Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 09/1809/1074. The contractual start date was in November 2009. The final report began editorial review in April 2013 and was accepted for publication in July 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Soper et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
CLAHRC aims and functions
In 2008 the National Institute for Health Research (NIHR) established nine Collaborations for Leadership in Applied Health Research and Care (CLAHRCs) to develop forward-looking partnerships between universities and local NHS organisations focused on improving patient outcomes through the conduct and application of applied health research. 1 The NIHR made £88 million available over 5 years for this initiative with the requirement that each CLAHRC also obtained matching funding from local NHS organisations. The aims of the CLAHRCs, as defined in the original call for proposals for external evaluations of the CLAHRC initiative, were:2
-
to secure a step change in the way that applied health research is done and applied health research evidence is implemented locally
-
to increase capacity to conduct and implement applied health research through collaborative partnerships between universities and NHS organisations
-
to link those who conduct applied health research with all those who use it in practice across the health community covered by the collaboration
-
to test and evaluate new initiatives to encourage implementation of applied health research findings into practice
-
to create and embed approaches to conducting and implementing research that are specifically designed to take account of the way that health care is increasingly delivered across sectors and across a wide geographical area
-
to focus on the needs of patients, and particularly on research targeted at chronic disease and public health interventions and
-
to improve patient outcomes across the geographic area covered by the collaboration.
The CLAHRCs’ remit was to identify and address problems facing the NHS and population health more widely. This involves three interlinked functions: conducting high-quality applied health research; supporting the ‘translation’ of research evidence into practice; and increasing the capacity of NHS organisations to engage with and apply research. The focus was therefore not only on the translation of research (whether undertaken locally or elsewhere) but also on developing ways of doing applied research that maximise its chances of being useful to the service and of being implemented.
From the start the CLAHRCs were encouraged to develop a community-wide outward-facing approach based on partnerships between academia and the NHS across the widest possible local geographical area, that also actively involved patients and the public and other relevant stakeholders. 3 They were also intended to be experimental, conceived as pilot projects with a common vision but considerable discretion as to how they achieved their goals.
Policy context and the emergence of the CLAHRCs
There has been long-standing recognition of the gap between findings generated by research and their implementation in daily practice. It was against this background that countries have set up programmes to encourage the implementation of research findings that is directly relevant to health care through collaboration,4 including the 10-year Quebec Social Research Council grant programme to encourage collaboration between researchers, practitioners and policy-makers set up in 1992,5 the Quality Enhancement Research Initiative (QUERI) programme launched in 1998 by the US Veterans Health Administration6 and the Need to Know project in Manitoba, funded in 2001 by the Canadian Institutes of Health Research. 7 In 2001, the US Institute of Medicine further highlighted the gap between research findings and health-care practice, in the context of its seminal work on quality improvement in health care,8 and it subsequently set up a clinical research round table that identified two ‘translational blocks’ or ‘translational gaps’ in clinical research:9
-
the transfer of new understandings of disease mechanisms, gained in the laboratory, into the development of new methods for diagnosis, therapy and prevention, and their first testing in humans
-
the translation of results from clinical studies into everyday clinical practice and health decision-making.
In the UK, the NHS Research & Development (R&D) programme was launched in 1991 to strengthen public health and health services research and ensure that the content and delivery of health care were based on high-quality research. 10 It built on previous government attempts to generate research to meet the needs of policy-makers which had emphasised the importance of users of applied health research and researchers working closely together. 11 The NHS R&D programme was intended to be driven by the needs of the service and be fully integrated into its management structure, with regional R&D offices providing a local focus for collaboration. 12,13
However, in practice, effective collaboration between researchers, clinicians and managers has sometimes proved elusive and the UK experience illustrated how entrenched cross-cultural differences and ongoing reorganisations of NHS structures hindered the full realisation of the hoped-for exchanges. 12
The establishment of the CLAHRCs represents one of the more recent attempts to integrate the health research system into the health-care system. 14 It followed the launch, in 2006, of a new 5-year research and development strategy for the NHS in England which aimed to create a health research system in which the NHS supported leading-edge research that focused on the needs of patients and the public. 15 This led directly to the creation of the NIHR. In the same year, the Cooksey Report on UK health research funding highlighted, among other findings, the two gaps in translation of health research previously identified by the Iinstitute of Medicine. 16 Specifically, it noted that a crucial stage in the second gap was the identification and evaluation of new interventions that are effective and appropriate for everyday use in the NHS, and their implementation into routine clinical practice.
Meanwhile, in 2007, the High Level Group on Clinical Effectiveness, which had been asked by the Chief Medical Officer to suggest a programme of action to enhance the effectiveness and efficiency of clinical care, recommended in the field of health research that ‘the health service harnesses better the capacity of higher education to assist with this agenda through promoting the development of new models of community-wide “academic health centres” to encourage relevant research, engagement and population focus and embed a critical culture that is more receptive to change’ (p. 14). 17
Parallel efforts to strengthen translation of research into patient benefit and promote innovation following the Cooksey Report included the establishment, in 2007, of 12 NIHR-funded biomedical research centres. 18 These were designed to address the first translation gap, drive innovation in the prevention, diagnosis and treatment of ill health, and translate advances in biomedical research into benefits for patients. Shortly afterwards, 16 smaller and more specialist biomedical research units were established with the same remit and a similar focus. 19
There was also continuing activity in the NHS, and the 2008 NHS Next Stage review addressed the same broad themes. 20 Specifically, it argued that there were cultural, professional and organisational barriers to effective innovation and relevant research, which would require new initiatives; these included academic health science centres and health innovation and education clusters (HIECs). In 2009, five UK-based academic health science centres were designated by the Department of Health with the aim of focusing on world-class research, teaching and patient care and competing internationally with comparable centres in the USA, Canada, Singapore, Sweden and the Netherlands. 21 The HIECs initiative was launched in 2009/10, with 17 HIECs set up across England for an initial period of 2–3 years. 22 These sought to promote innovation in the NHS by combining the expertise of industry, health and education at a local level.
Collaborations for Leadership in Applied Health Research and Care were originally foreseen as NIHR ‘Academic Health Centres of the Future’. 3 However, against the background of other ongoing initiatives, there was a perceived need to identify a designation that would more appropriately emphasise the collaborative nature of the proposed partnerships and their role in applied health research and the implementation of research evidence, as well as avoiding ‘any confusion with Academic Health Science Centres’ given their different purpose and structure. 23 The distinctive feature of CLAHRCs was that they had a wider, integrating role in promoting collaboration across a range of local organisations, including NHS trusts, primary care trusts, universities and industry, and a key focus on addressing the second translation gap. Depending on local circumstances, they might also relate to the work of other parts of the landscape such as biomedical research units/centres. In Chapter 5 we will return to the question of how CLAHRCs have assumed a unique role in this wider, and constantly evolving, landscape, and discuss their role in relation to developments in both the health research system and the health service.
The conceptual background
A wide range of thinking about the conduct and translation of research informed the development of the CLAHRCs and considerations of how their role is best interpreted. However, the literature on the diffusion of health-care research, knowledge transfer and dissemination is complex, reflecting the contributions made from a variety of disciplines, each bringing their own conceptual frameworks and terminology, such as ‘research’, ‘evidence’, ‘knowledge’ or ‘innovation’, and ‘diffusion’, ‘dissemination’, ‘exchange’, ‘transfer’ or ‘learning’. While we acknowledge this complexity and the resulting difficulties of summarising this literature without losing significant detail and risking misinterpretation, we also believe that there was a need to draw on insights from a wide range of theories and approaches in order to guide our work and help interpret observations from CLAHRCs as they evolved. Building on a targeted review of the literature which we undertook early in the evaluation,24 and which we have updated in light of more recent evidence, we describe here different insights from some key approaches that have explored the causal relationship between research production and research use.
Research diffusion and knowledge utilisation
Research diffusion and knowledge utilisation are concepts central to the working of CLAHRCs. Two key papers are discussed here. Estabrooks et al. suggest that research on knowledge utilisation has evolved through a series of paradigms in which certain disciplines seem to have dominated at different stages. 25 In contrast, Greenhalgh et al. suggest that many streams of research have explored research diffusion in parallel and attempt to identify the interactions and linkages between them, developing ‘a unifying conceptual model’ to consider the diffusion of innovations in health-care organisations. 26 Both groups of authors emphasise the wide range of research traditions involved and explain how an early emphasis on diffusion research (Greenhalgh et al. ) or knowledge utilisation (Estabrooks et al. ) broadened to cover other fields. Greenhalgh et al. cite the emergence of development studies (covering the different contexts and meaning or value of innovations) and health promotion;26 Estabrooks et al. note the emergence of diffusion of innovations and technology transfer. 25 Both comment on the emergence of evidence-based medicine in the mid-1980s, and Greenhalgh et al. also discuss the relevance of the organisation and management literature. 26
Greenhalgh et al. ’s attempt to provide an underlying framework was ambitious, and their suggestions for (and against) further research have been helpful. They highlight the importance of context and ‘confounders’, which ‘lie at the very heart of the diffusion, dissemination, and implementation of complex innovations’ and how these are ‘not extraneous to the object of study; they are an integral part of it’. 26 Therefore, future research should be multidisciplinary and multimethod, meticulously detailed and participatory, and should acknowledge the central importance of context. They further suggest that the next generation of research on the diffusion of health service innovations should be empirically driven but theory-guided so that consistent processes can emerge.
We were persuaded by the arguments brought forward by Greenhalgh et al. and informed by their recommendations on how research translation should be studied. For CLAHRCs, the important lesson is that when discussing research diffusion and knowledge utilisation there is no single, stable and agreed conceptual framework and this requires being sensitive to how terms are being used and recognising that the same concept may have different meanings. It also means that there is no off-the-shelf conceptual model that can be used without the potential for confusion.
Implementation and the use of theory
Eccles et al. also call for greater use of theory in promoting the uptake of research findings, and describe the current situation as ‘an expensive version of trial-and-error, with no a-priori reason to expect success or to have confidence of being able to replicate success if it is achieved’. 27 Following other work, they describe theory as ‘a coherent and non-contradictory set of statements, concepts or ideas that organises, predicts and explains phenomena, events, behaviour, etc.’ (p. 108), and, along with Ferlie and Shortell,28 note that interventions that seek to improve health care operate at four levels: the individual health professional, the health-care group or team, the organisation providing health care (e.g. NHS trusts) and the larger health-care system or environment in which individual organisations are embedded. In a comment that could have been tailored specifically for the CLAHRCs, Eccles et al. also note: ‘Because implementation research lives in a policy-relevant context where clinicians, managers, and policy makers may erroneously believe that they already know what is best to do, it will always be prey to the demands for a quick fix and the political solution’ (p. 111). 27
In a similar vein, Grol et al. refer to the need for a ‘better understanding of the black box of change in health care’ and also call for a more systematic use of theories in planning and evaluating improvement interventions in clinical practice. 29 Following other work, they describe ‘theory’ as ‘a system of ideas or statements held as an explanation or account of a group of facts or phenomena’, and distinguish two types:
-
impact theories: hypotheses about how specific interventions will facilitate a desired change, as well as the causes, effects and factors determining success (or the lack of it) in improving health care
-
process theories: how implementation activities should be planned, organised and scheduled in order to be effective (the organisational plan) and how a target group will utilise and be influenced by the activities (the utilisation plan).
According to Grol et al. ,29 the ideal model for change in health care would encompass both types of theory. They summarise and recommend a set of 16 theories about change in health care, and, in a taxonomy that closely reflects that used by Eccles et al. ,27 differentiate these by ecological level (individual professional, social setting, organisational context, political and economic context). Cognisant of the limited empirical evidence of the effectiveness and feasibility of theoretical approaches to produce the intended change, they emphasise the need to draw on different theoretical perspectives simultaneously to inform change plans.
Building on Greenhalgh et al. ’s26 work, Damschroder et al. developed a consolidated, metatheoretical framework for implementation research that is based on 19 published theories. 30 This again is a very broad approach (the authors use the term ‘theory’ to refer to published models, theories and frameworks) that encompasses five major, interactive domains:
-
intervention characteristics: source, evidence base, relative advantage, adaptability, trialability, complexity, design quality and packaging, and cost
-
outer setting: economic, social and political context in which organisation resides
-
inner setting: structural, political and cultural contexts through which the implementation will proceed
-
characteristics of the individuals involved: knowledge and beliefs about implementation, belief in own capabilities, identification with organisation and other personal attributes such as tolerance of ambiguity, intellectual ability, motivation, values, competence, capacity, innovativeness, tenure and learning style
-
process of implementation: planning, engaging, executing, reflecting and learning.
The aim was to provide a pragmatic structure for identifying potential influences on implementation and organising findings across studies.
Knowledge mobilisation and research utilisation: the potential contribution of the management literature
The relevance of the organisation and management literature is explored more fully by Crilly et al. ,31 who note that there is a well-established literature on the utilisation of clinical evidence in health care but that there has been less consideration of the utilisation of management evidence and research by health-care organisations. Crilly et al. 31 identify 10 thematic categories from the management literature: the nature of knowledge and knowing; information systems and technology; communities of practice; organisational form; organisational learning; resource-based view of the firm; critical theory; knowledge transfer and performance; barriers and facilitators; and culture. A review of the health and social science literature identified two further domains: the evidence-based movement and ‘super structures’, which they define as ‘the infrastructure of institutions and funding that commission healthcare research’ (p. 45). 31
Based on their review, the authors provide a series of propositions, including the general thesis that productivity and efficiency will become increasingly important in the context of spending restrictions in England, and that, as a result, knowledge transfer and the diffusion of innovations will be crucial to the sustainability of NHS organisations. Overall, they argue, the NHS would need to consider how knowledge and information can be used to improve productivity, innovation and performance. These arguments have been adopted in the establishment of Academic Health Science Networks (AHSNs) in England in 2013,32 to which we return later in this report.
Crilly et al. 31 also put forward propositions that are more specific to entities such as the CLAHRCs. They highlight the lack of consensus on what constitutes evidence-based management and suggest that ‘all management knowledge is contested’ (p. 216). 31 They draw on evidence about barriers to, and facilitators of, transfer, and propose that knowledge mobilisation is not just a mere technical activity, arguing that it is also cultural and political. A further proposition that Crilly et al. 31 put forward is extremely germane to the CLAHRCs: they suggest that partnership and network-based organisational forms are more effective at knowledge-sharing than markets or hierarchies and they emphasise the value of collaboration. This last proposition was also identified as important in studies of organisational culture, which we discuss further below. 33
Crilly et al. 31 observe that learning processes and their relationship with organisational design emerged as an important theme in their review. However, it is their further observation that is particularly telling, especially in relation to the CLAHRCs. Crilly et al. 31 note that the question of organisational form has received little attention in the health-care literature despite major reorganisations designed to promote bench to bedside research translation and organisational learning.
Knowledge transfer and exchange
A closely related field is the ongoing work on knowledge transfer and exchange (KTE), which Mitton et al. define as ‘an interactive process involving the interchange of knowledge between research users and researcher producers’ (p. 729). 34 In a wide-ranging review that examined the evidence base for KTE, the authors note that knowledge transfer emerged in the 1990s as a process by which research messages were pushed by the producers of research to the users of research but that, more recently, knowledge exchange emerged as a result of growing evidence that the successful uptake of knowledge requires more than one-way communication, calling instead for genuine interaction among researchers, decision-makers and other stakeholders. They also note a growing emphasis on generating knowledge that can have a practical impact on the health system, which has been a key driver of the CLAHRC scheme.
Mitton et al. list the key KTE strategies mentioned in the literature, including:34
-
face-to-face exchange (consultation, regular meetings) between decision-makers and researchers
-
education sessions for decision-makers
-
networks and communities of practice
-
facilitated meetings between decision-makers and researchers
-
interactive, multidisciplinary workshops
-
capacity building within health services and health delivery organisations
-
web-based information, electronic communications
-
steering committees (to integrate views of local experts into design, conduct and interpretation of research).
They also identify a variety of mechanisms to facilitate KTE, such as joint researcher–decision-maker workshops, the inclusion of decision-makers in the research process as part of interdisciplinary research teams, a collaborative definition of research questions and the use of intermediaries who understand both roles, known as ‘knowledge brokers’.
These lists suggest that a possible blueprint might be emerging for subsequent programmes (such as the CLAHRCs) to follow. However, Mitton et al. reiterate the concern about the lack of empirical evidence raised by others, noting that ‘despite the rhetoric and growing perception in health services research circles of the “value” of KTE, there is actually very little evidence that can adequately inform what KTE strategies work in what contexts’ (p. 756). 34
Research dissemination
There is some overlap between Mitton et al. ’s34 work on knowledge transfer and exchange and a review undertaken by Wilson et al. on the conceptual or organising frameworks relating to research dissemination. 35
While their focus is on dissemination, Wilson et al. 35 reiterate the debate about terminology mentioned earlier and note that the terms ‘diffusion’, ‘dissemination’, ‘implementation’, ‘knowledge transfer’, ‘knowledge mobilisation’, ‘linkage and exchange’ and ‘research into practice’ are all used to describe overlapping and interrelated concepts and practices. The authors define ‘dissemination’ broadly as ‘a planned process that involves consideration of target audiences and the settings in which research findings are to be received and, where appropriate, communicating and interacting with wider policy and health service audiences in ways that will facilitate research uptake in decision-making processes and practice’ (p. 2)(a formula that resonates with CLAHRC objectives). They note that there are currently a number of theoretically informed frameworks available to researchers that could be used to help guide their dissemination planning and activity, and identify 33, of which 28 are underpinned at least in part by one or more of three theoretical approaches: persuasive communication, diffusion of innovations theory and social marketing.
The authors do not provide a blueprint, although they caution against over-reliance on linear models of health communication. They also reiterate the need to use theoretically informed strategies and, specifically, suggest that funding agencies could consider encouraging grant applicants to develop theoretically informed plans for research dissemination.
Knowledge translation
The call for applications to establish the CLAHRCs stressed their role in addressing the second translation gap. 3 However, the terms ‘translation’ and ‘translation gap’ can be variously interpreted. Moreover, additional gaps have subsequently been identified to complement (and complicate) the two identified by the US Institute of Medicine 8 and the Cooksey Report. 16 Thus Westfall et al. propose a third translational step involving research in ambulatory clinical practices. 36 This proposal is based on the observation that much of clinical research is undertaken in an academic clinical setting whereas the majority of patients receive medical care in a primary care setting. It is at this interface, Westfall et al. 36 argue, that practice-based primary research is required to support primary care physicians to incorporate new discoveries into daily clinical practice, with the third translational step involving dissemination and implementation research. Khoury et al. add a fourth step that, beyond implementation, considers the impact of a given ‘discovery’ on population health outcomes. 37
However, it is increasingly recognised that this terminology may be unhelpful, and that a linear, basic-to-applied model which assumes that ‘gaps’ can somehow be ‘bridged’ does not fully capture the complexities of moving knowledge into action. 38 The translation and implementation of research in practice depends, in part, on the relevance, quality and usefulness of the research itself to service needs. That, in turn, depends on the ways in which research agendas are set, research processes implemented and research knowledge communicated and exchanged. Generating, translating and adopting knowledge is likely to involve iteration and feedback between multiple actors involved to varying degrees in different phases; therefore, implementation activity cannot be studied in isolation from research generation activity.
Research impact assessment
There is growing interest in understanding and measuring the return on investment in medical research. In a systematic review of the associated literature, Hanney et al. identified 200 papers, but relatively few were empirical studies. 39 One approach has been the descriptive categorisation of payback and the payback analytical framework developed by Buxton and Hanney,40 which originally assessed the impact or payback from health services research funded by the health department in England but is now applied more widely. The categorisation covers a wide range of measures of impact, including knowledge, benefits to future research and research use, informing policy and product development, health sector benefits and broader economic benefits. The payback framework focuses attention on the whole process including research production and use. Of specific relevance to the CLAHRCs and their potential influence in local health economies is another study identified in the review. This assessed the impact of the NHS South and West Region’s Development and Evaluation Committee’s technology appraisal reports and compared the impact in the south-west with that elsewhere in England. 41 It found considerable impact in the south-west but less elsewhere, suggesting that having local authors known to local decision-makers was influential in encouraging translation, a finding of interest given the local remit of the CLAHRCs.
Capacity building: collaborative research and absorptive capacity
The main purpose of the CLAHRCs was to develop collaborations that are a ‘mutually beneficial, forward-looking partnership between a university and the surrounding NHS organisations, focused on improving patient outcomes through the conduct and application of applied health research’ (p. 2). 3 Denis and Lomas traced the development of a collaborative approach to research in which researchers and potential users work together to identify research agendas, commission research and so on. 4 They identified the 1983 study by Kogan and Henkel of the R&D system of the health department in England42 as an important early contribution. According to Kogan and Henkel, a critical feature of the collaborative approach, as applied to research and policy-making, is that researchers and policy-makers should join forces ‘to identify research needs against policy relevance and feasibility’ (p. 143). 42 Work to analyse and operationalise this collaborative approach was subsequently undertaken by the Canadian Health Services Research Foundation, led by Lomas, whose concept of ‘linkage and exchange’ between users and researchers has been particularly influential. 43,44 Collaborative approaches to research somewhat mirror the concept of ‘Mode 2′ research: research that is context-driven, problem-focused and interdisciplinary. 14,45–47
The CLAHRCs were also required to increase ‘the capacity of NHS organisations to engage with and apply research’ (p. 4). 2 The concept of absorptive capacity was first described by Cohen and Levinthal in the context of industrial research;48 they suggested that conducting R&D within a firm helps that firm to develop and maintain its broader capabilities to assimilate and exploit externally available information from research. 49,50 The original theory could apply at different levels, including individual and organisational levels, and it can be argued that, when clinicians and managers in a health-care system are seen as stakeholders in the research system, their engagement in research is a way of enhancing their ability and willingness to use research from wherever it might originate. For example, Buxton and Hanney51 include increased capacity to use research as one of the benefits identified in their multidimensional categorisation of benefits from health research,40,51–53 and this approach is replicated in other health research impact assessment frameworks that build on the payback framework. 54–56 Part of the theoretical underpinning that research engagement contributes to building absorptive capacity is the notion that, in practice at least, knowledge is not a pure public good but instead requires a level of understanding of research before it can be absorbed. 57 Such understanding can be built up by undertaking research.
Cultural change
Another requirement of the CLAHRCs was to ‘embed a critical culture [in the NHS] that is more receptive to change’ (p. 14). 17 Shortell et al. 58 explored the relationship of organisational culture, quality improvement and selected outcomes in hospitals in the USA, showing that an organisational culture characterised as participative, flexible and risk-taking was significantly related to quality improvement implementation. More recently, Mannion et al. classified the extant cultures in NHS organisations into four types – clan, hierarchical, developmental and rational – and explored how these cultures change over time. 33 In general they identified ‘developmental’ culture, characterised by innovation, dynamism, growth and entrepreneurship with an external, relational focus, as one in which change was viewed as a ‘positive organisational attribute . . . [and there was a] . . . willingness of senior management to embrace innovative approaches to delivering services’ (p. 209). 33 It is this developmental culture that most closely matches the culture the CLAHRCs are seeking to instil. This is a considerable challenge; Mannion et al. found that this development culture was dominant in only a small percentage of NHS hospital trusts and general practitioner (GP) practices. 33 However, they also suggest that cultural change can happen when it is triggered by a perception of crisis, initiated and shaped by strong leaders, consolidated by perceived success and mediated by relearning or re-education.
Organisational change and system shift
Some health-care organisations have paid particular attention to the role of research in their overall approach to improve performance. 59 For example, the Veterans Administration in the USA sought to promote research engagement throughout its health-care delivery system as part of a comprehensive re-engineering exercise designed to improve the quality of the health care provided. 60 Veterans Administration investigators are nested in a fully integrated health-care delivery system with a stable patient population with a high prevalence of chronic conditions, which provides them ‘with unparalleled opportunities to translate research questions into studies and research findings into clinical action’ (p. I–10). 61 One way in which this integration has been achieved is through the aforementioned QUERI programme. Launched in 1998, it sought to accelerate the implementation of new research findings into clinical care by creating strong links between those performing research and those responsible for health systems operations: a remit that resonates strongly with that of the CLAHRCs. An evaluation of the QUERI programme described this approach as achieving a ‘paradigm shift to an action-oriented approach that meaningfully engages clinicians, managers, patients/clients, and researchers in research-driven initiatives to improve quality’ (p. 1). 62 In language that echoes that later used by the CLAHRCs, the authors concluded that this shift is towards coproduction of knowledge, or ‘Mode 2′ knowledge production.
Organising for quality
In the context of CLAHRCs, work on quality improvement also provides important insights. Bate et al. ,63 in a study of the quality of nine high-performing health-care organisations in the UK and the USA, took an approach that was grounded in the examination of actual processes at different organisational levels. Reflecting the observations of Grol et al. described earlier in this section,30 Bate et al. point to the underuse of theory in the quality improvement literature and note that much of the evidence that is available is descriptive rather than explanatory. 63 Furthermore, they contend that quality improvement has been dominated by a form of ‘menu mentality’,63 characterised by lists of factors seen as important, such as leadership support, team-based structures and composition, and information technologies (and their failings), instead of focusing on the processes that will bring these factors together to achieve change.
Emphasising that quality improvement has to be seen as a complex process, they suggest that the keys to quality improvement lie in the distinct characteristics and dynamics of organisational and human processes. In theoretical terms this is a shift from a variance or variables theory (e.g. more of X and more of Y produce more of Z) to a process theory (e.g. do A and then B to get to C). In empirical terms it is the shift from seeing quality improvement merely as a method, technique, discipline or set of skills to seeing it as a human and organisational achievement, that is a social process. Bate et al. identify six common challenges that all the organisations they studied faced, which they describe as structural (organising, planning and co-ordinating quality improvement), political, cultural, educational, emotional, and physical and technical. 63
Like others, Bate et al. 63 argue that there is no single best way to achieve service excellence. The case studies they report underscore the notion that quality improvement processes are interconnected and symbiotic. Organisational processes may form cycles or closed loops, which may be virtuous (upward improvement) or vicious (downward degrading) spirals. This step beyond the ‘menu mentality’ focuses on sequencing and transformation, and provides important insights for the CLAHRCs about the need to examine organisational processes and their interactions over time.
Normalisation process theory
Normalisation process theory (NPT) was developed by May et al. 64,65 and is concerned both with the implementation of new ways of thinking, acting and organising in health care and with the integration (‘routine embedding’) of new systems of practice into existing organisational and professional settings. NPT proposes what May and Finch refer to as a ‘working model of implementation, embedding and integration in conditions marked by complexity and emergence’ (p. 535). 66 It covers the relationships between a complex intervention and the context in which it is implemented. It is interested in the processes by which implementation proceeds – including interactions between people, technologies and organisational structures – and the work that proceeds from these. It proposes that (1) innovations become embedded in practice as a result of people working, individually and collectively, to implement them; (2) the work of implementation is operationalised through four generative mechanisms identified as coherence, cognitive participation, collective action and reflexive monitoring; and (3) organising structures and social norms specify the rules and roles that frame action. 66 The four mechanisms are described further as:64,67
-
coherence or sense-making: how complex interventions are formed in ways that hold together and people make sense of, and specify, their involvement in it
-
cognitive participation: how communities of practice are built and sustained, that is how actors enrol themselves and others into a complex intervention
-
collective action: the collective work that people do to enact a set of practices
-
reflexive monitoring: the appraisal that people make to understand the ways in which a new set of practices affects them and those around them.
May considers NPT a generic and middle-range theory of implementation that examines what people do and how they work. 64 This distinguishes it from theories of the cultural transmission of innovations (such as diffusion of innovations) that seek to explain how innovations spread, theories of collective and individual learning and expertise that seek to explain how innovations, are internalised, and theories of the relationships between individual attitudes and intentions, and behavioural outcomes. NPT emphasises the need to look for processes. It provides an important frame for CLAHRCs in that the outcomes of the CLAHRCs can be seen to result from the integration of a complex intervention into a complex system achieved by the accomplishments of its stakeholders.
Conclusions
This section has discussed theories of the diffusion of innovation, research use, quality improvement, collaboration and process theory that can inform CLAHRCs’ activities and their evaluation. The main observations are further summarised in Table 1. While we would not want to place too much weight on this brief overview, we believe that a number of key lessons can be learned:
| Approach | Focus | Features/strategy | Strengths |
|---|---|---|---|
| Implementation | |||
| Diffusion of innovation | Conceptual framework for implementation developed by Greenhalgh and others26 based on systematic literature review | Captures many of the features of implementation in the health services context and identifies some key attributes for success | Health-service specific Builds on a range of existing literature Broad and generalisable |
| Research use, includes research-based practitioner model, embedded research model and organisational excellence | Implementation by various groups/at various levels | Responsibility for implementation is at various levels, with an emphasis on creating a research-oriented mind-set | Context-driven Emphasises capacity building May help to clarify thinking about research uptake |
| Quality improvement | Several different models | Clear definition of the necessary, but not sufficient, conditions for the implementation of change | Importance of a combined approach, using relevant aspects from various models |
| Collaboration | |||
| Linkage and exchange, and knowledge brokering | Theoretical model focusing on personal interactions | Emphasis on frequent interpersonal interactions as crucial for learning | Recognises the importance of learning and capacity-building |
| Process | |||
| Organising for quality | Focusing on the characteristics and dynamics of organisational processes | Emphasis on key constituent processes in organisations and their interrelations over time | Sees improvement as a social process as well as a set of techniques or methods |
| NPT | Theoretical model focusing on process evaluation | Emphasis on what people do and how they work | Specifically aimed at the implementation and integration of complex interventions in health-care settings in relation to the work that it involves |
-
There is no ‘industry standard’ to guide the CLAHRCs; CLAHRCs are involved in both developing their own solutions and delivering these.
-
The causes of problems are understood differently, and consequently solutions vary (although these are often at a high level of abstraction).
-
It is widely recognised that context is very important.
-
There is a general scepticism about overly rigid linear models (but in all there is a sense that processes can be managed to make progress over time).
-
It is likely that successful change will be multifaceted and therefore evaluations must be equally multifaceted if they are to understand the range of processes involved.
We have identified a body of literature reflecting an area of research characterised by conceptual pluralism, alternative ways of framing the evidence and competing causal explanations. The conceptual terrain might be described as dynamic, pluralistic and competitive. With terminologies that evolve over time and compete one with another we need to define our terms with care. Given the wide range of theories and metatheories it is not always clear how to translate research into practice, although three general messages do emerge. The first is that context is increasingly identified as crucial to shaping outcome. If practitioners do not understand the context within which they operate, and evaluators fail to assess this accurately, then it is unlikely that we will develop a good understanding of why the CLAHRCs work in some contexts and not in others. Secondly, while there is a flow of knowledge it is not always clear that this is simply from research to practice and, even when this is largely the case, there will be a variety of ways in which information flows ‘back’ the other way. In the language of economists, there will be supply push as well as demand pull. Thirdly, and following from the first two, the metaphor of a single bridge, linking research to practice and with a steady flow of traffic moving one way, is unhelpful. Competing metaphors might include an ecosystem or a marketplace. 68
Structure of this report
This introductory chapter briefly set out the aims of and the policy context within which the CLAHRCs were established, as a means to illustrate the complexities involved and the innovative nature of the initiative. It also summarised the conceptual background against which the CLAHRCs were developed. Chapter 2 describes the methods used, setting out our approach and the phased nature of the work undertaken. Chapters 3 and 4 present the core findings of the work, with Chapter 3 presenting the observations from phase 1 of our evaluation while Chapter 4 focuses on findings emerging from phase 2 and is structured according to major themes that were identified in phase 1 of the study. Chapter 5 discusses our overall findings, seeking to relate them to the wider literature on research use and impact. We also review current developments in the NHS, in particular the new AHSNs, and explore how they, and the CLAHRCs in their second round of funding, have been tasked to work together in an integrated and synergistic way. Finally, we draw some general conclusions, highlight some practical implications and make recommendations for further research in an area that is continuing to evolve.
Chapter 2 Methods
This evaluation explored how effectively the CLAHRCs supported the translation of research into patient benefit, and how they developed ways of doing applied research that maximised its chances of being useful to the service and the capacity of the NHS to respond.
In developing the design for our study we sought to take account of the evolving and changing nature of the context within which CLAHRCs were established. We note how there were many paths that CLAHRCs could have taken to generate knowledge and enable its adoption for the improvement of patient care. Against this background, our approach to evaluation had to be emergent and ready to develop with the CLAHRCs’ phases. We thus adopted a tiered design to enable an adaptive and emergent approach69 and incorporated the formative evaluative components that were requested in the NIHR’s research brief for the evaluation of CLAHRCs. We did this to ensure that findings from the evaluation informed learning as the CLAHRCs evolved in the early years of their implementation. 2
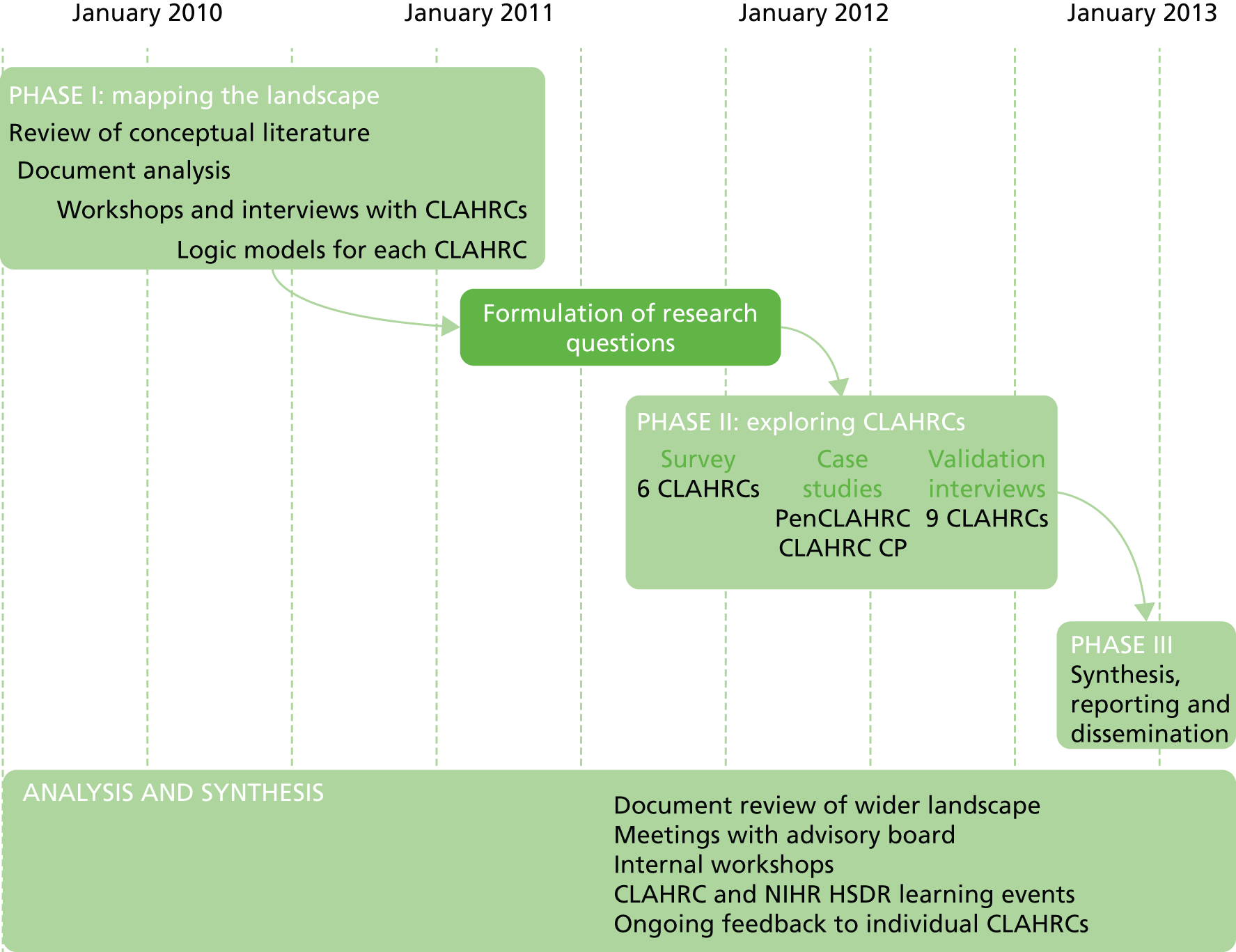
Recognising the breadth and complexity of the CLAHRC initiative, we developed a ‘research map’ to guide our work (Figure 1). This allowed us to formulate the preliminary evaluation questions that constituted a generic starting point for the analysis of specific CLAHRCs and the identification of specific research questions. These were:
FIGURE 1.
Key evaluation questions guiding the study.

Overarching research question: How, and how effectively, do CLAHRCs address the second translation gap?
Subsidiary questions:
-
How, and how effectively, do CLAHRCs support local health research?
-
How, and how effectively, do CLAHRCs build local infrastructures to utilise globally and locally generated health research for local patient benefit?
-
Does bringing together activities for health research and activities for delivering health research benefit both sets of activities?
In line with the tiered approach, the study consisted of three phases, each building on the insights from the preceding phase. Phase 1 sought to map the landscape of the nine CLAHRCs and the context in which they were established. Through this mapping exercise, and in consultation with the nine CLAHRC directors and the Health Services and Delivery Research Programme (HSDR), we identified three core research questions, which we explored in detail in phase 2, using qualitative and quantitative methods. These were:
-
How does the NHS influence CLAHRCs’ evolution, outcomes and impact (and indeed how does having a CLAHRC influence NHS behaviour)?
-
How are effective multistakeholder and multidisciplinary research and implementation teams for service improvement built: what can we learn from the CLAHRC model and what mechanisms are being used to enable it?
-
What can we learn from the CLAHRCs that can provide new understanding of how to use research knowledge and evidence to change commissioning and clinical behaviour for patient benefit?
The final phase of the study, phase 3, sought to synthesise the findings. Figure 2 illustrates how the three phases of our study interlinked and facilitated the emergence and refinement of our research questions over time. This approach was devised in response to the initial research brief,2 which also meant adapting the research protocol as the study evolved, in consultation with the advisory board to the project and following agreement by NIHR HSDR. The final revised research protocol is presented in Appendix 1 to this report.
FIGURE 2.
Study design and timeline. CP, Cambridgeshire and Peterborough; PenCLAHRC, South West Peninsula Collaboration for Leadership in Applied Health Research and Care.
Phase 1: mapping the CLAHRC landscape
We drew on a theory-of-change-led realist evaluation framework to help inform the identification of the various strategies that different CLAHRCs were pursuing to generate and use new forms of knowledge. 70 Specifically, we sought to understand the CLAHRCs by exploring their perceptions and behaviours, in order to reveal some of the implicit assumptions underlying the approaches adopted by individual CLAHRCs. Thus, we did not set out with pre-specified hypotheses on how CLAHRCs would evolve, and seek to test them, because we expected that such hypotheses would become outdated and made irrelevant almost as quickly as they were formulated.
Phase 1 of the study considered all nine CLAHRCs, and involved the collection of data to identify and make explicit the diversity of strategic approaches being used, and identify how the strategies were being implemented.
Before describing our approach to data collection in phase 1, it is important to reiterate that NIHR HSDR commissioned four teams to evaluate aspects of CLAHRCs. 71 There was, therefore, a need to minimise unnecessary duplication of data collection so as to not overburden CLAHRCs, in particular in the early phases of their establishment. As a consequence, the quantity and range of evidence collected in the first phase of our evaluation varied. However, we were able to collect sufficient data that allowed us to understand the key resources being used, the range of CLAHRC activities, the outputs achieved and the intended outcomes of all nine CLAHRCs, and the facilitators and barriers encountered.
Data collection primarily included document analysis, interviews with senior individuals, workshops or mini-conferences with some CLAHRCs and non-participant observation of key meetings in others, as well as drawing on existing literature in implementation science and the sociology of knowledge to inform our enquiries. Documents reviewed included CLAHRCs’ individual application forms to the NIHR and other documentation; Table 2 provides an overview of the range of interviews and workshops we carried out across the nine CLAHRCs.
| CLAHRC | Interview participants | Workshop and events |
|---|---|---|
| Birmingham and Black Country (CLAHRC-BBC) | 4 | Limited their involvement to interviews |
| Cambridgeshire and Peterborough (CLAHRC-CP) | 8 | Half-day workshop |
| Greater Manchester (CLAHRC-GM) | 4 | Non-participant observation at board and theme leads meeting |
| Leeds, York and Bradford (LYB-CLAHRC) | 7 | 2-hour workshop and attendance at business meeting |
| Leicestershire, Northamptonshire and Rutland (LNR-CLAHRC) | 8 | CLAHRC mini-conference and half-day workshop |
| North West London (Northwest London) | 7 | Half-day workshop |
| Nottinghamshire, Derbyshire and Lincolnshire (CLAHRC-NDL) | 3 | CLAHRC conference and mini-session |
| South West Peninsula (PenCLAHRC) | 5 | Half-day workshop |
| South Yorkshire (SY-CLAHRC) | 2 | Limited their involvement to interviews |
| Total number of interviews | 48 |
In-depth interviews
Interviews in the first phase of the evaluation sought to provide background information on the details of CLAHRC implementation strategies, approaches and activities, motivations for the selection of specific strategies and activities to achieve the CLAHRC goals, processes and structures in place for managing and delivering the activities, expected milestones and targets for outputs, and the nature and role of local and national factors as enablers or potential barriers to success.
We purposely sampled senior individuals who were likely to play a key role in implementing CLAHRC interventions across all nine CLAHRCs. We sought to interview three or four senior people per CLAHRC, covering clinicians, academics, managers and commissioners. Potential interviewees were identified in consultation with individual CLAHRCs. As indicated above, the final number of individuals agreeing to be interviewed varied across CLAHRCs, from two participants in South Yorkshire CLAHRC to eight participants representing Cambridgeshire and Peterborough (CP) CLAHRC and eight representing Leicestershire, Northamptonshire and Rutland CLAHRC (Table 2); roles and functions covered CLAHRC directors, clinical leads and theme leads. Interviews were conducted face to face or as telephone interviews, lasting an average of 60 minutes (the interview protocol is presented in Appendix 2). Interviews were recorded and transcribed following prior permission by the participant. Transcripts were analysed according to the themes guiding the interviews.
Workshops
The workshops sought to develop the themes identified in interviews with senior CLAHRC individuals. Specifically, the workshops aimed to explore innovative ways of delivering CLAHRC activities as well as the facilitators and challenges/barriers to their success, expected or intended outcomes, early and future impacts, and views on how to improve each CLAHRC’s performance. Participants were also asked to suggest issues on which the evaluation might focus in the succeeding period. An outline of the workshop agenda is presented in Appendix 3.
Our aim was to hold one workshop with each CLAHRC, which was to take place at the lead institution and involve five or six representatives of different stakeholder groups and organisations within the CLAHRC. However, as indicated in Table 2, the number and format of workshops varied, with two CLAHRCs limiting their participation in our evaluation to interviews only. Following the workshops, the evaluation team prepared a workshop report which summarised the issues discussed and the findings. These were shared with workshop participants to validate the evaluation team’s report.
Synthesis
Drawing on the primary and secondary data collected, we sought to identify and make explicit the theories of change and intervention logic of each CLAHRC. Specifically we explored:
-
the types of intervention being used to identify problems and promote evidence-generation and evidence-based improvement in health-service practice
-
the mechanisms through which these interventions operated (interactions, social influence, facilitation, etc.)
-
the diversity of stakeholders involved in the intervention approaches
-
the various levels at which these interventions operated:
-
the micro level, that is interventions that promoted improvements in the identification, conduct, application and integration of research by individual researchers, managers, practitioners and patients within a single organisation
-
the meso level, namely interventions that promoted improvements in the identification, conduct, application and integration of research by researchers, managers, practitioners and patients across different organisations
-
the macro level, interventions that promoted improvements in the identification, conduct, application and integration of research from organisation to organisation and across research and health-care sectors.
-
Guided by this information we developed logic models for each of the nine CLAHRCs, to illustrate and explore the theories of change underlying each CLAHRC.
In keeping with the formative emphasis of the evaluation, we fed early findings back to all the CLAHRCs, NIHR HSDR and other key stakeholders at a dedicated learning event in early 2011. We also provided a detailed report to the NIHR and others on progress achieved in the first year of the evaluation. 24
In addition to identifying and make explicit the diversity of strategic approaches adopted by individual CLAHRCs, phase 1 of our study also sought to identify the most pertinent research questions for detailed exploration in phase 2 of the evaluation. Informed by work undertaken in phase 1 and guided by the overarching question of how, and how effectively, CLAHRCs address the second translation gap, we identified a set of priority areas for further exploration. These priority areas were further informed through consultation with the advisory board to our study, and by consideration of the focus of the three other NIHR HSDR-commissioned evaluation teams. 71 Following this process, we identified three core areas for further analysis in phase 2 of the project, which we described in the introduction to this chapter:
-
How does the NHS influence CLAHRCs’ evolution, outcomes and impact (and indeed how does having a CLAHRC influence NHS behaviour)?
-
How are effective multistakeholder and multidisciplinary research and implementation teams for service improvement built: what can we learn from the CLAHRCs model and what mechanisms are being used to enable it?
-
What can we learn from the CLAHRCs that can cast new understanding on how to use research knowledge and evidence to change commissioning and clinical behaviour for patient benefit?
Phase 2: exploring CLAHRCs
Stakeholder survey
To better understand the inter-relations between the NHS and the CLAHRCs, the (perceived) effectiveness of multistakeholder and multidisciplinary research for service improvement, and how research knowledge and evidence can be used to inform commissioning and clinical behaviour for patient benefit, we carried out a survey of CLAHRCs (see Appendix 4).
Against the background of the CLAHRCs as a complex intervention, and the interest in learning about how this model might be used in future, the design of the survey instrument was informed by the theory of the normalisation of complex interventions (NPT),54,65,72 which we discussed in Chapter 1 of this report. In developing the survey instrument, we drew on the four components of the NPT and mapped these against the core research questions guiding phase 2 of the evaluation:67
-
coherence and sense-making: why people believe CLAHRCs to be distinctive and have value
-
cognitive participation: how individuals and groups participating in CLAHRCs come to see the role they can play to achieve the value on offer
-
collective action: how individuals and groups participating in CLAHRCs are able in practice to collaborate in pursuit of the goals of the CLAHRC
-
reflexive monitoring: how improvement achieved by CLAHRCs can be sustained by learning and adapting a multifaceted and evolving approach.
Informed by the NPT, our survey examined the diversity of interventions taking place in CLAHRCs as they related to our three core areas of interest, alongside practical insights into how people work, and perspectives on effectiveness and impact. Using this approach, we identified five cross-cutting themes: building awareness of the intervention; creating buy-in and mobilisation; sustaining engagement with the intervention; learning from the experience of the intervention; and acting on learning. These themes were adapted to the CLAHRC-specific context, with additional questions included on issues that needed to be explored in more depth.
Each of the nine CLAHRCs was invited to participate in the survey, with six agreeing to do so: CP; Leeds, York and Bradford; North West London; South West Peninsula (PenCLAHRC); Nottinghamshire, Derbyshire and Lincolnshire; and Leicestershire, Northamptonshire and Rutland.
The survey was conducted online, using SelectSurvey (SelectSurvey.NETv4.126.000, ClassApps.com, Overland Park, KS, USA), a survey software that provides a web interface for creating, administering, deploying and monitoring the uptake of the survey, and analysing results. Prior to roll-out, the survey instrument was piloted with two members of CLAHRC-CP. The participating CLAHRCs were then asked to circulate a link to the survey, together with an explanatory section, to prospective respondents from a number of stakeholder groups involved with their respective CLAHRC. Data were collected over a 4-month period from October 2011 to January 2012.
Key characteristics of survey respondents
The number of potential respondents invited by the six CLAHRCs ranged from 43 to 145 individuals; of the approximately 500 people who were invited to participate in the survey, a total of 242 across the six CLAHRCs responded.
The number of respondents varied across CLAHRCs, from 22 to 79, with response rates ranging from 28% to 51%. There was an average of 40 respondents per CLAHRC (see Appendix 5). Of the 242 respondents, almost half reported spending most of their time working in the NHS (n = 103), with the remainder working predominantly in academia (n = 113) (the remaining 26 respondents did not respond to this question) (Figure 3). This proportion of respondents from the NHS and academia was also reflected across the majority of individual CLAHRCs (data not shown).
FIGURE 3.
Number of respondents across NHS and academia.
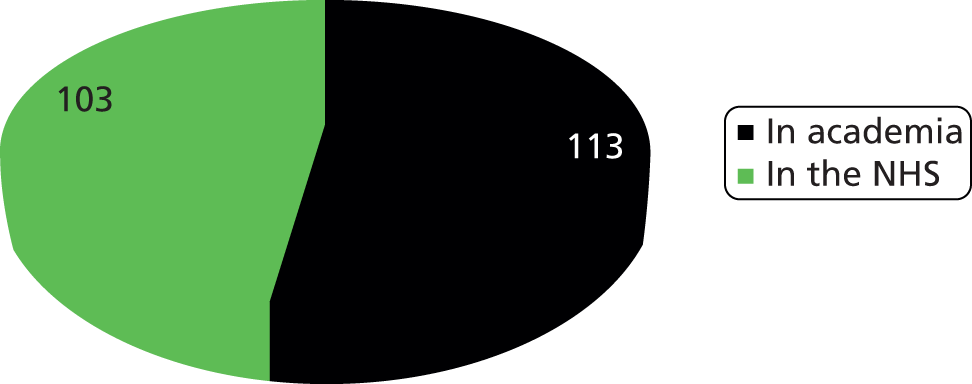
Figure 4 shows the nature of respondent involvement in the CLAHRCs where respondents reported this information (n = 163). A diverse range of job titles were cited, with the highest number being project team members, followed by theme leads, members of the CLAHRC board and research fellows.
FIGURE 4.
Respondent’s nature of involvement in the CLAHRC. PhD, doctor of philosophy; PPI, patient and public involvement.

Case studies
In order to develop a richer and more nuanced understanding of our areas of enquiry, we conducted case studies of two CLAHRCS. As noted earlier, the NIHR HSDR commissioned four teams to evaluate aspects of CLAHRCs. 71 HSDR’s key objectives throughout were to spread the evaluative effort evenly across the CLAHRCs, and to encourage the four HSDR-funded research teams to collaborate with each other so that the different parts of the evaluation were well co-ordinated and there was minimal duplication. All four research teams planned to undertake case studies with selected CLAHRCs. The selection of case study CLAHRCs was discussed by HSDR representatives and the four external evaluation teams at a start-up meeting in October 2009, and took into account the need to ensure an appropriate spread across all nine CLAHRCs and to ensure manageability for CLAHRCs and for researchers. Considerations about the nature and scope of individual CLAHRCs and more pragmatic reasons, such as geographical location, all played a role. As a result we agreed with HSDR that our evaluation should cover two case studies, CLAHRC-CP and PenCLAHRC.
Case studies comprised reviews of documentation relating to the two CLAHRCs, interviews with staff and a 1-day workshop with each CLAHRC to refine and validate emerging insights.
In-depth interviews
The in-depth interviews sought to explore the three core research questions guiding phase 2 of the study: the nature of the relations between the NHS and the CLAHRCs; how multidisciplinary teams for service improvement had been built; and how the CLAHRCs had promoted the use research evidence to influence commissioning and clinical behaviour for patient benefit. Participants were identified based on our prior knowledge of personnel involved with the CLAHRCs as identified in phase 1 of the evaluation, and in consultation with the CLAHRCs themselves. The selection of participants was intended to ensure representation of a wide range of individuals from academia and the NHS, including CLAHRC directors and managers, theme leads, management leads, programme leads, patient and public involvement (PPI) representatives and other stakeholders. Interviewees were contacted directly by the evaluation team with prior agreement of the two CLAHRCs.
We conducted a total of 29 interviews (CLAHRC-CP, n = 12; PenCLAHRC, n = 17). Interviews were semistructured in nature and lasted an average of 60 minutes (the interview protocol is presented in Appendix 6). Interviews for CLAHRC-CP were held face to face in February and March 2012, with 12 of the 16 individuals contacted agreeing to participate. Interviews for PenCLAHRC were conducted in March and April 2012; the majority were conducted face to face (or by telephone where this was not possible), with 17 of the 20 individuals contacted agreeing to participate. The majority of interviews were conducted by one researcher from the evaluation team, and all interviews were recorded and transcribed with prior permission. The transcripts were analysed using a uniform data extraction template structured according to the three research questions and, within each, clustered according to themes developed in the interviews.
CLAHRC workshops
The workshops served to refine and validate insights emerging from interviews in a collaborative way, and aimed to reflect on the evolution and progress of the CLAHRCS to (1) learn from the past and gain summative insights and (2) provide formative value for CLAHRCs to draw upon in informing any renewal of the initiative in the future. A total of 25 persons participated in the CLAHRC-CP workshop, and 14 persons participated in the PenCLAHRC workshop. The list of participants invited to the workshops largely reflected the individuals invited for interview. In the case of CLAHRC-CP, additional staff were approached by the CLAHRC in consultation with the evaluation team. Again, the primary objective was to ensure the presence of a wide range of individuals from both academia and the NHS.
Workshop discussions were facilitated by members of the evaluation team, following a structured protocol as detailed in the workshop agenda (see Appendix 7). Discussions were documented by workshop participants (flipcharts) and facilitators (notes) and the principal data points were organised according to the three research questions guiding phase 2 of the evaluation and, within each, clustered further into common themes.
Validation interviews
Informed by the survey and the case studies, we developed a number of deductive propositions which we sought to test and validate through a final set of interviews with representatives from all nine CLAHRCs. Eighteen interviews were conducted as part of the validation stage during September and October 2012. Interviewees included the directors from each of the nine CLAHRCs; senior members of the CLAHRCs affiliated to the NHS (in seven of the nine CLAHRCs); and representatives from the funder (NIHR). The interview protocol was structured to elicit the views of respondents on four emerging propositions relating to the CLAHRCs that had emerged from the case studies:
-
The task of the CLAHRCs is not just improving health-care research and not just improving patient outcomes, but a combination of both.
-
CLAHRCs are rooted in local relationships (some in place prior to the CLAHRC, providing a platform on which to build, others created during the CLAHRC) and build on local capacities, with implications for critical size and remit.
-
The collaborations CLAHRCs are building are ones that seek to promote integration and culture change, and are not designed simply to develop arrangements for brokerage (including knowledge brokerage) and linkage and exchange.
-
CLAHRCs legitimise a degree of experimentation in finding new ways of identifying and addressing NHS research needs, encouraging the emergence of research questions from the service and from its patients, which can then be funded by the CLAHRC but also by others.
The interviews also aimed to gain insights into how the CLAHRCs had evolved over time, including establishing the collaboration (e.g. the extent to which the original model for the CLAHRC persisted over time); leadership and developing the collaboration (including the scope of the individual CLAHRC and perceived risks surrounding the collaboration); and sustainability (e.g. did interviewees regard CLAHRCs as a persisting entity that would continue to broker the collaboration between the NHS and academia, or as a shorter-term catalyst to encourage a collaboration that could eventually stand on their own?). The full interview protocol is presented in Appendix 8.
Interviews were semistructured in nature and conducted by phone. The majority of interviews were conducted by one researcher from the evaluation team, and lasted an average of 60 minutes. All interviews were recorded and transcribed with prior permission. Interviews were analysed separately by two evaluation team members, using qualitative data analysis software (NVivo version 9, QSR International, Burlington, MA, USA), in order to identify content relating to our research questions and emerging propositions, and to capture any new themes arising from the data. The resulting analyses were cross-checked by the second team member.
Document review
Also as part of phase 2, we conducted two separate document reviews. The first of these aimed to review the wider landscape in which the CLAHRCs were operating, in order to place them in context and provide insights on the future role and potential of the CLAHRCs. To inform the review of the wider landscape throughout the period of the project, we regularly monitored the websites of the Department of Health and the NIHR and the most relevant programmes within them, and, using snowballing, identified documents produced by both the NIHR and the NHS, especially those related to the translation of research. We also conducted web searches to identify, and then review, proposals made in response to the call in 2012 for proposals to establish AHSNs. 73 Key findings from this review are presented in Chapter 5 and Appendix 9 of this report.
In addition, we conducted a document review to complement the validation stage of the study. This was intended to test our emerging propositions by cross-referencing with the documents produced by each of the nine CLAHRCs. We included documents available on the websites of all individual CLAHRCs and also contacted CLAHRC managers to obtain further documents, including publication lists and annual reports. This component of the study did not seek to provide an exhaustive assessment of all documentation produced by CLAHRCs. Its main purpose was to provide additional contextual information to inform our results further.
Phase 3: synthesis
The third phase sought to synthesise the findings from the overall study. It also constituted the reporting and dissemination phase.
Ethics approval
This study was granted ethics approval by Cambridgeshire 4 Research Ethics Committee on 1 July 2010.
Patient and public involvement
Patient and public involvement did not form a significant component of our study. This reflected the funder’s requirements that we keep a certain distance from the activities of the CLAHRCs and resist seeking close involvement in their day-to-day activities in order not to overburden managers and other key CLAHRC staff. However, we did strive to incorporate the views of PPI representatives where possible and explore the CLAHRCs’ role in engaging patients and the wider public in CLAHRC activities. Thus, we interviewed PPI representatives from CLAHRC-CP and PenCLAHRC as part of our case studies; they were also present at the workshops for both CLAHRCs. In addition, we attended a meeting of the Peninsula Public Involvement Group (PenPIG, PenCLAHRC’s user involvement group) in order to inform the case study further.
Chapter 3 Results phase 1: mapping the CLAHRC landscape
This chapter describes the findings from phase 1 of our evaluation, which was completed in the second year of the CLAHRC programme. 24 As noted in Chapter 2, a key aim of phase 1 was to identify the main logics of interventions underlying each of the nine CLAHRCs. Drawing on data derived from document review, interviews with senior individuals involved in the implementation of CLAHRCs and workshops with individual CLAHRCs, we explored how the partnerships were set up, their governance arrangements and the contexts in which CLAHRCS were implemented, alongside their aims and objectives, their overall approach (including any theories of change they identified) and the research and implementation themes they covered.
We here present a summary overview of our findings. The detailed accounts of each CLAHRC that emerged are summarised in Appendix 10, alongside the logic models that sought to capture the logic of intervention in each CLAHRC.
This initial overview was designed to obtain a broad picture of all nine CLAHRCs as they were in the second year after their establishment. In what follows we discuss these initial findings, distinguishing between those that were unique to specific CLAHRCs and those that were common, and describe how we used these findings, in discussion with the funder and the CLAHRC directors, to shape phase 2 of our evaluation.
The key themes of the CLAHRCs
A shared vision, but contrasting interpretations
The CLAHRCs involved collaboration between different stakeholders in health research and the NHS. They were intended to be vehicles for improving patient care through efficient and effective services built on improved generation, translation and adoption of knowledge. In this spirit we were interested not simply in the CLAHRCs as emerging forms of collaboration but also in how, through all their diverse impacts and activities, we could learn more about how a closer engagement between communities of researchers, health practitioners, health managers and others might lead to improved patient outcomes. From the detailed summaries (see Appendix 10) it was clear that all the CLAHRCs shared a vision and a vocabulary about the long-lasting change in the NHS that could be achieved by establishing new relationships between applied researchers and NHS decision-makers and new behaviours within each of these groups. There was shared optimism about the new pathways that could be forged, linking applied health-care research and medical research to patient outcomes and experiences. However, along with the similarities there were also more nuanced differences. Table 3 presents the broadly shared story of the CLAHRCs, using the data we obtained from all nine CLAHRCs. In Appendix 11 we show some of the ways in which individual CLAHRCs compare and contrast with others. The structure that we use to organise these summary tables draws upon a conceptualisation widely used to understand ‘improvement journeys’ in the health sector, reminding us that the ultimate aim of the CLAHRCs is to improve health care. See, for example, Bate et al. , who argue that there are six core challenges to organising for quality, and that these are structural, political, cultural, educational, emotional, and physical and technological. 63
| Structural and political | Cultural, educational and norms | Infrastructure: financial and physical | |||
|---|---|---|---|---|---|
| Governance and accountability | Organisational structure of CLAHRCs including activities and themes | Societal attitudes and behaviours | Individual attitudes and behaviours | Infrastructure (including technology) | Use of resources |
| What needs to be done to bridge the second translation gap? | |||||
|
|
|
|
|
|
| System shifts | |||||
|
|
|
|
|
|
| Vision for success | |||||
|
|
|
|
|
|
Governance, accountability and organisational structure
Governance and management arrangements involve the formal structures through which resources are allocated, decisions taken and disputes resolved. They also establish who should be accountable to whom and on what basis. From the outset, all the CLAHRCs involved leading figures with experience in establishing and running such arrangements across academic and service–delivery boundaries. All the CLAHRCs also shared the governance and management challenges that are unavoidable consequences of working in this terrain. These include navigating and managing dual R&D governance systems (NHS and academia) within a single structure and developing capacity, systems, provisions and contingency plans to adapt and respond to changing health-system landscapes (such as changes in the nature of commissioning and uncertainty about long-term funding availability). There were, however, differences in the way in which the fundamental governance principles of transparency, accountability and responsibility were operationalised. Some CLAHRCs had centralised ownership, control and management arrangements, while others devolved significant amounts of responsibility and provided substantial autonomy to constituent partner organisations or to differentiated functional committees. The administrative support in each CLAHRC was, therefore, diverse both in nature and in levels of centralisation.
Table 3 identifies the set of widely shared activities. There was a concern with effective leadership, a need to balance central direction with professional autonomy and experimentation, a need to align with local and national priorities (which may not always sit comfortably together) and a need to allocate responsibilities and rights within a system of accountability. Organisationally, the CLAHRCs opted to ‘chunk’ their workload into particular themes, building upon pre-existing relationships linked to clinical areas or to implementation themes. They then established mechanisms for learning and sharing insights among these themes. Within this broadly shared set of parameters, Appendix 11 illustrates how specific CLAHRCs have addressed the issues, some favouring more experimentation and variation and others more concerned with aligning and steering.
The focus of some CLAHRCs was on specific health areas (e.g. mental health across the life course) while others tackled a broad range of regional priorities (e.g. chronic diseases or chronic and acute care). Some CLAHRCs had common implementation frameworks across different thematic groupings, while others were tailored to specific projects and themes. All were trying to integrate activities that emphasised applied health research projects with those that had an explicit focus on implementation, and to do so by creating environments that enabled joint working and knowledge exchange. The ways in which such environments were brought to life and organised differed. For example, fellowships and studentships in applied health research and implementation science were one of the more common approaches (e.g. postdoctorates, research degrees, medical degrees). Short training courses for researchers and practitioners were also established, and these varied in nature across the CLAHRCs depending on their thematic focus. Dedicated funding to buy out time from the NHS to enable research activity by clinicians and nurses was another common approach. Some CLAHRCs relied on mixed project teams of clinicians and academics from diverse disciplines (including those that are non-traditional for health services research, such as systems engineering), and sometimes also including patients, as the primary means of bringing about cultural change, while others emphasised the roles of ‘boundary spanners’, ‘knowledge transfer associates’ or ‘diffusion fellows’ embedded in trusts. All the CLAHRCs supported meetings to encourage knowledge exchange and bridge professional and disciplinary gaps. Emphasis on evaluation activities designed to create self-improving, reflexive systems varied substantially, as did the stage of development and maturation of evaluation frameworks.
Changing individual and group attitudes and behaviours
We know from the discussion of the literature presented in Chapter 1 that developing shared norms and embedding behaviour change are central to improving the quality of health services. Common to all the CLAHRCs were efforts to change or modify the behaviours and attitudes of researchers and practitioners (or, at an organisational level, academia, service providers and commissioners) towards a more common vision of the role of research in improving services. This required building a shared language and understanding of the functions and working methods of different academic and clinical professions and disciplines, as well as of respective responsibilities along the pathway from research production and implementation to improvement in patient care. It also required an understanding of the constructive roles that patients can play. In particular, all the CLAHRCs tried to raise the profile of research in the NHS, as well as awareness in academia of the importance of doing research that is driven first and foremost by the needs of service providers and users. Prioritisation processes for projects within the CLAHRCs tended to be driven by a combination of population needs and the availability of skills, experience and resources to address them in the local research and innovation communities.
Changing the attitudes of individuals depends not only on those individuals but also on the flexibility and responsiveness of existing organisational-level attitudes and behaviours. High levels of NHS involvement underpinned the CLAHRCs’ ethos and theories of change. The CLAHRCs also sought to encourage public and patient engagement, and worked to communicate the value of their involvement in research to them and, more generally, to NHS decision-makers and the research community. They disseminated information on CLAHRCs’ activities, outputs and impacts widely.
However, the ways through which the public were involved, as well as the intensity of their involvement in different stages of the research cycle, varied. Some CLAHRCs tried to engage service users throughout, encouraging them to identify research questions and get involved in research design, and to remain involved during the production of research and the adoption of research findings. They developed research training and induction programmes for service users, and supported formal patient or public representative posts within the CLAHRC. Other CLAHRCs placed less emphasis on active public involvement in research design and implementation, and engaged the public mostly through the dissemination of public information about CLAHRC activities as part of an awareness-raising strategy.
Across the CLAHRCs there were conscious efforts to change the language and culture of those engaged in research and practice. This was pursued through active leadership, and by developing compelling narratives of successful projects, providing training and creating opportunities to meet and discuss. Evidence from the interviews and workshops in phase 1 suggested that some of the individuals most closely involved may indeed have changed their relationship to research and/or health care. All the CLAHRCs sought to create environments that encouraged knowledge exchange, communication and learning within and between different communities of practice. They created opportunities for new groups to join existing networks, and raised expectations that behaviours within and across organisations would change. However, realising such expectations required some degree of direction, and an ability to align, lead and shape groups and behaviours. The CLAHRCs did not necessarily have the resources or the authority to direct and control groups of researchers explicitly, or to micro-manage NHS clinicians and managers. Consequently, we would argue that the CLAHRCs should be seen less as unified and homogeneous organisations and more as terrains upon which compromises, trade-offs and tensions are played out.
Infrastructure and use of resources
All the CLAHRCs pursued their activities through a combination of funding from the NIHR and matched funding from local organisations (predominantly NHS trusts). The sustainability of the CLAHRC approach depends in part upon being able to demonstrate the benefits and manage the costs so that the approach is absorbed into the mainstream of provision and research. The physical infrastructure available to participants in the CLAHRCs was in some cases geographically dispersed across a region, and in others more centralised with the colocation of different research and implementation teams in shared spaces. Many reported on the benefits of colocation.
Online resources are a way of reaching out to, and engaging, external stakeholders. All the CLAHRCs used resources to improve information and communication systems in order to promote more timely and efficient sharing of knowledge and data across stakeholders. This led to changes in the ways in which the skills, expertise, influence and authority of diverse stakeholders were mobilised in research and implementation agendas, from commissioners and NHS managers to patients and the public.
System shifts
In their initial proposals all the CLAHRCs reported that they were hoping to achieve a system shift through their activities. Their aspiration was to create a new generation of researchers and clinicians with changed professional identities and motivations who were supported by a different set of incentives and drivers, both national and local, and a commissioning approach that was committed to reinforcing the aims of the CLAHRC. Table 3 suggests the system-level changes required if the implementation of research findings is to happen more efficiently and with shorter time lags, and if research is to match real-world service needs continuously.
For example, clearer and stronger incentive structures for NHS and academic staff across academic and health service sectors are needed to sustain cultural change, but these cultural changes also need to become normalised within a new system of health care and research. Creating opportunities for the participation of NHS staff across different stages of research is another area meriting system-level attention. A more explicit policy position and a better-co-ordinated national strategy for engaging patients and the public in research and implementation activities would help to ensure and sustain their meaningful contributions to service improvement, and central to any such strategy is active communication and demonstration of the benefits of research implementation for the quality of care that individuals and communities receive.
To build a critical mass of NHS and academic staff thinking in the CLAHRC way takes time, but proactive efforts to share and exchange insights between the CLAHRCs, and with the broader health-care landscape nationally and internationally, are important for learning and feedback, for ensuring that best practice is implemented, spread and sustained, and for future resource allocation. Related to this is the need to share information better about the link between different translational research and implementation initiatives in the overall health-system landscape. We return to these issues below and in Chapter 4.
Phase 1: conclusions
We know from the literature that there is a need for more theory-based, context-sensitive, embedded evaluation in this area. The CLAHRCs offer an important opportunity to understand further both the theory and the practice of reshaping the activities of research producers and research users (and the boundaries between them) with the intention of improving health care and health outcomes. Phase 1 of our evaluation provided us with a detailed understanding of the activities involved in achieving this, the context of these activities and some of the criteria seen to be associated with success. Creativity and effort had been applied to develop different models of change.
Two conclusions emerge. First, the CLAHRCs will not resolve the lack of consensus raised by the literature about the ‘best’ approach to mobilising knowledge to improve health care, but they do provide an opportunity to look carefully at specific dimensions of the problems and develop a scientific basis for addressing them. Second, the CLAHRCs cannot, on their own and once and for all, bridge what has been called (however inappropriately) the second translation gap, but they can help to bring about system shifts that bring the health and health-research systems closer together.
Emerging questions: shaping phase 2 of the evaluation
In phase 1 of our evaluation we sought to provide an overview of the background, development and future plans and aspirations of each of the nine CLAHRCs. We could not explore in detail every dimension of the improvement journeys being pursued. However, we identified a number of key questions which we thought would cast further light on that wider picture and which were:
-
relatively under-researched (as identified through our literature review)
-
potentially high-impact with transferable lessons
-
relevant to the success of the CLAHRCs
-
not being covered by one of the three other evaluations
-
capable of being researched across the CLAHRCs to support comparisons and contrasts.
These questions are listed in Box 1 starting with more macro-level questions about the relationships between the CLAHRCs and, on the one hand, the broader translational landscape and, on the other hand, the NHS. More meso-level questions concern issues such as governance and operational flexibility, and towards the end there are more micro-level questions about engagement and participation. This ordering is not intended to suggest any order of importance; there were macro-, meso- and micro-level dimensions to each of these questions.
-
How do CLAHRCS fit into the broader translational research and implementation landscape of the NIHR (and other funders) at present, and how might they fit in the future?
-
High levels of NHS involvement underpin the CLAHRC ethos and theories of change. What is the real scale of NHS involvement in CLAHRCs, and at what levels?
-
What is the impact of different governance and management structures on CLAHRCs’ activities and outputs?
-
What levels of operational flexibility do CLAHRCs need in order to deliver on their goals effectively and how is such flexibility best enabled and nurtured?
-
How are effective multistakeholder and multidisciplinary research and implementation teams for service improvement built? What can we learn from the CLAHRC model and what mechanisms are being used to enable this?
-
What are the different models of public and patient engagement at play in CLAHRCs? What value has PPI brought?
-
How can knowledge and evidence to inform service improvements be best communicated and disseminated to those who need to hear it in policy and practice circles?
-
What value does a CLAHRC bring to the different stakeholders involved? What does it mean to different parties?
As indicated in Chapter 2, we discussed phase 1 findings at a learning event with the CLAHRC directors and the NIHR. Our aim was, with their help, to identify three questions for more detailed investigation in phase 2. We describe these in detail in Chapter 4.
Chapter 4 Results phase 2: exploring the CLAHRCs
This chapter presents the findings of phase 2 of the study, bringing together observations from the stakeholder survey, the case studies and the validation interviews. We organise the data according to the three core questions that guided the second stage of the study:
-
How does the NHS influence CLAHRCs’ evolution, outcomes and impact (and indeed how does having a CLAHRC influence NHS behaviour)?
-
How are effective multistakeholder and multidisciplinary research and implementation teams for service improvement built: what can we learn from the CLAHRC model and what mechanisms are being used to enable it?
-
What can we learn from the CLAHRCs that can provide new understanding of how to use research knowledge and evidence to change commissioning and clinical behaviour for patient benefit?
For each question, we draw on data from three sources. We first report on the stakeholder survey, providing insights across six CLAHRCs. We then go into some depth, reporting on the findings from the two case studies, CLAHRC-CP and PenCLAHRC. We describe the principles that underpinned each CLAHRC: coproduction in the case of CLAHRC-CP and ‘Engagement by Design’ process in PenCLAHRC. We note how both CLAHRCs went well beyond a linear model in which knowledge is a product of research that passes from researchers to users by diffusion and can be generalised across contexts, and adopted holistic approaches to research and implementation that sought to promote integration and cultural change through learning and adaptation. Finally, we discuss the extent to which the findings from the case studies were validated and enhanced by the experiences of other CLAHRCs.
The findings presented below are based on data that were collected at slightly different points in time, starting with the stakeholder survey, which was undertaken from October 2011 to January 2012; case studies conducted in spring 2012; and validation interviews carried out in autumn 2012. All the while, the CLAHRCs continued to evolve within a changing NHS and economic environment. Apparent differences in the insights derived from different sources might not, therefore, necessarily represent a true difference between views but simply reflect the evolutionary process. We comment on relevant observations where possible and appropriate. Furthermore, in our survey analysis we differentiate between participants primarily affiliated with the NHS and those primarily affiliated with academia, highlighting commonalities and differences between the two groups. However, we recognise that, in practice, staff within the CLAHRCs often worked in both academic and NHS domains.
How does the NHS influence CLAHRCs’ evolution, outcomes and impact (and indeed how does having a CLAHRC influence NHS behaviour)?
The purpose of the NIHR CLAHRCs as set out in the original call for proposals to establish CLAHRCs was to ‘forge a mutually beneficial, forward-looking partnership between a university and the surrounding NHS organisations, focused on improving patient outcomes through the conduct and application of applied health research’ (p. 2). 3 One of the three core questions explored in our evaluation was the nature and development of these ‘mutually beneficial partnerships’, and the extent to which the CLAHRCs had an impact on the practice and culture of the NHS while themselves developing effective ways of working within the wider architecture of the NHS and universities.
Perspectives of NHS and academic staff across six CLAHRCs
The survey sought to explore how NHS and academic staff perceived the aims of their CLAHRC. It showed that NHS and academic respondents strongly supported CLAHRC aims of increasing the capacity to carry out and use applied health research in the NHS, and to foster a culture of collaboration between the academic and service delivery sectors (Figure 5). However, a smaller number of respondents (around 40%) also saw the involvement of commissioners and NHS managers in the formulation of research questions and the implementation of findings as a core aim of CLAHRCs. The majority of respondents (76%) were in full agreement with the formal aims articulated by their CLAHRC (see Appendix 5, Figure 27).
FIGURE 5.
Perceived aims in relation to integrating NHS staff with research activities.

When asked about their motivations for engaging in the CLAHRCs initiative, over 60% of NHS respondents cited a desire to improve clinical effectiveness by applying existing research better (Figure 6). NHS respondents also expressed an interest in the production of research and in encouraging the pursuit of research relevant to practice. These motivations were also commonly cited by academics, in addition to the desire to spend more time on applied research.
FIGURE 6.
Motivation for getting involved in CLAHRC.
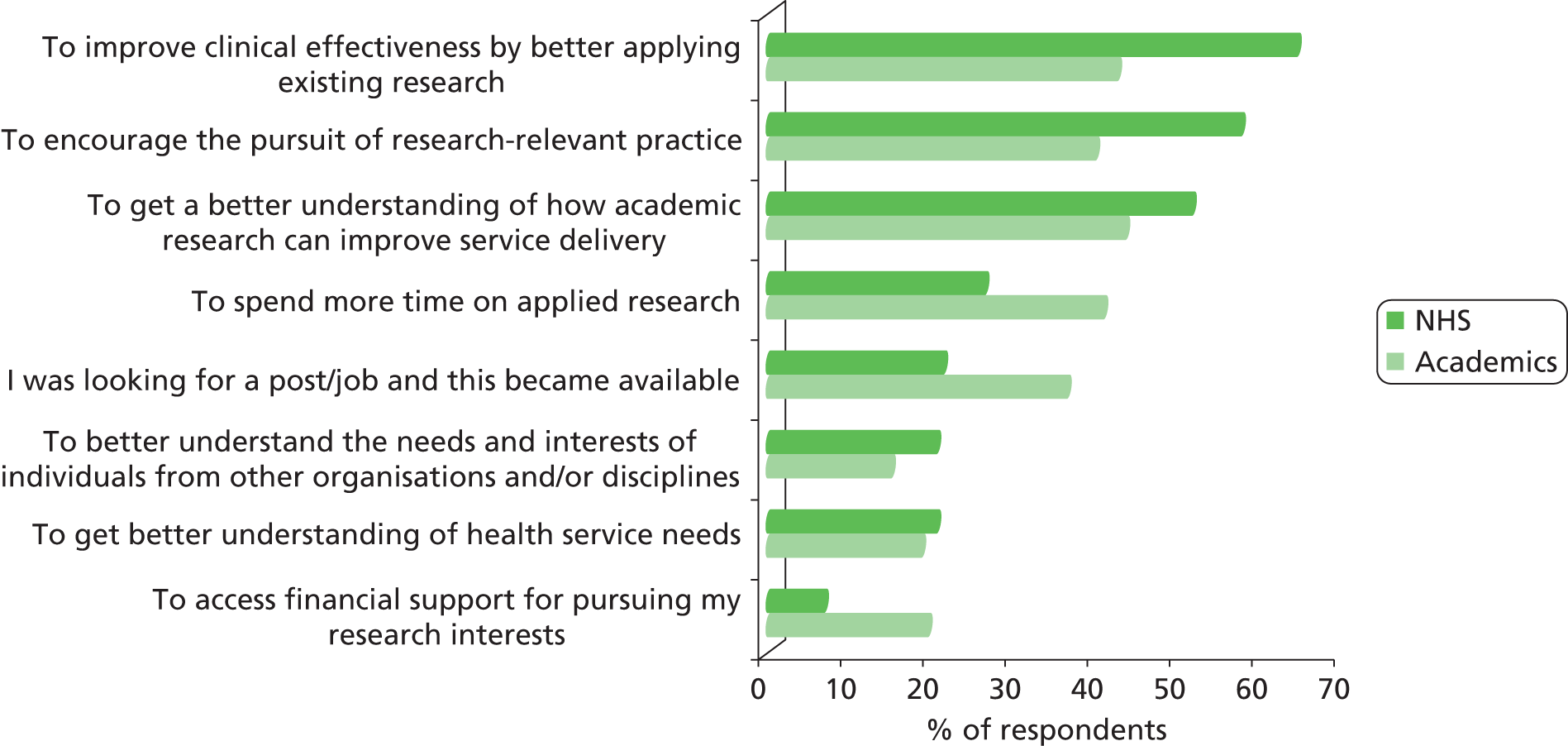
Respondents across all six CLAHRCs attributed NHS influence on their CLAHRC to a number of factors, including the involvement of clinicians in research design and in research implementation, and the existence of long-standing relationships between academic and NHS members of the CLAHRC (Figure 7). A relatively small number (10%) reported that this question was not applicable. It is difficult to assess, from these data, whether or not this implies that, in the view of these respondents, the NHS had not been influential in shaping CLAHRC activity. We explore this question further below.
FIGURE 7.
Reported reasons for the NHS being considered currently influential in shaping CLAHRC’s activities.
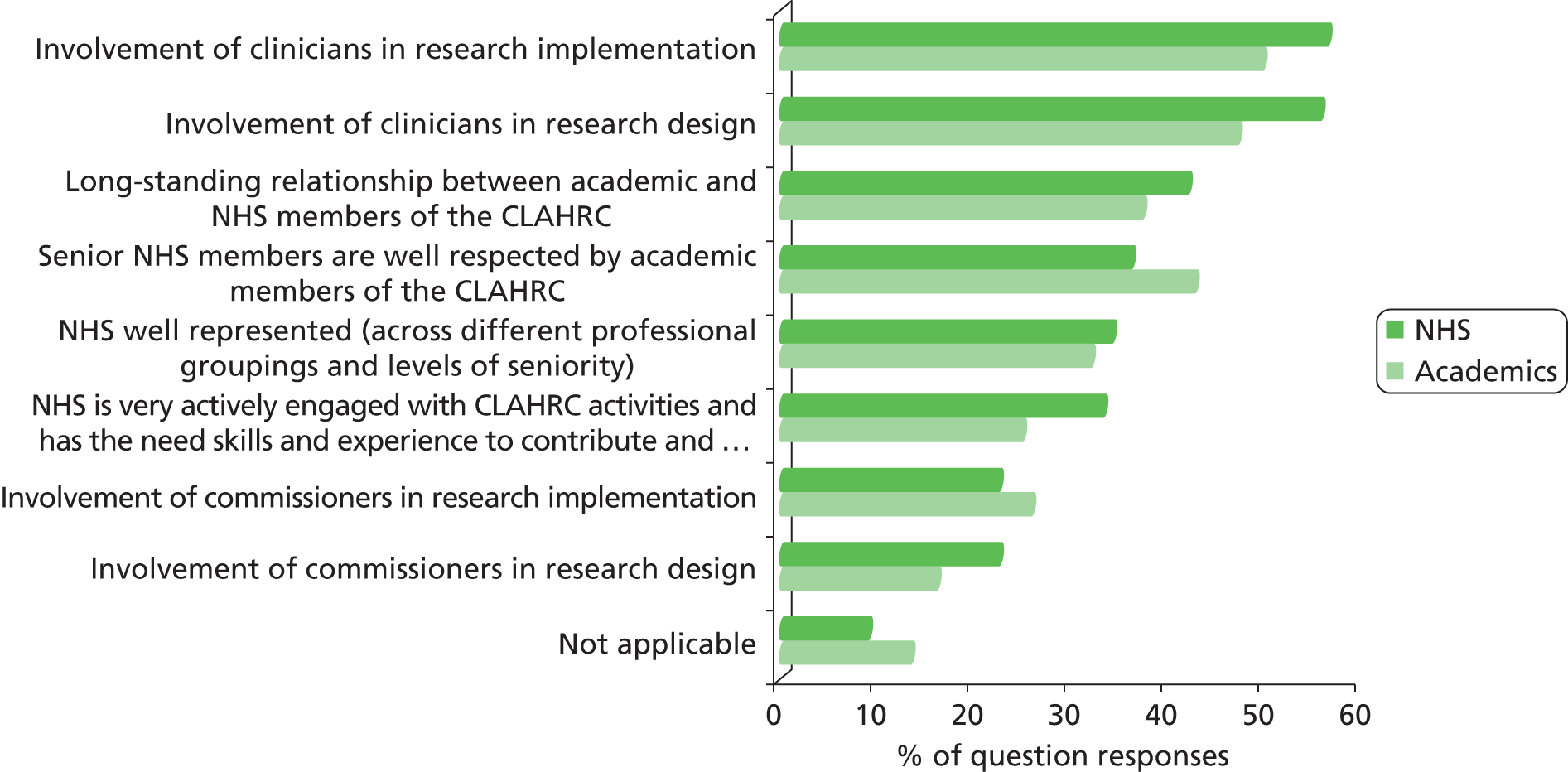
A key determinant of NHS influence on the CLAHRCs was the nature of the groups that shaped CLAHRC decision-making (Figure 8). Respondents suggested that seniority was important, including senior academic staff, senior NHS clinicians and senior NHS management. Conversely, junior NHS clinicians were judged to be the group with least strategic influence.
FIGURE 8.
Perceived extent to which different groups within local NHS and university are influential in shaping CLAHRC’s strategy, decisions, activities and choice of outputs.
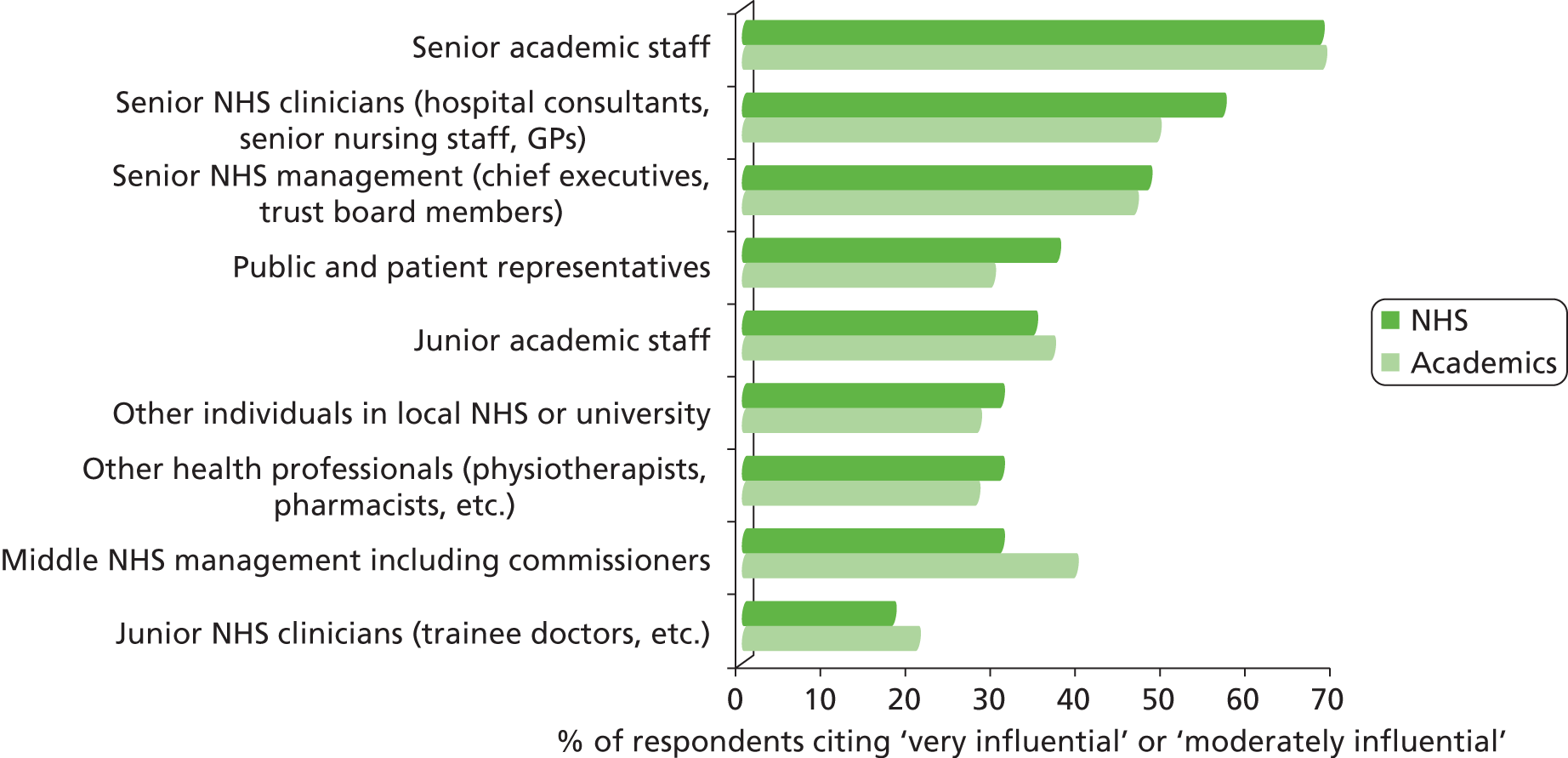
As indicated in Figure 7, a minority of respondents believed that the NHS had not been influential in shaping the activities of their CLAHRC. Where this was the case, respondents were asked to identify whether this was because of a predominance of academic staff in the CLAHRC or a lack of buy-in from senior NHS leadership. Most respondents attributed this lack of influence to the former (Figure 9). Similar concerns were reported by NHS respondents as a significant barrier to the success of the CLAHRC in meeting its objectives (see Appendix 5, Figure 57).
FIGURE 9.
Stated reasons why the NHS may not be influential in CLAHRC activities.
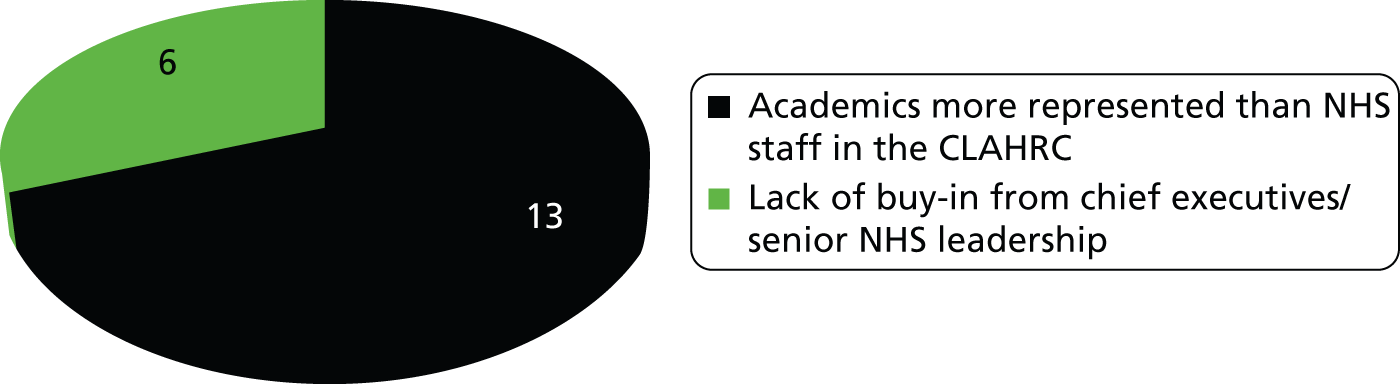
On the issue of how having a CLAHRC might influence NHS behaviour, over 80% of respondents across all six CLAHRCs were confident that their CLAHRC would lead to changes in NHS behaviour over time (Figure 10). However, when disaggregated by individual CLAHRC the levels of confidence expressed by NHS staff and academics were more varied (between 45% and 90%; data not shown).
FIGURE 10.
The CLAHRC will lead to changes in practice/will influence NHS behaviour.

A majority of respondents also thought that, at the time of the survey, some change had already happened, with 65% of NHS respondents and 57% of academics believing that CLAHRC’s activities and projects had influenced the way they worked outside the CLAHRC. Where this was felt to be the case, nearly 60% of NHS staff attributed it to easy applicability of the research undertaken by the CLAHRC (Figure 11).
FIGURE 11.
Stated reasons why information received about CLAHRC’s activities and projects did influence behaviour and ways of working.
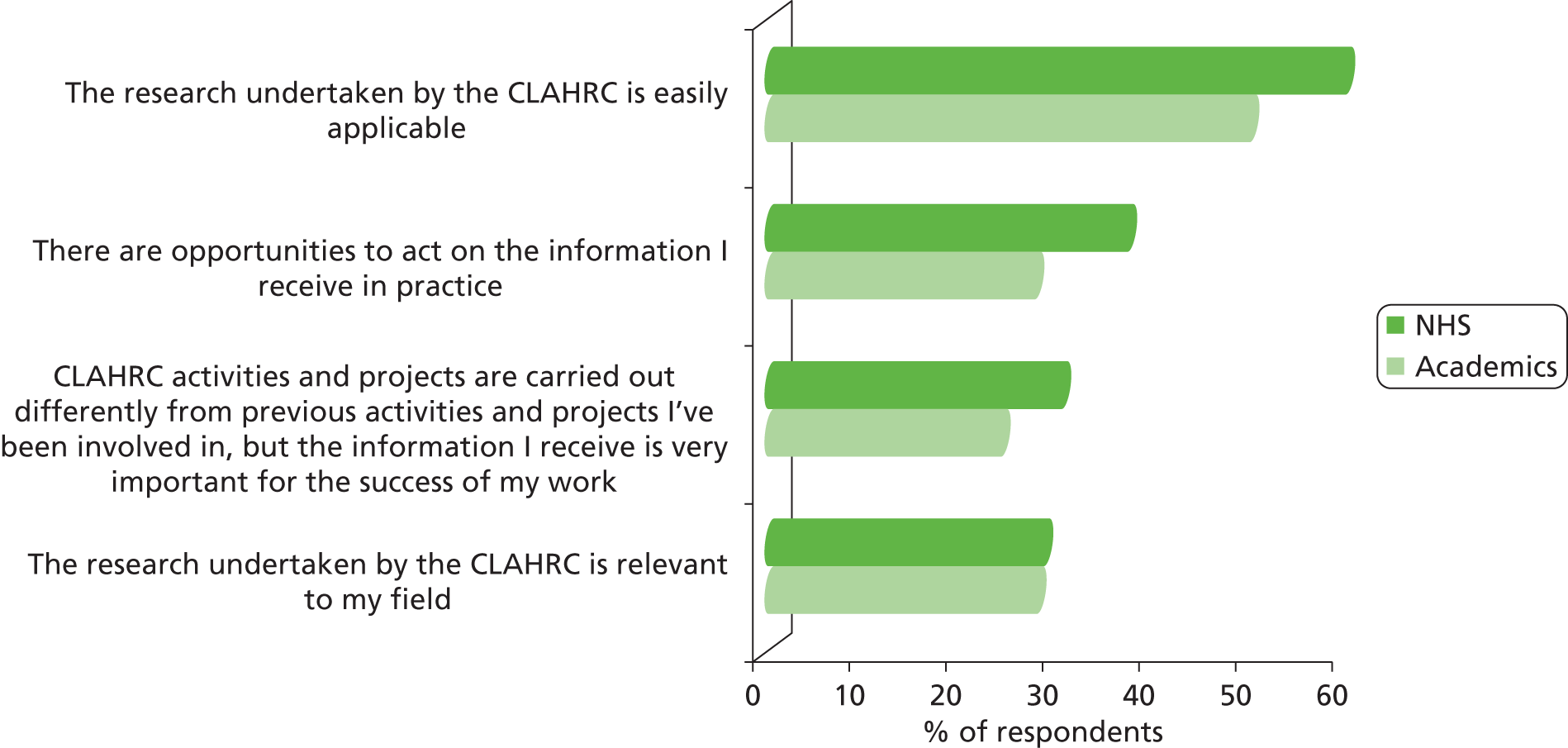
In line with the aims of the CLAHRCs, a majority of NHS respondents reported that they had developed new research skills as a result of working within the CLAHRC (Figure 12). There was also a sense that the innovative ways of working fostered by the CLAHRCs were engendering new skills in both groups, and over 40% of academic respondents reported that they had developed new communication skills. The findings also suggest that NHS respondents were starting to develop new ways of thinking about service provision and the use of evidence in practice, with a majority stating that working within the CLAHRC was enabling them to think about challenges in their work from different perspectives.
FIGURE 12.
Perceived difference in working within CLAHRCs from working outside it.
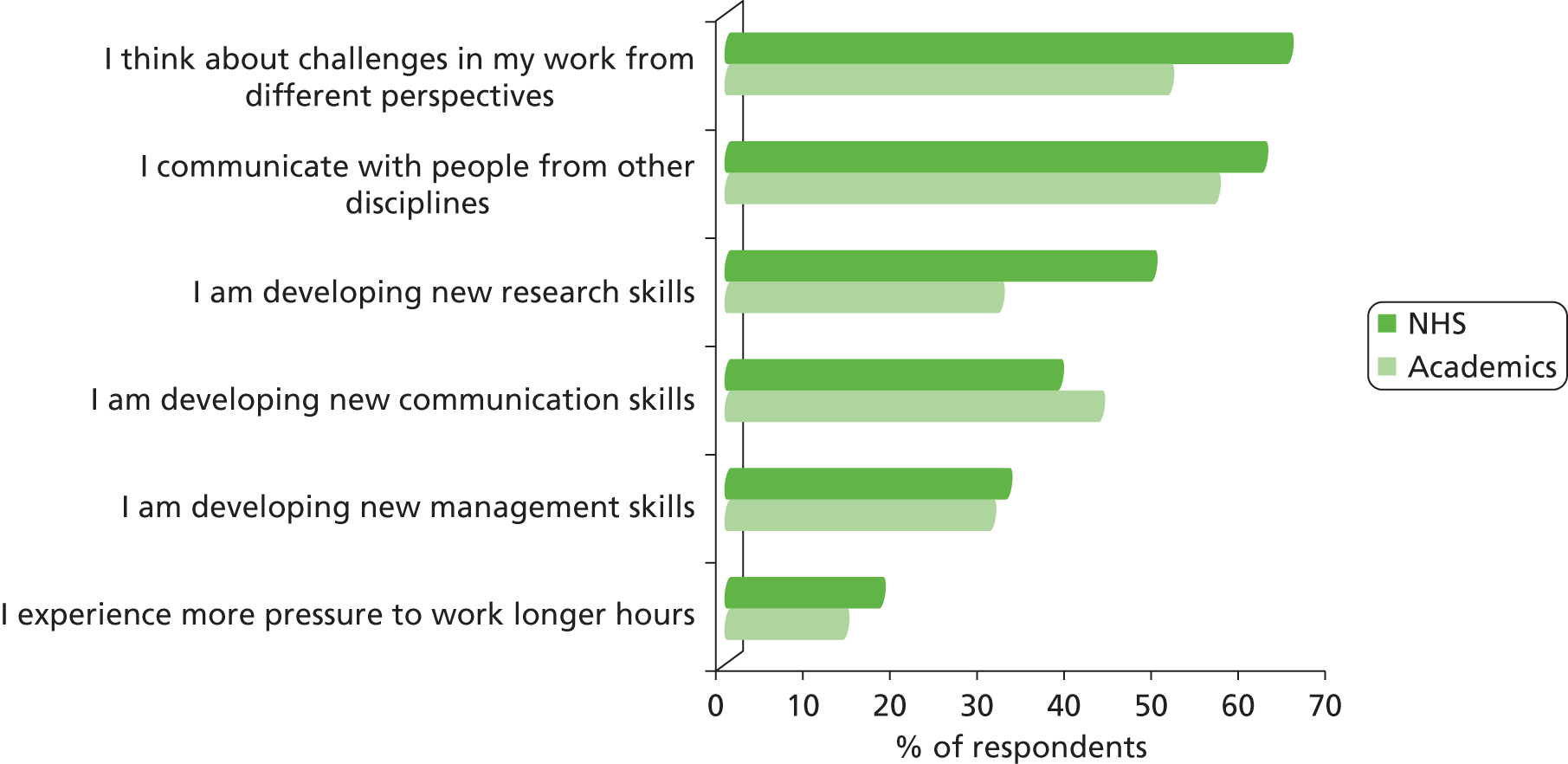
Experiences in CLAHRC-CP and PenCLAHRC
Our two case studies explored the influence of the NHS and the CLAHRCs on each other further. We identified four overarching themes: the local remit, the role of matched funding, the integrating nature of the collaboration and system change. In the following section we explore these issues, drawing on the experiences of CLAHRC-CP and PenCLAHRC. We also consider how the findings from the case studies are confirmed by the wider CLAHRC experience. We conclude each subsection with a short summary of key points observed.
Local remit
The two case studies of CLAHRC-CP and PenCLAHRC demonstrated the importance of having a strong local base and being able to build on existing goodwill, especially in the early phase of the CLAHRCs when they had yet to deliver and their ambitions had to be taken on trust. Both the CLAHRCs were able to develop and strengthen those existing relationships and build on existing research expertise, as well as building new relationships. While highlighting the significance of the local base (‘It’s hugely important that CLAHRCs have a local remit’) one interviewee placed equal importance on the CLAHRC’s ability to develop these existing relationships and to take them in new directions: ‘although they build on local capacities, the thing that CLAHRCs were able to do is bring in enough resource to put a bit of extra into the system, and have flexibility about how to spend it’ (PenCLAHRC interviewee 1).
Thus CLAHRC-CP built on established local research strengths in life-course approaches to mental health and illness, and supported existing streams of research as well as developing new ones, such as mapping mental health pathways. The CLAHRC exploited existing local capacity, such as the East of England Evidence Adoption Centre,74 which undertakes systematic reviews, and the Institute of Public Health at Cambridge University; and strengthened links with groups with expertise in implementation and service design at the Engineering Design Centre and in service change and evidence-based innovation at the Judge Business School. 75
Similarly, PenCLAHRC built on existing local relationships, such as the South West Peninsula Clinical Research Collaboration,76 on existing local research strengths, including the Peninsula Clinical Trials Unit and the Peninsula Technology Assessment Group, which had close links with the national Health Technology Assessment (HTA) programme, and on the goodwill generated between the NHS and local universities during the establishment, in 2000, of the Peninsula College of Medicine and Dentistry. An 8-year programme of work on patient involvement in the South West (through Folk-us77) provided a robust basis for PenPIG.
We observed examples of how local relationships underpinned and supported PenCLAHRC’s work and its projects. For example, an early PenCLAHRC project successfully encouraged the use of tranexamic acid in emergency care. This project has since been widely publicised and taken up across PenCLAHRC, and has informed recommendations for tranexamic acid to be introduced to all NHS ambulance services and hospitals in the UK. 78 The changes sought involved health professionals working in the local ambulance trust, with which good relations had already been developed through PenCLAHRC evidence-based practice training, and the fact that these staff already knew about PenCLAHRC and trusted its approach was identified as a factor in getting them to change their practice.
These observations from the two CLAHRC case studies were reflected in the general experience of the CLAHRCs that we identified through the validation interviews with directors and senior NHS staff in all nine CLAHRCs. Thus, a senior member of one of the other seven CLAHRCs noted how ‘There were some established trusted partnerships already and linkages that were quite well established, some of them were embryonic but looking promising and some of them were developed as an opportunity because of the CLAHRC funding’ (senior NHS-affiliated CLAHRC member 1). There was a recognition that pre-existing local relationships facilitated the establishment of the collaboration ‘because by necessity it had to, it had to be put together so quickly’ (senior NHS-affiliated CLAHRC member 2), and that new relationships developed as the collaborations evolved. Here, a core feature as identified by one interviewee was ‘the credibility of the individuals who are trying to build the relationships’ (senior NHS-affiliated CLAHRC member 2).
There was some perception of a ‘thirst’ for collaboration: ‘in terms of building capacity, it [the CLAHRC] does that, local capability, and it does build on local relationships. It’s a collaborative. And there’s a thirst for collaboration I’m finding’ (senior NHS-affiliated CLAHRC member 3). However, building the collaboration took time, and it also required effective and responsive leadership. Different CLAHRCs did it differently, and needed flexibility, and the freedom to experiment, learn and adapt as they developed:
One of the beauties of CLAHRCs is that they’re all quite different and they’re developed according to local structures and processes and that’s really helped. What wouldn’t have helped is if you push the same thing onto everybody and so you have to do exactly the same thing because I think that would be quite difficult.
Senior NHS-affiliated CLAHRC member 4
Summary
All the CLAHRCs were rooted in local relationships and through these focused on what was relevant and what worked locally. This was one of their defining features. This local remit and the differences between the CLAHRCs engendered as a result were, along with the lack of any single clear ‘roadmap’ for getting research into practice, important justifications for the experimental approach adopted in the NIHR CLAHRC programme. However, the CLAHRCs also had to meet other requirements: the research they supported had to be generalisable and relevant to people in a similar setting elsewhere; similarly the learning from their implementation activities had to be available to inform others more widely. The CLAHRCs needed to be relevant outside their own locality, and therefore needed freedom to go beyond their own boundaries.
Matched funding
The CLAHRCs were required to match their NIHR funding with funding from other sources. This deliberately gave partner organisations a strong stake in the CLAHRCs. The matched funding was expected ‘to enhance the activities of the CLAHRC, particularly by effecting cultural change and creating a magnet for staff’ (p. 5),3 and initially came largely from local NHS organisations, much of it in kind in the form of released time for NHS staff, allowing them to become actively involved in the collaboration. However, as the CLAHRCs became established and developed their research programmes, they were also able to obtain research funding from other sources. PenCLAHRC, for example, attracted over £17 million in external research grant funding between October 2008 and early 2013 (S. Logan, PenCLAHRC, 9 April 2013, personal communication).
South West Peninsula CLAHRC received matched funding from a variety of different NHS sources. This brought in many NHS partners and reduced concerns that funding might disappear following structural reorganisation and the closure of particular institutions. In CLAHRC-CP there was a different pattern. This CLAHRC focused on one clinical area (mental health) and received matched funding from a more limited range of NHS partners. Although this was seen to be advantageous in keeping oversight of the work, it was also more likely to (over)burden NHS colleagues: [‘we’ve kind of saturated our NHS colleagues with research and evaluation’ (CLAHRC-CP interviewee 3)], while also creating uncertainties for the CLAHRC when there were ‘major structural reorganisations’ (CLAHRC-CP interviewee 4) and changes in senior NHS staff in this one institution, which were seen to pose a ‘huge challenge’ (CLAHRC-CP interviewee 4).
These experiences were reflected in the wider CLAHRC community. Thus, while there was general agreement about the use and usefulness of the matched funding model in theory, its implementation into practice was seen as rather more complex:
The original call was fine, it explained exactly that this was relationships between and who should be in it and so on and so forth. I think the remit was good, they knew exactly what we were supposed to be doing. It was based on the Canadian model, the Jonathan Lomas model and the Cooksey Report, it was very clear what we had to base our collaboration on. I think they didn’t fully understand the complexities of the business model, the matched funding model and how tricky that was.
CLAHRC director 1
There was some concern about the ‘two-sidedness’ of the funding; that is, ‘NHS partners have to be able [to] see that they are getting something out of it. If you’re going for matched funding the risk is always that your partners will decide well this is not something I want to do’ (senior NHS-affiliated CLAHRC member 5). As with CLAHRC-CP, others also highlighted the potential risk in relying solely on only one type of NHS organisation. For example, one CLAHRC was largely orientated towards one care sector and arranged matched funding (as direct funding rather than in kind) with the relevant commissioning organisations. However, the subsequent restructuring of the health and social care system in England was experienced as having thrown ‘a spanner into the works’ (senior NHS-affiliated CLAHRC member 5) because some of the commissioning organisations felt they could no longer meet their commitment. As a consequence, the CLAHRC had to adjust its plans and seek matched funding from other NHS sources.
On the other hand, the matched funding model could also make things happen and increase people’s involvement and commitment:
If you are developing a collaboration there has to be a purpose of doing that and if you have got real money with an expectation of matched funding that is the mechanism that glues the collaboration together . . . In the traditional funding mechanisms what you have is, there is a call, it seems important, we will make the effort to put some work in together, it may or may not get funded.
Senior NHS-affiliated CLAHRC member 1
While the aforementioned example of relying on one type of organisation as a source for matched funding posed a real risk, the possibility of receiving funding from all partner organisations was seen to hold substantial potential:
I think this was serendipitous in as much as I went everywhere to get money and got quite a mixed bag, and thought at the time that that might be a weakness, but actually it turned out to be a strength. So when I say I got a mixed bag, I got investment from partner NHS organisations but also from large charities and from the strategic health authority. And also I had [funding] in kind, so I had organisations that said well yes okay we will work with you but that’s going to be my clinical effectiveness officer or my research co-ordinator will now work in your group, so it’s whole-time equivalent posts rather than real money . . . And that’s been hugely successful because, as PCTs [primary care trusts] dissolve, there is no money from them.
CLAHRC director 1
Moreover by acting as the ‘glue of the collaboration’, matched funding underpinned the commitment of the NHS to the CLAHRC; and, as NHS organisations came to recognise the value of the CLAHRCs, they offered additional funding: ‘our matched funding has more than doubled during the last three and a half years’ (CLAHRC director 2).
Getting and developing that commitment of the NHS to the CLAHRCs was, and remained, the rationale for the matched funding model:
The CLAHRC model has to be something which can exist and continue to operate when the CLAHRC funding has come to an end. Otherwise in a sense it hasn’t achieved its objective . . . If you say the CLAHRC has to have control of the money you have to imagine a world in which NIHR stops funding CLAHRCs as such and NHS managers still want to put all their money into a single pot and not have to control it. It’s hard to imagine that happening.
CLAHRC director 2
However, although matched funding was perceived as important, senior CLAHRC members highlighted that expanding the scope of the CLAHRC was important even when it was not possible for all partner organisations to provide matched funding:
In truth the partnership in the current environment is far more important than the money. What’s important is maintaining the partnership because without partners, CLAHRCs are just research outfits. Obviously not investing financially can put a very different power dimension on a partnership but we’ve had to be flexible and we’ve increased our partners.
CLAHRC director 3
Summary
Matched funding took two forms: direct funding and in-kind funding (usually the release of the time of NHS staff). There was initial concern about risks, particularly that this commitment might be withdrawn at a time of NHS reorganisation and budgetary constraints. The CLAHRCs’ experience as explored here suggests that these risks were greatest when matched funding was direct and came from a limited number and type of NHS sources. However, these risks were balanced by gains, which included the early commitment of NHS organisations and their early involvement in setting the CLAHRC agenda, thereby ensuring that it addressed (and was seen to address) issues that mattered to the service. Some CLAHRCs reported that their matched funding increased over time. Overall, the evidence compiled from our two case studies and the wider CLAHRCs experience suggests that this funding model helped to develop and sustain NHS commitment.
Promoting integration
The CLAHRCs sought to link those who conduct applied health research with those who use it in practice and to develop the capacities of NHS staff and patients to understand, engage with and implement research. In order to do this they mobilised individuals who can bridge the disciplinary and professional boundaries between academic and service delivery sectors (e.g. as theme leads). They also empowered future ‘knowledge exchange champions’ through training activities, and ran evidence-based training courses and regular CLAHRC-wide learning events. Related to these activities was a belief in the need to involve clinicians and managers in research activities in ways that allow them to introduce evidence-based change while remaining active in practice, and a commitment to providing people with opportunities to learn and adapt in the light of good practice elsewhere. As mentioned in the previous section, matched funding from the NHS facilitated this by enabling the CLAHRCs to buy out some of the time of key NHS staff.
At an early stage PenCLAHRC identified six ‘locality leads’. These were, in the words of a senior CLAHRC member, respected senior clinicians from NHS trusts who also worked part-time for PenCLAHRC. They encouraged their colleagues to become involved in question-generation and in clinical decision-making courses, and generally helped them think about evidence-based practice and become more research-aware. Their job was therefore not just to act as mere ‘knowledge brokers’ but to be deeply involved with clinicians throughout the research and implementation cycle:
What we try to do is allow these locality leads to help clinical groups to formulate issues in a way that makes sense to them, but also makes sense to us at the more research end. But then they keep involved in the process . . . So instead of saying, ‘Give us your questions and now we’ll take them off and do something’, we try to work with them, but also keeping these locality leads, who are grounded in practice, involved throughout.
PenCLAHRC interviewee 1
Among PenCLAHRC’s members these locality leads were seen as crucial to what the CLAHRC did. After its first year, PenCLAHRC added a small number of managerial locality leads, and also attempted to recruit some locality leads from general practice. One senior director also suggested that all CLAHRC staff and many of those involved in the CLAHRC (such as the members of PenPIG) could, potentially, act as informal locality leads in their own particular fields: ‘we do have the equivalent to the locality leads amongst patients’ (PenCLAHRC interviewee 1).
Other ways of promoting integration included training schemes to facilitate better understanding of the links between research and practice and help to strengthen those links. For example, CLAHRC-CP established a CLAHRC Fellowship scheme which aimed to get clinicians, health and social care practitioners and managers involved in research and promoted the use of research-based evidence, and details of this are available on the CLAHRC-CP website. 79 Both CLAHRCs also convened regular CLAHRC-wide learning events to help to promote better understanding between partner organisations. These events were seen as crucial to the development of the collaboration:
We invited people from trusts and the NHS to come to a knowledge exchange forum. And we talked about the kind of things we might be able to do to help them, which they might be interested in. And gradually they’ve taken that over. They come to us and say, these are the kind of questions we might like answered, or these are questions that are concerning to us, so could we find a way of answering them. And that’s provoked an interesting discussion. And we’ve had a few of these knowledge exchange fora now, and they’ve led to some interesting work.
PenCLAHRC interviewee 1
The experiences of CLAHRC-CP and PenCLAHRC were echoed by the wider CLARHC experience. Thus, all the CLAHRCs had some type of facilitator, people who, like the PenCLAHRC locality leads, worked as integrators or ‘knowledge brokers’ (we here follow the literature80,81 and use the latter term to cover all these roles). These individuals were intended to create a link between the CLAHRC and those working in practice.
However, although there was general agreement that this function was vital, there was much variation across the CLAHRCs about who were recruited to these roles, how they operated and what they were called. While we could not explore this important aspect across all CLAHRCs in detail, we did identify some of the approaches taken and some of the issues raised.
Thus, like PenCLAHRC, other CLAHRCs initially recruited senior clinicians in the trusts to work part-time as knowledge brokers, for example as ‘diffusion fellows’:
[You] get individuals in often quite senior roles within clinical services to go into a research environment, understand critical appraisal, understand the latest thinking for their services, then go back into their services with a couple of researchers, make them look good, make themselves look good, and actually innovate and put new practice in. I think that’s what CLAHRCs are about . . . one of the criteria for diffusion fellows was to have them reasonably senior so they could come back, and if they change their practice, they have a real influence in the areas they were working, and others would have to follow suit. They’re real opinion formers . . . you get your best people, your busiest people to do this.
Senior NHS-affiliated CLAHRC member 3
It was generally agreed that knowledge brokers needed to have credibility within the service in order to establish leadership:
If people feel that the diffusion fellows are recent graduates without any big exposure to the NHS then they have very little credibility. All you have done is displace the problem, and they become as alien as academics were to the service. Whereas if you ‘curate’ NHS staff who are already there doing the work, even though it’s much harder, that in the long term will pay dividends.
CLAHRC director 4
It was, therefore, important that they were the right appointments and could operate at the right level. Like the locality leads in PenCLAHRC, the diffusion fellows were seconded from NHS organisations on a part-time basis to act as change agents and champions for innovation. They assisted with the design of studies to ensure they solved practice-based real-world issues and remained involved throughout the research project. 82
However, this role is still relatively unfamiliar,82 and it was set up in ways that worked better in some CLAHRCs than others:
There are some things that we put in place to try and reinforce our relationship with other organisations that may not have been as much a success as they could have been. We had a series of what we called CLAHRC co-ordinators who we employed to work with some of our stakeholder trusts and I think that that was variably successful and I think that we might have reformatted that if we were doing it again.
Senior NHS-affiliated CLAHRC member 2
It was equally important to recruit knowledge brokers from a variety of backgrounds who could work across the service, reaching managers and commissioners as well as clinicians, operating across various communities of practice. One director made a point of saying that their CLAHRC had ‘got a diffusion fellow who works specifically with the [clinical commissioning groups]’ (CLAHRC director 3).
In addition, and again reflecting the experience of CLAHRC-CP and PenCLAHRC, other CLAHRCs experimented with different forms of training and exchange programmes in order to promote integration between the NHS and academia. Examples include the establishment of NHS CLAHRC Associates,
who come into contact with and contribute to the CLAHRC. In our case what we are offering is access to our high-quality research training programmes, which are configured in a very flexible way so they don’t take over your life.
CLAHRC director 4
A further example was the Research into Practice placements developed by another CLAHRC, involving
nurses and allied health professionals and so on who want to implement research into their current practice or develop a small piece of research in their current practice that would benefit the patient experience. These are specifically for non-medical staff. We had 37 applications and funded 13 people, and some of the outputs are just incredible.
CLAHRC director 3
These programmes were seen to have resulted in real change:
This is the closest they’d seen to real improvement science on the ground. You’ve got a whole host of researchers, a whole host of NHS people having a discussion about NHS issues and research. So I think that’s the type of infrastructure that we’ve created with this sort of . . . that’s sort of less of a tangible outcome.
Senior NHS-affiliated CLAHRC member 4
Summary
Overall, these examples illustrate how knowledge brokers and knowledge exchange and training programmes were used to involve NHS staff in research activities and foster a culture of collaboration between academia and the service. They suggest that knowledge brokers need to be well respected by their colleagues and relatively senior; remain grounded in practice (the locality leads were part-time appointments); and be well supported by the research and health systems in which they operate. This last point is important. The CLAHRC knowledge brokers were not single ‘change mechanisms’ working in isolation; they were supported by NHS matched funding (a second CLAHRC ‘mechanism’) and operated within the overall framework provided by each CLAHRC.
System shifts and complexity
We noted at the beginning of this section that, as both CLAHRCs in our case studies developed, they went beyond a linear model in which knowledge is seen as a product of research that passes from researchers to users by diffusion and can be generalised across contexts, and adopted relationship approaches to research and implementation that focused on interactions among people in which knowledge from multiple sources is exchanged and adapted to local circumstances. PenCLAHRC adopted an iterative question-generation process that involved ongoing feedback through a series of cycles (the ‘Engagement by Design’ model) and CLAHRC-CP used an approach that emphasised whole-system re-engineering and ongoing coproduction of research.
There was a clear message from both CLAHRC-CP and PenCLAHRC about how necessary, and how complex, these processes were:
I knew from the start that the ‘Engagement by Design’ model wasn’t linear, but I really know now that it’s not linear. It’s not about a guy with the knowledge in the laboratory which he sends out through various hurdles to people who do things. It’s about how the people doing the work can use research knowledge and help generate new research knowledge and understanding that’ll help them make better decisions.
PenCLAHRC interviewee 1
As one senior leader in PenCLAHRC pointed out, people do not make decisions in isolation. Complex health-care challenges require complex multilevel solutions tailored to specific settings. 83 What is needed is a capacity to think about how the system operates as a whole and consider the interactions between numerous players in multiple settings that take place within a specific legal, statutory and financial framework. The ongoing challenge for the CLAHRCs was to find ways to identify and demonstrate the complex and context-dependent pathways between research and health outcomes in ways that collaboration partners (patients, researchers, health-care practitioners and managers) could understand and use to guide research and practice. As indicated by the survey findings reported in Figure 12, individuals working within the CLAHRCs had already developed an understanding of new ways of working, and change had started to take place across the system.
Cambridgeshire and Peterborough CLAHRC also sought to challenge their thinking by involving staff from local academic institutions such as the Cambridge Engineering Design Centre and the Judge Business School:
The type 2 [translation] gap involves a great many players and an understanding of how to move ideas around a system. In fact, it’s a sophisticated systems engineering and management problem . . . What we’ve learned is that there are principles to short-circuiting having an idea and getting it into the hands of people who can use it. 84
These insights about the need to understand the CLAHRCs as complex interventions operating within highly complex health-care research systems were confirmed by other CLAHRCs:
One of the things that say a randomised control trial project will try and do is almost take some of the complexity out . . . can we be clear, does this drug work or not? Whereas essentially with quality improvement methods what you need to say is it needs to work in a highly complex NHS environment. So there’s no point taking a complexity out if a project’s going to be sustainable, it needs to deliver in that complex environment.
CLAHRC director 1
Collaborations for Leadership in Applied Health Research and Care need to work as part of those systems, which now include the AHSNs. These new bodies were seen to have the potential, in association with the CLAHRCs, to strengthen further the links between research and service-wide improvement: ‘One of the commitments of our AHSN is that organisations will bind themselves so if something works in one place they will all do it’ (PenCLAHRC interviewee 1). This potential was also identified by other CLAHRCs – ‘[the CLAHRC] does need to work it as part of the system, and how you define the system is important . . . CLAHRCs are very useful. I think AHSNs will make them universal’ (senior NHS-affiliated CLAHRC member 3) – highlighting that their reach can go beyond the local NHS organisations and extend to wider NHS practice.
Summary
The perceptions of key stakeholders about the nature of CLAHRCs as collaborations and the scope (and complexity) of the tasks they were set go to the heart of what this evaluation was seeking to explore. We noted earlier (see Chapter 1) that the language used in the original applications for the CLAHRCs was that of ‘bridging translation gaps’. This was also the language used in the NIHR call for evaluations of the CLAHRCs2 and in our own proposal for this study. However (and as we suggested in Chapter 1), this language did not fully capture the ambitions of the NIHR CLAHRC programme. The CLAHRCs recognised this at an early stage, appreciating that the simple linear model suggested by the terminology of bridges and gaps was not adequate and that what they were seeking to promote were complex system shifts.
Conclusions
In this section we have explored how the NHS has influenced the evolution of CLAHRCs and how the presence of a CLAHRC has affected the practice and culture of the NHS. We have identified four themes that characterise the nature of this mutual influence. First, we noted the importance of a local remit for the scope and work of the CLAHRCs. The CLAHRCs are rooted in local relationships, build on local capacity and expertise, and have relied on local relationships and capacity to shape their research projects. This has also meant that they have focused the outcomes of their projects across the widest possible local area through engagement with the local NHS providers and commissioners. Second, we noted how the requirement to attract matched funding provided opportunities (e.g. by creating NHS resources for projects through ‘in kind’ funding) and challenges (e.g. caused by health sector restructuring, which affected commitment). Third, the CLAHRCs have demonstrated a clear drive to promote integration through the creation of ‘integrating roles’ such as locality leads or diffusion fellows, as well as encouraging those not directly involved in the CLAHRC to engage with their activities as, for example, CLAHRC Associates. Finally, we explored the nature, and potential, of the CLAHRCs as complex interventions operating within highly complex health-care and health-research systems.
How are effective multistakeholder and multidisciplinary research and implementation teams for service improvement built: what can we learn from the CLAHRC mode and what mechanisms are being used to enable it?
The second core question explored in our evaluation concerned the multistakeholder and multidisciplinary teams for service improvement that have been built by the CLAHRCs. NIHR funding for the CLAHRCs was provided to
support a critical mass of people focused on the conduct of applied health research and the uptake of research evidence into practice; and attract the foremost individuals to produce reliable, relevant research evidence and translate this evidence into improved patient outcomes across the widest possible geographic area.
pp. 2–33
The findings from the two case studies illustrate how each CLAHRC encouraged NHS staff and patients to raise issues of concern and to get engaged in setting the research agenda and in the production and implementation of research.
Perspectives of NHS and academic staff across six CLAHRCs
The findings of the CLARHC-wide survey (Figure 13) show that both academic and NHS respondents believed that they were working towards the same long-term goal: to improve health services and patient outcomes. Both groups also regarded capacity building and developing new skills as important aims of their CLAHRC. More NHS respondents than academics thought that the creation of a sustainable research infrastructure focused on the needs of the service and patients was important, but both groups supported the aim of increasing NHS responsiveness to individual patients’ needs.
FIGURE 13.
Perceived aims in relation to longer-term outcomes and impacts.

One important concern among respondents was how effective the CLAHRCs were in taking the views of all their stakeholders into account in the day-to-day delivery of their activities (Figure 14). We found a high level of agreement among NHS and academic respondents that the views and concerns of clinicians, commissioners and patients involved in CLAHRC activities were taken into account. However, the findings also suggest that there was scope for improvement in responding to the wider public and patients.
FIGURE 14.
Perceived effectiveness of the CLAHRC taking into account the views and concerns of its stakeholders in the day-to-day delivery of its activities.

When asked about the level of participation of different groups in the CLAHRC, there was consensus among respondents that senior and junior academic staff and senior NHS clinicians had had high levels of involvement (Figure 15). There appeared to be less agreement among academic and NHS respondents about the involvement of junior clinicians and NHS middle management, with academics tending to ascribe these groups a higher level of involvement. Although respondents thought that NHS senior management and public and patient representatives had had some level of engagement, there appeared to be scope for closer involvement.
FIGURE 15.
Perceived extent to which relevant people within CLAHRC’s local NHS/university actively involved in CLAHRC.
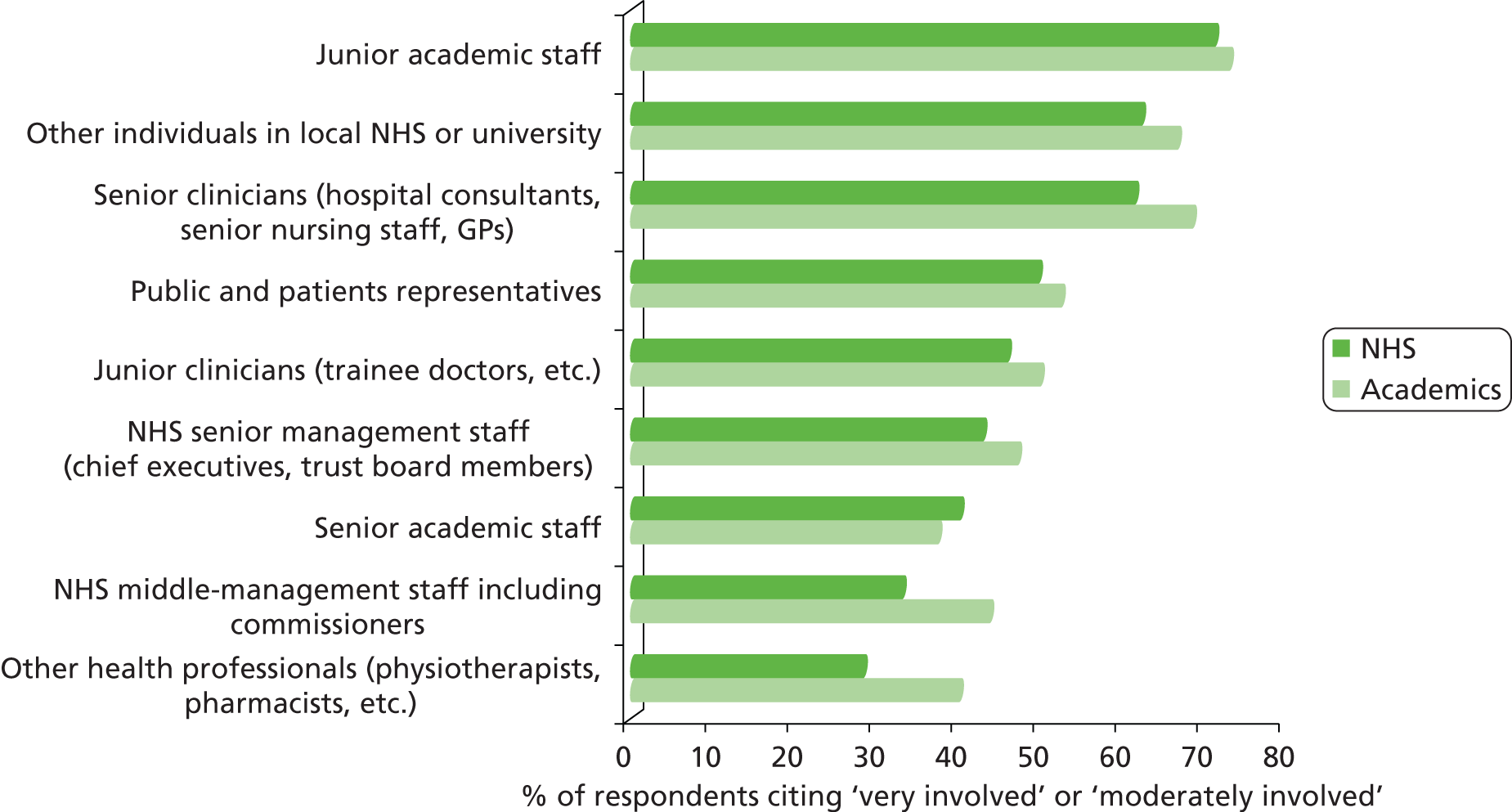
Respondents reported that people from the local NHS were actively involved in their CLAHRC primarily through the following three activities: working with academics on project teams; attending CLAHRC meetings and seminars; and having a place on the CLAHRC board (Figure 16). The availability of formal training courses and opportunities to solicit research projects based on NHS needs and consult academics also played a role in encouraging involvement.
FIGURE 16.
Reported reasons why relevant people within CLAHRC’s local NHS are actively involved in CLAHRC. MSc, Master of Science; PhD, doctor of philosophy.
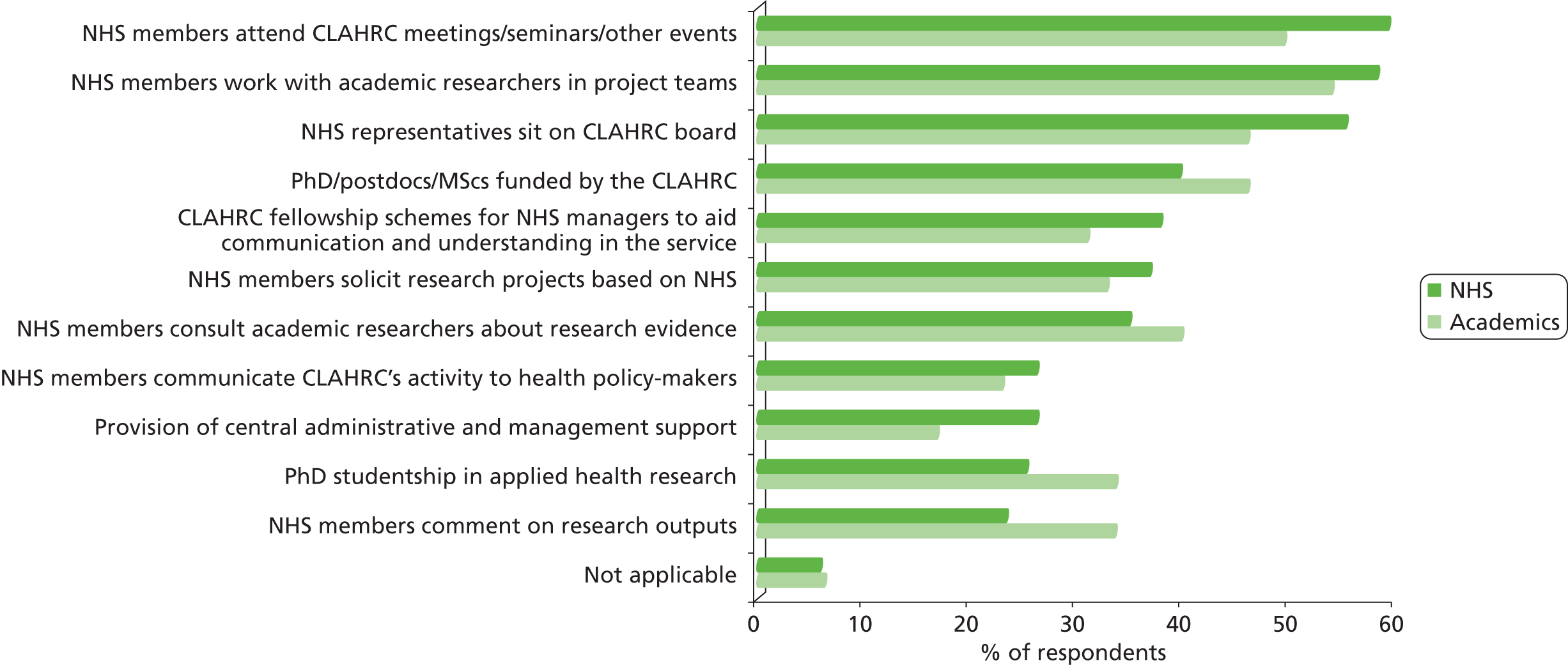
We also sought to understand why people in the local NHS had not become involved in the CLAHRC, with a number of respondents citing an enduring focus on traditional research, at the expense of applied research (data not shown). This sentiment was particularly pronounced among academic respondents, and complements the finding that one of the ways that CLAHRCs were able to influence behaviour was by undertaking research that is easily applied [see Chapter 4, How does the NHS influence CLAHRCs’ evolution, outcomes and impact (and indeed how does having a CLAHRC influence NHS behaviour)?, Perspectives of NHS and academic staff across six CLAHRCs]. In combination, these findings imply that when CLAHRCs focused on research that can be applied (as was consistent with their aims) they were perceived to have facilitated engagement, and that the reverse is also true.
When asked what had enabled the CLAHRCs to meet their objectives, respondents emphasised the skills, expertise, motivation and commitment of people involved with the CLAHRC (see Appendix 5, Figure 54). Funding availability, good buy-in from key individuals and good pre-existing networks were commonly cited, in keeping with the nature of CLAHRCs as collaborations rooted in local relationships.
In this context we also sought to understand the perceived barriers to meeting the CLAHRCs’ objectives. The most commonly cited by both NHS and academic respondents were existing incentive structures, such as the focus on the Research Excellence Framework (REF) criteria for university researchers and the lack of recognition of research involvement in career progression for NHS staff (Figure 17). There was also a perception that insufficient NHS involvement in identifying research topics was a barrier. There was a difference of opinion regarding the extent to which the lack of commitment of key individuals was a problem, with over 30% of NHS respondents regarding poor buy-in as a barrier compared with 15% of academics.
FIGURE 17.
Perceived elements of CLAHRC and wider landscape that provide a barrier to meeting its objectives. IT, information technology.

Experiences in CLAHRC-CP and PenCLAHRC
We explored the development of effective multistakeholder and multidisciplinary teams further through our case studies and identified three overarching themes: getting people involved and changing attitudes; the CLAHRC ethos of experimentation and learning; and the time required for change.
Getting people involved and changing attitudes
We describe what we found from the case studies about the CLAHRCs’ efforts to get people involved and change attitudes. Although engagement efforts overlapped across different groups, we describe these engagement processes as they relate to the following stakeholder groups: NHS clinicians, NHS managers, commissioners, academics and other stakeholders, including local authorities and the third sector, and patients and the wider public.
NHS clinicians
The stakeholder survey suggested that senior clinicians had considerable strategic influence over the CLAHRC (see Appendix 5, Figure 53). In CLAHRC-CP and PenCLAHRC most of the senior staff (including the PenCLAHRC locality leads) were well-respected clinical academics, and senior clinical staff in NHS trusts, from whose ranks these leaders were drawn, were often relatively quick to see value in the CLAHRC and come on board.
Other efforts to involve clinicians at all levels included training and fellowship schemes described earlier to enable exchange across the collaboration. The CLAHRC-CP fellowship scheme was aimed at individuals from a wide range of backgrounds, including junior clinicians, GPs and registered nurses. Thirty-two fellowships had been awarded by 2012/1379 and it was reported that ‘CLAHRC-CP fellows are making an invaluable contribution, acting as local “research champions”, and helping the CLAHRC connect with healthcare practitioners in the community’. 84
However, several interviewees in PenCLAHRC said that engaging GPs had been particularly challenging. The CLAHRCs were established at a time when considerable organisational change was about to be implemented across the health and social care systems, and people in primary care were at the forefront of many of these changes. Senior CLAHRC members also suggested that one difficulty was the way in which the system would encourage GPs to act as individuals who work in their own practices to address the problems of specific patients, with little time to think more strategically about service delivery. At an early stage delivery, PenCLAHRC appointed a senior lecturer in primary care and in 2010 further increased its links with general practice, borrowing strength from a successful system established by the local primary care research network [National Institute for Health Research. Collaborations for Leadership in Applied Health Research and Care: Progress Report for Second Award Year. The NIHR CLAHRC for the South West Peninsula (Peninsula CLAHRC). Unpublished, 2011], but it proved impossible to buy-in GP time and establish GP locality leads.
While we have not explored primary care engagement across all the CLAHRCs in detail, not all CLAHRCs reported the same challenges. Thus, one CLAHRC interviewee noted how they have been able to
engage a lot of different organisations and particularly general practices in applied research and implementation projects that they have never done before. So speaking personally I am working with 50 general practices in [location] who have never been involved in research ever. So that is a complete culture change for them and the concept of being involved in a study, being randomised into a study, having an intervention team working in the practice. This is something they have never done before so it is a complete shift in their working, in a way.
Senior NHS-affiliated CLAHRC member 2
It is difficult, on the basis of these observations, to infer with certainty why different CLAHRCs had different experiences when they tried to engage people from primary care. However, it underlines our earlier reflection that the CLAHRCs had different strengths to start with, chose to focus on different sectors of the service initially and have been subject to different local constraints and opportunities.
NHS managers
The requirement to obtain matched funding from the NHS meant that local NHS organisations had a financial commitment to the CLAHRCs from the start. However, interviewees in both CLAHRC-CP and PenCLAHRC also described initial uncertainties about how the CLAHRCs were going to achieve their objectives and about the exact nature of the NHS role in all this. One senior NHS manager in PenCLAHRC commented on a difficulty ‘in getting direction from the NHS about what exactly the NHS wanted to achieve’, and in CLAHRC-CP initial NHS reactions were described as ‘hesitant’ and ‘sometimes downright hostile’. These reactions changed as the CLAHRCs evolved: CLAHRC-CP members described how some senior NHS management staff started off as ‘aggressive and quite cynical’, but were ‘completely turned around’ when they saw the value of CLAHRC-CP work for local services.
There was evidence of a similar change in PenCLAHRC, with a senior member noting how:
[a] few weeks ago one of the chief execs of one of the local trusts gave an evening talk . . . and one element of it was ‘why I was originally very indifferent to PenCLAHRC and why I’m now persuaded of its importance.’ And that was a really fantastic thing to hear . . . [the chief executive] felt that it took a very long time to get going and it took time for [the chief executive] to see the potential and to see what PenCLAHRC was actually achieving and to feel that it actually was delivering something [that the chief executive] wanted to see delivered.
Senior NHS-affiliated CLAHRC member 2
This chief executive had been convinced by mainstream CLAHRC projects (not all of which were directly relevant to his/her own operations), by the systematic reviews that had been made available to support decision-making, and by the work of the Peninsula Collaboration for Health Operational Research and Development (PenCHORD), a PenCLAHRC initiative that was launched 2 years into the CLAHRC to help local trusts use modelling, simulation and other operational research techniques to improve patient care. 85 Overall, the chief executive felt that PenCLAHRC had helped the NHS to think about the right questions, and that there had been a genuine involvement of patients.
However, middle managers, who face urgent day-to-day concerns and are often subject to pressures over which they have no direct control, were more difficult to involve systematically rather than on a project-by-project basis. But there was also evidence from our case studies that over time this group too could be reached, albeit with difficulty: ‘In [location] we’ve really gone in quite deep with that group, middle management, and it’s been very, very, very helpful; but in other places not very far at all’. The same interviewee also suggested that the AHSNs might be able to help:
That is one of the things the AHSN will aim to do, build a system across NHS organisations where there’s some degree of pooling of service improvement people across providers and commissioners. That will make it a whole lot easier because at the moment there are a couple of rather isolated people in an organisation, particularly in smaller organisations.
PenCLAHRC interviewee 1
Our survey findings also alluded to the challenges of getting NHS middle management involved (Figure 15), and these challenges were confirmed by the wider CLAHRC community; interviewees mentioned ‘that barrier between the top and the kind of the people who are the coal face’ (senior NHS-affiliated CLAHRC member 6). However, the CLAHRCs were also prepared to keep trying and to do the
face-to-face legwork and talking it through and making sure that people did understand what we were about and where we were trying to get to and that we did actually mean business and things of that sort and that helps people to sort of come on board and say, yeah we are going to invest time because we want this to happen.
Senior NHS-affiliated CLAHRC member 4
NHS commissioners
Interviewees in PenCLAHRC and CLAHRC-CP reported that NHS commissioners could be hard to reach, especially as PCTs were to be replaced by clinical commissioning groups. However, members of PenCLAHRC also said that they had some success with senior people, through an initiative with the Peninsula Health Technology Commissioning Group to provide rapid assessments of new technologies (such as pharmaceuticals) supported by PenCHORD. This initiative was seen to have had a direct impact on the nature of specific commissioning (for further detail see Box 2). 86 Another initiative involved a PenCLAHRC collaboration with the National Institute for Health and Care Excellence (NICE) and with local clinicians, commissioners and patients on a project that sought to identify ineffective procedures which the NHS should discontinue funding. 87
South West Peninsula HTA Commissioning Group was charged, on behalf of all local PCTs, with reaching joint decisions about the use of new technologies. The group worked with PenCLAHRC to establish a facility to provide locally relevant cost-effectiveness models to underpin consistent joint commissioning decisions. The four PCTs in Devon and Cornwall, in response to research carried out in the Peninsula Medical School, established a co-ordinated framework to assess new health technologies (predominantly drugs) and make a single commissioning decision. The assessed technologies identified were selected on the basis of their importance to commissioners. PenCLAHRC staff were actively involved in the decision-making process: one of the deputy directors was a member of the HTA Commissioning Group and chairs the planning group which set the work programme. This academic/NHS partnership was supported by PenCHORD, and was seen to have had a direct impact locally on the quality of specific commissioning and to have helped to increase receptivity among NHS partners to the explicit use of evidence in decision-making. 86
Source: Adapted from PenCLAHRC. The NIHR CLAHRC for the South West Peninsula (Peninsula CLAHRC). In National Institute for Health Research, editor. Collaborations for Leadership in Applied Health Research and Care: Progress Report for Second Award Year. Unpublished, 2011.
The wider CLAHRC community reported a similarly mixed picture of relations with commissioners: ‘we have got links with them and having said that, you know they are jolly preoccupied at the moment just trying to get the basics in place’, but also:
in some way from the restructuring point of view the creation of clinical commissioning groups for us is as much an opportunity as anything else so we had pretty good relationships with one of the sort of pre-clinical commissioning groups [. . .] and managed a number of demonstration projects with them really, which, some of it, is very exciting.
CLAHRC director 6
Academics
The CLAHRCs encouraged academics to do research that relates directly to the needs of the service and its patients. Some academics were more comfortable with this than others. In PenCLAHRC there were initial concerns among senior university staff that PenCLAHRC would not deliver research that matched the REF agenda. However, over time, and with the help of external factors such as a new ‘impact’ element in the REF and the push to get universities more ‘community involved’, and given PenCLAHRC’s demonstrable success in attracting external peer-reviewed funding as described earlier (see Chapter 4, Experiences in CLAHRC-CP and PenCLAHRC), the PenCLAHRC research agenda became increasingly acceptable to the local universities and of interest to more academics. This finding was confirmed in other CLAHRCs.
Indeed, as this different way of working becomes more acceptable, it could in itself provide a new way of measuring research performance. Thus, a senior member of CLAHRC-CP noted that academic researchers
still do some pure knowledge production but when they’re doing work that’s aligned with the CLAHRC, largely they do think about ‘where is this work going, who do I need to work with and am I, have I coproduced this etc., am I going to exploit the new partnerships that we’ve made through the CLAHRC to get this work implemented or is it being pulled through by my new partners?’ So when they don’t behave like that then we notice it, so I think that’s a kind of unexpected performance indicator.
CLARHC-CP interviewee 6
This change in attitudes among academic researchers was reported across the CLAHRCs, and highlights the importance of having the right ‘infrastructure’ in place to ‘enable some of these discussions [to] happen and actually change culture.’ Part of that infrastructure was the availability of funding:
Money matters in the institution, there is money and resource and kudos and recognition to be had in this field of how service is researched. So that shifted their thinking that the CLAHRC funding did make them acknowledge that actually [location’s] greatest strength in research terms were in applied health services research, not in the basic biomedical research in some areas.
Funder 1
However, it was also recognised that, while the CLAHRCs had an important catalytic function in prompting a change in attitudes among researchers, there had been other influences as well:
One of the many positive aspects of the CLAHRC programme has been a recognition on the part of academics that if, for example, they are providing an evidence-synthesis service, it’s got to be provided in a really crisp and intelligible manner and at a time of the NHS partners’ choosing, answering questions that the NHS has framed . . . culture change has definitely taken place in academia. It is not just because of the CLAHRCs, although they’ve had a very positive and important effect.
CLAHRC director 4
It was appreciated that this shift had been of crucial importance, but also that it was early days and further progress was needed:
In my own institution over the last 10 years there’s been a real shift in thinking but it’s not gone as far as I think it needs to or I would like it to, but we now have seen people promoted, including promoted to professor, on the basis of their contribution to knowledge transfer.
Funder 1
Other stakeholders
Cambridgeshire and Peterborough CLAHRC focused on mental health. In this field, local authority and third sector involvement is crucial, and there is evidence that in CLAHRC-CP this was successfully achieved:
The greatest impact of the CLAHRC to date has been, and continues to be, the gradual enlightenment on the part of our local authority, voluntary sector and clinical colleagues of the potential value of high-quality research to their work.
CLARHC-CP interviewee 6
A senior academic who worked closely with the local authorities to explore how research could inform decision-making in CLAHRC-CP noted how:
It’s more apparent and it’s more impressive in the way in which we’ve changed our working relationship with Cambridgeshire Social Services . . . It’s us now coproducing a programme of evaluation which is funded by social services and will be supported by our infrastructure and I think we could say without hesitation that this would not be happening if it wasn’t for the CLAHRC. I think it’s the biggest multiagency success of my career.
CLAHRC-CP interviewee 3
This perception was echoed by social care staff:
I’m grateful to the relationships that we had in the CLAHRC that just made us begin to think a little bit differently, otherwise we wouldn’t be investing the money that we are doing in trying to create an evidence base for social work . . . we do feel as if we’re breaking new ground so it’s exciting.
CLAHRC-CP interviewee 5
The case studies also provided evidence that people’s views about the merits and possibilities of involving patients and the public in research changed, both among CLAHRC staff and among other CLAHRC partners. PenCLAHRC developed a strong PPI programme, and their internal evaluation found that the programme had developed
a life of its own. The whole point of involving patients is that new things are brought in and some of them may be quite challenging . . . if they’re not free to challenge us or to challenge the professionals then in a way we’ve failed. But they’re doing that, creative things are happening.
PenCLAHRC interviewee 3
An internal evaluation further identified factors that were seen to have helped to promote change, such as adequate funding for PPI, building on what was already there, and getting patients to help develop the partnership.
The lessons that emerge from these accounts are that getting people involved is an incremental process and that it is important to demonstrate ‘impact’ in order to get the different stakeholders on board:
I think they’ve always been involved. But their buy-in, their actual understanding of what PenCLAHRC does, how it is making a difference – all of that has shifted. They were always involved but more hesitant at the beginning. When you start to give examples, like the tranexamic acid one, they automatically see it – both the NHS and higher education and others . . . and, therefore, are much more engaged because they truly see the value.
PenCLAHRC interviewee 1
Summary
It is difficult to draw general conclusions from what was, and remains, a long and persistent effort across the CLAHRCs to engage large numbers of people from a variety of backgrounds in the NHS, academia and beyond, but we can make the following observations:
-
It was an incremental process that took time and considerable persistence, but it did appear to gain momentum as the CLAHRCs developed.
-
Demonstrating ‘impact’ was important, and it was also important to demonstrate that this impact was associated with CLAHRC activities.
-
Efforts to engage people needed to be made on several fronts (the aim being to build multidisciplinary teams) but it was not possible for each CLAHRC to seek to engage all potential stakeholders at the same rate and at the same time. Each CLAHRC had to use its relatively limited resources selectively.
-
Where the CLAHRCs had an existing expertise and strong existing relations (such as CLAHRC-CP in social care, PenCLAHRC in PPI and others in primary care) they could, and did, build strong relations with stakeholders.
-
Where these pre-existing factors were lacking, or there were operational or structural constraints in the research and health systems, the task was more challenging.
-
System shifts, although challenging, could sometimes help to facilitate the engagement of previously hard-to-reach groups.
The ethos of the CLAHRCs: experimentation and learning, responsiveness and flexibility
As noted earlier, the CLAHRCs were originally envisaged as pilots. 3 What we understood from our case studies was that the initial vision was clear but that there was little certainty at the start about how the aspirations set out in the call for proposals could or should be achieved in practice, nor was there much central prescription. The approaches taken were shaped by the local context and local capacities, and by the people who led the CLAHRC application. As a result there was considerable variation between individual CLAHRCs. Overall, the CLAHRCs were set up in such a way that they had to be prepared to explore, seek their own way, take some risks and exploit unforeseen opportunities, learn from failure and success, and adapt: ‘We said from the beginning that we were going to “suck it and see”, and made it clear from the beginning that we were going to change; and then we had some really crashing failures which were enormously influential’ (PenCLAHRC interviewee 1).
The evolving changes in the health and social care system also required ongoing responsiveness: ‘Questions emerge, new partners emerge, new researchers, new partners on the knowledge production side emerge, new techniques, new ideas. We need to be able to contain all those emergent issues’ (CLARHC-CP interviewee 5).
This was not just a matter of containment. CLAHRC funding was small in comparison with local NHS budgets, but it was flexible and could therefore have leverage:
The thing that CLAHRCs were able to do is bring in enough resource to put a bit of extra into the system . . ., and have flexibility about how to spend it. We have enough money to manoeuvre. . . . And so those little bits of flexible stuff that the CLAHRC could do – bringing in a statistician or a health economist to evaluate the situation – that gave us a disproportionate amount of leverage in the system.
PenCLAHRC interviewee 1
The CLAHRCs were set up to respond to the research needs of the service and its patients. Responsiveness also characterised how relationships developed and were handled within the CLAHRCs. What we saw in the case studies was genuine dialogue between the different partners within the collaborations, and previous sections have highlighted how the CLAHRCs listened to their stakeholders and worked with them to identify and address their concerns. Joint CLAHRC-wide events provided regular opportunities to share learning from CLAHRC initiatives and adapt.
These findings from the case studies were confirmed by the wider experience of the other CLAHRCs. Responsiveness was seen as a core feature of success:
The very responsive CLAHRCs are the more successful CLAHRCs. The ones that have got the good relationships and can maintain those relationships are the ones that will be successful and sustainable.
CLAHRC director 1
This required a good understanding of stakeholders, and a commitment to engage with them and hear their concerns in order to develop the research most appropriate to local service needs:
We’re listening to you, we have some ideas but we want to hear from you: what do you think the problems are and what do you think we can do to resolve those and here’s some evidence or here’s the way we want to look at things, we think there’s good evidence to support these. But it was very much trying to be very sensitive to that context and to stakeholders.
Senior NHS-affiliated CLAHRC member 5
Summary
Given their overall brief and the lack of any definitive roadmap of how to achieve their goals, NIHR established the CLAHRCs as natural experiments with a good deal of autonomy. This enabled them to be responsive to the concerns of all their partners and flexible in their approach. The evidence from the case studies and the wider CLAHRC experience gathered through validation interviews suggests that these characteristics were, and continue to be, crucial to the CLAHRCs’ success.
Time required to achieve change
Participants at our workshops in the two case studies and interviewees across the other CLAHRCs highlighted the importance of allowing time for the CLAHRCs to build relationships in which people could develop trust in each other and be willing to share information. The clear message was that ‘real’ engagement occurs at an individual level and over time, and requires patience, mutual understanding and a willingness to listen and respond to others.
The time scales to which managers, commissioners, clinicians and academics work differ, often considerably. The CLAHRCs sought to find a middle ground and develop awareness of the pressures on others. Specific barriers within the NHS that were identified in our two case studies were a general short-termism and a rapid turnaround of senior staff, resulting in a lack of capacity in the NHS to translate strategic vision into decision-making: ‘in the NHS, the capacity to take the long-term strategic views is . . . limited by the short lifespan of the chief executive; and the short term is engendered by the way the system is set up’ (PenCLAHRC interviewee 1).
There is a need to balance the requirement to undertake and use rigorous and relevant research with the pressures of immediate day-to-day decision-making. Primary academic research often follows long time-scales, and the studies that produce the quick wins needed to convince NHS managers and commissioners have hitherto had little credence among academics, in part because of the reward structures within the academic environment, such as the publication requirements within the REF. All the CLAHRCs recognised that if they were to establish a sustainable structure they needed to develop a ‘plurality of activities’, allowing for both long and short turnarounds. The aim was to create a win–win situation for both academics and NHS staff, recognising that the concept of a ‘win’ differs on both sides, and that ‘seeking a win–win has to be a process of negotiation’. But this takes time:
Over 5 years you’re not going to change, you’re going to maybe increase the opportunities for collaboration but I’m not sure you’re going to really change the culture when push comes to shove, particularly when they feel threatened, they’re asked to make all kind of efficiency cost savings.
Senior NHS-affiliated CLAHRC member 5
Summary
There are no quick fixes when it comes to creating real engagement among a wide and diverse group of stakeholders. The CLAHRCs argued this strongly, and successfully, when they sought further funding for a second term.
Conclusions
In this section we investigated how multistakeholder and multidisciplinary teams for service improvement have been built by the CLAHRCs. We showed how, despite initial challenges, CLAHRCs succeeded in engaging different stakeholder groups including clinicians, managers, commissioners, academics and others, such as people from social services and the public, although the pattern of that engagement varied across the CLAHRCs. There was recognition that getting the different stakeholders on board was an incremental process, with partnership working and the coproduction of research at the core of promoting and sustaining engagement. We noted how responsiveness was an essential component of effective multistakeholder and multidisciplinary working, in particular against a background of a changing health and social care system, and that the need (and ability) to experiment was a crucial pre-condition for the CLAHRCs. We also saw that responsive partnership working needs to be based on trusting relationships, and that these take time to build and foster.
What can we learn from the CLAHRCs that can provide new understanding of how to use research knowledge and evidence to change commissioning and clinical behaviour for patient benefit?
The third question explored in the evaluation was about how the CLAHRCs can inform understanding of how research knowledge and evidence are used to change commissioning and clinical behaviour for patient benefit.
Perspectives of NHS and academic staff across six CLAHRCs
A key aspect of influencing practice is to make evidence available in a format that potential users find helpful. 35 The stakeholder survey therefore assessed how well information about CLAHRC activities and projects was communicated, the impact of what was communicated and the intended target audience. Views on whether or not information on CLAHRC activities was communicated well outside the CLAHRCs varied among respondents, with about a third of respondents from the NHS and academia not able to say (Figure 18). While it was not possible to explore the underlying reasons from the survey data, this finding suggests that a considerable proportion of NHS and academic staff were not effectively reached by the communication strategies of the CLAHRCs at the time of the survey.
FIGURE 18.
Information related to CLAHRC activities and projects is well communicated outside CLAHRC.

However, although respondents had different views about whether or not their CLAHRC communicated well with external audiences, there was consensus about the purpose of this communication. The primary aim of communicating information externally was identified as raising awareness of CLAHRC activities. Such communication was also thought to have helped to support the development of the collaboration and enhanced implementation of CLAHRC findings (Figure 19). Primary means of communicating this information were identified as the CLAHRC website and presentations from CLAHRC representatives (see Appendix 5, Figure 45).
FIGURE 19.
Perceived impact of disseminating the information outside CLAHRC.
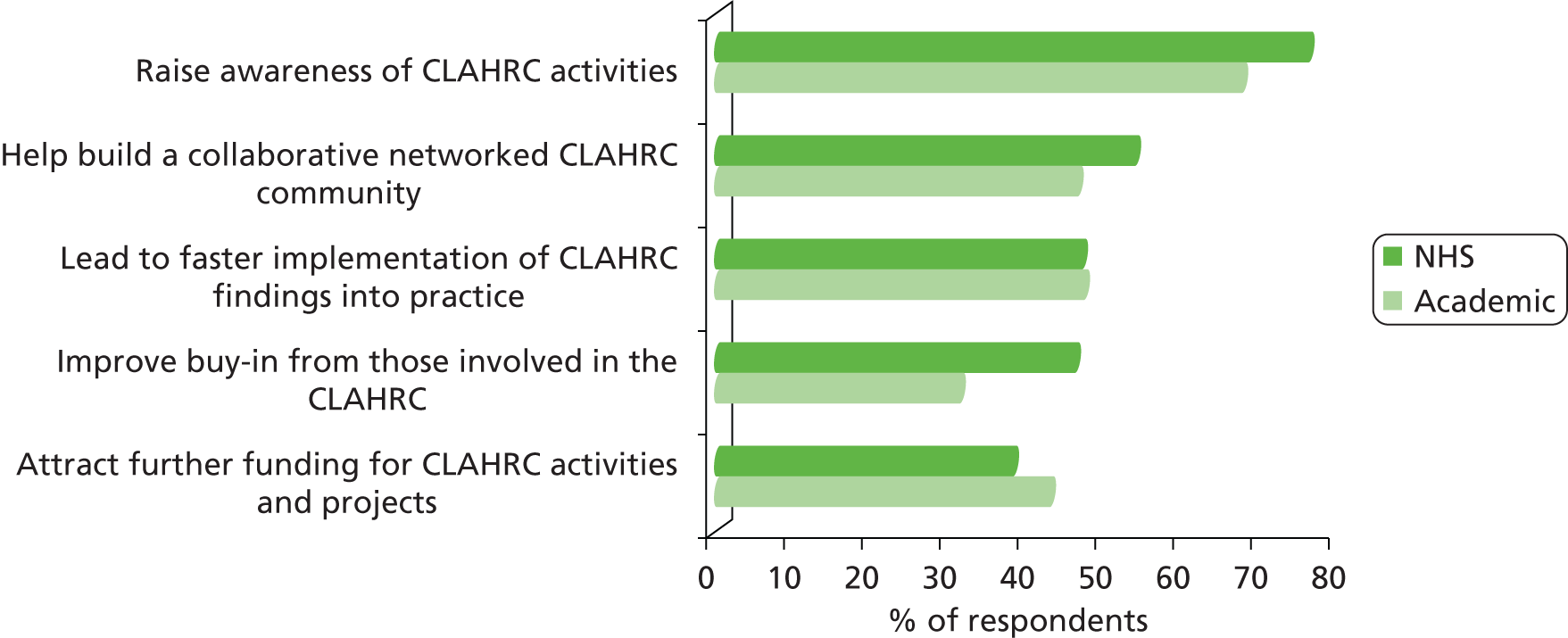
Both NHS staff and academics saw clinicians and commissioners as the key target audiences for information communicated outside the CLAHRC (Figure 20).
FIGURE 20.
Reported target audiences for information related to CLAHRC activities and projects outside CLAHRC.

Experiences in CLAHRC-CP and PenCLAHRC
Building on the findings from the stakeholder survey, we explored how the CLAHRCs sought to encourage the use of research knowledge to change behaviour and influence practice, describing the approaches taken and some of mechanisms used in the two case studies. We identified three overarching themes: shifting academic paradigms; communicating with commissioning; and informing clinical practice. In the following section we analyse these further. We also consider how the findings from the case studies were supported by the wider CLAHRC experience.
Shifting academic paradigms: broadening methodological expertise
The CLAHRCs were required to focus on improving patient outcomes through the conduct and application of applied health research. 3 There were three challenges: delivering the research evidence required to address the needs of the service; supporting the implementation of that research; and achieving an appropriate balance between these activities.
The preceding sections highlighted how the CLAHRCs encouraged academics and NHS staff and patients to understand and become more involved in applied health research and implementation. As they did so, the different agendas of these groups became clearer. NHS clinicians and patients tended to raise concerns about the treatment of particular conditions or new forms of care that were familiar to clinical researchers, whereas NHS managers were more likely to ask operationally related questions about how to organise services effectively and efficiently, questions that were largely outside the scope of clinical research and required a different set of skills. It was clear from the case studies that the CLAHRCs quickly recognised the need to identify and use new types of research and new methodologies to meet these different needs. Participants at a PenCLAHRC workshop commented that the CLAHRC needed to be able to address the research questions raised by all NHS stakeholders and that the CLAHRC should address a full spectrum of clinical, operational and system issues; this was the rationale for the development of PenCHORD, which was designed to apply operational research techniques to system problems. CLAHRC-CP sought to strengthen links with groups with expertise in implementation and service design (at the Cambridge University Engineering Design Centre) and in service change and evidence-based innovation (at the Judge Business School).
A similar pattern was evident in the other CLAHRCs. They also brought in expertise from disciplines outside health research, and there was general recognition that there was value in identifying and using a wide range of research approaches and methodologies: ‘that’s been the innovation in the CLAHRC, taking . . . different methodologies and introducing them into the health environment’ (CLAHRC director 1). Overall, this was a shift in the way research was shaped and conceptualised. One senior member of CLAHRC-CP noted that research success was initially conceptualised as performing longitudinal studies and randomised controlled trials, as suggested in their original proposal. However, as the CLAHRC evolved, this shifted to demonstrating ‘NHS staff engagement’ as a marker of success. 88 Academics in CLAHRC-CP also reported that they had had opportunities to be introduced to ‘real-world research’ and to experiment with methods from other disciplines, and that there was a general appreciation of the value and satisfaction of engaging with NHS staff.
In their proposals all the CLAHRCs identified separate research and implementation themes (see Appendix 10). In CLAHRC-CP the focus was on three applied research themes with two cross-cutting implementation themes. PenCLAHRC planned to develop a common system for the identification and structuring of research and implementation within the framework provided by its ‘Engagement by Design’ model. However, what is evident from the case studies (and from the accounts given in Appendix 10) is that the distinctions that the CLAHRCs made between research and implementation themes in their original proposals were not always clear cut, and were influenced by factors such as the expertise and working identity of CLAHRC members. There were mixed views across the CLAHRCs about the boundaries between research and implementation and some uncertainty about what had been expected by the funder.
Despite these different views, over time all the CLAHRCs came to appreciate how closely linked these two activities are. One director noted that ‘there has been an evolution in terms of we were driven by the original call to have specific themes around implementation and specific themes around research, but they’ve become much more integrated’ (CLAHRC director 1). Another said that ‘if you’re just doing applied health research, you know, you’re not doing the implementation bit then that’s not how I understand the purpose of CLAHRC’ (CLAHRC director 3).
It also became clear from the validation interviews that different approaches remained in place as the CLAHRCs developed: either implementation was kept as a separate theme spanning other themes within a CLAHRC, or it formed an integral activity or focus within each research theme. Either way, there was agreement that producing change in clinical and managerial practice through the implementation of existing research was just as important as producing good-quality research, and that there was a need to keep ‘implementation’ as a core activity within the CLAHRCs. Crucially, this meant supporting implementation through, for example, evaluation of different implementation approaches, but not doing it (which is the role of the service).
Summary
The academic paradigms on which the CLAHRCs were initially based differed and were challenged as their programmes developed. In particular, the boundaries between research, implementation and research on implementation are not always clear cut and can be areas of disputed responsibility. The CLAHRCs’ interpretation of the relation between research and implementation within their programmes varied. However, the arrangement through which the CLAHRCs received NIHR funding and funding from the local NHS, and deliberately sought support in both sectors, also put them in a strong position to explore those boundaries and strengthen the interface between research and implementation, aided by ongoing discussions among themselves about the pros and cons of their different approaches.
Communicating with commissioning
Both CLAHRC-CP and PenCLAHRC emphasised the importance of relating to and influencing commissioners, noting the need for multiple mechanisms to raise awareness of CLAHRC activities, increase the profile of the CLAHRC generally and disseminate information from and about research studies. However, as we noted in Chapter 4, How are effective multi-stakeholder and multi-disciplinary research and implementation teams for service improvement built: what can we learn from the CLAHRC mode and what mechanisms are being used to enable it?, both CLAHRCs were also concerned about the difficulty of engaging commissioners at a time of ongoing change in NHS organisations and in the commissioning structure. The case studies illustrated how these challenges were addressed.
One way in which the CLAHRCs could provide support for commissioners was by acting as an interface at joint meetings with them and service providers. To do this successfully the CLAHRCs had to offer something. One PenCLAHRC member noted that the CLAHRCs could play a role at such meetings through ‘illustrating, making things clearer and offering models that provide a way to discuss the issues rather than definitively pumping out numbers and outputs and so on’ (PenCLAHRC interviewee 4). As we saw above, both CLAHRCs specifically equipped themselves to do this: PenCLAHRC set up a designated unit (PenCHORD) to address operational problems; CLAHRC-CP involved academics from outside health research at an early stage, and they encouraged that CLAHRC to explore the complexities of the ‘sophisticated systems engineering and management problem’ that the CLAHRCs were facing in a structured way. 84
It was this expertise that was the key. When the CLAHRC-CP workshop discussed the notion of ‘complexity’ that is inherent in the CLAHRC model, participants commented that what they had learnt about dealing with complex issues as a CLAHRC could also help commissioners facing complex decisions. One interviewee described the support provided to a strategic multistakeholder workshop in the following terms:
I ran a workshop yesterday for [Improving Access to Psychological Therapies project] commissioners, clinicians, service managers, clinical leads, researchers from the CLAHRC . . . It was about, given the restraints of the funding for the NHS and all the changes that are going on over the next 12 months, what are we going to prioritise? How can we work as a region to support each other, share best practice, learn from each other? So that was a really useful workshop, and obviously, basing our decisions on some of the CLAHRC research as well, of best practice and things like that.
CLAHRC-CP interviewee 2
Another example of the support that the CLAHRCs provided is given in Box 2. Here the main role of the CLAHRC was to communicate the results from research in a way that made sense to the commissioners, and, specifically, to provide them with rapid fit-for-purpose local assessments of new technologies. 86
The survey findings confirmed the importance that all the CLAHRCs attached to engaging commissioners [see Chapter 4, How does the NHS influence CLAHRCs evolution, outcomes and impact (and indeed how does having a CLAHRC influence NHS behaviour)?, Perspectives of NHS and academic staff across six CLAHRCs], and the validation interviews with other CLAHRCs provided additional, often trenchant, insights:
Commissioners are front and centre. They’re the payers. So absolutely they [are] critical . . . I think they should be better at recommissioning from what we’ve learnt and they’ve learnt about us.
CLAHRC director 5
The validation interviews also provided more examples of how the CLAHRCs could support commissioning decision-making, such as helping with service redesign:
The commissioners had a real issue about the eating disorder service for adolescents and they needed help to redesign that service. The CLAHRC was able to respond and provide a research-based evaluation, the findings from which were implemented in the redesign of the service.
CLAHRC director 4
In addition to providing workshops, joint meetings and methodological support, the CLAHRCs recognised the need to portray a consistent programme style and develop a recognisable CLAHRC brand. They clearly saw branding as a powerful tool through which to improve communication and dissemination, demonstrate achievements and increase their influence: ‘having a project [such] as CLAHRC branded can create a “knowledge opportunity” and reframe, presenting opportunities for engagement; CLAHRCs has become a name’ (CLAHRC-CP interviewee 3). Mechanisms of and approaches to dissemination evolved over time, with interviewees citing the need for varied products if they were to engage commissioners and the wider health-service community:
They [commissioners] don’t want to read a document that’s 50 pages and talks about something that was happening 2 years ago really. They want two sides of A4 that tells them the key messages, the evidence that supports their decisions, and that’s what they want to use.
CLAHRC-CP interviewee 2
To address this need, in September 2011, one CLAHRC developed two-page evidence summaries of CLAHRC projects called the CLAHRC BITEs (Brokering Innovation Through Evidence). These summaries highlighted the most important findings from published research and projects, providing links for more in-depth information for the relevant audience, and were subsequently produced by other CLAHRCs: ‘So we started these BITEs, which are accessible emerging findings which don’t compromise further publication. They’ve gone down a storm, it’s now a national initiative, all the CLAHRCs are doing them and there’s a national CLAHRC library’ (CLAHRC director 3). This was, therefore, an area in which inter-CLAHRC collaboration proved fruitful, albeit at a relatively late stage in the overall programme. PenCLAHRC and CLAHRC-CP, for example, produced their first BITEs in 2012, and our document review indicated that, by December 2012, 59 CLAHRC BITEs had been produced across the CLAHRCs. The actual format used and the number of BITEs produced differed between the CLAHRCs, and details are given on their respective websites (a slightly outdated list putting the total number of CLAHRC BITEs produced at 77 is available on the Health Services Research Network website89).
The wider CLAHRC group also stressed the importance of being responsive and listening to the commissioners to find out what they wanted:
Because we used that workshop and the health inequalities workshop to ask the CCG [Clinical Commissioning Group] leads ‘What are the big ticket items that bother you and how can the CLAHRC work with you, through the CLAHRC’s current programmes? And is there stuff that we could do within our CLAHRC challenge fund that you’d be particularly interested in contributing to?’ To make that offer was possibly revelatory to them. It was a different sort of language to ‘Here’s a piece of research; we need you to help us.’
CLAHRC director 1
Summary
The case studies and the validation interviews suggest that it was the activities of these CLAHRC taken together – the combination of providing opportunities for dialogue, effective support for decision-making and a focus on well-synchronised, well-branded communication – which served to engage commissioners in CLAHRC activities, and to set the direction for further research projects within the CLAHRCs.
Informing clinical practice
An important aim of the CLAHRCs was to influence clinical practice [see Chapter 4, How does the NHS influence CLAHRCs evolution, outcomes and impact (and indeed how does having a CLAHRC influence NHS behaviour)?, Perspectives of NHS and academic staff across six CLAHRCs]. It was beyond the scope of our evaluation to assess systematically the actual impacts of research undertaken within the CLAHRCs on clinical practice and population outcomes; this was largely a matter for the CLAHRCs’ own internal evaluations. Instead, we here present selected projects from our two case studies to illustrate the way local expertise and relationships were used to inform clinical practice locally and elsewhere. These include the Improving Access to Psychological Therapies (IAPT) programme by CLAHRC-CP (a new innovation researched at speed within the CLAHRC and implemented in practice; see Box 3) and a PenCLAHRC project on thrombolysis for ischaemic stroke (Box 4). Another PenCLAHRC project on the use of tranexamic acid in emergency services was described in Chapter 4, Local remit.
The IAPT programme aims to provide quick access to cost-effective talking therapies to people who have common mental health problems. 90 As part of the programme, a low-intensity cognitive–behavioural therapy delivered over the telephone was tested in order to enhance access to treatment for those who would otherwise be less able to attend because of transport problems, work commitments, physical disability or other reasons. The research, which was published in a peer-reviewed journal,91 involved the development of a telephone training skills scheme, which was taken up swiftly across the locality and beyond:
I then developed a telephone training skills programme, and developed some core skills and developed a bespoke training programme, rolled it out to 150 therapists across the region, got amazing feedback from it that said everybody should go on this training, it’s improved our confidence and the way that we manage people on the telephone, and services have said . . . we can do three times as many contacts and all the rest of it. I’ve taken that to the Department of Health IAPT team, and rolled it out nationally.
CLAHRC-CP interviewee 2
The highest-priority topic for PenCLAHRC in its first round of topic identification and prioritisation concerned the organisation of services to maximise the benefit of thrombolytic therapy for acute ischaemic stroke. Within this context, PenCLAHRC initiated ‘Modelling approaches to the delivery of thrombolysis for acute ischaemic stroke’, which involved computer simulations that explored the different ways in which people who had suffered a stroke were managed between arriving at hospital and receiving thrombolytic treatment. Using locally available data, the simulation model provided a framework for the engagement of professionals and facilitated an exploration of the likely outcomes of alternative models of care. The trust which was involved in the study recognised the value of the initiative and seconded relevant managers and informatics staff in support. Local data indicated potentially significant gains from re-engineering the in-hospital pathway, and work is rapidly progressing towards this. The project, initially conducted at the Royal Devon and Exeter Hospital, was subsequently rolled out to the other acute hospitals in Devon and Cornwall in collaboration with the Peninsula Heart and Stroke Network
Source: Adapted from PenCLAHRC. 92
The success of the training programme described in Box 3 was attributed to the interactive and flexible nature of the project:
But what happened . . . I had a person who was in my team and in the CLAHRC’s team and going back and forth between the two, I could on a daily basis change, say well, ‘that’s really interesting, all that stuff’s great, but actually we want to know a bit more about that, just look at that in more detail and forget that . . .’. And so we were able to constantly, in real time, have an impact and an influence about it was that was the most important thing.
CLAHRC-CP interviewee 1
This observation highlights the key roles of partnership working, shared learning and dialogue in the coproduction of research.
Box 4 illustrates how the commitment to finding out the hospital’s requirements from the start facilitated further engagement by hospital staff once the project was under way. Senior staff in other CLAHRCs made the same point:
So it is a really sensitive negotiation sometimes and there are two cultures, they sometimes clash. So from that sense one of the things that we’ve seen is that real need to bring at maybe an earlier stage, well certainly at an earlier stage to when you’re planning research to get more NHS input because they’re going to be doing things . . . We know how to do good research but it’s about making the research a bit more responsive to the needs of the NHS and finding ways to work with competing priorities.
Senior NHS-affiliated CLAHRC member 5
This responsiveness to NHS needs extended well beyond the identification of research topics. As and when necessary, the CLAHRCs also provided ongoing support during a project:
If you want people to be able to effect change quite quickly, it’s probably more appropriate for us to work with them to develop that journey than it is to assume that they’ll get there on their own providing we give them the right background. It’s a balance. An example would be our use of the action effect diagram and variation on the driver diagram: the reality being that teams find that quite difficult to do on their own and often get it wrong or it ends up being more complex than it need be. If we facilitate that it means that we get the aim clarified with them much more quickly, which means we also get the measures identified much more quickly, which means the project moves more quickly.
CLAHRC director 6
Summary
The examples in this section illustrate three findings from the case studies that were also confirmed in the validation interviews: first, that working with clinical staff to identify research topics relevant to them worked well as a means of engaging and retaining their interest; second, that ongoing support from the CLAHRC during a project could speed change; third, that providing the right support at the right point needed to be done sensitively – it was a balance, a negotiation.
Conclusions
In this section we explored the extent to which research knowledge and evidence is being used to change behaviour and influence practice. The survey findings focused primarily on communication and dissemination of CLAHRC activities, including the evidence generated through CLAHRC projects. However, in our case studies and validation interviews, we investigated other ways in which research knowledge and evidence were shared to support changes in practice. Three processes were observed: shifting academic paradigms, communicating with commissioners and influencing clinical practice. Academics within the CLAHRCs were exposed to people from other disciplines and other backgrounds, and this helped to broaden their understanding of ‘implementation’ and of other research fields and methodologies. Communication with commissioners was supported by the development of a CLAHRC ‘brand’, which helped to identify CLAHRC products and give them credence. The projects described in this section illustrate how the CLAHRC way of working was helping to improve clinical practice, and how these improvements were being spread across the service.
Chapter 5 Discussion, conclusions, practical implications and research recommendations
In this chapter we explore how our findings answer the questions we sought to address at the start of our evaluation about how effectively the CLAHRCs address the second translation gap, discuss what they tell us about the three research questions considered in phase 2, and consider some of the main issues raised. We also discuss the potential role of the CLAHRCs in the future, given current developments such as the emergence of the AHSNs. Finally we draw some general conclusions, summarise the implications for practice and offer recommendations for further research. But first, and before we discuss our findings, we highlight some of the limitations of our study.
Limitations of the study
Our study was one of four commissioned by the NIHR HSDR to evaluate the CLAHRCs. 71 Given the diversity and complexity of the CLAHRC experiment, NIHR’s decision to adopt a multiple-evaluative approach was, we believe, justified. However, as we highlight earlier in this report, in order to optimise the evaluation effort and minimise the data collection burden on individual CLAHRCs, each evaluation team was required to concentrate on a subset of the CLAHRCs for detailed investigation. Two CLAHRCs were selected for in-depth review in this study. To allow broader generalisable lessons to be learned and to satisfy the formative element of our evaluation, our data collection also covered varying numbers of CLAHRCs at different points in time. We provided feedback of emerging findings to CLAHRC directors and NIHR HSDR at three of their regular meetings, six of the nine CLAHRCs took part in our survey, and representatives from all nine CLAHRCs (and NIHR HSDR) participated in the validation interviews. Thus, while we were not able to study each of the nine CLAHRCs to the same level of detail, we are confident that many of our findings will resonate across the CLAHRCs. However, it was also the case that some of our richest data were derived from the two case studies, and we are, therefore, unable to claim that the results presented in this document will carry equal validity for all the CLAHRCs.
It is also important to highlight that, in the context of the concerns about a possible ‘overevaluation’ of the CLAHRCs in the presence of four external evaluation teams and CLAHRCs’ own internal evaluations, there were constraints on the level of interaction of evaluation teams with each CLAHRC and their personnel. This has meant that recruitment of interviewees and workshop participants, which formed part of phase 2 cases studies, had to be based, in part, on our prior knowledge of personnel involved with the CLAHRCs from phase 1 of the evaluation, and in consultation with the CLAHRCs themselves. While we cannot exclude the possibility that our approach to recruitment may have biased our findings, we believe that the views captured through the various data collection exercises both within the case studies and in the wider CLAHRC environment provide a reasonably accurate account of the CLAHRCs’ experiences.
A further limitation was that it proved to be too resource intensive to conduct a full counterfactual analysis and attempt a comparison of areas that were part of a CLAHRC with those that were not. Throughout the evaluation we did, however, monitor and review the wider context, or landscape, of developments in the health-research system and the health service into which the CLAHRCs were introduced. This helped us to identify how far the CLAHRCs were making a contribution that could not (or was unlikely to) have been made by existing organisations and structures. This review is presented as Appendix 9 and it is drawn on in Future developments below, where we draw together ideas about the contribution the CLAHRCs are making to the health research and health systems and their potential role as those systems continue to evolve.
Phase 1: refining the evaluation questions
The CLAHRCs’ remit was to encourage the use of research in the NHS and develop ways of doing applied research that maximised its chances of being useful to the service and the capacity of the NHS to respond. This involved three interlinked functions: conducting high-quality applied health research; supporting the translation of research evidence into practice; and increasing the capacity of NHS organisations to engage with and apply research. The focus was not only on the translation of research (whether undertaken locally or elsewhere) but also on developing ways of doing applied research that maximises its chances of being useful to the service and of being implemented.
Our evaluation sought to explore how effectively the CLAHRCs supported the translation of research into patient benefit and developed ways of doing applied research that maximised its chances of being useful to the service and the capacity of the NHS to respond. Initially we identified one overarching and three subsidiary questions:
Overarching question: How, and how effectively, do CLAHRCs address the second translation gap?
Subsidiary questions:
-
How, and how effectively, do CLAHRCs support local health research?
-
How, and how effectively, do CLAHRCs build local infrastructures to utilise globally and locally generated health research for local patient benefit?
-
Does bringing together activities for health research and activities for delivering health research benefit both sets of activities?
The first phase of the evaluation was designed to provide an overview of the background, development and future plans and aspirations of each of the nine CLAHRCs, and explore the contextual backdrop of research and practice within which they were operating. In the light of a targeted literature review, we examined the CLAHRCs’ governance, accountability and organisational structures, discussed their plans to change individual and group attitudes and behaviours, and described the infrastructure and resources available to them. We found that the nine CLAHRCs shared a common vision and were hoping to achieve a system shift through their activities. Their aspiration was to create a new generation of researchers, clinicians and managers with changed professional identities and motivations who were supported by a different set of incentives and drivers, both national and local, and a commissioning approach that was committed to reinforcing the aims of the CLAHRC. They had, however, contrasting views about how to achieve these goals (Table 3).
Two general conclusions emerged from phase 1. First, the CLAHRCs would not resolve the lack of consensus identified in the literature about the ‘best’ approach to mobilising knowledge to improve health care, but they did provide an opportunity to look at specific dimensions of the problems and develop a scientific basis for addressing them. Second, the CLAHRCs could not, on their own and once and for all, bridge what had been called (however inappropriately) the second translation gap, but they could help to bring about system shifts that bring the health and health-research systems closer together.
We also concluded that, even in the two case studies, we could not hope to explore every dimension of the improvement journeys being pursued in detail. With the help of the CLAHRC directors and our NIHR funders, we therefore identified three key questions to be explored in phase 2 which we thought would cast further light on that wider picture. These were:
-
How does the NHS influence CLAHRCs’ evolution, outcomes and impact (and how does having a CLAHRC influence NHS behaviour)?
-
How are effective multistakeholder and multidisciplinary research and implementation teams for service improvement built: what can we learn from the CLAHRC model and what mechanisms are being used to enable it?
-
What can we learn from the CLAHRCs that can provide new understanding of how to use research knowledge and evidence to change commissioning and clinical behaviour for patient benefit?
Phase 2: how does the NHS influence CLAHRCs’ evolution, outcomes and impact, and how does having a CLAHRC influence NHS behaviour?
NHS influence on the CLAHRCs
The CLAHRCs were encouraged to develop innovative models for the conduct and application of applied health research, building on existing local research strengths. 3 Our analysis of the CLAHRCs’ early plans (see Chapter 3 and Appendix 10) demonstrated that the research strengths that the CLAHRCs identified when they made their original applications were largely strengths in clinical research, and that they intended to build on existing programmes of work on long-term conditions such as diabetes or chronic kidney disease. They also drew on their understanding of, and expertise in, fields such as implementation, quality improvement and innovation.
However, the CLAHRCs were intended to be more than just clinical/academic partnerships; they were also required to meet local research needs and involve a wide range of stakeholders, including NHS managers, commissioners, GPs and patients, and to seek matched funding from local NHS organisations. These arrangements potentially gave NHS organisations and their staff significant influence over the CLAHRCs’ emerging programmes. To identify and meet the research needs of all these groups, the CLAHRCs needed to address organisational and managerial concerns as well as clinical concerns, and, therefore, to draw on research approaches from a wide range of academic disciplines. In response, the CLAHRCs established links with business schools and with other groups with expertise in implementation and service design, and in operational research. Some CLAHRCs, such as CLAHRC-CP, did this at the outset in order to challenge their own thinking. Others did so over time as NHS staff (including managers) began to realise what the CLAHRCs had to offer and started to exercise more influence over the research topics that were selected and the way in which that research was undertaken and disseminated. Their involvement revealed gaps, such as the lack of sufficient research expertise to address the problems facing NHS managers, a challenge to which the CLAHRCs needed to respond: PenCLAHRC, for example, established a modelling and operational research facility (PenCHORD) in 2010. 85
It also became clear that something other than peer-reviewed publications was needed to bring the findings from CLAHRC projects to the attention of NHS decision-makers, and the CLAHRCs developed short evidence briefings and two-page summaries of successful projects (the CLAHRC BITEs). 89
In summary: the CLAHRCs were established to respond to NHS needs. They could do this effectively only if they were open to the influence of the service and tailored their research agendas and their research and implementation practices accordingly. They needed to be responsive and flexible.
CLAHRC influence on the NHS: capacity building and culture change
We saw in Chapter 3 how CLAHRC-CP and PenCLAHRC had changed the attitudes, and sometimes the behaviour, of those who had been directly involved in CLAHRC activities and projects. However, while this showed that the CLAHRCs could achieve positive change among those most directly involved, the broader question was if the CLAHRCs could influence others in and across the NHS. On this question, and after only 5 years of CLAHRC activity, we can provide no definite answer. The CLAHRCs themselves felt that 5 years was too short a time in which to embed their approach and change the norms of the service, and NIHR has provided further funding for a second round of CLAHRCs (see also Future developments). 93
The time it takes to achieve this sort of change is a common theme in the literature. 94,95 As we note earlier in this report, a recent study of change in management culture and organisational performance by Mannion et al. identified four distinct cultures within NHS organisations. 33 One of these, the development culture, is characterised by innovation, dynamism, growth and entrepreneurship with an external, relational focus in which ‘change was viewed as a positive organisational attribute . . . [and a] willingness of senior management to embrace innovative approaches to delivering services’. 33 The development culture has, in other words, all the hallmarks of the culture the CLAHRCs were seeking to instil across the NHS. However, the difficulties of doing so can be judged from other findings reported by Mannion et al. 33 During the time covered by their study (2001–8), the development culture was dominant in approximately 20% of NHS trusts, and, tellingly, this proportion remained largely unchanged during that period. If there was no movement towards a development culture in the NHS between 2001 and 2008, how could the CLAHRCs hope to make that change happen?
Mannion et al. suggest that culture change is triggered by a perception of crisis, initiated and shaped by strong leaders, consolidated by perceived success, and mediated by relearning or re-education. 33 As we saw from our case studies, and also from the wider CLAHRC experience, the CLAHRCs had strong, focused leadership, they relatively rapidly produced a portfolio of ‘quick wins’ that helped to convince sceptical NHS managers and commissioners, and they used their internal reviews and evaluations as a basis for learning and adaptation. Moreover, the NHS at this time faced a large-scale reorganisation and accompanying budget constraints which created significant uncertainty across the service. To this extent Mannion et al. ’s33 conditions for triggers of change were fulfilled. However, the time it takes to achieve change is not the only or even the main issue. The question of CLAHRC influence over the NHS is part of a wider debate about the role of CLAHRCs within the health research system generally, and the role of that system within the NHS.
Overall, this discussion suggests that the CLAHRCs’ goal of culture change is achievable (as the early evidence from our evaluation also confirmed), but after only 5 years the long-term aim of a NHS-wide change in attitudes towards research and its use in decision-making has not yet been achieved. The CLAHRCs’ experience therefore reinforces previous messages about the need to allow sufficient time for system change.
Phase 2: how are effective multistakeholder and multidisciplinary research and implementation teams for service improvement built: what can we learn from the CLAHRC model and what mechanisms are being used to enable it?
The relevance and importance of the local remit
The CLAHRCs were partnerships between local universities and local NHS organisations across a clearly defined geographic area. This local remit enabled the CLAHRCs to build on existing local relationships to get people in the NHS interested in how they could work with researchers to address knowledge gaps, since the CLAHRCs could become known across their local ‘patch’ in a way that would not have been possible if they had been more centralised and more distant. It was local clinicians, patients and managers who were spreading the word about the CLAHRC and its potential (see next section). It was local needs that were being identified and addressed, and matched funding from the local NHS that supported those activities; and even those who were not involved in specific CLAHRC projects had access to local evidence-based courses and to local learning events. All these were powerful influences.
Overall, the local remit was a defining characteristic of the CLAHRC initiative. It supported the development of collaboration, encouraged responsiveness to local research needs and shaped the separate character of each individual CLAHRC. However, what was equally important was that all this took place within the wider framework of the CLAHRC initiative as a whole, with the opportunities this provided for dialogue with other CLAHRCs, and the requirements this imposed to produce generalisable research and scale up successful projects. The CLAHRCs also needed to work beyond their own boundaries.
The practical implications of these findings are complex. The local remit was an important factor in the initial success of the CLAHRCs in meeting their goals and was, therefore, a helpful approach. However, and as we discuss further below, there can be tensions between addressing local research needs and producing generalisable findings that are useful to others. Attention also needs to be paid to the requirements of the research and health systems within which the CLAHRCs operate.
The complex challenges of knowledge mobilisation
[T]he inner workings, implicit rules, cultures, and realities that dominate the day to day lives of people working in the health system and those doing research on that system remain, for the most part, mysteries to people on the other side. 80
Complex health-care challenges require complex, multilevel solutions that are tailored to specific settings. 83 A key message that emerged from both phases of our evaluation was that a linear, basic-to-applied model which assumes that ‘gaps’ can somehow be ‘bridged’ does not fully capture the complexities of moving knowledge into action. The idea of building a single fixed bridge between two otherwise unchanging sides had little resonance with the CLAHRCs from the outset, and as they developed and the challenges they faced became clearer, there was an increased understanding of the complexities involved. All the CLAHRCs adopted relationship models that focused on interactions between people through which knowledge from multiple sources could be exchanged and adapted to local circumstances through a collaborative production–synthesis–integration cycle,43 and recruited people who could bring understanding of research to the service and vice versa. In one sense all CLAHRC staff acted as research champions, but many CLAHRCs also specifically recruited knowledge brokers (locality leads, diffusion fellows, CLAHRC associates and so on) to fulfil this function.
However, while a focus on multidisciplinary relationships was necessary, it was not, on its own, sufficient (see Chapter 4, How are effective multistakeholder and multidisciplinary research and implementation teams for service improvement built: what can we learn from the CLAHRC mode and what mechanisms are being used to enable it?). As the CLAHRCs were aware from the start, attention also needed to be paid to the systems within and through which these relationships operated, and to how system shift could be achieved.
This insight is reflected in recent literature. Using similar language to that used by the CLAHRCs, Best and Holmes describe a systems approach to getting evidence into policy in which knowledge is generated, assessed and used within specific contexts and cultures dominated by different priorities. 96 This knowledge cycle is mediated throughout by relationships and must be understood from a perspective that takes account of the organisation and its strategic purposes. Glasgow and Chambers38 also argue that if health-research results are to become more usable and timely, what is needed is a systems perspective that recognises that context is critical, that most problems and interventions are multilevel and complex, and that more emphasis needs to be placed on inter-relationships among system elements and system rules. They spell out what, in their view, needs to be done to make implementation science more rapid, rigorous and relevant. Their list could read as a list of CLAHRC objectives: more research needs to be undertaken that is pragmatic or practical, that evaluates participation and representativeness, that makes comparisons between real alternatives, and that collects cost and economic data; it needs to assess multiple outcomes, often using mixed methods; the research design should fit the question; and reporting should be transparent.
In summary, we note that when the CLAHRCs were established in 2008 there was no single roadmap to guide them. This is still the case, and what the experience of the CLAHRCs, taken as a whole, suggests is that the search for a single approach is probably a chimera. However, since 2008 thinking has moved on. As the two papers cited above indicate, there is now more understanding of the complexities of knowledge mobilisation and what these entail for practical programmes. In practical terms, the CLAHRCs have begun to make a contribution to these debates. They have demonstrated what it takes to identify, produce and implement research that is pragmatic and practical and which fits the question; they have assessed multiple outcomes and used mixed methods, and they have sought to produce clear, accessible reports; and they have shown how all this can be done in different ways in different contexts. Above all, they have brought the concept of linkage and exchange to life,43 and shown how individuals and organisations can build effective collaborations to address health-care research needs.
Phase 2: what can we learn from the CLAHRCs that can cast new understanding on how to use research knowledge and evidence to change commissioning and clinical behaviour for patient benefit?
‘What constitutes evidence and when do we have enough evidence to translate?’97
As we saw above, the CLAHRCs were rooted in local relationships and had a focus on what is relevant and what works locally. But it was also a requirement of NIHR funding that the research they supported be generalisable. There has been much discussion in the literature and among the CLAHRCs about the tension between producing ‘quick wins’, research that is in some sense ‘good enough’ to support health service decision-making (relevance), and the longer time scales of generalisable, peer-reviewed research (rigour). Rigour is typically thought of as a focus on experimental control and internal validity. Relevance is commonly associated with studies that have external validity; that is, they identify causal relationships that can be generalised to different measures, persons, settings and times. 98 These two qualities are often seen to conflict.
However, there is some evidence that improving attention to external validity need not be at the expense of internal validity. The Veterans Administration in the USA, for example, faced the problem of the balance between rigour and relevance in its QUERI programme, and found that ‘both are possible and that benefits can be translated in a timely manner when there is active dialogue among clinicians, researchers and policy-makers’ (p. 69). 99 Other commentators go further and reject the dichotomy between rigour and relevance altogether. Glasgow and Emmons97 suggest that one of the reasons that research fails to get translated into practice is that the programmes and methods used fail to address contextual factors. They argue that there is a need ‘to address context and to utilize research, review, and reporting practices that address external validity issues – such as designs that focus on replication, and practical clinical and behavioural trials’ (p. 413). 97 In other words, what is needed is more consideration of external validity in the funding, reporting, synthesis and application of research to create a better balance of research that is both credible and relevant to decision-makers in the health service. In the USA some journal editors have already responded and made recommendations about how to improve attention to external validity (or applicability) in the research reports that they publish. 98,100
Some of the CLAHRCs changed their views about the relations between applied research and implementation as their understanding of their remit developed. These CLAHRCs had initially seen these two activities as separate phases in which research first produces findings and these are then implemented, but they came to understand (as some of their colleagues had understood from the start) that these two activities need to be closely integrated within one overall iterative process if research findings are to be used effectively in a timely fashion. Where necessary, the CLAHRCs adjusted their programmes accordingly. Moreover, as NHS staff from clinical, managerial and commissioning backgrounds became more involved in the CLAHRCs, the diversity of the concerns they raised required a rethink about the types of research and research methodologies that were needed to produce the evidence required.
Overall, we find that the debate about the nature of evidence continues. The challenges identified above, and the richness of the various responses across the CLAHRCs, warrant more detailed investigation.
Communicating with commissioners
In 2010, a large-scale reorganisation of the NHS that would include a complete overhaul of the commissioning function from 2013 was announced. 101 At the same time, the health service was required to make substantial efficiency savings. This created a difficult environment in which to get people’s attention and explain ideas that would not obviously help them to handle immediate pressures. The fact that the CLAHRCs did manage to communicate with, and involve, commissioners (albeit with difficulty and as the result of much perseverance) is an important justification of their local remit and their local role. In Chapter 3 we described how in the two case studies the CLAHRCs built on existing local collaborations with commissioners, and across the CLAHRCs we heard how they were able to maintain relations with local commissioning staff even as the organisations for which those people worked were reshaped.
We also found that the scale of the changes created opportunities as entrenched practices were disrupted and people looked for new ideas. Here the flexibility of the CLAHRCs, their commitment to learning and adaptation, the matched funding model and the CLAHRCs’ understanding of the need for short-term as well as long-term research and implementation projects were all crucial. The CLAHRCs were able to be opportunistic and provide support when it was needed, not 6 months down the line. The CLAHRCs exploited early ‘quick wins’ and developed simple user-friendly research briefs to spread the word about their activities and their potential. Over time they developed a strong local brand that enabled local NHS staff to recognise CLAHRC products even if they had not been involved in generating them. At the same time, the matched funding model of co-investment began to force NHS organisations to think prospectively about the business case for investing in research and knowledge mobilisation and become more active and discerning partners in the CLAHRCs. 102 Overall, what the CLAHRCs were seeking to achieve here was a shift not only in individual attitudes and behaviour but also in the workings of the commissioning function within the NHS, a system shift. The local and national contexts in which they operated played an important role, as did the CLAHRCs’ commitment to responsiveness and flexibility, their understanding of the complexities of their role, and all their various activities, taken as a whole.
Informing clinical practice
It was beyond the scope of our evaluation (even in the two case studies) to systematically assess the actual impacts of research undertaken within the CLAHRCs on clinical practice and population outcomes, largely because this was something the CLAHRCs were doing themselves through their own internal evaluations. However, we were able to explore how some of the successful projects achieved their results, and we described three of these in Chapter 4 (What can we learn from the CLAHRCs that can provide new understanding of how to use research knowledge and evidence to change commissioning and clinical behaviour for patient benefit?).
In each case the people involved in the projects stated what they thought had contributed to success. The CLAHRC-CP IAPT project showed how the CLAHRC-CP coproduction approach worked in practice: there was considerable interaction between those conducting the study and the CLAHRC team overseeing it with ongoing (and useful) discussions about what the study was finding and whether or not that was what the service wanted. Moreover, and reflecting the thoughts above about external validity, the large and diverse sample meant that the results were widely applicable, and therefore contributed to scale-up across the CLAHRC and nationally. 91 The PenCLAHRC stroke pathways project illustrated how modelling approaches using locally available data could assist service redesign and capture the interest of the trust involved. And the success of the PenCLAHRC project on the use of tranexamic acid [described in Chapter 4, How does the NHS influence CLAHRCs evolution, outcomes and impact (and indeed how does having a CLAHRC influence NHS behaviour)?, Experiences in CLAHRC-CP and PenCLAHRC] was attributed to, among other things, the fact that the staff involved already knew about PenCLAHRC and trusted its approach. Another important facilitator was an existing operational mandate: patient group directions were in place in the ambulance service that allowed ambulance personnel to use generic prescriptions.
The way in which the tranexamic acid project was facilitated by an existing operational mandate shows how improvement interventions can successfully exploit opportunities within the system. Equally, barriers within the system can impede change. One CLAHRC project on falls prevention among older people involved changes in the treatments delivered by numerous health-care professions in multiple settings, and it proved impossible to align the competing requirements of different service providers and different patient groups.
There is a growing literature on these issues. One study identified health-care organisations that found and used evidence at multiple levels and in an ongoing, integrated fashion, and compared them with those that did not. 103 Echoing the experience of the Veterans Administration we briefly reflected on in Chapter 1 (see The conceptual background, Organisational change and system shift; also Appendix 12), this study found that one determinant of success was the ‘integration of evidence-based practice into the routine fabric of the organization; also known as normalization’ (p. 3). 103 But exactly what this means in terms of tailoring interventions to fit into the existing fabric, the various NHS professional and organisational systems, is still something of a mystery. A review of studies of interventions tailored to overcome identified barriers to change found evidence that tailored interventions can change professional practice, but insufficient evidence about effective approaches to tailoring. 104
In summary, what the CLAHRCs were seeking to achieve here was a shift in the individual attitudes and behaviour of NHS clinicians and managers and, ultimately, their patients. As with the commissioners, what that also involved was an appreciation of the challenges and opportunities posed by the various systems (organisational, professional, economic and so on) within which people work and are treated. In the three CLAHRC projects described above, things aligned well and change followed. In other circumstances unforeseen barriers emerged and more complex changes in, for example, organisational or professional responsibilities and patterns of working (system shifts) were needed before improvements could be made.
Other issues raised by our findings
An experimental approach: varieties of CLAHRC but a common ethos
The NIHR call for applications for the CLAHRCs was clear about what they were expected to do: the aims of the CLAHRCs were to increase the capacity to undertake and use applied health research in the NHS and to foster a culture of collaboration between the academic and service delivery sectors. 3 These aims were well understood by the CLAHRCs. However, although this vision was clear, there was considerable uncertainty about how to achieve it in practice. Programmes in other countries have attempted to do something similar (see Appendix 12). But the contexts in which these programmes operated and the remits to which they worked were very different. So, while lessons could be learned, these programmes could not provide definitive guidance. Moreover, and as we mentioned above (see Chapter 4, What can we learn from the CLAHRCs that can cast new understanding on how to use research knowledge and evidence to change commissioning and clinical behaviour for patient benefit?, Experiences in CLAHRC-CP and PenCLAHRC), the experience of the CLAHRCs support the view that there is no single ‘right’ model: ‘It is likely that there is no single or simple answer to the question, “how best to organise the implementation of large scale improvement programmes for health and social care”’ (p. 184). 105
This (inevitable) uncertainty was the rationale for the experimental approach that was adopted across the programme and by the CLAHRCs. NIHR did not prescribe how the individual CLAHRCs should achieve the goals they had been set. Instead, the CLAHRCs were encouraged to develop (and evaluate) innovative models for the conduct and application of applied health research. 3
The approaches adopted by individual CLAHRCs varied. The different principles that underpinned CLAHRC-CP and PenCLAHRC were described in Chapter 3: CLAHRC-CP was committed to the coproduction of research, and PenCLAHRC worked through the processes of ‘Engagement by Design’ to promote and support the explicit use of evidence as a norm among practitioners and organisations. The published protocols of other CLAHRCs describe their approaches (and where these were made explicit in their proposals as described in Appendix 10). Leicestershire, Northamptonshire and Rutland CLAHRC adopted an approach that was influenced by an organisational excellence model described by Nutley et al. 106 and by the experiences of the aforementioned US Veterans Health Administration’s QUERI. 107 The CLAHRC for Nottinghamshire, Derbyshire and Lincolnshire developed an approach that was based on organisational learning theory and used diffusion fellows and communities of practice as mechanisms to encourage change. 108 The CLAHRC for South Yorkshire incorporated implementation themes that built on the knowledge to action approach developed in Canada and on local work to develop evidence-based clinical effectiveness. 109 This diversity within the common CLAHRC programme should, over time, provide rich data about the advantages and disadvantages of different approaches.
In summary, notwithstanding their differences in approach, the CLAHRCs faced common challenges and shared a common ethos that included a willingness to negotiate and maintain a genuine dialogue between different partners, to listen and be responsive, and to adapt on the basis of ongoing evaluation and learning in the face of a constantly changing environment. The CLAHRC interviewees recognised these characteristics and valued them highly; they talked about the need to be flexible and nimble, and to respond serendipitously to unexpected opportunities and challenges. If the CLAHRCs’ achievements are to continue in the second round, an ongoing flexibility and a continuing openness to experimentation and learning are not only desirable but essential.
Flexible comprehensiveness
In Chapter 4, How are effective multi-stakeholder and multi-disciplinary research and implementation teams for service improvement built: what can we learn from the CLAHRC mode and what mechanisms are being used to enable it?, Experiences in CLAHRC-CP and PenCLAHRC, we suggested that the question of CLAHRC influence over the NHS was part of a wider debate about the role of CLAHRCs within the health research system generally, and the role of that system within the NHS. The experience of the QUERI, which was established by the US Veterans Administration to accelerate the implementation of new research findings into clinical care,6 suggests that, when the research function is fully integrated into the organisational structure of a health system, performance is improved. 62 The CLAHRC initiative was premised on the use of health-system resources (NHS matched funding) alongside research and development resources (NIHR funding), and in one sense this can be seen as a small move in that same direction. Throughout the CLAHRCs we saw this innovative funding arrangement beginning to work well. 102 Patients and NHS clinical and managerial staff were encouraged to become involved in research, their research needs were recognised and there was a move towards research-informed decision-making. However, as the Veterans Administration experience also demonstrates, many factors shape health-care performance, often in unknown and unintended ways. Like QUERI, the CLAHRCs were complex interventions that operated within complex systems. 38 In doing so, they pursued a strategy that can be categorised as one of flexible comprehensiveness; that is, their programmes were flexible and responsive and they used a range of approaches that sought to match the diverse aspects of the complex issues they faced. 110 Moreover, in future they will be expected to work with, and within, the AHSNs to produce a step change in the scale and pace of innovation in the NHS, adding opportunities for success but also further complexity.
Based on the discussion presented here, we conclude that what the CLAHRCs’ efforts to influence the NHS have achieved is ground-breaking. They have shown that it is possible to align research spending more closely with health-care spending and provide better support for health-care decision-making. 102 To date, the CLAHRCs have done this on a project-by-project basis. The challenge the second-round CLAHRCs, and the new AHSNs, now face is to convert that success into system-wide change.
Sustainability and scaling up
It was an NIHR requirement that effective improvement interventions that had been successfully implemented and evaluated locally should be sustainable, and should be spread, or ‘scaled up’, across the CLAHRC and the health service. 2 There is evidence from the CLAHRCs that they had some success in scaling up some projects, though it was generally too early to assess sustainability.
The CLAHRCs were new entities and initially their role in implementation was not necessarily well understood by their NHS colleagues, leading to some confusion and some disappointed expectations, although NIHR and the CLAHRC directors were clear from the start that making service improvements was a NHS responsibility and that the CLAHRCs were not funded to do this. The role of the CLAHRCs was to support implementation. This involved helping the service to identify, produce and disseminate the user-friendly evidence needed to support the development of effective improvement interventions. It also meant working with the service to evaluate new ways of implementing those interventions, and disseminating the findings from those studies. The CLAHRCs developed a substantial body of published projects in the peer-reviewed literature. They also developed evidence briefs and two-page publications aimed at decision makers (the CLAHRC BITEs, see Chapter 4, What can we learn from the CLAHRCs that can cast new understanding on how to use research knowledge and evidence to change commissioning and clinical behaviour for patient benefit?), which were made widely available through the CLAHRC websites. 89 They held large-scale CLAHRC-wide learning events. Through these efforts to communicate and disseminate information about their programmes and projects, the CLAHRCs sought to encourage NHS organisations and staff across their own locality (and sometimes beyond) to get engaged and to use interventions that had been successfully implemented elsewhere. 73,93
However, defining exactly what role the second-round CLAHRCs should play in sustainability and scale-up is still new territory. Glasgow et al. 111 describe sustainability and scaling up as areas where there are key opportunities to advance dissemination and implementation research, and suggest (in terms that would be familiar to any CLAHRC) that ‘further advances in the field will be achieved by focusing dissemination and implementation research on five core values: rigor and relevance, efficiency, collaboration, improved capacity, and cumulative knowledge’ (p. 1274). 111 More radically, Scheirer and Dearing suggest we should view ‘sustainability research as a further stage in the translation or dissemination of research-based interventions into practice’ (p. 2059). 112 A further issue is the sustainability and scale-up of the CLAHRC approach itself across the NHS. What the CLAHRCs were trying to promote was the explicit use of research evidence as a norm among NHS decision-makers, so that it is habitual for NHS staff to turn to research when they are seeking to improve services, and for academics to respond. The CLAHRCs have shown that it is possible to bring these two communities closer together. Through matched funding, the CLAHRCs have also demonstrated that it is possible to align research spending more closely with health-care spending and provide better support for health-care decision-making.
To summarise, the first-round CLAHRCs prepared the ground for closer integration of the research system and the health-care system. The challenge for the second-round CLAHRCs is to add scale and pace to CLAHRC activities within the context of the ASHNs. It is to these developments that we turn in the next section.
Future developments
The evidence we gathered in our evaluation indicates that our initial assessment that the CLAHRCs were playing a valuable integrating role was generally correct and that, while there were some partial overlaps, no other organisation was duplicating the overall contribution that the CLAHRCs were making (see Appendix 9). Nevertheless, concern about the translation of evidence into practice in the NHS continued. In 2011 the NHS Chief Executive launched the Innovation, Health and Wealth review with the aim of accelerating adoption and diffusion in the NHS. 113 In their collective evidence to the review the CLAHRCs highlighted what they saw as their success: ‘NHS Partners can use the example of the NIHR CLAHRCs as a model to combine NHS, academic and industry stakeholders in their structures, governance and daily-operations’ (p. 3). 114
Among its recommendations, the Innovation, Health and Wealth review called for the creation of AHSNs across the country. According to the review ‘AHSNs will present a unique opportunity to align education, clinical research, informatics, innovation, training & education and healthcare delivery . . . Every local NHS organisation should aspire to be affiliated to its local AHSN’ (p. 13). 113 The review also listed the various bodies with which it expected the AHSNs would work closely: Academic Health Science Centres, NIHR Biomedical Research Units and Biomedical Research Centres, NIHR CLAHRCs, HIECs, and NHS Innovation Hubs. However, the review noted there was a need to revisit the landscape because so many new organisations charged with improving innovation in the NHS had emerged that the landscape was ‘fragmented, cluttered and confusing’. The review therefore announced the NHS would conduct a ‘Sunset Review’ of ‘all NHS/DH funded or sponsored innovation bodies and make recommendations as to their future form and funding’ (p. 20). 113
The Department of Health responded to the report in June 2012, setting out a draft designation and establishment process for AHSNs and sought expressions of interest by 20 July 2012. In addition to defining the aims of the AHSNs it also referred to the ‘Sunset Review’ and suggested that local organisations would be able to use their AHSN application process to identify opportunities to simplify their local arrangements and structures. Under the heading ‘Translating research and learning into practice’ the June 2012 document stated that:
AHSNs will play a central role in the translation of research into practice [. . .] so it can ‘pull through’ innovations leading to adoption at scale that benefits the whole population thus addressing the T3 (dissemination and implementation) and T4 (scaling up including though government policy) gaps. The NIHR Collaborations for Leadership in Applied Health Research and Care (CLAHRCs) make an important contribution to this activity (p. 11). 73
This quote is significant in several ways for our evaluation of the CLAHRCs’ role in narrowing the second translation gap. First, it recognises that it is no longer helpful to refer just to the first and second translation gaps (T1 and T2) – although we would also contend it is not helpful either to complicate the analysis by increasing the number of so-called translational gaps, or, indeed, to use this language at all. 115 Second, it recognises the contribution the CLAHRCs are making to research translation.
Given the CLAHRCs’ role and their focus on their local geographical area, a central concern has been their limited number. If the CLAHRCs are doing useful things that cannot be done by other bodies then should not their number be increased so that the whole NHS has the opportunity to be involved in a CLAHRC? The CLAHRCs were initially set up as pilots and were later described as a natural experiment. This is important and helps to explain the flexibility the CLAHRCs have enjoyed and the scope they have had to evolve, both reasons why it has been so appropriate to adopt our own emergent evaluation approach. In the interviews with CLAHRC directors it became clear that the CLAHRCs have been evolving away from being largely conceptualised in academic terms towards more emphasis on a collaborative response to service needs and improved knowledge mobilisation. Now, with the NHS-funded AHSNs, there is an opportunity for national coverage through the development of a NHS-wide initiative that is intended to promote research engagement and translation, and to which the NIHR-funded CLAHRCs can make a unique contribution.
It is notable that the AHSN proposals that came from areas containing CLAHRCs drew heavily on the contribution their CLAHRCs had made already, and on the value of having that continuing contribution to the proposed AHSN. For example, the preface to the prospectus from Imperial College Health Partners listed the various organisations with which it was actively engaging, and the CLAHRC was first on the list: ‘We are actively engaging with North West London organisations including the CLAHRC, CLRN [Clinical Research Network], BRC [biomedical research centre], BRU [biomedical research unit], and the LETB [Local Education and Training Board], who will be integral pieces in the AHSN vision’ (p. 3). 116
Here we give a few more details from the AHSN proposals covering the two CLAHRCs where we conducted case studies. The South West Peninsula AHSN begins by referring to its strong track record in research delivery through networks dating back to the original Cancer Research Network. It continues, ‘Peninsula’s Collaboration for Leadership in Applied Health Research (PenCLAHRC), Peninsula Clinical Trials Unit (PenCTU), our Comprehensive Local Research Network and Cancer Network are known for their prominent successes in catalysing innovation through successful partnership working’ (p. 3). 117 It also lists a range of mechanisms established by PenCLAHRC on which the AHSN will draw (including PenCHORD, the PenCLAHRC Evidence Synthesis Team and local expertise in patient and public involvement in research). It further states that ‘PenCLAHRC has been a valued focus for innovation and collaboration but the establishment of the AHSN will bring a step change in the commitment of NHS organisations to work together to change practice based on research’ (p. 18). 117
The prospectus from the Eastern AHSN similarly drew on the experience of CLAHRC-CP, although inevitably, given CLAHRC-CP’s focus on mental health, a wider range of other organisations contributed, including the Cambridge Academic Health Science Centre and a biomedical research centre. Despite this, major contributions from the CLAHRC were described, such as that the CLAHRC had increased the capacity for applied health research and innovation through CLAHRC Fellowships and that it had increased the range of decision tools to help inform decisions on the potential innovations that were expected to lead to best value for the NHS and social care. 118 The Eastern AHSN also identified three priorities, and the first was mental health. The prospectus further set out how links with Eastern AHSN would support the forthcoming application to NIHR for the second round of funding for CLAHRC-CP.
Overall, however, a major endorsement of the role played by CLAHRCs, and of their potential in relation to the new AHSNs, is that the NIHR decided to fund a second phase of CLAHRCs whereas other initiatives such as the HIECs are being phased out, despite acknowledgment of useful work having been achieved.
Applicants for the second round of CLAHRC funding were told that their first aim should be to ‘develop and conducting applied health research that would be relevant across the NHS, and to translate research findings into approved outcomes for patients’ (p. 2). 93 But the relationship with the AHSNs was also highlighted as being of considerable importance in several ways:
-
One of the aims set out for CLAHRCs in the second round is to ‘create and embed approaches to research and its dissemination that are specifically designed to take account of the way that health care is delivered across the local AHSN’ (p. 2). 93
-
CLAHRC applicants were also told that their role would include incorporating ‘integrated and synergistic working with the relevant AHSNs’ (p. 3), and the guidance also stated that ‘Applicants need to have the backing and support from the relevant AHSN Board or other equivalent appropriate nascent AHSN governance structure’ (p. 3). 93
In the question-and-answer session held for potential applicants for the second round of CLAHRC funding in February 2013, the questions included ones asking for clarification about the functional difference between the AHSNs and the CLAHRCs, and if there were some activities that could be seen as part of both organisations. The answers highlighted some major differences between the two types of organisation. First, the universal geographical coverage of the AHSNs contrasts with that of the CLAHRCs. Second, the CLAHRCs will have a somewhat narrower, and research-oriented, role, which will focus on funding and translating applied research on chronic diseases and public health interventions, in contrast to the broader remit of the AHSNs. Nevertheless, it was stated that ‘There is clear complementarity between the aims and objectives of the NIHR CLAHRCs and the AHSNs in their remits of translating research and learning into practice’ (p. 2). 93
In practice, it is likely that some uncertainties about the precise boundaries around the work of the two types of organisation will remain, and there is likely to be continuing discussion and negotiation, in the geographical areas where both organisations exist, about how the local strengths of the CLAHRCs can be complemented by the role of the AHSNs. Some of the previous concern about the limited coverage provided by the CLAHRCs is now being addressed by the responsibility the AHSNs have for translation and delivering innovation in every geographical area across England. In response to a question about what had changed between the pilot CLAHRCs and the new CLAHRCs competition, the NIHR noted that the NHS landscape had changed significantly and that the innovation environment would continue to evolve with new structures, such as AHSNs responsible for delivering innovation into the NHS. 93 However, one thing is clear, collaboration will be an important aspect of the AHSNs just as it has been the defining characteristic of the CLAHRCs.
Conclusions, practical implications and research recommendations
In an essay published in 2007 that explored the relationship between health research and health services (or lack thereof), and the need to move towards better research-informed decision-making, Lomas argued that there was a need to revisit the reward systems in universities and in the health services in order to improve interactions between the processes that create the facts (research) and the ones that incorporate the values (decision-making). 80
To allow this to happen, he argued that universities as the producers of research should reward:
-
research that includes decision makers in research processes
-
the creation of centres that link researchers directly with clinicians, managers and policy-makers
-
the synthesis of different bodies of knowledge into actionable messages that are relevant to health-service questions
-
dissemination of brief, plain-language research summaries through face-to-face exchanges between the ‘doers’ and users of research.
Likewise, the health service should reward:
-
the active involvement of clinicians, managers and policy-makers in research that is relevant to (urgent) health-service questions
-
the support for operational research and development on its own activities
-
change management driven by evidence based on research
-
the inclusion of researchers in decision-making processes. 80
The call for the evaluations of the CLAHRCs recognised this important contribution,2 and it is no accident that this list reads like the brief for the CLAHRCs. The analysis of the CLAHRCs’ experience in this report found that the CLAHRCs (as collaborations between local universities and the local NHS) had achieved many of these goals. They included NHS decision-makers in research, and researchers in service decision-making, and delivered research findings in actionable forms. The multidisciplinary teams developed by the CLAHRCs produced innovative research projects that directly addressed local NHS needs and were widely implemented across their local patch, and sometimes across the NHS. The CLAHRCs obtained matched funding from the NHS that encouraged the active involvement of NHS staff, and also generated significant external funding for CLAHRC-inspired projects. Research capacities in academia and capacities in the NHS to engage effectively with research were expanded, and there was increased support for operational research and new opportunities for researchers to advise on change management were created.
The CLAHRCs also went further. They sought to change the culture in universities and the NHS so that the explicit use of research evidence in the service became a norm, and there is evidence that this was achieved to some extent, although there is still a long way to go. They threw some light on the complexities of knowledge mobilisation and what these entail for practical programmes, reinforcing the view that there is no single fixed ‘right’ approach. In addition, CLAHRCs demonstrated that a collaborative approach that is comprehensive and flexible, operates on several fronts simultaneously, is responsive and willing to experiment and learn, and can achieve change at individual and organisational levels within complex systems. Most importantly, they laid the groundwork for closer integration between the research and health-care systems.
Implications for practice
In summary, the following factors, working together, are thought to have contributed to the CLAHRCs’ achievements:
-
A focus on research relevant to the NHS and its patients.
-
Strong leadership allied with a significant degree of devolved responsibility to people such as research theme leaders and knowledge brokers.
-
A collaborative approach characterised by flexibility, responsiveness to the needs of partners and an ongoing ability to exploit foreseen and unforeseen opportunities. In practice this meant:
-
developing relationship models that focused on interactions between people through which knowledge from multiple sources could be exchanged and adapted to local circumstances through a collaborative production–synthesis–integration cycle43
-
recruiting people who could bring understanding of research to the service and vice versa: all CLAHRC staff acted as research champions; many CLAHRCs also recruited knowledge brokers to fulfil this function
-
developing research awareness and capacity through the coproduction of research and implementation projects, training and exchange programmes, regular cross-CLAHRC knowledge exchange meetings and user-friendly publications.
-
-
Matched funding from the service, which helped to promote initial NHS buy-in, allowed scope for adaptability and responsiveness to the needs of the service, and encouraged NHS organisations to think prospectively about the business case for investing in research and knowledge mobilisation and become more active and discerning partners in the CLAHRCs. 102 However, the disadvantage of this funding model, that is the risks associated with involving NHS organisations of only one type in a NHS environment subject to ongoing change, needs to be considered from the outset.
-
A continuing openness to experimentation and learning. The CLAHRCs had feedback from their own internal evaluations (including the evaluations of CLAHRC-funded projects), from the formative elements of the NIHR-funded external evaluations and, in some cases, from external interim reviews of progress.
Overall, the CLAHRCs’ experience suggests that programmes with similar goals need to adopt a systems perspective that recognises that context is critical, that most problems and interventions are multilevel and complex, and that more emphasis needs to be placed on inter-relationships among system elements and system rules and how system shift can be achieved. In practice this means developing programmes that can:
-
produce and exploit research that is pragmatic and practical, encourages participation and representativeness, makes comparisons between real alternatives, collects cost data and assesses multiple outcomes, often using mixed methods
-
identify and respond to the challenges and opportunities posed by the various systems (organisational, professional, economic and so on) within which NHS clinicians, managers and commissioners work
-
include short-term as well as long-term research and implementation projects and adopt an early focus on ‘quick wins’
-
consider external validity in the funding, reporting, synthesis and application of research as well as internal validity
-
commit to the full and transparent reporting of research findings through effective communications, including user-friendly publications
-
clarify, and strengthen, the roles of different players in research, implementation and service improvement.
Research recommendations
We have identified five overarching research areas and, within these, seven research questions from the evidence presented in this report that a future research programme could appropriately explore to further inform ongoing efforts within the health-research and health-service systems in England to promote the effective translation of evidence into practice.
-
Understanding the counterfactual. The second round of funding for the CLAHRCs provides an endorsement of their activities in the first round, and the development of the AHSNs helps to alleviate some of the concerns about the partial geographical coverage of the CLAHRCs. At the same time, the parallel development of the AHSNs and the second round of the CLAHRCs provides an important research opportunity to compare areas with both an AHSN and a CLAHRC, and areas with just an AHSN. Such a research programme would present an opportunity to explore the counterfactual, that is to understand the extent to which the CLAHRCs are making a contribution to furthering applied health research and its translation into patient benefit. Q: To what extent are the CLAHRCs furthering applied health research and its translation into patient benefit?
-
Understanding implementation. The role of the CLAHRCs was to support implementation and they were successful in helping the service to identify, produce and disseminate the user-friendly evidence needed to support the development of effective service improvement interventions, as well as evaluating new ways of implementing those interventions and subsequent dissemination of these evaluation findings.
-
However, the requirement that evidence be generated that is relevant to local service needs while at the same time generalisable beyond the locality means that there is a need to consider internal and external validity when designing research projects. There is, therefore, a need to explore and evaluate different implementation theories to advance understanding of how to achieve a balance between rigour and relevance in order to improve the applicability of research findings.
Q: What lessons can be learned from the CLAHRCs about how to balance rigour and relevance in research projects and improve the applicability of the findings?
-
There is also a need to identify the systemic barriers to, and facilitators of, implementation.
Q: What lessons can be learned from the CLAHRCS about how to tailor the implementation of research findings to different settings while retaining fidelity?
-
-
Achieving sustainability and scale-up.
-
We have shown how the CLAHRCs successfully influenced the culture in the NHS and in academia, and sought to ensure the explicit use of research evidence as a norm in the NHS. There is a need to understand the factors that support this normalisation better, and, in particular, the roles of communication and dissemination and of knowledge brokers.
Q: What lessons can be learned from the CLAHRCs about the mechanisms through which the use of research evidence is promoted in the NHS?
-
We have seen how the CLAHRCs were able to scale up some of their successful implementation projects across their own localities and across the NHS more generally. It has also been suggested that ‘sustainability research’ should be considered as a further stage in the translation or dissemination of research-based interventions into practice. 112 However, further work is required to advance our understanding of the processes and mechanisms that are needed to support the system-wide sustainability and scale-up of implementation projects.
Q: What factors support, and what factors hinder, the sustainability and scale-up of successful implementation projects?
-
-
The role of patient and public involvement. In this report we present some, albeit limited, evidence that the involvement of patients and the public as partners in the CLAHRCs was uneven. We have not been able, in the context of this evaluation, to study approaches to and processes of engaging patients and the wider public in the CLAHRCs, as partners, users and/or coproducers of research and its implementation. There is a need to understand more about the key enablers and barriers of successful patient and public engagement in the processes of research production and implementation in collaborative partnerships such as the CLAHRCs. Such an understanding will require a more systematic assessment of the (expected) outcomes of involving patients and the wider public in the collaboration; the level of involvement (e.g. to inform priority setting, resource allocation, service delivery, etc.); their role (e.g. advisory, participatory, coproduction, etc.) and representation; and the extent to which involvement promotes equity. 119
Q: What are the key enablers of, and barriers to, successful patient and public engagement in research production and implementation in collaborative partnerships such as the CLAHRCs?
-
The relation between CLAHRCs and NHS commissioners. We have seen that the CLAHRCs did not always find it easy to involve commissioners but that when they did so they found it, to use their own term, ‘exciting’. Given the recent changes in commissioning within the NHS and the opportunities these provide, it would be useful to explore how the developing relation between the CLAHRCs and local commissioners can be supported, how it operates and what it achieves.
Q: Have NHS commissioners used CLAHRCs? If so, how and with what results? If not, why not?
Acknowledgements
We would like to thank our scientific advisory group, comprising Professor Peter Jones, Dr Chris Henshall, Professor Justin Keen and Professor Martin Buxton. Their insight and experience has been of great benefit to us. Over the course of the project, Dr Steven Wooding, Dr Susan Guthrie and Professor Joanna Chataway have provided very helpful quality assessment advice, responding to tight deadlines with good humour. We should especially like to thank the 95 interviewees and the over 100 people who participated in our workshops through the course of the project. Finally, we would like to thank the CLAHRC directors and the NIHR HSDR programme for their ongoing engagement and support.
Below we provide a list of contributing authors to this report. In addition, we would like to express our gratitude to researchers who contributed substantially to earlier stages of this project. These were:
-
Professor Tom Ling (formerly RAND Europe), principal investigator until March 2012
-
Claire Celia (formerly RAND Europe)
-
Anais Reding (formerly RAND Europe).
Contribution of authors
Dr Bryony Soper (Associate Professor, Health Services Research) was co-applicant, was involved in study design, data collection and analysis, and is lead author of this report.
Dr Saba Hinrichs (Analyst, Health and Healthcare) was involved in data collection and analysis, and in the preparation of the report.
Samuel Drabble (Associate Analyst, Evaluation and Performance Management) was involved in data collection and analysis, and in the preparation of the report.
Dr Ohid Yaqub (Analyst, Innovation and Technology Policy) was involved in data collection and analysis, and in the preparation of the report.
Dr Sonja Marjanovic (Senior Analyst, Innovation and Technology Policy) was co-applicant and was involved in study design, data collection and analysis, and in the preparation of the report.
Professor Stephen Hanney (Professorial Research Fellow, Health Services Research) was co-applicant and was involved in study design, data collection and analysis, and in the preparation of the report.
Dr Ellen Nolte (Director, Health and Healthcare Policy) was principal investigator on the project as of March 2012. She was involved in data collection and analysis, and in the preparation of the report.
Publication
Soper B, Yaqub O, Hinrichs S, Marjanovich S, Drabble S, Hanney S, et al. CLAHRCs in practice: combined knowledge transfer and exchange strategies, cultural change, and experimentation. J Health Serv Res Policy 2013;18(Suppl. 3):53–64.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- National Institute for Health Research . NIHR Collaborations for Leadership in Applied Health Research and Care (CLAHRCs) n.d. www.nihr.ac.uk/infrastructure/Pages/CLAHRCs.aspx (accessed April 2013).
- Evaluating Partnerships between Universities and NHS Organisations: Learning from the NIHR Collaborations for Leadership in Applied Health Research and Care (CLAHRC). Research Brief (cla258). Call for Proposals. London: National Coordinating Centre for the Service Delivery and Organisation (NCCSDO) research programme; 2008.
- Collaborations for Leadership in Applied Health Research and Care (previously known as Academic Health Centres of the Future): Call for Proposals to Establish Pilots. London: National Institute for Health Research; 2007.
- Denis JL, Lomas J. Convergent evolution: the academic and policy roots of collaborative research. J Health Serv Res Policy 2003;8:1-6. http://dx.doi.org/10.1258/135581903322405108.
- Antil T, Desrochers M, Joubert P, Bouchard C. Implementation of an innovative grant programme to build partnerships between researchers, decision-makers and practitioners: the experience of the Quebec Social Research Council. J Health Serv Res Policy 2003;8:35-43. http://dx.doi.org/10.1258/135581903322405153.
- United States Department for Veterans Affairs . Quality Enhancement Research Initiative (QUERI) n.d. www.queri.research.va.gov/about/overview.cfm (accessed April 2013).
- Bowen S, Martens P. The need to know team: demystifying knowledge translation. Learning from the community. J Health Serv Res Policy 2005;10:203-11. http://dx.doi.org/10.1258/135581905774414213.
- Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001.
- Woolf S. The meaning of translational research and why it matters. JAMA 2008;299:211-13. http://dx.doi.org/10.1001/jama.2007.26.
- Research for Health: A Research and Development Strategy for the NHS. London: HMSO; 1991.
- Kogan M, Henkel M, Hanney S. Government and Research: Thirty Years of Evolution. Dordrecht: Springer; 2006.
- Black N. National strategy for research and development: Lessons from England. Annu Rev Public Health 1997;18:485-50. http://dx.doi.org/10.1146/annurev.publhealth.18.1.485.
- Peckham M. Developing the National Health Service: a model for public services. Lancet 1999;354:1539-45. http://dx.doi.org/10.1016/S0140-6736(99)08417-2.
- Hanney S, Kuruvilla S, Soper B, Mays N. Who needs what from a national health research system: lessons from reforms to the English Health Department’s R&D system. Health Res Policy Syst 2010;8. http://dx.doi.org/10.1186/1478-4505-8-11.
- Best Research for Best Health: A New National Health Research Strategy. The NHS Contribution to Health Research in England. London: Department of Health; 2006.
- Cooksey D. A Review of UK Health Research Funding. London: HM Treasury; 2006.
- Report of the High Level Group on Clinical Effectiveness. London: Department of Health; 2007.
- National Institute for Health Research . Biomedical Research Centres n.d. www.nihr.ac.uk/infrastructure/Pages/infrastructure_biomedical_research_centres.aspx (accessed April 2013).
- National Institute for Health Research . Biomedical Research Units n.d. www.nihr.ac.uk/infrastructure/Pages/infrastructure_biomedical_research_units.aspx (accessed April 2013).
- High Quality Care for All: NHS Next Stage Review Final Report. London: Department of Health; 2008.
- Kmietowicz Z. England gets five academic health science centres to compete on global stage. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b1005.
- Lessons from Health Innovation and Education Clusters. London: NHS Confederation; 2012.
- Caldwell S, Mays N. Studying policy implementation using a macro, meso and micro frame analysis: the case of the Collaboration for Leadership in Applied Health Research & Care (CLAHRC) programme nationally and in North West London. Health Res Policy Syst 2012;10. http://dx.doi.org/10.1186/1478-4505-10-32.
- Ling T, Soper B, Marjanovic S, Celia C, Yaqub O, Reding A, et al. Delivering the Aims of the CLAHRCs: Evaluating CLAHRCs’ Strategies and Contributions. Interim Report: Phase 1. Cambridge: RAND Europe; 2011.
- Estabrooks C, Scott S, Squires J, Stevens B, O’Brien-Pallas L, Watt-Watson J, et al. Patterns of research utilization on patient care units. Implement Sci 2008;3. http://dx.doi.org/10.1186/1748-5908-3-31.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. http://dx.doi.org/10.1111/j.0887-378X.2004.00325.x.
- Eccles M. Changing the behaviour of healthcare professionals: the use of theory in promoting the uptake of research findings. J Clin Epidemiol 2005;58:107-12. http://dx.doi.org/10.1016/j.jclinepi.2004.09.002.
- Ferlie E, Shortell S. Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Q 2001;79:281-315. http://dx.doi.org/10.1111/1468-0009.00206.
- Grol R, Bosch M, Hulscher M, Eccles M, Wensing M. Planning and studying improvement in patient care: the use of theoretical perspectives. Milbank Q 2007;85:93-138. http://dx.doi.org/10.1111/j.1468-0009.2007.00478.x.
- Damschroder L, Aron D, Keith R, Kirsh S, Alexander J, Lowery J. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-50.
- Crilly T, Jashapara A, Ferlie E. Research Utilisation & Knowledge Mobilisation: A Scoping Review of the Literature. London: King’s College London; 2010.
- NHS England . New Academic Health Science Networks Announced n.d. www.england.nhs.uk/2013/05/23/acc-health-sci-ntwrk/ (accessed 20 September 2013).
- Mannion R, Davies H, Harrison S, Konteh F, Greener I, McDonald R, et al. Changing Management Cultures and Organisational Performance in the NHS 2010. www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1501-94_V02.pdf (accessed June 2013).
- Mitton C, Adair C, McKenzie E, Patten S, Waye Perry B. Knowledge transfer and exchange: review and synthesis of the literature. Milbank Q 2007;85:729-68. http://dx.doi.org/10.1111/j.1468-0009.2007.00506.x.
- Wilson P, Petticrew M, Calnan M, Nazareth I. Disseminating research findings: what should researchers do? A systematic scoping review of conceptual frameworks. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-91.
- Westfall J, Mold J, Fagnan L. Practice-based research: ’Blue Highways’ on the NIH roadmap. JAMA 2007;297:403-6. http://dx.doi.org/10.1001/jama.297.4.403.
- Khoury M, Gwinn M, Ioannidis J. The emergence of translational epidemiology: from scientific discovery to population health impact. Am J Epidemiol 2010;172:517-24. http://dx.doi.org/10.1093/aje/kwq211.
- Glasgow R, Chambers D. Developing robust, sustainable, implementation systems using rigorous, rapid and relevant science. Clin Transl Sci 2012;5:48-55. http://dx.doi.org/10.1111/j.1752-8062.2011.00383.x.
- Hanney S, Buxton M, Green C, Coulson D, Raftery J. An assessment of the impact of the NHS Health Technology Assessment Programme. Health Technol Assess 2007;11. http://dx.doi.org/10.3310/hta11530.
- Buxton M, Hanney S. How can payback from health services research be assessed?. J Health Serv Res Policy 1996;1:35-43.
- Dixon S, Coleman P, Nicholl J, Brennan A, Touch S. Evaluation of the impact of a technology appraisal process in England: the South and West Development and Evaluation Committee. J Health Serv Res Policy 2003;8:18-24. http://dx.doi.org/10.1258/13558190360468182.
- Kogan M, Henkel M. Government and Research: The Rothschild Experiment in a Government Department. London: Heinemann; 1983.
- Lomas J. Using ‘Linkage and Exchange’ to move research into policy at a Canadian foundation. Health Affairs 2000;19:236-40. http://dx.doi.org/10.1377/hlthaff.19.3.236.
- Lomas J. Finding audiences, changing beliefs: the structure of research use in Canadian health policy. J Health Polit Policy Law 1990;15:525-42. http://dx.doi.org/10.1215/03616878-15-3-525.
- Gibbons M, Limoges C, Nowotny H, Schwartzman S, Scott P, Trow M. The New Production of Knowledge. London: Sage; 1994.
- Ferlie E, Wood M. Novel mode of knowledge production? Producers and consumers in health services research. J Health Serv Res Policy 2003;8:51-7. http://dx.doi.org/10.1258/135581903322405171.
- Nowotny H, Scott P, Gibbons M. Re-thinking Science: Knowledge and the Public in an Age of Uncertainty. Oxford: Policy Press; 2001.
- Cohen W, Levinthal D. Absorptive capacity: a new perspective on learning and innovation. Adm Sci Q 1990;35:128-56. http://dx.doi.org/10.2307/2393553.
- Cohen W, Levinthal D. Innovation and learning: the two faces of R & D. Econ J 1989;99:569-96. http://dx.doi.org/10.2307/2233763.
- Rosenburg N. Why do firms do basic research (with their own money)?. Res Pol 1990;19:165-74. http://dx.doi.org/10.1016/0048-7333(90)90046-9.
- Buxton M, Hanney S. Evaluating the NHS research and development programme: will the programme give value for money?. J R Soc Med 1998;91:2-6.
- Buxton M, Elliott R, Hanney S, Henkel M, Keen J, Sculpher M, et al. Assessing Payback from Department of Health Research and Development. Vol 2: 8 Case Studies. Uxbridge: Brunel University; 1994.
- Hanney S, Grant J, Wooding S, Buxton M. Proposed methods for reviewing the outcomes of health research: the impact of funding by the UK’s ‘Arthritis Research Campaign’. Health Res Policy Syst 2004;2. http://dx.doi.org/10.1186/1478-4505-2-4.
- May C, Mort M, Williams T, Mair F, Gask L. Health Technology Assessment in its local contexts: studies of telehealthcare. Soc Sci Med 2003;57:697-710. http://dx.doi.org/10.1016/S0277-9536(02)00419-7.
- Frank C, Nason E. Health research: measuring the social, health and economic benefits. CMAJ 2009;180:528-34. http://dx.doi.org/10.1503/cmaj.090016.
- Making an Impact: A Preferred Framework and Indicators to Measure Returns on Investment in Health Research. Ottawa, ON: CAHS; 2009.
- Callon M, Bowker G. Is science a public good? Fifth Mullins Lecture, Virginia Polytechnic Institute, 23 March 1993. Sci Techn Human Val 1994;19:395-424. http://dx.doi.org/10.1177/016224399401900401.
- Shortell S, O’Brien J, Carman J, Foster R, Hughes E, Boerstler H, et al. Assessing the impact of continuous quality improvement/total quality management: concept versus implementation. Health Serv Res 1995;30:377-401.
- Hanney S, Boaz A, Jones T, Soper B. Engagement in research: an innovative three-stage review of the benefits for health-care performance. Health Serv Deliv Res 2013;1.
- Oliver A. The Veterans Health Administration: an American success story?. Milbank Q 2007;85:5-35. http://dx.doi.org/10.1111/j.1468-0009.2007.00475.x.
- Kizer K, Demakis J, Feussner J. Reinventing VA health care: systematizing quality improvement and quality innovation. Med Care 2000;38:I-7. http://dx.doi.org/10.1097/00005650-200006001-00002.
- Graham I, Tetroe J. Learning from the U.S. Department of Veterans Affairs Quality Enhancement Research Initiative: QUERI Series. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-13.
- Bate P, Mendel P, Robert G. Organising for Quality: The Improvement Journey of Leading Hospitals in Europe and the United States. Oxford: Radcliffe Publishing; 2008.
- May C. Towards a general theory of implementation. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-18.
- May C. A rational model for assessing and evaluating complex interventions in health care. BMC Health Serv Res 2006;6. http://dx.doi.org/10.1186/1472-6963-6-86.
- May C, Finch T. Implementing, embedding, and integrating practices: an outline of Normalization Process Theory. Sociology 2009;43:535-54. http://dx.doi.org/10.1177/0038038509103208.
- May C, Murray E, Finch T, Mair F, Treweek S, Ballini L, et al. Normalization Process Theory On-Line Users’ Manual and Toolkit n.d. www.normalizationprocess.org (accessed April 2013).
- Frederiksen L, Hansson F, Wenneberg S. The Agora and the role of research evaluation. Evaluation 2003;9:149-72. http://dx.doi.org/10.1177/1356389003009002003.
- Soper B, Buxton M, Hanney S, Oortwijn W, Scoggins A, Steel N, et al. Developing the protocol for the evaluation of The Health Foundation’s ‘Engaging with Quality’ initiative: an emergent approach. Implement Sci 2008;3. http://dx.doi.org/10.1186/1748-5908-3-46.
- Mayne J. Addressing attribution through contribution analysis: using performance measures sensibly. Can J Program Eval 2001;16:1-24.
- NIHR Health Services and Delivery Research Programme . HS&Amp;DR Project Portfolio: CLAHRCs n.d. www.netscc.ac.uk/hsdr/projlisting.php?srtid=31 (accessed April 2013).
- May C, Harrison R, Finch T, MacFarlane A, Mair F, Wallace P. Understanding the normalization of telemedicine services through qualitative evaluation. J Am Med Informat Assoc 2003;10:596-604. http://dx.doi.org/10.1197/jamia.M1145.
- Department of Health . Academic Health Science Networks: Request for Expressions of Interest to Create AHSNs n.d. www.gov.uk/government/publications/academic-health-science-networks-request-for-expressions-of-interest-to-create-ahsns--2 (accessed April 2013).
- East of England Evidence Adoption Centre . Home n.d. www.eac.cpft.nhs.uk/ (accessed October 2012).
- NIHR CLAHRC for Cambridgeshire and Peterborough . Collaborators n.d. www.clahrc-cp.nihr.ac.uk/partner-organisations (accessed April 2013).
- NIHR CLAHRC for the South West Peninsula . The NIHR CLAHRC for the South West Peninsula: Proposal n.d. http://clahrc-peninsula.nihr.ac.uk/includes/site/files/files/PenCLARHC%20executive%20summary%20version%20for%20directors.pdf (accessed April 2013).
- Folk-us . Folk.Us Homepage n.d. www.folkus.org.uk (accessed March 2013).
- NIHR CLAHRC for the South West Peninsula . CLAHRC BITE: Bringing Tranexamic Acid (TXA) into Practice Safely, Quickly and Efficiently n.d. http://clahrc-peninsula.nihr.ac.uk/includes/site/files/files/Bites/BITE%2001%20-%20Tranexamic%20Acid.pdf (accessed March 2013).
- NIHR CLAHRC for Cambridgeshire and Peterborough . CLAHRC Fellowships n.d. www.clahrc-cp.nihr.ac.uk/sample-page/clahrc-fellows (accessed April 2013).
- Lomas J. The in-between world of knowledge brokering. BMJ 2007;334:129-32. http://dx.doi.org/10.1136/bmj.39038.593380.AE.
- Ward V, House A, Harner S. Knowledge brokering: the missing link in the evidence to action chain?. Evid Policy 2009;5:267-79. http://dx.doi.org/10.1332/174426409X463811.
- Rowley E. Protocol for a qualitative study exploring the roles of ‘Diffusion Fellows’ in bridging the research to practice gap in the Nottinghamshire, Derbyshire and Lincolnshire Collaboration for Leadership in Applied Health Research and Care (CLAHRC-NDL). BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2011-000604.
- Speechley M. Knowledge translation for falls prevention: the view from Canada. J Safety Res 2011;42:453-59. http://dx.doi.org/10.1016/j.jsr.2010.09.004.
- NIHR CLAHRC for Cambridgeshire and Peterborough . With the People, for the People: Applying Mental Health Research n.d. www.cam.ac.uk/research/news/with-the-people-for-the-people-applying-mental-health-research (accessed April 2013).
- NIHR CLAHRC for the South West Peninsula . PenCHORD n.d. http://clahrc-peninsula.nihr.ac.uk/penchord.php (accessed March 2013).
- Peninsula Health Technology Commissioning Group . The Annual Report of the Peninsula Health Technology Commissioning Group 2011–2012 n.d. www.devonpct.nhs.uk/Library/SWPHTCG/PHTCG_Annual%20_Report_2011_12_final.pdf (accessed April 2013).
- NIHR CLAHRC for the South West Peninsula . NICE Disinvestment Project Protocol n.d. http://clahrc-peninsula.nihr.ac.uk/includes/site/files/files/NICE%20Disinvestment%20project%20Protocol.pdf (accessed April 2013).
- NIHR CLAHRC for Cambridgeshire and Peterborough . Key Performance Indicators n.d. www.clahrc-cp.nihr.ac.uk/about-us/clahrc-board/key-performance-indicators (accessed April 2013).
- Health Services Research Network . BITES Categorised by CLAHRC n.d. www.hsrlive.org/page/bites-categorised-by-clahrc (accessed April 2013).
- NIHR CLAHRC for Cambridgeshire and Peterborough . Improving Access to Psychological Therapies: Briefing Paper 2 2012. www.clahrc-cp.nihr.ac.uk/wp-content/uploads/2012/11/CLAHRC-IAPT-briefing_CH-Nov19.pdf (accessed April 2013).
- Hammond G, Croudace T, Radhakrishnan M, Lafortune LW, Watson A, McMillan-Shields F, et al. Comparative effectiveness of cognitive therapies delivered face-to-face or over the telephone: an observational study using propensity methods. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0042916.
- NIHR CLAHRC for the South West Peninsula . CLAHRC BITE: Operational Research Seeks Benefit for Stroke Victims n.d. http://clahrc-peninsula.nihr.ac.uk/includes/site/files/files/Bites/BITE%2002%20-%20Stroke%20Pathways.pdf (accessed April 2013).
- National Institute for Health Research . Collaborations for Leadership in Applied Health Research and Care: Invitation to Submit an Application; And Competition 2013: Questions and Answers n.d. www.ccf.nihr.ac.uk/Pages/CLAHRC2013Competition.aspx (accessed April 2013).
- Graham I, Logan J, Harrison M, Straus S, Tetroe J, Caswell WR, et al. Lost in knowledge translation: time for a map?. J Contin Educ Health Prof 2006;26:13-24. http://dx.doi.org/10.1002/chp.47.
- Scott T, Mannion R, Davies H, Marshall M. Implementing culture change in health care: theory and practice. Int J Qual Health Care 2003;15:111-18. http://dx.doi.org/10.1093/intqhc/mzg021.
- Best A, Holmes B. Systems thinking, knowledge and action: towards better models and methods. Evid Policy 2010;6:145-59. http://dx.doi.org/10.1332/174426410X502284.
- Glasgow R, Emmons K. How can we increase translation of research into practice? Types of evidence needed. Ann Rev Public Health 2007;28:413-33. http://dx.doi.org/10.1146/annurev.publhealth.28.021406.144145.
- Green L, Glasgow R, Atkins D, Stange K. Making evidence from research more relevant, useful, and actionable in policy, program planning, and practice slips ‘twixt cup and lip’. Am J Prev Med 2009;37:S187-91. http://dx.doi.org/10.1016/j.amepre.2009.08.017.
- Francis J, Perlin J. Improving performance through knowledge translation in the Veterans Health Administration. J Contin Educ Health Prof 2006;26:63-71. http://dx.doi.org/10.1002/chp.52.
- Glasgow R, Green L, Ammerman A. A focus on external validity. Eval Health Prof 2007;30:115-17. http://dx.doi.org/10.1177/0163278707300627.
- Equity and Excellence: Liberating the NHS. London: Department of Health; 2010.
- Walshe K, Davies H. Health research, development and innovation in England from 1988 to 2013: from research production to knowledge mobilization. J Health Serv Res Policy 2013;18:1-12. http://dx.doi.org/10.1177/1355819613502011.
- Stetler C, Ritchie J, Rycroft-Malone J, Schultz A, Charns M. Improving quality of care through routine, successful implementation of evidence-based practice at the bedside: an organizational case study protocol using the Pettigrew and Whipp model of strategic change. Implement Sci 2007;2. http://dx.doi.org/10.1186/1748-5908-2-3.
- Baker R, Camosso-Stefinovic J, Gillies C, Shaw E, Cheater F, Flottorp S, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2010;3. http://dx.doi.org/10.1002/14651858.CD005470.pub2.
- Ovretveit J, Klazinga N. Linking research to practice: the organisation and implementation of The Netherlands health and social care improvement programmes. Health Policy 2013;109:175-86. http://dx.doi.org/10.1016/j.healthpol.2012.11.005.
- Nutley S, Walter I, Davies H. Using Evidence: How Research can Inform Public Services. Bristol: Policy Press; 2007.
- Baker R, Robertson N, Rogers S, Davies M, Brunskill N, Khunti K, et al. The National Institute of Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for Leicestershire, Northamptonshire and Rutland (LNR): a programme protocol. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-72.
- Rowley E, Morriss R, Currie G, Schneider J. Research into practice: Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for Nottinghamshire, Derbyshire, Lincolnshire (NDL). Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-40.
- Mawson S, Scholefield H. The National Institute for Health Research; Collaboration for Leadership in Applied Health and Care for South Yorkshire. J Res Nurs 2009;14:169-74. http://dx.doi.org/10.1177/1744987108101752.
- Soper S, Yaqub O, Hinrichs S, Marjanovich S, Drabble S, Hanney S, et al. CLAHRCs in practice: combined knowledge transfer and exchange strategies, cultural change, and experimentation. J Health Serv Res Policy 2013;18:53-64. http://dx.doi.org/10.1177/1355819613499903.
- Glasgow RE, Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. National Institutes of Health approaches to dissemination and implementation science: current and future directions. Am J Public Health 2012;102:1274-81. http://dx.doi.org/10.2105/AJPH.2012.300755.
- Scheirer M, Dearing J. An agenda for research on the sustainability of public health programs. Am J Public Health 2011;101:2059-67. http://dx.doi.org/10.2105/AJPH.2011.300193.
- Innovation Health and Wealth, Accelerating Adoption and Diffusion in the NHS. London: NHS Improvement & Efficiency Directorate, Department of Health; 2011.
- NIHR CLAHRCs Directors . Response to NHS Chief Executive’s Open Call for Evidence and Ideas n.d. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_131396.pdf (accessed April 2013).
- Trochim W, Kane C, Graham M, Pincus H. Evaluating translational research: a process marker model. Clin Transl Sci 2011;4:153-62. http://dx.doi.org/10.1111/j.1752-8062.2011.00291.x.
- Imperial College Health Partners . AHSN: Prospectus 2012. www1.imperial.ac.uk/resources/C79F6656–340A-496F-84DB-E2D394EF0D73/ (accessed March 2013).
- South West Peninsula Academic Health Science Network . South West Peninsula Academic Health Science Network: Prospectus and Business Plan 2012. www.rdehospital.nhs.uk/docs/trust/pr/2013/SWP%20AHSN%20Prospectus.pdf (accessed April 2013).
- Eastern Academic Health Science Network . Eastern Academic Health Science Network: Prospectus and Business Plan 2012. www.cuhp.org.uk/publications/EAHSN-Prospectus-and-Business-Plan-2012.pdf (accessed March 2012).
- Conklin A, Morris Z, Nolte E. Involving the Public in Healthcare Policy: An Update of the Research Evidence and Proposed Evaluation Framework. Santa Monica, CA: Rand Corporation; 2010.
- Priorities in Medical Research: HL Paper 54–1. London: The Stationery Office; 1988.
- Pang T, Sadana R, Hanney S, Bhutta ZA, Hyder AA, Simon J. Knowledge for better health: a conceptual framework and foundation for health research systems. Bull World Health Organ 2003;81:815-20.
- Delivering Health Research: National Institute for Health Research Progress Report 2008/9. London: National Institute for Health Research; 2009.
- National Institute for Health Research . Research Design Service n.d. www.ccf.nihr.ac.uk/Pages/RDSMap.aspx (accessed April 2013).
- Breakthrough to Real Change in Local Healthcare. A Guide for Applications to Create Health Innovation and Education Clusters (HIECs). Leeds: Department of Health; 2009.
- Denis J, Lehoux P, Hivon M, Champagne F. Creating a new articulation between research and practice through policy? The views and experiences of researchers and practitioners. J Health Serv Res Policy 2003;8:44-50. http://dx.doi.org/10.1258/135581903322405162.
- Soper B, Hanney S. Lessons from the evaluation of the UK’s NHS R&D Implementation Methods Programme. Implement Sci 2007;2. http://dx.doi.org/10.1186/1748-5908-2-7.
- Atkins D. QUERI and implementation research: emerging from adolescence into adulthood: QUERI series. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-12.
- Powell A, Rushmer R, Davies H. A Systematic Narrative Review of Quality Improvement Models in Health Care. Edinburgh: NHS Quality Improvement Scotland; 2009.
- Bartunek J, Trullen J, Bonet E, Sauquet A. Sharing and expanding academic and practitioner knowledge in health care. J Health Serv Res Policy 2003;8:62-8. http://dx.doi.org/10.1258/135581903322405199.
Appendix 1 Research protocol
Evaluation protocol_v2_06/06/2011
Version 2
6 June 2011
Narrowing the second translation gap: evaluating CLAHRCs’ potential, strategies and contributions
Background
Nine Collaborations for Leadership in Applied Health Research and Care (CLAHRCs) were established in October 2008 by the National Institute for Health Research. Their aim is to encourage and strengthen collaborations between Universities and local NHS organisations. These collaborations are focused on improving patient outcomes through changing the way applied health research is conducted, and strengthening the use of research results in health care practice. Each of these collaborations share some overarching purposes, but there are also many differences reflecting local circumstances, including local research and health care priorities and historic strengths. RAND Europe and the Health Economics Research Group at Brunel University have been commissioned by the NIHR Service Delivery Office as one of four teams evaluating CLAHRCs.
The Cooksey Report on UK health research funding (HM Treasury, 2006) identified two gaps in the translation of health research into practice. The first gap is in translating ideas from basic and clinical research into the development of new products, technologies and approaches to the treatment of disease and illness. The second gap is in implementing these products, technologies and service approaches in clinical practice.
Our evaluation of CLAHRCs focuses on the second translation gap. In an approach that will evolve as the CLAHRCs establish their ways of working, we will explore the various interventions and strategies being adopted by CLAHRCs to address the second gap. We will identify common features between CLAHRCs, explore promising ideas, and examine the strengths and weaknesses of distinct interventions. Our style of working will be collaborative, and we hope to contribute to shared learning and improvement during the lives of the CLAHRCs. Through doing so, we hope to provide pragmatic support to future decisions in this important area.
Aims
Our project aims to:
-
Improve understandings of attempts to bridge the second translation gap in ways that make sense to policy-makers, practitioners, and academic researchers
-
Contribute to recommendations that are evidence based, acceptable and feasible given health research and practice architectures and policy drivers
-
Contribute to the methodologies used in studying the translation gap, and multi-agency and evolving interventions/programmes.
Key research questions
This project will seek to answer one overarching and three subsidiary questions:
-
How, and how effectively, do CLAHRCs address the second translation gap?
-
How, and how effectively, do CLAHRCs support local health research?
-
How, and how effectively, do CLAHRCs build local infrastructures to utilise globally and locally generated health research for local patient benefit?
-
Does bringing together activities for health research and activities for delivering health research benefit both sets of activities equally (e.g. by stimulating local research that is more relevant to the needs of patients or by encouraging a ‘research-literate’ local community)?
Study design and methods: summary
This is a three year project with three phases. Our approach will be to better understand the sequence of activities supported by CLAHRCs and to assess how far they contribute to bridging the second translation gap. We will draw upon some of the concepts and analytical approaches developed in literature on how to manage innovation, and on how knowledge is produced and used in organisations.
In phase one we will identify types of interventions (and combinations of interventions) used by the CLAHRCs to address the second translation gap, and examine the logic behind their approach. We will do this through drawing upon existing research, analysing documentation from the CLAHRCs, and learning from workshops with multiple stakeholders in each CLAHRC. We would like to develop a typology of interventions the CLAHRCs are using to encourage and increase the adoption or research and innovations in health care practice. We are assuming that some approaches will be used in many CLAHRCs and some might be used only in isolated cases. In Phase II, we will explore in more detail some of the issues and factors identified in Phase I as likely to influence the CLAHRCs’ evolution and performance in relation to bridging the second translation. This Phase of the work will include an online survey of all CLAHRCs, a case study phase focusing on 2 to 3 CLAHRCs, a validation phase and a broader phase looking to situate the CLAHRCs within the broader NHS landscape. In phase III we will draw together the data and analyses and identify lessons learnt, before developing conclusions and recommendations.
Outputs
NIHR has made a significant investment in CLAHRCs on the understanding that these sorts of interactive collaborations can make an important contribution to the use of research. The outputs of this study should be relevant to the NIHR and other health research funders, healthcare practitioners, academics and policy-makers. Through a combination of reports, briefs and workshops, we will regularly feedback of our emerging findings to the SDO (Service Delivery and Organisation programme), other evaluation teams and to CLAHRCs. We will also actively participate in conferences, as well as forums with policy-makers and healthcare practitioners, and intend to publish our findings in peer-reviewed journals. Our final outputs form this project will also include documents tailored to the unique discourse and priorities of academic, practitioner and policy communities.
Details of each phase
Each phase of the study is detailed below.
PHASE I
During the first phase, we will work collaboratively with all CLAHRCs to build a taxonomy of their approaches to the second translation gap (i.e. the gap in health research translation that refers to implementing research-informed product and service innovations into clinical practice). Each CLAHRC is likely to have more than one approach to the second translation gap, and each approach may be present in more than one CLAHRC. We will look at the approaches being adopted by CLAHRCs, identifying and exploring: (a) the types of interventions being used by CLAHRCs to promote practice change and the mechanisms through which they operate (e.g. interactions, social influence, facilitation, etc.) and (b) the various levels at which these interventions will be used to promote change in practice (e.g. individual, organisational, and system-wide), and c) the logic behind the intervention (i.e. why the CLAHRC believes that implementing certain interventions, in certain contexts and with specific inputs, should result in specific outcomes).
Our concern will be to capture initiatives to support improvements in clinical practice at:
-
a micro-level, i.e. interventions that promote translation among individual practitioners within a single organisation (e.g. targeting research findings on doctors and nurses in a primary care practice setting, coupled with feedback opportunities),
-
a meso-level, i.e. interventions that promote translation among researchers, managers and practitioners working in different organisations. Among these we include interventions that aim to enhance the roles service managers can play in supporting improvements in clinical care; and
-
a macro-level, i.e. interventions that promote translation designed to facilitate organisation to organisation partnership, e.g. across research and health care sectors (such as the CLAHRCs themselves).
At the end of Phase I we will draft a First Interim Report, and feedback our early findings to all CLAHRCs, to the SDO, and the wider community of policy-makers and practitioners in and around the SDO.
The core methods to be used in phase I include literature review, document review and primary data collection through workshops/interviews with CLAHRCs. More details on different components and timelines for phase I are provided below:
Refining the evaluation design: it is important that the initial design and approach has been scrutinized by academics and practitioners within CLAHRCs (November–December 2009).
Reviewing key literature and assessing its significance for the evaluation project (November 2009–March 2010).
Kick-off meetings with SDO and CLAHRCs: The SDO organised kick off meetings with all the funded evaluation teams and with the CLAHRC Directors in October 2009 and February 2010 respectively. At these meetings, discussion and consensus building took place on issues of coordinating evaluation activities, minimising burden on CLAHRC time, and maximising learning.
Reviewing background information/CLAHRC documentation to assist in the scoping of CLAHRC ways of working and as inputs for data gathering at workshops/interviews (November 2009–end February 2010). Scoping the ways of working/logic models with each CLAHRC through meetings with each CLAHRC team and key informant interviews. These will be coordinated with other SDO-funded evaluation activities to minimize unnecessary burden. In terms of workshops, there will be 1 workshop at each CLAHRC to take place at the lead institution, and to involve approximately 5–6 representatives of different stakeholder groups and organisations within a CLAHRC (May 2010–September 2010).
Using meetings with CLAHRCs, their application forms, and CLAHRCs’ own developing documentation, we will model the logic(s) of intervention/ways of working for each CLAHRC. This will include describing the existing inputs, the processes (implementation plans) through which the second translation gap is to be addressed by the CLAHRC, and the expected outputs/outcomes from CLAHRC activity (September–November 2010).
We will then hold a national ‘learning’ event for CLAHRCs, SDO, other SDO-funded evaluation teams (involving also our Advisory group). We will disseminate and discuss our emerging findings, and identify questions which would benefit from further investigation (November 2010).
We will then meet with our Advisory group consider the significance of different intervention approaches and hold an initial discussion about which approaches to investigate further in phase two (November 2010).
Produce First Interim Report: identifying key models/ways of working, their significance, and the agenda for further evaluation in Phase Two (December 2010).
Quality Assurance on First Interim Report by two peer reviewers (December 2010).
PHASE II
In phase I, the RAND/HERG (Health Economics Research Group) team examined the CLAHRC landscape, and identified the various logics of intervention that different CLAHRCs are pursuing. CLAHRCs are each seeking to change the way research is done and the way the NHS uses research in commissioning, managing and delivering services. Our phase I work identified some similarities between the approaches of different CLAHRCs but also significant differences in areas such as operational approaches, disease focus, structures/governance approaches and stakeholder dynamics (as some examples). A range of interesting questions/themes around factors which are likely to influence CLAHRC evolution and performance emerged from our ‘landscape mapping’ in phase I.
In phase II we will explore some of these questions in more detail. The core questions to focus on were selected from the long list of questions, in consultation with our Advisory Board and some CLAHRCs (those who responded to our survey consultation). They were selected with the following criteria in mind:
-
be relatively under-researched (as identified through our literature review)
-
have a potentially high impact with transferable lessons
-
be relevant to the success of the CLAHRCs
-
not be covered by one of the three other evaluations (at least not as a central question)
-
be capable of being researched across more than one CLAHRC to support comparisons and contrasts.
In light of the above, we will be examining three interrelated aspects of CLAHRCs processes in more detail.
-
Core question: How does the NHS influence CLAHRCs evolution, outcomes and impact (and indeed how does having a CLAHRC influence NHS behaviour)? This requires examining and specifying the nature and extent of NHS involvement, including to what extent rhetoric matches reality.
-
Complementary question A: How are effective multi-stakeholder and multidisciplinary research and implementation teams for service improvement built: what can we learn from the CLAHRCs model, and what mechanisms are being used to enable it?
-
Complementary question B: What can we learn from the CLAHRCs that can cast new understanding on how to use research knowledge and evidence to change commissioning and clinical behaviour for patient benefit?
A number of assumptions related to our phase I findings are driving the questions above. These assumptions include:
-
High levels of NHS involvement underpin the CLAHRC ethos and theory of change.
-
Collaboration between multiple stakeholders in academic research and service provision can lead to service improvements and a better healthcare system. Important stakeholders in this respect include: academics; NHS executives; clinicians; senior, middle and front-line managers; patient and public representation groups; commissioners etc.
-
It is not enough to generate ‘good evidence’ for it to be adopted and lead to improved service. In addition to producing relevant and implementable research, a range of approaches and conducive infrastructures need to be in place for it to lead to service improvement.
Study design: we propose a four-step approach in phase II as illustrated in the figure below.
FIGURE 21.
Phase II study design.
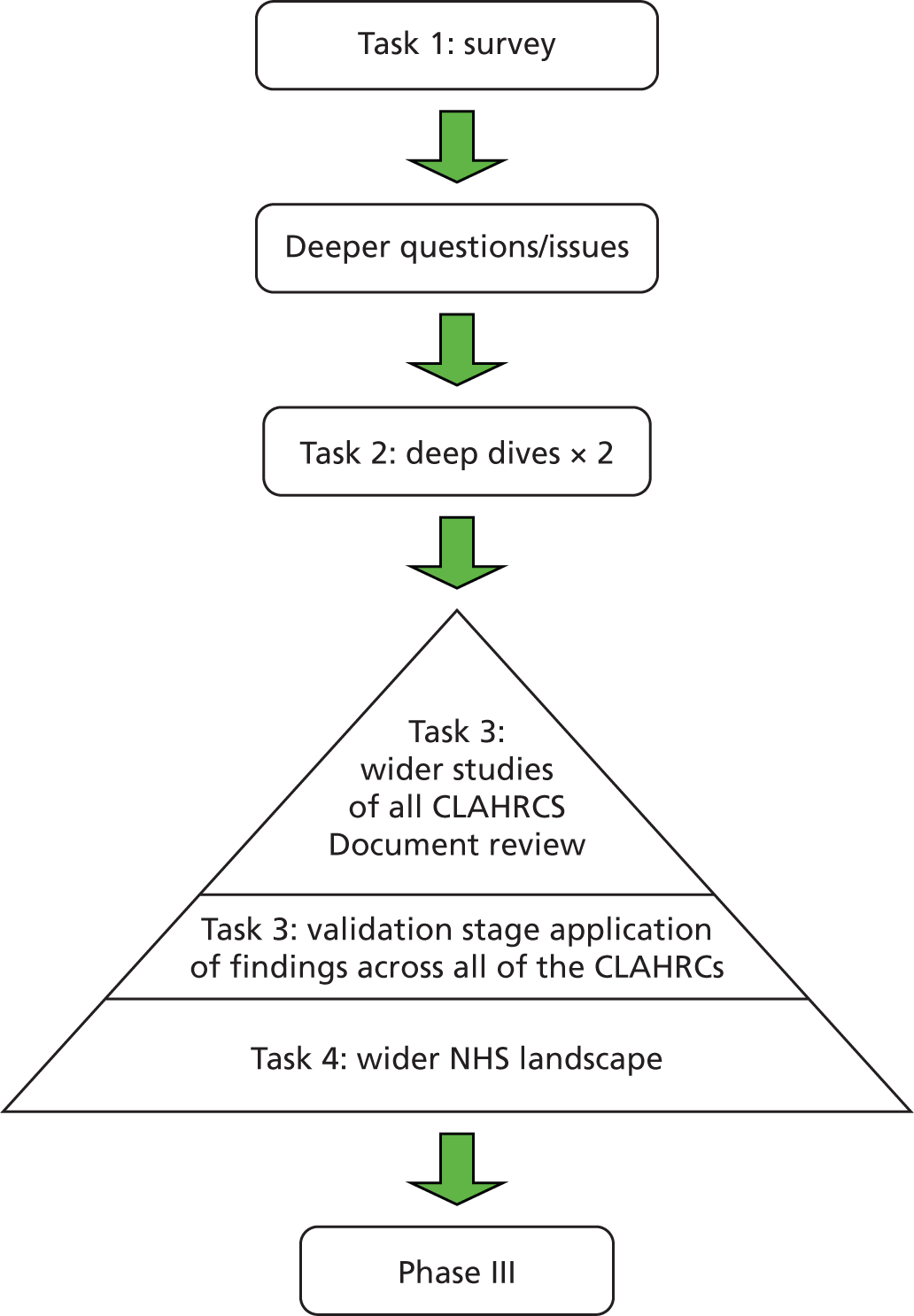
The section below provides more detail about each of the tasks to be undertaken in Phase II. We have also included indicative timescales for when we expect these tasks to be undertaken. Given the range of methodologies being used in this phase of the work, some of the components of these tasks will be carried out in parallel as reflected in the overlapping timelines given for some of these tasks. Should these timescales be required to be readjusted significantly due to delays associated with undertaking the online survey, we would seek approval from our funder (the SDO) and would duly notify the research ethics committee of these delays in our next progress report.
TASK 1: stakeholder survey across CLAHRCs (from April 2011 to February 2012)
In this phase we would design and conduct an online survey across all CLAHRCs who agree to participate and with different stakeholders in each. This survey would help generate insights about core issues related to our three questions (NHS involvement, multi-stakeholder research and implementation teams, and evidence adoption) across the CLAHRC landscape. We will investigate the interventions CLAHRCs are implementing as associated with all three questions; the contexts and variables that influence their actions; and the effects of the various interventions. We will do so in a way that can capture the multiple perspectives of different actors that constitute CLAHRCs: researchers, clinicians, NHS managers, commissioners, academic leadership, Trust executive leadership and patient/public representatives. Based on the insights that emerge from this survey, we would select specific ‘sites’ to dig deeper into through a case-study approach.
The key steps in task 1 include:
-
survey design
-
survey pilot
-
survey administration
-
survey results analysis
-
internal team analysis workshop
-
advisory board meeting.
In order to increase buy-in for the online survey, we envisage asking CLAHRC managers to send the link to the survey to relevant respondents. We would also seek to obtain an email/letter endorsed by the National Institute for Health Research to inform potential respondents about the importance of the survey for this research.
TASK 2: deep dives – interviews and workshop (from November 2011 to April 2012)
We will select 2 case-studies/sites exemplifying distinct types of interventions/combinations of interventions related to our research questions (likely to be two or maybe three sites). Site selection will be driven by the results of the CLAHRC survey and pragmatic concerns. Issues to consider include: focusing on sites which are addressing the questions we are researching in relatively novel, unexplored and/or promising ways; not overlapping with sites that other teams are researching (i.e. coordination).
The ‘deep dives’ would be implemented through a combination of document reviews (CLAHRCs own documents/grey literature); interviews (semi-structured, either face-to-face or telephone), and on-site workshops. The interviews will help refine the task 1 survey results by enriching earlier findings with more contextual data, and test the views/approaches of the selected CLAHRC against the perspectives of other CLAHRCs (based on survey results). The CLAHRCs documentation and interviews will set the scene for the workshops. The workshops would need to bring together representatives of multiple partners in a CLAHRC and attendants should come from different levels of the CLAHRC’s hierarchy. The workshops would focus on understanding the implicit assumptions and causal mechanisms at play in the CLAHRCs, as they relate to our research questions. They will focus not only on ‘the what’, but in depth on the how, why and ‘so what’/effects.
The key steps in task 2 include:
-
Deep dive site document reviews.
-
Interview template development.
-
Interview conduct.
-
Interview transcription.
-
Workshop preparation.
-
Workshop delivery.
-
Administration related to workshop organisation.
-
Analysis and synthesis of interview and workshop data.
-
Internal reflection and learning workshop.
-
A brief executive summary to use in soliciting validation interviews in task 3.
-
Advisory Board meeting.
TASK 3: validation stage (from June 2012 to December 2012)
The findings from our deep dives would be further enriched by a validation interview round with all (willing participant) CLAHRCs to test what emerged for transferability and generalizability, and to refine our insights further. We may also interview external stakeholders to get their views on our findings. In addition to interviews, this stage of the work will also include a review of all CLAHRCs’ relevant documentation to supplement our interview findings.
The key steps in task 3 include:
-
A review of relevant documents produced by all CLAHRCs.
-
Interview administration (soliciting participants).
-
Telephone validation interviews – template development.
-
Interview conduct.
-
Interview transcription.
-
Analysis of interviews.
-
Internal team workshop.
TASK 4 (led by HERG): the wider translational research and implementation landscape in the UK (and interpretation of phase II findings in this context)
In this task, we would produce a review of how CLAHRCs fit into the broader translational research and implementation landscape of the NIHR (and other funders) at present and how they relate to other initiatives. This is a complementary task and will actually be used in the final outputs of phase III. But if possible, we could explore whether and how phase II findings relate to the wider translational research landscape context, and what they imply for it. It may be possible to include some comparative analysis between CLAHRC and non-CLAHRC sites into this.
Outputs of phase II
The results of phase two would be communicated through:
-
Participation at SDO learning events.
-
Phase II interim report (submitted in May 2012).
PHASE III
The third phase will explore the implications of our findings for improving current policy and practice in the establishment of ‘beneficial forward-looking partnerships between universities and their surrounding NHS organisations’, including contributions to increase the capacity of NHS organisations to engage with and apply research (‘absorptive capacity’) and to encourage the effective involvement of patients and the public. We will demonstrate how this adds to, challenges, or reinforces existing international research. Throughout we will seek to work interactively with CLAHRCs to support learning. We will write a Final Report and a short Briefing Document, and will conduct a series of meetings to discuss our findings with policy-makers, relevant academics, NHS practitioners and managers, and representatives from patient and public associations. These interactions will be conducted in liaison with SDO. We will hold a final workshop with all CLAHRCs and the SDO to discuss our findings. We will also prepare papers and presentations for peer reviewed journals and conferences, and prepare and present policy-oriented briefings for the Department of Health and organisations such as the Nuffield Trust, funder-oriented material for the funders of medical research (such as NIHR, Wellcome, MRC, The Health Foundation, medical research charities), and management-oriented material for forums such as The NHS Confederation.
The core methods to be used in phase III include workshops and interviews with stakeholders, and triangulation of evidence from previous work packages and the literature. More details on different components and timelines for phase III are provided below. (These timelines are currently based on our original timelines for Phase II and could be subject to changes should the tasks in Phase II be delayed by the process of gaining further ethical approval for this study.)
Preparing and writing Final Report and Briefing Document (June–November 2012).
Quality Assurance on Final Report and Briefing Document by two peer reviewers (November 2012).
Final meeting with Advisory Group to discuss findings and dissemination strategy (October 2012).
Preparing and presenting articles for peer reviewed journals/conferences (June–December 2012).
Presenting findings to policy-makers and policy-researchers (DH, NHS Confederation, Nuffield Trust, Health research charities etc.) (May–July 2013).
Workshop with CLAHRCs and SDO to discuss findings (August–November 2012).
Presentation of final report and budget to SDO (December 2012).
Collaborating with SDO in overall presentation of findings from across the evaluation (August–December 2012).
Appendix 2 Phase 1 interview topic guide
The first phase of the project is to identify and assess the strategies CLAHRCs are developing, teasing out the (perhaps implicit) causal pathways being explicitly used or implicitly assumed. We also wish to understand how CLAHRCs understand the contexts in which they are working, and what they see the enabling and barrier factors in these contexts to be. We would also like to explore any interplay between distinct strategies being adopted in CLAHRCs, where these are being implemented in combination or in parallel. For example, are they developing a portfolio of activities that are only loosely related under the umbrella of the CLAHRC, or is the package of activities selected in order to get some value added by doing them together?
Interview guidance
-
What attracted you to the idea of becoming a CLAHRC?/Why did you choose to become involved?
-
What are your core objectives and implementation activities, and how do you think these specific activities will lead to the realisation of objectives? Can you please clarify your implementation strategy (note: we need to understand in director’s terms what they will actually be doing so we have guidance for the taxonomy) and how this may have changed since proposal/application phases?
-
How has the portfolio of activities been selected?/How will it be selected? What do you think is the added value of doing all of these simultaneously? Or is the CLAHRC more of a helpful umbrella for establishing a bundle of activities that are only loosely related?
-
If the CLAHRC was successful, how would things be different in, say 3, 5 or 10 years’ time?
-
Do you think that there are any local factors that will help you to succeed? And are there local barriers to overcome?
-
What are the national factors that will help/be barriers to achieving your CLAHRC’s objectives?
-
What do you expect to be the main contributions of your CLAHRC? Why do you think they will succeed?
Appendix 3 Phase 1 workshop outline
| Activity | Timing (estimates) |
|---|---|
| Welcome and outline of the workshop | 10 minutes |
| Warm-up discussion (issues to be covered include what participants find most exciting about working with the CLAHRC, intended outcomes of the CLAHRCs, opportunities, etc.) | 1 hour 20 minutes |
| Mapping the activities of the CLAHRC | |
| Break | 15 minutes |
| Exploring innovative ways of delivering the CLAHRC’s activities as well as facilitators and challenges/barriers to their success | 1 hour 40 minutes |
| Discussion about intended outcomes, early and future impacts | |
| Discussion on what could be done differently to improve the CLAHRC’s performance and input into what would be most helpful for the evaluation team to look at in the coming year | |
| Workshop closes | 5 minutes |
Appendix 4 CLAHRC survey questions
RAND Europe/HERG – national CLAHRC evaluation – online survey
Introduction
Thank you for agreeing to complete this survey, the survey will remain open until Tuesday, October 25th, 2011.
It is part of a wider evaluation of the CLAHRCs funded by the Department of Health’s Service Delivery Programme. Information resulting from this survey is likely to be beneficial in informing how your CLAHRC evolves looking forward. It will also help us understand the evolution of activities across all the CLAHRCs. The questions were arrived at as a result of our initial appraisal of the issues facing the CLAHRCs and also reflect our current evaluation focus.
Aggregate results and fully anonymised results for the initiative (i.e. findings across all of the CLAHRCs completing the survey) will be freely available to all participants. The responses of individuals completing this survey will not be accessed by anyone outside the RAND Europe/HERG research team.
The survey should take 15 to 20 minutes to complete. Many thanks in advance for your participation,
Tom Ling,
Chief investigator on behalf of the RAND Europe/HERG evaluation team.
Should you require any further information, please contact the evaluation team on clahrcevaluation@rand.org.
Survey questions
-
With which CLAHRC are you involved?
-
NIHR CLAHRC for Birmingham and the Black Country
-
NIHR CLAHRC for Cambridgeshire and Peterborough
-
NIHR CLAHRC for Greater Manchester
-
NIHR CLAHRC for Leeds, York and Bradford
-
NIHRC CLAHRC for Leicestershire, Northamptonshire and Rutland
-
NIHR CLAHRC for North West London
-
NIHR CLAHRC for Nottinghamshire
-
NIHR CLAHRC for South West Peninsula
-
NIHR CLAHRC for South Yorkshire
-
-
What is your job title within your CLAHRC?
-
Director of the CLAHRC
-
Manager of the CLAHRC
-
Member of the CLAHRC Board Theme lead
-
Project team member
-
Advisor
-
Other, please specify:
-
-
Where do you work most of the time?
-
In the NHS
-
In academia
-
Other, please specify:
-
-
What were your motivations for getting involved in your CLAHRC?
Please select all that apply.
-
To encourage the pursuit of research relevant practice
-
To improve clinical effectiveness by better applying existing research
-
To access financial support for pursuing my research interests
-
To spend more time on applied research
-
To get a better understanding of health service needs
-
To get a better understanding of how academic research can improve service delivery
-
To better understand the needs and interests of individuals from other organisations and/or disciplines
-
I was looking for a post/job and this became available
-
Other, please specify:
-
Building teams for service improvement
Aims of your CLAHRC
-
In your view, what is your CLAHRC aiming to achieve in relation to integrating NHS staff with research activities?
Please score each option on a scale of 1 to 5 where 1 is ‘not trying to achieve’ and 5 is ‘definitely trying to achieve’.
-
Foster a stronger culture of collaboration between the academic and service delivery sector
-
Increase and integrate capacity for doing, translating and using applied health research and evidence in service delivery across the NHS
-
Stimulate interest in applied research in universities
-
Raise awareness of applied research among clinical staff
-
Involve commissioners and NHS managers in identifying research questions, addressing them and implementing results
-
Other
-
-
If you indicated ‘other’ in the previous question, please specify below:
-
What do you think the sharing of knowledge and information across your CLAHRC and its relevant stakeholders aims to achieve?
Please score each option on a scale of 1 to 5 where 1 is ‘not trying to achieve’ and 5 is ‘definitely trying to achieve’.
-
Encourage the use of locally produced technologies, new processes or innovation in local clinical practice
-
Encourage the use of locally produced technologies in wider clinical practice
-
Contribute to the effective communication and dissemination of knowledge
-
Contribute to peer-reviewed publications
-
Contribute to the public and patients being better informed about health research and the possible benefits from health research
-
Other
-
-
If you indicated ‘other’ in the previous question, please specify below:
-
In your view, what is your CLAHRC aiming to achieve in relation to building the capacity of the NHS to carry out evidence-based service improvement?
Please score each option on a scale of 1 to 5 where 1 is ‘not trying to achieve’ and 5 is ‘definitely trying to achieve’.
-
Contribute to building a more needs-driven system with input from the NHS at the start of research projects
-
Establish new evidence to improve the working of the local health system
-
Make better use of existing evidence about care to improve service delivery
-
Increase the number of research aware individuals in the NHS
-
Empower front-line staff to engage and deliver service improvements
-
Decrease time lags between research, translation and adoption
-
Build NHS capacity to evaluate its own performance in using research and influencing the direction of research
-
Other
-
-
If you indicated ‘other’ in the previous question, please specify below:
-
In your view, what is your CLAHRC aiming to achieve in relation to longer term outcomes and impacts?
Please score each option on a scale of 1 to 5 where 1 is ‘not trying to achieve’ and 5 is ‘definitely trying to achieve’.
-
Improve health services and patient outcomes
-
Improve patient self-management and healthcare provision
-
Improve NHS responsiveness to the needs of individual patients
-
Reduce inequalities in patients’ access to care
-
Produce more public and patient-needs focused research
-
Create a sustainable research infrastructure focused on the needs of the health service and patients
-
Build up new capacity and new blends of skills (e.g. CLAHRC fellows with both research and implementation skills)
-
Other
-
-
If you indicated ‘other’ in the previous question, please specify below:
-
To what extent do you personally agree or disagree with the aims of your CLAHRC?
-
Fully agree
-
Moderately agree
-
Neither agree nor disagree
-
Moderately disagree
-
Strongly disagree
-
-
Has your confidence in the ability of your CLAHRC to deliver its aims grown or reduced over time?
-
Grown over time
-
Stayed the same
-
Reduced over time
-
-
Have you become more or less involved in your CLAHRC since you first participated?
-
More involved over time
-
Same involvement over time
-
Less involved over time
-
Impact of your CLAHRC on working practices
-
In your view, to what extent is the experience of working within your CLAHRC different from working outside it?
-
Very different
-
Moderately different
-
Somewhat different
-
Not at all different
-
-
In what ways is your experience of working within your CLAHRC different from working outside it?
Select as many options as applicable.
-
I communicate with people from other disciplines
-
I think about challenges in my work from different perspectives
-
I am developing new research skills
-
I am developing new management skills
-
I am developing new communication skills
-
I experience more pressure to work longer hours
-
Other, please specify:
-
-
Would you say that being involved in your CLAHRC has influenced the way you work outside your CLAHRC as well?
-
Yes
-
No
-
Don’t know
-
Not applicable, I work full time for the CLAHRC
-
Ongoing support for your CLAHRC
-
Overall, to what extent do you feel your CLAHRC is being supported by its senior leadership (i.e. CLAHRC board, CLAHRC director, CLAHRC manager and theme leads)?
-
Supported fully
-
Supported moderately
-
Supported weakly
-
Not supported
-
Don’t know
-
-
To what extent do you feel the following resources are adequate to your CLAHRC’s delivery of its activities? (Very adequate, Moderately adequate, Somewhat adequate, Not adequate, Don’t know)
-
Existing physical infrastructure
-
Existing relationships and networks
-
Administrative support
-
Management support
-
Human resources (i.e. staff)
-
Financial resources to do research
-
Expertise and skills in undertaking research
-
Expertise and skills in the implementation of research
-
Other resources
-
Overall resources
-
Communication, dissemination and learning
Information about your CLAHRC’s activities: Learning, linkage and exchange
Communication within your CLAHRC
-
In your experience, is information about your CLAHRC activities and projects communicated well within your CLAHRC?
-
Yes
-
No
-
Don’t know
-
-
What type of information is communicated well within your CLAHRC?
-
General information about the CLAHRC
-
Specific information about the CLAHRC’s activities
-
Information on CLAHRC progress and achievements
-
Information on different projects/topics
-
Information on publications coming out of CLAHRC activity
-
Information on forthcoming events
-
Information on press coverage
-
Information on recruitment
-
Information on CLAHRC’s members/staff
-
Other, please specify:
-
-
From your personal experience, what are the three means through which information is most often communicated and disseminated within your CLAHRC?
Select no more than 3.
-
CLAHRC website
-
Email distribution of newsletter
-
Presentations by CLAHRC representatives
-
Press releases
-
Publications
-
Word of mouth
-
Formal meetings
-
Informal discussions/opportunistically
-
Workshops
-
Other, please specify:
-
-
In your view, what is the impact of disseminating the information within your CLAHRC?
Please tick all options that apply.
-
Raise awareness of CLAHRC activities
-
Lead to more collaboration and joint-working within the CLAHRC
-
Improve buy-in from those involved in the CLAHRC
-
Help build a collaborative networked CLAHRC community
-
Other, please specify:
-
-
To what extent is the information you receive about your CLAHRC’s activities and projects influential towards your behaviour and ways of working?
-
Very influential
-
Moderately influential
-
Somewhat influential
-
Not influential at all
-
-
Please specify why you feel the information you receive about your CLAHRC’s activities and projects do not influence your behaviour and ways of working?
Please tick all options that apply.
-
The research undertaken by the CLAHRC is not relevant to my field
-
The research undertaken by the CLAHRC is not easily applicable
-
Limited opportunities to put research into practice and act on information in my job/organisation
-
CLAHRC activities and projects are carried out in the same way as previous activities and projects I have been involved in
-
Time constraints and/or competing priorities
-
Other, please specify:
-
-
Please specify why you feel the information you receive about your CLAHRC’s activities and projects influence your behaviour and ways of working?
Please tick all options that apply.
-
The research undertaken by the CLAHRC is relevant to my field
-
The research undertaken by the CLAHRC is easily applicable
-
There are opportunities to act on the information I receive in practice
-
CLAHRC activities and projects are carried out differently from previous activities and projects I’ve been involved in, but the information I receive is very important for the success of my work
-
Other, please specify:
-
Communication outside your CLAHRC
-
In your experience, is information related to CLAHRC activities and projects well communicated outside your CLAHRC?
-
Yes
-
No
-
Don’t know
-
-
Who are the current target audiences for this information?
Please check all the options that are applicable.
-
Commissioners
-
Funders
-
Policy makers
-
Clinicians and other front-line staff (not part of your CLAHRC at present)
-
The general public
-
Patients
-
Other NHS Trusts than those involved in the CLAHRC
-
Other academic institutions than those involved in the CLAHRC
-
Other, please specify:
-
-
For the following type of information communicated outside your CLAHRC, please indicate how effectively you think it is being communicated: (Very effectively, Moderately effectively, Somewhat effectively, Not effectively, Not communicated at all, Don’t know)
Please check all options that are applicable.
-
General information about the CLAHRC
-
Specific information about the CLAHRC’s activities
-
Information on CLAHRC progress and achievements
-
Information on different projects/topics
-
Information on publications coming out of CLAHRC activity
-
Information on events
-
Information on press coverage
-
Information on recruitment
-
Information on CLAHRC members/staff
-
-
From your personal experience, what are the three means through which information is most often communicated and disseminated outside your CLAHRC?
Select no more than 3.
-
CLAHRC website
-
Email distribution of newsletter
-
Presentations by CLAHRC representatives
-
Press releases
-
Publications
-
Word of mouth
-
Formal meetings
-
Informal discussions/opportunistically
-
Meetings
-
Workshops
-
Other, please specify:
-
-
In your view, what is the impact of disseminating the information outside your CLAHRC?
Please tick all the options that apply.
-
Raise awareness of CLAHRC activities
-
Lead to faster implementation of CLAHRC findings into practice
-
Attract further funding for CLAHRC activities and projects
-
Improve buy-in from those involved in the CLAHRC
-
Help build a collaborative networked CLAHRC community
-
Other, please specify:
-
-
Do you think your CLAHRC will lead to changes in practice/will influence NHS behaviour?
-
Yes
-
No
-
Don’t know
-
-
Please provide a brief explanation below for why you think your CLAHRC will lead to changes in practice and in the NHS or not.
-
In your view, how effectively does your CLAHRC take into account the views and concerns of its stakeholders in the day-to-day delivery of its activities? (Very effectively, Moderately effectively, Somewhat effectively, Not effectively, Don’t know)
-
The public
-
Patients targeted by CLAHRC activities
-
Patients more generally
-
Commissioners
-
Clinicians
-
Other stakeholders
-
NHS involvement in your CLAHRC
-
In your view, to what extent are relevant people within your CLAHRC’s local NHS and university actively involved in your CLAHRC? (Very involved, Moderately involved, Somewhat involved, Not involved, Don’t know)
-
NHS senior management staff (chief executives, Trust board members)
-
NHS middle management staff including commissioners
-
Senior clinicians (hospital consultants, senior nursing staff, GPs)
-
Junior clinicians (trainee doctors, etc.)
-
Other health professionals (physiotherapists, pharmacists, etc.)
-
Public and patient representatives
-
Senior academic staff
-
Junior academic staff
-
Other individuals in local NHS or university
-
-
In your view, what are the reasons why you feel the relevant people within your CLAHRC’s local NHS are not actively involved in your CLAHRC?
Please tick all the options that are applicable.
-
Not applicable, I did not select options indicating that relevant people within my CLAHRC’s local NHS are ‘not involved’ previously
-
CLAHRC too focused on traditional research rather than applied research and implementation or CLAHRC research not relevant to NHS needs
-
Not enough time for NHS staff to get involved
-
Not enough interest from NHS staff to get involved in the CLAHRC
-
Not enough interest from the CLAHRC to involve NHS staff in its activities
-
Incentive structure for NHS staff is not conducive to the NHS being involved in its activities
-
NHS staff are unsure of how to get involved in the CLAHRC
-
Other, please specify
-
-
In your view, what are the reasons why you feel the relevant people within your CLAHRC’s local NHS are actively involved in your CLAHRC?
Please tick all the options that are applicable.
-
Not applicable, I did not select options indicating that relevant people within my CLAHRC’s local NHS and university are ‘very involved’, ‘moderately involved’ or ‘somewhat involved’ previously.
-
PhD/Postdocs/MScs funded by the CLAHRC
-
CLAHRC fellowship schemes for NHS managers to aid communication and understanding in the service
-
PhD studentships in applied health research
-
Provision of central administrative and management support
-
NHS representatives sit on CLAHRC Board
-
NHS members work with academic researchers in project teams
-
NHS members attend CLAHRC meetings/seminars/other events
-
NHS members solicit research projects based on NHS needs
-
NHS members consult academic researchers about research evidence
-
NHS members comment on research outputs
-
NHS members communicate CLAHRC’s activity to health policy makers
-
Other, please specify:
-
-
In your view, to what extent are different groups within your local NHS and university influential in shaping your CLAHRC’s strategy, decisions, activities and choice of outputs? (Very influential, Moderately influential, Somewhat influential, Not influential, Don’t know)
-
Senior NHS management (Chief executives, Trust Board members)
-
Middle NHS management including commissioners
-
Senior NHS clinicians (hospital consultants, senior nursing staff, GPs)
-
Junior NHS clinicians (trainee doctors, etc.)
-
Other health professionals (physiotherapists, pharmacists, etc.)
-
Public and patient representatives
-
Senior academic staff
-
Junior academic staff
-
Other individuals in local NHS or university
-
-
In your view, what are the reasons why you feel the NHS is currently influential in shaping your CLAHRC’s activities?
Please tick all the options that are applicable.
-
Not applicable, I did not select options indicating that my local NHS was ‘very influential’, ‘moderately influential’ or ‘somewhat influential’ previously.
-
Involvement of commissioners in research design
-
Involvement of commissioners in research implementation
-
Involvement of clinicians in research design
-
Involvement of clinicians in research implementation
-
NHS well represented (across different professional groupings and levels of seniority)
-
NHS is very actively engaged with CLAHRC activities and has the needed skills and experience to contribute and influence
-
Senior NHS members are well respected by academic members of the CLAHRC
-
Long standing relationship between academic and NHS members of the CLAHRC
-
Other, please specify:
-
-
If you feel that the NHS is not influential in shaping your CLAHRC’s activities, why do you think that is?
-
Not applicable, I did not select options indicating that my local NHS was ‘not influential’ previously.
-
Academics more represented than NHS staff in the CLAHRC
-
Lack of buy-in from Chief Executives/senior NHS leadership
-
Other, please specify:
-
The wider context: enablers and challenges
-
In your view, which elements of your CLAHRC and wider landscape are enabling it to meet its objectives?
Please select all the options that apply.
-
Good buy-in from key individuals who have the ability to make things happen
-
Funding availability
-
Good motivation and commitment of individuals working in the CLAHRC
-
Supportive infrastructure (i.e. physical buildings, materials for doing research, IT systems, etc.)
-
Appropriate incentive structure for individuals and organisations taking part in the CLAHRC
-
Enabling national policy and developments
-
Enabling local and/or regional policy and developments
-
Good pre-existing networks and relationships between partner organisations and individuals involved
-
Well-developed existing research and evidence-base
-
Appropriate skills and expertise of those involved
-
Other, please specify:
-
-
In your view, which elements of your CLAHRC and wider landscape are barriers to meeting its objectives?
Please select all the options that apply.
-
Poor buy-in from key individuals who have the ability to make things happen
-
Inadequate funding
-
Lack of motivation and commitment of individuals working in the CLAHRC
-
Inadequate infrastructure (i.e. physical buildings, material for doing research, IT systems, etc.)
-
Inappropriate incentive structure for individuals and organisations taking part in the CLAHRC (e.g. focus on Research Excellence Framework criteria for university researchers)
-
Unsupportive national policy and developments
-
Unsupportive local and/or regional policy and developments
-
Poor pre-existing networks and relationships between partner organisations and individuals involved
-
Gaps in existing research and evidence base/underdeveloped base for CLAHRC
-
Inadequate skills and expertise of those involved
-
Not enough NHS involvement at the time of deciding on research projects
-
Lack of understanding that implementation can work in the NHS as it does in other fields
-
Other, please specify:
-
Closing questions
-
Please let us know if you have any further comments about the survey or your CLAHRC in particular:
-
If you are willing to be contacted about your responses, please let us know by providing your contact details below:
Email address:
Telephone number:
Many thanks for taking the time to fill in this survey.
Appendix 5 CLAHRC survey results
We here present further findings from the survey across six CLAHRCs, disaggregated where relevant to distinguish between respondents from academia and the NHS. Six of the CLAHRCs agreed to participate, which were as follows: CLAHRC-CP; Leeds, York and Bradford; Northwest London; PenCLAHRC; Nottinghamshire, Derbyshire and Lincolnshire; and Leicestershire, Northamptonshire and Rutland. Survey findings are provided in the order of questions in the online survey.
FIGURE 22.
Respondents by CLAHRC affiliation.
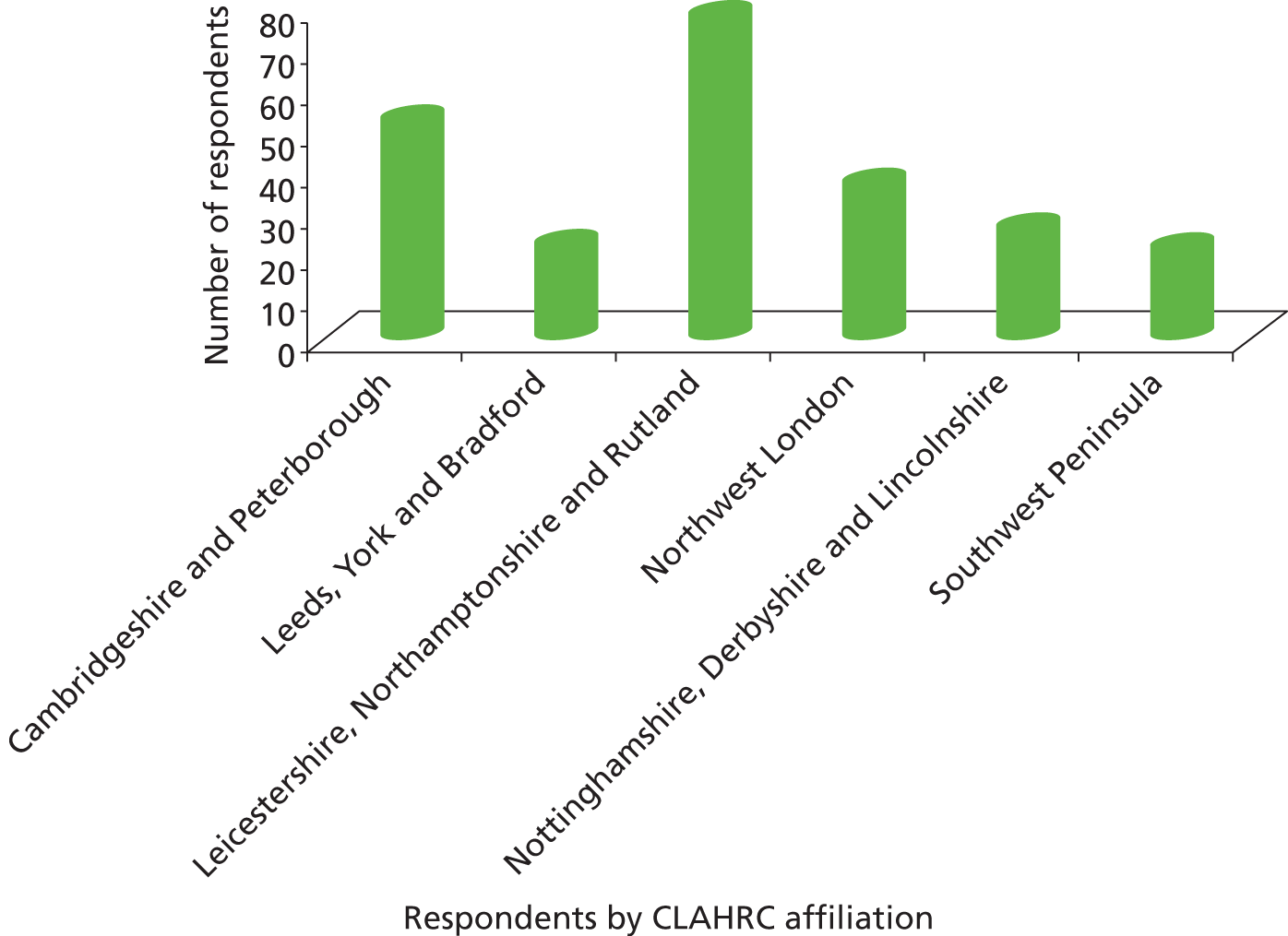
FIGURE 23.
Motivation for getting involved in CLAHRC.
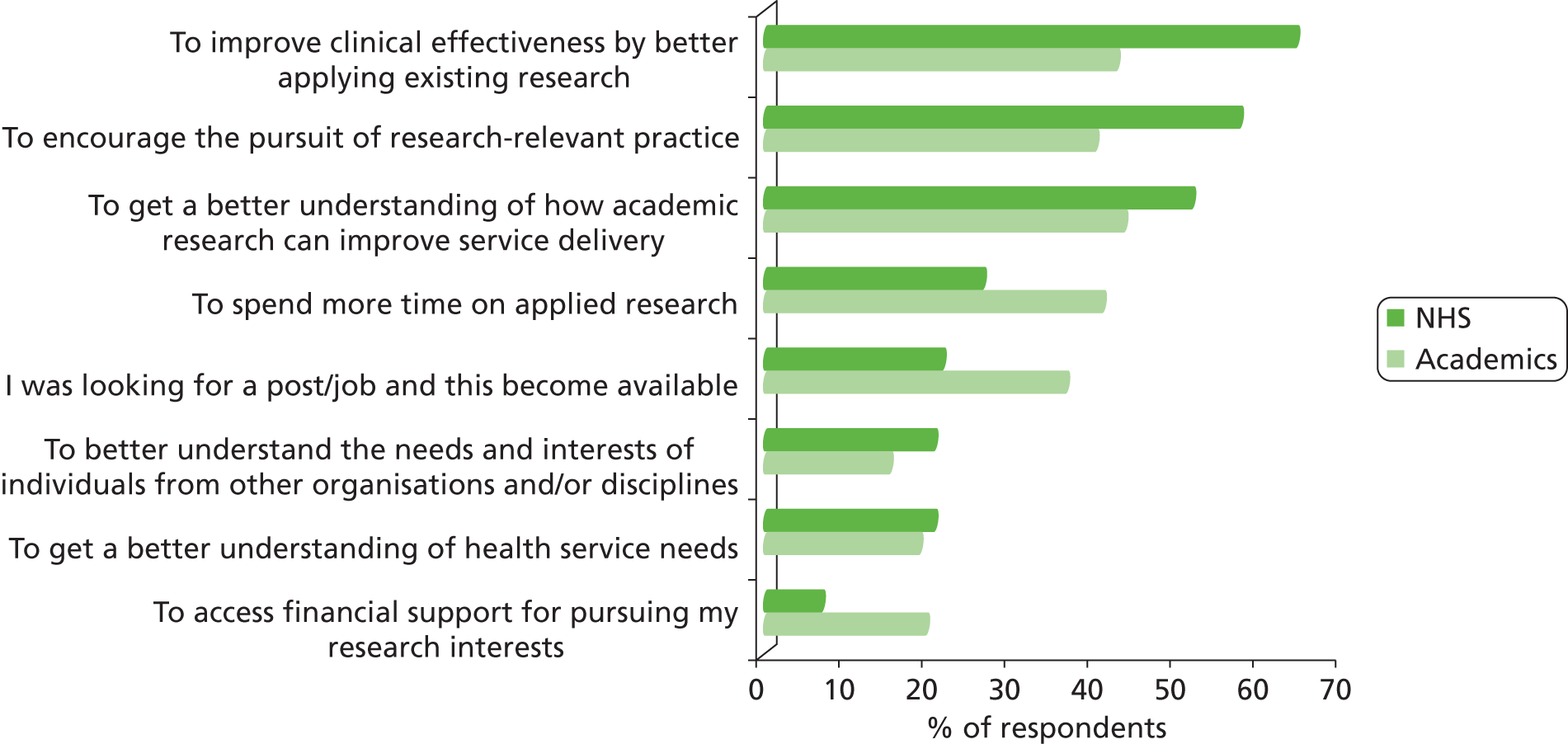
FIGURE 24.
Perceived aims in relation to integrating NHS staff with research activities.
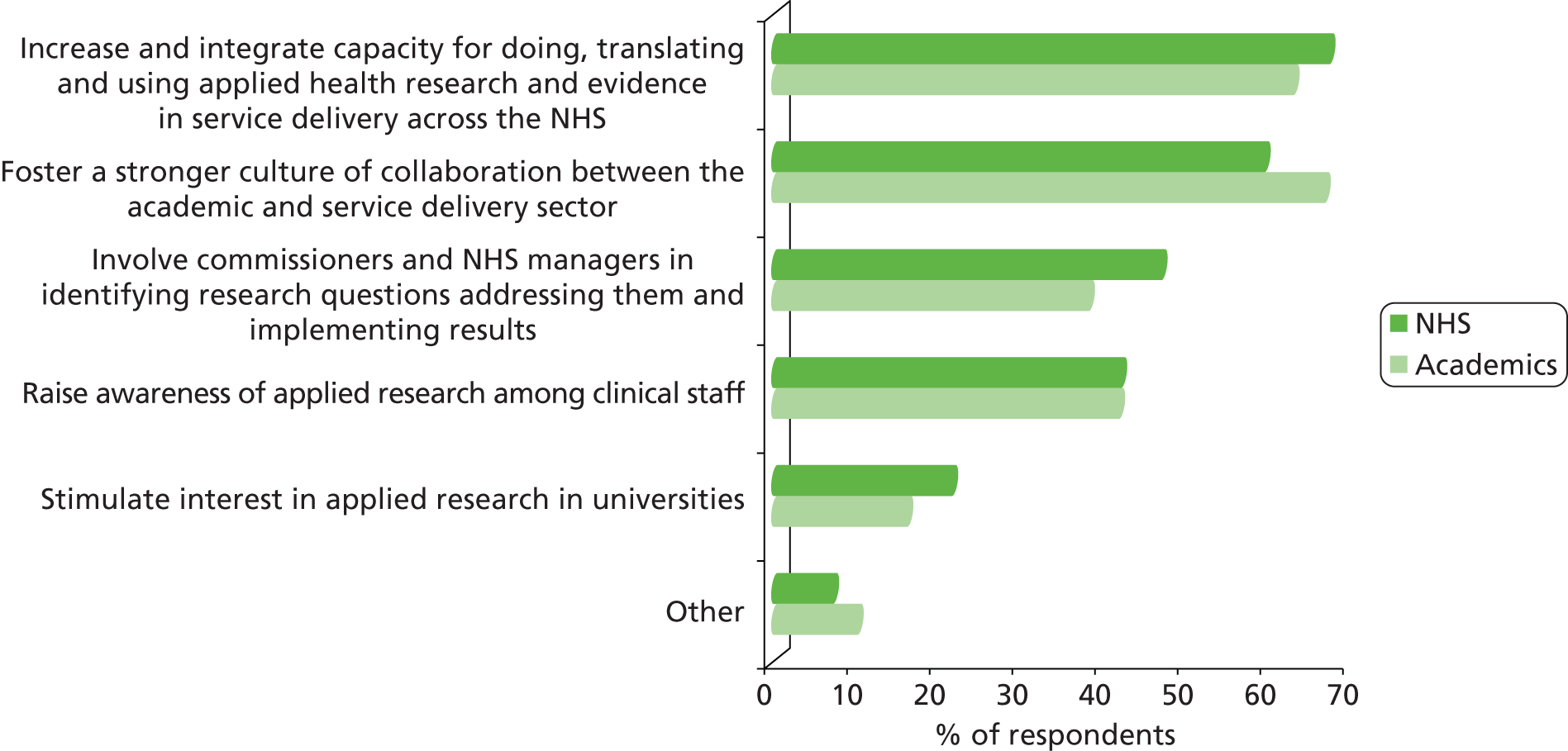
FIGURE 25.
Perceived aims of sharing of knowledge and information across CLAHRC.
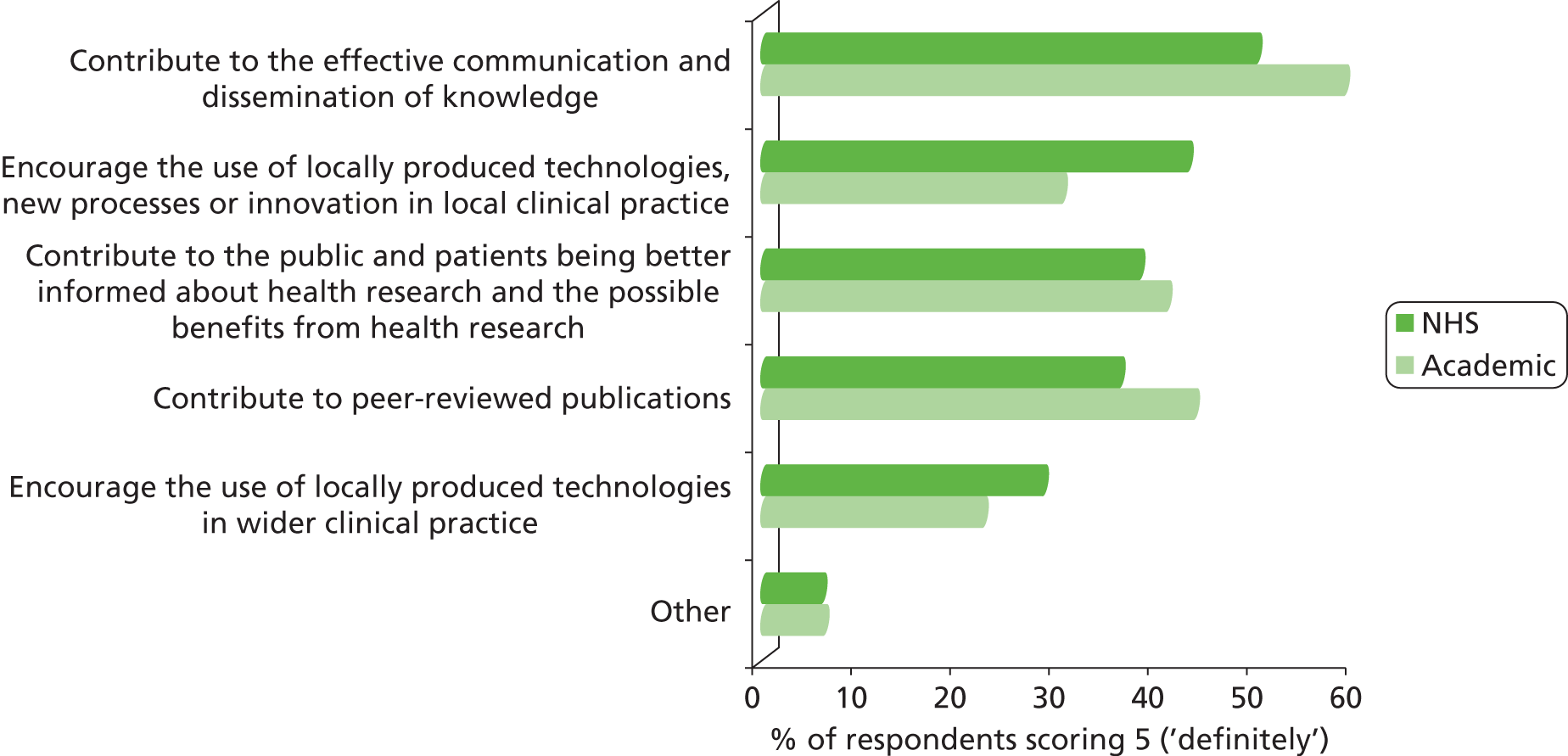
FIGURE 26.
Perceived aims in relation to building NHS capacity of the NHS for evidence-based service improvement.
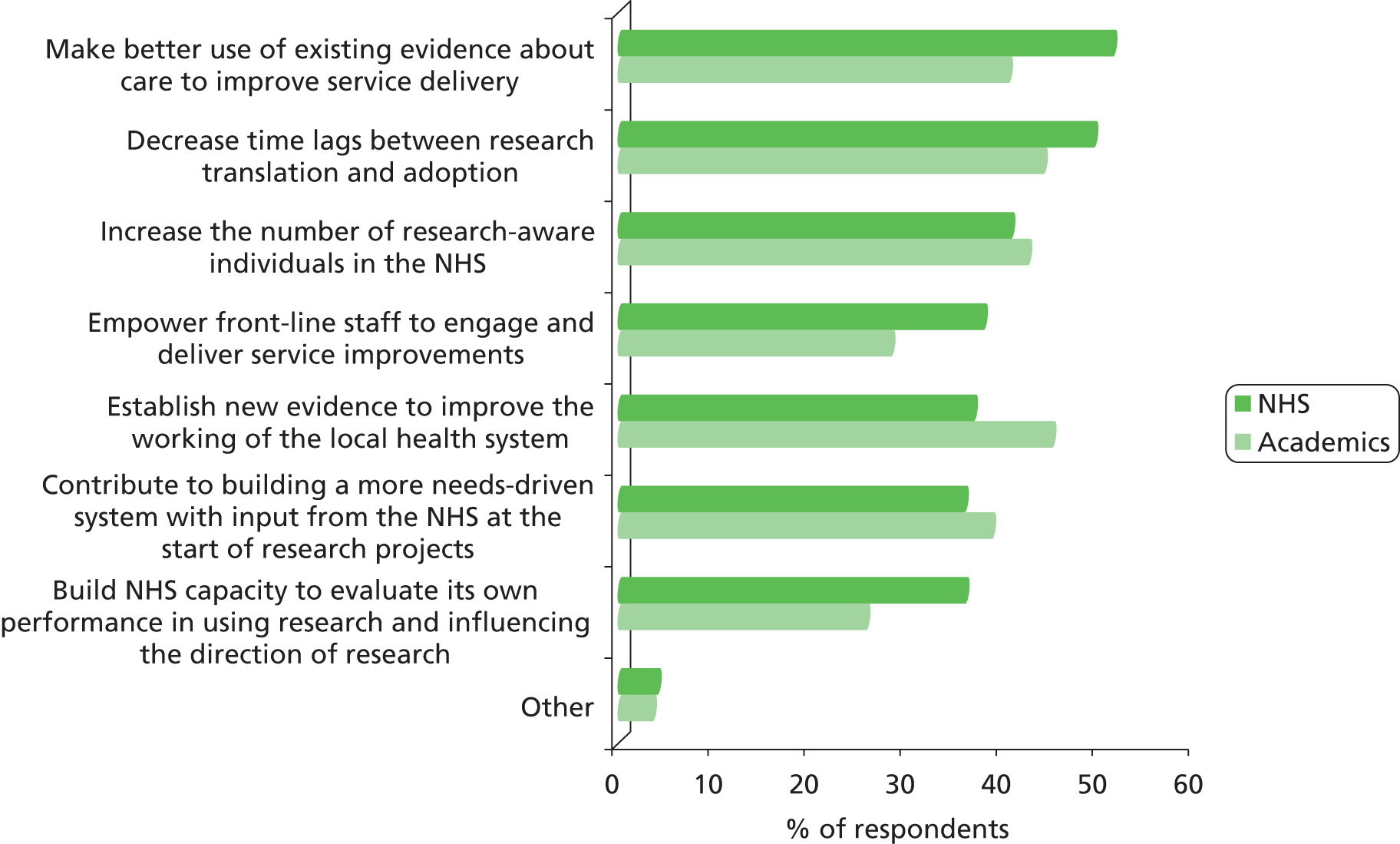
FIGURE 27.
Perceived aims in relation to longer-term outcomes and impacts.
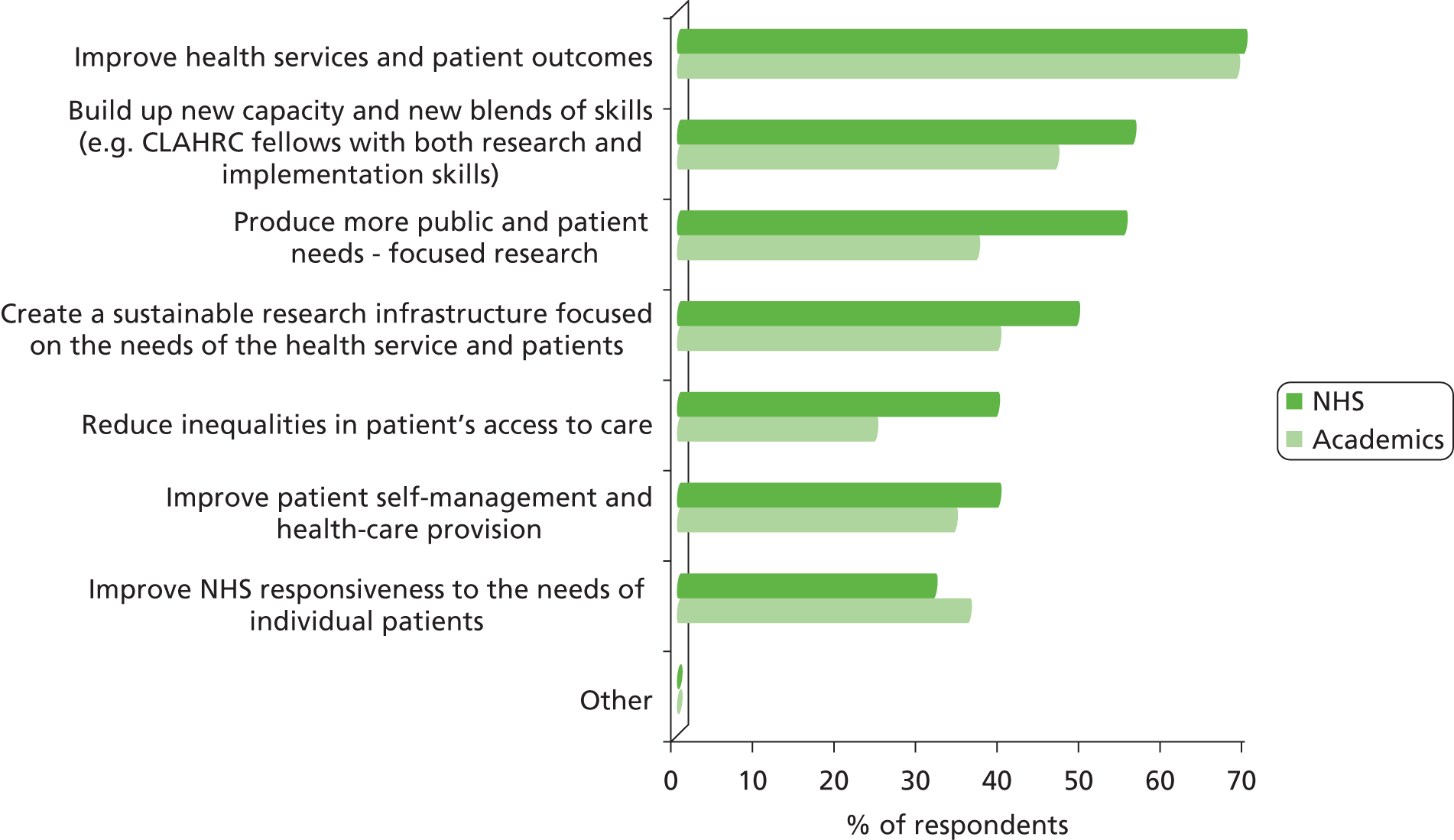
FIGURE 28.
Level of agreement with the aims of CLAHRC.
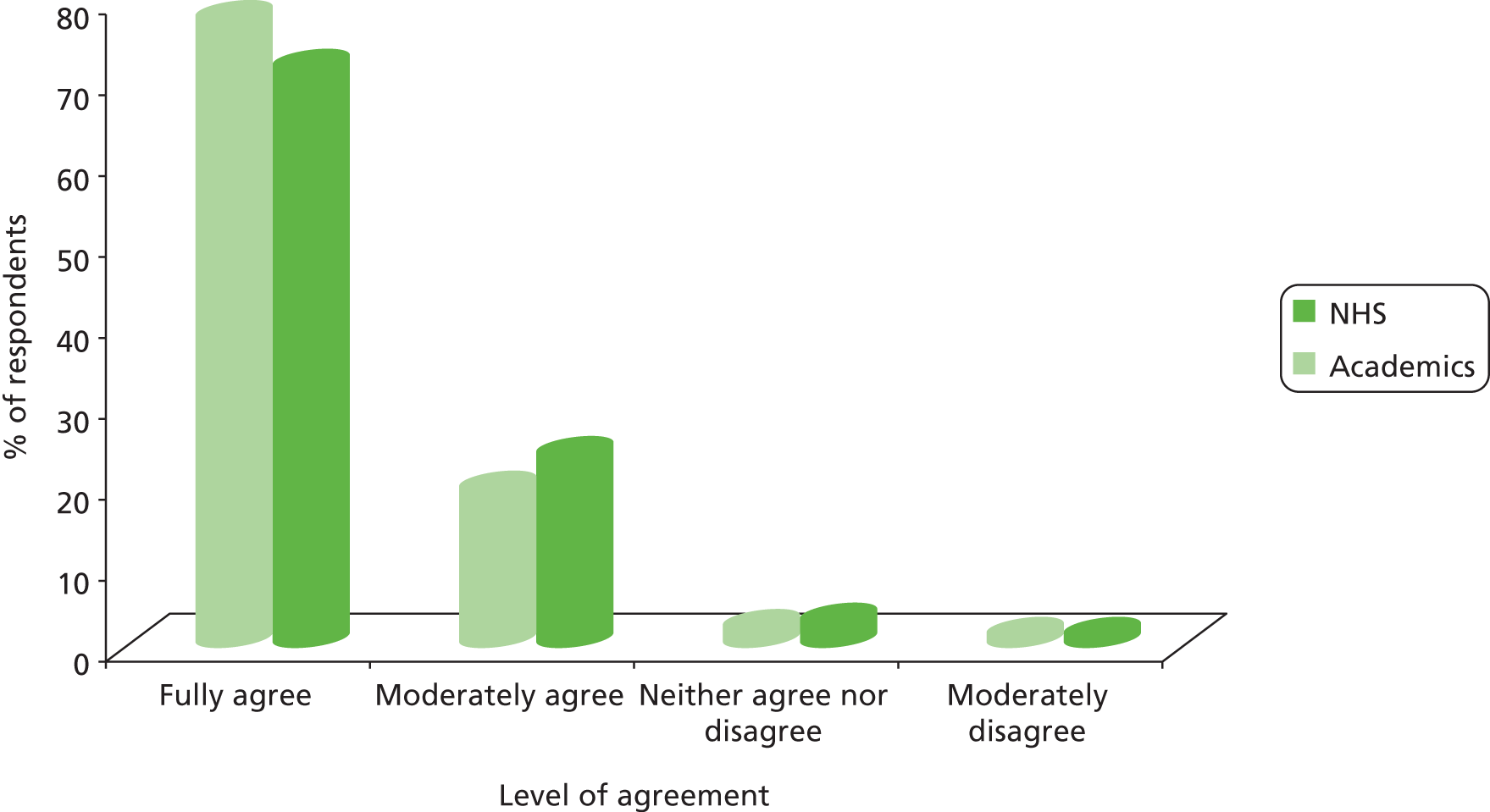
FIGURE 29.
Reported change in confidence in the ability of CLAHRC to deliver its aims.
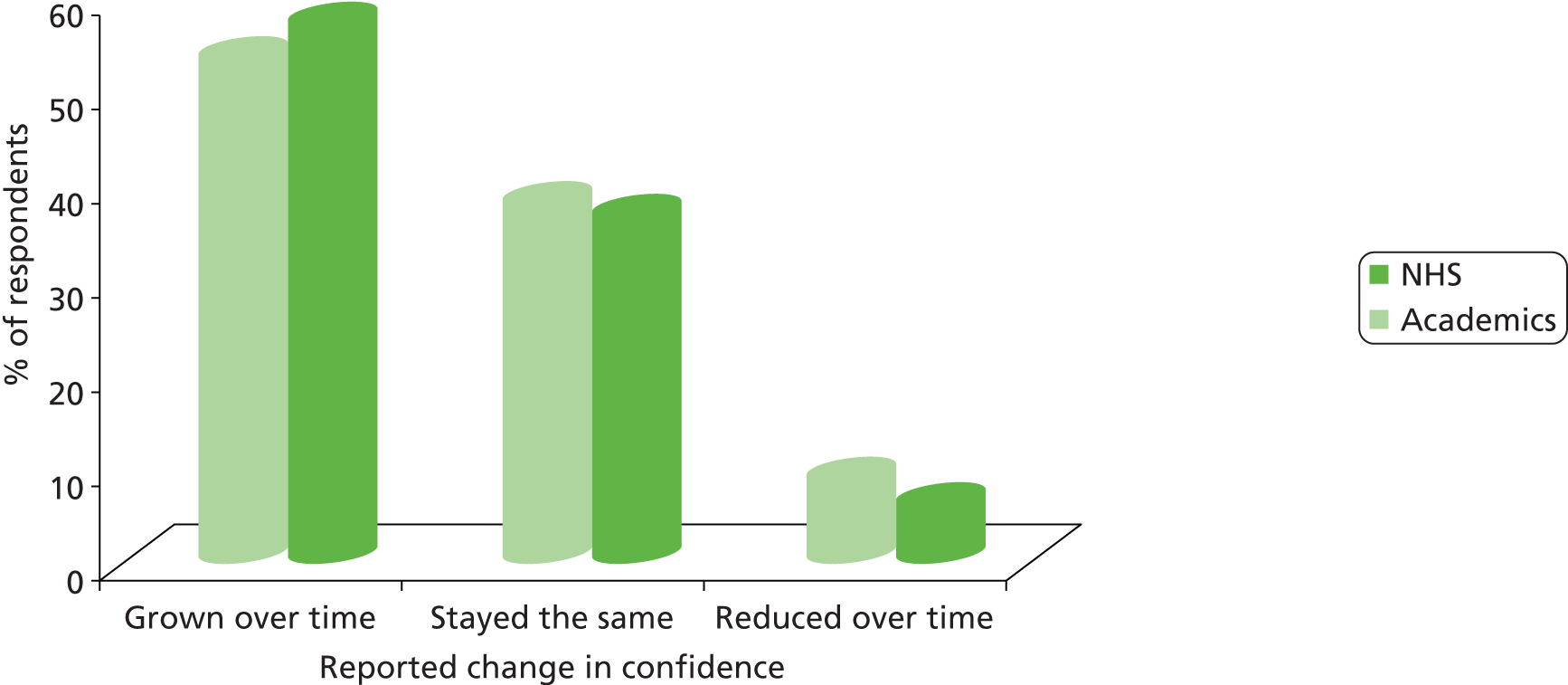
FIGURE 30.
Reported level of involvement in CLAHRC since first participation.
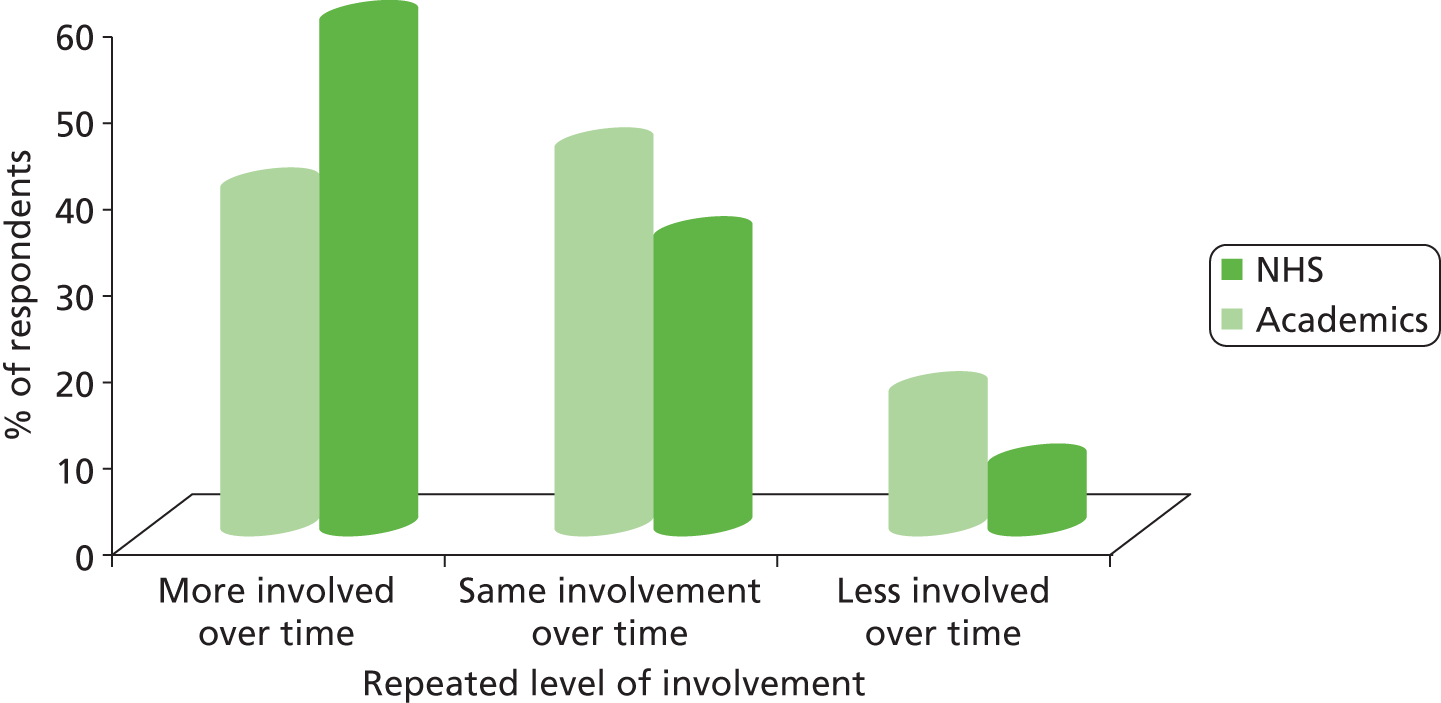
FIGURE 31.
Reported difference between experience of working within CLAHRC and working outside it.
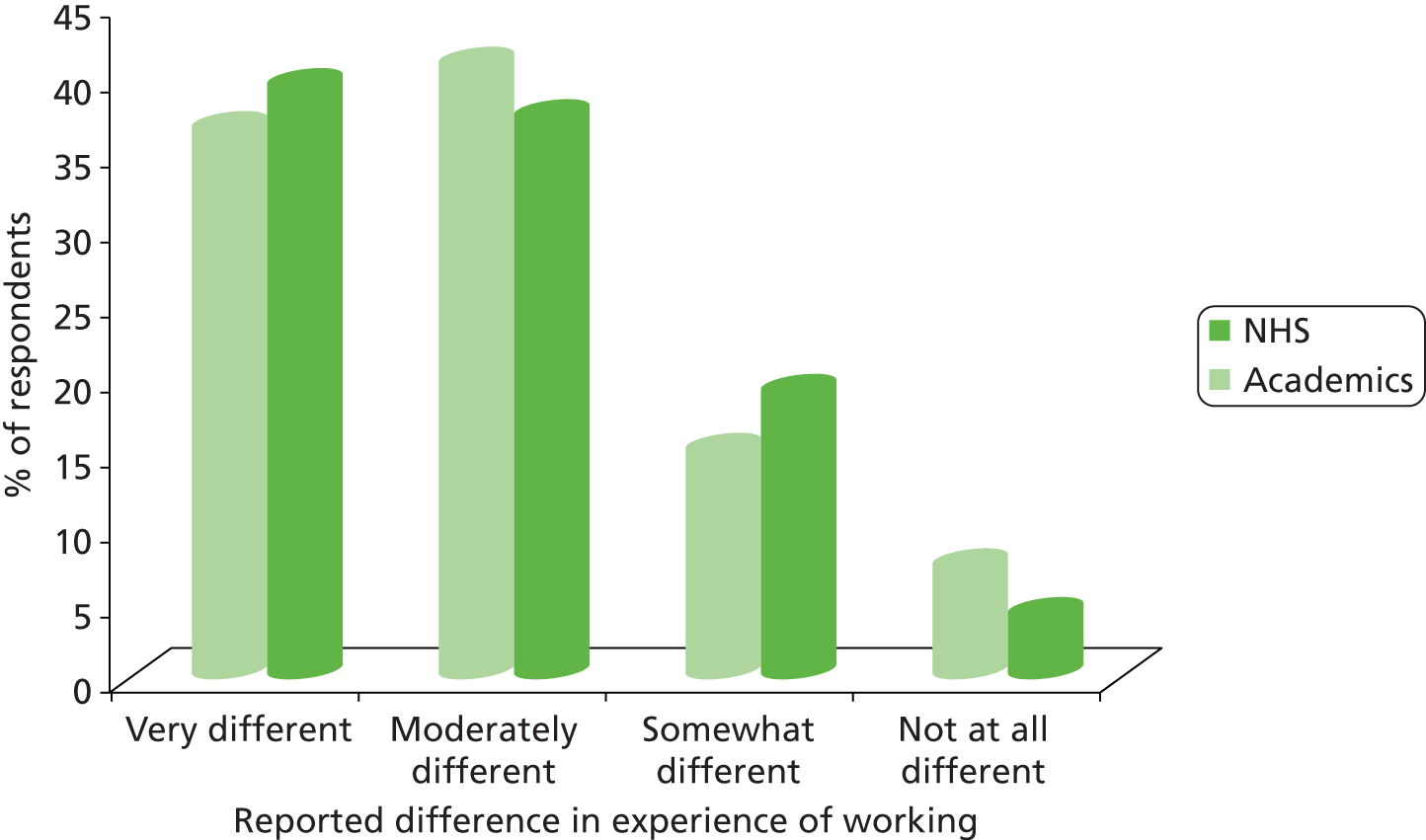
FIGURE 32.
Perceived difference in working within CLAHRCs from working outside it.
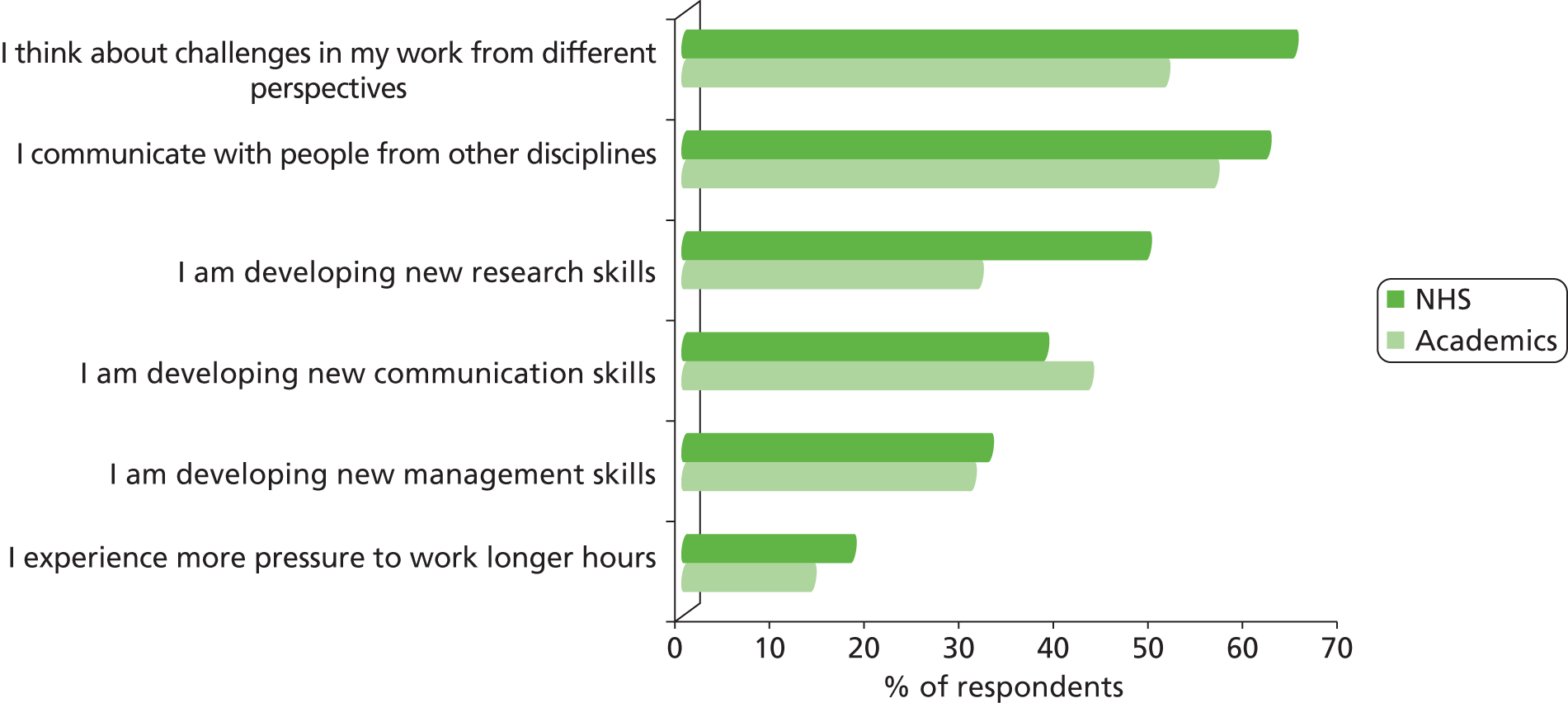
FIGURE 33.
Involvement in the CLAHRC has influenced way of work outside CLAHRC.
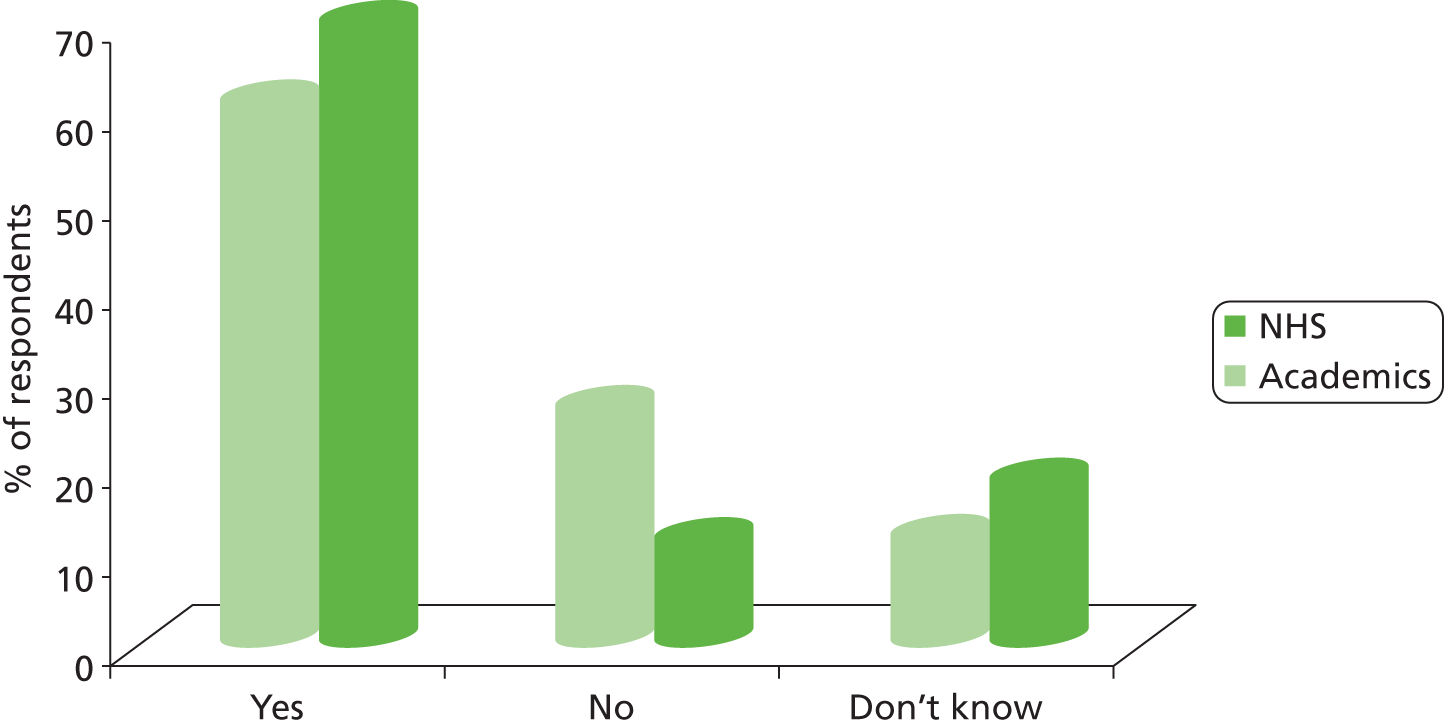
FIGURE 34.
Perceived support of CLAHRC by its senior leadership (i.e. CLAHRC board, CLAHRC director, CLAHRC manager and theme leads).
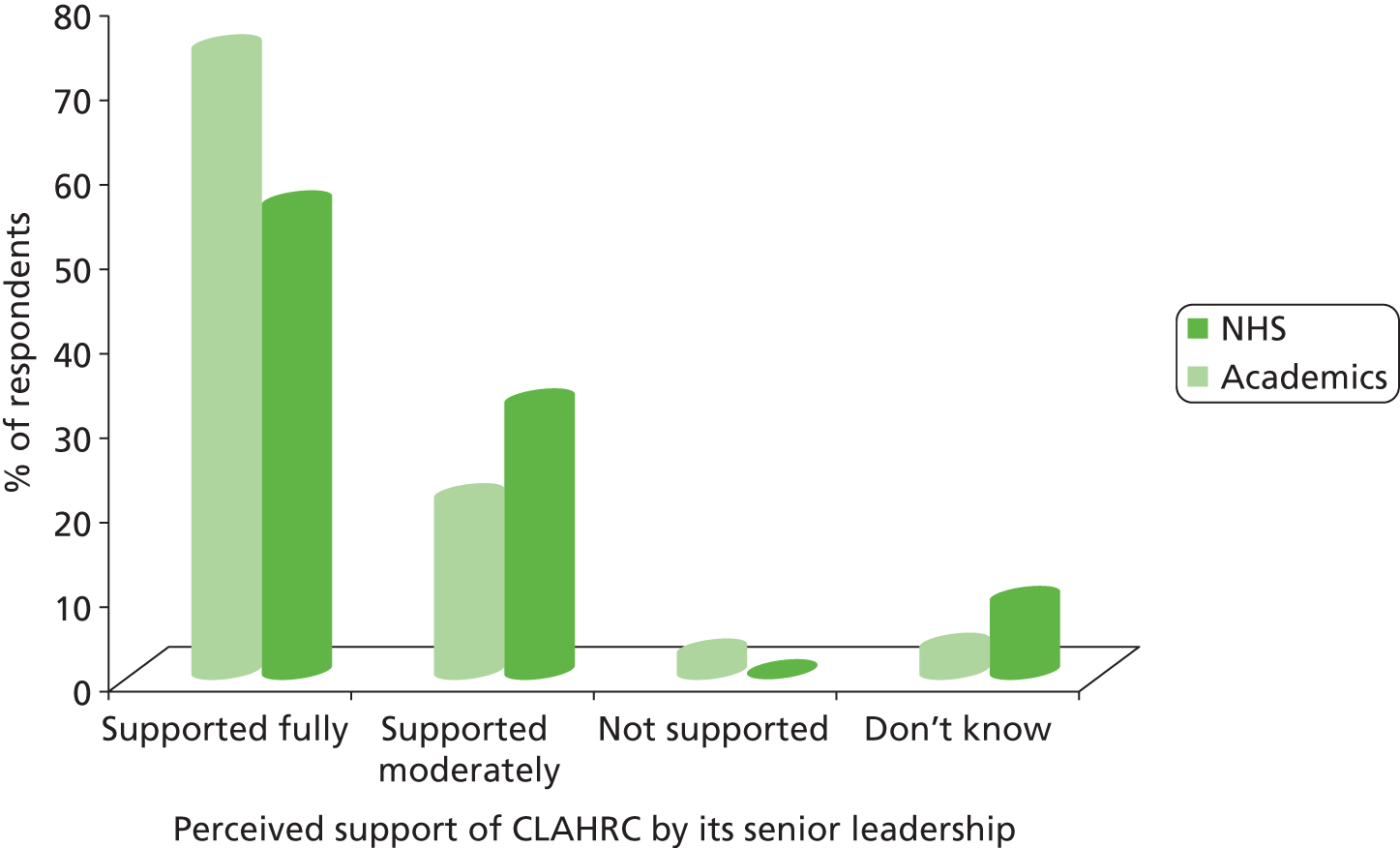
FIGURE 35.
Level of agreement that different types of resources are adequate to CLAHRC’s delivery of its activities.
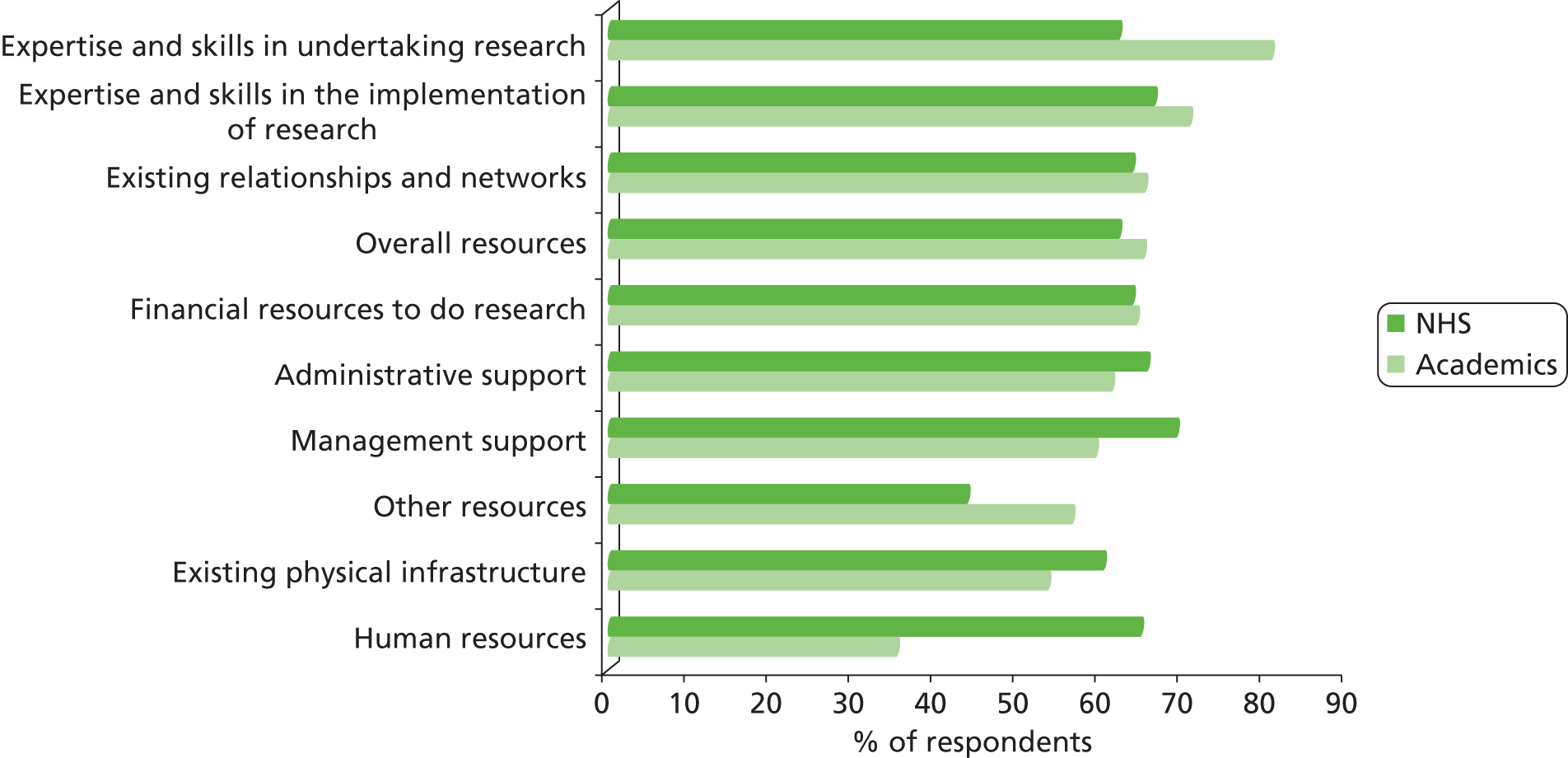
FIGURE 36.
Information about CLAHRC activities and projects communicated well within the CLAHRC.
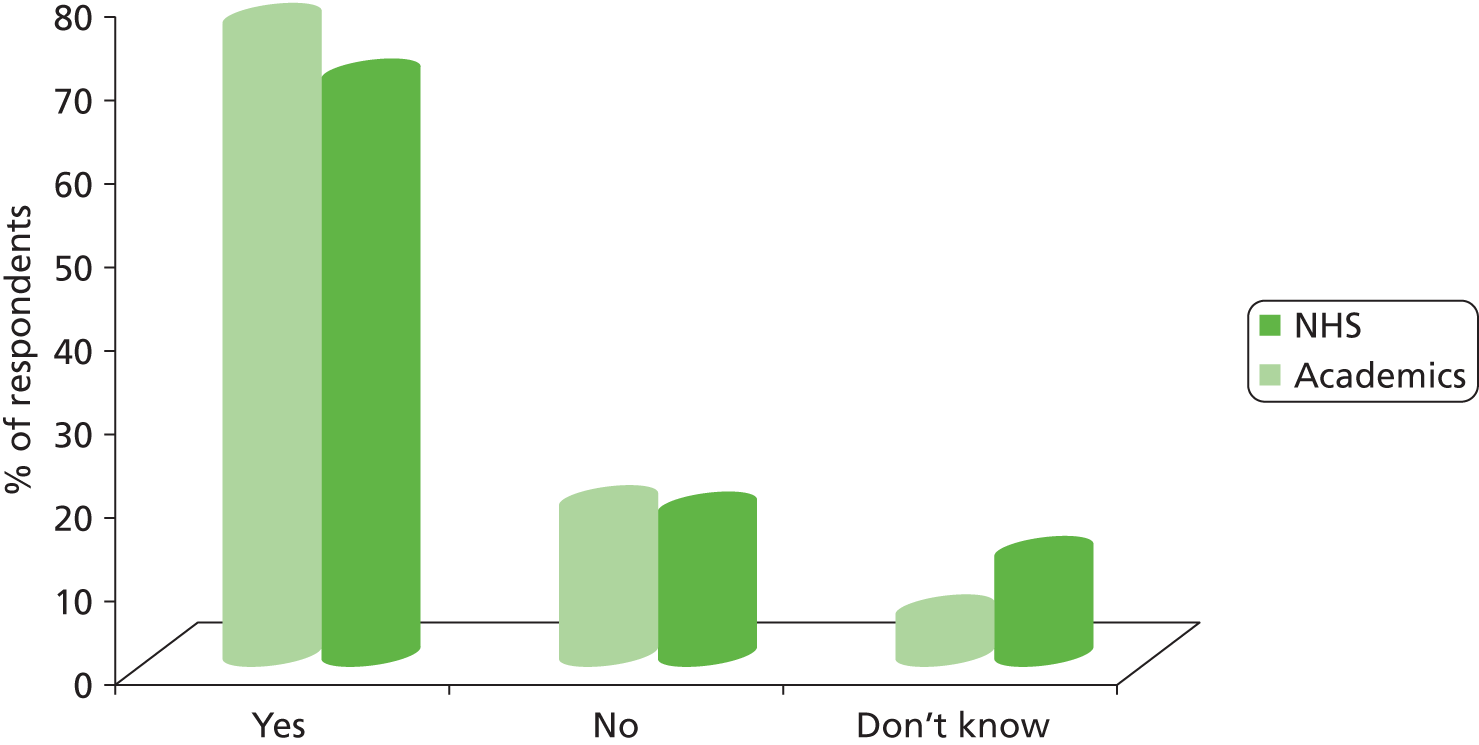
FIGURE 37.
Type of information that is communicated well within CLAHRC.
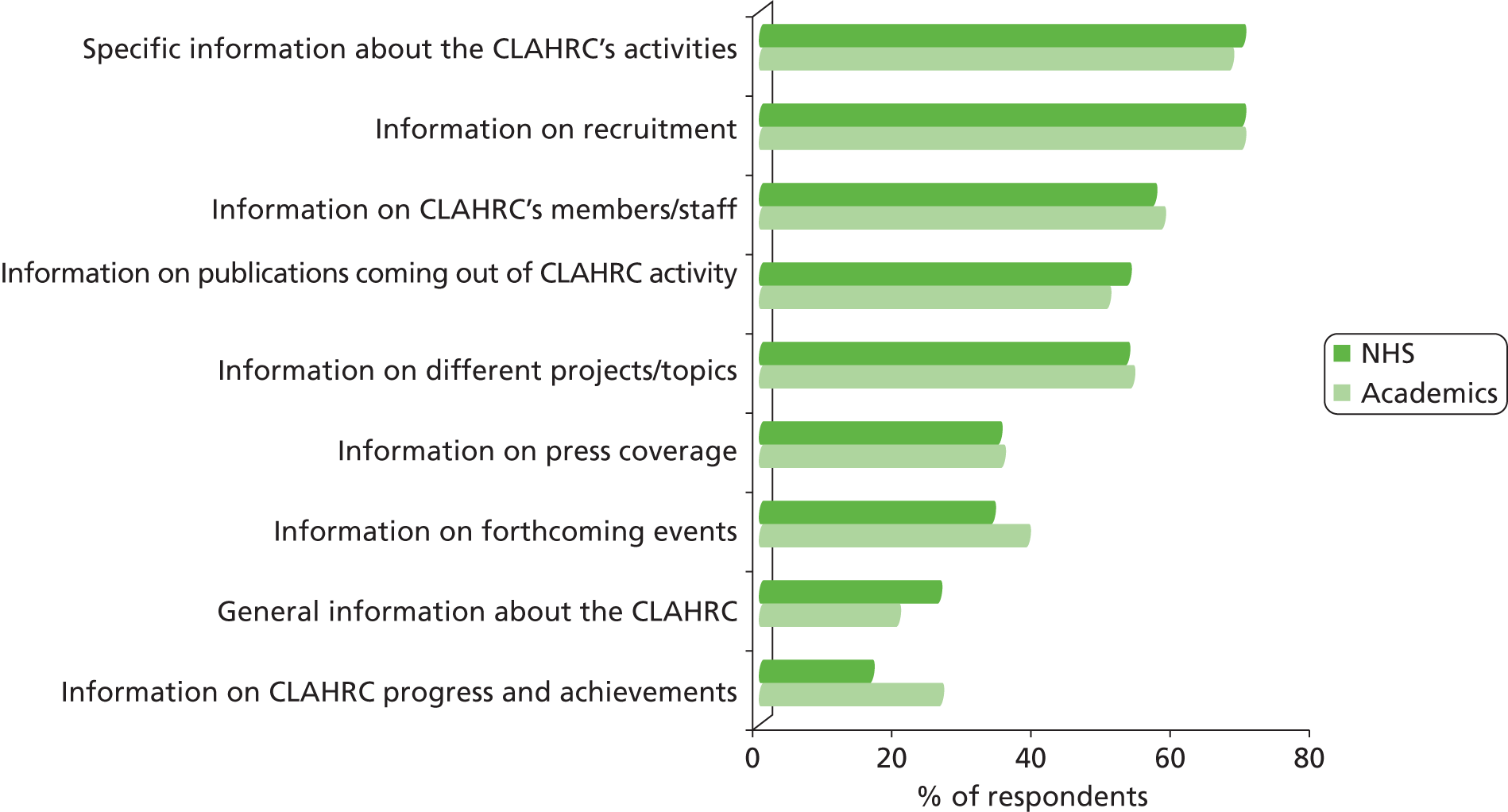
FIGURE 38.
Reported main ways through which information is most often communicated and disseminated within CLAHRC.
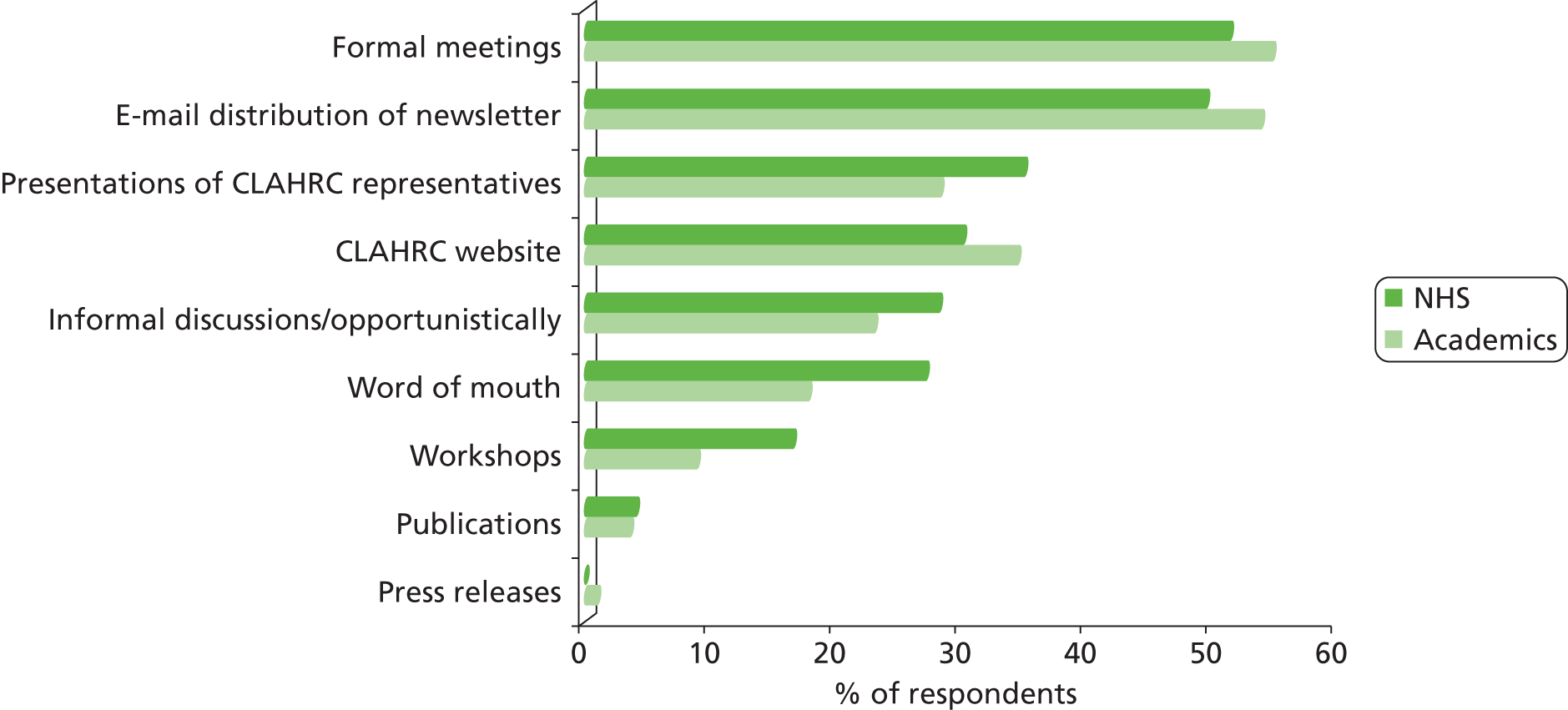
FIGURE 39.
Perceived impact of disseminating information within CLAHRC.
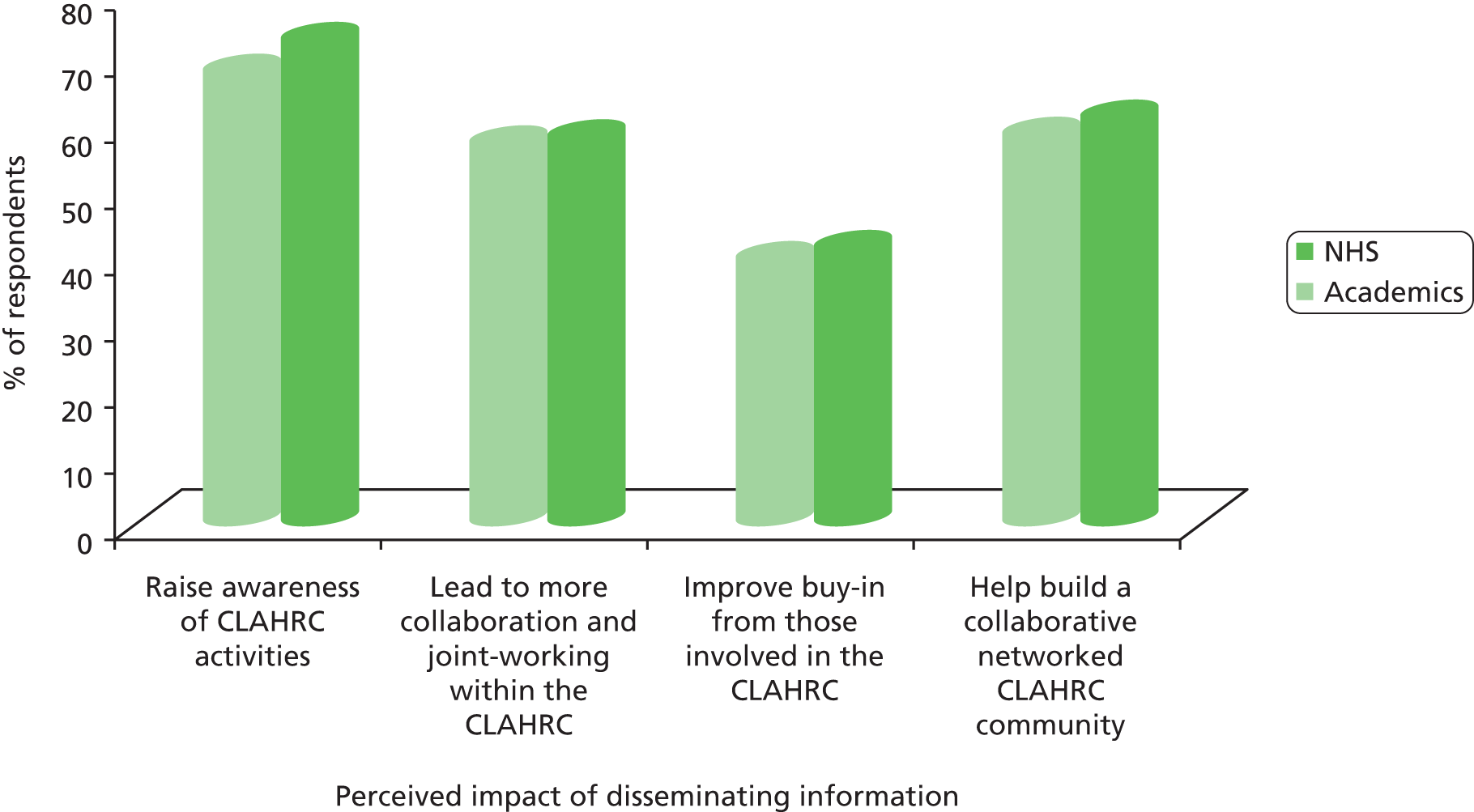
FIGURE 40.
Perceived extent to which information received about CLAHRC’s activities and projects has influenced personal behaviour and ways of working.
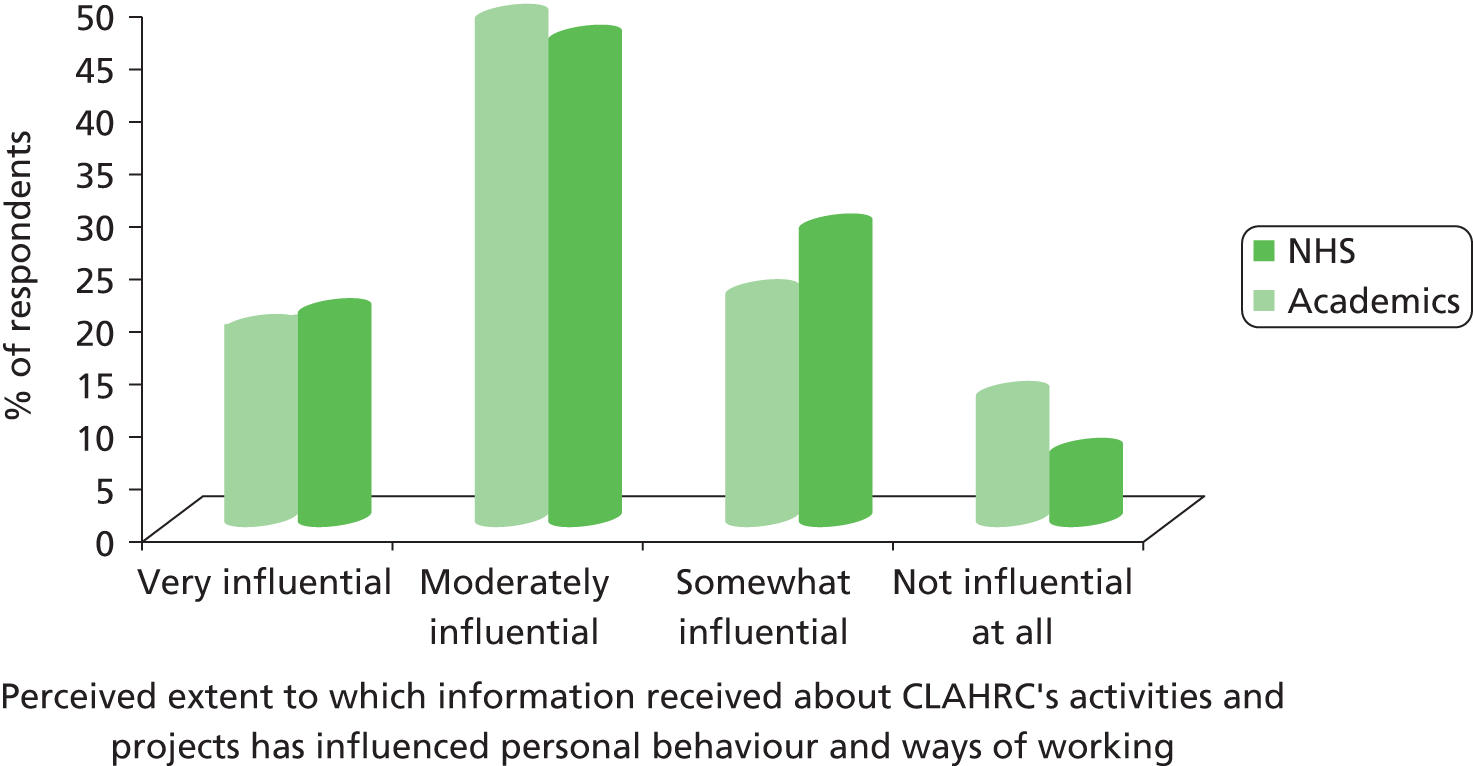
FIGURE 41.
Stated reasons why information received about CLAHRC’s activities and projects did influence behaviour and ways of working.
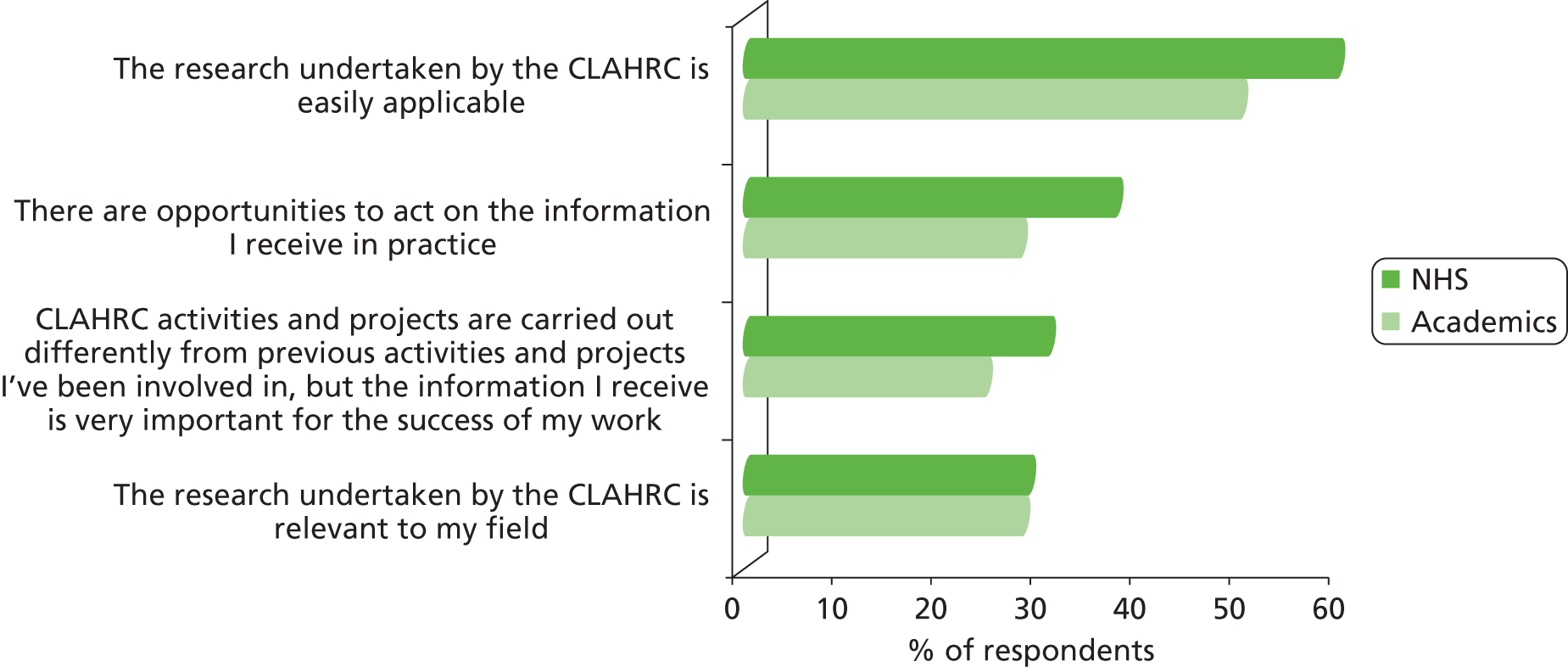
FIGURE 42.
Stated reasons why information received about CLAHRC’s activities and projects did not influence behaviour and ways of working.
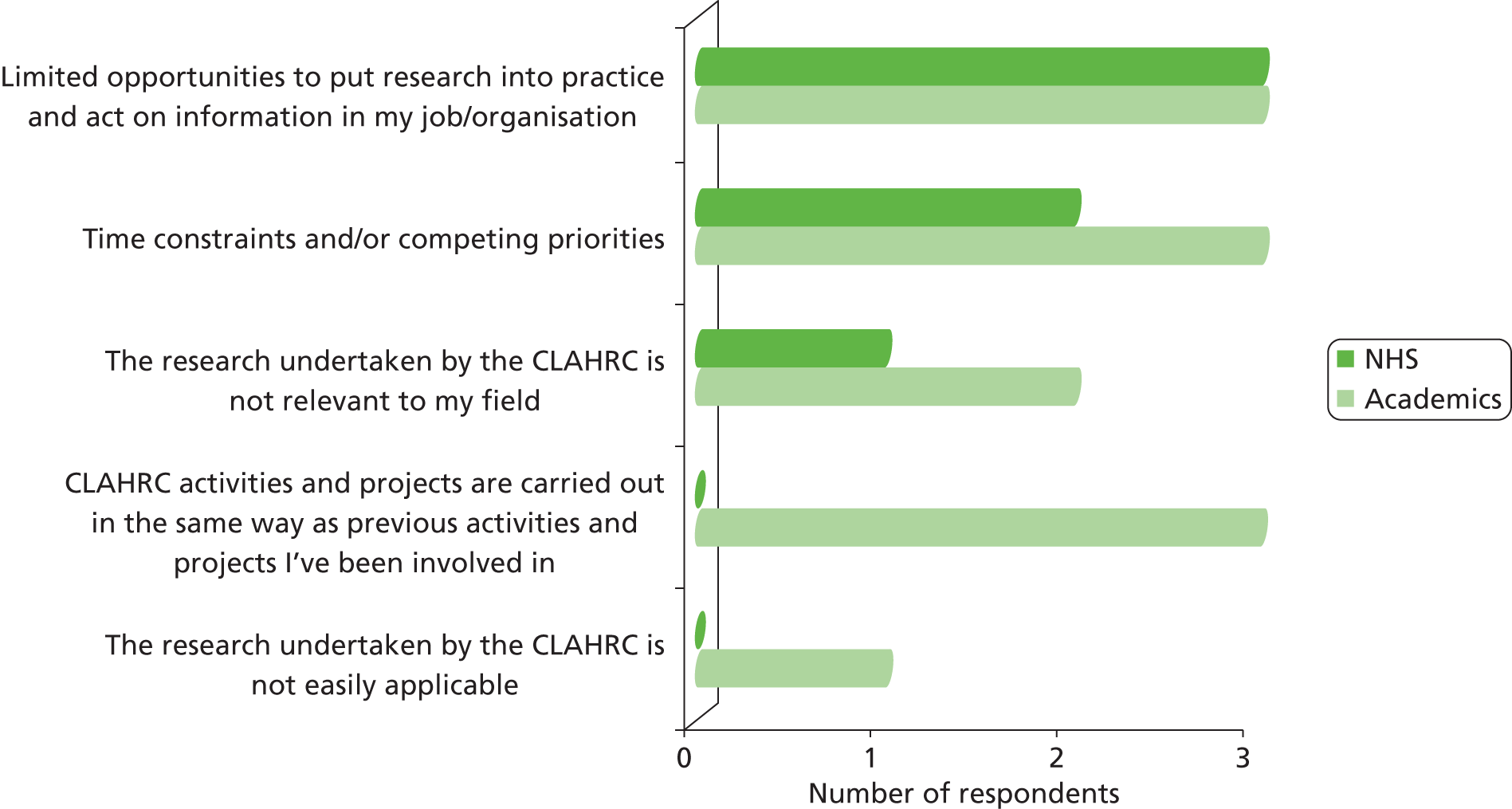
FIGURE 43.
Information related to CLAHRC activities and projects is well communicated outside the CLAHRC.

FIGURE 44.
Reported target audiences for information related to CLAHRC activities and projects outside the CLAHRC.
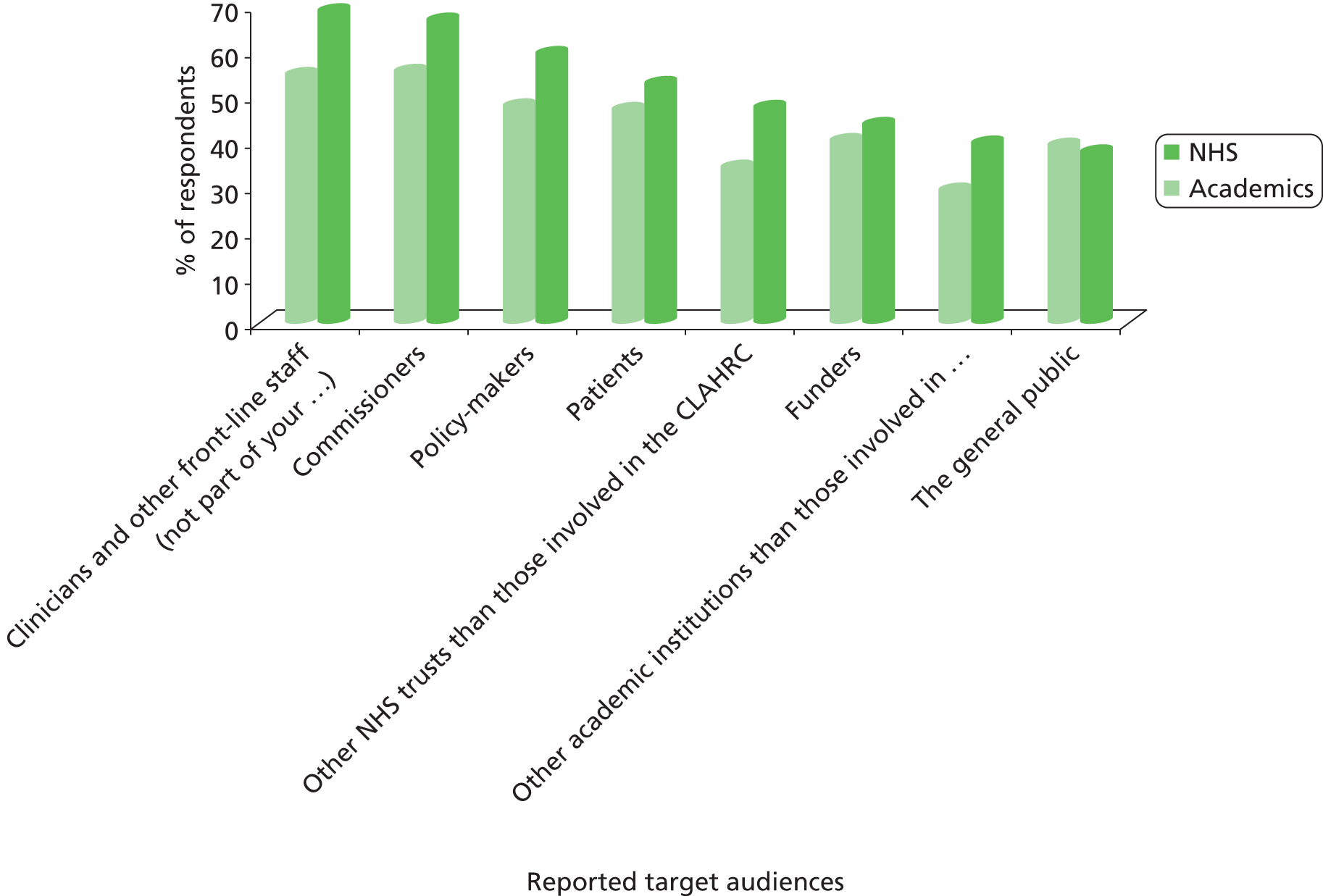
FIGURE 45.
Perceived effectiveness of communication of different types of information outside the CLAHRC.
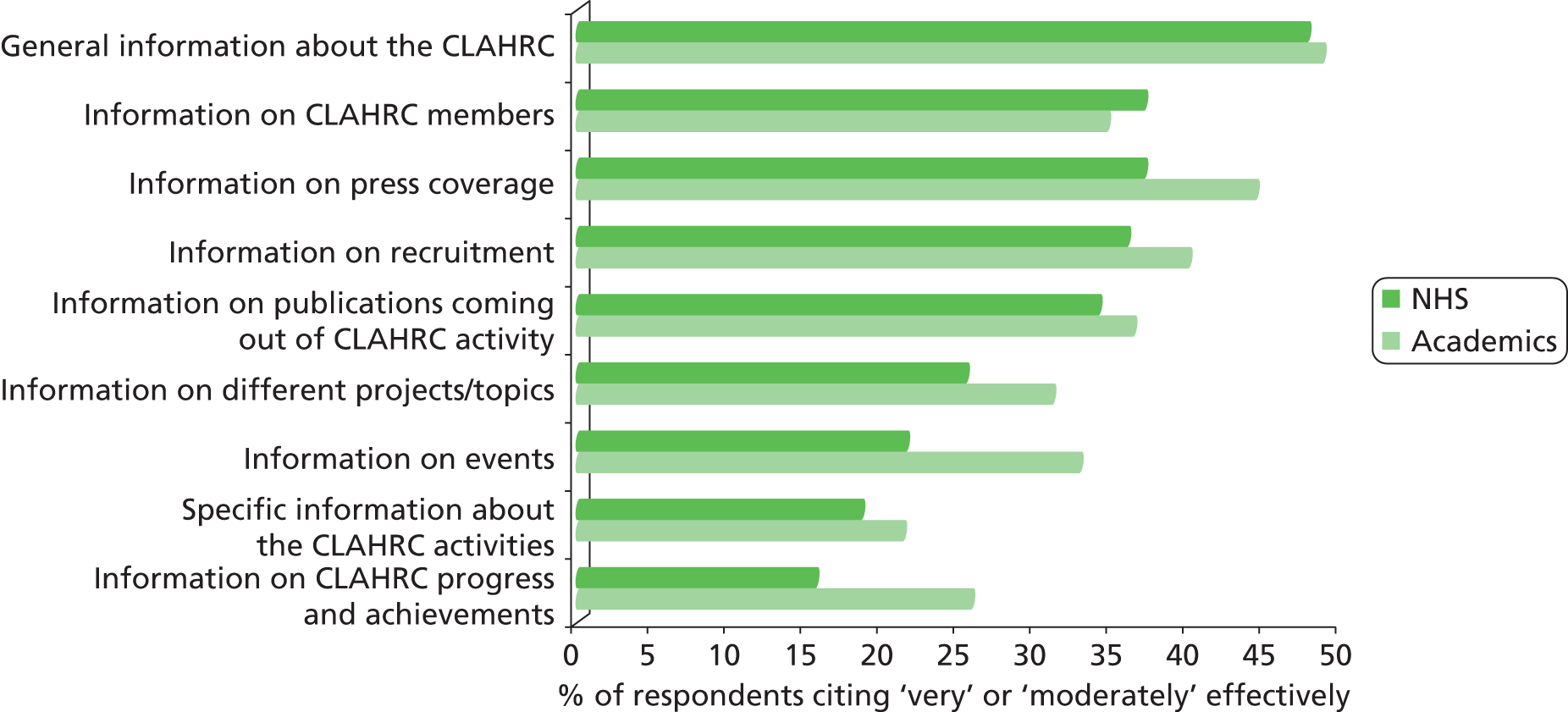
FIGURE 46.
Ways through which information is most often communicated and disseminated outside the CLAHRC.
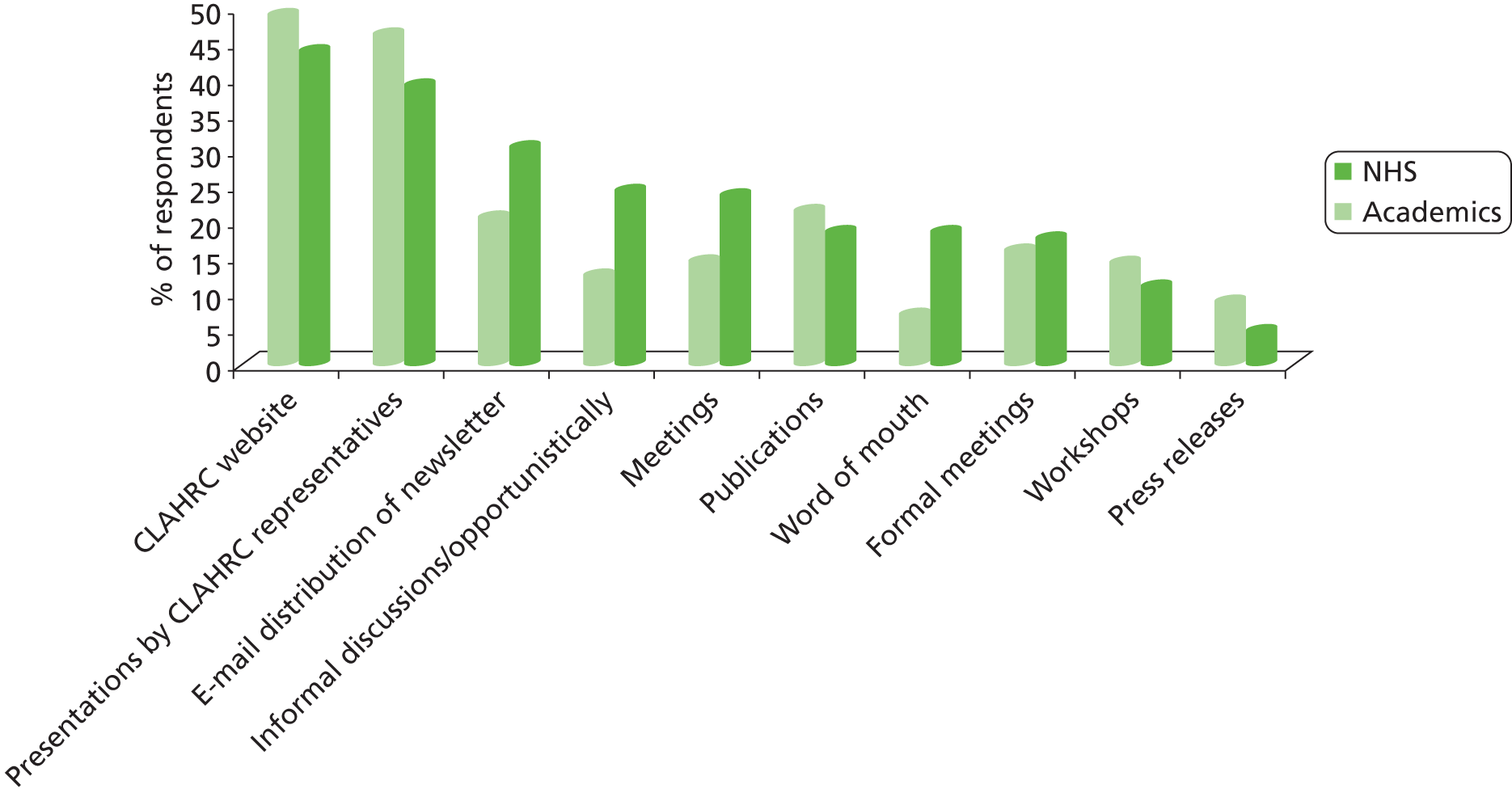
FIGURE 47.
Perceived impact of disseminating the information outside the CLAHRC.
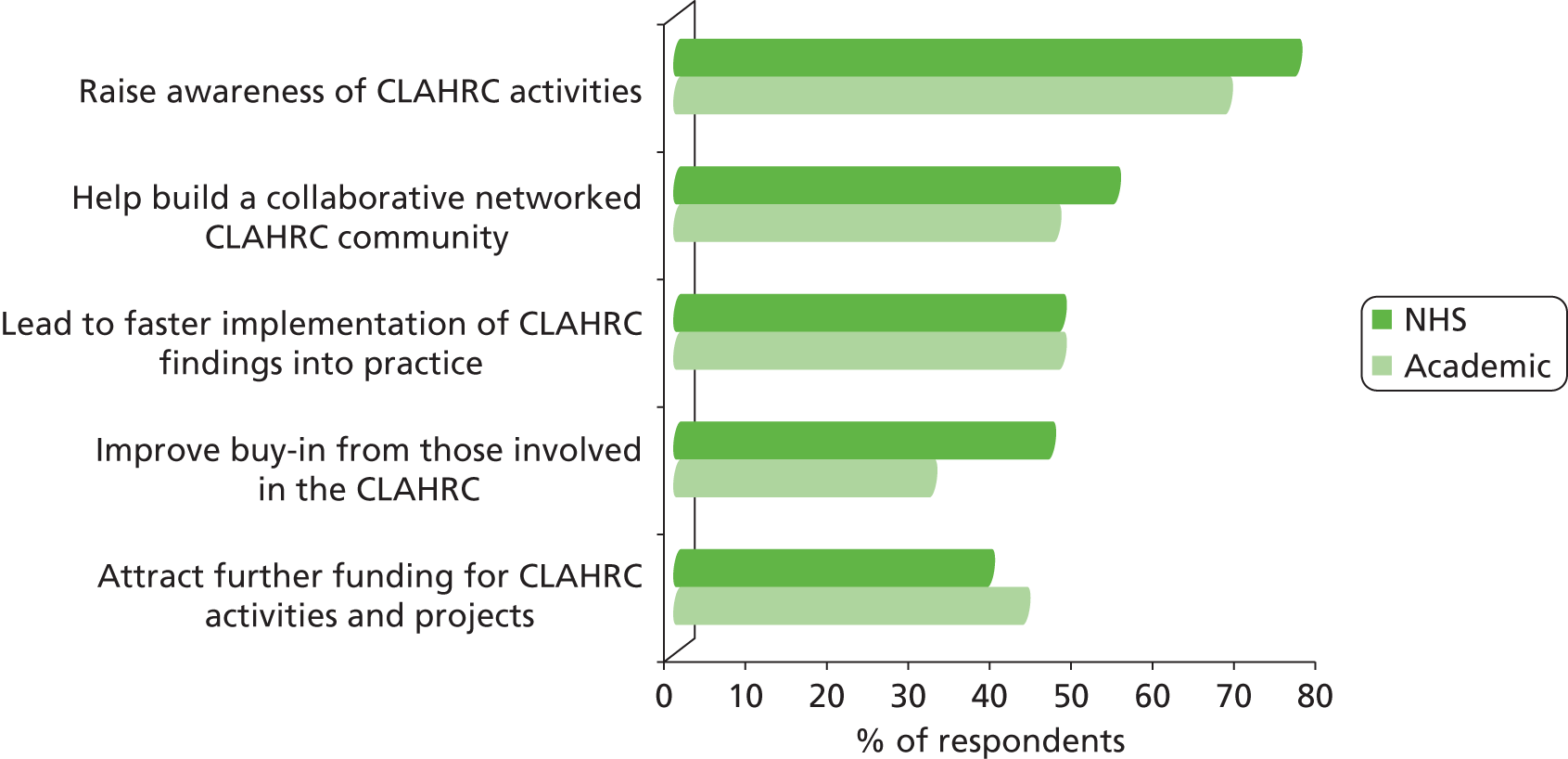
FIGURE 48.
The CLAHRC will lead to changes in practice/will influence NHS behaviour.

FIGURE 49.
Perceived effectiveness of the CLAHRC taking into account the views and concerns of its stakeholders in the day-to-day delivery of its activities.
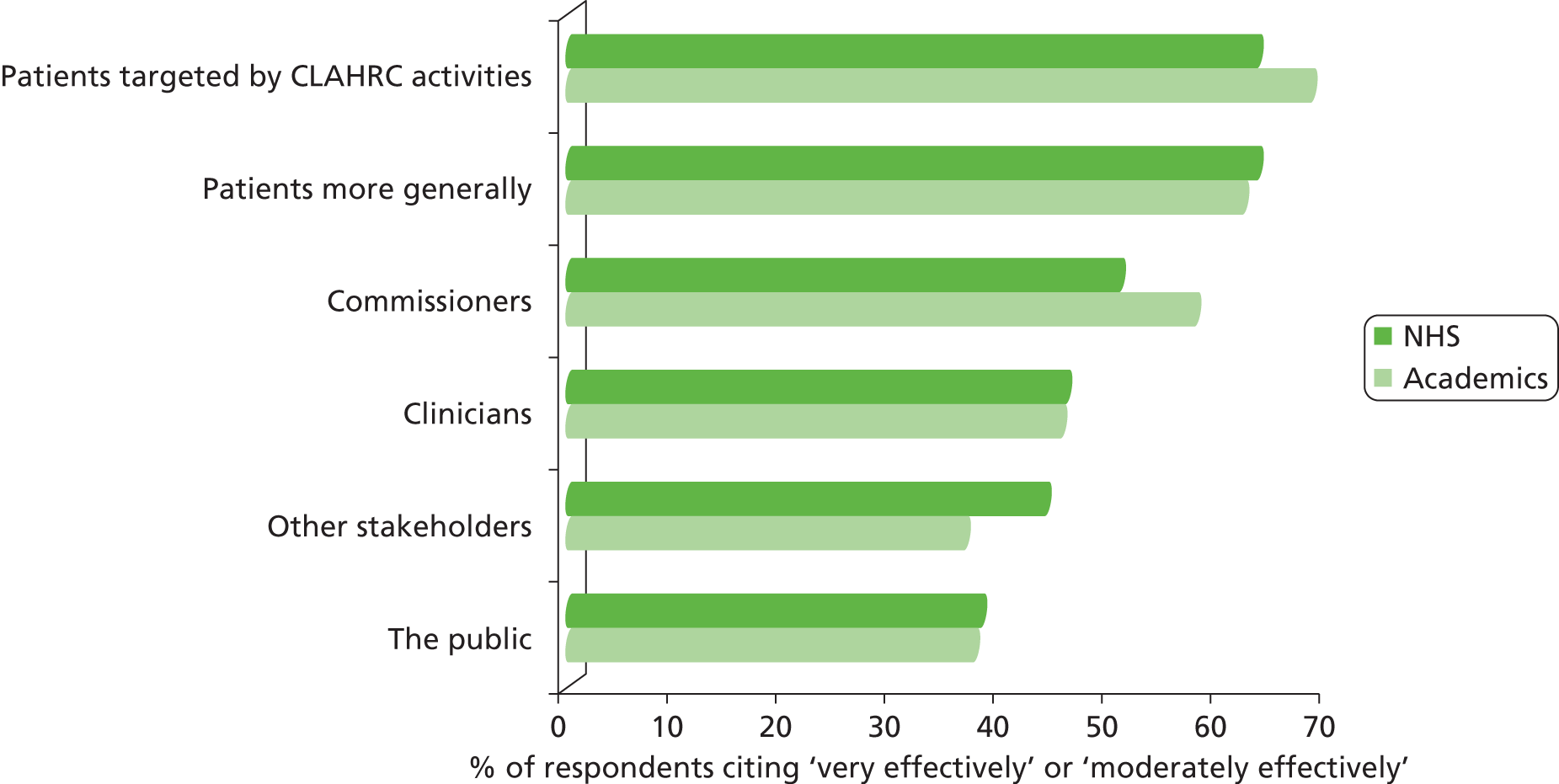
FIGURE 50.
Perceived extent to which relevant people within CLAHRC’s local NHS/university are actively involved in CLAHRC.
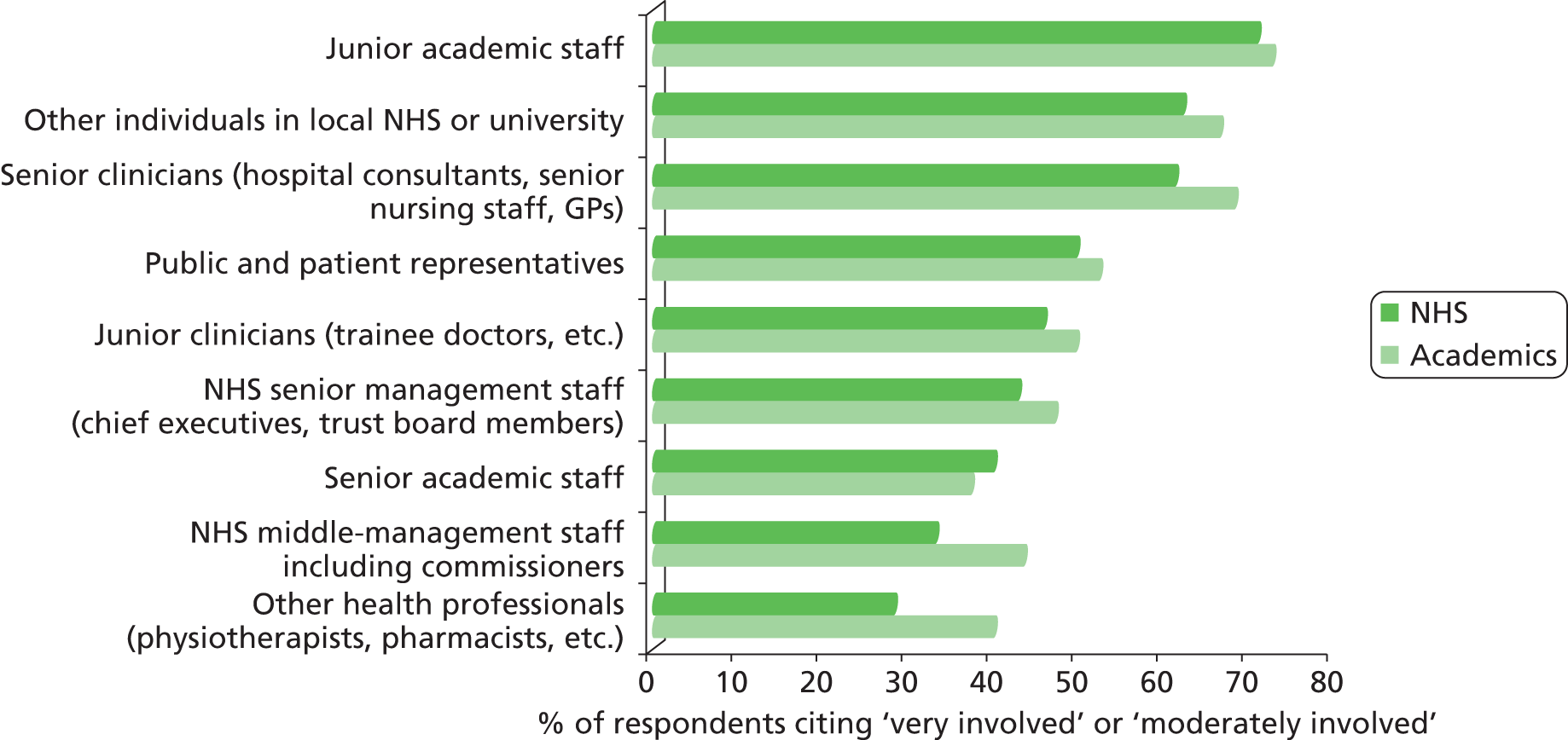
FIGURE 51.
Reported reasons why relevant people within CLAHRC’s local NHS may not be actively involved in CLAHRC.
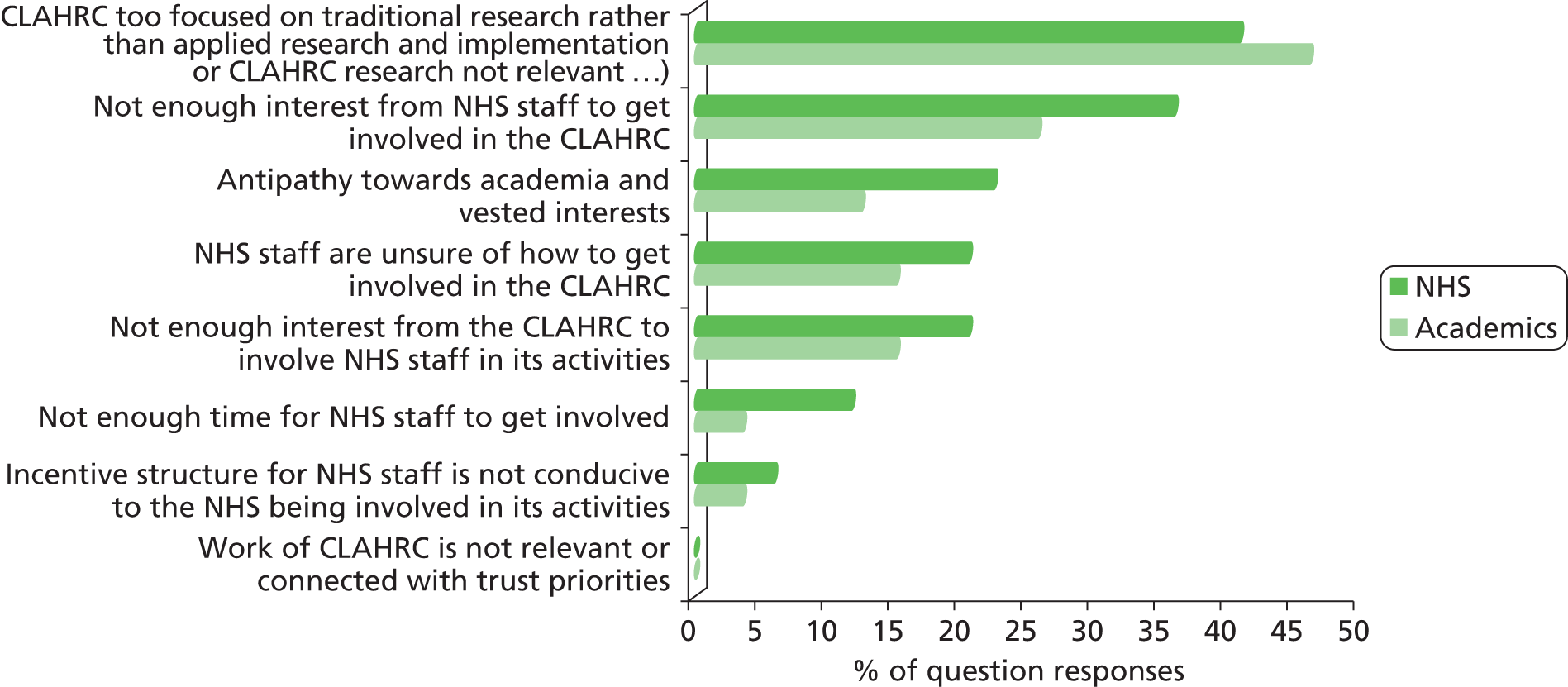
FIGURE 52.
Reported reasons why relevant people within CLAHRC’s local NHS are actively involved in CLAHRC. MSc, master of science; Phd, doctor of philosophy.
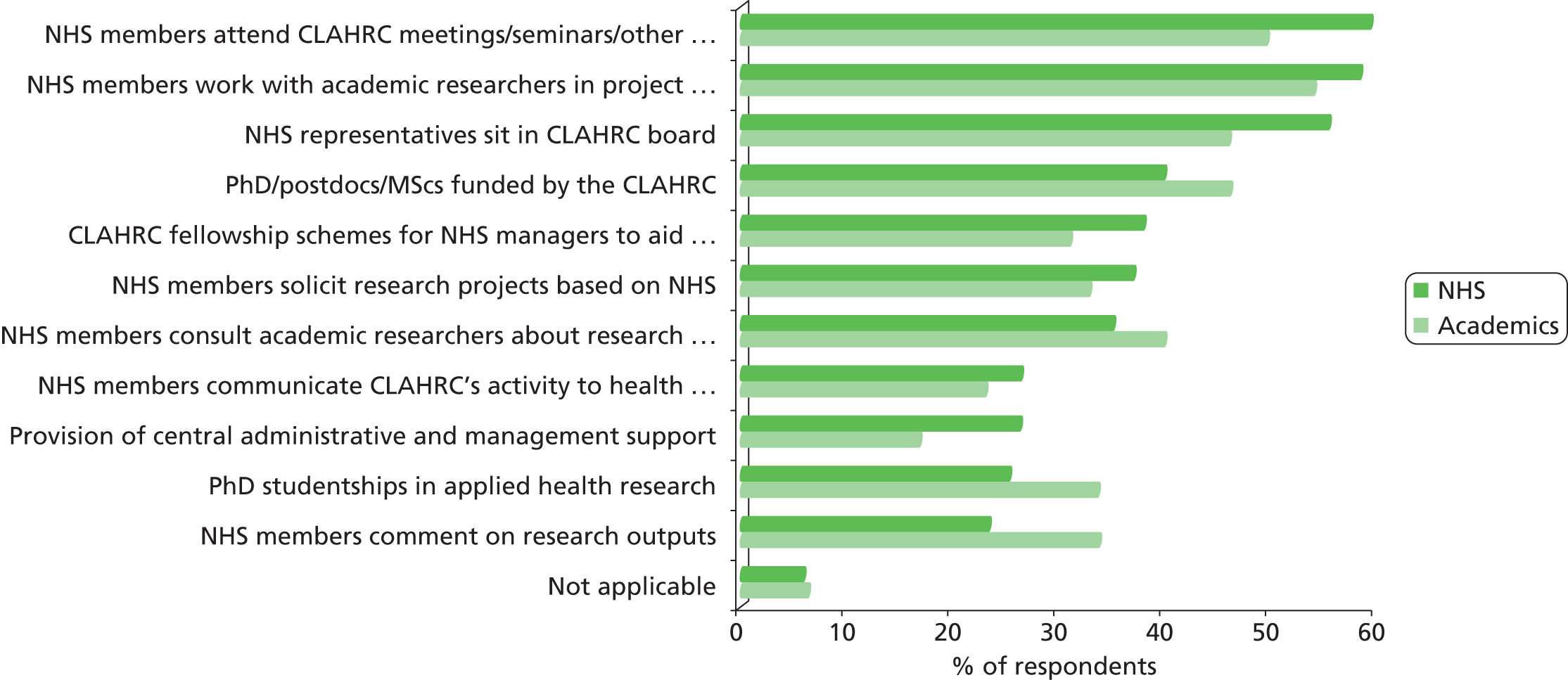
FIGURE 53.
Perceived extent to which different groups within local NHS and universities are influential in shaping CLAHRC’s strategy, decisions, activities and choice of outputs.
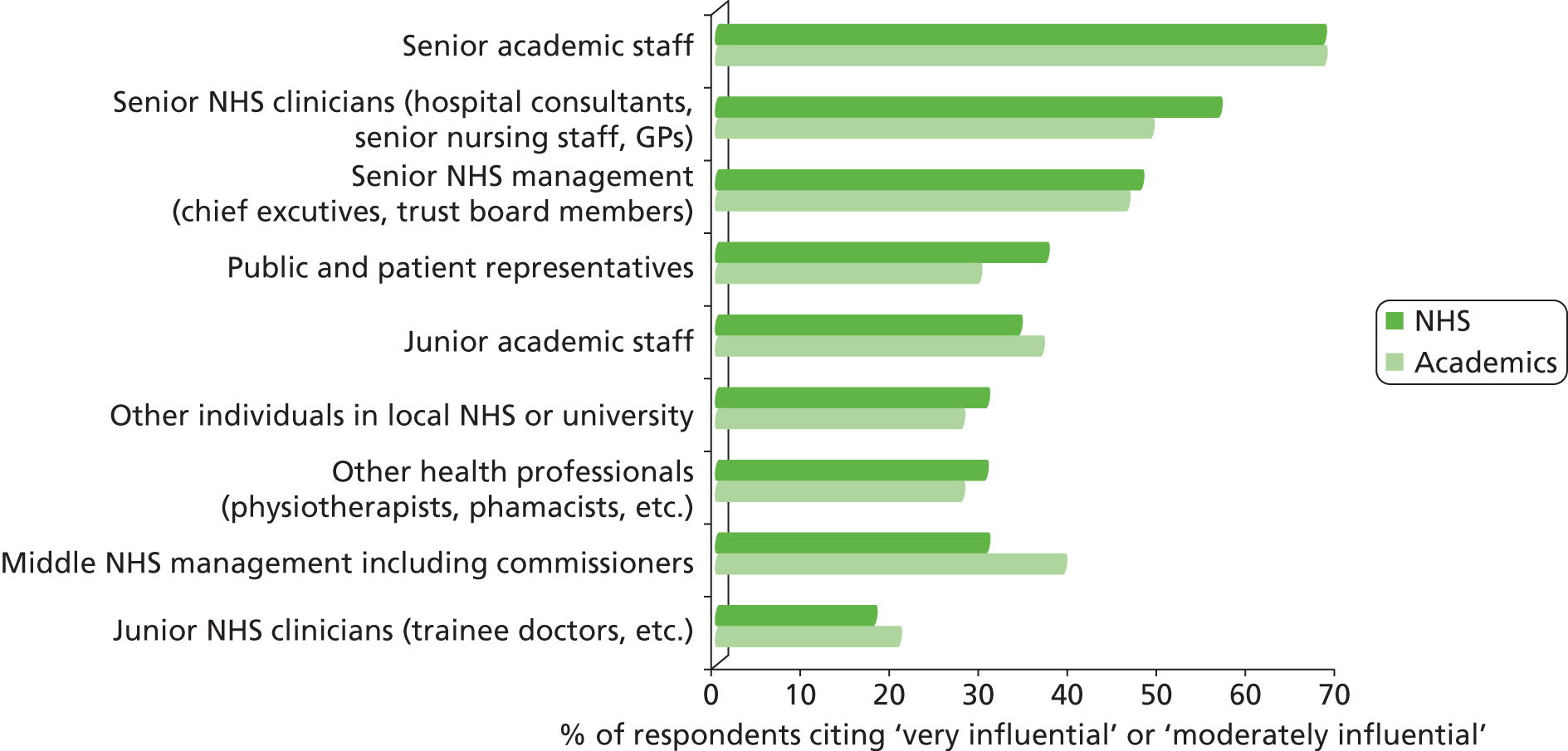
FIGURE 54.
Reported reasons for the NHS being considered currently influential in shaping CLAHRC’s activities.
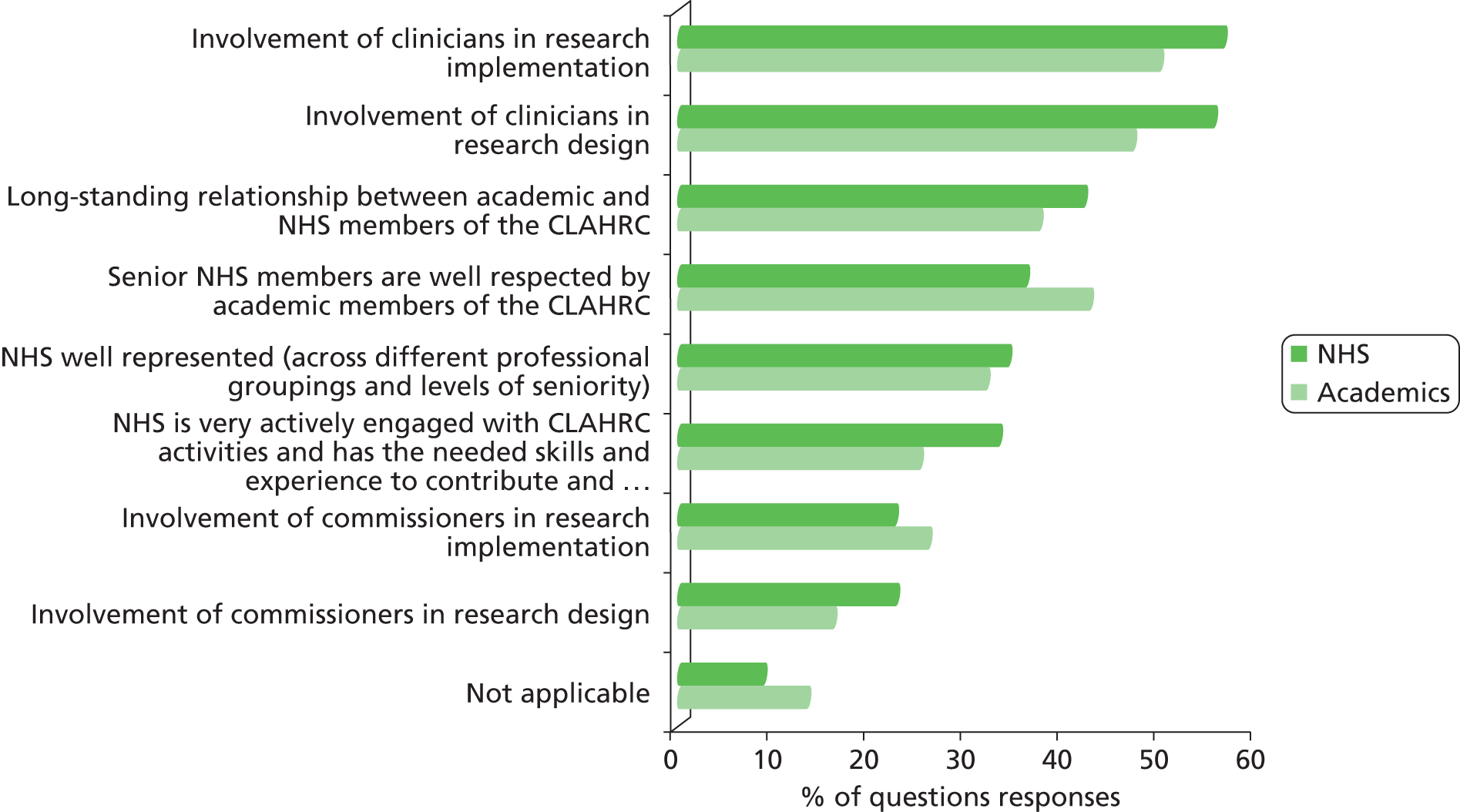
FIGURE 55.
Perceived reasons why the NHS may not be influential in shaping CLAHRC’s activities.
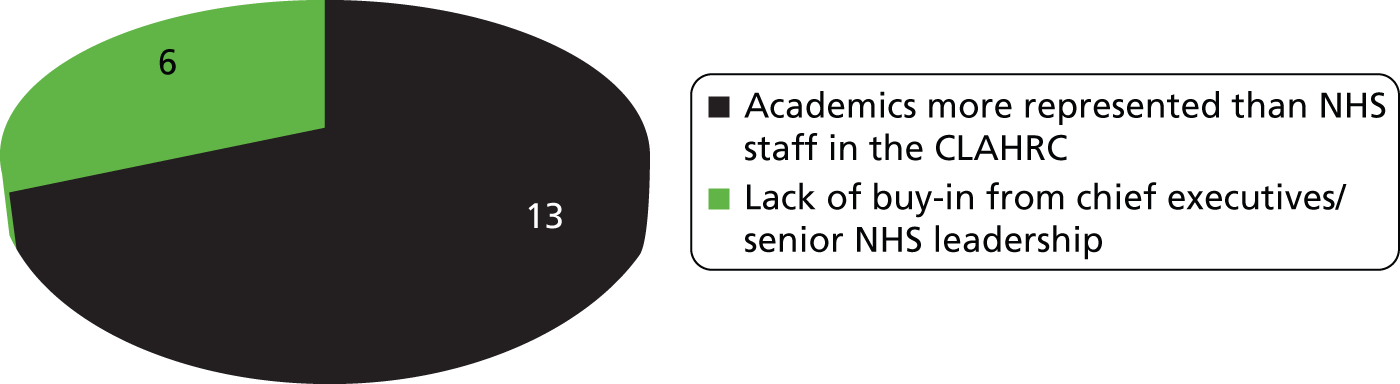
FIGURE 56.
Perceived elements of CLAHRC and wider landscape that enable it to meet its objectives. IT, information technology.
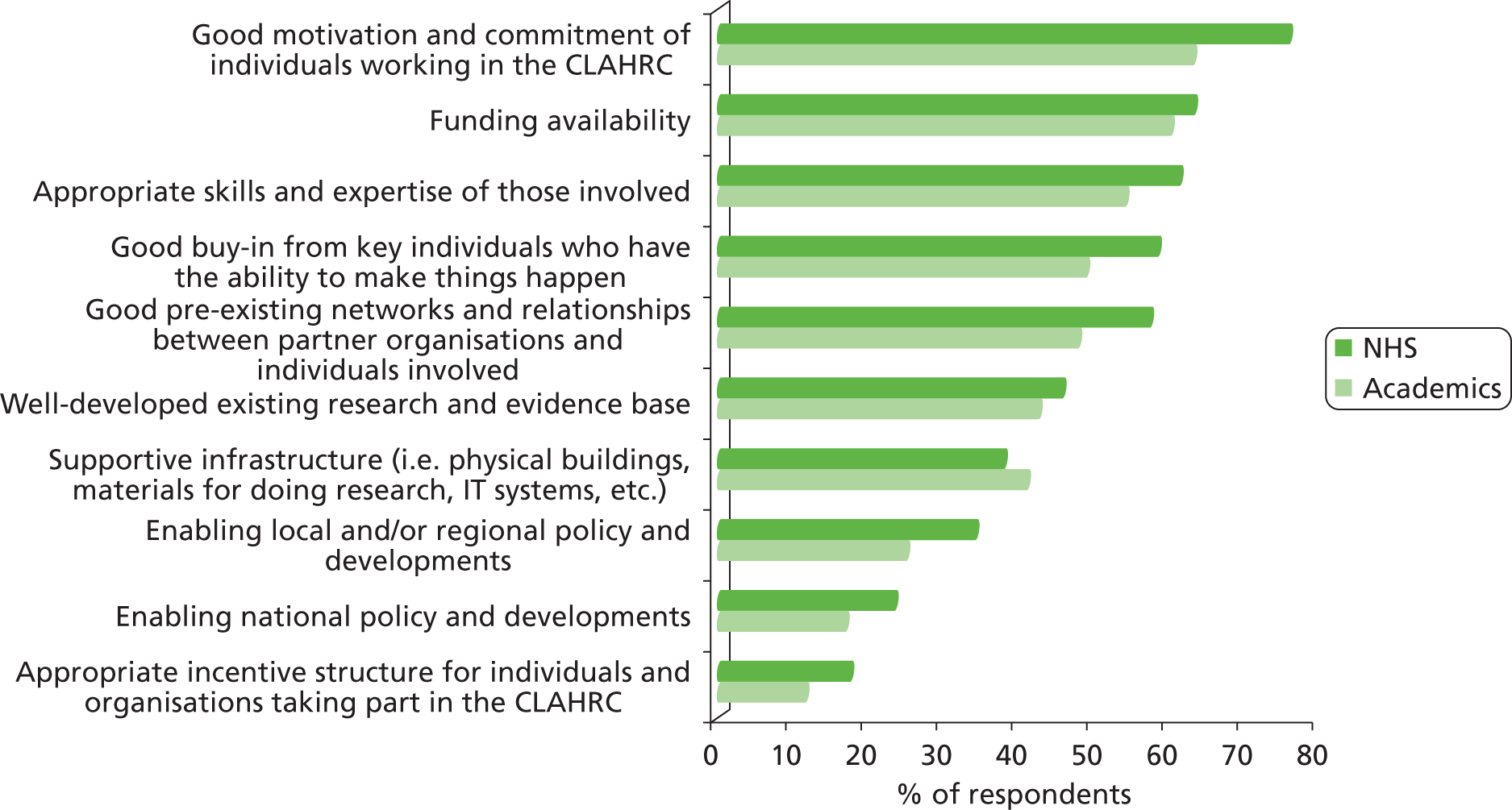
FIGURE 57.
Perceived elements of CLAHRC and wider landscape that provide a barrier to meeting its objectives. IT, information technology.
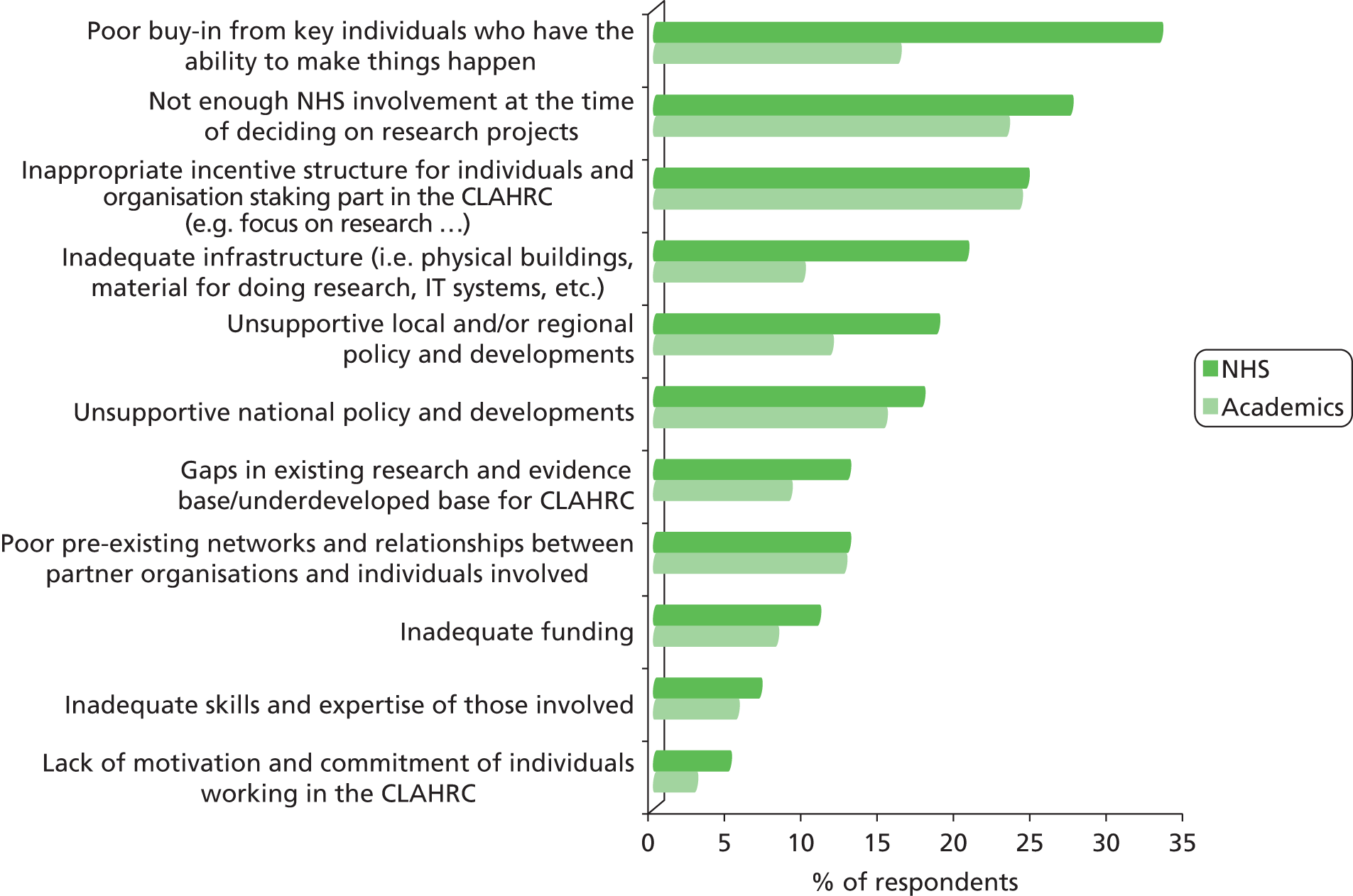
Appendix 6 Phase 2 case study interview protocol
The interview protocol presented in this appendix was used for CLAHRC-CP and PenCLAHRC participants. Interviews were approximately 1 hour in length and semistructured in nature, allowing the interviewer to direct the conservation according to each interviewee’s particular knowledge and expertise.
Theme 1: NHS influence on CLAHRCs evolution, outcomes and impact
Based on your experience and knowledge, has there been change over time in the levels of your CLAHRC’s emphasis on (i) conducting new research and maturing research streams of relevance for the NHS, in comparison to (ii) better applying existing research to improve clinical effectiveness?
Has there been a change in how different professional groups in the NHS have been involved with and working with the CLAHRC over time, and if so why do you think this is the case? What has worked particularly well in terms of engagement from these NHS groups and what hasn’t, and why?
Has the way the NHS partners have engaged with the CLAHRC had an effect on the scale and nature of the NHS influence on CLAHRC directions, agendas and areas of focus over time? If yes, in what way?
And in similar light, do you think having a CLAHRC has influenced changes in NHS behaviour locally (if so how and why)?
The results of our survey suggest that although the NHS partners have been engaged with the CLAHRC, that academic partners are overall more influential on the CLAHRC evolution, strategy, activities and outputs than the NHS? Would you agree? If so, why do you think this is the case? What do you think could be done to strengthen the influence of the NHS? If you disagree, why?
Have any non-NHS and non-academic stakeholders been particularly strongly involved with the CLAHRC over time, and if yes, what have the impacts of this been? Have levels of their engagement changed over time and if so why?
How have wider national and regional policy environments (including changes in them) impacted on the CLAHRC? And are there any examples of the CLAHRC influencing regional and national policy environments?
Theme 2: how are effective multidisciplinary and multi-stakeholder teams and collaborations built and sustained
Our survey results suggest that members of the CLAHRC think that working within the CLAHRC is quite different to working outside of it. Would you agree? If so, how is it different and why do you think that is the case? Can you provide some examples based on your personal experience? And has the way you work in the CLAHRC influenced how you work outside the CLAHRC?
Based on your experience, how is collaborative working between multiple disciplines and stakeholders in the CLAHRC enabled – through which concrete mechanisms? Which mechanisms do you think have been most effective and why? Have any specific groups/posts had strong boundary spanning roles in bringing together disciplines, academic and service delivery sectors?
Has the scale of collaboration between academics and clinicians from different disciplines changed over time? If yes, what has driven and enabled this and what have the impacts been?
Theme 3: information communication and dissemination
Based on your knowledge and experience, what do you think have been the most important and effective channels for sharing information about CLAHRC-wide activities within the CLAHRC and building a ‘knowledge community’, and why? Has this had influence on your own work?
Have you personally developed any new communication skills through the CLAHRC? What has enabled this and how do you think it has been manifested?
What do you think have been the most important and effective channels for sharing information about CLAHRC-wide activities and outputs externally? What has been the impact from these means of communication been – any examples?
Concluding questions
At the end of the first phase of the CLAHRC, what would you think are/will be the key legacies?
Finally in reflection of all we’ve discussed to today about the evolution of your CLAHRC, if you were doing things all over again, what would (i) you personally do differently with the benefit of hindsight? (ii) And is there anything you think could/should be done differently even if it is not directly related to your personal actions?
Appendix 7 Phase 2 case study workshop outlines
Agenda for the CLAHRC-CP workshop, as circulated to the 25 participants. The workshop was held at Douglas House, Cambridge, on 20 April 2012.
| 8:45–9:00 | Coffee and tea |
| 9:00–9:15 | Welcome and outline of the day |
| 9:15–9:40 | Setting the scene: background and context Overview of RAND/Health Economics Research Group (HERG) evaluation project, progress to date and plans looking forward Feedback on CP-CLAHRC survey results |
| 9:40–9:50 | Discussion and clarification of activities |
| 9:50–12:30 | Core session (1) The CLAHRC-CP theory of change over time: learning about pathways to impact from the CLAHRC-CP experience Session purpose: This session focuses on refining insights about pathways to impact and examining whether CLAHRC-CP assumptions about these pathways have shifted since earlier phases of CLAHRC existence, and if so how and why. Drawing on the above, the results of the session will provide new learning on three core questions relevant to CLAHRC strategy and wider translational research and implementation policy: (1) How does the NHS influence CLAHRC-CP evolution, outcomes and impact (and indeed how does having the CLAHRC influence NHS behaviour?; (2) What can we learn from CLAHRC-CP about how effective multi-stakeholder and multidisciplinary research and implementation teams for service improvement are built?; (3) What can we learn from CLAHRC-CP that can cast new understanding on how to use research knowledge and evidence to change commissioning and clinical behaviour for patient benefit? Session organisation: The session will involve a combination of individual work, parallel group sessions and plenary Individual work: Participants will be asked to first individually reflect on the CLAHRCs original theory of change and intervention logic (which the RAND/HERG team will share materials for) to see the extent to which they feel it still holds true, and to consider any fundamental changes and particularly important elements that have worked well or where there is scope for improvement. (9:50–10:10) Parallel session station work: Workshop participants will work in groups based on their professional affiliations (e.g. NHS, academic, CLAHRC ‘central’) and reflect on three core themes central to the CLAHRC’s strategy and goals: (i) interactions with the NHS; (ii) the development, nurturing and contributions of multi-stakeholder and multi-disciplinary teams and relationships to CLAHRC objectives; (iii) mechanisms of using evidence generated by the CLAHRC to influence commissioning and clinical practice. For each of these three themes, participants will through facilitated sessions be asked to consider the diversity of mechanisms through which activities in a theme take place and evidence of the effect of these interventions; what has worked well, what hasn’t; and what have been major changes in the CLAHRC over time as they relate to a particular theme. (10:10–11:40) 11:40–11:50 Comfort break Plenary: Participants will share their insights from the parallel sessions and engage in discussion focused on learning about pathways to impact in CLAHRC-CP over time. This will enrich insights on the added-value of the CLAHRC model for increasing local capacities to do and use research for patient benefit, particularly through the three key areas of interest (i.e. NHS involvement, multi-stakeholder and multidisciplinary relationships, effective mechanisms of using research evidence to change behaviours). This will also contribute to better understanding what is unique about the CLAHRC model and what could not have been done without it. (11:50–12:30) |
| 12:30–1:15 | Lunch |
| 1:15–3:30 (with 15 minute comfort break) | Core session (2) Learning from the past to inform future actions and CLAHRC-CP sustainability Session purpose: This session has formative elements and will enable participants to reflect on the past to inform future actions. As such, this addresses the RAND-HERG team’s commitment to a formative evaluation and in addition the CLAHRC-CP may find it useful to inform the case for future funding. Participants will consider what they would like the CLAHRC to look like should there be another phase, and what actions they could take in the shorter (6 months) and longer term (5 years) to realise this vision Session organisation: Participants will be divided into four stakeholder groups according to their role. The groups will consist of (i) Senior and general NHS managers, SHA [strategic health authority] (for the time being), commissioners; (ii) front line NHS staff (e.g. clinicians and GPs, allied health professionals); (iii) academia and the research community; (iv) PPI and service users Each group will in facilitated break-out sessions be asked to discuss and consider actions for the future in three key thematic areas of importance for the CLAHRC’s future strategy: these could be (i) breadth versus depth in a future CLAHRC thematic focus and geographical reach; (ii) CLAHRCS influence on the role of commissioners in driving evidence-based practice; (iii) the balance of doing research versus using existing research evidence in a future CLAHRC strategy In plenary, stakeholder group representatives will take turn to present and discuss their suggested actions. The ‘audience members’ will provide feedback and engage in discussion around the feasibility, suitability, importance and acceptability of the suggested actions in light of a future CLAHRC-CP agenda The session will be organised around the selected themes so that each group spends 20 minutes per theme and then 20 minutes in plenary on that theme. Given three themes, this will last 2 hours, and there will be a 15 minute comfort break |
| 3:30–3:40 | Coffee and tea |
| 3:40–4:10 | Conclusions, reflections and next steps Thanks and departure |
Agenda PenCLAHRC workshop, held at the Vesey Centre, Exeter, on 11 May 2012. With 14 participants, a half-day workshop was considered appropriate.
| 8:45–9:00 | Coffee and tea |
| 9:00–9:30 | Welcome and setting the scene Overview of RAND/HERG evaluation project, progress to date and plans looking forward Feedback on PenCLAHRC survey results |
| 9:30–11:00 | Core session (1) The PenCLAHRC model: learning about pathways to impact from the PenCLAHRC experience Session purpose: This session will focus on refining insights about pathways to impact and examining whether PenCLAHRC assumptions about these pathways have shifted since earlier phases of CLAHRC existence, and if so how and why Session organisation: Participants will work in two groups to reflect on: (a) PenCLAHRC’s original model – ‘Engagement by Design’ – to see the extent to which this still holds true, and to consider any fundamental changes and particularly important elements that have worked well and where there is still scope for improvement (b) the diversity of mechanisms through which (i) the universities and the NHS interact; (ii) multi-stakeholder and multi-disciplinary teams are developed and nurtured; (iii) evidence generated by PenCLAHRC (through reviews and research) has influenced commissioning and clinical practice, and to consider what has worked well, what hasn’t, and the major changes in PenCLAHRC over time. (9.30–10.15) Plenary: To share insights from the parallel sessions. (10.15–11.00) |
| 11.00–11.15 | Coffee break |
| 11:15–12:45 | Core session (2) Learning from the past to inform future actions Session purpose: This session will enable participants to reflect on the past to inform future actions. Participants will consider what they would like PenCLAHRC to look like should there be another phase, and what actions they could take to realise this vision Session organisation: Participants will be divided into two groups. In facilitated break-out sessions each group will be asked to consider actions for the short term future (6 months) and over the full 5 years in three key thematic areas of importance for the CLAHRC’s future strategy: These could be: (a) breadth versus depth in a future CLAHRC thematic focus and geographical reach; (b) PenCLAHRC’s influence on the role of commissioners in driving evidence-based practice; (c) the balance of doing research versus using existing research evidence in a future PenCLAHRC strategy. (11.15–12.00) Plenary: Group representatives will take turns to present and discuss their suggested actions. All will consider the feasibility, suitability, importance and acceptability of suggested actions in light of a future PenCLAHRC. (12.00–12.45) The session will be organised around three selected themes so that each group spends 15 minutes per theme and 15 minutes in plenary on that theme. Given three themes, this will last 1½ hours |
Appendix 8 Phase 2 protocol for validation interviews
Interview brief and questions for validation interviews
Background
Through our CLAHRC-wide survey and two in-depth case studies (at CLAHRC-CP and PenCLAHRC) we have developed a number of broad propositions about the nature of the collaborations developed by the CLAHRCs, and what is special about them. It is these that we would like to explore through this interview, especially to see how far our emerging findings from the two in depth studies might be applicable more widely to CLAHRCs.
CLAHRCs (our emerging view)
-
Their task is not just improving health-care research and not just improving patient outcomes, but a combination of both.
-
They are rooted in local relationships (some in place prior to the CLAHRC providing a platform on which to build, others created during the CLAHRC) and build on local capacities, with implications for critical size and remit.
-
The collaborations CLAHRCs are building are ones that seek to promote integration and culture change, not only to develop arrangements for brokerage (including knowledge brokerage) and linkage and exchange.
-
CLAHRCs legitimise a degree of experimentation in finding new ways of identifying and addressing NHS research needs, encouraging the emergence of research questions from the service and from its patients, which can then be funded by the CLAHRC but also by others.
Interview questions
A. Establishing the collaboration
Q1. Background
-
To what extent has the original vision/model that shaped your CLAHRC at the start persisted and been an important aspect of the CLAHRC?
-
In what form and to what extent has it persisted and to what extent has it changed, and who/what has driven that change? If it has changed, what has replaced it and why?
-
In both cases, to what extent were changes forced or imposed (e.g. by change of personnel at the top or by external circumstances outside the CLAHRC’s control) or were they evolutionary?
-
What qualities are required in CLAHRC directors, and have these changed over time?
-
Can you comment on proposition (i) above? Do you feel that your CLAHRC has achieved the right balance between these two objectives?
Q2. Context
-
How did the original context (nationally but, perhaps more interestingly, locally) influence the way the CLAHRC was set up?
-
To what extent have national and local contextual changes since 2008 shaped the CLAHRC?
-
To what extent has your CLAHRC been able to exploit these changes (and if so can you give an example)?
-
In this context, what is your view on the proposition that CLAHCRs are rooted in local relationships and build on local capacities, with implications for critical size and remit (see proposition ii above)?
B. Developing the collaboration
Q3. Scope
-
How helpful were the original decisions/thoughts from NIHR about:
-
–the scope of the CLAHRC geographically,
-
–the remit of the CLAHRCs to address applied health research and implementation, and the balance between the two,
-
–the extent of the collaboration (e.g. including LAs and social care as well as all NHS colleagues),
-
–the involvement of different stakeholder groups (e.g. patients, GPs, commissioners)?
-
-
In relation to each of the above, what main lessons have you learnt, and can you give examples of specific achievements?
-
In relation to each of the above, what would you, with hindsight, have done differently?
Q4. Risk
-
What were the main concerns about risk to the CLAHRC as a collaboration originally?
-
Were these concerns justified, and if so how were they handled?
-
To what extent has your CLAHRC encountered any tension between academic research needs and applied HSR needs and the different incentive structures at play, and, if it has, how has it been able to navigate between the two? (FOLLOW-UP QUESTION: How far is the new REF emphasis on ‘impact’ is one mitigating factor).
-
What tolerance has there been of failure(s) within the CLAHRC, i.e. has failure been seen as useful in any sense?
-
To what extent has the CLAHRC provided a ‘safe haven’/good environment for health services research?
-
In the context of your replies to Qs 3 & 4, what are your views on:
-
the proposition that the collaborations CLAHRCs are building are ones that seek to promote integration and culture change, not only to develop arrangements for brokerage and linkage and exchange (proposition iii above)?
-
the proposition that CLAHRCs legitimise a degree of experimentation in finding new ways of identifying and addressing NHS research needs (proposition iv above)?
-
C. Sustainability
Q5. How, originally, did you see the future of the CLAHRC: (a) as a persisting entity that would continue to broker the collaboration between the NHS and academe, or (b) as a shorter-term catalyst to encourage a collaboration that could eventually stand on its own?
-
If the latter, what will/would keep the collaboration going?
-
To what extent has the rapidly changing NHS environment provided an opportunity for your CLAHRC to develop a stabilising function/notion of continuity and how?
-
What impact is (or will) the development of the AHSNs having (have) on your CLAHRC?
Q6. What, from your perspective, constitutes a successful CLAHRC? What do you see as key measure/s of success?
And for those directors who have not already answered this question for us
Q7. What are the top three legacies of your CLAHRC to date?
D. Further help
Q8. On a more mundane level, we are planning a document review of all the CLAHRCs:
-
What documentation about CLAHRC plans and activities is available (and where), e.g. management board meetings, annual reports, etc. that you would be able to share?
-
Is there likely to be anything forthcoming in the near future from the CLAHRC’s own internal evaluation that you would be able to share?
-
Is there a list of publications from the CLAHRC that you would be able to share?
Appendix 9 The place of CLAHRCs in the wider landscape
Some of the issues CLAHRCs address about integrating the health research system into the health service, and encouraging knowledge brokerage, have been concerns in the English health R&D system for many decades. 14,42,120 We conducted an exploration of the wider landscape of the health-research system in order to develop a fuller understanding of how the CLAHRCs fitted into, and considerably enhanced, efforts to make the health-research system more fully meet the needs of the health service.
As we noted in the introduction to this report, the CLAHRCs were established following three policy initiatives that analysed the need to encourage more applied health research to respond to the needs of the local NHS, the need to promote more effective and rapid implementation of high-quality research and the need to increase collaboration across the NIHR, the NHS and higher education institutions to achieve these first two aims. These objectives, especially the first two, had long been aims of the Department of Health/NHS’s R&D division. In consequence there was an existing range of programmes within the NHS and NIHR designed to achieve them, and a potential overlap with the remit of the new CLAHRCs. In addition, and in response to the same policy drivers, other NHS and NIHR initiatives were set up after the CLAHRCs and were tasked with achieving similar aims.
This appendix provides further detail of this wider NHS/NIHR landscape and, in particular, informs the analysis of how far the CLAHRCs have played a unique role that could not be made by other NHS/NIHR initiatives. This is, in part, a historical analysis. It considers the other programmes that existed in 2008 when the CLAHRCs were established, traces new initiatives that started after the creation of the CLAHRCs and sets the scene for the analysis in the main report of the developments in 2012/13 as the CLAHRCs came towards the end of their initial 5-year funding. But it also attempts to address the counterfactual, that is how far existing arrangements might have allowed the institutions/people participating in the CLAHRCs to make the progress they have made if there had not been CLAHRC funding.
Inevitably, various developments are considered with the benefit of hindsight, but this throws useful light on the relation between CLAHRCs and the new AHSNs. As noted previously, the original designation for the CLAHRCs was NIHR Academic Health Centres of the Future. 3 This name was rapidly dropped because of potential confusion with the Academic Health Science Centres (see below), but, as the CLAHRCs have evolved and plans for the new AHSNs have developed, arguably it does in fact capture key aspects of the contribution the CLAHRCs are now making and could continue to make in the future.
An analysis of 30 years of development of the approach to R&D funding adopted by the English health department and the NHS14 applied the definition of a health-research system used by the World Health Organization that claimed such a system can include the ‘mechanisms adopted to encourage the utilization of research’ (p. 816). 121 The analysis of the English health-research system explored how it had evolved with a variety of funding initiatives and programmes designed to meet the diverse needs of an increasing range of stakeholders. The CLAHRCs emerged from that analysis as an initiative addressing concerns that had been central for many years, but which had proved difficult to tackle; namely meeting the research needs of the local health service and its patients and, more generally, facilitating the translation of evidence into practice.
As we have noted in the introduction (see Chapter 1), the call for the applications to establish the CLAHRC pilots was informed by three policy reports. 3 Two of these related to the health-research system;15,16 the third report was by a High Level Group for the Chief Medical Officer and addressed the issue of clinical effectiveness in the NHS. 17 This showed that there was:
a wide range of activities aimed at supporting clinical effectiveness ongoing within the NHS, but the degree to which they are fully integrated and aware of each other’s activities is not clear. Additionally, it is not clear which organisation has lead responsibility for the several dimensions of clinical effectiveness.
p. 1617
By the time the High Level Group’s report was published, the decision to establish the CLAHRCs had been made and in his foreword to the High Level Group’s report the Chief Medical Officer welcomed the NIHR’s decision to establish CLAHRCs as initiatives that ‘will develop innovative models for conducting applied health research and translating research findings into improved outcomes for patients, through partnerships between academia and the NHS’ (p. 3). 17
In 2008 the CLAHRCs were established as a new and separate programme within the NIHR (with matched funding from local NHS bodies). Reflecting their wider remit and role in promoting collaboration, and recognising the complex landscape in which they were being established, applicants were asked in their proposals to describe the partnership’s strategy in relation to:
engaging health care users and the general public; engaging, as appropriate, health care planners and policy makers; and linking, as appropriate, with other DH [Department of Health] and NIHR programmes and institutions, including the HTA and SDO [Service Delivery and Organisation] Programmes, CRD [Centre for Reviews and Dissemination], Cochrane Centre, NICE, and UKCRN [UK Clinical Research Network]. 3
In 2009, the NIHR produced a figure showing the place of various NIHR/NHS initiatives on the innovation pathway and where they all fitted together. 122 The CLAHRCs stand out because they cover a broader part of the pathway than any other initiative; that is, they cover three of the four main headings: evaluation, adoption and diffusion. Some of the overlaps between the CLAHRCs and other NIHR programmes were also shown: those programmes closest to the CLAHRCs on the innovation pathway were Service Delivery and Organisation (SDO), HTA, Centre for Reviews and Dissemination (CRD) and the Cochrane Centre.
Box 5 provides an overview of the key NIHR and NHS programmes that existed when the CLAHRCs were established and summarises their main activities and overlaps with the CLAHRCs. For example, the HTA and SDO programmes, the UK Clinical Research Network (UKCRN) and INVOLVE all played a part in setting research agendas and/or conducting research that was relevant to the needs for the NHS and patients, although since the abolition of regional R&D funds such needs assessment has been national rather than local. The CRD, the Cochrane Centre and NICE played various roles in making evidence available for translation into practice and in promoting translational processes.
Cochrane Centre: Established in the UK in 1992, it inspired the international Cochrane Collaboration, which consists of many groups who conduct systematic reviews and meta-analyses of evidence from RCTs and inform evidence-based practice.
Health Technology Assessment (HTA) Programme: Established in 1993, it produces research about the effectiveness of different health-care treatments and tests for those who use, manage and provide care in the NHS. It identifies the most important questions to which the NHS needs answers by consulting widely with these groups.
Centre for Reviews and Dissemination (CRD): Established in January 1994, it aims to provide research.
INVOLVE: This was established in 1996 to support greater public involvement in NHS, public health and social care research.
Service Delivery and Organisation (SDO) Programme: Launched in 2000, its remit included specific organisational issues of concern to managers as well as key policy issues of concern to the NHS. It consulted with potential users in the NHS on research topics and in 2012 became part of the Health Services and Delivery Research Programme (HSDR).
UK Clinical Research Network (UKCRN): This consists of a series of research networks established during the 2000s to provide an infrastructure for clinical trials spread widely throughout the NHS. Within the NIHR Comprehensive Clinical Research Network (CCRN) there are 25 Comprehensive Local Research Networks (CLRNs). There is also a Primary Care Research Network that has eight local networks, and six Topic Specific Networks that have local networks in parts of England. The six are cancer, dementias and neurodegenerative diseases, diabetes, medicines for children, mental health, and stroke.
Biomedical Research Centres (BRCs)/Biomedical Research Units (BRUs): Established from 2007, their research was more targeted at the first translational gap.
NHS organisations and programmes existing prior to the establishment of CLAHRCsNational Institute for (Health and) Clinical (from 2013: Care) Excellence (NICE): This was set up in 1999 to provide guidance to support health-care professionals and others to make sure that the care they provide is of the best possible quality and offers the best value for money.
NHS Innovation Hubs: These were set up from 2004 with support from the local NHS and the NHS Institute for Innovation and Improvement to champion the cause of innovation and to identify, develop and commercialise innovations and intellectual property created by NHS staff. The Institute was also responsible for the Commission for Quality and Innovation.
In our first report to the NIHR HSDR (previously SDO) we discussed the relationships between the CLAHRCs and existing NIHR and NHS initiatives in their local areas. 24 Box 6 provides examples of how the CLAHRCs referred to these links: it is clear that every CLAHRC was able to build on some level of previous collaboration with NIHR and NHS initiatives. In our report we also noted that: ‘The distinctive feature of CLAHRCs within this landscape was that they should have a wider integrating role across a wide range of local organisations, potentially including NHS Trusts, Primary Care Trusts, universities, and industries (p. 3).’24
CLAHRC-CP: This described how in reaching out to its user communities it would build on existing public engagement efforts such as INVOLVE, and in building internal evaluation capacity it would be supported by SDO academic fellowships.
PenCLAHRC: This was based on the South West Peninsular Clinical Research Collaboration which was a partnership of local NHS trusts and included the NIHR Comprehensive Local Research Network (CLRN) in the south west. The Peninsula Technology Assessment Group was also a key component bringing close links with the HTA programme and with NICE, and there was also engagement with the local NHS Innovation Hub in the South West.
Birmingham and Black Country (BBC): It referred to examples of past collaboration including two West Midlands research networks: Mental Health, and Medicines for Children.
Greater Manchester (GM): This had links with various networks including the Manchester Stroke Network and the Diabetes and Obesity Research Network. The Cooksey Report had earlier highlighted Greater Manchester as a good example of partnerships working.
Leeds, York and Bradford (LYB): This included the CRD based at York, and various CLAHRC staff had key roles on the West Yorkshire Clinical Research Network Board. Existing links included those with HTA, SDO, Cochrane and NICE.
Leicester, Northamptonshire and Rutland (LNR): Many of the partners within the CLAHRC had previous networks and relationships including the LNR CLRN, the South Midlands Diabetes Network and the East Midlands and South Yorkshire Primary Care Research Network.
North West London (NWL): The CLAHRC partners were jointly involved in similar work. Various examples are listed including that Chelsea and Westminster and Imperial partnered with the NHS Institute for Innovation and Improvement to provide training modules, and Imperial and all the Trusts involved are part of North West London CLRN.
Nottinghamshire, Derbyshire and Lincolnshire (NDL): The University of Nottingham hosts Trent CLRN, Mid-Trent Cancer Research Network, Trent Stroke Network and one for Medicines for Children.
South Yorkshire (SY): This had a history of strong collaboration prior to the inception of the CLAHRC, for example South Yorkshire CLRN was a key partner.
Source: Ling et al. 24 based on document review and interviews.
As noted above, almost as soon as the CLAHRCs were established there were further initiatives which to some extent overlapped with their activities. One change in the NIHR occurred at the same time as the CLAHRCs were introduced. In October 2008 the NIHR Research Design Service took the place of the former Research and Development Support Units (RDSUs). 123 One Research Design Service was established in each strategic health authority (SHA) area to provide expert advice to researchers on all aspects of preparing grant applications for applied research in health and social care. The South West Research Design Service, for example, played a part in PenCLAHRC’s efforts to identify and undertake research of relevance to the local NHS.
However, most of the initiatives that were introduced after the CLAHRCs came from the NHS and were intended to improve clinical effectiveness and encourage greater translation of research findings. Some of these had origins that pre-dated the establishment of the CLAHRCs: for example, starting in 2007 with Imperial College and Imperial College Healthcare NHS Trust, some health-care providers and universities began to come together to self-designate as academic health science centres. A review of the NHS led by Lord Darzi reported in 2008 and stated the Department of Health’s intention to promote academic health science centres in order ‘to bring together a small number of health and academic partners to focus on world-class research, teaching and patient care . . . [and] compete globally with established centres such as those in the United States, Canada, Singapore, Sweden and the Netherlands (p. 57).’20 Five academic health science centres were designated by the Department of Health in 2009, the year after the CLAHRCs started operating. 21 While they included universities, the academic health science centres were not formally part of the NIHR and did not receive NIHR funding.
However, it has also been reported that there was not complete unity within the Department of Health about how to respond to the call in the Cooksey Report to close the second translation gap. 23 For example, Caldwell and Mays quoted one interviewee as saying that:
although there’s been a lot of rhetoric about the second gap in translation and research about the reasons for it, there was no consensus view of what needed to be done and who the key players were and what the key levers were.
(p. 5)23
The consequence was that other initiatives were developed under a separate process, such as the HIECs. These were partnerships between NHS organisations (primary, secondary and tertiary care), the higher education sector (universities and colleges), industry (health-care and non-health-care industries) and other public and private sector organisations that were set up in 2009 with the aim of supporting the spread and adoption of innovation in care, treatments and processes (such as patient pathways). The Department of Health’s invitation for applications for HIECs stated that a HIEC should have ‘explicit and coherent relationships with other parts of the innovation landscape, e.g. AHSCs [academic health science centres] and CLAHRCs’ (p. 9). 124
Appendix 10 Phase 1 CLAHRCs’ descriptions and logic models
Summary accounts of all the nine CLAHRC partnerships presented in this appendix are based on information collected in phase 1 of our evaluation (the second year of the CLAHRC programme). Each summary describes the governance arrangements of each CLAHRC and the contexts in which they were established, their main aims and chief objectives, their overall approach (including any theories of change they had explicitly identified at that point), and the research and implementation themes they covered. Details are also given of their comments on the outputs and outcomes each CLAHRC was already achieving, or expecting, and their thoughts on the challenges faced and emerging lessons. Each description is completed by a logic model illustrating the underlying logic of intervention. These were produced by the evaluation team and shared with the CLAHRCs.
Birmingham and Black Country CLAHRC (CLAHRC-BBC)
Partnership and governance structures
University Hospital Birmingham NHS Foundation Trust is the lead NHS organisation and the University of Birmingham is the lead higher education institution. This core partnership is complemented by the West Midlands Strategic Health Authority (SHA). The main PCTs and secondary care trusts from the region are also part of the initiative. CLAHRC-BBC partners have a long history of collaboration with the University of Birmingham and the West Midlands SHA.
There are three levels of management, overseen by the CLAHRC director and the programme manager.
-
Nine theme management groups are responsible for the overall co-ordination and monitoring of each research theme. Each meets at least four times a year and reports to the programme management committee, outlined below, on a monthly basis. The administrators working for each theme are supported by a project management group co-ordinated by the programme manager.
-
The programme management committee oversees the delivery of the whole programme and optimises integration and synergy between themes. As well as monitoring the finances of the programme, the programme management committee plays an important role in reviewing and appraising the research proposals that are developed within each theme. It convenes each month and comprises theme leaders, lead researchers and financial and operational personnel.
-
The programme steering committee reports on the progress of the programme to the NIHR, provides strategic advice on the management of the research programmes, undertakes financial monitoring and is responsible for external relations and the dissemination of results.
Geographical context
Birmingham and Black Country CLAHRC covers all the Birmingham PCTs and extends into the area covered by two of the four Black Country PCTs. A highly diverse population is served.
High-level aims and key objectives
The main objective is to conduct needs-based applied health research to generate evidence that can be rapidly translated into routine practice to improve patient care. CLAHRC-BBC aims to reduce inequalities in and improve the quality of health-care provision, and to enhance safety and reinforce preventative services. Four core ideas build on each other:
-
The NIHR funding and matched funding will support service interventions that will be evaluated prospectively.
-
Complementary activities across themes and linked projects within themes will be conducted to help provide evaluations and an evidence base.
-
Research programme and management of staff careers will aim to generate sustainable capacity over the area.
-
The partnership will aim to capitalise on this capacity by developing further topics for research and by expanding its geographical reach further within the Birmingham and Black Country area.
CLAHRC-BBC approach
All the research and implementation themes focus on systems-level interventions intended to improve services. The CLAHRC has a strong commitment to evaluation, using a mixed-methods approach. The research studies are expected to identify factors that determine success or failure, and the various themes share findings and expertise in order to add value to each other and promote learning across the CLAHRC.
Research and implementation themes
Birmingham and Black Country CLAHRC comprises nine individual research or implementation themes addressing national health policy initiatives and reflecting local policies and priorities. Choice of the themes was driven by national and local priorities but was also opportunistic to the extent that it was seen as an opportunity to support local service development with research.
The research themes are, to that extent, based on service need, designed to promote relevance and information exchange.
Research themes:
-
health-service redesign
-
evaluation of paediatric outreach service
-
early detection and intervention in psychosis
-
assessment of the effects of new housing interventions
-
redesigned maternity support services for multiethnic disadvantaged groups
-
investment in prevention (evaluation of targeted prevention of cardiovascular disease in primary care)
-
optimisation of the management of stroke and transient ischaemic attack.
Implementation themes:
-
implementation of effective community care for diabetes
-
study of an evolving information technology system to improve patient safety.
Expected outputs/outcomes
-
Effective and appropriate service change: things that do not work are discontinued and things that do work are widely implemented.
-
An entrenched system for identifying and evaluating prospective service changes.
-
Good governance will allow a distributed leadership and will be supported by central administrative and management support. This will facilitate a culture of collaboration, stimulating closer ties between researchers and service delivery sectors, shorter time lags between research and application, and a base for securing further funding to support CLAHRC-like efforts.
-
Compared with other CLAHRCs, there is a particular emphasis on the importance of evaluation as a means of creating a self-improving and reflexive system. In time this will lead to improved services, a sustainable bridge between research and delivery sectors making both more responsive and timely. Meanwhile there will be spill-over effects on the local economy.
Challenges
-
Tensions between academic and NHS cultures: between producing papers and developing a focus on work of more immediate practical value that leads to soundly based, sustainable change. There is a related issue of getting the right people in CLAHRC posts who can work across the academic/service divide.
-
Differing interpretations of the CLAHRC remit.
-
Getting (and retaining) NHS management buy-in.
-
Communications, and specifically raising awareness in NHS trusts and engaging all trust staff.
-
Policy and finance-driven changes in local and NHS bureaucracies, such as the disappearance of the PCTs. There is a risk of the CLAHRC itself becoming overly bureaucratic.
-
Information sharing, governance problems and dealing with local bureaucracies
-
Getting genuine and real user participation.
-
The long time-scales to produce results.
Emerging lessons
-
Need to research service interventions properly in a timely fashion and learn as you go. Keys are producing timely data and working to appropriate time scales.
-
Need to help managers and commissioners to be more literate about research methods and appreciate the value of research, and to do this more systematically. Need to help managers, commissioners and clinicians understand the key levers of change.
-
Developing communications and building awareness about what the research is for and the best way of doing it; using some extra funding to raise knowledge about research through fellowships, secondments, etc. This requires a change of culture and to engage all trust staff.
-
Need for flexibility and working together, getting NHS people and researchers together to brainstorm possible service changes.
-
Value in having multidisciplinary teams working on CLAHRC themes, but this is challenging. There was a perception that the CLAHRC did provide a platform that brought together different research paradigms, allowing debate, exchange and exploration of areas of shared interest. It also helps to develop stronger links with people in other sectors, such as social services.
-
Means of getting and retaining NHS management buy-in, including:
-
matching funding
-
exploiting initiatives, such as the CQUIN (Commissioning for Quality and Innovation) framework and the new public health focus of local authorities
-
developing synergies with NHS bodies, such as SHAs.
-
-
A secondary value in exploiting wider economic potential; for example, local jobs can be created to develop health technologies being trialled locally.
FIGURE 58.
Birmingham and Black Country CLAHRC logic model of the theory of change.
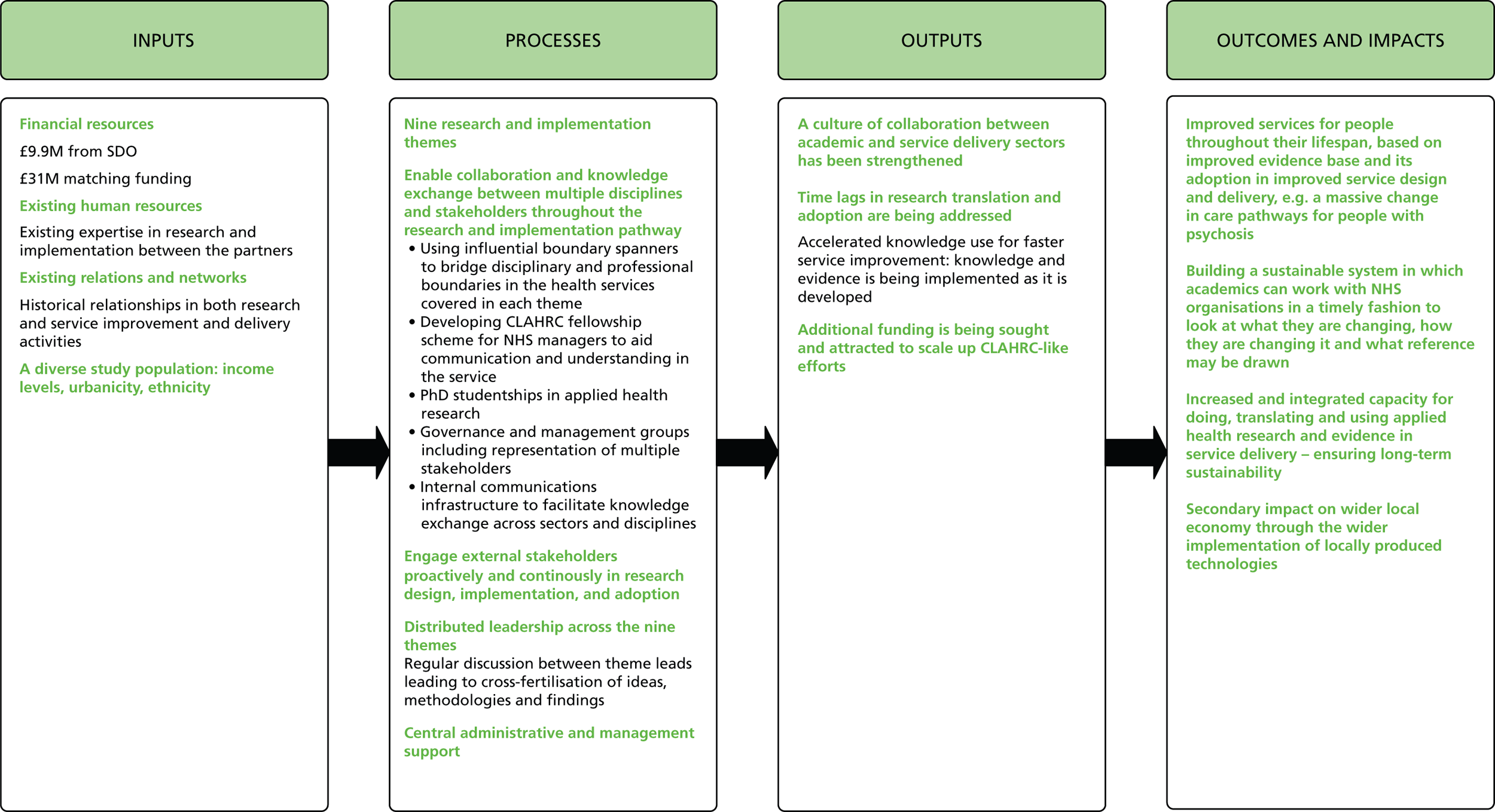
Cambridgeshire and Peterborough CLAHRC (CLAHRC-CP)
Partnership and governance structures
Cambridgeshire and Peterborough Mental Health Partnership NHS Trust, Cambridgeshire PCT, Peterborough PCT, NHS East of England Public Health Commissioning Network, University of Cambridge, Anglia Ruskin University, Cambridgeshire County Council and Cambridgeshire Community Services, supported by the UK Clinical Research Network (UKCRN) Mental Health Research Network East Anglia Hub, Eastern Region Public Health Observatory and the East Anglia Primary Care Research Network.
Many of the partners in CLAHRC-CP have a history of working together locally in research and care delivery initiatives. CLAHRC funding has enabled the consolidation of existing relationships, integration of fragmented efforts, bringing in additional expertise from new partners, and increasing regional participation and the coverage of diverse populations with varying needs. This included developing new partnerships with primary and social care providers and commissioners, and with organisations with expertise in change implementation.
The CLAHRC board is responsible for overall implementation and direction, and includes representatives from different academic disciplines, service providers, commissioners and local authorities. The CLAHRC executive group takes operational responsibility for the initiative and monitors the progress of the themes and implementation of research findings. Members include the theme leads, senior managers from the NHS, social care partners and the University of Cambridge. A governance group includes NHS R&D leads and ensures research governance, management and infrastructure support across the CLAHRC. Within a framework of central co-ordination and formal procedures for intertheme collaboration, there is also flexibility in terms of leadership, management and organisation within themes (distributed leadership).
Geographical context
The CLAHRC covers a population of over 1 million people living in both urban and rural environments across Cambridgeshire and Peterborough, with very diverse socioeconomic status and ethnicity.
High-level aim and key objectives
The mission of CLAHRC-CP is to improve the quality of community mental health and well-being, aiming to understand better the ways in which services are designed and delivered, examine them critically, and gradually improve services based on existing and new evidence on best practice. The CLAHRC’s focus is on people with mental illness, learning disability and acquired brain injury, and on end-of-life care. Within this broad field, CLAHRC-CP is building on established strengths of partners in life-course approaches to health and illness, focusing in particular on challenges at the points of transition. Specific objectives are to:
-
Create an environment that encourages interactions within and between thematic programmes: those working in implementation themes are conducting implementation science research, and will work with the research themes to inform research agenda-setting based on service needs, and enable the translation of research outputs into improved mental-health service delivery.
-
Facilitate knowledge exchange and build capacity to conduct, integrate and use health research to improve services and the quality of patient care.
-
Develop collaborative projects involving multiple stakeholders in an iterative manner, from design to dissemination; this includes academic researchers, clinicians, managers, commissioners, users and local authorities.
-
Mobilise individuals who can bridge disciplinary and professional boundaries between academic and service delivery sectors (e.g. as theme leads) and trying to empower future ‘boundary spanners’ and ‘knowledge exchange champions’ through its capacity in building and training activities. Related to this is a belief in the need to involve clinicians in research activities in a way that enables them to remain active in clinical practice (and teaching).
-
Share and disseminate learning widely, including beyond local and regional levels. This is grounded in the understanding that, although the CLAHRC’s direct and immediate focus is on local service delivery improvement, this should not compromise an academic ethos of sharing and communicating lessons learnt and research findings.
CLAHRC-CP approach
Cambridgeshire and Peterborough CLAHRC’s theory of change is based on a number of inter-related assumptions:
-
Effective mental-health services need to be designed in a way that considers the patient’s needs throughout their life. Improved practices in service provision are needed in particular at points of transition.
-
Improvement in practices requires a detailed understanding of the mental-health system pathway from the perspectives of different actors in the system (across professional groups and disciplines), so that areas in need of research-, policy- and practice-related attention are made explicit, and research and change implementation activities are framed accordingly.
-
Service improvement requires integrating doing research with translating and using applied health research.
-
The effective translation of research into practice is an iterative process with feedback loops between different stages. This requires close collaboration and knowledge exchange throughout all stages of research generation, maturation and utilisation processes.
CLAHRC-CP aims to establish and nurture strong and sustainable learning and exchange linkages between diverse stakeholders in the mental-health services pathway, including academic researchers, clinicians, NHS managers, local authorities, GP practices, commissioners and service users. Senior staff from all PCTs and the county council sit on the CLAHRC board, and heads of service commissioning sit on the executive group. The CLAHRC is also bringing together new combinations of disciplines, professions and individuals in research and implementation teams (in engineering, business, public health, general practice and psychiatry). This plurality is expected to enable the process of generating, communicating, disseminating and adopting research findings to be better tuned to the health-care system, and increase the relevance, usefulness and adoptability of outputs. The translation gap is not seen to be unidirectional, and CLAHRC-CP intends to involve stakeholders throughout different stages of the research and implementation processes.
Research and implementation themes
The CLAHRC aims to harness local research strengths in life-course approaches to health and illness, and focus on ‘pinch-points’ in service provision (such as transition between adolescent and adult services, social care and health, and end-of-life care) for some of the most vulnerable members of society.
There are three research themes:
-
adult disorders, focusing on learning disability and long-term outcome of head injury
-
child and adolescent mental health, focusing on transitions between these services and adult systems, with some work on autism
-
mental health and disability in old age, including end-of-life care and a development of clinical academic old age psychiatry.
There are two cross-cutting implementation themes:
-
public health, focusing on population health and commissioning
-
design, focusing on health systems analysis, education and training for managers, commissioners and clinicians, and investigation of the spread of innovation and ideas in health systems.
The expected outputs/outcomes are:
-
A more collaborative culture with a capacity to address issues in new ways: health services will become more evidence based and will draw upon research more quickly. This will create a platform for securing further future funding.
-
Outcomes including improved experiences and outcomes for service users, more appropriate applied research, more evidence-based services, a sustainable network of organisations to support this, and contributions to the national and international understanding of the theory and practice of how to bring research and practice together for the benefit of service users and society.
Challenges
-
Cultural, administrative and practical differences between the main organisations: there is a need to manage and navigate dual governance systems (i.e. academia and NHS).
-
Engaging the main players in the CLAHRC vision of integrated collaborative research, and sustaining partner enthusiasm and commitment to delivery on agreed objectives and responsibilities (including from senior levels in the NHS).
-
PPI is not easy (there were recruitment challenges to get a lead for PPI in post).
-
Getting buy-in at middle management and senior levels in universities and NHS trusts.
-
Navigating and responding to changing socioeconomic, political and NHS landscapes – related to this is the need for flexibility from all CLAHRC stakeholders.
-
Finding ways to balance and manage the academic ambitions of research groups with time commitments and emphasis on impact of research on services.
-
Clarity and management of expectations about the timelines needed for demonstrable change and wide-scale service improvement.
-
Continuation of the CLAHRC or CLAHRC-like funding beyond the first phase of initiative existence.
Emerging lessons
-
Central management and co-ordination capacity for complicated collaborative initiatives such as the CLAHRC is important (e.g. ethics, financial management, communications, appointments).
-
It is also important to develop leadership capacity through a commitment to distributed leadership.
-
Key performance indicators may further support this and can be a way of building consensus on goals, commitments and expectations from all participants (across organisations and disciplines).
-
Good public relations/website/communications are important if internal and external stakeholders are to engage effectively with the CLAHRC.
-
It is important to engage diverse stakeholders from the onset of the research process, not only at the end: i.e. in research agenda setting, implementation and adoption (e.g. local authorities, service users). Creating formal and informal opportunities for interpersonal and interorganisational exchange is important.
-
There is a need to identify and support champions of change: those who can use knowledge to affect service delivery and implement change (commissioners, managers, clinicians, social care practitioners, end users).
-
Physical proximity and colocation are important facilitators of multidisciplinary and multistakeholder collaboration.
-
There are practical organisational barriers for colleagues with split roles: it is difficult to work out how time is covered under each role. There is an associated issue of releasing time for people to be out of their normal team and in the CLAHRC (this is particularly relevant for applied health professionals). It is necessary to examine what types of support are needed to sustain split roles.
-
Building and working in multidisciplinary teams (especially if they bring together groups that had previously not worked together) requires time and repeated interactions (formal and informal), an openness to learn from each other, and positive attitudes to plurality and different working styles.
FIGURE 59.
Cambridgeshire and Peterborough CLAHRC logic model of the theory of change.
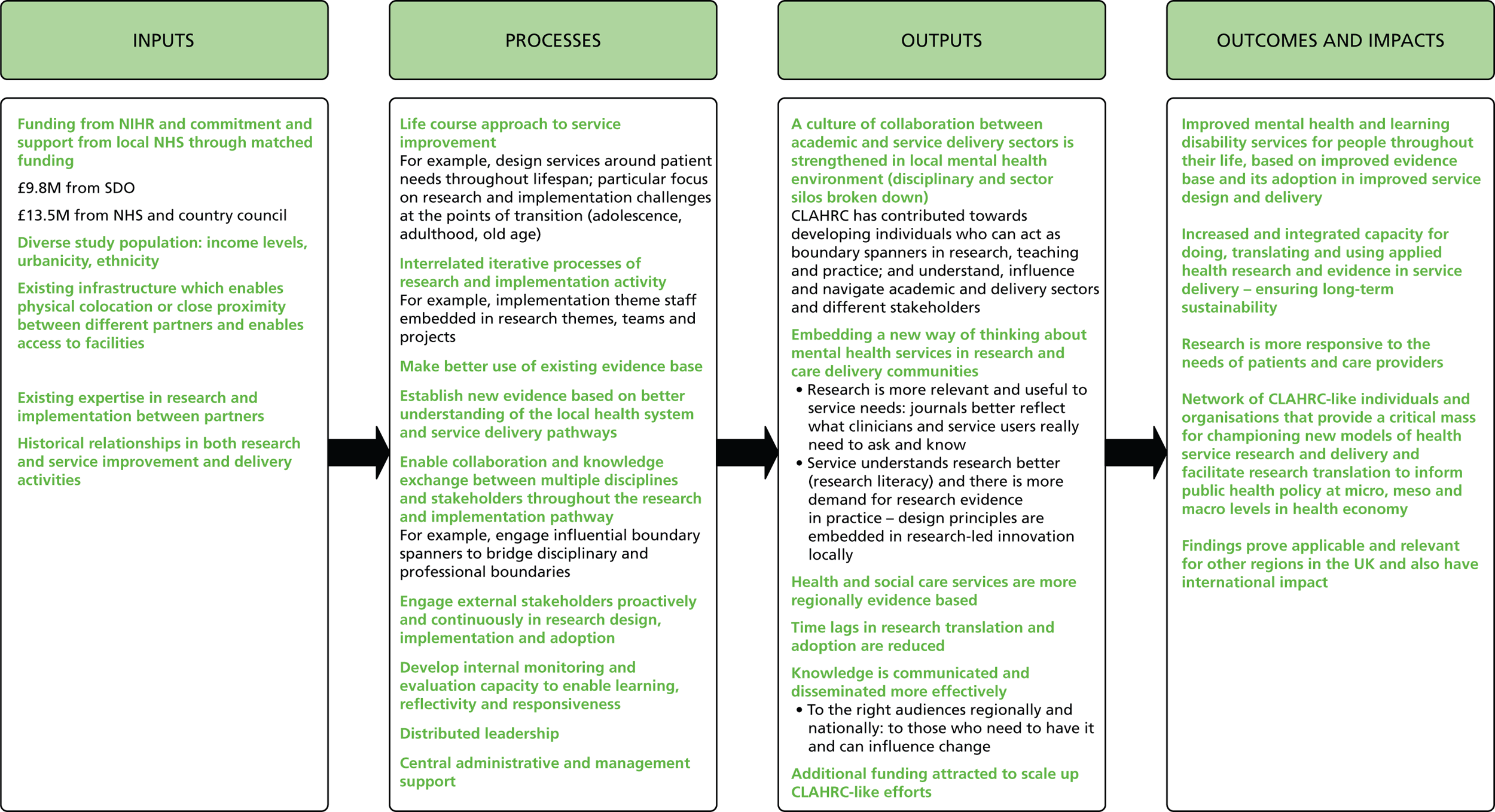
Greater Manchester (CLAHRC-GM)
Partnership and governance structures
Manchester University, 10 PCTs, six hospital trusts, three mental-health trusts and an ambulance service: it is led by the Salford Teaching PCT. There is a long history of collaboration between the University of Manchester and local NHS organisations, and all the local trusts have previously worked together to improve the quality, relevance and impact of NHS research for the public.
Greater Manchester CLAHRC has a central leadership and secretariat. It also includes studentships and 24 knowledge transfer associates. Its governance is made up of the following elements:
-
A steering group that is chaired by the lead trust meets twice annually to approve the CLAHRC’s budget and programme. The lead trust is responsible for managing finances and subcontracts with partners and providing general administrative support.
-
A research and implementation group meets quarterly to review progress across all themes and ensure integration of the work. It is composed of the theme leaders, the chief operating officer and the CLAHRC director as chair. The theme leaders meet monthly and manage day-to-day theme work.
-
The CLAHRC director is accountable to the NIHR and steering group for overall management and performance, and chairs the research and implementation group.
-
The chief operating officer is responsible for day-to-day management, including research governance and research protocols, and reports to the director.
Geographical and demographic context
Greater Manchester has more than 2.56 million residents and is the third largest metropolitan area in the UK. It is characterised by poverty (75% of wards in bottom fifth for England), ethnic diversity with a relatively high representation of Asian (approximately 6.5%) and black (1.7%) people, poor health (lowest life expectancy in England for men, 72.5 years; second lowest for women, 78.3 years; and a high incidence of cardiovascular disease) and inequalities in health/health-care provision.
High-level aims and key objectives
The overall goal is to improve the health of people in Greater Manchester by enhancing the quality of care in terms of safety, efficacy, efficiency, patient-centredness, timeliness and equality through the application of world-class research.
The overall objectives are to:
-
develop and evaluate a series of interrelated interventions to support patient self-management and improve the quality of care for people with chronic vascular disease
-
implement these and other evidence-based interventions in NHS trusts across Greater Manchester to improve patient health and reduce inequalities in healthcare provision
-
build local NHS capacity to plan and implement evidence-based changes in care pathways for people with vascular disease through close working and knowledge transfer between university researchers and NHS providers and commissioners.
CLAHRC-GM approach
-
Research approach: CLAHRC-GM notes that current approaches to chronic disease focus on developing evidence-based standards of care, as found in clinical guidelines. However, research that improves patient self-management may significantly reduce the burden of NHS service consumption. Recent research has shown that patient self-management can be improved by enhancing patient knowledge and coping strategies in a systems approach. This research approach can be implemented in six steps: agreeing what is to be accomplished; determining how the impact of change will be measured; identifying what changes should be made; implementing change using plan–do–study–act cycles; sustaining and spreading the changes; and evaluation of implementation.
-
The strategy for the implementation theme rests on the recognition that successful implementation requires multifaceted interventions across whole systems and is not a linear or technical process.
-
The research theme findings will feed into the implementation themes and knowledge transfer partnerships to facilitate change and build leadership capacity in implementation.
-
The CLAHRC aims to develop existing systems of partnership working among NHS trusts and the University of Manchester through closer alignment of research with NHS needs and priorities, facilitating the uptake of research into practice.
-
This approach involves both research and implementation themes and building capacity to generate and disseminate knowledge. The creation and application of knowledge is fundamental to the approach, and the knowledge transfer partnerships are an important aspect of this.
Research and implementation themes
There are four research themes and four implementation themes, focusing on patient self-management of chronic diseases.
Research themes:
-
People with long-term conditions: To elicit the needs, social and health contexts, and receptivity (to information) of socially disadvantaged people with vascular conditions in order that information can be developed, integrated and evaluated within an existing evidenced-based approach to guide self-management support.
-
Health-care practitioners: To promote better patient-centred care by practitioners through the development and testing of new approaches to the management of depression in patients with long-term conditions.
-
Health-care services: To contribute to the promotion of self-management through the development of new patient-centred systems of access to specialist care and through the development of allied programmes of training for specialists. Combined with the self-care information resources from the first research theme, this will generate whole-systems intervention.
-
Health information systems: Will develop the information systems needed to improve health-care planning by monitoring variations and inequalities in health-care provision for people with chronic vascular disease, and assessing the likely impacts of interventions to improve patient care and public health.
Implementation themes:
-
Coronary heart disease: To enhance NHS capacity to translate research findings into improved outcomes for patients by the improvement of services for people with heart disease.
-
Chronic kidney disease: To enhance NHS capacity to translate research findings into improved outcomes for patients by improving services for people with chronic kidney disease.
-
Diabetes: To translate research findings into improved outcomes for patients with diabetes by developing and improving services for people.
-
Stroke: To enhance NHS capacity to translate research findings into improved outcomes for patients by the improvement of services for people with stroke.
Expected outputs/outcomes
-
Outputs are focused on the production and creative use of information sources, including cost–benefit information, simulation models (allowing commissioners to engage with the evidence base by simulating the likely impact on costs of changing pathways) and peer-reviewed publications. Alongside these, and closely related to them, is the production of workforce development plans to support redesigned pathways and improved ways to access care.
-
Knowledge is therefore intended to play a key and transformative role in achieving ambitious impacts, more effective treatment, reduced (inappropriate) demand and improved access, improved patient self-management, a more responsive NHS, reduced inequalities and increased capacity in the NHS to plan and implement evidence-based changes.
-
The intended outcomes are firmly focused on transforming NHS services.
Challenges
-
Researchers and practitioners have different ways of working.
-
Having many different kinds of people working together involves practicalities and logistics, including pragmatic issues such as planning meetings, the number of meetings, lengthy and uncertain recruitment processes, and increased bureaucracy and governance.
Lessons emerging
-
There is an inherent tension between the research and service delivery worlds, one factor being that they work at different paces. CLAHRC-GM funded consecutive rounds of evidence-based innovation projects with a quick turn-round, allowing faster answers to be provided, while building on previous knowledge in future work. In other words, the research setting can be reorganised to respond to different time frames without losing the long-term accumulation of knowledge that lies at the heart of the scientific process.
-
Funding that forces interaction between researchers and research users may sometimes be successful. The success of the CLAHRC may depend upon the transformative power of knowledge, but it also recognises the need to support this with incentives and guidance.
-
Greater Manchester CLAHRC can synthesise information on how to bring research and practice into a more mutually beneficial relationship in a reliable and accessible way. In this sense CLAHRCs have a metafunction: supporting learning about learning.
-
There are dangers in trying to link everything with everything, and there is a need to retain focus; otherwise there may be a series of unproductive meetings and little else. The issue here is how priorities can be identified, agreed and acted upon within a distributed leadership.
-
Greater Manchester CLAHRC has had to emphasise that it is not about running services: it is about informing the way in which services are run and supporting evidence-based change.
FIGURE 60.
Greater Manchester CLAHRC logic model of the theory of change.

Leeds, York and Bradford CLAHRC (CLAHRC-LYB)
Partnership and governance structure
There are four core partners: the Universities of Leeds and York, and the Leeds and Bradford teaching hospital trusts. The core partnership was determined on the basis of the ambition to bid with the two strongest academic and NHS components in the region. These partners are also linked to the Leeds Partnerships NHS Foundation Trust, Bradford Metropolitan District Council, NHS Bradford and Airedale Teaching PCT, Leeds City Council, NHS Yorkshire and the Humber SHA, the NHS Innovation Hub for the Yorkshire and Humber region and the Yorkshire regional development agency (Yorkshire Forward).
Leeds, York and Bradford CLAHRC partners have worked together for many years in a variety of ways.
The governance of CLAHRC-LYB aims to provide central direction through a CLAHRC-LYB board (with input from public and patients) and a CLAHRC-LYB executive group (supported by an infrastructure group and a scientific steering committee) while giving the various themes freedom in running their work. Appointments to the various themes mainly come from the four core partners, but members also come from the other sectors on which the CLAHRC draws.
Geographical and demographic context
The CLAHRC covers a population of around 5 million people who have a range of socioeconomic, ethnic and cultural backgrounds.
High-level aims and key objectives
Leeds, York and Bradford CLAHRC aims to build capacity to innovate into NHS commissioning and service delivery in a cost-effective way. Specific objectives include:
-
building the research capacity of the NHS
-
building researchers’ ability to respond to front-line needs
-
building commissioners’ and NHS staff’s ability to communicate front-line needs
-
building the capacity of commissioners and those delivering health-care services to innovate – by tying research to outcomes, changing relationships and networks, and communicating on the topics of interest to commissioners
-
evaluating the cost-effectiveness of work
-
informing practice on the basis of rigorous evidence.
CLAHRC-LYB approach
The CLAHRC aims to respond to local and chronic health conditions distributed unequally in the population. It is driven by two key ideas:
-
The research themes are the starting point for developing local NHS capacity to drive the research cycle, starting with identifying questions, reviewing the literature to find out whether they have been answered, designing studies, undertaking them and interpreting the results. There are plans to develop NHS staff to the point where they can drive these cycles, with appropriate support from academics.
-
The implementation themes are concerned with the other aspect of innovation, with creating the capacity to incorporate new knowledge and practices safely and effectively into routine service delivery. NHS teams will seek to develop new ways of working and achieve cost reductions and improvements in quality and safety. CLAHRC-LYB will be responsible for ensuring that the teams have the tools/resources they need, and will work with NHS managers to remove barriers to change where necessary.
Leeds, York and Bradford CLAHRC builds change within the NHS by involving individuals who are in authority and in a position because of their place within networks to cascade the research and its outputs throughout the service. CLAHRC-LYB also seeks to involve commissioners, as well as clinicians, in order to build long-term capacity to integrate the clinicians and researchers’ knowledge into clinical research and practice: it sees commissioners as key to the sustainability of the CLAHRC legacy. PPI is also important to CLAHRC-LYB, as demonstrated through the board’s relationship with patients and the public and through the individual themes.
Research and implementation themes
Two research themes draw on local expertise and are intertwined:
-
The physical health and addiction theme will explore cost-effective interventions which can be routinely implemented in the acute care setting.
-
The vascular disease theme will investigate prevention, through a range of lifestyle-change advice programmes to at-risk communities; and treatment, exploring the reasons for poor medicines adherence.
There are three implementation themes: implementation-driven research (in maternal and child health and in stroke), and the Translating Research into Practice in Leeds and Bradford (TRiP-LaB) programme.
-
The child and maternal health theme will develop and implement research-calibre information systems that will focus on addressing inequalities in antenatal health (exposures to risk factors in utero), infant and child feeding and obesity, maternal mental health, and access to health and social care services.
-
The stroke care theme will seek to uncover the reasons for poor stroke care by routinely collecting data on hard-to-capture measures such as information on stroke care delivered, stroke care organisation and delivery structure, the unique characteristics of patients and the outcomes of care on patients, as described by them.
-
The TRiP-LaB programme will explore the hypothesis that multifaceted and theoretically informed interventions targeting different barriers to change are more likely to be effective than single interventions for getting evidence into practice, examining questions such as: What should a change strategy look like? What sorts of barriers can be overcome and how? How will we know if what we can achieve is worth it?
Projects will apply a range of theories to underpin their rationale, which may allow TRiP-LaB to draw conclusions regarding the application of different theoretical approaches. The projects will all focus on making access to care more equitable across communities, in particular for chronic disease, and cost-effectiveness will be a strong element.
Expected outputs/outcomes
-
The CLAHRC is expecting improved knowledge of the cost-effectiveness of certain interventions, better outcome measures and a better understanding of what the public wants. Capacity building includes embedding research and evaluation capacities in the NHS and embedding the needs of the NHS in researchers’ approaches. It also seeks to understand better what works in bridging the second translation gap.
-
The intended outcome is a structural and cultural change in the NHS, in academia and in commissioning, resulting in a new and sustainable relationship between researchers and practitioners.
Challenges
-
Providing clinicians with the time to engage in research through funding streams is not sufficient; it may be difficult to backfill their position.
-
Relationships and networks need to be built amidst a changing health-service landscape. This may confuse the direction of effort as well as the willingness and commitment of health-service providers to engage.
-
The impending abolishment of the PCTs had substantial implications, with NHS Bradford PCT being one of CLAHRC-LYB’s primary partners.
-
Funding has been delayed (allegedly because of the difficulty of fulfilling the novel CLAHRC human-resource funding approach) which has meant that certain outputs may not be achievable within the set time frame.
-
As yet, CLAHRC-LYB partners do not have a fully shared view of what the CLAHRC identity is/should be.
-
There are cultural barriers and differences between the NHS and academia to overcome, including:
-
Conceptual barriers – the sectors do not necessarily understand terminology and concepts in the same way;
-
Differences in ambition – practitioners are driven by different ambitions. These are not incompatible but they do imply different priorities; there need to be practical compromises;
-
Differences in work environment – clinicians and researchers do not generally grasp the day-to-day activities and the possibilities and constraints of each other’s work. This is an obstacle to successful collaboration.
-
Differences in time scales – researchers’ time scales are generally much longer than clinicians’, who have a fire-fighting capacity.
-
-
In seeking to bridge the second translation gap, clinicians and other NHS practitioners are expected to ask questions that will still be relevant to them in the future, while researchers are expected to be flexible and pursue research that can start providing answers relatively quickly.
-
The optimal way to achieve PPI is not clear.
-
The CLAHRC rests on deep collaborations. These rely on an element of trust between partners. This trust can take time to build, as partners have their personal ambitions and reason for being protective of these. This suggests that collaborations will take time and may have uncertain consequences.
-
Demonstrating impact: there are a number of tangible outcomes that may be measured, but much of the core of the CLAHRCs includes intangibles.
Emerging lessons
-
Networking is key to achieving collaboration and an understanding of ‘the other’s’ work environment, ambitions, possibilities and constraints. It is one of the hardest and most time-consuming activities, but is crucial to success. It is important to use people who are already embedded in the organisation and understand the culture and where the leaders are.
-
Buy-in from the chief executives is a key factor that can make the CLAHRC’s relationship brokering and pursuit of various activities more seamless.
-
There is a need to exploit clinical leadership and build on existing strands of expertise; this helps to build credibility and interest.
-
There is a need to develop a close relationship with commissioners, with mutual commitment to listening and integrating the other’s advice.
-
The fact that the CLAHRC initiative did not provide support costs was a concern at first but has since been considered a positive element, forcing researchers to ensure the usefulness and feasibility of the research. Field diaries can be a useful way of capturing these intangible aspects of CLAHRC activities.
-
It is important to engage, build and sustain a critical mass of change-capable agents.
FIGURE 61.
Leeds, York and Bradford CLAHRC logic model of the theory of change.
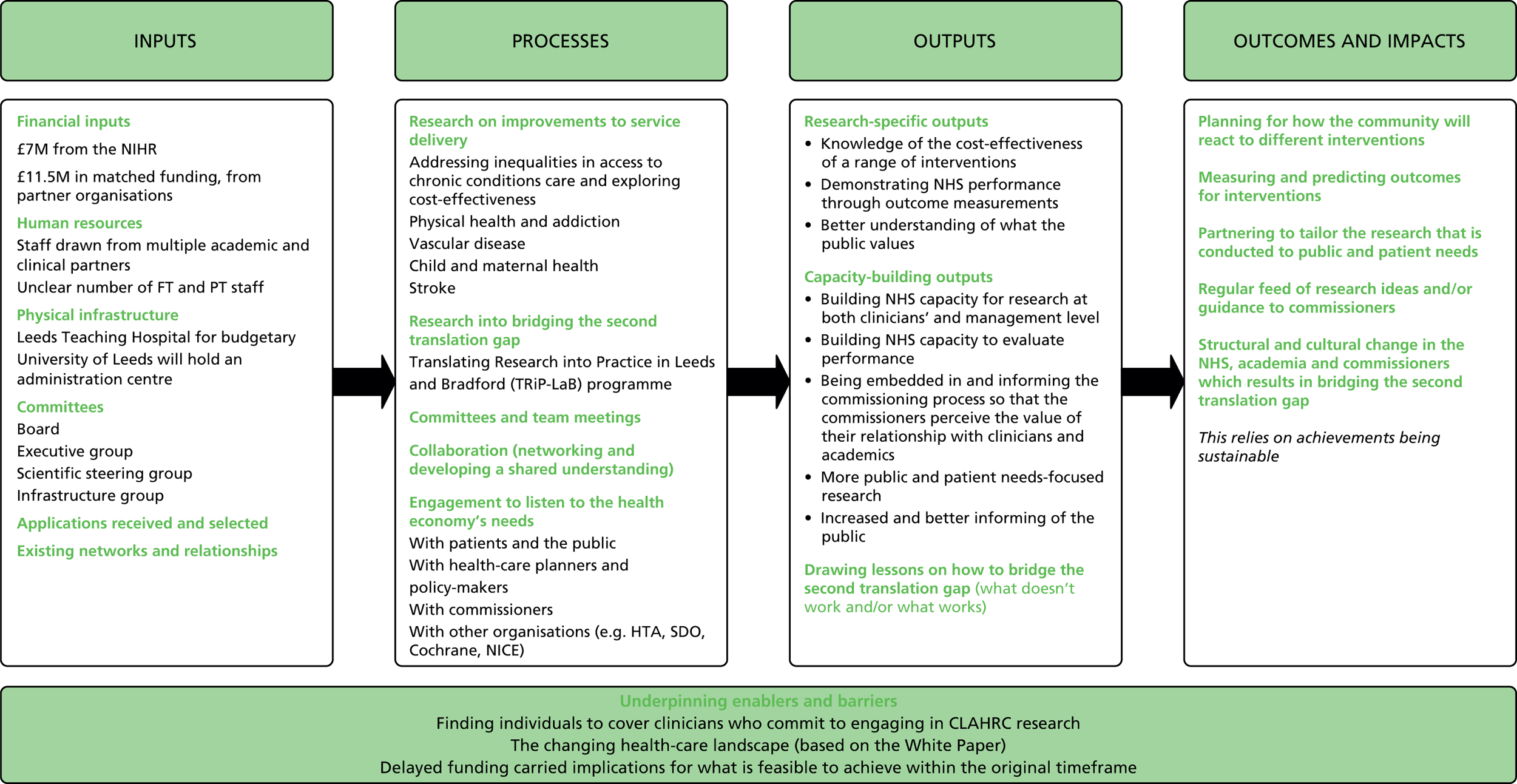
Leicestershire, Northamptonshire and Rutland CLAHRC (LNR-CLAHRC)
Partners and governance structure
University Hospitals of Leicester NHS Trust, Northampton General Hospital NHS Trust, Kettering General Hospital, Leicester City PCT, Leicestershire County and Rutland PCT, Northamptonshire Teaching PCT, Leicestershire Partnership Trust, Northamptonshire Healthcare NHS Trust, University of Leicester. The CLAHRC has access to a large number of GP practices and builds on previous networks. Relationships include the LNR Comprehensive Local Research Network, the South East Midlands Diabetes Network and the East Midlands and South Yorkshire Primary Care Research Network.
The CLAHRC board includes chief executives and senior people from the trusts including R&D leads. CLAHRC staff include a core team of director, deputy director, five theme leads, five deputy theme leads and five theme managers.
Geographical and demographic context
The counties of Leicestershire, Northamptonshire and Rutland cover a population of approximately 1.6 million. A large percentage of the population in some areas is from ethnic minorities (e.g. 34% in Leicester). Indicators of health are similar to the average for England and the East Midlands region, but there is wide variation, with significant levels of deprivation and poor health in some areas.
High-level aims and key objectives
To conduct applied health research (in long-term care) in new ways that can more rapidly inform practice, and to increase research capacity in the NHS. This means enabling partner NHS organisations to generate new research evidence, make use of existing research evidence and develop systems and structures for the application of knowledge and for the translation of research evidence into more effective and efficient health-care policy and practice. These high-level aims are underpinned by a set of nine objectives:
-
Secure a step change in the way that applied health research is conducted and health research evidence is put into practice.
-
Increase capacity to conduct and implement applied health research through education and collaboration.
-
Increase the involvement of stakeholders from the local health community, including the public, in the design, conduct and application of health research.
-
Link those who conduct applied health research with those who use it in practice.
-
Test new initiatives to encourage the use of applied health research findings in health-care practice.
-
Create and embed approaches to research that are specifically designed to take account of the changing ways in which healthcare is delivered.
-
Focus on the needs of patients.
-
Improve the health of the local population.
-
Make a significant positive impact on the health of the people of its region and contribute to a better understanding of the mechanisms for sustaining that improvement.
LNR-CLAHRC approach
The overall approach is influenced by the organisational excellence model described by Nutley et al. 106 and by the experiences of the Veterans Administration QUERI programme. 107
-
Engage NHS partners in all CLAHRC activities and at all stages of the research cycle, so they are encouraged to see research as part of their day-to-day work, with useful outputs that can be practically implemented.
-
Involve the public, patients and clinicians in research and CLAHRC activities so that the research the CLAHRC produces is directly relevant to them and has greater drive.
-
Develop guidelines locally and involve local partners.
-
Provide trusts with research that is tailored to their needs and those of their patients, using existing local knowledge where possible and ‘piggy backing’ on existing activities to make outputs relevant.
-
Use CLAHRC co-ordinators embedded in the trusts and translational teams in decisions on research.
-
Spread the relevance of the CLAHRC’s work by training people to deliver a model of education developed by the CLAHRC to support its aims.
-
Achieve buy-in from clinicians and the support of NHS management. The CLAHRC board includes chief executives and senior people from the trusts including R&D leads, which makes it powerful and gives it legitimacy; some of the ideas driving the CLAHRC come from them and, overall, their involvement makes it possible to get things done in the trusts.
Research and implementation themes
Four applied research themes focus on different stages of treatment (early detection of chronic disease, self-management and education in long-term conditions, prevention of chronic disease and its associated comorbidity, rehabilitation).
One implementation theme aims to improve the uptake of evidence-based practice, promote the implementation of LNR-supported research and develop an evidence base for effective implementation through evaluation.
Expected outputs/outcomes
-
Intended outputs include securing further funding, improving the availability of data to clinicians so they know when they are departing from evidence-based practice and guidelines. New and usable evidence is to be created along with an infrastructure to support the implementation of locally produced research.
-
Outputs already achieved included the ‘Detect Tool’ and articles in peer-reviewed journals.
-
Outcomes already achieved included raising awareness, bringing clinicians who were previously non-researchers into research activities and developing strengths in new areas of research. In the longer term, the CLAHRC hoped to achieve better health outcomes for patients, improved ways of working and sustainable behaviour change among NHS staff and researchers.
Challenges
-
There are geographical variances in engagement with the CLAHRC: different trusts have different levels of interest as well as varying levels of previous experience and expertise in research. Different tailored approaches are needed to achieve buy-in from all partners involved.
-
There are different incentives and time scales for researchers and for NHS staff: NHS staff often lack the time to stop and reflect on their practices, and NHS resources are seldom dedicated to evaluating current practice owing to the short time scales they operate on as well as frequent changes in management (if a research finding can make a difference but only in a few years, it is likely that the leadership of the trust will change and so will its priorities).
-
The CLAHRC operates in an environment where it is competing for the attention of all sorts of people, and current changes in the NHS landscape mean that involving commissioners in research is increasingly complex; the people the CLAHRC needs to engage are changing, and their priorities are changing because of current pressures.
-
There are staffing and recruitment problems: because of the bureaucratic processes involved and difficulty of defining some CLAHRC posts, such as CLAHRC co-ordinators.
-
It is difficult to get ethics approval for some studies.
-
There were unrealistic expectations of what the CLAHRC could achieve. A large grant was awarded to the CLAHRC, but it was relatively small compared with the region it covered and the changes it would like to bring about in the system. The CLAHRC cannot solve everyone’s problems and that was sometimes not well received. In addition, although the CLAHRC had been able to put together an infrastructure to make changes happen, these changes would be realised in the long term rather than straight away.
-
The CLAHRC research studies did not have research portfolio status and are therefore not eligible for support from the local research networks; CLAHRC studies competing with other prospective research studies that do have this status are at a disadvantage.
-
There is some concern that there is too much emphasis on applied research and too little on implementation, and concern that the applied themes are very close to traditional research.
FIGURE 62.
Leicestershire, Northamptonshire and Rutland CLAHRC logic model of the theory of change.
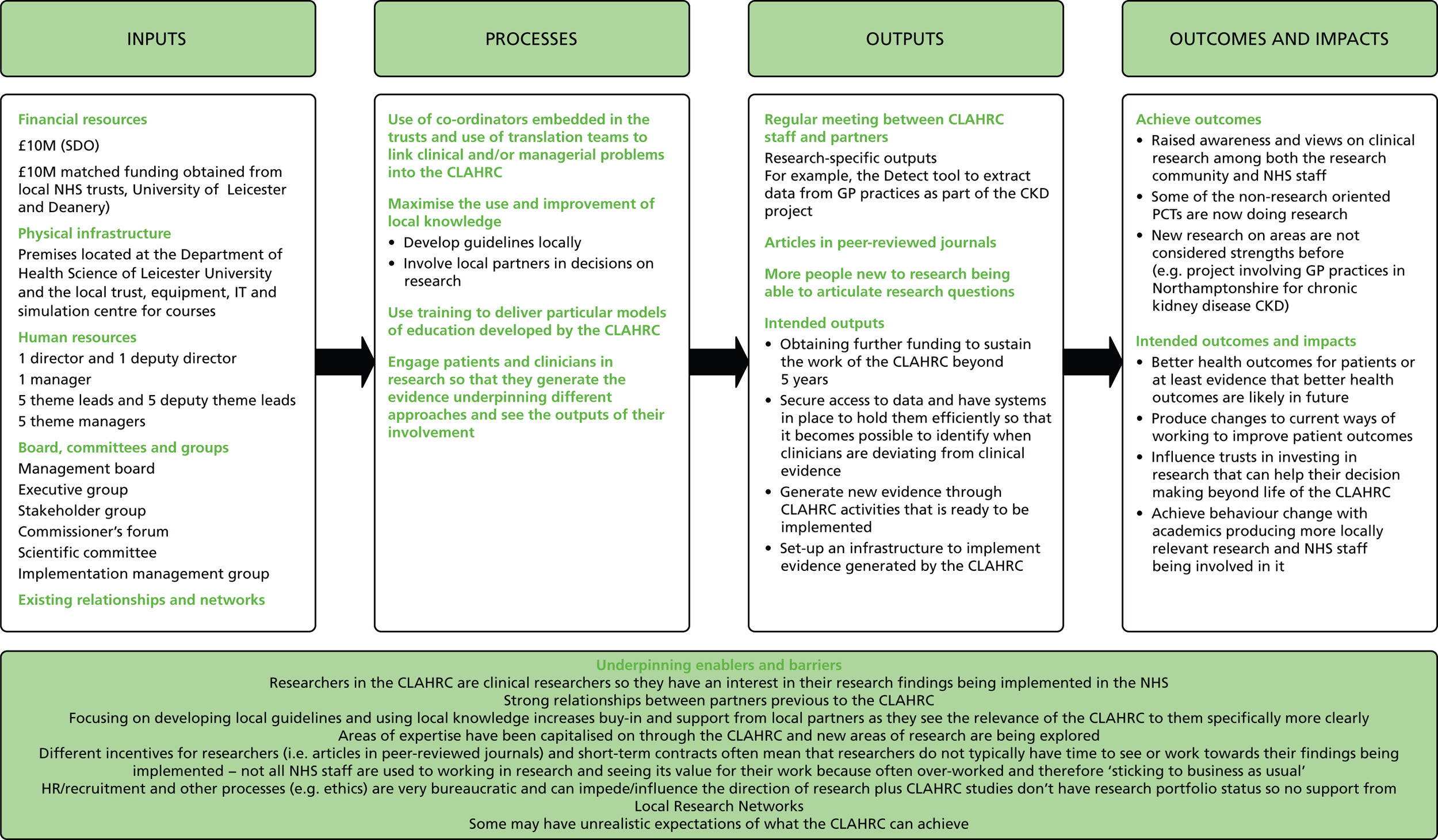
Northwest London CLAHRC
Partners and governance structure
The lead NHS organisation is Chelsea and Westminster NHS Foundation Trust; the lead higher education institution is Imperial College London, complemented by the main PCTs and social care trusts of the region, and supported by the London SHA and the West London Research Network. The CLAHRC partners have been jointly involved in similar work previously, targeting research and change management.
Governance is centralised with around 20 full-time staff for governance, management, administration and leadership of the themes funded. Twenty full-time research staff at the doctorate level are indirectly funded through research projects. The fully funded staff represent only a fraction of all those involved with the CLAHRC, estimated at around 500. A number of the key CLAHRC staff had/have appointments in both the clinical and research sector, and the CLAHRC’s core team come from a range of backgrounds including academic, NHS, PCT and frontline medical and nursing practice.
Geographical and demographic context
It covers a specific geographical area in London with 1.9 million individuals of whom 35% come from ethnic minorities (mainly Asian and black), 23% are under the age of 20 years and 12% are over the age of 65 years.
High-level aims and key objectives
Northwest London CLAHRC aims to devise and evaluate a systematic approach to the implementation of novel interventions. An action research programme will be used to facilitate rapid adoption and engage those directly involved in health-care delivery. Both the programme and research projects will be evaluated using quantitative and qualitative approaches as necessary to ensure outcomes are clear and hence help build a strong evidence base to deliver improvements in health care and patient experience. Specifically, the aim is to bring about institutional change in the NHS by building the capacity and knowledge of specific groups who in turn will be able to build the capacity and knowledge of their colleagues and bring about a comprehensive system change by enabling the principles, processes and skills to be transferred continuously and sustainably. As the system change being sought relates to the patient’s journey, the CLAHRC has put patients in the centre of its activities. The focus is on using projects to learn, feed back and build knowledge.
Specific objectives are:
-
monitoring the cost-effectiveness of clinical interventions
-
enhancing and speeding up uptake of clinical cost-effective interventions
-
improving the patient journey across interfaces
-
changing the culture and empowering individuals to design, influence and implement change programmes.
Northwest London CLAHRC approach
-
Within this CLAHRC the funding of research projects is an activity in itself, rather than an input. Northwest London CLAHRC provides training to prospective applicants (who have passed the screening stage) in the key principles underpinning the CLAHRC. In so doing, they are building some capacity that will not be directly captured at output/outcome stage, since not all applicants will eventually be funded.
-
The research projects selected are seen primarily as experiments to test new models for bridging the second translation gap. The CLAHRC’s core focus is on how the models fare, and it reflects and builds on the research project experiments through its implementation themes. There is a large number of committee, theme and CLAHRC-wide meetings (weekly and quarterly) to discuss experiences, successes and challenges, allowing for close monitoring. Data on outputs are collected on a weekly basis.
-
The CLAHRC engages with key stakeholders such as health-care planners and policy-makers as well as industry in order to inform them about their results and implement improvements in service delivery and caution about directions that appear to be either unproductive or counterproductive. This includes building cross-organisational networks to encourage sustained collaboration and exchange.
Expected outputs/outcomes
-
Northwest London CLAHRC sees these processes (training applicants, testing models through research projects, reflection and building on these research projects through collaboration, evaluation and engagement with stakeholders) as the means to gain insight into how to bridge the second translation gap, produce research-specific findings (i.e. the direct results of the research projects) and build capacity, especially in the NHS, to inform, conduct and integrate research into practice.
-
The CLAHRC hopes to achieve a systematic approach to education, knowledge and transfer from its collaborations, and thereby continue and sustain improvements in patient care. The CLAHRC also hopes that through its collaborations it will generate a critical mass of researchers and clinicians who understand one another and can work together to achieve products of shared benefit.
Research and implementation themes
There are two research themes:
-
chronic (human immunodeficiency virus testing in PCTs and the management of complex-needs patients)
-
acute care (mostly focused on the issues of medicines management and care bundles in chronic obstructive pulmonary disease and pneumonia).
There are three implementation themes:
-
collaboration, learning and delivery (develops and helps the application of a systematic approach to implementing and adopting new practice, providing educational and training programmes on improvement and research methodology, and on the value of public patient involvement; also provides tailored advice and support, and helps research teams collaborate and co-operate)
-
PPI (looks into methods that can be used to understand patient needs and opinions; provides an induction and training programme to empower the public to become involved in research into service delivery: both activities underpinned by public open days to develop knowledge about these opportunities)
-
evaluation (focuses on monitoring change programmes, assessing their outcomes and impacts, and drawing lessons from these to feed into future change programmes).
The research themes are, primarily, seen as the means to experiment and evaluate different systems to bridge the second translation gap, and the implementation themes support them through knowledge transfer and capacity building. The CLAHRC encourages larger teams than necessary to allow building a critical mass of skills, knowledge and interest, and it funds research projects in three rounds, thereby retaining flexibility over its activities. This provides the opportunity for the team to learn lessons from past experimental research projects and build on this in future projects, and for the implementation themes to continuously adapt the support they offer.
Challenges
-
Research projects need to be according to plan.
-
Staff turnover and retention: the CLAHRC places a large emphasis on people (notably through a large number of recruitments).
-
Sustainability relies on two key elements: the CLAHRC developing a clear identity; and the funding environment, which can keep initiatives going, aligning with the user focus as the CLAHRC does.
-
The CLAHRC aims to bring people out of their comfort zone, which means there can be misunderstandings and tensions between those involved, e.g. researchers, who may not grasp the importance of PPI.
-
There are inherent tensions between the research and service delivery worlds, which work at different paces. The CLAHRC has sought to address this by funding consecutive rounds of evidence-based innovation projects with a quick turn-round. It allows provision of faster answers, while still building on previous knowledge in future work.
-
The language barrier between different sectors means that there are different understandings of the same term.
Emerging lessons
-
A sense of group achievement is key to maintaining momentum of effort.
-
A useful aspect of the CLAHRC is its reliable and accessible synthesis of the large body of information on how to bridge the second translation gap.
-
Bridging the second translation gap starts not at the findings stage of research, but at the proposal stage. This allows service delivery processes to be integrated into the research through, for example, action research methodology.
-
Any effort at bridging the translation gap benefits strongly from being underpinned by strong collaboration/co-operation and evaluation. It allows learning and sharing from those lessons.
-
Communication is most successful when it is between individuals who relate to and respect each other.
-
Matched funding can usefully increase organisational involvement.
FIGURE 63.
Northwest London CLAHRC logic model of the theory of change.
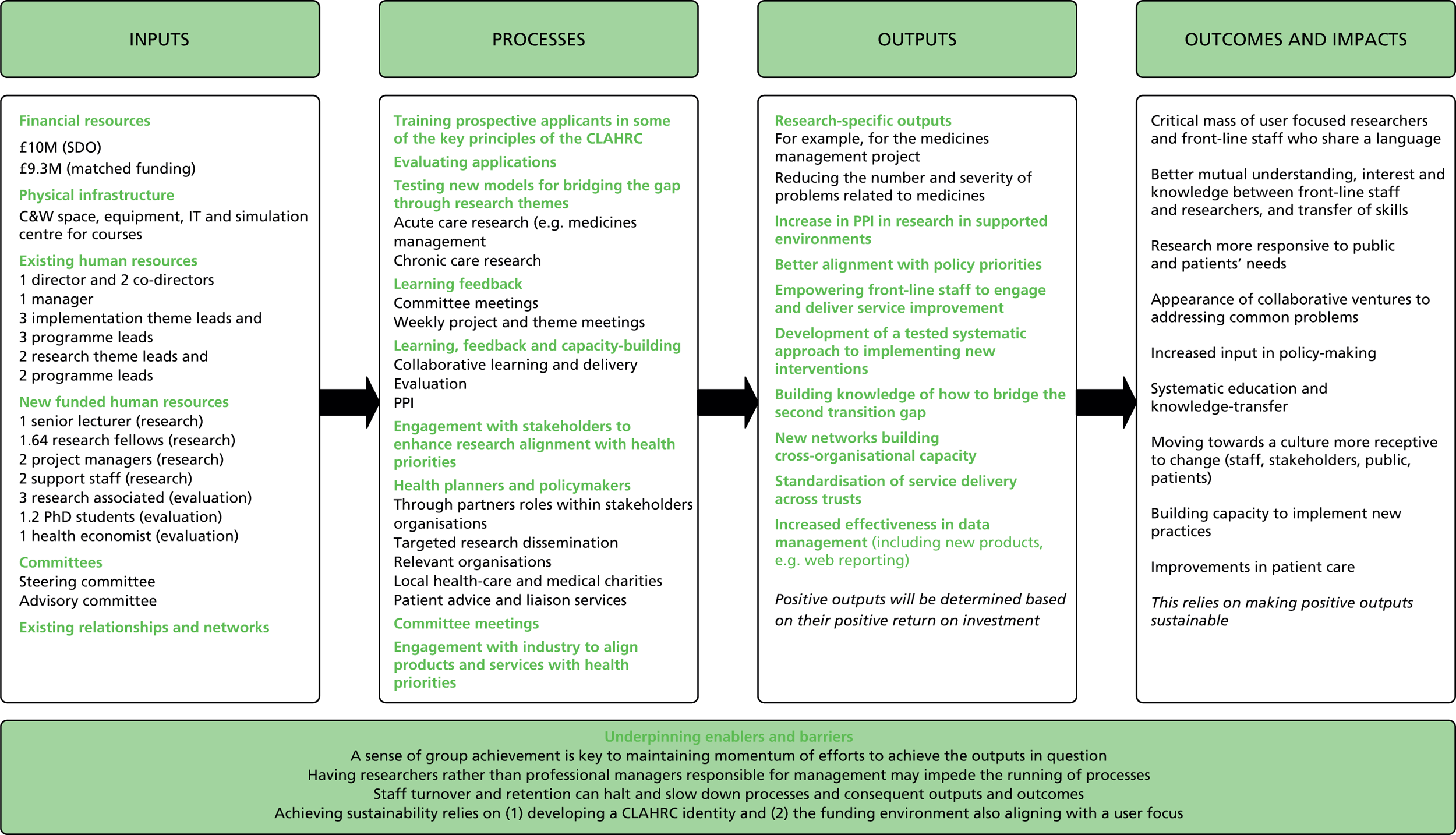
Nottinghamshire, Derbyshire and Lincolnshire CLAHRC (CLAHRC-NDL)
Partnership and governance structure
University of Nottingham, Nottinghamshire University Hospitals NHS Trust, Nottingham County Council, Nottingham City Council, Derbyshire Mental Health NHS Trust, NHS Nottingham City, Lincolnshire Partnership Foundation NHS Trust, NHS East Midlands, Bassetlaw PCT, Derbyshire County PCT, Nottinghamshire University Hospital NHS Trust, Nottinghamshire Healthcare NHS Trust, NHS Nottingham County and NHS Derby City. The partners had working relationships before the formation of the CLAHRC, and had already been engaged in translational research.
Oversight is from a governing board called BOAST (Behavioural medicine, Organisation science and Applied research Synergy in the Trent region) made up of four elements:
-
Operational executive: this meets monthly to supervise, co-ordinate and lead the detailed operation of BOAST themes and the wider relationship to the local health economy. It implements policies and project proposals agreed by the BOAST board and NIHR.
-
Theme structures and management: this ensures that themes and projects run to agreed timetables and budgets, meet all regulatory ethical and clinical governance requirements and report in a timely way. Training and support are offered by a senior trials manager. Each theme has an quarterly executive committee meeting.
-
Research support: trial management, administration, statistics, health economics and health psychology input into the studies constituting the research and implementation themes are centrally provided, sharing methodologies, protocol and procedures.
-
Engagement of service in research and research in service: 1 day each week, 20 to 25 diffusion fellows encourage research-based innovations in clinical practice and work with clinical staff to stimulate research. Associate fellows receive monthly e-mail updates and can become involved in a variety of activities hosted by BOAST, including a road show to take lessons learnt from BOAST to other parts of the East Midlands.
There are three governance centres:
-
Centre governance is to establish memoranda of understanding between partners, meet quarterly to set general strategy and plan updates, ensure clarity of roles, manage risk and outputs, oversee forward planning and sign off annual reports. Members are representatives from the SHA, local authorities and trusts.
-
Research governance is undertaken by research leaders from outside and inside the region. There is also a scientific committee chaired by an external expert to oversee the scientific quality of research, ensuring projects are peer reviewed and conducted in accordance with prevailing ethics and research procedures.
-
Partnership governance: two board subpanels, one looking at commissioners and one at health service users, carers and the public, ensure that the board is aware of priorities, issues and concerns identified by service users, the public and commissioners. Members are elected.
The CLAHRC has a chair, director, manager, two engagement fellows and 20 to 25 diffusion fellows.
Geographical and demographic context
The CLAHRC covers half of the population of the East Midlands SHA, which in total includes Leicestershire, Rutland and Northamptonshire as well as Nottinghamshire, Lincolnshire and Derbyshire. The SHA is responsible for around 4.3 million people.
High-level aims and key objectives
The overall goal of CLAHRC-NDL is to improve patient care by demonstrating the feasibility and usefulness of organisational learning in the NHS, and build capacity to apply organisational learning in the NHS. The overall strategy is to couple organisational learning and behavioural medicine (which combines behavioural, social and organisational science) to improve patient outcomes. Specific objectives include:
-
addressing cross-cutting themes of universal relevance concerning access to health care and occupational engagement, as a means to promote engagement and diffusion in the NHS workforce, service users and other stakeholders such as local councils
-
sustaining a coherent platform for future health gains in the East Midlands through developing capacity at the organisational and individual level in the local health economy, enabling the NHS to take the lead on future implementation research.
CLAHRC-NDL approach
The overall approach is based on organisational learning theory and uses diffusion fellows and communities of practice as mechanisms to encourage change:108
-
Employ and develop diffusion fellows seconded by practice partners in BOAST.
-
Engage health-care practitioners and managers as BOAST associates, and involve health professionals and other local stakeholders in research and implementation activity.
-
Set up research themes focused on chronic illness in the areas of mental health, stroke rehabilitation, young people and primary care.
-
Set up research-based implementation themes looking at implementation research and educational developments, and at engagement, synthesis and diffusion.
-
Engage commissioners through governance procedures and support the development of commissioning competencies through organisational learning that drives system-wide change.
-
Set up focused research projects to meet local research priorities.
Research, dissemination and engagement themes
The research theme focuses on four areas (primary care, mental health, children and young people, stroke rehabilitation) and has three aims:
-
To improve clinical care to at least the best current national standard by studying issues identified as local priorities and open to change. Studies attempt to identify where patient care is failing because of unsatisfactory interventions or unsatisfactory service provision.
-
To explore if organisational learning research is feasible, informative and of additional use to the process of commissioning and delivery of NHS services.
-
To develop capacity in the NHS workforce so that NHS commissioners and providers can undertake organisational studies research with minimal academic supervision.
The implementation theme aims to:
-
identify barriers and facilitators to implement innovations
-
identify how barriers and facilitators might be mediated or leveraged
-
provide local-level ‘situated’ educational support and national-level postgraduate programmes
-
engage, develop and sustain capacity within the NHS to implement and evaluate innovation among those delivering services
-
develop measures to evaluate the effectiveness of BOAST.
The engagement theme seeks stakeholder engagement in CLAHRC work and in the synthesis and dissemination of CLAHRC work, with a focus on access to care and occupational outcomes.
Expected outputs/outcomes
-
The outputs will be publications in peer-reviewed journals, clear and relevant recommendations, ‘evidence to practice’ guides and a systematic approach to communication, engagement and diffusion. The outcomes will be changed practice in selected sites, a national contribution to guidelines and knowledge of good practice, a change to NHS services reflecting findings, and an enhanced training and education capacity.
-
The approach depends (among other things) upon the quality and relevance of the research along with the innovative use of engagement and diffusion fellows. The BOAST synthesis and diffusion themes will therefore be especially important outputs. The quality and peer-reviewed nature of the research is seen as important both to reinforce local adoption and to contribute to national guidance and appraisal.
Challenges
-
Collaboration tensions: researchers and practitioners have different ways of working; practitioners tend not to understand what researchers are thinking, and researchers tend not to appreciate the problems practitioners face.
-
Community engagement: prompting users to define the problems they face is difficult and not always helpful.
Emerging lessons
-
There are limits to the codification of knowledge, and some knowledge must be transferred in person; interpersonal contact is important.
-
The CLAHRC can usefully bring together a range of activities: for example, RCTs can be a learning as well as an implementation effort.
-
Not all users’ experience is useful. Distinguishing between experience that does not seem to contribute much and experience that is useful is difficult but necessary, otherwise user involvement risks becoming a tick-box exercise.
Translation seems to differ significantly by therapeutic area.
FIGURE 64.
Nottinghamshire, Derbyshire and Lincolnshire logic model of the theory of change.

CLAHRC-Peninsula (PenCLAHRC)
Partnership and governance structures
Universities of Exeter and Plymouth and all the NHS trusts in the far south-west. The partnership has been facilitated by the local SHA (NHS South West) and is complemented by the NIHR CLRN in the south-west. Most of the CLAHRC partners have a history of recent and explicit collaboration, and PenCLAHRC builds on the strong joint research governance structures that were already in place across the Peninsula College of Medicine and Dentistry and its NHS partners.
The PenCLAHRC management board consists of 23 senior members with representatives from all the NHS trusts, the universities and patients. The director of PenCLAHRC chairs the executive group, which includes the PenCLAHRC project manager and the research and implementation theme leaders; the director oversees day-to-day management issues and ensures good communication and project integration. Each implementation theme has a theme lead and a separate theme management group.
Geographical context
The CLAHRC covers the south-west peninsula, with a population of 1.6 million people.
High-level aims and key objectives
The goal of PenCLAHRC is to improve health outcomes for patients and the public through the conduct and translation of patient-focused research. This goal embraces both clinical and cost-effectiveness in the use of evidence-based implementation, and PenCLAHRC strives for national as well as regional impact. More specifically, the objectives are:
-
to support the identification of research questions that address clinical concerns (within the four key research themes)
-
to support and undertake research that tests treatments, interventions and new ways of working in specific clinical areas, to see if they are effective and appropriate for everyday use in the health service
-
where effective interventions are identified, to support research into how NHS staff can implement them into their everyday working practices, so that patients across the local community and beyond receive a better standard of health care
-
through PenCLAHRC research and educational activity, to embed and fuel the partnership between the NHS and academia, building research capacity in applied health research and implementation
-
to treble the partnership’s involvement in applied health research to enable it to become a major sustainable contributor to this field for the future
-
to promote engagement and involvement in research that reflects real clinical concerns, contributing to the creation of a research-receptive culture in the local NHS.
PenCLAHRC’s priorities are aligned with the priorities of NHS South West.
Research and implementation themes
-
The four formal research themes are diabetes and cardiovascular health, mental health and neurology, development and ageing, and environment and human health. These themes reflect the existing research strengths within the partnership and include many of the major problem areas for public health and chronic disease and the bulk of NHS expenditure.
-
However, different projects take place at different stages of the research process so some of the projects are projects which could be characterised as implementation projects. A large component of funded work comes from the question generating and prioritisation, and there is a common system for the identification and structuring of research and implementation.
-
By colocating multiple implementation initiatives from different areas of practice within a single overarching group, the implementation group seeks to derive generalisable evidence for the whole health-care community.
PenCLAHRC approach
The model adopted, ‘Engagement by Design’, builds on the previous experience of the academic leads of working closely with clinicians, service users, and NHS and social care organisations. All these stakeholders are involved at all stages of the research process, from the generation of research questions, through the design and conduct of research, to the design and evaluation of implementation strategies.
-
Academics, clinicians and managers working in NHS organisations and the social care sector, and patients, the public and third-sector organisations work together to identify key research/implementation questions.
-
A rapid review process identifies what is known about a potential research issue and where key information gaps exist.
-
Depending on the results of the review, this may lead, if the evidence is clear, to the design of implementation strategies or, if evidence is not apparent, to primary or secondary research.
-
The design of these research or implementation projects will continue to involve those who originally generated the research question to ensure that projects remain grounded in service requirements and that the need for effective implementation guides research design.
-
PenCLAHRC is supported by a prospective, internal, formative evaluation.
Intended outputs and outcomes
-
The CLAHRC aims to produce some movement in the culture so that collaborative working between different stakeholder groups (including patients and the public) becomes embedded.
-
It seeks to delineate research questions, some of which will be taken up by other funders, some of which will lead to local studies.
-
It will rapidly review evidence already available.
-
It will help NHS partners to implement research findings from elsewhere
-
It aims to develop specific tools for implementation based on implementation research.
-
It will build capacity, which includes the development of skills among the public, clinicians, academics and managers.
-
The CLAHRC will be valued as a priority resource for NHS commissioners and providers, and as a means of making sure that their priority research needs are addressed by the university. This advantage will be available to the whole south-west region.
Challenges
-
Initial uncertainty about the CLAHRC’s remit.
-
Tensions between academic and NHS cultures: between producing academic papers and developing a focus on work of real, practical and immediate value that produces soundly based, sustainable change.
-
Keeping it real and staying relevant.
-
Linking to local health properties.
-
Integration with commissioning.
-
Fast prioritisation of decisions about research.
-
Getting (and retaining) NHS management buy-in, garnering organisational commitment.
-
Developing the capacity to respond fast to the problems of the day.
-
NHS trusts’ abilities to provide input into the PenCLAHRC question-generating model, and to get a perceived return on their matching funding.
-
Adequately exploiting other NHS initiatives, such as Quality, Innovation, Productivity and Prevention.
-
Debates with trusts about which outcomes should be measured.
-
Weakness of research implementation in trusts.
-
Raising expectations that PenCLAHRC cannot fulfil; for example, developing research questions through their model which they cannot use themselves.
-
The new world of no PCTs.
-
Special position of the district general hospitals, which tend to express little interest in research.
-
Research bureaucracy; for example, research governance and ethics arrangements, not being able to get CLAHRC projects adopted under the clinical research network portfolio and the deeper issue of how the various government initiatives (clinical research networks, HIECs, etc.) work together with the CLAHRCs.
Emerging lessons
-
Addressing people’s actual concerns:
-
Need to involve patients adequately: a very high proportion of interventions are never used; they are prescribed but they are not used by the end user if the patient is not convinced that the benefits will outweigh the costs. There is a need to involve patients to help develop the partnership, and fund this adequately.
-
Clinicians and policy-makers: there is a perception that clinicians as well as policy-makers seek to achieve specific outcomes and there is a need to communicate them appropriately. PenCLAHRC has used clinical locality leads – clinicians who can spread the word about the CLAHRC and work with clinical teams to develop researchable questions.
-
NHS management: the PenCLAHRC operational research facility (PenCHORD) is one response; it has recognised the need to work alongside NHS managers and clinicians to transform the ways in which care is organised and delivered.
-
-
The importance of marketing and of early dissemination of findings.
-
The need for flexibility when working together and the importance of having an emergent approach based on learning.
FIGURE 65.
South West Peninsular CLAHRC logic model of the theory of change.

South Yorkshire CLAHRC (SY-CLAHRC)
Partners and governance structure
Higher education institutions – University of Sheffield, Sheffield Hallam University; NHS foundation trusts – Sheffield Teaching Hospitals, Barnsley Hospital, Rotherham NHS Foundation Trust, Sheffield Children’s Hospital, Doncaster and Bassetlaw Hospitals, Sheffield Health and Social Care; NHS PCTs – Barnsley, Doncaster, Rotherham, Sheffield. The partnership is supported by the South Yorkshire NIHR CLRN. There is a local history of strong collaboration, including the Sheffield Health and Social Research Consortium, which has been in existence since 2001.
The SY-CLAHRC Board is chaired by a senior NHS academic who is independent of the CLAHRC. An executive committee chaired by the clinical director reports to the board and is charged with overseeing progress with project milestones and deliverables within each theme; it is supported by a committee of theme leads. The CLAHRC director is supported by an operational team and an associate director. Each theme has a designated steering group.
Geographical context
The CLAHRC covers the whole of South Yorkshire. This area has a population of 1.3 million and covers 1559 km2. This region experiences poorer health outcomes than other regions in England.
Aims and objectives
The CLAHRC focuses on enabling patients with long-term conditions to self-manage their care and aims to reduce health inequalities across South Yorkshire and to promote and support networks through which peer-review processes will be strengthened, international links developed, front-line staff and commissioners engaged, and academic and other partners secured to assist knowledge transfer and improved business development.
The mission of CLAHRC-SY is to undertake high-quality, strategic, applied research and related education in order to enable a step change in the way research is delivered and services are designed in South Yorkshire; and to foster knowledge transfer that will improve the quality and effectiveness of health-care delivery across South Yorkshire.
Specific objectives are:
-
to improve the health and well-being of people with long-term conditions in South Yorkshire through a distributed model of health research
-
to implement an innovative model for conducting applied research and translation which is embedded in the self-management and technology agenda for people with long-term conditions
-
to provide leadership in the governance of applied research and operate according to rigorous principles
-
to promote the transfer of knowledge from applied research into practice and facilitate the implementation of new knowledge into health service policy and practice
-
to encourage commercial exploitation, where appropriate, for the benefit of the South Yorkshire economy
-
to use existing advances in health technologies within the care pathways of South Yorkshire, enhancing self-management and improving access, choice and personalised care for people with long-term conditions
-
to work together as an organisationally robust and creative collaboration of higher education institutions and NHS leaders who will foster capacity and innovation in applied and translational research
-
to inform and respond to the needs for service commissioning within South Yorkshire
-
to ensure that the modern NHS workforce fully embraces both the self-care and the technology agendas for long-term conditions.
CLAHRC-SY approach
The overall approach incorporated implementation themes that built on the knowledge to action approach developed in Canada and on local work to develop evidence-based clinical effectiveness. 109
-
To integrate applied research into the business development and planning processes of health-service partners. By doing this, it is hoped that health service organisations will reduce the risks that are associated with the introduction of new initiatives by basing decisions on evidence-based planning and conducting rigorous evaluation of service changes and new interventions.
-
To capitalise on the expertise of academic partners in knowledge transfer and research implementation to work in collaboration with health service partners. There is an expectation that such an approach might help promote the delivery of effective care along the patient pathway and lead to enhanced outcomes and better quality of care overall.
-
To involve front-line clinical and managerial staff to improve the relevance of the research produced.
Research and implementation themes
South Yorkshire CLAHRC divides its activities into 12 themes that build on existing research strengths:
-
eight research themes focusing on self-management and self-care of long-term conditions (depression, chronic obstructive pulmonary disease, diabetes, stroke, obesity, attention deficit hyperactivity disorder), the application of technologies and genetics
-
four implementation themes focusing on research translation, particularly user-controlled health-care design, intelligent commissioning, knowledge into action and inequalities in health.
Expected outputs/outcomes
Research outputs include a screening tool, revised guidelines and other interactive tools for engaging individuals and organisations. Tangible outputs include a new website, newsletters and training. Other outputs concern a more effective business innovation and communication strategy, improved collaboration with partners and new ways of engaging individuals. The outcome is to integrate these programme outputs into the daily practice of NHS and research bodies in the partnership.
Challenges
-
Recruitment, which took longer than expected.
-
Changes in the NHS and in particular the restructuring of PCTs.
-
Concerns that some of the research priorities set may be more in line with areas of research expertise of those leading than with the priorities and challenges faced by health service partners.
FIGURE 66.
South Yorkshire logic model of the theory of change.
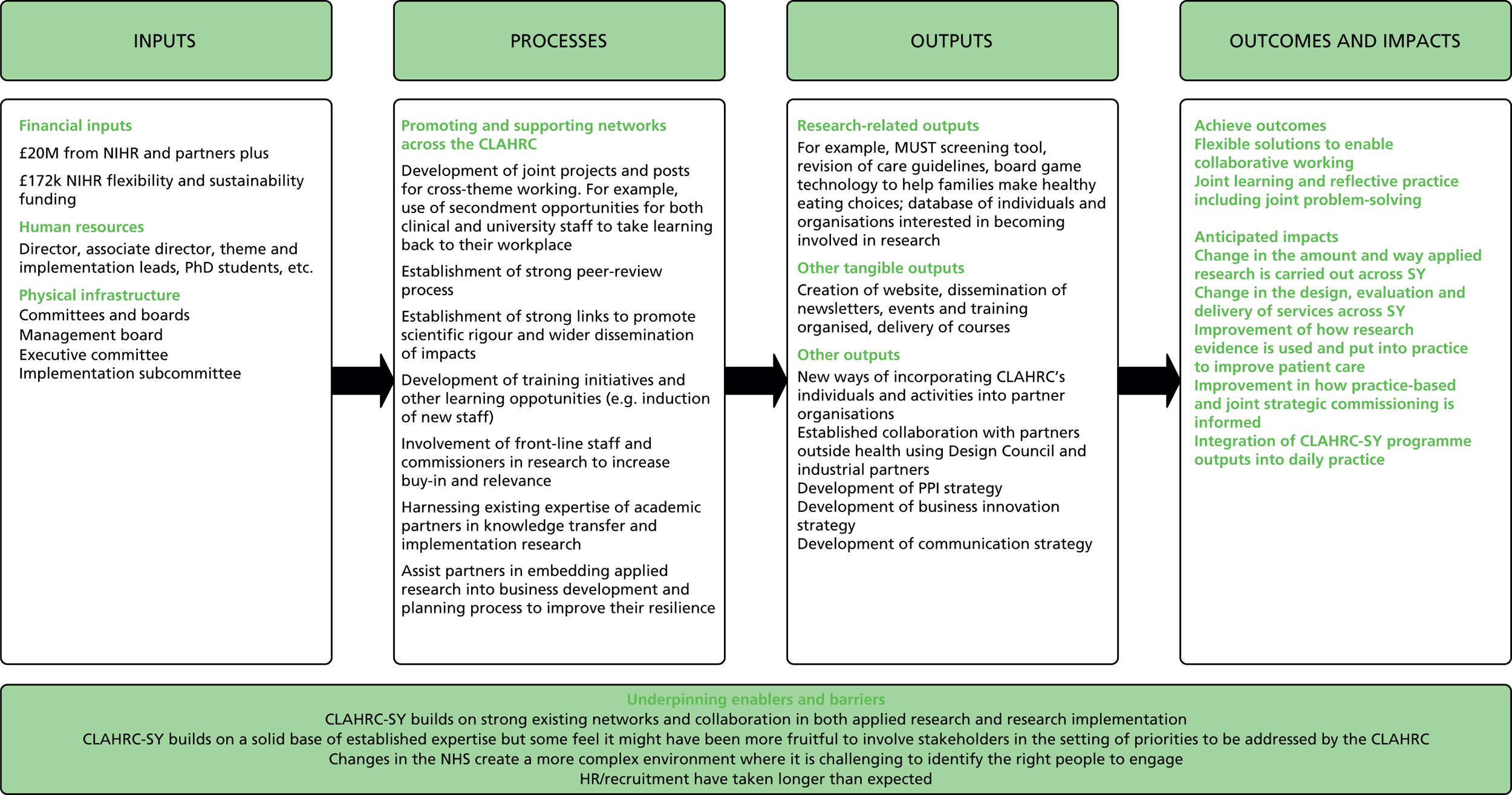
Appendix 11 Individual CLAHRC approaches and system shifts
Table 4 summarises the accounts of each of the nine CLAHRCs provided in Appendix 10. It is adapted from an earlier report of the evaluation following completion of phase 1, which was shared with NIHR HSDR and other stakeholders. 24 The table should be read in conjunction with Table 3 in the body of the report (see Chapter 3).
| CLAHRCs | Structural and political | Cultural, educational and emotional | Infrastructure: financial and physical | |||
|---|---|---|---|---|---|---|
| Governance and accountability | Organisational structure of CLAHRCs including activities and themes | Societal attitudes and behaviours | Individual attitudes and behaviours | Infrastructure (including technology) | Use of resources | |
| What needs to be done to bridge the second translation gap | ||||||
| Birmingham and Black Country | Management arrangements informed by the Engineering and Physical Research Council (EPRC) guidelines Distributed leadership across themes Driven by academics with relevant service experience Retain NHS management buy-in |
Focus on preventative services, on preimplementation evaluation of interventions and on capturing potential effects of service delivery interventions ‘Unique themes’:
|
Raise awareness of CLAHRCs in NHS Trusts Build links with people from other sectors including social services Assist managers and commissioners to become more research literate |
Use of influential ‘boundary spanners’ (individuals that can bridge disciplinary and professional boundaries between academia and service delivery sectors) CLAHRC fellowship schemes for NHS managers PhD students in applied health research |
Hosted by the University Hospitals Birmingham NHS Foundation Robust internal communications infrastructure to facilitate communications between all partners |
Prospective evaluation of service change – 50% of resources dedicated to evaluation Seeking to obtain additional funding to sustain activities |
| Cambridgeshire and Peterborough | Central management and support system to free up researchers’ time Governance group takes the lead in putting in place systems to support research governance and infrastructure Scientific advisory group consists of individuals with leading reputations in health research and health service provision. It is responsible for methodologies used in the programme of work |
Focus on community mental health across the life course Involvement of local authorities Focus on established strengths in life course approaches to mental health Involvement of partners with expertise in implementation and in service change and evidence-based innovation Driven by needs of service users and providers rather than academic interest – focus on areas with least research attention and biggest need for improved services |
Internal and external communications strategy to ensure all are aware of developments and progress | Use of ‘boundary spanners’ and ‘knowledge exchange champions’ CLAHRC fellowship scheme for clinicians and NHS managers PhD students and CLAHRC visiting fellows Secondment opportunities for nurses and practice assistants for consultants to engage in research |
Physical colocation of CLAHRC staff | Involvement of commissioners in meetings and research agenda settings Cross-disciplinary training programme Seeking to attract additional funding to sustain activities Building internal evaluation capacity Systematic review to identify current best practice and focus resources |
| Leeds, York and Bradford | Clinical leadership to ensure the research retains its clinical focus Scientific steering group has oversight of research methodologies used in themes. Group comprises academics with international reputation |
Themes draw on established expertise but also reflect patient pathways rather than organisational interests Particular focus on chronic diseases Outputs assessed against a series of performance indicators including measurable patient benefit, publications, grant income and research fellowships |
Secure involvement of patients and the public in research LYB-CLAHRC will work through the new Local Involvement Networks (LINks), which aim to give citizens a stronger voice in how their health and social care services are delivered |
Secure commissioners’ involvement | Physical administrative centre based at the University of Leeds | Secure additional funding to sustain capacity beyond initial funding period |
| Leicestershire, Northamptonshire and Rutland | Scientific committee advises executive group and revises detailed plans of research studies before launch. Committee is also responsible for reviewing outputs | Focus on conducting applied health research into long-term conditions in new ways Research themes focused on different stages of care and on implementation rather than on specific diseases Evaluation embedded within some of these themes Research focus driven by patient needs and areas of public health importance Interaction with experts in translation both in the UK and abroad to disseminate experience and draw on the experiences of others |
Involvement of patients, the public and clinicians in research Use of training to deliver models of education developed by the CLAHRC |
Use of co-ordinators embedded in the trusts Use of ‘translation teams’ to create ownership of the research within the NHS Important to involve ‘clinical researchers’who have an interest on both sides (i.e. academia and the NHS) |
Secure additional funding to sustain capacity beyond initial funding period | |
| Northwest London | Centralised governance Core staff with a history of working across the NHS and academia |
Focus on interventions’cost-effectiveness and monitoring Focus on chronic and acute care as well as PPI and evaluation ‘Unique themes’:
|
PPI is facilitated through the use of an induction and training programme to empower the public to become involved in service delivery research | Focus in early days on hiring large number of applicants at management and doctoral levels Provision of training for prospective applicants seeking to do research for the CLAHRC Creation and support of diverse project teams with tools and skills to rapidly deliver and evaluate change and support sustainable health-care delivery |
Funds research projects in three rounds to retain flexibility Seeks to secure additional funding |
|
| Greater Manchester | Steering group holds the director to account for the management and performance of the CLAHRC including oversight of finances and implementation of policies and procedures | Initial focus on vascular diseases as the single most important source of morbidity and premature mortality in the area Support patients’self-management Emphasis on the development and evaluation of inter-related interventions to support self management and improve quality of care |
Training associates including clinicians through knowledge transfer partnerships Training PhDs and medical doctors through implementation themes |
Building interactive simulation models to assist commissioners in assessing costs and patient outcomes resulting from changes in care pathways | Common implementation framework for disease themes | |
| Nottinghamshire, Derbyshire and Lincolnshire | Governance consists of three overlapping systems: centre governance, research governance and partnership governance Partnership governance structured through two board subpanels focused on commissioners, health-service users, carers and the public |
Approach characterised as ‘proof of concept’with exploration of how feasible and useful the organisational learning approach is Focus on chronic illness in mental health, stroke rehabilitation, young people and primary care Focus on local priorities Involvement of local authorities |
Involve health professionals and other stakeholders in research Involve service users meaningfully in research |
Use of diffusion fellows who focus on research-based innovations in clinical practice and make clinical staff more research facing through joint working Teaching PhD students to implement and evaluate innovations Importance of interpersonal contact to achieve successful diffusion of knowledge |
Identify where patient care is failing Use of ‘lessons learnt road shows’ Focus on dissemination through the website, annual conferences, diffusion fellows, publication of evidence to practice guides and public lectures |
|
| Southwest Peninsula | All partners are represented on the management board Patient- and carer-led advisory group to ensure adequate account is taken of the need for involvement in all aspects of the CLAHRC’s work Central administrative and management support Leads have previous experience of working across boundaries Importance of internal formative evaluation |
Focus on particular populations Focus on areas that can bring the most health gain/focus on areas of clinical concerns Themes built to contain substantial overlap Those identifying areas for research remain involved throughout to ensure projects remain grounded in service requirements Emergent approach based on learning |
Use of ‘champions’ or ‘locality leads’ to spread the word about the CLAHRC Work with clinical teams to formulate research questions ‘Question workshops’ for clinicians and managers within partner organisations as part of the evidence-based practice initiative Opportunities for public engagement |
Use of clinical academics as ‘boundary spanners’ to support the identification, prioritisation and development of research questions PhDs and postdoctorates in applied health research |
Colocation of multiple initiatives from different areas of practice within a single overarching group (implementation group) to produce general sable evidence for the whole health-care community Online community to disseminate outputs |
Less focus on substantive areas and more focus on process of engagement Identification of gaps in areas of focus and what is already known to focus resources either on the design of implementation strategies or on primary/secondary research if evidence is not apparent Seeking additional funding for projects it is not able to fund Dissemination through publications Ensure NHS management buy-in through involvement in research and return on matched funding |
| South Yorkshire | Board provides governance and strategic steer for the programme PPI strategy group advises on public and patient involvement in the CLAHRC Strong peer-review process in place to ensure high quality of CLAHRC research |
Central model is based on concepts of self-management and self-care Focus on enabling patients with long-term conditions to self-manage their care Capitalise on expertise of academic partners in knowledge transfer Establishment of strong international links and partnerships outside health |
Involvement of front-line staff and managers to produce research that is relevant Involvement of patients and the public through PPI strategy |
Secondment opportunities for both clinical and university staff to enable them to learn about each other | Encourage commercial exploitation of research outputs where appropriate | |
| System shifts | ||||||
| Birmingham and Black Country | Knowledge and evidence implemented as it develops as opposed to only at the end of the pipeline | |||||
| Cambridgeshire and Peterborough | Flexible and resilient structure for a changing environment Balance and manage ambitions of research groups |
Address challenges in arbitrary transition from children to adult services | ||||
| Leeds, York and Bradford | Research generated by CLAHRC directs commissioning of clinical services | |||||
| Leicestershire, Northamptonshire and Rutland | Chief executives of partner trusts are involved in the research process to ‘get things done’ | Change current ways of working to improve patient outcomes Produce more locally relevant research with the involvement of NHS staff |
Integrate needs of clinicians into the research process | Influence trusts to invest in research that can help their decision-making beyond CLAHRC | ||
| Northwest London | Create mass of researchers and clinicians with shared understanding Accelerate uptake of interventions into practice Patients at the centre of research |
Utilising information to drive evidence-based implementation and practice by adopting industrial standards of quality in the NHS | ||||
| Greater Manchester | Shift focus to improving patients’self-management and self-care | |||||
| Nottinghamshire, Derbyshire and Lincolnshire | Provide new approaches to care that commissioners may want to commission Change the culture of the local NHS by developing and demonstrating the effectiveness of a multimethod diffusion strategy to teach stakeholders to utilise organisational learning |
|||||
| Southwest Peninsula | Change the way applied health research is conducted and valued by the health community (and external research funders) such that it is sustainable beyond the life of the CLAHRC | |||||
| South Yorkshire | Incorporation of evidence-based planning and evaluation into applied research | Change the way research is delivered by focusing on knowledge transfer to improve care | ||||
| Vision for success | ||||||
| Birmingham and Black Country | Address time lag between research translation and adoption | Building sustainable systems for academia and NHS to work together Achieving increased and integrated capacity to improve service delivery Impact on local economy through implementation of locally produced technologies Overcome information-sharing and governance problems |
Generation of sustainable applied research capacity of region covered Implementation of initiatives and practice that works and abandonment of those that do not work |
|||
| Cambridgeshire and Peterborough | Sustain interests of partners in applied research beyond the CLAHRC Build capacity of clinicians and NHS managers to consume research evidence for service delivery Make research more responsive to the needs of patients and care providers |
Application of findings and best practice generated by the CLAHRC nationally | ||||
| Leeds, York and Bradford | Build capacity of the NHS Build researchers’ ability to respond to frontline needs Build capacity of commissioners and service providers to innovate Tackle health inequalities and improve patient outcomes |
Evaluation of cost-effectiveness of initiatives and research findings to check if can be routinely implemented into practice Inform practice based on evidence |
||||
| Leicestershire, Northamptonshire and Rutland | Increase research capacity in the NHS Increase the involvement of all stakeholders in research, including the public Best practice in LNR disseminated widely as local population representative of wider population |
|||||
| Northwest London | Patients experience a seamless journey with consistent delivery of high-quality care that is evidence-based | Empower individuals to design, influence and implement change | Build and test a systematic approach for the rapid adoption of clinically effective interventions Develop a model for the conduct and application of health research that is transferable across the NHS |
|||
| Greater Manchester | Build local NHS capacity to plan and implement evidence-based changes in care pathways | |||||
| Nottinghamshire, Derbyshire and Lincolnshire | Improve the standard of routine care Develop a NHS workforce able to carry out organisational learning research and implementation with minimal academic support |
Enable services to adopt/implement innovations | Demonstrate feasibility and usefulness of organisational learning in the NHS | |||
| SouthWest Peninsula | Improve health outcomes for patients and the public regionally and nationally Build capacity for carrying out applied health research |
Aim to treble the partnership’s involvement in applied health research in order to create economy of scale and competitiveness to be a major sustainable contributor to the field in the future | ||||
| South Yorkshire | Reduce inequalities across the region | |||||
Appendix 12 Programmes relevant to the CLAHRCs that were developed elsewhere and models that informed the CLAHRCs
The summary accounts of programmes relevant to CLAHRCs that are presented in this appendix are based on a targeted literature review undertaken during phase 1 of our evaluation. These programmes formed part of the contextual backdrop of research and practice within which the CLAHRCs were operating, and provided useful information about the barriers, facilitators and success factors previously identified. The review was intended to provide insights and questions to help us identify what was important, distinctive and especially interesting about the CLAHRCs.
Previous programmes
Quebec Social Research Council (CQRS) Programme Grants
In 1992 the Quebec Social Research Council (CQRS) introduced a grant programme to encourage researchers, practitioners and policy-makers with the aim of delivering health benefits. The programme’s aims were to:
-
introduce a culture of research within action settings, which are often isolated from social sciences
-
introduce a culture of action into research settings, increasing the pertinence and usefulness of the research produced
-
create an improved context for the training of young researchers and practitioners.
The 10-year programme offered infrastructure funding for research teams interested in developing programme-based partnerships between university researchers and the institutional sector. It introduced a range of requirements for the organisational structure of the partnerships (codirection from a researcher and practitioner, independent secretariat, etc.) to ensure effective integration, as well as offering long-term funding to ensure stability.
Antil et al. analysed the implementation of the CQRS (based on consultations with key informants from the programme). 5 Their analysis did not assess the impact of the CQRS on the quality, application and productivity of social research, but it noted that the teams supported by the CQRS were involved in the research and development of many innovative social programmes that were widely implemented across Quebec, that the principal stakeholders considered it to be a success and that the CQRS model had influenced other research foundations in Canada.
The following factors were thought to have explained the success of the CQRS programme:
-
Leadership and coherence in implementation: all the partners found benefits in the programme, thus ensuring buy-in. The flexibility and long-term nature of the funding provided time and space to build partnerships. It provided effective and inspiring institutional leadership by presenting a well-designed programme and executing it effectively and efficiently.
-
Favourable political and social conjuncture: it was linked to a broader strategic framework, and the partnerships were required to provide demonstrable proof of their results.
-
Ability to respond to the needs of institutions providing services and formulating policy: it improved access to useful research for health-service providers and policy-makers through increased contact and interaction with researchers, and was also effective in bringing together the different cultures of action-based policy-makers and health-care practitioners and university-based researchers. Decision-makers’ receptive capacities for research results were improved.
-
Responsive to the needs and expectations of universities: it gave universities leverage to obtain other funding, and made them more receptive to collaborative schemes.
Denis et al. explored the views and experiences of the researchers and practitioners involved in the CQRS programme, with similar findings. 125 The programme was viewed positively by participants and had significant outcomes in terms of building the skills and mind-sets to facilitate future collaborations, as well as building a culture of experimentation. There were positive changes in the attitudes and receptiveness of both researchers and practitioners, and a convergence of views about the importance and value of collaborative research.
NHS R&D Implementation Methods Programme
The NHS R&D Implementation Methods Programme (IMP) was set up in 1994. It was the last of a series of time-limited topic-specific R&D programmes that were otherwise developed largely with clinical research in mind, covering fields such as mental health and cancer. The IMP spanned a wider range of research fields, including social science, policy and management. With a budget of £4 million, the IMP funded 36 time-limited projects exploring issues of research implementation. It ended early because of external changes to the structure and remits of the NHS, and the full programme was never realised.
An evaluation carried out in 2002 regarded the programme as highly innovative. 126 Some of the projects funded had considerable impact but the IMP as a whole was hampered by not being well understood by the largely clinically based researchers who responded to the call for proposals. Specific difficulties (and insights of importance for initiatives such as CLAHRCs) were:
-
tensions between the perceived need for immediate demonstrable relevance to practice and more academic methodological/conceptual issues
-
the low quality of many applications
-
the lack of a programme-wide tailor-made communication strategy to support interactions among stakeholders, including the potential users of research findings.
The last of these was a significant shortcoming; such a strategy was planned but not realised because the IMP ended earlier than planned. Many of the problems encountered by the IMP came about because the state of knowledge at that time could not fully support its ambitions. The evaluators suggested that it might have been better to build the programme more gradually, learning from experience as it developed.
Quality Enhancement Research Initiative programme
The Quality Enhancement Research Initiative programme was launched in 1998 as part of a restructuring of the US Veterans Health Administration. It continues to this day. QUERI seeks to accelerate the implementation of new research findings into clinical care by creating a bridge between those performing research and those responsible for health system operations. QUERI researchers collaborate with policy-makers and health-care professionals to implement evidence-based practices into routine use, working within disease- or condition-specific units. The model is based on six logical steps:127
-
Identify high-risk/high-volume diseases or problems.
-
Identify best practices.
-
Define existing practice patterns and outcomes and variation from best practice.
-
Identify and implement interventions to promote best practices.
-
Document that best practice improves outcomes.
-
Document that outcomes are associated with improved quality of life.
The implementation stage (step 4) is generally subdivided into four phases to ensure effective roll-out (the planned action model):
-
single-site pilot
-
small-scale multisite trial
-
large-scale, multiregion trial
-
system-wide roll-out.
An overall evaluation of the programme and the many papers it has produced has been published. 62 This found that the programme had represented a ‘paradigm shift to action-orientated research’ and had utilised and substantially contributed to the implementation literature. The QUERI programme demonstrated the extent to which change takes time and persistence; benefits in terms of health gain were starting to emerge only in 2009, when this evaluation was published. The evaluation also found that the QUERI approach had been a significant contribution to the field of implementation and had contributed to debates about the ethical issues relevant to implementation research, the need for economic evaluations and the need to sustain change. The overall conclusion of the evaluation was resoundingly positive.
The QUERI programme can be considered a national case study that reveals that changing a health-care and research system by reorienting efforts towards the implementation of best practices is a complex, long and never-ending process, but the potential gains in health outcomes make it worth it. The QUERI programme also illustrates the value of working top down and bottom up, if not simultaneously, then iteratively. In other words, clear vision and leadership, supported by frameworks and tools, as well as a responsive collaborative team-focused work force, is a winning combination for innovation within the health system.
Atkins notes that the QUERI programme and implementation research have both come of age, and discusses some of the challenges to come. 127 These are as follows:
-
Tying implementation science to more effective implementation: going beyond basic discovery (i.e. listing lessons learned) and using and testing the increasing number of theoretical implementation models described in the literature.
-
Methodological debate: ensuring that evidence is both valid and acceptable, and that all relevant methodologies are considered without prejudice in order to foster timely improvements in care while protecting against ineffective or even harmful change.
-
Ensuring that implementation research becomes more relevant to the daily decisions of key stakeholders: aligning the priorities of research and the health-care system as early as possible.
-
Developing adequate and useful economic evaluations of implementation interventions: Promoting economic analyses and aligning economic models more closely with the budgeting and decision-making processes.
-
Developing capacity: Nurturing new implementers (front-line connectors) and new implementation researchers.
-
Strengthening connections to other operational and research activities that influence change in the health-care system, such as quality improvement, continuing education and health informatics: aligning with existing priorities.
-
Managing expectations: being realistic about what success looks like and transparent about goals and objectives.
-
Demonstrating impacts on health and healthcare that are meaningful to key stakeholders: showing what difference implementation research makes.
Need to Know Project
In 2001 the Canadian Institutes of Health Research funded the Need to Know project in Manitoba. This project built on an existing relationship between the Manitoba Centre for Health Policy and the provincial health authority, Manitoba Health, and was designed to address the need for research to support the decision-making of rural/northern regional health authorities, to promote and develop models of collaborative research and, ultimately, to improve health outcomes.
An evaluation of the Need to Know project was published in 2005. 7 This concludes that much of what was discovered through this project about knowledge translation was not new and, after initial scepticism, turned out to be equally well understood by researchers and community partners. There were clear messages about:
-
the importance of building trust between partners through formal and informal contacts
-
the need to overcome institutional barriers (such as understanding the time and resource limitations of partners)
-
the need to develop a common language and culture
-
recognising that time is required to build relationships and generate useful outcomes.
Participants regarded the relationships created by the project as its most significant outcome, and their creation as one of its most difficult challenges. The emphasis on capacity building included helping practitioners to engage better with research, helping researchers to understand more fully the practicalities of health care and the needs of patients, and building organisational capacity in all the partner organisations to identify, develop and implement well-founded and useful research.
Key lessons from these programmes
-
The aims of the CQRS programme were very similar to those of the CLAHRCs and its success factors were highly relevant to the latter. They included leadership and coherence in implementation; a favourable political and social conjuncture; an ability to respond to the needs of institutions providing services and formulating policy; and responsiveness to the needs and expectations of universities.
-
The IMP was the first attempt in England to set up a programme of implementation research. It followed the applied, needs-based emphasis of the NHS R&D programme and concentrated largely on what was later identified as the second translation gap. What the experience of the IMP highlights is the danger of having insufficient time to develop capacity among all partners in the programme, to promote strong and productive interaction between different groups and to develop a robust communication strategy.
-
The QUERI programme has generated a large literature and been very influential; its experiences were drawn on by the CLAHRCs, either explicitly in their published protocols107 or implicitly in their programmes. The experience of the QUERI programme confirms that a long time-scale is required to see systemic change, and, therefore, suggested from the start that the CLAHRCs were unlikely to produce measurable health gains over a 5-year period and that health impacts would become evident only later.
-
The Need to Know project also reinforced the message about the time and effort it takes to build effective relationships between professional groups and stakeholders.
Models of implementation, collaboration and process, and their use
Diffusion of innovation
Arising out of their review of the literature on research diffusion, Greenhalgh et al. developed a multifaceted evidence-based model of the diffusion of innovations in health-service organisations. 26 The broad scope of this model can be seen from its main components (Box 7).
The attributes of the innovation: 11 are cited, such as relative advantage, compatibility (being in line with adopters’ values and perceived needs) and low complexity (perceived simplicity of use).
Adoption by individuals: seven aspects of adopters and the adoption process are cited, such as psychological antecedents, meaning for the intended adopter.
Assimilation by the system: adoption by the team, department or organisation in which various changes in structures or ways of working will be required.
Diffusion and dissemination: seven components are cited, such as network structure, opinion leaders, champions and boundary spanners.
System antecedents for innovation, including administrative intensity, centralisation (which has a negative correlation), complexity, external communication, functional differentiation, internal communication, managerial attitudes towards change, professionalism, adequate resources, specialisation, technical capacity, absorptive capacity for new knowledge, and receptive context for change.
System readiness for innovation: this depends on the tension for change, innovation–system fit, assessment of implications, support and advocacy, dedicated time and resources, and capacity to evaluate the innovation.
Outer context, including informal interorganisational networks and collaboration, intentional spread strategies or formal networks, the wider environment and political directives or mandates.
Implementation and routinisation: this is nonlinear in process and depends on organisational structure, leadership and management, human resource issues, funding, intra-organisational communications, intraorganisational networks, feedback and ability to adapt or reinvent an innovation.
The links between these individual components form an important part of the model. They include linkage at the development stage between the developers and potential users of an innovation, a positive and supportive change agency and effective external change agents.
Key lesson for practitioners and policy-makers
Greenhalgh et al. were ‘struck by the number of studies that had been undertaken without a comprehensive review of the existing relevant research, many of which asked what appeared to be obsolete questions’ (p. 618). 26 For practitioners, the significant point is the multifaceted nature of the diffusion model, which requires alignment of activities and decision-making across a range of institutions. In turn this requires some shared incentives or sense of purpose to sustain it. This speaks to the experience of the CLAHRCs in having to conduct a variety of activities simultaneously and the sense that maintaining forward momentum in each CLAHRC requires a variety of skills, information, and alliances and incentives.
Research use
Nutley et al. identify three models of research use:106
-
Research-based practitioner model
-
In this model, individual practitioners seek out and keep themselves informed about the latest research to inform their decision-making. The origins of this model lie in evidence-based medicine and its focus is on enabling the practitioner to access good-quality research and develop the skill to appraise this evidence critically.
-
-
Embedded research model
-
In this model, relationships between the research and the clinician/manager are mediated by a number of organisational factors. Practitioners rarely engage directly with research findings, and the responsibility for developing and ensuring research-based practice lies with local and national policy-makers and service-delivery managers. The model’s approach depends on the widespread adoption of research-informed guidelines and tools, and it therefore tends to restrict rather than emphasise practitioner autonomy. The guideline movement to some extent reflects this model.
-
-
Organisational excellence model
-
At the core of this approach is a recognition that actions undertaken by individual practitioners are influenced by organisational, procedural and cultural service structures and policies. The focus is on changing the culture and context of the organisation; initiatives to adapt research findings to this context will take place at the local level, relying on partnerships with universities and other bodies to facilitate cross-pollination and the effective use of knowledge. The model contains many parallels to the CLAHRC scheme, and was specifically identified as an important influence by CLAHRC-LNR.
-
Key lesson for practitioners and policy-makers
All three perspectives and models are valuable and they need not be mutually exclusive; rather they offer a range of options to be used and evaluated.
Quality improvement
Quality improvement initiatives are another means through which research finds its way into routine practice. Powell et al. 128 describe five models of quality improvement (Total Quality Management/Chartered Quality Institute, Business Process Reengineering, IHI and rapid cycle change, lean thinking, Six Sigma) and five system-wide multimodel approaches (Jönköping County Sweden, Kaiser Permanente, QUERI, Organising for Quality case successes, IHI’s 100,000 Lives campaign). The models share a set of necessary, but not sufficient, conditions for the successful implementation of change. These are:
-
active engagement of health professionals
-
active participation of middle and senior managers and the support of board members
-
use of different approaches to intervention and allowing sufficient time for prolonged action
-
alignment of the process of implementation with the broader goals of the organisation
-
embedding of implementation as a part of everyday work of all staff.
Information technology support and sufficient training and development also matter.
However, crucially, Powell et al. 128 conclude that there is no one ‘right’ approach. Models should be selected in relation to circumstance and applied flexibly over a sustained period in order to engage staff at all levels and achieve desired outcomes.
Key lesson for practitioners and policy makers
Powell et al. 128 advocate an approach that the CLAHRCs adopted in practice: the use of different models to build a combined approach to fit the specific context. An important test of this approach is the goodness of fit of these combined models to particular cases. Quality improvement also, typically, seeks to integrate a number of processes, much as the CLAHRCs sought to do. Here again the need to balance a multifaceted approach with the need for coherence is apparent.
Collaboration
There are two key features of collaboration models,4 both of which underpin the work of the Canadian Health Services Research Foundation, which was established in 1997 to facilitate evidence-based decision-making in Canada’s health system:43
-
Linkage and exchange between researchers and decision-makers, ‘[Here] the primary motivation for collaboration comes from the demonstration that a major predictor for the application of research to practice is the extent of interaction throughout the research process between the researchers and the practitioners who could potentially use the results’ (p. 2). 4
-
The collaborative, or interaction, model aims to increase the implementation of research by encouraging applied health research that is directly relevant to the health-care system.
-
-
Knowledge brokering – bridging the know–do gap (a component of the linkage and exchange model)
-
Here research use is defined not just in terms of process change but also in terms of changes in understanding. In knowledge transfer there is a perceived need for frequent personal interactions; hence the importance of collaborative working, including the colocation of health-care professionals and researchers,129 and the use of knowledge brokers to bridge the know–do gap. 80
-
Key lesson for practitioners and policy makers
Ongoing linkage and exchange between researchers and decision-makers is widely seen as a crucial component of capacity building: it has been claimed that research funded under this model is four times more likely than that funded by traditional means to be actively disseminated and implemented. 94 This relationship model, with its emphasis on direct personal involvement and knowledge brokering, was an important influence on the thinking behind the CLAHRCs as they were being established.
Appendix 13 Detailed research questions derived from phase 1 of the evaluation
-
How do CLAHRCS fit into the broader translational research and implementation landscape of the NIHR (and other funders) at present, and how might they fit in the future?
-
Is the place of CLAHRCs in the broader translational research and implementation landscape clear? How much co-ordination versus duplication, collaboration versus competition, and sharing, learning and exchange is there between different initiatives (e.g. biomedical research centres, biomedical research units, HIECs, clinical research networks) nationally and locally?
-
To what extent are CLAHRCS focusing on generating new research and to what extent are they translating and implementing existing bodies of research evidence to improve services?
-
To what extent are CLAHRCs a temporary platform for spring-boarding wider-scale change or a longer-term initiative?
-
Are CLAHRCs scalable? To what extent are specific models dependent on disciplinary/health area focus and/or geography? How important is it that CLAHRCs are seen as relating to particular health economies?
-
-
High levels of NHS involvement underpin the CLAHRC ethos and theory of change. What is the real scale of NHS involvement in CLAHRCs, and at what levels?
-
Which elements of the NHS are involved: managers, commissioners, providers?
-
Are CLAHRCs leading to organisational-level changes in cultures and attitudes or only to changes in pockets within organisations and specific individuals?
-
How can CLAHRCs engage NHS managers at the highest and middle levels and ensure their buy-in for CLAHRC activities?
-
Why is this important for sustainability and impact?
-
What is driving NHS interest in CLAHRCs and why?
-
-
What is the impact of different governance and management structures on CLAHRCs’ activities and outputs?
-
What are the distinguishing features of different governance and management arrangements which exist across CLAHRCs?
-
How can dual R&D governance systems (academia and NHS) be managed within a single structure? What are the lines of accountability in CLAHRCs?
-
How important are centralised management and co-ordination platforms (e.g. for financial management, communications, human resources, ethics) for CLAHRC activities?
-
How much of management and leadership activity is centralised rather than distributed across different CLAHRC organisations (and within them)?
-
How important are formal procedures as opposed to informal mechanisms of management?
-
What types of advisory board arrangements exist and how do CLAHRCs use their advisory boards?
-
How can individuals with dual commitments (e.g. to NHS, academia, CLAHRC) be best supported through governance and management arrangements?
-
What suite of key performance indicators is most likely to support learning and accountability?
-
-
-
What levels of operational flexibility do CLAHRCs need in order to deliver on their goals effectively, and how is such flexibility best enabled and nurtured?
-
How much adaptation and change (deviation from original plans) takes place across CLAHRCs?
-
In what areas of CLAHRC activity is there most adaptation, and why? What drives the need for adaptation?
-
How are requisite levels of flexibility and adaptiveness enabled and nurtured in CLAHRCs (in terms of both formal structures and practices and informal behavioural norms)? What roles do absorptive capacities and combinative capabilities play?
-
-
How are effective multistakeholder and multidisciplinary research and implementation teams for service improvement built? What can we learn from the CLAHRC model and what mechanisms are being used to enable this?
-
What are the barriers to cross-organisational cross-stakeholder/multidisciplinary working? What incentives and motivations exist, and what are the enabling mechanisms?
-
How are CLAHRCs contributing to a critical mass of ‘NHS-savvy’ academic researchers and ‘research-savvy’ NHS practitioners?
-
Who are champions of change/boundary spanners in CLAHRCs and what is the scope of their influence on change implementation and service improvement? What roles do these people play? What are some of their traits? What levels in a hierarchy are they from? What do their backgrounds tend to be? How are they identified and nurtured? What skills and mechanisms of influence do they use?
-
How sustainable are the changes CLAHRCs are making and to what extent are they succeeding in embedding a new, more collaborative way of doing things?
-
-
What are the different models of public and patient engagement at play in CLAHRCs? What value has PPI brought?
-
To what extent are patients/the public really involved?
-
How are they involved (through which mix of mechanisms)?
-
At what stages of CLAHRC activity are they involved and what is their role? What value do they bring to addressing the second translation gap?
-
-
How can knowledge and evidence to inform service improvements be best communicated and disseminated to those who need to hear it in policy and practice circles?
-
Who is the audience for CLARHC evidence?
-
What is the diversity of communication, dissemination and engagement channels? (A crucial component of this is the balance CLAHRCs achieve between communicating with and exciting people and managing expectations.)
-
-
What value does a CLAHRC bring to the different stakeholders involved? What does it mean to different parties?
-
To what extent are individual and collective perceptions of value aligned and compatible? How does this influence the way the CLAHRC is evolving and pursuing the vision and goals originally set?
-
List of abbreviations
- AHSN
- Academic Health Science Network
- BITE
- Brokering Innovation Through Evidence
- CLAHRC
- Collaboration for Leadership in Applied Health Research and Care
- CP
- Cambridgeshire and Peterborough
- GP
- general practitioner
- HIEC
- health innovation and education cluster
- HSDR
- Health Services and Delivery Research programme
- HTA
- Health Technology Assessment
- IAPT
- Improving Access to Psychological Therapies
- KTE
- knowledge transfer and exchange
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NPT
- normalisation process theory
- PCT
- primary care trust
- PenCHORD
- Peninsula Collaboration for Health Operational Research and Development
- PenCLAHRC
- South West Peninsula Collaboration for Leadership in Applied Health Research and Care
- PenPIG
- Peninsula Public Involvement Group
- PPI
- patient and public involvement
- QUERI
- Quality Enhancement Research Initiative
- R&D
- research and development
- REF
- Research Excellence Framework