Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/1024/08. The contractual start date was in February 2013. The final report began editorial review in May 2014 and was accepted for publication in October 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Dr Gemma Trainor is employed as a consultant nurse in child and adolescent mental health services.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Hannigan et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Mental health in children and young people
One in 10 children and young people between the ages of 5 and 16 years living in Britain has a diagnosable mental health problem. 1 In England the total number affected is projected to increase by over 13% in the period to 2026. 2 In this context a priority for the NHS and its partner agencies is to make sure that the needs of each child are met in a tailored and timely way. To this end, child and adolescent mental health services (CAMHS) in England and Wales continue to be organised using a tiered approach. 3,4 This is represented in Box 1.
Tier 1: child and adolescent mental health services are provided by professionals whose main role and training is not in mental health, such as GPs, health visitors, paediatricians, social workers, teachers, youth workers and juvenile justice workers.
Tier 2: tier 2 CAMHS are provided by specialist trained mental health professionals, working primarily on their own, rather than in a team. They see young people with a variety of mental health problems that have not responded to tier 1 interventions. They usually provide consultation and training to tier 1 professionals. They may provide specialist mental health input to multiagency teams, for example for children looked after by the local authority. Tier 2 also consists of those practitioners and services from specialist CAMHS that provide initial contacts and assessments of children and young people and their families.
Tier 3: tier 3 is reserved for those more specialised services provided by multidisciplinary teams (MDTs) or by teams assembled for a specific purpose on the basis of the complexity and severity of children’s and young people’s needs or the particular combinations of comorbidity found on specialist assessment.
Tier 4: tier 4 services are very specialised services in residential, day patient or outpatient settings for children and adolescents with severe and/or complex problems requiring a combination or intensity of interventions that cannot be provided by tier 3 CAMHS. Tier 4 services are usually commissioned on a subregional, regional or supraregional basis. They also include day-care and residential facilities provided by sectors other than the NHS such as residential schools, and very specialised residential social care settings including specialised therapeutic foster care.
Source: information in this table has been directly extracted from the Wales Audit Office/Healthcare Inspectorate Wales document Services for Children and Young People with Emotional and Mental Health Needs,4 and is Auditor General for Wales and Crown copyright.
Inpatient child and adolescent mental health services: a component within a complex system
With multiple groups of people and organisations located at different tiers, all interacting in mutual interdependence, CAMHS are an example of a complex system. 5–7 Within this system, as Box 1 shows, the most specialised services are available at tier 4 to young people with the greatest need. Those who use services at this level often have multiple disorders and difficulties, and, until relatively recently, tier 4 was largely synonymous with hospital care. 8 New service developments reflect the idea that care at this highest level should be provided in the least restrictive environment possible. Against this background a team funded by the National Institute for Health Research (NIHR) Service Delivery and Organisation programme systematically reviewed alternatives to hospital admission for children and young people and the evidence of their effectiveness, acceptability and cost. 9 This team described a number of alternatives to inpatient care in a typology of evaluated models, and from its mapping exercise reported a variety of services in use across the UK.
This evidence, plus evidence secured by the independent CAMHS review team3 and by the National CAMHS Support Service,8 points to a diversification at tier 4 which includes an expanded array of highly specialised and/or intensive community and out-of-hospital services. However, inpatient CAMHS units continue to play a major part in overall systems of mental health care, and, reflecting the terms of the NIHR Health Services and Delivery Research (HSDR) programme’s call under which this project was funded (NIHR HS&DR 11/1024: Innovations in secondary mental health services), it is hospital services that have exclusively been focused on here. Over the lifetime of this evidence synthesis, important reminders have appeared of the need for locally accessible, age-appropriate, hospital-based mental health care for children and young people. New data published in February 2014 following a joint British Broadcasting Corporation (BBC)/Community Care investigation pointed to the continuing problem of young people being admitted to adult wards and to wards many miles from their homes, with detrimental effects on individuals and on the maintenance of relationships with family and friends. 10 This, plus the fact that highly specialised, institutional health care also constitutes a substantial component of health service costs, makes this evidence review in the tier 4 hospital services field particularly timely.
At the turn of the new century it was estimated that over 2000 young people are admitted to English and Welsh CAMHS inpatient units each year, with the majority of specialist centres catering exclusively for those over 11 years old. 11 Variations in the characteristics of young people admitted are believed to exist, reflecting differences in the socioeconomic features of regions and differing levels of bed availability. Pressure on inpatient beds is considerable, and many who are referred for inpatient treatment are not accepted. 12 The admission of young people to adult mental health wards has been recognised as a problem for some time,13 with the recent BBC/Community Care investigation including vivid first-person testimony of the difficulties this causes. The increased use of adult wards in England has also happened in the face of active monitoring by the Care Quality Commission, which requires services to report each occasion on which an under-18-year-old is placed on a ward intended for adults for a continuous period of more than 48 hours. 14
It is notable that, until relatively recently, little was known of the actual interventions offered to young people admitted to mental health hospitals or the advantages of providing inpatient care. This general situation is changing, helped by the commissioning (including by the NIHR Service Delivery and Organisation programme, the predecessor to the body funding this current evidence synthesis) of investigations such as Tulloch et al. ’s15 into costs, outcomes and satisfaction in inpatient CAMHS. The wider evidence base has also been strengthened by new knowledge of systems and processes supporting young people making the transition from CAMHS to adult mental health services. 16 What has not been attempted hitherto is a synthesis of the evidence in the area of risk in the way that has been accomplished here.
Identifying, assessing and managing risk: the case for an evidence synthesis
Within the inter-relating CAMHS system, the identification, assessment and management of risk are key considerations for practitioners and managers working at the interface between community and hospital services. Work across this interface includes making decisions on the transfer of young people from one tier to another. Decisions made at this juncture, and risk-related decisions made in the within-hospital context, can have lasting consequences for young people, families and services. In preparing our bid for NIHR support we were aware of individual (and sometimes small-scale) investigations being conducted in the areas of risk identification, assessment and management in inpatient CAMHS. To the best of our knowledge, however, no previous studies have systematically brought together research and other evidence in the way that has been done here.
The word ‘risk’ in everyday mental health services is overwhelmingly used as a shorthand referring primarily to the possibilities of direct harm to self or others, or harm through self-neglect and physical deterioration. Risk-management interventions, including the admission of people to hospital as places of safety in which round-the-clock care and observation can be provided, are then introduced as means of minimising the likelihood of harm happening. Action in response to identified risks of this type is vitally important for young people. Beyond this, an ambition of this project has also been to search for evidence in the area of inpatient CAMHS risk where risk is understood in the broadest of senses, with the word itself having a number of different meanings. ‘Risky behaviour’ and ‘posing a risk’ are two, correlating closely with the dominant ways in which risk is thought of in mental health services but contrasting with the ideas of ‘risk factors’ and ‘being at risk’. 17 To this Coleman and Hagell17 add the idea of ‘risk reframing’, through which behaviours typically seen as risky might be reinterpreted as opportunities to develop resilience. In the mental health service context, this connects with the idea of ‘positive risk-taking’,18 used as a route to the promotion of individual responsibility and personal development.
As a project team we view risk as complex and multifaceted. Our original case for funding support included the idea that, in addition to the risks of harm to self and others and self-neglect, attention ought also to be given to the identification, assessment and management of other, less obvious, risks for young people using inpatient mental health services. In a context of bed scarcity and regional variations in patterns of provision, it is known, for example, that CAMHS clinicians describe the most significant reasons for hospital admission as a young person’s high risk of suicide, risk of physical deterioration owing to mental illness, need for round-the-clock observation and the presence of serious deliberate self-harming behaviour. 12 Pursuing the example of self-harm is illustrative of the thinking behind this study. Although good practice involves care and treatment in the least restrictive environment possible, for young people who seriously self-harm, safety can be difficult to achieve in the community, making this risk a common trigger for hospital referral. Anecdotal, practice-based evidence included in our original bid for support suggests that managers and professionals in hospitals also find self-harm difficult to manage because of problems of contagion. Contagion is the copying of harmful behaviours and, while important, is a risk that may not feature highly when hospital admission decisions are made. It is also a risk that may be underexamined in the research context, and about which little is therefore known.
Informing this project is also the idea that mental ill-health and hospital admission present risks to young people’s achievement of developmental milestones, psychological maturity, educational attainment, social integration with family and peers, and personal physical well-being. This overall perspective has informed the production of an evidence synthesis which embraces a broad view of risk, along with the idea that action to reduce the chances of one type of unwanted event happening potentially increases the chances of another occurring. For example, admitting a young person to hospital may represent a reasoned response to the risk of harm to self but is also an action potentially increasing the risk of other, undesired, events happening (including contagion, but also disruption to family and friendship networks, educational continuity and increased stigma). Just as risks are connected, so too are the people and services who might collectively respond to them. Addressing the full range of risks for young people admitted to mental health hospital is likely to draw on the efforts of workers located across the system: in health, social care and education services. The intention in this report has been to bring together the available evidence in ways that are helpful to this broad group of workers and to young people using services and their families.
Overarching research question and objectives
This project was funded under a NIHR HSDR programme call focusing on innovations in secondary mental health services in order to answer the overarching research question:
What is known about the identification, assessment and management of risk (where ‘risk’ is broadly conceived) in young people (aged 11–18 years) with complex mental health needs entering, using and exiting inpatient child and adolescent mental health services in the UK?
Objectives for the overall project were:
-
to summarise and appraise the evidence for the identification, assessment and management of risk for young people: as they make the transition into inpatient CAMHS; as they are cared for in inpatient CAMHS; as they make the transition from inpatient CAMHS to the community; and as they make the transition from inpatient CAMHS to adult mental health services
-
to identify and describe any underlying theoretical explanations for approaches used in the identification, assessment and management of risk
-
to understand the views and experiences of risk of young people (aged 11–18 years) with complex mental health needs using inpatient mental health services, and of those involved in the identification, assessment and management of risk in these settings
-
to synthesise the evidence for the identification, assessment and management of risk in young people (aged 11–18 years) with complex mental health needs entering, using and exiting inpatient services
-
to synthesise the evidence on the costs and cost-effectiveness to the NHS of different approaches to identifying, assessing and managing these risks
-
to identify the future priorities for commissioning, service development and research for young people (aged 11–18 years) with complex mental health needs entering, using and exiting tier 4 inpatient services.
A two-stage framework to evidence synthesis: the Evidence for Policy and Practice Information and Co-ordinating Centre approach
The project team was commissioned to meet these objectives using a specific approach to the identification, review and synthesis of the evidence. In recent years a variety of review approaches suitable for the health-care field have emerged,19 of which the EPPI-Centre (Evidence for Policy and Practice Information and Co-ordinating Centre) framework is one. This has developed over a period of two decades, led by researchers located primarily at the Institute of Education at the University of London and their affiliates. Documents outlining EPPI-Centre methods (and other materials) are freely available from http://eppi.ioe.ac.uk/cms/, where reviews informed by this framework are intended to have particular utility in informing policy and practice for public services. Recent published examples modelling varying degrees of detail and complexity completed by EPPI-Centre members and their collaborators include syntheses of the evidence for the socioeconomic value of nursing and midwifery,20 on commissioning in health, education and social care21 and on the effectiveness of interventions to strengthen national health service delivery in low- and lower middle-income countries. 22 Previous examples also exist of NIHR-funded projects using the broad EPPI-Centre approach. These include an HSDR programme project addressing self-care support for children and young people led by a member of the current research team (SP),23 and a Public Health Research Programme review into the effects of schools and school environment interventions on health. 24
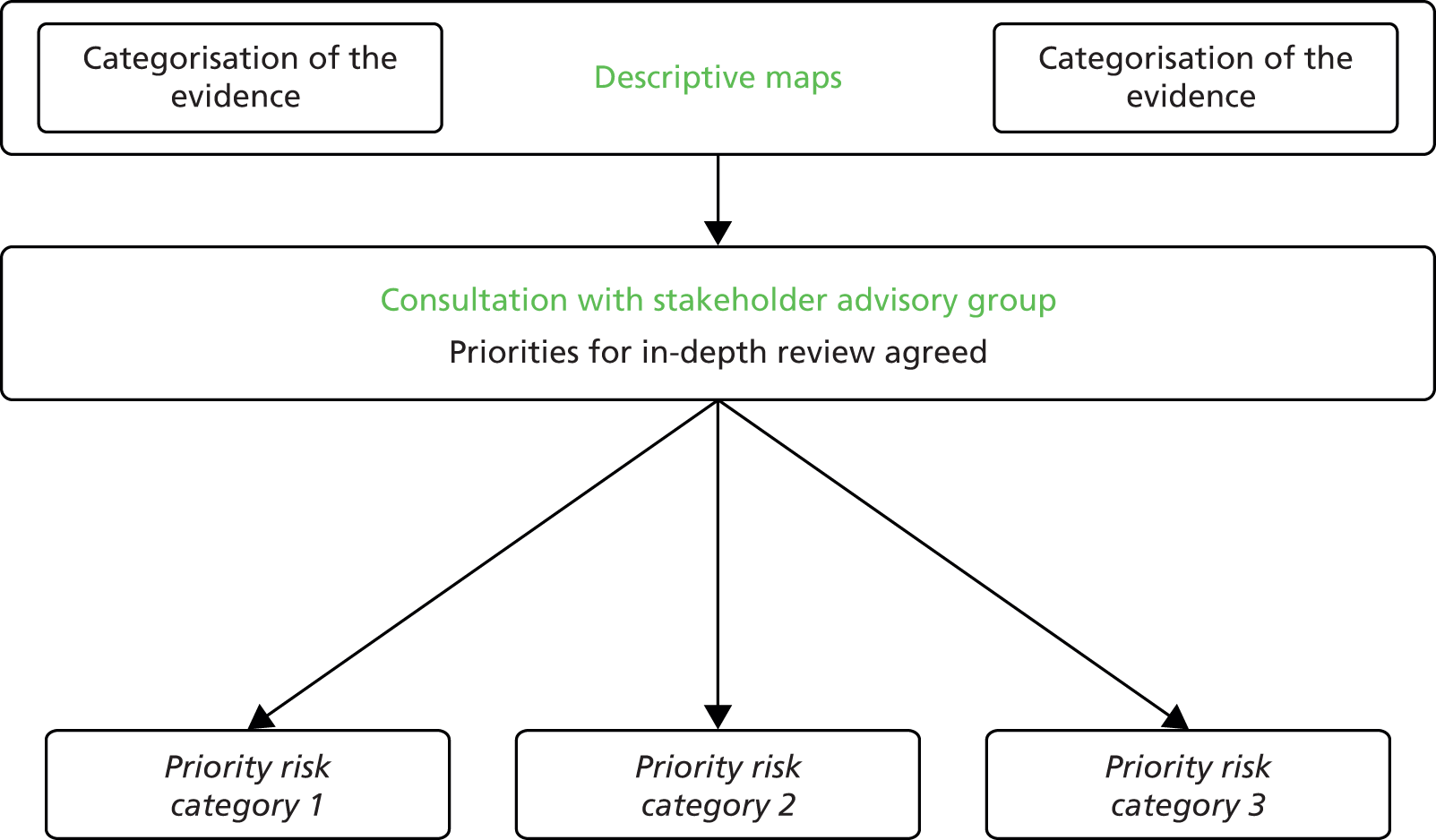
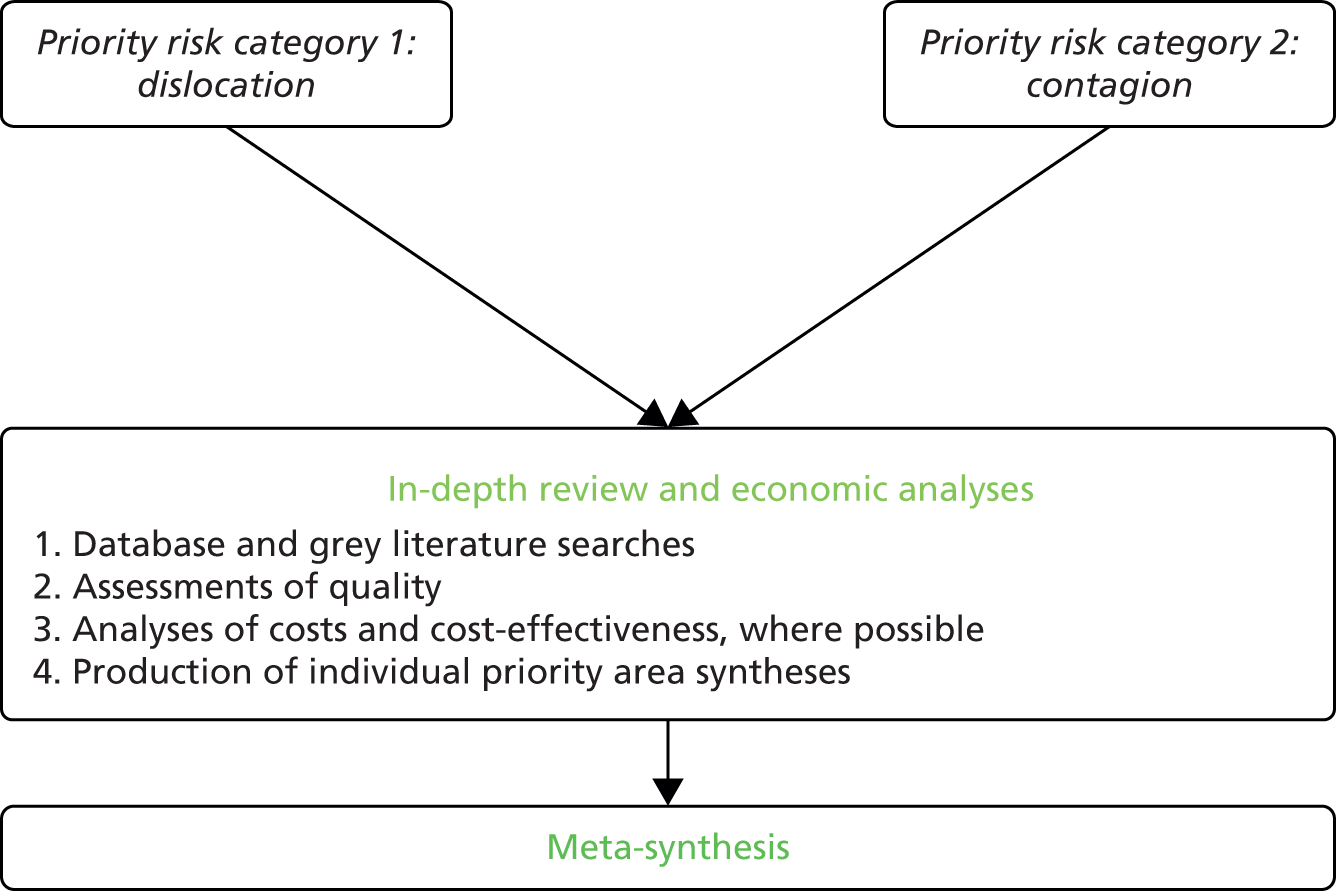
Our use of the EPPI-Centre approach throughout the totality of this project is summarised in Figure 1.
Like other frameworks guiding the review and synthesis of evidence, the EPPI-Centre approach stresses the importance of transparency and rigour. It also has a number of distinct, novel features. A first is an explicit acknowledgement that choice of research topic and specific focus (in the cases of both primary studies and syntheses of existing evidence) reflect particular sets of values and interests. 26 Research questions are not self-evident, but are constructed by particular people for particular purposes. In the case of the child and adolescent mental health field, the range of people with active interests in this complex system is wide indeed, potentially yielding a large variety of candidate priority research topics. Managers, practitioners from different backgrounds, commissioners, policy-makers, young people, families and others may have varying ideas on what kinds of research questions ought to be asked and what methods should be used to answer them. Often the authority to shape priorities remains limited to a relatively powerful few. These ideas underpin the observation that:
Involving representatives of all those who might have a vested interest in a particular systematic review helps to ensure that it is a relevant and useful piece of research.
(p. 1)26
In any project informed by the EPPI-Centre approach a crucial task must therefore be the effective engagement of concerned people. Involvement in an EPPI-Centre synthesis is typically secured through the setting up of an advisory group or something similar, in which representatives of groups with clear interests and experiences relevant to a study’s broad focus and eventual findings participate. In reviews conducted in the health-care field, members of advisory groups are likely to be drawn from communities of practitioners and managers as well as from those with direct experience of using services. A representative stakeholder advisory group, in turn, assumes particular responsibilities at key moments in the lifetime of a project. One critical moment for a group’s involvement is the point at which major decisions need to be made on the direction of travel an evidence synthesis is about to take.
This idea that in-progress decisions have to be made on the future direction an evidence synthesis will take is a second hallmark of the EPPI-Centre framework. This is particularly evident through the EPPI-Centre’s commitment to the combining of an initial scoping and mapping phase with a second, more targeted, review in one or more negotiated priority areas. In EPPI-Centre reports a detailed account is often included of how an initial mapping of the territory (in our case, the territory relating to risk in inpatient CAMHS) has been presented to stakeholder participants drawn from across a system, and how this has been used as the basis for the considered selection of candidate subareas for subsequent, detailed, quality review and synthesis.
A third component of the EPPI-Centre framework relates to the sharing of information on a project’s methods and findings in ways that are sensitive and accessible to the needs of larger stakeholder groups. Representatives of these groups are offered opportunities to advise project members on the most suitable ways of disseminating new knowledge, through the use of varieties of media including briefing summaries, online materials and articles of varying lengths and complexity tailored for particular audiences. Again, in this report we show how we worked with stakeholders to develop strategies to share what we learned. We also include plans for further work in this area once this final report has been accepted for publication as an NIHR journals library monograph.
Structure of this report
This opening chapter has set the scene for this evidence synthesis in the area of risk for young people moving into, through and out of tier 4 inpatient child and adolescent mental health services. It has introduced the CAMHS system as a tiered one, in which hospitals fulfil important functions within a dynamic and inter-related network of services. The existence of risks, both obvious and less so, has been introduced and a case made for a project of this type. An overarching research question has been given, along with a series of objectives. The project team’s commitment to the EPPI-Centre approach to evidence synthesis has been stated, and an overview given of some of the key distinguishing characteristics of this framework. In the chapter immediately following, methods and findings are given of the project’s phase 1 scoping and mapping exercise. Chapter 3 describes the approach taken to working with stakeholders, and the process through which priority categories of risk were identified and carried forward into the second, in-depth, phase of the project. Chapter 4 addresses the concepts and methods used in the phase 2 review, beginning with a summary of the research questions and objectives guiding this segment of the project. Chapter 5 synthesises the evidence in the phase 2 priority risk areas. Chapter 6 discusses the study overall and its findings. It includes a single-page matrix summarising the project overall and outlines plans for dissemination and knowledge exchange informed by discussions with stakeholder collaborators. It also draws out the implications of this project for policy, services and practice and makes recommendations for future research.
Chapter 2 Scoping exercise
Using the EPPI-Centre framework to map risk in inpatient child and adolescent mental health settings
The team’s use of the EPPI-Centre framework commenced with a scoping exercise (see Figure 2) to identify the broad contours of the research field relating to risk in inpatient child and adolescent mental health settings. The aim of this first phase was to identify and categorise research and other evidence at the intersection of the four key areas of young people, mental health, inpatients and risk (see Figure 3). During this phase no attempts were made to assess the quality of materials retrieved, the aim being instead to scope and map out the existing evidence at the meeting point of the areas lying at the heart of this project. In this initial searching, scoping and mapping, no attempts were made to determine which types of risk should be either included or excluded, and no attempts were made to identify underpinning theory or to identify costs or cost-effectiveness.
FIGURE 2.
Phase 1 of the EPPI-Centre framework in action.
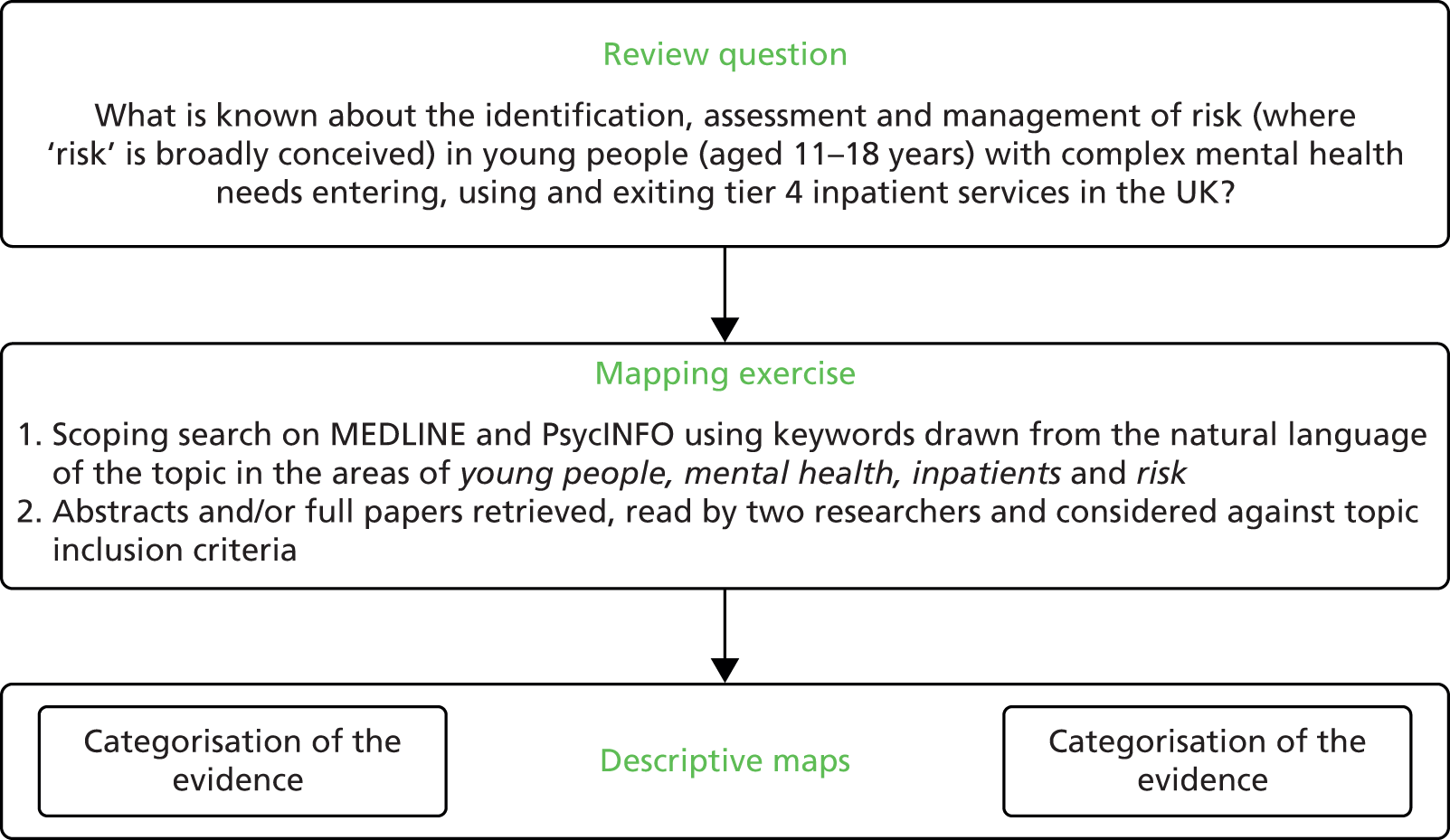
FIGURE 3.
Phase 1 search.
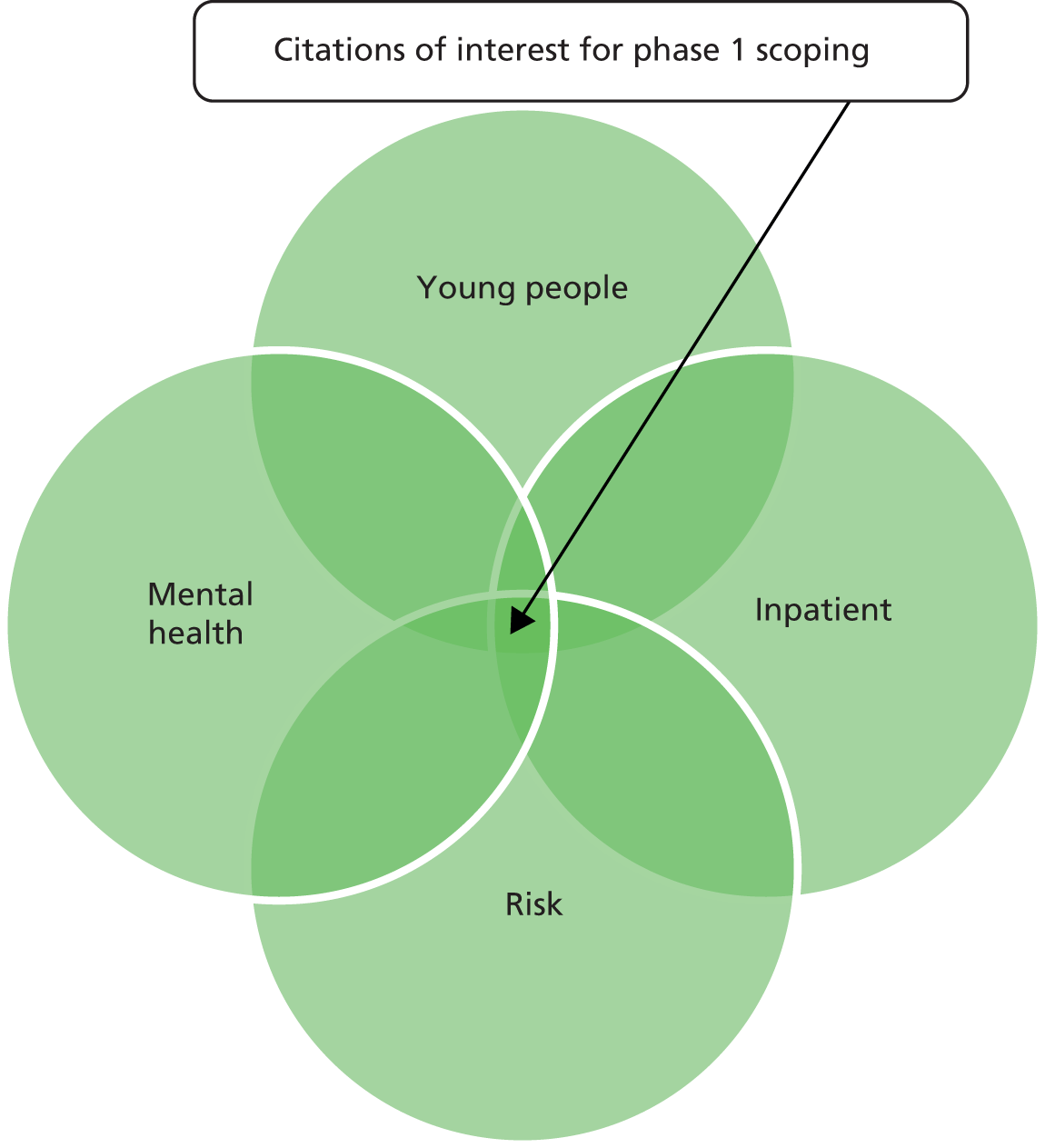
As per the study’s commissioned protocol, searching for papers was conducted using the electronic databases MEDLINE and PsycINFO. For these two databases, controlled vocabulary and free-text terms which covered the four key areas above were combined. Details of the search strategies used are given in Appendix 1 (MEDLINE) and Appendix 2 (PsycINFO). This search was guided by a set of inclusion and exclusion criteria described immediately below and (in summary) by the four-arm strategy depicted in Figure 3. The end date for searching was March 2013.
Inclusion and exclusion criteria
To be included in this scoping exercise, a citation (which could be a research report, a review paper, a discussion piece, a published opinion, an editorial or something similar) had to:
-
Be written in the English language.
-
Focus on young people aged 11 to 18 years by:
-
focusing exclusively on young people aged 11 to 18 years or
-
focusing on a wider age group but including sufficient detail to enable the accurate identification of data relating to young people specifically or
-
relating to a study sample where the mean age was between 11 and 18 years.
-
-
Focus on moving into (admission), through and/or out (discharge) of inpatient mental health services. As not all citations retrieved included unambiguous descriptions of service types, the decision was taken to consider ‘inpatient mental health services’ as any inpatient hospital services (and, in the case of US citations, residential treatment centres) staffed by mental health professionals.
-
Address risk identification and/or risk assessment and/or risk management. Reflecting the purpose of the review, risk was viewed in broad terms, with no a priori exclusions placed on citations because of the way risk was thought about and/or used by authors. Citations were therefore included which addressed the risks of (for example) harm to self or harm to others, but also the risks mental ill-health and hospital admission pose to young people’s physical, psychological, social and educational development.
All citations retrieved were downloaded into Endnote Web™ (2013, Thomson Reuters, New York, NY, USA) and duplicates removed. For the purpose of this scoping exercise, all citations to dissertations, theses or books were excluded. Each remaining citation retrieved was independently assessed for relevance to the review by two members of the study team, using the information provided in the title and abstract. Where any doubt existed, the full text was retrieved. In all cases, the full text was retrieved for all citations that at this stage appeared to meet the scoping review inclusion criteria.
Describing relevant papers
To achieve a high level of consistency, reviewers screened each retrieved citation for inclusion using a purposely designed form (see Appendix 3). Disagreement was resolved by discussion with a third reviewer. This phase 1 form included space for the extraction of key data from each citation: the country in which the study (in the case of research reports) had been carried out; if the citation focused on moving into (admission), through or out of (discharge) inpatient mental health services, or any combination thereof; the characteristics of the population studied (if relevant); the type of risk focused on; and, in the case of original research, the design used (e.g. cohort study, longitudinal study).
Evidence map
Figure 4 illustrates the flow of citations through the scoping exercise and shows how 124 individual items were eventually identified for inclusion. Details of the included papers are given in Appendix 4. Of these, the majority were primary research papers (115 articles describing 118 studies). The remaining papers (n = 9) described the development of guidelines (n = 1) or were a recommendation statement (n = 1), general discussions (n = 4), reviews (n = 2) and a letter (n = 1). In the following section we describe the characteristics of the 118 research studies according to the country in which projects were undertaken, the age of study participants, research design, the size of study populations and the year of publication.
FIGURE 4.
Flow of citations through phases of the scoping review.

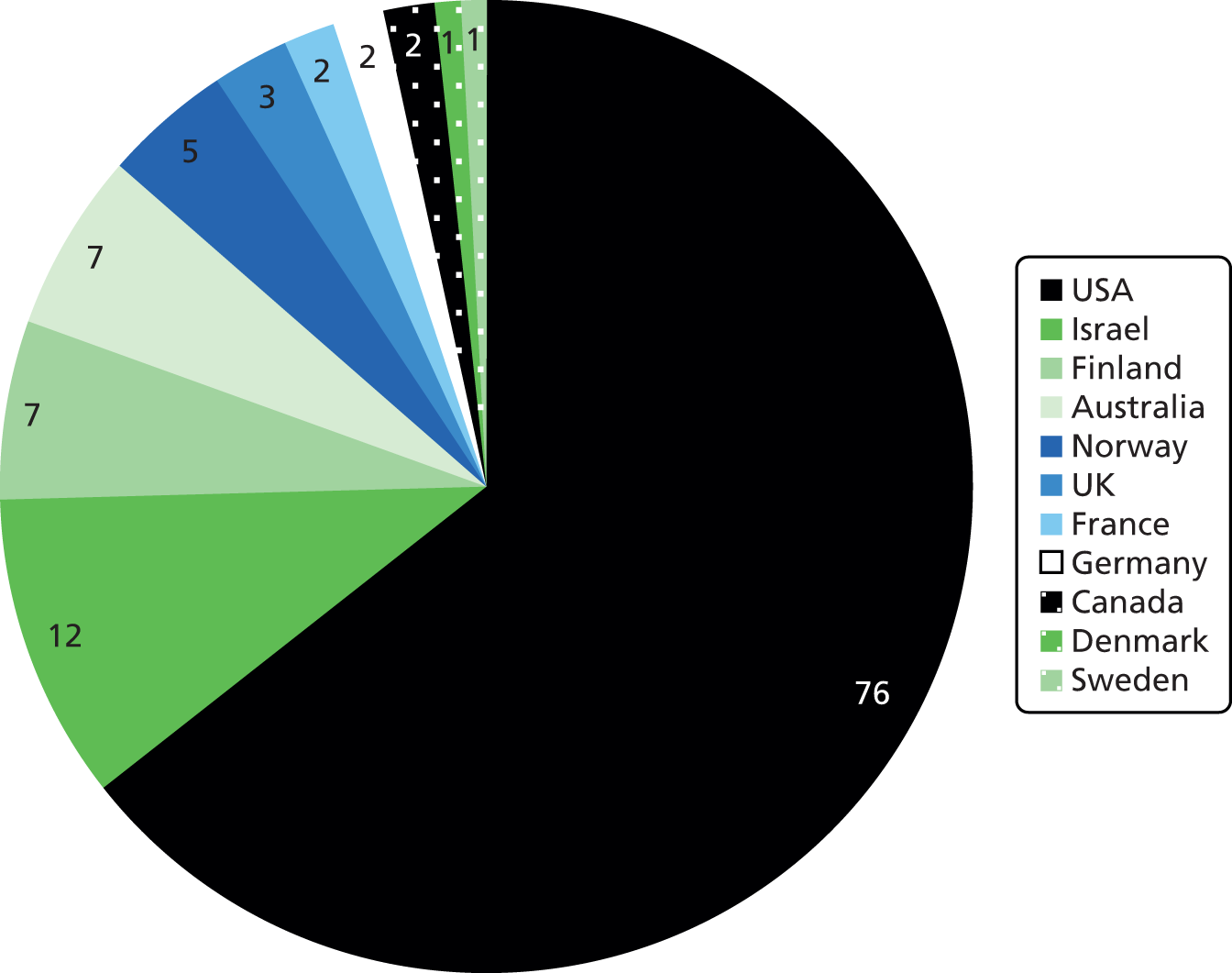
Country where research was undertaken
Information on the country in which each research study had been carried out was obtained from the methods section of the retrieved full-text version of each paper, or where this information was not directly given from the country location of the corresponding author. The distribution of research by country in Figure 5 shows that by far the largest number of studies (over 60%) were conducted within the USA, with only 2.5% conducted within the UK. This preponderance of studies from the USA may reflect the limiting of the phase 1 scoping search to English-language citations only, this having a direct effect on the country of origin of papers retrieved.
FIGURE 5.
Country of origin of the 118 studies included in the scoping review.
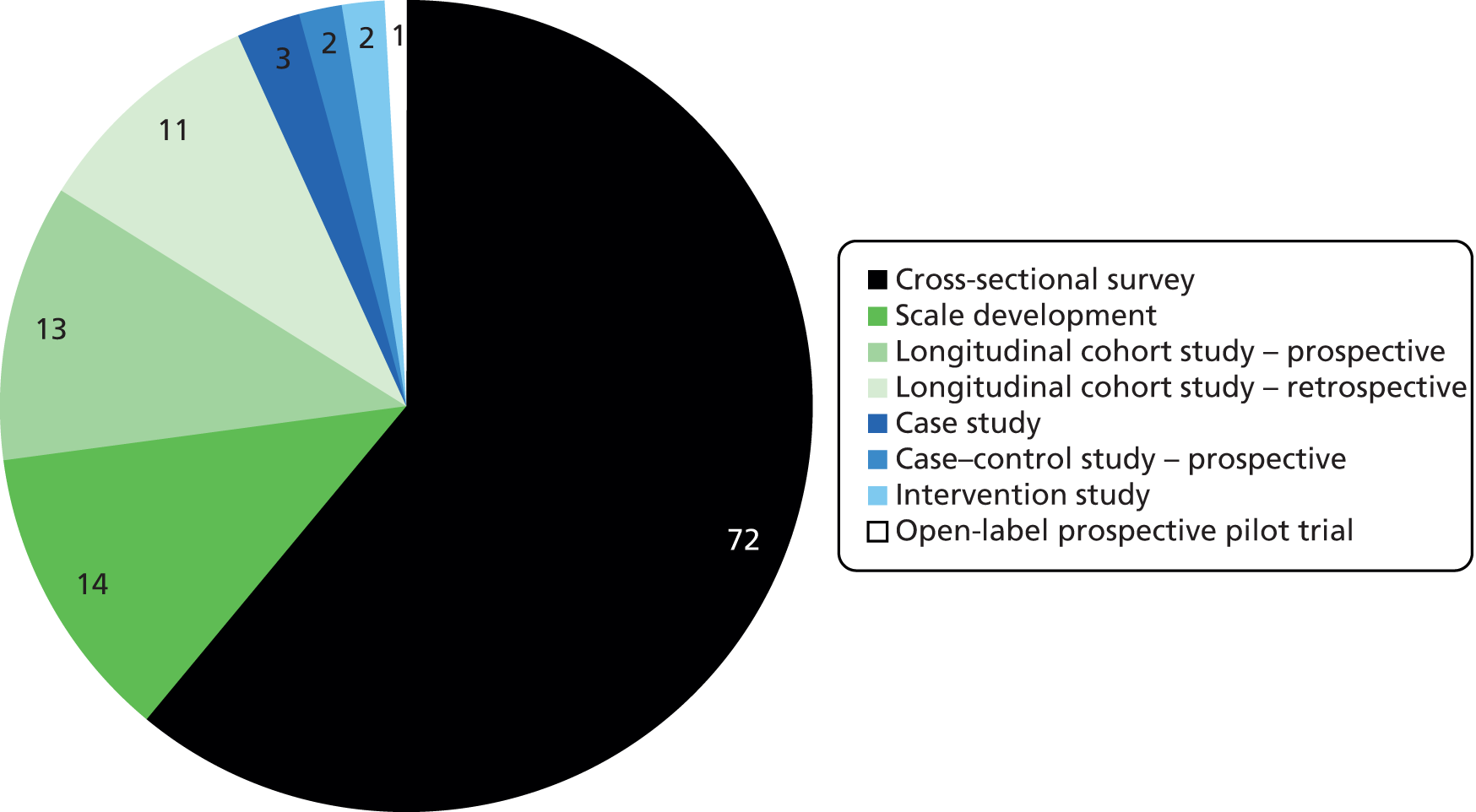
Research design
Figure 6 summarises the research design used in the 118 research studies included in the phase 1 scoping exercise. Seventy-two of the studies used a cross-sectional design, of which 24 involved the collection of retrospective data from young people’s inpatient medical notes or charts.
FIGURE 6.
Research design used in the 118 research studies included in the scoping review.
Age of study participants
The mean age of the young people whose data were included in each of the 118 studies in the phase 1 scoping fell between 11 and 18 years. The age ranges of young people participating, or whose data were used, in individual studies are summarised in Table 1.
| Age range (years) | Number of studies |
|---|---|
| 11 to 18 | 13 |
| 12 to 18 | 27 |
| 13 to 18 | 14 |
| 14 to 18 | 6 |
| 15 to 18 | 4 |
| 16 to 18 | 2 |
| 11 to > 18 | 3 |
| 12 to > 18 | 10 |
| 13 to > 18 | 8 |
| 14 to > 18 | 1 |
| 16 to > 18 | 1 |
| < 11 to 18 | 10 |
| < 11 to > 18 | 9 |
| Age not specified but sample described as adolescents | 10 |
| Total number of studies included in phase 1 | 118 |
Size of study populations
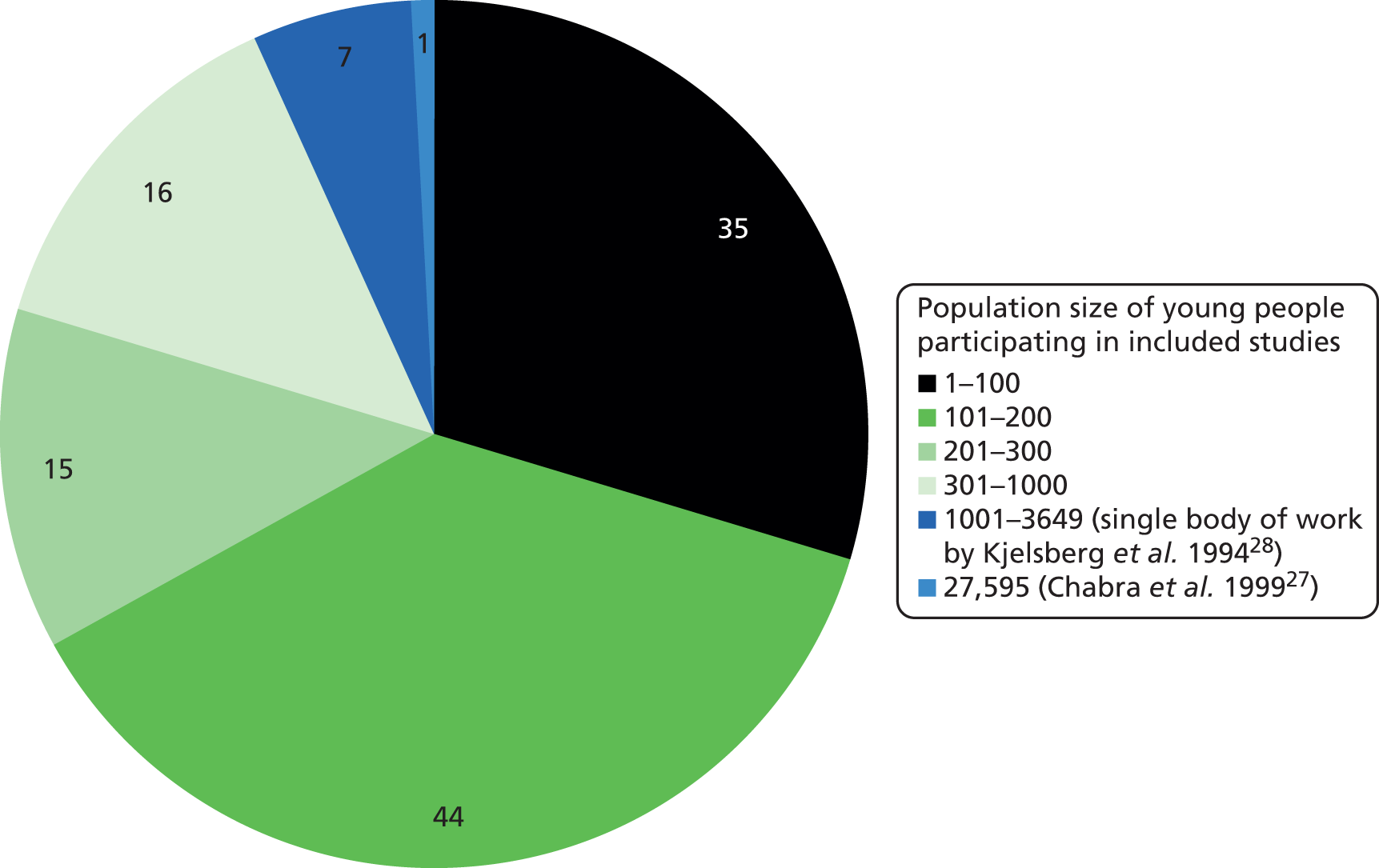
The size of the populations included in each of the 118 phase 1 studies varied, with the largest number being 27,000 included in the single study by Chabra et al. 27 Figure 7 summarises this information.
FIGURE 7.
Size of the populations participating in phase 1 included research studies.
Year of publication
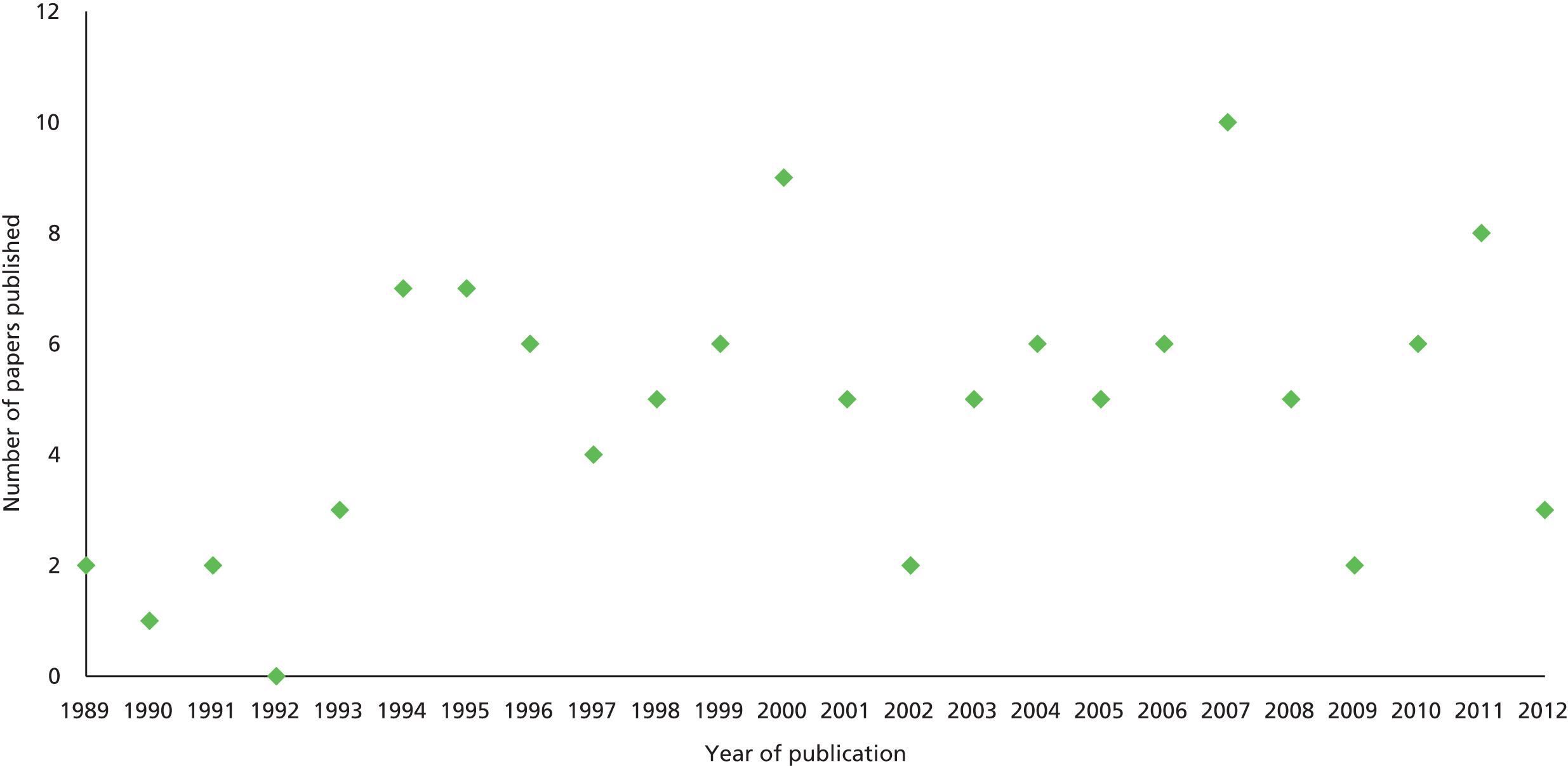
Data on the year of publication of the 115 papers reporting findings from the 118 studies included in phase 1 are given in Figure 8.
FIGURE 8.
Year of publication of phase 1 included papers.
Mapping exercise
As a way of presenting the evidence located and included in this phase 1 scoping, a number of broad, descriptive maps of the different ways in which risk has been identified, assessed and managed in the inpatient CAMHS area were produced. These are presented in this report as Figures 9–17. To group included papers thematically, an initial typology of risks was used, drawing on the work of Subotsky. 29 Subotsky uses four categories of risk: harm to self; harm to others; harm from others; and harm from the health-care system and its staff. In order to capture the full range of risks addressed across all 124 included papers, further categories were added by the project team as necessary, each reflecting the content of papers retrieved. Examples included the category of longer-term risks found at follow-up of young people previously admitted to inpatient CAMHS units, and risks of early disengagement from services. This full range of risks identified is reproduced in the figures immediately below, where the content of each map thematically summarises the main areas addressed by the papers included in each category.
FIGURE 9.
Descriptive map of ‘harm to self’.
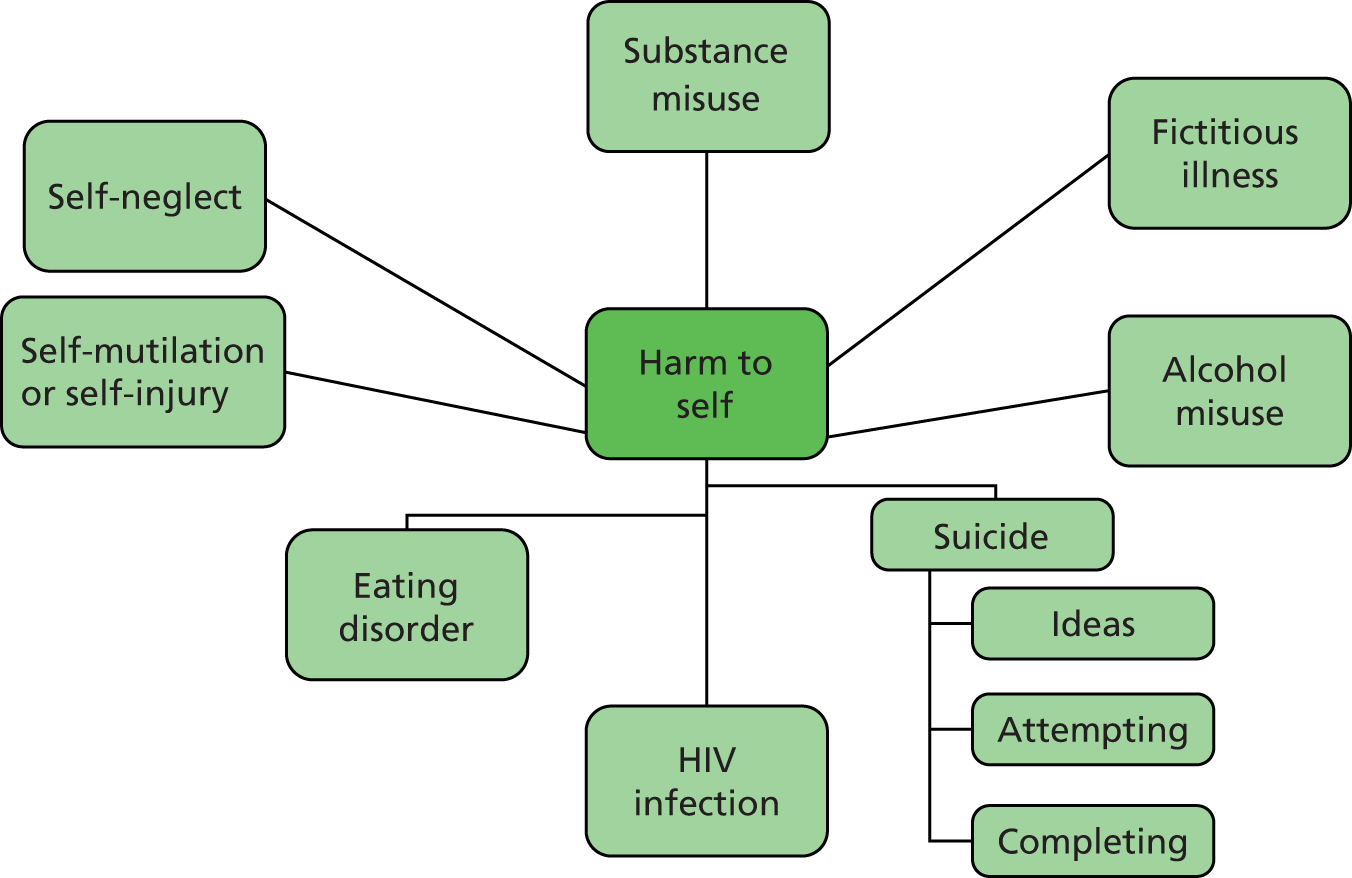
Risk of harm to self (65 papers)28,30–93
Given what is known about the general usage of the term ‘risk’ in mental health services and the types of risk that attract most attention in policy and practice, it was not surprising to the project team to find that the category with the largest number of included phase 1 papers addressed the risks of harm to self (see Figure 9 for the associated descriptive map). Of the 65 papers included here, overwhelmingly most (n = 53)28,30–81 were concerned with the identification and/or the assessment and/or the management of suicide risk, followed by the risks to self which are associated with alcohol and drug abuse (n = 7). 82–88 Smaller numbers of included papers focused on general self-harm (n = 3)89–91 and the risks associated with human immunodeficiency virus (HIV) infection and acquired immunodeficiency syndrome (AIDS) (n = 2). 92,93 Noting the high volume of papers addressing risks associated with suicide, a decision was made to produce a separate descriptive map for this area alone (see Figure 10).
FIGURE 10.
Descriptive map of ‘suicide’.
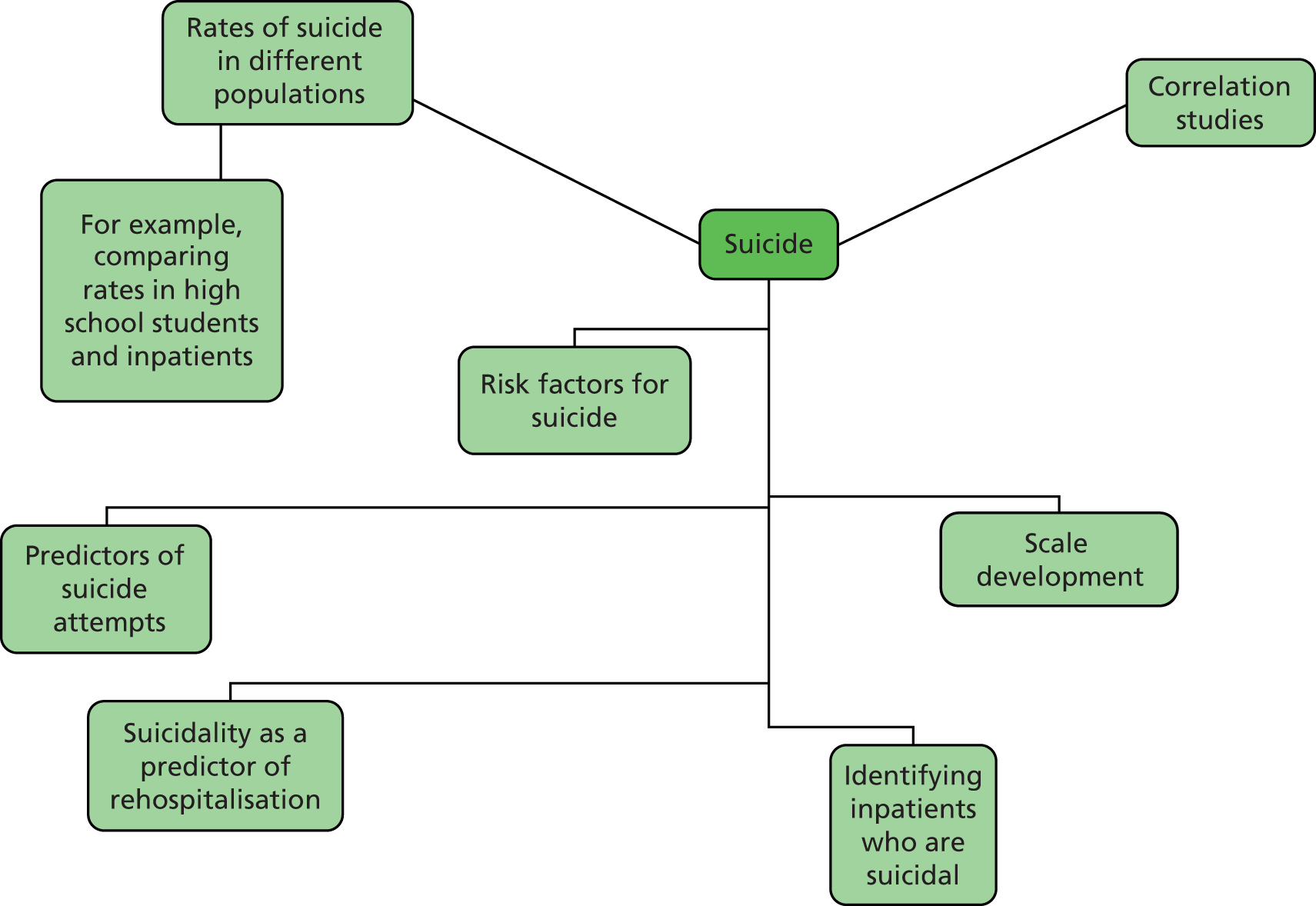
Suicide (53 papers)28,30–81
As noted above, the volume of papers addressing the identification, assessment and management of suicide risk in young people moving into, through and out of inpatient mental health services warranted a separate thematic map. This is reproduced in Figure 10. Papers included in the correlation studies category investigated the associations between suicide and a variety of personal and clinical characteristics (e.g. depression, delinquency).
Harm to others (20 papers)94–113
This category included a large number of papers addressing the risk of harm to others, with papers focusing on both aggression and violence (n = 18)94–111 and bullying (n = 2)112,113 (see Figure 11).
FIGURE 11.
Descriptive map of ‘harm to others’.

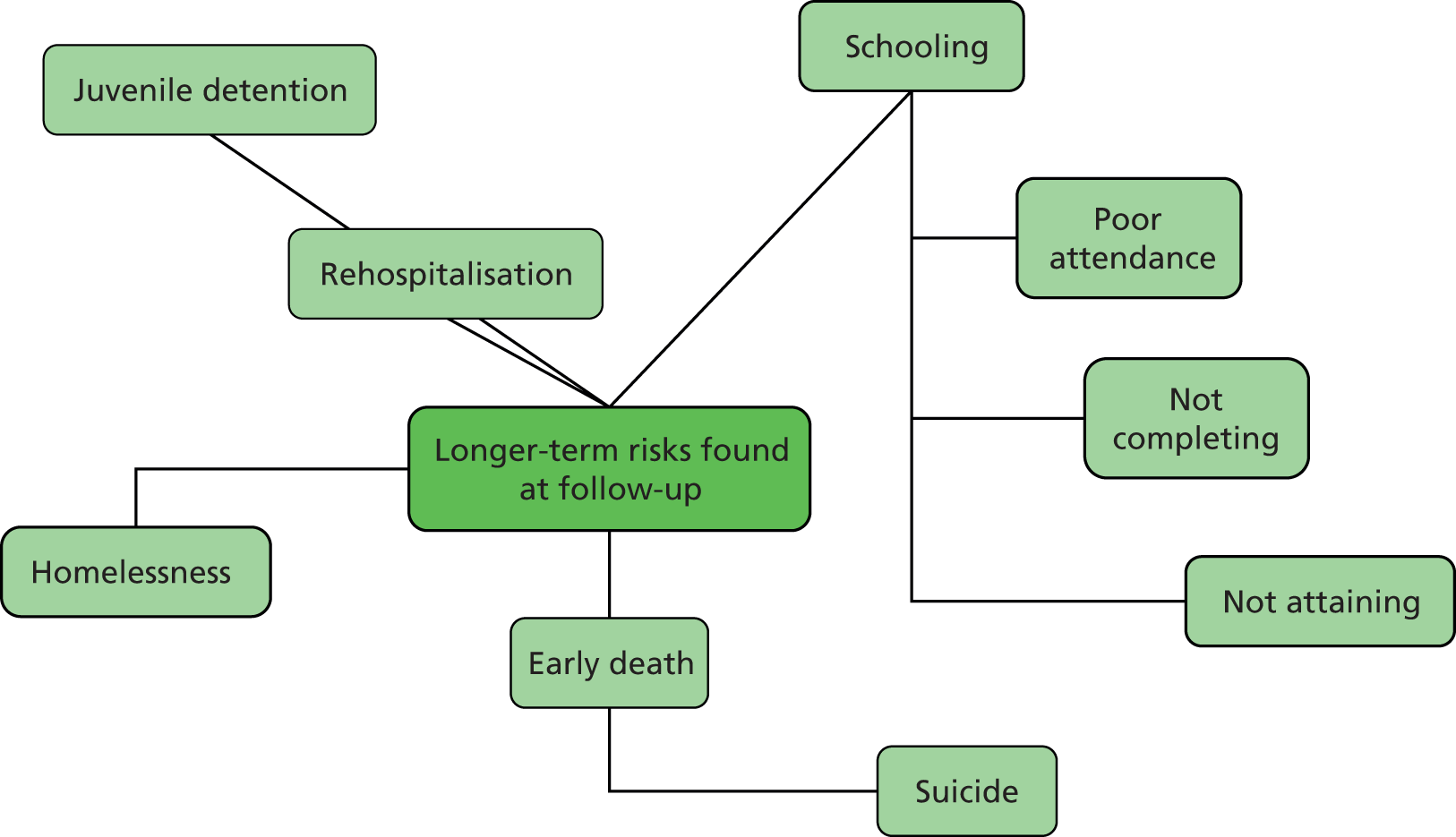
Longer-term risks found at follow-up (15 papers)114–128
This category was independently created by the project team to group together a series of papers focusing on the longer-term risks of being admitted to inpatient CAMHS units (see Figure 12). Included papers variously addressed the risks of readmission (n = 9),114–122 early death (n = 2),125,126 disrupted schooling (n = 2),127,128 homelessness (n = 1)123 and delinquency (n = 1). 124
FIGURE 12.
Descriptive map of ‘longer-term risks found at follow-up’.
Early disengagement from services (five papers)129–133
This category is depicted in Figure 13 and was developed by the project team to bring together papers concentrating on the risk of young people running away (n = 3),129–131 being discharged against medical advice (n = 1)132 and dropping out from treatment (n = 1). 133
FIGURE 13.
Descriptive map of ‘early disengagement from services’.

Risk factors influencing admission and length of stay (five papers)27,134–137
This category is depicted in Figure 14 and was created to bring together papers addressing factors influencing admission to, and length of stay in, inpatient CAMHS care. Factors identified included gender, ethnicity, general predisposing factors, and young people being adopted and living in disrupted family homes.
FIGURE 14.
Descriptive map of ‘risk factors influencing admission and length of stay’.

Risk of harm from the system (five papers)138–142
Directly drawn from Subotsky’s29 typology, this category includes the negative effects of treatment along with the risks of other adverse consequences of inpatient admission, such as loss of educational continuity, or exposure to risks, such as abuse by staff. Included in the mapping (see Figure 15) were papers dealing with the side effects of medication (n = 3),138–140 sexual abuse by staff (n = 1)141 and contagion (n = 1). 142
FIGURE 15.
Descriptive map of ‘risk of harm from the system’.

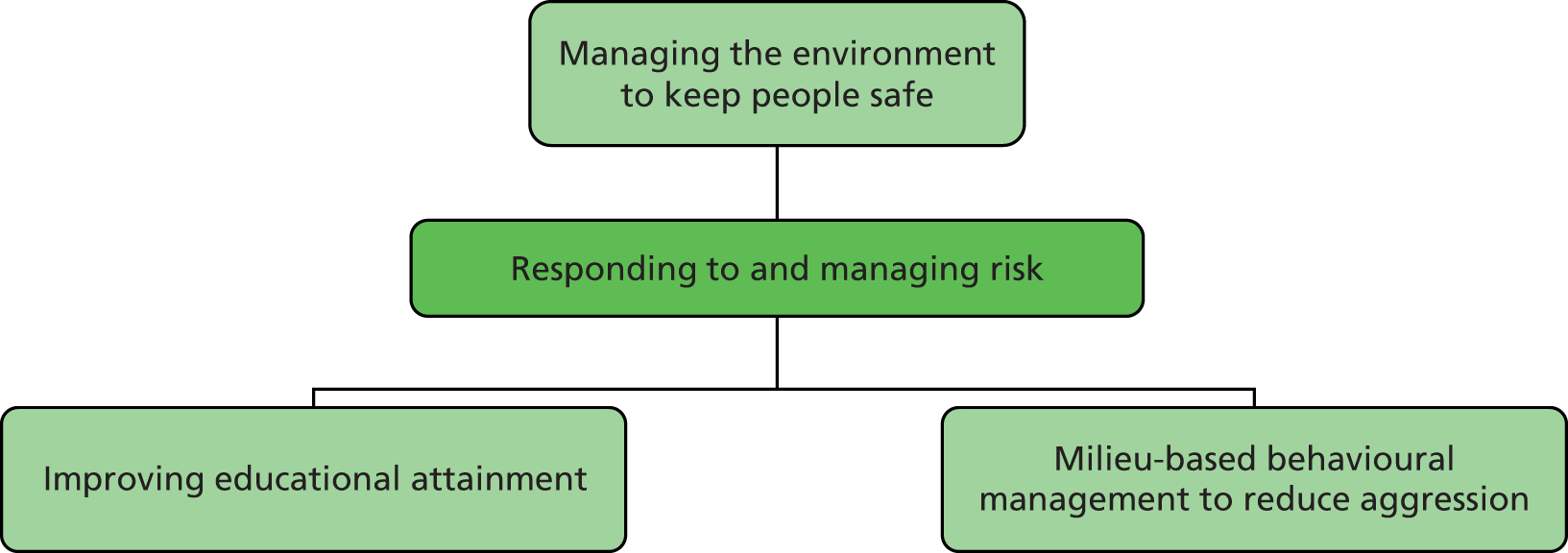
Responding to and managing risk (three papers)143–145
A small number of papers were brought together in this category, created by the team for the purposes of this mapping because they specifically addressed actions designed to manage or reduce risk (see Figure 16). These papers variously addressed improving educational attainment (n = 1),143 managing the environment to keep people safe (n = 1)145 and milieu-based behavioural management to reduce aggression (n = 1). 144
FIGURE 16.
Descriptive map of ‘responding to and managing risk’.
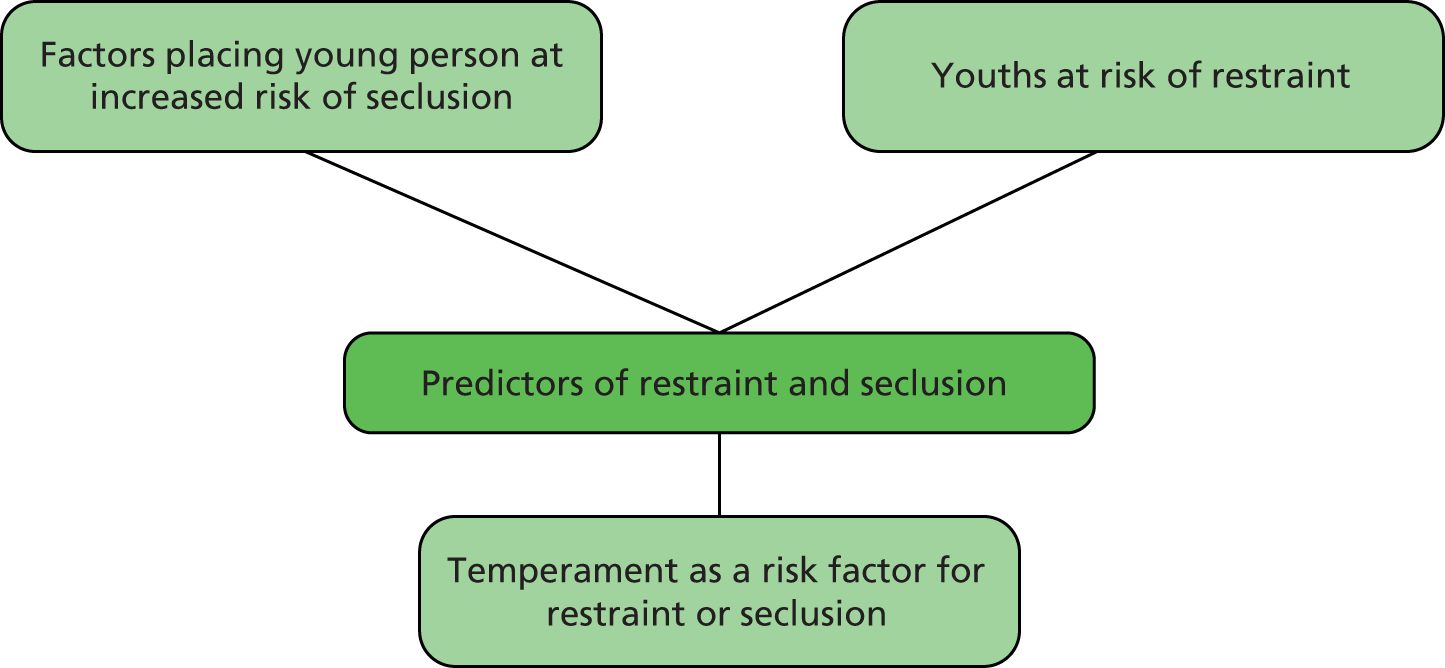
Predictors of restraint or seclusion (three papers)146–148
This set of three papers looked at predictors of restraint, seclusion or both (see Figure 17). Specifically, they sought to identify the factors that place a young person at increased risk of seclusion during his or her admission (n = 1),146 to establish whether or not a particular group of young people are at risk of restraint (n = 1)147 and to examine whether or not temperament characteristics (e.g. fear, anger) are risk factors for restraint and seclusion for young people in inpatient mental health hospital (n = 1). 148
FIGURE 17.
Descriptive map of ‘predictors of restraint or seclusion’.
Other
Three final papers were included, none of which could be mapped to the categories above and each of which addressed a distinct area. One paper focused on the risk of functional impairment, reporting on two studies which assessed the validity of a measure (the Functional Impairment Scale for Children and Adolescents). 149 The second reported from a study into the risks to, and the effects of, young people in inpatient mental health services playing fantasy role-playing games. 150 The third was a non-empirical paper included because it scoped the challenges facing inpatient CAMHS mental health services. 151
Summary of phase 1 findings
Each of the 124 papers included in phase 1 of this project was identified following a search of two databases combining terms from four arms (mental health, young people, inpatients, risk). Each was reviewed by at least two members of the study team, who agreed that it met the project’s criteria for inclusion. Data (e.g. focus of paper, country of origin, type of study in the case of papers reporting original research) were extracted from each and summarised.
The central purpose of this first phase of our overall evidence synthesis was to scope and map out the territory in the area of risk for young people moving into, through and out of inpatient mental health services. This was achieved by grouping together included papers using categories developed by Subotsky,29 and by using new categories created specifically for this study by the project team. This theming of retrieved papers demonstrated that, overwhelmingly, it is clinical risks (particularly the risks of suicide, self-harm and harm to others) that have featured most prominently in published papers (or, at least, in the papers published in journals indexed in the two databases searched in this phase of the project).
This was not an unexpected finding. It suggests that the risks that dominate policy and practice in mental health services are the risks that occupy most researchers and writers in the field. With regard to the characteristics of the research in this area, few papers retrieved reported data from inpatient CAMHS risk studies conducted in the UK. Most papers reported findings from prospective or retrospective cross-sectional surveys designed to establish associations between the personal and clinical characteristics of young people using inpatient CAMHS and the chances of certain unwanted events (e.g. self-harm, violence, running away) happening. Very few papers were directed at establishing what might be done to respond to or manage risk.
Chapter 3 Consulting with stakeholders and determining priorities for in-depth review
Using the Evidence for Policy and Practice Information and Co-ordinating Centre framework to consult with stakeholders
The EPPI-Centre approach obliges researchers to pause at the point where the territory has been scoped and mapped out, and to consult with people with interests in the field. The purpose of this consultation is to share knowledge of what has been found and to invite views to be given on the priority areas to be taken forward into the in-depth phase of the review which follows. In this project, key groups to involve in the consultation process included young people with personal experience of using inpatient mental health services; family members; service managers; practitioners drawn from different occupational groups; and workers from non-statutory organisations campaigning for young people’s mental health and the development of services. Figure 18 illustrates the use of the EPPI-Centre framework in this phase of the project.
FIGURE 18.
Using the EPPI-Centre framework to consult and determine phase 2 priorities.
Young people
In order to engage with young people with experience of using inpatient mental health services, members of the project team formed an early collaboration with representatives of the leading mental health charity YoungMinds. To inform our involvement strategy more generally, project members also consulted with two Cardiff University colleagues otherwise unconnected to the study but with expertise in involving young people in the research context (Professor Lesley Lowes in the School of Healthcare Sciences and Professor Sally Holland in the School of Social Sciences). From the project’s initial meetings onwards, members of the team were determined that the approach to working with young people should be sensitive to experiences, informed by an awareness of relative power relations and (during face-to-face project-related meetings) interactive in style. 152
The earliest approach to YoungMinds was made during the preparation of the project’s outline proposal for funding. It was set in the context of an existing collaboration between this organisation and a member of the project team (SP) in another, then-current, NIHR HSDR programme study involving young people with mental health needs. 23 YoungMinds was approached because it is the UK’s leading charity in its field, describing itself as:
committed to improving the emotional wellbeing and mental health of children and young people. Driven by their experiences we campaign, research and influence policy and practice. 153
Following confirmation of this project’s funding award, a key meeting was held in Cardiff at the beginning of March 2013 involving team members (BH, DE and NE) and YoungMinds’ then national Training and Development Coordinator (Matthew Daniel). This was convened with a view to mapping the fine detail of how young people might most effectively be engaged in the work of determining phase 2 priorities. Project team members were aware of the pitfalls of inviting young people to formal advisory group meetings without support, in which other contributors were likely to be drawn from more powerful groups such as management and the professions. An important guiding principle, therefore, was to agree an approach to involvement that ensured that the voices and experiences of young people were properly heard and their priorities around risk attended to.
At this key planning meeting, a number of strategies were considered and a two-part plan negotiated drawing on YoungMinds’ expertise in participation and consultation. First, the document specifying YoungMinds’ contribution emphasised the plan to involve experienced staff from the organisation’s national young people’s participation project and from its training and development team. It also emphasised YoungMinds’ then-current Very Important Kids (VIK) project, funded by the National Lottery and established with one aim of increasing young people’s involvement in service design and delivery. The VIK project enabled regionally based workers to support and engage with groups of young people affected by mental health difficulties, to both hear and represent their views and experiences. With staff already skilled in involvement work, and with networks of young people already engaged with YoungMinds, it was agreed that the part of the project budget devoted to involvement would first be used to support YoungMinds to conduct a series of independent priority-setting consultations with young people on the project team’s behalf. With our project classified as an evidence synthesis, rather than as a primary research study, we were clear to distinguish this consultative activity from the activity of directly participating in research. NHS or university research ethics committee approval is always needed for primary, data-generating, studies where people are recruited as research participants. Active involvement in projects to help identify and prioritise research topics and/or to join advisory groups is a different type of participation, a distinction made clear in national guidance. 154 Second, it was agreed that YoungMinds’ Training and Development Coordinator would participate in the project’s formal priority-setting event and, through his organisation’s networks, invite a number of young people to join him.
Following this planning meeting and throughout the remainder of March 2013, YoungMinds conducted a series of five separate consultative conversations with young people who had previously been admitted to inpatient CAMHS. Identification of people was made using YoungMinds’ existing networks. Broad questions guiding these discussions were agreed in advance by project team members (BH, DE and NE) collaborating with our YoungMinds colleague Matthew Daniel, and were explicitly designed to inform the process of research priority setting as opposed to eliciting research data. These focused on understanding young people’s perceptions of risks and what is done about them, including (reflecting current concerns in the CAMHS field) risk for young people admitted to adult wards. Noting the purpose of these consultations in the context of this as a two-phase evidence synthesis, a clear request was also put to young people taking part to identify those risks that the project team should focus on in the second phase of the overall study.
The five consultation questions put to five young people are reproduced here:
-
What do you think the risks to children and young people in inpatient settings are?
-
How do you think those risks are assessed?
-
What do you think is done about those risks?
-
Do you think there are a different set of risks for young people who are inpatients in adult wards?
-
What risks do you think the research team should focus on in its in-depth review?
To facilitate a record and to inform the study’s priority setting, each consultative conversation was audiorecorded and segments transcribed, so that young people’s ideas could be drawn on to stimulate debate and discussion among members of the project team and stakeholder advisory group. A formal report on this consultation was also delivered to the project team (see Appendix 5), in preparation for tabling at the subsequent priority-setting meeting of the combined project team and stakeholders for phase 2. The summary from this report included this extended section:
Though we spoke to a relatively small number of young people there were some clear themes that emerged from all of the conversations and those themes came out of the direct experiences of the young people. They told us that there were a number of risks that were not adequately being assessed or addressed and that this might be because of a lack of resources or training. All of the types of risks that we discussed were seen as equally important and the assessment of risk was highlighted as an area that needed to be carefully considered, as a poorly done risk assessment could feel extremely punitive and could therefore have a negative effect on the individual’s emotional wellbeing. Most of the young people talked extensively about the risk of emotional harm caused through exposure to distressing experiences as well as negative peer group influences. The young people also mentioned the risk of having their social lives put on hold indefinitely and the lack of opportunity to get any high quality educational provision. One young person used the term ‘fragmented’ to describe how what had happened to their life felt and the result of this fragmentation was their self-identification as ‘ill’. This new identity was seen as damaging as it prevented recovery and made it more difficult for the young people to move back into a ‘normal’ life off the ward. The young people said that they were put on wards to get better but that in many cases there were reasons why being placed in an inpatient setting was in fact detrimental to them. However they also recognised that leaving too early was equally damaging. The risks are present in the immediacy of the inpatient setting but the failure to address those risks has severe implications on both the young people and services as not addressing them leads to increased emotional distress as well as the increased likelihood of a readmission.
Carers
Along with involving young people to help shape this project, the team was also concerned to involve parents or other carers. One member of the project team combines identities as a mental health professional, academic and carer of a young person with mental health difficulties. An invitation to participate in our planned priority-setting stakeholder advisory group meeting was also extended to a mother whose child had recently been admitted to mental health hospital. This carer was identified as someone interested in participating in broader consultative and influencing activities by the project team’s senior practitioner member (GT). In the event, this person’s preference was to discuss risk in inpatient CAMHS settings and priorities for our in-depth evidence synthesis in a private, one-to-one conversation. This conversation took place in April 2013, involving one team member (BH), and focused on this carer’s views of the risks to young people entering, using and leaving hospital and on identifying phase 2 priorities.
Notes taken during this consultative conversation were prepared for tabling via oral presentation at the planned face-to-face stakeholder meeting. Key carer messages included that admission to inpatient CAMHS can be damaging, with planned short admissions turning into longer spells in which risks of harm to self can increase through the learning of abnormal, dangerous behaviours and the forming of new, unhelpful friendships (i.e. contagion). A further risk identified by this mother was at the transition from hospital to home, where concerns focused on the risks of young people remaining in touch with people met in hospital and thus extending unhelpful relationships.
Stakeholder advisory group meeting: agreeing risk priorities for phase 2
In preparation for a first combined project team and stakeholder advisory group (SAG) meeting, a set of documents was prepared for invited members and posted out in advance. Included were an accessible overview of the project (see Appendix 6), a proposed set of terms of reference for SAG members (see Appendix 7) and an agenda (see Appendix 8). The meeting itself was convened in Cardiff on 24 April 2013, organised for the express purpose of generating candidate categories of risk to serve as priorities for the second, in-depth, phase of this review. The event was chaired by Dr Michael Coffey (Associate Professor, Swansea University), an academic with expertise in mental health services but not associated with the study in any other way.
Decisions on the full range of stakeholders to include in the SAG, and the identification of actual representative individuals to invite, were taken collectively by the project team, drawing on our understanding of the CAMHS system, our knowledge of specific inpatient units and our working relationships with managers, practitioners and others. In addition to members of the project team, participants (drawn from South Wales and Greater Manchester, reflecting the locations of project members) included Matthew Daniel, collaborating representative from YoungMinds (who had already completed the consultation exercise reproduced in Appendix 5); two young people with experiences of using CAMHS; a senior NHS CAMHS manager; a senior child and adolescent psychiatrist; a senior CAMHS therapist; and a senior nurse with inpatient CAMHS responsibilities. Invitations were also extended to individuals with backgrounds in child and adolescent mental health social work, clinical psychology and teaching in inpatient CAMHS settings.
The principles of nominal group technique were drawn on in planning the process designed to lead to the identification of priority risk categories for phase 2 of the project. This is an approach to group decision-making introduced in the early 1970s by Delbecq and Van de Ven,155 which places weight on all participants having an equal opportunity to express a view. Since its emergence it has been successfully used in the research context, including in a study funded by the NIHR Health Technology Assessment (HTA) programme involving a member of this current project team (ML) as a co-investigator. 156 In this current project, the use of an approach explicitly designed to avoid letting group decision-making become dominated by one or more vocal individuals appealed to the team, given our concern that young people, in particular, might find it difficult to contribute in the presence of professionals, managers and academics.
The SAG meeting opened with an overview of the project, along with a presentation of the broad themes arising from the phase 1 scoping and mapping exercise. To facilitate later discussion and priority setting, our maps remained on display throughout the duration of the event, each depicted on an individual sheet of A1 flipchart paper. A presentation from YoungMinds followed, centring on a summary of the outcomes of the consultation exercise previously conducted with young people.
Following a natural break in the meeting, participants were invited to record independently written responses to the question ‘What do you think the risks for young people are as they make the transition into, through and out of inpatient CAMHS?’
The idea of inviting written responses, without conferring, was used as a nominal group strategy to ensure that as a project team we had access to the full range of views available in the room in enduring form once the meeting had ended. With a member of the team (NE) acting as facilitator, all SAG and project team members were then invited to share their written responses individually. These were recorded on flipcharts using the words directly spoken by the participants, and, during this round, the views of the carer who had previously been consulted were also reported and recorded. In the facilitated discussion following, opportunities were taken to seek explanations or further details about any of the ideas that participants had produced that were not clear to all. In this segment of the meeting our aim was to generate as comprehensive a list as possible of the full range of risks associated with inpatient CAMHS, including (but not limited to) the risks which our phase 1 scoping and mapping had identified as occupying the interests of researchers.
By the end of this process, meeting participants had access to a range of materials and ideas presented and discussed in the earlier part of the day. These included the pre-prepared series of maps displaying the themed overview of existing research; the account of the YoungMinds pre-meeting consultation with young people; and a series of flipcharts carrying the words of individual stakeholders (and a carer, previously consulted) in response to the invitation for people to identify the risks facing young people as they make the transition into, through and out of inpatient CAMHS. In a second round of activity informed by nominal group principles, project team and stakeholder group members were then asked to rank, in writing, their personal priorities for the categories of risk to take forward into the second, in-depth, phase of the project. The preamble to this exercise invited people to draw as widely as they wished on the full range of risks as previously described and discussed.
This first combined project team/stakeholder meeting closed with the collection of lists of individually generated, ranked phase 2 priority categories of risk produced by each person taking part. To this collection of lists were added carer priorities previously identified and a composite list of priorities extracted from the YoungMinds consultation report. This exercise gave project team members a long list of candidate categories of risk for the in-depth segment of the project ordered by individual researcher and SAG member, and from the young people collectively consulted (see Appendix 9). From this collated list the top three ranked priorities were taken from each individual (and from the YoungMinds consultation collectively) to produce a new, shorter, list of 45 individual items. In order to group these items under broader categories, this list was independently coded by two members of the project team (DE and NE), who then met to discuss and agree on their categorisation. This joint categorisation was then checked and agreed on with the involvement of a third member of the team (BH).
This process led to the identification of eight ranked priority categories of risk, each having a count of the number of items from the total of 45 subsumed within it (see Appendix 10). This information was included in a summary document for SAG members, which was circulated for final responses before the initiation of phase 2 of the review, and is also summarised in Table 2. Further details are given in Appendix 11.
| Area of risk | Number of times identified |
|---|---|
| Dislocation | 16 |
| Contagion | 6 |
| Harm from organisation | 6 |
| Institutionalisation | 5 |
| Self-harm | 4 |
| Decision-making | 3 |
| Suicide | 2 |
| Aggression | 1 |
| Other: managing dissonance/ambivalence (n = 1) and psychological risks (n = 1) | 2 |
The document for SAG members noted that the top risk category priorities for the in-depth segment of the review were all examples of ‘less obvious’ risks, and, as such, were unlike many of the more ‘clinical’ risks identified in the phase 1 mapping of the literature. The project team’s categorisation of these less obvious risks included a version of this summary information, along with plans for the initiation of the next phase of the synthesis overall:
-
Dislocation is the word the project team has used to describe the top priority emerging for the second phase of this review. This category of risk includes the ideas of young people being removed from ‘normal’ life, of being ‘different’ and of experiencing ‘fragmentation’.
-
Dislocation as a category of less obvious risk also captures the ideas of being stigmatised and discriminated against, and of young people losing their previous identities, social contacts and friendship groups. It includes isolation from, and within, families.
-
Dislocation also includes the risks presented to young people’s educational, psychological and social development.
-
Dislocation implies unhelpful loss, and contagion (the second category of risk prioritised for the next phase of the review) implies unhelpful gaining: the risk of being exposed to and of learning abnormal behaviour, and of new and unhealthy friendships.
The project team’s plan presented to SAG collaborators indicated the aim of taking both dislocation and contagion forward as the two, linked, priority risk categories for the second phase of this evidence synthesis. Team members were aware of an equal number of items having been brought together under the categories of ‘contagion’ and ‘harm from organisation’, but noted that, in consulting with a carer, the risks from contagion (learning new and harmful behaviours) were a particular priority. This informed the plan, also included in the report to collaborators, to take this area forward into the next study phase. The report also drew attention to the fact that the proposed phase 2 plans implied a move away from the more ‘clinical’ risks identified in the phase 1 mapping towards a consideration of some of the ‘less obvious’ risks, and in this context invited feedback on three questions:
-
Have we reflected stakeholders’ priorities accurately?
-
If we have reflected the priorities for the in-depth part of our review accurately, then we welcome ideas on where we need to go for evidence in these areas. If we are gathering information on how the risks of ‘dislocation’ and ‘contagion’ are identified, assessed and managed as young people move into, through and out of inpatient CAMHS, then where should we look and whom should we approach?
-
What other words can you think of that reflect the ideas of ‘dislocation’ and ‘contagion’, which we might use to continue to search for evidence?
One stakeholder participant from our April 2013 meeting responded to the summary and phase 2 initiation document by advising the team to be mindful of the dangers of ‘demonising tier 4 admissions’, noting that hospitals are a crucial and very scarce resource playing an important part in overall systems of care. Our response as a team, then and now, is that we concur: inpatient admission for young people with mental health difficulties is indeed sometimes necessary, as it is here that round-the-clock specialist care is provided to people with the greatest need. What the consultation exercise indicated, however, was an appetite among project members and collaborating stakeholders for a phase 2 review of some of the risks less often considered for young people passing into, through and out of inpatient care.
Summary of consultation with stakeholders
Following EPPI-Centre principles, a series of broad, phase 1 maps of the literature on risks for young people admitted to mental health hospitals were taken to a stakeholder advisory group with a view to determining the focus for the second, in-depth, phase of this study. Project team members engaged with the charity YoungMinds, which conducted a consultation on the team’s behalf. A series of maps arising from the phase 1 scoping exercise were devised and presented to people taking part in a key stakeholder advisory group meeting convened in April 2013. Collaborators were then asked to identify what they thought the risks to young people moving into, through and out of mental health hospital were. Responses were displayed alongside the risks occupying earlier teams of researchers identified from the scoping exercise. Informed by nominal group techniques, all team members and collaborators were invited individually to rank the categories of risk they saw as priorities for the in-depth phase of the project. These priorities were grouped together under a series of broader categories, with a large number of risks brought together under the umbrella category ‘dislocation’. The team determined to make this a first priority risk category for phase 2 alongside a second category, ‘contagion’.
Chapter 4 Phase 2 in-depth evidence synthesis: concepts and methods
Introduction and conceptual framework
During the phase 1 scoping of the literature using two databases, a preponderance of research and other outputs was found that concentrated on the clinical risks to young people admitted to mental health hospitals, and particularly in relation to the risks of suicide and self-harm. Typically, it is in response to these risks that young people are admitted to tier 4 inpatient settings, as it is in hospitals that round-the-clock specialist care and treatment in conditions of safety can be provided. The risks of suicide, self-harm, physical deterioration and harm to others are vitally important ones: for young people, their families, friends, practitioners, managers and the wider society. Nonetheless, the steer from young people contributing to the YoungMinds consultation exercise conducted on the project team’s behalf, and from stakeholders participating in the end-of-scoping priority-setting meeting, was to conduct a search and synthesis of the evidence across a series of other, less obvious, risks.
This part of the project was again informed by the idea that inpatient CAMHS units exist within a larger, complex and inter-related system of people and organisations. Young people themselves are part of this system, as are their families and friends, the schools they attend and the community-based health services they may use. Decisions to admit young people to mental health inpatient units are often made in the context of high levels of clinical risk, and have important consequences: for the individuals admitted, for families and friends and others immediately surrounding, and for those providing direct services. Hospital admission also has consequences at the system level, at which services are organised and delivered: where teams and workers in inpatient and community health and social care services, in schools and elsewhere have responsibilities to manage young people’s transitions into, through and out of hospital in as seamless and integrated a manner as possible. In this context a consideration of the broader, less obvious, risks of ‘dislocation’ and ‘contagion’ for young people and those around them is consistent with a systems perspective and it is these largely non-clinical risks that form the focus of this part of the project.
Having identified dislocation and contagion as the categories of risk to prioritise, the task of searching comprehensively for research and other evidence in these areas in the context of young people passing into, through and out of inpatient mental health hospital proved challenging. This segment of the report sets out the research questions guiding phase 2. It also addresses the approach used in the interrogation of databases, and the sequential strategy developed for sifting through citations and making decisions on including and excluding materials identified. Reflecting EPPI-Centre commitments to seeking out evidence of the widest variety (rather than research outputs alone), a description is also given of the steps taken to locate and secure grey literature, clinical case reports and reports of local practice initiatives on how inpatient CAMHS units identify, assess and manage the categories of ‘less obvious’ risk focused on in phase 2. A detailed account is then given of the materials included in this in-depth component of the project and how decisions were made on the quality of these.
Phase 2 research question and objectives
The research question for phase 2 was:
What is known about the identification, assessment and management of dislocation and contagion in young people (aged 11–18 years) with complex mental health needs entering, using and exiting tier 4 inpatient services in the UK?
Objectives for the in-depth evidence synthesis were:
-
to identify and appraise the evidence for the identification, assessment and management of the risks of dislocation and contagion for young people using inpatient CAMHS
-
to identify and describe any underlying theoretical explanations for approaches used in the identification, assessment and management of the risks of dislocation and contagion
-
to understand the views and experiences of dislocation and contagion of young people (aged 11–18 years) with complex mental health needs using inpatient mental health services, and of those involved in the identification, assessment and management of these risks in these settings
-
to synthesise the evidence for the identification, assessment and management of dislocation and contagion in young people (aged 11–18 years) with complex mental health needs moving through inpatient services
-
where possible, to synthesise the evidence on the costs and cost-effectiveness to the NHS of different approaches to identifying, assessing and managing the risks of dislocation and contagion for young people using inpatient mental health services.
Review design
As with the first phase of the project, the design of this second segment was informed by the approach developed by the EPPI-Centre, as Figure 19 illustrates.
FIGURE 19.
Phase 2 of the EPPI-Centre framework in action.
Review methods
As per the approach described in the project protocol, once we had agreed the focus for this second phase of the project, work commenced with electronic searches of specified databases. In the case of citations finally included, reference lists were searched to identify additional materials for possible inclusion (back-chaining). Searches were conducted for UK-only grey literature, and the project team published (and widely circulated) a call for evidence. This requested examples of local service responses to the less obvious risks and was sent to all NHS and non-NHS inpatient CAMHS units in the UK and was additionally distributed via online discussion and mailing lists.
Types of participants
To be included, research and other materials needed to be written in the English language and to focus on young people aged 11–18 years by:
-
focusing exclusively on young people aged 11–18 years or
-
focusing on a wider age group but including sufficient detail to enable the accurate identification of data relating to young people specifically or
-
relating to a study sample where the mean age was between 11 years and 18 years.
Types of intervention and phenomena of interest
All citations were considered which addressed ‘dislocation’ and ‘contagion’ for young people moving into, through and out of inpatient mental health services.
Context
All citations were considered where care was provided in inpatient mental health services. Following the decision made in phase 1, ‘inpatient mental health services’ was defined in this phase of the study as any hospital setting staffed by mental health professionals. In the case of US studies retrieved, the decision was again taken to include citations centring on residential treatment centres (RTCs) or residential treatment programmes. These facilities are comparable to hospitals, with the American Academy of Child and Adolescent Psychiatry defining them as providing:
intensive help for youth with serious emotional and behaviour problems. While receiving residential treatment, children temporarily live outside of their homes and in a facility where they can be supervised and monitored by trained staff.
(p. 1)157
Types of evidence
This part of the review considered a variety of types of evidence: published and grey literature original research; review, discussion and opinion papers; reports of local practice initiatives or service developments; clinical case studies; and policy and guidance documents. All evidence relating to outcomes, views and experiences, costs and cost-effectiveness, policies, and service and practice responses in the areas of ‘dislocation’ and ‘contagion’ for young people (11–18 years) with complex mental health needs using inpatient mental health services was sought. Materials published in the English language since the introduction of the tiered system in CAMHS in 1995 were sought.
Exclusion criteria
Excluded materials were those not in the English language; addressing inpatient mental health services for adults over 18 years; centring on inpatient mental health services for children under the age of 11 years; relating to any community-based mental health services (e.g. outpatient, day care or wraparound); addressing juvenile justice services.
Search strategy
Preliminary scoping searches of MEDLINE and PsycINFO performed for phase 1 of the project (see Chapter 2 and Appendices 1 and 2) highlighted a number of potential challenges to be considered when developing the in-depth searches required for phase 2, principally surrounding the use of the term ‘risk’. The outputs from phase 1 had predominantly focused on the clinical risks to young people in inpatient mental health settings, such as the risk of suicide and self-harm. Comparatively little evidence was found focusing on the less obvious risks such as the risk to young people admitted to mental health hospital of negative peer group influences or the loss of educational opportunities. The priority risk categories, to be taken forward to the second, in-depth, phase of the study and decided in consultation with the stakeholder advisory group, were all examples of these less obvious risks. An examination of the papers known to the investigators from phase 1 discussing these less obvious risks confirmed the challenge ahead, with very few using the term ‘risk’ and the language used within each varying considerably.
Led by one member of the project team (EG), an initial attempt was made to try to define and describe the two priority areas of ‘dislocation’ and ‘contagion’, with the intention of directly including these in one arm of the phase 2 search strategy. Potential keywords reflecting these areas were generated, drawing on contributions from the project team and from members of the stakeholder advisory group. Examples of candidate keywords connected to the priority risk areas are given in Table 3.
| Areas identified | Keywords for stage 2 |
|---|---|
| Dislocation | |
| Dislocation (loss or gain) | Dislocation, disrupt*, disconnect*, fragmentation |
| Removal from ‘normal life’ | Life in proximity to normal, abnormal. ‘Fitting in’, marginali?ation |
| Losing out educationally | Education or school in proximity to achievement, attendance, performance, progress, continuity, interruption*, attainment |
| Falling behind in psychological and social development | Social in proximity to network, support, development, relations, influences, isolation, media. Development* in proximity to milestone*, psychological, social, education*, risk |
| Being stigmatised/discriminated against | Stigma*, discrimination |
| Loss of previous identity | Identity, social contact*. Friend* or peer* in proximity to missing, loss, separation |
| Isolated within families | Family or parent* in proximity to breakdown, relationship*, dislocation, missing, separation, problem*, support, change, isolation |
| Contagion | |
| Contagion | Contagion, copy, mimic, imitate |
| Developing new and unhealthy friendships | Friend* or peer* in proximity to loss, separation, bad, manipulative, abnormal, detrimental, harmful, disruptive, negative, damaging, pressure |
However, testing these terms in pilot searches produced an unmanageable volume of citations. Following consultation with colleagues, including Mala Mann [an information specialist associated with the Systematic Review Network (SysNet) at Cardiff University], the decision was made to remove this arm of the search entirely. This decision produced a highly sensitive final search strategy for phase 2 comprising three arms: (1) young people, (2) mental health and (3) inpatient. This was recognised as the best approach to capturing all relevant material, leaving project investigators the task of reviewing all search results and manually identifying citations that also addressed the priority risks of dislocation and contagion, from which any papers addressing costs and cost-effectiveness could also be located. Searches were developed using a combination of controlled vocabulary [e.g. medical subject headings (MeSHs) in MEDLINE] and text words, and, before proceeding, this strategy was thoroughly tested to ensure that it retrieved all of the core papers identified as relevant during the phase 1 scoping. Information on search strategies used across all databases is provided in Appendix 12. The 17 individual databases searched were:
-
American Economic Association Database (EconLit)
-
Applied Social Sciences Index and Abstracts (ASSIA)
-
British Nursing Index (BNI)
-
Cochrane Library (including the Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, Cochrane Methodology Register, HTA and NHS Economic Evaluation Database)
-
Cumulative Index to Nursing & Allied Health Literature
-
Education Resources Information Center (ERIC)
-
Excerpta Medica (EMBASE)
-
Health Management Information Consortium (HMIC)
-
Medical Literature Analysis and Retrieval System Online (MEDLINE)
-
PsycINFO
-
Scopus
-
Social Care Online
-
Social Services Abstracts
-
Sociological Abstracts
-
System for Information on Grey Literature in Europe (OpenGrey)
-
Turning Research into Practice (TRIP) Plus
-
Web of Science.
To ensure that the project remained manageable in the time frame given, a number of limits were also applied to contain the number of results. Text word searching was used for titles and abstracts only, and, as per the inclusion criteria given in Types of evidence above, the search was limited to English-language publications from 1995 to September 2013. When numbers of results were particularly large, the option of restricting the search to ‘human’ was also utilised.
As described in our Review methods section above and in Call for evidence below, a range of snowballing techniques were also used to increase the sensitivity of the search. References from citations located and included in phase 2 were searched for additional studies (back-chaining), and the Journal of Child and Adolescent Psychiatric Nursing, European Child and Adolescent Psychiatry and Psychiatric Services were hand-searched for the previous 2 years to ensure that any relevant papers that may not have been indexed in the major databases were located. Searches for relevant grey literature were conducted using directories of conference proceedings, HMIC, OpenGrey and Index to Theses. A search was also made using the website of the NIHR, including for information on studies funded by the HSDR programme and its predecessors.
Searching for policy and guidance
As per the study protocol, searches were made of organisational websites to locate and include important contextual material (such as policy drivers, standards and cross-UK priorities for inpatient CAMHS), along with new material to include as direct evidence. Lists of current and archived websites to search were generated by project team members drawing on their understanding of the field. Those searched were:
-
CAMHS Outcomes Research Consortium
-
Care Services Improvement Partnership
-
Centre for Mental Health
-
Child and Maternal Health Observatory
-
Children and Young People’s Mental Health Coalition
-
Department of Health, England
-
Joint Commissioning Panel for Mental Health
-
Mental Health Foundation
-
Mental Welfare Commission
-
National CAMHS Support Service
-
National Institute for Health and Care Excellence
-
National Mental Health Development Unit
-
Northern Ireland Executive
-
Quality Network for Inpatient CAMHS
-
Royal College of Psychiatrists
-
Scottish Executive
-
Social Care Institute for Excellence
-
Solutions for Public Health
-
Welsh Government
-
YoungMinds.
Call for evidence
A single-side call for evidence was produced (see Appendix 13). This introduced the study and invited recipients to forward evidence relating to the identification, assessment and management of the categories of less obvious risks focused on in this phase of the review. This call was sent in the second half of 2013 to all NHS and non-NHS inpatient CAMHS units identified within the UK. In January 2014 the same call for evidence was electronically circulated via the Child and Adolescent Mental Health Service National Academic Mailing List Service discussion list (see www.jiscmail.ac.uk/cgi-bin/webadmin?A0=CAMHS). Contact was made with the Royal College of Psychiatrists’ Quality Network for Inpatient CAMHS (QNIC), and through the group’s Deputy Programme Manager the call for evidence was forwarded to all members. The team was unable to also circulate this call to members of the Royal College of Nursing’s Children and Young People forums (as had initially been intended and written into the study protocol) as no online forum was found to exist. Instead, snowball sampling was used to continue the circulation of the study among members of the nursing profession. Contact was made with the Royal College of Nursing’s Mental Health Advisor (who has UK-wide responsibilities), and then with a former National Nursing Officer in England with mental health responsibilities, for onward distribution via their lists. The call was also circulated to all members of Mental Health Nurse Academics UK (MHNAUK, an organisation with representatives of over 60 universities; see http://mhnauk.swan.ac.uk/main.htm), and to members of the All Wales Senior Nurse Advisory Group for Mental Health.
Screening citations: a staged approach
The reference management software package EndNote (Version X7.1, Thomson Reuters, New York, NY, USA) was used to manage all citations found through the team’s database searching. First, duplicates were removed. Because of the large volume of retrieved citations remaining, a staged approach to screening was then conducted. In an initial round, the title of each citation was read by two members of the review team to determine whether or not the item fell at the intersection of ‘young people’, ‘mental health’ and ‘inpatient services’. For citations included at this stage, abstracts where available were read by two members of the team to determine whether or not items fell at the intersection of ‘young people’, ‘mental health’, ‘inpatient services’ and, now, the additional category of ‘risk’, broadly defined. Abstracts were then screened a final time to determine whether or not citations were concerned with the ‘less obvious risks’ forming the focus of this phase of the overall review. Where any doubt existed, full texts of articles were retrieved.
The full texts of all citations included at this stage were screened independently by two reviewers using a screening tool to aid this process (see Appendix 14). Multiple articles by the same authors reporting findings from the same study were linked together to help inform decisions on which studies to include. At all stages of this screening process, any citations that reviewers were unsure of were taken through to the next stage to allow a further round of consideration. Disagreement on the inclusion of citations at any of the stages based on topic relevance was resolved by discussion with a third member of the review team. Studies identified from the back-chaining of reference lists were assessed for relevance based on publication titles, and then on the retrieval of full texts. Following the retrieval of back-chained full text publications, citations were managed in the same way as citations retrieved via database searching.
Policies and guidance, reports of practice initiatives, clinical case studies and other non-research materials found in the grey literature were also read by two members of the project team and considered against the topic inclusion criteria, with disagreements resolved as above. Initial judgements, using the criteria developed by the National Institute for Health and Clinical Excellence (now the National Institute for Health and Care Excellence) in 2006,158 were:
-
category A (accepted): material judged to be of sufficient quality to be included in the next stage of the selection process
-
category B (background): material judged to provide background or contextual information
-
category R (rejected): material judged to be of no use for the purposes of this review.
Figure 20 shows the flow of citations through each stage of this overall process. Despite interest being shown in the project from individual respondents (some of whom forwarded published papers to the team), no local policies, practice initiatives or service developments were secured in response to our call for evidence (see Appendix 13). Searching of websites for policy and guidance found a total number of 20 documents assessed as relevant to the review.
FIGURE 20.
Flow of citations through the phase 2 in-depth review.
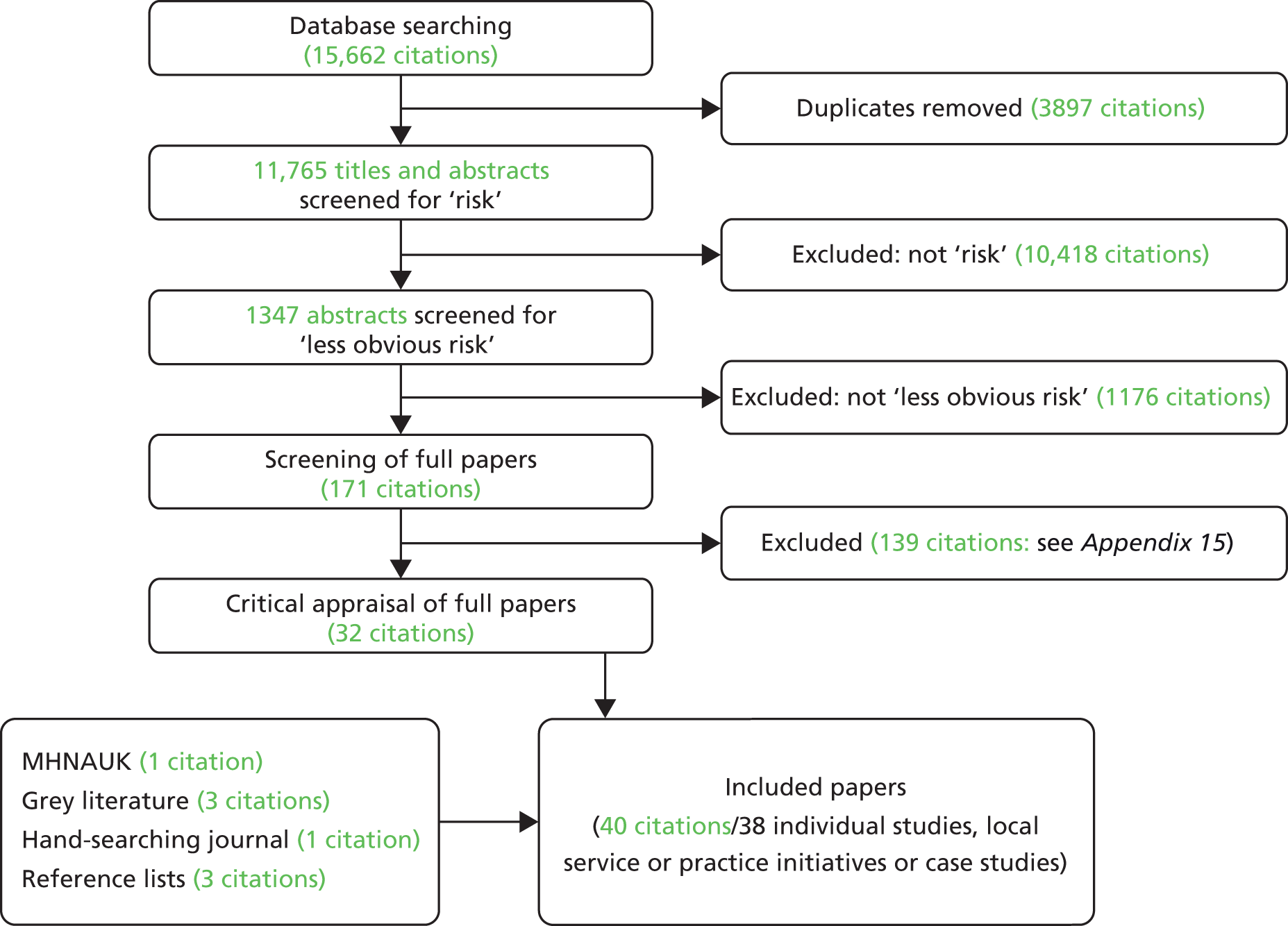
Data extraction
Each of the 40 citations and 20 policy and guidance documents was allocated to a member of the research team. Data from each were extracted and entered into a series of electronic tables. Table format followed guidance issued by the Centre for Reviews and Dissemination,159 with choice of table reflecting the type of material considered (see Appendices 16–21). Data extraction was independently checked for accuracy and completeness by a second researcher (DE), with any disagreements noted and resolved by consensus. A record of corrections was kept. Where multiple publications from the same study were identified, data were extracted and reported as a single study.
Quality assessment
As per the study protocol, each included study that passed the initial topic inclusion screening process was read and assessed independently for quality by two team members using one of a number of agreed appraisal checklists. For studies using an experimental design, the Effective Public Health Practice Project (EPHPP) tool was used. 160 This is a generic instrument which has been used to evaluate a variety of studies using an intervention design and has been deemed acceptable for use within systematic reviews. 161 Study quality is assessed using six criteria:
-
selection bias: the extent to which study participants were representative of the target population
-
study design
-
control of confounders
-
blinding: whether or not outcome assessors, intervention providers and participants were aware of the research question
-
data collection methods
-
withdrawals and dropouts.
An overall assessment of the quality of each study is also calculated, based on ratings of ‘weak’ through ‘moderate’ to ‘strong’ across each of the six criteria. Further study quality criteria are also included in this tool (including intervention integrity and statistical analysis), but these do not affect the overall assessment.
For studies using a survey design we used the checklist designed by Rees et al. ,162 and for qualitative studies the appropriate checklist available from the Critical Appraisal Skills Programme (CASP). 163 In order to calculate an overall assessment for both surveys and qualitative studies, appraisals were then considered alongside these criteria adapted from Kirk et al. :164
-
clear statement of the aims of the study
-
adequate description of the context for the study
-
clear specification of research design and its appropriateness for the research aims
-
reporting of clear details of the sample and method of recruitment/sampling
-
clear description of data collection
-
clear description data analysis provided
-
attempts made to establish rigour of data analysis
-
discussion of ethical issues/approval details
-
inclusion of sufficient original data to support interpretations and conclusions.
Based on the assessments of studies across all of these nine criteria, reviewers judged each study in terms of overall quality as ‘low’ (achieving quality ratings of 1–5), ‘medium’ (achieving quality ratings of 6–7) and ‘high’ (achieving quality ratings of 8–9). Resolution of discrepancies in the independent assessments of quality within each pair of reviewers was resolved through discussion, and, in a small number of cases, a third member of the team was invited to help achieve consensus and to arbitrate. No studies were excluded based on quality assessment ratings alone, although quality was used to inform the interpretation of findings.
Economic analysis
The plan for the economic analysis was sensitive to the type and quantity of evidence found. Where evidence of effectiveness in retrieved papers was accompanied by robust costing and/or cost-effectiveness analyses, our intention was, led by the health economist member of the project team (ML), to use the Drummond checklist165 to assess the quality of this. If little or no such economic evidence was found, attempts were to be made to estimate the cost of the most effective alternative approaches using resource data from the published/grey sources together with the most appropriate unit costs (e.g. Curtis;166 NHS Reference Costs, available at www.gov.uk/government/collections/nhs-reference-costs). Initial plans to add costs and economic terms to the search strategy to identify documents including an economic component were modified in light of the development of the three-arm search strategy already described above.
Data synthesis
Following the searching, sifting and appraising of the evidence, included materials (see Appendices 16–21) were brought together in a series of individual syntheses. Each of these focused on a priority risk category: a type of dislocation or contagion. Researchers informed by the EPPI-Centre approach recognise that a number of different synthesis strategies exist, with decisions on which to adopt reflecting the types of evidence located, theoretical orientations and overall review purpose. 26 Here, a configurative synthesis approach167 was used, a style suited to projects in which research and other materials from different contexts need to be meaningfully and coherently combined in narrative form.
Findings extracted from included citations (see Appendices 16–21) were inspected by members of the project team, and codes were applied to denote the category (or categories) of less obvious risk that each addressed. Available codes were created deductively, to reflect the categories and concepts arising from the joint project team and stakeholder consultation:
-
Dislocation: Normal Life
-
Dislocation: Identity
-
Dislocation: Stigma
-
Dislocation: Friends
-
Dislocation: Families
-
Dislocation: Education
-
Dislocation: Psychological Development
-
Dislocation: Social Development
-
Contagion.
The contents of policy and guidance documents (see Appendix 21) were inspected by members of the project team working individually, and information was coded as above. For each category of risk for which materials had been found, findings and extracts from relevant policies and guidance documents were grouped together. This grouping resulted in the identification of six types of dislocation risk (Normal Life; Identity; Stigma; Friends; Families; Education) and the risk of contagion. No material was coded as either Dislocation: Psychological Development or Dislocation: Social.
Led by the project manager (DE), as per the study protocol, packages of category-specific materials were distributed to review team members. Initially working independently, each reviewer inspected the detailed findings of each included study, clinical case report or practice initiative (see Appendices 16–20) and the relevant contents of policy and guidance (see Appendix 21). Subcategories were created in inductive fashion as reviewers developed familiarity with the materials assembled, an EPPI-Centre approach described by Gough et al. 168 This is consistent with the configurative synthesis approach used here, is recommended for reviews including mixtures of research evidence and policy,169 and is suited where a wide variety of study designs are being considered within tight time frames. 170 Each category-specific narrative synthesis summarising findings from included studies, juxtaposed with the relevant policies and guidelines, was then forwarded to two project members (DE and BH) for review and editing.
The strength of synthesised findings for stream 1 (intervention studies) was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach,171 where certainty of evidence is reported as being high, moderate or low/very low. Confidence in synthesised qualitative and survey findings was assessed using the Confidence in the Evidence from Reviews of Qualitative research (CERQual) tool, which uses a similar approach to GRADE. 172 The original CerQual approach was designed for qualitative findings and we used the same process but included findings from surveys in the assessment of confidence. Confidence in findings is described as high, moderate or low.
Results
Characteristics of included studies
Information on the characteristics of included studies, including assessments of quality, is given in Table 4.
| Author(s) (year) Country |
Participants | Setting | Length of stay (days) | Age (years) | Gender (% male) | Focus | Quality |
|---|---|---|---|---|---|---|---|
| Prospective cohort study | |||||||
| Best et al. (2004)127 USA |
Hospital: Ad (n = 70) High school: Ad (n = 76) |
Psychiatric units (n = NS) matched with one high school in same area | Range 37–921; mean 198 | Hospitalised: mean 14.1 ± 1.0; range 11.8–15.9 High school: mean 14.5 ± 0.4; range 13.8–15.8 |
Hospitalised: 56 High school: 46 |
Dislocation: Ed | Strong |
| Before-and-after study (no control group) | |||||||
| Singh et al. (2002)173 USA |
Study 1, HCP: pre (n = 18); post (n = 18) Study 2, HCP (n = 5) |
Study 1: inpatient unit (n = 1) Study 2: inpatient unit (n = 1) |
Study 1: NA Study 2: NA |
Study 1: NA Study 2: NA |
Study 1: NA Study 2: NA |
Study 1: Dislocation: Fa Study 2: Dislocation: Fa |
Study 1: weak Study 2: weak |
| Quasi-experimental multiple time series (retrospective) | |||||||
| Simmerman (1997)174 USA |
Ad (n = 107) | RTC (n = 1) | NS | Range 12–19 years | NS | Dislocation: Ed | Weak |
| Qualitative studies | |||||||
| Buston (2002)175 UK (Scotland) |
Ad (n = 12) | Previously inpatients | NA | Mean 17.3; range 14–20 | 34 | Dislocation: Fa, Fr, Ed | A, B, C, E, F, G, H, I High |
| Claveirole (2005)176 UK (Scotland) |
Ad (n = 18); P (n = 16); HCP (n = 23) | Inpatients (n = NS) | NS | Mean 16; range 12–21 | 33 | Contagion Dislocation: Fa, Fr, NL, St, Ed |
A, B, C, D, E, F, G, H, I High |
| Clemens et al. (2010)177/(2011)178 USA |
HCP (n = 14) | Inpatient units (n = 4) | Range 5–7 | NA | NA | Dislocation: Ed, Fr | A, B, C, E, F, G, H, I High |
| Colton and Pistrang (2004)179 UK (England) |
Ad (n = 19) | Inpatient units (n = 2), eating disorders | Range 35–140 | Mean 15.4; range 2–17 | 0 | Contagion Dislocation: Fa, Id, Fr |
A, B, C, D, E, F, G, I, High |
| Haynes et al. (2011)180/Painter (2008)181 UK (England) |
Ad (n = 10) | Inpatient units (n = 2) | Range 4 weeks to 36 months | Range 13–19 | 40 | Dislocation: Fr, St, Ed, NL, Id | A, B, C, E, F, G, H, I High |
| Moses (2011)182 USA |
Ad (n = 80) | Inpatient unit (n = 1) | Mean 7.6 ± 3.9; range 3–31 | Mean 15.3; range 13–18 | 59 | Dislocation: Fr, NL, St | A, B, C, D, E, F, G, H, I High |
| Offord et al. (2006)183 UK (England) |
Ad (n = 6) | Inpatient units (n = 6), eating disorders | NS | Range 16–23 | 0 | Contagion Dislocation: Fa, Id, Fr, Ed, St, NL |
A, B, C, D, E, F, G, H, I High |
| Puotiniemi and Kyngas (2004)184 Finland |
Ad (n = 1); P (n = 1) | Previously an inpatient | NS | 16 | 0 | Dislocation: Fa, Fr | A, B, C, E, F, H Medium |
| Longitudinal descriptive survey (prospective) | |||||||
| Anderson et al. (2008)185 USA |
Ad (n = 424); FU (n = NS) | Inpatient units (n = 5), substance abuse | NS | Mean 15.9 ± 1.3; range 13–18 | 49.5 | Dislocation: Ed | A, B, C, D, E, H Medium |
| Brinkmeyer et al. (2004)186 USA |
P (n = 47); FU-1 (n = 34); FU-2 (n = 25) | Inpatient unit (n = 1) | Median 6 | Mean 13.11 ± 2.89; range 7–17 | 56 | Dislocation: Fa, Ed | A, B, C, D, E, F, I Medium |
| Charlemagne (2011)187 USA |
P (n = 167); FU (n = 134); HCP (n = 27) | Inpatient unit (n = 1) | Mean 5.9 ± 3.4 | Range 13 ± 2.7 | 48.5 | Dislocation: Fa | A, B, C, D, E, F, G, H, I High |
| Czyz et al. (2012)188 USA |
Ad (n = 448); FU (n = 338) | Inpatients (n = NS) | NS | Mean 15.6 ± 1.41; range 13–17 | 29 | Dislocation: Fa, Fr | A, B, C, E, F, G, H, I High |
| Larzelere et al. (2001)189 USA |
Ad (n = 43); FU (n = 43) | RTC (n = 1) | Range 18–505; mean 181; median 15 | Mean 13.0; range 6–17 | 48 | Dislocation: Ed | B, C, E, F, I Low |
| Moses (2014)190 USA |
Ad (n = 102); FU (n = 80) | Inpatient unit (n = 1) | NS | Mean 15.3 ± 1.6; range 13–18 | 35 | Dislocation: St | A, B, C, D, E, F, G, H, I High |
| Parmelee et al. (1995)191 USA |
Ch and Ad (n = 90); FU (n = 77) | Inpatient unit (n = 2) | NS | Mean 2.2 ± 3.5; range 4–17 | 64 | Dislocation: Fa | A, B, C, D Low |
| King et al. (1995)142 USA |
Ad (n = 57); FU (n = 57) | Inpatient unit (n = 1) | Mean 24.9 ± 10.7 | Mean 15.8 ± 1.3; range 11.5–17.8 | 42 | Contagion | A, B, C, E, F, G, I Medium |
| Longitudinal descriptive surveys (retrospective) | |||||||
| Cawthorpe et al. (2003)192 Canada |
Ad (n = 198) | Inpatient unit (n = 1) | Males: mean 95.67 ± 56.87; range 1–337 Females: mean 79.82; range 3–254 |
Males: mean 14.89 ± 1.28; range 12–18 Females: mean 14.77 ± 1.17; range 12–18 |
64 | Contagion | A, B, C, D, E, F, I Medium |
| Shabat (2008)193 USA |
Ch and Ad (n = 457) | RTC (n = 50) | Mean 90.6 | Range 6–20 | 61 | Dislocation: Ed | A, B, C, E, F, G, H, I High |
| Lakin et al. (2004)194 USA |
Ch and Ad (n = 89) | RTC (n = 1) | Mean 58.6 ± 35.1; range 7–243 | Mean 11.7; range 5–17 | 67 | Dislocation: Fa | A, B, C, D, E, F, H, I High |
| Halfon et al. (1995)128 France |
Ad (n = 137) | Inpatient unit (n = 1) | Mean 10 months 10 days ± 9.3 | Mean 17.8 ± 1.5; range 14–21 | 54 | Dislocation: Ed | A, B, C, D, F, I Medium |
| Cross-sectional descriptive surveys | |||||||
| Moses (2011)195 USA |
Ad (n = 102) | Inpatient unit (n = 1) | Mean 7.6 ± 4.2; range 3–31 | Mean 15.3 ± 1.5; range 13–19 | 91.3 | Dislocation: St | A, B, C, D, E, F, H, I High |
| Thurber et al. (2007)196 USA |
Ch and Ad (n = 50); P (n = 75); HCP (n = NS) | Burn unit (n = 1); paediatric rehabilitation unit (n = 1); inpatient psychiatric unit (n = 1) | Median 20; mean 24 ± 25; range 4–174 | Mean 11 ± 3.5; range 3.9–18.6 | 70 | Dislocation: Fa | A, B, C, E, G, I Medium |
| Longitudinal descriptive survey (prospective) | |||||||
| Taiminen et al. (1998)197 Finland |
Ad (n = 12) | Inpatient unit (n = 1) | Mean 91.9 ± 73.2; range 7–200 | Mean 15.5; range 12.3–17.9 | 0 | Contagion | A, B, C, D, E, I Medium |
| Grey literature reports | |||||||
| Street and Svanberg (2003)198/Svanberg and Street (2003)199 UK (England and Wales) |
Ad (n = 107); P (n = 35); HCP (n = 115); interviews; questionnaire | Inpatient units (n = 10); paediatric wards (n = 2); adult psychiatry ward (n = 1); ‘one-stop’ service for young homeless people (n = 1) | NS | Mean 16.4 | 32 | Contagion Dislocation: Fa, Fr, NL, Ed |
A, B, C, D, E, F, H, I High |
| Tulloch et al. (2008)15 UK (England) |
HCP (n = 42); questionnaire | Independent and public CAMHS in England (n = 42 of 55, 76%) | Median 79 | Median: 12 years (lower end of the range – 38% of units); 18 years (upper end of the range – 77% of units) | NS | Dislocation: Ed | A, B, C, D, E, F, G, H, I High |
| Tulloch et al. (2008)15 UK (England) |
Ad (n = 19); P (n = 12); interviews; questionnaire | Independent and public CAMHS in England (n = 42 of 55, 76%) | NA | NA | NA | Dislocation: Fa | A, B, C, D, E, F, G, H, I High |
| O’Herlihy et al. (2001)11 UK (England and Wales) |
CAMHS units (n = 66); questionnaire | Independent and public CAMHS in England and Wales (n = 66 of 80, 82.5%) | NS | Mean 115 ± 181; range 0–2194 | NS | Dislocation: Ed, Fa | A, B, C, D, E, F, G, H, I High |
| O’Herlihy et al. (2001)11 UK (England and Wales) |
HCP (n = 245); questionnaire | Independent and public CAMHS in England and Wales (n = 80) | NA | NA | NA | Dislocation: Ed | A, B, C, D, E, F, G, H, I High |
| Mental Welfare Commission for Scotland (2009)200 UK (Scotland) |
Ad (n = 29); HCP (n = 11); interviews; case note review | All independent and public CAMHS in Scotland (n = NS) | NS | NS | NS | Dislocation: Ed, Fa | The study method is not fully detailed (e.g. sampling recruitment, participants age, gender, type of analysis) |
Box 2 summarises the policies and guidance documents included in phase 2, for which no quality assessment was undertaken.
Treatment that enables them [children and young people] to lead as normal a life as possible.
(p. 32)201
Links with home and the community should be maintained. 202
Ensure that children and young people in hospital continue to have access to a wide range of meaningful and culturally appropriate occupations and activities 7 days per week, and not restricted to 9am to 5pm. These should include creative and leisure activities, exercise, self-care and community access activities (where appropriate).
(p. 33)203
There may be a loss of potential, and hopes and gains may be unrealised. 201
Dislocation: IdentityNone.
Dislocation: Friends Relationships with young people outside hospitalA suitable location/designated private space should be provided for friends to visit. 204
There are unit policies and procedures on visiting. 204
Treatment should enable improved peer relationships. 205
Relationships with young people in hospitalNone.
Dislocation: StigmaStigma should be recognised as an issue for uses of mental health services. 201,206–212
Services should be provided in a non-stigmatising manner/environment8,204,213 and education should be provided to health care and social care professionals. 212
Dislocation: Education Education provision and facilitiesThe educational staff maintain communication with the young people’s parents/carers. 204
Inpatient services should provide access to education. 203,205,213
Education should be an integral part of the service provision and be provided during normal academic term. 205
Units should provide appropriate education facilities/classroom space204,214 and young people should have the educational materials they need for continuing their education for key stages 1–4204 and for those over 16 years to have access to educational materials they need. 204
Adolescents with eating disorders should have age-appropriate facilities which have the capacity to provide appropriate educational and related activities. 215
All young people have an individual education plan204 and education which is tailored to the individual’s need, age and stage of development. 205,216
Inpatient services will provide educational sessions203–205 which provide the full National Curriculum (or local equivalent) at the appropriate key stages,203,204 and, for those with psychosis and schizophrenia, should take account of their illness and degree of impairment. 203
Where the unit caters for young people over the age of 16 years, young people are able to continue with postcompulsory education. 204
The unit provides the core educational subjects: maths, English and science. 204
Treatment for adolescents with eating disorders should be balanced alongside the educational and social needs of the young person. 215
During admission following self-harm, consultation should take place with education staff as appropriate. 212,217
Treatment should enable improved family relationships. 205
Quality of inpatient educationEducation is provided by trained teachers who have additional training in all aspects of child and adolescent psychiatry. 202,205
For every eight places within a psychiatric inpatient unit, there should be at least one full-time teacher with at least one other whole-time-equivalent post comprising subject specialists at secondary stage. 202
Academic progressThe unit is a registered examination centre. 204
Reintegrating with school after dischargeEducation or training providers should support students to remain on the course or hold their place open for them whenever possible. 210
Working in partnership with education services/systems is important201,202,206,207,209,217–219 in order to maintain continuity of education provision at admission202,204 and to enable reintegration at discharge. 204,205,216
There is a key worker/named nurse to undertake this role especially at discharge and admission. 202
Dislocation: Families Impact on family relationshipsIt is recognised that one of the disadvantages of inpatient care is the effects of admission on family life. 8
A parent/carer support group should be available. 204
Consider alternatives to inpatient care when the inpatient unit is a long way from where they live. 203
Family involvementWork in partnership/collaboration with families205,218 and in development of the young person’s care plan. 204
Involve parents/carers in decisions about care after discharge. 204
Families should be involved. 201
During admission following self-harm, consultation should take place with the family as appropriate. 217
Ask the person who self-harms whether or not they would like their family to be involved in their care and, subject to consent, encourage the family to be involved where appropriate. 212
Maintaining contact with familiesOffer provision of family meetings within one week of admission and continuing thereafter as needed. 205
Flexible arrangements should be made for family contact. 202
Services are offered as near to home as possible, enabling frequent family visits/contact206,218 and appropriate family interventions. 218
There are unit policies and procedures on visiting. 204
Provide a suitable location/designated private space for family contact to take place. 204,205
Provide accommodation for families who have to travel a significant distance. 202
Parents/carers have access to refreshments at the unit. 204
ContagionNone.
Quality assessment
The methodological quality of the four experimental studies was judged against the six quality criteria, and is summarised in Table 4 below. All four studies127,173,174 were included in the narrative synthesis (see Chapter 5), although the quality of the studies varied as is summarised below:
-
Best et al. 127 – strong
-
Singh et al. 173 (study 1) – weak
-
Singh et al. 173 (study 2) – weak
-
Simmerman174 – weak.
No studies employed a randomised trial design. One was a prospective cohort study,127 and two were before-and-after studies with no control groups completed by the same researchers and reported in a single publication. 173 The final included study used a retrospective quasi-experimental multiple time series design study. 174 None of the studies reported any data on cost-effectiveness.
The paper by Singh et al. 173 reported two studies (study 1 and study 2) that rated the family-friendliness of the admissions treatment team process prior to and following different types of training intended to enhance family-friendliness. The sample sizes of the first before-and-after study (study 1) were small, with only 18 participants before and 18 after. For the second before-and-after study (study 2) the number of participants was not specified. The sample in one study was assumed to be representative of the RTC population, although no randomisation took place. 174 Three studies did not describe any characteristics (i.e. age, gender) of the young people in the sample. 173,174 The characteristics of the young people and their families taking place in the observed mindfulness sessions for study 2 were not described. There were very few original data presented to verify the statistical analysis. No ethical approval data were reported for either study.
The quality of the single prospective cohort study127 was judged to be strong, having a 20-year follow-up period. Data were first collected between 1978 and 1981 (during a period when inpatient care was different from that which exists today), and follow-up data collected 20 years later in 2001. The sample in this study was from psychiatric inpatient units in one metropolitan area of north-west USA, matched with one high school in the same area.
The methodological quality of each of the eight qualitative studies was judged against nine quality criteria, and each was then further classified as being of high, medium or low quality (see Table 4). The majority of qualitative studies included in this review were considered to be of high quality175–183 and one of medium quality184 because it was not clear how the family had been recruited and the study lacked rigour.
The methodological quality of each of the 15 non-experimental studies was judged against nine quality criteria and each was then further classified as being of high, medium or low quality (see Table 4). Of the non-experimental studies, six were considered to be of high quality,187,188,190,193–195 seven of medium quality128,142,185,186,192,196,197 and two of low quality. 189,191
For the large mixed-methods studies, the individual components were quality-assessed based on study design. The National In-Patient Child And Adolescent Psychiatry Study (NICAPS)11 had two components that were relevant to this project and included two surveys administered using questionnaires, both of which were considered to be high quality. The Costs, Outcomes and Satisfaction for Inpatient Child and Adolescent Psychiatric Services (COSI-CAPS)15 study had a survey administered using questionnaires and interviews, both of which were considered to be of high quality. The YoungMinds study also used questionnaires and interviews and was considered high quality. 198,199 However, the qualitative study undertaken by the Mental Welfare Commission Study200 did not detail the study methods and so the quality could not be graded.
No methodological quality assessments were conducted for the reports of local service or practice developments, or the case reports.
Study characteristics
Study design
Thirty-eight studies, reports of local initiatives or clinical case reports were included in the review, where the word ‘study’ or ‘studies’ is used here to refer to all as a shorthand. Eight studies (reported in 10 items) used a qualitative approach,175–184 four used an experimental design127,173,174 and 15 a non-experimental design. 128,142,185–197 Four (reported in five items) were reports of large-scale projects that used a variety of methods,11,15,198–200 two were published journal articles describing local initiatives and practice143,220 and five were clinical case reports221–225 of young people’s journeys into, through and out of the system where the less obvious risks were considered.
Of the 15 non-experimental studies, nine were prospective longitudinal descriptive surveys,142,185–191,197 four were retrospective descriptive surveys128,192–194 and two were cross-sectional surveys. 195,196
Intervention/programme details of experimental studies
Two of the studies contained findings that were extracted into the category Dislocation: Education. 127,174 The prospective cohort study127 included data on high-school completion and educational attainment over a 20-year period, whereas the single retrospective quasi-experimental multiple time series study174 compared a (previous) self-contained classroom format with the current rotating multiclass format for young people in a RTC in the USA. With the previous format, the young people remained in one classroom for the entirety of the school day and were confined in a single space for several hours. Teachers were expected to provide materials and instruction for all subject areas across grades 7–12. The current programme, however, consisted of four classrooms and separate teachers, making classes smaller and more specialised. Data from records over the 10 months before and 10 months after the programme change were collected.
One paper by Singh et al. 173 contained findings from two studies that were extracted into the category Dislocation: Families. These rated the family-friendliness of hospital admissions prior to and following different types of training intended to enhance family-friendliness. In study 1 the intervention was structured role-play training and in study 2 the intervention was mindfulness training.
Country of research
Of the 38 included studies, 22 were conducted in the USA. 127,142,143,173,174,177,178,182,185–191,193–196,220,223,224 Ten studies reported in 12 items were conducted in the UK. 11,15,175,176,179–181,183,198–200,221 Two studies were conducted in Finland95,184 and two in Canada. 192,222 One study each was conducted in Norway225 and France. 128
Year of publication
Three studies were reported on two occasions. 177,178,180,181,198,199 There were three studies reported in 1995,128,142,191 one in 1997,174 one in 1998,197 three in 2001,11,189,225 three in 2002,173,175 one in 2003,192 five in 2004,127,179,184,186,194 two in 2005,176,223 three in 2006,143,183,224 three in 2007,196,220,221 three in 2008,15,185,193 one in 2009,200 one in 2010,223 two in 2011,182,195 two in 2012187,188 and one in 2014. 190
Setting
The majority of studies (n = 34) were conducted in inpatient settings11,15,127,128,142,143,173,175–188,190–192,195–200,220–225 and four were conducted within RTCs in the USA. 174,189,193,194
Length of stay
There were 20 studies where the length of stay was not reported. 143,173–176,183–185,188,190,191,198–200,220–225 Of the remaining studies, short inpatient stays (< 1 month) were recorded in six (and reported in seven) studies: median 6 days;186 mean 5.9 days;187 5–7 days;177,178 24.9 ± 10.7 days;142 3–31 days;182 3–31 days. 195 There were inpatient stays exceeding 1 month in 12 studies reported in 13 items: 37–921 days;127 1–337 days;192 5–20 weeks;179 mean 10 months and 10 days;128 4 weeks to 36 months;180,181 7–243 days;194 18–505 days;189 mean 115 days;11 mean 90.6 days;193 7–200 days;197 4–174 days;196 median 79 days. 15
Participant characteristics
The largest group of studies (n = 24, reported in 25 items) involved only young people as the participants. 127,128,142,143,174,175,179–182,185,188–190,192,193,195,197,200,220–225 Four of these studies reported on the care of one young person only, the ages of the young people participating being 13,221 15,222 15223 and 16 years. 184 One reported on three young people (two 16-year-olds and a 17-year-old). 224 Apart from the case studies, 14 studies (reported in 15 items) included only participants who were within the precise range specified in this project’s inclusion criteria (11–18 years). 15,127,142,176,179,182,185,187,188,190,192,196–199
Six studies (reported in seven items) included participants older than 18 years in their samples128,175,180,181,183,193,195 and four studies included participants under 11 years old. 186,189,191,194 These studies were included because the mean age of participants fell within the 11–18 years range or because separate results could be extracted for the young people only. Four studies also included the views of parents of young people184,187,191,196 and seven studies (reported in eight items) included the views of health-care professionals who work alongside young people in inpatient units. 11,15,173,176–178,198,199
The exact ages of participants were not reported for a further six studies (reported in eight items). 143,174,177,178,200,220,225 These studies were included because the participants were described as adolescents.
Summary of phase 2 concepts and methods
A research question and associated objectives were devised to guide phase 2 of the project, centring on the search for evidence relating to the identification, assessment and management of the risks of dislocation and contagion for young people using inpatient mental health services. A comprehensive search strategy was devised to secure evidence of a variety of types. Multiple databases were searched for published and grey material, using combinations of words. The reference lists of included papers were scrutinised for possible additional citations and key journals were hand-searched. Government websites and the websites of relevant organisations were searched, and a call for evidence was prepared and sent to all NHS and non-NHS inpatient CAMHS units identified in the UK. This same call for evidence was circulated via discussion lists and directly to members of organisations with interests in the CAMHS field, and to targeted individuals for onwards distribution via their networks.
Evidence identified was screened through a number of sequential filters. Forty citations (reporting on 38 research studies, reports of local initiatives or clinical case reports) were finally included, alongside 20 policy and guidance documents. Data from the 40 citations were extracted, and quality was assessed using appropriately selected appraisal checklists. The characteristics of included studies were summarised, in preparation for the production of a series of individual syntheses, each focusing on a priority risk category: a type of dislocation, or contagion. These syntheses are reproduced in Chapter 5.
Chapter 5 Synthesising phase 2 findings
Introduction
This chapter brings together findings from the series of separate syntheses of the evidence, each addressing one category of less obvious risk. Where findings were reported across two publications, data were extracted as follows: the study by Haynes180 is reported in greater detail in the thesis by Painter,181 and all data are extracted from the longer document; the YoungMinds report authored by Svanberg and Street is published across two outputs, the first reporting methods198 and the second reporting findings. 199 All data are extracted from the second document only. In the case of the study by Clemens, two publications177,178 reporting different findings from the larger study are included, and data have been extracted from each separately. In reporting statistical information from the included studies, as much detail has been included (e.g. p-values and effect sizes) as was given by authors of the original papers.
Table 5 summarises the categories and subcategories of less obvious risk for which evidence has been brought together in this chapter.
| Categories of risk | Subcategories |
|---|---|
| Dislocation: Normal Life | (1) Everyday life and interactions in hospital |
| (2) Missing out on life outside and transition home | |
| Dislocation: Identity | (1) Mental health problems as identity-changing |
| (2) Responding to threats to identity | |
| Dislocation: Friends | (1) Relationships with young people outside hospital |
| (2) Relationships with young people in hospital | |
| Dislocation: Stigma | (1) Young people’s experiences during admission |
| (2) Young people’s experiences after discharge | |
| Dislocation: Education | (1) Education provision and facilities |
| (2) Quality of inpatient education | |
| (3) Academic progress | |
| (4) Reintegrating with school after discharge | |
| Dislocation: Families | (1) Impact on family relationships |
| (2) Family involvement | |
| (3) Maintaining contact with families | |
| Contagion | (1) Experiences of contagion |
| (2) Evidence of contagion |
Dislocation: Normal Life
Five of the included studies report findings related to the risk to young people in inpatient mental health hospital of dislocation from normal life. 176,181–183,199 Three of the policy and guidance documents address this area. 201–203
Two subcategories were created within Dislocation: Normal Life. These were (1) everyday life and interactions in hospital and (2) missing out on life outside and transition home.
Everyday life and interactions in hospital
It is recommended that children and young people in inpatient settings should lead lives as normal as possible, with admission representing a potential risk to the hopes and gains associated with everyday life. 201 Emphasis is placed on the importance of hospitals providing access to creative, leisure, exercise and self-care activities. 203 Three studies reported findings on everyday life and interactions. 182,183,199 In one,199 young people talked at length about what daily life was like in hospital, and many expressed the need for normalisation within inpatient units. Young people and staff spoke of the problems of there not always being enough to do, of boredom and of staff shortages affecting the activities that could be offered. For example, one 17-year-old is quoted as saying ‘There’s lots of time where there’s nothing to do. Boredom is a huge factor . . .’ (p. 27). 199 An 18-year-old said ‘There’s quite a lot of the time I think where you just spend it doing nothing . . . It makes me focus on my negative feelings and that. It’s not very good for me’ (p. 27). 199 Staff saw it as their responsibility to provide activities that provided a sense of normality. For example, one staff member commented:
I think it’s our responsibility not to make it a boring environment. It has to be an exciting, therapeutic, hospitable, understanding, creative, age appropriate environment, so we are working on that.
(p. 27)199
In the same study another said ‘We are not ignoring that we provide therapy here . . . but if we can put this therapy under the umbrella of normality for them it would be great’ (p. 27). 199
Young people valued everyday interactions, with younger staff in particular, where talk could be about ‘normal’ things (pp. 379–80). 183 For some young people the sustained attention that staff members gave to talking about mental health issues was unhelpful, with some preferring opportunities to engage in normal chats. A 17-year-old said ‘It can be bad if all you are doing is focusing on your illness – you can focus too much and make it too serious. It’s important to keep hold of your real life’ (p. 27). 199 Many young people felt that they were actively discouraged from engaging in real-world activities such as their hobbies and school work, which, in the case of young people with eating disorders, included activities not linked to exercise or their particular mental health difficulties. 183
One-third of the young people in one study182 complained about periods of being confined in their rooms and missing everyday interactions, with one-fifth describing being prevented from being able to access valued, everyday objects such as mobile phones and painting equipment. The terms ‘rigidity and confinement’ (pp. 129–30)182 are used to refer to those aspects of the inpatient experience found by young people to be ‘unnecessary, unreasonable or aggravating’ (p. 129). Some young people described as unhelpful the existence of institutional rules, which made for patterns of interaction unlike those found in everyday life. 182,183 Young people talked of staff often failing to offer adequate explanations for doing certain things, creating upset and confusion. 183 They were also expected to take part in organised group activities but were not able to participate in normal interactions with other young people, reflecting rules on restricted physical contact. 182 In some instances young people describing being too medicated or feeling too unwell to join in with activities and then losing privileges as a result. 182
Missing out on life outside and transition home
It is important that links be maintained with home and the community while the young person is in an inpatient unit. 202 Missing out on life outside the unit and the subsequent difficulties experienced on returning home were explored across three studies. 176,181,183 Young people identified feeling that their normal lives had been suspended,183 and that they had missed out on the rhythms, routines and relationships of life including birthdays, hobbies and just ordinary everyday activities. 181 For example, one young person (Cameron) said:
I mean not that long ago I went out into the community for the first time, and I was surprised all the stuff I’d forgotten, people doing their daily stuff . . . just seeing people gardening, walking the dog, waiting for the bus, driving about.
(p. 87)181
Several people felt that encouraging some form of ‘normal’ activity outside the unit would have helped their transition following discharge and served as an incentive to get well. 183 The dislike of the inpatient treatment regime could also act as a spur for young people to co-operate in order to be discharged. 176 One young person said how:
I want to be with my family and friends and have a more normal life than sitting in a hospital to get told when to sit down and what to eat and how long I can go out for. Sometimes it’s not much of a life . . .
(p. 114)176
Some young people described the difficulties of reintegrating into normal life after discharge and commented on the extreme differences between the high level of structure and support found in the unit and the outside world. 183 Transitions that were planned in a gradual and collaborative manner were more positively experienced; for example, Kate said:
everything, was slowly introduced, so we decided that in x amount of weeks I was going to leave and . . . it was sort of . . . slowly done, instead of saying, this weekend you’re going home, next weekend you’re going to school, week after you’re gonna leave, it was done slowly.
(p. 380)183
Dislocation: Identity
Three of the included studies report findings related to the risk to young people in inpatient mental health hospital of experiencing identity dislocation. 179,181,183 No policy documents were found addressing this area.
Two subcategories were created within Dislocation: Identity. These were (1) mental health problems as identity-changing and (2) responding to threats to identity.
Mental health problems as identity-changing
Two studies report findings on mental health problems as identity-changing for young people with eating disorders. 179,183 Young people with eating disorders described themselves as being confused about anorexia and not understanding it while also recognising that it had come to exert considerable control. One person said ‘it does control you and you don’t, even though I didn’t see it, looking back now after being in here I have seen that it did control my life and that’s how I ended up here’ (pp. 310–11). 179
Anorexia was described as identity-changing in that it functioned both as a ‘friend’ and as something to hide behind and to take confidence from, as well as simultaneously being an ‘enemy’. One person said ‘I think for me it numbs a lot of my emotions, it protects me from feeling all that’ (p. 130). 179 For one young person, ‘It’s like a monster like this big thing with claws wrapped around you . . . and it’s like you can’t get out and you can’t breathe because you’re trapped there’ (p. 310–11). 179 Eating-related difficulties for this group could be an identity-changing struggle, with good and bad elements co-existing. As one person put it:
the bad bits and the good bits just contradict each other all the time and I don’t know what to do. And when I do something good the bad bit feels guilty and when I do something bad the good bit gets angry.
(p. 311)179
Young people talked of the risks of being treated in conveyor belt fashion rather than as an individual. 179 One said, ‘it’s just like everything’s anorexic and everything you do’s anorexic everyone always says you can’t trust an anorexic’ (p. 311–12). 179 The idea of individual identity being eroded during admission was an issue for some,183 with the process of getting well during inpatient treatment for others being bound up with identity-related conflicts and ambivalence. 179 For example, a young person said:
I don’t want to get better so, that’s a bit hard, ’cause I have to want to do it. I have to wait ’till I am ready, but I’m not at the moment, so I don’t think they are going to be able to help me.
(p. 311)179
Many young people talked about aspects that they felt were unhelpful, which included staff making unhelpful assumptions about young people with anorexia and the lack of individualised care, leaving people sometimes feeling punished for the behaviour of others within their diagnostic group. In contrast, helpful aspects of inpatient treatment were those which conveyed to young people that they were unique and in need. 183 One young person, Chloe, described an incident when she was in acute distress and was being restrained, but which she saw as being a supportive action valuing her as an individual fighting against eating-related difficulties:
I felt so sort of safe that, cos I just felt like the anorexia is just getting so much, and they were just like, ‘It’s ok’, you know, ‘we’re here’, and it felt like they were helping you try and get the anorexia away . . .
(pp. 381–2)183
Responding to threats to identity
One study reports findings on young people’s responses to the threats to their identity. 181 Young people described themselves as protecting their identities in the face of admission and/or receiving a diagnosis by categorising other patients, but not themselves, as ‘mentally ill’ (p. 97). 181 For example, one young person (Mags) said ‘I don’t think I’m mentally ill, I’ve just got behaviour problems’ (p. 97),181 and another (Mike) (in response to the question ‘So would you say you’ve made friends here or?’) said ‘No they’re all mental. They’re all mentally ill people’ (p. 167). 181
Young people described engaging in identity-protecting strategies involving qualifying their diagnoses or externalising their symptoms. For example, one young person (Chris) said ‘I have borderline personality, but I don’t have what most people have with it, I just have the attention part’ (p. 97),181 while another (Holly) said ‘The panic attacks like aren’t who I am, they’re just like a part of me’ (p. 98). 181 Strategies used by young people to adjust to identity challenges are also identified,181 with examples including young people extricating themselves from previous friendship groups (see section on Dislocation: Friends) allowing the ‘wrong friends’ (p. 98) to become linked to hospital admission in the first place. For others, the management of identity was helped through accepting that problems existed and that help was available. 181 For example, one young person (Keira) said:
At first I thought I was kind of just attention-seeking and I was doing things just for no reason, but being here has made me think that I actually am ill. So I know it’s not an excuse or anything but it’s made me not feel as bad.
(p. 99)181
In some young people, accepting difficulties and diagnoses was associated with feelings of negativity.
Dislocation: Friends
Ten of the included studies report findings related to the risks around Dislocation: Friends. 175–177,179,181–184,188,199 One of the included clinical case reports addressed this category, giving an account of a 13-year-old boy’s journey through hospital, including a consideration of peer group identity. 221
Two subcategories were created within Dislocation: Friends. These were (1) relationships with young people outside hospital and (2) relationships with young people in hospital. Policy and guidance documents addressing these subcategories are included in each relevant section below.
Relationships with young people outside hospital
The importance of maintaining relationships with outside friends is noted in two policy and guidance documents,204,205 which argue for the provision of private spaces for friends to visit, the creation of unit-level policies and procedures on visiting,204 and treatment that enables improved peer relationships. 205
Seven studies report findings regarding pre-existing friendships with other young people outside the inpatient setting. 177,181–184,188,199
Young people in hospital valued pre-existing relationships with friends at home, which they wanted to maintain through phone calls and letter writing. For example, Natalia commented:
I’ve been away from them for so long now I don’t speak to them really, but they write to me and they phone me up and it’s nice to know they still care.
(p. 162)181
However, contact of this type did not always happen, and, as a result, relationships were often difficult to sustain during longer-term admissions, leaving the young person feeling distressed when these disintegrated. 181 For example, one young person said:
I had this group of friends . . . I said ‘right you all have to write to me ’cause I’m gonna have a month (in hospital)’ . . . and then none of them wrote to me, and I was just like ‘oh ok great’ . . . I felt really quite betrayed and stuff.
(p. 162)181
In some cases young people described a distancing from their peers prior to their admission and related this to being entrenched in their illness, as well as to a general lack of understanding by peers about how to relate to people with mental health difficulties. 183 For example, one young person (Chloe) commented ‘‘Cos you isolate yourself from your friends when you’re getting ill’ (p. 380). 183
Being admitted to a mental health unit appeared to contribute in particular to the deterioration of friendships. 177,181,184 For example, Holly commented:
I don’t think many people are quite open-minded about people going to a psychiatric hospital. I think they probably thought I was going crazy or something . . . I think maybe they just wanted to distance themselves from me because of it.
(p. 86)181
Others expressed discomfort that visiting friends saw them in a mental health facility. 182 For example, one young man (age 14 years) said ‘I didn’t really like that when my friends come to visit they see this giant sign “Psychia, psycha, Psychology” thing right in the front where you’re walking in’ (p. 132). 182 Other young people experienced rejection by their former friends from outside hospital. For example, a practitioner said that ‘They don’t need them as a friend any more because they’ve gotten a new friend since they’ve been gone’ (p. 255). 177 In one study184 it was noted that friendships had been broken off when it was discovered the young person was in a mental health unit. The young person here was described as having ‘prayed to find a friend’.
In contrast, some young people described deliberately disconnecting from their relationships with friends outside the unit. This was part of their recovery process because of the perceived role those friends held in causing and maintaining their individual difficulties prior to admission. For example, one young person (Phoenix) commented:
I was involved with a group that basically they were going down and they were trying to drag me down with them, a lot of drugs and alcohol and stuff, so I just come down here, and I’ve just cut off all contact with them, I didn’t want that . . .
(p. 87)181
In the sixth edition of the QNIC standards204 it is acknowledged that there are benefits for young people in hospital in maintaining relationships with friends, but that, despite recommendations that both inpatient facilities and their procedures should support this, a number of obstacles exist. These include rules within units about friends being allowed to visit,181 the conflicting priorities of young people’s hospital and home lives181 and the geographical distance between inpatient units and young people’s homes. 181,199 It was also clear from some young people that it could be helpful to be away from home, to have some time out from the pressures or difficulties in their lives,199 and that it was a young person’s parents who ended up having to provide lifts so that friends could visit. 181
Concern around reconnecting with their friends after being discharged from hospital was important for some young people. 177,181–183 They were worried about explaining where they had been177 and that friends would treat them differently181,183 or even reject them. 177 Some did not want their friends to know where they had been and were worried that they would find out. 182 A school counsellor described young people facing the same social problems that existed prior to their hospitalisation, difficulties in being able to explain absences to peers and concerns over the impact on their friendships. 177
Other young people talked about the ways in which relationships with peers outside the hospital environment change following discharge. 183 For example, Katie, a young person with an eating disorder, commented:
They seemed to act differently around me . . . I don’t know whether that was them, cos I’d been away for so long, ’cos it was weird seeing me and seeing me at a different weight and not being like a stick.
(p. 383)183
Young people’s ‘connectedness’ with both friends and families, described as the way in which young people perceived their relationships with their friends as close, confiding, satisfying and supportive, was found to change after being on an inpatient unit, and affected levels of depression and suicide attempts. 188 An increase in connectedness with peers was significantly associated with less severe depressive symptoms at 3 months after hospitalisation (p = 0.003) as well as a lower likelihood of attempting suicide during the entire follow-up period [odds ratio = 0.55, 95% confidence interval (CI) = 0.32 to 0.94]. However, the effect of increases in connectedness with peers being associated with less severe depressive symptoms was short-lived (6 months, p = 0.652, and 12 months, p = 0.763) after hospitalisation.
Relationships with young people in hospital
Seven studies report findings on young people’s relationships with other inpatients. The influence of living with other young people who have the same/similar conditions within the inpatient unit was described as being positive. 175,176,179,181–183,199 Young people enjoyed the support of inpatient peers,179,181,182,199 their companionship182 and the advice others offered179,182 and felt a sense of genuine acceptance. 183 Developing supportive relationships with other inpatients appeared to help young people cope with the negative emotions associated with hospitalisation, often through the simple process of listening and talking. 181,199 For example, one 16-year-old said:
I think it’s good to share experiences, because there’s people here that have had the same experiences as me and I find it easier to talk to people that have shared the same rather than people like my mum and dad because they don’t understand fully.
(p. 18)199
Support could also take a more active form. For example, Britney described how a group of residents helped one individual with the experience of feeling disconnected:
On her birthday as well nobody phoned her . . . none of her family sent her cards or anything . . . we threw a little party, and like we joined, all us girls went into Kirsty’s dorm ‘cause it was the biggest, then we pushed the beds against the wall and put some music.
(p. 93)181
Sometimes young people felt that staff actively discouraged friendships with other inpatients, for reasons that were unclear. Some young people reported that having anorexia nervosa meant staff treated them very differently from other patients, leading some to feel that they were not part of the inpatient community. 183
Living with other young people with mental health difficulties also had negative aspects. 175,179,181,182,199 This could result in increasing distress,179,181,182 especially when dealing with violent or bizarre behaviour which was not understood. 199 For example, one 16-year-old girl said, ‘It’s quite scary – I’m not used to being round people like that and I don’t understand their problems. It would be useful to know about [other people’s] problems’ (p. 18). 199 In another study, Holly said ‘It was just really scary, to see someone act like and just be completely like zoned out kind of thing . . .’ (p. 164). 181 Further worries over the benefits of having a group of young people with different difficulties, but all vulnerable, in one place emerged from parents199 and some young people. 175,199 For example, one young person commented ‘I would like to be in a place where’s there’s nothing the matter with nobody. Do you know what I mean? . . . there were some right odd bods in there’ (p. 238). 175
Dislocation: Stigma
Six of the included studies report findings related to the risk of stigma for young people admitted to inpatient mental health hospitals,176,181–183,190,195 and 11 policy and guidance documents address this area. 8,201,204,206–213 These documents recognise stigma as an issue for users of mental health services201,203,206–211 and that services should be provided in a non-stigmatising environment. 8,209,213
Three of the included papers provided descriptions of the term ‘stigma’. Terminology used and reported included ‘general devaluation’,190,195 ‘disrespect’, ‘emotional insult’, ‘underestimation by others’,190 ‘rejection’, ‘exclusion’, ‘people looking down on you when they find you are in treatment’195 and ‘being treated differently to other patients’. 183 Studies included also address both the apprehension of stigma among young people recently discharged195 and experiences of actual or enacted stigma. 190
Two sub-categories were created within Dislocation: Stigma. These were (1) young people’s experiences during admission and (2) young people’s experiences after discharge.
Young people’s experiences during admission
Four papers detailed specific stigmatising experiences felt to be a result of, or occurring during, inpatient admission. 176,181–183 Only a small fraction of young people (3.8%) reported stigma associated with being in hospital. 182 For those who did feel stigmatised while in hospital, their perception was that they were being stigmatised by a variety of different people, including the ‘outside world’,176,183 family members181 and staff. 183
One young person (Natalia) explained her experience of stigma from a family member and how her parents had decided to keep her admission a secret from her extended family, as they felt ‘embarrassed’, which caused Natalia herself to feel ‘upset’ (p. 86). 181 In contrast, one young person with an eating disorder detailed special practices, particularly around mealtimes, which often led to a sense of stigmatisation. These led some to feel that their problems were exposed, unlike those of other patients. The young person (Anna) highlighted that this sense of segregation and exposure of her problems was one of the most unhelpful aspects of her experience in a general adolescent unit: ‘it was really demoralising. I felt like I wasn’t human. Like I was some kind of, I, like I’d got leprosy or something and nobody would come near me’ (p. 384). 183
Some young people in two studies highlighted the stigmatisation often felt from the outside world/wider community, comparing this with the ‘strong sense of community’ (p. 384)183 and ‘companionable quality of unit life’ (p. 272)176 felt within the inpatient setting. Friendships with other patients/peers was seen as important, with several young people in one study stating that it offered them a sense of genuine acceptance183 (see discussion on Dislocation: Friends).
Young people’s experiences after discharge
Two linked studies looked at young people’s experiences of stigma after discharge. 190,195 Young people generally did not report a great deal of ‘stigma apprehension’. 195 The most common experiences were the feeling of being looked down on during treatment, and young people were least concerned with their friends rejecting them. A number of significant links were found between a young person’s personal circumstances and attributes and his or her feelings of ‘stigma apprehension’. Factors that were found to significantly predict (R2 = 0.46, p < 0.001) stigma apprehension were sex (female), age at first mental health treatment (being younger at initiation of treatment), need for others’ approval for self-worth (greater), discrimination against youth with mental health problems, and quality of friendship support. 195 Six months later, following their discharge from psychiatric hospitalisation, 70% of the same young people reported experiencing one or more aspects of enacted mental illness stigma (general devaluation, disrespect, emotional insult and being underestimated by others). Significant predictors of enacted stigma at follow-up were number of friends with psychological problems, affiliation with popular peers and school disciplinary problems (R2 = 0.36, p < 0.001). 190
Dislocation: Education
Seventeen of the included studies report findings related to the risk to young people in inpatient mental health hospital of dislocation from education,11,15,127,128,174–178,181,183,185,186,189,193,199,200 as did 15 of the policy and guidance documents. 93,201–207,210,213–218 One of the included clinical case reports addressed this category, giving an account of a 13-year-old boy’s journey through hospital including a consideration of school provision,222 and one of the included practice initiatives addressed this category. 221
Four subcategories were created within Dislocation: Education. These were (1) education provision and facilities, (2) the quality of inpatient education, (3) academic progress and (4) reintegrating with school after discharge. Policy and guidance documents addressing these subcategories are included in each relevant section below, along with the single practice initiative.
Education provision and facilities
Seven studies investigated education provision11,15,174,176,193,199,200 and this is also an area addressed by five policy and guidance documents. 202–205,212 Policy is clear that inpatient units working in partnership with education services/systems is important,201,202,204,206,212,216–218 including in the case of providing age-appropriate facilities for young people with eating disorders specifically. 215
The nationwide UK study known as COSI-CAPS15 obtained information about education provision from 29 units and found that these described two types of principal education delivery model. The first was a school integrated into the inpatient unit (72%); the second was provision outside the unit but within the bounds of the hospital site (28%). In the Mental Welfare Commission report it was found that all units in Scotland had specialist inpatient education provision on site. 200 One US study described full or partial attendance at a mainstream school for young people with conduct disorder hospitalised in a RTC, and found no significant change in either their school performance or attendance during the admission period (p > 0.05). 193
In some UK units a mainstream school ethos was explicit (to normalise the young people’s school days as much as possible), even to the point of having a full rather than part day at school. 176 Health professionals emphasised the importance of teachers having expertise in both teaching and in mental health: ‘Our ethos would mirror mainstream school ethos . . . We try and make them feel that no matter what is wrong at the moment they have got a future’ (p. 239). 176 In another study, a 14-year-old said ‘[It’s] a lot more comfortable here when I’m doing lessons, because I’ve got more support’ (p. 30). 199 In the NICAPS study11 two-thirds of teachers reported that young people who were inpatients had access to local school facilities as required; a member of unit staff in another study said that ‘It offers the possibility for young people to experience a normalisation of their lives’ (p. 30). 199 A member of staff also said ‘The content of the curriculum is not as important as the process’ (p. 30),199 while a 16-year-old said ‘I think we should have study sessions a few times throughout the day because 1 hour a day is not enough to keep up with the 6 hours that I would be doing at school’ (p. 30). 199
Where a hospital unit caters for young people over the age of 16 years, policy and guidance state that inpatients should be able to continue with postcompulsory education while hospitalised204 and that education and training providers should support students to remain on their course or hold their place open for them whenever possible. 210 The situation regarding those over 16 years may have become more pressing recently, however, because the raising of the school-leaving age to 17 years in 2013 and to 18 years in 2015 under the terms of the Education and Skills Act (2008) means that there will be a legal obligation to provide education and training for those under 18. In the UK, education provision appears to be less developed for those older than 16 years. One study found, for example, reported that educational support for hospitalised young people over 16 years was very limited,199 although the NICAPS study,11 which looked at inpatient units across the UK, found that most patients over 16 years were receiving some kind of educational input if they were well enough to attend.
In policy and guidance it is clear that inpatient units should provide access to education, including appropriate education facilities/classroom space. 203,204,206,213,214 However, no UK studies were found that looked at this area. One US RTC study174 found that smaller, multiclass, specialist teaching was effective in increasing the amount of work young people were able to produce while in hospital (p = 0.01), an outcome explained by increased opportunities for one-to-one consultation and teacher subject expertise. The value of having explicit staff–student ratios was questioned in another study, however, because it can lead to education authorities making staffing decisions on the basis of numbers rather than need. 199
Policy and guidance make clear that appropriate resources should be available to meet the demands of national curricula at the appropriate key stages205,216 and should provide the core educational subjects of maths, English and science. 204 In the NICAPS study,11 more than one-half of schools (35 of 62; 56%) did not have the educational resources to cover anything more than the core aspects of the National Curriculum, although they all met the key stage demands for the age groups being treated in the units. The number of specialist subjects the teachers in each unit were trained to teach at secondary school level ranged from 2 to 16 with a mean of 8.6.
Policy is also clear that inpatient units working in partnership with education services/systems is important,201,202,204,206,216–218 including in the case of age-appropriate facilities for young people with eating disorders specifically. 215 Partnership is specifically in order to maintain continuity of education provision at admission,202,204 with a key worker/named nurse to undertake this role,202 as well as to maintain communication with the young people’s parents/carers. 204 The COSI-CAPS study15 reported that most inpatient units had good relationships with their respective education authorities [mean score 2.2 on a scale from 0 (no contact) to 3 (excellent access)].
Quality of inpatient education
The quality of inpatient education provided to young people in inpatient mental health hospital compared with conventional schooling was investigated in two studies,175,199 and four studies explored issues around teaching staff. 11,15,176,199
The quality of schooling for young people while hospitalised is considered important and addressed by two policy and guidance documents. 202,205 Young people seem to enjoy and appreciate the supportive aspect of education,199 with only small numbers expressing concerns about the quality of schooling while being on an inpatient unit. 175
The training needs of the teacher within the unit as the one who provides the education is seen as important and highlighted across two policy and guidance documents which recommend that, as in conventional schools, teaching staff should have formal teaching qualifications. Additional training in child and adolescent mental health is seen to be beneficial. 202,205 Teachers who had worked at the units for a long time said that they kept up with training through study days and conferences, both in education and in mental health, with the result that they felt that they understood young people’s needs and problems. 176
The number of teachers employed in relation to the number of young people on the unit (staff/student ratios)11,15 and teacher shortages in inpatient units199 have been a focus of investigation. Current policy recommends not less than a 1 : 8 staff–student ratio. 76 Within England and Wales, the majority of units (n = 31) reported have a 1 : 3 staff–student ratio and a small number of units (n = 9) report ratios between 1 : 4 and 1 : 10. 202 In England alone, ratios are reported to be significantly lower (p < 0.05) in NHS units [mean 4.8, standard deviation (SD) 2.6] than in independently managed units (mean 8.7, SD 4.7). 11 Some unit staff felt that they needed more staff than they had access to on certain occasions, as a staff member said:
We can have seven kids . . . and be unable to take more because of the severity of those cases, even though there are beds free. The consequence is that the numbers are seen to drop – so the education authority says the numbers don’t justify two teachers, so removed one.
(p. 30)199
A 17-year-old in this study said:
There’s only two teachers, you need more support staff for the school. They try and find you work to your ability but it gets difficult for the teachers, especially with the older patients.
(p. 30)199
Most teachers reported that they had a good working relationship with young people’s parents,11 although parents themselves reported:
[school liaison] is often very poor in that teachers do not send work regularly. This makes it harder for the young person to re-integrate. It would be nice if the odd teacher might consider writing to her, or even visiting her!
(p. 30)199
A 17-year-old said ‘It would have been good if there had been more contact with school and college to prevent losing touch with them – they didn’t understand the seriousness of the problems’ (p. 30). 199
Academic progress
Nine studies explored issues regarding the academic progress of young people,11,127,128,176,177,180,185,186,189 and two explored how hospitalisation can have a significant effect on young people’s achievements and long-term goals. 176,181 Young people commented in the following way:
Is there anything else you’ve missed, or feel like you’ve missed out on while you’ve been here?
A chance to get my education.
And:
I’ve missed exams (.) so I’ve fallen behind on school.
Is that worrying you or?
Yeah ’cause I’m gonna have to re-sit the whole year.
(p. 163)181
The sixth edition of the QNIC service standards states that inpatient units should be registered as examination centres. 204 The nationwide NICAPS study11 explored this issue, finding that the majority of teachers reported that there were opportunities for young people who were inpatients to take exams, with only one unit reporting that this was not possible. Hospitalised young people on entering treatment often have pre-existing academic issues. 177,185 They typically receive below-average grades,185 and, in one study, 79% reported on discharge that they were doing the same or better in school than they had been prior to admission. 189 When young people have been followed up a number of years later to see what has happened to their educational attainment it has been reported that they have been significantly less likely than non-hospitalised young people to complete high school (p < 0.001), to get a bachelor’s degree (p < 0.001) or graduate degree (p < 0.001),127 less likely to take up a career after discharge128 and more likely to be expelled from school. 186 Exposure to substances in the year after treatment and younger age at treatment were significant predictors (R2 = 0.07, p = 0.00) of academic functioning (composite of school attendance 1 year after treatment, grades in school and attitudes towards school). 185
Reintegrating with school after discharge
Perhaps the most significant barrier to the academic progress of hospitalised young people is the difficulty encountered in re-entry and reintegration into school following discharge, and this is an issue that has been explored across five studies. 11,177,178,183,199 It is of extra concern when the young person has been placed in an inpatient unit far from home. 199 In policy and guidance it is recognised that education or training providers should support students to remain on the course or hold their place open for them whenever possible. 210
It is suggested that successful re-entry and reintegration into school requires partnership between schools (both in-unit and mainstream schools), the hospitalised young person, their parents and carers, and the mental health services involved. 178 Indeed, a partnership approach is endorsed by much of the policy literature reviewed (see also discussion under Education provision and facilities above). Commissioning policy205 covers reintegrating back into school after discharge and highlights effective liaison with schools on discharge to ensure successful reintegration, and documents emphasise the importance of working in partnership with education services/systems201,202,204,206,209,216,218,219 in order to maintain continuity of education, including with the help of a key worker/named nurse202 and specifically to enable reintegration at discharge. 204,216
A particular emphasis in one study is that there should be a focus on re-entry and reintegration into school at the point of admission. 178 Often, the focus of admission is on allowing the young person time to recover, but hospitalised young people seem to enjoy and appreciate the supportive aspect of education,176,199 and a lack of education support has been associated with discharge delays in a sizeable minority of young people. 11 Jointly agreed plans for re-entry into school should be made and followed through, but should also be flexible, because discharge from hospital does not necessarily mean that the young person is ready for re-entry into school. 177
Health-care professionals177 and young people183 described the experience of school re-entry from an academic viewpoint, describing how school absences result in getting behind and young people as a result getting stressed about the amount of work that they would need to catch up on. A health-care professional said:
they are stressing out about being here, trying to take care of themselves, but they’re also stressing out about the amount of work they’re got to make up whenever they get out of here.
(p. 251)177
For some young people, this was also linked to their friends moving on with their lives and going on to university without them. For example, a young person said:
they were getting on with their lives . . . they were doing their ‘A’ levels, they were gonna be going off to university at the end of the year, and that was really hard for me cos I had fears of everybody going . . . and I’d never catch up.
(p. 380)183
Health-care professionals indicated that, when there is co-ordination among education personnel, students are more able to reintegrate into school successfully. Clarifying roles was seen as helpful by a school counsellor who indicated that ‘sometimes roles get muddied in terms of who should be doing what’ (p. 206),178 as was keeping teachers informed when a young person is ready to go back to school. For example, an outpatient psychologist said:
If teachers were informed that there are some special circumstances and they could diminish the consequences of late work, if they could provide additional emotional support or energy and understanding in terms of allowing the student to catch up.
(p. 207)178
Health-care professionals also suggested that students benefit from an identified, adult support person in the school. For example, a school counsellor said:
Just knowing that there’s an adult that’s supporting them. Most of the times I think it helps kids with their confidence. I really think it’s just a sense of relief that they don’t have to go it alone.
(p. 207)178
For a number of reasons, open and honest communication is identified as a key element in partnership. 178 It allows the voices of young people to be heard; it enables school staff and parents to understand what it is like to be hospitalised (and to have to follow specific lines of treatment that may require taking medication with unpleasant side effects); it creates space for unrealistic expectations from all parties to be tackled (especially when resources are limited); and it promotes continuity of care. Effective liaison with the young person’s mainstream school is identified as a vital element in continuity of care, although some parents reported that mainstream teachers did not always send work for the young person on a regular basis and that, where the young person’s school was a distance away from the inpatient unit, maintaining links could be difficult. 199 However, the majority of teachers working within inpatient units in the UK were found to liaise with the young person’s own school. 11 Parents, in particular, see liaison with mainstream education as a route for reintegration into the wider community and not just into education. 199
A variety of different approaches to managing school reintegration have been described. 143,178 Those involved with this process have suggested school-based re-entry programmes and/or step-down programmes and re-entry options, with an emphasis placed on the importance of following through on interventions and asking students what is important. 178 For example, a middle school counsellor said ‘I’d like it to be student driven – for them to say that they can identify their needs because I think that’s really important’ (p. 207). 178 Step-down programmes and re-entry options differ from re-entry interventions in that they make available alternatives to immediate reintegration into the school setting in which the young person was placed before hospitalisation. Although not all young people may need to access such services, health professionals recognised the benefits of having the flexibility to meet the needs of those who were students. For example, one said:
I feel like it would be really cool if a kid could ease back into the situation instead of going back to [his or her] old life as it was. So that’s not the easiest thing to have happen in a traditional high school.
(p. 208)178
In a report of a local initiative, a programme in which young people are provided with intensive support in school and care co-ordination for a period of between 6 weeks and 10 weeks following hospital discharge is described. 143 Routine data indicating the use of this programme by 99 young people are given, and success in resuming their studies is described for all 67 students for whom educational status data were available.
Dislocation: Families
Seventeen of the included studies report findings related to the risk to young people in inpatient mental health hospital of dislocation from families. 11,15,173,175,176,179,183,184,186–188,191,193,194,196,199,200 Five of the included clinical case reports221–225 and one of the included practice initiatives addressed this category. 220 Jones221 gives an account of a 13-year-old boy’s journey through hospital, including a consideration of family functioning; Wilkinson225 describes the principles and practice of involving family members in an inpatient unit; and LePage222 describes the impact of early family participation in inpatient assessment and treatment of youth diagnosed with a first episode psychosis and includes the case of a 15-year-old boy. Nejtek et al. 223 present a case study of a 15-year-old boy and focus on issues around maternal non-compliance, and Olson224 discusses engagement using a parent/adolescent activity group and provides a case description of two 16-year-old boys and a 17-year-old girl.
Three subcategories were created within Dislocation: Families. These were (1) impact on family relationships, (2) family involvement and (3) maintaining contact with families. Policy and guidance documents addressing these subcategories are included in each relevant section below, along with the single practice initiative.
Impact on family relationships
One of the disadvantages of inpatient care recognised in policy and guidance is the effects of admission on family life. 8 The goal of treatment should be that it enables improved family relationships,205 with the sixth edition of the QNIC service standards recommending the availability of parent/carer support groups. 204 Six studies explored this issue from the perspective of the young person176,179,183,184,196,199 and two also from the perspective of their parents. 176,184
Young people who are in hospital for extended periods of time experience homesickness. 176,196,199 For example, one young person commented that ‘I hate being so far away from home, I feel homesick every day, I just want to be with my family’ (p. 9). 199 Other young people felt that being placed on an inpatient unit made it seem as if their families no longer cared for them; they often felt a sense of rejection179 or isolation183 and they felt as if their families had a negative attitude towards them. 184 For one young person, Anna, this isolation from her family also affected her sense of self and belonging:
I had quite a low self-esteem . . . and I felt, I didn’t, that’s it, I didn’t feel like I belonged anywhere. Because hospital’s hospital and I’d go home at weekends, but because I was only with my family at weekends I didn’t really feel like I belonged in the family either.
(p. 380)183
The way in which young people perceive their ‘connectedness’ with their families was found to change after being on an inpatient unit and affected levels of depression and ideas about suicide. 188 A significant increase in family connectedness following hospitalisation was associated with lower levels of depressive symptoms (p = 0.004), and a greater increase in connectedness with families 3 months after hospitalisation predicted less severe suicidal ideation for follow-up after 1 year but only for young people without multiple attempt histories (β = −4.10, p = 0.0005). More severe depressive symptoms at baseline were associated with more severe symptoms of depression at follow-up (β = 0.19, p < 0.0001), and greater family connectedness at baseline was related to less severe depressive symptoms at follow-up (β = −2.01, p = 0.021).
Parents’ perspectives of their need for support from within the inpatient unit176 and from extended friends and family184 have been explored. Some parents described getting support while others felt that they did not get it in the unit. 176 In some instances, relationship also broke down with wider family members and parental friends. For example, one young person said:
It used to be fun to go visiting, and we had family acquaintances . . . but there is nothing now, nothing left of that . . . I mean he does not want to go. and then we had this quarrel with my relatives.
(p. 679)184
Family involvement
Current policy and guidance urge family involvement,201 and that working in partnership with families is the way forward,205,218 including during the development of the young person’s care plan and in making decisions on care after discharge. 204 In particular, policy and guidance refer to the importance of consultation with families, particularly following episodes of self-harm. 212,217 It is suggested particularly for people with psychosis and schizophrenia that alternatives to inpatient care be considered when the inpatient unit is a long way from home. 203
Two intervention studies, both reported in one paper,173 explored the family-friendliness of the admission process and investigated the effectiveness of training staff in this area through role plays and mindfulness. Role plays had no significant impact on the family-friendliness of the treatment teams, but mindfulness did and appeared to have been sustained and maintained during a 6-month follow up period, although this was not tested for significance.
Five studies explored family involvement. 176,186,187,191,194 Family involvement has been conceptualised across studies as parents having visited their child during the hospitalisation period;187,194 the frequency with which parents visited the unit;186 participation in inpatient activities;187 going on planned therapeutic absences;194 participation in treatment planning;187,191 discussing treatment progress and challenges;186,187 taking part in family sessions;186,187,194 discharge planning;187 and an absence of parent hostility towards unit staff. 186
Health-care professionals report that obstacles to family involvement include confidentiality (including young people’s requests for treatment to be kept from family); parents’ own varying ability to get involved; lack of resources (including not having the time to be available); no formal structures in place to enable family involvement; and distances. 176
Young people whose parents got involved had a significantly better prognosis of maintaining their therapeutic gains in the community,194 and were significantly more likely to use aftercare services. 191 Psychiatric rehospitalisation for young people was associated with poorer family engagement in treatment (p > 0.05). 186 With parents who felt more empowered during the young person’s psychiatric treatment, rehospitalisation increased (odds 42%, p < 0.006). 187
In the single report of a local practice initiative included in this subcategory, the use of films to promote family engagement during young people’s stay in hospital was described. 220 This concluded with the idea that films can help engagement, and, if chosen carefully, empower families during periods of crisis.
Maintaining contact with families
Policy and guidance indicate that there should be unit policies and procedures on visiting,204 and that flexible arrangements should be made for family contact. 202 The provision of family meetings offered within 1 week of admission and continuing thereafter is recommended,205 as is the idea that services should be offered as near to home as possible, enabling frequent family visits and contact206,218 and appropriate family interventions. 218 Young people, when asked, said they would like to keep in touch with their families183,200 and that, although some units offer a flexible approach to visiting and family contact,200 this was not the same for all. 183
It is known that some young people are placed in inpatient units located at a distance from their homes, making it difficult to have regular contact with families. 15,175,176,199,200 In policy and guidance it is recognised that alternatives to inpatient care should be considered particularly when hospital is a long way from where a young person lives. 203 One young person stated that ‘They visit on visiting days, but it’s hard – they live one and a half hours away. We talk on the phone’ (p. 85). 15 Telephone was identified as an important way of staying in touch in other studies. 176,200 However, for some young people the break away from their environment and circumstances was also beneficial. One 18-year-old said ‘I don’t like it, it makes me feel quite bad sometimes, but sometimes it does the opposite, I’m glad to be away from the place’ (p. 9). 199 For others, the quality of care at the inpatient unit was considered to be more important than the distance from the hospital to their family home,15,200 and for some parents distance did not significantly affect the level of parent engagement or satisfaction (p > 0.05). 186
Providing facilities for families when visiting inpatient units is identified as important in policy and guidance. Recommended facilities include making available private space for family contact to take place;204,205 accommodating families who have to travel a significant distance;202 and allowing parents and other carers access to refreshments at the unit. 204 Parents15 and young people175,199,200 talk about the financial costs involved in being placed in inaccessible locations. One young person (Mark) said ‘my mum drove up most of the time. She eventually stopped it, ’cause of the petrol money, and then she only came up at weekends and things’ (p. 239). 175 A 14-year-old said ‘My mum couldn’t really afford petrol to come and see me much’ (p. 9). 199 In some instances, inpatient units had access to financial support to help families receiving welfare benefits to visit, especially if they had to travel a distance. 200 Some provided overnight facilities for parents visiting from distant parts of the catchment area11,200 and provided the opportunity for parents to make refreshments when needed and to use a family room for privacy. 11
Location was also an issue for staff engaged in working with local partners. In one study, a worker drew attention to the consequences of distance for interagency working:
I don’t know if it’s a good idea withdrawing a patient from their own home area, it’s very difficult to get them back, very difficult for Health Authorities to [take them] again . . . that is one of the big difficulties.
(p. 9)199
Contagion
Seven of the included studies report findings related to the risk of contagion for young people in inpatient mental health hospital. 142,176,179,183,192,197,199 No policy or guidance documents addressed this area.
Within the literature examined, two aspects of unhelpful behaviour acquired through the process of contagion were identified: deliberate self-harming behaviour in the forms of ‘self-mutilation by skin cutting’ or ‘blood-letting’, and suicidal behaviour. 197 Deliberate self-harming contagion was defined as two or more acts of deliberate self-harming behaviour that involved two or more young people and occurred on the same day or consecutive days. Suicide contagion was described by King et al. 142 as when one completed suicide triggers a cluster of subsequent suicidal behaviours among the contacts of the person who has died. One study192 set out to examine the spontaneous occurrence of self-harm among inpatients without a history of self-harm, but did not define the concept of behavioural contagion. Two studies addressed, briefly, the sharing of unhelpful eating behaviours. 179,183
Two subcategories were created within Contagion. These were (1) experiences of contagion and (2) evidence of contagion.
Experiences of contagion
Four studies touched on young people’s, carers’ and professionals’ experiences of contagion. 176,179,183,199 Health professionals and parents were found to have concerns about young people acquiring unhelpful, destructive behaviours while they were inpatients, particularly in the areas of suicide and self-harm176 or even just ‘picking up problems from others in the units’ (p. 18). 199 Health-care professionals suggest that the failure of treatment for some young people is when they learn bad habits and witness disturbing events. 176 Young people themselves described their experiences in this area, with one saying how ‘You see other people doing something, and you think maybe I should do that to myself as well’ (p. 19). 199
Young people with eating disorders are described in two studies as very quickly copying the behaviour of those around them with the same condition,179,183 including making comparisons with others and competing to be thin. 179 One young person said:
I questioned myself and I decided that I hadn’t been doing this eating disorder thing right at all, and I got worse. I started things like walking the longest way round things . . . things I hadn’t even thought of.
(p. 383)183
Some young people with eating disorders described themselves as becoming iller, not only in relation to eating behaviour but in relation to engaging in self-harm behaviours which they had not engaged in previously. 179 For example, one young person said, ‘I didn’t really know . . . about self-harm, um, about pacing to stop your weight going up, you know, walking around, exercise. I soon cottoned on’ (p. 311). 179 For some, living in the same location as other people with difficulties was followed by unhelpful thoughts, comparisons and competition. Sarah, one young person, said:
When I was there I was the ‘best anorexic’ because I wasn’t gaining as much weight as the others, I was, which was feeding my illness and letting it win, which now I see didn’t help me at all.
(p. 384)183
However, the experience of being in the same location as others with similar difficulties was positive for some young people (see Dislocation: Friends) in terms of support and identification. 28 Katie, a young person, commented that:
I think it was helpful, because it’s . . . you learn about, from other people, you learn how different people cope with things . . . so then you can take what they use and see if it works for you.
(p. 383)183
Evidence of contagion
The evidence from included studies for contagion in inpatient mental health facilities for young people is mixed. Taiminen et al. 197 identified the possibility of deliberate self-harm (DSH) contagion and that one type of self-harming behaviour could trigger another. A decrease in self-harming behaviour was noted among young people who were inpatients who had previously engaged in this behaviour,192 whereas for those on a short-stay unit no evidence of contagion was found. 142 The risk ratio among males representing the occurrence of inpatient self-harm behaviour, given no past self-harm behaviour, was 0.03 [standard error (SE) = 0.02, 95% CI 0.01 to 0.12]. The risk ratio among females representing the occurrence of inpatient self-harm behaviour, given no past self-harm behaviour, was 0.13 (SE = 0.09, 95% CI 0.03 to 0.48). Males and females with no prior history of DSH were significantly less likely to exhibit self-harm behaviour as inpatients, suggesting that the ‘spontaneous occurrence of self-harm’ among inpatients without a history of self-harm is low. 192
The incentives for young people who have been involved in contagion episodes of DSH vary, but are identified in one study as relieving anxiety or anger and feeling part of a group. 197 For some young people in this study, self-cutting and bloodletting became part of an initiation process promoting group cohesion based on the shared experience of relief following instances of self-harm. 197
Economic analysis
None of the studies reported above included an economic analysis or an economic evaluation of alternative ways of identifying, assessing and managing less obvious risks for young people using tier 4 inpatient CAMHS. This is not surprising considering that many studies used qualitative designs and focused mainly on the identification phase of the less obvious risks prioritised by the SAG. The data derived from these studies could not be used to inform an economic modelling exercise of likely NHS costs and analysis of cost-effectiveness. The health economist member of the project team (ML) contacted internationally leading health economists with expertise in the mental health field for specialist advice, and from Professor Martin Knapp (The London School of Economics and Political Science) two additional papers reporting on the economic impact of childhood mental disorder on public services were identified. 226,227 In the study reported in the first,227 of the 445 children with psychiatric disorder included, only three had been admitted to an inpatient psychiatric unit, meaning this paper could not be used to inform our economic analysis. The second227 used data from the same epidemiological survey and could not be used either.
The documents included in this review and summarised in Appendix 21 suggest, however, that the less obvious risks identified in this report exist and are recognised by the Department of Health. This additional economics paper includes the observation that health services in the UK (as in many other countries) are under tremendous financial constraint, dictating that NHS resources be allocated efficiently. 226 In the context of mental health care and services, study designs traditionally thought of as gold standard (i.e. randomised controlled studies) are not always possible and the use of alternative designs should be considered. 228 Modelling exercises are one way of generating evidence in these circumstances, but they rely on good-quality primary data of a type not available to the project team in this synthesis.
Conclusion
This chapter has presented seven individual, contextualised, syntheses of the evidence in the series of priority risk areas focused on in phase 2 of the review. In the chapter following, these are brought together in a metasynthesis, and, in the light of discussions held at a second SAG meeting, plans are outlined for the sharing of this project’s findings and promoting knowledge exchange. Strengths and weaknesses of this project are identified, and implications for future services, practice and research drawn out.
Chapter 6 Discussion and conclusions
Introduction
Findings from phases 1 and 2 are first brought together in this closing chapter in a matrix, which summarises what has been learned in accessible, single-page style. Key findings are then reviewed and set in a systems context. The project’s original overarching research question and objectives are returned to and reviewed, and, in the light of discussions held at a second SAG meeting, plans are outlined for the sharing of the project’s findings and the promotion of knowledge exchange. Strengths and limitations of the project are considered, implications for services and practice drawn out and recommendations for future research made.
Summary: what has been learned?
This project has been completed at a time when promoting the health and well-being of children and young people is an absolute priority. 229 The matrix in Figure 21 summarises findings from both the phase 1 scoping review and the phase 2 priority area syntheses. A headline is that, although this review has focused on a series of ‘less obvious’ risks which are important to people with stakes in the child and adolescent mental health system, little evidence to guide services and practice in these areas exists.
FIGURE 21.
Using the EPPI-Centre framework to summarise and synthesise all findings.
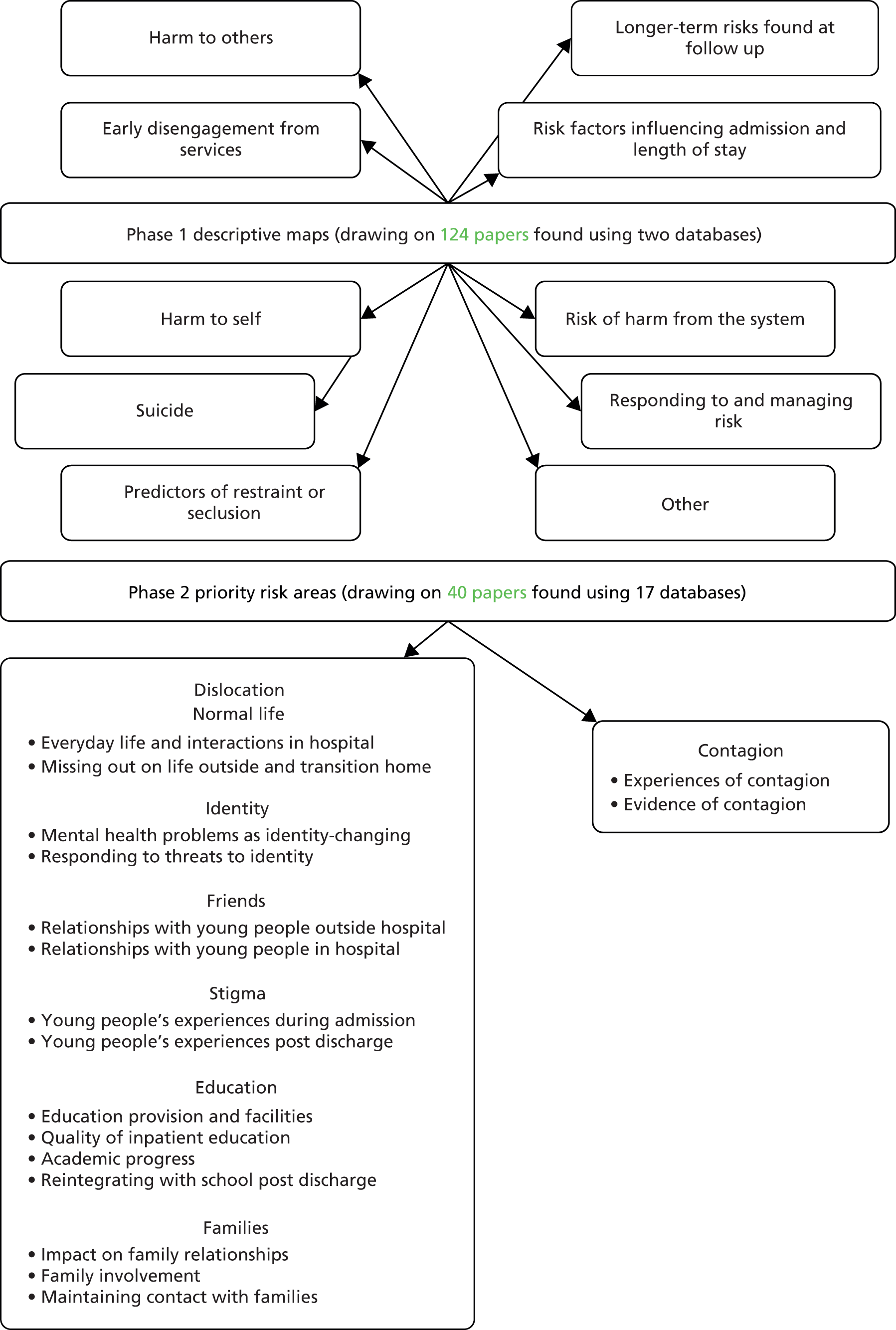
A first, and obvious, observation is to draw a contrast between the types of risk identified in the phase 1 scoping and the types of risk addressed in the in-depth phase 2 review and synthesis. It is clinical risks, relatively narrowly defined, which occupied the majority of researchers whose outputs were located in the initial segment of this project. As a project team we recognise the importance of research that improves the identification, assessment and management of clinical risks (including the risks of self-harm, suicide and harm to others) in the case of young people with mental health difficulties. As we acknowledged in our original proposal for funding using the NICAPS study11 in support, these are also precisely the types of risk that most often bring young people to the attention of hospital services. Inpatient child and adolescent mental health hospitals exist because it is here that high levels of skilled, continuous care can be provided to young people with the greatest need whose difficulties challenge the capacity of community-based workers. 230 Noting all of this, we are nonetheless also struck by the appetite of the stakeholder representatives we worked with for the prioritisation of a largely different set of risks to take forward into phase 2. Inpatient CAMHS play a vital, but changing, part in complex systems of care (for a discussion, see McDougall et al. 231) and the identification of a series of ‘less obvious’ risks for this project’s in-depth review points to an awareness that inpatient admission can have wider, and long-lasting, consequences about which more needs to be known.
In the areas of risks to normal life and identity policy and guidance was sparse but did recognise that young people undergoing treatment within inpatient settings should be able to lead as normal a life as possible. Views and experiences were reported in rich detail and young people and health-care professionals described boredom, stringent ward rules and routines, and a lack of opportunity for everyday interactions (CerQual – high). Feeling separated from life outside and the subsequent difficulties experienced on returning home were identified as pressing issues by some young people and health-care professionals (CerQual – high). Young people with eating disorders talked about mental health problems eroding their identities (CerQual – moderate), along with the experience of not being treated as individuals (CerQual – low). For other young people it was a struggle to manage threats to the sense of self during admission and treatment (CerQual – low). There were no intervention studies found that focused on the testing of actions to mitigate the risks to normal life or to identity.
In the case of risks associated with friendships and peer relations, policy and guidance are limited to making recommendations on inpatient units having space for visitors. The evidence included in this segment of the project pointed to the difficulties (and ambivalence) young people can experience in maintaining home friendships at a distance (CerQual – high) and in reconnecting with their friends after discharge (CerQual – high). In some cases, connections with friends were significantly associated with levels of postdischarge depression and suicidal ideation (CerQual – low). No intervention studies were found investigating actions to help young people in hospital maintain good relations with their peers at home. Evidence was found pointing to young people’s positive views of being with others in a similar position during hospital care and treatment, in terms of mutual support and companionship (CerQual – high). Young people also spoke of the negative aspects of living with other young people with mental health difficulties (CerQual – high). Some parents were found to be concerned about their children’s sharing of living space with other vulnerable people and at least some young people expressed ambivalence (and even fear) in their relationships with other inpatients (CerQual – low). No intervention studies were found investigating actions to promote positive peer relations among young people who were inpatients.
Managing the risks of stigma and discrimination is a high priority for policy-makers. Young people felt that stigmatising experiences can occur as a result of being admitted, as well as during their inpatient stay (CerQual – moderate) and at discharge (CerQual – low). Being with similar young people can also lead to feelings of acceptance, in contrast with the experience of being rejected in the community (CerQual – low). No intervention studies were found evaluating actions to mitigate the risks of stigma or discrimination to young people admitted to mental health hospital.
Hospital admission poses risks to young people’s schooling. Health-care professionals, parents and young people all recognise the importance of educational provision with appropriate facilities for young people in inpatient CAMHS (CerQual – high), which is also identified as a policy and guidance priority. Smaller class sizes utilising a multiclass format with specialist teaching have been shown in a study involving young people in a RTC in the USA (GRADE – low) to be effective in increasing the amount of work young people are able to produce while in hospital. In the UK, education is provided as standard across inpatient units, but in a majority of hospitals only core National Curriculum subjects are taught (CerQual – high). Improving quality and maintaining good communication and co-ordination across hospitals and schools feature prominently in policy. Within units in the UK, varying teacher/student ratios are found in NHS and non-NHS units (CerQual – high), and good (but not universally so) relations between parents and teachers have been reported (CerQual – low).
One of the disadvantages of inpatient care recognised in policy and guidance is the effects of admission on family life. Training inpatient staff working with young people and their families through the use of role plays or mindfulness did not have a significant impact on the family-friendliness of the admission process (GRADE – low). While on an inpatient unit, young people often feel homesickness (CerQual – high) and experience a range of negative feelings (CerQual – moderate). Associations between family connectedness and postdischarge depression and suicidal ideation have been reported (CerQual – low). Some family members need additional support during their children’s admission (CerQual – low).
Partnership with families during inpatient care is strongly recommended in policy and guidance. Young people whose parents do get involved make significant improvements across a range of treatment and postdischarge outcomes (CerQual – low) but health professionals report that a number of obstacles exist to enable this to take place (CerQual – low).
Whether or not families are fully involved in a young person’s care, the evidence suggests that units should have procedures on visiting and that flexible arrangements should be made for family contact. A particular risk of family dislocation is reported in instances where young people are admitted to hospitals located far from home, in terms of keeping in touch and cost (CerQual – high). For some, the quality of care at inpatient units is considered to be more important than the distance from the hospital to the family home (CerQual – moderate). Some young people also appreciated being away from the home environment (CerQual – low).
The risks of young people in hospital learning harmful behaviours was a priority area for phase 2 of this project, but no policy or guidance was found addressing this. Health professionals and parents have concerns about young people acquiring unhelpful, destructive behaviours while they are inpatients (CerQual – moderate). Young people with eating disorders very quickly copy the behaviour of those around them with the same condition (CerQual – moderate). There is mixed evidence of recorded contagion in inpatient mental health facilities for young people (CerQual – low), with no fixed definition of what constitutes ‘contagion’. No evidence was located investigating actions to mitigate the risks of contagion in inpatient settings.
None of the studies reported above included an economic analysis or an economic evaluation of alternative ways of identifying, assessing and managing less obvious risks for young people using inpatient CAMHS. This body of evidence suggests that this area of research is still in its embryonic stage, where hypothesis generating and exploratory work needs to be carried out to inform the design of large longitudinal studies. Economic analyses would not normally be carried out at this stage, as the size of the problem still needs to be quantified and alternative models of addressing the problem have to be formulated.
Systems and theory
Across the materials brought together in this report, the limited evidence of approaches explicitly used to identify, assess and manage the less obvious risks of dislocation and contagion challenged any attempt to locate and describe any underlying theory informing action in these areas. More generally, underpinning this project has been a recurring concern to set findings in a complex systems framework,5–7 and where possible to develop new theory associated with our narrative synthesis. Our contribution to theory particularly lies in our development and deployment of ‘dislocation’ as a broad class of risk, within which we identified a number of identifiable subdivisions. This concept building guided our phase 2 searches and our subsequent narrative syntheses. It allowed us to organise meaningfully our assembled reports of participant views and experiences, descriptions of services at national or local levels, descriptions and/or evaluations of local initiatives, and quantitative investigations (prospective, retrospective or cross-sectional) into aspects of young people and their care and/or outcomes.
Our commitment to existing theory extends to a reiteration of the idea that inpatient mental health units for children and young people must be thought of as being just one part of a larger, interacting network of services. 231 This system includes community CAMHS, but also, for example, schools. It was in synthesising the evidence surrounding the risks hospital admission poses to education that the clearest appreciation was found (by researchers, policy-makers and standard-setters) of the importance of working across health and education organisational boundaries during young people’s journeys through the system. This kind of thinking also draws attention to the highly specialised, geographically dispersed character of inpatient CAMHS units within the larger systems of which they are a part. Admission to hospital may be clinically necessary and helpful, but the distances units may be located from young people’s homes risk dislocation from family and friends, as well as from school.
A systems approach of this type can also be applied to the more microscopic understanding of young people’s experiences, and of those surrounding them. The evidence synthesised across all the phase 2 priority risk areas reveals the extent to which hospital admission can be disruptive and have major consequences for young people viewed in the context of family and friendship networks, and implications for identity and peer and community acceptance.
Reviewing the overarching research question and project objectives
This project was commissioned to summarise and appraise the evidence in the area of risk for young people moving into, through and out of inpatient mental health care. This has been achieved using a two-phase approach, beginning with a scoping of the literature using selected databases followed by a comprehensive search and in-depth review for evidence in a number of priority areas determined in collaboration with stakeholder representatives.
Specific objectives for the project are stated in Chapter 1 above, and these are reviewed here against the progress made in meeting each. The first objective, relating to summarising the evidence, has been addressed across both phases of the study, but the objective of appraising the evidence has been confined to the second (in-depth) phase. The attempt to identify underlying theory (objective 2) was also confined to phase 2 and was challenged by the limited evidence of approaches explicitly used to identify, assess and manage the risks of dislocation and contagion. Objective 3, relating to views and experiences, has been addressed in the appraisal and synthesis of evidence contained in phase 2 (and particularly the qualitative evidence located and included). Objective 4 has been comprehensively met in phase 2, and in Chapter 5 specifically. The synthesis of costs and cost-effectiveness (objective 5), where the evidence located supports this, has been confined to phase 2, where the limited literature located meant that no economic analysis proved possible. Implications and future priorities (objective 6) have been identified in the concluding section of this chapter, below.
Promoting knowledge mobilisation
As per this project’s commissioned protocol, a second stakeholder advisory group was held with the explicit purpose of sharing progress and discussing strategies for the dissemination of the review’s findings. This was convened in Cardiff on 31 March 2014, and all members of the SAG were again invited. Dr Michael Coffey, from Swansea University, once more acted as independent chair.
A key message arising from this meeting was the value of using a range of available media, both traditional and non-traditional, to promote the reading and uptake of summary and detailed findings. The project protocol refers to the production of accessible summaries, and the team’s intention is that these be produced (drawing on, for example, the single-page matrix reproduced as Figure 21) following peer review and acceptance of this report for the NIHR Journals Library. Care will be exercised to avoid duplicate or redundant publication, and advice will be taken where necessary, but the plan remains to prepare findings and process papers for high-impact journals (with at least one paper published in gold open access format) and in print and online publications targeting practitioners, managers, and young people and their parents. Abstracts have been submitted to conferences, and the first presentation at a national-level event has been made.
Strengths and limitations
This project has succeeded in bringing together and narratively synthesising the evidence in an area which has been largely overlooked in everyday practice and services: the identification, assessment and management of the less obvious risks for young people moving into, through and out of the inpatient component of the inter-relating CAMHS system. Our findings in no way undermine the importance of attending to the more obvious, clinical, risks: but they do alert people with interests in the CAMHS field to the importance of a broader constellation of risks associated with hospital admission. Recognising the importance of these less obvious risks as priorities for the second phase of the review was made possible only because of a close collaboration (in EPPI-Centre style) between members of the project team and stakeholders at a key decision-making event following an initial scoping of the literature. The CAMHS arena is populated by people with a variety of backgrounds and expertise, not all of whom have routine opportunities to shape the direction of policy, services or research. In this context we consider it a strength that this study was informed to the degree it was by the views, experiences and recommendations of people using and working in the system.
The importance to stakeholders of the identification, assessment and management of the less obvious risks to young people moving into, through and out of mental health hospital contrasts with the limited quantity and quality of completed research capable of informing policy, services and practice in these areas. Having first found an under-recognised area for our evidence synthesis, we now find ourselves unable to make comprehensive suggestions for improvement. This recognises, in particular, that very little evidence was found to support actions designed to mitigate the less obvious risks to young people admitted. We return to this theme in our section Implications for health care and recommendations for research below.
This project also has limitations. The limiting of all searches to English-language publications is one, with obvious implications for the non-retrieval of potentially relevant materials from teams possibly working in the non-English-speaking parts of the world. Another relates specifically to phase 1, where the search strategy used included the term ‘risk’. As we later found in phase 2, papers reporting on the less obvious risks do not necessarily use the language of ‘risk’ at all, and a different search strategy (across different or additional databases) might have yielded a series of phase 1 maps of a different character. This leads to a further potential limitation, which relates to our use of umbrella terms and concepts for phase 2. We developed the idea of ‘dislocation’ as an overarching construct to bring together a variety of risks. This helped us to connect different types of evidence across a number of distinct but relatable areas and gave us a robust framework for both searching and synthesising. However, we recognise that the idea of ‘dislocation’ is not a self-evident one. Our processes for searching and sifting materials were scrupulous, but we recognise that degrees of interpretation were used in the identification of evidence judged to make a contribution to knowledge in this broad, constructed, area.
Two final limitations remain. The first relates to the disappointing lack of information retrieved from NHS and non-NHS inpatient CAMHS units, and from others with interests and expertise in the field, in response to our widely circulated call for evidence. Enthusiastic responses to the focus of the study were received, and published papers were sometimes sent to us, but no written local service responses about the less obvious risks were sent. We return to this in Implications for health care and recommendations for research below. Second, the paucity of evidence on alternative approaches to identifying, assessing and managing the less obvious risks of dislocation and contagion challenged our aspiration of conducting a robust health economics analysis.
Implications for health care and recommendations for research
At the risk of overstating, we reiterate that nothing in this evidence synthesis should be interpreted as undermining the value of hospital services for young people with the greatest level of mental health need. However, the trend observed in Chapter 1 towards the diversification of tier 4 services to include specialist, intensive care provided in the community is one that we applaud. We therefore suggest that:
-
One way of mitigating the less obvious risks associated with hospital admission is to admit only when all other options have been exhausted, for periods as short as possible and close to home.
The evidence synthesised in this review has implications at the point that judgements are being made on admitting young people to the inpatient component of the CAMHS system. It suggests that:
-
As routine, explicit attention be paid to the assessment of the risks of dislocation and to the proactive planning of care which mitigates these.
The evidence suggests that, for young people in hospital:
-
Services should balance structured therapeutic activity with space for normalising, everyday interactions.
This review also suggests that:
-
Services should be able to help young people in hospital keep in touch with both family and friends, including in the case of admission to units located a long way from home.
The evidence found and included also underlines that:
-
It is important to help young people continue with their education during periods spent in hospital, and proactive care planning includes preparation for school reintegration.
Other evidence found suggests that:
-
Behaviour by staff (e.g. at mealtimes) can reveal the character of young people’s specific mental health difficulties and this can be experienced as stigmatising.
From the evidence located and synthesised in this review:
-
There is no clear support for the implementation of any specific menu of interventions to manage the less obvious risks (as many studies were isolated and of variable quality, sometimes conducted in different parts of the world, where health systems are different from those in the UK, limiting their direct applicability, and knowledge has not accumulated).
What this review therefore does is lay bare areas of real importance for young people’s health-care experiences, and for their longer-term flourishing, about which little evidence to guide services and practice exists. We therefore recommend that:
-
Research is needed into the risk of inpatient contagion, where the current evidence on the existence of this is equivocal.
-
High-quality studies are also needed to inform action to identify, and mitigate, the risks of dislocation associated with hospital admission; to assess the costs to the NHS of different approaches; and to place service commissioning and provision on a more evidence-based footing.
To this we add the suggestion that:
-
Studies should equally address the assessment, identification and management of the less obvious risks across all tiers and components of the CAMHS system (including newer, specialised community services such as those for young people with eating disorders or with challenging behaviours), reflecting the extent to which services are entirely interlinked.
We therefore see that:
-
There is a place for a programme of research which begins with the careful exploration of current services and practice with a view to identifying those features found locally to be helpful.
We do not interpret the absence of written policies and service specifications from local CAMHS units in response to our call for evidence as signifying an absence of actions routinely taken to offset the less obvious risks. Describing what happens and what helps to mitigate these, including actions which are not committed to paper in the form of formal policy or standards, would represent a reasoned first step towards isolating and potentially testing specific interventions.
Acknowledgements
Contributions of authors
Dr Ben Hannigan (Reader in Mental Health Nursing) screened, selected, appraised and synthesised materials, and wrote for and edited the final report.
Mrs Deborah Edwards (Research Fellow) screened, selected, appraised and synthesised materials, and wrote for and edited the final report.
Dr Nicola Evans (Lecturer in Mental Health Nursing) screened, selected, appraised and synthesised materials, and wrote for the final report.
Mrs Elizabeth Gillen (Subject Librarian, Healthcare Sciences) led the development of search strategies, screened, selected, appraised and synthesised materials, and wrote for the final report.
Dr Mirella Longo (Senior Research Fellow in Health Economics) led the health economics analysis, screened, selected, appraised and synthesised materials, and wrote for the final report.
Professor Steven Pryjmachuk (Professor of Mental Health Nursing Education) screened, selected, appraised and synthesised materials, and wrote for the final report.
Dr Gemma Trainor (Consultant Nurse in Child and Adolescent Mental Health Services) screened, selected and appraised materials, and commented on the final report.
The project team acknowledges the help of:
Dr Michael Coffey (Associate Professor, College of Human and Health Sciences, Swansea University) for independently chairing the meetings of the project team and stakeholder advisory group.
Mr Matthew Daniel (Training and Consultancy Manager, YoungMinds) for conducting the series of consultations with young people to inform the identification of priorities for the second phase of the project.
Professor Sally Holland (Professor of Social Work, Cardiff School of Social Sciences) for sharing her experiences and expertise in involving young people in research.
Professor Martin Knapp (Professor of Social Policy, The London School of Economics and Political Science) for his help identifying papers reporting the economic aspects of child and adolescent mental health needs and services.
Professor Lesley Lowes (Florence Nightingale Foundation Chair of Clinical Nursing Research, School of Healthcare Sciences, Cardiff University) for sharing her experiences and expertise in involving young people in research.
Ms Mala Mann (Information Specialist/Systematic Reviewer, Cardiff University) for her help refining the phase 2 search strategy.
All members of the stakeholder advisory group, who helped identify priorities for the second phase of the project, informed plans for dissemination and knowledge mobilisation and generated ideas for future research.
Funding
This project is funded by the National Institute for Health Research Health Services and Delivery Research programme (project number 11/1024/08). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the HSDR programme, the NIHR, the NHS or the Department of Health.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Green H, McGinnity A, Meltzer H, Ford T, Goodman R. Mental Health of Children and Young People in Great Britain 2004. Basingstoke: Palgrave Macmillan; 2005.
- McCrone P, Dhanasiri S, Patel A, Knapp M, Lawton-Smith S. Paying the Price: The Cost of Mental Health Care in England to 2026. London: The King’s Fund; 2008.
- Davidson J. Children and Young People in Mind: The Final Report of the National CAMHS Review. London: Department of Education; 2008.
- Services for Children and Young People with Emotional and Mental Health Needs. Cardiff: Auditor General for Wales; 2009.
- Plsek PE, Greenhalgh T. The challenge of complexity in health care. BMJ 2001;323:625-8. http://dx.doi.org/10.1136/bmj.323.7313.625.
- Geyer R, Rihani S. Complexity and Public Policy: A New Approach to 21st Century Politics, Policy and Society. London: Routledge; 2010.
- Chapman J. System Failure: Why Governments Must Learn to Think Differently. London: Demos; 2004.
- Kurtz Z. The Evidence Base to Guide Development of Tier 4 CAMHS. London: Department of Health; 2009.
- Shepperd S, Harris L, Bull L, Doll H, Fitzpatrick R, Gowers S, et al. Systematic Review and Mapping Study of Alternatives to Inpatient Care for Children and Adolescents with Complex Mental Health Needs. London: National Coordinating Centre for NHS Service Delivery and Organisation programme; 2008.
- Buchanan M. Rise in Children Treated on Adult Mental Health Wards 2014. www.bbc.co.uk/news/education-26255533 (accessed 29 April 2014).
- O’Herlihy A, Worrall A, Banerjee S, Jaffa T, Hill P, Mears A, et al. National In-Patient Child And Adolescent Psychiatry Study (NICAPS). London: Royal College of Psychiatrists; 2001.
- O’Herlihy A, Lelliott P, Cotgrove A, Andiappan M, Farr H. The Care Paths of Young People Referred but Not Admitted to Inpatient Child and Adolescent Mental Health Services. London: Royal College of Psychiatrists; 2008.
- Pushed into the Shadows: Young People’s Experiences of Adult Mental Health Facilities. London: Hard Copy; 2007.
- Statutory Notification: Regulation 18(2)(h),Care Quality Commission (Registration) Regulations 2009. Admission of a Child or Young Person to an Adult Psychiatric Ward. London: Care Quality Commission; 2013.
- Tulloch S, Lelliot P, Bannister D, Andiappan M, O’Herlihy A, Beecham J, et al. The Costs, Outcomes and Satisfaction for Inpatient Child and Adolescent Psychiatric Services (COSI-CAPS) Study. London: National Coordinating Centre for NHS Service Delivery and Organisation programme; 2008.
- Singh SP, Paul M, Islam Z, Weaver T, Kramer T, McLaren S, et al. Transition from CAMHS to Adult Mental Health Services (TRACK): A Study of Service Organisation, Policies, Process and User and Carer Perspectives. Southampton: National Institute for Health Research Service Delivery and Organisation programme; 2010.
- Coleman J, Hagell A. Adolescence, Risk and Resilience: Against the Odds. Chichester: John Wiley and Sons; 2007.
- Morgan S. Positive risk-taking: an idea whose time has come. Health Care Risk Report 2004;10:18-9.
- Pope C, Mays N, Popay J. Synthesizing Qualitative and Quantitative Health Evidence: A Guide to Methods. Maidenhead: Open University Press; 2007.
- Caird J, Rees R, Kavanagh J, Sutcliffe K, Oliver K, Dickson K, et al. The Socioeconomic Value of Nursing and Midwifery: A Rapid Systematic Review of Reviews. London: Institute of Education, University of London; 2010.
- Newman M, Bangpan M, Kalra N, Mays N, Kwan I, Roberts T. Commissioning in Health, Education and Social Care: Models, Research Bibliography and In-Depth Review of Joint Commissioning between Health and Social Care Agencies. London: Institute of Education, University of London; 2012.
- Willey B, Smith Paintain L, Mangham-Jefferies L, Car J, Armstrong Schellenberg J. Effectiveness of Interventions to Strengthen National Health Service Delivery on Coverage, Access, Quality and Equity in the Use of Health Services in Low and Lower Middle Income Countries. London: Institute of Education, University of London; 2013.
- Pryjmachuk S, Elvey R, Kirk S, Kendal S, Bower P, Catchpole R. Developing a model of mental health self-care support for children and young people through an integrated evaluation of available types of provision involving systematic review, meta-analysis and case study. Health Serv Deliv Res 2014;2.
- Bonell C, Jamal F, Harden A, Wells H, Parry W, Fletcher A, et al. Systematic review of the effects of schools and school environment interventions on health: evidence mapping and synthesis. Public Health Res 2013;1.
- Harden A, Popay J. Moving beyond Effectiveness in Evidence Synthesis Methodological Issues in the Synthesis of Diverse Sources of Evidence. London: National Institute for Health and Clinical Excellence; 2006.
- EPPI-Centre Methods for Conducting Systematic Reviews. London: Institute of Education, University of London; 2007.
- Chabra A, Chavez G, Harris E, Shah R. Hospitalization for mental illness in adolescents: risk groups and impact on the health care system. J Adolesc Health 1999;24:349-56. http://dx.doi.org/10.1016/S1054-139X(98)00116-5.
- Kjelsberg E, Neegaard E, Dahl A. Suicide in adolescent psychiatric inpatients: incidence and predictive factors. Acta Psychiatr Scand 1994;89:235-41. http://dx.doi.org/10.1111/j.1600-0447.1994.tb01507.x.
- Subotsky F. Clinical risk management and child mental health. Adv Psychiatr Treat 2003;9:319-26. http://dx.doi.org/10.1192/apt.9.5.319.
- Osman A, Gutierrez P, Schweers R, Fang Q, Holguin-Mills R, Cashin M. Psychometric evaluation of the body investment scale for use with adolescents. J Clin Psychol 2010;66:259-76. http://dx.doi.org/10.1002/jclp.20649.
- Adams D, Overholser J, Lehnert K. Perceived family functioning and adolescent suicidal behavior. J Am Acad Child Adolesc Psychiatry 1994;33:498-507. http://dx.doi.org/10.1097/00004583-199405000-00008.
- Apter A, Gothelf D, Offer R, Ratzoni G, Orbach I, Tyano S, et al. Suicidal adolescents and ego defense mechanisms. J Am Acad Child Adolesc Psychiatry 1997;36:1520-7.
- Apter A, Gothelf D, Orbach I, Weizman R, Ratzoni G, Har-Even D, et al. Correlation of suicidal and violent behavior in different diagnostic categories in hospitalized adolescent patients. J Am Acad Child Adolesc Psychiatry 1995;34:912-18. http://dx.doi.org/10.1097/00004583-199507000-00015.
- Brent D, Perper J, Goldstein C, Kolko D, Allan M, Allman C, et al. Risk factors for adolescent suicide: a comparison of adolescent suicide victims with suicidal inpatients. Arch Gen Psychiatry 1988;45:581-8. http://dx.doi.org/10.1001/archpsyc.1988.01800300079011.
- Brent D, Kolko D, Wartella M, Boylan M, Moritz G, Baugher M, et al. Adolescent psychiatric inpatients’ risk of suicide attempt at 6-month follow-up. J Am Acad Child Adolesc Psychiatry 1993;32:95-105. http://dx.doi.org/10.1097/00004583-199301000-00015.
- Brinkman-Sull D, Overholser J, Silverman E. Risk of future suicide attempts in adolescent psychiatric inpatients at 18-month follow-up. Suicide Life Threat Behav 2000;30:327-40.
- Brunstein-Klomek A, Orbach I, Meged S, Zalsman G. Self complexity of suicidal adolescents. Int J Adolesc Med Health 2005;17:267-73.
- Cohen Y, Spirito A, Sterling C, Donaldson D, Seifer R, Plummer B, et al. Physical and sexual abuse and their relation to psychiatric disorder and suicidal behavior among adolescents who are psychiatrically hospitalized. J Child Psychol Psychiatry 1996;37:989-93. http://dx.doi.org/10.1111/j.1469-7610.1996.tb01495.x.
- Danielson C, Overholser J, Butt Z. Association of substance abuse and depression among adolescent psychiatric inpatients. Can J Psychiatry 2003;48:762-5.
- D’Eramo K, Prinstein M, Freeman J, Grapentine W, Spirito A. Psychiatric diagnoses and comorbidity in relation to suicidal behavior among psychiatrically hospitalized adolescents. Child Psychiatry Hum Dev 2004;35:21-35. http://dx.doi.org/10.1023/B:CHUD.0000039318.72868.a2.
- DiFilippo J, Overholser J. Suicidal ideation in adolescent psychiatric inpatients as associated with depression and attachment relationships. J Clin Child Psychol 2000;29:155-66. http://dx.doi.org/10.1207/S15374424jccp2902_2.
- Eltz M, Evans A, Celio M, Dyl J, Hunt J, Armstrong L, et al. Suicide probability scale and its utility with adolescent psychiatric patients. Child Psychiatry Hum Dev 2007;38:17-29. http://dx.doi.org/10.1007/s10578-006-0040-7.
- Gasquet I, Choquet M. Hospitalization in a pediatric ward of adolescent suicide attempters admitted to general hospitals. J Adolesc Health 1994;15:416-22. http://dx.doi.org/10.1016/1054-139X(94)90267-4.
- Goldston D, Daniel S, Reboussin D, Kelley A, Ievers C, Brunstetter R. First-time suicide attempters, repeat attempters, and previous attempters on an adolescent inpatient psychiatry unit. J Am Acad Child Adolesc Psychiatry 1996;35:631-9. http://dx.doi.org/10.1097/00004583-199605000-00018.
- Goldston D, Daniel S, Reboussin B, Reboussin D, Kelley A, Frazier P. Psychiatric diagnoses of previous suicide attempters, first-time attempters, and repeat attempters on an adolescent inpatient psychiatry unit. J Am Acad Child Adolesc Psychiatry 1998;37:924-32. http://dx.doi.org/10.1097/00004583-199809000-00012.
- Goldston D, Daniel S, Reboussin D, Reboussin B, Frazier P, Kelley A. Suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study of risk during the first 5 years after discharge. J Am Acad Child Adolesc Psychiatry 1999;38:660-71. http://dx.doi.org/10.1097/00004583-199906000-00012.
- Gothelf D, Apter A, Brand-Gothelf A, Offer N, Ofek H, Tyano S, et al. Death concepts in suicidal adolescents. J Am Acad Child Adolesc Psychiatry 1998;37:1279-86. http://dx.doi.org/10.1097/00004583-199812000-00011.
- Greenham S, Bisnaire L. An outcome evaluation of an inpatient crisis stabilization and assessment program for youth. Resident Treat Child Youth 2008;25:123-43. http://dx.doi.org/10.1080/08865710802310012.
- Grilo C, Sanislow C, Fehon D, Lipschitz D, Martino S, McGlashan T. Correlates of suicide risk in adolescent inpatients who report a history of childhood abuse. Compr Psychiatry 1999;40:422-8. http://dx.doi.org/10.1016/S0010-440X(99)90085-8.
- Haavisto A, Sourander A, Ellila H, Valimaki M, Santalahti P, Helenius H. Suicidal ideation and suicide attempts among child and adolescent psychiatric inpatients in Finland. J Affect Disord 2003;76:211-21. http://dx.doi.org/10.1016/S0165-0327(02)00093-9.
- Horesh N, Zalsman G, Apter A. Suicidal behavior and self-disclosure in adolescent psychiatric inpatients. J Nerv Ment Dis 2004;192:837-42. http://dx.doi.org/10.1097/01.nmd.0000146738.78222.e5.
- Huth-Bocks A, Kerr D, Ivey A, Kramer A, King C. Assessment of psychiatrically hospitalized suicidal adolescents: self-report instruments as predictors of suicidal thoughts and behavior. J Am Acad Child Adolesc Psychiatry 2007;46:387-95. http://dx.doi.org/10.1097/chi.0b013e31802b9535.
- Ilomaki E, Rasanen P, Viilo K, Hakko H. Study-Workgroup . Suicidal behavior among adolescents with conduct disorder: the role of alcohol dependence. Psychiatry Res 2007;150:305-11. http://dx.doi.org/10.1016/j.psychres.2006.02.011.
- Joiner TJ, Rudd M, Rouleau M, Wagner K. Parameters of suicidal crises vary as a function of previous suicide attempts in youth inpatients. J Am Acad Child Adolesc Psychiatry 2000;39:876-80. http://dx.doi.org/10.1097/00004583-200007000-00016.
- Kirkcaldy B, Brown J, Siefen R. Disruptive behavioural disorders, self harm and suicidal ideation among German adolescents in psychiatric care. Int J Adolesc Med Health 2006;18:597-614. http://dx.doi.org/10.1515/IJAMH.2006.18.4.597.
- Larsson B, Ivarsson T. Clinical characteristics of adolescent psychiatric inpatients who have attempted suicide. Eur Child Adolesc Psychiatry 1998;7:201-8. http://dx.doi.org/10.1007/s007870050068.
- Lukonis C, Lustig S, Brant R, Goldman S, Vaughan B. Suicide, substances, and stories: treating a teenager in trouble. Harv Rev Psychiatry 2001;9:302-9. http://dx.doi.org/10.1080/10673220127911.
- McCarthy J, Nahas A, Welson R. Suicidal and assaultive behavior in hospitalized adolescents: incidence and co-occurrence with psychiatric disorders. Res Commun Biol Psychol Psychiatry 1995;20:69-80.
- O’Brien P, Wilkes T. An adolescent psychiatric unit’s responses to patient suicides. Fam Ther 2004;31:1-16.
- Ofek H, Weizman T, Apter A. The child suicide potential scale: inter-rater reliability and validity in Israeli in-patient adolescents. Isr J Psychiatry Relat Sci 1998;35:253-61.
- Ohring R, Apter A, Ratzoni G, Weizman R, Tyano S, Plutchik R. State and trait anxiety in adolescent suicide attempters. J Am Acad Child Adolesc Psychiatry 1996;35:154-7. http://dx.doi.org/10.1097/00004583-199602000-00007.
- Osman A, Kopper B, Barrios F, Osman J, Besett T, Linehan M. The Brief Reasons for Living Inventory for Adolescents (BRFL-A). J Abnorm Child Psychol 1996;24:433-43. http://dx.doi.org/10.1007/BF01441566.
- Osman A, Gilpin A, Panak W, Kopper B, Barrios F, Gutierrez P, et al. The multi-attitude suicide tendency scale: further validation with adolescent psychiatric inpatients. Suicide Life Threat Behav 2000;30:377-85.
- Osman A, Bagge C, Gutierrez P, Konick L, Kopper B, Barrios F. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment 2001;8:443-54. http://dx.doi.org/10.1177/107319110100800409.
- Osman A, Barrios F, Gutierrez P, Wrangham J, Kopper B, Truelove R, et al. The Positive and Negative Suicide Ideation (PANSI) inventory: psychometric evaluation with adolescent psychiatric inpatient samples. J Pers Assess 2002;79:512-30. http://dx.doi.org/10.1207/S15327752JPA7903_07.
- Osman A, Gutierrez P, Barrios F, Bagge C, Kopper B, Linden S. The Inventory of Suicide Orientation-30: further validation with adolescent psychiatric inpatients. J Clin Psychol 2005;61:481-97. http://dx.doi.org/10.1002/jclp.20086.
- Overholser J, Adams D, Lehnert K, Brinkman D. Self-esteem deficits and suicidal tendencies among adolescents. J Am Acad Child Adolesc Psychiatry 1995;34:919-28. http://dx.doi.org/10.1097/00004583-199507000-00016.
- Overholser J, Freiheit S, DiFilippo J. Emotional distress and substance abuse as risk factors for suicide attempts. Can J Psychiatry 1997;42:402-8.
- Pfeffer CR, Newcorn J, Kaplan G, Mizruchi MS, Plutchik R. Suicidal behavior in adolescent psychiatric inpatients. J Am Acad Child Adolesc Psychiatry 1988;27:357-61. http://dx.doi.org/10.1097/00004583-198805000-00015.
- Pfeffer CR, Newcorn J, Kaplan G, Mizruchi MS, Plutchik R. Subtypes of suicidal and assaultive behaviors in adolescent psychiatric inpatients: a research note. J Child Psychol Psychiatry 1989;30:151-63. http://dx.doi.org/10.1111/j.1469-7610.1989.tb00774.x.
- Pinto A, Whisman M. Negative affect and cognitive biases in suicidal and nonsuicidal hospitalized adolescents. J Am Acad Child Adolesc Psychiatry 1996;35:158-65. http://dx.doi.org/10.1097/00004583-199602000-00008.
- Rice B, Woolston J, Stewart E, Kerker B, Horwitz S. Differences in younger, middle, and older children admitted to child psychiatric inpatient services. Child Psychiatry Hum Dev 2002;32:241-61. http://dx.doi.org/10.1023/A:1015244626238.
- Schwartz-Stav O, Apter A, Zalsman G. Depression, suicidal behaviour and insight in adolescents with schizophrenia. Eur Child Adolesc Psychiatry 2006;15:352-9. http://dx.doi.org/10.1007/s00787-006-0541-8.
- Shoval G, Zalsman G, Sher L, Apter A, Weizman A. Clinical characteristics of inpatient adolescents with severe obsessive–compulsive disorder. Depress Anxiety 2006;23:62-70. http://dx.doi.org/10.1002/da.20135.
- Shoval G, Feld-Olspanger J, Nahshoni E, Gothelf D, Misgav S, Manor I, et al. Suicidal behavior and related traits among inpatient adolescents with first-episode schizophrenia. Compr Psychiatry 2011;52:596-9. http://dx.doi.org/10.1016/j.comppsych.2011.01.005.
- Steer R, Kumar G, Beck A. Self-reported suicidal ideation in adolescent psychiatric inpatients. J Consult Clin Psychol 1993;61:1096-9. http://dx.doi.org/10.1037/0022-006X.61.6.1096.
- Fehon D, Grilo C, Martino S. A comparison of dependent and self-critically depressed hospitalized adolescents. J Youth Adolescence 2000;29:93-106. http://dx.doi.org/10.1023/A:1005125322629.
- Kroll L, Green J. The therapeutic alliance in child inpatient treatment: development and initial validation of a family engagement questionnaire. Clin Child Psychol Psychiatry 1997;2:431-47. http://dx.doi.org/10.1177/1359104597023009.
- Pfeffer CR. Studies of suicidal preadolescent and adolescent inpatients: a critique of research methods. Suicide Life Threat Behav 1989;19:58-77.
- Engel Z, Mitrani M, Zalsman G. Prevention of suicide in an inpatient adolescent unit by environmental safety modification. Int J Adolesc Med Health 2005;17.
- Greenhill L, Waslick B. Management of suicidal behavior in children and adolescents. Psychiatr Clin N Am 1997;20:641-66. http://dx.doi.org/10.1016/S0193-953X(05)70335-X.
- Meyers K, McLellan A, Jaeger J, Pettinati H. The development of the comprehensive addiction severity index for adolescents (CASI-A): an interview for assessing multiple problems of adolescents. J Subst Abuse Treat 1995;12:181-93. http://dx.doi.org/10.1016/0740-5472(95)00009-T.
- Becker D, Grilo C. Ethnic differences in the predictors of drug and alcohol abuse in hospitalized adolescents. Am J Addict 2007;16:389-96. http://dx.doi.org/10.1080/10550490701525343.
- Evans A, Spirito A, Celio M, Dyl J, Hunt J. The relation of substance use to trauma and conduct disorder in an adolescent psychiatric population. J Child Adolesc Subst Abuse 2007;17:29-4. http://dx.doi.org/10.1300/J029v17n01_02.
- McKay J, Murphy R, Rivinus T, Maisto S. Family dysfunction and alcohol and drug use in adolescent psychiatric inpatients. J Am Acad Child Adolesc Psychiatry 1991;30:967-72. http://dx.doi.org/10.1097/00004583-199111000-00015.
- Becker S, Nargiso J, Wolff J, Uhl K, Simon V, Spirito A, et al. Temporal relationship between substance use and delinquent behavior among young psychiatrically hospitalized adolescents. J Subst Abuse Treat 2012;43:251-9. http://dx.doi.org/10.1016/j.jsat.2011.11.005.
- Shoval G, Zalsman G, Apter A, Diller R, Sher L, Weizman A. A 10-year retrospective study of inpatient adolescents with schizophrenia/schizoaffective disorder and substance use. Compr Psychiatry 2007;48:1-7. http://dx.doi.org/10.1016/j.comppsych.2006.05.002.
- de Kloet L, Starling J, Hainsworth C, Berntsen E, Chapman L, Hancock K. Risk factors for self-harm in children and adolescents admitted to a mental health inpatient unit. Aust N Z J Psychiatry 2011;45:749-55. http://dx.doi.org/10.3109/00048674.2011.595682.
- Wheatley M, Waine J, Spence K, Hollin C. Characteristics of 80 adolescents referred for secure inpatient care. Clin Psychol Psychother 2004;11:83-9. http://dx.doi.org/10.1002/cpp.398.
- Askenazy F, Sorci K, Benoit M, Lestideau K, Myquel M, Lecrubier Y. Anxiety and impulsivity levels identify relevant subtypes in adolescents with at-risk behavior. J Affect Disord 2003;74:219-27. http://dx.doi.org/10.1016/S0165-0327(02)00455-X.
- Aruffo J, Gottlieb A, Webb R, Neville B. Adolescent psychiatric inpatients: alcohol use and HIV risk-taking behavior. Psychosoc Rehabil J 1994;17:150-6. http://dx.doi.org/10.1037/h0095547.
- King C, Ghaziuddin N, McGovern L, Brand E, Hill E, Naylor M. Predictors of comorbid alcohol and substance abuse in depressed adolescents. J Am Acad Child Adolesc Psychiatry 1996;35:743-51. http://dx.doi.org/10.1097/00004583-199606000-00014.
- Brown L, Kessel S, Lourie K, Ford H, Lipsitt L. Influence of sexual abuse on HIV-related attitudes and behaviors in adolescent psychiatric inpatients. J Am Acad Child Adolesc Psychiatry 1997;36:316-22. http://dx.doi.org/10.1097/00004583-199703000-00009.
- Antonius D, Fuchs L, Herbert F, Kwon J, Fried J, Burton P, et al. Psychiatric assessment of aggressive patients: a violent attack on a resident. Am J Psychiatry 2010;167:253-9. http://dx.doi.org/10.1176/appi.ajp.2009.09010063.
- Barnett S, dosReis S, Riddle M. Maryland Youth Practice Improvement Committee for Mental Health: improving the management of acute aggression in state residential and inpatient psychiatric facilities for youths. J Am Acad Child Adolesc Psychiatry 2002;41:897-905. http://dx.doi.org/10.1097/00004583-200208000-00007.
- Barzman D, Brackenbury L, Sonnier L, Schnell B, Cassedy A, Salisbury S, et al. Brief Rating of Aggression by Children and Adolescents (BRACHA): development of a tool for assessing risk of inpatients’ aggressive behavior. J Am Acad Psychiatry Law 2011;39:170-9.
- Boxer P. Aggression in very high-risk youth: examining developmental risk in an inpatient psychiatric population. Am J Orthopsychiatry 2007;77:636-46. http://dx.doi.org/10.1037/0002-9432.77.4.636.
- Boxer P. Covariation of self- and other-directed aggression among inpatient youth: continuity in the transition to treatment and shared risk factors. Aggress Behav 2010;36:205-17. http://dx.doi.org/10.1002/ab.20343.
- Dean A, Duke S, Scott J, Bor W, George M, McDermott B. Physical aggression during admission to a child and adolescent inpatient unit: predictors and impact on clinical outcomes. Aust N Z J Psychiatry 2008;42:536-43. http://dx.doi.org/10.1080/00048670802050587.
- Hanssen-Bauer K, Heyerdahl S, Hatling T, Jensen G, Olstad P, Stangeland T, et al. Admissions to acute adolescent psychiatric units: a prospective study of clinical severity and outcome. Int J Ment Health Syst 2011;5. http://dx.doi.org/10.1186/1752-4458-5-1.
- Kerr D, Washburn J, Feingold A, Kramer A, Ivey A, King C. Sequelae of aggression in acutely suicidal adolescents. J Abnorm Child Psychol 2007;35:817-30. http://dx.doi.org/10.1007/s10802-007-9132-5.
- Knox M, Carey M, Kim W. Aggression in inpatient adolescents: the effects of gender and depression. Youth Soc 2003;35:226-42. http://dx.doi.org/10.1177/0044118X03255007.
- Phillips N, Stargatt R, Fisher L. Risk assessment: predicting physical aggression in child psychiatric inpatient units. Aust N Z J Psychiatry 2011;45:638-45. http://dx.doi.org/10.3109/00048674.2011.587396.
- Vivona J, Ecker B, Halgin R, Cates D, Garrison W, Friedman M. Self- and other-directed aggression in child and adolescent psychiatric inpatients. J Am Acad Child Adolesc Psychiatry 1995;34:434-44. http://dx.doi.org/10.1097/00004583-199504000-00010.
- Phillips N, Stargatt R, Brown A. Risk assessment of self- and other-directed aggression in adolescent psychiatric inpatient units. Aust N Z J Psychiatry 2012;46:40-6. http://dx.doi.org/10.1177/0004867411430876.
- Cautin R, Overholser J, Goetz P. Assessment of mode of anger expression in adolescent psychiatric inpatients. Adolescence 2001;36:163-70.
- Grosz D, Lipschitz D, Eldar S, Finkelstein G, Blackwood N, Gerbino-Rosen G, et al. Correlates of violence risk in hospitalized adolescents. Compr Psychiatry 1994;35:296-300. http://dx.doi.org/10.1016/0010-440X(94)90022-1.
- Fehon D, Grilo C, Lipschitz D. Gender differences in violence exposure and violence risk among adolescent inpatients. J Nerv Ment Dis 2001;189:532-40. http://dx.doi.org/10.1097/00005053-200108000-00006.
- Fehon D, Grilo C, Lipschitz D. A comparison of adolescent inpatients with and without a history of violence perpetration: impulsivity, PTSD, and violence risk. J Nerv Ment Dis 2005;193:405-11. http://dx.doi.org/10.1097/01.nmd.0000165294.41091.fc.
- Gammelgard M, Koivisto A, Eronen M, Kaltiala-Heino R. The predictive validity of the Structured Assessment of Violence Risk in Youth (SAVRY) among institutionalised adolescents. J Forensic Psychiatry Psychol 2008;19:352-70. http://dx.doi.org/10.1080/14789940802114475.
- Walker S, Kelly M. The introduction of an early warning signs journal in an adolescent inpatient unit. J Psychiatr Ment Health Nurs 2011;18:563-8. http://dx.doi.org/10.1111/j.1365-2850.2011.01705.x.
- Luukkonen A, Rasanen P, Hakko H, Riala K. Study Workgroup . Bullying behavior is related to suicide attempts but not to self-mutilation among psychiatric inpatient adolescents. Psychopathology 2009;42:131-8. http://dx.doi.org/10.1159/000204764.
- Luukkonen A, Riala K, Hakko H, Rasanen P. Study Workgroup . Bullying behaviour and substance abuse among underage psychiatric inpatient adolescents. Eur Psychiatry 2011;25:382-9. http://dx.doi.org/10.1016/j.eurpsy.2009.12.002.
- Pogge D, Insalaco B, Bertisch H, Bilginer L, Stokes J, Cornblatt B, et al. Six-year outcomes in first admission adolescent inpatients: clinical and cognitive characteristics at admission as predictors. Psychiatry Res 2008;160:47-54. http://dx.doi.org/10.1016/j.psychres.2007.06.024.
- Fontanella C. The influence of clinical, treatment, and healthcare system characteristics on psychiatric readmission of adolescents. Am J Orthopsychiatry 2008;78:187-98. http://dx.doi.org/10.1037/a0012557.
- Fontanella C, Bridge J, Campo J. Psychotropic medication changes, polypharmacy, and the risk of early readmission in suicidal adolescent inpatients. Ann Pharmacother 2009;43:1939-47. http://dx.doi.org/10.1345/aph.1M326.
- Barker D, Jairam R, Rocca A, Goddard L, Matthey S. Why do adolescents return to an acute psychiatric unit?. Australas Psychiatry 2010;18:551-5. http://dx.doi.org/10.3109/10398562.2010.501380.
- James S, Charlemagne S, Gilman A, Alemi Q, Smith R, Tharayil P, et al. Post-discharge services and psychiatric rehospitalization among children and youth. Adm Policy Ment Health 2010;37:433-45. http://dx.doi.org/10.1007/s10488-009-0263-6.
- Arnold E, Goldston D, Ruggiero A, Reboussin B, Daniel S, Hickman E. Rates and predictors of rehospitalization among formerly hospitalized adolescents. Psychiatr Serv 2003;54:994-8. http://dx.doi.org/10.1176/appi.ps.54.7.994.
- Abrantes A, Palm K, Strong D, Ramsey S, Brown R. Treatment utilization after psychiatric inpatient hospitalization among adolescents with and without substance use disorders. Addict Disord Treat 2007;6:147-56. http://dx.doi.org/10.1097/ADT.0b013e31802e9a24.
- Fontanella C, Zuravin S, Burry C. The effect of a Medicaid Managed Care Program on patterns of psychiatric readmission among adolescents: evidence from Maryland. J Behav Health Serv Res 2006;33:39-52. http://dx.doi.org/10.1007/s11414-005-9004-0.
- Pedersen J, Aarkrog T. A 10-year follow-up study of an adolescent psychiatric clientele and early predictors of readmission. Nord J Psychiatry 2001;55:11-6. http://dx.doi.org/10.1080/080394801750093643.
- Embry LE, Vander Stoep AV, Evens C, Ryan KD, Pollock A. Risk factors for homelessness in adolescents released from psychiatric residential treatment. J Am Acad Child Adolesc Psychiatry 2000;39:1293-9. http://dx.doi.org/10.1097/00004583-200010000-00017.
- Kjelsberg E, Dahl A. A long-term follow-up study of adolescent psychiatric in-patients. Part II: predictors of delinquency. Acta Psychiatr Scand 1999;99:237-42. http://dx.doi.org/10.1111/j.1600-0447.1999.tb07218.x.
- Kjelsberg E, Sandvik L, Dahl A. A long-term follow-up study of adolescent psychiatric in-patients. Part I: predictors of early death. Acta Psychiatr Scand 1999;99:231-6. http://dx.doi.org/10.1111/j.1600-0447.1999.tb07217.x.
- Kjelsberg E. Adolescent psychiatric in-patients: a high-risk group for premature death. Br J Psychiatry 2000;176:121-5. http://dx.doi.org/10.1192/bjp.176.2.121.
- Best K, Hauser S, Gralinski-Bakker J, Allen J, Crowell J. Adolescent psychiatric hospitalization and mortality, distress levels, and educational attainment: follow-up after 11 and 20 years. Arch Pediatr Adolesc Med 2004;158:749-52. http://dx.doi.org/10.1001/archpedi.158.8.749.
- Halfon O, Laget J, Barrie M. An epidemiological and clinical approach to adolescent suicide: a comparison between suicidal and non-suicidal clinical groups in a health foundation center for French students. Eur Child Adolesc Psychiatry 1995;4:32-8. http://dx.doi.org/10.1007/BF01987964.
- Siegel M, Callesen M. Adolescent runaway behaviour from an inpatient setting. Resident Treat Child Youth 1993;10:5-19. http://dx.doi.org/10.1300/J007v10n04_02.
- Berman L, Goodrich W. Running away from treatment: observations and admission predictors for hospitalized adolescents. Adolesc Psychiatry 1990;17:279-304.
- Kleis L, Stout C. The high-risk patient: a profile of acute care psychiatric patients who leave without discharge. Psychiatr Hosp 1991;22:153-9.
- Vander Stoep A, Bohn P, Melville E. A model for predicting discharge against medical advice from adolescent residential treatment. Hosp Commun Psychiatry 1991;42:725-8.
- Wallier J, Vibert S, Berthoz S, Huas C, Hubert T, Godart N. Dropout from inpatient treatment for anorexia nervosa: critical review of the literature. Int J Eat Disord 2009;42:636-47. http://dx.doi.org/10.1002/eat.20609.
- Leon S, Snowden J, Bryant F, Lyons J. The hospital as predictor of children’s and adolescents’ length of stay. J Am Acad Child Adolesc Psychiatry 2006;45:322-8. http://dx.doi.org/10.1097/01.chi.0000194565.78536.bb.
- McGilloway S, Donnelly M, Scott D. Teenagers in adult psychiatric inpatient care in Northern Ireland. Ir J Psychol Med 2000;17:54-8.
- Kaltiala-Heino R. Involuntary commitment and detainment in adolescent psychiatric inpatient care. Soc Psychiatry Psychiatr Epidemiol 2010;45:785-93. http://dx.doi.org/10.1007/s00127-009-0116-3.
- Leon S, Uziel-Miller N, Lyons J, Tracy P. Psychiatric hospital service utilization of children and adolescents in state custody. J Am Acad Child Adolesc Psychiatry 1999;38:305-10. http://dx.doi.org/10.1097/00004583-199903000-00018.
- Fleischhaker C, Heiser P, Hennighausen K, Herpertz-Dahlmann B, Holtkamp K, Mehler-Wex C, et al. Weight gain in children and adolescents during 45 weeks treatment with clozapine, olanzapine and risperidone. J Neural Transm 2008;115:1599-608. http://dx.doi.org/10.1007/s00702-008-0105-9.
- Shoval G, Nahshoni E, Gothelf D, Manor I, Golobchik P, Zemishlany Z, et al. Effectiveness and safety of citalopram in hospitalized adolescents with major depression: a preliminary, 8-week, fixed-dose, open-label, prospective study. Clin Neuropharmacol 2011;34:182-5. http://dx.doi.org/10.1097/WNF.0b013e31822cb863.
- US Preventive Services Task Force . Screening and treatment for major depressive disorder in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics 2009;123:1223-8. http://dx.doi.org/10.1542/peds.2008-2381.
- Berland D, Guskin K. Patient allegations of sexual abuse against psychiatric hospital staff. Gen Hosp Psychiatry 1994;16:335-9. http://dx.doi.org/10.1016/0163-8343(94)90020-5.
- King C, Franzese R, Gargan S, McGovern L, Ghaziuddin N, Naylor M. Suicide contagion among adolescents during acute psychiatric hospitalization. Psychiatr Serv 1995;46:915-8. http://dx.doi.org/10.1176/ps.46.9.915.
- White H, Langman N, Henderson S. A school-based transition program for high-risk adolescents. Psychiatr Serv 2006;57.
- Dean A, Duke S, George, Scott J. Behavioral management leads to reduction in aggression in a child and adolescent psychiatric inpatient unit. J Am Acad Child Adolesc Psychiatry 2007;46:711-20. http://dx.doi.org/10.1097/chi.0b013e3180465a1a.
- Delaney K, Hardy L. Challenges faced by inpatient child/adolescent psychiatric nurses. J Psychosoc Nurs Ment Health Services 2008;46:21-4. http://dx.doi.org/10.3928/02793695-20080201-04.
- Bridgett D, Valentino K, Hayden L. The contribution of children’s temperamental fear and effortful control to restraint and seclusion during inpatient treatment in a psychiatric hospital. Child Psychiatry Hum Dev 2012;43:821-36. http://dx.doi.org/10.1007/s10578-012-0298-x.
- Delaney K, Fogg L. Patient characteristics and setting variables related to use of restraint on four inpatient psychiatric units for youths. Psychiatr Serv 2005;56:186-92. http://dx.doi.org/10.1176/appi.ps.56.2.186.
- Fryer M, Beech M, Byrne G. Seclusion use with children and adolescents: an Australian experience. Aust N Z J Psychiatry 2004;38:26-33. http://dx.doi.org/10.1111/j.1440-1614.2004.01294.x.
- Frank S, Paul J, Marks M, Van Egeren L. Initial validation of the functional impairment scale for children and adolescents. J Am Acad Child Adolesc Psychiatry 2000;39:1300-8. http://dx.doi.org/10.1097/00004583-200010000-00018.
- Ascherman L. The impact of unstructured games of fantasy and role playing on an inpatient unit for adolescents. Int J Group Psychother 1993;43:335-44.
- Geller J, Biebel K. The premature demise of public child and adolescent inpatient psychiatric beds. Part II: challenges and implications. Psychiatr Q 2006;77:273-91. http://dx.doi.org/10.1007/s11126-006-9013-z.
- Kirby P. A Guide to Actively Involving Young People in Research for Researchers, Research Commissioners and Managers. Eastleigh: INVOLVE; 2004.
- YoungMinds . About Us n.d. www.youngminds.org.uk/about (accessed 26 February 2015).
- Patient and Public Involvement in Research and Research Ethics Committee Review. Eastleigh and London: INVOLVE and The National Research Ethics Service; 2009.
- Delbecq AL, Van de Ven AH. A group process model for problem identification and program planning. J Appl Behav Sci 1971;7:466-92. http://dx.doi.org/10.1177/002188637100700404.
- Gregory JW, Robling M, Bennert K, Channon S, Cohen D, Crowne E, et al. Development and evaluation by a cluster randomised trial of a psychosocial intervention in children and teenagers experiencing diabetes: the DEPICTED study. Health Technol Assess 2011;15. http://dx.doi.org/10.3310/hta15290.
- Residential Treatment Programs. Washington, DC: American Academy of Child and Adolescent Psychiatry; 2011.
- McGrath Y, Sumnal H, Edmonds K, McVeigh J, Bellis M. Review of Grey Literature on Drug Prevention among Young People. London: NICE; 2006.
- Systematic reviews – CRD’s Guidance for Undertaking Reviews in Health Care. York: Centre for Reviews and Dissemination, University of York; 2009.
- Effective Public Health Practice Project . Quality Assessment Tool for Quantitative Studies n.d. www.ephpp.ca/tools.html (accessed 26 February 2015).
- Deeks J, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al. Evaluating non-randomised intervention studies. Health Technol Assess 2003;7. http://dx.doi.org/10.3310/hta7270.
- Rees A, Beecroft C, Booth A, Gerrish K, Lacey A. The Research Process in Nursing. Chichester: Wiley-Blackwell; 2010.
- Critical Skills Appraisal Programme . Critical Appraisal Skills Programme Checklists 2013. www.casp-uk.net/#!casp-tools-checklists/c18f8 (accessed 26 February 2015).
- Kirk S, Beatty S, Callery P, Milnes L, Pryjmachuk S. Evaluating Self-Care Support for Children and Young People with Long Term Conditions. London: National Institute for Health Research Service Delivery and Organisation programme; 2010.
- Drummond MF, Jefferson TO. Guidelines for authors and peer reviewers of economic submissions to the BMJ. BMJ 1996;313:275-83. http://dx.doi.org/10.1136/bmj.313.7052.275.
- Curtis L. Unit Costs of Health and Social Care 2011. Canterbury: PSSRU, University of Kent; 2011.
- Gough D, Thomas J, Oliver S. Clarifying differences between review designs and methods. Syst Rev 2012;1. www.systematicreviewsjournal.com/content/1//28 (accessed 26 February 2015).
- Gough D, Oliver S, Thomas J. An Introduction to Systematic Reviews. London: Sage; 2012.
- Oliver S, Rees RW, Clarke-Jones L, Milne R, Oakley AR, Gabbay J, et al. A multidimensional conceptual framework for analyzing public involvement in health services research. Health Expect 2008;11:72-84. http://dx.doi.org/10.1111/j.1369-7625.2007.00476.x.
- Carroll C, Booth A, Cooper K. A worked example of ‘best fit’ framework synthesis: a systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol 2011;11. http://dx.doi.org/10.1186/1471-2288-11-29 (accessed 26 February 2015).
- Guyatt G, Oxman A, Akl E, Kunz R, Vist G, Brozek J, et al. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383-94. http://dx.doi.org/10.1016/j.jclinepi.2010.04.026.
- Glenton C, Colvin CJ, Carlsen B, Swartz A, Lewin S, Noyes J, et al. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis (review). Cochrane Database Syst Rev 2013;8. http://dx.doi.org/10.1002/14651858.CD010414.pub2.
- Singh N, Wechsler H, Curtis W, Sabaawi M, Myers R, Singh S. Effects of role-play and mindfulness training on enhancing the family friendliness of the admissions treatment team process. J Emotion Behav Disord 2002;10:90-8. http://dx.doi.org/10.1177/10634266020100020301.
- Simmerman S. A comparison of educational programs at an adolescent residential treatment center. Resident Treat Child Youth 1997;15:1-9. http://dx.doi.org/10.1300/J007v15n01_01.
- Buston K. Adolescents with mental health problems: what do they say about health services?. J Adolesc 2002;25:231-42. http://dx.doi.org/10.1006/jado.2002.0463.
- Claveirole A. Listening to the Voices in Four Scottish Adolescent Mental Health Units: Young People, Their Carers and the Unit Cultures. Edinburgh: Napier University; 2005.
- Clemens E, Welfare L, Williams A. Tough transitions: mental health care professionals’ perception of the psychiatric hospital to school transition. Resident Treat Child Youth 2010;27:243-63. http://dx.doi.org/10.1080/0886571X.2010.520631.
- Clemens E, Welfare L, Williams A. Elements of successful school reentry after psychiatric hospitalization. Prev School Fail 2011;55:202-13. http://dx.doi.org/10.1080/1045988X.2010.532521.
- Colton D, Pistrang N. Adolescents’ experiences of inpatient treatment for anorexia nervosa. Eur Eat Disord Rev 2004;12:307-16. http://dx.doi.org/10.1002/erv.587.
- Haynes C, Eivors A, Crossley J. ‘Living in an alternative reality’: adolescents’ experiences of psychiatric inpatient care. Child Adolesc Ment Health 2011;16:150-7. http://dx.doi.org/10.1111/j.1475-3588.2011.00598.x.
- Painter C. Surviving an Alternative Reality: A Qualitative Analysis of Adolescents’ Experiences of Psychiatric Hospitalisation 2008.
- Moses T. Adolescents’ perspectives about brief psychiatric hospitalisation: what is helpful and what is not. Psychiatr Q 2011;82:121-37. http://dx.doi.org/10.1007/s11126-010-9151-1.
- Offord A, Turner H, Cooper M. Adolescent inpatient treatment for anorexia nervosa: a qualitative study exploring young adults’ retrospective views of treatment and discharge. Eur Eat Disord Rev 2006;14:377-87. http://dx.doi.org/10.1002/erv.687.
- Puotiniemi T, Kyngas H. The coping of an adolescent who has been in psychiatric inpatient care and her mother in everyday life. J Psychiatr Ment Health Nurs 2004;11:675-82. http://dx.doi.org/10.1111/j.1365-2850.2004.00781.x.
- Anderson K, Ramo D, Schulte M, Cummins K, Brown S. Impact of relapse predictors on psychosocial functioning of SUD youth one year after treatment. Subst Abuse 2008;29:97-106. http://dx.doi.org/10.1080/08897070802093411.
- Brinkmeyer M, Eyberg S, Nguyen M, Adams R. Family engagement, consumer satisfaction and treatment outcome in the new era of child and adolescent in-patient psychiatric care. Clin Child Psychol Psychiatry 2004;9:553-66. http://dx.doi.org/10.1177/1359104504046159.
- Charlemagne S. Family Involvement, Clinician Beliefs and Child Psychiatric Rehospitalization. Loma Linda, CA: School of Science and Technology, Loma Linda University; 2011.
- Czyz E, Liu Z, King C. Social connectedness and one-year trajectories among suicidal adolescents following psychiatric hospitalization. J Clin Child Adolesc Psychol 2012;41:214-26. http://dx.doi.org/10.1080/15374416.2012.651998.
- Larzelere R, Dinges K, Schmidt M, Spellman D, Criste T, Connell P. Outcomes of residential treatment: a study of the adolescent clients of Girls and Boys Town. Child Youth Care Forum 2001;30:175-85. http://dx.doi.org/10.1023/A:1012236824230.
- Moses T. Determinants of mental illness stigma for adolescents discharged from psychiatric hospitalization. Soc Sci Med 2014;109:26-34. http://dx.doi.org/10.1016/j.socscimed.2013.12.032.
- Parmelee D, Cohen R, Nemil M, Best AM, Cassell S, Dyson F. Children and adolescents discharged from public psychiatric hospital: evaluation of outcome in a continuum of care. J Child Fam Stud 1995;4:43-55. http://dx.doi.org/10.1007/BF02233953.
- Cawthorpe D, Somers D, Wilkes T, Phil M. Behavioral contagion reconsidered: self-harm among adolescent psychiatric inpatients: a five-year study. Can Child Adolesc Psychiatry Rev 2003;12:103-6.
- Shabat J, Lyons J, Martinovich Z. Exploring the relationship between conduct disorder and residential treatment outcomes. J Child Fam Stud 2008;17:353-71. http://dx.doi.org/10.1007/s10826-007-9146-1.
- Lakin B, Brambila A, Sigda K. Parental involvement as a factor in the readmission to a residential treatment center. Resident Treat Child Youth 2004;22:37-52. http://dx.doi.org/10.1300/J007v22n02_03.
- Moses T. Stigma apprehension among adolescents discharged from brief psychiatric hospitalization. J Nerv Ment Dis 2011;199:778-89. http://dx.doi.org/10.1097/NMD.0b013e31822fc7be.
- Thurber C, Patterson D, Mount K. Homesickness and children’s adjustment to hospitalization: toward a preliminary model. Child Health Care 2007;36:1-28. http://dx.doi.org/10.1080/02739610701316753.
- Taiminen T, Kallo-Soukainen K, Nokso-Koivisto H, Kaljonen A, Helenius H. Contagion of deliberate self-harm among adolescent inpatients. J Am Acad Child Adolesc Psychiatry 1998;37:211-16. http://dx.doi.org/10.1097/00004583-199802000-00014.
- Street C, Svanberg J. Where Next? New Directions in In-Patient Mental Health Services for Young People. Report 1: Different Models of Provision for Young People: Facts and Figures. London: YoungMinds; 2003.
- Svanberg J, Street C. Where Next? New Directions in In-Patient Mental Health Services for Young People. Report 2: Issues Emerging: Views from Young People, Parents and Staff. London: YoungMinds; 2003.
- Report from Visits to Children and Younger People Who Use Mental Health Services. Edinburgh: Mental Welfare Commission for Scotland; 2009.
- No Health without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages. London: Department of Health; 2011.
- Child Health Support Group: Inpatient Working Group – Psychiatric Inpatient Services for Children and Young People in Scotland: A Way Forward. Edinburgh: Scottish Executive; 2005.
- Psychosis and Schizophrenia in Children and Young People: The NICE Guideline on Recognition and Management. London: The British Psychological Society and The Royal College of Psychiatrists; 2013.
- Solomon J, Thompson P, Collins E. Service Standards. London: QNIC; 2011.
- NHS Standard Contract for Tier 4 Child and Adolescent Mental Health Services (CAMHS): Children’s Services. London: NHS England; 2013.
- National Service Framework for Children, Young People and Maternity Services: The Mental Health and Psychological Well-Being of Children and Young People. London: Department of Health; 2003.
- No Health without Mental Health: Delivering Better Mental Health Outcomes for People of All Ages. London: Department of Health; 2011.
- Tackling Stigma: A Practical Toolkit. London: National CAMHS Support Service; n.d.
- Street C, Herts B. Putting Participation into Practice. London: YoungMinds; 2005.
- Together for Mental Health: A Strategy for Mental Health and Wellbeing in Wales. Cardiff: Welsh Government; 2012.
- Antisocial Behaviour and Conduct Disorders in Children and Young People: Recognition, Intervention and Management. London: NICE; 2013.
- Self-Harm: The NICE Guideline on Longer-Term Management. London: NICE; 2004.
- Specialist NHS Child and Adolescent Mental Health Services: Professional Advice for Service Planners. Cardiff: Welsh Government; 2013.
- Bridging the Gaps: Health Care for Adolescents. London: Royal College of Psychiatrists; 2003.
- Eating Disorders: Core Interventions in the Treatment and Management of Anorexia Nervosa, Bulimia Nervosa and Related Eating Disorders. London: NICE; 2004.
- National Service Framework for Children, Young People and Maternity Services in Wales. Cardiff: Welsh Government; 2005.
- Self-Harm: The Short-Term Physical and Psychological Management and Secondary Prevention of Self-Harm in Primary and Secondary Care. Cardiff: NICE; 2004.
- Acute In-Patient Psychiatric Care for Young People with Severe Mental Illness: Recommendations for Commissioners, Child and Adolescent Psychiatrists and General Psychiatrists. London: Royal College of Psychiatrists; 2002.
- Mental Health (Wales) Measure 2010. Cardiff: Welsh Government; 2010.
- Garrison D. The use of movies to facilitate family engagement in psychiatric hospitalization. J Am Acad Child Adolesc Psychiatry 2007;46:1218-19. http://dx.doi.org/10.1097/CHI.0b013e318095a3c4.
- Jones S. Negotiating time: the significance of timing in ending inpatient work. J Child Psychother 2007;33:325-44. http://dx.doi.org/10.1080/00754170701667205.
- LePage S. Family intervention in first episode psychosis: expanding and integrating the partnership and family consultation models. J Fam Psychother 2005;16:85-104. http://dx.doi.org/10.1300/J085v16n03_07.
- Nejtek V, Hardy S, Winter S. Adolescent mental health: challenges with maternal noncompliance. Neuropsychiatr Dis Treat 2010;6:67-9. http://dx.doi.org/10.2147/NDT.S8649.
- Olson L. Engaging psychiatrically hospitalized teens with their parents through a parent–adolescent activity group. Occup Ther Ment Health 2006;22:121-33. http://dx.doi.org/10.1300/J004v22v03_08.
- Wilkinson S. Developing practice on a ward for adolescents with psychiatric disorders. Clin Child Psychol Psychiatry 2001;6:151-63. http://dx.doi.org/10.1177/1359104501006001012.
- Snell T, Knapp M, Healey A, Guglani S, Evans-Lacko S, Fernandez JL, et al. Economic impact of childhood psychiatric disorder on public sector services in Britain: estimates from national survey data. J Child Psychol Psychiatry 2013;54:977-85. http://dx.doi.org/10.1111/jcpp.12055.
- Knapp M, Snell T, Healey A, Guglani S, Evans-Lacko S, Fernandez J-L, et al. How do child and adolescent mental health problems influence public sector costs? Inter-individual variations in a nationally representative British sample [published online ahead of print date on 29 September 2014]. J Child Psychol Psychiatry n.d. http://dx.doi.org/10.1111/jcpp.12327.
- Green J, Jacobs B, Beecham J, Dunn G, Kroll L, Tobias C, et al. Inpatient treatment in child and adolescent psychiatry: a prospective study of health gain and costs. J Child Psychol Psychiatry 2007;48:1259-67. http://dx.doi.org/10.1111/j.1469-7610.2007.01802.x.
- Annual Report of the Chief Medical Officer 2012. Our Children Deserve Better: Prevention Pays. London: Department of Health; 2013.
- Building and Sustaining Specialist CAMHS to Improve Outcomes for Children and Young People: Update of Guidance on Workforce, Capacity and Functions of CAMHS in the UK. London: Royal College of Psychiatrists; 2013.
- McDougall T, Worrall-Davies A, Hewson L. Tier 4 child and adolescent mental health services (CAMHS): inpatient care, day services and alternatives – an overview of Tier 4 CAMHS provision in the UK. Child Adolesc Ment Health 2008;13:173-80. http://dx.doi.org/10.1111/j.1475-3588.2007.00481.x.
- King C, Kramer A, Preuss L, Kerr D, Weisse L, Venkataraman S. Youth-nominated support team for suicidal adolescents (version 1): a randomized controlled trial. J Consult Clin Psychol 2006;74:199-206. http://dx.doi.org/10.1037/0022-006X.74.1.199.
- Makikyro T, Hakko H, Timonen M, Ilomaki E, Lappalinen J, Martunen M, et al. Smoking and suicidality among adolescent psychiatric patients. J Adolesc Health 2004;34:250-3. http://dx.doi.org/10.1016/S1054-139X(03)00284-2.
- Prinstein M, Nock M, Simon V, Aikins J, Cheah C, Spirito A. Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. J Consult Clin Psychol 2008;76:92-103. http://dx.doi.org/10.1037/0022-006X.76.1.92.
- Kjelsberg E. Adolescence-limited versus life-course-persistent criminal behaviour in adolescent psychiatric inpatients. Eur Child Adolesc Psychiatry 1999;8:276-82. http://dx.doi.org/10.1007/s007870050102.
- Abeles P, Holmes E, Wadge M. CAMHS dependency scoring: clarity and clinical relevance of the CAMHS-AID. Paediatr Nurs 2008;20:30-2. http://dx.doi.org/10.7748/paed2008.03.20.2.30.c6527.
- Adrian M, Zeman J, Erdley C, Lisa L, Homan K, Sim L. Social contextual links to emotion regulation in an adolescent psychiatric inpatient population: do gender and symptomatology matter?. J Child Psychol Psychiatry 2009;50:1428-36. http://dx.doi.org/10.1111/j.1469-7610.2009.02162.x.
- Adrian M, Zeman J, Erdley C, Lisa L, Sim L. Emotional dysregulation and interpersonal difficulties as risk factors for nonsuicidal self-injury in adolescent girls. J Abnorm Child Psychol 2011;39:389-400. http://dx.doi.org/10.1007/s10802-010-9465-3.
- Allen D. Adult wards are no place for children. Ment Health Pract 2009;12:6-7.
- Allen J, Hauser S, Bornman-Spurell E. Attachment theory as a framework for understanding sequelae of severe adolescent psychopathology: an 11-year follow-up study. J Consult Clin Psychol 1996;64:254-63. http://dx.doi.org/10.1037/0022-006X.64.2.254.
- Anderson R, Huff N, Hodgson J. Medical family therapy in an inpatient psychiatric setting: a qualitative study. J Collaborat Fam Healthc 2008;26:164-80. http://dx.doi.org/10.1037/1091-7527.26.2.164.
- Anderson D, Davis L, Keehn K, Palazzolo L. Classifying psychiatric inpatient pediatric populations. Nurs Manage 2012;43:42-8. http://dx.doi.org/10.1097/01.NUMA.0000421674.95475.4e.
- Ayton A, Meads G. The implementation of the Care Programme Approach in the West Midlands CAMHS: the impact of organisational diversity on patient safety – an extended audit. Int J Clin Leadersh 2012;17:185-200.
- Bean P, White L, Neagle L, Lake P. Is residential care an effective approach for treating adolescents with co-occurring substance abuse and mental health diagnoses?. Best Pract Ment Health 2005;1:50-6.
- Bechberger A. The Role of School Psychologists in Partial Hospitalization Program-to-School Transitions 2012.
- Bettmann JE, Jasperson R. Adolescents in residential and inpatient treatment: a review of the outcome literature. Child Youth Care Forum 2009;38:161-83. http://dx.doi.org/10.1007/s10566-009-9073-y.
- Bickerton A, Hense T, Benstock A, Ward J, Wallace L. Safety first: a model of care for working systemically with high risk young people and their families in an acute CAMHS service. Aust N Z J Fam Ther 2007;28:121-9. http://dx.doi.org/10.1375/anft.28.3.121.
- Cahalane H. Relationship Between Family Satisfaction and Outcome for Children and Adolescents in Inpatient Psychiatric Treatment 1997.
- Carek D, Hand L. Current child and adolescent inpatient psychiatric treatment: evolution or regression?. J S C Med Assoc 1995;91:5-8.
- Chesson R, Harding L, Hart C, O’Loughlin V. Do parents and children have common perceptions of admission, treatment and outcome in a child psychiatric unit?. Clin Child Psychol Psychiatry 1997;2:251-70. http://dx.doi.org/10.1177/1359104597022006.
- Chung W, Edgar-Smith S, Palmer R, Bartholomew E, Delambo D. Psychiatric rehospitalization of children and adolescents: implications for social work intervention. Child Adolesc Soc Work J 2008;25:483-96. http://dx.doi.org/10.1007/s10560-008-0147-8.
- Clarke D, Winsor J. Perceptions and needs of parents during a young adult’s first psychiatric hospitalization: we’re all on this little island and we’re going to drown real soon. Issues Ment Health Nurs 2010;31:242-7. http://dx.doi.org/10.3109/01612840903383992.
- Cook-Darzens S, Doyen C, Mouren-Simeoni M-C. A ‘joint family consultation’ approach to the initial treatment of early onset anorexia nervosa in a French pediatric hospital. J Fam Psychother 2001;12:55-76. http://dx.doi.org/10.1300/J085v12n03_04.
- Curran G, Walter G, Soh N, Herman M, Baker M, Paton M, et al. Staff experience, knowledge and attitudes regarding the management of adolescent patients in adult mental health units. Australas Psychiatry 2011;19:420-5. http://dx.doi.org/10.3109/10398562.2011.602079.
- Daniel S, Goldston D, Harris A, Kelley A, Palmes G. Review of literature on aftercare services among children and adolescents. Psychiatr Serv 2004;55:901-12. http://dx.doi.org/10.1176/appi.ps.55.8.901.
- Delaney K, Engels-Scianna B. Parents’ perceptions of their child’s emotional illness and psychiatric treatment needs. J Child Adolesc Psychiatr Nurs 1996;9:15-26. http://dx.doi.org/10.1111/j.1744-6171.1996.tb00269.x.
- den Dunnen W, St Pierre J, Stewart S, Johnson A, Cook S, Leschied A. Predicting residential treatment outcomes for emotionally and behaviorally disordered youth: the role of pretreatment factors. Resident Treat Child Youth 2012;29:13-31. http://dx.doi.org/10.1080/0886571X.2012.642268.
- Dicker R, Morrissey R, Abikoff H, . Hospitalizing the suicidal adolescent: decision-making criteria of psychiatric residents. J Am Acad Child Adolesc Psychiatry 1997;36:769-76. http://dx.doi.org/10.1097/00004583-199706000-00013.
- Drell M. ‘Sweet are the uses of adversity’: a transition program for children discharged from an inpatient unit. Psychiatr Services 2006;57:31-3. http://dx.doi.org/10.1176/appi.ps.57.1.31.
- Duffy F, Skeldon J. Innovations in practice: the impact of the development of a CAMH Intensive Treatment Service and service redesign on psychiatric admissions. Child Adolesc Ment Health 2013;18:120-3. http://dx.doi.org/10.1111/j.1475-3588.2012.00659.x.
- Duthie P. In-patient adolescent services. Psychiatr Bull 2001;25. http://dx.doi.org/10.1192/pb.25.9.360.
- Fishman MJ, Lewis L. Psychiatric medication compliance following adolescent inpatient addiction treatment. J Addict Dis 1998;17.
- Fontanella C. Psychiatric Readmission of Adolescents in the Public Mental Health System. College Park, MD: University of Maryland; 2003.
- Foster E. Does the continuum of care improve the timing of follow-up services?. J Am Acad Child Adolesc Psychiatry 1998;37:805-14. http://dx.doi.org/10.1097/00004583-199808000-00010.
- Foster EM. Do aftercare services reduce inpatient psychiatric readmissions?. Health Serv Res 1999;34:715-36.
- Galasso J. From Resilience to Recovery: Protective and Risk Factors that Influence Recovery for People Treated as Inpatients During Adolescence. San Diego, CA: Alliant International University; 2008.
- Garrison D, Daigler G. Treatment settings for adolescent psychiatric conditions. Adolesc Med Clin 2006;17:233-50.
- Geraghty K, McCann K, King R. Sharing the load: parents and carers talk to consumer consultants at a child and youth mental health inpatient unit. Int J Ment Health Nurs 2011;20:253-62. http://dx.doi.org/10.1111/j.1447-0349.2011.00730.x.
- Ghaziuddin N, King C, Hovey J, Zaccagnini J, Ghaziuddin M. Medication noncompliance in adolescents with psychiatric disorders. Child Psychiatry Hum Dev 1999;30:103-10. http://dx.doi.org/10.1023/A:1021950301932.
- Gorske T, Srebalus D, Walls R. Adolescents in residential centers: characteristics and treatment outcome. Child Youth Serv Rev 2003;25:317-26. http://dx.doi.org/10.1016/S0190-7409(03)00014-8.
- Gowers S, Rowlands L. Inpatient services. Curr Opin Psychiatry 2005;18:445-8. http://dx.doi.org/10.1097/01.yco.0000172066.24391.be.
- Gowers S, Clarke J, Alldis M, Wormald P, Wood N. In-patient admission of adolescents with mental disorder. Clin Child Psychol Psychiatry 2001;6:537-44. http://dx.doi.org/10.1177/1359104501006004007.
- Green J, Kroll L, Imrie D, Frances FM, Begum K, Harrison L, et al. Health gain and outcome predictors during inpatient and related day treatment in child and adolescent psychiatry. J Am Acad Child Adolesc Psychiatry 2001;40:325-32. http://dx.doi.org/10.1097/00004583-200103000-00012.
- Gross V, Goldin J. Dynamics and dilemmas in working with families in inpatient CAMH services. Clin Child Psychol Psychiatry 2008;13:449-61. http://dx.doi.org/10.1177/1359104507088350.
- Gullick K, McDermott B, Gibbon P, Stone P. Seclusion of children and adolescents: psychopathological and family factors. Int J Ment Health Nurs 2005;14:37-43. http://dx.doi.org/10.1111/j.1440-0979.2005.00353.x.
- Gunter M, Karle M, Kleefeld H, Werning A, Klosinski G. Psychiatric–psychotherapeutic crisis intervention for inpatient adolescents. J Crisis Interv Suicide 1999;20:71-7. http://dx.doi.org/10.1027//0227-5910.20.2.71.
- Harpaz-Rotem I, Blatt SJ. Changes in representations of a self-designated significant other in long-term intensive inpatient treatment of seriously disturbed adolescents and young adults. Psychiatry 2005;68:266-82. http://dx.doi.org/10.1521/psyc.2005.68.3.266.
- Hawkridge S. What if this were your child?. S Afr J Psychiatry 2002;8:4-6.
- Heinberg L, Haug N, Freeman L, Ambrose D, Guarda A. Clinical course and short-term outcome of hospitalized adolescents with eating disorders: the success of combining adolescents and adults on an eating disorders unit. Eat Weight Disord 2003;8:326-31. http://dx.doi.org/10.1007/BF03325035.
- Hodges K, Doucette-Gates A, Liao Q. The relationship between the Child and Adolescent Functional Assessment Scale (CAFAS) and indicators of functioning. J Child Fam Stud 1999;8:109-22. http://dx.doi.org/10.1023/A:1022902812761.
- Hofstra M, Flos M, Van Sloten N, Wielemaker J, Verheij F, Verhulst F. The Clinical Course of Inpatient Treated Children in a Child Psychiatric Unit in the Netherlands n.d.
- Jacobson C, Leaf-Farrell C, Meyer T. A Comparison of Children and Adolescents Funded by Medicaid and Commercial Insurance in an Inpatient Psychiatric Facility n.d.
- Johnson B. The service use of African-American and white adolescent girls prior to psychiatric hospitalization and attitudes of their social network. Psychopharmacol Bull 1996;32.
- Joiner T, Jr, Katz J, Lew A. Self-verification and depression among youth psychiatric inpatients. J Abnorm Psychol 1997;106:608-18. http://dx.doi.org/10.1037/0021-843X.106.4.608.
- Joiner T. Defensiveness predicts peer rejection of depressed children. Behav Res Ther 2001;39:929-38. http://dx.doi.org/10.1016/S0005-7967(00)00066-8.
- Jonikas J, Laris A, Cook J. The passage to adulthood: psychiatric rehabilitation service and transition-related needs of young adult women with emotional and psychiatric disorders. Psychiatr Rehabil J 2003;27:114-21. http://dx.doi.org/10.2975/27.2003.114.121.
- Kaplan T, Racussen L. A crisis recovery model for adolescents with severe mental health problems. Clin Child Psychol Psychiatry 2013;18:246-59. http://dx.doi.org/10.1177/1359104512449320.
- Kashani J, Jones M, Borduin C, Thomas L, Reid J. Individual characteristics and peer relations of psychiatrically hospitalized aggressive youths: implications for treatment. Child Psychiatry Hum Dev 2000;30:145-59. http://dx.doi.org/10.1023/A:1021327120547.
- Kavanaugh B, Holler K. Executive functioning in psychiatrically hospitalized adolescents with mood disorders. Clin Neuropsychol 2012;26:460-1.
- Kennedy R. Adolescence in psychiatric hospitals: a psychodynamic approach to evaluation and treatment. Br J Psychiatry 1999;175.
- Kerr D, Preuss L, King C. Suicidal adolescents’ social support from family and peers: gender-specific associations with psychopathology. J Abnorm Child Psychol 2006;34:103-14. http://dx.doi.org/10.1007/s10802-005-9005-8.
- King CA, Hovey JD, Brand E, Wilson R, Ghaziuddin N. Suicidal adolescents after hospitalization: parent and family impacts on treatment follow-through. J Am Acad Child Adolesc Psychiatry 1997;36:85-93. http://dx.doi.org/10.1097/00004583-199701000-00021.
- King CA, Hovey JD, Brand E, Ghaziuddin N. Prediction of positive outcomes for adolescent psychiatric inpatients. J Am Acad Child Adolesc Psychiatry 1997;36:1434-42. http://dx.doi.org/10.1097/00004583-199710000-00026.
- Kiser L, Millsap P, Hickerson S, Heston JD, Nunn W, Pruitt DB, et al. Results of treatment one year later: child and adolescent partial hospitalization. J Am Acad Child Adolesc Psychiatry 1996;35:81-90. http://dx.doi.org/10.1097/00004583-199601000-00016.
- Kjelsberg E. Delinquency, disability, and mortality in earlier adolescent psychiatric inpatients. Nord J Psychiatry 1998;52.
- Kolakoski R. A Group Therapy Manual Using Commercial Film Vignettes to Address the Stigmatization of Mental Illness With Inpatient Adolescent Boys 2000.
- Lamb C, Hall D, Kelvin R, Van Beinum M. Working at the CAMHS/Adult Services Interface: Good Practice Guidelines for the Provision of Psychiatric Services to Adolescents/Young Adults. London: Royal College of Psychiatrists; 2008.
- Lambe J. Admission of adolescents to psychiatric units. Australas Psychiatry 2012;20:164-5. http://dx.doi.org/10.1177/1039856212437260.
- Landers G, Zhou M. An analysis of relationships among peer support, psychiatric hospitalization, and crisis stabilization. Commun Ment Health J 2011;47:106-12. http://dx.doi.org/10.1007/s10597-009-9218-3.
- Laws S. Consulting children and young people on what they want from mental health services. Ment Health Care 1998;2:63-6.
- Leal C. Stigmatization of Hispanic children, pre-adolescents, and adolescents with mental illness: exploration using a national database. Issues Ment Health Nurs 2005;26:1025-41. http://dx.doi.org/10.1080/01612840500280695.
- Leavey J, Davidson J. Building best practice mental health care for youth aged 0–16 experiencing first episode/break symptoms and emerging mental health problems: developing a clinical research program at children’s hospital, Vancouver, BC, Canada. Acta Psychiatr Scand 2006;114.
- Lee B. Testing Peer Contagion in Youth Mental Health Services 2007.
- Leon S, Lyons J, Uziel-Miller N, Rawal P, Tracy P, Williams J. Evaluating the use of psychiatric hospitalization by residential treatment centers. J Am Acad Child Adolesc Psychiatry 2000;39:1496-501. http://dx.doi.org/10.1097/00004583-200012000-00009.
- Lepper J. Recovery in the right place. Child Young People Now 2007;11:24-5.
- Lewis S. Children. Consulting children and young people on what they want from mental health services. Ment Health Care 1998;2:63-6.
- Lintsi M, Liivamagi J, Aluoja A, Kaarma H. Some biological factors in school age boys treated in psychiatric hospital in Tartu. Nord J Psychiatry 1998;52.
- Lopez N. Adolescent Experiences of Psychiatric Hospitalization 2000.
- Lundberg B, Hansson L, Wentz E, Bjorkman T. Sociodemographic and clinical factors related to devaluation/discrimination and rejection experiences among users of mental health services. Soc Psychiatry Psychiatr Epidemiol 2007;42:295-300. http://dx.doi.org/10.1007/s00127-007-0160-9.
- Mackrell L, Lavender T. Peer relationships in adolescents experiencing a first episode of psychosis. J Ment Health 2004;13:467-79. http://dx.doi.org/10.1080/09638230400006775.
- Mattejat F, Hirt B, Wilken J, Schmidt M, Remschmidt H. Efficacy of inpatient and home treatment in psychiatrically disturbed children and adolescents: follow-up assessment of the results of a controlled treatment study. Eur Child Adolesc Psychiatry 2001;10:I71-9. http://dx.doi.org/10.1007/s007870170008.
- McDougall T, Scott S. Too much too young? Under 18s on adult mental health wards. Ment Health Pract 2008;11:12-5. http://dx.doi.org/10.7748/mhp2008.03.11.6.12.c6485.
- McDougall T, O’Herlihy A, Pugh K, Parker C. Young people on adult mental health wards. Ment Health Pract 2009;12:16-21. http://dx.doi.org/10.7748/mhp2009.05.12.8.16.c7002.
- McNamara D. Mental health legislation in child and adolescent psychiatry in England and Wales. Ir J Psychol Med 2002;19:66-9.
- Mears A, Worrall A. A survey of psychiatrists’ views of the use of the Children Act and the Mental Health Act in children and adolescents with mental health problems. Psychiatr Bull 2001;25:304-6. http://dx.doi.org/10.1192/pb.25.8.304.
- Good Practice Guide: Young People in Adult Mental Health Wards. Edinburgh: Mental Welfare Commission for Scotland; 2006.
- Miller T, Robbins J, Thompson J, Aitken M, Kramer T. Patterns of psychiatric comorbidity in hospitalized youth. Pediatr Res 2004;55.
- Moses T. Being treated differently: stigma experiences with family, peers, and school staff among adolescents with mental health disorders. Soc Sci Med 2010;70:985-93. http://dx.doi.org/10.1016/j.socscimed.2009.12.022.
- Myers K, Storck M, George R, Lindsay K. Maintaining the youth’s system of care during prolonged psychiatric hospitalization. Telemed E-Health 2008;14.
- Niedermeier C, Searight H, Handal P, Manley C. Perceived family functioning among adolescent psychiatric inpatients: validity of the Family-of-Origin Scale. Child Psychiatry Hum Dev 1995;25:253-65. http://dx.doi.org/10.1007/BF02250993.
- O’Brien P. Reflections of a facilitator for a parent support group in an adolescent in-patient psychiatric program. Fam Ther 2002;29:141-51.
- O’Herlihy A, Worrall A, Lelliott P, Jaffa T, Hill P, Banerjee S. Distribution and characteristics of in-patient child and adolescent mental health services in England and Wales. Br J Psychiatry 2003;183:547-51. http://dx.doi.org/10.1192/bjp.183.6.547.
- Oleniuk A, Duncan C, Tempier R. The impact of stigma of mental illness in a Canadian community: a survey of patients experiences. Commun Ment Health J 2013;49:127-32. http://dx.doi.org/10.1007/s10597-011-9453-2.
- Ornstein R, Lane-Loney S, Hollenbeak C. Clinical outcomes of a novel, family-centered partial hospitalization program for young patients with eating disorders. Eat Weight Disord 2012;17:e170-7. http://dx.doi.org/10.1007/BF03325344.
- Park C, McDermott B, Loy J, Dean P. Adolescent admissions to adult psychiatric units: patterns and implications for service provision. Australas Psychiatry 2011;19:345-9. http://dx.doi.org/10.3109/10398562.2011.601311.
- Parry-Jones W. Treating children and adolescents in residential and inpatient settings. Br J Psychiatry 1997;171.
- Petit-Zeman S. Finding the right words. Nurs Times 2001;97.
- Phillips C. Comparison of Teachers’ Ratings and Therapists’ Ratings Completed on Adolescents in a Psychiatric Hospital Using the Revised Behavior Problem Checklist 1996.
- Pridgen B. Navigating the internet safely: recommendations for residential programs targeting at-risk adolescents. Harv Rev Psychiatry 2010;18:131-8. http://dx.doi.org/10.3109/10673221003684000.
- Prinstein M, Boergers J, Spirito A, Little T, Grapentine W. Peer functioning, family dysfunction, and psychological symptoms in a risk factor model for adolescent inpatients’ suicidal ideation severity. J Clin Child Psychol 2000;29:392-405. http://dx.doi.org/10.1207/S15374424JCCP2903_10.
- Prinstein M, Heilbron N, Guerry J, Franklin JC, Rancourt D, Simon V, et al. Peer influence and nonsuicidal self injury: longitudinal results in community and clinically-referred adolescent samples. J Abnorm Child Psychol 2010;38:669-82. http://dx.doi.org/10.1007/s10802-010-9423-0.
- Puasiri S, Sitthimongkol Y, Tilokskulchai F, Sangon S, Nityasuddhi D. Adaptation of Thai families with mentally ill young people. Pacific Rim Int J Nurs Res 2011;15:137-50.
- Pugh K. Getting ready for change. Ment Health Today 2008:29-31.
- Puotiniemi T, Kyngas H, Nikkonen M. The resources of parents with a child in psychiatric inpatient care. J Psychiatr Ment Health Nurs 2002;9:15-22. http://dx.doi.org/10.1046/j.1365-2850.2002.00397.x.
- Reilly J. Admission to adolescent units: patients’ and parents’ views. Nurs Times 2006;102:33-4.
- Rutkowski B. The Effects of Emotional Autonomy and Family Support on an Individual’s Self-Reported Motivation to Change in an Adolescent Inpatient Unit. Ann Arbor, MI: Roosevelt University; 2011.
- Sawyer M, Kosky R. Approaches to delivering child and adolescent mental health services: the South Australian experience. Aust N Z J Psychiatry 1995;29:230-7. http://dx.doi.org/10.1080/00048679509075915.
- Schnell G. Monitoring the progress of young people’s occupational performance in an inpatient mental health setting. N Z J Occup Ther 2008;55:4-10.
- Scott D, McGilloway S, Donnelly M. Young people’s experience of adult in-patient psychiatric care: a Northern Ireland case study. Ment Health Learn Disabil Care 2001;4:305-8.
- Sheftall A, Mathias C, Furr R, Dougherty D. Adolescent attachment security, family functioning, and suicide attempts. Attach Hum Dev 2013;15:368-83. http://dx.doi.org/10.1080/14616734.2013.782649.
- Shulman S, Horesh N, Scharf M, Argov Y. Close relationships and social competence of hospitalized and nonhospitalized adolescents. J Nerv Ment Dis 2000;188:688-94. http://dx.doi.org/10.1097/00005053-200010000-00007.
- Simon J, Savina E. Facilitating hospital to school transitions: practices of hospital-based therapists. Resident Treat Child Youth 2005;22:49-66. http://dx.doi.org/10.1300/J007v22n04_04.
- Simon J, Savina E. Transitioning children from psychiatric hospitals to schools: the role of the special educator. Resident Treat Child Youth 2010;27:41-54. http://dx.doi.org/10.1080/08865710903508084.
- Slowik M, Willson S, Loh E-C, Noronha S. Service innovations: developing a parent/carer support group in an in-patient adolescent setting. Psychiatr Bull 2004;28:177-9. http://dx.doi.org/10.1192/pb.28.5.177.
- Smith H. Age-appropriate care environments for children and young people. Ment Health Pract 2010;14. http://dx.doi.org/10.7748/mhp2010.10.14.2.35.c8012.
- Sourander A, Piha J. A short-term, family-oriented, child and adolescent psychiatric inpatient treatment program. Fam Process 1996;35:103-11. http://dx.doi.org/10.1111/j.1545-5300.1996.00103.x.
- Stage S. Predicting adolescents’ discharge status following residential treatment. Resident Treat Child Youth 1999;16:37-56. http://dx.doi.org/10.1300/J007v16n03_03.
- Steel J, Ofield A. Empowering children in a hospital school. Young Mind Mag n.d.;35:14-5.
- Street C, Svanberg J. Listening to young people. Ment Health Today n.d.:28-30.
- Street C. In-patient mental health services for young people: changing to meet new needs?. J R Soc Promot Health 2004;124:115-18. http://dx.doi.org/10.1177/146642400412400311.
- Sutherland M, Harkness S. At home in an institution: daily life on a pediatric inpatient psychiatric unit as viewed through the developmental niche framework. Occup Particip Health 2007;27:93S-95S. http://dx.doi.org/10.1177/15394492070270S119.
- Tan E, Hannah D, Chant D, Martin G. Gundhu adolescent wing: providing adolescent beds in a rural acute mental health unit. Australas Psychiatry 2004;12:396-400. http://dx.doi.org/10.1080/j.1440-1665.2004.02134.x.
- Thompson S. Age suitable environments: the new duty of care. Every Child J 2010;1:56-60.
- Tonin V. Young people seeking mental-health care. Lancet 2007;369:1239-40. http://dx.doi.org/10.1016/S0140-6736(07)60375-4.
- van Bokhoven I, Matthys W, van Goozen S, van Engeland H. Adolescent outcome of disruptive behaviour disorder in children who had been treated in in-patient and day-treatment settings. Eur Child Adolesc Psychiatry 2006;15:79-87. http://dx.doi.org/10.1007/s00787-006-0490-2.
- Walter U, Petr C. Promoting successful transitions from day school to regular school environments for youths with serious emotional disorders. Child Sch 2004;26:175-80. http://dx.doi.org/10.1093/cs/26.3.175.
- Welsh J. In whose ‘best interests’? Ethical issues involved in the moral dilemmas surrounding the removal of sexually abused adolescents from a community-based residential treatment unit to a locked, forensic adult psychiatric unit. J Adv Nurs 1998;27:45-51. http://dx.doi.org/10.1046/j.1365-2648.1998.00502.x.
- Wood R, Wood A, Mullins D. Back to school: recommendations to assist mentally ill, post-incarcerated youth return to school. J Sch Health 2008;78:514-17. http://dx.doi.org/10.1111/j.1746-1561.2008.00337.x.
- Worrall A, O’Herlihy A, Banerjee S, Jaffa T, Lelliott P, Hill P, et al. Inappropriate admission of young people with mental disorder to adult psychiatric wards and paediatric wards: cross sectional study of six months’ activity. BMJ 2004;328. http://dx.doi.org/10.1136/bmj.38058.605787.AE.
- Yonge O. Power of irony in an adolescent residential psychiatric program. J Psychosoc Nurs Ment Health Serv 2007;45:46-52.
- Out of the Shadows?. London: YoungMinds; 2008.
- Zaitsoff S, Fehon D, Grilo C. Social competence and social-emotional isolation and eating disorder psychopathology in female and male adolescent psychiatric inpatients. Int J Clin Health Psychol 2009;9:219-28.
- Zilikis N, Abatzoglou G, Iacovides A, Ierodiakonou C. Adolescent admissions in psychiatry: reconsidering clinical and institutional parameters on the occasion of a report of a Greek experience. Adolesc Psychiatry 2011;1:340-8.
- Code of Practice to Parts 2 and 3 of the Mental Health (Wales) Measure 2010. Cardiff: Welsh Government; 2012.
Appendix 1 Phase 1 search strategy and results using MEDLINE (via Ovid)
URL: www.ncbi.nlm.nih.gov/pubmed
Date range searched: 1995 to September 2013.
Date search: 12 September 2013.
Records retrieved: 3933.
-
exp Adolescen/ (1,505,077)
-
exp Young Adult/ (260,419)
-
young person.mp (523)
-
young people.mp (13,422)
-
young adult.mp (273,560)
-
teen*.mp (18,861)
-
juvenil*.mp (60,114)
-
adolescen*.mp (1,525,896)
-
AYA.mp (110)
-
young patient.mp (364)
-
young wom#n.mp (18,910)
-
young m#n.mp (12,987)
-
youngster.mp (158)
-
youth.mp (32,711)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 (247,271)
-
exp Mental Health/ (19,337)
-
mental health services/ (69,938)
-
exp mental disorders/ (878,770)
-
mental* ill*.mp (26,830)
-
mental health.mp (98,794)
-
CAMHS.mp (305)
-
psychiatr*.mp (214,304)
-
16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 (603,230)
-
exp Risk/ (747,208)
-
exp Risk Assessment (157,275)
-
exp Risk Management (184,033)
-
risk*mp (216,990)
-
24 or 25 or 26 or 27 (1,372,225)
-
exp inpatients/ (11,000)
-
in-patient*.mp (973,174)
-
in-patient* (59,908)
-
exp Hospitals. Psychiatric/ (21,716)
-
exp Patient Admission/ (17,161)
-
exp Patient Discharge/ (17,105)
-
29 or 30 or 31 or 32 or 33 or 34 (1,068,105)
-
15 and 23 and 28 and 34 (3606)
Appendix 2 Phase 1 search strategy and results using PsycINFO (via Ovid)
URL: www.ovid.com/site/catalog/databases/139.jsp
Date range searched: 1995 to September 2013.
Date of search: 12 September 2013.
Records retrieved: 1875.
-
Adolescen*.mp (179,468)
-
young people.mp (15,519)
-
young adult.mp (7971)
-
young person.mp (735)
-
teen*.mp (15,245)
-
juvenil*.mp (27,387)
-
AYA.mp (50)
-
young patient.mp (217)
-
young wom#n.mp (5868)
-
young m#n.mp (4462)
-
youngster.mp (297)
-
youth.mp (51,581)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 (247,271)
-
exp Mental Health/ (35,835)
-
mental health services/ (30,246)
-
exp mental disorders/ (403,143)
-
mental* illness (38,046)
-
mental health (129,429)
-
CAMHS.mp (305)
-
psychiatr*.mp (214,304)
-
14 or 15 or 16 or 17 or 18 or 19 or 20 (603,230)
-
exp risk assessment (7970)
-
exp risk management (3085)
-
risk*mp (216,990)
-
22 or 23 or 24 or 25 (216,990)
-
exp hospitalize patients/ (9988)
-
inpatient*.mp (36,905)
-
in-patient*.mp (65,851)
-
admission*.mp (27,054)
-
admit*.mp (22,754)
-
discharge*.mp (25,454)
-
26 or 27 or 28 or 29 or 30 or 31 (154,419)
-
13 and 21 and 25 and 32 (933)
Appendix 3 Phase 1 screening tool
Appendix 4 Included papers in phase 1 scoping exercise
| Author(s) and date Country Aim |
Sample size Age (years) |
Recruitment Time of assessment |
Methods | Analyses |
|---|---|---|---|---|
| Risk of harm to self: suicide (n = 53) | ||||
| Osman et al. (2010)30 USA To examine the psychometric properties of the Body Investment Scale |
Study 1: n = 197 (hospital)/n = 204 (school); 14–17 years/mean 15.4 ± 1.0 (hospital), 14–17 years/mean 15.6 ± 1.4 (school) | Study 1: recruited from a state psychiatric hospital and a public high school Time of assessment not given |
Scale development | Study 1: factor analysis, Body Investment Scale |
| Study 2: n = 205; 14–17 years, mean 15.5 ± 1.0 (males_, mean 15.4 ± 1.0 (females) | Study 2: recruited from two inpatient units Time of assessment not given |
Study 2: factor analysis, subgroup analysis; suicide attempter group, suicide threat/plan group, psychiatric control group | ||
| Adams et al. (1994)31 USA To examine how adolescent suicidal behaviour is related to adolescents’ perceptions of family functioning and parent–adolescent relationships |
n = 64 (inpatients), n = 70 (community high school students); 13–18 years/mean 15.4 ± 1.3 | Mixed sample, consecutive inpatient admissions, high school students recruited from local school Within first 5 days |
Cross-sectional survey | Subgroup analyses: n = 37 (student non-suicidal control), n = 29 (inpatient non-suicidal controls), n = 33 (student suicide ideators), n = 35 (inpatient suicide attempters) |
| Apter et al. (1997)32 Israel To identify defence mechanisms that characterise adolescents with a range of suicidal behaviours and to differentiate them from non-suicidal adolescents |
n = 223 12–19 years/mean 16 + 2.6 (admit suicide), 12–19 years/mean 16 + 3.0 (admit other), 13–18 years/mean 15.5 ± 2.3 (school) |
Mixed sample, consecutive admissions over 12 months, high school population in same catchment area Within 10 days |
Cross-sectional survey | Subgroup analyses: n = 55 (admitted suicide), n = 81 (admitted reasons other than suicide), n = 81 (high school population) |
| Apter et al. (1995)33 Israel To determine the relative importance of aggression and depression in adolescent suicide within different diagnostic categories |
n = 176: schizophrenia n = 49, conduct disorder n = 45, major depressive disorder n = 24, anxiety disorder n = 22, anorexia nervosa n = 16 12–18 years/mean 14.1 |
Consecutive admissions Within 10 days |
Cross-sectional survey | Subgroup analyses: suicide/violent behaviour, fire setting/gang activities, bullying/persistent physical fighting/runaway overnight, vandalism/cruelty to animals, delinquency/homicidal acts |
| Brent et al. (1988)34 USA To determine, among a clinical population already at high risk of suicide, which patients are at highest risk |
Suicide completers n = 27/35; parents of adolescents ≤ 19 years Suicidal inpatients n = 38; 13–19 years |
Suicide completers: consecutive series of adolescent suicide victims December 1984 to June 1986; interview with parents 6–12 weeks after death Suicidal inpatients: from inpatient facility; within first 6 weeks |
Prospective, case–control study | Predictors of high suicide risk, logistic regression |
| Brent et al. (1993)35 USA To identify risk factors for suicidal behaviour at follow-up |
n = 134 13–18 years |
Hospitalised and assessed between July 1986 and August 1988 and followed up December 1986 and January 1989 Within 2 weeks and followed up 6 months later |
Prospective, longitudinal cohort study | Subgroup analysis: n = 48 (suicide attempters), n = 33 (suicidal ideators), n = 53 (no suicidality); predictors of suicidality at follow-up; logistic regression and survival analyses |
| Brinkman-Sull et al. (2000)36 USA To examine the ability of several individual and family variables to predict suicidal behaviour in former adolescent psychiatric inpatients and to investigate whether or not positive changes over time in family functioning could protect an adolescent from a future suicide attempt |
n = 60/102 12–18 years/mean 15.46 ± 1.20 |
Recruited from a previous project group, n = 102,67 for this follow-up study Length of follow-up 11–22 months |
Prospective, longitudinal cohort study | Predictors of suicide attempts |
| Brunstein-Klomek et al. (2005)37 Israel To examine the positive and negative self-complexity of suicidal adolescents |
n = 96 13–20 years/mean 16.4 ± 1.5 |
Recruited from inpatient units and a community sample of volunteers Not specified |
Cross-sectional survey | Subgroup analyses: n = 32 (suicidal group), n = 32 (non-suicidal – psychiatric group), n = 32 (control group community sample) |
| Cohen et al. (1996)38 USA To examine the associations between sexual and physical abuse and psychiatric symptomatology in adolescents who are psychiatrically hospitalised |
n = 105 12–18 years/mean 14.7 ± 1.6 |
Consecutive admissions First few days of admission |
Cross-sectional survey | Subgroup analyses: n = 35 (no abuse), n = 17 (sexual abuse), n = 20 (physical abuse), n = 31 (sexual and physical abuse) |
| Danielson et al. (2003)39 USA To determine whether or not depression levels differ among suicide-attempting and non-suicide-attempting adolescent inpatients in relation to their alcohol use |
n = 98 13–18 years/mean 15.4 ± 1.3 |
All admissions over a 2-year period Retrospective chart review |
Cross-sectional survey | Subgroup analyses: n = 76 (suicide attempters), n = 21 (non-attempters); correlational analyses: suicide-attempting status and drinking status |
| D’Eramo et al. (2004)40 USA To examine the relations between suicidal behaviour history and psychiatric functioning |
n = 104 12–17 years/mean 14.6 |
Consecutive admissions Retrospective chart review |
Cross-sectional survey | Subgroup analyses: n = 27 (non-suicidal), n = 30 (ideation only), n = 19 (suicide attempters), n = 28 (multiple attempters) |
| Di Filippo and Overholser (2000)41 USA To examine suicidal ideation in adolescent psychiatric inpatients as associated with depressive symptoms and attachments in mothers, fathers and peers |
n = 59 (response rate 76%) 13–17 years/mean 15.6 ± 1.2 |
Consecutive admissions Within first 5 days |
Cross-sectional survey | Predictors of suicidal ideation logistic regression |
| Eltz et al. (2007)42 USA To examine the factor structure, reliability and validity of the suicide probability scale |
n = 226 11–18 years/mean 14.8 ± 1.5 |
Consecutive admissions over 1 year (n = 419) who completed both intake and discharge ratings on the scale (n = 226) Within 1 week (usually 3 days) |
Scale development | Factor analyses |
| Gasquet and Choquet (1994)43 France To identify the specific role played by the paediatric ward in the care of hospitalised adolescent suicide attempters |
n = 430 13–19 years/mean 16.5 |
All units of 164 general hospitals Time of assessment not given |
Cross-sectional survey | Subgroup analyses by unit of hospitalisation: n = 174 (admitted to paediatric ward), n = 251 (other departments); factors influencing management of suicide attempters; logistic regression |
| Goldston et al. (1996)44 USA To describe the clinical characteristics of different groups of suicidal and non-suicidal youths |
n = 225 12–18 years/mean 14.8 |
Consecutive admissions, August 1989 to February 1992 Between days 3 and 5 |
Cross-sectional survey | Descriptive statistics |
| Goldston et al. (1998)45 USA To examine the rates of psychiatric disorder of different groups of suicidal and non-suicidal adolescents |
n = 269 12.0–19.4 years/mean 14.96 |
Consecutive admissions, September 1991 to November 1995; study population overs by 17.8% overlaps with Goldston et al. (1996)44 Between days 3 and 5 |
Cross-sectional survey | Descriptive statistics |
| Goldston et al. (1999)46 USA To examine risk of suicide attempts among 180 consecutively referred adolescents during the first 5 years after discharge from an inpatient psychiatry unit |
n = 180 12–18 years, mean 14.8/median 14.8, at time of admission |
Consecutive admissions, April 1991 to April 1995 and recruited from Goldston et al. (1998)45 1.5 years and every 6 months for 5 years after discharge |
Prospective, longitudinal cohort study | Periods of risk of suicide after hospitalisation, Cox regression models |
| Gothelf et al. (1998)47 Israel To test the hypothesis that suicidal adolescents would be more preoccupied with death and would perceive death as more pleasurable and reversible than would non-suicidal adolescents |
n = 51 12–19 years/mean 16 |
Mixed sample: consecutive admissions over a 1-year period for suicidal and non-suicidal adolescents; consecutive admissions to emergency room because of a suicide attempt but not requiring psychiatric hospitalisation; controls – high school population from same catchment area With 2 weeks of admission |
Prospective, case–control study | Subgroup analyses: n = 51 (suicidal inpatients), n = 102 (non-suicidal inpatients), n = 36 (suicidal emergency room patients), n = 81 (normal controls); death concepts |
| Greenham and Bisnaire (2008)48 Canada To describe characteristics and outcomes of youths aged 7–17 years who received inpatient psychiatric mental health services along different clinical pathways of a new service delivery model |
n = 211/342 7–17 years/mean 14.9 ± 1.8 |
Consecutive admissions to the crisis stabilisation and assessment service, October 2000 and October 2001 At admission, at 2 weeks and at discharge |
Cross-sectional survey | Subgroup analyses, categorised according to services used: n = 96 (crisis group), n = 90 (assessment group), n = 25 (transition group) |
| Grilo et al. (1999)49 Canada To examine correlates of suicide risk in psychiatrically hospitalised adolescents with a reported history of childhood abuse |
n = 127 12–18 years/mean 15.8 ± 1.5 |
Nearly consecutive series of admissions to the evaluation and crisis intervention unit | Cross-sectional survey | Subgroup analyses: n = 74 (abused), n = 53 (depressed/non-abused) |
| Haavisto et al. (2003)50 Finland To study the prevalence of suicidal ideation and suicide attempts among child and adolescent inpatients during hospital treatment |
n = 263 2–12 years/13–18 years; mean ns |
All admissions during 1 day in January 2000 in all psychiatric wards in Finland Throughout study period |
Cross-sectional survey | Factors associated with suicidality |
| Horesh et al. (2004)51 Israel To evaluate the correlation of self-disclosure with suicidal behaviour in adolescents |
n = 80 13–19 years/mean 16.9 ± 3.2 |
Consecutive admissions Not specified |
Cross-sectional survey | Correlation analyses: suicide and self-disclosure |
| Huth-Bocks et al. (2007)52 USA To examine the validity and clinical utility of the Reynolds Adolescent Depression Scale, Beck Hopelessness Scale, Suicidal Ideation Questionnaire – Junior and Suicide Probability Scale (SPS) in suicidal adolescents |
n = 289 (rr = 35%) 12–17 years/mean 15.3 ± 1.5 |
Admitted over 2 years, 1998–2000, to a RCT232 Follow-up assessment 5.0 to 8.7 months after discharge |
Scale development | Predictors of suicidality, hierarchical logistic regression analyses |
| Ilomaki et al. (2007)53 Finland To investigate the association between alcohol dependence and suicidal behaviour among female and male adolescents suffering from conduct disorder |
n = 141 with conduct disorder 12–17 years |
Those with DSM-IV diagnosed conduct disorder from the STUDY-70233 project, which was all admissions between April 2001 and 2005 On admission |
Cross-sectional survey | Subgroup analyses: n = 48 (alcohol dependence), n = 93 (no alcohol dependence) |
| Joiner et al. (2000)54 USA It was hypothesised that multiple attempt status would relate significantly to intensity of suicidal crises and would relate more strongly to intensity than to duration of crises. The aim was therefore to test these predictions in a sample of children and adolescents specifically referred for suicidal behaviour or severe ideation |
n = 50 11–17 years/mean 14.64 ± 1.54 |
From admissions who were routinely screened for suicidal symptoms On admission and discharge |
Cross-sectional survey | Correlational analyses: suicide attempt status with severity of depression |
| Kirkcaldy et al. (2006)55 Germany To examine the unique and shared risk factors for suicidal behaviour, self-injury and externally focused aggressive behaviour among German youths and adolescents of both sexes |
n = 3649 3–24 years/mean 13.4 ± 3.3 |
Admissions 2000–3 Not specified |
Cross-sectional survey | Subgroup analyses by gender for determinants of suicidal behaviour, self-injurious behaviour, disruptive behaviour |
| Kjelsberg et al. (1994)28 Norway To investigate the incidence of and predictive factors for suicide in youth psychiatric inpatients |
n = 1792 of 1969 12–18 years |
All admissions 1963–91 who could be traced through the Norwegian Central Bureau of Statistics at follow-up Mean follow-up time 15 years (median 0–32) |
Retrospective, longitudinal cohort study | Predictive factors for suicide at follow-up, logistic regression |
| Larsson and Ivarsson (1998)56 Sweden To examine (1) clinical characteristics and psychosocial factors in regard to frequency and severity of suicide attempts among adolescent psychiatric inpatients and (2) predictors of suicide attempts shortly prior to hospitalisation and frequency of lifetime attempts made by inpatients |
n = 191 11–18 years/mean 15.4 |
Admission from two inpatient samples Within 3 days |
Cross-sectional survey | Frequency of suicide attempts, predictors of suicide attempts, logistic regression |
| Lukonis et al. (2001)57 USA Report of a 15-year-old transferred to an inpatient unit after receiving medical treatment for a serious suicide attempt |
n = 1 15 years |
Transferred to an inpatient unit after receiving medical treatment for a serious suicide attempt Time of assessment not given |
Case study | Case study |
| McCarthy et al. (1995)58 USA To clarify the extent of suicidal behaviour among hospitalised adolescent patients with affective disorders, conduct disorders and other diagnoses |
n = 181 12–18 years/mean ns |
Currently discharged consecutively admitted patients Retrospective chart review 6 months prior to date of admission |
Cross-sectional survey | Subgroup analyses: assaultive behaviour, no assaultive behaviour; suicide attempts, no suicide attempts |
| O’Brien and Wilkes (2004)59 USA To review the impact of completed suicides in the context of an adolescent in-patient psychiatric unit, including the impact on the family, on the staff of the programme and on the treatment community |
n = 4 13–18 years |
Completed suicides over past 12 years in the Young Adult Program actively in treatment or within 12 months after the end of treatment Retrospective chart review |
Cross-sectional survey | Descriptive analyses Factors involved |
| Ofek et al. (1998)60 Israel To evaluate the psychometric properties of the Hebrew version of the child suicide potential scale for use with psychiatrically hospitalised adolescents |
n = 185 12–21 years/mean 16.6 ± 1.6 |
Consecutive admissions On admission and 6- to 12-month follow-up |
Scale development | Correlational analyses |
| Ohring et al. (1996)61 Israel To determine whether or not there are age continuities in the relationship between trait anxiety and suicidal behaviour across the developmental spectrum |
n = 46 (suicide attempters) 12–19 years/mean 15.7 ± 1.4 n = 72 (no history of suicide) 12–19 years/mean 16.3 ± 2.09 |
Recruited from consecutive admissions Retrospective chart review |
Cross-sectional survey | Subgroup analyses: suicide attempters, no history of suicide |
| Osman et al. (1996)62 USA To construct a brief version of the Reasons for Living Inventory and to examine the initial psychometric properties of the Reasons for Living Inventory |
n = 120 15–17 years/mean 16.0 ± 0.8 |
Recruited from consecutive admissions Within 1 week |
Scale development | Factor analysis |
| Osman et al. (2000)63 USA To examine the construct validity and psychometric properties of the Multi-Attitude Suicide Tendency Scale in adolescent psychiatric inpatients |
n = 180 14–17 years/mean 16.1 ± 0.8 (males), mean 15.9 ± 0.9 (females) |
Recruited from consecutive admissions Within 2 weeks |
Scale development | Factor analysis |
| Osman et al. (2001)64 USA To examine the reliability and validity of a brief self-report measure of past suicidal behaviour, the Suicidal Behaviours Questionnaire – Revised |
n = 65 (males)/n = 55 (females) 14–17 years/mean 15.6 + 1.0 (males), mean 15.6 + 1.0 (females) |
Mixed sample, consecutive admissions, adult psychiatric inpatient unit and adolescent psychiatric inpatient unit, high school, university Within 1 week |
Scale development | Receiver operating characteristic analysis |
| Osman et al. (2002)65 USA To evaluate the factor structure of the Positive and Negative Suicide Ideation Inventory, examine reliability and test–retest estimates for the two scales and evaluate evidence for known-groups discriminant and concurrent validity of the scales in samples of psychiatric inpatient adolescents recruited from two adolescent units of a state psychiatric hospital |
n = 107 (males), n = 88 (females) Mean 15.5 ± 1.1 (males), mean 15.4 + 1.1 (females) |
Consecutive admissions to two separate adolescent inpatient units of a state psychiatric hospital Within 1 week |
Scale development | Correlational analysis, logistic regression analysis |
| Osman et al. (2005)66 USA To examine the construct validity of the Inventory of Suicide Orientation-30 measure with a sample of adolescent inpatients |
n = 202 14–17 years/mean 15.6 ± 1.0 |
Recruited from consecutive admissions Within 2 weeks |
Scale development | Hierarchal logistic regression |
| Overholser et al. (1995)67 USA To examine self-esteem deficit as related to suicidality among adolescents |
n = 524 Mean 15.2 + 1.4 (inpatients), mean 15.2 + 1.5 (high school students) |
Mixed sample: inpatients, high school students Assessed during first week |
Cross-sectional survey | Subgroup analysis: low self-esteem, high self-esteem |
| Overholser et al. (1997)68 USA To examine the relationship between substance abuse, emotional distress and suicidal intent among 115 adolescent psychiatric inpatients who had attempted suicide |
n = 115 12–17 years/mean 15.3 ± 1.5 (males), mean 15.2 ± 1.3 (females) |
Participants in an ongoing research project67 | Cross-sectional survey | Correlational analysis: emotional distress with substance abuse |
| Pfeffer et al. (1988)69 USA To evaluate factors associated with suicidal behaviour |
n = 200 13–19 years/mean 16.8 ± 1.9 |
Consecutively admitted adolescents in 1983 Retrospective chart review |
Cross-sectional survey | Regression analysis |
| Pfeffer et al. (1989)70 USA To identify the variables that are related to the risk of suicidal behaviour, violent behaviour or both in adolescents |
n = 129 13–19 years |
Consecutive admissions Retrospective chart review |
Cross-sectional survey | Subgroup analyses: n = 10 (suicidal and assaultive), n = 57 (non-suicidal and non-assaultive), n = 47 (suicidal only), n = 13 (assaultive only) |
| Pinto and Whisman (1996)71 USA To examine interactive effects of suicidal behaviour and gender on negative affect and cognitive biases in hospitalised adolescents |
n = 288 13–18 years/mean 15.1 (ideators), 15.4 (attempters), 15.0 (non-suicidal) |
Consecutive admissions Within a few days of admission |
Cross-sectional survey | Subgroup analyses: n = 68 (ideators), n = 90 (attempters), n = 70 (non-suicidal) |
| Rice et al. (2002)72 USA To assess whether or not hospitalised preschool, school-age and young adolescents have different clinical characteristics, family environmental backgrounds and risk factors |
n = 1136 (3–16 years)/mean 10.5 ± 2.9 n = 128 (random sample 1993, 95, 96 and 97 children 11–16 years)/mean 13.1 ± 2.9 (11–16 years) |
Consecutive admission over a 5-year period, January 1993 to December 1997 Retrospective chart review |
Cross-sectional survey | Subgroup analyses: n = 99 (under 6 years), n = 100 (7–10 years), n = 128 (11–16 years) |
| Schwartz-Stav et al. (2006)73 Israel To investigate the inter-relationships between depressive symptoms of adolescent schizophrenia, PPD, negative signs, suicidal behaviour and insights into the disease |
n = 48 13–19 years/mean 17.5 |
Sampled from consecutive admissions, matched groups 2 weeks to 1.5 months |
Cross-sectional survey, major depressive disorder (n = 16) | Subgroup analyses: with schizophrenia who developed PPD in the month following an acute psychotic episode (n = 16); with schizophrenia who did not develop PPD in the month following an acute psychotic episode (n = 16) |
| Shoval et al. (2006)74 Israel To evaluate the clinical characteristics of adolescents with severe OCD who require hospitalisation |
n = 342 of 348 patients selected in previous study, n = 87 community controls Mean 16.4 ± 1.7 |
Mixed sample: consecutive admissions 1996–9, community controls Retrospective chart review |
Cross-sectional survey | Subgroup analyses Severe OCD |
| Shoval et al. (2011)75 Israel To compare suicide-related traits between subjects with first episode schizophrenia and those with other psychopathology |
n = 53 Adolescents, age ns |
Admission, no further details Within 4 weeks |
Cross-sectional survey | Subgroup analyses: n = 25 (first episode schizophrenia), n = 28 (controls) |
| Steer et al. (1993)76 USA To determine whether or not hopelessness is related to suicidal ideation in adolescents when depression is controlled for |
n = 108 12–18 years/mean 15.08 ± 1.55 |
Consecutive admissions Within 3 days |
Cross-sectional survey | Predictors of suicidal ideation, logistic regression |
| Fehon et al. (2000)77 USA To identify and describe potential dimensional differences in the personality patterns and clinical symptoms of patients who report high levels of dependency and self-criticism as assessed by the DEQ-A |
n = 194 12–18 years/mean = 15.8 ± 1.6 |
Nearly consecutive admissions Within 1–2 days admission |
Cross-sectional survey | Subgroup analyses: n = 37 (self-critical), n = 47 (dependent); correlational analyses: DEQ-A and self-criticism with dependency factors |
| King et al. (1997)59 USA To learn more about the Diagnostic Interview Schedule for Children as a tool for assessing severity of depression and suicidality from a dimensional perspective and for diagnosing depressive disorders |
n = 265 of 278 12–18 years/mean 14.9 ± 1.4 |
Consecutive eligible admissions over a 2-year period Not specified |
Scale development | Logistic regression |
| Pfeffer (1989)79 USA To evaluate the research methodology of investigations of suicidal pre-adolescents and adolescents who were admitted to medical inpatient facilities |
Not applicable Pre-adolescents and adolescents |
Not applicable | Review | Not applicable |
| Engel et al. (2005)80 USA To comment on a study of suicide prevention |
Not applicable Adolescents |
Not applicable | Letter | Not applicable |
| Greenhill and Waslick (1997)81 USA To undertake a review of the literature of the management of suicidal behaviour in children and adolescents |
Not applicable Children and adolescents |
Not applicable | Discussion article | Not applicable |
| Risk of harm to self: alcohol and drug abuse (n = 7) | ||||
| Meyers et al. (1995)82 USA To develop the Comprehensive Addiction Severity Index for Adolescents |
n = 102 12–18 years/mean 15.7 + 1.4 |
Receiving psychiatric treatment or substance abuse treatment, or both Over a 1 week period and retrospective chart review |
Scale development | Validity Internal consistency |
| Becker and Grilo (2007)83 USA To examine selected psychosocial correlates of substance abuse in psychiatrically hospitalised adolescents |
n = 458 12–19 years/mean 15.8 + 1.5 |
Nearly consecutive admissions Within 1–4 days |
Cross-sectional survey | Subgroup analyses: n = 367 (European Americans), n = 44 (Latino Americans), n = 47 (African Americans); psychosocial predictors of substance abuse; multiple regression |
| Evans et al. (2007)84 USA To better understand the relationship of substance abuse with conduct disorder and trauma |
n = 192 11–17 years/mean = 14.5 + 1.5 |
Consecutive admissions Intake evaluation and retrospective chart review |
Cross-sectional survey | Subgroup analyses: n = 78 (no CD/no PTSD), n = 29 (no CD/PTSD), n = 58 (CD/no PTSD), n = 27 (CD/PTSD) |
| McKay et al. (1991)85 USA To determine whether or not the degree of substance use and abuse by adolescent psychiatric inpatients is related to the functioning of their families |
n = 45 13–17 years/mean 14.6 + 1.16 |
Admissions, no further details Second or third week |
Cross-sectional survey | Correlations between family functioning and substance use, predictors of substance use, regression analyse |
| Becker et al. (2012)86 USA To examine the temporal ordering of substance use and delinquent behaviour in a sample of psychiatrically hospitalised early adolescents |
n = 108 at baseline, n = 83 at 9 months, n = 81 at 8 months 12–15 years/mean 13.5 |
Methods detailed in previous study by Prinstein et al. (2008)234 Baseline, 9 months and 18 months |
Prospective, longitudinal cohort study | Predictors of substance use and delinquent behaviour, modelling |
| Shoval et al. (2007)87 Israel To identify clinical correlates and characteristics of adolescent psychotic inpatients with and without comorbid substance use |
n = 188 diagnosed with schizophrenia/schizoaffective disorder 12.6–23.2 years/mean 17.4 |
Adolescents admitted to adolescent inpatient unit 1994–2004 Retrospective chart review |
Cross-sectional survey | Subgroup analyses: n = 135 (non-substance users), n = 53 (substance users) |
| King et al. (1996)92 USA To identify clinical profiles discriminating depressed adolescents on the basis of comorbid alcohol/substance use disorders |
n = 103 of 111 Range ns 15.9 + 1.31/mean 15.9 + 1.52 |
Consecutive admission with major depression Within 5 days |
Cross-sectional survey | Subgroup analyses: n = 30 (depressed with alcohol/substance use disorders), n = 73 (depressed without alcohol/substance use disorders) |
| Risk of harm to self: general self-harm (n = 3) | ||||
| de Kloet et al. (2011)88 Australia To identify risk factors for self-harm for children and adolescents in a mental health inpatient unit |
n = 206; self-harm group n = 150, 6–16 years/mean 14; non-self-harm group n = 56, 7–17 years/mean 13 | All admissions January 2006 to December 2009 Retrospective chart review |
Cross-sectional survey | Predictors of self-harm, logistic regression |
| Wheatley et al. (2004)89 UK To describe some of the key characteristics of 80 young people referred from around the UK for medium secure health care |
n = 80 13–19 years |
All admissions over a 30-month period | Cross-sectional survey | Descriptive statistics |
| Askenazy et al. (2003)90 France To explore and describe the relationship between anxiety, impulsivity and the major at-risk behaviours and the main axis I DSM-IV diagnoses |
n = 69 12–18 years/mean 15.4 + 1.6 |
Consecutive admissions over a 1-year period 2–4 days after admission |
Cross-sectional survey | Subgroup analyses: n = 21 (impulsive and anxious), n = 15 (impulsive and non-anxious), n = 15 (non-impulsive and anxious), n = 18 (non-impulsive) |
| Risk of harm to self: HIV/AIDS (n = 2) | ||||
| Aruffo et al. (1994)91 USA To evaluate the relationship between knowledge of HIV/AIDS, locus of control, alcohol and drug use, and risk-taking behaviours reported by psychiatrically hospitalised teenagers |
n = 100 Mean 14.8 years |
Consecutive admissions over a 6-month period Within 10 days of admission |
Cross-sectional survey | Correlational analysis: AIDS knowledge with sexual activity and alcohol and drug use |
| Brown et al. (1997)93 USA To investigate the associations between sexual abuse and HIV-related attitudes and behaviours in adolescents with a psychiatric disorder |
n = 100 12–17 years/mean 14.6 |
Inpatient, no details Within 42 hours |
Cross-sectional survey | Subgroup analyses: n = ns (abused), n = ns (non-abused) |
| Risk of harm to others: aggression (n = 18) | ||||
| Antonius et al. (2010)94 USA To present a case of a young adult inpatient with a long history of antisocial and assaultive behaviour who struck and injured a psychiatric resident |
n = 1 18 years |
Inpatient Over period of hospitalisation |
Case study | Case study |
| Barnett et al. (2002)95 USA To develop a guide to improve the management of acute aggression |
Not applicable Youth (age not specified) |
Not applicable | Guideline development | Not applicable |
| Barzman et al. (2011)96 USA To evaluate the Brief Rating of Aggression by Children and Adolescents Version |
n = 418 3.5–19.1 years |
Consecutive admissions from emergency department over 6 months On admission |
Scale development | ROC analyses |
| Boxer (2007)97 USA To examine the utility of clinical records of psychiatrically hospitalised youth for predicting critical incidents during treatment |
n = 484 10–17 years/mean 13.94 |
Consecutive admissions Retrospective chart review |
Cross-sectional survey | Predictors of seclusion/restraint, logistic regression |
| Boxer (2010)98 USA To examine the relationships that self- and other-directed aggression would tend to covary and display continuity from pre-treatment to in treatment |
n = 476 10–17 years/mean 13.94 |
Sample taken from previous study97 Retrospective chart review |
Cross-sectional survey | Indicators of aggression, correlational analyses |
| Dean et al. (2008)99 Australia To identify predictors of aggression in a child and adolescent inpatient unit and examine differences in clinical outcomes between aggressive and non-aggressive patients |
n = 134 5.8–18 years/mean 13.8 ± 2.9 |
Admissions October 2004 to December 2005 On admission and discharge |
Cross-sectional survey | Change in HoNOSCA scores over time; subgroup analyses: n = 20 (persistent aggression), n = 114 (no persistent aggression); predictors of aggression; logistic regression |
| Hanssen-Bauer et al. (2011)100 Norway To investigate the characteristics and clinical outcomes of a cohort of patients at four Norwegian units |
n = 192 10–18 years/mean 15.7 ± 1.4 |
Admissions over 1-year period Pre-test 72 hours of arrival, scoring period 2 weeks before; post-test day of discharge, scoring period 3 days before |
Prospective, longitudinal cohort study | Change in HoNOSCA scores |
| Kerr et al. (2007)101 USA To examine whether or not the severity of aggression among adolescents at acute risk for suicide predicted future suicidality, and to consider the long-term impact of aggression on problem trajectories and adverse life events |
n = 218 suicidal adolescents 12–17 years/mean 15.3 ± 1.5 |
Recruited 1998–2000, previously took part in RCT52,232 T1 baseline (n = 270), T2 6 months (n = 270), T3 minimum 10.7 months after T2 (n = 218) |
Prospective, longitudinal cohort study, intervention, psycho-education support for 6 months after discharge | Risk of suicidality, hierarchical linear models, logistic regression |
| Knox et al. (2003)102 USA To compare depressed inpatient youth with non-depressed inpatient youth to determine whether or not rates of aggression are higher in treatment-seeking adolescents with depressive disorders and whether or not these differences are gender-specific |
n = 84 13–17 years/mean 14.64 ± 1.35 |
Consecutive admissions over 1 year Time frame ns |
Cross-sectional survey | Subgroup analyses: depression, gender |
| Phillips et al. (2011)103 Australia To examine the predictive validity of unstructured clinical risk assessment and associated risk factors for aggression in predicting physical aggression in children admitted to an Australian psychiatric inpatient facility |
n = 127 8–13 years/mean 10.35 + 1.32 |
Admissions September 2006 to July 2009 Retrospective chart review |
Cross-sectional survey | Predictors of aggression, logistic regression |
| Vivona et al. (1995)104 USA To examine self- and other-directed aggression in children and adolescents on a psychiatric inpatient unit |
n = 89 of 98 (nine patients excluded as complete data set not available) 5–15 years/mean 11.8 ± 2.10 |
Consecutive admissions during a 12-month period Retrospective chart review |
Cross-sectional survey | Subgroup analyses: n = 35 (mixed aggression), n = 34 (other-directed aggression), n = 20 (no aggression) |
| Phillips et al. (2012)105 Australia To examine the predictive validity of unstructured clinical risk assessment and associated risk factors for aggression in predicting self- and other-directed aggression |
n = 197 13–18 years/mean 15.46 + 1.25 |
Admissions September 2006 to July 2009 Retrospective chart review |
Cross-sectional survey | Predictors of other-directed and self-directed aggression, logistic regression |
| Cautin et al. (2001)106 USA To investigate how internalised and externalised anger are related to substance misuse and suicidal behaviour |
n = 92 12–17 years/mean 15.4 |
No details First week |
Cross-sectional survey | Subgroup analyses: n = 34 (low internalised anger, low externalised anger), n = 21 (high internalised anger, low externalised anger), n = 23 (high internalised anger, high externalised anger) |
| Grosz et al. (1994)107 USA To identify additional correlates of violent behaviour in a sample of hospitalised adolescents |
n = 76 12–17 years/mean 13.8 ± 1.4 (violent), mean 4.1 ± 1.5 (non-violent) |
Consecutive admissions Within 2 weeks |
Cross-sectional survey | Subgroup analyses: n = 40 (violent), n = 36 (non-violent) |
| Fehon et al. (2001)108 USA To examine gender differences in violence exposure and violence risk among adolescent inpatients |
n = 130 12–18 years/mean 15.9 |
Nearly consecutive admissions 1–3 days after admission |
Cross-sectional survey | Subgroup analyses: victim and/or perpetrator of violence, gender |
| Fehon et al. (2005)109 USA To examine the issue of violence exposure and violence risk among adolescent inpatients who have a history of physical and violence perpetration |
n = 130 12–18 years/mean 15.9 |
Nearly consecutive admissions 1–4 days after admission |
Cross-sectional survey | Subgroup analyses: n = 52 (violence perpetrator), n = 78 (non-perpetrator) |
| Gammelgard et al. (2008)110 Finland To examine the short-term predictive validity of the Structured Assessment of Violence Risk in Youth (SAVRY) in a sample of institutionalised adolescents |
n = 208: two psychiatric wards n = 51, three correctional schools n = 110, forensic unit n = 47 11–18 years/mean 15.2 ± 1.0 |
Mixed sample, consecutive adolescents from two psychiatric wards over 6-month period Within 1 month and retrospective chart review |
Scale development | ROC analyses |
| Walker and Kelly (2011)111 UK To study the use of a journal to identify early warning signs of episode of psychosis |
n = 2 Case study 1 age 15, case study 2 age 16 |
On admission No further details |
Case study Journal keeping |
Descriptive |
| Risk of harm to others: bullying (n = 2) | ||||
| Luukkonen et al. (2009)112 Finland To study the association between being bullied, being a bully or being a bully-victim and subsequent criminality |
n = 508 12–17 years/mean 15.5 + 1.3 |
Admissions April 2001 to March 2006, part of study 70 project233 During hospitalisation |
Cross-sectional survey | Subgroup analyses: n = 423 (no crimes), n = 45 (non-violent crimes), n = 50 (violent crimes) |
| Luukkonen et al. (2011)113 Finland To study the association between being bullied, being a bully or being a bully-victim and subsequent criminality |
See Luukkonen et al. (2009)112 | See Luukkonen et al. (2009)112 | Cross-sectional survey | Predictors of criminality, logistic regression |
| Long-term risks found at follow-up: readmission (n = 9) | ||||
| Pogge et al. (2008)114 USA To examine clinical symptoms and cognitive performance at the time of first admission and at 6-year follow-up |
n = 102 of 389 13–17 years on admission/mean 14.4 + 2.5 |
First-admission psychiatric patients who had been discharged from the hospital at least 5 years before the study and who had undergone a complete psychological assessment during hospitalisation 6-year follow-up |
Retrospective, longitudinal cohort study | Predictors of readmission, stepwise regression analyses, correlational analyses, HoNOSCA at follow-up and diagnoses, clinical symptoms and severity |
| Fontanella et al. (2008)115 USA To examine predictors of readmission in adolescent inpatients at 1 year |
n = 522 11–17.99 years |
Consecutive admissions to three psychiatric hospitals and covered by Medicaid at time of admission, July 1997 to June 1998; retrospective chart review and Medicaid claims files 1-year follow-up |
Retrospective, longitudinal cohort study, same sample as Fontanella et al. (2006)196 | Predictors of readmission, Cox regression models |
| Fontanella et al. (2009)116 USA To examine whether or not psychotropic medication changes and polypharmacy are associated with 30-day readmission rates for suicidal adolescents |
n = 354; same sample as Fontanella et al. (2006)121 and who were admitted for suicidal ideation or attempted suicide 11–18 years/mean 14.30 + 1.70 |
Consecutive admissions to three psychiatric hospitals and covered by Medicaid at time of admission, July 1997 to June 1998 Followed for 30 days, retrospective chart review and Medicaid claims files |
Retrospective, longitudinal cohort design | Early readmission, Cox proportional hazard models |
| Barker et al. (2010)117 Australia To examine demographic and clinical factors associated with readmission to adolescent psychiatric hospitals within 12 months of discharge |
n = 112 11–17 years/mean 15.3 + 1.5 |
Consecutive admissions January 2005 to December 2005 Retrospective chart review, 1-year follow-up |
Retrospective, longitudinal cohort study | Subgroup analyses: n = 35 (readmitted), n = 77 (not readmitted); predictors of readmission; logistic regression |
| James et al. (2010)118 USA To examine the risk and determinants of rehospitalisation of children and adolescents following a first psychiatric hospitalisation |
n = 189/200 < 18 years/mean 13.6 + 2.8 |
First psychiatric hospitalisation January 2002 to December 2005 Phase 1 over 13 months, random sample of structured telephone interviews with caregivers; phase 2 over 30 months, retrospective chart review |
Prospective, longitudinal cohort study | Predictors of psychiatric rehospitalisation, Cox regression models |
| Arnold et al. (2003)119 USA To examine the rate of rehospitalisation among adolescent psychiatric inpatients and to assess potential predictors of rehospitalisation |
n = 180 (response rate 84%) 12–19 years/mean 14.8 |
Hospitalised between September 1991 and April 1995 and followed up for 10.3 years On admission and every 6–8 months |
Prospective, longitudinal cohort study | Predictors of rehospitalisation, Cox regression models |
| Abrantes et al. (2007)120 USA To examine rates of treatment service utilisation in the 12 months after hospitalisation among adolescents with and without substance use disorder |
n = 191 13–17 years/mean 15.4 + 1.3 |
Consecutive admissions February 1998 to April 2001 Assessments conducted while an inpatient and 1, 6 and 12 months after discharge |
Prospective, longitudinal cohort study | Rates of treatment utilisation and inpatient hospitalisation at 1, 6 and 12 months; subgroup analyses: n = 136 (suicidal), n = 54 (non-suicidal) |
| Fontanella et al. (2006)121 USA To describe the pattern of psychotropic medication treatment and discharge-planning practices used to stabilised adolescents during the index hospitalisation, with special emphasis on the extent of change in adolescents’ medication regimens and living situations and to examine the impact of these stabilisation strategies on early readmission |
n = 517 11–18 years/mean 14.3 + 1.7 |
Medicaid-covered adolescents admitted to three psychiatric hospitals from July 1997 to June 1998 Followed for 30 days, retrospective chart review and Medicaid claims files |
Retrospective; longitudinal cohort study | Cox proportional hazard models of the effect of stabilisation strategies on early readmission |
| Pedersen and Aarkrog (2001)122 Denmark To assess outcome, measured as the frequency of later psychiatric admissions for major diagnostic groups |
n = 488 Adolescents, age range ns |
Consecutive first admissions between 1968 and 1988 (n = 839); a subsample of all patients discharged 10 years or more before a specific date Retrospective chart review, 10- to 21.5-year follow-up |
Retrospective; longitudinal cohort study | Long-term risk of readmission, discriminant analyses, lifetable analyses |
| Long-term risks found at follow-up: homelessness (n = 1) | ||||
| Embry et al. (2000)123 USA To measure incidence of homelessness among youths discharged from an inpatient facility as well as to identify factors that place the youths at risk of homelessness |
n = 86 17.0 years entry, 19.9 years discharge |
Consecutive discharges over a 5-year period, 1981–7 admission data Retrospective chart review, interviewed annually within 1 month of discharge date (5 years) |
Prospective, longitudinal cohort study | Predictors of homelessness, principle component analysis |
| Long-term risks found at follow-up: delinquency (n = 1) | ||||
| Kjelsberg and Dahl (1999)124 Norway To identify predictors of later delinquency in adolescent psychiatric inpatients |
n = 932 of 1276 11–22 years at admission/mean 14.9 |
All consecutive admissions during 1936–81 Followed up 15–33 years after discharge through record linkage to the National Crime Register |
Retrospective, longitudinal cohort study | Predictors of delinquency, Kaplan–Meyer Survival analysis, Cox regression |
| Long-term risks found at follow-up: early death (n = 2) | ||||
| Kjelsberg et al. (1999)125 Norway To identify predictors of early death in former adolescent psychiatric inpatients |
n = 1095 of 1276 11–22 years on admission/mean 15.0 + 1.6 |
See Kjelsberg (1999)235 Followed up 15–33 years after discharge through record linkage to the National Death Cause Registry |
Retrospective, longitudinal cohort study | Predictors of early death, Kaplan–Meyer Survival analysis, Cox regression |
| Kjelsberg (2000)126 Norway To investigate excess mortality by calculating standardised mortality ratios relative to cause of death, diagnosis, cohort and age |
n = 1095 of 1276 11–22 years on admission/mean 15 + 1.6 |
See Kjelsberg (1999)235 Followed up 15–33 years after discharge through record linkage to the National Death Cause Registry |
Retrospective, longitudinal cohort study | Calculation of the expected deaths by cause of death, mental disorder, cohort and age for each gender |
| Long-term risks found at follow-up: schooling (n = 2) | ||||
| Best et al. (2004)127 USA To examine early adulthood outcomes of psychiatrically hospitalised adolescents |
n = 146: inpatients n = 70, 11.5–16 years/mean 14.1 ± 1; high school students n = 76, 3.8–15.8 years/mean 14.5 ± 0.4 | Mixed sample, consecutive admissions, 1978–81, ninth-grade students from a public high school in an adjacent community Three time points: recruitment, 11-year follow-up and 20-year follow-up |
Prospective, longitudinal cohort study | Cohorts compared for mortality, emotional distress levels, high school completion, complete completion, graduate school completion, degree attainment |
| Halfon et al. (1995)128 Finland To examine the major sociological family, clinical and schooling features of adolescents with psychiatric disorders |
n = 137 14–21 years/mean 17.8 ± 1.5 |
All hospitalised patients discharged January 1999 to December 1993 Not specified |
Cross-sectional survey | Subgroup analyses: n = 61 (suicidal), n = 76 (non-suicidal) |
| Early disengagement from services: running away (n = 3) | ||||
| Siegel and Callesen (1993)129 USA To identify those factors which place an adolescent at risk of running away from an inpatient treatment programme |
n = 102 12–18 years: mean 14.9 (runaway), mean 14.6 (control) |
Consecutive admissions October 1984 and October 1986 Retrospective chart review |
Cross-sectional survey | Subgroup analyses: runaway, control |
| Berman and Goodrich (1990)130 USA To predict which patients admitted might be the one to run away while undergoing treatment |
n = 118 9.2–21.3 years/mean 15.9 |
All patients admitted, treated and discharged between 1975 and 1976 | Cross-sectional survey | Linear discrimination function analyses, patterns of runaway behaviour |
| Kleis and Stout (1991)131 USA To examine some of the variables encountered in the patient at risk of elopement |
n = 16 13–17 years |
Patients who eloped April 1988 to December 1989 Retrospective chart review |
Cross-sectional survey | Descriptive statistics, characteristics of people who run away |
| Early disengagement from services: discharge against medical advice (n = 1) | ||||
| Vander Stoep et al. (1991)132 USA To identify factors that would enable clinicians to predict, at admission, the probability of a patient’s discharge against medical advice |
n = 81 Median age 17 years |
All patients discharged January 1983 to June 1988 Within 1 week and every 30 days, retrospective chart review |
Cross-sectional survey | Subgroup analyses: n = ns (planned discharges), n = ns (unplanned discharges) |
| Early disengagement from services: treatment dropout (n = 1) | ||||
| Wallier et al. (2009)133 France To review the literature concerning dropout from inpatient treatment for eating disorders |
Seven studies retrieved One paper within age range, with mean 16.7 ± 2.0 |
Not applicable | Review | Not applicable |
| Risk factors influencing admission and length of stay (n = 5) | ||||
| Chabra et al. (1999)27 USA To determine the extent and cost of hospitalisations for mental illness among adolescents and to identify differences in acute care hospital use by gender and between racial/ethnic groups |
n = 27,595 10–19 years |
Hospital discharge tapes for all hospitalisations for adolescents during 1994 | Cross-sectional survey | Relative risks for hospitalisation stratified by years of age Relative risks for hospitalisation stratified by gender Relative risks for hospitalisation stratified by gender and years of age Relative risks for hospitalisation stratified by diagnosis and years of age Relative risks for hospitalisation stratified by race/ethnicity Relative risks for hospitalisation stratified by race/ethnicity and diagnosis |
| Leon et al. (2006)134 USA To predict psychiatric hospital length of stay across 4 fiscal years |
n = 208 5–15 years/mean 13.6 + 3.5 |
Data collected from 1930 hospital episodes across 44 hospitals 1998–2011 | Cross-sectional survey | Predictors of length of stay, multiple regression |
| McGilloway et al. (2000)135 Northern Ireland To investigate the nature and pattern of teenage admission (13–18 years) to the 14 adult psychiatric units in Northern Ireland between 1989 and 1995 |
n = 443 (43% of all teenage admissions), n = 40 admitted to Young People’s Centre, n = 10 agreed to be interviewed, n = 7 took part within time frame of project 16–23 years |
All admissions of those aged < 18 years between 1994 and 1997 receiving adult psychiatric inpatient care; referrals from general hospital psychiatric-based unit to the Young People’s Centre Time after discharge when interviews were conducted not specified |
Retrospective Longitudinal cohort study Chart review (adult psychiatric inpatient care) Interviews (Young People’s Centre) |
Descriptive data of factors preceding admission |
| Kaltiala-Heino (2010)136 Finland To evaluate whether or not adolescents committed to psychiatric inpatient care are the most disturbed, and whether or not psychosocial factors are associated with commitment to and detainment in psychiatric are among adolescents |
n = 187 13–17 years |
All admissions 2004–6 identified from hospital databases Retrospective chart review |
Cross-sectional survey | Subgroup analyses: n = 93 (referred involuntarily), n = 94 (voluntary), n = 42 (detained involuntarily), n = 145 (treated voluntary) |
| Leon et al. (1999)137 USA To examine factors related to decision to admit and length of stay of children in a large mid-western state |
n = 2666 5–10 years 10–15 years/mean 13 (SD 3.4) |
Screened January 1997 to September 1997 to determine if they were in need of psychiatric hospitalisation | Cross-sectional survey | Factors predicting admission, logistic regression |
| Risk of harm from the system: side effects of medication (n = 3) | ||||
| Fleischhaker et al. (2006)138 Germany To improve and evaluate the practicability of a methods for the assessment of drug-associated side effects |
n = 51 9–21 years/mean 16.1 ± 2.1 |
Adolescent inpatients from four child and adolescent psychiatric departments who had started treatment with clozapine, olanzapine and risperidone during a 26-month study period | Prospective, longitudinal cohort study | Subgroup analyses: n = 16 (clozapine), n = 16 (olanzapine), n = 19 (risperidone) |
| Shoval et al. (2011)139 Israel To evaluate both the efficacy and the safety of citalopram for treatment of major depressive disorder and anxiety symptoms in adolescent inpatients |
n = 10 Mean 16.6 ± 1.99 years |
Adolescent inpatients | Open label, prospective pilot trial | Repeated measures, citalopram at baseline and 8 weeks with depression and anxiety symptoms |
| US Preventive Services Task Force (2009)140 USA To develop a guideline which talks about the harm of selective serotonin reuptake inhibitors and the risk of suicidality |
Not applicable 12–18 years |
Not applicable | Recommendation statement | Not applicable |
| Risk of harm from the system: sexual abuse by staff (n = 1) | ||||
| Berland and Guskin (1994)141 USA To determine prevalence and characteristics of patient allegations of sexual abuse against psychiatric hospital staff |
110 (43%), with 14 reports of allegations in the 10–19 years age group | Every fifth hospital from a commercially prepared list of 1279 hospitals with inpatient psychiatric units | Cross-sectional survey | Descriptive statistics |
| Risk of harm from the system: contagion (n = 1) | ||||
| King et al. (1995)142 USA To investigate whether or not exposure to other suicidal adolescents led to suicidal contagion among patients hospitalised on an acute adolescent psychiatric inpatient unit |
n = 57 11.5–17.8 years/mean 15.2 ± 1.3 |
Admissions over an 8-month period At admission and within 3 days of discharge |
Prospective, longitudinal cohort study | Descriptive statistics |
| Responding to and managing risk (n = 3), improving educational attainment (n = 1), managing the environment to keep people safe (n = 1), Milieu-based behavioural management to reduce aggression (n = 1) | ||||
| White et al. (2006)143 USA To provide a programme that provides intensive school-based support and care coordination during the first 6–10 weeks after discharge |
n = 99 No ages given |
Discharges October 2003 to November 2005 3-month follow-up |
Intervention study: intensive school-based transition programme of 2–20 weeks (median 8) | No details given; educational status |
| Dean et al. (2007)144 Australia To evaluate the impact of a milieu-based behavioural management programme on the frequency of aggressive behaviour in a child and adolescent mental health inpatient unit |
n = 151: before intervention (n = 65), 4.0–18.5 years/mean 13.61; after intervention (n = 86), 4.7–18.0 years/mean 13.59 | Ward outcomes extracted from clinical records for 6 months before and after Retrospective chart review |
Pre–post test, intervention study, behavioural management programme February 2004 | Change in HoNOSCA scores over time |
| Delaney and Hardy (2008)145 USA To examine how the dimensions of ideology, people, space and time relate to safety in CAMHS units |
Not applicable Child and adolescent psychiatric inpatient units |
Not applicable | Discussion article | Not applicable |
| Predictors of restraint and seclusion (n = 3) | ||||
| Bridgett et al. (2012)146 USA To examine temperament characteristics as risk factors for restraint and seclusion events in psychiatrically hospitalised youth |
n = 52 7–17 years/mean 14.1 + 2.3 |
Residents in a psychiatric inpatient hospital for youth at time of the study After 2-week initial evaluation period |
Cross-sectional survey | Predictors of restraint/seclusion, logistic regression |
| Delaney and Fogg (2005)147 USA To determine whether or not a particular group of youths was at risk of restraint |
n = 100 7–19 years/mean 13.9 |
Youths who were hospitalised and had been restrained, December 1998 to January 2000 Retrospective chart review |
Cross-sectional survey | Subgroup analyses: n = 31 (never restrained), n = 57 (restrained), n = 12 (restrained > 3 times) |
| Fryer et al. (2004)148 Australia To identify the factors that place a child or adolescent at increased risk of seclusion during admission |
n = 105 Mean 14.06 + 2.72 |
All admissions over a 1-year period Retrospective chart review |
Cross sectional survey | Descriptive statistics; reasons for seclusion; subgroup analyses: previous history of abuse |
| Functional impairment (n = 1) | ||||
| Frank et al. (2000)149 USA To assess the validity of the Functional Impairment Scale for Children and Adolescents (FISCA) |
Study 1: n = 804; 84% aged 11–18 years/mean 13.4 ± 3.0 | Study 1: hospitalised patients participating in an outcomes study for a mental health corporation | Scale development; FISCA: covers functional domains of school, home, delinquency, thinking, control of aggression, feelings and moods, self-harm, and alcohol and drugs | Study 1: factor analyses |
| Study 2: n = 330 | Study 2: follow-up study for above (n = 255) and additional follow-up patients from another hospital (n = 75) | Study 2: discriminant analyses | ||
| Impact of playing fantasy and role-playing games (n = 1) | ||||
| Ascherman (1993)150 USA To review the literature concerning the impact of playing fantasy and role-playing games on an inpatient unit for adolescents |
Not applicable 15–18 years |
Not applicable | Discussion article | Not applicable |
| Current challenges overview (n = 1) | ||||
| Geller and Biebel (2006)151 USA To examine the current challenges inherent in serving children and adolescents with serious emotional disturbances |
Not applicable 5–19 years |
Not applicable | Discussion article | Not applicable |
Appendix 5 YoungMinds consultation report
Appendix 6 Accessible overview of the project
Appendix 7 Stakeholder advisory group terms of reference
Appendix 8 Agenda for first stakeholder advisory group meeting
Appendix 9 Candidate areas for phase 2 review
Ranked priorities extracted from meeting participants, the YoungMinds consultation document and the carer consultation (each list from one participant at the stakeholder meeting):
-
Bad influences, unhelpful friendships, new peer norms.
-
Imitating other patients.
-
Attitudes of staff/therapists, dysfunctional systems, lack of staff training to deal with such behaviour.
-
Early discharge/making decisions about discharge without consulting patient.
-
Not acknowledging risk factors that are important to the young person’s well-being.
-
Transition back into community/adult services. Not enough planning or coping strategies in place to help patient.
-
Unable to engage with staff members/being isolated increases bad feelings, disempowerment of family members.
-
Self-injury.
-
Suicide.
-
Disempowerment/distress/no responsibility towards self, no motivation to recover.
-
Violence from patients.
-
Unhelpful friendship with other young people on the unit.
-
Having a new network of friends that all have mental health problems.
-
Contagion: learning and emulating behaviours witnessed in other patients.
-
Risk to education.
-
Stigma on return to mainstream education.
-
Unmonitored visitors taking advantage of young people’s vulnerability (abuse).
-
Losing ‘normal’ identity.
-
Not having the chance to achieve educationally.
-
Risk adverse culture leads to lack of progress and increased readmission.
-
Risk of losing connection to social group leads to a longer recovery time.
-
Risk of family breakdown/friends lost.
-
Emotional harm from being in hospital.
-
Increased symptoms severity and breadth.
-
Not feeling safe while an inpatient.
-
Institutionalisation.
-
Identification with mental disorder.
-
Loss of social contacts/context.
-
Parental disempowerment.
-
Gaining unhealthy friendships.
-
Learning unhealthy behaviour.
-
Traumatisation from admission.
-
Use of compulsory treatment and experience of coercion.
-
Escalation of risky behaviours.
-
Risks to educational progress.
-
Risks associated with discharge planning.
-
Risks to ‘being normal’/stigmatisation.
-
Lack of support/resilience.
-
Risks associated with ‘too much risk aversion’.
-
Environmental risk.
-
Psychological risks.
-
Self-harm.
-
Harm to others.
-
Transition.
-
Stigma/discrimination.
-
Self-harm.
-
Suicide.
-
Treatment risks: iatrogenesis.
-
Social support risks.
-
Educational risks.
-
Identity.
-
Self-mutilation/self-injury: overdose, cutting.
-
Aggression, violence.
-
Contagion.
-
Discharge planning.
-
Disruption to education.
-
Rehospitalisation.
-
Risk assessment triggering admission.
-
Risk assessment in discharge planning.
-
Risk of harm from the system.
-
Emulating self in others’ symptoms whereby risk-taking behaviours increase.
-
Families who cannot support the recovery process.
-
Inpatient environment feels more secure than home, hence risk-taking behaviour increases at point of discharge transition.
-
Lack of joint working.
-
Transitional difficulties into the community/education/lower tiers of CAMHS.
-
Identity.
-
Institutionalisation.
-
Stigmatisation.
-
Family/parent re-education, parental change (young people originally coming from a family background where the likelihood of problems have arisen).
-
Competition from peers (i.e. self-harm, eating disorders).
-
Socialisation.
-
Education.
-
Disempowerment of young people and families.
-
Contagion/imitation/’copycat’.
-
Staff culture, dysfunctional systems.
-
Managing dissonance/ambivalence.
-
Displacement.
-
Disempowerment of parents/carers.
-
New peer norms.
-
Stunted developmental trajectory.
-
Aftercare management.
-
Transitions.
-
Not acknowledging the importance of protective factors.
-
Dislocation from peers and family.
-
Parents not involved in decision-making.
-
Contagion.
-
Risks to development trajectories in terms of identity formation, educational achievement, social development, maturity and decisional capacity.
-
Flipside of risk is management of anxiety: of young person, their parents, their schools, social services, mental health professionals. Very high ‘objective’ markers of risk need not lead to admission or prevent discharge. If anxieties can be contained, this reflects resources, training, therapeutic relationships, level of experience and ‘normality’ of risk to professionals.
-
Risk of exposure to highly abnormal behaviours, etc. Normalisation of abnormality/pathology (including to professionals/parents).
-
Risk of inpatient admission disempowering parents and parental authority. May be helpful in some cases but often not.
-
Harm from organisation: restraint, risk assessment.
-
Dislocation from ‘normal’ life: friendship groups and education.
-
Institutionalisation: unit a safe place.
Appendix 10 Priority areas for phase 2
Appendix 10 groups together the items given by stakeholders and listed in Appendix 9.
| Coding | Item |
|---|---|
| Dislocation (n = 16) |
|
| Contagion (n = 6) |
|
| Harm from organisation (n = 6) |
|
| Institutionalisation (n = 5) |
|
| Self-harm (n = 4) |
|
| Decision making (n = 3) |
|
| Suicide (n = 2) |
|
| Aggression (n = 1) |
|
| Managing dissonance/ambivalence (n = 1) |
|
| Psychological risks (n = 1) |
|
Appendix 11 Phase 2 summary document
Project aim
The overall aim of this project is to synthesise the international research evidence and the UK grey literature relating to the identification, assessment and management of ‘risk’ in young people (aged 11–18) with complex mental health needs using inpatient mental health services, and to establish what is known about the costs and cost-effectiveness to the NHS of different approaches.
Objectives
Specifically, the project is examining and synthesising the evidence for, and the costs to the NHS of, approaches to risk used as young people:
-
make the transition into inpatient CAMHS;
-
are cared for in inpatient CAMHS;
-
make the transition from inpatient CAMHS to the community;
-
make the transition from inpatient CAMHS to adult mental health services.
Acknowledgement and disclaimer
This project is funded by the National Institute for Health Research Health Services and Delivery Research Programme (project number 11/1024/08).
The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the HS&DR Programme, NIHR, NHS or the Department of Health.
Background to the project
One in 10 children and young people between the ages of 5 years and 16 years has a diagnosable mental health problem.
NHS services are provided using a tiered approach.
The most specialised child and adolescent mental health services (CAMHS) are available at tier 4 to young people with complex and/or severe needs.
Tier 4 services have diversified, but inpatient CAMHS units continue to have an important place.
Often ‘risk’ is used as a shorthand to refer to the possibilities of direct harm to self or others, or harm through self-neglect.
These are important areas but, in this study, we are also interested in other, less-recognised, risks (e.g. to the achievement of developmental milestones, psychological maturity, educational attainment, social integration with family and peers, and personal physical well-being).
Methods
We are conducting an evidence synthesis guided by the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre) framework.
This approach is particularly recommended for reviews where the findings are destined for practical use by policy-makers, managers and other decision-makers.
The EPPI-Centre approach is two-stage, transparent, rigorous and sensitive to stakeholders.
Stage 1: Conceptual mapping of risk [February to April 2013]
We have conducted an initial scoping search using two databases: MEDLINE and PsycINFO.
We made no attempts to define the word ‘risk’.
Abstracts for each paper were read (and, where not available, full papers were retrieved) by two members of the team and considered against the inclusion criteria: the publication must address risk identification and/or risk assessment and/or risk management in the case of young people moving into, through and/or out of mental health hospital/inpatient mental health services.
An initial map was produced of the different ways in which ‘risk’ has been conceptualised, investigated and otherwise written about in the international literature, and what is currently known in the risk identification, assessment and management field in the inpatient CAMHS area.
We have grouped the 124 journal papers included in this part of the study under these themes:
Risk of harm to self (n = 65): Suicide (n = 53), Alcohol and drug abuse (n = 7), General self-harm (n = 3), HIV/Aids (n = 2)
Risk of harm to others (n = 20): Aggression (n = 18), Bullying (n = 2)
Longer-term risks found at follow-up (n = 15): Readmission (n = 9), Early death (n = 2), Disrupted schooling (n = 2), Homelessness (n = 1), Delinquency (n = 1)
Early disengagement from services (n = 5): Running away (n = 3), Discharge against medical advice (n = 1), Treatment dropout (n = 1)
Risk factors influencing admission and length of stay ( n = 5)
Risk of harm from the system (n = 5): Side effects of medication (n = 3), Sexual abuse by staff (n = 1), Contagion (n = 1)
Responding to and managing risk (n = 3): Improving educational attainment (n = 1), Managing the environment to keep people safe (n = 1), Milieu-based behavioural management to reduce aggression (n = 1)
Predictors of restraint and seclusion ( n = 3)
Functional impairment ( n = 1)
Impact of playing fantasy and role-playing games ( n = 1)
Current challenges overview ( n = 1)
Consultation with young people, conducted through YoungMinds [March 2013]
In preparation for our first project team/stakeholder meeting, over the course of a week collaborators working for the charity YoungMinds conducted a series of consultations with young people with experience of inpatient services.
Young people were asked to say what they saw as the ‘risks’ to children and young people in inpatient settings, how these were assessed, what was done about them, and what the research team should focus on in its in-depth review.
A report was delivered to the project team, which included this as a summary:
Though we spoke to a relatively small number of young people there were some clear themes that emerged from all of the conversations and those themes came out of the direct experiences of the young people. They told us that there were a number of risks that were not adequately being assessed or addressed and that this might be because of a lack of resources or training. All of the types of risks that we discussed were seen as equally important and the assessment of risk was highlighted as an area that needed to be carefully considered, as a poorly done risk assessment could feel extremely punitive and could therefore have a negative effect on the individual’s emotional wellbeing. Most of the young people talked extensively about the risk of emotional harm caused through exposure to distressing experiences as well as negative peer group influences. The young people also mentioned the risk of having their social lives put on hold indefinitely and the lack of opportunity to get any high quality educational provision. One young person used the term ‘fragmented’ to describe how what had happened to their life felt and the result of this fragmentation was their self-identification as ‘ill’. This new identity was seen as damaging as it prevented recovery and made it more difficult for the young people to move back into a ‘normal’ life off the ward. The young people said that they were put on wards to get better but that in many cases there were reasons why being placed in an inpatient setting was in fact detrimental to them. However they also recognised that leaving too early was equally damaging. The risks are present in the immediacy of the inpatient setting but the failure to address those risks has severe implications on both the young people and services as not addressing them leads to increased emotional distress as well as the increased likelihood of a readmission.
Carer consultation [March 2013]
A member of the project team consulted with a parent whose child has used inpatient CAMHS to hear this person’s views of the risks to young people entering, using and leaving hospital.
Key messages from this consultation included the idea that admission to inpatient CAMHS can increase risk through the learning of abnormal, dangerous, behaviours and the forming of new, unhelpful, friendships.
Stakeholder meeting [April 2013]
An independently chaired project team/stakeholder meeting was convened in Cardiff.
In addition to the project team participants included: a collaborating representative from YoungMinds, young people with experiences of CAMHS, a senior NHS CAMHS manager, a senior child and adolescent psychiatrist, a senior CAMHS therapist, and a senior nurse with inpatient CAMHS responsibilities.
An overview of the project along with the broad themes arising from the stage 1 mapping exercise was presented. Themes were displayed visually around the room on flip charts in the form of individual descriptive maps.
A presentation from YoungMinds was given drawing on the consultation exercise conducted with young people.
Participants were invited to record independently written responses to the question, ‘What do you think the risks for young people are as they make the transition into, through and out of inpatient CAMHS?’ before sharing their ideas, and a facilitator recorded these on a flip chart using the words spoken by the participants.
The views of the carer, previously consulted, were reported.
A facilitated group discussion followed, to seek explanations or further details about any of the ideas that participants had produced that were not clear to all.
Participants were then asked to write their personal priorities (where 1 was the most important) for the in-depth, second, stage of the project: drawing on both the descriptive maps capturing existing research and on the risks independently identified by individual participants and by people previously consulted.
Stage 2: Identifying priorities [ongoing]
Following the April meeting the project team collated all the responses from this priority-setting activity and took the first three priority areas from each participant (n = 14).
The project team took the top three priorities as identified by YoungMinds during their pre-meeting consultation with young people (n = 3).
These 45 top priority responses were coded independently by two members of the project team, and verified by a third.
Priority areas were identified and the number of times an area was identified was counted:
-
dislocation (n = 16)
-
contagion (n = 6)
-
harm from organisation (n = 6)
-
institutionalisation (n = 5)
-
self-harm (n = 4)
-
decision-making (n = 3)
-
suicide (n = 2)
-
aggression (n = 1)
-
other [managing dissonance/ambivalence (n = 1) and psychological risks (n = 1)].
The top priorities are all examples of ‘less obvious’ risks, and, as such, are unlike many of the more ‘clinical’ risks identified in our stage 1 mapping of the literature.
Dislocation is the word the project team is using to describe the top priority emerging for the second stage of this review. This includes the ideas of young people being removed from ‘normal’ life, of being ‘different’ and of experiencing ‘fragmentation’.
Dislocation also captures the ideas of being stigmatised and discriminated against, and of young people losing their previous identities, social contacts and friendships groups. It includes isolation from, and within, families.
Dislocation also includes the risks presented to young people’s educational, psychological and social development.
Dislocation implies unhelpful loss, and Contagion (the second emerging priority for the next stage of the review) implies unhelpful gaining: the risk of being exposed to and of learning abnormal behaviour, and of new and unhealthy friendships.
Stage 2: Mapping priorities to keywords
Dislocation and Contagion are broad terms, and the project team has been identifying other, related, keywords that will allow us to search for research papers, policy documents, reports of service developments (etc.) in these linked areas.
We have been testing out combinations of these keywords in databases to see what evidence we can find.
Stage 2: Requesting feedback from the stakeholder group
At this stage the project team plans to take both Dislocation and Contagion forward as the two, linked, top priorities for the second phase of this evidence synthesis.
This implies a move away from the more ‘clinical’ risks identified in our stage 1 mapping to a set of ‘less obvious’ risks.
We welcome your feedback on these three questions:
Have we reflected stakeholders’ priorities accurately?
If we have reflected the priorities for the in-depth part of our review accurately, then we welcome ideas on where we need to go for evidence in these areas. If we are gathering information on how the risks of ‘dislocation’ and ‘contagion’ are identified, assessed and managed as young people move into, through and out of inpatient CAMHS, then where should we look and who should we approach?
What other words can you think of that reflect the ideas of ‘dislocation’ and ‘contagion’, which we might use to continue our search for evidence?
Appendix 12 Phase 2 database searches
Applied Social Sciences Index and Abstracts (via Proquest)
URL: http://search.proquest.com/assia/advanced
Date range searched: 1995 to September 2013.
Date search: 12 September 2013.
Records retrieved: 663.
-
su.Exact(“adolescents”)
-
su.Exact(depressed adolescents”)
-
(adolescen* or teen* or “young adult*” or “young people” or “young person” or youth* or juvenile*).ti, ab.
-
1 or 2 or 3
-
su.Exact(“mental health”)
-
su.Exact(“mental health care”)
-
(mental* or psychiatr* or “tier 4”).ti, ab.
-
5 or 6 or 7
-
4 and 8
-
(CAMHS or “child and adolescent mental health service*).ti, ab.
-
9 or 10
-
su.Exact(“inpatients”)
-
su.Exact(“hospital discharge”)
-
su.Exact(“admission”)
-
(inpatient* or admission* or admitt* or discharge* or transition* or transfer*).ti, ab.
-
12 or 13 or 14 or 15
-
11 and 16
-
17 Limited to 1995-2013
* The BNI and ERIC were also searched using Proquest using a very similar/slightly adapted search to the one above.
Cochrane Library: to include Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, Cochrane Methodology Register, Health Technology Assessment and Economic Evaluation Database
Date range searched: 1995 to September 2013.
Date of search: 16 September 2013.
Records retrieved: 949.
-
MeSH descriptor: adolescent
-
MeSH descriptor: young adult
-
(adolescen* or teen* or “young adult*” or “young person” or “young people” or youth* or juvenile*).ti, ab, kw.
-
1 or 2 or 3
-
MeSH descriptor: mental health
-
MeSH descriptor: mental health services
-
MeSH descriptor: mental disorders
-
(mental* or psychiatr*or “tier 4”).ti, ab, kw.
-
5 or 6 or 7 or 8
-
4 and 9
-
MeSH descriptor: Adolescent Psychiatry
-
(CAMHS or “child and adolescent mental health services”).ti, ab, kw.
-
11 or 12
-
10 or 13
-
MeSH descriptor: inpatients
-
MeSH descriptor: patient admission
-
MeSH descriptor: patient discharge
-
MeSH descriptor: transition to adult care
-
(inpatient* or admission* or admitt* or discharge* or transition* or transfer*).ti, ab.kw.
-
15 or 16 or 17 or 18 or 19
-
14 and 20
-
MeSH descriptor: hospitals, psychiatric
-
4 and 22
-
21 or 23
Cumulative Index to Nursing & Allied Health Literature (via EBSCOhost)
URL: www.ebscohost.com/nursing/products/cinahl-databases/cinahl-complete
Date range searched: 1995 to September 2013.
Date of search: 13 September 2013.
Records retrieved: 1148.
-
(MH “Adolescence”)
-
(MH “Young Adult”)
-
(adolescen* or teen* or “young adult*” or “young people” or “young person” or youth* or juvenile*).ti, ab.
-
1 or 2 or 3
-
(MH “mental health”)
-
(MH “mental health services”)
-
(MH “psychiatric patients”)
-
(mental* or psychiatr* or “tier 4”).ti, ab.
-
5 or 6 or 7 or 8
-
4 and 9
-
(MH “Adolescent Psychiatry”)
-
(CAMHS or “child and adolescent mental health service*”).ti, ab.
-
11 or 12
-
10 or 13
-
(MH “inpatients”)
-
(MH “patient admission”)
-
(MH “patient discharge”)
-
(MH “transfer, discharge”)
-
(transition* or transfer*) N5 “adult care”.ti, ab.
-
15 or 16 or 17 or 18 or 19
-
14 and 20
-
(MH “Hospitals, Psychiatric”)
-
4 and 22
-
21 or 23
-
24 limited to English language 1995–2013
EMBASE (via Ovid)
URL: www.ovid.com/site/catalog/databases/903.jsp
Date range searched: 1995 to September 2013.
Date of search: 13 September 2013.
Records retrieved: 3617.
-
exp Adolescent/
-
(adolescen* or teen* or young adult* or young people or young person or youth* or juvenile*).tw.
-
1 or 2
-
exp Mental Health/
-
exp Mental Health Service/
-
(mental* or psychiatr* or tier 4).tw.
-
4 or 5 or 6
-
3 and 7
-
(CAMHS or “child and adolescent health service*”).tw.
-
8 or 9
-
exp Hospital Patient/
-
exp Hospital Admission/
-
exp Hospital Discharge
-
exp Transition to adult care/
-
inpatient*.tw.
-
11 or 12 or 13 or 14 or 15
-
10 and 16
-
exp Mental Hospital
-
3 and 18
-
17 or 19
-
Limit 20 to (human and English Language and yr=1995-current)
Health Management Information Consortium
URL: www.ovid.com/site/catalog/databases/99.jsp
Date range searched: 1995 to September 2013.
Date of search: 16 September 2013.
Records retrieved: 1053.
-
exp Young People/
-
(adolescen* or teen* or young adult* or young people or young person or youth* or juvenile*).tw.
-
1 or 2
-
exp Mental Health/
-
exp Mental Health Services/
-
(mental* or psychiatr* or tier 4).tw.
-
5 or 6 or 7
-
3 and 7
-
(CAMHS or “child and adolescent health service*”).tw.
-
8 or 9
-
exp In Patients/
-
exp Patient Admission/
-
exp Patient Discharge/
-
(transition* or transfer*) adj5 “adult care”.tw.
-
11 or 12 or 13 or 14
-
10 and 15
-
exp Mental Health Hospitals/
-
exp Mental Health Units/
-
exp Psychiatric Units/
-
17 or 18 or 19
-
3 and 20
-
16 or 21
-
Limit 22 to (English language and yr=“1995-Current”)
MEDLINE (via Ovid)
Date range searched: 1995 to September 2013.
Date of search: 12 September 2013.
Records retrieved: 3830.
-
exp Adolescent/
-
exp Young Adult/
-
(adolescen* or teen* or young adult* or young people or young person or youth* or juvenile*).tw.
-
1 or 2 or 3
-
exp Mental Health/
-
exp Mental Health Services/
-
exp Psychiatric Nursing/
-
(mental* or psychiatr* or tier 4).tw.
-
5 or 6 or 7 or 8
-
4 and 9
-
exp Adolescent Psychiatry/
-
(CAMHS or “child and adolescent health service*”).tw.
-
11 or 12
-
10 or 13
-
exp Inpatients/
-
inpatient*.tw.
-
exp Patient Admission/
-
exp Patient Discharge/
-
exp Transition to Adult Care/
-
15 or 16 or 17 or 18 or 19
-
14 and 20
-
exp Hospitals, Psychiatric/
-
4 and 22
-
21 or 23
-
Limit 24 to (English language and humans and yr=”1995-Current”)
PsycINFO (via Ovid)
URL: www.ovid.com/site/catalog/databases/139.jsp
Date range searched: 1995 to September 2013.
Date of search: 12 September 2013.
Records retrieved: 1875.
-
(adolescen* or teen* or young adult* or young people or young person or youth* or juvenile*).tw.
-
exp Mental Health/
-
exp Mental Health Services/
-
exp Psychiatric Patients/
-
(mental* or psychiatr* or tier 4).tw.
-
2 or 3 or 4 or 5
-
1 and 6
-
exp Adolescent Psychiatry/
-
(CAMHS or “child and adolescent health service*”).tw.
-
8 or 9
-
7 or 10
-
exp Hospital Admission/
-
exp Hospital Discharge
-
inpatient*.tw
-
(transition* or transfer*) adj5 “adult care”.tw.
-
12 or 13 or 14 or 15
-
11 and 16
-
exp Psychiatric Hospitals/
-
exp Psychiatric Hospitalization/
-
exp Psychiatric Hospital Admission/
-
exp Psychiatric Hospital Discharge/
-
18 or 19 or 20 or 21
-
1 and 22
-
17 or 23
-
Limit 24 to (human and English Language and yr=“1995 to Current”)
Keyword searches performed in the remaining databases
To include Scopus, Social Care Online, Social Services Abstracts, Sociological Abstracts, Turning Research into Practice Plus and Web of Science.
British Nursing Index
URL: www.proquest.com/products-services/bni.html
Date range searched: 1995 to September 2013.
Date of search: 16 September 2013.
Records retrieved: 120.
Turning Research into Practice
Date range searched: 1995 to September 2013.
Date of search: 16 September 2013.
Records retrieved: 15.
Web of Science
Date range searched: 1995 to September 2013.
Date of search: 16 September 2013.
Records retrieved: 437.
Scopus
URL: www.scopus.com/
Date range searched: 1995 to September 2013.
Date of search: 13 September 2013.
Records retrieved: 525.
Health Management Information Consortium
URL: www.ovid.com/site/catalog/databases/99.jsp
Date range searched: 1995 to September 2013.
Date of search: 16 September 2013.
Records retrieved: 75.
Social Care online
URL: www.scie-socialcareonline.org.uk/
Date range searched: 1995 to September 2013.
Date of search: 16 September 2013.
Records retrieved: 497.
Social Services Abstracts
URL: www.proquest.com/products-services/ssa-set-c.html
Date range searched: 1995 to September 2013.
Date of search: 13 September 2013.
Records retrieved: 364.
Sociological Abstracts
URL: www.proquest.com/products-services/socioabs-set-c.html
Date range searched: 1995 to September 2013.
Date of search: 13 September 2013.
Records retrieved: 364.
EconLit
URL: www.ebscohost.com/ACADEMIC/econlit
Date range searched: 1995 to September 2013.
Date of search: 13 September 2013.
Records retrieved: 15.
-
(adolescen* or teen* or “young adult”* or “young people” or “young person” or youth* or juvenile*).kw.
-
(mental* or psychiatr* or “tier 4”).kw.
-
(inpatient* or admission* or admitt* or discharge* or transfer* or transition* or hospital*).kw
-
1 and 2 and 3
Appendix 13 Call for evidence for phase 2
Appendix 14 Phase 2 screening tool
Appendix 15 Phase 2 excluded studies
| Study | Reason for exclusion |
|---|---|
| Abeles et al. (2008)236 | Psychometric assessment: CAMHS dependency scoring |
| Adrian et al. (2009)237 | Correlation study: emotion regulation and family and peer influences |
| Adrian et al. (2011)238 | Correlational study: non-suicidal self-injury and family and peer influences |
| Allen (2009)239 | Not inpatient: news article reporting on a policy document already sourced |
| Allen et al. (1996)240 | Not less obvious risks: follow-up study |
| Anderson et al. (2008)241 | Not adolescents: 25–51 + years |
| Anderson et al. (2012)242 | Not risk: development of a patient classification system |
| Ayton and Meads (2012)243 | Not risk: concerned with care programme approach |
| Bean et al. (2005)244 | Not risk: effectiveness of residential care |
| Bechberger (2012)245 | Not inpatient: partial hospitalisation programme |
| Bettmann and Jasperson (2009)246 | Review: relevant references extracted |
| Bickerton et al. (2007)247 | Not inpatients: outpatients |
| Cahalane (1997)248 | Not risk: family satisfaction |
| Carek and Hand (1995)249 | Not risk: change over time in one unit |
| Chesson (1997)250 | Not adolescents: mean age 9.3 years |
| Chung et al. (2008)251 | No disaggregated findings for adolescents in sample: rehospitalisation and parental influence |
| Clarke and Winsor (2010)252 | Not adolescents: 18–25 years |
| Cook-Darzens et al. (2001)253 | Not risk: family therapy for eating disorders |
| Curran et al. (2011)254 | Not less obvious risk: adult wards |
| Daniel et al. (2004)255 | Not risk: review of aftercare services |
| Delaney and Engels-Scianna (1996)256 | Not risk: parents’ perceptions of child’s emotional illness and treatment needs |
| den Dunnen et al. (2012)257 | Not risk: factors influencing long-term follow-up |
| Dicker et al. (1997)258 | Not less obvious risk: family support and admission |
| Drell (2006)259 | Unable to determine age of adolescents: text refers to sample throughout as adolescents |
| Duffy and Skeldon (2013)260 | Not risk: development of child and adolescent mental health intensive treatment service |
| Duthie (2001)261 | Not less obvious risk: adult wards |
| Fishman and Lewis (1998)262 | Not risk: medication compliance |
| Fontanella (2003)263 | Not less obvious risks: predictors of readmission |
| Fontanella (2008)115 | Not less obvious risk: predictors of readmission |
| Foster (1998)264 | Not less obvious risks: timing of follow-up services |
| Foster (1999)265 | Not risk: readmission and aftercare services |
| Galasso (2008)266 | Not risk: resilience |
| Garrison and Daigler (2006)267 | Not risk: discussion of treatment settings |
| Geraghty et al. (2011)268 | No disaggregated findings for adolescents in sample: peer support service (consumer consultants); children and youth of an inpatient unit aged 0–17 years |
| Ghaziuddin et al. (1999)269 | Not risk: predictors of medication non-compliance |
| Gorske et al. (2003)270 | Not inpatients: no disaggregation of community from RTC patients |
| Gowers and Rowlands (2005)271 | Not less obvious risk: general description of inpatient services |
| Gowers et al. (2001)272 | Not risk: general data on inpatient admissions |
| Green et al. (2001)273 | Not less obvious risk: health gain and costs/therapeutic alliance |
| Green et al. (2007)228 | Not less obvious risk: health gain and costs/therapeutic alliance |
| Gross and Goldin (2008)274 | No disaggregated findings for adolescents in sample: working in families of children and adolescents in an inpatient child and adolescent mental health facility; single case study of girl aged 13 years but no data relevant to the evidence synthesis |
| Gullick et al. (2005)275 | No less obvious risk: seclusion |
| Gunter et al. (1999)276 | No less obvious risk: reasons for admission |
| Harpaz-Rotem and Blatt (2005)277 | Not risk: psychopathology |
| Hawkridge (2002)278 | Not risk: availability of beds |
| Heinberg et al. (2003)279 | Not less obvious risk: adult wards |
| Hodges et al. (1999)280 | Psychometric assessment: utility of the Child and Adolescent Functional Assessment Scale in assessing functional status in youth with serious emotional disturbance |
| Hofstra et al. (2011)281 | Not risk: psychopathology and family factors |
| Jacobson et al. (1996)282 | Not risk: comparison of children and adolescents funded by Medicaid and commercial insurance |
| Johnson (1996)283 | Not inpatient: outpatient service |
| Joiner et al. (1997)284 | Correlational study: self verification and depression |
| Joiner (2001)285 | Correlational study: defensiveness and peer rejection |
| Jonikas et al. (2003)286 | Not risk: general transition into adulthood |
| Kaplan and Racussen (2013)287 | Not risk: crisis recovery model |
| Kashani et al. (2000)288 | Not less obvious risk: aggression |
| Kavanaugh and Holler (2012)289 | Not risk: executive functioning |
| Kennedy (1999)290 | Not risk: treatment approaches |
| Kerr et al. (2006)291 | Correlation study: suicide and family and peer support before admission |
| King et al. (1997)292 | Not less obvious risk: suicide |
| King et al. (1997)293 | Not less obvious risk: suicide |
| Kiser et al. (1996)294 | Not inpatient: partial hospitalisation programme |
| Kjelsberg et al. (1999)125 | Not less obvious risk: long-term risks at follow-up |
| Kjelsberg (1998)295 | Not less obvious risks: long-term risks at follow-up |
| Kolakoski (2000)296 | Not available: US thesis |
| Kroll and Green (1997)78 | Psychometric assessment: development and initial validation of an instrument to measure family alliance |
| Kurtz (2009)8 | Not risk: service provision |
| Lamb et al. (2008)297 | Not less obvious risk: adult wards |
| Lambe (2012)298 | Review: relevant references extracted |
| Landers and Zhou (2011)299 | Not adolescents |
| Laws (1998)300 | Review: relevant references extracted |
| Leal (2005)301 | Not risk: stigma of mental illness in Hispanic children aged 2–17 years as it relates to primary payer, admission source and length of stay; secondary analysis of inpatient data linking to concept of stigma in discussion |
| Leavey and Davidson (2006)302 | Not adolescents: 0–16 years |
| Lee (2007)303 | Unavailable: US thesis |
| Leon (2000)304 | Not less obvious risk: harm to self/aggression |
| Lepper (2007)305 | Not risk: report on two examples of early intervention services in the light of new policy/guidance |
| Lewis (1998)306 | Not risk: views of mental health services in general |
| Lintsi et al. (1998)307 | Not risk: weight and height of school boys |
| Lopez (2000)308 | Not available: US thesis |
| Lukonis et al. (2001)57 | Not inpatient: suicide risks in the community setting |
| Lundberg et al. (2007)309 | Not adolescents: 18–84 years |
| Mackrell and Lavender (2004)310 | Not risk: peer relationships in general |
| Mattejat et al. (2001)311 | Unavailable: insufficient information and reference to German-language thesis |
| McDougall and Scott (2008)312 | Not less obvious risk: adult wards |
| McDougall et al. (2008)231 | Not risk: overview of tier 4 services |
| McDougall et al. (2009)313 | Not less obvious risk: adult wards |
| McGilloway et al. (2000)135 | Not less obvious risk: adult wards |
| McNamara (2002)314 | Not risk: discussion of working within the law |
| Mears and Worrall (2001)315 | Not less obvious risk: Children Act and Mental Health Act |
| Mental Welfare Commission for Scotland (2006)316 | Not less obvious risk: adult wards |
| Miller et al. (2004)317 | Not risk: patterns of comorbidity |
| Moses (2010)318 | Not in-patient: wraparound programme – community-based intervention |
| Myers et al. (2008)319 | Not available: unable to locate via interlibrary loan |
| Niedermeier et al. (1995)320 | Psychometric assessment: validity of Family-of-Origin Scale |
| O’Brien (2002)321 | Not risk: parent support group – facilitator’s perspective |
| O’Herlihy et al. (2003)322 | Not adolescents: children and adolescents |
| Oleniuk et al. (2013)323 | Not adolescents: children and adolescents |
| Ornstein et al. (2012)324 | Not inpatient: partial hospitalisation |
| Park et al. (2011)325 | Not less obvious risk: adult wards |
| Parry-Jones (1997)326 | Not risk: treatment |
| Petit-Zeman (2001)327 | Not mental health: cancer patients |
| Phillips (1996)328 | Not less obvious risk: behaviour ratings by teachers and therapists |
| Pogge et al. (2008)114 | No less obvious risks: 6-year outcomes after treatment |
| Pridgen (2010)329 | Not risk: skills-based internet curriculum |
| Prinstein et al. (2000)330 | Correlational study: peer functioning and suicidal ideation in an inpatient sample |
| Prinstein et al. (2010)331 | Correlational study: peer influence as a potential risk factor for adolescent non-suicidal self-injury; study 1, community sample; study 2, inpatient sample; not related to actual inpatient experience; authors wanted a clinical sample to study longitudinally |
| Puasiri et al. (2011)332 | Not risk: family adaption to their child with a mental illness |
| Pugh (2008)333 | Not risk: broad-based discussion of impending legislation |
| Puotiniemi et al. (2002)334 | Not adolescents: mean age of sample 10.7 years |
| Reilly (2006)335 | Not risk: views and experiences of the inpatient admission process |
| Rice et al. (2002)72 | Not less obvious risk: factors influencing admission |
| Rutkowski (2011)336 | Not available: US thesis |
| Sawyer and Kosky (1995)337 | Not risk: broad-based discussion on South Australian experience of CAMHS effectiveness |
| Schnell (2008)338 | Not risk: occupational performance |
| Scott et al. (2001)339 | Not less obvious risk: adult wards |
| Sheftall et al. (2013)340 | Not risk: attachment theory |
| Shulman et al. (2000)341 | Correlational study: how hospitalised and non-hospitalised adolescents perceived their relationships with a close friend |
| Simon and Savina (2005)342 | Unable to determine age of children: mental health therapists working with children in inpatient settings; age of children not specified – author contacted and such data not collected |
| Simon and Savina (2010)343 | Unable to determine age of children: hospital-to-school transitions of children with mental health disorders; focused on perspectives of special education teachers; age of children not specified – author contacted and such data not collected |
| Slowik et al. (2004)344 | Unable to determine age of children: open group for parents and carers of children on two inpatient units |
| Smith (2010)345 | Not risk: discussion article on age-appropriate care environments – points to policy documents |
| Sourander and Piha (1996)346 | No disaggregated findings for adolescents in sample: family-orientated treatment programme for inpatients aged 7–14 years |
| Stage (1999)347 | Not risk: family therapy |
| Steel and Ofield (1998)348 | Unavailable: unable to locate via interlibrary loan |
| Street and Svanberg (2003)349 | Discussion of findings from previously published study report that was not relevant: YoungMinds, Meeting the Needs of Children and Young People with Serious Mental Illness |
| Street (2004)350 | Discussion of findings from previously published study reports that were not relevant: YoungMinds, Whose Crisis Report; YoungMinds, Where Next Report |
| Sutherland and Harkness (2007)351 | Not risk: description of daily life in a mental health unit |
| Tan et al. (2004)352 | Not risk: description of service provision |
| The Children’s Commissioner for England (2007)13 | Not less obvious risk: adult wards |
| Thompson et al. (2010)353 | Not less obvious risk: adult wards |
| Tonin (2007)354 | Not risk: opinion article on young people and the mental health-care system |
| van Bokhoven et al. (2006)355 | Not adolescents: mean age of sample 10.1 years |
| Walter and Petr (2004)356 | Not risk: transition to standard schools from special school |
| Welsh (1998)357 | Not less obvious risk: adult wards |
| Wood et al. (2008)358 | Not inpatient: young offenders |
| Worrall et al. (2004)359 | Not less obvious risk: adult wards |
| Yonge (2007)360 | Unable to determine age of adolescents: text refers to sample throughout as adolescents |
| YoungMinds (2008)361 | Not less obvious risk: adult wards |
| Zaitsoff et al. (2009)362 | Not risk: social competence in eating disorders |
| Zilikis et al. (2011)363 | Not risk: admission parameters |
Appendix 16 Phase 2 data extraction research papers (qualitative studies) (n = 8)
| Author (year of publication) Country Research aim Focus |
Design and methods Population |
Demographic details | Key findings relevant to the review |
|---|---|---|---|
| Buston (2002)175 UK (Scotland) To explore the health-related views and experiences of adolescent users of mental health services through semistructured interviews with 32 14- to 20-year-olds who had been diagnosed with a mental illness Dislocation: Education; Dislocation: Families; Dislocation: Friends |
Qualitative: semistructured interviews; grounded theory approach Adolescents |
Location: inpatients across mental health units in Scotland Sample: adolescents who had been diagnosed with a mental illness a year or more previously (n = 32); of those, 12 had been admitted as inpatients at some point (n = 12) Length of stay: not applicable Sample: see above Age (years): mean 17.3, range 14–20 Gender: male 34% |
165 substantive comments or dialogues relating to experiences of health care appeared in the 32 transcripts. 61 of the comments were coded as positive, 104 as negative. These relate to the doctor–patient relationship, treatment received, the health-care system and the environs of the hospital/clinic |
| Claveirole (2005)176 UK (Scotland) ‘To explore young people and their carers’ experience regarding treatment and participation in decision-making in four Scottish adolescent inpatient or day-care mental health units’ Contagion; Dislocation: Education; Dislocation: Families; Dislocation: Normal Life; Dislocation: Stigma |
Qualitative; ethnography: interviews (‘guided conversations’); unit documents; participant observation (21 weeks written up in 93,000 words of fieldnotes) Adolescents: interviews; parents: interviews; staff: interviews |
Location: intensive mental health treatment units for adolescents, both inpatient and day-care settings Sample: adolescents (n = 18), day patient (n = 11), inpatient (n = 7); parents (n = 16); staff (n = 23) Length of stay: not specified Age (years): mean 16, range 12–21 Gender: male 33% |
The findings suggest that the young people valued the personalised relationships they developed with the staff and their peers and that, if these relationships were empowering, they facilitated both treatment and participation in treatment. The findings also show that the parents and staff members were sometimes disempowered and that this impaired the overall participative nature of the units. The unit culture was an important contributor to the effectiveness of young people and parent involvement |
| Clemens et al. (2011)178 USA To identify constructs that detract from and are facilitative for successful reintegration to school after a psychiatric hospitalisation Clemens et al. (2010)177 USA To explore mental health-care professionals’ perceptions of the experiences and needs of adolescents as they transition from psychiatric hospital to school (Two papers from the same study) Dislocation: Education; Dislocation: Friends |
Qualitative: interviews; ‘consensual qualitative research’ HCPs |
Location: four different psychiatric hospitals located in three states and encompassing four school districts Length of stay: average 5–7 days Sample: mental health professionals who had recent experience working with adolescents who have transitioned from a short-term psychiatric hospitalisation back to their previous school (n = 14) |
Clemens et al. (2011): five domains emerged from the participants’ descriptions of factors that are related to success of adolescents’ school re-entry: school-based factors, student factors, familial factors, mental health-care factors and systemic factors Clemens et al. (2010): three domains emerged from the participant descriptions of adolescent school re-entry after psychiatric hospitalisation: academic, social and emotional |
| Colton and Pistrang (2004)179 UK (England) To provide a detailed description of how adolescents on inpatient, specialist eating disorder units view their treatment Contagion; Dislocation: Families; Dislocation: Friends; Dislocation: Identity |
Qualitative: interviews; time frame not specified; ‘discovery oriented, phenomenological approach’ Adolescents |
Location: recruited from two 10-bed, inpatient, eating disorder units for adolescents Length of stay: 5 to 20 weeks Sample: 19 young people from a total inpatient number of 25 Age (years): mean 15.4, range 12–17 Gender: female 100% |
Themes:
|
| Haynes et al. (2011)180 and Painter (2008)181 To explore adolescents’ experiences of psychiatric hospitalisation Dislocation: Education; Dislocation: Friends; Dislocation: Identity; Dislocation: Normal Life; Dislocation: Stigma |
Qualitative: interviews; grounded theory approach Adolescents |
Location: one adolescent inpatient unit and one adolescent unit in an independent hospital Length of stay: 4 weeks to 36 months Sample: adolescents who have been resident at a psychiatric inpatient unit for at least 2 weeks in the last 18 months (n = 10) Age (years): 13–19 years Gender: male 40% |
The core category and process model: Living in an alternative reality: a process model was developed consisting of seven main categories that related to the core category, either as contributory or outcome categories, as follows. Contributory categories: feeling restricted; feeling disconnected; negotiating new relationships. Outcome categories: developing supportive relationships; recreating reality; intellectualising; avoiding harm |
| Moses (2011)182 USA To conduct an in-depth examination of the range and meaning of adolescents’ subjective accounts of the most helpful and unhelpful/harmful aspects of their first psychiatric inpatient treatment Dislocation: Friends; Dislocation: Identity; Dislocation: Normal Life; Dislocation: Stigma |
Qualitative: interviews within 7 days of discharge; thematic analysis Adolescents |
Location: community-based hospital with a child and adolescent inpatient programme Length of stay: 7.6 ± 3.9 days, range 3–31 days Sample: adolescents (ages 13–18 years) entering their first psychiatric hospitalisation (n = 80 of 213, 38.5%) between June 2007 and March 2010 Age (years): mean 15.3 Gender: male 59% |
Most helpful experiences: peers: support and normalisation 58.8%; staff: support and interpersonal relationships 45.0%. Least helpful, harmful or disliked aspects: being away from home 6.3%; stigma related to being in hospital 3.8%. Most descriptions of unhelpful experiences fell into three categories: (1) perceived rigidity or confinement, (2) perceived lack of treatment responsiveness and (3) frightening or anxiety-provoking experiences |
| Offord et al. (2006)183 UK (England) To add to the current literature by asking a group of young adults their views on the treatment they had received while admitted to a general adolescent psychiatric unit; to elicit participants’ views regarding the impact their admission had on issues such as control and self-esteem, and their views regarding the process of discharge and subsequent adjustment to life back in the community Contagion; Dislocation: Education; Dislocation: Families; Dislocation: Friends; Dislocation: Identity; Dislocation: Normal Life; Dislocation: Stigma |
Qualitative: interviews; all had been discharged from inpatient care 2–5 years prior to the study; interpretative phenomenological analysis Adolescents and young adults |
Location: general adolescent units (n = 6); adult outpatient eating disorder services (n = 1) Length of stay: not stated Sample: participants were recruited either from past inpatient records from general adolescent units (n = 6) or by face-to-face contact with clinicians in adult outpatient eating disorder services (n = 1) Age (years): 16–23 Gender: female 100% |
Four superordinate themes emerged from participants’ accounts of their experiences of treatment and discharge:
|
| Puotiniemi and Kyngas (2004)184 Finland To describe the coping of an adolescent who had been in psychiatric inpatient care and her mother in everyday life Dislocation: Families; Dislocation: Friends |
Qualitative: Three interviews over 2 years 1999–2001; inductive content analysis Adolescent; parent |
Location: previously been an inpatient Sample: n = 1 Length of stay: not stated Age (years): 16 Gender: female |
Coping strategies and resources of an adolescent who has been in psychiatric inpatient care and her mother |
Appendix 17 Phase 2 data extraction research papers (experimental studies) (n = 4)
| Author (year of publication) Country Research aim Focus |
Design and methods Population |
Demographic details | Outcome Measures |
Key findings relevant to the review |
|---|---|---|---|---|
| Best et al. (2004)127 USA To examine early adulthood outcomes of psychiatrically hospitalised adolescents Dislocation: Education |
Prospective cohort study: admission, 11-year follow-up (95% response rate), 20-year follow-up (95% response rate); statistics, analytical statistics Adolescents |
Location: psychiatric units in one metropolitan area of north-west USA (1978–81) matched with one high school in same area Length of stay: hospital stays ranged from 37 to 921 days (mean 198 days) Sample: hospitalised adolescents, consecutive admissions to traditional psychiatric inpatient wards during a 2-year period (n = 70); high school adolescents, ninth-grade students recruited from a public high school in an adjacent community (n = 76) Age (years) on recruitment: hospitalised adolescents mean 14.1 ± 1.0, range 11.8–15.9; high school adolescents mean 14.5 ± 0.4, range 13.8–15.8 Gender: hospitalised, male 56%; high school, males 46% |
Outcomes: death; emotional distress; high school completion; educational attainment Measures: death, through newspaper reports and follow-up contacts; emotional distress, Derogatis Symptom Checklist; high school completion and educational attainment, self-reported and coded 1–6 (1, less than high school; 2, general equivalency diploma; 3, high school graduate; 4, postsecondary education; 5, college graduate; 6, graduate degree) |
High school completion: hospitalised adolescents (64%) were less likely to complete high school than high school adolescents (91%) (p < 0.0001) Educational attainment: hospitalised adolescents (64%) were less likely to gain a bachelor’s degree (6%) than high school adolescents (93%) (p < 0.0001); hospitalised adolescents (64%) were less likely to gain a graduate degree (2%) than high school adolescents (33%) (p < 0.0001) |
| Singh et al. (2002)173 USA (based on authors’ affiliations) A report of two studies that rated the family-friendliness of the admissions treatment team process prior to and following different types of training intended to enhance family-friendliness Study 1: to assess the effects of structured role play training on enhancement of family-friendliness of admissions treatment teams Dislocation: Families Study 2: to assess the effects of mindfulness training on the enhancement of family-friendliness of an admissions treatment team in the delivery of mental health services Dislocation: Families |
Study 1, before-and-after study (no control group): intervention, structured role play training, pre-training observation (n = 18), post-training observation (n = 18); statistics, analytical statistics HCPs |
Study 1 Location: an inpatient child and adolescent psychiatric hospital Sample: children and adolescents (n = 36) admitted to an inpatient child and adolescent psychiatric hospital and whose primary caregiver could be present during the treatment-planning meeting at the time of admission. Two admissions treatment teams (numbers not given) Age (years): before training, 11.3; after training, 11.6 Gender: before training, male 55.6%; after training, male 55.6% |
Study 1 Outcome variable: family-friendliness Measures: Family Assessment Planning Team (FAPT) – adapted for inpatients; introduction; meeting management; case presentation/discussion; service plans; tact and technicalities |
Study 1 Family-friendliness: introduction; pre 0.79, post 0.78; t-value 0.18, p = 0.86 Meeting management: pre 0.85, post 0.93; t-value –1.56, p = 0.13 Case presentation/discussion: pre 0.80, post 0.82; t-value –0.71, p = 0.49 Service plans: pre 0.67, post 0.48; t-value 2.80, p = 0.01 Decline in family friendliness: tact and technicalities; pre 0.73, post 0.69; t-value 0.72, p = 0.47 Role plays did not impact on the family-friendliness of the treatment teams |
| Study 2, before-and-after study (no control group): baseline observations (n = not specified), follow-up observations (once a month for 6 months) (n = not specified); intervention, mindfulness training; statistics, descriptive statistics HCPs |
Study 2 Location: an inpatient child and adolescent psychiatric hospital Sample: children seeking services and their primary caregivers were included in each training session. Members of one admission treatment team (n = 5) |
Study 2 Outcome variable: as per study 1 Measures: as per study 1 |
Study 2 Family-friendliness: introduction; baseline 79%, training 97.7%, follow-up 100% Meeting management: baseline 88%, training 100%, follow-up 100% Case presentation/discussion: baseline 82%, training 94.7%, follow-up 100% Service plans: baseline 54.3%, training 75.3%, follow-up 90.5% Tact and technicalities: baseline 69.1%, training 84%, follow-up 93.5% Increases in family-friendless were evident across the five components of treatment team meetings. The gains were substantial and maintained during a 6-month follow-up period |
|
| Simmerman (1997)174 USA To identify some of the factors that appear to assist students in an adolescent residential treatment centre to accomplish more academically in spite of the emotional issues they are also dealing with; to assess any improvements in grades and number of earned credits Dislocation: Education |
Quasi-experimental multiple time series (retrospective): data drawn from records over the 10 months before and 10 months after the programme change. Intervention: compared a (previous) self-contained classroom format – remained in one classroom for entirety of the school day, students confined in single space for several hours, teachers expected to provide materials and instructions for all subject areas grades 7–12 – with (current) rotating, multiclass format; divided the programme to include four classrooms and teachers, classes smaller and more specialised Adolescents |
Location: residential treatment centre Length of stay: not stated Sample: 107 subjects drawn from students attending the RTC. Only requirement for eligibility is to have been a resident in the programme. Individuals have a variety of psychological difficulties Age (years): age of subjects in the treatment centre stated to be 12–19 years but age of the actual sample not indicated Gender: not stated |
Outcome measures: assessment of grades and credits taken from records of written assignments, exercises, projects, etc. | Previous programme: mean number of credits earned per student over entire stay, 20.86; mean number of credits earned per day, 0.37; academic average, 87.06 Current programme: mean number of credits earned per student over entire stay, 31.57; mean number of credits earned per day, 0.51; academic average, 87.02; t-value between credits in the class conditions over entire stay 2.85, p < 0.01; t-value between credits earned per day in the class conditions 2.69, p < 0.01; t-value between academic averages in class conditions was p = 0.03 |
Appendix 18 Phase 2 data extraction research papers (non-experimental studies) (n = 15)
| Author (year of publication) Country Research aim Focus |
Design and methods Population |
Demographic details | Variables Measures |
Key findings relevant to the review |
|---|---|---|---|---|
| Anderson et al. (2008)185 USA To examine how personal, environmental and substance use factors predicted psychosocial functioning for youth with alcohol and drug problems Dislocation: Education |
Longitudinal descriptive survey (prospective): on admission, 1 year post discharge; statistics, regression analysis Adolescents |
Location: five inpatient adolescent mental health and substance abuse treatment programmes; consecutive admissions to each treatment centre Length of stay: not specified Sample: adolescents (n = 424) with substance use disorder, details at follow-up not provided Age (years): mean 15.9 ± 1.3, range 13–18 Gender: male 49.5% |
Intake variables: demographics/family history, psychopathology, conduct disorder symptoms, internalising symptoms, alcohol expectancies, motivation, self-esteem, substance involvement. Post-treatment variables: aftercare services, exposure to substances. Outcome variables: academic functioning, family relations, social functioning, health status, mental health treatment Demographic questionnaire, including mental health history of child |
Academic functioning: at baseline, adolescents entering treatment were most likely to report getting below average grades (Ds and Fs 53%). The post-treatment variables (aftercare services and exposure to substances) accounted for 7% of the variance in academic functioning. Exposure to substances in the year post treatment was a predictor of academic functioning (p = 0.00). Younger age at treatment onset was associated with better academic functioning (p = 0.00) |
| Brinkmeyer et al. (2004)186 USA To examine the association between family engagement and consumer satisfaction for children and young people admitted to an psychiatric inpatient unit Dislocation: Education; Dislocation: Families |
Longitudinal descriptive survey (prospective): admission, discharge, 9 months post discharge; statistics, analytical statistics Parents, HCPs |
Location: one child and adolescent psychiatric unit Length of stay: inpatient – short stay, median 6 days Sample: the parents/guardian of children and adolescents (n = 47) on admission (n = –47), at discharge (n = 34) and at 9-month follow-up (n = 25) Age (years): mean 13.11 ± 2.89, range 7–17 Gender: male 56% |
Outcome variables: satisfaction and engagement with service; child mental health Parents: CBCL, IPSI; phone follow-up included questions about rehospitalisation, expulsion from school, arrest, suicide attempt. HCPs: FEQ |
Family engagement: on the FEQ (administered only at time 1), total scores ranged from 34 to 72 out of a possible 72 (mean 57.64, SD 9.46) Distance from unit: the distance families lived from the inpatient unit was not related to parent engagement or satisfaction Schooling: 12% had been expelled from school Hypothesis 1: partly supported. Satisfaction was negatively correlated (r = –0.542) with clinician ratings of parent hostility (p < 0.001). Parent satisfaction ratings were positively correlated (r = 0.737) with clinical ratings of parent alliance (p < 0.05). Satisfaction ratings were not related to therapist ratings of child engagement Hypothesis 2: partly supported. Parent reports of child externalising behaviour were not correlated with therapist-rated child alliance, although they were positively correlated (r = 0.388) with therapist ratings of child hostility (p < 0.05) Hypothesis 3: partly supported. Total engagement, child alliance, child confiding and parent satisfaction were lower and parent hostility was higher for families with prior inpatient hospitalisations. These findings were not statistically significant, although their moderate to large effect sizes suggest that they would attain statistical significance with a larger sample. Parents who go into their child’s hospitalisation with positive expectations are more likely to participate meaningfully than those whose expectations are negative. By the same token, when parents participate meaningfully in their child’s care, they are likely to be more satisfied with the care. It appears that parents’ satisfaction with their child’s treatment depends more on their own participation in treatment than their child’s |
| Cawthorpe et al. (2003)192 Canada To examine the occurrence of behavioural contagion among inpatient adolescent psychiatric patients in terms of past self-harm-related behaviours Contagion |
Longitudinal descriptive survey (retrospective): admission, discharge; statistics, analytical statistics Adolescents |
Location: inpatient psychiatric assessment and treatment unit for adolescents; consecutive admissions over a 5-year period between 1983 and 1988 Length of stay: males 95.67 ± 56.87 days, range 1–337 days; females 79.82 days, range 3–254 days Sample: adolescents (n = 198) Age (years): mean 14.89 ± 1.28 (males), 14.77 ± 1.17 (females), range 12–18 Gender: male 64% |
Outcome variables: deliberate self-harm; suicidal ideation; gestures; attempts; self-destructive behaviour without expressed suicidal intent (e.g. self-mutilation, self-harm occurring both prior to and during the course of admission) Data extracted from medical records |
Ideation: past 34.6% (male), 53.5% (female); inpatient 18.2% (male), 31% (female) Gesture: past 19.7% (male), 42.2% (female); inpatient 9.5% (male), 18.3% (female) A proportion of individuals persist in the expression of self-harm after admission for treatment, although on the whole less intensely than in the past. Not tested for significance Six naive subjects out of 198 exhibited self-harm behaviours as inpatients. 55% of males with past self-harm behaviours exhibited self-harm behaviour as inpatients. 4% without past self-harm behaviours exhibited self-harm behaviours as inpatients. The risk ratio among males representing the occurrence of inpatient self-harm behaviour, given no past self-harm behaviour, was 0.03 (SE = 0.02, 95% CI 0.01 to 0.12). Males who were behaviourally naive (i.e. no past self-harm behaviours) were significantly less likely to exhibit self-harm behaviour as inpatients. 53% of females with past self-harm behaviours exhibited self-harm behaviour as inpatients. 12% without past self-harm behaviours exhibited self-harm behaviours as inpatients. The risk ratio among females representing the occurrence of inpatient self-harm behaviour, given no past self-harm behaviour, was 0.13 (SE = 0.09, 95% CI 0.03 to 0.48) |
Charlemagne (2011)187 USA
|
Longitudinal descriptive survey (prospective): phase I, discharge; phase II, during hospitalisation; phase III, 3-month follow-up; statistics, logistic regression analysis Children and adolescents, parents, HCPs |
Location: child and adolescent inpatient psychiatric unit serving children (8–13 years) and adolescents (14–17 years) Length of stay: mean 5.9 ± 3.4 days Sample: convenience sample parents/caregivers of child and adolescent patients (n = 167); purposive sample clinicians (n = 27) multidisciplinary clinical team providing services 67% (n = 134) response rate at 3-month follow-up Gender: male 48.5% Age (years): 13 ± 2.7 |
Outcomes variables: parent visitation, parent participation in inpatient activities, parent perceptions of provider helping (supportive, transparent, empower, unsupportive). Covariates (research question 3): child age, sex, ethnicity, previous hospitalisation, psychosocial risk, length of stay, diagnosis Phase I: parents: FII, HBCL. Phase II: clinicians: PBAP – adapted. Phase III: parents: child and adolescent services assessment. Phase IV: children and adolescents: medical records |
Most parents reported participating in about three inpatient activities during their child’s hospital stay Previous hospitalisation, psychosocial risk and parent perceptions (empower) significantly predicted psychiatric rehospitalisation. Regression results indicated that the overall model was reliable in distinguishing between rehospitalised and non-rehospitalised children and adolescents (–2 log-likelihood = 156.336; Cox & Snell R2 = 0.160, Nagelkerke R2 = 0.234; χ2 (12) = 27.874, p < 0.006). The model correctly classified 77.5% of the cases The odds ratio indicated that, for children who were previously hospitalised, the odds of psychiatric rehospitalisation increased 2.98 times. In addition, for every unit increase in psychosocial risk, the odds of psychiatric rehospitalisation increased by 59%. Finally, the odds ratio indicated that, for every unit increase in parent perceptions (empower), the odds of psychiatric rehospitalisation increased by 42% Research question 4: clinician beliefs about parents do not predict psychiatric rehospitalisation |
| Czyz et al. (2012)188 USA To examine posthospitalisation change in connectedness with family, peers and non-family adults predicted suicidality in former inpatient adolescents Dislocation: Families; Dislocation: Friends |
Longitudinal descriptive survey (prospective): baseline, within 1 week of hospitalisation; 3, 6 and 12 months post hospitalisation; statistics, regression analysis Adolescents |
Location: inpatients from either a university hospital or a private hospital Length of stay: not specified Sample: the data for the present study were drawn from a larger study investigating the efficacy of a social support intervention – Youth-Nominated Support Team-II – for suicidal adolescents following hospitalisation. The original study included 448 adolescents, aged 13 to 17 years, who had been psychiatrically hospitalised because of acute suicidal ideation or attempts. The present study was restricted to adolescents who had completed at least one follow-up assessment 3, 6 or 12 months after hospitalisation (n = 338) Age (years): mean 15.6 ± 1.41 Gender: male 29% |
Outcome variables: connectedness – the degree to which respondents perceive their relationships as close, confiding, satisfying, and supportive; suicide attempts; suicidal ideation; depressive symptoms Connectedness, PEPSS; suicide attempts, DiSC; suicidal ideation, SIQ-Jr; depressive symptoms, youth self-report |
Predictors of depression: regardless of gender or multiple attempt status (of suicide) an increase in family connectedness following hospitalisation was associated with lower levels of depressive symptoms (p = 0.004). These results suggest that more severe symptoms of depression measured at baseline were associated with more severe symptoms of depression at follow-up (β = 0.19, p < 0.0001) and that greater family connectedness with family at baseline was related to less severe depressive symptoms at follow-up (β = −2.01, p = 0.021). The effect of increase in connectedness with peers was more shortlived, significant at 3 months (p = 0.003) but not sustained 6 (p = 0.652) and 12 months (p = 0.763) after hospitalisation Predictors of suicidal ideation: greater increase in connectedness with family 3 months after hospitalisation predicted less severe suicidal ideation for the year (p = 0.0005). No effect of peer connectedness on suicidal ideation at 6 months for either gender. The significant interaction between change in family connectedness and multiple attempt status suggests that greater increase in connectedness with family 3 months following hospitalisation predicted less severe suicidal ideation during the entire 1-year follow up period, but only for adolescents without multiple attempt histories (β = −4.10, p = 0.0005) Predictors of suicide attempts: change in peer connectedness was associated with a lower likelihood of making a suicide attempt during the follow-up period. Specifically, after adjusting for the effect of gender, multiple attempt status, treatment group and baseline peer connectedness, the odds of attempting suicide following hospitalisation were reduced by approximately one-half (OR = 0.55, 95% CI = 0.32 to 0.94) for adolescents who reported greater, versus lesser, increase in posthospitalisation connectedness with peers |
| Larzelere et al. (2001)189 USA No explicit aim – implicitly an evaluation of a residential treatment centre Dislocation: Education |
Longitudinal descriptive survey (prospective): admission, discharge, follow-up (6–21 months); statistics, descriptive statistics Adolescents |
Location: first 43 youths admitted to a RTC Length of stay: 18–505 days, mean 181 days, median 15 days Sample: severely disturbed youths (n = 43) with a mixture of MH problems Age (years): mean 13.0, range 6–17 Gender: male 48% |
Outcome variables: problem behaviours, level of functioning, restrictiveness of living environment, youth satisfaction Intake (pre) measures: ROLES, CBCL, CGAS, YSS. Discharge (post) measures: ROLES, CBCL, GCAS, YSS. Follow-up measures: CBCL, in school/employed, use of MH services |
96% either were going to school (89%) or had graduated and were working. Of those asked (n = 19), 79% were reported as doing the same in school as, or better than, they had been before the RTC treatment |
| Moses (2011)195 USA To establish to what extent young people discharged from brief hospitalisation feel apprehensive about being stigmatised, and to what extent the level of stigma apprehension is related to personal characteristics, collective stigma representations and interpersonal support Dislocation: Stigma |
Cross-sectional descriptive survey: within 7 days of discharge; statistics, analytical statistics, regression analysis Adolescents |
Location: community-based hospital with a child and adolescent inpatient programme Length of stay: 3–31 days, mean 7.6 ± 4.2 Sample: adolescents following first admission (n = 102 of 265, 38.5%) with a mixture of mental health problems (June 2007 to July 2010) Age (years): mean 15.3 ± 1.5, range 13–19 Gender: male 91.3% |
Dependent variable: stigma apprehension. Predictor variables: personal characteristics including clinical and demographic factors; collective representations and personal stigma experiences; interpersonal support – family, friends and school Author-developed stigma apprehension questionnaire; peer group identification – identify peer groups (they) identify with most from choice of 12; social affiliation – represent each participant’s percentage of friends with mental health problems; self-identification – extent to which participants identify as having significant mental health problems; domain identification – each participant was asked to rate how important is having mental health problems to their sense of who they are or the way that they think about themselves; self-worth contingency – approval from others subscale of the CSWS; perceived societal devaluation – seven items adapted from PDDS; personal rejection – six items, four of which were adapted from RES; general family functioning – general functioning subscale of the FAD; relationships with friends – includes nine items from IPPA; School Attachment Scale |
To what extent did adolescents report stigma apprehension? Respondents did not report a great deal of stigma apprehension; most common stigmatising experience was ‘people look down on you when they find you are in treatment’; least stigmatising experience was friends rejecting you after they find out about treatment What circumstances and attributes relate to youths’ stigma apprehension? Bivariate analysis showed that participants who reported identifying with ‘peers with emotional problems’ and ‘kids who get into trouble’ scored significantly lower on stigma apprehension (p = 0.007 and p = 0.001 respectively). The proportion of participants’ friends with perceived/known mental health problems was inversely related to their level of stigma apprehension (p = 0.005). Adolescents scoring higher scores on ‘need for others approval’ also scored higher on stigma apprehension (p < 0.001). Women reported significantly more stigma apprehension than men (p = 0.01). Adolescents who reported more perceived societal devaluation of youth with mental health problems in society (p = 0.01) and more experiences of personal stigmatisation in the past (devaluation, rejection, exclusion; p < 0.001) reported higher stigma apprehension after discharge from hospital. Multivariate model – accounted for 46% of the variance of youths’ reported stigma apprehension. Factors that demonstrate unique contributions to explaining stigma apprehension include sex (female), age at first mental health treatment (being younger at initiation of treatment), need for others’ approval for self-worth (greater), a discrimination against youth with mental health problems and quality of friendship support (R2 = 0.46, p < 0.001) |
| Moses (2014)190 USA To examine social and clinical factors that predict enacted stigma Dislocation: Stigma |
Longitudinal descriptive survey (prospective) (follow up of Moses195 – anticipatory stigma): within 7 days of discharge (time 1), 6 months later (time 2); statistics, analytical statistics, regression analysis Adolescents |
Location: community-based hospital with a child and adolescent inpatient programme Sample: adolescents following first admission (n = 102 of 265, 38.5%) with a mixture of mental health problems at time 1 (June 2007 to July 2010) and study retention at time 2 was 80 of 102, 78.4% Age (years): mean 15.3 ± 1.6, range 13–18 Gender: male 35% |
Predictor variables at time 1 (immediate post discharge): social context, clinical symptoms, school functioning. Outcome variable at time 2: stigma Family support – general functioning subscale of the FAD; quality of relationship with friends – includes nine items from IPPA; number of friends; peer group identification – identify peer groups (they) identify with most from choice of 12; number of friends with MH problems; symptom severity – two broad subscales of YSF; grade achievement; school discipline problems; special learning needs; enacted social stigma – four out of five items adapted from RES; perceived public stigma – 14 items of which half are adapted from PDDS |
6 months following their discharge from psychiatric hospitalisation, 70% of adolescents reported experiencing one or more aspects of enacted mental illness stigma. Most of the stigma reported was not outright social rejection, but rather general devaluation, disrespect, emotional insult and being underestimated by others. Significant predictors of enacted stigma at follow-up: number of friends with psychological problems, affiliation with popular peers, and school disciplinary problems; the model explained 36% of the variance |
| Parmelee et al. (1995)191 USA To identify demographic, clinical and service history characteristics of children and adolescents following discharge from hospital Dislocation: Families |
Longitudinal descriptive survey (prospective): baseline, 3 and 12 months, after discharge; statistics, analytical statistics Children and adolescents, parents |
Location: two state hospitals in Virginia Sample: all children and adolescents admitted within a 3-month period (n = 90) at 1-year follow-up (n = 77) Age (years): mean 12.2 ± 3.5, range 4–17 Gender: male 64% |
Outcome variables: a series of follow-up questionnaires Parents: CBCL. Data sources included medical records while the child was in hospital, clinician discharge plan and records from the community mental health clinic for postdischarge data. Telephone interviews were also conducted at 3 and 12 months after discharge with the parents/legal guardians |
Family involvement in the treatment planning during hospitalisation (p = 0.004) and living with a family member at time of hospitalisation (p = 0.011) was significantly associated with the use of aftercare services at 3-month follow-up |
| Thurber et al. (2007)196 USA To understand the role of homesickness in children’s adjustment to hospitalisation Dislocation: Families |
Cross-sectional descriptive survey: second or third day of hospitalisation or sometimes longer; statistics, analytical statistics Children and adolescents, parents, HCPs |
Location: three hospital units: a burn unit (n = 13), a paediatric rehabilitation unit (n = 13) and an inpatient child psychiatric unit (n = 49) Length of stay: median 20 days, mean 24 ± 25, range 4–174 days Sample: parents of children aged 3–18 years (n = 75); children and adolescents aged 8–18 years (n = 50) Age (years) (n = 75): mean 11 ± 3.5, range 3.9–18.6 Gender (n = 75): male 70% |
Predictor variables: demographics, socioeconomic status, weeks of previous hospitalisation, weeks of previous separation from home, number of times in foster care, number of trips away from home without parents/guardians Parents: MSAS, CBCL. Children aged 8 years or over: RYDR, CHA, SRASP, CDI. HCPs: CSRS, CGF |
88% of the participants reported some homesick feelings during hospitalisation. Mean self-reported homesickness, calculated by averaging eligible respondents’ scores on the RYDR homesickness scale across all administrations was 15.3 ± 10.6. The mean score on the pain scale was 10.2 ± 9.3. Adjusted to the same 0–30 point range, the Positive Emotion and Negative Emotion scale means were 17.8 ± 6.5 and 8.7 ± 6.6 respectively. There were no differences among the three hospital units in self-reported homesickness, negative emotion or positive emotion. On the psychiatric unit, homesickness was not correlated with the severity of children’s problems, as indexed by the admitting psychologist’s or psychiatrist’s global assessment of functioning rating (Axis V on the DSM-IV-TR’s multiaxial assessment system; r = –0.02, p = 0.92). Positive correlation between homesickness and number of weeks of previous separations from home (r = 0.31, p < 0.05) |
| Shabat (2008)193 USA To investigate the differential response to residential treatment in youths with and without conduct disorder in a large state system Dislocation: Education |
Longitudinal descriptive survey (retrospective): day 30, every 6 months until discharge; conducted using the residential treatment outcome system (RTOS), which gathers demographic, assessment and outcome data about Department of Child and Family Services (DCFS) wards; statistics, analytic statistics Children and adolescents |
Location: 50 RTCs and group homes Length of stay: mean 90.6 days Sample: children and adolescents who were wards of the DCFS (n = 457) between January 2002 and January 2004 Age (years): 6–20; 6–11, 12–14, 15–17, ≥ 18 Gender: male 61% Diagnosis: conduct disorder (CD) n = 90 (26.3%); without conduct disorder (non-CD) n = 239 (73.7%) |
Outcome variables: mental health functioning; school attendance Mental health functioning: CFARS (work or school function within last 3 weeks). School attendance: percentage of school attendance calculated from the data in RTOS; school attendance calculated from data regarding the number of school days attended out of the number of school days scheduled in both on-site and off-site schools |
The relationship between CD group membership and change in performance in work or school depended on age range as measured on day 30 of treatment (F = 5.36, p = 0.005) and on discharge (F = 3.36, p = 0.036). Further analysis revealed that changes in work or school performance (worsened) were found for youths between the ages of 6 and 11 years at 30 days (F = 10.51, p = 0.003) and on discharge (F = 4.55, p = 0.041). No change for youths aged 12–14 years or 15–17 years. The relationship between CD group membership and school attendance was not dependent on age range as measured on day 30 of treatment (F = 1.05, p = 0.370) and on discharge (F = 1.00, p = 0.395) |
| King et al. (1995)142 USA To investigate whether or not exposure to other suicidal adolescents led to suicide contagion among patients hospitalised on an acute adolescent psychiatric unit Contagion |
Longitudinal descriptive survey (prospective): on admission and within 3 days of hospital discharge, 8-month period of data collection; statistics, descriptive statistics Adolescents |
Location: adolescent inpatient psychiatric unit Length of stay: 24.9 + 10.7 days Sample: adolescents admitted during an 8-month period (n = 57) Age (years): mean 15.8 ± 1.3, range 11.5–17.8 Gender: male 42% |
Measures: patient’s exposure to other self-harmful or suicidal patients recorded. Depression – CDRS-R; suicidal ideation – SIQ-Jr (covered 1 month before hospitalisation); suicidal behaviour – SSB (covered 6 months before hospitalisation) | No completed suicides and no suicidal behaviours with clear suicidal intent during the study period. 7% (n = 4) engaged in self-cutting without clear suicidal intent and these behaviours did not cluster. Suicidal thoughts or the overt expression of these thoughts did increase among 26% of adolescent inpatients during hospitalisation |
| Lakin et al. (2004)194 USA To determine if patients with greater parental involvement would have a lower recidivism rate than those patients with less parental involvement Dislocation: Families |
Longitudinal descriptive survey (retrospective): time frame of data collection not specified; statistics, analytical statistics; parental involvement – length of stay had to be long enough to allow for phone calls, visits, therapeutic absence and therapy – three subjects excluded from this part of the analysis Children and adolescents |
Location: RTC Length of stay (days): mean 58.6 + 35.1, range 7–243 Sample: children and adolescents admitted between 1 December 1998 and 30 April 2000 (n = 97). Eight excluded (reasons given) = 89 Age (years): mean 11.7, range 5–17 Gender: male 67% Diagnosis: severe behavioural problems |
Outcome variables: recidivism; parental involvement Medical record review; demographics; frequency of weekly parent phone calls; frequency of weekly parent visits; therapeutic absences (special passes so that young people may leave the facilities or grounds with their families for an allotted period of time); participation in weekly family therapy sessions; family APGAR scores (A, adaption; P, partnership; G, growth; A, affection; R, resolve); CFARS; CAFAS |
The mean number of physical parent contact per week (visits and therapeutic absence) was 2.1 (range 0.5), and the mean number of total parent contacts per week (physical contact plus phone calls) was 3.9 (range 0–8). A significant relationship was found between physical parent contacts and family functioning at discharge, r = 0.42, p = 0.001. A significant relationship was found between total parent contacts during the patients’ stay and family functioning at discharge, r = 0.41, p = 0.001. Patients who returned to the hospital (either to acute or to RTC) had significantly lower levels of family functioning (APGAR scores) at discharge than patients who did not return, t = 2.16, p < 0.05 |
| Halfon et al. (1995)128 France To examine the major sociological, family, clinical and schooling features of adolescents with psychiatric disorders Dislocation: Education |
Longitudinal descriptive survey (retrospective): time frame of data collection not specified; statistics, descriptive statistics, analytic statistics Adolescents |
Location: psychiatric unit for adolescents Length of stay: mean 10 months and 10 days ± 9.3 Sample: all adolescents hospitalised who were then discharged, January 1991 to December 1993 (n = 137) Age (years): mean 17.8 ± 1.5, range 14–21 Gender: male 54% |
Outcome variables: school performance; academic progress at discharge; patient and family characteristics No specific tools or measures, just basic data collection |
28% admitted to a higher grade or were successful in their final exams; 18 of 137 graduated; 99 of 137 failed to fulfil their academic project; 43 of 137 left the centre with no educational or career project; 64 of 137 left to be admitted to a normal school environment; 30 of 137 took up a career after discharge |
| Taiminen et al. (1998)197 Finland To determine the quantitative importance of contagion of deliberate self-harm among adolescent psychiatric inpatients; to clarify the psychological mechanisms behind contagion by interviewing subjects involved in DSH contagion incidents Contagion |
Longitudinal descriptive survey (prospective): data collected over 1 year, questionnaire completed by semistructured interviews (open and closed questions); statistics, analytic statistics Adolescents |
Location: inpatient adolescent psychiatric ward Sample: adolescents treated on the ward during a 12-month period (n = 51). During the 12 months, 64 acts of DSH were performed by 12 adolescents. These were the subjects within the study Of the 12 patients involved in DSH: Age (years): mean 15.5, range 12.3–17.9 Gender: female 100% (total sample 35 female and 16 male) Length of stay: 91.9 days ± 73.2, range 7–200 days Seven subjects were involved in four or more contagion incidents. These subjects were invited to interview but one refused. Interviews were carried out with six subjects |
Outcome variable: DSH Interviews covered questioning of patient’s personal history of DSH, patient’s subjective affective states during the acts of DSH, patient’s estimation of her own motivation for DSH, patient’s impression of why other adolescents on the ward had been involved in DSH, patient’s relationships with other patients involved in DSH and patient’s judgement of the role of imitation or identification in acts of DSH on the ward |
During the 12 months of the study, 64 acts of DSH were performed by 12 adolescents. Ten of the 12 patients were involved in contagion episodes. Seven patients were involved in four or more contagion episodes (range from 4 to 17 contagion episodes), three patients in two contagion episodes each and two patients in none. The seven patients involved in four or more contagion episodes were invited to interview but one refused. Of the six subjects interviewed, five were influenced by others. Self-mutilation did relieve anxiety or anger for five of seven patients. Patients (two of seven) were involved in DSH mainly because they did not want to feel themselves outsiders. Three of seven had a peculiar habit of storing blood in their wardrobes. For only one did blood storage serve as a ‘transitional object’ and for the other two the main incentive was imitationSkin cutting and blood letting had become an initiation right that strengthened group cohesion however it seems that a pre requisite for the feeling of togetherness was a shared emotional experience of relief after an event of DSH(p. 215)From the discussion: micro-level contagion of DSH occurs in psychiatric units for adolescents. Results suggest that a majority of DSH incidents on an adolescent psychiatric ward may have been influenced by contagion. The study also demonstrates that one type of DSH behaviour, for example self-mutilation by skin cutting, may trigger another type of DSH behaviour, for example parasuicide by drug overdose in another individual In discussing social factors: it is possible that social isolation and social stress created by the overpopulation of the closed ward, together with a population exceptionally vulnerable to imitation, exposed the ward to contagion incidentsOne subject which did not feel any relief from self mutilation was openly treated with contempt for four of the subjects and was labelled by them as a fake or a pretender(p. 215) |
Appendix 19 Phase 2 data extraction grey literature report (n = 4)
| Author (year of publication) Country Research aim Focus |
Design and methods Population |
Demographic details | Variables/measures | Key findings relevant to the review |
|---|---|---|---|---|
| Street and Svanberg (2003),198 Svanberg and Street (2003)199 UK (England and Wales) To give young people and families using inpatient CAMHS a ‘voice’; to add to the knowledge base about inpatient CAMHS; to identify innovation and change; to examine barriers to service development and the challenges facing service providers; to disseminate good practice Contagion; Dislocation: Education; Dislocation: Families; Dislocation: Friends; Dislocation: Normal Life |
Mixed methods, cross-sectional descriptive survey, qualitative: interviews, questionnaire; statistics, descriptive statistics Adolescents, parents, staff |
Location: six established in-patient units – four CAMHS, one independent and one multiagency (health, social services and education); two newly opened units – one CAMHS, one independent; one CAMHS unit working with younger children; one CAMHS unit working with older adolescents (18–21 years); two paediatric wards; one adult psychiatry ward; one ‘one-stop’ service for young homeless people Length of stay: not specified Sample: staff (on average, 14 members of staff were interviewed from within the sample units, and interviews from surrounding services averaged nine); adolescents (n = 107) Age (years): mean 16.4 Gender: male 32% |
Measures Adolescents: 61 were interviewed in person, 28 completed a questionnaire only and 18 gave their views in a group setting. Secondary user evaluation data were gathered from a further 15. Retrospective data were collected by postal questionnaire from 10 young people who had been discharged in the 6-month period before the fieldwork commenced (a 10% response rate). A follow-up questionnaire distributed 2 months after discharge was returned by 15 young people (38% response rate) Staff: a total of 115 staff from within residential provision, including the main sample units, were interviewed for the study. For surrounding services, the total was 54 Parents: a total of 35 parents were interviewed from the main and subsample units. Of this number, 8 were interviewed in person, 13 were interviewed by telephone and 20 completed a questionnaire. (There is some overlap in that some people completed a questionnaire as well as undertaking a telephone interview) |
Key issues identified in the study fell under the following areas:
|
| Tulloch et al. (2008)15 UK (England) To carry out the costs, outcomes and satisfaction for inpatient child and adolescent psychiatric services study (COSI-CAPS) and answer the questions: Which types of CAMHS inpatient care produce better clinical and social outcomes? What is the cost-effectiveness of adolescent units, paediatric wards and adult acute inpatient wards? How do independent and NHS sector providers compare? Which types of service offering acute treatment and care are preferred? Dislocation: Education |
Mixed methods, cross-sectional survey HCPs |
Locations: CAMHS inpatient GAUs and specialist EDUs in England; independent and public CAMHS in England (n = 42 of 55, 76%) Sample: ward managers/senior staff in participating services. 42 of the 55 eligible units in England agreed to take part in the study. Mainly adolescents aged between 12 and 18 years. Five centres admitted children younger than 12 years |
Measures: a questionnaire used was adapted from the NICAPS study and included:
|
Age: the median is 12 years for the lower end of the range (38% of units) and 18 years for the upper (77% of units). At the extremes, two independent sector EDUs would admit young people between the ages of 8 and 18 years and one independent sector EDU would admit young people between the ages of 13 and 25 years. Two other services, both NHS GAUs, will admit people older than 18 years (19 years and 23 years) Length of stay: the median for the whole cohort is 79 days. For young people with an eating disorder, there was no difference in length of stay between those admitted to a GAU (mean 138.2 days, SD 88.1, median 120 days) and those admitted to an EDU (mean 139.5 days, SD 68.6, median 125 days) (Mann–Whitney U-test: z = –0.61, p = 0.54). For young people with a diagnosis other than an eating disorder, the length of stay for those admitted to an NHS unit (mean 101.2 days, SD 78.6, median 86 days) is significantly longer than for those admitted to an independent sector unit (mean 87.2 days, SD 74.7, median 67 days) (Mann–Whitney U-test: z = –2.9, p < 0.01) Educational provision: 29 units provided information about their educational provision. All provide some form of facility for the appropriate educational level (‘Key Stage’) of young people resident in the unit. 21 units (72%) describe their provision as ‘within the unit’ and eight (28%) as ‘outside the unit but on the hospital site’. Day patients share the educational facilities in 15 units. Pupils are typically taught in ‘mixed-ability’ groups (n = 25, 86%) but with consideration of pupils’ emotional and behavioural needs (n = 24, 83%). 18 (62%) units also provide one-to-one teaching. In 27 (93%) units, teachers contribute towards policy-making. Table 3.9 in the report shows the mean number of teaching staff, expressed as whole-time equivalents (wtes), providing input to units. The number of pupils per teacher in NHS units (mean 4.8, SD 2.6) is significantly lower (t = –2.6, df = 24, p < 0.05) than in independently managed units (mean 8.7, SD 4.7). Units rated the quality of their relationship with external services [e.g. education services scored 2.2 on a scale from 0 (no contact) to 3 (excellent access)] Costs: costs were estimated for 31 of the 42 units. The median costs per inpatient day were only slightly lower than the mean (median £343, n = 317). Mean length of stay was 97 days (SD 76.4, range 1 to 411, n = 273). See report for additional information on costs |
| Tulloch et al. (2008)15 UK (England) To carry out the costs, outcomes and satisfaction for inpatient child and adolescent psychiatric services study (COSI-CAPS) |
Prospective cohort study: admission, discharge, 6 months after discharge | Not relevant to present study so no further details extracted | ||
| Tulloch et al. (2008)15 UK (England) To carry out the costs, outcomes and satisfaction for inpatient child and adolescent psychiatric services study (COSI-CAPS) Dislocation: Families |
Mixed methods, qualitative, semistructured interviews, satisfaction scale Adolescents, parents |
Location: CAMHS inpatient GAUs and specialist EDUs in England; independent and public CAMHS in England (n = 42 of 55, 76%) Sample: convenience sample, 19 young adults and 12 parents |
Measure: CAMHSSS | Themes emerging from qualitative interviews with young people and parents:
|
| O’Herlihy et al. (2001)11 UK (England and Wales) To carry out a detailed review of a stratified sample of 15–20 child and adolescent psychiatric inpatient units in England and Wales, including an evaluation of standards of care, and safeguards, against explicit standards; the National In-Patient Child and Adolescent Psychiatry Study (NICAPS) Dislocation: Education; Dislocation: Families |
Mixed methods, evaluation study CAMHS units |
For the visits, 18 general psychiatric inpatient units were sampled according to stratifying criteria which included age range; 5- or 7-day opening; NHS or independently funded; location (in terms of both geographical spread and deprivation); and Office for National Statistics families and groups | The service standards were adapted into interview schedules and checklists for use in the site visits. Data sources and methods most appropriate for each standard were identified. For example, to collect data about the facilities a checklist was designed to use on a tour of the premises, whereas to collect data on patient involvement in their treatment decisions patients themselves were asked in a short interview. This selection of standards kept data collection time to a minimum and enabled each visit to be conducted in 1 day. In all, eight data-collection tools were developed including interview schedules for the consultant psychiatrist, charge nurse, head teacher, therapists, social worker, patients and trust management, and a checklist for the site inspection. All schedules and checklists were piloted in a 1-day visit to a single unit. Standard to Appendix 9.4 of full report | Standards relevant to our review question. Units are parent-friendly (standard 21). Before discharge, decisions are made about meeting any continuing needs (standard 23). School work (standard 32) |
| O’Herlihy et al. (2001)11 UK (England and Wales) To investigate the characteristics and the use of child and adolescent psychiatric inpatient units in England and Wales; to identify and describe all child and adolescent psychiatric inpatient units in England and Wales No focus as not relevant |
Mixed methods, cross-sectional descriptive survey Outpatient psychiatrists, lead consultants and charge nurses |
Not relevant to present study so no further details extracted | ||
| O’Herlihy et al. (2001)11 UK (England and Wales) To investigate the characteristics and the use of child and adolescent psychiatric inpatient units in England and Wales; to identify and describe all child and adolescent psychiatric inpatient units in England and Wales No focus as not relevant |
Mixed methods, cross-sectional descriptive survey: postal survey HCPs |
Not relevant to present study so no further details extracted | ||
| O’Herlihy et al. (2001)11 UK (England and Wales) To investigate the characteristics and the use of child and adolescent psychiatric inpatient units in England and Wales; to identify and describe all child and adolescent psychiatric inpatient units in England and Wales No focus as not relevant |
Mixed methods Follow-up study of those referred but not admitted to 18 units |
Not relevant to present study so no further details extracted | ||
| O’Herlihy et al. (2001)11 UK (England and Wales) To investigate the characteristics and the use of child and adolescent psychiatric inpatient units in England and Wales; to identify and describe all child and adolescent psychiatric inpatient units in England and Wales Dislocation: Education |
Mixed methods, cross-sectional descriptive survey HCPs |
Royal College of Psychiatrists’ Child and Adolescent Faculty members, n = 245 of 454 (60%) | Postal questionnaire | Problems identified by respondents: lack of emergency beds and facilities (36%); insufficient number of beds (25%); poor provision for severe or high risk cases (24%); poor liaison with other services (20%) |
| O’Herlihy et al. (2001)11 UK (England and Wales) To investigate the characteristics and the use of child and adolescent psychiatric inpatient units in England and Wales; to identify and describe all child and adolescent psychiatric inpatient units in England and Wales Focus: Dislocation: Education; Dislocation: Families |
Mixed methods, cross-sectional descriptive survey: a general unit survey of all 80 units; a 1-day census of beds, staff and patients in the 80 units; a 6-month activity study of referrals to, admissions to, and discharges from the 80 units CAMHS units |
The general survey questionnaire, sent out to all 80 units, included questions about the educational provision within inpatient services. The results presented here refer to educational provision in the 66 units (response rate 83%) that answered the relevant questions. 63 (94%) responding units reported that they provided an educational facility or had on-site access to an educational facility (i.e. off premises but on site). The three units that reported not having an educational facility were primarily adult wards with a licence to treat young people under the age of 18 years | Unit survey questionnaire: the purpose of this questionnaire was to collect information about the characteristics of the unit and it included questions on the following topics:
|
Length of stay: the mean length of stay for cases discharged during the study period was 115 days (3.7 months), with a standard deviation of 181 days (5.9 months) and a range of 0 to 2194 days. The range, excluding the six (1%) long-stay inpatients (2 to 6 years), fell between 0 and 717 days (23 months), with a mean length of stay of 103 days (3.3 months) and a SD of 108.38 days (3.5 months). The six long-stay patients (2 to 6 years) were over 18 years old at the time of discharge and were inpatients in two types of specialist units: five were resident in a secure adolescent unit and one in a learning disability psychiatric unit. Delay in discharge owing to difficulty arranging local follow-up or community support was reported for four of these cases. These four cases were discharged to low and medium secure units. Specifically for general psychiatric units the mean length of stay was 104 days, with a SD of 106 days, and the range was from 0 to 680 days. 4% stayed between 1 and 2 years. There was a significant association between diagnosis and length of stay in general psychiatric units (Fisher’s Exact Value = 97.79) Results presented under the following headings:
|
| Mental Welfare Commission for Scotland (2009)200 UK (Scotland) To visit all specialist child and adolescent inpatient facilities in Scotland on an annual basis, as part of the normal visiting programme Dislocation: Education; Dislocation: Families |
Qualitative: interviews Adolescents, HCPs |
Location: all independent and public CAMHS in Scotland Sample: young people (n = 16) in different units across Scotland were interviewed; case files of young people (n = 13) were retrieved; staff across units (n = 11) were interviewed Study method: visits with specialist inpatient facilities; visits with young people admitted to non-specialist wards over a 3-month period (where this was not possible the medical and nursing notes relating to the admission were reviewed); meetings with representatives from CAMH services and local authorities in each of the 11 NHS Board areas in mainland Scotland |
Variables of interest: contact with family; education | Contact with family: young people were asked if they were able to keep in touch with families, and they all said they could; visiting policies within the specialist units varied, with some units having core visiting times but offering flexibility to families if required and actively encouraging family contact and involvement; involvement of families in family therapy was provided for the majority of services Education: all specialist inpatient units have education provision on site |
Appendix 20 Phase 2 data extraction (clinical case reports and practice initiatives) (n = 7)
| Author (year of publication) Country Focus |
Description and key findings relevant to the review |
|---|---|
| Jones (2007)221 UK Dislocation: Families; Dislocation: Friends; Dislocation: Education |
Clinical case report. Looks at the patient’s journey through a tier 4 NHS children’s psychiatric inpatient unit for 7- to 14-year-olds. Presents a case illustration of a 13-year-old boy and considers, in brief, family functioning, suitable school provision and identity of child within a peer group |
| Wilkinson (2001)225 Norway Dislocation: Families |
Clinical case report. Describes the therapeutic principles and practice on a psychiatric inpatient unit for young people, which include the involvement of family members |
| LePage (2005)222 Canada Dislocation: Families |
Clinical case report. Describes the impact of early family participation within inpatient assessment and treatment of youths diagnosed with a first episode psychosis at a regional children’s psychiatric centre for young people aged 0–18 years. A case of a 15-year-old male is presented |
| Nejtek et al. (2010)223 USA Dislocation: Families |
Clinical case report. Presents a case study of a 15-year-old male and pulls out issues of maternal non-compliance |
| Olson (2006)224 USA Dislocation: Families |
Clinical case report. Discusses engaging adolescents with their parents through a parent/adolescent activity group and provides a case description of two 16-year-old males and a 17-year-old female |
| White et al. (2006)143 USA Dislocation: Education |
Local practice initiative. Report on a ‘program [which] provides intensive school-based support and care coordination during the first six to ten weeks after discharge’. Refers to preparatory work before discharge involving care co-ordinator liaison with students, families, the school and the hospital. Return to the classroom is followed by ongoing support. Cites routine data indicating the use of this programme by 99 young people between October 2003 and November 2005, and success in resuming their studies for all 67 students for whom educational status data was available |
| Garrison (2007)220 USA Dislocation: Families |
Local practice initiative. Described the development of an exercise that involved the use of movies to facilitate family engagement in hospitalised adolescents. Concluded that ‘movies can engage adolescents and families in treatment quickly’ and ‘with thoughtful movie selection and targeted discussions to address communication and the family’s own crises, the movie intervention can help empower a family to navigate its way through a crisis together’ |
Appendix 21 Phase 2 policy and guidance documents
| Document details | Extracted material relevant to the review |
|---|---|
| NHS Commissioning Board (2013)205 NHS Standard Contract for Tier 4 Child and Adolescent Mental Health Services (CAMHS): Children’s Services Focus: Dislocation: Families; Dislocation: Friends; Dislocation: Education |
Aims and objectives of service:Providing treatment in a safe, age appropriate, child friendly environment where risks are managed proactively and in the least restrictive way ensuring the safety of the child and othersp. 3Providing treatment that will result in improved function and safe and sustainable recovery and improved resilience as shown by improved mental well-being, increased social inclusion, increased access to education and improved peer/family relationshipsp. 3Working collaboratively with parents/carers to provide family centred carep. 3Treatment and care programme approach:All families will be offered Family meetings which will start within one week of admission and should continue at a frequency determined by the child’s needsp. 8Service environment:Facilities which include a room which is suitable for contact between children and their families and is available at weekends and eveningsp. 11Education:All day/in-patient services will provide educational sessions during normal academic term. Education should be an integral part of the service provision. The Provider educational provision should be The Office for Standards in Education (OFSTED) registered. The Provider educational provision will be funded by re-charge of the patient’s home-base Local Authorityp. 11Discharge planning and discharge:The service will ensure high levels of liaison with schools to ensure educational reintegration is successfulp. 11Treatment and interventions:Whilst day/in-patients the child/young person shall receive education specifically tailored to individual need and provided by teachers skilled in special needs teaching. There should also be a programme of suitable activitiesp. 32ANNEX 1 TO SERVICE SPECIFICATION: PROVISION OF SERVICES TO CHILDRENAims and objectives of serviceFamilies with children have easy access to hospital facilities for children without needing to travel significantly further than to other similar amenitiesp. 36 |
| Department of Health (2003)206 National Service Framework for Children, Young People and Maternity Services: The Mental Health and Psychological Well-Being of Children and Young People [now archived] Focus: Dislocation: Stigma; Dislocation; Family; Dislocation: Education |
1. Introduction1.1 The National Service Framework for Children, Young People and Maternity Services establishes clear standards for promoting the health and well-being of children and young people and for providing high quality services which meet their needsp. 31.2 There are eleven standards of which this is the ninth. They cover the following areas:Standard 9 The Mental Health and Psychological Well-being of Children and Young People6.2 Many children, young people and their families who could benefit from mental health services for assessment and treatment are not accessing services. There are a variety of reasons for this: a lack of trust in statutory services; a wish to solve problems themselves; a lack of recognition and agreement that a problem exists; a fear of being teased and stigmatised; a fear of confidentiality being broken and a belief that nothing can be done. These can all affect the take-up of helpp. 156.3 It is often the children and young people about whom there is most concern, and who are likely to experience the poorest outcomes, who are most reluctant to seek help. Services therefore need to respond flexibly and creatively in order to be able to meet their needs. The setting in which the first contact is made may make a difference e.g. in school which may be seen as less stigmatising for some or, where confidentiality is of particular concern, away from school for a young person who fears being teasedp. 15Services are offered as near to home as possible and in a number of settings to take account of the different needs and choices of children, young people and their parents or carers. They should include locations such as schools, homes and family centres, which may be perceived as less stigmatising, as well as traditional clinic settingsp. 16Standard:All children and young people, from birth to their eighteenth birthday, who have mental health problems and disorders have access to timely, integrated, high quality, multi-disciplinary mental health services to ensure effective assessment, treatment and support, for them and their familiesMental health problems in children are associated with educational failure, family disruption, disability, offending and antisocial behaviour, placing demands on social services, schools and the youth justice system. Untreated mental health problems create distress not only in the children and young people, but also for their families and carers, continuing into adult life and affecting the next generationp. 6Where a child or young person needs to be placed in an in-patient unit, every effort is made to find a place that is close to home, so that contact with the family can be maintainedp. 19Tier 4 CAMHS refers to the highly specialised provision that may be required by these children and young people. The different range and prevalence of serious disorders in childhood compared with adolescence means that services for these two broad age groups have to cater for a different range of needs, which need to be reflected in the specific skills of the staff working with them. The Department of Health has defined highly specialised services (www.dh.gov.uk) for the minority of children and young people who may need them. The needs of the young people and their families may be met by these services in a variety of ways through intensive outpatient services, assertive outreach, inpatient psychiatric provision, residential and secure provision or other highly specialised assessment consultation and intervention services. Amongst the highly specialist services, inpatient psychiatric units for both children and adolescents, but separately provided to ensure that the developmental needs of different age ranges are met, are essential resources, representing ‘the intensive care of child mental health’. 9.9 Due to the insufficient numbers of adolescent beds, some young people are being cared for inappropriately in adult psychiatric beds. In addition, children and young people who are psychotic or who have complex, persistent and severe behaviour disorders and who first present in accident and emergency departments may then be admitted to paediatric wards. A children’s ward is not usually the best place for such patients, who may need to be in a children’s or adolescent psychiatric unit or other appropriate, jointly agreed, alternative facilities as soon as possiblep. 31It is important to recognise that supporting children and young people with mental health problems is not just the responsibility of specialist CAMHS. In many cases, the intervention that makes a difference will come from another service. For example, a child presenting with behavioural problems may make better progress if his/her literacy problems are also addressed, in which case an input is required from education. The lack of provision in one service may impact on the ability of other services to be effective. Partnership working is an essential requirement of high quality service provisionp. 7 |
| Department of Health (2011)201 No Health without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages (current MH policy for England) Focus: Dislocation: Education; Dislocation: Families; Dislocation: Stigma; Dislocation: Normal Life |
Complex system: 1.26 Such cross-cutting strategies recognise that the Government can achieve more in partnership with others than it can alone, and that services can achieve more through integrated, pathway working than they can from working in isolation from one anotherp. 11We all need to take responsibility for caring for our own mental health and that of others, and to challenge the blight of stigma and discriminationp. 5Sixth agreed objective:(vi) Fewer people will experience stigma and discriminationPublic understanding of mental health will improve and, as a result, negative attitudes and behaviours to people with mental health problems will decreasep. 63.58 Tackling stigma and discrimination and promoting human rights are at the heart of this strategy. A number of mental health trusts currently undertake local anti-stigma and discrimination activities, gaining additional benefit by encouraging service user involvement, thereby aiding their recoveryp. 293.59 However, to shift public attitudes substantially requires a major and sustained social movement. Recognising that children and young people can suffer greatly from the effects of mental health stigma, YoungMinds has prioritised combating stigma in their Children and young People’s Manifestop. 293.12 young people’s ideas about body image and what looks good are strongly influenced by fashion and friends; and body image is linked to self-esteem. Eating disorders have a peak age of onset in adolescence. For more information see No Health Without Mental Health: Delivering better mental health outcomes for people of all agesp. 194.16 Choice is fundamentally about the objectives and circumstances of treatment and care. It is just as relevant for children and young people as for adults. It includes treatment in age- and developmentally-appropriate settings, care designed to enable children and young people to be at home with their families as much as possible, and treatment that enables them to lead as normal a life as possible, at school or college and with their friendsp. 321.1 Mental health is everyone’s business – individuals, families, employers, educators and communities all need to play their partp. 51.15 Mental health problems can also contribute to perpetuating cycles of inequality through generations.* However, early interventions, particularly with vulnerable children and young people, can improve lifetime health and wellbeing, prevent mental illness and reduce costs incurred by ill health, unemployment and crime.** Such interventions not only benefit the individual during their childhood and into adulthood, but also improve their capacity to parent, so their children in turn have a reduced risk of mental health problems and their consequencesp. 9(ii) More people with mental health problems will recoverMore people who develop mental health problems will have a good quality of life – greater ability to manage their own lives, stronger social relationships, a greater sense of purpose, the skills they need for living and working, improved chances in education, better employment rates and a suitable and stable place to livep. 211.19 There are also the further, incalculable costs to the individual, their family and their community of lost potential and unrealised hopes and goals. The majority of mental health problems affect people early, interrupting their education and limiting their life chancesp. 105.11 For adolescents, multi-systemic interventions that involve young people, parents, schools and the community have been shown to reduce conduct disorder, improve family relationships and reduce costs to the social care, youth justice, education and health systems. Families often experience multiple problems, such as substance misuse or mental health problems, parenting problems, child neglect and behaviour problems in school, or involvement in offending. Evaluation of family intervention has shown reductions in mental health problems, drug or substance misuse and domestic violence.72 More details are given in No Health Without Mental Health: Delivering better mental health outcomes for people of all agesp. 405.44 The development of meaningful, high-level outcomes for children and young people is still at an early stage. The Department of Health is very aware of the need to develop a considered way forward – working with its partners in the Department for Education and elsewhere – building on the learning from, for example, the proposed Adult Social Care Outcomes Frameworkp. 475.45 It will be a priority to agree key outcome measures with service users, including children, young people and their families, and with the sector as a wholep. 475.60 These arrangements will promote further integration of health with adult social care, children’s services (including education) and wider services, including disability services, housing, employment support and the criminal justice system. This has the potential to meet people’s needs more effectively and promote the best use of public resourcesp. 50 |
| Department of Health (2011)207 No Health without Mental Health: Delivering Better Mental Health Outcomes for People of All Ages Focus: Dislocation: Education; Dislocation: Families; Dislocation: Stigma |
2.3 Different approaches are required for children, young people and adults, although some interventions are effective in reducing distress and improving functioning across all age groups. Stigma and discrimination create barriers for people with mental health problems of all ages and their families and carers. The principles of the recovery approach, which emphasises the equal importance of good relationships, education, employment and purpose alongside reduction in clinical symptoms, apply equally to children and young peoplep. 306.10 A number of mental health trusts currently undertake local anti-stigma and discrimination activities with the active involvement of service users. This can have the added benefit of supporting their recoveryp. 846.11 While stigma can affect people of any age, the impact on children and young people at a time when their brains, identities and social skills are still developing can be considerablep. 84Body image and eating disordersChildren and young people learn about what is considered normal behaviour and what society values from the people close to them, their surroundings and the media messages to which they are exposed. In the same way, young people’s ideas about body image and what looks good are strongly influenced by fashion and friends, and body image is linked to self-esteem. Young peoples’ diet and appetite can be affected by stress, worry or tiredness. Worries about weight, shape and eating are common, especially among young girls. Nearly 1% of women in the UK between the ages of 15 and 30 suffer from anorexia nervosa, and between 1% and 2% have bulimia nervosa. Eating disorders start most commonly in adolescence and are associated with high levels of mortality, physical health problems and psychological distress, as well as impaired quality of lifeAccess to high-quality mental health care, based on the best available evidence and delivered by staff with an appropriate range of skills and competencies, is critical to meeting the specific needs of this group of young people. The Government is bringing together a group of experts to identify non-legislative ways of tackling low levels of body confidencep. 18 |
| Department of Health (Kurtz) (2009)8 The Evidence Base to Guide Development of Tier 4 CAMHS Focus: Dislocation: Stigma |
1) In order to be accessible, acceptable and effective, services for child and adolescent mental health may need to be delivered in a non-stigmatising environment often through the voluntary sector or universal provision such as schools. It may be necessary to visit families at home, to offer outreach facilities, and to provide active support to a young person or their family in using other services with which they may be unfamiliarp. 111) The effectiveness of interventions to meet the complex and often entrenched mental health needs of children and young people depends upon these young people taking up the appropriate service, engaging with the therapeutic activity and staying with it. Therefore whatever is needed has to be delivered in a style that promotes take-up: non-stigmatising venue (outreach in community settings or home; voluntary sector front; prefer to be regarded as ‘bad’ not mad); convenient time and place; involving young person in deciding on the type of intervention and in monitoring his or her progress; building a trusted relationship with the young personp. 12Disadvantages of inpatient care include:• Loss of support from the child’s local environment• Presence of adverse effects within the inpatient environment• Effects of admission on family lifep. 7Effectiveness of Inpatient and Day patient treatmentThe overall efficacy of Inpatient care across a range of disorders has been shown in rigorous research studies which have also shown the following predictors of outcome:• High levels of aggressive antisocial behaviour and organic symptoms, as in schizophrenia predict poor outcome. Emotional disorders do better• Intelligence measured as IQ shows a moderate positive effect but functional achievement may be more critical• Pretreatment family functioning is a key predictor of outcome• Longer treatment stays are, in general, associated with improved outcome• For eating disorders, there are widely differing results• For depression, suicidality and psychosis little beneficial effects of inpatient psychiatric care have been shown• For conduct disorder, multimodal day treatment for children with disruptive disorders has produced significantly greater improvement in behaviour than in a control group• In substance misuse, research shows additional benefits from community treatment• For obsessive, compulsive disorder, poorer outcomes are found among those needing admission compared with those treated as outpatientsp. 87Inpatient admission allows detailed assessment in a controlled environment and away from the family. The individualised assessment and intensive educational input possible within the inpatient unit can make a major impact with young people, often whose social adaptation within their community has broken down and who have a history of school failurep. 7 |
| Royal College of Psychiatrists (2002)218 Acute In-Patient Psychiatric Care for Young People with Severe Mental Illness: Recommendations for Commissioners, Child and Adolescent Psychiatrists and General Psychiatrists Focus: Dislocation: Education; Dislocation: Families |
Service Principlesp. 7Adolescence is a time of rapid developmental change. In addition to physical, intellectual, emotional and social development, adolescents are also managing the transition from the world of the child and family to that of the independence of adulthood. All these factors mean that a specialist adolescent mental health service should have expertise in:• the assessment, management and treatment of severe mental illness• adolescent development• working in partnership with family, educational and social welfare systemsProvision for those young people who require in-patient care should include:• prompt admission• a suitably safe and appropriately staffed ward environment which conforms to agreed quality standards (http://www.rcpsych.ac.uk/cru/qnic.htm)• geographical proximity to family allowing frequent contact and appropriate family interventions• minimisation of health and safetyYoung people aged under 16 years should not be admitted to adult psychiatric wardsp. 8Executive summaryThe report notes that the principles of specialist provision for adolescents with serious mental illness should include: prompt admission; a suitably safe and appropriately staffed ward environment (which conforms to the agreed standards); geographical proximity to the family home (enabling frequent visits and appropriate family interventions); and minimisation of health and safety risks from other patients and availability of drugs and alcoholp. 5 |
| Royal College of Psychiatrists (2003)214 Bridging the Gaps: Health Care for Adolescents Focus: Dislocation: Education |
Recommendations for inpatient care– All such units should be provided with appropriate education facilities and access to transition to employment schemesp. 44 |
| Scottish Executive (2005)202 Child Health Support Group: Inpatient Working Group – Psychiatric Inpatient Services for Children and Young People in Scotland: A Way Forward Focus: Dislocation: Education; Dislocation: Families; Dislocation: Normal Life |
7.2 Because a child or young person is not independent, and usually lives with a family or carers, it is imperative that, when planning services, account is taken of the need for regular family work – an evidence-based therapeutic intervention which requires resources. It is also important to provide accommodation for families who have to travel a significant distancep. 21Recognise the significance of home, family and other carers: Flexible arrangements must be made for family contact and links with home and the community should be maintainedp. 32In an inpatient setting, a key worker/named nurse also has the task of liaising effectively with wider systems such as schools, colleges, social work and other health and nonhealth agencies. These nurses will often be the people who undertake preparatory work prior to admission and carry out rehabilitation and preparation for dischargep. 50TeachingLike Social Workers, teaching staff are not employed by the health service, but are vital for the safe and efficient running of the unit. Teachers in Hospital Education Services all hold graduate and post graduate Diplomas in Education. They are employed by local authority education departments. In addition to their primary education or specialist secondary subject skills, teachers receive continuous professional development in their own academic area, and in aspects of child and adolescent psychiatry. Teaching staff should be dedicated to child and adolescent mental health teams. For every 8 places within a psychiatric inpatient unit, there should be at least one full-time teacher with at least one other whole time equivalent post comprising subject specialists at secondary stagep. 52In addition to providing the curriculum education for patients in liaison with the pupil’s mainstream school, teaching staff advise clinical staff on the educational elements of treatment, liaise with schools, further education establishments and other child and adolescent mental health outpatient staff and teachers. They are involved in inter-disciplinary work in assessment and planning for an individual’s treatment programme. They should be involved in admission planning and are pivotal in the discharge processp. 53 |
| YoungMinds (Street and Herts) (2005)209 Putting Participation into Practice Focus: Dislocation: Stigma |
The stigma that still accompanies discussions of ‘mental health’, ‘mental illness’ or poor emotional health which can make it hard to engage children, young people and their families directly – and can result in many wanting to detach themselves from services as quickly as they can, once their needs have been addressedp. 5The evaluation findings highlight the following as the key elements in a service that ‘works’ – services need to be acceptable, to be provided in a non-stigmatising environment, to be welcoming, respectful and empowering; they need to seek to engage children, young people and their parents/carers, with professionals in services being committed to consulting with and acting on children’s and families’ viewsp. 8 |
| QNIC (Solomon et al.) (2011)204 Service Standards (sixth edition) Focus: Dislocation: Education; Dislocation: Families; Dislocation: Friends; Dislocation: Stigma |
The detailed service standards produced by the Quality Network for Inpatient CAMHS (QNIC), and published by the Royal College of Psychiatrists, address risks to Dislocation: Education, Dislocation: Families, Dislocation: Friends and Dislocation: Stigma |
| Welsh Government (2013)213 Specialist NHS Child and Adolescent Mental Health Services: Professional Advice for Service Planners. CAMHS National Expert Reference Group Focus: Dislocation: Education; Dislocation: Stigma |
Promote positive health and avoid unnecessary stigmatisation or labellingp. 8Inpatient services are a necessary environment for assessing and treating young people with the most complex needs. Current evidence suggests that the adolescent inpatient unit has a particular ability to provide stabilisation and rapid reduction of symptoms and riskIn patient services should provide . . . Access to educationp. 24The transition from childhood, through adolescence to adulthood is a crucial stage of social, personal and emotional development. Many severe mental health disorders present in this time and the traditional models of Adult Mental Health and CAMHS Services mean that gaps in provision exist. (p28) but no mention of anything further about education, family etc.Youth Mental Health Service (16–25 years) . . .Key principles for a successful youth mental health service: . . . An emphasis on supporting young people towards getting on with their lives’pp. 29–30Outcomes and monitoring frameworkService user involvement frameworkA framework, agreed with the appropriate planning board across all service elements, should ensure that service users, young people and/or their families and carers are involved in all aspects of service development; that delivery is consistent; and of an acceptable standardInformation to support this may include:Child/survey perceptions before entering the service and after contact to encourage feedback on servicep. 30 |
| Welsh Government (2012)210 Together for Mental Health: A Strategy for Mental Health and Wellbeing in Wales Focus: Dislocation: Stigma; Dislocation: Education |
Reducing stigma and discriminationPeople with other health problems do not usually face the same stigma and discrimination as those with a mental illness. In children and young people, this can often lead to bullying. Stigma and discrimination can further lead to secrecy and unwillingness to discuss mental health problems or to seek help when mental health problems and early signs of dementia arise. They can also give rise to self-stigma, loss of hope and reduced self-esteem in people with a mental illnessThe media: Negative portrayals of people with mental health problems and dementia in both print and broadcast media can lead to an ungrounded fear, misunderstanding and mistrust. Too often media coverage fails to cover those incidents when people with mental illness are victims of crime, focussing instead on the far rarer occasions when they are perpetrators. This in turn leads to discrimination towards people experiencing mental health problems, resulting in reduced access to work, education, housing and leisure opportunities. Inappropriate or irresponsible media reporting of suicides can also risk copycat behaviourWithin services: Any stigma or discrimination by staff supporting people who have mental health problems must be identified and addressed, and the staff involved given appropriate training. Staff working within mental health services may also face stigma from their peers in other disciplines and action should be taken to address thisThe population more widely: We have demonstrated our commitment to ending mental health discrimination in Wales through support of Time to Change Wales (TTCW) supported by BIG Lottery and Comic Relief. TTCW aims to transform public attitudes and behaviour towards mental health and reduce the stigma and discrimination experienced by people with mental health problems. Annual surveys will measure progress and TTCW Champions will be identified in each Health Boardpp. 31–2In-patient care: For children and young people: Age-appropriate environments should be provided, and children and young people should not be admitted to adult wards except in the most exceptional circumstances. Where such an admission is unavoidable, it should be treated as a serious incident, in line with the Welsh Government guidance. The approach should be to work with the child and their family to manage and address distress and issues of attachment appropriatelyp. 39Not specifically on in-patient care but ‘Our Programme for Government describes how we will ‘help everyone reach their potential, reduce inequality and improve economic and social wellbeing’. We have published an Implementation Plan setting out the course of reform through to 2015 to achieve improvements in educational standardsEvidence has demonstrated poorer educational outcomes for those with mental health problems and an increased potential for not being in education, employment or training at a young age. The initial onset of severe mental illness is particularly prevalent at school age or when people are first engaged in higher or further education. This can interrupt people’s schooling or education causing permanent disadvantage. Education or training providers should support students to remain on the course or hold their place open for them whenever possiblep. 52 |
| Welsh Government (2005)216 National Service Framework for Children, Young People and Maternity Services in Wales Focus: Dislocation: Education |
Welsh Government:Standard that ‘Service providers work together to ensure the successful reintegration of children and young people who have been absent from school due to hospital episodes or other long term illness, pregnancy, care or custodial placements away from their family and community, mental health problems, personal difficulties or a period of exclusion’p. 37An appropriate amount of on-going education, in a suitable environment, is provided to all children and young people who are well enough to receive it, including those in hospital. Education is provided in liaison with each child’s school, and is appropriate to their age and stage of development. (Section 19 of the Education Act 1996)p. 65 |
| Welsh Government (2012)364 Code of Practice to Parts 2 and 3 of the Mental Health (Wales) Measure 2010 Focus: Dislocation: Education |
2.17 In relation to the assessment of children and young people (within the context of Part 2 of the Measure), practitioners undertaking assessments should consider the child in the context of their developmental level and seek to view problems and issues in the ways in which children experience them. In addition, they should ideally empower good parenting, include a focus on prevention and health promotion and aim to develop relationships that aid children in tackling their problems. Consideration needs to be given to establishing:–a) who has parental responsibility for the child and the needs of the carers to enable them to provide care;b) the ability of the child to make their own decisions in terms of emotional maturity, intellectual capacity, mental state and their competence;c) The involvement and role of other statutory services in the support of the child such as education or local authority children’s social services |
| NICE (2013)211 Antisocial Behaviour and Conduct Disorders in Children and Young People: Recognition, Intervention and Management Focus: Dislocation: Stigma |
NICE:Be aware that parents and carers of children and young people with a conduct disorder might feel blamed for their child’s problems or stigmatised by their contact with services. When offering or providing interventions such as parent training programmes, directly address any concerns they have and set out the reasons for and purpose of the interventionWhen working with children and young people with a conduct disorder and their parents or carers: take into account that stigma and discrimination are often associated with using mental health servicep. 16 |
| NICE (2004)215 Eating disorders: Core Interventions in the Treatment and Management of Anorexia Nervosa, Bulimia Nervosa and Related Eating Disorders Focus: Dislocation: Education |
In children and adolescents with anorexia nervosa, the need for inpatient treatment and the need for urgent weight restoration should be balanced alongside the educational and social needs of the young personp. 11Admission of children and adolescents with anorexia nervosa should be to age-appropriate facilities (with the potential for separate children and adolescent services), which have the capacity to provide appropriate educational and related activitiesp. 14 |
| NICE (2004)217 Self-Harm: The Short-Term Physical and Psychological Management and Secondary Prevention of Self-Harm in Primary and Secondary Care Focus: Dislocation: Education; Dislocation: Families |
During admission to a paediatric ward following self-harm, the Child and Adolescent Mental Health Team should undertake assessment and provide consultation for the young person, his or her family, the paediatric team and social services and education staff as appropriatep. 30 |
| NICE (2012)212 Self-Harm: The NICE Guideline on Longer-Term Management Focus: Dislocation: Stigma; Dislocation: Families |
Health and social care professionals working with people who self-harm should be aware of the stigma and discrimination sometimes associated with self-harm, both in the wider society and the health service, and adopt a non-judgemental approachp. 106Health and social care professionals who work with people who self-harm (including children and young people) should be: educated about the stigma and discrimination usually associated with self-harm and the need to avoid judgemental attitudesp. 108Families, carers and significant others:10.1.22 Ask the person who self-harms whether they would like their family, carers or significant others to be involved in their care. Subject to the person’s consent and right to confidentiality, encourage the family, carers or significant others to be involved where appropriatep. 283 |
| NICE (2013)203 Psychosis and Schizophrenia in Children and Young People: The NICE Guideline on Recognition and Management Focus: Dislocation: Education; Dislocation Family; Dislocation: Normal Life |
Recommendations:4.7.10.1 If a child or young person needs hospital care, this should be in a setting appropriate to their agep. 314.7.10.2 Before referral for hospital care, think about the impact on the child or young person and their parents, carers and other family members, especially when the inpatient unit is a long way from where they live. Consider alternative care within the community wherever possible. If hospital admission is unavoidable, provide support for parents or carers when the child or young person is admittedp. 324.7.10.4 Undertake shared decision-making routinely with children or young people in hospital who are of an appropriate developmental level, emotional maturity and cognitive capacity, including, whenever possible, those who are subject to the Mental Health Act (1983; amended 1995 and 2007). Include their parents or carers if appropriatep. 324.7.10.5 Ensure that children and young people of compulsory school age have access to a full educational programme while in hospital. The programme should meet the National Curriculum, be matched to the child or young person’s developmental level and educational attainment, and should take account of their illness and degree of impairmentp. 324.7.10.6 Ensure that children and young people in hospital continue to have access to a wide range of meaningful and culturally appropriate occupations and activities 7 days per week, and not restricted to 9am to 5pm. These should include creative and leisure activities, exercise, self-care and community access activities (where appropriate). Activities should be facilitated by appropriately trained educational, health or social care professionalsp. 32 |
| National CAMHS Support Service (no date)208 Tackling Stigma: A Practical Toolkit Focus: Dislocation: Stigma |
A practical toolkit for tackling stigma with examples of use within a variety of inpatient settings |
Glossary
- Contagion
- This is the term used by the project team to describe the second priority guiding the second phase of this evidence synthesis. It is used to refer to the risks to young people admitted to mental health hospital of being exposed to abnormal behaviour, of learning it and of developing new and unhealthy friendships.
- Dislocation
- This is the term used by the project team to describe the top priority guiding the second phase of this evidence synthesis. It is used to refer to the risks to young people admitted to mental health hospital of being removed from normal life, of being different and of experiencing a sense of fragmentation. It captures the ideas of being stigmatised and discriminated against, and of young people losing their previous identities, social contacts and friendship groups. It includes isolation from, and within, families and the risks presented to young people’s educational, psychological and social development.
- Less obvious risks
- This is the umbrella term used by the project team to bring together the risks of dislocation and contagion, distinguishing them from clinical risks such as suicide, harm to others or physical deterioration.
List of abbreviations
- AIDS
- acquired immunodeficiency syndrome
- ASSIA
- Applied Social Sciences Index and Abstracts
- BBC
- British Broadcasting Corporation
- BNI
- British Nursing Index
- CAMHS
- child and adolescent mental health services
- CERQual
- Confidence in the Evidence from Reviews of Qualitative research
- CI
- confidence interval
- COSI-CAPS
- Costs, Outcomes and Satisfaction for Inpatient Child and Adolescent Psychiatric Services
- DSH
- deliberate self-harm
- EPPI-Centre
- Evidence for Policy and Practice Information and Co-ordinating Centre
- ERIC
- Education Resources Information Center
- HIV
- human immunodeficiency virus
- HSDR
- Health Services and Delivery Research
- HTA
- Health Technology Assessment
- MeSH
- medical subject heading
- MHNAUK
- Mental Health Nurse Academics UK
- NICAPS
- National In-Patient Child and Adolescent Psychiatry Study
- NIHR
- National Institute for Health Research
- QNIC
- Royal College of Psychiatrists’ Quality Network for Inpatient Child and Adolescent Mental Health Services
- RTC
- residential treatment centre
- SAG
- stakeholder advisory group
- SD
- standard deviation
- SE
- standard error
- VIK
- Very Important Kids
- BH
- Ben Hannigan
- DE
- Deborah Edwards
- EG
- Elizabeth Gillen
- GT
- Gemma Trainor
- ML
- Mirella Longo
- NE
- Nicola Evans
- SP
- Steven Pryjmachuk
