JF. The multiply injured patient. Found Years 2008;4:314–18 | 2 |
| Sirbaugh PE, Bradley RN, Macias CG, Endom EE. The Houston flood of 2001: the Texas Medical Center and lessons learned. Clin Pediatr Emerg Med 2002;3:275–83 | 2 |
| Sklar DP, Crandall CS, Zola T. 99: Emergency physician perceptions of patient safety risks. Ann Emerg Med 2008;51:501 | 2 |
| Skouloudis A, Evangelinos K, Kourmousis F. Assessing non-financial reports according to the Global Reporting Initiative guidelines: evidence from Greece. J Clean Prod 2010;18:426–38 | 1 |
| Slabbert JA, Smith WP. Patient transport from rural to tertiary healthcare centres in the Western Cape: is there room for improvement? Afr J Emerg Med 2011;1:11–16 | 7 |
| Slaven K, Hobbs JN. The air in there. JEMS 1995;20:13–14 | 4 |
| Sloane EB, Liberatore MJ, Nydick RL, Luo W, Chung QB. Using the analytic hierarchy process as a clinical engineering tool to facilitate an iterative, multidisciplinary, microeconomic health technology assessment. Comput Oper Res 2003;30:1447–65 | 2 |
| Stephen DS. Simulation applications for human factors and systems evaluation. Anesthesiol Clin 2007;25:237–59 | 7 |
| Smit EM, van Beek EJ, Bakker AJ, Reekers JA. Hemodynamic effects and image quality of low-osmolar ionic and nonionic contrast media during pulmonary angiography. Acad Radiol 1995;2:609–13 | 2 |
| Smith PC, Mossialos E, Papanicolas I, Leatherman S. Performance Measurement for Health System Improvements – (Part III Analytical Methodology for Performance Measurement). WHO Regional Office for Europe. Copenhagen: WHO; 2011 | 4 |
| Smith M. Vital signs. Shared public safety network. Emerg Med Serv 2000;29:26–7 | 4 |
| Smith Jr SC, Feldman TE, Hirshfeld Jr JW, Carabello BA, Erwin JP, Guyton RA. ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). J Am Coll Cardiol 2006;47:e1–121 | 2 |
| Smith RD, Chanda R, Tangcharoensathien V. Trade in health-related services. Lancet 2009;373:593–601 | 1 |
| Smith M. Build a safety net. It’s prudent, professional and practical. EMS Mag 2010;39:22 | 4 |
| Snooks H. Safer (support and assessment for fall emergency referals) trial: study design. Emerg Med 2009;26:4 | 5 |
| Solberg LI, Asplin BR, Weinick RM, Magid DJ. Emergency department crowding: consensus development of potential measures. Ann Emerg Med 2003;42:824–34 | 2 |
| Solheim J, Papa A. Cutting-edge discussions of management, policy, and program issues in emergency care. J Emerg Nurs 2011;37:90–5 | 2 |
| Somnay AR, McDermott PN, Alecu R. 101 Clinical implementation of the varisource high dose rate remote afterloader. Radiother Oncol 1996;39(Suppl. 1):S26 | 1 |
| Søreide E, Deakin CD. Pre-hospital fluid therapy in the critically injured patient – a clinical update. Injury 2005;36:1001–10 | 4 |
| Soufir L, Auroy Y. Champ 2. Épidémiologie (erreurs médicales et événements indésirables patients). Ann Fr Anesth Reanim 2008;27:e59–63 | 2 |
| Soufir L, Auroy Y. Sécurisation des procédures à risque en réanimation (risques infectieux exclus). Réanimation 2008;17:517–21 | 2 |
| Soulat L. For which Patient is it Necessary to Give Prasugrel in Pre-Hospital Sitting? Congres thrombose et urgences coronaires. Paris: SAMU; 2011 | 8 |
| Soyka PA, Feldman SJ. Capturing the business value of EH&S excellence. Corporate Environ Strategy 1998;5:61–8 | 2 |
| Spector P. To the editor: my patients’ safety, as well as my own, is in jeopardy. Revolution 1995;5:5 | 4 |
| Spedding LS. Environmental due diligence and risk management: sustainability and corporate governance. In Spedding LS. Due Diligence Handbook: Corporate Governance, Risk Management and Business Planning. Oxford: CIMA Publishing; 2009. pp. 535–64 | 4 |
| Stefanidis D, Swiderski DM. Carolinas Simulation Center. J Surg Educ 2010;67:262–4 | 7 |
| Stern AW. 10 ways to control errors in EMS. Learning from and preventing mistakes. JEMS 2005;30:70–9 | 4 |
| Sterud B. Prehospital trauma management in northern Norway: where are the weak links in rural areas? Can we improve? Acta Anaesth Scand Suppl 2001;115:43 | 6 |
| Stewart RD. Things are seldom what they seem . . . . Ann Emerg Med 1989;18:1015–17 | 4 |
| Stewart JA. Delayed defibrillation caused by unexpected ECG artifact. Ann Emerg Med 2008;52:515–18 | 7 |
| Stewart RM, Geoghegan K, Myers JG, Sirinek KR, Corneille MG, Mueller D. Malpractice risk and cost are significantly reduced after tort reform. J Am Coll Surg 2011;212:463–7 | 2 |
| Stillsmoking KL. Simulation scenario building. In Kyle R, Bosseau Murray W. Clinical Simulation. Oxford: Academic Press; pp. 535–40 | 4 |
| Stoker MR. Care and monitoring of the anaesthetized patient including the prevention of injuries. Surgery 2002;20:60–6 | 2 |
| Strange JW. Assessment and management of acute coronary syndrome. Found Years 2008;4:99–105 | 4 |
| Stuart R. The challenges and opportunities of the Chemical Hygiene Officer. J Chem Health Saf 2009;16:11–15 | 1 |
| Strong C, Thompson CB. Documentation of decision-making during air transport. Air Med J 2000;19:77–82 | 9 |
| Subhas K, Appleby I. Traumatic brain injury: initial resuscitation and transfer. Anaesth Intensive Care Med 2011;12:201–3 | 4 |
| Sun LL, Song KJ. Optimal Control of Active Ambulance Stretcher Suspension. Materials Science Forum 2004;471–2:312–616 | 4 |
| Sun BC, Mohanty SA, Weiss R, Tadeo R, Hasbrouck M, Koenig W. Effects of hospital closures and hospital characteristics on emergency department ambulance diversion, Los Angeles County, 1998 to 2004. Ann Emerg Med 2006;47:309–16 | 1 |
| Suresh MS, Munnur U, Wali A. The patient with a full stomach. In Carin A, Hagberg MD, eds. Benumof’s Airway Management. 2nd edn. Philadelphia, PA: Mosby; 2007. pp. 756–82 | 2 |
| Sutherland JW. A prospective on macrocybernetic process management systems. Technol Forec Soc Change 1997;55:215–48 | 7 |
| Sutton J, Valentine J, Rayment K. Staff views on the extended role of health care assistants in the critical care unit. Intensive Crit Care Nurs 2004;20:249–56 | 2 |
| Szucs P, Richman P, Mandell M. Triage nurse application of the Ottawa knee rule. Acad Emerg Med 2001;8:112–16 | 2 |
| Taheri PA, Butz DA, Anderson S, Boothman R, Blanco OL, Greenfield LJ, et al. Medical liability – the crisis, the reality, and the data: the University of Michigan story. J Am Coll Surg 2006;203:290–6 | 1 |
| Tam CM, Tam VWY, Tsui WS. Green construction assessment for environmental management in the construction industry of Hong Kong. Int J Proj Manag 2004;22:563–71 | 1 |
| Telion C, Carli P. Prehospital and emergency room pain management for the adult trauma patient. Tech Reg Anesth Pain Manag 2002;6:2–9 | 4 |
| Terlaak A, King AA. The effect of certification with the ISO 9000 Quality Management Standard: a signaling approach. J Econ Behav Organ 2006;60:579–602 | 1 |
| Anonymous. AMR, AEV & safety experts create safer ambulance. EMS Insider 2004;31:7 | 4 |
| Thevenin A, Chenet V, Schlumberger S, Fischler M. Expérience d’un système de recueil d’évènements indésirables en anesthésie. Ann Fr Anesth Reanim 2009;28:838–43 | 2 |
| Thomas L, Pollak PT. Delayed recovery associated with persistent serum concentrations after clozapine overdose. J Emerg Med 2003;25:61–6 | 7 |
| Thomas HA, Binder LS, Chapman DM, Kramer DA, LaMantia J, Perina DG. The 2003 model of the clinical practice of emergency medicine: the 2005 update. Ann Emerg Med 2006;48:e1–17 | 7 |
| Thomas HA, Beeson MS, Binder LS, Brunett PH, Carter MA, Chisholm CD. The 2005 model of the clinical practice of emergency medicine: the 2007 update. Ann Emerg Med 2008;52:e1–17 | 7 |
| Thomas Roger E, Russell M, Lorenzetti D. Interventions to increase influenza vaccination rates of those 60 years and older in the community. Cochrane Database Syst Rev 2010;9:CD005188 | 1 |
| Thompson L. Patient safety and risk management. Ther Wkly 2004;30:12–13 | 2 |
| Thomsen TW, Sayah AJ, Eckstein M, Hutson HR. Emergency medical services providers and weapons in the prehospital setting. Prehosp Emerg Care 2000;4:209–16 | 3 |
| Thorby R, Maybin J. A High-Performing NHS? A Review of Progress 1997–2010. London: The King’s Fund; 2010 | 7 |
| Tiah L, Wong E, Chen MFJ, Sadarangani SP. Should there be a change in the teaching of airway management in the medical school curriculum? Resuscitation 2005;64:87–91 | 3 |
| Tiefenbrunn AJ, Sobel BE. Thrombolysis and myocardial infarction. Fibrinolysis 1991;5:1–15 | 4 |
| Taylor TB. Emergency Medical Treatment and Labor Act (EMTALA). In Jill MB, Md, Mbe, eds. Pediatric Emergency Medicine. Philadelphia, PA: W.B. Saunders; 2008. pp. 1053–61 | 4 |
| Touati N, Pomey M-P. Accreditation at a crossroads: are we on the right track? Health Policy 2009;90:156–65 | 1 |
| Trossman S. A move toward safety. Am J Nurs 2006;106:81–3 | 3 |
| Trucco P, Cavallin M. A quantitative approach to clinical risk assessment: the CREA method. Saf Sci 2006;44:491–513 | 2 |
| Terence MCT, Chuang CC, Chi CH. Utilization of communication technology to improve team recall efficiency. Prehosp Disaster Med 2002;17(Suppl. 2):S85 | 2 |
| Tsiknakis M, Kouroubali A. Organizational factors affecting successful adoption of innovative eHealth services: a case study employing the FITT framework. Int J Med Inf 2009;78:39–52 | 7 |
| Tzeng S-F, Chen W-H, Pai F-Y. Evaluating the business value of RFID: evidence from five case studies. Int J Prod Econ 2008;112:601–13 | 7 |
| Udaeta ME, Weiner GM. Alternative ventilation strategies: laryngeal masks. Clin Perinatol 2006;33:99–110 | 2 |
| Umble M, Umble EJ. Utilizing buffer management to improve performance in a healthcare environment. Eur J Oper Res 2006;174:1060–75 | 4 |
| Usagawa T, Iwatsubo Y, Nishimura T, Nishimura Y, Chiaski Y. An Active Control System of Ambulance Siren by means of Loudspeakers Mounted in Headrest. Noise control engineering. Proceedings of inter-noise, CD-ROM edition. N565. Inter-noise 2003 Secretariat; International congress and exposition; 32nd, Noise control engineering: Seoul; 2003 | 1 |
| Vaillancourt C, Charette M, Kasaboski A, Maloney J, Wells GA, Stiell IG. Evaluation of the safety of C-spine clearance by paramedics: design and methodology. BMC Emerg 2011;11:1 | 6 |
| Valenzuela TD, Criss EA, Spaite DW, Meislin HW. Evaluation of EMS management training offered during emergency medicine residency training. Ann Emerg Med 1989;18:812–14 | 1 |
| Valunzuela TD. EMS data collection: filling in the dots. Ann Emerg Med 1991;20:1381–2 | 4 |
| Varghese M. Technologies, therapies, emotions and empiricism in pre-hospital care. In Mohan D, Tiwari GN, editors. Injury Prevention and Control. Abingdon: Taylor and Francis; 2000 | 4 |
| Verschoor AH, Reijnders L. Toxics reduction in ten large companies, why and how. J Clean Prod 2000;8:69–78 | 1 |
| Vicente V, Ekebergh M, Castren M, Sjöstrand F, Svensson L, Sundström BW. Differentiating frailty in older people using the Swedish ambulance service: a retrospective audit. Int Emerg Nurs 2012;20:228–35 | 7 |
| Vilke GM, Brown L, Skogland P, Simmons C, Guss DA. Approach to decreasing emergency department ambulance diversion hours. J Emerg Med 2004;26:189–92 | 4 |
| von Goedecke A, Wenzel V, Hörmann C, Voelckel WG, Wagner-Berger HG, Zecha-Stallinger A, et al. Effects of face mask ventilation in apneic patients with a resuscitation ventilator in comparison with a bag-valve-mask. J Emerg Med 2006;30:63–7 | 1 |
| Vourvahakis D, Giannakoudakis N, Pyrros D, Panagopoulos D, Gatsouli M, Lampakis S. Trauma in East Crete. Prehosp Disaster Med 2002;17(Suppl. 2):S10 | 7 |
| Wade EL. Computer applications. Going mobile: first responders get information in the palm of their hand. Occup Health Saf 2002;71:30–2 | 4 |
| Wagner MJ, Wolf S, Promes S, McGee D, Hobgood C, Doty C. Duty hours in emergency medicine: balancing patient safety, resident wellness, and the resident training experience: a consensus response to the 2008 institute of medicine resident duty hours recommendations. J Emerg Med 2010;39:348–55 | 2 |
| Wagner W. Drug safety in the emergency service. Arzneimittelsicherheit Im Rettungsdienst [German]. Deutsche Apotheker Zeitung 1992;132:2297–301 | 4 |
| Wagner-Berger HG, Wenzel V, Stallinger A, Voelckel WG, Rheinberger K, Augenstein S. Optimizing bag–valve–mask ventilation with a new mouth-to-bag resuscitator. Resuscitation 2003;56:191–8 | 7 |
| Wagner-Berger HG, Wenzel V, Stallinger A, Voelckel WG, Rheinberger K, Stadlbauer KH. Decreasing peak flow rate with a new bag-valve-mask device: effects on respiratory mechanics, and gas distribution in a bench model of an unprotected airway. Resuscitation 2003;57:193–9 | 7 |
| Walden V, Lamond EA, Field SA. Container contamination as a possible source of a diarrhea outbreak in Abou Shouk Camp in Darfur Province, Sudan. Prehosp Disaster Med 2005;20(Suppl. 2):s128–9 | 1 |
| Wall IF. Lack of training in custodial medicine in the UK – a cause for concern? J Forensic Leg Med 2008;15:378–81 | 2 |
| Anonymous. Patient-handling mishaps top cause of injury claims. EMS Insider 2007;34:1, 10 | 4 |
| Wang HE, Fairbanks RJ, Shah MN, Abo BN, Yealy DM. Tort claims and adverse events in emergency medical services. Ann Emerg Med 2008;52:256–62 | 1 |
| Wankhade P. Performance measurement and the UK emergency ambulance service: unintended consequences of the ambulance response time targets. Int J Public Sector Manag 2011;24:384–402 | 7 |
| Watt K, Enraght-Moony E. Transportation of aggressive patients to hospital: rage against the machine. J Emerg Prim Health Care 2007;5:1p | 7 |
| Watterson D, Cleland H, Darton A, Edgar D, Fong J, Harvey J, et al. Developing clinical quality indicators for a Bi-National Burn Registry. Burns 2011;37:1296–308 | 1 |
| Webb PJ. Information gathering, site characterization, and information resources. In William FM, Michael G, eds. Protecting Personnel at Hazardous Waste Site. 3rd edn. Woburn: Butterworth-Heinemann; 2000. pp. 23–50 | 1 |
| Webster S, Malone G. 2000 Olympic Games: the Sydney experiences in large-scale preparation for major incidents and counter terrorism. Prehosp Disaster Med 2002;17(Suppl. 2):S53 | 1 |
| Weekes AJ, Quirke DP. Emergency echocardiography. Emerg Med Clin N Am 2011;29:759–87 | 7 |
| Weinger MB, Vredenburgh AG, Schumann CM, Macario A, Williams KJ, Kalsher MJ. Quantitative description of the workload associated with airway management procedures. J Clin Anesth 2000;12:273–82 | 7 |
| Weinstein EP, Sayre MR, Mistler AF, Evans JL, Kramer AT, Pancioli AM. Endotracheal intubation by basic EMTs. Ann Emerg Med 1998;32:391–2 | 4 |
| Weitemeyer L. Prehospital treatment of patients with obstructive lung disease. Acta Anaesth Scand Suppl 2001;115:76 | 1 |
| Welch S, Savitz L. Exploring strategies to improve emergency department intake. J Emerg Med 2012;43:149–58 | 2 |
| Werfel P. Case of the month. When trauma masks a medical emergency. JEMS 2002;27:24 | 4 |
| Werman HA. Medical direction of air ambulance services. Top Emerg Med 1994;16:10–20 | 4 |
| West K. Ryan White Notification Law for emergency response employees deleted: 10 reasons why we need it back. EMS Mag 2008;37:24 | 3 |
| Westbrook MT, Braithwaite J, Travaglia JF, Jorm C, Iedema RA. Promoting safety: longer-term responses of three health professional groups to a safety improvement programme. Int J Health Care Qual Assur 2007;20:555–71 | 7 |
| Weydahl PG. Prehospital reversion of a heart attack. A matter of team work along the chain of survival. Acta Anaesth Scand Suppl 2001;115:42 | 9 |
| Whately J, Plummer R. Helicopter emergency medical services. More than just a change in uniform. JEMS 1994;19:38–40, 43–44 | 4 |
| White BA, Brown DFM, Sinclair J, Chang Y, Carignan S, McIntyre J, et al. Supplemented Triage and Rapid Treatment (START) improves performance measures in the Emergency Department. J Emerg Med 2012;42:322–8 | 2 |
| Whiteley D. Report on the Lessons Learned from the Summer 2007 Flooding Experiences from an Estates and Facilities Perspective. London: Department of Health; 2008 | 1 |
| WHO. Report of the Second Session. WHO Regional Office for Europe. Copenhagen: WHO; 2005 | 7 |
| Widner-Kolberg MR. Immobilizing children in care safety seats – why, when, and how. J Emerg Nurs 1991;17:427–8 | 4 |
| Wik L, Hansen TB, Fylling F, Steen T, Vaagenes P, Auestad BH, et al. Delaying defibrillation to give basic cardiopulmonary resuscitation to patients with out-of-hospital ventricular fibrillation: a randomized trial. JAMA 2003;289:1389–95 | 9 |
| Willems HGM. Turning environmental concerns into environmental care in the chemical industry in the Netherlands. J Clean Prod 1994;2:173–9 | 1 |
| Williams KA, Rose WD, Simon R. Teamwork in emergency medical services. Air Med J 1999;18:149–53 | 4 |
| Williams D, Padmanabhan V. Substance misuse and intoxication in adolescents. Found Years 2009;5:67–71 | 1 |
| Williams NN, Mittal MK, Dumon KR, Matika G, Pray LA, Resnick AS, et al. Penn Medicine Clinical Simulation Center. J Surg Educ 2011;68:83–6 | 2 |
| Williams S, Coombs M, Lattimer V. Workforce Planning for Critical Care: A Rapid Review of the Literature (1990–2003). London: Department of Health; 2003 | 2 |
| Williams S. Speaking up saves lives: the National Patient Safety Agency. J Clin Excellence 2003;4:272–4 | 4 |
| Williams DM, Zalar CM. The risky side of response. Increasing fatalities underscore the need for reconciled safety practices of ground & air ambulances. JEMS 2007;32:58, 60–64, 67 | 1 |
| Williamson J. IAHCSMM annual meeting roundup. [German, English]. Int J Sterile Supply 2011;19:224–7 | 1 |
| Willis CD, Gabbe BJ, Cameron PA. Measuring quality in trauma care. Injury 2007;38:527–37 | 7 |
| Wilson R. Improving clinical handover in emergency departments. Emerg Nurse 2011;18:22–6 | 2 |
| Wiskow C, Albreht T, de Pietro C. How to Create an Attractive and Supportive Working Environment for Health Professionals. WHO Regional Office for Europe. Copenhagen: WHO; 2010 | 7 |
| Wolfberg D. Legal consult. Medical errors: saying ‘I’m sorry’ under the law. EMS Insider 2011;38:2–3 | 4 |
| Wood IV. Medical affairs an attractive option for pharmacists. Pharm J 2008;280:120 | 2 |
| Woodhall LJ, Vertacnik L, McLaughlin M. Implementation of the SBAR communication technique in a tertiary center. J Emerg Nurs 2008;34:314–17 | 2 |
| Worley GH. Helicopter air medical transport safety: what is the role of the emergency nurse? J Emerg Nurs 2009;35:152–3 | 1 |
| Wretstrand A, Petzall J, Bylund PO, Falkmer T. Reducing non-collision injuries in special transportation services by enhanced safety culture. Med Eng Phys 2010;32:254–62 | 7 |
| Wright AS, Kim S, Ross B, Pellegrini C. ISIS: the Institute for Simulation and Interprofessional Studies at the University of Washington. J Surg Educ 2011;68:94–6 | 1 |
| Wright RS, Burdumy TJ. Acute endotracheal tube occlusion caused by use of an esophageal detector device: report of a case and a discussion of its utility. Ann Emerg Med 2004;43:626–9 | 2 |
| Wright D. Safety management vs. picking leaves. J Air Med Transport 1991;10:11–12 | 1 |
| Wu Y-CJ, Lee P-J. The use of patent analysis in assessing ITS innovations: US, Europe and Japan. Transport Res Part A Policy Pract 2007;41:568–86 | 7 |
| Wu J-R, Moser DK, Riegel B, McKinley S, Doering LV. Impact of prehospital delay in treatment seeking on in-hospital complications after acute myocardial infarction. J Cardiovasc Nurs 2011;26:184–93 | 1 |
| Yealy DM. Prehospital pain research. Ann Emerg Med 1996;27:471–3 | 1 |
| Youngs P. Anaesthetic priorities in pre-hospital trauma care. Anaesth Intensive Care Med 2008;9:384–6 | 4 |
| Zafar N, Mohammad A, Jlala H, Winter B. Checking pupils from the head-end of a patient during an ambulance transfer. J Intensive Care Soc 2010;11:10–12 | 4 |
| Zavod RM. Professionalism, programs, and perspectives. Curr Pharm Teach Learn 2009;1:65 | 3 |
| Zeller SL, Rhoades RW. Systematic reviews of assessment measures and pharmacologic treatments for agitation. Clin Ther 2010;32:403–25 | 2 |
| Zehner J. Health information management and the EMR. In Thomas P, ed. Practical Guide to Clinical Computing Systems. New York, NY: Academic Press; 2008. pp. 157–69 | 2 |
| Zhang C, Thompson S, Miller C. A review of simulation-based interprofessional education. Clin Sim Nurs 2011;7:e117–26 | 3 |
| Zigmont JJ, Kappus LJ, Sudikoff SN. Theoretical foundations of learning through simulation. Semin Perinatol 2011;35:47–51 | 7 |
| Zimmermann PG. Cutting-edge discussions of management, policy, and program issues in emergency care. J Emerg Nurs 2006;32:178–85 | 2 |
| Ziv A, Rubin O, Sidi A, Berkenstadt H. Credentialing and certifying with simulation. Anesthesiol Clin 2007;25:261–9 | 1 |
| Ziv A, Erez D, Berkenstadt H. Clinical simulation on a national level: Israel. In Kyle R, Bosseau Murray W. Clinical Simulation. Oxford: Academic Press; 2008. pp. 371–5 | 4 |
| Zonfrillo MR, Mello MJ, Palmisciano LM. Usefulness of computerized pediatric motor vehicle safety discharge instructions. Acad Emerg Med 2003;10:1131–3 | 1 |
| Digital ECG Transmission from Ambulance Cars with Application of the European Standard Communications Protocol SCP-ECG. Computers in Cardiology. Bethesda, MD: IEEE Computer Society Press; 1994 | 9 |
Appendix 5 Reasons for exclusion and numbers of papers excluded
| Reason for exclusion | Number of excluded papers (n = 1025) |
|---|---|
| Off topic, for example road traffic collisions | 254 |
| Considered the wrong setting | 207 |
| Considered the wrong population, for example related to the safety of staff rather than patients | 52 |
| Did not provide research methods, overviews, opinion, letters, comments, etc. | 281 |
| Research was reported elsewhere | 13 |
| Study was in progress or planned with no preliminary findings reported | 10 |
| These studies were not specific to ambulance services but covered general care/guidance instead | 188 |
| English abstract was not available | 3 |
| Research had been superseded | 12 |
| Disaster or military context | 4 |
| Retracted paper | 1 |
Appendix 6 Annual report data extraction sheets
Annual report data extraction sheet for ambulance services 1–4
| Ambulance service | ||||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| Patient safety mentioned | No | Twice | 1 × in statement of internal control | Whole chapter ‘Clinical care and patient safety’ dedicated to patient safety |
| Patient safety issues mentioned | ||||
| Cleanliness/infection | In internal control section | Cleanliness audits for vehicles | Fleet maintenance team follow thorough maintenance schedule. Deep clean of stretcher, trolleys and other big equipment, supply of spill kits and sanitising wipes. Employment of ambulance hygiene assistants | |
| Safeguarding | In internal control section | Committed to safeguarding, training for trust board and executive team, level two training for front-line staff, executive safeguarding lead | Independent consultant to review safeguarding procedures, increase of staff awareness through training resulted in increase of referrals | |
| Response time targets | ||||
| Category A (life-threatening): 75% within 8 minutes | Met category A performance standard B, 78.2% | 74.6% | 73.72% | 75.8% |
| Category A (life-threatening): 95% within 19 minutes | 95.6% | 97.38% | 98.53% | |
| Category B (non-life-threatening): 95% within 19 minutes | 93.1% | 93.69% | 93.4% | |
| Others | Mental health and end-of-life care | Improve management of pain as a result of interviews and patient experiences (including paediatrics) | Improved pain relief | Managing medicine group. Data protection, sharing info and keeping it safe |
| Improved care | ||||
| NHS pathways/alternative pathways | TIA patient care pathway | Referral to alternative pathways, nursing and care home support | ||
| PRF | Electronic patient care record rolled out to improve patient experience and patient safety, collecting real time clinical data to measure clinical performance and patient outcome | |||
| See/hear and treat/referral | Taking stroke patients to stroke units – specialist centres, major trauma centres and local trauma units, specialist centres for cardiac care, extended hear and treat/referral for less serious conditions | Clinical support desk to enhance telephone triage for less serious conditions, thrombolysis services | Clinical hub (call centre) for non-life-threatening conditions | |
| Others | Defibrillators in public places | Emergency care assistants, training paramedics for enhanced triage assessment, computerised-assisted dispatch, 91 new PTS vehicles for more comfort, 56 new A&E vehicles, roll out of mobile data system for more effective communication, a PCR submission audit tool for intranet to improve quality of completed PCR and patient handover, resuscitation training | New operational models: rapid response vehicle to most incidents then determine next level of care, enhanced training for front-line staff (including obstetrics) and additional paramedics; working with hospitals on service changes; radio tracking for cycle response unit; virtual call centre – calls answerable by other call centres; roll out of digital radios for better communication; updated dispatch system; electronic link with NHS direct for seamless data transfer; mobile data terminals; PTS improved and upgraded; 40 new ambulances for efficient and comfortable transport, two 4 × 4s, five PTS stretcher vehicles and 89 defibrillators | Continued use of NHS pathways; accredited as NHS pathways training site, introduction of 111 service as pathfinder. Roll out of ePRF for more robust recording and validating patient info. Reinforcement around the see and treat procedure. Enhancement of community first responder scheme; transformation of the PTS fleet maintenance; guide to using ambulance service for pregnant ladies and GPs developed to reduce the use of emergency ambulance service |
| SUIs | Two reported | None | ||
| Incidents reporting | 200 incident reports from other health and social care agencies | Serious incidents, n = 5; patient safety incidents, n = 35; clinical negligence, n = 7; transparent and thorough reporting well-establish policy and procedure. Incidents reported to Governance and Risk Committee, then to Quality Committee. Methods of reporting: clinical risk register; general incident reporting system; using incident report form; whistle blowing policy (three incidents reported); incidents investigated by root cause analysis panel. Examples of learning from incidents: improvement in standard of completed PRF; reinforcement around the See and Treat procedure; learning academy for new call handler; coaching for those call handlers needing on-going support; reflection and learning events; reorganisation and revision of jobs. Any incidents reported to NPSA ( n = 43), automatically uploaded and electronically transferred after validation | ||
| Complaints | About n = 500. Improving service through response to feedback | n = 530. Set up of learning group to deal with info from complaints, incidents and performance indicators | n = 210, includes types of complaints. Complaints policy working to ‘principles for remedy’, examples are given to illustrate learning from complaints, for example Clinical Practice Circular. Amended wording used in triage. Audits for complaints. ‘Experience, complaints, litigation, incidents and PALS’ Group introduced which is accountable to Quality Committee | |
| CQC compliance status | Unconditional registration | Unconditional registration | Unconditional registration | Unconditional registration |
| NHSLA level | Level 1 | Level 1 | ||
| Recognition of new clinical indicators | Yes | Yes | Yes | Not mentioned |
| Public involvement/patient experience | LINk involvement; publication of case studies on website | LINk involvement; blood pressure checks, and stroke info at different events; discovery interviews to get patient experiences | LINk involvement | Public involvement in foundation trust bid: visits to public about accident prevention, safety workshops for children what to do in case of emergency. Creating ways of collecting patient experiences. LINk involvement |
| End-of-life care | Information about end-of-life care included in the computerised assisted dispatch | End-of-life transport policy updated | ||
| Patient safety activities | ||||
| Awareness campaign | Facilitated eight NIHR studies | |||
| Research | ‘Research-friendly’ environment | |||
| Others | Master degree course funding for paramedics – research is crucial to improving patient outcome | |||
| Safety culture; non-punitive reporting system; being open culture | Committed to safety and public accountability by being open about matters when something goes wrong | Complies with code of practice on openness, public can gain information | Director of Clinical Care and Patient safety. Establishment of Quality Committee reviewing issues on clinical care and patient safety; being open and accountable; encouragement and support of staff to report incidents; implementing a proactive patient safety culture; and receive and contribute alerts and guidance from/to Central Alerting System. Carried out 16 clinical audits resulting in changes such as introduction of Quality Improvement Officer; staff clinical practice circular, quality improvement workshops. Clinical audit on performance in line with five national clinical performance indicators | |
| Internal control | Since 2010 new post: Director of Health Promotion and Quality to manage risks concerning infection prevention and control and safeguarding. Systems are in place to monitor compliance throughout the year with CQC compliance. Actions to minimise risk: 390 new model defibrillators, CPR training to the public, 72 new modern ambulances, clinical care pathways are being developed, action plans being prepared to address weaknesses in respect of stock holding, reporting of losses and monitoring of losses, and implementing new computer-aided dispatch system. Complaints, incidents, patient experiences and claims are all indicators of risk and are managed and reported in line with our policy. We operate a policy of openness and transparency, Learning from Experience group, and two serious incidents concerning patient information took place | Takes holistic approach to risk, risk management committee in place. The medical director has lead responsibility for clinical risk management and patient safety, ensuring that all clinical procedural documents are maintained and current. Major risks identified: risk of failing response time targets and the potential adverse impact on clinical outcome. Mitigated a risk by upgrading computer-aided dispatch system to deliver consistent and efficient response service. One SUI; fully compliant with CQC standards. Trust board: monthly performance reports outlining achievement against key performance, safety and quality indicators | Governance and Risk Committee and Quality consider non clinical and clinical risks. Risks are identified via system of risk registers and incident reporting system and quantified with Risk Scoring Matrix. Clinical Risk is monitored via Quality Committee; clinical risk is everyone’s responsibility and is managed by operational staff and specialist managers. Quality Committee monitors quality of patient care (safety, effectiveness, experience), to learn from letters of appreciation and complaints. Limited number of gaps in assurance and/or control in areas of operation, urgent care reform, workforce planning, training, information clinical governance, finance and preparation for foundation status, not classed as significant, with plans to address issues | |
| Foundation trust status | Application in process, aim for early 2012 | Application in process, aim for early 2013 | Application in process, aim for 2012 | Foundation trust status will improve patient outcomes and experiences. Hoping for authorisation in autumn 2011 |
Annual report data extraction sheet for ambulance services 5–8
| Ambulance service | ||||
|---|---|---|---|---|
| 5 | 6 | 7 | 8 | |
| Patient safety mentioned | 1 of 3 quality priorities in quality report section | Yes (whole chapter ‘Quality and safety’ dedicated to patient safety) | The paragraph under nursing and quality directorate | Twice |
| Patient safety issues mentioned | ||||
| Cleanliness/infection | ‘Cleaner Care’ initiative, deep clean of ambulances every 8 weeks | Reduced health-care acquired infections, through our ‘Make Ready’ scheme | New audit programme focused on cleanliness of premises, vehicles and observed practice of staff. Strategic infection, prevention and control group | IPC responsibility of all, one station clean contract, new audit programme, expansion of make ready programme |
| Safeguarding | Staff are supported to attend reviews following incidents as often as possible in order to enhance learning and improve practice in safeguarding | Safeguarding awareness campaign, increased uptake of safeguarding training, observed practice audits and the introduction of clinical supervision. Two full-time leads for safeguarding appointed. The change in the safeguarding reporting process to a verbal referral through a dedicated number. Development of the safeguarding database | Safeguarding responsibility of all, advice and information on staff intranet | |
| Response time targets | ||||
| Category A (immediately life-threatening) 75% in 8 minutes | 76.86% | 77.5% | 72.38% | 74.3% |
| Category A (immediately life-threatening) 95% in 19 minutes | 96.11% | 95.3% | NR | 95.1% |
| Category B (serious but not immediately life-threatening) 95% in 19 minutes | 95.58% | 91.4% | 88.28% | 91.38% |
| Others | Falls is patient safety priority for 2011/12: enhance falls referral system and increase in non-conveyance | Drive to reduce hospital handover delays | Asthma care | Dementia (raised staff awareness) and pain management in people with cognitive impairment (assessment tool implemented). Asthma, diabetic care, cardiac arrest and heart attack |
| Improved care | ||||
| NHS pathways/alternative pathways | NHS pathways (software decision-making package) to enable patients to receive the right response to their call. Fall patients referred to falls service and fall alert pathway to be developed. Engagement with local trauma networks | Appropriate pathways are used for patients, directed either on scene or on the phone, highest non-conveyance rate | Clinical assessment and advice service (nurse led) providing patients with alternative care pathways | Individualised care plans held for > 2000 people about alternative care pathways. Developing a clinical desk to identify alternative care pathways for patients to avoid hospital admission |
| PRF | Electronic care system to electronically capture patient data to improve data flow and analysis | Electronic patient records to connect with GP, ability to access patients’ summary care record. This will improve patient safety as staff will know about pre-existing medical conditions, medications and allergies, and patient’s wishes, such as end-of-life care | Laptops and computer system to access patient records for out-of-hours service | |
| See/hear and treat/referral | Safety netting to be put in place for non-conveyed patients to further patient safety. Three digit number service. ‘Single point of access’ service | The introduction of the clinical support desk in the triaging of calls improved patient experience and outcome. Assessment and treatment without conveyance. Clinical support desk staffed by nurses and ECPs for assessment, advice and referral | PPCI catheter suits; stroke centres; improving patient care by non-conveyance | Prioritise non-emergency calls, advise and refer; new model of service delivery to better match patient needs; triage software for category C calls for advice and signposting to alternative pathways; crew referral pathways are devised for see and treat |
| Others | Provide/replace all PTS vehicles with external defibrillators. Ambulance radio project: airwave system radios for vehicles to enable real time communication with control rooms. Pathways support vehicles; category C audit to improve patient experience and reduce avoidable admissions. Medicines management implementation plan: development of enhanced policies and procedures including standardised format for providing clinical updates to ED to ensure patient safety; 280 medication errors reported; employment of ambulance pharmaceutical advisor. Manual handling equipment (compressed air lifting cushions) introduced for improved patient comfort; investment in high-tech fleet; enable ambulance care assistants to progress to paramedics through training; and recertification training for ambulance staff, skill enhancement of paramedics. Improved pain management: develop and train staff in scoring system, include patients with learning disability and dementia | Introduction of Virtual Computer-aided Despatch, sharing of resources between two call centres. Participated in pilot of 111 urgent care service number. New vehicles including wheelchair accessible vehicles and 4 × 4s. Airwave radio system included in vehicles | Automated external defibrillators in public places. New 4 × 4s, planning replacement of solo response vehicles and ambulances. New PTS vehicles and keeping fleet of emergency and support vehicles up to date and on the road with patient safety always in mind. Taking part in 111 pilot | |
| SUIs | ||||
| Incidence reporting | 280 medication errors reported | Effective incident reporting system, good level of reporting (in statement of internal control) | All staff trained in risk assessment, incident reporting and patient safety, awareness campaign for recognising and reporting patient safety incidents, patient safety champions, safety projects set up four work streams – safe care, safe service, safe fleet and safe staff – introduction of Patient Stories to Board, development of a safety culture and monthly Patient Safety Visits by Board members | n = 22 SUIs. 2000 incidents reported; reported through the adverse incident reporting system. Demonstrates a culture in which staff are receptive to reporting incidents. To improve safety of all our patients we regularly report all patient safety incidents to the NPSA. Nine incidents of confidentiality breaches; 282 complaints – committed to learn from these; learning from the experiences and feedback of complainants and developing a culture of continuous improvement. Results from learning include: protocols for our call handlers have been reviewed to better identify stroke cases at an early stage and recruit and train additional staff |
| Complaints | n = 489 complaints. Learning from experience group brings together issues from adverse incidents, litigation, comments, concerns, complaints, compliments, audits, major incidents, safeguarding and information governance issues. Trust-wide learning through clinical articles and advisory documents | Listen to and learn from comments and complaints, complaints were outweighed 4 : 1 by compliments | n = 228; learning review groups to learn from incidents and complaints, PALS process made more streamlined risk management and patient safety team restructured to strengthen ability to deliver the risk management and patient safety work programme | |
| CQC compliance status | Unconditional registration | Unconditional registration | Full compliance | Full compliance |
| NHSLA level | Level 1 | Level 1 for 2 years | Level 1 aiming for level 2 | Level 1 aiming for level 2 |
| Recognition of new clinical indicators | Yes | Took part in developing, measuring, improving and piloting new clinical indicators for ambulance services | Yes | |
| Public involvement/patient experience. End-of-life care | Surveys carried out to improve patient experience. Know your blood pressure campaign; ‘You said, we did’ posters on website giving feedback to public; Senior Quality Experience Manager appointed to develop feedback service; involvement of LINk; ‘Respect and dignity leaflet’ on website in response to category C survey; and implementation of end-of-life care strategies and quality markers | Public involvement in foundation trust bid; involvement of LINk and public involvement panel | Public involvement: employment of a patient experience lead. Introduced patient stories to the board. Captured patient experience though shadowing patients on their journey. Regularly survey of category A, B and C calls and PTS patients. EoL care: to be included in ePRF single, standardised Do Not Resuscitate form to be used; developed end-of-life care registration system, which raised staff awareness | Know your blood pressure campaign; patient opinion website for online patient feedback; involvement of LINk; patient representative group – external reference group; surveys of PTS and category C patients |
| Patient safety activities | ||||
| Awareness campaign | Patient safety first campaign and patient safety awareness week: asthma | |||
| Research | Contributed to two UK CRN portfolio projects; participated in industry funded trial (patient outcome using mechanical chest compression device vs. standard CPR); study on head injury in children; research facilitator post funded externally | Focus on quality improvement and translational research, several publications: pain management, overdose and cannulation | Profile of research raised. High-quality research: NIHR – airway management during pre-hospital cardiac arrest; NIHRi4i – design for better cervical collar | |
| Others | Participate in quality improvement initiative to improve care for stroke and heart attack patients | Patient questionnaire on patient satisfaction | ||
| Safety culture; non-punitive reporting system; being open culture | In internal control | Development of a safety culture. Introduction of a being open policy | Committed to providing an open and non-judgemental approach to complaints | |
| Internal control | Director of corporate services leads responsibility for risk management. Induction workbook for all new staff with risk management section: the identification, rating and prioritisation of risk; incident reporting; and management of risk (including slips, trips and falls). Trends in incidents, complaints and claims are also considered in depth by the learning from experience group and lessons disseminated through newsletters and publications. Quality and Governance Committee: development and review of quality improvements including patient experience; patient safety; health and safety reports; risk management; identification of new risks; NHSLA implementation; learning from experience; infection prevention and control; implementation of NICE guidelines; clinical audit and effectiveness; clinical and non-clinical training; fleet; compliance; safeguarding updates; and feedback from subgroups | Integrated approach to risk management bringing together complaints, PALS, health and safety, security management and patient/clinical safety including child protection, infection control and medicines management. Under leadership of the Director of Patient Care, supported by Head of Governance and Risk Management, Head of Clinical Effectiveness, Consultant ECP and a Pharmacy Advisor. Developed a fair open reporting culture which encourages health professionals to report errors and ‘near misses’ without fear of blame or reprisal. Encourages both reactive and pro-active risk reporting from staff in order that learning and continual improvements can be made. Trust has in place induction training programme for all new staff, which includes health and safety, awareness of risk, and incident reporting and investigation. Trust’s Quality and Safety Committee is responsible for monitoring clinical performance, patient safety and the patient experience, providing assurance on these matters to the trust board. The Risk Management Policy provides guidance for managers and staff on incident reporting, investigation and risk assessment. The trust has in place an effective incident reporting system. There is evidence of a good level of staff both proactively and reactively reporting risks and incidents. The trust is committed to creating a culture which encourages reporting and is supportive of any member of staff that does so. The trust has in place a whistle blowing policy. A comprehensive web-based risk management database is in place that enables analysis and divisional benchmarking of adverse incidents, complaints, PALS enquiries and vehicle accidents. All serious incidents are reported, investigated and then reviewed by a group. A strategic risk register is in place. Expansion of ‘hear and treat’ and ‘see and treat’ services that avoid ED admission. Patient experience review group to review outcomes from compliments, complaints and PALS enquiries | Takes a holistic view of risk including the management of clinical risk as well as operational, financial, human resource and data security risks and includes identification of risk; analysis, control and treatment of risk; incident reporting and investigation; claims and complaints management; establishment and management of risk registers; educating staff on issues of risk; reporting incidents to the relevant external authorities; and achieving compliance with relevant statutory legislation | |
| Foundation trust status | Achieved | Application in process | Application in process, aim for early 2013 | Application in process, aim for Oct 2012 |
Annual report data extraction sheet for ambulance services 9–11
| Ambulance services | |||
|---|---|---|---|
| 9 | 10 | 11 | |
| Patient safety mentioned | No | Yes – whole chapter ‘Quality and safety’ dedicated to patient safety | Yes |
| Patient safety issues mentioned | |||
| Cleanliness/infection | Make Ready programme continued to be rolled out to minimise cross-infection and maximise patient safety | Make Ready programme continued to develop to minimise cross-infection and maximise patient safety | |
| Safeguarding | Safeguarding protocols recognised as best practice. Management of safeguarding referrals through a single point of access | Safeguarding policy and procedures have been reviewed and updated | |
| Response time targets | |||
| Category A: 75% in 8 minutes | 73.64% | 67.8% | 76.02% |
| Category A: 95% in 19 minutes | 95.66% | 98% | 97.68% |
| Category B: 95% in 19 minutes | NR | 95% | 94.29% |
| Others | Work with PCTs and acute trusts to manage demand and flow of patients to hospital and improve turnaround times at hospital. Completed installation of hospital arrival screens in A&E, provides hospitals with advance notification of ambulance activity. Turnaround times is a system issue with detrimental effect on ambulance availability and ability to deliver effective patient care | Patient falls identified as patient safety issue, learning through incidents resulted in 27% decrease in harm through falls | Raised awareness and understanding of staff in mental health. Training on information governance compliance rolled out |
| Improved care | |||
| NHS pathways/alternative pathways | Developing NHS pathways | Utilising clinical support desk. Clinicians will direct patients to the most appropriate point of care. Development of clinical pathways for heart attack, stroke and asthma patients. Primary PCI centre | New clinical triage system (NHS pathways) will replace current AMPDS system including NHS primary care services. Includes directory of health and social care services. Pre-hospital stroke pathways. Collaboration with NHS organisations to develop care pathways |
| PRF | Regional access to patient notes | Web-based access to patient clinical records | |
| See/hear and treat/referral | Senior clinical advice in control centres. Referral management team | ||
| Others | More efficient single command and control system in control centre for PTS. Education programmes for frontline staff in partnership with universities | Site assurance visits by non-executive directors in relation to patient safety and quality control | Critical care paramedics contribute to improved patient safety and outcome. New single computer-aided dispatch system was introduced to dispatch most appropriate care to patients. Numbers of paramedic practitioners grow, have undertaken further higher education to enable them to manage patients, ensure that patients are cared for in the community if possible, avoiding A&E. Introduced patient group direction medicines including painkillers and antibiotics. ‘Telemedicine’ pilot for patients with burns, plastic surgery needs and hand injuries to send clinical photographs to the specialists who provide advice, treatment and referral options. Increasing number of critical care paramedics, ultrasound training course for CCPs. CCPs are attending an increasing amount of critical incidents and are contributing to improved patient safety and outcomes. Weight reduction in the latest batch of ambulances to reduce the effect of harmful emissions while, at the same time, ensuring that patient safety is not compromised. New vehicles delivered included 64 A&E ambulances, 30 PTS vehicles, one HART vehicle and 28 response cars. Standardisation of vehicles, equipment and supplies |
| SUIs | No SUIs | ||
| Incidents reporting | n = 27 (14 related to delays at hospitals, no data security incidents). The trust’s risk team ensures all serious incidents are thoroughly investigated, root causes established and actions implemented to reduce future risk. Nursing and quality directorate is focused on developing the analysis and learning from all reported incidents | Eight personal data related incidents. The trust reports the Information Governance SUIs, all incidents of losses of personal data rated as 1–5, to the SHA through the Strategic Executive Information System reporting process. The information commissioner will be informed of all category 3–5 incidents. The decision to inform any other bodies will also be taken, dependent on the circumstances of the incident, for example if this involves risks to the personal safety of patients, the NPSA may also need to be informed | |
| Complaints | n = 483 including 12 failure to convey complaints. Information on complaints is regularly reviewed and action plans monitored by an incident learning forum. Apply the ‘principles for remedy’ to produce reasonable, fair and proportionate remedies during its complaints handling processes | n = 273 | n = 321. Learning from complaints: weekly staff bulletin gives examples of complaints/incidents/near misses so that everyone can learn from these; operational staff attend key skills updates every year for additional training on issues raised by complaints/incidents; standardised report provided to trust board, commissioners, and risk management and clinical governance committee once every 2 months; apply the ‘principles for remedy’ to handle complaints; and established an incident review group which looks at serious issues and investigations and makes any additional recommendations |
| CQC compliance status | Unconditional registration | Full compliance | Full compliance |
| NHSLA level | |||
| Recognition of new clinical indicators | Yes | Yes | |
| Public involvement/patient experience | Patient experience programme. Activities under the leadership of Director of performance and patient experience. To gain insight into patient experience and feedback: established a communities subcommittee that monitors patient and public engagement activities; ‘crowd sourcing’ programme; face-to-face engagement with emergency service patients; web surveys; LINk involvement; ‘Listening to You’ section on website; and single number service for the patient experience team | Online feedback service for patient views | Patient experience workshop, where the complaints and PALS information we compile and share was discussed and debated with patient/public representatives, directors and managers of the trust. New interactive website. Three workshops took place with > 100 participants helping to identify practical mechanisms to enable ambulance service to better support the survivors of violence and early identification of violence. CPR demonstrations and workshop for resuscitating infants. See the Internal control row |
| End-of-life care | |||
| Patient safety activities | |||
| Awareness campaign | Patient safety campaign was launched that included improvements in training and education, closer monitoring and a general awareness of risk factors of patient falls | ||
| Research | |||
| Others | |||
| Safety culture | Promote an open and fair culture | Being open and accountable | |
| Non-punitive reporting system | |||
| Being open culture | |||
| Internal control | Directors, managers and staff have been provided with training, awareness and/or instruction with regard to risk management. Risk management is an integral part of good management practice and to be most effective should become part of the trust’s culture. Approved risk management policy. Identification of risks through incident reporting. Identified risks: harm through non-conveyance because of lack of clinical expertise; patient delays; lack of trained paramedics; failure to meet national targets; risk moderation subcommittee in place; and introduced a holistic approach to risk management across the organisation, including financial, organisational, clinical and non-clinical risks | Ownership of risk management has been improved through the revised committee responsibilities. Staff are provided with training and education to enable them to manage risks. Relevant themes and lessons arising from adverse incidents are taken into account in the focus of training programmes. Identified the following risks as potentially significant: failing to meet the nationally set standards for responding to emergency and urgent calls resulting in delay to patient care and loss of reputation; failing to deliver high quality safe and effective clinical care resulting in adverse effect on patients; failing to deliver education and training. Staff are unable to deliver a safe and effective service; and failing to provide a skilled workforce resulting in failure to deliver a safe service and poor patient outcome | Risk management is corporate responsibility. Board is committed to the continuous development of a framework to manage risks in a structured and focused way, in order to protect the trust from losses, damage to its reputation, or harm to its patients, staff, public and other stakeholders. Risk Management and Clinical Governance Committee oversees the management of all areas of risk; fully developed, maintained and comprehensive risk register a trust-wide database recording corporate risks identified from whatever source, the assessed level for current risk, and details of control measures or an action plan to reduce the risk; facilitate the SECAmb patient and public liaison group, and has three public opinion groups; engages with the public and patients through LINks and specific SECAmb workshops and events; and regular review and reports on the position of the risk register |
| Foundation trust status | Application in process, aim for Oct 2012 | Application in process, aim for end of 2012 | Achieved in March 2011 |
Appendix 7 Case descriptions for cases awarded ≥ £100,000 in damages from 1995/96 to 2010 (n = 15)
| Award | Outcome | Description of incident |
|---|---|---|
| £100,000 | Fatality | Called to a 35-year-old male with pain in his arm and chest. The patient suffered cardiac arrest and died |
| £100,000 | Fatality | Called to a patient who subsequently suffered a cardiac arrest; the patient was not transferred to further care |
| £100,000 | Fatality (child)/psychiatric/psychological damage (parents) | Called to a patient (child) with breathing difficulties. Parents attempted to clear airway. A paramedic and technician transferred patient to hospital but did not initiate resuscitation; resuscitative efforts at hospital were unsuccessful |
| £120,000 | Brain damage | Called to a patient (child) not breathing; CPR undertaken. The patient sustained brain damage |
| £120,000 | Fatality | Called to a patient but not transferred to further care; a second call 23 days later found the patient dead |
| £142,408 | Brain damage | Delay in transferring the patient to further care |
| £150,000 | Fatality | Called to a patient (adult) with a muscular injury. The patient was advised to consult their GP the next day; the patient consulted after 4 days and radiographs demonstrated a fractured hip. Failure to transfer the patient to further care was cited as negligence |
| £150,000 | Fatality | Called to a patient (adult) who was a known asthmatic. The patient inhaled furniture polish and was suffering increased breathlessness. The ambulance crew administered steroids and the patient was requested to walk to the ambulance. While being transferred to further care, the patient suffered a convulsion that led to respiratory and then cardiac arrest; advanced life support was undertaken en route |
| £115,000 | Unnecessary pain | Called to a patient; the crew did not transfer the patient to further care or complete the paperwork. The patient died the same day with an overdose of prescription medicine and alcohol abuse |
| £174,574 | Fatality | Called to a patient (child) suffering an asthmatic attack. Delayed response was cited as the cause of death |
| £190,000 | Fatality | Failure to transfer the patient to further care |
| £300,000 | Brain damage | Called to a patient (adult) in cardiac arrest. A delay in attending resulted in the patient, who is now in a permanent vegetative state, suffering brain damage. No details of the cause of the delay |
| £300,000 | Unnecessary pain | Patient suffered cardiac arrest while being transferred to further care |
| £500,000 | Brain damage | Called to an intoxicated patient with a head injury. The patient was transferred to further care without ‘back boarding’. The patient was found to have a fracture of the cervical spine and is now tetraplegic/quadriplegic |
| £2.8M | Brain damage | Called to a patient with an overdose. An airway adjunct was incorrectly inserted and the patient sustained irreversible brain damage |
Appendix 8 Medical directors’ questionnaire
Perceptions of Key Safety Issues in the Ambulance Service
Instructions
Please rate the items listed below in terms of your view of the degree of risk they present to the Ambulance Service, with 1 = very little to 10 = a great deal. Please circle the position that best represents your view. All responses will remain entirely confidential. We ask only for the name of the Ambulance Service responding. Please return to Professor Peter Spurgeon, Medical School, Warwick University, Gibbet Hill Road, Coventry, CV4 7AL.
Many thanks for your assistance.
Please state the name of your service here:
Please rate each item in terms of the degree of risk to the Ambulance Service in the following issues.
| Question | Very little | A great deal | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1) Delay in gaining access to hospital | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 2) Equipment failure/shortage | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 3) Call handling triage/categorisation | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 4) Decision to leave at home | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 5) Medication errors | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 6) Skill mix of staff available | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 7) Increased clinical intervention | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 8) Handover process in A&E | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 9) Resources available to respond | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 10) Allocation of patients at co-located sites (A&E/Minor Injury Units) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
Do you feel there are any other key safety issues not covered by this list? Yes/no
If yes please identify them:
Appendix 9 Areas of concern rated in the top five by ambulance personnel
Vehicle deep clean.
Paramedic knowledge.
Respondent 2More training on how to handle and speak to patients.
Respondent 3Staff are not fatigued as a result of long shiftworking.
Clinical knowledge factors: assessment, clinical decision-making ability, etc.
Level of education and training.
Patient language and communication.
Safety culture and priorities.
Respondent 4Protocols and guidelines: known and easily used (training/revalidation).
Communication: user/carer to ambulance staff (language?).
Use of correct vehicles.
Skill mix dispatched: appropriate?
Learning from mistakes: personal and organisational levels.
Respondent 5Communication (team, between staff and patients).
Staff physical and mental health.
Level of clinical knowledge and assessment skills.
Patient condition and illness.
Organisational culture.
Respondent 6Infection control.
Accessibility (especially for powered wheelchairs).
Training on hidden impairments, for example autism and other neurological conditions.
Patients who have particular allergies to allopathic medicines where the patient was unable to explain and was put at risk.
Respondent 7Training of all staff (clinical): ongoing/updating and poor attendance.
Staff with appropriate skills.
Long shifts.
Communication: people whose first language is not English.
Ensuring appropriate care for people with serious mental health problem.
Respondent 8Staff attitude.
Equal opportunities awareness.
Language and communication (other languages).
Professional knowledge.
General safety awareness.
Respondent 9Patient condition/illness.
Clinical assessment skills.
Promotion of the right culture (safety culture).
Public involvement.
Availability and accuracy of test results.
Appendix 10 Questions in the 2011 Care Quality Commission NHS staff survey
My employer is committed to helping staff balance their work and home life.
My immediate manager helps me find a good work-life balance.
I can approach my manager to talk openly about flexible working.
Working flexi-time.
Working reduced hours.
Working from home in normal working hours.
Working to annualised hours.
Working during school term-time only.
My team makes its own decisions about rotas.
Job sharing.
Not used any flexible working options.
Have you done any taught courses?
Have you received any supervised on-the-job training?
Have you received mentoring?
Have you done any shadowing?
Have you received e-learning or online training?
Have you kept up to date with developments in your work?
Have you used other methods of training, learning or development?
Have you had equality and diversity training?
Have you had health and safety training?
Have you had training in what to do in a major incident?
Have you had training in how to handle violence and aggression?
Have you had training on infection control?
Have you had computer skills training?
Have you had training on how to handle confidential information?
Have you had training on how to give information to patients?
Have you had training on how to undertake CPA?
Have you had training on how to conduct a mental health risk assessment?
Have you had training on how to identify patients at risk of committing suicide?
Have you had training on how to assess and support carers of patients?
Have you had training on how to assess and treat patients with dual diagnosis?
Have you had training on psychological therapy?
My training, learning and development has helped me to do my job better.
My training, learning and development has helped me stay up to date with my job.
My training, learning and development has helped me stay up to date with professional requirements.
My supervisor encourages those who work for her or him to work as a team.
My supervisor can be counted on to help me with a difficult task at work.
My supervisor gives me clear feedback on my work.
My supervisor asks for my opinion before making decisions that affect my work.
My supervisor is supportive in a personal crisis.
Have you had an appraisal in the last 12 months?
Did the appraisal help you to improve how you do your job?
Did the appraisal help you agree clear objectives for your work?
Did the appraisal leave you feeling valued by your employer?
Have you agreed a PDP in the last 12 months?
Have you received the training, etc., identified in the PDP?
Has your manager supported you in accessing this training?
Do you work in a team?
Team members have a set of shared objectives.
Team members often meet to discuss the team’s effectiveness.
Team members have to communicate closely with each other to achieve the team’s objectives.
I have, clear, planned goals and objectives for my job.
I often have trouble working out whether I am doing well or poorly in this job.
I am involved in changes that affect my work area.
I cannot meet all the conflicting demands on my time at work.
I have adequate materials, supplies and equipment to do my work.
There are enough staff at this trust for me to do my job properly.
I am able to do my job to a standard I am personally pleased with.
I often think about leaving this trust.
I will probably look for a new job in the next 12 months.
As soon as I can find another job, I will leave this trust.
How satisfied are you with the recognition you get for good work?
How satisfied are you with the support you get from your manager?
How satisfied are you with the freedom you have to choose your own method of working?
How satisfied are you with the support you get from work colleagues?
How satisfied are you with the amount of responsibility you are given?
How satisfied are you with the opportunities you have to use your abilities?
How satisfied are you with the extent to which your employer values your work?
How satisfied are you with your level of pay?
I always know what my responsibilities are.
I am consulted about changes that affect my work area.
I do not have time to carry out all my work.
I get clear feedback about how well I am doing my job.
Relationships at work are strained.
I can decide on my own how to go about doing my work.
The people I work with treat me with respect.
The people I work with seek my opinions.
I am trusted to do my job.
I feel I belong to a team.
I often do more than is required.
I try to help colleagues in my trust whenever I can.
Senior managers here try to involve staff in important decisions.
Communication between senior management and staff is effective.
Senior managers encourage staff to suggest new ideas for improving services.
On the whole, different parts of the organisation communicate effectively with each other.
Care of patients/service users is my trust’s top priority.
I know who the senior managers are here.
Senior managers where I work are committed to patient care.
Patient information is treated confidentially by staff in this trust.
Staff are kept informed about important changes by trust headquarters.
Communication between trust headquarters and other parts of the trust is good.
Does your employer act fairly with regard to career progress?
Have you experienced discrimination in the last 12 months from patients/clients, relatives or other members of the public?
Have you experienced discrimination in the last 12 months from manager or other colleagues?
Have you experienced discrimination on the ground of: ethnic background?
Have you experienced discrimination on the ground of: gender?
Have you experienced discrimination on the ground of: religion?
Have you experienced discrimination on the ground of: sexual orientation?
Have you experienced discrimination on the ground of: disability?
Have you experienced discrimination on the ground of: age?
Have you experienced discrimination on the ground of: other?
If you were concerned about fraud, malpractice or wrongdoing, would you know how to report it?
Would you feel safe raising your concerns?
Would you feel confident that your trust would address your concerns?
Ambulance vehicles are kept in a good state of repair.
Ambulance vehicles provide a safe working environment.
There are opportunities for me to progress in my job.
I am supported to keep up to date with developments in my field.
I am encouraged to develop my own expertise.
There is strong support for training in my area of work.
I would recommend my trust as a place to work.
If a friend or relative needed treatment, I would be happy with the standard of care provided by my trust.
I am satisfied with the quality of care I give to patients/service users.
I feel that my role makes a difference to patients/service users.
I am able to deliver the patient care I aspire to.
I am able to make suggestions to improve the work of my team/department.
There are frequent opportunities for me to show initiative in my role.
I am able to make improvements happen in my area of work.
Health-care professionals and managers in non-clinical roles work well together in my area of work.
Senior managers act on staff feedback.
I look forward to going to work.
I am enthusiastic about my job.
Time passes quickly when I am working.
In the last month, have you seen errors or near misses that could hurt staff?
The last time you saw an error or near miss that could hurt staff, did you or a colleague report it?
In the last month, have you seen errors or near misses that could hurt patients?
The last time you saw an error or near miss that could hurt patients, did you or a colleague report it?
My trust treats fairly staff who are involved in an error, near miss or incident.
My trust encourages us to report errors, near misses or incidents.
My trust treats reports of errors, near misses or incidents confidentially.
My trust blames or punishes people who make errors, near misses or incidents.
When errors, near misses or incidents are reported, my trust takes action to ensure that they do not happen again.
We are informed about errors, near misses and incidents that happen in the trust.
We are given feedback about changes made in response to reported errors, near misses and incidents.
Experienced physical violence from patients/clients, relatives or other members of the public?
Experienced physical violence from manager/supervisor or colleagues?
In the last 12 months, how many times have you experienced physical violence from patients/clients, relatives or other members of the public?
The last time you experienced physical violence did you or a colleague report it?
Experienced bullying or abuse from patients/clients, relatives or other members of the public?
Experienced bullying or abuse from manager/supervisor or colleagues?
The last time you experienced bullying or abuse did you or a colleague report it?
My employer takes effective action if staff are physically attacked by patients/clients, relatives or other members of the public.
My employer takes effective action if staff are physically attacked by other members of staff.
My employer takes effective action if staff are bullied, harassed or abused by patients/clients, relatives or other members of the public.
My employer takes effective action if staff are bullied, harassed or abused by other members of staff.
Do you have access to counselling services at work?
Do you have access to occupational health services at work?
Have you been hurt due to moving and handling?
Have you been hurt due to needlestick and sharps injuries?
Have you been hurt due to slips, trips or falls?
Have you been hurt due to exposure to dangerous substances?
Have you been ill due to work related stress?
Hot water, soap and paper towels, or alcohol rubs are available when they are needed by staff.
Hot water, soap and paper towels, or alcohol rubs are available when they are needed by patients.
Hot water, soap and paper towels, or alcohol rubs are available when they are needed by visitors.
The trust does enough to promote the importance of hand washing to staff.
The trust does enough to promote the importance of hand washing to patients, service users and visitors.
Infection control applies to me in my role.
Overall, how would you rate your health during the past four weeks?
During the past four weeks, how much difficulty did you have doing your daily work, both at home and away from home, because of your physical health?
During the past four weeks, how much did personal or emotional problems keep you from doing your usual work or other daily activities?
In general, my job is good for my health.
My immediate manager takes a personal interest in my health and well-being.
In the last three months have you ever come to work despite not feeling well enough to perform your duties?
Have you felt pressure from your manager to come to work (when ill)?
Have you felt pressure from colleagues to come to work (when ill)?
Have you put yourself under pressure to come to work (when ill)?
Key finding 1: satisfied with quality of work?
Key finding 2: role makes a difference?
Key finding 3: feel valued by colleagues?
Key finding 4: quality of job design?
Key finding 5: work pressure felt?
Key finding 6: work in a real team?
Key finding 7: quality of work-life balance?
Key finding 8: work extra hours?
Key finding 9: used flexible working?
Key finding 10: good opportunities to develop? Potential?
Key finding 11: received training, learning and development beneficial to career development in last 12 months?
Key finding 12: had appraisal in last 12 months?
Key finding 13: had good quality appraisal in last 12 months?
Key finding 14: agreed PDP in last 12 months?
Key finding 15: support from supervisor
Key finding 16: had health and safety training in last 12 months?
Key finding 17: suffered work-related injury in last 12 months?
Key finding 18: suffered work-related stress in last 12 months?
Key finding 19: availability of hand-washing materials
Key finding 20: seen at least one error that could harm patients or staff?
Key finding 21: last error seen reported?
Key finding 22: action taken following errors
Key finding 23: experienced violence from patients/relatives in last 12 months?
Key finding 24: experienced violence from colleagues in last 12 months?
Key finding 25: experienced harassment from patients/relatives in last 12 months?
Key finding 26: experienced harassment from colleagues in last 12 months?
Key finding 27: effective action from employer towards violence/bullying/harassment?
Key finding 28: general health and well-being?
Key finding 29: presenteeism among staff?
Key finding 30: good communication between managers and staff?
Key finding 31: can contribute towards improvements?
Key finding 32: staff job satisfaction?
Key finding 33: staff intention to leave?
Key finding 34: would recommend trust as place to work or receive treatment?
Key finding 35: staff motivation at work?
Key finding 36: had equality/diversity training in last 12 months?
Key finding 37: trust provides equal opportunities to staff?
Key finding 38: suffered discrimination in last 12 months?
Glossary
- Alternative pathways
- Pathways that involve taking a patient to a service other than an accident and emergency department, such as out-of-hours care, rapid response teams and emergency care practitioners.
- Ambulance bypass
- Transfer of patients to the most appropriate, but not necessarily closest, hospital for their condition.
- Ambulance diversion
- Diversion of an ambulance to a distant hospital because of a lack of clinical resources at the closest hospital.
- Dispatch
- Allocation of the ambulance service resources to cover the demands placed on the service.
- Hear and treat
- Assessment and treatment of a patient over the telephone, without sending ambulance staff to see the patient.
- Level 1 trauma centre
- A trauma centre that provides the highest level of surgical care to trauma patients.
- Non-conveyance
- The decision not to convey a patient from the scene to a hospital or other health-care provider facility.
- Rule 43 coroners’ reports
- Details of coroners’ reports and responses received from organisations asked to consider action to prevent future deaths.
- See and treat
- Assessment and treatment of a patient by ambulance staff at the scene, without transporting the patient to hospital.
- Telemedicine
- The use of telecommunication and information technologies in order to provide clinical health care at a distance.
- Treat and leave
- See ‘see and treat’.
- Triage
- The process of determining the priority of patients’ treatments based on the severity of their condition.
List of abbreviations
- A&E
- accident and emergency
- AE
- adverse event
- AHRQ
- Agency for Healthcare Research and Quality
- ATMIST
- age, time, mechanisms, injury, signs, treatments
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CPR
- cardiopulmonary resuscitation
- CQC
- Care Quality Commission
- ECG
- electrocardiogram
- ED
- emergency department
- EMS
- emergency medical services
- GP
- general practitioner
- MaPSaF
- Manchester Patient Safety Framework
- MeSH
- medical subject heading
- NHSLA
- NHS Litigation Authority
- NPSA
- National Patient Safety Agency
- NRLS
- National Reporting and Learning System
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
- randomised controlled trial
- SBAR
- situation, background, assessment, recommendation
- SD
- standard deviation
- SPSS
- Statistical Product and Service Solutions